WOMEN'S HEALTH ARTICLES
Item
- Title
- WOMEN'S HEALTH ARTICLES
- extracted text
-
RF_WH_.11_8_SUDHA
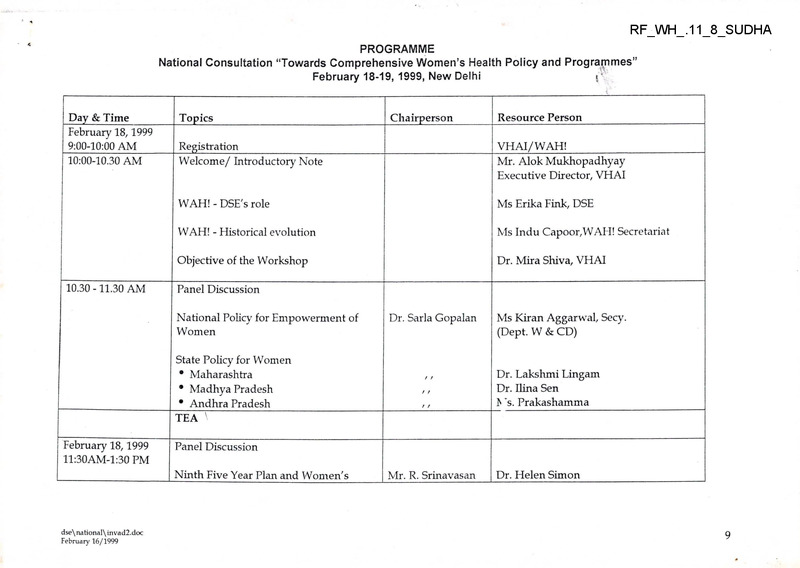
PROGRAMME
National Consultation “Towards Comprehensive Women’s Health Policy and Programmes”
February 18-19, 1999, New Delhi
i‘
Day & Time___
February 18,1999
9:00-10:00 AM
10:00-10.30 AM
10.30 -11.30 AM
Topics
Chairperson
Regis ti’ation_______________
Welcome/ Introductory Note
VHAI/WAH!__________
Mr. Alok Mukhopadhyay
Executive Director, VHAI
WAH! - DSE's role
Ms Erika Fink, DSE
WAH! - Historical evolution
Ms Indu Capoor,WAH! Secretariat
Objective of the Workshop
Dr. Mira Shiva, VHAI
Panel Discussion
National Policy for Empowerment of
Women
Dr. Sarla Gopalan
State Policy for Women
• Maharashtra
• Madhya Pradesh
• Andhra Pradesh
TEA \
February 18,1999
ll:30AM-l:30 PM
Ms Kiran Aggarwal, Secy.
(Dept. W & CD)
Dr. Lakshmi Lingam
Dr. Ilina Sen
F Ts. Prakashamma
Panel Discussion
Ninth Five Year Plan and Women's
dse\ na Honal\ invad2.doc
February 16/1999
Resource Person
Mr. R. Srinavasan
Dr. Helen Simon
9
Health
National Health Policies and
Programmes from women's perspective
Mr. R. Srinivasan
Women's Health Policy
Mr. R. Srinavasan
Dr. Imrana Qadeer
-■
Dr. Sundari Ravindran
Hoar.
2.15 - 3.30 PM
Panel Discussion
Economic Policy & Women's Health
Prof Ranjit Roy
Chowdhury
Drug Policy & Women's Health
Education Policy & Women's Health
3.30 - 5.30 PM
Ms. Kumud Sharma
Dr.Mira Shiva
Prof.. Usha Nayyar
Dr.Vimla Ramachandran
Dr.Y.N. Chaturvedi
Dr.Nirmala Murtv
Dr.Abhijit Dasgupta
Dr.Shanti Ghosh
Dicussion______
TEA___________
Panel Discussion
Reproductive & Child Health Policy &
Programme
Nutrition Policy & Women's Health
Traditional System of Medicine (TSM)
Policy & Women's Health
//
Dr. H. Sudershan
Dr.Veena Shatrughan
Dr.Shanta Shastri
Dr.G.G. Gangadharan
Ms. Philomena Vincent
Discussion
dse\national\invad2.doc
February 16/1999
10
Day & Time
February 19z 1999
9.00-9.30 AM
Topic
____
Mainstreaming Gender in Development
9.30 -11.45 AM
Panel Discussion
Chairperson
Ms. Binoo Sen
Policy
Resource Person
Dr.Sujata Rao
Ms.Sarojini Thakur
'XrG?c)
Ms Mohini Giri
Dr. Padma Seth
Laws Affecting Women's Health (WH)
Ms. Amita Dhanda/Dr.Bharghavi
Mental Health Concerns in WH
Ms Jasjit Purewal/
Ms.Hiti Mahendru
Violence & Women s Health
Dr. Padmini Swaminathan
Occupational Health Hazards of Women
TEA
11:45-1.:15 PM
Panel Discussion
Women & Panchayati Raj Institutions
Ms. Nirmala Buch
h s. Aleyamma Vijayan
District Level Planning for WH
Women and Media
1.15-2.15 PM
Dr. Susheela Kaushik
Dr. Rami Chabra
Ms. Akhila Shivdasa
LUNCH BREAK
11
■ ’-P.dnf-
c
2.15 - 3.45 PM
Training for Women's Health
Dr. Helen Simon
Gender & Power Issues in Medical
Education
Women's Perspective & Gender
Sensitization in Health Care
Ms.Pallavi Patel
Dr. Mira Sadgopal
•r.Thelma Narayan
Ms. Sarojini
Thakore
Ms.Shumita Gosh
Ms.Saulina Arnold
Dr.Srilekha Ray
Dr. Sarla Gopalan
Ms.Renu Khanna
Discussion
3.45 - 4.00 PM
TEA
4.00 - 5.30 PM
Issues for Advocacy
Work
5.30 PM
Conclusion
dse\national\invad2.doc
February 16/1999
Strategy - Group
Dr. Mira Shiva
12
SUPPLEMENT TO MANUAL FOR HEALTH WORKER (FEMALE)
S—33
instructions for filling rIN MONTHLY REPORT FORM
FOR HEALTH WORKERSj (MALE AND FEMALE)
You will complete this form at the end of each month and hand over a copy to your supervisor in the first week of (he next month.
.......... Yo11 wil1 nmintnin one copy in your own file at the sub
centre.
The monthly report form will mdicate the extent of work carried out by you during the month
“'k"‘ (M,">
mltted""',h’ ”” °ry°",
I.
‘l»
reported P, tJe He.S wX
the Repo,, „ het.g !ub.
■nd P',C “d tto m“'h f"
Immunizations
1.
±”y
‘"“’-S
—* ■«<
2.
p™, :»r " «■ “"S
3.
D.P.T. : Enter number of persons given first dose of DPT vaccine during the
given second and third doses of D^acciite^ £
vaccine during the month and
dose of DPT during the month.
Umber glven booster
4.
Poliomyelitis : Enter number of persons given first dose of poliomyelitis vaccine
month, number given second and third doses of vaccine during th<
booster dose during the month.
5.
er
Tetanus Toxoid : Enter number of pregnant women ; '
given first dose of T.T. during the month,
and number given second dose of T.T. during the month.
Enter number of persons other than pregnant women given T.T. during the month.
nun’ber of persons given other immunizations and specify which,
6-
H.
Communicable Diseases
I.
Malaria :
1.1 Enter number of fever cases seen during the month.
1.2 Enter number of blood films taken from fever cases during the month.
1.3 Enter number of cases showing blood films positive for malaria parasites.
NOTE : These may include positive films taken during the previous month from fever
cases, but of which the report is received only during the month under report.
1.4
Sh0Wing eaCh type Of SpeCieS Of ma,aria Parasi,e as mentioned in the
ep it of the blood smears, i.e. number of cases showing Plasmodium vivax in the smear,
tber showing Plasmodium falciparum, number showing Plasmodium malariae and
number showing any other Plasmodium.
1.5 Enter number of fever cases given presumptive treatment for malaria by you.
1.6
ianrCMaler"
rad'Cal treatment by ,he Health Assis-
I
MANUAL FOR HEALTH WORKER (FEMALE)
S—34
Smallpox :
2.1 Enter number of cases of fever with rash which you have detected and reported during
the month.
2.
2.2 Enter number of those cases of fever with rash which have been confirmed by the Medical
Officer as cases of smallpox.
2.3 Enter number of cases of smallpox contained during the month.
Cases
Cases of
of Other
Other Notifiable
Notifiable Diseases:
Diseases : Note
Note whether there have been cases of any other noti
fiable diseases in your area during the month and if so, specify which disease and what control
3.
measures have been taken.
TH. Vital Statistics
if Enter the number of live births of male children, female children and total children during
/
2.
the month.
Enter the number of deaths among males in each of the five age groups i.e °-l year, >1-5
years >5-15 years, >15-44 years and >44 years. Enter the number of deaths among females
in each of these age groups, and the total number of deaths in each of these age groups.
3.
S cify the signs and symptoms preceding death wherever the information is available but
especially in age groups 0-1 year and >1-5 years, and among pregnant women.
IV. Family Planning
1. Eruer the total number of eligible couples registered for your area at the end of the month.
NOTE ' " i sum of the total number of eligible couples stated by each of the two Health Wor
kers (Male) of the subcentre in their reports should equal the total number of eligible
couples stated by the Health Worker (Female) in her report.
2.
Use of Family Planning Methods :
area on whom vasectomy was performed during the
2.1 Enter the number of cases from your i
month.
area on whom tubal ligation (tubectomy) was per2.2 Enter the number of cases from your
formed during the month.
i • the
me uuiuwui
2.3 Enter
number vf
of cases from jyour areai in whom the intra-uterine device was inserted
during'the month. Give separate figures for the insertion of Lippes loop and Copper T.
2 4 Enter the number of pieces of Nirodh which were distributed to couples in your area during
the month (either at the subcentre, or by you on your home visits, or by the depot holders).
2.5 Enter the number of diaphragms fitted in your area during the month.
the number of tubes of jelly distributed to couples in your area during the month,
2.6 Enter
2.7 Enter the number of vials or packets of foam tablets distributed to couples in your area
during the month.
2.8 Enter the number of packets of oral contraceptives distributed to couples in your area
during the month.
3.
Depot Holders :
3.1 Enter the total number of depot holders of Nirodh in your area at the end of the month.
3.2 Enter the number of pieces of Nirodh distributed to the depot holders in your area during
the month.
I
SUPPLEMENT TO MANUAL FOR HEALTH WORKER (FEMALE)
V. Maternal,
1.
and
S—35
Child Health
Prenatal care :
1.1 Enter the new cases of pregnancy in the area during the month. Also enter the number
of cases of pregnant women carried forward from the previous month, i.c. all those who
have not yet delivered. Enter the total number of pregnant women in the area during the
month.
1.2 Enter the new cases registered in your area during the month for prenatal care. Also
enter the number of registered prenatal cases carried forward from the previous month,
and the total cases registered.
1.3 The Health Worker (Female) will enter the number of prenatal cases from her whole area
(intensive and twilight) referred to the Health Assistant (Female) during the month.
1.4 The Health Worker (Male) will enter the number of prenatal cases from the twilight area
referred to the HeaUh Worker (Female) during the month.
2.
Intranatal care :
2.1 Enter the number of pregnancies ending in live births, i.e. infants born alive—cases regis
tered (R) and cases not registered (NR).
..2 Enter the number of pregnancies ending in still birth, i.e. infants born dead—cases regis
tered (R) and cases not registered (NR).
2.3 Enter the number of pregnancies ending in abortion, i.e. pregnancy terminating prior
to the period of viability, viz., before 28 weeks of pregnancy.
2.4 Enter the number of pregnancies ending in Medical Termination of Pregnancy (MTP),
i.e. deliberate planned interruption of the pregnancy by the doctor before 28 weeks and
generally before 12 weeks.
In each case enter how many deliveries were conducted by the Health Worker (Female), by
trained dais, by untrained dais, and by other persons, e.g., medical practitioners in the area, or
female relatives. Enter how many pregnant women in the area were referred for delivery to
the PHC'/Hospital.
3.
Postnatal care :
3.1 Enter the number of cases from the area registered during the month for care after delivery.
3.2 Enter the number of ca^es or their husbands who accept a method of family planning during
the first six weeks after delivery.
4.
Infant care :
4.1 Enter the number of new cases of infants (zero to one year) from your area registered
during the month for infant care. Also enter the number of infants carried forward from
the previous month for infant care, and enter the total number of infants registered for
infant care.
5.
Care of pre-school children :
Enter the new cases of pre-school children (one to five years) registered during the month for
child care.. Also enter the number of pre-school children carried forward from the previous
month for child care, and enter the total number of pre-school children registered for child
care.
6. Nutrition :
6.1 Enter the number of cases of anaemia in mothers and in children detected in your area
during the month.
6.2 Enter the number of cases of anaemia in mothers and children referred for treatment to
the PHC during the month.
manual for health worker
Si-36
(female)
6.3 Enter the number of cases of malnutrition in mothers and children detected in your area
during the month.
6/ Enter the number of cases of malnutrition in mothers and children referred for treatment
to the PHC during the month.
6.5 For each of the groups mentioned, (i.e. pregnant and nursing mothers, children zero to
five yea. and family planning adopters to be given iron and folic acid, and children one to
five years to be given vitamin A solution), enter the number of new cases, carried forward
cases and total cases given nutritional supplements (i.e. iron and folic acid tablets, and
Vitamin A solution) during the month.
"
VI.
ONMENTAL SANITATION
1.
-nter the number of wells chlorinated in your area during the month.
2.
Enter the number of soakage pits constructed in your area during the month.
3.
Er er the number of latrines constructed in your area during the month.
4.
Enter the number of kitchen gardens started in your area during the month.
5.
Enter the number of compost heaps supervised by you in your area during the month.
Enter the number of smokeless chulhas installed in your area during the month.
7.
Enter the number of water pumps out of order in your area at the end of the month.
VU. Treatment of Minor Ailments
1.
2.
Enter the number of persons treated by you for various ailments, e.g., headache, cuts, burns,
etc. in the five age groups, i.e. 0-1 year, > 1-5 years, >5-15 years, >15-44 years and >44 years
in your area during the month.
Enter the number of persons from your area referred by you for treatment either to the PHC
or hospital or to a local practitioner.
VIH.
Health Education Activities
Enter the number of group meetings, mass meetings and film shows held by you during the month
and under the remarks column enter any relevant remarks, e.g., as to the topic of the meeting, atten
dance, reaction of the audience, etc.
IX.
Home Visits
1
Enter the total number of home visits made by you during the month.
2.
Enter the number of families visited by you during the month.
NOTE : You may visit the same family more than once during the month so that the number of
home visits paid will be more than the number of families visited during the month.
Other Activities
Mention any other activities carried out by you during the month, e.g., base-line survey of a
village, assistance in vasectomy camps, assistance in spraying operations, involvement in special
X.
campaigns for control of communicable diseases, etc.
Enter the date of completing the report, your name, designation and the name of your subcentre and PHC.
I
(
K
i
ANNEXURE 9.2
ANTEN^ AL CARD
Date of Enrolment
Age
PHC :
Card No.
Name
PREVIOUS PREGNANCIES :
Number
Pregnancy
Delivery
♦
♦
Puerperium
*
Result
Subcentre
Village No.
Address
Use abbreviations HISTORY OF PAST ILLNESS (TB, STD,
♦N = Normal
Heart, Diabetes, Abdominal Operation, etc.)
Place of
delivery By whom
C = Complicated
Home/
delivered
**L = Liveborn
Hospital
S = Stillborn
A = Abortion
LABORATORY TESTS :
Add (P) for
premature
c
tfl
2
tn
Z
H
O
>
z
d
£
"fl
o
73
TETANUS IMMUNIZATION
Date
Whether put on Iron tablets
PRESENT PREGNANCY : First day of last menstruation :
General Nutrition :
Anaemia :
Tongue :
Teeth :
Pyorrhoea :
Breasts :
Varicose Veins :
Bowels :
Institutional delivery recommended :
Reason for recommendation :
S
ra
>
YES/NO
Expected date of delivery
a
*
o
73
*m
73
Heart :
Lungs :
Liver :
Spleen :
Vomiting :
Oedema :
Vaginal discharge :
Bleeding :
M
2
>
S'
I
Contd.
Obs trie Examin tk is
Date
C*/H
Height
I
Weight
Urine
Hb.
B.P.
Week of ■ Fundal
Height
gestation
Presentation
Engaged-Free
Foetal
movements
Oedema
OO
>
%
♦C=Clinic
H=Home
■ Progress notes : Progress, complications, advice, drugs & diet supplements - treatment etc. given :
Signature
•n
o
X
Date :
TO
f
X
o373
7?
M
75
Delivery by PHC I 1 Subcentre CZZ]
Premature
Abortion IZ3
END OF PREGNANCY : Full Term
Dai I 1
Others (specify)
Mother : Alive I I
Died during labour 1 I Child : Alive I I
Still born
Died immediately after birth
POST NATAL EXAMINATION : (6 weeks after delivery) : Breasts, abdomen,
and child.
Family Planning adopted :
Card closed : Date :
Nirodh
Diaphragm
IUD
Sterlization |
Hospital E3
perineum, pelvic organs, lactation, general health of mother
| Others
(Mark the appropriate box.)
Signature
’ll
W
g
Pl
ANNEXURE 9.3
DELIVERY CARD
No.:
PHC
Subcentre
PREVIOUS PREGNANCIES
No.
Result
♦
Nat-re of
pregnancy
PN |—|
only
Date of
enrolment
Village No.
Name
A. N.
'ard No.
best ieFisetsssam joizj
Indiv. No.
Age
Nature of
delivery**
ANTENATAL CARE : By this PHC
other qualified |
c
■T3
| none
m
2
m
Z
BIRTH ATTENDANT (signature, designation)
Birth attendant called (day, hour)
In-patent, admitted (day, hour)
arrived
left
O
discharged
>
31
Z
d
£
General appearance
o
50
State of membranes
Show or vaginal bleeding
X
ra
I
|
>
qX
Week of gestation
o
5
MEDICAL EXAMINATION
50
nT
ra
2
>
•S*L = Liveborn
S = Stillborn
A = Abortion
LL = Liveborn
twins,
etc.
Add P for prematurity
**N = Normal
C = Complicated
Date and Signature
C/2
Contd.
L
LABO JR
Day
Hour
rwiiMi
i'emp.
Pulse
Urine
Contractions
intervals/
duration
Lie-
sentation
Enga
ged,
free
Foetal
heart
i
■cations, treatment (drugs).
Rectal or vaginal examination if necessary
Co i
z
c
o
75
s
SUMMARY OF LABOUR
MODE OF DELIVERY :
Other
£
Day
Hour
Onset of labour
o
Normal
Delivery of placenta
Spontaneous I
Complete
Delivery of membranes :
Complete
1
----
Rupture of membranes
assisted
incomplete I
incomplete I
I
I
Beginning of second stage
2
Delivery of child
rrt
Delivery of placenta
and membranes
Injury to mother
Abnormal blood loss I
75
m
I
Total time of labour
Contd.
(
THE BABY
LivebornO Stillborn
Sex
Birthweight
.
Medical care of baby
^raaraassE.
«s»- tjsssujbc
Eye propbylax's
Condition : Asphyxia; spina bifida, anencephalus, clubfoot, cleft palate/lip, polydactyly, etc.
co
C
PUERPERIUM
•xj
^3
FT}
Date
Temp.
z
zH
Date
4 2 -
Fundal height
41 o 8
6
4
2
Co
-
40 o -
8 6 -
O
Cm
z
14
>
I
12
10
39 o -
6
8 6 -
4
38 o -
37 o Z
8 6 -
38
q
o
5«
8
-
8
6
4
2
*TJ
x
o
2
5
Symphysis pubes
50
*n'
m
-
Z
>
r
«
Pulse
Lochia
Urine
Contd.
I
Child
Mother
"Date”*
or
plications, treatment, advice
rogress, oi p!
♦
Progress, complications, treatment, advice
Signature
g
z
C
•n
o
73
Condition on discharge
Condition on discharge
X
tn
POSTNATAL EXAMINATION 6 weeks after delivery (breasts, abdomen, perineum, internal examination, lactation, general health
of mother and child)
o
*
tn
73
Family Planning adopted : IUD I
I
tn
Nirodh
Diaphragm
died during labour
Cause of death :
Mother
Sterilization
Others
r
tn
Mother was alive 6 weeks after delivery
died within 6 weeks after delivery
L I
Unknown I ~1
Survival of liveborn child (ren)
after delivery (Twin)
7 days after : Alive
□□
[Alive
dead [—|j
dead
dead O
I I
[Alive
dead I
28 days after : Alive
O
dead
Child
Card closed date :
Signature
*C or H (Clinic or Home)
k
|]
SUPPLEMENT TO MANUAL FOR HEALTH WORKER (FEMALE)
S—43
ANNEXURE 9.4
CHILD CARD
PHC
Subcentre
Child Card No.
Mother’s Card No.
Name :
Religion :
Male/Female :
Number of brothers :
Date of birth :
Number of sisters :
Birth order :
Name of father :
Birth attendant :
Occupation :
Birth weight :
Name of mother :
Date of enrolment :
Occupation :
Address :
Milestones
Immunization® Date Date Date
Diseases
Yes* Age
Yes£ Age
Holds head up
Measles
Sits
Chickenpox
Smallpox
Examng.
of scar
Revaccination
Smallpox
B.C.G.
Crawls
Diphtheria
Teething
Whooping Cough
Stands without support
Typhoid fever
ED
Examng.
of scar
D.P.T.
Keratomalacia
Walks without support
Speaks syllables
(Triple)
D.T.
Marasmus
Feeding :
Kwashiorkor
Typhoid
Fed on breast milk
Poliomyelitis
Supplement introduced EZ]
Others (specify)
Milk
Pulscs/Cereals
Laboratory examinations—Dates & results
Fruits/Vegctabies
Breastfeed stopped
Eats family food
EZJ
Family Planning Status of Parents :
♦Mark x/in the box if the milestone is observed and give the age in months.
£Mark y/in the box if the child suffered from the disease and give the age at which it suffered.
©Enter the date on which the inoculations were given and dates of examining the scars.
Mention if the parents are practising F. P. If so, the method. If not the action taken.
This card should be maintained from birth to five years of age.
Contd.
S—44
Femember
to examine
the
following
MANUAL FOR HEALTH WORKER (FEMALE)
♦
Date
C/H
Height
in cm
Weight Findings-diagnosis-advice & treatment
in kg
Fontanelle
Eyes
Fars
Nose
Throat
Mouth
Teeth
Feeding
Bowels
Nutrition
Skin
Muscles
Clands
Genitals
Walk
Speech
Cleanliness
aess
F. . Status
of parents
I
*C—Centre
H—Home
Contd.
SUPPLEMENT TO MANUAL FOR HEALTH WORKER (FEMALE)
S—45
CHILD CA-RD---- CONTINUATION CARD
Remember
to examine
the
following
V-
Fontanelle
Eyes
Ears
Nose
Throat
Mouth
Teeth
Feeding
Bowels
Nutrition
Skin
Muscles
Glands
Genitals
Walk
Speech
C' uanliness
Illness
F.P. Status
of parents
*C—Centre
H—Home
♦
Date
C/H
Height
in cm
Weight Findings-diagnosis-advice & treatment
in kg
1
I'l
s-
MANUAL FOR HEALTH WORKER (FEMALE)
ANNEXURE 10.1
House
EHHble
Couple Number
Number
ELIGIBLE COUPLE
Name of Husband (H)
Name of Wife (W)
Age
Address
Number of living
children
H
M
u
F
W
(I)
(2)
(3)
(4)
(5)
(0
(7)
I
I
I
S—47
SUPPLEMENT TO MANUAL FOR HEALTH WORKER (FEMALE)
REGISTER
Age of Pregnant.
youngest novv
child
with sex Yes No
(8)
(9)
Whether using i. If yes,
family pan
method
ning method (s) used
ii. If no,
Yes
reasons
No
(10)
(U)
Remarks
Date
(12)
(13)
Obser
vations Date
Obser
vations
(15)
(16)
(14)
■
S—48
MANUAL FOR HEALTH WORKER (FEMALE)
INSTRUCTIONS FOR MAINTAINING ELIGIBLE COUPLE REGISTER
The Eligible Couple Register is intended to keep a record of all currently married women
between the ag:s of 15 to 44 years. The objectives of the Eligible Couple Register are :
i.
To find out the eligibility of the couples for family planning.
11.
To identify the priority groups of couples for various methods in order to approach
them for motivation and ultimate adoption of the method.
iii.
To follow up the acceptors of the various family planning methods in order to find
out about the regularity of use, satisfaction or dissatisfaction with the method, and
complaints as a result of the use of the method.
i
/
I
In this Register particulars of all the currently married women in the age group 15 to 44 years
should be entered. The missing information should be collected during the course of the follow
up of contacts. During these visits the particulars collected earlier may also be verified.
Absence of the wife to visit her parental home, or the husband for employment in another
place, constitute only a temporary separation. In such cases the spouse present should be inter
viewed. Guests and casual visitors to the house should not be interviewed and should not be re
corded in this register.
At the time of conducting the initial survey, three copies of the Eligible Couple Register
should be prepared village-wise, of which one set should be kept by the Health Worker (Male),
One should be given to the Health Worker (Female), and one should be kept at the Primary Health
Centre. Additional pages should be left blank for entering future additions to the eligible couple
list. A separate Eligible Couple Register should be kept for each village for easy reference.
i
The Eligible Couple Register should be updated at least once a year.
Column 1 : Eligible couple number : This should be a running number starting from one (1)
‘ the village where survey is undertaken. For instance if there are 250 couples in a village, the
k .her will start from 1 and end at 250. If there are more than one couple in the house, where the
wife’s age is between 15 to 44 years, each couple should be given a separate number and the
rticulars of all the couples in the house should be entered separately, one line of the register being
allotted to each couple.
Column 2 : House number : If the houses have already been numbered by the panchayat for
the malaria programme, the existing number of the houses should be recoided. If the houses aic
not numbered, all the houses should be serially numbered. These numbers should be painted on
small iron plates, which should be fixed on the right-hand upper corner of the main door frame of
inch house. In case iron plates are not available the number should be painted in fast colour
on the right-hand upper corner of the door. The same number should be entered in this column.
Column 3 : Name of Husband) Wife : The name of the husband along with the name of the
should be given in this column. The name of the husband should be written above the line
ar^
u of the wife below it. If the husband has more than one living wife staying with him, her
r.. jc should also be entered below the first wife’s name.
■
C. ./< 4 . Address : The full address indicating the street, lane and village should be entered.
T-- - -’’ess should be complete so as to facilitate the location of the house in subsequent visits for
follow-up.
Column 5 : Age of Husband) Wife : In this column, the age of the husband should be entered
in complete years above the line and that of his wife below it.
SUPPLEMENT TO
MANUAL FOR HEALTH WORKER (FEMALE)
S—49
Columns 6 and 7 .• Number of living children : The number of living children, male and female,
should be entered irrespective of the fact whether or not they are living with the couple. If the
person has marricu more than cnce, the number of living children from all marriages should be en
tered and the fact of two or three marriages should be given in the remarks column. If the hus
band has more than one wife living with him, the number of children from the second wife should
also be mentioned separately against her name.
Column 8 : Age of youngest child with sex : The age of the youngest child should be entered
in years and months and the sex of the child may be indicated by ‘M’ for males or ‘F’ for females
after the age. For instance, if the age of the youngest child, who is a boy, is found to be three years
4
and four months, it should be written as : 3-|2_M
Column 9 : Pregnant now 'Yes' or 'No' : The entry should be ‘Yes’ or ‘No’ according to
whether 05. not the wife is reported to be pregnant.
Column 10 : Whether using family planning method(s) : The entry should be ‘Yes’ or ‘No*.
Column 11 ; If the reply to W is ‘Yes’, it means that the wife/husband is sterilized, or the wife
is fitted with an IUD, or the couple is using some other method. This fact should be indicated by
the following abbreviations :
(1) Vasectomy
V
(2) Tubectomy
T
(3) Intra-utcrine device
IUD
(4) Nirodh (condom)
N
Foam tablet
FT
(5)
(6) Jelly/Cream
J
(7) Diaphragm
D
(8) Safe period or rhythm
R
(9)
Withdrawal
W
If the reply to column 10 is ‘No’, it means that the couple is not using any method and, there
fore, the reason(s) should be indicated in brief (for the investigator's guidance only). The reason(s)
for not using family planning methods may be of the following types : (i) sterility, (ii) wanting a
child, (iii) ill health of husband or wife, or (iv) husband away for long period.
she
Column 12 : Remarks : In this column any relevant observations, not covered elsewhere,
be recorded.
Columns 13 and 15 : Date : The date along with the month and year on which a suosequent
visit for follow-up is made, should be entered.
Columns 14 and 16 : Observations : After the completion of the Eligible Couple Register, the
couples should be followed-up at regular intervals. Observations with regard to regularity of use
of a method, difficulties in use, complications as a result of the use, and other problems of the couples
should be noted in this column. Observations such as ‘Neither of the spouses found at home’,
‘4 iouse locked’, ‘Loop expelled’, ‘Discontinued using Nirodh’, ‘Changed method’, etc.,
which may be found on subsequent visits should also be recorded here. Any other observation
not covered in previous columns may be entered here, e.g., if any advice or method is given; if one
of the spouses is sterilized, the date of sterilization; if an IUD is fitted, the date of insertion; if
separated, the date of separation; if one of the spouses has died, the date of death.
S—jO
MANUAL FOR HEALTH WORKER (FEMALE)
NOTE : If a family has shifted from the area, the serial number of the family in column 1
should be circled. The fact that the old family has vacated the house should be
mentioned in the remarks column. In case a new family has occupied the vacant
house, the entry of the new family should be made after the last entry in the Eligible
Couple Register and a new serial number should be assigned. In order to facili
tate cross reference, the serial number of the new family should also be indicated
in the remarks column against the old family. For instance, the family living
in house number ‘X* at serial number 19 has left the area and a new family has occu
pied the house and has been entered at serial number 507. The entry in the remarks
column against serial number 19 will read as follows :
‘Family left the area. Particulars of new family occupying house number ‘X*
given at serial number 507’.
1
SUPPLEMTs r TO MANUAL FOR HEALTH WORKER (FEMALE)
S—51
ANNEXURE 11.8
FORMS A, B AND C FOR VITAMIN A DEFICIENCY PROPHYLAXIS
PROGRAMME
Form A :
.C
REGISTER OF BENEFICIARIES UNDER THE VITAMIN ‘A’ DEFICIENCY
PROPHYLAXIS PROGRAMME
SI.
No.
Date of
Regis
tration
Child
Card
No.
Name
(1)
C2)
(3)
(4)
Address Age Date of Administration Remarks Initials
of the
1 2 3 456789 10
worker
(5)
(6)
(7)
(9)
(8)
I
Form 8 : STOCK REGISTER OF RECEIPTS AND ISSUES OF VITAMIN
o
‘A’ SOLUTION
Date
Receipt
Issue
Balance
Remarks
Initials
(I)
(2)
(3)
(4)
(5)
(6)
MANUAL FOR HEALTH WORKER (FEMALE)
S- -52
PROPHYLAXIS AGAINST BLINDNESS IN CHILDREN
VITAMIN ‘A’ DEFICIENCY
Form C :
19
eport for the month ending
CAUSED BY
for the State of.
Statement of Beneficiaries
Category
Age of children
(years)
No. covered during
the month
Progressive total
for the year
Remarks
(1)
(2)
(3)
(4)
(5)
i
i
I
1-2
(I) Children
given
1st
2-3
3-4
i
4-5
(Total 1-5 yrs.)
1-2
(2) Children
given
2nd dose
2-3
3-4
4-5
(Total 1-5 yrs.)
(2)
Position Regarding the Receipt and Issue of the Drug
!
. -ling Mance
o the 1st day of the
nth in mill'htres
(1)
Receipt during
the month in
millilitres
Issued during
the month in
millilitres
(3)
(2)
On hand on the last
day of the month in
millilitres
(4)
Remarks
(5)
♦
j
Age break-up of children may be given. If the break-up is not available then the total children
in 1-5 years age group should be given.
Place
Signature
Date
Designation
I
S—53
SUPPLEMENT TO MANUAL FOR HEALTH WORKER (FEMALE)
J
ANNEXURE 11.9
I
J
FORMS A, B AND C FOR NUTRITIONAL ANAEMIA PROPHYLAXIS
PROGRAMME
Form A :
SI.
No.
REGISTER OF BENEFICIARIES UNDER THE NUTRITIONAL ANAEMIA
PROPHYLAXIS PROGRAMME
Card
No.
(2)
(1)
Date
of
enrol
ment
Name
(3)
(4)
Age
Category
Mother Child
(5)
(6)
(?)
Family
Planning
accep
tor
Date of Re
cessa marks
tion of
treat
ment
(8)
(9)
(10)
)
I
Initials
of
worker
I
(H)
!
I
i
Form B :
STOCK REGISTER OF IRON AND FOLIC ACID TABLETS
Date
Receipt
Issue
G)
(2?
(3)
Balance
i
Initials
■
(4)
(5)
I
ik J
I
I
I
I
MANUAL FOR HEALTH WORKER (FEMALE)
S—54
Form C :
PROPHYLAXIS AGAINST NUTRITIONAL ANAEMIA AMONG MOTHERS
AND CHILDREN
Report for the month ending
(D
£
• ’ .*
'■'h
19
'i
for the State of
Statement of Beneficiaries
SI.
No.
Category of
beneficiaries
(2)
1.
Mothers
2.
F.P. cases
No. on
1st day
of the
month
No. of
cases
enrolled
during
the
month
No. of
cases
dropped
during
the
month
No. of
cases
remain
ing at
the end
of the
month
Progres
sive
total for
the year
(3)
(4)
(5)
(6!
(7)
Remarks
•:
(8)
1
t
■IUD
Tubectomy
1
Others
3.
Children
der 5
years of
age)
i
3
4.
1
Position of Receipt and Issue of the Drug
O :mng balance
on the first day
of the month
Receipts during
the month
Issues during
the month
On hand on
the last
day of the
month
Remarks
(1)
(2)
(3)
(4)
(5)
>•
1' .i'.
■
L
Signature
Date
Designation
• _
MGIPLP(FBD)-101/M of H*FW (ND)/77------ 22-11-78------- 25,000
■
■uJ
APPENDIXES
A—1.3
1 enema can with tubing, connector, clamp and rectal tube
18. Plastic mackintosh (1 metre square)
19. Plastic apron
20. Soap dish with soap
21. Towel
22. Nail brush
23. Torch
24. Safety pins
25. Baby weighing spring scale
26. Containers for drugs :
17.
\
i. 5 plastic bottles of suitable sizes with water-tight caps for liquid medicines
ii. 1 amber coloured bottle with dropper cap
iii. 3 plastic containers of suitable sizes for tablets, powders and ointments.
27. Kit box
28. Medicines :
For internal use
i. Ergot tablets
ii. Mist chloral hydrate
iii. Injection methyl ergometrine maleate (methergen).
For external use
iv. Antiseptic lotion
v.
vi.
vii.
viii.
ix.
x.
Liquid paraffin
Mercurochrome 2 %
Methylated spirit
Silver nitrate eye drops 1 %
White vaseline
Zinc boric dusting powder.
APPENDIX 2
LIST OF ALLOPATHIC MEDICINES USED AT SUBCENTRE LEVEL
2.1
MEDICINES TO BE CARRI^p BY HEALTH WORKER (FEMALE)
For Internal Use
1. Aspirin, Phenacetin and Caffeine (APC) tablets
2. Belladonna and phenobarbitone tablets
3. Chloroquine tablets
4. Dried aluminium hydroxide tablets
5. Ergot tablets
6. Iron and folic acid tablets
7. Magnesium hydroxide tablets
8. Magnesium sulphate
9. Mepyramine (Antihistamine tablets)
10. Mist bismuth kaolin
11. Phthalyl sulphathiazole tablets
12. Piperazine citrate tablets
13. Rehydration powder
14. Tincture codeine co.
15. Triple-sulpha tablets
16. Vitamin A solution
For External Use
17. Antiseptic lotion
18. Benzoic salicylic ointment
19. Benzyl benzoate emulsion
20. Ephedrine nasal drops
21. Gentian violet 2%
22. Mercurochrome 2 %
23. Methyl salicylate liniment
24. Potassium permanganate crystals
25. Silver nitrate eye drops 1 %
26. Sulphacetamide eye and ear drops 10%
27. Sulphanilamide skin ointment
28. Sulphonamide dusting powder
29. Tetracycline eye ointment
30. White vaseline
Reagents
31. Benedict’s qualitative reagent
32. Acetic acid 5%
2.2
MEDICINES TO BE KEPT AT SUBCENTRE
For Internal Use
1. Biphenium hydroxy-naphthoate granules
2. Calcium gluconate tablets
3. Liquid paraffin
4. Mist, alkaline
5. Mist, carminative
6. Mist, chloral hydrate
7. Mist, sedative expectorant
8. Multivitamin tablets (A, B, C, D)
I
1
A—2.2
MANUAL FOR HEALTH WORKER (FEMALE)
9.
10.
Prochlorperazine tablets (emidoxyn)
Syrup ferric citrate
11. Vitamin C tablets
12. Injection methyl ergometrine maleate (methergen)
For External Use
13. Boric acid powder
14. Calamine lotion
15. Methylated spirit
16. Tincture benzoin co.
17. Tincture iodine
18. Zinc boric dusting powder.
SUPPLEMENT TO MANUAL FOR
HEALTH WORKER (FEMALE)
ANNEXURE 4.1
HOUSEHOLD AND FAMILY RECORD
General Information
I.
1.
House No. :
2.
Village :
3.
Name of PHC :
4.
Block :
5.
District :
6.
State :
7.
Name of head of family :
8.
Religion :
9.
Scheduled Caste/Scheduled Tribe :
10.
SI.
No.
19.
11.
Name
of
family
member
12.
Rela
tion
ship
to
head
of
family
Source of income :
13.
14.
Age
Sex
Non-vegetarian >—.
(fish or meat) —
|
18.
Re
marks
per month
19.2 casual employment :
19.3 self employment :
Rs.
Rs.
per month
per month
Rs.
per month
Dietary habits of family :
Partly vegetarian 1
(eggs)
17.
Occu
pation
Rs.
19.5 Barter payment :
Purely vegetarian
16.
Edu
cation
19.1 regular employment :
19.4 Total
20.
15.
Mari
tal
status
S—2
II.
MANUAL FOR HEALTH WORKER (FEMALE)
Immunization Status
1.
SI.
No.
2.
Smallpox
3.
B.C.G.
Pock Pri Revac 1st Booster 1st
marks mary cinat
vac ion*
cina
tion
(2.1) (2.2) (2.3) (3.1) (3.2) (4.1)
4.
D.P.T.
5.
Poliomyelitis
2nd Boos 1st 2nd Boos
and ter
and ter
3rd
3rd
7.
6.
Other
T.T.
(specify)
in
pregnancy
1st 2nd
(4.2) (4.3) (5.1) (5.2) (5.3) (6. 1) (6.2J
* Within the last 3 years
III.
Maternal and Child Health
1. Mother :
1.1 No. of times pregnant :
1.2 Pregnant at present :
1.3 If yes, duration of pregnancy
1.4 Presence of anaemia :
1.5 Under treatment for anaemia :
Yes
No
weeks
Yes
Iron and folic acid :
Yes
Yes
Other :
Mild
1.6 Presence of malnutrition : Absent EZJ
1.7 Under treatment for malnutrition :
Yes
2. Children (0-5 years) :
2.1 Presence of anaemia :
2.2 Under treatment for anaemia :
Yes CZI
Iron and folic acid :
Yes I |
Yes
Other :
Mild F I
2.3 Presence of malnutrition : Absent
2.4 Getting nutritional supplements : Vitamin A solution
Yes □□
Yes O
Other :
No
CZJ
No
No
Severe
No
No
No
No
Severe i
:
No
No
I
SUPPLEMENT TO
S—3
MANUAL FOR HEALTH WORKER (FEMALE)
Family Planning
IV.
1. No. of living children : Male
2. Age of last child :
3. Couple eligible for family planning :
4. Use of Family Planning Methods :
SI.
No.
Family Planning
Methods
Ever
used
Yes
(2)
(1)
Female
Years
Yes
Period
of use
Presently
using
(4)
(5)
Total
Months
ZJ No
Discon
tinued
Since
when
Reasons
for dis
conti
nuing
(6)
(7)
(8)
No
(3)
4.1 Vasectomy
4.2 Tubal ligation
4.3 Intra-uterine
device
4.4 Oral contraceptive
4.5 Condom (Nirodh)
4.6 Diaphragm
4.7 Jelly
4.8 Foam tablets
4.9 Other
4.10 No method used at present
4.11 No method ever used
4.12 Remarks :
V.
Environmental Sanitation
1.
House :
I 1
f I
Reason
Reason
1.1 Pucca : with thatched roof
without thatched roof
1.2 Kutcha : with thatched roof
without thatched roof
1.3 No. of rooms :
2.
Smokeless chulha used :
Yes
3.
Water supply :
3.1 Community supply
3.2 Source :
Tap
3.3 Source : Sanitary
3.4 Storage of water :
Pump |
4.
Sanitary
No
|
|
|
Household supply CZJ
Well I | Other (specify)
Insanitary QU
Insanitary | |
Excreta disposal :
4.1
Household latrine
Communal latrine Q
4.2 Type of latrine : latrine with water seal I I
latrine without water seal | |
bucket latrine | |
other (specify)
4.3 Sanitary | |
Insanitary
No latrine |
facilities
|
/
MANUAL FOR HEALTH WORKER (FEMALE)
5.
6.
Sullage water disposal
5.1 Soakage pit :
5.2 Kitchen garden :
5.3 Open drain :
Yes
Yes
Yes
No
No
No
EZI
Sanitary
Sanitary
Sanitary
□□
Insanitary
Insanitary
□□ Insanitary
EZJ
Refuse disposal :
6.1 Method :
6.2 Sanitary
composting
| |
1 1
Insanitary
burning
tipping
7. Livestock and poultry :
7.1 Livestock kept on the premises :
7.2 Maintenance and housing of livestock :
7.3 Poultry kept on the premises :
7.4 Maintenance and housing of poultry :
Yes
I—I
Sanitary I I
Yes
Sanitary | |
No
I—I
Insanitary
No
O
Insanitary I I
VI. Communicable Diseases
SI. No.
Disease
(1)
(2)
1.
Tuberculosis
2.
Leprosy
3.
Trachoma
4.
Malaria
5.
Filariasis
6.
Sexually transmitted
diseases (specify)
Date :
Name of persons in
household known to
be suffering from
the disease________
(3)
Under treatment Treatment dis
continued
since when
since when
(4)
Name of the Health Worker :
Designation :
Subcentre :
PHC :
(5)
supplement to
manual for health worker
(female)
HOUSEHOLD AND FAMILY RECORD FOLLOW-UP SHEET
Date of follow up
I.
General Information
10 to 18. Change in
family members :
II.
Immunization
2 to 7. Change in
immunization status :
2. Smallpox
3. B.C.G.
4. D.P.T.
5. Poliomyelitis
6. T.T.
7. Other (specify)
III.
Maternal and Child Health
1.2 Wife pregnant :
Yes
No
IV.
Family Planning
3. Couple eligible for
family planning :
Yes
No
4. Family Planning method
presently used :
4.1 Vasectomy
4.2 Tubal ligation
4.3 Intra-uterine device
4.4 Oral contraceptive
4.5 Condom (Nirodh)
4.6 Diaphragm
4.7 Jelly
4.8 Foam tablets
4.9 Other
4.10 Nil
I
MANUAL FOR HEALTH WORKER (FEMALE)
S—6
Date of follow up
V.
Environmental Sanitation
Change in environmental
sanitation :
1. Housing
2. Smokeless chulha
3. Water supply
4. Latrine facilities
5. Sullage water disposal
6. Refuse disposal
7. Livestock and’ poultry
VI.
Communicable Diseases
Change in persons in house
hold suffering from follow
ing communicable diseases :
1. Tuberculosis
2. Leprosy
3. Trachoma
4. Malaria
5. Filariasis
6. S.T.D.
Remarks
Signature
SUPPLEMENT TO
S—7
MANUAL FOR HEALTH WORKER (FEMALE)
INSTRUCTIONS FOR COMPLETING HOUSEHOLD
AND FAMILY RECORD
This form is to be filled in for each household in your area during the initial or base-line
survey. The information is meant to give you a comprehensive picture of each family—its socio
economic status, the size of the family, the health of the family members, and the environmental
conditions in which the family lives.
A family unit consists of the husband, his wife and children. Besides the family unit, other
relatives, e.g., an aged parent or an unmarried brother or sister, who are permanently residing in
the house, are also included in the household. If a married son or daughter or a younger married
brother or sister continues to reside in the house with his or her spouse and/or children, a separate
form should be filled for each family unit under the same household number. For example, if
there are three family units in household No. 77, there will be three Household and Family Record
Forms numbered 77A, 77B and 77C, and on form 77A a note will be entered: ‘See forms 77B-77C*.
I.
General Information
1. Enter the house number if it has already been numbered, e.g., by the malaria survey.
If there is no number, mark your own number on each house and use this number in your record.
2-6. Enter the name of the village, the location of the PHC which covers the area, and the
block, district and State in which the PHC is situated.
7. Enter the name of the husband.
8. Enter the religion of the family, e.g., Hindu, Muslim, Christian, Sikh, Jain, Parsi, Neo
Buddhist, etc. If the husband and wife belong to different religions, mention, e.g., Hindu (H)/
Muslim (W).
9.
Scheduled Caste/Scheduled Tribe : Strike off whichever does not apply.
10. & 11. Enter all the members of the family unit starting with serial number 1 as the
husband (head of the family), then the wife, and unmarried children. Add any other relatives (not
forming separate family units) who are permanently residing in the household.
12. Enter the relationship of each family member to serial No. 1, i.e. wife, daughter, brother,
mother, father-in-law, etc.
13. Mention age in years or, if below two years, in years and/or months.
able, mention date of birth.
Wherever avail
14.
State whether Male (M) or Female (F).
15.
State whether Married (M), Single (S), Widowed (W) or Divorced (D).
16.
State level of education completed up to date, i.e.
Post-graduate degree, e.g., M.A. (Soc.).
ii.
Graduate degree, e.g., B.Ed.
iii.
College level, e.g., 1st Year Arts.
iv.
School level, e.g., S.S.C. or 9th Std.
17. Mention actual occupation, e.g., farmer, weaver, shopkeeper, teacher, etc. In the case
of a woman who is not earning, mention ‘housewife*. In the case of children attending school or
college, mention ‘attending school’ or ‘attending college’.
i
I
S—8
MANUAL FOR HEALTH WORKER (FEMALE)
18. Remarks : Any relevant remarks may be entered against any particular family member,
e.g., as regards his or her state of health, occupation, impending marriage, etc.
A specimen form may read as follows :
10.
11.
12.
1.
2.
\a!^
3.
So-n
4PahA/iJc
16.
13.
14.
41
A7
SSC
F
75^.
15.
I(d
3
/Z
S
64
F
h/
17.
18.
ScK&trC
Ndi
19. State approximate earnings of the family in rupees per month against one or more of the
types of employment listed.
19.1
Regular employment : e.g., those in service or holding regular jobs with a monthly
salary, such as teachers, clerks, factory workers, etc.
19.2
Casual employment : e.g., those who arc daily wage labourers, porters, etc.
19.3
Self employment : e.g., those who have their own business such as shopowners,
farmers, potters, etc.
19.4
Total : The total income of the family in rupees (/>. 19.1, 19.2 and 19.3) is cal
culated.
19.5
Barter payment, i.e. payment in kind in exchange for work, e.g., grain, vegetables,
etc.
20. Check off in the appropriate box whether the family is purely vegetarian, i.e. no eggs,
meat or fish are eaten by any member of the family unit, or partly vegetarian, i.e. the diet consists
mainly of cereals, vegetables and fruit but eggs are eaten by some or all members of the family unit,
or non-vegetarian, i.e. meat or fish are eaten by some or all members of the family unit.
11.
Immunization Status
1.
2.
The same serial numbers as in Section I should be used.
Smallpox :
2.1 Pock marks : Mention whether or not the individual has pock marks (state ‘yes’
or ‘no’).
2.2 Primary vaccination : Indicate whether or not primary vaccination has been given
as ‘yes’ or ‘no’ and, where available, mention the date. Check for scars of primary
vaccination and note if they are seen.
2.3
3.
Revaccination : Note whether or not the person has been revaccinated within the last
three years and mention ‘yes’ or ‘no’.
B.C.G. vaccination :
3.1 First dose : indicate whether given or not (‘yes’ or ‘no’) and, where available, mention
approximate date.
SUPPLEMENT TO
3.2
4.
MANUAL FOR HEALTH WORKER (FEMALE)
S-9
Booster dose : Indicate whether given or not (‘yes’ or ‘no’), and, where available,
mention approximate date.
Diphtheria, Pertussis and Tetanus (Triple) vaccination :
4.1 First dose : Indicate whether given or not (‘yes’ or ‘no’) and, where available, men
tion approximate date.
Second and third doses : Indicate whether given or not (‘yes’ or ‘no’) and, where
available, mention approximate date.
4.3 Booster dose : Indicate whether given or not (‘yes’ or ‘no’) and, where available,
mention approximate date.
5. Poliomyelitis vaccination :
5.1 First dose : Indicate whether given or not (‘yes’ or ‘no’) and, where available, mention
the date.
5.2 Second and third doses : Indicate whether given or not (‘yes’ or ‘no’) and, where
available, mention the date.
5.3 Booster dose : Indicate whether given or not (‘yes' or ‘no’) and, where available,
mention the date.
Tetanus
Toxoid in pregnancy :
6.
6.1 First dose : Indicate whether given or not (‘yes’ or ‘no’) and, where available, men
tion the date.
6.2 Second dose : Indicate whether given or not (‘yes’ or ‘no') and, where available, men
tion the date.
6.3 Booster dose : Indicate whether given or not (‘yes’ or ‘no’) and, where available,
mention the date.
4.2
7.
Other :
Indicate any other immunization which the individual may have had during the
last 12 months, e.g., Typhoid, Cholera, etc., and, where available, mention the date.
Maternal and Child Health
III.
1.
2.
Mother :
1.1
Mention the total number of pregnancies of the wife, including those that ended
in live births, still births, spontaneous or induced abortions. If the wife is pregnant
at the time of survey, the present pregnancy should also be included.
1.2
Check of! whether or not the wife is pregnant at present.
1.3
If yes, mention the period of pregnancy in weeks.
1.4
Check off whether or not the wife is anaemic as judged by the colour of the con
junctiva, lips and nails. If haemoglobin estimation has been carried out, note the
haemoglobin level.
1.5
1.6
Check off whether or not the wife is receiving iron and folic acid tablets or any other
treatment for anaemia.
Check off whether malnutrition is absent or present and if the latter, whether mild or
severe. Presence of malnutrition would include any of the symptoms, viz., cracks
at the corners of the mouth, red glossy tongue, presence of rickets or osteomalacia, etc.
1.7
Check off whether or not the wife is receiving treatment for malnutrition.
Children (zero to five years), i.e. from birth up to and including the 5th birthday :
2.1
Out of the total number of children aged zero to five years in the family unit, include
in each box the number who have anaemia and the number who do not.
S—10
MANUAL FOR HEALTH WORKER (FEMALE)
2.2
Include in the appropriate box the number of children who arc under treatment for
anaemia (i.e. either receiving iron and folic acid tablets or syrup, or any other treat
ment), and the number who are not.
2.3
Include in each box the number of children who do not have malnutrition and the
number who have mild or severe malnutrition. The presence and degree of mal
nutrition may be gauged by measuring arm circumference.
Include in the appropriate box the number of children who are getting nutritional sup
plements (vitamin A solution or other nutritional supplements) and the number who
are not.
Family Planning
2.4
IV.
1.
Enter in the appropriate box the number of male, female and total living children.
Note the age of the youngest living child in years and months.
3. Note whether or not the couple is eligible for family planning, i.e. they are currently
married and the wife is between 15 and 44 years of age.
4. Against each method of family planning, note whether or not the method has ever been
used and if so, the duration of use, and whether it is still being used or has been discontinued, Jf
the method has been discontinued, note since when it has been discontinued and the reason for
discontinuing.
A specimen form may read as follows :
4. Use of Family Planning Methods :
o
SI. No.
Family Plan
ning Method
Ever used
Yes
(1)
(2)
Vasectomy
Tubal ligation
Intra-uterine
device
4.1
4.2
4.3
I YZ|
Diaphragm
Jelly
Foam tablets
Other
V.
(5)
Disconti- Since
nued
when
I
No method used at present
No method ever used
Remarks : yo
| (3
(6)
Reasons
for dis
conti
nuing
(8)
(7)
□
E]
4.6
4.12
(4)
(3)
Oral contraceptive I I
Condom (Nirodh) |v/~|
4.10
|4.11
Presently
using
No
4.4
4.5
4.7
4.8
4.9
Period
of use
‘—I
as
Reason:
Reason :•
Environmental Sanitation
1. Housing : Check off whether pucca : i.e. built of bricks, wood, cement or stone, with or
without a thatched roof, or kutcha : i.e. built of mud, straw, tin sheets, etc. with or without a
thatched roof.
SUPPI.FMFNT 1O
MANUAL FOR HEALTH WORKER (FEMALE)
S—11
Mention the number of rooms (separated by walls or partitions).
2.
Smokeless chulha used: Mention whether or not the house has a smokeless chulha.
NOTH : If tho household is using some other form of fuel, c.g., gobhar gas or a kerosene stove,
make a note of this.
3.
Water supply :
3.1
Check off whether the household has its own water supply or uses the common water
supply of the village.
3.2
Check off whether the water used by the household comes from a tap, pump, well
(tube well or ordinary well) or other source (specify whether a pond, river, reservoir,
canal, etc.).
Check off whether the source of water supply is sanitary or insanitary.
3.3
3.4
4.
Check off whether the water is stored by the household in a sanitary or insanitary
way.
Excreta disposal :
Check off whether the household has its own latrine, or uses a common latrine or has
no latrine facility at all.
4.2 If there is a household or common latrine, check off whether the latrine is one with
a water seal, one without a water seal, or a bucket latrine. If it is of some other type,
specify.
4.3 Check off whether the latrine used by the household is sanitary or insanitary.
4.1
5.
Sullage water disposal :
5.1 Check off whether or not the household has a soakage pit and if so, whether or not it
is sanitary.
5.2 Kitchen garden : Check off whether or not the household has a kitchen garden and
if so, whether or not it is sanitary.
5.3 Open drain : Check off whether or not the household has an open drain to carry off
sullage water and if so, whether or not it is sanitary.
6.
Refuse disposal :
6.1 Check off the method of disposal of refuse, whether by composting, burning, or
tipping.
6.2 Note whether the method used is sanitary or insanitary.
7.
Livestock and poultry :
Check off whether or not livestock are kept on the premises.
If yes, check off whether or not the maintenance and housing of livestock are sani
tary.
7.3 Check off whether or not poultry are kept on the premises.
7.4 If yes, check off whether or not the maintenance and housing of poultry are sani
tary.
7.1
7.2
VI.
Communicable Diseases
If there are any persons in the household suffering from tuberculosis, leprosy, trachoma,
malaria, filariasis or specific sexually transmitted diseases, note in column 3 the name of each person
suffering from the disease, in column 4 whether the patient is under treatment and if so, since when,
and in column 5 whether the patient has discontinued treatment and if so, since when.
NOTE : If any particular disease is endemic in an area and information on the incidence
of the disease is required, it can be added to section VI.
S—12
MANUAL FOR HEALTH WORKER (FEMALE)
Fill in the date on which the household has been interviewed, your name and designation,
and the location of your subcentre and PHC.
HOUSEHOLD AND FAMILY RECORD FOLLOW-UP SHEET
In order to keep your records up to date it is necessary to enter any new information as regards
general socio-economic conditions, immunization status, use of family planning methods, inforn. ion regarding MCH, environmental sanitation and communicable diseases of the households
in your area. A follow-up sheet is provided with columns in which at regular intervals, e.g.,
monthly or three monthly, you can enter any new information gathered since the time of the base
line survey. All information collected on a particular visit is entered in one column. The numbers
for e?ch item are the same numbers used in the Household and Family Record.
I.
General Information
10-18. Any changes in the household since the last visit are recorded, e.g., the birth of a baby,
or the death of a family member, or the marriage of a son or daughter, brother or sister. In the
last case, if the newly married couple is staying in the household a separate form with the same
household number will be prepared.
II.
Immunization
2~7. Note if any more family members have received any of the immunizations listed.
III.
Maternal and Child Health
1.2 Note whether or not the wife is pregnant.
IV.
Family Planning
3.
4.
V.
Note whether or not the couple arc still eligible for family planning.
Note what family planning method is presently used by the couple.
Environmental Sanitation
1-7. Note any change in housing, the acquisition of a smokeless chulha, any improvement or
deterioration in source of water supply, the construction of a latrine, the construction of a soakage
pit, or the commencement of a kitchen garden, and a change in method of refuse disposal or in the
maintenance and housing of livestock and/or poultry.
Communicable Diseases
1-6. Note if any family member previously suffering from tuberculosis, leprosy, trachoma,
malaria, filariasis or specific sexually transmitted diseases has completed or has interrupted treatment,
or if any other family member is now suffering from one of these diseases.
VI.
Enter any pertinent remarks and your signature.
S—13
SUPPLEMENT TO MANUAL FOR HEALTH WORKER (FEMALE)
ANNEXURF. 4.2
VILLAGE RECORD
I.
General Information
1.
Name of village:
3.
Block_____
6.
Distance from subcentre:
7.
Distance from PHC‘
8.
Date of commencement of
9.
Date of completion of
2.
4. District:
5. State:
base-line survey:.
base-line survey:
10.
Total number of households;
12.
Population according to religious group :
Others
13.
11.
Muslim
Hindu
Total number of families:
Christian
Sikh
Total
Population according to age and sex :
SI. No.
Age group
Male
Female
Married
(13.1)
(13.2)
(I)
0-1 year
(2)
>1-5 years
(3)
>5-15 years
(4)
>15-44 years
(5)
>44 years
(6)
Total
14.
Subcent rc:
(13.3)
Total
Unmarried
(13.4)
(13.5)
Number of couples according to number of living children :
SI. No.
Number of living children
(14.1)
(14.2)
(I)
0
(2)
1
(3)
2
(4)
3
(5)
4
(6)
5
(7)
6 and above
(8)
Total
Number of couples
(14.3)
I-
■
.
S—14
MANUAL FOR HEALTH WORKER (FEMALE)
15. Private medical practitioners :
Qualifications
Address
SI. No.
Name
System
(15.1)
(15.2)
(15.3)
(15.4)
(15.5)
SI. No.
Name
Trained
Untrained
Address
(16.1)
(16.2)
(16.3)
(16.4)
(16.5)
16. Dais :
17. Community leaders and Community Health Workers:
SI. No.
Name
(17.1)
(17.2)
Occupation/Designation
(17.3)
Address
(17.4)
18. Depot holders (Nirodh) :
SI. No.
Name
Sex
(18.1)
(18.2)
(18.3)
Occupation/Designation
(18.4)
Address
(18.5)
19. Community resources and agencies (Youth Club/Mahila Mandal/Bhajan Mandal/Young
Farmers’ Club/Drama Club/Balwadi/Cooperative, etc.)
SI. No.
Type of resource
Address
(19.1)
(19.2)
(19.3)
I
. j"
supplement to
manual for health worker
Facilities
Address
(I)
(2)
(3)
20.1
Primary Schools
20.2
Secondary Schools
20.3
Post Office
20.4
Police Station
20.5
Panchayat Office
20.6
Places of Worship
20.7
Other (specify)
SI. No.
21.
Communications :
21.1
Village connected to subcentre by :
pathway
bus route |
other (specify)
]
Village connected to PHC by :
road
21.3
S—15
Public facilities :
20.
21.2
(female)
bus route
train
waterway 1
other (specify)
I
Nearest telephones available :
Address
(1)
21.4 Village electrified :
II.
Family Planning
1.
Total number of eligible couples
Telephone number
(2)
Yes
No EZ1
S—16
MANUAL FOR HEALTH WORKER (FEMALE.)
Couples presently using family planning methods :
2.
SI.No.
Method
(1)
O)
Number of couples currently practising with number of living
children
0
(3)
2.1
Vasectomy
2.2
Tubal ligation
2.3
Intra-uterine device
1
(4)
2
(5)
3
(6)
4
(7)
5
(8)
6+
Total
(9)
(10)
Oral contraceptive
2.5
Condom (Nirodh)
2.6
Diaphragm
2.7
Jelly
2.8
Foam tablets
2.9
Other (specify)
2.10
Nil
III.
Immunization Status of Community :
1. Smallpox
Pock Primary
Marks vacci
nation
(2)
(0
3. D.P.T.
2nd Booster
and
3rd
(3)
(I) (2)
_2. B.C.G.
1st Booster 1st
Re
vacci
nation*
(I)
(3)
(2)
4. Poliomyelitis
1st
Booster
2nd
and
3rd
(3)
(1) (2)
* Within the last 3 years.
IV.
Environmental Sanitation :
1.
Housing :
1.1 Pucca : with thatched roof
without thatched roof
1.2 Kutcha : with thatched roof
without thatched roof
2.
Source of water supply :
2.1
Number of wells :
Household :
Communal :
sanitary
insanitary
total
sanitary
insanitary
total
I 1
EH
EH
EE
I I
EZJ
5. T.T. in
pregnancy
2nd
1st
(1)
(2)
SUPPLFMFNT IO
2.2
Number of pumps :
S—17
MANUAL FOR HEALTH WORKER (FEMALE)
Household :
in working order
out of order
total
in working order
out of order
total
Comnuinal :
2.3
Number of ponds/tanks :
2.4
Other sources (specify) :
protected
unprotected
total
protected
unprotected
total
3.
Number of latrines :
(1)
Type
(2)
3.1
Latrine with water seal
3.2
Latrine without water seal
3.3
Bucket latrine
3.4
Other (specify)
SI. No.
Household
(3)
Communal
(4)
Total
(5)
3.5
Number of households with no latrine :
4.
Number of households with soakage pits :----------sanitary
insanitary □□
Number of households with kitchen gardens :
sanitary
insanitary Q]
Number of households with open drains :
sanitary
ihsanitary 1
5.
6.
7.
Number of households with smokeless chulhas :
Date :
Name of health worker :
Designation :
Subcentre :
PHC :
1
S—1ft
MANUAL LOR IIFAI.TH WORKER (I FMAI.E)
VILLAGE RECORD FOLLOW-UP SIIEI I
Date of follow-up
I.
General Information
10.
Total number of
households
11.
Total number of
families
12.
Population
religionwise :
Hindu :
Niuslim :
Christian :
Sikh :
Others :
Total :
13.
Population
agewise :
Male
Female
Married
Unmarried
Male
Female
Married
Unmarried
0-1 year
>1-5 years
>5-15 years
> 15-44 years
>44 years
I
Total
14.
Number of
couples with
living children :
0 child
1 child
2 children
3 children
i
I
I
4 children
Contd.
SUPPLEMENT TO
MANUAL FOR HEALTH WORKER (FEMALE)
S—19
5 children
6 or more
children
Total
15.
Change in private
m c d i ca I practitioners
16.
Change in dais
17.
Change in community
leaders and Community
Health Workers
18.
Change in depot
holders (Nirodh)
19.
Change in community
resources and agencies
20.
Change in public
facilities
21.
Change in communi
cations
II.
Family Planning
I.
Total number of
eligible couples
2.
Couples presently
using family
planning methods
No. of couples currently
practising with number
of living children
0 1 2 3 4 5
6+ Total
No. of couples currently
practising with number
of living children
0 1
2 3 4 5 6-]- Total
2.1 Vasectomy
2.2 Tubal ligation
2.3 I.U.D.
2.4 Oral contraceptive
2.5 Condom (Nirodh)
Contd.
S—20
2.
MANUAI. FOR Hr.Al.TlI WORKER (fEMAT.E)
Couples presently
using family
planning methods
No. of couples currently
practising with number
of living children
0 1 2 3 4 5
6 + Total
No. of couples currently
practising with number
of living children
0 1 2 3 4 5 64 Total
2.6 Diaphragm
2.7 Jelly
2.8 Foam tablets
2.9 Other (specify)
2.10 Nil
111.
Immunization Siatus
of Community
Number of persons
protected by :
I.
Smallpox vaccination :
1.1 Pockmarks
1.2 Primary vaccination
1.3 Revaccination
2.
B.C.G. :
2.1 1st dose
2.2 Booster
3.
D.P.T. :
3.1 1st dose
3.2 2nd and 3rd doses
3.3 Booster
4.
Poliomyelitis :
4.1 1st dose
4.2 2nd and 3rd doses
4.3 Booster
Contd.
SUPPLEMENT TO MANUAL FOR HEALTH WORKER (FEMALE)
5.
S—21
Tetanus Toxoid :
(in pregnancy)
5.1 1st dose
5.2 2nd dose
IV.
Environmental Sanitation
I.
Housing :
1.1 Pucca :
1.2 Kutcha :
2.
Thatched
Not thatched
Thatched
Not thatched
Water supply:
2.1 No. of wells
Household
Communal
Household
Communal
Sanitary :
Insanitary :
Total :
2.2 Number of pumps:
in order :
Out of order :
2.3 No. of Ponds/Tanks :
Protected :
Unprotected :
i
2.4 Other sources :
Protected :
Unprotected :
3.
Number of Latrines :
3.1 With water seal :
Household :
Communal :
Total :
Contd.
S—22
MANUAL FOR HEALTH WORKER (FEMALE)
3.2 Without water seal :
Household :
Communal :
Total :
3.3 Bucket latrine :
Household :
Communal :
Total :
3.4 Other (specify) :
Household :
Communal :
Total :
3.5 Number of households
with no latrine :
4'
Number of households with
soakage pits :
Sanitary :
Insanitary :
5.
Number of households with
k.tvhen gardens :
Sanitary :
Insanitary :
6.
Number of households with
open drains :
Sanitary :
Insanitary :
7.
Number of households with
smokeless chulhas :
Remarks
Signature
Designation
1
suphtment to manual for health worker
(female)
S—23
INSTRUCTIONS FOR COMPLETING VILLAGE RECORD
This form is to be filled in for each village in your area and is a summary record of all the
Household and Family Records filfcd in during the base-line survey of that particular village. The
information is meant to give you a comprehensive picture of the village—the number of households,
the population distribution according to religion, age, sex and number of living children, the health
facilities, community resources and communications available, the health status of the community
and the environmental sanitation in the village. Use these data for preparing maps of your area
indicating the various factors you wish to demonstrate.
I.
General Information
1—5.
Enter name of village, location of subcentre and name of block, district and State in which
the village is situated.
6-7.
Note the distance of the village from the subcentre and from the PHC.
8-9.
Enter the date of commencement and completion of the base-line survey of the village.
10.
Enter the total number of households in the village.
11.
Enter the total number of family units in the village.
NOTE : There may be two or more family units sharing one household.
12.
Population according to religious group : Enter the total number of persons in each religious
group in the village.
13.
Population according to age and sex :
Enter the number of males in each of the five age groups, (Ac. 0-1, >1-5, >5-15, >15-44
and >44 years) and the number of married females and unmarried females in each of these
five age groups. The total (line 6) of the population in these five age groups (Ac. lines 1 to 5)
should tally with the toial (col. 13.5) of the population in the two sex groups (Ac. cols. 13.3
and 13.4).
NOTE : Age group (1) includes children from birth up to and including the first birthday;
age group (2) includes children from the day after the first birthday up to and in
cluding the 5th birthday; and so on.
14.
Number of couples according to the number of living children :
Indicate how many of the couples in the village have no living children, one living child, two
living children, three living children, four living children, five living children, or six or more
living children. Note that the total of these couples may not tally with the total eligible coup
les as some couples may be beyond the age group, (i.e. 15-44 years), specified for eligible
couples.
15.
Private Medical Practitioners :
Enter in series the name of each medical practitioner in the village, the system of medicine
practised, viz., Allopathy, Ayurveda, Homoeopathy, etc., the qualifications held by the practi
tioner, c.g., M.B.,B.S., D.H.M., Ayurvedacharya (B.A.M.S.), etc. and the full address of the
practitioner.
16.
Dais :
Enter in series the name of each dai (indigenous midwife) in the village, whether or not she
has received dais’ training, and her full address.
manual for iifai.th worker
S—24
(female)
Community leaders and Community Hcnltli Workers :
7.
Enter in series the name of each of the community leaders and Community Health Workers
in the village. Enter each person’s occupation and his or her designation if any, r.g., farmer/
numberdar, or shop owner/sarpanch, or teacher. Enter each person’s full address.
1 .
Depot holders (Nirodh) :
Enter in series the name and sex of each person who is serving as a depot holder for Nirodh
in the village, his or her occupation and designation if any (see 1.17) and full address.
•o
Community resources and agencies :
Enter in series the type of community resources and agencies in the village such as the youth
clubs (yuvak mandals), women’s clubs, (mahila mandals), bhajan mandals, vyayam mandals,
young farmers’ clubs, drama clubs, balwadis, cooperatives, etc., with the full address of each.
2r’.
Public facilities :
Enter the address of the various public facilities in the village, i.e. the primary schools, secon
dary schools, post office, police station, panchayat office, places of religious worship, (i.e.
temple, mosque, gurudwara, or church), and any other specific facility which the village may
I
have.
21.
Communications :
21.1
Note whether the subcentre can be reached from the village by pathway, i.e. a beaten
track, or whether there are buses running from the village to the subcentre, or whether
any other form of communication such as a ferry across the river is available.
21.2
Note whether the PHC can be reached from the village by road, whether there are
buses running from the village to the PHC, whether there is a railway station nearby
from which people from the village can go to the PHC, whether there is a ferry service
which can take the people from the village to the PHC or whether there is some other
means of communication with the PHC.
21.3
Note the address of any place in the village or near the village where there is a telephone
and note the telephone number.
21.4
Note whether or not there is electricity in the village.
II.
Family Planning :
1.
Note the total number of eligible couples in the village, i.e. the number of currently married
couples where the wife is between 15 to 44 years of age.
2.
Note the number of couples currently using each of the family planning methods mentioned.
Against each method, enter the number of couples having no living children, one living child,
two living children, three living children, four living children, five living children and six or
more living children. If the couples are using any other method, c.g., withdrawal or rhythm,
enter under 2.9 (Other) and specify. If the couples are not at present using any method at
all and are not sterilized, enter under 2.10 (Nil).
III.
Immunization Status of Community :
Enter the total number of persons protected by :
1.
Smallpox vaccination :
(1) Those showing pock marks.
(2) Those who have had primary vaccination. Note whether the scar is present.
!
SUPPLEMENT TO MANUAL FOR HEALTH WORKER (FEMALE)
S—25
(3) Those who have been revaccinated within the last three years.
2.
B.C.G. vaccination :
Enter separately the number of persons who have received the first and booster doses of
B.C G. vaccine. Note whether the scar is present.
3.
D.P.T. vaccination :
Enter separately the number of persons who have received the first, second, third and booster
doses of Diphtheria, Pertussis and Tetanus (Triple) vaccine.
4.
Poliomyelitis vaccination :
Enter separately the number of persons who have received the first, second, third and booster
doses of poliomyelitis vaccine.
5.
Tetanus toxoid in pregnancy :
Enter separately the number of women who have received the first and second doses of
tetanus toxoid during pregnancy.
IV.
Environmental Sanitation :
1.
Housing : Note the number of pucca houses and the number of kutcha houses. Mention
under each the number of houses with thatched roofs, and without thatched roofs.
2.
Sources of water supply :
2.1 Note the number of sanitary and insanitary household wells and sanitary and insanitary
communal or public wells and enter the total number of sanitary and insanitary wells
in the village.
2.2 Note the number of pumps which arc in working order and the number which are out
of order, and enter the total number of pumps in the village.
2.3 Note the number of ponds or tanks which are protected and those which are unprotected.
2.4 Specify any other source of water supply of the village, e.g., rivers, canals, reservoirs,
lakes, etc., and not? if the source is protected or unprotected. Enter the total number of
such sources.
3.
Number of latrines :
Note the number of household latrines and communal latrines which have a water seal and
those which do not have a water seal, and enter the total number of these latrines in the
village. Note the number of bucket latrines in the households, the number of communal
bucket latrines, and the total number of bucket latrines in the village. Note the number of
any other type of latrine in the village and specify what type is available. Note the number
of households which have no latrine at all.
4.
Number of households with soakage pits :
Note the number of households which have sanitary soakage pits and the. number of house
holds which have insanitary soakage pits.
5.
Number of households with kitchen gardens :
Note the number of households which have sanitary kitchen gardens and the number of
households which have insanitary kitchen gardens.
6.
Number of households with open drains :
Note the number of households with open drains which are in a sanitary condition and the
number of households which have insanitary open drains.
S_ 26
manual for health worker
(female)
Number of households with smokeless chulhas :
Note the number of houses in which there are smokeless chulhas.
7.
Enter the date, your name and designation and the name of your subcentre and PHC.
VILLAGE RECORD : FOLLOW-UP SHEET
From the time.of carrying out the initial base-line survey, many changes take place in a village,
t.g., old people die, children are born, new couples become eligible for family planning advice,, more
couples
children are immunized against the various communicable diseases, and more c*■
;,“ undergo
sterilization, while others change the method of contraception.
In order, therefore, to keep up to date the information obtained during the base-line survey
about each village in your area, it is necessary for you to summarize the available data from the
household and family records at regular intervals, e.g., every six months, or every year, and to enter
this on the village record follow-up sheet. The necessary changes should also be made in the map
of your area. The numbers for each item are the same numbers used in the village record.
Record the date of making the follow-up entry.
General Information :
I.
10.
Enter the total number of households in the village.
II.
Enter the total number of families in the village.
12.
13.
Enter the religionwise distribution of population in the village.
Enter the agewise distribution of population in the village.
Enter the distribution of couples according to the number of their living children.
15.
Enter the names and addresses of any new medical practitioners in the village, or mention
if any practitioner has moved away from the village or died.
Enter the name, address and training received of any new dais in the village and mention if
any of the dais previously listed have moved out of the village, or have died.
4
16.
17.
Enter the name, occupation, designation and address of any new community leader or
Community Health Workers in the village and mention if any of those previously listed
18.
have moved away or died.
Enter the name, sex, occupation, designation and address of any new depot holders estab
lished in the village. Mention if any of the depot holders previously listed have discontinued
functioning as depot holders, or have moved away from the village, or have died.
19.
Enter the name and address of any new organizations set up in the village, or mention if any
of the organizations previously listed have discontinued functioning.
20.
Enter any new public facilities in the village, e.g., schools.
Enter any change in communication between the village and the subcentre and PHC, and any
21
change in telephone numbers.
II.
Family Planning :
1.
2.
Enter the total number of eligible couples up to date.
Enter the number of couples presently using each of the family planning methods listed and
the breakdown of the couples according to the number of their living children.
III.
Immunization Status of the Community
Enter the number of persons protected by smallpox, B.C.G., D.P.T. and poliomyelitis vaccination, and the number of pregnant women immunized with tetanus toxoid.
/
SUPPLEMENT TO MANUAL FOR HEALTH WORKER (FEMALE)
IV.
S—27
Environmental Sanitation :
Enter the current information about the houses, water supply, latrine facilities and number of
houses with soakage pits, kitchen gardens, open drains and smokeless chulhas.
Enter any pertinent remarks and your signature.
i
.
)
i
J
MANUAL FOR HEALTH WORKER (FEMALE)
S—28
ANNEXURE 4.3
MONTHLY REPORT FORM
FOR HEALTH WORKERS (MALE AND FEMALE)
Subcentre :
PHC :
Month :
I.
Immunizations
1.
Smallpox :
1.1 Primary vaccination :
1.2 Revaccination :
2.
B.C.G. :
2.1 1st dose :
2.2 Booster :
3.
D.P.T. :
3.1 1st dose:
3.2 2nd and 3rd doses :
3.3 Booster :
4.
4.2 2nd and 3rd doses
Poliomyelitis : 4.1 1st dose :
4.3 Booster :
5.
Tetanus toxoid: 5.1 to pregnant women : 5.1.1
1st dose :
5.1.2 2nd dose :
5.2 to others :
6.
Other immunizations (specify )
IL
Communicable Diseases
1. Malaria
1.1 Fever cases
1.2 Blood films taken
1.3 Positive cases
1.4 Type of species
1.4.1 P. vivax
1.4.2 P. falciparum
1.4.3 P. malariae
1.4.4 Any other
1.5 Presumptive treatment given
1.6 Radical treatment given by Health
Assistant (Male)
2.
Smallpox :
2.1 Cases of fever with rash detected
and reported
2.2 Cases confirmed by M.O. as smallpox
Number
S—29
SUPPLEMENT TO MANUAL FOR HEALTH WORKER (FEMALE)
2.3 Cases contained
3.
Other Notifiable Diseases :
3.1 Number of cases of other notifiable diseases (specify)
SI. No.
Disease
Number of cases
(1)
(2)
(3)
3.2 Action taken for control :
in. Vital Statistics
1.
No. of births :
1.2 Female :
1.1 Male :
1.3 Total :
0-1 yr.
(1)
2.
>1-5 yrs. >5-15 yrs.
—(3)
(2)
> 15-44 yrs.
(4)
>44 yrs.
”(5)
No. of deaths :
2.1 Male :
2.2 Female :
2.3 Total :
3.
