NUTRITION ASSESSMENT
Item
- Title
- NUTRITION ASSESSMENT
- extracted text
-
RF_NUT_7_SUDHA
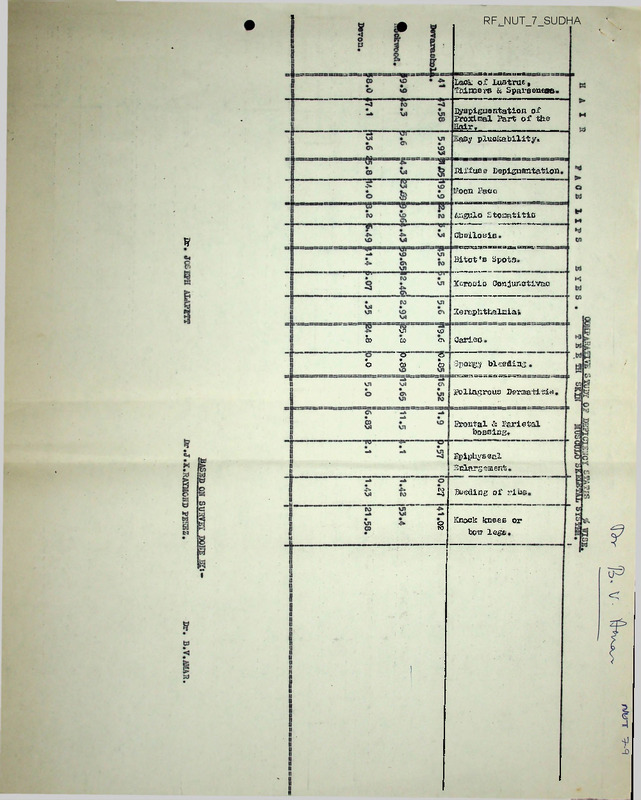
Lack of Lustrue,
Thinners & Sparseness.
Eyspigmentation of
Proximal Part of the
Hair.________
;«a£»y pluckability.
Diffuse Depignantation
Koon 1’aoo
Angulo stomatitis
ChciloBis
%
Bitot’s Spots.
Xerosis Conjunctivae
Xerophthalmia.
'Ll
to
b
00
<n
Sarles
b
*~5T
b
o
b
Spongy bleeding
Pellagrous Penaatitie
Frontal & Parietal
bossing.
Epiphyseal
Enlargement
3
Beetling of ribs.
8
Knock knees or
bon lege
clinical assessment survey- 197fr»79
(Devarashola, Rockwood,
Doveon and All-Indla).
—
H A I Hl
Jr- li Xeare»8
Deverashola.
Rockwood.
Devon.
Kean for the group.
• All-India.
FA C E
_
Total Ko. of-Lack of lustre Thinners
Children, and Sparseness
Easy Pluckability
Diffuse
Depigacntation.
Ho. of Sign
of Children.
No. of
Percen
sign of
tage.
Children.
Ko. of
Sign of
Children,
Per
cen
tage.
53
46
27
126
ityspigmontation of
X’roxiraal part of hair.
Percentage Mo. of sign percen
tage.
of Children.
Mota Face,
No. of sign Per
of Children cen
tage.
1
2
3
4
5
6
7
8
9
10
21
14
U
49
39.6
30.4
51.9
38.9
6.3
27
9
15
51
3.9
19.6
55.6
40.5
5.8
2
2
4
8
3.8
4.3
14.8
6.3
3
11
10
3
34
-
20.8
21.7
11.1
19
*
8.
8.
6
22
-
15.1
17.4
22.2
17.5
1.4
20
17
8
55-6
42.5
50
2
2
1
5.6
5
6.3
11
14
4
30.6
35
25
9
6
5
25
15
31.3
45
48.9
7
5
5.4
2.9
29
*
31.5
•*
20
—
21.7
2.4
4
6
16.2k
16
9.3
12.2
16.2
12.4
13
21
16
50
30.2
42.9
43.2
38.8
13
12
8
33
30.2
24.5
21,6
15.6
1.6
-
*■
-
3.4
5.3
2.3
12.5
5.2
1.2
11
12
4
27
*
28.9
27.9
25
27.8
-
6
11
3
20
—
15.8
25.6
18.8
20.6
4.9
——
Deverashola.
Rookwood.
Devon.
16
40
16
18
17
5 '
50.00
Mean for the group.
All India-
92
40
43.5
4.4
42.5
31.5
------- -
——
------ ------ -
2 - 2-?? Years*Tteverashola.
w Rockwood.
Devon.
Moan for the group.
All-India.
2j.. xlJ&gFLte
Devarashola.
Rookwood.
Devon.
Mean for the group.
All-India.
43
49
37.
129
26
20
1?
63
60.5
40.8
45.9
48.8
—
—
3.6
38
43
16
97
•»
13
19
5
37
*■
34.2
44.2
33.3
38.1
6.1
24
26
♦5.1
66
55.8
53 .1
45.2
51.2
6.6
14
15
4
33
-
36.8
34.9
25
34
6.6
2
1
2
5
•»
CKINICAB ASSESSHTMT SURVEY-. 1978"I5x
(Deverashola, Hockwood, Devon and All~In<Jia»)
____________________________________
H A I
R
Total Ho. of lack of lustre, thinness and Sparseness.
Children,
Percentage.
Signs of
Children.
2
1
*
______________
Dyspignention of proximal pari of hair
Signs of
Children.
3
Percentage.
4
Easy pluckability.
Signs of
Children.
5
Percentage
6
ZLsJLXearPir
Deveraohola.
Rockwood.
Devon.
Mean fbr the Croup.
All-India:
96
106
80
282
-
42
39
29
110
-
43.75
36.79
36.25
39.00
2.9
44
47
41
132
-
45.83
44.33
51.25
46.80
3.8
7
4
9
20
4
7.29
3.77
11.25
7.09
1.00
Deverashola.
Rookwood.
Devon.
Mean for the Group.
All-Indiaj
85
102
53
240
-
27
36
25
88
-
31.76
35.29
47.16
36.66
1.5
38
47
22
107
-
44.70
46.07
41.50
44.58
1.6
4
f
5
14
-
4.70
4.90
9.43
5.83
0.5
•
ck
ai
s
ss ss
cssESssrsssssacsss » s ssjssa«»»53s= XSSlSSjxttUSSES essscssssswais! aa ss
Total No.
of Children,
•
3r4X.efi.rsL*
Deverashola
Rookwood.
Davon.
Mean for the Group.
All-India.
1jxxxuso Bopif^mentation
Sign of
Percen
Children.
tage.
96
106
80
282
85
002
53
240
w
Moon Pace ______ Xerosis
Percen
Sign of
Sign of
Children
tage,
Children
' 1 "........
2
3
4
31
42
27
100
32.29
39.62
33.75
35.46
23
27
9
59
•
23.95
25.47
11.25
20.92
3.5-
—
4 r. j..Xc££S?.=
Devarashola.
Rookwood.
Devon.
Mean for the Group.
All-lndla.
ss «s 33SS3Ssa»»SSS3 -nsaonssasisa sssssxssssassx
“~5
9
14
5
28
*>
Percen
tage.
g—~
9.37
13.20
6.25
9.92
5.5
Xeropthalmia
Sign of
percen
Children. tage.
37.64
45.09
32.07
39.58
•
a X s c:
Bitot's spot.
Sign of
Children Percen
tage.
7.....
I8
!5
10
7
«
*
11
7.29
3.77
3.90
51
61
37
149
53.12
57.54
46.25
52.83
3.3
42
74
25
141
-
49.41
72.54
47.16
58.75
4.8
—
<—
32
46
17
95
•
» -x s x
11
16
8
35
•
13.41
16.68
15.09
12,41
1.8
5
15
1
19
3.52
14.70
1.88
7.91
5.8
7
2
*
9
—
8.23
1.96
—
3.75
•
CLINICAL ASSESSHEHT
(Devaraehola, Rockwood, Devon anfl All-India.)
T E B TE
Total No. Carle s
of Chil
dren.
sign of percen
Children tage...
1
2
6666
1 - 1j Years;Dovara choir.
Rockwood.
Devon.
Lloan for the group.
All-India.
3.8
2.2
—
2.4
-
GUMS
Spongy bleeding gune
_____ SKI. H
pelKgrous-dermtoala
B O HE.
Frontal and Parietal
BoBeing.
Sign of
Children.
3
Sign of
Children.
5
Sign of
Children.
7
Percen
tage.
8
—
—
-
Percen
tage.
4
53
46
27
126
•
2
1
3
-
Devaraehola.
Rockwood
Devon.
Keen for tie group.
All-India.
36
40
16
92
-
4
4
8
-
10
25
8.7
0.4
2 - aiTeargtItevaran tola.
Dockwood.
Devon.
Mean for the Group.
AAll-India.
43
49
37
129
-
5
9
8
22
-
11.6
13.4
21.6
17.6
2.0
1
1
-
—
23.7
9.3
25.0
17.5
4.1
1
2.6
flfl*
—
—
—
-
1’ercen. tage.
6
Dpiphysaal enlaro»-nwnt.
Sign of
Ghildr»n.
9
Peroei>
10
8
6
2
16
—
15.1
13.00
7.14
12.7
0.2
2
5
3
10
-
3.8
10.09
11.1
7.9
2.23
*
5
2
4
11
-
13.9
5
25.0
12
0.4
1
2
4
7
-
2.8
5
25.0
7.6
2.23
*
2
2
-
*
5,0
—
2.2
6
5
1
13
*
14
12.2
2.7
10.1
0.4
2
6
2
10
•
4.7
12.2
5.4
7.8
2.25
1
1
5
-
2.3
2.0
8.1
3.9
1.3
3
3
*
6
—
7.9
7.0
—
6.2
0.4
«
7
1
8
-
16.3
6.25
8.2
2.23
1
3
—
4
-
2.6
7.0
—
4.1
1.3
»
2
-
*
4.3
*
1.6
1.3
i
2i - 3 YOfigB t DevaraBhola.
Rockwood
Devon.
Mean for -the group.
AlL-lndi.ru
39
43
16
97
—
9
4
4
17
-
—
*
—
W
-
-*
fl*0.1
•
—
-
1
-
-
2
0.8
0.8
—
—
1.0
1.2
w
>
1.31
SURVEY- 1978-7&
CLU1ZCAL
(Dcveraehola, Roaisrood, Devon & Ali-india).
lips.
eyes
total So. of XeroBiB Conjunctivae. Xsr cphttialaid'(Inola*”"
Children.ding Keratomalacia)»
Sign of
Percentage
Sign of
PcroenChildren
Children
tags.
1
V ~ H fraraiD veraohola
5
_
tpot
Sign of
Children
Percentag©.
. 4
___ 5______
6
___ 7____ 8
Sign Of
Children
____ 9___10___
53
5
5.7
1
30.19
2
3.8
2
3
-
4.5
11.1
1.5
1
•
1.9
2.2
0.1
16
46
27
23DEWhEXX±Mx&ESE?3 All-InfliasJtfcg
14
2
*
30.4
7.4
6
1
-
3.7
1.6
1
1
-
2.2
3.7
.4
Mean for tho Group.
126
8,
6.5
2
1.6
52
25.4
>
2.4
2
1.6
Deveraahola.
Rockwood.
Devon.
56
40
16
1
2
2
2.8
5.00
12.5
1
-
2
-
16
22
4
44.4
55.00
28.00
3
-
8.3
7.5
-
1
2
-
2.8
5.00
-
Mean for tho group.
All-Indin:
92
-
5
-
5.4
2.2
1
-
1.1
-
42
-
45.7
1.5
6
-
6.5
3.8
3
-
3.3
0.6
2=2^YearEl~
Dcveraehola.
Rockwood.
Devon.
Mean for the group.
All-Indiat
45
49
57
129
*
3
6
5
12
7
12.2
8.1
9.5
5.5
2
1
4
*
4.7
4.1
19
57
7
63
-
44.2
75.5
18.9
48.8
1.9
2
3
6
11
*
4.7
6.1
16.2
8.5
3.4
4
3.
-
9.4
6.1
58
45
4
6
•
10
10.5
15.00
—
10.5
4.2
3
2
5
7.9
4.7
5.2
15
21
10
46
«■»
39,5
48.8
62 .5
47.4
3.1
8
4
12
21.1
9.3
12.4
6.1
1
2
3
Rockwood.
Devon.
I
2
Cheilitaia.
_
Percen- Sign of Peroen
tage.
Children tags.
Angular Stomatltio
lOotT's
-
-
Ikr. 2..Xems.r...
2j- 5
YearsiDeverashola.
Rockwood.
Devon.
Mean for the Group.
All-India.
«e
m
-
ssiBn».Tr-.T ssts sskk:=»3S^===:sts, sssssasase: =s
«twswMBtsffiUMtBsxcMSiann sxsxsxascsxs^cxsssCTMnBTgaso
3.1
-
jsoaassca- HXSiS3S3 £2fT? S3-C3C5® 2222®~~SSIa sssa S3 XS SSSJwWSSS XUSxx
-
»»s:=s3S3sx=aecU3SSSSSES3SSSS3
—
5.4
1.2
2.6
12.5
3.1
1.5
asasssa
CLINICAL ASSESSm^T SURVEY- 1918-79
(Severashola, Rockwood,
Devon and All-India.)
