TOBACCO HEALTH-CANCER-CONTROL REPORTS EPIDEMIOLOGICAL-FACTORS ETC.
Item
- Title
- TOBACCO HEALTH-CANCER-CONTROL REPORTS EPIDEMIOLOGICAL-FACTORS ETC.
- extracted text
-
RF_PH_7_SUDHA
c/XNCEK J>A'fTerjes
NC-^P -
B^^f\i-C> R.P- I1&2-
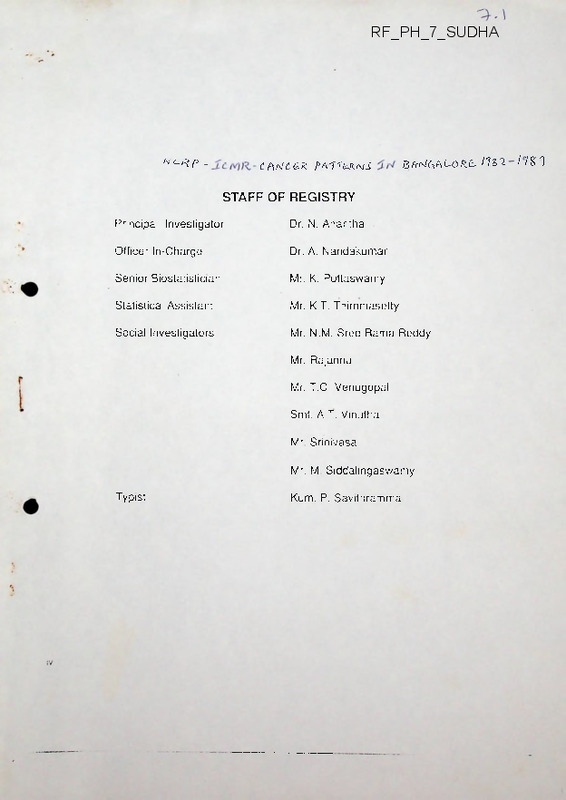
STAFF OF REGISTRY
Principal Investigator
Dr. N. Anantha
Officer In-Charge
Dr. A. Nandakumar
Senior Biostatistician
Mr. K. Puttaswamy
Statistical Assistant
Mr. K.T. Thimmasetty
Social Investigators
Mr. N.M. Sree Rama Reddy
Mr. Rajanna
Mr. T.C. Venugopal
Smt. A.T. Vinutha
Mr. Srinivasa
Mr. M. Siddahngaswamy
Typist
Kum. P. Savithramma
//S’*)
POPULATION-BASED CANCER REGISTRY BANGALORE
Year: 1989
Sex: Female
INCIDENT CASES OF CANCER BY MOST VAUD BASIS OF DIAGNOSIS AND SITE (ICD.9)
ICD
9TH
SITE
140 LIP
141 TONGUE
142 SALIVARY GLANDS
143 GUM
144 FLOOR OF MOUTH
145 OTHER MOUTH
146 OROPHARYNX
147 NASOPHARYNX
148 HYPOPHARYNX
149 PHARYNX ETC
150 OESOPHAGUS
151 STOMACH
152 SMALL INTESTINE
153 COLON
154 RECTUM
155 LIVER
15S GALL BALDDER
157 PANCREAS
158 RETROPERITONEUM
159 OTHER DIS SYS
160 NASAL CAVITY
161 LARYNX
162 LUNG
163 PLEURA
164 THYMUS
165 OTHER RES SYS
170 BONE
171 CONNECTIVE TISS
172 SKIN MELANOMA
173 SKIN OTHER
174 BREAST FEM
179 UTERINE UNS
180 CERVIX UTERI
181 PLACENTA
182 BODY UTERUS
183 OVARY
184 VAGINA
188 URI BLADDER
189 KIDNEY
190 EYE
191 BRAIN
192 NERVOUS SYSTEM
193 THYROID GLAND
194 OTH ENDO GLANDS
195 ILL DEF SITES
196 SEC LYMPH NODES
197 SEC RES ETC
198 SEC OTHER
199 PRIM UNK
200 LYMPHOSARCOMA
201 HODGKINS DIS
202 OTH LYMPHOMA
203 MULT MYELOMA
204 LEUK LYMPHATIC
205 LEUK MYELOID
206 LEUK MONOCYTIC
207 LEUK OTH SPE
208 LEUK UNS
ALLSITESTOTALS
%
MICROSCOPIC
n
%
8
5
24
3
68
5
3
7
75
27
0
19
17
5
4
5
2
6
13
4
1
0
12
16
227
5
253
0
21
42
5
5
20
0
46
2
8
6
4
1
3
10
21
5
8
23
0
0
4
1085
77.22
100.00
80.00
83.33
88.89
75.00
80.95
100.00
60.00
58.33
50.00
71.43
56.25
0.00
76.00
70.83
33.33
62.50
36.36
100.00
50.00
100.00
85.71
68.42
80.00
100.00
0.00
85.71
100.00
100.00
88.89
88.67
71.43
86.94
0.00
95.45
80.77
100.00
71.43
100.00
100.00
71.43
0.00
97.87
100.00
88.89
100.00
87.50
57.14
1.25
100.00
100.00
84.00
71.43
88.89
88.46
0.00
0.00
40.00
X-RAY
n
%
0
0
0
3
0
0
12
4
0
0
0
0
0
2
0
1
0
0
2
0
0
0
0
0
0
3
0
0
0
0
0
0
0
0
-o
3
0
0
0
0
1
0
3
0
0
1
0
0
0
0
0
0
CLINICAL ONLY
n
%
0
0
0
2
0.00
0.00
0.00
3.70
0.00
3.57
0.00
0.00
8.33
0.00
11.43
8.33
0.00
0.00
0.00
0.00
0.00
18.18
0.00
25.00
0.00
0.00
10.53
0.00
0.00
0.00
9
0
2
3
0
12
0
4
3
2
0
0
0
0
0
0
0
0
0
o
21
0
33
0
0
0.00
0.00
0.00
1.17
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
10.71
0.00
0.00
0.00
11.11
0.00
12.50
0.00
3.75
0.00
0.00
4.00
0.00
0.00
0.00
0.00
0.00
0.00
0
2
0
0
0
0
1
0
0
0
0
2
0
0
0
0
1
0
0
0
0
0
39
2.78
117
8.33
81
0.00
0.00
0.00
7.41
25.00
10.71
0.00
40.00
25.00
0.00
11.43
22.92
0.00
16.00
12.50
16.67
12.50
9.09
0.00
25.00
0.00
0.00
5.26
0.00
0.00
0.00
0.00
0.00
0.00
0.00
8.20
0.00
11.34
0.00
0.00
7.69
0.00
28.57
0.00
0.00
0.00
0.00
2.13
0.00
0.00
0.00
0.00
28.57
0.00
0.00
0.00
0.00
14.29
0.00
0.00
0.00
0.00
0.00
OTHERS
n
%
D.C.O.
n
%
0
0
0
0
0
0
0
0
0
0
2
0
0
0
2
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
3
0.21
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
1.90
0.00
0.00
4.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0
0
0
0
1
4
6
1
4
6
2
0
0
0
1
3
1
0
0
0
0
2
5
2
5
6
0
0
0
5
0
0
0
0
0
0
76
0
0
3
1
•j
3
0
0
6
161
11.46
0.00
20.00
16.67
0.00
0.00
4.76
0.00
0.00
8.33
50.00
3.81
12.50
100.00
4.00
16.67
50.00
25.00
36.36
0.00
0.00
0.00
14.29
15.79
20.00
0.00
0.00
7.14
0.00
0.00
1.95
28.57
1.72
100.00
4.55
11.54
0.00
0.00
0.00
0.00
17.86
0.00
0.00
0.00
0.00
0.00
0.00
14.29
95.00
0.00
0.00
12.00
14.29
11.11
11.54
0.00
0.00
60.00
TOTALS
n
%
10
6
27
84
5
5
12
2
105
48
25
24
12
8
5
4
7
19
5
0
14
18
256
7
291
22
52
14
7
5
28
0
47
2
9
6
8
80
3
10
25
7
9
26
0
0
10
1405
100.00
100.00
100.00
100.00
100.00
100.00
100.00
100.00
100.00
100.00
100.00
100.00
100.00
100.00
100.00
100.00
100.00
100.00
100.00
1 oo.oc
100.00
100.00
100.00
100.00
100.00
100.00
0.00
100.00
100.00
100.00
100.00
100.00
100.00
100.00
100.00
100.00
100.00
100.00
100.00
100.00
100.00
100.00
0.00
100.00
100.00
100.00
100.00
100.00
100.00
100.00
100.00
100.00
100.00
100.00
100.00
100.00
0.00
0.00
100.00
BANGALORE - 1989
MOST COMMON FORMS OF CANCERS
[males |
STOMACH
OESOPHAGUS
LUNG
PROSTATE
HYPOPHARYNX
TONGUE
RECTUM
LARYNX
[females |
CERVIX UTERI
BREAST
MOUTH
OESOPHAGUS
OVARY
STOMACH
THYROID GLAND
COLON
* AGE-ADJUSTED (WORLD POPULATION)
82
.
-
■ '
'
Trends Over Time
■ able G 3 gives the Age Adjusted Incidence Rales (AAR) and three year Moving Averages (MA) ol tobacco related
sues of cancer lor different years. The same is graphically represented in Fig 6.1 There is a clear rising trend in the
overall incidence of these cancers in males, whereas in females the rates are about the same over the ye'ars 1982
to 1989 The values of AAR for specific tobacco related sites is given in Tables 6.4 and 6.5.
Table 6.3
TOBACCO RELATED CANCERS - TRENDS OVER TIME : 1982 - 1989
ALL SITES OF CANCER ASSOCIATED WTIH USE OF TOBACCO - MALES AND FEMALES
Table gives figures ol AAR and 3 year Moving Averages (MA) of AAR
YEAR
1982
1983
1984
1985
1986
1987
1988
1989
1982-89
49.68
45 90
39.94
42.08
MALE
38.11
41.92
40.73
40.51
37.94 *
MA
40.3
41.1
39.7
L2.7
44.5
FEMALE
27.35
23.58
2625
22.86
24.93
MA
25.7
24.2
24.7
24.2
25.2
45.2
24.79
25.83
27.47
25 40
26.0
Fig 6 1
TOBACCO RELATED CANCERS - TRENDS OVER TIME ; 1982 - 1989
ALL SITES OF CANCER ASSOCIATED WTIH USE OF TOBACCO - MALES AND FEMALES
Figure shows line graphs ol 3 year Moving Averages of AAR
VLAR
Male
Female
Tobacco Related cancers (TRC):
>cancers of the oral cavity,pharynx,
and urinary
bladder
larynx,
oesophagus,
considered
are
as
the
cancer
lung
6a
sites
related to Tobacco use.The paportion of these cancers by sex
is shown below.
Tobacco related cancers by sex
EMALE
MALE
% TO
NO.
SITE
TRC
ALL SITES
TOTAL
% TO
NO.
% T
NO.
TRC
ALL SITES
TRC
AL
Oral cavity
386
24.5
12 16
553
58 2
14.87
939
37.2
Pharynx
503
31.9
15 84
97
10 2
2.60
600
23.8
Oesophagus
318
20.2
10 01
238
25 0
6.40
556
22.0
Larynx
157
10.0
4 94
17
1 9
0.46
174
6.9
Lung
187
11.9
5 89
37
3 9
1.00
224
8.9
Uri.Bladder
24
1.5
0 76
8
0 8
0.22
32
1.3
Total
1575 100.0
49 6
950 100 0
25.5
2525
100.0
All sites
3174
6892
3718
Tobacco related cancers constituted 37% of all cancers in
both
sexes.
males
and
It
26%
accounted
in
for
females.
No
about
50%
of
significant
all
cancers
change
in
in
the
relative proportions in the TRC have been observed over the
years. Among males,
one third of TRC were cancer of pharynx
followed by cancers of the oral cavity & oesophagus.
It can be observed that,
■
among Tobacco
Related Cancers
of
oral cavity in females was more than double compared to
the proportion
in
males.
This
could
be
mainly
due
to
the
habit of chewing which is very common in females more so from
the rural folk.
TOBACCO RELATED CANCERS
HOSPITAL CANCER REGISTRY 1995, KIMIO
■ males
MALES-1575(49.6%): FEMALES-950(25.5%)
O females
cancer incidence rate was observed in each registry. While in Barshi (rural) , on an average one out of 24 to 25
persons get cancer in their lifetime. While in Connecticut (USA) and in United kingdom (Oxford), on an average one
out of 6 to 8 persons get cancer (0-64 years).
2.8
MOST COMMON FORMS OF CANCERS
The most common forms of cancers observed in men and women in Bangalore, Bombay, Madras, Delhi Bhopal
and Barshi areas are presented in Table 2.8.
TABLE 2.8 : MOST COMMON FORMS OF CANCERS (1989) - MALES
RANK BANGALORE
BOMBAY
MADRAS
DELHI
BHOPAL
BARSHI
1.
Trachea, Bronchus
& Lung (14.6)
Oesophagus
(11-5)
Larynx
(8.8)
Hypopharynx
(8.2)
Stomach
(7.0)
Prostate
(6.9)
Tongue
(6.5)
Mouth
(5.8)
Stomach
(16.5)
Trachea, Bronchus
& Lung (13.5)
Oesophagus
(10.2)
Mouth
(7.3)
Hypopharynx
(6.5)
Larynx
(5.5)
Tongue
(5.3)
Rectum
(4.5)
Trachea, Bronchus
& Lung (11.9)*
Larynx
(8-6)
Tongue
(7.7)
Oesophagus
(6.4)
Prostate
(6.3)
Uri. Bladder
(5.6)
Lymphoma
(5.1)
Brain
(3.4)
Stomach
(3.4)
Trachea, Bronchus
& Lung (14.1)
Tongue
(13.2)
Mouth
(10.4)
Hypopharynx
(8.4)
Oesophagus
(7.7)
Prostate
(5.6)
Rectum
(5.5)
Stomach
(3.7)
Oesophagus
(6.7)
Penis
(51)
Rectum
(4.7)
Hypopharynx
(3.5)
Mouth
(3.4)
Skin,other
(2.7)
Liver
(26)
Stomach
(3.4)
RANK BANGALORE
BOMBAY
MADRAS
DELHI
BHOPAL
BARSHI
1.
Cervix Uteri
(26.4)*
Breast
(223)
Mouth
(11-1)
Oesophagus
(10.2)
Ovary
(4.7)
Breast
(26.1)
Cervix Uteri
(19.4)
Oesophagus
(8.2)
Ovary
(7.0)
Mouth
(3.9)
Cervix Uteri
(43.5)
Breast
(24.6)
Mouth
(8.2)
Oesophagus
(7.7)
Stomach
(7.1)
Cervix Uteri
(30.1)*
Breast
(28.3)
Ovary
(8.7)
Gall Bladder
(6.6)
Oesophagus
(4.6)
Cervix Uteri
(26.2)
Breast
(6.8)
Bone
(2.4)
Skin,other
(23)
Rectum
(1.7)
6.
Stomach
(4.3)
Trachea, Bronchus
& Lung(3.7)
Ovary
(6.0)
Brain
(2.6)
Cervix Uteri
(24.3)
Breast
(21.9)
Mouth
(6.8)
Ovary
(6.2)
Oesophagus
(5.2)
Gall Bladder
(5.2)
Body Uterus
(4.2)
7.
Thyroid Gland
(3.2)
Stomach
(3.4)
Hypopharynx
(2-7)
8.
Colon
(23)
Rectum
(26)
Rectum
(2.6)
Body Uterus
Trachea, Bronchus
(2.5)
4 Lung (3.2)
Mouth
(2.5)
Stomach
Colon
(2.4)
(2.1)
Lymphoma
Thyroid Gland
(2.4)_____________ (2.1)
2.
3.
4.
5.
6.
7.
8.
Stomach
(9.5)*
Oesophagus
(9.4)
Trachea, Bronchus
& Lung (8.6)
Prostate
(7.1)
Hypopharynx
(5-9)
Tongue
(4-7)
Rectum
(4.3)
Larynx
(4.1)
FEMALES
2.
3.
4.
5.
‘Age-adjusted (world population) cancer incidence rate, per 100,000 persons.
12
Oesophagus
(1-4)
Lymphoma
(1-4)
2.9
SOME OBSERVATIONS ON SELECTED CANCER SITES
2.9.1
Lip, Oral Cavity and Pharynx (ICD.9 : 140-149)
Malignant tumours of the lip, oral cavity and pharynx are the most common site group of cancers in the Indian
registries i.e., Bangalore, Bombay, Madras, Delhi, Bhopal and Barshi (Table 2.9.1).
The total incidence of the lip, oral cavity and pharynx cancers disguise very large differences in the individual
sites in the Indian registries. The tongue (mainly base tongue), mouth, oropharynx and hypopharynx are the
predominant sites in this group.
There is also a marked variation in the incidence of lip, oral cavity and pharynx cancer in different countries.
Indian registries display much higher age adjusted and truncated rates than those reported by other registries in
Cancer Incidence in Five Continents (Vol. V,1987). Although this grouping includes cancers of quite distinct etiology
(e.g. cancers of the oral cavity, nasopharynx and hypopharynx). The global picture is dominated by the incidence of
oral cancer in Southern Asia and of oral cavity plus nasopharynx cancer in South-Eastern Asia.
Oral cancer is one of the 10 most common cancers in the world. In India, Bangaladesh, Pakistan and Srilanka,
it is the most common and accounts for about a third of all cancers. More than 100,000 new cases occur every year
in south and South-East Asia, with poor prospect of survival (Bull. WHO, 1984).
TABLE 29.1 : LIP, ORAL CAVITY AND PHARYNX (ICD 9:140-149)
MALES*
ICD.9
SITE
140-149 Lip, Oral Cavity
& Pharynx
140
Lip
141
Tongue
142
Salivary Glands
143-145 Mouth
146
Oropharynx
147
Nasopharynx
148
Hypopharynx
149
Pharynx Etc.
BANGALORE
BOMBAY
MADRAS
DELHI
BHOPAL
BARSHI
17.5
26.8
23.6
19.4
38.8
10.8
0.4
4.7
0.8
3.0
1.9
0.6
5.9
0.2
0.3
6.5
0.4
5.8
3.2
0.6
8.2
1.8
0.6
5.3
0.4
7.3
1.9
0.6
6.5
1.0
0.5
7.7
0.8
3.7
3.2
0.6
2.3
0.6
0.2
13.2
0.5
10.4
3.8
0.0
8.4
2.3
0.0
2.1
0.5
3.4
0.0
0.0
3.5
1.3
BANGALORE
BOMBAY'
MADRAS
DELHI
BHOPAL
BARSHI
14.9
9.5
14.7
6.4
10.4
1.1
0.1
1.0
0.5
11.1
0.5
0.4
1.2
0.1
0.2
1.9
0.3
3.9
0.6
0.2
1.5
0.9
0.3
2.1
0.2
8.2
0.4
0.3
2.7
0.5
0.3
1.3
0.5
2.5
1.0
0.2
0.6
0.0
0.0
1.4
0.0
6.8
0.5
0.5
0.8
0.4
0.0
0.0
0.0
0.6
0.0
0.0
0.5
0.0
FEMALES*
ICD.9
SITE
140-149 Lip, Oral Cavity
& Pharynx
140
Lip
141
Tongue
142
Salivary Glands
143-145 Mouth
146
Oropharynx
147
Nasopharynx
148
Hypopharynx
149
Pharynx Etc.
‘Age-adjusted (world population) cancer incidence rate, per 100,000 persons.
Relative risk of oral cancer in people with various tobacco habits, as well as the frequency of those habits, based
on retrospective case control studies in India and Srilanka are noteworthy. There is a wide variation in frequencies
and risks in different regions, but certain conclusions stand out. Approximately, 90% of oral cancers in south and
south-east Asia can be attributed to tobacco chewing and smoking habits (Bull. WHO, 1984).
Case-control studies conducted in different parts of India have demonstrated that cancers of the oral cavity and
pharynx are associated to a wide variety of tobacco chewing (pan chewing and betel nut with tobacco, lime and other
ingredients) and smoking habits prevalent among men and women. These associations are statistically significant.
Although it is difficult to obtain precise estimates of the risk for oral cancer associated with specific substance, it is
clear that almost all of the risk is due to smoking of tobacco and the chewing of quids of various kinds. Notani et al.
(1989) estimated the attributable risks associated with these habits as 61 % for oral cancer (81 % for males, 36% for
females) and 79% for cancers of the pharynx and larynx (90% for males, 30% for females).
The most obvious and efficacious measure of control for oral cancer in I ndia would be the elimination of chewing
and smoking habits. I ntervention studies carried out in some parts of I ndia show that leukoplakia, a possible precursor
of oral cancer, does regress rapidly after cessation of betel chewing (Mehta et al., 1982). Education programmes
which reduced the prevalence of chewing and smoking tobacco also seem to have had an effect in reducing rates
of leukoplakia (Gupta et al., 1990).
TABLE 2.9.1b: COMPARISON OF LIFE TIME CUMULATIVE CANCER INCIDENCE RATES (0-64 YEARS), 1989.
UP, ORAL CAVITY AND PHARYNX (ICD-9 ; 140-149)
CUMULATIVE RISK
(%)
REGISTRY
2.9.2
ONE IN HOW MANY
PEOPLE WILL GET CANCER
IN THEIR LIFE TIME
MALE
FEMALES
MALE
FEMALE
BANGALORE
1.2
0.8
83
125
BOMBAY
1.8
0.6
56
167
MADRAS
1.6
1.1
DELHI
1.3
0.5
62
77
200
BHOPAL
2.8
1.0
36
100
BARSHI
0.9
0.1
111
1000
91
DIGESTIVE ORGANS AND PERITONEUM (ICD9 :150-159)
In the digestive system, the oesophagus and stomach are the most frequently affected sites in the Indian
Registries (Table 2.9.2).
TABLE 2.9.2 : DIGESTIVE ORGANS AND PERITONEUM (ICD 9:150-159) -1989.
(a) MALES*
ICD.9
SITE
BANGALORE
150-159 Digestive Organs 33.0
& Peritoneum
Oesophagus
9.4
150
Stomach
151
9.5
Small Intestine
0.0
152
Colon
2.7
153
Rectum
154
4.3
Liver
155
3.2
Gall Baldder
0.5
156
Pancreas
1.7
157
Retroperitoneum
0.9
158
Other
0.8
159
BOMBAY
MADRAS
DELHI
BHOPAL
BARSHI
35.5
37.0
22.3
25.4
18.6
11.5
7.0
0.5
4.0
3.9
3.5
1.6
2.5
0.3
0.7
10.2
16.5
0.1
2.0
4.5
1.9
0.3
1.4
0.1
0.0
6.4
3.4
0.2
2.0
3.0
2.2
1.9
2.3
0.3
0.6
7.7
3.7
0.0
1.4
5.5
2.1
2.6
2.4
0.0
0.0
6.7
1.2
0.0
2.0
4.0
2.6
0.0
0.0
2.1
0.0
* Age-adjusted (World Population) Incidence Rate, Per 100,000 Persons.
14
(b) FEMALES*
ICD.9
SITE
BANGALORE
150-159 Digestive Organs 22.8
& Peritoneum
150
Oesophagus
10.2
151
4.3
Stomach
152
Small Intestine
0.0
2.3
153
Colon
154
Rectum
2.2
1.0
155
Liver
0.8
156
Gall Bladder
157
Pancreas
1.0
0.5
158
Retroperitoneum
0.5
159
Other
BOMBAY
MADRAS
DELHI
BHOPAL
BARSHI
23.9
20.2
20.6
15.5
5.5
8.2
3.4
0.3
2.4
2.6
1.8
2.3
1.8
0.6
0.5
7.7
7.1
0.0
0.8
2.6
0.6
0.6
0.7
0.1
0.0
4.6
2.4
0.2
2.0
1.8
1.1
6.6
1.3
0.3
0.3
5.2
1.1
0.0
2.1
0.0
1.1
5.2
0.8
0.0
0.0
1.4
1.3
0.0
0.5
1.7
0.0
0.0
0.6
0.0
0.0
* Age-adjusted (world Population) Incidence Rate, Per 100,000 Persons.
2.9.2.1
Cancer of the Oesophagus (ICD.9 :150)
Oesophageal cancer is characterised by an extreme diversity of rates throughout the world. There are usually
more cases among males then females (Table 2.9.2.1).
It is interesting to observe that the cancer of the oesophagus in India mainly occur in the persons who are 30
years and above and age-specific incidence rates vary between 1 and 75 per 100,000. In 1989, age-adjusted
incidence rates of cancer of the oesophagus in males are Bangalore (9.4), Bombay (11.5), Madras (10.2), Delhi (6.4),
Bhopal (7.7) and Barshi (6.7), While in females, the rates are lower than males, except Bangalore (10.2); in other
centres rates are Bombay (8.2), Madras (7.7), Delhi (4.6), Bhopal (5.2) and Barshi (1.4).
One of the prominent epidemiologic characterstics of the oesophageal cancer isthe great variability in sex ratios
reported in different geographical regions of the world. The typical pattern of male preponderance has been noted
by several registeries. The sex ratios in urban areas in India vary between (M/F = 0.9 : 1) and (M/F = 1.5 : 1). In
Barshi rural population the sex ratio is (M/F = 5.6 :1).
TABLE 2.9.2.1: INTERNATIONAL COMPARISON OF AGE-ADJUSTED (AAR) AND
TRUNCATED TR) (35-64 YEARS) INCIDENCE RATE PER 100,000 PERSONS.
OESOPHAGUS CANCER (ICD.9:150)
(a) MALES
YEAR STUDIED
REGISTRY
AAR*
TR*
1978-82
1978-82
1978-81
1978-82
CHINA (SHANGHAI)
SINGAPORE (CHINESE)
JAPAN (MIYAGI)
USA (CONNECTICUT) WHITE
BLACK
UK (OXFORD)
FINLAND
INDIA
BOMBAY
MADRAS
BANGALORE
BHOPAL
DELHI
BARSHI
20.8
13.5
13.3
5.1
24.0
3.6
3.7
21.0
13.9
14.5
6.2
47.8
2.8
3.4
11.5
17.3
10.2
9.4
7.7
6.4
6.7
19.6
14.3
13.4
10.7
10.4
1979-82
1977-81
1989
15
FEMALES
YEAR STUDIED
REGISTRY
AAR*
TR*
1978-82
1978-82
1978-81
1977-81
1979-82
1978-82
CHINA (SHANGHAI)
SINGAPORE (CHINESE)
8.9
3.5
9.7
4.1
JAPAN (MIYAGI)
FINLAND
UK (OXFORD)
• USA (CONNECTICUT) WHITE
BLACK
INDIA
BANGALORE
BOMBAY
MADRAS
BHOPAL
DELHI
3.1
2.4
2.9
1.5
6.0
2.5
1.8
3.6
1.9
11.8
10.2
8.2
7.7
5.2
4.6
1.4
20.8
15.8
16.1
11.1
10.0
2.0
1989
BARSHI
* World Population
Source : Cancer Incidence In Five Continents, Vol. V.1987. NCRP Data, 1989
In Bombay, where oesophageal cancer is almost as common as in men as in women, drinking of the local
alcoholic brews and smoking of bidis & cigarettes are associated with particularly high risks in men, but chewing of
tobacco quids, smoking and drinking explain only a small fraction of the incidence in women (Jussawalla &
Deshpande, 1971). Notani et al. (1989) estimated that 34% of oesophageal cancer in India is related to tobacco use,
although the percentages for males (50%) and females (13%) are very different.
2.9.2.2. Cancer of the Stomach (ICD.9 : 151)
In 1980, stomach cancer was estimated to be the single most common form of cancer in the world, accounting
for some 670 000 new cases per year (10.5% of all cancers) (Parkin etal., 1988). It is probably now the second most
common cancer, after lung cancer. The highest incidence rates occur in Japan (Males - 79.6; Females - 36.0 per
100,000) and lowest rates in Kuwait (Males - 3.7, Females -1.6) (Table 2.9.2.2).
Age-adjusted incidence rates of stomach cancer in India are low. In 1989, the rates in men in Madras (16.5) is
iTOre than Bangalore (9.5), Bombay (7.0), Bhopal (3.7), Delhi (3.4) and Barshi (1.2). Thus stomach cancer, in men,
in Madras is frequent where the incidence is almost 1.5 times than Bangalore, double that in Bombay and over three
times as frequent as in Delhi and Bhopal. The female incidence rates are lower than males: Madras (7.1), Bangalore
(4.3), Bombay (3.4), Delhi (2.4), Bhopal (1.1) and Barshi (1.3).
The incidence and mortality rates in males are approximately double those for females in both high-risk and
low-risk countries.
The most remarkable feature of the epidemiology of gastric cancer is the universal decline in its incidence and
mortality. The decline is about 2-4% per year, but there is a lot of variation between different countries. Rates are
falling more rapidly for females than for males.
Christopher et al (1986) have indicated that, between 1950 and 1979, the Scandinavian countries, Switzerland
and the USA exhibited the greatest percent decrease (65% - 73%) in their gastric cancer mortality rates. Western
Euporean countries showed the next greatest percent decrease (59% - 62%), followed by Australia (56%). The
countries that demonstrated the smallest percent change in gastric cancer mortality over the 29-year period were
Japan and Italy (44%), and Northern Ireland (41%). The authors conclude that the major etiologic influences in gastric
cancer are environmental rather than genetic.
Data from cancer registries indicate that the temporal changes in the incidence of gastric cancer in Norway
(Munoz & Asvall, 1971) and Japan (Hanai et al., 1982) are due largely to the disappearance of the'intestinal' type
16
of gastric cancer as opposed to the 'diffuse' type.
Case-control and cohort studies in a wide variety of populations have shown increased risk associated with
more frequent use of starchy foods (such as corn, wheat, rice, potatoes, and beans), smoked, salted and fried foods,
and a decreased risk associated with the more frequent intake of green leafy vegetables, citrus fruits and dairy
products (Hirayama, 1980).
TABLE 29.2.2: INTERNATIONAL COMPARISON OF AGE-ADJUSTED (AAR) AND
TRUNCATED (TR) (35-64 YEARS) INCIDENCE RATE PER 100,000.
STOMACH CANCER (ICD-9 :151)
MALES
YEAR STUDIED
REGISTRY
AAR*
TR*
1978-81
JAPAN (MIYAGI)
FINLAND
UK (OXFORD)
USA (CONNECTICUT) WHITE
BLACK
KUWAIT: KUWAITIS
INDIA
MADRAS
BANGALORE
BOMBAY
79.6
24.6
20.2
111.8
10.8
19.4
3.7
11.5
22.0
4.1
32.6
16.3
BHOPAL
DELHI
16.5
9.5
7.0
3.7
3.4
BARSHI
1.2
1977-81
1979-82
1978-82
1979-82
1989
25.7
225
9.5
8.5
6.2
3.9
FEMALES
YEAR STUDIED
REGISTRY
AAR*
TR*
1978-81
1977-81
1979-82
1978-82
JAPAN (MIYAGI)
FINLAND .
UK (OXFORD)
USA (CONNECTICUT) WHITE
BLACK
KUWAIT: KUWAITIS
INDIA
MADRAS
36.0
12.9
7.8
4.3
9.1
1.6
50.5
13.7
6.8
4.5
11.3
2.0
7.1
4.3
3.4
24
1.1
1.3
17.4
8.4
1979-82
1989
BANGALORE
BOMBAY
DELHI
BHOPAL
BARSHI
6.1
5.0
3.0
4.1
* World Population
Source : Cancer Incidence In Five Continents, Vol. V.1987. NCRP Data, 1989
2.9.3
RESPIRATORY AND INTRATHORACIC ORGANS (ICD 9 : 160-165)
In the respiratory and intrathoracic organs, cancers of the larynx and trachea, bronchus and lung are the most
affected sites (Table 2.9.3).
17
TABLE 2.9.3a : RESPIRATORY AND INTRATHORACIC ORGANS (ICD 9:160-165) -1989.
MALES*
ICD.9
SITE
BANGALORE
BOMBAY
MADRAS
DELHI
IBHOPAL
BARSHI
160-165 Respiratory
13.7
25.1
17.6
21.3
19.0
3.3
0.3
4.1
8.6
1.4
8.8
14.6
0.6
5.5
11.1
0.5
8.6
11.9
1.6
2.9
14.1
0.0
1.3
2.0
0.6
0.1
0.0
0.2
0.1
0.0
0.2
0.2
0.0
0.2
0.1
0.0
0.4
0.0
0.0
0.0
0.0
0.0
163
164
165
& Intrathoracic
Nasal Etc.
Larynx
Trachea, Bronchus
& Lung
Pleura
Thymus etc.
Other
ICD.9
SITE
BANGALORE
BOMBAY
MADRAS
DELHI
BHOPAL
BARSHI
160-165 Respiratory
3.3
6.3
2.8
4.6
4.6
0.0
0.4
0.7
1.6
1.0
1.3
3.7
0.8
0.3
1.7
0.4
1.8
2.2
0.4
0.5
3.2
0.0
0.0
0.0
0.5
0.1
0.0
0.2
0.1
0.0
0.0
0.0
0.0
0.2
0.0
0.0
0.5
0.0
0.0
0.0
0.0
0.0
160
161
162
•
FEMALES*
160
161
162
163
164
165
& Intrathoracic
Nasal etc.
Larynx
Trachea, Bronchus
& Lung
Pleura
Thymus etc.
Other
* Age-adjusted (World Population) Incidence Rate, Per 100,000 Persons
2.9.3.1 Cancer of the Larynx (ICD.9 : 161)
The age-adjusted incidence rate of laryngeal cancer in Indian material is high in men than women. Among men,
the highest incidence rates are in Bombay (8.8 per 100,000) and Delhi (8.6 per 100,000), during the period 1989.
•
TABLE 2.9.3.1 : INTERNATIONAL COMPARISON OF AGE-ADJUSTED
(AAR) AND TRUNCATED (TR) (35-64 YEARS) INCIDENCE RATE PER 100,000.
LARYNX CANCER (ICD-9:161)
(a) MALES
YEAR STUDIED
REGISTRY
AAR*
TR*
1978
1978-82
BRAZIL (SAO PAULO)
17.8
USA (CONNECTICUT) BLACK
WHITE
FINLAND
UK (OXFORD)
SWEDEN
INDIA
12.6
7.7
4.5
4.2
2.8
27.6
24.8
12.4
7.1
5.8
4.1
8.8
8.6
5.5
4.1
2.9
1.3
15.6
19.7
8.9
8.3
5.3
4.1
1977-81
1979-82
1978-82
1989
BOMBAY
DELHI
MADRAS
BANGALORE
BHOPAL
BARSHI
18
(b) FEMALES
YEAR STUDIED
REGISTRY
1978-82
USA (CONNECTICUT) BLACK
1978
WHITE
BRAZIL (SAO PAULO)
UK (OXFORD)
1979-82
1977-81
1978-82
1989
AAR*
TR*
2.7
1.7
4.4
3.0
1.3
0.5
2.8
0.8
0.7
0.7
0.3
0.3
FINLAND
SWEDEN
INDIA
DELHI
BOMBAY
BANGALORE
BHOPAL
MADRAS
BARSHI
1.8
1.3
0.7
0.5
0.3
0.0
4.0
1.8
1.6
0.0
0.5
0.0
* World Population
Source : Cancer Incidence In Five Continents, Vol. V, 1987. NCRP Data, 1989
The rates in other centres are: Bangalore (4.1), Madras (5.5), Bhopal (2.9) and Barshi (1.3). While in females,
laryngeal cancer age-adjusted incidence rates are very low in all the centres (vary between 0.0 and 1.8 per 100,000).
International comparisons are done in Table 2.9.3.1 for selected countries.The highest incidence rate of
laryngeal cancer world wide have been reported from Sao Paulo (Brazil) in males (Males - 17.8 and Females-1.3
per 100,000) and the lowest rate reported for European populatins in Sweden (Males - 2.8, Females - 0.3).
Jayant et al. (1977) estimated the proportion of cases of laryngeal cancer in Bombay that could be attributed
to chewing tobacco quid and/or smoking. The attributable risk for these two exposures combined was 78%; 28% of
the cases occurred in chewers who were nonsmokers, 38% in smokers who did not chew and 34% in cases who
admitted to both habits. The smokers mostly smoked bidis and the chewers used pan with betel nut, tobacco and
lime. Only 11 % of the cases were nonchewers and nonsmokers compared to 46% of the controls.
2.9.3.2
Cancer of the Trachea, Bronchus & Lung (ICD.9 :162)
Cancer of the lung is of epidemiological interest because of the wide spread geographical and racial variations
observed and steadily increasing incidence and mortality noted in the West. This increase has so far been noticed
particularly in men, but recently women have also begun to present a similar rising trend.
Age-adjusted and truncated incidence rates of lung cancer are much lower in I ndia than the corresponding rates
reported world wide by other countries in Cancer Incidence in Five Continents (VoLV, 1987). Age-adjusted incidence
is higher in the male population : Bombay (14.6), Bhopal (14.1), Delhi (11.9), Madras (11.1), and Bangalore (8.6).
Lung cancer is in the first rank in Bombay, Delhi and Bhopal, but it is not in the first eight ranking sites in the Barshi.
While in Indian women, incidence is low (ranges between 1.7 and 3.7 per 100,000).
The highest rates for cancer of the bronchus and trachea in people of European stock are 100.4 in males in
western Scotland and 33.3 among white females in San Francisco (Bay Area); the lowest rates are found in Iceland
in males (24.7) and in Doubs, France, in females (2.8), indicating a potential for prevention of 75% in males in western
Scotland, and 92% in females in San Francisco (Tomatis et al., 1990). Theoverall incidence of the disease is much
higher in the industrialised countries.
A large number of epidemiological studies in the West has shown that there is a progressive and absolute risk
in its incidence which has occurred over the past few decades and that it is clearly linked to cigarette smoking and
environmental pollution.
The association of cigarette smoking with lung cancer has now been universally accepted. The U.S. Surgeon
General’s Advisory Committee concluded that cigarette smoking is causally related to lung cancer in men and that
its effect far outweighs all other probable etiological factors. The risk increases with the duration of smoking habit
19
and the number of cigarettes smoked daily. A heavy smoker (more than 50 cigarette per day) runs a 20 times higher
risk of developing lung cancer, than a non- smoker. The increasing incidence of lung cancer in women in the West
is clearly linked with the steep increase registered in cigarette smoking by women during the sixties.
Many specific occupations and occupational exposures have been associated with elavated risks for lung
cancer, and in a number of cases the link has been clearly established to be causal. Clearly identified occupational
lung carcinogens are asbestos, coal-tars and soots, arsenic and arsenic compounds, nickel compounds, mustard
gas and radon. Increased risk for lung cancer have also been found to be causally associated with occupational
exposure in aluminium production, in coal gasification and coal production, in iron and steel founding etc. (IARC,
1987).
TABLE 2.9.3.2: INTERNATIONAL COMPARISON OF AGE-ADJUSTED
(AAR) TRUNCATED (TR)(35-64 YEARS) INCIDENCE RATE PER 100,000.
TRACHEA, BRONCHUS & LUNG (ICD.9:162)
MALES
YEAR STUDIED
REGISTRY
AAR*
TR*
1979-82
1977-81
1979-82
1978-82
1978-82
UK (WEST SCOTLAND)
FINLAND
UK (OXFORD)
USA (BAY AREA) WHITE
USA (CONNECTICUT) WHITE
BLACK
COLUMBIA (CALI)
INDIA
BOMBAY
100.4
74.2
68.8
65.8
64.3
120.7
93.2
68.1
84.0
81.1
89.8
19.5
140.1
25.5
14.6
14.1
11.9
11.1
8.6
2.0
24.7
24.5
233
23.2
13.2
3.9
1977-81
1989
BHOPAL
DELHI
MADRAS
BANGALORE
BARSHI
FEMALES
YEAR STUDIED
REGISTRY
AAR*
TR*
1978-82
1979-82
1978-82
USA (BAY AREA) WHITE
UK (WEST SCOTLAND)
USA (CONNECTICUT) WHITE
BLACK
UK (OXFORD)
33.3
28.6
25.3
21.9
19.5
FINLAND
COLUMBIA (CALI)
7.0
5.4
54.4
46.3
41.5
41.1
25.6
10.0
9.5
3.7
3.2
2.2
1.7
1.6
0.0
5.3
6.3
4.5
4.5
4.1
0.0
1979-82
1977-81
1972-76
1989
INDIA
BOMBAY
BHOPAL
DELHI
MADRAS
BANGALORE
BARSHI
* World Population
Source : Cancer Incidence In Five Continents, Vol. V.1987.
20
TABLE 2.10.1 : TRENDS IN AGE-ADJUSTED (WORLD POPULATION) CANCER INCIDENCE RATES
BANGALORE*
SEX: MALES
YEAR : 1982-1989
1982
1983
YEAR OF DIAGNOSIS
1984
1985
1986
1987
1988
1989
140
0.2
Lip
141
Tongue
4.5
142
Salivary Gland
0.4
143-145i Mouth
4.0
146
Oropharynx
2.2
147
Nasopharynx
0.9
148
Hypopharynx
4.9
149
Pharynx Uns
0.4
150
Oesophagus
8.4
151
Stomach
11.0
152
Small Intestine
0.0
153
Colon
2.0
154
Rectum
3.0
155
Liver
4.0
156
Gallbladder
0.0
157
Pancreas
0.7
158
Peritoneum
1.0
160
Nose Etc
0.2
161
Larynx
4.5
162
Lung
5.3
163
Pleura
0.7
164
Other Thoracic
0.4
170
Bone
1.0
171
Connective Tissue 1.5
i /z
Skin Melanoma
0.5
173
Skin Other
2.7
175
Breast
0.3
185
Prostate
4.1
186
Testis
0.7
187
Penis Etc
2.3
188
Bladder
3.3
189
Kidney
1.2
190
Eye
0.7
191-192 Brain-Ns
1.8
193
Thyroid Gland
0.9
194
Endocrine Other
0.2
201
Hodgkins Disease 1.5
200-202 Non-Hodg Lymphoma 3.1
203
Mult Myeloma
0.7
204
Leuk Lymphoid
0.9
205
Leuk Myeloid
1.0
206
Leuk Monocytic
0.0
207
Leuk Other
0.0
208
Leuk Uns
0.6
Primary Unk
12.5
0.0
4.0
0.4
4.9
2.0
0.4
6.0
0.4
6.3
10.9
0.2
2.0
2.3
1.5
0.3
1.2
1.0
0.2
4.9
8.8
0.4
0.2
1.6
1.2
0.7
0.9
0.6
3.2
0.3
2.8
4.5
0.8
0.1
2.6
0.4
0.4
' 1.4
3.1
0.5
0.7
1.0
0.0
0.3
0.5
6.6
0.0
3.0
0.0
3.6
2.3
0.7
6.6
0.8
8.2
10.5
0.0
2.4
2.3
3.7 ■
0.2
0.7
0.5
0.5
4.0
9.2
0.2
0.2
1.1
1.3
0.0
1.7
0.3
4.2
0.9
2.0
2.9
1.0
0.1
1.1
0.4
0.1
1.0
3.4
1.1
1.1
1.2
0.0
0.1
0.4
5.5
0.0
2.6
0.3
4.5
1.3
0.7
6.0
0.7
7.3
12.1
0.1
2.6
3.4
3.6
0.3
0.7
1.1
0.8
3.7
11.8
0.5
0.2
1.1
0.8
0.0
0.9
0.3
5.6
0.7
2.3
2.8
1.8
0.2
1.7
1.1
0.0
1.4
2.9
0.8
1.0
0.8
0.2
0.3
0.3
7.6
0.1
2.8
0.4
3.1
1.9
0.4
5.2
0.3
7.6
9.9
0.4
2.4
3.5
2.8
0.7
0.8
0.5
0.6
4.1
10.0
0.5
0.1
0.5
0.3
0.5
1.4
0.5
5.0
1.0
1.0
3.0
1.9
0.3
3.0
1.7
0.0
1.6
3.2
1.0
1.2
1.0
0.0
0.0
0.5
10.4
0.0
4.5
0.5
5.4
1.9
0.3
7.5
0.7
11.1
9.3
0.0
2.1
3.4
3.4
0.7
1.4
0.7
0.9
4.8
10.8
0.3
0.2
0.5
1.6
0.1
1.4
0.5
5.5
0.7
1.4
3.1
1.5
0.1
2.2
0.6
0.1
1.5
1.7
0.9
0.8
1.5
0.0
0.0
0.5
14.3
0.1
2.9
0.7
3.4
2.5
0.2
7.3
0.6
9.9
13.6
0.2
2.6
3.6
2.8
0.4
2.3
0.7
0.6
4.4
11.7
0.5
0.1
1.3
0.6
0.0
2.5
0.4
4.9
0.3
2.2
3.3
0.6
0.1
3.5
1.2
0.0
1.2
4.2
0.3
1.2
0.9
0.0
0.0
0.2
14.7
0.4
4.7
0.8
3.0
1.9
0.6
5.9
0.2
9.4
9.5
0.0
2.7
4.3
3.2
0.5
1.7
0.9
0.3
4.1
8.6
0.6
0.1
1.3
0.6
0.1
2.0
0.2
7.1
0.6
1.8
2.7
1.1
0.2
4.0
0.9
0.1
2.4
3.1
0.6
1.6
2.3
0.1
0.0
0.7
15.2
92.5
90.6
98.7
97.0
110.7
114.6
112.2
ICD9
SITE
ALL SITES
100.2
* Incidence Rate Per 100,000
30
TABLE 2.10.2 :TRENDS IN AGE-ADJUSTED (WORLD POPULATION) CANCER INCIDENCE RATES
BANGALORE*
SEX: FEMALES
YEAR: 1982-1989
1982
1983
YEAR OF DIAGNOSIS
1984
1985
1986
1987
1988
1989
140
0.1
Lip
141
Tongue
1.1
142
Salivary Gland
0.2
143-145 Mouth
13.4
146
Oropharynx
0.4
147
Nasopharynx
0.1
148
Hypopharynx
1.3
149
Pharynx Uns
0.3
150
Oesophagus
7.1
151
Stomach
6.0
152
Small Intestine
0.1
153
Colon
1.5
154
Rectum
2.6
155
Liver
1.4
156
Gallbladder
0.0
157
Pancreas
0.4
158
Peritoneum
1.6
160
Nose Etc
0.7
161
Larynx
1.3
LUNG
162
1.4
163
Pleura
0.4
164
Other Thoracic
0.1
170
Bone
1.2
171
Connective Tissue 1.1
172
Skin Melanoma
0.5
173
Skin Other
1.9
174
Breast
17.3
179
Uterus Uns
0.2
180
Cervix Uteri
35.6
181
Placenta
0.2
182
Corpus Uteri
1.8
183
Ovary etc
5.0
184
Other Fem Genital 2.3
188
Bladder
0.7
189
Kidney
1.7
190
Eye
0.3
191- 192 Brain-Ns
1.2
193
Thyroid Gland
2.5
194
Endocrine Other
0.0
201
Hodgkins Disease 0.4
200-202 Non-hodg Lymphoma 1.4
203
Mult Myeloma
0.2
204
Leuk Lymphoid
0.5
205
Leuk Myeloid
0.9
206
Leuk Monocytic
0.2
207
Leuk Other
0.0
208
Leuk Uns
0.3
Primary Unk
10.0
0.1
1.4
0.5
9.6
0.4
0.5
1.7
0.4
7.3
6.0
0.2
1.1
1.9
1.2
0.6
0.4
0.7
0.4
0.8
1.7
0.4
0.0
0.4
0.7
0.4
2.4
17.6
0.2
33.7
0.2
2.2
4.3
1.2
0.4
0.9
0.2
1.0
2.7
0.2
0.3
1.6
0.1
0.3
1.0
0.0
0.3
0.7
6.1
0.3
1.0
0.6
10.2
0.3
0.3
1.6
0.0
9.5
5.7
0.4
1.2
2.8
0.6
0.3
0.3
0.7
0.1
0.6
2.2
0.4
0.0
1.3
0.9
0.4
2.1
18.5
1.0
31.0
0.0
1.6
5.5
1.2
0.5
0.4
0.0
1.1
3.4
0.1
0.3
1.7
0.7
0.5
0.9
0.0
0.0
0.1
3.9
0.1
1.2
0.2
9.2
0.2
0.0
1.2
0.6
7.2
7.0
0.3
1.5
2.5
0.8
0.4
1.3
0.1
0.7
0.9
1.7
0.4
0.1
0.2
0.7
0.3
1.2
17.8
0.4
29.5
0.2
1.0
3.1
0.8
0.6
0.6
0.2
1.6
3.1
0.0
0.9
1.0
0.6
0.8
1.4
0.0
0.0
0.0
5.1
0.1
0.8
0.3
10.4
0.4
0.1
0.6
0.5
10.1
4.7
0.1
2.2
3.2
0.9
0.2
0.5
0.7
0.7
0.7
1.4
0.3
0.0
0.6
0.8
0.2
1.3
15.9
0.5
28.7
0.4
1.3
5.3
1.5
0.2
0.8
0.1
1.4
1.7
0.0
0.4
2.5
0.6
0.6
1.3
0.0
0.0
0.3
. 10.5
0.1
1.1
0.9
8.9
0.1
0.1
1.2
0.2
9.8
5.2
0.1
2.6
3.0
1.1
0.8
1.0
0.2
0.2
0.6
2.3
0.3
0.1
0.7
1.0
0.1
0.7
20.9
0.8
32.4
0.1
2.0
5.9
1.5
0.7
1.1
0.2
1.8
3.0
0.1
0.7
2.0
1.0
0.4
1.5
0.0
0.1
0.4
10.4
0.2
1.2
0.2
11.2
0.5
0.3
1.5
0.3
8.1
6.3
0.1
2.4
3.6
1.5
0.7
0.7
0.7
0.5
0.5
1.5
0.2
0.1
0.8
0.5
0.2
2.5
20.4
0.1
32.2
0.0
0.9
4.7
1.9
0.8
0.5
0.4
1.3
3.4
0.1
1.0
1.3
0.5
0.5
2.1
0.0
0.1
0.6
12.9
0.1
1.0
0.5
11.1
0.5
0.4
1.2
0.1
10.2
4.3
0.0
2.3
2.2
1.0
0.8
1.0
0.5
0.4
0.7
1.6
0.5
0.1
0.9
0.3
0.1
1.6
22.3
0.6
26.4
0.0
2.0
4.7
1.4
0.8
0.4
0.0
1.7
3.2
0.1
0.7
2.1
0.7
0.6
2.0
0.0
0.0
0.9
10.5
129.0
116.2
116.3
108.7
115.9
129.5
132.3
124.7
ICD9
SITE
ALL SITES
* Incidence Rate Per 100,000
31
TABLE 2.10.3 rTRENDS IN AGE-ADJUSTED (WORLD POPULATION) CANCER INCIDENCE RATES
BOMBAY*
SEX: MALES
YEAR: 1982-1989
SITE
1982
1983
YEAR OF DIAGNOSIS
1984
1985
1986
1987
1988
1989
140
Lip
141
Tongue
142
Salivary Gland
143-145 Mouth
146
Oropharynx
147
Nasopharynx
148
Hypopharynx
149
Pharynx Uns
150
Oesophagus
151
Stomach
152
Small Intestine
153
Colon
154
Rectum
155
Liver
156
Gallbladder
157
Pancreas
158
Peritoneum
160
Nose etc
161
Larynx
162
Lung
0.3
7.1
0.6
5.7
3.3
0.9
9.5
2.6
11.2
7.4
0.2
2.5
4.0
3.8
0.7
2.2
0.5
1.1
7.0
13.7
0.4
7.2
0.5
5.9
2.7
1.1
7.7
2.3
9.9
7.4
0.2
2.9
3.1
3.3
0.6
1.7
0.1
0.8
8.9
14.7
0.3
7.8
0.4
5.0
3.8
0.5
8.6
1.6
12.1
7.1
0.3
2.5
3.5
3.3
1.1
2.2
0.2
1.1
8.1
13.4
0.3
7.9
0.4
6.9
3.6
0.7
8.1
2.4
11.6
7.3
0.2
2.6
3.2
3.3
1.2
3.2
0.3
1.0
7.8
14.2
0.4
7.8
0.5
5.9
2.7
0.8
8.0
2.6
11.4
7.9
0.5
3.5
2.9
3.7
1.0
2.7
0.3
0.9
9.8
13.1
0.3
6.3
0.5
5.6
3.3
0.5
8.3
2.1
11.8
6.8
0.2
4.5
3.2
3.2
1.1
2.6
0.4
1.1
9.9
14.8
0.2
5.9
0.5
6.1
3.5
0.6
9.4
1.8
11.4
7.7
0.2
3.0
3.3
3.5
1.2
2.3
0.6
0.7
8.1
14.0
0.3
6.5
0.4
5.8
3.2
0.6
8.2
1.8
11.5
7.0
0.5
4.0
3.9
3.5
1.6
2.5
0.3
1.4
8.8
14.6
163
Pleura
164
O ther Thoracic
170
Bone
171
Connective Tissue
172
Skin Melanoma
173
Skin Other
175
Breast
185
Prostate
186
Testis
187
Penis etc
188
Bladder
189
Kidney
190
Eye
191-192 Brain-Ns
193
Thyroid Gland
194
Endocrine Other
201
Hodgkins Disease
200-202 Non-hodg Lymphoma
203
Mult Myeloma
204
Leuk Lymphoid
205
Leuk Myeloid
206
Leuk Monocytic
207
Leuk Other
208
Leuk Uns
Primary Unk
0.1
0.1
0.9
1.0
0.3
1.9
0.2
5.4
0.8
2.2
3.4
1.1
0.2
1.8
0.6
0.1
1.1
2.6
1.2
1.7
1.5
0.1
0.0
0.4
6.6
0.0
0.0
0.8
1.2
0.2
1.6
0.1
5.7
1.0
1.7
3.1
1.5
0.5
1.8
0.9
0.1
1.3
3.4
0.9
1.1
1.4
0.0
0.1
0.5
6.8
0.1
0.1
0.9
1.8
0.4
1.4
0.5
6.9
1.1
2.1
4.0
1.5
0.2
2.8
0.8
0.1
1.0
3.3
0.7
2.2
2.1
0.0
0.0
0.6
6.8
0.3
0.1
0.9
1.1
0.3
2.6
0.3
8.3
0.9
1.7
3.2
1.1
0.3
2.7
0.6
0.1
1.4
4.1
0.9
1.7
1.9
0.0
0.0
0.5
8.5
0.5
0.1
0.9
1.4
0.2
2.1
0.3
6.1
1.1
2.2
3.8
. 1.5
0.2
2.0
1.0
0.2
1.2
3.6
0.8
1.5
1.9
0.0
0.0
0.58.9
0.5
0.2
0.9
1.3
0.1
1.9
0.6
7.3
1.0
2.0
4.1
1.5
0.3
2.6
0.7
0.2
1.0
4.4
0.9
1.4
1.7
0.0
0.1
0.6
9.0
0.5
0.1
0.8
1.3
0.5
2.0
0.4
8.2
0.9
2.0
4.5
1.6
0.1
2.8
0.7
0.3
1.1
3.1
0.8
1.7
1.7
0.0
0.1
0.4
10.0
0.2
0.1
0.8
1.5
0.3
1.3
0.3
6.9
0.9
1.6
4.2
1.4
0.4
3.1
0.7
0.2
1.2
4.0
1.3
1.6
1.9
0.0
0.2
0.3
9.7
119.9
116.5
123.9
129.5
128.5
130.4
129.6
130.4
ICD9
ALL SITES
* Incidence Rate Per 100,000
32
TABLE 2.10.4 iTRENDS IN AGE-ADJUSTED (WORLD POPULATION) CANCER INCIDENCE RATES
BOMBAY*
SEX: FEMALES
YEAR: 1982-1989
1982
1983
YEAR OF DIAGNOSIS
1984
1985
1986
1987
1988
1989
140
0.1
Lip
141
Tongue
2.9
142
Salivary Gland
0.7
143-145 Mouth
4.5
146
Oropharynx
0.5
147
Nasopharynx
0.5
148
Hypopharynx
2.1
149
0.4
Pharynx Uns
150
Oesophagus
8.4
151
Stomach
5.4
152
Small Intestine
0.5
153
Colon
2.3
154
Rectum
2.4
155
Liver
2.7
156
Gallbladder
1.0
157
Pancreas
1.4
158
Peritoneum
0.2
160
Nose Etc
0.8
161
Larynx
1.2
162
Lung
3.3
163
Pleura
0.1
164
Other Thoracic
0.1
170
Bone
0.7
171
Connective Tissue 1.0
172
Skin Melanoma
0.1
173
Skin Other
1.3
174
Breast
21.4
179
Uterus Uns
1.5
180
Cervix Uteri
18.5
181
Placenta
0.3
182
Corpus Uteri
2.1
183
Ovary etc
5.9
184
Other Fem Genital 1.6
188
Bladder
0.7
189
Kidney
0.5
190
Eye
0.2
191-192 Brain-Ns
1.3
193
Thyroid Gland
1.5
194
Endocrine Other
0.0
201
Hodgkins Disease 0.6
200-202 Non-hodg Lymphoma 1.8
203
Mult Myeloma
0.6
204
Leuk Lymphoid
1.0
205
Leuk Myeloid
1.4
206
Leuk Monocytic
0.1
207
Leuk Other
0.1
208
Leuk Uns
0.4
Primary Unk
4.9
0.4
2.4
0.3
4.2
0.7
0.4
1.3
0.5
7.4
3.7
0.3
2.7
2.3
1.5
1.6
1.3
0.3
0.6
2.0
3.2
0.0
0.0
0.8
0.8
0.0
0.9
21.6
1.2
18.5
0.2
2.2
6.3
1.2
1.0
0.7
0.3
1.2
1.3
0.1
0.5
2.0
0.8
0.7
1.3
0.0
0.0
0.5
4.8
0.2
2.0
0.4
3.9
0.3
0.2
2.0
0.9
8.4
3.9
0.3
2.8
2.3
1.4
1.4
. 1.2
0.5
1.0
1.3
4.1
0.0
0.0
0.9
0.7
0.2
1.2
23.6
1.2
19.6
0.2
2.1
6.2
1.4
0.9
0.7
0.1
1.5
1.4
0.2
0.7
2.4
1.0
0.8
1.7
0.0
0.1
0.3
6.7
0.2
2.5
0.3
4.4
1.0
0.2
2.6
0.7
8.9
4.2
0.2
2.5
2.5
2.2
1.9
1.9
0.6
0.9
1.4
2.7
0.3
0.1
0.6
1.1
0.5
2.0
26.4
1.4
19.3
0.3
2.0
6.7
1.1
1.3
0.8
0.1
1.7
1.5
0.2
0.7
2.0
1.1
0.9
1.4
0.1
0.0
0.4
7.1
0.3
3.2
0.5
4.5
0.6
0.3
1.9
0.5
8.3
4.9
0.2
2.4
2.6
2.5
1.5
1.1
0.5
0.9
1.6
2.0
0.4
0.1
0.8
0.7
0.2
1.6
26.7
1.7
19.9
0.1
2.7
6.0
1.2
0.9
0.7
0.1
1.6
1.8
0.1
0.3
2.3
0.8
1.3
1.4
0.0
0.0
0.4
6.7
0.3
2.5
0.3
4.4
0.7
0.1
1.8
0.9
8.8
4.8
0.2
2.8
2.8
1.7
2.0
2.0
0.4
0.7
1.6
2.9
0.1
0.0
0.6
0.6
0.1
1.7
24.2
1.1
19.1
0.2
2.4
7.3
1.7
0.7
0.6
0.3
2.3
1.7
0.0
0.6
2.8
0.8
0.9
1.5
0.0
0.0
0.3
5.4
0.3
2.2
0.3
4.7
0.6
0.3
2.2
0.6
8.0
4.3
0.3
2.7
2.3
1.9
2.1
1.9
0.3
0.3
1.5
3.6
0.2
0.1
0.6
0.9
0.2
1.1
25.0
1.3
21.0
0.2
2.2
7.6
1.6
1.3
0.7
0.4
1.7
2.0
0.1
0.5
2.6
0.8
1.1
1.4
0.0
0.0
0.5
6.9
0.2
1.9
0.3
3.9
0.6
0.2
1.5
0.9
8.2
3.4
0.3
2.4
2.6
1.8
2.3
1.8
0.6
1.0
1.3
3.7
0.2
0.1
0.7
0.9
0.3
1.2
26.1
1.5
19.4
0.1
2.2
7.0
1.7
1.3
0.8
0.2
2.3
2.0
0.1
0.7
3.0
0.6
1.1
1.3
0.0
0.1
0.4
6.1
106.3
113.8
122.9
120.9
118.8
122.7
120.4
ICD9
SITE
ALL SITES
111.2
* Incidence Rate Per 100,000
33
TABLE 2.10.5 :TRENDS IN AGE-ADJUSTED (WORLD POPULATION) CANCER INCIDENCE RATES
MADRAS*
SEX: MALES
YEAR: 1982-1989
1982
1983
YEAR OF DIAGNOSIS
1984
1985
1986
1987
1988
1989
140
0.4
Lip
141
Tongue
3.8
142
Salivary Gland
0.3
143-145 Mouth
6.7
146
Oropharynx
1.8
147
Nasopharynx
0.7
148
Hypopharynx
3.7
149
0.6
Pharynx Uns
150
Oesophagus
6.3
151
Stomach
12.1
152
Small Intestine
0.3
153
Colon
1.5
154
Rectum
2.7
155
Liver
1.7
156
Gallbladder
0.1
157
Pancreas
1.0
158
Peritoneum
0.7
160
Nose Etc
0.6
161
Larynx
4.2
162
Lung
5.1
163
Pleura
0.0
164
Other Thoracic
0.0
170
Bone
0.9
171
Connective Tissue 0.6
172
Skin Melanoma
0.2
173
Skin Other
0.9
175
Breast
0.3
185
Prostate
2.8
186
Testis
0.6
187
Penis etc
2.9
Bladder
188
1.8
189
Kidney
1.7
190
Eye
0.5
191-192 Brain-Ns
1.3
193
Thyroid Gland
0.7
194
Endocrine Other
0.2
201
Hodgkins Disease 2.3
200-202 Non-hodg Lymphoma 2.3
203
Mult Myeloma
0.4
204
Leuk Lymphoid
1.2
205
Leuk Myeloid
1.4
206
Leuk Monocytic
0.3
Leuk Other
207
0.0
Leuk Uns
208
0.6
Primary Unk
3.4
0.2
3.5
0.8
6.1
1.7
0.6
5.4
1.0
6.1
14.2
0.5
2.1
2.1
1.6
0.4
1.0
0.3
1.1
3.9
7.3
0.1
0.1
1.1
1.1
0.6
1.0
0.4
2.1
0.3
3.7
0.8
0.7
0.4
2.3
0.9
0.0
1.8
1.8
0.5
1.0
0.9
0.0
0.0
0.5
6.1
0.1
4.0
0.7
5.6
1.4
0.9
4.2
0.4
7.6
13.8
0.2
0.7
2.6
2.5
0.3
1.1
0.5
0.7
4.8
8.5
0.0
0.0
1.0
1.1
0.3
1.3
0.3
1.3
0.5
3.0
1.9
0.6
0.1
2.8
0.5
0.1
1.3
2.0
0.8
1.3
1.1
0.0
0.0
0.2
5.5
0.5
5.5
0.7
6.7
1.1
0.8
3.8
0.4
7.7
15.7
0.1
1.7
2.1
3.1
0.4
0.9
0.4
0.7
4.6
8.0
0.2
0.1
0.7
0.6
0.2
1.7
0.1
1.5
0.9
1.9
1.4
0.9
0.3
1.7
0.8
0.3
1.4
3.2
1.0
1.4
1.1
0.0
0.0
0.3
5.4
0.1
5.0
0.4
7.4
2.0
0.8
5.9
1.2
7.2
17 1
0.0
1.7
2.6
2.1
0.3
1.2
0.4
1.2
4.3
9.9
0.1
0.2
0.1
0.9
0.3
1.4
0.5
3.1
0.8
2.5
1.8
1.7
0.6
2.1
0.6
0.0
1.7
2.7
0.6
1.1
1.2
0.0
0.0
0.1
6.4
0.5
5.1
0.7
8.1
2.2
0.4
6.6
0.9
9.5
14.3
0.2
1.3
2.5
2.4
0.9
1.5
0.3
0.6
4.6
8.8
0.1
0.1
0.7
0.9
0.4
1.4
0.1
2.6
0.5
2.6
3.C
1.5
0.4
2.4
0.7
0.1
1.7
3.4
0.5
1.0
1.4
0.0
0.0
0.6
6.6
0.5
8.2
0.9
9.8
2.9
1.4
7.8
1.2
10.4
15.1
0.2
1.9
3.7
3.9
0.5
0.3
1.6
5.5
11.4
0.4
0.0
1.4
1.5
0.1
1.5
0.1
2.9
0.7
4.0
2.3
0.4
0.9
2.7
0.8
0.2
1.6
3.5
0.9
1.4
0.9
0.0
0.0
0.2
8.5
0.6
5.3
0.4
7.3
1.9
0.6
6.5
1.0
10.2
16.5
0.1
2.0
4.5
1.9
0.3
1.4
0.1
0.6
5.5
11.1
0.2
0.2
0.9
1.0
0.3
2.2
0.7
3.6
1.1
2.8
3.8
0.9
0.3
1.8
0.9
0.1
1.7
3.9
0.5
1.5
1.4
0.2
0.0
0.3
10.4
88.7
87.6
92.2
101.3
104.4
125.2
118.5
ICD9
SITE
ALL SITES
81.6
Incidence Rate Per 100,000
to
TABLE 2.10.5 .'TRENDS IN AGE-ADJUSTED (WORLD POPULATION) CANCER INCIDENCE RATES
MADRAS*
SEX: MALES
YEAR : 1982-1989
1982
1983
YEAR OF DIAGNOSIS
1984
1985
1986
1987
1988
1989
140
0.4
Lip
141
Tongue
3.8
142
Salivary Gland
0.3
143-145 Mouth
6.7
146
Oropharynx
1.8
147
Nasopharynx
0.7
148
Hypopharynx
3.7
149
Pharynx Uns
0.6
150
Oesophagus
6.3
151
Stomach
12.1
152
Small Intestine
0.3
153
Colon
1.5
154
Rectum
2.7
155
Liver
1.7
156
Gallbladder
0.1
157
Pancreas
1.0
158
Peritoneum
0.7
160
Nose Etc
0.6
161
Larynx
4.2
162
Lung
5.1
163
Pleura
0.0
164
Other Thoracic
0.0
170
Bone
0.9
171
Connective Tissue 0.6
172
Skin Melanoma
0.2
173
Skin Other
0.9
175
Breast
0.3
185
Prostate
2.8
186
Testis
0.6
187
Penis etc
2.9
188
Bladder
1.8
189
Kidney
1.7
190
Eye
0.5
191-192 Brain-Ns
1.3
193
Thyroid Gland
0.7
194
Endocrine Other
0.2
201
Hodgkins Disease 2.3
200-202 Non-hodg Lymphoma 2.3
203
Mult Myeloma
0.4
204
Leuk Lymphoid
1.2
205
Leuk Myeloid
1.4
206
Leuk Monocytic
0.3
207
Leuk Other
0.0
208
Leuk Uns
0.6
Primary Unk
3.4
0.2
3.5
0.8
6.1
1.7
0.6
5.4
1.0
6.1
14.2
0.5
2.1
2.1
1.6
0.4
1.0
0.3
1.1
3.9
7.3
0.1
0.1
1.1
1.1
0.6
1.0
0.4
2.1
0.3
3.7
0.8
0.7
0.4
2.3
0.9
0.0
1.8
1.8
0.5
1.0
0.9
0.0
0.0
0.5
6.1
0.1
4.0
0.7
5.6
1.4
0.9
4.2
0.4
7.6
13.8
0.2
0.7
2.6
2.5
0.3
1.1
0.5
0.7
4.8
8.5
0.0
0.0
1.0
1.1
0.3
1.3
0.3
1.3
0.5
3.0
1.9
0.6
0.1
2.8
0.5
0.1
1.3
2.0
0.8
1.3
1.1
0.0
0.0
0.2
5.5
0.5
5.5
0.7
6.7
1.1
0.8
3.8
0.4
7.7
15.7
0.1
1.7
2.1
3.1
0.4
0.9
0.4
0.7
4.6
8.0
0.2
0.1
0.7
0.6
0.2
1.7
0.1
1.5
0.9
1.9
1.4
0.9
0.3
1.7
0.8
0.3
1.4
3.2
1.0
1.4
1.1
0.0
0.0
0.3
5.4
0.1
5.0
0.4
7.4
2.0
0.8
5.9
1.2
7.2
17.1
0.0
1.7
2.6
2.1
0.3
1.2
0.4
1.2
4.3
9.9
0.1
0.2
0.1
0.9
0.3
1.4
0.5
3.1
0.8
2.5
1.8
1.7
0.6
2.1
0.6
0.0
1.7
2.7
0.6
1.1
1.2
0.0
0.0
0.1
6.4
0.5
5.1
0.7
8.1
2.2
0.4
6.6
0.9
9.5
14.3
0.2
1.3
2.5
2.4
0.9
1.5
0.3
0.6
4.6
8.8
0.1
0.1
0.7
0.9
0.4
1.4
0.1
2.6
0.5
2.6
3.C
1.5
0.4
2.4
0.7
0.1
1.7
3.4
0.5
1.0
1.4
0.0
0.0
0.6
6.6
0.5
8.2
0.9
9.8
2.9
1.4
7.8
1.2
10.4
15.1
0.2
1.9
3.7
3.9
0.5
0.3
1.6
5.5
11.4
0.4
0.0
1.4
1.5
0.1
1.5
0.1
2.9
0.7
4.0
2.3
0.4
0.9
2.7
0.8
0.2
1.6
3.5
0.9
1.4
0.9
0.0
0.0
0.2
8.5
0.6
5.3
0.4
7.3
1.9
0.6
6.5
1.0
10.2
16.5
0.1
2.0
4.5
1.9
0.3
1.4
0.1
0.6
5.5
11.1
0.2
0.2
0.9
1.0
0.3
2.2
0.7
3.6
1.1
2.8
3.8
0.9
0.3
1.8
0.9
0.1
1.7
3.9
0.5
1.5
1.4
0.2
0.0
0.3
10.4
88.7
87.6
92.2
101.3
104.4
125.2
118.5
ICD9
SITE
ALL SITES
81.6
* Incidence Rate Per 100,000
34
to
TABLE 2.10.6 : TRENDS IN AGE-ADJUSTED (WORLD POPULATION) CANCER INCIDENCE RATES
MADRAS*
SEX: FEMALES
YEAR: 1982-1989
1982
1983
YEAR OF DIAGNOSIS
1984
1985
1986
1987
1988
1989
140
0.3
Lip
141
Tongue
1.7
142
Salivary Gland
0.2
143-145 Mouth
8.6
146
0.8
Oropharynx
147
Nasopharynx
0.2
148
Hypopharynx
1.1
149
Pharynx Uns
0.1
150
Oesophagus
3.3
151
Stomach
5.9
152
Small Intestine
0.1
153
Colon
0.5
154
Rectum
1.3
155
Liver
0.6
156
Gallbladder
0.2
157
Pancreas
0.3
158
Peritoneum
0.2
160
Nose Etc
0.3
161
Larynx
0.5
162
Lung
1.1
163
Pleura
0.0
164
Other Thoracic
0.1
170
Bone
0.7
171
Connective Tissue 0.9
172
Skin Melanoma
0.0
173
Skin Other
0.7
174
Breast
18.8
179
Uterus Uns
0.6
180
Cervix Uteri
41.6
Placenta
181
0.4
182
Corpus Uteri
1.4
183
Ovary etc
4.1
184
Other Fem Genital 1.8
188
Bladder
0.9
189
Kidney
0.4
190
Eye
0.4
191-192 Brain-Ns
0.8
193
Thyroid Gland
1.4
194
Endocrine Other
0.1
201
Hodgkins Disease 0.5
200-202 Non-hodg Lymphoma 1.0
203
Mult Myeloma
0.1
204
Leuk Lymphoid
0.3
205
Leuk Myeloid
0.3
206
Leuk Monocytic
0.1
Leuk Other
0.0
207
Leuk Uns
0.4
208
Primary Unk
2.8
0.6
1.5
0.4
8.4
0.3
0.3
1.8
0.3
5.8
6.4
0.2
1.5
1.0
0.7
0.4
0.3
0.2
0.4
0.4
1.4
0.0
0.0
0.7
0.8
0.5
0.6
18.7
1.2
44.8
0.5
1.0
4.6
2.0
0.8
1.3
0.3
1.1
1.7
0.2
0.7
1.2
0.4
0.5
0.6
0.2
0.1
0.3
5.0
0.1
1.1
0.5
7.4
0.3
0.4
1.4
0.4
5.9
6.0
0.1
1.9
2.3
0.6
0.6
0.4
0.4
0.9
0.6
0.9
0.1
0.0
1.0
0.8
0.3
0.9
19.2
1.1
43.3
0.3
1.6
6.0
2.1
0.7
0.5
0.3
1.6
1.4
0.0
0.6
0.8
0.2
0.5
0.8
0.1
0.0
0.3
3.5
0.3
1.8
0.4
7.7
0.3
0.4
2.5
0.3
5.6
6.7
0.2
1.4
2.2
1.0
0.5
0.5
0.5
0.1
0.5
1.7
0.2
0.1
0.8
0.5
0.4
1.3
19.5
0.8
48.5
0.4
1.8
5.7
2.1
0.8
0.6
0.2
1.0
1.8
0.0
1.0
1.3
0.2
0.9
1.1
0.0
0.1
0.1
2.6
0.2
1.1
0.4
8.8
0.7
0.4
2.2
0.4
7.6
7.4
0.1
1.2
1.8
1.0
0.5
0.7
0.1
0.7
0.8
1.5
0.0
0.0
0.6
0.6
0.2
1.0
20.9
0.9
52.6
0.3
1.5
6.0
1.8
0.4
0.1
0.6
0.7
2.5
0.0
0.4
1.8
0.6
0.7
1.2
0.0
0.0
0.0
2.8
0.3
1.6
0.9
9.3
0.4
0.3
1.8
0.3
6.3
7.0
0.1
1.6
2.4
0.6
0.5
1.5
0.3
0.6
0.6
1.4
0.0
0.0
0.4
0.8
0.2
1.6
20.8
1.1
46.2
0.1
2.4
5.9
3.1
0.5
0.6
0.4
1.7
1.3
0.0
0.6
0.9
0.7
0.7
1.1
0.0
0.0
0.3
4.0
0.3
1.2
0.4
8.6
0.5
0.3
2.8
0.1
7.2
6.9
0.0
1.3
1.9
0.7
0.2
0.8
0.2
1.0
0.9
1.2
0.1
0.0
0.5
1.1
0.2
1.2
24.6
0.4
41.5
0.1
2.7
4.8
1.8
0.7
0.4
0.1
1.0
1.6
0.0
0.5
1.7
0.8
0.7
0.7
0.0
0.0
0.1
5.9
0.3
2.1
0.2
8.2
0.4
0.3
2.7
0.5
7.7
7.1
0.0
0.8
2.6
0.6
0.6
0.7
0.1
0.8
0.3
1.7
0.0
0.0
0.6
0.7
0.2
0.7
24.6
0.4
43.5
0.2
1.9
6.0
2.0
1.1
0.7
0.6
0.8
1.1
0.1
0.7
1.8
0.2
0.5
0.9
0.2
0.0
0.2
7.7
121.9
120.0
128.3
135.7
133.4
129.7
135.0
ICD9
SITE
ALL SITES
108.1
* Incidence Rate Per 100,000
35
INCIDENCE RATE PER 100,000
TIME TRENDS IN AGE ADJUSTED INCIDENCE RATES OF CANCER
1982 - 1989
BANGALORE — MALES
CANCER SITE
—TONGUE
—'
OESOPHAGUS
MOUTH
LARYNX
STOMACH
INCIDENCE RATE PER 100,000
PROSTATE
CANCER SITE
— mouth
OESOPHAGUS
BREAST
STOMACH
UTERINE CERVIX
* WORLD POPULATION
SOURCE : NCRP DATA : 1982-1989
37
TIME TRENDS IN AGE ADJUSTED INCIDENCE RATES OF CANCER
1982 - 1989
BOMBAY — MALES
CANCER SITE
-------
TONGUE
~MOUTH
OESOPHAGUS
LARYNX
~LUNG
PROSTATE
-®-
STOMACH
FEMALES
YEAR OF DIAGNOSIS
CANCER SITE
MOUTH
-e~
—OESOPHAGUS
~STOMACH
UTERINE CERVIX
BREAST
SOURCE : NCRP DATA : 1982-1989
‘WORLD POPULATION
38
INCIDENCE RATE PER 100,000
TIME TRENDS IN AGE ADJUSTED INCIDENCE RATES OF CANCER
1982 - 1989
MADRAS — MALES
YEAR OF DIAGNOSIS
CANCER SITE
-------
TONGUE
—LARYNX
—•—
MOUTH
OESOPHAGUS
—LUNG
~STOMACH
PROSTATE
60
INCIDENCE RATE PER 100,000
50
40
30
20
10
0
'982
1983
1984
1985
1987
1986
1988
1989
YEAR OF DIAGNOSIS
CANCER SITE
-------
MOUTH
_~s~
BREAST
—
OESOPHAGUS
~STOMACH
UTERINE CERVIX
* WORLD POPULATION
SOURCE : NCRP DATA : 1982-1989
39
2.11 BURDEN OF TOBACCO RELATED CANCERS IN INDIA
NCRP has provided incidence rates of cancer in Bangalore, Bombay and Madras areas for eight years
(19S2-1989). Based on these figures, the burden of tobacco related cancers in India has been estimated.
TABLE 2.11: BURDEN OF TOBACCO RELATED CANCERS IN INDIA,
ESTIMATES FOR 1982 (AS ON JULY 1)
Total Population (millions)*
Crude Rate Per 100,000
Number Of New Cancer Cases Per Year
New Cases Related To Tobacco Habits Per Year:
Mouth
Pharynx & Larynx
Oesophagus
Lung
Others
Total - Tobacco Habits
Related Cancers
MALES
FEMALES
TOTAL
450
70
315,000
412
80
329,600
644,600
36,200
49,200
23,700
27,800
15,000
151,900
(48.2%)
27,000
10,600
16,500
5,100
7,200
66,400
(20.1%)
63,200
59,800
40,200
32,900
22,000
218,300
(33.8%)
862
_
* As on July 1,1992
Estimates are shown separately for males and females for commonly affected sites namely, mouth, pharynx &
larynx, oesophagus and lung (Table 2.11). Some other sites related to smoking habits known from the experience
of the west such as bladder, pancreas etc. are taken as others. Although stomach and uterine cervix cancers are
appear to be associated with the bidi and cigarette smoking, but they are not taken into account. It is also possible
that tobacco chewing and bidi smoking may show risks for cancers not studied so far. From these considerations,
the present estimate of tobacco related cancers is a conservative one (Sanghvi, 1989).
In India, cancer morbidity cases related to tobacco habits, per year, are 151,900 (48.2%) in men and 66,400
(20.1 %) in women with an overall estimate of 218,300 (33.8%) for the two sexes. Of 218,300,74.7% cancers related
to tobacco were found in mouth, pharynx & larynx and oesophagus; lung cancer accounted for only 15% of cases.
2.12 INCIDENT CASES OF CANCER BY YEAR 2001 A.D.
Incident cases of cancer by year 2001 A.D. (as on July 1) has been estimated as given in theTable 2.12. These
estimates are based on averages of crude incidence rates for Bangalore, Bombay and Madras registries for the year
11989. India’s population was projected, by sex, for the year 2001 A.D. (as on July 1), using 1981 and 1991 (provisional)
censuses and applying the exponential rate of growth. The present estimates of cancer cases may be considered
as a conservative one.
TABLE 2.12: ESTIMATED NUMBER OF INCIDENT CANCER CASES FOR SELECTED SITES, ALL AGES, BY
THE YEAR 2001 AD. (AS ON JULY 1), IN INDIA*
SITE (ICD.9)
MALES
FEMALES
TOTAL
Lip, Oral Cavity (140-145)
Pharynx & Larynx (146-149,161)
Oesophagus (150)
Stomach (151)
Lung (162)
Breast (174)
Cervix Uteri (180)
Others
39,000
53,000
31,000
35,000
34,000
—
—
201,000
31,000
14,000
26,000
16,000
7,000
80,000
100,000
139,000
70,000
67,000
57,000
51,000
41,000
80,000
100,000
340,000
TOTAL
393,000
413,000
806,000
'Estimates are based on crude cancer incidence rates for Bangalore, Bombay, Madras and Delhi.
Source : NCRP Data, 1989.
40
REFERENCES:
1.
Armstrong B. K. et al. Time trends in prevalence ofcervical cytological abnormality in women attending a sexually
transmitted diseases clinic and their relationship to trends in sexual activity and specific infections. Br. J. Cancer,
54, 669-675, 1986.
2.
Christopher P. Howson et al. The decline in gastric cancer : epidemiology of an unplanned triumph.
Epidemiologic Reviews, vol. 8, 1986.
3.
Cancer Incidence in Five Continents, Volume V. IARC Scientific Publication No. 88, 1987.
4.
Day N. E. A new measure of age-standardised incidence, the cumulative incidence rate. In: Cancer Incidence
in Five Continents, vol. Ill, IARC Scientific Publication No. 15, pp 443-445, 1976.
5.
Ernster V. L. etal. Cancer incidence by marital status. J. Nat. Cancer Inst., 63,567-585, 1979.
6.
Gupta P. C. et al. A primary prevention study of oral cancer among Indian villagers. Eight-year follow-'jn -e^iits.
In: Evaluating Effectiveness of Primary Prevention of Cancer. IARC Scientific Publications No. 1 LL,, 1990.
7.
Hirayama T. etal. The cancer risks by site. UICC,Geneva, 1980.
8.
Hanai A. et al. Trend of stomach cancer incidence and histological types in Osaka. In : Trends in Cancer
Incidence, 1982.
9.
Henderson et al. An epidemiologic study of breast cancer. J. Nat. Cancer Inst.,53, 609-614, 1974.
10.
Institute of Cytology and Preventive Oncology, Annual Report, ICPO (1990-1991).
11.
IARC Monographs on the Evaluation of Carcinogenic Risk of Chemicals to Humans, Volume 14, Asbestos,
1977.
12.
IARC Monographs on the Evaluation of Carcinigenic Risk of Chemicals to Humans, Volume 37, Tobacco Habits
Other than Smoking; Betel-quid and Areca-nut; and Some Related Nitrosamines. IARC, 1985.
13.
IARC Monographs on the Evaluation of Carcinogenic Risk of Chemicals to Humans, Volume 38, Tobacco
Smoking. IARC, 1986.
14.
IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. IARC, 1987.
15.
Jayant K. Cancers of the cervix uteri and breast: changes in incidence rates in Bombay over the last two
decades. Bull. WHO, 64(3), 431-435, 1986.
16.
Jayant K. etal. Quantification of the role of smoking and chewing tobacco in oral, pharyngeal, and esophageal
cancers. Br. J. Cancer, 35,232-235, 1977.
17.
Jayant K. & Yeole B. B. Cancer of the upper alimentary and respiratory tract in Bombay, India : a study ot
incidence over two decades. Br. J. Cancer, 56, 847-852, 1987.
18.
Jussawalla D. J. et al. The diagnosis and management of cancer. Orient Longman, 1983.
19.
Jussawalla D. J. and Deshpande V. A. Evaluation of cancer risk in tobacco chewers and smokers : an
epidemiologic assessment. Cancer, 28, 244-252, 1971.
20.
MacMahon B. et al. Epidemiology, Principles and Methods, 1970.
21.
MacMahon B. etal. Age at first birth and breast cancer risk. Bull. World Helath Organisation, 43,209-221,1979.
22.
Mehta F. S. et al. An intervention study of oral cancer and precancer in rural Indian populations; a preliminary
report. Bull. World Health Organisation, 60, 441-446,1982.
23.
Munoz N. and Asvall J. Time trends of intestinal and diffuse types of gastric cancer in Norway. Int. J. Cancer,
8,
144- 157,1971.
24.
Notani P. et al. Assessment of morbidity and mortality due to tobacco usage in India. In: Tobacco and Health
1989.
25.
National Cancer Control Programme, July 1984. Directorate General of Health Services, Ministry of Health and
Family Welfare, Government of India.
41
26.
National Cancer Registry Project, Annual Reports 1982-1988, Indian Council of Medical Research, NewDelhi.
27.
Parkin D. et al. Estimates of the worldwide frequency of sixteen major cancers in 1980. Int J. Cancer, 41,
184-197, 1988
28.
Richard Doll and Richard Peto. The causes of cancer. Oxford University Press, 1981.
29.
Rotkin I. D. A comparison review of key epidemiological studies in cervical cancer related to current searches
for transmissible agents. Cancer Research, 33, 1353-1367, 1973.
30.
Sanghvi L. D. Tobacco related cancers. In : Tobacco or Health - The Indian Scene, pp 9 -15, 1989.
31.
Schlesselman James J. Case-Control Studies, 1982.
32.
Tomatis L. et al. Cancer: Causes, Occurrence and Control. IARC Scientific Publications No. 100. 1990.
33.
Tuyns A. J. Oesophageal cancer in non-smoking drinkers and in non-drinking smokers. Int. J. Cancer, 32,
443-444, 1983.
' 34.
Tuyns A. J. Salt and gastrointestinal cancer. Nutrition Cancer, 11, 229-232, 1988
35.
US Department of Health and Human Services, The Health Consequences of Smoking: Cancer. A Report of
the Surgeon General, Washington DC, US Public Health Service.
36.
US Department of Health, Education, and Welfare, ICD-0 to ICD-9, Public Health Service, National Institutes
of Health, 1979.
37.
World Health Organisation ICD-0 International Classification of Diseases for Oncology, 1976.
38.
World Health Organisation Cancer Statistics, Technical Report Series, 632, 1976.
39.
World Health Organisation ICD-9 International Classification of Diseases, 1975 Revision, Volume 1, 1977.
40.
World Health Organisation ICD-9 International Classification of Diseases, 1975 Revision, Volume 2, 1978.
42
ReJcv*ncc to Human Cancer of N-Nitroso Compounds,
Tobacco Smoke and Mycotoxins.
Ed. I.K. O’Neill. J. Chen and H. Bartsch
Lyon, International Agency for Research on Cancer
© 1ARC. 1991
LUNG CANCER AND THE CHANGING CIGARETTE
D. Hoffmann, I. Hoffmann & E.L. Wynder
Naylor Dana Institute for Disease Prevention,
American Health Foundation, Valhalla, NY, USA
Epidemiological studies have shown that the long-term smoker of low-yield cigarettes
has a 20-50% lower risk of lung cancer than the smoker of high-yield cigarettes. This risk
reduction is attributed to changes in the make-up of cigarettes and especially to the
introduction of filter tips. Other changes relate to the use of tobaccos that produce lower
smoke yields, including reconstituted and expanded tobaccos, as well as utilization of
porous cigarette paper and perforated filter tips. New developments in the make-up of
commercial cigarettes must be monitored in order to prevent unfavourable introductions.
Although a smoke-free society should be the major public health goal, recent consumer
statistics do not support this goal. Thus, a strong social case is made for further
developments in the low-yield cigarette.
In 1961, Wynder and Day offered three postulates for the causation of noncommunicable
diseases, including cancer:
(1)
The greater and the more prolonged the exposure to the factor, the greater the
risk of a population involved.
(2)
The epidemiological pattern should be consistent with the distribution of the
factor.
(3)
Removal or reduction of the risk factors for a given population group should be
followed by a reduction in the incidence of disease.
More than 100 epidemiological studies from various countries have demonstrated a
dose-response relationship between the number of cigarettes smoked and the risk for
cancer of the lung (IARC, 1986; US Department of Health and Human Services, 1989).
Laboratory studies have substantiated these findings by documenting the dose-response
relationship between exposure to cigarette smoke and tumours of the upper respiratory
tract in hamsters (Dontenwill, 1974) and that between application of smoke condensate to
the skin of mice and rabbits and tumour yield at the site of application (Wynder &
Hoffmann, 1967). These findings clearly satisfy postulate (1) for a causative association
between cigarette smoking and lung cancer.
Postulate (2) is sustained by the correlation between age at onset of cigarette smoking
and depth of inhalation with risk for lung cancer. Further support is gleaned from the
observation that, by comparison to cigarette smokers, primary cigar and pipe smokers have
-449-
450
D. Hoffmann et al.
a lower risk for cancer of the lung but the same risk for cancer of the oral cavity (US
Department of Health and Human Services, 1989).
The observed decrease in lung cancer risk upon cessation of cigarette smoking supports
postulate (3) for cancer causation. More importantly, it also has major public health
implications. Independent of the length of smoking history, the risk for tobacco-related
diseases diminishes further as the period of abstention from smoking increases (Table 1).
Thus, the demand for a smoke-free society by the year 2000 (Koop, 1986) deserves the full
support of the medical and scientific community. Unfortunately, the recent statistics on
tobacco use do not support this goal. Between 1971-75 and 1979-81, the percentage
increase in cigarette consumption in all parts of the world, except Europe, exceeded the
increase in population (Fig. 1).
Figure 1. Change in apparent cigarette consumption and adult population size, by region;
1971-75 to 1979-81"
• From World Health Organization (1986)
These data on cigarette consumption reinforce the need for health education about the
harmful effects of cigarette smoking and for the widest availability of smoking cessation
programmes. However, these figures also show that a strong case can be made for less toxic
cigarettes, since far too many people seemingly cannot or will not give up the smoking habit.
The changing cigarette — epidemiological observations
Since the early epidemiological studies on the association of cigarette smoking and lung
cancer clearly showed a dose-response relationship, product modification was seen as one
possible approach to reducing exposure (Wynder & Hoffmann, 1962). Changes in the
design of cigarettes, most notably use of filter tips but also alterations of the composition
of cigarettes, were implemented in several countries in the late 1950s and early 1960s. Since
then, the yields of smoke condensate (‘tar’) and of nicotine in the smoke stream have fallen
drastically. For example, between 1960 and 1984, sales-weighted average ‘tar’ delivery of
cigarettes in the USA, the UK and the Federal Republic of Germany decreased from 26,
31 and 25 mg to 14.2,13.7 and 12.8 mg, respectively, that is, a reduction of 45-50%. During
IJ. HuJJinann el al.
and nicotine values are based on standardized machine-smoking of cigarettes, and (ii) most
smokers of low-yield cigarettes compensate for the reduced nicotine delivery by smoking
more, by drawing puffs more frequently and more intensely, and by inhaling more deeply
(Herning et al., 1981: Haley etal., 1985: Augustine el al., 1989).
Epidemiological studies have also reported a reduction in the risks for cancers of the
larynx and urinary bladder for long-term smokers of filter cigarettes (Wynder & Stellman.
1979; Vineisera/., 1984; Wynder er a/., 1988).
In addition to comparing the cancer risks of smokers of plain and filter cigarettes,
epidemiological studies have been concerned with the relative risk of smoking black
cigarettes versus blended or bright cigarettes. It was found that smokers of cigarettes made
exclusively of black tobaccos, such as those that are commonly smoked in France, North
Africa and Cuba, are at higher risk for cancers of the lung, larynx and urinary bladder than
are smokers of blended or bright cigarettes (Joly el al.. 1983; Vineis et al., 1984, 1985;
Benhamou et al.. 1985. 1987: DeStefani el al.. 1987).
The changing cigarettes — technical developments
The introduction of cigarettes with filter tips in North America and Europe around 1940
represents the first major change in the make-up of machine-made cigarettes. However.
it was not until the first reports on smoking and lung cancer in the early 1950s that
consumers demanded cigarettes with reduced ‘tar’. In response, cigarettes with cellulose
acetate filter tips were offered. These filter tips are usually 17-30-mm long and contain a
few per cent of plasticizers such as glyceryl triacetate. In 1988, 96% of the cigarettes sold
in the USA had filter tips; about half of them were 85-mm long and about one-third were
100-inm long (US Department of Agriculture. 1989). Similar developments were seen in
other American countries, in Japan and in some parts of Europe, while in 1987 filter-tipped
cigarettes in China accounted for only 26% and in the USSR. 27% (Anon., 1988).
The degree to which 'tar' and nicotine can be retained by conventional filter tips is
limited to about 50%, primarily due to the fact that cigarette smokers will usually not accept
a draw resistance above 140 mm (Kuhn & Klus, 1976). Apart from removing ‘tar' and
nicotine from the smoke, cellulose acetate can selectively remove up to 80% of certain
hydrophilic, volatile smoke components, such as phenols and volatile Af-nitrosamines
(Wynder & Hoffmann. 1967; Brunnemann cl al.. 1977).
The introduction of perforated filter tips around 1968 had a profound impact on the
cigarette market (Norman. 1982). In general, such filter tips have one or more rows of
perforation in the wrapper at the half-way point of the filter column. As a result, the smoke
is diluted by air entering through the holes during puff-drawing without causing an increase
in draw resistance. Enhancing the air dilution of the smoke stream by optimal perforation
of the filter tip diminishes the velocity of the air that enters the burning cone. This, in turn.
reduces the oxygen deficiency of certain zones in the burning cone, which results in the
selective reduction of CO. nitrogen oxides and volatile aldehydes in these cigarettes
(Newsome & Keith. 1965: Baker, 1984).
Even though cigarette length has increased from 70 mm to 85 mm. and even to 100 mm
and 120 mm, the average weight of the tobacco in the typical US cigarette has decreased
from 1300 mg in the 1940s to 750 mg in the 1980s (Norman, 1982). This is due mainly to
Lung cancer and the changing cigarette
455
Table 3. Composition of a typical US blend for cigarettes"
Component
%
Flue-cured leaf
Burley leaf
Maryland leaf
Oriental leaf
Cut, rolled stems
Reconstituted sheet
Dip casing
Flavours/humcctants
32
20
2
10
6
22
4
4
' From Pcrfelti (1987)
(Wynder & Hoffmann, 1962; Hoffmann et al., 1980). Various processes have been tested
for their efficacy by initially analysing the smoke of the modified cigarettes for ‘tar’.
nicotine, CO, benzo[a|pyrene and tobacco-specific rV-nitrosamines (TSNA). When this
analytical profile showed a reduction in the smoke yields, determinations of volatile
aldehydes, volatile (V-nitrosamines. cyanide, phenols and catechol were made.
Experimental cigarettes with significantly changed analytical smoke profiles were then
designated for evaluation of the toxicity and tumorigenic potential of their smoke. Such
bioassays were done with ‘tars’ as well as with smoke itself (Wynder & Hoffmann. 1967;
Dontenwill, 1974), as summarized in Table 4. Several of the modifications described here
have been incorporated in the design of present-day low-yield cigarettes. Modifications in
cigarette make-up have also led to the selective reduction of certain smoke constituents and
have specifically contributed towards lowering the toxic and tumorigenic potential of
cigarette smoke. The decline of benzo[u|pyrene levels in the smoke of a leading US
non-filter cigarette as measured over 1958-79 is one indicator of selective reduction of a
carcinogen; while ‘tar’ and nicotine in the smoke of this cigarette were reduced by 31 % and
39%. the reduction in benzo[a|pyrene was from 36 to 16 ng/cigarette. i.e„ 56% (I loffmann
etal., 1980).
In evaluating preventive strategies that involve product modification, it is important to
monitor not only specific indicators but also the overall chemical composition of the smoke
of commercial cigarettes. Use of nitrate-rich tobaccos and ribs increases the potential for
higher smoke yields ofTSNA(Brunnemann et al., 1983). Consequently, low-yield cigarettes
can deliver higher amounts of carcinogenic TSNA than some plain cigarettes, as was
recently shown for some cigarettes in the Federal Republic of Germany by Fischer et al.
(1989). Another concern is the addition of flavouring agents to the tobacco of low-yield
cigarettes (LaVoie et al., 1985). These few citations underscore how important it is that
nonindustrial scientists monitor new developments in the make-up of cigarettes.
Outlook
Future research and development will probably bring about new features in the design
of commercial cigarettes. Plans have been announced for the marketing of filter cigarettes
made with tobaccos from which the bulk of the nicotine has been removed by supercritical
extraction with CO2 (Grubbs & Howell. 1987). This development is potentially beneficial
Lung cancer and the changing cigarette
453
the utilization in present-day cigarettes of tobacco material with higher filling power,
namely reconstituted tobacco, tobacco ribs and expanded tobacco. Reconstituted tobacco
sheets are made from tobacco dust and fines and from opened ribs. They can be prepared
by slurry or paper-like processes. Expanded tobacco is obtained by a freeze-drying process
(Wynder & Hoffmann, 1967; Perfetti, 1987).
The composition of cigarette smoke and its toxicity and carcinogenic potency are aiso
very much affected by the tobacco type(s) used. The composition of the tobacco filler in
cigarettes in different countries is primarily the result of traditional usage and availability
of tobacco types. In the USA, the Federal Republic of Germany and Scandinavia, blends
of the four major tobacco types are used; in China, flue-cured tobacco is the dominant type
for cigarettes; while cigarettes made exclusively from flue-cured tobaccos are preferred in
the UK and Finland. A large segment of cigarette smokers in France, Italy, North Africa
and several Central and South American countries prefer black tobaccos.
Bright tobaccos contain generally high levels of reducing sugars (15-20% of dry weight)
and carbohydrates but relatively lower amounts of di- and tricarboxylic acids (<4%) and
nitrate (<0.1%), while burley and black tobaccos are low in reducing sugars (<2%),
relatively high in di- and tricarboxylic acids (> 10%) and high in nitrate (> 1%); this is
especially true for the ribs. Oriental and Maryland tobaccos are minor components of
cigarette blends because of their specific smoke flavours. Their leaves contain moderate
amounts of reducing sugars (10-15%) and of di- and tricarboxylic acids (< 10%), while their
nitrate content is low (Neurath & Ehmke, 1964; Tso, 1972). The nicotine concentration of
the leaves depends on the variety chosen; however, bright, oriental and Maryland tobaccos
contain less nicotine (<2%) than burley and black tobaccos (Tso, 1972).
The composition of a typical blend currently formulated for US cigarettes is shown in
Table 3 (the composition of expanded tobaccos is described by Perfetti. 1987). Other
changes in the make-up of commercial cigarettes include the use of cigarette paper of
higher porosity as well as reduction of the circumference of some cigarettes (DeBardeleben
et al., 1978; Owens, 1978). Together, all of these changes have led to a gradual decrease
in the sales-weighted ‘tar’ and nicotine yields in the smoke of commercial US cigarettes
(Figure 2).
The changing cigarette — effect on turnorigenicity of smoke
As discussed earlier, smokers of low-yield cigarettes tend to compensate for the reduced
delivery of nicotine and perhaps other smoke components; however, they do not
compensate fully. The 20-50% reduction in risk for lung cancer of long-term cigarette
smokers supports the concept that low-yield cigarettes have reduced carcinogenic potential.
The IARC monograph on tobacco smoking states: ‘no substantial cause (or cofactor) has
so far been identified that offers a plausible explanation for the observed magnitude of the
reduction of risk for lung cancer, other than changes in the cigarette design which include
reduction in tar content.’ (IARC, 1986).
Whether other factors are indeed responsible for the reduced carcinogenic potential of
the changed cigarette can at this time be evaluated only in laboratory studies. Concepts of
‘less harmful’ cigarettes have frequently been devised by investigators outside the industry
D. Hoffmann et al.
Table 2. Relative risk for lung cancer by type of cigarette smoked (filter versus nonfilter) in
men
Reference
Type of study
Relative risk
Hawthorne & Fiy (1978)
Rimington (1981)
Brass & Gibson (1968)
Wynder et al. (1970)
Dean et al. (1977)
Wynder & Stellman (1979)
Lubin (1984)
Cohort
Cohort
Case-control
Case-control
Case-control
Case-control
Case-control
0.8
0.7
0.6
0.6
0.5
0.6-0.9"
0.6*
* Depending on number of cigarettes smoked daily
* Men who smoked only filter cigarettes
Lung cancer and the changing cigarette
457
in that it promises a selective reduction in the major habituating agent of tobacco and a
precursor for carcinogenic TSNA. A recent attempt to market a modified cigarette that
‘heats rather than bums tobacco’ has not been accepted by consumers (RJ. Reynolds
Tobacco Co., 1988).
Because large numbers of people continue to smoke cigarettes, dc.elopment of less
harmful cigarettes should not be rejected per se. One may agree with a«recent editorial in
the New York Times (Anon., 1989), which reads in part, ‘Obviously, no smoking is better
than smoking, but the best should not be the enemy of the good. There is a strong social
case for encouraging manufacturers to develop safer cigarettes that will sell.’
Acknowledgements
We are most grateful to many colleagues at the American Health Foundation who have
made significant contributions to our research programme in tobacco carcinogenesis. We
thank Mrs Bertha Stadler for editorial assistance. Our studies are supported by research
grants No. CA-17613, CA-29580 and CA-32617 from the US National Cancer Institute.
References
Adlkofcr. E,Scherer. G.&Thurau. K.(1988)Rauchcn undGesundhcil: Chanccwdurch Produktmodifikation.
In: the ‘Deutsche Lcbcnsmittclchcmikcrtag 1988', Bremen, FRG. Sept. 14-16, 1988, p. 22
Anon. (1988) Percentage share of filler cigarettes compared with total production. Tab. J. Int.. S. 362
Anon. (1989) Safer cigarettes. New York Times, 3 March, p. A38
Augustine, A., 1 larris. R.E. & Wynder. E.L. (1989) Compensation as a risk factor for lung cancer in smokers
who switch from nonfiltcr to filler cigarettes. Am. J. Public Health, 79, 188-191
Baker, R. (1984)'Hie effect of ventilation on cigarette combustion mechanics. Recent Adv. Tob. Sci., 10,88-150
Bcnhamou, S„ Bcnhamou, E., Tirmarchc, M.& Ramant, R. (1985) Lung cancer and use ofcigarcttcs: a French
case-control study. J. Natl Cancer Inst., 74, 1169-1175
Bcnhamou, E.. Bcnhamou. S. & Hamanl, R. (1987) Lung cancer and women: results of a French case-control
study. Br J Cancer, 55. 91-95
Brass, I.DJ. & Gibson, R. (1968) Risk of lung cancer in smokers who switch to filter cigarettes. Am. J. Public
Health, 58, 1396-1403
Brunncmann, K.D, Yu, L. & Hoffmann, D. (1977) Assessment of carcinogenic volatile N-nitrosamincs in
tobacco and in mainstream and sidestream smoke of cigarettes. Cancer Res, 37,3218-3222
Brunncmann. K.D, Masaryk. J. & Hoffmann, D. (1983) The role of tobacco stems in the formation of
JV-nitrosamincs in tobacco and cigarette mainstream and sidestream smoke. J. Agric. Food Chcrn, 31.
1221-1224
Dean, G, Lee, P.N., Ibdd. G.F. & Wicken, AJ. (1977) Report on a Second Retrospective Study in Northeast
England. Part I. Factors Related to Mortality from Lung Cancer, Bronchitis, Heart Disease and Stroke tn
Cleveland County with Particular Emphasis on the Relative Risks Associated with Smoking Filter and Plain
Cigarettes (Research Paper 14), London. "Utbacco Research Council
DcBardclcbcn, M.Z., ChaBin, W.E. & Gannon, W.F. (1978) Role of cigarette physical characteristics on smoke
composition. Recent Adv. Tob. Sci., 4, 85-111
DcStcfani, E, Correa, P, Orcggia, F, Leiva, J., Rivero, S, Fernandez, G, Dcneo-Pcllcgrini. H, Zavala. D.
& Fontham, E. (1987) Risk factors for laiyngcal cancer. Cancer, 60. 3087-3091
Dontcnwill, W.P. (1974)Tbmorigcnic effect of chronic cigarette smoke inhalation on Syrian golden hamsters.
In: Karbc, E. & Park,J.F, cds. Experimental Lung Cancer. Carcinogenesis and Bioassays, New York, Springer.
pp. 331-359
Fischer, S, Spicgelhaldcr, B. & Prcussmann, R. (1989) Tobacco-specific nitrosamincs in mainstream smoke
of West German cigarettes - tar is not a sufficient index for the carcinogenic potential of cigarette smoke.
Carcinogenesis, 10, 169-173
Grubbs, HJ. & Howell. T.M. (1987) Process for the Removal of Basic Materials from Plata Products (European
Patent Office Publ. No. 0 280 817)
458
D. Hoffmann et al.
Haley, NJ., Sepkovic, D.W., Hoffmann, D. & Wynder, E.L (1985) Compensation with nicotine availability as
a single variable. Clin. Pharmacol. Ther, 38, 164-170
Hawthorne, V.M. & Fry, J.S. (1978) Smoking and health: the association between smoking behavior, total
mortality and cardiorespiratory disease in West Central Scotland./ Epidemiol. Commun. Health, 32,260-266
Heming, R.I., Jones, R.T., Bachman, J. & Mines, A.H. (1981) Puff volume increases when low-nicotinc
cigarettes are smoked. Br. Med. J., 283, 187-189
Hoffmann, D„ Ito. T.C. & Gori. G.B. (1980) The less harmful cigarette. Prev. Med., 9, 287-296
1ARC (1986) IARC Monographs on the Evaluation of the Carcinogenic Risk of Chemicals to Humans. Vol. 38.
Tobacco Smoking, Lyon
Joly, O.G., Lubin, J.H. & Caraballoso, M. (1983) Dark tobacco and lung cancer in Cuba. J. Natl Cancer Inst.,
70, 1033-1039
Koop, C.E. (1986) The quest for a smoke-free young America by the year 2000. J. School Health, 56, 8-9
Kuhn, H. & Klus, H. (1976) Possibilities for the reduction of nicotine in cigarette smoke. In: Wynder, E.L.,
Hoffmann. D. & Gori, G.B., eds. Proceedings of the Third World Conference on Smoking and Health, Vol. 1.
Modifying the Risk for the Smoker (DHEW Publ. No. (NIH) 76-1221), Washington DC, US Department of
Health, Education, and Welfare, pp. 463-494
LaVoic, EJ., Shigcmatsu, A., TUcciaronc. P.L, Adams, J.D. & Hoffmann, D. (1985) Comparison of
steam-volatile components in commercial cigarette, pipe, and chewing tobacco. J. Agric. Food Chcm., 33.
876-879
Lubin, J.H. (1984) Modifying risk of developing lung cancer by changing habits of cigarette smoking. Hr. Med.
J., 289, 92
Ncurath, G.& Ehmkc. H. (1964) Study of nitrate content of tobacco (in German). Beitr Tabakforsch., 2,333-334
Newsome, J.R. & Keith, C.H. (1965) Variation of the gas phase composition within a burning cigarette. Tob.
Sci.. 9, 65-69
Norman, V. (1982) Changes in smoke chemistry of modem day cigarettes. Recent Adv. Tob. Sci., 8, 141-177
Owens, W.E, Jr (1978) Effect of cigarette paper on smoke yield and composition. Recent Adv. Tob. Sci, 4, 3-24
Perfctti, T.A. (1987) Measurement of the quality of cigarette products. Recent Adv. Tob. Sci., 13. 119-161
R.J. Reynolds 'Ibbacco Co. (1988) New Cigarette Prototypes that Heut Instead of Rum Tobacco. Winston-Salem,
NC
Rimington, J. (1981) The effect of filters on the incidence of lung cancer in cigarette smokers. Environ. Res.
24. 162-166
’Iso, TC. (1972) Physiology and Biochemistry of Tobacco Plants. Stroudsburg, PA, Dowden. Hutchinson & Ross,
p. 393
US Department of Agriculture (1989) Tobacco Products (Tobacco — Situation Outlook Rep.. TS-206).
Washington DC, Economic Research Service, pp. 4-8
US Department of Health and Human Services (1982) The Health Consequences of Smoking. Cuncer A Report
of the Surgeon-General (DHHS Publ. NO. (PUS) 82-50179). Bethesda. MD
US Department of Health and I luman Services (1989) Reducing the Health Consequences of Smoking. 25 Years
of Progress. A Report of the Surgeon-General (DHHS Publ. No. (CDC) 89-8411). Bethesda. MD
Vincis, P., Esteve, J. & Tcrracini. B. (1984) Bladder cancer and smoking in males: types of cigarettes, age at
start, effect of stopping and interaction with occupation. Int. J. Cuncer, 34. 165-170
Vincis, P., Ciccone, G. & Ghisetti, V. (1985) Cigarette smoking and bladder cancer in females. Cancer Lett.
26, 61-66
Weber, K.H. (1972)Utr and nicotine in German cigarettes. Prev. Med.. 1. 446-450
World Health Organization (1986) Change in apparent cigarette consumption and adult population size, by
regions, 1971-75 to 1979-81. In: WHO Health Statistics. Geneva, pp. 16-19
Wynder, E.L & Day, E. (1961) Some thoughts on the causation of chronic disease J. Am Med Assoc 175
997-999
Wynder, E.L & Hoffmann, D. (1962) Present status of laboratory studies on tobacco carcinogenesis Acta
Pathol. Microbiol. Scand., 52, 119-132
Wynder, E.L & Hoffmann, D. (1967) Tobacco and Tobacco Smoke. Studies in Experimental Carcinogenesis. New
York, Academic Press
Table 4. Reductions in the biological activity of smoke from experimental cigarettes"
Method
Agricultural
Tobacco type (bright-burlcy^
New cultivars
Fertilization (nitrate)
Tobacco processing
Cut
Use ol tobacco midribs
Reconstituted tobacco
sheets (RTS/
RTS/paper process
Expanded tobacco laminae
Expanded tobacco midribs
Cigarette production
Paper porosity
Cellulose acetate Filters
Charcoal filters^
Perforated Filters
Smoke constituents
Selective reduction in
biological activity*
•Tar’
Nicotine
Benzo[a [pyrene
Carcinogenicity
+
4+
+
4.
-
44.
4-
44-
±
±
4-
±?
4. 4.
4. +
9
Tumour
promotion
+
9
9
4-
4-
i
4.
-
+ +
+
+
44r 4-
+
4-
4. 4.
±
±?
4- 4-
9
+
+
+
+ +
4.
4.
4-
4.
44.
+ +
±
±
±
±
+ 4-
Remarks^
+ 4-f-
Increase in TSNA
Increase in TSNA
Some RTS give high CO
9
±
±
±
Smoker’s compensation
' Adapted from Wynder & Hoffmann (1982> Methods known to be applied to commercial US cigarettes. Reductions: + +. > 50%; +. significant; ±?.
questionable; ?, unknown
* Comparison of gram-to-gram Itari on mouse skin tests and'or smoke inhalation with hamsters
e TSNA. tobacco-specific N-nilrosamines
' Replacing bright with burley tobaccos
* Data given for RTS relate to those not made by the paper process
1 Reductions in ‘tar’, nicotine, benzo(a]pyrene (and other nonvolatiles) and volatile .V-nitrosamincs are generally greater with cellulose acetate filters than
with charcoal filters.
Lung cancer and the changing cigarette
Wynder, E.L. & Hoffmann, D. (1982) Tbbacco. In: Schottenfeld, D. & Fraumeni, J.F., Jr, cds, Cancer
Epidemiology and Prevention, Philadelphia, Saunders, pp. 277-292
Wynder, E.L. & Kabat, C. (1988) The effect of low-yield cigarette smoking on lung cancer risk. Cancer, 62.
1223-1230
Wynder, E.L. & Stcllman, S.D. (1979) The impact of long-term filter cigarette usage on lung and larynx cancer
risk: a case control study. J. Natl Cancer Inst., 62, 471-477
Wynder, E.L., Mabuchi, K. & Beattie, EJ., Jr (1970)1116 epidemiology of lung cancer. Recent trends. J. Ant.
Med. Assoc., 213, 2221-2228
Wynder, E.L., Augustine, A., Kabat, G.C. & Hebert, J.R. (1988) Effect of the type of cigarette smoked on
bladder cancer risk. Cancer, 61, 622-627
Important Advances m Oncalogy 1995. edited by Vincent T. De Vita.
Samuel Hellman, and Steven A. Rosenberg. (j.B. Lippincott Com
pany. Philadelphia 0 1995)
Dimitrios Trichopoulos
Risk of Lung Cancer
and Passive Smoking
6
Introduction ■
This Chapter concisely presents evidence indicating
that exposure to environmental tobacco smoke (ETS).
also termed involuntary or passive smoking, increases
the risk of lung cancer, and can be considered as one
of the causes of this disease. Several major reports
of authoritative bodies that have addressed the question
are available.1-5 but this chapter is useful to clinicians.
epidemiologists, and other health professionals who
wish to familiarize themselves with the issues
surrounding this important topic in modem public
health.
Mainstream smoke (MS) is the tobacco smoke that is
generated during a puff and is drawn through the butt
end into the smoker’s respiratory system. Sidestream
smoke (SS) is emitted directly from the burning end
of the cigarette, cigar or pipe. ETS is produced by
smokers mostly in enclosed spaces and is inhaled by
nonsmokers as well as by the smokers. ETS contains
a vapor and a particulate phase and its main source
is SS (about 80%), with exhaled MS, smoke that comes
from the nonbuming end but is not inhaled by the
smoker, and smoke that diffuses through the paper
wrapper of the cigarettes contributing the rest. Spe
cifically, SS contributes almost all of the vapor phase
of ETS and more than half of the particulate mat
ter.6-7
Composition and Respiratory
Deposition of Sidestream Smoke ■
At the time and point of generation, SS is characterized
by higher concentrations of many of the definitely.
probably or possibly carcinogenic compounds8 found
in MS, including benzene (5-fold), formaldehyde (2fold). hydrazine (3-fold), butadiene (3-fold). N-nitrosamines (20-fold), aniline (30-fold), 2-napthylaminc
(30-fold), 4-aminobiphcnyl (30-fold), bcnz[a|antraccne
(3-fold). benzo[a)pyrcnc (3-fold), and NNK (a tobacco
specific carcinogenic nitrosamino, 2-fold). SS also con
tains higher concentrations than MS of several toxic
compounds, including carbon monoxide (3-fold), am
monia (4-fold), nicotine (3-fold) and particulate matter
(tar, 1.5 fold). These data arc abstracted from several
references >-2-5-7 and are based on the work of many in
vestigators. The SS/MS ratios vary considerably, most
ly because MS composition varies substantially by puff
volume, filter characteristics and ventilation, and type
of cigarette. By contrast, the variability of SS composi
tion is limited and use of filtered, rather than unfiltcrcd,
cigarettes had little influence on the concentration of
compounds in SS.7 As might be expected from the
relative concentrations of established and probable car
cinogens in SS and MS, condensates of SS have dem
onstrated higher mouse skin tumorigcnicity per unit
weight than MS condensates.9 Chemical characteriza-
77
78
Risk of Lung Cancer from Passive Smoking
lions of ETS, rather than SS, are limited, but the find
ings are essentially compatible with predictions based
on SS composition.5-7
^The different composition of SS and MS at the time
and point of generation is caused by differences in tem
perature (lower in SS) pH (higher in SS) and oxygen
concentration (substantially lower in SS). The rapid di
lution of SS is accompanied by marked reduction in the
concentration of all its constituents; however, about
half of the tobacco in a cigarette is eventually con
sumed to form SS.1
Panicles as SS are, originally, only slightly smaller
than those as MS. Particles of MS, however, grow in
size by coagulation, whereas particles of SS are rapidly
diluted and their size distribution is shifted to smaller
values. These changes are accompanied by changes in
phase distribution of several constituents. Thus, nico
tine exists mostly as particulate in MS, but mostly as
gas in SS. The different particle size distribution and
the different breathing patterns of smokers and nonsmokers explain the different deposition rates of MS
and SS particles in the respiratory tract (more than 50%
vs. about 10%. respectively). The deposited ETS parti
cles, because of their small size, are likely to be found
peripherally, rather than in the nasopharynx and the
large conducting airways.15'
Chemical Indicators of
Environmental Tobacco Smoke ■
The difficulty in assessing exposure to mixtures is well
recognized.lu-11 In assessing concurrent personal expo
sure to ETS, as distinct from actual absorption of ETS
constituents, stationary measurements coupled with
time-activity patterns of the subjects under consider
ation can be studied, or personal monitors can be used.
Several factors can affect ETS concentrations, includ
ing the generation rate of the contaminants, the space
volume, and the ventilation or air infiltration rate. Prox
imity of a subject to a smoker can also be a major
determinant of exposure to passive smoking.
Several compounds have been measured as indica
tors of microenvironmental tobacco smoke pollution.
including some of the established or probable carcino
gens in ETS. N-nitrosamines and 4-aminobiphenyls are
important in this respect because they are found in
much higher concentrations in SS than in MS at the
point of origin, they are generally considered as carci
nogenic. and they are ETS-specific in the nonoccupational indoor environment.5-7 However, these com
pounds cannot be measured easily, accurately and cost
effectively, and thus fail to satisfy an important crite
rion for the selection of an appropriate ETS indicator.
Among the many compounds that were used or sug
gested for use, nicotine has emerged as the most conve
nient indicator for the vapor phase constituents of ETS,
whereas respirable suspended particulates (RSP, medi
an mass diameter s 2.5 pm) has become the indicator
of choice for the particulate phase constituents of ETS.
Although nicotine is specific to tobacco products, RSP
are not and background levels must be accounted for
before they can be utilized as a valid indicator of ETS
particulate pollution. For both nicotine and RSP, indoor
levels from less than 1 pg/m3 to more than 1000
pg/m3 have been reported, although usual nicotine val
ues are below 15 pg/m3 and usual RSP values below
50 pg/m3.5-7
Sialic environmental measurements do not adequate
ly reflect personal exposures. Modeling effective expo
sure as a function of several static measurements and the
corresponding time-activity pattern represents an im
provement, but personal monitors allow a better integra
tion of the time-weighted individual exposures. How
ever, personal monitors cannot account for interperson
variations in ventilation rates, breathing patterns, and
deposition factors. This limitation notwithstanding,
studies using personal monitors have provided valuable
data concerning exposure to airborne nicotine and RSP
in the workplace,12-13 and to RSP during a whole 24
hour day.14
Biomarkers of Environmental
Tobacco Smoke Absorption ■
Biomarkers of exposure to ETS are good indicators of
uptake and represent close correlates of effective indi
vidual exposure. Among the biomarkers proposed as
indicators of ETS absorption, serum thiocyanate is not
sufficiently specific, whereas the relatively short half
life of carboxyhemoglobin and nicotine (about 4 and 2
hours, respectively) limits their utility, unless attention
is focused to a very recent exposure.
Cotinine, a major metabolite of nicotine, can be ac
curately measured in blood, saliva and urine in concen
trations down to 1 ng/ml, is sufficiently specific for
tobacco products, and has a half-life of about 24 hours,
allowing its use as a biomarker of exposure to ETS over
a period of about 48 hours. Cotinine has been exten
sively used for the validation of questionnaires assess
ing exposure to ETS15-16 and in several surveys exam
ining factors affecting the levels of this biomarker in
biologic fluids.15-17-18 These studies have demonstrated
that self-reported exposure to ETS during the recent
past is reasonably valid, and that 5-fold differences in
Questionnaires for Past Long-term Exposure to Environmental Tobacco Smoke
a) Sampling categories
of exposure
b) Self-reported
exposure
79
c) Self-reported
extreme patterns
of exposure
FIG. 6-1 Average cotinine/creatinine levels (ng/mg) for groups of nonsmoking women denned either by
sampling categories of exposure or by self-reporting exposure to ETS from different sources during the four days
preceding collection of a urine sample.15
levels of effective exposure to ETS are not unusual in
everyday life (Fig. 6-1).
Cotinine studies suggest that exposure to ETS is
equivalent to about 1% of exposure to active smoking.
This, however, is only true with respect to cotinine and
its parent compound nicotine, the concentration of
which in SS is only 3 times higher than in MS (see
p. 77). If, instead of nicotine a protein adduct, the
4-aminobiphenyl adduct of hemoglobin were used (4ABP), exposure to ETS would have been estimated as
close to 10% of that of active smokers, since the SS to
MS ratio for 4-ABP is about 30 (see p. 77).,9-20 II is
also relevant that the increase of urine mutagenicity
after passive exposure to cigarette smoke is about 4%
of the increase found in active smokers.21 ETS is a
mixture of more than 4000 compounds, variably related
to each other and to their sources (MS or SS) and with
different physicochemical properties and possibly inter
active health effects. Therefore, concepts like “cigarette
equivalent" and expressions in relation to active smok
ing arc meaningful only with respect to single com
pounds and specific biomarkers.
Questionnaires for Past Long-term
Exposure to Environmental Tobacco
Smoke ■
For chronic diseases with long latencies like lung can
cer. biomarkers and static environmental measurements
are not directly useful, since they refer to the very re
cent past. As indicated (see p. 78), questionnaire-based,
self-reported exposure to ETS correlates well with ob
jective evidence of such exposure, as documented
through cotinine in biologic fluids, and other bio
markers.15'18 By contrast, questionnaire-derived infor
mation concerning long-term exposure to ETS is diffi-
80
Risk of Lung Cancer from Passive Smoking
cult to integrate over time and almost impossible to
validate with an appropriate “gold standard." Never
theless, the validity of self-reported exposure to ETS
in the recent past argues in favor of the validity of
questionnaire-assessed exposure to ETS over prolonged
periods in the remote past.
Most studies concerning diseases of long latency,
like cancer of the lung, have focused on risk compari
sons between nonsmoking women married to husbands
with different smoking habits. This is justifiable because1-22-24: (1) Among older people tobacco smoking
has been more common in men than in women, partic
ularly in traditional societies; (2) A smoking husband is
the main source of passive smoking for an older wom
an, particularly for a housewife who is estimated to
spend more than 80% of her lime at her home; (3)
Information concerning the smoking behavior of a
spouse is usually more reliable than that concerning
other relatives, friends and colleagues; (4) Nonsmokers
married to smokers are likely to be more tolerant to
ward other sources of passive smoking; (5) Finally,
since smokers tend to socialize with other smokers, and
vice versa, the absolute difference of exposure to ETS
between nonsmoking women married to smokers, rath
er than nonsmokers, tends to be amplified.
Tobacco smoking habits of cohabitants other than the
spouse and recollection of ETS inhalation at work and
other places outside the home have also been used, as
secondary exposure variables, in some lung cancer
studies. However, the irregular use of these variables
and the possibility of inconsistent reporting of the cor
responding data, limit the interpretability of the respec
tive results.
Prediction of Lung Cancer Risk and
Passive Smoking ■
Data from large analytic epidemiologic studies of the
association between active smoking and lung cancer
have consistently demonstrated dose-dependent rela
tionships that extend to minimal exposure levels and
have no apparent threshold.25-2" The patterns that have
been empirically demonstrated in four major studies are
shown in Figure 6-2.29 Doll and Peto30-31 have argued
that the true association between active smoking of the
long-used high-tar cigarettes and lung cancer may be
much stronger, with a relative risk for smokers of more
than 1 pack of cigarettes per day exceeding 20. These
authors also have pointed out that the unavoidable mis
classification of exposure to the relevant carcinogenic
compounds in MS at critical lime periods, is bound to
reduce the true slope of the regression of lung cancer
relative risk on the amount of tobacco smoke reportedly
consumed.30-31 In any case, the epidemiologic evidence
indicates that there is no safe level for tobacco smoking
in relation to lung cancer risk. This is what should be
expected from the known composition of MS, which
contains several compounds with initiating carcinogen
ic potential and no demonstrable threshold.8
Since SS is qualitatively similar to MS and is readily
absorbed in the body, an excess lung cancer risk from
exposure to ETS should have been assumed even if
there were no conclusive epidemiologic evidence. The
situation is similar to what is known and assumed about
the carcinogenic potential of ionizing radiation at vari
ous levels. High doses of ionizing radiation have been
shown to cause cancer and, in the absence of a thresh
old, it is generally accepted that low doses from cosmic
radiation or even diagnostic radiographs should cause
some cases of cancer, even though this has never been
empirically demonstrated in adult human beings. With
respect to passive smoking a legitimate question is not
whether it can cause lung cancer but whether the ex
pected excess risk from long-term exposure to ETS is
substantial enough to be empirically demonstrable with
existing epidemiologic methods.
Extrapolations of the dose-response curves linking
active smoking to lung cancer risk at the low ETS ex
posure levels, as assessed through nicotine absorption
and continine excretion, generate relative risk estimates
for passive smoking too low to be detected by conven
tional epidemiologic studies.1-24-32-33 However, if urine
mutagenicity or carcinogen-hemoglobin adducts are
used as indicators of ETS exposure, higher relative risk
levels for passive smoking are predicted.20-21 Further
more, exposure to ETS may start soon after birth,
whereas active smoking usually starts in the teen-age
years or later, since lung cancer risk is an exponential
function of the duration of exposure,30-31 the early ex
posure to ETS is likely to have disproportional risk
implications.24 In addition, the delayed clearance of
nicotine among passive smokers, in comparison to ac
tive smokers, may lead to increased rate of formation of
endogenous tobacco-specific nitrosamines with carci
nogenic potential.I-5-24-34 Finally, and perhaps more
importantly, predictions of relative risk for lung cancer
in association with passive smoking are based on mod
els derived from studies of active smoking. In these
studies the referent baseline group encompasses all
smokers, including nonsmokers passively exposed to
ETS. Theretore the baseline risk is regularly overesti
mated which leads to underestimation of relative risk
values associated with active smoking, and similar un
derestimation of model-derived predictions of relative
risk associated with passive smoking.24-35 When the
required adjustments are made the relative risk for lung
Epidemiologic Studies
81
• X Canadian Veterans
FIG. 6-2 Mortality ratios of deaths from lung cancer in
men. Data from four large prospective studies.25 2R
cancer in association with passive smoking is substan
tially elevated and should be demonstrable in well de
signed epidemiologic studies.24-15-16
Epidemiologic Studies ■
At the time of this review (March 1994), 29 case
control studies and 4 cohort investigations have been
reported in the literature.-17-71 Their findings are sum
marized in Table 6-1. The results have been abstracted
from the original publications or from derivative calcu
lations presented in earlier reports.I-5-24-74
In January 1981, Trichopoulos et a!.31 and Hirayama40 reported simultaneously (within 2 days) and quite
independently the results of the first two studies explor
ing the role of passive smoking in the etiology of lung
cancer. One study-17 was of case-control design and was
specifically undertaken in Greece to estimate the rela
tive risk for lung cancer, other than adenocarcinoma or
alveolar carcinoma, of nonsmoking women married to
smokers, rather than nonsmokers. The other study40
was based on women participating in a multipurpose
cohort investigation in Japan. Both studies reported sta
tistically significant and dose-dependent associations.
The results of Garfinkel,42 based on a cohort study by
the American Cancer Society and published soon after
ward were equivocal but not incompatible with a slight
increase of lung cancer risk among persons exposed to
ETS.
Between 1982 and 1994, 30 additional studies were
published,4-1-7-1 whereas Trichopoulos et al.3*-39 and
Hirayama41 reported additional results from their re
spective studies. Most studies were done in nonsmok-
82
Risk of Lung Cancer from Passive Smoking
Table 6-1
Epidemiologic Studies of Passive Smoking in Relation to Lung Cancer
Authors (year)
Trichopoulos et al. (1981, 1983, 1984)
Hirayama (1981. 1984)
Garfinkcl (1981)
Chan and Fung (1982)*
Correa el al. (1983)
Buffler et al. (1984)*
Gillis « al. (1984). Hole er al. (1989)’
Kabar and Wynder (1984)
Garfinkel el al. (1985)
Wu et al. (1985)
Lam (1985)
Akiba et al. (1986)
Lee et al. (1986)
Koo et al. (1987)
Lam et al. (1987)
Pcrshagcn et al. (1987)
Brownson et al. (1987)
Gao et al. (1987)
Humble et al. (1987)
Buller (1988)
Geng et al. (1988)
Inoue and Hirayama (1988)
Kalada et al. (1988)
Shimizu et al. (1988)
Svensson et al. (1989)*
Wu-Williams and Samel (1990)
Kalandidi et al. (1990)
Janerich et al. (1990)
Sobue (1990)
Liu et al. (1991)*
Foniham et al. (1991, 1994)
Stockwell et al. (1992)
Brownson et al. (1992)
Reference
Number
37, 38. 39
40. 41
43
44
45
46, 47
48
49
50
51
52
53
54
55
56
57
58
59
60
61
62
63
64
65
66
67
68
69
70
16,71
72
73
ing women and in most of them the principal exposure
of interest was the smoking habits of the husband, i.e.,
the variable generally considered as the most valid indi
cator of long-term exposure to ETS. It is of interest that
among the 6 studies that reported a point estimate of
relative risk below 1 (inverse association), only 3
(50%) have used, as they should, spouse smoking hab
its as the principal exposure variable, whereas among
the 27 studies that reported a point estimate of relative
risk above 1 (positive association) the corresponding
number was 25 (93%). In 12 of the positive studies
there was clear evidence of a dose-response trend,
whereas in no study was there evidence for substantial
confounding by any of the co-variates that were exam
ined, including age, socioeconomic status, occupation.
and diet.5-74
Several meta-analyses of the available epidemiologic
data at various points in time have been undertake'n.
(No.)
77
200
153
84
22
41
14
134
29
60
94
32
86
199
67
19
436
20
8
54
•>?
17
90
34
417
90
191
144
54
653
210
432
Controls
(No.)
Cohon
Cohort
139
133
196
Cohort
25
402
62
144
270
66
136
335
347
47
605
162
Cohort
93
47
17
163
174
602
1)6
191
731
202
1253
301
1402
Relative
Risk
90% Confidence
Interval
2.08
1.38
1.17
0.75
2.07
0.81
1.99
0.79
1.31
1.20
2.51
1.50
1.03
1.55
1.65
1.20
1.31-3.29
1.03-1.87
0.89-1.53
0.48-1.19
0.94-4.52
0.39-1.66
0.33-11.92
0.30-2.04
0.93-1.85
0.65-2.23
1.49-4.23
1.00-2.50
0.48-2.20
0.98-2.44
1.21-2.21
0.75-1.92
0.49-4.79
0.87-1.63
0.90-5.50
0.60-6.81
1.21-3.84
0.90-7.20
0.49-23.80
0.70-1.68
0.65-2.48
0.64-0.98
1.13-3.25
0.57-1.29
0.83-1.54
0.35-1.68
1.08-1.55
0.94-2.72
1.21-2.69
1.19
2.20
2.02
2.16
2.55
3.40
1.08
1.26
0.79
1.92
0.86
1.13
0.77
1.29
1.60
1.80
Estimates of the relative risk for lung cancer contrasting
individuals exposed to ETS (mostly women married
to smokers) with individuals not so exposed (mostly
women married to nonsmokers) were 1.34,2 1.30,75
1.44.76 1.35,77 1.17,78 and 1.25.5 All these estimates
are significantly different from the null value of 1, even
though in none of the respective analyses was dose
dependent trends accounted for (had they been the re
sults would have deviated more clearly from the null
value). There is no conclusive evidence that the relative
risk linking ETS to lung cancer is different for ade
nocarcinoma and other histologic types.5-16-57-71-74 al
though early reports37-56 and studies in China58-61-66-70
suggest that the relative risk may, perhaps, be slightly
lower for adenocarcinoma.
Meta-analyses are of questionable value when ap
plied to observational data generated under variable
conditions through very different study designs. Nev
Environmental Tobacco Smoke as a Cause of Lung Cancer
ertheless, the fairly consistent overall pattern (Table 81). the identification of significant positive trends in
almost half of the reasonably powerful studies, the ro
bustness of the relative risk estimates to adjustments for
several factors,5-74 and the converging results generated
by all cohort studies41-42-47-60 and most case-control
studies that were specifically undertaken to examine
the ETS-lung cancer association49-52-56-67-71-73 indi
cate that the overall association is not due to chance and
is not confounded by any of the known risk factors for
lung cancer.
The main objections raised against the causal inter
pretation arc. allegedly, publication bias against studies
showing no association between ETS and lung cancer.
bias introduced in both cohort and case-control studies
by misclassification of smokers or former smokers
among the nonsmokers, and differential information
bias in case-control studies.
Publication bias would be generated if papers report
ing positive associations between ETS and lung cancer
were more likely to be submitted and accepted for pub
lication than papers reporting no such associations. 79
Selective publication could be a legitimate concern
with respect to secondary indicators of exposure to
ETS. for example, at work and from cohabitants other
than the spouse, or when men. rather than women, rep
resent the study base. For this reason this review, as
well as several others, have focused on studies of wom
en characterized according to their husbands' smoking
habits.
Publication bias can be detected using a statistical
technique in which relative risk estimates are plotted
against an indicator of study power. In the absence of
publication bias the relative risk estimates should be
normally distributed around the true value, with de
creasing variability with increasing study power. Devi
ations from the expected funnel-like plot can be inter
preted as indications of selective publication. Using this
procedure, Vandenbroucke80 found no evidence of
publication bias for studies based on women and eval
uating the relative risk for lung cancer in relation to
husbands’ smoking habits. Wells81 and Woodward and
McMichael82 have also examined this issue and have
found no evidence for selective publication in the exist
ing literature.
Misclassification of smokers and former smokers as
nonsmokers can introduce bias in both case-control and
cohort studies, since these persons arc at increased risk
for lung cancer and tend also to be married to, or live
with, smokers.83-84 The magnitude of this bias depends
on the values of four necessary and sufficient parame
ters: the overall proportion of ever smokers, the propor
tion of misclassified ever smokers, the risk for lung
cancer among those misclassified, and the aggregation
83
of smokers. Using realistic values for these variables
Wald et of.85 have estimated that about 15% of the
excess lung cancer risk associated with passive smok
ing could indeed be attributed to this bias. Correction
for misclassification of ever smokers among nonsmok
ers has been incorporated in several mcta-analyses2-5
but. as expected, had little effect. A point of interest is
that those willing to invoke this bias in order to explain
part of the reported excess risk for lung cancer among
self-declared passive smokers, must also accept that
active smoking increases substantially the risk for lung
cancer. This is, of course, established, but has yet to be
accepted by some tobacco smoking promoters. Finally,
information bias could not exist in the early studies37-40
and cannot account for the results of prospective cohort
investigations.40-42-47-60
Environmental Tobacco Smoke as a
Cause of Lung Cancer b
Several criteria have been used by various authors in
their efforts to operationalize the establishment of cau
sality. To this reviewer, the criteria of causality can be
reduced to just two: the relative risk gradient in relation
to exposure, as generated by the collective epidemio
logic evidence, and the biologic plausibility. On the one
hand, causality should be seriously considered when
there is a sharp relative risk gradient, even when etiol
ogy is not biologically plausible. On the other hand, a
weak empirical association should be considered as
causal only when the biologic evidence is overwhelm
ing. The association of ETS with lung cancer falls into
the second category. The collective epidemiologic evi
dence indicates that ETS is positively associated with
the relative risk for lung cancer to a highly significant
degree. Usually the relationship is dose-dependent and
remains statistically significant even when bias and
confounding arc accounted for. Nevertheless, the asso
ciation is weak, and the firm conclusion for causality is
based, to a large extent, on the converging and over
whelming biologic evidence: the qualitative similarity
of sidestream and mainstream smoke, their unquestion
able no-threshold carcinogenicity, and the extraordi
narily strong causal link of active smoking with lung
cancer. Recent evidence that passive smoking is associ
ated with epithelial possibly precanccrous lesions of the
lung in an autopsy study86 and suggestive results link
ing exposure to ETS with canine lung cancer risk87
provide additional, but hardly necessary, support for a
causal link. The strength of the biologic evidence dis
tinguishes lung cancer from other cancers and several
nonrespiratory conditions that have also been fre-
84
Risk of Lung Cancer from Passive Smoking
quently associated with passive smoking (reviewed
in88).
References ■
U.S. Department of Health and Human Services. The health
consequences of involuntary smoking. A report of the Surgeon
General. U.S. DHHS, Public Health Service, Office of the Assis
tant Secretary for Health, Office of Smoking and Health, Wash
ington DC. DHHS Pub. No. (PHS) 1986:87-8398.
2.
National Research Council. Committee on Passive Smoking. En
vironmental Tobacco Smoke: Measuring exposures and assess
ing health effects. Washington DC: National Academy Press,
1986.
3.
World Health Organization. Tobacco Smoking. I ARC Mono
graphs on the Evaluation of the Carcinogenic Risk of Chemicals
to Humans; Vol. 38. Lyon, France: World Health Organization.
I ARC. 1986.
4.
Office of Technology Assessment, US Congress. Passive smok
ing in the workplace. Special Projects Office. Health Program.
Washington DC, 1986.
5.
United States Environmental Protection Agency. Respiratory
Health Effects of Passive Smoking: Lung Cancer and Other Dis
orders. EPA/600/6-90/006F. Washington. DC, 1992.
6.
Baker RR, Proctor CJ. The origins and properties of environmen
tal tobacco smoke. Environ Int 1990:16:231-245.
7.
Guerin MR. Jenkins RA. Tomkins BA. The chemistry of envi
ronmental tobacco smoke: composition and measurement.
Chelsea, Ml: Lewis Publishers. 1992.
8.
Tomatis L, ed. Cancer: causes, occurrence and control. Lyon:
IARC Scientific Publication 100:1990:97-125.
9.
Wynder EL, Hoffmann D. Tobacco and tobacco smoke: studies
in experimental carcinogenesis. New York: Academic Press,
1967.
10.
Leaderer BP. Assessing exposures to environmental tobacco
smoke. Risk Analysis 1990;10:19-26.
11.
Axelson O, Fajen J, Feron V el al. Approaches and processes
used to evaluate the carcinogeneity of mixtures and groups of
chemicals. International Agency for Research on Cancer Work
ing Group. IARC Internal Technical Report No. 88/002. Lyon:
IARC, 1988.
12.
Mattson ME, Boyd G, Byar D et al. Passive smoking on com
mercial airline flights. JAMA 1989;261:867-872.
13.
Coultas DB, Samel JM. McCarthy JF et al. A personal monitor
ing study to assess workplace exposure to environmental tobacco
smoke. Am J Public Health 1990;80:988-990.
14.
Spengler JD, Trictman RD, Tosteson TD et al. Personal expo
sures to respirable particulates and implications for air pollution
epidemiology. Environ Sci Tcchnol 1985:19:700-707.
15.
Riboli E, Preston-Martin S, Saracci R et al. Exposure of non
smoking women to environmental tobacco smoke: a 10-country
collaborative study. Cancer Causes Control 1990;1:243-252.
16.
Fontham ETH, Correa P, Wu-Williams A et al. Lung cancer in
nonsmoking women; a multicenter case-control study. Cancer
Epidemiol Biomarkers Prev 1991;1:35-43.
17.
Jarvis MJ, Russell MH. Passive exposure to tobacco smoke Br
Med J 1985:291:1646.
18.
Cummings KM. Markello SJ, Mahoney MC et al Measurement
of current exposure to environmental tobacco smoke. Arch Envi
ron Health 1990;45:74-79.
19.
Maclure M. Katz RB-A, Bryant MS et al. Elevated blood levels
of carcinogens in passive smokers. Am J Public Health
1989;79:1381-1384.
1.
Hammond SK. Coghlin J, Gann PH et al. Relationship between
environmental tobacco smoke exposure and carcinogenhemoglobin adduct levels in nonsmokers. J Natl Cancer Inst
1993:85:474-478.
21.
Bos RP. Henderson PT. Genotoxic risk of passive smoking. Rev
Environ Health 1984;4:161-178.
22.
Wald NJ. Ritchie C. Validation of studies on lung cancer in
nonsmokers married to smokers. Lancet 1984:1:1067.
23.
Quackenboss JJ, Kanarek MS, Spengler JD et al. Personal mon
itoring for nitrogen dioxide: ^Methodological considerations for a
community study. Environ Internal 1982;8:249-257.
24.
Trichopoulos D. Passive smoking and lung cancer: The Ipsen
Lecture 1987. Scand J Soc Med 1988;16:75-79.
25.
Best EWR. A Canadian Study of Smoking and Health. Ottawa.
Department of National Health and Welfare, Epidemiology Divi
sion, Health Services Branch, Biostatistics Division, Research
and Statistics Directorate. 1966:65-86.
26.
Doll R. Peto R. Mortality in relation to smoking: 20 years’ obser
vations on male British doctors. Br Med J 1976;2:1525-1536.
27.
Hammond EC. Seidman H. Smoking and cancer in the United
Slates. Prev Med 1980;9:169-173.
28.
Rogot E. Murray JL. Smoking and causes of death among U.S.
veterans: 16 years of observation. Pub Health Rep 1980:95:213222.
29.
U.S. Department of Health and Human Services (U.S. DHHS).
The health consequences of smoking: cancer. A report of the
Surgeon General. U.S. DHHS, Public Health Service, Washing
ton DC. 1982.
30.
Doll R. Peto R. Cigarette smoking and bronchial carcinoma:
Dose and lime relationships among regular smokers and lifelong
non-smokers. J Epid Comm Health 1978:32:303-313.
31.
Doll R. Peto R. The causes of cancer Quantitative estimates of
avoidable risks of cancer in the United Slates today. J Natl Can
cer Inst 1981:66:1191-1308.
32.
Lee PN. Passive smoking. Food and Cosmetics Toxicology
1982;20:223-229.
33.
Matsukura S, Taminato T, Kitano N et al. Effects of environmen
tal tobacco smoke on urinary cotinine excretion in nonsmokers:
Evidence for passive smoking. N Engl J Med 1984:311:828832.
34.
Hoffmann D. Haley NJ. Adams JD et al. Tobacco sidestream
smoke. Uptake by nonsmokers. Prev Med 1984;13:608-617.
35.
Vutuc C. Quantitative aspects of passive smoking and lung can
cer. Prev Med 1984.13:698-704.
36.
Repace JL. Lowrey AH. A quantitative estimate of nonsmokers ’
lung cancer risk from passive smoking. Envir Inti 1985; 11:3-22.
37.
Trichopoulos D, Kalandidi A, Sparros L et al. Lung cancer and
passive smoking. Int J Cancer 1981;27:1-4.
38.
Trichopoulos D. Kalandidi A. Sparros L. Lung cancer and pas
sive smoking: conclusion of Greek study. (Letter] Lancet
1983:667-668.
39.
Trichopoulos D. Passive smoking and lung cancer [Letter]. Lan
cet 1984;1:684.
40.
Hirayama T. Nonsmoking wives of heavy smokers have a higher
risk of lung cancer a study from Japan. Br Med J 1981 ;282:183185.
41.
Hirayama T. Cancer mortality in nonsmoking women with smok
ing husbands based on a large-scale cohort study in Japan. Prev
Med 1984;13:680-690.
42.
Garfinkel L. Time trends in lung cancer mortality among nonsmokers and a note on passive smokine. J Natl Cancer Inst
1981;6:1061-1066.
43.
Chan WC. Fung SC. Lung cancer in nonsmokers in Hong Kong.
In: Grundmann E. ed. Cancer campaign. Vol. 6. Cancer epidemi
ology Stuttgart. West Germans. Gustav Fischer Verlag. 1982:
199-202.
20.
References
■U. Correa P. Fontham E, Pickle L et al. Passive smoking and lung
cancer. Lancet 1983:2:595-597
45 Buffler PA. Pickle LW. Mason TJ et al The causes of lung cancer
in Texas. In: Mizell M. Correa P. eds. Lung cancer: causes and
prevention. New York: Verlag Chemie International. 1984;pn.
83-99.