Signs and symp
toms preceding
death :
3.1 Male
3.2 Female (not
pregnant)
3.3 Female
(pregnant)
IV.
Family Planning
1.
Total number of eligible couples registered at end of month :
2.
Use of Family Planning Methods :
2.1 Vasectomy : No. of cases on whom vasectomy was performed during
the month :
2.2 Tubal ligation (tubectomy) : No. of cases on whom tubal ligation was performed
during the month :
Total
(6)
S—30
MANUAL FOR HEALTH WORKER (FEMALE)
2.3 Intra-nterine device : No. of cases in whom IUD was inserted during the month :
Lippes loop :
Copper T :
2.4 Nirodh : No. of pieces distributed to couples during the month :
2.5 Diaphragm : No. of pieces fitted during the month :
2.6 Jelly : No. of tubes distributed to couples during the month :-------------------2.7 Foam tablets : No. of vials/packets distributed to couples during the month :
2.8 Oral contraceptives : No. of packets distributed during the month
3.
:
Depot holders :
3.1 Total number of depot holders of nirodh at end of month :
i
3.2 No. of pieces of nirodh distributed to depot holders during the month :
V.
Maternal and Child Health
1.
Prenatal care :
1.1 No. of cases of pregnancy :
New :
Carried
forward :
Total :
1.2 Number of cases registered for
New :
prenatal care :
Carried forward :
Total :
1.3 No. of cases referred to Health Assistant (Female) :
1.4 No. of cases referred to Health Worker (Female) :
NOTE : 1.3 to be completed by Health Worker (Female)
2.
Ro
1.4 to be completed by Health Worker (Male)
Tntranatal care :
SI. No.
(2)
Type of
Termination
(4)
Delivered by
(3)
Total
No.
Health
Worker
(Female)
(i)
Z1
Trained
Dai
Untrained
Dai
Other
(ii)
(iii)
(iv)
Referred to
PHC/
Hospital
(v)
No. of live
births
R
NR
2,2
No. of still
births
R
NR
2.3
No. of
abortions
2.4
No. of MTP
I
SUPPLEMENT TO MANUAL FOR HEALTH WORKER (FEMALE)
3.
Postnatal care :
3.1 No. of cases registered :
3.2 No. of cases/husbands accepting
4.
S—31
family planning :
Infant care :
New :
4. i No. of cases registered :
Carried forward :
Total :
5.
Care of pre-school children :
New :
5.1 No. of cases registered :
Carried forward :
Total :
6.
Nutrition :
Mothers :
6.1 Number of cases of anaemia detected :
Children :
Mothers :
6.2 Number of cases of anaemia referred to PHC :
Children
Mothers :
6.3 No. of cases of malnutrition detected :
Children :
Mothers :
6.4 No. of cases of malnutrition referred to PHC :
Children :
6.5 No. of cases given nutritional supplements :
(1)
SI. No.
(2)
Nutritional
supplement and
group to which
given
(3)
No. of cases
New
(i)
6.5.1
Pregnant & nursing women
(2)
Children 0-5 years
(3)
Family planning adopters
(1)
Total
(iii)
Iron & Folic acid tablets :
(1)
6.5.2
Carried
forward
(ii)
Vitamin A solution :
Children 1-5 years
VI.
Environmental Sanitation
1.
No. of wells chlorinated
2.
No. of soakage pits constructed :
3.
No, of latrines constructed
4.
No. of kitchen gardens started :
:
.1
!
1
I
MANUAL FOR HEALTH WORKER (FEMALE)
S—32
5.
No. of compost heaps
6.
No. of smokeless chulhas installed :
No. of water pumps out of order :
7.
Treatment of Minor Ailments
VII.
1.
supervised :
No. of persons treated.:
F
2.
1.1
0-1 year :
1.2
1-5 years :
1.3
1.4
5-15 years :
15-44 years :
1.5
44 years :
No. of persons referred
Health Education Activities
VIII.
Total
f
!
1.
Group meetings :
2.
Mass meetings :
3.
Film shows : —
IX.
Home Visits
1.
No. of home visits made during the month :
2.
No. of families visited during the month :
X.
Other Activities (Specify)
Date :
Remarks
F
I
Name of health worker :
Designation :
Subcentre :
I
PHC :
i
APPENDIX 1
SUGGESTED LISI OF CONTENTS OF KU FOR
HEALTH WORKER (FEMALE)
1.1
SUGGESTED LIST OF CONTENTS OF GENERAL KIT FOR HEALTH WORKER
(FEMALE)
1. Manual for Health Worker (Female)
2. Records (health cards, diary)
3. Health education materials on MCH, family planning and nutrition (charts, pamph
lets, IUD)
4. Microscope slides
5. Slide box to hold 10 slides
6. Cleaning cloth for slides
7. Hagedorn needle in spirit bottle
8. Cotton wool—one small packet
9. Gauze dressings
10. 1 triangular bandage
11. 1 roller gauze bandage
12. Adhesive plaster
13. Stick swabs
14. Razor blade
15. Safety pins
16. Pencil
17. Teaspoon (5 ml)
18. Graduated medicine glass
19. 1 pair blunt pointed scissors
20. 1 pair blunt, non-toothed dressing forceps
21. Soap dish with soap
22. Nail brush
23. Nail clipper
24. Towel
25. Plastic sheet
26. Tallquist haemoglobin colour scale and papers
27. Arm circumference scale
28. Clinical oral thermometer
29. Clinical rectal thermometer
30. Spirit lamp
31. Wind-shield
32. Matches
33. Tape measure
34. Contraceptives :
i.
ii.
iii.
iv.
35.
36.
37.
38.
39.
Nirodh packets : 50
Foam tablets : 1 tube
Jelly tubes with applicators : 1
Oral contraceptive packets : 1
2 test tubes
Test tube holder
1 pair artery forceps
De Lee mucus catheter (16 Fr)
Female rubber urethral catheter (16 Fr)
MANUAL FOR HEALTH WORKER (FEMALE)
A—1.2
40.
41.
Cord ligatures
4 cloth or plastic bags (20 cmx 15 cm)
42.
Containers for drugs :
43.
44.
i. 10 plastic bottles of suitable sizes with water-tight caps for liquid medicines.
ii» 3 bottles (one amber coloured) with dropper caps.
iii. 17 plastic containers of suitable sizes for tablets, powders and ointments.
Drugs according to list (see Appendix 2).
Kit bag : light yet strong with compartments, pockets and straps, for carrying drugs,
dressings, instruments, etc.
Additional material to be carried when necessary
1. Syringes and needles :
i. 2 syringes (1x2 ml; 1x5 ml) with hypodermic needles (I packet 23 gauge: I
packet 22 gauge; 1 packet 20 gauge) in sterilizing box.
ii. 2 tuberculin syringes with hypodermic needles (26 gauge 1 cm) in sterilizing
box.
2. Bifurcated needles in container.
3.
1.2
Vaccines :
i. Smallpox vaccine
ii. DPT vaccine
iii. Poliomyelitis vaccine
iv. BCG vaccine
v. Tetanus toxoid
vi. Cholera vaccine
vii. Typhoid vaccine
4. File for opening ampoule
5. Vaccine carrier
6. Vaccine holder
7. Thermos
8. Needle sharpening stone
9. Rubber rings and rubber tubing.
SUGGESTED LIST OF CONTENTS OF MIDWIFERY KIT
1. Sterile cotton wool swabs
2. Sterile gauze dressings
3. Sterile perineal pads
4. Cord ligatures
5. 1 pair blunt pointed scissors
6. 1 pair sponge holding forceps
7. 2 pairs artery forceps
8. 2 syringes (2x2 ml) with hypodermic needles (20 gauge; 22 gauge; 23 gauge) in steri
lizing box
9. Ampoule file
10. Clinical oral thermometer
11. Foetoscope
12. De Lee mucus catheter (16 Fr) with suction bulb
13. Female rubber urethral catheter (16 Fr)
14. 1 pair rubber gloves
15. 2 bowls
16. 1 kidney tray
THE MADHYA PRADESH WOMEN’S POLICY: A STATUS REPOiri
BY
ILINA SEN
Prepared for the
National Consultation Towards
Comprehensive Women’s Health Policy and Programmes
BY
VHAI-WAHI-DSE
Held in VHAI, New Delhi.
February 18-19, 1999
I®
THE MADHYA PRADESH WOMEN’S POLICY: A STATUS REPORT.
ILINA SEN, A 26, HOUSING BOARD COMPLEX, KATORA TALAB,
RAIPUR, M.P.
The process:
The Madhya pradesh policy for women (MPWP) was prepared and
ratified in 1995, in the context of two major developments in the area of
Women’s empowerment, one of them national, and the other international.
The national context was provided by the 73rd amendment to the
constitution and consequent codification of state laws, which provided for
elections to the three tier institutions of the Panchayati Raj with 33 %
reservation for women at each level.This development brought women into
effective politics on a scale and at levels that had never till now been
experienced. Because of the traditionally subservient position that women
occupied in many parts of the state of M.P., this development did not take
place without trauma. In the northern parts of the state,effective
participation of women in Panchayati Raj Institutions (PRIs) was the
hardest to achieve. In the south eastern parts, and in the Chhattisgarh
region, where women traditionally play a more important role in public life,
transition to the new regime was relatively smoother, although even now,
is by no means complete.
The international context to the MPWP was the activities connected with
the culmination of the international decade for women and the Fourth
World Conference of Women at Beijing, in August, 1995. It was the stated
intention of the state Chief Minister to release the MPWP before the
Beijing conference. However, although the document was prepared in time
for it to be ratified by the state Assembly prior to the conference, the
Women and child development Minister of the state who was statutorily
required to sign the document before placing it for discussion in the
Assembly, sat on the file until November, as the entire process of
preparation of the policy draft had bypassed her and had been controlled
directly by the office of the Chief Minister.
':L
The actual preparation of the document was undertaken by a team of senior
state level bureaucrats with the help of an NGO consultant. The team
studied the directives and policies of the different government
departments, and recommended changes in each for inclusion in the
document. The two existing Women’s policy documents, viz., Maharashtra
and Tamil Nadu were also studied in some detail.
Through advertisements in the major newspapers,and letters addressed to
NGOs and Women’s groups, the government invited suggestions on the
proposed policy from the people of the state, and over 200 letters with
suggestions were received in response. After the policy document was
fmlized, there was some dissatisfaction expressed by some NGOs that they
were not part of a consultative process in the finalization of the document.
This was countered by the state government on the ground that the NGOs
were free to give their suggestions in writing. Once the document was
prepared it was circulated to selected women activists and subject
specialists for comments, and was also presented to a large convention of
women members of the PRIs for comments and suggestions.
The Document:
The actual document asserted the government’s commitment to ensuring
equality for women in all walks of life, and to improve their condition in
the political, economic, social and cultural spheres.The broad objectives
were stated to be the evolution of programmes and strategies for women’s
empowerment, ensuring of women’s full and equal participation in social
life, the active promotion of an ideology of women’s equality, and the
provision of positive discrimination where necessary, to fulfill these goals.
The goals of the policy were comprehensive and included protection of
female life, prevention of atrocities on women,and ensuring their visibility
in all walks of life. A twenty point strategy towards these aims was laid
down, and included the revamping of data collection systems to ensure
women’s visibility,acitve support to women in their role as'economic
producers,protection of the girl child, recognition to women headed
households, the upgradation of women’s technical and managerial skills,
and the recognition of women as major stakeholders in the development of
common property resources.
The document includes specific sections on the political, economic, and
physical and social empowerment of women, and these are worth
considering in somewhat greater detail.
The section on political empowerment is built around the achievements of
the state government in holding elections to the PRIs with reservation for
women, and seeks to remove impediments for women’s effective
participation in the PRIs by holding trainings, and through awareness
building.
The section on economic empowerment begins with the recognition that
women will never be strong unless the material basis of their life and
livelihood is strengthened.In the sub-section on women in agriculture, the
government agrees to recognize women as farmers in their own right, and to
reorient extension programmes to cater to the needs of women farmers.In
the agriculture and allied sector
marketing bodies and supportixe
organizations, it asserts its commitment to increase women’s membership to
50 % and above.In the matter of land rights, it proposes to extend co
parcenary rights to women, and to vest at least 50% of the village common
lands in the joint ownership of all adult women of the village for suitable
developmental activity. The document also proposes to streamline credit
flow to women,and to include women in managerial positions in forest co
operatives and tendu leaf collection centres.
Other highlights of the section on economic empowerment are the
proposals to halt female retrenchment from industry, and provide technical
training opportunities for women to facilitate their integration into
industry.The policy includes specific programmes for the social security of
women who have to leave the state as migrant workers.
The section on physical and social
empowerment includes major
recommendations in the areas of health, education, drinking water, and for
the girl child.In the health section the main focus is on strengthening
vertical programmes like ICDS and childhood survival and safe
motherhood, to improve women’s nutritional status and better address their
reproductive health needs.Education for the girl child is declared a priority
area, special
efforts are promised for women victims of violence, safe accomodation for
women in service in remote parts of the state is declared a priority area of
government activity,and alcoholism is recognised as a major contributor to
the violence that women face in domestic and public life.The policy
promises that if over 50% of the women in a village or urban
neighbourhood want a liquour outlet removed, the government would be
committed to removing the outlet within a period of fourteen days.
Finally, no additional financial allocation is made for implementing the
MPWP, but the intention is expressed that with better management of
existing resources, it will be possible to implement the main directions of
the policy .
The Implementation:
Three years later, one can take stock of the extent to which the provisions
of the MPWP have been put into pracitce. A document from December
1997 sums up the status of implementation as at that time.
The state government seems to have demonstrated its commitment to the
MPWP by extending land rights to women .According to a government
order of 1996, the land records of the state are to be amended to include
the names of the wives of men who may have been hitherto registered as
single owners. Older land records are to be brought up to date in this
respect. Girls are given full inheritance rights in land and other property.
The government has also effected a 30 % reservation for women in all
government jobs, and enforced a 10 year relaxation in age requirement as a
form of positive discrimination. Mandatory women’s membership of
cooperative and marketing bodies has been extended to 50%.
Among other measures,pensions of Rs 150/ pm has been announced for
destitute widows, and data collection systems have been instructed to
collect data on women’s work separately from that of men. Women’s co
operative banks have been given priority in document processing,an
expanded ICDS programme has been launched with UNICEF support,
women have been given priority in the drinking water committees of the
panchayts, they are being trained in handpump maintainance.
Post 1997, the major achievement seems to be the constitution of a State
Women’s Commission (SCW)
in 1998, although, since this is not here a
statutory body, the roles and functions of the SCW are yet to be clearly
defined.
An assessment:
Although the MPWP is a fairly broad based document, in actual fact not
too much has been done in terms of achieving the broader goals of the
policy, viz., ensuring women’s full and equal participation in the social and
economic life of the state. It is an of course an open question whether this
can be achieved by executive fiat at all. But even if we do not look at the
fundamentals,we find that while there was extreme alertness in the drafting
of the document, and an effort was made to make it as comprehensive as
possible, the alertness has not been of a similar magnitude in the matter of
implementation.There was a problem of additional resource allocation in the
first place. Having made a comprehensive statement of intent in the draft
document, the government more or less spiked it by definition by inserting
in the final paragraph the clause on no additional resource allocation.
There are some peculiarly circuitous arguments in the document on
achievements of the MPWP referred to above, which is the single
document to date that discusses the concrete realities of the Women’s
Policy. For eg., in the matter of political empowerment, the government
claims to have
demonstrated its commitment in the matter through
ensuring elections with 33 % reservation for women to the PRIs. This is of
course, historically incorrect, as the PRI elections predate the drafting of the
MPWP. There is again the matter of the extension of ICDS services in the
state. This extension of the programme, funded by the UNICEF and the
World Bank, was also pre-negotiated by the major players even prior to the
drafting of the MPWP.Nothing has been done to ease the conditions of
migrant women, and nothing at all to include women in the management
of forests and tendu leaves, except the tokenist membership of joint forest
(JFM) committees.The last again, was at the funders’ (World Bank)
initiative, more thaan anything else. The so called achievements, thus,
appear to be flaky except in the matter of reservation and age relaxation for
jobs.
I n contrast, there are some areas where the the promises have clearly not
been kept.The MPWP bravely promises to remove particular liquor outlets
if over 50 % of the women in a particular locality demand so. A recent
press
release by the excise department reveals that only one outlet has been so
removed since the policy came into effect. Living in Raipur, one is familiar
with the frequent dharnas by the women of the region for the removal and
banning of liquor outlets. This has obviously fallen on deaf ears.
The Digvijay Singh government will go down in history as the greatest
policy maker of all. There has been the Women’s Policy, the Housing
Policy,
the Industrial Policy, and two departmental sponsored editions of the MP
Human Development Report.The current status of the Women’s Policy
indicates however, that
the bureaucracy cannot substitute for the
movement,and that cheap radicalism cannot substitute for political process.
Ik
The Andhra Pradesh Women’s Health Policy:
A Review
By
M. Prakasamma
Paper Prepared for the
National Consultation Towards
Comprehensive Women's Health Policy And Programmes
BY
VHAI-WAH'-DSE
Held in VHAI, New Delhi.
on February 18 - 19, 1999
The Andhra Pradesh Women's Health Policy :
A Review
M. Prakasamma
Professor, Reproductive Health Studies
Indian Institute of Health and Family Welfare
Vengalrao Nagar, Hyderabad
Summary :
Andhra Pradesh announced a Women's Health Policy in 1996. The policy had a
rapid decline. Though this paper does not attempt at a policy analysis, it tries to study and
review the Policy Statement in the context in which it was prepared. The sociopolitical
context in which it was formulated is first reviewed. Developments in the last few years
which influenced the policy are also assessed. The paper also presents the key components
of the Policy statement and assesses their relevance today in the context of later
developments and field realities. Finally some comments are offered on what could be
included in a comprehensive women's health policy and how advocacy for the
comprehensive policy can be mobilized and sustained.
i
1
i
Formulation of the Women's Health Policy in Andhra Pradesh
The Andhra Pradesh Government decided to announce a Policy on Women in the
year 1 995. The combined force of several sociocultural and political changes at that time
influenced the decision. It is therefore appropriate to review the scenario during the last
five years in order to place the development and demise of the Andhra Pradesh Policy on
Women.
**■
1. Political Scenario :
The State Government was once again headed by a new and popular Chief Minister
(Mr. N. T. Rama Rao) in December, 1 994 as a result of the Assembly elections. As promised
during election speeches he introduced prohibition of alcohol in the State immediately
on taking the reins of the Government into his hands in response to the massive movement
against liqour by women in the entire State. Women had become the decisive group in
the change of government. However, in less than a year after assuming office, he was
ousted by his son-in-law, Mr. N. Chandrababu Naidu who became the Chief Minister of
the State in September 1995.
2. Women's movement and developments:
The anti-liquor protest which started in a village in Nellore district in 1 993 soon
became a spontaneous mass movement all over the State. It involved large scale
mobilization and organization of women. Several women's groups and activists soon
joined the movement and helped in providing a direction in order to advocate not only
for anti alcohol laws but for overall gender equality and women's empowerment. The
movement was sustained in coverage and intensity for more than a year. Media and political
parties (TDP and Left parties) supported the voice of the women. Women activities were at
a cross roads with a supportive international environment due to the Cairo Conference
on Reproductive Rights just completed.
The success of the women's movement in the form of a government action and the
introduction of prohibition encouraged women activists and supporters to advocate for a
better deal for women in the State. The Fourth World Conference on Women at Beijing
and the pre and post debates and discussions kept the mood for gender equality and
women's empowerment alive. This was the period of maximum visibility to women and
women's issues due to the media coverage about Beijing and post Beijing meetings and
discussions.
The change of leadership at this time was critical and conducive to the introduction
of a Policy on Women in the State. The leadership realised the importance of women in
perceptions and emotions to rally support to the Government. The factors leading to the
policy on prohibition forced state policy makers to appreciate the importance of the women
voters. The time was perceived to be ripe for pro women policies and programmes, and
several of these were launched.
The 73rd amendment and reservations for women:
According to the policies prior to the 73 amendment women had 9% reservation
in elected bodies in mandal and zilla praja parishads in Andhra Pradesh. As a result of this
2
measure, the elections in 1986 saw two women as Zilla Parishad Presidents in Nizambad
and Srikakulam districts which had a favourable sex ratio to women. During this term
there were also 96 women mandal Praja Parishad Presidents. These women elected leaders
were in power for five years from 1987 to 1992. Even though it was a small beginning,
many of these women gradually became vocal and some of them continued to be active
in politics.
The 73 amendment was introduced and was being debated all over the Country at
this time. As soon the new Government came into power (headed by Mr. .T. Rama Rao),
series of elections to local bodies were held. As a result of the positive political leadership
and the 73rd amendment, one third of the Panchayat members in the March 1 995 elections
were women. A massive women's representation was seen. Many who had participated
actively in the anti-alcohol movement were elected.
There were 14,300 MPTC members and 361 out of 1092 ZPTC members in the
new local bodies. Even though there are several criticisms regarding the role and functioning
of these bodies, it is a fact that several women gained a voice due to this system. In every
district the grass roots base of women elected members and women's leadership increased.
In every district there were an average of 1 515 panchayat members, 21 7 MPTC members
and 8 ZPTC members. In the newly formed Panchayats, there were 6506 women
sarpanches, 364 mandal presidents and 7 zilla parishad chairpersons. Though initially
hesitant, non-vocal dummies of their male family members or political guardians many of
these women came into their own and started exercising more right and responsibility
in the Panchayat system.
gradually
;
The need to consolidate on the broad based grassroots support and gain their
approval continued with the change in the head of Government from Mr. N.T. Rama Rao
’ to Mr. Chandrababu Naidu.The new Chief Minister built on and introduced a series of
measures to bridge the gap between the government and the people. Some of these are:
Government to the People in November,1995 (Prajala Vaddaku Palana); Self reliance and
voluntary work donation in January, 1997 (Shramadan and Janmabhoomi).
Along with grassroots activities policies were being formulated and strategies
designed for overall development in other spheres. The AP State Policy on Women was
the first of these to be introduced. A Steering Committee on Women was formed with well
known women. This Committee took up the matter of formulating a Women's Policy and
several sub committees were constituted to deal with each key issue. The AP Women's
Policy document in released in 1 996.
The Women's Health Policy statement and implementation strategy were part of
this overall Women's Policy. The entire document was presented by the State and opened
for debate and discussion at a State Seminar to which experts from all over the country
were invited.
The policy however had a premature demise due to several problems the foremost
of which have been the flaws within the statement itself and also the gaps between stated
policies and actual intentions. The meeting and agreement among the various stakeholders
was difficult to achieve. The Steering Committee became dysfunctional
3
I
Table - 1: Indicators of Andhra Pradesh in relation to other Major States
Indicator
Crude Birth
Rate
(CBR, 1994)
Total Fertility
Rate
(TFR, 1993)
Crude Death
Rate
(CDR, 1994)
Infant Mortality
Rate
(IMR, 1994)
Couple
Protection
Rate (1991)
Sex
Ratio
(1991)
Males
Females
(1991)
Uttar Pradesh
35.4
5.2
11.0
88
35.5
879
55.73
25.31
19.1
Rajasthan
33.7
4.5
8.9
84
29.0
910
54.99
2044
17.9
Madhya Pradesh
32.8
4.2
11.5
98
40.3
931
58.42
28.85
18.6
Bihar
32.5
4.6
10.4
66
26.0
911
52.49
22.89
18.8
India
28.6
3.5
9.2
73
44.1
927
64.20
39.19
19.5
Orissa
28.0
3.1
11.1
103
41.0
971
63.09
34.68
19.8
Gujarat
27.1
3.2
8.7
64
57.8
934
73.13
48.64
20.2
West Bengal
25.1
3.0
8.3
61
33.7
917
67.81
46.56
19.3
Punjab
25.0
3.0
7.6
53
75.8
882
65.66
50.41
20.4
Maharashtra
24.9
2.9
7.4
54
56.2
934
76.56
52.32
18.9
Karnataka
24.9
2.9
7.8
65
46.9
960
67.26
44.34
19.4
Andhra Pradesh
23.7
2.6
8.3
63
44.3
972
55.13
32.72
18.2
Tamil Nadu
19.0
2.1
7.9
59
57.3
974
73.75
51.33
20.3
Kerala
17.3
1.7
6.0
16
55.6
1036
93.62
86.17
22.0
4
Literacy Rate
Age at
Marriage
I
ANDHRA PRADESH WOMEN'S HEALTH POLICY - THE CONTEXT
^■Overall DevG/(
' VISION 2020
Status of
Women
A.P Women's
Policy
Political
Scenario
Health
Problems
and Services
WOMEN’S
HEALTH
POLICY
Health
Programmes
Andhra Pradesh
Population
Policy
Demographic
Scenario
Socio-economic
Scenario
I
Summary of Andhra Pradesh Women's Health Policy (refer to annexure - 1)
Objectives:
1. To reduce maternal mortality to 1 00 per 1 00,000 live births by 2000 A.D
2. To improve the sex ratio by 1 0 points by 2000 AD
3. To improve utilization of health services by women
Key components of AP Women's Health Policy
1.Family Planning
a) Women's burden of responsibility for birth control shall be reduced: The
implementation strategy focuses on male methods
b) Participatory and informed choice in decisions on birth control for women: The
implementation strategy states that women will be equipped with knowledge to make
decisions.
c) Emphasis on quality rather than on quantity: The implementation strategy talks of
reviews based on quality indicators.
II.Women's Health
a) The girl child and adolescent: The implementation strategy emphasizes the village
wise analysis of cause of death of girls below five years, laws against sex determination,
immunization, sex education, literacy and schooling.
b) Maternal health: Access to maternal services to be improved and strengthening of
midwifery services
c) Reproductive health: All women shall have access to reproductive health services.
There is a special focus on AIDS and women
d) General health of women
111.Referral System
Referral services from village upwards shall be strengthened
IV. Personnel Policies: gender sensitization training to all staff
V. Medical Technology
VI. Women's Health at the Workplace
VII. Women's Participation
Andhra Pradesh Population Policy : The Population Policy was formulated during 1997
and is being disseminated to all sections. The policy has several implications for women's
health and sets the trend in the State regarding women's health (refer to annexure-ll).
Vision 2020 : Swarna Andhra Pradesh: Vision 2020 is a perspective and statement for
overall development of Andhra Pradesh with effective utilization of resources. The vision
was formulated in 1998 and released on 26th January, 1999.
5
Discussion
Adetailed review and retrospective analysis of the Andhra Pradesh Women's Health
Policy document shows
several problems in its conception and design.
It contains
simplistic statements of unrealistic objectives. The policy statements and the strategies for
implementation are internally inconsistent and shaky.
Unrealistic objectives:
The maternal morbidity and mortality has not been studied in Andhra Pradesh just
as in other states of the Country. No accurate figures for maternal mortality are available.
The ones being used are those obtained from national surveys or small localised studies.
Even if the figure estimated by the National Family Health Survey of 1 992 is considered,
the maternal mortality ratio is 470 per 1 00, 000 live births. To set a goal to reduce maternal
mortality to 1 00 within a few years seems extremely unrealistic and hoping for miracles.
The second goal of improving sex ratio by 1 0 points by 2000 AD is also unrealistic.
The sex ratio in Andhra Pradesh, though better than the all India average has been steadily
declining during the last century. To raise the ratio of women to 1 000 men by ten points
would mean taking it from the current 972 to 982 as well as counteracting the steady
decline which has been the trend for a century (refer table below).
Table 2 : Sex ratio of Andhra Pradesh and India
Year
Andhra Pradesh
India
1901
985
972
1911
929
641
1921
993
955
1931
987
950
1941
980
945
1951
986
946
1961
981
941
1971
977
930
1981
975
934
1991
972
927
Just as in the rest of the country in AP also, differential mortality levels for boys and
girls start in infancy and childhood itself due to preferential treatment for boys. Mortality
levels among the 1 to 5 year old children are higher for girls than for boys - 27.6 for girls
and 21.5 for boys. According to NFHS (1992) less number of girls suffering with fever are
6
taken for treatment than boys - 66 for girls and 73 for boys in AR According to the current
sex ratio 9.5 lakh women are missing women in AR according to the current sex ratiof
refer Andhra Pradesh at 50, p. 89).
Internal inconsistencies in the policy
Leaving aside the unrealistic objectives of the Women's Health Policy, one sees
the true goal as one reads the document. The preoccupation with demographic goals and
population control is reflected in the women's health policy. Though the objectives do
not mention population control, when the details of the statement are read one sees that
family planning is the first statement.
This becomes much clearer when one looks at the very first sentence in the
Population Policy of the State. The Chief Minister's Foreword to the Policy starts with,
"Population control remains the most challenging task before our nation and our state
today" In the very next paragraph it is stated, "Fertility reduction is at the heart of the
development of the State" (Govt, of AP, 1997). However statistics clearly indicate that
Andhra Pradesh is a state in demographic transition with declining fertility and mortality
rates and moving towards adulthood. The median age of the population which was
estimated at 22.3 years in 1995 is expected to increase to 32.3 years by 2020. (AP at 50)
The policy is fragmented. Certain components alone are given emphasis. There is
no scope for comprehensive and basic health. No scope is provided for obtaining and a
women's perspective to their health problems.
Here are a few examples of internal inconsistencies in the policy document:
Quality is stated as an essential aspect under the family planning in the document and
not in other areas. Here too, the implementation strategy is vague.
The statement refers to strengthening of midwifery services but the implementation strategy
does not mention this aspect at all
The implementation strategy states th at every case of maternal mortality shall be identified
and analysed but does not provide for strengthening of services to support this.
Ambitious nature of the statement and strategies
It proposes to convert 450 primary health centres in the State to women's health
centres and the visit of a paediatrician and obsterician\gynecologist twice a week. It also
states that women's health groups shall be trained in each of the villages in these PHCs
and that weekly clinics shall be conducted in the villages. It states that there will be a fully
qualified nurse midwife and public health nurse in every mandal
7
I
In summary the AP Women's Health Policy was meant to facilitate empowerment
and gender equality through reduction in maternal mortality, improvement in sex ratio
and facilitate a higher level of utilization of health services. However it did not have clear
cut and concrete strategies for undertaking activities to achieve the stated objectives.
Political will and advocacy campaigns could not be sustained either by the system or the
women's groups. Retrospective analysis reveals theft a comprehensive and pragmatic policy
conceived through a detailed dialogue with women's groups, government departments,
political opinion makers would have laid stronger foundation. As it is, the shaky and
internally inconsistent policy could not be strengthened and nurtured.
The conception and development of the Andhra Pradesh Population Policy soon
took precedence and its formulation, printing and dissemination became the main focus
in the State.
Towards a Comprehensive Women's Health Policy
The role of public policies is to redress the balance in favour of the underprivileged
and marginalized sections, in this case women. The inequalities created by an injust social
system are often corrected by a positive and facilitative policy (World Bank, 1995). A
positive public policy lays the foundation for designing concrete and favourable strategies
for equity, and ensures that these are implemented through regulatory mechanisms. It is
expected that a positive women's health policy formulated by the government would
attempt at redressing the inequitable health services to women and address issues of poor
access and availability of services to women, facilitate their effective utilization and
neutralise over-technical or biased health technology and health services.
What should a comprehensive women's health policy contain? Definitely, clear
policy statements and measurable objectives. Besides, the policy should contain in detail
the strategies for implementation commensurate with the objectives. The tone of the policy
should be towards gender equity and redressal, equal opportunity and measures for
facilitating the availing of that opportunity. It should contain the essential missing links to
make the utilization a reality.
Umbrella of women's health services
Should the emphasis be on maternal health or comprehensive women's health?:
Though women are most vulnerable and require specific and life saving services during
the period of maternity, it is a well known fact that maternal health services have come to
be equated with women's health services in most parts of the developing world. This
concept encourages a narrowing of women's health services to converge at the time of
pregnancy and childbirth and therefore reducing importance to and even neglecting
8
women's general health problems. Even within the maternity phase, women's health
problems are ignored whether they are related to pregnancy or not. What happens then,
to those women who do not enter the maternal phase of the life cycle either because of
problems of infertility or because of being single, widowed? Introducing the life cycle
approach to women's health into the general health care delivery system would be more
appropriate than concentrating maternal health services alone.
Women suffering with tuberculosis, malaria and other disorders require special
attention because of the lower level of nutrition and heavier burden of work. However
though there are national programmesand huge infrastructure for these diseases, no special
attempt is made to coordinate these with women's health services.
A positive and holistic policy for women's health would contextualize maternal
health services within a comprehensive women's health approach. This would take care
of all problems affecting women's health and well-being.
The different issues to be seriously considered for inclusion in a comprehensive
women's health policy are presented below.
Sex differentials in morbidity and mortality
Though infant mortality is lower in female infants as compared to male the mortality
levels are reversed in the toddler and preschool child in Andhra Pradesh, just as in the rest
of India. Child mortality is 28 for girls and 22 for females. There is a higher percent of
undernourished girls than boys (69 for girls and 61 for boys). This needs to be considered
actively in measures to redress the balance of numbers of male and female and 'find the
missing women' in India's population.
Table 3 : Sex differentials on key Indicators
Female
1.
2.
Sex Ratio (number of women per 1 000 men) ___________ 972
a) Infant Mortality Rate
_____________ 69
b) Child (age 1 to 4) mortality rate :
28
3.
Percent of Children under nourished
69
4.
Percent of Children immunised
a) against all 6 diseases
b) against none
5.
1000
__ 78
22
61
44
20
47
61
62
66
59
64
74
73
62
15
Percent of sick children taken to hospital for
a) Diarrhoea
b) Cough and fast breathing
c) Fever
6.
Male
Longevity (in years)
9
Girls are taken for treatment less than boys when they have diarrhoea, cough and
fast breathing or fever. NFHS results for AP show that when attacked with cough and fast
breathing only 62 percent of girls compared to 74 percent of boys are taken for treatment
(NFHS(1992).
Service availability, accessibility and utilization
Accessibility and availability are two critical issues in utilization of health services
by women. Stringent strategies need to be designed for enhancing access to services for
women. All aspects of access need to be considered: time, distance, economic access,
financial access, attitudinal access, social and cultural access and informational or
knowledge access. These become specially important with regard to utilization of services
related to reproductive tract infections, abortions and infertility.
Linkages and collaboration
Most issues related to women's health have social implications with
multidimensional relations. How can age at marriage be raised and at the same time the
fear of parents regarding the safety of their daughters during adolescence period be
alleviated? A linkage needs to be forged between education, rural development and women
and child welfare departments and the health department.
The policy has to clarify positions taken by each department, identify and thrash
out differences, turfs and boundaries, and finally forge strong linkages with common
objectives in order that the policy may be realized.
Work, work place and women's health
Hazardous occupations to women not just because they are the vehicles of the
next generation but because of their own health: smoking, and specially passive smoking
and cooking fuel; beedimaking and working with tobacco need to be seriously considered
and included in the policy. Women's health cannot be separated from women's work
since most women bear a double.burden.
Myths, mysteries and norms about women's health
Perceptions that women can bear pain better and that they have a greater tolerance
for pain because of labour pains, or that pain during menstruation is common and women
and girls should learn to accept it are detrimental to women seeking treatment for their
problems. Another accepted norm is that adolescents girls should be slender leading to
less nutrition at a critical stage of growth of girls. Yet another example is that a pregnant
woman should not gain much weight since she will have a difficult delivery if the child
weighs more. Such perceptions, myths and norms need to be surveyed, assessed and
10
measure taken for devolving them.
Gendered health occupations:
Women health care providers are by virtue of job requirement specially related to
family planning, positioned as antagonists of women, because of their large families, non
acceptance of family planning and non utilization of health services, and non compliance
of treatment and instructions like swallowing the iron and folic acid tablets. This needs to
be addressed and a positive relationship needs to be fostered between the two if the ANM
is to deliver women's health services.
Empowering women health care providers (ANMs) by equipping them with skills
and capacity is necessary if they are to function independently. Gendered occupations
like those of midwives and ANMs have not been getting due support though they have
been burdened with achieving national goals at the field level.
The increasing burden of work of female care providers needs to be rationalized
and they need to be strengthened with technical skill and supportive guidance. Female
health workers should be given the recognition that is their due and adequate remuneration
and career advancement policies should be designed. At the same time the role of the
male health staff needs to be clarified.
Medicalization of women's health :
Women's health and specially maternal health have been medicalized with highly
technical interventions and diagnostic and therapeutic services. Attempts at
institutionalizing childbirth further need to be clearly studied and the reasons for this shift
understood before this is advocated as a policy. Which environment - the home or the
hospital - is conducive to the woman and keeps her options open? Who benefits most by
which option. What type of deliveries or treatments really require hospitalization and
i
higher level treatment? Attempts to keep women's health in women's hands should be
made.
Survey into what women want:
Closely related to medicalization of childbirth is the issue of what women's
perspectives are regarding family planning, abortion services, RTIs, operative interventions,
health care services, maternal health and comprehensive health care. A comprehensive
women's health policy should attempt at understanding these and incorporating them in
the services.
11
Women's health knowledge: Women as primary care providers and also as survivors
have enmassed a vast knowledge of health, health problems and remedial measures.
These should be assessed and incorporated if effective into the health care delivery system.
Nutrition and health linkages health:
It is a well known fact that poor nutrition is the root cause of most of women's
health problems. This leads to the increased episodes of illness among girl children, poor
development in adolescent girls, anemia in pregnant women, nutritional deficiencies
among middle aged women and early menopause in rural poor women. Like the weathering
hypotheses (Sen and Snow, 1 994) the influence of poor nutrition among girl children and
adolescent girls the final malnutrition during pregnancy are incremental and result in high
risk pregnancy and labour.
Burden of gynaecological illnesses:
Most gynaecological illnesses among women are a result of reproduction and
childbearing - prolapse, calcium deficiencies, fistula, infections, cancers and others. These
need to be given special attention while advocating for a policy on women's health.
Advocacy for a comprehensive women's health policy can be planned and carried
out in a sustained and effective manner only if strong proponents can be identified. In the
Indian context, it is the politicians and the media. During the women's movement in
Andhra Pradesh which ultimately resulted in the formulation of Women's policy it was
the systematic supportive stand takemby local widely circulated papers that the moemtum
was built an carried on. It was again political will that decided on a women's policy and
later undermined it by giving greater priority to the population policy and within this to
the demographic goals rather than to women's health.
1I
.
■
•»
12
h
i.
J
References:
Government of Andhra Pradesh, 1996. Andhra Pradesh Women's Policy. Hyderabad:
Government of AP
Government of Andhra Pradesh, 1997. Janmabhoomi Health booklet Hyderabad:
Government of AP *
Government of Andhra Pradesh, 1996. Vision 2020 : Swarna Andhra Pradesh.
Hyderabad: Government of AP
j
Government-of Andhra Pradesh, 1997. Andhra Pradesh Population Policy.
Hanumantharao, V. N.K. Acharya and M.C Swaminathan, 1998. Andhra Pradesh at
50. Hyderabad: Data News Features.
Sen, G and R‘. Snow. 1994. Power and Decision: The Social Control of Reproduction.
Boston: The Harvard school of Public Health.
World Bank. 1995. Towards Gender Equality: The Role of Public Policy. Washington
D.C. The World Bank.
Handbook for elected representatives 1996, APARD (Mana Paripalana Vidhanam,
Telugu).
List of annexures
i.
1. AP. Women's Health Policy, 1996
2. Andhra Pradesh Women's Policy 1996
3. Andhra Pradesh Population Policy, 1997
•A
13
MAHARASHTRA STATE POLICY FOR WOMEN (1994 & 1998):
ANALYSIS OF THE OLD AND NEW DOCUMENTS
Lakshmi Lingam1
The state of Maharashtra brandishes several firsts to its credit. Significant
among these are the legislation regulating sex detection techniques - the
Maharashtra Regulation of the Use of Pre-natal Diagnostic Techniques Act,
1988 and the Policy for Women, 1994. A fresh draft of the policy titled
'New Policy for Women : An Overview’ was released in July, 1998. The
1994 policy document (hereafter referred to as 'old') was prepared by the
Congress Government at the State whereas the 1998 document (hereafter
referred to as new') was prepared by the Shiv Sena- BJP combine
Government at the State. The electoral opportunism of viewing women as a
significant vote bank by both the political parties has to be observed.
The present paper attempts to highlight (a) the salient points of the new
policy document, and (b) the points of agreement or departure from the old
policy document. The significance of the statements in the light of empirical
evidence of women's status in Maharashtra, will be provided at relevant
places.
NEW POLICY DOCUMENT
This document states emphatically that the Government of Maharashtra is
keen on enhancing women's status by empowering them through a special
focus on law, economic programmes, education and health. It is important to
note that nearly 34 Government Orders (GOs)( 15 in 1994; 4 in 1995; 11 in
1996 and 4 in 1997) have been passed that attempt to operationalise the
statements made in the 1994 document. There is no clue about the
implementation of these GOs.
Salient Points in Law
> To set up more Family Courts, in the interim period regular courts to
devote one day in a week to deal will cases of marital discord, divon c.
and so on.
> To deal with sexual harassment at the work place.
1 Reader. Women’s Studies Unit. Tata Institute of Social Sciences . Mumbai.
Draft Paper presented at the VH AI-WAHPNational Seminar on Women. Health & Development', 18-19
February. 1999. New Delhi.
i
> To eliminate upper limit for alimony but fix a lower limit. Further, to
deduct alimony from the salary at source.
Ado change adoption laws to provide natural parenthood to father and
mother.
Salient Points in Economic Programmes
lhe sections under this theme deal with organised and the unorganised
sectors under separate heads.
In the organised sector the points in a nutshell are:
> Continuity of service of working women, who take a break due to
pregnancy and child care.
>• The need to create ease of entry into the labour market by increasing the
age limit for women.
> Creche facilities to be provided in the premises of Municipal schools.
While the earlier two points make good sense, the third point raises several
questions about - what about ensuring creche facilities at the workplace ? or
community based creche facilities which are supported by sectors that hire
women? Many aspects such ‘^declining work opportunities, lack of
unionisation in the organised sector; provision of support structures for
working women, opportunities for training to attain mobility and the like
have been completely left out from the document.
Home based self employment is identified as an important economic
programme for women in the unorganised sector. The document states that
many women :annot go out of their homes, hence the Kama Dhenu scheme
will help them earn while at home. The public and private sectors could
utilise women's skills at home. The statement in tliis section that majority of
women stay at home is empirically incorrect. Only sections of the urban and
rural middle classes are exclusively located at home/private domain.The vast
numbers of poor women and small number of educated pursuing careers are
enmeshed in the public domain. Therefore, this policy priority has a limited
scope.
A Mahila Sahayogini at the district level and Anganwadi functionary and
Maliila Mandals at the village level are seen as focal points to disseminate
information, form self help groups and facilitate economic empowerment of
rural women.
2
In view of the increased involvement of the Anganwadi functionary in
economic programmes over and above women and child health programmes,
the document states that increase in honorarium will be considered.
However, struggles by anganwadi women functionaries for recognition as
workers and payment of salaries in the place of honorarium are ongoing.
Women's multiple work roles; issues of domestic drudgery; unequal sexual
division of labour; technologies that displace women; training and credit
needs; occupational hazards and health; security of a living wage, and so on
are completely missing in the document.
SalieiH Points in Education
Typically the discussion on women's education highlights the positive
benefits of it to women 's self- confidence, increase in age at marriage, to
limit family size and improve chances of employment in the organised
sector.
The sections in this theme focus on:
r Adult education - to focus on personal hygiene, storage of water, use of
toilet, home remedies and symptom identification of primary illnesses,
and property rights of women.The Anganwadi Centre and the Maliila
Mandals will be encouraged to run the adult education centres.
> Girls education will be addressed by providing special tutions to school
drop outs, by extending scholarship to classes 5th and above. Sex
education ^nd hygiene (moral) education to be taught at girls hostels.
Economic aid to be provided to families below poverty line to encourage
the education of their girl children.
> Maliila Mandals and Village Education Committees to collaborate to
ensure the performance of literacy and primary education.
> Technical Education for girls will be encouraged through increase in
seats reserved for girls; girls hostels to be constmcted and scholarships
to be given. Scholarship fund to be raised from industrialists.
The statements on education vouch for the lack of an integrated approach to
women's and girl child education. Issues of quantity and quality of
education, the increasing privatisation of education even at the primary
levels, the irrelevant curriculum, lack of opportunities to maintain reading
3
and writing abilities, the apathetic parental attitude towards girl child
education, sex abuse and violence, have not formed the analytical
background of these formulations.
Salient Points in Health of Women
The health section reiterates the focus on Reproductive and Child Health
components. It highlights the importance of healthy mothers for child's
health and welfare. The points in this section are:
a i o improve male responsibility by providing for paternity leave.
> To evolve a policy to deal with maternal and infant mortality.
> To develop education modules to impart knowledge on factors that
determine the sex of the foetus.
To train traditional birth attendants for healthy and safe deliveries.
1 o focus on mental and physical health of adolescent girls and boys
To impart knowledge of HIV/AIDS, responsible behaviour and to set up
counselling Centres with the permission of parents in schools.
> To impart awareness of HIV/AIDS, STDs to vulnerable women, shim
women, adivasi women, SCs, STs, Dalits and Devdasis.
T^o expand the ambit of ICDS programme to newer districts.
> To impart knowled.Ige on healthy diet through out the life cycle.
The state to take lead in generating a debate about the population
problem.
r To give priority to women headed households in water and sanitation
programmes.
To construct public baths in cities and villages.
To constuct separate toilets for boys and girls in schools.
Despite rhetoric
women’s neaitn
health has to be viewed beyond maternal role,
iHviouc that
inar womens
the policy statements do not depart from old addiction. The RCH
programme, has important new components to be included in tire
constellation of services in Family Welfare Programme. However, women's
health will remain a distant drcam if RCH is not integrated into a
comprehensive health care package which is sensitive to women's status
related issues.
1 he training of traditional birth attendants, important though would only
partially address the issue of untrained attendance at birth. Empirical
evidence indicates that majority of the home births are attended by female
relatives and not even untrained dais. Safe child birth, crisis or distress at
4
childbirth, identifying 'at risk' mothers, benefits of colostrum, healthy infant
feeding practices need to be designated as community issues, just as
drinking water and sanitation.
Issues such as the resurgence of communicable diseases; the support that the
State would provide to HIV positive men and women; rural poverty, male
migration, and STDs/AIDS disease burden in the villages are completely out
of the purview of this document. Maharashtra is considered to the leading
Stale in HIV positive cases. It also has a large single male migrant
population in urban areas and at least tliree male migr ation endemic districts.
COMPARISON OF THE OLD AND THE NEW DOCUMENTS
The old document came in at a time of structural adjustment, globalisation
and liberalisation advanced by the State as inevitable and irreversible. The
document echoed the language of neo- liberalism and utility maximising
individualism through the deployment of women's special economic agency.
The new document emerged on the scene in the post 73rd and 74th
Amendment and the UN Conference on Women, Peace and Development,
held at Beijing. The economic agenda had not changed, though the party in
porver has. However, the social and political context has deteriorated with
dubious constructs of what constitutes national identity, Indian culture,
religion and their representations. Communalism and fundamentalism of all
hues are taking deep roots. Oblivious of this background, the new document
is pitched in a decontextualised terrain, with no reference to the socio
economic and political scenario or the differential positioning of women in
terms of caste, class and religion. The document, in a piece meal fashion,
essentially spalls out a statement of intent in the form of few ideas and
schemes to be implemented in the next two years. The difficulties in
implementation have also been acknowledged in the document, without any
analysis of the reasons.
The common contours of both documents are as follows:
> Both the documents are replete with tenns like 'development', 'welOj /,
'empowerment', providing enabling environment for women, 'womencentredness', 'participation', 'collaboration', etc. Poor women are made
out to be efficient or promising managers of poverty. It is ironical that
the conditions of poverty arc not alleviated, but women are targetted
through schemes to manage poverty.
5
|
|
Issues ol: employment, secure conditions of work, living wage, etc.,
have been replaced in the globalisation context with a significant focus
on efficiency' to be achieved through self-help, self - employment,
entrepreivuership, micro credit and micro entreprise.
y lhe community, village level committees, rnab.ila mandals and women's
groups have been discovered as the change agents. This fits in with the
development sector jargon of democratic decentralisation, role of civil
society, institution building, etc., which facilitate the rolling up of the
State. However, development is increasingly being referred to as a social
issue rather than an economic or political one.
Apart from occasional references to advasi women, dalit women, women
headed households and women from vulnerable groups, the documents
tend to treat women as a homogenous group.
In terms of differences:
> the old document addressed - eliminating violence against women,
ensuring equality through law; improving the economic status of
women; appropriate use of media; increase participation of women in
local sell government and enhancing community participation in
Government activities. The new document focuses only on law,
economic issues, education and health.
X While the old document introduced the concept of 'flexitime' for
oiganisec* sector working women (which received mixed reactions), the
new document did not touch the issue.
1 he nev' document positioned home based self employment as
importair. Ihis makes 'sound economic sense’ in the liberalisation
environment, where production is steadily shifting from the 'public' to
the'private'domain.
CONCLUSION
The policy documents on women seemingly progressive, provide spaces for
lobbying and advocacy at one level but constrain options at another level.
The language of the documents also signify the political culture and
economic priorities of the State. In this paper, an attempt has been made td^'
reve.d the lack of conceptual clarity and empirical correctness of (he
documents, further, the silence with regards to monitoring mechanisms and
indicators either by design or by default, contribute to non assessment of the
policy either by the State or by the women’s movement.
6
)6
Education Policy and Women’s Health
There Are No Linkages
By
Vimala Ramachandran
Paper Prepared for the
National Consultation Towards
Comprehensive Women's Health Policy And Programmes
BY
VHAI-WAHl-DSE
Held in VHAI, New Delhi.
on February 18 - 19, 1999
V
EDUCATION POLICY AND WOMEN'S HEALTH1
THERE ARE NO LINKAGES!
Vimala Ramachandran
Since Independence in 1947, the debate on women’s education was centred on the
“universal good” of education for men and women, role of education in fighting
obscurantist practices and in modernisation and the importance of education in India’s
march towards equality. In the 1970s Government policy and the plan documents linked
women’s education to fertility rate, maternal and child health. It also explored the notion of
‘functional literacy’ as an instrument or tool to gain access to developmental resources,
maintain accounts, read information on contraceptives, child care, nutrition etc. This was the
peg on which women’s education was hung. It is quite interesting to note that women’s
education was not linked to women’s own welfare — her economic status, her bargaining
power and of course her own health. The focus was on fertility control and related issues namely child survival and safe motherhood. It was only in 1986 that the education policy
linked to education, equality and empowerment
a concept that should ideally subsume
women’s health.
Government’s population policy and to some extent health policy (not education policy)
argued about the centrality of women’s education in achieving national demographic goals
and in improving the health status of the family. Women were projected as primary care
givers in the family. Government documents stress the importance of education in bringing
about changes in child rearing practices. Demographic profiles were plotted linking
educational status of the mother to child survival indicators. Similar profiles were done
linking fertility rate with educational status. Most recently, almost all health and family
welfare initiatives of the Government point out the importance of education in promoting
good health and nutrition practices. In the last fifteen years the urgency to increase the age
of marriage, reduce maternal mortality linked to teenage pregnancies and delay the age first
conception has brought home the centrality of universal primary education in India. The
spectacular success recorded in Tamil Nadu, Himachal Pradesh, Mizoram and Kerala is' •
attributed to almost universal enrolment and retention of girls in school.
This approach was greatly influenced by demographers who were the single most important
lobby that influenced India’s population programme. Anirudh Jain and M Nag’s argument
reproduced below is illustrative and representative of the arguments put forth through out
the 1980s and the 1990s. “The reason for expecting a negative influence of primary
1 In this paper the author has drawn from the following:
Vimala Ramachandran: The Indian Experience in “Bridging the gap between intention and action —
girls and women’s education in South Asia; ASPBAE Mumbai and UNESCO-PROAP Bangkok
June 1998
’
Vimala Ramachandran: Girls and women’s education — policies and implementation mechanisms,
UNESCO-PROAP, Bangkok, September 1998
Vimala Ramachandran: Literacy, development and empowerment — conceptual issues; in Rekha
Wazir’s forthcoming edited volume on girls and women’s education, 1999
2
education on fertility is that primary education, by providing basic functional literacy and
numeracy, enhances women’s status within and outside the family and increases their
exposure to information and ideas disseminated through printed material, and improvements
in female education can be expected to influence fertility behaviour even widiout
simultaneous change in other factors such as increased opportunities for the to participate in
paid labour force.” (Quoted in Jeffery and Basu, 1996). Schooling was almost promoted as
contraception by international and multilateral agencies funding India’s population
stabilisation programme. Notwithstanding intense international and national lobbying — the
Education sector thankfully stopped at paying lip service to women’s education as a strategy
for population stabilisation. This was perhaps because many of the influential people
engaged with education policy believed in the universal good of women’s education and did
not want to link it to fertility control. Our policies also made no connection between
women’s education and women’s health as such.
This paper:
Given this reality, it is not possible to find policy or programmatic linkages between
education policy and women’s health. Therefore this paper traces the evolution of
Government education policy with special focus on external aid and the adult literacy
programme of the Government.
Educational policies and programmes - a critical overview:
Almost every conceivable strategy and approach have been covered in policy documents of
the Government of India. All policy documents recognise that the first stumbling block is
poverty and that women from poor communities, especially in rural areas need special
attention. The second stumbling block is social status - with children from disadvantaged
communities (Scheduled Castes. Scheduled Tribes, some minority groups, nomadic tribe).
The Seventh and Eighth Five Year Plan documents recognise that national developmental
and demographic goals cannot be achieved unless women’s education is taken up on a
priority basis. All possible strategies, starting from flexible school timings to decentralised
planning and administration have been recommended over and over again.
What are these policies? Scanning though documents of the Government from 1854 to the '
present, it is quite apparent that there is no dearth of pohey recommendations. They are:
•
Provide schools within walking distance, closer to the place of dwelling, if necessary
satellite schools for remote hamlets,
•
•
Provide child care facilities / creche within school premises,
Escort for girls, if school is away from the village or hamlet,
•
•
0
•
Introduce flexible school timings and region specific school calendar,
Provide alternative modes / forms of schooling, combine formal with non-formal,
condensed coursed for drop-outs, residential schools (Ashram Shala) for special focus
groups like nomadic tribes etc.,
Appoint more women teachers in rural areas and provide them with secure residential
accommodation.
Expand pool of women teachers by lowering qualifications, intensive training (near the
place of dwelling), provide regular educational support, organise special condensed
coursed for drop-outs who can be trained to work as teachers, provide secure
3
•
•
•
o
•
•
•
•
•
•
•
accommodation for out-station teachers, etc.
Make curriculum relevant to the lives of poor women who are engaged in battle for
survival,
Recognise the problem of working children, provide special facilities with flexible
calendar and timings,
Introduce facilities for “bridge programmes” to enable dropouts to re-'enter the school
system.
Provide incentives like uniforms, textbooks, exercise books, attendance scholarship, free
bus passes etc.
Involve the community in managing the school through advocacy, mobilisation and
formation of village education committees with at least 50% women members,
Improve quality of education, motivate teachers to make learning a joyful exercise,
Decentralise educational planning and administration, bring it closer to people so that it
reflects the special needs and aspirations of tire community,
Create village level education committees to plan, support, encourage and monitor basic
education;
Address management issues that inhibit the implementation of government policy, like
grievance redressal, administrators and teachers union’s resistance to flexible timings,
school calendar, recruitment of women with lesser qualifications from rural areas,
recruitment of local youth in remote areas where teacher absenteeism is rampant,
appointment of teachers to a specific school and so on, and
Mobilise public opinion for primary education and universal literacy in general and
women’s education in particular. Advocate for greater political will and administrative
commitment.
Make it a national mission with time-bound goals and targets through National Literacy
Mission (NLM), District Primary Education Projects (DPEP) and National Elementary
Education Mission (NJJEM).
The National Policy on Education (1986, revised in 1992) is perhaps the most lucid
document on women’s education. It was hailed as a major breakthrough in addressing
gender issues in government policy. The chapter titled “Education for Women’s Equality”
states: “Education will be used as an agent of basic change in the st^Jfts of women. In order
to neutralise the accumulated distortions of the past; there will be a. well-conceived edge in
favour of women. The National Education System will play a positive, interventionist role in
the empowerment of women. It will foster the development of new values th ough
redesigned curricula, textbooks, the training and orientation of teachers, decision-mak&s -Arid
administrators, and the active involvement of educational institutions. This will be an act of
faith and social engineering...The removal of women’s illiteracy and obstacles inhibiting their
access to, and retention in, elementary education will receive overriding priority, through
provision of special support services, setting of time targets, and effective monitoring....”
This document was developed after nation-wide debate through a Government document
titled — “Challenge of Education”. University teachers and students, school teachers, training
institutions, NGOs, newspapers and a wide range of formal and informal groups /
organisations were invited to comment on and debate India’s new policy. This process was
initiated in 1985 and continued for a year. The National Institute of Educational Planning
4
and Administration (NIEPA) sifted through, compiled and edited the recommendations
made by a wide range of people across the country. This process was unprecedented in India
and generated a great deal of enthusiasm for education in general. The National Policy on
Education was accepted by the Parliament in 1986. Due to political compulsions arising put
of change of governments, this policy was debated again in 1992 and accepted with njinor
modifications. The section on Education for Women’s Equality was brought forward frpm
being Chapter IV of the 1986 Programme of Action to Chapter I in the 1992 version. The
following rider was inserted: “Education for Women’s Equality is too important to be left to
the individual proclivities of persons in charge of implementation. It should be incumbent
on all actors, agencies, and institutions in the field of education at all levels to be gender
sensitive and ensure that women have their rightful share in all educational programmes and
activities..(Programme of Action, National Policy on Education, GOI, 1992)
The period from 1986 to 1991 was, perhaps, a very creative period in the history of basic
education and women’s education in India. Six new initiatives were launched by the
government, namely: British ODA supported Andhra Pradesh Primary Education Project
and Swedish aided Rajasthan Shiksha Karmi project in 1987; Netherlands supported Mahila
Samakhya - Education for Women’s Equality in Karnataka, Uttar Pradesh and Gujarat in
1988; UNICEF funded Bihar Education Project and World Bank supported Uttar Pradesh
Basic Education Project in 1990; and Swedish aided Rajasthan Lok Jumbish in 1992. All
these externally aided education projects explored alternative administrative mechanisms for
flow of funds and administration. Shiksha Karmi programme was the first to be
administered through an autonomous body the Shiksha Karmi Board. This, it was argued,
provided the project the necessary flexibility to run a community based education
programme while retaining the legitimacy and authority of a government department. Similar
implementation mechanisms were adopted in all subsequent externally aided programmes.
While basic education was opened up to external assistance, adult literacy remained a
national commitment. In 1988-89 the Government of India launched the National Literacy
Mission. That was not all, this period, i.e. 1986-1991 witnessed three other national initiatives
to promote basic education, with a focus on greater participation of girls and women.
Operation Blackboard was launched in 1987 with national resources. This programme .
focused on construction of school buildings and appointment of a second teacher in single
teacher schools. The Non-Formal Education (NFE) initiative was also launched with
government’s own resources. Taking cue from the erstwhile NAEP, this scheme provided
grant-in-aid to state governments and NGOs to start NFE centres for out-of-school
children. 100 per cent central funds were promised for NFE centres for girls. A similar
scheme was also launched for innovations in elementary education. These two NGOs
oriented schemes created space for innovation and experimentation.
In 1991-92 there was intense speculation over the impact of Structural Adjustment loan on
the social sectors. In particular, there was some apprehension about decreased government
spending on elementary education. As a result of global advocacy on the harmful
consequences of Structural Adjustment Policies, the World Bank and Government of India
agreed on a Social Safety Net programme. It was agreed that a certain proportion of the loan
will be spent on the social sectors, namely basic education, primary health, public
distribution of subsidised food grains and nation renewal fund for re-training of labour
forced rendered unemployed. As a result of this agreement Government of India proposed
5
District Primary Education Project (DPEP) in 1992. This was envisaged as an intensive area
specific and “decentralised” effort to revitalise the primary education system. This strategy
was seen as an answer to criticism of a fragmented approach to basic education. DPEP, it
was hoped, will provide multidimensional inputs in the same geographic area, thereby giving
basic education a big push. DPEP was formally launched in 1994 with three corner stones of
the programme being sustainability, equity and local ownership. Bridging the gender gap is
subsumed in the equity agenda, alongside social and economic backwardness.
With the exception of DPEP and the UP Basic Education Programme (now subsumed in
DPEP), all the other externally assisted projects are run with the help of bilateral aid and in
the case of the Joint UN System project which is funded by the UN System. 1 he
Government through its own resources funds all the national initiatives mentioned above.
Expenditure on education now stands at 3.9 per cent of GNP with a total investment of Rs
44,583 million by the States and Rs 34,410 million by Government of India in 1996-97
(Source: Towards the next millennium - India Status Report, GOI, September 1997). I he
DPEP initiative has estimated an expenditure of Indian Rupees 400 million per district over
the project period of five years. This is a soft loan from the World Bank, which the
Government will repay over a long period. It is difficult to estimate the investment in girls’
education.
External assistance (aid and loan) in basic education:
Till the mid-1980s Government of India did not reach out to external funds for elementary
education. From the era of Jawaharlal Nehru to that of Indira Gandhi the Government took
a policy decision to this effect. This decision was reviewed after 1985. The first elementary
education project to be funded by an external donor was the DFID supported Andhra
Pradesh Primary Education Project (1986) followed by the Sida assisted Rajasthan Shiksha
Karmi Project (1987). It can be safely argued that the National Policy on Education of 1986
reopened the debate on external funding. It was during the Rajiv Gandhi era when Mr. P V
Narasimha Rao was the Minister for Human Resource Development that the Government
took a decision to invite external funding in elementary education. Since then there has been
no looking back. A interesting range of special projects were introduced with external funds
between 1987 and 1992, namely:
• Andhra Pradesh Primary Education Project with British ODA support in 1986 (in 199293 this was subsumed under DPEP)
• Rajasthan Shiksha Karmi Project with Sida support in 1987 (Swedish aid withdrawn in
1998 after the Nuclear tests)
• Mahila Samakhya (Education for Women’s Equality) was launched with Assistance from
the Netherlands in 1988-89
• Bihar Education Project with UNICEF support in 1990
• Uttar Pradesh Basic Education Project with World Bank aid in 1991 (later subsumed into
DPEP)
• Rajasthan Lok Jumbish with Sida support in 1992 (Swedish aid withdrawn m 1998 after
the nuclear tests)
• District primary Education Project with World Bank loan and with bilateral assistance
from DFID, EU and other bilateral agencies in 1993-94
•
Joint UN System primary education initiative in 1996-97
6
During the period 1992-97 external assistance in education contributed less that 5% of the
total of Indian Rupees 9201 Crore spent by the Government (Central and State
Governments) on elementary education. Out of this a major chunk of Indian Rupees 450
Crore was taken as loan from die World Bank. According to GO1 estimates, during the 9
Five Year Plan (1997-2002) external assistance is estimated to increase significandy to Indian
Rupees 4300 Crore, out of which the loan component from the World Bank is Indian
Rupees 3700 Crore.
Eighth Plan Ouday (1992-97) of externally aided projects in the elementary education sector
was Indian Rupees 613.62 Crore as compared to the Seventh Plan (1987-1992) was a very
modest amount of Indian Rupees 8.62 Crore. Project-wise expenditure during the eighth
plan was as follows2: ,
_______ Indian Rupees in Crores
Actual Expenditure
Approved Outlay
Name of Project_______________________________
29.41____________
35.00__________
Rajasthan Shiksha Karmi (Sida)____________________
63.93
90.00
Rajasthan Lokjumbish (Sida)
Bihar Education Project (UNICEF)________________
Mahila Samakhya (Netherlands Government)________
U P Basic'Education Project (World Bank)__________
South Orissa Project (Source of funding not available)
District Primary Education Projects (Multiple Sources)
Total
118.00
51.00__________
1.00___________
5.00___________
230.00
530.00
58.96
18.44
0.20____________ _
0.20___________ •
512.99
683.33
In addition to the above there are a few other small scale externally aided projects, namely
Population Education in Adult Education is supported by UNFPA and routed through the
National Council for Educational Research and Training (NCERT). Similarly the UNFPA
and UNICEF also support specific activities like training, material production, study tours
and so on in India. However this assistance is small and channelled to specific project
components in different institutions in India.
Within the overall budget, it is difficult to pinpoint the proportion of resources channelled to .
girls and women’s education. With the exception of Mahila Samakhya project, which is a
women’s empowerment programme - other elementary education projects are meant for
girls and boys.
Adult literacy and women's empowerment:
In the mid-seventies, when the women’s movement was just gathering momentum, die
world was waking up to the centrality of adult literacy in the struggle for equality and
empowerment. Adult educadon came to be accepted as a very political activity. This was
validated through experiments with popular education in Brazil, Cuba and Mexico. Its
centrality was accepted in workers struggles and radical movements across the third world.
In India the decision of the Government to entrust the newly emergent voluntary sector
with the task of adult education was hailed as a very radical step in the immediate post
emergency era (1977). The NAEP initiative of the Government provided for the first time
2 Source: Government of India, Department of Education, New Delhi
7
an opportunity to develop teaching and learning material for adult women. State Resource
Centres across the country tried to integrate message on health, contraception, child rearing
and nutrition into adult education primers. For example, Literacy House of Lucknow
produces very interesting material on health education. Similarly, the State Resource Centre
of Rajasthan produced innovative health awareness material. There was also a lot of criticism
that adult literacy material continue to focus on women as mothers, care providers and
cooks. Women’s organisations and the nascent women’s movement were quite critical of the
adult education materials for women.
The National Literacy Mission was established in 1988. There were some spectacular
successes. Kottayam City in Kerala was made fully literate in 100 days in April-June 1989.
Ernakulam District also in Kerala was made fully literate in one year January-December
1989. The government withdrew NAEP and moved full steam into a mission mode to
‘eradicate illiteracy’ in 1990. Initial scepticism gave way to euphoria in 1990-92 and the
Literacy Mission forged ahead. Like the NAEP, voluntary organisations, social action
groups and village-based social animators were the mainstay of the literacy campaign - but
with a difference. Having learnt a bitter lesson from the erstwhile NAEP programme, the
literacy mission (popularly known as TLC) was positioned as a time bound campaign
involving a wide range of actors as ‘partners’ in social mobilisation. The centre-based
approach gave way to intensive time-bound literacy classes through volunteers. District
Literacy Societies were created to bring together people from the administration, voluntary
groups, social activists and national resource agencies like the Bharat Cyan Vigyan Samitis
(BGVS).3 This structure was created to transfer initiative to die community and generate a
momentum for literacy through creative environment building through Jatlias,4 identification
and training of literacy volunteers and post-literacy centres called Jana Shikshan Nilayam.5
Leadership and dynamism of the District Collector6 was the key to success.
Starting with an ambitious plan to mop up all illiterates in the 6-60 age group the literacy
mission gradually narrowed its focus to the 15-35 age group. While die entire movement was
constructed in gender-neutral framework, the government was surprised to note that women
came out in large numbers making the movement a potential force for women’s
empowerment. This realisation gave the movement a boost. Somewhere along the way
organisations and people working with women realised the tremendous potential of literacy
campaigns for women’s mobilisation. The few unexpected spin-offs of the literacy
movement emerged as its greatest validation. In an otherwise bleak scenario, this aspect of
3 Bharat Cyan Vigyan Samiti was the national equivalent of Kerala Sasthya Sahitya Parishad involved
in people’s science movement, spreading education and awareness though folk media, rural
campaigns which used theatre, processions, music, dance and so on to propagate scientific temper.
The BGVS was in the forefront of the Literacy Campaign in the early years and was the chief advisor
to the Department of Education on the Literacy Campaign. It represented the radical and secular
constituency in politics. It is also linked to the Communist party of India (Marxist).
4 Cultural procession using theatre, music, dance etc. This form of social mobilisation is quite
popular in many radical movements across the country.
5 People’s Reading Room/Library and centre for educational activities
6 Chief Executive Officer of the Government at the District level. He/she has both administrative
and judicial powers. He/she is also in-charge of all developmental work in the District. For all
practical purposes, he/she is the most senior official of the state at that level.
8
f
the literacy campaign reopened the debate on education as a tQol for women’s
empowerment and equality. Even the BGVS — a creative offshoot of the communist
movement in Kerala - grudgingly acknowledged ‘gender’ as a significant variable in
mobilisation for literacy. The women’s movement, which had hitherto had an ambiguous
stand on adult education and literacy, took note of unprecedented mobilisation of women in
Puddukottai in Tamil Nadu and Nellore in Andhra Pradesh.
Nellore, a coastal district of Andhra Pradesh was witness to one of the most spectacular
campaigns. The initial social mobilisation for literacy in 1991 was successful and many
women came forward to participate in literacy classes. One seemingly unimportant chapterdescribed the effect of alcoholism on the family and the efforts in some parts of the country
to fight against alcoholism. Maybe the time was just right or maybe the women of Nellore
were quite fed up with the havoc alcohol has created in then- lives. This provided a trigger.
Within no time thousands of women came out of their homes. The ‘anti-#r/w£’7 movement
was born in 1992. District officials involved in the literacy campaign were not only
sympathetic to the movement but actually encouraged them and praised their courage. This
movement picked up momentum and the Government of Andhra Pradesh declared the state
an alcohol-free area in April 1993 — i.e. declared prohibition. Changing government policy
was a heady experience and during one of the victory celebrations women discovered the
magic formula of self-help groups. The savings movement was thus born and in almost a
record time of two years almost 6,000 savings groups called ‘Podupulakshmi’ came up. While
women were savouring their new-found strength and the meaning of power as a positive
force for social transformation, the government decided to create a Women’s Bank. Women
who were now used to handling their own money and who had experienced the power of
decentralised decision-making were reluctant to hand over their savings to an impersonal
banking system. This vibrant movement gradually faded away from public eye.
During group discussions on "women's ailments" in Nellore in 1995, it emerged that as
women gain greater self-confidence they begin to value themselves, they become more
articulate. Women who had accepted abdominal pain, discharge, discomfort, etc as being a
"curse all women have to bear" started breaking this silence. Analysing the loans taken by
women it became evident that as income levels go up and women have control over their.
earning, they actively seek medical help. Approximately 40% of consumption loans taken by
women were spent on health. In most cases, they borrowed money for treatment of family
members (husbands, sons and daughters). Many women had also taken loans of Rupees
2000/- to 4000/- for hysterectomy operations. The worrying aspect was that in the absence
of reliable primary health care facilities and government hospitals, women went to private
practitioners. It may be difficult to ascertain the proportion of women who were subject to
unnecessary operations - but it became more than evident that hysterectomy was popular in
that region8. Literacy volunteers also reported perceptible change in nutrition patterns. For
example, women grew and consumed more vegetables, recognised the value of unpolished
rice and took care of their adolescent girls’ nutrition.
7 Arrack is a local alcohol that is brewed and sold locally.
8 For more details on the credit movement see Vimala Ramachandran (January 1996) Critical
Consciousness, credit and productive assets - key to sustainable livelihood”, Monograph UNICEF
New Delhi.
9
Puddukottai, an impoverished District in Tamil Nadu was in the spotlight for yet another
innovative literacy movement. The campaign led to unprecedented mobilisation of rural
women in 1992 — almost the same period of the anti-liquor movement of Nellore. The
symbol of power adopted by women in this area was cycling. Thousands of women learnt to
ride the bicycle. Acquiring literacy skills alongside the means for greater mobility was the
distinguishing feature of this unique campaign.
Large-scale campaigns do infuse dynamism and the will to change. This was more than
demonstrated in some Districts. Literacy and the associated practice of group discussion,
experience sharing, access to information, collective action generates its own momentum.
Evaluation reports and travel notes of those who visited the TLC districts show that
traditionally disadvantaged groups like scheduled caste people and those from scheduled
tribes participated in* large numbers. Women jumped into it with great enthusiasm.
Notwithstanding some spectacular success stories, the literacy mission lost its zest in 1993.
There was also a realisation that many districts were floundering and the campaign did not
have the desired impact. Therefore the government launched ‘Operation Restoration’ in
1994. Twenty-five districts, mosdy from the ‘resistant’ states were selected (with the
exception of Karnataka where Bijapur, Kolar and Bangalore were chosen).
The literacy mission was not a complete blank. It showed to the world that given the right
environment and the right stimulus the state machinery could be galvanised into creative
action. It also demonstrated beyond doubt that people were not apathetic to education and
learning. Beyond a particular stage in life they may find literacy skills difficult to memorise
and retain, but enthusiasm for learning and acquiring knowledge was tremendous. Women
participated in large numbers, not because they wanted to learn the 3 Rs, but because it
opened a window to the world outside. It created an invigorating environment for accessing
information and finding out about the larger world. It also brought home the point that
literacy is but a sub-set of education. Women may not have learnt to read and write, but they
certainly learnt to think, introspect, speak their mind and come together.
Another missed opportunity to link education to women's empowerment:
Let us take the now legendary Nellore or the spectacular Puddukottai campaigns discussed in
the earlier section of this paper. In a very short span of time, thousands of women came
together. Poor rural women got a glimpse of a New World. In Nellore the literacy campaign
sparked off an anti-^mzf^ (anti-liquor) movement. Women came out of their homes, made
alliances, worked closely with the administration and tried, albeit short-lived, to change
government policy. This created greater awareness about social issues and encouraged the
women to think strategically. The anti-liquor movement gradually gave way to savings
movement. Women formed groups to pool their savings, rotate them for consumption and
production loans. It was estimated in April 1995 that there were 6,600 groups, bringing
together 204,000 women. They had mobilised Rs 6 Crores9 through their savings groups and
accessed Rs 3.75 Crores through IRDP (Integrated Rural Development Programme) and
DWCRA (Development of Women and Children in Rural Areas). There was tremendous
enthusiasm and the Government of Andhra Pradesh was euphoric. It was the greatest
success story of the decade. There was a move to initiate a movement called ‘People’s health
9 Rs 1 Crore is equal to 10,000,000 Rupees.
10
in people’s hands’. The environment could not have been more favourable.
What happened next? Adult educators gloated over their success, the anti-^mz^ movement
was their crown feather. Here were thousands of women’s groups consisting of barely
literate women engaged in savings - a golden opportunity for meaningful continuing
education. But that was not to be. Adult educators and campaign managers packed their bags
and left. A ready and eager village-level institutional base to encourage life-long learning was
not acknowledged. The campaign could have been used as a very effective medium to
educate women on health and nutrition. There were thousands of informal groups in many,
districts — a rich base to forge effective linkages between education, empowerment and
health. 1’he women of Nellore are definitely richer by way of experience. The confidence
they gamed through the literacy campaign, anti-^mz^ movement and the savings movement
is still with them. But they have lost their collective strength. There is an element of tragedy
in the Nellore story - education could have made a difference, but that was not to be.
Women in Puddukottai narrate similar experiences. Cycling was just a symbol of mobility
and empowerment. It was not an end in itself. However the administrators involved in this
campaign moved on after initiating and nurturing these spectacular road shows. The women
of Nellore and Puddukottai were left behind.
Why were we not able to convert these wonderful experiences into opportunities for life
long learning? Where did we go wrong? Talking to a wide range of actors involved at
different stages of the literacy campaign it became apparent that there was no strategic think
ing. District Collectors, like most career civil servants, have a short horizon. They like to leap
into prominence like shooting starts, make a splash and move on. The painstaking process of
nurturing a movement, helping ordinary people consolidate their new found identity and
strength and build sustainable organisational structures - are alien to the civil service. The
literacy campaign was launched and justified as a ‘quick’ movement, a magic formula to
eradicate illiteracy. It was never conceived as a spark drat would ignite a movement for life
long learning. It was a quick-fix technology mission. In the tumultuous 1970s the population
bomb exploded on India. Family Planning was taken up with renewed vigour. The
Emergency Years of 1975-77 brought population control on the national agenda. Unlike
strategies adopted in the 1950s or even the 1960s, the magic formula to control population
growth was sterilisation. Thousands of men and lesser number of women were bullied,
cajoled, dragged for sterilisation operations. There was a feeling in India that population
stabilisation could be achieved through sterilisation targets.
During this period, there was also a confidence that child survival could be assured through
immunisation drives and Oral Rehydration Therapy. Malaria could be eradicated by pumping
DDT aimlessly. Self-sufficiency in food grains and edible oil could be achieved through
intensive chemical fertilisers pumped into degraded land (never mind the long-term impact).
Primary schools could be fixed though Operation Blackboard. Yes, the list of such quick-fix
magic bullets is long. Long-term planning and strategic planning was given up in the 1970s.
I his approach to development issues continued through the 1980s and 1990s. Little wonder
that the Literacy Campaign ot the 1990s is a saga of missed opportunities.
11
There are no linkages!
Reviewing policies and programmes of the Government it becomes quite apparent that there
is really no conscious link at the policy level between women’s education and health.
However, the adult literacy programme linked education to health awareness - leading to
appreciable change in health seeking behaviour and also in nutrition and child rearing
practices. Unfortunately, tins aspect of successful interventions has not been highlighted either by the Government or by commentators. It will be a long time before Governments
make policies in a truly holistic manner - linking one dimension of people’s existence with
another. Organisations and people working with women realise that they cannot separate
health and education of women - the two are linked inextricably. This malice is not limited
to Governments alone. Donor agencies - bilateral and multilateral (including the Bank) also
work in watertight compartments. The education division rarely knows what the health
division is doing. The population division talks about multisectoral approach (especially after
Cairo) and ends up funding reproductive health and family planning. Even HIV and AIDS is
not seen as being a part of the health and family welfare programme - it is with the health
department! Women’s credit, education, health care, mobility, and rights - all these are dealt
with by different units. Breaking this mindset will not be easy.