IfflSOULAR
Total No. of
Children.
SKELETAL
AND
Bleading of Ribs.
SYS TEE.
Knock-knee© or Dow lege.
Sign of Children
Percentage.
>—
*
—
0.4
13
11
1
25
*
24.5
23.9
3.7
19.8
9*07
•w
5
*
2.2
0.4
9
16
7
32
-
25.00
40.00
43.8
34.8
0.07
«w
*
0.4
14
28
8
50
-
32.6
57.1
21.6
38.8
0.07
—
17
14
7
38
-
44.7
32.6
43.8
39.2
0.07
Sign of Children Percentage
1- HYears:Iteveraeiiola.
Rockwood.
Devon.
Mean for the group.
All-India:
53
46
27
126
-
H -2 Years:Deveranhola.
Rockwood.
Devon.
llean for the group.
All-India:
—
■»
2
36
40
16
92
—
2
-
—
- rTu i
2 - 2{:- Years:Devorashola.
Rockwood.
Devon.
Mean for the group.
All-India:
43
49
37
129
-
2?> - 3 Tears:Devcrashoiu
Rockwood.
Devon.
Llean for tho group.
All-India.
36
43
16
97
•
S
53 S3 S3 S3 £5 SX
-
—
—
—
'f
—
—
-
*
*
0.4
= a = =saeaaaa = — as
as
ss as
nzcasEfias -
s» ss a o c s »
ss ss ss
ASSESSMENTS 19lg~Z2i.
(Devarashola Group of Estates.).
_________ ____ _______________ MtAQAJW„ age m,
_________ _____ ______________________________________________
0-3
3-6
6-9
9/12-1
li^xJJS^- 2-2* Yrs. 2^.-3 Yrs . 3 - 4
4 - . yrs. ._
Months. Months. Koniho.
Year.
mle Pejaale Lislepeaalo aale 3‘emale Male Eemale HaleItenale
mla /©male.
Devcsnehola.
2.5
5.9
$.6
7
7.7
7.4
8.3
8.4
9.8
9.1
10.9
10.7
11.5
10.8
13.1
12.6
W6ckwood.
3.1
9.3
6.5
6.9
8.3
7.4
9.0
8.4
9.8
8.8
11.3
9.9
12.1
11.4
12.9
12.6
Devon.
4.0
8t6
9.3
9.3
7.6
7.3
5.1
7.7
5.1
9j>
10 5
10.2
11.2
11.£
13.2
13.4
AU-India.
-
-
-
-
7.8
7.3
8.5
8.0
9.4
9.0
9.8
9.7
11.1
10.7
13.2
12.6
Doveraehola.
51.0
60.9
63.5
66.7
70.8
70.3
74.0
75.0
79.3
79.2
86.0
82.8 89.0
86.7
95.2
92.3
Booktood.
51.5
55.7
63.7
63.9
98.6
66.6
72.9
72.3
78.2
76.9
83.6
81.3 84.3
85.6
92.1
91.9
Devon.
57.0
57.2
64.5
68.3
73.7
71.8
78.0
77.2
75.4
78.0
85.5
85.1
87.4
87.3
93.2
95.1
',11-India.
—
—
-
—
70.8
69.3
74.2
73.3
78.2
77.1
81.3
85.8
86.2
84.9
93.9
92.6
Doveraslwla,
37.1
41.2
42.5
43.2
45.6
43.8
45.9
^j.O
46.5
46.3
48.0
47.2 47.9
47.3
48.9
48.3
Bockwood.
35.5
39.6
41.8
43.1 ■
44.4
41.6
44.4
|44.2
46.4
45.8
46.6
45.7
47.1
46.4
47.5
47.4
47.1
1-4.3
46.6
45.8
47.0
46.3
48.4
47.0
48.9
47.4
45.1
I4.O
45.5
44.6
46.3
45.4 47 .a
46.1
47.9
47.1.
Ci'S1OOggEXESl I
5Y UI j>
13.2
12.6 Ji2*7
12.7
14,1
14.3
WEIGHT AGAINST AGE G-HOU?;
AGE BZ HEAD CIWCWIJWiCE
41.0
Devon.
All India.
-
IWeraahola.
39.7
-
42.8
-
43.8
-
45.2
43.9
43.8
43.0
13.1
13.0
15.6
13.5
13.8
13.5
13*5
13.4
14.1
13.4
14.0
14.5
14.3
14.2
12,6
12.5
13.0
12.3
12.8
12.9
13.1
13.5
12.7 K5- 15.0
AGE BY CHEST aihWMFERENcji/ “ “ •
45.0 J'43.7
44.6
44,0
47.8
12.8
13.0
13.0
13.4
13.4
14.0
13.9
45.9
4818
47.9 49.6
49.1
51.0
50.7
Bo ck wood.
13.5
13.1
13.6 Jp3.3
Devon.
12.9
11.2
11.4 hl.6
All-Indla
1*. «» «RT
•pevareehola.
Bookwocd.
mb
■»*
m*
w
12.5
12.1
44.6
42.4
45.9 ,W 45.9
48.0
46.4
48.5
48.0 49.5
48.5
49.7
49.4
Devon.
44.9
44.1
47.3 /■ 43.6
47.4
46.4
48.5
47.4
50.0
48,3
49.9
49.4
All India.
43.1
42.1
45.5
48,1
46.9
49.6
48.6
44.5 ‘4M
45.4
44.4
46.6
Nutritional assessment of under fives belonging to three estates
* in Gudulur Taluk.
-z-z. zZ--3-3,
Survey done by: Dr. Joseph Alapatt.
Dr. B.v.Amar.
Dr. Raymond X. Perez.
SUMMARY: Large majority of children are suffering from malnutrition
Anthropometrical measurement shows close parallel to the all India
mean and falls ^elow the normal growth curves. Clinical assessment
supports these ^sctsjT’most of those, examined showed deficiency
signs. Practice of bad food habits and unhealthy housing and
sanitation has contributed to the high degree of malnutrition
among the under Fives. Ill^tracy also plays an important role.
INTRODUCTION: Good nutrition is of prime importance in attaining
normal growth and development and maintenance of health throughout
life. During our stay in the estates we noticed that most of the
mothers go for work leaving behind their children in the Creeches
I and paying little attention to their diet. 1979 being the Inter
national Year of the Child we decided to look into the nutritional
status of these children*Ue participated in similar surveys during
our "Social Paediatrics" posting which gave us the impetus to attempt
this survey.
OBJECTIVES: Objectives are as follows:1)
Anthropometrical and Clinical Assessment of
nutricional status.
2)
having found the deficiency/malnutrition; to
assess the impact of existing, curative and
educational /standards of the health care in the
estates.
wW ?
MATERIALS AND METHODS 8
PERSONNEL:!) Medical adviser ( CLWS, UPASI)
~
)■
2) One health worker ( —" —•)
3)
Balasevikas and the compounder of the respective
estates.
A proforma containing anthropometrical measurements and various
signs of nutritional deficiency states was prepared for each child.
We instructed ^supervised the balasevikas, health worker, and
the compounder in the use of measuring tape, weight, balance and height
scale in taking anthropometrical measurements while we carried out
the clinical assessment of children.
Advance notice was given to all the workers to bring their
children to tTie resPsctive creeches/schools for assessment. Defaulters
were covered by line to line approach, The hospital in-patients were
also examined thereby obtaining 100% coverage
the children in
these estates.
- 2 -
ANALYSIS!
Key to the Graphs
: ANTIffidPOMiiTTICAL MEASUREMENTS!
1.
2.
Weigh t/age study in male.
Weight/age study in female.
3.
Ht/age study mules.
4.
5.
Ht/age study feraalf1".
Chest oircumference/age male.
6.
7.
8.
9.
Chest circumferenee/age female,
Head cLrcoEiference male.
Head circumference female*
Midarm clrctaiferenoe male.
10.
Midarm circumference female.
Graph 1 A 2;-
All the three estates and the Indian mean appear to be much
below the norftal co ad to health standards.
'
2 - 2J- year aga group, both boys and girls have not registered
any weight gains all of growth curve also occurs iu Rockwood estate
at 4th yeai'.
In Devarahola 3 years 4ysurs age group show only bare,
minimal weight gain.
Graph 3 & 4?.~
Growth curves of all 3 estates drop at the age of 4 years
Growth curve which sre wall below ths standards begin to full-
one thinks it is time to worry.
1£ “
years ag-' group i" Devon (both b&ya and girls) show
a stepp fall in the growth curve, thereby suggesting that weaning
period and their customs contribute to a great many
of PCM in
this estate.
The vegetarian food habits of this community also
contributes.
Graphs 5,6t7,8 & 11,
At birth, the head oiroumfex'enoe is much greater than the
chest circuEifex'snce but depending upon the mental gxowth, the two
curves meet aadh other sooner or later and the Chest circumference
overtakes the Iwsi circumference at the age of 2 years in Indian
children and 9 month or so among American children, Thia hae been
linked up with malnutrition prevailing in our country. Among the
estates, in hevsrshole, the crossing takes plf.ce at the age of
2| years.
In Rockwood, the head circumference always remains
lowers in Devon, they cross at 1 year.
- 3 -
’
Based upon this we find that in Rockwood, - from "birth, the
child is at a dieadvantage(therefore interbreeding among the Maplhas
is very common and polygamy is the rule) and continues to be deprive
them from growing up normal citizens of India.
DEVARSHOLA:
Ac for as the data collected, thid is perhaps the only
estate amongst these three estates which shows signs of promise and
this is due to
(1) The group Manager is incharge of this estate.
(ii) The group medical officer (CM3) and his AMO are residing
there, having a group hospital with OT facilities.
Head and chest circumference cross each other at a later age
than the mean, Indian child does (2 years), as this is an indication
of the prevailing nutrititional status of children, this goes to
show the situation st Devarshola estate.
A
Graphs 9 & 10:
Midarm circumference in devon is well below that of All India
mean, whereas Rockwood and Devarshola are above it.
boys in Bevan, there is fall in circumference.
years
DISCUSSION
BAR DIAGRAM:
% of diflciency status in each estate.
On observing the tables the bar diagram, protien calorie deficiency
(
is prevalent in ail 5 estates, Rockwood and Devarshola have high
incidences (47.50$ ami 42.5$ resp) of protine dificieney as compared
to Devon where protin calorie deficiency is more, explaining the
fact that there are more vegetarians in Devon estate.
£
Vit * A* : dificieney is prevalent in all, amounting to more than 40$.
But in Rockwood, it is nearly 60$, This high incidence of Vit ‘A*
dificieney may be explained due to their cooking habits (Prolonged ----- 7
boiling of vegltables).
The car&dane intak of Devon appears to be
much more than the other tow estates - may be due to their food habits
(vegetarians).— ?
Vit *B* ;
deficiency appear to be more in Devarshola.
Vit * C* ; deficiency does not seen to exist as citrus fruits are
*7
easily available amidst the hills.
(------------------------------------------------------------As far as Vit *D*;
deficiency is concerned it is double that of
Devon in Rockwood, and Devershola estates. The $ of attendance in
creches and schools in Devon estate is comparitivety low and the
child is carried on the back of the mother explaining the following.
PCM because they do not get enou^i supplement from creche or
scnoola.
Vit "D’ deficiency is less than elsewhere ie.t u v light
exposure is more than the other tw0 estates reflecting the low
attendance in school and creches in Devon estate, where they are
given Mid Day Meal which for some form they only Balance diet.
- 4 The elirnnte and the natural
up io not allow enough euilight
resulting in the deficiency of Vit ’D' in all three estates.
BEOOMMBNDATIONS?
1.
Education is a in tint People there lack literacy.
be able to read, write, and understand.
the health education will be abortive.
2.
They should
Unless there la basic education
Family Planning shouldbe introduced and encouraged there.
For a few, it is against their religions customs,
The cause of
this failure can also be explained by the fact that after the age
of 10, he/she in the family becomes one of the earning members in
the house. Naturally, an earning member is as asset to the family
and they would like to have as many as possible. (They should be
encouraged to have less but healthier and better educated children
there by, increasing eai'ning capacity.)
h
3. Early marriage should be discouraged.
4. biiring our line to line visit we observed that, the lines
7
are crowded and the houses are not adequate enough to accomodate
the Icing slaefamilies. Sanitation is very poor and the surrounding
are not kept clean.
The house lack adequate ventilation.
Health education should Ls baaed ou the followings-,
1.
3.
Family Planning.
Food habits.
2. Sanitation.
4. Chnsanguityr— >
/
/
During our assessment we cane across, few cases of gross mental
retardation congenital heart diseases, CDS, and TEV - may be due to
coneanguity,
)
5. Rockwood needs a full time MO as it is far from the group
hospital and the Medical Officers arc not staying in an approachable
distance.