46. Gillis CR. Hole DJ. Hawthorne VM et al The effect of environ
mental tobacco smoke in two urban communities in the west of
Scotland. Eur J Respir Dis 1984.133(Suppl): 121-126.
47. Hole DJ, Gillis CR. Chopra C et al. Passive smoking and cardio
respiratory health in a general population in the west of Scotland.
48. Kabar GC. Wyndcr EL. Lung cancer in nonsmokers. Cancer
1984;53:1214-1221.
49. Garfinkel L. Auerbach O. Joubert L. Involuntary- smoking and
lung cancer, a case-control study. J Natl Cancer Inst 1985:75:
50. Wu AH. Henderson BE. Pike MD et.al. Smoking and other nsk
factors for lung cancer in women. J Natl Cancer Inst 1985:74;
51. Lam WK. A clinical and epidemiological study of carcinoma of
lung in Hong Kong [doctoral thesis]. Hong Kong: University of
Hong Kong. 1985.
52. Akiba S. Kato H. Blot WJ. Passive smoking and lung cancer
among Japanese women. Cancer Res 1986;46:4804-4807.
53. Lee PN. Chamberlain J. Alderson MR. Relationship of passive
smoking to risk of lung cancer and other smoking-associated
diseases. Br J Cancer 1986;54:97-105
54. Koo LC. Ho JH. Saw D et al. Measurements of passive smoking
and estimates of lung cancer risk among nonsmoking Chinese
females. Int J Cancer 1987;39:162-169.
55.
Lam TH. Kung ITM. Wong CM et al Smoking, passive smok
ing. and histological types in lung cancer in Hong Kong Chinese
women. Br J Cancer 1987;6:673-678
56.
Pershagen G, Hrubec Z, Svensson C. Passive smoking and lung
cancer in Swedish women. Am J Epidemiol 1987;125:17-24.
57.
Brownson RC. Rief JS. Keefe TJ et al Risk factors for adenocar
cinoma of the lung. Am J Epidemiol 1987;125:25-34.
58.
Gao Y. Blot WJ. Zheng W et al. Lung cancer among Chinese
women. Int J Cancer 1987;40:604-609.
59.
Humble CG, Samet JM. Pathak DR. Marriage to a smoker and
lung cancer risk. Am J Public Health 1987;77:598-602.
60.
Buller TL. The relationship of passive smoking to various health
outcomes among Seventh-Day Adventists in California [disserta
tion]. Los Angeles: University of California at Los Angeles.
1988.
61.
Geng G, Liang ZH. Zhang GL, On the relationship between
smoking and female lung cancer. In: Smoking and health.
Elsevier Science Publishers. 1988;pp. 483-486.
62.
Inoue R. Hirayama T. Passive smoking and lung cancer in wom
en. In: Smoking and health. Elsevier Science Publishers. 1988;
283-285.
63.
Katada H, Mikami R. Konishi M et al. Effect of passive smoking
in lung cancer development in women in the Nara region. Gan
No Rinsho 1988:34:21-27.
64.
Shimizu H. Morishita M. Mizuno K et al. A case-control study of
lung cancer in nonsmoking women. Tohoku J Exp Med 1988;
154:389-397.
65.
Svensson C. Pershagen G. Klominek J. Smoking and passive
smoking in relation to lung cancer in women. Acta Oncol
1989;28:623-629.
66.
Wu-Williams AH. Samel JH. Environmental tobacco smoke.
85
exposure-response relationships in epidemiologic studies. Risk
Anal 1990:10:39-48.
67. Kalandidi A. Katsouyanni K. Vbropoulou N et al. Passive smok
ing and diet in the etiology of lung cancer among nonsmokers.
Cancer Causes Control 1990; 1:15-21.
68.
Janerich DT. Thompson WD. Varela LR et al. Lung cancer and
exposure to tobacco smoke in the household. N Engl J Med
1990:323:632-636.
69.
Sobue T. Suzuki R. Nakayama N et al. Passive smoking among
nonsmoking women and the relationship between indoor air pol
lution and lung cancer incidence—results of a multicenter case
controlled study. Gan No Rinsho 1990;36:329-333.
70.
Liu Z. He X. Chapman RS. Smoking and other risk factors for
lung cancer in Xuanwei. China. Int J Epidemiol 1991:20:2631.
71.
Fontham ETH. Correa P. Reynolds P et al. A multiccntcr study of
environmental tobacco smoke and lung cancer in nonsmoking
women. JAMA 1994;271:1752-1759.
72.
Stockwell HG, Goldman AL. Lyman GH et al. Environmental
tobacco smoke and lung cancer risk in nonsmoking women. J
Nail Cancer Inst 1992;84:1417-1422.
73.
Brownson RC. Alavanja MCR. Hook ET et al. Passive smoking
and lung cancer in nonsmoking women. Am J Public Health
1992.82:1525-1530.
74.
Trddaniel J. Boffcta P, Saracci R. Hirch A. Environmental tobac
co smoke and the risk of cancer in adults. European Journal of
Cancer I993;29A:2O58-2O68.
75.
Blot WJ. Fraumcni JF Jr. Passive smoking and lung cancer. J
Natl Cancer Inst 1986;77:993-1000.
76.
Wells AJ. An estimate of adult mortality in the United States
from passive smoking. Environ Int 1988:14:249-265.
77.
Saracci R, Riboli E. Passive smoking and lung cancer: current
evidence and ongoing studies al the International Agency for
Research on Cancer. Mutation Res 1989;222:117-127.
78.
Tweedie RL. Mcngerscn KL. Lung cancer and passive smoking:
reconciling the biochemical and epidemiological approaches. Br
J Cancer 1992:66:700-705.
79.
Mantel N. Lung cancer and passive smoking. Br Med J
1987:294:440-441.
80.
Vandcnbroucke JP. Passive smoking and lung cancer, a publica
tion bias? Br Med J 1988;296:391-392.
81.
Wells AJ. Passive smoking and lung cancer: a publication bias?
Br Med J 1988:296:1128.
82.
Woodward A. McMichael AJ. Passive smoking and cancer risk:
the nature and uses of epidemiological evidence. Eur J Cancer
1991:27:1472-1479.
83. Lee PN. Lung cancer and passive smoking: association and arte
fact due to misclassification of smoking habits? Toxicol Lett
1987:35:157-162.
84. Lee PN. Passive smoking and lung cancer association: a result of
bias? Hum Toxicol 1987;6:517-524.
85. Wald NJ. Nanchanal K. Thompson SG et al. Does breathing
other people’s tobacco smoke cause lung cancer? Br Med J
1986:293:1217-1223.
86. Trichopoulos D, Mollo F, Tomatis L et al. Active and passive
smoking and pathological indicators of lung cancer risk in an
autopsy study. JAMA 1992:268:1697-1701.
87. Reif JS. Dunn K. Ogilvie GK et al. Passive smoking and canine
lung cancer risk. Am J Epidemiol 1992;135:234-239.
88. Whiddcn P. Tobacco-smoke pollution. The association for non* smoker’s rights. Edinburgh. Scotland: Melgund Centre. 1993;
I -68.
Control of Tobacco-related Cancers and Other Diseases.
Intern?, ional Symposium, 1990. Prakash C. Gupta, James E. Hamnf.r, III
and P.R. Murti, eds. Oxford University Press, Bombay, 1992.
Lung cancer and other diseases related to
passive smoking: a large-scale cohort study
Takeshi Hirayama
Institute of Preventive Oncology, Tokyo, Japan
In 1981, we demonstrated an elevated risk oflung cancer among nonsmoking wives of husbands
who smoke; subsequently, there have been several studies on this topic. Seventeen out of the 22
studies published in 1989 showed elevated risks; in seven studies, the risks were statistically sig
nificant. The risks in 10 selected studies were mostly higher when husbands smoked more heavily,
the average relative risks for lung cancer in nonsmoking women with nonsmoking husbands, light
smoking husbands and heavy smoking husbands being 1.00, 1.41 and 2.38, respectively. In addi
tion to lung cancer, our cohort study revealed significantly elevated risks for nasal sinus cancer,
brain tumour, post-menopausal breast cancer and ischaemic heart disease in nonsmoking women
with heavily smoking husbands as compared to those with nonsmoking husbands. These effects
are due to carcinogens and other toxic substances, which are present in higher concentration in
sidestream smoke than in mainstream smoke.
INTRODUCTION
Since our report on the effect of husbands'
smoking on the lung cancer risk in nonsmoking
wives (1), many studies have been conducted
to examine the passive smoking-lung cancer
hypothesis. The results of most of these studies
were in line with our report, as reviewed by the
US Surgeon-General (2) and others (3-7).
The purpose of this paper is to summarize
the results of our study in Japan, with special
reference to lung cancer and other selected
causes of death the risk of which is elevated by
passive smoking.
MATERIAL AND METHODS
In our large-scale cohort study in Japan, 9106
deaths were recorded among 91 450 nonsmok
ing wives whose husbands’ smoking habits
were known during the 16-ycar follow-up
(1966-81). The risk of nonsmoking wives dying
from lung cancer (n=200), ischaemic heart
disease (n=494) and other selected causes of
death was measured according to the extent of
the husbands’ smoking habit.
RESULTS
The results arc summarized in Tables 1-4.
Those diseases that showed a significant eleva
tion in risk in nonsmoking wives with hus
bands who smoked 20 or more cigarettes daily
are listed in Tables 1 and 2; associations
with the extent of husbands’ smoking (dose
response relationships) are shown in Tables 3
and 4.
Lung cancer: Out of 429 female lung cancer
deaths that took place during the 16-year
follow-up period, 303 were in nonsmokers.
Of these women, 200 were from 91 450
130
Hi rayama
Effects of passive smoking
131
Table 1
Table 2
Relative risks" ofcancer ofselected sites for nonsmoking wines with heavily smoking husbands (20 or more cigarettes daily). Risk
for wives with nonsmoking husbands = 1.00. Cohort study, 1966-81, Japan
Relative risks" of selected causes of death for nonsmoking wives with heavily smoking husbands (20 or more cigarettes daily).
__________________ Risk for wives with nonsmoking husbands = 1.00. Cohort study, 1966-81, Japan
n
Relative
risk
90%
Confidence limits
One-tailed
;>
Bile duct/Gallbladder
34
28
51
200
115
85
226
17
273
91
4.78
3.29
2.04
1.90
1.73
1.58
1.31
1.31
1.28
1.25
1.62 - 14.11
1.36- 7.96
1.09- 3.82
1.94- 2.70
1.12 - 2.66
0.89 - 2.81
0.94- 1.82
0.33 - 5.21
0.95 - 1.74
0.79 - 1.98
0.008
0.013
0.030
0.001
0.018
0.096
0.094
0.373
0.089
0.215
All sites
2705
1.21
1.10 -
1.32
0.000
Colon
Ovary
Urinary organs
Upper digestive tract
Rectum
Stomach
Pancreas
142
54
49
80
112
854
127
1.11
1.08
1.03
1.01
1.01
1.01
0.87
0.77 - 1.61
0.54- 2.15
0.50 - 1.91
0.58- 1.78
0.64- 1.60
0.86- 1.19
0.56- 1.34
0.318
0.428
0.468
0.486
0.484
0.463
0.295
Site of cancer
Brain tumour
Nasal sinus
Leukaemia
Lung
Breast
Malig. lymphoma
Liver
Bone
“Adjusted for husband's age by the Manlel-Haenzel method
Cause of death
n
Relative
risk
90%
Confidence limits
One-tailed
Stomach ulcer
Subarachnoid haemorrhage
Emphysema
Suicide
Hypertensive disease
Ischaemic heart disease
Hypertensive heart disease
Cerebral haemorrhage
Nephritis, nchprosis
Gastritis, enteritis
Diabetes
Cancer
Ill-defined
cerebrovascular disease
57
126
106
200
61
494
226
1179
128
57
227
2705
438
All sites
9106
1.19________ ________ 1.13 - 1,26
0.000
Other heart disease
Pneumonia
Tuberculosis
Cholelithiasis
Arteriosclerosis
Cerebral thrombosis
Chronic rheumatic heart disease
Senility
Liver cirrhosis
680
258
100
30
68
992
106
164
180
1.19
1.15
1.15
1.04
1.01
1.00
0.86
0.81
0.75
0.073
0.232
0.321
0.476
0.399
0.493
0.286
0.204
0.094
1.73
0.80 - 3.75
1.69
_________ 1.08 - 2.65
1.49
0.92 - 2.39
1.46
_________ 1.07 - 1.63
1.46
0.77 - 2.77
1.31
_________ 1.06 - 1,63
1.29
0.93 - 1.78
1.25
_________1.08 - 1,43
1.27
0.83 - 1.93
1.23
0.70 - 2.16
1.23
0.89 - 1.69
1.21________ ________ 1.10 - 1,32
1.20
0.95 - 1.51
0.97 - 1.44
0.84 - 1.59
0.71 - 1.86
0.35 - 3.07
0.60 - 2.01
0.85 - 1.17
0.55 - 1.34
0.53 - 1.24
0.52 - 1.08
0.121
0.026
0.085
0.019
0.166
0.019
0.100
0.036
0.399
0.277
0.147
0.000
0.097
“Adjusted for husband’s age by the Mantel-Hacnzel method
Fig. I. Mortality ratios for lung cancer in nonsmoking wives by husband’s smoking habit (prospective
study, 1966-81, Japan)
nonsmoking wives whose husbands’ smoking
habits were known. The extent of the elevation
in risk for lung cancer in nonsmoking wives
was studied in relation to the smoking habits of
the husbands.
The standardized mortality ratios :"or lung
cancer in nonsmoking women were 1.G0, 1.36,
1.42, 1.58 and 1.90 when their husbands were
nonsmokers, ex-smokers, daily smokers of
10-14, 15-19 and 20 or more cigarettes per day,
respectively (/> for trend: 0.00178). A similar,
significant dose-response relationship was
observed by age and by occupation of hus
bands, by age of wives, and in each period of
observation (Fig. 1), and also when other risk
factors such as diet, prefecture and population
density were adjusted for (Fig. 2) (8,9).
No other characteristic of the husbands or
wives themselves, other than the amount of
husbands’ smoking, was found to elevate the
risk of lung cancer in nonsmoking partners
(Fig. 3).
Similar studies have been conducted
in many countries. Most were case-control
studies (10-27), and only a few were cohort
studies (28,29). The results of most (17 out of
22 reported by 1989) were in line with the
results of our study in Japan (Tables 5 and 6)
(external consistency).
The earlier the age of marriage to hus
bands who smoked, higher was the risk for
lung cancer in nonsmoking wives, suggesting
the importance of duration of exposure to pas
sive smoking (Fig. 4) (30). It was also observed
that the risk for lung cancer in nonsmoking
husbands was significantly higher when their
wives were smokers rather than nonsmokers.
Therefore, nonsmokers with a nonsmoking
132
Hirayama
Effects of passive smoking
their husbands’ smoking were ischaemic heart
disease, subarachnoid haemorrhage, cerebral
haemorrhage, s’ icide -nd all causes of death
(Table 4). '
The risk for breast cancer, although of
border'inc significance, when analysed by age
groups of wife or standardized by occupation
of husbands, revealed a significant dose-rcsponse relationship. At age 50-59 years when
husbands smoked 1-19 and 20 or more ciga
rettes daily, the relative risk for mortality from
breast cancer was 1.3 and 2.68, respectively (p
for trend: 0.00969) (Fig. 6). The effect was
independent of each of the other risk factors for
wives, such as number of children (Fig. 7).
DISCUSSION
The validity of interview-based information on
exposure to passive smoking, on which the cur
rent study was based, was clearly demon
strated by recent I ARC studies (31) that were
conducted in 13 centres in 10 countries by
measuring urinary cotinine levels.
Other causes of death: Other causes of death
in which the risk in nonsmoking wives is
significantly associated with the amount of
spouse should be selected as the unit risk group
in order to study the clffct of exposure to
tobacco smoke on lung cancer, either actively
or passively (Fig. 5).
Other cancers: For most other sites, no signi
ficant association was observed between the
risk in nonsmoking wives and the amount of
For lung cancer, enough evidence to sat
isfy epidemiological criteria such as consistency
Table 3
Fig. 2. Relative risk for lung cancer in nonsmoking
wives by smoking habit of husbands.
Comparison of 200 lung eaneer cases and
age-occupation matched controls.
Observation by selected life style and
demographic variables (prospective study.
1966-81, Japan)
133
Relatii'f risks of cancers at selected sites for nonsmoking wives by husbands’ smoking habits; dose-response relationship.
Cohort study, 1966-81, Japan
Fig. 4. Lung cancer risk in nonsmoking wives by
husbands' smoking habit and by age at
marriage (prospective study, 1966-81,
Japan)
smoking of husbands. However, a significant
elevation of risk for cancers of the paranasal
sinuses, breast and brain, and leukaemia in
nonsmoking wives was detected, according
to the amount of the husband’s smoking
(Table 3).
Husbands’ smoking habit_____
Site of cancer
Nonsmokcr
1-19 daily
»20 daily
Mantel
extension chi
One-tailed
Lung
Nasal sinus
Brain
Breast
Leukaemia
1.00
1.00"
1.00
1.00
1.00’
1.44
2.28
4.01
1.12
1.79
1.90
3.29
4.78
1.73
2.04
2.990
2.064
2.069
1.795
2 009
0.001
0.019
0.019
0.036
0.022
All sites
1.00
1.11
1.21
3 143
0.000
"Including ex-smoking husbands
Table 4
Relative risks of selected causes of death for nonsmoking wives by husbands* smoking habits; dose-response relationship.
Cohort study, 1966-81, Japan
Husbands' smoking habit
Site of cancer
Fig. 3. Lung cancer mortality
in nonsmoking
women. Ratio by
selected risk factors
(prospective study,
1966-81, Japan)
Nonsmoker
1-19 daily
5=20 daily
Mantel
extension chi
One-tailed
Cancer
Ischaemic heart disease
Subarachnoid haemorrhage
Cerebral haemorrhage
Suicide
1.00
LOO
LOO
1.00
LOO
1.11
1.14
1.52
1.31
1.34
1.21
1.31
1.69
1.25
1.46
3.143
2.164
1.846
2.680
2.030
0.000
0.015
0.032
0.036
0.021
AB causes
1.00
1.15
1.19
5.449
0.000
P
134
Effects of passive smoking
Hirayama
135
Table 5
Relative risks for lung cancer among nonsmoking women, according to number of cigarettes smoked per day by their husbands
Husbands’ smoking status
Author(s)
Correa et al.
Trichopoulos et al.
Inoue el al.
Pershagen et al.
Akiba et al.
Wu el al.
Garfinkel et al.
Hirayamma*
Koo et al.
Garfinkel*
Ref. no.
Nonsmoker
Light
Heavy
14
26
19
24
10
27
16
8
21
28
1.0
1.0
1.0
1.0
1.0
1.0
1.0
1.0
1.0
1.0
1.2
2.4
1.2
1.0
1.4
1.2
1.1
1.4
1.9
1.3
3.5
3.4
3.4
3.2
2.1
2.0
2.0
1.9
1.2
1.1
‘Prospective study; all others are case-control studies.
Table 6
Relatioe risks (R) for lung cancer in women who had never smoked but had smoking husbands
Senior author
Ref.
no.
Lung
cancers
R
Inoue
Geng
Trichopoulos
Correa
Lam
Humble
Brownson
Lam
Koo
Hirayama
Avika
19
17
26
14
36
18
1]
22
21
1,8
10
22
54
77
22
60
<28
19
199
88
183
94
2.25
2.16—
2.11“
2.07*
2.01“
1.80
1.68
1.65“
1.64
1.63“
1.50
Senior author
Ref.
no.
Lung
cancers
R
Garfinkel
Wu
Pershagen
Gao
Garfinkel
Shimizu
Gillis
Lee
Kabat
Bufiler
Chan
16
27
24
15
28
25
29
23
20
12
13
134
<29
67
226
153
90
8
32
24
41
84
1.31’
1.20
1.20
1.19
1.17
1.10
1.00
1.00
0.79
0.78
0.75
Fig. 5. Active and passive smoking and lung cancer mortality (prospective study. 1966-81. Japan)
*Signilicant only in trend analysis or in subjects validated as heavy smokers
‘•Significant at 95% confidence level in comparison of exposed and non-exposed subjects
Modified from ref. (7)
of association, specificity of association and
dose-response relationship has already been
accumulated in the literature to evaluate the
risk of nonsmoking women with smoking
husbands.
A different histological pattern of lung
cancer in women than in men, e.g., predomi
nance of adenocarcinoma, is considered to
be due to the higher proportion of passive
smoking-related cases in women than in men.
The results of our large-scale cohort study
in Japan further showed an elevated risk
for cancers of the nasal sinus, breast and
brain and leukaemia in addition to lung
cancer.
Others
1.92(0.61-6.04)
1.00
Husband smoke
20 or more/daily
6.63(2.19-20.01)
4.31(2.07-8.96)
An elevation in risk for nasal sinus cancer,
as in the case of lung cancer, is compatible
with the existence of potent carcinogens in
sidestream smoke, which is inhaled through
the nose in even higher concentration that- in
mainstream smoke.
Fig. 6. Rate ratio for death from breast cancer
in nonsmoking women by husbands’
smoking habit
Fig. 7. Relative risk for breast cancer (age 50-59)
in nonsmoking women by number of
children and by husbands' smoking
habit
A significant elevation in risk due to pas
sive smoking was reported for childhood brain
tumours (32,33); a similar elevation related to
passive smoking was also observed for adult
brain tumours.
For breast cancer, the observed associa
tion is similar to that reported by Sandler et al.
Effects of passive smoking
136
137
Hiravama
14.
(34). In our study, the association with the
smoking habits ofhusbands was observed most
strikingly in
nonsmoking women
at
peri-
menopausal age, 50-59 years. The association
was also observed to be independent of repro
ductive history. Epidemiological patterns of
breast cancer are more or less similar to those
of lung cancer (urban-rural relationship, inter
national variation, increasing trend, etc.) may
be due, at least partly, to the common associa
tion with passive smoking.
For leukaemia, in view of the recent report
on the positive association between the disease
and active smoking (35), intensive studies will
be necessary to confirm the existence of an
association with passive smoking as well.
The risks of ischaemic disease, subarach-
noid haemorrhage, cerebral haemorrhage and
suicide in nonsmoking wives were also signifi
cantly associated with their husbands’ smok
ing habit. Most of these associations can be
explained by the higher concentrations of car
bon monoxide, nicotine and other toxic sub
15.
Correa P, Picklf. LW, Fonthan E, Lin Y,
Haenszel W. Passive smoking and lung can
cer. Lancet 1983; ii:595-7.
Gao Y-T, Bi.ot WJ, Zheng W, et al. Lung
cancer among Chinese women. Int J Cancer
16.
stances in sidestream smoke than in main
17.
Meanwhile, in view of the enormous size
of the population at risk, intensive efforts
should be made to reduce the chances of expo
sure to passive smoking in onr environment as
low as possible in order to reduce the risk of
these selected cancers and certain other dis
eases of vital importance.
Hiravama T. Non-smoking wives of heavy
smokers have higher risk of lung cancer: a
study in Japan. Br Med J 1981; 282:183-5.
2.
US Surgeon-General. The Health Consequen
ces of Involuntary Smoking. A Report of the
Surgeon-General. Rtx'kvillc, Maryland. US
Public Health Service. DHHS (C1X1) 1986;
87-8398.
3.
National Research Council. Environmental
Tobacco Smoke, Measuring Exposures and
Assessing Health Effects. National Academy
Press. Washington 1X1. 1986.
4.
Wald NJ, Nanchanal K, Thompson SG,
Cuckle HS. Does breathing other people’s
tobacco smoke cause lung cancer? Br Med J
1986; 293:1217-22.
5.
Blot WJ, Fraumeni JF. Passive smoking
and lung cancer. J Nall Cancer Inst 1986;
77:993-1000.
6.
Wells AJ. An estimate of adult mortality in
the United States from passive smoking. J
Environ Int 1988; 14:249-65.
7.
Lee P. Passive smoking and lung cancer; fact or
Action? In: Bieva CJ, Courtois Y, Govaerts
M, eds. Present and Future of Indoor Air
Quality. Elsevier Science Publishers BV.
Amsterdam: 1989. pp. 119-28.
Hiravama T. Cancer mortality in non
smoking women with smoking husbands based
on a large-scale cohort study in Japan. Prev
Med 1984; 13:680-90.
9.
Hiravama T. Dietary habits arc of limited
inqxirtance in influencing the lung cancer risk
among Japanese females who never smoked.
In: Bieva CJ, Courtois M, Govaerts M,
eds. Present and Future of Indoor Air Quality.
Elsevier Science Publishers BV. Amsterdam:
1989. pp. 77-82.
10.
Akiiia S, Kato H, Blot WJ. Passive smoking
and lung cancer among Japanese women.
Cancer Res 1986; 46:4804-7.
11.
Brownson RC, Reif JS, Keefe TJ,
Ferguson SW, Pritzl JA. Risk factors for
adenocarcinoma of the lung. Am J Epidemiol
1987; 125:25-34.
12.
Buffler PA, Pickle LW, Mason TJ,
Contant C. The causes of lung cancer in
Texas. In: Mizell M, Correa P, eds. Lung
Cancer; Causes and Prevention. Verlag
Chemie International. New York: 1984;
pp. 83-99.
13.
Chan WC, Func SC. Lung cancer in nonsmokers in Hong Kong. In: Grundman E, cd.
Cancer Campaign, Cancer Epidemiology. Vol
6. Gustav Fischer Verlag. Stuttgart, 1982.
pp. 199-202.
75:463-9.
Geng G-Y, Liang ZH, Zhang AY, Wu GL.
On the relationship between smoking and
female lung cancer. In: Aoki M, Hisamichi S,
Tominaga S, eds. Smoking and Health 1987.
Elsevier Science Publishers BV. Amsterdam:
1988. pp. 483-6.
18.
Humble CG, Samkt JM, Pathak DR.
Marriage to a smoker and lung cancer risk. Am
19.
References
1.
Shimizu H, Morlshita M, Mtzu.no K,
Masuda T, Ogura Y, Santo M. A case
control study of lung cancer in non-smoking
women. Tohoku J Exp Med 1988; 154:389-97.
26.
Trichopoulos D, Kaiandidi A, Sparros L.
Lung cancer and passive smoking; conclusion
of the Greek study. Lancet 1983; ii:677-8.
27.
Wu AH, Henderson BE, Pike MC, Yu MC.
Involuntary smoking and lung cancer: a case
control study. J Nall Cancer Inst 1985;
stream smoke. Further studies will also be
necessary for these causes of death to clarify
the mechanism of the association.
1987; 40:604-9.
Carfinkel K, Auerbach O, Joubert L.
25.
8.
J Public Health 1987; 77:598-602.
Inoue R, Hiravama T. Passive smoking
and lung cancer in women. In: Aoki M,
Hisamichi S, Tominaga S, eds. Smoking and
Health 1987. Elsevier Science Publishers BV.
Amsterdam: 1988. pp. 283-5.
KabatGC, Wvnder EL. Lung'canccr in nonsmokers. Cancer 1984; 53:1214-21.
21.
Koo LC, Ho JHC, Saw D, Ho C. .Meas
urements of passive smoking and estimates of
lung cancer risk among non-smoking Chinese
females. Int J Cancer 1987; 39:162-9.
22.
Lam TH, Kung 1TM, Wong CM, et al.
Smoking, passive smoking and histological
types in lung cancer in Hong Kong Chinese
women. Br J Cancer 1987; 56:673-8.
23.
Lee PN, Chamberlain J, Alderson MR.
Relationship of passive smoking to risk of lung
cancer and other smoking associated disease.
28.
66:1061-6.
Gillis CR, Hole DJ, Hawthorne VM,
Boyle P. The effect of environmental tobacco
smoke in two urban communities in the west of
Scotland. Eur J Resp Dis 1984; 65:121-6.
30.
Hiravama T. Duration of exposure as a deter
minant of lung cancer risk in passive smokers.
Environ Tech Letters 1988; 9:731-2.
31.
Riboi.i E, Preston-Martin S, Saracci R, el
al. Exposure of nonsmoking women to environ
mental tobacco smoke: a ten-country collabo
rative study. Cancer Causes Control 1990;
29.
20.
24.
Br J Cancer 1986; 54:97-105.
Pershagen G, Hrubec Z, Svensson C.
Passive smoking and lung cancer in Swedish
women. Am J Epidemiol 1987; 125:17-24.
Smoking and other risk factors for lung cancer
in women. J Natl Cancer Inst 1985; 74:747-51.
Garfinkel L. Time trends in lung cancer
mortality among non-smokers and a note on
passive smoking. J Natl Cancer Inst 1981;
32.
1:243-52.
Preston-Martin S, Yu MC, Benton B,
Henderson BE. W-nitroso compounds and
childhood brain tumors: a case-control study.
33.
Cancer Res 1982; 42:5240-5.
Gold E, Gordis L, Tonascia J, Szklo M.
Risk factors for brain tumors in children. Am J
34.
Epidemiol 1979; 109:303-19.
Sandler DP, Everson RB, Wilcox AJ.
Cigarette smoking and breast cancer. Am J
35.
Epidemiol 1986; 123:370-1.
Kinlen LJ, Rocot E. Leukaemia and smok
ing habits among United States veterans. Br
36.
Med J 1988; 297:657-9.
Lam WK. A clinical and epidemiological study
of carcinoma of lung in Hong Kong. Thesis,
University of Hong Kong, 1985.
470
PC. Gupta
Gupta, P.C.. Aghi. M.B.. Bhonslc, R.B., Murti. P.R., Mehta, F.S., Mehta, C.R. & Pindborg. JJ. (1986a)
Intervention study of chewing and smoking habits for primary prevention of oral cancer among 12 212
Indian villagers. In: Zaridze, D.G. & Peto, R., eds, Tobacco: A Major International Health Hazard (IARC
Scientific Publications No. 74), Lyon, IARC, pp. 307-318
Gupta. P.C., Mehta, F.S.. Pindborg. J J.. Aghi. M.B.. Bhonslc, R.B., Murti, P.R., Daftary, D.K., Shah. H.T. &
Sinor, P.N. (1986b) Intervention study for primary prevention of oral cancer among 36,000 Indian tobacco
users. Lancet, I. 1235-1238
Gupta. P.C., Mehta. F.S., Pindborg. J J., Daftary, D.K., Aghi, M.B., Bhonslc, R.B. & Murti. P.R. (1989a) A
primary prevention study of oral cancer among Indian villagers. Eight-ycar follow-up results. In: Hakama,
M., Bcral, V., Cullen, J. & Parkin. M.. eds. Evaluating Effectiveness of Primary Prevention of Cancer (IARC
Scientific Publications No. 103), Lyon. IARC. pp. 149-156
Gupta, P.C., Bhonslc, R.B., Muni, P.R., Daftary, D.K., Mehta, F.S. & Pindborg, JJ. (1989b) An epidemiologic
assessment of cancer risk in oral prccanccrous lesions in India with special reference to nodular
leukoplakia. Cancer, 63, 2247-2252
IARC (1985) IARC Monogaphs on the Evaluation of the Carcinogenic Risk of Chemicals to Humans, Vol. 37,
Tobacco Habits other than Smoking Betel-quid and Areca-nut Chewing and Some Related Nitrosamines, Lyon
Mehta. F.S., Pindborg. J J., Gupta. P.C. & Daftary. D.K. (1969) Epidemiologic and histologic study of oral
cancer and leukoplakia among 50,915 villagers in India. Cancer, 24, 832-849
Mehta. F.S., Gupta. P.C., Daftary, D.K.. Pindborg. J J. & Choksi. S.K. (1972) An epidemiologic study of oral
cancer and prccanccrous conditions among 101.761 villagers in Maharashtra. India. bit. J. Cancer, 10,
134-141
Mehta, F.S., Aghi. M.B.. Gupta. P.C.. Pindborg. J J.. Bhonslc. R.B., Jalnawalla. P.N. & Sinor. P. (1982) An
intervention study of oral cancer and prccanccr in rural Indian populations: a preliminary report. Bull World
Health Organ., 60. 441-446
Mehta. F.S.. Gupta. P.C.. Bhonslc. R.B.. Murti. P.R.. Daftary. D.K. & Pindborg. J J. (1986) Detection of oral
ctmccr using basic health workers in an area of high oral cancer incidence in India. Cancer Detect. Prev., 9.
219-225
Murti. P.R., Bhonslc. R.B.. Pindborg. JJ.. Daftary. D.K.. Gupta. P.C. & Mehta. F.S. (1985) Malignant
transformation rate in oral submucous fibrosis over a 17-ycar period. Commun. Dent. Oral Epidemiol, 13,
340-341
Wamakulasuriya. K.A.A.S. (1984) Utilization of primary health care workers for early detection of oral cancer
and prccanccr cases in Sri Lanka. Bull. World Health Organ , 62. 243-250
World 1 Italth Organization (1984) Control of oral cancer in developing countries. Report of a Wl IO meeting.
But! World Health Organ . 62. 817-830
n<c io Human Cancer of N-NItroso Compounds.
** /co Smoke and Mycotoxins.
T
O'Neill. J. Chen and H. Bartsch
! ‘on International Agency for Research on Cancer
€ IARC. 1991
LUNG CANCER: POLITICAL MEASURES
J.M. Mackay
Asian Consultancy on Tobacco Control, Hong Kong
In countries where prolonged smoking of manufactured cigarettes is a widely established
luibit. it is responsible for about 90% of lung cancer. As lung cancer is usually incurable,
r.cn with expensive technology, the key to its control lies in prevention. World experience
bus shown the crucial need for government commitment, funding and action in controlling
■ be epidemic of tobacco-related disease. It is recommended that each country establish a
national council of ‘tobacco or health’ to coordinate a comprehensive tobacco control
programme. This programme should incorporate data collection, including evaluation of
specific anti-tobacco measures; legislative measures, including strong, rotating health
warnings, limits on harmful substances, establishment of smoke-free areas, bans on any
new forms of tobacco use, and a total ban on all direct or indirect promotion of tobacco
products; health education campaigns; and taxation and price policies. The support and
involvement of the medical profession is vital. Obstacles to success include the effect of
advertising revenue in silencing the media, the inertia of governments and the medical
profession, but most importantly the tobacco industry — the largest, wealthiest, most
determined and strongest opposition to tobacco control worldwide.
In countries where tobacco smoking is an established habit, it is responsible for about
90% of lung cancer. As lung cancer is rarely curable, even with expensive technology, the
key to reducing its frequency lies in prevention. While the prevalence of cigarette
consumption is decreasing in industrialized countries, it is increasing in nonindustrialized
countries which have fewer legislative controls and other measures that, in industrialized
countries, limit the use of tobacco. Different countries are at very different points in the
five-stage process of lung cancer prevention: epidemiology, social science, action, decrease
in smoking prevalence and, finally, reduction in lung cancer mortality.
Science and epidemiology
Conclusive data on the hazards of tobacco exist on which preventive public health action
can be based now, without waiting for further research. Continuing surveys on tobacco
prevalence, mortality and morbidity related to tobacco use, attitudinal surveys and the
economic impact of tobacco remain necessary, however, in order to assess the scope of the
problem in each country, to illustrate the necessity of preventive measures and to evaluate
the most effective of these measures.
m
Lung cancer: political measures
J. M. Mackay
Preventive measures
World experience has shown the crucial need for government commitment, funding and
action in establishing a national programme to reduce the tobacco epidemic. It is important
that all countries establish a national focal point to stimulate, support and coordinate
anti-tobacco activities. The experience of such bodies is that it is not possible to cooperate
with the tobacco industry, which is committed to the opposite goal — of increasing tobacco
sales.
Ban on all tobacco promotion, advertising and sponsorship
Advertising conveys the message that smoking is associated with success, pleasure,
relaxation, machoism, sports, freedom, beauty in nature, slimness, sophistication and
sexuality. Castleden (1983), Charlton (1986) and Aitken et al. (1988) have shown that
children are aware of and are influenced by tobacco advertising. Roemer (1986) reported
that in 20 countries there was a total ban on advertising, in 17 there were strong partial bans,
and in 21 there were moderate, partial bans. Partial bans have only partial effects and are
frequentiy circumvented by ingenious, indirect advertising and sponsorship. A total ban
allows children to grow up free from all commercial pressure to smoke and, as Bjartveit
and Lund (1987) have shown in Norway, this leads to a decrease in the numbers of children
who smoke.
Ban on sales to youth
Banning sales to young people may be good in principle, but in practice it is difficult to
enforce. The countereffect is that, by suggesting that smoking is an adult activity, some
youths, who wish to appear adult or daring, may even be encouraged to smoke. Saito (1987)
reported that, in Japan, where persons under 20 years of age are not allowed to smoke, the
adult rates of smoking -are nevertheless established in the teenage years, indicating the
ineffectiveness of that law.
Effective, rotating health, warnings
Roemer (1986) noted that in 53 countries health warnings are required. Ramstrom
(1980) in Sweden has shown that smokers read and are aware of informative, rotating
warnings. In many countries, governments are moving from single, mild warnings, such as
‘Smoking may harm your health’, to tougher, rotating health warnings, such as: ‘Smoking
kills,’ ‘Smoking causes lung cancer,’ ‘Tobacco is addictive,’ ‘Smoking in pregnancy harms
your baby,’ ‘Smoking causes heart disease,’ and ‘Quit smoking and feel healthier.'
Limits on harmful substances
Lowering the levels of tar in cigarettes can prevent about one-third of cases of lung
cancer, although quitting can prevent more. A ceiling of about 10-15 mg tar per cigarette
is a reasonable current aim. Smokers have an exaggerated perception of the benefits of
low-tar cigarettes, however, so the tobacco industry should never be allowed to suggest that
a lower tar cigarette is a ‘safe’ cigarette — especially since cigarettes kill even more people
by other diseases than by lung cancer, and such evidence as is available on these other
diseases suggests that differences in machine-measured tar delivery may involve little
difference in risk.
473
Ban on new forms of tobacco
New forms of manufactured tobacco products are constantly being launched.
Pre-emptive bans are true preventive health measures in that they avoid an additional range
of cancers.
Smoke-free areas
Smoking is not only unpleasant to nonsmokers but may also give them cancer (IARC.
1986). In many countries, smoking has been banned in public areas, public transport, places
of work (especially health premises), schools and government offices. Most people are
nonsmokers: thus, the freedom of the majority to breathe clean air is an important
consideration. Bans also help smokers: the creation of smoke-free areas encourages
smokers to cut down or quit, thus helping them to make a decision in the best interest of
their own health.
Price policy
Increasing taxes on cigarettes is a very effective way of reducing smoking without loss
of revenue to governments. Most smokers give cost and health as the two main reasons for
quitting. Lewit el al. (1981) and Warner (1984) reported that in the USA. for example, for
every 10% increase in tax there is a 4% decrease in the number of smokers and a 14%
decrease in the number of teenage smokers. The World Health Organization (1984) noted
that ‘Millions of lives could be saved if steep taxes were imposed on tobacco.' Grossman
(1983) concluded that increasing taxes has a particularly beneficial effect upon young
people and the poor, who have less money to spend and are therefore more likely to quit.
Health information and education
Health information and education form an important part of a comprehensive
anti-tobacco programme, by educating both decision makers and the population to
understand and accept legislative and other anti-tobacco measures. In contrast to the
attractive ‘Come and join us' images used by the tobacco industry, many health educators
have traditionally used depressing, boring health statistics and finger-wagging ‘Don’t
smoke’ messages, which may encourage adults to quit but seem to have little effect in
preventing young people from starting to smoke. Health education — especially that geared
to youth — is now moving towards positive, healthy images.
Overcoming the obstacles
The media, the medical profession and politicians must be persuaded that smoking is
harmful and that action is needed; yet these groups are often obstacles to tobacco control.
The media
Varner (1985) stated that ‘Studies dating back to the 1930s provide evidence that the
media’s dependence on revenue from cigarette advertising has repeatedly led to
suppression of smoking and health matters,’ concluding ‘It seems likely that there are more
people who smoke today than there would be in an environment of responsible media
coverage. The result is an avoidable excess burden of suffering and premature death. As
474
J. M. Mackay
long as cigarette advertising remains legal and widespread, its influence on editorial
coverage of smoking and health is likely to persist.'
As well as avoiding financial pressures that distort media coverage, it is important to
avoid the pressure to regard tobacco-related issues as stale news. Simply saying that
smoking causes cancer does not produce front-page headlines. Doctors involved with
anti-tobacco programmes must learn to become public relations experts, to write press
releases, to nurture journalists, to highlight newsworthy items and, perhaps most difficult
of ail, to drop their professional jargon and find lively ways of presenting complicated
medical statistics accurately — roles for which we have received little training.
The health profession
Doctors are more often involved with cure than with prevention. Medical societies
usually have little money in comparison with the wealth of the tobacco industry. Both
individual doctors and medical societies are often reluctant to be involved in political issues
or public confrontations with the well-groomed representatives of the tobacco industry.
Tobacco is a health problem, but the resolution of this problem is political. Decisions on
nationwide containment of tobacco use. for example by legislation, lie with governments
not with hospitals. If doctors are in the business of prevention, however, they also are in
the business of politics. Doctors who do not address the political dimensions of the tobacco
epidemic cannot hope to contribute substantially to reducing the scope of this epidemic.
The support of medical organizations to national anti-tobacco efforts is essential: in
giving health information to the public, in advising governments and in participating in
anti-tobacco actions. Statements from international and national health organizations can
have an influential effect by indicating solidarity on this issue. In Hong Kong, all 65 medical
societies have agreed in writing that tobacco is harmful to health — a powerful statement
of support. Medical meetings can be declared‘smoke-free meetings’. Individual doctorscan
set an example by not smoking, making their offices smoke-free, displaying posters, giving
out pamphlets on howto quit, participatingin anti-smoking efforts, refusing tobacco money
and not buying shares in the tobacco industry.
Walking a more lively path, one finds organizations like ‘BUG A-UP’(Billboard Utilising
Graffitists Against Unhealthy Promotions), spawned in Australia, and ‘DOC (Doctors
Ought to Care) in the USA. These groups comprise health professionals and others who
have become weary of the inactivity of governments on this public health issue. Staging
eye-catching ‘re-facing- of billboards, using catchy slogans, cheerfully disrupting
tobacco-sponsored events and promotional displays with alternative messages and
appearing dressed in skeleton suits, these groups certainly focus media and public attention
on tobacco.
Governments and politicians
Governments are often worried about ‘losing’ immediate tax revenue, and politicians
may have pressure put upon them by large tobacco companies. In fact, tobacco use drains
the economy by medical and health costs, lost productivity, welfare costs, costs of fires and
cost of the use of land that could be used to grow food.
Lung cancer: political measures
475
The tobacco industry
The international tobacco industry is the largest, most determined and strongest
opposition to tobacco control. It is organized globally, commands considerable political
influence and continues to deny the main evidence about the health effects of tobacco. It
has vast amounts of money to sponsor sport, the arts, academic institutions and many other
organizations, and sponsorship of institutions makes them less likely to speak out against
tobacco.
Nowadays, a country in which effective legislation is attempted can expect a coordinated
and intensive confrontation with the international tobacco industry, and use of double
standards. The international tobacco companies, although based in countries with
long-established bans, strenuously fought Hong Kong’s ban on tobacco advertising on
television. The same companies are breaking the stated regulations of China by advertising
cigarettes.
Sections of the US government have threatened trade sanctions against Hong Kong.
Japan, the Republic of Korea, Taiwan and Thailand if those countries do not open their
markets to the sale or advertising of US cigarettes. McNeil (1988) reported a comment of
the Philip Morris tobacco company: ‘The suspension of the tariffs in Japan and the recent
opening of the market in Taiwan are the direct result of effective negotiations by the Office
of the US Trade Representative [of the US government].’ The political coercion of trace
sanctions is noteworthy by an industry that so often speaks of freedom. The tobacco
companies make no apology for this. Chan (1988) reported that a representative of the R.J.
Reynolds company even said ‘We expect such support [from the US government]. That’s
why we vote them in.’
A class action suit has been brought in the Philippines against US tobacco companies
for failure to provide the same level of protection for Filipino children as that provided for
children in their country of origin. If successful, this would result in a ban on television
advertising, health warnings and enforcement of the same tar levels as in the same cigarettes
sold in the USA. This case has implications for many developing countries.
Litigation is a more recent and interesting development in the ‘tobacco war’. Ramstrbm
(1986) reported that compensation had been awarded for the harmful effects of passive
smoking in causing lung cancer in Sweden; there has recently been a similar case in
Australia; and headline-catching cases are now in progress in the USA (Eichenwald, 1988).
which reverberate on tobacco shares on Will Street. The number of such cases will
undoubtedly increase over the next few decades and could possibly bring the tobacco
industry to its knees financially.
A note of optimism
Is it possible to be optimistic about tobacco control? Worldwide, the health statistics give
little comfort, and death and disability from tobacco will certainly increase over the next
few decades. The behaviour of the tobacco industry gives no comfort either. But optimism
stems from several points: data on health effects are slowly being collated — a crucial first
step. While some countries have still taken virtually no action against tobacco, health
concerns are mobilizing in many others. Remarkably similar battles are being fought all
over the world. There is now sharing of international expertise in countering the tobacco
476
J- M. Mackay
industry at the political and legislative level. Roemer (1986) reported that, by mid-1986,
over 70 countries had enacted legislation to control smoking and many had strengthened
existing legislation — a continuing process. An ancient Chinese saying goes: ‘A journey of
10 000 miles begins with a single step.’The first steps in cancer reduction have already been
taken, but there are many miles ahead.
Relevance to Human Cancer of //-Nitroso Compounds,
Tobacco Smoke and Mycotoxins.
Ed. I.K. O’Neill, J. Chen and H. Bartsch
Lyon. International Agency for Research on Cancer
© IARC. 1991
References
Aitken, P.P., Leather, D.S., Scott, A.L- & Squair. S.I. (1988) Cigarette brand preferences of teenagers and
adults. Health Promotion, 2, 219-226
Bjartvcit. K. & Lund, K.E. (1987) Smoking Control in Norway, Oslo, National Council on Smoking and Health,
PP- 1-4
Castlcdcn, W.M. (1983) Advertising, cigarettes and young smokers. Med. J. Aust., 1, 196-197
Chan, G. (1988) Tbbacco giants and COSH trade fiery words over smoking. South China Morning Post, October
16, p. 4
Charlton, A. (1986) Children’s advertisement-awareness related to their views on smoking. Health Educ. J.,
45, 75-78
Eichenwald, K. (1988) Tbbacco case verdict hailed. Report on Rose Cipollonc case from New York Times. Hong
Kong Standard, June 16
Grossman, M. (1984) Taxation and cigarette smoking in the United Slates. In: Proceeding? of the 5th World
Conference on Smoking and Health (Winnipeg. 10-15 July, 1983), Ottawa, Canadian Council on Smoking and
Health, Vol. 1, pp. 483-487
I ARC (1986) 1ARC Monographs on the Evaluation of the Carcinogenic Risk of Chemicals to Humans, Vol. 38.
Tobacco Smoking, Lyon
Lcwit, E.M., Coatc, D. & Grossman, M. (1981)17)0 effects of government regulation on teenage smoking.
J. Law Econ., 24, 545-569
McNeil, M. (1988) Cigarette firms look overseas as the market dries up in the US. South China Morning Post,
January 26, p. 4
Ramstrom, L.M. (1980) The Swedish programme for smoking control - current progress and future plans. In:
Ramstrdm, UM., cd.. The Smoking Epidemic. A Matter of Worldwide Concern, Stockholm, Almqvist &
Wikscll
Ramstrom, L.M. (1986) A case of lung cancer classified as occupational injury due to passive smoking at the
workplace - a ruling by the Swedish Insurance Court of Appeal. Press Release, National Smoking and
Health Association, Sweden; January 13
Rex:mer, R. (1986) Recent Developments in Legislation to Combat the World Smoking Epidemic
(WHO/SMO/HLE/86.1), Geneva, World Health Organization
Saito, R. (1987) Smoking among young women in Japan. In: Aoki. M., Hisamichi, S. & Tominaga, S., eds.
Smoking and Health 1987 (Excerpta Medico International Congress Series 780), Amsterdam, Elsevier, 517-519
Wald, NJ., Nanchahal, K., Thomson, S.G. & Cuckle, H.S. (1986) Does breathing other people’s tobacco smoke
cause lung cancer? Br. Med. J., 293, 1217-1222
Warner, K.E. (1984) Cigarette taxation; doing good by doing well. J. Public Health Policy, 5, 312-319
Warner, K.E. (1985) Cigarette advertising and media coverage of smoking and health. New Engl. J. Med., 312,
384-388
World Health Organization (1984) World tobacco tax could help save millions of lives. WHO Tobacco Alert
Series 1, Vol. 2, No. 4:1
ANALYSIS AND PYROLYSIS OF SOME N-NITROS AMINO ACIDS
IN TOBACCO AND TOBACCO SMOKE
K.D. Brunnemann, M.V. Djordjevic, R. Feng & D. Hoffmann
Naylor Dana Institute for Disease Prevention.
American Health Foundation, Valhalla. NY. USA
A new tobacco-specific nitrosamine, 4-(A'-nitrosomcthyIamino)-4-(3-pyridyl)butyric acid
(iso-NNAC), has been identified in tobacco, and its structure was confirmed by gas
chromatography-mass spectrometry following enrichment of a tobacco extract. The levels
of iso-NNAC ranged from 0.01 to 0.95 ppm. It does not induce DNA repair in primary rat
hepatocytes and is inactive as a tumorigenic agent in strain A mice. In order to study the
fate of nitrosamino acids during smoking, we spiked cigarettes with the following
A-nitrosamino acids: iso-NNAC, 3-(nitrosomethylamino)propionic acid (NMl’A),
4-(nitrosomethylamino)butyric acid (NMBA), /V-nilrososarcosine (NSAR) and N-nitrosoproline (NPRO). NMl’A and NMBA were partially transferred, unchanged, during
smoking and partially formed the corresponding methyl esters, while pyrolysis of NSAR
and NPRO resulted mainly in their decarboxylating products. This is the first time that the
pyrosynthesis of methyl esters has been observed during smoking.
We have isolated and identified a new tobacco-specific nitrosamine (TSNA) and consider
it a potential biomarker for exposure to TSNA. In addition, we studied the fate of certain
nitrosamino acids during the burning of a cigarette in order to determine how they
contribute to the formation of volatile nitrosamines and to the carcinogenic potential of
cigarette smoke.
Tobacco-specific nitrosamines
Nitrosation of nicotine with sodium nitrite (Figure 1) in vitro gives rise to three TSNA:
N'-nitrosonornicotine (NNN), 4-(nitrosomethylamino)-l-(3-pyridyl)-l-butanone (NNK)
and 4-(nitrosomethylamino)-4-(3-pyridyl)butanol (NNA; Hecht et al.. 1978). Although
NNA was found in neither tobacco nor tobacco smoke, its reduction product,
4-(nitrosomethylamino)-4-(3-pyridyl)-1-butanol (iso-NN AL), has been identified in dry and
moist snuff together with
the reduction
product of NNK, 4-(nitrosomethylamino)-l-(3-pyridyl)-l-butanol (NNAL; Brunnemann et al., 1987). The identi
fication of iso-NNAL led to the hypothesis that 4-(N-nitrosomethylamino)4-(3-pyridy!)butyric acid (iso-NNAC), an oxidation product of NNA, would be present in
tobacco.
We developed an analytical procedure for the determination of iso-NNAC in tobacco.
consisting of an aqueous extraction of tobacco and subsequent solvent partition with ethyl
-477-
478
K.D. Brunncmann et al.
acetate at pH 2 (nitrosamino acid fraction). pH 9 (TSNA fraction) and pH 4 (iso-NNAC
fraction). The final fractions were methylated and analysed by gas chromatography-thermal
energy analyser (GC-TEA Djordjevicera/., 1989).7hble 1 presents the levels of iso-NNAC
and other nitrosamino acids in different tobaccos. 3-(NitrosomethyIamino)propionic acid
(NMPA) and Mnitrosoproline (NPRO) were the most abundant nitrosamino acids in all
tobaccos analysed; 4-(nitrosomethyIamino)butyric acid (NMBA) was present at lower
levels, and iso-NNAC at concentrations of 0.01-0.95 ppm. The ranked order of abundance
of the nitrosamino acids in tobacco was: NPRO > NMPA > NMBA > iso-NNAC.
Figure 1. Formation of tobacco-specific A'-nitrosamines
NICOTINE
479
Nitrosamino acids in tobacco
Table 1. Contents of nitrosamino acids in different tobacco products
Product
type
Sample
Nitrosamino acids (pg/g dry weighty
_________________________________________________
NMPA
NMBA
NPRO
iso-NNAC lolal
Chewing
tobacco
KY 1S1
A
1.0
0.6
0.05
0.03
0.7
0.2-
0.03
0.02
1.8
0.8
Moist
snuff
KY 1S3
A
E
KY 1S2
A
B
4.6
3.2
11.0
13.1
1.2
4.5
0.40
0.26
0.12
1.54
0.14
0.46
6.6
4.5
15.4
3.0
8.1
0.13
0.05
0.21
0.95
0.05
0.21
11.8
10.6
15.8
31.0
4.4
13.3
KY 1R1
KY 1R4F
A
0.16
0.63
3.10
ND
ND
0.17
0.59
0.57
2.62
0.01
0.01
0.05
0.76
1.21
5.94
Dry snuff
Cigarette
tobacco
* Abbreviations: NMPA. 3-(nitrosonicthylamino)propionic acid. NMBA. 4-{nitrosomcthylaniino)butyric acid: NPRO.
N-nitrosoprolinc; ND. not detected
In order to verify the structure of iso-NNAC, we analysed the enriched pl I 4 fraction by
capillary gas chromatography-mass spectrometry (GC-MS). The compound isolated from
tobacco was confirmed as iso-NNAC. In order to study the biological activity of iso-NNAC.
we employed the rat hepatocyte primary culture/DNA repair test (Djordjevic et al., 1989;
Williams el al., 1989); in addition, iso-NNAC was bioassayed for lung adenomas in strain
A/J female mice (Rivenson et al., 1989). Iso-NNAC did not induce DNA repair in primary
rat hepatocytes and. at 200 pmol/mouse, did not increase the rate of lung adenomas.
Pyrolysis studies
Carcinogenic volatile iV-nitrosamines, such as N-nitrosodimethylamine and
A/-nitrosopyrrolidine, have been detected in tobacco and tobacco smoke. We postulated
that they may be formed by decarboxylation of nitrosamino acids occurring in tobacco. We
therefore selected NMPA, NMBA. Af-nitrososarcosine (NSAR) and NPRO and applied 5
mg of each dissolved in 50 pJ water to the tobacco column of 20 cigarettes. The cigarettes
were then smoked under standard conditions and the smoke analysed by GC-TEA
NMPA did not yield its decarboxylation product but partially formed its methyl ester
(Figure 2). This fraction was further enriched by rotary thin-layer chromatography, and
subsequent GC-MS analysis confirmed the structural identity of the methyl ester of NMPA
(Figure 3). In addition, we observed that some NMPA was carried over intact into the
mainstream smoke. Pyrolysis of NMBA on a tobacco column also resulted in formation of
the methyl ester, asconfirmed by GC-MS. NMBA was also decarboxylated and was carried
over into the smoke to some extent. NSAR was primarily decarboxylated to form
N-nitrosodimethylamine. NPRO was decarboxylated to a large extent to form
N-nitrosopyrrolidine, although some methylation and transfer into the smoke occurred.
This is the first time that pyrosynthesis of methylesters has been observed during smoking.
Interestingly, when iso-NNAC was pyrolysed on a tobacco column, it did not undergo
decarboxylation but its condensation product was formed (0.07%); 0.9% of iso-NNAC was
transferred unchanged into the mainstream smoke.
In order to study the mechanism of formation of these esters, we spiked cigarettes with
3-(N-nitrosoethylamino)propionic acid, which resulted in the formation of both the methyl
and ethyl esters at a ratio of 2:1. Additional mechanistic studies with deuterated
3-(Af-nitrosoethylamino)propionic acid are under way.
Future studies
Future studies will focus on the conditions leading to the endogenous formation of
iso-NNAC and its analysis in urine. Iso-NNAC may serve as a biomarker for measuring
exposure to TSNA and/or the extent of endogenous formation.
K.D. Brunnemann et al.
Nitrosamino acids in tobacco
Figure 2. Gas chromatography-thermal energy analyser (TEA) traces of volatile
A'-nitrosamine
reference
mixture
(top)
and
of
pyrolysis
fraction
of
3-(\-nitrosomethylamino)propionic acid (bottom)*
Figure 3. Mass spectra of the methyl ester of 3-(nitrosomethylamino)propionic acid: A,
reference; B, isolated from tobacco smoke
480
100
CH.-N-CH CH CO.CH,
B0
100 120 140 160 180 200
80
100 120 140 160 180 200
' Abbreviations: NOMA. At-nitrasodimethylaminc; NDEA. A'-nitrosodiethylamine.' NDPA. N-nitnx<xlipropylaminc;
NDBA. JV-nilrosodibutylamine; NP1P, Mnilrasopiperidinc; NPYR. N-nitn»opym>lidine; NMOR. N-nilnsomorpholine
Acknowledgement
This study was supported by Grant CA-29580 from the US National Cancer Institute.
References
Brunnemann, K.D., Gcnoblc. I_ & Hoffmann, D. (1987) Identification and analysis of a new tobacco-specific
N-nitrosamine, 4-(mcthyInitrosaminoH-(3-pyridyl)-l-bulanol. Carcinogenesis. 8, 465-469
Djordjevic, M.V., Brunnemann, K.D. & Hoffmann, D. (1989) Identification and analysis of a nicotine-derived
N-nitrosamino acid and other nitrosamino acids in tobacco. Carcinogenesis, 10. 1725-1731
Hecht. S.S., Chen, C.B., Ontaf, R.M.. Jacobs, E„ Adams. J.D. & Hoffmann, D. (1978) Reaction of nicotine
and^sodium mtntc: formation of nitrosamines and fragmentation of the pyrrolidine ring. J. Org. Chem.. 43.
Rivenson, A., Djordjevic, M.V., Amin. S. & Hoffmann. D. (1989) A study of tobacco carcinogenesis. XIIV.
Bioassay in A/J mice of some N-nitrosamines. Cancer Lett., 47, 111-114
Williams, G.M., Mori, H. & McQueen. C.A. (1989) Structure-activity relationships in the rat hepatocyte
DNA-repair test for 300 chemicals. Mutal. Res., 221. 263-286
’
Studics in tobacco carcinogenesis
483
of rooms polluted with tobacco smoke we found 7-36 pg/m3 benzene and 0.8-4.5 pg/m3
butadiene.
1.3-
Effect of catechol on the metabolism of benzo[a]pyrene
STUDIES IN TOBACCO CARCINOGENESIS
D. Hoffmann, AA. Melikian & K.D. Brunnemann
Naylor Dana Institute for Disease Prevention,
American Health Foundation. Valhalla, NY, USA
The vapour phase of freshly generated cigarette mainstream smoke, of sidestream smoke
and of environmental tobacco smoke was analysed for such tumorigenic agents as benzene,
U-butadicne and acrolein with a newly developed, highly sensitive gas chroma
tography-mass selective detection method. The major carcinogen in tobacco smoke,
catechol, was studied in regard to its specific action on the metabolism of bcnzo[a]pyrene in
mouse lung and mouse skin. The major tobacco-specific carcinogens in tobacco and its
smoke are the nicotine-derived A'-nitrosaniines, A'-nitrosonornicolinc and 4-(nitrosomelhylamino)-l-(3-pyridyl)-l-butanone. A third nitrosamine that can be formed in vitro by
nitrosation of nicotine is l-(nitrosomethylamino)-l-(3-pyridyl)butylaldehydc. This alde
hyde is not present in tobacco products, but its noncarcinpgenic oxidation product,
4-(nitrosomethylamino)-l-(3-pyridyl)bulyric acid, was found in tobacco and can be formed
from the major nicotine metabolite, cotinine. It is also likely that this acid can be formed by
endogenous reactions.
The objective of our studies in tobacco carcinogenesis lies in the elucidation of
mechanisms of carcinogenesis and the determination of bioactive constituents in tobacco
and tobacco smoke. This paper describes some of the chemical-analytical, biochemical and
biological evaluations in progress.
Analysis of the vapour phase of tobacco smoke
fhe vapour phase of cigarette mainstream smoke and of sidestream smoke contains
known tumorigenic agents (IARC. 1986). An analytical procedure was developed for the
determination of selected gas-phase components in unaged smoke, utilizing cryofocusing
capillary gas chromatography and mass selective detection. The latter was used in the
selective ion monitoring mode, allowing us to scan for three selective ions, typical for each
compound, during specific ‘time windows'. Mainstream smoke was analysed via a ten-port
gas sampling valve on a puff-by-puff basis. The concentrations of benzene and
butadiene
1,3increased only slightly with progressive numbers of puffs, except for
cigarettes with charcoal-containing filter tips when volatiles that have been selectively
retained in the filler from early puffs are released into the mainstream of later puffs. The
mainstream smoke of one cigarette contains 6-73 pg benzene, 5-88 pg toluene, 16-70 pg
butadiene.
1,390-1060 pg isoprene and 8-260 pg acrolein. The sidestream smoke of one
cigarette contains 350-650 pg benzene and 200-360 pg 1.3-butadiene. In the ambient air
-482-
Bioassays have revealed that catechol (1.2-dihydroxybenzene), a major phenolic
constituent of tobacco smoke, is a potent carcinogen and a weak co-initiator with
benzo|a]pyrene (BP). The mechanism underlying these biological phenomena is not
known. In vivo, catechol alters the penetration of BP into mouse skin as well as its
metabolism. Specifically, catechol suppresses secondary steps in the metabolism of BP.
namely epoxidation of 7,8-dihydroxy-7,8-dihydro-BP (BP-7,8-diol) to 7,8-dihydroxy9.10-epoxy-7,8,9,10-tetrahydro-BPs (BPDEs). Co-application of catechol with BP or with
BP-7.8-diol also decreases the speed with which the hydrocarbons penetrate skin. When
applied to mouse skin with the racemic BP-7,8-diol, catechol is as potent a cocarcinogen
as it is with BP itself. However, we found differences in the effects of catechol on the extent
of metabolic activation of racemic and enantiomeric BP-7,8-diols and also with regard to
DNA binding. Catechol suppresses epoxidation of the moderately carcinogenic
(+ )-BP-7,8-diol to a greater extent than that of the more active (-) enantiomer. In the
presence of catechol, less of the major adduct is formed between metabolites of the
( + )-BP-7,8-diol and DN A. while the presence of the phenolic compound has no significant
impact on formation of the major DNA adduct derived from the (-) enantiomer.
Consequently, catechol affects the proportion of major adducts derived from ( + )- and
(-)-BP-7,8-diols in mouse skin.
Tobacco-specific N-nitrosamines
N-Nitrosation of nicotine in vitro leads to three tobacco-specific N-nitrosamines.
A''-nitrosonornicotine (NNN), 4-(nitrosomethylamino)-l-(3-pyridyl)-l-butanone (NNK)
and 4-(nitrosomethy!amino)-4-(3-pyridyl)butylaIdehyde (NNA; Figure 1). While tobacco
and tobacco smoke contain significant amounts of the highly carcinogenic NNN and NNK.
NNA has not been identified in any tobacco product. However, both the reduction product
of NNA, 4-(nitrosomethylamino)-l-(3-pyridyl)-l-butanol (iso-NNAL; 66-2500 ng/g) and
the oxidation product of NNA, 4-(nitrosomethylamino)-4-(3-pyridyl)butyric acid
(iso-NNAC; 10-950 ng/g) have been identified in processed tobacco. This acid is not
genotoxic, nor does it induce tumours in mice. Iso-NNAC is also formed in vitro from the
major nicotine metabolite, cotinine. Biochemical studies in progress indicate that
iso-NNAC may also be formed in vivo after N-nitrosation of cotinine and cotinine acid.
Acknowledgement
Our studies in tobacco carcinogenesis are supported by grants No. CA-29580 and
CA-43910 from the US National Cancer Institute.
Reference
I ARC (1986) IARC Monographs on the Evaluation ofthe Carcinogenic Risk of Chemicals to Humans, Vol. 38, Tobacco
Smoking Lyon
D. Hoffmann et al.
Figure 1. A-Nitrosation products of nicotine0
Relevance to Human Cancer of N-Nitroso Compounds,
Tobacco Smoke and Mycotoxins.
Ed. I.K. O’Neill, J. Chen and H. Bartsch
Lyon, International Agency for Research on Cancer
© IARC, 1991
CARCINOGENIC SUBSTANCES IN SOVIET TOBACCO PRODUCTS
D.G. Zaridze', R.D. Safaev', G-A. Belitsky',
K.D. Brunnemann2 & D. Hoffmann2
'Department of Epidemiology and Prevention. All-Union Cancer
Research Centre, the USSR Academy of Medical Sciences.
Moscow, USSR; and ^Naylor Dana Institute for Disease Prevention.
American Health Foundation, Valhalla, NY. USA
' NNN. N -nitrosonomicotine: NNA, 4-{ni(rosomelhylamin<>y4-(3-pynUyl)butylaldchy<Jc; NNK. 4-(nilrosomclhylaminoVl^S-pyridylV 1-bulanonc; NNAC. Hnitrosomclhylamiru>)-^3-pyridyl)-butyric acid: NNAI, 4-(nitro«>incthy|.
amino>l<3-pyridyl>-l-butanol
Chemical carcinogens were determined in mainstream smoke from nonfilter cigarettes
produced and consumed in the USSR and in nass, a mixture of tobacco, lime, ash and cotton
oil. Cigarettes contained high levels of tar (23-25 mg/cigarette) and nicotine (1.5-1.9
mg/cigarette) and, generally, a high content of polycyclic aromatic hydrocarbons, which are
major epithelial carcinogens, A-nitrosuinines, which are organ-specific carcinogens, and
some carcinogenic metals, such as arsenic and chromium. Nass contained the
tobacco-specific A-nitroso compounds, A'-nitrusonurnicotine, A'-nitrosoanatabine,
A'-nitrosoanabasine and 4-(A-nitrosomethylamino)-l-(3-pyridyl)-l-butaii<>ne, as well as
volatile A-nitrosamines, but at levels lower than in other types of chewing tobacco and
snuff. The low levels in nass are due to the short ageing process used, in contrast to
commercially produced chewing tobacco and fine-cut snuff, which are highly processed
products requiring long ageing and fermentation.
In the USSR, the proportion of filter cigarettes smoked increased from 0.3% in 196.3 to
21.3% in 1982; however, 90% of the cigarettes consumed in this country fall within the
category of ‘high-tar’ cigarettes (Zaridze et al.. 1986a). In some areas of the USSR.
particularly in the central Asian republics, a smokeless tobacco product, nass. is widely used.
Use of nass has been associated with a high incidence of oral cancer and a high prevalence
of leukoplakia (Zaridze el al., 1986b).
Carcinogens in cigarette smoke
TXvo types of nonfilter cigarettes were smoked according to ISO requirements
(International Standards Organization. 1986) in a 20-port smoking machine (Borgwald).
The concentration of polycyclic aromatic hydrocarbons was determined by
spectroluminescence (Khesina et al., 1983), metals by atomic emission spectroscopy
(Westcott & Spincer, 1974; Jenkins, 1986). and carcinogenic nitrosamines by gas
chromatography-thermal energy analysis (Brunnemann et al., 1977; Adams et al., 1983).
The cigarettes contained high levels of tar (23-25 mg/cigarette) and nicotine (1.5-1.9
mg/cigarette), and the smoke contained very high concentrations of some carcinogenic
polycyclic aromatic hydrocarbons (Thble 1). The concentrations of metals in Soviet
-485-
grievance to Human Cancer of //-Nitroso Compounds.
Tobacco Smoke and Mycotoxins.
Ed IK. O'Neill, J. Chen and H. Bartsch
[.von. International Agency for Research on Cancer
C IARC. 1991
TOBACCO-SPECIFIC NITROSAMINES IN COMMERCIAL
CIGARETTES: POSSIBILITIES FOR REDUCING EXPOSURE
S. Fischer, B. Spiegelhalder & R. Preussmann
Institute of Toxicology and Chemotherapy, German Cancer
Research Center, Heidelberg, Germany
Tobacco-specific nitrosamines (TSNA) are powerful carcinogens found in tobacco and
tobacco smoke in relatively high concentrations. Tar delivery, which is generally accepted
as an index for the carcinogenic potential of cigarette smoke, must be declared in most
European countries. In this investigation of more than 170 types of commercial cigarettes
from several European countries and the USA, no correlation was observed between tar
delivery and mainstream smoke concentration of A'-nitrosonomicotine (NNN) and
4-(A'-nitrosomethylamino)-l-(3-pyridyl)-l-butanone (NNK). Therefore, although crucial,
tar delivery alone is not a sufficient index for the carcinogenic potential of cigarette smoke.
It is proposed that TSNA concentrations be determined for characterization of the
carcinogenic potential of cigarettes with low and ultra-low tar yields and that these be
declared by an additional and adequate parameter. The mainstream smoke concentrations
of NNN and NNK are given by the amounts of preformed compounds in tobacco, which is
dependent on the nitrate content of the tobacco and the tobacco type. A further important
determinant of the exposure of smokers to TSNA is the total volume drawn through a
cigarette while smoking, which is dependent on puff volume and puff frequency and which
directly influences TSNA transfer. Smokers inhale higher volumes when smoking
low-nicotine cigarettes, so that low NNN:nicotine and NNK:nicotine ratios result in
decreased exposure to TSNA. Reduction of exposure to TSNA can be achieved by selecting
tobaccos with low levels of preformed TSNA (low nitrate content, small amounts of burley
tobaccos and stems) and by manufacturing cigarettes with low NNNmicotine and
NNK:nicotine ratios.
Tobacco-specific nitrosamines (TSNA), which are powerful carcinogens, have been
found in tobacco and tobacco smoke in relatively high concentrations (Hoffmann & Hecht,
1985). In order to reduce smokers’ exposure to TSNA, we have investigated the main factors
that influence their concentrations in mainstream smoke. Since tar delivery is generally
accepted as an index of the carcinogenic potential of cigarette smoke, and must be declared
in most European countries, this measure was compared with the amounts of TSNA, and
especially N'-mtrosonornicotine (NNN) and 4-(N-nitrosomethylamino)-l-(3-pyridyl)1-butanone (NNK), in cigarettes.
More than 170 types of commercial cigarettes from Austria, Belgium, Germany, France,
Italy, Poland, Switzerland, the United Kingdom, the USA and the USSR were analysed for
-489-
1
490
S. Fischer et al.
TSNA in tobacco and in mainstream smoke as well as for nitrate in tobacco, by the methods
of Spiegelhalder et al. (1989) and Fischer and Spiegelhalder (1989). The declared values
of tar and nicotine were used. The results are presented in Thble 1.
Thr delivery, which is widely considered to reflect the carcinogenic potential of cigarette
smoke, did not correlate with the amounts of the strong carcinogens NNN and NNK in
mainstream smoke (NNN: r2 = 0.18; NNK: r2 = 0.14). Furthermore, there was no
correlation between nicotine andTSNAdeliveries(NNN:r2 = 0.13: NNK: r2 = 0.10).Thus,
the concentration of TSNA should also-be determined and declared by an additional and
adequate parameter (Fischer et al., 1989a).
The mainstream smoke concentrations of NNN and NNK strongly depend on tlje
amounts of preformed NNN and NNK in tobacco (Fischer et a/., 1989b). We saw a constant
ratio between the two concentrations, which was not dependent on the level of nitrate in
tobacco, except for NNK in nitrate-rich, dark tobacco cigarettes, nor on the nicotine level.
Spiking the cigarettes with the nitrosamine precursors nicotine (at 10 mg/cigarette) and
nitrate (at 4-20 mg/cigarette) prior to smoking did not significantly change the mainstream
smoke concentrations of NNN and NNK (Fischer et al.. 1989b). These data indicate that
NNN is not formed during smoking, and synthesis of NNK is very unlikely, at least for
tobaccos with low nitrate levels. Thus, the NNN and NNK found in mainstream smoke is
derived from preformed nitrosamines in the tobacco (Fischer er a/., 1989b).
The amount of preformed TSNA in tobacco is determined mainly by the nitrate level
in the tobacco (Fischer et al., 1989c), and this depends on the tobacco type, especially for
NNK. The lowest TSNA concentrations were observed in oriental-type cigarettes, which
contain little nitrate. In low-nitrate, Virginia-type cigarettes, the TSNA concentrations were
also low, but NNK was present at the same or much higher concentrations than NNN.
whereas in other cigarettes NNN levels exceeded NNK levels. The highest TSNA
concentrations were found in cigarettes made of dark tobaccos, which are high in nitrate.
In blended cigarettes, both high and lowTSNA concentrations were found, correlating with
the nitrate level of the tobacco composition.
A further important determinant of TSNA concentration in mainstream smoke is the
total volume drawn through a cigarette while smoking, which is dependent on the puff
volume and the puff frequency and which directly influences TSNA transfer (Fig. 1: Fischer
et al., 1989d). Since the smoker’s interest is to maintain an adequate nicotine intake.
smokers inhale higher volumes from low-nicotine cigarettes, resulting in higher intakes ol
TSNA and tar in relation to standard smoking conditions. Thus, with low ratios of
NNNmicotine and NNKmicotine, the smoker’s exposure to TSNA is decreased.
A reduction in the exposure of smokers to TSNA could be achieved by selecting
cigarettes made of tobaccos with low concentrations of preformed TSNA, i.e., those with
a low nitrate content, and containing little burley tobaccos and stems, and by manufacturing
cigarettes with low ratios of NNNmicotine and NNK:nicotine.
Tobacco-specific nitrosamines in cigarettes
491
Figure 1. Dependence of concentration of W'-nitrosonornicotinc (NNN;O) and
4-(A-nitrosomcthylamino)-l-(3-pyridvl)-l-butanone (NNK, ®) in mainstream smoke on the
total volume drawn through a low-tar, blended filter cigarette
. ,aacc to Human Cancer of //-Nitroso Compounds.
Smoke and Mycotoxins.
1 I X O'Neill, J. Chen and H. Bartsch
!
International Agency for Research on Cancer
/[a’rC. 1991
OCCURRENCE OF AND EXPOSURE TO //-NITROSO
COMPOUNDS IN TOBACCO
A.R. Tricker & R. Preusstnann
Institute of Toxicology and Chemotherapy, German Cancer
Research Center, Heidelberg, Federal Republic of Germany
The concentrations of 21 A-nitroso compounds in smokeless tobaccos are presented.
Inbacco-specific nitrosamines accounted for 70-90% of the total identified A-nitroso
compounds. Daily exposure of smokeless tobacco users to preformed A-nitroso compounds
?00
400
600
800
1000
Fischer. S. & Spicgclhaldcr. B. (1989) Improved method for the determination of tolxicco-spccific nitrosamines
tn tobacco smoke. Hear Tubukforsch.. 14. 145-153
Fischer. S.. .Spicgclhaldcr. B. A: Prcussrnann. R. (1989a) liibacco-specific nitrosamines in West German
cigarettes - tar alone is not a sufficient index for the carcinogenic potential of cigarette smoke.
Carcinogenesis. 14. 169-I73
Fischer. S.. Snu-fHh .M.T l< a- i................... •»
’
................... .
OI looacco-spccitic
n smoke of cigarettes. Cun mo^nrsis (submitted for publication)
k Prcussrnann. R. (1989c) Preformed tobacco-specific nitrosamines in tolxicco
nee of tobacco Ivor. (‘tin-innwnr»e in isi i.kii
tobacco-specific nitrosamines in cigarette smoke
10. 1059- l(k><>
I loffmann. I). & I lecht. S.S. (1985) Nicotine derived Mnitrosamincsand tobacco related cancer: current status
and future directions. Cancer lbs., 45. 935-944
Spicgclhaldcr. B., Kubacki. SJ. & Fischer. S. (1989) A method for the determination of tobacco-specific
nitrosamines. nitrate and nitrite in tobacco leaves and processed tobacco. Hcitr. Tabukforsch . 14, 135-144
may exceed 200 pg/day in certain populations.
We have identified 21 volatile, nonvolatile and tobacco-specific A-nitrosamines(TSNA)
in smokeless tobacco products available commercially in 1987-88 (Tricker & Preussmann.
1088. 1989). Selected representative data are presented in Table 1. Currently.
.V-nitrosodimethylamine. A-nitrosoethylmethylamine, A-nitrosopiperidine and A-nitrosopyrrolidine are the most commonly found volatile nitrosamines; traces of
V-nilrosodipropylamine and A-nitrosodibutylamine are present in heavily cured and/or
tcimented tobacco products. Trace levels of A-nitrosomorpholine are still found in some
l iK and Swedish oral tobacco products packed in waxed containers. The most commonly
found nonvolatile A-nitrosamino acids and their derivatives are A-nitrosoproline.
V-nitrosopipecolic acid, A-nitrosohydroxyproline, A-nitrososarcosine, 3-(A-nitroso-Amethylamino)propionic acid and 4-(A-nitroso-A-methylamino)butyric acid. Some heavily
cured/fermented tobaccos, in particular zarda and some American moist snuffs (data not
presented), were found to contain A-nitrosoazetidine 4-carboxylic acid (<200 pg/kg) and
A-nitrosothiazolidine 4-carboxylic acid (< 280 pg/kg). The presence of other nonvolatile
A-nitrosamines, amenable to gas chromatography-thermal energy analysis only after
methylation or silylation, were also found. TSNA are by far the most abundant A-nitroso
compounds present in tobacco and usually account for 70-90% of the total.
•t-(A-Nitrosomethylamino)-4-(3-pyridyl)-l-butanol (<8100 pg/kg) has been detected in
about 60% of all tobacco samples analysed (n = > 120), including various forms of smoking
tobacco, indicating far greater exposure to this compound than previously reported (Hecht
& Hoffmann. 1988).
In order to make a rough estimate of potential exposure to carcinogenic A-nitroso
compounds, and in particular to 4-(A-nitrosomethylamino)-l-(3-pyridyl)-l-butanoI and
A'-nitrosonornicotine during use of smokeless tobacco, mean daily exposure to the
identified A-nitroso compounds was estimated by multiplying the concentrations of
individual compounds by the average amount of tobacco consumed by the tobacco-using
population (Thble 2). This method of calculating exposure is based on the assumption that
-493-
494
A.R. Tricker& R. Preussmann
N-Nitroso compounds in tobacco
100% of TSNA are extracted from saliva. Osterdahl and Slorach (1988) have shown that
this is not true in Swedish snuff dippers, whose saliva contains higher levels of TSNA than
can be accounted for by levels of preformed nitrosamines in tobacco. Thus, endogenous
formation of TSNA in saliva (Osterdahl & Slorach. 1988) and under simulated gastric
conditions (TYicker et al.. 1988) probably results in higher exposure to TSNA than indicated
in Thble 2.
Feasibility of a prospective study of smoking
Relevance lo Human Cancer o( X-Nitro»o Compounds,
Tobacco Smoke and Mycotoxins.
Ed. I.K. O’Neill. J. Chen and H. Bartsch
Lyon. International Agency for Research on Cancer
© IARC. 1991
Table 1. TYends in manufactured cigarette sales in Qidong
FEASIBILITY OF A PROSPECTIVE STUDY OF SMOKING
AND MORTALITY IN QIDONG, CHINA
Year
Total sales of
manufactured
cigarettes (millions)
Annual sales
per person
Daily sales
per person
jU49
W50
|951
97
195
243
304
338
359
376
463
392
382
381
378
153
76
195
361
611
342
388
425
607
638
656
631
664
599
747
730
708
721
680
688
778
729
1009
920
1092
1294
160
314
382
466
492
508
528
615
509
493
480
475
191
90
224
405
668
365
407
437
608
627
637
608
634
566
700
678
654
661
621
627
706
656
905
822
973
1150
0.44
0.86
1.05
1.28
1.35
1.39
1.45
1.69
1.40
1.35
1.32
1.30
0.52
0.25
0.61
J.G. Chen’, R. Peto*, Z.T. Sun” & Y.R. Zhu’
'Qidong Liver Cancer Institute. Jiangsu, China;2 ICRF Cancer Studies Unit,
University of Oxford, UK: and 'Cancer Institute, Chinese Academy
of Medical Science, Beijing. China
Qidong is a rural county in eastern China with particularly good facilities for
epidemiological research: cigarette use by adult males is widespread (70% now smoke),
male lung cancer rates already appear to be rising, the population is stable and well served
by a county-wide network of health care facilities, and systematic county-wide registration
of all deaths has existed since the mid-1970s, causes currently being assigned according to
the 9th International Classification of Diseases.
1b help assess the feasibility of a prospective study of smoking and tobacco-related
disease in rural China, we describe the current prevalence of smoking, the history of
tobacco use. the age-specific mortality rates from lung cancer and the overall mortality rates
from various broad groups of disease in one particular county, Qidong. Qidong is a
low-lying, densely populated agricultural county located at the mouth of the Yangtze River,
in Jiangsu province, just north of Shanghai municipality. There is little turnover of
population: almost all the adults were born in the county and will probably continue living
there. A central registry, with age. sex and ICD coding of the causes of all deaths in Qidong,
is maintained by the Qidong I aver Cancer Institute. Direct information on tobacco
consumption before 1949 is not available, although retrospective questioning of old people
about their previous habits has been attempted. Since 1959, manufactured cigarette sales
to the county as a whole have been recorded. The Qidong Statistics Bureau reported that
the population of Qidong has about doubled, from 620 000 in 1950 to 1 130 000 in 1986;
and that annual cigarette sales in 195(1, 1960, 1970 and 1986 were 195, 378. 638 and 1294
million pieces, respectively (Table 1). The mean daily sales of manufactured cigarettes per
person reached 3.15 in 1986, as against only 0.86 in 1950. Almost all of the cigarettes are
consumed by men, so although no exactly representative survey of age- and sex-specific
smoking habits is available, the consumption per adult male is probably well over 10/man
per day.
All causes of death coded in ICD9 for 1987
A population-based registry system of all causes of death has been established in Qidong
since 1974, although registration may have been seriously incomplete in the mid-1970s. In
-502-
503
1087. the causes were classified according to the 9th International Classification of Diseases
(It’D 9). as recommended by the Health Ministry of China. The leading causes of death
m Qidong in 1987 are given in Table 2. In classifying causes of death, particular attention
is given to cancers, most of which are diagnosed at the county hospital, which is adjacent
to the Qidong Liver Cancer Institute that houses the death registry.
<
p)$K1‘Xil)
1(X»2
l*Xi7
i’M
1970
1971
1972
1973
1974
1975
1976
1977
1978
1979
1980
1981
1982
1983
1984
1985
1986
1.83
1.00
1.11
1.20
1.67
1.72
1.74
1.67
1.74
1.55
1.92
1.86
1.79
1.81
1.70
1.72
1.93
1.80
2.48
2.25
2.67
3.15
504
J.G. Chen et al.
Feasibility of a prospective study of smoking
Table 2. Causes of death in 1987 in Qidong county, China, as recorded by the Qidong Live,
Cancer Institute registry
Cause of death
9th ICD category
Age
>.70
M
Oil: Pulmonary tuberculosis
Rest of 001-138 (infectious and parasitic
diseases
ISO: Cancer of oesophagus
151: Cancer of stomach
155: Cancer of liver
162: Cancer of lung
Rest of 140-230-4 (malignant neoplasms)
430-438: Stroke
410-414: Ischaemic heart disease
Rest of 390-439 (vascular diseases)
466, 490-3, 496: Bronchitis, emphysema.
asthma
Rest of 460-519 (other respiratory
diseases)
571: Cirrhosis
Rest of 520-579 (other digestive diseases)
Rest of 001-799 (other medical causes)
800-999: External causes
All causes
(Rate per 100 000)
7
—
13
138
192
538
(147)
45
2
12
93
109
352
(97)
230
8
156
48
66
100
1620
(943)
12
42
16
9
2
1
2
8
1
1
3
5
13
36
103
28
65
59
319
89
101
18
21
45
13
36
92
417
110
131
92
642
523
10
72
36
77
54
886
(501)
44
61
47
37
77
88
198
302
47
62
1910 1972
(9338) (6036)
Age-specific mortality from lung cancer
During ,1972-86. a total of 2572 deaths were attributed to lung cancer (although there
is inevitably some under-registration, and, conversely, there is some possibility of confusion
between primary and secondary disease, since many cases were diagnosed only by radiology
and symptoms). During this period, the crude mortality rate attributed to lung cancer was
16/100 000 (22/100 000 males and 10/100 000 females).
The age-specific lung cancer mortality rates recorded in 1972-86 among females r'o not
appear to be increasing. The age-specific rates for males were already higher than those
for females in 1972-74, and the male rates increased significantly between 1972-74 and
1984-86.
Prevalence of smoking among male adults
A sampling survey on smoking prevalence was completed in 1987 among male peasants
aged over 30 years: 70% are current smokers, 5% being heavy smokers (over 23 pieces/day)
and 32% being light smokers (1-7 pieces/day); 69% of current and ex-smokers started to
smoke before 24 years of age, the median age of starting being 22.
505
Manufactured cigarettes are the main type of tobacco used in Qidong. In 1987, the
prevalence of cigarette smoking was 69% among adult males, while that of water-pipe
smoking was 11%. Most water-pipe smokers, however, also smoke cigarettes.
Table 3, which is based only on retrospective recall of previous habits by adult males in
1987, suggests that the prevalence of smoking may have approximately doubled over the
past few decades, but the limitations of such retrospective enquiries are obvious.
Tktble 3. Retrospective estimation of the prevalence of smoking in different periods in
Qidong county, China
Year
1987
1976
1966
1958
1949
(1939)
No. then smoking
No. of males
interviewed at age
over 15 years a
Cigarette
Water pipe
694s
694<■
566
426
293
(161)
476 (69%)
447 (64%)
420 (74%)
245 (58%)
154 (53%)
(50) (31%)
74
69
63
40
(4)
Pipe
6
(1)
* Intimated from thoac aged over 30 years at present
* Over age 30 in 1987
* Over age 19 in 1976 (and hence over Hgc 30 in 1987)
Potential epidemiological enquiries
It has been estimated (Peto, 1987) that current Chinese smoking habits may eventually
cause a total of about two million deaths a year from various neoplastic, vascular and
respiratory diseases during the second quarter of the next century. This study indicates that
lung cancer is already a common cause of death in Qidong (Table 2). and there has recently
been a substantial further increase in cigarette consumption (Table 1). Male lung cancer
death rates are increasing, and, even though liver cancer is particularly common in Qidong,
lung cancer may eventually overtake it as a cause of death.
Qidong is in many ways a particularly suitable area for prospective, or other, field
research on smoking and disease in rural China: (i) a county-wide network of health care
has been in place since the early 1970s, and information on all causes of death is now
collected routinely (Chen. 1987); (ii) these causes are already registered in such a way they
could routinely be linked with personal identifiers; and (iii) there is a high prevalence of
smoking, particularly of cigarettes. Qidong is, moreover, one of the 65 Chinese counties
fo which diet, life style and mortality rates were described extensively in a recent monograph
(Chen et al., 1990), and comparison of the characteristics of Qidong with those of other
counties may be of further assistance in planning epidemiological studies.
Acknowledgement
This work was supported by National Natural Science Foundation of China.
References
Chen, J.G. (1987) Experience with the method of classifying death-causes that has been used in Qidong for
the past 12 years (in Chinese). Chin. J. Health Stat. 4. 52-54
528
U.J. Nair et aL
c ^fTeCt °f ?ietary vi,amin A s,atus on urinarr excretion of mutagens detected in the
Ames Salmonella/microsome assay after metabolic activation
otrain
Treatment0
TA98
(SR - 30)
None
DMSO
TE
None
DMSO
NNN
TA100
(SR - 100)
No. of rcvertants/plalc*
Vitamin A-sufficient
Vitamin A-dcficicnt
32±1
32 ± 1
39 ± 6
137 ± 8
>34 ±15
146 ± 14
28 ± 4
.
64 ± 4
165 ± 11 *
122 ± 7
120 ±2
459 ± 16*
' DMSO. dimethyl sulfoxide; TE. tobacco extract; NNN. N’-nitnsonomicotine
2^x8108Pcelk/ml>m *W°
CXPCr*mcnls’s^0013000*15
Relevance to Hunwn Cancer of N-Nitroso Compounds.
Tobacco Smoke and Mycotoxins.
£d. I.K< 0‘NclllJj- Chen and H. Bartsch
Lyon. Inlcrnalionil Agency for Research on Cancer
OIARC. 1991
INHIBITION OF TOBACCO-SPECIFIC NITROSAMINE
d-(/V-NITROSOMETHYLAMINO)-l-(3-PYRIDYL)-l-
were not subtracted; viab
‘ p < 0.005 as compared to DMSO controls
References (contd)
Hu, M.W., Bondinell, W.E. & Hoffmann, D. (1974) Chemical studies on tobacco smoke. XXIII. Synthesis ol
carbon-14 labelled myosmine, nomicotinc and N’-nitrosonomicotinc. J Labelled Conipd Rudiopharm.. 10.
79-88
Lowry. O.H., Rosebrough, RJ., Farr, A.L. & Randall, RJ. (1951) Protein mesurement with a folin phenol
reagent. J. Biol. Chem., 193, 265-275
Maron, M.S., De Pierc, J.W. & Manncrwich, B. (1979) Levels of glutathione, glutathione reductase and
glutathionc-S-transfcrasc activities in rat lung and liver. Biochem. Biophys. Acta, 582, 67-78
Nceld, J.B., Jr & Pearson, W.N. (1963) Macro- and micromethods for the determination of serum vitamin /X
using trifluoroacctic acid. J. Nutr, 79, 454-462
Omura, J. & Salo, R. (1964) The carbon monoxide binding pigment of liver microsomes. I. Evidence for its
hemoprotcin nature. J. Biol. Chem., 239, 2370-2378
Santhanam, U.» Nair, UJ. & Bhide, S.V. (1988) Effect of vitamin A deficiency on induction of enzymes
metabolizing different carcinogens. Indian J. Exp. Biol., 26, 337-340
Yamasaki, E. & Ames, B.N. (1977) Concentration of mutagens from urine by adsorption with the nonpolar
resin XAD-2: cigarette smokers have mutagenic urine. Proc. Nail Acad. Sci. USA, 74. 3555-3559
BUTANONE (NNK) TUMORIGENESIS WITH AROMATIC
ISOTHIOCYANATES
M.A. Morse, K.I. Eklind, S.S. Hecht & EL. Chung’
Section of Nucleic Acid Chemistry. Division of Chemical
Carcinogenesis, American Health I'oundation. Valhalla. NY. USA
4-(/V-Nitro|omcthylaniino)-l-(3-pyridy!)-l-butanone (NNK) is a potent tobacco-specific
carcinogenic nitrosamine. At low doses, it induces primarily lung tumours in mice,
hamsters and rats, regardless of the route of administration. Its unique organ specificity
and potency suggest its possible role in the high incidence of lung cancer in smokers. The
goal of this sludy was to find agents that would potentially prevent NNK tumorigenesis.
Previous results led us to test phenethyl isothiocyanate (PEITC) on NNK tumorigenesis in
a two-year bipassay in Fischer 344 rats. The NNK-treated group developed 80% lung
tumour incidence, whereas NNK-treated rats fed PEITC diets had only 40% lung tumour
incidence. Incidences in other organs were not affected by this treatment. We also tested
PEITC in a Ifrwcek, short-term bioassay against NNK-induced lung adenomas in A/J mice.
Pretreutmentpf mice with PEITC by gavage at four daily doses of 5 pmol or 25 pmol reduced
the formation,of NNK-induced lung adenomas by 70% or 100%, respectively. Interestingly,
benzyl isothiocyanate and phenyl isothiocyanate, the lower homologues of PEITC, were
Inactive in this bioassay. Using a protocol similar to that used in the bioassays, PEITC was
shown Io decrease DNA methylation by NNK in the lungs of rats and mice and suppress
the metabolism of NNK by mouse lung microsomes. These results are consistent with the
previous data, suggesting that the inhibition of NNK-induced lung tumour formation by
PEITC is a consequence of reduced DNA methylation caused by inhibition of NNK
metabolism. As an extension of the structure-activity study, we also tested phenylpropyl and
phenylbutyl bothiocyanate in the A/J mouse bioassay. These isothiocyanates were
remarkably potent inhibitors of NNK-induced lung adenoma: at doses of 5 pmol, they
completely inhibited lung adenoma formation caused by NNK treatment These results
provide a basjs for future chemoprevention studies on lung cancer induction associated
with exposure: to NNK in tobacco smoke.
■To whom correspondence should be addressed
-529-
%
4-(A,-Nitrosomethylamino)-l-(3-pyridyl)-l-butanone (NNK; Figure 1) is the most potent
carcinogenic N-nitrosamine so far found in tobacco and tobacco smoke (Hecht &
Hoffmann, 1988). The organ-specific effect of NNK in the induction of lung tumours in all
species tested indicates its possible role in the development of lung cancer among smokers
(IARC, 1985). Therefore, it would be of great importance to find compounds, either
synthetic or dietary-related, that can counteract the carcinogenic action of NNK.
Our previous studies demonstrated that pretreatment of rats with a diet containing «
phenyl isothiocyanate (PITC), benzyl isothiocyanate (BITC) or phenethyl isothiocyanate .4)
(PEITC; Figure 1) resulted in reduced metabolic demethylation of NNK in hepatic ®
microsomes as well as a decrease in hepatic DN A methylation by NNK (Chung eta/., 1985), l-Vf
suggesting that these aromatic isothiocyanates can potentially inhibit NNK carcinogenesis, -!y
In this study, we examined the effects of PEITC on NNK tumorigenesis in Fischer 344 rats //•
and of PITC, BITC and PEITC on NNK tumorigenesis in A/J mice. We compared these . .?■
results to their effects on NNK-induced DNA methylation in liver, lung and nasal cavity of
rats and in lung of mice, all target tissues of NNK tumorigenesis. In a separate bioassay,
we also evaluated phenylpropyl- and phenylbutylisothiocyanates (PPITC and PBITC),
higher homologues of PEITC, and oxopyridylbutylisothiocyanate (OPBITC). an
isothiocyanate related to NNK. for their effects on NNK tumorigenesis in A/J mice. Both
PBITC and OPBITC are newly synthesized arylalkyl isothiocyanates.
Figure 1. Structures of isothiocyanates and of 4-(/V-nitrosomethylamino)-l-(3-pyridyl)-l-butanone (NNK)“
^\^CH,CH,CH,CH?N-C-S
0
PBITC
/\.CH2N.C.S
-X
0
11
/x^CCH,CH,CHjN.C.S
&OPBITC
^zXx^CHjCHjN.C-S
lQT
PBITC
0
II
X'-'S^CCH,CH,CH,NCHJ
.-7
n-0
/X^CHjCH.CHjN.C-S
(qt
PPITC
• Abbnviations PITC. phenyl isothiocyanate; BITC. benzyl isothiocyanate; PEITC. phenethyl isothiocyanate. PPITC.
phenylpropyl isothiocyanate. PBITC. phenylbutyl isothiocyanate; OPBITC, oxopyndylbulylisothiocyanatc
Table 1 shows the tumour incidences in lung, liver and nasal cavity of Fischer 344 rats
after treatment with NNK. NNK plus PEITC or PEITC. The tumour incidences induced
by NNK alone were within the range expected on the basis of the results of previous
bioassays. Only 43% of rats fed a diet containing PEITC before and during NNK treatment
developed lung tumours, whereas 80% did so in the group fed the control diet. The PEITC
diet did not alter the incidences of tumours in the liver or nasal cavity induced by NNK.
,;3g
Inhibition of NNK tumorigenesis
Table 1. Incidences of lung, liver and nasal cavity tumours after treatment with NNK, N N K plus PEITC or PEITC'
M.A. Morse et al.
530
531
-Si
Inhibition of NNK tumorigenesis
monary adenomas, with a multiplicity of 10.7 tumours/mouse in only 16 weeks. The 5-pmol
daily dose (20 pmol total) of PEITC did not significantly reduce the proportion of mice that
developed pulmonary adenomas, but resulted in an approximately 70% reduction in
tumour multiplicity. The 25-jtmol daily dose (100 jimol total) of PEITC resulted in a 70%
reduction in the percentage of mice that developed tumours and nearly complete inhibition
of tumour multiplicity. However, pretreatment with BITC or PITC at 5 jimol/day resulted
in no significant change in the percentage of mice that developed tumours or in tumour
multiplicity. Both BITC and PITC proved too toxic to be tested at a daily dose of 25 jimol.
The effects of these isothiocyanates on NNK-induced O6-methylguanine (O6-MeG) in
A/J mouse lung DNA were also investigated. The same dosing regimen as employed in the
pulmonary adenoma assays was used. Six hours after NNK administration, the 5-jimol daily
dose of PEITC had resulted in an 87% reduction in (96-MeG levels, while the25-pmol daily
dose gave undetectable levels. Neither BITC nor PITC pretreatment resulted in a
significant reduction in 05-McG levels. The effects of the isothiocyanates on NNK-induced
06-MeG formation are thus in good agreement with their effects on NNK lung
Table 2. DNA methylation in rats treated with 4-(Ar-nitrosomcthylamino)-I-(3pyridyl)-l-butanone O'INK) and fed control or phenethyl isothiocyanate (PEITC) diets"
Diet
7-Mcthylguaninc (gmol/mol guanine)
Lung
Liver
Nasal mucosa
Control
10.4 ± 1.3*
20.6 ± 0.9*
21.5*
PEITC
5.9 ± 0.6''
22.8 ± 0.7
31.5
“ Groups ofsix male Fischer 344 rats fed control or test diets con!aining3pimol/g of diet PEITC for 2 weeks. Heginningonday
11 of feeding. [3H-CH3JNNK was administered subcutaneously daily at a dose of 0.6 mg/kg body weight for four consecutive
days. Four hours after the last NNK dosing, rats were sacrificed and tissue I)NA was isolated for analysis of 7-methylgu;unnr
* Mean ± SE for six rats
* Mean of two pooled preparations (two to three rals/pool)
Jp < 0.05 compared to values in control group
Table 3. Effects of isothiocyanates on adenomas induced by 4-(/V-nitrosomcthylamino)-l(3-pyridyl)-l-butanone(NNK)and on formation ofof O6-methylguanine(O6-MeG) in lungs
of A/J mice”
Group
no.
Pretreatment*
i
2
None
PEITC
PEITC
BITC
PITC
4
533
M^4. Morse et al.
To determine the effects of PEITC on the formation of DNA adducts by NNK, we used
experimental conditions analogous to those used in the bioassay. Thble 2 shows the effects
of two weeks’ feeding of PEITC on DNA methylation by NNK in liver, lung and nasal
mucosa of rats. The levels of 7-methyiguanine in DNA of the liver and nasal mucosa of rats
were not affected; in lung, however, the levels were reduced from 10.4 to 5.9 pmol/mol
guanine, a reduction of nearly 50%.
In the A/J mouse bioassay, we examined the effects of PEITC and its homologues PITC
and BITC on NNK-induced lung adenomas (Thble 3). A single intraperitoneal
administration of NNK at a dose of 10 jimol/mouse resulted in a 100% incidence of pul-
532
Daily
dose
(gmol)
5
25
5
5
No. of
mice
Mice with No. of
tumours
tumours/
(%)
mouse4’
CAMeG
(pmol/mol
guanine)^
30
18
20
20
20
100
89
30J
100
100
30.9' ± 5.9
3.9* ± 1.2
ND'
26.1' ±6.7
29.7’ ± 4.4
10.7' ± 0.8
2.6* ± 0.4
0.3* ±0.1
7.6' ± 0.5
9.5’ ± 1.2
Groups of 20-30 female A/J mux. maintained on A1N-76A diet, were administered coni oil or isothiocyanates by gavage
daily for four consecutive days. Two hours after the final gavaging. a single dose of NNK (10 pmol/mousc) was administered
intraperitoneally. Sixteen weeks after NNK administration, mice were sacrificed and pulmonary adenomas were counted
For assay of O^-McG, groups of five mice were administered com oil or isothiocyanates by gavage for four consecutive days.
Two hours after the final gavaging. NNK was administered intraperitoneally at a dose of 10 pmol/mouse. Mice were
sacnficcd 6 h after NNK administration. DNA was isolated from lung and hydrolysed in 0.1 N HC1 for 60 min. 0*-MeG was
analysed by strong cation exchange high-performance liquid chromatography and fluorescence detection.
* PEITC, phenethyl isothiocyanate; BITC. benzyl isothkvyanate: PITC. phenyl isothiocyanate
* Mean i SE; mean bearing different superscripts under each column are statistically different (p < 0.05) from one another
as determined by analysis of variance followed by Newman-Keul's ranges test
'Significantly (p <0.01) less than that of group 1 as determined by the chi-square test
' Not delected
tumorigenicity.
Our results indicate an upward trends in inhibitory potency as the alkyl chain length
increases. To test this hypothesis, we assayed NNK using PPITC, PBITC. OPBITC. PITC,
BITC and PEITC as inhibitors (Table 4). PPITC and PBITC exhibited remarkable
inhibitory activities; both were considerably more potent than PEITC, and at a daily dose
of 5 jimol for four days, they completely prevented the development of lung tumours by
NNK. OPBITC was inactive. As in previous bioassays. PITC and BITC were inactive.
whereas PEITC reduced lung adenoma multiplicity by 60-70%. The multiplicity and
tumour incidences in the groups treated only with isothiocyanates were similar to those in
a corn oil control group.
DNA methylation by NNK was reduced in the lungs of rats and mice administered
PEITC; however, it was not affected in the liver and nasal cavity of rats fed PEITC or in
the lungs of mice fed PITC and BITC. These effects are consistent with the effects of these
isothiocyanates on tumorigenicity induced by NNK in the two species and clearly suggest
that the protective effect of PEITC against NNK-induced lung tumours is due to its ability
to inhibit DNA methylation by NNK. Since there is a parallel relation between NNK
tumorigenicity and DNA methylation, ability to inhibit DNA methylation could be used as
a means of screening potential inhibitors of NNK carcinogenicity.
These data represent the first demonstration of inhibition of NNK tumorigenesis by any
compound (Morse et al., 1989a,b). PEITC is a product of the hydrolysis of gluconasturtiin,which is commonly found in turnips and rutabagas (Tookey et al., 1980). PPITC
and PBITC are both synthetic compounds. The goals of our future studies are to develop
inhibitors of higher efficacy by structure-activity studies and. ultimately, to test them in
high-risk groups such as heavy smokers.
534
AM. Morse et al.
Tabic 4. Effects of isothiocyanates on pulmonary adenoma
4-(A'-nitrosomethyla mino) l-(3-pyridyl)-l-butanone (NNK) in A/J mice”
Treatment*
No.
Com oil + saline
Com oil + NNK
ITTC + NNK
HFIV + NNK
PETI’C + NNK
PPITC + NNK
PBITC + NNK
OPBHC + NNK
induction
01 mice
Weight (g:
mean ± SE)
N-x of tumours/
mouse (mean ± SE)r
Mice with
tumours (%)
29
39
30
29
28
30
28
28
24.2 ±0.6
21.9 ±0.3
23.4 ± 0.4
22.1 ±0.4
22.4 ± 0.3
22.0 ±03
22.2 ±0.5
23.1 ±0.4
0.3'±0.1
9.2’±0.5
9.8? ± 0.9
10.4^0.7
33> ± 0.4
0.4' ±0.1
0.4’ ±0.1
7.9’±1.0
31
100
100
100
93
374
32
96
by
' Groups of 20-40 ?VJ mice were administered com oil or isothiocyanate (5 gmol/mousc per day) by gavage daily for four
consecutive days. Two hours after the final dose of corn oil or inhibitor, a single dose of saline or NNK (10 gmol/mousc) in
saline was administered intraperitoneally. Sixteen weeks after NNK administration, mice were sacrificed and pulmonary
adenomas were counted.
* PI 1C. phenyl isothiocyanate; BITC. benzyl isothiiKyanatc. PEITC. phenethyl isothiocyanate; PPITC. phcnylpmpyl
isothiocyanate; PBITC, phcnylbutyl isothaxyanatc; OPBITC. oxypyridylbutyl isothiocyanate
' Means in this column that bear different supersapts arc significantly different from one another as determ incd by analysis
of variance followed by Newman-Kenis ranges test. Saline-treated groups and NNK-treated groups were tested separately.
'Significantly different from the appropriate control group as determined by the chi-square test
References
Chung. EL.. Wang. M & Hecht. S S. (1985) Effects of dietary indoles and isothiocyanates on
N-nilrosodiincthylaminc and 4-(mcthylnitrosamino)-l-(3-pyridyl)-l-butanonc a-hydroxylation and DNA
methylation in rat liver. Carcinogenesis. 6. 539-543
Hecht. S.S. & Hoffmann. I). (1988) liibaixo-spccific nitrosamincs: an important group of carcinogens in
tobacco and tobacco smoke. Carcinogenesis. 9. 875-884
I ARC (1985) IARC Monographs on the Evaluation of the Carcinogenic Risk of Chemicals to Humans. Vol. 37,
Tobacco Habits Other than Smoking: betel-quid and Areca-nut Chewing and Some Related Nitrosamines. Lyon,
pp. 209-224
Morse. M.A., Wang. ('.X . Stoner. (LI).. Mand.il. S.. Conran. P.B.. Amin, S.G.. Hecht, S.S. & Chung. EL.
(1989a) Inhibition of 4-(methylnitrosamino}-l-(3-pyridyl}-l-butanonc-induccd DNA adduct formation and
tumorigcnicity in the lung of F344 rats by dietary phenethyl isothiocyanate. Cancer Res . 49. 549-553
Morse, M.A., Hecht, S.S. & ('hung. EL (1989b) Effects of aromatic isothiocyanates on tumorigcnicity.
(^-mclhylguaninc formation, and metabolism of the tobacco-specific nitrosaminc 4-(methylnitrosamino)-l-(3-pyridyl)-l-butanonc in A/J mouse lung. Cancer Res., 49. 2894-2897
Rxikey. H.L., VanEtten. C.H. & Daxcnbichlcr. M.E. (1980) Glucosinolatcs. In: Licncr, I.E., cd., Toxic
Constituents of Plan! Foodstuffs. 2nd cd.. Ch. 4. New York, Academic Press, pp. 103-142
Relevance to Human Cancer of N-Nitroso Compounds.
Tobacco Smoke and Mycotoxins.
I d I.K. O'Neill, J. Chen and H. Bartsch
I »on. International Agency for Research on Cancer
t IARC. 1091
-------- MODULATION OF GENOTOXIC ACTIVITY OF TOBACCO SMOKE
I
R.M. Balansky', P.M. Blagoeva & Z.I. Mircheva
Laboratory of Chemical Mutagenesis and Carcinogenesis.
National Centre of Oncology, Sofia, Bulgaria
Tobacco smoke (TS) caused a three- to nine-fold increase in the frequency of his +
revertants in Salmonella typhimurium TA98 but not in TA97a, TA100 or TA102. Activation
by a post-mitochondrial fraction obtained from the liver of rats pretreated with
Aroclor-1254 or methylcholanthrene was required; fractions from phenobarbitalpretreated or untreated rats had no effect. Vitamins A and E, but not ascorbic acid,
inhibited the TS-induced mutagenesis by up to 63%, whereas glutathione and cysteine
increased it slightly. Na2SeO3, but neither C0CI2 nor caffeine, inhibited the mutagenic
effect of TS by 46-56%. In Chinese hamster ovary cells, both Na2SeO3 and caiTcine strongly
potentiated the number of chromosomal aberrations induced by TS, while theophilline
slightly reduced its clastogenic effect. Treatment of mice with TS for 60 min/day increased
the frequency of micronuclei in polychromatic erythrocytes in bone marrow and in fetal
liver and the number of NCE micronuclci in peripheral blood by four to five fold.
Simultaneous treatment of mice with TS and Na2ScC>3 reduced the clastogenic effect ofTS.
Ascorbic acid had no effect on clastogcnicity but reduced toxicity as measured by body
weight loss. Both NajSeOs and ascorbic acid suppressed the induction of TS-induced
hyperplastic and metaplastic changes in bronchial mucosa but had no effect on the number
of urethane-induced lung adenomas. Vitamins A and E and ascorbic acid may have a
protective effect against the toxic and genotoxic activities of TS.
Chemoprevention of genotoxicity due to tobacco smoke (TS) might contribute to
reducing the cancer risk linked to tobacco smoking. Thus, a better understanding of the role
of modifiers in this process is needed.
Modulation in vitro of TS-induced mutagenesis in bacteria
We have seen previously a three- to nine-fold increase in mutation rate in Salmonella
typhimurium TA98 but not inTA97a,TA100 or TAKE treated withTS (Balansky et al.. 1987,
1988). The addition of an exogenous metabolic activation system, obtained from the livers
of Aroclor-1254 or methylcholanthrene pretreated rats was required; no activation was
produced with liver from phenobarbital-pretreated or untreated rats. A dose-dependent
' lb whom correspondence should be addressed
-535-
R.M. Balansky et al.
Modulation of genotoxic activity of tobacco smoke
inhibition of TS-induced mutagenesis up to 57-63% (p < 0.05) was seen in S. typhimurium
TA98 treated with vitamins A or E (0.08-0.8 mg/plate) (Figure 1). Inhibition of 46-56% (p
< 0.05) was observed when Na2SeO3 (25-100 ng/plate) was added to the top agar (Figure
1). Neither ascorbic acid (0.2-2.0 mg/plate). CoCl2 (0.2-1.0 mg/plate) nor caffeine (0.2-0.8
mg/plate) influenced this process. However, the addition of glutathione (0.6-2.4 mg/plate)
or cysteine (0.12-0.48 mg/plate) increased TS-induced mutagenesis slightly.
Na2SeO3 and TS decreased the number of NCE micronuclei as compared with that in mice
given TS alone; ascorbic acid did not have a similar effect (Figure 2). Ascorbic acid slightly
reduced the toxicity of TS, as measured by body weight loss.
Supplementation of the diet with vitamins A, and E and ascorbic acid might have a
protective effect against the toxic and genotoxic activities of TS.
536
Figure 1. Dose-dependent inhibition of mutagenesis induced by tobacco smoke (TS; 240 cm3
in a 16-1 glass chamber) in Salmonella typhimurium TA98 by Na2SeO3 and vitamins A arid
E; spontaneous mutation rate, 33-41 his+ revertants per plate
NarSeOa (jig/plate)
Vitamin A (mg/plate )
Figure 2. Numbers of micronuclei in the peripheral blood of mice treated with tobacco
smoke (TS; 600 cm3 in a 14-L glass chamber, four exposures of 15 min each with 1-min
intervals during which a total air change was made); Na2Se€>3 and ascorbic acid were
added to drinking-water starting ten days before the first TS exposure and continuing up
to the end of the experiment.
Vitamin E (mg/plato )
Modulation in vitro of TS-induced clastogenicity in Chinese hamster ovary cells
Direct treatment of Chinese hamster ovary (CHO) cells with TS enhanced the number
of metaphases that had chromosomal aberrations (breaks and exchanges). Treatment ol
CHO cells with Na2SeO3 (2.0-5.0pg/ml)2-4 h before or 18 h after exposure to TS increased
the chromosome damaging effect of TS by 80.9-92.3% (p < 0.05). Similar treatments wit,'.
caffeine (0.1-0.2 mg/ml) potentiated TS-induced clastogenicity by 97-141% (p < 0.01). In
contrast, treatment of cells with theophilline (0.05-0.2 mg/ml) 4-15 h before exposure to
TS caused a 31-53% (p < 0.01) decline in the frequency of TS-induced chromosomal
aberrations.
Modulation in vivo of TS-induced clastogenicity in bone marrow, peripheral blooa
and fetal liver of mice
Single or multiple treatment of BDF, (C57B1 x DBA2) mice with TS (60 min/day) caused
a dose-dependent, four- to five-fold increase in the number of polychromatic and NCE
micronuclei in mouse bone marrow and peripheral blood, respectively (Balansky et al.
1988). In addition, TS was shown to have transplacental clastogenic activity in fetal live:
after single or multiple treatment of pregnant mice during the last third of gestation. Four
months’ treatment of mice with TS (60 min/day) did not change significantly the number
of lung adenomas induced by urethane (1.0 g/kg). Ascorbic acid (0.04-0.3%) and Na2SeO3
(5-10 ppm) did not influence adenoma formation but suppressed TS-induced hyperplastic
and metaplastic changes in bronchia; mucosa. Simultaneous treatment of mice with
TS treatment ( days )
TS treatment (days )
Acknowledgements
Supported in part by the Ministry of Culture, Science and Education, grant 317. Part of
this investigation was carried out under the tenure of a Research Fellowship awarded by
the International Agency for Research on Cancer, l.yon. France, and spent at the British
Columbia Cancer Research Centre. Vancouver. BC. Canada.
References
Balansky, R.M.. Blagocva. P.M. & Mircheva, Z.I. (1987) Investigation of the mutagenic activity of tobacco
smoke. Mutat. Res.,
13-19
Balansky, R.M., Blagocva, P.M. & Mircheva, Z.I. (1988) Ihe mutagenic and clastogenic activity of tobacco
Mutat. Res.
237-241
smoke.
188,
208,
napio^a^ cancel
- yc mr
BA^^ore.- ^§2-\<^ .
CArJC^K pattern
6. Tobacco Related Cancers (TRC)
Sites of cancer that have been attributed to use of tobacco include oral cavity, oropharynx, hypopharynx, pharynx.
oesophagus, larynx lung and urinary bladder Accordingly, the number (#). proportionof cancers of these sites
relative to cancers of all sites, the Crude Rate (CR;. Age Adjusted Incidence Rates (AAR) and Truncated Rate (T R
are indicated in Table 6 1. Cancers due to use of tobacco constitute 37 85% and 19% of all sites of cancers in ma!es
and females respectively
Table 6 1
TOBACCO RELATED CANCERS
s
%
CR
AAR
TR
Males
Females
3285
37.8
22 6
42 1
75 5
1856
190
14.2
25.4
52.1
Table 6.2gives the number (#) and proportions (%; of individual specific sites of the TRC indicated above The values
given for the first proportion (%at are relative to all sites of cancer and those of the second proportion (%b) are relative
to all tobacco related sites The most important of the tobacco related sites in males are lung, oesoptiagus and oral
cavity which together account for over 60% <62.2%) of all tobacco related cancers. Among females 80% of the
tobacco related cancers are those of cancers of the oral cavity and oesophagus.
Table 6.2
TOBACCO RELATED CANCERS (TRC) : 1982 - 1989
Numbers (-) & Proportions i%:
Males
Females
Site --------------
a
#
%•
%“
Oral cavity
Oropharynx
Hypopharynx
Pharynx
Oesophagus
Larynx
Lung
U. Bladder
632
157
466
43
676
329
737
245
7.27
1.81
5.36
0 49
7 78
3.78
8.48
2.82
19.2
4.8
14.2
1 3
20 6
10.0
22 4
. 7.5
TRC*’
3285
37.78
100.00
1856
19 03
100 00
All Sites
8694
100.00
100.00
9754
100 00
100 0
% of total numbers of all sites of cancers
% u! loLil numb'!., jl nil fnbJt'co Halnlfj (\m< »*r
#
%a
%b
859
24
OR
8 81
0 25
0.97
0 26
6 42
0.57
1.32
0.43
46 3
1 3
5.1
1 3
33 7
3.0
70
23
25
626
56
129
42
Trends Over Time
Table 6.3 gives the Age Adjusted Incidence Rates (AAR) and three year Moving Averages (MA) of tobacco related
sites of cancer for different years. The same is graphically represented in Fig 6 1. There is a clear rising trend in the
overall incidence of these cancers in males, whereas in females the rates are about the same over the years 1982
to 1989. The values of AAR for specific tobacco related sites is given in Tables 6.4 and 6.5.
Table 6.3
TOBACCO RELATED CANCERS - TRENDS OVER TIME : 1982 - 1989
ALL SITES OF CANCER ASSOCIATED WTIH USE OF TOBACCO - MALES AND FEMALES
Table gives figures of AAR and 3 year Moving Averages (MA) of AAR
YEAR
1982
1983
1984
1985
1986
1987
1988
1989
1982-89
49.68
45.90
39.94
42.08
MALE
38.11
41.92
40.73
40.51
37.94
MA
40.3
41.1
39.7
42.7
44.5
FEMALE
27 35
23.58
26.25
22.86
24.93
MA
25.7
24.2
24.7
24.2
25.2
45.2
24.79
25.83
27.47
25.40
26.0
Fig. 6.1
TOBACCO RELATED CANCERS - TRENDS OVER TIME : 1982 - 1989
ALL SITES OF CANCER ASSOCIATED WTIH USE OF TOBACCO - MALES AND FEMALES
Figure shows line graphs of 3 year Moving Averages of AAR
TOBACCO RELATED CANCERS ■ TRENDS OVER TIME : 1982 1989
Table gives figures of AAR tor different years
TABLE 6 4
SPECIFIC SITES OF CANCER ASSOCIATED WTIH USE OF TOBACCO - MALES
1982
1983
1984
1985
1986.
1987
1988
1989
1982-89
Oral. Cavity
Oropharynx
Hypopharynx
Pharynx
Oesophagus
Larynx
Lung
U.Bladder
8.78
2.24
4 87
0.37
8 35
4 47
5 47
3.56
896
2.02
6 04
0.36
6.34
4.93
8.77
4.50
6 65
2 29
6.68
0 78
8 21
4 03
9 17
2 92
7.14
1 29
5.95
0.71
7.28
368
11 67
2.79
6.02
1.85
5.23
0.40
7.61
4.08
9.78
2.97
9.87
2.06
741
0.69
10.96
4 81
10.75
3.13
6.47
2.46
7.25
0 64,
9.87
4.34
11.44
3.43
8.12
1 90
5 86
0 24
8 57
4 04
8 57
2.64
7.74
2.01
6 19
0.53
8.57
4 29
9 53
3.22
TRC Sites
38 11
41.92
40.73
40.51
37.94
49.68
45.90
39 94
42.08
TABLE 6.5
SPECIFIC SITES OF CANCER ASSOCIATED WTIH USE OF TOBACCO - FEMALES
1982
1983
1984
1985
1986
1987
1988
1989
1982-89
Oral Cavity
Oropharynx
Hypopharynx
Pharynx
Oesophagus
Larynx
Lung
U. Bladder
14 66
0.44
1.30
0.28
7.25
1.27
1 36
0 79
10.98
0.41
1.70
0.36
7.27
0.78
1.71
0.37
11 54
0.34
1 59
0 00
9 52
0.49
2 24
0 53
10 57
0.15
1.22
0.56
7.16
0.88
1 71
0.61
11 27
0.36
0.55
0.46
10.02
0.69
1.42
0.16
9 88
0.12
1.20
0.24
9.74
0.60
2 34
0.67
12.51
0.45
1 52
0 32
8 18
0.50
i 51
0.84
12.31
0.53
1 21
0 14
10 18
0.74
1 60
0 76
11.69
0 35
1.28
0.29
8.73
0.73
1.74
0.59
TRC Sites
27 35
23.58
26.25
22.86
24.93
24.79
25.83
27.47
25 40
Age Specific Incidence Rates (ASR)
Table 6.6 gives values of age specific rates and the corresponding line graph is depicted in Fig 6.2. The curves on
ASR show that as early as the age of 25 years in females and 30 years in males the curves start rising Similar curves
across religious groups show the lower rate of these cancers in Muslim women of all age groups though in terms ol
proportion of total cancers in Muslim females and males they are fairly comparable to that in Hindus.
Table 6.6
TOBACCO RELATED CANCERS ■ AGE SPECIFIC INCIDENCE RATE (ASR):1982 - 1989
ALL SITES OF CANCER ASSOCIATED WTIH USE OF TOBACCO - MALES AND FEMALES
Table gives figures ol AS T, Crude Rate (CR), AAR. Truncated RAte (TR) and number (») of cases
AGE GROUP
MALE
FEMALE
0-4
5-9
10-14
15-19
20-24
25-29
30-34
35-39
40-44
45-49
50-54
55-59
60-64
65-69
70-74
75+
0.5
0.0
0.0
0.1
0.9
1.0
1.5
7.1
19.5
46.2
86.3
129.1
209.3
275.5
336.5
237.3
0.2
0.1
0.0
0.3
08
2.1
5.1
9.7
25.7
45.8
69.2
86.6
108.9
146.6
106.2
108.3
CR
22.58
14.19
AAR
42 08
25.40
TR
75.49
52.08
It
3285
1856
Fig. 6.2
TOBACCO RELATED CANCERS ■ AGE SPECIFIC INCIDENCE RATES (ASR) 1982 ■ 1989
ALL SITES OF CANCER ASSOCIATED WTIH USE OF TOBACCO - MALES AND FEMALES
□
Age Group (In years) --->
MALE
♦FEMALE
Religious Groups
The AAR of TRC combined and for specific sites by religious group is given in Table 6.7 and the age specific rates
of TRC according to religious group is presented in Table 6.8. The overall AAR is lower in Muslims especiall0n women
and for cancers of the oral cavity and oesophagus However Muslim men have comparable and slightly higher rates
of lung cancer than Hindu men. The curves of age specific incidence rates in males (Fig 6.3) are not very different
in the three religious groups, but these are considerably lower in Muslim women compared to Hindu and Christian
women.
Educational Status
Table 6.9 gives the number (#) and relative proportion (%) of cases according to known educational status. Table
6:9 (a) is for thetobacco related sites and 6.9 (b) is for all other sites. The proportion of illiterates among those who
have tobacco related cancer sites is substantially greater than for all other sites of cancer in both males and females
Table 6.7
TOBACCO RELATED CANCERS (TRC) : 1982 - 1989
AAR ACCORDING TO RELIGIOUS GROUPS
Female
Male
Hindu
Muslim
Christian
Hindu
Muslim
Christian
Oral cavity
Oropharynx
Hypopharynx
Pharynx
Oesophagus
Larynx
Lung
U. Bladder
8.06
2.04
6.48
0.48
9.69
4 26
9.42
3.20
5.53
2.00
5.42
0.85
4.77
3.77
10.24
2.78
9.17
1.40
4.85
0.37
5.32
5.58
10.39
4.08
13.47
0.37
1.47
0.35
9.98
0.89
1.66
0.63
4.87
0.12
0.80
0.10
4.42
0.26
1.94
0.26
8.47
0.61
0.51
0.17
4.92
0.00
2.42
0.82
TRC
43.63
35.36
41.16
28.82
12.77
17.92
All Other Sites
64.37
42.34
59.27
103.23
59.22
102.94
All Sites
108 00
77.70
100.43
132.05
71 99
120.86
Hindu
FEMALE
Muslim
Christian
0.1
0.0
0.0
0.2
0.9
2.5
5.5
11.3
28.7
53.4
78.3
98.5
121.5
165.5
120 8
123.3
0.4
0.4
o.o
0.5
1.0
0.5
2.2
3.3
14.6
19.4
48.1
43.9
59.8
49 7
65.5
38.6
Table 6.8
TOBACCO RELATED CANCERS (TRC) : 1982 - 1989
ASR ACCORDING TO RELIGIOUS GROUPS
A
Age Group
Hindu
MALE
Muslim
Christian
0-4
5-9
10-14
15-19
20-24
25-29
30-34
35-39
40-44
45-49
50-54
55-59
60-64
65-69
70-74
75+
0.1
0.1
0.1
0.4
1.4
1.3
3.3
8.7
23.1
56.4
94.3
158 9
204.6
265.8
292.7
238.9
0.0
0.0
0.0
0.4
0.4
1.0
3.0
2.7
26.8
46.5
72.6
140.7
162.5
234 5
224.8
159.0
0.0
0.0
0.0
0.0
0.0
1.0
5.1
7.5
13.6
41.4
78.8
127.5
146.8
357.8
199.2
362.8
CR
23.49
19.02
21.21
16.09
7.27
9.60
AAR
43.63
35.34
41.16
28.82
12.77
17.92
TR
79.24
65.58
60 64
59.09
28.37
32.16
a
2624
420
212
1609
144
_______ 93
0.0
0.0
0.0
0.0
0.0
0.0
3.0
8.6
17.5
25.3
23.7
57.9
84.6
152.3
51.5
108.9
Hindu
Ago Group (In yrs.) -•>
♦
Muslim
Christian
Table 6.9 (a)
Number (#) and Proportion (%) of TOBACCO RELATED CANCERS according lo Educational Status
#
%
Female
#
%
Illiterate
Literate
Primary
Middle
Secondary
Tec. Aft
College
Others
Unknown
806
415
489
275
552
67
163
14
504
24.54
12.63
14.89
8.37
16.80
2.04
4.96
0.43
15.34
1145
153
140
79
91
10
18
1
219
61.69
8.24
7.54
4.26
.4.90
0 54
.0.97
0.06
11.80
Total
3285
100.00
1856
100.00
Male
Table 6.9 (b)
Number and Proportion of all other sites according to Education
Male
#
illiterate
Literate
Primary
■Middle
Secondary
’ec Aft
College
Others
Unknown
Total
%
Female
it
To
800
530
593
383
865
131
399
44
1664
14.79
9.80
10.96
7.08
1599
2.43
,7 38
G 81
30.76
3203
619
769
473
944
52
268
i7
1553
40.55
7.84
9.74
5.99
.11.95
0.66
3.39
0.22
19 66
5409
100 00
7898
100 00
io’
“7‘?5r“s‘n c*831t iteatea patients with hypertension, but
c evoked J <S;?
^individuals were selected for study because their indirect..___ —William P. Castelli ■
Robert J. Garrison . ; ■
sc paticift'®;
r'Sture. readings seemed inappropriately high . when
Patricia M. McNamara' . ■.
Thomas R. Dawber
imbulatc:; .TOsidered against a general absence of target organ damage;
Manning Feinlf.ib
William B; Kannf.l. :
3 mmHg:!;,sthe same study a good correlation was observed between
Framingham Heart Study, National Heart, Lung, and Blood
jKn-lrtenal blood pressures and cuff pressures as obtained
Institute, Framingham, Massachusetts; Biometrics Research Branch,
ps I andl-fc■7 the general practitioner or in the hospital setting in
National Heart, Lung, and Blood Institute, Bethesda', Maryland; and
■g/ml)ind£:Kjbedected untreated subjects with hypertension. However, a
Boston University Medical Center, Evans Research Foundation',
JO pg/nil vj[Jet study, which selected untreated subjects without clinical
Boston, Massachusetts, U.S./!; '
'
d the meat ?.■■sdence of target organ damage, did show mean waking
ial pressure^"
alri-atterial pressures to be significantly less than mean
Summary
Long-term-follow-up of the Framingham
i:Thisw»>■tttpalient blood pressures, by 18 mm Hgon average.*7
1115
10
8
*14
12
The
cohort for coronary heart disease (CHD)
mm Hg v f £®son for the discrepancy between cuff and ambulatory
end-points has made it possible to test the hypothesis that
psaings is not clear. These observations arc important in the
those who smoke filter cigarettes arc less likely to get clinical'
its whJ^^Sion to treat subjects with mild or moderate hyperton
manifestations of CHD than' those who smoke non-filter
«tory
ia. 20 of our 59 subjects fulfilled the conventional defl
cigarettes. Men were "classified at. the 7th biennial
357±9-W ation of hypertension but their average ambulatory mean
examination (1963-64) according to-whether they smoked *
.’em!pressure throughout the waking day was less than 108
filter or non-filter cigarettes. 58% of the cigarette-smoking
« pysisttf £jrnHgfi.e., equivalent to 140/90 mm Hg) and even lower'
men under age 55 at this examination smoked filter cigarettes. '
15 patient’.!.'caiag sleep when the average mean arterial pressure fell
These men had slightly lower prior smoking exposure than •
iges, or IS’’i■ eptoxitnately 25% for waking levels.
smokers of non-filter cigarettes. Despite what seemed to be a
■cafdiogrsih; ;
1 Both the American hypertension detection and follow-up
favourable cigarette-smoking history, the filler-cigarette
19%) oftlajE
riegram16 and the Australian therapeutic trial17 showed the
smokers did not have lower CHD incidence rates than non0-001,'xJl?
.stfit oftreatment in reducing the morbidity and mortality
filter smokers. This finding was unchanged even after
y the ciosec iTcild hypertension. A noteworthy difference between these
multivariate logistic regression analysis to adjust for the
.S?r6trials was the smaller mortality from cardiovascular
slight differences in age, systolic blood pressure, and serum
JLrsase in the placebo group of the Australian study when
cholesterol between the two groups.
. f -•ipared to either the “stepped care” or the “referred care"
T pressur^^tc-up ofthe hypertension detection and follow-up program.
roup I) or.r
W2S suggested17 that the inclusion of some patients with
s (group pjhSjkaily detectable end organ damage in the American trial
•ups were
have selected subjects with a higher degree ofcardiovas■s, but-.lk.^.bArrisk. The Australian subjects, interestingly, had a lower
Hg lowert'.J h'dtl mean arterial pressure (119 mm Hg) than our own
of
subjects. One possibility, therefore, is that the be(tcr
and plM-agpojnosis in both the placebo and treated groups of the
>ose of.’ .',-stralian study, and the lack of apparent benefit of therapy
muli. lSy<npmnts'under 50 years of age in both trials may have been
1 arithr^^.betoalowcr, perhaps even normal, ambulatory blood presilasma-nts^jsi.-tinasignificant proportion of these individuals.
g bicyclinfgSTfereisnodoubt that cuff pressures give a reasonable preure was afef j ihiiia ofcardiovascular risk. We suggest, however, that the
-:viation)vi?;?'thdonship between arterial pressure and subsequent cardio;
objects wfel^TiOTlat'mcibid events might well be even greater if a more
. latory ratejgnwte assessment of true arterial pressure and its daily flue
changes
Mons, could be obtained on a wider scale than is possible
their higis^vili present techniques.
e> thefefok.|>;.
may Qddre,lcd to Prof. P. Sleight, John Radcliffe
aveen an
.*■Sfc&nl, Readington, Oxford OX3 9DU.
y reflect
ted pressusSr
'
references
* uJ
idto'W. Honour AJ, Sleight P, Stott FD. Continuous recording of direct arterial
QOeS
- ptynfcindelectrocardiogram In unrestricted man. Be MedJ 1972; l(j: 76-78.
,plicati6n®rWlsfe*S.B’.i»EN,P»»caul AV, Matice .M, Hannon L, HunyorSN, Sandler LN. Home
r
"3/. ;F.wd pruture determination: value in borderline (‘labile*) hypertension. JAMA
■f &*&i14;229: 66J-66.
30d'Pf^^’F-^»~a KD’ Gerrard DJ, Fisher L. Comparison of clinic and home blood pressure
• Indi to essential hypertenaion and variables associated with clinic-home differ*
ie stuay
CimD;, |980.33. l97_206.
(
tSlOn
SAale* M, Werdeg:r D, Kain HK, Hinman AT. Relationship between blood
Trnm 1 SC# £•’' JTtKtrtmciiurcdcimjolly and by portable recorders and severity ofcomplications
ironi m
Lmuniijlhypertension. C/Wuru'-r |966|34t 379-H9.
e related
at, Honour aj. stmt j-d. Direct arterial pressure recording In unrestricted
h this»•* )3’-<1
l irn- i-'-U"-’1 HowwAJ. Pulley DJ, Sleighl P. Conlinuolu recording ot.lirrcr jrtcrul
jrVOlS Ur.-y. . pcsirt iaunrr,:r.nrd pcricni). >r> role In lhe Ji.eno.i, and rn.n.Kcnrcor »thirch
,-fleet the
;sure dllUJC
tlw. prawn CmJjn«« WSiSli 1101-06.
■
iRtfereiica di.;;t.ucd at fool of next column.
Introduction
Till; introduction of low-tar and low-nicotine cigarettes
was partly prompted by the finding that number of cigarettes
smoked is positively related to subsequent disease. This dose
response relation suggested that cigarettes would be made
less hazardous by removing, by filtration or other means,
those substances responsible for the increased fates ofcancer,
pulmonary disease, and coronary heart disease (CHD). Ofthe
more than 4000 chemical substances in cigarette smoke,
nicotine and carbon monoxide arc the most likely to be
responsible for the cardiovascular consequences of smoking.
Some studies show a parallel fall in nicotine and carbon
monoxide in the low tar-low nicotine cigarettes whilst others
show a rise in carbon monoxide dose with a,,fall in nicotine.
DR FLORAS AND OTHERS: REFERENCES—continued
7. Keith NH, Wagener HP, Barker NW. Some_diffcrcnt types of essential hypertension.
their course and pro^pMtsrHmJ'AfcJSci 1939; 197: 332-43.
8. McPhie J. Left vejurfcular hypertrophy: Electrocardiographic diagnosis, Autt Ann
Med 1958;7:317-27. "
.
surcments./lm Heart J1942
10. Henry DP, Starnun BJ, Johnston DG, Williams RH. A sensitive radio enzymatic assay
for norepinephrine in tissues and plasma. Life Sei 1975; 10: 375-84.
11. Sleight P, Floras J, Jones JV. Autom-'ic analysis of continuous intra-arterial blood
pressure recordings. Index: blood pressure variability' (Clement DI., cd.).
12. Watson RD, Stallard TJ, Flinn RM, Littler WA. Factors determining direct arterial
pressure and its variability in hypertensive man. Hypertension 1980; 2: 333-41.
I). Gribbin B, Pickering TG, Sleight P. The effect of age and high,blood pressure on
baroreflex sensitivity in man. Cite Res 1971; 29: 424-31.
14. Ayman D, Goldshine AD. Blood pressure determinations by patients with essential
hypertension I. The difference between clinic and home recordings before treat* ’
15. Editorial. Home Blood pressure recording!. Lancet 1975; I; 259-60,
finding! of (he hypcrteniinn detection and follow up program, I. Rtduciion In
mortality of per sons with high blood pressure. including mild hypertension. Jzl.t lei
17. Australian Therapeutic Trial in Mild Hypertension, Report by the Management Com* .
The measurement of clinical disease end-points is the
ultimate test of whether any alteration in the dose of noxious
elements is beneficial. So far few large-scale studies have
assessed CHD end-points. The very large American Cancer
Society study1 showed that low tar/nicotine smokers had a
20% lower rate of CHD mortality in 6 years than high
tar/nicotine smokers. Three prospective surveys in Scotland2
showed a slightly higher rate of ischaemic heart disease
mortality among filter cigarette smokers. An English study,
sponsored by the Tobacco Research Council, reported a 25%
fall in risk of coronary heart disease in smokers of filter
cigarettes?
j
In our prospective survey reported here rates of CHD
among Framingham Heart-Study men were related to type of
cigarette smoked (filter or non-fiiter). It also compares the
smoking history of individuals who switched to filter
cigarettes with those who continued to smoke regular
cigarettes, and tests for the contribution of filter use to the
prediction of CHD in multivariate analysis.
Methods
Framingham Heart Study Cohort participants have undergone
physical examinations every 2 years since 1948? Data presented.
here include those which were collected at the 1st examination and
at the 7th to 14th examinations, inclusive. Details asked about
cigarette-smoking history at the 1st examination included the
number of cigarettes smoked daily and the duration (years) of
cigarette smoking. The first.timc a question about filter cigarette use
was asked was the 7th examination, which took place during the
2-ycar period starting in September,' 1963. The most recent
examination for which cigarette-smoking data is available is
examination 12. At this follow-up questions were asked about filter
use, frequency of cigarette use per. day, maximum cigarette
consumption per day for any 1-year period, and number of years
previous cigarette smokers had not smoked. For this report the 7th
examination was the baseline at which individuals were classified
according to smoking habits. Thus, only those who underwent
examination 7 are considered in the tables that present data from the
1st, 12th, or other follow-ups. Blood pressure, measured with the
subject seated, and total serum cholesterol, measured by the AbellKendall method,5 were recorded at the 7th biennial examination.
These measurements, together with age in years, were used as
independent variables in multivariate logistic regression analyses
since they are consistent and powerful predictors of CHD risk.
Regression coefficients (/J,) of the logistic function were calculated
by maximum likelihood methods? The standardised regression
coefficients represent the relative strength of each independent
variable in a given estimated equation as a predictor of the CHD
end-point under-consideration. The-significance test associated
. with each’ cocfficient’indicates whether that variable contributes
independent information, apan from that contributed by other
variables in the equation, to the prediction of disease. .
. Diagnoses of clinically apparent CHD were made according to
methods and criteria that have been described.7 Only individuals
who were .free of pre-existing CHD at the 7th examination are
considered in this report, and they were followed-up for the next 14
years (up to the 14th examination) for occurrence of new disease.
The specific CHD end-points considered in this report are CHD
death (both sudden and non-sudden death), myocardial infarction
(MI) (all proven MI, whether fatal or not fatal), and total CHD (MI,
coronary insufficiency, angina pectoris, and all CHD deaths).
Results
1605 men and 2132 women, aged 41-74 years, underwent
the 7th biennial examination. Only the youngest women
smoked cigarettes. Therefore no test of the hypothesis that
filter and regular cigarettes differ in their relation with CHD
was possible among women. The men were divided into a
TABLE 1-DISTRIBUTION OF SMOKING BEHAVIOUR OF MEN j,
EXAMINATION 12 IN RELATION TO SMOKING HABITS AT
EXAMINATION 7
Smoking status at exam 12 ■■■'
(n=1590)
Smoking status at
Age <55 yr (n ■ 846) ,
Filter (n = 295)
. Regular (n = 214) •
Non-smoker (n=337) *
^>55yr(n=744)
Filter (n= 178)
Regular (n=137)
Non-smoker (n=429)
Filter
Reiular smoker
examini
36-6%
29-8%
2-1%
3-4%
22-0%
0-6%
42*0%
33-2%
86-1%
20 -OS,
15-0*
ir.d
25-6%
19-7%
0-2%
2-9%
11-0%
0-2%
37-2%
27-0%
67-7%
31-3»
42-35,
31-W
•Plain or untipped.
group who were above and a group who were below 55y
of age at examination 7, this age being approximately
midpoint of the age-range then. 60%ofthe younger grbu
men smoked cigarettes at examination 7, and 58-0% of
cigarette smokers smoked filter cigarettes (table I). Altho
fewer of the older men smoked cigarettes, a "sin
proportion of smokers (56 • 5%) used filters. In both?
groups nearly all. men who smoked filter cigarettes'.,
continued to smoke carried on using filter'cigarettes. M
■ than half of the smokers of regular cigarettes (untipp«|
examination 7 who'were smoking cigarettes 10 years'!!
were still smoking regular cigarettes. Otherlcomparisoni
exposure between the filter and regular cigarette groups
shown in tables II and III. Although a slightly hig
proponion of filter smokers had stopped smoking cigara
by examination 12 (table 1) there were no significdifferences between filter and non-fiiter smokers in durap
of cessation of smoking among those who stopped smote
Nor was therea difference in thenumberofeigarettessiiraj
TABLE 11—SMOKING STATUS AT EXAM 13* FOR MEN 11Y AGE AM
SMOKING STATUS AT EXAM 7.
Smoking stums at exam1 12
Smoking status . No. of cigarettes
smoked-}* • ’
Age <55 yr
Filter ...
Regular
Age ^55 yr
Filter ' 1
Regular •
'■
No. ofy^l
Aiaximnn no-, of
non-smoki^J
cipxencs
smtksdj* ‘ ■ before examj-|
23'9(112)... .
24-6(7///
30-3(7//) ■
30-2 (110)
18-2 (51)
18-4 (42)
25-2(51)
27-5(42)
■ ‘1
5-4»
■'s-omi
'
’■ 6-5(%gj
No. of observations in parentheses/
-■<
‘Only those who underwent exam. 12 are induced in these calculation
•j-Smokers only
\
.
.
^Quitters only
TABLE III—SMOKING STATUS* AT EXAM 1 33R MEN BY AC E AT?
7 AND TYPE OF CIGARETTE SMOKED AT EXAM 1
Smoking status at
Age <55 yr
’Filter (n = 295)
•Regular (n«=214)
Age ^55 yr
Filter (n= 178)
Regular (n= 137)
Smoking stums at exam 1
Percentage of
men smoking
Average no. of Avenge^
at exam 1
cigarettes smoked ofsinokinj!
93-2
96-7
21-9
24-0
89-9
94-9
19-3
23-1
w nCRATE PER 1000 AFTER 14 YEARS OF OBSERVATION FOR Ml,
v •.1- a!D death, and total chd for men by age and smoking
STATUS AT EXAM 7*
Age<55
Rate
-Xoa-CTOxer
F Regubr smokers
Filter smokers
CHD fa*
Sr Son-smoker
i Regular smokers
£< Fiher
ifTotal CHD
g- Non-smokers.
X Regular smokers
t FD er smokers
g.
Age ^5+
No. of cases
No. ofcases
Rate
20
40
147
146
ISO
63
20
32
58
9
9
11
101
131
90
43
IS
16
119
2)6
210
40
44
62
269
2S5
242
115
39
43
59
112
- . 136
27
S «Those with CHD at examination 7:arc not included.
9 by those who continued to smoke, or the mxximum number
of cigarettes ever smoked over one year. Comparison of
V smoking behaviour at examination 1 reveals differences
3 bctws^gjlter and non-filter smokers (table ill)—a higher
propoWR of non-filter smokers at examination 7 had
SS- .smoked cigarettes at examination 1. Furthermore, those who
smoked regular cigarettes at examination 7 and who smoked
Ij.at examination 1 seemed to have done so longer and were
/. .smoking more cigarettes at examination 1 than participants
who smoked filter cigarettes at examination 7.
£;• Table IV shows the 14-year rates of occurrence per 1000
f men for myocardial infarction, coronary heart disease (CHD)
..death,'and total CHD by age and smoking status at the 7th
jjjTexatSnation. Among the younger men non-smokers had the
«■ lowest rates, and filter cigarette smokers the highest. No clear
trend was observed among the older men. Differences in rates
^•ybetweenynon-smokers and smokers (filter and regular
^.dgarettes combined) after adjustment for other risk factors
g.-.were" tested’ by multivariate logistic regression and are
gr presented in table v, which shows a strong relation between
i7 dgareue smoking and CHD in middle-aged men. Although
coefficients are also positive for the older, men, none are
statistically different from zero. It should be noted that
among the older men smoking cigarettes at examination 7,
less than one third continued to smoke cigarettes until
examination 12 (table I). Also, those who continued to smoke
reduced their daily consumption.
The hypothesis that MI, CHD death, or total CHD rates
differ between men who smoked filter cigarettes and those
who smoked regular cigarettes was tested by multiple logistic
regression analyses (table VI) based on data for men who
smoked at examination 7 but were free of pre-existing CHD.
Thus, the positive standardised coefficients for the middleaged men (<55 years group) indicate that filter cigarette
smokers have higher rates of MI than smokers of untipped
cigarettes, after considering any differences in total
cholesterol, systolic blood pressure, and age. These
coefficients parallel the difference in univariate rates
presented, in table IV. There are no statistically significant
differences between filter use and MI, CHD death, or total
CHD.
Discussion - .
Information about the timing of the “switch” to filter
cigarettes in Framingham is not available but.is assumed to
have taken place fairly soon after the introduction of filter
cigarettes in 1950. By 1964 filter cigarettes took 65% of the
cigarette market.8 A similar proportion was smoked by our
subjects at examination 7, although differences would have
been expected in view of the older age-structure of the
Framingham sample compared with the general population.