Should we then be surprised that there are really no policy level linkages between education
policy and women’s health!
12
HEALTH POLICY AND PROGRAMMES- WOMEN’S HEALTH
BY
DR. HELEN SIMON
Prepared for the
National Consultation Towards
Comprehensive Women’s Health Policy and Programmes
BY
VHAI-WAH!-DSE
Held in VHAI, New Delhi.
On February 18-19, 1999
Health Policy and Programmes - Women’s Health
Introduction
India has a rich , old heritage of Medical and Health Sciences and nourishing, scientific traditions in
ancient and medieval period. The concern for health development and primary health care in India dates
as far as vedic period. In 3000 B.C, Indus Valley Civilisation showed relics of planned cities and drainage,
houses and public bath built of baked bricks on excavation of the Indus Valley (eg. Mohenjodaro and
Harrapa), environment sanitation by ancient people. Later Aryans had invaded India, bringing Ayurveda
and Siddha systems of medicines to India. Ayurved or science of life developed a comprehensive/holistic
concept of health. Our ancient tradition in the scientific health care of our people include Physiology of
Ayurveda and surgical skills developed by Charaka and Sushrutha.
During post vedic period (600 B.C.-600A.D.) religious teachings of Buddhism and Jainism had dominated.
Medical Education was introduced in the ancient universities of Takshasila and Nalanda. Atterya was the
first great Indian Physician and Teacher in the ancient university of Takshasila. Hospital system was
developed during the rule of Rahul Sukrityana ( Son of Buddha) for men, women and animals and the
systems was continued and expanded by King Ashoka. King Ashoka during 226 B.C. and other Buddhists
Kings developed Ayurveda as state medicine and Public Hospitals. Around 1000 A.D., Muslim rulers
introduced, the Arab system of medicine, popularly known as unani system, the origin of which was
traced to greek medicine. Unani system since then has become one of the Indian systems of Medicine.
Only in 1 Sth century. British had introduced Allopathic medicial services primarly to provide health care
to British Army Personnel and Civil Servants. However, phenomenal growth and development of modem
system of medicine occured during the 19th century. The fact remains that as late as beginning of the 19th
century the only medical practice used for health care and treatment of sickness in our country was
mostly through Traditional Indigenous System of Medicine.
Development of Healh Policy in India
The state of Public Health in British India was very low. There was wide preveliance of diseases like
Malaria, Tuberculosis, Cholera, Plague and consequent high rates of mortality in the community.
Crude death rate was 22.4/1000
Infant Mortality 162/1000 live births (Bhore Committee Voll, 1946)
Services were mostly available in general hospitals located in big cities and commercial centres were
largely curative. Lati ’ some preventive measures were instituted for the control of epidemics. Some
dispensaries were also established in some remote villages. Provincial health department was established
in 1919. But neither health planning nor medical education was related to Health needs of the people in
the community (Ray 1985).
Medical services were scattered inadequately and in certain areas, rural population did not have any
medical services.
In united provinces- status regarding health Personnel One Institute served a population of 1,05,626 personnel in about 202 villages.
73000 hospital beds were available, making an average of 0.24 per thousand population. A ratio of
One doctor to 6000 population
One nurse to 43,000 population
One health visitor to 4,00,000 population
One midwife to 60,000 population
One qualified Pharmacist to 40.00.000 population
One dentist to 3,00,000 population
It IS note worthy that efforts to develop a National Health Policy were initiated prior to Independece alone
with the growing national movement. Historically, the first committee to study and evolve a policy and
1938OTh
?1S
COnStltUtl0n 01 sub comi«itee under the Chairmanship of Pandit Jawarhal Lal Nehru
93 . The sub comimittee was headed by Col. Santok Singh Sokhey. The interim report was submitted hi
J and was published m 1948. Major recommendations contained in the interim report were as follows
Integiated Services of preventive services.
Maintenance of the health of the people was the responsibility of the slate.
Need for training large number of the Health workers in practical, in community and Personal
aspecls“'d “I"-'”"5
'”n6 “ on ,he
On health worker for every 1000 of population, (he norm to be attained within five years.
se'Ze 8 °f Se‘eCted health W°rkcrS at Suilable intervais so that they might be better trained for this
One qualified medical doctor for every 1000 population .
One bed for eveiy 600 population.
Tn arm at one medical doctor for every 3000 population and one bed for I SOO population.
While these reports were under publication, II,e next major development was lhe appointment of the
Health Survey and Development committee in 1943 under lhe chairmanship of sT Joseph Bho e
Subsequent developmnts m lhe field of health has been based mainly on Ibis report.
Ihecomnuitleobseiyed “.f lhe nations- health is to be built, the health programmes should bedeveloped
on the foundatron of prevent,ve health work and that such activities should process side by side wiU,
recommendations of Bhore
Ofpa,i“,s’' So™ «l the
Each primary centre in rural area to cater to
d population of 40,000 with the secondary health
centres to serve as a supervisor.
-
Setting up of primary health unit with 75 bedded hospital for each 10,000 to 20,000 population.
SSKST Com,”i"“ “ *“■'aai,e co-o'™tro"
'
mXure0"
of Public"
’ '1“Or W''° Sl,°l"<l
Ph,Si"” Wh°
b»th “ative and preventive
Hea“h B"d f°raCh d,S'riC1 Wilh DiS,ria Health Offi°als and responsibilities
10 ensure suitable housing, sanitary surroundings, safe drinking water supply eliminaation of
unemployment and lay special emphasis on preventive work.
™tion of
Intersectoral approah to health services development
....... .
individual Elomnalton ol illhealtb, improvement ofpublic health and assurance ofgmeral Ztit fora'll
men and women are some of the imporatant aims of the constitution.
f
The Constituent Assembly adopted the constitution of India on 26th November 1949 when India solemnly
resolved “to secure for the people of India justice - social, economic and political liberty of the thought,
expression, belief, faith and worship equality of status and of opportunity and to promote among them all
fraternity assuring the dignity of the individuals and the unity and integrity of the nation”. Article 21 of
the constitution ensured the “Right to life of the citizens. Article 47 under the directive Principle of the
state policy stated that the state shall regard the raising of nutrition and the standard of living of its people
and improvement of Public Health as among its primary duties. Under article 246, all the health subjects
under were enumerated in the seventh schedule under three lists, union list, concurrent list and state list.
The constitutional mandate is the yardstick to evaluate our country’s performance in the past.
After adopting the constitution which came into force on January 26th 1950 when India became Republic
in Commonwealth. Govt of India set up Planning Commission which immediately set to work after
revieweing the poor state of Public Health.
The first five year plan laid down following priorities in the health plan (1) Provision of Water Supply and
sanitation (2) Control of Malaria (3) Preventive I lealth Care of the rural population through health units
and mobile units. (4) Health Services for mother’s and children (5) Education and Training and Health
Education (6) Self sufficiency in drugs and equipments and (7) family Planning and Population Control.
Thus comprehensive health programmes during the first five year plan phase(l 951 -56) and subsequent
expansion of health and family planning infrastructure in the second five year plan (1957-62) paved the
way for systematic health planning in India. In addition developments in this field were influenced by
reports of various committees headed by Dr. A.L. Mudaliar in 1959 and the other headed by Dr.J.B.
Srivastava in 1984. Mudaliar Committee had recommended radical revision of primary health centre
programme and suggested medical coverage to rural areas through mobile health vans from District and
Taluq hospitals instead of multiplying primary health centres on the pattern already existing which were
not constituted and staffed as envisaged by the recomendations of Bhore Committee. The Mudaliar
Commitee also observed that the norm set by Bhore Committee regarding bed per population was not
practical and recommended one bed for 1000 population over the two or three plan periods.
The Srivastava Commiteee had recommended and advocated community health approach which finally
led to the community health workers scheme (subsequently renamed as the community health voluntary
scheme) which was launched in 1977 and later modified in 1980. Subsequently during the sixth plan
period emphasis was on public health and eradication of communicable diseases. Empahasis was to provide
safe drinking water in the villages, improvement of environment and sanitation and high priority to
family welfare.
Need for evolving the National Health Policy
Having committed to the goals of HFA bvy the year 2000 A.D. through Primary Health Care approach it
became imperative to consider regarding complete restructuring of the existing systems of health care
delivery and educationa nd training of the health personnel, further taking into consideration the varieties
of inputs to the health, the need for complete integration of all the plans for health and human development
with the overall process of national development was recognised. It necessitated a closer collaboration
with health related sectors, particularly pharmaceuticals, food and agriculture, nutrition, rural development,
education, social welfare, housing, water supply, sanitation and preservation of the environment. Therefore,
the disease control approach in the planning and adhocism in decision making regarding health had to be
given up and a holistic approach to the health was considered necessary.
The thrust of the nation’s basic development was determined under the revised 20 Points Programme of
the Prime Minister. It attributed high priority to the promotion of family planning as peoples’ programme
on a voluntary basis, augmentation and provision of primary health care on universal basis, control of
leprosy, tuberculosis and blindness, acceleration ofwelfare programme for women and children and nutrition
improve their health status. Recently ministry of Health and family welfare along with their previous
ongoing programmes where women are also covered, initiated many new women specific programmes.
At the same time, to achieve total development of women various other ministries/departments like : the
Education, Labour, Industry; Welfare, Agriculture, Rural Development etc. have also together initiated
women’s specific programmes from sixth five year plan onwards which coincided with Internaitonal
Womens’ year and first report of status of women in India. The women’s development programmes had
gained momentum. Subsequent a women’s bureau was set up within the department of women and child
development which was specifically created under Human Resources Development Ministry to promote
devleopment of women and children. The Ministry of Human Resource Development is the Nodal Agency
for monitoring and supervision of all programmes covering women and run by various ministries including
Health and Family Welfare.
Some of the interventions on some critical issues related to women’s health.
Medical Termination of Pregnancy Act 1972
This is inacted by the parliament in 1971 and implemented in all states and union territories in April
1972. This was inacted mainly to safeguard maternal health and to reduce maternal morbidity and mortality
due to unsafe abortions. However even after over two dacades, counscelling and safe abortion services
with technically skilled medical personal arc not within reach of the most of the women especially in rural
areas.
2. Prenatal Diagnostic Techniques (regulation and prevention of misuse) Act 1994 Being concerned about the sex ratio amd misuse ol'modern diagnostic techniques for determination of sex
to abort female foetuses. Government of India had enacted the above act, which permits the modern
Diagnostic techniques for sex determination in approved institutions only in certain circumstances especially
to diagnose certain genetic disorders. Eventhough penalities have been prescribed for violation of law to
the owners of Institutions, doctors and other staff for conducting the test, for family members of pregnant
woman and also the pregnant woman. Successful implementation depends upon the cooperation of the
approved institutions, staff, law enforcing agencies and general public. A massive media campaign with
involvement of village level women organisations is essential to bring changes in social attitudes towards
girl child prevention and female infanticide. In 1992 studies were conducted in 9 states - Andhra Pradesh,
Bihar, Gujarat, Haryana, Madhya Pradesh, Punjab, Rajasthan, Tamil Nadu and Uttar Pradesh sponsored
by Dept, of Women and Child Development to assess the extent of prevalence of female infanticide in
these states. 65 districts of these states where sex ratio of the population 0-6 years was 1100, revealed that
female infanticide is practiced only by certain communities in Bihar and Tamil Nadu, whereas it was not
practiced in states of Andhra Pradesh and Gujarat. National Plan of Action for SAARC decade for girl
child, special schemes for Adolescent Girls through 1CDS and Reproductive Health Programme are also
being carried out for the development of children, adolescents and women.
Present Status of Women and Health
National Family Health Survey 1992-93 shows that inspite of the Govt. Polices, programmes and efforts,
still the women’s status is low in our country.
61 percent of girls were in school compared to 75% of boys during the age group 6-10 years and 55% of
girls were in school compared to 76% of boys during the age group 11 -14 yrs - However, the percentage
varies in various states, more than half of girls arc not in school in Bihar, Rajasthan and Uttar Prtadesh
whereas 86 percent of girls aged 6 to 14 attend schools in Kerala. Goa, Nagaland, Mizoram, Himachal
Pradesh, Manipur and Delhi.
It was found that major state like Bihar, Uttar Pradesh, Rajasthan, Madhya Pradesh, Orissa and Assam
lag behind in relation to socio-economic development, female literacy, maternal mortality, infant mortality,
percentage of women who have antenatal1 care, institutional deliveries. NHbS has shown that the education
and female literacy is most crucial for improving status of women and health.
Gender discrimination still exsist inspitc of the efforts made by Govt, till now. Studies have shown the
discrimination against girls still exist and about 13.90,593 missing girls 0-6 yrs in 1991 was reported by
UNICEF in 1995.
Still women are not allowed to make decisions regarding their own life, and they are also not allowed to
participate in the decision making in the families and in the communities. Very few women are allowed to
effectively participate in decision making at national level even when they are in high political or
administrative positions. Unless a woman is allowed to make decisions regarding her education, participation
in labour force, marriage, reproductive career and participate in family and community in important
decision making, mere positional status does not improve her status. There is a great need to bring about
a change in mind set of men and women i n the families and communities and later at national level. Inspite
of the 73rd constitutional amendment and reservation of 1/3 rd seats lor women, tire elected women members
are still not allowed to function by the male members. Unless these women are empowered to take part in
governance of their Panchayats without obstruction, thinks will be still status quo in Panchayats without
relevant development in education, health, environment, sanitation in their local areas according to then
local needs. As women status is closely linked with her health status, the priority m the country is to strive
towards raising the status of the woman in our country.
Sex Ratio
The Female: male ratio continues to be adverse (929:1000). This is mostly due to discrimination against
girl child, female foetocide, less access to healthcare etc.
Life expectancy :
The girl child and women in early reproductive age still have lower life expectancy but the life expectancy
ApAMpr
oop omnn
of elder age
group wnnie.n
women c.onsiderabl
considerablyv improved
improved slightly
slightly more than that of the males i.e. 62.1 fot fema es
compared to 61.4 for males (1996).
Maternal Morality :
Even though correct data is not yet available, the official estimates show 4-5 per 1000 live births. For each
women dying due to pregnancy related causes 18 women suffer morbidity due to various causes. Anaemia,
haemorhage, toxae-a sepsis and abortion are still the major causes of maternal mortality'. NFHS estimates
that 1,00,000 women die every' year due to pregnancy related causes. The maternal mortality rate is moie
in rural areas where 42% of women have no antenatal care compared to 18% in urban areas. Still 7 o
deliveries occur at home with only 36% deliveries attended by trained birth attendants. Majority of the
maternal deaths are preventable. Still health care delivery system in public sector does not cater lor the
needs of the women due to various reasons as they are not established to give women oriented quality care
About 17% of adolescents still marry before 1 8 yrs and about 8% of births occur in this group. Maternal
mortality and morbidity is higher in this age group
Infant Mortality (IMR)
Studies show that even though infant mortality is more ini rural areas compared to urban areas, theie is no
in certain states due to female foetocide,
marked gender di fl erence in IMR except in some communities
c
neglect of health and nutrition of the girl.
Nutritional Status of Women
than 145 cms Jorming a high risk group during pregnancy. In low rncome groups the calone ml
lower in women, pregnant and lading motheis.
Family Welfare Measures
Still the programmes for Family Welfare/Keprododive Irealih only have “^“P'^XlTlesfo
tametted towards women, even though attempts are made to popularise use of condo
>
prevent HIV infection and also to popularise male permanent sterilisation through no scalpel techmqu .
Accessibility to health care and family welfare facilities
Accessibility to health care is very limited to women in rural areas due to their preoccupation with then
domestic responsibilities and also due to low priority accorded to health needs of girls and women
Lilies and societies. Lack of transport, long distance of the health care delivery unit and fixed timings
are some of the factors which make health care less accessible to women.
Thus the situational analysis of women’s health clearly indicates their poor health status and an imbalance
between the both sexes. Health status of the women is intertwined with socio-cultural and ec0™1
conditions in a particular society along with social relations. Son preference to carry the family nan e
for old age support/security due to the traditional patriarchial society in our country has created imbalanc
SXS' Tl«. nil, io be life cycle approeeb fo»n conception to the time ofdeath to tmprove
women’s health status.
Occupational Health Hazards
Cooking with fire wood with smoke causes irritation of eyes and eye ailments and blowing to keep the fire
burning can be one of the caustive factors for prolapse of uterus in multiparous women. Beedi making
also cause lung problems due to the dust. Various industries where chemicals are used can cause imtation
of skin and cause various skin problems are inhalation of their toxic products may cause varioushe
disorders Young children and girls are used for various domestic chores and in various factories tmd
industries for chean labour. About 60% of children employed in child labour aie girls. The; string
measures and the child labour abolition act needs to be effectively implemented on a war footing as
Lal TaXveZm n otirl child will be adversely affected. Various forms of girl child abuse at home,
byuelafisls^pL^Lid^he society need to be properly understood and preventive and therapeutic measures
need to be instituted for proper physical and mental development.
Mental health of women
Many women and adolescent girls develop mental depression due to family related problems in rural .
areas Cruel practices are undertaken, believing that they are possesed by the evil spirits. 1 here is an
urgency and great need to integrate mental health services with primary health care service - as envisaged
in National Health Policy and National Mental Health Programme.
Elderly Women
There are no organised health care services to the women in this age group who often face psychological
problems and other physical disabilities due to osteoporosis, cardiovascular diseases, cancers, hormon
problems etc. They need to be completely dependent upon relatives or society. 1 he recently enacted act
welfare of elderly should address to the health needs of the elderly women.
I
1
Welfare Measures for Working Women
j.
Extcnde&maternily leave, creches at work place or flexibility in working hours to promote breast feeding
and other welfare measures need to be instituted to ensure better health status of women. Sexual abuse at
work place should be strictly condemned and women should be encouraged to report such cases in the
light of the legal support extended to them by the recent judgement ol supreme court.
Violence against women
Women are beaten in their homes by their partners/mlaws and many are sexually harassed and raped. In
particular communities in some states in India especially tribals practice genital mutilation in females.
■ Harassment due to dowry, forceable prostitution, customs and religious sanctions like devadasis, jogins
etc. for young girls and girl children, forced children prostitution and begging need to be immediately.
Therefore there is a great need to formulate a women’s health policy in the country to make the health
system responsive to the women’s health need taking into account impact of discrimination against women
and its illeffects on women’s well being.
9
• Unnl-
I .
National Health Policy - Health Priorities
and Needs
Establishment of preventive, promotive and public health
services
Provision ol primary health care with special emphasis
on the preventive, promotive and rehabilitative aspects.
Reorganisation of curative services to prevents, control
and treat diseases.
Restructuring ol medical and health education as per
national health priorities and needs:
Re-orientation of existing health personnel
Integration ol the indigenous and modern systems
Utilisation ol practitioners of indigenous and other
systems of ipcdicine and their role in health care.
Material and
programmes.
child
health
including imnmnizatioii
Strategies to ensure adequate nutrition to all especially
those in rural areas and urban slums.
Prevention of food adulteration and maintenance.
Provision of safe drinking water.
Sanitary disposal of waste water, human and animal
waste both in urban and rural areas.
--- ; with
health
education
programmes
Nation wide
ach health
appropriate communication strategies approa —
form, to motivate
information in easily understandable
t----development of an attitude for
lor healthy living.
Establishment of an effective health information system.
To Imild-up sound technological and nianiilacturmg
capability in (he field of drugs, vaccine, biomedical
equipments etc.
To device well considered health insurance schemes on a
statewise basis.
To work towards a unified, comprehensive legislation in
health field.
balanced development of
Medical research to aim at
oriented operational icseaich.
basic, clinical and problem
To ensure effective coordination between health and its
more intimately related sectors.
11
To monitor and periodically review, the success, o.l the
effort made and results achieved.
ACHIEVEMENTS AND GOALS
Past levels/achvt.
Cui'rent level
146(1951-1901
72(190G)
Crude Death Rate
25.1(1951)
8.9(1996)
Maternal Mortality Rate
NA
4.37(1992-93)*
Total Fertility Rate
6.1(1951)
3.5(1993)
Male
37.1(1951)
61.5(1996)
Female
36.1(1951)
62.1(1996)
Crude Birth Rate
40.8(1951)
27.4(1996)
Effective Couple Protection Rate
10.4(1970-71)
46.5(1996)
TT (for pregnant women )
40(1985-86)
76.73(1996)
Infant (BCD)
29(1985-86)
93.12(1996)
44(1987-88)
78.91 (1996)
Indicator
Infant Mortality Hate
■
Life Expectancy at Birth (Years):
Immunization status (% Coverage)
Measles
* National Family Health Survey 1992-93
National Healtli/llealth Related Programmes
National tuberculosis Programme
c?'*
National Malaria Eradication Programme
National Kalazar Control Progranime
National Leprosy Eradication Progranime
National Programme lor Control of Blindness
National Cancer Control Prom amme
National iodine Deficiency Disorder Control Programme
National Mental Health Programme
National AIDS Control Programme
Prevention of Food Adulteration Progranime
Central Bureau of Health Intelligence for Development and
monitoring health management information system.
Health Sector Disaster Management
Programmes concerning Indian Systems of Medicine and
Homoeopathy
Strengthening of Drug Quality Control Programme
Nationwise Disease Surveillance Programme
National Family Welfare Programme/Reproductive Child
Health Programme
Universal Immunisation Programme
Diarrhoea Control Programme
Control of Acute Respiratory Infections
Integrated Child Development Services
Supplementary Nutrition Programme
Waler and Sanitation Programme
'environment Protection and Pollution Control Programme
Reft-l TP
•>
H-upof^rN
TWfO STRO C-TiXC
£> e^LELoPcc?
I N
Resource
ti £"C /\ [>gS ,
1-leallli Inliastiucture
1,31,9UU
22,156
2,377
13,692
27,403
4,235
8,377
Sub-centres
Primary Health Centres
Community Health Centres
Hospital
Dispensaries
Government 1 lospitals
Government Dispensaries
1 Inman Resource lor 1 leal th
28,135
2,585
5,658
15,196
19,045
1,32,950
20,172
10,715
11,653
1,200
Medical Officers
Specialists
Block Extension Educators
Male Supervisors
Female Supervisors
Female l lealth Workers
Pharmacist
Dab. Technicians
Nurse Midwives
Radiographers
»
Training Facilities
Medical Colleges
Post-graduate 'Training Facilities in about medical colleges
General Nursing Training Schools/Colleges,
Midwifery Training Schools
ANM Training Schools
Health Supervisors (F) Training Schools
160
116
493
297
498
26
Human Resource for Health Developed Annually
Medical doctors,
Medical Doctors with Post-graduate degrees
Doctors with Post-graduate Diplomas
Dentist with B.D.S.
Dentist M.D.S. Degrees
Nurses
Mid-wives,
Auxiliary Nurse Midwives
Health Visitors Trained Annually
1J Regional Institutes of Ophthalmology
Upgraded Medial Colleges
District I lospilals,
Paramedical Ophthalmic Assistant 1 raining Centres
Eye Banks for Special Ophthalmic Services
13,000
2,075
1,064
819
96
10,753
7,852
10,890
754
11
81
418
39
166
Medical Personnel Registered with the Relevant Councils
Medical Doctors
Dentists
Nurses
Auxiliary Nurse Midwives
Health Supervisors (F)
ISM and 1 lomoeopathy Practitioners in the Rural Areas
4,74,200'
11,300
j,40,208
1,50,658
17,302
5,65,000
Statement Prepared for National Consultation ‘Towards
Comprehensive Women’s Health Policies and Programmes’
VHAI / WAH!! DSE, 18-19 February 1999, New Delhi
Recommendations for Integrating Traditional Systems
of Medicine (TSM) within National Health Policy,
especially relating to Women
z
cc
Pl-aH.-LH. I/
’/ 1 o. __
8op
The underlying aim of the WAH! (Women and Health) Programme is...
v
NlO
to ensure primary health care which is women-sensitive and comprehensive throughoout
the life cycle through empowerment of women and communities drawing upon local
health traditions and practices.
Hence, supporting Traditional Health Systems or TSM is one of the three foundational
‘pillars’.
We stress traditional medicine because it is close to women - it is accessible,
understandable, affordable, and effective. Despite such benefits, economic changes
and the aggressiveness of western medicine threaten to snuff out healing systems and
ways of life which have developed over thousands of years. Unfortunately, this is a trend
in all countries of the world which have surviving traditional populations. ...Women and
men have passed on local health traditions for countless generations. Bearing them
forward now to meet health needs is important for women’s empowerment and
appropriate development of communities.*
The Current Government Position
Support of TSM in the Ninth Five Year Plan is meagre and vague. It does not provide
any link between TSM and mainstream ‘medicine’ in the national health programme. For
example only around 3 percent of the current National Health Budget is allocated to
TSM, hoping to achieve total health care coverage of our population.
However, the National Health Policy of 1983 recognises the key role of TSM in health
care:
‘The country has a large stock of health manpower comprising of private practitioners in
various systems, for example, Ayurveda, Unani, Siddha, Homeopathy, Yoga,
Naturopathy, etc. This resource has not so far been adequately utilised. The
practitioners of these various systems enjoy high local acceptance and exert
considerable influence on health beliefs and practices. It is, therefore, necessary to
initiate organised measures to enable each of these various systems of medicine and
healthcare to develop in accordance with its genius. Simultaneously planned efforts
should be made to dovetail the functioning of the practitioners of these various systems
and integrate their services at the appropriate levels within specified areas of
responsibility and functioning in the overall health care delivery system, specially in
regard to the preventive and promotive public health objectives. Well considered steps
b .-i
would also require to be launched to move towards a meaningful phased integration of
the indigenous and modern systems.1 (GOI, National Health Policy, 1983)
The National Health Policy, although passed in Parliament, has not been implemented,
and in its place a series of vertical policies and programmes are in operation. Along with
this, there has been a shift towards ‘curative’ care based on western medicine rather
than ‘preventive’ solutions. Consequently, indigenous systems encompassing
preventive, promotive and curative healthcare have been marginalised. Therefore, in
view of the increasing drug-dependence and rising medicare costs, it is necessary to
revive local health traditions to deal with common health problems which can be treated
cost-effectively and safely at the community level.
To summarise, the aims as laid out in the NHP are”
❖
To utilise the vast TSM resources
To enable each TSM to develop appropriately, and
To integrate the TSM services in the overall healthcare system.
Importance of TSM in Primary Health Care
WHO experts at a Working Group Meeting held after the historic Alma Ata Declaration of
1978 arrived at the following definition of TSM:
Traditional medicine is the sum total of all the knowledge and practices, whether
explicable or not, used in diagnosis, prevention and elimination of physical, mental, or
social imbalance and relying exclusively on practical experience and observation handed
down from generation to generation whether verbally or in writing.
Traditional medicine is already practiced by the communities and accepted by them. It is
an integral part of people’s culture and heritage, therefore, it should be promoted and its
potential developed for wider use and benefit.
India is a country of mega-biodiversity with more than 25,000 species of higher plants,
as per the ongoing All-lndia Ethno-Botanical Survey under the ‘Man and Biosphere’
Programme under the Ministry of Environment & Forests, GOI. More than 8,000 species
are medicinally used by 441 ethnic communities in the country. Out of these, around
2,500 species find reference in various classical health texts.
There is evidence to suggest that over seventy percent of healthcare needs of the
country are met by TSM. There are around
4,00,000 registered practitioners of ISM
(Ayurveda, Unani, Siddha, Tibetan (Amchi), Yoga, Naturopathy, etc.)
❖
over 6,00,000 traditional birth attendants (dais).
❖
over 60,000 indigenous bonesetters
❖
thousands of local specialists, such as those in vishachikitsa (poisonous bite
healers).
In fact, there are countless unregistered non-professionai folk healers and millions of
women treating common ailments in their homes and neighbourhoods. A micro-study
conducted by Academy of Development Sciences (ADS, 1990) in Raigad District of
Maharashtra reveals that ordinary village women know how to manage more than 50
common health problems using local resources and home remedies. Similar findings
have emerged from micro-studies conducted by AIKYA (1996) in Chikmagalur District in
Karnataka, by Stree Sangshema Trust (SST, 1998) in Anantpur District of Andhra
Pradesh, and the multiregional action-research experience of the Shodhini Collective
(1992).
The value of TSM in primary health care can be summarised as follows. The traditional
systems are:
❖
Culturally in tune with local communities
❖
Related to local resources, food-habits, life-style and environment
❖
Promotive, preventive and curative
Decentralised, self-reliant and empowering, and
❖
Cost-effective and sustainable.
Recommended Aspects of Policy and Programme Strategies
On the basis of the history and field experience referred to above, we make the following
recommendations for incorporating TSM within the Health Policy, especially relating to
women:
>
Find ways to recognise and make use of the local expertise and experience available
with traditional practitioners. For example, the Government might consider instating a
graded registration system for TSM practitioners (A = graduates, B - diploma
holders, C = recognised local healers, with specific roles).
>
Instate orientation programmes for registered TSM practitioners to involve them in
the mainstream health programmes, using their own knowledge and resources.
>
Build and maintain local databases of medicinal plants used in TSM and disseminate
the information at appropriate levels for sustainable use, for example, to be used by
practitioners, households, schools and researchers.
>
Educate the public about the role and value of TSM in promoting and sustaining
health, and to break the myths and misinformation spread by vested interests.
>
Bring about a shift in research priorities and methodologies acknowledging the
foundational principles and worldview of TSM so that it can originally contribute to
the world of medicine.
>
Restrict the indiscriminate use of plants, especially RET/s
encouraging them to cultivate the same.
k
>
Stop multinational companies and other vested interests from appropriating the
traditional knowledge and resources.
>
Make available the TSM remedies in simple locally packaged form for public and
primary health care systems.
ides, by industry while
Make larger proportionate budget allocation for the contribution of TSM to PHC, for
R&D, for medicinal plant cultivation and conservation, for public health education and
for support of the local healing community including midwives.
13
POLICY ON WOMEN’S HEALTH
BY
DR. IMRANA QADIR,
JNU
Prepared for the
National Consultation Towards
Comprehensive Women’s Health Policy and Programmes
BY
VHAI-WAH!-DSE
Held in VHA1, New Delhi.
On February 18-19, 1999
t
as mciIanci" (2). Infectious processes were rightly understood to harm the foetus and the mother, if exposed In
the seventies, the broad based perception of maternity health continued. Nutrition and infections were regarded
as critical but, at the same time, hazardous and excessive reproduction was seen as a burden on women.
In 1976, though Primary Health Care and education of mothers was added to the core of services, “unplanned
reproduction” and the need to regulate fertility acquired significant importance.(3) This heralded a shill in
emphasis from the integrated concept of maternity to selected intervention for high risk cases. Though
apparently rational, this strategy de-emphasised expressed needs as well as structural and administrative problems
of the health services and gave a biological till to maternity care. Later, the term maternity health was
incorporated into the broader terminology of reproductive health’ that the WHO adopted.(4) Other than
maternity, this covered abortion, contraception, 11IV, AIDS, reproductive tract infections, and sterility services.
While, for the developed world, these shifts were a logical expansion of the initial concept of maternity care, it
was not the same for the third world. For the latter, starting from a meaningful focus on maternity, WHO chose
to dissolve that focus by broadening the scope to reproductive health when its strategies for improved maternity
care did not succeed! This was done despite sufficient evidence of the importance of communicable and
nutritional diseases or women’s general and maternal health (5) and despite knowing that programmes against
these lacked resources and suffered from poor implementation (6).
In recent years WHO has not only crystallised its Reproductive Health (RH) strategy for women’s health but it
has also accepted major transformation of its approach to Primary Health Care. Accepting the constraints of
SAP, it emphasises growth with equity. It proposes that as the present patterns of production cannot be
interfered with, therefore we need to change life styles’ and focus on individual action. Thus, it proposes
citizen’s action to create healthy cities and healthy communities (7)! This shift of approach has many serious
implications.
Since the role of the state is reduced, the marginalisation of public sector in health, where investment has
drastically declined to 1.2% of the GNP in the case of contemporary India, is ignored.
The state is treated as one of the many partners in achieving health rather than the central actor which has to
monitor and moderate.
Within the present overall structural reforms, where the brunt of the cuts on subsidies affects food security
systems and employment of the poorest segments, the intersectoral emphasis of Primary Health Care is diluted.
Primary Health Care then acquires the ' selective’ mould where technocentricity and population control through
RH become central.
This leads to narrowing the efforts to achieve women’s health to maternity and reproductive aspects alone, at the
cost of her full health as a social being.
By overplaying the socio-economic basis of health, the WHO swings the pendulum from medical technocentricity
to achieving SAP which is seen as the long-term answer to ill health of the poor. This ignores the need for
recognising the fact that, (a) the transformation of the economy through SAP is not ensured as shown by the
South Asian Economic crisis, (b) that 40% of those living below poverty line many not be able to sustain
themselves through this harsh period of transformation, © that all talk of social security net has up till today been
only on paper and food and employment securities are dwindling for the poor.
This then, cannot be the direction or nature of development for the third world, particularly India, nor can it be
the basis for health of the Indian poor, specially women. The other important international organisations that
have more or less pushed India in a similar direction are the UNFPA and the World Bank.
UNITED NATIONS FUND FOR POPULATION ACTIVITIES (UNFPA)
In its document, “ India: Towards Population and Development Goals, 1996” (8) UNFPA places a lot of
emphasis on gender and RH related health indices Though it recognises the importance of unsustainable
consumption and production patterns and unsustainable use of natural resources for environmental degeneration,
it ignores the linkages between these processes and poverty. Poverty, gender inequity and demographic changes
are measured and presented but their causes and linkages are not made explicit.
The undue emphasis on demographic analysis uses declining sex ratios.to focus on the need for technological
interventions for mortality control for women in different age groups. Without denying the importance and
urgency of this intervention, it needs to be pointed out that UNFPA, despite accepting the fact that “public health
programmes continue to effect declines in mortality levels”, does not examine declining sex ratios along with
declining mortality rates. The two together emphasise the social constraints within which the same interventions
produce dincrenlial impacts on the mortality rates of men and women. No amount of counting numbers and
increasing technocentric approaches to fertility or mortality control will bridge this gap unless social and
economic structural issues are addressed. UNITA not only underplays the importance of such analysis, it also
ignores general health which is central to a populations development.
Except for reproductive health indicators no data is analysed on communicable or non-communicable diseases
(except for disability). Thus, even diseases that cause the bulk of the health problems, and which are amenable to
technological interventions, arc left out of the discussion. This is primarily due to the acceptance of the fact that
the present distribution of health expenditure between private and public sector of 3:1 cannot be reversed.
Within the guidelines provided by health-sector reform policies, the greater focus is on cost recovery, which
ultimately pushes the public services out of reach of the poor.
UNFPA’s emphasis in public health is on reproductive health and family planning, immunization, disabilities, and
environment pollution due to transportation. Food and nutrition and safe drinking water arc there but not as key
factors. This selective emphasis is obviously indicative of a new paradigm of public health where choices for
intervention are based not on epidemiological criteria, or perceived needs of different sections, but on what is
practical and profitable, “cost clfective” without creating any structural instabilities. Human interests are thus
made subservient to the interests of international capital, which operates on the basis of monetary gains alone.
WORLD BANK
The World Development Report, 1993 (9), in its effort to cut back State investment, proposed clinical and public
health ‘packages’ where family planning was perceived as the second most critical input into women’s health
through fertility control. Absolute numbers of 430,000 deaths due to child bearing in developing countries were
used as ‘evidence’ of the dangers of pregnancy but no effort was made to see the relative position of maternal
mortality and the nature of other dangers to women’s health. The concern for women’s nutrition was expressed
but the answers were sought in micro-nutrient supplementation, rather than making food availability the central
concern. The WDR argued that, except under the extraordinary conditions of famine, the government must not
interfere with food markets. This meant supporting export oriented agriculture production strategies at the cost
of food security systems.
Instead of emphasising communicable disease control as a whole, the public health package talked of AIDS alone
and of mass chemotherapy for worm infestation, immunization, health education, and reducing alcohol and
tobacco consumption. It also talked of pollution but, unlike UNFPA, its emphasis was on indoor pollution. It
then proposed a privatised system of services including water and health.
The essential clinical package again included maternity care, family planning services, paediatric care, TB 8l STD.
The second list of priorities included treatment of chronic diseases such as diabetes, schizophrenia, manic
depressive illnesses, and cancers. These priorities, based on the DALYS calculations, have little to do with
epidemiological priorities, or principles of public health practice, that demand discreet use of curative
interventions at a large scale to control and prevent spread of diseases. In the Bank’s essential package the
concern is either with population control strategies or with creating markets for technology, inespective of their
preventive potential. For instance, there is no recognition that the rise in cancer is an outcome of indiscreet use
of chemicals in industry that pollute the environment.
This goes unchallenged in third world countries. Thus detection and treatment (with poor results) can only help
the medical establishment, and not the alfcctcd population. In any case, early diagnosis and treatment facilities are
available to very few and it only adds to curative inputs and does not promote prevention. Similarly, mental
illnesses which are rooted in rising social tensions due to economic pressures, migration, destabilisation of whole
communities and breaking up of families, cannot be tackled through drugs alone, flic World Bank’s strategy
actually mcdicaliscs a social problem and adds market value to it.
With this perspective towards health, it is obvious that the World Bank too emphasises the reproductive health of
women and leaves out the other dimensions, such as general and occupational health, to the mercy of curative
markets.
The irrational emphasis on privatisation was partly curtailed during later efforts by the Bank to intervene in
India’s health sector planning. For example, a World Bank’s publication on, “Development in Practice,
improving Women’s Health in India” (10) accepts that the public sector will continue to play a key role in
providing services such as family planning, maternity care and control of communicable diseases
” (11) At the
same time, it makes no move to increase the share of health sector funding beyond the existing 1.3%. In
addition, in actually working out the details, its entire emphasis is on Family Welfare and Maternity. This leaves
communicable diseases out of women’s health concerns. The document discusses postural and nutritional
problems, violence against women, and weight - bearing problems more than death and morbidity from
communicable diseases. Thus while problems rooted in social realities are dragged into health sector for ‘cure’,
those that can actually be cured by technology, and therefore, lead to prevention, are neglected.
We see a common thread in the shifts affecting the very definition and content of Primary Health Care. A narrow
technocentric Reproductive Health is being given a push that marginalises other programmatic inputs more
critical for women’s health. In the following sections we examine the process of health planning in India and the
international influences on it.
II.2
INDIAN PLANNING
THE: EARLY DECADES
Independent India’s most prominent problem was its widespread and deep poverty. This was reflected in very
high morality and morbidity profiles. In 1943, the Government of India appointed the National Health and
Development Committee (Shore Committee) to survey the health situation in the country and make
recommendations for future planning.
The Shore Committee was apparently influenced by the Beveridge Committee in England (which had given birth
to the National Health Service in that country) and by the extraordinary progress of health services in the
Soviet-Union. The Shore Committee made long term recommendations guided by two over-ridding principles.
First, the provision of health services was the responsibility of the state. Second, comprehensive health care was
the right of all irrespective of their ability to pay. The blue print for the future development of health services had
projections of two kinds: the long term projection for twenty to forty years; and short term project for 10 to 20
years. This committee worked out or three tier organizational set-up at the district level with a health committee
of five to seven volunteers to help in the regulation of the activities of the primary health unit. For each PHC,
which would cater to a total population of 40,000 with a total staff strength of 35, there were to be four beds
specially earmarked for maternity cases. Every four such primary health units were, to have a thirty-bed hospital
with a special medical officer for MCH work. Sy the end of the 40s there were 5000 mid-wives and around 750
Lady Health Visitors. The number of working doctors, however, was not more than 4,000, of whom hardly
2,000 were in private practice and only 1,000 in public service. The rest did not practice at all. Due to this
shortage of trained personnel what was actually possible in terms of an infrastructure in earb^50s was much less
than the Shore Committee’s recommendation. The Factory’s Act of 1934, that provided fomnaternity care for
factory labour, was seen as a way to strengthen women’s health. It was also proposed to provide creches for
children under six years of age wherever there were 50 or more women workers (12). The National Planning
Committee of the Indian National Congress set up a Sub-Committee on Health in 1943, the Sokhe Committee?
Its report was published in 1948 (13). The group realised the importance of a centralised authority to provide
services for mothers and children, the need for a national level minimum infrastructure, and the need to train
paramedical workers and traditional Dais to provide natal, ante-and post-natal services. These, in fact, became
the basis for a Maternity and Child Health focus within India’s General Health Services.
FIVE YEAR PLANS AND SPECIAL COMMITTEES
Health Planning in India has been part of overall development. Though the recommendations of the Shore
Committee were accepted by the Government, allocations during the First and the Second Plan periods were only
3.3% and 3.1% of the total outlays respectively. This was one-third, or less than one-third, in contradiction to
the irreducible minimum of 10 per cent as recommended by the Shore Committee. Fifty five to sixty percent of
these resources were, in turn, allocated to curative health services and medical education, which became a trend
for the future (14)( 15). Initially 'maternal health’ got prominence but then it became secondary to family
planning, which was perceived as an urgent national need. The shift in the strategy of planning for MCH was
determined by the priority given to MCH in achieving the goals of Family Planning Programme (FPP). The
development of the infrastructure for MCH was also influenced by the policies of integration of services. Even
within MCH, more weightage was given to child health in comparison to the mother as 1MR was linked to
fertility and maternal to mortality was not! This continued till the eighties. In the beginning, investment on
‘Family Welfare’ was lower than health per se, but the gap between the two has been reduced over time.
generating demands lor lainily planning services. The latter report was particularly emphatic about proper
gcnciaung
policies lor welfare, specially in the area of nutrition, and taking people’s perceptions, cultures and history into
account when planning their participation. In contrast to these the National 1 Icalth Policy of 1983 despite its
concern for providing for the unmet met needs, reiterated the need for opening medical care to non-governmental
and private sector investment (43).
I he Seventh Plan was a continuation of the same trends except that the will to restrain vertical FPP and invest in
a more integrated welfare strategy was lost and resource investment in FPP again started increasing. For MCH,
this Plan emphasized child survival, inter-sectoral co-ordination and strengthening of infrastructure. It admitted
that the performance of the MCI 1 services in the area of immunization and anti-natal care despite the U1P and the
GOBI-FFF approaches, which were in operation since seventies, was far from satisfactory. It proposed raising
the health consciousness among women through education and communication programmes. No specific
measures were proposed lor general health of the women except for those mentioned above. Instead, organising
women around economic activities was proposed to enable their participation in socio-economic development.
Over the next ten years, however, women have only been pushed into the unorganised sectors of industry and
agriculture. The plan also proposed better use of MTP Act (1971) for improving maternal health through the
stipulation of conducive condition under which pregnancies may be terminated by well trained doctors (44).
During the Seventh Plan period AIDS emerged as a new public health problem and the National AIDS control
programme was launched in 1986 with loans from US and World Bank (45). While the old vertical disease
control programmes remained intact, such as those for the control of Malaria, Filariasis, Leprosy etc., new ones
like Blindness and non-communicable disease were added. A technocentric approach to Ischaemic Heart
Diseases, Rheumatic Heart Diseases, Cancer and Mental Health was proposed. In other words the Seventh Plan
not only reverted to the initial balance of resources between health and family planning, it also introduced purely
technocentnc emphasis to non-communicable disease control the contribution of working conditions and social
tensions in the increasing prevalence of these diseases was thus ignored.
'I he Eight Plan was conceived over a very critical period when India formally accepted Structural Adjustment
Policies (SAP) prescribed by the IMP and the World Bank. Its main features in health sector were: sharp cuts in
wcllare sector investments, specially health sector; privatisation of medical care; opening up of public sector in
health to private investments; and massive cuts on public distribution systems (PDS) This was called health
sector ‘reforms’! The implications of these so-called ‘reforms’ for health planning were serious, from providing
basic minimum facilities to all, specially the women and children, the Eighth Plan focused on the under-privileged
among this high-risk group. Thus, within the health for all strategy, ‘health for under privileged’ became its
theme. 1 his shrinking focus was accompanied by a strategy to consolidate and not expand PHC network. This
meant strengthening physical and technical aspects such as supply of equipment and drugs, education and
provision of training of personnel.
A negative impact ol this strategy was that poor States which had inadequate infrastructures suffered, as they got
comparatively lesser investments for consolidation. The plan openly confessed its inability to provide for the
infra-structural backlog in these Stales. It proposed a review of the existing population coverage by the PHC
network. It called for promoting privatisation and, at the same time, proposed making services accountable to
local Panchayats and strengthening referral systems at secondary and tertiary levels. The resource requirements
or these conflicted with the policy of cutbacks. The vertical approach to disease control continued and Family
Planning Programme acquired yet another hike in resource allocation (Table I). It was during this plan that
emphasis on female literacy, employment, improved social health and nutritional status, and increase in the age of
marriage was recognised as important. Yet, social development was left to the ‘pool of fragmented schemes’,
while health policy focused on provision of contraceptives, sterilisation, safe motherhood, and child health
services (46).
I his period saw three other policy documents. The Country Statement from India al the ICPD made all the
correct political statements and then reverted to calling family planning as the ‘basic need’ Apart from accepting
the use ol surer, but less safer, contraceptives in the name of giving a wide rang of choices, it also used the threat
of instability (born out of implementation of SAP) to demand ‘significant concessional funding from multilateral
agencies and bilateral donors’ (47). The draft population policy made even more radical proposals such as a
non-target approach, better inheritance laws for women, integration of health and family planning and MCH
sei vices, gender sensitive sustainable and equitable development. At the same time it retained the primacy of
population control for which it suggested legislative steps including culling off of employment and piornotional
and electoral avenues lor those who had more than two children. Il even suggested the use of army in promoting
small family norms (48)! The Country Statement for Beijing elucidated the Government of India’s commitment
to Reproductive Health approach (49) and, finally, in 1996 the Draft Population Policy was accepted by the
Government of India with some modifications and dilution of its positive features retaining the emphasis on
women and reproductive health (50).
I he Ninth Plan, due to the changing political leadership, remains an uncertain exercise. The Janta Party’s
approach paper realises the severe implication of increasing labour time unemployment rate for male workers, the
increasing inter-regional disparities and the importance of improving quality of life along with increase in growth
rates as well as employment. It targets the under privileged and the vulnerable and places participatory processes
al the centre of social planning. It emphasises food security and basic minimum services but continues to
dissociate the issue of population numbers from health and socio-economic development (51). Its health sector
plan is for “population, Family Welfare, and Health” RCH and prevention of IMR and MMR, filling gaps in
infrastructure and manpower, increasing the efficiency of the system, and providing Family Welfare coverage
through private and other sectoral linkages are its central focus.
bor health, the 9lh Plan’s Approach Paper focuses only on the underserved and under privileged. It promises
primary Health Care, particularly to the rural population and urban slums. As a part of the vulnerable
underprivileged, women do get attention but more for fertility control. For their health no special inputs or
out-reach programmes are conceived to reduce differential access to existing general health services.
1 he perspective paper has a major problem. It reallocates the earlier Plan priorities of Health and Family Welfare
to sectoral planning for Population, Family Welfare and Health. In other words, it not only dissociates the two
but also puts Fertility Control as the most crucial priority. The emphasis on numbers is clear, not only front the
shift in the title, but also from the content, where every effort is promised to provide for “all the unmet need for
spacing and terminal methods” and RCH. For health however, the plan addresses only the under privileged
segments. Perhaps this is due to the assumption that the health of others will be taken care of by the private
sector! What the perspective paper does not realise however, is that the National Programmes for Disease
Control become victims of such dichotomies. The total lack of control over private sector makes standardisation
of treatment, diagnosis, and monitoring totally impossible. Since most national disease control programmes are
based on curative strategies, they arc bound to get dissipated or converted into one-time campaigns likely to fail
in absence of sustained efforts at detection, care and monitoring. The approach paper also fails to see the
connection between RCH and disease control programmes, even though it acknowledges that communicable
diseases continue to be a major cause of mortality and morbidity in India.
Even for fertility control, the approach paper recognises unmet need (due to poor provision of services) and high
wanted fertility due to prevailing high IMR, It thus emphasises concerted intervention at these levels. However,
it pays no attention to the fact that high fertility is also linked to the desire for larger families in sections where
due to economic constraints, family labour is critical. Among the middle and small farmers and artisans this
factor is important. Unless the technological and monetary constraints of these sections are met with, in the
prevailing economic frame their family sizes will remain high. In addition, unless the issue of status of women’s
education, economic independence, participation in decision making etc. is linked to a strategy for fertility
control, the 9lb plan’s strategy will be no different.
11.3 PROGRAMMES FOR WOMEN’S HEALTH
In the process of planning, a set of programmes evolved that were critical for women’s health. However, the
official emphasis for women s health has been rather narrow. The MCH, nutrition and immunisation programmes
were brought into the frame of the family Welfare Programme (FWP) over the years and have been finally
transformed into the Reproductive and Child Health (RCH) strategy. RCH along with the ICDS, provided a
range of services to women. What is not realised by the official policy is the impact of effective general health
services for women. We briefly highlight these in the following section.
INTEGRATED CHILD DEVELOPMENT SCHEME (ICDS):
Started in 1975, the ICDS programme provides not only ante-natal, nutritional and maternity assistance, but also
education inputs. An extensive survey performed by the Central Technical Committee of the Integrated Mother
and Child Development Organisation in 1996(52) provides data on the programme performance. In all areas of
activity among women, ICDS blocks show better results as far as coverage is concerned (figure 1-2). In terms
of impact however, while evaluations have shown improved nutritional and immunisation status, assessment of
1 lie inadequate number ol PI ICs marginalised the impact of the planned sei vices. Aller twenty years of effort the
number of Pl ICs became 5,216 but their coverage remained one lakh of population, in contrast to the
recommendations ol the Bhore Committee, which had visualized a population coverage of 40,000 per P11C.
More than half of the Pl ICs were constructed by funding agencies, specially UNICEF. The government
constructed only 2067 PHCs.(16,17) The numbers of sub-centres were 20,991, not even half of the required
amount, and the total number of t rained doctors in 1967 was only 27,000. Achievement in terms of paramedical
personnel was no different. The total number of LIIVs and ANMs was 1 1,572 and 54,621 respectively.
It is worth noting that the basis on which the total numbers of midwives were estimated by the Bhore Committee
was one midwife for the total of 100 births per year. For 10 million births each year, they estimated a total
requirement of 10,0000 midwives. The number of midwives required in 1961 would, thus, be 166,820. But the
achievement was not satisfactory even in 1967. In terms of total paramedical personnel for a 439 million
population with a birth rate of 38 (as in 1961), India had only about 55 per cent of the required midwives! This
thin crust of infra-structural facilities was given the credit for the decline in infant and maternal mortality!
In the 1 bird Plan, health allocation decreased up to 2.63 per cent of the total allocation (18). The allocation for
family planning shot up to 50 crores as against 65 lakhs in the First and 5 crores in the Second plan. Il is
apparent that it was not until the third Plan that family planning programme received a great deal of emphasis.
This was due to the higher rate of population growth shown by 1961 census. The Clinic Approach was
abandoned in favour of the ‘Extension Education Approach’ in what was called the ‘Reorganized Programme’.
Io the Extension Education Approach was added the ‘Reinforced Programme’ at the behest of international
agencies. I he propagation and the use of IUCD was a major component of the ' Reinforced Programme’.
I he official acceptance of this policy came through the Mukherjee Committee Report (19) which also
recommended specific targets and incentives. The then Director General of Health Services, in a special report,
recommended addition of 4-6 Auxiliary Nurse Midwives, 4 Family planning Health Assistants and a Block
Extension Educator at the PHC, who were to work only for the Family Planning Programme (20). The UN.
Advisory Missions (21) also recommended the dc-linking of MCH from family planning services. The reason
given was “the programme may otherwise be used in some States to expand the much needed and neglected
Mother and Child Welfare Services.” Thus the experts chose to de-link MCI I from Family Planning. I lowever,
due to the close linkage between MCI I and Family Planning, very soon, ‘‘with a view to giving a broader base to
the FPP”, it was decided in 1967 that MCI I be integrated with FPP.(22) Shilled from general health services and
used as a prop for the FPP, the maternity services became lopsided. Even the narrow goal of “linking up the
MCH services with the primary health units, with extended health facilities in referral and district hospital”(23)
remained a far cry.
What was seen in the third plan period was the reflection of the recommendations of the Health Survey and
Planning Committee (24), known as the Mudaliar Committee. This Committee recommended that expansion of
services be stopped and the existing PHCs (less than 2000) be consolidated. Its logic was that the staffing of the
existing PHCs was inadequate, they were not oriented to maternity care and public health, and that the onslaught
of curative demands was excessive. The Committee further noted, that only “when facilities in regard to
personnel, finance and other requirements arc sufficiently enlarged then the Bhore Committee formula for the
PI ICs be adopted.” It proposed mobile dispensaries for far Hung areas where no PI ICs existed and it assumed
that the growing urban services and communication and transformation network would help rural populations in
availing of urban medical care services. It recommended establishment of specialist services including Paediatric
and Maternity hospitals in urban areas and emphasised on professional higher education.
Its recommendations gave no clue as to when and how the proposed suspension of the PHC network expansion
would be withdrawn and how MCH and Public health would come centre stage if urban medical services and
professional training was to be the focus in conditions of resource crunch. It then pioposed that a large
population be left waiting for crucial health services. 1 hough never fully accepted, its recommendations became
the force which set the trend of a shill in favour of urban areas at the cost of rural areas. Thus, during the third
plan period, the attempt at integrating the services for family planning, control of communicable diseases and
MCH at the PHC level, did not succeed fully and, in the process, MCH was ignored due to the over emphasis and
target oriented approach of the family planning work.
In the Fourth Plan period, the budget allocation for health further decreased while, for the FPP, there was a
phenomenal rise. Health obtained Rs 433.5 crores whereas FP got Rs. 3 15 crores which were 2.12% and
1.76% of the total outlay respectively. During the Fourth plan period the major thrust was on vasectomy and this
was through the ‘Camp Approach’ (25). The IUCD programme had suffered a setback as a result of reported
side efiects like bleeding and pain and it was replaced by mass vasectomy camps, pioneered in Kerala. These
camps got financial support from a host of international aid agencies. The target oriented, coercive Family
Planning programme got a major jolt when I 1 vasectomised men died in a eamp in Gorakhpur in 1972. The
dissent within the policy makers became sharper and the focus of the programme on sterilisation was questioned
Communication experts like Kakar argued that just throwing a slogan can not solve the problem, but birth
control needs to be presented to the people, as part of the larger package of welfare.(26) At the end of the
Fourth Plan, the targets were fixed in accordance with the MCI! Advisory Committee. These targets were for
immunization of pregnant mothers against tetanus, and for the prophylaxis of nutritional anaemia (27). Intensive
District Programmes were initiated to cover the 'most populous’ states alone (28) and contraceptive projects
introduced in 1967 focused on female conception (29). Even the legislation for abortion was not spared and by
introducing ‘failure of contraceptives’ (30), abortion was made a possible strategy for family planning. This
thrust ensured that services developed in the name of maternity care would, in fact, benefit the FPP more than the
women themselves.
Towards the end of this Plan period, MCH was over-shadowed by FPP. •Then the Kartar Singh Committee in
1973, (31) recommended the integration of the workers at the grass root level and designated them as
Multipurpose workers. In this scheme, maternal health work became one of the many activities of the female
multipurpose workers(32).
Another scheme that was proposed to strengthen MCH services was the Integrated Child Development Scheme
(1CDS), where mothers were also targeted for nutrition and education (33). Run by the Social Welfare
department the scheme ran into many problems due to double control by two departments. The Fifth Plan made
an effort to integrate FPP, MCH and Nutrition Services through the ICDS (34).
The outlay for FP was increased to Rs. 516 crores in the Fifth Plan and health got Rs. 797 crores. The Plan
noted that “the primary objective is to provide minimum public health facilities integrated with family planning
and nutrition for vulnerable groups.” This shift was a manifestation of the changing perspective on
developmental. The Minimum Needs Programme was launched taking into account the needs of the poorest. The
population policy pronounced in 1976 talked about female education and raised the age of marriage to reduce
birth rates (35).
The whole scenario changed after the promulgation of Emergency which called for a direct attack on the
population problem. During this period even before the new perspective could manifest as concrete programmes,
the Ministry of Health & Family Planning opted for compulsory sterilisation which led to major political turmoil
(36). Due to the excesses under the family planning programme the Government was thrown out of power in the
1977 general elections.
The next government announced that the Family Planning Programme was a voluntary programme, an integral
part of a ‘comprehensive policy’ covering education, health, MCH and nutrition. In 1977, the Srivastava
Committee (37) argued that medical education is dependent upon one vision of a health care system. It
recommended the strengthening of rural health care services. The Government introduced the CHV scheme in
1977. The Community Health Volunteers (CHV) joined the PHC network to make health services more
meaningful, with the slogan ‘People’s 1 leallh in People’s I lands’. The people oriented strategics of‘Health for
All by 2000 AD’ of Alma Ata were accepted by India in 1978 when FP and MCH became a part of basic health
services (38). Adoption of CHV scheme, the MPW scheme, the Reorientation of Medical Education (ROME)
scheme and Expanded Programmes of Immunization were considered a part of Primary Health Care approach.
Enthused by the Alma Ata declaration, a draft policy in 1979 not only accepted Primary Health Care as central
but also proposed “bold attempts to ensure 100% health coverage in the next 10-15 years for children”. It
expressed concern for high maternal mortality but the main focus remained on child survival (39)1
The Sixth plan emphasized on infra-structural development and integration of services at the PHC level. The
share of MNP in the health budget rose from 17 percent in the fifth plan to 31 percent in the sixth plan (40).
This helped in expanding the PHC network, where a population coverage of 30,000 for PHC and 5,000 for SC,
was proposed. In addition, a 30 bedded CHC with six basic speciality services including gynaecology, obstetrics
and paediatrics was proposed. This plan bravely attempted to curtail the unbridled rise of resource investment in
Family Planning and increased inputs in Programmes for disease control. It proposed to bring down infant and
maternal mortality through extension programmes such as Extended Programme for Immunisation, Anemia
Prophylaxis, Supplementary Feeding and ICDS. Despite this emphasis, it was during this period that the CHV
scheme was dumped and medical care was opened to the non-governmental sector including private sector.
There are three important documents which need special mention here, two were published in 1980. One was the
Report of the Working Group on Population (41) and the other was a Report on Health by a joint 1CSSR and
1CMR committee (42). Both talked of inter-sectoral development as a prime need for health and population
planning. They emphasised the need for integrated health care services and Maternity and child care services for
IN I'LGIAAinO CHILD DIaVUL()PMEN I\SCJ ILML1!CDS):
Started in 1975, the ICDS programme provides not only ante-natal, nutritional and maternity assistance, but also
education inputs. An extensive survey performed by the Central Technical Committee of the Integrated Mother
and Child Development Organisation in 1996(52) provides data on the programme performance. In all areas of
activity among women, ICDS blocks show better results as far as coverage is concerned (figure 1-2). In terms
of impact however, while evaluations have shown improved nutritional and immunisation status, assessment of
maternal mortality or morbidity is lacking (53). Women’s services in ICDS however, do not cover women’s
general health needs. The latter, though never debated, are critical for women’s health.
REPRODUCTIVE AND CHILD HEALTH (RCH):
As it exists today, RCH is necessary but not sufficient. The policy shifts over the last decade have some positive
aspects. It calls for a target free’ approach, emphasis on ‘Safe Motherhood’, and ‘empowerment’ of women,
along with inputs to improve child health. Thus RCH, which in 1996 was seen as a paradigm shift (54), became
the official policy of the Government of India. It however, did not extend beyond the Department of Family
Planning even though RCH was concerned with ‘empowerment’ of women, their good health and self respect
based on social recognition. This called for a multipronged strategy that effectively improved women’s economic
and social status and created opportunities for education, employment and security for their families.
Instead of developing into a fully integrated service system, the Family Welfare Programme restricted its
integrative efforts to bring together the disaggregated and vertical programmes within its domain. This, as we
have shown earlier, undermined RCH itself by neglecting the major causes of poor health of girls and women.
Secondly, RCH medicalises deliveries as it attempts to push hospital deliveries irrespective of‘risks’ involved.
This is contrary to the principle of reducing unnecessary burden on institutions by providing good home delivery
facilities through trained personnel, good referral services for institutional care, and capacity building for
supervised home deliveries by trained personnel including traditional dais. The practice of hospitalisation for
normal deliveries in cases other than a primi is uncalled for. It invalidates the past efforts at improving the
practices ot traditional practitioners and undermines the value of their empirical knowledge. Also, by increasing
workload of institutions, it undermines their ability to provide good care to high-risk cases or complicated
deliveries.
f hirdly, the content of RCH continues to talk of ante and post-natal care without examining their content. In the
four components of RCH recognised as ‘essential’, treatment and prevention of anemia finds no place! RCH,
therefore, needs to be fully integrated into disease control and nutritional programmes. It needs to expand its
focus from 1MR and M.MR to lowering child death rates and communicable disease death rates among women
and young girls.
An analysis of the expenditures on MCH reveals that over the 90s, despite the professed emphasis on maternity,
the proportionate expenditure on MCH has actually declined till 94-95. Only in 1996-97 it goes up to 22.5% of
the total FP expenditure (Table II).
GENERAL HEALTH SERVICES:
Over the time National Health Programmes that remained vertical were the ones for Leprosy elimination, Kala
Azai control, Filaria control, and blindness control. Only the National Malaria Control Programme was
integrated. National Tuberculosis Programme was actually modified into a more or less vertical programme.
Directly observed treatment (DOTS) with multidrug regimes became a part of the strategy. The shifts proposed
were based more on the experience of the developed countries. They lacked epidemiological basis, as neither is
bacterial resistance epidcmiologically significant in India nor is the national health infrastructure fully equipped to
provide and monitor DOTS In fact, the standard regimes continue to be relevant and necessary for Indian
conditions (55).
10
The vertical programme for Leprosy lias, at best, reduced severity of morbidity for Leprosy, but elimination
remains a distant goal (56). Most of these programmes need a thorough epidemiological i eview and
restructuring, with a view to integrate them into General Health Services Without this exercise, increasing
investments will add to waste of resources. For improving the health of the women this remains a basic
requirement.
The present programmes for women’s health are thus based on the 1CDS and the restricted R.CH strategies,
rooted in the linear and purely technological approach which focuses on (i) women as targets; (ii) NGOs as
providers; (iii) privatised medical care including obstetric and gynaecological care; and (iv) reproductive health of
women. We examine these official concerns in the following section.
11.4 THE MAIN TRENDS IN POLICIES
FOCUS ON WOMEN.
Programmes promoting women’s welfare lagged behind as they got caught in the conflict between welfare and
SAP. The FPP’s experiment with popularizing vasectomies was brief. It soon revived its focus on women,
excluded their ill-health, and dealt with their reproductive capacity. The logic behind the approach is stated to be
the greater extent of suffering borne by women as a consequence of frequent pregnancies and births. It is also
argued that ill effects of currently introduced hormonal contraceptives (HCs) are likely to be much less than the
negative impact of numerous pregnancies.
The HCs considered for extensive use were Depot medroxyprogesterone acetate (DMPA), NET-EN and
Norplant. Of these, Norplant was the most favored one and has been claimed as safe, reversible and long acting
(57). There are problems with these assumptions and they need to be examined. Brushing aside side effects as
being less problematic than the complications of pregnancy itself has some basic problems:
Assuming safety of the new HCs on the basis that in poor countries, MMR is much higher than the
possible mortality due to HCs, is incorrect for two reasons. Firstly, the limited data on HCs trial precludes a
thorough understanding of the complications that may develop over time. Such a comparison in fact, treats
lightly the side effects reported by the trials. Secondly, women who are already suffering need relief through
better services, not even more harmful techniques to suffer from.
International trials of Norplant report high prevalence of menstrual problems and side effects such as
ii)
headaches, skin reactions, weight gain, depression, mood changes and dizziness. These are labelled as minor
problems (58). These side effects, in fact, assume a serious dimension in the Indian context where women
are known to have a high prevalence of conditions such as anaemia, where HCs are contra indicated.
Norplant used on a large scale here may cause serious complications.
iii)
fhc pre-introduction trials in 46 countries (59) were conducted largely in the urban centres where
side-effects could be tackled. In India, where emergency maternal care and follow up services are weak
(60), the implications are obvious.
The limited data from India already indicates that the number of users experiencing complications is
iv)
going to be high. 40 percent women under ICMR trials of Norplant2 discontinued its use after 36 months
due to menstrual problems while 10 percent women were lost to follow up. Once the trial was stopped,
none of the 1466 women under trial were followed up. (61)
Anthropological data shows that the events that affect women’s daily routines can seriously influence
v)
the acceptance patterns. This is particularly true of menstrual disturbances which create special problems in
carrying out her functions - domestic, religious and social - particularly in the LDCs (62) where traditional
social norms prevail. The so-called minor problems and all types of menstrual problems brought on by HCs
can have far-reaching consequences for acceptance.
vi)
The Population Council trials for developing the Norplant system used IUD users as controls. Problems
like bleeding, rejection and infections are very high in the case of IUD. Therefore, when in comparison to
IUD, Norplant is projected as safe, it does not say very much (63).
i)
Despite all these problems, the official experts have justified the use of Norplant. Bleeding due to Norplant is
said to pose no risk to health. “In fact implant reduces the risk of anaemia by overall reduction in blood
loss”(64). In other words, for Indian women it is better to have amenorrhoea as a protection from anaemia and
Norplant offers an advantage rather than a risk. Il is also argued that in the LDCs, irrespective of the medical
11
infrastructure, the women can take hormonal contraceptives (oral pills) as, “For those few women for whom they
are contraindicated, pregnancy or illegal abortion is even more dangerous (65).
This choice to 'protect’ “some” women at the cost of “others”, may appear statistically rational, but it neglects
the fact that the vulnerable women will definitely have more complications. Their suflering can become a cause
for rejection of HCs by other women in the community. This was the case when IUD induced bleeding became
the source of rumours and rejection of IUD in the villages.
The so-called ’protection’ of the majority from the dangers of pregnancy may actually be an added danger for
women using Norplant who have poor access to the health services and higher prevalence of conditions in which
HCs are contraindicated. Even the post-introduction trials of Norplant in 100 medical colleges covering 20,000
women (66) arc not sufficient, for they do not test F1C in the rural setting where they are ultimately to be
delivered.
These lessons could have been easily learnt from the experience of IUDs inclusion in the FPP. In 1965, IUD was
provided on an extensive scale immediately after some pilot studies in urban centres and city populations. In the
rural areas its acceptance declined within five years of introduction because of the serious nature of complications
and lack of infrastructure to take care of users.
Though the hormonal contraceptives arc being pushed in the name of woman’s right to have more choices, it is
clear that she has no role in the making of these choices. The funding agencies arc calling the shots and setting
directions of research. Thus, while traditional and barrier methods - that contributed to the demographic
transition in the West -have been neglected, HCs have been patronized. The Population Council has spent 20
million dollars to develop and introduce Norplant (67).
Other than Norplant were the experiments with anti-fertility vaccines whose rationale as well as safety has been
questioned (68). Still more harmful is the use of Quinacrinc as a contraceptive which, despite being highly
dangerous, is being supplied through private routes without the permission of the drug controller of the approval
ofthelCMR! (69).
Women are thus denied the chance of using a really safe and user controlled contraceptive, because research
funds are diverted to find surer, though not safer, contraceptives which are provider-controlled and which make
women dependent. This lechnocentricity of a woman centred population policy is in fact damaging the health of
women rather than improving it.
FOCUS ON NON-GOVERNMENT ORGANISATIONS.
The latest strategy of funding voluntary agencies to open clinics and operation theatres to provide sterilization,
IUD and spacing service, is yet another attempt to avoid confronting the challenge of enhancing informed
choices, providing safe contraceptives and integrated services, specially for rural areas and slums. By shifting
responsibility, this strategy raises a host of questions. Can the Government actually prevent diversion of these
resources into private practice? Can the inadequacy of Primary Health Centres be made up by opening
sterilization wards? Where will these resources come from? What is the logic of investing in independent
institutions at the cost of PHC network? The official documents are silent on these questions.
Only the initial failure of the FPP led to some efforts at integration in the early seventies. I lowever, the primacy
of this programme was never questioned. The post-Emergency shock led to withdrawal, but very soon better
techniques of force were discovered to push for targets. Thus, whatever the strategy choices, the use of
dangerous but more definite methods, inadequate information and tagging fertility control to a variety of health
programmes became common. And when nothing worked, independent non-goveinment agencies were tapped to
bail out the programme.
NGOs then have a dichotomous relationship with official institutions. They need funds and at the same time need
to keep their structures independent to retain their creativity and autonomy. Being close to communities they can
act as providers of information and organisational support. The bureaucracy wishes to use them as cheap
providers of their programmes and wants them to remain under official control and monitoring. The conflict
therefore changes with the nature of the NGO, as there is no uniformity within the NGO sector.
This strategy however, is riddled with problems because most NGOs work in specialized areas and are in no
position to offer comprehensive services. Secondly, given the inability of the state to exercise any control over
these, there is no way to ensure standardised quality.
12
PRIYATLZATLQN Oil Ml'DICAI, CARL
While the Bhore Committee explicitly proposed banning of private practice by government doctors it assured the
private practitioners a space within the total health care system. The Mudaliar Committee, in fact, went on to
recommend that the private practitioners be used by government hospitals and be subsidised. It was in the 1979
Draft Health Policy document that three propositions were put forward, in addition to strongly recommending an
end of private practice by public hospital doctors.
Guaranteed health services to all segments through the introduction of national health insurance.
Co-ordination between private, public and voluntary sector to regulate services provided by each sector.
Attempts at self-regulation of the high fee in the private and even in the voluntary sector.
Despite these policies, over years the private sector acquired a substantial size as well as clout in the political and
professional spheres. It acquired a variety of subsidies and support from the government and at the same time
avoided taking any responsibility for long-term investments in public health. Medical care which ensured quick
and high profit became its forte. In fact a large number of big business houses opened up charity hospitals which
earned them goodwill along with tax exemptions.
Over the past ten years there has been an increasing pressure to give up the commitment that independent India
made, i.e., provision of health care irrespective of one* paying capacity. Two basic arguments have been put
forward to support this.
There is a significant proportion of the population that can pay for services and does not need subsidised care. If
they go to the private sector then the public sector will be able to provide adequately for the poor.
Tertiary level care, which is the most expensive and most used by the well-off, draws resources off primary health
care and undermines it. Hence we need to invest only in Primary Health Care and cut down on tertiary level care.
These simplistic assumptions have been questioned by evidence that shows the implications of privatisation of
medical care on National disease control programmes. Most communicable disease control programmes are
based on secondary prevention. Hence, privatisation of medical care completely dislocates all efforts at
standardisation of treatment, epidemiological monitoring, and adequate coverage in poor countries where
40-50% of the population lives below the poverty line and cannot seek medical care (70). In India the problems
created by private sector treatment strategies in tuberculosis and malaria are well known where irrational use of
drugs plays havoc (71).
The undermining of tertiary level health care in public sector is yet another blow to the very concept of Primary
Health Care. It converts it into an issue of ‘levels’ of care where Primary means the lowest level. This has
nothing to do with the original concept evolved at Alma Ata where a set of basic services were to be supported
by two special measures. One, developmental inputs such as food, employment, sanitation, housing, roads and
other welfare services; and the other, adequate support from tertiary and secondary health care services. Without
these Primary Health Care was not complete. Thus cutting at tertiary care indiscreetly only undermines Primary
Health, and does not strengthen it. In addition to these two arguments privatisation has also been supported by
arguments such as :
Scarcity of resources in the public sector and the need for opening it up to private investment.
Need to improve the efficiency of health care and reduce wastage.
Evidence however, shows that introduction of user fee has only worked against the poor who can no more have
access to these services. The well-off therefore monopolise both the private as well as the public sector (72).
There is also no evidence to establish that quality of care is better in the private sector despite the unsubstantiated
claims of the World Bank (73). The basic problem here is that both ‘efficiency’ and ‘quality’ are defined in
economic terms, in a way that has nothing to do with a public health perspective of quality. ‘Efficiency’ is
defined as maximum output with ‘minimum’ resource input and output is measured through DALYS, and the
notion of national and epidemiological priorities is completely lost. Also, saving money becomes a greater
priority than controlling diseases and having long-term policies.
for example, these notions of efficiency have led to conceptualization of‘clinical’ and ‘public health’ packages as
i f the two are independent of each other. Efficiency is being measured only for technological interventions
without taking into account the implications of increasing unemployment, marginalisation of women workers.
13
s
receding PDS system, and increasing costs of basic goods as well as education. This approach is totally
detrimental to the conceptualization of a health care system that takes a comprehensive view of health itself.
DALYS, which assess diseases as independent entities and are unable to bring out the links between diseases
such as diarrhea, pneumonia and malnutrition, which do not make a distinction between morbidity and mortality,
which completely reject the values of diverse cultures and perceptions of different communities by imposing the
‘experts’ perceptions and which use the totally inapplicable economic notion of‘discount rate’ for measuring
value of life, are a tool made especially to promote the economic notion of efficiency. Once its biases are
understood the calculated efficiency models fall flat and we have to rethink (74).
The implications of these for women’s health and programmes to promote it are obvious. The tertiary and
secondary level care, especially emergency care, has to be quantified and provided through public sector. If it is
left to the private sector the implications for women’s health, especially the poor, are going to be serious.
The private sector that works for profit cannot be expected to provide for epidemiologically significant priorities,
which do not necessarily manifest as expressed wants. For example, treatment of anemia, good ante-natal care,
basic immunisation services, provision of information to women, and preventive activities for disease control
must continue to be a function of the public sector.
Within the RCH there is a need to pay heed to what the women are saying and asking for, a matter that has not
been paid adequate attention and has affected the programme negatively. Studies demonstrate that the nature of
ante-natal and natal care needs to be altered and based on women’s expressed needs and conditions rather than
the medicalised view of the professions (75). This calls for strengthening the cadre of female health workers who
are closest to women and can act as mediators between them and the health service system. This is possible only
within a well though out public sector and not a private sector of health care. The cuts on health sector
therefore, need to be checked and maldistribution within it needs correction.
The prioritisation within disease control programmes, family planning programmes and infrastructure building is
crucial and needs to be addressed. Table III presents the distribution of resources in some of these programmes
over the 90s and reveals that their investment pattern are not based on epidemiological rationality. These
misplaced thrusts in fact, detract from the real issues of women’s health which lie in the overlap between
occupational, maternity and general ill health of women in India. It also impedes the emergence of a
comprehensive strategy for successful FWP. Despite clear historical evidence that FPP can not succeed except as
a fully integrated strategy of the total Health Services system, the state continues to push it as a vertical and
isolated programme. A women centred FPP needs to be even more sensitive to the health of women. We
present here a critique of the policy of RH, based on epidemiological insights into women’s health and a public
health approach.
II.5 REPRODUCTIVE HE/\LTH - THE EPIDEMIOLOGICAL BASIS
Reproductive health is defined as a state of complete physical, mental and social well-being and not merely the
absence of disease or infirmity, in all matters relating to the reproductive system and to its functions and
processes. It is obvious then, that it leaves out all other aspects of health and well being. Only a full grasp of all
dimensions of health can lead to adequate prioritisation of problems and a desirable policy. To examine the
epidemiological priorities, the Model Registration Scheme offers valuable insights despite its limitations. An
analysis of deaths from 1982-1993 shows that deaths due to childbirth constitute 2.1 to 2.9 percent of the total
female deaths (Table - IV). MCH then tackles only these deaths and leaves out 98% of female deaths! The main
causes of death among women remain respiratory diseases, causes peculiar to infancy, diseases of the circulator
system (which includes anaemias), fevers, and digestive disorders. Time trends show very little decline in these
proportions. The proportion of death due to injuries actually increases slightly and those due to fevers decline
over the entire period. For causes falling within the purview of Maternal and Child Health (childbirth and
pregnancy, causes peculiar to infancy and diseases of the circulatory system including anaemia), there is an initial
decline in proportions till 1988-89. Then a slight but consistent reversal of this trend sets in.
To acquire a better idea of the distribution of causes we have identified from each group specific communicable
diseases. Deaths due to Gastro-enteritis, Cholera, Dysentery, Tuberculosis, Pneumonia, Whooping Cough,
Meningitis, Jaundice, Tetanus, Chicken Pox, Measles and Polio Myelitis have been clubbed together to look at
three specific groups of causes of death - communicable diseases, maternal deaths (deaths related to pregnancy
and child birth), and anaemia. Table - V presents the age specific death load for these three groups. The
important features of this analysis arc that in all age groups communicable diseases cause the highest proportions
14
of deaths. In the 15-44 years age group these maternity deaths range between 11% - 18% but there is no definite
pattern. A visible trend is the virtual stagnation of the pattern of distribution of deaths within this age group.
I he slight decline in the proport ion of deaths due to communicable diseases in the 15-44 ycai age gioup is
compensated by the slight increase in the proportions of maternal deaths. The non-communicable disease and
anaemia deaths show little change except over the years 1992-93, which needs cautious interpretation.
When we look at deaths due to anaemia in the 15-44 years age group (Table - V), we find that as a complication
of pregnancy it has certainly not declined, as its share has come down from 3.4% to 1.93% in 1988 and then
again risen to 3.07% in 1993. General Anaemia (without pregnancy) is an equally serious threat to women’s
lives. Even if the 1993 figures are treated with caution, the rising contribution of general anaemia to deaths
cannot be denied.
If we add to this the low levels of average calorie intake, as shown by the National Monitoring Bureau data, the
picture of general health becomes very poor. For example, in 9 major states, for 1975-78, the women who were
sedentary workers (requiring 1900 calories) showed a mean calorie intake of 1307-1816 in all states except one.