An annual objective review by the Medical Officers to assess the
response to the health education should be carried out.
A closer participation of the estate beaurocracy is indicated.
AOiOiOWLaD GEMi& To?
We thank first and foremost, our Community Medicine Department
for having given us this exeellant opportunity of studying the
workings of the Tea estates and its workers.
We thank them also for
their guidance and full Co-operation in having made the project a
success.
We thank Dr. M&4. Rahamaihullah,
Dr. S. Pothl and the CLWS
workers, for their guidance and organisation.
□or heartful thanks to ths froup Medical Officer, and the
Medical Officer for their help, encouragement and guidance.
- 5 -
We are feaiful to the Manager, Balasevikas, and Compounders
of the respective estates, for helping us to obtain insight into
the problem.
BIOLOGRAPHY
Text Bosk of preventive and social medicine - Part.
National Pls n of action for international year of the child 1979.
Text Bosk of Paediatsiss- nelson,
Text Book of Pediatries - Aohar.
Outline of Paediatrics
- Slobody.
PKuGRAl! COMPONENT
I'ight st the outset of our interchip, we wore informed about
the need of bias io health doctors' appreciation and involvement in
the following,
1. Prevecitics:
1
a) Eviornmental sanitation.
b) Im'scnleation of under 5s.
2.
Ke al th education of the masses.
3.
4.
Family Planning.
Curtice work.
EHPIK.13:;S?'TA]j 3’ITATIJKs-
Xa th-: estates of Xtlgiris, we noticed
poor housing, inadequate ventilation and lighting, improper disposal
of waste and axercto.
tTs p:>^*nhle wr;*:r lo *.Inible f$r the c&aenmptioh of the workers
We udrisnd the *r;tnte M.-marrsr and lick workers, how to circumvent
the vace,
IMHdSIuATIOih I haring cur social paedlatoro posting, before, we
embarked to the estates, we inntoiaed 1058 children belonging to
our neighbouring villages, <3uddag?Jhte- paiyg, Gurapu pslya and
providence school) with Df'T & JPV,
We did a study of the innufflerisatioa coverage among the CIWS
estates, with hr. dahaiathullab, the figoraa of which, she presented
during th® child haslth conference, at Ccocoor,
HEALTH EDUCATIVE s- During our Bocxal peadlatx’ics posting, we educated
the pax'euts of the aei^jbouring villages with the help ;f charts,
the need for
i) proper disposal of waste and excreta.
ii) the need for IraaunismtioB
ill) Balanced diet.
iv) anti helminthtio precautions.
v) Portable water.
It: the estate,s we educated, the link workers by giving them
simpxe data about nutrition, sanitation, Inuuunisatiu and common
diseases, who intern are sappased to educate the workers.
Suring our clinical asscuement of children, ’.-re inforised th®
parents, of the sailuxwa*3 inadequacies, their eauste and co ruction,
FAMILY PWKINGj-
Chrativa work:-
be handled the out patient clinic
in Goonoci-, dozing the moming hours.
Boring the IfFMI week, w© were the medical officcra who were
posted at different sport venues.
The congenital heart disease, TEV, Qi>H, these cases we reffered
tn the Coimbatore District Hospital for the necessary treatment.
We brought to the notice of th® Medical Officer, oases which needed
treatment in the estates.
- 2 Oar interest in social paediatries was eahaaced daring SJMC
Hospital posting where— we have already mentioned, we assessed
nutritional status of children among the neighbauring villages,
we were askecTta da a study an the foilawing amongst the estate
warkers.
1. Bauble checking the ICMR pilat project.
2, Respiratory disorders amongst the insecticide sprayers.
J. Link warkers scheme.
We finished the double checking af the ICMR pilot project.
We could not carry aut a study an the inseeticide, sprayers
as all the male Workers are employed in apreying as a part af the
task work. We attended the link voters meeting at different
estates and educated them.
We prepared the falders and its contents for the 'Child Health
Conference’ which was held at UP AS I @n September 2, 1979.
As instructed and guided by Dr, Dara,
S.?Amar, w started
examining children f®r the incidence af aieabrics and pedioulasn
in Glendall estate. But, befare we could camplete the survey we
were requested by Dr. Mrs. Rahamathullah, to assess the Nutritional
status of children belonging to the Devarshola group of estates.
We assessed all the children (100$)
FaAjLY PLANNING*- During sy Family Planning postings, I did 4
tubtfetomies. £k I did not get an opportunity for vasectomy.
Durink my da a no or postings, I did 7 Tub^atomies making it a
total ©f 11 Tubeetomies.
UM
2^
■ J
tew
gSSgS
nnn
pill
ns
iios
I • OS'f)
llllilibSSliiBli
/ A e V M P C -fi(r tv (l
■
1101
- Qihj
1111*
fi'illl
■
(7 ^
!
Mid- mn
ciRccMPe/e^Aj c&
£1
>
IZn>v
siifflBSil
NUTHTTIONAl assessment.
Clinical Analysis of Highwayye—Group, Pff-j-atates*
Name of the estateB,
; Age group.
0-J months*
j
Cloudland.
i
Highwavye.
Upper Maneleer*
Manalaar.
Venniar I.
Venniar II,
Venniar III.
8
8
1
7
]
j
j
Total number
i of children.
4
5
1 a
1 b
1 o
1 d
1
1
..
1
..
..
2 a
2 b
••
••
3 a
3 d
••
3
Hair.
I
Face.
’
i
'
Eyes.
lips.
I
4 a
4 b
I
Teeth.
i
Bin.
I
..
6 a
6 b
8 a
8 b
••
••
9 a
• •
..
I
Najl.
A A
A ‘ti
AA
Mugcular_&
skeletal
gystems.
' 1
••
■•
A*
••
••
A A
AA
••
A*
• A
*A
A A
..
••
••
••
0
;
I
AA
a a
••
••
••
- a
*A
••
1
I
Pyoderma *
P
I
•' «
I
Otitjp.
i
|
..
11 a
11 d
11 8
11 h
11 f
L
.a
••
Pb
••
!
Mo
•*
Soabieo*
..
A* A
i
I
I
••
_k¥TJ.
••
••
••
I
I ••
••
••
••
••
• •
••
••
••
1
••
I
••
••
••
••
i
I
NUTRITIONAL ASSESSMENT.
Clinical Analysis of Highwavys Group__of Elates
I
Name of the estates.
Age group.
Cloudland•
Highwavys•
Manalaar.
Upper Manalaar.
Venniar I.
Venniar II,
Venniarlll
4
5
. . .
Total number
of children.
9
9
9
14
7
1
1
1
1
F
[
I
Hair.
a
b
c
d
3
• •
..
4
2
6
2
ii
Face.
2
••
..
••
• •
I
1
| ■
2 a
2 b
..
• •
Eyes.
..
3 a
3 d
I
Lips.
• •
I
4 a
4 b
••
..
••
Teeth.
B
6 a
6 b
••
..
8 a
8 b
• •
Skin.
■
••
■
''
I
• •
I
Nail.
9 a
..
..
a
d
g
h
f
••
A.
• •
• •
••
• •
0
• >
I
..
••
••
a.
a •
•«
-.
• •
• a
• •
• •
• •
••
••
• •
••
• •
• •
••
••
••
• •
••
••
**
••
Muscular &
skeletal
systems.
11
11
11
11
11
--
1
-.
...
Otitis.
••
••
Pyoderma.
P
LRTI
••
••
1
••
••
• •
••
Scabies.
S
• •
••
Pb
••
••
Me
••
•*
.•
• •
••
I
NUTRITIONAL ASSESSI-IEN.
Clinical Analysis of_Kighwa^s.. Grpup_<^.^o.tes .
Name of the estates.
6-9 months.
Highwavys.
Cloudland.
Manalaar.
Upper Manalaar.
Venniar I.
Venniar II.
Venniar III
i
i
i
Total number
of children.
5
12
7
12
3
7
10
3
6
1
8
1
2
3
4
**
*i
Hair.
1 a
1 b
m
r
~
1
c
d
::
I
i
Pace .
2 a
2 b
i
••
••
Eyes .
..
3 a
3 d
Lips.
4 a
4 b
Teeth.
6 a
6 b
A
••
..
Skin.
8 a
8 b
1
Nail.
9 a
Muscular &
skeletal
figstarns.
i
11 a
11 d
11 ff
11 h
11 f
*i
z
I
Otitis.
0
-
1
Pyoderma..
P
i
••
1
"
LRTI.
1
1
Scabies.
S
Ph
__
I
!
J
i
-----------------------
I
::
...
••
i
NUTRITIONAL ASSESSMENT,
Clinical Analysis of Highws.V£P—P?QUP—PJ ^BtateR.
Name of the estates
Age group
9-12 months.
Upper Manalaar.
Highwavys.
Cloudland.
Manalaar.
j
Venniar I.
Venniar .11 .
Venniar III.
I
1
Total number
of children.
5
13
6
6
3
11 dc
3
.a
••
• •
o a
••
2 a
2 b
• •
-•
3 a
3 d
..
• • •
4 a
4 b
••
24
3
5
1 a
1 b
ml
F
r
8
1
He. ir .
15
3
2
••
6
1
••
• •
Face .
..
••
••
!
..
Eyes .
••
Lips .
• •
••
••
• •*
6 a
6 b
B
a•
• •
!
8 a
8 b
••
9 a
••
••
..
• •
••
..
• •
Skin.
'
I
1
Teeth.
1
..
...
i
• • •
|
Neil.
• •
•.
••
Muscular &
skeletal
systems.
11
11
11
11
11
a
d
g
h
f
|
••
••
•’
1
1
m *
•.
a •
••
Otitis.
Ii
I
i
••
1
1
•a .
*•
••
.*
• a
**
• •
• .
. •
••
•.
••
••
••
••
I
••
..
2
• •
••
••
••
• •
1
. .
• •
••
1
••
••
..
..
••
• •
1
••
S
••
..
..
••
• •
..
Pb
1
..
••
• •
..
Me
1
••
**
••
0
j
Pyoderma.
P
LREI.
I
j
I
Scabies.
i
I
i
I
••
••
I
i
;
>
!
NUTRITIONAL ASSESSMENT.
Clinical Analysis of Highwayye Orgur O.£_gptates.
1
Name of the estates,
Age group.
1-1/2 years.
____ ______ ._______________________________________ ______________ ___ .______
Cloudland.
I
Highwayye.
F
M
F
9
12
17
2
«=>
7
M
F
M
F
M
7
9
9
13
13
4
8
1
6
5
9
6
SB
am
so
'SB
—
ca
Venniar I.
Manalaar.
Upper Manalaar.
M
Venniar II.
M
F
M
F
7
13
6
10
6
6
•
SB
i
Total number
of children.
Venniar III.
F
Hajr.
1 a
1 b
I ■
—
-
1
-
2 a
2 b
—
•
Sb
*
-
I
1
-
3
<a»
<->
*
6
■■
n
8
sb
■B
«•
«=»
■
*
-
1
-
-
1
mm
—
•
*
•
•
•
2
Face.
I
—
—
—
-
-
W
a.
—
I -
6
*
Eyep.
3 a
3 d
-
—
m
—
am
—
—
*
-
■B
-
■B
-
-
•
—
«•
'-a
•
__
—
—
—
—
—
•
•
-
-
-
•
«»
•
so
-
am
SB
—
i
iiR£.
*
•»
—
-»
—
—
—
-
-
-
-
8 b
SB
•
*
—
—
1
1
—
—
•B
9 a
—
mb
—
•
*
•
—
-
-
-
—
*
—
*
•»
*
—
—
*
1
*
1
*
SB
Sb
*
SB
SB
«•
*1
■»
SB
es
«m
-
SB
SB
a*
«»
—
—
—
am
•
M*
•
•»
*»
—
m.
1
1
4 &
4 b
Teeth.
6 a
6 b
I
I
Skin.
—
—
SB
•
—
—
-
M4
ern
—
•
•
SB
•
•
SB
•
MB
MS
*
SB
-
•
1
1
•
Najl.
Muscular A
skeletal
systems.
11
11
11
11
11
a
d
e
h
f
MB
,MB
—
—
I
i
I
1
ate
am
-
sb
MS
•
<a*
OB
otitis.
0
*
■fycdermy..
F
1
•
-
LET I.
i
1
1
-
—
•
1
1
-
-
—
•
-
*
—
•
«»
me
—
*
Scabies,
S
Eb
Me
•
1
-
-
-
—
•
«•
-
—
j
-
|
**
-
I
-
i
i
SB
-
«•
—
—
i
i
Sb
NUTRIIIONAI. ASSESSMENT.
Clinical Analyais of Highwevys Grpup 2.f_Eatgt£g
Name of the estates,
Age group.
1/2-2 years.
Cloudland.
M
Highwavye.
M
F
F
Manalaar.
Upper Manalaar.
M
M
F
F
Venniar I.