The nicotine content of the cigarettes that were smoked by
the subjects of this report can be inferred from sales-weighted
average nicotine deliveries of filter and regular cigarettes for
the U.S.’ Between 1963 and 1977 (the period of follow-up
covered in this report) the average nicotine delivery was 1-75
mg, for regular cigarettes and 1 - 3 mg for filter cigarettes.
Although the nicotine content of regular cigarettes remained
fairly constant over the period, averages for filter cigarettes
declined from about 1 • 4 mg to 1 • 1 mg in 1977. Most of this
Eji table V-STANDARDISED MULTIVARIATE LOGISTIC REGRESSION COEFFICIENT^ AND l-VALUES FOR MEN WHO HAD NEW Ml. CHD DEATH AND
NEW CHD BETWEEN EXAMINATIONS 7 AND 14Age ^53 (n = 752)
Age <55 (n=>853)
'• —''2r’3b-c
f, Total cholesterol
fclvSjstolic blood-pressure .
; __Ciga:et’.est
•
„ t
Coefficient
i ■
Coefficient
0-345
0-303
-0-049
0-409
3-22
2-80
-0-41
3-13
-0-014
0-293
’ 0-057
o\)53
-0-14
3-05
0-55
0-52
0-168
0-299
0-201
0-198
2-12
3-86
1-87
1-91
0-054
0-36S '
'0-035
0-092
0-46 *
3-36
0-29
0-77
0-175
0-432
0-407
0-186
0-52
3-85
0-94
3-35
0^043
0> 299
-0-002
o-dos
0-242
0-322
0-216
0-154
* 'No; ofcases
CTDisri
yToia! cholesterol ”
.Systolic blood-pressure
| Ggareuesf
1. No. of cases’ 1
.
70
36
0-438
0-340
'0-0S9
0-333
rk-
TS-nuk-n^ CHP al examination 7 were excluded.
WCT« given a value of 1, and non-smokers a value ofO. for this variable. \
v
t
4-16
2-52
'2-50/..
1-84
5-00
3-95
1-82
115
-0-03
0-09
200
/'
202
116
86
0-324
0-556
0-345
0-376
• No. of cases .
i.-VruCHD
. Total cholesterol
S.'xtobc blood-pressure
■-^61)
_ ^garenesf •
All ages (n = 1605)
Coefficient
3-98
5-37
3-35
351
TABLE VI—STANDARDISED MULTIVARIATE LOGISTIC REGRESSION COEFFICIENTS AND t-VALUES FOR MEN WHO SMOKED CIGARETTES AT EX^ •
AND WHO HAD NEW MI, CHD DEATH AND NEW CHD BETWEEN THEN AND EXAMINATION 14’
* •
r
NenAfZr
Total cholesterol
Systolic blood-pressure
Age Gt) ■
Filter cigarettes!
0-261
0-141
-0-042
0-120
2-08
1-08
-0-31
0-87 .
No. ofcases
/
CHD deaths:
Total cholesterol
Systolic’ blood-pressure
Age Gt)
Flier cigarettes!
No. of cases
Coefficient
0-100
0-491
• -0-126
0-116
2-40
2-89' /
1-85
0-66
0-313
0-240
-0-212.
-0-206 ’
3-38
2-21
0-58.
0-‘19
.0-109
• 0-331
-0-141 ■
-0-150
Coefficient
t
0-63
3-34
-0-77
0-72
0-190
0-321
0-020
o-hs
1-94 .
••
■
-
0-20’W
i-i2%g
1,4
1-67
1-36
-1-08
0-367
0-360
0-289
-0-024
33
. 26
0-370
0-239
0-066
0-021
106.
t
50
6-1
. 0-419
*0-507
0-402
0-143
No. of cases ’
New CHD:
■ ■ ■.
Total cholesteroJSystolic blood-pressure
Age Gt)
Filter cigarettes!
All ages (n-814)
Age >55(n = 310)
Age <55 (nB5O4)
Coefficient
Independent variable
2-95M
2-99
2-14.M
“O'17!®
59
0-82 ‘ ■
2-57
' -1-04 .
-1-14
79
_
- 0-270
5-22^3
• 0-291
0-048./;
-0-047 's
3-50
0-56^3
“°’55^
185.-
.
. .-Q
■ ’Those with CHD at examination 7 were excluded. .
!Fher cigarette smokers were given a value of 1, and regular cigarette-smokers a value of 0, for this variable.
’ decline in average filter cigarette yield was probably due to . arrhythmias.20 Nicotinc-.stimulated catecholamine relsj
’ rapid increase in sales of “ultra” low tannicotine
’
may increase platelet stickiness and aggregation.2.1 Initia®
I the
formation, decreased fibrinolysis, decreased clotting tiae
I cigarettes.10 Thus, the rapid change to filter cigarettes in the
change in the rate of initial clo' formation, maximum cb
j late 1950s and early 1960s and the apparent uniformity of
I cigarette nicotine content provide somjjgsurance that the ■ tensile strength, and clot retraction,21 along with (anti
1 comparisons made in this report (dcspitetn^^j^aSeptcific . relating to platelet function, have been considered in weds
the pathogenesis of atherosclerosis.22
.brand information) between filter and regular cigarettes
Carbon monoxide has an affinity for haemoglobin thaj
reflect true differences in exposure to nicotine. Data on the
245 times that of oxygen, so it can severely reduce oxjjt
relative uniformity and differences in. carbon monoxide
delivery to the myocardium. This interference in oxyg
exposure among filter and regular cigarette smokers are not
transport
is increased by the way carboxyhaemoglobins®
available, but studies in England covering this period show
the oxyhaemoglobin dissociation curve to the left.2’ Carts
no change' in carbon monoxide delivery between filter.and
monoxide alsocombines with myoglobin thus impairingW
regular cigarettes. (Wald NJ, Coll R, personal communi-•
diffusion ofoxygen to mitochondria in heart muscle, andyt
. cation).
” .
.
cytochrome oxidase, thus slowing oxidation at an enzymes
Filter-cigarette smokers have consistently been shown to
have a lower cancer mortality1,11,12 than non-filter-cigarette ' level.21 By decreasing left ventricular end-diastolic press
left ventricular1; stroke index and cardiac index it®
smokers; This decrease has been attributed to the reduction
decidedly negative inotropic effect on the myocardium^
in tar exposure, which is thought to be causally related to high
patients with angina, carboxyhaemoglobin signified
cancer rates in cigarette smokers. However, the total impact
ofcigarette smoking on the health of individuals needs to be . shortens exercise time-and the product of systolic!)®
pressure
considered before drawing conclusions about the benefits of
r----- and rate (the double product) needed toprodite'
filter cigarettes. There is very little known, for example,
ischaemic S-T segment' depression is redup®
Carboxyhaemoglobin
lowers the threshold for ventrig
about the specific constituents in tobacco smoke that might
L
contribute to atherosclerosis or aggravate existing coronary fibrillation in monkeys,26 and exposure' of rabbits to carle
or cardiovascular pathology. Only a dozen or so of the- monoxide results in prominent ultrastructural changes
heart.27 Carboxyhaemoglobin increases vessel wall hyPr
■ thousands of compounds’in cigarette smoke have shown a
and permeability;28 such increased' permeability^
possible connection with coronary heart disease, and only
lipoproteins may promote atherosclerosis.25 Wald-p?
two, nicotine and carbon monoxide; have been looked at.in:
reported a stronger association between carboxyhaemogls
any depth.
and coronary heart disease than between smoking history*5
Nicotine acutely raises systolic blood pressure, heart rate,
coronary heart disease.10 "
and
cardiac
output
and. ' causes
cutaneous.
The present results indicate that nicotine lowering do*6
vasoconstriction,I1,14 probably by increasing catecholamine
have much effect on CHD risk in filter-cigarette smoke*..
secretion.15 It acts directly on the myocardium to produce
such results may be compatible with the growing susp,of
positive chronotropic and inotropic cardiac muscle actions.15
that carbon monoxide is probably one of the more
The rise in free fatty acids, also probably due to
constituents in tobacco smoke. Cigarettes which havens
catecholamine stimulation,16 may aggravate cardiac
yield of tar. and nicotine may not necessarily produce./
dysfunction17 and contribute to the fatty cellular lesions of
yields
of carbon monoxide. Indeed ordinary filter cig31*?.
atherosclerosis.18 Nicotine increases the diurnal secretion of
without perforations in the filter lead to increased expos0,'
cortisol,15 which has been associated with myocardial
and
higher
levels
infarction and with more frequent and complex ventricular ’ carbon ' monoxide
^£ANCET,JUt.Y18,19SI
catbbxyh3emog'°b‘n’ • - while low tar and nicotine
cigarette? with perforations in the filter have lower carbon
^'poxidc >'ields?2 Whc;her lhe ultra-low tar and nicotine
cigarettes or the perforated filter will reduce CHD risk is not
Known- The most optimistic data, published by the Tobacco
Research Council, suggest only- about a 25% decrease in
Cabbnn’onoxi^c exposure from such cigarettes.
'..The rnultivariate analysis is an attempt to “control” for
biher factors known to be strongly related to CHD but which
roay differ between filter and regular cigarette smokers,
although ■ other “confounding” variables, such as
hiuneasured lifestyle differences, may obscure the true
rdations. between filter use and CHD. Furthermore, a
.substantial proportion of the older age-group had stopped
smoking before the 7th biennial examination and therefore
the power to detect differences in event rates between filter
and regular cigarettes in this group is diminished. The high
proportion of former smokers among the “non-smokers” makes the purity of the comparison between smoking and
mdn-smoking men in the older age-group.subject to some
question. However, the comparison between filter and
■regular rj^is not influenced because it is an “internal” .
comparis^^comprised of only men who are long-term
; cigarettesmokers. Although the slightly higher rates of MI
among'filter cigarette smokers suggest a possible deleterious
impact of filters, most of this difference results from higher
’rates very early in the follow-up period. It is not possible to
".resolve whether this is due to a “harvesting” effect of filter
•.cigarettes or to selection of filter cigarettes by men who have
bad subclinical “warning” of CHD. The latter seems most
unlikely because most of the men had been smoking filter
’.cigarettes for a number of years before examination 7. The
■ tendency for filter cigarette smokers at examination 7 to have
a more favourable smoking history, although consistent with
' most,other data, also, suggests that these men should have
| mdreJayourable CHD outcomes. Since they do not, more
suspicion, should be raised about potential benefit of filter
cigarettes-. The promise of the filter philosophy is that the
toxins winch cause degradation of lung function, cancer, and
:.GHD ,can be. identified and removed, leaving a “safe”
| agaret'te. There is no evidence that the filter cigarettes ofthe
.; 60s and early 70s conferred any protection from coronary
• heart disease for men in the Framingham Study.
K ■: Requesl^yr eprinls should be addressed io W. P. Q, Department ofHeallh
-.Hu^Mtervices, Framingham Heart Studv, 118 Loncoln Street,
; ramagb^Massachusetts 01701, U.S.A.
“Society, increasingly impressed with the seemingly unending
achievements in medicine, has developed an almost insatiable
appetite for health services and is now faced with' the dilemma of
decision as to the fraction ofthe nation’s gross national product to be
devoted to the enterprise we now call ‘medical care’ What is it that so
' seriously burdens the health care system? It is not those diseases
which, thanks to successful research, can be prevented or
cured—pernicious anaemia, tuberculosis, smallpox, pneumonia
and many others: It is the management of those diseases which we
cannot cure and, inst-.ad, the victims are offered' expensive
supportive but temporary measures; among them I would include
heart transplantation, tl c treatment of many forms of cancer, and
most virus diseases for .vhich we lack immunising procedures. I
venture to predict that this half-way medical technology will
increase its pseudo-curaiive offerings, that these will be demanded
by an inadequately informed public, and that no health care system
in the world will be able to afford them. Those who state that we
now spend too much on -.esearch and who wish to deflect such funds
into the health care system could noi be more wrong! Our only hope
is to seek with renewed vigour the ultimate understanding which
. will lead to rational pre ventive or curative treatments as successful
as those we have gained for the infections and other diseases..
Sir Andrew Watt Kav, regius professor of surgery, Universitv of
Glasgow. Graduation speech, July 11, 1981.
Jin-Ling Tang, Joan K Morris, Nicholas J Wald, David Hole, Martin Shipley, Hugh Tunstall-Pedoc
Department of
Environmental and
Preventive Medicine,
Wolfson Institute of
Preventive Medicine, St
Bartholomew’s Hospital
Medical College, London
EC1M6QB
Jin-Ling Tang, research
fellow
Joan K Morris, statistician
Nicholas J Wald, professor
West ofScotland Cancer
Surveillance Unit, Greater
Glasgow Health Board,
Ruchill Hospital, Glasgow
G20 9NB
David Hole, principal
epidemiologist
Department of
Epidemiology and Public
Health, University College
London Medical School,
London WC1E6BT
Martin Shipley, statistician
Cardiovascular
Epidemiology Unit,
Nincwclls Hospital and
Medical School, Dundee
DD19SY
Hugh Tunstall-Pedoe,
Correspondence to:
Professor Wald.
BA fjl995;3tl 1530-3
1530
Abstract
Objective—To investigate relation between tar
yield of manufactured cigarettes and mortality from
smoking related diseases.
Design—Prospective epidemiological study of
four cohorts of men studied between 1967 and 1982.
Setting—Combined data from British United
Provident Association (BUPA) study (London),
Whitehall study (London), Paisley-Renfrew study
(Scotland), and United Kingdom heart disease pre
vention project (England and Wales).
Subjects—Of the 56255 men aged over 35 who
were included in the studies, 2742 deaths occurred
among 12400 smokers. Average follow up was 13
Main outcome measures—Relative mortality from
smoking related diseases according to tar yields of
cigarettes smoked.
Results—Age adjusted mortality from smoking
related diseases in smokers of filter cigarettes was
9% lower (95% confidence interval 1% to 17%) than
in smokers of plain cigarettes (P=0*047). Mortality
from smoking related diseases consistently
decreased with decreasing tar yield. Relative
mortality in cigarette smokers for a 15 mg decrease
in tar yield per cigarette was 0*75 (0*52 to 1*09) for
lung cancer, 0*77 (0*61 to 0*97) for coronary heart
disease, 0-86 (0’50 to 1*50) for stroke, 0*78 (0*40 to
1*48) for chronic obstructive lung disease, 0*78 (0*65
to 0-93) for these smoking related diseases com
bined, and 0*77 (0*65 to 0-90) for all smoking related
diseases.
Conclusion—About a quarter of deaths from lung
cancer, coronary heart disease, and possibly other
smoking related diseases would have been avoided
by lowering tar yield from 30 mg per cigarette to
15 mg. Reducing cigarette tar yields in Britain has
had a modest effect in reducing smoking related
mortality.
Introduction
The average tar yield of cigarettes in Britain has
steadily reduced from 32 mg per cigarette in 1965 to
14 mg in 1987.' Nicotine levels have also declined.
However, because of compensation—cigarettes with
- ■
lower tar yields being smoked more intensely- (JS2uitmen
reduction in risk of smoking related diseases is liU ^observat
be less than expected from the reduction in tar jx i^ium
In addition, some other toxic components of cign an
smoke have not been reduced in the same property rduths
'.J^years
tar.' If is therefore important to quantify the S
effects of reduction in tar yield on mortality fr tM(mg,'cigar
smoking related diseases.
j
It is reasonably certain that lower tar yields i
associated with reduced mortality from lung one rio smoked :
The position is less clear with other smoking re
diseases, particularly coronary heart disease.”*4 .(/subjects w€
/deaths per It
describe the results of the tar pooling project, inr -nation
_.^ion (on tar
data from four prospective studies were combi^ .
investigate the effects of tar yield on smoking rci _
diseases.
l—Numbe,
Subjects and methods
INDIVIDUAL STUDIES
We collected data on men from four pros?: i
studies—the British United Provident Assoot ■—(BUPA) study (London), the Whitehall c ‘
(London), the Paisley-Renfrew study (Sco,dan£.
■Renfrew
the United Kingdom heart disease prevention F **ase preven
(England and Wales). Table 1 shows details c---studies’: the BUPA study recruited predon#
business and professional men who attended .—
BUPA Medical Centre in London for a compre^ ___
medical examination; the Whitehall study cons?
^Relative r
civil servants; the Paisley-Renfrew cohort wasfrom population registers of the relatively $
economically deprived towns of Renfrew and rin the west of Scotland; and the men in the t
Kingdom heart disease prevention project werec
aged industrial workers from the south of
south Wales, the Midlands, and Manchester- •
studies are described in more detail elsewhere. ^eartdiseas<
?tetructive lur
related
........ —
---------------------------. ..^ng
'••‘yreiateo
Information on smoking was collected throuf ^causes
administered questionnaire completed on entry’
study. Men were classified into four cate? s__
,s*
lifelong non-smokers, former smokers, sm°* **er, coronary
manufactured cigarettes, and other smokers. *»jor
,X5rssmoking r.
non-smokers had never regularly smoked tob*
BMJ VOLUME 311
9DECBM’S •01UME311
any form (more than one cigarette a day, or more than
two cigars a week, or more than '/< ounce of tobacco a
week for as long as one year). Former smokers had
previously smoked some form of tobacco but had given
up completely. Smokers of manufactured cigarettes
smoked only manufactured cigarettes at entry to the
study. Men who smoked hand rolled cigarettes, cigars,
or pipes were grouped as other smokers regardless of
whether they also smoked manufactured cigarettes.
Smokers of manufactured cigarettes were further
categorised according to whether the cigarettes were
plain or filter. A tar yield was estimated for each
smoker from the cigarette brand that was smoked
the longest (was currently smoked in the BUPA study)
using the tar yields published in UK Smoking Stat
istics.' The classification of tar yields was based on the
values at entry to the study. Men for whom the number
or tar yield of cigarettes smoked was not known were
vKZy^Selected details of the four individual studies of the tar pooling project
rpective study
1
BUPA
study
unstall-Pedi’
.
utentry (years)
smoked more intensely—ufreenjitment
•king related diseases is lidyi ^(observation (years):
om the reduction in tar yidl totaum
toxic components of cigars “ft
iuced in the same propomefl’j
portant to quantify the EU ^ed mortality!
i tar yield on mortality
W|mg/Cigarette)*:
Whitehall
study
Professional
and business
men
Civil servants
19167
21398
35-64
36-78*
1975-82
1967-70
245443
1240
314 702
4730
Heart disease
Paisleyprevention
Renfrew study
project
Total
Residents
6591
45-64
1972-6
10-8
1451
workers
9099
1971-3
56255
35-78
1967-82
100
87 604
830
718992
8251
4-36
1-35
22-0
Lain that lower tar yield* I *
80
100
82
100
d mortality from lung cancer,1 ihosmoked > 18 mg/day (%) 48
ear with other smoking rein
_ ^subjects were within age range 40-64.
oronary heart
-v-..disease.
---- ■■—’ . ■ ^deaths per 1000 person years standardised for age.
..he tar pooling project, in wta Hiationontaryieldscouldbedeterminedfor12400of 14372 smokers of manufactured cigarettes.
ctive studies were combined!
of tar yield on smoking rdrj
il—Numbers of men in tar pooling project according to study and smoking status
excluded. The analysis of relative mortality in smokers
of plain and filter cigarettes was based on 14327 men,
and the analysis of mortality according to tar yield was
based on 12 400 smokers.
DEFINITION OF CAUSES OF DEATH
Men from each cohort were flagged at the Office of
Population Censuses and Surveys or the National
Health Service Central Records (Scotland), which
notified all deaths and causes of death. For this
analysis, the causes of death were coded according to
the International Classification of Diseases, eighth
revision (ICD-8). Lung cancer (ICD code 162),
ischaemic heart disease (codes 410-414), chronic
obstructive lung diseases (codes 491-492, 519), and
stroke (codes 430-438) were grouped as “four major
smoking related diseases.” Twenty other diseases for
which excess mortality in smokers was suggested by
the International Agency for Research on Cancer to
be partly or wholly attributable to smoking” were
grouped as “other smoking related diseases.” “All
smoking related diseases” consisted of both the four
major smoking related diseases and the 20 other
smoking related diseases. Other causes of death were
grouped as “the remaining causes.”
STATISTICALANALYSIS
Relative risks were estimated with proportional
hazards regression analysis to adjust for potential
confounding factors such as age and the number of
cigarettes smoked. For each relative risk, 95% con
fidence intervals were calculated, and intervals that
excluded 1 -00 were significant (P < 0’05).
Results
NUMBER OF SUBJECTS AND DEATHS
Table 2 shows the number of men in each study
according to smoking habits. Of the total of 56255
men, 38% were from the BUPA study, 34% from the
Whitehall study, 12% from the Paisley-Renfrew study,
and 16% from the heart disease prevention project.
At entry to the studies, 11 794 (21%) of the men
were lifelong non-smokers, 15 996 (28%) were former
smokers, 14 327 (25%) were smokers of manufactured
cigarettes, and 14 138 (25%) were other smokers. Of
the smokers of manufactured cigarettes, 11 708 (82%)
smoked filter cigarettes and 2619 (18%) smoked plain
cigarettes. No data on smoking were available for 45
men.
There were 8251 deaths observed during an aver
age of 13 years of follow up, of which 5995 were from
smoking related causes.
Smokers of manufactured
Lifelong
cigarettes
Former
---------- Other
smokers smokers
Filter
smokers
on men from four prospCT I
United Provident Assocta
6586
262
3 666
4 519 21398
6365
ndonl^e WhitehaU m
3110
5 275
1216
4 458
5108 19167
-Renfr^Ktudy (Scotland),*
? Renfrew
2124
2346
262
6 591
heart disease prevention pm feascprevention project 1074
4 249
9 099
2011
527
1238
RELATIVE MORTALITY ACCORDING TO FOUR MAJOR
Table 1 shows details ot t _
SMOKING CATEGORIES
study recruited predoffln®
11794
15996
2 619
11708
14138 56 255
Table 3 shows the number of deaths from specific
sional men who attended t
e in London for a compedu®
the Whitehall study connsid ^-Relative mortality (95% confidence interval) of smokers compared with non-smokers from specific causes (adjusted forage and study)
sley-Renfrew cohort was •
psters of the relatively £
Smokers of manufactured cigarettes
d towns of RenfreLifelong
,a; ano u» --in,h£S
Other smokers
No of deaths
non-smokers
Former smokers
Plain
.nd; and the men
prevention project were
----2-23 (206 to 2 41)
1-68 (1-55 to 1-82)
1-23(1-1310 1-33)
2-34 (2-12 to 2-58)
8251
rs iiuju
from the —
southi of«
ers
13-58 (8-31to22-18) 12-85 (808 to 20-43) 8-57 (5-37 to 13-68)
836
3-16(1-9410 5-14)
Manchester.
dlands, and Manchester
1-94
(1-70
to
2-21)
1-56
(1-36 to 1-78)
•yheart
disease
2931
1-21
(1-06
to
1-38)
2-05(1-7310
2-42)
n more detail elsewhere.
1-62 (1-19 to 2-21)
1-98 (1-36 to 2-88)
489
1-00 (0-73 to 1-36)
1-17(0-8510 1-61)
6-44 (3-55 to 11-71) 3-95 (2-13 to 7-35)
2-18 (1-16to 4-09)
obstructive lung disease
283
.NG CATEGORIES AND TAR^, •'•eking related diseases
2-61 (207 to 3-30)
2-32(1-92 to 2-79)
1-80 (1-49 to 2-18)
1-21 (1-00 to 1-46)
1456
1-32 (1-14 to 1-52)
1-16 (1-02 to 1-33)
2256
.□king was collect1-90 (1-69 to 2-13)
4539
1-30(1-1610 1-45)
°rsmoking related diseases*
onaire completed on
2-47 (2-25 to 2-72)
1-87 (1-70 to 2-06)
269 (2-39 to 302)
5995
1-27 (1-15 to 1-40)
tlassificd into four
*?Cer' coronary heart disease, stroke, and chronic obstructive lung disease.
s, former smokers, s®1<T
^jor smoking related diseases plus other smoking related diseases.
ttes, and other
■ver regularly smoked
9 DECEMBER 1995
1531
Table 4— Relative mortality (95% confidence interval) of smokers of filter cigarettes compared wfri'
cigarettes from specific causes (adjusted for age, study, and number of cigarettes smoked a day)* ..
No of filter cigarettes smoked a
1-10
11-20
0-83 (0-68 to 1-00)
0 99 (047 to 2-12)
0-76 (0-56 to 1-03)
1-06 (0-54 to 209)
076 (0-33 to 1 76)
0-76 (0-48 to 1-19)
0-87 (0-59 to 1>30)
0-83 (0-64 to 1-06)
0-81 (0-65 to 101)
0-93 (0-83 to 1-05)
1-01 (073 to 1-39)
0-91 (0-75 to 1-11)
0-74 (0-46 to 1-19)
0-87 (0 77 to 1-45)
0-87 (0-66 to 1-15)
1*03(0*82 to 1-31)
0-91 (0-78 to 1*06)
0-90 (0-79 to 1-03)
Cause of death
All causes
Lung cancer
Coronary heart disease
Stroke
Chronic obstructive lung disease
Other smoking related diseases
Remaining causes
Four major smoking related diseases!
All smoking related diseases!
>20
S
1 04 (0-90 to 1*217^
0-87 (0-61 to 1 22)
1-11 (0-84 to 1-46)
|
0-77 (0-43 to 1*36)
1*33 (0-61 to 2-92)
0-94(0-66to1-33) Jj
1-32 (0-94 to 1-85) aa
1*00 (0 82 to 1-24) 1
0-98 (0-83 to 1*16) £
•Smokers of manufactured cigarettes only.
Rung cancer, coronary heart disease, stroke, and chronic obstructive lung disease.
!Four major smoking related diseases plus other smoking related diseases.
causes and the mortality rates (adjusted for age and
study) for the four smoking categories expressed rela
tive to the lifelong non-smokers. In current smokers
(of tobacco of any form) mortalities from all causes,
lung cancer, ischaemic heart disease, stroke, chronic
obstructive lung diseases, and the group of the 20 other
smoking related diseases were significantly higher than
those observed for lifelong non-smokers. Ischaemic
heart disease and stroke showed an interaction with
age. The relative risk of both diseases in cigarette
smokers compared with lifelong non-smokers declined
with increasing age: the risk of ischaemic heart disease
was 2-66 (95% confidence interval 2-1 to 3-4) in those
aged <50, 1-53 (1-3 to 1-8) in those aged 50-59, and
1 -30 (1 • 1 to 1 -6) in those aged 60 or more, while the risk
of stroke was 2-2 (1-0 to 4-8), 1-46 (0-99 to 24), and
1 -06 (0*7 to 1 *6) in the three age groups.
RELATIVE MORTALITY IN PLAIN AND FILTER CIGARETTE
SMOKERS
Table 4 shows the relative mortality rates (adjusted
for age, study, and number of cigarettes smoked a day)
in smokers of filter and plain cigarettes according to
levels of cigarette consumption. Point estimates for
mortality from each category of smoking related dis
eases were consistently lower in smokers of filter
cigarettes than in smokers of plain cigarettes, but only
the relative mortality for all smoking related diseases
was significantly different (P=O047).
RELATIVE MORTALITIES ACCORDING TO TAR YIELD
Table 5 shows the relative mortalities due to a
decrease in tar yield of 15 mg per cigarette. In the
American Cancer Society study low tar cigarettes were
defined as having, on average, 17-6 mg of tar per
cigarette and high tar cigarettes had, on average,
25-8 mg per cigarette? In our study the mean differ
ence in tar yield between high and low tar cigarettes
Table 5—Relative mortality from specific causes due to decrease in tar yield of 15 mg per
cigarette
Causes of death
All causes
Lung cancer
Coronary heart disease
Stroke
Chronic obstructive lung disease
Other smoking related diseases
Remaining causes
Four major smoking related diseases*
All smoking related diseases!
No of deaths
Relative mortality
(95% confidence interval)
P value
2742
366
917
163
127
486
683
1573
2059
0-80 (0-70 to 0-92)
0*75 (0-52 to 1-09)
0*77 (0-61 to 0-97)
0-86 (0-50 to 1*50)
0-78(0-41 to 1-48)
0-73 (0-53 to 1-02)
0-93 (0-70 to 1-23)
0-78 (0-65 to 0-93)
0-77 (0-65 to 0-90)
0-0014
0-13
0-026
0-61
0-45
0-060
0-64
0-0051
0-0008
•Lung cancer, coronary heart disease, stroke, and chronic obstructive lung disease.
!Four major smoking related diseases plus other smoking related causes.
1532
was about 15 mg per cigarette. Thii
express relative mortalities in ten3
difference. There was a consistent^
mortality from smoking relatedjdj
creasing tar yields; this was signi&S
heart disease, four major smokingf
combined, all smoking related dis
causes. The relative mortality from all 1
diseases due to a decrease of 15 nj
cigarette was 0'77 (0-65 to 0-90). The<
cancer mortality was not significant'
1-09)) because of the relatively small a
from lung cancer (366). No trend wa
mortality from causes not related tdl
Discussion
Mortality from all smoking relateda
lower in smokers of filter cigaretttfi
smokers of plain cigarettes (95% Ctffi
1% to 17%). A decrease in tar jiddj
cigarette was associated with a 23Wu
decrease in relative mortality. We WOt
crease (48% decrease to 9% inaeW
mortality rate from lung cancer fWfl
decrease in tar yield of 15 mg per Qpgg
consistent with other studies. In the I2JI
up of 120 000 male cigarette smokerttprf*
same reduction in tar yield was assocuv*'reduction in mortality from lung ctnctf. A review of the evidence on lower W!**
and ischaemic heart disease concluded W
one study (the largest, the American u*
study), reductions in tar and nicoufttj*’
effect on the risk of coronary disease^
accumulation of further data has
Two case control studies incilC3tc?!^2
lower tar yields.”20 Petitti and Fned®*^;
a 5 mg decrease in tar yield was aw*.
decrease in risk of cardiovascular
showed that cigarette smokers with auy *.
7-5 mg had a 10% lower nskolno
infarction than smokers with
13-3 mg.” Our findings have rewW
The relative mortalin- from ischaow^
reduced by 23% (3% to 39%) h>
of 15 mg per cigarette.
The original uncertainty over „ "
cigarettes on heart disease *
findings. Firstly, in the early
cigarettes with lower tar yre
had higher carbon monoxide )
results of the Framingham snW
of filter cigarettes did not have-®
myocardial infarction y13" ^y"
rettes.” During the 1960s and
BMJ VOLUME 3W
almost complete switch from plain to filter cigarettes,
so that comparisons between plain and filter became
less relevant. By the late 1970s most of the differences
between smokers in tar yield reflected differences in
filter cigarettes alone, and among filter cigarettes there
was, and still is, a high correlation between yields of
tar, nicotine, and carbon monoxide.
Data on the effect of tar yield on the risk of chronic
obstructive lung diseases,2’21 stroke, and other smok
ing related diseases are sparse. In our study death rates
from these diseases were associated with tar yield, but
the association was not significant. The position there
fore remains uncertain.
POTENTIAL SOURCES OF BIAS
Two sources of bias may have underestimated the
association between tar yield and mortality in our
study. Firstly, smokers often do not identify their
brand of cigarette with sufficient accuracy,” and
brands with similar names can have different tar yields.
Secondly, in the studies we used, tar yields were higher
before entry into the study and in the earlier years of
the subjects’ smoking history. The studies recorded
only the tar yields of cigarette smoked at entry to the
study, yet the subsequent tendency was to switch to
lower yield cigarettes. With the reduction in the
average tar yield of cigarettes sold in Britain over the
past two decades, the range of tar yields would also
have become narrower. The range of death rates from
smoking related diseases that were recorded were
therefore incorrectly related to the range of tar yield on
entry to the study rather than to the narrower range
during follow up. This may be important since recent
exposure to cigarette smoke is more relevant to risk.26
Confounding by social class did not seem to be a
problem. Data from the Whitehall and the RenfrewPaisley studies indicated that social class had little
effect on the estimate of the effects of tar yield on
mortality.
Our results indicate that the reduced tar yield of
British cigarettes over recent decades has reduced
mortality from smoking related diseases. The potential
for further reductions in mortality from further tar
yield reductions may be more limited. Very low tar
cigarettes have not been widely accepted.2’ In Britain,
in spite of the increasing number and advertising of low
tar brands, the percentage of smokers who smoke
cigarettes of tar yield below 10 mg per cigarette has
remained small and has hardly changed since 1978.'
Tar yields from British cigarettes are currently limited
by regulation to 15 mg per cigarette, and this will fall to
12 mg per cigarette at the end of 1997. Future public
health policy would be best directed mainly towards
preventing cigarette smoking through public edu
cation, tobacco taxation, stricter legislation (including
control over advertising of cigarettes), and measures
that will discourage children and young adults from
taking up the habit.
We thank Cheryl Swann and Robert Waller for their'
comments.
Funding: Tobacco Products Research Trust and BUPA
Medical Research and Development.
Conflict of interest: None.
CONCLUSION
About a quarter of deaths from lung cancer, coron
ary heart disease, and possibly other smoking related
diseases could be avoided by switching from higher tar
cigarettes (30 mg/cigarette) to lower tar ones (15 mg/
cigarette). This is consistent with studies of compen
satory smoking; switching to cigarettes of half the tar
yield reduces tar intake by about a quarter rather than
a half.2
Key messages
• It is reasonably certain that smoking low tar
cigarettes rather than high tar cigarettes reduces
risk of lung cancer, but the position is less clear
with other smoking related diseases, particularly
coronary heart disease
• We used data from four large British cohort
studies to investigate effect of lowering tar yield
on smoking related diseases
• Mortality from smoking related diseases was
reduced by about 23% for a reduction in tar yield
of 15 mg per cigarette
• Mortality from ischaemic heart disease was
also reduced by 23%, and mortality from lung
cancer was reduced by 25%
• Britain’s policy of reducing the tar yield
of cigarettes has been associated with modest
benefits, but these benefits are much less
than that associated with stopping smoking
completely
(Accepted28 September 1995)
°LUME 311
9 DECEMBER 1995
1533
PAPERS
:ttcs; and a.L
ng at sponi,s£M
t related t0
and hats. vsg|
o include a
ompanies
3m) advert
Cigarette smoking, tar yields, and non-fatal myocardial infarction
14000 cases and 32 000 controls in the United Kingdom
S Parish, R Collins, R Peto, L Youngman, J Barton, K Jayne, R Clarke, P Appleby, V Lyon,
S Cederholm-Williams, J Marshall, P Sleight for the International Studies of Infarct Survival (ISIS)
Collaborators
for under agc
*
ibutors, and rttS’I
bacco ccmpajgSB
companies, iMr/*!
.on Tobacco q
□mpany is
ZJI
ie
Food and
orth Carolina,
bl
1
an is impeding
n the
—
is by
„
Henges the admiatj
overstep its botsdjl
,e, medical proi,-..
I companies by os
r tobacco.
.1
Congress to teas
sals will go forrat!
eked completdy.Jii
cs predict that MrQ&IU11 Senice Unit
promised his dais■jUtenological
Democrats and Rp Writ, Nuffield
u the southern dal net ofClinical
red his proposals
la.Raddiffe
ia’s Republican s? wy,Orford
^enMohn
*^Orford
on, said that it
Congress to dead *
non could go.-» p.teuA Heart
journalist, Bost®
^sorofmedical
Bitfidemiology
umor research
administrator
administrator
BOrdtfellow
^erth fellow
fellow
*faor emeritus of
Oxford
Abstract
Objectives—To assess the effects of cigarette
smoking on the incidence of non-fatal myocardial
infarction, and to compare tar in different types of
manufactured cigarettes.
Methods—In the early 1990s responses to a postal
questionnaire were obtained from 13 926 survivors of
myocardial infarction (cases) recently discharged
from hospitals in the United Kingdom and 32 389 of
their relatives (controls). Blood had been obtained
from cases soon after admission for the index
myocardial infarction and was also sought from the
controls. 4923 cases and 6880 controls were current
smokers of manufactured cigarettes with known
tar yields. Almost all tar yields were 7-9 or 12-15
mg/cigarette (mean 7-5 mg for low tar (< 10 mg) and
13*3 for medium tar (2^10 mg)). The cited risk
ratios were standardised for age and sex and com
pared myocardial infarction rates in current
cigarette smokers with those in non-smokers who
had not smoked cigarettes regularly in the past
10 years.
Results—At ages 30-49 the rates of myocardial
infarction in smokers were about five times those in
non-smokers (as defined); at ages 50-59 they were
three times those in non-smokers, and even at ages
60-79 they were twice as great as in non-smokers
(risk ratio 6*3, 4-7, 34, 2*5, and 1*9 at 30-39, 40-49,
50-59, 60-69, 70-79 respectively; each 2P< 0-00001).
After standardisation for age, sex, and amount
smoked, the rate of non-fatal myocardial infarction
was 10-4% (SD 5-4) higher in medium tar than in low
tar cigarette smokers (2P=0-06). This percentage
was not significantly greater at ages 30-59 (16-6%
(7-1)) than at 60-79 (1-0% (8-5)). In both age ranges
the difference in risk between cigarette smokers and
non-smokers was much larger than the difference
between one type of cigarette and another (risk ratio
3-39 and 3-95 at ages 30-59 for smokers of similar
numbers of low and of medium tar cigarettes, and
risk ratio 2-35 and 2-37 at ages 60-79). Most possible
confounding factors that could be tested for were
similar in low and medium tar users, with no
significant differences in blood lipid or albumin
concentrations.
Conclusion—The present study indicates that the
imminent change of tar yields in the European Union
to comply with an upper limit of 12 mg/cigarette will
not increase (and may somewhat decrease) the
incidence of myocardial infarction, unless they
indirectly help perpetuate tobacco use. Even low tar
cigarettes still greatly increase rates of myocardial
infarction, however, especially among people in
their 30s, 40s, and 50s, and far more risk is avoided
by not smoking than by changing from one type of
cigarette to another.
19 august 1995
Introduction
In countries such as the United Kingdom, where
cigarettes have been used widely for several decades,
tobacco now accounts for about 30% of all deaths in
middle age, with lung cancer and coronary heart
disease the most common fatal conditions. Over the
past few decades cigarettes have been altered in various
ways, reducing die so called yields of tar and nicotine
when smoked in a standard way by a machine. Typical
British cigarettes had tar yields of 25-35 mg during the
1950s and 5-15 mg in 1990/ But, partly because
the chief toxins in cigarette smoke are uncertain and
partly because smokers may compensate for reduced
yields (or other changes) by smoking cigarettes more
actively,the health effects of alterations in cigarette
manufacture are unpredictable. Low tar cigarettes do
cause substantial risks of cancer and heart disease,
although the risk of lung cancer is less than with high
tar cigarettes? “‘14 For heart disease, however, there
remains uncertainty,’■,7 about whether the rates have
been decreased, increased, or not changed by alter
ations in cigarette composition over the past few
decades. National heart disease mortality rates and
trends are not informative because other factors cause
such large differences in coronary heart disease
between different populations and time periods.
Instead, concurrent epidemiological comparisons
within one population are needed.
But, although tobacco is a major cause of heart
disease, particularly among young and middle aged
adults, it is difficult for conventional prospective or
retrospective studies to compare the risks from dif
ferent types of cigarette. Only a narrow range of
cigarette tar yields is concurrently available within one
population, and the tar yields of cigarettes smoked by
people in 1990 might correlate poorly with the tar
yields smoked by these people years earlier. Hence,
even large differences in risk between prolonged use of
low, medium, and high tar cigarettes might produce
only small differences in risk between current use of
low and medium tar cigarettes. At younger ages the
proportional difference in rates of coronary heart
disease between smokers and non-smokers is particu
larly extreme, so any effect of cigarette type may also
be extreme. Thus, to minimise the chances of a false
negative result in a study of tar yields, the number of
cases of myocardial infarction in middle aged cigarette
smokers should be large—preferably several thousand
—with at least as many controls. We achieved this
by studying subjects from the United Kingdom
who participated in the large ISIS (international
studies of infarct survival) trials of the treatment
of acute myocardial infarction,by using postal
questionnaires (copies available on request), rather
than interviews, and by simplifying blood collection
procedures.
Patients and methods
CASES AND CONTROLS
Cases were the survivors in the United Kingdom
aged 30-79 from the ISIS-3 or ISIS-4 trials who
completed an epidemiological questionnaire sent to
them a few months after their infarction. Those who
were asked to complete it were all the survivors from
ISIS-3, but from ISIS-4 only the survivors aged 30-59
who on admission to hospital were reported to be
cigarette smokers. Thus, although only cases from
ISIS-3 can be used to compare smokers with nonsmokers, the cases from ISIS-4 strengthen the analyses
of tar yields among smokers aged 30-59. The ISIS-3
questionnaire asked the cases to identify all their
brothers, sisters, and children aged at least 30
who were resident in the United Kingdom. A
similar “control” questionnaire was then sent to
such relatives, accompanied by a second copy, which
the relatives, if married, were to ask their spouse to
complete. One reminder was sent to cases and relatives
who did not reply, and inconsistencies or omissions
were queried once.
Of the 20 681 ISIS-3 patients in the United King
dom, 19065 who were not known to be dead were
posted the case questionnaire, of whom 1346 were
found to be dead and 13969 (79% of presumed
survivors) completed it. The control questionnaire was
sent to 30247 relatives of ISIS-3 cases, of whom 75
were found to be dead and 21 995 (73% of presumed
survivors) and 14245 of their spouses completed it.
Patients with a history of stroke, gastrointestinal
bleeding, or ulcer tended not to have been recruited
into the ISIS-3 trial,” and so people with such condi
tions were not eligible as cases or controls. Of those
who completed questionnaires, 2002 cases and 3851
controls were excluded because they were under 30,
over 79, or of unknown age or because they had a self
reported history of “definite stroke” or of “bleeding or
ulcer in (or near) the stomach.”
ISIS-4 patients in the United Kingdom aged 30-59
who were described at trial entry as current smokers
were also sent the questionnaire. The response rate
for such patients was similar in both trials. Any of
these ISIS-4 patients whose questionnaire response
indicated that they were not cigarette smokers at the
time of their infarction were excluded. ISIS-4 (and, to
some extent, ISIS-3) tended to exclude patients with
shock or persistent hypotension,20 but such exclusions
should not bias the epidemiological analyses of tobacco
use.
BLOOD SAMPLES
Blood was to be taken from patients in ISIS-3
immediately after randomisation but before the trial
treatments and collected in a 10 ml vacutainer con
taining 0-12 ml preservative (15% potassium EDTA
with aprotinin 0-34 mmol/1: Becton Dickinson). On
returning their questionnaire, controls were sent an
identical container for their general practitioner to
collect blood. Case and control containers were sent by
first class post to Oxford. Controls were sent one
reminder about giving a sample. After a mean of two
days in the post the blood was centrifuged, the packed
cell volume was recorded, and the plasma and bufiy
coat were aliquoted for storage at -40°C. Blood arrived
from 97% of ISIS-3 cases and 45% of controls, but
breakages or haemolysis rendered 6% of these samples
unusable. The present blood analyses involve only
correlations of smoking with blood biochemistry
results, and these analyses should not be materially
biased by low response rates.
Plasma cotinine concentration was measured in
controls who were current cigarette smokers, and in
a 3% sample of controls who reported no current use
of tobacco, by means of antibodies developed by Knight
ct al in a modification for plasma
radioimmunoassay. 21 Results with
correlate closely with those with gas
Beckman CX-4 and CX-5
for measuring concentrations of
albumin (both with Beckman
proteins AI and B (with Immuno
for discoloration from haemolysis,
reading was subtracted from the final
from a large plasma pool were
analytical run, yielding coefficients of
for cholesterol and albumin and
proteins.
QUESTIONNAIRES
Information was sought on sex,
smoking, drinking, past health, and
were asked about their habits and
their index myocardial infarction
heart attack may alter a patient’s
were asked about their present
lions to cases often began, “Befo
admission. . . .” Both cases and
to list how many relatives of certain
but only cases were to provide
other respects case and control
identical. The medical history
technical and recorded various
be associated with exclusion from the
(see above) or that might affect, or be
smoking. After the question
smoked regularly (ie on most days
the rest of the cigarette section was to be
only by those who replied “yes.”
which the subject had first and last
whether any cigarettes had been smoked
vious month, the number smoked per day wfc
subject had last smoked cigarettes regularfyS
way in which cigarettes were smoked. Pcopkw
tick against 137 detailed brand names the m
when they last smoked, they usually smoked oat
or, if it was not on the list, to write out its
(and, whenever possible, to enclose the padd
that brand with the questionnaire). For the W
listed more than one brand, the average of thty
was taken. Ninety eight per cent of controls efi
of cases who currently smoked only manata
cigarettes with a known tar yield, and both
using their current brand for, on average, the|N
or 11 years.
DEFINITIONS OF CIGARETTE SMOKING STATUS 3
Respondents were classified as current dp
smokers (26% of the controls: those who had S1
^•Tciacco use in case.
cigarettes in the previous month, plus the
failed to answer this yes/no question but grt1
evidence of current cigarette use); other tobacrfl
(3%: pipes, cigars, or smokeless tobacco in &
Manufac
year); or as not using tobacco (71%: all odra
table I these are further subdivided. Became*
possible confusion between those who
smoking many years ago and those who never R
688(
cd*
the main comparison group was defined
* k 3o_59
218‘
ularij $
30-59
smokers who had not used cigarettes regur
326*
| **79
563
past 10 years.
.*5 **79
ESTIMATED 1990 TAR YIELDS
*59
The United Kingdom’s government ch&&
858
ducts surveys of common cigarette brands, fl* * *79
tar, nicotine, and carbon monoxide yields,
(R Waller, personal communication).
* £59
1980s the annual decrease in sales weighted P* gg
about 2-3% for tar, 1-2% for nicotine, an<L
11803
carbon monoxide (J Rentoul, personal co^
tion).« Most ISIS-3 cases replied in 1990 abo*
’’odnon-ujcra.
i
BMJ
volume 311
19AlJ
before their myocardial infarction (mean date of
infarction: February 1990), most controls replied in
1990-1 (mean: November 1990), and most ISIS-4 cases
replied in 1992-3 (mean date of infarction: July 1992).
To avoid secular trends in yields introducing minor
biases, the mid-1990 survey results for each cigarette
brand were used (R Waller, personal communication).
If a brand was assayed only earlier or later than mid1990, yields from the closest survey were extrapolated
to mid-1990 by annual decreases of 2-5% in tar and
1-5% in nicotine.
RESURVEY OF CONTROLS A FEW YEARS LATER
To check reproducibility, about 2000 controls
who originally returned both questionnaire and blood
sample (and whose replies indicated no previous
vascular disease) were sent the same questionnaire and
blood kit again about 2-3 years later. To avoid oversampling young controls, the random sample was
stratified with respect to sex and age in groups of five
years. Seventy per cent (1388/1996) returned the
questionnaire, 95% (1324/1388) of whom gave blood.
STATISTICAL METHODS
The analyses are all unmatched—that is, they
compare cases with all controls, not just with their own
relatives—and for tar yield analyses among smokers
the controls are as relevant to ISIS-4 as to ISIS-3 cases.
All analyses of myocardial infarction rates were strati
fied either for sex and five year age group or for
these factors and amount smoked (five categories; see
below). Calculations of risk ratios—or, equivalently,
relative risks—entailed unmatched stratified logistic
regression (fined by unconditional maximum likeli
hood), with one extra term included for each stratum.
Risk ratios are often given with 95% confidence
intervals. Two sided probability values (2P) are used.
fig 1—Replies by controls who smoked manufactured cigarettes only.
(a) Reported daily cigarette use (34% reported 20 cigarettes per day,
and 85% reported 10-30). (b) Taryields in 1990 ofthe brands reported
tion of (a) the reported number smoked per day and (6)
the estimated 1990 tar yield. Self reported cigarette
consumption was categorised as 1-9, exactly 10,11-19,
exactly 20, and >21 cigarettes a day; 85% reported
smoking 10-30 cigarettes a day. The tar yields show a
bimodal distribution, with commonest values 7-9 or
12-15 mg/cigarette. Tar yields of TO mg were, rare,
which makes this a natural point of subdivision,
unaffected by any slight differences in dates of case and
control responses, to define two main categories: low
tar (< 10 mg, mean 7-5 mg) and medium tar (> 10 mg,
mean 13-3 mg). Medium tar is sometimes split into 1012,13, and > 14 mg/cigarette. This definition of low tar
is also used by the Department of Health (R Waller,
personal communication). 4 Twenty five per cent of the
smokers in figure lb use low tar cigarettes, as in the
nationally representative survey in 1990?’ Almost all
Results
FREQUENCY DISTRIBUTIONS OF SMOKING HABITS
Table I shows the numbers of controls and cases in
various categories of tobacco use subdivided by sex and
by age. The age range of chief relevance to the tar yield
analyses is 30-59, and among controls in this range 28%
both of men and of women were current cigarette
smokers, in close agreement with nationally represen
tative, interviewer administered surveys in the early
1990s.” Twenty two per cent of these controls were
current users of manufactured cigarettes only with
known tar yields.
Figure 1 gives, for controls who currently used
manufactured cigarettes only, the frequency distribui-Tobauo use in cases and controls aged 30-79 with questionnaires returned
Current cigarette smoker
Manufactured cigarettes and no
other tobacco
known
30-59
Tar
unknown
Not using tobacco
Other tobacco
Other
cigarette
users
Now
using any
cigarettes
Smoking pipe
or cigar but no
cigarettes
Using
26
28
28
20
21
38
48
60
27
35
—
—
—
1031
676
11
337
71
40
859
405
o
450
4
_
_
—
28
2
48
">6
0
20
2
_
_
—
-
1890
119
6880
2184
3264
563
869
3453
1351
520
858
724
1470
1117
353
162
35
60
21
46
65
23
16
18
34
29
5
1389
958
153
251
27
1063
619
33
382
29
455
430
25
11803
261
2907
Former regular cigarette smoker
regular
<10 years ago
& 10 years ago
smoker
Total*
3181
1128
1145
465
443
1311
424
98
537
252
_
—
5502
1785
1385
1506
826
2070
467
47
1268
288
_
_
—
14173
4357
6559
906
2351
3098
804
236
1171
887
_
_
—
32389
11163
12578
4077
4571
11967
4119
942
4702
2204
1959
1576
383
4492
7572
17271
46315
non-usets.
311
19 august 1995
473
In figure 2b the mean cotinine vaju '^1
third higher among the controls who
tar cigarettes (low tar 217 ng/ml *****
292 ng/ml). But the smokers of 1O^
reported smoking 15-8 cigarettes a day '
18-7 a day for those in the medium t?
standardisation for age, sex, and an
however, the mean plasma cotinine co
still 19% higher with medium tar
difference in cotinine is still hiahV
(2P< 0-00001), which helps validate the 9
of tar yield based on the questionnaire
extreme than the difference of over 50%
yield per cigarette measured by machine (
1-18 mg). This may be partly because tW
tion of tar yields is imperfect, and •*.smokers of low yield cigarettes comp
in more smoke per cigarette. But, since thS
tion predicts highly significant biochemical
in blood taken months later (figure 2b) Ft
validity.
FIG 2—Cotinine by cigarette
smoking habit in controls, (a)
Cotininc versus daily cigarette
use. (b) Cotinine versus taryield
of reported brand. In the low and
medium tar smokers whose blood
samples were assayed, mean
plasma cotinine concentrations
were 217 and 292 ng/ml, mean
18-7, and mean yields per
tar, 0'75 and 1'18 mg nicotine,
monoxide. Blood was taken on
average ofeight months after
293 whose questionnaire had
table n—Non-fatal myocardial infarction: age-specific effect of cigarette use in people with no history of
major neoplastic or vascular disease
Myocardial infarction*
Risk ratio (95%
confidence
Age (yean)
30-39
40-49
50-59
78
293
435
1784
1497
861
35
190
508
4873
4306
2701
30-59
806
4142
733
11880
60-69
70-79
60-79
416
111
527
653
163
816
707
369
1076
2299
942
3241*6
CIGARETTE USE AND NON-FATAL MY
INFARCTION
When those using manufactured d
were compared with non-smokers who had n«
cigarettes regularly in the past 10 years (
both cases those using any other type oftob^
relative risks for non-fatal myocardial i
people with no previous neoplastic or major
disease depended strongly on age (table II, fig
the case for mortality from coronary heart
the risk ratio comparing smokers with no
was greater at younger ages, reinforcing the to'
the relevance of tar yields to be considered
younger and older ages.
TAR YIELDS AND NON-FATAL MYOCARDIALINFA^j &'•' X ■
Information about the relevance of tar yid&g E
from current users of manufactured cigaretttug
these, much the most informative are the j
30-59, rather than the 3000 aged 60-79. Thhbifc
because the numbers are larger but also btttt
risk ratio when smokers are compared
ter
Myocardial Infarction and cigarette smoking:
. 12 000 cases and 32 000 controls
fNumber ofstandard deviations by which the logarithm ofthe risk ratio differs from zero.
used filtered brands (100% of the low tar group, 96%
of the medium tar group), so filters accounted for little
of the difference in yields between low and medium tar
cigarettes in 1990.
RELATION BETWEEN QUESTIONNAIRE AND COTININE
CONCENTRATIONS
Figure 2 shows the relation between plasma cotinine
concentrations and (a) reported daily cigarette use and
(6) tar yield for controls reporting use of manufactured
cigarettes only or no current tobacco use. The mean
cotinine concentration was very low in the self reported
non-smokers, which helps validate both questionnaire
and laboratory results. Among cigarette smokers there
was a strong relation between cotinine concentration
and the amount reported to be smoked, which again
helps validate the questionnaire. The downward
curvature in figure 2a suggests that those who smoke
more cigarettes may absorb less nicotine from each one
or that those reporting large numbers include dispro
portionately many who overreported, or both. Either
way, self reported cigarette consumption provides only
approximate information about the real doses of
nicotine and of other substances.
Age 30-59
Risk ratio 3.85
fig 3—Cigarettes and non-fatal myocardial infarction"
risk ratios at various ages. Results in people with nfP’r
major neoplastic or vascular disease. Each risk ratio «
sex: and
a::df::
for quinquennium of
:f age, and compares
lured
cd cigarettes only with those who were not currt^Lf
tobacco and had not been regular cigarette smokeri^jKi
past 10 years. Risk ratio is given within each colu*~^p
recruited from ISIS-4 were cigarette smokers, this pS^
onlyfrom ISIS-3)
BMJ VOLUME 311
311
tinine values Werc'JJH
toIs who smoky
,7 ng/ml v
was much larger than the difference between one type
of cigarette and another: the risk ratios were 3.39 and
3-95 for smokers of similar numbers of low and of
medium tar cigarettes at ages 30-59 and were 2-35 and
2-37 at ages 60-79. (Table III shows that results were
similar when these comparisons were based on the
smaller numbers of cigarette smokers with no reported
history of neoplastic or major vascular disease.)
xttes a day conv>?M
t medium tat
■ex, and amount
cotinine concena^\
dium tar cigate^W|
s still highly
s validate the catejS?
questionnaire. But
of over 50%inthe^
1 by machine (075^*
rtly because the cs2^
2®®
1
ettes compensatebj>?
e. But, since this ptJj
ant biochemical disj?
er (figure 2b), it
es, reinforcing the tri
o be considered sepin^ d v—Reproducibility ofsmoking classification
Response to original questionnaire
t MYOCARDIAL INFARCUX
-elevance of tar yields a
ufactured cigarettes 01)
formative are the 90001 ^2-3 years law
0 aged 60-79. This ism ------------------larger but also beaux atari cigarettes only
s are compared wiih 1
Not using tobacco “
Currently using tobacco
Manufactured
cigarettes
only
tobacco
user
Former cigarette smoker
CiOyears
>10 years
Never
cigarette
smoker
99*
9
5
0
1
86
7
3
3
12
50
11
0
8
n~~~l Excess with ogvea ra of these had known tar yield at both enquiries (65 cla
slew then low, 8 as medium then low, 3 as low then mcdiui
r—! Not caused by sax
smokers is more extreme in middle than in old age.
As there was no significant difference between the tar
yields of cases aged 30-59 in ISIS-3 and in ISIS-4
(table III), the groups were combined.
Table III provides age-sex standardised compari
sons of non-fatal myocardial infarction in smokers of
low tar versus smokers of medium tar cigarettes.
Overall, there were only slight effects of the tar yield.
The mean daily number of cigarettes smoked was
slightly higher in the medium tar than in the low tar
cigarette smokers (19-0 v 17-1). When standardised
not just for age and sex but also for the daily number of
cigarettes smoked, the incidence of myocardial infarc
tion was 104% (SD 5-4) higher in medium than in low
tar cigarette smokers (2P=0-06). This difference was
non-significantly greater at ages 30-59 (16-6% (7-1)
higher; 2P=002) than at 60-79 (1-0% (8-5) higher;
2P>0*l) (fig 4). As these two results are not signific
antly different from each other, they do not prove that
tar yields are of greater proportional importance to the
cardiotoxicity of cigarettes in middle than in old age,
especially since the smoker versus non-smoker risk
ratios are less extreme in old age. In both age ranges the
difference between cigarette smokers and non-smokers
.VMB3H
I9a^<uME31I
19 august 1995
____
POTENTIAL CONFOUNDING FACTORS
Table IV relates smoking to blood lipid concentra
tions among ISIS-3 cases entering the trial within 0-4
hours of pain onset whose blood spent only one or two
days in the post, and among one randomly chosen
control per case (matched for age, sex, and days sample
spent in the post). Apolipoprotein A. was 1-2% lower
and apolipoprotein B 2-4% higher in smokers than in
non-smokers, but these differences are too small to
account for much of the excess risk among smokers.
There were no significant differences in blood lipid
concentrations (or albumin concentration, data not
shown) between smokers of low and of medium tar
cigarettes, either overall or in those aged 30-59 (data
not shown). For many factors there were likewise
no significant differences between smokers of low
and medium tar cigarettes. These include self
reported height, weight, loneliness, depression,
worry, insomnia, teenage acne, tea consumption,
alcohol consumption, and whether living with a
spouse. For a few factors, however, there were definite
differences even after standardisation for age and sex.
(Multivariate adjustment for these observed differ
ences would make little difference, but these
differences point to the possibility of others existing.)
Those who smoked low tar cigarettes were, on average,
almost six months older when they left full time
education (mean leaving age 15-9 years for low tar
group v 15-5 years for medium tar), were more likely to
say that they had matured physically “later than
average” (13-4% v 10*5%), had “softer hands than
average” (14-4% v 11*0%), had been regular drinkers
of coffee (75% v 67%), were older when they started to
smoke (18*8 v 17-9 years old), and had changed to their
current brand more recently (7'9 v 10-1 years pre
viously). These suggest a general tendency for those
who smoke medium tar cigarettes to include a slightly
larger proportion of manual workers, and to have
slightly less education. (Likewise, unpublished
analyses by M Jarvis of the 1990 and 1992 general
household surveys in the United Kingdom found
significantly higher “indices of deprivation” in users
of medium than of low tar cigarettes.)
REPRODUCIBILITY OF SMOKING CLASSIFICATION
A total of 1388 controls repeated the questionnaire a
few years later, and table V compares their two replies.
When subdivided three ways (manufactured cigarettes
only; other tobacco or ex-cigarette smoker < 10 years;
remainder), 90% remained in the same category; of the
97 who smoked only manufactured cigarettes with tar
known on both occasions, 89% had continued to smoke
medium or low tar cigarettes as originally. Overall,
there was a 5% shift towards the low tar category, in
line with national trends, and the correlation co
efficient between the two assessments of tar yield was
0-71.
Discussion
When cigarette smokers are compared with nonsmokers the risk ratio for myocardial infarction is
much more extreme in early adult life than in old age.
The numbers contributing to figure 3 are unusually
large (12000 cases and 32000 controls) and so the
pattern of steadily increasing risk ratio with younger
475
age is particularly reliably demonstrated, as are the
hazards at the extremes of the age range of 30-79. The
risk ratio is twofold at ages 70-79, but it is almost
fourfold at ages 30-59 (threefold at 50-59 but fivefold at
30-49). Even these large differences have probably
been somewhat diluted by the misclassification of some
smokers or non-smokers. Had it been possible, with no
classification errors, to compare persistent cigarette
smokers with lifelong non-smokers then the risk ratios
would probably have been still more extreme than
those in figure 3, and would have been at least fourfold
at ages 30-59. As most of the excess risk associated with
smoking is caused by smoking,'1 this fourfold risk
ratio implies that about three quarters of the
myocardial infarctions among cigarette smokers aged
30-59 were caused by tobacco (two thirds at ages 50-59,
but four fifths at ages 30-49).
Any differences in the risk of heart disease between
those who are smoking different types of cigarette must
be much less extreme than the differences between
smokers and non-smokers, so especially large studies
are needed to assess them. Moreover, epidemiological
studies that were undertaken when tar yields below
15 mg were still uncommon (N J Wald et al, un
published data)2*-50 are of limited contemporary
relevance in countries such as the United Kingdom
where tar yields above 15 mg have already virtually
disappeared (fig lb) and where a European Union
upper limit of 12 mg is soon to be enforced. As no other
large recent studies are available, our current findings
stand alone.
For tar yields the central finding is that after
standardisation for age, sex, and number of cigarettes,
the incidence of non-fatal myocardial infarction
seemed to be about 10% greater with medium tar than
with low tar cigarettes (95% confidence interval 0 to
22%, table HI). Even if this 10% difference was highly
statistically significant (which it is not: 2P=0-06) it
would still not be epidemiologically secure. It is
uncertain how much selective emphasis to put on the
data at ages 30-59 as opposed to those at 60-79, how
much selective emphasis to put on the data from people
with no previous disease, and how much to emphasise
Myocardial infarction and cigarette tar yield
Low tar (< 10 mg, mean 7.5 mg)
Medium tar (> 10 mg, mean 13.3 mg)
FIG 4—Cigarette tar yields and risk of non-fatal myocardial infarc
tion. Standardised for age, sex, and amount smoked, comparisons at
ages 30-59 indicate that non-fatal myocardial infarction rates were
1-166 (SD 0-071) times as great among medium tar as among low tar
cigarette smokers (2P=0-02; table III). The same standardised
comparisons at ages 60-79 give 1-010 (0-085) (NS). These two
estimates (1 -166 and 1-010) are combined with the risk ratios of 3-85
and 2-37 for cigarette smokers versus non-smokers (fig 3) to yield the
cited risk ratios for smokers of low and medium tar cigarettes: 3-39 and
3-95 at ages 30-59 and 2-35 and 2-37 at ages 60-79
476
Key messages
• Non-fatal myocardial infarction L
times as great among cigarette snto *
non-smokers at ages 30-49, three"
at ages 50-59, and twice as great
• Among cigarette smokers fotn- ^
myocardial infarctions at ages 30-4qgjji
by tobacco, two thirds at ages 50-50*™*
ages 60-79
• The risks seem to be slightly
medium tar than with low tar ci
difference is not definite
• Differences in risk between cigarette
and non-smokers are far greater thati i
ences in risk between one type of
another
• Far more myocardial infarctiont'^L
avoided by not smoking than by chswO
one type of cigarette to another
^Xumber
analyses that are standardised for the atnotgi
(Those using low tar cigarettes reporttd
slightly fewer than those smoking
cigarettes, and if lower daily consumption^
consequence of lower yields of tar, nicotine,
smoke components then it should not be ai
ised for.) Hence, table IH repons seven!
comparisons of disease rates in smokers
smokers, with differences that are sometimes^ f
sometimes less than 10%. Also, there wa j,
tendency for tar yields to be inversely nkeducation and to various other aspects of soa‘.
is difficult to see how some of these uncermsaj ■
resolved: large scale randomisation is imps.
and even if the present study could have been .
larger, thereby .narrowing the confidence innrt
possibility of confounding would remain.
•
Despite these uncertainties, however,
results provide some reassurance to those if
ment or in industry who could direct des:,
cigarette tar yields to reduce cancer indte
They indicate that such changes will not icbfv
increase the incidence of myocardial intae
may well decrease it. Thus, the limit of 12 tn$k»
on tar yields that is now being introdwrfl
European Union should help limit the
premature deaths from tobacco, unless govts?
smokers come to regard reductions in at F
substitutes for the avoidance of cigaretftj
developed countries tobacco remains mud:*
important cause of premature death. This* J j
larly so for men, with tobacco now causst*
third of all deaths in middle aged men.
women have been smoking cigarettes for sect.
(as, for example, in the United Kingdom or®'
States) tobacco also already causes about if
all the deaths in middle aged women.'
Public
For the general population, therefore, P ’kksc, Mj
important finding is not the slight and * ^ftsctlce,
difference in figure 4 between one type
another but the large and definite diff«eD*
90220
3 between cigarette smokers and W*;
particuularly in early middle age. 1^'
whether low or medium tar cigarettes are &
laa"
three quarters of the smokers who have a
^de^^
in their 30s, 40s, or 50s need not have dont .
more heart attacks could be prevent.
prevented by “ ’to:
than by reducing cigarette tar yields.
The chief acknowledgment is to the pa
BMJ
volume 311
relatives who collaborated in this study, and to the medical
and nursing staff from more than 100 hospitals in the United
Kingdom listed in the ISIS reports.”10 We particularly thank
Peter Froggatt, Cheryl Swann, and Robert Waller of the
Independent Scientific Committee on Smoking and Health,
Department of Health; Keith Darrall of the Laboratory of the
Government Chemist; Martin Jarvis of the Imperial Cancer
Research Fund; and Kuldip Bhamra, Vanessa Boag, Lee
Buckingham, Mary Burton, Sarah Clark, Sarah Edwards,
Sheila Foster, Heather Halls, Mavis King, Karen Kourellias,
Christine Marsden, Gale Mead, Kevin Murphy, Martin
Radley, and Karl Wallendszus of the Oxford Clinical Trial
Service Unit and Epidemiological Studies Unit.
Funding: The ISIS trials and epidemiological studies were
supported by the manufacturers of the study drugs”20 and by
the British Heart Foundation, Imperial Cancer Research
Fund, Medical Research Council, and Tobacco Products
Research Trust of the Independent Scientific Committee on
Smoking and Health, Department of Health.
Conflict of interest: None.
12
13
14
Kaufman DW, Palmer JR, Rosenberg L, Stolley P, Warshauer F Shaoiro S.
Tar content of cigarettes in relation to lung cancer. Am v
1989;129:703-11.
J Epidermal
Stellman SD, Garfinkcl L Lung cancer risk is proportional to cig,rcnc ...
yield: evidence from a prospective study. Prev Med 1989;18:518-25.
Wynder EL, Stellman SD. Impact of long-term filter cigarette usage on lung
and larynx cancer risk: a case-control study. J Natl Cancer Inst 1979;g2-
15 Kaufman DW, Hclmrich SP, Ro’cnberg L, Miettinen OS, Shapiro s.
myocardial infarction in young men. N EnglJ Med 1933;308:409-l 3.
16 Palmer JR, Rosenberg L, Shapiro S. "Low-yield“ cigarettes and the risk of
non-fatal myocardial infarction in women. N EnglJ Med 1989;320:1569-73.
acute myocardial infarction. BMJ 1993^06:1567-70.
18 ISIS-2 (Second International Study of Infarct Survival) Collaborative Group.
Randomised trial of intravenous streptokinase, oral aspirin, both, or neither
I988yi:349-60.
19 ISIS-3 (Third International Study of Infarct Survival) Collaborative Group.
20
I Peto R, Lopez AD, Boreham J, Thun M, Heath C Jr. Mortality from smoking in
vs anistreplasc and of aspirin plus heparin vs aspirin alone among 41,299
cases of suspected acute myocardial infarction. Lancet 1992;339:753-70.
ISIS-4 (Fourth International Study of Infarct Survival) Collaborative Group.
mononitrate, and intravenous magnesium sulphate in 58,050 patients with
suspected acute myocardial infarction. Lancet 1995;345:669-85.
Knight GJ, Wylie P, Holman MS, Haddow JE. Improved ‘“iodine
radioimmunoassay for cotininc by selective removal of bridge antibodies.
ClinChem 1985^1:118-21.
Fcyerabend C, Russell MAH. A rapid gas-liquid chromatographic method for
2 Doll R, Peto R, Wheatley K, Gray R, Sutherland I. Mortality in relation to
smoking: 40 years' observations on male British doctors. BMJ 1994^09:
901-11.
21
International Agency for Research on Cancer, 1986. (IARC scientific
publications No 74.)
4 Wald N, Nicolaides-Bouman A. UK smoking statistics. 2nd ed. Oxford: Oxford
Pharmacol 1990;42:450-2.
23 Department of Health. Statistics on smoking: England 1974 to 1993. London:
Government Statistical Service, 1994.(Statistical Bulletin 1994/14.).
nicotine. N Engl J Med 1983;309;
Community Health 1981^5:16-22.
25 Wynder EL, Hoffman D. Tobacco and health: a societal challenge. N Engl J
Med 1979;300:894-903.
6 Wald N, Froggatt P. Nicotine, si
Oxford University Press, 1989.
smoking behaviour, total mortality and cardiorespiratory disease in west
central Scotland. J Epidemiol Community Health 1978;32:260-6.
8 Woodward M, Tunstall-Pcdoc H, Smith WCS, Tavendale R. Smoking
J Clin Epidemiol 1991 ;44:1405-10.
9 Woodward M, Tunstall-Pedoc H. Do smokers of lower tar cigarettes consume
lower amounts of smoke components? Results from the Scottish Heart
Health Study. BrJAddict 1992;87:921-8.
Scottish Heart Health Study. Addiction 1993;88:821-30.
22
27
28
29
Petitti DB, Friedman GD. Cardiovascular and other diseases in smokers of
low yield cigarettes. J Chron Dis 1985;38:581-8.
Castelli WP, Garrison RJ, Dawber TR, McNamara PM, Feinleib M, Kannel
Lanc«198l;ii:109-13.
Higgenbottom T, Shipley MJ, Rose G. Cigarettes, lung cancer, and coronary
heart disease: the effects of inhalation and tar yield. J Epidemiol Community
Health 1982^6:113-7.
(Accepted 28July 1995)
A 28 year follow up of mortality among women who smoked during
pregnancy
Paula Rantakallio, Esa Laara, Markku Koiranen
'I
g'^ll
Abstract
Objective—To investigate long term mortality
among women who smoked during pregnancy and
those who stopped smoking.
Design—A follow up of a geographically defined
cohort from 1966 through to 1993.
Subjects—11994 women in northern Finland
expected to deliver in 1966, comprising 96% of all
women giving birth in the area during that year.
Smoking habits were recorded during pregnancy but
not later.
Main outcome measure—Mortality by cause (571
deaths).
Results—The mortality ratio adjusted for age,
place of residence, years of education and marital
status was 2-3 (95% confidence interval 1-8 to 2-8) for
the women who smoked during pregnancy and 1-6
(14 to 2*2) for those who stopped smoking before the
second month of pregnancy, both compared with
non-smokers. Among the smokers the relative
mortality was higher for typical diseases related to
tobacco intake, such as respiratory and oesophageal
cancer and diseases of the cardiovascular and
digestic organs and also for accidents and suicides.
Conclusion—The risk of premature death seems
19 august 1995
to be higher in women who smoke during pregnancy
than in other women who smoke. This may be
explained either by the low proportion of those who
stop later and the high proportion of heavy smokers
or by other characteristics of these subjects that
increase the risk.
Introduction
The consequences for the child of maternal smoking
during pregnancy have been well documented,1 but
less interest has been directed towards the mothers’
prognosis. We analyse here 28 year mortality data on a
geographically defined population of women who
smoke during pregnancy; many background variables
were recorded prospectively.
Methods
Population—The cohort consisted of 12055
pregnant women (13 of them delivering twice) in the
two most northern provinces in Finland, Oulu and
Lapland, whose expected dates of delivery fell in 1966
and when the pregnancy resulted in a birth. The cohort
covered 96% of all deliveries in the region in 1966? The
PAPERS
Cigarette smoking, tar yields, and non-fatal myocardial infarction:
14 000 cases and 32 000 controls in the United Kingdom
S Parish, R Collins, R Peto, L Youngman, J Barton, K Jayne, R Clarke, P Appleby, V Lyon,
S Cederholm-Williams, J Marshall, P Sleight for the International Studies of Infarct Survival (ISIS)
Collaborators
ISIS, BHF/ICRF/MRC
' Clinical Trial Service Unit
and Epidemiological
Studies Unit, Nuffield
Department of Clinical .
Medicine, Radcliffe
Infirmary, Oxford
0X2 CHE, and
Cardiac Department, John
Radcliffe Hospital, Oxford
. OX3 9DU
: S Parish, senior research
fedow
; R Go|os, British Heart
■ F^^ion senior research
Hbt,
■ ■ RPeto, professor of medical
" statistics and epidemiology
' LYoiingman, senior research
.- feP.ow
*--—
: J Barton, senior administrator
K jayne, senior administrator
R Cktte, research fellow
P Appleby, research fellow
V Lyon, research fellow
P Sleight, professor emeritus of
cardiovascular medicine
. Oxford Bio-Research
Laboratory, Magdalen
Science Park, Oxford
0X4 4G A
' S Cederholm-Williams,
director
- J Marshall, researchfellow
Correspondence to:
Dr Parish.
'•';ai(71W53il:471-1
BMJ
volume 311
Introduction
In countries such as the United Kingdom, where
cigarettes have been used widely for several decades,
tobacco now accounts for about 30% of all deaths in
middle age, with lung cancer and coronary heart
disease the most common fatal conditions.1-’ Over the
past few decades cigarettes have been altered in various
ways, reducing the so called yields of tar, and nicotine
when smoked in a standard way by a machine. Typical
British cigarettes had tar yields of 25-35 mg during the
1950s and 5-15 mg in 1990.* But, partly because
the chief toxins in cigarette smoke are uncertain and
partly because smokers may compensate for reduced
yields (or other changes) by smoking cigarettes more
actively,5-10 the health effects of alterations in cigarette
manufacture are unpredictable. Low tar cigarettes do
cause substantial risks of cancer and heart disease,
although the risk of lung cancer is less than with high
tar cigarettes.’"-l* For heart disease, however, there
remains uncertainty”-1’ about whether the rates have
had not smoked cigarettes regularly in the past
been decreased, increased, or not changed by alter
10‘years.
ations in cigarette composition over the past few
Results—At ages 30-49 the rates of myocardial decades. National heart disease mortality rates and
infarction in smokers were about five times those In trends are not informative because other factors cause
non-smokers (as defined); at ages 50-59 they were such large differences in coronary heart disease
three times those in non-smokers, and even at ages between different populations and time periods.
60-79 they were twice as great as in non-smokers Instead, concurrent epidemiological comparisons
(risk ratio 6-3, 4'7, 3-1, 2'5, and 1-9 at 30-39, 40-49, within one population arc needed,
50-59, 60-69, 70-79 respectively; each 2P< 0-00001).
But, although tobacco is a major cause of heart
After standardisation for age, sex, and amount disease, particularly among young and middle aged
smoked, the rate of non-fatal myocardial infarction adults, it is difficult for conventional prospective or
was 10-4% (SD 5-4) higher in medium tar than in low retrospective studies to compare the risks from dif
tar cigarette smokers (2P=0-06). This percentage ferent types of cigarette. Only a narrow range of
was not significantly greater at ages 30-59 (16-6% cigarette tar yields is concurrently available within one
(7-1)) than at 60-79 (1-0% (8-5)). In both age ranges population, and the tar yields of cigarettes smoked by
the difference in risk between cigarette smokers and people in 1990 might ■ correlate poorly with the tar
non-smokers was much larger than the difference yields smoked by these people years earlier. Hence,
between one type of cigarette and another (risk ratio .even large diffcrcncds in risk between prolonged use of
3-39 and 3-95 at ages 30-59 for smokers of similar low, medium, and high tar cigarettes might produce
numbers of low and of medium tar cigarettes, and only small differences in risk between current use of
risk ratio 2-35 and 2-37 at ages 60-79). Most possible low and medium tar cigarettes. At younger ages the
confounding factors that could be tested for were proportional difference in rates of coronary heart
similar in low and medium tar users, with no disease between smokers and non-smokers is particu
significant differences in blood lipid or albumin larly extreme, so any effect of cigarette type may also
be extreme. Thus, to minimise the chances of a false
concentrations. '
Conclusion—The present study indicates that the negative result in a study of tar yields, the number of
imminent change of tar yields in the European Union cases of myocardial infarction in middle aged cigarette
to comply with an upper limit of 12 mg/cigarette will smokers should be large—preferably several thousand
not increase (and may somewhat decrease) the —with at least as many controls. We achieved this
incidence of myocardial infarction, unless they by studying subjects from. the United Kingdom
indirectly help perpetuate tobacco use. Even low tar who participated in. the large ISIS (international
cigarettes still greatly increase rates of myocardial studies of infarct survival) trials of the treatment
infarction, however, especially among people in of acute myocardial infarction,,,-!0 by using postal
their'30s, 40s, and 50s; and far more risk is avoided questionnaires (copies available on request), rather
by not smoking than by changing from one type of than interviews, and by simplifying blood collection
procedures.
cigarette to another.
Abstract
Objectives—To assess the effects of cigarette
smoking on the incidence of non-fatal myocardial
infarction, and to compare tar in different types of
manufactured cigarettes.
Methods—In the early 1990s responses to a postal
questionnaire were obtained from 13 926 survivors of
myocardial infarction (cases) recently discharged
from hospitals in the United Kingdom and 32389 of
their relatives (controls). Blood had been obtained
from cases soon after admission for the -index
myocardial infarction and was also sought from the
controls'. 4923 cases and 6880 controls were current
smokers of manufactured cigarettes with known
tar yields. Almost all tar yields were 7-9 or 12-15
mg/cigarette (mean 7-5 mg for low tar (< 10 mg) and
13-3 for medium tar (3= 10 mg)). The cited risk
ratios were standardised for age and sex and com
pared. myocardial infarction rates in current
cigarette smokers with those in non-smokers who
19 august 1995
_.. <.y v.i;n
v.u.-. gj.s ..tronuteg.Beckman CX-4 and CX-5 autoanalyscrs were used
for measuring concentrations of cholesterol and
albumin (both with Beckman reagents) and apolipo
proteins A, and B (with Immuno reagents). To correct
for discoloration from haemolysis, an initial blank
reading was subtracted from the final reading. Samples
from a large plasma pool were included in each
analytical run, yielding coefficients of variation of 2%
for cholesterol and albumin and 4% for apolipo
proteins.
/f
aged 30-79 from the ISIS-3 or ISIS-1 trials who
completed an .epidemiological questionnaire sent to
them a few months after their infarction. Those who
were asked to complete it were all the survivors from
ISIS-3, but from ISIS-4 only the survivors aged 30-59
who on admission to hospital were reported to be
cigarette smokers. Thus, although only cases from
ISIS-3 can be used to compare smokers with nonsmokers, the cases from ISIS-4 strengthen the analyses
of tar yields among smokers aged 30-59. The ISIS-3
questionnaire asked the cases to identify all their
’ brothers, sisters, and children aged at least 30
who were resident in the United Kingdom. A
similar “control” questionnaire was then sent to
such relatives, accompanied by a second copy, which
the relatives, if married, were to ask their spouse to
complete. One reminder was sent to cases and relatives
who did not reply, and inconsistencies or omissions
were queried once.
Of the 20681 ISIS-3 patients in the United King
dom, 19 065 who were not known to be dead were
posted the case questionnaire, of whom 1346 were
found to be dead and 13 969 (79% of presumed
survivors) completed it. The control questionnaire was
sent to 30247 relatives of ISIS-3 cases, of whom 75
were found to be dead and 21 995 (73% of presumed
survivors) and 14245 of their spouses completed it.Patients' with a" history of stroke, gastrointestinal
bleeding, or ulcer tended not to have been recruited
into the ISIS-3 trial,” and so people with such condi
tions were not eligible as cases or controls. Of those
who completed' questionnaires, 2002 cases and 3851
controls were excluded because they were under 30,
over 79, or of unknown age or because they had a self
reported history of “definite stroke” or of "bleeding or
ulcer in (or near) the stomach."
ISIS-4 patients in the United Kingdom aged 30-59
who were described at trial entry as current smokers
were also sent the questionnaire. The response rate
for such patients was similar in both trials. Any of
these ISIS-4 patients whose questionnaire response
indicated that they were not cigarette smokers at the
time of their infarction were excluded. ISIS-4 (and, to
some extent, ISIS-3) tended to exclude patients with
shock or persistent hypotension,” but such exclusions
should not bias the epidemiological analyses of tobacco
use.
Information was sought on sex, age, body size,
smoking, drinking, past health, and relatives. Cases
were asked about their habits and history just before
their index myocardial infarction (because having a
heart attack may alter a patient’s habits), while controls
were asked about their present habits. Hence, ques
tions to cases often began, “Before your recent hospital
admission. . . .” Both cases and controls were asked
to list how many relatives of certain types they had,
but only cases were to provide contact details. In
other respects case and control questionnaires were
identical. The medical history section was non
technical and recorded various conditions that might
be associated with exclusion from the randomised trial
(see above) or- that might affect, or be affected by,
smoking. After the question of whether they had “ever
smoked regularly (ie on most days for at least a year)”
the rest of the cigarette section was to be completed
only by those who replied “yes.” It dealt with the age at
which the subject had first and last smoked regularly,
whether any cigarettes had been smoked in the pre
vious month, the number smoked perl day when the
subject had last smoked cigarettes regularly, and the
way in which cigarettes were smoked. People were to
tick against 137 detailed brand names the one that,
when they last smoked, they usually smoked most of—
or, if it was not on the list, to write our its exact name
(and, whenever possible, to enclose the packaging of
that brand with the questionnaire). For the few who
listed more than one brand, the average of the yields
was taken. Ninety eight per cent of controls and 98%
of cases who currently smoked only manufactured
cigarettes with a known tar yield, and both reported
using their current brand for, on average, the past 10
or 11 years.
BLOOD SAMPLES
DEFINITIONS OF CIGARETTE SMOKING STATUS
QUESTIONNAIRES
Blood was. to be taken from patients in ISIS-3
Respondents were classified as current cigarette
immediately after randomisation but before the trial smokers (26% of the controls: those who had smoked
treatments and collected in a 10 ml vacutainer con cigarettes in the previous month, plus the few who
taining 0-12 ml preservative (15% potassium EDTA failed to answer this yes/no question but gave other
with aprotinin 0-34 mmol/1: Becton Dickinson). On evidence of current cigarette use); other tobacco users
returning their questionnaire, controls were sent’ an ’ (3%: pipes, cigars, or smokeless tobacco in the past
identical container for their general practitioner to year); or as not using tobacco (71%: all others). In
collect blood. Case and control containers were sent by table I these are further subdivided. Because of the
first class post to Oxford. Controls were sent one possible confusion between those who stopped
reminder about giving a sample. After a mean of two smoking many years ago and those who never smoked,
days in the post the blood was centrifuged, the packed the main comparison group was defined as noncell volume was recorded, and the plasma and bufiy . smokers who had not used cigarettes regul trly in the
coat were aliquoted for storage at -40°C. Blood arrived past 10 years.
from 97% of ISIS-3 cases and 45% of controls, but
breakages or haemolysis rendered 6% of these samples ESTIMATED 1990 TAR YIELDS
unusable. The present blood analyses involve only
The United Kingdom’s government chemist con
correlations of smoking with blood biochemistry ducts surveys of common cigarette brands, measuring
results, and these analyses should not be materially tar, nicotine, and carbon monoxide yields, twice a year
biased by low response rates.
(R Waller, personal communication). During the late
Plasma cotinine concentration was measured in
1980s the annual decrease in sales weighted yields was
controls who were cutrent cigarette smokers, and in about 2-3% for tar, 1-2% for nicotine, and zero for
a 3% sample of controls who reported no current use carbon monoxide (J Rentoul, personal communica
of tobacco, by means of antibodies developed by Knight tion).* Most ISIS-3 cases replied in 1990 about habits
BMJ
VOLUME 311
19 ALCL’ST.1995
replied :n 1092-3 (mean date of infarction; July 1992).
T o avoid secular trends in yields introducing minor
biases, the mid-1990 survey results for each cigarette
brand were used (R Waller; personal communication).
If a brand was assayed only earlier or later than mid1990, yields from the closest survey were extrapolated
to mid-1990 by annual decreases of 2-5% in tar and
1-5% in nicotine.
O
j
curettes only
;
o 20-
S
<£ 10-
RESURVEY OF CONTROLS A FEW YEARS LATER
_rvJU-n
To check reproducibility, about 2000 controls
who originally returned both questionnaire and blood
sample (and whose replies indicated no previous
vascular disease) were sent the same questionnaire and
blood kit again about 2-3 years later. To avoid oversampling young controls, the random sample was
stratified with respect to sex and age in groups of five
years. Seventy per cent (1388/1996) returned the
questionnaire, 95% (1324/1388) of whom gave blood.
15
10
20
25
30
35
£40
STATISTICAL METHODS
The analyses are all unmatched—that is, they
compare cases with all controls, not just with their own
relatives—and for tar yield analyses among smokers
the controls are as relevant to ISIS-4 as to ISIS-3 cases.
All analyses of myocardial infarction rates were strati
fied either for sex and five year age group or for
these factors and amount smoked (five categories; see
below). Calculations of risk ratios—or, equivalently,
relative risks—entailed unmatched stratified logistic no I—Replies by controls etho smoked manufactured cigarettes only.
regression (fitted by unconditional maximum likeli (a) Reported daily cigarette use (3d% reported 10 cigarettes per day,
and &5%avported 10-30). (b) Taryieldsitl 1990 ofthe brands reported
hood), with one extra term included for each stratum.'
Risk ratios are often given with 95% confidence
intervals. Two sided probability values (2P) are used. tion of (u) the reported number smoked per day and (f>)
the estimated 1990 tar yield. Self reported cigarette
consumption was categorised as 1-9, exactly 10, 11-19,
Results
exactly 20, and &21 cigarettes a day; 85% reported
FREQUENCY DISTRIBUTIONS OF SMOKING HABITS
smoking 10-30 cigarettes a day. The tar yields show a
Table I shows the numbers of controls and cases in bimodal distribution, with commonest values 7-9 or
various categories ofXobacco use subdivided by sex and 12-15 mg/cigarcttc. Tar yields of 10 mg were rare,
by age. The age range\of chief relevance to the tar yield which makes this a natural point of subdivision,
analyses is 30-59, and among controls in this range 28% unaffected by any slight differences in dates of case and
both of men and of women were current cigarette control responses, to define two main categories: low
smokers, in close agreement with nationally represen tar (< 10 mg, mean 7-5 mg) and medium tar (& 10 mg,
tative, interviewee administered surveys in the early mean 13-3 mg). Medium tar is sometimes split into 101990s.;’ Twenty two per cent of these controls were 12,13, and & 14 mg/cigarette. This definition of low tar
current users of manufactured cigarettes only with is also used by the Department of Health (R Waller,
personal communication).* Twenty five per cent of the
known tar yields.
Figure 1 gives, for controls who currently used smokers in figure lb use low tar cigarettes, as in the
manufactured cigarettes only, the frequency distribu- nationally representative survey in 1990.“ Almost all
-Tobacco use in cases and controls aged 30-79 tenth questionnaires returned
Not using tobacco
Manuiacrureo cigarrnes ana no
otner rooaccu
known
Tar
unknown
cigarette
1389
958
153
251
Mffl1’’ 30-59
Women 30-59
Men
60-79
Women 60-79
i;IS-3 cases:
Men
30-59
Women 30-59
Men
60-79
Women 60-79
SIS-4 cases:
Men
30-59
Women 30-59
6880
2184
3264
563
869
3453
1351
520
85S
724
1470
1117
353
162
35
60
21
46
65
23
8
16
18
29
5
1063
.bl9
' 33
382
29
455
430
; 25
otal
11803
261
^07
■1MJ
VOLUME 311
19 AUGUST 1995
using any
cigarettes
28
28
20
21
38
48
60
35
—
—
—
-
Smoking pipe
or cigar but no
cigarettes
" smokeless
tobacco only
71
40
1
28
2
48
Former regular cigarette smoker
<10 years ago
& 10 years ago
5502
1785
1385
1506
826
2070
467
7572
—
-r—
—
—
—
3181
1128
1145
465
443
1311
424
98
537
252
—
—
—
1890
119
4492
1031
676
11
337
859
405
0
450
4
20
1268
288
—
—
—
cigarette
smoker
Total’
—
32389
11163
12578
4077
4571
11967
4119
942
4702
2204
1959
1576
3S3
17271
46315
14173
4357
6559
906
2351
3098
804
236
1171
887
—
473
third higher among the controls who smoked medium
tar cigarettes (low tar 217 ng/ml v medium ta
292 ng/ml). But the smokers of low tar cigarette
reported smoking 15-8 cigarettes a day compared witl
18-7 a day for those in the medium tar group. After
standardisation for age, sex, and amount smoked
however, the mean plasma cotinine concentration was
still 19% higher with medium tar cigarettes. This
difference in cotinine is still highly significant
(2P< 0-00001), which helps validate the categorisation
of tar yield based on the questionnaire. But it is less
extreme than the difference of over 50% in the nicotine
yield per cigarette measured by machine (0-75 mg and
1-18 mg). This may be partly because the categorisa
tion of tar yields is imperfect, and partly because
smokers of low yield cigarettes compensate by taking
in more smoke per cigarette. But, since this categorisa
tion predicts highly significant biochemical differences
in blood taken months later (figure 2b), it has some
validity.
fig 2—Corinine by cigarette
smoking habit in amrrols. (a)
Codnine versus dznfy cigarette
use, (b) Cotinine versus taryield
ofreported brand. In the low and
CIGARETTE USE AND NON-FATAL MYOCARDIAL
INFARCTION
i
tar, 0-/5 ana I-18 mg nicotine,
and 8-4 and 15-0 mg carbon
average of eight months after
questionnaire, and in'12 out of
293 chose questionnaire had
indicated no smoking cotinine
concentration (mean 2G8,ng/ml)
indicated current tobaecc use
0
5
10
Tar yield (mg/cigareae) .
IS
Ion-fatal myocardial infarction: age-specific effect of cigarette use in people with no history of
Non-smoker with no regular
cigarette use in past 10 years
When those using - manufactured cigarettes only
were compared with non-smokers who had not smoked,
cigarettes regularly in the past 10 years (excluding im
both cases those using any other type of tobacco), the'
relative risks for non-fatal myocardial infarction in
people with no previous neoplastic or major vascular
disease depended strongly on age (table II, fig 3). Asis
the case for mortality from coronary heart disease,*2.
the risk ratio comparing smokers with non-smokers
was greater at younger ages, reinforcing the need for
the relevance of tar yields to be considered separately at
younger and older ages.
Myocardial infarction*
TAR YIELDS AND NON-FATAL MYOCARDIAL INFARCTION
Risk ratio (95%
confidence
interval)
Information about the relevance of tar yields comes'
from current users of manufactured cigarettes only. Of
these, much the most informative are the 9000 aged
30-59, rather than the 3000 aged 60-79. This is not only
because thi numbers are larger but also because the
risk ratio tWien smokers are compared with non- I
Test
statistic!
30-39
40-59
50-59
293
435
1784
1497
861
35
190
508
4873
4306
2701
6-33 (4-22 to 9-51)
4 66 (3-82 to 5*69)
3 10 (2 64 to 3-65)
8-9
15‘ 1
13-7
30-59
806
4142
733
11880
3-85 (3-41t‘o4-34)
22-1
60-69
70-79
60-79
416
111
527
653
163
816
707
369
1076
2299
942
3241
2-54 (2-16 to 2-98) . i i.i
4*6
1-92 (1-45 to 2-54)
2-37 (2 06 to 2-72) 121 .
i
I
Myoardfal infarction and cigarette smoking:
12 000 cases and 32 000 controls
’Smoker v non-smoker rates standardised for age and sex.
fNoraber of standard deviations by which the logarithm of the risk ratio differs from:zero.
used filtered brands (100% of the low tar group, 96%
of the medium tar group), so filters accounted for little
of the difference in yields between low and medium tar
cigarettes in 1990.
RELATION BETWEEN QUESTIONNAIRE AND COTININE
CONCENTRATIONS
Figure 2 shows the relation between plasma cotinine
concentrations and (a) reported daily cigarette use and
(6) tar yield for controls reporting use of manufactured
cigarettes only or no current tobacco use. The mean
cotinine concentration was very low in the self reported
non-smokers, which helps validate both questionnaire
and laboratory results. Among cigarette smokers there
was a strong relation between cotinine concentration
and the amount reported to be smoked, which again
helps validate the questionnaire. The downward
curvature in figure 2a suggests that those who smoke
more cigarettes may absorb less nicotine from each one
or that those reporting large numbers include dispro
portionately many who overreported, or both. Either
way, self reported cigarette consumption provides only
approximate information about the real doses of
nicotine and of other substances.
Age 30-59
Risk ratio 3.85
'
Age 60-79
Risk ratio 137
fig 3—Cigarettes and non-fatal myocardial infarction as a first events
risk ratios al various ages, Results in people trick no previous history
major neoplastic or vascular disease. Each risk ratio is standardisedfor
sex and fonquinquennium of age, and compares those using manufac
tured cigarettes only with those who were not currently using any
tobacco and had not been regular cigarette smokers al any time tn the
past 10 years. Risk ratio is given within each column. (As all cases
recruited from ISIS-4 were cigarette smokers, this figure involves cases
onlyfrom ISIS-3)
BMJ
’1
was much larger than tne oxicrer.ce between one type
of cigarette and another: the risk ratios were 3-39 and
3-95 for smokers of similar numbers of low and of
medium tar cigarettes at ages 30-59 and were 2-35 and
2-37 at ages 60-79. (Table HI shows that results were
similar when these comparisons were based on the
smaller numbers of cigarette smokers with no reported
history of neoplastic or major vascular disease.)
of medium ur v smokers of low:
(with 95% confidence interval anc
infarctioa’ infarction’
(no
ISIS-4
ISIS-3
infarction)
\ge 30-59:
Law tar
Medium tax
AseSO-79:
Medium tar
«e 30-79:
Low tar
• Medium tar
1196
359
1512
—
43S
1144
433
999
2656
1701
5179
1196
1-203
1-166
1-075
(1061tol-364) (1-025 to 1-326) (0-900 to 1-283)
2P=0-004
2P=0-02
2P>01
1-046
1-010
1-010
(0-890 to 1-230) (0-856 to 1-191) (0-771 tol-323)
2P>0-l
2P>01
2P>01
1-142
1-104
1-055
(1-034 to 1-260) (0-998 to 1-222) (0-910 to 1-223)
2P=0008
2P>01
2P=0-06
1268
4180
. medium tar cigarettes were similar in ISIS-4 and ISIS-3: after
oked, the odds ratio comparing the two tar yield categories in the two
1 studies was 1-000 (SD 0-091).
fFor comparison of the effects of different tar yields, inclusion of pauents with some previous neoplastic or vascular
disease may well produce no material bias and helps stabilise the estimates.
table rv—Associations between smoking habits and blood lipid concentrations. Values are means (SE)
Standardisedfor age, sex, and case-control status
Cigarette tar yield
(^295)
Cholesterol (mmol/1)
Apolipoprotein A, (gfl)
Apolipoprotein B (g/1)
5-92 (0-03)
1-273(0-006)
1-194(0-008)
NS
2P=O-O5
2P-0004
5-91 (0-02) .
1-288(0004)
1-165 (0-005)
Medium tar
(n=942) Significance
6 01(006) 6-02(0-03)
1-266(0 013) 1-264 VO-007)
1-222(0-016) 1-226^0-009)
NS
NS
NS
-Reproducibility ofsmoking classification
Responde to original questionnaire
1
Currently uising tobacco
Not using tobacco
Other
tobacco
user
Former cigarette smoker
Never
<10 years
>10 years
smoker
0
Response to repeat
questionnaire 2-3 years later
Manufactured
cigarettes
only
Manufactured cigarettes only
99’
9
8
5
Other tobacco user
Former cigarette smoker.
. ‘<10 years
1
86
7
3
3
22
12
50
11
0
18
9
37
-
. .>10years
Never dgartne smoker
370
;
591
’Ninety seven of these had known tar yield at both enquiries (65 classified as medium tar originally and medium tar
later, 21 t^Hhthen low, 8 as medium then low, 3 as low then medium).
smokers is more extreme in middle th.m in old age.
As there was no significant difference between the tar
yields of cases aged 30-59 in ISIS-3 and in ISIS-4
(table III), the groups were combined.
Table HI provides age-sex standardised compari
sons of non-fatal myocardial infarction in smokers, of
low tar versus smokers of medium tar cigarettes.
Overall, there were only slight effects of th: tar yield.
Tne mean daily number of cigarettes smoked was
slightly higher in the medium tar than in the low tar
cigarette smokers (19-0 v 17-1). When standardised
not just for age and sex but also for the daily number of
cigarettes smoked, the incidence of myocardial infarc
tion was 10-4% (SD 5-4) higher in medium than in low
tar cigarette smokers (2P=0-06). This difference was
non-significantly greater at ages 30-59 (16-6% (7-1)
higher; 2P=0-02) than at 60-79 (1-0% (8-5) higher;
2P>0-l) (fig 4). As these two results are not signific
antly different from each other, they do not prove that
tar yields are of greater proportional importance to the
cardiotoxicity of cigarettes in middle than in old age,
especially since the smoker versus non-smoker risk
ratios are less extreme in old age. In both age ranges the
difference between cigarette smokers and non-smokers
POTENTIAL CONFOUNDING FACTO RS
Table TV relates smoking to blood lipid concentra
tions among ISIS-3 cases entering the trial within 0-4
hours of pain onset whose blood spent only one or two
days in the post, and among one randomly chosen
control per case (matched for age, sex, and days sample
spent in the post). Apolipoprotein A, was 1-2% lower
and apolipoprotein B 2-4% higher in smokers than in
non-smokers, but these differences are too small to
account for much of the excess risk among smokers.
There were no significant differences in blood lipid
concentrations (or albumin concentration, data not
shown) between smokers of low and of medium tar
cigarettes, either overall or in those aged 30-59 (data
riot shown). For many factors there were likewise
no significant differences between smokers of low
and medium tar cigarettes. These include self
reported height, weight, loneliness, depression,
worry, ■ insomnia, teenage acne, tea consumption,
alcohol consumption, and whether living with a
spouse. For a few factors, however, there were definite
differences even after standardisation for age and sex.
(Multivariate adjustment for these observed differ
ences would make little difference, but these
differences point to the possibility of others existing.)
Those who smoked low tar cigarettes were, on average,
almost six months older when they left full time
education (mean leaving age 15-9 years for low tar
group v 15-5 years for medium tar), were more likely to
say that they had matured physically “later than
average” (13’4% v 10'5%), had “softer hands than
average” (14-4% v 11-0%), had been regular drinkers
of coffee (75% v 67%), were older when they started to
smoke (18-8 v 17-9 years old), and had changed to their
current brand more recently (7-9 v 10-l years pre
viously). These suggest a general tendency for those
who smoke medium tar cigarettes to include a slightly '■
larger proportion of manual workers, and to have
slightly less education. (Likewise, unpublished
analyses by M Jarvis of the 1990 and 1992 general
household surveys in the United Kingdom found
significantly higher “indices of deprivation” in users '
of medium than of low tar cigarettes.)'
REPRODUCIBILITY OF SMOKING CLASSIFICATION
A total of 1388’controls repeated the questionnaire a
few years later, and table V compares their two replies.
When subdivided three ways (manufactured cigarettes
only; other tobacco or ex-cigarette smoker <10 years;
remainder), 90% remained in the same category; of the
97 who smoked only manufactured cigarettes with tar
known on both occasions, 89% had continued to smoke
medium or low tar cigarettes as originally. Overall,
there was a 5% shift towards the low tar category, in
line with national trends, and the correlation co-t
efficient between the two assessments of tar yield was,
0-71. ,
Discussion
When cigarette smokers are compared with non-^
smokers the risk ratio for myocardial infarction is
much more extreme in early adult life than in old age.
The numbers contributing to figure 3 are unusually
large (12 000 cases and 32000 controls) and so the
pattern of steadily increasing risk ratio with younger
at me extremes of the age range of 30-79. The
risk ratio is twofold at ages 70-79, but it is almost
fourfold at ages 30-59 (threefold at 50-59 but fivefold at
30-49). Even these large differences have probably
been somewhat diluted by the misclassification of some
smokers or non-smokers. Had it been possible, with no
classification errors, to compare persistent cigarette
smokers with lifelong non-smokers then the risk ratios
would probably have been still more extreme than
those in figure 3, and would have been at least fourfold
at ages 30-59. As most of the excess risk associated with
smoking is caused by smoking,11 this fourfold risk
ratio implies that about three quarters of the
myocardial infarctions among cigarette smokers aged
30-59 were caused by tobacco (two thirds at ages 50-59,
but four fifths at ages 30/49).
Any differences in the risk of heart disease between
those who are smoking different types of cigarette must
be much less extreme than the differences between
smokers and non-smokers, so especially large studies
are needed to assess them. Moreover, epidemiological
studies that were undertaken when tar yields below
15 mg were still uncommon (N J Wald et al, un
published data)'*-” are of limited contemporary
relevance in countries such as the United Kingdom
where tar yields above 15 mg have already virtually
disappeared (fig lb) and where a European Union
upper limit of 12 mg is soon to be enforced. As no pthef
large recent studies are available, our current findings
stand alone.
For- tar yields the central finding is that after
standardisation for age, sex, and number of cigarettes,
the incidence of non-fatal myocardial infarction
seemed to be about 10% greater with medium tar than
with low tar cigarettes (95% confidence interval 0 to
22%, table III). Even if this 10% difference was highly
statistically significant (which it is not: 2P=0'06) it
would still not be epidemiologically secure. It is
uncertain how much selective emphasis to put on the
data at ages 30-59 as opposed to those at 60-79, how
much selective emphasis to put on the data from people
with no previous disease, and how much to emphasise
Myocardial infarction and cigarette tar yield
Low ar(<10 mg, mean 7.5 mg)
Medium tar (> 10 mg, mean 13.3 mg)
Flo 4—Cigarette tar yields and risk of non-fatal myocardial infarc
tion. Standardised for age, sex, and amount smoked, comparisons at
ages 30-59 indicate that non-fatal myocardial infarction rates were
1'166 (SD 0'071) times as great among medium taros among low tar
cigarette smokers (2P=0 02; table III). The same standardised
comparisons at ages 60-79 give 1'010 (0-085) (NS). These two
estimates (T166 and 1-010) are combined with the risk ratios of 3'85
and 2-37 for cigarette smokers versus non-smokers (fig 3) to yield the
cited risk ratios for smokers of low and medium tar cigarales: 3-39 and
3-95 at ages 30-59 and 2-35 and 2-37 ar ages 60-79
Key messages
• Non-fatal myocardial infarction rates are five
times as great among cigarette smokers as among
non-smokers at ages 30-49, three times as great
at ages 50-59, and twice as great at ages 60-79
o Among cigarette smokers four fifths of
myocardial infarctions at ages 30-49 were caused
by tobacco, two thirds at agespO-59, and half at
ages 60-79
°
• The risks seem to be slightly greater with
medium tar than with low tar cigarettes, but this
difference is not definite .
• Differences in risk between cigarette smokers
and non-smokers are far greater than any differ
ences in risk between one type of cigarette and
another
• Far more myocardial infarctions could be
avoided by not smoking than by changing from
one type of cigarette to another
analyses that are standardised for the amount smoked.
(Those using low tar cigarettes reported - smoking
slightly fewer than those smoking medium tar
cigarettes, and if lower daily consumption is chiefly a
consequence of lower yields of tar, nicotine, and other
smoke components then lit should not be standard
ised for.) Hence, table III reports several different'
comparisons of disease rates in smokers and in non-smokers, with differences that arc sometimes more and
sometimes less than 10%l Also, there was a slight
tendency for tar yields t<^ be inversely related to
education and to various other aspects of social class. It
is difficult to see how some of these uncertainties can be
resolved: large scale randomisation is impracticable, ,
and even if the present study could have been much
larger, thereby narrowing the confidence intervals, the
possibility of confounding would remain.
Despite these uncertainties, however, the present
results provide some reassurance to those in govern
ment or in industry who could direct decreases in
cigarette tar yields to reduce cancer incidence.’
They indicate that such changes will not substantially
increase the incidence of myocardial infarction and
may well decrease it. Thus; the limit of 12 mg/cigarette ,
on tar yields that is now being introduced in the.
European Union should help, limit the number of.
premature deaths from tobacco, unless governments or
smokers come to regard reductions in tar yield as
substitutes for the avoidance of cigarettes, for in
developed countries tobacco remains much the most
important cause of premature death. This is particu
larly so for men, with tobacco now causing about a
third of all deaths in middle aged meh. But where
women have been smoking cigan ties for some decades
(as, for example, in the United K ngdom or the United
States) tobacco also already causes about a quarter of
all the deaths in middle aged women.1
For the general population, therefore, the most
important finding is not the slight and uncertain
difference in figure 4 between one type of cigarette and
another but the large and definite difference in figure
3 between cigarette smokers and non-smokers,
particuularly in early middle age. Irrespective of
whether low or medium tar cigarettes are used, about
three quarters of the smokers who have a heart attack
in their 30s, 40s, or 50s need not have done so, and far
more heart attacks could be prevented by not smoking
than by reducing cigarette tar yields.
The chief acknowledgment is to the patients and their
-r.J. mirsmi: staff from mure chan 100 hospitals in die United
Kingdom listed in the ISIS reports.*' • We particularly thank
Frogg-iu, Chen I Swann. and Robert Waller of the
Independent Scientific Committee on Smoking and Health,
Department of Health; Keith Darrall of the laboratory of the
Government Chemist; Martin Janis of the Imperial Cancer
Research Fund; and Kuldip Bhamra, Vanessa Boag, Lee
Buckingham, Mary Burton, Sarah Clark, Sarah Edwards,
Sheila Foster, Heather Halls, Mavis King, Karen Kourellias,
Christine Marsden, Gale Mead, Kevin Murphy, Martin
Radley, and Karl Wallcndszus of the Oxford Clinical Trial
Service Unit and Epidemiological Studies Unit.
Funding: The ISIS trials and epidemiological studies were
supported by the manufacturers of the study drugs1’20 and by
the British Heart Foundation, Imperial Cancer Research
Fund, Medical Research Council, and Tobacco Products
Research Trust of the Independent Scientific Committee on
Smoking and Health, Department of Health.
Conflict of interest: None.
12 Rjufnun IW, Palmer JR. Rmcnbctt I- St.
and larynx cancer nsk.- a case-control «udy. J S'ad Cancer Inst 1979,62.
15 Kau&nan DVC, Helmrich SP, Roscnb
myocardial infarction in young men. K Er.giJ.Ited 1983308:409-13.
16 Palmer JR, Rosenberg L, Shapiro S. "Low-yiekl" cigarettes and the risk o
non-fatal myocardial infarction in women. X EnglJ Med 1989320:1569-73.
behalf of GISSI-EFRLM Investigators. Tar yield of cigarette
acute myocardial infarction. BMJ 1993306:1567-70.
18 1S1S-2 (Second International Study of Infarct Survival) Collaboi
ISIS-3: A randomised trial of streptokinase s-s tissue plasminogen activator
20 ISIS—4 (Fourth International Study of Infarct Survival) Collaborative Group.
mononitrate,
msa 1995345:669-85.
Phamatol 1990;42:450-2.
smoked. J Epidemiol
AW 1979300:894-901.
(AccreditJuly 1995)
______ 5-------------------------------------------------------------------------------------------------------------------------------\
A 28 year follow up of mortality among women who smoked during
pregnancy
Paula Rantakallio, Esa Laara, Markku Koiranen
Abstract
to be higher in women who smoke during pregnancy
Objective—To investigate long term mortality than in other women who smoke. This may be
among women who smoked during pregnancy and explained either by the low proportion of those who
those who stopped smoking.
stop later and the high proportion of heavy smokers
Design—A follow up of a geographically defined or by other characteristics of these subjects that
cohort from 1966 through to 1993.
increase the risk.
Subjects—11994 women in northern Finland
expected to deliver in 1966, comprising 96% of all
women giving birth in the area during that year. Introduction
Smoking habits were recorded during pregnancy but
The consequences for the child of maternal smoking
not later.
during pregnancy have been well documented,' but
Main outcome measure—Mortality by cause (571
less interest has been directed towards the mothers’
deaths).
prognosis. We analyse here 28 year mortality data on a
Results—The mortality7 ratio adjusted for age, geographically defined population of women who
place of residence, years of education and marital smoke during pregnancy; many background variables
status was 2-3 (95% confidence interval 1-8 to 2-8) for were recorded prospectively.
the women who smoked during pregnancy and 1-6
(1 -1 to 2-2) for those who stopped smoking before the
second month of pregnancy, both compared with Methods
non-smokers. Among the smokers the relative . Population—The cohort consisted of 12 055
mortality was higher for typical diseases related to pregnant women (13 of them delivering twice) in the
tobacco intake, such as respiratory and oesophageal two most northern provinces in Finland, Oulu and
cancer and diseases of the cardiovascular and Lapland, whose expected dates of delivery fell in 1966
digestic organs and also for accidents and suicides.
and when the pregnancy resulted in a birth. The cohort
Conclusion—The risk of premature death seems covered 96% of all deliveries in the region in 19 66.: The
'fy- 7-0
I
nt results a
is a majoresq
in middle-ad
fthofalldeS
■oWng.lW.
king, howeti
uencesofS
ortality Attributable to
KcCTarette Smoking in China
items aieO
iven there-'., M
~
,
U.^XgLam, MD; Yao He, PhD; Lan Sun Li, MD; Liang Shou Li, MD; Shu Fang He. MD; Bao Cling Liang. MD
led men in Fi-14
'' 'l4fclftSW.a(t.—The few published prospective studies of smoking and mortality in
.'.'iiaSyii^F--'e reported low relative risks, but the durations of follow-up were short.
dcstoroi cor.5®ective.—To assess the mortality of ever- and never-smokers in a cohort af'
’ears °* l°llow’uPJfeign, Setting, and Subjects.—A cohort analytic study in a machinery factory
“■
id. nigareite^fei, China, involving 1696 people aged 35 years or older (1124 men and 572
' r>si-3°&jA’r’ 'v examinecl in May 1976.
•>up of CHD.cflj-1 Outcome Measures.—All-cause and tobacco-associated mortality. i myorardiaiM^iJts.—A total of 56% of the men and 12% of the women were ever-smokers
V 'sium'ra y~’
ns Tnr0LJ9h August 31.1996. 218 persons (173 men and 45 women) had
cioi-sandcari'iMIhe relative risks (95% confidence intervals (Clsj) for ever smoking (after ad
mit. j Cftrawfig-gfof age, marital status, occupation, education, diastolic blood pressure, and
dahn e WenWS®'!je and cholesterol levels) for deaths resulting from all causes, all cancer,
. Cigarette sr.-’. Jsonary heart disease were, respectively, 2.42 (95% Cl, 1.72-3.42), 2.50 (95%
2O-.G38-654.
)'■ 41-4.43), and 3.61 (95% Cl, 1.35-9.67) in men and 2.32 (95% Cl, 1.18-4.56),
Cl, 0.50-7.92), and 4.67 (95% Cl. 0.78-27.8) in women.
Seclusions.—Previous prospective studies of smoking-related mortality in
aiineiWB,Borj^atenc|ecj t0 underestimate the risks, probably because of short durations of
,vKJa,im. b&P- We have demonstrated that smoking is a major cause of death in China,
Jijtfie risks are similar to those seen in the United States and the United KingurmainH, tjens^Thus, about half of the 300 million smokers in China will eventually die of
idy'.'slWiBLY wing-related diseases if urgent tobacco-control measures are not instituted to
Spent this growing epidemic.
I « ir «
nnl.M QnHnrt’iatireS.
|31DENCE OF the adverse health eftj-analysisofrefflaj attributed to smoking derives
<1 stroke.BMJ.Vsp.,T,
.,
. ,
.
L
..
.■BBlyfrom epidemiologic studies, par. ct al. HypertaifiiSifeit.prospective studies from the
ein a-i as risk faffed Kingdom and the United States,
199122^03-3Mfcj the epidemic of tobacco-related
cached its peak in the 1980s.
lidemiologieatdiB.SW, China ,s now the largest
35:170S-1713. . ; bafo-producing country in the world,
Hong SG,
the most smokers—over 300
Smoking prevalence in China
■aUucreased rapidly tn recent decades,
coking and aussjfe, tompared with the West, China is
years ofobscr.xv.-:
’""lihmon JF~i t All* Department of Community Medicine. Uni-Vi.trr 177 ' *tw*HoigKong.HongKong(DrsLamandY.He).
’ ‘; ', ■
j „• J'teH-.s of Epidemiology (Drs Y Ho and Liang
bmoktng anauk jfel?aMCaiai0|0g,/(Dr
Sun L1) Fourth Military
ninths of follo*3gaSaUtetsav.Xi'an, and Der.anmant of Medicine
<1:1159-1172.
•>,! F. He and bang). Kun Lun Machinery Factory
ownsend M, Brotne 4
. The cpidcmio1®7;.} Saar fa Hng Lan. MD. Doparlmont ol CommoDinortalliyinlteV 3».t?xre.Un.-«ra',yolHaigkoin). Patrick Manoon
I Trial. AmXaJkT'A 'b^SouJtVtog. 7 Sassoon Rd. Hong Kong. China
(':'<'KeiftsK.-jri'ucc hku.hr1
in Cnina-Chen^jl^IbCTner 12, 1997-Vol 278. No. 18
■ irr.e
1508
only at the early stage of the epidemic.
Data from a large case-control study in
China estimated deaths from smoking at
about 500 000 per year.2
and mortality in China have been
published; one recently appeared in
a major international journal;' and
several have appeared in Chinese
journals.1' All had a short duration of
follow-up (4 to 13 years), and some were
limited to men only.3’’7 One study com
pared tobacco-related mortality in
Shanghai and the United States and con
cluded the risk of mortality in the Chi
nese was lower.3 However, as the study
from Shanghai only described the early
stage of the Chinese epidemic’1 and as
the risk estimates might have been un
derestimated, comparison of risk esti
mates from a developing nation in the
early stage of the epidemic with those
be premature.
Our objective in this cohort study in
Xi’an, China, was to examine the rela
tionship between smoking and mortal
ity in men and women after 20 years of
follow-up.
METHODS
Subjects
From March to May 1976, a cross-sec
tional survey of risk factors and preva
lence of coronary heart disease was car
ried out in a machinery factory in Xi’an
by both the teaching hospital of the
Fourth Military Medical University and
the workers' hospital of the factory. AU
employees of the factory aged 35 years
or older were included. A total of 1842
persons (1179 men and 663 women) were
examined, accounting for 90% of work
ers (96% of those aged 40 years or older).
See also pp 1500 and 1531.
In early 1994, we began to review the
records created at baseline and found
that 1696 persons (1124 men and 572
women) had data on birth month and
year, sex, marital status, education level,
occupation, systolic and diastolic blood
pressure, serum cholesterol and triglyc
eride levels, and smoking history (never,
current, or ex-smoker; amount smoked
daily; years of smoking). No baseline
data were found for 146 subjects. We
suspect theifrecords were discarded be
cause of incomplete data collection at
baseline. These 146 subjects were not
included in the present studyi
Blood pressure measurement followed
the 1974 Chinese national standards
(take the measurement on the right arm,
with the subject sitting, using a mercury
sphygmomanometer; use the mean of 2
readings that must not differ by 4 mm Hg
or more). Serum lipid analyses were per
formed on samples obtained after a 12hour fast and were carried out in the labo
ratory of the teaching hospital. The
Salkowski test (Fc [SO.|]2) was used for
total cholesterol, and the 1-Iontzsch test
Smoking and Mortality in China—Lam cl al
1505
i*ie 1 —Characteristics of 1124 Men oind 572 Women in the Cohort .r. Basel. ne in 1976'
Men. No. (%)
45.4 (6 6)
Characteristics
Manta' status
S^Qle______________________
Dv creed_____________________
Widowed
Occupation
Cadre
Worker
Education, y
0-3_________________________
4-6_________________________
7-9_________________________ ,
9-12________________________ ?
;
a 13
Sood pressure, mm Hg
Diastolic, mean (95% Cl)t__________
Systolic, mean (95% Cl)__________
Total cholesterol, mean, mmol/L (95% Cl)
pg-dL
"■-^[ycerides. mean, mmol/L (95% Cl)
pgdL
Smoking habit
Current smoker_________________
Ex-smoker
Ever-smoker (current and ex-smokers)
Women, No. (%)
43 3 (4 6)
1 (0.1)
1017(90.5)
21 (1.9)
85 (7.6)
____ 0]0)____
487(85.1)
6(1.4)
77 (13.5)
150(13.3)
403 (36.3)
566 (50.4)
60(10.5)
86(15.0)
426 (74.5)
34 (3.0)
258 (23 0)
470(41.8)
210(18.7)
152(13.5)
78(13.6)
220 (38.5)
150 (26.2)
87(15.2)
37 (6.5)
83.2 (62.5-83.9)
125 2(124.1-126.4)
4.63 (4.58-4.69)
179
1 17(1.14-1 20)
104
82.1 (81.0-83.1)
126.3(124.4-128.1)
4.62 (4.55-4.69)
178
1.13(1.09-1.17)
100
607 (54.0)
25(2.2)
632 (56.2)
63(11.9)
3 (0.5)
71 (12.4)
tCI indicates confidence interval
(acetylacetone) was used for triglycer
Fourth Military Medical University
ides."'’ Factory physicians classified only
teaching hospital and then coded accord
~2r'< of subjects, according to their work
ing to the International Classification of
sites, as being exposed to factors that
Diseases, Ninth Edition.
posed occupational hazards, such as
The data were entered (double entry,
chemicals like solvents, paints, tint! gases
once in Xian and once in Hong Kong)
(3.7%) and physical factors such as noise
and managed by Foxbase 2.1 (Fox Hold
(2.4%) and high temperature (1.1%). Be
ings Inc. Perrysburg, Ohio). Only the
cause so few subjects were exposed, the \
' baseline data from 1976 were used to excontribution of Occupational exposure to \ amine the mortality of ever-smokers (in
mortality could not be examined.
cluding current and ex-smokers) com
Vital status was assessed through Au
pared with never-smokers. Kaplangust 31, 1996. Two senior physicians at
Meier survival analysis and log-rank
the factoiy hospital were responsible foi;
tests were used to compare cumulative
overseeing the follow-up. Interviewers
survival. The Cox regression model was
were recruited from retired female cad
used to estimate relative risk (RR) and
res or technicians who had postsecond
95% confidence interval (95% CI) after
ary education. Training sessions for as
adjusting for potential confounders (age,
certainment of vital status and pilot study > marital status, occupation, education, di
testing of the interview instrument were
astolic blood pressure, and triglyceride
canned out before the main field work.
and total cholesterol levels) for each sex
Vital status was traced from personnel
separately. The date of death, the last
files and union records. Face-to-face or
date of known survival, or the last date
telephone interviews were conducted
of follow-up for those who were alive on
with all accessible subjects. Those who
that date (August 31.1996) was used as
were alive but had left Xi’an were traced
the right censored date in the propor
by letters; Vital status was also confirmed
tional hazards analysis as appropriate.
through interviews of coworkers or rela ■ The likelihood ratio test and the global x2
tives. If vital status was unknown, the
were used to test the Cox regression
last date the subject was known to be
models. All statistical analyses were car
alive was recorded. For those who died
ried out using SPSS for Windows (6.1)."'
after May 31, 1976, cause of death was
,
obtained from medical records ofthe hos- ' RESULTS
pital or death certificates in the local po-'
The study entry date for- all subjects
lice departments. This information was . was set as May 31, 1976. Through Aureviewed by 2 senior physicians of .the
gustSl. 1996,1471 subjects (945 menand
1505 JAMA. N
:er 12.1997—Vol 278. No '8
526 women > were alive, and 2111
and 45 women) had died. Seven
(6 men and 1 woman) were lost fz
up. and their last day at the fa^5
known date of survival) was co •
the censored date. The numbed
son-years of follow-up was Sb
the mean duration was 19 Iven-"'
0.9-20.2 years).
’
Causespf death were assign^
versity teaching hospitals or host*"
the city hospital level or above r
deaths (84%); for 17 deaths (8%)
of death were assigned at hospS
the county level. Seventeen Lp
(8%) died at home; the causes of;
were determined from the diaaiS
the last hospital admission, anti thf
cause of death was recorded in thet
certificate.
Demographic characteristics' di
cohort at baseline in 1976 are she*4
Table 1. The mean seram cholegl
concentrations for men (4.63 ns^
[179 mg/dLl) and women (4.62
[178 rng/dL]) were similar. -7^
At baseline, 54% of the menand jlj.'
of the women were cuirentsmokei£i
cause there were so few ex-smok^M
persons only), they were grouped fa
current smokers as ever-smokers(®j
in men and 12.4% in women). Thepra
lence of ever smoking 1 to 19 cigarefi,
per day and 20 cigarettes or morej.;
day was 32.S% and 23.4% in matt;
10.5% and 1.8% in women, respective^
For male ever-smokers, the arap
amount smoked and duration of sh'Jr,,
was 14.5(95% CI. 14.0-15.0) cigarettes?#.
day and 25.1 (95%C1.24.4-25.7)yeaS|
spectively. The female evei'-smok^a
average, smoked 9.4 (95% CI,
cigarettes per day for 252 (95% CI,?-' i
26.8) years. The mean age for stars |
smoking in men was 22.0 years (955® ;
21.6-22.4) and in women. 22.1 yearsf*:
CI, 20.8-23.4). No association wastebetween the age for starting smo&?? |
the amount smoked daily. The25nak.it l
smokers had stopped smoking, on.’’;
age, 6.8 years (SD, 6.5 years) priogs| ■
baseline study; the 3 female ex-sffljg ■
had stopped, on average, 3 years (9y ;
years) prior.
-5
Crude mortality rates in men.2s®
cancer, coronary’ heart disease,’a-b’F
cular diseases, chronic obstruct)'*Ct
monary disease, and all causes
nificantly higher in ever-smoked |
in never-smokers (Table 2). Th®1* I
12 lung cancer and 8 stomach
.
deaths observed in ever-smokeib
no cases were observed in ne'’erX:) j
ers. The RRs were indeterm*11*
these 2 cancels, but they '*e
nificant when 0.5 case was as^U ;|
have occurred in never-si’’®1'
women, significant excess de
I
0(0)
_______________
0(0)
73.5(7) .
l
_______________
________ ____
21.0(2)
SSsd40-808)_________
168.0(161
<Sdisease
.^ggybeartdisease (410-414)
52.5 (5)
115.5 (11)
tMgjjar disease (390-459)
163.0(16^Obstructive pulmonary
42.0 (4)
^J490^95)___________
472.5 (45)
P
Never-Smokers, ‘
Rate
(No. Who Died)
q
Ever-Smokers,
Rate
(No. Who Died) •
ft
Never-Smokers.
Rate
(No. Wno Died)
H i
cguss of Death
i/CD-S Code)
P
! -
P
RR (95% Cl)f
102.0(12'
68.0 (8)
76.5 (9
85.0(10
408.2 (48»
.008;
Undefined
.047+
Undefined
on
1.07 (0.40-2.91)
.07
4.30(0.93-19.9)
.002 2.50(1.41-4.43)
40.7 (4)
0(0)
10.2(1)
0(0)
101.8(10)
75.5(1)
0(0)
0(0)
0(0)
225.4 (3)
.56
1.75 (0.17-18.1)
22
1.98 (0 50-7 92)
178'6 (211
187.1 (22i
374.1 (4.ii
161.6(19'
.01
17
61.1 (6)
61.1 (6)
142.6(14)
20.4 (2)
226.4 (3)
150.9 (2)
452.8 (6)
150.9 (2)
.06
.26
.005
.01
3.61 (1.35-9.67)
1.54 (0.72-3.28)
2.29(1.27-4 12)
4.05(1.31-12.50)
.04
4.67 (0 78-27.8)
1.81 (0.31-10.6)
2.44 (0.83-7.18)
26.61 (2.08-339)
1088.4 (123)
<.00t
2.42 (1.72-3.42)
325.9 (32)
981.1 (13)
<.001
2.32(1.18-4.56)
RR (95% Cl)+
y-^lotal person-years of follow-up: men who never smoked, 9523: men who e-er smoked. 11 7 50; women who never smoked. 9820; and women who ever smoked. 1325.
r^cinicaies International Classification of Diseases. Ninth Edition; RR. ’elative rise Cl. confidence interval; and ellipses, not applicable.
\^swere adjusted for age. marital status, occupation, education, c astohc biooo treasure. and triglyceride and total cholesterol levels.
' Isvate calculated after assuming that 0.5 case had occurred tn me never-smoie'5.
Survival Time, y
Survival Time, y
Survival Time, y
Snwa! functions for death resulting from all causes (left), all cancer (center), and coronary heart disease (right) (or ever-smokers and nevensmokers.
irer-smokers were observed for all vas»!ar diseases, chronic obstructive pul
monary disease, and all-cause deaths.
arrival function curves for deaths re
ntingfrom all causes, all cancer, and
sronary heart disease are shown (Fig*o).WithU^xception of the category
’“all can^^eaths” in women, all the
t?111 t.ests were significant.
rec adjusted RRs for ever-smoking
i5® Cox regression analysis are shown
■'.Table 2. No significant interactions
observed between ever smoking
the other 3 risk factors (total choleslevel, triglyceride level, and diastolic
j Pressure), and all the Cox models
■C.atistieally sigtlificant. For men.
& * J^stec'for e'«' smoking for all
?^Wthswas 2.501;95% CI. 1.41-4.43)
rti ra-i coronai'y heart disease deaths.
CI> 1-35-9.6:) (P=.O1); all vas<!2)(P?a^ deaths, 2.29 (95% Cl. 1.27tcr,.
chronic Obstructive puhno^)(^deaths«5% CI,.1.3.1'5't pj 7®); and alllcause deaths. 2.42
M. /2-3.42J (Pk.001). The attrib
utable risk from smoking, based on the
adjusted RR. in ever-smokers for all
causes was 58.7% (95% CI, 41.9%-70.8%).
For women, the adjusted RR for coro
nary heart disease deaths was 4.67 (95%
CI, 0.78-27.75); for chronic obstructive
pulmonarv disease. 26.61 (95% CI. 2.08339.82) (P=.003); and for all causes. 2.32
(95% CI. 1.18-4.56) (P<.001). The attrib-.
utable risk from smoking for all-cause
deaths was 56.9% (95% CI. 15.3%-78.1%).
The 95% Cis for the risk estimates in
women were wide because of the small
number of deaths.
The population-attributable risks (for
all the study subjects) for all causes of
death, based on the formula [Pe (RR-1)]/
[ 1 + Pe (R R-1)] (where Pe is the propor
tion of ever-smokers and RR is the ad
justed RR). were 44.4% (95% CI. 28.8%57.6%) in men and 14.1% (95%CI.2.2%30.6%) in women!
COMMENT
Results from several prospective
studies of the effect of smoking in Chi
nese cohorts have been inconsistent. In a
study from Shanghai by Yipin et aP that
followed up IS 244 men for an average of
5.4 years, significant RRs of death re
sulting from ever smoking (after adjust
ing for age and alcohol consumption)
were found for all causes (1.4), all cancer
(1.9), ischemic heart disease (2.0), and
other heart diseases (2.4). These authors
concluded that 21% of all deaths in the
study subjects could be attributed to
cigarette smoking, and the RR for total
mortality (1.4) of Shanghai smokers vs
never-smokers was lower than that in
the United States (2.3).*i3*&
Our study provides further evidence
that smoking is a major cause of death in
China. Furthermore, our risk estimates
for total mortality are higher than those
from pre vious st tidies in China. For men.
we calculated an RR. of 2.42 (95% CI.
1.72-3.42), which is ne'ar that estimated
for smokers in the United States (2.3)
and the United Kingdom (2.0). In the
United Kingdom, a 40-year follow-up
study of male British physicians demon-
strated that during the period 1951
through 1971, death rates in cigarette
smokers were about double those in nonsmokers throughout middle age; din ing
the period 1971 through 1991, the corre
sponding difference was nearly triple."
In the United States, a study of 1 million
US adults found that the HR of death in
male smokers was 2.8 for those aged 35
to 69 years and about 2.(kin those aged 70
to 79 years.2 Yuan et al .ittributed their
lower risk estimates to the later age for
starting smoking in Shanghai (46% be
gan smoking at age 25 years or older in
Yuan’s cohort, as compared with virtu
ally no new smokers after age 25 years in
the U nited States2; 32% of male smokers
in our cohort started at age 25 years or
older). But a cohort with a later age for
starting smoking must be followed up
for an even longer duration—until the
true magnitude of risk can manifest.
Studies with an insufficient length of fol
low-up may underestimate the risks of
smoking on disease and death.
To examine the effect of the duration
of follow-up on the risk estimates for to
tal mortality, we repeated our analysis
using different durations of follow-up. I n
men. the adjusted RR estimates dbr a
follow-up duration of 5 years, 10 years,
15 ■.cm;-.,;md20years were 1.15(95%CI,
0.49-2.71), 1.95 (95% CI, 1.10-3.45), 1.84
(95% CI, 1.22-2.76), and 2.42 (95% CI,
1.72-3.42), respectively. In women, the
corresponding figures were 1.64 (95%
CI, 0.27-10.09), 2.20 (95% CI, 0.70-6.93?
2.30 (95% CI, 0.93-5.66), and 2.32
CI, 1.18-4.56). The results on crude RRs
were similar (data not shown). Thus, as
the duration of follow-up increased, the
RRs also increased."
Based on an RR of 2 from a US cohort,
Peto et al2estimated that about halfofall
young men who become regular ciga
rette smokers will eventually be killed
by tobacco. Our risk estimate is in line
with the estimate made by Peto et al,2 so
that at least half of the male smokers in
China will eventually die of smoking-re
lated causes.
Chinese women, though they smoke
in smaller absolute numbers, will not be
spared. A recent study from Shanghai
by Gao et al12 reported a significant ex
cess in total mortality (RR, 1.19) in wom
en smokers, but this risk could also be an
underestimate because their duration of
follow-up was only 5 years. Our RR was
higher (2.32) and nearerto thatfrom the
US American Cancer Society cohort
(2.15).- There was a long delay between
the male and female epidemics in the
United Kingdom and the United Suites,
where smoking prevalence in females
now approaches that in males.2
It should be noted that the risk esti
mates for active smoking arc bnsgiLon
comparing smokers-wivlrhonsmokers as
the reference, assuming that the latter
are not exposed. However, nonsmokers
who are exposed to environmental to
bacco smoke have an increased risk Of
tobacco-related diseases such as I”
cancer.” If many nonsmokers in' ’
mence group were
sed '
.ssive
References
1. Zhang YE. Make every effort for a tobacco-advertising-free China by the year 2000. In: Proceed
ings of 1006 Conference on Smoking and Health.
Hong Kong. China: Hong Kong Council on Smoking
and Health; 1996:17-20.
2. I'eloR.Lopez.DA,BorchamJ.ThunM.I! ■
Jr. Mortality From Smoking in Penelopro .-atries. imo-mii. Oxford, England: Oxford
rsily Press: 1991.
X* Yuan JM. Ross RK. Wang XL, Gao Y'l.
-rson li It. Yu MC. Morbidity and mortality
ton
to cigarette smoking in .Shanghai, China::
. -clive male cohortstuily.JrUM. 1996:276::
6511.
I. Wu XU, Lu CQ. Zhang XG. Xu Y.S,
SY.
Zhang YS. Coronary heart disease amor
kers
in a steel plant: a follow-up study of thirl. I four
years I in Chinese) Cluing lino llsin li.Knar
Ping Tso Chili. 1979;7:I6-’1-I(W.
5. I.IW.X, Wang WZ.JingHG. Qin W, . . .-i X ..
smoking, the RRs from actives?
would be underestimated. InCbi
heart disease in nevcr-smokingJ !
—
,
™ki"4 LOiK’
ronary he?:--.
Effet
in H
total mortality attributed to tote
eluding both active and passive!
ing) could have been underestimz
the effect of passive smoking hi
been taken into account inn they:
”
f'f’WY|
study or in other previous: studies
s
In conclusion, results from ours
suggest that Chinese (particularly:
who smoke like smokers in the) Trip F)i
(particularly in the United State ;'J
United Kingdom) will die of sirti
related causes similar td'theh’We Robert H. K
counterparts, although the relate
jjortance of specific diseases may; /Alice
$ice A.
A' Do
Uo'
Urgent and stringent tobaccos
measures are needed to prevesfi Context
growing epidemic in China amlinrs^-has not [
developing countries.
tjyperlipiderr
; Objective
This sillily was supported by a grant fa intake restrif
Committee via
v>wiHiTnvrcv
on Research
numaai vu un.i
and Conference^
ConfercnceQ: 1.. naeinn
ripqinn_
the University of Hong Kong, Hong Konjlg. ueb,9"and another grant from the Research Graft': tu SsttlDCJ.—
> oft he I’eopie-s Lk -. partici pa I
e's studies in Hotjifi Avi'eve'i-s ai?
?nYalScnVisita4te)
HnoflhoFaciillrdipWelS leSS tl
Identic (HC)
were definei
Interventi
pnd4taug
Shdomized
partners in f
Main Out
cage, III: SI’
Tlality in relation to smoking: 40 year/j s ' Results.ergy to 27%
ms on male Bnlish doctors. BMJ.
u YT. DengJ. Xiang Y B, cl ul. Sm^ K® 3
iihc.Tsandot
t*rs and othe
hcrilisfaaea
r <1 isenses—resullofik
rcsullofik W-4 '°+ 14.6
up of 210000 adults in Shanghai,Cs 7.0%x16.2°
' '
.........
i. Hong Kong.
,
s
cut 1 instar.
jideHCgrou
urn: Hong kwgCBKT. , ,a
.uviromnenlai Protection Agcn^y.fts1 instance). T
Ollier Disorders. Washington, DC:U$i$3 and 4, 2
'pHigh-densib
fassivcsiKjdiets 3 and
'"“"S Conclusi.
Chinese women who have never sinokctl.B.WS
308:380-384.
i.pieaningful
■ ductions in 1
Me further
‘in'HC subje
k From the No
< Knopp and MC
: Dowdy). Depai
z-toors and Mss
r-Cafdiovasculai
tejj&itmentof Psy
i.McCann), Uni*
1508
JAMA. November 12. 1907 -Vol 278. No. 18
Smoking and Mortality in China-lai; JAMA, Novem
u SudoO- S
uaoooodadu?
Fibrosis
C Oral Submucous
) sou &es?oodu3 Scotts de.jjatj sracaob-
Extracts from the article "ORAL SUBMUCOUS FIBROSIS" '
Tobacco and vitamin (’eficiencies have also been incriminated as
causes of Sub Mucous Fibrosi
Chewing of betel nuts and Areca nuts have
now taken the attention of the workers all over the world working in this field.
OSF is an insidigus disease which is progressing all over the country with the
event of many newer eating habits including 'Pan Masalas, Gulkas and
Kaporis with and without tobacco interspersed in them.
Its further
development should be arrested epidomiologically as well as.cUnically.
... When the detailed history was recorded, a significant observation made
was that 9 out of 10 patients were habitual takers of different types of pan
masalas available at least for one year, with 5 of them ieven taking 'Gutkas'.
I he Report may also-highlight certain important aspects from the
ar tide written by Soma Babu, and others. The relevant extracts may be:
"A study was carried out to examine the comparative inwivo_effacts_oLp.an
masala / qutkha vis-a-vis betel quid chewing QQ_buccaI--mucosal cytology^ Ln
patients of oral submucous fibrosis(OSF). The nucleolated intermediate cells
which constitute proliferating ratio o’f~(he cells in the buccal mucosa was
- 2 significantly higher in all habitual chewers. more so in pan masala / gulkha
consumers. The group which chewed pan masala /' gutkha alone had
developed OSF within
whereas betel quidInduced OSf_
between 2 and 25 years. It, therefore, appears that habiutual chewing of pan
masala / gutkha could induce OSF earlier than beteiquid.
exist.
It is estimated that in India alone around two million cases of OSF
---------------- -------------------------------- ---------
In India, the use of betelcuid can be traced back to more than 2000
years. In recent years, the traditional betelcuid is gradually being replaced
by a new product called 'Pa'n Masala / Gutkha'. Pan Masala contains all the
ingredients of traditional, betelquid except betel leaf, while gutkha contains
tobacco in addition to other ingredients of pan masala.
The present study was carried out to compare the clinico-pathological
features of OSF in subjects habituated to consumption of either betelquid
and / or pan masala / gutkha.
In general pan masala usage was seen predominantly in younger age
group. The mean ace of pan masala chewers with SE is 24.9 + 0.87 years
Tney~developed OSF after chewing for a mean duratiorFof 2.7 + 0.61 years,
whiie beteiquid chevzers, who are older with a mean age of 34,3 + 3.63 years
had developed OSF after a_mean duration of 8,6 +2.30 years of" habitual
chewing. The age analysis showed that 80% of pan masala and pan masala
+ betelquid chewers were below o(J years,'Whereas in betelquid group only
28% vzere below 30 years. The important observation is that pan masala
alone or combined usage of pan masala and betelquid induced OSF changes
in oral mucosa much earlier as compared to traditional betel quid chewing.
The severity of restriction in the opening of the mouth i.e. inter incisal
distance is almost same among all the habitual chewers but significantly
reduced when compared to non-chewers.
Clinical and histological features observed in the present study
showed that, the habitual chewing of betelhUtTlobacco Fbetelquid or pan
masala__/ gutkha is associaled with USE. Z7Sihce~~tbbodco~i‘S—'one or the
constituents of gutkha, its consumption probably results in O5R————
the addition of tobacco to betelquid increased the risk from 4 (without
tobacco) to as much as 29~~times with addition. ...the tissue collagen
increased "significantly in buccal mucosa oiopsy samples obtained from
patients who chewed belelnuts / pan masala and developed OSF.
It may be mentioned here that traditionally in India, adults only after
marriage are consumers of betelquid. The children and unmarried persons
by social customs refrain from such habits of chewing. However, during
recent yeais with the advent of attractive, conveniently packed sachets and
mass media adveilisement. consumption of pan masala by younger people
has considerably increased.
3
The group which chewed pan masala / gutkha and who had OSF, were
consuming it for a period of 4 months to 4 years with a mean duration of 2.7j;
0.61 years whereas habitual chewers of betelquid were bertween 2 to 25
years with a mean duration of 8.6 + 2.30 years. This indicates that pan
masala / gutkha chewing may induce OSF in a shorter period compared to
belelquid chewing. The combined chewing of pan masala and berelquids
also had a mean duration of 3.5 + 0.62 years. ... Another possible reason for
delayed effect of betelquid in the development of OSF compared to pan
masala chewing'could perhaps be due to composition of betelquid.... The
average betelquid weighing 3.8 gms has 70% moisture,, whereas the pan
masala / gutkha sachet weighing 3.5 gms. has 7% moisture. The general
impression among the habitual chewers is that,’one who consumes 2 to 10
betelquids per day can conveniently and comfortably eat equal numbner of
pan masala sachets. It appears that 3 to 4 gms quantity of either betelquid or
pan masala can provide mouthful satisfaction for habitual chewers. Based on
this observation and taking into account the moisture content, in the persons
who consume one sachet of pan masala, the intake of active ingredients will
be approximately 3 times higher than betelquid. Therefore, the induction of
OSF is possibly more rapid with pan masala as compared to betelquid
chewers.
It can be concluded that habitual chewing of pan masala / gutkha can
induce OSF at a faster rate compared to conventional betelquid, the reasons
being the absence of betel leaf and low moisture presence in the pan masala
I gutkha.
2017
7Hho»encsis of OSF/Pillai et al.
wtigens?14"1’* a similar association has been sought
far OSF.
In an elegant study of 50 unrelated patients of In
dian origin with OSF. Canniff et a/?17 showed increased
frequencies of A10, B7, and DR3. It is c: interest that inWian populations HLA A10, BS, zr.d DR3 occur in
tvsitive linkage disequilibrium?1* The finding reported
FyCanniri et c\.?17 that A10 and DR3 were increased
ejnificantly in a. croup of patients whh OSF, suggests
^possibility that a haplotype encoding these antigens
associated with the susceptibility to OSF. It has been
apn-n recently that particular haplotypes, rather than
rdividual antigens, are associated with susceptibility to
cmimatoid arthritis?1’ insulin-dependent diabetes
sellites?” and gold-induced nephropathy?^0 The de-
sctsin cellular immunity seen in OSF3:'7’*”,n are fur- *
; her suggestive of an autoimmune phenomenon. Morei *rr, the presence of autoantibodies against gastric
.?&, smooth muscle, and nuclei also has been docurznted 121 Studies on serum from our Laboratories also
■jvt shown elevated levels of immunoglobulins G and •
A.”5* A similar finding is seen in'scleroderma, a disease
■Kembhng OSF histologically in that epithelial atrophy
»c dermal fibrosis are associated with 3 chronic inflamaitory infiltrate and an increased frequency of HLADrJand the haplotypic pair BS/DRo?22-123
Conclusions
hem the data currently available or. OSF, it appears
pise dear thatxthe disease is multifactorial, as is the
05? with oral cancer and most of its precursor lesions. It
iboeppears that people in whom OSF develops have a
imetic predisposition, which could render the oral mu.-oy more susceptibltt to chronic inflammatory changes
.xiexposure to carcinogens. The latter definitely would
rriede betel quid components including tobacco. As
•sc.-ssec earher, Detel nbt extracts czn stimulate col 1 a synthesis .inc fibroblast proli^e^£.ri□r.?^•>^, In addi>.<n. these extracts also canSstabilize the collagen fibrils
nd render them resistant Co enzymatic degradation,
"r.e role of genetic abnormalities apzr: :rcm major his-.ccmpatibility complex (MHQ varisb".:ry still needs to
:? denned for OSF. Alsc relate^ to this is the role of
rases and their oncog'nic potent:’’.. Ji appears that
nr.une dysfunction is a common\a~or and could be
ihied to any of the factors discussed so far. Based on
fine factors, we have suggested a possible model fur
a?pathogenesis of OSF, as illustrated in Figure 4. The
r*cel is indeed speculative and needs to be completed.
1 Search into genetic, viral, and immunologic aspects is
xscing in our laboratories. These, along with similar
;pro.iches elsewhere, should provide valuable infor
mation on this disease, which rapidly is becoming an
excellent.model for studying genetic-environmentalimmunologic-nutritional interactions in disease patho
genesis. .
References
£c.4jV)orf
‘•ORAL. SUBMUCOUS- ’FIBROSIS
—A NEW APPROACH TOWARDS ITS MANAGEMENT
AUTHORS
Dr. PRADEEP JAIN. M.D.S.
Dental Wing
V S M.S. Medical Collegr
-JAIPUR
Submucous Fibrosis was first described by Schwartz1* in 1952 as_ a’
Clinical entity showing thickening of
Oral Mucosa and restricted Mouth
opening*. He termed it as Atrophia
idiopalhica (tropica) Mucosae 0r i s _b u t
Joshi’ in 1953 is credited to be the
firslP«.rson_whq_d_escribed_it and gave
the present term. Though this disease
is prevalent in Indian Sub-Continent,
been
many
cases
I
reoorted from all
world.
. .Dr, VINOD KUMAR: SUMAN, b.D.S.
•
«
Senior Demonstrator: ■ •
Dental Wing:
S.M.S. Medical College .
..JAIPUR!