For moderate female workers too, all except one of the nine states had values less than the required 2200 calories
and here too the range of mean intakes was 1141-1976 (76). This reflects the severe deprivation of adult women
in Kerala, Tamil Nadu, Andhra, Mahrashtra, Gujarat, Madhya Pradesh, West Bengal and Uttar Pradesh. In 1996,
among the sedentary workers, the mean calorie intake went above the recommended levels in two out of 8
States, and for moderate women workers 4 States had values above the required. In the 1996 data however,
U P. and West Bengal were replaced by Karnataka and Orissa (77)!
LINKS BETWEEN MATERNAL MORTALITY AND DISEASES
Women’s poor nutritional status, high prevalence of anaemia, and communicable diseases complicate
Reproductive Health. This fact needs to be highlighted. Unfortunately very little recent national level data exists
to demonstrate the association. During the sixties however, when reporting systems were more open, the
Ministry of Health and Family Planning published some useful statistics on this problem which were subsequently
discontinued.
For the years 1966, '67 and 68, we present cumulative data on deaths due to toxaemia, haemorrhages,
complication of pregnancy, sepsis, abortion, and post-natal complications. Along with these we also examine
maternal (obstetric) deaths with associated medical conditions such as tuberculosis, anaemia, dysentery, and
smallpox. A majority of these were certified by doctors but some were not. We club this data in Table - Vll and
find that, among the total registered maternal deaths, up to 16.39% mortality is caused by complications due to
associated causes. Given that all deaths were not certified by medical personnel, and complications such as
cerebro-vascular diseases, diabetes, etc. have not been considered, the detection of associated causes can only be
an under-estimate. In other words, the under-estimation of the underlying ill-health associated with obstetric
deaths is not an insignificant issue. Even though such data for the present is not available, given the almost static
levels of mortality and the return of epidemics of Malaria, Kala Azar, Hepatitis, Plague, and Dengue, grave
doubts exist that the 90s present a more hopeful scenario.
The Model Registration data thus emphasises the following :
1 .The importance of dealing with the health problems of under 15 year old girls, who bear a high load of
mortality, and who enter reproductive age with a disadvantage.
2. The importance of the communicable diseases, which not only kill the young but remain the second major
killers of women in the 15-45 years age group.
3. The inappropriateness of exclusive Reproductive Health interventions for women in the reproductive age group
when communicable diseases, anaemia, and malnutrition are their major killers across all age groups.
4. The need to retain the focus on maternal mortality, before opting for broadening the base of Maternal and Child
Health services in the face of severe cuts in health sector investment. .This broadening into peripheral areas of
Reproductive Health will dilute the efforts of the public sector which, through the FPP, is already
concentrating investment in contraceptive services.
5 .The need to recognise the impact of general illness on maternal health as the complications caused add to
maternal mortality.
This data gives a clear basis for policy level interventions in the area of public health. It also explains partly
the 'silence’ of poor Indian women on the issue of Reproductive Health and rights other than basic Maternity
Services.
15
II.6 THE NEGLECTED AREAS OF POLICY
Apart from the problems that are inherent in the emerging trends, a major weakness is total neglect of certain
key areas of concern. These include women’s occupational health problems, availability of food, and
legislative provision.
OCCUPATIONAL HEALTH AND DISEASE
Our review of policies shows that, in the process of planning, Maternity Health of women has received the
maximum attention of planners. Emphasis on occupational health was limited and is reflected in the
introduction of legislation such as Maternity Benefit Act, ESI Act and protective legislation in terms of hours
of work, timing and work specification. Despite these positive steps and the recommendations of the National
Commission on Self Employed Women and women in the informal sector, the actual policy statements on
acceptance and implementation of these recommendations by the government are lacking. The National
Commission highlighted the importance of poor working conditions and low wages of women in unorganized
sector (78). It pointed out:
that 1/3 of them were the sole owners and therefore fully responsible for the survival of the family.
they were fully responsible for reproductive labour and looking after the sick and household work which
trebled their burden,
• the health problem were related to long hours of work and postural problems bom out of hard labour in
stooping positions, as in rice plantation or Beedi, Zari and carpet makers.
• workers’ exposure to toxic substances and dust such as chemical fumes in electronic industry, tobacco
and silica dust, wood smoke, carbon monoxide etc.
• high risk of lung infections.
• that women needed improved working conditions and not just medical technological inputs.
The recommendations of the National Commission were:
•
•
1
Ensuring them fuel, fodder and water to meet their basic requirements;
2.
Strengthening their existing employment by providing appropriate support in the areas of skill, training,
credit and marketing;
3.
Protecting their employment in the sectors where it is declining due to technological advancement;
4.
Creating new employment opportunities for them based on local markets for mass consumption goods;
5.
Protecting women workers from casualisation and contractualisation, which lead to their exploitation;
6.
Providing supporting senices to women like housing, toilets and child-care facilities;
7.
Proper and effective implementation of industrial and protective legislation.
It needs to be recognized that as more and more women are pushed into the unorganized sector, where
legislation is ineffective, the health problems are going to increase and will get reflected in health indicators.
While ESI services for women need to be strengthened, the importance of broader policies regarding working
conditions cannot be overemphasized.
An important area of occupational health is problems of reproductive health. It is important to realize that
tackling these through the technocentric RH approach can only be a short term limited intervention as the real
answer is in long term policies on women’s work and working conditions, protective legislation, and recognition
of the value of their labour.
Yet another problem associated with rising tension levels of displaced families and working women is the
increased emphasis on mental illnesses (79). It is important to realise that occupational and mental illnesses are
rooted in social conditions and no amount of pills can cure them. Often enthusiastic NGOs and women’s groups
contribute to the medicalisation oi these social problems. They do so without realising that they arc only helping
the drug lobby by opening up yet another area of social health to markets.
16
These observations based on various studies illustrate the overlap between working and living conditions of
women and therefore call for a comprehensive policy on health,
NATURE OF WORK DURING PREGNANCY
Women’s work have been seen as household labour and has therefore largely remained out side the sphere of
social legislation. Only the recognition of her contribution to social production, her major role in the
unorganised sector ( both agriculture and industry) and the expansion of the home based industry where women
are the primary producers has focused on the need for regulation of her work. Given the problems of definition
of an industry and the current protective legislation, most women have no protection. Even where maternity
benefits are available in the interest of infant care women prefer to work till the last day of pregnancy.
Legislation therefore has made no difference to the quantity and quality of work that women do during
pregnancy. The ILO recommendations for maximum load bearing and-hours of work prevail only in the organised
sector and are used more as instruments for exclusion of women rather than their protection. At the same time ,
in the unorganised sector no heed is paid to these recommendations.
FOOD AND NUTRITION
The present nutritional status of women is yet another matter of concern. The National Nutrition Monitoring
Bureau (NNMB) data reveals that 24.2% women suffer from second and third degree chronic energy deficiency
while first degree energy deficiency is prevalent in 25.9% women. Thus only 44.8 % are normal in 1988-90.
There was a direct relationship between energy deficiency and occupation. Thus laborers with chronic energy
deficiency constituted 60.3% of the landless agricultural labour, with men being equally affected. Among the
artisans and the cultivators, the prevalence of chronic energy deficiency was 45.6 and 49.4%. The levels of
anaemia in pregnant women was 87.5% with 46.7% women showing moderate to severe anaemia and the rest
having mild anaemia. (80)
Evaluation studies of nutrient distribution programmes, such as VitA and Iron distribution, show that the impact
of these programmes is insignificant due to poor implementation (81,82). While the feeding programmes have
their problems the PDS systems are becoming less accessible. For any affirmative policy therefore, the
recognition of these limitations of the present policies is critical.
In the face of the given problems, the policies over the first four decades of independent planning seem to be
narrow and focused on maternity issues. Over the 90’s there is an effort to broaden the perspective. There is
however, a danger in this kind of broadening, where the initial core services that are basic are threatened by
dilution. There should be no undermining of the basic maternity services and Communicable Disease Control
Programme within the health sector. Broadening the scope of the basic services has to be based on
epidemiological and sociological date on need assessment. The health sector inputs need to be supported by
better PD systems and food security systems.
Development that is equitable and provides basic means of survival to all is critical but it must not deny the
importance of state run welfare services for all. There is enough evidence to prove that the poorest sections need
this most as they are unable to access private services. For women’s health the two basic prerequisites are : (i) a
multipronged attack on poverty, social injustice and cultural myths; (ii) identification of critical areas of health
needs and developing PHC services for these.
Our concern for women’s health should be expressed in policies for gainful employment for all women and men.
This is critical in the light of the fact that in India the minimum wage of a single individual is calculated on the
assumption that both adults of a nuclear family are employed. One person’s wage is therefore half the family’s
requirement. In view of the high proportion of single parent families, rising unemployment, shrinking welfare
investment, and a dwindling food security system, even partial employment can play havoc with families, specially
of the poor and with women as the head.
It is therefore, necessary to call for stopping wasteful over exploitation of natural resources such as land, forests
and water, which constitute the livelihood of a large number of people, building food security systems, and
ensuring that people retain their rights over natural resources that are central to their survival and health.
17
LEGISLATION AND WOMI-N'S I IF.ALTI I
Legislative measures that influence women’s health have evolved as a part of the struggle for welfare. With the
weakening of the workers' organisations, efforts to improve or strengthen legislation or to see that mechansims io
implement them are strengthened, have slowed down. For example:
The pre-natal Diagnostic Techniques (Regulation and prevention of Misuse) Bill, 1991, became inadequate even
before it was passed due to the use of ultra-sound, but nothing has been done about it (83).
The Medical Termination of Pregnancy Act, 1971 pushed the safe limit beyond the initial 12 weeks to 20 weeks
to accommodate population control planners. This is causing serious injury to the health and life of women (84).
1 he Maternity Benefits Act, 1961, provides for a 12 week maternity leave for women alone and only to those
who have put in 160 days of work with the employers within 12 months of the expected date of delivery. This
leads to very low utilisation of the benefit as most women in unorganised sector never manage to retain
continuous employment. Secondly, the rate of benefit is counted on the basis of her average daily earning three
months prior to her maternity leave. This ensures low wages as only her work with pregnancy is counted and not
her average performance otherwise. The Act is restricted to women alone and hence treats pregnancy as her
personal responsibility rather than the social responsibility of a couple. Another reflection of this attitude is the
fact that pregnancy is treated as a disease.
Despite the existing Drug and Cosmetics Act a number of harmful drugs are sold openly in the market without
warning. Often this is dangerous for pregnant women and children.
The main occupation related legislation that cover women as well as men are the Factories Act, the Workman’s
Compensation Act, the ESI Act, the Construction Workers Act and the Act for regulating work conditions of
Bidi Workers. The Factory Act provides for separate toilets for women, resting places for them, and exemption
from working at night and from hazardous work. It also claims to provide safety by prohibiting their employment
in cleaning, oiling or repairing moving machines, and lifting heavy weights. The Mines Act prohibits employment
of women for underground work. These provisions however, have acted more as a deterrent for women’s
employment than as protective measures for the safety of women industrial workers.
Apart from inadequate legislation, there are critical areas that actually need legislative intervention. For example,
the 1992 Draft Population policy proposed legislative measures to give land rights to women but the 1996
ministry document on population policy ignored it. Though large number of women are being pushed into the
unorganised sector these sectors are beyond the pale of legislative control such as Minimum Wages, ESI,
Workman’s Compensation etc. Absence of legislative control over human population research makes women
into guinea pigs, as in the case of the Quinacrine trials (85). Last, but not the least, monitoring and guiding
private sector through legislation is an area that cannot be ignored.
II.7 ABORTION:
Indian policy in this area has been relatively progressive. Not only was the 1971 MTP Act a bold step, its
implementation too has been active. The actual numbers of legal abortions however, are estimated to be 2-5
times more than the reported. In addition about 4 million illegal abortions were estimated. According to other
estimates, this number ranges between 3-6 million illegal abortions in India. The fact that 6-9% of abortions are
in adolescent girls and 20-34 year old women contribute 16% of it shows the need for adolescent health care and
the use of abortion as a Family Planning technique. A negative development has been its linkup with sex
selected foetal destruction, and the growth of clinics which make use of abortion services for foeticide. This
calls for a careful MTP Programme as a part of the Safe Motherhood strategy, supported by provision of
information and public education to build awareness regarding safety use of MTP. To achieve this goal a strong
Primary Health Care programme alone will provide the back up.
18
11.8 AN EVAIAJA riON (H HEALTH AND FAMILY WELFARE POLICIES
Our review of policies and programmes delineates the main constraints of the planning process which have
serious implications for women’s health. For any future health planning therefore, these have to be directly
addressed. We briefly enumerate them as the following :
There is an essential dichotomy in conceptualisation of the problem. Changes in health and population numbers
arc seen as two independent processes As a result, fertility related technological interventions are promoted
without grasping the links between population, general health, and the nature and content of development itself,
particularly employment and food security.
Due to this conceptual inadequacy (despite sufficient socio-historical and demographic evidence) the process of
integration of services also has been partial and therefore ineffective. The main weaknesses in the policy for
integration have been that : (a) structural integration has been attempted in absence of conceptual integration of
problems; (b) the priorities have been set by planners without any incorporation of the perceptions of different
sections; Q as a result, all the benefits of integration have gone to the programme with the highest priority
(FWP) while others have suffered; (d) the non-performance of disease control programmes is, therefore, an
outcome of partial integration and priority setting without epidemiological basis.
Integration therefore, needs to be clearly defined as planning and resource allocation by a unified authority with
full grasp of the populations’ total health problems, its epidemiological dimensions, and the needs and perceptions
of different sections. Within this definition, the vertical approach to disease control needs to be questioned and
links within programmes that mutually influence each other need to be recognised. This alone can be the basis for
shared manpower and programme structures that are economic as well as more efficient. In other words,
conceptual integration along with a fully integrated structure that is responsive to a variety of health needs is a
necessary pre-requisite for improving health service system. Since, in the planning exercise, integration was more
a result of successive failures of vertical programmes such as National Malaria Eradication Programme and FPP,
there has been very little debate on the subject. Integration has been limited to the activities within the health
sector and never beyond.
The socio-economic correlates of health have been acknowledged by Bhore Committee itself, but only in 1978
did the concept of Primary Health Care actually incorporate them into health planning in the form of intersectoral
development to provide comprehensive facilities for livelihood. Though accepted in principle, the imposition of
SAP has made it difficult to achieve. Available evidence reveals that technocentric services by themselves are not
sufficient to achieve good health. For the health of women this neglect becomes even more critical, given their
secondary position in the family and their caring responsibilities. Without ensuring women their share in
employment, adequate availability of food through strengthening food security systems, education, and
supportive legislation, health policies and programmes will continue to lack comprehensiveness.
The single most critical programme for women’s health has been the FPP. It not only appropriated MCH but
also reproductive health. It did not permit a genuine realisation of the approach that tackles all aspects of
women’s health, including their occupational, general, and nutritional health. Maternity and reproductive health
have become vehicles for FPP rather than its objectives. The obsession with fertility control makes women the
target for population control rather than subjects involved in their development and empowerment, including
control over their own fertility. Though much is being said at present about social opportunities, economic
development with equity, and women’s empowerment, the macro economic policies are against the interests of
the underprivileged. At the same time there is no evidence of even the 'safety net’ that was prescribed for the
poor. Without this the welfare sector continues to be starved of resources, particularly the health sector where
investments are now as low as 1.2% of the total.
The massive investment in FPP has led to distortion of resources allocation at the cost of women’s health. This
is reflected in poor inputs into MCH programmes and communicable disease control. The cuts on Malaria
Control, the near stagnation in TB control, and excessive increase in AIDS control (for which no control
measures are available except for good health care and education) reveals the unbalanced resources distribution
when epidemiological priorities are assessed (Table III). Thus both intra-scctoral resources distribution and
sectoral investment in health need to be corrected and expanded.
19
’■’A--
li
The content of RCH and its epidemiological basis needs thorough review to ensure supportive and referral
services within public sector, strengthen positive traditional knowledge and practice, and correction of priorities.
Thus, emergency and gynaecological services should be ensured and not just RT1 and STD treatment. ICDS and
RCH need to enrich each other and their separate emphasis needs to be equalised. An inbuilt system for
monitoring coverage, quality and impact must be built to unify these programmes and make them broad based as
well as more effective
There is pressure on India to incorporate non-communicable diseases in its public sector health programmes.
This needs to be reviewed on two grounds, (a) The genesis of these illnesses lies in environment that influences
human genetics and its manifestation. Without taking into account the environmental factors, using molecular
epidemiology and gene replacements is yet another way of remaining technocentric. Similarly, rising prevalence
of chronic heart diseases and hypertension are not just diseases of affluence. They are also linked with the
patterns of production systems that spread pollution, toxic damages and tensions. Facing environmental issues
means facing issues linked to the nature of development itself. This, though critical, is an issue that cannot be
dealt with within the boundaries of the health sector. At best health sector as of today offers curative services
and therefore, has a limited role in prevention. Problems such as hypertension and Chronic Heart diseases
(CHD), where risk factors are known and health education has a place, are amenable to public health action but
curative strategies for Diabetes, Mental illnesses and cancers will have to be tackled judiciously. The real
answers to these lie in changing the course of development, reduce social tensions and environmental pollution by
hazardous substances, and not in expanding the medical market.
If the public sector has to improve its performance it must be strengthened through training and filling of posts of
paramedical workers, provision of basic drugs, laboratory facilities, and well established epidemiological
monitoring systems.
The strengthening of secondary and tertiary level support systems within public sector are crucial as primary
health care is not a notion about levels. It is the optimum care for the highest priority problems (based on
epidemiological assessment) within a given situation It calls for Secondary and Tertiary level support for
peripheral units within a district health service where referral systems are well established. These support systems
should not be built on demands of the urban or rural elite.
The present policies do not provide any strategies for monitoring and control of private sector which is now
dominating medical care. Since most disease control programmes are based on curative strategies, it is necessary
for their success to develop legal mechanisms for (a) standardisation of the quality of treatment, (b) transfer of
information about coverage from private sector to public health monitoring units, © coordination for preventive
interventions, (d) training and information dissemination, and (e) cost control.
Legislations that influence women’s health, employment and rights are weak and cumbersome. Primary Health
care is not yet a basic right. Both these need to be changed.
HL WOMEN’S GROUPS ,\ND POLICY MA KING:
Women’s groups’ in India have been primarily responsible for focusing upon the plight of women and their poor
health. Their active and constructive participation at ICPD, Cairo and Women in Beijing is a clear evidence of
their effective and important role. Some of the groups have also contributed in a significant way to the
understanding of women’s health through their action research. This has gone a long way into policy making.
Over the past eight years their involvement in policy making has been encouraged. It must be noted therefore
that it is not sufflcient to invite women’s groups to participate in policy making, they need to be adequately
equipped with methodologies of policy making. The short training being offered in issue based advocacy are not
sufficient for this. If women’s groups have to participate in health policies then they must be familiar with the
various dimensions and determinants of health and the process and tools of planning. Without these, the danger
of these groups being used to push inadequate strategies and methodologies is alive and needs to be curbed by
women’s groups themselves through equipping themselves for the task.
IV. SPECIFIC GOALS FOR WOMEN’S HEALTH
20
There have been targets for Family Planning and later for MCH (such as the number of beneficiaries, and the
number of deliveries Ante and Post Natal Care and the number of women and children being immunised ).
However, there have been no targets for women’s health. Even the current efforts to fix the targets for the
coverage of population in RNTCP (Revised National tuberculosis Control Program ) and NLEP (National
Leprosy Eradication Program) pays no attention on women per se even though it is well known that their access
to services is poor.
V. PUBLIC DEBATES ON WOMEN’S HEALTH ISSUES
The issues in women’s health policy that have drawn public attention are varied. For example the MTP Act itself
was the outcome of the debate on abortion. The use of medical technology for reasons other than the welfare
of women- as in the case of sex determination-also became public debates. This was particularly so when the
1991 census showed a very poor sex ratio which had in fact worsened . This triggered the debate on the
socio-demographic implications of the dwindling size of the female population.
The third most critical issue in public debate has been the problem of child abuse particularly in girl child. The
women’s groups played a key role in making this debate public. A less debated issue but one which did come
up was the issues of rape and the legalities involved in the procedures adopted while verifying the case. The
double trauma that the victim went through was the key issue which forced legislators to re-look at the
procedures involved.
The current Population Policy itself was vigorously debated both by the general public as well as the women’s
groups. A component of this public debate and action has been the use of dangerous contraceptives. Currently,
a public interest litigation was filed and won through public intervention to stop the use of Quinacrine as
contraceptive pellets as the drug has not been approved and has harmful effect on direct use. The total
hysterectomies performed on mentally retarded girls also become a hotly debated issue wherein it was argued
that a State Institution can and must provide the basic services necessary and protect the young women rather
than hide their callousness by performing hysterectomies. This debate got linked to the debates on trafficking of
women and their sexual exploitation in absence of social and economic security, and the issue of recognition of
prostitutes as “Sex .workers”.
VI. MEDICAL EDUCATION AND GENDER ISSUES
Though among institutions of higher learning, Women’s Studies/Gender studies have found a place, and the
University Grants Commission is promoting such centres of research and teaching, the medical colleges still
remain tied to their biological orientation. A curriculum weak in social sciences ensures that social articulation
of sex roles in societies and its significance for health sciences remains outside the domain of medical education.
The need for such a reorientation is obvious. There is also a need to strengthen social science inputs to help
understand social determinants of disease and provide an overall context without which gender sensitisation has
little meaning and can be counter productive by undermining caste - class issues.
VII. RECENT REFORMS OF WOMEN’S HEALTH SERVICES
The effort to ensure safe motherhood and reproductive health through RCH approach is new. RCH is a step
forward from what FTP was earlier. Its target free approach, its effort to involve users and providers by
focusing on improved quality of MCH and self assessment of goals by the ANMs certainly gives FPP a new
turn. However, from the point of view of women’s health, this still remains a limited view of her problem, as it
leaves out the major cause of women’s-mortality and morbidity - the communicable diseases.
21
RCH therefore must take this final leap of integrating FPP, RCH, Nutrition and Communicable Diseases Control
Programmes.
VIII. POLICY RECOMMENDATION
Health then is no simple issue of distributing pills (be they nutrient, curative or contraceptive. It calls for ensuring
full employment and women’s right to protect themselves, their jobs, their land, & their children. It required that
women To have access to public distribution systems and welfare services that extensively cover the deserving
and cater to their needs.
Central to health are the following:
•
•
•
•
•
Provision of potable water supply which is gradually becoming a scarce resource threatened or polluted by
the uncontrolled growth of hazardous industries.
Better living and working conditions for women who are increasingly being pushed to take up jobs in the
unorganized sectors of industries at low wages and high risks to their health.
Social justice for women through revamping legal and institutional support structures.
Education for the sake of learning and not only as a means to bring down fertility and control births.
Provision of Comprehensive Primary Health Care (PHC), with a special focus on making health services
accessible to those women who are the first to get marginalised in conditions of scarcity and financial
constraints, and not the Selective PHC which emphasizes population control strategies.
Adequate intersectoral inputs - such as agriculture, housing, transports drinking water supply etc, to make the
Comprehensive Primary Health Care Services effective.
Within this broad policy framework it is recommended that women’s health can be promoted only if: 1. The separate departments of Health and Family Welfare are fully integrated into a single department of Health
and Family Welfare.
2. Under the Commission for Women, a sub committee is created to constantly review and monitor the
intersectoral planning for health.
3. A policy statement on Health and Family Welfare is reworked on the basis of the links between the two.
4. Mechanisms are developed to monitor and guide standardisation of treatment, information pooling and quality
of care, both in private and public sectors.
5. Legislative measures are taken regarding access to information, right to provision of Primary Health Care, and
improvement in existing legislation.
6. The vertical nature of health programmes is replaced by ongoing integrated programmes evolved on the basis
of health-systems approach with epidemiology-guided give monitoring.
7. Increase in the share of health sector inputs to strengthen public sector, which alone can reach out to the
underprivileged.
8. Emphasis on training and improving the working conditions of the paramedical staff.
9. Provision of basic drugs, equipment, and laboratory facilities to primary and secondary units. Judicious
investment in tertiary units.
10. Recognising the strengths of traditional systems, particularly the empirical knowledge of traditional dais.
Creating spaces for them and mechanism for mutual enrichment.
REFERENCES
22
•L-.
World Health Organisation (1952). “Expert Committee on Maternity Care : First Report - A Preliminary.
Survey”, Geneva, WHO, pg.3 (WHO Technical Report Series No.51)
World Health Organisation (1969) : “The Organisation and Administration of Maternal and Child Health
Services. Fifth Report of the WHO Expert Committee on Maternal and Child Health”, Geneva, WHO, pg.9
(WHO Technical Report Series No.428).
World Health Organisation (1976) : “New Trends and Approaches in the Delivery of Maternal and Child Care in
Health Services. Sixth Report of the Expert Committee on Maternal and Child Health”, Geneva, WHO pg. 15
(WHO Technical Report series No.600).
World Health Organisation (1985), “Women, Health and Development: A Report by the Director General”,
Geneva, WHO, pg. 5.
Qadeer, Imrana (1995) Women and Health : A Third World Perspective, Lokayan Bulletin, Vol. 12, Nos. 1/2,
July-Oct, pp. 111-119.
Indian Council of Medical Research (1989) : “Evaluation of the National Nutritional Anemia Prophylactic
Programme”, New Delhi, ICMR.
World Health Organisation (1989): “Challenges of Epidemiology : Issues and Selected Readings”, Washington,
PAHO WHO.
Srinivasan, K. and Shariff, A (1997) :”I ndia : Towards Population and Development Goals” UNFPA for United
Nations System in India, Delhi, Oxford University Press.
World Bank (1993): “World Development Report 1993: Investing in Health”, New York, Oxford University
Press.
World Bank (1996): “Development in Practice : Improving Women’s Health in India”, Washington, World Bank.
World Bank (1996) : Ibid, pg. 10
Government of India (1996): “Report of the Health Survey and Development Committee, Bhore Committee”,
Vol. 1, Delhi, Manager of Publications.
National Planning Committee, Sub-Committee on National Health (1948) : “Report, Sokhey Committee”,
Bombay, Vora.
Government of India (1951): “First Five Year Plan”, New Delhi, Planning Commission
Government of India (1956): “Second Five Year Plan”, New Delhi, Planning Commission.
Government of India (1968) : “Annual Report 1967-68”, New Delhi, Ministry of Health, Family Planning and
Urban Development; pg. 139.
Government of India (1966) : “DGHS Report, 1964-66”, New Delhi, DGHS, pg. 143.
Government of India (1965): “Third Five Year Plan”, New Delhi, Planning Commission.
Government of India, Ministry of Health and Family Planning (1966) : “Report of the Committee on Basic Health
Services (Mukherjee Committee)”, New Delhi, Ministry of health and Family Planning.
Raina, B.L. (1963): “Family Planning Programme: Report for 1962-63”, New Delhi, Ministry of Health and
Family Planning.
UN Advisory Mission (1966), “Report of the Family Planning Programme in India”, New York, UN Advisory
Mission.
Government of India (1968) op.cit: p. 195
Government of India (1963) Summary Proceedings of the special Meeting of the Central Council of Health, held
in New Delhi, April, 9-10, 1963, New Delhi, Ministry of Health, p.36, 1963.
Government of India Ministry of Health (1962): Report of the Health Survey and Planning Committee (Mudaliar
Committee) New Delhi, Ministry of Health, vol. 1
23
th
Government of India, Planning Commission (1969) “Fourth Five Year Plan 1969-74”, New Delhi, Planning
Commission.
Government of India (1978) Population Communication in India (V.N. Kakar), New Delhi, Ministry of Health
and Family welfare.
Government of India (1973) Annual Report of Swasthya Aur Parivar Niyojan Mantralaya, New Delhi, pp-76-78.
Government of India (1973), “Outline of the Master Plan for the Provision of Health, Medical and Family
Planning Services in Rural Areas”, New Delhi, Ministry of Health, Family Planning, Works, Housing and Urban
Development, pp. 10-11
National Institute of Health and Family Welfare (1989), “Contraceptive Technology Past, Present and Future”,
New Delhi, N1HFW, pg. 23, (NIHFW Status Report Series no.l).
Government of India (1971) “The Medical Termination of Pregnancy Act, 1971”, New Delhi, Ministry of Health
and Family Planning.
Government of India, Ministry of Health and Family Planning (1973), “Report of the Committee on
Multi-Purpose Workers Under Health and Family Planning Programme (Kartar Singh Committee)”, New Delhi,
Ministry of Health .
Government of India (1973); Ibid.
Government of India (1975); “Integrated Child Development Services in India” New Delhi, Planning
Commission.
Government of India (1974) “Fifth Five Year Plan”, New Delhi, Planning Commission, pp.232, 271.
Government of India (1976): “National Population Policy”, New Delhi, Ministry' of Health and Family Planning.
Government of India, Ministry of Home Affairs (1978) “Report of the Shah Commission of Inquiry”, Vol. 111,
New Delhi, Ministry of Home Affairs
Government of India, Ministry of Health and Family Planning (1975) Health Services and Medical Education “ A
Programme for Immediate Action: Report of the Group on Medical Education and Support Manpower”, New
Delhi Ministry of Health.
Government of India (1981) “Report of the Working Group on Health for All by 2000 A.D.” New Delhi,
Ministry of Health and Family Welfare.
Government of India (1979) “Draft National Health Policy”, New Delhi, Ministry of Health and Family welfare.
Government of India (1981) “Sixth Five Year Plan”, New Delhi, Planning Commission.
Government of India, Planning Commission (1980): “Report of the Working Group on Population Policy”, New
Delhi, Planning Commission pp. 4-14
Indian Council of Social Science Research and Indian Council of Medical Research (1981), Health for All : An
Alternative Strategy-Report of a Study Group set up jointly by ICSSR and ICMR, Indian Institute of Education,
Pune
Government of India (1983) “National Health Policy”, New Delhi, Ministry of Health and Family Welfare.
Government of India (1985), “Seventh Five Year Plan”, New Delhi, Planning Commission, p.280
Government of India. Ministry of Health and Family Welfare (1993), “National AIDS Control Progammc, India
Country Scenario : An Update”, New Delhi, NACO.
Government of India (1992) “Eighth Five Year Plan”, New Delhi, Planning Commission
Government of India (1994) “India - Country Statement”, International Conference on Population and
Development, Cairo, New Delhi, Dept. Of Family Welfare.
Government of India (1994) “Expert Group on Population Policy - Draft National Population Policy (Chairman,
M.S. Swaminathan)”, New Delhi, Ministry of Health and Family Welfare.
Government of India (1994) “Country Paper India - A Draft for Fourth World Conference on Women, Beijing
1995”, New Delhi, Dept. Of Women and Child Development.
24
Ij
Government of India (1996) “Draft Statement on National Population Policy”, New Delhi, Ministry of Health
and Family Welfare.
Government of India (1996): “Approach Paper to the Ninth Five Year Plan (1997-2000)”, New Delhi, Planning
Commission
Central Technical Committee, “Integrated Mother and Child Development (1996): Survey Evaluation and
Research System in Integrated Child Development Services, 1975-1995”, New Delhi, Central Technical
Committee.
Punhani, Rita and Mahajan, Rachna (1989) : “Research on ICDS : An overview, Vol. 1, (1975-85)”, New Delhi,
National Institute of Public Co-operation and Child Development.
Government of India (1996) : “A Paradigm Shift - National Family Welfare Programme - India”, New Delhi,
Dept, of Family Welfare.
Banerji, D (1997) : “Summary Report of the Expert Committee on Review of the Revised National Tuberculosis
Control Programme”, New Delhi, VHAI and Nucleus for Health Policies and Programmes.
Tare, S.P. (1990): How far the Goal of leprosy Eradication by 2000 A.D. is Achievable, Sawsth Hind, January,
pp.14-16.
Population Council (1990) “Norplant Levonorgestral Implant : A Summary of Scientific Data”, New York,
Population Council, p. vi - viii.
Population Council (1990); Ibid.
Population Council (1990); Ibid.
Indian Council of Medical Research (1989) : “Evaluation of Quality of Maternal and Child Health and Family
Planning Services in Primary Health Centres and suggested strategies for their Improvement: Summary Report”,
New Delhi, ICMR.
Malini, Karkal (1992): “Norplant: A long Acting Contraceptive Implant : A Critical Review” March 1992,
Bombay, pp.2-3.
Buckley, T and Gothlock, A (ed.) (1988) : “Blood Magic: The Anthropology of Menstruation”, Berkley,
University of California Press.
Mintzes, Barbara, Hardin Anita and Hanhart, Jannemicke (ed.) (1993) : “Norplant, Under Her Skin”, The
Netherlands, Eburn, p. 11.
Roy, Somanth (1987): “Introduction of Contraceptives in National Family Planning Programme : Injectables and
Implants”, New Delhi, NIHFW (N1HFW Technical Paper No.3).
Government of India (1993); “Model Scheme for Promotion of Small Family Norm and Population Control”,
New Delhi, Dept, of Family Welfare, Ministry of Health and Family Welfare.
Malini Karkal (1992); op.cit, p.3
Population Council (1990); op.cit.
Judith Richter (1996), “Vaccination against Pregnancy - Miracle or Menace” Zed Books, London.
Berer, Marge (1995): “The Quinacrine Controversy Continues” Reproductive Health Matters, 6, Nov. PP 142 144.
Qadeer, Imrana (1994) : “The World Development Report 1993 : The Brave New World of Primary Health
Care”, Social Scientists, vol. 22, No.9-12, Sept-Dec., pp.27-39.
Phadke, Anant, et al (1995), “A study of Supply and use of Pharmaceuticals in Satara District”, Bombay, FRCH.
Krishnan, T.N. (1994): “Access to Health and Burden of Treatment in India”, UNDP Research Project, CDS,
Thiruvananthapuram, (Studies on Human Development in India Series No.2)
World Bank (1993); op.cit.
Kothari, V.N. and Gulati, I.S. (1997), “Disability Adjusted Life Year as a Guide for Health Policy”: Economy
and Political Weekly, Vol. 32, No. 41., Oct. 11-17, P. 2612-2617.
25
I
&
Alpana Sagar (1997) : Improving Women’s Health through the Reproductive Health Package under the
structural Adjustment Program : A Chimera: Paper presented at the International Seminar on Impact of SAP on
Health in South Asia, Sept. 24-26, 1997, New Delhi, CSMCH, SSS, J.N.U.
National Nutrition Monitoring Bureau (1980): “Report for the year 1979”, Hyderabad, NIN.
National Nutrition Monitoring Bureau (1996): “Nutritional Status of Rural Population, Additional Tables”,
Hyderabad, NIN, A 18.2, A 19.2
National Commission on Self Employed Women (1988): “Report of the Task Force on Health - Occupation and
Health Issues of Women in the unorganized sector”. New Delhi, Dept, of Women and Child Development.
Government of India (1992); op.cit.
National Institute of Nutrition (1993): “Nutrition Trends in India”, Hyderabad, NIN, pp. 33-37.
Vijayaraghavan, K and Pralhad Rao N (1982) An Evaluation of the National Prophylaxis Programme against
Blindness due to Vit A Deficiency, Nutrition Reports International, Vol. 25, No.3, March.
ICMR (1989); op.cit.
Voluntary Health Association of India (1991) : “Amniocentesis”, New Delhi, VHAI, Public Policy Division
Kabra, S.G. (1997), “Health Legislation in India”, Health for the Millions, Vol. 23, No.4, pp. 24-25.
Mohan Rao (1997) : “Surreptitious Sterilization: An Endangering Process”, Health for the Millions, vol. 23,
No.4, pp.26-28. •
c:\whd\irnra see.doc
26
■MH ■
’
■■
•
Reproductive and Child Health Programmes
Learning from the field
Nirmala Murthy
RCH programme: Policy Background
The Indian family welfare programme has helped India bring down the total fertility
rate from 6 in 1950's to 3.4 in 1993-94. During the same period, 1MR declined by
about half, from 146 to 79; maternal mortality from 8 to 4.2 per 1000 births, and the
life expectancy at birth doubled, to slightly over 60, primarily due to reduction in the
infant mortality rate. Nearly half the married couples use contraception, over 60
percent children protected against vaccine preventable diseases (NFHS, 1993). 1 hese
health statistics indicate that though India is slowly marching towards the Health for
All Goals for Year 2000, announced in the Health Policy document of 1983, the
progress is slow, falling short on all important goals by 20-30 percent.
Though the Indian family welfare programme has many strengths such as its size and
number of services provided, its main weaknesses are inadequate population coverage
and poor service quality. Various evaluation studies have attributed these to lack of
staff, equipment, and supplies in the programme, and also to the government's policy
of using contraceptive targets and incentives to pursue the fertility i eduction goal.
Contraceptive targets were particularly blamed for poor service quality and for
diverting health staffs attention away from health sendees. Early in the program,
targets were adopted as a management tool to bring fertility rates down rapidly.
Unfortunately, some irrational practices crept in to the target setting process and the
'carrot and stick' approach used to implement them, encouraged health workers to use
any means - giving women incentives, false promises, using pressure, and ignoring
other services.
Particularly affected were the maternal health services, for many reasons. One reason
was the gender bias prevalent in India. There is a gender bias in perception of illness,
male illness get more attention than female illness. Even then, morbidity rates among
women in the reproductive ages 25-44 are much higher as compared to males— almost
100 percent higher in the rural and 50 percent higher in the urban areas (Duraisamy
1998). Poor maternal health results in about 30 percent babies being bom with lowbirth weight and over 50 percent children under 5 are under-nourished, though NFHS
did not find gender bias in nutrition deficiency (NFHS, 1993).
Another reason was the policies of donor agencies which fund various programmes.
India has been quick in responding positively to various international policy shifts. For
example, after the Alma Ata declaration of Primary Health Care, India adopted the
comprehensive PHC strategy and appointed multipurpose health workers and
community health volunteers to deliver primary health care at the door step of the
people. But within a year of signing that declaration. Selective Primary7 Care approach
was proposed as a cost effective alternative to the comprehensive PHC approach
(Walsh & Warren 1979). It was quickly accepted by major donor agencies. UNICEF
introduced a service package containing growth monitoring, oral re-hydration, breast
feeding and immunisation as its child survival program. Even within that package, the
expanded programme on immunisation (EPI) was given primacy by all donors.
Maternal health services did not get that kind of support even in the UNICEF's Child
Survival and Safe Motherhood initiative that is until 1994, when the International
Conference on Population Development (ICPD) at Cairo, Egypt urged the countries
to make reproductive health services available through their primary health care
system. The government of India (GOI) once again responded rather quickly by
deciding to convert its family welfare programme into a Reproductive and Child Health
(RCH) programme and to abandon its target based approach to implementation, to be
consistent with the spirit of ICPD.
Under the RCH programme, GOI is committed to providing a package of reproductive
services such as safe delivery, pre and post natal care, abortion, treatment of
reproductive track infections and sexually transmitted diseases, counselling on
sexuality and responsible parenthood, and contraceptive services. Some of these
services are currently available, some need strengthening and some are to be newly
introduced in the programme (Pauchuri,1998). The change was also envisaged in the
way this package of services was to be delivered - through local health planning,
improving service quality and increasing client satisfaction with the services. This
decision was a result of many years of lobbying and sustained dialogue between
different stake holders - service providers, women's advocates and program
administrators.
This paper describes the current field situation in the context of RCH, how the latest
policy changes are being implemented, the role played by public and private service
providers in service delivery, as well as the role of women in improving the range and
quality of RCH services.
Historical context of RCH
RCH
is aa programme
being built
built on the earlier family welfare program, which in turn
RCH is
programme being
was the old family planning program. Until 1971, MCH and family planning were
separate vertical programs, MCH was in the state sector and family planning in the
central. There were MCH sub- centres and FP sub-centres, depending on where the
funds came from. ANMs from both types of centres were expected to provide similar
services - care for mothers, children and family planning However, for historical
reasons MCH sub-centres provided more of mother and child care while FP sub
centres stressed on family planning. ANMs in MCH sub-centres were generally older,
better trained and more respected because they delivered babies, compared to ANMs
in the family planning centers, who were younger and provided mainly contraceptives
services.
During the late 60’s large vasectomy camps became a very familiar sight Preparation
for these camps in terms of finding ’’cases” overshadowed regular activities of the
2
health centres. Typical fallout of these camps were widely publicised infected cases not
properly attended, wrong men were being sterilised for incentive money, and promises
that were not kept. Predictably enough the reputation of the family planning workers
sank low. They could not motivate cases because they had nothing to give in return,
they said. They wanted to distribute medicines and vaccines like the health workers. Or
they wanted the "power" to certify ration cards or issue birth certificates to increase
their status in the community. These demands contributed to the government's decision
in the early 70's to integrate health and family planning and creating a cadre of
multipurpose workers who would deliver health and family planning services in a
smaller area of 5000 population.
Family planning workers were happy with this change, health workers were unhappy
that they were given the unpopular task of achieving family planning targets. Next
came the Emergency period (1975-77), when the MCH services were as good as
suspended. In the aftermath of the emergency, family planning became family welfare,
to signal reorientation of the program, in which MCH and family planning would get
equal priority
But until 1996, family planning was dominating the family welfare programme
Workers had to meet sterilisation targets, even if it meant ignoring MCH services
ANMs were conducting fewer and fewer deliveries because they were busy searching
family plannhg cases. Many families avoided them for fear of family planning method
getting thrust. Even as recently as in 1993, some studies noted that women did not
allow ANMs to examine their young daughters- in-law for antenatal care, for fear of
family plannirg (FRHS, 1994).
In fact when family planning became family welfare, nothing much changed The
service package remained the same, priorities were the same, approaches to service
delivery were also the same — persuasion, incentives and pressures. Only two things
changed — program's name and the responsibility for contiaception shifted from men
to women.
The skill to perform vasectomy disappeared from the primary' health centres If a man
wanted to undergo sterilisation he was discreetly advised "it is better if your wife did it,
there will be less chance of a "social" problem t she becoming pregnant after husband's
operation)". Mile doctors were afraid to touch a vasectomy cases With women they
had no fear. .
Women could te approached during the prenatal period and persuaded to accept,
family planning after delivery. Maternal services therefore began to be seen as a
strategy to promote family planning. There were written and unwritten instructions to
doctors to "persuade" all women delivering in the government hospital to accept some
contraceptive method. Women who were not ready for sterilisation should get IUD or
condoms. Abortions were not to be conducted unless the women agreed to accept
IUD or the Oral Pill.
As a result, family welfare programme lost its welfare connotation It became an
euphemism for family planning. Media brought before ones eves pictures of
sterilisation camps where bicycle pump was used to pump air into women's bodies or
"speed doctors" were performing 300-500 female sterilisation in 10 hours in a single
day (Banarage, 1998). In monthly review meetings, district officers would reprimand
ANMs saying "what's the use of providing ANC services if women don't accept
sterilisation?" One of the "dynamic" health secretaries told me very seriously, " you
makes too much about maternal care, what if some women die, it is good for family
planning"
This has been the history, the RCH program has inherited. In that history all kinds of
services and schemes have been used as gimmicks to increasing contraceptive use.
Now RCH is coming with two new packages - essential obstetric care and emergency
obstetric care (WB 95). How can we be ensure that these also don't get used as means
to fertility control?
Field Situation in the context of RCH
ANM. is the most important service provider in the RCH program There is an ANM
for every 5000 population (per 3000 population in tribal areas). She ii expected to
conduct deliveries or supervise deliveries conducted by a dai (traditional birth
attendant), provide post-natal services, immunise children, treat mina’ ailments, and
provide family planning services.
Young and unmarried ANMs have difllculty living alone in the villages. Married
ANMs have family constraints - husbands' employment, children's education, other
family obligations which make living in the rural area difficult In addition caste
determines their position in the villages. ANMs generally belong to lower castes and
carry little credibility with clients from higher caste. Local leaders ana officials are
known to take unfair advantage of them, subjecting them to sexual and other
harassment. As a result, ANMs do not feel safe in the villages or at the subcenters
(Mishra, 1997). They prefer to commute from nearby towns which means that less
time is available for services; visits to villages are uncertain and infrequent, and village
women cannot depend on them for delivery which may occur at any time.
The next pivotal functionary for RCH is a PHC doctor, preferably a hdy doctor 1 heir
availability is severely curtailed because not many doctors are willing to join the
government services. Those who join prefer and manage hospital poUings. 1 hose
posted in rural PHC complain about lack of facilities and supplies. ANMs areal least
15 percent less than the required number Shortage of supervisors and medical oHicers
is 25-30 percent (Dept.of FW, 1996). These shortfalls are either because required
posts have not been sanctioned or not filled.
Even if all positions arc filled that docs not indicate their availability As one study
reported, only 60 per cent clients reported staff availability, though all Stall positions
were filled. The reason, a PHC has only doctor In addition to attending clinics, he has
to attend meetings, make court appearances for medico-legal cases, attend training
programmes, undertake field supervision of the stall and also needs some lea e and
A
holidays. For these reasons, even with best of intentions, PHC doctors are available
only half the time (Murthy and Vasan, 1998).
Studies have also reported rude behaviour of health staff as a major reason for low
utilisation of government health services. In a study in Gujarat 20 percent respondents
complained that the staff at the primary health centre did not talk to them properly and
that they had to wait too long. Nearly 60 percent reported going to private doctors
because private doctors, they believed, provided better quality services, even though
government hospitals had better diagnostic equipment and better- trained doctors
(Visaria & Visaria, 1990).
Service providers' attitudes in family welfare program have been shaped by years of
pursuing contraceptive targets. To meet the targets, the health staff was resorting to
practices such as not informing clients about possible side effects, not screening for
contraindication, not giving clients choice in contraception, and ignoring other health
services with impunity. Over the years people have come to look upon primary health
centres' role only in the context of family planning and not in health The program also
had other limitations such as services like emergency obstetric care and treatment of
RTI/STI were not available, maternal care was minimum, health centres were not
properly equipped, and the staff lacked technical training (World Bank 1995)
Therefore the GOI decided to decided to take a comprehensive approach to improve
RCH services which included stopping the three decade old practice of setting
contraceptive targets, introducing the Community Needs Assessment (CNA) approach
to convey the message that community health needs and not the contraceptive targets,
will be the driving force in the RCH programme, and augment resources and training
specific to RCH services.
RCH: Implementation Experience
GOFs decision to discontinue the practice of setting targets represented a paradigm
shill in which programme's orientation was to be shirted from reaching demographic
goals to meeting couples' health and family planning needs. The GOI issued guidelines
to health workers on how to assess community's health needs The steps involved were
conducting household survey, discussing local needs with local functionaries like the
angemwadi workers, health committee members, private doctors and panchayat
members; estimating service requirements based on birth rate estimates, and finally
arriving at a realistic estimate of "needs". These needs were to be treated as targets
against which workers' performance was to be monitored (GOI, 1996)
GOI tried to disseminate these guidelines by preparing a manual and by holding
numerous state and district level workshops. Though most states found this approach
"too complicated" and "too time consuming", they eliminated the word "target" from
their official reports and replaced it with "estimated need" "Needs" for maternal and
child immunisation were uniformly estimated as equal to expected number of
pregnancies based on birth rate estimate. Methods used to estimate the need for family
planning varied from state to state. In some states workers took average of previous
three years' performance as the need. In some others workers carried out hous to
house surveys to identify couples with unmet need for sterilisation and for spacing
methods (i.e. couples who want to stop or delay pregnancy but not using
contraception). Some states told the workers to calculate the need as 10 per
thousand population.
In Tamil Nadu, workers used birth-order distribution as a basis to determine need for
family planning. All deliveries of parity 3 and above, and half of parity 2 deliveries
were assumed to have "need" for sterilisation. This way, a district with higher birth rate
and more high order births would have higher contraceptive targets. This method,
though did not reflect couples' felt need for contraception, was easy to sell to the
workers and was more acceptable to the officers, who were weary of using client
survey data collected by workers themselves.
The states of Rajasthan and Maharashtra who carried out the needs assessment
surveys, found those to be time consuming and were under-estimating "need" lor all
services by about 30 percent. On the positive side, the surveys made health workers
somewhat client oriented, workers' communication with client improved, they were
able to identify specific health education needs in their area. Some workers reported
that the exercise of data gathering and data analysis stimulated their mind and they felt
responsible for meeting clients' needs.
This CNA approach helped increase health worker's awareness of the range of
services they needed to provide since they are expected to estimate needs for as many
as 18 services (box 1). Of these, 3 relate to family planning and the rest to
reproductive health services. Initially the programme is trying to focus on improving
performance of safe deliveries, measles immunisation and on reducing unmet need for
family planning, in that order. Though it is too early to say when the programme s
focus might revert back to family planning. Some states are already giving (or
arranging to give) attractive incentives to sterilisation acceptors Use of spacing
methods is increasing, but how much of it is because people want them and how much
because those are thrust upon them, is difficult to tell
Impact of the CNA on RCH
The CNA approach is almost 30 month old and attempts to evaluate its impact on the
RCH service delivery have already begun. Some of the positive outcomes noted as a
result of this approach are: improvement in MCH services coverage, increased
importance of safe deliveries, increased acceptance of spacing methods among
younger and low parity couples, reduced tendency to inflate performance data Some
states have also reported improvement in household visits by health workers (Khan &
Townsand, 1998).
The CNA was earlier called TFA, the Target Free Approach. The term was causing
problems in all states, to varying degrees. Immediately after the TFA came in efiect m
April 1996, almost all states reported decline in sterilisation operations In the fust year
A
of RCH programme this decline was alarming, ranging from 10 to 50 percent The
states with low decline attributed it to reduction in fake reporting Those with
substantial decline, attributed it to the TFA. "Without targets it is very difficult to
extract work from the woikeis". they icpoitcd Io the GOI
Not just the health workers but even doctors from district hospitals tended to cancel
sterilisation camps because there were no targets. Ironically, when the targets were in
force, health staff was after the clients, now that the targets were removed, clients
seemed to be at the receiving end. Some ANMs reported taking women to private
doctors because PHC doctors were not operating regularly or rejecting cases on
smallest pretext. Removing targets, it seemed, did not automatically guaranty that
clients' health needs will be met or that their access to services will improve
As a reaction to this decline in sterilisation performance some states once again
imposed targets. Others sent messages that "% needs mef" will be reviewed seriously
and also started institution-wise performance review, not just for family planning but
also for institutional deliveries and maternal deaths. Either as a result of such reviews
or because everyone began to understand the real meaning of TFA, that in the second
year, family planning performance improved and the positive trend has continued in
1998-99.
Not forgetting the main agenda behind the policy shift, the GOI for the first time,
included quality indicators like contraceptive failures and contraceptive side effects in
its regular monitoring system (Box 2: critical indicators). This was to be a signal that
these events are not to be ignored. How often these events will get reported and what
actions will follow, remains to be seen. If the actions become punitive then these
events will not get reported, if the staff gets credit for reporting and treating such
cases, it will be a major step towards improving quality
Technical skill training is an important component of this programme such that all
primary health centres should be able to handle complicated deliveries, abortion,
treatment of RTI/STI, Sterilisation and IUD insertions The program's aim is to make
all health centres "fully functional" meaning having full compliment of trained staff,
required equipment, medicines and supplies and to minimise situations like a health
centre has trained staff but no equipment or has a vehicle but no driver To monitor
health centres' "functionality", a system of facility survey through external agencies,
has been instituted. The GOI has high expectations from this monitoring system, but is
also aware of the fact that many problems uncovered by this system will not have easy
solutions. For example, a Taluk hospital functioning as a first referral unit for RCH,
has no anaesthetist but a trained anaesthetist is functioning as a PHC medical officer in
the same district because his wife has a nursing home near by. Such human problems
though result in irrational distribution of resources, are difficult to resolve through
policy instruments.
Use of service protocols and technical assessment is also a component of this
programme. Past experience with such instruments however has not been too
encouraging because supervisors do not take them seriously ( Ramana, 1997)
Notwithstanding these experiences some of the more developed states have decided to
w'
use them partly to send down the message that "quality matters" and partly to give
workers an operational definition of expected quality.
Even so, the service quality may not improve for quite some time, at least not until the
inputs such as staff, training and equipment as per the norms, are in place. And there
are significant gaps in these inputs (Verma, 1994). The softer dimensions of quality,
such as improved privacy, convenient timings, behaviour with the clients, informing
clients about their entitlements and giving them choices, are not even on the planning
horizon. Though these changes require very little additional resources they call for
changes in attitudes of programme administrators and service providers First we have
to deal with the widely held belief among administrators that notions of quality belong
to urban middle class women, and not relevant to rural poor I have been told several
times that rural men and women do not mind waiting at the health centres, they dont
want a choice in contraception, they are happy if a choice is made for them, expecting
friendly behaviour from health staff is impractical, their clinics are crowded, people are
uneducated and do not follow instructions.
Some health staff openly say that government services are free therefore people have
no right to expect good quality services (Ramasundaram 1994) Private doctors are
friendly with patients, because they have to extract large fees from them Why would a
government doctor want to be friendly9 asked a PHC doctor. Under these conditions,
improving interaction between clients and service providers is a Herculean task These
interactions take place at numerous places, under varied conditions and therefore
cannot be supervised. The only way out may be is to give clients powers over the
service providers.
Many women see a connection between rude behaviour of government doctor and
their private practice in the evening. In one village I visited recently, many women said
that they were using oral pill not for spacing but because they did not like the lady
doctor and did not trust her skills in sterilisation operation. They recounted many
instances of failed sterilisation operations performed by her in the camps (observation
confirmed by the ANM). ” She wants us to come to her nursing home, there she will
be nice" they said.
Rural women, obviously, do have strong ideas of what is good or bad for them, who
they can trust and who they cannot. Such information travels through their informal
network and difficult to capture through formal surveys. ANMs who do not become a
part of women’s informal network do not know what her clients really think
Government staff conveniently blames poor service quality on lack of facilities and
medicines forgetting that their own attitudes and behaviours affect sen ice quality,
specially their lack of respect for the poor, the illiterate, and socially disadvantaged
groups.
Systemic Impediments
The government investment in primary health centres and sub-centres is justified on the
grounds that health services have to reach the poorest of the poor But these centres
seemed to be perpetually afflicted by problems such as shortages of medicines, lack of
transport, and de-motivated staff. In addition, this system is accused of being corrupt,
mismanaged and wasting resources. When it comes to curative care, these centies ate
not the first choice of anybody, not even the poor. Over 80 percent of illnesses are
treated by private doctors, both in urban and rural areas The poor generally are not
aware of qualifications of the various kinds of private doctors around them 1 hey rely
on proximity and recommendations of their friends in selecting doctors Cost comes
much lower as a criteria for selecting doctor (Murthy and Barua 1997)
The poor returns from this investment, is not only because of inadequate resources but
also because of administrative constraints and procedural bottlenecks that hamper
smooth functioning of the services. For example, health workers do not make outreach
visits because they are not paid travel for months Repairs of vehicles and maintenance
require long bureaucratic procedures. Work distribution among the staff is lopsided female workers are over-worked and male workers are under utilised, there are no
incentives for good work and no threats for poor performance (OHFWP. 1996) The
system is not accountable to the clients but to the political bosses who control
transfers and other benefits.
Therefore even though the government is investing in the primary health care, pool
patients are paying high fees to untrained practitioners who fail to cure them It can be
argued that the well-being and health of the poor could be improved, il the
government centres made a full range of medicines available at reasonable prices A
small experiment in a few villages in Andhra Pradesh has found that medicine
requirement for a typical sub-centre could be about Rs 1500-2000 per month, which is
10 times the medicine budget of the government sub-centre People are willing and
able to pay reasonable charges for getting good quality service ( Prakasamma 1990)
But government's current policy of "free services" at the government health facilities is
only benefiting the private sector
Role of Private Sector
More and more women obtain services from private sector, both in urban and ruial
areas and from among the poor and not- so- poor The notion that service quality is
better in private than in public hospitals is widely and unci itically accepted by people
In one survey of health workers in rural area in Maharashtra, most ANMs said that if
they had any health problem they go to private doctors Government doctors around
them, they said, were not competent enough In this suivey, over 60 percent of the
women with complications during pregnancy reported going to private doctor tor
treatment - in some cases they were referred there by the ANMs
Rapidly growing number of private nursing homes and hospitals in urban and periurban areas is an indication of growing demand for their services Use ot these facilities
>
soeciallv among young women is rapidly increasing - first for sex determmat ion and
second for delivery complications like caesarean delivery. In another study, again m
rural Maharashtra, about 50 percent adolescent pregnant women rePO^^°^ hersprivate doctor to "confirm" pregnancy at the suggestion of their husb nds. mothers
Law. Though they did not mention sex determination test, the private doctor they
consulted was well known in the area for SDT (Barua 1998)
In more developed Indian states it is a common practice among young women to
register with a private nursing home for antenatal care when they go to their na al
home for delivery. This is a precaution against unanticipated complication in dehvety
needing hospital services, because many private nursing homes i efuse admission
cases not registered with them for antenatal care. Extent of caesarean operatic
these institutions is not known, though believed it is to be high Our recent
observations in cities like Hyderabad and Bangalore suggest that even in government
hospitals, caesareans deliveries are increasing, and the staff claim that clients ask
them.
Most deliveries in fact take place in the private sector, if one included dais the
private sector, as they should be. Information from various group discussions^ case
studies and informal talks with dais reveal that they charge anywhere between 00 to
1500 per delivery. ANMs charge between Rs 500-1000 when they conduct deUvtrv
privately Private clinics charge 1500 for normal delivery and upwards of 3000 for
complicated delivery. Women expect to pay for delivery whether in private or publ
insHtXns They prefer institutional delivery for first pregnancy or when they dec.de
Xo
Th,!refore;staKS llke '
,u
where two children is becomins a norm, up to SO percent deliveries are institutional
and more than half take place in private institutions
One of the main objectives of the RCH programme is to increase the all India
percentage of safe deliveries from 30 percent to 40 per cent, by year 200. Sale
deliveries are defined as all institutional deliveries, and home deliveries conducte y
midwifery trained persons. Mainly North India is lagging behind on this indicator for
many reason - lack of awareness, fewer facilities and trained persons, low status of
women men not aware of health risks during delivery. An NGO in Gujaiat, afie.
recognising the men's role in getting hospital treatment for women, introduced a
system of sending a post card to the male head of the family, informing hmi about he
health problem his wife or daugher-in-law, asking him to bring her in for treatn ent
That idea worked. Most women who earlier would not have come foi treatment, we
brought by the family to the hospital (Murthy, 1991)
With increased level of mass communication on women's health problems, this
constraint is likely to be reduced over time, all over India We are likely to witness
increased demand for institutional deliveries, as is seen in the southern states W
that happens, one can depend on the private sector to respond rapidly and set-up
nursing homes and small hospitals to serve the market. Would developing the capacity
of sub-centres, PHC and CHC for providing delivery services contain the private
sector?
I
1
Some case-based evidence is already showing that iinal hcallh lai ihli< aic not being
used lor dcliveiics because slulf is nol available foi .’ I horns Piivale nuisinp homes
are coming up next door, where ANMs refer deliveries and even conduct them there
for a fee. If this is going to be the scenario of the future, we need to address issues
like, should the government facilities be allowed to charge moderate fee9 Should these
facilities be handed over to "not-for-profit” voluntary organisations to compete with
the "for profit" sector. Should the government think of a financial package only for the
very poor, so women can avail good quality services at places of their choices
RCH and Gender Issue
Considerable hope has been pinned on women's involvement in providing good quality
care to women and children. That hope is based on the 33% reservation for women at
all levels in the Panchayat system, resulting in their empowerment and increased
participation in local decisions. The experience in this respect so far has been mixed In
states where social status of women has been traditionally better, with higher literacy
and greater participation in work force and in public affairs, women have been able to
take advantage of the reservation policy. In states where these conditions do not exist,
mostly the north India states, reservation measure has not produced much change (
Pai, 1998).
Women in the north have relatively little autonomy in terms of freedom of movement,
inheritance rights, control over economic resources, and support from their natal home
after marriage. In contrast women in south India have been better oft in all these areas.
A few available health indicators as if, reflect the disparities in the levels of autonomy.
In UP, life expectancy is about 5 years higher for men as compared to women (54, 49
), while in Tamil Nadu it is 61 for both men and women Maternal mortality ratio is
over 900 in UP and about 300 in Tamil Nadu. Women in UP are more vulnerable and
powerless and therefore suffer more from higher fertility, mortality and mortality
(Jejeebhoy, 1998).
In addition to lack of autonomy, their lack of knowledge and awareness about
reproductive health are other factors that determine the quality of care they get and the
preventive measures they can take. But focusing on women's awareness alone is not
the solution because awareness among men on whose co-operation women depend,
matters a great deal. Traditionally, men are not suppose to know much about womens
problems, its not their domain. But if husbands know about these problems, then they
are more likely to support their wives decision to seek tieatmcnt and likclv to piovide
money and escort to seek treatment (Barua A 1998)
Interestingly though, the medical technology is an unwitting partner in perpetuating
gender bias. Son preference in India is well documented Now there is ample evidence
that families are abusing medical technology such as differential contraception, sex
determination test, and selective abortion, to convert this preference into reality A
small but carefully documented data from Rural Haryana reported families wanting
women to undergo sex determination test (SDT). Only if it was a boy. was the need
for ante-natal care raised. More and more doctors were buying ultrasound machines
//
and some were taking them in cars to villages The only impact oi banning the SDI m
1994 was that its cost doubled. The doctors justified selective abortion as a way to
improve status of women. The study reported that the Post Graduate Medical Institute
had decided to suspend training in mid-trimester abortion but had to restart it when the
hospital started getting referrals of botched abortions from their alumni (Sabu
Dahiya, 1998).
Is the
the RCH
programme ready
to deal
deal with
with the
the iissues of sex determination and selective
Is
RCH programme
ready to
abortion? Tamil Nadu has launched a massive educational campaign dealing with
female infanticide and sex discrimination. At the same time the number of SDI clinics
in the state have increased manifold As long as these services are available in pnvate,
public facilities are likely to be under-utilised.
Discussion & Recommendations
The preceding review of field level experiences in implementing the RCH programme
denotes several salient points which need attention
So far RCH is programme is mainly grappling with the issues ot whether to remove
the target, what will replace them, what effect that will have and how to neutralise tha
effect. The CNA approach has tried to deal with those issues rather well But
/ is
not the RCH programme. The experience so far shows that its not the target alone ut
the attitude of health staff, policies and procedures, have to be reformed
Administrative constraints and procedural bottlenecks which hampet smooth
functioning of the programme, need to be tackled urgently These will require systemic
reforms. The decentralised planning implied under the CNA is inadequate to ea wi
these constraints. In fact CNA puts planning responsibility on the ANMs and on the
PHCs which is disproportionate to the power and resources they control States and
districts have no role in planning when they control the resources and the policies ns
anomaly needs to be removed, states and districts have to play more managerial role.
We also have to recognise that the RCH program has inherited a past in which all
kinds of ideas and schemes have been used as gimmicks to increasing contraceptive
use. Those administering this program still have those ideas" how to mampti ate
people in doing what we want". There is no guaranty that the services packages
offered in the RCH programme will not get used the same way CNA in itself will not
ensure service quality and access, unless clients gain some control over the service
provider
Most important weakness in RCH design to my mind, is the inadequate recognition to
the role of private sector. The underlying uncritical assumption is that poor people
prefer public institutions over private if they are well equipped But experience in al
sectors show otherwise. As demand for RCH services increase, growth in private
sector is inevitable. The government needs to develop containment strategies sue i as
(a) develop regulatory mechanisms
■ ■iiHiBin _
...
- -
(b) strengthen not-for- profit sector to compete with the for -profit sector
(c) develop financial packages and community insurance only for the poor
This is particularly important because the next strategy shill that is likely to allect the
health services in the near future is the World Bank's suggestion that states should
divest from curative tertiary care and allow curative services to be more or less
privatised. This suggestion is based on policy instrument currently being used called
DALY, disability adjusted life years, suggesting that public expenditure should
concentrate on those health services in which DALY gain is the highest (World
Bank,1993). This approach may exclude the poor, old and may be women from access
to curative care ( Emmel, 1998).
And finally we must understand that the programme is still new, the full package is not
in place, its operational details are yet to be worked out and its implications are yet to
be seen. At this stage, it is important for the researchers and activists to remain
vigilant, observe the field realities, and listen to the voices from below At the same
time, be patient so that this unique opportunity to give fundamental reorientation to the
Indian family welfare program, is not lost
‘3
References
Barua, Alka (1998), Use of reproductive health semces by marriedI adolescem
females, findings from a study in rural Maharashtra, a paper presented at the ICRW
workshop, Bangalore
Banarage A (1998), Women, population amid global crisis. Zed books, London
Department of FW, Family Welfare Programme in
in India, Year Book, 1995-96, New
Delhi, Akshadeep Printers.
Duraisamy P (1998), Morbidity in Tamil Nadu: levels, differentials and determinants,
Economic and Political Weekly 33(17) April-May, 982-990
Emmel N D (1998), Health for All for 21st Centure: Demise of primary health care.
Economic and Political Weekly, 33 ( 11), March, pp 577-580
Futures Group International, 1998, "Targets for Family Planning inJndia an analysis
of policy change, consequences and alternative choices, the Policy Project. 4,_ S <
Niketan New Delhi, India, pp 3
FRHS (1994) Operations Research in Health System Development: a report on the
barline survey, Monograph, Foundation for Research in Health System, Ahmedabad
GOI (1996), Manual on Target Free Approach in Family Welfare Programme,
Ministry of Health and Family Welfare, New Delhi, pp 35-36
Jejeebhoy S,(1998) Wife-beating in Rural India: a husband s right9, EPW.33(15).
April 1998, pp 855.
Khan M E and Townsand J, "Has the Indian family welfare programme lost
momentum under the TFA? Emerging evidence", presented at the wotks (
TFA approach, by the Population Council, Agra
Mishra. R 1997. Female Health Workers: problems and implicahons. Economic and
Political Weekly 32(43), 2791-2793.
Murthy Nirmala (1991) "A case study of Society for Education Welfhre and Action
(SEWA-Rural)", in A review of selected innovative projects mi amily we fare
programme in India, Monograph, Foundation for Researc in ea
ys
Ahmedabad
Oxford University Press, Delhi, 291-309
14
Murthy N V»s»n A (1998). Decentralized Planning Methodology lor
“ltire
aeXs' experience and lessons Iron, a district in South Indta. tout.tai ol Health
MiuuigcmciH, (Io* Ihcoiinup,)
National Family Health Survey (1992-93), International Institute for Population
Sciences Bombay, pp 283
Orissa Health and Family WeUare Project. -Impact Assessment Study ofPh.ses 1 & II.
Institute for Health Service Development, Bhubaneshwar 19 6
reproductive health package for India
Oxford University Press, New Delhi, 310-339.
Pai Sudha (1998), Pradhanis in New Panchayats: field notes from Meerut district,
EPW, vol 33, No. 18, May 1998, ppl009.
Ramana GNV (1997, "India: Improving Quality of Care
Center, Andhra Pradesh, Population Manager 5: 23-42
at Shamirpet Primary Health
Sabu George and Ranbir Dahiya, Female foeticide in Rura! Haryana, Economic and
Political Weekly 33 (32) Aug 1998, pp 2191-2198.
Verma Ravi Roy T.K., Saxena P C. 1994 Quality of Family Welfare sendees and
Care in Selected Indian States, International Institute of Population Studies.
Visaria L & Visaria P, 1990, Quality of services and family planning in Gujaiat State,
working paper no. 34, Gujarat Institute of Development Researc )
Walsh JA and Warren KS(Selective primary health care, New England journal ot
medicine, 301 (18):967-74, 1979),
World Bank (1993). World Development Report, investing in health. Oxford
University Press, Bombay , pp 26.
The World Bank, 1995, India's Family Welfare Programme, towards a rePr0^,,ve
and child health approach. Population and Human Resource pei ations
South Asia County Department II
TI1P World Bank(1997) Project Appraisal Document. India Reproductive and C luld
Heato project, Population and Human Resource Operations Division, South Asia
County Department II, pp 105-109
JI
IMPACT OF LAWS ON WOMEN’S HEALTH
BY
DR. PADMA SETH
Prepared for the
National Consultation Towards
Comprehensive Women’s Health Policy and Programmes
BY
VHAI-WAHI-DSE
Held in VHAI, New Delhi.
On February 18-19,1999
IMPACT OF LAWS ON WOMEN'S HEAL HI
By Dr. Padma Seth
• Laws pertaining to health alone do not ensure women's health
• Laws affecting her welfare in the family, in society her status
as a girl child have enormous bearing on her health
• Starting from marriage laws, laws regarding divorce, custody,
maintenance, property rights - guardianship, adoption affect
women's health
• Laws regulating and protecting employee women - their
violation and non-compliance do affect her health and well
being
• Laws protecting her, person, maintaining her dignity and
status - her equal rights are in her favour - totally violated
affecting her mental and physical health
• Laws against physical, mental and sexual exploitation,
trafficking - are unimplementable due to lack of will on the
enforcement/establishment and has become a perennial source
of income and pleasure - totally dishonored and violated
• Where can health be protected in such situations?
• Laws protecting the most vulnerable in destitute homes mental
asylums and custodial institutions including Jails if violated
there no 'Health 'for women
• Violence - atrocities - crimes on women and girls - lead to
innumerable mental and physicaltailments
• Ineffective Juvenile Justice Act - delivery of Justice - cannot
help girls in a big way - neglected.children does cover children
pushed into prostitution - But JJ Act often ignores such girls /
such cases
• Personal laws of inheritance, property rights, marriage
customs/traditions have reduced women to non-entities
• Malpractices in the name of tradition like Devdasis, Jogins,
Basaris - though restricted by law - is rainphant as a tradition
amongst certain tribes and Scheduled Castes. There are no
medical records kept or check-ups done
1
• Total dishonouring and violation of constitutional
mandate/fundamental rights to life, equal protection and equal
opportunities are non-contributory to good health
• In caste, battering, domestic violence are suppressed in the
name of family honour.
• Reflection of societal ethos in court judgements - often
insensitive to women's issues - have reduced women as
receivers of social grace/alms instead of participants in
development
• Unless Panchayati Raj becomes a functional reality power
cannot be truly decentralized. Women members of Panchayats
and municipalities have important roles to play in group
impetus to women's health
- Licensing laws to contractors selling arrack and alcoholic
drinks and psychotropic substances - have to be.severely put an
end to improve the health of women
• Laws by themselves can be amended and reinterpreted
• It is the lack of win to enforce the laws
• Laws affecting food, nutrition, public distribution system,
regulatory laws and procedures to certain hoarding of essential
commodities - all impact on women's health
• Directive Principles of state policy can be made effective by
public taking it to courts unless strict and severe sentencing
policies are evolved against indecent representation of women
in the various media - women's image is demolished - her right
to equal status is impaired - so also her right to access to health
and allied needs
• A holistic approach to health needs - a new perspective in
health policy can be effective with a women's health legislation
- that can be a comprehensive health code for women and girls
• Right to education will reduce ill health, improve better
awareness about health - and will exercise the right to demand
better services for health care for women and girls
• RiyliL Lu buLLur uiiviruiimunl
• Right to easy access to health services in the villages
• Will ensure better health
I
• Laws prohibiting child labour, bonded labour, laws against
sexual exploitation - to be strictly enforced for better societal
health and those of women
• Laws to be made and enforced - for better and adequate support
services to women labour, work force
• Social security through law to the unorganized women in
agriculture and other occupations - will bring better impact on
women’s health
• 'Health Volunteer Force' to be enacted by law to help volunteers
to serve women and girl children
Laws to be reviewed reharshed, amended - re-structured for the
benefit of women and health
Contrary to current rhetoric; health for all by 2000 A.D., health
care is still not a right and that no government programme
however organized and funded, can realistically hope to provide
universal access to minimum health to face these facts squarely,
we are missing our limited resources to best advantage.
A legal discourse on gender in the areas of women's health will
help to unravel the complex interface of law, tradition and culture
to explore the potential of law as an instrument of social change.
1 he changes brought about by law affects the single most
important fact of existence. Psychology, government, social
expectations almost everything we behave or do.
It is also to be noted how laws are undone by executive inaction,
delay and lack of enforcement.
The mere lacunae in the laws are not the only reason for non
implementation of the laws, though anomalies and gaps render
the laws ineffective.
Laws are made to condition social and individual's action,
behaviour and demand performance and accountability It is the
benchmark of violated can result in punishment. It is a deterrent
i
<
Z-
an educative force and abo^e all a leveler. Its objective is social
justice, and any sane and rational person will dread to overlook it.
The other side is the paeeivity-jMlcuu one invokes it like involving
a Government, it will not act ohits own. This characteristic of the
law has given room for criminals and violators to have a field day.
On the one side, the Directive Principles of State Policy as
enshrined in Chapter IV of the Indian Constitution speaks
volumes of secure social order. Welfare of the people, equal justice:
and free legal aid village panchayats, right to work, health and I
strength of workers men and women, right to education and public
assistance, maternity relief, living wages, economic interests of !
the deprived classes and of fundamental duties of citizens. Law
can also alter the structure of power in the community,
consciences people with a view to organize them into action awareness generation and training, part mobilization for
adherence to legal mandates include in the process.
With all these laudable attributes, one wondei's how laws are not
able to help people; instead people by and large are aware of the
constraints posed by law rather than its advantages.
Law often becomes the last resoi’t/recourse by common people.
"The Directive Principles of State Policy are not enforceable by
any court, but the principles there in laid down are nevertheless
fundamental in the governance of the country and it shall be the
duty of the state to apply these principles in making laws".
Besides, no person shall be deprived of his/her life or personal
liberty except according to procedure established by law.
The Indian Constitution not only prohibits the state from
discrimination against any citizen grounds of sex but at the same
time empowers the state to make special provisions for the well
being of women. To give effect to the aforesaid mandate of the
Constitution, legislation and amendments to existing legislation
i
have been directed towards bringing down inequalities against
women. Article 15 (3) specifically mentions gender thus :
"Prohibition of discrimination on grounds of religion,
race, caste, sex, plate of. birth"
nothing in this article shall prevent the state from making any
special provision for women and children. Article 16 deals with
equality of opportunity in "public employment" clause (2) of this
article specifically mentions women.
<
In keeping with the constitution, the state has passed a large
number of laws in every possible sphere for the benefit of women.
They can be categorized1 ks
| criminal laws, labour laws, family laws
and other civil laws, etc.
Are these legal provisions actualized by women and children is the
basic question? A quick scanning of the laws affecting women
reveal not merely judicial insensitivity in interpreting the spirit of
the law but the laws themselves are truly discriminatory in
nature.
Looking at the Medial termination of Pregnancy (MTP) Act 1971,
there appears, a right to a choice, since MTP can be performed
only under Section 4, it can only be performed in a place or
hospital approved by Government for this Act - for distant women
living in rural areas, this facility is not adequately available.
Besides it is often the choice exercised by the male.
Pre-natal diagnostic techniques (Regulation and Prevention Act)
1994 though regulates. The vai’ious types of techniques including
ultrasound a nd also prescribes penalties for the doctor for
revealing the sex of the foetus to the pregnant woman or her
relatives, there is flagrant violation of the law. The evidence is in
the progressive decrease in female child ratio vis-a-vis male birth
rate. The preference for boys and the social pressures on the girls
parents to reject the girl child are some of the reasons for
1
■
misusing this diagnostic facility. There- are negligible if not nil
cases where erring doctors have been punished by the law courts.
The girl child in the womb's survival is threatened as also the
mother is not able to save the foetps because she is not allowed to
take a decision.
Maternity Benefits Act 1961 to provide leave before and after
child birth. This Act if truly has to be supported by breast feeding
practices. The leave should not be less than six months. And who
enforces the law and see that this benefit is not violated by
contractors and private employers? So many cases where
maternity leave is not granted and pregnant women are refused
employment and the working mothers are neither provided creche
facilities nor allowed time for breast-feeding. To add to this in
certain factories, unless the woman has worked for a little less
than 100 days, she is not entitled. Devians ways are adopted to
make the act unworkable for large number of needy women.
Contract labour (Regulation and Abolition Act) 1970, separate rest
rooms for women, creches for the children, shady open play
ground for children are to be provided but who does it and if not
how to enforce and if so why the violators are let Scot fiee?
While talking of women's health, both her psychological and .
physical health are overlooked by the family, the society, at the
work place, by employers - there is yet to have a integrated health
policy - that can mandate enforcement of positive laws for the
benefit of women.
Equal Remuneration Act, 1976 though in existence is not enforced
- the court of the first class magistrate and the labour office have
the power to inspect and file complaints etc. For non payment of
equal wages can be fined upto 10,000 - even voluntary
organizations can complain - but for fear of losing the job though
with unequal and less pay no woman dares to complain.
1
Fmployees State Insurance Act, 1948 provides for employers of
factories and uatublishments earning less than 1600 p.m. But the
women iri the unorganized sector are art of the pale of this benefit
comprehensive maternity protection Act Fund/Scheme for all in
the unorganized sector - only a very few states after nutrit ional
support ■ ICD3 though as a policy is going to bo universalized the
reach art is yet not adequate.
The Factories Act, 1948 in section 19 provides for separate
latrines and urinals foi* women and washing facilities - no women
tn work hetween 7 p ra, to 6 a.m. These etill remain cn
on pa
paper.
What is the fault of the law? It is the lack of enforcement.
Minimum Wages Act, 1948, Plantation Labour Act 19nl, Trade
Viwsn Aot K?36( Worlimnn'o Compensation Act 1923 till maku
employers bablo but
Besides the labour laws which are <often violated
11
by the employers,
there arc laws protecting vulnerable women in special
circumstances like.