M
1
9
4
10
3
3
em
me
cm
-
8
•
*
1
8
M
F
M
F
12
11
4
10
8
cm
7
•
3
•m
7
••
me
me
em
me
**
3
me
m.
cm
*
*
—
•
me
•
—
*
*
me
1
—
1
1
•
—
6
15
14
11
13
3
3
cm
em
6
•
12
1
me
cm
-
—
6
•
■»
1
5
m»
«•
—
^7'
me
cm
cm
me
cm
8
1Venniar III.
J
I
Total number of
children.
Venniar II.
F
Hf;lr.
1 a
Jm
11 bo
wF
1
d
5
1
*
1
-
Fee?.
2 a
2 b
•»
me
«=»
-
-
1
3 e
*
*
■e
-
1£®£.
3 a
•
4 a
am
C»
4 b
•
•
6 a
6 b
*
8 a
*
am
me
me
•
-
am
-
me
I
line.
i
me
1
7!*
I
—
A*
*
<m
cm
1
-
1
am
me
—
1
me
*
•
*
w
1
1
Teatfa.
f
P
I
cm
1
•
Skin.
I
8 b
/
4
*
-
•fl
am
me
T
1
K>
me
Wail.
9 a
-
i
Muscular &
Skeletal
systems.
11a
11 d
11 g
11 h
11 f
j
/
cm
cm
*
me
me
me
cm
-
—
*
am
me
me
me
cm
me
me
me
*
am
me
me
«.
1
cm
m
ami
*
*
•
*•'
-
•
-
*
1
1
—
me
1
*
3
«
i
2
■m
me
-
*
Otitis.
0
1
1
j1
2S21.
|=
Scab!eg.
i
1
1
1
1
1
2
-
me
- ■
-
-
i
i
Pyoderma.
2
1
me
am
*
1
—
-
ir
-
•
8
-
*
•
-
-
•
-
-
-
Fb
-
-
•
me
-a
-
-
-
-
•*
•
-
*
•
F
Me
i
*
*
—
cm
I
-
j
-
-
•
•
i
-
1
-
•
I
“
.
-
—
*
T
!
-
NUTRITIONAL ASSESSMENT.
Clinical Analysis pf Hi^hwavys Group, of &afatep
Name of the estates.
Age group.
2-2/2 years.
Cloudland.
M
:
Upper Manaleer.
Highwavys.
T
M
F
M
:
<
F
Venniar I.
Manalaar.
M
F
M
Venniar III
Venniar II.
F
M
F
M
F
3
6
,0
2
2
7
1
i
t
3
12
13
9
8
3
6
a*
10
•
•
2
•
—
-
4
-
1
6
I
i
«•
1
s
7
2
5
9
3
-
’
—
-
;
—
1
*
*
5
—
1
-
-
-
—
—
I
-
—
-
■
I
A.
-
-
face.
2 a
2 b
1
-
-
1
-
I
Eyes.
—
-
I
I
-
I
3 a
3 d
-
•
-
-
-
—
1
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
-
Lips.
-
-
•s
—
-
-
*
-
-
-
4 a
4 b
Teeth.
I
6 a
6 b
-
1
1
—
-
Skin.
8 a
8 b
-
-
1
2
—
—
1
1
1
—
1
-
-
1
-
2
I
—
-
-
1
1
-
-
-
-
-
*
-
-
-
-
-
-
-
-
-
-
-
—
•m
*
*
—
—
—
_
*
—
—
a*
-
-
-
-
-
*
•
-
«*
1
-
-
-
-
-
-
-
-
1
—
-
-
-
-
-
1
-
-
Nail.
-
-
Muscular ft
skeletal
systems.
—
—
-
1
••
—•
—
1
!•
2
—
1
-
«>
•
-
-
Fyoderma.
f
lrti.
■Scabies.
S
-
-
-
2
1
—
—
-
-
-
-
•
-
-
•
-
-
-
•
•
I
-
1
-
1
_
-
—
i
1
-
—
*
-
1
—
•
-
-
•
-
-
-
NUTRITIONAL ASSESSMENT.
Clinical Analysis of Highwayyg Grpup. of ggtat^p..
Name of the estates,
V
( Age group,
; if 2 - 3 years,.------------------------------------------------------------------- --------------------------------------------------------------------- ~-------Cloudland•
M
Manalaar.
Upper itonalaar.
Highwavys.
|
Venniar I.
Venniar II.
Venniar III,
F
M
F
M
F
M
F
IH
F
M
>■
M
F
5
9
10
12
11
8
12
3
3
4
5
10
5
2
•a
7
—
2
-
3
3
4
2
1
—
as
■s
as
*
mb
<=»
1
*
*
3
•B
1
•
•B
2
■a
*
1
*
1
—
-
*
■
Total number
of children.
2
i
Hair.
1 a
1 b
1 c
1 d
1
*»
—
2 a
2 b
*
«-
—
*
•»
•B
SB
MB
MB
-
*•
?£££*
as
—
—
•
-
*
M
T
-
—
«M
-
BM
*
*
*
1
as
I
*
*
“
I
Eyes ,
•
-
*
•
•
-
M
SB
n.
as
*
•
as
3 a
3 d
*
!
se
*
as
mb
•
-
Lipp.
4 a
4 b
an
M
<s»
as
•s
1
1
1
•
—
1
,
■B
*
•
•U,
*
1
MB
I
Teeth.
I
6 a
6 b
*
1
1
-
—
-
-
MS
1
st
as
—
•
Skin.
SB
8 a
8 b
■SB
1
*■
1
n
1
•
1
1
1
j
Mail.
*
09
1
•
I
i
a>
9 a
Muscular &
Skeletal
pystemp.
11
11
11
11
11
a
d
g
h
f
MB
—
•a
•»
•
!
0
—
*
«B
as
an
m
■»
*
•s
as
■a
*
*
*
*
'SB
*
•i
-
•
1
1
-
*
*
•
—
•
-
-
1
-a
—
MB
1
*
-
-
as
-
SB
1
-
as
SB
«a
*
SB
I
as
SB
a
•a
1
MB
MS
•
*
*
*
»
MB
M.
-
•
•
*B
•
SB,
-
«W
1
•
SB
*
•
i
*
!
Pyoderma.
£
LRTI.
-
—
M
•
!
1
-
as
’
-
-
-
•
•
-
*
!
I
1
Scabjeg.
S
-
-
—
Pb
*
-
•
Mo
|
I
—
1
I
-
SB
-
•
*
SB
-
-
•
-
-
-
-
•
*
-
•
NUTRITIONAL ASSESSMENT .
Clinical Analyste c>f E ighwavys_ Group Q^-EstgteB•
Name of the estates •
Age group.
3-4 years.
I
■
.
;
Upper Manaleer.
Highwavye.
Cloudland•
Venniar I.
Manalaar.
F
M
F
I
M
F
M
F
M
15
16
21
16
13
23
37
23
9
t
5
2
7
7
14
-
-
1
:
’
F
17
7
Venniar II. j
Hair.
17
6
Venniar III.
I
M
F
9
15
11
5
2
4
1
—
1
-
i
!
Total number
of childrezi.
a
F
:
■
2
1
b
a
r
•
1
,
1
d
-
Face.
2
!
—
*
-
-
i
2
•
2
1)
-
Eyea.
-
3
5 d
-
-
-
-
1
-
-
-
i
-
i
1
I
-
I
2
I
-
1
-
2
”
Lips.
4 a
4 b
Seeth.
6
6 b
B
—
—
*
•
—
2
3
2
1
2
-
1
2
1
—
SB
SB
—
—
w
1
1
•
3
-»
-
—
—
—
—
4
1
•
•
—
-
—
—
2
1
1
-
-
w
2
i
Skis.
8 a
8 b
-
—
1
SaU-
I
0
F
1
w.
—
—
*
—
*
«»
—
-
-
1
"•
1
-
2
3
-
-
2
1
1
*
2
*
I
*
2
1
i
—
!
—
*
1
—
—
*
*
*
—
1
*
I
i
2
1
1
-1
1
I
Sb
I
e
MB
i
-
-
1
-
-
-
-
-
I
'
1
5
i
I
I
2
1
■»
!
i
1
—
|
I
5
1
i
I
"
*
—
*
I
I
I
-
1
-
1
•
1
-
-
*
•
•*
•*
1
-
I
s
Eb
*
I
Scabies.
* i
1
3
I
FyodermiL.
LET I.
-
5
(
Muscular &
skeletal
systems.
otit14.
I
i
o
11 A
11 d
11 g
11 U
—
4
1
-
1
-
-
-
-
I
I
I
I
i
-
-
-
-
-
*
-
-
-
—
-
1
NUTRIIIONAL ASSESSMENT.
Clinical Analysis of Hjghwavys Group of JBgt^tes.
!
J
I Clcudlana.
.Ago group.
4-5 year
Iteme of the estates,
Eighwavys.
Manalaar.
Upper Manalaar.
!Venniar I.
Venniar II.
Venniar III.
M
F
M
F
M
F
M
F
M
F
M
F
K
F
6
13
23
20
15
13
37
48
7
8
13
22
8
16
a
b
c
d
•»
••
—
4
1
••
—
2
*
11
—
2
*
*
•
4
a
m
<•
11
-
—
«•
—
22
2
••
—
—
••
6
—
—
1
2 a
2 b
—
-
*
—
*
—
a.
—
-
*
«e
-
1
<»
—
3 a
3 d
-
-
<=>
1
-
1
Total number
of childrei1>
Sala:.
1
*
1
2
I
1
••
—■
2
*
i
*
*
face .
-
Syeg.
1
-
•
Teeth.
-
-
-
•
-
1 3
1
2
1
5
z
1
3
1
1
-
|
I
1
-
I
6
6 b
U
w
i
I
2
1
!
Iiips .
4
4 b
2
—
\
*
2
1
5
1
2
2
1
2
I
8 a
8 b
-
—
j
1
—
—
4
—
8
i.
2
4
r
i I
9a
—
-
-
-
•*
!
!
11
! i-
11
—
-
!i
-
-
—
—
Ptitis.
I
3
2
1
-
-
—
—
—
—
—
*
1
:
—
—
P
;
1
—
-
-
1
•
-
8
-
-
-
-
Pb
1
-
-
-
1
1
2
\
—
3
3
I
a.
* -
-
I
-
I
-
-
—
1
-
-
I
!
*
-
w
«a
i
1
1
-
2
-
1
i
—
-
1
j
I
flEpder^a •
1221.
’
I
-
•
0
2
.1
. -
I
i
i
iKpletal
gyptems.
d
S
h
f
-
- ’■
I
Nail.
-
;
-a
•
1
-
1
2
Scabies.
/'
Mo
-
-
■
-
-
I
-
I
-
—
-
-
.
—
•
-
]
i
•
-
2
KEYtHair.
1 a 1b1c1 d -
Lack of lustre Thinness end sparseness.
Dyspigmentation of proximal part of hair.
Flag sign.
Easy pluckability.
Face.
2 a - Diffuse depigmentation.
2b- Naso-labial dysseb&cea.
Eyes.
3a- Xerosis conjunctivae.
3d- Angular palpebritis.
Lips.
4 a - Angular stomatitis.
4b- Angular scars.
Teeth.
6 a - Caries.
6 b - Mottled enamel.
Skin.
8 a - Xerosis.
8b- Follicular hyperkeratosis, types 1
Mail.
9 a - Kollonyohia.
Muscular and Skeletal_systems.
11
11
11
11
11
a
d
g
h
f
0
P
LRTI
S
Pb
Me
ss.
27-2-1980.
- Frontal and parietal bossing.
- Knock-knees or bowlegs.
~ Eiseon chest.
- HariBson'e sulcus.
-
Otitis.
Pyoderma.
Lower Respiratory tract infection.
Scabies.
Mo Hue cum ContaglOB,„m.
and 2.
HEIGHT
Name o_C jj/S’ta'te/
Division.
0-3 months.
N
207
51.75
Total
Mean.
N
Total
Mean.
9 N
12 months
’Total
Mean.
GROUP___ ~___ 12121
1 yeat to 11/2 years.
172 years to 2 years.
Male
Female
Male
Female
NTT6tal~l "Flean? nTTo^ aTTean? -N~TTo^aI” "Mean N |T6EaI Mean?
9
525
58.3
5
314
62.8
5
342.5 68.5
7
501.5
71.64
9
638
70.9
9
695
77.2
8
628
78.5
5
272.5 54.5
9
532
59.1
12
786
65.5
13
892.5 68.7
9
639
71
13
921
70.84
4
298
74.5
0
751
75.1
Manalaar
8
423
52.88
14
841
60.07 12
770
65.16 24
1638
68.25 12
864
72
17 1188
69.88
15
1129
75.27
1016
72.57
Upper Manalaar
3
158
52.66
7
408
58.3
7
431
62.71
6
403
67.16 13
927
71.3
9
616
68.44
8
615
76.87 6
431
71.83
Venniar I (a)
3
153
51
5
291
58.2
3
187
62.33
3
195
65
2
129
64.5
5
350
70
4
295
73.75 8
580
72.5
Venial-
5
24-3
48.6
4
230
57.5
-
2
129
64.5
1
70
70
2
138
69
7
535
76.42 5
358
71.6
Veniar II
1
53
53
4
222
55.5
7
451
64.43
8
522
65.25 13
875
67.31
6
425
70.83 12
861
Veniar III
7
358
51.14
5
295
59
10
631
63.1
8
532
66.5
692
69.2
6
398
66.33
4
292
71.75 11
73
j' 10
805
714
73.18
71.4
1867.5 51.88 57
3344
58.67 56
3570
63.75 69
4654
67.44 67 4697.5
70.1
67 4674
69.76 63
4720
74.9 ; 72 5283
73.38
- .