Soon there is progression towards.
stiffness of oral, mu cos a_an cLsarne. even’
have dilficulty in protruding thejongue.Referred pain to the ear Er deafness dueto obstruction of Eustachean tube werereported by Rao1*-11 in 1SG2. On exami
nation the patient had generalized stom-.
alities & Vesicle formasje^njwith ulccj>_
leather like showing typical fibrous
bands which extend from the pharynxto
retromolar area Er pterygomand. raphae
involvcmcnl of
Occasionaly “proceeded by
vesicle formation, always associated
with fibrous bands and a Juxta epith
elial inflammatory reaction followed by
a fibro-elastic change of the lamina
properia with epithelial atrophy leading
to stiffness of the oral mucosa, trismus
Jr I
several Cms. depending on the severity
of the disease.
Etiology :
The exact ciioiogy of this condition
is still uncertain though many factors
have been thought to be the causative
The most common initial symptom
Submuccus
Fibrosis
collagen
disorder.
Prolong Chronic irritation by
on the ears of Swiss white mice failed
to show a high incidence of cancer...
chillies, tobacco^ alcohol & betclnut is
suspected to be th^ prime cause. Since
Histopathology :
the disease occuves
predominantly
among the Indians, a possible allergen
has been suspected In their common
diet. Spices being an\essential ingre
dient
in
Indian
disnes,
Tobbacco & Vitamin!
■■■ •
the early st a g es, fine (fibril I a^j
(jpollagen^seen dispersed in connective
tissue along with marked r^cdema^.
especially
chillies & peppers, ate supposed to be a
chief or supporting etiologic factor
Sirsat & Khanolkar” has! demonstrated
changes similar to human Sub Mucous
Fibrosis' alter painting ra't palates for
8-28 weeks with a 2% concentrated
capsaicin, the active irritant substanco
in chillies.
In
presence of few inflammatory cells. In
the advanced cases the oral (^hheiTurn\
is almost invariably ext rente lycajrophic^
' with
complete
loss
of iftetepegfr;.
Epithelial atypia may also be present.
Tho underlying connective tissue shows
severe hyalinization with homogenisation
of collagen bundles. ' Fibroblasts are
marke-dly reduced in number and blood
vessels are completely obliterated or
narrowed. Some chronic inflammatory
cells may be seen. The melanin con
.
deficiencies
have also been incriminated as causes
of Sub Mucous Fibrosis. \ Chewing of
betal nuts & Areca nuts haOe now taken
the attention of the workers all over the
world woiking in this field. Though
the animal studies such as ihose invol
taining cells in lamina propria become
surrounded by dense collagen which
explain the clinically observable loss of
pigment.
Treatment :
ving the application of arecoline, the
alkaloid isolated from Betelryjts. on the
oral Mucosa of Rats have failed to yield
This dis order has been treated by
various workers on following lines of
treatments with indifferent success.
positive results for Sub Mucous Fibrosis.
so far.
Sub Mucous Fibrosis & Cancer
of the Mouth
Sub Mucous Fibrosis of the oral
cavity ' is considered to be a Precan
cerous lesion. The_ first report was
mentioned by Pay,Master*.in 1956.__ In
1966, Pindborg and Sirsat”, 15 reported
a 9% epithelial atypia changes in 101
cases of Sub Mucous Fibrosis.._TheStudy
by Kwan1’ found thatjj3r4% of patients
with ora I MeLjgnan.cies had the betel nut
chew'yjgr habit. Lab. tests to induce
cancer by applying betcl/tobncco quid
39
1.
Restriction of the habits
2.
Local injections bf fibrinolytic
agents,.’,",li.u
(Collagenase, Trypsin, Hyaluronidase, Fibrinolysine)
3.
Corticosteroids - locally/Systemically5,14
4.
Gold or high doses of vitimin
A & E
5.
Injections of Senotyphoid
large doses of Iodides’
6.
Surgical splitting
Bands1/,”
of
&
Fibrous
. ' —
—
B6
Nicotinamide
Ca. Pantothenate ■ —
0.3 Mg
15.0 Mg
1.0 Mg
The combination of iodine compound.
with Vit. B-complex is responsible for
the stimulation of metabolic processes
and enzymatic processes within the body
(Oxygen reduction, transamination, etc)
Moreover association - with Vitimin B '
Complex potentiates the iodine action
2.
& makes its use non-toxicand hepato-
protective which is
extremely valuable.
therapeutically
Administration
Treatment is initial
ed with Intramuscular lnj< of Smaller
doses and continued with the larger
doses of iodine (10,25 50,75 & 125 mg,
in 2 ml ampoules) daily. The course of
5 injections is repeated after 7 daysi
.Placenta Extract (Inj Placentrex)
It is an aqueous extract of human placenta.
It contains :
—Nucleotides
:
—Enzymes
: .Alkaline & acid phosphatase. Glutamic oxalo-acetic acid
—Vitimins
;
RNA. DNA, ATP
transaminase, glutamic acid Pyruvic acid transaminase.
Vit. E, 81, B2 B6, B12.
:
’
• Pantothenic acid, nicotinic acid, biotin, PABA, Folic acid.
— Aminoacids
—Steroids
17 Kejosteroids Cholastrian, Cholesterol.
Its action is essentially "BIOGENIC2
STIMULATION”", it is suggested that it
stimulates the pituitary, adrenal cortex
and' regulates
the metabolism
of
tissues. It is also proved to increase
the vascularity of tissues. Its use is
based on the new method of 'TISSUE
THERAPY' introduced by Filatov in 1933,
and later developed in 1953..
His
theory was that "Animal & vegetable
tissues when severed from the-parent.
body and exposed to conditions un
favourable. -but not mortal to their
existence undergo biological readjust
ment leading to development of sub
stances in state of their survival to
ensure their vitality biogenic stimula
tors.
Such
tissue" extracts when
implanted into the body after resist
ances to pathogenic . factor stimulates
metabolic ' or
regenerative
process
therapy favouring recovery”".
Administration: The regionaffected
with Sub Mucous Fibrosis was divided
into 5 regions. Each region was locally
injected, if possible around . fibrous
bands presents, intramucously at the
interval of 3 days 'for 15 days. Each
time 2 Ml. of solution was deposited ail
round the specific region on both sides.
This course can be repeated after a
month if required.
3-5
of
Fluorouracil (FFU)‘,:o :
It is a fluorine substituted analog
uracil pyramidine derivative.
Its
The present study shows the sue-
cesiul treatment by the new approach.
All the cases responded favourably. The
minimum mouth opening-achieved was.
4 mm and maximum of 25mm.
the severity grades were
When
assessed, it
was found that in 3 cases with severe
trismus mouth opening to the extent
of 20-30mm was achieved. When the
Mucosal colour. Burning sensation and
Stomatitis were compared, it was found
that In 90% of cases. Burning sensa
tion and Stomatitis completely dis
appeared while the white patch decrea
sed to a great extent.
Fibrosis is without any doubt, though
advanced cases have also shown consi
derable improvement.
Even
though
encouraging
results
were obtained with the drugs, it will
be erroneous to say it to be a treatment
of choice because the sample size being
too small and duration of results does
not guarantee it
It is felt that theseprocedures may be of greater value if
they are followed up for a long time in
a larger group of patients to keep the
degree of trismus under arrest for a long
time. The side effects of FFU and
Piacentrex should be noted down in
more
details;
The
epidemiologic
studies should be carried our in the
main centres of dental research all
The improvements seen In these
cases compares favourably with the
Studies done with other drugs including
corticosteroids, though
results with
surgery wero belter than this study.
But surgery was helpful in only very
the country to establish the
of' Submucous Fibrosis even
though to some extent, various prepa
round
cause
localised lesions, while Chemotherapy
rations
has to be resorted in generalised
lesions. Its use (combination therapy)
at the early stage cases of Submucous
of
Betelnuts,
Arecanuts
&
Tobbacco available in the market can
be incriminated.
43
t
cOcmr
</£>LaJ’AJ MEMoRjA t~ frJ S’ftf,J'f<=- OF Cj r>J C 0 LX> Crf
an-njal report IHT
2.8 SOME OBSERVATIONS ON SELECTED CANCER SITES
2.8.1 Lip, Oral Cavity and Pharynx (ICD.9 :140-149)
Malignant tumours of the lip. oral cavity and pharynx are the most common site group of cancers in the three
registries i e , Bangalore , Bombay and Madias
There is also a marked variation in the incidence of lip, oral cavity and pharynx cancer in different countries.
Indian registries display much higher age adjusted and truncated rates than those reported by other registries in the
Cancer Incidence in Five Continents (Vol. V.1987). Although this grouping includes cancers of quite distinct etiology
re q. cancers of the oral cavity, nasopharynx and hypopharynx). The global picture is dominated by the incidence of
oral cancer in Southern Asia and of oral cavity plus nasopharynx cancer in South-Eastern Asia.
Oral cancer is one of the 10 most common cancers in the world. In India, Bangaladesh, Pakistan and Srilanka,
it is the most common and accounts for about a third of all cancers. More than 100,000 new cases occur every year
in south and South-East Asia, with poor prospect of survival (Bull. WHO, 1984).
Epidemiological studies conducted in different parts of India have demonstrated that cancers of the oral cavity
and pharynx are associated to a wide variety ol tobacco chewing (pan chewing and betel nut with tobacco , lime and
other ingredients) and smoking habits prevalent among men and women. These associations are statistically
significant.
The total incidence of the lip, oral cavity and pharynx cancers disguise very large differences in the individual
sites in the three Indian registries The tongue (mainly base tongue), mouth and hypopharynx are the predominant
sites in this group.
The relative risk of oral cancer in people with various tobacco habits, as well as the frequency ol those habits,
based on retrospective case control studies in India and Srilanka by Hirayama (1966) has made interesting
observations. There is a wide variation in the frequencies and risks indifferent regions, but certain conclusions stand
out. Approximately, 90% of oral cancers in south and south-east Asia can be attributed to tobacco chewing and
smoking habits (Bull. WHO, 1984).
AVERAGE ANNUAL AGE-ADJUSTED (WORLD POPULATION) INCIDENCE RATE PER
100,000 (1982-1987) LIP, ORAL CAVITY AND PHARYNX (ICO 9:140-149)
____________ MALES____________________ FEMALES________
BANGALORE BOMBAY MADRAS BANGALORE BOMBAY MADRAS
ICD.9
SITE
140-149
Lip, Oral Cavity & Pharynx
Lip
Tongue
Salivary Glands
Mouth
Oropharynx
Nasopharynx
Hypopharynx
Pharynx etc.
140
141
142
143-145
146
147
148
149
27.2
0.3
7.0
0.4
5.5
3.1
0.7
80
2.2
16.1
0.1
3.3
0.3
4.0
1.8
0.5
5.6
0.5
19.7
0.3
4.4
0.6
6.6
1.6
0.7
4.8
'07
12.9
0.1
1.0
0.4
9.4
0.3
0.2
1.2
0.3
10.4
0.2
2.4
0.4
4.1
0.6
0.3
1.8
0.6
COMPARISON OF LIFE TIME CUMULATIVE CANCER INCIDENCE RATES (0-74 YEARS)
LIP, ORAL CAVITY AND PHARYNX (ICD-9 :140-149)
CUMULATIVE RISK
(%)
ONE IN HOW MANY PEOPLE
WILL GET CANCER IN THEIR
LIFETIME
REGISTRY
MALE
FEMALE
MALE
FEMALE
BANGALORE
2.0
1.5
50
67
BOMBAY
3.3
1.3
30
77
MADRAS
24
1.5
42
67
13.0
0.3
1.4
0.5
8.0
0.5
0.3
1.7
0.3
2.8.2
Cancer of the Oesophagus (ICD.9 :150)
In the digestive system, the oesophagus is clearly the most frequently affected site in Bombay.
It is interesting to observe that lhe disease mainly occur in the persons who are 30 years and above and the
ASR vary between 1 and 75 per 100,000.
One of the prominent epidemiologic characterstics of the oesophageal cancer is the great variability in sex ratios
reported in different geographical regions of the world. The typical pattern of male preponderance has been noted
by several registeries in Cancer Incidence in Five Continents (Vol. V, 1987). But unlike as at other registries, Bombay
presents high AAR together with a low sex ratio (M/F = 1.4 :1). In Madras, sex ratio is lower (M/F = 1.3 : 1) than
Bombay. While in Bangalore the sex ratio is almost equal to one (M/F = 0.96 :1).
Although tobacco in its various forms is clearly associated with the disease; however, it does not provide an
explanation for the sex ratio.
INTERNATIONAL COMPARISON OF AGE-ADJUSTED (AAR) WORLD POPULATION) AND
TRUNCATED (TR) (WORLD POPULATION) (35-64 YEARS) INCIDENCE RATE PER 100,000
OESOPHAGUS CANCER (ICD.9 :150)
MALES
YEAR STUDIED
REGISTRY
AAR
TR
1978-82
China (Shanghai)
20.8
21.0
1978-8
Singapore (Chinese)
1978-81
Japan (Miyagi)
1978-82
USA (Connecticut)
.
13.5
White
Black
13.9
13.3
14.5
5.1
24.0
6.2
47.8
2.8
3.4
1979-82
UK (Oxford)
3.6
1977-81
Finland
3.7
1982-87
India
16.8
14.6
14.3
Bombay
Bangalore
Madras
10.8
7.6
7.2
1986-87
Bhopal S
8.8
16.1
1987
Delhi $
4.2
8.6
■
FEMALES
1978-82
China (Shanghai)
8.9
9.7
1978-82
Singapore (Chinese)
3.5
4.1
1978-81
Japan (Miyagi)
3.1
2.5
1977-81
Finland
2.4
1.8
1979-82
Uk (Oxford)
2.9
3.6
1978-82
USA (Connecticut)
1.5 ,
6.0
1.9
11.8
1982-87
India
Bangalore
Bombay
Madras
7.9
7.9
5.5
15.7
14.6
2.3
1986-87
Bhopal $
5.3
9.1
1987
Delhi $
3.3
6.4
White
Black
$ PROVISIONAL
SOURCE CANCER INCIDENCE IN FIVE CONTINENTS. VOL V. 1987 NCRP DATA. 1982-1987
2.8.2
Cancer of the Oesophagus (ICD.9 :150)
In the digestive system, the oesophagus is clearly the most frequently affected site in Bombay.
It is interesting to observe that the disease mainly occur in the persons who are 30 years and above and the
ASR vary between 1 and 75 per 100,000.
One of the prominent epidemiologic characterstics of the oesophageal cancer is the great variability in sex ratios
reported in different geographical regions of the world. The typical pattern of male preponderance has been noted
by several registeries in Cancer Incidence in Five Continents (Vol. V, 1987). But unlike as at other registries, Bombay
presents high AAR together with a low sex ratio (M/F = 14: 1). In Madras, sex ratio Is lower (M/F = 1.3 : 1) than
Bombay. While in Bangalore the sex ratio is almost equal to one (M/F = 0.96 :1).
Although tobacco In its various forms is clearly associated with the disease; however, it does not provide an
emanation for the sex ratio.
INTERNATIONAL COMPARISON OF AGE-ADJUSTED (AAR) WORLD POPULATION) AND
TRUNCATED (TR) (WORLD POPULATION) (35-64 YEARS) INCIDENCE RATE PER 100,000
OESOPHAGUS CANCER (ICD.9 :150)
MALES
'
YEAR STUDIED
REGISTRY
AAR
1978-82
China (Shanghai)
20.8
21.0
1978-8
Singapore (Chinese)
13.5
13.9
1978-81
Japan (Miyagi)
13.3
14.5
1978-82
USA (Connecticut)
5.1
24.0
6.2
47.8
1979-82
UK (Oxlord)
3.6
2.8
1977-81
Finland
3.7
3.4
1982-87
India
Bombay
Bangalore
Madras
103
7.6
7.2
16.8
14.6
14.3
Bhopal $
8.8
16.1
Delhi $
4.2
8.6
1986-87
1987
■
White
Black
-
TR
FEMALES
9.7
1978-82
China (Shanghai)
8-9
1978-82
Singapore (Chinese)
3.5
1978-81
Japan (Miyagi)
3.1
1977-81
Finland
2.4
1.8
1979-82
Uk (Oxford)
2.9
3.6
1978-82
USA (Connecticut)
1.5
6.0
1.9
11.8
1982-87
India
Bangalore
Bombay
Madras
7.9
7.9
5.5
15.7
14.6
2.3
1986-87
Bhopal $
5.3
9.1
1987
Delhi $
3.3
6.4
White
Black
.
4.1
2.5
$ PROVISIONAL
SOURCE : CANCER INCIDENCE IN FIVE CONTINENTS. VOL V. 1987 NCRP DATA. 1982-1987
13
2.8.4
Cancer of the Larynx (ICO.9 :161)
The age-adjusted incidence rate of laryngeal cancer in Indian material is high in men than women. Among men
the highest incidence is in Bontay (rates vary between 6.7 & 8.4 per 100,000 during the period 1982 through 1987).
The AAR are low in Madras (rates vary between 3.7 & 4 6 per 100, 000) and Bangalore (rates vary between 3.1 &
4.9
per 100,000). Among females, laryngeal cancer age-adjusted rates are very low in Bangalore (rates vary between
0.3 & 1.2 per 100,000), Bombay (rates vary between 1.2 and 2.3 per 100.000) and Madras (rates vary between 0.4
& 0.7 per 100. 000).
International comparisons are done for selected countries. The highest incidence rate ot laryngeal cancer world
wide has been reported from Sao Paulo (Brazil) in males. (Males -17.8 and Females -1.3 per 100,000).
The ratio of laryngealcancerto lung cancer incidence, In men, ordinarily ranging from 1:5 to 1:20, is 1:1.6 in
Bombay, 12.2 in Bangalore and 1:1.8 in Madras.
WThe strong relation between tobacco use and laryngeal cancer has long been known.' Much of the association
seen for is demographic factors such as sex, race and geographic location is probably attributable to the effects of
tobacco, alcohol and occupational exposure.
INTERNATIONAL COMPARISON OF AGE-ADJUSTED (AAR) (WORLD POPULATION) AND
TRUNCATED (TR) (35-64 YEARS) (WORLD POPULATION) INCIDENCE RATE PER 100,600.
LARYNX CANCER (ICD-9 :.161)
MALES .
' REGISTRY
YEAR STUDIED
AAR
TR
17.8
27.6
12.6
7.7
24.8
12.4
4.5
7.1
1978
Brazil (Sao Paulo)
1978-82
USA (Connecticut)
1977-81
Finland
1979-82
UK (Oxford)
4.2
5.8
1982-87
India.
Bombay
Madras
Bngalore
8.2
13.9
7.4
7.1
.1986-87
1987 '
. .
■
Black
White
4.0
Bhopal $
3.7 ’
6.7
Delhi $
5.7
11.0
FEMALES
AAR
TR
2.7 •
■;
1.7 ■ • ’ a’
4.4
3.0
Brazil (Sao Paulo)
1.3
2.8
UK (Oxford)
0.5
0.8
Finland
0.3
0.7
India
Bombay
Madras
^Bangalore
1.4
o.5
0.7
1987
Delhi $
0.6
1.4
1986-87 - . . -'
Bhopal $
0.0
0.0
REGISTRY
YEAR STUDIED
' 1978-82
.
USA (Connecticut)
1978 '
1979-82
......
1977-81
_
’
1982-87
Black
White
,-1E
J PROVISIONAL'
SOURCE : CANCER INCIDENCE IN FIVE CONTINENTS. VOL. V. 1907 NCRP DATA. 1902 07
2.5
1.2
1.2
Cancer of the Trachea, Bronchus and Lung (1CD.9 ; 162)
2.8.5
Cancer of the lung is ol epidemiological interest because of the wide spread geographical and racial variations
observed and steadily increasing incidence and mortality noted in the West. This increase has so tar been noticed
particularly in men, but recently women have also begun to present a similar rising trend.
The AAR and TR of lung cancer are much lower in India than the corresponding rales reported by other countries
in Cancer Incidence in Five Continents (Vol.V).
Lung cancer is one of the most common and lethal malignant tumours known. It occurs mainly in urban areas
through out the industrialised world. In India, its incidence is higher in the male population (ranges between 10 and
13 per 100,000 in the three centres) than females. Among Indian women incidence is very low (ranges between 1
and 3 per 100,000). In white American males & females (USA-Connecticut), the incidence is 64.3 and 25.3 per
100,000. The male-female ratio thus works out to 2.5 :1. The overall incidence of the disease is much higher in the
industrialised countries
,
■" '
A large number of epidemiological studies in the West has shown that there is a progressive and absolute risk
in its incidence which has occurred over the past few decades and that it is clearly linked to cigarette smoking and
environmental pollution.
The association ol cigarette smoking with lung cancer has now been universally accepted . The U.S. Surgeon
General’s Advisory Committee concluded that cigarette smoking is causally related to lung cancer in men and that
its effect far outweighs all other probable etiological factors The risk increases with the duration of smoking habit and
the number of cigarettes smoked daily A heavy smoker (more than 50 cigarette per day) runs a 20 times higher risk
of developing lung cancer, than a non-smoker. The increasing incidence of lung cancer in women in the West is
clearly linked with the steep increase registered in cigarette smoking by women during the sixties.
Atmospheric pollution from industry and automobile exhausts is also considered to be a significant etiological
factor
There are several studies in the West on industrial lung cancers arising in workers associated with certain
occupations, such as :
(i)
Asbestos miners and textile workers.
Manufacturers and handlers of arsenic ■ containing insecticides and those working as arsenic smelters.
(ii)
■
(iii)
Chromium refining workers and nickel & iron ore miners
(iv)
Uranium and Cobalt miners
(v)
Radon daughter products
INTERNATIONAL COMPARISON OF AGE-ADJUSTED (AAR) (WORLD POPULATION) AND TRUNCATED
(TR)(35-64 YEARS) (WORLD POPULATION) INCIDENCE RATE PER 100,000.
TRACHEA, BRONCHUS & LUNG (ICD.9 :162)
MALES
FEMALES
YEAR STUDIED
REGISTRY
AAR
TR
AAR
TR
1979-82
UK (Oxford)
68.8
68.1
25.3
41.5
1977-81
Finland
1978-82
USA (Connecticut)
1977-81
Columbia {Cali)
1982-87
India
While
Black
74.2
93.2
21.9
41.1
64.3
89.8
81.1
140:1
19.5
7.0
25.6
10.0
19.5
25.5
5.4
9.5
Bombay
Bangalore
Madras
'l3.3
8.7
7.7
21.4
16.1
17.2
2.9
1.7
1.3
4.6
3.1
2.9
1986 87
Bhopal $
10.3,
19.0
1.9
3.0
1987
Delhi $
8.8
14.7
1.7
3.2
S PROVISIONAL
SOURCE CANCER INCIDENCE IN FIVE CONTINENTS VOL V, 1987 NCRP DATA. 1982-1987
2.9
BURDEN OF TOBACCO RELATED CANCERS IN INDIA
NCRP has provided incidence of cancer in Bangalore, Bombay and Madras areas for the years 1982-1987.
Based on these figures, the burden of tobacco related cancers in India has been estimated as given below in the
table.
BURDEN OF TOBACCO RELATED CANCERS IN INDIA,ESTIMATES FOR 1990
MALES
FEMALES
TOTAL
Total Population (millions)
430
410
840
Crude Rate per 100,000
70
80
75
301,000
328,000
629,000
61,500
Number of New Cancer cases per Year
New Cases Related Io Tobacco Habits:
.
34,500
27,000
Pharynx & Larynx
47,000
10,400
57,400
Oesophagus
22,600
16,400
39,000
Lung.
26,400
5,000
31,400
Others
14,500
7,200
21,700
TOTAL
145,000
(48%)
66,000
(20%)
211,000
(33%)
Mouth
Estimates are shown separately for males and females for commonly affected sites namely, mouth, pharynx &
larynx, oesophagus and lung. Some other sites related to smoking habits known from the experience of the west
such as bladder, pancreas etc. are taken as others. Although stomach and uterine cervix cancers are appear to be
associated with the bidi and cigarette smoking , but they are not taken into account. It is also possi ble that tobacco
chewing and bidi smoking may show risks tor cancers not studied so far. From these .considerations, the present
estimate of tobacco related cancers is a conservative one (Sanghvi, 1989).
in India, cancer morbidity related to tobacco is 48% in men and 20% in women with an overall estimate of 33%
for the two sexes. 75% cancers related to tobacco were found In mouth, pharynx & larynx and oesophagus; lung
^cancer accounted for only 15% of cases.
2.10
Incident Cases of Cancer By Year 2000 A.D.
Incident cases of cancer by year 2000 A.D. has been estimated as given in the table. These estimates are based
on weighted averages of crude incidence rates for Bangalore, Bombay and Madras registries. India's population was
projected, by sex and age, for the year 2000 A.D., using 1971 and 1981 censuses and applying the linear rate of
growth..The present estimates of cancer cases may be considered as a conservative one.
ESTIMATED NUMBER OF INCIDENT CANCER CASES FOR SELECTED SITES, ALL AGES,
BY THE YEAR 2000 A.Di, IN INDIA
SITE-
(ICD.9)
MALES
FEMALES
TOTAL
Lip, Oral Cavity
Pharynx & Larynx
Oesophagus
Stomach
Lung
Breast
Cervix Uteri
Others
(140-145)
(146-149,161)
(150)
(151)
(162)
(174)
(180)
45000
60000
30000
33700
33700
—
—
.
172100
32000
16000
20000
16000
8000
72000
104000
131200'
77000
76000
50000
49700
41700
72000
104000
303300
374500
399200
773300
TOTAL
ESTIMATES ARE BASED ON WEIGHTED AVERAGES OF CRUDE INCIDENCE RATES FOR
BANGALORE. BOMBAY AND MADRAS
SOURCE : NCRP DATA. 1982-1987.
TABLE 4
ALL CANCER PATIENTS TYPE OF TREATMENT RECEIVED HCRs, 1987
Chandigarh
Ditxugarh
Trivandrum
Mate Female Mate Female Male Female
%
%
%
%
%
%
Bombay
Type of
Bangalore
Treatment
Male Female Male Female Male Female
%
%
%
%
%
%
Madras
14.6
10.8
9.7
24.0
6.0
7.4
Surgery (S)
7.8
4.0
21.9
21.1
6.9
2.1
44.9
55.5
81.4
53.3
62.2
61.4
Radiotherapy (R)
36.2
61.6
44.1
48.6
71.9
71.1
18.9
13.2
3.7
12.4
'8.0
8.5
(S) + (R)
4.9
3.9
97
7.3
6.1
2.1
5.5
4.5
2.6
5.0
5.1
29
Chemotherapy (C)
24.2
13.4
10.4
5.8
3.5
2.7
3.1
3.7
1.8
3.3
2.0
2.2
(S)HC)
3.6
2.6
3.3
6.1
1.9
0.5
7.1
2.1
0.7
2.1
14.1
8.4
(R) + (C)
19.6
7.4
8.6
3.1
7.3
8.5
3.0
4.4
0.2
0.0
1.5
3.0
(S) + (R) + C)
2.6
2.1
1.1
2.8
1.6
6.5
2.8
5.5
0.0
0.0
1.1
6.2
Others
1.2
4.8
0.8
5.2
0.5
6.6
1603
2852
2388
737
1181
732
748
547
242
1245
1060
Total No. of
Cases Trated
1133
Tobacco Related Head and Neck Cancers
Analysis o( head and neck cancers (ICO 9:140-149) in the hospital registries according to the 4th digit code of
the ICD9 has a significant effect on the ranking of common cancers particularly in men. Pharynx comes out as a
leading cancer site in men in five out of six registries (Table 5). This is in contrast to the 3-digit classification which
shows oral cavity as a leading cancer site in three out of six registeries, pharynx In two and lung in one registry. The
major reason for such a change is the shift of base tongue cancers from the oral cavity to the oropharynx where they
really belong. Since base tongue is identifiable only by the 4th digit ICD9 code, such classification is needed if oral
cavity and pharynx, aetiologicaliy and biologically different, are to be distinguished. Chewing tobacco causes oral
cancer; bidi smoking is related to pharyngeal cancer.
Overall about 85-90% of oral and pharyngeal cancers are evaluated and more than 60% get cancer directed
treatment. The proportion of patients treated is generally higher in general hospitals than in cancer centres; this is
also reflected in the different categories of cancer spread.
Breast and Cervical Cancers :
Overall about 50% of breast cancer patients could be and were evaluated for cancer spread. Of these 40%
received cancer directed treatment. In contrast almost 90% of cervical cancer patients could be and were evaluated
and 60% wre treated. There are two major difference viz. (i) surgery is the first choice of traetment in breast cancer.
(ii) surgical facilities are widely available outside reporting institutions so that breast cancer patients have often already
had this before they come to reporting institutions; (iii) breast cancer is more common in upper socio-economic
classes.
■' Pattern of treatment for breast and cervical cancer show a higher proportion of patients have been treated in
general hospitals than in cancer centres in all the three categories (localised, regionally and distantly spread) of cancer
spread. This proportion is highest for patients which localised cancers followed by regionally spraed cancers
Additional studies into patient noncompliance/compliance and of therapeutic facilities available outside reporting
institutions are needed.
TABLE 5
LEADING CANCERS USING 1CD 9 ■ 3-DIGIT AND 4-DIGIT
CLASSIFICATION CODES -HCRs, Males-1987
REGISTRY____
3-DIGIT
4-DIGIT
General Hospital
Chandigarh
(12.2)
(9-9)
Pharynx
Lung
Larynx
i
Oesophagus)
Lung
Oral Cavity
Pharynx
Oesophagus 1
Larynx
J
(9-9)
(9.8)
Brain
"
Pharynx
Oesophagus
Oral Cavity
Lung
Larynx
Stomach
(26.1)
(19.7)
(12.9)
(14.9)
(5.5)
Dibrugarh
Pharynx
Oesophagus
Oral Cavity
Lung
Larynx
Stomach
(32.9)
(19.7)
. (6-2)
(4.9)
(4.2)
Oral Cavity
Lung
Pharynx
Oesaphagus
Brain
(22.6)
(12.4)
(8.5)
(5-9)
(4.2)
Trivandrum
Oral Cavity
Lung
Pharynx
Oesaphagus
Brain
(20.3)
(12.4)
(10.8)
(5.9)
(4.2)
Pharynx
Oral Cavity
Oesophagus
Lung
Stomach
(15.1)
(14.8)
(11.4)
(8.3)
(5.3)
Bangalore
Pharynx
Oesophagus
Oral Cavity
Lung
Stomach
(20-5)
(11.4)
(9.4)
(8-3)
(5.3)
Oral Cavity
Pharynx
Oesophagus
Lung
Larynx '
(18.6)
(11.8)
(7.7)
(69)
(6.7)
Bombay
Pharynx
Oral Cavity .
Oesophagus.
Lung
"
Larynx
(18.5)
(11-9)
(7.7)
(6.9)
(6.7)
Oral Cavity
Pharynx
Oesophagus
Stomach
Lung
(21.5)
(11.6)
(9.3)
(7-7)
(5.4)
Madras
Pharynx
Oral Cavity .
Oesophagus
Stomach
Lung
(17.0)
(16.1)
(9.3)
(7.7)
(5-4)
(7-3)
(3.5)
(5-7)
Cancer Centre
Regional Cancer Registry— Expansion of the Hosital Registry into a Network :
T
sl
Dibrugarh Hospital registry of Assam Medical College has taken initiative and provided additional data from the
D.B. Barooah Cancer Institute at Guwahati. The data from these two sources in Assam complement each other. This
is a welcome begining towards the development of a regional cancer registry composed of a group of registries ir
different hospitals.
Acknowledgements :
To registries, for cooperation and prompt despatch of data; Mr. M.D. Singh for statistical assistance; Ms. C
Stewart for computer programme generation; Ms. V. Krishnan for correction of errors and generation of tables; M
M. Gujarathi for typing assistance; messrs R. Keni and T. Sable for circumstantial support.
Reference :
82
National Cancer Registry report for 1986; Indian Council of Medical Research. New Delhi. 1989.
A study of certain's epidemiological
factors on blood pressure distribution
and prevalence of hypertension
in a rural • community of
Pondicherry (S. India)
DISSERTATION SUBMITTED TO THE
UNIVERSITY OF MADRAS
IN PARTIAL FULFILMENT OF THE REQUIREMENTS
FOR
M.D. [Br. XV] COMMUNITY MEDICINE
Mhe
Or-
MARCH 1986
5
No.l:
TO STUDY CERTAIN EPIDEMIOLOGICAL
FACTORS LIKE AGE, SEX , MARITAL STATUS,
OCCUPATION , INCOME, HEIGHT, WEIGHT
AND HABITS LIKE SMOKING AND DRINKING
ALCOHOL ON BLOOD PRESSURE DISTRIBUTION.
No.2:
TO ESTIMATE THE PREVALENCE OF HYPERTENSION
AND TO STUDY THE EPIDEMIOLOGICAL FACTORS
IN CASES OF HYPERTENSIVES THUS DETECTED .
?3
Smoking and Blood PressureS
Kannovan M. et al in 1959 conducted a
blood pressure survey in Finland to study the
relationship to study the relationship between,
cigarette smoking, serum cholesterol and blood
pressure .
In this study it was observed that cigarette
smoking varied inversely with the level of blood
pressure.
The level of blood pressure depended on
the years of smoking.
Another study was conducted by Blackburn
et al in Finland in i960. The study population consisted
of 1618 men aged 17-67 years.
The level of smoking
was divided into light less than 10 cig/day, Moderate
ll-2o per day and High more than 20 per day.
The
study population included various categories.Afaongst
studdnts and businessmen it was observed that smoking
and blood pressure did not have any relationship. But
on examination of data from broader studies of
population , there was a tendency towards lower systolic
and diastolic pressure in smokers.
This was statistically
significant in the three groups.’
Goteberg's btudy in Sweden showed that
the frequency of smoking and level of blood pressure
showed a inversed relationship with each other,
Sive's study
among Israeli men showed that
smoking had a-negative effect on the level of blood
pressure.
Gyntelberg* s study in Copenhagen males
aged 40-59 years showed that smokers had lower blood
pressure levels than non-smokers.
The level of smoking
was divided into 3 categories - High more than 10 perday
Moderate 5-10 per day
Light less than 5 per day
The levels.of blood pressure showed a decrease with
increase in the frequency of smoking.
Poulter's study in an African tribe in 1980
showed that there was no apparent association between
blood pressure and reported level of smoking.-
Alcohol and Blood Pressure:
Goteberg's study revealed that there was a
significant increase in the levels of blood pressure in
case of drinkers compared to non-drinkers.
The level
of blood pressure increased with level of drinking.
In Gyntelberg's study it was observed that
there was a significant increase in the levels of both
systolic and diastolic blood pressure among drinkers.
Also a statistically significant increase in both
systolic and diastolic blood pressure was found with an
increased alcohol consumption.
1594 male employees in Chicago People gas
light and Coke Company, was studied for relationship
The study was conducted in the Jawaharlal
Institute Rural Health Centre (JIRHC) Ramanathapuram
from 1st October,1984 to 30th September,1985.
This
is situated at a distance of 15 Kms from Pondicherry
the headquarters of the Union Territory of Pondicherry.
The population of the state was 6,04,471 according to
1981 c nsus.
The JIRHC caters to a population of 14,562
residing in fourteen villages (JIRHC, Annual report,
1983). The centre has got a good documentation system
(Datta et al 1965).
Details of the population of the
14 villages are given below:
Males
Females
Total
283
635
684
1319
353
990
886
1876
Osudur
24
65
73
138
Pilliarkuppam
287
784
757
1541
Coodapakkam
768
2126
2106
4232
Koneri kuppam
81
220
185
405
Karasur
169
430
410
840
Thuthipet
73
179
190
369
Agaram
85
258
228
486
Poraiyur
157
481
424
905
01aivakkal
Sedarapet
36
414
107
1158
89
1097
196
2255
Village
No. of
Familes
Ramanathapuram
Thondamanatham
Total number of familie s - 2730
Males
- 7433
Female s
- 7129
.30
Study sample ;
taken as '
family
The sampling unit was
This was because
i) All the families in the study villages
have been given folder numbers which could be
conveniently used for choosing the study population
by sampling.
ii) All the members in a family could be
surveyed and any family history of hypertension
could be studied.
It has been found in most Indian studies
that incidence of hypertension was minimal before
the age of 20 years ( Padmavathi 1959, Ranganathan
et al 1975).
Therefore the study was restricted to
persons 20 years and above.
Sample size: According to the prevalance
studies conducted in rural areas of India, hyper
tension prevalence ranges from 0.17% (Padmavathi,
1959) to 8.1%.
An average prevalence value of 4%
was taken for calculating the sample size for the
present study.
The sample size was calculated based on
the formula 4PQ
p2
where 'P» was the prevalence
rate.
An error of 30% was allowed on either side
of the values.
Confidence limit was 95%.
31
Accordingly, the sample size was calculated
as 1100. 100 more subjects were included for chances
of drop outs.
Hence 1200 subjects were required for
the study.
Since the average family size in the study
area is 5.3 and 52% of the total population are aged
20 years and above, to get the required study unit of
1200, 500 families were required to be selected.
The 500 families were chosen from all the
families (2730) residing in the 14 villages giving
proportionate representation to all the villages
according to the number of families in the village.
The study families were chosen from each of the
villages by simple random sampling.
The number of
families chosen from each of the villages are given below.
Village
No. of families
chosen
Ramanathapuram
52
Thondamanatham
65
Osudur
4
Pilliarkuppam
53
Coodapakkam
141
Konerikuppam
15
Karasur
31
Thuthipet
13
Agaram
14
Poraiyur
Olavaikkal
29
7
Sedarapet
Total no, of families
76
500
32
Data Collection; 1, House to house visit
of the sampled families was made and each family
member above 20 years in the family was contacted
and data collected regarding name, age, sex, caste,
marital status, income, habits like smoking and
drinking alcohol, height, weight and blood pressure
on a predesigned and pretested proforma (Annexure I).
If any member / members in a particular family could
not be contacted after three visits the particular
family was eliminated from the sample and the family
reiding next to it was taken into consideration.
The study was conducted in the morning
hours between 6 AM to 12 Noon and in the evening
hours between 4.30 PM to 7.00 PM.
2.
The following procedures for recordi
were followed for; recording blood pressure , weight
and height.
a) Recording of blood pressures
The
blood pressure apparatus was checked every day for
any leak in the mercury column or other problems
in the apparatus.
Blood pressure was recorded
using a mercury sphygmomanometer with a 12.5 cm
cuff with subject in a sitting position and the
left arm slightly flexed at heart level (Dasgupta
1982).
For this purpose a stool was carried to
33
Before recording of blood pressure
every house.
it was ensured that the subject was in a relaxed
If the subject was engaged in any
atmosphere.
physical activity or smoking he was made to
relax for 5-10 minutes and after filling up the
history and identification data, blood pressure
was recorded.
Systolic blood pressure was taken
as the pressure at which the ear distinguishes
the first arterial sound.
The point at which the
arterial sound disappears (Korotkoff's phase 5)
was taken as the diastolic blood pressure (TRS
628,1978).
Three readings were taken at an
interval of five minutes and the mean of the three
values was taken.
A case was diagnosed as hypertensive
if subject had systolic blood pressure 160<
mmHg
or more or diastolic blood pressure 95 mm Hg or
more or both (TRS 628,1978).
If the subject was
diagnosed as hypertensive, details regarding family
history, awareness and treatment details if any
were obtained.
b. Recording of weight?
This was recorded
with subject in minimal clothes by bathroom scales
weighing machine.
nearest kilogram.
The readings were taken to the
,34
c. Recording of height;
Height was
recorded by means! of a metal measuring tape, with
the subject standing against the wall of the house.
Readings were taken to the nearest centimetre.
3.
Data on (a) smoking habits:
Every
individual was enquired about their smoking habits.
If there was a positive history of smoking , details
of regarding type of smoking and amount smoked per
day was enquired.
Smokers were classified according to
i) number smoked per day.
Group I: Light ,Less than 5 per day
II; Moderate, 5-10 per day
III: High , More than 10 per day
(Gyntelberg 1962)
ii) type of smoking.
Group I: Beedi smokers
II: Cigarette smokers
III. Cigar smokers
(b) Drinking habits; If the subject was in
the habit of taking alcohol, details regarding
frequency of drinking and type (toddy, arrack,
IMFL) and amount of drinking were enquired and the
details classified according to
TABLE 1
DEMOGRAPHIC CHARACTERISTICS OF THE STUDY POPULATION
Number
(N=1262)
Percent
20 - 24
25 - 34
35 - 44
45- ’ 54
55 - 64
65 +
126
309
347
293
135
52
10.0
24.5
27.5
23.2
10.7
4.1
Males
Females
674
588
53. 4
46.6
135
1055
82
10.7
82.8
6.5
699
320
243
55.3
25.5
19.2
515
443
137
167
40.8
35.1
10.9
13.2
672
382
208
53.2
30.3
16.5
871
317
50
24
63.7
30.5
3.9
1.9
Demographic characters
1. Age (in years)
2. Sex
3. Marital status
Unmarried
Married
Widowed/separat ed
4. Ca st e:
Counders
Harijans
Others
5. Occupation
Agriculture
Housewife
Farmer
Others
6. Education
Illiterate
Read and Write & primary
Middle school and above
7. Percapita income per month
Less than Rs.50
Rs. 50 to 99
Rs. 100 to 149
Rs. 150 +
TABLE. 12
BLOOD PRESSURE DISTRIBUTION ACCORDING TO HEIGHT
DBP
SBP
S.D
Height in
eras
No.
Mean
S,D.
130 +
65
121
11.0
75
7.4
140 +
286
124
11.4
78.
7.2
150 +
434
124
10.1
78
6.9
160 +
312
123
10.8
77
6.8
170 +
165
125
10.8
79
7.1
Mean
TABLE. 13
BLOOD PRESSURE DISTRIBUTION ACCORDING TO
SMOKING HABITS AMONG MALES
DBP
SBP
Habit
No.
Smokers
NonSmokers
Mean
S.D
Mean
S.D
203
125
11.1
79
6.7
471
125
11.4
79
6.4
Even with 3 standard deviation the Quetelet's index
would remain at 0.25 indicating in the study sample
that no one was over weight as per the index.
This could be one of the reasons for the poor correlation
of Quetelet's index with blood pressure.
Smoking habits; Table 13 shows blood
pressure distribution according to smoking habits among
males.
None of the females in the study population
gave history of smoking.
Slight increase in the
values of both systolic and diastolic blood pressure were
seen among non smokers, but the difference in the means
were found to be not statistically significant.
J able 14 shows blood pressure distribution
according to frequency of smoking.
The values of
systolic and diastolic blood pressure show an uneven
distribution and the values were not statistically
signi ficant.
Table 15 shows blood pressure distribution
according to type of smoking.
Most of the smokers were
beedi smokers and only a small percentage of smokers
(13%) were cigarette smokers.
Kanovan (1959) observed that smoking varied
universely with blood pressure.' Blackburn (i960)
showed that the values of both systolic and diastolic
blood pressure values were lower amongst smokers.
(1962) and Goteborg (I960) also showed an inverse
relation with blood pressure amongst smokers.
Sive
TABLE 14
BLOOD PRESSURE DISTRIBUTION ACCORDING TO' FREQUENCY OF
\
SMOKING
DBP
SBP
frequency
No.
Mean
S.D
Mean
S.D
Mild
60
125
10.8
79
6.3
Moderate
109
124
11.7
79
7.2
41
125
12.1
79
7.4
Hi gh
TABLE 15
BLOOD PRESSURE DISTRIBUTION ACCORDING TO TYPE
OF SMOKING
Type
No.
SBP
DBP
Mean
S.D
Mean
S.D
Beedi
164
125
11.2
79
6.8
Cigarette
27
125
11.4
79
7.2
Cigar
12
124
11.9
79
6.9
TABLE 27
BLOOD PRESSURE DISTRIBUTION AMONG HYPERTENSIVES
ACCORDING TO ALCOHOL DRINKING
HABITS
Group
S B P
No
D B P
Mean
S.D
Mean
s,,D
Dri nker s
9
156
4.2
99
2,,0
Non
Drinkers
9
155
3.7
99
1 .3
TABLE 28
BLOOD PRESSURE DISTRIBUTION IN HYPERTENSIVES ACCORDING TO
AMOUNT OF ABSOLUTE ALCOHOL CONSUMPTION
S BP
Amount per
year
No
D B P
Mean
S.D.
Mean
S.D
1.8
5000
4
155
2.5
99
10000 4-
2
158
2.0
100
20000 +
3
155
5.2
97
1.9
1ABLE 29
BLOOD PRESSURE DISTRIBUTION IN HYPERTENSIVES ACCORDING TO
SMOKING HABITS
Group
No
SBP
Mean
S.D.
DBP
Mean
S.D.
Non smokers
8
155
4.9
99
1.7
Smokers
10
156
3.5
99
1.6
50
absolute alcohol show an uneven distribution. The
values are shown in Table 28.
Table '29 shows blood pressure distribution
according to smoking habits.
The values between
smokers and non smokers was not statistically
si gni f icant.
Awareness of hypertension?
6 persons
(18%) were aware of being hypertensive.
In this
only 50% were taking regular treatment.
The rest
were on irregular patient.
27 persons (82%)
who were not aware of being hypertensive, were found
to be asymptomatic and pursued with their physical
work though they were hypertensive.
Family history of hypertension; In the
present study, there was no family history of
hypertension among hypertensives.
This could be
because of the lack of knowledge of the hypertensives
regarding blood pressure status of their parents
or other relatives and may also be due to the small
number of hypertensives in the study.
The present stgdy was conducted in JIRHC,
Ramanathapuram with the aim of studying certain
epidemiological factors like age, sex, marital
status, occupation, income, height, weight and
habits like smoking and drinking alcohol on blood
pressure distribution and to estimate the prevalence
of hypertension and study the epidemiological factors
in cases of hypertensives thus detected.
Data was
collected from 1262 persons above the age of 20 years
by house visits.
Prevalence of hypertension; The prevalence
of hypertension was estimated to be 2.6% . Prevalence
of hypertension was slightly higher in males (2.7%)
than males (2.5%) though the differences between the
two proportions was not significant.
Epidemiological factors and blood pressure:
Age and Sex:
The levels of both systolic
and diastolic blood pressure increased with advancing
age.
A statistically significant positive correlation
in males were found for both systolic blood pressure
and diastolic blood pressure with age.
In case of
females, a statistically significant positive
correlation was.found only for systolic blood pressure.
Marital status: Unmarried individuals had
lower systolic blood pressure and diastolic blood
pressure compared to other groups (married group and
widowed group). The values were statistically significant.
Occupation ;
House wives had significantly
lower blood pressure values compared to other
groups.
The differences between the other groups
were not statistically significant.
Income:
Though values of blood pressure
showed slight rise in the higher income group, the
difference in the means were not significant.
Educational status?
Educational status
did not seem to have any apparent association with
the levels of blood pressure.
This may probably be
because of the low level of education of the group
studied.
Weight : There was a definite increase in
the values of both systolic and diastolic blood pressure
with increase in weight .
A statistically significant
positive correlation between weight and systolic blood
pressure and diastolic blood pressure in case of
males was observed.
In case of females though a
positive correlation was obtained, it was not found
to be significant.
Height; Values of both systolic and diastolic
blood pressure were least in the. 130 to 139 cm group.
This was significantly different from the other groups.
The difference in the values between the other
groups for both systolic blood pressure and diastolic
blood pressure were uneven and not significant.
53
Quetelet's index? Though positive
correlation was obtained between the quetelet's
index and blood pressure the values were not
significant.
Smoking t Both Systolic Blood Pressure and
Diastolic Blood Pressure did not show any relation ship between smokers and non smokers correlation
coefficient values were not significant .
Drinking; Though slight differences were
seen in the values of blood pressure between drinkers
and non drinkers, the differences were not significant.
Epidemiological factors among Hypertensives:
The prevalence of hypertension increased with
age in both the sexes.
The increase in the levels
were found to be statistically significant.
Mean blood pressure values did not show
significant differences between .the two sexes.
Mean values of blood pressure in hypertensives
did not show significant differences with height, weight
and habits like smoking and alcohol drinking.
Awareness of hypertension was found to be
in 18% of the hypertensives . Of these 50% were on
regular treatment and 50% were on irregular treatment.
No ■ family history of hypertension was
obtained in the hypertensive individuals which may be
due to lack of knowledge.
Also-not more than one
individual in a particular family was diagnosed as
hypertensive.
-2-HControl of I obacco-rclatcd Cancers and Other Diseases.
International Symposium. 1990. Prakash C. Gupta, James E. Hamner, III
and P.R. Murti, eds. Oxford University Press, Bombay, 1992.
Antitobacco campaign in Maharashtra, India:
achievements and perspectives
D. T. Joseph
Maharashtra Institute of Development Administration, Pune, India
Recognizing that cancer is a preventable disease, the Government of Maharashtra. India, under
took an aggressive anlitobacco campaign, consisting ofhealth education programmes, slogans and
billboards reminding nonnsers of their right to a tobacco-free environment; a counter-campaign
against cigarette advertisements was launched in Bombay Cits. Coupled with these activities, leg
islation was enacted making smoking in Government establishments and closed spaces in
Maharashtra an offense.
INTRODUCTION
Most public health programmes of the
Government of India arc directed to communi
cable diseases such as malaria, tuberculosis
and leprosy. The occurrence of certain diseases
due to life style has now been recognized,
and public health programmes are also being
mounted against them. Lung cancer is one
fatal but preventable life-style disease. The
Government of the State of Maharashtra,
India, thus initiated a campaign against smok
ing in 1986. The first reaction of smokers,
mostly from urban upper-middle classes, was
Mkc smoke because we like it. It is none of your
^mcern. After all, it is we who would suffer,
not you".
After experience of rejoinders of that
type, an aggressive antitobacco campaign was
launched in Maharashtra. This paper summa
rizes those activities and gives details of the
legislation enacted against tobacco.
antitobacco measures
Awareness of passive smoking: To counter
indifferent attitudes of the kind illustrat
ed above, the Public Health Department of
the Government of Maharashtra adopted the
slogan ‘Your smoking is injurious to out
health'. To support this line, a poster was
designed depicting a half-smoked cigarette.
with a man at one end and his wife and
young daughter at the other end, coughing.
This poster, which was displayed on the sides
of buses, led to awareness of the hazards of
sidestream smoke and of passive smoking. It
was assumed that realization of the fact that
smoking might be harmful to others in a family
would at least incite people to keep away from
children while smoking. Interestingly, nonsmokers began to use this slogan to counter the
indifference of smokers. Youngsters reading
this slogan aloud gave a clear but polite signal
to nearby smokers either not to smoke or to
move away. It also served to counter the rude
antagonism of smokers towards antismoking
activities.
In January 1987, the Tata Memorial
Hospital, Bombay, and the Public Health De
partment of the Government of Maharashtra
organized a two-day workshop on cancer
in collaboration with the UICC, where a plan
for a State cancer control programme was
adopted. One of the strategies was to launch
an aggressive anti-tobacco campaign. Perhaps
346 Joseph
the only action that had been taken against
tobacco use up to that time had been national
legislation in 1975 that all cigarette packets
and cigarette advertisements display a warn
ing to the effect that ‘Cigarette smoking is inju
rious to health’. Most manufacturers and ad
vertisers ran the sentence, but preceded it with
the words ‘statutory warning’.
Smoking as a criminal offense'. A move was
made to make smoking in Maharashtra Gov
ernment offices an offense. A proposal was
initiated by the Public Health Department
that resulted in billboards being put up in the
corridors of the State Secretariat to the effect
that 'Smoking is prohibited’. Predictably, how
ever. this measure did not prove to be effective,
indicating that an administrative order alone
would be of no great value. A more powerful
means of curbing smoking was found in certain
provisions of the ‘Bombay Police Act 1951’,
which read as follows: "Section I 16: No person
shall in any court, police station, police office,
building occupied by Government or building
occupied by any public body, smoke or spit
in contravention of a notice by a competent
authority in-charge of such places and affixed
to such court, station, office or building. Sec
tion 117: Any person contravening the provi
sions of section 99 to 166 (both inclusive) on
convic tion, be punishable by fine which may
extend to Rs. 100/-.’’
specified; since these boards were put up right
outside the gate, the campaign drew special
attention, (ii) An antismoking environment
was created by removing ashtrays from all
Government offices in Maharashtra, (iii) Even
cigarette and bidi kiosks within the premises of
Government offices were closed down.
Within two days after these orders were
issued, a small news item appeared opposing
them. ‘The workers in AiWt’-making units woukl
march to the secretarial to protest', the
item stated. The march did not materialize;
on the contrary, newspapers reported readers’
satisfaction about the Governmental action.
One letter read. "Why is it that Maharashtra
Government is selfish? Why do they take care
of their own employees? What about banning
smoking in public spaces?"
Health education: Smoking can perhaps be
prevented in Government offices by means of a
Government order, but an intensive public
education campaign is required to prevent
people from smoking in public places. It was
felt that, with a proper approach, such a cam
paign would incite a groundswell demanding
legislation to restrict tobacco use, sales, adver
tisement and even cultivation.
These provisions were explored to make
smoking and spitting within Government
offices a criminal offense. Applications were
made to the Home Department and to the
General Administration Department of the
Government of Maharashtra. Finally, approv
al by the Minister of State for Health and the
Health Minister was obtained, and orders
were issued on 5 August 1987. A copy of the
order is reproduced as Appendix.
‘Wills' is a popular brand of cigarette
manufactured by a leading firm, the Indit^H
Tobacco Company, a subsidiary of BritishAmerican Tobacco. They advertise their prod
uct with attractive models and the slogan
’Made for each other’, stating that the filler
and tobacco are well matched. The anti
smoking advertisement used the same format
but changed the content to imply that smoking
and cancer arc made for each other. A huge
hoarding was erected at one of the busiest
traffic roundabouts in Bombay (at Haji Ali)
on the night of 31 December 1987, as a New
Year’s gift to the citizens of Bombay!
I'he prohibition applies not only in
built-up areas but the premises, including
compounds, (i) The notice-boards, the colour
scheme and the material to be- displayed were
The Indian Tobacco Company, which
was in the process of putting up its usual
hoardings for ‘Wills’ in the same area, stopped
the painting midway. Instead it put up the
Anfitobarci) ram/mign
hoarding of another of its brands, ‘Bristol.’
with the message ‘I get what I want'. This was
counteracted with an anti-advertisement slo
gan ‘I get what I do not want — cancer'.
Another manufacturer uses the slogan * Taste
the spirit of freedom’. To neutralize this,
the visual content of (he advertisement was
changed to vultures and the caption to 1 Taste
the spirit of free. doom’.
Several other slogans and hoardings were
designed for the antismoking campaign. In an
attempt to enlist the support and services of
the women, one hoarding had ‘Smoker stinks.
Cigarette harms’ on one side, and ‘Be wise, live
longer, choose a nonsmokcr’ on tin* other
34/
campaign. It has banned smoking and spitt
ing in (Government offices and made these acts
a criminal offense. The orders are generallv
implemented properly, and inanv senior offi
cers in (Government departments in Bombav
have slopped smoking in their offices. The
penalty on conviction is a fine of onlv
Rs. 100/- (USS about 5); but the issue is one of
criminal conviction, There may be a few viola
tions. but the measure has created a fear of
being convicted and a feeling of guilt about
breaking the law. furthermore, the environ
ment for giving up tobacco use has become
more congenial. We believe (hat this approach.
with new slogans, new programmed and an
aggressive anlitobacco counter-campaign. has
resulted in the creation of greatei aw.uencss «»f
DISCUSSION
Maharashtra State is proud of its aggressive.
blunt, outspoken and innovative anlitobacco
the harmful elicits of tobacco and nonsmokris*
Appendix
Cancer Control Programme Ban on smoking and spilling in Govcrnment/Semi-Governmcnt oflices
and institutions
GOVERNMENT OE MAHARASHTRA
Public Health Department
Resolution No. CNG IO86/CR 24I/PH-6
Mantralaya. Bombay 400 032. dated 5 August, 1987
According to the estimates made by experts, there arc 1.5 million cancer patients in the country at
present. It is also estimated that 0.5 million new patients arc added every year. Taking into consid
eration the increased longevity of the citizens in the country and at this rate, the number of cancer
patients by 2000 AD is likely to have been tripled. According to the observations of the Indian
(ioimcil of Medical Research, out of the total number of cancer patients, cancer could be prevented
in respect ol 40% totally. In respect of 30% cancer patients it can be cured if it is detected in early
stages. Eor remaining 30% cancel patients, only long-term treatment/thcrapy can be given. TakProgramme is self evident.
Among cancer patients, the number of patients, who an* affected by cancer due to tobacco, is
large Smoking and tobacco-chewing not only cause cancer but also can cause respiratory and diges
tive system diseases. It is therefore* necessary to prevent citizens from these diseases and to motivate
them to refrain limn smoking and tobacco-chewing. Government has, therefore, as an important
pieventivc measure, decided to ban smoking and spitting in Government, Semi-Government,
/.ilia Parish.ids, Municipal Corporations. Municipal Council Offices and Institutions and Under
takings coming with in the purview of the Stale Government.
2. Bombay Point* Act 1951 has the following provisions:
Section 116- No person shall, in any Court, Police Station, Police Office, Building occupied by
the Govci nment or by any public body, smoke or spit in. contravention of a notice by a competent
authority in-charge of such places and affixed to such Court, Station, Office or Building.
Section 117: Any person contravening the provisions of Section 99 to 116 (both inclusive) on
conviction, be punishable by line which may extend to Rs. 100/-.
3. Government directs (hat competent authorities in all Government, Semi-Government
offices, Zilla Parishad, Municipal Council, Municipal Corporation Offices and Institutions, and
Undertakings shall lake recourse to the above provisions of Bombay Police Act, 1951 and should
ban smoking and spitting. While implementing this, the accompanying guidelines should be fol
lowed. ’fhe.se orders shall come into effect immediately.
All Mantralaya Departments should instruct the Heads of Oflices and Government Under
takings under their control to follow these orders.
By order and in the name of the Government of Maharashtra.
Sd/Arun Ghate
Section Officer
Antitobacco campaign
349
Accompaniment to Government Resolution, Public Health Department, No. CNC 1086/CR
241/PH-6, dated 5 August 1987.
(•uidelines for ban on smoking and spitting
(I) In every room of the office or institution a Board having the following words may be displayed.
Smoking strictly prohibited (Punishable under Section 116 and 117 of Bombay Police Act 1951).
I he size of the board should not be less than 15 x 45 cm.
(2) Similar boards should be displayed on the wall outside every room of the institution or office.
if there is ample vacant space available, for example, Corridor, Out-patient Department.
Meeting Hall. Such boards in Marathi and English as above should be displayed at a distance
of every' three metres.
At every entrance of the building, a board of the minimum size of 60 cm x 75 cm should be
displayed and the following words should be displayed in Marathi and English. Smoking
and Spitting strictly prohibited inside this building and compound.
(4)
A similar board of minimum size of 90 cm x 60 cm should be displaced at the entrance of the
compound of the building.
(5)
All these boards should be of permanent nature i.e. wooden, tin or of similar material. The
ground colour of the board should be red and the words in white. If some period is likely to be
taken for preparation of the permanent boards, temporarily, paper or card board Ixiards should
be displayed.
(6)
The boards on the wall should be at a minimum height of 1.5 metre.
(7)
If any ash-trays have been kept in any of the rooms or elsewhere in the institution or the office.
they should be removed.
(8)
If there arc any pan-bidi vendors in the building or in the compound of the building, they should
be moved outside the compound of the building.
Into national Symposium. 1990. Prakash C. Gupta, James E. Hamner. Ill
AND P.R. Murti, EDS. Oxford University Press, Bombay. 1992.
Controlling cancer by suing tobacco companies:
the potential for India in the light of
the US experience
Richard A. Davnard
Northeastern University School of Law, Boston, USA
Litigation on the liability presented by tobacco products is now widely recognized as providing
unique opportunities for discouraging tobacco use by raising product prices and focusing public
products. In view of the recent legal precedents from suits on motor accidents and the Bhopal gas
tragedy. India has potentially the most promising legal environment for bringing such litigation.
INTRODUCTION
Lawsuits against tobacco companies are
potentially powerful tools for controlling to
bacco consumption. They have also proven —
like most other such tools — to be difficult to
wield and slow to produce results. Recent legal
developments have made these cases easier to
bring and more likely to win in the USA;
Indian legal developments also suggest that
such lawsuits, perhaps in a slightly dinbrent
legal form, might also succeed.
4&TENTIAL BENEFITS
The benefits sought from litigation on tobacco
product liability include: (i) forcing the manu
facturers to raise the price of tobacco products
(to covet the expected cost of litigation and
judgment), thus discouraging consumption;
(ii) forcing the manufacturers to stop lying
about the dangers of their products and,
indeed, to ‘volunteer’ the truth about them;
(iii) discrediting the industry in the legislative
arena by releasing internal documents giving
details of their disinformation campaign and
their disregard of public health; and (iv) publi
cizing the dangers of tobacco use through
media publicity attendant upon the filing and
trial of such suits.
THE US EXPERIENCE
Difficulties that have arisen in bringing these
suits in the USA include: (i) the willingness of
the tobacco industry to spend endless amounts
of money to intimidate plaintiffs and delay
proceedings; (ii) the ability of the industry
to evoke ‘blame-thc-victim’ attitudes among
judges and jurors by exaggerating the extent of
both past and current public awareness of the
dangers of tobacco use and by presenting a
misleading picture of the amount of individual
choice involved in the continued use of tobacco
products; (iii) adversejudicial decisions result
ing from judges’ fears of a flood of litigation if
the suits are permitted to proceed; and (iv)
poor choice of plaintiffs in the first suits (weak
etiological evidence and no effort to quit even
after warnings received).
Recent, positive US legal developments
have made each of these difficulties much less
formidable. First, evidence about the knowl
edge and behaviour of the multinational to
bacco companies, developed by plaintiffs and
lawyers at great expense for use in their
trials, is now available cheaply from the
Tobacco Products Liability Project. Also, five
years of experience in fighting the tobacco
companies have prepared the plaintiffs’ bar for
dealing effectively with the defendants’ argu
ments and litigativc devices. Cases against
tobacco companies arc now no more expensive
to bring than other complex product liability
cases.
Second, the decision on 5 January 1990
of the US Court of Appeals in Cipollone vs.
Liggett Group, Inc. makes clear that juries will
have to compare knowledge of the dangers of
tobacco held by tobacco companies and by
individual consumers at specific times in the
past, rather than anachronistical!}’ evaluating
earlier behaviour in the light of current levels
of public knowledge. Furthermore, the 1988
US Surgeon-General’s Report on Nicotine
Addiction has helped change public conscious
ness on the amount of choice exercised by most
long-time smokers.
Third, the fact that the first plaintiffs ver
dict in June 1988 in the Cipollone case did not
lead to a flood of new cases has encouraged
courts to begin decide tobacco-related cases
consistently with the way they treat those on
manufacturers of other dangerous products.
Thus, the 5 January 1990 appellate decision
in Cipollone, although it reversed the USS
400 000 verdict and remanded the case for a
new trial, for the first time allowed the plaintiff
to use a risk-benefit analysis, which holds man
ufacturers liable whenever the risks of their
products to consumers exceed the benefits.
This holding, along with the court’s strength
ening of the ‘failure-to-warn’ and express war
ranty theories of action, opens up powerful
legal theories for plaintiffs' attorneys.
Finally,- plaintiffs’ attorneys have learnt
which cases to avoid.
The benefits achieved from tobacco litiga
tion in the USA to date include: (i) at least a
modest contribution to both snuff and cigarette
price increases (which the industry explained
were needed, in part, to cover litigation ex
penses); (ii) forcing the industry to adopt a
defensive public relations posture of ‘if you
die from smoking, it was your own choice’ —
hardly the best way to sell cigarettes; (iii)
releasing damaging internal documents which
discredited the industry politically; and (iv)
focusing public attention not just on statistics,
but on the fact that real individuals die fro,™
tobacco use.
THE INDIAN POTENTIAL
The Indian legal situation is quite different
from that of the USA, yet it appears to hold
substantial possibilities for producing similar
public health benefits from tobacco litigation.
While product liability actions — anti tort
claims in general — have traditionally been
rare, three recent legal developments in India
have made it a potentially hospitable envir
onment for litigation against multinational
tobacco companies.
First, in two 1987 cases, the Indian Su
preme Court articulated tort principles that
were more liberal even than the risk-benefit
test enunciated in the Cipollone case. Thus, in
Gujarat State Road Transport Corporation^^
Ramanbhai Prabhatbhai, the court held
the first time that ‘liability without fault’ was
‘a principle of social justice’ in automobile ac
cident cases. Then, in M.C. Mehta vs. Union
of India, involving a pre-Bhopal release of
toxic gases from a factory, the court articulated
its willingness to go beyond the principles of
liability applied in the United Kingdom and
other foreign countries, and it illustrated this
willingness by holding that: “If the enterprise is
permitted to carry on a hazardous or inher
ently dangerous activity for its profit, the law
must presume that such permission is condi
tional on the enterprise absorbing the cost of
any accident arising on account of such haz
ardous or inherently dangerous activity, as an
appropriate item of its overhead.
Cancer control by suing tobacco companies
While the immediate application of this
principle was to an industrial accident, the
principle itself and the underlying reasoning
were broad enough to encompass’ tobacco lia
bility cases.
Particularly encouraging for our purposes
is the paragraph of the Mehta opinion immedi
ately following this discussion:
“We would also like to point out that the
hcasure of compensation in the kind of cases
referred to in the preceding paragraph must
be correlated to the magnitude and capacity
of the enterprise because such compensation
must have a deterrent effect. The larger and
more prosperous the enterprise, greater must
be the amount of compensation payable* bv it
for the harm caused on account of an accident
in the carrying on of the hazardous or inher
ently dangerous activity by the enterprise.”
Philip Morris and British American To
bacco are both very large and very prosperous!
Second, while India does not permit con
tingency fees (which, in the USA, recruit
plaintiffs’ attorneys by offering them part of
the eventual recovery), the Indian Supreme
Court has in recent years recognized a catc•y of‘public interest litigation' in which it is
343
willing to order defendants to compensate pub
lic interest plaintiffs for their expenses. This
action, along with court rules which permit
class actions, could facilitate injunciivc actions
against abusive industry practices, as well as
perhaps carefully planned and respectably
sponsored test cases in the product liability
Finally, the political and legal ferment
around the Bhopal disaster, focusing on the
role of tort law both in deterring multinational
corporations from dangerous practices and in
providing compensation to large numbers of
victims, appears to have produced a new
receptivity among Indian judges, lawyers and
politicians to the need lor effective legal reme
dies for tortious acts injuring large numbers of
people. I assume (hat in India, unlike the
US/\, the tobacco industry could not plausibly
claim that everybody who uses tobacco prod
ucts should know (and should have known for
many years) of the attendant dangers; on the
other hand, there is abundant evidence that.
Philip Morris and British American Tobacco
should have known of these (Lingers for several
decades. In this context, a public advocacy of
tobacco product liability suits by respected
Indian public health authorities could produce
a positive public and judicial response.
Centro! of Tobacco-rclatcd Cancers and Other Diseases.
International Symposium, 1990. Prakash C. Gupta, James E. Hamner, III
and P.R. Murti, eds. Oxford University Press, Bombay, 1992.
The public health practice of tobacco control
Thomas E. Novotny
US Department of Health and Human Services, Rockville, USA
Twenty-five years after the publication of the first US Surgeon-General’s Report on the Health
Consequences of Smoking, considerable progress against tobacco use has been observed in the
USA. The public health practice of tobacco control has been refined during this period, and sev
eral essential elements in this practice may be identified: (i) surveillance systems, including behav
iour process and disease outcomes to control tobacco have been established; (ii) disease impact
estimates, i.e., smoking-attributable mortality, morbidity and economic costs, iiave provided
|x>lent information to policy makers and public health officials; (iii) policies that restrict smoking
in public places and the excess of minors to tobacco have assisted in changing .he social milieu
supporting tobacco use in the USA; (iv) community planning and coalition-building have become
mainstays in the.complcx task of tobacco controls; and (v) public information campaigns using
several different media have been extremely effective in changing the public’s perception of
tobacco. Despite the significant progress against tobacco, and downward trends in its use, 50 mil
lion Americans continue to smoke.
INTRODUCTION
As a public health problem, tobacco use may
not be unlike communicable disease, with
which practitioners of public health have great
familiarity. The public health practice of com
municable disease control incorporates strate
gy for surveillance, case finding, clinical
treatment, containment, immunization, public
policy development and goal-setting. Many of
these strategies can be applied to the control of
chronic diseases, especially those caused by
tobacco. Tobacco use is itself a disease of
addiction, and it is responsible for 2.5 million
deaths worldwide (1).
The 1964 Report of the Advisory Com
mittee to the US Surgeon-General provided
the scientific information needed to launch
an effective, sustained public health campaign
against tobacco (2). This campaign was
described most recently in the SurgeonGeneral’s 1989 Report, Reducing the Health
Consequences ofSmoking — 25 Years of Progress (3).
Despite the notable successes of the last 25
years, tobacco use is still widespread in the
USA.
Recently, tobacco prevention and control
activities have focused on the individual states.
It is within the states’ jurisdiction to protect
the public against environmental and infec
tious hazards.
This paper summarizes the progress made
against tobacco use, outlines the essential ele
ments of the public health practice of tobacco
control, and describes the future directions of
public health activities against tobacco use in
the USA.
TWENTY-FIVE YEARS OF PROGRESS
The 1989 Surgeon-General’s Report docu
ments that knowledge of the health conse
quences of tobacco use has expanded dramati
cally since 1964; programmes and policies for
controlling the hazards of tobacco use have
278
Novotny
also proliferated. The conclusions of the report
highlight important gains in preventing to
bacco use and tobacco-related disease and
emphasize areas of continuing concern. The
conclusions are: (i) The prevalence of smoking
among adults decreased from 40% in 1965 to
29% in 1987. Nearly half of all living adults
who ever smoked have quit, (ii) Between 1964
and 1985, approximately three-quarters of a
million smoking-related deaths were avoided
or postponed as a result of decisions to quit
smoking or not to start. Each of these avoided
or postponed deaths represented an average
gain in life expectancy of two decades, (iii) The
prevalence of smoking remains higher among
blacks, blue-collar workers and poorly educa
ted people than in the overall population. The
decline in smoking has been substantially
slower among women than among men. (iv)
Smoking begins primarily during childhood
and adolescence. The age of initiation has
fallen over time, particularly among females.
Smoking among high school seniors levelled off
from 1980 through 1987 after previous years of
decline, (v) Smoking is responsible for more
than one in every six deaths in the USA.
Smoking remains the single most important
preventable cause of death in our society (3).
The per-caput consumption of cigarettes in
the USA is a sensitive measure of the remark-
Fig. 1. Adult per-caput cigarette consumption and
major smoking and health events, USA,
1900-85 (source: USDA, 1989)
Public health practice of tobacco control
able change in smoking behaviour over the last
few decades (Fig. 1). Significant events in the
campaign against smoking included the first
scientific reports on tobacco and its association
with cancer, the release in 1964 of the SurgeonGeneral’s Advisory Committee Report (2), the
elimination of tobacco advertising from televi
sion (after the 'Fairness Doctrine’ had man
dated such effective anti-smoking television
spots that the tobacco companies volunta
rily agreed to accept the television advertis
ing ban), the nonsmokers’ rights movement
(accompanied by the proliferation of clean
indoor air policies), and the doubling of the
Federal excise tax on cigarettes. Economic
disasters such as the Great Depression of
1929-31 and World War II suppressed ciga
rette consumption because of decreased dis
posable consumer income. The current decline
in per-caput consumption cannot be attributed
to one event or even a series of identifiable
events. Instead, it reflects a changing social
milieu in which smoking is no longer seen as
fashionable, healthful and safe. With this psy
chosocial change in attitudes towards tobacco
use, the public health practice of tobacco con
trol has evolved.
ESSENTIAL ELEMENTS OF TOBACCO
PREVENTION AND CONTROL
Surveillance'. Surveillance of disease inci
dence and the prevalence of tobacco use is crit
ical to assessing the severity of the public
health problem and to evaluating changes in
disease status resulting from control measures.
Surveillance systems must be simple, informa
tive, uniform and sensitive to changes in dis
ease status. For tobacco use, the following sur
veillance items must be reported periodically:
Adult knowledge, beliefs and behaviour. This
information indicates the coverage of public
information and education campaigns and per
mits identification of subgroups that may need
additional attention.
In the USA, national surveillance of adult
smoking behaviour is accomplished through
the National Health Interview Surveys
(NH1S) and the Adult Use ofTobacco Surveys
(AUTS). Data from the NHIS (4) show that
smoking prevalencA declined for both men and
women between 1973 and 1985, with a steeper
rate of decline for men (Fig. 2). It is predicted
279
of a tobacco-use surveillance system. Useful
trend data have been provided by the National
Table 1
Percentage of US adults who believed ‘smoking causes
disease’ 1964 and 19861
Disease
-m- Women
Fig. 2. Prevalence of smoking among adults
20 yean old or older, USA, 1965-87
(source: ref. 3)
that by the late 1990s smoking will be more
common among women than among men in
the USA (5). Low educational status has been
found to be the single most important predic
tor of slow change in current smoking preva
lence (6). Thus, national goals should focus on
reducing smoking among women (especially
young women) and among all persons with low
educational attainment.
Year and
smoking status
Lung
cancer
Heart
disease
Lung
disease
1964
Smokers
Nonsmokers
53
74
32
41
42
55
1986
Smokers
Nonsmokers
85
95
71
83
85
91
■Source: Gfliceon Smoking and Health, adult use of
tobacco surveys, 1964 and 1986
Institute on Drug Abuse High School Seniors'
yearly survey (7). The prevalence of daily cig
arette smoking among high-school seniors
decreased from 29% in 1975 to 21% in 1980,
after which it levelled off at 18-21% (Fig. 3).
The prevalence of smoking among females has
consistently exceeded that among males since
1977, although a part of this difference may
be due to increased use of smokeless tobacco
The AUTS found (3) that knowledge of
the health consequences of smoking increased
significantly between 1964 and 1986 (Table 1).
The data show that progress is being made
with public awareness of the health conse
quences of smoking. Children and adolescents
may need additional educational efforts, so
that they also recognize the health hazards
before experimenting with tobhcco.
Adolescent knowledge, beliefs and behaviour. In
the USA, about 90% of smokers begin to use
tobacco before the age of 21 (3). Assessing
knowledge, beliefs and behaviour among chil
dren and adolescents is a critical component
Man
Woman
Fig. 3. Percentage of high-school seniors
reporting daily cigarette smoking,
USA, 1975-87 (source: ref. 7)
280
Public health practice oj tobacco control
Novotny
among young men over the last two decades
(8). The age of initiation for smoking is
decreasing (3), which indicates that national
programmes should target young persons.
The tobacco-control proceps (policies, laws, pro
grammes and educational programmes)-. In 1989,
the Association of State and Territorial Health
Officials (ASTHO) surveyed all state health
departments about public health control ac
tivities within each state. These activities
included developing tobacco or chronic disease
coalitions, tobacco-control plans, surveillance
systems, economic incentives and disincen
tives, clean indoor air policies, laws restricting
minors’ access to tobacco products, and others.
States can use the results of this survey when
comparing their activities with others, meas
uring the progress of programmes against
tobacco and evaluating behavioural outcomes
in different populations (9).
When national or state goals call for wide
spread policies, such as clean indoor air at all
worksites, then surveillance systems should be
established to follow the spread and coverage
of these policies. Data can be obtained from
sources such as business groups and unions. If
schools are to be tobacco-free, then school
boards may also wish to establish systems
by which progress towards these goals can
be measured. In 1989, the National School
Boards Association found that 95% of school
districts in the USA had a written policy on
smoking in schools and that 17% of schools
banned smoking on school premises or at
school functions (10).
Problem assessment: The second clement of
tobacco control activities in the USA is prob
lem assessment, which is a detailed analysis of
current behaviour, tobacco consumption, cur
rent programme capabilities and the disease
impact of smoking.
The disease impact measures used in the
USA are both epidemiological and economic.
The critical calculation in estimating disease
impact is the attributable fraction formula:
Smoking-attributable fraction =
/>(RR-1)
I) + l
where p is the prevalence of smoking and RR
is the relative risk of death from a particular
disease for smokers compared with ‘never-'
smokers’ (11). The relative risk for 14
smoking-associated conditions was reported in
the Surgeon-General’s 1989 Report (3). Using
those values and current smoking prevalence
data, it was estimated that 390 000 deaths
were attributable to tobacco use each year in
the USA (3).
Economic estimates have also been made
of the direct costs of medical care and indirect
losses due to disability and premature mortal
ity. One estimate is approximately USS 65 bil
lion in smoking-attributable economic losses
per year (12).
Each state has individualized its estimate
of the impact of smoking-attributable disease
by using software specifically designed for this
purpose (13). Results were reported to each
member of the US Congress by the Secretary
of Health and Human Services, and results
appeared in numerous local newsletters, state
medical journals, and state tobacco reports
(14). The data arc often very useful to policy
makers who need to quantify the disease
impact of smoking and compare it with other
risks (15).
Policies and programmes: Interventions
against tobacco must be multifaceted; no sin
gle intervention will be successful without
scientifically-based public education and com
munity-based activities, policies and legislative
support. Interventions can be promoted
through several channels (Table 2) and mea
sured through several resources. If a particular
goal is set — for instance, that all health care
providers will advise their patients to quit
smoking at every opportunity — then some
form of monitoring of this activity must occur.
Monitoring could take the form of public sur
veys or, for physicians, chart reviews.
281
In the USA, clean indoor air laws have
become more widesoread and stronger over
•he fast several years (Fig. 4). Thus, a trend
has begun that may help convince states to
strengthen their laws as part of a larger
Table 2
Examples of intervention activities
Health care system
• Motivate smokers to seek assistance for cessa
tion from health care providers.
« Train physicians, dentists and pharmacists in
cessation techniques.
« Expand cessation programmes and funding
sources.
Woi ksites
• Promote changes in smoking behaviour at the
worksite through presentations, posters and
newsletters.
• Support worksite cessation programmes by
offering self-help manuals, audiovisual activities
and economic incentives.
• Develop smoke-free worksite policies.
Community organizations
• Present information about the health and eco
nomic consequences of tobacco use at organiza
tion meetings.
• Promote community cessation resources and
self-help programmes of large organizations.
• Promote smoke-free meetings and events.
Schools
a Mandate tobacco prevention as part of the
school curricula.
• Train teachers in prevention and cessation
skills.
• Promote parental cessation through actions of
children.
• Promote smoke-free policies for school build
ings, sports events and other school activities.
national effort. However, the same trend is not
true for laws restricting access to tobacco by
minors. Very few states have even modestly
strong enforcement of restrictions on the pur
chase of tobacco products by minors (Table 3).
In future plans for improving tobacco-control
activities, additional attention must be given to
strengthening these restrictions and enforcing
them.
Fig. 4. Number of states with laws regulating
smoking in public places, by year and type
of law, USA, 1960-88
Table 3
Restriction imposed by laws on minors’ access to cigarettes
and other tobacco products
None
No restriction on sale of cigarettes or
other tobacco products to minors
Nominal
Law banning sale of cigarettes to
minors (minimum age requirement
stated). In some places, the law
applies to all tobacco products.
Basic
Statewide regulations for sale or
distribution of tobacco products
to minors (minimum age stated)
with penalties of either a fine and/
or imprisonment. Bans or restricts
access to vending machines by
minors
Basic regulations that also require
visible warning signs at points of
sale about the illegality of the sale
of tobacco products to minors.
Requires a license 40 sell tobacco
products that can be revoked or
suspended for selling to minors.
Moderate
Extensive
Moderate regulations with bans
on free distribution of tobacco sam
ples. Mandates enforcement and
commits resources for enforcement
through earmarked license fees
One effort that may inhibit young people
from smoking is increasing the excise tax on
282
Novotny
cigarettes (16). Currently, all states impose a
tax on each package of cigarettes sold. These
taxes range from 2 cents to 40 cents per pack,
and they are generally lowest in the tobacco
producing states (17). Recently, portions of
excise taxes have been earmarked by some
states to fund tobacco-control programmes.
Public information campaigns: Figure 1 and
Table 1 show that public information cam
paigns have considerable power. In the USA,
media campaigns have been developed for
specific groups (minorities, young women and
children). Unfortunately, the tobacco industry
has also targeted many of these same groups,
and analysis of this targeting reveals disturb
ing and insidious marketing techniques (18).
Communications systems among various
public health providers, advocacy groups and
non-governmental organizations need to be
developed and strengthened (19). These net
works permit the rapid dissemination of in
formation and exchange of ideas. Electronic
bulletin boards and monthly newsletters
have been developed in the USA to help these
processes. Training constituency groups (in
particular, health department personnel) in
media relations is another component of suc
cessful public health communications cam
paigns. These groups can then disseminate to
the public scientific information about
tobacco-related disease and the need for
tobacco-control programmes.
Social marketing is a technique for creat
ing a market for a particular product or service
(20). Social marketing can also create a milieu
in which tobacco use is no longer the norm,
thus facilitating change among users and dis
couraging young persons from beginning to
use tobacco. Public information campaigns are
the cornerstone of social marketing efforts.
Coalition building and community planning:
Coalitions have become an integral part of
tobacco-control activities in the USA. The fur
ther a coalition extends beyond the health
Public health practice of tobacco control
community, the greater ownership the entire
community exerts over tobacco-control initia
tives. Coalitions may represent public health
officials, health care providers, advocacy
groups, voluntary organizations, business
groups, religious groups, government officials,
the insurance industry, the legal profession,
the military, labour organizations, economists,
educators, advertisers and communications
specialists. Activities of coalitions include
developing and implementing tobacco-con
trol plans, public information programmes,
and public and professional education pro
grammes. Coalitions also sponsor research and
evaluation. Among the 50 states and the
District of Columbia, four states have no co
alition, 25 states have modestly strong
coalitions, 15 states have moderately strong
coalitions, and 7 states have strong coalitions
(21).
According to the ASTHO survey, nine
states have separate public health plans for
tobacco use, and 16 states address tobacco
use as part of another programme plan (21).
To assist states with tobacco-control plans,
ASTHO analysed existing plans and pub
lished a guide for their development (9,22).
The steps for developing a tobacco-control
plan include the following: take advantage of
national expertise; establish a coalition or
advisory group; assess the tobacco problem;
develop the mission, goals and objectives of the
plan; analyse existing tobacco-control poten
tials; package and market the plan; ami evalu
ate and revise the plan.
National objectives for the year 1990
included improved health status from' the
reduction of tobacco use, increased public and
professional awareness, improved services and
protection, and improved surveillance and
evaluation (23). Evaluation methods for to
bacco-control activities are still rather rudi
mentary. Evaluation is difficult because of the
unique nature of the tobacco-use epidemic.
First, outcomes change very slowly in response
to extensive campaign efforts. For example, the
prevalence of adult smoking is decreasing at
only 0.6% per year in the USA (4); even after
25 years of change, only recently has the lung
cancer mortality rate begun to level off among
men (23). A 20-30-year lag period in the
expression of chronic disease makes it difficult
to measure the success achieved during the last
25 years of changing smoking behaviour in the
USA.
Second, the rates of voluntary participa
tion in cessation activities arc low (80% of
smokers quit on their own) (25), and rates for
abstinence achieved through such programmes
are low (26). Moreover, medical insurance
docs not, as a rule, cover payment for such pro
grammes, and cessation programmes arc often
not appropriately designed for, nor accessible
to, the most resistent populations. Thus, the
proliferation of smoking cessation services may
not be associated with widespread behavioural
changes.
Third, behavioural change in response to
policies, such as those restricting smoking in
public places, is difficult to evaluate. In places
where evaluation studies have been carried out
(worksites), some policy changes have resulted
in no change in overall cigarette consumption,
some have been associated with a decrease in
the daily consumption of cigarettes, and some
have been associated with a decline in the
prevalence of smoking (27). Yet, such policies
contribute to an overall social norm of not
smoking.
Finally, the tobacco industry has mounted
a massive rear-guard action against restrictive
policies on smoking and against economic
interventions against the industry. About
USS 3.5 billion are spent yearly on tobacco
advertising; tobacco is the second most com
mon subject of advertising in the printed
media and the most common in the outdoor
(billboard) media (28). In addition, each state
and nearly every local jurisdiction considering
tobacco legislation is pressured by the power
ful tobacco lobby. Grassroot efforts, including
283
referenda, can be expensive and frustrating for
groups not funded for and not trained in polit
ical processes.
THE FUTURE OF TOBACCO-USE
PREVENTION AND CONTROL
Tobacco-control efforts in the USA will con
tinue to encourage state and local activities.
The American Stop Smoking Intervention
Study for Cancer Prevention (ASSIST) will
begin in 1993 (see paper by Glynn el al., this
volume). This multistate programme will coor
dinate, provide training for, and evaluate
efforts to prevent and control tobacco use ifl
20 areas (entire states or large metropolitan
areas) through 1998 (9).
California has achieved heretofore un
imaginable funding levels for tobacco control
through the passage of Proposition 99, a public
initiative that increased the state excise tax
on cigarettes, the revenues from which are
directed, in part, to tobacco-related education.
In the next few years, the question, ‘If we had
enough money, what could we do to prevent
tobacco use?’ may be answered in that State.
About US$ 155 million have been earmarked
for the health education component of the
appropriations bill attached to this successful
initiative. A substantial portion of these
funds will be directed to a communications
campaign that will be thoroughly evaluated
(29).
In 1988, the governors of eight western
states initiated the Rocky Mountain Tobaccofree Challenge, a regional effort intended to
reduce the prevalence of tobacco use and of
chronic diseases associated with it. The chal
lenge will continue until the year 2000; key ele
ments include increased community interest,
strengthened interstate and intrastate collabo
ration, promotion of state activities for reduc
ing tobacco use, and long-term evaluation of
tobacco-related policies. Other regions of the
country may adopt this innovative, competi
tive approach (30).
284
Novotny
International cooperation has begun be
tween the Office on Smoking and Health and
the Pan American Health Organization
(PAHO). In 1992, a joint report on smoking in
the Americas will be produced by the PAHO
and the US Surgeon-General. This report will
highlight the changing tobacco-use environ
ment in developing countries and emphasize
the need to prevent chronic diseases associated
with tobacco use. As tobacco use becomes less
common in the industrialized world, it is
becoming more of a problem in many non
industrialized countries (31).
CONCLUSIONS
Despite significant progress made against
tobacco use, over 50 million Americans con
tinue to smoke. The trend in tobacco use is
downward in the USA, and several high risk
groups, including young people, minorities,
people with low educational attainment and
Public health practice of tobacco control
pregnant women, have been Targeted for future
interventions. The public health practice of
tobacco control continues to evolve, and meth
ods for evaluating tobacco-control activities
need further development. Public health efforts
for controlling tobacco use differ somewhat
from those used to control infectious diseases,
but they incorporate several of the same princi
ples. These principles involve scientific infor
mation, public policy, mass media, social
marketing techniques and community-based
programmes to affect change. No single inter
vention will stop the tobacco epidemic. Public
health activities for controlling tobacco use
need continual assessment and evaluation; as
successful strategies emerge, they should be
adapted to different cultural and social envi
ronments. Unfortunately, the chronic diseases
resulting from the epidemic of tobacco use will
be measurable for decades, both in developed
and developing nations.
References
Maki.er H. Tobacco or health: choose health.
World Health Forum 1988; 9:78-83.
2. US Department of Health, Education, and
Welfare. Smoking and Health: A Report of the
Advisory Committee to the Surgeon-General of
the Public Health Service, Washington DC;
US Department of Health, Education, and
Welfare, PHS Publication No. 1103, 1964.
1. US Department of Health and Human Ser
vices. Reducing the Health Consequences of
Smoking — 25 Years of Progress: A Report of
the Surgeon-General, Washington DC: US
Department of Health and Human Services,
DHS Publication No. (CDC) 1989; 89-8411.
Fiore MC, Novotny TE, Pierce JP,
Hatziandreu EJ, Patel KM, Davis RM.
Trends in cigarette smoking in the United
States: the changing influence of gender and
race. J Am Med Assoc 1989; 261:49-55.
Pierce JP, Fiore MC, Novotny TE,
Hatziandreu EJ, Davis RM. Trends in ciga
rette smoking in the United States: projections
to the year 2000. J Am Med Assoc 1989;
261:61-5.
1.
6.
7.
8.
Fierce JP, Fiore MC, Novotny TE,
Hatziandreu EJ, Davis RM. Trends in ciga
rette smoking in the United States: educational
differences are increasing. J Am Med Assoc
1989;261:56-60.
Johnston LD, O’Malley PM, BachmanJG.
National Trends in Drug Use and Related
Factors Among American High School Stu
dents and Young Adults. 1975-1986. Rockville,
Maryland: National Institute on Drug Abuse,
1987.
Novotny TE, Pierce JP, Fiore MC, Davis
RM. Smokeless tobacco use in the United
States: the adult use of tobacco surveys. Natl
Cancer Inst Monogr 1989; 8:25-8.
Centers for Disease Control. State tobacco-use
prevention and control plans. Morbid Mortal
Wkly Rep 1990; 39:133-6.
10.
Centers for Disease Control. School policies
and programs on smoking and health —
9.
United States, 1988. Morbid Mortal Wkly Rep
1989; 38:202-3.
Walter SD. The estimation and interpreta
tion of attributable risk in health research.
Biometrics 1976; 32:829-49.
! '? US Office of Technology Assessment. Smok
ing-related Deaths and Financial Costs.
Washington DC: Health Program, Office of
Technology Assessment of the US Congress,
September 1985.
13.
ShultzJM. SAMMEC: smoking-attributable
mortality, morbidity, and economic costs
(computer software and documentation). Min
neapolis, Minnesota: Center for Non-smoking and Health, Minnesota Department of
Health, 1986.
14.
US Department of Health and Human
Services. Smoking and Health: A National
Status Report. A Report to Congress. 2nd cd.
Rockville, Maryland: US Department of
Health and Human Services, Public Health
Service, Centers for Disease Control. DHHS
publication No. (CDC) 87-8396, 1990.
15.
Warner KE. Health and economic implica
tions ofa tobacco-free society. J Am Med Assoc
1987; 258:2080-6.
16.
Lewit EM, Coate D. The potential for using
excise taxes to reduce smoking. J Health Econ
1982; 1:121-45.
17.
Tobacco Institute. The Tax Burden on
Tobacco. Historical Compilation, Volume 22.
Washington DC: Tobacco Institute, 1988.
18.
Davis RM. Current trends in cigarette adver
tising and marketing. New Engl J Med 1987;
316:725-32.
19.
US Department of Health and Human
Services. Making Health Communication
Programs Work: A Planner’s Guide. US
Department of Health and Human Services.
Public Health Service, National Institutes of
Health, Office of Cancer Communications,
National Cancer Institute. NIH publication
No. 89-1493, 1989.
20.
Bandura A. Social Foundations of Thought
and Action: A Social Cognitive Theory.
Englewood Cliffs, New Jersey: Prentice-Hall,
Inc., 1986.
21.
Novotny TE. Results of the ASTHO Survey
of State Tobacco Control Activities. In:
;l
22.
23.
24.
25.
26.
27.
28.
29.
30.
31.
285
Proceedings: ASTHO Conference on the
Public Health Practice of Tobacco Prevention
and Control. Rockville, Maryland: Office on
Smoking and Health, 1990.
Association of State and Territorial Health
Officials and National Cancer Institute. Guide
to Public Health Practice: Slate Health
Agency Tobacco Prevention and Control
Plans. McLean, Virginia: Association of State
and Territorial Health Officials, 1989.
US Department of Health and Human
Services. Promoting Health/Prevcnting Dis
ease: Objectives for the Nation. Washington
DC: US Department of Health and Human
Services, Public Health Service. DHHS, 1980.
American Cancer Society. Cancer Facts and
Figures — 1990. Atlanta Georgia: American
Cancer Society, Inc., 1990.
Fiore MC, Novotny TE, Pierce JP, et al.
Methods used to quit smoking in the United
States: do cessation programs help? J Am Med
Assoc 1990; 263:2760-5.
Schwartz JL. Review and Evaluation of
Smoking Cessation Methods: The United
States and Canada, 1978-1985. Bethesda,
Maryland: National Cancer Institute. NIH
Publication No. 87-2940, 1987.
Novotny TE. Passive smoking — beliefs, atti
tudes, and exposures in the United States. In:
Compendium of Technical Information on
Environmental Tobacco Smoke. Washington,
DC: Environmental Protection Agency (in
press).
Centers for Disease Control. Cigarette adver
tising — United States, 1988. Morbid Mortal
Wkly Rep 1990; 39:261-65.
Bal D. Proposition 99. In: Proceedings of the
ASTHO Conference on the Public Health
Practice of Tobacco Prevention and Control.
Rockville, Maryland; Office on Smoking and
Health, 1990.
Centers for Disease Control. State-based
chronic disease control: the Rocky Mountain
Tobacco-Free Challenge. Morbid Mortal Wkly
Rep 1989; 38:749-52.
Chapman S, Leng WW. Tobacco Control
in the Third World: A Resource Atlas. Penang,
Malaysia: International Organization of
Consumers Unions, 1990.
Control of Tobacco-rclatcd Cancel's and Other Diseases.
international Symposium, 1990. Prakash C. Guin a, James E. Hamner, III
and P.R. Murti, eds. Oxford University Press, Bombay, 1992.
Tobacco control in India: problems and solutions
Usha v. Luthra, V. Sreenivas, G. R. Menon, A. K. Prabhakar and K. Chaudhry
Indian Council of Medical Research, New Delhi, India
Tobacco conttol is a subject of worldwide importance. India is the third iarge't producer of
tobacco in the world, and the tobacco industry in our country is labour intensive and provides
employment to millions of people. It also earns the Government much revenue and foreign
exchange. Tobacco in any form, however, is detrimental to health: aboutJ3% of the estimated five
million deaths in the adult population can be attributed to tobacco use. A conservative estimate
of tl>e annual health care costs attributable to tobacco-related diseases exceeds the revenue earned
from tobacco by Rs. 6850 million (USS 403 million). The Government of India has initiated sev
eral measures to tackle the problem. The Cigarette Act of 1975 stipulates that packets of cigarettes
and cigarette advertisements display the statutory warning that cigarette smoking is injurious to
health. I-aws prohibit smoking in closed spaces such as cinemas, theatres, buses and on domestic
flights. Tobacco advertisements arc banned in state-controlled media. The National Cancer
Control Programme launched in 1984,. gave high priority to eliminating tobacco-related cancers.
Unfortunately, these measures arc yet to make a significant impact. A comprehensive programme
is described with the aim of creating a tobacco-free society in the country during the next century.
INTRODUCTION
Tobacco appears to be as old as human
civilization itself. Cultivation of the tobacco
plant probably dates back 7000 years: tobacco
seeds were discovered in archaeological exca
vations in Mexico and Peru, and the remains
^Lpermancnt settlements built around 3500
showed that tobacco was an important
article to the inhabitants (1).
Documented evidence of tobacco usage
has been available since the end of the 15th cen
tury. In 1499, Indians on Margarita Island, off
the coast of Venezuela, were observed chewing
a green herb which was carried in a gourd
around their necks. It was assumed that the
green herb, known as tobacco, was chewed
to quench thirst (2,3). Tobacco chewing ap
peared to be widespread in the late 1500s in
parts of southern America (1); men in Veragua
(presently Costa Rica) were also seen to be
chewing a dried herb (2). Tobacco smoking
was also popular in the 1500s: Columbus ob
served American Indians smoking thick bun
dles of twisted tobacco leaves wrapped in dried
palm or maize leaves (4).
Inhaling of powc.red tobacco (snufl)
seems to have come into vogue much later.
Snuff was prepared by grinding tobacco leaves
into a powder with a block and pestle of rose
wood (5). The Indians of Brazil were perhaps
the first to use snuff. In Haiti, it was used as a
medicine for cleaning nasal passages and as an
analgesic; Mexican Indians were known to
have used tobacco powder to heal burns and
wounds by the year 1519 (3) and also inhaled
powdered tobacco through a hollow Y-shaped
piece of cone or pipe called lobago or tobaca (6).
TOBACCO PRODUCTION AND USAGE
IN INDIA
Tobacco is now cultivated .and consumed in
various forms all over the world. India is one
Gvntrol of Tobacco-related Cancers and Other Diseases.
international Symposium, 1990. Prakash C. Gupta, James E. Hamner, III
ano P.R. Murti, eds. Oxford University Press, Bombay, 1992.
Tobacco control in India: problems and solutions
Usha v. Luthra, V. Sreenivas, G. R. Menon, A. K. Prabhakar and K. Chaudhry
Indian Council of Medical Research, New Delhi, India
Tobacco conttnl is a subject of worldwide importance. India is the third largest producer of
tobacco in the world, and the tobacco industry in our country is labour intensive and provides
employment to millions of people. It also earns the Government much revenue and foreign
exchange. Tobacco in any form, however, is detrimental to health: about!3% of the estimated five
million deaths in the adult population can be attributed to tobacco use. A conservative estimate
of the annual health care costs attributable to tobacco-related diseases exceeds the revenue earned
from tobacco by Rs. 6850 million (US$ 4U3 million). The Government of India has initiated sev
eral measures to tackle the problem. The Cigarette Act ofl975^stipulates that packets of cigarettes
and cigarc':c advertisements display the statutory warning that cigarette smoking is injurious to
health. Laws prohibit smoking in closed spaces such as cinemas, theatres, buses and on domestic
flights. Tobacco advertisements are banned in state-controlled media. The National Cancer
Control Programme launched in 1984,. gave high priority to eliminating tobacco-related cancers.
Unfortunately, these measures are yet to make a significant impact. A comprehensive programme
is described with the aim of creating a tobacco-free society in the country during the next century.
INTRODUCTION
Tobacco appears to be as old as human
civilization itself. Cultivation of the tobacco
plant probably dates back 7000 years: tobacco
seeds were discovered in archaeological exca
vations in Mexico and Peru, and the remains
^^permanent settlements built around 3500
^Bt showed that tobacco was an important
article to the inhabitants (1).
Documented evidence of tobacco usage
has been available since the end of the 15th cen
tury. In 1499, Indians on Margarita Island, off
the coast of Venezuela, were observed chewing
a green herb which was carried in a gourd
around their necks. It was assumed that the
green herb, known as tobacco, was chewed
to quench thirst (2,3). Tobacco chewing ap
peared to be widespread in the late 1500s in
parts of southern America (1); men in Veragua
(presently Costa Rica) were also seen to be
chewing a dried herb (2). Tobacco smoking
was also popular in the 1500s: Columbus ob
served American Indians smoking thick bun
dles of twisted tobacco leaves wrapped in dried
palm or maize leaves (4).
Inhaling of powdered tobacco (snufl)
seems to have come into vogue much later.
Snuff was prepared by grinding tobacco leaves
into a powder with a block and pestle of rose
wood (5). The Indians of Brazil were perhaps
the first to use snuff. In Haiti, it was used as a
medicine for cleaning nasal passages and as an
analgesic; Mexican Indians were known to
have used tobacco powder to heal burns and
wounds by the year 1519 (3) and also inhaled
powdered tobacco through a hollow Y-shaped
piece of cone or pipe called lobago or tobaca (6).
TOBACCO PRODUCTION AND USAGE
IN INDIA
Tobacco is now cultivated .and consumed in
various forms all over the world. India is one
242
Luthra et al.
of the principal tobacco producing countries,
ranking next to China and the USA. Tobacco
is cultivated on an area of over 450 000 ha,
with an annual production of 450-500 million
kg, constituting 7.6% of total world production
in 1987, The average yield per hectare in
creased from 750 kg in 1960-61 to 1199 kg in
1987-88 (7). Increases in the cultivated area,
production and yield of tobacco leaf per hect
are since 1949 are presented in Table 1. From
1967-68 onwards, the increase in the total area
under this crop can be seen to be marginal;
total production and average yield per hectare
increased by about 2% per annum, which is due
largely to better cultivation methods. When
Indian yield is compared with that in Taiwan
(2692 kg), Japan (2468 kg), Australia (2436
kg), Canada (2250 kg), the Republic of Korea
(2210 kg), Pakistan (1774 kg) and Burma
(1644 kg) (7), it is obvious that our productiv
ity is likely to rise further. This implies in
creased availability of tobacco in India in the
years to come.
Table 1
Alt-India compound growth rales (°/o) of area, production
and yield of tobacco*
Period
Production
Yield
2.79
2.15
2.16
0.96
2.11
1.47
X10’
1949-64
1967-85
1949-85
1.66
0.05
0.70
'Source: re:f. (7)
Tobacco is used in various forms in India
(see paper by Bhonsle et al., this volume).
Although there are no data on the extent of
tobacco use on a national basis, reports from
different parts of the country show that the
prevalence rates vary from 62 to 82% among
men and 15 to 67% in women (8). In a study
supported by the Indian Council of Medi
cal Research in Goa, 12% of school children
were found to be tobacco users (see paper by
Vaidya et al., this volume); in Bangalore, Delhi,
Diburgarh, and Ranchi, 56-64% of men over
20 years of age and 14-43% of women were
tobacco users.
TOBACCO ECONOMICS IN INDIA
Tobacco production is a major industry in
India. The current gross product value of man
ufactured tobacco is estimated to be of the
orderofRs. 36 000 miilionJUSS 2117 million).
Twelve companies with 20 factories manu
facture cigarettes in India. In 1987, 75 420
million cigarettes, 51% of which were fil^^
tipped, were produced in India (7). The ciga■rette industry is capital-intensive in the orga
nized sector, providing direct employment for
about 20 000 people and indirect employemcnt
for hundreds of thousands of people.
The bidi industry, which is essentially a
cottage industry, provides gainful employment
for more than three million people, mostly in
rural areas. Annual production of bidis is esti
mated to be over 550 000 million pieces. To
bacco is used not only for smoking, chewing in
various forms (see paper by Bhonsle et al., this
volume) and as snuff, but also for making sev
eral chemicals (see paper by Chari and Rao,
this volume).
The excise revenue earned from tobacco is second only to that from mineral oils, amount
ing to Rs. 15 515 million (USS 916 milli<4fen
1986-87 (7). Tobacco products are an impor-'
tant source of foreign exchange earnings in
India: during 1986-87, Rs. 1711 million (USS
101 million) were earned through the export of
unmanufactured tobacco and of manufactured
tobacco products like bidis, cigarettes, chew
ing tobacco, snuff, zarda and scented tobac
co. Interestingly, India also imports a limited
amount of tobacco and tobacco products: in
1984-85, tobacco products worth Rs. 3.8 mil
lion (USS 22 300) were imported (7).
NEED FOR TOBACCO CONTROL
In the past, tobacco use was considered by
some to be beneficial. In the USA during the
Tobacco control in India
19th and early 20th centuries, dental snuff was
used to relieve toothache and neuralgia, to
cure bleeding gums and scurvy, to preserve
and whiten teeth and to prevent tooth decay
.
(6)
The use of tobacco has, however, been
controversial since the beginning. Tobacco
was prohibited in Japan in 1590; and taxes on
tobacco were increased by 4000% by King
James VI ofScbtland. In 1633, Sultan Murad
IV of Turkey declared that the use of tobac
co in any form was a capital offense. During
1613-45, the Czar of Russia prohibited the sale
of tobacco. A major attitudinal change towards
tobacco chewing arose from the germ theory of
infection, tn the USA, spitting on the llobr'and
into brass cuspidors was considered a source of
contamination and disease spread, and by the
1890s public outcry made tobacco chewing a
socially unacceptable behaviour and it be
came unlawful in most public places (6). Anti
spitting laws were passed in New York and
’Philadelphia in 1896 and in Toronto, Canada,
in 1904 (9).
••
y
;
f;
In India, the earliest observation of the
harmful effects of tobacco was made by
Niblock (10), who observed in 1902 that can
cer of the cheek accounted for almost one-third
Aof all cancer admissions to a general hospital in
■.-‘ ^^the State of Madras (presently Tamil Nadu).
'
'
j.
He attributed this to the tobacco chewing
habit, which was prevalent in that region. In
1933, a case-control study indicating a link
between tobacco chewing and oral cancer was
reported (11). Much later, several epidemio
logical studies carried out in the Mainpuri district of Uttar Pradesh demonstrated that the
earlier the onset of tobacco chewing, the
greater the risk for oral cancer (12). The asso
ciation between tobacco use, oral cancer and
precancer was also reported from this area
(13-16). The. carcinogenic potential of tobacco
use has been described in other regions of
India as well. For example, in the Bombay
ana, bidi smoking was found to carry risks
243
for cancers of the oral cavity, pharynx and
oesophagus (17,18). A dose-response relationship between smoking and lung cancer in
India was also .demonstrated (19). Data from
the National Cancer Registry Project of the
Indian Council of Medical Research (20) -.
showed that 50% of all cancers in men and '
20% of those among women arc tobacco- I
related. Furthermore, the annual incidence of >
tobacco-related cancers was estimated to vary \
from 20 to 30 per 100 000 men and 12 to 14 per I
100 000 women. /Mthough the mortality rales
from these cancers are very high, no effective
cure is available, but these cancers can be pre
vented, simply by avoiding the use of tobacco.
It was estimated (21) that if a 20% reduc
tion in the use of tobacco were to be achiev
ed in 1985, as was envisaged, approximately
48 465 cancer cases could be prevented by
2000 z\D. In terms of cost economics, the dif
ference between the cost of treating these can- 1
cers and the cost of a primary prevention pro- I
gramme, i.e., the net savings, would be around I
Rs. 265 million (USS 15.6 million). Further
estimates indicate that the total annual costs -i
for health care (diagnosis and treatment) for
tobacco-related diseases (cancers, coronary ,
heart disease and chronic bronchitis) exceed .
the tobacco revenue by Rs. 6850 millions (USS ;
402.9 million). This is a very conservative es
timate, as the cost of establishing essential
health care facilities and the loss to the Cross
National Product due to tobacco use (disabil
ity, fetal loss/underweight) are not included.
Other diseases commonly associated with
tobacco use are chronic bronchitis, emphy
sema, ischaemic heart disease, chronic ob
structive pulmonary disease and pulmonary
tuberculosis. A cohort study showed that both
bidi and cigarette smokers had a three-fold
greater risk of developing coronary heart dis
ease or myocardial infarct than nonsmokers
(22).
The harmful effects of tobacco also
include increased risk oUow birthweight,
244
Luthra el al.
spontaneous abortion, stillbirth and neonataTdeaths. An excess rate of stillbirths was
observed among smokers (50 per 1000 births)
compared to nonsmokers (17 per 1000 births),
and babies born to mothers who smoked
weighed on average 100-200 g less than babies
born to mothers who did not smoke (23). In
another study (24), children born to mothers
who smoked weighed an average of 395 g less
than those born to nonsmoking mothers (sec
paper by Krishnamurthy, this volume).
Numerous biochemical investigations on
tobacco products also confirmed their harmful
nature. For example, carcinogenic and cocarcinogcnic polycyclic aromatic hydrocarbons
were found in substantial amounts in mishri,
which is applied to the teeth and gums, and in
snuff used for inhalation (25). Nicotine, carbon
monoxide, hydrogen cyanide, volatile phenols,
polycyclic aromatic hydrocarbons, acrolein
and acetaldehyde contribute to the toxicity/
carcinogenicity of tobacco smoke (26). Betel
quid also contains several carcinogenic sub
stances (sec paper by Hoffmann et al., on
smokeless tobacco, this volume). These find
ings indicate unequivocally that tobacco con
sumption in any form is a substantial health
hazard.
■
It is estimated that atJcast 630 000 deaths
among people aged 15 years and above in
India arc directly attributable to tobacco use;
this forms 23% of the total deaths among men
and 4% among women (8).
(
The tobacco industry spends Rs. 2682
(US$ 102) per ha, amounting to Rs. 1200 mil
lions (USS 70.6 million) per annum in curing the
tobacco. The major share of this, which is on
fuel, is Rs. 1598 (USS 94) per ha, totalling
Rs. 703 million (USS 41.3 million) per annum
.
(7)
These figures indicate that since the to
bacco industry requires considerable energy
resources for curing, it is also responsible to
some extent for deforestation in the country,
which will lead to ecological imbalance in the
years to come.
PROBLEMS AND POSSIBLE
SOLUTIONS FOR TOBACCO
CONTROL
Possible tobacco control measures can be split
broadly into (i) sociobchavioural aspects; (ii)
pharmacological and psychological aspects;
(iii) economic losses and gains; and (iv) politi
cal will.
Sociobehavioural aspects: Every effort should
be made to make tobacco use an antisocial
habit, be it al home, at work, in public places
or at social gatherings. Some state govern
ments in India — for example, those of West
Bengal, Tamil Nadu. Kerala, Karnataka,
Maharashtra and Gujarat — have promul
gated laws prohibiting smoking in enclosed
areas, such as cinemas, buses, educational
institutes and hospitals. Smoking is prohibited
currently on all domestic flights of Indian
Airlines. Any advertisement or even mention
of tobacco is banned on the broadcasts of All
India Radio.
To achieve the aim of a tobacco-free soci
ety, environmental situations must be created
in which nonsmokers arc given preference over
smokers. In order to achieve this, many grad
ual and carefully designed steps will have to be
undertaken. For instance, antitoba_ccp_cd_ucation, focused on young nonusers through an
extensive, persuasive campaign would be an
important step in that direction. Use of the
mass media, voluntary agencies, women’s
organizations, educational institutions, reli
gious organizations, shrines, no-tobacco days
for users and traders, and messages from
health-related institutions should be explored.
Periodic cross-sectional assessment to measure
the impact of such educational programmes
would be essential in order to make the mid
course corrections.
Pharmacological and psychological aspects:
Termination of nicotine ingestion, even after
intake of small quantities (daily dose, 0.002
mg/kg body weight), produced behaviour
al patterns associated with aggressiveness,
KOKfCI
Tobacco control in India
regional languages, as a weekly serial with 28
episodes, by all of the 104 broadcasting sta
tions, focusing on the rural community aged 10
years and over.
RESEARCH PRIORITIES
Operational research for antitobacco commu
nity education must be strengthened, and var
ious agencies can be used for this purpose. A
single approach will not be suitable for all pop
ulation groups, but packages for different areas
of the country could be devised and imple
mented. Research on tobacco usage would
247
help in deciding the most effective method of
community-based intervention.
z\ major hindrance to implementing anti
tobacco legislations is the fear of loss of
employment and the revenue .earned from
tobacco. As described above, however, the
amount spent on the treatment of tobaccorelated diseases outweighs the gains due to
tobacco revenue and export. The Indian
Council of Medical Research is initialing
studies on the cost of managing tobaccoreiated diseases, which will help in computing
the .tobacco economic,sJar the country more
accurately.
References
Voces E. The pleasure of tobacco — How it all
began and the whole story, 'fob J Im 1984;
1:80-2.
2.
Heiman RK. Tobacco and Americans, New
York, McGraw-Hill. pp. 8, 65, 118-119, 236,
1960.
3.
Stewart GG. z\ history of medicinal use of
tobacco. 1492-1860. Med Hist 1967; 11:228-68.
4.
Tso TC. Tobacco plants. In: Hand Book
of Tobacco and Tobacco Products: Beitrage
zur Tabakforschung International, Hamburg,
1986.
5.
Curtis MM. The Book of Snuff and Snuff
Boxes, New York, Bramhall House, pp. 20-7,
67, 1935.
6. Christen AG, Swanson BZ, Glover ED,
Henderson AH. Smokeless tobacco: the folk
lore and social history of snuffing, sneezing,
dipping, and chewing. J Am Dent Assoc 1982;
105:821-9.
, 7. .1 Direcorate ofTobacco Development, Ministry
-•
of Agriculture. Tobacco in India. In: z\ Hand
Book of Statistics, Government of India,
Madras, 1989.
8. Gupta PC. Health consequences of tobacco
use in India. World Smoking Health 1988;
13:5-10.
9. Kozlowski LT. The determinants of tobacco
use: cigarette smoking in the context of other
forms of use. Can J Public Health I98l;72:
396-101.
1.
It). Ni block WJ. Cancer in India. Indian Med
Gaz 1902; 37:161-5.
11.
Orr IM. Oral cancer in betel nut chewers in
Travancorc. Lancet 1933; ii:575-8O.
12.
Wahi PN. The epidemiology of oral and oro
pharyngeal cancer. A report of the study in
Mainpuri district, Uttar Pradesh, India. Bull
World Health Organ 1968; 38:495-521.
13. Wahi PN, Luthra UK, Lahiri B. factors
influencing oral and oropharyngeal cancer in
India. BrJ Cancer 1965; 19:642-60.
14. Wahi PN, Lahiri B, Luthra UK, Arora S.
Oral and oropharyngeal cancer in North India.
BrJ Cancer 1965; 19:627-41.
15. Wahi PN, Kapur VL, Luthra UK,
Srivastava ML. Submucous fibrosis of the
oral cavity and clinical features. Bull World
Health Organ 1966; 35:789-92.
16. Wahi PN, Luthra UK. Morphological and
cytochemical studies of exfoliated cells in oral
precancerous lesions. Acta Cvtol 1966; 10:
173-8.
17. Sanchvi LD, Rao KCM, Khanoi.kar VR.
Smoking and chewing tobacco in relation to the
cancer of the upper alimentary tract. Br Med J
1955; kill 1-4.
18. J Ussawalla DJ, Deshpande VA. Evaluation
of cancer risk in tobacco chewers and smokers:
an epidemiologic assessment. Cancer I97l;28:
244-52.
Tobacco control in India
hostility and irritability (28). Thus, nicotine
acts as a reinforcing agent in tobacco smok
ing. The nicotine withdrawal syndrome, which
includes sleep disturbances, changes in brain
wave-pattern, fall in pulse rate and blood pres
sure, anxiety, nervousness and fatigue, con
tributes to the difficulty in giving up tobacco.
Counselling centres for quitting the to
bacco habit, comprising psychological sup
port to tobacco users, would be necessary. In
some situations, the focus could be on mitiga
tion rather than on elimination. People con^nue to smoke because of dependency due to
cognitive helplessness: research must therefore
be undertaken to find ways to satisfy their
psychological and pharmacological needs. Nonsmokers’ rights in the face of the dangers of
passive smoking arc another important social
issue. In a large proportion of people, initiation
into alcohol and drug abuse starts after to
bacco use (28).
Economic aspects-. As discussed above, to
bacco contributes to both the negative and
positive aspects of the country’s economy, but
the losses to the economy far outweigh the
gains. Unfortunately, this fact is still not well
known and should be proven with sound data.
While the gains are clear, in the form of
employment generated by tobacco-related
activities and revenue and foreign exchange
^k nings, the losses occur in the form of costs
meurred in providing health care for people
with tobacco-related diseases due to loss of
productivity caused by decreased efficiency,
disability and premature death. The use of
wood in tobacco curing, resulting in environ
mental degradation and soil erosion, also has
serious economic implications.
A conservative estimate, based on the
impressions of a number of clinicians, of the
cost of treatment of three major tobaccorelated diseases, namely, cancers, heart dis
eases and bronchitis, is that it costs the govern
ment about Rs. 24 190 million (US$ 1422.8
million) annually, which is Rs. 6850 million
245
(USS 402.9 million) more than the revenue
and foreign exchange provided by tobacco to
the Government. As mentioned earlier, these
estimates do not include the cost of diagnosis
and treatment of otiier diseases and disorders
or the cost of establishing health care facilities
such as radiotherapy units and computerized
tomography scanners.
Experience all over the world has shown
that a gradual price rise is an effective means of
reducing the smoking habit. Thus, a gradual
increase in the prices of all tobacco products in
the country would be the right approach.
Political will: A necessary ingredient for the
success of any national programme is political
and administrative support. Politicians and
administrators must be convinced of the mag
nitude of tobacco-related problems, so that
they will promulgate and strictly enforce any
legislation directed towards tobacco control.
Politicians can also act as leaders for anti
tobacco programmes, and this increases their
chances of success. The political will can be
stimulated by close interaction between scien
tists (health, agriculture, industry), politicians
and administrators.
EFFORTS OF THE GOVERNMENT
OF INDIA TOWARDS TOBACCO
CONTROL
Realizing the magnitude of health problems
associated with tobacco usage, the Govern
ment promulgated The Cigarette Act, 1975
(regulation of production, supply and distribu
tion), which requires that all manufacturers or
persons trading in cigarettes display promi
nently a statutory warning, ‘Cigarette smoking
is injurious to health’, on all cartons and pack
ets of cigarettes that are put on sale. This, how
ever, made no significant dent in the smoking
habit; because (i) the statutory warning is lim
ited to cigarettes, which are consumed much
less than bidis, which are cheaper and more
harmful; and (ii) the printed warning can be
read only by literates.
246
Luthra el al.
It has been suggested that, in view of the
diverse forms of tobacco use, (i) the statutory
warning be extended to other tobacco prod
ucts; (ii) the warning be printed in local lan
guages; and (iii) the warning made more effec
tive by a pictorial depiction, for instance, in the
form of a skull-and-crossed-bones. The print
ing of more direct messages like ‘Tobacco can
cause cancers and heart diseases’ in local lan
guages might also be useful. Printing the tar
and nicotine levels on packets and cartons of
all tobacco products and fixing the maximum
permissible limits of these toxins for all tobac
co products should also be made mandatory.
High levels of taxation should be placed on
high-tar, high-nicotine tobacco products. Both
cigarettes and bidis should be required by law
to have effective filters.
On the recommendations of the LuthraBisht Committee in 1984, a national cancer
control programme was formulated, which
gave impetus to the antitobacco cause. Noting
that tobacco-related cancers account for about
one-third of all cancers in the country, primary
prevention of tobacccnrelated cancers consti
tuted a major objective of this programme.
Accordingly, the National Cancer Control
Board and state cancer_control-bdafds~Kave
given high priority to antitobacco educational
programmes for primary prevention of to
bacco-related cancers. To date, 17 states and
union territories in.the country have-consti
tuted such cancer control boards.
Monitoring and controlling scenes that
glamourize smoking in films, Doordarshan
(television) programmes and road-side adver
tisements constitute another important con
trol measure. As described earlier, a complete
ban on tobacco advertisements in government
media exists, and smoking is prohibited on
domestic flights.
It is realized, however, that such govern
mental steps, although commendable, are not
sufficient to make an impressionable dent on
the tobacco habit of the community: it is
necessary to have a comprehensive programme
for tobacco control. The main planks of such
a comprehensive programme should com
prise tougher antitobacco legislation, a gradual
price rise on tobacco, changes in agricultural
practices to replace tobacco by other crops,
finding alternative uses of tobacco, modifying
tobacco products to make them less harmful
and an aggressive health education campaign
to wean people away from tobacco. Other
steps that the Government should initiate
urgently are: protection of nonsmokers in gL
lie places from passive smoking; banimg
tobacco advertisements in all public places;
making it unlawful to sell tobacco items to peo
ple below the age of 18; sale of cigarettes and
bidis in packets, as opposed to selling them sin
gly; prohibition of the sale of tobacco in and
around educational, health and religious insti
tutions; and a ban on tobacco imports.
OPERATIONAL RESEARCH ON AN
ANTITOBACCO PROGRAMME
The experience all over the world is that
antitobacco education is an effective means of
stopping or curtailing tobacco use. Although
such efforts have to be targeted at users as well
as nonusers of tobacco, the most profitabletarget group is the young nonuser. An inter
vention study by the Tata Institute of ^hidamental Research, Bombay, showed that
9-17% of peopl<T"stbpped~ tbbacco use and
20-49% reduced their habit substantially after
five years of health education (27). The Indian
Council of Medical Research initiated a
multicentre study in Bangalore, Goa, Agra and
Trivandrum, utilizing the existing health infrastruefure. Workers at the Goa centre are also
studying the use of school children as a means
ofchanging tobacco habits in a community.
All-India Radio, in collaboration with the
Indian Council of Medical Research, will soon
initiate an educational programme on the haz
ards of tobacco, drugs and alcohol. This pro
gramme (Radio Date) will be broadcast in 17
248
Luthra el al.
Notani P, Sanghvi LD. A retrospective study
of lung cancer in Bombay. Br J Cancer 1974;
29:477-82.
20. Indian Council of Medical Research. National
Cancer Registry. Annual Report, 1986. New
Delhi, 1989.
,21. /Indian Council of Medical Research. Tobacco
Related Health Hazards. A Task Force of
Indian Council of Medical Research, 1989,
...__ New Delhi.
JJZ/Jayant K, Notani PN, Sanghvi LD. Health
consequences of tobacco smoking in two
socioeconomic classes in Bombay, India. In:
Forbes VVF, Fregker RC, Nosta ba keen D,
eds. July 10-15, 1983. Proceedings of the Fifth
World Conference on Smoking and Health
Winncpcg, Canada, 1983. Canadian Council
on Smoking and Health, Ottawa, Vol. I: pp.
149-56.
23. Krishna K. Tobacco chewing in pregnancy.
Br J Obstet Gynecol 1978; 85:726-8.
19
24. Agrawal P, Chansoriya M, Kaul KK.
Effect of tobacco chewing by mothers on pla
cental morphology. Indian J Pediatr 1983;
20:561-5.
25. Bhide SV, Kulkarni JR, Padma PR, d al.
Studies on tobacco specific nilrosamines and
other carcinogenic agents in smokeless tobacco
products. In. Sanghvi LD, Notani P, eds.
Tobacco and Health: The Indian Scene, UICC
Workshop. Tata Memorial Centre. 1989,
Bombay, pp. 121-31.
26. Wynder EL, Hoffmann D. Tobacco and
Tobacco Smoke Studies in Experimental Car__ * cinogenesis. Academic Press, New York: 1967.
c27.J Gupta PC, Mehta FS, Pindborg JJ, d al.
Intervention study for primary prevention of
oral cancer among 36 000 Indian tobacco
users. Lancet 1986; i: 1235-9.
. 28?) World Health Organization. Smoking and its
Effect on Health. WHO Technical Report
Series No. 568. Geneva, 1975.
Control strategies for tohaeco-related cancers
intervention and (v) intervention specially
directed to high-risk populations.
Tobacco cessation clinics'. Quitting the use of
tobacco is complex and requires continuous
support from various sources. Thus, tobacco
cessation programmes should include health
education, motivation and psychological, so
cial, family and sometimes pharmacological
support in order to bring attitudinal changes
and modification of behaviour. Implemen
tation of these programmes, therefore, must
be multidisciplinary, involving clinicians, psy
chologists, sociologists and family support in
a suitable environment. We envisage conduct
ing tobacco cessation clinics incorporating
the necessary infrastructure, especially for
heavy tobacco users. The reasons for the high
level of health awareness among some individ
uals may be applicable for primary prevention
in others. We will therefore collect this infor
mation from a sample of the 100 000 individu
als who registered themselves in the Kerala
government scheme ‘Cancer care for life'.
Chemoprevention: Chemoprevention is a
major experimental activity for the control of
oral cancer and precanccr at the RCC, which
is being conducted in collaboration with the
British Columbia Cancer Research Centre,
Vancouver, Canada. The main objective is to
determine whether micronutrients can lower
the risk of cancer by preventing or reverting
the process of carcinogenesis. The feasibility
of using micronucleated cells as intermediate
endpoints is being evaluated. B-carotene and
Vitamin A intake appear to result in higher
rates of regression of leukoplakia among heavy
chewcrs, smokers and alcohol users (6-8). The
optimal doses, spacing and maintenance of
these vitamins were also determined. Chem
opreventive agents are believed to act even
with the continued action of etiological factors;
however, whether these agents really reduce
the risk for cancer is yet to be determined from
long-term follow-up studies. At this stage, the
emphasis is on clinical trial; we hope to trans
late the experiences gained from these studies
251
into a full-scale chemopreventive intervention
trial.
Secondary prevention:
Use of primary health workers for early detection of
oral cancer: Studies conducted in Sri Lanka (9)
and in the Ernakulam district of Kerala (10)
demonstrated that primary health care work
ers can be used in oral cancer detection pro
grammes. A similar study is in progress in the
northern part of Trivandrum district: primary
health care workers in six primary health cen
tres were trained by the RCC to identify people
al risk and to examine their mouths to detect
oral cancer and prccancerous lesions. An area
covered by primary health care workers in the
southern part of the Trivandrum district has
been selected as the control area. It is proposed
to compare the numbers of oral cancer cases
arriving from these two areas to evaluate
whether early detection has been achieved in
the study area.
Use of unemployed youths for early detection
ofcancers: Some 92 unemployed youths belong
ing to a community of 1-1 000 persons were
informed about the seven warning signals of
cancer and were briefly trained to examine the
oral cavities of high-risk persons. These youths
then screened 13 959 people from that commu
nity and identified 397 high-risk individuals.
While examining the individuals, they also dis
seminated information on the seven warning '
signals. People who thought they might have
cancer on the basis of these signals and people
found by the unemployed youths to have a sus
picious oral lesion were advised to consult
physicians. Employing this method, nine can
cers, of which four were buccal cancers, and
169 prccancerous lesions and conditions were
detected, vindicating the feasibility of using
such young persons in oral cancer detection
programmes.
Use ofNational Service Scheme volunteers: The
National Service Scheme is a voluntary stu
dent organization which is involved in various
2.- 2-8
Control of Tobacco-rclatcd Cancers and Other Diseases.
International Symposium, 1990. Prakash C. Gupta, James E. Hamner, III
and P.R. Murti, eds. Oxford University Press, Bombay, 1992.
Control strategies for tobacco-related cancers
in Kerala, India
M. Krishnan Nair, B. Mathew, R. Sankaranarayanan and R. Lesley
Regional Cancer Centre, Trivandrum, India
Various cancer control activities undertaken by the Regional Cancer Centre, 1 rivandrum,
Kerala, India, include a novel method of utilizing the services of National Service Scheme volun
teers, primary health care workers, social workers and unemployed youth in both primary and
sccondat y prevention of cancer. These approaches were found to be effective.
INTRODUCTION
Cancer control implies a broad spectrum of
activities aimed at primary prevention, reduc
tion in morbidity and mortality and rehabilita
tion. The basis for cancer control is research in
basic sciences, cancer epidemiology, diagnos
tics, clinical oncology, social sciences, rehabili
tation, health care organization and health
delivery. Many countries have formulated can
cer control policies consistent with their needs
and priorities (1), and India is one of them
(2). Tobacco-related cancers constitute 50-55%
of cancers among men and 20-25% among
women in India (3,4). Accordingly, in the
blational Cancer Control plan, primary pre(Pition formed an important objective. In con
sonance with this objective, the State of Kerala
on the south-western coast of India has formu
lated its own cancer control programmes (5).
This paper gives an overview of the activities
conducted by the Regional Cancer Centre
(RCC), which is a major cancer treatment cen
tre in the State.
CANCER IN KERALA
Data from the RCC show that every year
15 000 new cancer cases occur in the State
(4). Of these, 17% among men and 11%
among women are oral cancers. Other common
cancers among men include cancers of the lung
(11.5%), oesophagus (5.8%) and larynx and
pharynx together (7%). Among women, the
common cancers include those of the uterine
cervix (25%) and breast (17%).
CONTROL STRATEGIES IN KERALA
To facilitate the planning of control strategies,
the following data were collected: (i) the pat
tern of tobacco usage in the community; (ii)
knowledge, attitude and perception of the gen
eral population; (iii) refeiral pattern; (iv) inci
dence rates of various cancers; (v) clinical
extent of cancer at first presentation; and
(vi) proportion of cases receiving radical
treatment.
Several measures are being implemented
in the State, but the major emphasis is on
primary prevention, with an interdisciplinary
approach utilizing health care delivery agen
cies and voluntary organizations. The vari
ous activities can be summarized as follows:
Primary prevention involves surveys of to
bacco use and of knowledge, attitude and
perception, cancer registration, health educa
tion, tobacco cessation clinics, chemopre
vention and legislation. Secondary preven
tion consists of utilization of primary health
250
Krishnan Nair el al.
workers, volunteers to the National Service
Scheme and unemployed youth, cancer detec
tion camps and peripheral centres for early
detection of cancer. Tertiary prevention in
volves therapeutic intervention, surgical recon
struction, clinical trials, pain clinics and psy
chosocial surveys of morbidity.
Primary prevention:
Tobacco surveys: Information on the prevalence
of tobacco use is important for planning con
trol measures and was obtained from different
parts of the State. For example, 13 000 people
in the south were interviewed by health and
social workers. These individuals represented
a 10% sample of the 278 census enumeration
blocks in each of which the entire population
was enumerated for tobacco habits. In central
Kerala, unemployed youth collected this infor
mation from 11 420 people; in Kottayam, all
individuals over the age of 21 were screened
by National Service Scheme volunteers with
regard to their tobacco habits and alcohol con
sumption, as part of an oral cancer screening
programme.
Tobacco smoking by itself or with chew
ing was common (46%) among men; only 9%
were exclusively chewers. An overwhelming
proportion (92%) of women in this group did
not use tobacco. Compared to data avail
able from other sources, these prevalences
are rather different. Information on alcohol
consumption was also collected from these
individuals.
Surveys of knowledge, attitude and perception:
Table 1 summarizes information collected on
knowledge, awareness and perception about
cancer among 600 individuals by hospital
social workers. A high level of awareness was
observed about cancer in general, about warn
ing signals and about the risk factors for oral
cancer. The knowledge of medical students
was monitored in another survey, and such
information is now being obtained from physi
cians and surgeons.
Table 1
Awareness about cancer among 600 individuals in Kerai
Criteria
Heard about cancer
Aware about at least one or more risk
factors for oral cancer
Aware about at least one or more risk
factors for lung cancer
Aware about at least one or more of the
seven warning signals of cancer
Aware about at least one or more
common cancers
Percent
100
67
28
75
65
Cancer registration: Since 1982, a hospital
based cancer registry has been functioning a
the RCC, which is the only cancer treatmen
centre in southern Kerala. Data from thi
source is used to compute the minimal inci
dence rates of different cancers in order t
study their trends. Information on referra
practices, the clinical extent of cancers at pres
entation, treatment modalities and prognosis i
also available from the registry.
Health education: Helping people to avoi
tobacco use is accorded high priority in th
cancer control programme. With that view
various health educational programmes ar
being undertaken at the Community Oncdiog
Centre of the RCC. Electronics and the pres
are being used to disseminate in^^natio
about tobacco related-cancers to the publi
Further, audiovisual programmes on canci
are being shown during cancer detection camj
in various parts of the state. School childrc
will be educated on the harmful effects «
tobacco and will be used later to spread tl
messages. Suitable material to be included i
the school curriculum is being developed. ?
part of self-help measures, pamphlets on exam
ining one’s own mouth are distributed perio<
ically, so that they will reach a large nun
ber of households. The various health edi
cation measures thus comprise (i) schoo
based intervention, (ii) self-help strategies, (ii
mass media approaches, (iv) community-bas<
252
Krishnan Nair el al.
developmental programmes in the community.
The organization has different levels of leader
ship and implements many socially relevant
schemes, such as teaching, hygiene and immu
nization, in the community. For the present
purpose, volunteers were instructed about the
seven warning signals of cancer and were also
trained to conduct oral examinations. They
have screened 4041 persons so far, and de
tected 15 oral cancers, 12 in clinical stages 1
and 2 and three in stages 3 and 4; they also
found 92 precancerous lesions and conditions,
which were confirmed by physicians. Thus, the
strategy of using National Service Scheme vol
unteers was found to be fruitful, and they are
now being used regularly in screening pro
grammes in Kottayam.
Clinical trials to assess the efficacy of
multi-modal treatment of advanced tobaccorelated cancers are in progress at the RCC.
The cancer surgery division uses an indige
nous reconstruction technique for oral and
head-and-neck cancers. Pain relief manage
ment consistent with that recommended by the
WHO global programme on cancer pain relief
is part of the treatment protocol at the RCC,
and this knowledge is disseminated to other
centres in the State. Objective and subjective
assessments of various pain relief methods are
also being planned. Psychosocial surveys
on morbidity of cancers of the head-andneck, breast and cervix arc being contem
plated.
Early detection centres and cancfr detection cam
paigns: Two peripheral centres for early detec
tion of cancer were established in Ernakulam
and Palghat by the RCC in collaboration with
the Kerala State Health Services Department.
The main purpose of these peripheral units is
to provide diagnostic services for cancers of the
head and neck, breast and uterine cervix (11).
The units also organize regular cancer detec
tion campaigns in the community in order to
examine high-risk individuals and to follow-up
cases of prccancer.
DISCUSSION
Tertiary prevention:
Tertiary prevention encompasses reconstruc
tion, rehabilitation and pain control therapy.
In order to provide optimal treatment and
minimal loss of structure, a combined ap
proach consisting of surgery, radiation and
chemotheraphy is used for treating cancer at
the RCC. Regular programmes propagate this
approach to other centres in Kerala.
Kerala is a small state with a high literacy rate
(65%), which is advantageous for raising the
health consciousness of the people. As else
where in the country, tobacco use is deeply
entrenched. In order to combat its health con
sequences, the RCC, in association with medi
cal colleges in the State, the Health Services
Department of Kerala Government, National
Service Scheme volunteers, unemployed youth,
general practitioners and various social organi
zations, has embarked on multifaceted cancer
control activities. The active concern of the
Government regarding the health conse
quences related to tobacco use and its support
ive action are encouraging. For instance, the
Government is contemplating measures to pre
vent tobacco from being available to children
and to deter tobacco use in public places, edu
cational institutions and Government offices.
It is hoped that these attempts will produce the
desired results in the near future.
References
1.
2.
US National Cancer Institute. Cancer Control
Objectives for the Nation: 1985-2000. NCI
Monographs No. 2, Bethesda, 1986.
Directorate General of Health Services. Na-
3.
tional Cancer Control Programme for India.
Ministry of Health and Family Welfare, New
Delhi, 1984.
Indian Council of Medical Research. Annual
Control strategies for tobacco- related cancels
!.
5.
6.
7.
Reports of National Cancer Registry Project of
India. New Delhi, 1982-87.
Regional Cancer Centre. Hospital Cancer Re
gistry. Annual Report. Regional Cancer Centre,
Trivandrum, 1987.
Krishnan Nair M. A Tcn-ycar Action Plan
for Cancer Control in Kerala, Regional Cancer
Centre, Trivandrum, 1987.
Stich HF, Rosin MP, Hornby AP, et al.
Remission of oral leukoplakias and micronuclei
in tobacco/betcl quid chewers treated with
betacarotcnc and with betacarotcnc plus vita
min A. Int J Cancer 1988; 42:195-9.
Stich HF, Hornby AP, Mathew B,
San KA RANARAYAN an R, KRISHNAN NaIR M.
Response of oral leukoplakias to the admin
istration of vitamin A. Cancer Lett 1988;
40:93-101.
8.
253
Stich HF, Mathew B, Sankaranarayanan
R, Krishnan Nair M. Remission of oral pre-
cancerous lesions of tobacco/arcca nut chewers
following administration of betacarotcnc or
vitamin A and maintenance of the protective
effect. Am J Clin Nutr (in press).
9. Warnakulasuriya KAAS, Ekanayake AN I,
Sivayoham S, et al. Utilization of primary'
health care workers for early detection of oral
cancer and precanccr cases in Sri Lanka. Bull
World Health Organ 1984; 62:243-50.
10. Mehta FS, Gupta PC, Bhonsi.e RB, et al.
Detection of oral cancer using basic health
workers in an area of high oral cancer inci
dence. Cancer Detect Prcv 1986; 19:219-25.
11. Regional Cancer Centre, Annual Report of the
Regional Cancer Center 1988-89. Trivandrum,
1989.
9-Cancer Causes and Control 1995, 6, 119-129
Efficacy of an anti-tobacco
community education program
in India
N. Anantha, A. Nandakumar, N. Vishwanath, T. Venkatesh,
Y.G. Pallad, P. Manjunath, D.R. Kumar, S.G.S. Murthy,
Shivashankariah, and C.S. Dayananda
(Received 21 September 1994; accepted in revised form 14 December 1994)
In a study on ‘Assessment of Efficacy of an Anti-Tobacco Community Education Program’ on Kolar District of
Karnataka, India, an experimental and two control areas were chosen based on comparable population, health,
and socioeconomic parameters. The two main objectives were to prevent individuals from taking up the tobacco
habit among those who currently did not smoke or chew tobacco, and to stop the tobacco habit in those who did
smoke or chew tobacco. A baseline tobacco-habit survey of the population was followed by anti-tobacco
education of the community in the experimental area only. Two years later, a repeat survey of the population
was conducted, followed by a final survey after a further three years. Methods of health education of the
community included screening of films, exhibits, and personal contact with a display of photographs of the
harmful effects of tobacco. The results were evaluated through changes in prevalence rates, quitters’ rates, and
initiation rate. The final survey showed that in the experimental area, the decline in the prevalence rate in the
combined sample compared with the baseline rates was 10.2 percent in males and 16.3 percent in females, with a
corresponding quitter’s rate of 26.5 percent in males and 36.7 percent in females. Among men, a higher
proportion (30.2 percent) had given up chewing compared with smoking (20.4 percent). Cancer Causes and
Control 1995, 6, 119-129
Key words: Anti-smoking education, India, program evaluation, tobacco control.
Introduction
Use of tobacco in various forms is widely prevalent in
the Indian subcontinent, although exact figures of
prevalence of the habit are available from only some
areas.' In these studies, there is a wide variation from
region to region in the prevalence and type of tobacco
used (62 to 82 percent in males and 15 to 67 percent in
females). The annual number of deaths in India
attributed to tobacco use is estimated to be between
630,000 to one million.3,4 The association between use of
tobacco and the occurrence of oral cancer was reported
over 60 years ago5 and since then, the burden of
tobacco-related cancers has been estimated6"9 at 40 to 42
percent of all cancers among males and 15 to 20 percent
of all cancers among females.
It is obvious, therefore, that education of the public,10
including selected target populations, on the harmful
effects of tobacco is of paramount importance. Few
studies have been conducted in this pan of the world in
Drs Anantha and Nandakumar are with the Coordinating Unit, National Cancer Registry Programme, Kidwai Memorial Institute ofOncology,
Bangalore, India Authors (AN., N.V., T.V., Y.G.P., PM, D.R.K., S.G.S.M, S., CS.D.) are with the Anti-Tobacco Cell, Kidwai Memorial Institute of
Oncology, Bangalore, India Address correspondence to Dr Nandakumar, Coordinating Unit, National Cancer Registry Programme of India,
Kidwai Memorial Institute ofOncology, Post Box No 2930, Hosur Road, Bangalore S60029, India The study was possible because ofthe financial
support provided by the Indian Council of Medical Research, New Delhi to Kidwai Memorial Institute of Oncology, Bangalore.
© 1995 Rapid Communications of Oxford Ltd
Cancer Causes and Control. Vol 6. 1995
119
N. Anantha et al
a systematic and evaluable way, so as to measure the
impact of such an education program and also to
examine whether this could be integrated into the
general health scheme of the community. This study
was conducted to assess the efficacy of such an anti
tobacco community-education program. It had two
main objectives. The first was to prevent the uptake of
the tobacco habit in persons who did not smoke or
chew tobacco, and the second was to stop the tobacco
habit in those who did smoke or chew tobacco—both
objectives being achieved through health education of
the community.
Materials and methods
An ‘Anti-Tobacco Community Education Program’ was
conducted as a demonstration-cum-research study by
Kidwai Memorial Institute of Oncology, Bangalore
through funding from the Indian Council of Medical
Research, New Delhi. It was carried out over a six-year
period between February 1986 and March 1992. The
work essentially involved a systematic survey of the
population for the prevalence of the tobacco habit in
three different areas. This was followed by intervention
through anti-tobacco community education of one area,
followed by two additional surveys in all three areas.
The impact of the education was measured through
tobacco-habit prevalence rates, the number and rates of
persons who had quit the habit, and the rate of uptake
of the habit by prior nonusers of tobacco.
Selection ofplaceIareas for study
The study was conducted in one experimental and two
control areas of Kolar District (population [pop] = 1.9
million [1981 Census]) in Karnataka State (pop = 37
million) of India. The district of Kolar was selected
because of the proximity of the district to Bangalore.
Three areas under the purview of the Primary Health
Centers of Dibbur (pop = 60,447), Malur (pop =
64,202), and Gudibanda (pop = 46,878) comprising
117, 136, and 120 villages, respectively, were chosen on
the basis of a fair degree of comparability of prevalence
of the tobacco habit, availability of educational
facilities, and socioeconomic infrastructure. Dibbur
was chosen as the experimental area (ExA), and Malur
and Gudibanda as control areas I (CoAl) and II
(CoAH), respectively.
Plan of survey
The survey was carried out three times. The first survey
was defined as the ‘baseline survey’ (BLS) and was
carried out before undertaking any educational
programs. The second survey was called ‘first repeat
survey’ (FRS) and was done two years after education
120
Cancer Causes and Control Vol 6. 1995
was imparted to the community covered by the ExA.
The ‘final survey’ (FS) was made three years after the
FRS. The actual survey was done in two sets of selected
villages in the three areas. The first set referred to as
‘panel sample’ (PS) consisted of 10 villages in the ExA,
five villages in CoAI, and 11 villages in CoAII. The
population in these villages, comprising the PS in the
experimental and control areas, was surveyed all three
times during baseline, first repeat, and final surveys. The
second set of villages referred to as the ‘non-panel
sample’ (NPS) consisted of 47 villages in ExA, 32
villages in CoAI, and 34 villages in CoAII. These villages
in the NPS were defined as those villages which were
surveyed only once during any of the surveys mentioned
above. Thus, of the 47 villages mentioned in the ExA, 19
were chosen for BLS, 14 for FRS, and another 14 for FS.
Similarly, the number of villages chosen during the
three surveys, respectively, for CoAI were 10, seven, and
15, and for CoAII were 17, eight, and nine. A stratified
random-sampling method was used to select the villages.
The above method of choosing one set of villages as PS
and another set as NPS was done to ensure as much
coverage of the population as was possible while at the
same time to observe the impact of education on people
in one set of villages. The results from the NPS also
eliminates any bias that may be associated with the
results in the PS from repeated tobacco surveys in the
same population. This needs to be emphasized, since the
PS was not exposed to any deliberate or planned
intervention vis-a-vis the villages under the NPS.
The number of villages chosen in the combined
sample (CS) (CS = PS + NPS) as well as for the panel
and non-panel samples during each of the three surveys
in the experimental and control areas with their
respective population according to the 1981 census is
shown in Table 1. However, the actual population of
the different villages at the time of the survey was higher
because of the period of time that elapsed between the
conduct of the census in 1981 and the time when the
surveys actually took place. The exact population at
the time of each survey is indicated in the subsequent
tables that give results of the survey.
Survey methodology
Three forms consisting of village appraisal, household
information, and tobacco habit were completed by
trained social investigators. The village appraisal form
consisted of the basic characteristics of the village in
terms of land available for cultivation, the literacy of the
population, education, and health, as well as commu
nication and transport facilities that were available. The
household survey form was used to identify the
household in the village, record income of the earning
members, and number of persons in the house who
Anti-tobacco education
Table 1. Number of villages (Vil) and their total estimated population (1981 census) in the combined sample, panel
sample, and non-panel sample during Baseline Survey (BLS), First Repeat Survey (FRS), and Final Survey (FS), India
Experimental area
No.
Vil
Male
Female
Total
Combined sample
BLS
29
FRS
24
FS
24
5,097
2,246
3,239
5,116
2,281
3,285
10,213
4,527
6,524
Panel sample
BLS
10
FRS
10
FS
10
1,228
1,228
1,228
1,249
1,249
1,249
Non-panel sample
BLS
16
FRS
FS
14
3,869
1,018
2,011
Total
6,898
47
Control area (II)
Control area (I)
Population
No.