The Orphanages and other Charitable Homes (Supervision &
Control) Act 1960 mandates minimum standards of service,
education and training to the inmates. This depends on the Board
of Control.
Protection of Civil Rights Act, 1955 prohibits preaching and
practice of untouchability the Scheduled Castes and Scheduled
Tribes (Prevention of Atrocities) Act 1989 provides stiffer
punishment for community crimes against SCs and STs, The
flagrant violations are ever increasing not allowing the women
access to drinking water sance, to cross the village fields for
naturecalls are denied - rending women many gastric problems
infections. AP Land Transfer Prohibition Act, 1970 prohibits
transfer of land from a ST to non-ST. But women have no right to
land.
1
■
I
Immoral Traffic Prevention Act, 1986 the girls are often caught
soliciting and no trafficker falls in the legal net. Police in action
and connivance and criminals/mafia are ever expanding their
trade - kidnapping/abducting girls and women and continue sale
of girls to brothels. Even if girls are raided and retrieved - where
is rehabilitation for them - the ever increasing number of young
girls and women in Prostitution proves the ineffective law. No
special courts are ever appointed to hand to these cases.
AP Devadasi (Prohibition of Dedication) Act, 1988 bans the
practice of dedicating girls/women but in surreptitious ways, the
practice is going on.
One wonders if any are of these laws are honoured? Only the
litigant rich and leisurely can fight the cases in Courts.
Where is the health of the woman when she is rocked by demands
for dowry. She is threatened to death if she cannot bring dowry no state has appointed dowry prohibition officers - the practice of
giving and demanding goes on - NCW recommended that the giver
should not be punished. But no Government seems to be
interested in these reforms. This dowry ill not merely affects the
mental but physical health of the married girl and her parents.
Commission of Sati (Prevention) Act, 1987 - young girls tried to
die along with the husbands pyre - they are drugged and forced
where very survival is threatened who talks of her health.
The Marriage and Divorce Laws are equally unfavourable to
women - Impotency on the part of the man is an optional condition
for divorce. Though the woman is thrown out for her infertility.
Epilepsy has been a condition for divorce now with NCWs
recommendation, this condition was abolished.
Hindu Succession Act, 1956 both boys and girls have equal share
in the self acquired property of the father - but the widow gets the
share along with her children only.
1
? ■
Even in the married women's right to property act, 1939, she can
only have life interest in the property of her deceased husband
she can insist upon partition, but .she is only a custodian. She has
no power of disposal of the ancestral property.
Coming to criminal laws a child can be kidnapped or a women
abducted - there is no punishment if there is no motive established
- though these crimes demand severe punishment.
Criminal force, molestation, rape fall in the series of Acts ending
up in rape/gang rape and even murder, These are dealt with by
courts HS Separate crimes - with sapArAtp
and required
evidence - they all put together deserve severe punishment - but
the law is such that it is faultily structured. Hence NCW has
recommended codification of criminal laws pertaining to women.
Until a decade ago downy death was not even treated at part with
murder - leave alone the battering she suffered all Ifcr life. Her
injuries both mental and physical leave irreparable scars - 498A of
IPC.has been a boon to women to complain against cruelty and
harassment to women within 7 years of marriage.
Let us look at the mental Health Act - under Section 3 of the Act,
it says the Court may visit a patient before consigning her to an
asylum - the Magistrate should visit "instead of may go any
number of times and meet the woman/patient before sending her
to the asylum. That too in the presence of parents or guardians
any NGOs.
Right to visii. by vn, NGO must be mado compulsory to report on
the condition of the woman in the mental asylum.
The case of AnaniLka an intelligent girl was tried to be proved as a
mental case by her husband/parent and psychriatists. If not for
the cover offered by the Court she would have been consigned to a
mental asylum for no fault of hers. What health are we discussing
when laws have gaps and mnrts are
to tricky ioouca?
1
For Custody and Maintenance of Children - the woman has to
undergo harassment, threat, trauma and financial bottlenecks.
Street children, children and women lepers, destitute and
, , deserted ones and beggars are social castaways no law is adequate
■ to offer protection and health to children. Added to poverty,
ondage, sexual exploitation leaves them with disease, aids and
c angerous diseases. Law by itself cannot help in a big way to
piotect woman s health, unless the society wakes up to this
inhuman discrimination practiced at every step - dehumanizing
t e woman and the girls child, reducing them to almost slaves and
second rate citizens.
10
•1
IJ
Women ana Panchayati Raj Institutions
(Special focus on health services)
By
Susheela Kaushik
Paper Prepared for the
National Consultation Towards
Comprehensive Women's Health Policy And Programmes
BY
VHAI-WAH1-DSE
Held in VHAI, New Delhi.
on February 18 - 19t 1999
J
■Il
JLiwi
INTRODUCTION
Unique among the nations of the world, India has followed the concept of
empowerment for its weaker sections, through a reverse discrimination has enabled its
women, along with members of other disadvantaged sections of India, to emerge as
their own decision makers, in a new form of self-government. Their experience and
performance, in the backdrop of a traditional, feudal and patriarchal set up, is bound to
have immense messages for the women's movement all over the world.
It is more than four years since the 73rd Amendment to the Constitution of India,
reconstituting and empowering the Panchayati Raj, came into being. Within a year, the
states had formulated their conformity legislations. By 1996, all the stales of India
(except Bihar and Assam) had completed their elections and brought the new
Panchayats into existence. For the first time in India, nearly eight lakhs of women had
become members/chairpcrsons at the three levels of Panchayati Raj, thanks to the
reservation which the 73rd Amendment had provided for. It included, as per the new
Act, the election of scheduled caste/scheduled tribe women to the extent of not less than
one third of total scheduled caste/schcduled tribe members/chairpcrsons.
This is, indeed, a unique experiment in the world of democracy, wherein women
at grassroot level, irrespective of their educational, professional and socio-economic
background, have been found suitable enough to occupy political positions and
participate in legislating, decision making and governance. For India, it is even more
noteworthy as the bulk of Indian women in grassroots level are not too literate and
socially backward. Strong religious and sociological foundations in the form of
customary, superstitious, unscientific norms and practices, caste and class hierarchies
and rural-urban dichotomies have been sharpest in an old civilisation like India. They
all have cumulatively contributed to preserving and strengthening the patriarchal forces
and practices. Not merely the civic society but even the state has often floundered on
this rock and prevented women from participating equally and eagerly in the decision
making processes and governance.
It is then worthwhile to take a look at the extent, level and nature of women's
participation in the Panchayat Raj, wherever they have been in positions for 2 to 4
years.
Over a period, quite a few micro studies based on research and training
interactions have emerged on the experience of women. Many seminar papers and oral
presentations, particularly by the Panchayat women themselves, have highlighted the
role, functions, achievement and limitations of the women, both as members and as
chairpersons.
1
The 73rd Amendment and Grass Roots Democracy:
In April 1993, the 73rd Amendment to the Constitution of India came into
operation, strengthening and constitutionalising the structure, powers and functions of
the local self-governments. With this empowering of the third tier of democracy, the
democratic process in India has received much thrust and world wide attention. It,
above all, has brought about devolution of powers and functions under Schedule 11 and
required the states to gradually decentralise by transferring 29 areas to the local bodies.
There is also the mention of committee system and the state legislations are expected to
prescribe the committees.
Devolution of Power : Despite the provisions in the Constitution for the transfer of
29 areas, not many states are able to devolve the developmental functions to the
panchayats. In addition under the 74th Amendment for the Urban Local Government
called the Municipalities Act, there is a provision for District Planning Committee.
This is a combined Planning Committee for Panchayat and municipal areas. Every
DPC will prepare a draft development plan for the district and forward it to the
Government of the State. The state legislature has the power to make laws for the
manner of composition and filling up of the seats in such committees, functions and the
procedure of election of the chairperson etc. Not less than 4/5 of the total number of
members of such committees are elected from amongst the elected members of
panchayats and municipalities in the district by the members themselves in proportion
to the ratio between the population of the rural and the urban areas in the district.
However, the record of the states willingly and promptly transferring the areas
to panchayats has been very dismal. The operation of PRI has confirmed that even if
constitutionally secured, it cannot be dissociated from the broader political imperatives
and manipulations. The commitment of the States too the spirit and objectives of local
self-governance is doubtful. Nor has much visible advance been made by way of
decentralisation of power and transfer of developmental schemes and resources to the
PRIs.
The government at the Centre, diverted to other issues, seems to give lesser
priority to the enforcement of Constitutional Amendments. An occasional statement
by the Prime Minister, his incentives by way of grants of MPs or even the latest move
to give developmental grant to select panchayats in the country, have not helped to
accelerate the implementation of the concept of local governance.
2
In the absence of a speedy enforcement of the Act and effective implementation
of the provisions in its letter and spirit, the participation of women and weaker sections
will be lurther reduced. No amount of education and training of women for political
empowerment will have any meaning or use if the broader Panchayati Raj movement
itself fails.
In select areas some state governments have made a beginning of an attempt. In
the case of West Bengal and Madhya Pradesh, primary education upto class 5 has been
transferred to panchayats. In Tamil Nadu education has been brought under Panchayat
Unions (bloc level). In West Bengal primary health care has been entrusted to
panchayats. In Kerala, a Local Development Planning Board has been set up to devise
such transfers.
In Madhya Pradesh and Orissa, the Women and Child Development Departments
run the DWCRA and the ICDS programmes and both are supposed to be supervised
and activated in close collaboration with the PRI institutions. The village anganwadi
also runs through this programme.
The state government has entrusted the
newly-elected panchayats with the task of completing rural development projects which
include electrification of villages and propagation of non-conventional sources of
energy. Besides, the panchayats have been given wide-ranging powers in the field of
social welfare, potable water supply, public health, family welfare, animal husbandry,
dairy and poultry development, education, pisciculture, horticulture, sports, public
distribution system, irrigation and welfare of SCs, STs and BCs. However, in most of
these instances it is decentralisation in monitoring and implementation rather than
policy making or programme formulation.
Committee System : Many states have introduced varied types of standing committees
to carry on the work of panchayats. It looks like there are more committees and they
are more active at the district and bloc level than at the panchayat level. However, no
where is there any mandatory provision for having women in these committees. It is
also surprising that while the Social Justice Committee and Social Welfare Committees
are common to all states, only Andhra Pradesh and Maharashtra seem to have specific
committees for women's and children's welfare, that too only at the zilla parishad level.
The Health Committees are, however, found in almost all the slates especially at the
Zilla Parishad level. In the gram panchayats and bloc level, there are Amenities
Committees in almost all states. Possibly sanitation and public toilets figure as
amenities. However there is no devolution as such, of public health and family welfare
to the panchayats, even though it figures as one of the 29 areas. PHCs, ANMs, ICDS
and Anganwadi workers figure as state government officials in almost all states.
3
Only in Orissa, the standing committees have prominent role for women. The
three standing committee meant for education, health and other distributive aspects
must have three women out of five members. Such a provision is generally not found
in other states; however, persons belonging to scheduled castes,- scheduled tribes or
other backward communities are preferred for the purpose.
These features have much relevance for the effective functioning of women in
the panchayats as well as the decisions they can make for the development of the people
in general and women in particular.
Population Policies: Two Children Norin: The committee on Population Policies
with Dr. M.S. Swaminathan as Chairperson recommended in 1994 that panchayats
should be utilised to make family planning popular among the masses seems to be the
one idea that struck the Central Government, working for devolution of functions and
power. The elected women of panchayats came to be viewed as agents to carry out
family planning.
However, soon this gave way to viewing the elected women as models for family
planning. In a short sighted view the state governments try to bring about small family
norm of imposing it on all the political aspirants to local government positions.
Haryana was one of the few states to attempt a notification on population
control. The Rajasthan government on 23rd April 1994, had issued an ordinance
stating that those who have more than two children would not be eligible to contest the
Panchayat and Municipal elections. If a third child was born to a member after being
elected, he/she would lose the seat.
The announcement was, of course, stoutly
opposed by the aspirants as well as others on various grounds and was not
implemented; it was held in abeyance for some time on the ground of giving at least
one year for the people to prepare themselves as candidates. In Delhi, Andhra Pradesh
and Orissa too, followed suit.
The whole policy, though propagated as a way of controlling population, thereby
promoting women's health and public participation, is actually anti-women. It will
debar a number of representatives of the weaker sections who are getting the
opportunity to contest elections to the Panchayats for the first time. The women
aspirants will be affected most as they have very little control within the families to
make such decisions. It will, further, prevent those women and men who having
married young as is the tradition in the rural areas may already have more than 2
children. It will also adversely affect the sex ratio which in India is already
unfavourable to women and stood at 929 women per 1000 males in 1991. The adverse
4
impact is already being felt, as one comes across instances of women being removed as
chairperson for having given birth to a third child (Sikar District in Rajasthan) or
threatened to be confronted with a no-confidence motion (
Rajasthan).
Functioning of the Elected Women:
The general opinion seems to be that the majority of rural women being
illiterate, they could only fix their thumb impression, and would be ignorant of the
ways of manipulative politics; of the intricate financial procedures and 'deals', and
complicated development schemes and processes; and that the women would be
constrained by the social norms and customs, and intimidated in the presence of elderly
men and senior relatives. Women, not having been used to equality and exercise of
their rights, would not be able to assert themselves or occupy positions in the PRIs.
The cynics and critics were particularly sceptical about women occupying the position
of chairpersons and vice-chairpersons of the three tiers of PRIs performing effectively.
It then becomes necessary to see the functioning of the new Panchayati Raj, to
what extent have the women come forward to utilise these new political opportunities.
Even more significantly, to what extent will the new political operations at the local
level allow them to do so.
Panchayats Activities: What are the activities of panchayats according to the elected
women? Or what are the ones in which they are involved? Most of the women
believed the more traditional spheres like provision of drinking water, road
construction, public works like maintenance of bridges, culverts and community hall,
electricity supply etc. as the activities in which panchayats are involving themselves. In
this they were not much different from the males.
The panchayat women elected in recent times have also some ideas for women's
development. They could spell out many special issues for women, in which they and
the panchayats should be concerning themselves. Quite a few elected women,
particularly from Tamil Nadu emerged as very conscious.
They brought out
differences in the point of view of both men and women as well as confirmed that
almost on all issues women emerged progressive and empowered. Possibly, the mass
literacy campaigns and media exposure had played a role in this modern outlook.
Many of them desired that the women's point of view should be reflected better in the
panchayats' decisions. Economic self-sufficiency and income generation, women's
education and schools for girls, emerged as major demands for women.
5
In many parts of India the panchayat women stressed a ban on alcoholism. In
some cases they also came out with issues like hostels for unwed mothers and homes
for abandoned children as an area for panchayat action. In states like Himachal
Pradesh, Haryana and Garhwal, there are instances of panchayat members and
chairpersons leading demonstrations and breaking pots and resisting the police.
How have the women performed in the panchayats?
All Women Panchayats and Developmental Planning:
The 73rd Amendment is a milestone in the history of legislation which has
ensured the coming of women to the leadership and decision-making positions, and it
has made such a role mandatory and universal in the whole of India. But in some areas
women had occupied such positions and performed effectively even before. In Andhra
Pradesh, Karnataka and Maharashtra, women had contested elections, occupied
reserved positions and contributed to the panchayats' functioning.
It is interesting to .note that the panchayat elections in India ever since the
seventies has been throwing up what is called "all-women Panchayats" wherein all the
members and chairpersons have been women. In Andhra Pradesh, there was one
all-women panchayat in Mathupalli in Kurnool district in the seventies and another at
Gandhinagaram in Warangal district in 1981. In Maharashtra there was one all-women
panchayat Nimbut in sixties and another at Vanjara in the seventies, and eight more
after the 1989 Gram Panchayat elections. In these elections, in nine villages all-women
panels contested the elections. In Madhya Pradesh in the village of Pidghara, 40 kms.
from Ratlam in Dhar district, all the 13 members elected in February 1989 were
women. In the present series of elections too, some of the States have given examples
of all-women panchayats. In West Bengal, the village Kultikri in Midnapur district had
elected an all-women panchayat. In Tripura, Mirza village of South Tripura district
elected unopposed all its nine women candidates. A village with near-total tribal and
SC population, the nine members (five STs and four SCs) belonged to the CPI(M). In
Karnataka, Mydolalu in Bhadrawati Taluq of Shimoga district has an all-women
panchayat. After the 1992 elections, Maharashtra has two all women panchayats at
Brahmanagar (Pune district) and Bhende Khurd (Ahmednagar).
Quite a few studies have pointed out to the difference that women members,
particularly in the all-women panchayats have made to the nature of the decisions, and
the process by which they were formulated. They had utilised their power to give
priority to issues like drinking water supply, installation of pumps, construction of
6
toilets and village wells and roads, appointment of teachers, closing of liquor shops etc.
There were instances, as in the Vitner village of Jalgaon district (Maharashtra), where
women got playgrounds built, land transferred to 127 women from their husband's
share and toilets constructed in the SC areas. Conscious of their increasing housework
and the need to save energy and have some free time, the women in Pidghara (Madhya
Pradesh) went for a 27 point action plan that undertook the building up of educational
and other community-based infrastructure.1 Similar has been the experience and action
agenda of the seven-member panchayat of Brahmanagar of Pune district.2
An interesting example is from a village called Erikuppam in Thiruvallur
district, where crude oil is obtained at four feet. As a result, the water problem had
become extremely acute. The women panchayat leader had got pipes laid from a
neighbouring village in order to provide water supply.
Even many men found a marked difference in the working of panchayats because
of chairpersons being women.3 They said women are more honest and sincere, active
and hard working in the village development activities. Corruption has also gone down
and more transparency in functioning has come about. It was evident that there are
positive changes in the society because of women's entry into panchayats.
The
prevailing situation is reflected by the words of a male member of a bloc in Tamil
Nadu, "Though some women are uneducated, they have learnt about the functions, and
even started getting educated. Sometimes they do better than us".
Constraints Before the Women:
In case the panchayat women have to play their leadership and decision making
roles effectively, they need to get the support of the officials and the male members.
The women feel very sore about the role of officials. The relationship between the
elected members/chairpersons and the corresponding set of officials has become a very
1.
2.
12 Feb.
Manjeet Singh, "We want to outdo the Males",
1989.
Reproduced in Aalochana, Women and Electora.1
Politics 1990-94, Newspaper clippings.
Ibid.
Vol 2; Subha Gandhari, "The Rule of the
(Bombay), December 1994.
Second
Sex" in Indian Express
3.
Opinions expressed in the NOW sponsored study of
"Panchayat! Raj:
A Stocktaking in Five
States",
compiled and edited by Susheela Kaushik for Centre for
Development Studies and Action, New Delhi.
7
thorny issue. The Acts themselves, in many states of India, by giving the implementing
and monitoring power to the officials, have made the latter somewhat superior.
Many women members particularly at gram panchayat and panchayat samiti
levels, have, of course, had no opportunity' to directly interact with the officials. The
members of panchayat samiti and zila panchayat come across them more often.
However, among those who had interacted with them, or who had heard about their
behaviour, many found the officials uncooperative. Many of them, they however felt
that the officials responded to male representatives immediately. A woman bloc
president from Tamil Nadu said, "whenever we pass a resolution in our panchayat on
works to be carried out and take it to the panchayat union office, they refuse to accept
it and impose a different decision on us".
How did the women perceive their own functioning, role and contribution as
local leaders and rulers? A majority of women consider themselves representatives of
people in general as well ass women's representatives. Many women are not satisfied
with their role and believe they are not able to work for the society adequately because
the functions and powers had not been delegated to them. They also could not allot as
much time to panchayat work as they were expected to do mainly because of family
pre-occupation (37%), inadequate transport (15%) and health conditions (7%).
However, a majority (61%) were happy with their own work and would like to come
again. The women find it difficult because of lack of adequate support structures. The
MP tribal women were particularly conscious of this. Many other women also
mentioned domestic assistance, child care facilities, transport, political information etc.
as the support which they required and which were lacking (Table 4.3). It was
interesting to see in one of the districts of Madhya Pradesh, Sidhi, sarpanches and
punches are getting together for networking through news letters to facilitate
information sharing.
The women chairpersons would particularly like to get some
a)
b)
c)
d)
e)
Help in maintenance of income and expenses accounts
How to generate finance
Leadership Training
Training for planning for development
Support staff
Despite this, many considered the present system of panchayats to be better, that
it is working for the betterment of the people and that the presence and participation of
the women have made all the difference to its functioning. They also believed that the
8
panchayats are now more transparent and representative of all sections, particularly SC
and ST. The outlook of most of the elected women was thus positive, confident and
assertive. They were prepared to face the obstacles and not be cowed down by their
limitations. These elected women had entered politics and would like to stay with it.
In addition of the democratic decentralisation and devolution of power have to
take place in its true sense, the elected women in the panchayats will need to interact
with the village women, be guided by their demands and needs, and be supported and
monitored by them. The formation and strengthening of the Mahila Mandals, and
empowering the village people are essential. Many organisations like SUTRA (H.P.)
with their projects like Sanjivini, Panchayat Mandalis, other NGOs training the
panchayat women all over India are attempting to back up the elected women. Health
care, schooling for girls, education and awareness of their own rights are definitely on
their agenda.
9
12-02-99
11:03
ra 91 11 6132922
C D S A
001
‘-5i 1-v.VrV t
Thuci
•J/LW
'2'
-x .
RECOMMENDATIONS
Panchayat Structures and Powers:
T-
More representation should be given to women in all legislative bodies of State
Assemblies and Parliament.
*
The Act which is powerful on paper, needs to be keenly implemented. Effective
rights should be given to the panchayat bodies; there should be more devolution
of functions and powers to the local bodies. Eleventh Schedule of the Act
should be enforced speedily. TRDP, Indira Avas, ICDS Education should be
transferred to the panchayat bodies.
*
Panchayat Samiti should be given more powers.
*
The government must specify clearly the powers of all the three tiers of the
panchayat.
One of the major problems which come up often is the lack of
coordination between the 3 tiers of the panchayat which has led to occasional
conflicts between them, There is a lack of clarity of powers particularly
regarding finance.
*
Village panchayat chairperson should
be made responsible to the Bloc
Panchayats; they arc not invited to the meeting, nor consulted. Thus they feel
clieated, as they are also direct representatives of the people. The sarpanch and
pradhan should be made members of the higher panchayat body. Tills is not
obtained everywhere. The Bloc Pramukh should be the regular member in
DR DA meetings.
There should be more transparency concerning the development schemes and
budget. Most of the sarpanchcs and P.S. members even, are ignorant of the
schemes and budget which has led to the manipulation by the officials, at times
in the form of commission from the panchayat.
*
Every panchayat should maintain a black board giving detailed information about
the budget, work done, schemes implemented etc. in Older to remove corruption
and ignorance.
*
Certain amendments must be mode in the Acts so that it becomes mandatory
for the sarpanch to consult other members of the panchayat. Powers should also
be delegated to panches and they should be involved in the development work in
the village.
I*
1
The chairpersons have to be made answerable to the members regarding ali the
developmental action and contracts. There is presently a lack of transparency.
In many places, this was used, to initiate no confidence motion against Lie
women irrespective of the fact that these women sarpanches were working for
the villages.
*
Panchayats should be entrusted with the legal powers (Judicial & Police Power)
to make it more effective.
*
No confidence motion should not be passed before two years against the women
sarpunch of panchayats. There should be some mechanism to ensure the security
of the women chairpersons so that such a motion is not used as a weapon by me
male members to throw them out, if she does not comply with their wishes, or
takes an independent stand.
Some even believed the pradhan should not be
removed by the panchayat members; she is directly elected by the people.
*
More finance should be given to the panchayat. Finance should be directly sent
across to bodies which are the final recipients.
t-
Formation of a committee for women and child development should be made
compulsory. Only a few' villages have a Committee on Women & Child
Development,
*
Every Committee should have adequate representation of women members.
t-
The quorum for every panchayat body should compulsorily include a woman and
a S.C. member.
*
Women’s representation in panchayats should be increased to 50 per cent so riat
they can voice women's issues better and get majority support.
*
Wherever there is no nyay panchayat provided in the State Acts, such nyay
panchayats should be revived, by an Amendment.
*
More information should be given to women.
*
There is a need for greater interaction and exchange of visits among women
belonging to various regions of India. The social variations and developmental
experiences, apart, from the travel and exposure, would help rhe elected women
compare and learn. Such interaction is needed among panchayat chairpersons
and members within the state as well as with those of other states.
*
For every panchayat body headed by a woman the corresponding official should
also be a woman.
2
t!
*
A newsletter is needed to keep the women informed about latest developments
new schemes and other details on a regional basis,
'
On Bureaucracy: The powers of the Bureaucracy should be well defined 1
so tliat they
are nor a hurdle in development work. The Bloc Pramukh should be die
-J regular
member, m DRDA meetings.
$
Bureaucrats should be more receptive to the demands of the women and their
functions should be made more transparent.
Support Services for Women: In order to ensure the effective participation of women
m panchayati raj, the necessary support services should be provided to them as most of
them are, taking part for the first time in the decision-making process in the cub ic
political sphere.
H “
Honorarium TA/DA: There should be some support in terms of the T.A. and D.A.
whenever they go out for official work,
In order to facilitate women attending meetings or training camps at a distance,
they should be either called in groups or the persons accompanying them should
also be given transport allowance.
*
The women also mentioned the need for domestic assistance by way of child care
facilities in the villages.
*
The chairpersons, particularly, needed some assistance in office work,
messenger to carry information to members, distribute meeting notices etc.
*
Literacy and adult education for women need to be encouraged,
2
The Block Pradhan and members should be provided residential accommodation
in the bloc, as they come from far off places: this causes problems of
accommodation especially for women.
Training: The women need training and technical advice immediately; otherwise she
is branded as a rubber stamp of her husband. There is a very thin line which divides a
woman taking advice from her husband when she docs not understand and the so called
phenomenon of "pradhan pati", but this difference is very important to make.
*
The government should organise training camps especially for the women
panchayat chairpersons and members, as to what their powers are and how they
can implement them and gel the various impediments removed.
3
' i between bureaucracy and the
In this training there should be interaction
panchayat members so that
t— the women, can overcome their hesitation.
*
Gender sensitization training should be given to the bureaucracy, as oftenthey
have very unsympathetic view regarding the women chairpersons and
of the panchayats. They do not listen to them and take advantage of thu:
$
ignorance.
Training must have suitable mechanisms so as help the bureaucrats momtor
empathetically the performance of women as well as refresh and upgrade their
information so as to help them understanding grassroots reality.
*
*
Elected women should be taken on a tour to other stales and panchayats which
are functioning successfully for on the spot training and interaction.
*
The training should be held at regular intervals so that additional information can
be given from time to time on panchayats.
should be held close to the villages so as to enable the women
Training
participate without being anxious about children, domestic and occupational
chores.
*
The training programmes conducted by the government and NGOs, need to be
improved and constantly monitored.
*
The content of the training workshop should also include, legal rights for
women, leadership training and training to speak m meetings, public relations
tic.
Community Participation: There should more community participation at die village
level, for the PRI to work efficiently.
*
*
People should seek information from the sarpanch. The villagers should be
helped to be more alert, active and participative in the
1 panchayat. They should
raise voice against corruption and oilier practices.
A board should be constituted in the village to assess the work of panchayat.
*
SL The formation of mahila mandals, wherever they do not exist, need
to be facilitated.
*
Schemes for mobilizing and organising the women need to be utilised.
4
/3
*
IS!","18 ffn""? NGOs’ 80vernm™ functionaries and panchayat animators
Miute % 'u PaDC, yaB ‘0 frganise pcri0‘lic
’abha meetings “5
rate a two way interaction between panchayat members and
panchayat members and bureaucracy.
c
e’
Moe und’diStrielZcirdmsiAg of conS^TdMdua^o^S
representatives and developmental functionaries.
T
P b
ieveia to «i£m a SS™
toTh^'’ ’"‘T
should undertake the collection and dhseXX Xata ' '
*
*
*
fe’ clected
““
Z1.“,mCW.sh0“ld ad™aB “d MP in organising support services like capacity
building, training, child care, TA/DA etc.
NCW, the central and state governments and NGOs should organise periodic
training and camps where elected women and chairpersons in particular can
come together, exchange their experiences and learn from one another.
1™^“ f°? WTCn and State S°ve™ ^ncies should
mon to; tire violence against elected women and their facilities. Machineries and
nechamsms should be evolved to deal with such violence against elect-d
women.
*
$
NCW, all the state women's commissions, NGOs and government departments
should organise awareness camps in die rural areas on gender sensitization, legal
rights and policies and programmes for women.
5
(‘t
A
Decentralised Planning for Women’s Health :
The Kerala Experience
By
Aleyamma Vijayan
Paper Prepared for the
National Consultation Towards
Comprehensive Women ’s Health Policy And Programmes
BY
VHAI-WAHl-DSE
Held in VHAI, New Delhi.
on February 18 - 19, 1999
Decentralised Planning for women's health
The experience of Kerala
1 Background
LI Kerala
kerala is one of the smallest states in India, comprising 1.2% of the countries total land
area and supporting 3.% of the population. Among other Indian states, it has the unique
position of having achieved all the major health parameters such as birth rate, death rate,
infant mortality rate and expectancy of life at birth. This uniqueness lies in the fact that
Kerala achieved this status in an environment of low per capita income and relative
economic stagnation.
Some of the significant outcome of this social development has been the demographic
transition observed in Kerala in recent decades, efficient public distribution system,
numerous welfare and social security programmes and recently a massive surge towards
people’s planning from the grass roots level upwards.
All studies on Kerala experience, without any exception , emphasizes the significant role
of the high female literacy as the crucial factor in achieving this major gains. Other notable
factors are the climatic and topographical conditions, availability of safe, potable drinking
water, hygienic and clean habits, sanitary facilities etc. Efforts made by the Government
in building up a sound infrastructure capable of delivering health care to all socio-economic
levels and to remotest rural areas are equally important. Private sector, specially missionaty
hospitals also played a crucial role in providing health care .
1.2 Emerging Concerns and issues in the health sector.
Although Kerala has made remarkable achievements in the health front, new chaUenges
emerge with the changes in the demographic profile of the state, economic and socio
cultural factors
According to Dr,Equbal, member of the state planning board ( handbook on Health )the
lollowing are some of the recent concerns facing the health sector.
The Government hospitals, are getting weakened. People are loosing faith in the Govt,
hospitals as they perceive signs of inefficiency and only 30% of people are using this
facility now.
• Private health care sector is growing very strong in Kerala and has become a big
business.
• Since private practice is allowed for Govt, doctors and since most of the investigation
like laboratory tests has to be done from outside, an internal process of privatisation is
taking place in the Govt, hospitals.
•
i
•
•
The growth of private hospitals has led to commercialisation and commodification of
health care. The aggregate bed strength in private hospitals has increased 40% from
1986-96 whereas that of the public sector went up by only 10%. The private sector
also outpaced the state sector in acquisition of medical technologies such as CT scans,
MRI and endoscopy units. The resultant outcome is cost escalation and the
marginalisation of the poor.
As a consequence of all of this, a consumer culture is growing in the Health sector with
its concomitant problems
Together with the economic problems created by privatisation, other problems like the
return of communicable diseases and emergence of new diseases , the increase in the so
called ‘life style’ diseases like cancer, heart diseases are the posing new challenges in the
health sector of Kerala. The present situation is one ‘/ow mortality, high morbidityr
syndrome. In the content of increased life expectancy, the problems of the elderly and
chronically ill also poses new challenges. With the increased educational standaids,
unemployment rate also is increasing. Large number of Keralites have migrated for work,
resulting in changes in the family structure. With increasing expectations brought about by
the affluent few and the great mobility of the people, tensions and frustrations also
increase. All this are creating serious problems in the mental health status . The rate of
suicides in Kerala is three times that of the national average.
1,3 Women's health situation in Kerala.
As indicated earlier, the maternal and child health situation in Kerala seems to be unique in
the country. 95% of deliveries takes place in the hospitals. The system of Traditional birth
attendants (TBA ) is almost disappeared. Yet morbidity is very high . Since a general
awareness on reproductive and sexual health and rights and women’s issues and concerns
are weak, these aspects gets veiy little attention in the policy making and planning process.
Although it is believed that infant mortality rates in Kerala are as low as in developed
countries, recent stadies by Dr.S.Irudayarajan and P.Mohanachandran ofCenter for
Development Studies, Trivandrum claims that Kerala’s Infant Mortality Rate (IMR ) is
as high as 37 per thousand and not 14 per thousand as claimed by the govt.1 and other
agencies. They used the census data to arrive at this conclusion. The study while analysing
the official statistics ( on which the govt, based its claims) in the 1996 Sample Registration
System (SRS) provided by the Registrar General of India found that out of 14 children
who died in Kerala within a year, 11 died within a week- a rate which is even higher than
the national average. According to these researches, even if' one accepts the IMR provided
by SRS was collect, still birth rates and prenatal mortality rates were also extremely higli.
Otherwise, it indicates another paradox of Kerala - low IMR, high still birth and one week
mortality.
Another recent disturbing factor in Kerala is the low birth weight of the new boms
Available studies indicate that the proportion of low birth weight babies was on the
increase. The average birth weight had declined from 2.81 kg in 1987-88 to 2.65 kg in
1992-93. In 1981-82 only 11% children were below 2.5kg and the rate at present is 24 %
7
This is disturbing and it shows the decline in the per capita average food consumption and
the consequence of the policies in the agricultural sector.
Yet another disturbing factor is the Privatisation of healthcare and its impact on the
women’s health. The whole process of pregnancy and delivery is higfily medicalised. Most
doctors prescribe two or three scans during pregnancy. Average visits to the doctor during
pregnancy is seven, which is higher than that of the west. Caesarean deliveries are
extremely high.
Privatisation of health care also means that the poor women’s health is neglected. There are
no facilities for delivery at the Primary Health centers. (PHC’s ). In a survey conducted
recently by us the women of the slums and coastal communities spoke of the inefficiency,
lack of infrastructure facilities, high rates of bribery, rude and unfriendly attitude^the
staff and lack of privacy in consulting rooms as problems faced by women in the Govt,
hospitals.
Although there is wide acceptance of family planning methods, it is a women centered
approach. Of the couples who adopt permanent methods, majority are tubectomies.
A serious problem affecting women in the state is the increasing sexual violence .
Organised sex rackets are flourishing in the state where unemployment also is very high
The awareness about sexual and reproductive health problems is low and women keep this
problems to themselves rather than consulting a doctor. This also is true for educated and
women of high income groups.
2. Decentralised planning process in Kerala
In accordance with the 73rd and 74th constitutional amendment, The Kerala Panchayat Act
Was passed in 1994, which paved the way for real ‘devolution of power’ to the local bodies
and to the people through "Grama sabhasf. In order to actively invoke the people in the
9* plan, a massive ‘People’s plan campaign’ was started in 1996. . About 40% of the
total plan fund is earmarked to be spend through local bodies.
The state planning board is pioneering this unique experiment of decentralised planning
process in Kerala. The various experiments in decentralised planning so far in thecountry
had focused on the district levels or the block levels. Here through appropriate acts and
rules the panning process is entrusted to the local panchayats and every citizen is
entitled to be a member of the planning process through their participation in the
Grama sabha.
'S
There are lot of hurdles to make this process a reality. The ‘devolution of power’Ki
means deployment of officials and their powers, funds etc. New rules are formulated for
this. People and the elected local body representatives are without any experience in
planning. So numerous training programmes at various levels are being conducted. Lack of
sufficient date at the local level, lack of technical skills etc were other major problems.
These are also being tackled gradually
“Decentralised planning process is generally categorised into need based and resource
based planning. In the need based process, acute problems faced by people are identified
■jlso
and resources to solve these problems are located and development programmes are
planned accordingly. In the second approach, human and other resources and their
potentials are visualized and appropriate plans are made. The basis of peoples plan is an
integration of this two approaches" ( People’s Plan- Theory and practice: Dr. T.M.
Thomas Issac : Kerala State Planning Board :1997 October )
In order to ensure that the decentralised planning process is transparent, scientific and time
bound, a 5 phase action programme is envisaged in the plan document.
Phase 1
Identification and prioratising local problems and needs by the people
themselves coming together in the grama sabha.. Eveiy voter in a ward of the panchayat
will constitute a grama sabha. . The people coming together in a grama sabha are divided
into 12 sub-groups or more as per the need. The 12 main groups are Agriculture and
irrigation; Animal husbandly and Fisheries ; Education; Industiy; Drinking water and
Public Health ; Transport and Energy; Housing and Social welfare; Culture; Women, SC&
ST welfare, Co-Operative sector; Resource mobilisation.
Phase 2
Development seminar. This process involves finding solutions to the
problems raised by the people with the help of relevant data, studies and the resources
available locally . In this seminar two people selected from each subgroup of the grama
sabha and other experts, resource persons etc. participate. An Action Committee is
constituted here to formulate projects based on the recommendations of the development
seminar..
Phase 3. Project formulation by the action committee. At the end of this a number of
projects suitable for each area will be ready
Phase 4
Select projects which can be executed by the panchayats with available
resources, with state and central assistance etc. A plan document is thus prepared.
Phase 5. In this phase, the village panchayat projects are coordinated at the block
level and the block level projects at the district level. Thus projects for the block and district
panchayats are prepared.
Expert committees are formulated at this level to examine the projects, recommend
*
changes and make them worthy of technical approval and then this are recommended to
the District Planning Committee (DPC )
2.1 Approach to health
Health is considered as the most important development sector in the service sector. There
is a general awareness that gains in the health sector cannot be sustained unless there are
improvements in the basic living conditions like drinking water, sanitation, housing, and
nutrition. Some of this can be addressed only through improving family income,
particularly income of women. Experts opine that emphasis should be given on ecological
and economic measures and not the further expansion of infra-structural facilities.
Two major aims of the projects in the health sector, as envisaged by the planning board, is
to improve the quality of care and increase the outreach of services provided.
4
The public health care system from the PHC to the district hospitals are now under the
three tier Panchayat system. The restructuring of the health sector with people’s
participation is beginning to take place.
If we examine the projects formulated in the decentralised planning process in Kerala in
the last year, the following were the priorities.
1. Most of the projects in this initial phase is to do with environmental hygiene and
sanitation, health surveys, improvement of the basic facilities in the PHC’s and
Community Health Centers ( CHC’s )
The ICDS programme is handed over to the local bodies. The ICDS supervisor is the
main functionary of the Mother and Child Health (MCH) programmes of the Panchayats
and Municipalities. The local bodies can earmark funds to supplement the nutrition
programme.
2. Since sufficient funds are earmarked for the health sector from the plan funds , the
resource crunch in the health sector is solved to a certain extent. In the 6th plan about
6000 crores is allocated for the service sector like the drinking water, sanitation,
education, environmental hygiene etc. Out of this about 500 crores will be spend in the
health sector alone. If in the 8th plan, only 2.20% was spend in this sector, in the 9th
plan it will be 5.02%.
3. In the rural areas a collective spirit is growing with the doctors, health workers, elected
members of the local bodies, and the public working together. They do not have to wait
for the bureaucratic delays. Many doctors feel that it is the first time that they get
involved in planning for the sector in which they work. One must admit that there are
also cases where the doctors feel upset to be under the local authorities and to be
accountable to the people
*
4. The peoples campaign for decentralised planning is giving opportunities to experiment
and execute new and innovative programmes. Health camps, blood donation camps,
health card distribution, surveys to identify health problems of the area, projects for the
rehabilitation of mental patients, mentally retarded children etc. are some of the
projects so far. Considerable voluntary labour is drawn into these activities.
A new approach is emerging with people taking responsibility and demanding
accountability from the public health personnel. Local specific problems are getting due
attention. A great deal of preventive health care is possible. Other health systems like
Ayurveda and Homeopathy are getting integrated . In some places, there are attempts to
study in detail the health problems of the general population of the area and then plan
projects accordingly.
s
An integrated approach proposed by the state planning board for the decentralised planning
is as follows.
Food
Drinking watei
sanitation
Health education
Housi
Health for all
common aim
Life expectancy ~ 72—80
Infant mortality rate=l 8—10
Birthrate
=18-10
Mortality rate
- (5-5
Treatment
preventive care
hygiene
- Income
2.2 Decentralised planning process and women's health
If we examine the plan documents and the hand book prepared by the planning board on
Women’s development, Mother and child health development and health, the following
factors emerge.
All these documents speak of the contradiction of high female literacy and rather poor
socio-economic status of women. It is emphasised that the decentralised planning process
should give special attention to study the status of women in their areas and evolve suitable
projects to increase the status of women. Since an evaluation of the 1st year plan s showed
lack of sufficient fund allocation, planning board made it mandatory that 10% of funds be
set apart exclusively for schemes for women and the district planning committee is
authorised to monitor and ensure this before final sanction is given.
Women’s health concerns are integrated with ICDS programmes and the Anganavadis are
expected to be the centers of health education and women’s joint actions. The ICDS
supervisors and the Anganavadi workers are expected to give leadership to get women into
neighbourhood groups
The following is the guideline for an integrated maternal and child development
programme
6
Nutritious food
People’s committee
Information center
special schemes for
children below 6
treatment
Preventive measures
Integrated
mother and child
primary health
care/
development
Improve infrastructure ___
facilities
Informal preschool
education
Special schemes for adolescence
women empowerment
center
Local specific data collectioi
guidance and counseling
center
special care for pregnan
and lactating mothers
Envormental hygiene
sanitation &drinking
water
In all this , reproductive health, sexual health and rights do not sufficiently get reflected.
The general lack of gender concerns and perspectives is reflected in tlie programmes
proposed in the first year.
Yet in the second year, some panchayats and blocks have prepared some good projects.
An example is the ‘Integrated social health scheme’ formulated by the Ponnani Block
Panchayat in North Kerala in collaboration with Indian Medical Association (IMA ) and
Mental Health Action Network. (MHAN ). In this Muslim dominated block, a major thrust
of the project is to discourage adolescent marriages, and give wider awareness on women’s
reproductive and sexual health. A hand book called ‘Mother’ is prepared and widely
distributed. As is said in the preamble of this booklet, Tt is hoped that awareness of one’s
body will help women for better family life and more control and power over their own
lives’
The Muncipality of the same area is doing a health survey and is planning to issue health
cards for women and children. Cervix cancer detection camps, special supplement nutrition
programmes, gender education programmes etc. are some other projects planned
7
2.3 Limitations
The decentralised approach is in place only since 2 years and hence it is too early to judge
its impact. It also has to be kept in mind that people are still in the old mindset of expecting
concrete individual benefits.
Although the plan documents and hand books makes special mention of gender concerns
this do not seem to have percolated to the local level planning process. The planning board
has set up a gender- impact monitoring cell and also has insisted that the District planning
committees pass only projects which has earmarked 10% of funds for women.
But these measures alone are not sufficient when deep and subtle patriarchal attitudes
prevail. In many panchayats, women had to fight to get this 10 % funds earmarked for
women specific projects as the men resented this and try to get general projects like
drinking water and sometimes even roads under them!. Most often people lacked ideas as
to what are appropriate and viable projects. They are never used to think with and for
women.
Even worse is the scenario of women’s health projects. Even the handbook prepared by the
planning board do not mention specifically about women’s health concerns, e^xcept anemia
and quality of maternal and child health services.
What gets reflected in the local plans and projects is what is discussed and proposed in the
grama sabhas or by the action committees .There is general complacency that everything
is well with the health status of women and their specific health issues remain invisible or
unspoken.
Now with HIV/ .Aids threat looming large in the state, more organisations have come
forward to work with sexual health issues..
3. Suggestions for Policy advocacy and programme intervention
3.1 General suggestions
•
•
Special efforts have to be made to make the public health system vibrant and able to
respond to the health needs of people. Special incentives be given to encourage
doctors to work in the rural areas (like tax subsidy on their earnings as suggested by
IMA)
All states should take steps to decentralise planning process . Necessary laws to be
enacted by the respective state Governments for this purpose and financial allocation be
made in this line. Intense campaigns be conducted so that the new thinking becomes
people’s own.
•
Comprehensive studies/ data collection needs to be undertaken to understand the
specific women’s health issues in the states, specially of the marginalised groups like
indigenous people, Dalit women, women of the fishing community etc.
•
Wider information dissemination of this concerns to planners and policy makers so that
these are reflected in the plans and programmes
•
Model projects to address women’s health concerns needs to be formulated and
proposed to the grama sabhas/ Action committees.
•
A state level consultative body of eminent doctors with gender sensitivity, women’s
health activists etc. can be constituted to suggest priority areas and monitor projects
•
The ‘Peoples Heath, action committee’ to be formed at each PHC and CHC level
consisting of doctors, para-medical staff, elected representatives, Anganawach workers,
representatives of women’s organisations, teachers etc. be authorised to Plan , suggest
and monitor local specific health action in consultation with grama sabhas to be
funded and supported by the local bodies .
3.2
•
•
•
•
•
•
•
•
•
Specific suggestions.
All the PHC’s should have facilities for normal deliveries. Other infrastructure facilities
be improved so that the place becomes attractive and pleasing. Local Panchayats
should earmark funds for the same.
The services of a gynecologist be made available at least in the community health
centers, with privacy for consultations
The timings of doctors be rearranged to suit the needs of the people or as is done in
Tamilnadu ( 24 hours)
Educational programmes using audio-visuals to help women to get a clear idea of their
body and its functioning’s
Indigenous health practices be documented and promoted in treating gynecological
disorders
Special efforts to make men responsible in women’s health and contraception. The
responsibilities of health workers be reorganised so that male health workers assume
more responsibility, specially in reprodetive health matters.
Women’s organisations should establish constant dialogue with policy makers and
planners so that women’s health concerns gets reflected in the planning process.
Use mass media for wider dissemination and public debate on women’s heath concerns
other than that of the population control angle
Special efforts be made to ensure and increase women’s meaningful participation in
the planning process. Audio-visuals, theatre , folk ait forms etc could be used
effectively.. Collaboration of NGO’s, women’s groups etc also should be sought.
9
•
It has to be remembered that women are not a homogeneous category and the health
needs of adolescents, older women etc ( life cycle approach ) and women of different
economic categories be addressed separately.
4. Conclusion
Although the concrete health situation of Kerala may be different from other states, the
general approach to the problem is applicable in all states of India.
The current paradigm of health sectors development, is raising inequalities and alienating
the poor and needy from the public health care system. The goal of universal primaiy
health care service cannot be achieved if policies favour privatisationof medical services
The decentralised Planning process offers an innovative approach to health care financing,
enhancement of quality health care, prominence of preventive over curative care, demand
accountability from health personnel, and last but not least empowerment of people. In the
degree in which the women are made aware of their health concerns and issues and
empowered to be active in the social and political process, their health concerns also will
find a place. This is the challenge to be faced by the women’s groups.
Let me conclude by a quotation from Comrade E.M.S Nmaboothiripad who was the
chairperson of the people’s plan campaign “ True development can be possible only with a
decentralised approach, where people take over the power to decide for themselves. If
departmentalism has to end, oldforb-esses of bureaucracy erected between people and
departments should be broken down. The humiliation suffered by ordinary people at the govt,
offices and the system ofbegging favoursfrom higher-ups should end. Each citizen shouldfeel
that he is part of the govt. The Govt, should have the will power to hand overpower to
people
”
Aleyamma Vijayan
Sakhi women’s resource center
Trivandrum. 695001
10
Abbreviations used
Primary Health Center
PIIC
Community health Center
CHC
Government
Govt.
Maternal and Child Health
MCH
Infant Mortality rate
IMP
Integrated Child Development Scheme
ICDS
References
Books
Department of health and family welfare: Govt, of Kerala; Health profile of Kerala
1989
Kerala state planning board and Health and Family welfare Dept.: Planning helper
3: Handbook on Health 1998 (Mai)
Kerala state planning board and social welfare dept. Planning helper 6: Handbook
on Maternal and child development sector 1998 (Mai)
Kerala state Planning board and social welfare dept. Planning Helper 11:
Women's development sector: 1998 (Mai)
Kerala Sastra Sahitya Parishat: The health status of Kerala (Malayalam) 1991
Thomas Issac T.M (Dr) People’s Plan: Theory and practice: Kerala state planning
board 1998.(Mai)
Ponnani Block Panchayat; Amma 1999 (Mai)
Zachriah K.C and Irudaya Rajan S: Kerala’s demographic transition: determinants
and consequences: 1997 sage publication
11
©
Decentralised Planning for women's health
The experience of Kerala
1 Background
1.1 Kerala
Kerala is one of the smallest states in India, comprising 1.2% of the countries total land
area and supporting 3% of the population. Among other Indian states, it has tlie unique
position of having achieved all the major health parameters such as birth rate, death rate,
infant mortality rate and expectancy of life at birth. This uniqueness lies in the fact that
Kerala achieved this status in an environment of low per capita income and relative
economic stagnation.
Some of the significant outcome of this social development has been the demographic
transition observed in Kerala in recent decades, efficient public distribution system,
numerous welfare and social security programmes and recently a massive surge towards
people’s planning from the grass roots level upwards.
All studies on Kerala experience, without any exception , emphasizes the significant role
of the high female literacy as the crucial factor in achieving this major gains. Other notable
factors are the climatic and topographical conditions, availability of safe, potable drinking
water, hygienic and clean habits, sanitary facilities etc. Efforts made by die Government,
in building up a sound infrastructure capable of delivering healtii care to all socio-economic
levels and to remotest rural areas are equally important. Private sector, specially missionary
hospitals also played a crucial role in providing health care .
1.2 Emerging Concerns and issues in the health sector.
Although Kerala has made remarkable achievements in the health front, new challenges
emerge with the changes in the demographic profile of the state, economic and socio
cultural factors
According to Dr,Equbal, member of the state planning board (handbook on Health )tlie
following are some of the recent concerns facing the health sector.
• The Government hospitals, are getting weakened. People are loosing faith in the Govt,
hospitals as they perceive signs of inefficiency and only 30% of people are using this
facility now.
• Private health care sector is growing very strong in Kerala and has become a big
business.
• Since private practice is allowed for Govt, doctors and since most of the investigation
like laboratory tests has to be done from outside, an internal process of privatisation is
taking place in die Govt, hospitals.
•
•
The growth of private hospitals has led to commercialisation and commodification of
health care. The aggregate bed strength in private hospitals has increased 40% from
1986-96 whereas that of the public sector went up by only 10%. The private sector
also outpaced the state sector in acquisition of medical technologies such as CT scans,
MRI and endoscopy units. The resultant outcome is cost escalation and the
marginalisation of the poor.
As a consequence of all of this, a consumer culture is growing in the health sector with
its concomitant problems
Together with the economic problems created by privatisation, other problems like the
return of communicable diseases and emergence of new diseases , the increase in the so
called ‘life style’ diseases like cancer, heart diseases are the posing new challenges in the
health sector of Kerala. The present situation is one "low mortality, high morbidity'
syndrome. In the context of increased life expectancy, the problems of the elderly and
chronically ill also poses new challenges. With the increased educational standai ds,
unemployment rate also is increasing. Large number of Keratites have migrated for work,
resulting in changes in the family structure. With increasing expectations brought about by
the affluent few and the great mobility of the people, tensions and frustrations also
increase. All this are creating serious problems in the mental health status . The rate of
suicides in Kerala is three times that of the national average.
1.3 Women's health situation in Kerala.
As indicated earlier, the maternal and child health situation in Kerala seems to be unique in
the country. 95% of deliveries takes place in the hospitals. The system of Traditional birth
attendants ( TBA ) is almost disappeared. Yet morbidity is very high . Since a general
awareness on reproductive and sexual health and rights and women’s issues and concerns
are weak, these aspects gets very little attention in the policy making and planning process.
Although it is believed that infant mortality rates in Kerala are as low as in developed
countries, recent studies by Dr.S.Irudayarajan and P.Mohanachandran of Center for
Development Studies, Trivandrum claims that Kerala’s Infant Mortality Rate (IMR ) is
as high as 37 per thousand and not 14 per thousand as claimed by the govt, and other
agencies. They used the census data to arrive at this conclusion. The study while analysing
the official statistics ( on which the govt, based its claims) in the 1996 Sample Registration
System (SRS) provided by the Registrar General of India found that out of 14 children
who died in Kerala within a year, 11 died within a week- a rate which is even higher than
the national average. According to these researches, even if one accepts the IMR provided
by SRS was correct, still birth rates and prenatal mortality rates were also extremely high.
Otherwise, it indicates another paradox of Kerala - low IMR, high still birth and one week
mortality.
Another recent disturbing factor in Kerala is the low birth weight of the new boms.
Available studies indicate that the proportion of low birth weight babies was on the
increase. The average birth weight had declined from 2.81 kg in 1987-88 to 2.65 kg in
1992-93. In 1981-82 only 11% children were below 2.5kg and the rate at present is 24 %
7
This is disturbing and it shows the decline in the per capita average food consumption and
the consequence of the policies in the agricultural sector.
Yet another disturbing factor is the Privatisation of healthcare and its impact on the
women’s health. The whole process of pregnancy and delivery is highly medicalised. Most
doctors prescribe two or three scans during pregnancy. Average visits to the doctor during
pregnancy is seven, which is higher than that of the west. Caesarean deliveries are
extremely high.
Privatisation of health care also means that the poor women’s health is neglected. There are
no facilities for delivery at the Primary Health centers. (PHC’s). In a survey conducted
recently by us the women of the slums and coastal communities spoke of the inefficiency,
lack of infrastructure facilities, high rates of bribery, rude and unfriendly attitude of the
staff and lack of privacy in consulting rooms as problems faced by women in the Govt,
hospitals.
Although there is wide acceptance of family planning methods, it is a women centered
approach. Of the couples who adopt permanent methods, majority are tubectomies.
A serious problem affecting women in the state is the increasing sexual violence .
Organised sex rackets are flourishing in the state where unemployment also is very high
The awareness about sexual and reproductive health problems is low and women keep this
problems to themselves rather than consulting a doctor. This also is true for educated and
women of high income groups.
2. Decentralised planning process in Kerala
In accordance with the 73rd and 74th constitutional amendment, The Kerala Panchayat Act
was passed in 1994, which paved the way for real ‘devolution of power’ to the local bodies
and to the people through '‘Grama sabhas \ In order to actively involve the people in the
9th plan, a massive ‘People’s plan campaign’ was started in 1996. . About 40% of the
total plan fund is earmarked to be spend through local bodies.
The state planning board is pioneering this unique experiment of decentralised planning
process in Kerala. The various experiments in decentralised planning so far in thecountry
had focused on the district levels or the block levels. Here through appropriate acts and
rules the panning process is entrusted to the local panchayats and every citizen is
entitled to be a member of the planning process through their participation in the
Grama sabha.
There are lot of hurdles to make this process a reality. The ‘devolution of power’ also
means deployment of officials and their powers, funds etc. New rules are formulated for
this. People and the elected local body representatives are without any experience in
planning. So numerous training programmes at various levels are being conducted. Lack of
sufficient date at the local level, lack of technical skills etc were other major problems.
These are also being tackled gradually
“Decentralised planning process is generally categorised into need based and resource
based planning. In the need based process, acute problems faced by people are identified
1
and resources to solve these problems are located and development programmes are
planned accordingly. In the second approach, human and other resources and tlieir
potentials are visualized and appropriate plans are made. The basis of peoples plan is an
integration of this two approaches” ( People’s Plan- Theory and practice: Dr. T.M.
Thomas Issac : Kerala State Planning Board :1997 October)
In order to ensure that the decentralised planning process is transparent, scientific and time
bound, a 5 phase action programme is envisaged in the plan document.
Phase 1
Identification and prioratising local problems and needs by tlie people
themselves coming together in the grama sabha.. Every voter in a ward of the panchayat
will constitute a grama sabha. . The people coming together in a grama sabha are divided
into 12 sub-groups or more as per the need. The 12 main groups are Agriculture and
irrigation; Animal husbandry and Fisheries ; Education; Industry; Drinking water and
Public Health ; Transport and Energy; Housing and Social welfare; Culture; Women, SC&
ST welfare, Co-Operative sector; Resource mobilisation.
PHASE 2
Development seminar. This process involves finding solutions to the
problems raised by the people with the help of relevant data, studies and the resources
available locally . In this seminar two people selected from each subgroup of the grama
sabha and other experts, resource persons etc. participate. An Action Committee is
constituted here to formulate projects based on the recommendations of the development
seminar..
Phase 3. Project formulation by the action committee. At the end of this a number of
projects suitable for each area will be ready
PHASE 4
Select projects which can be executed by the panchayats with available
resources, with state and central assistance etc. A plan document is thus prepared.
Phase 5. In this phase, the village panchayat projects are coordinated at the block
level and the block level projects at the district level. Thus projects for the block and district
panchayats are prepared.
Expert committees are formulated at this level to examine the projects, recommend
changes and make them worthy of technical approval and then this are recommended to
the District Planning Committee (DPC )
2.1 Approach to health
Health is considered as the most important development sector in the service sector. There
is a general awareness that gains in the health sector cannot be sustained unless there are
improvements in the basic living conditions like drinking water, sanitation, housing, and
nutrition. Some of this can be addressed only through improving family income,
particularly income of women. Experts opine that emphasis should be given on ecological
and economic measures and not the further expansion of inffa-structural facilities.
Two major aims of the projects in the health sector, as envisaged by the planning board, is
to improve the quality of care and increase the outreach of services provided.
4
The public health care system from the PHC to the district hospitals are now under the
three tier Panchayat system. The restructuring of die health sector with people’s
participation is beginning to take place.
If we examine the projects formulated in the decentralised planning process in Kerala in
the last year, the following were the priorities.
1. Most of the projects in this initial phase is to do with environmental hygiene and
sanitation, health surveys, improvement of the basic facilities in the PHC’s and
Community Health Centers ( CHC’s )
The ICDS programme is handed over to the local bodies. The ICDS supervisor is the
main functionary of the Mother and Child Health (MCH) programmes of the Panchayats
and Municipalities. The local bodies can earmark funds to supplement the nutrition
programme.
2. Since sufficient funds are earmarked for the health sector from the plan funds , the (
resource crunch in the health sector is solved to a certain extent. In the
plan about
6000 crores is allocated for the service sector like the drinking water, sanitation,
education, environmental hygiene etc. Out of this about 500 crores will be spend in the
health sector alone. If in the 8th plan, only 2.20% was spend in this sector, in the 9th
plan it will be 5.02%.
3. In the rural areas a collective spirit is growing with the doctors, health workers, elected
members of the local bodies, and the public working together. They do not have to wait
for the bureaucratic delays. Many doctors feel that it is the first time that they get
involved in planning for the sector in which they work. One must admit that there are
also cases where the doctors feel upset to be under the local authorities and to be
accountable to the people
4. The peoples campaign for decentralised planning is giving opportunities to experiment
and execute new and innovative programmes. Health camps, blood donation camps,
health card distribution, surveys to identify health problems of the area, projects for the
rehabilitation of mental patients, mentally retarded children etc. are some of the
projects so far. Considerable voluntary labour is drawn into these activities.
A new approach is emerging with people taking responsibility and demanding
accountability from the public health personnel. Local specific problems are getting due
attention. A great deal of preventive health care is possible. Other health systems like
Ayurveda and Homeopathy are getting integrated . In some places, there are attempts to
study in detail the health problems of the general population of the area and then plan
projects accordingly.
5
An integrated approach proposed by the state planning board for the decentralised planning
is as follows.
Food
Drinking wat<
sanitation
Health education
Housi
Health for all
common aim
Life expectancy ~ 72—80
Infant mortality rate=l 8—10
Birthrate
=18-10
Mortality rate
= 6-5
Treatment
preventive care
hygiene
Income
22 Decentralised planning process and women's health
If we examine the plan documents and the hand book prepared by the planning board on
Women’s development, Mother and child health development and health, the following
factors emerge.
All these documents speak of the contradiction of high female literacy and rather poor
socio-economic status of women. It is emphasised that the decentralised planning process
should give special attention to study the status of women in their areas and evolve suitable
projects to increase the status of women. Since an evaluation of the 1st year plan s showed
lack of sufficient fund allocation, planning board made it mandatoiy that 10% of funds be
set apart exclusively for schemes for women and the district planning committee is
authorised to monitor and ensure this before final sanction is given.
Women’s health concerns are integrated with ICDS programmes and the Anganavadis are
expected to be the centers of health education and women’s joint actions. The ICDS
supervisors and the Anganavadi workers are expected to give leadership to get women into
neighbourhood groups
The following is the guideline for an integrated maternal and cliild development
programme
6
Nutritious food
Information center
special schemes for
children below 6
treatment
Preventive measures
People's committee
Integrated
mother and child
primary health
care/
development
Improve infrastructure
facilities
Informal preschool
education
Special schemes for adolescence
women empowerment
center
Local specific data collectio]
guidance and counseling
center
special care for pregnan
and lactating mothers
Envormental hygiene
sanitation &drinking
water
In all this , reproductive health, sexual health and rights do not sufficiently get reflected.
The general lack of gender concerns and perspectives is reflected in the programmes
proposed in the first year.
Yet in the second year, some panchayats and blocks have prepared some good projects.
An example is the ‘Integrated social health scheme’ formulated by the Ponnani Block
Panchayat in North Kerala in collaboration with Indian Medical Association (IMA) and
Mental Health Action Network. (MHAN). In this Muslim dominated block, a major thrust
of the project is to discourage adolescent marriages, and give wider awareness on women’s
reproductive and sexual health. A hand book called ‘Mother’ is prepared and widely
distributed. As is said in the preamble of this booklet, Tt is hoped that awareness of one’s
body will help women for better family life and more control and power over their own
lives’
The Muncipality of the same area is doing a health survey and is planning to issue health
cards for women and children. Cervix cancer detection camps, special supplement nutrition
programmes, gender education programmes etc. are some other projects planned
7
2.3 Limitations
The decentralised approach is in place only since 2 years and hence it is too early to judge
its impact. It also has to be kept in mind that people are still in the old mindset of expecting
concrete individual benefits.
Although the plan documents and hand books makes special mention of gender concerns
this do not seem to have percolated to the local level planning process. The planning board
has set up a gender- impact monitoring cell and also has insisted that the District planning
committees pass only projects which has earmarked 10% of funds for women.
But these measures alone are not sufficient when deep and subtle patriarchal attitudes
prevail. In many panchayats, women had to fight to get this 10 % funds earmarked for
women specific projects as the men resented this and tiy to get general projects like
drinking water and sometimes even roads under them!. Most often people lacked ideas as
to what are appropriate and viable projects. They are never used to think with and for
women.
Even worse is the scenario of women’s health projects. Even the handbook prepared by the
planning board do not mention specifically about women’s health concerns, except anemia
and quality of maternal and child health services.
What gets reflected in the local plans and projects is what is discussed and proposed in the
grama sabhas or by the action committees .There is general complacency that everything
is well with the health status of women and their specific health issues remain invisible or
unspoken.
Now with HIV/ Aids threat looming large in the state, more organisations have come
forward to work with sexual health issues..
3. Suggestions for Policy advocacy and programme intervention
3.1 General suggestions
•
•
Special efforts have to be made to make the public health system vibrant and able to
respond to the health needs of people. Special incentives be given to encourage
doctors to work in the rural areas (like tax subsidy on their earnings as suggested by
IMA)
All states should take steps to decentralise planning process . Necessary laws to be
enacted by the respective state Governments for this purpose and financial allocation be
made in this line. Intense campaigns be conducted so that the new tliinking becomes
people’s own.
R
•
Comprehensive studies/ data collection needs to be undertaken to understand the
specific women’s health issues in the states, specially of the marginalised groups like
indigenous people, Dalit women, women of the fishing community etc.
•
Wider information dissemination of this concents to planners and policy makers so that
these are reflected in the plans and programmes
•
Model projects to address women’s health concerns needs to be formulated and
proposed to the grama sabhas/ Action committees.
•
A state level consultative body of eminent doctors with gender sensitivity, women’s
health activists etc. can be constituted to suggest priority areas and monitor projects
•
The ‘Peoples Heath action committee’ to be formed at each PHC and CHC level
consisting of doctors, para-medical staff, elected representatives, AnganayvadL workers,
representatives of women’s organisat ons, teachers etc. be authorised to Plan, suggest
and monitor local specific health action in consultation with grama sabhas to be
funded and supported by the local bodies .
3.2
Specific suggestions.
All the PHC’s should have facilities for normal deliveries. Other infrastructure facilities
be improved so that the place becomes attractive and pleasing. Local Panchayats
should earmark funds for the same.
• The services of a gynecologist be made available at least in the community health
centers, with privacy for consultations
• The timings of doctors be rearranged to suit the needs of the people or as is done in
Tamilnadu ( 24 hours )
• Educational programmes using audio-visuals to help women to get a clear idea of their
body and its functioning’s
• Indigenous health practices be documented and promoted in treating gynecological
disorders
• Special efforts to make men responsible in women’s health and contraception. The
responsibilities of health workers be reorganised so that male health workers assume
more responsibility, specially in reprodctive health matters.
• Women’s organisations should establish constant dialogue with policy makers and
planners so that women’s health concerns gets reflected in the planning process.
• Use mass media for wider dissemination and public debate on women’s heath concerns
other than that of the population control angle
• Special efforts be made to ensure and increase women’s meaningful participation in
the planning process. Audio-visuals, theatre , folk art forms etc could be used
effectively.. Collaboration of NGO’s, women’s groups etc also should be sought.
•
o
•
It has to be remembered that women are not a homogeneous category and the health
needs of adolescents, older women etc (life cycle approach ) and women of different
economic categories be addressed separately.
4. Conclusion
Although the concrete health situation of Kerala may be different from other states, the
general approach to the problem is applicable in all states of India.
The current paradigm of health sectors development, is raising inequalities and alienating
the poor and needy from the public health care system. The goal of universal primary
health care service cannot be achieved if policies favour privatisationof medical services
The decentralised Planning process offers an innovative approach to health care financing,
enhancement of quality health care, prominence of preventive over curative care, demand
accountability from health personnel, and last but not least empowerment of people. In the
degree in which the women are made aware of their health concerns and issues and
empowered to be active in the social and political process, their health concerns also will
find a place. This is the challenge to be faced by the women’s groups.
Let me conclude by a quotation from Comrade E.M.S Nmaboothiripad who was the
chairperson of the people’s plan campaign " True development can be possible only with a
decentralised approach, where people take over the power to decide for themselves. If
departmentalism has to end, oldfortresses ofbureaucracy erected between people and
departments should be broken down. The humiliation suffered by ordinary people at the govt,
offices and the system of begging favours from higher-ups should end. Each citizen shouldfeel
that he is part of the govt. The Govt, should have the will power to hand overpower to
people
”
Aleyamma Vijayan
Sakhi women’s resource center
Trivandrum. 695001
10
Abbreviations used
Primary Health Center
PHC
Community health Center
CHC
Government
Govt.
Maternal and Child Health
MCH
Infant Mortality rate
LMR
Integrated Child Development Scheme
ICDS
References
Books
Department of health and family welfare: Govt, of Kerala; Health profile of Kerala
1S§9
Kerala state planning board and Health and Family welfare Dept.; Planning helper
3: Handbook on Health 1998 (Mai)
Kerala state planning board and social welfare dept. Planning helper 6: Handbook
on Maternal and child development sector 1998 (Mai)
Kerala state Planning board and social welfare dept. Planning Helper 11:
Women's development sector: 1998 (Mai)
Kerala Sastra Sahitya Parishat: The health status of Kerala (Malayalam) 1991
Thomas Issac T.M (Dr) People's Plan: Theory and practice: Kerala state planning
board 1998.(Mal)
Ponnani Block Panchayat; Am ma 1999 (Mai)
Zachriah K.C and Irudaya Rajan S: Kerala’s demographic transition: determinants
and consequences; 1997 sage publication
ii
DILEMMAS OF ADVOCACY IN MENTAL HEALTH:
MAKING POLICY RECOMMENDATIONS FOR WOMEN
BY
BHARGAVIV. DA VAR
Prepared for the
National Consultation Towards
Comprehensive Women’s Health Policy and Programmes
BY
VHAI-WAH’-DSE
Held in VHA1, New Delhi.
On February 18-19, 1999
I
Paper prepared for the National Seminar on 'Health Policy and
Women’ at VHAI, Delhi, February 18-19, 1999
Dilemmas of advocacy in mental health:
Making policy recommendations for women.
Bhargavi V Davar+
I have throughout argued that making policy recom
mendations in the absence of baseline data and documenta
tion on Indian women’s mental health status is problematic.
Dhanda’s work (most recently, see her 1999) has led to
important and critical advocacy positions, while not forget
ting the legislative and policy vacuum within which such
positions have to be played out. Other campaigns for the
rights of the mentally disabled have highlighted the prob
lems of having to protest indignity in a completely nonsupportive and morally bankrupt political climate. In this
paper, I highlight some tentative suggestions and ideas that
have been debated, but only as a footstep for further ascendence into the space of mental health activism and ad
vocacy, especially as they pertain to women’s issues. As
such, this paper is summarily drawn from earlier work done
by not only myself, but several others actively involved in
advocacy for women, the mentally disabled & ill, and a list
of references has been appended for more detailed discus
sions.1
It is often assumed that advocacy means only legal re
form. However advocacy involves both legislative reform
as well as policy research. These are two different issues,
but equally important for advocacy. Legal advocacy in
volves examining legislative instruments & structures,
pressing for law reform, for humane adjudicatory processes,
etc. Policy advocacy involves looking at the national or
regional mental health policy documents, drug policies, etc.
and other service planning instruments, and the structures
and practices installed for using these instruments. This
distinction is an important one for wholistic activism in the
area of mental health.
+ Bhargavi V Davar, PhD
Bapu Trust for Research on Mind & Discourse
I Floor, SOONA Lodge
16/A Shankershet Road
Pune 411042 Maharashtra.
1 This paper has drawn from discussions and deliberations that
have happened in many parts of the country on Women & Mental
health in the last 5-6 years. It has also drawn from the lives, re
sources and perspectives of innumerable friends and colleagues
who have contributed to the debate on the subject in these years.
The many sided contributions to the debates have been acknowl
edged in detail in my recent book. However, 1 want to specially
thank Dr Amita Dhanda (Indian Law Institute, New Delhi) for her
influence on my thinking about mental health law & advocacy,
and many friends from Anveshi (Research Centre for Women’s
Studies, Hyderabad), and especially Veena Shatrugna, for their
influence on my thinking about feminism.
Dhanda (1993) argued that legal reform must keep
pace with scientific progress in diagnosis and treatment.
Davar (1997) argued that such legal reform must be sup
ported by real (and not simply paperwork) changes in pol
icy and services. Thus, for example, apex court decisions,
following recent PILs, to “release” the non-criminal insane
from jails in West Bengal (and also other parts of India)
were important legal victories from a “Rights” position.
However, these victories were forced to be morally com
promised (as happened in the West after the de
institutionalisation process) because policy support was
completely lacking from the state. The wrongly institution
alised persons were simply released into the streets without
any state initiatives for providing mental health care.
Mental health activism therefore should involve a two
pronged approach, one, targeting Legislation, and the other,
Policy. The Indian Lunacy Act (1902) was recently changed
to the Mental Health Act (1987). The Disability Act is also
being re-processed. The MHA also did not have a Rights
chapter, being, in letter and spirit, only a minimalist, cus
tody Act. Dhanda (through 1984 - 1999) has extensively
analysed the limitations of the MHA and has argued for a
maximalist law. Other international instruments include the
UN Principles for the rights of the menially ill, and such
instruments are also consistent with others such as the
CEDAW, Universal Declaration of Human Rights, etc. Es
pecially •promised in these instruments is the right of the
mentally ilJ person not to be discriminated against for being
a woman. However the reality is far from the promise.
From the policy side, there is the National Mental
Health Programme (1982). This document shifts the basis
of practice from the traditional (psychiatric) services to
community care. The NMHP is only a footnote to the na
tional health policy, not offering any (fiscal or technical)
supports for building community initiatives, and simultane
ously, leading to downsizing of already existing facilities.
Further, the priorities of NMHP (psychoses, epilepsy, psy
choneuroses... in that order) are such that interventions in
volve nothing more engaging or humane than drug dis
pensing. While in its philosophy, the policy signals
“revolutionary” ideas in community care, in practice, and
by the way that priorities are set up, the bio-medical model
is reinstated, that too, in its least rigorous and most prob
lematic form, i.e., through the PHCs.
Both the NMHP as well as the MHA limit themselves
to the case of those diagnosed with severe illness. The rea
son for this is that, insanity, especially of the severe type,
and criminality are close in terms of legal conceptualisation,
and both are brought to the forefront when law and order is
at issue. The so-called “societal burden” for the mentally ill
is also more acute in the case of severe illness. The defense
in the case of hysterectomies in Sirur was built upon feudal
notions of such (parental) burden in protecting the girl
child’s body/sexuality. Advocacy positions have empha
sised that both law and policy, as they exist now in India,
serve only to protect the interests of the state, the courts,
and the society, rather than the interests of the mentally
1
distressed. Thus, the available legal & policy instruments
facilitate social control over individual behaviour, and
maintains the state prerogative to take behavioural deviance
into custody, rather than facilitating adequate or humane
interventions.
Mental health advocacy has so far been loosely net
worked, issue based and mainly targeting law. However, I
have emphasised that legal advocacy must co-occur with
consumer pressure for policy changes and demand for state
supports in creating essential mental health services. The
services in India are so pathetically meagre, and the NMHP
has offered little to enhance services. Mental health advo
cacy must connect as a systematic and coherent movement,
with the consumer, health rights and women’s movements.
1. Prevalence data pertinent to women’s mental health.
Brief review.
♦ Samples from psychiatric surveys in rural/urban,
North/South Indian communities in India done between the
late 1960s and 1990, average a diagnostic rate of about
11%, with men averaging 10% and women, 15% (Review
in Davar, 1999).
♦ In these surveys, around 1% of men and 1.3% of
women received a diagnosis of Severe Mental Disorder
(SMD) (including organic brain syndromes, epilepsy, MR,
psychoses), whereas 6-7% of men and 10-11% of women,
received a diagnosis of Common Mental Disorder (CMD)
(including depression, anxiety, psycho-somatic and other
neurotic symptoms) (Chakraborty, 1990; Sandel, 1990;
Review in Davar, 1999).
♦ More women than men use the so-called indige
nous healing systems (shamans and mystics), are possessed,
or go into mystical trance.
CMD is of greater prevalence among women, and has
elicited feminist attention. Some emerging concerns in the
area of common mental distress among women are: The
mild to serious mental effects of victimisation by violence,
especially child sexual abuse; Self-injury and suicide, espe
cially among adolescent girls; Eating disorders, following
the post-liberalised media onslaught of images of thin and
ravishing women. The psychological impact of violence on
women are comparable to the effects of trauma, disaster or
war. Higher rates of suicide, greater use of health services,
and a range of diagnoses between anxiety to severe mental
illness may result from victimisation. It is estimated by the
World Bank 1993 report that 1 out of 5 healthy years is lost
to women in the 15-44 year range due to victimisation. The
health burden for victimisation is 9.5 DALY, comparable to
costs of HIV, TB, cardiovascular disease and maternal
morbidity. In the west, recent authors have emphasised’,
especially in the context of the astounding information on
victimisation by violence, that women’s mental health must
be overall seen within an epidemiological and public health
perspective (Lubotsky, et al, 1998). However, such re
organisation of priorities should not underestimate the life
situations nor the service needs of severely ill women. The
common menial health problems of the elderly women or
women suffering from disabling illness such as osteoporo
sis, cancer etc. is not known.
2. Gender, data and psychiatry.
♦ The statistical association between childbirth and
symptom formation is strong (Sandel, 1990:p.l74). A
small, but significant sample of women, develop post par
tum psychoses, which is often neglected (Chandra, Under
review).
While provisionally, the psychiatric survey data may
be considered as useful, many of the methods used can be
questioned for lack of gender-sensitivity. The earlier diag
nostic systems (DSM-III, used in many of the studies) used
diagnostic categories such as “hysteria”, “depression”, etc.
quite uncritically. Until date, barring a few exceptions, re
searchers in psychiatry, even on issues very close to
women’s lives such as depression, do not feel it is essential
to probe for the associations between illness experieric’t^. ••
and gender. Needless to say, other socio-political realities > /
underscoring Indian women’s lives, including victimisation
.
by violence, common mental health problems relating Jo ’ ’
sexuality and reproduction, possession and other dis^L\
tion experiences, and somatisation, have elicited
•
est in professional circles. While those rare mentaywltP’.
professionals (for example, Chakraborty, 1990; S^s'hWI,'
1994) have worked with a gender perspective in their inter
ventions, and have been friends of the feminist movement,.
the mainstream practice still asks, (as one highly functional
psychiatrist did to me), “What does gender have to do with
psychiatry?”
♦ 17.9% of women in the community report CMD,
using a gender sensitive questionnaire (Jaswal, Under re
view). There is a strong correlation between gynecological
morbidity and CMD.
In India, some suggestions which have come up in the
context of the ethics for education / research / publishing
regarding women’s mental health are the following:
♦ Independent (Indian) surveys on depression and
neuroses, show that a lot more women than men receive
diagnoses of CMD, such as anxiety, depression, somatisation, phobias and obsessive compulsion.
♦ Twice the number of women, than men, are be
lieved to be “depressed”. Depression is the 5th highest
ranking disorder in women across the world, according to
recent world data-bases (Desjarlais, et al 1995).
♦ 12% to 15% of women in community samples may
report pre-menstrual distress. For 13% of women reporting
such distress, the symptoms may be intolerable (Review in
Chandra, Under review). Post partum depression is com
mon, and in a small number of women, severe enough to
require intervention.
♦ Research interviewing, data processing, choosing
samples, framing explanatory models, etc. must be sensitive
I
to issues of gender. All research proposals, and also funding
for such proposals, should include criteria probing for gen
der sensitivity.