-
-
70.8
74.2 ;!
J
73.3
I
(b)
Group Total:-
36
Deli Study
57.4
All-India.
Name o±'
Estate/
Division.
'
N
-___ HIGH WAVYS
Highwavys
Cloudlgnd
1
Mean.
AGE
6—9 months.
3 - 6 months.
Total
FOR
-
-
-
-
!
____2’7 2 years to 3_years .___
2 years to 2^/2 years.
-----_ ___
N
Total
Mean.
N
Toia.1
Mean.
Total
N
Mean.
Total
N
Mean.
N
Total
Mean.
2002.5
87.06 37
3476
98.94 48
4923
102.56
2017
87.69
15
1400
93.33 13
1213
93.30
6
520
86.66
4
378
94.5
289
96.33
15
1325
88.3
82.8
21
1879
89.47
Manalaar.
6
466
77.67
552
78.86
8
681
85.13
12
982
81 .83 36
3309
Upp er: -Manalaar.
9
706
73.4
8
613
76.62 12
980
81.66 1 1
883
80.27 13
1135
1
80
30.0
4
301
75.3
2
169
84.5
77
77.0
792
88.0
1
6
,463
77.17
47
3704
78.8
Groy.p Total:-
Delhi Study.
All-India.
73.2
74
74.0
1
;
90
90.0
2
171
85.5
8
684
85.5
230
76.67
4
■
318
79.5
3
241
80.33
17
1497
10
756
75.6
i 10
830
83
5
4oo
80
88.06
I 87.07
52
4041
77.7
48
3971
77.9
i
82.73 49 3988
81.39
81 .8
85 • 8
1306
13
Mean,
87.30 23
81.2
828
___
Total
89.43 23
406
10
Veniar III.
N
94.4
5
82.33
77.89
Mean
94.35
31
741
83.0
87.7
Female
Total
1887
162
9
83
N
1227
2
81.38
701
Mean •
95.12 20
76.2
1058
1
4 years to 5 years.
Male
91.3
457
13
9
1403
-
L
548
6
80.83
Veniar II/
[16
Total
-
2188
78.3
970
9
N
=
6
235
Veniar l/b)
-
. 85.62 23
3
12
1
69.3
-
1370
Cloudland.
(^)
-
M ale___________________ Female_________
Highwavys.
Veniar I
-
_______ 3 years to 4 years.___
Male___________________ Femal_________
Female
Male
69.0
66.5
63.O
10
16
'
1
92
92.0
3
272
90.66
473
94.6
9
780
86.67 13
1233
94.85
12
2046
93.0
11
972
88.36
728
91
16
1493
93.3
135 11,927 33.35 105 9156.5 87.2
86.2
84.9- '
109
10,223 93.79
■
93.9
140 13,551
96.79
92.6
for
0
3 months.
3
-
Me an.
N
age
9 months.
6 months.
6
Total
Me an.
N
Total
Me an •
Name of Estate/Div.
N
Total
HIGIIUAVYS group -
-
1979.
,9 - 12 moriths. _ 1_ Year to 1''/2 years.
Male
Female
N" "To^al
w“ "ToTal"1 "Mean7
Mean.
N Total Mean.
11'2 years to 2 years.
Female
Male
FTotal
ean. "n To^al" Mean
.Cloud Land
4
17.5
4.33
9
5-1.7
5.74
5
32.5
6.54
5
37.0
7.4
7
55.7
7.96
9
69.2
7.7
9
84.6 9 4
8
74.7 9.33
High.'.Wavys
5
18.8
3.76
9
48.3
5.37
12
80.1
6.68
13
89.3
6.87
9
76.0
8.44
13
102.5
7.83
4
34.3 8 57
10
84.5 8.45
Manalaar
8
33.4
4.18
14
79.9
5.71
12
78. 1
5.58
24
185-9
7.75
12
97.9
8.16
17
131.5
7.74
15
138.4 9 23
14
1 14.2 8.16
Upper Manalaar
3
8.83 2.94
7
33.9
4.84
7
43.5
6.21
6
42.3
7.05
13
103.6
7.96
9
66.6
7.4
8
72.8 9 06
6
50.1
3
19.4
6.46
3
19.4
6.46
2
14.6
7.3
5
35.5
7.5
4
33 • 2 8 3
8
66.2 8.27
5
39.2 7.84
Veniar I
(a)
3
11.1
3•7
5
26.8
5.3o
Veniar I
(b)
4
19.6
4.9
-
-
-
2
13.4
6.7
1
7.5
7.5
2
15.0
7.5
7
62.8 8 97
17.6
4.4
7
46.9
6.7
8
54.3
6.79
13
100.0
7.69
6
45.4
7.57
12
97.7 8
5
25.2
5.04
10
62.1
6.21
8
59.6
7.45
10
78.7
7.87
6
42.1
7.02
4
32.1
57
311.0
5.46
56
362.6
6.48
69
501.2
7.26
67
533.9
7.97
67
507.8
7.58
63
-
-
-
-
-
-
7.8
-
-
7.3
-
-
5
17.5
3 •5
Veniar II
1
4.3
4.3
Veniar III
7
28.0
4.0
Group Total;Delhi Study
36
-
All-India
139.43 3.87
-
4.8
-
-
6.2
-
-
-
-
-
-
-
2 Years to 21/2 Years.
Name of Estate/Div.
"
6.9
21/2_years
Female
"Total] Mean.
Mai.e
“n“‘ tsezi "Mean.
-
N
-
-
7-6
-
-
-
-
-
to 3 Years.
3 Years to h years.
8 03
88.8 8.1
78.6 7.86
10
555.9 8 82 72 596.3 8.28
8 5
-
-
-
-
8.0
4 years to 5 years.___
Female
Male
iBSal" "Mean? " n“ "Total" "Mean
Female
"ToTal" "Mean?
Male
"Total" Mean •
-
14 11
8.35
_Male
Female
—v" "Total" Mean? "n"]T6T al Mean
Cloud Land
3
27.7
9.2
6
53.3
8.9
2
18.8
9.4
5
50.5
10.1
15
167.3
11.2
16
177.7
11
1
6
12.68
13 198.8
12.2
High Wavys
12
121.1
10.09
13
121.1
9.31
9
88.8
9.36
10
97.6
9.76 21
255.7
12.17
16
178.6
11
16
23
304.0 13.21
20 257.6
12.88
76.1
Manalaar
6
54.9
9.15
7
67.2
9.6
8
88.6
11.07
12
124.2
10.35 37
443.3
11.98 23
272.8
11
86.
37
505.7 13.66 48
638.7 1 1330
Upper Manalaar
9
88.3
9.8
8
72.0
9.0
12
124.9
io.4o
11
111.4
10.12 13
155.1
11.93 23
269.9
11
73
15
195.0 13.0
13
171.0
13.15
43
53.0 13.25
3
45.1
15.0
3
36.3 12.1
5
65.9
Veniar I
(a)
1
10.4 10.4
4
36.6
9.15
2
20.7 10.5
1
10.0
10.0
9
105.5
11.72
6
68.6
11
Veniar I
(b)
1
10.7 10.7
1
8.1
8.1
1
12.1
12.1
2
22.4
11.2
8
84.6
10.57
1
12.5
12 5
Veniar II
9
85.2
9.47
3
28.4
9.47
4
38.0
9.5
3
30.1
10.03
17
200.0
11.76
9
100.1
11
12
13
106.8 12.98 22 282.8
Veniar III
6
58.8
9.8
10
89.3
8.93
10
106.15 1 0x62
5
47.7
9.54 15
167.4
11.16 11
127.1
1 1 55
8
97.5 12.19
493.9
10.08 135
Group Total;-
47
457.11
Delhi Stury.
All-India.
-
9.73
52
476.9
78.2
-
-
77.9
-
-
-
-
9.15
48
-
498.1
10.38
-
81.8
-
-
49
-
85.8
1573.9 11.7
105
1207.3
-
-
-
-
-
-
-
86,2
-
-
1 1
5
109 1436.4 13.18
16
84 9
-
93.9
209.6 13.1
140 18?) .5
-
13.8
12.85
13.07
-
-
-
92.6
CHEST
lame of Estate/
Division.
Total
Mean.
N
Total
Mean •
N
Total
Mean.
- high wavys gaoup - 19?9»
N
Total
Mean.
1 year to 11/2 years.
- TotalMaAean.
Tota?a^Fiean.
N
N-
9 -
6-9 months,
3-6 months.
0-3 months.
N
CIA CL 2-xE2?A^=~~- CL I1 'oi< age
12 months
44.2
N
11/2 years to 2 years.
Totafle]ftean.
Me an •
N
Cloud Land.
4
143.5
35.88
9
352
39.1
5
203
40.6
5
217
43.4
7
309.5
9
337.5
43.1
9
426
47.3
8
372
46<2
High Wavys.
5
180.5
36.1
9
349
38.78
12
505.5
42.13
13
558.5
42.96
9
397.25 44.13
13
574
44.15
4
191.5
47.87
10
454
45.4
Manaliar.
8
282
35.25
14
545
38.93
12
488.5
40.7
24 104-9.5
44.15
Upper Manalaar. 3
110.5
36.83
7
272
38.85
7
287
41
6
(a). 3
101.5
33.83
5
195
39
3
122
4o.66
3
(b).
Veniar
(l)
43.73 12
519.5
43.29
17
732.5
43.08
15
663.5
44.25
14
574
249
41.5
13
569.5
43.8
9
382
42.4
8
365.5
45.68
6
260.5
43.41
125
41.66
2
84.5
42.25
5
21 1
42.2
4
176.5
44.1 2
8
349
43.63
83.5
5
1 71
34.2
155
38.75
-
-
2
41.75
1
44
44
2
87.5
43.75
7
323
46.85
5
221
44.2
Veniar II.
1
35
35
4
152.5
38.13
7
301.5
43.1
8
339
42.4
13
575.
44.2
6
267.5
44.58
12
549.5
45.79 11
493
44.82
Veniar III.
7
247
35.29
5
199
39.8
10
413
41.3
8
346
43.25 10
6-
262
43.67
4
182.5
45.63
443.5
44.35
Group Total;-
36 1271
All-India.
-
Veniar (l)
35.30 57 2219.5
-
-
38.93 56 2320.5
-
-
-
-
-
41.43 69 2937.5
-
-
42.57 67 2948.75 44.01
2 year’s to 2’72 years.
J
female
Male
- '“Tot all
'
Total
Mean
•
Mean.
n‘
Division.
2V2 years to
Male
"Total
Mean, _
-
-
-
43.1
67 2904
-
-
10
43.34 63 2883
45.76 72 3167
43.98
42.1
44.5
43.4
-
-
-
-
=== ======== ======*=== ===== = =:C=== = =S == b======= k===== L= = :i======= L=======J
s.'ZS-ss —=========== === ======== ====== === L= = ====== ======:=== fe======== ====== I= = :
Name of Estate/
449.5 44.95
i years to 4 years.
[ale
Jfemale
Total Mean. ~N~*"Total rMe an.
ye ars.
female
Total"' ‘Mean.
4 years
to
Male
N' "Tot al" f Mean"
5 years.
Femetie
N“ "Total" Me an.
6
13
Cloud Land,
3
140
46.70
6
270.50 45.10
2
47.50
239
4-7.80
731
48.70
16
760.50 47.50
High Wavys.
12
575
47.91
13
594.50 45.73
9
446.50 49.61
453
45.30
21
1043.5
49.69
16
769.5
48.09
Manalaar.
6
284
47.33
7
319.5
45.64
8
389
48.63
561.5
460.75
36
1758.5 48.84 23
1117.5
48 »58 36 1824.4
50.67 47 2310
557
95
301.50 50.25
1165.5
50.67 20
9
415
46.11
8
358.75 44.84 1 2
46.41
500.5
45.5
13
622.5 47.88 23
1098
47.73
15
738
49,2
Veniar I
(a).
1
45
45
4
175.5
43.87
2
93.5
46.75
46
46
9
425
47.22
6
281.1
46.91
4
196
49
Veniar I
(b).
1
50
50
1
46
46
1
50.5
50.5
97.5
48.75
8
390
48 • 75
1
.50
50
3
146.5
48.83
49.9
9
439.5
48.83
13
11
542.15 49.34
Uppez? Manalaar
9
430
47,78
3
143
47.67
4
192
48
142.5
47-5
17
834.5
Veniar III.
6
283
47.17 10
462
46.2
10
485
48.5
239
47.8
15
727.25 48.48
Group Total;-
47 2222
48.09
2279
46.51
134 6532.25 48.74 105 5058.