Vil
No.
Vil
Population
Female
Total
28
19
20
4,667
1,773
2,477
4,594
1,758
2,460
9,261
3,531
4,937
11
11
1,397
1,397
1,397
1,367
1,367
1,367
2,764
2,764
2,764
6,754
2,067
9,688
17
8
9
3,270
376
1,080
3,227
391
1,093
6,497
767
2,173
18,509
34
4,726
4,711
9,437
Female
Total
15
12
20
4,341
1,905
5,821
4,126
1,875
5,580
8,467
3,780
11,401
2,477
2,477
2,477
5
5
5
862
862
862
851
851
851
1,713
1,713
1,713
3,867
1,032
2,036
7,736
2,050
4,047
10
15
3,479
1,043
4,959
3,275
1,024
4,729
6,935
13,833
32
9,481
9,028
smoked or chewed tobacco. The individual survey
recorded details of the tobacco habit and level of
awareness about the harmful effects of tobacco.
Individuals of all ages were surveyed. Surveys took
about five to six months to be completed. Information
on the tobacco habit was elicited in-person by the social
investigators.
Anti-tobacco education
Education on the harmful effects of tobacco was carried
out in all the 117 villages (including 10 in the PS and 47 in
the NPS) within the experimental area, but not in any of
the villages in the control areas. Twenty-five junior
health-workers of the Primary Health Center and three
senior health-workers were involved in health education.
Each junior health-worker would cover each village
under his/her care once a week, and the senior health
worker once a month. Health education was imparted
to individuals or small groups by the junior health
worker, whereas group discussions which were held
once a month, were conducted usually in the presence
of the senior health-worker. The intervention com
menced soon after the completion of the baseline
survey and lasted for about three years. The following
health education materials were used to impart
education:
• Handbills —Summary about harmful effects of
tobacco on health. About 2,000 handbills were
used. These were distributed by the health workers
to households with literate persons;
Population
Male
Male
• Folders—Brief explanation about tobacco-habit
formation and misconceptions about tobacco
messages. About 500 folders were distributed by
the health workers to persons such as community
leaders in the village;
• Card Ifi" X 3W) with photographs of advanced
cancers of the oral cavity on both sides. A health
worker could carry this card easily in his/her
pocket and use it during person-to-person contact
in the community. Each health worker carried a
card which was replaced whenever necessary with
a fresh one. Approximately 100 cards were used;
• Photo album with 28 postcard-size photographs
with appropriate captions and messages on harmful
effects of tobacco and about cancer. Just as with the
cards above, one photo album was used by each
health-worker. In all, 40 photo albums were used;
• Portable display boards with messages about
harmful effects of tobacco and photographs on
cancer. Two sizes of boards one small (15w X 12M)
and the other larger (4x3) were used for group
discussions. Four sets of these boards were used;
• Audio-visual aids including 16 mm feature films—
These consisted of two separate films (duration 10
minutes each) on smoking and the other on
chewing in four languages (English, Kannada,
Hindi, and Telugu);
—the above also was prepared in the form of a
video casette along with another video casette
Cancer Causes and Control. Vol 6. 1995 121
N. Anantha et al
titled ‘Cancer is curable’ with highlights on
primary prevention of cancer, basic knowledge
on its treatment and terminal care of cancer
patients.
Films were screened at least twice during the
period of intervention, in each of the 117 villages in
the experimental area.
Statistical tables/methods
The findings of the study are expressed in quantitative
terms in the following ways:
o Prevalence rates: The prevalence of the tobacco
habit in the population as indicated by the number
of users of tobacco (for at least six months’
duration at the time of personal interview) per 100
persons (percent) in the population was calculated
for the three surveys (BLS, FRS, and FS). The
difference in the prevalence rates during the survey
periods was observed;
e Quitters’ rates: The number of persons among
the tobacco users who had quit the use of tobacco
(for at least six months’ duration at the time of
personal interview) was calculated for the surveys
(FRS and FS) done subsequent to the intervention
through health education of the community. The
rates were calculated as number of quitters per 100
(percent) ever-users of tobacco in the population.
This is the same as the ‘quit ratio’11 expressed for
smokers;
• Initiation rates: The number of persons among the
nonusers of tobacco who had taken up the tobacco
habit within the past six months at the time of
personal interview was calculated and the rates
expressed as the number of these new habituates
per 100 nonusers of tobacco in the population.
This was calculated for persons between 10 to 24
years of age. The influence of age, as demonstrated
by the age specific prevalence rates of tobacco
users and age-specific quitters’ rates, during the
different surveys was also compared;
• An attempt was made to determine which among
the health education materials used for interven
tion in the ExA had the most profound impact in
motivating persons to quit the habit.
Each of the above was calculated for the populations
in the villages selected for the combined sample and also
separately for those villages in the PS and NPS.
In males, the rates also were calculated separately for
chewing and smoking tobacco. Males who practiced
chewing alone as well as those who practiced chewing
and smoking were added in calculating the rates of
122
Cancer Causes and Control. Vol 6.1995
chewers. Similarly, only smokers, and smokers who
chewed tobacco were included in calculating the rates of
smokers.
The survey results on type of tobacco use showed
that over 99 percent of women, whether in ExA or
either of the control areas, were tobacco chewers and
the others were users of snuff. Thus, there were no
smokers among women in any of the areas. Conse
quently, the results presented for females pertains
exclusively to tobacco chewing.
Tests for statistical significance were calculated by
computing chi-squares of observed and expected values
in ExA compared with each of the control areas at the
time of FRS and FS in relation to that of the BLS.
This was done for the CS as well as for the panel and
non-panel samples. The level of significance was exam
ined by observing P-values of the chi-squares. Chisquares and the level of statistical significance were
calculated also for linear trend in the prevalence and
initiation rates in the ExA for the three survey periods.
Results
Prevalence rates
The population present at the time of the respective
survey, the number of users of tobacco, and their
prevalence rates (percent) in the population, in each of
the surveys at the Experimental and two Control Areas
are presented in Table 2. The proportions (percent) of
differences in the rates between surveys are shown in
Table 3.
Baseline prevalence rates. The prevalence rates in
percent of tobacco users (Table 2a) during the BLS in
the ExA is higher in both males and females compared
with that in CoAI and CoAII. Females show a higher
prevalence of tobacco use compared with males in
experimental and control areas. Examination of the
prevalence rates after stratifying according to villages
of the PS and NPS did not show any marked
difference.
Baseline prevalence of type of tobacco. Table 2b gives
the respective prevalence rates of tobacco chewers and
smokers among men in the experimental and control
areas during each of the surveys. In the BLS itself, the
type of tobacco habit of the population in the ExA and
in the two control areas shows some variation. Thus,
the ExA shows 16.4 percent of tobacco chewers com
pared with 7.7 percent and 8.4 percent chewers in CoAI
and CoAII, respectively. Similarly, the ExA shows 17.7
percent of smokers compared with 21.0 percent and 21.7
percent in CoAI and CoAII, respectively.
Anti-tobacco education
Table 2(a). Population (Pop) and prevalence rates (PR), in percent (%), of
tobacco users at the time of the three (BLS,a FRS,b FSC) surveys, India
ExAd
Combined sample
Males
BLS
FRS
FS
Females
BLS
FRS
FS
Panel sample
Males
BLS
FRS
FS
Females
BLS
FRS
FS
Non-panel sample
Males
BLS
FRS
FS
Females
BLS
FRS
FS
PR (%)
Pop
PR (%)
Pop
PR (%)
5,464
3,330
3,454
(30.9)
(19-6)
(20.7)
5,369
3,043
6,290
(27.0)
(26.0)
(24.9)
4,893
3,135
4,169
(29.1)
(30.3)
(28.6)
5,236
3,212
3,260
(38.5)
(21.3)
(22.2)
4,905
2,889
5,862
(28.7)
(26.2)
(25.8)
4,677
3,014
4,002
(30.4)
(30.6)
(29.8)
1,413
1,462
1,433
(30.5)
(21.5)
(17.4)
1,600
1,505
1,582
(28.3)
(26.0)
(28.3)
1,285
1,469
1,442
(33.6)
(30.5)
(32.7)
1,323
1,386
1,361
(40.1)
(21.6)
(18.2)
1,428
1,377
1,425
(24.6)
(22.7)
(25.5)
1,229
1,388
1,417
(36.7)
(33.7)
(34.2)
4,051
1,868
2,021
(31.1)
(18.1)
(23.0)
3,769
1,538
4,708
(26.5)
(26.2)
(23.7)
3,608
1,666
2,727
(27.5)
(30.1)
(26.5)
3,913
1,826
1,899
(38.0)
(21.0)
(25.0)
3,477
1,512
4,437
(30.4)
(29.7)
(25.9)
3,448
1,626
2,585
(28.2)
(28.0)
(26.9)
d ExA = experimental area.
6 CoAl = control area I.
1 CoAII = control area II.
° BLS=baseline survey.
b FRS — first repeat survey.
CFS = final survey.
Table 2(b). Prevalence rates (percent) of male tobaccochewers (PRCh%) and male tobacco-smokers (PRSm%)
at the time of the three (BLS,a FRS,b FSC) surveys, India
PRCh%
ExAd
Combined sample
BLS
16.4
FRS
9.4
FS
10.8
Panel sample
BLS
16.8
FRS
9.5
FS
8.1
Non-panel sample
BLS
16.2
FRS
9.4
FS
12.8
PRSm%
CoAI®
CoAII*
ExAd
CoAI6
CoAII1
7.7
8.4
6.5
8.4
9.0
8.4
17.7
12.1
12.0
21.0
19.0
19.8
21.7
23.6
22.5
6.9
6.6
7.1
11.4
9.9
11.4
17.2
13.5
11.1
22.5
19.9
23.1
23.8
22.9
24.9
8.1
10.1
6.2
7.3
8.4
6.8
17.9
11.0
12.5
20.3
18.1
18.7
20.8
24.3
21.2
6 BLS = baseline survey.
b FRS — first repeat survey.
bFS = final survey.
CoAII1
CoAI®
Pop
d ExA = experimental area.
6 CoAI —control area I.
1 CoAII = control area II.
Prevalence rates following intervention. Table 2 also
gives the prevalence rates of the tobacco habit during
FRS and FS following health education of the
community in the ExA. Table 3 indicates the
proportion of reduction in prevalence rates of the
tobacco habit between surveys. Comparison of results
of FRS between the ExA and two control areas
showed high statistical significance (P < 0.0001) in all
samples.
The proportion of decline in prevalence rates
between BLS and FS provides the overall picture of
the effect of intervention in the ExA in contrast to
nonintervention in the two control areas. The results
were again highly significant (P < 0.0001).
The decline in the prevalence of chewing in males in
the ExA was also statistically significant (P < 0.0001)
for the results in all samples of the FRS and for that of
CS and PS in the FS, but not significant in the NPS of
CoAI (P = 0.06). Similarly, for smoking, the results of
the PS in FRS were not significant (P = 0.3).
Otherwise, all the remaining samples in both FRS
Cancer Causes and Control. Vol 6. 1995 1 23
N. Anantha et al
Table 3(a). Proportion (%) of reduction in prevalence rate
of the tobacco habit between surveys (BLS,a FRS,b FSC),
India
Males
ExAd
Females
CoAl8
CoAII1
ExAd
CoAl®
CoAII*
2.5
0.4
2.9
-0.2
0.8
0.6
Combined sample
BLS-FRS
11.3
FRS-FS
-1.0
BLS-FS
10.2
1.0
-1.2
2.1
0.5
17.2
-0.9
16.3
Panel sample
BLS-FRS
FRS-FS
BLS-FS
13.1
2.3
-2.3
0.0
3.1
-2.2
0.9
18.5
3.4
21.9
1.9
-2.8
-0.9
3.0
-0.5
2.5
Non-panel sample
BLS-FRS
13.0
FRS-FS
-4.9
BLS-FS
8.1
0.3
-2.5
2.8
-2.6
3.6
1.0
17.0
-4.0
13.0
0.7
3.8
4.5
0.2
1.1
1.3
9.0
8 BLS = baseline survey.
6 FRS = first repeat survey.
' FS = final survey.
d ExA = experimental area.
’ CoAl = control area I.
1 CoAII = control area II.
and FS showed a statistically significant (P < 0.001)
decline in the prevalence rates of smoking.
Tests for a declining trend in prevalence rates in
ExA from BLS to FS, indicated a statistically signi
ficant trend only for the PS in males when the
tobacco habit was considered as a whole (chewing and
Table 3(b). Proportion (%) of reduction in prevalence rate
of the male tobacco-chewers and smokers between
surveys (BLS,a FRS,b FSC), India
Smokers
Chewers
ExAd
CoAl8 CoAII'
ExAd
CoAl®
CoAII*
Combined sample
BLS-FRS
7.0
—1.4
FRS-FS
5.6
BLS-FS
-0.7
1.9
1.2
-0.6
0.6
0.0
5.6
0.1
5.7
2.0
-0.8
1.2
-1.9
Panel sample
BLS-FRS
FRS-FS
BLS-FS
8.7
0.3
-0.5
-0.2
1.5
-1.5
0.0
3.7
2.4
6.1
2.6
-3.2
-0.6
0.9
-2.0
-1.1
Non-panel sample
6.8
BLS-FRS
-3.4
FRS-FS
3.4
BLS-FS
-2.0
3.9
1.9
1.6
0.5
6.9
-1.5
5.4
2.2
-0.6
1.6
-3.5
3.1
-0.4
7.3
* BLS = baseline survey.
b FRS = first repeat survey.
CFS = final survey.
124
-0.8
d ExA = experimental area.
’ CoAl = control area I.
1 CoAII = control area II.
Cancer Causes and Control Vol 6.1995
smoking) (P = 0.03) and in the PS for male smokers
(P < 0.004).
The prevalence rates of the FS also were compared
with that of the FRS, and tests for statistical significance
were carried out. Only the results of the PS showed a
statistically significant decline during the FS compared
with the FRS.
Age-specific prevalence rates. The baseline age-specific
prevalence-rates of the tobacco habit for the population
in the three areas did not show any variation among
males. In females, the age-specific curves in the control
areas were lower. In the ExA, in males and females, the
curves of the FRS (to a larger extent) and that of FS (to
a smaller extent) compared with that of BLS were at a
lower level, indicating a decline in the prevalence rates
in almost all age groups.
In the graphs for the PS, the age-specific rates in
persons less than 30 years of age during the FS was
lower than that seen in the FRS. Among males, the shift
of the age-specific chewing rates was greater than the
age-specific smoking rates. This effect was seen clearly
during the FRS, but not as well demonstrated during
the FS, except in the younger age groups of the PS.
Curves of the age-specific prevalence rates of the
tobacco-habit status during the three surveys showed
little or no change in the two control areas in both
genders.
Quitter's rates
Table 4a shows the number of habituates interviewed
during the three surveys, the number who had quit
the habit (for at least six months), and the rate
(percent) of such quitters among ever-users of
tobacco. The numbers and rate of persons who had
quit (‘quit ratio’) the habit at the time of FRS was
much higher in the ExA—where intervention
through health education was given—compared
with the control areas (in males, 26.5 percent in
ExA cf 3.2 percent and 1.1 percent in CoAl and
CoAII, respectively; and in females, 40.7 percent in
ExA cf 2.4 percent and 0.2 percent in CoAl and
CoAII, respectively). However, comparison of the
quitters’ rate between FRS and FS showed a decline
in the quitters’ rate in the ExA, although the actual
quitters’ rate itself was far higher than in the control
areas. Stratification according to the PS and NPS gave
a different picture of the difference in the quitters’
rate between FRS and FS. The results of the PS
showed an increase in the quitters’ rate by 12.4
percent in males and 7.6 percent in females in the
ExA, whereas there was a decline by 9.2 percent and
12.4 percent in the quitters’ rate in males and females,
respectively, in the NPS. A slight increase in the
Anti-tobacco education
Table 4(a). Number of tobacco habituates interviewed (HI), and the quitters'
rate (OR) percent (%) at the time of the three (BLS,a FRS,b FSC) surveys, India
ExAd
Combined sample
Males
FRS
FS
CoAII1
CoAl8
HI
QR (%)
HI
QR (%)
HI
QR (%)
853
946
(26.5)
(26.5)
806
1557
(3.2)
(1-1)
941
1,194
(1-1)
(1.1)
Females
FRS
FS
1,070
1,042
(40.7)
(36.7)
761
1,469
(2.4)
(1-5)
918
1,165
(0.2)
(0.5)
Panel sample
Males
FRS
FS
401
395
(26.9)
(40.2)
392
461
(3.6)
(3.7)
448
478
(2.0)
(2.3)
Females
FRS
FS
482
455
(43.6)
(51.2)
315
368
(3.8)
(6.0)
363
481
(0.4)
(0.8)
452
551
(26.2)
(17.0)
414
1,096
(3.0)
(0.0)
493
716
(0.2)
(0.3)
588
587
(38.0)
(25.6)
446
1,101
(1-0)
(0.0)
454
684
(0.0)
(0.4)
Non-panel sample
Males
FRS
FS
Females
FRS
FS
dExA = = experimental area.
’CoAl = control area I.
' CoAIII = control area II.
a BLS = baseline survey.
b FRS = first repeat survey.
c FS = final survey.
quitters’ rate also was observed in the control areas in
the PS but the reverse holds true for those villages in
the NPS.
Tables 4b and 4c show the quitters’ rate for males,
among tobacco chewers and smokers, respectively.
In the ExA, the rate of quitting the habit of chewing
was higher than the rate of smokers quitting the habit.
Tests showed a very high degree of statistical
Table 4(b). Number of male tobacco-chewers interviewed (Cl), and the quitters'
rate (QR) percent (%) at the time of the three (BLS,a FRS, FSC) surveys, India
ExAd
CoAII*
CoAl’
Cl
QR (%)
Cl
QR (%)
Cl
QR (%)
Combined sample
FRS
FS
463
535
(32.0)
(30.2)
260
410
(2.3)
(1.2)
286
354
(1’1)
(1.1)
Panel sample
FRS
FS
211
224
(34.2)
(48.2)
101
118
(2.0)
(4.2)
146
168
(1.3)
(2.4)
Non-panel sample
FRS
FS
252
311
(30.2)
(17.4)
159
292
(2.5)
(0.0)
140
186
(0.7)
(0.0)
a BLS = baseline survey.
b FRS=first repeat survey.
cFS = final survey.
d ExA = experimental area.
8 CoAl = control area I.
1 CoAII = control area II.
Cancer Causes and Control. Vol 6. 1995 1 25
N. Anantha et al
Table 4(c). Number of male smokers interviewed (SI), and the quitters’ rate
(QR) percent (%) at the time of the three (BLS,8 FRS,b FSC) surveys, India
ExA8
CoAII*
CoAle
SI
QR (%)
SI
QR (%)
SI
QR (%)
Combined sample
FRS
FS
495
534
(18.6)
(20.4)
597
1,257
(3.4)
(1-0)
746
950
(0.9)
(1.2)
Panel sample
FRS
FS
244
229
(18.8)
(28.8)
312
378
(3.8)
(3.4)
342
368
(2-0)
(2.4)
Non-panel sample
FRS
FS
251
295
(18.3)
(14.6)
285
879
(2.8)
(0.0)
404
582
(0.0)
(0.3)
d ExA = experimental area.
8 CoAl = control area I.
' CoAII = control area II.
“ BLS = baseline survey.
b FRS = first repeat survey.
8 FS = final survey.
significance (P < 0.0001) for the quitter’s rate in the
ExA compared with the two control areas, in all
samples in either gender and for results during both
FRS and FS.
The influence of age on quitting the habit was
examined by generating graphs of age-specific quitters’
rates during the FRS and FS, but the graphs did not
show any variation with age group.
In order to determine whether the duration of the
tobacco habit had any influence on quitting of the
habit, the mean of the duration of the habit was
calculated for quitters and also for those who had not
quit the habit. This was not significantly different in the
two groups.
Initiation rate
Table 5 gives the initiation rates of the tobacco habit
during the survey periods in the three areas in the 10
to 24 year age-group since initiation is expected to be
seen mainly in that age group. The baseline initiation
rates among males were comparable in experimental
and control areas, but were somewhat different among
females. In the ExA, the initiation rate dropped in
both males and females, but more in the latter, during
the FRS, but increased in the control areas. During
the FS, the initiation rate was higher than during
the FRS among males in the two control areas and
also in females in CoAI. Stratifying initiation rates
into PS and NPS gave very small numbers for any
Table 5. Number of non users of tobacco (NT) in the 10-24 year age-group, and
the initiation rate, percent (%), of tobacco (IRT) use, India
ExA8
Combined sample
Males
BLS
FRS
FS
Females
BLS
FRS
FS
Cancer Causes and Control Vol 6.1995
CoAII8
IRT
NT
IRT
NT
IRT
1,419
933
1,068
(0.2)
(0.0)
(0.4)
1,636
912
2016
(0.2)
(0.8)
(0.8)
1,406
862
1,251
(0.1)
(0.7)
(1-7)
1,257
767
902
(1-6)
(0.1)
(0.6)
1,294
758
1,623
(0.6)
(1.1)
(1.1)
1,229
740
1,033
(1.4)
(4.7)
(2.5)
8 ExA = experimental area.
b CoAI = control area I.
c CoAII = control area II.
126
CoAlb
NT
Anti-tobacco education
meaningful correlation. For the same reason of small
numbers, age-specific initiation rates could not be
calculated.
The initiation rates in the ExA showed a statistically
significant decline in males (P < 0.01) and females
(P = 0.005) during FRS. In the FS, males in CoAI did
not show a statistically significant decline in the
initiation rate (P = 0.16), but comparison with CoAII
and the FS results in females showed a significant
decline (P < 0.005).
Among males, the initiation rates of tobacco chewing
and smoking were compared. In the ExA, during the FS
the initiation rate of chewing was 0.2 percent and that of
smoking 0.1 percent. In CoAI, the initiation rate of
chewing was 0.1 percent compared with 0.3 percent for
smoking. In CoAII, these were 0.4 percent and 0.9
percent for chewing and smoking respectively.
Impact of health education material used
The different types of health education materials used
to impart messages about the harmful effects of tobacco
have been mentioned above. Essentially, these consisted
of three channels of communication. First, was the
method which could be read by the literate population.
The second was the audio-visual means which could be
understood by almost all the persons who saw it. The
last was interpersonnel communication, with the health
worker actually explaining the contents of the messages
and describing the photo albums and identity cards that
they carried.
In order to assess the impact of the health education
material ia helping individuals to quit the habit, the
proportiodfexposed to such material among the quitters
was compared with the proportion exposed among
non-quitters. There was no noticeable difference in this
proponion in the first and last methods of commu
nication listed above. However, in the audio-visual
means of education, during the FRS, 68.6 percent of
quitters had an opportunity to view the films on
chewing and smoking compared with 57 percent of
non-quitters of either gender. During the FS, 95.7
percent of quitters had viewed the films compared with
90 percent of non-quitters.
Discussion
With the initiation of several cancer-control programs
in India under its National Cancer Control Program,
knowledge of prevalence rates of tobacco usage,
including the various types used, is becoming increas
ingly important. Unless these baseline rates of the
population are known, the impact of any education
programs cannot be assessed. The present study has
shown ways of conducting tobacco-habit surveys in the
population, the impact of education on the community,
and methods of reporting such results.
Variation in the prevalence and type of tobacco used
even within the same district of a state is seen in this
study. The initial baseline prevalence-rates of the
tobacco habit, showed that, in both genders, the rates
were higher in the experimental than in either of the
control areas. This was despite the fact that the
experimental and control areas and the villages under
them were chosen on a random basis. However, among
males, when the type of habit was taken into account,
the prevalence rate of tobacco chewing in the
experimental area was almost twice that in the control
areas, whereas the prevalence rate of smoking was
marginally higher in the control areas compared with
the experimental area.
The results of the FRS showed a decline in the
prevalence rates by 11.3 percent in males and 17.2
percent in females in the experimental area. The
proportion of persons who quit the habit was 26.5
percent in males and 40.7 percent in females. Among
males, the decline by seven percent in the prevalence
rates of chewers is marginally higher than the decline of
5.6 percent among smokers. However, the difference in
the response of chewers and smokers towards giving up
the habit is observed better if one looks at the
proportion (32 percent) among chewers who have quit
the habit compared with the proportion (18.6 percent)
among smokers who have quit the habit. The former is
almost twice that of the latter. Thus the effect of anti
tobacco education, as provided in the results of the FRS,
is indeed considerable. Stratifying the results of the FRS
into panel and non-panel samples does not show much
difference.
If the results of the FRS in terms of response to the
intervention were remarkable, the sustenance of the rate
of decline in the habit appears missing from the findings
of the FS. Nonetheless, on examination of the stratified
sample, perceptible difference is seen between the panel
and non-panel samples. The figures of the panel sample,
do show a sustenance of the decline in the prevalence
rates between FRS and FS as also a further increase in
the proportion of people who have quit the habit
between FRS and FS. However, this is not the case in
the results of the non-panel sample.
Some reasons could be given for this difference in
findings between the panel and non-panel samples.
Even though the social investigators who worked on
this program were not imparting any direct education
to the community, their repeated visits to the villages
under the panel sample probably would have added to
the conscientiousness of the people and enhanced their
response to the anti-tobacco education. Another reason
could be because of the differences in educational,
Cancer Causes and Control. Vol 6. 1995 127
N. Anantha et al
socioeconomic, and cultural background among the
villages coming under the purview of the panel sample
on the one hand, and of the villages under the non
panel sample on the other. This factor probably could
not be eliminated completely by random sampling of
villages.
The results of the Anti-Tobacco Community
Education Program indicate that there has been a
substantial decline in the number of persons pursuing
the habit as indicated by a drop in the tobacco
prevalence-rates as well as in the proportion of persons
who quit the habit. The response, as indicated by these
two parameters, appears to be greater among women
than men and among males who were tobacco chewers
rather than smokers. The degree of the decline in the
habit was considerable between the BLS and FRS,
(regardless of whether the combined-sample results
were observed or panel and non-panel sample results
were seen) much less between the FRS and FS for the
villages under the PS and no decline in the habit for the
villages under the NPS. Any comparable decline in
the habit as measured by these parameters was not
observed in the control areas where no anti-tobacco
education was given.
The influence of age was assessed by examining the
age-specific prevalence and age-specific quitters’ rates.
There was a greater shift of the age-specific prevalence
rates towards the lower side in the younger age group
(<35 years) during the FS compared with the FRS, but
no such perceptible change was seen between BLS and
FRS in this age group. This suggests that persons below
35 years of age respond to the anti-tobacco education by
quitting the habit rather slowly compared with the
older age groups. The above effect of age was seen in
both genders and for both chewing and smoking in
males. It was more pronounced in the villages under the
PS than in the NPS.
A third, quantitative, statistical indicator that was
used to evaluate the impact of the program was the
rate of initiation of the habit. Among males, the
initiation rate was comparable during the BLS in
experimental and control areas, but in the subsequent
surveys, the increase in rates in the control areas was
steep, whereas this was not the case in the ExA. In
females, in the ExA, there was a decline in the
initiation rate and, in both the control areas, an
increase in the initiation rates. Thus, the anti-tobacco
community education not only saw a decrease in the
number of persons quitting the habit, but also saw a
decline in the uptake of the habit. The reverse was true
in the control areas where there was indeed an increase
in the rate of uptake of the habit during the surveys
following the BLS. A matter of concern about this
indicator is not only the high rate of uptake of the
128
Cancer Causes and Control Vol 6.1995
tobacco habit in the control areas, but a probable
increase in these rates with passage of time. The data
indicate that the initiation rate (despite small numbers)
of smoking among males within a period of six months
was about 0.8 percent. This means that the incidence of
smoking among males could be as high as 1.6 percent
or 1600 per 100,000 which is over 10 times the
estimated incidence of cancer in India.5 Since anti
tobacco education of the community generally is not
practiced routinely by the health workers, these figures
easily would be applicable to the general rural
population as a whole.
One of the outcomes of this study is to have a clear
method of reporting results of tobacco surveys, in the
form of prevalence rates, quitters’ rates, and initiation
rate. In this study, we used a minimum time-interval of
six months to define the above rates, respectively, as to
whether the person was a user of tobacco, a person
who had quit, or a person who had taken up the habit
during the interval. However, this time period could be
taken as one year in future studies since that way it
would be easier to calculate rates per annum, in
keeping with incidence, prevalence, and mortality rates
of cancer.
The package of health education material was
prepared mainly to impart knowledge to change mis
conceptions and negative attitudes about the harmful
effects of tobacco, through uniform and standardized
health education. The materials utilized to educate
literates were handbills and folders. The identification
card and photo album were used for interpersonal
education. The portable and exhibition panels and
films on chewing and smoking were used to educate
groups or large gatherings. Among all the educational
devices used for the anti-tobacco community education
program, the response appeared to be best in order of
importance for film on the harmful effects of chewing
and smoking, photo album, and identity card. The
other items used for education also had some effect but
perhaps not as marked, as indicated by the commu
nity’s response.
Anti-tobacco education of the community in this
study brought into focus the role of health workers in
conducting such education. The points to be considered
in this context include the concomitant healthcare
program that health workers routinely carry out and
the feasibility of their doing additional program on anti
tobacco education and cancer control. Further factors
that determine effective education and successful response
therefrom, include, the health workers’ educational
qualification and background, specific training received
by them, their professional responsibility and commit
ment, and lastly, but most importantly, the skill with
which they execute the work. However, the singlemost
Anti-tobacco education
important keystone towards the success of the program
is almost entirely dependent on the interest, commit
ment, and motivation provided by the medical officer at
the primary health center. As was done in this study, a
built-in method of evaluating, at every step, the
performance of health workers through details of
visits, number of persons whom they have not only
educated but also motivated, etc. is necessary.
Studies on the tobacco habit and the effect of educa
tion have been done earlier in different parts of this
country,13"15 but this is the first in the State of
Mehta FS, Pindborg JJ, Gupta PC, et al. Epidemiologic
study of oral cancer and leukoplakia among 50,915
villages in India. Cancer 1969; 25: 844-61.
3.
Gupta PC. An assessment of excess mortality caused by
tobacco usage in India. In-. Sanghvi LD, Notani P, eds.
Tobacco and Health: The Indian Scene. Bombay, India:
Tata Memorial Center, 1989: 57-62.
4.
Gupta PC, Bhonsle RB, Mehta DS, et al. Mortality
experience in relation to tobacco smoking and chewing
habits from a 10-year follow-up study in Emakulam
district Kerala. Int J Epidemiol 1984; 13; 184-7.
5.
Orr IM. Oral cancer in betel nut chewers in Travancore.
Lancet 1933; 2: 575-80.
6.
Sanghvi LD, Rao KCM, Khanolkar VR. Smoking and
Karnataka. The strength of this study is in its case
chewing of tobacco in relation to cancer of the upper
control design with both experimental and control
alimentary tract. Br Med] 1955; 1: 1111-4.
areas having an adequate sample size. The study has
7.
Sanghvi LD. Tobacco related cancers. In: Sanghvi LD,
demonstrated that it is feasible to conduct anti-tobacco
Notani P, eds. Tobacco and Health: The Indian Scene.
education programs through health workers and that
Bombay, India: Tata Memorial Center, 1989: 9-15.
8.
Annual Reports of the National Cancer Registry
there is substantial impact of such education on the
Programme of India. New Delhi, India: Indian Council
community. The response of women is greater than
of Medical Research, 1982-90.
that of men, and, among men, chewers seem to have
9.
Nandakumar A, Anantha N, Thimmasetty K. Cancer
responded better than smokers. The study also has
Patterns in Bangalore 1982-89. Bangalore, India: Depart
brought into sharp focus the extremely high rate of
ment of Population Based Cancer Registry, Kidwai
Memorial
Institute of Oncology, 1990.
initiation of the tobacco habit, calling for urgent action
10.
Pierce JP, Dwyer T, Frape G, et al. Evaluation of the
against this addictive habit at both levels concerning
Sydney “Quit. For Life” anti-smoking campaign. Med J
education and legislation.
Aust 1986; 144: 341-4.
11.
Pierce JP, Aldrich RN, Hanratty S, et al. Uptake and
Acknowledgements—Thanks are due to the health
quitting smoking trends in Australia 1974-84. Prev Med
1987; 16: 252-60.
services staff at Dibbur Primary Health Center. Dr
12.
Boyle P, Parkin DM. Statistical methods for registries. In:
Anwar Jan, Chief Medical Officer, as leader, provided
Jensen OM, Parkin DM, Maclennan R, Muir CS, Skeet
the inspiration for his team to undertake this additional
RD, eds. Cancer Registration: Principles and Methods.
work amidst their tight schedules. The members of the
Lyon, France: International Agency for Research on
Project Coordinating committee and Project Consulta
Cancer, 1991; IARC Sci. Pub. No. 95.
tive committee gave their expert technical guidance in
13.
Mehta FS, Aghi MB, Gupta PC et al. An intervention
planning and monitoring the project. The Director,
study of oral cancer and precancer in rural Indian
Kidwai Memorial Institute of Oncology, and the staff of
population: a preliminary report. Bull WHO 1982: 60:
the Anti-Tobacco Community Education Programme
441-6.
are grateful to them.
14.
Gupta PC, Mehta CR, Pindborg JJ, et al. Intervention
study for primary prevention of oral cancer among
36,000 Indian tobacco users. Lancet 1986; i: 1235-9.
References
15.
Gupta PC, Mehta FS, Pindborg JJ, et al. Primary
prevention trial of oral cancer in India; a 10-year follow
1.
Wahi PN. The epidemiology of oral and oropharyngeal
up study. / Oral Pathol Med 1992; 21, 433-9.
cancer. Bull WHO 1968; 38: 495-521.
2.
Cancer Causes and Control. Vol 6. 1995 129
The Effects of Parental Divorce on AdultTobacco and Alcohol Consumption-------- 255-
The Effects of Parental Divorce on Adult Tobacco and Alcohol
*
Consumption
NICHOLAS H. WOLFINGER
The University of Utah
Journal of Health and Social Behavior 1998, Vol 39 (September): 254-269
/ use data from the 1977-1994-National Opinion Research Council General
Social Survey to examine the impact ofparental divorce on the alcohol and
tobacco consumption of adult offspring. Divorce greatly increasesjhejikeljhoo^ofbeingjasmoker- and. for men. a problem drinker. Parental remarriage
completely offsets the effects ofparental divorce on men s drinkingdntt does not
substantially jaffeet cigarette. use~.Respondent socioeconomic characteristics
accountedfor a portion ofthe relationship between parental divorce and smok
ing but did not affect rates ofproblem drinking. Social control and psychoso
cial adjustment—two established—explanations for the effects of parental
divorce—could not adequately explain myfindings.
INTRODUCTION
1996. 1997a,b) and poor psychological health
(Amato 1991; Amato and Booth 1991;
Cigarettes claim hundreds of thousands of
Cherlin. Chase-Lansdale, and McRae 1998;
lives annually. Tens of thousands more people
Kuh and Maclean 1990; Roy J985: Schooler
die from alcohol-related accidents and dis
1972). Broadly speaking, marital instability
eases (sec United States Bureau of the Census and poor psychological health are signs of
1997). The associated medical costs are
maladjustment. Alcohol and tobacco use may
tremendous. For these reasons, it is important
well be two additional forms of maladjustment
to understand the etiology of alcohol and related to parental divorced.
tobacco use?
———-—______
I analyze data from the 1977-1994 General
In this paper I examine the likelihood that Social Survey (GSS) that are nationally repre
the adult children of divorced parents^ will
sentative^ Further, my data al!
differentiasmoke and abuse alcohol. Previous researchers '—tion- between parental death ..d parental
have established that parental divorce can have divorce, and contain detailed sociodemographmany lasting effects on the well-being of adult ic information. As such, they allow me to adju
offspring, including marital instability' (Amato dicate among several competing theoretical
1996; Glenn and Kramer 1987; Kulka and explanations for the relationship between fam
Weingarten 1979; McLanahan and Bumpass ily of origin and offspring substance use.
1988; Mueller and Pope 1977; Wolfinger
*1 thank Jessica Koff. the editor of Journal ot
Health and Social Behavior, and three anonymous
reviewers for their many useful suggestions. Thipaper was presented al the 1998 annual meeting o:
the America:', Sociological Association, an earlie.
draft was an honorable mention in the 199s
General Social Survey student paper competition
Address correspondence to: Nicholas 11.
Wolfinger. Department of family and ConsumeStudies. 225 1400 I.. Room 228. University of
Utah. Salt lake City. UT 8-1112 00X0: e-mail
Nick Wolfingetw fcs.utah.edu
THEORY
I expect parental divorce to increase alcohol
and tobacco consumption in adult offspring for
three reasons, outlined below, and derive hypo
theses to be tested in a multivariate analysis.
.So< ml Control
After a divorce almost every familial rou
tine is disrupted ■ Wallcrstctn'and Kellx 198th.
Recently divorced mothers2 often experience
considerable emotional distress, thus debilitating~their parenting skills (Dombusch et al.
1985; Wallcrstein and Kelly 1980). Moreover.
single mothers are likely to be working and
therefore jess able to supervise children
(McKeever and Wolfinger 1997). Visitation by
absent fathers tends to be infrequent and when
it does occur, it is often social in nature and not
related to the more serious tasks of childrear
ing (Furstcnbcrg and Nord 1985). For all of
these reasons, 1 expect parental control to
decrease in single-mother households.
In turn, lower levels of control afford chil
dren more opportunity io experiment with
alcohol and cigarettes (Resnick et al. 1997;
Kandel 1996), leading to an increased likeli
hood of substance use later in life. Adolescents
are especially at risk as the chances of initia
tion into .alcohol and tobacco use peaks at
about age 18 (Kandel and Yamaguchi 1985).
' According to the social control hypothesis.
parental remarriage should largely offset the
effects of parental divorce. In other words, the
offspring of step-families should be no more
likely to-smoke and abuse alcohol than their
counterparts from intact families. Although
family structure is weaker in reconstituted
families than in intact families (Cherlin~I978;
Fursienberg and Cherlin 1991; Cherlin and
Furstenberg 1994), J nevertheless expect to
find stronger social control in step-parent fam
ilies than in mother-only families. Whatever
the family dynamics, a step-parent provides a
second source of authority and discipline:
Socioeconomic Status
Socioeconomic status (SES) may affect the
relationship between parental divorce and
adult substance consumption in several ways.
Low levels of education increase the likeli
hood of divorce (Bumpass. Martin, and Sweet
1991), so divorced parents as a xx'hole com
prise a disproportionately uneducated group.
Due to their lower average level of education.
divorced parents may be relatively permissive
about smoking. In contrast, educated parents.
even if divorced, are more likely to dissuade
their children from smoking through both
exhortation and example. The absence of eigarettes in the house substantially decreases the
likelihood that offspring will smoke (Resnick
.■=_
In addition, levels of parental income may
affect the children of divorce through down
ward residential mobility. McLanahan (1983)
found that approximately 38 percent ofsingie
mothers moved within a year of getting
divorced, more than twice the overall mobil
ity rate. Moreover, single-mother families
are much more likely to live in depressed
areas than are intact families (McLanahan.
Astone. and Marks 1991). and children living in depressed areas inay have more, oppor
tunities to experiment with smoking and
drinking than children raised in affluent
neighborhoods. It is here that step-parenting
"impinges on the SES hypothesis; since step
parent families have incomes comparable to
those of intact families (Bachrach 1983; Mason
and Mauldon 1996). children with step-parents
may be less likely to be exposed to as much
drinking and cigarette-smoking as are children
in single-mother families.
Finally, parental divorce may affect tobacco
and alcohol consumption by reducing the
socioeconomic attainment of offspring.
Compared to people from intact families, the
children of divorce complete fewer years of
school (Blau and Duncan 1967; Krein 1986;
Krein and, Beller 1988; McLanahan 1985;
McLanahan and Sandefur 1994) and do less
well economically (Amato and Booth 1991;
Amato and Keith 1991a; Mueller and Cooper
1986) as xvell as occupationally (Biblarz and
Raftery 1993). This may affect their cigarette._ use, as smoking is strongly linked to both low if
education and low income (United States T?
Buriat: of the Census 1997;. On thc~other ' |
Iftmtir-alcohol ~usc increases with income-, i |
(United States Bureau of the Census 199"i.
Psychosocial Adjustment
A third theoretical perspective attributes the
proclivity for alcohol and tobacco consumption
to the social and psychological maladjustment
that can result from parental divorce. There is
little doubt that parental divorce often has pro
found social and psychological consequences
for children (Hetherington 1993; Wallerstein
and Kelly 1980).’ The conflict accomnaaxinc
divorce is especially traumatizing (Amato 199).
Amato and Keith 1991b; Emery 1982. 1988>
I’revious research shows that parental divorce
and conflict can mcrease_aleohoj and lobacc,
256
JOURNAL OF HEALTH AND SOCIAL BEHAVIOR
Baer et. al. 1987; Johnson and Pandina 1991;
Webb and Baer 1995). More generally, the chil
dren of divorce sometimes develop patterns of
behavior- that fit the classic sociological notion
of deviance (Hetherington. Cox. and Cox 1985;
Hetherington 1993; Wallerstein and Kelly
1980).
Unresolved, the troubles leading teenagers
to drink and smoke may contribute to high
rates of substance consumption in the adult
children of divorce. Some psychosocial effects
of parental divorce often persist into adult
hood. including poor mental health (Amato
1991; Amato and Booth 1991: Cherlin et al.
1998; Kuh and Maclean 1990; Rby 1985;
Schooler 1972) and difficulty in romantic rela
tionships (Amato 1996; Amato and Rogers
1997; Silvestri 1992; Webster. OrbUchTTmd
— House 1995). Causality here could be lec.piXH
cal: if the adult children of divorce drink heav
ily, their social and psychological well-being
may further deteriorate. Ifsubstance“corisumption in the children of divorce is related to poor
psychosocial adjustment and difficulty in their
own marriages, then variables measuring these
factors should mediate the relationship
between parental divorce and offspring sub
stance consumption. — Across a variety of outcomes,, children in
step-families do no better than those reared by
single mothers (Cherlin and Furstenberg.
.
1994)
According to the psychosocial-adjust
ment hypothesis, step-parenting should
increase the likelihood that the children of
divorce will become smokers and problem
drinkers, or, at best, will produce enough dis
ruption to offset the beneficial effects of
remarriage. Note that this prediction is the
opposite of that resulting from the social con
trol perspective.4
Why might remarriage not benefit children,
despite the higher incomes typical of reconsti
tuted families? Remarriage confuses traditional
familial roles, yielding complicated and often
problematic social dynamics (Cherlin 1978;
Cherlin and Furstenberg 1994; Furstenberg and
Cherlin 1991; but see MacDonald and DeMaris
.
1995)
Girls have a particularly difficult time in
step-families (Glenn and Kramer 1987;
..Hetherington 1993; Hetherington et al. 1985;
McLanahan _and Bumpass 1988), so women
whose divorced parents remarried may experi
ence especially high rates of alcohoj_and
—tobacco consumption.------ ..
PRIOR RESEARCH
Two prior studies of American adults show
that parental divorce increases smoking but
not alcohol consumption (DeFronzo and
Pawlak 1993; Tucker et al. 1995). However,
both studies have serious limitations.
DeFronzo and Pawlak (1993) do not distin
guish between divorcees and widows in spite
of research showing that parental death does
not have adverse effects on children. (Acock
and Kiecolt 1989; Amato 1988; Demo and
Acock 1988; Wolfinger 1997a) or affects them
much less severely than does divorce
(McLanahan 1985. 1988; McLanahan and
Sandefur 1994).'Tucker et al. (1995) distin
guish between death and divorce but use an
exotic and unrep entative data Set: 1,528 ~
high-IQ responder bom between J.904 aridc=_
1915. almost all white and middie-class, from _
Lewis Terman s longitudinal “genius” study.~
Perhaps even more important than'the unrepre
sentative character of their data, however, is
the fact that most of their respondents came of
age during Prohibition. Kuh and Mclean
(1990) find that parental divorce increase .
smoking and alcohol- consumption, but they
analyze a sample composed entirely of 36year-old women. Moreover, their research was
conducted in England, so their findings may
not apply to Americans. Finally, Tennant and
Bernardi (1988). using a clinical sample-of-^
120 Australian alcoholics and drug addicts,
found that a disproportionately high number of
subjects came from broken homes.
METHODS
----------- — ■
Data
My data comes from the General Social Survey (GSS) (Davis and Smith 1996), a
national probability sample of English-speak
ing households within the continental United
States conducted annually or biennially since
1972. I use data for, the years 1977-1994,
excluding the 1985 data (when questions bn
alcohol and smoking were not asked) and the
Black oversamples in 1982 and 1987.5 The
smoking and alcohol items were not used-in
1996 nor prior to 1977. With the exception of
the 1994 survey, containing 2,904 respon
dents, approximately 1,500 people were inter- __
The Effects of Parental Divorce on Adult Tobacco and Alcohol Consumption
viewed in each cross-section analyzed in this
study.
The GSS sampling unit is the household,
with sample weights available to adjust for
household size. Analyses using unweighted
data produced results similar to those obtained
with the weighted data, so I report the
unweighted results.
The final sample size is 11,268: 6408
women and 4860 men. Cases with missing
data were deleted listwise (except where
noted).
variables are retrospective, while all others
used are contemporaneous.
Cherlin and his colleagues (Cherlin et al. .
1991, 1998) have shown that children’s prob
lems often begin before the divorce. Along
similar lines, others (Amato, Loomis, and
Booth 1995; Mechanic and Flansell 1989) con
tend that the conflict accompanying divorce
(but sometimes also bedeviling intact mar
riages) is the primary source of children’s
woes. For these reasons, more detailed-infor
mation on respondent family background “
would be useful. However, divorce appears to
hurt children irrespective of conflict (Hanson
Variables
1993) or predivorce well-being (Cherlin et al.
1998). More generally, we can be certain that
1 use two dependent variables, one to mea . parental divorce is correlated with experiences
sure problem drinking and a second to mea inimical to children’s well-being, even iflevels
..
sure smoking. The GSS measures smoking- .ofrconflict-and predivorce functioning camrur
-—
with a single question asking if the respondent •be directly measured.
_
— —currently smoked.6 I created the problem
Parental education may offset the effects of
drinking variable by merging information from parental divorce. For respondents reared-in
two items, the first asking if respondents drank intact families and step-families Fuse the high
and the second ascertaining whether drinkers er level of education between the two parents.
ever felt that they drank more than they For respondents from mother-only families I
should.7 This yielded a single dichotomous use mothers’ education. Data on parental
measure of problem drinking. More detailed income or occupational status are not avail
information on alcohol consumption would be able. An item that asks respondents to recall
useful but is not available. My coding-for all their families’ economic well-being ajmost
variables is shown in Appendix A.
certainly-fails to provide accurate recollec
__ My GSS data include two items that mea tions. Finally, to ascertain whether the effects
sure the structure of respondents’ families of of parental divorce on substance use are sim
origin. Respondents were first queried about ply a product of diminished socioeconomic
household composition at age 16. If respon well-being I use two measures of respondent
dents were not living with both biological par socioeconomic status, education10 and occupa
ents, a second question ascertained the reason. tional prestige (Hodge, Siegel, and Rossi pres
My analysis is based on the 83 percent of GSS tige scores).11
respondents who reported three varieties of
I employ three measures of respondent psy
family structure: intact two-parent families, chosocial adjustment. The three measure “hap
mother-only families resulting from divorce or piness,” a belief that the world is a “fair place,”
separation, and mother/step-father families and an assessment of whether people in gener
resulting from divorce or separation.8 al are “helpful.” They allow me to see whether
- Respondents reporting other living-arrange the problem drinking associated with parental
ments (e.g., with fathers or relatives) were divorce is concomitant with other symptoms
omitted from the sample, as were those whose of poor psychosocial adjustment. Along simi
living arrangements at age 16 were the result lar lines, respondent marital status may be
of parental military service, incarceration, or related to alcohol consumption. Previous
death.9 Unfortunately, the GSS does not permit researchers have established that the children
identification of respondents bom out of of divorce are disproportionately likely to end
wedlock.
their own marriages (Amato 1996; Glenn and
T recoded the family structure items as two Kramer 1987; Kulka and Weingarten 1979;
dummy variables: respondent came from McLanahan and Bumpass 1988; Mueller and
mother-only family and respondent came from Pope 1977; Wolfinger 1996, 1997a,b). Could
mother/step-father family. The reference cate- increased..alcohol consumption_among the------- gory was respondent from-intact family. Theses children of divorce^hlylfollow-in the wake of
JOURNAL OF^EALTHAND-SOUWiWlAVIOR'.^feJ
a foiled matriage? 1 test this notion with a
dummy variable ascertaining whether or not
respondents have ever been divorced.
The liability of cross-sectior.al data emerges
most strongly in foe psychosocial adjustment
and marital status measures. It is impossible to
know for sure whether respondent substance
consumption causes or is caused by these variables. Nevertheless the variables will allow me
to see whether adjustment and marital status
play a role in foe relationship between parental
divorce and offspring substance use.
In all analyses I use four control variables.
First, I adjust for survey year to capture period
trends in alcohol and tobacco consumption. In
recent years, for instance, far fewer people
smoke "TUnited States Bureau of the Census
1997). On the basis of lowess1- plots (not
shown), 1 model survey year as a continuous
variable.1-' Second, I control for respondent
birth cohort as recent cohorts contain many
more people from divorced families (Bumpass
^anfo Sweet 1989).|z Lowess plots (not shown)
reveal a curvilinear relationship between birth
cohort and smoking, while cohort has a
monotonic but nonlinear impact on problem
drinking. Accordingly I model the former rela- tionship as a quadratic and foelatter as a piecewise linear spline.15 Based on preliminary
analyses. I include an interaction between
mother-only parenting and birth cohort in the
equation predicting men's problem drinking.
Third, I include a dummy variable to measure
urbanicity^since parental divorce and initiation
into-substance use may vary according to
-whBther-aTespondent was
red in a city.
Fourth, and finally, I control .or respondent
race by contrasting blacks with all other
respondents. Blacks are more likely to have
grown up in divorced families (Bumpass
1984) and use alcohol and tobacco at different
rates than other population groups (United
States Bureau of the Census 1997).
Analysis
I examine the impact of parental divorce and
remarriage on alcohol and tobacco consump
tion using bivariate probit models (Greene
1993:660-63). The probit specification is
appropriate because my measures of smoking
and problem drinking arc both dichotomies.
The bivariate probit allows two equations to be
estimated simultaneously with correlated
errors.~assuming that the errors have a bivariate normal distribution with equal variances .
and means of 0.1 assume that the errors will be
correlated because foe same unmeasured variables predict both smoking and problem drinking. With correlated errors, the bivariate probit
produces more efficient estimates of coefficients and standard errors than could be
achieved with separate probit equations.
I first examine the impact of family struc
ture on the propensity to smoke and engage in
problem drinking. Next 1 see whether the con
sequences of parental divorce persist while
controlling for parental education and respon
dent socioeconomic well-being. I then add the
variables measuring respondent psychological
well-being, allowing me to ascertain whether
the smoking and problem drinking resulting
from parental divorce arc associated with other
symptoms of poor psychosocial adjustment.
Finally, I introduce _the variable measuring
respondent divorce into the model to deter
mine whether substance use is an artifact of
the intergenerational transmission of divorce.
All analyses control for survey year, birth
cohort, race, and urbanicity. Preliminary
regressions with interaction terms revealed
significant sex differences in the effects of
parental divorce on substance consumption, so
I conduct separate analyses for men and
women. Models are estimated in Limdep.
RESULTS
~
-
Smoking
Table 1, Panel A shows bivariate probit esti
mates of the impact of parental divorce on
men’s substance consumption. For each of the
five models I present two columns of coeffi
cients. The left-hand column for each model
shows the'effects of parental divorce on the
likelihood of being a smoker. The large and
statistically significant coefficients in Model 1
indicate that both single-mother parenting and
step-parenting increase the chances of smok
ing in men. Panel B displays results for
women, which tell a similar story.
Probit coefficients are difficult to interpret
so I compute predicted probabilities from
regression standardization based on Model I.
The results are shown in the left-hand panel of
Table 2. Forty-six percent of men whose par
ents divorced smoke compared to only 35 per-
j
V
'
The Effects of PARENTALrpiv9ReE^ApytxXQBACcq and Alcohol Consume ion
259
centpf those raised in intact families. Parental divorce is related to psychosocial maladjust
divorce therefore increases foe risk of smoking ment. Inclusion of the psychosocial adjust
by a little less than one third for mem ment variables'(Model 4) did not affect the
Moreover, single-mother parenting_and step impact of parental divorce on cigarette use.
parenting produce the same risk of smoking. Controlling for respondent marital status
The results for women are slightly different. (Model 5) did not affect the results either.
Thirty-six percent of women raised by single _
'mothers smoke compared to 32 percent of
those whose divorced parents remarried. In Drinking
contrast, only 24 percent of women raised in
The second column for each model in
intact families became smokers. Again,
parental divorce produces about a one-third Table 1, .Panel A shows the effects of parental
increase in the likelihood of becoming a smok divorce on the likelihood that male offspring
er, but for women step-parenting slightly will become problem drinkers as adults. In
Model 1, the-positive and statistically signifi
dampens this effect.
Table 2 provides evidence against the cant coefficient indicates that single-mother
social control hypothesis: the presence of a parenting increases the odds of problem drink
step-parent, presumably a second agent of ing in men. In contrast, the coefficient for
parental authority, reduces the likelihood of step-parenting is much smaller and statistical
smoking'only for women. Moreover, women ly insignificant. For men, step-parenting
reared in step-families still smoke at a much apparently repairs some of the damage done by
higher rate than do women from intact fami parental divorce.
The-story is-quite different for women.
lies. On the other hand, parental education
accounts for a portion of the relationship According to Model 1 in Panel B of Table 1,
between divorce and smoking. The coeffi- neither_.single-mother parenting nor step
-cients for single-mother parenting and step parenting increase the likelihood of becoming
parenting decline somewhat from Model 1 to a problem-drinker; both coefficients are smal’
Model 2 (containing the variable for parental and insignificant.
I gauge the exact size of the effects of
education) for both men and women (Table 1,
divorce on alcohol consumption from predict
Panels A and B respectively).
Respondent SES plays a large role in the ed probabilities obtained from a regression
relationship between parental divorce and the standardization (Table 2, Panel B). Men from
chances of smoking. The coefficients measur intact families_report"sometimes drinking
ing family background decline considerably more thaitfoey-should approximately 43 per
-from Modcls 1 and 2 to Model 3 (containing^ cent of the timer In contrast, 57 percent of men
report
the variables measuring respondent education raisedLr6ySingie^"divorced pareand occupational prestige) for both men and . problem drinking, an increase of jt. .. under
women (Table 1. Panels A and B). In addition, one . third. Men whose mothers remarried
the negative impact of parental education on have the same level of problem drinking (43
smoking (Model 2) disappears when holding percent) as men from intact families. On the
respondent education constant (Model 3). other hand, for women step- and single-moth
Parental education only affects offspring er parenting result in levels of problem drink
smoking indirectly, through the intergenera ing similar to those of women from intact fam
tional transmission of socioeconomic attain ilies. It is noteworthy, though, that step-parent
ment. However, except for women from step ing produces rates of problem drinking higher
families, the coefficients for the family back than either mother-only parenting or intact
ground variables remain large and statistically parenting. I will return to this point in the dis
significant in Model 3. indicating that the cussion.
My results do not support any of the three
effects of family background on the propensi
ty to smoke cannot be explained entirely by the theoretical explanations for the relationship
reduced socioeconomic attainment often between parental divorce and offspring sub
stance consumption. Step-parenting almost
brought on by parental divorce.
My results offer little support for the psy completely offset the effects of divorce, but if
chosocial adjustment perspective, which states this were a product of social control, then step
that substance consumption in the children of parenting should also reduce the likelihood
260
TABLE 1.
JOURNAL OF HEALTH AND SOCIAL BEHAVIOR
The Efeeci s of Parental Dt.orcf. on Adult Tobacco an1D Al.COI IOL Consi :mption
261
Panel A: Bivariate Probit Estimates of Men's Smoking and Problem Drinking on Family
Structure of Origin
Model 1
Variable
Model 2
_________
Model 3
Model 4
Model 5
Problem
Drinking__________
Smoking
Problem .
Drinking •
Smoking
Problem
Drinking
Smoking
.25**
.29* •
—
.71 —
.02
—
.23.23*
—
.70**
.01
—
22**
22*
—
.71**
.01
—
.22**
.21*
—
.06***
.09-*
.06—
.09**’
.05*
.09***
-.0006**’"
.02***
-.0006***
.02***
-.0005***
.02***
Smoking
Problem
Drinkjng
Smoking
.29***
31*‘
—
.67—
.02
—
-
Parental Family Structure
Divorced Single Mother
Divorced Mother and Step-father
Intact Family
Birth Cohort / Birth Cohort 1889-1910
.04***
.09* **
.05* **
’.09***
Birth Cohort Squared / Birth Cohort
1911-1976
-.0004** •
.02***
-.0004-* **
- .02***
Birth Cohort 191 l-1976*Divorced Single
Mother
Parental Education
—
Parental Education Data Missing
.■
Respondent Education
Occupational Prestige
-.01*
-.01*
-
-J
.02
.14
-
__
-.09***
_ —
_—
—
—
Occupational Prestige Data Missing
—
—
_
.69-0.002
—
-
-.01*
-
-.01*
—
.01
.03
.01
.03
.01
.03
-.03 ’
-.25*
-.03
-.25*
’^-21-***-
.003
-.21***
-.001“ --—
-.004*
-.001
-- -.004*
-.32*
-.09
-.03
-.02
.06**
.02
---------- .01
-.003
.--23____ —
-.02
-=-------=^_..
_+ +
-
-.002
—
-.35*
_ _
—
_
— -
Problem
Drinking
-M*
- ‘
__-.12
-.35*
—
—
-.04
. -.03
.07**
-.01*
_-.0l .-
Psychosocial Adjustment
Happiness
People are Helpful ___ ■
The World is a Fair Place
Respondent is Divorced
Intercept __
—p
Log Likelihood
—
—
—
—.
—
—
—
—
—
—
—
—
—
— -
1.27***
.94*
.28***
-6085.05
--
.29***
-$067.26
—
. -
—
1.28***
.02
-.02
.01
.96*
__
1.02**
.29***
-5979.84
-
33***“
.32***
—
1.05**
..
"L02*__
29***
-5970.44
1. JO-
J.25**
28***
-593622
*p < .05; •• p < .01; ’“p < .001 (2-tailed tests)
Source: General Social Survey, 1977-1994.
Noles: All models control for survey year, race, and urbanicity at age 16. N for all models is 4,860.
that male offspring become smokers. However, ate the impact of parental divorce on alcohol
this was not the case.
consumption. Moreover, the intergencraAlso not supported by the data is the expla tional transmission of divorce could not
nation concerning the low SES often associat account for the relationship between family
ed with parental divorce. The introduction of structure and men’s alcohol consumption,
controls for parental and~respondent SES although being divorced has a large and sta
(Models 2 and 3, Table 1, Panels A) did not tistically significant impact on problem
affect the relationship between parental drinking (Model 5, Table 1).
divorce and problem drinking.
The final noteworthy result concerns the
The psychosocial adjustment perspective negative interaction between birth cohort and
states that the deviant ideation sometimes mother-only parenting. This interaction indistemming from parental divorce can account . cates that the relationship between parental
for the propensity to be a problem drinker. divorce and the propensity to become a prob
This perspective is also not supported, as the lem drinker has weakened for men bom since
controls for psychosocial adjustment 1910. In other-words,-divorce does not, at least
(Model 4, Table 1, Panel A) failed to attenu in this one respect, hurt children as much as it
once did. This finding, consistent with earlier
research (Amato and Keith 1991b; Wolfinger
,
1996)
can probably be.attributed to the nor
malization of divorce in contemporary
America (see Whitehead 199J7).
DISCUSSION AND CONCLUSION
My research shows that parental.divorce
increases the likelihood-that adult offspring
will be smokers and, for men, problem
drinkers. Parental remarriage almost com
pletely attenuates the impact of divorce on
men’s drinking but has Ifttle effect on-the rela
tionship between family background and ciga
rette use. I propose three mechanisms to
explain the connection between family of ori
gin and respondent substance consumption:
(1) decreased social control in single-parent
families; (2) the lower SES often associated
with parental divorce; and (3) poor psychoso
cial adjustment in the children of divorce.
These three mechanisms were generally
unsuccessful in explaining the results.
Although the decreased socioeconomic attain
ment often brought on by parental divorce
accounts for a portion of the relationship
between parental divorce and smoking, it does
not affect the impact of divorce on the procliv
ity to drink excessively. This result makes
sense. The majority of educated Americans
2b2
-^ZZZJOURNAUOL HEALl.H AND SOCIAL BEHAVIOR
Divorce on Adult Tobacco and Alcohol Consumption -
; -263 -
TABLE I.-Panel B: Bivariate Probit Estimates of Women’s Smoking and Problem Drinking on
__________ Family Structure of Origin
Model 1
Model 2
■
Models
Model 4
Problem.
• Drinking
Smoking
Problem
Drinking
Smoking
Problem
Drinking
.28***
.15
—
-.07
.08
—
.27***
.14
—
-.06
.08
—
.24***
.12
—
-.09
-.05
—
.08**
.07***
’ .08**
.02-
-.0006***
Smoking
.35*’*
.23**
—
- 11
.05
.32***
.23**
-.08
.07
—
Birth Cohort/ Birth Cohort 1889-1910
.05***
.OS**
.05***
Birth Cohort Squared / Birth Cohort
1911-1976
-.0004***
.03* **
-.0004**'
Smoking
Model 3
>•’
Smoking
Problem
Drinking
Problem
Drinking
Variable
'
•
Parental Family Structure
Divorced Single Mother
Divorced Mother and Step-father
Intact Family
Parental Education
-
-
-.09***
.06***
.004
Parental Education Data Missing
-
—
.18
-.51**
.04
Respondent Education
—
-
—
—
Occupational Prestige
-
—
—-
_
Occupational Prestige Data Missing
—
-
-
—
Respondent is Divorced
Intercept
P
Log-Likelihood
‘-.21***
—
-----
-.01**
.08**
.06***
.07* •
-.0006***
.02***
-.0005***
.02***
.06**
.01
.06**
.01
.06**
‘ -.48"*
.02
-.47**
.02
-.48* *
-• .03
-.20***
.02
-.20***
.03
-.002
-.01**
-.002
-.01**
<002
-.13
-.07
-.12
-.04__
'-.09
-.05**
-.01
.10***
.04
-.03
.02 '
-.05*
-.01.
.10***
.04
—
—
—
—
—
.33***
.34***
.32
.29
.49
.37
’
-.05
----- .
Psychosocial Adjustment
Happiness
People are Helpful
The World is a Fair Place
•
.07***
.02***
—
—
—
—
__
—
—
-
-
-
_
__
------
J7
.32***
-6577.75
_
29
.34***
-6543.59
_-
-
.36
- _
.43
35...-------- -
.34* •*
-6385.54
.35***
-6428.85
-6449.89
.02
*p < .05, ** p < .01; ***p.< .001 (2—tailed tests)
Source: General Social Survey, 197-7-1994.
Noies:-A\l models control for survey year, race, and urbanicity at age 16: N for all models is 6.408.
perceive-smek-ing as a serious health risk. In
contrast, irrespective of social background
most people drink at least occasionally (United
States Bureau of the Census 1997).
Single-parenting and step-parenting pro
duce almost identical increases in the risk of
smoking. This is evidence against the social
control argument: "the presence of a step
parent, no matter how ineffectual a disciplinar
ian. should provide an additional agent of
social control and thereby reduce initiation
into smoking.
Female respondents from step-families
report higher rates of problem drinking than
women from either intact families or motheronly families. In contrast, step-parenting
completely offset the large impact of parental
divorce on mens problem drinking. These
results are supported by Hetherington and
her colleagues (1985; Hetherington 1993).
who found that single-mother parenting was
harder on boys than on girls. Conversely.
step-parenting hurt girls but benefitted boys.
That my results fit this pattern supports the
claim that distinct antecedents of adult prob
lem drinking originate in the family processes
Hetherington and others describe (and not
from an inherited predisposition towards alco
holism. a point I will return to).
Finally, my results do not support the psy
chosocial adjustment theory. The controls for
psychosocial well-being did not attenuate the
impact of parental divorce on either alcohol or
tobacco consumption. Respondent marital sta
tus also could not explain the effects of
parental divorce.
Due to the cross-sectional nature of the data
it is impossible to ascertain whether these
potentially”'ihtervening- factors are actually
anterior to offspring substance consumption.
Panel data, with more refined measures of
psychosocial adjustment, would permit a bet
ter test of the adjustment theory.
My results could also be affected by the fact
that the GSS measures family structure at age
16. Some researchers (e.g.. Allison and
Furstenbcrg 1989; Amato 1996.- McLanahan
and Bumpass 1988: but see Stewart at al. 1997
and Wojtkiewicz 1993 for contrary findings)
contend that the effects of a parental divorce
may vary with.its timing, although little con
sensus exists as to whether older or younger
TABLE 2. Predicted Percentages for the Liklihood of Being a Smoker or Problem Drinker as a
Result of Parental Divorce
Problem Drinker________
Smoker
Family Structure of Origin
Intact Family
Divorced Single Mother
Divorced Mother and Step-Father
Men
Women
35%
46
46
■24
36
32
Men
•
43%
57
43
Women
24
_______ 26
Source: General Social Survey, 1977-1994.
Noles: Percentages are based on regression standardization, calculated from Model I, Table 1 Percentages control
survey year, race, urbanicity at age 16, and birth cohort.
JOURNAL OF HEALTH AND SOCIAL BEHAVIOR
264
The Effects of Parental Divorce on Adult Tobacco and Alcohol consumption
children tare better (Hetherington. Bridges. ing in respondents’ families of origin. This
and Insabella 1998). Offspring in step-families raises the possibility that parental divorce is
at age 16 may have experienced parental not the real story: alcohol problems may lead
divorce at any age prior to 16. In contrast. parents to divorce. The higher rates of problem
since two-thirds of divorcees eventually remar drinking in the children of divorce may only
ry (Cherlin and Furstenberg 1994). people in reflect an inherited propensity for alcoholism.
single-mother families at age 16 are more like
Although it is impossible to know the exact
ly to have experienced parental divorce as role played by the genetic transmission of
teenagers. Unmeasured differences tn divorce alcoholism. I am confident that it is not the
timing may therefore contribute to the differ only cause of dipsomania in the children of
ences in the effects of parental divorce based divorce. Step-parenting has such a great
on family type. Finally. I should note that all impact on problem drinking for both men and
children in step-parent families were first in women that a large portion of the propensity
mother-only families, if only for a short time. for alcoholism must be the product of environ
It is possible, perhaps, that the children of mental and not genetic factors.16
divorce often begin smoking before or soon
The lack of information on parental alco
after the breakup. Even if step-parenting helps
holism may be a limitation in explaining the
children in some ways it may not be enough to
findings but does not affect their implications.
keep them from smoking if they have already
The children of divorce are clearly at high risk
begun. For theerrreasons, 1 cannot arrive at a
to become smokers and problem drinkers/l'his
final- decision: abonrany of the three theoretifinding very clearly tells us where prevention
cal perspectives“based only orT'differences
efforts should be directed. This is an important
between step-parenting and single-mother par
issue in an age when more than haff of first
enting.
Other'iimitations of my study stem from marriages end in divorce (Martin, and
inadequate measures of alcohol consumption. Bumpass 1989).
Social_ scientists, have - documented many
First, the GSS measure of problem drinking is
not optimal. Recent estimates show that only lasting effects of parental divorce’ZMpst of
between seven percent and eight percent of the these concern demographic or psychological.
population fit DSM-IV criteria for alcohol outcomes. My study shows that parental
abuse (Grant et -aI.1994),so many GSS divorce has serious consequences for the phys
respondents who report sometimes drinking iological well-being of offspring. Needless to
more than they should are not true abusers. say, this is cause for both concern and further
However, therejsTOTeason to think that the- -research. Furthermore, on the basis of my
overestimation of problem drinking should findings, efforts at substance education and
depend on family background. A more serious prevention should concentrate on the children
limitation is the lack of data on problem drink of divorce.
APPENDIX A.
Continued
Occupational Prestige
(Hodge. Siegel, and Rossi scale)
Continuous variable; 1 00 point scale
Occupational Prestige Data Missing
Coded I if data are missing, 0 otherwise
Problem Drinking
Coded 1 if respondent feels s/he sometimes drinks
more than s/he should. 0 otherwise
Race
Coded 1 if black, 0 if non-black
__
Respondent Family Structure
at Age 16
Set of two dichotomous indicators, each coded
1 if family was: headed by a divorced single
mother, remarried divorced mother; intact
family is the reference category
Respondent Education" ~-----
Continuous variabler.l - not a high school graduate,
high school graduate,
lunior-college-graduate,
- = college graduate', 5 = post-graduate degree
Respondent Education Data Missing
Coded 1 if data are missingTO otherwise
Respondent Urbanicity at Age 16
Coded 0 if respondent lived in a city of
50,000 or more persons or in a suburb of
a larger city, coded 1 if respondent lived
~
in a town of under 50.000 persons or in a_
rural area
_____
Smoking —.
Coded 0 if nonsmoker, I if smoker - ----
Social Adjustment
Survey Year
~ -
—
Set of three items, each a 3 point Likert scale asking
respondents whether they agree wiih~items about
happiness, a sense that the world is a*fair-place, and
whether people in general are helpful
Continuous variable; the last two digits of the calendar year
APPENDIX A.
Coding of Variables for Multivariate Analyses
Coding
Variable
Birth Cohort
_
Continuous variable recoded as piecewise linear
splines, with knot at 10 (for equation predicting
problem drinking): continuous varisble-with squared
term (for equation predicting smoking)
Education of Head of Respondent
Parental Family
Continuous variable: 1 = not a high school graduate.
2 = high school graduate. 3 = junior college graduate,
4 = college graduate. 5 = post-graduate degree
Parental Education Data Missing
Coded I if data are missing, 0 otherwise
Number of Siblings--
Coded I if only child. 0 otherwise
NOTES
the children of divorce live with their moth
ers (Seltzer 1994).
There is copious research examining the 3.
Hetherington and Wallerstein note that the
impact of parental divorce and conflict on
upheaval associated with divorce often sub
adolescent alcohol and tobacco use.
sides after a year of two.-This is a mislead
However, with the exception of the studies
ing observation because many negative
cited here none have taken a life course
effects of parental divorce only become
perspective by examining the effects of
apparent in adulthood (see below).
parental divorce on adult substance con 4.
In other respects, though, a- lack of social
sumption. More generally, comparably lit
control in the family of origin may exacertle research has considered the long-term — bate the maladjustment produced by
consequences
of parental
divorce
parental conflict and divorce. In this sense,
- (Furstenberg and Seltzer 1986; Chasethere is some overlap in the social control
Lansdale and Hetherington 1990).
and psychosocial adjustment perspectives.
2.
The vast majority—about 85 percent—of 5.
Although .sampling design for the GSS has
1.
jt4UXfN-ATj-jjji.H HALjHiANl) SOCIAL-BEHAVIOR.
undergone various changes over the years,
divorce (e.g., McLanahan 1985^ 1988;
McLanahan and Sandefur 1994).
one constant’has been cluster sampling.
This presents a problem for most statistical
10.1
coded both parental and-respondent edu__ cation as continuous variables (see
packages, which assume simple random
sampling in the calculation of standard
Appendix A). I repeated the analysis with
dummy variables for education and
errors. Artificially inflated significance
levels may result from standard errors
obtained similar results.
11.1
chose not to use respondent income as a
derived from cluster-sampled data. To
variable because it is highly correlated
assess the bias induced by clustering, I con
with respondent marital status, another
ducted preliminary analyses using Huberindependent variable.
White standard errors (Huber 1967; White
12. Lowess (Cleveland, Grpsse and Shyu 1992)
1980; for overviews see Greene 1993;
uses a moving window to calculate a local
StataCorp 1995), making use of GSS data
regression line for each data point. The
on primary sampling units in order to
result is a nonparametric, graphical depic
account for between-cluster variation. I did
tion of the relationship between two varinot use Huber standard errors in the analy
ables. Lowess is therefore very useful for
ses reported here because they are not
ascertaining functional.form.
available in the Limdep software package.
13.1
tested interactions between survey year
The Huber standard errors yielded /-statis
and the dummy variables measuring
tics similar to those produced by conven
piarentardivorce, but they were insignifi
tional methods, so I concluded that the
cant and therefore omitted from the models
clustering did not affect my results.
presented here;—
6.
In 1977, 1978, 1980, 1983, and-1984
I47Rc'spondent birth cohort is almost perfect
respondents who smoked were also asked
ly correlated with respondent age (r = .97),
if they smoked cigarettes (presumably as
so any argument for using the latter in
opposed fo”or in addition to cigars or
place of the former (or vice versa) is irrel
pipes). The vast majority, ninety-three per
evant.
cent, smoked cigarette’s." In other years
15. Splines (Greene 1993) facilitate the model
respondents were not asked this question.
ing
of
nonlinear
relationships
by “cutting
To ascertain whether this omission is a
up” continuous variables into linear segsource of bias 1 repeated all analyses a
-ments. The knots are the points at* which
number of different ways: treating the
these linear segments, the pieces df’ffie
seven percent of pipe_pt cigar smokers as
spline, join. —
nonsmokers, missing data, or lumping
16.
It could be-argued that the impact of step—-L&emJnwith-those “identified as cigarette
parenfing on ^menfcprobiern drinking
smokers. The results were identical in all
might only be-a-producrofdivorcedjnothcases, so for the analyses reported here I
er’s selection out of remarriage. In other
used only the third solution.
words, if a divorced mother has a particu
7.
The precise text of these items is: “Do you
larly grievous drinking problem, she might
ever have occasion to use any alcoholic
be less likely to remarry. It would then be
beverages such as liquor, wine, or beer, or
the severity of her drinking problem that
are you a total abstainer?” and “Do you
produces both her failure to” remarry and
sometimes drink more than you think you
her son’s drinking problem. However, this
should?”
scenario seems unlikely. Step-parenting
8.
It is not a concern that the GSS conflated
increased by five percent the chances that
separated and divorced parents. Bumpass
female offspring would have drinking
et al. (1991) suggest that treating separa
problems. This is strong evidence against
tions as divorces is not likely to be prob
the notion of selection out of remarriage on
lematic.
the grounds of parental.alcoholism.
9.
Many researchers have shown that parental
death does not have adverse effects on chil
dren (e.g., Acock and Kiecolt 1989; Amato
REFERENCES
1988; Demo and Acock 1988) or affects
them much less severely than does parental Acock. Alan C. and K. Jill Kiecolt. 1989. “Is It
''THE'EFFECi^bF'T’AEENTAL-IJf^wCB cnjAdLlt Tobacco-and Alcohol Consumption—
- -267
Disruption: -A Replication and Update.”
Family Structure or Socioeconomic Status?
Demography. 21:71 -82. ‘
Family Structure During Adolescence and Adult
Bumpass, Larry L., Teresa Castro Martin, and
Adjustment.” Social Forces 68:553-71.
James A. Sweet. 1991. “The Impact of Family
Ahlgrcn, Andrew, Ardyth A. Norcm. Mark
. Background and Early Marita! Factors on
Hochhauser, and Joan Garvin. 1982. “Ante
Marital Disruption.” Journal of Family Issues
cedents of Smoking among Pre-Adolesccnts.”
12:22-42.
Journal ofDrug Education 12:325-40.
Allison, Paul D. and Frank F. Furstenberg, Jr. 1989. Bumpass, Larry L. and James A. Sweet. 1989.
“Children’s Experience in Single-Parent
“How Marital Dissolution Affects Children:
Families: Implications of Cohabitation and
Variations by Age and Sex.” Developmental
Marital Transitions.” Family Planning
Psychology 25:540-49.
Perspective 21:256-60.
Amato, Paul R. 1988. “Long-Term Implications of
Parental Divorce for Adult Self-Concept.” Chase-Lansdale, P. -Lindsay ' and E. Mavis
Hetherington. 1990. “The Impact of Divorce on
Journal of Family Issues 9:201-13.
Life-Span Development: Short and Long-Term
--------- . 1991. “Parental Absence During
Effects.” Pp. 105-50 in Life-Span Development
Childhood and Depression in Later Life.” The
and Behavior, vol. 10., edited by P. Baltes, D.
Sociological Quarterly 32:543-56.
Featherman and R.M. Lerner. Hillsdale, NJ:
--------- . 1993. “Children's Adjustment to Divorce:
Lawrence Erlbaum.
Theories, Hypotheses, and Empirical Support.”
Cherlin, Andrew J. 1978. “Remarriage as an
Journal ofMarriage and the Family 55:23-8.
Incomplete Institution.” American Journal of
--------- . 1996. “Explaining the Intergenerational
Sociology 84:634-50.
Transmission of Divorce”. Journal of Marriage
Cherlin, Andrew J., P. Lindsey Chase-Lansdale, and
and the Family 58:628-40.
Amato, Paul Jll. and Alan Booth. 1991.
Christine McRae. 1998. “Effects of Parental
Divorce on Mental Health Throughout the Life“Consequences of Parental Divorce and Marital
Course." American Sociological Review
Unhappiness for Adult Well-Being.” Social
—63:239.-49:—;
Forces 69:905-14._
Amato, Paul R. and Bruce Keith. 1991a. Cherlin, Andrew J. and-Frank F. Furstenberg, Jr.
1994. “Stepfamilies in the United States: A
• “Separation from a PareriTdunhg Childhood and
Reconsideration.” Annual Review of Sociology
Adult Socioeconomic Attainment.” Social
20:259-81.
Forces 70:187-206.
Cherlin,
Andrew J„ Frank E Furstenberg. Jr., P.
Amato, Paul R. and Bruce Keith. 1991b. “Parental
Lindsay Chase-Lansdale, Kathleen E. Kiernan,
Divorce and the Well-Being of Children: A
Philip K. Robins, Donna Ruane Morrison, and
Meta-Analysis.”
Psychological
Bulletin
Julien O. Teitler. 1991. “Longitudinal Studies of
H 0:26-46.
Effects of-Divorcc on Children mGreat Britain
Amato, Paul R., Laura Spencer Loomis, and Alan
and the United States.” Science‘252:1386-89.
Booth. 1995. “Parental.-Divorce, Marital
Conflict, arid Offspring Well-being during Early Cleyeland,.WiUiam S„ Eric Grosse, and Wiliam M.
Shyur-f992~“LocaI Regression Models.” Pp.
Adulthocd.”~5toCTu7'Forces 73:895—915.
309-76 in Statistical Models in S, edited by John
Amato, Paul-Pr^-and Stacy J.-Rogers. 1997. “A
M. Chambers and Trevor J. Hastie. Pacific
Longitudinal Study of Marital Problems and
Grove, CA: Wadsworth & Brooks.
Subsequent Divorce.” Journal of Marriage and
Davis, James A. and Tom W. Smith. 1996. The
the Family 59:612-24.
General Social Surveys: Cumulative Codebook.
Bachrach. Christine. 1983. “Children in Families:
1972-1996. Chicago: National Opinion
Characteristics of Biological. Step-, and
Research Center.
Adopted Children.” Journal ofMarriage and the
Family 4'5TL71-79._ '
_
DeFronzo, James and Rebecca Pawlak. 1993.
“Effects of Social Bonds and Childhood
Baer, Paul E., .Lisa B. Garmezy. Robert J.
Experiences on Alcohol Abuse and Smoking.”
McLaughlin, and Alex D. Pokorny. 1987.
The Journal ofSocial Psychology 133:635—42.
“Stress. Coping, Family Conflict, and Adoles
cent Alcohol Use." Journal of Behavioral Demo, David 11. and Alan C. Acock. 1988. “The
Impact of Divorce on Children.” Journal of
Medicine WM49-66
Marriage and the Family 50:619-48
Biblarz, Timothy J. and Adrian E. Raftery 1993.
“The Effects of Family Disruption on Social Dornbusch, Sanford M., J. Merrill Carlsmith,
Steven J. Bushwall, Philip L. Ritter. Herbert
Mobility." American Sociological Review
Leiderman, Albert H. Hastorf, and Ruth T.
58:97-109.
Gross. 1985. “Single Parents, Extended
Blau, Peter M. and Otis D. Duncan, 1967. The
Households, and the Control of Adolescents.”
American Occupational Structure. New York:
Child Development 56:326-41.
Wiley.
Bumpass. Larry L 1984. "Children and Marital Emery, Robert E. 1982. “Interparental Conflict and
nuil ofHealth dntFHuman Behavior) is published quarterly in March, JuncpScptcmber, and
:emb.cr by the American Sociological Association, 1307 New York Avenue NW, Suite 700,
shington, DC 20005-4701. JHSB is printed by Boyd Printing Company, Albany, New York.
t
The Impact of Education and Heart Attack on Smoking
Cessation Among Middle-Aged Adults*
LINDA A. WRAY
A. REGULA HERZOG
ROBERT J. WILLIS •
University ofMichigan
ROBERT B. WALLACE
University of Iowa
Manuscript Submission
ibmit manuscripts to: John Mirowsky, Editor, JOURNAL OF HEALTH AND SOCIAL
v.HAVIOR, Department of Sociology, The Ohio State University, 300 Bricker Hall, 190 North
Vai Mall, Columbus, OH 43210-1353; Phone: 614-688-8673; E-mail: JHSB@osu.edu. New
^missions must be accompanied by a SI5 processing fee. The processing fee may be paid by
heck or money order made payable to the American Sociological Association. The fee must
k>aid in order for the review process to begin. The fee is waived for student members of the
'A. This reflects a policy of the ASA Council and Committee on Publications affecting all
A journals. For detailed information about preparation and submission of manuscripts,
hors should consult the Notice to Contributors in the September 1998 issue.
I Advertisements, Membership Dues and Subscriptions, and Changes of Address
pit advertisements to: the Executive Office, American Sociological Association, 1307
| York Avenue NW, Suite 700, Washington. DC 20005-4701.
bership dues'and subscriptions: Annual membership dues in the ASA S36-S206 (S25 of
mount may cover a subscription to the Journal ofHealth and Social Behavior); Associate
iers; $62r Student members. S36. Subscription rate for members, 325, nonmem’uers, 350
1 the-USrS65 outside the US; institutions. S95 within the US, SI 10 outside the US;.single
available. New subscriptions and renewals will be entered on a calendar year basis only.
es of Address: Subscribers must notify the ASA Executive Office six weeks prior to a
i
of address. Notification must include both the subscriber’s old and new addresses.
fqr.undeliverable copies must be made within the month following the regular month of
st
in transit
a change
address. the ASA will replace copies of JHSB that have
tion.
When due
the to
reserve
stockofpermits,
’ht © 1998, American Sociological Association. Copying Bey ond Fair Use: Copies of
in this journal may be made for teaching and research purposes free of charge and with
iring permission, as permitted by Sections 107 and 108 of the United States Copyright
r all other purposes, permission must be obtained from the publisher.
[or thanks the Department of Sociology and the College of Social and Behavioral
at The Ohio State University’ for providing the journal’s office space and equipment.
Journal of Health and Social .Behavior 1998 (December): 271-294
Considerable evidence supports the premise that higher levels ofeducation lead
to enhanced health, including protective health behaviors. This paperfocuses on
how education affects one health behavior known to lead to enhanced health:
the cessation ofsmoking. In particular, the authors examine the extent to-which
education influences the decision by middle-aged adults to quit smokingfollow
ing a heart attack, a potentially life-threatening health'event. We first hypothe
size that middle-aged adults with moreformal education will stop smoking more
readily than people with less formal education following the experience of a
heart attack. Second, we ask what otherfactors might underlie and explain tliat
hypothesized effect. Using longithdinal data, the authors track changes in indi
vidual smoking behaviors after a heart attack among preretirement-age
Americans. We control for documented correlates of smoking and heart attack
plus otherfactors associated with education, heart attack, and smoking that may
also influence whether a person quits smoking. In addition to confirming evi-.
dence on the education-health association as well as the documented connection
between Kea'rFattack and smoking cessation, this study provides a-Surprising
twist_Ojtdho.se links: Our results how that the move to-quit smoking following
the experience of a heart attack . :ong middle-aged adults is significantly and
dramatically moderated by their level ofeducational attainment.
behaviors, in both' older and younger adults
t Adler et al. 1994; Antonov <ky 1967; Feinstein
1993; Feldman et. al. .19x9; Kitagawa and
Hauser 1973: Ross and Wu 1995: Syme and
Berkman
1976). This paper focuses more
•A preliminary version of this paper was presented
at the F. Thomas Juster Symposium held on closely on how education affects one health
December 13-14, 1996 at the University of behavior known to lead to enhanced health: the
Michigan. Ann Arbor. Michigan. Support for this cessation of smoking. In particular. we exam
research was provided by NIA Grant No. P20- ine the extent to which education influences the
AG12846, NIA Grant No. Utl 1-AG09740. and NIA decision to quit smoking by middle-aged adults
Grant No. T32-AG00117. The authors thank Duane following a heart attack- -a potentially life
Alwin. John Bound, and Dick Campbell for their threatening health event. Trits, we study one
insightful comments on earlier drafts of this paper. step in the process linkr education and
The authors also thank John Mirowsky and two enhanced health in a highly selective group of
anonymous reviewers for their helpful comments.
middle-aged smokers. Specifically, these
Correspondence should be addressed to: Linda A.
Wray. Institute for Social Research. University of smokers may differ from y . unger smokers in
several ways. They may re—esent a group <-f
Michigan. Ann Arbor. Ml 48106-1248.
Considerable evidence supports the premise
that higher levels of education lead to
enhanced health, including protective health
272
JOURNAL OF HEALTH AND SOCIAL BEHAVIOR
Impact of Education and Heart Attack on Smoking Cessation
273
quit smoking once they experience a heart smoking behavior. That is, perhaps education
longer-termed and, thus, more heavily addict stop smoking has increased consistently since
event compared to smokers who did not expe al attainment moderates the relationship
ed or otherwise committed smokers who have 1964 (U.S. Department of Health and Human
rience such an event (U.S. Department of between heart attack and smoking cessation so
successfully resisted.decades of widely avail Services 1990), the reasons why some people
Health and Human Services 1989). In addi that the move to quit smoking varies across
able information on the health dangers of cig quit and others continue to smoke are not
tion, the proportion of those quitting following levels of education. In particular, it may be that
arette smoking. Their unique characteristics entirely clear.
any heart event increases with the severity of higher levels of education produce more of the
may also contribute to their resisting current
Education clearly plays a role in smoking
the event (Baile et al. 1982). Given the well-’ necessary knowledge, skills, and abilities that
public health programs targeted to the smok cessation: The rates of quitting smoking since
established relationship between smoking and help a person to understand the link between
ing community at large or to younger smokers. the 1964 Surgeon GeneralVReport have conheart attack; smoking behavior may also be cigarette smoking and heart attacks and, in
This study aims to understand the role that sistehtly increased (and increased more rapid
affected indirectly by modifiable risk factors turn, the advisability of quitting smoking fol
higher levels of education may play in chang ly over time) for those with more education.
associated with the experience of heart attacks lowing the experience of a heart attack.
ing smoking behavior in the face of a health For example, although the overall quit rates
or other heart-related conditions such as physWe also consider the extent to which select
crisis.
have increased from 33 percent in 1965 to 44
ical'irfactivity, high blood pressure,_ahd ‘obesi- ed psychological, social environment,-and
Given the available literature, we-hypothe- percent in 1987, college graduates have quit at
ty (Brownso'n 'et alr’1996fBucWerahd Ragland resources consequences of education may”
size that middle-aged adults with more formal significantly higher rates than high-school
-1995; Wenger 1995; Winkleby et al. 1996) as mediate the process of quitting smoking. From
education will stop smoking more readily than graduates (U.S. Department of Health and
well as by enduring factors such as gender and a psychological perspective, acquiring-higher
middle-aged adults with less education follow Human Services 1990), suggesting that peoole
race/ethnicity (Brownson et al. 19967Nevid et levels of. education in childhood and young
ing the experience of a heart attack. Second, with higher educational attainment may have
al. 1996; Ransford-1986; Strecher et al. 1995). adulthood may reinforce or augment cognitive
we ask what other factors might underlie and better understood the risks of cigarette smokability in. adulthood^particularly in the explain such an effect;'~In~ exploring these— ing and acted on the Surgeon General’s recomdimension
’ Jmowiedge-baseu- Inteliigencc-^
issues .'.bring togeti er two voluminous bod- mendations.
(Perlmutter 1986^’ dr pro’dbcf Tntelhgepce”7
Education and Health .
■ —ies of ..teraftire that cr6~SS^cut7sucTFaireiplines ^—-Several other health as well as demographies —
(Salthouse 1991, 1996). People-who”fijhction ..
as sociology, psychology, medicin.e.-econom- environmental, and psychosocial factors may
Decades of studies fiave_documented that at a higher cognitive level may be better able to
ics, and epidemiology: one pertaining to the ~alsorinfluence smoking behavior. Studies have
—
higher levels of education are linked to a vari use their educational resources to apply the
predictors of smoking cessation and the other shown
’
■ ■ or quitting smoking
...is thatnot■ smoking
ety of measures of enhanced health, including ever-changing health data to their own liyes “
to the relationship between education rand highest among older adults, people who are—
protective-health behaviors such as weight (Kenkel 1991), thereby decreasing their
health. Using longitudinal data, we track not married to other smokers,-and workers not
management, regular exercise, and moderate propensity to smoke and, in turn, their risk for '
changes in individual smoking behavior after a employed in manufacturing or day labor jobs
drinking (Wray et al. 1996). Although the link heart attack (Hamilton 1972; Ippolito 4972L.
heart attack while controlling for documented (O’Loughlin et al. 1997; U.S. Department of
Lewit,
between
Coate’^and
education
Grossman
and 1981;
health
Schneider,
is wellcorrelaieTof smoking and heart-attack plus Health and Human Services 1990; Wister
established across academic disciplines, the" Klein, and Murphy 1981). Further, some
other factors associated .with education, heart 1996; Wray et al. 1996). In contrast, smokingTl-_
meaning of this association-is open to debate smokers with higher levels of educatiorT-arid,
attack, and smoking that may alsp-ihfluence
... cessation is lowest among people 'Xho are
(see Adler et al. 1994; Ettner 1996; Ross and relatedly, higher levels of cognitive ability may
whether a person quits.
depressed (AndaTWilliamson, and Escobedo
Wu 1996).
interpretations
of the associa have been more positively influenced, by evi3) (990; Glassman, Helzer,.and
CoveyFour
1990)
or
tion are possible: two suggesting direct rela dence that 10 to 15 years of abstaining~Troiri ~
heavy alcohol users (Breslau et al. 1996; U.S.
tionships between-education and health smoking returns the all-cause mortality-risksPREVIOUS RESEARCH
: Department of Health and Human Services
(Grossman and Kaestner. 1997), a third look of past smokers to those of non-smokers and—
1994)TSmoking “cessation may also be lower
ing at an indirect relationship due to the exis perhaps more saliently—that even one year of Previous studies dealing with smoking ces- among individuals with poorer self-assessed
tence of other factors that are associated with abstention significantly reduces the risks of
■ sation as well as the links between education health (Nevid, Javier, and Moulton 1996).
both education and health (Behrman 1997; dying from various diseases (Samet 1992; U.S.
and health are wide and varied. Each area is ’
'
More
heavily addicted' smokers—people who I
Cobum and Pope 1974; Grossman and Department of Healtfr’amrttnrnarrServices
summarized briefly below.
smoke more than one^paclT of cigarettes a
Kaestner 1997; Matthews et al. 1989; Ross and 1990).
day—are also”less”Iikely to quit (Marbella,
Ldyde, arid Remington f995)7”In addition, —'
Wu 1995, 1996) and a fourth examining a con
Another psychological factor that may
ditional relationship that indicates that educa explain a link among education, heart attack,
Smoking Cessation
studies have shown that smoking cessation
tion and health outcomes are associated only and smoking cessation is a personality charac
may_differ-by- gender, some indicating-that----under selected circumstances.
The first Surgeon General’s Report on women are more likely to quit smoking and
teristic that predisposes people to invest in the
Smoking and Health in 1964 as well as all sub- others that men quit more often (Escobedo and
The third and fourth possibilities—which future through “good” health behaviors in the
sequerit repofts from that office demonstrate Peddicord 1996;,Jarvis 1995;, Rogers, Nam,
have received far less analytic attention than present (Becker, Grossman, and Murphy-1991,
tire other two primarily due to data con 1994; Becker and Murphy 1988; Farrell and“
. that cigarette smoking is the foremosrpre- and Hummer 1995; U.S. Department of Health
I ventafito^use of deatE7in~&e United States^- and Human Services 1989; Wenger 1995),
straints—serve as the basis for this study’s Fuchs 1982; -Fuchs 1982; Grossman and
i and,'in’particuiar,~those'deaths.resulting from
In general, although smokers perceive their
conceptual framework. We begin by examin Kaestner 1997“Kenkel 1991; Rakowski efal;
I cardiovascular diseases and cancers, (Centers health risks for cardiovascular diseases and
ing whether heart attack or education exerts 1987). People with higher levels of education
(<- for Disease Control 1987; U.S. jDepartment of cancer to-be-greater than those of non-.
direct effects rarr smoking cessation among are more likely than people with lower levels
Health and Humah.Sep'iccsZjL989,kL990). smokers, they also underestimate their health
middle-aged smokers as demonstrated in the of education to engage in healthful .behaviors;
Although the 1990 SurgeomGeneral'sReporf risks (Strecher, Kreuter, and Kobriir
:
literature-for al! smokers:-of, alternatively, overall, including never smoking (Matthews et
indicates that theprop^cnf-ofsmokers who -Nevertheless, higher proportionrpf smokers,
whether they interact in some way? to change al. 1989; Wagenknecht et aH 990; Winkleby- *
~-^^RNA^ffi^HEAI.IHSiNDSOCIAL'BJillAVIOR
et al.. .1992), and thereby reducing their risk of tect against heart attack.cr encourage a deci
many diseases (Antonovsky 1967; Diez-Roux sion to quit smoking.following a heart attack.
et al. 1995; Wray et-al. 1996). They may doso
Whatever the true meaning of the education
because they are more willing to-plan or health association, increased years of educa
“invest” in the future rather than “consume" in tion are consistently found to be positively
the present Thus, we speculate that differences associated with many aspects of enhanced
in future orientation may explain the education health in both younger and middle-aged
health association.
adults. Whether education contributes directly,
Alternatively, a social-environment perspec indirectly, or conditionally to enhanced health
tive posits that educational levels may influ in the form of smoking cessation among a par
ence a person’s choice of where to live or work ticular group of older smokers is the question
that-may differentially reinforce beneficial that is the focus of this paper.
health behaviors or discourage harmful health
behaviors through “social control” in the form
of peer norms or values (Diez-Roux et al. METHOD
, 1995; Rogers et al. 1995; Ross and Wu 1995;
Umberson 1987). As noted earlier, smoking Data
I cessation is reported to be highest among peoThe lack of conclusive research on the
I pie whose spouse or other household members
I are nonsmokers (O’Loughlin et al. -1997-;- process by which education changes health
I Wister 1996). Similarly, rates of smoking vary behaviors-is-due in part to the paucity of data
| by job categories: Workers in professional or sets contalningjippropriate longitudinal data
I higher-status jobs are disproportionately nan- to studyTthis questionTldeally, such a data set
smokers compared to workers in lower-status would contain individual social, health, and
□jobs (Wray et al. 1996). Since less-educated economic characteristics as well as other indi
people tend to marry other people with dess vidual and environmental factors which may
education and work in jobs which require less influence making-certain behaviors and deci
education, it is~pbssible that they are faced sions. Thc”Health and Retirement Study
with disproportionately greater numbers of (HRS),.a large, nationally representative sam
pokers in their immediate environment. Tire ple of preretirement-age Americans, is unique
bwer-status jobs may also include more phys- _ ly suited.for exploring this study’s issues for
tally demanding and repetitive tasks as well two primary reasons. First, the HRS is rich in
— I less autonomy and flexibility, factors that information central toour interests, containing
py combine to increase job-related boredom considerable-socfodemographic, physical and
jd stress and,-potentially, the likelihood of- - emutionalrjieaIUuheJth-foehavior, functiloking to-counter.foe boredom and stress. "work-^d—retiremeny? income and ;iss«.
lus, people with lower levels of education health- and life-msurance data as well as mea
ty be more likely to start or continue smok- sures on cognitive ability, future orientation,
risk aversion, and subjective probabilities.
I not because of their levels of educational
inment per se but instead because of influ- Second; the HRS is a panel study that has col
:s in their social environment which are lected three waves of data to date,1 enabling us
to explore a range of dynamic processes relat
ed to educational level.
ing to health and economic decision-making
similar logic applies to a resources pertive; Higher levels of education may among preretirement-age individuals.
” better health through higher income and
h that then purchase more health insur
er greater access to high-quality healthiGrossman and Kaestner 1997; Patterson,
al, and White 1996; Schultz 1975; Welch
I. Rather than advanced education linking
ly to fewer heart attacks or to the cessaIf smoking, it may be that the greater
I or employer-provided health insurance
ated with higher levels of education pro
Questions and Hypotheses
Based on our review of studies on smoking
behavior and the health benefits of education,
we expect that education will be an impor
tant—and perhaps even predominant—predic
tor of smoking cessation among middle-aged
smokers. In addition, given the documented
link between the experience of a heart attack
and smoking cessation, we anticipate that edu- possible? explanations --for an education .or
cation will mteract-with the experience of-a- education-heart attack effect on smoking cesheart attack so that rates of smoking cessation sation. Two hypotheses test whether psycho
will differ acrosseducational levels. Because logical factors associated with education affect”
education is a proxy for knowledge, skills, and
abilities developed over half a lifetime in the
case of our HRS cohort, we also test whether
smoking behavior:
(4). Smokers with higher levels of cognitive
ability are more likely tn
to m<it
quit smoking
smnkino
thanare smokers with lower levels of cog
selected psychological, social environment,
nitive ability.
and resources factors perceived as conse
quences of education might explain any of the ((5) Smokers who are more future-oriented are
. more likely to quit smoking than are
—
effects of education or the interaction of edu
smokers who are less future-oriented.
cation and heart attack on the decision to quit
“Similarly, two hypotheses test whether
smoking. We anticipate that these educationrelated factors may be all the more important ,social-environment factors associated with
in decision-making for this particular group of (education influence smoking behavior:
Smokers who are not married to other
middle-aged smokers. Because they are more (6)
(
smokers are more likely to quit smoking
likely to be highly addicted to cigarettes after
thaiTare smokers married to other stnokmany smoking years, their smoking behavior
may also be influenced considerably more by
each of the education-related factors to which (7) Smokers who do/did not work as a
they have beemrxposed for longer periods of
machine operator or laborer are more like
time-compared with-their younger counter
ly to quit smoking than are smokers who”
worked as a machine operator or laborer.
parts.
In this paper, we ask the following questions
Finally, two hypotheses test the effects of
about middle-aged adults:
resourcesrfactors associated with education on
(1) Does education-affect smoking cessation? smoking behavior:
~~
Does the experience of a heart attack (8)
Smokers who report-greater net worth are
affect smoking cessation? Do education
more likely to quit smoking than are
and the experience of a heart attack inter
smokers who- report lower net worth.
act to affect smoking cessation such that (9)
Smokers who are covered by employerpeople-withrmore formal education are
provided health insurance are more likely
more likely to quit smoking following a
—to-quit smoking than are smokers without
heart attack than do people with less for' —employer-provided health insurance.
mal-cducatiohV
~~~
___ social environment, or resources factors
explaining an education or an education-
Samples
heart attack interaction effect on smoking
cessation?
Based on our study questions and the extant
literature, we test three primary hypotheses
relating-to smoking cessation among middleaged adults:- •----(1) Smokers with higher levels of education
are-more likely to quit smoking than are
smokers with lower levels of education.
(2) Smokers who have experienced a heart
attack are more likely to quit smoking than
smokers who have not experienced a heart
attack.
(3) Smokers with higher levels of education
are more likely to quit smoking than are
smokers with lower levels of education
following the experience of a heart attack.
Additional secondary hypotheses test six
Although a large body of past research has
consistently supported the strong negative
association between higher levels of education
and smoking, less conclusive evidence exists
on a causal relationship between years of edu
cation and quitting smoking, particularly
among middle-aged or older smokers (U.S.
Department of Health and Human Services
1989, 1990). In order to isolate the effect of
education on the process of modifying smok
ing behavior, we tracked the effects of educa
tion on smoking cessation following the expe
rience of a heart attack between 1992 and 1994
(when the data for HRS Waves 1 and 2 were
collected) among smokers age 51 to 61 in
1992.2 Heart attack was chosen as an example
of a major smoking-related health event that, if
JOURNAL OF HEALTH AND SOCIAL BEHAVIOR
diagnosed. can be reported with reasonable
prec-.sion tn surveys.
T*o primary respondent groups were drawn
for this study. First, a full sample included the
8.656 age-eligible respondents for whom we
have unambiguous smoking history data in
both 1992 and 1994 interviews. Among those
respondents. 3.216 reported they had never
smoked cigarettes or had smoked less than 100
cigarettes m their lives prior to 1992; 3,049
reported they had smoked in the past but had
quit by 1992; and 2.391 reported they were
current smokers in 1992 who had either continued to smoke or had quit smokihgby -1994.
The full sample provided us with data on the
relationships between smoking history and
various social, physical health, psychological,
and economic characteristics and helped us to
refine our major analytic models QiLsmdking
—cessation'. The second respondent group,
which included the 2,391 people who reported
they were current smokers in 1992 for whom
we had matching 1994 data on smoking status,
was the basis for our major analytic models.
The independent variables in our models of
smoking cessation were restricted to:
(1)
the measures of major analytic interest:
education, incident heart attack, and an
interaction term for education by heart
attack;
(2)’potential predictors that may explain the
education-heart attack effect-on smoking
cessation, including selected psychologi
cal, social-environment, and resources
factors;
(3)
the primary correlates of smoking cessa
tion: gender and measures of depressed or addictive personalities; and
(4)
additional correlates of heart attack:
race/ethnicity and specific measures of
heart-related health.
Among the independent variables of major
analytic interest, education is measured as the
number of years ’ education completed’ by-----1992 (0 to 17 yeai„, with 17 representifigrpost^"7
baccalaureate education), centered on 12-years—
of education. The measure of incidentheart
attack indicates whether or noT the respondent
reports having experienced a heart attack
between 1992 and 1994 (0 = no; 1 = yes). The
interaction term, representing the dependency
Analysis Plan
of education on heart attack, is measured as years of educationTnultiplied by the experi—
We tested multivariate models using various
ence of a heart attack (Jaccard, Turrisi, and
subgroups of the full and "smoking samples.
Wan 1990).
First, exploratory models tested-the effects of
The independent variables include six psy- '
education and other hypothesized predictors
chological, social-environment, and resources _
on three dichotomous outcomes: never srnokfactors that may explain the effects of-the “"
ing among all middle-aged adults, quitting interaction term on smoking cessation. These
prior to 1992 among middle-aged adults who factors were also measured at baseline in 1992.
had smoked in the past but were not current Among the psychological factors, cognitive
smokers in 1992, and having experienced a ability is a measure that combines the stan
heart attack between 1992 and 1994? Findings dardized total scores (Z-scores) from two cog
from these analyses informed the design of our nitive performance tests available" iri-the
analyses on smoking cessation.
HRS—the immediate and delayed word recall
Second, the models that focused on our tests as well as the WAIS-R word similarities
major analytic interest—smoking cessation test (0 to 54)? Future orientation is measured
between 1992 and 1994—were tested on the by whether or not the respondent reports a smokers sample only. Given the dichotomous short-term financial planning horizon (a few
outcome measure for this set of analyses as months to one year) or a medium-term finan
well, the models were tested using logistic cial planning horizon (a few years), with a
regression? In these primary analyses, we long-term planning horizon (more than five
regressed smoking cessation between 1992 years) being the reference category.
and 1994 on sequentially-entered blocks of
The social environment factors include
variables that test the relative contributions of whether the respondent’s spouse smokes (0 =
selected variables proposed to measure the no; 1 = yes) and whether the respondent
-educatioo-smoking behavior relationships, and worked as a machine operator or laborer (0 =
controlling for- documented correlates of yes; 1 = no). The resources factors include a
measure of logged net worth (centered on the
smoking cessation and heart attack.
Impact of Education and Heart Attack on Smoking Cessation
mean) and a dichotomous measure of whether Never smokers also experienced significantly
the respondent is covered by employer- fewer heart attacks prior to 1992, fewer heart
provided health insurance (0 = no; 1 = yes).
attacks between 1992 and 19'M, have a lower
Finally, we include documented correlates history of high blood pressure, drink less heav
of smoking cessation measured at baseline in ily, and report better self-assessed health as
1992: gender (0 = male; 1 = female); heavy well as fewer CES-D depressive symptoms
smoking measured as current cigarette dosage than do smokers in 1992 or 1994. Never smok
of greater than 25 per day (0 = no; 1 = yes); ers are also less likely to be married to smok
heavy drinking measured as currently drinking ers or to work as machine operators or laborers
more than two alcoholic drinks per day (0 = and are more likely to report higher networth
no; 1 = yes); and the number of Center for than are recent smokers. Past smokers—smok
Epidemiological Studies-Depression Scale ers who quit smoking priorto 1992—are sta
(CES-D) depressive symptoms experienced tistically similar to never smokers on many
most or all of the time in the past week (0 to 8), characteristics, including education, depres
centered on the mean number of CES-D symp sive symptoms, self-assessed health, cognitive
toms. Similarly, we include documented corre ability, spousal smoking, employer-provided
lates of heart attack measured at baseline: two health insurance, and net worth. Three signifi
measures of race/ethnicity (1 = African cant differences between those groups are
American or 1 = Latino; 0 = White or other . worth noting. Compared with never smokers,
race/ethnicity as the reference category); diag—: "past smokers are disproportionately men, peo
nosis of high blood pressure Tn the past (0 = ple who "experienced a heart attack" before
no; 1 = yes); obesity measured as greater than" 1992, and people who reported they drink
the third quartile of body mass"index for the heavily. These differences are significant at the
HRS respondents (0 = no; 1 = yes); irregular p < .05 level.
exercise measured as light exercise less than
In contrast, current smokers in 1992 and
once a week (0 = no’; 1 = yes); and two mea
1994 are less well-educated, heavier drinkers,
sures of self-assessed health status (1 = good report higher levels of depressive symptoms,
or 1 = fair/poor health; 0excellent/very good and test lower in cognitive ability than do
.as the reference category).
never or past smokers in those years. Smokers
in 1992 and 1994 are more likely to be married
to othersmokers and to report lower net worth
RESULTS
than never or past smokers. Importantly, peo
ple who quit smoking between 1992 and 1994
Correlates of Smoking History
also disproportionately report having experi
enced a heart attack during that same, period.
Table 1 describes the characteristics of four
subgroups of Americans age 51 to 61 in 1992,
arrayed according to their smoking history in Predictors of Never Smoking and Quitting
1992 and 1994: (1) respondents who reported . Among Past Smokers
in both 1992 and 1994 that they had never
smoked cigarettes; (2) those who reported in
Tables 2 and 3 present results of exploratory
1992 that they had smoked in the past but had analyses focusing on two of the smoking states
quit prior to 1992; (3) those who reported they illustrated in columns 1 and 2 of Table f—
were current smokers in 1992 but were not never smoking and having quit smoking prior
smokers in 1994; and (4) respondents who to 1992. The goal of each of these analyses is
reported they were current smokers in both to gain some understanding of the role of edu
1992 and 1994. As expected, in general, cation on pre-1992 smoking behavior while
middle-aged adults without any smoking his controlling on selected correlates of smoking
tory had fewer risk factors for heart disease in order to better design our major analytic
and more characteristics associated with high models concerning smoking cessation
er education than did smokers in 1992 or 1994. between 1992 and 1994. As shown in Models 1
For example, never smokers are disproportion through 4 in each table, blocks of variables
ately female with higher levels of education were entered sequentially:" (1) demographic
and cognitive ability compared.with their and status origin characteristics; (2) years of
counterparts who report a smoking history._ . education; . (3) measures of healthrbehaviors'
.278-.|
[
Journal of health and-social^eRavior
TABLE 1. Frequencies, Means, and Medians on Selected Characteristics of U.S. Adults Age 51-61,
by Smoking History
Characteristics’
Psychosocial Risk Factors
Female4
Race/Ethnicity4
White
African American Latino
Other
Father’s Education (mean, 0-17)4-'
Never
Smoked
Smoker Priorto 1992
Smoker in 1992
QuitbyT99'4
85.3
8.4
78.7
■ Smoker in 1992
and 1994
66.0
10.4
Education (mean, 0-17)4*
Heart Attack Prior to 1992b
Heart Attack 1992—1994”
High Blood Pressure11
Heavy SmokerlnTWHeavy Smoker Prior to 1992
Heavy Drinker4
Irregular Exerciser*'
Obese4
Self-Reported Health4
- Excellent/Very Good
__Good
~Fair/Poor
CES-D Symptoms (mean. 0-8)4e
Psychological Factors
Cognitive Ability (mean, 0-54)b t
Future Orientation11
Short-Term Planner
Medium-Term Planner
Long-Term Planner
.
40.3
50.3
' 25.4
56.:
26.:
20.4
43.228.7
28.1
18.6
25.7
33.7
38.7
Social-Environment Factors
Spouse Smokes4
BlurCqllafWorkeA
Net Worth-(median)b
Employee Healthinsurance4
30.1
39.6
27.7
38.5
32.1
28.5 _
-26.8
124,000
------- ------------------------------------------------3-216
120,000-----76.4
3,049
—72,000
70,000
402
1,989
Standard deviations are presented below means
and lifestyle as well as physical and emotional
health that may be associated with education;
and (4) selected psychological, social environ
ment, and resources consequences of educa
tion. For ease of interpretation, the tables pre
sent parameter estimates and t-statistics as
well as odds ratios.
As shown in Table 2, certain enduring char
acteristics of individuals that may be seen as
precursors to education are consistently asso
ciated with whether or not middle-aged adults
ever smoked. For example, being female or
Latino significantly increases the odds of
never smoking in Model 1. These factors
remain significant in Models 2-4 as well, even
after education, health, lifestyle, and education
consequences are introduced. Most central to
our interest is that education is highly signifi
cant across Models 2-4, increasing the odds of
never smoking by 5-8 percent for every addi
tional year of education beyond high school. In
other words, more highly educated people are
iMPACT OF-fertJCATION AND HEART ATTAOCON^MOKING CESSATION
279
less likely to have ever started smoking. In —1992 and 1994 (net of selected correlates of
both Models 3 and 4, other behavioral, social • heart attack) in order to compare our findings
environment, and health factors such as being on middle-aged adults with findings in the lita heavy drinker, married to a smoker, or hav .erature.
Surprisingly, neither education nor the con
ing experienced a heart attack prior to 1992 are
also significantly associated with never smok sequences of education appear to play a role in
ing. Interestingly, greater numbers of CES-D - the likelihood of an incident heart attack,
depressive symptoms contribute significantly ■counter to recent studies (Diez-Roux et al.
1995; Feinstein 1993; Feldman et al. 1989;
to decreased odds of never smoking. Model 4
also, shows that working as a machine operator Matthews et al. 1989). However, other find
or laborer decreases the odds of never.smoking ings shown in Table 4 demonstrate support for
other “existing literature. For example, being
while greater net worth increases the odds.
female or a heavy drinker significantly
Table 3 presents data for middle-aged adults
who ever smoked and contrasts those who quit decreases the odds of experiencing a heart
prior to 1992 with those still smoking in 1992. attack. In contrast, being a smoker in 1992,
Among the precursors of education shown in having been diagnosed-with high blood pres
Model 1, being female or African American sure, and reporting higher levels of CES-D
reduces the odds of past quitting. In contrast, • depressive symptoms increase the odds.
In sum, the three sets of exploratory analy
higher levels of father’s education (our mea
sure of status origins) is positively associated ses indicate that education is importantly
with prior quitting. When education is intro ;Tinked“ to never starting smoking but only
duced in Models 2-4, only- being female indirectly, tostopping prior to 1992 and to the
remains consistently significant-among the experience of an incident heart attack. The
preprecursors. Education itself is-significantly consequences of education—represented here
linked to past quitting as expected—those who - as lifestyle and health status as well as psy
are more highly educated are more likely to chological, social-environment, and resources
have quit smoking before 1992—but only in factors—suppress the association between
Models 2 and 3. Once the consequences of education itself and prior stopping. Other fac
education are entered into Model 4, education tors that are influential to both past smoking
itself loses significance. All of our health and state? include gender and race/ethnicity. In
lifestyle measures plus cognitive ability, net general7all of the potential predictors in these
worth, and employee health insurance are also exploratory models except father’s education
significantly associated with prior quitting-and are consistently associated with past smoking
alLin the direction we would expect fromjtbe. ' behaviot-Eewer of the potential predictors in
literature.. That is, higher levels of cognitive .■ourmodeis are significantly relate ' > incident
ability and net worth, having- employer- heart attack, but those that arc ge. ally sup
provided health insurance coverage, or having port the literature and also are associated with
been diagnosed with a previous heart attack or educational level. Although the findings from
high blood pressure contribute positively to the exploratory analyses are associational
having quit smoking prior to 1992. In contrast.
rather than causal, they provide us with useful
detrimental health behaviors such as irregular information on which to base and interpret our
exercise or heavy drinking are negatively asso models of smoking cessation between 1992
ciated with prior quitting.
and 1’994. The major analytic models that are
described below combine all of the potential
predictors of past smoking behavior and
Predictors of Incident Heart Attack
incident heart attack except father’s education.
Finally,' Table 4 presents results of
exploratory analyses focusing on the experi
ence of an incident heart attack. In addition to
trying to understand how education con
tributed to smoking behavior prior to 1992
(when the HRS started), we also wanted to
understand how education might have influ
enced the experience of a heart attack between
Predictors ofSmoking Cessation Between
1992-1994
In this section, we describe the results of the
multivariate analyses on those people we are
most interested in. those represented in
columns 3 and 4 of Table I—the people who
TABLE 2. Logit Equations Showing Never Smoking Regressed on Education, Incident Heart Attache, and Selected Predictors Among U.S. Smokers Age 51-61,
1992 and 1994
I
I
|
,
Intercept
Female
African Americanb
I I
Latino6
i
1 |
Father^ Education
, •.
Education
■1
■^ognitive Ability
Short-Tenn Planner*
1 i ’l- ■, ■
. i :« 'Medium-Term Planner6
|
Model 1
Parameter
Characteristics*Estimate
-1.003*’*
(24.811)
.865***
(17.930)
-.120
(.227)
.280**
(2.585)
.011
(1.668)
—r~
■
—r~
Mddel 2
,
j Parameter
Odds Ratio' Estimate
Odds Ratio
-1.150***
(25.372)
’ .899***
(18.446)
.120
(.226)
.471
(4.208)
-.012
(1.703)
.746***
(7.663)
2.375
.980
1.323
1.011
------ ■
1.020
1.601
I
.988
1.077.
------
—
•
____
—
-1.285”*
(15.934)
.878».’
(15.478)
.265*
(2.535)
.520*”
. (3.948)
1 -.021***
(2.618)
I'.feiO**
(4.895)
.
1005
(.264)
-.1027
1
(.398)
. r .O]70
,1(1.160;.
■ -.244"
'(3M9)','
1 .•w’
2.457
I
—
| i
1.304
1.682
1.063
.980
1.005
.973
—
■- -
In1 : 1Blue Collar Worker i
■
—
1 i 1
— ■ ■■
■ .
. ..
—
—
—
—
'.047 .
(.732)
—
—
—
——.
..
|
Net Worth
LI |
fflj, |
:'ii
Obese
—
—
—
—
^regular Exercise
—
—
—
Heavy Drinker
—
—
—
.-
—
■(
i
ll. 'l i Spouse Smokes
■
'
|'l
Heart Attack
L !
■ 1992-1994
|r
1.072
.783
1.117
1
Health Insurance
I’
____
i
Mi'■[ ■'Employee
' ' •
!'
—
-1.102’**
(12.391)
.810***
(13.899)
.214*
(2.010)
.501**
(3.749)
-.020*
(2.551)
.051***
(4.040)
.000
(.010)
.003
(.048)
.084
(1.381)
-.225**
(2.897)
.104***
(6.958)
2 405
■
—
■
—
------
1
j
j-—■
.040
(.618)
.100
(1 557)
.009
(.109)
-1.279***
(6.945)
-.709***
(9.157)
<
.I
1 '*—1
1
—
1.048
r
____
|
1
■II
ihii
Model 1
1
-.541***
(3.683)
2.247
1.239
1.651
.980
1.052
1.000
1 003
1.088
.799
1.109
1.041
1.105
1.009
.278
.492
.582
TABLE 3.
Impact of Educationand Heart Attack on Smoking Cessation--—higher levels of education increasing that
probability only very modestly (from 14 to
16 percent). In stark contrast, among indi-..
viduals who did "experience a heart attack
(top curve), higher levels of educational
attainment clearly play a role in smoking
cessation. Middle-aged adults with at least
some high school education had a 30 per
cent probability of quitting if they had a
heart attack, compared to a 53 percent prob
ability for those who completed high
school. 83 percent for those with a college
education, and 88 percent for those with a
postbaccalaureate education. People who
never attended any high school and also
experienced an incident heart attack were
about as likely to quit smoking as those who .
did not experience a heart attack between
1992 and 1994:
Table 6 shows that introducing additional
predictors of smoking cessation to Model 4
of Table 5 changes the story only slightly. In
general, the additional predictors do not
modify the powerful effect of educatiorTon
the impact of_heart attack on smoking ces
sation. Model 5 includes not only education,
heart attack, and the interaction of educa
tion and heart attack but also the primary
correlates of smoking cessation and heart
attack. In Model 6, we add the potential
explanations for an- education and heart
attack- interaction. In those two models,
heart, attack remains a significant (and
somewhat stronger) predictor of quitting,.
. compared with Model 4. Education as a
-main effect continues to be nonsignificant.
However, the'effect of the interaction
between education and heart attack remains
significant and virtually unchanged in
strength from its effect in the previous
Jjnodel without the-primary correlates.
Among-the correlates of smoking cessation,
only being a heavy smoker, obesity, and the
experience of heart attack are significant
predictors: heavy smoking decreases the
odds of quitting and being overweight or
having a heart attack increases the odds,
while all other factors are held constant. In
addition, among the explanatory factors
added in Model 6, medium- versus long
term financial planning significantly pre
dicts smoking cessation, strongly and unex
pectedly increasing the odds of smoking
cessation.
'
JOURNAL OF HEALTH AND SOCIAL BEHAVIOR
ct of Edi cation and Heart Attack on Smoking Cessation
285
Finally, in'Model 7, we add to our pre
vious model a set of interaction terms
representing the product of heart attack
by each of the psychological, social
environment, and resources factors. We
do this for two primary reasons. First,
because each of these factors represents
consequences of education, we wanted
to test the relative effects of education
and its consequences both separately and
as interaction terms.6 Second, we also
wanted to test the effect of the heart
attack-education interaction term after
including all other education-related
interaction terms. Model 7 indicates that,
even with all of the interaction terms
entered into the model, the results are
scarcely altered, with' one_exception.
Heart ar-ck by education hoHs-as the
only sigt
cant interaction_term,-butthc .;
main effect for heart attack loses signifi
cance as well as considerable^strength.
Heavy cigarette dosage, obesity, and
mid-term planning remain-solid as other
significant predictors.
DISCUSSJ2N
Age 51-61, 1992 and 1994______________
TABLE 4. Logit Equations Showing Experience of Heart Attack 1992-1994 Regressed on Selected Risk Factors and Correlates of Education Among U.S. Adults
284
This study’s analyses of the effecLof
education on smoking cessation among
middle-aged adults led to both expected
and unexpected results, providifig-at=
least partial support for our primary and
secondary hypotheses. Surprisingly, and
counter to previous research (Douglas
1998; U.S. Department of Health and
Human Services 1989) as well as one of
our primary hypotheses, education alone
was not a significant predictor of smok
ing cessation in middle-aged adults. In
contrast, heart attack was significant,
supporting both literature and one prL
mary hypothesis. More importantly, the
interaction of education and heart attack
was a powerful and significant predictor
of smoking cessation: Among smokers
who experienced a heart attack, higher
levels of education played a protective
role by increasing the likelihood that
they would quit smoking. Absent a heart
attack, higher levels of education had
virtually no effect on whether ormot a
person quit Although this'may-seem
contrary to the expectation that increas-
------ JOURNAL OF HEALTH AND SOCIAL BEHAVIOR
ing levels of formal education should
lead to participating in more protec~tive health behaviors (Fuchs 1982;
Kenkel 1991), it may also reflect the
fact that education had already exert
ed a major effect on smoking behavior
before 1992 in our middle-aged adults
by reducing the likelihood that a more
highly educated person would have
ever started smoking or would have
remained a smoker until 1992.
The dramatic influence of higher
levels of education following the
experience of a heart attack suggests
that more highly educated older
smokers “learn" from their heart
attacks and quit smoking. This result
is particularly striking given the selec
tion effect on smokers. As reported by
other studies and our exploratory
analyses, many people with higher
levels of education had never smoked
or, if they had smoked, had already
quit by 1992, quite possibly in
— _ response to three decades worth of
g
Surgeon General’s reports, smoking~ ' related health events, -and family or
:j workplace pressures. The highly=
educated people who were still smok_g
ers in 1992 may have been longers
term smokers or more heavily addictI ed to cigarettes than were their
| counterparts who quit and, thus, may
jg— have-found quitting under most cir.■g_cumstances to be espec: '!y difficult.
-g - -Alternatively,, they ma. have been
exposed to other life events and risks
£ or had different personality characterg
istics that impeded their quitting previously. Whatever their initial barriers
g to quitting, education apparently pre<
vailed over addiction and other factors
to impel the better-educated, middle?
aged individuals to quit smoking once
» g. faced with a heart attack.
SJ g
Second, we found partial support
f°r on'y one
our s’x secondary
;"Lc hypotheses testing possible psychological, social-environment, anu
° |J
resources explanations for an educa-
=
‘. 5 J
81£ g
g|
•
?
t>on or education-heart attack effect
on smoking cessation. In particular,
one of the psychological factors,
future orientation, helped us disentangle the effect of the heart attack-
Years of Education
FIGURE 1. Probability of Quitting Smoking by 1994, Given the Experience of a Heart Attack
1992-1994 in U.S. Adults Age 51-61 (Table 5, Model 4)'
education interaction. Being a medium- versus
long-term planner unexpectedly increased the
odds ef quitting smoking, counter tb the idea
that people who are morehfuture-oriented
should participate in more healthful and less
addictive behaviors (Becker’et al. 1991, 1994;
Fuchs 1982). Preliminary analyses not pre
sented here indicated that long-term planners
were generally more highly educated and less
likely to be smokers in the first place, com
pared with-medium-term planners. However,
long-term planners who were smokers in 1992
were also disproportionately heavy smokers,
compared with short- and medium-term plan
ners. It may be that the current smokers whose
behaviors were analyzed in this snidy were
affected by'their future orientation differently
than were past smokers. Their heavier cigarette
dosage may have raised the “cost” of quitting
to such an extent that their higher education or
degree of future orientation became less pro
tective. Alternatively, medium- versus long
term planning may reflect a more "realistic”
(ally of the costs and benefits associated with
smoking cessation in older age. For example,
middle-aged smokers may surmise that even—
though quitting considerably reduces the risks
of heart attack, lung cancer, and other diseases
within 5-15 years, the fact that these diseases
are generally associated with older age may
promote the belief that there is little e-.entual
health benefit in stopping a presumably plea
surable habit in later life (Douglas 19^S; U.S.
Department of Health and Human Services
1990).
No evidence w'as found in our analyses to
support the effects of cognitive ability nor the
social-environment or resources factors asso
ciated with education that we posited might
play a role in smoking cessation among
middle-aged adults and help us to explain the
heart attack by education interaction effect.
Despite their nonsignificance, the inclusion of
education consequences in our models—par
ticularly in interaction terms—did lessen both
significance and strength of the heart attack by
education interaction. Perhaps other measures
of psychological orientation, social er. iron-
JOURNAL OF HEALTH AND SOCIAL BEHAVIOR
Impact of Ed; cation and He art Attack on Smoking Cessation
289
o.g
hi
ment, or resources would have proved more
informative.
Finally, among the primary correlates of
smoking cessation, heavy cigarette smoking in
1992 negatively influenced quitting by 1994.
Since some people with higher levels of edu
cation continued to smoke despite widelyavailable'information in the community on the
dangers of cigarette smoking (Kenkel 1991),
factors other than-health information must
have, driven decisions to quit or continue
smoking. Our analyses pointed toward one
such factor: The odds of smoking cessation
decreased strongly among heavy smokers,
demonstrating that the cost of quitting may be
greater for more strongly addicted smokers,'
even after controlling for "education and the
experience of a heart attack. These results sup
port other recent research (e.g., Marbella et al.
1995) also finding heavy smokers to be less
likely to quit smoking.
girr
In addition, being overweight strongly..pre-
dieted smoking cessation, although physical
activity did not, lending partial support to the
notion that participation in some beneficial
health behaviors should increase the likelihood
of participating in other such behaviors
(Matthews et al. 1989; Wagenknecht et al.
1990; Winkleby et al. 1992). In particular,
middle-aged adults who are overweight may
recognize the need to eliminate or control one
risk factor for heart-related disease (smoking) ■
bnt not others (exercise or wtight manage-
ment), reasoning that smoking cessation may
be a more critical predictor of enhanced health
than either of the other health behaviors.
Additional factors identified in the literature
as associated with education, heart attack, and
smoking cessation (e.g., gender, race/ethnicity,
heavy drinking, history of high blood pressure,
_ ,-and depressive
„r
self-assessed health status,
symptoms) failed to reach significance in our
models, whether or not we controlled for additional education-heart attack “explanations.”
Z9U
■
TOURNALOEHHALTH AND SOCIAL^EHAVIOR.
.... Certain attributes of the study's data set may only those with an education of at least high
-.have limited our ability to identify these or school or beyond changed their smoking
’ other potential predictors of smoking cessa behavior. Each additional year of educational
tion. First, the HRS collects disease and' attainment-beyond high school dramatically
health-condition data by self report. Although raised the probability of quitting—from one in
experience with heart attack in the past two two for those with a high-school education to
years is likely to be remembered reasonably near certainty for those with postbaccalaureate
well by respondents and the HRS does ask education.
what year the heart attack occurred, the data
Although this study’s focus on change in
are only as good as the respondent’s recall. one health behavior following the experience
Second, our measure of smoking cessation is of a potentially life-threatening health event
static and indirect in that it is based on reports was intentionally narrow, our analyses shed
of current or past smoking behavior in 1992 some light on the association between educa
and 1994. If a respondent stopped smoking tion and health. Our probe of education’s
between 1992 and 1994, the HRS does not ask effects on smoking cessation demonstrated
when s/he quit. Thus, we cannot know whether that education alone did not always provide
a report of no longer smoking in 1994 means sufficient incentive to quit smoking among our
the person has quit for a day. a month, a year, group of older smokers. As noted, these smok
or permanently. Neither can we know for cer ers may be different from younger smokers in
tain that smoking cessation followed the heart many ways, resulting in their being more resis
attack in the case of those smokers who expe tant to-decades of public health messages
rienced incident heart attacks. Finally, we did _about the dangers of cigarette smoking. The
not consider the influence of other long-term higher levels of knowledge, skills, and abilities
or more recent health problems other than high proxied by educational attainment furnished
blood pressure on the decision to quit smok the-necessary justification for quitting in such
ing. Clearly, smoking cessation is a complicat individuals.only when they suffered the shock
ed decision-making process that defies simple of a life-threatening health event.-Future
analysis or interpretation in our cohort of research could add to our understanding in this
middle-aged adults.
area by exploring education’s effects on a
. CONCLUSION
wider range of health and economic outcomes
at different points across the lifecourse, incor
porating different moderating life events as
well as other potential mediators of those out
comes.
This paper started by acknowledging the
well-established positive association between
—higher levels
education and enhancedhealth, including protective health behaviors:—NOTES
Ultimately, our study results augmented The
wealth of evidence from various academic dis 1.
The public release data set for Wave 3 of the
ciplines in confirming that association. Higher
■ HRS is expected to be available in fall
levels of education do, in fact, play a role in
1998.
one health-enhancing behavior, at least under 2.
In order to retain as many of the cases of
.some circumstances among preretirement-'
incident heart attack as possible, all heart
aged Americans. Our study also supported the
attacks between 1992 and 1994 were count
documented connection between heart attack
ed among respondents for whom these
and smoking cessation. In addition, our study
heart attacks represented first heart attacks
provided a surprising twist on those links: The
as well as respondents for whom the heart
move to quit smoking following the experience
attacks represented subsequent heart
of a heart attack among middle-aged adults
attacks.
was significantly and dramatically moderated 3.
The exploratory models focused on three
by their level of educational attainment.
dichotomous outcomes: never having
Among older smokers without an incident
smoked, ruining prior to 1992, and experi
heart attack, the probability of quitting smok
encing a heart attack between 1992 and
ing was less than one in six. However, among
1994. These models were tested on four
older smokers who experienced a heart attack,
sequentially -entered blocks of variables. (I)
-------- impact ofEducation and Heart Atiack on'Smoking Cessation
291 --
concept. However, their moderate correla
demographic and status origin-characteris
tion (r = 0.44) suggests that they are still
tics; (2) level of education; (3)health status, .
measuring different traits. Similar analyses
health behaviors, and lifestyle variables;
were, conducted substituting interaction
and (4) selected psychological, social erviterms comprised of heart attack by each of
ronment, and resources factors. All of the
the other psychological, social-environ
variables except the measure of status ori
ment, and resources factors believed to be
gins—father’s educational attainment—
consequences of education. However, none
reached significance in most’ of the
of these other interaction terms proved to be
exploratory models. These variables were
significant predictors in the preliminary
included in the final models predicting
analyses.
smoking cessation-and are described in
detail in the paper’s text. Father’s education
al attainment was measured as the number
of years the respondent reports his/her- REFERENCES
father completed, centered on 12 years of
■Adler, Nancy, Thomas Boyce. Margaret A. Chesney.
education.
Sheldon Cohen, Susan Folkman, .Robert L.
4.
Smoking cessation has been documented to
Kahn, and S. Leonard Syme. 1994'.
be a dynamic process with alternating.
“Socioeconomic Status and Health: The
periods of quitting and relapse before per
Challenge of the Gradient.” American
manent abstinence "(UTS. Department of.
Psychologist 48:15-24.
Health and Human Services 1990). While Anda, Robert E, David E Williamson, and Luis G.
acknowledging that dynamic process=we_. - Escobedo. 1990. “Depre-ion and the Dynamics
of Smoking: A National Perspective." JAMA ~
are constrained irr'our analyses to using a
264:1541-45.
static measure-based on changes in self
reported smoking status at two points in Antonovsky, Aaron. 196". "Social Class. Life
Expectancy, and Overall .Mortality." Milbank
time, 1992 and 1994.
____
Memorial Fund Quarterly 45:31-73.
5.
We combine these scores in order to tap two
Baile. Walter E, George E. Bigelow. Sidney H.
dimensions of cognitive ability—fluid and
Gottlieb, Maxine L. Stitzer, and J. D. Sacktor.
crystallized abilities—that may'influence a
1982. “Rapid Resumption of Cigarette Smoking
person’s capacity for making informed
Following Myocardial Infarction: Inverse
decisions..Fluid ability measures process
“Relation to MI Severitv." Addictive Behaviors
ing capabilities that affect the ability to _ 7:373-80.
acquire new informations Often used-in -Becker, Gary S.. Michael Grossman. and Kevin M.
standardized cognitive-screens "for-older- - Murphy. 1991. “Rational Addiction and the
Consumption.” American— adults, the word recall tests^primafily -s— Effect of Price
41.
- —___
(although not exclusively^ assess -fluid- - Economic Review .
Becker,
Gary
S..
Michael
Grossman, and Kevin M. ability which may decline somewhat with
Murphy. 1994. "An Empirical Analysis of
aging. In contrast, crystallized ability mea
Cigarette Addiction." American Economic
sures the actual acquisition ofthat informa
Review 84:396—418.
tion in the form of knowledge-based Becker. Gary S. and Kevir. M. Murphy 1988. "A
abilities (e.g., verbal and abstract reason
Theory of Rational Addiction.” Journal oj' ing) which are closely tied to educational ■
Political Economy 96:6'5-700.
attainment, remaining stable or even increas Behrman. Jcre R. 199' “Conceptual and
Measurement Issues." Pp. 17-67 in Social
ing throughout the life course. Word simi
Benefits, edited by J. Behrman and N Stacey.
larities tests primarily measure crystallized
Ann Arbor. MI: University of Michigan Press.
ability.
Breslau.
Naomi. Edward Peterson. Lonni Schultz,
6.
Preliminary analyses that are not presented
Patricia Andreski, and Howard Chilcoat. 1996.
here demonstrated that a heart attack by
“Are Smokers With Alcohol Disorders Less
cognitive ability interaction term (as a sub
Likelv to Quit?” .4mcn.cn Journal of Public
stitution for a heart attack by education
Health 86:9S5-90.
interaction term) was a significant predictor Brownson. Ross C.. Carol A Smith. Michael Pratt.
of smoking cessation. That seemed a logical
Nilsa E. Mack. Jeannene Jackson-Thompson.
Cynthia G. Dean. Sue Dabney, and Joan C.
finding given that education and cognitive
Wilkerson. 199a "Presenting Cardiovascular
ability are often perceived as two sides of
Disease Through C.—nunity-Based Ri>k
the same coin, that is, tapping into a similar
NO TOBACCO CAMPAIGN
Smoking can also
cause brittle bones
Researchers in the United States
say they may have discovered why
women who smoke are much more
prone than non-smokers to develop
brittle bones, or osteoporosis, in old
age.
Scientists at the Argonne National
Laboratory said the link between
cigarettes and bone loss appears to
be cadmium^a heavy metal found in
trade concentrations in vegetables
and tobacco. Pack-a-day smokers
| have blood levels of cadmium that
F average 15 times the levels in nonsmokers or people who have quit.
Argonne biochemicists Maryka
Bhattacharya and David Peterson
fed mice a diet with elevated levels of
cadmium, raising the concentration
in their blood to a point comparable
to that found in smokers.
They found the hejghtenedleyelsjof.
cadmium led to bone thinning in
pregnant mice that had their ovaries
removed. This operation on the mice
cuts off their main source of the
female reproductive hormone estro
gen. making them physically compara
ble to post-menopausal women.
As the amount of cadmium in the
diet of the mice was increased, the
amount of bone loss increased
iproportionately, the scientist found,
"out only in the two groups of females
lacking estrogen.
Osteoporosis, or brittle-bone
disease, is one of the most common
perils of humans in old age, affecting
typically, post menopausal, small
boned, white women who have
smoked. As the bones are stripped of
calcium, they become thin and brittle,
breaking readily, leading to repeated
fractures, especially of the hip, wrist
and ankle and crushing of backbones
leading to a condition known as
Dowager's Hump.
"Because the amount of cadmium
introduced into the blood stream
through feeding produced blood
cadmium levels similar to those
found in the blood of smokers",
Bhattacharya said.
48 • HEALTH ACTION OCTOBER 1983
Bhattacharya said in an interview
to UPI that cadmium levels are
heightened in smokers because lung_
tissue absorbs cadmium from
tobacco smoke much more effecti
vely than the digestive tract absorbs
from vegetables.
But she said the first clues that
cadmium might be a factor in
osteoporosis actually came from a
tragedy that involved ingested, not
inhaled, cadmium.
Japanese researchers found that
post-menopausal women living in a
town downstream from lead and zinc
mines had very high incidence of
osteoporosis. They suspected the
high levels of cadmium in the
stream's water and their diet were
responsible for the women's brittle
bones, but the Argonne study
provides the first direct evidence
that cadmium was to blame.
The fact that post-menopausal
women and female mice in pregnancy
or with their ovaries removed show
the cadmium effect most strongly
indicates that estrogen is also
involved in the effects of cadmium on
the bones, Battacharya said. But she
does not yet know how.
Exercise, calcium supplements,
and the hormone estrogen are
typically prescribed to prevent bone
loss in women prone to osteoporosis.
Studies described elsewhere in the
United States showed sodium
fluoride may also help strengthen
thinning bones in the spine.
Meanwhile, a group of researchers
from the West Valley Medical
Center in Los Angeles studied 38
women to see how their production
of a key substance involved in dilating
blood vessels was affected in they
smoked and took birth control pills.
They found evidence offering one
possible explanation for why women
who smoke and use oral contracep
tive pills may have an increased risk
for heart disease.
The key substance, known as
prostacycliiywhich doctors believe
may help prevent heart attack and
other cardiac disorders, wasjowest
in women who took the pills and who.
had smoked for at least five years,
the researchers found.
These women were compared to
those who took birth control pills but
did not smoke, those who smoked
but did not take the pill and those who
did neither.
The analysis, led by Dr. Gil
Mileikowsky, suggests decreased
prostacyclin production is the cause
of increased cardiovascular risk.
Because prostacycline also decrea
ses the formation of blood clots.
Meleikowsky cautions that lower
levels of the substance pave the way
for dangerous blood clot formation.
These clots can circulate through
out blood vessels and land in the
lungs, thus creating pulmonary
embolisms", he said.
Embolisms diminish the capacity
of the lung to function and supply the
body with oxygen.
The study suggests steroids
contained in birth control pills may
work in tandem with substances in
tobacco to dramatically lower
prostacyclin levels.
— Deccan.Herald (Bangalore)
COVER STORY
CANCER
Smokeless Tobacco and Oral Cancer:
A cause for concern?
Nlinni Sood
Advertisements for smokeless
tobacco imply that the habit is less
harmful than smoking. Unfortunately
this impression is common among
the public and even among health
professionals.
It is instructive to consider data
available from India, where more than
48% of cancers are found in the oral
cavity. This high incidence of oral
cancer has led a number of
researchers to look for factors that
might account for the observed
morbidity. In a series of extensive
epidemologic studies, Pindborg and
co-workers followed Ao.OOOJndians
for five years and a group of 30,000
for 10 years^They concluded that
oral cancer and oral precancerous
lesions (leukoplakia)occurred almost
solely among tnose whohadtobacco
habits of one type or another. The
use of tobacco in various forms, such
as in cigarettes, cigars, and for
chewing, is widespread in India, with
between 47% and 73% of the
population indulging in the habit,
compared with approximately 36%
in the U.S. High incidence of oral
cancer in India is not a reflection of a
unique susceptibility or a more
pernicious lesion, but simply of the
very high prevalence of tobacco use.
It is well known that in India, as in
many parts of South-east Asia,
chewing tobacco is mixed with a
variety of other substances, the
most common additive being the nut
of the betel palm, betelleaf, and
slaked lime.
Further evidence that points to
tobacco as a major etiological factor
in the development of oral lesions and
emphasises the greater risk_of
chewing over smoking comes from
studies in both India and U.S. These
reports have calculated the relative
risk for tobacco use, a factor that
indicates the greater risk of
developing cancer for a tobacco user
compared with a non-user. The
Indian data suggest that the relative
risk of developing oral cancer is 2.82
for smoker and 5.98 for chewers.
The study by Winn et. al. of female
smokers and snuff dippers on the
south east U.S. showed that the
relative risk of developing cancer of
the gums and buccal mucosa is 4.6
for smokers and from 13 to 48 for
snuff dippers, depending on how long
the user had indulged in the habit.
(fig. 1). Thus both the American and
Indian studies point to a greater risk
of developing oral cancer among
users of snuff and chewing tobacco
than among smokers, despite the
differences in the way smoke-less
tobacco is used in the two
populations.
Unfortunately, both the general
public and health professionals are
largely unaware of these risks. There
is a great need of health education.
The dental profession can play a
jeading rolei in sucfT programmes by
promoting an awareness of the
cancer risks
from
smokeless
tobacco, by discouraging its uses,
and by vigilance in detecting early
mucosal lesions among those who
persist with the habit.
Smokeless Tobacco is____________________________________________
not Safe
Smokeless tobacco (snuff for
exarfiple) does not carry the health.
hazard warning that cigarettes do,
but it should. It’s tobacco just the
same and is habit forming. The
nicotine in it lifts you up first... then
lets you down. That high-low effect
on your nervous system sets you up
for a continued need. That's what the
ads are really doing — trying to get
you hooked!
But that’s all. Habitual use of snuff
ahd chewing of tobacco means there
are other health hazards also. The
habitual users of smokeless tobacco
lose their ability to smell and the
sense of taste. Hence they need
more salt and sugar in their food,
both of which are unhealthy if used in
excess. They also face dental
problems, such as receding gums
and greater wear and tear of tooth
enamel. These lead to both decay and
bad breath. Like most tobacco users
they too develop discoloured teeth.
.Smokeless tobacco plays worse
havoc inside our body. If the person is
in the habit of chewing tobacco, it
irritates the delicate mucosa of his
mouth and over the course of years
he developes a white patch. This
white patch generally occurs at a
place where the quid is kept. The
.white patch is known as leukoplakia.
Thisjeukoplakia is a very peculiar
thing. Nearly 95% of cancers in the
mouth start with this patch. If a
person stops using tobacco, this
leukoplakia does disappear but it
takes years. But once it disappears,
there is no danger of getting cancer.’
— Consumer Confrontation
HEALTH ACTION OCTOBER 1989 • 21
Oral Diseases (1998) 4, 200-206
0 1998 Stockton Press All rights reserved. I354-523X/98 $12.00
http://vvww.stockton-press.co.uk/od
Dietary factors in oral! leukoplakia and submucous fibrosis
in a population-based case control study in Gujarat, India
PC Gupta1, JR Hebert2, RB Bhonsle1, PN Sinor1, H Mehta1, FS Mehta1
'Epidemiology Research Unit, Tata Institute of Fundamental Research, Homi Bhabha Road, Bombay 400005, India; 2Division of
Preventive and Behavioral Medicine, Department of Medicine, University of Massachusetts Medical School, 55, Lake Avenue,
Worcester, MA 01655, USA
OBJECTIVES: To investigate the relationship of specific
nutrients and food items with oral precancerous lesions
among tobacco users.
DESIGN: A population-based case-control study.
SETTING: Villages in Palitana taluk of Bhavnagar district,
Gujarat, India.
SUBJECTS AND METHODS: An interviewer-adminis
tered food frequency questionnaire, developed and vali
dated for this population, was used to estimate nutrient
intake in blinded, house-to-house interviews. Among
5018 male tobacco users, 318 were diagnosed as cases.
An equal number of controls matched on age (±5 years),
sex, village, and use of tobacco were selected.
MAIN OUTCOME MEASURES: Odds ratios (OR) from
multiple logistic regression analysis controlling for rel
evant variables (type of tobacco use and economic
status).
RESULTS: A protective effect of fibre was observed for
both oral submucous fibrosis (OSF) and leukoplakia, with
10% reduction in risk per g day-1 (P < 0.05). Ascorbic
acid appeared to be protective against leukoplakia with
the halving of risk in the two highest quartiles of intake
(versus the lowest quartile: OR = 0.46 and 0.44, respect
ively; P < 0.10). A protective effect of tomato consump
tion was observed in leukoplakia and a suggestion of a
protective effect of wheat in OSF.