♦ Editorialising research conclusions in journal arti
cles often carry unlimited gender bias. When studies are
presented in official/academic journals or newsletters,
vague over- generalisations about women, the causes for
their mental illness, over-generalisations about “biological
vulnerability”, their “social roles”, their “hormones” etc.
should be avoided. More attention must be paid to the so
cio-political contexts of women’s mental experiences, their
emotions and their views and experiences about their bod
ies. More attention must be paid to women’s common
mental health problems.
♦ Many examples have been unearthed from the psy
chiatric literature and practise where a feudal morality and
sexism is unacceptably blatant. Forums for research pres
entations and publications in psychiatry & allied disciplines
must make it an official policy to avoid such language and
negative perceptions about women.
♦ Curricular changes in psychiatry & mental health
training & courses must be made to suit contemporary con
cerns about women’s issues. For example, relevant feminist
literature in psychology or therapy can be included.
♦ It is important to facilitate feminist / women’s lob
bies within the mental health professions, which is a pre
dominantly male domain, because of the priority of psy
chiatry, a medical discipline. It has been suggested that
women’s mental health concerns are better addressed by
psychological models than the psychiatric, thereby ques
tioning the current hegemony of psychiatry over the mental
health discourse.
3. Mental health services and women.
The in-patient facilities (private, public hospitals, gen
eral hospital psychiatric wards, other private residential
facilities) have fewer beds for women. Severely ill women
are often seen as genderless, in in-patient facilities. Espe
cially in mental hospitals such facilities do not serve the
special physical health needs, for example, pregnancy, gy
necological or menopausal problems, of women. Rape and
sexual abuse of institutionalised and ill women by hospital
superintendents, who are then sent for clandestine abor
tions, is not unknown. Women’s expression of disapproval,
anger or resistance within inpatient facilities is likely to be
interpreted as evidence of their illness. Strong gender
stereotypes operate within in-patient psychiatric settings
where “abnormality” and “cure” are defined in terms of
conformity to a notion of femininity.
Social reasons for incarceration of women within
mental hospitals are also against the women’s interests. See
Dhanda’s extensive work in this area. Women who deviate
from the feminine role (good wife, chaste mother, dutiful
daughter-in-law), infertile women, women from whom eco
nomic benefits are sought to be extracted, and women who
stood in the way of the husband’s second marriage, have
been trapped in insanity petitions for divorce. Women in
mental hospitals have fewer visitors, are abandoned or tend
to stay on longer than men within the institution. There arc
fewer voluntary patients among women than among men.
The risk of being abandoned, deserted, divorced or losing
their rights over children is higher among institutionalised
women.
CMD, common in women, are more amenable to
psych-j-therapy. However, gender sensitive psycho-therapy
options are yet to be articulated in mainstream practice. The
abuse of over the coupler medication is largely unre
searched, though experientially, feminists have always wor
ried about the over-prescription of tranquilizers, sedatives
and anti-depressants (Shatrugna, 1999). It is now known
that Indian psychiatrists over-prescribe drugs (Nunley,
1996), do needless psycho-surgeries and use ECT indis
criminately or in a cavalier way (Agarwal, et al, 1990,
1992), without taking consumer issues about providing in
formation or consent to treatment too seriously. The recent
APA (1990) sanction of ECT use is only likely to worsen
the situation further, because ethical codes for the safe ad
ministration of the treatment, and the technology required,
are near absent in Indian hospitals. In a recent study
(Agarwal et al 1997) of professional attitudes to ECT it was
found that an overwhelming
of psychiatrists fa
voured its use, while only 2.7^i*ad strong objections. A
majority disagreed that “ECT sholil’d be used only when all
else failed”. Relatives of patients, too, preferred ECT and
drugs overwhelmingly over psycho-therapy (Boral, et al,
1980). But not even one patient voluntarily chooses ECT
(Verghese et al, 1968), most of (hem passively accepting
what is chosen for them by professionals or relatives. The
arbitrary use of ECT in treating behavioural problems has
been discussed in detail in Davar (1999). It is not likely, as
in the west, that women are given more of these physical
treatments, because, excepting the community care settings,
women’s access to mental health care in India is meagre.
However, it is likely that those women who do enter treat
ment settings are regularly abused by ECT and are over
prescribed psycho-active drugs.
Suggestions that have come up for creating or im
proving services for women’s mental health:
In-patient / hospital care:
♦ Making available equitable, more transparent, user
friendly, accountable and open treatments in mental hospi
tals and other state supported in-patient facilities, through
legal and institutional processes that are adequately covered
by individuals’ & consumers’ rights paradigms.
♦ Instead of creating “model mental hospitals” out of
a few premier institutions that have show case value, efforts
must be made to force all Indian mental hospitals to con
form to the ethical standards of practice, in terms of tech
nology and infrastructure as we|Lfs in terms of administra
tion. Hospital reform which has SBrecent years elicited pro
fessionals’ pride should be enforced on each and every hos
pital.
4
♦ Open and non-paternalistic institutions for women,
where women can make their own decisions, have free mo
bility, can act in their own interest and be safe.
♦ Creating gender sensitive cross-refenal systems
within health services that offer comprehensive caie
(polyclinics, hospitals, etc.), including facilities for gyne
cological and general health care for hospital and other in
stitutionalised patients.
♦ Creating gender sensitive day care, counselling
and supportive therapy options in each and every mental
hospital and in-patient psychiatric facility.
♦ Setting up professional norms and standards lor
the rational and ethical practise of physical treatments, such
as drugs & ECT, especially the latter, in such a way that
women’s role in their own treatment is participatory and by
choice, and not under duress.
♦ National level debate and the formulation of ethi
cal codes and controls on the use of ECT, including speci
fying rationale for use, criteria for humane methods ol use,
treatment protocols, consent to treatment and right to in
formation.
♦ Preceding the ECT treatment, patients should be
informed about risks, alternatives, a detailed description of
the procedure until the patient understands, the option to
say no,
♦ A precise legal definition of “extreme cases”
when ECT will have to be used perforce.
♦ Upgrading technology and personnel training for
ECT use in all hospitals.
♦ Scrupulous maintenance of records regarding
every ECT use, including profile of patient, diagnostic de
tails, reason given for use, patient acceptance, side effects
and follow up. Such records should be made available to
the patient on demand.
♦ Setting up patients’ counselling and rights council
or a consumer council in every mental hospital facility.
♦ Providing social security and legal and institu
tional supports and safety nets for deserted, homeless men
tally ill women who are institutionalised or jailed.
♦ Rehabilitation programmes within mental institu
tions (including for the mentally disabled children) should
be gender sensitive, and creative for women. Such pro
grammes should be designed or planned on the basis of the
special requirements of and feedback from the in-patient
women, instead of adhoc administrative views about
“creativity”, which often reduces the women to making as
sembly line products.
♦ In an age of growing communal clashes and in
creasing violence against women, diagnosed, mentally
challenged, severely ill, or institutionalised children and
women are specially disadvantaged groups. Against an
alarming scenario of child sexual abuse, and the rape and
abuse of mentally challenged women, creating safe envi
ronments through not only legislative but also institutional
frameworks is the (hitherto neglected) responsibility of the
state.
Supports to be created in general health and cornnHinity.
care.
♦ Community care should be planned care, taking
into account local social needs, housing and empowerment
problems, conflict areas, etc. A good community oriented
policy would be comprehensive in a social sense, and not
just be a drug dispensing medical manual.
♦ Policy should specify not only the general objec
tives of community care, but also give supports for setting
up specific treatment protocols, resources and personnel
within community care settings. As it stands, the
(undertrained, often unmotivated and poorly supported)
PHC staffers are supposed to take on the responsibility of
case identification & referral.
♦ Providing state supports (technical as well as eco
nomic) for establishing and working of community initia
tives, support & advocacy groups for women who are men
tally distressed / ill.
♦ Creating gender sensitive counselling & mental
health care options in comprehensive health care settings
that are predominantly used by women, such as GP, gynae
cological clinics, burns, outpatient and other emergency
wards where women victimised by violence are regularly
treated.
♦ Of especial concern is the medicalisation of com
mon mental problems of women such as somatisation by
needless medication and sometimes even surgery, leading to
iatrogenic damage.
♦ Creating educational and training institutions fo
cussing more on psychotherapy, psychiatric nursing and
counselling.
Ethical audits and securities.
♦ In-patient facilities for the mentally ill and mental
health institutions are public institutions, offering services.
They should be accountable and open, with regular moni
toring and audits, involvement of patients and their views
about the services offered, and open access to audits.
While the mental hospitals have been disgraced by the
many reported horror stories, access to them even for re
search purposes is unbelievably difficult.
♦ Ethical audits and evaluative documentation for
treatments offered, especially ECT and other physical
treatments (as detailed above).
♦ A national level debate, evaluation and policy
making on the rational use of anti-psychotic, anti-depressant
and other prescriptions for mental disorders.
♦ Involving user participation in the design, process
and evaluation of every type of treatment or service being
offered for mental disorder.
5
♦ Setting up consumer centered norms & standards,
internal audits and codes of ethics within official psychiat
ric & related mental health forums, (including peer re
views), for monitoring and evaluation ol the sexual ethics of
individual professionals’ practise.
♦ Formulating legal definitions of abuse of mental
health practise in the community or in private practise, in
cluding sexual abuse of patients, and installing suitable
penalties and compensations, or what constitutes appropri
ate justice in the case of violations.
♦ In the west, the American Psychiatric Association
in 1973 proscribed professionals from (1) fostering tradi
tional sex-roles, (2) holding biased expectations from cli
ents (3) using psychoanalysis in a sexist way and finally (4)
responding to clients as sex objects (Holroyd, 1983). Ethi
cal codes for practise will enforce attitude changes in the
mental health profession.
♦ Providing social and legal safety nets for diag
nosed women, so that their rights to equal employment and
obtaining other social benefits of such employment (such as
insurance, promotions, leave, etc.), are protected.
4. Mental health law and women.
The problems of institutionalised women is well
documented (Mehra, 1995). Women, alleged to be men
tally ill or disabled, are brought within total institutions
such as mental hospitals, jails, orphanages, or remand
homes. Other than their personal and civil liberty being
taken away from them, they are often vulnerable for neglect
and abuse, including sexual abuse. PILs have only high
lighted the inadequacy of law to treat the mentally ill hu
manely. Campaigns against the jails in the north-east for the
abuse of non-criminal insane resulted in SC intervention.
The inquiry committees set up made many human rights
recommendations that the state ignored. The campaign
against the hysterectomy of the mentally challenged also
suffered setbacks because of the inadequacy of the law to
protect the rights of the disabled and the lack of policy to
install supportive services. The Anamika Chawla case
brought to the forefront the facile manner in which institu
tionalisation can be (and has been) effected in the case of
women. The limitations of the Mental Health Act has been
widely debated. Among its many problems, Dhanda has
noted the following: (1) The definition of the mentally ill
within law is more narrow than the scientific definition and
is ambiguous, confusing and ad hoc. (2) Leaving the right
of incarceration to relatives places too much trust in the
goodwill of relatives. (3) The Act has no rights chapter,
indicating the lack of state interest in the quality of lives
and personal liberties of the mentally ill. (4) Even gross
instances of institutional and professional abuse have not
invited appropriate justice. (5) Those diagnosed with men
tal illness in law are not considered legitimate persons/citizens, being deprived of civil liberties (such as right
to contract, own property, etc.), and state protection. The
MHA, simply giving the norms of institutionalisation
(admission & discharge) exists only to protect the interests
of the courts, the state and society, and not the interests of
the mentally b&.'pr disabled. As it stands, the MHA is an
extension of s aje’s power for taking inconvenient individu
als into custody, by seeing them as a “law & order” prob
lem. Dhanda lias- emphasised that, against this scenario,
bringing mentally distressed women within the purview ol
law in any context is a problem. Instead of empowering
them, the law is likely to disempower them further, rein
forcing already negative social stereotypes of the dangerous
and uncontrollable lunatic.
The MHA is not an acceptable law in its minimalist
form, as a custodial law. Arguments have been made to
reexamine MHA and make way for a maximalist law, which
will aim to protect the rights of the mentally ill. Suggestions
that have come up in this context are (broadly):
♦ Rationality & adjudicatory procedures of incar
ceration to be made precise, unambiguous and just, espe
cially in the context of women.
♦ Setting up legal audits for mental institutions to
regularly monitor for abuse of practise.
♦ Addressing the rights violations of non-criminal
mentally ill men and women in the Indian jails.
♦ Establishing a human rights & civil liberties
chapter in law for the mentally ill.
♦ Creating a patients’ counselling and rights cell in
every mental hospital.
♦ Creating legal safety nets and social securities for
the mentally Rl and disabled, especially the poor, wandering
or jailed women.
♦ Enforcing the creation and proper working of
mental health authorities in all states as promised.
♦ Changing divorce laws and other personal laws as
they pertain to mentally challenged women.
♦ Penalties and checks on sexual abuse-within instiititions.
Recent efforts to implement the Disability act brings
in rights related issues for the disabled, including the men
tally disabled. However, how this will interact with the
MHA in letter and practise is yet to be examined.
5. Women’s movement.
The suggestions above, as may be obvious, are not
suggestions for specific legal or policy reform, but rather in
the nature of re-examining and re-formulating the available
legal and policy documents. The documents, as they exist,
are a blot in the face of the state, which has promised pro
viding health care for all by the year end.
The advocacy for women’s mental health occurs
within the context of the women’s health movement, and
within wider debates about development, empowerment,
human rights and gender equality. For many diagnosed
women, and others who have suffered mentally from vari-
()
ous types of oppression, the women’s movement has been
a process of psychological empowerment. Women’s emo
tions (such as anger or sexuality) which in everyday con
texts are seen as pathological, are accepted within women’s
groups and given the experiential space that it deserves.
Certain skills that women are denied in society, such as
negotiating power, assertiveness, being in control of one’s
own body, etc. have been learnt by innumerable women
through the women’s movement. It is therefore possible to
see the women’s movement as a mental health movement. It
is only inevitable that the women’s movement will take
steps and initiatives in forming community support and
advocacy groups for mentally challenged women. Recently
there have been many efforts (including the WAH pro
gramme) to understand and integrate mental health ideas
and practices self-consciously and critically within the
feminist movement. In this paper, I have however high
lighted the areas whereby the state and the professions must
be negotiad with. This is not to belittle NGO work in the
mental health area. We must however be cautioned that the
state does not relinquish its responsibilities because of the
easy availability of humanpower and motivation in the
community oriented women’s health movement. From the
point of view of advocacy, much requires to be researched
and documented from the perspectives of the (women)
mental health consumers, about which so little is known.
Social studies in mental health care evaluation (in economic
terms such as existing budget allocations, audits of such
allocations, expense priorities of services, etc. as well as in
terms of outcome studies) are also required. Systematic
documentation of community initiatives and networking on
community mental health work will help in highlighting the
possibilities of such work as well as the problem areas2.
LIST OF RELEVANT LITERATURE.
1. Agarwal, A K & Andrade, C (1997) Indian psychiatrists’
attitudes towards electroconvulsive therapy Indian Journal oi
Psychiatry, 39( 1), 54-60
2. Agarwal, A K (1990). ECT. A need for reappraisal. Edito
rial. Indian Journal of Psychiatry, 32(4), 295-296.
3. Agarwal, A K , Andrade, C & Reddy, M V (1992). The
practice of ECT in India. Issues relating to the administration of
ECT. Indian Journal of Psychiatry, 34(4), 285-297.
4. American Psychiatric Association (1990). “The practice of
ECT. Recommendations for treatment, training and privileging.
Report of the task force of the APA on ECT.” Task Force Report.
14. Washington DC : APA Press.
5. Bhattacharya, R N & Chatterjee, S B (1978). Problems of
committed mental patients. Indian Journal of Psychiatry, 20(3),
267-273.
6. Boral, G C , Bagchi, R & Nandi, D N (1980). Anopinion
survey about the causes and treatment of mental illness and the
social acceptance of the mentally ill patients. Indian Journal of
Psychiatry, 22(3), 235-238.
7. Broverman, I K , Broverman, D M , Clarkson, F E Rosenkrantz, P S & Vogel, S R (1970). Sex-role stereotypes and clinical
judgments of mental health. Journal of Consulting and Clinical
Psychology, 34(1), 1-7.
8. Brown, GW & Harris, TO (1978). The social origins of de
pression: A study of psychiatric disorder in women. London: Ta
vistock.
9. Caplan, P J (1987). The name game. Psychiatry, misogyny,
and taxonomy. Women and Therapy, 6, 187-202.
10. Carmen, E H , Russo, N F & Miller, J B (1981). Inequality
and women’s mental health. An overview. American Journal of
Psychiatry, 138(10), 1319-1330.
1 1. Chakraborly, A (1967). A critique on the concept of menial
health. Indian Journal of Psychiatry, 9(3), 192-202.
2 In this paper, because of the lack of comprehensive view on the
subject, 1 have not reviewed the debates about mental handicap,
nor the case of hysterectomies on mentally challenged girls. Also,
there are many questions about how the recent disability act links
with the other legal instruments already in operation.
12. Chakraborly, A (1990). Social stress imd mental hcalih. A
social-psychiatric field study of Calcutta. New Delhi: Sage.
13. Chamberlin, J (1994). A psychiatric survivor speaks out.
Feminism and Psychology, 4(2), 284-287.
14. Chandra, P (Under review). The interphase between psychia
try and reproductive health. In Davar, B V [Ed.]. Mental health,
gender and society. Inter-disciplinary perspectives,
15. Davar, B V (1995a). Mental illness in Indian women. Eco
nomic and Political Weekly, 30 (45), 2879-2886.
16. Davar, B V (1995b). Gender politics in mental health care.
Radical Journal of Health, 1 (3), July-September, 183-207.
17. Davar, B V (1997). Evolving consumer perspectives in mental
health in India. Some preliminary notes on the interface between
users and policy. Paper presented at the International Conference
on Global Health Law, Indian Law Institute, New Delhi, Decem
ber.
18. Davar, B V. (1999). Mental health of Indian women. A femi
nist agenda. New Delhi: Sage Publications.
19. Dennerstein, L (1995). Mental health, work and gender.
International Journal of Health Services, 25(3), 503-509.
I
20. Dennerstein, L Aslbury, J & Morse, C (1993). Psychosocial
and mental health aspects of women’s health. WHO Report, Ge
neva.
37. Levine, SV, Karnin, LE & Levine, EL (1974). Sexism and
psychiatry. American Journal of Orthopsychiatry, 44(3), pp. 327336.
21. Desjarlais, R , Eisenberg, L , Good, B & Kleinman, A
(1995). World Mental Health. Problems and Priorities in LowIncome Countries. New York: Oxford University Press.
38. Lubotsky, BL, Blanch, AK & Jennings, A [Eds.]. (1998)
Women’s mental health services. A public health perspective.
Foreword by E H Carmen & P P Rieker. Thousand Oaks: Sage
Publications.
22. Dhanda, A (1995). Insanity, gender and the law. Contribu
tions to Indian Sociology, 29(1 & 2), 347-367.
23. Dhanda, A (1984). The mental health bill of 1981. A new
deal for the mentally ill. Supreme Court Cases, 2(8), 8-19.
24. Dhanda, A (1986). Non-communication between law and
psychiatry - A focus on the victims of this cold war. In Essays in
law and poverty. (Ed.). U Baxi (pp. 281-287). Bombay: Tripathi.
25. Dhanda, A (1987a). Rights of the mentally ill . A forgotten
domain. In U. Baxi [Ed.]. The right to be human, (pp. 147-160).
New Delhi: Lancer International.
39. Mechanic, D & Rochefort, DA (1990). Deinstitutionalization.
An appraisal of reform. Annual Review of Sociology 16:301-327.
40. Mehra, M. (1995). [Ed.]. Women and institutionalisation. A
report. Co-ordination unit. World Conference for Women, Bei
jing-95. New Delhi.
41. MIND (1995) Making sense of treatments and drugs series.
ECT. LondomMIND.
42. Murray, J. & Abramson, P.R. (1983a). [Eds.]. Bias in psy
chotherapy. New York: Praeger.
26. Dhanda, A (1987b). The plight of the doubly damned. The
mentally ill women in India, New horizons of law, 409, 187-198.
43. NMHP, (1982). The National Mental Health Programme. The
Directorate of Health Services. New Delhi: Government of India.
27. Dhanda, A. (1993). The lack of consonance between law and
psychiatry. In P. Mane & K. Gandevia. [Eds.]. Mental health in
India. Issues and concerns, (pp. 94-107). Bombay: TISS Publica
tions.
44. Nunley, M. (1996). Why psychiatrists in India prescribe so
many drugs? Culture, Medicine and Psychiatry, 20(2), 165-197.
28. Dhanda, A (1999) Legal order, mental disorder. New Delhi,
Sage Publications.
29. Ettore, E & Riska, E (1995). Gendered moods. Psychotropics
and society. London: Routledge.
30. Good, B.J. (1996a). Culture and DSM-IV. Diagnosis, knowl
edge and power. Culture, Medicine and Psychiatry, 20( 1), 127132.
31. Good, B.J. (1996b). Mental health consequences of displace
ment and resettlement. Economic and Political Weekly, 31(24),
June 15, 1504-1508.
32. Goodman, LA, Koss, MP & Russo, NF (1993). Violence
against women. Physical and mental health effects. Part I : Re
search findings. Part II: Conceptualizations of posttraumatic
stress. Applied & Preventive Psychology, 2, 79-89; 123-130.
33. Holroyd, JC (1983). Erotic contact as an instance of sexbiased therapy. In J. Murray & PR Abramson [Eds.]. Bias in psy
chotherapy. New York: Praeger.
34. Jamison, KR (1995). An unquiet mind. New York: Alfred A.
Knopf.
35. Jansen, E (1980). The therapeutic community. Outside the
hospital. London: Croom Helm.
36. Jaswal, S (Under review). Gynecological morbidity and com
mon mental disorders in a lower class urban community in Bom
bay. In Davar, BV [Ed.]. Mental health, gender and society. Inter
disciplinary perspectives.
45. Nunley, M. (1996). Why psychiatrists in India prescribe so
many drugs. Culture, Medicine and Psychiatry, 20(2), 165-197.
46. Prabhu, G.G., Raghuram, A., Verma, N. & Maridass, A.C.
(1984). Public attitudes toward mental illness. A Review.
NIMHANS Journal, 2(1), 1-14.
47. Russo NF & Green, BL (1993). Women and mental health.
In FL Denmark & MA Paludi (Eds.). Psychology of women.
Handbook of issues and theories. Westport, CN:Greenwood Press.
48. Russo, N F (1990). Overview; Forging research priorities for
women’s mental health. American Psychologist 45(3):March,
368-373.
49. Sandel, (1990). A study of neurosis in the women of Calcutta.
Appendix. In A Chakraborty (1990) Social stress and mental
health. New Delhi: Sage Publications.
50. Seshadri, S (1994). Report on child sexual abuse. Unpub
lished Observations. Dept, of Psychiatry, NIMHANS, Bangalore.
51. Shatrugna, V (1999) Foreword to Davar, BV Mental health
of Indian women. A feminist agenda. New Delhi: Sage Publica
tions.
52. Verghese, MM, Gupta, MN and Prabhu, GG (1968). The
attitude of the psychiatric patient towards electro convulsive ther
apy. Indian Journal of Psychiatry, 10(3&4), 190-197.
6
LINKING HEALTH & VIOLENCE:
TRACING SAKSHI’S JOURNEY
BY
JASJIT PUREWAL,
SAKSHI
Prepared for the
National Consultation Towards
Comprehensive Women’s Health Policy and Programmes
BY
VHAI-WAHJ-DSE
Held in VHAI, New Delhi.
On February 18-19, 1999
LINKING HEALTH & VIOLENCE:
TRACING SAKSHFS JOURNEY
JASJITFUREWAL
SAKSHI
J 39, NDSET
NEW DELHI 110 049
1999
X
Linking Health & Violence: Tracing SakshPs Journey
In 1992, Sakshi emerged a& a violence intervention center working with
women in situations of battery and sexual abuse. These womeir had
been subjected to sexual and emotional violation and had approached an
organization for help. Though initially, there was no clear indication as
to what we could do to help them, through our repeated experiences
with women in these situations, there emerged a clearer understanding
of their problems and needs.
Through the course of its work, Sakshr defined violence in its broadest
terms, which includes physical as well as more subtle forms of violence.
We feel that violence also has to be operationally defined in relation to
each individual woman’s experience since that will reflect the extent and
degree of her trauma and the symptoms thereof. It is important
therefore, to record what the women themselves perceived as violations
and how they impacted on her well being.
The Prevalence ofSexual Violence inChir Society’:
The following statistical table represents only the reported cases
documented by different information gathering agencies in Indiar
• 90 % increase in domestic violence between 1989 and 1990.
• 22,000 women in India were battered within the family in 1993.
• 1,28)881 cases ofrape reported all India between 1990 and 1994.
• According^ to the National Crime Records Bureau, Govt, of India,
a crime against a woman occurs every 7 minutes.
• In the United States, 35% to 51%) ofinpatient and out patient mentally
ill women report histories of childhood physical abuse; between 20%
to 54% report histories of child sexual abuse. (Harris 1997)
• Samvada3s study in Bangalore found that 83 °/o in a sample of348girls
had experienced some form of childhood sexual abuse.
L
2
o
Sakshi’s workshops with 675 girls aged 14-16 years in 14 New Delhi
schools indicate that 59 % have been sexually abused.
•
The same workshops brought to our notice the fact that 60% of the
perpetrators were known to the children, of which 20% were close
relatives, 19% were family friends or acquaintances, ll%y were male
friends, 6%) were teachers, and 4 % were servants.
The preceding statistics, culled from government and alternative
sources, indicate thatviolence against women and children is a very real
phenomenon that cannot be ignored. They represent tangible and
measurable forms of violence, but the invisible impact of inequality has
formed the basis for socio-psychological inquires in disciplines like
sociology, development economics, social anthropology etc. Herein
violence is being viewed in light of a larger system of discrimination and
inequality at all levels such as education, health and nutrition, the legal
system, family and marriage etc. It is seen as a long-term life experience
of women that adds up to feelings of inferiority, low self-esteem,
discrimination, and powerlessness (Coomaraswamy, UN Special
Rapporteur’s Report on Violence Against Women, 1995^. Therefore,
violence can assume broader dimensions and definitions that should be
considered in evaluating a woman’s life experiences1
Violence against women manifests itself in many Ways (infanticide, sex
selective abortion, and spousal violence such as wife battering, rape, eve
teasing, dowry, verbal abuse, and denial of food, education and
opportunities}. Eaclr act has an emotional consequence for the female
psyche. The impact of this violence on women can be viewed as a
spectrum, with the effects ranging from women being invisible as a
people, to murder. The health effects can be short-term or long-term,
immediate ordelayed.
1 Dobash & Dobash: Violence against Women & Social change. Routledge. 1976.
3
We began our intervention with the knowledge that violence in most
cases is protracted and not x one-off incident. With this knowledge
came the realization that in addressing violence we are in fact raising
questions about certain entrenched ‘practices’, that facilitated the
presence of violence.
OUR INTERVENTION
Our intervention strategies are centered largely on the victim and her
eventual empowerment. Immediately after Sakshi’s inception, the need
of the hour was giving victims a space to vent their emotions. It was
only after a couple of years while evaluating the impact of outwork, we
were confronted with the task of creating a composite intervention
strategy that would aid the victim on her way to healing.
Crisis counseling, legal redress were emergency measures and in course
of our work we kept feeling that we required long-term intervention
strategies which would empower the victim so as to enable her to lead
her own life. We devised intervention strategies that would address
violence in the ‘personal sphere’, at the community level and, at the
policy leveL
A) Counselings Holistic He^Hrtg^
Sakshi’s first foray into violence intervention was to create a safe space
for women to talk about their lives.
This in turn fashioned our
counseling norms. Our experiences with these women led us to realize
that the experience of violence, particularly when perpetrated by an
intimate person, has devastating effects on her health, particularly her
mental health, often causingpermanenttrauma. We recognized patterns
4
of behavior that emerged possibly as a reaction to her situation. Being
subjected to sexual violation influenced women’s expression, selfesteem, their life choices, and their relationships and the way in which
they viewed the world. A recurring factor that surfaced was the victims’
perception of possessing no control over their lives, a common feature of
learned helplessness.
As with all individuals, women in situations of violence adopted specific
coping mechanisms that reflected the "abnormality’ in their lives, a
reahty, social activists workingon women and violence can relate to. The
behavioral patterns that violated women display could possibly be their
means of dealing with the fear, the humiliation of being viofit^d, and the
trauma of being deprived of empathy, understanding, support from her
society and their families.
Sakshi’s counseling has significantly addressed victims of sexual assault.
We have witnessed the indelible impact violation leaves on a woman or a
child’s psyche. Therefore, in our eyes, their coping mechanisms seem to
be a logical extension of their experiences. Erasing the feeling of guilt
and responsibihty for the abuse has been a constant factor in our
counseling.
Our counsehng integrates mainstream concepts as well as !spiritual
healing to empower the "victim’. By counselling we seek to address the
trauma caused to the psyche. By empowerment, we mean the intrinsic
capacity of individuals to decide and act on their own. By healing, we
mean a process whereby the mind arises out of the morass of hurt, guilt
and self-blame to create a stronger individual.
W1-- •
5
B) Workshops^ Training and Awareness-raising campaigns:
Sakshi’s intervention has always been two pronged.
Along with
fieldwork, awareness raising and training programs, there is a research
wing, which substantiates the outreach programs with data on the
complexities in our target issues. The aim is to hone intervention
techniques through an inclusionist strategy. Through our outreach
programs with law-enforcement agencies and with psychiatrists and
other medical professionals, we have stressed the necessity of including
gender reality in their interventions.
Our stress on this aspect of intervention reflects our urge to broadbase
violence intervention in gender development. Sakshi’s attempts at
intervention have largely been based on the assumption that all women
must be provided with a non-judgmental and sensitive space to talk,
with therapy being directed at family and specific experiences which
they had found difficult to cope with. Constructive violence intervention
projects will yield results when caregivers intervene from the same
baseline of perspective.
An important aspect of our training programs is to inculcate in the
minds of community outreach workers and other primary health care
workers the fact that effective intervention will initiate a process of
interaction and work whereby the basic ‘sexual health’ of a woman and
an adolescent will be the target of community interventions. One of our
consistent efforts has been to define ‘reproductive health’ with a broader
perspective whereby it will address women and adolescents as
individuals who need to be informed, educated and consequently
empowered.
e>-
6
'If
We have designed workshops with grass roots organizations working in
the area of health. Our aim is to create a basic i "’demanding of violence
in women’s lives among the outreach workers TBy using examples from
daily life. The understanding will aid the health-workers to integrate
messages against violence in their work and detect instances of violence
in their communities.
C) Pro-Active Research
Integrating health with violence is perhaps most difficult when
attempted at the levels of policy decisions and government machinery.
Tfhe reason being that broad-basing violence within health represents an
inclusionist perspective; not present in governmental policy making or
implementation. As a violence intervention center our interaction with
mainstream health centers (hospitals both private and government,
clinicians, as well as grass root health functionaries and policy makers)
has proved that their understanding of women’s health and the impact of
violence on it is limited. Yet, in our interaction we have noticed the/
conspicuous absence of ^violence’ as a significant factor in cases of
medico-legal investigation, the dogmatic reiteration of a ‘gendered’
reality in cases of medical examination and complete disregard of the
victim’s psyche after assault.
Along with our regular gender sensitization trainings, we designed a
research project, which would look at the link^^s between violence and
women’s mental health. After interviewing’ jwomen inpatients and
psychiatrists, we could conjecture a tentative linkage between the
occurrence of violence and its impact on mental health. In most cases
there was a prevalence of violence, which created behavioral disorders or
resulted in other manifestations. Yet, diagnosis in most parts did not
acknowledge the significance of violence in creating these ‘ailments’. In
7
our experience, there has been a paucity of diagnoses that reflect the
inclusion of factors that define ‘a (woman’s) sense of self and self
esteem. There has been very limited acceptance that the factors
mentioned have a crucial role in circumscribing the individual’s sense of
despair and dis-empowerment and usually have long term mental health
effects.
We plan to publish our report with the aim of bringing mainstream
health practitioners together to address bias in the mainstream
disciplines. We seek from the mainstream a commitment, whereby it is
understood that psychological effects of abuse are far more
incapacitating than its physical effects. Through our work viz. crisis
intervention and counselling we know that women who are abused show
greater tendencies of dependency and suggestibility and find it difficult
to make decisions. In addition, there is also the relationship to the
abuser; primarily, the legal, financial and emotional attachments that
victims of marital violence often have to the perpetrator enhance their
feelings of vulnerability, loss, betrayal and hopelessness.
D) Working on Sexuality: Cutting Across onr Interventions
Working on sexual violence and in attempting to address the damages
wreaked by it, sexuality was one facet that needed to be looked into in
greater details. Violence or more specifically sexual violence has become
a ‘normal’ evil in our society. Women have been subjected to tlie
additional traumas of being fohaste’, ‘responsible’, “pure’ etc.
From time immemorial, it is the victim of sexual violence who has been
termed guilty, it is the victim’s sexuality, body and her existence that has
been declared ‘immoraP. These judgments have been codified in edicts
barring a gender all access to ‘forbidden’ knowledge. Sexuality happens
(4661) IPunoj uoneindod aqi
:3imiuiSoq jBOQOEjd y -qUBOH SAi^npojcfo^ piw .Mipaixag inoqs SunuBsq in JOipnjAI-Jioxia qin>i aag ,
z '^aypuapi
JOpHZiS pxiB |BnX3S JO sSxiipiIBJSJapiin {BUOSJQd pUB JBpOS 33B3J3
’joiABqoq jBnxos jo sSuuiboiu jBpos p3JBqs aip sb jpAk sBpjnsBQjd
joj sapioBdBO {BoisXqd sasuduioo jBq3 jdaauoo opsqoq b si jj ‘Ajapos
Xub ui uaiuoM puB U3ui jo suoi3B4uasajd3j pjoiSojopos puB JB3I§OJOqpXsd
^BOiSojoiq aqj sosssduiooua jBip uopBSjo pzpos b si XjijBnxag
^XjqBnxas
jaq si 3^q^ ‘uxcd put? suoisnjuoo qons aiepioixiE 01 sooeds 03 ssooor
dcjujom sjtiaAaid jvqa Aopos r Xq papunodiuoo sxqj; •sjuoppm aAisnqr
jo uoprqos^i pur s^oiwuadx^ j^q jo Sxnpurisj^pun QApisod r qjiAk
Xqjp?oq iou si ^ocds jBnxos jsj-j ‘(inooo 04 asoqs 3q4 ^uimojjb, joj 4pn§
qjm sd&qj^d) jpsj^q sai^ia ^qs Aioq pur ‘(juauqpjinj, q4iAi uopiqoiA puB
nopBjoiA q4m xas Suurnbo jo x^s waij jBAMupqqAk qxiAi sdBipdd) aoBds
{Buxss b ui j^uuBd b 04 sa4Bpj aqs Aioq ^^□uB4Sip jo uoispiAax sdBqjdd)
Xpoq Joq inoqB spaj ^qs Moq s^dBqs ij -XjqBnxos 03 uoii3tipoJ3ui 3Eq3
jo o§BSSBq 3q4 squjbo ppqo b sb pasnqB XqBnx^s u^aq SBq oqM ubuiom
b ^[duiBxo joj •BijB3itiaS jo uoixEJJOOjd jo nopou b uBqx SuissBduiooua
fpr ajoxxi qonui ajojpjaq3 si puB ‘-orp uopBuiuxuosip/oouajoiA
^gxxiuopxpuoo ‘SuiSbuh jo sjb^X jo Xio3isodaj oip si ^qBnxas
sjBnpiAipui uy -X3q^uosj^d aq4 jo sjoadsB j^ipo qB joj suoissnojadai
SBq qoiqAk ‘Buosiad {Bnxss oqj ui uoissaidxo puy XflBnsn q3iM
soaij {BtipiAipui ub 3Bq3 s^nunossui puB sjb3j ‘suiBd ^qj; ‘UOSJOd B JO 9JOO
isouu^inn aqj spajjoj 4Bq3 3do3iioo pBOiq b sb XxqBnxos jaimsuoo 3^
•aouajsixa jo uuoj slip sjuaqui aqs ji sb jsoujjb
si jj
qqB^q jBnxas j^q SuipJvSaj oduejoxiSi {ejoi jo ^qBUUOXiqr jo
ajq v aAq 04 p^uosop sj ubjlooal y aSpapioxiq ^uappiqjoj, qons auo aq 03
9
Sakshi’s exploration of men and women’s expressions of their sexuality.
is an attempt to understand more about sexual trends and patterns in our
society today. There is little primary data that records how men and
women relate to each other, the sexual scripts that exist in the
subcontinent, and the various metamorphosis people undergo over time
and by socialization. In discussing policy issues regarding reproductive
and sexual health, such information is crucial to understand the best
entry points for new attitudes, the concept of sexual responsibility, and
basic attitudes regarding sex and sexuality. Such important information .
about a community or society would prevent wasteful expenditure of
time and effort; understanding a people is necessary before programs are
designed to help them.
The study and investigation of human sexuality is an exercise that many
NGOs working on violence against women, reproductive health and
women issues have to consider as integral to their work. In a ^blinkered
society that recognizes sexuality only within legitimate’ spaces, and is
still unable to address the violence therein, the numbers of men, women
and children who remain invisible and in need are growing. An
individual’s sexuality is often seen in light of ‘abnormality’ and
‘problems’, most of these being arbitrarily defined by social prejudices.
With the threat of AIDS looming larger than ever over South Asia, and
Sexually Transmitted Diseases being more common than ever young
people at risk need to take responsibility for their own lives. One cannot
respect and protect the physical body if there is.no awareness and a
sense of comfort with it; sexuality has to be celebrated as a holistic entity
encompassing the entire being. Women come with the additional
baggage of having to accept a socially desirable notion of ‘femininity’
and sexuality, which precludes the option to be vocal about
discrimination and pressure to conform. Men have a similar set of
•3SIBJBUI 3JO3 S4I SI aOU^JOIA 41?lp JIUIpF OJ UOSV3J
p^apux pxw 4OKJ qSnoua si ^xaip uoip
oqqnd jo uvd f si ippaq
sjuoiuoAk jj ipjEaq uo 43«dxux 4ip ssssse ptw Xjpu^nb 04 auoui^josboui
jo sjoaj pur aouaps popps OAizq oxpi suepunp 4siuiuiaj Xq pwoddns
6A4oqAlXlOA^ SuiSIEJ
S4SIAI43E 4SUIUUOJ qoiqAY □Se^juij pjorjuo
^q4 si qipaq s4uquiom uo ^ou^joia jo 43^duii ^ip dn SuppiKj uoipjnj
ssausnopsuoD pur 94vq9p jo si^puoij aq4 saqn qoiqM jooqos quo aq4 si
UlSIUIIUaj JQAQMOJ-J ‘SQAIJ OlQlp XU UQUI Qip UIOJJ QOUQJOIA UIOJJ HOI43Q4Ojd
S^UQUIOM JO SUUQ4 UI 431U4Sip XfpJ^q UtQQS SUOUBU pjJOM pJiqjQ pUE 4SJIJ
•SQOuoixadxo uuojiun jo ppoji SuxXpuoq e dsui 04 pQ4JEis QAEq sqaij
S^UQUIOM w ^OUQJOIA JO 8314814^48 ‘OJOqMXlOAQ EpU3§E JEOWfOd [EUOI4EU
oq4 ui oouojoia osiej 04 unSoq OA^q sisiuuuaj ^3uig -Xoiuaiq pur qoej
CSSE|3 jpip JO 3AI43QdSQXU S3Aq S^UQUlOAl UI UUOU Oip XjJEQp SI QOUajOIA
NOlSmONOD
1
-i/
-Xjipjnxas jo sou®jou§i puE aouaps
jo XoeSoj aip xio Axrea cn jmcjJe iouueo oxpi dnoiS e air Xaqj; •saAjasuiaqj
jaajojd oj uouEtujojui jo sgpfs'-aip xnoipiM aauajoiA pire saards psnxas
01 ssaaa® si ajaq) asneoaq aauapiA jEnxas puE saiauruSajd pajuEMun
"sasrasiQ pawuusuEJX XpEuxag ‘SGIV JOJ
4® 3J®
‘uoiSajr siqj uj
ahaijoe jEnxas Jiaqj jdaooE oj aauEjanjaj axp 04 anp guiuuEjd Ajiuiej puE
qqraq aAijanpojdaj uo saaoeoxui {EjuaunuaAQS jsom Xq passaippE-un
uaaq aarq oqav uopEjndod e oje ajdoad Suno^ XuiouojnE ja}Eaj§ jo ajEjs
e spiEAioj aAoui 04 A\oq iuEa{ pUE ‘sxaqjo puE jjas aqi oj jnjuuEq aq Xeui
qaiq.w sJOjAEqaq aqj luEapm oj SuqjiAi puE uado aq oj uaiuoav puE uaiu
SunoX joj qnayjjp si 41 ‘auqrj jeoos sup uupjM pajEaxa pus ojui uoao/\\
•sdxqsuouEpj w ssojis jo ooej 3ip xri s^sxo Xwuapi jo JoiAisqaq
Suxi^auiuiop ‘oajsssjSSe j^ipp Suumcds uayo ‘03 dn OAq 04 suoimDadxa
01
•>
©
VIOLENCE AND WOMEN’S HEALTH
By Hiti Mahindroo
Women in India have become more violence prone today, as incidences of violence
against them have shown a marked increase in the last decade. In the land that has
produced Swami Vivekanand and Mahatma Gandhi, rising trends of torture and demand
for dowry, female infanticide and foeticide, rape, prostitution and criminalisation of
politics and its effect on women have become ‘hot’ issues that have moved the parliament
and judiciary, and roused the society. Atrocities against women occur at three levels, the
most primary being atrocities within the family, the second level being atrocities by
society, and the third is due to actions by state
Deprivation of women from economic, legal and social rights, such as education and
r
health , gives birth to these atrocities to occur and also to be tolerated by most women.
What is specific to women is that their oppression takes place not only in the field, the
factory but within the home itself. The family structure gives recognition to women
primarily as wives and mothers, both of which are considered subordinate positions in
family heirarchy. Control over the woman’s body becomes crucial since the line of
inheritance is carried through males. Female infanticide aand foeticide have become
common
“ it is better to spend Rs 800/- now than Rs 80,000/- on her dowry
especially in regions where the property rights are desired to stay with sons. Since these
atrocities occur within the walls of homes, it is a difficult task to document them
Moreover, the problems of women inside the family get personalised, and the women are
expected to fight their private battles with their families all alone.
Nutritionally, girls and women are discriminated against. Medical care is usually granted
only in severe cases. Emotional problems are moie likely to set in in the above
circumstances. Physical health of women is therefore likely to deteriorate . The fall in the
sex ratio is testimony to the alarming trends working against women.
The changing economic scenario has also contributed to increase in crimes against
women inflicted by society, leading to increasing number of cases of dowry harassment,
(and I would like to add here that tbe Burns Deptts need to be strengthened in the city
hospitals and more created at district levels), abetment to prostitution, selling of girls,etc.
It is felt that this changing economics of the
country allows criminal tendencies of the people to come to the fore more easily. 1 he
increase in the numbers of women in prostitution as well as ot unwed mothers is due to
the fact that women are generally uneducated and unskilled, and their welfare has
I
been completely sidelined when policies were made. It is to be hoped that future policies
will take into account the urgent and vital health care that the above group has to be
provided , not only for the women concerned and their children, but also for the society
at large. According to reports, India already has a sizeable number of people who have
been afflicted with STD and AIDS. Therefore it is needless to stress on the importance of
health care that has to provided here, considering that what exists is not adequate
Another important point that should be mentioned is that health care should be provided
within easy reach of the vulnerable group. If the government is unable to provide the
above health care, partnership to work closely with NGO’s and trained health workers
should be encouraged. Extra funds should be allocated to specific areas, if needed, for
health care. Awareness programs , counselling centres and help of media should be used
to let public know about the health care available.
State level policies have affected the cottage industries and the agreria sectors. Since
protection offered to these industries is gone, workers are defenceless in the face ol rising
prices. The weakest and the most helpless section of the workers are the women, who
have to leave behind their niches, and migrate to cities, unprepared and unprotected. This
group of migrant women has little or no access to health care in the cities. Being a daily
wage earner, it is difficult for her to reach the larger hospitals and private medical
practitioners prove to be very expensive for her. It is needed that smaller health care units
be set up in cities, such as near slum areas and ‘jhuggi’ clusters, where there is higher
probability of migrant people. It has also been noted that as of now, little or no
importance is attatched to the emotional health of women. Health care lays stress on the
physical state , but more effort is required on the part of health department and NGOs to
look after the emotional health of the women. Most women who have to leave their
homes, families, the young and old, suffer from trauma, which affects the physical health
A large number of women in the younger age group is included in the migrant labor. A
large number of rape cases are reported. There is absolutely no emotional help existing
for them. Urgent attention needs to be paid to rape victims especially victims of child
abuse.
We must also take a look at the women who have been left behind when the men go out
in search of work. The slowly dying village industries are forcing men to migrate to
larger industrial regions and the number of women-headed households has increased. It
has been a cause of concern for the women’s movement to note that the age ot marriage
of girls in women-headed households is now lower. In the recent past, efforts of women’s
groups had shown an encouraging rise in the age of marriage of young girls. However, in
the absence of menfolk, age of marriage has again fallen, as it is felt that it is safer to
have the girl married off, rather than leave her alone when the mother is away at work.
Future policies in health care should take into account the larger number of younger
mothers that is arising in rural areas.
Displacement of families, either due to urbanisation or by acquisition of land is yet
another cause of forcing women in a more diadvantaged position. Quick money earned
by them on sale of land is often squandered away. In most cases, alcoholism is
encouraged (as in the case of regions in Outer Delhi and regions on Haryana border,
where farmers had sold their land to DDA and took to drinking in absence of work and
availibilty of easy money). As
it is, there are hardly any deaddiction centres in the city, leave alone in the areas that
need them most. Cases of wife battering have increased and nutrition level has fallen in
such families.
People displaced from their homes (reasons being varied), need special health care
packages specially designed forthem. Women again become more vulnerable Trauma
on being forced to move
and alien suroundings account for deteriorating health.
Ignorance of the new flora and fauna leaves them with no
home remedies, on which they
depend to a large extent.
It should also be mentioned that little health care exists for the older women, who are
helpless and usually abandoned by their families and have little economic resources to
look after themseves . This is true
not only for rural areas
but also of urban areas, a point that should be noted by policy
makers. In its Health Policy 1988, Australia brought out a special incentive “Health of
Ageing Women”, thus separating it from “Health of Older Persons
Some statistics regarding violence against women
The crime chart brought out by National Crime Records Bureau 1995 shows.
Rape cases reported had gone up by 40.4% over 1991. dowry deaths had gone up by
3.2% over 1994, torture by 92% over 1991, molestation by 38% over 1991.
In 1995, the All India figure of reported case of crimes against women was 1,06,471,
with an upsurge of 7.6% over 1994. These are the reported figures, whereas the
unreported figures are far more.The number is growing. Moreover, even though the
total population of the country increased by 24.7%, but there was a fall tn sex ratio during
the same period, froom 934 to 927.
Some Suggestions:
1) The Health Policy should take into account the needs of women today. Policies should
study the changing social conditions . The crime chart clearly indicates that violence
against women is growing. Such women would require emotional health care.The health
policy lays stress on the physical (mainly gynaecological) aspect of women s health.
There is no thought provided for the emotional health of women, even though there ate
provisions for mental health. It is felt by those working in the area of violence agains
women that government pay special heed to the growing need of women for emotional
health services, which is a delicate state of health that affects physical health of women,
and could also help in preventing mental disorders.
2) Health policies have not only to be state specific, but district specific, maybe even
block specific. So the National Policy may not be able to be completely comprehensive.
For, example, according to reports, the majority of rape cases in Delhi occur in jhuggi
clusters. Such areas would specially need trauma centres and emotional health care.
Deaddiction centres also need to be area specific. Health care packages need to
NWl <0
to rtove
services. Area specific health care could prove to be more etlectlYC if the a^stanc? of
above is 19^1), not only -QVIbfi PUPOtnS
M
M MV Pl'HHR/F'WnlWUOn
Training needs to be given to health workers.
3) In all these positve efforts, women themselves have to be ‘takers’. In our society, most
women push themselves to a degree of self denial, which is self contradictory, smee they
know that denying themselves food is not good for them
/
Women’s movement had to work very hard to encourage women to come forward and
XgS^StS^
a few good judgements being delivered.
This is whst 1 mean tha. women themselves have to be takers for setviees iike .emotional
health Counselling and trauma eentres not only haave to be opened but also ' »de
acceptable. NGOs could play a major role in raising awareness levels of women
after their emotional health.
4) The National Heaalth Policy needs to look beyond the gynaecological aspects of
1
their Health Policy 1992. We need to introduce this concept in our Health I obey also.
J7
J ’ is
C>.>
„
VI t
r 0. 7/ /
c (Xr<-
J.
TRADITIONAL SYSTEMS OF MEDICINE (TSM) POLICY AND
WOMEN'S HEALTH
By Smt Shanta Shastry, Secretary, Department of ISM&H
Ministry of Health and Family Welfare.
Govt of India.
Paper prepared for the
National Consultation Towards Comprehensive women's health policy and
programmes.
organized by VHAI WAR! and sponsored by DSE.
VHAI, New Delhi - 18-19, February 1999.
TRADITIONAL SYSTEMS OF MEDICINE (TSM) POLICY
AND WOMEN S HEALTH
Man and Woman complement each other and together make life.
Traditionally woman has had the unique distinction of bringing out
the
progeny into the world. This child bearing role of woman continues. She
was treated with respect and dignity and has been glorified goddess. It was
said that even gods tread where women are worshipped (Yatra Nariyastu
Pujyante Tatra Ramante Devata). But with foreign invasions the woman
was confined to the hearth and restrictions of various kinds were imposed
on her freedom. She was
viewed as an ‘Abla’ (helpless, weak). Tulsidas
the author of Hindi Ramayana (Ramcharitmanas) described woman as fit
for being beaten up and equated her with Dhol(Drum), Ganwar( ignorant
an object of enjoyment and
person), Sudra and Pashu She remained
exploitation. Her status
declined. She
Her
was deprived of education,
health suffered both physically and mentally.
After independence women have been granted equal
status in law. The Indian constitution has provided
for gender equality
under its preamble, fundamental rights and directive
principles. Various
laws, developmental
policies, plans
and programmes have aimed
at
woman's advancement in different spheres. From the 5lh Five Year Plan
onwards there has been a marked shift in the approach to women's issues.
From a welfare approach the focus shifted to a developmental approach
towards women in the earlier
decades. Now- again the focus
empowerment of women. A National Commission
for Women
is on
was set
up in 1990 by an act of Parliament to safeguard the rights and legal
entitlements of women. The 73rd and 74th amendment to Constitution
provided for reservation of seats
for women in Panchayats and
Municipalties laying a strong foundation for their participation in decision
making at local levels. A bill providing for similar reservation in Parliament
and State Legislatures is pending. Concerted efforts are on at National and
International levels to give the woman her due status.
and
The Government of India too has introduced
implemented various schemes, projects and programmes for the all-round
development of women through various mimstnes/departments.
However, there still exists a wide gap between the
goals
enunciated
in the Constitution, legislation, policies, plans,
programmes and related mechanisms on the
one hand and the situational
reality of status of woman in India on the other hand. Women, particularly
in rural
areas and in the informal unorganised sector still do not have
adequate access to education health and productive resources. They have
remained
marginalised, poor and socially excluded. A draft policy
for
empowerment of women was drawn up to bring about the advancement of
development and empowennent of women. Among the various
issues
addressed in this policy document health also figures. The draft policy
talked of adopting a holistic approach to women’s health and giving
special attention to the needs of women throughout their life including in
terms
of nutrition and basic services during
infancy, childhood,
adolescence, reproductive years and services during old age.
Health cannot be viewed in isolation. It is linked up
like education, nutrition, sanitation, safe drinking
with various things
water, employment, economic development, etc. All these have a bearing
on the health of a person and much more so on the health of a woman who
has the special responsibility of bearing children. The prime period of a
woman’s life i.e.
from 16 years
to 45 years is the reproductive period.
Therefore, while other Ministries/Departments of Government of India
have been addressing issues relevant to them the Ministry of Health and
Family Welfare have the responsibility
women’s health. In
of taking
particular
the early stages due to concern over
care of
population
explosion, Government adopted various family planning measures. The
emphasis was on controlling
fertility. Woman was the target. Over a
period this programme led to excesses on women and malpractices. Taking
a lesson the approach
was modifed to combine fertility control measures
with certain welfare aspects so as not to affect the health of the woman.
The Department
came to be renamed as the Department of Family
Welfare. Now again
the Department of Family Welfare has launched on
a target free approach and has come out with Reproductive Child Health
Programme to safeguard the health of the woman even while trying to
control population.
All these efforts have no doubt brought about some
improvement as is reflected in the various
gams
in respect
of
women’s health
health indicators. Significant
status
have been recorded.
Expectation of life birth for female has risen steadily to 59.7 years. The
Marriage
Restraint Act 1976 has helped prevent child/early
marriages amongst
the girls. Education and employment have also helped
Child
in raising the age of marriage. Crude birth rate declined to 27.5. Total
fertility rate also declined to 3.5. Maternal mortality rate is still very high at
437 per one lakh live births and is
legalised. Sex ratio
a matter of concern. Abortion has been
has been exceptionally unfair. The reproductive tract
infection and sexually transmitted infection
of HIV/AIDS have been
are already very high. Cases
increasing among women. According to the
National Institute of Nutrition, Hyderabad 49.3% women were suffering
from various degrees of chronic energy deficiency and 87.5 % of pregnant
women were anemic in various degrees in 1989-90. All the same in spite
of spending large funds the desired results have not been achieved and the
health targets are eluding. This
is a matter of concern indeed and a
thought needs to be given to this serious problem.
It is observed
that in the various
schemes and
programmes for the health of women too much of dependence has been
placed on only one system of medicine, i.e., the modem allopathic system.
It is against this background that the role of ISM&H is
discussed
below.
It is
overlooked that there are Indian Systems
of
Medicine, like Ayurveda, Siddha, Unani, Yoga. Naturopathy as well as
Homoeopathy each having its own strengths and merits and capable of
making substantial contribution to the health care of women. In fact the
National Health Policy of 1983 emphasised the need for planned efforts to
dovetail the functioning
of the practitioners
of the ISM&H and to
integrate their services at appropriate levels within
specified areas of
functioning in the overall health care delivery system specially in regard
to preventive, promotive
and
public
health objectives. The policy
envisaged a meaningful phased integration of the services of these systems
and the modern system of medicine. Unfortunately, the policy did not get
operationalised though ad hoc sporadic measures
State Governments to involve
Kerala
were taken by some
the 1SM&H in the Primary Health Care.
is a leading State in the achievement of the Health parameters. A
close study of this study will reveal that the success could have been due to
the
fact that in addition to the allopathic system, in Kerala Ayurveda is
also
practised widely and it could also have contributed
health of the people in Kerala. It is, therefore,
tune that
solidly to the
the 1SM&H
should be given an opportunity to participate at par in the various health
programmes in a positive manner.
India has a rich heritage of medical systems of
Ayurveda, Unani and Siddha which are time tested
and are still popular
and acceptable to communities,
today
They are relevant
and will be
relevant in future.
Ayurveda, Siddha and Unam Systems are capable of
taking care of the health of women. In fact, women themselves get trained
naturally in these
systems because these systems are so much interwoven
in the culture and way of life of the communities that
the Indian Women
have been the custodians of the grandma’s recipes under ayurveda, siddha
and unam systems. The Indian kitchen and
dispensaries providing kitchen remedies
They show
the strong
kitchen gardens are mini
for day to day health problems
belief and tradition of health
care through
indigenous
food, diet and seasonal receipes. Dinacharya, ritucharya,
swasthavritta and
traditional
sadvritta are practised as a matter of routine in the
homes. These systems
and life style. They also
prescribe "Do’s and Don’ts’ of diet
go well with the budget
of the family. Minor
health problems are treated through some home remedies available
in the
vicinity and are acceptable to all. These systems
easily
have played an
important role where other health care facilities have been lacking. These
systems have also taken care
of the nutritional aspects
through the
kitchen preparations.
ISSUES RELATING TO HEALTH PARAMETERS
Sex Ratio
The
sex ratio has declined to 927 females per 1000
males. It is gradually decreasing. Instances of female infanticide continue in
some States. Foetal sex determination has led to foetal infanticide where
already more than one girl child exists. Infanticide is considered as a sin
according to the Indian culture. However, after legitimization
of medical
termination of pregnancy through the medical termination of pregnancy
Act, 1971, in stead of promoting
the health
affected have been the female infants. There is
of the woman the most
no moral
fear of sin
among mothers and doctors in killing the foetus. Also in spite of the Act
illegal operations still continue to be perfonned by unauthorised persons,
like
the local quacks and untrained persons in unhygemc and unsafe
conditions because of non-availability of medical termination of pregnancy
services within the easy reach of most of the rural population. It only adds
to the suffering of women. The Indian Systems of Medicine can help in
reducing foetus infanticide incidence. In ayurved there is a concept known
as pumsavana sanskar under which certain medication, food as well as
‘Do’s and Don’ts’ about sexual behaviour help to get a male child. The
purpose is not to increase male children but to provide a choice to desirous
couples. This will help to plan the family as per choice and also reduce the
trauma to the woman. Proper research needs to be earned out to validate the
practice of Pumsavana Sanskar.
MATERNAL MORTALITY
As has already been pointed out maternal mortality,
morbidity due to complications of pregnancy are still high in our country as
compared to many developing countries of the world. The main causes are
bleeding of pregnancy/purperium 28.9%, abortion 17.6%, Anaemia 17%,
texemia 9.9%, puerpenum cepsis 8.5%, malposition of child
4%, non-
classifiable 14%. The Indian Systems of Medicine can help reduce both
maternal mortality and morbidity through Masanumasic Garbhim Charya
which is just a monthly dietary and behavioural advice which can also
reduce threatened abortions.
The prescribed regimen if followed for 9
months can assure delivery of a healthy child and safe motherhood. Post
delivery practices of body massage, use of dashamool quath ajwain ark, hot
water bath, intake of certain food items can take care of a number of post
delivery complications and the health of the child. Dietary restrictions help
immenselv.
REPRODUCTIVE TRACT INFECTION AND S.T.D.
Reproductive tract infections due to various reasons
like unhygenic conditions of genitalia, etc. STD could be prevented by
following ‘Do’s and Don’ts’ as advised under the Indian Systems of
Medicine.
Traditionally ayurveda, siddha and unam medicines, like,
Panchvalkal quath for cleaning genitals and vagina are known to be very
effective in preventing various infections and discharge. There are quite a
few simple remedies of ISM to regulate menstruation and
to avoid
excessive bleeding and white discharge etc. Food habits are also important
and need elaborate publicity and propagation among the masses.
NUTRITION
Girls at puberty/onset of menstruation, pregnant
mothers and other women during fertility period require more nutrition more
of iron, calcium, minerals, etc. Yet discrimination is practised even now in
many places in the case of female child as compared to a male child.
Women and daughters-in-law will not take food well in time and in proper
quantity. Fasting also leads to deterioration in health. Girls and women
give away their shares to male children and men. Some of these traditional
notions need to be rationalised and girls and women need to be encouraged
to take proper and adequate food. Only healthy women can keep the home
happy and give birth to healthy children. Costly unwarranted fast food need
to be discouraged.
Food value of the traditional
seasonal foods, fruits,
vegetables needs to be highlighted. Fast food, soft drinks and other market
products are not only costly they also consume the share of nutritious food
of women and girls. Ayurved has a very good drug known as Punarvadi
Mandoor which contains iron for improving the aneamic conditions of
pregnant women. It has no major side effects. There are many other drugs
also which can add to the health of a pregnant woman
CONTRACEPTIVE CARE AND OTHER ISSUES
The population of our country is around 940 million.
This is posing a great threat to the health of not only women but also men
and children.
The major emphasis in the various Family Welfare
programmes has been placed on contraceptives and huge funds are spent on
providing condoms etc. Some of the measures , like, the insertion of copper
T had led to certain health problems. Lot of improvements have been
carried out and some safe condoms are being made available.
The
traditional systems also have devices for fertility regulation and elimination
of foetus. They are recorded in the ancient classics of ayurveda, unani, etc.
In fact the demerits of the big family are also indicated in these texts. The
specific formulations for contraceptives have been put forth in the 13th
century AD by Bhava Prakash.
Among them Pipliyadi Yog which is a
combination of Pipli, Vidanga and Tankan is a prominent one.
Lot of
research work is being conducted by the Central Council for Research in
Ayurveda and Siddha(CCRAS) on contraceptives. The Pipliyadi Yog has
been extensively studied by the council in fertile female volunteers for more
than a decade.
The study with a dose of 500 mg/bd from day one had
established the efficacy of Pipliyadi Yog in the prevention of child berth.
Even the prolonged administration of this drug has not shown any significant
side effects or toxic effects. Findings of this study have also been recorded
in standard text books of gynaecology. Recently a further clinical study has
been undertaken on pipladi yog. Some modern medicine hospitals are also
participating in this research project financed by the Department of Family
Welfare.
Separately the Defence Research Institute of Physiology and
Allied Sciences, Deepas has also been working at neem oil as a
contraceptive. In short there is immense potential among the ISM&H drugs
in controlling conception. Even the unani system of medicine has various
‘Do’s and Don’ts’ brought out in the form of a classical text for controlling
conception. These are very simple remedies.
Apart from the drugs, the concept of Brahmcharya has
been given a very important place in ayurveda. The object is to control the
sexual behaviour of the person. Unfortunately, this concept has not been
discussed though various other issues on sex education are deliberated upon
at various forums. Observance of Brahmcharya can also help the society in
many ways by limiting the spread of STD and HIV infections. These need
to be incorporated in all programmes of Family Welfare.
REPRODUCTIVE CHILD HEALTH
This programme covers the health of the woman during
their child bearing age as well as children upto the age of six. Ayurveda,
siddha and unani systems have a lot to contribute in this area.
In fact,
recently the Department of Family Welfare has incorporated a component of
ayurveda in the RCH programme. Ayurveda which is known as Ashtang
Ayurveda has eight specialities. Of these Kaumarya Bhntya is a speciality
which deals exclusively with women’s and children health and disorders.
Kashyap Samhita, Shushrut Samhita , Charak Samhita and Vag Bhatt have
given elaborate discussion
of women’s health and diseases and their
treatment. Siddha and unam systems also have specialities dealing with
women’s health independently.
The subject of safe health and happy
motherhood has been discussed in various ayurvedic classics under various
headings, like
(a)
Premature period, i.e., period before onset of menstruation;
(b)
Menstruation;
(c)
Impregnation;
(d)
Antenatal period;
(e)
Labour;
(f)
Puerperal period;(post delivery period);
(g)
Management of child after delivery;
(h)
Preventive aspects of health of a child.
Right from the conception to the safe delivery of the child and post
delivery care of mothers and children of various age groups are described at
great length in the classics of Ayurveda.
There is an increased pressure on the body of the woman during the
reproductive activities. It weakens the body. Menopausal stage also causes
a lot of imbalance in her health.
Some medicinal intervention and food
supplements are required in various conditions to provide proper nutrition to
such women. Simple home remedies use of ashvagandha, satavari. kuman,
ashok and chandan, etc. are used in a number of recipes to treat the woman’s
problems.
In fact, while in modem medical science the ante natal care
begins after conception, in ayurveda it begins much before conception
starting with menstruation stage.
Specific rules have been laid down
regarding when to have intercourse. Medications have been suggested for
those with specific problems.
Aphrodisiacs, relaxants and many such
medication can help in conceiving a male child or to ensure the health of the
foetus. Shushrut the father of modern plastic and reproductive surgery could
well have been awarded the title of father of obstetrics considering the thesis
he wrote on the stages of pregnancy.
He has described elaborately the
development of the foetus and the child on a month to month basis.
Similarly, good wholesome diet is prescribed during pregnancy. As a rule
medicines are to be avoided during pregnancy unless advised by a qualified
doctor.
Simple measures like oil enema were used in stead
of giving
laxatives. In short the Indian systems of medicine have the capability to
handle the health of the woman.
The woman has come out of her hearth and is now rubbing shoulders
with man.
She is advancing towards economic independence.
A large
section of women is working as professionals and are participating in
activities of nation building.
Though this has made the woman
economically independent and hence provided certain dignity to her, this
also has put burden on her physical and mental stamina. In turn it has given
rise to many problems of health for women. The stress and strain are also
affecting the woman. In addition ,today, women are being exploited more
and more. The trauma caused by rapes, etc., is equally telling on the health
of the woman. The Indian Systems of Medicine have something to offer
even for such conditions. Yoga can help women in putting up with the
stresses and strains of modem socio-economic life.
These systems,
therefore, can play a very important role along with modem medicine. The
goal of '‘health for all” can be reached faster and more effectively by
harnessing the services of the ISM&H.
CHAPTER 1
PERSPECTIVE, OBJECTIVES AND STRATEGY OF DEVELOPMENT
The Ninth Five-Year Plan is being launched in the 50th year of India’s Independence.
i.i
Much has happened in the intervening years.
The people of India have conclusively
demonstrated their ability to build up a nation overcoming all the divisiveness and to operate
a representative political system in the true spirit of democracy. The time has now come to
extend this spirit to the social and economic spheres in full measure, so that the poorest and
the weakest will be able to shape their destiny in an unfettered manner. This will require not
only higher rates of growth of output and employment, but an all-round human development
with stress on social sectors and a thrust on eradication of poverty, minimizing economic
disparities and correcting regional imbalances.
1.2
In this perspective, the Approach Paper to the Ninth Five Year Plan, adopted by the
National Development Council, had accorded priority to agriculture and rural development
with a view to generating adequate productive employment and eradication of poverty;
accelerating the growth rate of the economy with stable prices; ensuring food and nutritional
security for all, particularly the vulnerable sections of society; providing the basic minimum
services of safe drinking water, primary health care facilities, universal primary education,
shelter, and connectivity to all in a time bound manner; containing the, growth rate of
population; ensuring environmental sustainability of the development process through social
mobilization and participation of people at all levels; empowerment of women and
socially disadvantaged groups such as Scheduled Caste, Scheduled Tribes and Other
Backward Classes and Minorities as agents of socio-economic change and development;
promoting and developing people’s participatory .bodies like Panchayati Raj institutions,
co-operatives and self-help groups; and strengthening efforts to build self-reliance. These
very priorities constitute the objectives of the 9’ ‘ Plan'.
1.3 While the government will have to play a major role in promoting such development,
there will have to be an increasing reliance on peoples’ initiatives through institutionalised
structures at the grass-root level on the basis of co-operative federalism. Because of the
constraints of inadequacy of capital, large unemployment and wide technological gaps in
certain sectors, India’s economy will have to harmonize the roles of state, market and co
operatives. The investment patterns will inevitably have to be a blend of public and private
investments. Foreign investment will be welcome, particularly in the sectors with large
technological gaps.
1.4 Today India has a much more developed resource base, in terms of physical and human
capital, domestic savings and supply of foreign exchange. These resources still need to be
used optimally to achieve the objectives, minimising the cost in terms of efficiency and
productivity. The growth performance of the economy in recent years provides ample
evidence of the ability, resilience and innovative spirit of the Indian people and institutions to
follow this process with success.
i
1.5
While launching the Ninth Plan, \vc must take stock of the strength of our past
development strategy as well as its weakness and provide appropriate direction and balance
to the socio-economic development of the country. The principal task of the Ninth Plan will
be to usher in a new era of people-oriented planning, in which not only the Governments at
the Centre and the States, but the people at large, particularly the poor, can become effective
instruments of a participatory planning process. In such a process, the participation of public
and private sectors and all tiers of government will be vital for ensuring growth with justice
and equity.
Imperatives of State Policy and Public Action
1.6 Recognition of the complementarity of the state and private sector initiatives in the
development process docs not mean an abdication of the role of the state in economic
matters. Indeed, it would be naive to believe that free and unfettered market forces would
necessarily lead to an outcome which cannot be improved upon in any manner. There arc a
number of reasons why markets may not exist or, even if they do, may not work efficient:
and effectively. There arc also conditions under which unbridled operation of market forces
may give rise to outcomes which may be deleterious when seen in a national perspective.
Govcrmncnt intervention in such situations is no doubt imperative, but this docs not
necessarily mean a complete or even substantial abridgement of private initiative.
The
interventions have to be strategic and must emanate from a vision of the role and
responsibility of stale policy and public action in an imperfect market economy characterised
by large exclusions.
1.7
The Ninth Plan has been developed in the context of four important dimensions of
state policy, which may not necessarily be attained by the free operation of market forces.
These arc:, (a) quality of life of the citizens; (b) generation of productive employment; (c)
regional balance; and (d) self-reliance.
(a)
Quality of Life
LS
‘Quality of life’ is a multi-dimensional concept encompassing not only the economic
opportunities available to the people, but also their ability' so as to take advantage of these
opportunities; and the existence‘6f living conditions which arc conducive to a healthy and
productive life. Eradication’of poverty and provision of basic minimum services arc integral
elements of any strategy to'improve the quality of life. No developmental process can be
sustainable unless it leads to visible and widespread improvement in these areas.
-.b.'
1.9
There is by now enough evidence to show that rapid growth has strong poverty
reducing effects and, given a public policy stance which is sensitive to the needs of the poor,
a focus on accelerated growth will also help in realising the objective of alleviating poverty.
However, a growth process leading to high and accelerating inflation is inappropriate in the
context of wide-spread poverty; The positive relationship between growth and inflation that
is sometimes postulated is based on the forced extraction of savings, which enables a higher
rate of investment. On the negative side, high inflation tends to fall disproportionately on the
living standards of the poor, who do not have the economic power to protect their real
incomes from erosion. In the Indian context, however, voluntary savings of the households
arc high enough today to achieve and sustain adequate rates of growth without recourse to
2
inflation tax to extract forced savings lor generating investible resources, provided that the
available savings are utilised productively and efficiently. It is the responsibility of the
government to ensure that the growth process takes place in a framework of relatively stable
prices, with inflation held down to the minimum possible level consistent with the need to
realign relative prices both in the domestic and international markets when necessary.
1.10
I he shift in emphasis towards private initiative and reliance on the entrepreneurial
spirit of the people essentially seeks to create the conditions for rapid and sustained
growth. Nevertheless there are aspects of growth whiefa can be labour-displacing and
impoverishing. These arise essentially out of unequal initial endowments of physical
resources, human capital and information, which prevent segments of the society,
particularly women and other socially and economically disadvantaged groups like the
Scheduled Castes, Scheduled Tribes, Minorities. Other Backward Classes, disabled etc.
from taking advantage of the opportunities that become available or from protecting their
interests in an adequate manner. Much of these disadvantages have their roots in 1 smrical
c umstances and arc perpetuated through social and political factors. Market f< *ces left
to themselves may not correct these disparities, and indeed may accentuate them since there
would very likely be a tendency to exploit the weak and the disadvantaged by economic
alignments of the socially and politically advantaged. Public action will be necessary to
reduce and eventually eliminate these schisms through a focus on removal of the initial
handicaps and stringent protection of'the rights of tl^c disadvantaged.
1.11
It is important to emphasise that the process of elimination of historical
disadvantages such as gender, caste and other types of social and economic inequalities
should not be based on increasing dependency of these segments of the people on the
government. Sustainability of the growth process demands that they should be viewed as
active participants, and indeed as partners, in thj; process of development and not as
passive beneficiaries of public largesse. I he need therefore is io cieatc the conditions
by which the disadvantaged are not only empowered to take advantage of the opportunities
cf ted by the growth process but also to contribute actively in the process of creation of
wealth and well-being. For this purpose, the individual capabilities of the people have to
enhanced through education, information and access to appropriate technology.
Amelioration of the immediate deprivation through anti-poverty programmes should be
viewed only as a transitional arrangement, and every effort directed towards ensuring that
these can be phased out at the earliest.
1.12 Empowerment of the historically disadvantaged will require more than provision
of the basic capabilities for integrating them into the growth process. Appropriate
institutional structures will need to be created and encouraged in order to allow full play
to their productive and entrepreneurial energies. I he objective conditions of the Indian
economy arc such that the vast majority of the populace will continue to have to be
engaged in self-employment or casual employment in the foreseeable future. I hus any
effort at raising the growth rate of the economy through increases in productivity and
entrepreneurial dynamism would need to look beyond the usual fdrms of production
organisation. In order for such activities to be viable and remunerative in a market
framework, alternative forms of organisation will have to be recognised and nurtured.
These
organisational
structures not only
provide
the institutional basis for
channelising the productive energies of the people, but also provide the countervailing
forces which can prevent the emergence of the negative features of market-based systems.
In this context, revitalisation of the cooperative sector and other forms of economic
association of people is of great significance. Cooperatives have played an important role
in development and promotion of equity and social justice.
Some have grown into
substantial size, but there continue to be policy and procedural limits on their growth and
diversification. There is % nce'd to de-burcaucratisc and de-politicisc the operation of this
sector and to enable it to access resources from other sources on its own strength. It also
needs to be ensured that the errors committed in the process of formalising the
cooperative sector, particularly in excessive governmental control, arc not repeated in
the ease of other and more recent forms of people’s participatory institutions. More
flexible policies and procedures have to be evolved which would give greater operational
freedom to such organisations.
T.13 Of all forms of economic'activity in the country, agriculture has a special role to
play as the primary source of livelihood for the majority of the people. Studies have
shown that agricultural growth has stronger poverty reducing effects than growth in any
other sector. While private initiatives and investment have been the principal source of
agricultural growth, particularly in the recent past, and will continue to be so in the future,
public intervention is essential to correct certain existing infirmities and to impart added
dynamism to this sector. Cognisance needs to be taken of the small farmer nature of Indian
agriculture, which is both its spurce of strength and the rationale for public action.
There arc three dimensions which need to be recognised. 1’irst. in a land-constrained
economy, rapid agricultural growth can take place only on the basis of sustained increases
in productivity. For this, development and dissemination of agricultural technology is of
the essence. Although private efforts at agricultural research and development arc on the
increase and should be encouraged, the process of technological diffusion continues to
remain primarily in the public domain. Second, although the farmer bears the principal
responsibility for micro-lever land and water management, sustainable development of
command areas and watersheds and the need to expand irrigation potential require public
intervention in order to make the necessary investment and to prevent over-use and unequal
access. Ideally, such functions arc best carried out by farmers’ associations, but until such
time as these are established on a firm footing and appropriate rights and powers
conferred, the government' will have to play an active role. Third, in large parts of the
country, trade in agricultural produce is controlled by a small number of traders in a
monopsonistic manner. As a consequence, the fruits of productivity growth do not
accrue to the farmers in adequate measure. Public intervention is essential to eliminate
this stranglehold
through the development
ol
adequate
rural connectivity and
marketing support.
1.14 In the past, food and nutritional security has been largely interpreted to mean
adequate availability of basic food products in the country as a whole. The concept of food
security now needs to be broadened to include peoples’ access to basic nutritional
requirements, both physically and economically. This problem is particularly acute in the
vulnerable sections of society and in the deficit and inaccessible regions of (he country.
It is necessary to’develop Strategies by which such inadequacies can be overcome by
integrating the food production and distribution systems with the employment and
poverty alleviation programmes. In particular, the Public Distribution System (PDS) will
need to be restructured in order to provide foodgrains at substantially lower prices to the
■I
poor in a focused manner and to ensure availability of such commodities in the remote
and deficit areas of the country. Indian agriculture remains vulnerable to weather-related
shocks, albeit less than earlier, and periodic or localised shortages of essential
commodities cannot easily be ruled out at present. In such circumstances, reliance
cannot be placed on private food distribution systems, which may tend to act against the
interests of the poor. A wide-spread, well-established PDS is essential for ensuring food
security. Provision of pulses and iodated salt at subsidised prices are additional steps towards
nutrition security as would be fortification of salt with iron and its availability through the
PDS. This function alone justifies the existence of the PDS despite the costs that may
have to borne by the government during normal periods.
1.15
Economic growth and employment opportunities in themselves may not be
sufficient to improve the living conditions of the poor. They need to be accompanied by
measures which enhance the social and physical conditions of existence. Despite
considerable efforts, provision of social infrastructure and services remain inadequate.
These are areas which are in the nature of quasi-public goods and in which private
initiatives and the market are unlikely to play a significant role. Primary education,
primary healthcare, including the preventive and promotive, safe drinking water, nutrition
and sanitation require hea\y investment which has to be provided out of public funds.
However, since the requirements of social infrastructure vary significantly
across
regions, greater decentralisation of decision-making than exists at present is
desirable. Furthermore, recognising the localised nature of these essential services, it is
desirable that the control over the operation and maintenance of the facilities should be in the
hands of peoples’ institutions and local associations, with adequate resources being made
available either from the exchequer or through devolution of powers to raise such
resources.
1.16 In recent years the problems of rapid urbanisation has become acute. There has
been a progressive decline in the availability of essential services as well as in the quality
of life in urban areas. The urban poor have been the worst affected segment in this process of
decline. The health and environmental consequences of increasing population density,
lack of safe drinking water and inadequate urban sanitation are likely to become further
aggravated unless steps are initiated during the Ninth Plan to improve the situation through a
well considered and articulated
urbanisation policy with
identified
programme
components including those for disease surveillance, epidemic control and urban solid and
liquid waste management.