65
48.18
45.5
48.1
46.9
. Veniar II.
J
All-India.
47.27 52 2309-75 45.57 48 2308.5
45.4
-
:L= =
N
sspd.
19-2-1980.
-
44.4
46.6
= = =======
=
No,
of children.
657.5
50.58
410.5
51 .31
108 5439.
9
1
13
626.75 48 .20
973.5
48.67
'49.14
635.5
48.88
151.5
50.5
1032.55 46.93
798.5
49.9
50.36 139 6685.
48.82
49.6
48.6
16
4
MID-ARM
Name of Estate/
Division.
3-6 mon ths.
6-9 months.
Mean.
N
Total
Total
0-3 Months,
N
Total
CIRCUMFERENCE FOR AGS
Mean .
Mean •
-
HIGHWAVYS GROUP
9 -12 months .
N
Total
Mean.
N
1979.
-
____
1 Year to 11/2 Years.
Male.
Female.
Total" "Mean? “"n" Total" Me cin.
1'1/2 years to 2 years.
Male.
Femal e.
"ToEal" Mean'
N-'"Total"! "HeanV"""""
Cloud Land.
4
42.25
10.56
9
109.5
12.17
5
61.5
12.3
5
60.5
12. 1
7
89
12.7
9
111.5
9
115.5
12.8
8
104
13
High. Wavys .
5
50
10
9
102
1 1 .3
12
145.5
12.13
13
156.25
12
9
114.25
12.69
13
164.75 12.67
4
51.25
12.81
10
127
12.7
Manalaar,
8
83.5
10.44 14
161.5
11.54 1 2 145.5
12.12 24 300.25
12.51
12 149.5
12.46 17
212.5
12.5
15
1 94
12.93
14
165.5
12.73
Upper Maiaiaaar .
3
34
11.33
76.5
10.92
7
82
11.71
6
72.5
12.08
13
1 62.5
12.5
9
111
12.33
8
103
12.87
6
74
12.33
9.33
57
11.4
3
36
12
3
34.5
1 1.5
2
25.5
12.75
5
61
12.2
4
50.5
1 2.6g
8
100.5
12.56
11 .5
7
Veniar I
(a).
3
28
Veniar I
(b).
5
12.4
5
48.7
4
47.5
11.87
-
-
-
2
24
12
1
12
12
2
23
87
12.42
5
60.5
12.1
Veniar II.
1
10.5
10.5
4
42.5
10.63
7
88.25
12.61
8
95
11.88 13
159
12.24
6
72.25 1 2.04 12
145.5
12.13
11
133
12.09
Veniar III.
7
72.5
10.36
5
56»J
11.3
10
118
11.8
8
100.9
12.61
10
128.5
12.85
6
72
12
48
12
10
122.9
12.29
12.23 67
840.25
12.54 67
828
72
887.4
12.32
-
12.5
Group Total;Allilndia.
36 369.45
9.74
10.26 57
-
-
2 ye ars
Male.
Name of Estate/^
Division,
653
11 .45 56 676.5
-
-
0 21/2 years.
Female.
12.08 69 843.9
-
Male.
-
12.1
794.75 12.61
-
& years to 5 years.
Male.
Female.
3 years to 4 years.
Female.
N Total
Mean.
N
Total
N
Total
Me an.
Total
Mean.
15
196.25
13.1
16
214.95
6
81
13.5
177
13.6
127
12.7
21
282.5
1'3.45
16
216.75
13.54 23 323.75
14.07 20
277.5
13.87
157.75
13.15 36 482.75
13.4
23
315.7
13.72 36 502.3
13.95 47
652
13.87
1 1
144
13.09
13
13.88 23
302.5
13.15
207.5
13.83 13
187
14.38
12.5
1
■13
13
9 1 19
13.22
6
78
12
4
56
14
3
46
15.33
13
2
26.25
13.12
8
12.88
1
13
13
3
40.5
13.5
5
71
14.2
53.5
13.38
3
39.5
13.17 17 230.75
13.57
9
120
13.33
13. 013.25
13.33 22
307
13.95
10 135.5
13.6
5
67
13.4
11
148.25 13.48
8
107.25
13.41
16
225
14.06
639.75
13.05
13.42 108 1491 •
55
14.4
13.81
13C
1942.5 13.97
12.66
13
164
12.61
9 1 24
Manalaar.
6
77.5
12.92
7
92
13.14
106
Upper Manalaar.
9
118
13.11
8
105
13.12 12 155
12.91
Veniar I (a).
1
13.5
13.5
4
50.5
12.62
2
(b).
1
13.5
13.5
1
12
12
1
Veniar II.
9
115.5
12.83
3
38.5
12.83
4
Veniar III.
6
78.5
13.08
10
124.25
1 2.43
47 60 4
12.35 63
13.05
12 152
Group Total;-
-
Me an.
76
All-India.
■
65.25
6
Veniar I
Male.
12.5
Total
1 1.8
High Wavys.
-
-
12.5
Me an.
Total
-
Me an,
Me an • __ N __ Total
Total
3
-
21/2 years to 3 years.
Female.
35.5
Cloud Land.
-
4
25
25
13.77
10
13.25 1 2
12.85 52 662.75
12.74 48 637
13.27 49
13
12.8
13
13
180.5
103
201
13.4
13zI- 1795. 13.40
LL
13.4
105
1409.15
Me an«
14
'I
13.9
MID-ARM
N
0-3 Months,
r
TotalI Mean .
CIRCUMFERENCE FOR AGE
3-6 mon ths•
N
Total
Mean.
Total
Mean.
HIGHWAVYS GROUP
9-12 months .
6-9 months.
b
-
Total
Mean.
N
1979«
-
1 Year to 1-l/2 Years.
Male.
Female.
Total Mean.
N
Total
Mean.
l"/2 years
Ma le.__
"ToEal-'"Mean’
to 2 years.___
Femal e.
Total He an.
Cloud .Land.
4
42.25
10.56
9
109.5
12.17
5
61.5
12.3
5
60.5
12.1
7
89
12.7
9
111.5
1 2.4
9
115.5
1 2.8
8
104
13
High Wavys.
5
50
10
9
102
1 1 .3
12
145.5
12.13
13
156.25
12
9
114.25
1 2.69
13
164.75
12.67
4
51.25
12.81
10
1 27
12.7
Manalaar,
8
83.5
10.44
14
161.5
11.54 1 2 145.5
12.12 24 300.25
12.51
12 149.5
1 2.46
17
212.5
12.5
15
1 94
12.93
14
165.5
12.73
Upper MaAaAaaar .
3
34
11.33
7
7b. 5
10.92
7
82
11.71
6
72.5
12.08 13 1 62.5
12.5
9
111
12.33
8
103
12.87
6
74
12.33
9.33
5
57
11.4
3
36
12
3
34.5
11.5
2
12.75
5
61
12.2
4
50.5
12.6g
8
100.5
12.56
7
Veniar I
(a).
3
28
Veniar I
(b).
25.5
5
48.7
4
47.5
11.87
-
-
-
2
24
12
1
12
12
2
23
1 1 .5
87
12.42
5
Veniar II.
1
10.5
10.5
4
42.5
10.63
7
88.25
12.61
8
95
11.88 13
159
12.24
6
72.25
1 2.04 12
145.5
12.13
11
133
12.09
Veniar III.
7
72.5
10.36
5
56»5
11.3
10
118
11.8
8
100.9
12.61
10
128.5
12.85
6
72
12
48
12
10
122.9
12.29
12.23 67
840.25
12.54 67
828
794.75 12.61
72
887.4
12.32
12.7
4
-
1 2.5
Group Total;All-^India.
36 369.45
9.74
10.26 57
653
-
-
-
-
-
1 1.45 56 676.5
2 years to 2 72 years.
Female.
Male.
IS
Total
Mean.
35.5
K
Male.
Total
Mean.
-
-
-
-
£1/2 yea rs to 3 years.
Female.
N
Total
Me an <
25
-
Male .
N
Total
Mean,
N Total
Mean.
177
13.6
277.5
13.87
13.15 36 482.75
13.4
23
315.7
13.72 36 502.3
13.95 47
652
13.87
13.09 13
13.88 23
302.5
13.15
15 207.5
13.83 13
187
14.38
15.33
65.25
13.05
15 196.25 13.1
10
127
12.7
21
Manalaar.
6
12.92
7
92
13.14
8 106
13.25 12
157.75
Upper Manalaar.
9118
13.11
8
105
13.12 12 155
12.91
11
144
Veniar I (a) .
1
13.5
13.5
4
50.5
12.62
2
25
12.5
1
13
(b).
1
13.5
13.5
1
12
12
1
13
13
2
26.25 13.12
Veniar II.
9
115.5
12.83
3
38.5
12.83
4
53.5
13.38
3
39.5
13.17 17 230.75
Veniar III.
6
78.5
13.08
10
124.25
12.43
10 135.5
13.6
5
67
13.4
13
13
639.75 13.05
-
13.5
14.07 20
5
13.77
13.27 49
31
Totalj Mean.______
13.54 23 323.75
12.5
9 1 24
12.74 48 637
Me an.
13.4
2
12.61
12.8
Total
216.75
12.7
164
13
Mean. __ N
214.95
76
13
12.85 52 662.75
Total
16
6
12.66
47 6o4
N
16
11.8
Group Total;-
====== ======*====== :========
1'3.45
3
12 152
All-India.
12.1
4r years to 5 years.
Male.
Femal e.
3 years to 4 years.
Female.
Cloud hand.
Veniar I
-
12.5
High Wavys.
77.5
12.35 63
12.1
L=== = ======:==== = = :
:====== = = =:±======= ======= :=== ======== b=====
-== = :
-
-
=================='=== =--—-= 4=== ==:J===: = = == = = = !=====:
Name of Estate/.
Division.
12.08 69 843.9
4
60.5
13
282.5
180.5
13
9 119
13.22
6
78
12
4
56
14
3
46
8
12.88
1
13
13
3
40.5
13.5
5
71
14.2
13.57
9
120
13.33
13.0 1/3.25
13.33 22
307
13.95
11
148.25 13.48
107.25
13.41
16
225
14.06
1409.15 13.42 108 1491 •
55
1^.4
13.81
13C
1942.5 13.97
14
-
103
15 201
J
6
13.4
134 1795. 13.40 105
75~
13.4
-
8
-
5
13.9
3
SffAP
Name of Estate/
Division.
0_2_3_mc nths4_ __ _3 _2_6 mon ths.
N
Cloud .Land
4
High Wavys
;
Manalaar
1
Upper Manalaar
Total
Mean.
N
Total
143.5 37.13
9
362
183.5 36.7
9
£2fi-AGg , HXGHWAVYS GROUP - 1979
12jmonths.
I------- -- 9 months.
Mean.
N
Total
40.2
5
12
208
41.6
§
39.28
508
42.3
13
Mean.
N
Mean.
N
1 year to Tj/2_year S .
Male’
Female?
Total ‘Mean.
Total Mo an •
216
43.2
561.21 43.17
7
9
312.5 44.64
9
403.5 44.83 13
1051.8 43.82 12
.Total
— 1^2 years to 2! years.
Male.
Female?
•f—------- —
| Total f Me an.
Total Mean.
F2
389.5 43.28
44.07
573
9
4
415.'
182
46.2
45.5
8
10
8
295
36.88
14
556.5 39.75
12
501 .3 41.78 24
536
44.67 17
754
44.35 15
682.:
45.5
3
114.5 38,16
7
276
39.42
7
291 .5 41.64
6
253.5 42.25
13
577
44.38
9
386
42.88
8
362.5
45.31
5
200
4o
3
123.5 41.16
3
128
42.66
2
86.5 43.25
5
215
43
4
175.5
43.62
-
-
1
44
2
37.5 43.75
7
321
43.67 1 2
Veniar I
(a)
3
104
34.66
Veniar I
(b)
5
175
35
4
157
39.25
Veniar II
1
37
37
4
152
38
Veniar III
7
257.5
36.79
5
200.5 40.1
Group Total;-
36
36.53
57
2257.5 39.61 56
Delhi Study.
-
38.2
-
-
40.7
All-India.
-
-
-
-
-
1315
—
-
2
84. > 42.25
7
292
42.71
8
343.5 42.9
10
414.5 41 .45
8
345.5 43.19
2984.1
2338.8 41 .76 69
-
-
-
-
-
42.2
13
6
262
10
442.5 44.25
6
269.5 43.25
43.25 67
-
43.2
-
-
44
569.5 43.81
2971.5 44.35 6?
-
-
-
-
43.9
-
367
441
45.88
44.1
14
578
44.46
6
262
43.66
8
355
44.3 7
5
215.5 43.1
45.85
531
44.25
11
485.5 44.14
4
180.5
45.13
10
441
2936.4 43.83 63
2850.5
45.25 72
-
-
-
-
44.1
3145 "
43.68
43
45.1
44
= = =1
==================?==- ======= fc=====<== = =J======1====== i====d ======1====== ;s=——: :======-:===== k= = = =j============== = == = -:= = ====!:======«=
============ = = ===== =======&=======
Cloud land. .