CONCLUSION: In addition to tobacco use, intake of spe
cific nutrients may have a role in the development of oral
precancerous lesions.
Keywords: India; oral neoplasms; precancerous conditions;
nutrition; diet; /3-carotene; zinc; iron; ascorbic acid; submucous
fibrosis; leukoplakia; tobacco chewing; smoking
Introduction
Oral cancer is the sixth commonest cancer in the world
(Parkin el al, 1993). Its incidence is particularly high in
India, some other countries in Asia, and certain places in
Correspondence: Dr Prakash C Gupta, Epidemiology Research Unit, Tata
Institute of Fundamental Research, Homi Bhabha Road, Colaba, Mumbai400 005, India
Received 16 February 1998; revised and accepted 20 April 1998
the Western hemisphere, e.g., parts of France and Brazil.
In the Western hemisphere, smoking and alcohol drinking
are major risk factors, whereas in India, the chewing of
tobacco products, in addition to smoking in various forms,
is primarily responsible for the high incidence. The WHO
have estimated that 90% of oral cancers in India among
men are attributable to the chewing and smoking of tobacco
(WHO, 1984).
Nutritional risk factors have also been implicated in can
cers of the oral cavity. A number of studies have indicated
that the consumption of various vegetables and fruits
reduces risk. These relationships may be independent of
other risk factors and show a dose-response (Marshall el
al, 1982; Winn et al, 1984; Franco et al, 1989). However,
there is considerable potential for confounding, and this
may be difficult or impossible to control in most epidemiol
ogic studies on the subject (Marshall and Boyle, 1996).
Oral cancer is often preceded by oral precancerous
lesions and conditions (Pindborg, 1980). Conversely, the
relative risk of individuals with oral precancerous lesions
developing oral cancer has been demonstrated to be very
high, even after controlling for the use of tobacco (Gupta
et al, 1989). The association of oral precancerous lesions
with tobacco habits follows a pattern similar to that of oral
cancer (Gupta et al, 1980). Because the prevalence of oral
precancerous lesions is much higher than that of oral can
cer, these lesions provide useful clinical markers for oral
cancer. They have been used as such in large-scale inter
vention trials (Gupta et al, 1992a).
A focus on precancerous lesions avoids much of the
potential for measurement bias and confounding that affect
most studies of diet and oral cancer (Marshall and Boyle,
1996) because many of these conditions, such as oral leuko
plakia, would have no plausible effect on dietary intake. It
should be noted, however, that oral submucous fibrosis
(OSF) may affect intake to some extent because of associa
ted symptoms, a common one being a burning sensation on
intake of spicy food. An additional rationale for conducting
a study in an Indian population included a probable wide
range of variability in nutrient exposures (Rao, 1987;
NIN, 1991).
The primary goal of this research was to test the relation
ship between precancerous changes in the mouth and diet
ary intake of specific nutrients; in particular the antioxidant
vitamins, several minerals, the B-vitamins, and fibre
Dietary factors in oral leukoplakia and OSF
PC Gupta et oi
through a population-based case-control study. These nutri
ents were chosen based on the availability of nutrient con
tents of foods commonly eaten in India (NIN, 1993; Hebert
et al. 1998) and on a variety of laboratory (Shklar and
Schwartz, 1993; Kandarkar and Sawant, 1996) and human
experimental studies (Garewal and Schantz, 1995; Krishnaswamy et al. 1995; Prasad et al, 1995; Tanaka, 1995;
Maher et al. 1997) especially relevant to India. A food fre
quency questionnaire (FFQ) specific to this population was
developed and validated for collecting dietary information
necessary to estimate exposure to these and a variety of
other nutrients. In general, the results of the validation
study indicated a higher level of accuracy than what is
observed in studies conducted in the West. Besides examin
ing relationships between the lesions and these specific
(nutrients we also sought to investigate the potential role of
specific foods.
Subjects and methods
Subject recruitment/data collection
This study was conducted in one of the 12 taluks, Palitana.
of Bhavnagar district, Gujarat state. Among 92 villages in
this taluk, 20 that were geographically contiguous and not
included in earlier studies (Gupta et al, 1980, 1992a) were
chosen. A preliminary census was conducted for listing all
households along with the identification information for
each member of the household and their tobacco use status
in each selected village.
A team consisting of dentists, social scientists, field
investigators and a nutritionist visited each household on
the house lists. As the first step in the recruitment/data col
lection process, a field investigator interviewed the poten
tial study subject (males aged 15 years or over) and filled
out a questionnaire containing basic demographic infor
mation and details of tobacco habits. Only males were
included, as in earlier studies in Bhavnagar district very
few females reported using tobacco and were diagnosed
with oral precancerous lesions (Mehta et al, 1969b; Gupta
et al, 1980). The subject was then examined by one of the
authors (PNS) and an additional examining dentist for the
presence of oral precancerous lesions. After examination
by the dentist, the subject was classified as a case if he had
an eligible precancerous change (either OSF or leukoplakia)
or a lesion (an ulcer or a growth) suspicious of oral cancer.
The first male from the same village, examined sub
sequently and found to be free of any oral mucosal lesion,
and matched on age (±5 years) and tobacco use (yes/no)
was selected as a control. The potential control pool thus
consisted of all examined persons who were found to be
free of lesions. The recruitment was halted when we had
safely exceeded the predesignated goal of 250 cases and
250 matched controls. This was earlier than anticipated
because of an unexpectedly high prevalence of OSF found
during examinations.
The most common precancerous lesions in this region
are OSF and leukoplakia (Pindborg, 1980). Oral leuko
plakia was defined as a raised white patch 5 mm or more
in diameter which could not be scraped off and could not
be ascribed to any other diagnosable disease. OSF was
diagnosed on the basis of palpable fibrous bands (Pindborg,
1980). For lesions suspicious of being oral cancer, the diag
nosis was confirmed histologically.
Smoking of bidis and clay pipe (hookli) are the common
forms of smoking tobacco. Bidi is a smoking stick prepared
by rolling 0.15-0.25 g of sun-dried flake-form of tobacco,
in a rectangular dried piece of tembumi leaf (Diospyrous
melanoxylon). It is sold in bundles of 25. Mawa is a prep
aration containing thin shavings of areca nut (5-6 g) with
the addition of some tobacco (about 0.3 g) and few drops
of watery slaked lime. The contents, kept on a piece of
cellophane paper, are tied with a thread into a ball and the
packet is rubbed vigorously on the palm to homogenise the
contents. It is then opened and a portion, or the whole of
it, is placed in the mouth. Other tobacco habits practised
in the region are described elsewhere (Bhonsie et al, 1990).
The FFQ interview was conducted only if a subject was
selected as a case or a control and after obtaining informed
consent. To minimise the likelihood of bias, all data were
collected in a blinded fashion (i.e., the interviewer was not
aware of the status of the subject and the subject was not
told of the presence or absence of the lesion until com
pletion of the interview). Therefore, unlike most case
control studies, the FFQ was administered without anyone
involved in the collection of the dietary data having knowl
edge of the subject’s disease status.
The FFQ took about 25 min to complete. It consisted of
questions on the typical frequency and quantity of con
sumption of 92 food items representing >95% of exposure
to total energy, fat, fibre, iron, copper, zinc, calcium, ascor
bic acid, (3-carotene, and the B-vitamins in this population.
Statistical methods
Descriptive statistics were computed for all variables.
These consisted of standard parametric statistics for
continuous variables (e.g., the nutrient scores), and non
parametric frequency statistics for variables measured as
counts or on an ordinal or nominal scale. Each target nutri
ent score was also categorised into quartiles of its respect
ive distribution.
For this case-control study, the definitive multivariable
analysis was conducted using a logistic regression model.
Even though cases and controls were users of tobacco in
some form, because of the strength of association between
tobacco use and oral cancer and these precancerous lesions,
some designation of tobacco habit was fit in all models.
For leukoplakia, we fit one indicator variable indicating
smoking (whether or not the person also chewed tobacco)
versus chewing only (as the referent). For OSF, there were
two indicator variables: one for chewing mawa (with any
other tobacco exposure) and one for any chewing other than
mawa', with the referent being non-chewers (i.e., smoking
only). Any chewing in general, and mawa chewing in parti
cular (but not smoking), have been shown to carry high
relative risks for OSF (Sinor et al, 1990).
In most investigations of diet or smoking it is important
to account for social and economic variables that often
function as proxies for potentially important risk factors for
cancer and therefore can act as confounders of such analy
ses. For this population we defined three economic classes
described as follows. High status individuals were those:
possessing a concrete or tiled house; owning a farm
Dietary factors in oral leukoplakia and OSF
PC Gupta et al
employing servants; having a successful business or shop;
or being a government officer. Middle status individuals
were those: having a low-level government job; being a
primary school teacher; owning a small shop; owning a
house plastered with mud and cowdung; or owning a smallscale farm. Low status individuals were those marginally
employed or unemployed individuals who could neither
afford to live in their own house nor own their own
business.
Dietary data were fit both as nutrient scores and as fre
quency of exposure to specific categories of food items.
Nutrient scores and estimates of food frequency were fit
both as continuous data and as quartiles, in separate models.
Due to the fact that these dietary factors are highly corre
lated, it is important to model them separately from one
another.
Analyses were conducted for all lesions together and sep
arately for leukoplakia and OSF. Because dietary exposure
estimates may be biased by overall errors in reporting
(Willett, 1990; Bingham and Nelson, 1991) and some nutri
ents have a stoichiometric relation with total energy utilis
ation (Goodhart and Shils, 1980), we controlled for total
energy intake in the logistic regression models focusing on
nutrient exposures. All analyses were conducted using the
personal computer version of SAS (1997). All logistic
regression models were tested for goodness of fit using the
Hosmer and Lemeshow statistic (Hosmer and Lemeshow,
1989).
Results
Of 5018 male tobacco users examined, 323 were found to
have qualifying lesions, and thus met the criterion of being
a case. Out of these, 318 cases could be exactly matched
to an equal number of controls. These 636 study subjects,
out of a total of 666, were used for analysis. Shown in
Table 1, are the descriptive statistics of the study popu
lation, including the daily nutrient intakes, as estimated by
the FFQ. Because nutrient data were modelled as quartiles
of exposure, the cutpoints for the 13 nutrients of primary
interest in this study are shown in Table 2. The distribution
of lesions is also presented (Table 3).
All logistic models had diagnostics consistent with a
good model fit. Results from models in which a particular
nutrient or food category was found to be at least mar
ginally significantly associated (P =s 0.1) with either leuko
plakia or OSF are shown in Table 4 (for nutrients) or Table
5 (for foods). In all models, irrespective of specific nutrient
or food effects, virtually identical results were observed for
all control variables. For example, in OSF models in which
we controlled for dietary energy and no specific food or
nutrient: relative to smoking alone, mawa chewing was
associated with a marked elevation of risk (OR = 28.9; 95%
CI = 3.8, 222.0). For other forms of chewing the risk was
also elevated (OR = 10.4; 95% CI = 1.2, 89.8). Relative to
low economic status, for middle economic status the OR
was 0.90 (95% CI = 0.45, 1.83) and for high economic
status the OR was 1.11 (95% CI = 0.47, 2.60). Relative to
sedentary work, for occupations requiring physical activity
the OR was 0.85 (95% CI = 0.51, 1.43). For dietary energy
(kcal d-') the OR was 0.80 (P = 0.08). However, in the
Table 1 Descriptive statistics in diet and oral prccanccr study, Bhavnagar District, Gujarat*
Controls
Cases
Categorical variables*
Males
Occupation||
Active
Sedentary
Education
Illiterate
Primary
Middle
High School
College
Social category
Forward
Backward
Schedule
Socio-economic status
High
Middle
Low
Tobacco use
No areca nut^
Mawa
Areca nut with
tobacco
Mixed with smoking
Continuous variables/
Age (years)
Height (in ems)
Weight (in kgs)
Nutrientsti
Total energy (Kcal
d-’)‘
Total fat (g d ')
Fat (% Energy)
Fibre (g d1)
Iron (mg d_|)
Sodium (mg d-1)
Copper (mg d“‘)
Zinc (mg d-1)
Calcium (mg d~‘)
Ascorbic acid (mg
d-')§
/3-Carotene (gg
d-')§
Thiamin (mg d_|)
Riboflavin (mg d~‘)
n
W
(100.0)
318
(100.0)
(37.4)
(62.6)
112
206
(35.2)
(64.8)
137
101
50
24
6
(43.1)
(31.8)
(15.7)
(7.6)
(1.9)
126
111
51
27
3
(39.6)
(34.9)
(16.0)
(8.5)
(0-9)
199
106
13
(62.6)
(33.3)
(4.1)
207
86
25
(65.1)
(27.0)
(7.9)
53
188
77
(16.7)
(59.1)
(56.2)
64
194
60
(20.1)
(61.0)
(43.8)
164
131
2
(51.6)
(41.2)
(0.6)
175
102
14
(55.0)
(32.1)
(4.4)
n
(%)
318
119
199
21
(6.6)
27
(8.5)
Mean
38.1
164.1
51.2
(s.d.)
(14.7)
(5.5)
(9.4)
Mean
38.3
164.0
51.5
(s.d.)
(14.3)
(5.6)
(9.7)
2945
(942)
3051
(1056)
124.6
(50.6)
37.1
(5.8)
10.8
(4.3)
33.4
(9.7)
368.7
(227.2)
4.04
(1.24)
12.3
(3.6)
907
(425)
4.1
(0.6)
8.0
(0.5)
2.02
1.82
(0.63)
(0.70)
131.7
(56.5)
37.9
(5.8)
11.9
(5.4)
34.6
(11.2)
356.8
(190.6)
4.18
(1.41)
1 6
(4.0)
917
(396)
4.2
(0.6)
8.0
(0.5)
1.81
(0.72)
(0.68)
♦Values presented arc the number and percentages of all cases and controls
with the attribute
tValue is the mean and standard deviation (s.d.) by case and control status
^Nutrients are daily amounts as calculated from the food frequency ques
tionnaire, as described in the text
§Values for these nutrients are log transformed to normalise the distri
bution
((Categories arc defined as follows: Active included people engaged in
farming, merchandising, and any type of labour work, whereas sedentary
was defined as business men, professionals, skilled labourer (most of them
diamond cutters), secretary, clerk and householders
^Almost all of them (93%) were smokers. Rest were chewers of tobacco
with lime
Dietary factors in oral leukoplakia and OSF
PC Gupta el al
Table 2 Quartile designations of candidate nutrients, diet and oral prccancer study, Bhavnagar District, Gujarat*
Table 5 Adjusted odds ratios for foods in relation to submucous fibrosis
and leukoplakia in diet and oral precanccr study Bhavnagar District, Guja-
Percentile values
Food groups
25%
Total energy (Kcal d~‘)
Total fat (g d“’)
Fat (% Energy)
Fibre (g d1)
Iron (mg d~’)
Sodium (mg d ’1)
Copper (mg d “ ’)
Zinc (mg d“‘)
Calcium (mg d-1)
Vitamin C (g d ')
/3-Carotcne (/ng d-1)
Thiamin (mg d-1)
Riboflavin (mg d-')
2335.3
91.9
34.6
8.0
27.2
230.8
10.0
634.9
40.2
2195.6
1.6
1.4
2883.9
3535.0
154.2
41.1
13.7
39.8
448.8
4.8
14.4
1097.9
96.1
4237.3
2.4
2.1
38.4
10.4
32.4
317.4
3.9
12.0
834.8
65.9
3082.7
2.0
1.7
* Based on the food frequency questionnaire
Table 3 Distribution of lesion types in diet and oral precancer study,
Gujarat*
Male
n
(%)
Submucous fibrosis
Leukoplakia
Carcinoma!
149
168
1
(46.9)
(52.8)
(0.3)
Total number of subjects with qualifying
lesions
318
*Tabulatcd values are die number of subjects (cases) with each lesion.
The value in parentheses is the percent of total represented by this lesion
tPreviously undiagnosed. Suspected to be oral cancer on clinical examin
ation and later confirmed histologically
Table 4 Adjusted odds ratios for dietary nutrients in relation to submuc
ous fibrosis and leukoplakia in diet and oral precancer study Bhavnagar
District, Gujarat*
Submucous fibrosis?
Fibre (g/d)
Leukoplakia§
Fibre (g d-1)
Ascorbic acid (10 mg d_|)
Ascorbic acid
quartile 2
quartile 3
quartile 4
Odds Ratio (95%CI)
P-value
0.69 (0.43, 1.12)
0.49 (0.20, 1.17)
0.93 (0.86, 1.01)
0.85 (0.70, 1.04)
0.1
0.1
0.07
0.1
0.40 (0.15, 1.09)
0.63 (0.39, 1.03)
0.78 (0.61, 1.00)
0.32 (0.12, 0.87)
0.07
0.06
0.05
0.03
<0.01!
75%
50%
Odds Ratio (95% CI)
P-value
0.89 (0.81. 0.99)
0.02
0.87 (0.79, 0.97)
0.95 (0.89, 1.01)
0.01
0.01
<0.011
0.82 (0.45, 1.49)
0.48 (0.25, 0.95)
0.45 (0.21, 1.00)
♦Results are based on a logistic regression model fitting social
class/economic status, tobacco exposure, total dietary energy as control
variables
tThis is the P-value for the test of trend
iResults based on 149 cases and 149 controls
§Results based on 168 cases and 168 controls
Submucous fibrosis!
Roots & tubers
Onion
Wheat preparation
Fruit
Leukoplakia§
Pulse
Roots & tubers
Other vegetables
Tomato
Tomato
quartile 2
quartile 3
quartile 4
0.95 (0.53, 1.69)
0.66 (0.35, 1.23)
0.42 (0.22, 0.81)
♦Results are based on a logistic regression model fitting social
class/economic status, tobacco exposure and total dietary energy as con
trol variables
tThis is the P-value for the test of trend
iResults based on 149 cases and 149 controls
§Results based on 168 cases and 168 controls
model shown in Table 4, fibre removed the effect of total
energy.
In leukoplakia models in which we controlled for dietary
energy and no specific food or nutrient: smoking relative
to chewing alone showed an increased risk (OR = 8.69;
95% CI = 2.53, 29.79). Relative to low economic status,
for middle economic status the OR was 0.79 (95% CI =
0.46, 1.36) and for high economic status the OR was 0.45
(95% CI = 0.22, 0.91). Dietary energy (kcal d~') did not
affect the risk (OR = 1.00).
In the nutrient-based analyses for OSF, only dietary fibre
was significantly protective after accounting for relevant
covariates. It showed a strongly linear protective effect (OR
= 0.89 on a continuous scale (g d-1), P < 0.02, Table 4).
For leukoplakia, fibre was similarly protective (OR = 0.87,
P < 0.01). In addition, ascorbic acid appeared to be protec
tive in a linear fashion (OR = 0.95, P < 0.1), but it also
evinced a very strong trend in the quartile-based analyses
(P < 0.01).
For OSF, a variety of foods were found to be marginally
associated (P < 0.1) including roots and tubers, onion,
wheat preparations, and fruits (Table 5). For leukoplakia.
a number of foods were found to be significantly protective,
especially pulse and tomato (P < 0.02).
Discussion
Studies attempting to relate diet with oral cancer must con
front two major obstacles, one inherent in the relationships
among relevant risk factors and the other a consequence of
the distribution of oral cancer in human populations. In
most populations, oral cancer is strongly related to either
tobacco use or alcohol consumption or both (Marshall and
Boyle, 1996) and, typically, these two risk factors are
related to diet (Hebert and Kabat, 1990, 1991). As such.
they can confound the effect of dietary factors. For
203
Dietary factors in oral leukoplakia and OSF
PC Gupta et al
example, even in studies using serum levels of /3-carotene
(Zheng et al. 1993), unless smoking is carefully measured
and controlled in analyses, inferences regarding dietary /3carotene will almost certainly be confounded because
smoking is itself an important determinant of serum /3-carotene levels (Stryker et al, 1988; Hebert et al, 1994).
Due to the fact that oral cancer is a very rare disease in
most populations, it has been amenable to study using
mainly case-control designs. Such designs are subject to
biases in self-report, arising either directly or indirectly
from changes in exposure to risk factors concomitant with
the onset of disease symptoms (Hebert and Miller, 1988;
Marshall and Boyle, 1996), or to beliefs held by research
subjects regarding the causes of disease (Hebert et al,
1995). Because oral cancer is likely to affect the diets of
oral cancer patients and diet-cancer hypotheses have been
popularised in many populations, such studies are limited
by the potential for biased dietary recall among the cases
as compared to the controls (Marshall and Boyle, 1996).
There are no reports in the scientific literature of any belief
among Indian populations about diet causing cancer,
though there are widely held beliefs about the relationship
between food habits and health, more generally (Messer,
1997).
In this study, we were careful to enrol only users of tob
acco and then to measure their exposure to tobacco pro
ducts using methods that had been developed and refined
through years of study in the Bhavnagar district (Mehta et
al, 1969b; Gupta et al, 1980, 1992b). Gujarat traditionally
has been (and continues to be) a dry state, therefore alcohol
consumption is illegal, socially unacceptable, and the rate
of consumption is generally quite low. Besides, it is known
that alcohol intake is less influential for the risk of oral
leukoplakia in Indian populations (Gupta, 1984). Therefore,
we did not attempt to measure alcohol exposure in this
population.
In designing this study, a decision was made to focus on
precancerous lesions. In part, this was to increase outcome
yield and in part to reduce the probability of biased dietary
exposure estimates due to the presence of a condition that
could affect the physical sensation and payability of food
among the cases. OSF, however, does affect palatability of
food items to some extent, particularly due to associated
oral symptoms (the most common being a burning sen
sation on the intake of spicy food). The prevalence of this
condition in Bhavnagar district in an earlier study
(Pindborg et al, 1968) was only 0.16% but turned out to
be extraordinarily high in this study. This finding lends cre
dence to a suspicion of an evolving epidemic of OSF in
India (Babu et al, 1997).
Despite a possibility of a restriction in the intake of spicy
food among OSF cases and consequent bias, we decided to
include this condition in this study. This decision was based
on our prior research indicating high relative risks of
developing frank oral cancer in individuals with either leu
koplakia or OSF compared to individuals without any pre
cancerous lesion or condition, even after accounting for
tobacco use in the form of chewing or smoking (Gupta et
al, 1989). By studying these conditions earlier on in the
natural history of the disease, there would be a better
chance of determining diet during the more etiologically
relevant period. The one oral cancer included in this study
was early-stage disease without symptoms, but was con
firmed histologically. Finally, in order to further reduce the
probability of bias, we chose to withhold the diagnosis of
any lesion from both the subject and the interviewer until
the FFQ interview was completed.
This study used a custom-made FFQ with portion size
and recipe database to estimate nutrient exposure in the
target population. Because there is a sizeable fraction of
the adult population that is illiterate, it was decided to have
the FFQ administered by an expert interviewer. Previous
testing of this instrument in a group of subjects from vil
lages in the target population census area indicated a
reasonable level of agreement when comparing nutrient
consumption data derived from this FFQ to nutrient data
derived from 6 days of 24-h diet recall interviews adminis-.
tered over a 1-year period.
The strongest and most consistent relationships observed
in this study were the protective effects of fibre for both
OSF and leukoplakia. In a hospital-based case-control study
in China, it was found that dietary fibre derived from fruits
and vegetables showed a strong negative association with
oral cancer risk (Zheng et al, 1993), a result consistent with
the effect of overall vegetable intake here. In another case
control study in the USA, fibre was also found to be protec
tive (Marshall et al, 1992). Ascorbic acid was found to be
protective for leukoplakia, consistent with a wide range of
evidence (Marshall et al, 1982; Hinds et al, 1984; Verreault
et al, 1989). This protective effect, found at very low levels
of consumption in this population, is not inconsistent with
a lack of effect of ascorbic acid for reversing leukoplakia
that was reported at much higher doses (Kaugars et al,
1994, 1996). Thus, while reconfirming a previously
reported strong relationship in this population between
smoking and leukoplakia (Mehta et al, 1969a), and rnawa
chewing and OSF (Sinor et al, 1990), the present study
revealed a protective effect of ascorbic acid on leukoplakia
and of fibre on both leukoplakia and OSF.
The marginally protective effects of onion (and allium
vegetables generally), fruits, and pulses, is consistent with
a broad range of evidence concerning epithelial cancers
(Committee on Diet NaC, 1982; Byers, 1988; US Dept of
Health and Human Serv, 1988; Nat Academy of Sciences,
1989; AICR, 1997). Of all foods, the tomato was the most
strongly protective for leukoplakia. This is consistent with
other evidence in humans (Steinmets and Potter. 1996;
Gerster, 1997), its inhibition of proliferation in cell culture
(Levy et al, 1995), and its strong antioxidant properties
(Stahl and Sies, 1996). There is one recent report about the
possible effect of copper on OSF (Trivedy et al, 1997),
although this interpretation was questioned (Meghji et al,
1997). In our study, we did not observe any effect of copper
on OSF.
In summary, this study found protective effects of several
nutrients and categories of foods in both OSF and leuko
plakia. That we were able to observe these relationships
using a design that obviated many of the possible reporting
biases in conventional case-control studies of frank oral
cancer, underlines two very important things. The first is
the fact that these dietary factors play a role in the presence
of tobacco use, the dominant risk factor for these con
Dietary factors in oral leukoplakia and OSF
PC Gupta et al
ditions. The second is that the public health message must
be focused primarily on eliminating exposure to tobacco,
in any of the forms in which it is currently used.
Acknowledgements
This work was supported by the Special Foreign Currency Pro
gram of the Fogarty International Center (National Institutes of
Health). Grant number N-406-645, and a USIA Fulbright Senior
Research Fellowship to Dr James R Hebert for the 1997-1998
academic year through the US Educational Foundation in India.
The authors acknowledge the help of Dr VS Pawar, an examining
dentist in the field.
References
AICR (1997). Food, Nutrition and the Prevention of Cancer: A
I Global Perspective. American Institute for Cancer Research:
Washington, DC.
Babu S. Sesikeran B, Bhal RV (1997). Oral fibrosis among teen
agers chewing tobacco, areca nut. and pan masala. Lancet
318: 692.
Bhonsle RN, Murti PR, Gupta PC (1990). Tobacco habits in India.
In: Gupta PC, Hamner JE, Murti PR, eds. Control of TobaccoRelated Cancers and Other Diseases: Proceedings of an Inter
national Symposium: 15-19 January 1990. Oxford University
Press: Bombay. India, pp 25-46.
Bingham SA. Nelson M (1991). Assessment of food consumption
and nutrient intake. In: Margetts BM, Nelson M, eds. Design
concepts in nutritional epidemiology. Oxford University Press:
New York, pp 153-167.
Byers T (1988). Diet and cancer: any progress in the interim?
'Cancer 62: 1713-1724.
Committee on Diet NaC (1982). Diet, Nutrition and Cancer.
National Academy Press.
Franco EL, Kowalski LP, Oliveira BV et al (1989). Risk factors
for oral cancer in Brazil: a case-control study. Int J Cancer 43:
992-1000.
Garewal HS, Schantz S (1995). Emerging role of beta-carotene
and anitoxidant nutrients in prevention of oral cancer. Arch
Otolaryngol Head Neck Surg 121: 141-144.
Gerster H (1997). The potential role of lycopene for human health.
J Am Coll Nutr 16: 109-126.
Goodhart RS, Shils ME, eds (1980). Modern Nutrition in Health
and Disease. 6th edn. Lea & Febiger: Philadelphia.
Gupta PC (1984). Epidemiologic study of the association between
alcohol habits and oral leukoplakia. Community Dent Oral Epi
demiol 12: 47-50.
Gupta PC, Bhonsle RB, Murti PR et al (1989). An epidemiologic
assessment of cancer risk in oral precancerous lesions in India
with special reference to nodular leukoplakia. Cancer 63:
2247-2252.
Gupta PC. Mehta FS, Daftary DK et al (1980). Incidence of oral
cancer and natural history of oral precancerous lesions in a 10year follow-up study of Indian villagers. Community Dent Oral
Epidemiol 8: 287-333.
Gupta PC, Hamner JE. Murti PR (1992b). Control of TobaccoRelated Cancers and Other Diseases: Proceedings of an Inter
national Symposium: 15-19 January 1990. Oxford University
Press: Bombay, India.
Gupta PC, Mehta FS, Pindborg JJ et al (1992a). Primary preven
tion trial on oral cancer in India: a 10-year follow-up study.
J Oral Pathol Med 21: 433^139.
Hebert JR, Clemow L, Pbert L et al (1995). Social desirability
and approval biases in dietary self-report may profoundly
compromise the validity of diet-disease studies. Int J Epidemiol
24: 389-398.
Hebert JR, Gupta PC, Bhonsle RB et al (1998). Development and
testing of a quantitative food frequency questionnaire for use
in Kerala, India. Public Health Nutr (in press).
Hebert JR, Hurley TG, Hsieh J et al (1994). Determinants of
plasma vitamins and lipids: the working well study. Am J Epi
demiol 140: 132-147.
Hebert JR. Kabat GC (1990). Differences in dietary intake asso
ciated with smoking status. Eur J Clin Nutr 44: 185-193.
Hebert JR, Kabat GC (1991). Implications for cancer epidemi
ology of differences in dietary intake associated with alcohol
consumption. Nutr Cancer 15: 107-119.
Hebert JR, Miller DR (1988). Methodologic considerations for
investigating the diet-canccr link. Ain J Clin Nutr 47: 1068—
1077.
Hinds MW, Kolonel LN, Hankin JH et al (1984). Dietary vitamin
A, carotene, vitamin C, and risk of lung cancer in Hawaii. Am
J Epidemiol 119(2): 227-237.
Hosmer DW, Lemeshow S (1989). Applied Logistic Regression.
John Wiley & Sons: New York City.
Kandarkar SV, Sawant SS (1996). The effect of vitamin C on the
hamster cheek pouch treated with the water soluble carcinogen
4-nitroquinoline-l-oxide (4NQO). Eur J Cancer 32B: 230-237.
Kaugars GE, Silverman SJ, Lovas JG et al (1994). A clinical trial
of antioxidant supplements in the treatment of oral leukoplakia.
Oral Surg Oral Med Oral Pathol 78: 462^168.
Kaugars GE, Silverman SJ, Lovas JG et al (1996). Use of antioxi
dant supplements in the treatment of human oral leukoplakia.
Oral Surg Oral Med Oral Path 81: 5-14.
Krishnaswamy K, Prasad MP, Krishna TP et al (1995). A case
study of nutrient intervention of oral precancerous lesions in
India. Eur J Cancer 21B: 41-48.
Levy J, Bosin E, Feldman B et al (1995). Lycopene is a more
potent inhibitor of human cancer cell proliferation than either
alpha-carotene or beta-carotene. Nutr Cancer 24: 257-266.
Maher R, Aga P, Johnson NW et al (1997). Evaluation of multiple
micronutrient supplementation in the management of oral sub
mucous fibrosis in Karachi, Pakistan. Nutr Cancer 27: 41—47.
Marshall JR, Boyle P (1996). Nutrition and oral cancer. Cancer
Causes Control 7: 101-111.
Marshall JR, Graham S, Haughey BP et al (1992). Smoking, alco
hol, dentition and diet in the epidemiology of oral cancer. Eur
J Cancer 28B: 9-15.
Marshall J, Graham S, Mettlin C et a/ (1982). Diet in the epidemi
ology of oral cancer. Nutr Cancer 3: 145-149.
Meghji S, Haque MF, Harris M (1997). Oral submucosis fibrosis
and copper. Lancet 350: 220.
Mehta F, Pindborg J. Daftary D et al (1969a). Oral leukoplakia
among Indian villagers. The association with smoking habits.
Br Dent J 127: 73-77.
Mehta F, Pindborg J. Gupta P et al (1969b). Epidemiologic and
histologic study of oral cancer and leukoplakia among 50,915
villagers in India. Cancer 24: 832-849.
Messer E (1997). Inlra-household allocation of food and health
care: Current findings and undcrstandings-introduction. Soc Sci
Med 44: 1675-1684.
National Academy of Sciences (1989). National Academy of
Sciences Report on Diet and Health. Nutr Rev 47: 142-149.
National Institute of Nutrition (1991). National Nutrition Monitor
ing Bureau Report of Repeal Surveys (1988-90). Indian Coun
cil of Medical Research. Hyderabad, India: NIN.
National Institute of Nutrition (1993). Nutritive Value of Indian
Foods. Hyderabad, India: NIN.
Parkin DM, Pisani P. Ferlay J (1993). Estimates of worldwide
incidence of eighteen major cancers in 1985. Int J Cancer 54:
594-606.
Pindborg JJ (1980). Oral Cancer and Precancer. John Wright &
Sons, Ltd: Bristol.
Dietary factors in oral leukoplakia and OSF
PC Gupta et al
206
Pindborg JJ, Mehta FS. Gupta PC et al (1968). Prevalence of oral
submucous fibrosis among 50,915 Indian villages. Br J Cancer
22: 646-654.
Prasad MP. Mukundan MA, Krishnaswamy K (1995).
Micronuclei and carcinogen DNA adducts as intermediate end
points in nutrient intervention trial of precancerous lesions in
the oral cavity. Ear J Cancer 31B: 155-159.
Rao B (1987). Monitoring nutrient intakes in India. Indian J Pediatr 54: 495-501.
SAS (1997). SAS User's Guide - Statistics Vers 6.11. SAS Insti
tute: Caty, NC.
Shklar G, Schwartz J (1993). Oral cancer inhibition by micronutri
ents. The experimental basis for clinical trials. Eur J Cancer
29B: 9-16.
Sinor PN. Gupta PC. Muni PR et al (1990). A case-control study
of oral submucous fibrosis with special reference to the etio
logic role of areca nut. J Oral Pathol Med 19: 94-98.
Stahl W, Sies H (1996). Lycopene: a biologically important carot
enoid for humans? Arch Biochem Biophysics 336: 1-9.
Steinmetz KA. Potter JD (1996). Vegetables, fruit, and cancer pre
vention: a review. J Ant Dietet Assoc 96: 1027-1039.
Stryker WS, Kaplan LA, Stein EA et al (1988). The relation of
diet, cigarette smoking, and alcohol consumption to plasma
beta-carotene and alpha-tocopherol levels. Am J Epidemiol 127:
283-296.
Tanaka T (1995). Chemoprevention of oral carcinogenesis. Eur J
Cancer 31B: 3-15.
Trivedy C, Baldwin D, Wamakalusuriya S et al (1997). Copper
content in Areca catechu (betel nut) products and oral submuc
ous fibrosis. Lancet 349: 1447.
US Department of Health and Human Services (1988). The Sur
geon General’s Report on Nutrition and Health. DHHS (PHS
Publ No. 88-50210). Washington DC: U.S.G.P.O.
Verreault R, Chu J, Mandelson M et al (1989). A case-control
study of diet and invasive cervical cancer, hit J Cancer 43:
1050-1054.
WHO (1984). Control of oral cancer in developing countries: A
WHO Meeting. Bull WHO 62: 817-830.
Willett WC (1990). Nutritional Epidemiology. Oxford University
Press: Oxford.
Winn D. Ziegler R. Pickle L et al (1984). Diet in the etiology of
oral and pharyngeal cancer among women from the Southern
United States. Cancer Res 44: 1216-1222.
Zheng T, Boyle P, Willett WC et al (1993). A case-control study
of oral cancer in Beijing, People's Republic of China: Associ
ations with nutrient intakes, foods and food groups. Eur J Can
cer 29B: 45-55.
Authors are responsible for the accuracy of the references.
prevalence and Determinants of Coronary Heart
Disease in a Rural Population of India
Rajec’v Gupta,1' bi. Prakash. V. P. Gupta/ and K. D. Gupta1
"’JBUcnoN
Proforma
A detailed questionnaire was prepared according to guide
lines from the World Health Organization (WHO) [10]. the
United States Public 1 lealth ^Service [11], and a review oi
previous Indian studies [12]. The proforma elicited family
history oi hypertension and CRD; social factors such as edu
cation, housing, type of job, stressful life events, depression,
■and participation in religious prayer and yoga. Details of
conventional risk factors—smoking, alcohol intake,
amount of physical activity, diabetes, and hypertension—
were enquired. Blood pressure was measured using standard
ized mercury manometer. At least two recordings were made
at 5-minute intervals according to WHO recommendations
,
[10]
When high blood pressure ai4O/9O mmHg was noted,
a third reading was made after 30 minutes. Lowest of the
three was recorded. Weight in light summer clothing was
measured; in kilograms on a calibrated spring balance.
Height without shoes was measured in meters on a wallmounted scale. Standing hip measurement at intertroc:;.,:.teric level and supine waist measurement at the most promtitem portion of abdomen with the person breathing quietly
were taken. A 12-lead ECG using proper standardization
was performed on all persons. To obtain fasting blood sam
ple of 10% of the total study sample, a random 12% of the
study participants were approached [13].
Diagnostic Criteria
In India and in many developing countries tobacco is con
sumed in various forms (rolled tobacco leaves Ibidi], Indian
pipes [hpokahs], cigarertes, chewing tobacco, etc.) and some
people use it in more than one form. Hence, it is difficult
to accurately measure the amount of tobacco consumed. We
therefore categorised users of any form of tobacco along
with former smokers as “smokers.” Physical activity was as
sessed by asking about both work-related and leisure-time
activities as suggested by Paffenberger et al. [14]- Their crite
ria classify a person as leading a sedentary lifestyle who
walks <9 mi’es/week, climbs <20 flights of stairs/week, or
performs no moderately vigorous physical activity five days
a week.- In th: study area, which is a desert, farming activity
occurs only < uring two or three months of rainy season in
a year so that most of the time, the population is either
sedentary cr intermittently physically active.
Hypertension was diagnosed when either the person was
on antihyf-ertensive medication or systolic blood pressure
was a 140 mmHg and/or diastolic blood pressure a90
mmHg [15L Figures for WHO criteria [10] of hypertension
(£160 and/or 95 mmHg) used by most previous Indian
n2n,c|v- Minn,
,
, T"?versi°ninb?
\ i was ignored. In an uneducated rural populat•■
ria based on history mav result in OverdiaonA.- e? I
agnosts because of poor interpretation of sympt01 ' f
Statistical Analyses
The sample size was calculated by the formula-np).'Here n is sample size, t is normal variate ’
proportion of prevalence of disease, and e is ntargiFrom previous Indian studies in rural areas the p-.of CUD varies between 1.485’6 |9] and 2.26%. [$[0.02. Taking the margin of error c to be small (0
would be 202 5. We proposed a larger sample sited;
mately 3000 as suggested by a recent Indian study
Tire prevalence rates are in percent Mean-a!
given with 1 SD. Analy-is to determine significant
lions of coronary risk factors with Cl ID prevalence t
formed with logistic regression (SPSS V4-0.1,'5i
Chicago, USA). The dependent variable W3S pet
absence of CHD (diagnosed by Q-waves) and ind-z
variables were age, years of educat ion. smoking, pliv
tivity, prayer habit, body-mass index, presence of!i,
sion, and systolic ami diastolic blood pressure. Varj
smoking, sedentary habits, prayer habit, and hypt
were dichotomized (yes = 1, no = 0) and others;
continuous numbers. Odds ratios and 95% confideoi
vals were detennined for (a) all variables inA(b) after incorporating age as a continuous vans,.
equation (age-adjusted), and (c) after addition'
risk factors in the equation to determine die inJ4
determinants of CHD prevalence (multivarialf*
tailed p values less than 0.05 were taken as signi"--
RESULTS
A total of 314S persons were studied. The respond
90.6% (1982 of 2188) in males and 59.2% (1^
it fen ties. l~he overall CHD prevalence deterrn^
presence of clinical or ECG findings was 3.5% I11’
females 3.7%). ECG changes (ST, T, or Q) (SES
in 3.0% (males 2.8%, females 3.3%). Q-wavesch-’y
in 1.4% (males 1.6%, females 0.9%). The^^,
of CHD patients is shown in Table 1- The p^
CHD diagnosed by various criteria increased"'1^
ing age in both males and females (Mantel-H3'trend, p<-0.001).
36.81 * 3
1085 (93)
81 (7)
1146 (98)
10(1)
10(1)
180 (15)
19(2)
3 (.3)
31 (3)
933 (80)
608 (52)
304 (26)
194 (17)
30 (3)
970 (83)
111 (9)
85 (7)
22 (2)
423 (36)
1021 (12) '
145 (12)
689 (59)
410(35)
67 (6)
26 (2)
The standard coronary risk factors smoking, hypertension.
and sedentary lifestyle are widely prevalent. Significant pos
itive associations of CHD are with age, smoking (males),
and systolic blood pressure (females).
Hospital based data [17] and epidemiological meta-analysis [7] show that CHD occurs at a younger age in the Indian
population. Therefore we included’individuals 20-29 years
and results show that CHD exists in this age group also. In
the present study confirmation of CHD was based on pres
ence of Q-wave and using this criteria the CHD prevalence
is 1.6% in males and 0.9% in females. Earlier studies from
India used different criteria [3-5,8,9] and showed higher
CHD prevalence. When the diagnostic criteria in the pres
ent study are extended to include past documentation, re
sponse to WHO-Rose Questionnaire and ST-T wave
changes in ECG as done in previous studies, the prevalence
increases to 3.4% in males and 3.7% in females, which is
higher than in previous Indian rural studies [8,9]. However,
the validity of both the past documentation of CHD as well
as the affirmative response to WHO-Rose questionnaire
have been questioned [18]. This would be more so in die
case of an illiterate rural population where reliance on self-
p;.
I-1
„.
__
reported diagnosis of CHD may result m either ers
nosis or overdiagnosis. As diagnostic markers of Cif:
of the previous studies from India included such E(ria as the presence of left bundle branch block.heart block and presence of ST segment and
changes [3-5,7,8]. Many studies suggest that the ;
are not reliable enough to diagnose CHD and T
in females where ST-T changes may be non-sp-'-'
Dewan et al. [8] studied 1504 individualsJ'‘■'
(North India) while Jajoo et al. [9] studied 2433 f
Vidharbha (Central India). In both these studio.1-
diagnosed on the basis of presence of Q-wavest T wave changes or left bundle branch block[8] reported a CHD prevalence of 14.5/1°°° P
Jajoo et al. |9| 2O.6/1OOO. When we re.inalT-*1 -
Dewan et al. [8] basing diagnosis on rhe presentonly the prevalence decreased to 3.3/10°°-Jai'*,
not specify the prevalence of Q waves and furtn--
not possible.
Our results are not comparable wit!1 urban-h" '
from India not only because ours is a rural-b‘l>i''‘
also because of different and varying criteria
hivotham and Berry |3| studied a sample of 2030 periniore than 30 years in city of Chandigarh in North
reported a prevalence oi 66/1000. In this study,
: CHD was diagnosed on basis of either Q-waves or
sir complete heart block in ECG the prevalence was
COwhich is more than the present study. In a study
; Trlhi reported by Chadha ci al. [5], the criteria for
•• ■•■iilgCHD were entirely different. These authors in'■ i nil symptomatic cases as definite CHD and later
: -r/inptomatic individuals with either Q-waves or ST-and showed CHD prevalence as 96.7/1000. Sub■ of the Delhi data in asymptomatic individuals.
’ c-wave prevalence as 14.2/1000 in 5621 individuals
■r years of age [19]. Although this prevalence rate
- m our data, it is not comparable because of exclu'unptomatic persons. We recently reported CHD
••-e of 75.9/1000 and Q-wave prevalence ol 19.9/
■' 3n urban popujation of Rajasthan (n = 2212) [6[.
s'.ilence rate insignificantly higher than 13.«/1000
"'stent study.
sensidering all the criteria, the prevalence ot CHD
'• !Iudy is higher compared with previous Indian
■ • ■•■■tinn studies and less than in urban populations.
" ?’'f pp is a wel1 known phenomenon in the
">t CHD a?id could be an explanation tor this
- '.)inCe'
tl'le ot!ier hand, the Haryana [8] and
J I studies.'were reported twenty-two and eight
and the higher prevalence in the
> may m dn indication of the rising trend of
^^Populations |7[.
previous studies [3-5]. The mean -.rum lipoprotein lipid
levels are lower than those reported from the Western coun
tries [16], but are higher than a previously reported study
from North India [20]. This may reflect a rising trend in
lipid levels in the Indian population. The prevalence of
hypercholesterolaemia in our subjects is not comparable to
any other Indian study because of the newer criteria used
for classification. However, while the prevalence ot hyper
cholesterolaemia is less than in USA, as well as in several
European countries, it is similar to the prevalence in China
[21]. A low prevalence of diabetes could represent an arti
fact due to reliance on self-reported diagnosis in our study.
A study from USA has suggested that sell-reported diagnosis
of diabetes accurately reflects the true prevalence [22|.
We used stricter criteria for grading physical activity acompared with previous Indian studies [8,9]. Low grade
physical activity is universal in a rural agrarian population.
and moderate or high grade physical activity is related to
agricultural cycles. We used the 1’atfenbergcr |14| criteria
for physical activity assessment, validated in 'tudies from
I ISA andtother developed countries. 1 hese criteria may no:
accurately reflect physical activity m a semiliterate popula-
tion.
Univariate analyses confirm the importance oi classical
coronary risk factors, age and smoking. These factors are
also independently associated with CHD prevalence in men
as confirmed by multivariate analysis. Systolic bkxid pres
sure positively correlated with CHD in females. The sig'. nificance of truncal obesity and hyperinsuiinaemic states
i has recently been highlighted as an important coronary risk
' factor among South Asians living in Britain [23]. A precise
relationship between CHD with serum cholesterol, other
lipoprotein lipids, obesity, and truncal obesity has not been
demonstrated in our study as the proportions where such
measurements were made was small. Sedentary lifestyle has
not emerged as an important risk factor. The absence of any
significant association may reflect the protective influence
of intermittent physical activity.
CHD prevalence was significantly greater among unedu
cated versus educated persons. This observation is consis
tent with international data, which show that CHD and
coronary risk factors—smoking and hypertension-are more
frequent among the uneducated [24]. Men who engaged in
regular prayer had a significantly lower prevalence of CHD
Mental stress is important in rhe genesis as well as perpetua
tion of coronary atherosclerosis [25,26]; therefore mentallyrelaxing activities may be relevant in CHD. Our results
show that persons who pray regularly had a lower preva
lence of CHD. This was confirmed on univariate, as well
Risk factor
Odds ratio (95% CI)
p Value
Odds ratio (95% Cl)
P Value
study. Ind Hvs
WP, Orchard
1.05 (1.02-1.07)
1.05 (I.02-1.0S)
<0.001*
<0.001*
1.08 (1.04-1.13)
1.07 (1.03-1.12)
<0.001*
0.002*
19. Gopinath N, Kaul U, Chadha SI.
0.64 (0.45-0.92)
0.84 (0.57-1.01)
1.00 (0.66-1.51)
0.017*
(l 05 *
0.999
0.29 (O.O8-I.O5)
0.64 (0.16-2.52)
0.51 (0.11-2.32)
0.059*
0.524
0.385
0.28 (0.38-0.91)
0.26 (0.08-0.86)
0.28 (0.08-0.95)
n nt 5*
0.027*
0.041*
1.47 (0.45-4.84)
1.61 (0.48-5.43)
2.39 (0.64—8.88)
0.528
0.439
0.194
0.802
0.786
0.795
Age
c
men and women. J Clin Epidemit
Radhakrishnan S. Asymptomatic
Education
b
c
Ihi. Ind Heart J 1992; 44: 95-98
Gandhi BM. Lipoprotein composi
Ind ] Mr
21. People's Republi
Prayer habit
b
Smoking
b
c
2.95 (1.32-6.61)
2.56 (2.04-3.21)
2.50 (1.09-5.73)
0.008*
n ■ ■ ■- •
0.031’
0.01 (0.00-3.97) ■
0.01 (0.00-3.83)
0.01 (O.OO-7.O4)
1.63 (0.75-3.56)
1.79 (0.81-3.95)
1.18 (0.51-2.75)
L i '
0.147
0.698
1.18 (0.15-9.37)
1.60(0.19-13.2)
1.14 (0.13-10.0 .
0.873
0.661
0.906
c
Body-mass index
1
0.87 (0.76-0.99)
0.88 (0.80-1.04)
0.92 (0.80-1.04)
0.028*
; mi
0.172
1.01 (0.94-1.07)
1.00 (0.95-1.06)
1.00 (0.96-1.05)
0.828
0.921
0.824
1
1
1.00 (0.98-1.02)
0.99 (0.98-1.01)
1.00 (0.98-1.03)
0.974
0.394
O./48
1.02 (1.00-1.03)
1.02 (1.00-1.03)
1.04 (1.00-1.09)
\
0.031*
0.034*
0.057.
0.99 (0.96-1.02)
0.98 (0.95-1.00)
0.98 (0.94-1.02)
0.490
0.1 OS
0.249
0.98 (0.95-1.00)
0.98 (Q.9&-1.01)
1.05 (0.982-1.09)
0.209
0.134
0.205
1.69 (0.65-4.41)
2.47 (0.94-6.55)
2.23 (0.83-5.98)
0.284
0.068
0.112
1.86 (0.49-7.06)
0.85 (0.21-1.75)
0.90 (0.22-3.71)
0.363
0.820
0.885
Systolic BP
b
c
Diastolic BP
b
H-ypenension
b
c
iihandran K. A cross s,
aie in a community. In:
Sedentary habits
ib-
,.*G Blackbum H. Cardiovascular Sum Methods
Geneva; World Health Organization: 1:. _
Heart Study Group. The Strong Heart Study Manual.
jjiovascular disease in American Indians. Oklahoma
University of Oklahoma Health Sciences Center. 1989.
Cholesterol
Small numbers
Abbreviations: Cl = confidence intervals, BP = blood pressure, * = significant, a - unadjusted odds ratio, b
- age-adjusted odds ratio, c = odds ratio after;addition of al! the
variables in equation.
as multivariate analysis. The exact mechanism by which
prayer habit imparts protection against CHD is not clear
and unknown neuro-endocrine mechanisms may be in
volved.
In conclusion, analysis of rhe present epidemiological
data shows that there is a rising trend of CHD in the Indian
rural population. Coronary risk factors, smoking and hyper
tension, are widely prevalent and are important in the aetiopathogenesis of CHD in these persons as in any other popu
lation. In addition, social factors that are frequent in niral
communities in India but are also present elsewhere are sig
nificant. Increasing level of education and regular participa
tion in stress-reducing activities such as prayers appear to
be significant protective factors.
Supported by « grunt from Jan Mungo! Trust, Rnjnsth®’ I’1- I
dation, Jaipur 302004,
__ --
References
1. Leaf A, Ryan TJ. Prevention of coronary
medical imperative. N Engl J Med 1990; 323:: lit .
2. Reddy KS. Cardiovascular diseases in India- 1
Stat Q 1993-46: 101-107.
3. Sarvotham SG, Berry JN. Prevalence of cor0"arlu|,f
in an urban population in northern India. Circ
37: 839-846.
-> f
4. Gupta SP, Malhotra KC. Urban rural trends inj
of coronary heart disease. J Assoc Physie>anS
885-889. '
S
5. Chadha SL, Radhnkrishnan S, Ramachandr-’11 |j
'
miological study of ct
of China. Baseline Rei
----- ---------
Publishing House;
JkTl-39•taR, Gupta HP, Kumar N, Joshi AK. Gupta VP. Lipopro*
ia lipids and the prevalence of hyper!ipidaemia in rural In-
. J Cardiovasc Risk N94; 1: 179-184
■ knbergcr RS, Hyde RT. Wing AL. Lee IM. Jung DL,
G.npert ]B. The association of changes in physical activity
Ld and other lifestyle characteristics with mortality among
tn. N Engl J Med 199?: 328: 538-545.
T. Fifdr Report of the Joint National Committee on Detcca. Evaluation and Treatment of high blood pressure (JNCArch Intern Med 1995. 153: 154-183.
sle Expert Panel. Report of the Expert Panel on Detection,
i'.duation and Treatment of High Blood Cholesterol in
Ind 993: 41
Control of Tobacco-rcIatcd Cancers and Other Diseases.
International Symposium, 1990. Prakash C. Gupta, James E. Hamner, III
and P.R. Murti, eds. Oxford University Press, Bombay, 1992.
Role of diet and alcohol in tobacco-related cancer
at sites in the upper aerodigestive tract in an
Indian population
Perin N. Notani
Epidemiology Unit, Cancer Research Institute, Tata Memorial Centre, Bombay, India
('.sneers of the upper alirncnlary and respiratory tracts, for which tobacco is the major cause, con
stitute about one-third of all cancers among Indians. Probable changes in demography suggest
that the incidence of these cancers will increase. Since a large segment of tobacco users remain
cancer free, however, other factors may have a modifying effect on the risk of developing the dis
ease. The modifying effect of diet on the occurrence of oral cancer was observed in an exploratory
study in India in early 1970s. Subsequently, the role of various dietary factors and of alcohol were
studied for cancers of all sites in the upper aerodigestive tract. The results indicate that intake of
vegetables, fish and buttermilk (liquefied yogurt) was associated with a lower risk for upper
aerodigestivc tract cancers and that use of red chillie powder, a common spice used in Indian food,
was a risk factor in a dose-dependent manner. Alcohol intake had a limited but significant influ
ence on the risk for these cancers.
INTRODUCTION
Epidemiological studies indicate that 80-90%
of human cancers are attributable to environ
mental factors and life style. The major differ
ences in the incidence rates of various cancers
among different countries, between the gen
ders, and between migrant and native popula
tions, as well as time trends, implicate environ
mental factors in cancer causation.
In each country, there are characteristic
site patterns of risk due to local exposure fac
tors and life styles. For example, the rate of
cancers at all sites combined among Indian
males is quite low when compared with rates
for men in Connecticut, USA, Oxford, United
Kingdom, and Miyagi, Japan (1-6), where the
incidence rates are two- to three-fold higher
(Table 1). The incidence rates of cancers of the
oral cavity, pharynx and larynx in India, how
ever, are some of the highest in the world
(Table 1). The incidence of lung cancer,
although low by international standards, is
similar to that of oesophageal and pharyn
geal cancers in the national context. Thus,
in Indian males, cancers of the upper aero
digestive tract constitute 30-40% of all can
cers, whereas they constitute only 12, 6 and
8% of cancers in Connecticut, Oxford and
Miyagi, respectively. With the inclusion of
lung cancer, however, cancers of the upper
alimentary and respiratory tracts constitute
40-50% of cancer at all sites combined among
Indian males and about 20% of cancers among
Indian females.
The use of tobacco as a major risk factor
for cancers at these sites is well established
(7-10). Quantification of the risks associated
with different tobacco habits has also resulted
in high values. Even so, not all heavy chewers
and smokers develop cancer; thus, it is likely
150
Notani
Diet and alcohol in tobacco-related cancers
Table I
Table 2
Average annual age-adjusted incidence rates of cancers of the upper alimentary
■ and respiratory tracts in males per 100 000 population
Relative risk estimates for cancers of the upper aerodigestive trad (with 95% confidence intervals) associated
Registry
Oral Cavity'
(140-145)*
Pharynx
(146, 148)
Oesophagus
. ■ (150)
Larynx
(161)
Lung
(162)
usilfe consumption of different dietary items in Bombay, India"
AH sites
combined
(140-208)
India1*
Ahmcdabad
Bangalore
Bombay
Madras
Nagpur
Poona
21.1.
9.0
13.4
12.0
15.3
14.8
16.9
8.8
11.8
6.8
9.7
5.7
10.5
8.3
11.4
7.4
14.1
12.8
10.2
4.9
8.0
4.9
13.1
11.2
13.9
8.6
13.8
7.5
8.6
11.3
149.5
107.0
120.5
91.1
122.2
127.6
Others'
Connecticut, USA
Oxford, UK
Miyagi, Japan
10.6
5.2
1.9
3.7
1.2
0.4
5.3
3.8
13.8
8.2
3.9
2.2
60.9
69.3
25.5
303.0
268.5
208.9
‘Figures in parentheses are ICD codes: 9th for Indian registries; 8th for other registries, with codes 140-207 for
all sites instead of 140-208
“Source: refs. (1-5)
'Source: ref. (6)
that certain secondary factors, either external
or internal, may have modifying influences on
the risk, and diet and nutrition could be one
such factor. This paper reviews the role of diet
and also of alcohol in the pathogenesis of can
cers of the upper aerodigestive tract.
ROLE OF DIETARY FACTORS
Nutrition and diet can act in several ways.
Nutrients, food additives and contaminants
(like aflatoxins) can act as complete carcino
gens or pro-carcinogens. Dietary deficiencies
or excesses can lead to biochemical malfunc
tion, which in turn may initiate or promote a
neoplastic process; they may also impede or
enhance the delivery of carcinogens, to the
target tissue. They can result in metabolic ac
tivation or deactivation of carcinogens. Thus,
diet and nutrition can interact with the host
environment in several ways and alter the sus
ceptibility of tissues to cancer induction and
promotion (II). Generally, several dietary
components are considered to act more as
tumour promoters or antipromoters rather
than as direct carcinogens.
An exploratory analysis c-f data collected
in the 1950s in Bombay, India, indicated that
certain dietary components may modify the
risk of tobacco chewers and smokers for devel
oping oral cancer (12). This formed the basis
for a case-control study (13) conducted subse
quently for al) sites in the upper aerodigestive
tract. Some of the results abstracted from this
study are discussed below.
DIET AND CANCERS OF UPPER
AERODIGESTIVE TRACT
Cancers of the oral cavity, pharynx, larynx and
oesophagus formed the case group for this
study. Two control groups were used. The
results obtained with controls from the general
population (using electoral rolls) are shown in
Table 2. Information on usual diet before
disease onset, in terms of the frequency
and amount of intake, was obtained by a
Dietary item
(level of comparison)
Cereals and pulses
Cereals
(not daily vs. daily)
Pulses
(not daily vs. daily)
Vegetables and fruits
Vegetables
(not daily vs. daily)
Fruits (<l/wcek vs. &l/wcck)
Animal products
(<l/week vs. SI/week)
Meat
Fish
Poultry
Eggs
Dairy products
(not daily vs. daily)
Milk
Buttermilk
Fat
Groudnut oil (g/cu/month)
(<600 g vs. > 600 g)
Spices
Red chillie powder (g/cu/month)
< 75
75-99
100-149
2= 150
X1 trend test
Beverages
Tea
(>2 cups/day vs. « 2 cups/day)
____________________Cancer site
Oral cavity
Pharynx
Oesophagus
1.45
(0.8-2.5)
1.57
(I.0-2.5)
1.59
(0.9-2.9)
1.90
(1.2-3.1)
1.51
(0.9-2.7)
1.11
(0.7-I.8)
0.87
(0.4-1.9)
1.48
(0.8-2.8)
2.39
(1.4-4.0)
’ 0.89
(0.5-1.4)
2.65
(1.6-4.5)
0.99
(0.6-1.6)
2.62
(1.5-4.4)
1.23
(0.8-2.0)
2.75
(1.4-5.3)
2.00
(1.0-4.1)
1.21
(0.7-2.0)
3.28
(2.1-5.3)
0.78
(0.1-5.2)
0.83
(0.5-1.5)
1.13
(0.7-1.9)
2.23
(1.3-3.7)
0.90
(0.1-7.0)
0.43
(0.2-0.8)
1.46
(0.9-2.5)
3.77
(2.3-6.3)
3.50
(0.3-48.9)
0.79
(0.4-1.4)
1.12
(0.6-2 J)
3.94
(2.I-7.7)
(0.02-48.3)
0.64
(0.3-1.4)
1.11
(0.6-2.2)
3.71
(1.6-8.7)
1.13
(0.6-2.3)
3.68
(1.4-9.4)
1.47
(0.7-3.0)
2.44
(1.1-5.4)
0.78
(O.3-2.O)
11.09
(1.5-83.1)
2.91
(1.8-4.7)
2.93
(1.8-4.8)
1.99
(1.2-3.2)
2.61
(1.3-5.1)
1.00
2.61 •
3.79“
3.94“
<0.001
1.21
(0.8-1.9)
‘Source: ref (13): Comparison group; general population
Relative risk adjusted for age and tobacco use
*p < 0.05; ""p < 0.01
1.00
1.45
2.33
2.37“
<0.01
1.46
(0.9-2.4)
1.00
1.94
1.99
2.85“
<0.0!
2.39
(I.5-3.9)
1.00
2.05
3.39“
<0.10
1.10
(0.6-2.0)
15
152
Diet and alcohol in tobacco-related cancers
Notani
questionnaire. Findings from the analysis
based on the frequency of intake of several
dietary items (13) arc summarized in the table.
The results arc given in terms of relative risk
estimates that were adjusted for the two impor
tant risk factors, use of tobacco and age.
Adjustment was not required for sex or com
munity, as all the patients were men and they
belonged to one community with similar socio
economic status.
Cereals and pulses: These constitute the most
common food items for all segments of the
Indian population. Tabic 2 compares the risks
of those who did not consume these items daily
versus those who did. For those who did not
include pulses in their diet daily versus those
who did, the relative risk (1.9) was significant
for pharyngeal cancer.
Vegetables and fruits: A two- to three-fold in
crease in risk was observed for men who did
not consume vegetables daily versus those who
did, and these were highly significant. The
lower risks were consistent with the current
hypothesis that vitamin A, (J-carotenc and
vitamin G have protective effects. Intake of
fruits, however, showed no association; this
was not surprising, since both the control and
study groups were from the lower income stra
tum and, perhaps understandably, could not
afford this relatively expensive food item.
Animal products: Risks were also assessed for
men who ate meal, fish, poultry and eggs less
than once a week versus those who consumed
these items at least once a week. Only fish
intake showed a significant relative risk, which
was two- to four-fold higher for nonconsumers
than consumers.
Dairy products: Milk intake was found to be
relatively poor in both the study and control
groups, and the relative risks were not signifi
cant. Butter was consumed by only 0.2% of
the study group and was therefore not ana
lysed. Nonconsumers of buttermilk (liquefied
yogurt) were at significantly higher risk than
consumers.
Fat: Information was obtained on the con
sumption of various types of fats and oils, and
the quantity consumed was expressed in grams
per consumption unit (cu) (one for a member
of the family 12 years of age and above, half
otherwise) per month (g/cu/mth). Groundnut
oil was the most commonly used cooking
medium (81-86% in different groups), and
median consumption in the population control
group was 600 g per cu per month while that of
the whole study group was 400 g per cu per
month. Men who consumed less oil were at a
two-fold higher risk than those who used more.
In contrast to the western diet, in which fat
contributes 30-40% of the total caloric intake,
in an average Indian diet fat consumption is
low and contributes only 8-10% of the total
caloric intake. High fat consumption in west
ern countries was reported in several studies to
be associated with higher risks for cancers of
the colon and of endocrine-dependent sites
(14,15); so the risk elevation even with low
caloric intake from fat in this study is in
teresting.
Spices: Red chillic powder is an important
spice in Indian food, and this emerged as a risk
factor in a dose-dependent manner. With an
increase in chillic use from <75 g to 150 g or
more per cu per month, there was a one- to
three-fold increase in risk, which was signifi
cant for all sites except the larynx. This obser
vation is consistent with experimental findings
that red chillies are mutagenic in bacterial test
systems and are tumour promoters in vivo
(16,17).
Beverages: Barely 2% of the study group
drank coffee, but drinking of tea was common,
the median intake being two cups per day.
There was a significant, two-fold increase in
risk for oesophageal cancer among men who
drank more than two cups of tea a day as com
pared to those who drank two cups or less. For
pharyngeal cancer, the risk was 1.5, which was
only marginally significant.
When men who drank three, four, five or
more cups of tea per day were compared with
those who drank two cups or less per day, a
significantly increasing trend of relative risk for
oesophageal (2.0, 2.2 and 3.5) and pharyngeal
cancers (1.1, 1.8 and 2.3) was observed. It
is possible that it is the temperature of the
tea and not the tea itself that is relevant, but it
was not possible to study this aspect in our
investigation.
Since this is the only case-control study on
diet and cancer in India, the results need to be
interpreted with caution. Furthermore, it was
not possible al this stage to assess the attribut
able risks due to dietary factors, as has been
done for tobacco (18).
DISCUSSION
A number of studies have reported similar
results. In an extensive study by the In
ternational Agency for Research on Cancer,
the role of several food items was investigated
in the induction of oesophageal cancer in an
area of high incidence (165 per 100 000) in
Iran. Of the 45 food items listed (19), nine
showed a significant association with the dis
ease in both males and females. Tea drinking
was one of them; a significant, almost two-fold
increase in risk was observed among those who
drank hot tea compared to those who did not.
The other items included consumption of dairy
products, raw vegetables and fruit; these were
found to have a significant protective effect, the
risks for higher versus lower levels of consump
tion ranging from 0.42 to 0.69. Consumption of
meal, poultry and fish showed no association,
nor was there a significant association with
tobacco use or alcohol intake.
In a case-control study on oral and pha
ryngeal cancers in women in the southern
USA, Winn et al. (20) reported a significant
protective effect of vegetable and fruit con
sumption. A report from the Roswell Park
Memorial Institute (USA), where large-scale
questionnaire studies on diet are routinely
conducted, also revealed a protective effect of
vegetable and fruit intake, but not of meat or
153
fish intake, on the development of oesophag
eal cancer in a dose-dependent manner (21).
UsHg standard food composition tables, it was
shown that higher dietary levels of vitamins A
and C conferred protection. A similar protec
tive effect of vitamins A and C was reported for
laryngeal cancer (22), and the gradient in risk
persisted even after adjustment for the effects
of alcohol drinking and cigarette smoking.
It is not easy to quantify the contribution
of diet to cancer risk because of the complexity
and extreme difficulty of measuring in mean
ingful quantitative terms dietary intake prior
to disease onset. Moreover, dietary items inter
act not only with each otiicr but also with the
host environment. Despite these complexities,
certain consistent associations with specific
food items have been observed.
It may be concluded that, although to
bacco is known to be a major causal factor for
some human cancers and efforts must be made
to eliminate its use, the tumour promoting or
protective role of eerie.;.! dietary factors cannot
be ignored. It is therefoiv suggested that a bal
anced diet adequate in protein and nutrient
intake, especially fresh vegetables and fruits
rich in minerals and vitamins, coupled with
avoidance of high intake of fats and meal and
strict surveillance of quality, preservation and
storage practices, would be consistent with the
lowest possible risk for cancer and other dis
eases for the Indian population.
ROLE OF ALCOHOL
Alcohol plays an important role in the patho
genesis of cancers of the upper alimentary
tract, especially in conjunction with cigarette
smoking. In the present study, alcohol was
consumed in the form of a locally distilled
brew.
The risks of alcohol drinking and tobacco
smoking and chewing were assessed using
log-linear models, which were translated into
logistic regression models for the dichoto
mous response variable (23). Table 3 shows the
?H->154
Notan 1
Diet and alcohol in tobacco-related cancers
Table 3
Smoking and chewing of tobacco in relation to
cancer of the upper alimentary tract. Br Med J
1955; i:llll-4.
Cancer site_______________
8. Jussawalla DJ, Deshpande VA. Evaluation
Adjusted odds ratios
associated with
of cancer risk in tobacco chewers and smokers:
Oesophagus
Pharynx
Oral cavity
an epidemiologic assessment. Cancer 1971; 28:
244-52.
4.7
5.6
7.4
Smoking
9.
Notani PN, Sanchvi LD. A retrospective
4.9
11.4
6.8
Chewing
study of lung cancer in Bombay. Br J Cancer
2.2
1.3
Alcohol drinking
1974; 29:477-82.
'Source: ref. (23): Comparison group; genera) population controls
10.
Jussawalla DJ, Jain DK. Lung cancer in
bBecauseofan age-alcohol interaction term in the model, estimates of odds ratios differ with age group and are
Greater Bombay: correlations with religion and
2.7, 2.6 and 0.6 for age groups 40-49, 50-59 and & 60 years, respectively.
smoking habits. Br J Cancer 1979; 40:437-48.
11.
Doll R, Peto R. The causes of cancer: quanti
tative estimates of avoidable risks of cancer in
Pure ethyl alcohol is not likely to be careresults abstracted from this study. The risks
the United States today. J Natl Cancer Inst
nogcnic to man, since studies in animal sys
associated with alcohol intake perse were not as
1981; 66:1191-1308.
12.
Notani PN, Sanchvi LD. Role of diet in the
tems have invariably given negative results;
high as those associated with tobacco habits;
cancers of the oral cavity. Indian J Cancer
but the possibility cannot be ruled out. Con
for oral cancers, the adjusted odds ratio of reg
1976; 13:156-60.
taminants in alcohol might, however, play a
ular chewers was 11.4, arid that for regular
13.
Notani PN, Jayant K. Role of diet in upper
role in the pathogenesis of cancer. It has been
smokers was 7.4, while for alcohol consumers it
acnxligesiive tract cancers. Nutr Cancer 1987;
suggested that the mechanism of the alcoholwas only 1.3. Similarly, for pharyngeal can
10:103-13.
cancer association may be related to nutri
cers, the risk associated with alcohol drinking
14. Jain M, Cook GM, Davis FG, el al. i\ case
tional deficiencies, which would increase sus
was lower than those associated with tobacco
control study of diet and colo-rcctal cancer. Im
ceptibility to the carcinogenic potential of an
habits. Because of the presence of an ageJ Cancer 1980; 26:757-68.
alcohol interaction term in the model fitted for
external agent like tobacco. Alcohol may also
15. Miller AB, Kelly A, Choi NW, et al. A
oesophageal cancer, a single risk figure could
act as a solvent and enhance penetration of
study of diet and breast cancer. Am J Epi
not be obtained; these varied from 0.6 to 2.7 in
carcinogens into target tissues (25). Although
demiol 1978; 107:499-509.
16. Ackawai. RC, Hecker E, Wie.si.ER M, et al.
different age groups. The risks for a combina
the effect of alcohol in indt> 4m» cancers of the
Tumor promoting effect of chillie extract in
tion of habits can be obtained by multiplica
upper alimentary tract has been demonstrated
Balb/c mice. Im J Cancer 1986; 38:689-98.
tion, and they are high. In another study of
in several epidemiological studies, its mode of
17. Nacahiiushan M, BiiideSV. Mutagenicity of
oesophageal cancer from this region (24), sim
action in the carcinogenic process is still not
chilli extract and capsaicin in short-term tests.
clear.
ilar risks were reported.
Environ Mutagen 1985; 7:881-8.
Estimates of odds ratios associated with regular habits obtained under fitted logistic models'
References
1.
2.
3.
The Gujarat Cancer and Research Institute.
Biennial Report 1984-85. Population Based
Cancer Registry for Ahmedabad Urban Ag
glomeration Area. The Gujarat Cancer and
Research Institute, Ahmedabad. 1987.
Indian Council of Medical Research. National
Cancer Registry. Annual Report 1984. New
Delhi, 1987.
Jussawalla DJ, Deshmukh NTS, Gandhe
ML, el al. Cancer morbidity and mortality in
Nagpur City agglomeration 1980-1984. Indian
Cancer Society, Bombay, 1987.
4.
5.
6.
7.
Jussawalla DJ, Natu M, Yolk BB, el at
Cancer Morbidity and Mortality in Pooni
City, 1981-1985. Indiac. Cancer Socicts.
Bombay, 1988.
Indian Council of Medica' Research. Nation.!
Cancer Registry. Annual Report 1983. Nev
Delhi, 1986.
Waterhouse J, Muir C, Shanmugaratnah
K, el at. Cancer Incidence in Five Continent
Vol. IV. IARC Scientific Publication No. t.
IARC, Lyon, 1982.
Sanchvi LD, Rao KC.M, Kiianolkar VK
155
18. Notani PN, Jayant K, Sanchvi LD. As
sessment of morbidity and mortality due to
tobacco usage. In: Sanchvi LD, Notani PN.
cds, Tobacco and Health: The Indian Scene.
UICC Workshop, Tata Memorial Centre,
Bombay. 1989. pp. 66-78.
19. Cook-Mozaffari PJ. Azordecan F, Dav
NE, et al. Esophageal cancer studies in the
Caspian littoral of Iran: results of a case
control study. Br J Cancer 1979; 39:293-309.
20. Winn DM, Ziegler RG, Pickle LW, el al.
Diet in the etiology of oral and pharyngeal canccr among women from (hr southern United
States. Cancer Res 1984; 44:1216-22.
21. Mettlin G, Graham S, Priore R. et al. Diet
and cancer of the esophagus. Nutr Cancer
1981; 2:143-7.
22. Graham S, Meit lin C, Marshall J. el al.
Dietary factors in the epidemiology of cancer of
the larynx. Am J Epidemiol 1981; 113:675-80.
23.
Noiani PN. Role of alcohol in cancers of the
upper alimentary tract: use of imxlels in risk
assessment. J Epidemiol Communitv Health
1988; 42:187-92.
24.
Jussawalla DJ. Epidemiological assessment
of aetiology of esophageal cancer in Greater
Bombay. In: Jussawali.s DJ, Doll R. cds.
Monograph, International Seminar on Epide
miology of Esophageal Cancer. Indian Cancer
Society, Bombay, 1971; Vol. I. 20-30.
25.
International Agency for Research on Cancer.
IARC Monographs on the Evaluation of Car
cinogenic Risks to Humans. Vol. 44. Alcohol
Drinking. Lyon, 1988.
Cover
Story
I
—]
Risk Factors For
Coronary Heart Disease
— What Are They?
Dr Om Prakash, Head of the Department of Medicine, St Martha’s Hospital, Bangalore.
r. Srinivasan, 48 years, is a
businessman with a lot of
drive and has an aggressive
personality. He drinks only socially and
smokes about 25 cigarettes a day — a
habit he is unable to give up.
Five years ago he was noted to have
high blood pressure (160/106) but he is
irregular in taking his prescribed medica
tions. His work keeps him busy; he often
gets angry during the course of the day.
He also carries his business papers home.
He is reluctant to change his way of func
tioning.
Mr Srinivasan’s father died suddenly,
at the age of 44, presumably from a heart
attack. His mother has diabetes and is on
regular medication. While driving to
work one day, Mr Sreenivasan got severe
chest pain and he was sweating.
He was rushed to the nearby hospital
with a cardiac care unit. He was noted to
have acute myocardial infarction. He
was given a drug (streptokinase) and
M
other supportive measures. He made an
uneventful recovery. He is now awaiting
further tests to decide future treatment
plans.
Could Mr Srinivasan’s heart attack
have been prevented? Could he have
been more prudent and cautious? What
are the coronary risk factors, which are
commonly being talked about and writ
ten about?
A heart attack refers to a sudden and
complete blockage of one or more
branches of coronary arteries. It cuts off
the supply of oxygen and nutrients, giv
ing rise to death of part of the heart mus
cle. It is a potentially life- threatening
condition, calling for immediate medical
action.
Today, we have a better understand
ing of the condition and what causes it.
More important, we understand the
various factors which singly, and in com
bination, conspire to lead to coronary
atherosclerosis, (stiffening of the coro
nary arteries).
Such increasing knowledge of the
risk-factors has been of immense help in
preventing attacks, reducing the suffer
ing and deaths due to acute heart attacks.
Such reductions have been seen in the
Unites States of America and other west
ern countries.
Coronary risk factors include:
♦ Tobacco-smoking
♦ Hypertension
♦ Diabetes mellitus
♦ Obesity, and
♦ Cholesterol
Tobacco-smoking
We have such abundant evidence to
conclude that tobacco-smoking is a
major risk contributor in the causation of
Health Action • June 1994
coronary disease. Different mechanisms
play a part here. Even after two years of
stopping smoking your chances of get
ting a fatal heart attack become as low as
that of a life-time non-smoker.
In the United States of America, re
duction in smoking has resulted in a
gradual but substantial reduction in fatal
and nonriatal heart attacks. The message,
unfortunately, in our country has not yet
been registered by a large majority of
smokers.
Heart specialists in India feel that the
prevalence of heart attacks in the
younger populations may well be related
to the increasing smoking habit.
Cessation of smoking is necessary in
any primary preventive programme, es
pecially so in patients who already have
ischaemic hearts.
Apart from patient-education and em
phatic counselling, mass education cam
paigns and similar other efforts have to
be launched. Recourse may have to be
taken to means such as nicotine substitu
tion in the form of chewing gum or transdermal patches containing nicotine.
Hypertension
Elevated blood pressure is another
major factor increasing the risk of coro
nary artery disease. Hypertension is most
often symptomless. Hence, it is impera
tive that all adults have regular blood
pressure check-ups done. This will en
sure that hypertension that needs medical
treatment can be detected early enough
and appropriate action taken. Very often,
what is needed is a change in the food
habits and life-style.
Uncontrolled hypertension acceler
ates the process of atherosclerosis. FurContd. on p.22
7
Cover
Story
22
Health Action • June 1994
py
Offprint from
The National
Medical Journal
of India
Volume 11, Number 3
(May/June 19P8)
THE NATIONAL MEDICAL JOURNAL OF INDIA
VOL. 11, NO. 3, 1998
113
Original Articles
Oral submucous fibrosis in India: A new epidemic?
P. C. GUPTA, P. N. SINOR, R. B. BHONSLE, V. S. MWAR, H. C. MEHTA
ABSTRACT
Background. Oral submucous fibrosis (OSF) Is a precancerous condition caused by use of the areca nut. The reported
prevalence of OSF in Bhavnagar district during 1967 was
k0.16%. We investigated whether the Impression of an increase
in the incidence of the disease was real.
Methods. A house-to-house survey was conducted In
Bhavnagar district, Gujarat state. The use of areca nut-containing
products and tobacco was assessed through an Interviewer admin
istered questionnaire. The oral examination was done by dentists.
The diagnostic criteria for OSF was the presence of palpable
fibrous bands.
Results. A total of 11 262 men and 10 590 women aged
15 years and older were interviewed for their tobacco habits.
Among 5018 men who reported the use of tobacco or areca nut,
164 were diagnosed as suffering from OSF. All but four cases
were diagnosed among 1786 current areca nut users (age-adjus
ted relative risk: 60.6). Areca nut was used mostly In mawa, a
mixture of tobacco, lime and areca nut, and 10.9%of mawa users
had OSF (age-adjusted relative risk: 75.6). The disease as well as
areca nut use was concentrated (about 85%) In the lower (< 35
years) age group.
Conclusions. An increase in the prevalence of OSF, espe
cially in the lower age groups, directly attributable to the use of
^-eca nut products was observed. This could lead to an increase
in the incidence of oral cancer in the future.
Natl Med J India 1998;11:113-16
INTRODUCTION
Oral submucous fibrosis (OSF) is a chronic, progressive, debili
tating disease that was first reported from India in 1953.la
Initially the disease was found only amongst people living in the
Indian subcontinent or in Indian migrants to other countries.
Later, it was reported from many South-east Asian populations.
In this disease the oral mucosa loses its elasticity and fibrous
bands develop? The epithelium is atrophic and there is a marked
intolerance to spicy food. The opening of the mouth progressively
reduces and in extreme cases it may be difficult for even a straw
to pass into the mouth. The disease is precancerous4-5 and carries
a high relative risk (397.3 after controlling for tobacco use) for
Tata Institute of Fundamental Research, Homi Bhabha Road,
Mumbai 400005, Maharashtra, India
P.C. GUPTA. P.N. SINOR, R. B. BHONSLE, V. S. PAWAR,
H. C. MEHTA
Epidemiology Research Unit
Correspondence to P. C. GUPTA
© The National Medical Journal of India 1998
malignant transformation? Spontaneous regression has not been
reported and there is no effective or widely accepted treatment.
Several aetiological hypotheses for OSF have been proposed.
The most prominent among them was its relation with intake of
chillies. This was influenced by the fact that affected individuals
showed a high degree of sensitivity to chillies as well as its occur
rence mainly among Indians who used chillies liberally in their
daily diet. However, this and other hypotheses have not been
confirmed.
It has now been demonstrated that the chewing of areca nut is
the most important aetiological factor for OSF. In case-control
studies from Bhavnagar, Gujarat7 and Karachi, Pakistan? very
high levels of relative risk for areca nut chewing were reported
(109.6 and 94, respectively). A hospital-based prevalence study
of 1790 patients’ and a population-based prevalence study of
11 046 individuals,10 diagnosed 136 and 335 OSF cases, respec
tively, all of whom were areca nut chewers. In an intervention
trial, the incidence of OSF was lower (although not significantly)
in the intervention cohort where there was a substantial decrease
in smokeless tobacco and areca nut use due to health education,
than in the control cohort.11
The practice of chewing areca nut in a betel quid is at least two
millennia old.12 It remained a rather personal habit in which a user
purchased areca nut from the market or ordered a vendor to
custom-prepare a fresh quid. Tobacco was introduced about four
centuries back and currently almost all regular areca nut chewers
use it with tobacco. This necessitates frequent spitting of a red
colour juice, a scourge for almost all public places in India. This
practice appeared to be slowly decreasing with increasing educa
tion, urbanization and unacceptability of spitting behaviour.
During the last two decades, the situation has changed once
again and the practice of chewing areca nut has received a boost
with the advent of ‘pan masala’. These areca nut-containing
products are industrially manufactured and commercially market
ed. They are available in small convenient sachets and are backed
by high profile advertisement campaigns. As a result the use of
‘pan masala’ and similar mixtures containing areca nut has again
become quite common.
The prevalence of OSF was reported from population-based,
house-to-house surveys in rural areas of six districts in India.13’14
The highest prevalence (0.36%) was in Emakulam district and the
next highest, in Bhavnagar district (0.16%). The annual incidence
per 100 000 was 13.5 in Emakulam and 5.5 in Bhavnagar district.15
Thus, OSF did not appear to be a very common disease. However,
there is a widespread feeling among health professionals, especially
dentists and otorhinolaryngologists in northern India, that there is
a marked increase in the incidence of OSF.
The present study was undertaken in Bhavnagar district,
Gujarat to investigate whether there was any increase in the
114
THE NATIONAL MEDICAL JOURNAL OF INDIA
prevalence of OSF and, if so, could it be attributed to an increase
in the use of areca nut?
SUBJECTS AND METHODS
Bhavnagar district is located on the western coast of India in the
state of Gujarat and has an area of 9259 sq km. In Palitana taluka
ofthis district, 20 geographically contiguous villages were selected
and all individuals aged 15 years and older were included in the
study. A brief questionnaire on the use of areca nut and chewing
and smoking of tobacco was administered by trained investigators
to each individual during house-to-house visits. Those men who
reported some kind of chewing or smoking habit were examined
in natural daylight using two disposable wooden spatulas by the
authors (PNS, VSP) who had been conducting similar studies in
this area for many years. The visits and examinations were called
off after 5018 male tobacco users were examined as more than the
targeted oral precancerous lesions were accumulated.
The criteria for diagnosing OSF was the presence of palpable
fibrous bands in the oral mucosa. This criteria has been used
consistently in all our studies since 1966.”
The most popular method of areca nut use in Bhavnagar region
is the chewing of mawa. This is a combination of areca nut,
tobacco and slaked lime [Ca(OH)J. Areca nut is also chewed with
betel quid. Some people chew tobacco with lime without areca
nut. Application of commercially available dry snuff called bajar
is also popular, especially among women.
The most common method of smoking in this region was bidi.
This is made by putting a small amount (about 0.2 g) of coarse,
ground tobacco on a rectangular piece of dried temburni leaf,
hand-rolling it into a conical shape and securing the roll with a
thread. Its length varies from 4 to 7 cm. Another common method
of smoking tobacco was in a clay pipe. All these habits have been
described elsewhere.”
RESULTS
A total of 11 262 men and 10 590 women were interviewed for
their areca nut/tobacco habits. Figure 1 shows the age distribution
of the sample for both sexes. The pyramid first increases but then
tapers off rather steeply in older age groups.
Table I shows the distribution of tobacco habits among men
and women. Among women, almost the only tobacco habit preva
lent was oral application of bajar, practised by 11.6%. Tobacco
use was much more common among men (67.6%). A variety of
VOL. 11, NO.. 3, 1998
tobacco habits were prevalent, the most common being bidi
smoking (31.3%), followed by mawa chewing (18.9%). Smoking
was slightly more popular compared to smokeless tobacco use
(35% v. 27.7%) with 4.8% reporting both kinds of use. Cigarette
smoking was rather uncommon (0.2%).
Among women, thebajar habit was concentrated among older
age groups whereas among men, smokeless tobacco use was
concentrated in the lower age groups (Fig. 2), 76% of all smokeless
tobacco users were less than 35 years old.
OSF was diagnosed among 164 men. The age and tobacco
habit distribution shows that 70.7% were solely mawa chewers
and an additional 22% used tobacco in other forms as well (Table
H). Only 4 persons (2%) did not report any current areca nut use
(they were past users). The disease seemed to be concentrated in
lower age groups; 84.1 % of the cases were less than 35 years old.
The highest prevalence of OSF was amongmawa users (10.9%)
and the lowest among those who did not use areca nut (0.12%).
Compared to no areca nut use the age-adjusted relative risk foj*p
kind of areca nut use was 60.6 (Table HI).
Figure 3 shows the age distribution of the prevalence of OSF
among men with some kind of tobacco habit and those with
smokeless tobacco habit only. Among men with some kind of
tobacco habit, the prevalence was high in the lowest age groups
(15-19 and 20-24) and then fell sharply. In contrast, among
smokeless tobacco users the prevalence fell rather slowly.
Table I. Distribution of tobacco habits among men and women
Tobacco habit
Male
n (%)
Female
n (%)
Any smoking
Bidi
Cigarette
Pipe
3942
3526
19
397
(35.0)
(31.3)
(0.2)
(3.5)
16 (0.2)
15 (0.1)
- -
Any smokeless
Mawa
Betel quid
Tobacco
Bajar
3124
2127
171
799
27
(27.7)
(18.9)
(1-5)
(7.1)
(0.2)
Mixed
Any habit
No habit
Total
544 (4.8)
7614 (67.6)
3648 (32.4)
11262
1242 (11.7)
(0.07)
2 2 —
1231 (11.6)
1 1265 (11.9)
9325 (88.1)
10 590
AGE GROUP
85 +
80-84
75-78
70-74
8S-69
60-04
SS-S9
SO-54
45-49
40-44
35-39
30-34
25-29
20-24
15-19
25
% OF INDIVIDUALS
Fig 1. Age and gender distribution of the study population
AGE (IN YEARS)
Fig 2. Age distribution of the prevalence of smoking among men
and smokeless tobacco use among men and women
115
GUPTA et al. : ORAL SUBMUCOUS FIBROSIS
Table II. Age and tobacco habits of subjects with oral submucous
fibrosis
Age
Mawa
(years)
Mawa and
others
Areca nut
and others
No areca nut
15-24
59
25-34
42
9
35-14
45-54
5
1
55-64
Total 116
(70.7)
12
16
5
3
36
(22.0)
2
3
3
—
—
8
(4.9)
4
—
—
—
4
(2.4)
Total
73 (44.5)
65 (39.6)
17 (10.4)
8 (4.9)
1 (0.6)
164
(100)
Figures in parentheses are percentages
Table III. Prevalence of tobacco use among subjects with oral
submucous fibrosis (OSF)
RR
(age adjusted)
Areca nut
Users
OSF
Prevalence %
(age adjusted)
No areca nut use
3232
4
0.12 (0.16)
1.0
Areca nut use
Mawa
with tobacco
with smoking
Total
1786
1326
136
324
5018
160
144
2
14
164
9.0
10.9
1.5
4.3
3.2
60.6
75.6
9.4
31.3
(9.7)
(12.1)
(1.5)
(5.0)
(3.3)
DISCUSSION
The prevalence of OSF in Bhavnagar district is available from a
population-based house-to-house survey of 10 071 individuals
aged 15 years and older, carried out in early 1967 by the same
group of investigators.13 In that survey, a total of 16 OSF cases
were diagnosed; a prevalence of 0.16%. In the current survey
carried out in 1993-94, using the same criteria and with one
common examining dentist (PNS), 164 OSF cases were diagnosed
among 5018 individuals examined with tobacco/areca nut habits;
a prevalence of 3.2%. A total of 21 852 individuals were screened
and even if we make the most extreme assumption that no OSF
listed among the remaining 16 838 non-examined individuals,
e prevalence still is 0.75%.
The old and the new prevalence are not equivalent for compari
son because of the involved assumptions. Also in the older
sample, the villages were selected by random sampling giving a
representative sample of the entire district. In the current sample,
geographically contiguous villages were selected from one specific
taluka of the district. No other kind of selection, however, was
allowed. Although the examinations were stopped before complet
ing all villages, this is unlikely to have introduced any bias since
the villages were not being examined in any specific order. Also,
the age-sex distribution of examined individuals was compared
with that of the entire screened sample; and these were identical.
It seems unlikely that this sample selection procedure can
account for the large difference between the old and the new study
since the people studied are from the same district. Such a large
difference even on the most unfavourable assumption cannot be
an artifact either.
The real difference in the prevalence is higher than apparent at
first sight. In the older sample, not a single OSF case was found
among men although 5227 were examined out of which 71 % were
tobacco users.16 Thus among men, the prevalence increased from
zero in 1967 to at least 1.46% in 1993-94 (164 among 11 262
men, again making the extreme assumption of zero prevalence
among 6035 non-examined men).
K
Fig 3. Age distribution of the prevalence of oral submucous fibro
sis among all tobacco users and smokeless tobacco users only
Chewing of areca nut has been established as the main causative
factor for OSF.17 The present study shows that the trend in OSF
prevalence closely followed the trend in areca nut chewing. The
age distribution of OSF cases followed the pattern of smokeless
tobacco users rather than that of smokers or the general population.
OSF was diagnosed only among areca nut chewers since on
detailed questioning, all four patients not using areca nut presently
were past users. However, this information was not available for
the rest of the sample so no indication regarding the relative risk
for past areca nut use was possible. Thus while reconfirming the
role of areca nut in OSF, this study also emphasized earlier find
ings that areca nut chewing in India almost always involves
tobacco chewing as well.18
The findings in this study point towards an evolving epidemic
of OSF in the rural population of Bhavnagar district. OSF is a
progressive chronic disease with no known cure, yet 84.4%
patients in this population-based study were less than 35 years old
and 44.5% less than 25 years. The prevalence of areca nut chew
ing in the form ofmawa chewing, followed a very similar pattern.
The age-specific prevalence of OSF among smokeless tobacco
users demonstrated a close and direct link between the two.
The reasons for this increased prevalence of areca nut chewing
and consequent increase in OSF are not hard to locate. Areca nut
is the main constituent of all ‘pan masala’ (betel quid mixture) that
may or may not contain tobacco. Unlike for cigarettes, government
taxes are low on these products and for ‘pan masala’ that does not
contain tobacco, there is no restriction on advertising. This has led
to an enormous increase in the use of all types of areca nut and
smokeless tobacco in the Indian population, especially in north
India as almost the entire ‘pan masala’ industry is concentrated in
the north.
Thus, the perception of a substantial increase in the incidence
of OSF in the north Indian population appears to be real. Given the
degree of concomitant tobacco use among areca nut chewers and
the high relative risk of malignant transformation of OSF, there is
a possibility of an increase in the incidence of oral cancer. The
epidemic needs to be stemmed urgently by taking measures to dis
courage the use of products containing tobacco and/or areca nut.
ACKNOWLEDGEMENTS
We thank Drs Fali S. Mehta and P.R. Murti for their help and advice. The
116
THE NATIONAL MEDICAL JOURNAL OF INDIA
research was supported by funds from the National Institutes of Health Indo
U.S. fund Research Agreement No.N-406-645.
REFERENCES
Lal D. Diffuse oral submucous fibrosis. J All India Dent Assoc 1953;26:1-3.
Joshi SG. Submucous fibrosis of the palate and the pillars. Indian J Otolaryngol
1953;4:1-4.
Mehta FS, Hamner JE HI. Tobacco-related oral mucosal lesions and conditions in
India. A guidefor dental students, dentists and physicians. Bombay:Tata Institute
of Fundamental Research. 1993.
World Health Organization. Guide to epidemiology and diagnosis of oral mucosal
diseases and conditions. Community Dent Oral Epidemiol 1977;8:1-26.
Axell T, Holmstrup P. Kramer IRH, Pindborg JJ, Shear M. International seminar on
oral leukoplakia and associated lesions related to tobacco habits. Commun Dent
Oral Epidemiol 1984;12:145-54.
Gupta PC, Bhonsle RB, Murti PR, Daftary DK, Mehta FS, Pindborg JJ. An
epidemiologic assessment of cancer risk in oral prccancerous lesions in India with
special reference to nodular leukoplakia. Cancer 1989;63:2247-52.
Sinor PN, Gupta PC, Murti PR, Bhonsle RB, Daftary DK, Mehta FS, Pindborg JJ.
A case-control study of oral submucous fibrosis with special reference to the
etiologic role of areca nut. J Oral Pathol Med 1990;19:94-8.
Maher R, Lee AJ, Wamakulasuriya KAAS, Lewis JA, Johnson NW. Role of areca
nut in the causation of oral submucous fiUrosis—A case-control study in Pakistan.
J Oral Pathol Med 1994;23:65-9.
Babu S, Sesikeran B, Bhat RV. Oral fibrosis among teenagers chewing tobacco,
areca nut, and pan masala. Lancet 1997^50:220.
VOL. 11, NO.*3, 1998
Tang JG, Jian XF, Gao ML, Ling TY, Zhang KH. Epidemiological survey of oral
submucous fibrosis in Xiangtan city, Hunan Province, China. Community Dent
Oral Epidemiol 1997;25:177-80.
Murti PR, Gupta PC, Bhonsle RB, Daftary DK, Mehta FS, Pindborg JJ. Effect on
the incidence of oral submucous fibrosis of intervention in the areca nut chewing
habit. J Oral Pathol Med 1990;19:99-100.
12
Bhonsle RB, Murti PR, Gupta PC. Tobacco habits in India. In: Gupta PC, Hamner
JE, Murti PR (eds). Control of tobacco-related cancers and other diseases.
Proceedings ofan internationalsymposium, 15-19January, 1990. Bombay:Oxford
University Press, 1992:25-16.
13
Pindborg JJ, Mehta FS, Gupta PC, Daftary DK. Prevalence of oral submucous
fibrosis among 50,915 Indian villagers. Br J Cancer 1968;22:646-54.
14
Mehta FS, Gupta PC, Daftary DK, Pindborg JJ, Choksi S K. An epidemiologic study
oforal cancer and prccancerous conditions among 101,761 villagers in Maharashtra,
India. Int J Cancer 1972;10:134-41.
15
Gupta PC, Mehta FS. Daftary DK, Pindborg JJ. Bhonsle RB, Jainawalla PN, et al.
Incidence rates of oral cancer and natural history of oral prccancerous lesions in a
10-year follow-up study of Indian vi Hagers. Community Dent Oral Epidemiol 1980;
8:283-333.
16
Mehta FS, Pindborg JJ, Hamner JE, Gupta PC, Daftary DK, Sahiar BE, et al. Report
on investigations of oral cancer and prccancerous conditons in Indian rural
populations 1966-69. Copenhangen:Munksgard, 1971.
17
Murti PR, Bhonsle RB, Gupta PC, Daftary DK, Pindborg JJ, Mehta FS. Etiologj^^
oral submucous fibrosis with special reference to the role of areca-nut chewing^^
Oral Pathol Med 1995;24:145-52.
18
Gupta PC, Pindborg JJ, Mehta FS. Comparison of carcinogenicity of betel quid with
and without tobacco: An epidemiological review. Ecol Disease 1982;1:213-19.
10
11
Descriptive epidemiology of leukaemias in Greater Mumbai
B. B. YEOLE, D. J. JUSSAWALLA, S. H. ADVANI
ABSTRACT
Background. There is little data available on the occurrence
of leukaemias in India. This is despite a large number of patients
being diagnosed and treated at various cancer centres all over the
country. We, therefore, analysed the available data of the
Bombay Cancer Registry to ascertain the epidemiological
characteristics of leukaemias In India.
Methods. The incidence and mortality rates of leukaemias by
cell type and sex were obtained for the most recent 5 years
(1989-93). The data of the past 30 years were used to study
the time trends using a linear regression model based on the
logarithms of the incidence rates.
Results. Leukaemias constituted 3.9% of all registered can
cer cases and 5.4% of all registered deaths In Greater Mumbai.
Males were affected more frequently than females. Myeloid
Bombay Cancer Registry, Indian Cancer Society, Parel, Mumbai 400012,
Maharashtra, India
B. B. YEOLE
Lady Ratan Tata Medical and Research Centre, M. Karve Road,
Cooperage, Mumbai 400021, Maharashtra, India
D. J. JUSSAWALLA
Tata Memorial Hospital, Parel, Mumbai 400012, Maharashtra, India
S. H. ADVANI Department of Medical Oncology
Correspondence to B. B. YEOLE
© The National Medical Journal of India 1998
leukaemias were the commonest. A bimodal age incidence was
observed with the first peak in childhood, a trough bet ween^k
to 19 years of age and a slow rise thereafter. Among the vairos
religious groups Hindus had the highest rate. An increasing trend
In the incidence of all types of leukaemias was also observed.
Conclusion. The Incidence of leukaemias in Greater Mumbai
is comparable to world rates. There is a male preponderance in
all cell types and an Increase in incidence was observed over the
last 30 yeans. The higher Incidence of myeloid leukaemias
observed by us might be related to underreporting of chronic
lymphatic leukaemia.
Natl Med J India 1998;! 1:116-19
INTRODUCTION
Leukaemias are conventionally distinguished by cell type (lympho
cytes, myelocytes, monocytes) and clinico-pathological behaviour
(acute, subacute, chronic). A comparison of the different subtypes
is difficult because of the small number of cases and the varied
accuracy of diagnosis, with different proportions remaining
unspecified. As a group, leukaemias represent 3% of the world
incidence of cancer. There is relatively little variation in the types
of leukaemia occurring in different regions of the world. However,
some variation in the incidence pattern related to various subtypes
has been reported. There have been few reports on the epidemiology
of leukaemias from developing countries including India.
(-gutka industry come through?
opponents did their homework. ”
The industry has had to learn
several new lessons in the past
few days. Its biggest weakness
sources say, has been an inability .
to lobby effectively. “We do not
have an organised lobby”, says
Thakkar. According to Dhariwal,
“The industry is fragmented, with
many local level players. There
are at least five to six independent
associations. We have been trying
to organise more efficiently; the
idea of a single association was
mooted. But it may take time."
Right now there are only two
national players, Dhariwal, and
the around Rs 300 crore Kothari
Products, owned by MM Kothari.
The need to “ work together”
maybe important. It was only last
week, under threat of a ban, that
the first ever national meet of
gutka and masala manufacturers
took place in The New Delhi Hotel
in the capital. This when the org
anised sector market has around
400-500 players, with a combined
turnover of Rs 2,500 crore (An
estimated Rs 2,500 crore comes
from the unorganised sector).
The health ministry meeting
scheduled for 13 April was post
poned by five days. Why this
happened is as yet unclear, but
sources say that the panicked
industry had lobbied hard for the
postponement. In the past week,
the manufacturers have been
trying to come up with a survival
strategy. Industry lobbyists met
with Atal Bihari Vajpayee to
present their side of the case on
the 15th. Says Dhariwal: “He did
npt have much time, but Pramod
Mahajan gave us a hearing.”
The industry now says that the
ban on gutka and pan masala is
unfair because it is yet to be
proved that these are harmful. 1
“We don’t claim it is Chyawanprash,” says Dhariwal, “but it is
not as harmful as the tobacco
lobby is making out. We carry a
statutory warning on all ourproducts. Our manufacturing proce As the health ministry squares up to pan masala manufacturers, this could be a thing of the past
dures are open to examination by
the government. And ifgutka and * _noduce
r0(j.
in India annually. For out by the unorganised sector is a required to carry out a compre
masala are tobebanned, so should I .i^c
J js of farmers in Karnataka and real problem. Their solution; all hensive study of this industry.
cigarettes.” Says Thakkar: “Ciga- * Assamwearetheirmain
Assaj
source of ow the industry to organise better, And, the politicians we have met
rettes have a hundred per cent j income. Almost 50 per cent of the and implementrigidmanufactur- have assured us that they will not
tobacco content; gutka and masala j packaging industry is dependent ing practices on even the small shut down an industry that
vary between eight and 12. So if t on us, as is the attar/perfume manufacturers. "We are ready to employs so many people". Asa
you ban us, ban them as well. ”
sector. We contribute Rs 1,000 talk to the government; but are belligerent Lalwani states, “We
The AIPMTPA is also trying to crore in excise to the centre and they?" says Harishbhai Lalwani, never said this product is good for
ram home the point that it has ' states every year. It isn’t ghing to be owner of Prince Gutka.
your health — it isn't. But I chal
greater mass support, and lever that easy to implement a’ban."
For the moment, manufactur lenge anyone to try and ban it
age than one would suspect. “ At
The solution, the industry ers believe they have breathing Pen-pushers and politicians think
least one crore vendors depend on pays,
I
o> is to implement uniform
-------space. SaysDhariwal: “Weunder- they can take such decisions .But
this industry for their livelihood. ) l-manufacturingpractices. There is stand that the health ministry will they will not be able to handle the
We pickup almost 80 per cent, or-;
implicit acceptance that poor not take a decision on the coming consequences."
2,800 tonnes of the total arecanut Equality gutka and masala churned Monday. Some more time is
• MAN1SH KHANDURI
This phot
18
APR 1996
I
pan
A paranoid and belligerent favour of a ban say that the two
industry is now lashing out at products are directly responsible
cigarette manufacturers such as for cancer, especially of the oral
ITC and GTC for ‘initiating’ a tract. Thakkar disagrees vehe
sustained misinformation cam mently. “No report so far has con
paign. “According to the market clusively proved a causal link," he
information we possess,” says says. “There is no clear evidence.'”
Rasikbhai Dhariwal, president of
But towards the end of 1997
AJPMTPA, “cigarette manufac the H Narasimhaiah committee
turers are behind the move to ban recommended a complete ban on
this industry.” Dhariwal is the the manufacture, sale, storage and
owner of the Rs 350 crore Dhari exhibition of gutka and pan
wal Tobacco Products, India's masala. By then, also, the antilargest pan masala/gutka manu gu tka/pan masala movement had
facturer. “Cigarette manufacturers spread from Maharastra and
are running scared because we are Gujarat down to the South. In
eating into their market share.”
Kerala, for instance, the Cochin
Whatever the truth of that, municipality banned all adver
there’s no doubt that the industry tisement of the two products. !
has been caught napping. TheSoon after, in early 1998, ana
case for a ban has been building up on the basis of the Narasimhaiah
for some time now. In mid-1997 report, the Central Committee of
the Rajasthan High Court asked Food and Supplies recommend
the central government to ed that the health ministry ban all
conduct an enquiry into the possi chewing tobacco and gutka prod
ble deleterious effects ofgutka and ucts. This month the health
pan masala. This order, Thakkar ministry made out a notification
says, initiated the setting up of a to that effect. This order was to be
committee; and the start of a signed on April 13.
research campaign in various
For the industry it was a bolt
government laboratories.
from the blue. “ We came to know
The results of the research is of this notification 10 days ago”,
being contested heatedly even says Thakkar. Says an industry
now. Both the anti and pro- official, “It seemed as if the notifi
gutka/pan masala lobbies often cation was intended to be passed
cite the same report. Those in in a clandestine manner. Our
DOCrOST-CBD:
Will the ban
n two days from now, a flour
ishing, Rs 5000 crore industry,
directly employing an estimat
ed one lakh workers, could vanish
without a trace. On Monday, a toplevel meeting in the health
ministry will be held to decide the
fate of the pan masala and gutka
products industry. The first item
on their agenda; should this sector
be banned on the grounds that its
products are injurious to health?
The industry knows it is
crunch time. Already the Delhi
office of the All India Pan Masala
& Tobacco Products Association
(AIPMTPA) appears to be under
siege. Bharat Thakkar, coordina
tor, spends most ofhis time lobby
ing with politicians, calling up
journalists, and soothing the odd
panicky industrialist. “We have
presented our case to the prime
minister,” he says, “and politi
cians including Bansi Lal, Sush■ ma Swaraj and Maneka Gandhi.
We are trying to get an appoint
ment with George Fernandes. ” He
adds grimly, “But if this ban is
enforced, people have to realise
that this is not a question of 400500 manufacturers. Crores of
people depend on us. We will sit
in protest outside every Vidhan
Sabha in this country with our
lakhs of supporters.”
p h - y-.
_______________ -3 MAT 1998
Leading yon up the cancer path
availability of gutka has resulted in oral submucous fibrosis reaching epidemic
proportions, writes Sameera Khan
HEN
nine-year-old
Kania, a slum-dweller
doing menial household
jobs, recently visited the OPD of St
George's Government Hospital,
Mumbai, she could barely open her
mouth.
The culprit: the eight to 10 gutka
pouches she had consumed every
day over the past year.
The prognosis: Oral submucous
fibrosis (OSF) — a disease which
causes dense fibrous tissue bands to
develop in the oral cavity, thereby
damaging the inner lining of the
mouth. A progressive disease, it is
accompanied by soreness and a
burning sensation. Due to atrophy
(thinning) of the epithelium (inner
lining of mouth), hot and spicy
foods cannot be tolerated . The
tongue is also affected and speech
gels disturbed. Over a period of
the mouth opening may get so
^rouced that meals have to be taken
through a straw.
Doctors immediately advised
Kanta to give up the gutka habit
that was threatening not just to
close her oral cavity but also
increase her risk of getting oral can
cer. Unfortunately. Kanta never
returned for further treatment or
medical advice.
“We are today seeing an
increased incidence of OSF in the
community, especially among
younger people.” says Dr Surendra
Shastri, professor and head of
department of preventive oncology,
at Tata Memorial Hospital,
Mumbai. “It's due to the easy avail
ability and consumption of gutka
and pan masala.”
At the Tata Memorial OPD, it’s
now common to come across stu
dents of Class VII and VIII, who
consume a minimum of five gutka
^^tets a day, with signs of OSF.
e years ago. we saw no cases of
OSF in this young age group — now
we see about four cases in the daily
OPD." says Dr Shastri. “Clearly, it's
just the tip of the iceberg”
According to Dr Prakash Gupta,
senior research scientist, epidemiol
ogy unit of the Tata Institute of
Fundamental Research, OSF has
W
hat do you have to say
about the proposed ban on
gutka and tobacco chewing prod
ucts?
It is most unwarranted, and unfair
to say the least. Chewing tobacco
is part of our tradition. Our raja
maharajas and sadhu-sants patro
nised it from time immemorial.
There was never any opposition
to it. But today some vested inter
ests are trying to impose this ban.
In any case, there is no scientific
basis for it.
How can you say that? It has been
widely reported that the pro
posed ban was mooted to safe
guard public health. It is also
believed that these products arc
carcinogenic.
That's not true. Smoking tobacco
is far more harmful than chewing
tobacco. If the government is real
ly serious about people's health, it
should first ban cigarettes, which
have been proved to cause lung
cancer. Passive smokers are also
W
reached epidemic proportions in
India. “In the 1950s, the only cases
of OSF were among older people.
In the 1990s, the prevalence has
increased tenfold,” says Dr Gupta.
“And 80 per cent of these cases are
in the under-35 age group.”
The biologically active agents in
gutka are tobacco—with the addic
tive nicotine — and arecanut.
Regular chewing of these sub
stances causes OSF. A recent TIFR
population-based survey in villages
around Bhavnagar, Gujarat, reveals
that one in 30 of those who chew
gutka (tobacco and arecanut) are
prone to OSF. “The situation is
alarming because there are no
accepted lines of treatment for OSF,
except for some surgical interven
tions to relieve the painful symp
toms,” says Dr Gupta.
Gutka also puts a person at risk
for gingivitis (inflammation and
recession of the gums) and pre-cancerous lesions such as leukoplakia
(white patch) and crythroplakia
(reddish patch) on the inner lining
of cheek.
“Gutka also causes narrowing of
‘First ban cigarettes
Banning chewing tobacco will drive the
industry underground, activate the mafia,
and increase smuggling, M. M. Kothari of
Pan Parag tells Sakina Yusuf Khan
affected. There is no such danger
with chewing tobacco.
Besides, the government cannot
impose a ban without conducting
a proper epidemiological study
that definitively links oral cancer
with tobacco chewing.The clinical
studies on oral submucous fibro
sis patients carried out so far are
not enough evidence.
If it’s not health, what other rea
son could the government possi
bly have for proposing this ban?
After all, it will lose Rs 1,000
crore in excise duty and Rs 300
crore as sales tax.
True, it will be losing a lot of rev
enue. But it is contemplating the
ban because of pressure from
powerful multinational tobacco
companies. These companies want
to destroy this domestic industry
and and capture the market.
Do you think the industry might
go underground if the ban is
implemented?
It certainly will, thereby making
it even more hazardous as there
will be no quality control.
Smuggling across the border will
the blood vessels which can lead to
serious heart problems,” says Dr J.
Peter Rodrigues, honorary head of
department of ENT at St. George’s
Hospital. “But what’s really alarm
ing is that when left unchecked,
OSF can cause oral cancer.”
Already oral cancer tops the list
of cancers suffered by Indian men
and ranks third among Indian
women. About 1,00,000 Indians suf
fer annually from it. “Our greatest
concern is that we will see a lot
more cases of oral cancer in the
future,” says Dr Gupta. “The risk of
developing oral cancer is 400 times
higher among patients of OSF as
compared to patients without OSE”
According to estimates at St.
George’s Hospital, 7.6 per cent
cases of OSF finally get oral cancer.
Even those who chew non-tobacco pan masala are at risk. TIFR
studies have revealed that OSF is
more a result of the arecanut than
the tobacco present in gutka.
Besides, most non-tobacco pan
masala chewers eventually move
over to gutka.
“ The only way to stop OSF and
avoid the risk of oral cancer is to
stop eating gutka,” says Dr
Rodrigues But giving up the dan
gerous habit is a tough process and
many former addicts complain of
withdrawal symptoms, including
craving, irritation, and lack of con
centration.
“It's hard to give it up. Nicotine is
habit-forming,” says Dr Shastri.
“We have a de-addiction pro
gramme at the Tata Memorial
Hospital for tobacco and gutkausers but our success rate is as low
as 12 per cent.”
Still, there are those like Salma
who for ,two years chewed five
gutka packets a day. “I thought it
was a mouth freshner but then I got
addicted to it and couldn’t do with
out it,” she recalls. “When my
mouth started burning and gradual
ly closing. I was terrified. I made
myself give up gutka completely. It
was such a wise decision.” One, that
a lot more people in this country
need to make.
also increase. Since cultivation of
tobacco cannot be stopped with
one sweeping legislation, chewing
tobacco will become a commodity
in the hands of the mafia.
In any case, bans never work.
Prohibition in Andhra and
Haryana and their subsequent
withdrawal prove the incfficacy of
such shortsighted legislation.
If incentives arc given to switch to
other businesses within a reason
able time-frame, would you find
that acceptable?
We are not worried for ourselves.
Most of us (the 300-odd gutka
manufacturers in the country)
have other businesses alongside.
We are fighting for the 10 crore
tobacco and arcca-nut fanners,
processors, silver beaters, per
fumeries, packers transporters
and pan-shop owners who will be
adversely affected by this b>n.
Can the government guarantee j
alternative employment for all of i
them?
•'
Et PAAN MASALA
A New Way to Die?
Recent studies show India’s favourite condiments are heightening the risks of an
prabcancer epidemic. Doctors want an urgent restriction on sales and advertising.
By SAMAR IIALARNKAR
ver eaten dinner with
A straw? Anil Vaswani
does. Slowly, the 36-yearold hardware
store
sucks
in a bowl
of owner
bland.
watery gruel. His mouth is no more
than thesizeofa large button: themuscles have tightened into hard bands of
tissue, no longer so flexible as to open
wide enough to swallow the samosas
and dhoklas he loves so much. Through
his unnaturally pursed lips. Vaswani
painfully tries to explain how he came
to be this way. All (hat emerges is an in
comprehensible mumble.
Vaswani hasan extreme case ofsubmucous fibrosis, a silent ailment that is
spreading like wildfire through India.
l-'ar more frightening than struggling to
keep your mouth open, submucous fi
brosis is often a precursor to oral can
E
cer—victims have a 400 times greater
risk ofgetting this cancer than a norma I
person—a disease that literally eats
away your face and ends, inevitably, in
a slow, lingering death.
New evidence confirms what scien
tists long suspected: the disease springs
from those pint-sized, silver-foil or plas
tic sachets of paan masala—a powdery
mixture of arecanut (supari), lime, be
tel nut and a few other ingredients—
and its relative, gutka. A study done
jointly by the Regional Cancer Centre
and the John Hopkins University in the
US shows that 19 out of 22 popular
paan masala brands (see graphic) have
mutagens, substances that can trans
form ordinary human cells into un
controlled cancers.
Paan masala is a 1990s icon of In
dian society. It’s convenient to carry
and available anywhere—in the re
motest villages and even in medical
stores. Film stars like Vinod Khanna,
Shammi Kapoor and Ashok Kumar pro
mote it with glee, little realising they
may be endorsing a message of death.
"We are observing a big epidemic of
submucous fibrosis across India.” says
Dr Prakash Gupta, an epidemiologist at
the Tata Institute of Fundamental Re
search (tier) in Mumbai, who has stud
ied thedeleteriouseffectsofprtrm masala
for more than two decades. “We are
now afraid we will sec an epidemic of
oral cancer in the near future.” Gulka (it
contains tobacco: paan masala may or
may not have tobacco) creates cancer
in halfthc time that cigarettes taketodo
so, warn doctors. The cancer breaks out
any time from five to 10 years after the
advent of submucous fibrosis.
Oralcanccralready accounts for 10
per cent of all cancer cases, drastically
different from the West where such can
cers rarely occur. If paan masala's pro-
Graphic by JAf
Genesis of an Epidemic
Newstudies directly,
indict paan masala
and gutka for
jgra
causing
Arecanut triggers the synthesis of ■.
collagen, a tough,fibrous protein that
stiffens the muscles of the mou th. The
mbuth size shrinks. In extreme cases,
only a button-size opening is left?
jgK,.
submucous
fibrosis (smf),
an incurable,
'
disease. Victims
are 400 times
more at risk of
contracting oral
cancer—death is
slow and painful—
j
thananormal
person. Ten per cent J
i of all cahcer cases in :
India affect the .
\
mouth and tongue. In X
the.West, oral cancer is
not a public health problem.
The epithelium (skin cells) atrophies. As
the skin wastes away, carcinogens like
. ..
tobacco act easily. In
i
V? '.’
traditional paan, the leaf ; .
'betweenthe ingredientsandthesktn.
' A1
The tongue loses its rough outer. -. ’j
layer and becomes
smooth and white. .^8
An SMr patient ■
Bl
cannot consume
spices, and is
reduced to eating ''
bland food.
Note: Paan masala is a powdery mix of arecanut, lime, betel
nut and other ingredients. Gulka has all these and tobacco.
,
*
ey
ys
at
tedtla
re
of
(it
or
er
io
ut
'ie
0
iy
liferation is not checked, doctors fear
the deadly disease will begin peaking in
numbers after its incubation period is
over, around the turn of the cent ury.
The submucous fibrosis epidemic—
it runs into uncounted millions—is a
phenomenon directly related to the ex
ploding consumption of paan uinsn/a.
“There is incontrovertible evidence of
the link." says Gupta. “Paan masala must
be considered a hazardous product."
An unpublished tifr study in Gu
jarat shows just how the contagion has
taken hold. In 1967 Tll’R scientists
found that one in 800 people had sub
mucous fibrosis; today the incidence
has skyrocketed to one in 30. Other
kinds of tobacco use also cause the dis
ease, but nine out of 10 of the victims in
Gujarat are users of paan masala.
Little wonder. The paan masala in
dustry has grown from an estimated Rs
200 crore in 199 2 to well over Rs 1,000
crore today. There are no restrictions on
advertising, no standards and no test
ing protocols. The warning is mi
croscopic and often absent: “Chewing
of paan masala is injurious to health."
And that’s in English, a language alien
to most paan masala consumers.
Disturbingly, many of the brands
"If you thought smoking was bad, this is deadly.
Paan masala is even killing children.”
SuCHBTAN Pradhan, Prosthodontist, Mumbai
may not contain their prime ingredient,
paan, or betel nut. They contain only the
masala, which is an amalgam of ingre
dients, many unknown, says Dr Babu
Mathew, professor of community
oncology. Regional Cancer Centre,
Thiruvananthapuram. The flavouring
agents are trade secrets (the packet only
names major ingredients), but the two
main known disease-causing agents
are tobacco and arecanut.
A number of recent studies from In
dia and Pakistan confirm that arecanut
is the main cause ofsubmucous fibrosis,
inducing the production of a protein
that cripples the mouth's muscles. That
finding undermines a great social tra
dition: for the last 500 years, supnri has
not only been chewed but also forms an
important part ofreligious rituals, from
pujas to marriages.
“Anything taken in excess is harm
ful, even gulab jamuns and chocolate,”
says M.M. Kothari, manufacturer of In
dia’s largest selling brand. Pan Parag,
“Gulabjamuns and chocolates taken in excess
are also harmful. Why single out paan masala?"
M.M. Kothari, Manufacturer, Pan Parag
‘
and the father of the modern paan
masala industry. 1 Ie freely admits that
gutka is harmful, but points to the statu
tory warning carried on the packs.
Kothari, who’s built a multi-crore paan
masala empire from scratch in the last
decade, says, “We have no objection to
a ban, but then the Government must
stop cigarettes too." He knows that is
unlikely to happen in a hurry.
Despite the overwhelming evidence
of the damage that paan masala is caus
ing. the Government is clearly hesitant
to act against a powerful commercial
lobby. “Paan masala manufacturers are
growing rich at the expense of our
lives," Maharashtra Health Minister
Daulatrao Aher declared before the
state Assembly earlier this year. A vo
ciferous advocate of a ban on paan
masala, Aher can do little until the Cen
tre acts—and there’s no immediate sign
of any restrict ions being imposed.
Two years ago, the Rajasthan High
Court asked the Health Ministry to ex
amine the carcinogenicity of paan
masala. A committee constituted by the
Directorate-General of Health Services
is currently reviewing papers on the
subject. Officials say animal studies have
been cleared to lest the carcinogenicity
of paan masala ingredients, but they
haven't yet begun. None of this is re
quired, say researchers, who accuse the
Government of ignoring all available ev
idence against the concoction.
Meanwhile, the paan masala rage is
spreading, especially among the Indian
middle class and the rich. One reason is
that gutka is a form of tobacco that’s so
cially acceptable. As Kothari says, “A
son can offer gutka to his father, but he
cannot offer a cigarette.” Most worry
ing, say doctors, is gutka's gleeful adop
tion by the young: some chewers are no
more than six years old. “Paan masala
is killing them,” says an agitated
DrSuchetan Pradhan, a prosthodontist
who has been witnessing a “tremen
dous" increase in submucous fibrosis
among his patients in his upmarket
Mumbai clinic. “Ifyou thought smoking
was bad.” says Pradhan, “this is deadly."
The paan masala craze has hugely
displaced traditional paan chewing,
which ended up as red. dribbly spittle
splattered on walls and pavements.
Most new victims are below 3 5 years of
age. Even the south, traditionally a paan
masala-free area, has succumbed. “At
least a dozen boys below 17 (suffering
from submucous fibrosis) have been
registered as outpatients at our hospi
tal," says Mathew. "The youngest is 11
years old and he used to consume at
least six packets a day.”
Forget about a ban. It hasn't hap
pened with cigarettes, and it won’t hap
pen with paan masala. But what the
Government can do is to first ensure that
paan masala is not freely advertised and
promoted as it is today on the media, es
pecially television, which reaches into
the Indian hinterland. Manufacturers
use a loophole that frees non-tobacco
products from advertising restriction
like cigarettes. “But the paan masala sold
has tobacco ... there must be no adver
tising or promotion." says Gupta.
The Government can also make
consumption unattractive by simply
slapping hefty taxes onpaan masala.The
money can then be used on spreading
the message about its dangers—none
of that is done today. There are no taxes
on it, and the little sachets cost only a
couple of rupees. Unless at least this
much is done, millions of Indians could
be reduced to sustaining their lives at
the end of a straw—and adding on an
other way to die.
■
AUGUST 11. 1997 * INDIA TODAY 73
Control of Tobacco-related Cancers and Other Diseases.
International Symposium, 1990. Prakash C. Gupta, James E. Hamner, III
and P.R. Murti, eds. Oxford University Press, Bombay, 1992.
Mawa chewing and oral submucous fibrosis in
Bhavnagar, Gujarat, India
Pesi N. Sinor, P. R. Murti, R. B. Bho.nsle and P. C. Gupta
Basic Cental Research Unit and WHO Collaborating Centre for Oral Cancer Prevention,
Tata Institute of Fundamental Research, Bombay, India
Maura is an arcca-nut preparation containing tobacco and lime. Its use is very popular among the
youth in Bhavnagar. Recently, there has been an increased occurrence of submucous fibrosis in
this area. A vase-control study on submucous fibrosis in Bhavnagar showed a re’ -live risk of 109.6
for all forms of arcca-nut use, 106.4 for mawa chewing and 780.0 for chewing mawa as well as betel
quid (pan). The relative risks increased with the increase in the duration and frequency of arccanut chewing; a bivariate analysis also showed a multiplicative effect. Clinically, submucous
fibrosis in Bhavnagar differed in regard to age, sex and location distribution from cases in
Ernakulam. These variations could be due to the differences in the type of arcca-nut chewing in
these areas — mawa chewing in Bhavnagar and betel-quid chewing in Ernakulam. The findings
raise several research questions and indicate a need for public health measures against arcca-nut
containing products.
INTRODUCTION
Submucous fibrosis is a prccanccrous condi
tion. The malignant potential of this condition
is due to the atrophic epithelium that is often
seen in submucous fibrosis and the action of
carcinogens in tobacco upon it (1). Several
factors, ramcly, the use of chillies (Capsicum
annum and Capsicum frutescens) and nutritional
deficiency states, were thought to be involved
in its pathogenesis. Current epidemiological
evidence highlights arcca-nut (Areca catechu)
chewing as an etiological factor in this condi
tion (2-4).
A marked increase in the occurrence of
submucous fibrosis has been seen recently,
especially among the young, in Bhavnagar,
Gujarat. This increase corresponds to the in
creasing popularity of mawa chewing in the
population, especially among the youth. Mawa
>s a preparation containing thin shavings of
areca nut with the addition of some tobacco
and slaked lime (see paper by Bhonslc el al.,
this volume). A case-control study was con
ducted to investigate the association between
mawa and other forms of areca-nut chewing
and oral submucous fibrosis (5). In this paper
we describe some of the findings from that
study and the differences in the clinical charac
teristics of the disease associated with mawa
chewing in Bhavnagar and that with betel
quid (pan) chewing in Ernakulam district,
Kerala.
MATERIAL AND METHODS
Submucous fibrosis was diagnosed on the
basis of the presence of palpable fibrous
bands, as per the standardized criteria (6) (see
paper by Murti et al., this volume). The case
control study was conducted in a dental clinic
in Bhavnagar among 60 consecutive dental
patients diagnosed with submucous fibrosis.
Controls matched for age, sex, religion and
108
Mawa chewing and oral submucous fibrosis
Sinor et al.
occurred among people who were regular
chewers of areca nut in one form or another,
except one who was an occasional chewer. The
overall relative risks were 109.6 for areca-nut
chewing, 106.4 for mawa chewing and 780.0 for
chewing mawa and betel quid.
socioeconomic status were selected from
among patients attending the same clinic who
showed no evidence of oral submucous fibrosis
or any other tobacco-associated oral mucosal
lesion or condition. Prior to their examination,
information on the type of areca-nut chewing,
forms of tobacco use and other relevant infor
mation was recorded. All cases were photo
graphed in colour.
Table 2 gives the relationship between the
duration of chewing and its frequency per day.
The relative risks increased with duration and
frequency of the habits.
The clinical features recorded in Bhavnagar were compared with those of 64 cases of
submucous fibrosis reported earlier (3) from
various population-based studies in Emakulam district, which is about 2000 km south
of Bhavnagar.
Table 3 shows the results of a bivariate
analysis of the dose-response relationship ac
cording to duration and frequency. A multipli
cative effect between duration and frequency of
the chewing is clearly seen.
RESULTS
Table 4 shows the age and sex distribu
tion of submucous fibrosis cases in both areas.
Most of the (79%) individuals in Bhavnagar
were in the age range 15-34 years, while in
Ernakulam 94% were aged 35 years and over.
This condition occurred overwhelmingly (97%)
among men in Bhavnagar, whereas only 18%
of cases were in men in Ernakulam.
An overwhelming majority (97%) of the 60
individuals with submucous fibrosis in Bhav
nagar were men; some 79% of these were
under the age of 35 years.
There were no marked differences in the
smoking habits between the cases and controls,
implying that smoking is not an etiological
agent in this condition.
Table 5 shows the location of submu
cous fibrosis in the mouth in the two areas..
The buccal mucosa was affected more or less
Table 1. gives the relative risks for differ
ent types of areca-nut chewing habits. All cases
Table 2
Relationship between duration of chewing (in years), frequency of chewing (per day) and occurrence of submucous fibrosis
Cases
Chewing habit
No habit
Arcca nut (no mawa)c
Areca nut (no tobacco)11
Mawa
Mawa (with others)*
]b
5
4
30
20
2%
8%
7%
50%
33%
Overall
60
•100%
%
No.
%
Relative
risk
17
16
26
29%
27%
44%
10
5
6
47%
24%
29%
1.0
1.9
2.5
16
37
6
27%
63%
10%
10
10
1
47%
48%
5%
1.0
2.3
3.8
Total
59
100%
21
100%
‘Source: ref. (5)
Table 3
Dose-response relationship between chewing habits and submucous fibrosis*
Duration of chewing
=S5 years
Frequency of chewing (per day)
Cases
Controls
No.
39
7
2
11
1
%
Relative
risk
65%
12%
3%
18%
2%
780.0* •
60 _______ 100%
109.6**
"Source: ref. (5)
bOccasional areca-nut chewer
•Betel quid with tobacco; betel quid without tobacco + tobacco-lime
••/><0.01
““including betel quid without tobacco
'Mostly betel quid with tobacco
1.0
29.9«
78.0* •
106.4**
>5 years
RR
Cases
Controls
RR
•Source: ref. (5)
Age and sex distribution of submucous fibrosis patients in
Bhavnagar and Ernakulam districts
Controls
No.
%
Table 4
Cases
Chewing habits
Controls
No.
Duration (in years)
1-5
6-10
>11
Frequency (per day)
1-5
6-15
>16
Table 1
Association of submucous fibrosis with chewing habits*
109
Age (years)
Bhavnagar
Ernakulam*
15-24
25-34
35-44
>45
Mean age
13 (22%)
34 (57%)
10 (17%)
3 (5%)
29.1
4 (6%)
17 (27%)
43 (67%)
51
Men
Women
58 (97%)
2 (3%)
18 (28%)
46 (76%)
Total
60 (100%)
64 (100%)
Sex
‘Source: ref. (3)
equally in both areas, but its involvement in
Bhavnagar was generally restricted to the
posterior one-third (Fig. 1). In Ernakulam,
there was a more generalized involvement of
the buccal mucosa. The disease was clinically
advanced in Bhavnagar and less severe in
Ernakulam. Retromolar areas (100%), soft
palate (95%) and the uvula (55%) were very
frequendy affected in Bhavnagar (Fig. 2), but
less frequently in Ernakulam. The tongue and
the floor of the mouth were involved in 59%
and 22%, respectively, in Ernakulam, whereas
in Bhavnagar they were either not involved or
the involvement was negligible.
Seven individuals with this condition in
Bhavnagar were siblings from three families.
No similar observation was made in Erna
kulam district.
iio
SiNORrfa/.
Mawa chewing and oral submucous fibrosis
Table 5
Location distribution of submucous fibrosis in Bhacnagar and Emakulam districts
Location
Labial mucosa
Buccal mucosa
Retromolar area*
Hard palate*
Soft palate*
Uvula*
Tongue*
Floor of the mouth*
Ernakulam0
(n=64)
Bhavnagar
(n=60)
No.
%
No.
%
30
59
60
_
57
33
]
—
50%
98%
100%
41
62
14
12
8
5
38
14
64%
97%
22%
19%
12%
8%
59%
22%
95%
55%
2%
“Source: ref. (3)
Fig. 1. Involvement of posterior one-third of the
V<o.oi
DISCUSSION
This paper demonstrates that mawa and arccanut chewing in various forms arc strongly as
sociated with the occurrence of submucous
fibrosis in Bhavnagar and that this disease
exhibits specific regional variations in its clini
cal characteristics.
The upsurge of the mama habit is a recent
phenomenon in Bhavnagar. This habit, with
some minor variations and under different
names, is widely prevalent in other parts of
Gujarat and also elsewhere in India. The high
relative risks for different arcca-nut chewing
groups, observed for the first time, arc con
sistent with other epidemiological observa
tions which implicate areca-nut chewing in the
pathogenesis of this condition. For example,
Bhonsle el al. demonstrated in a review that
34-100% of individuals with submucous fi
brosis chewed areca-nut in various forms (3).
This habit was observed to be much more
prevalent among the eases than in the general
population (2), and the prevalence (7) and the
incidence rates (8) were higher among arecanut (betel-quid) chewers (see paper by Murti
et al., this volume). In the present study, chew
ing areca-nut alone, i.e., supari (see paper by
Bhonsle et al., this volume), was observed
buccal mucosa and retromolar area in a
in 8% of cases in Bhavnagar; but this habit
was practised by 67% of submucous fibrosis
patients in Pune reported in an earlier study
(3).
The above observations demonstrated a
strong association of this condition with arccanut chewing; similarly, a 10-year prospective
intervention study showed a fall in the inci
dence of submucous fibrosis (4). In this study
the annual incidence per 100 000 dropped from
21.3 among men and 45.7 among women in the
control cohort to 8 and 29 in the intervention
cohort, respectively. These findings also sup
port the etiological role of areca-nut chewing in
this condition.
It has been suggested that.there might be
a genetic susceptibility to areca-nut alkaloids
and tannins in individuals with this disease
(9,10). In this context, it must be noted that
seven individuals with this condition were sib
lings from three families, sharing perhaps the
same genetic predisposition and similar expo
sure to areca-nut chewing.
Submucous fibrosis exhibits notable re
gional differences in its age and sex distri
bution and its clinical characteristics; such
variations are attributable to differences in
mawa chcwcr
Fig. 2. Involvement of retromolar areas, soft
palate and the uvula in a mawa chcwcr
areca-nut chewing practices in different areas
(3). Similar observations were made in this
investigation. The contiguous involvement of
the posterior one-third of the buccal mucosa,
retromolar areas (Fig. 1), soft palate and uvula
(Fig. 2) in Bhavnagar could be due to the habit
of keeping the mawa quid in the posterior
part of the mandibular groove. In Ernakulam,
exposure of the buccal mucosa to the betel
quid is generalized; this may be responsible for
the more diffuse involvement of the buccal
mucosa.
111
Long-term studies on malignant transfor
mation rates of submucous fibrosis among
betel-quid chewers show that (see p'per by
Murti et al., this volume) the .near age (51
years) of individuals with this condition in
Emakulam was higher than that in Bhavnagar
(29 years). Correspondingly, the mean age of
individuals with this condition who developed
oral cancer (7.6%) in Emakulam was 64.6
years (11). In view of the very low mean age
(29 years) of the patients in Bhavnagar, it
would be important to find oct whether they
develop oral cancer at an earlier age. It would
also be important to know whether submucous
fibrosis among areca-nut chewers with no con
current tobacco use develops into oral cancer.
The health hazards of tobacco use are
well recognized; consequently, tobacco control
measures arc receiving priority. While epide
miological studies have revealed no significant
risk for oral cancer associated with areca-nut
chewing (12), this habit certainly appears to be
involved in tfre pathogenesis of oral submucous
fibrosis, which is itself often a progressive
disease with a burning sensation and dry
ness of the mucosa, with no effective cure.
Furthermore, a recent study demonstrated a
high relative risk (397.3) for oral cancer associ
ated with this condition (13).
The popularity of areca-nut containing
preparations such as pun masala (see paper by
Bhonsle el al., this volume) has increased tre
mendously within the last few years owing to
a very sophisticated marketing campaign. In
view of the serious consequences of submucous
fibrosis and the etiological role of areca-nut
chewing, a strict curb on the advertisement
and use of these products is warranted.
Acknowledgments
This study was supported by funds from
the National Institutes of Health, USA, under
Indo-US Fund Research Agreement No.
01-022 N.
112
Sinor et al.
References
1.
2.
3.
4.
5.
6.
7.
Pindborg JJ, Murti PR, Bhonsle RB, et al.
Oral submucous fibrosis as a precancerous con
dition. Scand J Dent Res 1984; 92:224-9.
Mehta FS, Gupta PC, Daftary DK,
Pindborg JJ, Choksi SK. An epidemiologic
study of oral cancer and precancerous condi
tions among 101 761 villagers in Maharashtra,
India. Int J Cancer 1972; 10:134-41.
Bhonsle RB, Murti PR, Gupta PC, et al.
Regional variations in oral submucous fibrosis
in India. Community Dent Oral Epidemiol
1987; 15:225-9.
Murti PR, Gupta PC, Bhonsle RB, et al.
Effect on the incidence of oral submucous
fibrosis of intervention in the areca nut chewing
habit. J Oral Pathol Med 1990; 19:99-100.
Sinor PN, Gupta PC, Murti PR, et al.
A case-control study of oral submucous fi
brosis with special reference to the etiologic role
of areca nut. J Oral Pathol Med 1990; 19:
94-8.
Mehta FS, PindborgJJ, Hamner JE,.Ill, et
al. Report on Investigations of Oral Cancer
and Precancerous Conditions in Indian
Rural Populations, 1966-69, Munksgaard,
Copenhagen, 1971.
Pindborg JJ, Mehta FS, Gupta PC,
Daftary DK. Prevalence of oral submucous
fibrosis among 50 915 Indian villagers. Br J
Cancer 1968; 22:646-54.
8.
Gupta PC, Mehta FS, Daftary DK, et al.
Incidence rates of oral cancer and natural
history of oral precancerous lesions in a
10-yr follow-up study of Indian villag
ers. Community Dent Oral Epidemiol 1980;
287-333.
9. Canniff JP, Harvey W. The etiology of oral
submucous fibrosis: the stimulation of collagen
synthesis by extracts of arcca-nut. Int J Oral
Surg 1981; 10: Suppl. 1. 163-7.
10. CanniffJP, Harvey W, Harris M. Oral sub
mucous fibrosis: I. Its pathogen-sis and man
agement. Br Dent J 1986; 160:429-34.
II. Murti PR, Bhonsle RB, Pini horg JJ, et al.
Malignant transformation rate in oral submu
cous fibrosis over a 17-yr period. Community
Dent Oral Epidemiol 1985; l3:3nO-l.
12. Gupta PC, Pindborg JJ, Mehta FS.
Comparison of carcinogcnesity of betel quid
with and without tobacco: an epidemiologic
review. Ecol Disc 1982: 1:213-9.
13. Gupta PC, Bhonsle RB, Murti PR, et al. An
epidemiologic assessment of cancer risk in cral
precancerous lesions in India with special ref
erence to nodular leukoplakia. Cancer 1989;
63:2247-52.
Control of Tobacco-rdatcd Cancers and Other Diseases.
Internatioral Symposium, 1990. Prakash C. Gupta, James E. Hamner, III
1992.
and P.R. Murti, eds. Oxford University Press, Bombay,
Tobacco-related cancers in Bombay, India:
a study of incidence over two decades
Kasturi Javant and B. B. Yeole*
Cancer R- search Institute, Bombay, India; and 'Bombay Cancer Registry, Bombay, India
A study of the site-specific incidence rates of cancers of the upper alimentary and respiratory tracts
over two decades among males in Bombay showed that the incidence of cancers of the tongue, oro
pharynx and larynx have decreased significantly, whereas that of ora! cancer excluding the tongue
has remained more or less stable. The incidences of cancers of the hypopharynx, oesophagus and
lung increased only marginally, but successive birth cohorts showed no consistent pattern.
Limited data on tobacco habits in Bombay indicate a marked decrease in the proportion of bidi
smokers in younger cohorts, which conforms with the observed decline in the incidence of those
cancers for which bidi smoking is the predominant risk factor. For cancers of the hypopharynx,
oesophagus and lung, for which tobacco chewing or cigarette smoking is an equally or more
important risk factor than bidi smoking, no consistent pattern was seen. Tobacco-related cancers
constitute about 50% of cancers among men in India. As the recent national trends in per-caput
consumption of tobacco arc different from those in Bombay, the decline in predominantly bidi
dependent cancers seen in Bombay cannot be extrapolated to the country as a whole.
Consequently, control programmes arc needed for all smokers in the country and especially for
cigarette smokers in urban areas.
INTRODUCTION
Tobacco is a major risk factor for cancers of the
upper alimentary and respiratory tracts, which
constitute about 50% of all cancers among
Indian men. This paper examines the trends in
the incidence of these cancers over the years.
TRENDS IN TOBACCO-RELATED
CANCERS
Data on site-specific incidence of cancer are
available from the Bombay Cancer Registry
for a period of over two decades (1,2), mak
ing it possible to assess trends in tobacco-relat
ed cancers. When the age-adjusted incidence
rates for these cancers in five-year periods
between 1964-82 (except 1964-66, which is a
'.hree-year period) were examined, the inci
dence of cancer of the tongue declined progres
sively, from 14 per 100 000 in the early 1960s
to 9.7 per 100 000 in the period 1978-82, while
those of cancers of other parts of the mouth
remained more or less stable over the years,
with an age-adjusted incidence rate of about 7
per 100 000 (Table 1). The rate for cancer of
the oropharynx declined from 6.1 per 100 000
to 3.5 per 100 000 over the years, the decline
being marked in the late 1970s and early
1980s. The incidence of cancer of the hypo
pharynx and oesophagus, however, increased
from 7.3 to 10.0 per 100 000 and from 13 to 15
per 100 000, respectively. The age-adjusted
incidence rate for cancer of the larynx declined
from 13.8 to 10.1 per 100 000, whereas that for
cancer of the lung increased marginally from
13.3 in the 1960s to 15.8 per 100 000 in the
1980s.
A clearer picture of changing incidence
rates was obtained for each site by fitting a
Tobacco-related cancers in Bombay
140 Jayant and Y eole
141
Table 1
Site-specific age-adjusted incidence rates far cancers at major tobacco-related sites in males in Bombay, 196d-82
Age-adjusted incidence rate (world) per 100 000 per year
1964-66
(ref- 1)
1968-72
(ref. 2)
1973-77
1978-82
Oral cavity
Tongue
Mouth (all other parts)
14.0
7.0
12.6
7.3
10.2
6.7
9.7
7.5
Pharynx
Oropharynx
Hypopharynx
6.1*
7.3
5.6
7.7
4.5
8.7
3.5
10.0
Digestive organs
Oesophagus
13.0
15.2
14.7
15.0
Respiratory organs
I-arynx
l-ung
13.8
13.3
13.6
13.5
12.4
14.7
10.1
15.8
All sites
139.5
143.1
142.1
147.4
Site of malignant neoplasm
*ICD 7, 145: tonsils and oral mesopharynx
log-linear polynomial of the first order, which
is the usual model for analysing trends in
cancer incidence (3). The average percentage
change in incidence was obtained and the
significance tested by Student’s I test.
For cancers of the tongue, oropharynx and
larynx, the average percentage changes in inci
dence were -4.39, -3.73 and -3.16, respectively,
and these were highly significant (Fig. 1). For
cancers of the hypopharynx, oesophagus and
lung, the average percentage changes were
1.23, 0.95 and 0.05, respectively, and these
were not significant (Fig. 2).
The decline in incidence of cancers of the
tongue, oropharynx and larynx has been repor
ted to be due to a cohort effect, younger five-year
birth cohorts in general having lower rates than
older cohorts (4). Hovvever, for cancers of the
hypopharynx and oesophagus, no clear pattern
was discernible; for lung cancer, there seemed to
be no cohort effect at all (Fig. 3).
We considered that a synoptic measure of
the experience of each birth cohort would lead
to better appreciation of the risk differentials
between birth cohorts. On examining the age
ranges for which the incidence data were avail
able for each cohort, it was found that each
cohort had two overlapping 15-year age inter
vals: one common to the five-year younger
cohort and the other, common to the fiveyear older cohort. For example, the 1933 birth
cohort had the age range 30-44 years common
to the 1938 birth cohort and the age range
35-49 years common to the 1928 birth cohort
(Fig. 4). Hence, a synoptic measure of risk
in each birth cohort could be obtained by
estimating the cumulative rate as defined by
Day (5) over an appropriate age range.
Accordingly, cumulative rates over an age
range common to the five-year older or youn
ger cohort were used to assess the risk differen
tials between adjacent cohorts.'
A diagrammatic representation of cumu
lative rates in pairs of adjacent cohorts for the
same age range is given in Figure 5 (4). It w.is
observed that for cancers of the tongue, oro
pharynx and larynx, in each of the pairs of
birth cohorts, the younger cohort had a lower
cumulative rate. However, for cancers of the
hypopharynx, oesophagus and lung, the pat
tern was not consistent; only cohorts born after
1928 seemed to have rates lower than those of
five-year older cohorts, but for those born
before 1928 the successive five-year younger
cohorts had either similar rates or showed a
reversal (i.e., younger cohorts having higher
rates).
INTERPRETATION OF TRENDS
The observed changes in the incidence rates
arc not likely to be artefacts, as various indices
have shown that the data of the Bombay
Cancer Registry are reliable (6). This chang
ing pattern, therefore, needs to be viewed on
the basis of changing exposure to etiological
factors. For that purpose, it is essential to know
the risk factors for cancers at each of the sites,
the associated risk ratios and the prevalence of
risk factors in the population over the years.
It must be pointed out that most Indian
oncologists pool cancers of the base of the
tongue with cancers of the oropharynx, as
it has been found that the clinical behavi
our, prognosis and etiology of cancers of the
base of the tongue are similar to those of
142 Jayant and Yeole
Tobacco-related cancers in Bombay
INCIDENCE PER IO S PER YEAR
25-29 30-34 35-39 40-44 45-49 50-54 55-59 60-64
1936
1933
1923
lies
1916
Fig. 4. Age ranges for which incidence data are
available for various birth cohorts
oropharyngeal cancer (7). This practice is in
contrast to the international classification, in
which the entire tongue used to be grouped
under one rubric. In Bombay, almost 75% of
lingual cancers occur at the base of the tongue.
It is therefore justifiable to consider that the
risk ratio for cancer of oropharynx inclusive of
the base of the tongue is appropriate for can
cers of both the tongue and oropharynx.
It is interesting that bidi smokers have a
much higher risk of cancers of the oropharynx
and larynx compared to cigarette smokers. For
cancer of the lung, bidi and cigarette smokers
in Bombay had two- to three- fold higher risks
(13). Furthermore, bidi smoking and tobacco
The risk ratios obtained in a Bombay
study for smokers and chcwcrs as compar
ed to nonusers of tobacco (8) arc shown in
Table 2. In this study, smokers who were
Table 2
Risk ratios in smokers and chewers fir tobacco-related cancers'
Type of tobacco usage6
INCIDENCE PER
10
PER YEAR
predominantly bidi smokers had strikingly
higher risks of cancers of the oropharynx,
including the base of the tongue (11.8) and lar
ynx (7.7), than chewcrs (3.3 and -r.u, respec
tively). In contrast, chcwers had a higher risk
for cancers of the oral cavity (excluding the
base of tongue) and hypopharynx (6.0 and 6.2,
respectively). Smokers and chewers had simi
lar risks for oesophageal cancer. Risks for oral,
pharyngeal and laryng-? .1 cancers specifically
among cigarette smokers are not available
from India. Two studies in the west showed
that the risk ratios for oral cancers in cigarette
smokers were about 1.5 (9) and 3 (10); the risk
for cancers of the pharynx taken as a group
was not significantly higher in smokers (11);
for cancers of the larynx, the ratio was between
3 and 6, depending on the frequency of ciga
rette smoking (12).