1.17
It should be realised, however, that social and demographic indicators cannot
improve merely through increased investment, but in addition require a significant
change in social attitudes and behavioural responses of the people. In order to achieve
these objectives, there is no alternative to social mobilisation and community participation.
In this process the role of women is critical. The process of empowerment of women at
the political level has already begun, but it needs to be carried forward into the social and
economic spheres as well. Special emphasis would have to be placed on ensuring that
control of social infrastructure, particularly in health and education, in the public domain
ls vested in women and women’s organisations.
5
■■HI
1-18 A synergy between environment health imt i
i
‘
recognised. No development process which leads to ,7° T™1
‘O bc CXplichly
sustained in aa situation
situation of deteriorating env‘ '1duilllltc clu;illly of life can be
Environmental degradation is usually the outcome of in'l t
CC°logical conditions,
take into account the externalities imnncr I
dividual actions which do not
market mechanism left to itself does not provide any metlmd of f ’
Thc
of these costs. Indeed, it mav actuallv r^inf
Y ■
, offorci,,K li)c internalisation
lie responsibility of the government to ensure thatint’em is’er botHI ' 1 “nSC,",cnc':- il is
environmental degradation and future generation.
t ’ b 1 thc current v,clims of
disrupting the process of growth and devrlo
<
adequately protected, without
for preservation of the environment rests on thc nc^
.Lvcnlually’ lhc responsibility
responsibilities to be properly discharged howcvcAl P<- . 'cmsc vcs
,n order for these
to be unambiguously assigned-through legislative ’ictioir ™ 1° 1C.a,!liy cnvir°nmcnt have
preservation of the environment fostered
through
sociaT " P^.^011 in
appropriate organisational structures.
L
mobilisation
and
under .he pressure ■
conflict with both me nX,""i.................... ..
While there is evidence that rapid growth aiid the longer-term interests of individuals. I
towards population containment the pace of sucl^r0]0^110'11 d0CS 8cncra,c P0Sllivc effects
of the pressures that are being^xperienccd on
±
T7 7 bC SUff,cicnt in view
Concerted public action both direct and im
creating thc conditions by’which thc countrv
be sustained in the long-tem
(b)
°n S lniltc^ nalllral resource base,
S a.'varcncss'bllI,ding’ is essential for
S,;ib,I'SC 'tS popi,la,ion a* a lcv^ ^at can
i
Employment
»r-n-being.
n IS also an integral element in nurturing nationaHdcnlity and MchrcohXfon^AfS'^h
rapid economic growth is thp eumet ™ i
.
■
concsion. Although
u!aS^r™p“dgrSh'rPlOy"“'
SrothPa„d skiu dXnem.'L'd TaZt"
(>
==?
mtervemion wi:l be necessary to ensure not only that adequate work opportunities are
creatsd. but also 'hat the labour force is able to access these opportunities.
1 •’- agricultural sector has historically played an extremely important role in
providing employment in India, and is likely to continue to do so at least for the next decade
or more. The skill profile of the emerging work-force is such that a large majority will have
to continue to seek work opportunities in this sector. In order to create such opportunities,
land and tenancy reforms are essential. The evidence strongly suggests that small farmer
agriculture, based on secure rights on the land, is not only more productive per unit of land
than either large farms or where the rights of the actual tiller are not well defined, but is
also more labour absorbing. Active government intervention, both in implementation of
existing laws and formulating new legislation for ensuring the tillers' rights, in these areas
will have to be taken up in earnest in order to create conditions of high labour absorption
with adequate productivity growth.
1.23 In a dynamic economic environment, restructuring or failure of firms and even
demise of certain economic activities is natural and to be expected. Efforts at preventing
such adjustments and failures in the interest of protecting employment has proven to be both
lefficient and ineffective. The welfare effects of such measures, in terms of the trade-off
Between the interests of the currently employed and those of either the unemployed or
the new entrants to the labour force are also not unambiguous. While providing avenues
for retraining, skill upgradation and reemployment, the focus of public policy needs to be
shifted from protecting specific jobs to protecting the interests of the work-force. This
has two dimensions. First, provision has to be rriade 'for the payment of the legitimate dues
of and for mitigating the hardships faced by the displaced work-force. Such systems by and
large exist for the organised sector, but the labour force in the unorganised sectors and the
self-employed arc presently uncovered. Providing such support is not easy to do without
the creation of appropriate people’s organisations with active government support.
Second, all efforts have to be made to find alternative occupation for the unemployed.
Although the minimum necessary condition for ensuring such reemployment is that the
growth rate of creation of work opportunities must exceed the growth rate of the labour
force, it is not sufficient. Existing workers embody a certain structure of skills which may
not be appropriate for the new work opportunities that may be created. The market by itself
y not be prepared to impart these skills to the displaced workers, since the preference
will generally be for training the younger, new entrants in the labour force, whose
potential life-time returns to the investment in human capital is likely to be significantly
higher. It is necessary, therefore, to establish systems in the public domain for retraining or
reskilling the displaced labour' force in line with the requirements of the economy.
1-24 However, even if the generation of work opportunitiesis adequate, the quality of
employment in terms of the incomes received and the work environment may leave much
to be desired, and may be likely to remain so without directed public action. It is
erefore necessary to shift the focus of employment strategies ftowards creating
conditions whereby
wherebv employment
emDlovment opportunities
onnortunitipc lead
Irad to
tn significantly
cianifirontk/ better
knHar living
andJ
working conditions of the people and to uphold the dignity of labour. In particular, the
incidence of scavenging and child labour which arise out of acute poverty and prevailing
social disabilities need to be eradicated keeping in mind the requirement of maintaining
iamily incomes. Public investment in modem sanitation systems, on one hand, and
7
of
^r.d
cr. •?.« cv^r. ci’ r.etxssary4 to tackle
ine first social evil. Insofar as the second is concerned, precipitate action may not
always achieve the objectives. A family-centric strategy and sensitivity to the needs of
the orphan or run-away, coupled with rigorous implementation of the existing laws will
need to be evolved to effectively tackle this problem.
1.25
Improvements in the quality of employment can be achieved only in a situation ol
rapidly growing productivity to which the labour can lay a just claim. However, it is not
enough to merely create the right kinds of employment opportunities, but also to provide the
people with the human capital by which they can take advantage of these opportunities.
Education and skill development are the essential features of such empowerment Free and
compulsory education for children, especially for the girl-child and other educationally
backward groups, supported by an adequate mid-day meal programme in schools is the
first step towards this end. Vocationalisation of the education system is essential
particularly since there is evidence tliat there arc a number of skills which arc in acute short
supply and for which there is a serious shortage of training facilities. In addition, special
programmes will have to be implemented to develop skills, enhance technological level'’ md
provide marketing channels for people engaged in traditional occupations. The eduumon
and training systems in the country if not reformed will begin to display a certain degree
of rigidity and get increasingly divorced from the needs of the economy and the
social infrastructure. This -trend needs to be reversed, and efforts will have to be made to
introduce a system by which the emerging skill requirements of the economy arc
anticipated and the education and training sys'ems reoriented accordingly. Although the
private sector, which will be the main source of work opportunities in the future, will
have an important role to play in this regard, the initiative will have to be taken by the
government since the bulk of the educational system in India is in the public domain.
1.26 Recognising the high incidence of underemployment and increasing casualisation
of labour, there is need to enhance employment opportunities for the poor, particularly for
those who are in seasonal occupations. The recent trend in lower labour force participation
rates among women is partly a reflection
ol the inadequacy of appropriate work
opportunities. In view of the observed relationship between women’s participation in the
labour force and ■ fertility, this trend has disquieting portents regarding the pa^_ of
reduction in the growth rate of population. There is need therefore for public intervention in
creating work opportunities which are sensitive to the seasonal and locational needs of the
underemployed, particularly women. Such opportunities should be demand-driven to the
extent possible. In this context, the effort to implement a national Employment
Assurance Scheme is of considerable significance.
(c)
Regional Balance
\.n
Balanced' regional development has always been an essential component of the
Indian development strategy in order to ensure the unity and integrity of the nation. Since
not all parts of the country are equally well endowed to take advantage of growth
opportunities, and since historical inequalities
have not
been eliminated, planned
intervention is required to ensure that large regional imbalances do not occur. With
greater freedom and choice of location that is now available to industry, it is more than likely
that some states would be able to attract more private investment than others. In such a
s
■ t situation it will be necessary to deliberately bias public investment in infrastructure in
favour of the less well-off states. It will also have to be ensured that the states which
benefit from this reorientation do not dilute their own efforts at generating investible
resources or divert their resources to other uses.
1.28 Efforts at attracting private investments by state governments has already led to a
certain degree of competition in granting of fiscal and other concessions. This tendency
is likely to be accentuated in the future as private investment becomes increasingly more
important. While a certain degree of competition in this regard may be desirable, in the
long-run it would adversely affect the fiscal viability of some of the states and (hereby
jeopardise the ability of these states to provide the basic social and economic
infrastructure. This would have serious implications regarding the future progress on
regional balance and would tend to accentuate regional disparities in quality of life. It is
necessary therefore for states to operate in a spirit of cooperative federalism and to arrive at a
set of public policy and action in which state-level initiatives at attracting private
investment in a competitvc manner will be acceptable, and those in which a common
position would be taken by all states in their collective interest.
1.29 There are also regions or pockets of poverty which are unable to benefit adequately
from the over-all growth process. For the most part such pockets of poverty reflect the
inadequate integration of the local economics in the wider growth process due to historical
reasons. There is a strong probability that even in the future, market-based growlh may
elude these regions unless active intervention is made by
the government.
Sustainable anti-poverty programmes in such regions would need to involve not only direct
employment and income enhancing policies to tide over the immediate deprivation, but
also measures by which the asset endowment of the poor can increase and such areas can
become better integrated with the rest of the economy for sustainable growth.
1.30 The focus regarding the issue of backwardness and regional balance has
traditionally been on industrialisation. The evidence, however, suggests that reduction
in regional disparities, particularly in average standards of living, may be better achieved
through greater focus on agriculture and other rural activities. I'or this it is necessary to not
only increase the productivity of agriculture in backward areas, but also to increase the
degree of integration between the rural areas and the rest of the country' through improved
connectivity in terms of transport and communications, and provision of marketing support.
In the absence of adequate public investment in such infrastructure, the prospects
of a disparity-reducing agricultural growth will recede.
1.31
In some regions of the country, relatively high levels of income continue to be
associated with low human development indicators and poor provision of social
infrastructure, such as safe drinking water, primary health and primary education
facilities. These are areas in which private initiatives arc unlikely to play any major role,
and it would be the primary responsibility of the government to ensure that appropriate
interventions are made. There is therefore a need to identify the minimum norms of
availability of such infrastructure and to accelerate public investment for achieving these
norms in a balanced and time-bound manner. The problem of shelter for the poor, both in
urban and rural areas, is particularly acute and a programme of providing assistance for
construction of houses will need to be implemented.
9
1 .32 The issue of regional balance operates at both the intcr-Statc and the intra-State
level and there is therefore the need to address it in a framework that is more flexible than
the political and administrative boundaries of each individual state.
Growth and
development are intimately related to the level of economic integration of the various parts
of the country and the linkages that arc formed between the backward and the more
developed regions. In view of this, it is necessary to move away from the concept of
competitive policy formulation to a framewdrk of cooperative federalism wherein
neighbouring states adopt a common set of strategies for development of their backward
areas in a coordinated manner and remove or reduce the barriers to inter-state commerce
that have been built up over the years. Cooperative action can not only prevent loss of
revenues to state and local governments that may arise from the reduction of existing
fiscal barriers, but actually augment the flow of resources.
1.33
in view of the resource constraints being faced by the Government at all levels,
the prioritisation of the various facets of quality of life would have to be carried out on
a region-specific basis. In particular, it will be necessary to identify those areas of the
country where the growth process will more or less take care of the problem of acute
deprivation. The focus of anti-poverty programmes would have to be shifted to those
other areas which are as yet inadequately benefited by the growth process. In such areas the
pre-conditions for a
market-based development strategy will have to be created
expeditiously, even if it means a certain degree of positive bias.
/
(d)
Self-reliance
1.34 India;, has embarked on a process of gradual and phased opening up of its economy
to take advantage of new opportunities in trade and investment. While this process
needs to be continued and taken forward, it should be from a position of strength and not
through cither external compulsions or a lack of alternatives. In this sense, self-reliance
must remain an important component of development policy and strategy. The Ninth
Plan will address the issues of external vulnerability and develop suitable strategies for
making India a strong and confident player in the international economy.
1.35 The first, and perhaps most important, component of self-reliance is to ensure
balance of payments sustainability and avoidance of excessive external debt. This end can
be best served by a focus on expanding the export base of the nation. Greater export
orientation may not be achieved by reliance on market-forces alone, and the government
will have to take active measures to enhance the attractiveness of export activities. This also
requires a commitment to sound and prudent niacro-cconomic policies, particularly in fiscal
and monetary management matters. In a market-based system, micro-level decision-making
by private economic agents can collectively lead to excessive draft on the foreign exchange
resources of the nation and growing external debt. It is the responsibility of the government^
to create the conditions, by which such tendencies can be corrected by the agents
themselves. A framework of prudent macro-management and greater reliance on non-defy
creating external flows for financing balance of payments needs are aspects of such?
conditions. In addition, it is necessary for the government to continuously monitor the
progress on the balance of payments front and to initiate action if there is dangq
of unsustainability.
?
I')
1.36 Accelerating the growth rate of the economy will require a significant step up in
-the availability of investible resources. Self-reliance demands that most of these resources
should be generated domestically and recourse to external sources be resorted to the extent
dictated by a sustainable proportion of external liabilities. There is need to link the inflow
of external resources to the level of domestic savings and the long-run ability to scrx'icc
external liabilities. This can only be done by the government.
1.37 Self-sufficiency in food is a basic element - in any strategy of self-reliance. In
view of the fluctuations in agricultural production arising out of weather-related factors.
India will have to target a secular growth rate of agriculture higher than that dictated by
the needs in order to prevent periodic large-scale imports and the vulnerability that it
entails. In order to support such growth rates, it will be essential to plan for regular and
sustained export of food products in normal years and to create the conditions necessary
for facilitating such trade. .Although the commercial aspects of such production and trade
can be left largely to private initiatives, the policy support and critical infrastructural
inputs, including technology, will have to be provided by the government.
1.38 Natural resources arc a patrimony of the nation and it would not be desirable to
.cessivcly deplete the natural resource endowments of the country and thereby expose
future generations to vulnerabilities over which they ma}1 have no control. Market
forces generally tend to have a shorter time-horizem than desirable from a national stand
point and can therefore result in faster depiction of resources. On the other hand, market
forces have played an important role all over the world in achieving more efficient
utilisation of raw materials and energy. The government will therefore have to lay stress on
conservation and optimal utilisation of natural resources, including herbs and plants of
medicinal value, keeping in view’ the international availability of such resources and the
need to maintain a viable balance of payments position.
1.39 A critical' element of self-reliance is self-reliance in technology. While it is desirable
to access the best and most appropriate technologies from wherever they arc available, in
the long-run it is necessary that domestic capacity is developed in respect of all critical
technologies needed by the country. This aspect has gained further importance in view of
the emerging global regimes restricting national autonomy and the unilateral restrictions
ng placed on a wide range of technologies on the grounds of “dual-use”. This situation
will have to be met. on the one hand, through a suitable international initiative and, on the
other, by strengthening indigenous capabilities and reinforcing the legal framework on
intellectual property rights. Nurturing the capabilities tor development of technology is a
long-term process, and the private sector may find it more expedient to rely on external
sources in the short-run. Public intervention may be required to provide the right incentives
for Indian firms to internalise their technology requirements more rapidly than would
otherwise be the case.
Objectives of the Ninth Plan
>•40 The Eighth PI an had identified “human development” as its main focus. There can
be no two opinions about this being the ultimate goal of all public action, including
planning and development strategy. The emphases and nuances, however, will need to
Vary from time to time depending upon the objective conditions of the economy and the
11
Qf;
ThR
rw-'i'iiitit.'n >1 'he hnej-ml ijnk. hej.vnen. nujkl
growth and improvement in the quality of life characterises the approach to the Ninth Plan. It
is also based on the collateral recognition of the need to pursue policies which arc pro-poor
and arc aimed towards correction of historical inequalities. Thus the focus of the Ninth Plan
can be described as : “Growth with Social Justice and Equity”. The specific objectives of
the Ninth Plan arising from the greater reliance on market forces and the imperatives for
public policy and action discussed above arc as follow .
(i)
Priority to agriculture and rural development with a view to
generating adequate productive employment and eradication
of poverty;
(ii) Accelerating the growth rate of (he economy with stable prices;
(iii) Ensuring food and nutritional security
the vulnerable sections of society ;
for all. particularly
(iv) Providing the basic minimum services of safe drinking water,
primary health care facilities, universal
primary education,
shelter, and connectivity to all in a time bound manner;
(v) Containing the growth rate of population;
(vi) Ensuring environmental sustainability of
process through social mobilisation
and
people at all levels;
the development
participation of
(vii) Empowerment of women and socially disadvantaged groups
such as Scheduled Castes, Scheduled Tribes and Other
Backward Classes and Minorities as agents of socio-economic
change and development;
(viii) Promoting
and
developing
people’s
participatory
institutions like Panchayati Raj institutions, cooperatives and
self-help groups;
(ix) Strengthening efforts to build self-reliance.
The Development Strategy ~
1.41 The gradual shift in development strategy that has occurred since the early 1980s in
India is now at a stage where it needs to be articulated fully and unambiguously. Although
India has always had a vibrant private sector and a functioning market economy, the role
of the government has been dominant, not only as a significant investor and producer of
goods and services in its own right, but also as an arbiter of the actions of the private
sector. The former role will have'to continue in the foreseeable future, since the economy
is still not at a stage where the most pressing needs of public goods and services have been
met in adequate measure. Nor for that matter arc the private sector and the peoples’
organisations at a stage where thev can shoulder the responsibilities of meeting these
12
needs. In so far as the latter role is concerned, it too will have to continue, but its manner
and content will need to change. In the development strategy of earlier years, government
intervention was overly focused on guidance through prevention’ As a consequence,
there was insufficient room for market signals to determine the course of private behaviour.
Greater reliance on market forces and people’s initiatives implies that the focus of
government action will have to shift towards evolving transparent and unambiguous policies
with limited scope for discretionary action, greater decentralisation and improved
monitoring and enforcement systems.
1.42 An important component of government intervention in markets is in the area of
promoting the degree of competition. For this purpose it is not .only necessary to enact
the appropriate legislation regarding monopoly and other restrictive practices, but to also
provide the institutional mechanism for adjudicating and enforcing such discipline. In
areas where abridgement ot competition can involve technological complexities, it
is preferable to establish independent regulator^’ authorities. In most other cases
transparent regulations combined with normal judicial and quasi-judicial processes would
be adequate.
1.43 An important source of inadequate competition and inefficient markets is the
lack of adequate and appropriate information being available to all concerned. This is
a particularly serious problem in India and little progress can be .achieved without active
government intervention. It is necessary for the Government not only to stipulate a
minimum level of transparency and information disclosure by economic agents but also to
have enforcement mechanisms to back them up. In addition, the single largest generator
of data and information in the economic system is the Government itself. More openness
and transparency in making such data available to the public is an area of immediate
concern. One ot the observed weaknesses of government programmes, particularly those
having to do with poverty alleviation and social services, is the lack of awareness among
; the target population about the scope and content of the various schemes and facilities.
Improving the level of such awareness needs to be of highest priority in the coming years
in order to improve the efficiency of these public efforts.
1.44 Greater reliance on the market is only one facet of the process of decentralisation
which is at the heart of the development strategy. Equally important is the
decentralisation within the government system itself. The Ninth Plan is based on the
concept or cooperative federalism whereby much greater freedom would be given to
states to determine not only their own priorities but also the modalities of public
intervention and provision of goods and services. This concept also embodies a higher
degree of dialogue and coordination between the states. The central government’s principal
role in this regard would be to raise the issues which appear to be of national interest and to
provide a forum for arriving at a consensus. These issues are dealt with in greater depth in
Chapter 6.
1.45 The other component of decentralisation, which is expected to become
Progressively more important in the coming years, is the role and function of the
Panchayati Raj Institutions (PRJs) within the overall structure of government decision
making and action. Past experience has shown that functions and services which are
ocalised in nature are most efficiently implemented by local political entities and other
13
1.
local bodies.
It is therefore necessary to devolve not only greater resources and
responsibilities to the I’Rls, but also to grant greater powers to them for raising their own
resources. In this context, programmes in the social sector which arc of national
importance, and therefore have a high level of central government involvement, but which
arc essentially localised in their delivery, would need to be operated through a more direct
relationship between the central government and the I’Rls in order to increase their
effectiveness. This mechanism is already operational in certain centrally sponsored schemes
(CSS), and needs to be extended to others as well. The transfer of some CSS along with the
funds, as already initiated, is a step in this direction.
1.46 The Eighth Plan had identified peoples’ initiative and participation as a key element
in the process of development, particularly in improving the effectiveness of
development outlays which has been declining over the years. Il had also recognised that
the role of the Government should be to facilitate the process of peoples’ involvement
by creating right types of institutional infrastructure, particularly in rural areas. The
progress on this front has not been entirely satisfactory principally due to the fact that the
other tiers of the Government were not fully integrated into the development strategy. The
process of social mobilisation and development of peoples’ initiatives cannot be achieved
without the active support and involvement of the political system at all levels. The
Panchayati Raj bodies in rural areas and Nagar Palikas in urban areas will have to be
directly involved in the development process. People’s involvement via their elected
representatives will be realised through genuine democratic decentralisation.
1.47 Other forms of peoples’-participation also need to be strengthened. Erom the early
days of planning, cooperatives have been perceived as the most important form of peoples’
institution for promotion of equity, social justice and economic development. Every effort
will be made to make the.cooperatives work. They need to be liberated from tight
bureaucratic control. Self-help Groups, Associations of Workers or Small Producers, etc.
are other forms of institutions which will be encouraged. Government will seek active
partnership with the voluntary sector in organising and promoting these institutions.
1.48 Indeed, in view of the shrinking share of public investible resources, every
effort needs to be made on improvement of the implementation and the delivery
mechanisms through which public goods and services arc provided to the people.
Decentralisation is only one of the modalities for effecting
such
improvements.
Improved transparency and information dissemination is another. However, emphasis has
also to be placed on better monitoring and the readiness to be more flexible in the
implementation methodology if circumstances so require. Ibis is one area where there arc
serious inadequacies, and which needs to be strengthened on an urgent basis.
1.49 The development strategy also has to take cognisance of the changing role of the
public sector in general in the allocation of responsibilities for harmonious development of
the economy. In order to effectively discharge the altered responsibilities, the structure
of not only public investment but also of public assets have to be changed in a significant
way. Investments which have been made in areas which can be effectively discharged
by peoples’ organisations and the private sector, need to be gradually turned over to the
appropriate organisations. The resources thus released can then be devoted to building up
assets and facilities in such areas where private investments arc likely to be either absent or
14
. inadequate. It is in this context that the portfolio of public sector undertaking
■Cenlrc and .ho Su.es would need .0 be examined aSd deeisiX
reorientation would need to be taken.
L uivcsiment and
Z
i reonenting
structure of the public sector, the conditions for enabling the
entry of private enterprises in these activities needs to be created and sufficient confidence in
attmetmg investment has to be achieved. Although the areas which are reseXed fo
public sector have been reduced significantly.' the remaining areas also have to be
reassessed with great care. More importantly, in the areas which have been dereserved
steps would need to be taken to ensure that private investments are economically viable In
particular, in such areas where the public sector will continue to be either the principal
customer or the main competitor to the private sector, it is necessary to establish independent
sXrs0^ 6 ieS WhlCh C3n
fa‘r comPetition hctwcen ^e public and private
1.51 In this context, provision of economic infrastructure needs particular mention
Adequate quantity, quality and reliability of infrastructure are essential pre-coZions
nly for economic growth and development but also to make the countrv
internationally competitive and attractive for investment. The investment needs in
Govenunent ^Th ° 3 mag.nitude .that are bey°nd the resources available to the
Government. There is an imperative need, therefore, to motivate the orivate sector tn
participate in the development process, if the infrastructure gap has to be bridged . The
benefit bZ"
haS
016 burden °f infrastructure development so fa/will also
benefit by the competition and partnership with the private sector. Successful development
of this crucial sector will require bold policy initiatives, framing of schemes and setting
cZt? inStlt^t,onaI environment which would provide a level playing field to ah
bZ
S kWhl St Simultaneously safeguarding the rights of consumers Legislative
baefang to these mst.tutional reforms would also require to be given ' While new
nitiatives are being taken for additonal investment, optimum utilisation of the existing
nfrastructure should not be neglected. This needs to be done bv technology upgradation
system improvement and ensuring public utilities function on commercial lines Most
unportantly, care should be taken to ensure that in the provision ofZseZvi es theZ
dieir nZs^0^^
-iZeXogy suZ^J
to review fceh
1
"“e been delice"scd 10 a =ubS.antial extern .here is need
prXb for .he
,?e Ve,S',£eS °f 'h<: licensing r^ime- Similar|y. ‘he reservation of
Str Of „ /
' SCa,e S“,or nceds 10 be reviewd- Th'ro is =videnee that for a
mon^olv wwereto
‘he Sn’d‘
1,35 °”ly rau“ed in gran'in8 u"d“e
« ve^X ’ hv the S “TT “""S' 'n OlhCr
d<:Spi,C "“tvations, there
approarh t
small scale for reasons either of technology or of markets The
XSt
,he !maI1 SCale sec'°r sl”“ld shift from pn^ective lo
ittveaXt ^,tPro-n’0'r '■ ”this C°nto“’the availahility of credit and even longer term
Provid^ ade^e res^ 8reat 'm,x>rtance- Sln<:e lhc ftnancial sector left to itself may not
™d ~'halT,n T7T Pn°'l'y SeC'°r lending by banks would have to be continued
PromMi^o i™e smaH seal
“
°f 'hC i’nancial SeC,or' The other
»f
lechnologies XnTh L , ! ‘S
Pr°V,dJ"8, access 10 b't<er
t™ appropriate
gies. Although the entrepreneaur should be left to select the technologv that is
15
f
more suitable, it is the responsibility of the Government to provide the institutional'
mechanism through which the information on available technologies, both in the
country and abroad, arc made readily available.
1.53 With the tremendous expansion that has taken place in information technology,
access to technological information is not difficult. What is required is a well organised
system by which international data sources arc accessed and made available to the potential
users. The spread of information technology in India is as yet inadequate, and specific
efforts would have to be made to^create a national network for information dissemination.
This would not only help the industrial sectors, but would also enhance the effectiveness of
dissemination of technologies for strengthening rural economic activities, including
agriculture, and social infrastructure and would also enable greater transparency in
the operation of Government schemes and programmes.
1.54 One sector which will become increasingly more important in the coming years is the
financial sector. Rapid growth and increasing complexity of the economy can be
supported only by highly sophisticated and integrated financial intermediation system.
At present the Indian financial sector is extremely fragmented and is not efficient enough
for the demands that arc likely to be placed on it. f inancial sector reform is only one aspect
of the measures necessary to strengthen this sector. Reorganisation and induction of new
skills and technologies arc equally important. I bis sector is prone to vulnerabilities
arising out of inadequate information and moral hazards. There is, therefore, ease that
deregulation of this sector would need to be accompanied by relatively more stringent
prudential norms and improved monitoring by the Government in order to protect the interest
of the savers and to prevent undue speculative and imprudent behaviour.
1.55 The responsibilities of the Government in a more market oriented economy have
already been discussed in the imperatives for public action and policy. These functions
however would need to be seen in the context of the principal responsibility of the
Government, which is to . maintain a stable macro-economic environment. Prudent
macro-economic management requires that the Government must carefully assess the
various responsibilities that it bears.and prioritise them in a manner which is consistent with
its ability to raise resources without stifling private initiatives, fhcrc arc number of
implications of this which need to be considered.
1.56
The fiscal deficit, particularly the revenue deficit, must be a central concern of
macro-economic management. The development strategy will have to recognise explicitly
the need to restore the fiscal health of the government at all levels and to regulate its
borrowings programme injsuch a manner as to maximise the productive potential of the
economy. An important component of this effort is to avoid excessively unrealistic
projections of public resources at all levels of the government, and to adhere as closely as
possible to these budgetary limits. Stress will have to be placed on evolving a long-term
fiscal policy stance in order to reduce the revenue deficits of the government, both Centre
and States. Commitment at all levels to implement these proposals is a prerequisite for
successful implementation of the proposed development strategy.
16
1.57 The need to contain the revenue deficit of the government has to be seen within
. the context of ensuring health and optimal utilisation of existing public assets and increasing
the effectiveness of social schemes/programmes. The development strategy will need to be
based on the premise that such measures, including emphasis on maintenance, are likely to
yield much greater dividends than outlays on new projects or schemes. Such proposals will
need to be strictly implemented and carefully monitored to ensure that the benefits of public
expenditures are maximised.
1.58 Over the years, a number of subsidies, both direct and hidden, have come into
existence. Fixation of administered prices on extra-economic considerations is an important
element of non-transparent subsidies. Such subsidies are open-ended and in some cases have
accrued to those who are not envisaged to be the real beneficiaries. There is a need to move
to a system of transparent subsidies directed towards specific target groups in a selective
manner.
f
1.59 A particularly disturbing aspect of the experience in recent years is that there has
been a decline in the share of States in total Plan outlay. In the Eighth Plan it has declined
• to 36.4 per cent as compared to the projected 41.5 per cent. What is a matter of concern
is that when the states’ share decline, the sectors which suffer more severely are
agriculture, basic minimum services, health, education, women and child development,
welfare and economic infrastructure such as electricity, etc. Given the emphasis that is
being placed on the importance of these sectors in Government action, this trend needs to
be halted and reversed. A thorough reappraisal of the priorities of Government action and
the distribution of responsibilities between the Centre and the States indicates that the role i
of the States in economic management and social service areas would become
progressively more important. In order to support this shift, the distribution of resources
would also need to be reoriented. Failure to do so may lead to a growing mismatch
between the responsibilities of the various wings of Government and the resources
available to carry them out.
-.60 The other aspect of the development srategy which is of crucial importance is to
evolve sound foreign trade and investment policies in order to promote rapid and
sustained export growth. There is need to enhance the technological strength and
economic efficiency of our domestic production, and to ensure a smooth and effective
t.ansition to a more open economy. The industrial and financial policy framework will
also have to be streamlined to promote rapid expansion of foreign direct investment flows
11 order to augment domestic investment and reduce reliance on external borrowings to
extent possible.
Domestic entrepreneurship, which is the backbone of the
oevelopment process, will be fully encouraged through measures to enhance their
competitive strength and to facilitate their growth and efficiency. In particular, the small
nnd viHage and home industries will have to be provided the proper environment for
diversification in a more open environment.
1.61- .’The maintenance of balance of payments stability would also depend upon the
growth rate of exports that can be achieved on a reasonable basis. It needs to be realised that
over 90 per cent of Indian exports originate from the manufacturing sector. Therefore,
Hnless a substantial shift can be effected in the export basket, the rate of growth of exports
would be limited by the infrastructure constraints and the profitability of manufactured
17
exports versus profitability of domestic sale of manufactured goods. In view of the faster
growth rate of imports that is expected, there is need to revitalise the export oriented schemes
so that the average export propensity of manufacturing rises significantly. In addition
measures would have to be implemented to diversify the export basket, particularly for
processed agricultural products.
1.62 The Eighth Plan has witnessed improvement in technology levels in the country,
particularly in the industrial sector. However, much of this dcvelopmcnt has been based
on continual import of technology rather than on adequate development of technological
capabilities within the country. This process cannot be carried on in the longer run and
steps will need to betaken to enhance the technological capabilities of the nation. To this
end, it is necessary to evolve a technology policy which would not only ensure adequate
growth in productivity and quality, but would enhance the competitiveness of Indian
products in the international market.
1.63 The Indian planning process has always laid emphasis on measures to ensure
sustainability of the development process not only in economic terms, but also in ter
of social and environmental factors. Much of the measures adopted in the Agenda 21 of
the United Nations Conference on Environment and Development already find
reflection in the Indian plans. The Ninth Plan will need to carry this tradition further
and consolidate on the creation of conditions for sustainable development. Rapidly
growing population, urbanisation* changing agricultural, industrial and water resource
management, increasing use of pesticides and fossil fuels have all resulted in perceptible
deterioration in the quality and sustainability of the environment. It is recognised that
environment protection docs not only involve a prevention of pollution and of natural
resource degradation, but has to be integrated with the over-all development process and the
well-being of people.
The Role and Methodology of Planning
1.64 The Planning Commission, believes that the principal task of planning in a federal
system is to evolve a shared vision of and a shared commitment to the national object’ 's
and the development strategy not only in the Government at all levels but also among all
other economic agents. No development strategy can be successful unless each component
of the economy works towards’a common purpose with the full realisation of the role that
has to be played-within an overall structure of responsibilities. The principal function
of the approach to the Ninth Plan is not only to articulate such a shared vision, but also to
ensure shared commitments.
1.65 Based on such a shared vision, the principal task during the Ninth Plan is to build on
the successes of the Eight Plans, while tackling the problems that have emerged,
particularly in areas such as capital formation in agriculture, living standards of the poor,
infrastructure, social sector, regional disparity, and fiscal deficits. Despite the considerable
progress that has been made by the Indian economy in both economic and social spheres,
the development task is far from complete and resources continue to be limited. Moreover,
as has been indicated, the Indian economy is still vulnerable and the operation of a more
open economic system has to be tempered by judicious public interventions to ensure that
these vulnerabilities are gradually overcome.
18
1.66 Recognising the federal nature of the Indian system, the planning process has to
.develop a common policy stance which would be adopted both by the Centre and the
States. I he role of planning would therefore involve considerable degree of policy
coordination between the Centre and the States, between the States, and between the
States and the sub-Statc level tiers of Government.
1.67 In light of the emerging situation, sectoral investment planning continues to form an
important component of the planning process. Individuals and entrepreneurs are frequently
unable to assess the areas of opportunities and anticipate likely problems. Investment
planning is a methodology to bridge this gap. The planning process also needs to take
stock of the resources for development and to indicate methods by which these resources
can be augmented in a sustained manner. Since planning is done for the entire nation, the
strategies for resource augmentation need to cover not only the government at all levels but
also those which would be available to other sections of people.
1.68 The other principal task of planning, particularly in a market oriented economy, is to
identify the areas of emerging vulnerabilities and to suggest measures to address them.
Although the specific policies would need to be worked out by the concerned ministries or
the States, the broad directions would have to be provided by the planninu system. Unless
such problem areas are placed within the wider macro-economic context, short-run fire
fighting measures can lead the economy in undesirable directions.
1.69 With the reduction in the instruments available 1to Government in controlling
economic matters and the greater degree
o - of
-- uncerjainities
----- ------- arc that
present in any market
based system, the methodology of planning will have to change if it is to retain its
relevance. The Eighth Five Year Plan had explicitly indicated a shift from directive to
largely indicative plan. There is considerable variance in the interpretation of this term.
The Ninth Plan is based on a more specific modality of planning which involves working
outofa consistent and desirable development path, the identification of emerging trends
and deriving policy measures to bring about a confluence between the two. The planning
process today, therefore, focuses on planning for policy so that the signals that arc sent to
the economic system induce the various economic agents to behave in a manner which is
consistent with the national objectives.
1-70 . The most important characteristic of the methodology adopted in the formulation of
the Ninth Plan is that it is not based on a deterministic relationship between the Plan
and economic performance. It is explicitly recognised that there are unccrtainitics in the
system and limitations in the ability of the planning system to accurately predict future
trends. Furthermore, it is also recognised that the effects ot Government policies and
interventions are not entirely predictable. This is certainly true of economic variables,
though it may not be so for the performance in social sectors such as health and
education. The planning approach adopted for the Ninth Plan therefore concentrates on
Pointing out the likely outcomes and suggests the directions for policy intervention. The
S of the actual policies and the manner of implementation will need to be worked out
rom time to time between the concerned Ministries. States and the Planning Commission.
19
Development Perspective and Sustainability of Growth
1.71 Development and growth arc long term processes, and a five year plan represents
only the characterisation of the economy and social processes over a period in which a fair
degree of reliance can be placed on estimates and projections.
The viability and
sustainability of the development strategy embodied in a five year plan needs to be seen in
the longer perspective in order to ensure that continuity of directions and the balance
between interests of the present and the future generations is maintained, fhc Indian Five
Year Plans have traditionally been embedded in a 15 year perspective period. The Ninth
Plan continues this tradition.
1.72 Since the principal objective of economic planning, is to fulfill the social and human
aspirations of the people, the basis for all planning efforts rests upon the projections of
future demographic trends, the requirement for work opportunities and the need to crrn/Jicatc
poverty. The factors which determine the long term conditions of growth, along with, the
size and skill profile of the work force, are the availability of investible resources through
domestic savings and prudent access to international investment funds, the basic resource
endowment of the country, the available and latent entrepreneurial abilities of the people
and the pace of technological development.
Population Growth & Demographic Profile
1.73 Population stabilisation is an" essential prerequisite for sustainability of the
development process. The "National Family Planning Programme was launched in 1952
with the objective of “reducing birth rate to the extent necessary to stabilise the population
at a level consistent with requirement uf national economy”. The technological advances
and improved quality and coverage of health care resulted in a rapid fall of mortality rate
from 27 in 1951 to 9.8 in'1991J‘In contrast, the reduction in birth rate has been less steep
declining from 40 in 1951 to 29.5 in 1991. As a result the annual exponential population
growth has been over 2% in the last three decades. The report and recommendations of the
NDC Committee on Population gave a new thrust and dynamism to the Family Welfare
Programme during the Eighth Plan period. As a result of these recommendations, the
centrally defined method-specific targets for Family Planning have been abolished and
decentralised area-specific need assessment to meet all the felt needs for contraception,
maternal and child health have been initiated. Indeed this was the basis on which one half of
the funds under the social safety net scheme was provided to districts with crude birtli rate
(CBR) over 39/1000 (as per the 1981 Census) to improve existing facilities for safe
delivery and child care Wthesc districts. During the Eighth Plan period the fall in birtli rate
has been steeper than that in the death rate; consequently annual growth rale is around 1.9%
during 1991-95. The projections of the major demographic indicators for the perspective
period arc presented in Table 1-1. It may be seen that the rate of decline in population
growth is likely to be accelerated during the Ninth Plan period and will continue to do so
during the perspective.
20
Table 1-1 : Major Demographic Indicators
1996
1. Population (million)
934.22
2. Urban Population (%)
27.23
3. Sex Ratio
107.9
(males per 100 females)
2 001
2006
Oil
1012,39
28.77
107.2
1094.13
30.35
106.6
1178.89
31.99
106.0
1996-200
4 . Growth rate of population
5. Expectation of life
at Birth (years'
Ma 1 e
Female
(^)
2001-06
1 . 62
62.3 6
6 5.2"'
Note :
* S9.3 based Abridged Life
General, India.
Tables z
2026-11
1.10
63.67
r c.
1939-93,
g ■>
65.65
6'’. 67
Registrar
SOURCE: Report of -he technical Group on Population
Projections
constituted
by ^Planning Commission,
published
as:
Population
■, Projections for India & States 1996-^2016,
Registrar
General,
India
(1996)
1.74 Although the above projections made by the Technical Group on
Population
rejections constituted by the Planning Commission in 1996 arc based on ’
well-accepted
and ume-tested methodology and should have a high degree of accuracv
thev
arc
nevertheless project.ons. Any such exercise is based on extrapolation of past trends
Retro t ■,0Urt; K
n-never ade^ateI-v caPturc possible departures from the trend
vXmU Tt ?eha2°Ur IS affeCted by an extreme'y complex set of economic and social
anTtheS't
?°US I 'S
t0 derive Precise reIationships between these variable
Xs In ntrt T r
SOme °f
HnkagCS arC
at mn
part,cuIar; [acIors such as female literacy, infant mortalitv rates averaee atte
consfchT • t
°Ur rf°rCC panic'Pation ralc for ^onten are believed to “exert
that is bem" pS™ ba"'
likC,y
SpCCia' Cmphasis
Ninth PH “ P
? i 5 ! minimum services and on empowerement of women in the
imnrn P r nay , Cad t0 sharper increase in thcsc variables and therebv to even more
mpressive fall In the growth rate of population than indicated in the table. '
consideringfTrTf
demographic behaviour which has been the cause for
orient cen^ from 9^ f^t
"T
‘f5
deCline in the Sex ratio durin8
from 972 femaies per thousand males in 1901 to 927 in 1991. The factors
responsible for this continued decline are
aS yet not clearly identified. However, it is well
recognised that the adverse sex ratio is a
refiection of gender disparity and appropriate
J ps to correct this trend will need to be 1
taken during the Ninth Plan period. It is expected
at the steps that are being proposed will lead
,"~'4 to an improvement in the sex ratio to about
oy the end of the perspective period. A
major component in the reversal of the sex
21
ratio trend would be a substantial reduction in maternal
At present the
maternal mortality.
mortality,
longevity at birth of women is only marginally higher (han that of men.
men. 1 lowcvcr, over the
next decade the difference in life expectancy between men and women is expected to
progressively increase.
1.76 The average growth rate of population during the 15 year perspective
|
period of 1.54
percent is distributed extremely unevenly between the different states of the nation,
Thestatcwisc estimates of the likely rates of growth of population arc ogiven
...................
.. 1-2.
in fable
As may be seen, there is a wide variation in the growth rates, varying between 0.89 per
cent per annum in Orissa to 2.22 percent per annum in Uttar Pradesh. As a consequence of
these differential population growth rates, the share of different states in the total population
of the country is likely to efiange quite substantially over the perspective period. In
particular, the population share of northern slates of Bihar, Madhya Pradesh and Uttar
Pradesh arc likely to increase substantially, whereas almost all other States would cither have
a constant or declining population proportion. A matter of greater concern relates to the
goal of population stabilisation. In recent years, the earlier approach of using the Net
Reproduction Rate of unity (NRR = 1) as the over-all indicator of the replacement level of
fertility has been changed to a Total Fertility Rate (H R) of 2.1. The projected level of the
TFR for the country as a whole in 2012 is 2.52, which is significantly higher than the
level required for attaining the replacement rate, and the desired rate may not be achieved
until 2026. As can be seen, if the country has to attain the desired replacement rate within
the perspective period, urgent measures at fertility reduction would need to be taken in
Bihar, Madhya Pradesh, Rajasthan and Uttar Pradesh.
Table 1-2 : Rate of Growth and Share of Projected Population
States
Rate
Share of population Year by whifh
of
to total
'i’ll’.-2.1 may
Growth
1997
2012
be arieved
(1997-2012)
Andhra Pradesh
Assam
Bihar
Gujarat
Haryana
Karnataka
Kerala
Madhya Pradesh
Maharashtra
Orissa
Punjab
Rajastan
Tamil Nadu
Uttar Pradesh
West Bengal
Rest of India
1.06
1.39
1.70
1.37
1.54
1.24
0.90
1.77
1.09
0.89
1.15
1.82
0.82
2.22
1.29
2.05
7.40
2.65
* 9.71
4.73
1.94
5.13
3.21
7.74
9.01
3.50
2.33
5.20
6.17
- .16.37
7.77
7.03
6.90
2.50
10.07
4.62
1.94
4.91
2.92
0.01
0.44
3.25
2.20
5.42
5.55
10.10
7.50
7.50
2002
All India
1.54
100.00
100.00
2026
2015
20 3 9
2 0 14
2025
2009
1900
2060»
2000
2010
2019
2040
1 99 3
2 1 00 »
2009
SOURCE: Report of the Technical Group on I'opulat ion I’i
t ions constituted
Planning Commission,
published
as: Populal ion PTOjnr f ir>nr. for India k
States 1 996-2016, Registrar General, India ( 1 f»96)
pp
by
1.77 The important socio-economic variables which are not only related to population
dynamics but also to the quality of life are given in Table 1-3. In recent years most of
these indicators have improved quite significantly. The birth rate has reduced from 29.9 in
1990 to 27.4. The death rate too has declined from 9.6 to 8.9 during the same period. In
particular, the infant mortality rate has come down from 80 to 72. Although the couple
protection rate has increased from 44.1 per cent in 1991 to 45.4 per cent in 1995, its pace of
increase is relatively slow and reflects in part the inadequacies that have been
experienced in meeting the demand for contraception. Despite this, the total fertility rate
has shown a fairly sharp reduction from 4.3 in 1985-to 3.5 in 1994. One of the reasons for
this could be the increase in the mean age of marriage of females from 18.3 in 1981 to 19.4
in 1994. However, these broad all-India numbers are not uniformly distributed between the
States, which is one of the principal reasons for the significant differences that have been
noted in the projections of population over the perspective period.
Tabs 1-3
:
Important Social and Demographic Indicators-Major States
States
Birth
Rate
(1996)
Andhra Pradesh
Bihar
Gujarat
Haryana
Karnataka
Kerala
Madhya Pradesh
Maharashtra
Orissa
Punjab
Rajastan
Tamil Nadu
Uttar Pradesh
West Bencal
All India
22.7
32.1
25.5
26.9
23.0
17.8
32.4
(2)
(1)
t
*
26.8
23.5
32.3
19.2
34.0
22 . 9
27.4
Death
Rate
(1996)
Infant
C-jrlcTotal
Lif°
Female
Mean
Mortality Frrterticn Fertrlty expectancy Literacy ace at
Rate
Rat*feam.es
feamles
Rate
Marriaoe
Rate
(rrc!
(TFP)
(8^-9?
'1991'
te^-9?’ ’
(IMF)
( 1 9?4 )
.
1
994)
(5)
(3[
8.3
10.2
7.6
8.1
7.6
6.2
11.1
7.4
10.7
7.5
9.1
7.9
10.2
7.8
3.9
66
(2
C9
3
4a
95
52
?5
55
Source: Col. 1,2,3,5 i 8 SRS Estimates
Col 4 Deptt of Family Welfare
Col 6 SP.S Based Abridged Life tables,
i
46 . 9
21 . 1
57.4
53.0
55.6
4 6.7
4'.4
51.2
39.5
’f. 9
'2.6
(6)
4.6
3.1
3.7
2.8
1 .7
_ m
(8)
(9)
61.5
33.7
23.1
48.5
40.9
44 . 3
*6.9
2? . 4
5C.5
34 . 4
49.7
20.8
52.3
26.0
4 .1
3 9.4
i'.e
18.6
20.4
19.2
19.4
22.3
18.8
19.1
19.5
20.3
1a.4
2 0.2
19.5
ia.5
19.4
57.2
61 . 1
63.■*
63.5
74.7
5 3.8
65.4
3.3
2.9
5 5.3
4 .5
59 . 5
37 . 2
.74.2
2.1
5.1
5.0
4 5.4
3.5
63.4
55 . 1
62 . 3
5 <4. 7
1989-53,
P.GI,
67.6
India
1-78 Though the decline in birth and death rates have occurred in all states, the rate of
decline was slower in some states like U.P. and Bihar; even within the same state there are
substantial differences between^ districts. The Family Welfare Programme, therefore
needs to be re-oriented to remove or minimise the inter- and intra-State differences, with
emphasis on improved access and quality of reproductive and child health sendees
through PHC-based decentralised area-specific microplanning without recourse to
specific centrally fixed targets. It is imperative that adequate data-base is available at the
PHC level on a yearly basis, both for need assessment and also to provide an independent
r mechanism for impact assessment and midcourse correction. This can be achieved only
through complete registration of all births and deaths. For this, it is necessary to strengthen
tiie. Civil registration system through involvement of ICDS workers, Panchayati Raj
institutions, as well as health personnel.
23
I 79 Simultaneously, the Ninth Plait will launch an intensive
intensive drive
drive to promote health
education particularly in reproductive health, so that India builds a sound foundation lor a ,
suc“ sfu preventive and promotive national health paradigm. Basic pnno.pks o
hveiaresandation, nutrilionf and prevention of illness and disease wrll be promo cd
through not only the educational institutions and (he adult education programme but a
tough Ihe 1CDS programme, tough counselling oilcred by the health workers at all
levels, and the mass media.
Sr/ast "pbk to£0Ce^eetos are presented in fable ! -4
that the growth rate of the population between the
.o
it wih be seen
5.90
“!Ltoe“he“ie contooni of the households should in,,,rove sign.f.oantly faster
than earlier.
Tabic 1-4 : Projected Arc structure (million) ns on 1st March
Year
under 15
15-59
60 r
Dependency ratios :
(a) Young
(b) Old
(c) Total
1997
2002
2007
2012
353.64
532.60
334.80
692.64
84.01
337.93
758.61
63.64
345.11
610.55
1 1 . 94
0.66
0.12
0.70
0.57
0.12
0.69
0.4 8
0.12
0.60
0.45
90.50
0.13
0.58
population to 15-59 population
Notc'.(a) dependency ratio for young is the ratio between under ;155
population to 15-59 population
(b) dependency ratio for old is the ratio between 6
I •
SOURCE: Report of the Technical Group on Population Projections
constituted by Planning Commission, pubJrsh.d as: Population
Projections for India i States 1996-2016, Registrar Generalr
India (1996)
1 81
While demographic transition rcnccts quanOiattvc and quahta tve change t in the
i
tinn
major
health
population nrnf.le'
profile, the
the "on-going
on-going changes
cnoig in disease burden is producing aand
projccted
StWlrsc^;
(DALYS) oy orudu
perinatal motbid.ty, presently5M P“
diseases eonslttute less1
JO r eent O c
f DAlYs, while non-communicable
™
•
non.c„mraunicble
. iy
......... -» -
24
the rapidly changing life styles both in ten^of^^
diseases 1 S>
' C°mmUnity educaliOn and early detection as w-cll as management of such
. 1.82 The details of the labour force participation fates and its likely evolution over time
are given in Chapter 4. However, the likely position of labour force growth relative to the
growth rate in population ts; given in Table 1-5. It will be seen, that the growth rate of
labour force is hkely to be h.ghest during the Ninth Plan period and onlv gradual decline
thereafter.
As a result, any planning over the perspective period will have ’ to have
c™
ped XreECZ17bT,sccn,rai rCs- If
°PP-™"''- 7 "ft
created, there would be growing incidence of unemplovmcnt in thc countrv and tn
increase in thc social tensions that arise therefrom.
Tabic
’
1-5 . Population and Labour Force during the Perspective period
Population
millions
% growth
197 8
1993
1994
1997
2002
2007
2012
’
637.6
725.7 t
893.7
94 9.9
1027.6
1111.4
1195.0
>
2.92
2.00
1.89
1.59
1. 58
1.46
Labour Force
millions
V growth
289.1
367 . 4
7 Q?
'•
4 50.2
5 0 9.4
■ r ■.
r.
; . ]f
2.32
2.43
2
C‘ 4
2.50
2 . C '•
Growth Target for Full Employment
T,he nTd fT PLr0Vldin8 adcquat= work opportunities for the erowinc labour force
pressing task foVdetc
°f Uncmp!o-Vment significantly has been taken as the most
The Znin fOr^tCrmin,n8 thc
required growth performance of the econcmv
persicTe n m°? hTTS 5123 y Sta'C gr0Wt11 Pa,hs hctWCCn thc ,erminal ' ear of thc
corXencvPCr'?d 3nd thC
‘T3 manncr which ensures both inter-sectoral
investible resources
bCtWCen thc Invcstment requirements and the availability of
constant sectoral ? ’ |L S'n8 C°nstant scctoral ‘ncremental capital output ratios (ICORs) and
of thS imnac nr Th
elastlc’ties> alternative growth paths can be evaluated in terms
the emnlovmpnt be generatl0n of work opportunities. Thc details ofthcICORS and
ynient elasticities are discussed in Chapters 2 & 4 respectively.
yicldiiSh6™ line,sccnim'° was developed on the basis of a steady stale growth path
eonsiam With ,h
aVTB' 6r0?'th P'r annum °vcr ll”: PcrsP“,ivc P'tiod. This was
Plan Period
he
rate that has been observed on thc average during thc Eighth
were such that th
f°U^d that thC W°rk °PPortunitics generated along this growth path
year of the N X ™CrnPl^’ment rate wouId actually increase from 2.06 per cent in the base
12). Tn ntbA n
10 “■5 PCr Cent 1,1 thc terrninal year of thc perspective period (2011r words, maintenance of the Eighth Plan growth performance is likclv to be
' 25
>
^3.4 HEALTH
14.1 The Centuries-old rich Indian heritage of holistic health care practice, as detailed
in Ayurveda and as evidenced from the relics of Indus Valley civilisation, was lost through
gradual deterioration in the quality of medical and health care during successive centuries,
more so during the colonial period. Further deterioration followed the inappropriate
uses
of scientific discoveries and the deleterious impact of colonial pattern of
industrialisation. All this led to an impoverishment of rural agricultural hinterland,
periodically recurrent famines, urban migration, widespread growth of slums, and
gross unhygienic sanitary environment in cities and towns, bringing in their wake disease
epidemics affecting large segments of population.
3.4.2 The health conditions of the people and the state of health sendees became an issue
of national movement much before Independence. The Indian National Congress in 1930
had set up the National Planning Committee (NPC) under the Chairmanship of Shri
Jawahar Lal Nehru. The sub-committee on National Health of the NPC was formed to
assess the health situation and sendees in the country7 under the Chairmanship of Col. S.S.
Sokhey. It submitted an interim report in 1940. The National Planning Committee
’opted a resolution on August 31, 1940, based on the interim report, urging the integration
of preventive and curative functions in a single State agency and the responsibility of the
State in the maintenance of the health of the people. This political commitment is
enshrined in the Constitution of India.
Health Planning in Independent India
3.4.3 At the time of Independence the status of public health was low as shown by high rates
of infant and under - five mortality, high fertility rate and ven7 low life expectancy. It
reflected the general state of the social sectors and underlined low literacy rate, a large
segment of population below the poverty line subjected to hunger and malnutrition,
indicating poor quality of human existence. It was in 1946, at a time thdt independence
of the country' was no longer a distant dream, that the Health Sun'ey and Development
Committee, headed by Sir Joseph Shore, submitted its report and recommended the
establishment of a well-structured and comprehensive health service with a sound basic
ilth care infrastructure, laying equal importance on the need for safe drinking water
supply, housing and sanitation. This report was not only a historical landmark in the
development of public health system in independent India but also laid down the blueprint
for subsequent health planning and development.
3.4.4 From the First Five Year Plan the Central and State Governments made efforts
to build up primary, secondary and tertiary care centres and to link them through
appropriate referral systems. Private and voluntary sector also tried to cater to the
health care needs of the population (Table 1). Efforts to train adequate number of medical,
dental and para-medical personnel were also taken up . National Programmes for
combating major public health problems were evolved and implemented during the last
fifty years. Improvement in coverage and quality of health care and implementation of
disease control programmes resulted in steep decline in the crude death rate (CDR) from
25.1 in 1951 to 9.8 in 1995. Life expectancy rose from 32 years in 1947 to 61.1 years in
145
1991-96 with female life expectancy (61.7 yrs) higher than the
male (60.6 yrs).
However, the morbidity due to common communicable and nutrition - related
------- 1 diseases
continue to be high. Morbidity due to inon-communicable diseases
j
is showing a progressive
increase because of increasing longevity and alterations in
in life style. During the Ninth
Plan
efforts
will
have
to
be
made
to
tackle
this
dual
disease
....
- -------------- ‘ burden effectively so that
there is sustained iimprovement in the health status of the population.
3.4.5 India today has a vast network of governmental health infrastructure manned by
large number of medical ;and' paramedical persons. This network is functioning suboptimally because of lack of essential infrastructure,suitable equipment and appropriate
manpower especially in some critical positions, and poor referral sendees. During the Ninth
Plan efforts will be further intensified to improve the health status of the population by
optimising coverage and quality of care by:
J
a) identifying and rectifying the critical gaps in infrastructure, manpower, equipment
essential diagnostic reagents and drugs;
b) enhancing the efficiency of the health system.
Approach During the Ninth Plan:
3.4.6 The approach during the Ninth Plan will be :
(i) an absolute and total commitment to improve access to. and enhance the quality
of, primary health care in urban and rural areas by providing an optimally
functioning primary health care system as a part of the Basic Minimum Services;
(ii) to improve the efficiency of existing health care infrastructure at primary,
secondary and tertiary care settings through appropriate institutional strengthening,
improvement of referral linkages and operationalisation of Health'Management
Information System (HMIS);
(iii) to promote the development of human resources for health, adequate in
quantity and appropriate in quality so that access to essential health care
services is available to all and there is improvement in the health status of
community; periodically organise programmes for continuing education in health
sciences, update knowledge and upgrade skills of all workers and promote
cohesive team work;
(iv) to improve the effectiveness of existing
programes for control
of
communicable diseases; to achieve horizontal integration of ongoing vertical
programmes at the district and below district level; to strengthen the disease
surveillance with the focus on rapid recognition, reporting and response at district
level; to promote production and distribution of appropriate vaccines of
assured quality at affordable-cost; to improve water quality and environmental
sanitation; to improve hospital infection control and waste management;
146
/
■ (v) to develop and implement integrated1 non-communicable disease prevention
and control programme within the
t*-~ existing health care infrastructure ;
•(Vi)
to undertake screening for common
S
nutritional deficiencies «P“>a11^
pr^X^X^1 — -s, including
micronutrient status of the population,
linkage between data from ongoing environmental monitoring and th
status of the population residing in the area,
vulnerable groups;
; at all levels for emergency and disaster prevention
(ix) to develop capabilities
implement appropriate management sy stems for emergency,
and management; to i .
disaster, accident and trauma care at all levels of health care:
; for food and drug safety:
(x) to ensure effective implementation of the
and drug administration both at the Centre and in the States.
strengthen the food <
(xi) ;o increase the involvement of ISM&H practitioners in meeting the health
care needs of the population.
(xii) ,0 enhance —pabUity
and health systems research aimed at improving me 4
at various levels of health care.
hnplementauon of health programmes and heahh-reiated acuvn.es;
(x,v) to enable the Panchayad Raj I—m
Sh ’’STdte 'opS greater Accountability 'to promote inter-sectora!
cootdinatior> and utilised and community resources for health care.
Health Care Infrastructure
Primary Health Care
care infrastructure provides the first level of contact between the
3.4.7 The primary health ; < providers upto and including primary health care physicians an
population and health care
147
forms the common pathway for implementation of all the health and family welfare
programmes in the country. It provides integrated promotive, preventive, curative and
rehabilitative services to the population close to their hearth and home. Majority of the
health care needs of the population are taken care of by the trained health personnel at the
primary health care level. Those requiring specialised care arc referred to secondary or
tertiary care. Thus, the three-tier system consisting of Primary, Secondary and Tertiary
care facilities with adequate referral linkages will provide essential health and family
welfare services to the entire population.
3 4 8 Realising that the goal of "Health for All (HFA) by 2000 AD" laid down in the
utional Health Pohcy (1983) was unlikely to be achieved within the time specified the
mnl J Ia" ^nsci°usly .rec°gnised and restated the goal as 'Health for Under-privileged
(HFU) by 2000 and consistently promoted health care to the under-privileged segments
of that vulnerable population.The focus during the Eighth Plan was on :
a) major investment in development and strengthening of primary health car^
infrastructure aimed at improving the quality and out reach of services/
b)
consolidation and expansion of the secondarv
keeping district as the focal point;
health
care infrastructure
c)
optimisation of the functioning of the tertiary care through efficient and
effective utilisation of human, technological and manpower resources; and
d) building up of referral linkages so that optimal utilisation of available
facilities at each level is possible .
Rural Priman Health Care Infrastructure
3.4.9 At the time of Independence, Health Care services were mainly urban-centred
and Hospital-based. Realising the importance of creating a functional Primary
Health Care infrastructure, national norms for the primary health care infrastructure
were drawn up. Earmarked funds were jprovided
’' ' under the Minimum Needs Programme ii
the State Plan allocations. The funds received from the Department of Family Welfare
and through the Externally Assisted Projects (EAPs) were utilised to build up the Rural
Health infrastructure. The current functional status of Primary’ Health Care infrastructure
a/.- Ce,ntreS’ Pnmary Health Centres 20(1 the Community Health Centres), and the
additional requirements, wherever necessary , to meet the nonns for population as on 1996
census are given in Table-2.
3.4.10 The national norm for a sub-centre vary between 3000-5000 population depending
On Similar considerations the norm for a Primary Health Centre
r t ’Ta,'
.population; for four PHCs there should be a Community Health
Centre.^ At the national level the total number of functional Sub centres and the PHCs
nearly meets the set norms for the population in 1996 (Table-2). However, there-are
marked disparities at the State and district level. It is a matter of concern that many of the
districts with poor Health Indices do not have adequate Health infrastructure/Taking
cognizance of the widening disparities among the States in the availability Zof Basic
148
Minimum Services (BMS), the Conference of the Chief Ministers in July 1996,
‘recommended that Additional Central Assistance (ACA) may be provided to the States for
correcting the existing gaps in the provision of seven Basic Minimum Services (BMS).
The modalities of implementation of the programme, are discussed in detail in the section
on Basic Minimum Services. Of these, access to primary health care, safe drinking water
and primary education were given higher priority with the mandate that universal access to
these services is to be achieved by 2000 AD. The States were given the choice of allocating
the ACA within the seven identified areas depending on their priorities. Available data
on sectoral allocation made by the States for the seven BMS sectors for 1996-97 shows
variability.
While Rajasthan had allocated nearly 40% of the BMS outlay for health
sector, states like Bihar with equally poor demographic and health indices and large
gaps in infrastructure have not allocated any amount from ACA for BMS to the health
sector During the Ninth Plan efforts will be made to bridge the gap bet-ween the need and
the availabilitv of Primary' Health Care services rapidly through optimum utilisation of
all available resources including the ACA under BMS. The possibility of joint discussion
between the Planning Commission and States may have to be considered during the Ninth
Plan period so that each of the identified priority sectors under BMS does get sufficient
allocation from the ACA. There is considerable backlog in. terms of construction of the
buildings for Sub Centres and PHCs. Some States have adopted innovative measures
including mobilisation of local resources to clear this backlog. Increasing involvement of
the people's representatives, voluntary organisations and the people themselves in these
activities will be further encouraged during the Ninth Plan.
Care Institutions (PHIs) are
3.4.11 In some areas, the existing Primary Health
functioning sub-optimally because of one or more of the following factors:
1.
Inappropriate location, poor access, lack of maintenance;
2. lack of professional and para-professional staff at the critical posts,
3.
mismatch between the requirement and availability of health professionals
especially physicians at PHC;
4. lack of funds for essential drugs;
5.
lack of First Referral Units (FRUs) for linkage of referral services.
3.4.12 These problems need urgent resolution at the local level through dequate provision
of resources and intervention of the PRI.
3.4.13 Unlike the SC and PHCs, the number of functioning CHCs which form the First
Referral Unit (FRU) is far below the projected requirement. This gap should be filled
quickly so that the PHCs and Sub Centres do have a nearby referral hospital for the
management of 'high-risk patients’ who are referred. In most of the States there are
functioning subdistrict and taluka hospitals. With the restructuring of the Primary Health
Care Institutions in the Seventh Plan, these Institutions were to be redesignated as CHCs
149
and suitably strengthened. The Eighth Plan had also reiterated this strategy. States which
had implemented this suggestion, report that these FRUs are well utilised as they are located
in towns which are well connected with villages by transport and are well known.
3.4.14 m During the Ninth Plan, all the States will restructure the existing sub-district, taluka
hospitals and block level PHCs into functioning CHCs (FRUs); it is expected that once
this restructuring is completed, the current large gaps in functioning CHCs will be narrowed
substantially. Similarly existing rural hospital and dispensaries have to be restructured
wherever possible to meet the requirements in PHC. Earmarked funds under BMS could
be utilised for completing the restructuring and strengthening of these hospitals/dispensaries.
Health Manpower in Rural Primary Health Care Institutions
3.4.15 Health manpower position in Primary Health Care Institutions in the last year of
the Eighth Plan period is indicated in Table-3.
Paramedical Personnel
3.4.16 As per the national norms, one male and one female multi-purpose worker should be
available at the Sub-Centre catering to the Health needs of 3000 to 5000 population. The
number of sanctioned posts of male multi-purpose workers is only half, the number
required. This has been cited as one of the major factors responsible for the sub-optimal
performance in Malaria and TB control programmes. The availability of the female multi
purpose workers in adequate number has been the major factor for the near universal
coverage under the Immunisation Programme and improve-ment in Ante-Natal care. The
vacancies as well as the lack of sanctioned posts of radiographers, lab-technicians and
other para-professionals have adverse impact on ongoing Health and Family Welfare
Programmes. These need to be rectified as rapidly as possible and funds provided under
BMS in 1996-97 have been utilised by some States to fill the critical gaps in health
manpower.
<
<
3.4.17 During the Ninth Plan, several of the Centrally Sponsored Schemes including
Family Welfare Programme,
Revised National Tuberculosis
Control
Programme
(RNTCP), National Malaria Eradication Programme (NMEP), will provide funds for
recruitment of appropriate manpower, if necessary on contractual basis. Funds provided
under ACA for BMS may also be utilised to fill the critical gaps in health manpower. Every
district will undertake district-level manpower survey and planning, so that funds from all
these sources are optimally utilised to fill the existing gaps in vital manpower and
unnecessary duplication is avoided.
3.4.18 So far, the national norms for manpower requirement have been computed on the
basis of the population. During the Ninth Plan the
requirement of personnel
will be
computed not only on the basis of population, but also on the basis of workload,
distance to be covered and difficulties in delivery of Health Services.
A flexible
approach to recruitment of staff, if necessary on contract basis, will be adopted to ensure
that the programmes do not suffer due to lack of key personnel.
150
• Physicians in PHCs
3.4.19 The number of PHC doctors at the national level exceed the requirement as per the
norms. However, there are marked differences in their distribution . About 10% of the
PHCs are without doctors, while a similar number have three or more doctors. The
PHCs without doctors are mostly located in remote areas where health care facilities
under voluntary or private sector are also limited. The State Governments are taking steps
to redeploy the PHC doctors so that the needs of the population in under-served areas are
met on a priority basis. Some of the innovative approaches to fill the vacancies in underserved areas currently being tried in some States include :
i) local recruitment of doctors, if necessary' on part-time or contractual basis;
ii) adoption of a village/PHC/district by industrial establishments, cooperatives,
self-help groups and religious/charitable institutions;
iii) permitting local practitioners to pay a rental and practice in the PHCs after OPD
hours.
3.4.20 During the Ninth Plan, the feasibility and usefulness of these approaches will be
evaluated and those found useful in any area will be utilised as a part of local area- specific
micro planning for effective delivery of essential Primary Health Care.
Specialists at CHCs
3.4.21 A substantial proportion of specialists posts even in the functioning CHCs is vacant.
Hence these CHCs are unable to function as First Referral Units. In view of the
serious implications of this lacuna in the establishment of referral system, as well as
effective provisions of health, MCH/FP care, there is an urgent need to rectify this.
Improving the service conditions and providing a conducive environment are essential to
ensure that specialists in CHCs do stay and provide the needed services. At the moment,
there is no post of Public Health Specialist or Anaesthetist, in the CHCs. Services
of Anaesthetist are vital because without an Anaesthetist, emergency/routme surgery
in CHCs will not be possible. Efforts will be made to provide this critical manpower, if
necessary on part-time contractual basis. As a long-term measure, sufficient number of
in-service candidates may be trained in this speciality. It is vital to provide inter
linkage between preventive, promotive and curative services in the CHCs so that health
and family welfare programmes, disease surveillance and response mechanisms get
strengthened. Until the specialists in public health get posted in CHCs, the existing
specialists in these Centres who presently are mainly responsible for curative services, will
have to be given Public Health orientation, training in Epidemiology and health
management so that each one of them assumes the responsibility of looking after the
Disease Control Programme in their respective f specialities e.g. Immunisation by
paediatrician and FP by the obstetrician.’ This would also improve the linkages between the
CHC and the PHCs.
151
Tribal Health
3.4.22 The Scheduled Castesand Scheduled Tribes constitute 16.48% and 8.08%
respectively of the total population of the country as per 1991 census. The highest
concentration of tribal population is found in the North Eastern States and also in the UTs
of Lakshdweep and Dadra and Nagar Haveli. High concentration of tribal population is
also present in the States of Madhya Pradesh, Orissa, Gujarat, Maharashtra and Bihar.
The factors that contribute to increased disease burden in these communities include:
a) poverty and consequent undemutrition;
b) poor environmental sanitation, poor hygiene and lack of safe drinking water,
leading to increased morbidity from water and vector-borne infections;
c) lack of access to health care facilities resulting in
duration of illness;
d)
increased severity and/or
social barriers preventing utilisation of available health care services;
e) specific diseases they are prone to such as genetic diseases (G-6 PD deficiency).
infections (Yaws) etc.
3.4.23 The tribal population is not a homogeneous one. There are wide variations with
regard to education and health status, access and utilisation of health services amongst
these tribal populations. The tribal population in North Eastern States have high literacy
levels, they access available health facilities, and hence their health indicators and
demographic indices are better than national levels inspite of the fact that the region is
endemic for malaria. On the other hand, the Onges in Andaman and Nicobar remain a
primitive tribe with very little access to either education or health care. Differential area
specific strategies will therefore have to be developed for each of the' tribal areas to
improve access and utilisation of health services.
3.4.24 The National Health Policy accorded a high priority to provision of health services
to those residing in the tribal, hilly and backward areas as well as to endemic diseases
affecting the tribal population. The strategy adopted for meeting the health care needs
during the Eighth Plan period included provision of preventive, promotive and curative
services through the primary health care institutions, and at the village level through health
guides and trained Dais. Keeping in view the far-fiung areas, forest land, hills and remote
villages, where most of the tribal habitations are concentrated, the population coverage
norms for PHIs is relaxed to one PHC for every 20,000 population and one Sub Centre
for 3,000 population. While choosing the villages for establishments of Sub Centres the
States have been advised to set up at least 15% of these in Scheduled Castes' habitations
or villages having 20% or more Scheduled Caste population and 7.5% in tribal areas.
3.4.25 Till June 30, 1996 there were 20097 sub-centres functioning against a requirement of
28383 sub-centres for tribal areas. The number of functioning PHCs were 3260 against a
requirement of 4180 and functioning CHCs were 446 against a requirement of 492 There
are also 1122 Dispensaries and 120 Hospitals in Modern Medicine, 78 Mobile Clinics in
" 152
the
KeJ in the countty. As many as
16.845 Sub Centres. 5987 PHCs and 373
CHCs have been established in Scheduled Caste Basties/Villages having 20% or more
Scheduled Caste population. In addition 980 Dispensaries in Modern Medicine, 1042
Ayurvedic Dispensaries, 480 Homeopathic Dispensaries, 68 Unam/Siddha Dispensaries are
functioning in the Scheduled Caste concentrated areas in the country
Mobi
dispensaries and camps were organised to provide health facilities wherever feasible.
3 4.26 Even though efforts have been made to create primary health care infrastructure
and sanction necessary manpower both under modern medicine and under ISM&H there is
lack of both professional and paraprofessional manpower, mainly because the State Govt,
personnel do not prefer to work in these areas. The State Governments are trying to
minimise vacancies by taking contractual staff in tribal areas. A Central Planning
Committee has been setup to review the health care activities in j 9 districts o
States with pockets of extremely backward tribal population. The States have been
reauested to restructure the existing primary health care institutions, redeploy existing
personnel and make them fully operational. After this is done, it will be possible to compute
the caps in manpower/infrastructure and take steps to ensure that these are filled. In
addition to State Government funds, allocation from appropriate Centrally Sponsored
Schemes will also be available for filling critical manpower gap. For example, un er
the National Malaria Eradication Programmes 100% Central assistance is being provi e
for fillinc critical manpower gaps, and for drugs and insecticides in North Eastern
States manv of which have predominantly tribal population. The Tribal sub-project of
RCHwill also provide funds for manpower, equipment, drugs and training of statt.
3 4 27 Priority was also accorded to research in diseases to which Scheduled Tribes/
Scheduled Castes are prone. The Indian Council of Medical Research, has set up ive
regional medical centres in tribal areas in the country one each at
Bhuvaneshwar, Jodhpur, Dibrugarh and Port Blair to carry out research on health
problems of people in these regions, especially the schedded tnbes- 7116
In
institute of Hygiene and Public Health has also initiated a project Integrated Health
Development of Scheduled Castes and Scheduled Tribes of Sunderbans area of West
Bengal^ The Central Council for Research in Ayurveda and Siddha has set up research
projects, and conducted service- oriented survey to provide medical aid to Scheduled n es
and Scheduled Castes.
3 4 78 A review of all these activities will be undertaken in the Ninth Plan so that
information generated so far is transformed into well structured action programme.
During the Ninth Plan period priority action will be:
153
speciSy relaxed
s18®"8 k*"™ °f S“b CentreS and PHCs wil1
and proNe^XkbteXry S “h’8 'n,° ““““H'
dim“^ id
b) implementation of all
monitored in these areas;
ongoing
programmes will be
intensified and closely
c) 100% assistance under NMEP to tribal districts in other States will be provided;
d) specific projects will be evolved to meet the
requirements for RCH care of
the tribal population in the States such as MP, Bihar and Orissa.
Urban Health and Family Welfare Services
last’dt^?
Population lives in urban areas. Urban migration over the
• fi , / i 3S rCSU te^ ln raPlcl growth of people living in urban slums. The masshe
O of the population has also resulted in the deterioration of living conditions in
the cities. Some of the available data on health and related indices in urban and rural
Popula -on .s given m Table-4. From the data it would appear that the urban popukZn
has better health facilities and health indices than the rural population. However in manv
towns and cities the health status of urban slum dwellers is worse than that of the
rural population. I he urban health facilities provide health care, especially tertiary care
to both the urban and rural population, lhe available urban health care infrastructure is
insufficient to meet the health care needs of the growing urban population.
3.4.30 Realising this the municipalities, State Governments and the Central Government
have tried to provide funds for building up urban health care. Unlike the rural health
services, there has not been any well planned and organised efforts to
secondary and tertiary care services in geographically delineated areas provide primary,
in urban health
care| Asa result; there is either non-availability or substantial under utilisation
of
an res Pr'n’a'’'
'Vi‘h " ovcr-‘:ro"'di"S at secondary and tertiary care
3.4.31 During the Ninth Plan period, efforts will be made to evolve a well stmetnr^
organisation of urban primary healthcare to remedy the existing situation A health care
delivery system aimed at providing basic health and family welfare service to the
1. adequate outpatient facility;
2^ In-patient facility (at least 10 beds of which four will be for maternity
the remaining beds will be for medical, surgical and paediatric care);
are and
3. supportive services including laboratory and radiology facilities and pharmacy;
4. provision for referral/ transport of patients.
154
3.4.32 The essential services, to be provided, will include :
' 1. medical and surgical services including eye and ENT care;
2. Obstetric care and new-born care and child health;
3. counseling for reproductive health and contraception
4. dental services;
5. emergency and trauma care;
6. prevention and control of communicable and noncommunicable diseases;
For effective integration of health-related services the
ordinate with other assigned social sector activities of
provision of safe drinking water and sanitation.
urban health centres will coNagar Palikas especially for
3.4.33 An
An overview
overview of
of all
all the
the facilities
facilities available
available in
in a defined geographical area will be
undertaken and appropriate linkages between primary', secondary and tertiary' care centres
in the area will be established so that provision of basic minimum health semces and
optimal utilisation of the available health care facilities for referral sendees will be
ensured. Earmarked funds under BMS and the ACA for BMS will be effectively utilised
to fill the critical gaps in health manpower and infrastructure in urban areas also so that
the performance of both health and family welfare programme improve.
Involvement of Local Self-Government Institutions
3.4.34 With the 73rd and 74th Constitutional amendments the Nagar Palikas and
Panchayati Raj Institutions, are becoming operational in many States. During the
Ninth Plan period, these institutions will play increasing role <in ensuring planning,
implementation and monitoring of health and family welfare services at the local
level. They will also ensure effective coordination of programmes at the local level
between related sectors such as sanitation, safe drinking water and women and child
development, so that optimal benefit from all these programmes become available to
the community and the vulnerable segments receive the attention that they need.
Secondary Health Care
3.4.35 The secondary health care infrastructure at the district hospitals today functions
both as primary health care infrastructure for taking care of the needs of the population
in the city/town in which it is located and as secondary care Centres. This dual role
dilutes its effectiveness. To remedy the situation, initiatives were taken during the Eighth
Plan to ensure that these hospitals are able to cope with the referred cases. Four States Andhra Pradesh, Kamataka, West Bengal and Punjab - have initiated Secondary Health
System Development Projects with special focus on strengthening the District
Hospital and the referral services. This step is expected to reduce the burden on the
tertiary care hospitals, besides providing a credible and effective linkage with Primary
Health Care Institutions. In order to raise resources to meet the recurring costs of good
155
quality diagnostic and curative services, the feasibility of collecting user charges* from
patients (except those below the poverty line) is also being explored. These experiences
will enable the States to evolve and implement appropriate schemes for strengthening
these hospitals so that they cater to the increasing need for secondary care services
during the Ninth Plan period.Increasing involvement of private and voluntary sector in
secondary health care has been reported from many states. The mechanisms by which
secondary health care services could be made readily available and affordable through
collaboration between Government,private and voluntary sector will be explored during
the Ninth Plan period.