High Wavys.
3
12
to
p
j.l<?an.
-
Y2,xea£ s_ t 0
years.
Femal.e •
To€a8T“ "(Tani
~Teah.
-
____ 3....X ea£ri__t;<? .4.. years.
3 yea rs.____
Male
1" "To faF ""iTeanT
-
-
N
Female
Male
■Tofar- rftS’aiT; —I" -TCHra-r- Ttean?
47.2
16
744.25 46.3
1
Male
x—
“n"' f'T'n-hai
-
?!
oH ip
2 years
.
. 189.5
6
to 5
rs.
Ale an.”
~~e‘aiT.“
48.25 13
620.5
47
48.34 20
949.5
47.47
48.48 47 2219.7
47.22
613.5
47.19
139.25
46.42
6
266.5
44.4
47.25
229.5
45.9
15 , 715.5
558
46.54
13
594
45.69 9 422
46.83' 10
446
44.6
21
1022.75 48.70 16
745
46.56 23 11112
45.28 8 334.5
41.81
12
553.5
46.13
36 1697.5 47.15 23
1102
47.91
36
1745 .5
45.86
13
611.5
>7.03 23
1071.5
46.58
15
706^5 47.08 13
2
94.5
Manalaar.
6
276
46
7
370
Upper Manaliar.
9
414.5
46.05
8
357.5
44.63 12 550.5
45.37
1 1
504.5
Veniar I
(a) .
46
46
4
177
44.3
2
90.5
45.25
1
47
47
9
419.5
46.61
6
277.5
46.25
4
191.1:
47.87
3
143
47.66
1
Veniar I
(b) .
46
46
1
46
46
1
47
47
2
93
46.5
8
377.5
47.18
1
48.5
48.5
3
140
46.66
5
136.5
47.3
1
139
46.33 4 185.5
46.38
3
134.5
44.83 17
797
46.88
9
412
45.78 13
450.5
45.05 10 468
46.8
5
230
46
702.5 46.8
I 1
514.5
46.77
8
4681
46.1
Veniar II.
9
#414.25 46.03 3
Veniar III.
6
274
Group Total;-
xfisihixSiadjcx
All-India.
47 2168
___
45-67 10
46.12 52 2347.5
45.5
-
-
45.14 48 2192.5
44.6
-
-
15
45.67 49 2238
45.67 134
46.3
45.4
=—======== :== = ==== =======
-
-
6343.75 47.34 105 4915.25
-
47.2
-
-
22 1039.5
47.25
335
16
757.5
47.47
10£
5293
-
49
1 39 6571.7
47.9 j
-
47.27
-
623.2:
:======== ====== ;==== ======= ====== ==== ======= ====== L-==l ======J
'UJ5.9I
47.1
======== =======
4
NUTRITIONAL ASSESSMENT.
Clinical Analysis of Highways Group. of States.
Name of the estate6.
Age group•
0-3 months,
Total number
of children.
Clouaiana,
Highwavys.
Upper Manalaar.
Manalaar.
Venniar I,
Venniar II.
Venniar III*
8
8
1
7
..
4
5
3
1
1
1
• o
9 9
9 9
9 9
a *
e 9
9 9
• 9
® 9
« ©
• -
•
A »
o.
• •
• *
Q »
• O
9 9
9 9
9 9
« •
9 9
9 9
Hair.
1
"
1
1
1
1
a
b
c
d
Face.
2 a
2 b
• 9
Eyes.
a o
3 a
3 a
9 O
o 9
9 O
..
• 9
••
••
« 9
9 9
Lips.
9 €
• 9
9 •
9 9
9 9
e •
9 *
9 «
O *
e »
••
9 9
9 »
0 9
4 a
4 b
Teeth.
6 a
6 b
9 •
Skin.
8 a
8 b
"
9 O
e <T>
a ®
• 0
9 9
9•
« 9
9 9
O 9
€ 9
••
• •
• 9
9 O
9 O
9 9
9 •
Nail.
9 a
• •
Muscular &
skeletal
systems.
11 a
11 a
11 g
11 h
11 f
a a
9 9
a .
a a
a a
9 9
9 9
a a
aa
aa
9 o
9 O
9 9
9 9
9 9
© e
••
«• e
• •
••
9 •
• •
a a
a a
a a
a a
a a
9 9
e •
• 9
• 9
a •
9 •
• 9
9 9
••
• •
••
• •
•*
••
1
i
Otitis.
0
Pyoderma.
••
••
••
•*
••
• 9
LRTI
••
• 9
9 9
• *
1
••
♦•
Scabies.
9 •
••
© 9
••
♦ *
• •
9 9
Pb
••
• 9
• 9
••
••
••
**
Me
••
•*
9 9
•*
♦ •
9 9
• *
P
NUTRITIONAL ASSESSMENT.
Clinical Analysis of Highwavys Group of Estates.
Name of the estates.
Age group.
3-6 months.
1
Cloudland.
Total number
of children.
Highwavys.
Upper Manalaar.
Manalaar.
Venniar I .
I
|
Venniar II.
Venniarlll
9
9
7
14
9
4
5
3
4
■» 9
2
6
• »
2
2
1
® o
o &
• «
..
..
•0
• •
••
Hair.
"
1 a
1 b
1 c
1 d
«• •
••
Face .
2 a
2 b
« 9
3 a
3 d
• •
4 a
4 b
• e
Eyes .
Lips.
Teeth.
6 a
6 b
w
Skin.
8 a
8 b
• a
9 a
A&
••
* 0
Nail.
•9
••
Muscular &
skeletal
systems.
11
11
11
11
11
a
d
g
h
f
*1
1
••
••
••
• .
• e
• •
e •
• •
. •
• •
•.
•♦
O a
• •
. .
••
••
• o
a o
9 •
• a
• »
• •
Otitis.
a a
0
Pyoderma.
P
LRTI
-
'a
1
a a
. .
••
••
••
••
• •
• •
..
••
Scabies.
'
S
a a
a a
a a
• •
Pb
••
• •
• •
••
Me
aa
a1
a a
a •
* *
!
••
••
• •
••
NUTRITIONAL ASSESSMENT
Clinical Analysis of Highway,ys Group of jgtates,
NUTRITIONAL ASSESSMENT.
Clinical Analysis of Hifthwavys Group of Estates
NUTRITIONAL ASSESSMENT
Clinical Analysis of Highwavye group of ggtates
Name of the estates.
Age group.
1-1/2 years.
Cloudland.
Highwavys.
Upper Manalaar.
Venniar I.
Manalaar,
Venniar II.
Venniar III.
M
F
M
F
M
F
M
F
M
F
M
F
M
F
7
9
9
13
13
9
12
17
3
7
13
6
10
6
1 a
1 b
1 c
1 d
4
—
—
-
8
1
6
—
—
-
5
«•
—
-
9
—
-=»
1
6
—
2
2
—
—
6
••
—
-
8
—
—
1
3
-
7
—
—
-
—
-
6
—
—
-
6
—
—
1
2 a
2 b
—
-
—
—
—
■ —
—
—
—
-
—
—
—
—
I
*
-
-
*
-
-
—
-
—
-
3 a
3 d
—
-
-
-
—
—
—
—
—
—
-
—
-
—
-
—
—
—
I
-
—
-
—
—
4 a
4 b
—
—
—
-
—
—
—
—
—
—
-
--
—
—
—
—
—
—
—
-
6 a
6 b
-
-
-
—
-
-
-
M.
-
—
-
—
—
-
-
—
*•
—
—
8 a
8 b
—
-
—
-
-
-
-
1
1
-
-
-
«.
-
—
-
—
—
—
—
9 a
-
-
-
-
-
-
-
-
-
-
-
-
-
—
—
—
—
-
—
—
-•
-
—
1
—
1
—
—
—
-
—
—
—
-
—
«=>
—
=»
—
-
-
—
-
1
»•
—
-
—
—
-
—
—
-
—
—
—
-
—
—
—
-•
—
—
—
—
—
-
-
-
-
-
1
-
-
1
-
-
-
••
-
-
-
1
1
Total number
of children.
Hair.
-
Face.
Eyes.
Lips.
Teeth.
}
-
Skin.
Nail.
Muscular &
skeletal
systems.
11 a
11 d
11 g
11 h
11 f
—
—
—
-
Otitis.
0
Pyoderma.
P
LETT.
1
-
-
1
-
-
-
-
-
-
-
-
-
1
1
-
-
-
-
-
-
1
-
-
-
-
-
-
-
-
-
-
-a
-
-
-
-
-
-
-
-
-
Scabies,
S
Pb
Me
-
-
—
-
-
-
-
NUTRITIONAL ASSESSMENT
Clinical Analysis of Highwavys.Group of Estates.
Name of the estates.
Age group.
1/2-2 years.
Cloudland.
Total number of
children.
Highwavys.
Upper Manalaar,
Manalaar,
Venniar I.
Venniar II.
F
M
F
M
F
M
F
15
14
11
13
12
11
4
10
6
12
1
6
5
8
7
3
7
M
F
M
F
M
F
M
9
8
4
10
8
6
5
1
3
3
8
3
3
Venniar III.
Hair.
1 a
1 b
1 c
1 d
1
1
1
3
Eace.
-
2 a
2 b
1
Eyes.
3 a
3 d
..
Z
:
1
Lips.
4 a
4 b
1
**
1
Teeth.
™
6 a
6 b
I
1
Skin.
8 a
8 b
1
1
1
3
2
Nail.
9 a
Muscular &
skeletal
systems.
11 a
11 d
11 g
11 h
11 f
1
1
1
1
Otitis.
0
1
1
1
1
1
2
1
Pyoderma.
P
LRTI.
2
1
Scabies.
S
Pb
Me
1
if
1
1
NUTRITIONAL ASSESSMENT
Clinical Analysis of Highwavys Group of Estates.
Name of the estates.
Age group.
F
3
6
12
13
1
3
1
6
10
tej
M
Manalaar.
M
F
C
O
F
!
6
7
^4.
M
Upper Manalaar.
3
3
-V 1
Total number
of children.
Highwavys.
g
Cloudland.
?
"
Venniar I.
M
2
Venniar II.
Venniar III.
F
M
F
M
F
5
9
, 3
6
10
1
5
2
2
7
1
a
1
1
1
b
c
a
IIIM
Hair.
P
-
1
-
1
1
||
2 a
2 b
II
Face .
-
||
3 a
3 d
II
Eyes.
-
—
—
-
:
-
!
4 a
4 b
—
—
II
II
Liss.
1
i
2
II
1
I
6 a
6 b
—
1
Teeth.
Ik
P
-
1
Skin.
II
II
1
2
8 a
8 b
1
1
1
1
Nail.
9 a
I|
Muscular &
skeletal
systems,
1
1
lllll
lllll
11 a
11 d
11 g
1 1 h
11 f
2
1
1
1
1
1
-
1
0
-*
Otitis.
2
1
1
II
P
LETT.
-*■
Pyoderma.
Me
1
Ill
S
Pb
iV l
Scabies.
■
------------------------ -
NUTRITIONAL assessment
Clinical Analysis of Highwavye Group of Estates.
Name of the estates.
Age group.
2/2-3 years.
Cloudland.
Highwavys.
Upper Manalaar,
|
Manalaar.
Venniar I.
Venniar III.
Venniar II.
M
F
M
F
M
F
M
F
M
F
M
F
M
F
2
5
9
10
12
11
8
12
3
3
4
3
10
5
1 a
1 b
1 c
1 d
1
-
2
2
7
3
4
1
2
1
1
3
-
1~
2 a
2 b
Z
-
3 a
3 d
:
z
Total number
of children.
Hair.
1
•
Face.
-
Eyes .
1
z
,
-
Li£S.
4 a
4 b
Teeth.
-------------- c
6 a
6 b
1
2
i
-
-
1
-
1
1
1
1
1
1
1
1
Skin.
8 a
8 b
1
1
1
Nail.
9 a
-
’
I
-
Muscular &
skeletal
systems•
1
11 a
11 d
11 g
11 h
11 f
z
z
-
'
2
2
-
Otitis.
0
;
1
1
1
1
-
i
Pyoderma,
P
LRTI.
i
1
-
.
-
t
Scabies.
S
Pb
Me
I
-
1
I
I
I
“
1
NUTRITIONAL ASSESSMENT
Clinical Analysis of Highwavys Group of Estates.
Name of the estates.
Age group.
3-4 years.
Total number
i of children.
•
j
M
F
15
16
I
Hair.
‘
M
I
Manalaar.
:
Venniar I.
I
j Venniar II.
F
M
F
M
F
M
F
M
F
! -
16
13
23
37
25
17
7
17
9
4
1
5
—
-
-
a
b
c
d
2
—
—
1
9
—
—
-
2 a
2 b
2
—
—
—
1
1
1
1
Upper Manalaar.
Highwavys.
Cloudland.
Venniar III.