AGE RANCE IN YEARS
BIRTN-YEAR
or
O1CRT
Site of cancer
S
C
SC
2.8
6.0
10.1
Pharynx
Oropharynx, including base of tongue
Hypopharynx
11.8
3.6
3.3
6.2
31.7
16.9
Oesophagus
2.2
2.5
6.2
Larynx
Lung
7.7
4.6
20.1
(Cigarettes)
CgS
1.5-3.0
Oral cavity
excluding base of tongue
(Bidis)
143
NS
3.4
2.4
'Calculated from data in refs. (8-13)
hS, smoker; C, chewer; SC, smoker-chewer; CgS, cigarette smoker
NS, not significant
I Risk ratios here refer to western studies
3-6c
10-15
Tobacco-related cancers in Bombay
144 J AVANT AND YeOLE
chewing were found to be major risk factors for
oral cancers and for cancers of the pharynx
and larynx, and the risks attributable to to
bacco usage were high, varying between 70
and 85%, depending on the site (14). Thus,
the observed changes in incidence rates proba
bly reflect the changes in tobacco usage that
occurred in this population some 20 years ago.
Data on the prevalence of tobacco usage in the
population of Bombay over the years are not
available to fully substantiate this hypothesis.
An attempt to estimate the pattern of tobacco
usage was made by considering limited data on
prevalence by age available from a cohort
study on blue-collar workers carried out in the
1970s (15). By approximating the habits in dif
ferent age groups to the habit pattern in the
corresponding birth cohorts, trends in the hab
its of cohorts born between 1921 and 1936 were
assessed. These were used to interpret the can
cer experience of cohorts born between 1913
and 1943.
Examination of the patterns in various
birth cohorts showed a marked decrease in bidi
smoking and a moderate increase in cigarette
smoking in successively younger birth cohorts
(Fig. 6). The pattern for those with dual hab
its, i.e., bidi smoking with tobacco chewing and
cigarette smoking with tobacco chewing, is
similar to that of people with the single habit of
145
smoking. This situation would lead to succes
sive younger birth cohorts having lower inci
dence rates of cancers in which bidi smoking is
the dominant risk factor. This may explain the
trends in the incidence rates of cancers of the
tongue, oropharynx and larynx, which are the
major AtWi-relatcd cancers in this analysis.
Tobacco chewing remained more or less
stable in various birth cohorts; and the inci
dence of oral cancer, excluding the tongue, for
which tobacco chewing is the dominant risk
factor, was also stable over the years. For lung
cancer, for which both bidi and cigaretfe smok
ing are risk factors, and hypopharyngeal can
cer, for which chewing is a more important risk
factor than smoking, it is difficult to explain
the lack of consistency in the pattern in succes
sive birth cohorts; it is probably due to the
paucity of data. Perhaps, detailed data on a
representative sample of the entire population
would provide a plausible explanation. For
oesophageal cancer, the risk attributable to
tobacco was only 50% (14), and no explana
tion of the trend (or rather lack of it) can be
given solely on the basis of the prevalence of
tobacco usage.
In order to assess whether the trends
observed continue in the same direction, the
latest five-year data were considered. Inter
estingly, the incidence rates for cancers of the
oropharynx and larynx have stabilized, at
about 3.5 and 10 per 100 000, respectively.
FUTURE CANCER PATTERN IN THE
COUNTRY
Fig. 5. Cumulative incidence rates over two overlapping 15-year age ranges for cancers of the tongue,
oropharynx, hypopharynx, oesophagus, larynx and lung for various birth cohorts
Fig. 6., Proportions of smokers and chewers in
cohorts born between 1936 and 1921
(blue-collar workers in Bombay)
The pattern of tobacco-related cancers ex
pected for the country as a whole on the basis
of estimates of per-caput consumption of raw
tobacco of different types, obtained from data
published by the Ministry of Agriculture, is at
variance with what was actually observed in
Bombay (16,17). For instance, during the
period 1951-81, the per-capul consumption of
bidi tobacco increased from 145 to 191 g anti
that of cigarette tobacco from 55 to 115 g.
146 Jayant and Yeoi.e
Tobacco-related cancers in Bombay
Table 3
Estimated pcr-capul consumption of raw tobacco (in grams) in India0
1951-52
1960-61
1970-71
1980-81
Cigarette
Chewing
145
55
140
168
97
143
155
133
94
191
115
54
Total
556
566
474
541
Tobacco type
Bidi
"Calculated from data in refs. (16, 17)
Consumption of chewing tobacco, however,
decreased from 140 to 54 g (Table 3). The pos
sible implications are that the incidences of
6i</i-rclatcd cancers, i.c., cancers of the tongue,
oropharynx and larynx, arc unlikely to show a
decline in the near future. There is thus an
urgent need to institute tobacco control pro
grammes especially directed to all smokers in
the country, with special emphasis on cigarette
smokers.
References
1.
2.
3.
4.
5.
6.
7.
Jussawalla DJ, Deshpande VA. Evaluation
Jussawalla DJ. Cancer Incidence in Grea
8.
ter Bombay (1964-66). The Indian Cancer
Society: Bombay, 1970.
WaierhouseJ, Muir C, Correa P, Powell
J, eds. Cancer Incidence in live Continents.
Vol. Ill, IARC Scientific Publications No. 15,
International Agency for Research on Cancer:
Lyon, 1976.
The Cancer Registry of Norway. Trends in
Cancer Incidence in Norway 1955-1978. Oslo,
1982.
Jayant K, Yeoi.e BB. Cancers of the upper
alimentary and respiratory tracts in Bombay,
India: a study of incidence over two decades.
Br J Cancer 1987; 56:847-52.
Day NE. A new measure of age-standardized
incidence rate. In: Waterhouse J, Muir C,
Correa P, Poweij.J, eds. Cancer Incidence in
five Continents Vol. Ill, p. 443, IARC
Scientific Publications No. 15. International
Agency for Research on Cancer: Lyon, 1976.
Yeoi.e BB, Jussawalla DJ. An assessment
of reliability and completeness of Bombay Can
cer Registry data. Indian J Cancer 1988;
25:177-90.
Paymaster JC. The importance of a uniform
clinical classification and staging of carcinomas
of the upper digestive tract. IndianJ Surg 1957;
19:1-6.
of cancer risk in tobacco chcwcrs and smokers:
an epidemiologic assessment. Cancer 1971 ;28:
244-52.
9. Rothman KJ, Keller A. The effect of joint
exposure to alcohol and tobacco on risk of can
cer of the mouth and pharynx. J Chronic Dis
1972;25:711-6.
10. Wyndf.r EL, Bross IJ, Feldman RM. A
study of the etiologic factors in cancers of the
•mouth. Cancer 1975;10:1300-23.
II. Elwood JM, Pearson JCG, Skippen DH,
Jackson SM. Alcohol, smoking, social and
occupational factors in the etiology of cancer
of the oral cavity, pharynx and larynx. Int J
Cancer 1984; 34:603-12.
12. Wyndf.r EL, Covey LS, Mabuchi K,
Mushinski M. Environmental factors in can
cers of the larynx: second look. Cancer 1976;
38:1591-601.
13. Notani PN, Rao DN, Sirsat MV, Sanchvi
LD. A study of lung cancer in relation to bidi
smoking in different religious communities in
Bombay. IndianJ Cancer 1977; 14:115-21.
14. Jayant K, Balakrishnan V, Sanghvi LD,
Jussawalla DJ. Quantification of the role of
smoking and chewing tobacco in oral, pharyn
geal and esophageal cancers. Br J Cancer 1977;
35:232-5.
15. Jayant K, Notani PN, Sanghvi LD. Health
consequences of smoking in two socioeconomic
classes in Bombay. In: Forbes WF, Frecker
RC, Nostbakken D, eds. Proceedings of the
Fifth World Conference on Smoking and
Health, Winnipeg, Canada, July 10-15, 1983.
Canadian Council on Smoking and Health,
Ottawa, Vol. 1: pp. 149-56.
147
16. Directorate of Tobacco Development. Indian
Tobacco Statistics. Ministry of Agriculture and
Irrigation, Government of India, New Delhi,
1975.
17.
Directorate of Tobacco Development. Tobacco
in India: A Handbook of Statistics. Ministry of
Agriculture and Irrigation, Government of
India, New Delhi, 1983.
Control of Tobacco-rclatcd Cancers and Ollier Diseases.
Inter.-lational Symposium, 1990. Prakash C. Gupta, James E. Hamner, III
AND P.R. Murti, EDS. Oxford University Press, Bombay, 1992.
Oral health consequences of tobacco vse in
Ei nakulam district, Kerala, India
P. R. Murti, R. B. Bhonsle, P. C. Gupta and D. K. Daftary
Basic Denial Research Unit and WHO Collaborating Centre for Oral Cancer Prevention,
Tata Institute of Fundamental Research, Bombay, India
Bidi smoking and betel-quid {pan) chewing arc the most common forms of tobacco use in
Ernakulam district. They arc strongly associated with oral cancer, various prccanccrous lesions
and conditions, and others which do not seem prccanccrous. Nodular leukoplakia and submucous
fibrosis arc a very high-risk prccanccrous lesion and condition, respectively; other clinical types of
leukoplakia also indicate a significant risk for ora! cancer. Malignant transformation was not asso
ciated with leukoedema, leukokcratosis nicotina palati, palatal erythema, central papillary atro
phy of the tongue, ^an-chcwcr’s lesion or oral lichen planus-like lesion. Most of these oral lesions
remained stationary, some regressed and few recurred; submucous fibrosis, however, did not
regress. Overall, tobacco use was found to influence the entire natural history of precancer, indi
cating the n-jed to implement tobacco control measures.
INTRODUCTION
Ernakulam district in the State of Kerala, is on
the south-western coast of India. In 1966, at
the time of initiation of our epidemiological
f>tudics, the district had an area of 3340 km2
and a population of 1 859 913 (1961 census).
Bidi smoking and bctcl-quid (pan) chewing
are the main forms of tobacco use in this area
(see paper by Bhonsle et al., this volume). In
this paper wc describe the oral health conse
quences of these forms of tobacco use on the
basis of various epidemiological studies con
ducted over the past 24 years.
prospective study of those examined in phase 1
(2). Phase 3 was an intervention trial in a new
sample of 12 212 tobacco users in 23 karas (3).
It consisted of a base-line survey and a 10-year
follow-up of these individuals. An additional
survey was carried out among 5099 people in
five karas in the Parakadavu area (4), and peo
ple with lesions and matched controls were
followed-up annually.
Prior to examination, the frequency of
tobacco use, i.e., the number of times per day
Table 1
MATERIAL AND METHODS
Three main studies were conducted in
Ernakulam district (Table 1). Phase 1 was a
cross-sec-ion;-.! study among 10 287 villagers
aged 15 years and over in 14 karas (kara is a
smallest sampling unit) selected by random
sampling (1;. Some 59% of these individuals
were tobacco users. Phase 2 was a 10-year
Main studies conducted in Ernakulam district
Studies
Population Tobacco
users (%)
(no.)
Phase 1 and 2 (1966-77)
10 287
59%
Phase 3 (1977-88)
12 212
100%
Parakadavu survey (1971)
5 099
55%
92
Oral health consequences of tobacco use
Murti et al.
an individual smoked or chewed tobacco, the
duration or such habits and other relevant
details were recorded by trained interviewers.
Examinations were conducted in a house-tohouse approach, and selected oral lesions were
recorded as per standardized criteria (1,5). All
lesions were photographed in colour at the
initial diagnosis and subsequently whenever
necessary. Several hundred oral lesions were
biopsied, and smears were obtained for cyto
logical examination as per the requirement of
the particular survey.
LESIONS ENCOUNTERED
Almost all of the oral lesions were observed
only among tobacco users. In this paper, the
lesions can be grouped broadly as shown below
on the basis of their frequency in groups with
different habits.
Predominantly associated with smoking: (i)
leukoedema; (ii) leukokeratosis nicotina palati;
(iii) palatal erythema; and (iv) central papil
lary atrophy of the tongue
Predominantly associated with chewing: (i)
pan-chewer’s lesion; (ii) oral lichen planus-like
lesion; and (iii) oral submucous fibrosis
Associated with smoking and chewing (mixed
habit): (i) leukoplakia and preleukoplakia; (ii)
oral lichen planus; and (iii) oral cancer
LESIONS PREDOMINANTLY
ASSOCIATED WITH SMOKING
As mentioned earlier, bidi smoking is the most
popular smoking habit, especially among men
in this area. Overall, 17% of the 10 287 indi
viduals examined in phase 1 smoked bidis (1).
Leukoedema: This is a chronic mucosal condi
tion in which the oral mucosa has a grey, opa
que appearance (Fig. 1) as though a greyish
film were hanging over it like a veil. When the
mucosa is stretched the lesion disappears, only
to reappear when it is relaxed.
Epidemiology. The prevalence of leuko
edema was 0.4%. About 16 (62%) of the 26
Fig. 2. Leukokeratosis nicotina palati in a
bidi smoker
Fig. 1. Leukoedema (L) in the buccal mucosa of a
bidi smoker
adjusted incidence rate among smokers was
1.7 per 1000; it was 0.7 per 1000 in those who
smoked and chewed (2).
leukoedemas were seen among bidi smokers
and the rest in people who smoked and chewed
(1). The annual age-adjusted incidence rate ofj
this lesion was 2.5 per 1000; it was 3.8 per 1000)
among smokers (2).
Natural history. Over a 10-year period,
66% of the 44’ lesions remained stationary,
34% regressed spontaneously and none show
ed malignant transformation (2).
Histologicalfeatures: Leukoedema was char
acterized by accumulation of spongy vacuo-!
lated cells in the superficial epithelial layer,
ballooning cells in the stratum spinosum and
epithelial hyperplasia (6).
Natural history. Of the 87 leukoedemas
(includes incidence lesions) followed-up over a
10-year period, 64% remained stationary and
36% regressed; no malignant transformation
was observed (2).
Leukokeratosis nicotina palati: This lesion
which is commonly seen among conventional
smokers, consists of a greyish-white palate
with small nodular excrescences having small
central red dots, corresponding to the inflamed
orifices of the minor salivary glands (Fig. 2).
Epidemiology. The prevalenc: of this lesion
was 0.3%; 52% of the 31 lesions occurred
among bidi smokers (1). The annual age
Leukokeratosis nicotina palati observed
among conventional smokers must be distin
guished from the palatal changes associated
with reverse chutta smoking (see paper by
Daftary et al., this volume). Palatal changes in
reverse smokers are multimorphic and precancerous, whereas leukokeratosis nicotina palati
exhibits neither great variability nor malignant
transformation.
Palatal erythema: Palatal erythema is marked
by a diffused erythematous hard palate (Fig.
3A), occasionally extending to the soft palate.
Epidemiology. Of the 69 lesions observed
among 7216 tbbacco users (Table 2), 87%
occurred among smokers, especially bidi smok
ers. This lesion was observed in only three
women, which corresponds to the low preva
lence of bidi smoking among women.
Clinical aspects: The lesion occurred either
independently or sometimes with other lesions.
Fig. 54. Palatal erythema in a bidi smoker
Fig.3B. Palatal erythema with papillary
hyperplasia in a bidi smoker
Fig. 3C. Regression of palatal erythema shown
in Fig. 5.4, following discontinuation
of smoking; note loss of
pigmentation
93
94
Oral health consequences of tobacco use
Murti el al.
restarted and stopped. These observations
clearly indicate that palatal erythema is caused
by smoking, particularly bidi smoking.
Table 2
Distribution of individuals with palatal erythema according
to habit and sex
Habit
Men
(n=6978)
Women
(n=238)
Total
(n=7216)
Smoking
Smoking &
chewing
58 (88%)
8 (12%)
2 (67%)
1 (33%)
60 (87%)
9 (13%)
Total
66 (100%)
3 (100%) 69 (100%)
About 10% of the lesions were associated with
palatal papillary hyperplasia (Fig. 3B) and
25% with central papillary atrophy of the
tongue and bilateral commissural leukopla
kias. This triad of lesions is comparable to the
‘multifocal candidiasis ’ described in western
literature (7).
Natural history. Over a 10-year period,
35% of the 69 lesions persisted, 56% regressed
and 9% were transient, i.e., they regressed,
recurred and regressed again (Table 3). In
terestingly, the highest percentage (60%) of
persistent lesions was seen among people who
did not give up their smoking habits, while the
highest percentage (75%) of regressed lesions
occurred among those who discontinued or
reduced smoking substantially (Fig. 3A and
C). Most of the transient lesions were asso
ciated with inconsistent habit practices,
i.e., among those who stopped their habits,
elongated; some were rhomboid or irregular
(8). The mean length was 2.7 cm and the
breadth, 1.3 cm. They were generally smooth,
but some were fissured. In 69% of cases the
lesion occurred independently; 14% had co
existent palatal erythema and 8% had leu
koplakia. A triad of central papillary atrophy,
bilateral commissural leukoplakia and palatal
erythema, comparable to the 'multifocal candi
diasis’ described in western literature (7) was
seen in 3% of cases. The remaining occurred
with other lesions. Central papillary atrophy of
the tongue must be distinguished from the
atrophic candidiasis reported among people
with human immunodeficiency viral infection
(9).
I
Central papillary atrophy of the tongue-. This
lesion has also been described in the literature
as median rhomboid glossitis and localized
atrophy of the tongue papillae (1). It consists
of a well-defined, oval, pink area in the centre
of the dorsum of the tongue devoid of lingual
papillae (Fig. 4A).
Epidemiology. The prevalence of this lesion
was 1%; it was present among 2.2% bidi smok
ers, 1.6% cigarette smokers and 0.3% non
users of tobacco (1). In the 10-ycar follow-up
study, the annual age-adjusted incidence rate
among smokers was 1.5 per 1000 as compared
to 0.8 per 1000 among nonsmokers (2).
Histological features: This lesion was mark
ed by the absence of tongue papillae, the
presence of slight parakeratinization of the epi
thelial surface, long slender reteridges and
occasional pseudocarcinomatous hyperplasia.
Chronic inflammatory cell infiltrate, chiefly of
lymphocytes, was usually present within the
epithelium and in the lamina propria. In a
single periodic acid-Schifl" section study of 12
biopsies, candidal hyphae were observed in
67% (8).
Etiology. Central papillary atrophy of the
tongue, is considered to be due to candidal
infection, smoking or both (8). In this study,
central papillary atrophy exhibited a strong
association with smoking, particularly bidi
smoking. This was exemplified by its higher
prevalence (I) and incidence rates (2) among
smokers, its long-term behaviour in relation to
the cessation or reduction of smoking (see
below) and the observation that' 87% of the
lesions occurred among bidi smokers (8).
Interestingly, very few women had this lesion,
due perhaps to the rarity of smoking among
women.
Table 3
Behaviour of palatal erythema according to change in tobacco use over a 10-year period
Tobacco use
Palatal erythema
Unchanged/
increased
Reduced/
stopped
"Not constant
No.
%
No.
%
No.
Persistent
Regressed
Transient
15
9
1
60%
36%
4%
9
30
1
23%
75%
2%
Total
25
100%
40
100%
Total
•%
No.
%
_
—
4
100%
24
39
6
35%
56%
9%
4
100%
69
100%
95
Fig. 4A. Central papillary atrophy of the
tongue in a bidi smoker
Fig. 4B. Regression (repapillation) of the lesion
shown in Fig. 4A following
discontinuation of bidi smoking
Clinical aspects: Most of the 182 lesions
studied were pink to dark-pink, oval or
Natural history: Some 50% of the 182
lesions that were observed for 10 years were
persistent (8), 43% regressed, i.e., repapillated, 5% regressed and recurred and 2%
showed inconsistent behaviour (regressed,
recurred and regressed). The highest percent
age (65%) of persistent lesions was found
among people who did not stop or reduce their
habits, while the highest percentage (87%) of
regressed lesions (Fig. 4A and B) was seen in
those who stopped their habits. None of the
lesions progressed to cancer.
LESIONS PREDOMINANTLY
ASSOCIATED WITH BETEL-QUID
CHEWING
Tobacco was most ofteh chewed as an ingre
dient in betel quid (pan) by 33% of the women
96
Oral health consequences of tobacco use
Murti et al.
and 35% men in Ernakulam district (see paper
by Bhonsle et al., this volume). Betel-quid
chewing inevitably stains the mucosa bright
red, due to the formation of o-quinone from
water-soluble polyphenols, notably, leucocynidins, at the alkaline pH of 8-9 via second
ary reactions (10). These stains can be washed
clean or disappear with abstinence from chew
ing; however, it is not unusual to see persons
with perpetually stained mucosa.
97
Natural history. Pan-chewer’s lesion is a
specific entity and rarely progresses to leuko
plakia. Over a three-year observation period,
26% of the 532 observed lesions were persist
ent, 45% regressed spontaneously and 29%
recurred; malignant transformation was not
observed in these lesions (2).
Oral lichen planus-like lesion: A characteristic
lesion consisting of white, wavy, parallel, non
elevated striae that do not crisscross (Fig. 6A)
(as in lichen planus) was observed. Some
times, these striae radiate from a central ery
thematous area (Fig. 6B) at the site of place
ment of the betel quid.
Fig. 5. Pan-chewer’s lesion
Epidemiology. The prevalence of this lesion
among 5099 individuals in Parakadavu was
0.7% (4). z\bout 89% of the lesions occurred
among betci-quid chewers and 11% among
people with mixed habits. In a 10-ycar follow
up study of 10 000 villagers in Ernakulam dis
trict, the annual age-adjusted incidence rates
among men and women were 0.7 and 2.2 per
1000, respectively (2). The peak incidence for
women was in the 45-54-year age group. The
incidence was zero among smokers and nonusers of tobacco; 4.3 per 1000 among women
who chewed. This lesion is thus entirely asso> i-
ated with betel-quid chewing.
Pan-chewer’s lesion: This lesion consists of a
thick brownish-black encrustation on the buc
cal mucosa (Fig. 5) at the site of placement of
the betel quid. It was often seen among heav
ily addicted betel-quid chewers. It could be
scraped off with a piece of gauze; it regresses
spontaneously, more frequently when the habit
is discontinued.
Epidemiology. The annual age-adjusted
incidence rate of this lesion was 28 per 1000
among male chewers and 17.4 per 1000 among
female chewers (2).
Histological features: These lesions showed
pale-staining parakeratin-like surface layers of
epithelium, containing round nuclear rem
nants, ballooning and vacuolated cells and
epithelial hyperplasia.
Clinical aspects: The striae seen in these
lesions were very fine, like fingerprints, ai d
always occurred in the buccal mucosa and
mandibular groove, locations which are in inti
mate contact with the betel quid.
Histologicalfeatures: The lesion shows para
keratinized atrophic epithelium, liquiietation degeneration of the basal-cell layer and a
band-like inflammatory cell infiltrate coptauiing lymphocytes and plasma cells (4). Unlike
lichen planus, this lesion shows hyper
parakeratosis, and plasma cells in the ;i x-
taepithelial region.
Natural history. A total of 42 lesions were
followed-up for four years: 79% remained s •>tionary, 21% regressed and two of the
Fig. 7. Buccal mucosal involvement with
blanching in oral submucous fibrosis
Fig. 6A. Oral lichen planus-like lesion in
buccal mucosa
Fig. 6B. Radiating striae from a central
erythematous area at the site of
placement of betel quid
nine regressed lesions recurred (2). Although
the histological features were similar to those
of oral lichen planus, in view of its complete
association with betel-quid chewing, it is
regarded as a specific entity.
Oral submucous fibrosis: This is a chronic oral
mucosal condition marked by rigidity of the
mucosa of varying intensity (Fig. 7) due to
fibro-elastic transformation of the juxtaepithelial layer, resulting in progressive in
ability to open the mouth (Fig. 8). When the
tongue is involved, it is shrunken and hard
(Fig. 9), with restricted mobility. Occasionally,
Fig. 8. Limited oral opening in submucous
fibrosis; also shows shrunken tongue with
impaired protrusion
pharyngeal and oesophageal involvement have
also been observed. Submucous fibrosis occurs
predominantly among Indians, Indians settled
abroad and to a lesser extent in other Asiatics.
Areca-nut (Areca catechu) chewing in any form
is currently believed to be the primary etiolog
ical agent for this condition (11-13) (see also
paper by Sinor et al., this volume); areca nut is
98
Oral health consequences of tobacco use
Murti et al.
an indispensable ingredient of betel quid (see
paper by Bhonslc et al., this volume).
Table 4
Prevalence of oral submucous fibrosis according
to tobacco habit*
Habit
Fig. 9.
Involvement of the tongue marked by
absence of lingual papillae and restricted
protrusion; note a homogeneous
leukoplakia (L) on the dorsum and loss of
pigmentation from the vermilion borders
Epidemiology: The prevalence (1,14) and
the incidence (2) rates of submucous fibrosis
arc high in Ernakulam district as compared to
other areas of India. The overall prevalence
was 351 per 100 000; it was highest (1090 per
100 000) among betel-quid chewcrs (Table 4).
The annual age-adjusted incidence rate was 7
per 100 000 among men and 17 per 100 000
among women (2); all new cases occurred
among betel-quid chewcrs. The prevalence
rates seem to be too high in comparison with
the incidence rates because this condition does
not regress like other prccancerous lesions.
Clinical aspects: Submucous fibrosis affects
people of each sex, but a definite female pre
dominance was observed in Ernakulam (2,14),
which was related to the extent of areca-nut
(betel-quid) chewing (12). For example, in this
area, most of the betel-quid chewers were
women, so there were more women with this
condition. Submucous fibrosis occurs in the
age range 20-40 years, with some regional var
iation; for instance, the mean age of individu
als with this condition in Pune was lower (37
years) than that in Ernakulam (51 years)
No.
examined
Prevalence
No.
Per 100 000
2b
No habit
Smoking
Chewing
Mixed
4 210
2 272
2 661c
1 106
—
29
5
48
—
1090
452
Total
10 249
36
351
"Source: ref. (1)
bPast chewcrs
c38 individuals who chewed pan without tobacco not
included
(12). The age of individuals with this condition
may also depend on the type of areca-nut
chewing habit and the age at initiation of the
habit.
Submucous fibrosis commonly affects the
buccal mucosa (Fig. 7), retromolar areas and
soft palate. The frequency of their involve
ment varies, however, with geographic area,
depending on the type of areca-nut chewing
(12). The earliest and commonest sign of this
condition is blanching (15), which imparts a
marble-like appearance to the mucosa. When
the disease is fully developed, palpable fibrous
bands develop in the buccal mucosa, soft pal
ate and rima oris; they run vertically in the
buccal mucosa and are circular around the
rima oris. As the disease progresses, the mu
cosa becomes stiff and the oral opening may be
restricted. Petechial spots resulting from the
breakdown of connective-tissue support of the
vasculature were observed in 11 % of cases in
one study (16). Submucous fibrosis is often
associated with leukoplakia (Fig. 9), oral can
cer and pigmentation changes (14). Most
patients complain of a burning sensation, often
aggravated by spicy food and excessive or
decreased salivation.
Histological features: The most common
histological features of this tondition are
epithelial atrophy with juxtacpithelial hyalinization and collagen of varying density. A
notable feature was the presence of epithelial
dysplasia in 26% of cases (17).
Natural history: Unlike other precancerous
lesions, submucous fibrosis does not regress,
either spontaneously or with discontinuation of
the habit. The most serious aspect of this con
dition is its precancerous nature (18). In a
17-year follow-up of 66 cases, oral cancer had
developed in 0.4% of cases at the end of 10
years (2), 4.5% at the end of 15 years (17) and
7.6% at the end of 17 years (19). In an eightyeai follow-up study of 25 cases, the relative
risk of malignant transformation for submu
cous fibrosis, compared to that of tobacco users
without any oral mucosal lesion or condition,
was 397.3 (20).
Primary prevention: As mentioned above
areca-nut chewing in any form is involved in
the pathogenesis of this condition. There is
no effective cure, so far, for this condition.
Discontinuation of all forms of areca-nut and
tobacco use would probably limit the extension
of this disease and prevent malignant transfor
mation. Stoppage of betel-quid chewing would
probably lead to a decrease in the incidence
of submucous fibrosis (21). This approach
assumes great importance in view of the
upsurge in mawa and pan masala usage in the
country (see papers by Bhonsle et al.; Sinor et
al., this volume).
LESIONS ASSOCIATED WITH
SMOKING AND CHEWING
The combined habit of smoking as well as
chewing tobacco, mostly in betel quid (pan),
was practised overall by 11% of the 10 287
individuals (I); almost all of them were men.
Leukoplakia: Leukoplakia, literally mpans a
white patch. It was hypothesized initially as
precancerous mainly because of its co
existence with oral cancer; it has a similar
intraoral location as that of oral cancer.
Leukoplakia is defined as a raised white patch
99
of oral mucosa measuring 5 mm or more,
which cannot be scraped off and which cannot
be attributed to any other diagnosable disease.
This definition does not carry any histological
connotation (5).
Epidemiology. The prevalence of this lesion
in Ernakulam district was 17 per 1000; it was
highest (61 per 1000) among people with
mixed habits (Table 5). The annual ageadjusted incidence rate was 2.1 per 1000
among men and 1.3 per 1000 among women;
the highest incidence (6.0 per 1000) was
among men who both chewed and smoked (2).
Table 5
Prevalence of leukoplakia according to tobacco habiP
Habit
Prevalence
Total no.
No.
per 1000
No habit
Smoking
Chewing
Mixed
4 210
2 272
2 661b
1 106
8
48
47
67
2
21
18
61
Total
10 249
170
17
"Source: ref. (1)
b38 individuals who chewed pan without tobac
co not included
Almost all leukoplakias in India occur
in tobacco users. A definite dose-response
relationship between leukoplakia and various
forms of tobacco use in this area has been
demonstrated (22). The dose-response rela
tionship was stronger for smoking habit than
for the chewing habit and remained significant
after taking account of age, sex and type of
tobacco habit.
Clinical aspects: Leukoplakias are classified
into (i) homogeneous; (ii) ulcerated; and (iii)
nodular types (5). Homogeneous leukoplakia
is characterized by a raised formation of
plaques or groups of plaques varying in size,
with irregular edges (Fig. 10A). The les
ions are predominantly white but may also be
■’WWIffgMEWW
100
Murti it al.
Oral health consequences of tobacco use
greyish-yellow. Ulcerated leukoplakia consists
of an area of ulceration sometimes surrounded
by keratinized areas, pigmentation or both
(Fig. 10B). Nodular leukoplakia shows many
small white nodules on a erythematous base
(Fig. 10C). Some 75% of the leukoplakias in
this region were homogeneous, 20% ulcerated
and 5% nodular leukoplakias (5). The risk for
cancer varies with clinical type of leukoplakia
(Table 6).
Leukoplakias occur from the age of 20
onwards. For men, the incidence increases
steadily from the age of 20; for women, how
ever, the peak incidence is in the age range
50-60 years, after which there is a drop (2).
Most (88%) leukoplakias are located on the
buccal mucosa, commissures and tongue (5).
Ulcerated leukoplakias are associated with bidi
smoking and are generally located in the com
missures, whereas homogeneous leukoplakias
associated with bidi smoking occur on the
commissures and anterior part of the buccal
mucosa; those associated with betel-quid chew
ing and mixed habits are often situated on the
posterior part of the buccal mucosa. As men
tioned above, in some instances commissural
leukoplakias among bidi smokers occurred with
palatal erythema and central papillary atrophy
of the tongue, a triad comparable to the
'multifocal candidiasis’ reported in western
literature (7).
Fig. 10B. Ulcerated leukoplakia
Histological features: Leukoplakias associa
ted with betel-quid chewing showed hyperor
thokeratosis in 82% and hyperparakeratosis
in 12%; those associated witii mixed habits
of smoking and chewing showed hyperorthckeratosis in 63% and hyperparakeratosis in
23% (1). Overall, epithelial dysplasia was
observed in 8%; nodular leukoplakias ac
counted for 71% ofdysplastic leukoplakias. In
a study of 723 leukoplakias in different areas of
India, 14% showed superimposed candidal
hyphae (23); nodular leukoplakias showed th;
highest frequency of candidal hyphae.
Fig. IOC. Nodular leukoplakia
Natural history. Of the 225 leukoplakias
studied over a 10-year period, cancer developed
Fig. 10A. Homogeneous leukoplakia
101
Table 6
Relative risk for malignancy associated with various precancerous lesions and conditions'
Precursor
lesion/
condition
Nodular leukoplakia
Submucous fibrosis
Others1”
Ulcerated leukoplakia
Homogeneous leukoplakia
Lichen planus
None of the above
Total
no.
Average
follow-up
period
(years)
No. of
oral
cancers
Transfor
mation per
100 000
per year
Relative
risk
13
25
26
105
489
344
’ 10 145
2.8
6.0
2.6
4.4
4.8
3.7
7.8
6
3
lc
1
3
1
4
16 216.2
1 986.7
1 515.2
218.8
128.1
78.9
5.0
3243.2
397.3
303.0
43.8
25.6
15.8
1.0
"Source: ref. (20)
bIncludes nonspecific diagnoses, such as red area,.ulcers and benign growth
•Preceding lesion, red area
in 4% cases, 47% remained stationary, 42%
regressed and 7% recurred (2).
Malignant transformation was most fre
quent (21%) in nodular leukoplakias (Fig. 11A
and B), as compared to 2% in homogeneous
leukoplakia (2). In another study (Table 6),
nodular leukoplakia showed the highest re
lative risk (3243.2) among all precancerous
lesions and conditions for developing into oral
cancer, as compared to the risk for people with
tobacco habits but no oral lesion.
Preleukoplakia: This lesion can be considered
a precursor lesion to leukoplakia. It consists
of a low-grade or very mild reaction of the
mucosa, appearing as a grey or greyish-white
but never completely white area with a slight
lobular pattern and indistinct borders blend
ing into the adjacent normal mucosa (5). The
prevalence of this lesion was 2.4%; it was seen
more often among people who chewed and
smoked (5). The annual age-adjusted inci
dence rate was 3.1 per 1000 among men and
0.2 among women; the incidence was high
est (5.6 per 1000) among men who smoked
and chewed (2); of the 309 preleukoplakias
followed-up over a 10-year period, 15% prog
ressed to leukoplakia and two cases to cancer.
Fig. HA. Nodular leukoplakia in the buccal
mucosa
Fig. I IB. Exophytic growth (g) that developed
in the lesion shown in Fi%. IIA
102
Oral health consequences of tobacco use
Murti cl al.
Oral lichen planus: Oral lichen planus is
primarily a dermatological disorder. Various
mucosal surfaces may be involved in this
condition, cither independently, concurrently
with cutaneous involvement or serially. Oral
mucosa, however, is, more frequently affected
mucosal location. Oral lesions are suspected to
possess some cancer potential. Interestingly, in
our study oral lichen planus was found to be
strongly associated with tobacco habits.
Epidemiology: The overall prevalence of
oral lichen planus was 1.5%; it was highest
(3.7%) in those people with mixed habits and
lowest (0.3%) in nonusers of tobacco (24). The
annual age-adjusted incidence rate was 2.1
and 2.5 per 1000 among men and women,
respectively. It was highest (8.2 per 1000)
among men who smoked as well as chewed
tobacco; among women it was highest (4.5 per
1000) in chcwcrs (2). The relative risk for oral
lichen planus was highest (13.7) among those
who smoked and chewed tobacco (25).
Clinical aspects: Oral lesions are diagnosed
on the basis of presence of Wickham’s striae.
Oral lichen planus occurred predominantly
among women. The buccal mucosa was the
most favoured location. Oral lichen planus
occurred in diverse morphological forms such
as reticular, annular, linear, erosive or ulcer
ated and pigmented forms; of these, 20% were
erosive or ulcerated lesions (24) and about
11% were associated with pigmentation (26).
Histological features: Sixty lesions were
studied microscopically and epithelial atrophy
was observed in 82%, hyperortho or hyper
parakeratosis in 90%, and Civatte bodies in
78%. Band-like juxtaepithelial inflammatory
cell infiltrate was present in all biopsies (24).
Natural history: Most oral lesions persisted;
some regressed and recurred. The regression
rates were highest in nonusers of tobacco and
lowest in people with mixed habits (2). The
malignant potential of this condition was
assessed in 722 affected individuals (27) : over a
precancerous lesion or condition (2,20). In a
10-year follow-up stud.;', all 12 oral cancers
developed from prccanr -ous lesions or condi
tions (2), while in an eight-year follow-up
study (20), 15 of the 19 oial cancers developed
from precancer, giving a relative risk of 69.2.
The relative risks for oral cancer associated
with various precancerous lesions were sig
nificant for nodular leukoplakia, submucous
fibrosis and others, including red area, ulcera
tions and ulcerated and homogeneous leuko
plakia. The risk was not significant for lichen
planus (Table 6).
10-year period (mean, 5.1 years), oral cancer
developed in three patients (0.4%) who had
erosive (atrophic) lesions; all of them used
tobacco. In an eight-year follow-up study of
344 individuals with oral lichen planus (20),
the relative risk for malignant transformation
was 15.8 (Table 6); this, did not, however,
attain the 5% significance level. Overall, the
high prevalence and incidence rates among
tobacco users as well as its natural history
strongly support the hypothesis that tobacco
does play an important role in this condition.
Oral cancer: The term oral cancer is used in
this paper to denote squamous-cell carcinoma,
which comprises over 95% of all oral malig
nancies in Kerala. This disease is the most
serious oral health consequence of tobacco
use. Earlier hospital-based studies showed oral
cancer to be the most frequent cancer in
Kerala (28,29). More recent data from the
National Cancer Registry show that among all
cancers, oral cancer ranks first and third
among men and women, respectively (30).
Epidemiology. In a cross-sectional study of
10 287 individuals in Ernakulam district, 12
oral cancers were diagnosed (117 per 100 000)
(1); six were diagnosed among 2661 (225 per
100 000) betel-quid chewers and six among
1106 (542 per 100 000) with mixed habits.
Although there was a substantial number of
(4210) nonusers of tobacco and (2272) bidi
smokers in this study, no oral cancer occurred
among them.
In a 10-year follow-up study of 10 000
individuals, the annual-age adjusted incidence
rate of oral cancer was 16 per 100 000; the in
cidence was highest (32 per 100 000) among
people with mixed habits (2). Interestingly,
although there were substantial person-years
of observation, none of the cancers occurred
among nonusers of tobacco or bidi smokers.
The average age of bidi smokers in this study
was low (31.2 years), as compared to 52.1
years for male chewers, and 43.8 years for
males who smoked and chewed (1); this
103
Fig. 12. Exophytic squamous-cell carcinoma in the
buccal mucosa with an associated
leukoplakia
perhaps explains the absence of oral cancers
among bidi smokers. Tobacco chewing and
smoking are recognized as causal factors for
oral cancer (31-33). Thus, the occurrence of
oral cancer exclusively among tobacco users in
Ernakulam substantiates the hazardous nature
of tobacco.
Clinical aspects: Oral cancer is predom
inantly a disease of the elderly. For exam
ple, the average age of oral cancer patients,
although based on small numbers, was 55
yeais (1). The age-specific incidence rates (2)
showed that the peak occurrence of 57 per
100 000 per year was among people aged 55
years and above. .
Oral cancer occurred more often among
men. The buccal mucosa was the most fre
quently involved location in this region, and it
often co-existed with leukoplakia (Fig. 12) or
submucous fibrosis; it mostly arose from a
POSSIBLE SOLUTIONS
This overview demonstrates that bidi smoking
and betel-quid chewing are detrimental to oral
health, as they are strongly associated with
oral cancer, precancerous lesions and other
mucosal pathologies. In view of these findings,
specific studies for primary and secondary pre
vention were undertaken. Primary prevention
was found to be feasible and effective (3,34,35)
(see also paper by Gupta et al., this volume).
In the above-cited studies, oral examinations
were conducted by dentists in a research
set-up. The possibility of early detection of oral
cancer by paramedical personnel in the gov
ernmental health care infrastructure was also
explored in this area (36), and the results
were encouraging (see paper by Mehta, this
volume).
Acknowledgments
This study was supported by funds from the
National Institutes of Health, USA, under
Indo-US Fund Research Agreement No.
01-022 N.
References
I.
Mehta FS, Pindborg JJ, Hamner JE, III,
el al. Report on Investigations of Oral Can
cer and Precancerous Conditions in Indian
2.
Rural Populations, 1966-69, Munksgaard,
Copenhagen, 1971.
Gupta PC, Mehta FS, Daftary DK, et al.
104
Murti el al.
Incidence rates of oral cancer and natural
history of oral precancerous lesions in a 10year follow-up study of Indian villagers.
Community Dent Oral Epidemiol 1980; 8:
287-333.
3. Mehta FS, Achi MB, Gupta PC, el al. An
intervention study of oral cancer and precan
cer in rural Indian populations: a preliminary
report. Bull World Health Organ 1982; 60:
441-6.
4. Daftary DK, Bhonsle RB, Murti PR,
Pindborg JJ, Mehta FS. An oral lichen
planus-like lesion in Indian betel-tobacco
chewers. Scand J Dent Res 1980; 88:244-9.
5. Mehta FS, Pindborg JJ, Gupta PC,
Daftary DK. Epidemologic and histologic
study of oral cancer and leukoplakia among
50 915 villagers in India. Cancer 1969; 24:
32-49.
6. Hamner JE, III, Mehta FS, Pindborg JJ,
Daftary DK. An epidemiologic and histo
pathologic study of leukoedema among 50 915
rural Indian villagers. Oral Surg 1971; 32:
58-65.
7. Hoi.mstrup P, Bessermann M. Clinical, ther
apeutic and pathogenic aspects of chronic
oral multifocal candidiasis. Oral Surg 1983;
56:388-95.
8. Mehta FS, Bhonsle RB, Murti PR, el al.
Central papillary atrophy of the tongue among
bidi smokers in India: a 10-year study of 182
lesions. J Oral Pathol Med 1989; 18:475-80.
9. Greenspan D, Greenspan JS, Schiodt M,
Pindborg JJ. Fungal infections. In: AIDS and
the Mouth. Copenhagen, Munksgaard, 1990.
pp. 91-102.
10. Bavappa KVA, Nair MK, Premkumar T,
eds. The Areca Nut Palm. Kasargod, Kerala,
Central Plantation Crops Research Institute.
1980. p. 241.
11. Mehta FS, Gupta PC, Daftary DK,
Pindborc JJ, Choksi SK. An epidemiologic
study of oral cancer and precancerous condi
tions among 101 761 villagers in Maharashtra,
India. Im J Cancer 1972; 10:134-41.
12. Bhonsle RB, Murti PR, Gupta PC, el al.
Regional variations in oral submucous fibrosis
in India. Community Dent Oral Epidemiol
1987; 15:225-9.
13. Sinor PN, Gupta PC, Murti PR, el al. A
case-control study of oral submucous fibrosis
Oral health consequences of tobacco use
with special reference to the etiologic rob: of
areca nut. J Oral Pathol Med 1990; 19:94-11.
14. Pindborg JJ, Mehta FS, Gupta PC,
Daftary DK. Prevalence of oral submucous
fibrosis among 50 915 Indian villagers. Br J
Cancer 1968; 22:646-54.
15. Pindborg JJ, Bhonsle RB, Muiiti PR el al.
Incidence rate and early forms of oral submu
cous fibrosis. Oral Surg 1980; 50:40-4.
16. Bhonsle RB, Murti PR, Pindborg JJ,
Daftary DK, Mehta FS. Focal vascul-r di
latations and petechiae in oral submucous fi
brosis. Scand J Dent Res 1981; 89 '170-4.
17. Pindborg JJ, Murti PR; Bhonsle RB, et al.
Oral submucous fibrosis as a precancerous con
dition. Scand J Dent Res 1984; 92:224-9.
18.
PindborgJJ. Is submucous fibrosis a preca.-icerous condition in the oral cavity? Int Deist J
1972; 22:474-80.
19. Murti PR, Bhonsle RB, PindborgJJ, el al. '
Malignant transformation rate in oral submu
cous fibrosis over a 17-yr period. Community
Dent Oral Epidemiol 1985; 13:340-!.
20. Gupta PC, Bhonsle RB, Murti PR, et al. Au
epidemiologic assessment of cancer risk in ora!
precancerous lesions in India with special inf
erence to nodular leukoplakia. Cai. er 1989;
63:2247-52.
21. Murti PR, Gupta PC, Bhonsle kii, et al.
Effect on the incidence of oral submucous fi
brosis of intervention in the areca nut chewing
habit. J Oral Pathol Med 1990; 19:99 100.
22. Gupta PC. A study of dose-response relation
ship between tobacco habits and oral leukopla
kia. Br J Cancer 1984; 50:527-31.
23. Daftary DK, Mehta FS, Gupta I’.!,
PindborgJJ. The presence of Candida in 7'13
oral leukoplakias among Indian village.^.
Scand J Dent Res 1972; 80:75-9.
24. Pindborg JJ, Mehta FS, Dafiaky Di'.,
Gupta PC, Bhonsle RB. Prevalence if ci .-.l
lichen planus among 7639 Indian villagers in
Kerala, South India. Ac.a Dermauni::.;;
(Stockholm) 1972; 52:216-20
25. Bhonsle RB, Pindborg JJ, Gupta I..',
Murti PR, Mehta FS. Incidence rate of <. J
lichen planus among Indian village.-s. A. -.
Dermatovener (Stockholm) 1979; 59:2' >
26. Murti PR, Bhonsle RB. D.u fa? .•
Mehta FS. Oral lichen piano associat d w -.
pigmentation. J Oral Med I9?9; 34:23-4.
I
27. Murti PR, Bhonsle RB, Daftary DK, et al.
Malignant potential of oral lichen planus:
observations in 722 patients from India. J Oral
Pathol 1986; 15:71-7.
28. Somervell TH. Recent advances in the treat
ment of carcinoma of mouth and jaws. Br J
Surg 1944; 32:35-43.
29. Pindborg JJ, ZachariahJ. Frequency of oral
submucous fibrosis among South Indians with
oral cancer. Bull World Health Organ 1965;
32:750-3.
30. Indian Council of Medical Research. National
Cancer Registry. Annual Report 1986. New
Delhi, 1989.
31. International Agency for Research on Cancer.
IARC Monographs on the Evaluation of the
Carcinogenic Risk of Chemicals to Humans.
Vol. 37. Tobacco Habits other than Smoking;
Betel-quid and Arcca-nut Chewing and Some
Related Nitrosamines. Lyon, 1985.
32. Internationa) Agency for Research on Cancer.
IARC Monographs on the Evaluation of the
105
Carcinogenic Risk of Chemicals to Humans.
Vol. 38. Tobacco Smoking. Lyon, 1986.
33. World Health Organization. Control of oral
cancer in developing countries. Bull World
Health Organ 1984; 62:817-30.
34. Gupta PC, Mehta FS, Pindborg JJ, el al.
Intervention study for primary prevention of
oral cancer among 36 000 Indian tobacco
users. Lancet 1986; i: 1235-9
35. Gupta PC, Mehta FS, PindborgJJ, et al. A.
primary prevention study of oral cancer among
Indian villagers. Eight-year follow-up results.
In: Hakama M, Berai. V, Cullen JW,
Parkin DM, eds. Evaluating Effectiveness of
Primary Prevention of Cancer. IARC Scientific
Publications No. 103, International Agency for
Research on Cancer, Lyon, 1989. pp. 1-19-56.
36. Mehta FS, Gupta PC, Bhonsle RB, Murti
PR, Daftary DK, PindborgJJ. Detection of
oral cancer using basic health workers in an
area of high oral cancer incidence in India.
Cancer Detect Prev 1986; 9:219-25.
Cciu.ol of Tobacco-related Cancers and Other Diseases.
International Symposium, 1990. Prakash C. Gupta, James E. Hamner, III
1992.
ako ? R. Murti, eds. Oxford University Press, Bombay,
A. 10-year follow-up study for primary prevention
of oral cancer among Indian villagers
Prakash C. Gupta, F. S. Mehta, J. J. Pindborg*, R. B. Bhonsi.e, P. R. Murti and M B. Achi
,Basi< Denial Research Unit and WHO Collaborating Centre for Oral Ca-cer Prevention,
Tata Institute of Fundamental Research, Bombay, India
'Department of Oral Pathology, Royal Dental College Copenhagen and Dental Department, Rigsr.ospitalet,
Copenhagen, Denmark
Oral cancer is caused by tobacco chewing and smoking. In (his behavioural intervention study in
Eriiakulam district, 12 000 tobacco users were interviewed about their tobacco habits, examined
for the presence of oral prccanccrous lesions and exposed to an intensive pro; '?mmc of health
education on tobacco habits. The control cohort was a subset from an earlier study which used a
similar methodology but with minimal behavioural intervention. Results after 10 years of
follow-up showed that a higher percentage of individuals stopped using tobacco completely in the
intervention cohort than in the control cohort. Several other indicators also showed that the inter
vention had been effective. As a result, the annual incidence of the most common oral prccancerous lesion, leukoplakia, decreased substantially in the intervention cohort. Since most oral cancers
arc known to be preceded by oral prccanccrous lesions, the results demonstrate that primary pre
vention of oral cancer is feasible and practicable.
INTRODUCTION
It is a v/ell-acccpted fact that a high incidence
of oral cancer in India and in several other
South-East Asian countries is caused by the
use of tobacco in the form of chewing and
smoking. Most of this oral cancer, as much as
90% according to WHO estimates, is directly
at'.ri but able to the chewing and smoking of
tobacco (1). This indicates that oral cancer is
amenable to primary prevention. The current
study was undertaken to assess the feasibili
ty and effectiveness of a primary prevention
programme for oral cancer in a rural Indian
population.
follow-up study of 30 000 individuals in three
areas showed that all new cases of oral cancer
and prccancer developed exclusively among
tobacco chewers and smokers, although a large
proportion of the cohort consisted nonu^ers
of tobacco. In addition all new cases of oral
cancers developed among individuals with a
prior diagnosis of oral precancerous lesions
(4). When tobacco use was stopped or reduced
substantially, the regression rates of oral pre
cancerous lesions increased significantly (5).
These results establish an almost complete
association between tobacco use, oral cancer
and prccancer.
In large scale house-to-house cross-sec
tional surveys of over 150 000 individuals in
rural India, the habits of tobacco chewing
and smoking were strongly associated with
oral cancer and precancer (2,3). A 10-year
The present study was undertaken with
two objectives: (i) to find out whether individ
uals in rural areas can be motivated to give
up their tobacco habits through a concentrat
ed programme of health education and (ii)
308
Primary prevention of oral cancer
Gupta el al.
whether this programme would affect the inci
dence or risk of oral cancer. This study was
conducted in three districts of India (see paper
by Mehta, this volume) and the results from
Ernakulam district in the State of Kerala in
southern India where the incidence of oral can
cer and precancerous lesions is known to be
high, arc discussed in this paper.
MATERIAL AND METHODS
Two distinct cohorts were selected and fol
lowed up at annual intervals for 10-years in
Ernakulam district. In both cohorts, the base
line and annual follow-ups consisted of an
interview and a clinical mouth examination
for each individual in house-to-house surveys.
In follow-up surveys, each individual was
identified before the interview and examina
tion from an alphabetical list of names crossindexed with addresses and other identifying
information.
The commonest method of tobacco smok
ing was bidi smoking and tobacco was chewed
most commonly in pan (betel quid) (see paper
by Bhonsle el al., this volume). The commonest
oral precancerous lesion was leukoplakia (see
paper by Murti el al., this volume).
The survey teams that went house-tohouse consisted of dentists, interviewing clerks,
drivers and local help. For the intervention
study a social scientist was also a member of
the team. The intervention cohort was sub
jected to a concentrated programme of health
education about tobacco use in various differ
ent forms (see paper by Aghi et al., this vol
ume), whereas the control cohort was sub
jected to no such campaign.
Intervention cohort: The populations from
selected ‘karas’ (smallest population unit
available through census publications) in
Ernakulam district were screened, and all
available tobacco users aged 15 years and
over were chosen (12 212 individuals) as the
study sample. Only temporary residents, very
old, sick, infirm or psychologically disturbed
people and those treated for oral cancer were
excluded. The base-line survey for this in
tervention cohort was conducted in 1977-78,
and 10 annual follow-ups were conducted
thereafter.
Intervention: Special studies revealed that
many people began to use tobacco and very
often continued it because of its perceived
medicinal value for disorders such as tooth
ache and gastric disturbances (see paper by
Bhonsle et al., this volume). There was almost
no awareness of any possible health conse
quence of tobacco use. The health education
programme therefore consisted of two broad
categories: (i) information for creating aware
ness regarding the relationship between to
bacco use and oral cancer and convincing the
target population of this relationship, and (ii)
helping individuals to stop their tobacco use.
In the health educational campaign, both per
sonal and mass media communication were
employed. For details see the previous paper
by Aghi et al. in this volume.
The health educational programme was
ongoing, dynamic and responsive to feed-back
from the target population. All the interven
tion inputs were pretested before implementa
tion and modified if necessary. The entire
health education material was based solely
upon scientific facts.
Control cohort: For this cohort, 'karas' were
selected by random sampling and the entire
population aged 15-years and over was exam
ined. The base-line survey was conducted in
1966-67 and the first follow-up survey threeyears later. Eight annual follow-up surveys
were conducted, providing 10-year (bllow-up
results. For the purpose of this report, only a
subset of the original cohort is included,
namely tobacco users in the base-line survey.
Intervention: Although health education
was not actively attempted in the control
cohort, the conduct of the study itself provided
some intervention input. The association
between oral cancer and tobacco habits was
explained to patients, especially while inter
viewing and conducting oral examinations.
The examining dentists routinely advised
patients to give up their tobacco habits, more
forcefully if the patient had an oral precancer
ous lesion.
Statistical analysis: The incidence rates of leu
koplakia were calculated using person-years
method. The numerator for the incidence rate
consisted of individuals with'a diagnosis of oral
leukoplakia in any of the follow-ups, but with
out a diagnosis of oral leukoplakia, submucous
fibrosis or oral cancer in any previous exami
nation. The denominator consisted of.pcrsonyears of observation among individuals with
no prior diagnosis of oral leukoplakia, sub
mucous fibrosis or oral cancer. Variations
with time in age and tobacco use were taken
into account. Stoppage of tobacco habit was
defined as complete discontinuation of any
form of tobacco use at least six months prior to
the interview.
309
Table 1
Follow-up details after 10 years for intervention and control
cohorts
Follow-up
details
Intervention
cohort
(n= 12 212)
(%)
Control
cohort
(n=6075)
(%)
Re-examined’*
Died*
Maximum followed up
Lost to follow-up
93.2-81.2
0.7-11.7
98.4
0.9
74.8-71.4
2.9-10.3
87.2
9.9
"The range is from die first to the last follow-up.
The percentage decrease in the individuals re
examined and increase in deaths was fairly steady.
The first follow-tip of the control cohort was done
three years after the base-line survey.
RESULTS
Table 1 shows the cohort size and the
follow-up details for the intervention and con
trol cohorts. The control cohort was half the
size of the intervention cohort. The loss to
follow-up was higher in the control cohort
(9.9% vs 0.9%), and correspondingly follow
up percentages were higher in the intervention
cohort.
Fig. I.
Percentages of men reporting stoppage of
their tobacco use at each follow-up in the
intervention and control cohorts
Fig. 2.
Percentages of women reporting stoppage
of their tobacco use at each follow-up in the
intervention and control cohorts
Figures 1 and 2 show the percentages of
men and women who reported stopping of
tobacco use at each follow-up in intervention
and control cohorts. In the control cohort,
there was some variation but no discernible
trend. In the intervention cohort, there were
very clear, significant, substantial positive
trends for both men and women. Among men,
the trend was almost constant throughout the
10-year period, whereas among women there
was a decrease in the trend after six years.
Table 2 shows the number and percentage
of men and women who reported stopping
Ft>LLOW-UP( ANNUAL)
310
Primary prevention of oral canter
Gupta el al.
311
Table 2
Comparison of stoppage of tobacco habit for 2, 3 and 4 successive sears in the intervention and control cohorts
Stoppage
Intervention cohort
Control cohort
Followed up
No.
Stopped
%
Followed up
No.
Stopped
%
8279
3466
11.2
22.9
3320
1778
2.2
7.1
8081
3391
8.3
18.0
3208
1720
1.7
5.3
7901
3336
6.3
14.5
3086
1676
1.0
4.0
2 years
Men
Women
3 years
Men
Women
4 years
Men
Women
their tobacco habit for two, three, and four
consecutive years. These percentages were
much higher in the intervention cohort than in
the control cohort, showing that more people
discontinued their tobacco habit for a longer
time in the intervention cohort. The ratios
were higher for men than for women.
Figures 3 and 4 compare distributions of
the age at starting tobacco use of (hose individ
uals who stopped their tobacco use and those
who did not, in the intervention and control
cohorts, respectively. Those who started their
5
10 15 20 25 30 35 40 45 50 55
AGE AT WHICH TOBACCO HABIT STARTED
Figures 5 and 6 compare the distribution
of frequency of tobacco smoking per day in the
base-line survey and after 10-years in the inter
vention and control cohorts, respectively.
Figures 7 and 8 provide the same information
for tobacco chewing. Some individuals in the
control cohort did stop tobacco use as indica-
60
Comparison of distribution of age at
starting the tobacco use for those who
stopped their tobacco use and those who
did not, in the intervention cohort
Fig. 6.
Distribution of frequency of smoking per
day in the base-line and 10th follow-up
surveys in the control cohort
Fig. 8.
Distribution of frequency of chewing per
day in the base-line and 10th follow-up
surveys in the control cohort
PERCENTAGE
tobacco habit later in life were better able to
discontinue than those who started using it
earlier. The pattern is similar in both cohorts,
but the difference is less pronounced in the
intervention cohort.
PERCENTAGES
Fig. 3.
Distribution of frequency of smoking per
day in the base-line and 10th follow-up
surveys in the intervention cohort
Fig. 5.
AGE AT WHICH TOBACCO HABIT STARTED
Fig. 4.
Comparison of distribution of age at
starting the tobacco use for those who
stopped their tobacco use and those who
did not, in the control cohort
0
Fig. 7.
5
10
IS
20
25
30
35
40
FREQUENCY OF CHEWING PER DAY.
45
Distribution of frequency of chewing per
day in the base-line and 10th follow-up
surveys in the intervention cohort
ted by zero frequency, but there was very little
change in the frequency distribution after 10
years. In the intervention cohort, however, not
only many more individuals stopped their
tobacco habit, but there was a clear and sig
nificant shift towards the left for both smokers
and chewers, demonstrating that their fre
quency of tobacco use had decreased.
Table 3 shows the age-specific incidence
rates of oral leukoplakia in the intervention
and control cohorts. It is clear that the inci
dence rates in the intervention cohort were
substantially lower than in the control cohort.
DISCUSSION
The results described above corroborate the
findings reported earlier after, one, five and
Table 3
Annual age-specific incidence rates (per 100 000) of leuko
plakia in the intervention and control cohorts
Intervention
cohort
Control
cohort
<34
35-44
45-54
55-64
2=65
77
256
262
373
234
255
677
846
756
507
Total
Age adjusted
236
186
586
470
Age group
(years)________
312
Gupta et al.
eight years of follow-up (6-8). Notably, the
percentage of individuals who stopped their
tobacco habit in the intervention cohort in
creased in successive follow-ups. This demon
strates that the effect of health education was
cumulative over the years and helped not only
in stoppage but even more in continued absti
nence from tobacco.
Multiple logistic regression analysis of the
five-year follow-up data showed that men who
chewed were a difficult subgroup for stoppage
of tobacco use, and the educational interven
tion helped them most (7). Interestingly, the
trend in stoppage remained fairly constant for
men over the 10-year period, but there was a
decrease in the trend for women after six years.
further, this analysis showed that individuals
in the higher age groups and those with a
shorter duration of tobacco use were more
likely to stop their habit. The present analysis
demonstrates that it is easier to stop tobacco
use if the individual started using it late in life.
This confirms and explains the earlier finding.
The objective of the behavioural interven
tion programme was to stop tobacco use, and
this was achieved to a fair degree. The edu
cational programme helped in reducing the
frequency of tobacco use in the intervention
cohort, and this difference was as much or
more pronounced in comparison with the con
trol cohort as the stoppage of tobacco use.
In this study the comparison is not be
tween the intervention and no intervention,
but rather between programmed intervention
and minima] intervention. It can be hypothe
sized that in the absence of such minimal inter
vention, the differences between the interven
tion and control cohorts would have been more
pronounced.
As has already been demonstrated, leuko
plakia is the most important oral precancerous
Primary prevention of oral cancer
lesion (see paper by Murti et al., this volume),
in that it is the most common and is the point
of origin for most oral cancers (4,9). Therefore
a decrease in the risk of leukoplakia can be
construed as decreasing the risk of oral cancer.
This study shows that primary prevention of
oral cancer is a feasible and practicable propo
sition, even among populations who have many
misconceptions about the beneficial effects of
tobacco.
The study has some limitations. The most
important, perhaps, is the non-concurrence of
the intervention and control cohorts. In terms
of calendar time, the difference between the
intervention and control cohort was ten years.
Therefore the possibility that the observed dif
ferences were due to differences in time trends
cannot be entirely ruled out. There is, how
ever, no specific indication that time trend dif
ferences exist, or that they affect the validity of
the conclusions in any way.
Although the possible benefits of health
education in this study have been assessed :n!y
in terms of a decrease in the risk of oral can
cer, it should be remembered that tobacco use
is responsible for increase in the risk of
many diseases, such as other cancers, especial
ly those occurring in the aerodigestive tract,
heart disease and respiratory disease. It has
been estimated that in India tobacco use is
responsible for at least 630 000 extra deaths
every year (10). Thus, the positive effects of
health education would undoubtedly be far
greater than simply a decrease in the risk for
oral cancer.
Acknowledgments
This study was supported by funds from the
National Institutes of Heajth, USA, urder
Indo-US Fund Research Agreement No. 0i022-N.
313
References
I.
2.
3.
4.
5.
6.
World Health Organization. Control of oral
cancer in developing countries. Bull World
Health Organ 1984; 62:817-30.
Mehta FS, Pindborg JJ, Gupta PC,
Daptary DK. Epidemiologic and histologic
study of oral cancer and leukoplakia among
50 915 villagers in India. Cancer 1969;
24:832-49.
Mehta FS, Gupta PC, Daptary DK,
Pindborg JJ, Choksi SK. An epidemiologic
study of oral cancer and precancerous condi
tions among 101 761 villagers in Maharashtra,
India. Int J Cancer 1972; 10:134-41.
Gupta PC, Mehta FS, Dafiary DK, el al.
Incidence rates of oral cancer and natural
history of oral precancerous lesions in a 10year follow-up study of Indian villagers.
Community Dent Oral Epidemiol 1980;
8:287-333.
Mehta FS, Aghi MB, Gupta PC. et al. An
intervention study of oral cancer ami precancer
in rural Indian populations: a preliminary
report. Bull World Health Organ 1982;
60:441-6.
Gupta PC. Mehta FS, Pindborg JJ, el al.
Intervention study for primary prevention of
oral cancer among 36 000 Indian tobacco users.
Lancet 1986; i: 1235-9.
7.
Gupta PC, Aghi MB, Bhonsle RB, et al. An
intervention study of tobacco chewing and
smoking habits for primary prevention of oral
cancer among 12 212 Indian villagers. In:
Zaridce DG, Peto R, eds. Tobacco: A Major
International Health Hazard. IARC Scien
tific Publication No. 74, Lyon. International
Agency for Research on Cancer, 1986; pp.
307-18.
8. GurrA PC, Mehta FS, Pindborg JJ, et al. A
primary prevention study of oral cancer among
Indian villagers. Eight-year follow-up results.
In: Hakama M, Berai. V, Cullen JW,
Parkin DM, eds. Evaluating Effectiveness of
Primary Prevention of Cancer. IARC Scien
tific Publication No. 103, Lyon. Ipternational
Agency for Research on Cancer, 1990; pp.
149-56.
9. Gupta PC, Bhonsle RB, Murti PR,
Dafiary DK, Mehta FS, Pindborg JJ. An
epidemiologic assessment of cancer risk in oral
precancerous lesions in India with special ref
erence to ntxlular leukoplakia. Cancer 1989;
63:2247-57.
10. Gupta PC. Health consequences of tobacco
use in India. World Smoking Health 1988;
13:5-10.
Contiol cf Tobacco-related Cancers and Other Diseases.
Internanonal Symposium, 1990. Prakash C. Gupta, James E. Hamner, III
AND P.R. Murti, eds. Oxford University Press, Bombay, 1992.
Epidemiology of tobacco habits in Goa, India
Sharad G. Vaidva, N. S. Vaidva and U. D. Naik
Goa Cancer Society, Dona Pavla, Goa, India
The Goa Cancer Society has conducted several epidemiological studies in Goa, India, -o deter
mine the prevalence of tobacco habits among schoolchildren and adults; to educate schoolchildren
through a specially designed school curriculum on tobacco habits and intervention; and to assess
the feasibility of using schoolchildren to bring about cessation of tobacco use by their parents or
in the community. About 13.4% boys and 9.5% girls used tobacco, mostly smokeless tobacco.
Usually, they had begun its use by the age of 5, and generally family members or .i lends had ini
tiated them to tobacco. Among adults, nearly 33% of men and 20% of women used tobacco;
smoking was the most common habit among men, while smokeless tobacco use was most common
among women. Schoolchildren who received health education on tobacco and intervention meth
ods were instrumental in achieving stoppage rate of9.7% among adults. Furthermore, health edu
cation imparted a negative attitude to tobacco among the children.
INTRODUCTION
The State of Goa, which lies on the west
coast of India tucked between the states of
Maharashtra and Karnataka, became a part of
the Indian Union in 1961 after being a Por
tuguese colony for several hundred years. As in
many other parts of India, tobacco use is com
mon in Goa. The prevalence of various types of
tobacco habits and the practice of d/iumli smok
ing in this area was reported by Bhonsle et al.
(1).
In Goa, children seem to be a special tar
get for tobacco advertising. Sweets and candies
are sold which look exactly like cigarettes and
are wrapped in packages similar to cigarette
packets (Fig. 1). During the last few years,
a tobacco product in paste form, described
as ‘creamy snuff, has been marketed in
toothpaste-like tubes (Fig. 2) under various
brand names. Initially, this product is used
as a toothpaste; but soon it becomes addic
tive. Although it costs more than twice a regu
lar toothpaste, its use has become popular.
Fig. 1. Candies that look like cigarettes
Ironically, unlike regular toothpaste, there is
no sales tax on this product.
The Goa Cancer Society has undertaken
several studies to elucidate the epidemiology of
tobacco use in Goa and to explore strategies for
316
Fig. 2. Creamy snulT in a toothpaste-like tube
effective intervention. Children are considered
effective agents for change, particularly in
rural India where a school-going child may be
the only literate member of the family. In this
study, they were educated specifically with a
view to conveying intervention messages to
their parents.
MATERIAL AND METHODS
For this study, the State of Goa was divided
into three zones: north, central and south, with
rural populations of 227 000, 213 000 and
244 000, respectively. The requisite number of
villages was selected by random sampling from
each zone (21 from the north, 25 from the cen
tre and 27 from the south), from which a pop
ulation of 50 000 was selected. There were 73
schools in these 73 villages; 31 schools were
selected by random sampling, and a question
naire was distributed to 6271 schoolchildren in
grades 5-10. Information was collected on age,
gender, kinds of tobacco habits, age at starting
those habits and the possible influence of par
ents and family members on the habit. This
survey was done in 1986-87.
In 1987-88, another survey of a total of
29 713 individuals over the age of 15 years
in three zones was done through house-tohouse visits by selecting a 40% systematic
sample from the 73 villages mentioned above.
Information on age, gender and details of
tobacco used was collected by trained investi
gators from 10 009, 9801 and 9903 individuals
in each zone, respectively.
317
Tobacco habits in Goa
Vaidya el al.
In 46 selected villages in the north and
central zones, education about tobacco habits
was given through children. Two booklets, one
for 4th and 5th grade students and one for 6th
to 9th grade students, were introduced during
the academic year 1987-88. These booklets
contained information on the history of to
bacco, its ill-effects and advice on giving up
tobacco habits. Class teachers were given a
three-hour course on how to teach this infor
mation in four periods, each of 45 min. Il was
expected that children would not only benefit
from this education but would convey the mes
sages to their parents and spread the infor
mation in the community. In 25 villages of
the central zone, the information was also
spread by multi-purpose health workers and
Anganwadi (child welfare) workers. The re
maining 27 villages in the southern zone served
as controls.
A sample of 448 boys and 332 girls from
the intervention area were re-interviewed and
a sample of 432 boys and 289 girls from the
non-intervention area were interviewed after
two-years to assess the changes in their atti
tude towards tobacco. These interviews were
through self-administered questionnaires.
For the community-based intervention,
results are available on 1159 tobacco users in
the intervention area of the northern zone and
659 from the control area after about 1.5 years
of the base-line survey.
Table 1
Table 2
Prevalence of tobacco use according to age and sex among
schoolchildren aged 10-18 years
Prevalence of different types of tobacco habits among
schoolchildren
Age
10-14
15-18
Total
Boys (%)
(n=3443)
Girls (%)
(n=2828)
Total (%)
(n=627I)
10.6
15.4
9.4
9.7
10
12.7
13.4
9.5
11.7
No.
%
No.
%
Creamy snuff
Chewing
Single
Multiple
13
256
212
66
388
73
3
56
46
14
84
16
5
177
128
36
219
51
2
66
47
13
81
19
Total
461
100
270
100
Smoking
Mishri
higher in the age group 15-18 years (15.4%)
than in the age group 10-14 years (10.6%).
Table 2 shows the types of habits preva
lent in the 731 tobacco users among the 6271
schoolchildren. Most (98%) of the boys and
girls used tobacco in smokeless form, the com
monest being mishri, followed by tobacco paste,
i.c., creamy snuff, and chewing.
On the question of age at starting tobacco
use, the response rate was low: 48% of boys
and 52% of girls. Among those who respon
ded, nearly one-third of the 223 boys and onehalf of the 152 girls said that they hail begun to
use tobacco before the age of 5.
The response rate to the question about
the people who influenced initiation of tobac
co use was also not very high, namely, 62%
among boys and 56% among girls. Family
members were most influential for initiating
tobacco use (boys, 60%; girls, 84%), although
among boys other persons like friends (17%)
and teachers (10%) were also influential.
Table 3 shows the distribution of the prev
alence of tobacco use according to age among
29 713 individuals in the community. z\bout
one-third of the men and one-fifth of the
women used tobacco. The prevalences in
creased rapidly up to the age of 44 among men
and 64 among women; but prevalence rates
among women were almost half of those
observed in men up to the age of 44.
Table 3
Prevalence of tobacco habits according to age and sex
Table 1 shows the prevalence of tobacco
use according to age and sex among the 6271
schoolchildren. The prevalence was higher
(13.4%) among boys than girls (9.5%) and
Women
Men
RESULTS
Tables 1 and 2 give the results from the self
administered questionnaire among 6271 school
children. Tables 3-6 and Fig. 1 give results
from a community survey of 29 713 adults.
Table 7 assesses the effect of the educational
intervention in the community.
Girls
Boys
Habit
Age
(years)
No.
Prevalence (%)
(n=4778)
No.
Prevalence (%)
(n=3152)
15-24
25-34
35-44
45-54
55-64
>65
4 815
2 894
2 159
1 952
1 505
1 038
3.9
24.6
49.3
63.8
62.7
53.3
4 027
3 497
3 043
2 297
1 578
908
2.3
11.8
25.9
35.4
41.9
42.3
Total
14 363
33.2
15 350
20.5
■318
VAiDYAda/.
Tobacco habits in Goa
Table 4 shows the distribution of different
types of tobacco use among men and women.
Smoking was most common (82.8%) among
men, while smokeless tobacco use was most
common (67.3%) among women.
tobacco use due to a friend’s influence and
22% just to pass time. More women started
using tobacco either for perceived medicinal
Table 5
Altitude of schoolchildren to the question ‘Are you likely to lake uf> tobacco use in future?’
-----------------Attitude
Table 4
Intervention
Men
Girls (%)
(n=332)
Boys (%)
(n=432)
Girls (%)
(n=289)
80
9
87
6
7
62
14
24
65
14
23
Definitely not
May not
All others
Women
No.
%.
No.
%
Smoking only
Chewing only
Afuhri only
Creamy snuff
Multiple
3957
217
163
71
370
82.8
4.5
3.4
1.5
7.8
1 031
1 476
349
62
234
32.7
46.9
11.1
2.0
7.3
Total with habits
Total without
tobacco habits
4778
9585
100
3 152
12 198
100
X5Boys=8.2 with df=2
x’Girls=14.9 with df=2
Attitude of schoolchildren to the question ‘What would you do if a friend!relative offered you a tobacco product?’
Intervention
Attitude
Boys (%)
(n=448)
Girls (%)
(n=332)
Definitely refuse and advise
82
89
Definitely refuse but not advise
10
8
All others________________ ___ ______________ «__________ 4
Non-intervention
Boys (%)
(n—432)
Girls (%)
(n=289)
59
16
27
60
15
25
x’Boys=!6.2 with df=2
X2Gitis=23.O with df=2
Big- 4. Age at initiation of tobacco use among
adults
Figure 4 shows the cumulative percentage
of men and women starting tobacco use by
a given age. Over one-third of individuals
started tobacco use before they attained 20
years of age and most of them before they were
30 years old.
Figure 5 shows the reasons for start
ing tobacco use. About 28% of men started
Table 6
EDUCATION
Big- 3. Tobacco use according to educational level
Bidi smoking was the commonest smoking
habit among men (63%) as well as women
(60.8%). The second commonest smoking habit
among men was cigarette smoking >24%),
while among women it was dhumti smoking
(27.3%).
figure 3 shows the prevalence of tobacco
use according to educational level and gender.
Tobacco use decreased sharply with increase
in the educational level; for example, among
men the prevalence was 64% among illiterates,
46% among those with primary education and
14% among those with middle-school educa
tion. Among women, it was 38% for illiterates,
11 % in those with primary education and
3% among those with middle-school educa
tion.
Non-intervention
Boys (%)
(n=448)
Distribution of various tobacco habits according lo sex
Habit
319
Big- 5. Reasons for starting tobacco use in a
community
reasons (24%) or through family influence
(21%).
Tables 5 and 6 show the differences in the
attitudes of children in schools where educa
tional intervention was performed after about
two years, compared to those in schools where
there was no intervention. The attitudes were
determined by analysing responses to two
questions: ‘Are you likely to take up tobacco
use in future?’ (Table 5) and ‘What would you
do if your friend/relative offered you a tobacco
product?’ (Table 6). Although answers were
given on five-point and six-point scales, respec
tively, they are presented in the tables, in
terms of three categories by combining all
extremes due to small numbers. For both ques
tions, the difference between intervention and
non-intervention schools was significant for
boys as well as girls (/><0.001).
Table 7
Rates of stopping tobacco habits among men and women
Cohort
Intervention
Followed-up
Quit
Men
Women
Total
705
63
(8.9%)
454
50
(11%)
1159
113
(9.7%)
378
24
(6.3%)
281
16
(5.7%)
659
40
(6.1%)
Control
Followed-up
Quit
320
Vaidya el al.
Table 7 shows rates of stopping tobacco
use in the intervention and control areas in the
community according to gender. Overall, a
significantly higher percentage (9.7%) of men
and women stopped their tobacco use in the
intervention area compared with the control
area. The difference was significant for women,
but not for men.
DISCUSSION
This investigation showed that tobacco use in
different forms is very common in Goa and its
use generally starts at a very young age, mostly
influenced by family members and friends.
The finding that smoking is the most common
habit among men and tobacco chewing is more
often practised by women is similar to that of
an earlier study in this region (1) and of stud
ies in other parts of India (2). The present
findings are also consistent with those of
studies (3-5) in other parts of ti e country: that
it is possible to motivate people in rural areas
of India to quit their tobacco habits (see paper
by Gupta el al., this volume). Furthermore, the
present investigation focused on -he impor
tance of desirability of including he dth educa
tional material on tobacco in school curricula.
It highlights the findings that such material is
useful in shaping the children s attitude
towards tobacco in a proper perspective and in
propagating the intervention messages to their
parents.
•>
Acknowledgments
This study was supported by a grant from
the Indian Council of Medical Research,
New Delhi, India. Our grateful thanks go to
Drs P. C. Gupta, R. B. Bhonsle. and P. R.
Murti for their valuable suggestions and
help.
References
I.
2.
3.
Bhonsle RB, Murti PR, Gupta PC, Mehta
FS. Reverse dhumti smoking in Goa: an epide
miologic study of5449 villagers for oral precancerous lesions. Indian J Cancer 1976; 13:301-5.
Mehta FS, Pindborg JJ, Gupta PC,
Daptary DK. Epidemiologic and histologic
study of oral cancer and leukoplakia among
50 915 villagers in India. Cancer 1969; 24:
832-49.
Mehta FS. Achi MB, Gupta PC, el al. An
intervention study of oral cancer and precancer
in rural Indian populations: a preliminary
report. Bull World Health Organ 1980; 60:
441-6.
4.
5.
Gupta PC, Mehta FS, Pindborg JJ. el alIntervention study for primary prevention of
oral cancer among 36 000 Indian t.ib. ecu users.
Lancet 1986; i: 1235-9,
Gupca PC, Mehta FS, Pindboi.-.: J J, el al. A
primary prevention study of oral cancer among
Indian villagers. Eight-year follo-.r-Vp results.
In: HakaM/\ M, Beral V, Cuilen JW,
Parkin DM, cds. Evaluating El!'.e;.v<mcss of
Primary Prevention of Cancer. IzX IC Scientific
Publication No. 103, Lyon,
rnational
Agency for Research on Cancer . 19‘JO. pp.
149-56.
POLICY AND LAW
Anticarcinogenic effects of betel leaf extract
Relevance to Human Cancer of N-Nitro»o Compounds.
Tobacco Smoke and Mycotoxins.
Ed I.K. O'Neill. J. Chen and H. Bartsch
Lyon. International Agency for Research on
© IARC. 1991
ANTIMUTAGENIC AND ANTICARCINOGENIC EFFECTS OF BETEL
LEAF EXTRACT AGAINST THE TOBACCO-SPECIFIC NITROSAMINE
4-(ArMTROSOMETHYLAMINO)-l-(3-PYRIDYL)-l-
Table L Effects of betel leaf extract (BLE) and hydroxychavicol (HC) on the
concentration-dependent mutagenicity of 4-(/V-nitrosomethylamino)-l-(3-pyridyl)-lbutanone (NNK) in Salmonella typhimurium strain TA100 with posi.nitochondrial rat liver
fraction
No. of his+ rcvcrtants/plalc
.jg/plate)
NNK alone
+ BLE
(200 jig/ml)
+ HC
(200 jig/ml)
123 ± I
320 ±9
499 ±41
824 ± 26
124 ±7
284 ± 8
301 ± 10
471 ±4
89±4
124 ± 14
222 ± 17
374 ± 19
BUTANONE (NNK)
S.V. Bhide', P.R. Padma' & A J. Amonkar'
'Carcinogenesis Division and }Bio-organic Unit,
Cancer Research Institute. Tata Memorial Centre,
Parel. Bombay, India
Earlier studies showed that betel leaf inhibits the mutagenic action of standard
mutagens like benzo[a]pyrene and dimethylbcnz[a]anthraccnc. Since tobacco-specific
nitrosamincs arc the mtjor carcinogens present in unburnt forms of tobacco, we studied
the effect of an extract of betel leaf on the mutagenic and carcinogenic actions of one of the
most potent, 4-(A-nitrosomethylamino)-l-(3-pyridyI)-l-butanone (NNK). Betcl-lcaf extract
and hydroxychavicol suppressed the mutagenicity of NNK in both the Ames and the
micronuclcus test. In studies in mice, betel-leaf extract reduced the tumorigcnic effects of
NNK by 25%. Concurrent treatment with the extract also inhibited the decreases in levels of
vitamin A in liver and plasma induced by NNK. Betel leaf thus has protective effects
against the mutagenic, carcinogenic and adverse metabolic effects of NNK in mice.
I he habit of chewing tobacco has been shown to be associated causally with oral cancer
(Sanghvi. 1981; Bhide et al.. 1984; Winn. 1984). In addition, people who chew tobacco with
lime have a higher risk for oral cancer than those who chew tobacco in a betel quid
(Khanolkar. 1944, 19?0). suggesting that betel quid contains some protective factor. We
showed earlier that betel-leaf extract (BLE) inhibits the mutagenicity of benzo[a|pyrene
and dimethylbenz|a|anthracene (Nagabhushan et a!.. 1987). Since tobacco-specific
N-nitrosamines are the only carcinogens present in unburnt tobacco products like chewing
tobacco (IARC, 1985). we tested the effect of BLE on the mutagenic and carcinogenic
effects of 4-(N-nitrosomethylamino)-l-(3-pyridyl)-l-butanone (NNK), which is a strong
tobacco-specific carcinogen. We also tested the effects of hydroxychavicol, a phenolic
antimutagen present in betel leaf (Amonkaretal., 1986, 1989), against the effects of NNK.
NNK was synthesized according to the method of Hecht et al. (1983). BLE and
hydroxychavicol were prepared according to procedures described earlier (Amonkar et al..
1989; Padma er a/., 1989).
Antimutagenicity studies
The antimutagenic effects of BLE and hydroxychavicol against NNK were tested in the
Ames test (Maron & Ames, 1983) and in the micronucleus test (Schmid, 1975). At a dose
-520-
521
>( "’00 pg/plate (Padma et al., 1989), both BLE and hydroxychavicol suppressed the
mutagenic action in Salmonella typhimurium strain TA100 of all three concentrations of
\NK tested (Table 1) in the presence of an exogenous metabolic activation system.
0
250
MX)
iixxi
\ lines are means dt SE of eight plates from two independent experiments
In the micronucleus test, NNK at 500 mg/kg body weight induced 1.3 ±0.05 micronuclei
per 100 polychromatic erythrocytes as compared to 0.3 ± 0.02 in controls given distilled
water. In the presence of BLE and hydroxychavicol, the numbers of micronuciei were 0.5
1 0.04 and 0.9 ± 0.05. respectively, which were significantly different from that in
NNK-treated animals. Animals treated with only BLE and hydroxychavicol showed 0.4 ±
0.025 and 0.42 ± 0.025 micronuclei, respectively.
■inticarcinogenic effects
I he anticarcinogenic effect of BLE against NNK was tested in long-term studies on
inbred male Swiss mice. NNK (1 mg/day three times a week; total dose. 22 mg) was
administered on the tongues of mice following a 3-4 h administration of atropine (1% in
drinking-water) to decrease salivation and facilitate retention of the nitrosamine in the oral
cavity, as is the case with chewers. BLE was supplied in drinking-water (2.5 mg/animal per
day) for the duration of NNK treatment. After treatment, animals were killed periodically
to monitor tumour incidence or when moribund. All dead animals were autopsied and
tissues fixed in 10% formalin for histological analysis.
In the group treated with NNK alone, 19/29 (65.5%) animals had tumours (17 lung
adenomas, three forestomach papillomas and two hepatomas) while in the group treated
with NNK and BLE, 11/27 (41%) animals had tumours (eight lung adenomas, three
forcstomach papillomas and one hepatoma). The per cent decrease in tumour incidence
is not statistically significant.
Effect of BLE on vitamin A status in liver and plasma
The levels of vitamin A in both liver and plasma have been shown to be depleted by
treatment with NNK (Padma, 1988). We studied the effect of BLE at 12-14 and 20-22
months on vitamin A levels, using the method described by Neeld and Pearson (1963). The
results are shown in Table 2. Animals treated with BLE alone had significantly higher levels
pH-a--
522
S.VBhide et aL
of liver vitamin A than untreated animals at both time points, while the levels in plasma
were elevated only during the earlier period.
Table 2. Levels of vitamin A in the liver and plasma of Swiss male mice treated with
4-(A'-nitrosomethyIamino)-l-(3-pyridyl)-l-butanone (NNK) alone or in combination with
betel-leaf extract (BLE)
Treatment
Vitamin A levels at
12-14 months
20-22 months
Untreated controls
NNK alone
BLE alone
NNK + BLE
Plasma
208.2 ± 10.8
327 ± 1.4
261.1 ± 13.2
148.8 ± 26
196.1 ±6.4
573 ± 4.0
245.3 ± 8.8
135.9 ± 3.9
Untreated controls
NNK alone
BLE alone
NNK + BLE
91.1 ± 1.3
34.1 ± 13
216.6 ± 122
93.0 ± 1.9
100.4 ± 3.0
59.2 ± 6.2
105.2 ± 5.5
110.1 ±5.9
Anticarcinogenic effects of betel leaf extract
We found that vitamin A levels were elevated in both liver and plasma of BLE-treated
animals. It has also been observed that BLE induces a significant increase in liver ascorbic
acid levels (Padma, 1988). Vitamin A has been shown to exert a protective action against
carcinogens (McCormick & Moon, 1982; Goodwin etal., 1986), and ascorbic acid has been
shown to prevent the initiation of skin tumours following the application of a promoter
(Slaga & Bracken, 1977). The protective effect may therefore be mediated partly by vitamin
A and ascorbic acid.
Thus, the inclusion of betel leaf may reduce the carcinogenic risk of tobacco chewers,
and these results support the hypothesis that betel-quid chewers may have some protection
against cancer (Khanolkar, 1944, 1950).
Liver
Results are means for six animals ± SE
The levels of vitamin A in the livers of the animals treated with NNK and BLE were
significantly lower than those in untreated controls at both times, but the levels were
significantly higher than those in animals treated with NNK alone. The levels of circulating
vitamin A in animals treated with NNK and BLE were comparable to the control levels at
both intervals but were significantly higher than those in animals treated with NNK alone.
Potential use of BLE as an anticarcinogen
Our study shows that BLE is nonmutagenic in both the Ames and micronucleus tests.
These results are consistent with previous reports in which betel leaf was found to be
nonmutagenic in the Ames test (Shirname etal., 1983; Nagabhushan el al., 1987) and in the
V79 and human lymphoblastoid cell lines (Umezawa et al.. 1981). Our observation that
betel leaves are not carcinogenic is also consistent with the results of previous studies in
mice (Bhide et al., 1979) and rats (Mori et al., 1979).
BLE has been shown to suppress the mutagenicity of polycyclic aromatic hydrocarbons
(Nagabhushan et al., 1987), as well as that of NNK and N'-nitrosonornicotine (Padma
1988), and to be anticarcinogenic against benzo[a]pyrene in the hamster cheek pouch
model (Rao, 1984) and in the forestomach tumour model in mice (Padma, 1988), against
dimethylbenz[a]anthracene in the rat mammary tumour model (Rao et al. 1985) and
against A/'-nitrosonornicotine in Swiss mice (Padma, 1988). The antimutagenic and
anticarcinogenic action of BLE against this wide variety of agents may be attributed to the
presence of compounds like chlorophyll, phenolics like eugenol and hydroxychavico'
(Amonkar et al., 1986) and vitamins like A, ascorbic acid (Aykroyd, 1963) and vitamin 1
(unpublished data) in betel leaves.
References
Amonkar, AJ.. Nagabhushan, M„ D’Souza. A.V. & Bhide. S.V. (1986) Hydroxychavicol: a new phenolic
antimutagen from betel leaf. Food Chem. Toxicol. 24. 1321-1324
Amonkar, AJ., Padma. P.R. & Bhide. S.V. (1989) Protective effect of hydroxychavicol, a phenolic compment
of betel leaf, against the tobacco specific carcinogens. Mutat. W-.r.. 210, 249-253
Aykroyd, W.R. (1963) ’Ihblc of food values. III. Vitamins. In: Go|»lan, C. & Balsubramanian. S.C., cds. The
Nutritive Value of Indian Foods and the Planningof Satisfactory Diets. New Delhi. Indian Council of Medical
Research, pp. 114-133
Bhide, S.V., Shivapurkar. N.M.. Gothoskar, S.V. & Ranadive. KJ. (197*)) Carcinogenicity of betel quid
ingredients: feeding mice with aqueous extract and the polyphenol fraction of betel mil. Hr J Cum er. 40.
922-926
Bhide, S.V., Shah. AS., Nair. J. & Nagaraj Rao, D. (1984) Epidemiological and experimental studies on
tobacco-related oral cancer in India. In: O’Neill, I.K.. von Borstel. R.C.. Miller, ( . I., I .ong, J. & Bartsch,
H. eds, N~Nitroso Compounds: Occurrence. Biological Effects and Relevance to Human Cancer (IARC
Scientific Publications No. 57). Lyon, IARC, pp. 851-857
Goodwin. WJ., Jr, Bordash. G.D., Huijing. E & Altman. N. (1986) Inhibition of hamster longue carcinogenesis
by selenium and retinoic acid. Ann. Otol. Rhinol. luiryngol. 95. 162-166
Hecht, S.S., Lin, D. & Castonguay. A (1983) Effects of o-dcuterium substitution on the mutagenicity of
4-(methylnitrosamino)-l-(3-pyridyl)-l-butanone (NNK). Carcinogenesis, 4. 305-310
Khanolkar. V.R. (1944) Oral cancer in Bombay, India: a review of 1000 consecutive cases < oncer Rrs . 4.313-319
Khanolkar, V.R. (1950) Cancer in India. Acta Unio Int. Contra Cancrum. 6. 881 -890
Maron, D.M. & Ames, B.N. (1983) Revised mcthtxls for the Salmonella mutagenicity test. Mulut Res, 113.
173-215
McCormick, D.L. & Moon, R.C. (1982) Influence of delayed administration of retinyl acetate on mammaiy
carcinogenesis. Cancer Res, 42. 2639-2643
Mori. H.. Matsubara, N., Ushimaru, Y. & Hirino. I. (1979) Carcinogenicity examination of belle nuts and Piper
belle leaves. Experienlia, 35, 384-385
Nagabhushan, M., Amonkar, AJ.. D’Souza, AV. & Bhide. S.V. (1987) Nonmutagenicity of betel leaf and its
antimutagenic action against environmental mutagens. Neoplasm, 34. 159-167
Neeld J.B. & Pearson, W.N. (1963) Macro- and micro-methixls for the determination of serum vitamin A
trifluoroacetic add. J. Nutr., 79. 454-462
Padma P.R. (1988) Mutagenicity and Carcinogenicity of N’ •Nitrosonomicotine and 4-(Methyinitrosamino)-l-(3-p)ridyl)-l-butanone. and their Mechanism of Action. PhD Thesis submitted to the
University of Bombay, India
Padma. P.R.. Amonkar. AJ. & Bhide, S.V. (1989) Anbmutagnic effects of betel leaf extract against the
mulagenidty of two tobacco-specific N-nitrosamines. Mutagenesis, 4, 154-156
Rao, AR. (1984) Modifying influences of betel quid ingredients on B(a)P induced carcinogenesis on the buccal
pouch of hamster. Int. J. Cancer, 33, 581-586
Rao AR., Sinha. A & Selvan, R.S. (1985) Inhibitory action of Piper belle leaf on initiation of
7 12-dimethylbcnzanthracene induced mammary carcinogenesis. Cancer Lett.. 26. 207-214
Betel quid and oral cancer
Relevance to Human Cancer of .V-Nitroso Compounds.
Tobacco Smoke and Mycotoxins.
Ed. I.K. O'Neill. J. Chen and H. Bartsch
Lyon. International Agencv for Research on Cancer
C 1ARC, 1991
BETEL QUID AND ORAL CANCER: PROSPECTS FOR PREVENTION
P.C. Gupta
Basic Dental Research Unit. WHO Collaborating Center for
Oral Cancer Prevention. Tata Institute of Fundamental
Research. Bombay. India
Betel-quid chewing is an ancient and socially accepted practice. The introduction of
tobacco reinforced this practice, and now almost all habitual chewcrs of betel quids include
tobacco. It is well established that chewing of betel quid with tobacco causes oral cancer
and is largely responsible for the high incidence of oral cancer in several South Asian
countries. The feasibility of primary prevention of oral cancer was studied in a
population-based prospective intervention study. A cohort of 12 212 betel-quid chewcrs and
smokers was exposed to a programme of health education for stopping chewing and
smoking and subjected to annual examinations for detection of oral prccancerous lesions.
Evaluations after one, five and eight years showed that primary prevention of oral cancer
is feasible and practicable. Early detection of oral cancer is an important control measure.
In a secondary prevention study, 53 basic health workers were trained in the detection and
referral of lesions suspected of being oral cancer. Over one year, they examined more than
39 000 high-risk individuals, resulting in the detection of 20 cases of oral cancer. The
sensitivity and specificity of their diagnoses was assessed through a re-examination of a
5% sample: we concluded that it was possible to incorporate a secondary prevention
programme into the existing health care system.
The chewing of betel quid is a very ancient practice in India and many other South Asian
countries. References to this habit in stone and other inscriptions are about a millenium
old, and literature references are about two millennia old. Betel-quid chewing has been part
of religious and cultural rituals and enjoys complete social acceptance.
Basically, the betel quid consists of betel leaf, areca nut, lime and condiments, and
sweetening and flavouring agents, which depend upon individual and local preferences.
Tobacco was introduced into India, as everywhere else, from the New World in the sixteenth
century by Europeans. It soon became an ingredient of the betel quid and because of this
association enjoyed social acceptance.
The relationship between betel-quid chewing and oral cancer was postulated in the late
nineteenth and early twentieth centuries by British surgeons, who noted that oral cancer
was rare in Great Britain but common in India. Subsequently, several studies have been
made of this association. The terms used to describe the habit have not been consistent,
however, and the same terms have been used differently in different studies. This has
resulted in a considerable amount of difficulty in interpretation. A major source of
-466-
467
confusion was the description of the habit as ‘betel-nut’ chewing, with the occasional
addition of tobacco. This description led to the impression that the addition of tobacco to
the chewing quid was of little or marginal prevalence. This impression was corrected
comparatively recently by population-based house-to-house surveys of chewing habits in
six different areas of India. Chewing habits were widespread in three of the six areas, and
m these three areas 92-98% of chewers who did not smoke included tobacco in their quid
(Mehta et al., 1969, 1972). These findings demonstrate that the betel-quid chewing habit
is usually the habit of chewing betel quid with tobacco.
'Chewing habit’ is another loose term, which may include areca-nut chewing,
tobacco-lime chewing and betel-quid chewing. Unless otherwise specified, the term
betel-quid chewing implies the chewing of betel quid containing tobacco. Although the
prevalence of tobacco chewing has been declining over the last few decades, it is estimated
(hat there are still at least 40 million regular tobacco chewers in India.
Betel quid and oral cancer
The relationship between betel-quid chewing and oral cancer has been reviewed
extensively (I ARC. 1985). The association has been demonstrated in numerous case-control
and cohort studies, and evidence from experimental studies points in the same direction.
I he overall evaluation of the I ARC working group was that the evidence is sufficient for
the carcinogenicity of betel quid with tobacco, meaning that chewing of betel quid with
tobacco causes oral cancer. Neither the epidemiological nor the experimental evidence for
the carcinogenicity of betel quid without tobacco was sufficient (Gupta et al.. 1982). This
does not mean, however, that the chewing of betel quid without tobacco is an innocuous
habit. Areca nut in betel quid causes oral submucous fibrosis, which is a debilitatingdisea.se
with no known cure (Bhonsle et al., 1987); it is also a precancerous lesion (Murti etal., 1985).
A person with submucous fibrosis who is exposed to carcinogens in tobacco in the form of
chewing or smoking has a higher risk of developing oral cancer than persons without the
disease.
It has been estimated that about 30% of oral cancer can be attributed to the habit of
chewing betel quid with tobacco (World Health Organization, 1984). Betel-quid chewing
and tobacco smoking have a synergistic effect on the risk for oral cancer, and the combined
habits of chewing and smoking are quite common. Thus, an additional 50% of oral cancers
can be attributed to the combination. It is therefore clear that betel-quid chewing is the
single most important factor responsible for the high incidence of oral cancer in India and
other South Asian countries.
Betel quid and oral precancer
Betel-quid chewing is strongly associated with white lesions of the oral cavity, the most
important of which is leukoplakia. In several hospital-based studies in India, leukoplakia
was found to be highly prevalent among people who chewed betel quid and rare among
those who did not chew betel quid and did not smoke. These findings were confirmed in
population-based cross-sectional studies (Mehta et al., 1969, 1972). The most compelling
evidence came from a ten-year prospective study of a random sample of 10 287 individuals
in Emakulam district with annual follow-ups (Gupta et al., 1980). Not a single new
leukoplakia was diagnosed among individuals who did not chew or smoke, although there
ph-9-Control of Tobacco-related Cancers and Other Diseases.
International Symposium, 1990. Prakash C. .Gupta, James E. Hamner, III
ANO P.R. Murti, EDS. Oxford University Press, Bombay, 1992.
Population impact of adverse reproductive
outcome attributable to maternal tobacco use
in India
Sarai.a Kr.lSHNAMURTHY
National Cancer Registry Project (ICMR), Tata Memorial Hospital, Bombay, India
The prevalence of tobacco use among women in India ranges from 10 to 62%. Tobacco is used
by women predominantly in its smokeless forms; overall, an estimated 10%' of Indian women
chew tobacco and 2.5% smoke bidis. Nevertheless, the potential health hazards of maternal
tobacco use to reproductive outcome arc not well documented. Preliminary estimates showed
a three-fold risk of stillbirths among women in India who chewed tobacco during pregnancy
anc a two fold increase in perinatal mortality for babies born to bidi smokers in Bangladesh.
The odds ratio for low birthweight (2.5 kg or less) associated with mishri use during pregnancy
was 3.2 for all babies in Bombay, 6.96 for girls and 1.6 for boys. From the.c estimates, about
17% of stillbirths, 9% of perinatal mortality and 17% of birthweights of 2.5 kg or less arc
attributable to maternal tobacco use during pregnancy. Estimates for 1986 showed that nearly
457 000 deaths among infants and children under five years could be attributed to maternal
tobacco use. Additional indirect effects may be increased infant mortality due to premature birth
and diversion of income from nutritional needs to tobacco. These estimates emphasize the neces
sity for stopping tobacco use during pregnancy and the need for appropriate antenatal efforts.
INTRODUCTION
Maternal cigarette smoking is harmful to the
unborn fetus, newborn, neonate and growing
child in various ways. Cigarette smoking dur
ing pregnancy adversely affects the growth of
the unborn fetus, resulting in low birthweight,
increased numbers of stillbirths and increased
perinatal, neonatal and infant mortality (1).
It is also associated with a decrease in the
maletfemale ratio of newborns (2,3) and with
an increased prevalence of infections (4).
Further, it slows or adversely affects the re
spirator)’, mental, emotional and behavioural
development of the child at newborn, infant,
under-five and over-five stages (1,4).
Tobacco is used in various forms through
out India and South-East Asia (see papers by
Bhonslc et al.; Pindborg el al.; this volume), but
very little is known about its adverse effects on
pregnancy, a topic which has been reviewed
recently (5,6). Studies from Pune (7) and
Jabalpur (8) in India rnd from Bangladesh (4)
showed that maternal tobacco chewing (7,8)
and bidi smoking (4) during pregnancy result
in offspring of low birthweight. A three-fold
increase in the number of stillbirths was seen
among tobacco chcwers (7), and increased pla
cental weights were also reported (9,10). A
two-fold increase in perinatal mortality was
associated with bidi smoking (4). Perinata1
mortality was twice as high among illiterate
and less well educated women than among
educated women and among those who had
had little or no antenatal care compared
to those who had sought antenatal care. Less
well educated women were more likely to be
bidi smokers and to have sought no or less
168
Reproductive outcomes of maternal tobacco use
Krishnamurthy
antenatal care. Thus, lack of education, bidi
smoking and lack of antenatal care seem to be
interrelated. Furthermore, the scarce income
of poorer, less well educated women may be
diverted from nutritional and other needs
to the purchase of tobacco (11), which would
add indirectly to the adverse effects of
tobacco.
Relative risk estimates for the effects of
maternal use of smokeless tobacco during preg
nancy arc available from a preliminary study
in Bombay, India (12). In this study, 33% of
the 500 women were mishri users, and they had
a nearly three-fold greater risk of bearing an
offspring with low birthweight (2.5 kg or less)
than nonusers of tobacco. Female babies had
a nearly seven-fold risk of weighing less than
2.5 kg (/><0.0005); for male babies, the birth
weights showed no significant difference. The
relative risk for having a baby weighing 2 kg or
less was 5.4, and that for having a baby weigh
ing 2-2.5 kg was 2.76.
This paper assesses the extent of prema
ture births and other adverse effects associated
with maternal tobacco use during pregnancy
in India.
MATERIAL AND METHODS
In order to estimate the population impact of
adverse reproductive outcomes due to mater
nal tobacco use in India, one must know the
prevalence of tobacco use among women dur
ing pregnancy and the relative risk estimates.
Relative risk estimates are available from the
studies (4,7,8,12) described above. There has
been no nationwide prevalence survey of
tobacco use in India, but studies in some
selected rural areas show that 10-62% of
women use tobacco in one form or another
(13,14). Overall, it has been estimated that at
least 10% of women use smokeless tobacco,
and an additional 2.5% smoke (15). Thus, it
can be calculated that, in 1986, about 20.5 mil
lion women of reproductive age (15-44 years)
were using tobacco in India.
RESULTS
Table 1 shows the population attributable
risks associated with tobacco use for stillbirth
and birthweight of 2.5 kg or less in all babies
Table 1
Estimated impact on reproductive outcome attributable to
maternal tobacco use in India, 1986
Population attributable
risl (%)
Odds
Reproductive
outcome
Bidi
less
smokers
tobacco
users
■t
Stillbirth’
<2.5 kg birthweight’’
(both genders)
<2.5 kg birthweight1*
(girls)
<2.0 kg birthweight*’
2-2.5 kg birthweight
Perinatal mortality'
16.7
4.8
4.8
7
37.5
13.0
5.4
2.8
2
30.5
15.3
9.0
9.9
4.3
2.4
3
according to gender. Some 9% of perinatal
mortality and nearly 17% of stillbirths could
be attributed to tobacco use during pregnancy.
The estimated population load of such
adverse reproductive outcomes is shown in
Table 2. Overall, 457 000 deaths, of which
124 000 were stillbirths, 194 000 prematurityrelated deaths, and 139 000 perinatal mortal
ity, were estimated to have occurred in 1986
due to maternal tobacco use during pregnancy.
DISCUSSION
Our analysis shows that nearly half a million
deaths among infants and children aged less
than five years might be due to maternal to
bacco use during pregnancy. This is likely to
1.
“Source: ref. (4)
Deaths (X |Q3) due to
Smokeless Smoking
tobacco
use
Stillbirth @ 25/1000
livebirths’
Prematurity-related
deaths @ 41 %b
Perinatal mortality @
53/1000 livebirths'
Total
96
28
Herriott A, Bh.i.ewicz WZ, Hvi ien FE.
Cigarette smoking in pregnancy. Lancet 1962;
i:771-3.
3.
Ravenholt RT, Levinski MJ, Neli.ist DJ,
Takenaca M. Effect of smoking on reproduc
tion. Am J Obstet Gynecol 1966; 96:267-81.
4.
Coleman S, Piotrow PT, Rinehart W.
Tobacco hazards to health and human repro
duction. Pop Rep 1979; L:l-37.
5.
Krishnamurthy S. Tobacco use in pregnancy
and reproductive outcome. In: Sanchvi LD,
Notani P, eds. Tobacco and Health: The
Indian Scene. UICC Workshop. Tata Memo
rial Centre, Bombay, 1989. pp. 48-56.
Both
124
151
43
194
no
29
139
.357
ICO
457
6.
’Source: ref. (16)
’’Source: ref. (17); figures for prevalence of |.ren'..-
lure births not available
‘Source: ref. (17)
US Department of Health and Human Ser
vices. Reducing die Health Consequences of
Smoking — 25 Years of Progress: A Report of
the Surgeon General. Washington DC: US De
partment of Health and Human Services DHHS
Publication No. (CDC) 1989; 89-8411.
2.
Estimated deaths from adverse reproductive outcomes due to
tobacco use in pregnancy, India, 1986
Reproductive
outcome
be an underestimate, since the risks for
stillbirths were calculated on the basis of 25
stillbirths per 1000 in Bombay City (16) and
stillbirths may be underreported, since all
deliveries do not take place in hospital.
The higher death rates due to premature
birth among female infants and children under
the age of five may be due to the low birth
weight of female babies, which in turn could be
the outcome of maternal use of smokeless to
bacco (12). As these relative risk estimates
may change in the future with the availability
of additional data, the present restdts must be
viewed with caution. They nevertheless pro
vide an estimate of the size of the problem and
signal the need for action.
References
‘‘Source: ref. (7)
’’Source: ref. (12)
Table 2
169
Krishnamurthy S. Potential public health
impact of maternal tobacco use and repro
ductive outcome in India and Bangladesh.
In: Aoki M, Hisamichi S, Tominaca S,
eds. Smoking and Health, 1987. Elsevier
Science Publishers BV, Amsterdam: 1988; pp.
487-90.
7.
Krishna K. Tobacco chewing in pregnancy.
Br J Obstet Gynaecol 1978; 85:726-8.
8.
Verma VC, Chanmiriya M, Kaui. KK.
Effect of tobacco chewing by mothers on Ictal
outcome. Indian J Pediatr 1983;20:105-10.
9.
Acrawai. P, Chansoriya M, Kaui KK.
Effect of tobacco chewing by mothers on pla
cental morphology. Indian J Pediatr 1983;
20:561-5.
10.
Krishna.murthi S. Strength of association of
increased placental weight and smokeless
tobacco use in pregnancy. Indian J Pediatr
1991; 58:863-5.
11.
Cohen N. Smoking, health and survival: pros
pects in Bangladesh. Lancet 1981; i:1090-3.
12.
Krishnamurthy S. Joshi S, Mehta AC.
Gender differences and low birthweight with
maternal smokeless tobacco use in pregnancy J
Tropical Pediatr (in press).
13.
Mehta FS, Pindborg JJ, Gupta PC,
Daitary DK. Epidemiologic and histologic
study of oral cancer and leukoplakia among
50 915 villagers in India. Cancer 1969; 24:
844-61.
14.
Bhonslb RB, Murti PR, Gupta PC, Mehta ■
FS. Reverse dhumli smoking in Goa: an •'
170
Krishnamurthy
epidemiologic study of 5449 villagers for oral
precancerous lesions. Indian J Cancer 1976;
13:301-5.
15.
Notani P, Jayant K, Sanchvi LD. As
sessment of morbidity and mortality due to
tobacco usage in India. In: Sanchvi LD,
Notani P, cds. Tobacco and Health: The
Indian Scene. UICC Workshop. Tata Memo
rial Centre, Bombay, 1989. pp. 62-78.
Bombay Municipal Corporation. Annual Re
port of the Executive Health Officer for the
Year 1981. Bombay Municipal Corporation,
Bombay, 1985.
17.
Directorate-General Health Services. Central
Bureau of Health Intelligence: Health In
formation India-1988. Ministry of Health and
Family Welfare, Government of India, New
Delhi.
16.
Tobacco-Related Cancers :
Portends for the Future
Drs. Cherian M. Koshy and Rachel Cherian Koshy
“Fire at one end and fool at the
other", was how this cylindrical
contraption was defined much be
fore the health warning was made
mandatory on cigarette packs.
^Christopher Columbus found the
natives using tobacco in much the
same way as it is used today, and
being led to believe in its possible
medicinal value, it was carried to
France, Spain, Europe and the rest
of the world, wherever colonies
were established. Grown in more
than 120 countries today, China
leads, followed by the USA, India,
Brazil and Turkey.
Tobacco belongs to the night
shade family Solanaceae, and the
genus, Nicotiana was named after
Jean Nicot, French Ambassador to
Portugal (1559-1561). Many varie
ties developed subsequently and a
South American variety N. Tabacum
is the major source of today’s
^commercial varieties. Nicotine and
other alkaloids which are nitrogen
containing organic compounds are
recognised as habit forming. The
seeds are extremely tiny, one table
spoon can easily grow enough seed
lings in 6 acres and harvesting takes
place between 70-130 days after
transplanting. After a process called
‘curing’ (wilting, yellowing, colour
ing and drying), it is ready. James
A Bonsack in the US patented a
Health for the Millions • Sept-Oct 1998 * 18
machine in 1880 in which cigarette
paper was filled with tobacco,
formed, pasted, and cut into proper
length by a rotary machine. Today
it is a multimillion dollar industry,
more than 7 million tons of tobacco
are produced annually and more
than 4 trillion cigarettes sold yearly.
Nearer home it occupies prime spot
through hoardings at traffic inter
sections. The industry owns luxury
hotels, sponsors sports events and
advertises it as the icon of the
macho male whom the woman seeks!
Today thanks to ceaseless efforts
by the transnational tobacco con
glomerates, production, distribution
and marketing of cigarettes contin
ues to grow. Cigarette advertise
ments continued in the pages of the
‘Journal of the American Medical
Association’ until 1954, and even
the American Cancer Society (ACS)
has been cautious and conservative
in challenging its $390 million an
nual tobacco industry!
The Health Hazard
Of the 676,000 annual newly diag
nosed cases of lung cancer in men
worldwide, 85% is attributable to
cigarette smoking, and compared to
men, women have a higher risk of
developing cancer, and although
the diagnostic and treatment meas
ures have greatly improved along
Drs. Cherian M. Koshy and
Rachel Cherian Koshy are
with the Department of
Surgical Oncology and
Anaesthesia at the Regional
Cancer Centre,
Thiruuananthapuram.
side the understanding of smokingrelated cancers, the risk is still
dependent on the extent of expo
sure to tobacco smoke. Cigarette
smoking is a major cause of cancer
of the larynx, approximately 80%
directly attributable to smoking,
and a similar risk exists in those
who smoke pipes or cigars, thus it
is imperative to explode a myth!
Regarding oral cancers a dose rela
tion exists between the number of
cigarettes smoked per day and
cancers of the lip, tongue, salivary
gland, floor of mouth, and
hypopharynx, esophagus. Tobacco
in its varied forms is responsible for
90% of cancers of the oral cavity. In
1992 the National Cancer Institute
(NCI) of the US through a popula
tion based case-control study con
firmed that cigarette smoking is a
major cause of cancers of the renal
pelvis, ureters, bladder and pros
tate. A case-control study of stom
ach cancer in Japan suggests that
cigarette smoking plays a signifi
cant role in its causation. The
strength and consistency of asso
ciation of pancreative, colonic can
cer, in smokers, and the epidemio
logical association between smok
ing and lymphoid and myeloid
leukemia have resulted in identify
ing tobacco metabolites in bile and
blood as the causative agents.
In the eighties smoking
caused approximately
315000 deaths yearly in
the US, which is greater
than all the drug and alco
hol and drug-abuse deaths,
seven times more than
automobile fatalities, and
more than all American
military fatalities of both
the World Wars, and Viet
nam combined! China, the largest
producer of tobacco, is also the
largest consumer. Smoking in the
US is declining marginally, but the
tobacco produced in the US finds its
way elsewhere. In fact tobacco
moghuls there have the clout to the
extent that exports of various com
modities from countries like Tai
wan, Korea, Philippines etc. are
linked to the import to these coun
tries of the US brand of cigarettes.
Urge and Scourge ■ Why?
“Smoking relieves stress” - the stress
that is relieved is that which
resulted from being dependent
on nicotine - the essence of addic
tion. Sales gimmicks are responsi
ble for propagating the lure. Every
documented report of health haz
ard has been countered by the
promoters. Virginia Slims adver
tised that smoking keeps you slim
and trim, aiming at the female
clientele. Advertising strategies suc
ceeded in boosting target sales in
the US through catchy slogans.
India never lagged behind in adver
tisement strategy.
Brands with purportedly low lev
els of tar and nicotine were pro
moted to calm widespread fears of
lung cancer development from smok
ing when the first medical reports
were published in 1964. Tar is a
composite of more than 4000 solid
products of combustion, containing
nearly 40 known carcinogens. Simi
lar adverse reports were offset by
the introduction of the filtered
brands with risk reducing claims. Of
late considerable resources have
been invested by tobacco compa
nies in the development of cigarette
prototypes in which tobacco is not
burned, instead heated so as to
provide with nicotine and flavour.
Personalised approaches
from all health care givers
and individualisation of such
messages is the cornerstone
Passive Smoking
of success. Prevention
Documented reports suggest that
two-thirds of smoke from a burning
cigarette never reach the smoker’s
lungs but instead go directly into
the air. Environment tobacco smoke
(ETS) also called ‘second-hand
smoke’ is defined as the combina
tion of sidestream smoke emitted
thus from a cigarette between puffs
and the fraction of mainstream
smoke exhaled by one who smokes.
Considerable evidence is available
to the effect that nonsmokers ab
sorb and metabolise significant
amounts of ‘second-hand smoke'
and even reports of possible in
creased relative risks of lung cancer
and other diseases in the nonsmoker are available.
Cessation Strategies
Around three hundred cessation
strategies have been reported,
from group therapy and hypnosis
to over-the-counter pharmaceutical
products
either
containing
nicotine analogues or aversive
chemicals. The Physicians’ active in
volvement is vital of course. From
pack-year history, today the meta
phor is the ‘inhalation count’. To
put it this way, a pack-a-day smoking
patient will breathe as many as one
million doses of cyanide, ammonia,
carcinogens and carbonmo-noxide
in less than 15 years, not including
the inhalation of other people’s
smoke.
nevertheless is better than
cure, and like charity which
has to begin at home, let all
who have anything at all to
do with health, stay away
from tobacco.
Urgent versus Important
It is not enough that our country
bans cigarette advertisement in tel
evisions or the cigarette pack carry
the ‘health warning'. Common myths
have to be debunked, that smoking
relaxes you, relieves stress and so
on. The fact that smoking causes
cancer has to be impressed upon
through positive strongly worded
strategies through the media, be it
radio or television. The life of an
Indian is as important or more so,
than the Indian tiger or our ecology.
which seem to be a matter of prior
ity, more to the powers that be. Ap
propriate measures to limit tobacco
sales should be undertaken. Smokingshould be banned in public places,
much less in government offices and
institutions. The right to smoke
should not infringe upon the right of
those who desire a smoke free envi
ronment. Breach of freedom is a crime
and therefore through appropriate
legislation smoking which violates
an adopted code of conduct should
be made punishable. “Knowledge
puffeth off but wisdom lingereth". ■
DR. MANOJ SHARMA BAGS 1998 OSU ALUMNI AWARD
Manoj Sharma, Ph.D. Assistant Professor of Health
Education at the University of Nebraska at Omaha,
received the William Oxley Thompson Award for
professional achievement by young alumni from the
Ohio State University Alumni Association Inc., at its
annual recognition banquet on 16 October, 1998.
Sharma earned his Ph.D in preventive medicine/
behaviour and health promotion from Ohio State in
1997. He has already made many contributions to the
advancement of public health through his actions,
research, and publications, and it is for these
achievement that he was honoured.
The Ohio State University Alumni Association Inc.,
is a dues-supported organisation of graduates, former
students, and friends of the university with more than
121000 members. Each year, the Association presents
awards in several categories to honour those living
alumni who personify Ohio State’s tradition of excel
lence.
The VHAI family is proud of one of its former
members getting such an esteemed recognition at an
international level.
Health lor the Millions • Sept-Oct 1993 • 11
pH'
THE NAffoNAL MEDICAL JOURNAL OF INDIA
VOL. 11, NO. 6, 1998
299
Correspondence
Oral submucous fibrosis, areca nut and
pan masala use: A case-control study
Oral submucous fibrosis (OSF) is a chronic debili
tating disease in which fibrous bands develop in
the mouth. There is a marked intolerance for spicy
food and opening the mouth becomes progres
sively more difficult. This disease does not regress
and has no known cure. The most serious aspect of
the disease is its precancerous nature. In a cohort
study, the relative risk for development of oral
cancer among OSF cases was 397.3 compared to
individuals without any oral precancerous lesions
after controlling for tobacco use.1 Several aetiological factors have been proposed, and the current
consensus seems to be the habit of chewing areca
nut.2 There is great concern about the increasing
^^kridence of this disease in India, especially among
WKolescents and young adults.3,4
A case-control s’tudy was undertaken in the
Government Dental College and Hospital, Nagpur,
Maharashtra where 200 consecutively diagnosed
outpatients with OSF over a period of one year
(June 1996-May 1997) were selected as cases.
Every fifth outpatient was designated as a poten
tial control, roughly matched for age. Almost all
patients and controls were in the age range of
15-54 years and 16% of cases and 38% of controls
were women. Details of areca nut and tobacco use
were obtained by an interviewer-administered,
structured questionnaire in a face-to-face inter
view.
A wide variety of areca nut and tobacco chew
ing habits were reported; the most common (50%)
being the use of pan masala. Pan masala, which
literally means betel quid mixture, is a commer
cially manufactured product almost always con
taining tobacco and areca nut. This is widely
advertised, aggressively marketed and the indus
try has grown from scratch to almost a billion
rupees within a few decades. The next most popu^BBabit among patients was the use of kharra, a
WEl preparation containing pieces of areca nut
(7-8 g), a small amount of tobacco flakes, and
drops of slaked lime, mixed, homogenized and
wrapped in a cellophane paper ball. Other chew
ing habits were tobacco-lime and betel quid in
different combinations. Table I shows the number
of cases and controls according to the daily freq
uency of use of areca nut-containing products and
the relative risk.
The relative risk and the trend for dose-res
ponse were highly significant (p<0.01). The relaTable I. Relative risk of oral submucous fibrosis
by the daily frequency of areca nut use
Frequency/day
Cases
No areca nut use
5
1
11
2-3
65
4-5
61
2.6
58
Any areca nut use 195
Total ________ 200
•p<0.01, p for trend <0.01
Controls Relative risk
110
1.0
24
10.1*
42
34.0*
16
83.9*
5
255.2*
87
49.3*
197_____________
tive risks were of the same order of magnitude as
reported in earlier case-control studies.3,6
The likelihood of an emerging epidemic of OSF
seems to be justified by the present data. Over 70%
of the cases were less than 35 years of age. Since
almost all OSF cases use tobacco as well—and
OSF is a high-risk pre-cancerous condition—an
increase in the incidence of oral cancer can be
predicted. In this study, 5.5% cases had associated
oral cancer and 3.5% had associated leukoplakia.
Urgent regulatory actions are, therefore, warranted
to control the manufacture, marketing and consumption of products containing areca nut and/or
tobacco, especially pan masala.
Vinay K. Hazare
Ruchi R. Goel
Government Dental College and Hospital
Nagpur
Maharashtra
Prakash C. Gupta
Tata Institute of Fundamental Research
Mumbai
Maharashtra
2 October 1998
REFERENCES
1 Gupta PC, Bhonsle RB, Murti PR, Daftary DK. Mehta
FS.PindborgJJ. Anepidemiologicassessmentofcancer
risk in oral precancerous lesions m India with special
reference to nodular leukoplakia. Cancer 1989;63:
2247-51.
2 Murti PR. Bhonsle RB, Gupta PC, Daftary DK, Pindborg
JJ, Mehta FS. Etiology of oral submucous fibrosis with
special reference to the role of areca nut chewing. J Oral
Pathol Med 1995;24:145-52.
3 Babu S, Sesikeran B, Bhat RV. Oral fibrosis among
teenagers chewing tobacco, areca nut and pan masala.
Lancet 1 ; : 92.
4 Gupta PC, Sinor PN, Bhonsle RB, Pawar VS, Mehta
HC. Oral submucous fibrosis in India: A new epidemic?
Nail Med J India 1998;11:113-16.
5 Sinor PN. Gupta PC. Murti PR. Bhonsle RB, Daftary
DK, Mehta FS, el al. A case-control study of oral submucous fibrosis with special reference to the etiologic
role of areca nut. J Oral Pathol Med 1990:19:94-8.
6 Maher R, Lee AJ. Wamakulasuriya KAAS, Lewis JA.
Johnson NW Role of areca nut in the causation of oral
Medical education and health needs
of a community
There is disenchantment with the existing system
of medical education in many developing countries because of its irrelevance to the prevailing
health situation. Medical education must be based
on the health needs of a community and requires
to be modified based on a critical assessment of
programme requirements and staff and system
performance within the existing stracture of health
services. Health problems vary with the socioeconomic and political situation in a country.
Continuous situation analysis, planning, programming, implementation, management evaluation,
reprogramming, and revaluation are necessary.
Unfortunately, the health services sector and medical education lack interaction. As a result, the
producer and the user are at cross-purposes. The
outcome is a health scenario inconsistent with
expectations. Today, India has the largest medical
manpower in the world, but the health situation is
far from satisfactory. Thus, the education of doctors and allied health professionals needs a thorough overhaul; a balance between technological
and humanistic medicine, a more holistic approach covering promotive, preventive, curative
and rehabilitative medicine, a suitably evolved
health system with strong pillars of medical and
ethical values, based on human suffering but withQut sacrificing scientiflc slandards.
25 December 1998
S. Chhabra
Department of Obstetrics and Gynaecology
Mahatma Gandhi Institute of Medical Sciences
Sevagram
Wardha
Maharashtra
The me(Jical examination system
All countries spend a lol of money on technical
education. Training medical personnel is more
expensive than training other technical personnel.
Undeniably, India needs more doctors who can
dcliver quality care t0 patients. Therefore, training of doctors is a hot and cold topic of discussion
among medical personnel, hot because urgent
e b
......
. r
reforms are needed and cold because of the frustralion experienced by medical professionals over
the listlessness that prevails.
The most important component in the training
process is our system of examinations. Students in
particular have lamented that the examination at
end of each course has assumed more than the •
nec
importance. This strikes an instant chord
With teachers as wel! as students. The main reason
for the negative reaction evoked by this important
exercise is the flawed and sloppy manner in which
it is conducted at all levels—undergraduate and
postgraduate—throughout the country.
Students feel more strongly than their teachers
aboul 1116 urgency of reforms in the examination
system. Understandably so, as they suffer the ills
of the system while teachers are passively respon
sible. Yet, most teachers valiantly protect the
flawed system' baulking any improvement in it.
WhaI are the ills? Typically, the theory examination consists of either essay-type or short note
questions, which are impossible to evaluate objecbvely and fairly. The objective type questions,
more commonly referred to as multiple choice
questions (MCQs) are superior and more objective in testin8 theoretical knowledge, but as very
few ‘eachers are trained in the art of formulating
MCQs, these have been ignored. Surely, faulty
MCQS
worse than the good old essay system.
At the same time, training teachers in making
psychiatry, 3rd cd. Oxford: Blackwell Scientific, 1903: 200-29.
11 Smith M, Bentorim A. Sexual abuse. In: Rutter M, Taylor E,
Hersov L» cds. Textbook on child and adolescent psychiatry, 3rd cd.
Oxford: Blackwell Scientific, 1993: 230-51.
12 Voss L, Walker J, Lunt H, Wilkin T, Betts P. The Wessex growth
study, first report. Acta Paediarr Scand 19S9; 349: 65-72.
13 Voss L> Mulligan J, Bens PR, Wilkin TJ. Poor growth in school
entrants as an index of organic disease: the Wessex Growth Study.
BMJ 1992; 305:: 1400-02.
14 Runer M, Tizard J, Whitmore K. A children’s behaviour questionnaire
for completion by parents. In: Rutter M, Tizard J, Whitmore K, eds.
Education, health and behaviour. London: Longman, 1970:
412-21.
._«:/■
15 Runer ML A’children’s behaviour questionnaire for completion by
teachers: preliminary findings. J Ch^d Psychol Psychiatry 1967; 8: 1-11.
16 Wechsler D. Wechsler Preschool arfd Primary Scale of Intelligence:
revised UK edition. New .-York: Psychological Corporation, 1990.
17 Wechsler D. Wechsler Intellligence Scale for Children: revised UK
edition. New York: Psychological Corporation, 1976.
18 EUion CD, Murray DJ, Pearson LS. British Ability Scales. Windsor.
NFER-Nelson, 1983.
19 Cameron N. The measurement of human growth. London: Croom
Helm, 1984.
20 Cole TJ, Freeman JV, Preece MA. Body mass index reference curves
for the UK, 1990. Arch Dis Child 1995; 73: 25-29. ;
21 Shah A, Stanhope R, Matthew D. Hazards of pharmacological tests of _
growth hormone secretion in childhood. BMJ1992; 304: 173-74.
. 22 Chatfield_C. The analysis of time series. London: Chapman & Hall,
1984.
Ruction
"°z 198s';
02,n? e (IHD) compared with most other ethnic groups.
^^reason for this increased risk, which has been
25
Butler MG. Prader-Willi syndrome: current understanding or . .
^ ded both amonS south Asian migrants to other
and diagnosis. Am J Med Genet 1990; 35: 319-32.
26
Skonewska A, Lal S, Waserman J, Guyda H. Abnormal food./ < •^°’triesM and among Indians in urban India,M is
behavior after surgery for craniopharyngioma-hyperphagia. <^3:
. - prevalence of conventional risk factors such as
Xamopsychobiology 1989; 21: 17-20.
king, hypertension, and hypercholestcrolaemia is no
27
Schachar R, Runer M, Smith A. The characteristics of situatin' ’’»9
■^her'in. south Asians than in other ethnic groups.
and pervasively hyperactive children: implications for syndrom
defininon. J Child Psychol Psychiatry 1981; 22: 375-92.
-r
/Jrj^ triglyceride concentrations, low concentrations of
28
Money J, Wolff G, Annecillo C. Pain agnosia and self-injury in th’ • ’ iSl’density-lipoprotcin (HDL) cholesterol, increased
syndrome of reversible somatotropin deficiency (psychosocial ' ■
-^rid fat, and insulin resistance are more prevalent
dwarfism). J Aut Child Schizo 1972; 2: 127-39.
29
Samuel .AM, Deshpande UR. Growth hormone levels in protein '' A'ong south Asians, and these factors have been proposed
calorie malnutrition. J Clin Endocrinol Metab 1972; 35: 863.
aS reasons for the higher risk of IHD.,A6-7-* However, a
30
Skuse D. Epidemiological and definitional issues in failure to th •
variable that is more common among south' Asians may
Child Adolesc Psychiatr Clin N Am 1993; 2: 37-59.
nbt
'necessarily be associated with IHD risk. Conversely, a
31
Dowdney L, Skuse D, Heptinstall E, Puckering C, Zur-Szpim
Growth retardation and developmental delay amongst inner-ritv Ts ■factor that is not more common among south Asians may
children. J Child Psychol Psychiatry 1987; 28: 529-11.
: ■ /*•?]
stilj’have an important relation with IHD. Further, since
Woolstpn JL Benign nutritional dwarfing. Eating and growth di$^? most studies have been based on migrants to western
32
in infants and children. Newbury Park: Sage Publications, 199] > ■
counfries; the findings may not necessarily apply to the
65-68.
s
- ...
33
Yamanaka C, Momoi T, Fujisawa I, et alfAcquired growth honnost ‘? vast majority of South Asians who live in their own
deficiency due to pituitary stalk transection after head trauma in
countiies: Therefore, we conducted a hospital-based case
children. EurJ Paediarr 1993; 152: 99-101.
control study of patients with a first myocardial infarction
in Bangalore, India, to assess the relative importance of
the risk factors for IHD among south Asians.
Participants and methods
Risk factors for acute myocardial infarction in Indians: a
case-control study
■
Cases
- 200 consecutive patients aged 30-60 years (inclusive) admitted to
the coronary care unit of St John’s ^Medical College Hospital with
an acute myocardial infarction (AMI) were prospectively
recruited as cases. AMI was defined as typical chest pain lasting at
•|east320' min and an electrocardiogram (ECG) showing ST
elevation of at least 2 mm in two or more contiguous leads with
’ Prem Pais, J Pogue, H Gerstein, E Zachariah, D Savitha, S Jayprakash, P R Nayak, Salim Yusuf
subsequent evolution of the ECG and diagnostic enzyme changes
^doubling, of creatine kinase with at least 10% MB fraction).
-Patients
were excluded if they had a history of heart disease,
Summary
beedis (a local form of tobacco! with Individuals wlfc j currently smoked 10 or more per day having an OR of^ri ■' idinical’evidence of liver disease, a change in diet in the previous
month; or.if a fasting blood sample could not be taken within 24 h
Background South Asians who have settled overseas and
(p<0-001). History of hypertension and of overt diabetes^ of the onset of chest pain. ‘
those in urban India have an increased risk of ischaemic
heart disease (IHD). Reasons for this increased risk are
unclear.; Most studies have been based" on migrants, to
western nations, so their findings may not apply to most
■ south Asians, who live in their own countries. Therefore, we
assessed.,the relative importance of risk factors'for IHD
among South Asians in Bangalore, India.
Methods We conducted a prospective hospital-based case
control study of 200 Indian patients with a first acute
"myocardial infarction (AMI) and 200 age and sex matched
• controls. We. recorded prevalence of the following risk
factors for IHD: diet, smoking, alcohol use, socioeconomic
status, waist to hip ratio (WHR), blood glucose, serum
insulin, oral glucose tolerance test, and lipid profile.
Findings The most important predictor of AMI was current
smoking (odds ratio [OR] 3-6, p<0 001) of cigarettes or
Departments of Medicine (P Pais mo. E Zachariah pno.
D Savitha asc), and Cardloto./y (S Jayprakash om, P R Nayak om).
Epidemiology Research and Training Centre, St John's Medical
College, Bangalore 560034. India; and Divisions of Cardiology
(J Pogue MSc, Prof S Yusuf *-rcp), and Endocrinology
(H Gerstein frcpc), McMaster University and the Hamilton Civic
Hospitals Research Centre, Hamilton General Hospital,
237 Barton Street East, Hamilton, Ontario, Canada L8L 2X2
Correspondence to: Prof Salim Yusuf
35R
Age In years
47-3 (SO 80)
Male (%)
189(95)
Religion
Hindu
Muslim
Christian
146
' 24
30
Marital status
Single
Married •
Widowed. .
Income per month
<Rs 1999
Rs 2000-3999
&RS4000 .
47-0 (SO 3D
■________
US (95)
1
151
14
f 35
3-5,* 0174
j
'
4
190
6
9
187
4
91
81
28 ’
74 "
78
10-66.* 0005
21
95
84
6-39.* 0041
"\
Level of education
None
■■■;'.■ ’ .
School
College
Serum Hplds (mean, SD)f
Total cholesterol (mrnol/L)
Median (range)
HDL cholesterol (mmol/L). .
Median (range).
17
118
65 \
;
!
2-86.‘O239
•
.
’ 4-64. 096
0-08
4-83,1-17
.4-71 (2-25-9-19) 4 69 (2-10-7-59)
1.15,6-27
0-98
1-16,0-26 ;'
1-09 (065-2-43) 1-09 (073-2-59) .
2-68,082
" .0-14
\ 2-76.098
\2-73 (0-67-5-36) 2-75(065-5-02) '
4-3,1-14 ’’
4-2.117
043
4-2(l-O-7-3) .. 4-111-6-8-3)
1-77.097
-Oil ...
Triglycerides (mmol/L)' ' 200.1-37
1-51(044-7-36)
•—
Median (range)
1 • - 1-68(037-7-57)
•p=2 df, tslgn rank test in paired case-ccnuols.
Table 1: Demographic, socioeconomic, and lipid data
LDL cholesterol (mmol/L)
Median (range) ’ ,
Total/HDL cholesterol.
Median (range)
•—•-.— ..
Fasting blood glucose and lipids (total, low-density-lipoprotein
[LDL) and HDL cholesterol, and triglycerides) were measured in
all participants. Fasting serum insulin was measured in
individuals without a history of diabetes; they also had a 75 g oral
glucose tolerance test with measurement of a 2-h blood glucose
(PPBG). In cases, fasting blood for. lipids was taken within 24 h of
onset of chest pain. Blood for fasting glucose, serum insulin, and
PPBG was taken on the 9th. or 10th day after admission. In
controls, the blood tests were done on the same day as the lipid
measurements; if patients were scheduled to have surgery, studies
were completed before operation.t Blood glucose, total
mellitus were, also independent r sk factors (ORv^o tcholesterol, and triglycerides were estimated on an automated
[p=0'001] and 2-64 (p=0-004], respectively). Amongjalb; K?pniro/s
:•
■:
system with standard kits • (Boehringer. Manheim GmbH).
individuals, fasting blood glucose was a strong prediefonof,, t
controls were prospectively selected either from individuals
Enzymic, methods were used: cholesterol oxidase/peroxidaserisk over the entire range, including at values usu^ l
hospital outpatients clinic (for refraction,
aminophenazdne for cholesterol and glycerol phosphate.
regarded as normal (OR adjusted for’smoking, hypertens® fepg^nolaiyngology
|
evaluation, or a general physical examination
oxidasc/peroxidase-aminophenazone -for trigyIcerides. HDL
requested) or from patients admitted for elective
cholesterol was.estimated .with, the precipitation method and
and WHR. 1-62 for 1 SD.increase,'- p<0-001). Abdor^ ra^;ftey.,had
i
glucose .by the glucose oxidase method; Analyses were done on a
-conditions that were unlikely to confound a
obesity (as'measured by WHR) was also a stra^ ?;
| t;^parativC ■ analysis (eg, cataract and herniorrhaphy).
Beckman Synchron CX4 Random Analyzer. LDL cholesterol wras
independent predictor across the entire range of measifej
^vith any previous diagnosis of heart disease, history of
calculated *as‘ totals cholesterol : minus (HDL cholesterol
(OR
adjusted
for----------smoking,
hypertension, and bloodVO^^^vP^^chest
+triglyceride/5). Serum insulin was’ estimated by RLA (Radio
feSWpnal-chest-pain,
clinicalevidence
evidenceotofliver
liveraisease,
disease,oiciaiy
dietary
'
—,------- —
--------------------------------------’pain, clinical
• the previous month, or a 12-lead
- - , , ECG showing
.i--- •_
2-24 for 1 SD increase; p<0-001). Compared.;.<changcs • in
Immuno Assay Kit-1, the Board’of Radiation and Isotope
individuals
with
no
risk
factors,
individuals
with
niyltipJ^^ihological
Q
waves,
ST
segment
deviation,
T
wave
inversion,
Technology,.
Bombay, India), which uses ‘^I-labelled insulin. All
iiiuiviuuais wun
nsK Taciors, maiviauais wim
'
V waves, o i segment ucvwuvn, *
...
r
.
.....
___
risk factors had greatly increased risk of AMI (eg,
'yFj •p«e Jhnch or atrioventricular block, tachyarrhythmia other . biochemical' analyses were.done' without knowledge of clinical ;
information. The laboratory, takes pan regularly in an external
‘isolated 'atrial ectopics, or chamber hypertrophy were
10-6 for the group with smoking and elevated. gluc0,^<|:;
. quality, assessment programme for lipids and glucose with
Lipid profile was not associated with AMI. In univanaJSfe ?Clu.'?Sd" Controls were matched to cases for age and sex.
' satisfactory results. . ' '
‘ .
analyses, higher socioeconomic'(income) status (OR.
Yariab/es '
p=0 005 highest vs lowest; OR 0-75 middle vs lowest) aj' itir. ‘.Dau wer*» ’
Statistical methods
■panjq--- ' Prospectively recorded with standard forms. Ln all
vegetarianism (0R=0-55, p=0-006), seemed
protective. The impact of^ vegetarianism was
correlated with blood glucose,and WHR.
h
le^la8e> sex, religion, monthly income, and educational
KI
ahd\r^COr^C<^ l08ether
details of diet, smoking, alcohol
• height •
^storT °f diabetes mellitus and hypertension.
each’e^t’ 3nd wa,st
h’P circumferences were recorded
Interpretation Smoking cessation, treatment of
• ^^Towes: df”0”’ Waist circumference was measured at the
tension, and reduction in blood glucose and central
ii
. eter between the costal margin and the iliac crest,
(perhaps through dietary modification) may be import^J^g ’
th^rcum^erence was measured at the greatest diameter
preventing IHD in Asian Indians. ,
..>^2utwcks- An interviews and anthropometric
were carried out by the same research assistant.
Lancet 1996; 348: 358-63
' Vol 3-18 •
.? •• ,‘gust 10, 1996
Comparisons of mean or median .values or prevalence of a risk
factor were conducted after matching" each case with the next
control subject recruited of the same sex and age within 5 years. A
comparison of discrete variables in cases and controls was done
with logistic regression accounting for the matching of cases with
controls. Estimates of relative risk and 95% Cis were also done.
For continuous variables, non-parametric analyses on paired
values were used because of the skewed values obtained for many
variables—eg, triglycerides. Multivariate analyses were conducted
359
Category
Smokers’
Never
Former
AH current
Cunent <10/day
Current >10/day
Cases
(n=200)
Controls
(n=200)
OR
55\ Cl
68.(34%)
22(11%)
110 (55%)
30(15%)
80 (40%)
|
1-Ot
1-9 '
3-6
1-6
6-7
0-93-3-90
2 20-6-03 <0-001
0-84-3-07
3-51-12-8 <0-001
S,
23(12%)
58(29%)
36 (18%)
22(11%)
p
Type of tobacco
*
Cigarettes alone
Beedis atone
Both
78 (39%)
54(27%)
1-81-8-95
29 (15%)
16(8%)
2-08-13-6 <0-001
25(12%)
11(6%:
5-3
'Combined data tor beedis and cigarette smoking tor never smoked at any time
(never), smoked In the past (tormer), and any current smoker ofcigarettes/beedrs
(cunent), tReferent. JData are tor category by-bpe of smoking, including former and
current smokers.
Table 2: Smoking and risk o^AMI
with logistic regression methods on transformed values. The SAS
(SAS Institute, Cary, NC) and BMDP (BMDP Statistical
Software Inc, Los Angeles, CA) statistical packages were used for
analyses, p values were two tailed. However, for data in which the
overall sample of 400 subjects was divided by tertiles or by
diabetic status, unmatched analyses were conducted. Analyses for
the multiple logistic regression model excluded fasting insulin and
PPBG concentrations because they were measured only in
patients without diabetes
Results
The demographic characteristics and lipid data of-the 200
cases and 200 controls are shown in table 1. Cases had
significantly lower monthly incomes than controls, and'
significantly fewer of them had a college education. The
odds ratio (OR) for AMI was 0 32 (95% CI 0-16-0-66) for
the highest versus lowest income group and 0-75
(0-48-1-17) for the middle versus lowest income groups.
Life-style and diet
■Smoking was an important risk factor. 132 (66%) cases
and 82 (41 %)'controls had smoked or were current
smokers of cigarettes or beedis (a local type of tobacco)
(OR 3-1, 95% CI 1-94-4-90). This increased risk was also
seen in those who qnly smoked beedis (table 2). When the
data on cigarette and beedi smokers were combined, a
dose-response'- effect was evident. .Although alcohol was
consumed by more cases (87, 44%) than controls (62,
31%) when the data were adjusted for the effect of
smoking, alcohol was no longer a risk factor (p=0-221).
The high risk of IHD in Indians has been attributed to
ghee (clarified butter) consumption,11 but in our study
regular use of ghee was broadly similar in the two groups
(20/144, 13-9% in cases, 22/165, 13-3% in controls;
p=0-739). Individuals were classified as being vegetarian
or non-vegetarian by a simple questionnaire. 59 (30%)
cases and 84 (42.1) controls were Veget
Vegetarianism had a protective effect (OR 0-55, 95y 31’-.
0-35-0-85; p=0-006), which persisted after adjust^?
smoking, blood glucose, HDL and LDL cholesterol
triglycerides but not after incorporating waist to hir>’ ’N
(WHR) into the analysis.
P 2gjg
Glucose metabolism, WHR, and/iypertension
'
36 cases (18%) were known to be diabetic compared 18 controls (9%) (OR 2-64, 95% CI 1 -31-5-30; p=o-S
Overall, cases had a higher fasting blood glucose Ssl
controls. This finding was expected since there were m
known diabetics among the cases. After exclusion'
*
patients with known diabetes, mean fasting blood glue - '
was higher in cases than in controls (p=0-003) (table t)
PPBG was 8-49 mmol/L (3-46) and 6-61 mmol/L (3.’fj®|
respectively (p<0-0001). Even after subjects with impair^
glucose tolerance (PPBG 2=7-77 mmol/L) were excluder
fasting blood glucose remained significantly higher^'
cases (p<0-0001). Overall, after adjustment for smoking
hypertension, and WHR, a 1 SD increase in fasting blood"
glucose was associated with a 1-62 increase in risk of AML
.jest for trend.
Cases had higher fasting plasma insulin (which was not
measured in known diabetics) than controls (p=0-039)-- J Table 4: Relative risk In groups by tertile of fasting blood
this difference was abolished after exclusion of patients j glucose (FBG) and Insulin
with impaired glucose tolerance, p=0-239 (table 3). For
fasting blood glucose and insulin, separate analyses were I was no pattern of risk when cases and controls were
done for all participants together, for those not known to I divided by tertiles according to the various lipids (data not
be diabetic, and for those with a PPBG of 7-77 mmol/L'or' | shown).- ■ !
less (table 4). All these analyses indicated a progressively.increasing risk of AMI with increments of fasting blood | Stepwise-wise regression analysis
glucose even within the range regarded as euglycaemic.."-. [ Stepwise logistic regression analysis was carried out for
Although the body-mass index of cases and controls mm I continuous variables (WHR; fasting blood glucose; total,
similar (22-8 [SD 3-25] and 22-6 [4-06], respectively), the'. . HDL, and LDL cholesterol; and triglycerides) and for
WHR was significantly greater in cases (0-92 [0-06]/ti': categorical variables (any smoking, history of diabetes
0-89 [0-06], p<0-0001). When patients were divided irito: mellltus and hypertension, income, and education level).
tertiles on the basis of WHR, fasting-blood glucose,' and';
The 'most predictive independent variables were smoking
fasting plasma insulin, there was a progressive increase in p :(p<0-001), WHR (p<0-001), fasting blood glucose
risk- for AMI with each increment in WHR and fasting;
blood glucose. Compared with those in the lowest tertile' 5 (p=0-003), history of hypertension (p=0-017), and income
for WHR (cut-off values: «0-89, 0-90-0-93, 2=0-94),‘.the< j A(p=0;015). Smoking and WHR were associated with the
ORs for those in the second and highest tertiles were 2T9.-. ; highest risks. With receiver-operating-characteristics
(95% CI 1-33-3-58) and 3-84 (2-33-6-32), respectively^ -curves, cut-off values were chosen for high WHR and
After adjustment for smoking, hypertension, and blood. .'.fasting Blood glucose on the basis of the highest
glucose, a 1 SD increase in WHR increased the OR.hy.-' ^proportion of correctly classified cases and controls. To
detemtine the. effect of these risk factors, we considered
2-24.
A history of hypertension was significantly niorep
common in cases than in controls (37, 19% vs 15, 8%: 9^7
Adjusted OR (95% Cl)
Model
2-69, 95% CI 1-42-5-11; p<0-001).