Tertiary Health Care
3.4.36 Along with the emphasis on enhancing the outreach and quality of primary’health
care services and the strengthening of linkages with secondary care institutions, there is a
need to optimise the facilities available in the tertian’ care Centres. At this level, there is
an ever widening gap between what is possible and what is affordable either for the
individual or for the country. Majority of the tertiary care institutions in governmental
sector lack adequate manpower and facilities to meet the rapidly growing demand for
increasingly complex diagnostic and therapeutic modalities. Over the last two deca'1 s
these institutions have been facing increasing resource crunch and have not been able io
obtain spares for equipment maintenance, to replace obsolete equipment, to maintain
supply of consumables and to upgrade the infrastructure necessary7 to provide high
technology, high quality care at affordable cost to meet the ever increasing needs and
rising expectation of the population. Several States have started levying user charges
for the diagnostic and curative services offered in these institutions from people above
the poverty line,to meet some of the recurring costs in providing such services. During the
Ninth Plan, efforts will be made to provide a one time support to selected tertiary care
institutions in each State and Union Territory to update their technical capabilities and to
evolve and implement a rational user charge policy that would enable these institutions to
provide high quality tertiary care at affordable cost. Some of the States are also taking
up experimental projects of establishment of pay clinics/ pay cabins for generating
funds required by the institutions. Necessary amendments have been made to enable these
hospitals to retain the funds generated by these activities so that they could be utilised to
improve quality of services available; If found successful it might also be possible
use the income from pay clinics as cross subsidy for treatment of patients below poverty
line. ; Other States are exploring the feasibility of providing land, water and
electricity at lower cost to private entrepreneurs for setting up tertiary care/super speciality
institutions if these entrepreneurs agree to provide 30% in-patient facilities and 40% of
the out-patient /diagnostic services free of cost for people below poverty line. Exemption
from import duty for import of diagnostic equipment has been given in the past to
private/ voluntary’ agencies who had agreed to provide diagnostic services to poor patients
free of cost. The advantages, disadvantages in these experiments need to be documented
and those found useful replicated in other settings.
Quality and Accountability in Health Care
3.4.37 Ensuring quality and bringing in accountability in health care provided is of utmost
importance. In recent years, there has been increasing public concern over these issues
156
because of both increasing awareness of the population and mushrooming growth of
institutions providing health care especially in the private sector. The” Consumer
Protection Act provides one mechanism for redressal of grievances pertaining to quality
of care. Some States have attempted to provide a legal frame work for the functioning of
private health care institutions on the lines of Bombay Nursing Home Registration Act
1949. Until now these legislative measures have not been effectively implemented mainiv
because of lack of objective criteria for defining 'quality of care’ and the possible
impact of such regulations on cost .of care.The cumulative experience generated thus far
will be utilised to evolve norms for quality and cost of health care and ensure
accountability in a uniform standardised manner.
Bio-medical and Health Care Technologies
3.4.38 Development and utilisation of appropriate technologies for diagnosis and
management of patients at priman; secondary and tertiary care is an essential pre
requisite for improvement in quality of health services without unnecessary escalation in
cost of health care. Realising the need for an in-depth review of the requirement for
supportive and diagnostic services at primary, secondary and tertiary care a separate
Working Group on this subject was constituted prior to the formulation of the Ninth
Plan.
3.4.39 During the Ninth Plan period the recommendations of the Working Group
regarding diagnostic and supportive services at each level, technologies and equipment
appropriate for each of these levels and maintenance of these will be implemented. In all
major institutions, a technical appraisal committee will be constituted to assess the
essential requirements and prioritise the same according to funds available. A national
mechanism for total quality appraisal of new technologies will be established. Efforts will
be made for the development and testing of appropriate inexpensive technologies for
1. measuring weight and height to facilitate early detection of under nutrition in adults
and children;
2.
colourimeters for bio-chemical test to improve diagnostic facilities at PHCs;
accurate self-recording instruments for measuring arterial blood-pressure for
use by ANMs/male multi-purpose workers;
4.
hand-held electronic data entry machines for ANM/MMPW to enable record
maintenance and updating for health and Family Welfare Programmes.
Health Insurance
; 3.4.40 Surveys carried out by NSSO indicate that the high cost of hospitalisation is one of
the factors leading to indebtedness especially among low and middle income group
population. Health insurance to meet the cost of hospitalisation for major illness will
ensure that health care costs do not become a major financial burden or cause of
indebtedness among these patients or‘their families. Over the last two decades several
health insurance schemes have been introduced. There are individual, family and group
insurance schemes for health care, senior citizens insurance and for specific diseases.
157
Some of the currently operationalised insurance schemes include Mediclaim, Group
Medical Insurance Scheme, Group Health Insurance Scheme, Bavishya Arogya
(Insurance for senior citizens), Senior Citizen Unit Plan, Cancer Insurance, Asha Deep
and Jan Arogya Bima Policy. The experience gained in the implementation of these
schemes will provide useful inputs for planning health insurance schemes during the
Ninth Plan period. The premium of health insurance may have to be adjusted on the basis
of health status of the person and age.of the person and his /her family at the time of
entry into health insurance. Yearly 'no claim bonus’/ adjustment of the premium could be
made on the basis of previous years hospitalisation cost reimbursed by the insurance
scheme. This would be a mechanism through which the health education messages
regarding the importance of remaining healthy through optimum utilisation of the
preventive and promotive services as well as adopting a healthy life style get reinforced by
economic incentives. Guidelines regarding what are the services for which
reimbursement of treatment cost will be borne by the insurance company may have to
be discussed, drawn up and implemented. Appropriate mechanisms through which the
insurance premiums for the people below the poverty line arc to be met will have to be
evolved, tested and implemented.
DEVELOPMENT OF HUMAN RESOURCES FOR HEALTH
3.4.41 The outcome and impact of any health programme depends on the competencies
and skills of the personnel who implement it. Both in the State and in the Central sector,
over 75% of the funds provided are spent to meet the salary of the employees.
Personnel costs form a major portion of investment in health service delivery in
voluntary and private sector. Unlike health service planning, health manpower planning
in India has not received adequate attention. There has been ven' little attempt to assess
the requirement in manpower and to match health manpower production with
requirement. While the production of physicians and specialists has been more than the
estimated requirement, dental and para-professional manpower production has lagged far
behind the present and projected needs. The curricula have not kept pace with the changing
health care requirements of the population or skills and attitudes required for
implementation of health and family welfare programmes. Continuous updating of
skills and knowledge have not been made an essential mandatory requisite for all
practicing health professionals. There are regional disparities both in quantity and
quality of available
health care professionals. These factors constitute a major
impediment to effective implementation of the health and family welfare programmes.
3.4.42 During the Ninth Plan, the objectives will be:
1. to establish an Education Commission of Health Sciences with the assigned
responsibility of planning and producing health manpower that is appropriate in
quantity to the
present and projected needs of the health system;
2. to strengthen the educational process*for all categories of health professionals at all
levels so that health care professionals possess necessary knowledge and have
appropriate skills, health programme_orientation and people orientation;
158
3'. to ensure continuing knowledge and skill upgradation of all health care providers
through Continuing Education. Programmes with emphasis on multi-professional
problem_splving learning strategies.
National Education Policy in Health Sciences
3.4.43 The need for National Education Policy in Health Sciences was emphasised in the
reports of Medical Education Review Committee 1983 and Expert Committee on Health
Manpower Planning, Production and Management 1986. A draft National Education Policy
in Health Sciences was prepared by a Consultative Group under the Chairmanship of
Member(Health). This draft Policy was adopted in the meeting of the Central Council of
Health and Family Welfare held in 1993 and its salient features shall be implemented
during the Ninth Plan. The Council recommended urgent action with respect of
establishment of Education Commission in Health Sciences.
Education Commission in Health Sciences
3.4.44 The Committee on Health Manpower Planning. Production and Management and
he Ninth Plan Steering Committee on Human Resource Development for Health
recommended that
Education Commission in Health Sciences (ECHS) must be
established as a Central Organisation on the lines of UGC to provide requisite financial
and technical support for professional and para-professional education in health
sciences, to provide realistic projection for national health manpower requirement and
to establish suitable mechanism to continuously review the projections based on felt
needs.
3.4.45
Major functions of the Education Commission to be constituted during Ninth
Plan shall include :
I
(1) provision ojjealistic prajections for national health manpower requirements hnd to
recommend the establishment of mechanism(s) through which such projections could
be continuously reviewed in the context of evolving social epidemiological and
demographic requirements.
crea-°—~f—durational institutions and facilities, or strengthening of such
facilities in already existing educational institutions through adequate financial and
technical support so as to facilitate the production of projected health manpower
and establishment of one or more Universities of Health Sciences in all States/regions.
(3) implementation
hanges required
implementation of
ot desired
desired, cchanges,
required to be brought about in the
curricular contents and training programmes of medical and allied health professionals
at various levels of functioning, to optimise health care delivery system.
(4) planning and implementation of appropriate, changes in the educational system
that would facilitate the establishment of essential inter-linkages between health
functionaries of various grades.
(5) establishment of a continuing review mechanism for the strengthening of health
related pedagogic communication and information technologies; development of
159
such health-related community educational programmes, using distance education
mode that could effectively and optimally utilise these technologies.
(6) development of in-built mechanism of reviewing, monitoring, and mid-course
corrections through financial and technical assistance so as to ensure expeditious
implementation of recommendations and decisions.
(7) co-ordination
-ordination of intersectoral health systems research by interlinking
education of suitable manpower with mission oriented research needs.
the
3.4.46 The Commission will in consultation with the Universities and Professional
Councils concerned, take all such steps as they may deem appropriate for the promotion
and coordination of Education in Health Sciences, including medical sciences at all
levels, nursing, pharmaceutical and dental sciences and other categories of health care
providers.
3.4.47 The Central Government has already initiated the process for obtaining approval
for establishment of the Commission as a statutory body. Due to paucity of funds only a
token provision of Rs.l crore was made for establishment of the Commission during 199697. Sufficient funds shall be provided during the Ninth Plan to make the Commission
fully operational.
Universities of Health Sciences
3.4.48 The Universities of Health Sciences will be the implementing arm of ECHS for
production, evaluation and sustenance of health manpower policy. The aim of the
Universities of Health Sciences is to create a physical and academic environment where
all Faculties of Health Sciences an interact together and provide a model for the education
and training of health care teams, through multiprofcssionaL and inter-professional
education. Inorder to achieve this it was recommended by the Bajaj Committee that such
Universities of Health Sciences be established in the country, one in each region to begin
with and subsequently one for each major State. The Universities will affiliate all Medical
Colleges, Dental Colleges, Para professional Colleges and Nursing Colleges, besides
possibly considering grant of affiliation to Colleges of ISM&H, imparting graduate level
education in the State. These Universities may have one or more constituent
professional colleges, and a number of study centres and field project areas. Three
Universities have already been established in Andhra Pradesh, Tamil Nadu and Karnataka
and another is being started in Punjab. Networking of these Universities with each other
and through the ECHS shall be established. Attempts will be made to establish at least one
University of Health Sciences in each region during the Ninth Plan period.
Health Manpower Planning
3.4.49 The Shore Committeejwas_the2fksLtp_recommcnd a population-based norm, for
medical (1/1500) and juirsing personnelfl/500). The Mudaliar Committee made
realistic
recommendations for progressive improvement in health manpower.
A
comprehensive situation analysis is available in the 1987 Report of the Expert
Committee on Health Manpower, Planning Production and Management (Bajaj
Committee). This Committee suggested that for assessment of health manpower
160
requirement several parameters including functionary to population ratio, inter
professional ratio and manpower-mix must be considered. It was further emphasised that
health manpower requirements would vary depending upon the income-elasticity and the
public and private expenditure on health. During the Ninth Plan, health manpower
planning will be linked to the needs and demands of health services. In addition, a fine
timing will be undertaken regarding health manpower development required for
specific components of the programme and health manpower requirements in voluntary
and private sector.
Health Manpower Production
3.4.50 The changes in medical, dental and nursing personnel over the last decade are
given in Fig-1. The Eighth Plan clearly stated that "the existing facilities for training of
medical graduates has outstepped the needs . No new medical college or an increase in
the admission capacity of the existing colleges will be supported during the Eighth Plan".
The Indian Medical Council Act was amended in 1993. According to this amendment
"no person shall establish a medical college and no medical college shall open a new or
a higher course of study or training including a post graduate course of study or
training or increase in its admission capacity in any course of study or training ,
without the prior permission of the Central Government". The Central Government
after due clearance from the Medical Council of India may grant permission for
establishment of new Medical Colleges if there was a requirement for manpower in the
field of practice of medicine and if other conditions specified in the enabling provisions of
the Act are fulfilled. A strict compliance of these provisions is called for.
3.4.51 The current stock of medical, dental, nursing and para-professionals in the
country, the number of training institutions, annual admission capacity for each
category are given in Table-5. During the Ninth Plan, no new medicaj college wall be
opened nor wall there be any expansion in the admission capacity of existing institutions as
there are adequate number of doctors in the country. Already, over two-third of the
doctors are undergoing post graduate training. Hence there is no need for any addition to
existing number of seats in various post graduate institutions, except for identified
specialities with unmet manpower needs.
3.4.52 There is an acute shortage of dental manpower in the country. There is a need to
ensure that adequate number of dental professionals of appropriate quality are trained. The
dental colleges are unevenly distributed in the country7. As many as 41 out of 96 dental
colleges are in one State. The quality of dental education needs to be reviewed and
appropriate remedial measures instituted.
3.4.53 Nursing education and nursing services have been given a high priority in order
to bridge the large gap between requirement and availability of nurses and ensure
quality of nursing training. These efforts will be continued during the Ninth Plan. In
addition, efforts will be made to . meet the increasing demand for nurses with
specialised training in speciality and' sub-speciality areas intensive medical and
surgical care in hospitals and for public health nurses in health care system.
3.4.54 Many programmes are faltering because of lack of critical para-professional
manpower. Over the last three decades, there has been an increasing requirement of several
161
categories of para-medical persons such as male multipurpose worker, laboratory ,
technicians, radiographers. Their availability and requirement vary from State to State
and from time to time. Till the Eighth Plan the medical colleges, dental colleges and
nursing training institutions have been the major training institutions for para
professionals. During the Eighth Plan the Open University system and the vocational
training courses at 10 + 2 stream have provided two additional mechanisms for education
and training of para-medical manpower. During the Ninth Plan the State manpower cells
will assess the changing requirements for para-professionals, preferably at the
district level and take necessary steps to meet the requirement through all available
training channels.
The Universities of Health Sciences (UHS) will ensure that
appropriate curricula are evolved dnd followed. The State Governments will make
necessary amendments in recruitment rules for these posts so that those who qualify
through vocational courses and open university system become eligible for the jobs in
Government, voluntary and private sectors. The feasibility of introducing pre-vocational
courses at the 9th and 10th standards will be explored.
Bio-Informatics, Telematics and Distance Education
3.4.55 As early as 1986-87, the Expert Committeei on Health Manpower Planning,
Production and Management (Bajaj Committee) recommended: ’’for an effective support
to the health manpower management, information system is vital for managerial
efficiency. The health manpower information should encompass all the components of the
health manpower management. The Committee recommends development of national
health manpower information system as an important support to the health manpower
development strategies." While recommending the establishment of Universities of
Health Sciences, it was further emphasized that "it is entirely likely that several new
faculties will grow in the University of Health Sciences : It is expected that a faculty of
health information systems shall also be established in the Health Science Universities .
3.4.56 In spite of these far reaching recommendations, necessary action plans have yet to
the concretised. Information Technology (IT) is now becoming one of the major
components of the technological infrastructure for health management. All sub-sectors
dealing with the generation, transmission and utilisation of demographic and
epidemiological data such as
bio-informatics, bio-statistics,
health management
information system (HMIS) and decision support systems (DSS) are finding increasing
use in health planning and management. With the nation-wide network, NICNET, under
the Planning Commission, giving health information support through its MEDLARS, Bio
Medical Informatics Programme and Tele-Medicine Programme, a viable nucleus has
already been set up which will be enhanced during the Plan period to cover all the Primary
Health Centres and district hospitals. MEdNET, when operational, shall become a major
instrumentality of continuing multiprofessional
education and distance
learning.
Policy initiatives shall be undertaken during the Ninth Plan with the aim of developing
clinical leadership, deciding which applications arc to be supported, providing the
appropriate technology, gaining clinician acceptance, setting up in Universities of
Health Sciences one or more clinician-driven academic unit(s) and nctwork(s) that are
multidisciplinary and multisite to provide support for new and existing biomedical
applications.
162
Health Manpower Information System
3.4.57 At the moment only infrastructure and manpower at the primary health care
institutions are monitored and information periodically updated. There is no mechanism
for obtaining and analysing information on health care infrastructure and manpower in
private and voluntary sectors in the district. Unless this information is available it will
not be possible to undertake any effective area-specific microplanning so that the health
manpower required to meet the local health needs of the population is provided. This
exercise becomes even more important in the current context when the population is
undergoing a demographic, health and economic transition and there are marked
differences in the health profile between States and districts. There is also the need for
aggregating this data at the State and Central level so that appropriate policy and
programme initiatives can be undertaken and adequate resources allocated.
3.4.58 During the Ninth Plan, attempts will be made to create a district data base on
health manpower belonging to various categories (including the 1SM&H practitioners)
working in Central and State Government, voluntary, private sectors, defense services
and Railways and public sector undertakings. The District Manpower Cell will assess
district manpower requirement and availability and assist the Stale in manpower planning
at district level. District-based manpower profile data will be updated at least once in
an year. Health manpower planning exercise at district. Stale and regional level by the
University of Health Sciences will be carried out utilising this data and the information
on the health care needs of the population and health facilities available. The Education
Commission for Health Sciences (ECHS) will act as the nodal agency for the exercise at
the national level.
3.4.59 The Health Manpower Planning, Production and Management Committee in 1987
recommended that the ECHS must be established as a central organisation on the lines of
UGC for professional and para-professional education in health sciences, inter alia to
provide realistic projection for national health manpower requirement and suitable
mechanism to continuously review the projections based on felt needs. During the Ninth
Plan period, the ECHS' will promote all educational activities for all categories of
health manpower at all levels. The UHS will develop newer faculties such as health
management, health economics, social and behavioural sciences. UHS will also
initiate necessary steps to enhance computer literacy among medical students and
expose them to emerging technologies of informatics and telematics which are likely to
the base and basis for 21st century mode of communication through telemedicine and
distance learning by open learning system in medicine and health sciences.
Health
manpower cells in the States will coordinate collection of data on manpower at district
level and implement the recommendations of UHS for health manpower production.
Quality of Education in Health Sciences
3.4.60 One of the important reasons for the -sub-optimal per-formance of health care
institutions is the poor quality and inappropriateness of the education and training of
health care providers, resulting in a lack of problem-solving competencies and skills .
During the Ninth Plan period, appropriate changes in syllabi, curricula, teaching methods
and assessment system will be made through various professional Councils to improve
the undergraduate and post-graduate training so that the medical and dental graduates as
163
well as allied health professionals acquire necessary technical knowledge and managerial '
skills to solve health problems and implement ongoing major national health and
family welfare programmes within the existing constraints.
3.4.61 Medical colleges are periodically inspected by the Medical Council of India (MCI)
regarding both the
physical facilities and training process. During the Ninth Plan
Plan,
inspection by the MCI will be inot only
* for
" initial
‘ ‘
recognition but also for continued
recognition as medical colleges and admissions will not be permitted unless the college i:
is
recognised. Attempts will be made to reorient education in health sciences so that the
health care system becomes more efficient and effective. The existing professional
Councils and any other Council which may be established in the future, will be
responsible for ensuring the quality of medical and para-medical
education, training
and ethics of conduct and practices as per the statutory requirements.
Continuing education for health professionals
jAb2 In the context of the rapidly evolving technology, demographic transition,
changing lifestyles and disease patterns it is imperative that the process of continuing
education is internalised throughout the working career of all health professionals so
that their knowledge and skills are updated. Currently, in-service training courses in
^nous institutions, thematic CME programmes conducted by National Academy of
Medical Sciences, National Board of Examinations, and various professional bodies
and associations have played a major role in CME. All these programmes will be
expanded and intensified during the Ninth Plan. In addition. Open Universities will play a
major role in periodically updating the skills and knowledge of various categories of
ealth personnel. The Open University mechanism can efficiently and cost effectively
provide specific training programmes where there is a major component of didactic
earning eg. epidemiology, hospital administration and health management. It is also
likely to be one of the most effective, efficient and cost-effective method of CME
involving practitioners in Government, private and voluntary sectors and hence requires
increased utilisation.
M
. .63 During the Ninth Plan, a major programme of multi-professional and inter
professional education will be initiated for training the members of health care delivery
team, so as to enable them to accomplish group tasks in providing health care in the
community. At the national level there will be training of the trainers in newer
echnologies national programmes on emerging diseases and their management. At the
State level there will be a similar training of personnel with special reference to the State's
requirement. At the district level two types of training programmes have to be
undertaken 1) the multi-professional health team training in delivery' of integrated
health and family welfare service at the primary health care level; and 2) the training of
e multi-professmnal team for the delivery of evolving programmes eg. the delivery of
RCH care programme.
J
3.4.64 In addition, there will be training of the health professionals working in the
government voluntary and die private sectors together as a team to ackle the identified
health problems in the district. Inter-sectoral training of personnel from related sectors
eg nutrition, agriculture , water resource management and environmental sanitation
Will be undertaken as and
- ’ when
’
necessary.
164
Control of Communicable Diseases
3.4.65 At the time of Independence communicable diseases were the major cause of
morbidity and mortality in the country. Efforts were therefore initially directed towards
their prevention and control. Smallpox, a major killer in pre-Independence era has been
eradicated. In 1953, malaria affected over 75 million and killed 0.8 million people.The
National Malaria Control Programme, which was launched in 1953, successfully
brought down the incidence of malaria to 0.1 million cases with no death by 1965.
Subsequently, there has been a resurgence of malaria. The Modified Plan of
Operation has, however, succeeded in keeping morbidity and mortality at relatively low
levels. The use of antibiotics has resulted in a substantial reduction in deaths due to
common infections. Effective therapy for infections and vaccines for prevention of
infection were the major factors responsible for the steep fall in crude death rate from
25.1 in 1951
to 8.9 in 1996. However, the morbidity due to communicable
diseases continues to be high. Deteriorating urban and rural sanitation, poor liquid and
solid waste manacement and overcrowding have resulted in an increasing prevalence of
common communicable diseases. TTe re-emergence of diseases like Kala Azar, and
emergence of new infections like HIV have added to the existing disease burden due to
communicable diseases. Control of communicable diseases is becoming more difficult
because of emergence of drug-resistant pathogens and development of insecticide-
resistant vectors.
i
3.4.66 Even though health is a State subject, the Central Government has over the last
forty years provided additional funds through Centrally Sponsored Schemes (CSS) for
control of some of the major communicable diseases. Of these, the National Leprosy
Eradication Programme is likely to achieve its objective of reduction in leprosy prevalence
to below 1 per 10000 by the end of the Ninth Plan. However, malaria, tuberculosis and
HIV infection require vigorous and intensified efforts for their containment and control.
3.4.67 The performance in, and shortcomings of, these National Programmes have been
evaluated during the Eighth Plan period by Expert Committees. Accordingly, following
remedial measures will be taken during the Ninth Plan period to:
1. rectify the identified defects in the design and delivery of these programmes,
2. fill the critical gaps in infrastructure and manpower;
3. improve the operational efficiency and the quality of sendees;
4. make service delivery system more responsive to users
needs;
5. ensure that health care providers have the necessary
including referral facilities and supplies they need;
165
skills and
support,
6. improve the community awareness of the existing services through IEC
efforts so that there is optimal utilisation of available services.
3.4.68 External assistance has been obtained to augment available funds for implementing
these programmes. These National Programmes will continue as CSS during the Ninth
Plan period.
New initiatives during the Ninth Plan
Horizontal Integration of Vertical Programmes:
3.4.69 Initially, when sufficient infrastructure and manpower were not available for
management of major health problems, several vertical programmes eg. National
Malaria Eradication Programme (NMEP), National Leprosy Eradication Programme
(NLEP) were initiated. Subsequently, over the years a three- tier health care infrastructure
has been established. During the Ninth Plan period, efforts will be made to integrate the
existing vertical programmes at district level and ensure that primaiy health care
institutions will provide comprehensive health and family welfare services to the
population.
3.4.70 In order to assist the PHC/ CHCs officers to effectively implement such a horizontal
integration, the middle level public health programme managers who ar
arc currently heading
the vertical programmes at district level will be given
--- the
--- additional
----------- 1 task of ensuring
coordination and implementation of integrated Health and Family Welfare Programme at
Primary Health Care institutions in defined blocks. Involvement of the public health
specialists at the subdistrict level will also improve data collection, reporting,
strengthening HMIS, improving the supply of essential drugs/devices for all programmes
at PHCs/CHCs and enabling operationalisation of the disease surveillance and response
at district level.
Disease Surveillance & Response
3.4.71 Given the existing conditions of poor environmental sanitation and the
weakness ofthe public health system it may not be possible to completely prevent
outbreaks
of communicable diseases in the near future. Delays in recognition and
reporting of focal outbreaks, absence of functioning HMIS and disease surveillance system
result in delays in implementation of appropriate response and consequent high morbidity
and even mortality. The Expert Committee on Public Health Svstem chaired by Member
(Health), Planning Commission recommended the establishment of an epidemiological
surveillance system. During the Ninth Plan, establishment of a functioning system for
early detection and prompt response for rapid containment and control of the disease
out reak will receive high priority. Disease surveillance and response will be at district
level to ensure prompt, effective, efficient remedial action utilising the existing
infrastructure. This system will be given the necessary back-up,
laboratory
and
epidemiological support so that containment measures are based on sound data and
scientific rationale. This back-up system will be evolved by strengthening and optimal
utilisation of the facilities and expertise available in the national institutions/medical
colleges.
166
3.4.72 The regulations governing notification of diseases vary widely between States.
There is an urgent need to develop a uniform regulation for notification of diseases in all
States. The diseases that are to be covered under the notification system should consider
adequately the problems of new, emerging and re-emerging infections so that appropriate
response could be generated to tackle the situation.
Hospital Infection Control and Waste Management
3.4.73 Increasing incidence of hospital-acquired infections and accidental infection in
health care providers and waste disposers, renders it imperative that efforts are made to
improve infection control and waste management through utilisation of appropriate,
affordable technology at all levels of health care. During the Ninth Plan period, infection
control and waste management in all health care institutions will receive due attention
and adequate funding.
National Malaria Eradication Programme (NMEP)
3.4.74 In the early fifties, malaria was not only a major cause of morbidity and mortality
in the country but also one of the constraints for ongoing developmental efforts. Illness
due to malaria was a major cause of absenteeism in agricultural and industrial labour
and in irrigation and construction workers in the fifties. The National Malaria Control
Programme, the first of the Health Sector CSS, aimed at reduction of the morbidity and
mortality due to malaria, was launched in 1953. It is noteworthy that even though there
was no well established health infrastructure in rural areas, the number of cases came
down from 70 million in 1950 to 0.1 million by 1965. However, subsequently, there
was a resurgence of malaria. In 1976 over 6.7 million cases were reported. From 1977,
the NMEP started implementing a Modified Plan of Operations for control of
malaria. After the initial success the number of cases have remained at over 2 million
(Fig-2). <. Initially, malaria in India, was mainly a rural disease.^ Subsequently, due to
major ecological changes five more eco-types have been recognised viz., forest and forest
fringe malaria; rural malaria; urban malaria; industrial malaria; border malaria and
migration malaria.
3.4.75 The North Eastern (NE) States have high incidence of P.falciparum malaria.
High morbidity, mortality due to malaria and emerging problem of drug resistance are
reported. A major initiative during the Eighth Plan (1994) was to provide 100% Central
Assistance for NMEP in NE States so that financial constraints do not come in the way
of effective implementation of the NMEP. The performance of NMEP during the Eighth
Plan period is indicated in Table-6. There has been an increase in the number of cases of
malaria reported during the Eighth Plan period. The proportion of Pf infection has
increased to 40 per cent. Many of the fever patients are not screened, diagnosed and
effectively treated primarily because of lack of male multipurpose worker and
laboratory technicians. Not all the diagnosed cases are reported to the programme
authorities. Residual insecticide spraying is often not done at appropriate time.
Community involvement in spray operations and the bioenvironmental measures for
control of mosquito breeding are poor. Some of the vectors of malaria have developed
resistance to one, two or three of the currently used insecticides.
167
3.4.76 There is an urgent need to intensify the malaria control activities during the Ninth
Plan period especially in the States which had been reporting large number of malaria cases
(Fig-3). The NMEP has, therefore, drawn up a programme for intensive and effective
implementation of the Modified Plan of Operation (MPO) in malariogenic areas in the
country during the Ninth Plan. Financial assistance has been procured from the World
Bank for augmenting domestic funds available for implementation of the programme.
3.4.77 The criteria for selecting the areas for intensive implementation of MPO during
the Ninth Plan are:
&
(i) annual parasite incidence of more than 2 for the last 3 -years;
(ii) Pf. rate of more than 30%;
(iii)deaths due the malaria reported
(iv) tribals form more than 25% of the population.
The areas identified on the basis of these criteria arc the 7 North Eastern States and 100
districts spread over the States of Andhra Pradesh. Bihar, Gujarat, adhya Pradesh
Maharashtra, Orissa and Rajasthan.
3.4.78 The ongoing programme with 100 percent Central assistance in the seven NorthEastern States will be continued during the Ninth Plan. Additional inputs will be
provided to the 100 hardcore and tribal districts identified on the basis of the above
criteria. Enhanced malaria control programme will also be implemented in 19 cities/
towns which have rising slide-positivity rate and in areas where there have been
focal outbreaks of malaria in the previous year.
3.4.79 The main components of MPO which will be strengthened In these areas are:
1. early diagnosis and prompt treatment,
passive surveillance and laboratory diagnosis;
through
strengthening of active and
2. selective vector control by integrating various vector
promotion of personal protection methods;
control approached and,
3. prediction, early detection and effective response to malaria outbreaks;
4. intensified information, education and communicable campaign.
3.4.80 In spite of the reported increase in drug resistance, Chloroquin will remain the
first line drug for presumptive treatment and Primaquine will be given for radical
treatment. Sulpha pyrimethamine drug combination will remain as the second line of
treatment especially for Pf cases in areas where drug resistance is reported and selective
use of quinine will continue for treatment of severe and complicated malaria.
3.4.81 The village will be the unit for residual insecticide spray operations. DDT will
continue to be the insecticide of choice in areas where vector is sensitive because of its
efficacy and cost effectiveness. In areas where DDI is ineffective, Malathion maybe
168
used. Synthetic pyrethroids will be used only in areas where triple insecticide resistance
are reported. Personal protection through use of insecticide impregnated bed nets will be
advocated. In urban areas stringent measures to prevent stagnation of water, ensure
covering of overhead tanks and drains and enforcing periodic cleaning will be attempted.
3.4.82 With effective implementation of the Programme, it is expected that by the end of
the Ninth Plan the following targets will be achieved in malariogenic areas: 1. ABER of
over 10%; 2. API less than 0.5% and 3. 25% reduction in morbidity and mortality
due to malaria.
Kala-azar
3.4.83 Available data indicates that Kala-azar is endemic *ini 36 districts in Bihar and 10
^1 (population
75 million). Periodic outbreaks of Kala-azar with
districts in West “Bengal
(
increase iin morbiditv and mortality continue to occur in these States. Over 90% of the
reported cases and over 95% of the reported deaths are from Bihar. Over two third of the
cases in Bihar are reported from 7 districts.
3.4.84 The Government of India is implementing a CSS for control of Kala-azar in Bihar
and West Bengal. Following reported increase in the number of cases and deaths due to
Kala azar in 1989-91, an intensive programme for containment of Kala-azar was launched
i
in 1992.
i
3.4.85 The strategy for control of infection includes, interruption of transmission through
insecticidal spraying with DDT and early diagnosis and treatment of Kala-azar cases.
The Government of India is providing insecticides and anti Kala-azar drugs. The State
Governments meet the expenses involved in the diagnosis and treatment and insecticide
spraying operations.
< 3.4.86 Effective implementation of the programme resulted in a decline in both Kalaazar cases and deaths during 1993-95. However, there were delays and inadequacy of
be
the insecticidal spray operations during 1995-96' the decline could not
maintained(Table-7).
3.4.87 During the Ninth Plan, the focus will be on ensuring effective implementation
of the programme so as to prevent outbreaks and eventually to control infection. DDT
will continue to be the mainstay for insecticide spray as the vector (Phlebotomus
argentipes) is still susceptible to DDT.
Other Vector-borne Diseases
Filariasis
3 4 88 Filariasis is endemic in Southern, Eastern, Western and Central Indian States. It is
estimated that about 428 million (113 urban, 315 rural) people are living in areas
where filariasis is endemic.'Reports from 13 States and UTs covering about 48 million
population indicate that annually 6 million persons suffer from acute lymphangitis due
to filariasis. Chemotherapy and vector control measures have succeeded in reducing
169
TRAINING ON WOMEN’S HEALTH
BY
T. K. SUNDARI RAVINDRAN
&
&
Prepared for the
National Consultation Towards
Comprehensive Women’s Health Policy and Programmes
BY
VHAI-WAH!-DSE
Heid in VHAI, New Delhi.
February 18-19. 1999
TRAINING ON WOMEN S HEALTH
TK Sundari Ravindran
This is a statement and elaboration of the conceptual framework underlying training on
women's health conducted by me for a wide range of groups: community health workers of
Rural Women’s Social Education Centre, Chengalpattu, doctors training for a Masters in
Public Health in Kerala; District health service managers from Southern Africa attending a
course on gender issues in health; and programme officers of a donor agency funding
community health projects in developing countries.
\
I. Conceptual framework for the training/course:
The entire approach to gender issues in health adopted in the various training workshops/
courses is informed by the discourse which views health as more than a medical issue confined
to natural and biological factors amenable to medical interventions.
How we live, what we do, who we interact with, and the nature of these interactions and
relationships - all these affect our health. Feeling healthy is closely associated with feeling
relaxed, productive and useful; living in healthy and pleasant surroundings, and amidst
supportive relationships with people we enjoy being with. Thus, health is a socially
constructed reality, a product of the physical and social environment in which we live and act,
which are in turn affected by the global and local environment: social, cultural, economic and
political. Inequalities in health arise largely as a consequence of differentials in social and
economic status, and differential access to power and resources.
Within this framework, the need to address gender issues in health is evident. Biological
differences that lead to gender- based differences in health needs are well acknowledged. But
this is not all. Women and men have differential access and control over resources; differing
roles and responsibilities and different social realities. This directly influences the risks they are
exposed to, their ability to stay well. Moreover, male and female socialisation processes and
social identities are so vastly different that they often have differing definitions of health and
ill-health, and differing perceptions of what they are entitled to, when they fall ill. This again
influences their health seeking behaviour.
Access to and utilisation of health services (formal or informal) is an important mediating
factor influencing the outcome of an illness event. There are two sets of factors which would
affect women’s access to and utilisation of health services. The first set of factors are the same
as those outlined above: whether women recognise the need to seek help; feel entitled to do
so; and have the means to access health services. The second is the nature and characteristics
of the health care system itself: whether it has a wide and equitable coverage, is public or
private, available free of cost/at subsidised prices, the range and quality of services provided;
and the gender ideology it reflects (treating women only as mothers; women as incapable of
making independent decisions or articulating their health problems reliably, etc.)
In understanding the determinants of women’s health, it is important to disentangle those that
relate to women’s 'condition’: their class, race, ethnicity or position in the social hierarchy as
member of a community, which they share with the men in their households - and those that
relate to women’s ‘position’: their relative status within the household in terms of power and
J tv'
control over resources. It would be naive to talk of-women’s’ health in general - we need Io
acknowledge inequalities and differentials across different groups of women-.by caste, class,
ethnicity, place of residence, to mention only a few.
Factois operating at the individual, household (position) and community (condition) level
are themselves subject to the influence of the national and the global environment. A
community s access to resources is a function both of the country's level of prosperity (the
size ol the cake) as well as on the community’s relative power in the national scenario ( its
distribution). Similarly, international forces such as a slump in the export prices of agricultural
commodities may cause widespread unemployment in a local community and in turn affect the
resources available to a household and to its women.
The variables identified in this framework are very many; however, these may be reduced to
four major groups of factors:
1 Backgiound factors - operating at the international, national and local levels, which affect a
household s access to and control over resources
2. Health service factors - at the national and local levels
j. Women’s status - autonomy, access to resources, power and authority, and
4. a) Women’s illness burden
b) Women’s health seeking behaviour
The mterlinkages between these factors and how they relate to women’s health status at any
given point in time is depicted in Figure 1.
II. Designing a course based on the above framework:
fheie are at least three essential modules that would constitute a course based on the above
framework, and a fourth module pulling together the first three:
Module 1: a) Gender analysis - understanding differentials by sex as arising from differentials
in access to and control over resources; and as sustained and perpetuated by the patriarchal'
k eology that accepts as the natural order of things men’s superiority and the privileges
ensuing.
°
b) Control over women’s sexuality and reproduction as an important component of
the patriarchal ideology
Module 2: Social determinants of health and illness
a) Introduce health as a development issue; illustrate the social determinants of illness: class,
race, caste, and introduce gender as one determinant of health, but different from the above
because it cuts across ail the above categories. Introduce literature that shows gender
diffeientials to persist across class groups, or other sources of inequality in health.
b) intioduce the various levels at which health determinants operate (international, national,
community, household, etc), underscoring the role of political power, and provide at least one
clear-cut example of how GENDER determines health status at each of the various levels.
Module 3: Analysis of the health care system: Formal and informal/public and private and
traditional and modern sectors; organisation of the formal health care system: ideological
premise, finances, coverage, range of services, quality, and attitude to women (sexism in
medicine); how this translates into availability or non-availability of health care for women at
the local level.
Module 4 Understanding factors influencing women’s health : a) those that contribute to their
illness burden and b) those that affect their access to health services ; and planning
interventions at various levels, to both reduce women’s illness burden and improve their access
to quality health services which are gender-sensitive and responsive to women’s needs.
Optional Module: To run concomitantly with 4: A gender analysis of the etiology of women’s
health issues through their life cycle which take into account their CONDITION and
POSITION, and their PRODUCTIVE, REPRODUCTIVE AND COMMUNITY ROLES.
For example, analysing nutritional status in childhood, adolescence and adult years, explicitly
taking into consideration how women’s productive and reproductive roles at each stage would
affect it, for women from various class/caste groups.
/■'
I
■
"H
o
Q Background Factors
c
n
ft
J
3
f
International
N-S power relations
influencing trade, aid. and
national economic policies
2
transnational pharmaceutical
and medical suppfies industry;
population coning lobby'
Health Service Factors
I
National
organisation; financing; coverage and
distribution; priorities and quality of care
National
l<ll
o
political structure; social
stratification; resource base;
resource distibution
o
Local
tn
Local
community structure;
• power distribution;
resource base:
.
access to services: physical,
economic 'and social
CD
to
pnonties and quality of care
5"
ra
resource distribution
!o
community heafth culture
I
□
El
women's status (Autonomy, access
to resources; power and authority)
women’s health
seeking behaviour
1'
f
illness burden
Is
health status of women
il
g
WOMEN’S HEALTH POLICIES:
ORGANISING FOR CHANGE
BY
T. K. SUNDARI RAVINDRAN
’repared for the
National Consultation Towards
Comprehensive Women’s Health Policy and Programmes
BY
VHAI-WAHJ-DSE
Held in VHAI, New Delhi.
On February 18-19, 1999
Introduction
Womens Health Policies:
Organism for Change
T K Sundari Ravindran
!
I
i
\7~ W1HE 1970s saw the emergence of organised
Women's health policies
efforts by the feminist movement to
Brazil was the first country to create a
demand changes in legislation, policies,
comprehensive women's health policy in 1983.
-LL programmes and services in many areas
Since then, Australia and Colombia have also
affecting women's reproductive health formulated national policies. A comparison of
abortion, birth control, shelters for battered
the subjects of these policies show s, as do the
women, rape crisis centres, and sexual selfdraft policy proposals recently put together by
determination - as well as other aspects of women in South Africa, that women's health
women's lives, such as economic independence.
agendas have much in common despite the
Services to meet women's health needs set up by
widelx- varying social contexts from which they
women appeared in many parts of the world.
originate. They address the fact of gender-based
The campaigning and service delivery
discrimination and other social disadvantages
experiences during that decade led to the
imposed on women, which are a major part of
conceptualisation of women's health and
the reason why these policies are needed. They
recognition of the need to make health care
go beyond conventional medical concerns,
women-centred and gender-sensitive. These
which centre around illness management, to
experiences have occurred side by side with the
address issues such as violence against women,
involvement of feminists in influencing policy
mental health, occupational health, the
and in more recent years, their participation in
consequences for women of ageing, the health
national and global policymaking, programme
effects of sex-role stereotyping, ethical and
design and implementation, and provision of political issues - as well as medical concerns.
education and services. Ideas emerging from the
For example, in Australia five key action areas
feminist health movement have influenced
were identified:
women working in policy, law and health service
systems considerably, and vice versa, encourag
• improvements in health services for women,
ing change both from within and without.
• provision of health information for women,
This issue of Reproductive Health Matters
• research and data collection on women's
focuses on the policies that have emerged from
health,
these ongoing processes. They reflect on how
• women's participation in decision-making in
policy formation occurs, the forces that have
health, and
facilitated or hindered change, the myriad
• the training of health care providers.
considerations that go into policymaking, and
(Wainer and Peck)1
what needs to be done alter policies are in place.
These are stories of success, lack of success, and
Reproductive and sexual health constitute the
successes derailed. More than anything, they
core of women's health policy. This is not merely
highlight how complex the achievement of an
because women bear a greater burden of illintegrated women's health policy is.
health from childbearing. Rather, the focus on
reproductive and sexual health has emerged
_______ _________ r* *'j______
7
Ravind ran
International Conference on Population and
Development (ICPD). Yet reproductive and
sexual health and rights issues have been
advocated by women's health advocates for
many decades now, going back far into the last
century and more. For example, Pearson
describes how the National Women's Health
Network in the US has worked with and tried to
influence US Food and Drug Administration
policy since the 1970s; Wainer and Peck give a
brief history of feminist health movement
activities in Australia in the same period; and
Laura Kaplan's book tells the history of Jane,
probably the world's first abortion underground
network, in the US (Round-Up).
The ICPD Programme of Action was influ
enced considerably by the women's health
movement; many other factors also played a role.
The AIDS pandemic and the resulting concern
with sexual behaviour was one. Another was
dissatisfaction among service providers with the
limitations of existing family planning and
maternal/child health (MCH/FP) programmes.
from the conceptualisation and articulation of
women's lack of control over their bodies, their
fertility and their sexual lives - and therefore
their health. For example, social control over
women's sexuality has taken various forms, eg.
criminalisation of abortion, demographically
driven population control programmes, female
genital mutilation and other forms of violence,
and forced marriages, all with impact on fertility
control.
'Reproductive health is not now, and never has
been, simply a matter of preventing disease. This
is because a woman's ability to bear children is
linked to the continuity of families, clans, and
social groups; the control of property; the
interaction between human communities and
their environment; the relationship between men
and women; and the expression of sexuality. It is
therefore valuable currency in every society and
the object of regulation by families, religious
institutions and governmental authorities.'
(Maine et al)
The scant regard accorded to women's
experiences in the formulation and implemen
tation of health policy has been and continues to
be a fundamental concern of the women's health
movement. To redress this situation implies
nothing short of a radical departure from current
strategies and changes in the whole mind-set
governing the design of health programmes and
service delivery. Influencing mainstream health
services to make them bottom-up and gender
sensitive as well as more humane, constitutes an
important component of the policy work
discussed in these pages.
One way this may be done is illustrated in the
paper on the Proyecto Madre (Project Mother)
initiative in Bolivia (Bender et al), in which health
service providers change the way they provide
care for women, working as a team in a
participatory process which starts with going
into the community to meet women and hold
discussion workshops about health care.
A* .
.
‘
What is this reproductive health
THING?
Reproductive health policy is much more than a
reproductive health approach to family planning.
The latter represents a limited and limiting
medical approach, focused on adding a few
additional services such as the control of
reproductive tract infections to existing MCH/FP
programmes. A reproductive health policy based
on the premise of respect for women's
reproductive rights, as the authors in this journal
explain, would recognise the central role of
women's status and well-being and would:
• pursue approaches which enhance women's
information base, and enable women's
control over their fertility and sexuality; better
self-care and prevention and management of
reproductive and other health problems.
• adopt a life-cycle approach to reproductive
health needs starting before menarche and
continuing post-menopause, instead of being
ric^owly focused on the pregnant woman and
the faTnily planning adopter.
• rely- bn holistic and integrated solutions that
take into account the social, biological as well
as psychological causes of illness, and seek to
Where did it all start?
These issues were suddenly elevated to centre
stage by the media and by international
participants (governmental and NGO) who
worked on the Programme of Action for the
8
t
Hcproductive Health Mullvis. No 6, November 1995
promote public health overall
• plan from the grassroots up, respect women's
knowledge and definition of their health
needs, and provide good quality services in a
humane and caring setting.
t-
danger that nothing more than the minimum
may ever be implemented. In a time of scarce
resources and growing tension between fiscal
constraints and the pressures created by new
technology, conflict between the 'economically
attainable' and the 'medically possible' has
inevitably arisen.2
To have to do less than what is technically
possible, and putting lives and well-being at risk
thereby, is not an easy role to shoulder. On the
other hand, policy commitments that promise
too much and do not deliver are also risky, as
Kennedy et al show in their paper on maternal
and congenital syphilis. Can we eradicate it in the
Americas, they ask, and should we try?
Clinics for women in Brazil and Sierrdeone
(Round-Up) among many others have had nearly
a decade of experience in providing womencentred reproductive health services which
adhere to these principles. They have important
lessons to offer on how much can be done with
limited resources.
The focus, however, must be to apply such
models at a national scale, so that all women can
be served. A strategic decision is whether to set
up a parallel system of services for women's
health, or to integrate these within the
mainstream health system. The Australian
experience described by Wainer and Peck offers
an example of women-specific services alongside
of integrating the knowledge and resources
gained into mainstream services.
Perhaps the most difficult task at national level
is allocating resources across competing claims, a
task that is compounded in the present economic
climate, where countries are facing a serious
resource crunch, stripping of public assets,
rejection of social welfare on grounds of cost and
privatisation of public and social services.
Focusing on women's needs
Women's health advocates believe programmes
should be based on women's needs. In practice
however, policymakers and programme man
agers rarely start from this premise in order to
decide what needs to be done. Instead, they stan
by asking what services already exist and how
'more' can be accomplished with the least
possible disturbance to the existing system.
Unless this difference in perspective is explicitly
acknowledged, women's health advocates and
policymakers will always be talking at cross
purposes, no matter what 'buzz words' they use
in common to describe policy objectives.
Being guided by women's decisions is a good
priaciple, but it may not be enough to make
allocation of scarce resources happen in a just
and ethical way. The problem remains how to
strike the right balance between the common.
recurrent health problems affecting the majorir.
of women versus those that are serious, life
threatening, chronic and disabling, which are
suffered by a minority; between prevention and
educational initiatives and effective tertiary care
The magnitude and epidemiological profile c:
some women's health problems are well known,
but there are others, equally serious, about which
little is known. Priorities can vary dramatical;.
between localities, and policies and programmes
have to allow for decentralised decision-makinc
Many women do not have access u
information that would enable them to make
valid risk/benefit assessments regarding thenown health and treatments. Data barely exist i.n
most (Countries on the prevalence of common
Setting priorities
Bishop et al, Kennedy et al and Maine et al put
forward guidelines for programme planning and
priority setting. Public health policy may be
based on epidemiological data regarding the
needs of the population as a whole, while dpctors
go by the needs of individual patients, and these
often conflict with each other. The dilemmas
inherent in making policy choices become
apparent when Bishop et al examine cervical
cancer screening and treatment options. Of what
use are model policy recommendations when
they are unavailable to most women in most
developing countries and some in developed
countries too.
Does a country start by providing the bare
minimum, to benefit at least the majority of
women to some extent? Taking this pragmatic
approach and pursuing a minimal package,
which has to be better than nothing, poses the
9
Ravi ndrun
health problems women suffer from, such as
menstrual
disorders
and
premenstrual
syndrome (Round Up). A great deal needs to be
done in the realm of research - as Bulut et al
show, for example, there are not even standard
definitions of what constitutes reproductive tract
infection, let alone what tests and measurements
should be used or how best to find out whether a
woman has one or not.
Research would help to identify the best wafys
of communicating existing and new information
to women, as well as service providers and
policymakers. What women perceive as
important health needs and why they do or do
not use services, is another important area for
research. Glasier's review looks at why women
are choosing medical rather than surgical
abortion, and shows how research can provide
insights into how and why women make the
choices they do.
Organising for change
Women's health policies have often been put into
place successfully as a result of a dynamic
women's movement combined with a favourable
political climate. The fate of these policies has,
however, been very different. In Colombia, the
lack of sustained effort combined with changes
in political leadership need to be overcome if the
national policy is ever to become more than an
'interesting and rare government document with
a gender perspective'. (Plata et al)
The significance of a supportive political
climate comes through yet again when Klugman
et al describe their experience in South Africa of
formulating women's health policies in the midst
of social and political transformation. An
important element of that initiative was its
inclusive nature, using processes which cut
across barriers of race, class and ideology to
reach consensus, minimising the scope for
derailment. Coney, on the other hand, describes
a classic case of policy derailment in New
Zealand in relation to recommendations on
protecting patients' rights following ethical
abuses during research, in the face of a
conservative and defensive medical profession,
health service re-structuring and changes in
political leadership.
The strengths of inclusive process are vividly
brought home when Nunes and Delph describe
I 10
how one group organised to support abortion
law reform in Guyana. The Pro-Reform Group
made a conscious attempt to minimise
differences and to build bridges with those who
opposed law reform. The 'pro-life, pro-choice,
pro-reform' slogan they used to this end proved
to be a brilliant strategic move.
Throughout this issue of the journal,
formidable forces opposed to the reproductive
rights of women appear: anti-abortion groups,
fundamentalist political and religious leaders.
Their opposition to the consensus at Cairo and
Beijing, as Petchesky points out, was formidable
and must continue to be addressed at national
level. A media-based campaign, apparently
launched by Human Life International, success
fully shut down anti-tetanus immunisation
campaigns in four developing countries this
year, and is perhaps the most shocking story in
this issue. Milstien et al and Tan describe how the
power of the Catholic church was misused to
create mistrust and fear. They not only falsely
accused WHO and UNICEF of 'lacing' tetanus
toxoid vaccines with non-existent contraceptix e
vaccine to cause miscarriages and sterility, but
also by implication the health workers
administering the immunisation campaigns.
. lives have been put on the firing line, all in the
name ofpreserving life.' (Tan)
In most societies, in spite of the ravages of
AIDS, the environment is still not conducive to
candid discussion of sexual behaviour and
practices. What a relief that Tan can make us
laugh at the fraught responses to such grave
policy questions as whether or not flavoured
condoms should be banned. Yet condom use is a
deadly serious issue.
While conservative forces want to cut-off
access to fertility regulation altogether, women's
health and reproductive rights are under attack
from a diametrically different side as well: those
who disregard women's dignity altogether in the
course providing 'services', as Ramanathan et al
observe in a sterilisation camp in Kerala state in
India. It is in the* very philosophy of tjiese
programmes that women's interests should be
subordinated to demographic goals*
Shallal's paper on the continued use of
quinacrine sterilisation in Chile illustrates how ;
political, medical and religious forces may
7
"———— --------
Reproductive Health Matters, No 6, November 1995
collude to deny women reasonable choices. With
abortion illegal and with surgical sterilisation
severely restricted in law thanks to anti-choice
influence, and only easily obtainable privately,
women are offered quinacrine as a fast-track
means of birth control.
Political survival in a country where such
forces are dominant make a liberal and 'pro
women' stance difficult. Would attempts at
organising for women's health policies succeed?
Would it be in women's interests to seek
consensus and inclusiveness, i.e., compromise,
with those who oppose women's reproductive
rights in such circumstances?
While policymaking from the grassroots up is
in principle highly desirable, grassroots partici
pation may not be easy to achieve. First, the lack
of information on the part of women being called
upon to make choices and decisions must be
acknowledged and dealt with. For example, even
though Kerala has an exemplary tradition of
people's participation in political processes, the
women attending the sterilisation camp descri
bed here were apparently not aware of the
minimum standards of care due to them. In Chile,
again, women opting for quinacrine have not
been informed about the controversy over its use.
Under these circumstances, women are unlikely
to demand changes. Thus, important issues may
not find a place in the needs they articulate.
Second, women's health advocates and others
involved in organising for change need to
grapple with the ethical issues involved in mass
organisation for policy changes in any country
riddled with ideological factionalism, and where
people's organising efforts have been con
sistently thwarted. It is the responsibility of
leadership to help women appreciate the
strength of the forces they are up against and the
risks involved, and to strategise not only for a
successful outcome, but also what to do in case of
failure. There is now considerable organising
experience from which these lessons can be
learnt so that mistakes are not repeated.
Third, those involved in policymaking have to
contend with the hard decisions involved in the
setting of priorities. When all is said and done,
the needs of some women would still have to
come before the needs of others. Disenchant
ment among and alienation of those sections of
women whose expectations have not been
fulfilled may follow.
11
There are a number of important policy issues
that have not been addressed in this issue of the
journal - significant among these are HIV/AIDS
and women, and infertility and assisted con
ception. There is also a far greater coverage of
experiences of organising and formulation of
policy than of implementation of national
women's health programmes, a reflection of the
limited experience that exists with the latter.
This is a critical juncture in the long history of
organising for women's health policies. Post
Cairo, there is an apparent willingness on the
part of policymakers to formulate reproductive
health policies and implement programmes. The
search is on in country after country for an
appropriate reproductive health services pack
age. We hope that those involved in this process
take note of a recurrent theme in many of the
papers here: that women's struggle for better
reproductive and sexual health is a political
struggle for control over their bodies, and not
merely a demand for 'adding on' services
without making fundamental changes to the way
programmes are formulated and managed, and
the way services are delivered.
References
1. All quotes come from papers in this issue.
2. Orosz E, 1994. The impact of social science research
on health policy. Social Science and Medicine.
39(9):1287-93.
J^eproductive
Health Matters
We would welcome submissions for
the following issues of the journal:
Number 7, May 1996
Men
Number 8, November 1996
Fundamentalism, women's
empowerment and reproductive rights
Features
Making Abortion Law Reform Happen
in Guyana: A Success Story
Frederick E Nunes and Yvette M Delph
On 4 May 1995, after two years of intense public debate, the National Assembly of Guyana passed
the Medical Termination of Pregnancy Bill, making Guyana the second country m theEnghs
speaking Caribbean to introduce such legislation. For the entire two years scarcely a day went by
without letters or articles in the press, and at least once a week there was a programme on
television and radio. This paper describes the history and content of the campaign> ^uPPort
the new law by the Pro-Reform Group, whose mam slogan was Pro-Life, Pro-Choice Pro
Reform'. This^ampaign sought common interests with the opposition, their public education was
based on research among health and legal professionals, students and the public and on facts
about abortion and women's experiences. It was carried out mainly through the media. The paper
ends with a description of the new law and efforts to begin implementing it.
'FN 1971, four years after the UK passed the
1967 Abortion Act, Guyana became the first
Caribbean country to initiate public
_. _discussion about abortion law reform. The
People's National Congress (PNC) appointed a
Special Select Committee to examine the need to
liberalise the law but although they held several
hearings, they failed to submit a report.
In 1974 Caribbean Common Market
(CARICOM) Health Ministers passed a resolu
tion to review legislation essential for improving
maternal health.
In 1983, a Medical Termination of Pregnancy
Act was passed in Barbados. Shortly afterwards,
the Health Desk in the Secretariat of CARICOM
sent copies to all Permanent Secretaries in
Ministries of Health in the English-speaking
Caribbean, urging them to use the opportunity to
act on the 1974 resolution. Nothing happened.
In 1985, the PNC Government in Guyana
prepared a draft bill on abortion that was almost
identical to the 1983 Barbados Act.
In 1988 they began a process of public
consultation about the bill. In an effort to respond
to concerns raised by various interest groups,
the contents were expanded to include clauses
on counselling, approval of medical institutions
and limiting terminations to 28 weeks. The
compact form of the earlier draft had yielded to
cumbersome comprehensiveness. Concerns for
——-
administrative control overshadowed the focus
on women's health.
Although this Bill was approved by the PNC
Cabinet in 1989, it was never advanced to the
National Assembly. It was shelved and never
voted on, probably in deference to the general
election that was expected the following year,
and possibly also in response to religious
opposition, or both.
The PNC had held power continuously from
Guyana's independence in 1966 until they were
voted out of office in October 1992 and replaced
by the People's Progressive Party (PPP), the main
opposition party.
The new PPP Minister of Health demonstrated
remarkable courage in the face of this highly
controversial subject when, in May 1993, she
announced her intention to review the law
relating to abortion, which she described as 'a
law which no-one cares to obey and no-one
dares to enforce'.
She promised an open public debate on the
abortion bill which had been left by the previous
PNC administration and invited a wide range of
interest groups to join in the creation of a
Ministerial Committee. A commitment to trans
parency was manifested in her bold design of
this Committee, which included more than 30
members from religious, legal, medical, and
women's organisations and which held public
I
GENDER AND POWER ISSUES IN MEDICAL EDUCATION
Paper prepared for the at National Consultation on
“Towards Comprehensive Women’s Health Policy and Programmes”,
Organised by Voluntary Health Association of India, New Delhi,
18th-19lh February 1999
by
Dr. Thelma Narayan,
Coordinator,
Community Health Cell,
Society for Community Health Awareness, Research and Action,
NO.367, ‘Srinivasa Nilaya, Jakkasandra I Main, I Block, Koramangala,
Bangalore - 560 034.
Phone : (080) 553 15 18 & 552 53 72
Fax : (080) 553 33 58 (Mark Attn. CHC)
Email: sochara@blr.vsnl.net.in.
GENDER AND POWER ISSUES IN MEDICAL EDUCATION
/Currently gender is recognised as a term that reflects the complex social relations
between men and women (Kannabiran 1997, Bhasin 1997, WHO-SEARO, 1998).
Accepting biologically determined differences as being more unchangeable, the focus
is on socially constructed roles that have developed historically within and across
cultures. This process of socialization has lead to the generally inferior positioning of
women within families and in all other institutional groupings that exist in society. The
underlying issue of power equations in the relationship, that manifests itself in terms of
dominance, subordination, equality, inequality, role in decision making, control over
resources, division of labour and access to services, is one that needs to be constantly
reflected upon to ensure that the interests of more powerless and vulnerable groups are
not made subservient to those that are dominant. Cross-cutting linkages with other
power structures in society such as class and caste or ethnicity adds additional
oppression to the position and condition of women in particular social groupings. The
internalization of these social relations, roles and attitudes is deeply ingrained through
socialization processes during childhood and adulthood. They are reinforced by culture,
traditions and religion, such that both women and men usually implicitly accept given
roles.
These social relationships with their inherent hierarchies and positions of
privilege are characterized by conflict, often with the use of overt force and violence.
A veneer of harmony may mask much subterranean ‘silent suffering’ which is part of
the glorified and sanctified role assigned to women. However, social constructions are
products of the human mind and though they may be reinforced by strong beliefs and
ideologies, they can be deconstructed.
The Position of Women in India as reflected through Health
Indicators and Medical Practice
A vailable health indicators (more accurately indicators of levels of death and
zvdisease) provide evidence of the position of women in India. While globally the
gender ratio (number of women per 1000 men) favours women because of certain
biological strengths, the ratio in India from the turn of the century is adverse to women.
More alarming is the fact that it has been consistently declining, despite fifty years of
political freedom, decades of development efforts, and the spread of education. It has
continued inspite of awareness created during the International Decade of Women and
the efforts of women’s groups throughout the country. All these liberative forces have
not been able to dislodge sets of factors that seem to be very deeply embedded in our
society. The continuing high rates’of maternal mortality and high rates of anemia
among women point to deprivation of basic physical needs.
/George S and others have researched and documented the prevalence of female
vJfoeticide in Haryana and Tamil Nadu. It has also been reported from Maharashtra
and Rajasthan and probably occurs all over the country. Medical technology in the
form of diagnostics, particularly ultrasound and amniocentesis is used for sex
determination, despite the national legislation passed in 1992 banning its practice. The
finding of a girl foetus is usually followed by performance of a Medical Termination of
Pregnancy (MTP), often by qualified obstetricians, a practise legalised by the MTP
2
Act. The selective abortion of girl foeteses is justified as an exercise of free choice by
the parents and the mother. The medical ethical issues underlying these practices by
medical professionals do not seem to find a place in the professional discourse of
bodies like the Federation of Obstetricians and Gynaecologists, many of whose
members are women themselves. It is hypothesized that the practice of female
foeticide is one of the reasons for the declining gender ratio. Private ultrasound and
MTP services have been mushrooming even in small towns and large villages, though
in contradiction, at the same time shortages of simple iron and folic acid tablets for
anemia (required particularly by pregnant women and costing just a few paise) have
been reported from all over the country in 1997 and 1998. This contradiction raises
questions regarding the actual interests of both private and public sector health care
services vis-a-vis women’s health needs.
A Talini Karkal (1996) based on years of research observes that asymmetric gender
IVXrelations often cause discriminatory treatment of daughters within the parental
family, and that this is further strengthened by marriage practices. It has been found
that bums comprise one of the largest causes of death in young women aged 15-35
years, even more than pregnancy related causes. One study in Mumbai found that 60%
of deaths due to bums occurred in the parental home and not in the in-law’s house as
commonly believed. Karkal (1996) also hypothesises that patriarchy operates on age
hierarchy with ageing enhancing a women’s position in the family. Hence, the support
for patriarchy by older women.
TTigh stress levels, due to playing multiple roles, causes women to have an increased
£1 vulnerability to mental illness with feelings of helplessness, worthlessness, apathy,
depression and sometimes suicidal behavior (CHETNA 1996, from Indian NGO’s
Report on CEDAW, published by Coordination Unit for Beijing Conference, 1995).
Girls and women are socialised to tolerate discomfort and pain, often leading to delays
in seeking care, support and treatment, with resultant progression of underlying disease
processes.
A ccess to care is lower for women, as has been found in some studies looking at
Zvutilisation of inpatient and outpatient medical services (FRCH). It is suggested
that part of the cultural definition of being a women in India is her association with the
“inside” namely within the confines of the home and the family (WB 1991). This
restricts knowledge and access to services including to health care, but also to the
“outside” world where political and economic power is exercised (ibid). The poor
health status of women in India and their limited access to care is part of the overall
inequitous social position of women. While medical and health care can potentially
liberate women through reduction of pain, suffering and death, medical professionals
have sometimes misused medical technology to perpetuate an anti-women bias as is
particularly evident in the widespread practice of female foeticide and in the promotion
of a family planning programme in pursuit of state demographic goals at the cost of
women’s health.
'T'here is evidence of lack of power of women in India in other spheres as well. For
1 instance, in general, women do not own land, they have less access to markets,
3
about 75% are illiterate, and 90% of rural and 70% of urban women workers are
unskilled (WB 1991). These factors along with low purchasing power, lack of food
security, poor access to safe water and sanitation, impact more adversely on the health
of women, and vulnerable groups than do individual germs and bugs. One needs to
assess how much and how seriously medical education addresses these underlying
social/societal factors that impinge so greatly on health.
Gender and Medical Education
A Tedical Education, both graduate and post-graduate, forms medical professionals,
JLVjLand along with research, informs medical practice. It also sets the guidelines and
tone for education and training of allied health professionals. How does medical
education confront and address gender issues? Is it sensitive and responsive to
women’s health concerns? Or is it another institutional arena in which gender issues get
played out without being challenged?
nphough medicine is commonly associated with objective scientific thought and
methods in its practice, there is little rationale in the structure of medical education.
Historical factors relating to the growth, acceptance and dominance of certain
disciplines, as well as the prestige attached to them at that time, resulted in greater or
lesser allocation of time for their study. Thus Anatomy receives of larger time share,
while psychology and psychiatry are still struggling for their space. Sociology has not
yet found a strong entry point and medical ethics is still on the fringes. The
foundations of ‘modem’ medical education occurred during the period of ‘scientific
optimism’. There was little space for the social sciences or for the experience of
medical practitioners through their interaction with reality, to be able to raise questions
concerning the social roots of disease and ill health or the relevance of medical
prescriptions to the lives of people, particularly of women.
'“phus, for instance, medical students spend the first one-third of their taught underJL graduate course with cadavers, frogs and biochemical experiments that bear
relatively little relevance to their practice as healers. These are probably early steps in
the process of dehumanization, which later leads to a fragmented focus on organs and
systems rather than on the whole human person who is suffering and in need of care
besides cure. Medicine and medical education, through described as a social science
took a scientific trajectory and grew by reducing the problems being addressed to more
and more specific detail of their biological components. The growth and faith in
molecular biology and genetic intervention is evidence of this. Modem medicine has
thus not related adequately to social end cultural reality, to intra and interpersonal
behavioural factors and much less to conflictual social relations. A major lacuna in
this regard is the lack of recognition given to women’s health and gender issues.
Historical Developments
y~ historically, modem medicine and medical education came to India through the
JllEuropean colonial powers of the time (Portugese and British). A process of
gradual marginalisation of the Indian Systems of Medicine (ISM’s) and folk health
practices followed. The ISM’s though also urban based and to some extent elite, had a
4
more wholistic approach to the sick person as a total being and attempted to maximise
and build up the healing powers within the persons body. An extensive pharmacopea
and surgery had been developed by the ISMs over centuries of empirical observation,
classification and codification. However, it appears that the approach to women’s
health focussed largely on her role in child-bearing and motherhood. More
importantly, the ISM’s had traditional cultural links with local indigenous healing
practices including dietary and other preventive practices which were widespread
throughout the countryside. Women were largely the bearers of these local knowledge
systems and practices.
Western medicine, including gynaecology, “gradually
marginalised midwives (dai’s or traditional birth attendants), medicine women, women
healers; they declared women’s indigenous knowledge as non-knowledge” (Bhasin,
1997, p 23). The marginalisation of ISMs occurred even in health planning and policy
and this continued even after gaining political Independence. Even today, ISMs receive
about 5% of the budgetary outlays for health at national level. At the state level, some
states accord ISM’s slightly greater priority though the major allocations still go to
modem medicine. Western or allopathic medicine by asserting and establishing a
hegemonic dominance in India, has negated local systems of knowledge and medical
practice and denied them a legitimacy that is theirs by right.
Policy Guidelines for Medical Education
A review of the Medical Council of India (MCI) Recommendations on Graduate
ZvMedical Education (MCI, 1981) is revealing regarding its gender sensitivity:
a) While mention is made that “the importance of social factors in relation to the
problem of health and diseases should receive proper emphasis throughout the
course”, specific social factors such as gender are not mentioned. That social
factors can be a cause of ill health and disease is also not considered.
b) The importance of population control and family planning for health and
development has been strongly emphasized, with a detailed curriculum for the
teaching of Family Planning methods. A strong demographic agenda is evident,
related to ‘the needs of the country’ as understood, determined and defined by
the state. That women’s health needs and interests may differ from state
interests is not considered. Women have been made targets (Prakash, 1983) and
objects of methods that in themselves are an iatrogenic cause of ill health, due
to the side-effects of most of the available contraceptive methods.
c) Obstetrics and Gynaecology in Phase III focuses largely on the obstetric, child
bearing aspects. Thus “not less than 2/3rd of hours of clinical instruction shall
be given to Obstetrics including Antenatal Care, Newborn care and maternal
health”. Notice the lack of emphasis on the whole woman, and on the total
dimensions of her health and well-being at all ages.
d) During internship, the posting in OBG is to be focussed on “Antenatal care,
family planning, contraceptive technology, operative techniques, sterlization,
newborn care, well baby clinic and paediatrics”. Again a large lacuna persisted
5
in the understanding and approach to women’s health. Gender sensitivity was
completely missing.
The gender bias in the content of the curriculum received comment from the
Medico Friend Circle, an all India ‘thought-current’ of persons interested in health
issues affecting the majority population, the poor. The MFC was and is interested
in socially relevant medical education and in women’s health issues. There was no
other social grouping in India then that took up this issue. (Narayan, 1991).
Dialectical discussions on the presence or absence of a ‘sexist bias’ in the teaching
and practice of Obstetrics & Gynaecology also took place (MFC, 1983).
rp^he next revision of the MCI Recommendations termed MCI Regulations (MCI
1 1997) made remarkable shifts in statements from disease to health and from
hospital to community, with an emphasis on being relevant to service situations as
obtaining in the country. It recognised the health rights of all citizens and called on
doctors to fulfill their social obligations, to observe medical ethics; to appreciate sociopsychological, cultural, economic and environmental factors affecting health and to
develop humane attitudes. This is indeed a positive change and in the right direction.
However, again it is silent regarding the broader, total dimensions of women’s health.
Obstetrics and gynaecology continues to be biologically oriented and confined to the
reproductive system. Five of eight teaching objectives relate to pregnancy, with only
one “to identify common gynaecological diseases and describe their principles of
management”. Here again, the medicalisation of problems occurs.
While Pharmacology specifically mentioned the prescription of drugs during pregnancy
and lactation, infancy and old age, Psychiatry had no special mention concerning
women’s mental health.
Additionally, the emphasis on “analytical, logical, scientific thought and independent
judgment” (MCI 1997) while useful, is too left brained or masculine and needs to make
space for integrative and collective learning, and intuitive creative abilities.
These new regulations seem to offer an opportune moment for greater interaction
between Universities, those responsible for medical education and women’s health and
gender sensitive activists and scholars, to evolve gender sensitive curricula and
methods.
^Content of Medical Education
V6'
1
£.<-rT''here is need for further work to review the syllabus of each subject from a gender
1 perspective and to make positive suggestions as to the elements that need to be
introduced, deleted or modified. While obstetrics and gynaecology, pharmacology and
psychiatry could be the subjects to start with, the exercise needs to be done for all the
disciplines. For instance, all doctors in all departments need to be sensitised to the
issue of domestic violence which may underlie a presentation of a woman with injuries
at the surgical or orthopaedic OPD or in the casualty. The underlying real cause may
not be divulged unless the physician has the sensitivity and skill to get such a history.
The support, care and professional intervention that is required in such a case is much
6
more than just treating the wound surgically. Similarly a young girl or woman may
present with bums - underlying the treatment of bums is the deep socio-psychological
trauma that may prevent her from telling the truth or it may even force her to make a
false dying declaration. In other instances, women who are raped need the professional
advice of a forensic expert and of the local general practitioner. Paediatricians are
faced with girl children who are brought late for treatment or in worse situations with
children who are sexually abused. Dermatologists need to treat children and innocent
women who have STDs. Research and other insightful studies have raised questions
concerning common medical / surgical procedures performed on women such as the
practice of routine episiotomies for all primies, the increasing rate of caesarian sections
and hysterectomies and the use of the lithotomy position for normal deliveries. Thus,
every aspect of medical practice and therefore of medical education comes face to face
with gender issues. Medical professionals and even more so all allied health
professionals are in a unique position where they can go beyond the immediate to
address some of the deeper causes of gender related health consequences. For this,
there is a need for mainstream education to take in the learnings from the women’s
movement and from research studies.
Methods of Medical Education
IV Tethods need to move beyond didactic, hierarchical, exam and theory oriented
IVJLteaching to use interactive, participatory, problem based learning methods, that
are centred on student growth but also equally importantly relate to social context and
health needs of people.
A number of innovative experiments have been tried in India (Narayan, et al 1993).
IkSome of these are not widely known or are lost to history. However, there is a
stream within mainstream medical education that has always sought social relevance
and has tried community based or community oriented approaches. These are the
natural allies through whom gender sensitive approaches could be introduced into
medical education. Globally there is the Network of Community Oriented Educational
Institutions for Health Sciences. It was initiated with the help of WHO and continues
to have its active support. At their Annual Meeting in 1994, a suggestion was made
from Pakistan and India to have a women’s health cell. This could be further pursued.
Their journal is appropriately titled Education for Health. There are a few Indian
institutions and individuals who are members. Some Indian Universities have taken a
lead in introducing progressive changes. Mumbai University is introducing women’s
studies as an integral component of several of their courses. The Rajiv Gandhi
University of Health Sciences - Karnataka, in Bangalore, is restructuring the
curriculum based on the 1997 MCI Guidelines. It is one of the first Universities to
introduce the teaching of Medical Ethics throughout the course. Thus, there are
windows of opportunity that need to be used to promote an understanding of gender
and power issues in medical education that will also translate into action into the
educational programs offered.
7
Values in Medical Education
■Cl. ixr
A
II Tith current global and national trends towards globalization, liberalization and
VV commercialization which includes the commodification of women and of
medical care it is important to emphasise and reiterate in medical education certain
basic values in health. These include equity, sociaLjustice^^thics, gender sensitivity,
sustainability and self-reliance. There could be many others such as respect for plural
peoples health traditions, and cultural sensitivity.
Women in Medical Education and Medical Care
detailed review of medical education found increasing numbers and proportions
of women medical students gaining admission and graduating from medical
colleges across India (SOCHARA, 1995). From 21.5% in 1971-72 admissions of
women students were 39.8% in 1989-90. There are gender differences in admission to
the prized post-graduate specialities of surgery and medicine. Gender discrimination is
reported to occur in promotions, with women considered to be unavailable to handle all
the responsibilities due to the double burden of also managing their families and homes.
This as in all other occupations raises the issue of joint responsibility for child care and
home management. Women physicians in Delhi have been reported to have a better
status than in the past, also occupying leadership, and decision making positions as
heads of departments and institutions. However, they are still viewed as occupying
specializations that are less academic and inferior (Abidi 1993). There are still
marginal numbers of women in cardiology, neurology, medicine, surgery, disciplines
that are seen as requiring greater abilities (ibid). Studies abroad show that women are
concentrated in primary care including family medicine, paediatrics and psychiatry
(Notzer & Brown, 1995). They report that repeated studies have found women doctors
to have a more humanistic and personalised approach to patient care (ibid).
A brief literature review found sexual harassment experienced by women medical
students during their under-graduate and post-graduate period and registrarship. This
includes psychological abuse and discrimination because of sex. It has been reported
from Canada (Myers, 1996, Philips, 1996 ) and elsewhere. This dimension is not
researched in India and hence one cannot estimate its extent. However, its occurence
itself reflects the position of women in society.
Conclusion
fT^here is tremendous need for further work on gender and power issues in medical
1 education. Besides research and analyses, the coming together of different streams,
with networking and sharing of experience between the groups is required. Most
importantly, there is need for engagement with bodies concerned with medical
education, such as the Medical Council of India, Health and other Universities and the
Indian Medical Association.
8
References:
1. WHO-SEARO, 1998, Regional Health Report 1998 - Focus on Women, WHOSEARO, New Delhi.
2. World Bank, 1991, Gender and Poverty in India - A World Bank Country Study,
The World Bank, Washington DC.
3. CHETNA, 1996, Convention on the Elimination of all forms of Discrimination
Against Women (CEDAW) - An Alternative Report by NGOs, Article 12 Health
Care Services - summary.
4.' Malini Karkal (Ed), 1995, Our Lives Our Health, Coordination Unit, World
Conference on Women - Beijing, 1995, New Delhi.
5. WHO-SEARO, 1993, National Meeting on Women, Health and Development, New
Delhi.
6. VHAI, 1994, Women & Health Report - Women’s Health is a Human Right,
VHAI, New Delhi.
7. WAH! Secretariat, 1997, Approach Document - The Women and Health
Programme (WAH!), India & Nepal, CHETNA, Ahmedabad.
8. MCI (Medical Council of India) 1981, Recommendations on Graduate Medical
Education, MCI, New Delhi.
9. MCI, 1997, Regulations on Graduate Medical Education, MCI, New Delhi.
10. Bhasin K, 1997, Gender Training Endangered by Fragmental Thinking : A View
from the South, SEARCH Bulletin 12, 4, p 20-24.
11. Kannabiran V, 1997, Sharing the Fish Head : The Philosophy and Practice of
Gender Training in South Asia, SEARCH Bulletin, 12, 4, 25-45.
12. Narayan R, Narayan T, Tekur S.P., 1993, Strategies for Social Relevance and
Community Orientation in Medical Education, Community Health Cell,
SOCHARA, Bangalore.
13. SOCHARA, 1995, Perspectives in Medical Education - A Report prepared for the
‘Independent Commission on Health in India’.
14. Narayan R, 1991, Medical Education Alternatives - Anthology of Ideas in Medical
Education Re-examined, Medico Friend Circle, 1991.
15. MFC (Medico Friend Circle) Bulletin, March 1983, Prejudice against Women in
Health Care - Report of the discussion during the Ninth MFC Annual Meet at
Anand, Gujarat in January 1993.
16. Prakash P, 1983, F.P. Programme, Women as ‘Targets’, Background paper for
Ninth MFC Annual Meet, MFC, Pune. (See also other background papers).
17. Myers MF, 1996, Abuse of Residents : its time to take action, editorial comment,
Can. Med. Assoc. J, 154 (11), 1705-8.
18. Nigar Fatima Abidi, 1993, Women Physicians - A Study in Roles and Role
Conflict, Manak Publications, Delhi.
19. Noizer Nand Brown S, 1995, The feminization of the medical profession in Israel,
Medical Education 1995, 29(5), 377-81.
20. Philips S, 1996, Sexual Harassment of Female Physicians by Patients. What is to
be done? Can Fam Physician, 42, 73-8 (only an abstract was available on Medline).
9
- Media
 RF_WH_.11_8_SUDHA.pdf
RF_WH_.11_8_SUDHA.pdf
Position: 1080 (11 views)