Coefficients
SE
There were no significant differences between cases am|
controls in any of the lipid variables (table 1), and
_______ —-33
Patient group
All participants
Age (years)
Mean (SD)
Median (range)
FBG (mmol/L)
Mean (SD)
Median (range)
Insulin (mU/L)
Mean (SD)
Median (range)
Not known diabetic
mmol/L
Controls (n»200)
Cases(n=164)
Controls (n=182)
Cases(n=90)
Controls (n=l<jt49
47-3 (80)
48 (30-60)
47-0 (8-1)
48 (30-60)
46-2 (8-2)
46 (30-60)______
46-3 (8-0)
47 (30-60)
45 0 (8-1)
45(30-60)
45 9 (8 2)
46(30-6°)
6-77 (3-31)
5-55 (3 00-26-09)
5-55 (2-36) •
4-77 (3-05-18-65)
5-83 (2-16)
5-24 (3-00-20-31)
5-16 (1-84) •
4-72 (3-05-18-65)
6-05 (2-65)
5-36(3-22-2031)
4-83 (1-65)' '.A
4.66(30^869;-
25-5 (18-5)
20-5(1-9-101-7)
24-3 (26-7) t
17-2 (3-9-217)
23-3 (17-7)
17-6 (1-9-90-8)
*220(22-1) ..
15-8(3-9-2^>-;
.-'J
''
ND
ND
ND
ND
p values (cases vs controls) were -p<00001, tP<0-S5. and *p>0-05. Ntfanot done.
Table 3: Fasting blood glucose (FBG) and serum insulin
360
PPBG 37
*77
Cases(n=200)
. - Smoking "
-^HR feO-92 , .
'..typertensionV FBG >4-94 mmol/L
/erne <4000 rupee*/mo
^getarian
P=l-136
P=l-094
* P =1-042
0-298
0-279
0-280
0-406
3-12 (1-80-5 40)
2 67 (1-20-5-94)
1-23 (0-70-2-19)
preser :e of sin2!e risk ,actor can calculated from ar.j.og ui
e freoefficier is. To calculate adjusted OR for combination of two risk factors.
’ (B
and calculate antilog. For example, in individuals who smoke
c&ti ♦ 1and ^ave * n elevated fasting blood glucose (FBG) (P4=l-042/. the OR is
ated as e ,‘K“ w ilch is e J “^iO-6.
*jre-IS ^3Sed On naW<
*
case-control analysis. Data on fasting insulin and PPBG
’ fcistit-01'nCluded •'!in:e they were unavailable in diabetics. Recalculation of multiple
. PtoJ^Sression m pdeI without matching but a'so including fasting insulin and
’ SE=n^?ed 0,6 ^Wowing results- intercepts-1-327. SE=0-237: smoking: P.=l-252.
Il-tel27,0R 3-£- (2-24-5-47); FBG ^4-94 mmo!/L. p =1 219. SE=0-299.0R=3-3S
r<£Z09,: tyP^insion p =1-064. SE 0-354. OR 2-90 (1-44-5-82):
SeJ^anism ? =0-410. SE 0-228.0R=l-51 (0-96-2-36); WHR ^0-92 p =0-244.
Tabi 8’0R1'38'l0'67'2'4'1)'
e 5: cnect
Effect of multiple
multiple risk
risk factors,
factors, moaeiiei
modelled with logistic
esslon: prediction of cases versus controls
resaw
'=13.|§
'August 10, 1996
smoking, hypertension, income, non-vegetarianism, WHR
of 0-92 or more, and fasting blood glucose of 4-94 mrnoLL
or more. Table 5 shows the adjusted OR for each variable,
with the independent predictive effect of each risk factor
controlling for all others in the model. With the
information in this table, the independent effect of risk
factors and various combinations can be calculated. For
example, individuals who smoke and have a raised glucose
'have an OR of 10-6. For an individual with the three risk
factors of smoking, raised glucose, and hypertension, the
ORis31-7.
Discussion
Our study, which is probably the first prospective case
control study aimed at identifying the relation between
risk factors and AMI in south Asians in India, shows that
tobacco smoking, a history of hypertension, a high
prevalence of diabetes, increased fasting blood glucose
(even in those who are not diabetic), and an increased
ratio of visceral to total body fat (WHR) are independent
risk factors for AMI. Patients with multiple risk factors
have a substantially increased risk for AMI.
Our study was conducted in a tertiary care hospital
serving an urban and suburban population in Bangalore, a
large south Indian city. Since the cases are confirmed
cases of AMI not known to. have had previous heart
disease, the study avoids the' problem of misdiagnosis
associated with sole use of ECG diagnostic criteria (as has
beer, done in prevalence studies) and of modification of
risk factors by treatment of IHD. We also avoided
problems associated with migration and acculturation
since the study was done in India; it also allows
comparison of risk factors among individuals within a
relatively homogeneous ethnic origin and geographic
region with and without AMI, rather than between
popmations.
\
Tobacco smoking is\in important modifiable risk factor
for IHD in western countries." Studies on migrant Indian
populations have not ^emphasised the importance of
smoking?-11 The prevalence of smoking is increasing in
Intis even as it decreases; in developed countries. Our data
shosr that it was the most important risk factor with a
dose-related risk (cigarettes and beedis). McKeigue and
colleagues'- reported a similar relation between smoking
and IHD among south Asians in the UK. Our study
supports the conclusion that tobacco control programmes
in India and other countries of the region could have an
important public-health impact.
Despite low meat and fish consumption, even among
non-vegetarians in India, our findings point to a significant
protective effect of vegetarianism, which persisted after
adj-nttment for smoking, lipids, and glucose
conmntrations. That the inclusion of WHR in the model
subtcantially explained the potential impact of
vegemrianism suggests possible ways for reducing the risk
associated with central obesity. Vegetarianism among
Inmans is generally life long and is not necessarilv
assotiated with other healthy behaviours (eg, less smoking,
mere exercise) and therefore our data are less subject to
—g-.n abnormalities are a widely accepted risk factor for
LHD. Studies on Indian populations in other countries
hr.v reported than Indians generally do not have higher
:rts_ cr LDL cholesterol concentrations than white or
-Acr.-Car.bbean populations. They do, however, have
vise—
.. ,
.
lower HDL cholesterol and higher triglyceride
depends on the state of the economic development’ll
concentrations?... .
Although the mean HDL
country. In developing countries IHD is thought to"'-I i^uf data suggest that smoking cessation programmes
cholcstcrol was low and triglycerides were high in our
predominantly a disease of the upper income groups W • ed at controlling both cigarette and beedi use, control
cases, they were not significantly different from controls.
development progresses this relation may reverse."*'?; ?blood glucose, treatment of hypertension, and
In a survey of Asian men in Britain, McKeigue et al'
findings that cases of AMI had a lower income and 1
i “Suction of visceral obesity, perhaps by diet, are likely to
reported that presence of major Q waves on ECG was
education than controls accords with a recent c°^ ' ^j-ay factors in the prevention of premature IHD in
associated with increased total cholesterol and
sectional study conducted in a/ural area of Rajasthah” >th Asianstriglycerides but not with reduced HDL cholesterol. Two
which the prevalence of ECG abnormalities was jnve’
small studies from India (Chaddha et al” with 11 cases
related to the level of education.” Our data are unlikes and Dhawan et al” with 28) showed that total cholesterol
be biased since hospital fees for patients admitted^ Srenc^
and triglycerides were higher in individuals with IHD than
u Keiffue PM, Miller GJ, Marmot MG. Coronary heart disease in
elective surgery are similar to those for emergency
in those without IHD. The data from our much larger
Asians: a review. J Cltn Epidemic! 1989; 42: 579-609.
such as AMI. However, controls from outpatient c]? '1 so^h
study do not show significant differences in the
c as EA Yusuf S, Mehta JI— Prevalence of coronary arterv disease in
who request a general physical examination may have hi 2 San Indians. Am J Cardiol 1992; 70: 945-49.
concentrations of any of the usual lipid fractions in
Carvotham
SG, Berry JN. Prevalence of coronary heart disease in an ,
a
different
social
background.
Of
the
200
controls'
ig
patients with and without AMI; this may indicate that in
were in this category. If these 18 controls are exclude < urban population in Northern India. Gradation 1968; 37: 939-53.
our population the serum lipids that we measured did not
■ Chadha S, Radhakrishnan S, Ramachandran K, Kaul U, Gopinath N. .
from the analysis, the findings remain largely imchangffi • Eoidemiological study of coronary heart disease in urban population in
have an important causal role. Our study had 80% power
By contrast, Chadha et al* in a study from Delhi reported’to detect 11 mmoVL (6%) relative differences in total
&& Indian J Med Res 1990;92:424-30.
lower prevalence of ECG abnormalities among people of? f - Anon Coronary heart disease in Indians overseas. Lancet 1986; i:
cholesterol. AMI alters serum lipids but this change
1307-08.
occurs after the first 48 h whereas all our blood samples
lower socioeconomic status than among those of a higher
, McKeigue PM, Adelstein AM, Shipley MJ, et al. Diet and risk, factors
status. McKeigue and Marmot” found no difference fo I for CHD in Asian Indians in Northwest London. Lancet 1985; ii:
were taken within the first 24 h.”1’ In addition, the fact.
prevalence of IHD among South .Asians in Britain' from I J086-90.
that infarction tends to lower HDL cholesterol and raise
different socioeconomic backgrounds. These conflicting^ \ .Miller GJ, Kotecha S, Wilkinson WH, et al. Dietary and other
triglycerides should exaggerate any difference in the
/.characteristics relevant for CHD in men of Indian, West Indian and
concentrations of these lipid fractions. However, some of
data suggest that India may be in a state of transition from,
European descent in London. Atherosclerosis 1988; 70: 63-72.
the cases in our study did receive intravenous heparin soon
.a pattern of disease seen in developing countries to that:' 8 Reddy S, Sanders TAB. Lipoprotein risk factors in vegetarian women
after admission which may lower serum triglycerides but
seen in the more developed ones.
oflhdian descent are unrelated to dietary intake. Atherosclerosis 1992;
95: 223-29.
' \
not the other lipids.”
-Our study may have some of the limitations inherent ia
9 McKeigue PM, Ferric JE, Pierpoint T, Marmot MG. Association of
Known diabetes mellitus was a significant risk factor for
a case-control design. Although the controls were hospital
'.early onset coronary’heart disease in South Asian men with glucose
AMI in our study, and both serum glucose and insulin
based, we'carefully defined a group of individuals drawn
intolerance and hypcrinsulinemia. Circulation 1993; 87: 152-61.
were higher in cases than in controls. Although transient
from the same catchment area for whom enhancement or- 10 Jacobsen MS. Cholesterol oxides in Indian ghee: possible cause of
■ unexplained high risk of atherosclerosis in Indian immigrant
hyperglycaemia occurs in AMI, it is accompanied by a
avoidance of putative risk factors were unlikely. Althoughpopulation. Lancet 1987; ii: 656458.
concomitant fall in serum insulin, in contrast to our
controls from the community would have been ideal,'- 11 Farmer
JA, Gotto AM. Risk factors for coronary artery disease. In:
findings. How long lasting are these transient AMI-related
hospital-based controls were easier to recruit and generally
Braunwald E, ed. Heart disease. A textbook of cardiovascular
medicine. 4th ed. Philadelphia: WB Saunders, 1992: 1125-O0.
changes in insulin and glucose is unclear. According to
belonged to the same population as hospital-based cases...
Ryder et al,” blood sugar returns to normal in 3 days.
Further, all cases were defined prospectively with accepted? 12 BeckJes GLA, Miller GJ, Kirkwood BR, Alexis SD, Carson DC,
' Byam NNTA. High total and cardiovascular disease mortality in adults
Serum insulin is low in the early hours after AML and
criteria and all controls were carefully screened clinically,.' •; of Indian descent in Tnnidad unexplained by major coronary risk
returns to normal in a few hours to a few weeks.10-'1 If
to eliminate those who may have had subclinical diseased? . factors. Lancet 1986; i: 1298-301.
assessment of glucose tolerancA is delayed after an AMI
The values for several variables (eg, lipids, glucose, bbdyj: 13 Miller GJ, Becklcs BLA, Maude GD, ct al. Ethnicity and other
characteristics predictive of CHD tn a deseloping community:
values may be altered by diet and changes in life style.
mass index) that we obtained in our controls are similar.®
.
principal results of the St James survey, Trinidad, bit J Epidemiol 1 989;
Therefore, we measured blood sugar and serum insulin on
those from an independent large cross-shctional study of'S
j. 18:80S-17.
the 9th and 10th day after admission. Fasting blood
5455 (2488 of whom were male) urban and rural/ I 14 Thomas I, Gupta S, Sempos C, Cooper R. Serum lipids in Indian
glucose was higher in cases'-than in controls even among
individuals in north India (K S Reddy, All India Institutes i ■ . physicians living in the US compared to US bom physicians.
Atherosclerosis 1986; 61: 99- 106.
of Medical Sciences, New Delhi, India). Without?®
patients not previously known to be diabetic and in those
15 Chadha SL, Gopinath N, Ramachandran K. Epidemiological study of
without impaired glucose tolerance. Our findings accord
prospective cohort study, it is difficult to assess*^/:
with several previous repons indicating a high prevalence
potential impact on risk factors, if any, of pre-exisang? of non-insulin dependent diabetes mellitus in Asians”*”
silent IHD, changing risk factors among cases, and any...
and two previous studies showing the importance of
treatment for diabetes mellitus and hypertension toy ■
diabetes and impaired glucose tolerance as risk factors for -patients may have received. However, such factor
IHD.*'’ Our observation of increasing risk with increasing
generally tend to reduce differences between cases w.;
blood glucose concentrations suggests that even high
controls. Finally, the patients in this study
blood glucose within the euglycaemic range identifies
predominantly male and any extrapolation to wotto;
individuals at higher risk of IHD. This is consistent with
should be done cautiously.
data from the Framingham Heart Study indicating a
Our findings suggest that, in addition to smoking
relation between glycosylated haemoglobin and IHD.”
hypertension (which are important risk factors for IHD
The lack of an association of fasting insulin levels (a crude
most populations), central obesity and raised b'°° ■.
glucose are important across a wide range of values “LA
measure of insulin resistance) with AMI in the
euglycaemic group suggests that glucose may be more
south Asians. Although glucose intolerance, ‘nsU.c','»
relevant to the development of IHD than hyperresistance, hypertension, central obesity,
triglycerides, and low HDL cholesterol occur together ao^.l
insulinaemia in this population.
The WHR is a measure of abdominal obesity and a
are associated with an increased prevalence ..
surrogate measure for visceral fat deposition.” McKeigue
cardiovascular disease, the mechanism of the increaS^.'.
et al’ found a significantly higher prevalence of major Q
vascular disease associated with these syndromeS .
,
waves and positive ECG but not symptomatic IHD across
unclear.’-” In our study vegetarianism seemed to h <.
a protective effect against AMI that was unrelated.1’ t
tertiles of body-mass index and WHR. Central obesity is
generally regarded as a more important predictor of IHD
risk factors other than WHR. This finding sug^,$S t
than is generalised obesity.” \
that modifications in diet among non-vegetan ,_.j e
362
Vol 348 • Autnist
abnormalitic
in India witn coronajj
Ryder REJ, Hayes TM, Mulligan IP, Kingswood JC, William S,
Owen DR. How soon after myocardial infarction should plasma lipid
values be assessed? BMJ 1984; 289: 1651-53.
18
Gore JM, Goldberg RJ, Matsumoto AS, Castelli WP, McNamara PM,
Dalen JE. Validity of total cholesterol level obtained within 24 hours of
acute myocardial infarction. Am J Cardiol 1984; 54: 722-25.
19
Leidig GA Jr, Pasternak RC, Horowitz G, Ginzburg GS. Effects of
heparin and cardiac catheterization on serum lipoprotein and
triglyceride levels. Am J Cardiol 1994; 74: 47-52.
20
Verter NJ, Strange RC, Adams W, Oliver MF. Initial metabolic and
hormonal response to acute myocardial infarction. Lancet 1974; i:
284-88.
21
Ceremuzynski L. Hormonal and metabolic reactions evoked by acute
myocardial infarction. CircRes 1981; 48: 767-71.
22
.McKeigue PM, Shah B, Marmot MG. Relation of central obesity and
insulin resistance with high diabetes prevalence and cardiovascular rsk
in South Asians. Lancet 1991; 337: 382-86.
23
Seedat YK, Mayet FGH, Khan S, Somers SR, Jourbert G. Risk factors
for coronary artery disease in Indians of Durban. S Afr MedJ 1990;
78:447-54.
’
,
24
Ramchandran A, Jali MV, Mohan V, Snehlatha C, Vishwanathan M.
High prevalence of diabetes in an urban population in South India.
BMJ 1988; 297: 587-90.
25
Singer DE, Nathan DM, Anderson KM, Wilson PWF, Evans J.
Association of HbAu with prevalent cardiovascular disease in the
original cohort of the Framingham Heart Study. Diabetes 1992; 41:
202-08.
26
Kvist H, Chowdury B, Grangard V, Tylen V, Sjostrom L. Total and
visceral adipose tissue volumes derived from measurements with
computed tomography in adult men and women: predictive cquaucen.
Am J Clin N'tttr 1988; 48: 1351-61.
27
Lapidus L, Bengtsson C, Larsson B, Pcnnert K, Rybo E, Sjostrom 1_
Distribution of adipose tissue and risk of cardiovascular disease and
death: a 12 year follow up of participants in the population study of
women in Gothenburg, Sweden. BMJ 1984; 289: 1257-61.
28
McKeigue PM, Sevakk L Coronary heart disease in South Asian
communities. A manual for health promotion. London: Health
Education Authority, 1994.
29
Davey Smith G, Shipley MJ, Rose G. Magnitude and cause of
socioeconomic differentials in mortality: further evidence from the
Whitehall Study. J Epidemiol Commun Health 1990; 44: 265-70.
30
Gupta R, Gupta VP, Ahluwalia NS. Educational status coronary hear:
disease and coronary risk factor prevalence in\a rural population in
India. BMJ 1994; 307: 1332-36.
\
31
McKeigue PM, Marmot MG. Mortality from coronary heart disease c
Asian communities in London. BMJ 1988; 297: 903.
32
Rcaven GM. Role of insulin resistance in human disease. Diabetes
1988;37: 1595-607.
x
I
33
Frayn KN, Coppack SW. Insulin resistance adipose tissue and
coronary heart disease. Clin Sa 1992; S2: 1 -8.
17
HOW TO STOP SMOKING
PREPARATION OF SURROUNDINGS
»»■ Two weeks prior to grz/Zdate, limit your smoking to one room in your home.
iw
Clean and. remove the smell of cigarette smoke from your home.
PREPARATION OF YOUR PHYSICAL SELF
w
Get your teeth cleaned. With tar and nicotine removed from your teeth.
r>- Monitor your alcohol consumption.
w
Reduce your caffeine consumption prior to quitting
Get plenty of rest. Your body needs time to readjust without the drug,
nicotine
Drink plenty of fluids.
Use healthy oral substitutes.
PREPARATION OF YOUR EMOTIONAL SELF
pr
Repeat to yourself your reasons for needing to quit smoking
w
Plan activities for your first smoke-free week.
Occupy your hands with other objects when you feel something is missing
without a cigarette.
Beware of cigarette advertisements.
Never allow yourself to think that one cigarette won’t hurt.
w
ENLISTING SOCIAL SUPPORT FOR YOUR t2£//7"DATE.
<«r
"r
w
Remind your friends and family that you are' going through the quitting
process and that it is important to you that they support you.
Be assertive and direct when asking for support.
Working with a smoker. It is important to make a request for support or at
the very least for respect of your efforts to quit smoking by not smoking in
your presence. You may also ask for a transfer to a work area that is somke
free.
COMMUNITY HEALTH CELL
2
You’r quit date, and the weeks that follow.
1.
Visualize and reinterpret your physical systems as “Symptoms of recover^'.
Initial phase of quitting; you may experience a list of nicotine withdrawal
symptoms (i.e.
Restlessness, irritability, difficulty in concentration, sleep
disturbances, dry mouth or sore throat, fatigue, coughing and Nicotine
"Craving”. These symptoms are short-term and necessary to the healing
process. Try to think about them as symptoms of recovery”. When you are
feeling irritable and restless or having a "Craving” remind yourself that your
body is healing.
Imaginary exercise of healing process......!!
Close your eyes and imagine your lungs. See the black tar sitting on the tiny
little air sacs that makes it hard for you to breathe at times. Each time you feel
“uncomfortable" imagine this tar gradually being lifted off your lungs. Each
breath that you take feels easier. You feel the clean air healing the wounded
lung tissue.
You see the 4,000-plus particles that are floating in your
bloodstream being washed away. You feel your arteries relaxing and allowing
blood to pass more readily through, cutting your risk for strokes and heart
attacks. With each passing day you see more and more healing occurring inside
your body.
2. Pay attention to your “high risk" situations. These are times, such as when
you are stressed at work or finishing a meal, when you are most likely to desire
a cigarette. Try either to avoid these situations or at the very least to have
alternative strategies available.
3. Use distraction techniques.
When you find yourself tempted to smoke a
cigarette get some distance from the thought or situation.
wonderful technique for preventing impulsive smoking.
4. Reinforce your reasons for needing to quit smoking.
Distraction is a
Remember, these
reasons need to be specific and personal to you. These reasons will help get
you through the periods of temptation.
5. Repeat to yourself the benefits of quitting smoking. Repeat the following
list of benefits to yourself several times a day.
COMMUNITY HEALTH CELL
3
BENEFITS OF QUITTING SMOKING
1
2.
3.
4.
5.
6.
7.
8.
9.
10.
Circulation improves.
Significantly decreases your risk for lung cancer and emphysema.
Increases lung and breathing capacity
Decreases allergies
Eliminates chronic bronchitis (which decreases energy level, resistance to
infection, and predisposes one to emphysema) in a few months after cessation.
Reduces number of cavities and increases chance of keeping your own teeth
(smokers have three times more cavities and gum disease than non-smokers)
Decreases risk of esophageal cancer by 500 percent.
Decreases risk of kidney cancer by 50 percent
Decreases frequency and intensity of headaches.
Decreases risk of osteoporosis
QUICK FIX COPING STRATEGIES.
Things You Can Do
l
2.
3.
4.
5.
6.
7.
8.
9.
Do relaxation exercises.
Go to a place where smoking is not allowed.
Take a walk.
Exercise.
Listen to your favorite music.
Drink fruit juice, water, or soda with lemon.
Take a hot bath.
Call a friend for support
Do some gardening.
THINGS TO THINK ABOUT OR SAY TO YOURSELF
l
2.
3.
4.
5.
6.
7.
8.
9.
10.
Think about how many ways quitting will improve your health.
Think about how not smoking will help your loved ones.
Go over your reasons for quitting.
Imagine yourself as a non-smoker.
Think about how much better food tastes when you are not smoking.
“I can manage this without a cigarette."
“I have made it this far."
“My lungs are getting healthier."
“I can breathe better."
“NO!!!!"
COMMUNITY HEALTH CELL
MANAGING SYMPTOMS OF ANXIETY RELATED TO NICOTINE
WITHDRAWAL
The symptoms of anxiety that you are experiencing are caused by the physical
withdrawal process from nicotine.
2.
This is your body’s way of healing itself. The discomfort you are feeling will
lead to overall healing and improved health. It is "good” pain.
3.
These symptoms of anxiety will last for only a couple of weeks. The worst
feeling will be around the third or fourth day after your last cigarette.
4.
Practise visualizing how nicotine increases your heart rate and blood pressure.
1.
Next visualize how without nicotine your heart rate and blood pressure will
return to normal.
5.
You may want to picture your anxiety as a wave. You can feel it rise - but as
you ride it out you can feel it subside. It passes without any action on your part.
Steps to Beating Depression - Related to Nicotine Withdrawal
w
<«r
w
Recognize your triggers to depression
Avoid isolating yourself.
Push yourself to engage in small tasks. Depressed individuals often
complain of no energy or interest in activities. Set small but reasonable
goals for yourself. For example, force yourself to go to the grocery store or
to a social function.
Get support from those you trust.
Seek professional help. You don’t necessarily have to wait until the
depression gets really bad to get professional help. The longer you wait to
treat depression the worse it can get, and subsequently the harder it is to
beat.
Compiled By
S. D. Rajendran.
Community Health Cell, #367, “Srinivasa Nilaya”, 1st Main, 1st Bloc,
Koramangala, Bangalore - 560 034. Ph : 5525385. Email: sochara@vsnl.com
Source : “HOW TO STOP SMOKING” - Lori Stevie-Rust & Anita Maximin.
COMMUNITY HEALTH CELL
-naaner. hpaitg amg r$pyp;
am imtrohijctiom
Jeff Coliin
Centre on Global Change and Health, London School of Hygiene & Tropical Medicine
The World Health Organisation (WHO) is in the process of negotiating its first
international public health treaty, a proposed Framework Convention on Tobacco
Control (FCTC). A major stimulus to this initiative has been recognition of the
escaiaiing burden arising from tobacco consumption and production in low- and
middlG-incomG countries with serious 2nd diverse sociel, economic 2nd
environmental impacts in addition to enormous implications for global health. With
one or two exceptions, however, the development community has generally been
slow to respond both to the challenges posed by the tobscco industry and to the
opportunities presented by the FCTC process. This short paper highlights the
importance and value of engaging with tobacco control for NGOs working with
development issues, 2nd provides links to easily accessible sources of further
information. It serves as an introduction to key issues that will be developed during
discussions, at the forthcoming meeting of the Health and Development Forum to be
held at the London School of Hygiene and Tropica! Medicine on September 12th 2002
at 1.30pm.
Tobacco, Health anti Equity
it is estimated that some 4 million deaths per year can currently be attributed to
tobacco, or about 1 in 10 of ail adult deaths. Such figures aie set to rise dramatically
such that by 2030 the annual death total will stand at around 10 million or 1 in 6 adult
deaths. Consequentiy, around 500 million people alive today will eventually be killed
by tobacco.
"*"nis burden is becoming increasingly inequitable in its distribution. Smoking related
deaths were once largely confined to men in high-income countries, but the marked
shift in smoking patterns to middle and low-income countries is being accompanied
by rapidly rising trends in death and disease.
9
•
•
Around half of all deaths from tobacco occur in the developing world, but this will
rise to 70% by 2030.
in China smoking accounts for around i in 3 of all adult male deaths, or around
100 million of the 300 million Chinese males now aged 0-29.
Tobacco will kill around 80 million Indian males currently aged 0-34
Selling tobacco products to women has been described as the single largest product
marketing opportunity in the world. While the epidemic may be in gradual decline
among men, it will not reach its peak among women until well into the 21■ century.
and it is predicted that the current world total of around 187 million women smokers
will reach 532 million by 2025. Such an increase, driven by economic and social
change and by increased targeting of women by major tobacco companies, is liable
to have enormous consequences for health, incomes and families across developing
countries.
Sources:
WHO Tobacco Free Initiative (2001) Burden of Disease
http://www5.who.int/'tobacco/page.cfm?sid=47
Gajalakshmi CK et al (2000) Global patterns of smoking ano smoking-attributable mortality in
jha P and Cnaioupka F (eds) Tobacco Control in Developing Countries available at'
http://v.VAv1.y<orldbank.prg/tobacco/tcdc/0.09T0040,_PDF
krJ
Same’ J and Yoon S eds. (2001) Women and the Tobacco Epidemic: Challenges for the 21s
Century (Geneva: World Health Organization)
http:niobacco.who.int/documents/WoMonograph01 .pdf
The Economics of Tobacco Control, Tobacco Production and Development
A. fundamental obstacle to the development of comprehensive tobacco control
programs has been the misolaced belief in the value of tobacco production and
consumption to national economies. As a result of research led by the World Bank, it
is increasingly dear that, for the vast majority of countries, increased taxation of
tobacco products would not cause long-term job losses. Tobacco control actually
presents policy rnokors with s virtuous circle, often combining substentie! benefits for
public health through reduced consumption with an expansion in revenues via
increased taxation.
Notwithstanding the broadening evidence base that tobacco control makes good
economic sense it is clear that some countries are significantly reliant on tobacco
production. Rea! dependence on the crop is however far less common than is often
suggested. Of the 141 countries that export tobacco only Io derive more than 1% of
their total exnort earnings from it, and tobacco accounts for over 5% of export
earnings in only 4, namely Kyrgyzstan, Macedonia, Zimbabwe and Malawi (at 8%,
16%, 32% and 58% respectively).
Importantly, however, improved tobacco control is not going to result in a sudden
collapse. Rather, the number of people using tobacco products is expected to
increase by over 500 million during the next quarter of a century. Tobacco control
efforts do not focus on reducing supply, and any decline in overall consumption that
could undermine employment in tobacco farming will occur over several generations.
Sources.
World Bank (1999) Curbing the Epidemic: Governments and the Economics of Tobacco
Control http://www1.worldbank.org/tobacco/reports.htm
Campaign for Tobacco Free Kids (200 i) 'Golden Leaf, Barren Harvest: The Costs of Tobacco
Farming’ http://tobaccofreekids.org/campaiqn/global/FCTCreport1.pdf
Globalisation, Trade and the Tobacco Epidemic
Globally, the tobacco industry is increasingly dominated by a handful of major
companies. 75 percent of the world cigarette market is now controlled by just four
companies: Philip Morris, British American Tobacco (BAT), Japan Tobacco and the
China National Tobacco Corporation. Recent years have also seen the number of
major companies involved in the purchasing, processing and shipment of raw
tobacco faii from eight to three. The period from 1994-97 witnessed a 12,5%
increase in unmanufactured tobacco exports globally, following a decade of
negligible growth. Cigarette exports were relatively stable between 1975 and 1985,
began to steadily rise thereafter, and grew by 42% between 1993-96.
Both the consolidation and expansion of the tobacco industry have boon driven by
trade liberalization.
The opening of cigarette markets in Asia has been particularly
significant, as shown by the impact of the so-called Section 301 agreements in
Japan, South Korea, Taiwan and Thailand. Access to these markets was gained
following threatened trade sanctions by the US and, in the Thai case, adjudication by
GATT, it has been estimated that the opening of these markets increased per capita
cigarette consumption by an average of 10% by 1991.
r? particularly important to note the inequitable impacts of trade liberalisation on
lOvacco consumption. Trade liberalisation has led to increased consumption of
tobacco overall out, while it has no substantive effect on higher-income countries, it
has had a large and significant impact on smoking in low-income countries and a
significant, if smaller, impact on middle-income countries.
Sources:
Faylor A et ai (2000) ‘The impact of trade liberalization on.tobacco consumption' in Jha P and
Chaloupka
F
eds.
Tobacco
Control
in
Developing
Countries,
available
at:
■2iffiFif^£^..Jwori<^ank.o.rg/tobaccg/tcdc/343T0364tPpF
Hammond R (1998) 'Consolidation in the tobacco industry', Tobacco Control, 7: 426-428
(Winter), httpj7tc.bmjiournals.eom/cqi/context/full/7/4/426?
Transnational tobacco companies and development
The tobacco industry has undoubtedly contributed to the widespread failure to
perceive tobacco as a significant development issue, particularly in seeking to
undermine the credibility of WHO’s work to promote tobacco control. An examination
WHO ComrnUt©© of tExpsns
by
industry occumonts msdc svsiisbio vis sitiejstion
revealed the scale of efforts to portray such activities as a ‘First World’ agenda
carried out at the expense of developing countries. Documents have identified the
explicit use of the international Tobacco Growers Association as a front group for
industry lobbying, a clear concern to stop developing countries becoming committed
to tobacco control, to restrict WHO’s funding and divide it from other UN agencies,
and the creation of an international consortium to mobilize officials from developing
countries to advance pro-tobacco positions.
Underlying such tactics has been a broad strategy of attempting to present the
concerns of small tobacco farmers in developing countries as fundamentally aligned
with those of tne enormous transnational tobacco companies based in the United
States, the UK and Japan. The extent of divergence in interests is becoming
apparent, with increasing evidence of the poor economic returns, environmental
damage and health impacts associated with tobacco production:
•
•
*
•
In Brazil, a report by Christian Aid highlighted the role of BAT’s local
subsidiary Sousa Cruz in controlling the livelihoods of small-scale contract
farmers and raised serious concerns about the health impacts of pesticides
sold by the company.
In Uzbekistan, where BAT has made a substantia! investment, the British
Helsinki Human Rights Group identified exploitation of local farmers
amounting to de facto slave labour.
in Kenya, there is rising concern about the substantia! death toll from
pesticide use and the rapid rate of deforestation attributable to tobacco.
Cigarette companies are using progressively less tobacco per cigarette,
adopting techniques such as using expanded or reconstituted tobacco,
increasing profitability while reducing demand for raw tobacco.
Sources:
WHO Committee of Experts (2000) 'Tobacco Company Strategies to Undermine Tobacco
Control Activities zt the World Health Organization'
h11p.!!m!e.31ore.w■ io. int/ • w!jo/»jo•Tie/tobacco/tobacco.pdf
Christian Aid/DESER (20u2) Hooked on Tobacco report on BAT subsidiary Sousa Cruz
http:/AeAnA',cJrrjstian-2id,prq.uk.'indepth/02qibat/inc!exJitm
British Helsinki Human Rights Group (2002) Uzbekistan 2002: British American Tobacco
Campaign for Tobacco Free Kids (2001) Factsheets: ‘Tobacco and the Environment1.
‘Tobacco Industry Manipulation of Agricultural issues' and ‘Lowering Leaf Content, Boosting
r i Ci no i mp
lOOaCCOn ccrxi vS.Orp/Cg/i jpg iG p/GiObai/
Towards tf?e Framework Convention on Tobacco Control
i he process of negotiating the rC i C was established by a unanimous resolution of
the World Health Assembly in 1999. initiating a two-step process of Working Groups
(iivB). Seini-annuai negotiating sessions of the INB have been heid in Geneva since
November 2000. with the fifth round set for October 2002. The FCTC is expected to
take the form cf a broad convention outlining legal parameters, structures and
general obligations for all signatories, in combination with a number of protocols
detailing more specific commitments to which states can choose to accede on a
csso-by-csss bssis Ths ob’sctivo is for a negotiated convention to be ready for
presentation to the WHA in May 2G03.
The FCTC process has been characterised by an attempt to secure broad
participation both by member states and by civil society. One notable development
has been the negotiation of coordinated positions among regional groupings prior to
the INB meetings. The Johannesburg Declaration on the FCTC, for example, was
adopted by the 21 countries of WHO's African Region in March 2001. This common
front was widely perceived as having added weight to their contributions to the first
INB session, emphasising a commitment to progressive control measures in
combination with calls for assistance in agricultural diversification.
The FCTC process has aimed to encourage the participation of actors traditionally
excluded from the state centric politics of UN governance. Public Hearings held in
October 2000 provided an opportunity for interested groups to register their views
prior to the start of inter-governmental negotiations. Over 500 written submissions
were received, 'while i'll organisations provided testimony during the 2 day hearings,
encompassing i iCs. state tobacco companies and producer organisations as well
as diverse public health agencies, womens’ groups and academic institutions.
i he iole of NGOs in the process has centred on the development and activities of the
Framework Convention Alliance. This grouping of over 160 increasingly diverse
NGOs was crested io improve communication between those groups already
engaged in the FCTC process and to address the need for a systematic outreach to
smaller NGOs in developina countries. It has developed a valuable series of briefing
papers and identified key issues in support of developing a strong Framework
Convention.
Sources:
WHO (2002) 'Framework Convention on Tobacco Control: An Introduction' with links to all
documentation and draft Chairs text http://tobacco.who.int/en/fctc/index.html
Bates C (2001) Developing countries take the lead on WHO convention. Tobacco Control, 10
(3): 209 http://www.ash.ora.uk/html/international/html/inb2review.html
Framework Convention Alliance (2002) Briefings on Trade, Advertising, Smuggling and
Packaging and Labelling, together with a list of 10 key issues for global tobacco control and
the FCTC, available at www.fctc.orc)
Special Theme - Tobacco
Building the evidence base for global
tobacco control
Mario Ann Corrao,1 G. Emmanuel Guindon,2 Vilma Cokkinides,3 & Namita Sharma4
The tobacco control movement needs a global information system permitting routine monitoring of the tobacco
trade, tobacco farming, the tobacco industry, the prevalence of tobacco use, associated mortality, and national
resources for combating tobacco. The Tobacco Control Country Profiles database, a data collection initiative led by
the American Cancer Society in collaboration with WHO and the Centers for Disease Control and Prevention,
represents the first step in the development of such a system. Baseline data on several indicators of tobacco use
were obtained from 191 Member States of WHO, two Associate Members, Hong Kong Special Administrative
Region of China (Hong Kong SAR), China (Province of Taiwan) and the West Bank and Gaza Strip. The methods
used to compile the data are described in the present paper.
Selected indicators from the database were analysed in order to demonstrate the potential utility and value of
data derived from an information system devoted to tobacco control. The analyses covered gender-specific smoking
prevalence by WHO Region, per capita cigarette consumption by Human Development Index (HDI) category, and
average real annual percentage changes in cigarette prices between 1990 and 1999 for selected countries in each
category. In 1998, men were almost four times more likely than women to be smokers. The prevalence of smoking
among men was highest in the Western Pacific Region. The differential in gender-specific smoking prevalence was
narrowest in the Region of the Americas and the European Region. It was wider in the South-East Asia Region and
the Western Pacific Region. The lowest and highest per capita consumption of manufactured cigarettes occurred in
the lowest and highest HDI categories respectively. In the medium HDI category, China's growing cigarette
consumption after 1975 had a major bearing on the rise in per capita consumption. Cigarette price trends suggest
that there is considerable scope for increasing taxes on tobacco products, particularly in low or medium HDI
countries. The implications of the findings for future tobacco control efforts are discussed, as are issues surrounding
the quality of available data, priorities for future data collection and the need to maintain and improve the
information system in order to support such efforts.
Keywords: smoking, statistics; smoking, epidemiology; tobacco, statistics; prevalence; commerce; databases,
factual, utilization; information.
Voir page 889 !e resume en frangais. En !a pagina 889 figura un resumen en espanol.
Introduction
It has been estimated that some three million deaths
are attributable to smoking annually and that the
number could rise to ten million within 30 to 40 years
(7). Effective action against tobacco requires coun
tries to understand the magnitude of the adverse
effects of smoking on their populations. As country
representatives negotiate WHO’s Framework Con
vention on Tobacco Control, the need for reliable
and timely data on tobacco and its use is greater than
ever before. The effects of tobacco use could be
1 Program Manager, Tobacco Control Country Profiles, American
Cancer Society, 1599 Clifton Road NE, Atlanta, GA 30329-4251, USA.
Correspondence should be addressed to this author.
2 Economist, Tobacco Free Initiative, World Health Organization,
Geneva, Switzerland.
3 Director, Risk Factor Surveillance, American Cancer Society Atlanta
GA, USA.
4 Presidential Management Intern, Office on Smoking and Health,
Centers for Disease Control and Prevention, Atlanta, GA, USA.
Ref. No. 00-0648
884
‘ World Health Organization 2000
monitored through a global system routinely assem
bling information on the tobacco trade, tobacco
farming, the tobacco industry, the prevalence of
tobacco use, associated mortality, and national
resources for combating tobacco. Anticipating the
demand for a global information system to support
new tobacco control efforts, WHO and the Centers
for Disease Control and Prevention initiated the
development of the National Tobacco Information
Online System (known provisionally as NATIONS)
in 1998. The baseline data for this system were
collected for the Tobacco Control Country Profiles
(TCCP) project, led by the American Cancer Society'.
The project has produced a monograph to be
presented at the 11 th World Conference on Tobacco
or Health (Chicago, 6-11 August 2000).
In order to demonstrate the potential utility of
the data available from the TCCP project and later
from NATIONS, we have analysed gender-specific
smoking prevalence, per capita cigarette consumption,
and changes in cigarette prices. The analyses illustrate
the type of comparison that can easily be made
between regions and countries by means of data from
Bulletin of the World Health Organization, 2000,78 (7)
Building the evidence base for global tobacco control
the TCCP project, which represents the first step in the
development of a global tobacco infonnation system.
In addition, we highlight issues surrounding the quality
of available data, priorities for future data collection,
and the need to maintain and improve the system in
order to support tobacco control efforts.
Methods
For analyses of smoking prevalence we categorized
191 Member States of WHO, two Associate
Members, Hong Kong SAR, China (Province of
Taiwan) and the West Bank and Gaza Strip, thus
allowing comparison with previous studies con
ducted by WHO. For analyses of manufactured
cigarette consumption we categorized countries
according to the Human Development Index
(HDI) (2), whereby 174 countries are placed in high,
medium or low categories based on life expectancy,
educational attainment and income, giving a better
measure of basic human capabilities or deprivation
than income alone. This made it possible to examine
how manufactured cigarette consumption varied
with basic standards of living.
Country-specific statistics on smoking preva
lence in the TCCP database were obtained through
Medline literature searches, personal contacts with
investigators and nongovernmental organizations en
gaged in tobacco control, and reports from health
ministries, national statistical offices and WHO country
representatives. The minimum inclusion criteria for a
survey were the following items ofinformation: date of
the survey or its publication; characteristics of
respondents (age and sex distribution); a description
of sampling and data collection methods; and the
questions used in assessing smoking behaviour.
When several studies from the same country
met these criteria they were compared with respect to
geographical coverage, dates, sample sizes, response
rates and methods. Wherever different sources yielded
contradictory data on prevalence, historical data were
reviewed and expens working in the country were
consulted. The most recent and representadve studies
on adult smoking prevalence were included.
Regional estimates of smoking prevalence were
derived on the assumption that all studies reported
current daily and occasional smoking among persons
aged 15 years and older and that they reflected the
smoking statuses of the populations in 1998. The
gender-specific prevalence estimates for each coun
try were weighted by the size of the male and female
populations aged 15 years and above. The values
were averaged so as to obtain WHO weighted
regional prevalence estimates. Each of these was
assumed to apply to an entire WHO region. The
number of smokers in each region was estimated by
multiplying the prevalence by the total population
aged 15 years and above.
Data on per capita cigarette consumption in the
TCCP were derived from production, import and
export data in several electronic databases and national
Bulletin of the World Health Organization, 2000,78 (7)
statistical yearbooks available for public scrutiny.
Statistics on cigarette imports, exports and production
were obtained from the United Nations Statistical
Division’s Commodity'Trade Statistics, the Industrial
Commoditv Production Statistics databases, the Uni
ted States Department ofz\griculture, and the Food and
Agricultural database.1 For countries where these data
were unavailable, figures from national statistical
agencies and private research firms were used.
Cigarette consumption in each country was
calculated as productionplus imports minus exports, using a
three-vear moving average for the y’ears 1975 and
1985. For high development countries, consumption
was also calculated for 1995, a year in which trade and
production data were not available for most countries
in the medium and low development categories. In
the medium development category', consumption
was calculated for 1994, and in the low development
category' it was calculated for 1991. Average per
capita consumption was estimated within each HDI
category by combining the country-level consump
tion figures and dividing by the population aged
15 years and above. Adult per capita cigarette
consumption in the medium development category
is presented both including and excluding China and
is calculated separately for China.
Data on cigarette prices, reflecting prices in the
autumns of 1990 and 1999 unless otherwise noted, are
presented by HDI category in USS on the basis of
values in local currencies and exchange rates in force
when surveys were conducted (price and exchange
rate data were obtained from the Economist Intelli
gence Unit). For countries where prices were sampled
in more than one city, averages of all the city prices
were calculated. Average annual real percentage
changes in price between 1990 and 1999 were
calculated using the percentage difference in local
currency' prices while taking into account or discount
ing for inflation. These calculations were facilitated by
creating an inflation index based on estimates
provided by the Economist Intelligence Unit.
Results
Prevalence of smoking
Data on smoking prevalence were available from
countries with populations representing 55.4 % of
the African Region, 96.3% of the Region of the
Americas, 88.7% of the Eastern Mediterranean
Region, 88.8% of the European Region, 96.9% of
the South-East Asia Region and 99.3% of the
Western Pacific Region (Table 1).
Men were almost four times as likely to smoke as
women, yet 23% of females were smokers in the
Region of the Americas and 23.4% were smokers in the
The following product codes were used to identify data for analysis
in each of the sources: code 1222, COMTRADE Standard International
Trade Classification (Revision 2); code 3140-07, UNSD Production
International Standard Industrial Classification of all Economic
Activities (Revision 2); code 828, FAOSTAT.
885
Special Theme - Tobacco
European Region. Smoking prevalence among men
was highest in rhe Western Pacific Region and lowest
in the Eastern Mediterranean Region. Among women,
smoking prevalence was highest in the European
Region and lowest in the Western Pacific Region.
There were about 1.235 billion adult smokers in a total
world population of 5.926 billion (US Central
Intelligence Agency’s estimate of the world’s popula
tion in 1998). ()n the assumption that there will be no
change in the global prevalence of smoking, it can be
expected that the number of cigarette adult smokers
will reach 1.278 billion this year (2000) and 1.671 billion
in 2020 because of changes in the world population (3).
Per capita consumption
The percentages of populations in the calculations of
per capita consumption varied by HDI category and
by year (Table 2). Fig. 1 presents estimates of per
capita cigarette consumption for over 15-year-olds in
1975,1985 and 1995 by HDI category.
The estimates for countries in the medium
category are presented with and without China and
separately for China. The highest per capita consump
tion of manufactured cigarettes occurred in the high
development category and decreased between 1975 and
1995. Countries in the medium development category
experienced a progressive 46% increase in consump
tion between 1975 and 1994, reaching 1139 cigarettes
per capita in 1994. China experienced an increase in per
capita consumption at a greater rate than that of the
medium development category as a whole from 1975 to
1994. In total, China experienced a 128% increase in per
capita consumption between 1975 and 1994. Without
China’s contribution to the medium development
category, its per capita consumption would have
decreased slightly between 1985 and 1994. Per capita
cigarette consumption in the low development category
remained fairly constant from 1975 to 1991.
Price of cigarettes
Table 3 presents trends in cigarette prices in various
countries. Substantial increases in real cigarette
prices, adjusted for inflation, occurred in only France,
South Africa, the United Kingdom, and the USA. No
increase or a substantial decrease in cigarette prices
occurred in more than half the countries listed. This
was especially true of imported brands.
Discussion
Using the TCCP database to support
tobacco control
The analyses presented above demonstrate the utility
of the data available in the database for supporting
programme and policy planning for tobacco control.
For instance, analyses of smoking prevalence and
cigarette consumption can assist in identifying the
countries with the greatest need for resources
devoted to tobacco control efforts. Globally, some
30% of adults were estimated to be smokers in 1998.
By 2020 the number of smokers will have increased
by 35% if global smoking prevalence remains the
same. Per capita cigarette consumption trends over
20 years, however, demonstrate the changing nature
of the pandemic. If consumption trends continue as
they have been since 1975, an increase in cigarette
consumption will occur in economically developing
countries and a gradual decrease will occur in
economically developed countries. The countries
with the greatest expansion in the cigarette market
will be those with the smallest resources available for
tackling the health problems associated with tobacco
use. While these analyses used very broad economic
categories, the TCCP database allows comparisons
between countries, geographical regions or other
groupings which might lend support to tobacco
control initiatives.
Analyses of average real percentage changes in
cigarette prices help to identify policy areas in which
national governments can improve their efforts in
tobacco control. The cigarette price trends in our
study suggest that there is scope for increasing taxes
on tobacco products, most notably in countries
belonging to the low and medium HDI categories,
Table 1. Gender-specific smoking prevalence by WHO Region, 1998
Weighted prevalence estimate
(%)____________
Region
Male
Estimated numbers of smokers
(millions)
Female
Total
Male
Female
Total
Number
of studies
% of total
population
represented
by studies
36.2
Africa
34.7
The Americas
34.2
Eastern
Mediterranean
43.5
Europe
South-East Asia 48.2
Western Pacific 62.3
9.4
23.0
8.7
22.9
28.7
21.8
59.6391
98.0754
49.7699
15.1086
67.8454
11.9266
74.7477
165.9209
61.6965
15
30
17
55.4
96.3
88.7
23.4
8.2
5.8
33.0
28.6
34.4
144.3112
242.6307
387.2792
84.6990
39.4710
34.9310
229.0102
282.1017
422.2101
40
6
23
88.8
96.9
99.3
47.9
12.4
30.2
981.7055
253.9816
1235.687
131
92.3
Total
Sources: American Cancer Society and World Health Organization, TCCP database.
Note: Several small countries for which population figures were not available did not contribute their population weight to the analysis.
886
Bulletin of the World Health Organization. 2000,78 (7)
Building the evidence base for global tobacco control
where cigarette prices have failed to keep up with
increases in the general price level of goods and
services. Cigarettes were more affordable in 1999
than at the beginning of the decade. Increasing the
price of tobacco products is arguably one of the most
effective means of curbing their consumption (•/). On
average, a price increase of 10% can be expected to
reduce the demand for cigarettes by about 4% in
high-income countries and bv about 8% in lowincome and middle-income countries (5). The young
{6, 7) and the poor (8, 9) tend to be more responsive
to price changes than other groups of people.
Analyses using data from the TCCP database, and
later from NATIONS, can provide evidence in
support of the World Bank’s tobacco tax and price
increase strategy and related policies.
Using the TCCP database for needs
assessment
In addition to providing an evidence base for tobacco
control, the database identified disparities between
countries in regard to the amount and quality of data
available for analysis. This indicated priority areas for
future data collection and tobacco control surveil
lance efforts. For instance, smoking prevalence
statistics were not found for 33% of the countries,
provinces and territories. The prevalence of smoking
in the African Region has probably been influenced
by the lack of data because only half the Regional
population contributed to the estimate, whereas the
data for the other regions cover more than 85% of
their populations. Compared to previously reported
statistics the representativeness of Africa’s regional
smoking prevalence data has improved. In 1997, for
example, WHO’s Tobacco or Health Programme
analysed regional smoking prevalence in the early
1990s (70). The new estimate covers 22% more of
the African Region’s population. The validity of
estimates in developing regions can be expected to
improve with increased access to country-specific
data and increased capacity and resources for
monitoring risk factors. Standardized survey meth
ods would also increase the utility of regional
estimates. In all regions there were variations
between countries in the survey methods employed,
and regional estimates were affected by the compar
ability of country-specific data.
The TCCP database made it possible to see
ways in which consumption estimates could improve
through standard reporting of country-level data to
an information system. The accuracy of most per
capita consumption estimates is limited by the
information not included in each country’s official
trade and production statistics. In countries where
the preferred cigarettes are not of the manufactured
kind the TCCP data underestimate consumption.
Country-level data related to the consumption of rollyour-own, bidi and kretek cigarettes would usefully
supplement information on manufactured cigarettes
from databases of the United Nations and the United
States Department of Agriculture. This is particularly
Bulletin of the World Health Organization, 2000,78 (7)
Table 2. Population coverage by Human Development Index
category in 1975,1985 and 1995
Level of human development 1975
1985
1995
97.8%
83.1%
77.2%
97.3%
85.9%
81.6%
87.6%
85.5%a
73.7%b
High
Medium
Low
a Population coverage in 1994
b Population coverage in 1991.
Source: American Cancer Society and World Health Organization, TCCP database.
Note: Coverage represents the percentage of the total population within each category that
also reported consumption figures. Within each level of human development no population
figures were available for certain countries, and these were not taken into account in the above
calculations.
Fig. 1. Annual per capita consumption by Human Development Index
category (three-year moving average)
;
3500
3000
2500
2000
1500
1000
500
0
N°'e: bD«a!oN9M
@
E3
High
Medium
S
Low
Medium
w/o China
China
Source: American Cancer Society and World Health Organization, TCCP database.
relevant to the Eastern Mediterranean Region and
Central and Southern Asia, where tobacco consump
tion is likely to be underestimated if traditional forms
of use are excluded from the calculations.
Routine data collection is less likely to provide
the means of overcoming certain additional obstacles
to estimating consumption, indicated below with a
view to aiding the interpretation of TCCP data.
The calculations we used did not account for
factors that increase or decrease the true volume of
trade and production, such as smuggling and tax
exemption. The consumption formula does not
account for cigarette stocks held in reserve by cigarette
wholesalers and retailers. This factor only becomes
apparent if a very large net change in stock volume
occurs from one year to the next. The per capita
consumption calculation includes only persons aged
15 years and older in its denominator and thus does
not account for younger smokers. The importance of
this factor is greatest in certain developing countries
where the largest proportion of the population
consists of people under 15 years of age.
887
Special Theme - Tobacco
Table 3. Cigarette prices in selected countries by human development level: 1990-99
Marlboro (USS per pack of 20 cigarettes)
Local brand (USS per pack of 20 cigarettes)
1990
1999
Average
real annual
% change
1990
1999
Average
real annual
% change
High human development
3.85
Canada
1.78
Czech Republic
4.64
Denmark
1.98
France
2.86
Germany
1.75
Japan
2.63
New Zealand
1.34
Poland
3.90
Sweden
3.40
United Kingdom
United States of America 1.74
3.50
1.29
4.37
3.26
2.87
2.58
3.81
1.21
4.32
6.27
3.16
-0.18
-5.66
-0.69
7.40
-0.19
1.01
4.78
-5.90
3.20
7.46
4.72
3.40
1.05
4.55
1.20
2.75
1.61
2.67
0.26
3.72
3.40
1.71
2.67
1.15
4.30
2.76
2.79
2.30
3.62
0.99
4.20
6.27
3.04
-1.67
-2.88
-0.67
14.86
-0.09
0.70
3.78
10.55
3.45
7.46
4.39
Medium human development
1.49
China
0.89
Costa Rica
1.47
Egypt
1.46
Hungary
2.15
Kenya
0.52
Mexico
0.96
Malaysia
2.21
Morocco
1.07
South Africa
1.16
Thailand
1.66
Turkey
0.46
Venezuela
1.83
0.69
1.16
1.01
1.59
1.07
1.11
2.84
1.37
1.09
1.32
1.44
0.55
-4.74
-6.52
-6.03
-3.09
0.16
1.74
-0.76
4.45
-0.97
-6.06
3.06
0.96
0.70
1.10
0.52
0.65
0.45
0.89
0.98
0.68
0.50
0.92
0.46
1.73
0.64
1.16
0.89
0.80
0.86
0.76
1.45
1.37
0.73
0.99
1.28
5.97
-3.63
-4.99
1.43
2.13
-0.70
-1.50
0.78
13.48
4.67
-4.44
1.49
Low human development
1.41
Bangladesh
1.87
C6te d’Ivoire
1.26
Nigeria
1.15
Senegal
0.89a
Zambia
1.37
0.94
0.83
0.80
2.03
-1.25
-4.72
-4.13
-1.07
-12.09
1.13
1.54
0.44
0.77
0.74a
0.85
0.78
0.83
0.32
0.64
-3.50
-4.67
8.83
-5.09
-14.93
Country
4 1993.
Source: Economist Intelligence Unit; calculations made by World Health Organization.
Both the wide range of analyses possible using
TCCP data and die limitations of these data indicate a
need for standardized data collection techniques at the
country level and greater access to data by researchers
working outside each country. In the future, NA
TIONS can be expected to increase access to data. The
svstem will integrate information systems and data
sources electronically to facilitate the tracking of
country-specific information across a wide range of
indicators, including smoking prevalence and tobacco
consumption, laws and regulations, morbidity and
mortality’, industrial organizations, tobacco econom
ics, and programmatic interventions against tobacco
use. NATIONS will report time-trend data for each
indicator and will update them periodically. In this
wav, the evidence base for tracking the progress of
tobacco control policies will be increased and the
common electronic framework necessary for storing
and updating data, making information easily acces
888
sible to researchers, tobacco control advocates, and
policy-makers over the Internet will be provided.
Conclusion
The results of these analyses using data from the
TCCP database demonstrate the potential applica
tions of an information system devoted to tobacco
control. Because TCCP compiled data on a wide
variety' of indicators, from employment in tobacco
manufacturing to pharmaceutical treatments for
tobacco dependence, future analyses are not limited
to the type of prevalence, tobacco consumption and
price comparisons presented here. Nor are they
restricted to groupings by WHO Region and HDI
level. Unfortunately, neither TCCP nor NATIONS
can directly meet the need for standardized survey
and data collection methods at country level. This
Bulletin of the World Health Organization, 2000, 78 (7)
Building the evidence base for global tobacco control
provide an incentive for improving and increasing
tobacco control efforts by making the results of
independent research available to the global tobacco
control communitv. H
requirement is best tackled through capacity-building
at local level with leadership from WHO and others
in accordance with defined principles (//). The
establishment of a permanent electronic framework
for data management and retrieval, however, may
Resume
[.'information au service de la lutte antitabac
Le mouvement de lutte antitabac a besoin d’un systeme
d'information mondial sur la culture et le commerce du
tabac, I'industrie du tabac, la consommation de tabac et la
mortalite qui lui est associee, ainsi que sur les moyens
existant au plan national pour la lutte centre le tabac. La
base de donnees par pays (Tobacco Control Country Profiles
- TCCP) mise en place par I'American Cancer Society en
collaboration avec I'OMS et les Centers for Disease Control
and Prevention constitue une premiere etape vers
I'etablissement d'un tel systeme. Des donnees de base sur
une serie d'indicateurs relatifs a la consommation du tabac
ont ete recueillies aupres de 191 Etats Membres de I'OMS,
de deux Etats Membres associes, de deux provinces de
Chine et de trois territoires occupes. Le present article decrit
les methodes utilisees pour synthetiser les informations.
II analyse egalement les indicateurs employes pour
les TCCP, de fagon a mettre en evidence I'utilite et la
valeur potentielles des donnees fournies par un systeme
d'information specifiquement voue a la lutte antitabac.
Cette analyse porte sur la prevalence du tabagisme par
sexe et par Region OMS, sur la consommation de
cigarettes au regard de I’indicateur du developpement
humain (HDI) et sur devolution annuelle moyenne en
valeur reelle du prix des cigarettes entre 1990 et 1999.
L'artide met egalement en avant certains problemes
concernant la qualite des donnees et la necessite de
maintenir et d'ameliorer le systeme d'information afin de
faciliter les efforts de lutte contre le tabagisme.
Globalement, les hommes etaient pres de quatre fois
plus nombreux que les femmes a fumer en 1998. C'est dans
la Region du Pacifique occidental que le pourcentage
d'hommes consommant du tabac etait le plus eleve.
S'agissant de la proportion respective de fumeurs et de
fumeuses, c'est dans les Ameriques et en Europe que I'ecart
entre les hommes et les femmes etait le plus faible, et dans
les Regions de I'Asie du Sud-Est et du Pacifique occidental
qu'il etait le plus marque. En ce qui concerne les cigarettes
industrielles, la consommation la plus faible et la plus elevee
par habitant cdincidaient avec I’indicateur le plus faible et,
respectivement, le plus eleve du developpement humain.
Dans la categorie moyenne, I'augmentation globale de la
consommation enregistree depuis 1975 en Chine correspondait a une augmentation par habitant. Quant au prix des
cigarettes, son augmentation etait inferieure a la moyenne
du rencherissement des biens et services, ce qui fait que les
cigarettes etaient relativement plus abordables en 1999
qu'en 1990. Ces indications confirment qu'il existe une
importante marge potentielle d'augmentation des taxes sur
les produits du tabac, notamment dans les pays ou
I’indicateur du developpement humain est faible a moyen.
L'analyse met egalement en lumiere la contribu
tion potentielle de la base de donnees TCCP au
developpement des programmes et politiques de lutte
antitabac. Ainsi, les statistiques de la consommatioh des
cigarettes permettent d'identifier les pays oil le besoin de
ressources dans ce domaine est le plus aigu. Les pays oil
le marche de la cigarette connait la plus forte expansion
sont a ('evidence ceux qui disposent des ressources les
plus faibles pour faire face aux problemes associes au
tabac. De meme, l'analyse de 1'evolution du prix des
cigarettes et autres donnees connexes permet de definir
des domaines d'intervention dans lesquels les gouvernements pourraient renforcer leur contribution a la lutte
antitabac, par exemple en augmentant le prix des
cigarettes afin de faire baisser la consommation.
Le projet TCCP a revele des disparites entre les pays
en ce qui concerne le volume et la qualite des donnees
disponibles pour l'analyse et permis d'identifier un certain
nombre de priorites pour les futures activites de collecte de
donnees et de surveillance. Ainsi, on n'a pas pu etablir la
prevalence de la consommation de tabac dans 33 % des
pays, provinces et territoires occupes englobes dans I'etude.
Dans la Region africaine, cette indication a ete biaisee par le
fait que seule la moitie de la population a ete prise en compte
dans les estimations. Les estimations relatives a la
consommation de cigarettes pourraient etre ameliorees
grace a des systemes de collecte de donnees standardises au
plan national. Dans les pays oil les cigarettes les plus
consommees ne sont pas les cigarettes industrielles, les
donnees TCCP sous-estiment la consommation des
populations concernees. Des statistiques sur la consomma
tion des cigarettes roulees, des bidistf. des cigarettes kretek
permettraient de dresser un tableau plus complet que les
donnees limitees aux cigarettes industrielles.
Le large eventail d'analyses autorisees par les
donnees TCCP et les limites de ces memes informations
confirment la necessite de techniques de collecte des
donnees normalisees au plan national et d’un meilleur
acces aux donnees par des chercheurs travaillant en
dehors des pays concernes.
Resumen
Acopio de datos estadisticos para la lucha antitabaquica mundial
El movimiento contra el tabaco necesita un sistema
mundial de informacidn para vigilar regularmente el
Bulletin of the World Health Organization, 2000,78 (7)
comercio, el cultivo y la industria de ese producto, asi
como la prevalencia del habito de fumar, la mortalidad
889
Special Theme - Tobacco
asociada y los recursos Rationales para la lucha
antitabaquica. La base de datos sobre las caracteristicas
de los paises en relation ton la lucha antitabaquica, una
initiative de recopilacidn de datos toordinada por la
Asociacidn Estadounidense de Lucha eontra el Canter en
colaboracidn ton la OMS y los Centres para el Control y
la Prevention de Enfermedades, representa el primer
paso en el desarrollo de dicho sistema. Se obtuvieron
datos tomparativos sobre varios inditadores del •
tonsumo de tabato de 191 Estados Miembros de la
OMS, dos Estados Miembros Asodados, dos provintias
de China y tres territorios otupados. Los metodos
utilizados para tompilar los datos se destriben en el
presente dotumento.
A fin de demostrar la utilidad y el valor potentiales
de los datos derivados de un sistema de information
deditado a la lutha antitabaquica, se analizan los
inditadores arriba mendonados. Los analisis versan
sobre la prevalenda de tabaquismo por sexos por region
de la OMS, el tonsumo de cigarrillos per capita por
tategoria del indite de desarrollo humano (IDH) y los
tambios portentuales anuales reales promedio de los
pretios de los tigarrillos entre 1990 y 1999. Se destatan
temas reladonados ton la talidad de los datos y la
netesidad de mantener y mejorar el sistema de
information para respaldar la lutha antitabaquica.
A nivel mondial, los hombres tenian una
probabilidad de fumar tasi tuatro vetes mayor que las
mujeres en 1998, y la prevalentia mas alta de
tabaquismo mastulino se registrd en la Region del
Patifico Occidental. Las diferencias de prevalentia de
tabaquismo por sexos eran menores en la Region de las
Americas y la Region de Europa y mayores en la Region
de Asia Sudoriental y la Region del Pacifico Occidental.
Con respetto a los tigarrillos elaborados, el tonsumo per
capita mas bajo y el mas alto se registraron en las
categories mas baja y mas alta, respectivamente, del
Indite de desarrollo humano. En la tategoria de IDH
medio, el consumo creciente de cigarrillos en China
despues de 1975 tuvo una influencia predominante en el
aumento del consumo per capita. Los pretios de los
cigarrillos no aumentaron tan rapidamente como el nivel
general de los pretios de los bienes y servicios, y en
consecuencia los cigarrillos fueron mas asequibles en
1999 que en 1990. Estos resultados indican que hay un
margen considerable para aumentar los impuestos que
gravan los productos del tabato, panicularmente en los
paises de IDH bajo y medio.
Los analisis muestran el potential que encierra la
base de datos sobre las caracteristicas de los paises para
apoyar la planificacion de programas y politicas. Por
ejemplo, los analisis del consumo de cigarrillos pueden
contribuir a determinar en que paises se necesitan
muchos recursos para la lucha antitabaquica. Los paises
con mayor expansion del mercado de los cigarrillos son
evidentemente aquellos que tienen menos recursos
disponibles para abordar los problemas asociados con el
tabato. El estudio de la variation porcentual de los
pretios de los cigarrillos y los analisis conexos pueden
ayudar a identificar las esferas normativas en las que los
gobiernos pueden mejorar sus esfuerzos de lucha
antitabaquica, por ejemplo aumentando el precio de
los cigarrillos como medio para reducir el consumo.
El proyecto reveld dispandades entre los paises en
cuanto a la cantidad y la talidad de los datos disponibles
para efectuar analisis y mostrb esferas prioritarias para los
fines futures de la recopilacidn de datos y los esfuerzos de
vigilancia. No se encontraron estadisticas sobre la
prevalentia del tabaquismo en un 33% de los paises,
provintias y territorios otupados considerados. El analisis
de la prevalentia del tabaquismo en la Region de Africa
estuvo muy determinado por la falta de datos, ya que las
estimaciones se realizaron solo con la mitad de los
habitantes de la Region. Los calculos sobre el consumo de
cigarrillos podrian mejorar mediante una notification
normalizada de los datos sobre los paises. En los paises
donde los cigarrillos preferidos no son los elaborados, los
datos que aporta esta base sobre consumo de cigarrillos
por la poblacidn dan lugar a subestimaciones. Si se
reunieran datos sobre el consumo de cigarrillos confeccionados manualmente y de cigarrillos de bidi y de kretek, se
podria obtener un panorama mas complete que el que
ofrecen los datos sobre consumo de cigarrillos elaborados.
La amplia variedad de analisis posibles a partir de
los datos de la base sobre las caracteristicas de los paises
y las limitaciones de estos datos muestran la necesidad
de tecnicas estandarizadas de recopilacidn de datos a
nivel de pais y de un mejor acceso a los datos para los
investigadores que trabajan fuera de determinados
paises.
References
1.
Peto R et al. Mortality from smoking worldwide. British Medical 7.
Chaloupka FJ, Pacula RL Sex and race differences in young
Bulletin, 1996, 52 (1): 12-21.
people's responsiveness to price and tobacco control policies.
United Nations Development Programme. Human
Tobacco Control, 1999, 8:373-377.
development report, 1999. New York, UNDP, 1999.
8.
Townsend J, Roderick P, Cooper J. Cigarette smoking
3.
United Nations Population Division. Worldpopulation
by socioeconomic group, sex and age: effects of price, income,
prospects 1950-2050. New York, United Nations, 1998.
and health publicity. British Medical Journal, 1994,309 (6959):
4.
Warner KE. The effects of the anti-smoking campaign on
923-927.
cigarette consumption. American Journal ofPublic Health, 1977,
9.
Centers for Disease Control and Prevention. Response
67:645-650.
to increases in cigarette prices by race/ethnicity, income, and
5.
Curbing the epidemic: governments and the economics of
age groups - United States, 1976-1993. Morbidity andMortality
tobacco control. Washington DC, World Bank, 1999
Weekly Report, 1998, 47 (29): 605-609.
(Development in Practice Series).
10.
Tobacco or health: a global status report. Geneva, World
6.
Harris JE, Chan SW. The continuum-of-addiction: cigarette
Health Organization, 1997.
smoking in relation to price among Americans aged 15-29.
11.
Guidelines for controlling and monitoring the tobacco epidemic.
Health Economics, 1999, 8 (1): 81-86.
Geneva, World Health Organization, 1998.
2.
890
Bulletin of the World Health Organization, 2000,78 (7)
pH
of Cancer Control in India
TOBACCO CONTROL IN INDIA
Kishore Chaudhry
Tobacco use has not been considered as a good habit by many
societies, right from its introduction in 16th century. Availability of
irrefutable scientific evidence on its health hazards from well-conducted
cohort and case-control studies during 1950s supported the pleas for
tobacco control. However, the anti-tobacco movement acquired a
global nature after the publication of the official reports on the subject
by the Royal College of Physicians1 and the US Surgeon General2.
Subsequently, thousands of scientific investigations have confirmed
the association of smoking with various diseases, and have provided
additional evidence implicating cigarette smoking as a cause of
coronary artery disease, stroke, obstructive airway disease, peripheral
vascular disease, pregnancy complications including intra-uterine
growth retardation and a variety of neoplasms including cancers of
oral cavity, larynx, oesophagus, urinary bladder, kidney, stomach,
pancreas, cervix and more recently of haematopoietic system3.
A long-term British study4 that followed 34,439 male doctors for
40 years, concluded that about 50% of all smokers will eventually die
from their habit. The median survival of smokers was 7.5 years shorter
compared to non-smokers, and the decrease in survival was also
dose-dependent. Review of the health hazards of exposure to
environmental tobacco smoke (or passive smoking) shows that it
damages the respiratory tract of adults, adversely effects the
cardiovascular system and results in lung cancer5. Children of smokers
have an increased frequency of respiratory and middle ear infections
and are at risk of impaired lung function. Passive smoking increases
the frequency & severity of asthmatic episodes, both in children and
adults. Newer epidemiological studies are substantiating the risk of
coronary heart disease due to passive smoking. Many hazardous
substances have been identified in tobacco3, but it has’ not been
possible to identify all the components, which result into cancers or
other diseases. Nicotine, tar, HCN, volatile aldehydes, nitrosamines
are some of the identified hAyarrinns substances in tobacco smoke.
50 Years of Cancer Control in India
Despite progress made in identification of these hazardous
substances, it has not been possible to identify chemicai(s) whose
removal may render tobacco safe. Thus, the most effective preventive
measure for control of tobacco related diseases is to avoid tobacco
use.
The total number of tobacco users in the World has been
estimated at 1.2 billion, which is expected to rise to 1.6 billion during
2020s6. At present, tobacco use causes death of 3.5 to 4 million people
globally, which is expected to increase to about 10 million during
2020s. Developing countries need to be concerned because 7 million
of these deaths would be occurring in these areas, mainly due to
increasing trends of tobacco use.
Indian studies have also recognized tobacco use as a major
health hazard in India. Association of smokeless tobacco use with
oral cancer was pointed out as eariy as 19087. Subsequent Indian
studies on tobacco have amply shown its association with major
diseases entities, both in smoking as well as in smokeless form.
Tobacco is used for smoking as well as in smokeless form in India8.
Smoking of tobacco is mainly in the form of bidi, followed by cigarette,
hukah, chilum, chutta, etc. The habit of smokeless tobacco (also
referred as tobacco chewing) is also very common. Some common
forms of smokeless tobacco include khaini, Mainpuri tobacco, mawa,
mishri, etc. Careful review of Indian studies concluded that bidi
smoking is also associated with the diseases caused by cigarette
smoking and results in similar physiological changes9. Association of
smokeless tobacco has been observed with cancers of oral cavity,
pharynx, larynx and oesophagus, and precancerous lesions of oral
cavity.
Prevalence of Tobacco Use in India
Information on prevalence of tobacco use in India is available
from surveys carried out in general community. As per various
surveys carried out during 1980s, the prevalence of tobacco use
among men above 15 years of age varied between 46% and 63% in
urban areas and between 32% and 74% in rural areas. Among women
it varied between 2% and 16% in urban areas and between 20% and
50% in rural areas10- A survey in Mumbai city showed the prevalence
197
50 Years of Cancer Control in India
of tobacco use to be 69.3% among men over 35 years of age and
57.5% among women above 35 years11. A large survey in 2001
showed that the prevalence of current tobacco use above 10 years
of age in Uttar Pradesh was 50.0% among men & 9.1% among
women; whereas the prevalence in Kamatka was 41.0% among men
& 14.9% among women12.
Two nationwide surveys have been carried out in India for
prevalence of tobacco use13'14 covering rural as well as urban areas.
The second and the most recent nationwide survey (earned out from
July 1993 to June 1994) revealed that 23.2% males (any age) and
4.0% females (any age) consumed tobacco in any form in urban
areas13. In rural areas the prevalence of tobacco use in any form
was 33.6% among males and 8.8% among females. The reported
prevalence of tobacco use in 1993-94 is less than the prevalence
reported in the first national level survey (1987-88), which showed
the prevalence of tobacco use among men to be 25.7% and 35.3% in
urban and rural areas, and among women to be 5.95% and 11.1% in
urban and rural areas, respectively. The reason for this decline is not
clear. Based on age & sex specific rates for tobacco use in urban
and rural areas, as reported in the second national level survey, it is
estimated that in 1996, 184 million persons (150 million males and 34
million females) in India used tobacco15. It has also been estimated
that about 112 million persons smoked tobacco, while 96 million used
it in smokeless form.
Deaths due to Tobacco in India
Information on mortality rates associated with tobacco use in India
is available from three cohort studies. The age adjusted relative risk
of mortality due to tobacco use and the prevalence of tobacco use,
applied to overall mortality of the country, suggested that at least
630,000 persons died in 1986 due to tobacco use16. Median risks as
observed from these cohort studies, and the prevalence of tobacco
use as found in the first nationwide survey of National Sample Survey
Organization14, when applied to the 1996 population, showed that about
800,000 persons in India died due to their tobacco habit in 199617.
Recent studies18'19 indicate that the risk of death due to tobacco use
may in fact be more than that identified earlier16.
198
50 Years of Cancer Control in India
Magnitude of the Tobacco Related Diseases in India
Magnitude of three major tobacco related disease entities was
estimated based on a careful review of Indian literature on risk
estimates for development of these diseases; magnitude of these
disease in India; and prevalence of tobacco use in the country15.
Three disease entities under consideration were coronary artery
disease, chronic obstructive lung diseases and cancers of oral cavity,
pharynx, larynx, lungs & oesophagus. The prevalence of tobacco habit
(smoking or smokeless form as applicable for the disease entity) was
taken from the second nationwide survey on tobacco use (1993-94)
by the National Sample Survey Organization13. The exercise revealed
that the tobacco results into enormous morbidity in the country, being
responsible for 42 lakh existing cases of coronary artery disease and
37 lakh existing cases of chronic obstructive lung diseases. It also
caused about 154,000 incident cases of cancers in 1996.
Diseases due to Tobacco in India, 1996
Disease Entity
Tobacco related cancers
Total number
Cases due to
in India
tobacco use
209,810
154,320
15,700,000
4,200,000
14,000,000
3,700,000
(Incident cases)
Coronary artery disease
(Prevalent cases)
Chronic obstructive lung diseases
(Prevalent cases)
Economic considerations of tobacco in India
The Ministry of Health & Family Welfare constituted an expert
• committee to undertake a comparative study on the economics of
tobacco use inter-alia examining the tax revenue and foreign exchange
earnings, employment and consumer expenditure on the one hand
and the cost of tertiary level medical care facilities for treatment of
tobacco-related diseases, losses due to fire hazard, ecological damage
due to deforestation and disposal of tobacco-related waste on the
other hand with a view to making an economic study of the impact of
199
50 Years of Cancer Control in India
tobacco consumption. The committee had members from the field of
economics, health, health services, epidemiology, agriculture, tobacco
trade, tobacco industry and trade unions. The committee suggested
that tobacco economics should be studied in relation to it being a
“de-merit good”. The short-run, indirect macro economic, secondary
benefits of tobacco use are easily outweighed by the conservatively
estimated costs of three major diseases associated with the use of
tobacco, as shown by an ICMR study. The report underlined the public
health angle as critical to an approach towards tobacco use, while
not ignoring the short run, secondary and indirect benefits to economy
other than tobacco consumers who bear the brunt of the addiction15.
The committee noted that information on costs due to tobacco
related cancers, coronary artery disease and chronic obstructive lung
diseases, are available through a study of the Indian Council of Medical
Research. The average cost due to a case of tobacco related cancers
(as experienced by the cohort20) for the year 1990-91 was Rs. 134,449.
The average cost of a case of chronic artery disease13 for 1992 was
Rs. 14,909, whereas the average cost of a case of chronic obstructive
lung disease was Rs. 11,952. Using the same discounting rate as
used in ICMR study, the average cost of tobacco related cancers,
coronary artery disease, and chronic obstructive lung disease, for the
year 1999 was estimated to be Rs. 350,000, Rs. 29,000, and Rs.
23,300. The total cost to the country for the year 1999 due to these
three disease entities was estimated at Rs. 27,761 crore21.
Cost of Major Diseases due to Tobacco Use in India
Tobacco Related Diseases
Cancers
Coronary Artery
Disease
Chronic Obstructive
Lung Diseases
Number due to tobacco use
1996
1999
154,300
163,500
4,200,000
4,450,000
3,920,000
Average Cost (1999) (Rs)
350.000
29,000
23,300
Total Cost India (1999)
57225
129.05
91.336
3,700,000
Billion Rupees
Total Loss (1999) = Rupees 277.611 Billion or US $ 6.5 B
Source : Rath GK & Chaudhry K2’.
50 Years of Cancer Control in India
The economics of tobacco use needs to be considered at the
consumer level as well as its economy wide effects, including linkages
and externalities to other sectors15. The commonly identified benefits
of tobacco (like employment, contribution to GDP, export earnings,
public earnings, inter-industry linkages, etc.) are at macro level and
for the government (except for the perceived benefit for the users),
while the costs are incurred by the tobacco users. For an existing
product like tobacco, any change in pattern of use is likely to upset
the regional/ local economies. Addictive properties of this de-merit good
influences the rationality of choice for tobacco. India is the third
largest producer of tobacco in the world. Tobacco provides on an
average, 10% of India’s total excise revenue, of which 88% is
contributed by cigarettes. The economics of tobacco use has to take
note of the multi-sectoral connections of tobacco. The returns to the
farmers from tobacco cultivation are high, but the cost of production
is also high and thus, the relative return from the crop may not be
highest for tobacco. The expert committee on economics of tobacco
use in India noted that in 1993-94, total tobacco employment was
over 35.59 lakh.
Major efforts for tobacco control in India
Warning on cigarette packages/ advertisements: Recognizing the
health hazards of tobacco, the Government of India promulgated The
Cigarette (Regulation of Production, Supply and Distribution) Act 1975.
Under the act, all packages and advertisements of cigarettes are to
carry a statutory warning, “Cigarette smoking is injurious to health”.
The Act provides specific instructions related to minimum font size,
colour contrast, etc. However, the Parliament's Committee on Sub
ordinate Legislation in its 22nd report (December 1995) on this
legislation, observed that these guidelines were often not followed22.
Considering the issue of tobacco in totality, the Committee made wideranging recommendations, including, strong & rotatory warning in
regional languages on tobacco products; ban on direct as well as
indirect advertisement of tobacco products; prohibition of smoking in
public places; initiation of measures for awareness on tobacco through
health infrastructure, educational institutions and mass media; and
initiation of efforts for persuasion of farmers to switch over to alternate
crops. These recommendations of Parliament's committee resulted in
201
50 Years of Cancer Control in India
modification of the proposed comprehensive legislation on tobacco
control.
Warning on smokeless tobacco products: In India, nearly half of
the tobacco users consume tobacco in smokeless form. Realizing
the need for a warning on smokeless tobacco products (which are
classified as food material), the provisions under the Prevention of
Food Adulteration Rules (1955) were applied in 1990, which
necessitates that every package and advertisement of smokeless
tobacco product should have a warning stating that “chewing of
tobacco is injurious to health”. Packages of arecanut should also state
that “chewing of supari may be injurious to health". An expert
committee of Directorate General Health Services also provided the
minimum font size and other guidelines for this purpose.
Cabinet guidelines for smoking in public places: Cabinet secretariat
by an administrative order in 1990, prohibited smoking in certain places
such as hospitals, dispensaries, educational institutions, conference
rooms, domestic air flights, A/C sleeper coaches in trains, sub-urban
trains, A/C buses, etc. State Governments were also advised to
discourage sale of tobacco products in and around educational and
health related institutions. Direct advertisements of tobacco products
had already been prohibited in government media, including
Doordarshan and All India Radio. These cabinet guidelines were
reiterated in 1998.
Comprehensive legislation on tobacco control: In view of various
recommendations and experience on relative inefficacy of the existing
legislation (the Cigarette Act), the Ministry of Health & Family Welfare
initiated the process of formulation of a comprehensive legislation for
replacement of the Cigarette Act (1975). The draft legislation had to
undergo a second round of inter-ministerial consultations, in view of
the recommendations of the Parliament's Committee on Sub-ordinate
Legislation (22nd report - December 1995). The draft has undergone
changes as per the suggestions of the Rajya Sabha’s Standing
Committee and currently proposes a ban on tobacco advertising; clear
health warnings on all tobacco products; limit on levels of tar & nicotine;
ban on smoking in public places: and ban on sale of tobacco products
to minors. The legislation is expected to help in reduction of tobacco
202
50 Years of Cancer Control in India
use and in generating a social environment conducive to tobacco
control. Legislation has also been promulgated by the states of Delhi,
Kerala, Goa and Rajasthan, aimed mainly on prohibition of smoking in
public places. Recently, many states such as Tamil Nadu, Maharashtra,
Andhra Pradesh, etc., have imposed a ban on production and sale of
gutka and pan masala-containing tobacco, as a short-term measure.
Multi-sectoral approach for tobacco control: The problem of
tobacco in India is complex, in view of the varied nature of its use;
association of a large number of sectors like health, agriculture,
finance, mass media, labour, education, industry, welfare, etc.;
unorganized nature of work for many tobacco products; dependence
of a large number of people on tobacco production & processing; and
need for action by many agencies. The situation necessitates multi
sectoral approach, wherein different sectors (government as well as
non-govemment) identify themselves as contributor to a radical social
change leading to tobacco control.-
A major exercise involving different sectors was organized in
July 1991, through organization of a national conference on tobacco
or health. The conference recognized tobacco as a major public health
hazard and noted that consumption of tobacco is not compatible with
the goal of “Health For AIT. It also realized that an integrated
educational, legislative and agro-economic strategy with an operational
framework and political, administrative, financial & research support
is needed. The conference recommended establishment of a National
Tobacco Control Commission to plan, coordinate and monitor tobacco
control activities; Prohibition of smoking in certain public places as
per Cabinet Secretariat O.M 27/1/3/90 (7.9.90); Ban on consumption
of tobacco products in other public places; Ban on sale of tobacco to
minors; Ban on advertising; Statutory warning on all tobacco products;
Printing of tar & nicotine levels; Compulsory licensing of tobacco
products; Afforestation by tobacco producers; Regulation of tobacco
production; Preference for non-smokers in certain jobs; Study of
tobacco economics; varied economic and agro-industrial restructuring
measures aimed at reduction of involvement of government, Reduction
of tobacco crop with rehabilitation of concerned, Removal of subsidies
& guarding against involvement of foreign players, Increased taxation,
etc.; Health education through various strategies; Involvement of
203
50 Years of Cancer Control in India
NGOs; Research; Development of a National action plan; and
preparation of a White paper on government policy on tobacco.
The multi-sectoral and inter-sectoral approach by the
Government of India is amply demonstrated through inter-ministerial
consultations, consultations with non-governmental organizations and
public hearings related to the development of development of the
comprehensive legislation on tobacco control; follow up actions on
the recommendations of the Parliament's committee on sub-ordinate
legislation (22nd report); study on economics of tobacco use in India;
and development of a country stance for the framework convention
on tobacco control by the World Health Organization. The Indian
Council of Medical Research (ICMR) conducted operational research
project for involving schools and community volunteers in anti-tobacco
community education. The ICMR's collaborative project with All India
Radio also showed the mechanism of inter-sectoral collaboration in
cost-effective education through radio.
Community education on tobacco: In view of the deep-rooted
nature, the eradication of tobacco habit would require concerted action
resulting into a social change. Community education regarding tobacco
and its health hazards would necessarily be an integral component of
such an action plan. Anti-tobacco education needs to be targeted at
decision-makers, professionals and the general public, especially the
youth. Efficacy of educational activities in tobacco cessation had amply
been demonstrated by various organizations. A study by Tata Institute
of Fundamental Research, Mumbai, showed that after an intervention
of ten years, a significantly higher proportion of persons in the
intervention group stopped tobacco usage as compared to a control
cohort23. No Tobacco Day (31st May) activities have been a regular
feature since 1988, which generally comprise of educational
advertisement(s) in newspapers along with a programme/ workshop
in Delhi and at other centres by states. Tobacco has been included
as a topic in books brought about by NCERT. National Cancer Control
Programme also stresses on anti-tobacco education, in view of the
fact that half of the cancers among men and about one fifth of the
cancers among women in India pertain to tobacco related sites. The
anti-tobacco community education activities have been initiated in about
60 districts through district level projects for control of cancers. India
204
50 Years of Cancer Control in India
participated in WHO’s SEAAT Flame project, under which an anti
tobacco flame traveled by road from Delhi to Calcutta and from Delhi
to Thiruvananthapuram. Educational programmes on tobacco through
television have also been initiated.
The Indian Council of medical research (ICMR) carried out
operational research studies on anti-tobacco community education
through involvement of existing infrastructures. The studies involved
radio, health infrastructure, schools and community volunteers. The
primary health workers in the areas utilizing health infrastructure also
examine the oral cavities for presence of any pre-cancerous lesions24.
The intervention through schools resulted in overall reduction of
tobacco habit by 11.8% among men and 9.1% among women in one
intervention zone and by 13.4% among men and 13.3% among women
in a second intervention zone as compared to a decrease of 2.0%
among men and 10.2% among women in control zone. Based on the
experience of this project, Ministry of Education, state of Goa, included
an 8 hour course on tobacco as a part of co-curricular activities for
standard five and above. One-year intervention through community
volunteers resulted in 26.3% males and 10.5% females quitting tobacco
habit with another 10.1% males and 4.3% females being likely quitters
(6 months had not passed since tobacco cessation). Intervention
through health infrastructure achieved a reduction of tobacco habit in
experimental area, amounting to 5.7% in the males and 6.9% in the
females, as compared to an increase of 3.8% among male and 7.8%
among female in one control area and an increase of 2.9% among
males and 4.6% decrease among females.
205
50 Years of Cancer Control in India
The collaborative project of ICMR and All India Radio (Radio
DATE - acronym for Drugs, Alcohol, and Tobacco Education) was in
the form of 30 weekly episodes of 20 minutes each25. Ten episodes
focused on tobacco. The episodes were broadcast from 84 stations
of All India Radio (out of 104 existing at that time) at prime time,
simultaneously in sixteen languages. The Hindi prototype was sent
to selected radio stations of All India Radio for translation in regional
language, as per the specified guidelines. The broadcast was during
a specified time (between 8.00 A.M. and 9.00 A.M. on Sundays, with
a repeat broadcast during the week, generally in the evening). Two
community based surveys in rural areas with no organized anti-tobacco
programmes ahowed that about 4% tobacco users in rural Goa and
about 6% users in rural Karnataka quit their habit after hearing the
programme. About 32% of the potential listeners in Karnataka and
about 27% of the potential listeners in Goa had heard at least one
episode on tobacco.
Proprorion of Persons Hearing the
Programme in Rural Goa
Heard Programme ■ Did not Hear
EITect of Radio DATE in Rural Coa
Proproliou of Persons I louring die
Programme in Rural KarnalJsx
| □ Hoard Programme BDId not Hoar
LITocl of Radio DATE in Rural Kaniatka
None
Planning m Quit
■ Quit Uubil
206
Reduced Frequency i
PhnningfoQuit
■ Quil Uiibil
■ No Comments
Reduced Frequency
50 Yeas of Cancer Control in India
Coverage of entire country for anti-tobacco education is a
formidable job and can not be achieved without active support from
Non-Governmental Organizations and mass media. They however,
need support from the health departments for availability of reliable
and impartial information on the subject Support would be needed
not only from health related non-govemmental organization but also
from other related sectors like education, economics, agriculture,
welfare, etc.
Expert committee on health hazards of pan masala
containing tobacco
The Directorate General of Health Services constituted a
committee to examine the scientific literature on health hazards of
pan masala-containing tobacco. The committee realized that if this
substance is a causative factor for oral cancer, then most of the users
of this substance would be in incubation period and thus,
epidemiological data not likely to represent correct picture. The
committee examined scientific literature from point of view of in-vitro
studies, animal studies, epidemiological data on combination of various
substances in pan-masala-containing tobacco and data on tobacco
mixtures similar to pan masala-containing tobacco. The committee
recognized Pan Masala-containing tobacco to be an important cause
of oral sub-mucous fibrosis and cancer. Based on this report, the
Central Committee on Food..Standards, recommended a ban on
chewing tobacco, which was considered by the Government from
logistic point of view. Various state Governments have banned the
sale and production of such products as a short-term measure, till a
long-term strategy for dealing with this substance is finalized.
Tobacco Control Cell
A Tobacco Control Cell has been established in the Department
of Health, New Delhi, since August 2000, under Deputy Secretary
(PH), with the aim of coordination of activities related to tobacco
control, with the help of a 7 member Advisory Board. The current
activities initiated through this cell include, educational programmes
through mass media and schools, strategy papers for alternate crops
and bidi workers, advocacy workshops for non-health sectors, and
establishment of tobacco cessation clinics.
207
50 Years of Cancer Control in India
2.
US Department of Health and Human Services. Smoking and
health. Report of the advisory committee to the Surgeon General.
Washington DC: US Government Printing Office (PHS publication
no 1103), 1964.
3
US Department of Health and Human Services. The health
consequences of smoking: 25 years of progress. A report of the
Surgeon General. US Department of Health and Human
Services, Public Health Service, Center for Disease Control,
Center for Chronic Disease Prevention and Health Promotion,
Office on Smoking and Health, 1989; DHHS Publ No. (CDC)
89-8411, 1989.
4.
Doll R, Peto R, Wheatley K, Gray R, and Sutherland I (1994). Mor
tality in relation to smoking: 40 years’ observations on male British
doctors. BMJ, 1994; 309: 901-11.
5.
Wiebel FJ. Health effects of passive smoking. In: Bolliger CT, &
Fagerstrom KO (eds.) (1997). The tobacco epidemic. Progress in
respiratory researchVo\ 28, Karger, Basel, 1997; p 107-21.
6.
Peto R, & Lopez AD (1990). Worldwide mortality from current smok
ing patterns. In: Durston B & Jamrozik K (eds.), The Global war;
Proceedings ofthe seventh world conference on tobacco and health,
Perth, Western Australia, 1990; p 66-8.
7.
8.
Niblock WJ. Cancer in India. Indian Med Gaz, 1902; 37:161-5.
Bhonsle RB, Murti PR, and Gupta PC (1992). Tobacco habits in
India. In: Gupta PC, & Hamner JE III (eds.), Control of tobacco
related cancers and other diseases. International Symposium, 1990.
Oxford University Press, Bombay, 1992; p 25-46.
9.
Sanghvi LD & Notani PN (eds.) (1989). Tobacco and Health: The
Indian Scene. International Union Against Cancer & Tata Memorial
Centre, 1989.
10
Chaudhry K, Prabhakar AK, & Luthra UK (1990). Tobacco control
in India - Search for strategies. In: Durston B & Jamrozik K (eds.),
The Global war; Proceddings of the seventh world conference on
tobacco and health, Perth, Western Australia, 1990; p 363-6.
209
50 Years of Cancer Control in India
11.
12.
Gupta PC (1996). Survey of sociodemographic characteristics of
tobacco use among 99,598 individuals in Bombay, India, using hand
held computers. Tobacco control, Summer 1996; 5(2): 114-20.
Chaudhry K, Prabhakar AK, Prabhakran PS, Singh K, et al.
Prevalence of tobacco use in Karnataka and Uttar Pradesh. Final
report of the study by the Indian Council of Medical Research and
World Health Organziation, SEARO. 2002.
13.
NSSO (1998). Sarvekshana, Journal of the National Sample
Survey Organization, Department of Statistics, Ministry of
Planning, Government of India, January-March 1998;p 76.
14.
NSSO (1991). Sarvekshana, Journal of the National Sample
Survey Organization, Department of Statistics, Ministry of
Planning, Government of India, July-September 1991; XV(1): p
375 & 406.
15.
Government of India. Report of Expert Committee on economics
of tobacco use in India. Ministry of Health & Family Welfare,
Government of India, February 2001.
16.
Gupta PC (1988). Health consequences of tobacco use in India.
World smoking and health, Spring 1988; 5-10.
17.
CMR. Tobacco Plain Facts (1996). Division of Noncommunicable
diseases, Indian Council of Medical Research, New Delhi, India,
1996.
18.
Gajalakshmi CK. Tracking the epidemic: Tobacco control activities
in Tamil Nadu. Lifeline, a quarterly from WHO South-East Asia
region on tobacco & alcohol issues. March 2000; Vol 3: 4-5.
19.
Gupta PC and Mehta HC. Cohort study of all-cause mortality
among tobacco users in Mumbai, India. Bulletin of the World
Health Organization, 2000: 78(7): 877-83.
20.
Rath G.K. and Chaudhry K. Estimation of cost of tobacco related
cancers - Report of an ICMR task force study (1990-96). Indian
Council'of Medical Research, New Delhi, 1999.
21.
210
Rath GK and Chaudhry K. Cost of tobacco related diseases.
Paper presented during the WHO international conference on
50 Years of CancerControl in India
global tobacco control law: towards a WHO framework convention
on tobacco control, at New Delhi India, 7-9 January 2002.
22.
Lok Sabha Secretariat. Commfoee on Subordinate Legislation
(10th Loksabha) Rules/ regulations framed under The Cigarette
(Regulation and Production, Supoly and Distribution) Act, 1975.
Lok Sabha of India, December 1995.
23.
Gupta PC, Mehta FS, Pindborc JJ, Bhonsle RB, Murti PR and
Aghi AB. A 10-year follow-up study for primary prevention of oral
cancer among Indian villagers. In: Gupta PC, Hamner JE II and
Murti PR (eds). Control of tobacco-related cancers and other
diseases. Oxford University Press, Bombay, 1992; p 307-13.
24.
ICMR. Cancer research in ICMR. http//www.icmr.nic.in. 2000.
25.
Rath GK and Chaudhry K. Estimation of cost of tobacco related
cancers. Report of an ICMR task force study (1990-1996). Indian
Council of Medical Research, New Delhi, 1999.
211
pH-^-
AHEmCAN
LUNG
ASSOCIATION
t
If you've just quit smoking,
or are about to, you deserve
a lot of credit. It's not easy to
do—you can face a lot of
hurdles along the way. But 46
million ex-smokers have
shown that it can be done,
and without a doubt is one of the best things
you can ever do for yourself and those you
love.
Concern about gaining weight is a
hurdle for most smokers. Some smokers
refuse to quit smoking because they're
afraid that they'll gain a lot of weight. Some
others return to smoking after stopping for
awhile, because they gain some weight and
think they're better off smoking.
Cigarette companies have taken
advantage of this for years. In the 1930’s
their ads told people to "Reach for a Lucky
instead of a sweet." Today they tell you that
“Slim" is the way to be. They want you to
smoke as a way of controlling weight and
coping with life's pressures—regardless of
the consequences.
But the truth is you’re never better off
smoking. There are better ways to cope.
Although it will take some work and take
some time, you can quit smoking and conti^J
your weight for good.
Gain Your
Freedom—
Control
Your
Weight
O
Scientists have found that
smokers are apt to weigh less
than nonsmokers of the same
sex, age and height, and that
many smokers gain weight
when they quit smoking.
Smoking may affect the
amount and types of food that smokers eat,
and how their body processes the food,
causing them to have a lower body weight.
How
Stopping
Smoking
Affects
Weight
©2000 American Lung Association
Quitting smoking can trigger changes in
eating habits and the body's processing of
food, resulting in weight gain.
quitting smoking, they probably will avoid
much of the weight gain, too.
• Metabolic changes.
Changes in the body's metabolic rate (the
rate at which the body bums calories) may
account for why many smokers gain a few
pounds soon after quitting smoking.
Snaking increases the smoker’s metabolic
rt® and seems to make it easier for the
body to expend calories and harder for it to
store them—contributing to a lower body
weight for smokers. When the smoker quits
smoking, more calories are converted into
tissue, resulting in some weight gain.
Exercise is an effective way to combat these
metabolic changes.
There are many things you
can do to help yourself
succeed at quitting smoking
and controlling your weight.
But before you make
changes in your diet and exercise, you have
to make changes in your outlook—the way
you look at smoking, weight and yourself.
Too many people get trapped in a
vicious cycle of quitting smoking, gaining
weight, and going back to smoking.
• Eating more.
It is likely, however, that smokers who
gain a substantial amount of weight after
quitting smoking also increase the amount of
food they eat. Food in general may seem to
taste and smell better, leading to bigger
portions and extra helpings. Snacking may
become a substitute for smoking and a new
crutch in dealing with stress and other
string triggers.
• Eating more sweet foods.
Current research indicates that many
smokers develop cravings for sweet (highsugar, high-calorie) foods after quitting
smoking, and that eating more sweets is a
significant factor in their weight gain. Some
scientists think that nicotine affects the level
of blood sugar (glucose) in the body, so that
nicotine withdrawal triggers an increased
craving for sweet foods. These scientists
suggest that if a smoker avoids sweets after
What You
Can Do
About It
2)
The key to breaking the cycle
is to first make not smoking
your #1 priority.
Do what you can now to
avoid weight gain. But accept the fact that
you still may gain a few pounds as a result of
quitting smoking. If you do, chances are
good that you can lose it after a few months,
when you’ll have control of not smoking and
be better able to lose weight.
Keep in mind that you’re only fooling
yourself if you think that you can continue
to smoke and stay healthy. Or that you’ll be
better able to quit smoking in a few years.
So quit smoking now and for good. The
American Lung Association is ready to help.
Breaking
The Cycle
0
10 Steps For
Keeping The
1) Make not smoking your
#l Priority-
Weight Off
Maintain yOur freedom from
4)
Exercise regularly.
Exercise is a big help in controlling
v^^ht and quitting smoking. Research
s^fests that exercise is a key factor in losing
weight and, more important, in maintaining
the loss.
Exercise can change your body
composition, which in turn will help increase
the rate at which your body burns calories,
making it easier to keep the weight off.
Physical activity helps you lose fat and
develop muscle. It helps reduce tension and
stress; you feel more relaxed and alert rather
than exhausted and vulnerable to eating
binges.
Your choices are infinite. You could take
a walk after dinner or learn something new
and different, like karate or dancing.
Aerobic-type exercises, such as walking,
jogging, swimming, bicycling and cross
country skiing, are best for improving your
c^io-respiratory endurance.
Consult your doctor and plan a program
tailored to your age and physical condition.
Start out slow, make it fun, and stick to it.
3)
smoking by using new ways
to cope with life’s pressures. Contact your
local American Lung Association for
weight once you’re in control of not
smoking.
maintenance strategies for dealing with
stress, using relaxation techniques and
assertiveness, and coping with urges and
feelings. Don’t let concern about weight get
in your way.
Monitor your weight.
Weigh yourself regularly—at least once
a week, under the same conditions—in order
to note and respond to any changes in your
weight. Gaining a few pounds after quitting
smoking is common. Do what you can now
to avoid weight gain and then lose any extra
4
Know what you’re eating.
Just as it’s important in quitting smoking
to learn when and why you smoke, it’s
important in controlling weight to know
what foods you’re eating, how much, when,
and why. Think about what triggers your _
eating.
W
5)
Eat well-balanced meals regularly.
Weight control does not mean
dangerous diets, skipping meals, and bad
food. It means a healthy, balanced eating
plan you can stick with.
Making smart food choices is the secret
to controlling your weight. Simply “going on
a diet” by cutting calories isn’t the answer. If
you cut calories too drastically, you won’t get
enough food to be satisfied, and you may
not get enough of certain nutrients. Cutting
calories also promotes temporary loss of
fluids, instead of permanent loss of fat.
Instead, you’ll need to change your basic
eating habits.
Use the Food Guide Pyramid to guide (
you in your daily food choices from the six
basic food groups. Make sure your meals are
satisfying, to make up for the satisfaction
you used to get from smoking. The
government recommends that you eat 6-11
servings from the bread, cereal, rice and
pasta group; 3-5 servings from the vegetable
group; 2-4 servings from the fruit group; 2-3
servings from the milk, yogurt and cheese
group; 2-3 servings from the meat, poultry,
fish, dry beans, eggs and nuts group; use fats,
oils and sweets sparingly.
snacks at hand: raw vegetables, unbuttered
popcorn, fruits that must be peeled. Drink
water and low-calorie beverages without
caffeine.
The Food Guide Pyramid
KEY
O Fat (naturally occurring
and added)
These symbols show fats,oils,
him or her from breathing secondhand
smoke. If you're pregnant or nursing, be
sure to talk to your doctor about a proper
diet before trying to control or lose weight.
and added sugars in foods.
V Sugars(added)
8) Avoid sweets and alcohol.
Avoid sweet high-calorie foods and
refined sugars. Try fresh fruits such as
berries and grapes to satisfy cravings for
sweets. Most alcoholic drinks contain 100®
200 calories each, but no nutrients.
Substitute calorie-free iced tea, mineral
water, or seltzer with a squeeze of lemon or
lime.
9) When you eat out, eat well.
6) Cut down on fat.
Focus on limiting fat to no more than 30
percent of daily calories. Fat is the biggest
source of calories. Reducing calories from
fat lets you eat more foods rich in nutrients,
such as whole grains, fruits and vegetables.
Switch to leaner cuts of meat and low-fat
®biry products. Broil instead of fry, and
eliminate high-fat foods such as creams and
oils. Serve and eat reasonable portions, no
second helpings. Use smaller plates and
bowls to give the impression of more food.
Controlling your weight
along with quitting isn’t
always an easy thing to do. It
may take some extra time
and effort. But making the
effort could mean the
difference for you in getting
off the “smoking and weight merry-goround” for good. Don’t be discouraged if
you do gain a little weight. Chances are
good that you can lose what you gain after
three to six months, when you’ll have
control of not smoking and be better able to
lose weight.
Remember that you are better off—in
terms of your health, appearance, your
sense of self-control—not smoking. So, be
good to yourself and those you love. Stick
with it! Stay free from smoking and do your
best to control your weight. Call your local
American Lung Association if you need
®elp.
Whatever
Happens,
ju’re Better
Off Not
Smoking
Order wisely in restaurants. Ask for
foods without extra oils and sauces; get salad
dressing and butter on the side or not at all.
Don’t use high-calorie food or alcohol as a
crutch in social situations.
It’s okay to eat high-calorie foods on
special occasions now and then, but plan
ahead and fit them within your daily calorie
quota.
10) Eat slowly.
e
Wfe need your support to fight lung disease, the
third leading cause of death in the U.S. Call your
local American Lung Association to find out how
you can help.
g
Chew slowly. Rest your fork and knife
between bites. Give your body 20 minutes to
digest the meal and tell you it’s satisfied.
Call 1-800-LUNG-USA
(I -800-586-4872)
National Web Site:
www.lungusa.org
7) Snack well.
Being pregnant or a new
If You're
parent is a great reason to
Pregnant
quit smoking, for you and
Or A New
your baby. Smoking during
Parent
pregnancy can be very
harmful to the fetus. After
your baby is bom, it’s important to protect
Limit your snacking by eating good
regular meals. Learn new ways to cope with
snacking triggers such as anxiety and
boredom: try “deep breathing” and other
relaxation exercises. Keep “safe” nutritious
6
When You Can’t Breathe,
Nothing Else Matters®
^AMERICAN LUNG ASSOCIATION®
7
2102
10/00
TOBACCO CONSUMPTION PATTERNS AND IT’S HEALTH
IMPLICATIONS: THE INDIAN SCENARIO
By
Rijo M Johnf
Indira Gandhi Institute of Development Research, Mumbai
Oct. 2003
Abstract
Tobacco has become a major cause of death across the entire world. Around 9-lakh
people die in India every year due to tobacco related diseases. In this context this paper
tries to analyze the tobacco consumption pattern and its health implications in India
using the latest National Sample Survey data on tobacco consumption. The paperfinds
that though there is reduction in tobacco consumption in India as a whole the rural India
is showing a sort ofsubstitution between different tobacco products. It has been also
observed that the consumption of tobacco is more among the poor in India pointing to the
fact that the consequent higher health care spending leaves them worse off. Thus the
paper concludes that in spite of the huge Tobacco industry that isflourishing in India and
the economic gains it gives to the country the burden it imposes on the country and it's
masses in the form of various diseases and high morbidity is immense. Hence government
policy needs to be targeted towards an effective control of Tobacco use.
Keywords: Tobacco, Consumption, Health, India
JEL Code: 112,118, R22
f Address of correspondence: IGIDR, Film City Rd., Gen. A.K. Vaidya Marg, Goregaon
(E), Mumbai 400065,
India. E-mail: rijo@igidr.ac.in
1. Introduction
It is well known that tobacco use in any form is potentially harmful from both
economic and human development considerations. Tobacco has become a major cause of
death across the entire world. It is estimated that by 2030, it would account for the death
of about 10 million people per year; half aged 35-69. This is a matter of serious concern
for the developing countries where more than 82 per cent of the world smokers reside.
Incidence of daily tobacco consumption is about 50 per cent among males in low-income
countries, which is in fact increasing over time (www.worldbank.org). The costs and
consequences of this phenomenon are manifold. It leads to high morbidity due to ill
health from tobacco use and hence, increased death rate. This would call for replacement
of productive labor and thereby impose heavy economic costs on the society in the form
of high spending on health care, training labor force for replacement etc. These factors
could prove a serious threat to the development process of the poor countries. Hence
much of the cost in the form of disease and death could be avoided with policy action
aimed at regulating tobacco consumption.
Government of India has passed certain legislations in the past to curb tobacco
use. But unlike in the past, legislation for curbing tobacco use has taken a qualitative
change in the recent times mainly with the introduction of Cigarette and other tobacco
Products (Prohibition of Advertisement, Regulation of Trade and Commerce, Production,
Supply and Distribution) Bill, 2001. Nevertheless the Bill is yet to be implemented.
Many state governments are also enacting various legislations to curb tobacco use in
recent times. But in spite of all these tobacco use is widespread and continues unabated in
India. This would raise a number of policy relevant questions: What is the pattern of
tobacco consumption across various regions and social groups? Is it the poor or the rich,
who consumes more of tobacco and thereby susceptible to various health calamities, bear
the consequent economic costs? In this context we make a simple attempt to analyze the
incidence of tobacco consumption at various levels and the associated health implications
in India, which may help to underline the need for effective policy intervention by the
government.
2.Tobacco economy in India
Some important features of the tobacco economy in India, which make a case for a
serious academic study, are as follows:
• India is the second largest producer and fourth largest exporter of tobacco in the
world. (Sundaram, 2003)
• In India an estimated 65% of all men and 33% of all women use some form of
tobacco. (Shimkhada et al. 2003)
• tobacco is raised on an area of about 4 lakh hectares;
• Six million farmers are engaged in tobacco leaf production in India; and
• tobacco Industry supports nearly 100 million people in India either directly or
indirectly. (Gupta Indrani & Shankar Deepa, 2001)
While these statistics depict a strong tobacco industry that is flourishing in India it
has got a lot of health implications too. tobacco use has taken epidemic dimensions in
India. This will reflect in a high burden of disease for the country not immediately but at
a future date. The following statistics depict its severity in India.
• Around 9 lakh people die in India every year due to tobacco related diseases
(The Hindu, June, 05, 2001)
• tobacco related cancers account for nearly half of all cancers among men and onefourth
among women. (Shimkhada et al. 2003)
• India has one of the highest rate of oral cancers in the world
• Oral cancer accounts for one-third of the total cancer cases in India, with 90% of
the patients being tobacco chewers. (www.cdc.gov/tobacco/who /india.htm)
• An estimated 8.3 million cases of coronary artery diseases and chronic obstructive
airway diseases are attributable to tobacco every year. (Shimkhada et al. 2003)
• The treatment of tobacco related diseases in India costs 135.7 billion Rupees ($2.9
billion) every year and this is much more than the nationwide sale value of all
tobacco products. (Pramod Mahajan, Hon’ble Minister, Gol, Jan 6,2001)
Given the above facts it is worthwhile to look at the prevalence of tobacco in India and
also the associated health impacts. An analysis of this kind will really help in directing
policy in such a way that maximum social benefits are achieved. Using NSS data for
various years we try to analyze this.
The
3.
consumption patterns (National Scenario)
In India National Sample Survey Organization (NSSO) collects data on the prevalence
of tobacco use along with its consumption expenditure surveys in India. Among the many
million tobacco users in India 48% of them use Bidis, 38% use different chewing items
and the rest 14% are Cigarette smokers (Sundaram, 2003). Following table gives the
change in pattern of consumption of different tobacco products in India over the last
decade as obtained from different NSSO quinquennial surveys.
Table 1: Trends in Per Capita Qty. & value of consumption of various
tobacco Products per 30 days in Rural & Urban India*
All-India Rural
55th round, 1999-2000 50th round, 1993-94 43rd round, 1987-88 Item
Qty. (no) Value (Rs.) Qty. (no) Value (Rs.) Qty. (no) Value (Rs.)
Pan 0.83 0.78 0.64 0.39 0.65 0.21
Bidi 38.18 4.91 45.74 3.7 49.5 1.93
Cigarette 0.96 0.88 0.8 0.45 1.05 0.27
All-India Urban
Pan 1.2 1.76 1.39 1.16 1.7 0.7
Bidi 22.13 3.12 32.39 2.79 38.67 1.6
Cigarette 3.24 3.68 3.65 2.45 4.89 1.47
♦Source: NSS Report No.461 (55/1.0/4), 1999-2000.
The table clearly shows the differences in the consumption patterns of rural and the urban
household in India. The table also shows the decreasing tendency in the consumption of
tobacco products between both the groups. The main observations that one can make
from this data are:
• Bidi is predominantly consumed in the rural areas. It could be because of the low
unit value of the Bidi and the low income of the rural mass.
• Bidi consumption has been steadily declining in both rural and urban areas.
• It is also interesting to note that the percentage decline in per capita Bidi
consumption was more in urban (42,77%) than in rural (22,87%) India over this
period of analysis. (Suryanarayana, 2002)
• Another interesting feature is that this decrease in Bidi consumption is more or
less compensated by an increment in the consumption of pan in the rural areas.
That is consumption of pan has increased in the rural areas. Where as this sort of
a shift is not seen in the urban population. So it may be a sign that the urban
populace, in general, is gradually decreasing the consumption of various tobacco
products relative to their rural counterparts.
• Per capita number of Cigarette consumption, on the other hand, is more in urban
India than in rural India. One obvious reason could be the higher price of
Cigarette. It may be also due to some cultural factors, e.g. the taboo associated
with smoking Cigarettes among some villagers (Sinha et al. 2002)
• There is a consistent decrease in Cigarette consumption in urban India where as,
even though it has decreased in rural India over the period, it shows an increasing
tendency in the last period of the study. From the year 1987-88 to 99-2000 the
percentage decrease in Cigarette consumption was also very high (33.74%) in
urban India compared to rural India (8,6%).
• The Pan consumption also has been steadily increasing in rural India while it
showed a declining trend in urban area.
In sum one can safely conclude from the above statistics that the tobacco
consumption habit of the urban household is showing a declining trend on the whole,
while that of the rural household is showing a substitution between various tobacco
products. The possible reasons for this kind of behaviors can be given only by further
studies. One may think of the possible reasons like changes in the cultural aspects,
tendency of rural population to imitate the urban mass, general changes in the
consumption patterns, the effect of advertisements, lack of proper awareness etc.
Consumption
4.
Patterns at the state level
Now let us look at the behavior of consumption of various tobacco products at the state
level. The following table shows change in the per capita annual consumption of Bidi and
Cigarette at the state level calculated from the NSS reports for both the urban and rural
population. A careful analysis of this table can shed a lot of light into understanding the
problem at a disaggregated level.
Table 2: Per Capita Monthly tobacco consumption of different states both in Urban and
Rural areas (in qty.)*
Rural India Urban India
Bidi (No) Cigarette (No) Bidi (No) Cigarette (No)
State 1993-94 1999-'00 1993-94 1999-00 1993-94 1999-00 1993-94 1999-00
Andhra Pradesh 48.06 38.95 2.80 3.52 25.47 14.27 7.86 8.03
Arunachal Pradesh 28.46 14.43 1.71 0.37 22.30 5.59 7.52 4.91
Assam 33.19 13.83 1.16 0.57 17.07 7.29 8.31 4.01
Bihar 10.63 6.92 0.13 - 6.57 - 1.15 0.93
Goa 34.84 16.55 4.54 3.78 31.01 14.14 4.21 1.78
Gujarat 74.17 63.84 0.16 - 47.12 31.57 0.90 0.41
Haryana 80.50 80.01 0.12 0.42 58.86 51.73 1.81 1.67
Himachal P 72.67 62.60 0.93 1.66 50.01 29.15 6.68 7.35
J& K 70.72 32.30 3.04 7.45 33.79 10.44 7.79 10.60
Karnataka 51.55 42.63 0.65 0.67 32.09 19.70 2.59 2.31
Kerala 45.09 26.35 3.35 4.95 32.70 17.65 5.27 5.66
Madhya Pradesh 52.46 42.23 0.17 - 38.38 - 1.58 1.27
Maharashtra 22.17 16.43 0.39 0.01 15.52 9.84 2.81 1.99
Manipur 51.05 27.85 2.40 2.39 39.97 19.98 3.16 4.08
Meghalaya 37.07 49.24 4.67 2.73 24.31 19.52 23.17 9.24
Mizoram 10.12 9.08 0.98 5.17 1.04 2.03 6.37 12.57
Nagaland 63.07 37.53 5.78 0.85 47.39 36.05 12.87 2.67
Orissa 14.24 9.45 0.17 - 14.64 5.69 3.70 1.06
Punjab 22.77 13.40 0.82 - 32.02 22.25 2.22 0.94
Rajasthan 87.34 78.60 0.43 - 56.95 40.74 1.99 1.55
Sikkim 20.48 8.12 2.85 1.95 13.82 9.21 3.87 3.67
Tamil Nadu 26.90 35.03 1.77 2.32 21.73 12.70 4.26 5.49
Tripura 94.66 79.29 3.32 2.11 57.76 55.40 15.02 15.18
Uttarpradesh 54.94 46.520.26-36.21 31.56 2.00 1.23
West Bengal 65.96 61.61 0.89 0.66 45.57 42.79 8.20 8.43
A&N Island 24.09 13.73 4.29 0.84 18.65 6.61 9.78 2.54
Chandigargh 84.32 54.93 0.15 2.49 79.71 35.71 3.92 3.57
Dadra& N.Haveli 26.37 28.02 0.37 - 35.78 19.90 1.62 2.29
Damen&Diu 63.93 11.16 0.72 0.98 34.54 21.08 1.14 1.35
Delhi 125.29 27.84 4.36 2.43 56.31 19.72 5.43 3.81
Lakshadweep 39.62 36.18 1.09 4.68 43.12 30.60 4.77 9.57
Pondichery 16.09 15.36 0.28 1.29 7.33 3.89 2.40 5.26
All India 45.74 38.18 0.80 0.96 32.39 22.13 3.65 3.24
*Source: NSS Report No. 461(55/1.0/4) for year 1999-200; Survekshana Oct- Dec 1996
for the year 1993-1994;
The behavior of the rural and urban households at the state level is very much in
accordance with the National level statistics. It reflects an over all decline in the per
capita consumption of tobacco in general with slight differences in rural areas. The main
observations are as follows.
• Among the rural households Meghalaya, T.N & Dadra Nagar Haveli are the only
states/UT, which showed an increase in the Bidi consumption. Whereas 13 states
(rural) show an increase in the Cigarette consumption, which is also the national
level trend.
• Coming to the urban households Mizoram is the only state, which shows an
increase in the Bidi consumption.
• The rural households of 11 states including 3 UT’s have shown an increase in
Cigarette consumption in the 55th round compared to the 50th round, which is in
accordance with the national scenario.
• It is interesting to note that in both T.N & Dadra N Haveli consumption of both
Bidi and Cigarette have gone up among the rural population.
♦ Similarly in Mizoram Consumption of both Bidi & Cigarette has gone up among
the urban population.
• Haryana, Tripura & Rajasthan are the states with very high per capita
consumption of Bidi.
• J&K, Tripura, Meghalaya, Kerala & Mizoram are the states with very high per
capita consumption of Cigarette.
• It is interesting to note that in some of the states like Arunachal Pradesh,
Maharashtra, Assam & Nagaland Cigarette consumption has fallen drastically.
This kind of information is good from the policy point of view in the sense that the
states in which the consumption of both Cigarette and Bidi has increased, policy can be
directed towards a desirable path. It may be also interesting to see why Cigarette
consumption has fallen in certain states while it increased in most of the states between
the last two rounds. Studying the associated health statistics for these states along with
this can give us an insight into the relationships existing between the tobacco
consumption and health hazards. Lack of proper data at a disaggregated level makes these
kinds of analysis nearly impossible. But even the limited data from various case studies
can be of good help in this regard.
4.Consumption Patterns among different socio economic & age groups
The classification of tobacco consumption at such disaggregated levels is not
available for the period of study conducted so far. But based on the data available for the
period 1995-96 (52nd round) one can analyze the behavior of tobacco consumption of
various socio economic and age groups. The following table will help us to understand
the consumption patterns among males and females belonging to different age groups.
The distribution of total tobacco consumption that we see in this table can help one to
understand the nature of different socio economic groups in consuming various tobacco
products.
Table 3: tobacco use prevalence (for 1000 population) among different
Socio-economic groups. *
10-14 Yrs 15-24 Yrs 24-44 Yrs 45-59 Yrs 60+ All
RURAL MALE
Any tobacco 19 281 664 800 878 521
Smoking 10 220 488 680 626 397
Smokeless 11 81 324 300 450 232
RURAL FEMALE
Any tobacco 12 112 151 139 346 137
Smoking 3 9 59 44 54 38
Smokeless 10 105 134 102 300 118
URBAN MALE
Any tobacco 6 162 523 452 171 350
Smoking 3 41 345 393 125 227
Smokeless 4 129 306 92 66 193
URBAN FEMALE
Any tobacco 3 13 68 101 118 53
Smoking 1 2 4 25 25 7
Smokeless 2 11 65 79 95 47
* Source: NSS 52nd round (1995-96) calculated from Gupta et al. (2002)
Here again, as we saw in the tables above, the tobacco consumption in both smoking
and nonsmoking form is more prevalent in rural India than in urban India. The following
main observations can be made from the above table
• The prevalence of all forms of tobacco is more in the age group 24 years and
above. But some WHO studies these days shows that the consumption by the
lower age group is increasing.
• In all most all the age groups the male groups consume more of tobacco of any
form compared to their female counterparts. This can be easily attributed to the
social set up in the country.
• But interestingly the gap in consumption between male and female is much less in
smokeless tobacco compared to smoking.
—
• In case of the 15-24 & 60+ age groups the prevalence of smokeless tobacco
consumption is more among-females than among the.males?
~
• Fbrthe age groupsl 0-14 & 15-24 the prevalence of smokeless tobacco
consumption is more than smoking, except for the rural male. The higher
smoking prevalence compared to the smokeless tobacco in this age groups may be
attributed to the fact that Bidi, which may be cheaper product, is the main
constituent of smoking among this category. Adjusting for this factor one may
like to conclude that smokeless tobacco is more prevalent than smoking among
children and youngsteFs.This could beniaihly’due'to'the’sociaTsanctions on this
group against smoking: ■
We can also have a look at the nature of consumption of different income classes and
communities from the NSS 52nd round.
Table 4: The prevalence of tobacco consumption among different income
groups and communities. *
Smoking Smokeless Any form
KIDWAI MEMORIAL INSTITUTE OF ONCOLOGY
fl2H3
DEPARTM ENT OF EPIDEMIOLOGY AND BIOSTATISTICS
pH-*!-
(HOSPITAL BASED CANCER REGISTRY)
KIDWAI MEMORIAL INSTITUTE OF ONCOLOGY
Dr.C. Ramesh: PROF. & HEAD
WORLD: It is estimated that about 9 million new cancer cases are diagnosed every year and over 4.5
million people die from cancer each year in the world.
INDLA: The estimated number of new cancers in India per year is about 7 lakhs and over 3.5 lakhs
people die of cancer each year. Out of these 7 lakhs new cancers about 2.3 lakhs (33%) cancers are
tobacco related.
KARNATAKA: There would be about 1.5 lakhs cancer cases at any given time in Karnataka and about
35,000 new cancer cases are added to this pool each year.
"he Department of Epidemiology and Biostatistics comprises of both the Hospital Based Cancer
Registry and Population Based Cancer Registry. The Hospital Based Cancer Registry collects
information on each and every patient registered at Kidwai Memorial Institute of Oncology in a
predivised questionnaire devised by the National Cancer Registry Programme Project of the Indian
Council of Medical Research. The Registry Provides Information on the Magnitude of cancer patients
attending KIM1O, various types of cancers, the treatment particulars and its outcome, which enables
the Insitution to plan for the management / control of the cancer disease. The information so
collected by the registry enables initiation of epidemiological studies to find out various causative
factors for different cancers and also play an important role in Cancer Control Activities. Over 16,000
new cases are registered every year with more than 20 % from neighbouring states of Andhra
Pradesh andTamil Nadu and Kerala.
The Faculty staff of the Department is also involved in teaching students of Undergraduate,
Postgraduate students and also for Superspeciality courses in addition to involvement in many of the
Research Projects / Clinical Trials conducted by various departments of the Institute.
Research Activities - Projects:
1. Cancer Atlas Project: The HBCR is involved in the Cancer Atlas Project of the WHO,
ICMR under taken by the NCRP since 2001 and provide information on all non resident
cases registered at KMIO.
2. Pattern of Care and Survival Studies: The HBCR has taken up the project titled
"Pattern of Care and Survival Studies in Head and Neck Cancers, Cancers of Cervix and
Breast".
All though thousands of cancer patients are receiving treatment from various cancer hospitals in
India, no scientific evaluation of therapeutic efficacy in terms of pattern of care and survival has been
done. The data from HBCRs of India has shown that Cancer of Cervix (28%) and Breast (16%) in
women are most common and cancer of Head and Neck region constitute about 30 % of all cancer in
kiijv.ai.kar.nic.in/statistics.him
174
KIDWAI MEMORIAL INSTITUTE OF ONCOLOGY
7/2/13
males and females. Realising the problem of follow-up of cancer patients wherein huge number of
patients dropout from regular follow-up visits. ICMR decided to initiate pattern of care and survival
studies on three of the most common cancers i.e Cancer of Cervix, cancer of Breast and Head and
Neck Cancers. The project being carried out in all the HBCRs of India where Cancer Registry are
established.
OBJECTS OF THE PROJECT:
I. To obtain core indentifying and diagnostic information in all patients in the particular
/ Institution with cancer cervix / breast / head and Neck.
center
2. To record details of clinical stage and types of treatment of patients included.
3. To have periodic follow-up and record the patient and disease status in all patients suffering
from these cancers so as to have clinical stage and treatment based on survival on these sites
of cancer.
The project has already been in progress with grants funded by the ICMR. The duration of the project
is of 3 years.
•
Two epidemiological studies - One on Oral Cancers and another one on Pharyngeal cancers are in
progress which are aimed at investigating various risk factors in the causation of these two major
sites of cancer.
Leading Sites of Cancer - Male:
Pharyngeal cancers (excluding cancer of nasopharynx) continue to be the most common
form of cancers among males and accounts for 14.1% of the total cancers in males.
Among Pharyngeal cancers, cancer of the Hypopharynx is the most predominant site of
cancer accounting for over 68 % of the Pharyngeal cancers. The other common cancers
among males in order are oral cavity (11.2%), Leukaemias (8.4%), Oesophagus (8.3%) and
Lung (6.8%)
Leading Sites of Cancer - Female:
Cancer of the cervix uteri continues to be the most predominant site of cancer and
accounted for 26.7% of all cancers in females. Cancer of the breast is the second most
common site (16.6%) followed by cancers of oral cavity (11%), Oesophagus (5.7%) and ovary
(5%). Over the years, a gradual decrease in the proportion of cervical cancers and
marginal but steady increase in the numbers and relative proportion of breast cancers is
observed.
Common Cancers:
The Commonest cancers among Males and Females seen at KMIO-2004-05 are as below:
MALE
kicUa.kar.nic.in7statistics.htm
FEMALE
Pharynx
Cervix
Oral Cavity
Breast
2/4
KIDWAI MEMORIAL INSTITUTE OF ONCOLOGY
r/2/13
Leukaemia
Oral Cavity
Oesophagus
Oesophagus
Lung
Ovary
Lymphoma
Leukaemia
Stomach
Thyroid
Brain & Ner.Sys
Stomach
Larynx
Lymphoma
Liver
Pharynx
DEPARTMENT OF EPIDEMIOLOGY AND BIOSTATISTICS
(POPULATION BASED CANCER REGISTRY)
Kidwai Memorial Institute of Oncology
Dr.K.Ramachandra Reddy:Prof. & Head
The Population Based Cancer Registry at Kidwai Memorial Institute of Oncology was established
during the year 1981 with the main objective of assessing the incidence/magnitude and type of
various cancers in Bangalore and to provide a framework for controlling the impact of cancer on the
community. The registry was included under the network project of the National Cancer Registry
Programme (NCRP) of Indian Council of Medical Research (ICMR) and the actual registration of cancer
cases was commenced in the year 1982. The registry covers the resident population of Bangalore
Urban Agglomeration which has an area of 741 sq.kms and has an estimated population of 7.0 million
as of 2007. The inclusion criteria for registration of cases is that patients who have lived in the
defined areas of Bangalore Urban Agglomeration for a minimum period of one year at the time of fist
diagnosis of cancer. The registration of cancer cases is done by active registration method. The staff of
the registry visits all hospitals, nursing homes, diagnostic labs besides the base institution and death
registration units in the defined areas to elicit the required information from cancer patients in a
standard format. On an average about 5000 new cancer cases are registered in the registry area per
year. During the period from 1982 through 2004 a total number of 73524 (34045 males & 39479
females) cases of cancers were reported to the National Cancer Registry Programme by the Population
Based Cancer Registry of Bangalore. The average annual age adjusted rates of cancer among males &
females were 96 and 120 per 100,000 persons respectively. Tobacco related cancers accounted for 34%
of all cancers in males and 16% of all cancers in females and paediatric cancers accounted for 3% of
all cancers in males and 2% of all cancers in females.
LEADING SITES OF CANCER
kdwai.kar.nic.in/statistics.htm
3/4
//2T3
KIDWAI MEMORIAL INSTITUTE OF ONCOLOGY
The first ten leading sites of cancer among males and females are shown in table. Ranking of these
sites'’are based on the frequency of their occurrence. Among males, cancer of the stomach is the
nfost predominant site of cancer constituting 9% of the total cancers among males followed by cancers
of the lung (7.0%), oesophagus (6.6%), prostate (5.3%) and NHL (4.6%). Among females, cancer of the
breast is the predominant site of cancer and has accounted for 24.6% of the total cancers in females
followed by cancer of the cervix (15.9%), ovary (4.9%), oesophagus (4.7%) and mouth cancers (4.6%).
The incidence of breast cancer among females in Bangaloreans is showing a steady and statistically
significant increase as is the case in other Urban cities. Altogether, the first ten leading sites of
cancers among males and females accounted for 53.1% of the total cancers in males and about 70.9%
of the total cancers in females.
CUMULATIVE RISK : In the absence of other causes of death, the risk of developing cancer by an
individual among Bangaloreans would be 15.1% in males and 16.8% in females (cumulative risk). In
other words, one in six persons in either sex has the risk of developing cancer during their life time.
kdwai.kar.nic.in/statistics.htm
4/4
pH -B
Consortium for Tobacco Free Karnataka condemns
BBMP move with tobacco manufacturer
Sunilha Rao R. TXN >'
;
Tags:
Consortium for Tobacco Free Karnataka |
BBMP
BANGALORE: As the BBMP decided to tie up with the ITC in its Zero waste management,
and work on segregation of waste at source, the members of Consortium for Tobacco Free
Karnataka (CFTFK) have taken objection.
"It's ironic but a fact that the theme for this year's World No Tobacco Day is prohibition on
Tobacco Advertisement, Promotion and Sponsorships (TAPS) and a state-level consultation
on ban on TAPS has been planned this week. In fact, BBMP itself is a district anti tobacco
cell for the Bangalore Urban district," said an official release from the CFTFK.
Number of member organizations of CFTFK have written letters to the BBMP
Commissioner expressing their concern over such collaboration.
According to S J Chander of CFTFK, such collaboration is sheer violation of section 5 of
Cigarettes and Other Tobacco products (Prohibition of Advertisement and Regulation of
Trade and Commerce, Production, Supply and Distribution) Act, as well as article 5.3 of the
Framework Convention on Tobacco Control (FCTC) signed by Government of India, as it
enhances public image of a tobacco company and amounts to an indirect promotion of
tobacco.
Palike move to tie up with ITC flayed
Bangalore, July 1,2013, DHNS :
The move by BBMP to tie up with ITC for its Zero Garbage Model programme, which was launched
on July 1, has been strongly opposed by the Consortium for Tobacco Free Karnataka (CFTFK).
A number of NGOs, academic institutions and healthcare delivery organisations that make up the
consortium have demanded that the BBMP immediately disassociate itself from the tobacco company.
The consortium has said that any collaboration by the government with a tobacco firm, as is the case
here, will mean an indirect promotion for the latter.
'While we appreciate the Palike’s efforts to control tobacco use, it is ironical that it being the District Anti
Tobacco Control Cell (Bangalore Urban), the Palike should encourage the efforts of such tobacco
companies in promoting their image,” said Upendra Bhojani of CFTFK.
Enarada, Bangalore, July 1, 2013:
The recent decision by the Bruhat Bangalore Mahanagara Palike (BBMP) to tie up with a tobacco company (ITC) for
its Zero Garbage Model programme has received objections from many corners.
Members of the Consortium for Tobacco Free Karnataka (CFTFK), that comprises NGOs, academic institutions and
healthcare delivery organisations, today demanded that the BBMP disassociate itself immediately from the tobacco
company.
It’s ironic but a fact that the theme for this year's World No Tobacco Day is prohibition on tobacco advertisement,
promotion and sponsorships (TAPS) and a state-level consultation on ban on TAPS has been planned this week. In
fact, BBMP itself is a district anti tobacco cell for the Bangalore Urban district
CFTFK members were concerned over the media reports on BBMP’s collaboration with ITC (Indian Tobacco
Company) for Zero Garbage Model programme launched on 1 st July, 2013. Mr S J Chander of CFTFK explained
that "such collaboration violates section 5 of Cigarettes and Other Tobacco products (Prohibition of Advertisement
and Regulation of Trade and Commerce, Production, Supply and Distribution) Act, as well as article 5.3 of the
Framework Convention on Tobacco Control (FCTC) signed by Government of India, as it enhances public image of a
tobacco company and amounts to an indirect promotion of tobacco."
ITC is the largest manufacturer of cigarettes in India. It is estimated that more than 10 lakh people die every year due
to the use of tobacco in India. More than 1.5 crore people use tobacco in Karnataka.
“Such collaboration between government agency and a tobacco company not only enhances public image of tobacco
company but also creates opportunities for tobacco companies to influence and interfere with public policies in
general” Dr. Prem Mony of CFTFK added.
In past (2010), Karnataka high court had directed another government agency (Indian Tobacco Board, Ministry of
Commerce and Industry, GOI) to withdraw its partnership with other tobacco companies for an event in Bangalore
(Institute of Public health, Bangalore Vs Union of India and others), terming such partnership as indirect promotion of
tobacco. The proposed collaboration would also amount to surrogate advertisement of tobacco.
Many member organisations of CFTFK have written letters to BBMP Commissioner expressing their concern over
such collaboration. “While we appreciate BBMP’s efforts to control tobacco use, being the District Anti-Tobacco
Control Cell (Bangalore Urban) itself, the Palike should discourage tobacco companies’ efforts in promoting their
image through 'so called’ corporate social responsibility (CSR).
As per WHO, activities that are described as “socially responsible” by the tobacco industry, aiming at the promotion of
tobacco consumption, is a marketing as well as a public relations strategy", said Dr. Upendra Bhojani of CFTFK.
The day when the Bruhat Bangalore Mahanagara Palike (BBMP) launched, with much fanfare, the
Zero Garbage project in partnership with ITC Ltd., the Consortium for Tobacco-Free Karnataka
(CFTFK) demanded the civic authority dissociate itself from the tobacco company.
In a press release in Bangalore Monday, CFTFK objected to the BBMP’s partnership with ITC for the
project.
Pointing out the irony of this partnership, it the theme for the year’s World No Tobacco Day was
prohibition on tobacco advertisement, promotion and sponsorship, and a state-level consultation on
such a ban was planned for this week.
Besides, the BBMP was a district anti-tobacco control cell while ITC was the largest manufacturer of
cigarettes in India.
According to S.J. Chander from CFTFK, BBMP’s partnership with ITC “violates section five of
Cigarettes and Other Tobacco Products (Prohibition of Advertisement and Regulation of Trade and
Commerce, Production, Supply and Distribution) Act, as well as Article 5.3 of the Framework
Convention on Tobacco Control signed by government, as it enhances public image of a tobacco
company and amounts to an indirect promotion of tobacco”.
In 2010, the Karnataka High Court had directed another government agency (Indian Tobacco Board,
Ministry of Commerce and Industiy) to end its partnership with tobacco companies for an event in
Bangalore. It had termed such partnership as indirect promotion of tobacco, the release added.
“While we appreciate BBMP’s efforts to control tobacco use...the civic body should discourage
tobacco companies’ efforts in promoting their image through so called corporate social
responsibility,” said Upendra Bhojani of CFTFK.
Keywords: BBMP, Zero Garbage project, anti-tobacco control cell, tobacco
consumption, CFTFK, ITC, BBMP-ITC partnership
Kidwai Memorial Institute of Oncology
The Kidwai Memorial Institute of Oncology being a Regional Cancer Center, located in South of
India, KMIO is catering to the poor and needy cancer patients from Karnataka and neighboring
states. We register approx 17000 new cancer patietns each year. The Cancer Control Activitieswere
establishment for our State. Mobile Cancer Education & Detection Unit (MCEDU), Cancer Detection
Clinic:Community Programmes. In order to help thousands of poor and deserving cancer patients
who need costly anti-cancer drugs for treatment "Kidwai Cancer Drug Foundation(KCDF)" was
started from December 1991 and provided these medicines at 50% low cost than the market price.
An ANTI-TOBACCO CELL:
The staff of Anti-tobacco Cell is involved in bringing about awareness among different categories of
persons in the community on the harmful effect of tobacco usage through education wherever
possible.Activities:Adoption of Schools/Colleges for anti-tobacco education.Organising & conducting
training programmes for health personnel, teachers, VHG, etc. Conducting programmes to convey
Anti-tobacco messages through guest lectures, exhibition, workshops, debates & painting
competition. Adoption of taluk for Anti-tobacco education. Development of health education materials
to the target group
Conducting tobacco related studies .
The Institute has initiated a program of Professional education, technology and expertise transfer
through short-term education/training programme for undergraduate, postgraduate and staff of
medical colleges/district hospitals and Primary Health Centres. The main objective of this training
programme would be to train the medical personnel in prevention, diagnosis and treatment of cancer
in early stages in their respective areas. This Institute is running postgraduate courses in MD
(Radiotherapy) from the year 1987. Super Speciality Courses viz. M.Ch (Surgical Oncology) & D.M.
Medical Oncology), PG diploma in DNM (Diploma in Nuclear Medicine) & DRP (Diploma in Radiation
Physics), B.Sc. Medical Technology (Laboratory/Radiotherapy/Radio diagnosis) have also been
started from 1, Sept. 1989. These courses are affiliated to Rajiv Gandhi University of Health
Sciences, Bangalore and recognised by the Medical Council of India, New Delhi. Several
multidisciplinary - multi centric global studies are on-going.
Finance:KMIO is recognised as a Charitable Institute by the Endowment Department of Karnataka,
considering its commitment for services to poor cancer patients. The charges levied for cancer
investigations and treatment, are well with in the reach of poor patients. In cases where the total
treatment cost becomes too heavy such patients are financially assisted by various schemes like
Free drugs from the Institute, Karnataka Chief Minister's Medical Relief fund, Poor Patients Welfare
Fund, children Welfare Fund, Kidwai Cancer Drug Foundation, etc.,. The anti-cancer drugs sold at
Kidwai Cancer Drug Foundation' are 40 to 60% cheaper than the market rates.
The annual budget of the Institute is about Rs.19 Crores out of which about Rs.9.50 Crores in spent
on Salaries and Administrative over heads. The other items essential for patient care and hospital
maintenance are drugs, diet, linen, surgical sutures, x-ray films, blood bank materials, laboratory
reagents, hospital necessaries, water & electricity, maintenance of medical equipments and hospital
buildings, replacement of obsolete equipments, etc.,, which cost annually at about Rs.9.50 Crores.
KMIO is recognised as one of the regional cancer centres by the Government of India. Patients not
only from Karnataka but also from the adjacent areas of the neighboring States of Tamilnadu, Andra
Pradesh, etc., In case of the latter the patients number is about 40% of the total no. of patients
treated. The Government of Karnataka is extending substantial financial support to the Institute
through Grant-In-Aid, annually, to the extent of about Rs. 10.00 Crores. Annually the Government of
India is releasing Rs.75.00 lakhs for purchase of Medical equipments. Since the Institute is levying
treatment charges at a very reasonable rate the revenue earned out of it is not substantial for the
maintenance of the Hospital.
Health Systems Global
Improving performance
through research and policy
pH-7!
The Health Systems
Global Thematic
Working Groups
The thematic working groups are an important part of the society’s operations. They provide a platform for member
interaction and the exchange of experience on particular issues in health systems research. There are currently eight
thematic working groups created and run by Health Systems Global members.
This flyer provides an overview of the eight groups, their aims and activities. You can also find more information about
the thematic working groups and how to contact the coordinators on the Health Systems Global website
(www.healthsystemsglobal.org).
If you have any questions or queries about the thematic working groups or if you wish to establish one, then please
contact the Secretariat (healthsystemsresearch@cphiv.dk ).
Supporting and Strengthening the
Role of Community Health Workers in
Health System Development
Community health worker programmes rely on staff
who live and work at the community level. There is true
potential for these services to strengthen delivery of
health services through tailoring services to meet the
needs and realities of individuals and households, and
making more appropriate links between the community
and the formal health system.
We are working to support the generation, synthesis
and communication of evidence on the roll-out and
functioning of community health worker programmes
and to enable learning across geographical and political
contexts.
This work includes: supporting dialogue online; arranging
events; facilitating learning across the group; supporting
research; and publishing and translating evidence into
products which meet the needs of diverse audiences.
Ethics of Health Systems Research
The overall goal of the Ethics of Health Systems Research
TWG is to initiate critical thinking and dialogue on the
ethics of health systems research in low and middle
income countries. It aims to explore what ethical issues
arise in relation to health systems research in low and
middle-income countries, how they should be addressed,
and by whom. Thematic working group activities include
hosting webinars, workshops, meetings at bioethics
and global health conferences, conference panels, and
Google Group discussions.
Health Systems in Fragile and
Conflict Affected States
Improvements in health systems in fragile and conflict
affected states will not be possible with a 'business as
usual’ approach. These settings need special attention,
policies and programming. The Health Systems in Fragile
and Conflict Affected States Thematic Working Group
brings together key actors interested in this area.
We promote the creation of new knowledge, improved
policy and better communication among stakeholders
to contribute to the development of responsive health
systems. Our aim is to strengthen the research base and
encourage the use of evidence in decision-making.
Medicines in Health Systems
Medicines play crucial clinical, public health, social,
economic, political, and ethical roles in achieving the
goals of health care delivery and financing systems.
When used appropriately, medicines contribute to the
health and well-being of individuals and populations; and
they waste scarce resources when used unnecessarily or
incorrectly. The thematic working group on Medicines in
Health Systems will define medicines-focused activities
that add value to ongoing global and national efforts
to improve medicines availability, access, affordability,
and use. Activities may include: facilitating constructive
dialogue among stakeholders within and across systems;
strengthening capacity of practitioners in generating
evidence on medicines in health systems; disseminating
applied research evidence early and efficiently to each
relevant system stakeholder.
Health Systems Global
Improving performance
through research and policy
SHaPeS: Social Science Approaches
for Research and Engagement in
Health Policy & Systems
SHaPeS aims to strengthen and raise the profile of
social science approaches within the wider field of
health policy and systems research. The group is
particularly interested in qualitative and participatory
approaches to research and analysis, and in conceptual
and philosophical perspectives. Our primary interest is
questions about health system performance that are
difficult to study with the dominant health research
methods. SHaPeS convenes a range of activities and
discussions structured around four methodological
clusters of engagement: participatory action research;
policy analysis; theory-driven research; complexity
science and systems thinking. There are several cross
cutting discussion areas: conceptualizing health policy
and systems; research quality and rigour; linking
research with policy and action; power in health policy
and systems; capacity building; and working across
disciplines.
Teaching and Learning Health Policy
and Systems Research
The thematic working group is organized around ways to
improve the teaching and learning of Health Policy and
Systems Research (HPSR). The group will focus on issues
in teaching and learning HPSR at educational institutions
around the world, with an emphasis on research and
its application in low and middle-income countries and
disadvantaged populations, and address global, regional,
and local policy and program priorities. Responding to
interests of its members, the group is currently working on:
• Mapping out current approaches to teaching and
learning HPSR around the world;
• Collecting and sharing curricula, courses, and other
teaching and learning offerings in HPSR;
• Supporting ways to develop approaches to teaching
multi-disciplinary research on health systems and
policy for different target groups (undergraduate,
graduate and post-graduate students, program
managers, policy-makers);
• Supporting innovations in pedagogical approaches to
teaching HPSR.
The Private Sector in Health
The non-state sector plays a significant role in delivering
health care to people in developing countries. This poses
both challenges and opportunities in terms of the quality,
cost and availability of health services. The Private Sector
Thematic Working Group seeks to enhance the quality,
quantity, and accessibility of knowledge and evidence
around the potential role this diverse set of actors has in
delivering healthcare to the poor. The group will actively
involve health researchers, practitioners, and policy
makers to encourage translation of research into policy
and practice.
Translating Evidence into Action
The need for strong evidence to support health systems
strengthening efforts globally has gained increasing
attention in past years. However, there continues to be
a gap between the creation of new and solid evidence
■ from health systems research efforts and the translation
of that same evidence into policy action. Policy-makers
struggle to find, collect and understand context-specific
evidence to support their own decision-making needs,
despite existing knowledge. These challenges are not
inevitable, and we propose that with the right level
of support and interaction between researchers and
decision-makers, the translation of research findings
into actionable policy and programmatic guidance is an
achievable goal.
This thematic working group focuses on the translation
of health systems evidence Into action, and support
mechanisms to share best practices, lessons learned,
and practical guidance and tools. The overall aim is to
decrease the current gap between what we know and
what we do.
We set out to:
• Enable researchers to support the use of health '
systems research by policy-makers and other
stakeholders;
• Raise awareness among policy-makers, programme
implementers, providers, citizens and the press/media
about the need to value, demand and use evidence;
• Create opportunities for all Health Systems Global
members to dialogue and share best practices in
evidence translation;
• Collaborate with other Health Systems Global
thematic working groups to promote evidence
translation.
www.healthsystemsglobal.org ■ healthsystemsresearch@cphlv.dk
And engage with us online: www.facebook.com/healthsystemsglobal • Twitter: @H_S_Global
- Media
 RF_PH_7_SUDHA.pdf
RF_PH_7_SUDHA.pdf
Position: 2552 (4 views)