M
F
15
11
2
—
—►
-
4
1
—
-
I
14
—
-
6
—
—
-
2
—
—
-
6
—
—
-
5
I
-
—
-
—
-
—
—
—
I
—
—
1
-
-
•
-
—
I
-
—
2
—
2
—
7
—
1
-
7
—
—
-
-
—
—
—
1
Face .
—
Eyes .
3 a
3 d
—
—
1
-
—
-
—
—
—
2
—
4 a
4 b
-
-
1
-
-
-
1
-
-
»
-
«
-
-
-
6 a
6 b
2
—
3
—
2
-
-
1
—
—
3
—
-
4
—
1
—
2
1
1
—
8 a
8 b
1
—
2
-
1
2
1
-
1
-
5
2
1
4
-
3
3
1
2
2
-
-
-
-
-
-
-
-
-
-
—
—
1
—
■
—
—
—
-
—
—
—
—
—
1
—
—
—
—
1
—
—
—
—
2
-
1
1
-
5
1
1
Lips .
-
-
Teeth.
—
Skin.
Nail.
9 a
i
I
-
—
Muscular &
skeletal
systems.
11
11
11
11
Otiti^L
a
d
g
*/
i)
1
2
•i
—
0
2
1
—
;
1
—
—
—
•
1
-
1
■»:
-
-
-
1
—
-
Pyoderma.
P
LRTI.
•
-
—
—
1
-
-1I
1
1
—
-
-
3
2
i
1
-
-
L
1
—
-
-
Scabies.
S
•_
-
-
-
-
-
Pb
1
-
-
-
-
-
-
-
-
-
-
-
-
-
Me
-
-
-
-
-
-
-
-
-
-
-
—
NUTRITIONAL ASSESSMENT.
Clinical Analysis of Hiphwavys Group o,£_Estates «
FOR
HEIGHT
Nano of Estate/
Division.
6 - 9 months.
I
3—6 months.
__N_ Total- Moan. __N_ Total —Mean.
-12 months
1979*
1 yeat to 1 '/2 years.
Malo
Fomal.e
"To Tai "EloanZ
n~ "ToTal" “rieanZ
N_ Total__ Mean,
Total_ Moan.
-
1'72years to 2 years.
Female
Male
To Tai ■MoanZ
’Tolal^ "Mean
32Z
9
525
58.3
5
314
62.8
5
342.5 68.5
7
501.5
71.64
9
638
70.9
9
695
77.2
8
628
78.5
272.5 54.5
9
532
59.1
12
786
65.5
13
892.5 68.7
9
639
71
13
921
70.84
4
298
74.5
• 0
751
75.1
69.88 15
Cloudland
4
207
Highwavys
5
51.75
Manalaar
8
423
52.88
14
841
60.07 12
770
65.16 24
1638
68.25 12
864
72
17 1188
1129
75.27 if
1016
72.57
Upper Manalaar
3
158
52.66
7
408
58.3
7
431
62.71
6
403
67.16 13
927
71.3
9
616
68.44
8
615
76.87 6
431
71.83
Vanniar I (a)
3
153
51
5
291
53.2
3
187
62.33
3
195
65
2
129
64.5
5
350
70
4
295
73.75 8
580
72.5
Veniar
5
243
48.6
4
230
57.5
-
-
.-
2
129
64.5
1
70
70
2
138
69
7
535
76.42 5
358
71.6
1
53
53
4
222
55.5
7
451
64.43
3
$22
65.25 13
875
67.31
6
425
70.83 12
861
71.75 11
805
73.18
51.14
5
295
59
10
6^1
63.1
8
398
66.33
4
292
73
10
714
71.4
1367.5 51.88 57
3344
58.67 56
3570
69.76 S3
4720
74.9
72 5283
-
-
-
-
-
-
74.2 |
-
-
73.3
I (b)
Veniar II
Voniar III
358
7
Group Total;-
►
0-3 months.
Gil OOP
-
AGE
Deli Study
All-India.
36"’
-
-
57.4
-
-
-
-
-
-
-
================ ====: bccss=ss=S5’ ====== —-—
63.0
4654~~
63.75 69
-
-
66.5
-
-
-
-
-
-
-
=======
—
= = == = = =':=====
66.5
10
692
69.2
6
67.
67
1697.5
70.1
67 4674
69,0
-
-
-
-
-
-
-
70.8
-
-
69.3
"
___ ---- ===— B----
______ 2 years to 2^/2 years.___________
________ 21/2 years to 3 years.
Estate/
Division.
Male
N
Total
Female
Mean.
H
Total
Male
Mean.
N
Total
Mean.
N
— —.. -=—-======== --- ===== ===!
Total
Mean.
ssssss:===£=======:=======
4 years to 5 years.
3 years to 4 years.
Fema lo
Male
Female
Male
Femal
I
73.33
N
Total
Mean.
N
Total
Mean.
N
Total
Mean
N
Total
Mean.
3
1227
94.4
Cloudland.
3
235
78.3
6
457
76.2
2
162
81
5
406
81.2
15
1325
no q
OO • J
16
1403
87.7
6
548
91.3
Highwavys.
12
970
80.83
13
1058
81.38
9
741
82.33
10
828
82.8
21
1879
89.47 16
1370
85.62
23
2188
95.12 20
1887
94.35
Manalaar.
6
466
77.67
7
552
78.86
8
631
85.13
12
982
81.83 36
3309
89.43 23
2002.5
87.06 37
3476
98.94 48
4923
02,56
Upp or Mhaalaar.
9
706
78.4
8
613
76.62 12
900
81.66
11
883
80.27 13
1135
87.30 23
2017
87.69
15
1400
93.33
13
1213
93.30
Veniar I (&)
1
80
80.0
4
301
75.3
2
169
84.5
1
77.0
9
792
88.0
6
520
86.66
4
378
94.5
3
289
96.33
’ veniar l(b)
77
1
83
83.0
1
74
74.0
1
90
90.0
2
171
85.5
8
634
85.5
1
92
92.0
3
272
90.66
5
473
94.6
Veniar Iljf
9
701
77.89
3
230
76.67
4
318
79.5
3
241
80.55’. 17
1497
88.06
9
780
86.67 13
1233
94.85 12
2046
93.0
6
3463
77.17
10
756
75.6
10
830
83
_5_
400
_S0____ 15
1306
87.07 11
972
88.36
8
723
91
16
1493
93.3
GroUp Total;-
47
3704
78.8
52
4o4l
77.7
48
3971
82.73 49 3988
109
10,223 93.79
Delhi Study.
-
-
78.2
-
-
77.9
-
-
81.59 135 11,927 88.35 105 9156.5 87.2
85.8
-
-
-
-
-
-
All-India.
-
-
-
-
-
-
-
------ «
84.9
-
-
93.9
-
-
92.6
Veniar III.
___
ssssssssssssssasflsftssftssssstssss!
--------
81.8
-
-
-
6=3S3 XS S£SC*SS!Stt
-
-
86.2
------ -=35S—33——— ~ —
-
-
140 13,551
96.79
WEIGHT
0
-
3 months.
6 months.
3
—
Total . Mean.
Mean.
FOR
AGE
- .JJIgH/AVYS GROUP - 1979.
-12 mqnths.
N
Total
Moan.
Year to 11/2 years.
Male
Female
NTToTal Mean.
E"1~T6Tal1“MoanT
9 months.
6
-
Mean.
Namo of Estate/Div.
1
11/2 years to 2 years.
Male__ _ __
Female
N-|~T6EalTTlean “nTTo^ aTTjiean
N
Total
N
Total
Cloud Land
u
17.5
4,38
9
51.7
5.74
§
32.5
6.§4
5
37.0
7.Il
7
55.7
7.96
9
69.2
7.7
9
84.6 9.4
8
74.7 9.33
MighiWavyS^
5
18.8
3.76
9
48.3
5.37
12
80.1
6.68
13
89.3
6.87
9
76.0
8.44
13
102.5
7.8S
4
34.3 8.57 10
84.5 8.45
Manalaar
8
33.4
4.13
14
79.9
5.71
12
78.1
5.58
24
185.9
7.75
12
97.9
8.16
17
131.5
7.74
15
138.4 9.23 14 114.2 8.16
N
50.1 8.35
Upper Manalaar
3
8.83 2.94
7
33.9
4.84
7
43.5
6.21
6
42.3
7.05
13
103.6
7.96
9
66.6
7.4
8
72.8 9.06
6
Voniar I (a)
3
11.1
3.7
5
26.8
5.36
3
19.4
6.46
3
19.4
6.46
2
14.6
7.3
5
35.5
7.5
4
33.2 8.3
8
66.2 8.27
Veniar I (b)
5
17.5
3.5
4
19.6
4.9
-
2
13.4
6.7
1
7.5
7.5
2
15.0
7.5
7
62.8 8.97
5
39.2 7.84
Voniar II
1
4.3
4.3
4
17.6
4.4
7
46.9
6.7
S
54.3
6.79
13
100.0
7.69
6
45.4
7.57
12
97.7 8.14 11
88.8 8.1
Veniar III
7
28.0
4.0
5
25.2
5.04
10
62.1
6.71
8
59.6
7.45
10
78.7
7.87
6
42.1
7.02
4
32.1 3.03 10
78.6 7.86
57
311.0
5.46
.56
362.6
7.26
67
533.9
7.97
67
507.8
7.58
63
7.6
M.
—
—
—
—
—
—
7.8
-
-
7.3
36
Group Total:Delhi Study
-
All-India
-
at sa so S3 =s cs x==s axes ~
139.43 3.87
4.8
6.2
-
-
-
6.48
69
501,2
-
-
6.9
-
-
•* ,,
*“
—
—
-
—
—
—
_
3.5
-
-
8.0
~=s ss sa tx ~ ~=: ssss =3 ====s=s: ss as ss==—
s=si==~ s
—
Name of Estate/Div.
555.9 8.82 72 596.3 8.28
—
2 Years to 2V2 Years.
Male
~n"' Total Mean.
------- ———
21/2 ye ars to 3 Years,_
Female
Total
N
Mean.
Male
“foEal-
Femala. j
Moan? '“n“
—
3 Years to 4 years.
Male
"Mean? ”n“' -T6TS1" Me an •
4 years to 5 ye ars„
Female
N “ToEaT" “Mean
Female :
.Male
N* “Total' 'Mean? "“Tola”!Mean
76.1
12.68 13 198.8 12.2
Cloud Land
3
27.7
9.2
6
53.3
8.9
2
18.8
9.4
5
50.5
10.1
15
167.3
11.2
16
177.7
11.1
6
High Wavys
12
121.1
10.09
13
121.1
9.31
9
88.8
9.86
10
97.6
9.76 21
255.7
12.17
16
178.6
11.16
23
304.0 13.21
Manalaar
6
54.9
9.15
7
67.2
9.6
8
88.6 11.07
12
124.2
10.35 37
443.3
11.98 23
272.8
11.86
37
505.7 13.66 48 638.7 1 1330
Upper Manalaar
9
88.3
9.8
8
72.0
9.0
12
124.9 io.4o
11
111.4
10.12 13
155.1
11.93 23
269.9
11.73
15
195.0 13.0
13 171.0 13.15
Veniar I
(a)
1
10.4 10.4
h
36.6
9.15
2
20.7 10.5
1
10.0
10.0
9
105.5
11.72
6
68.6
11.43
4
53.0 13.25
3
45.1 15.0
Veniar I (b)
1
10.7 10.7
1
8.1
8.1
1
12.1
12.1
2
22,4
11.2
8
84.6
10.57
1
12.5
12.5
3
36.3
5
65.9; 13.8
Veniar II
9
85.2
9.47
3
28.4
9.47
4
38.0
9.5
3
30.1
10.03
17
200.0
11.76
9
100.1
11.12
13
106.8 12.98 22 292.8 ’ 12.85
Veniar III
6
58.8
9.8
10
89.3
8.93
10
106.15 10162
5
47.7_
9.54 15
167.4
11.16 11
127.1
11.55
8
47
457.11 9.73
9.15
48
498.1
49
493.r
10.08 135
1578.9 11.7
105
1207.3
11.5
-
-
-
-
-
-
-
-
84.9
-
-
93.9
Group Total:-
Delhi Stury.
All-India.
-
SIffli.SSSSSSSS-SSaeSCiSSSSKfiSSSSSSSJSSSS :===: =======
52
476.9
78.2
-
-
77.9
-
-
-
-
-
-
=55333 =S==S
10.38
85.8
81.8
---- —————— ssxssa
-•
sscssaxsi Saaa^s:s==5S?sbc:=s;=====
-
-
z
86,2
12.1
20 257.6, 12.88
97.5 12.19 16
109 1436.4 13.18
209.6
140 1329.5 ! 13.07
-
I
- 1 92.6
——————iSSSSSSfiI===sa===
2
CHEST
Name of Estate/
Division.
Cloud Land.
CIRCUMEERE2TCE FOR AGE - Ig gi WAVYS GROUP - 19?9,
9 -
Total ■Moan.
39.1
5
203
40.6
38.78
12
505.5
42.13 13
Total
Moan. _N_
Total I Mean.
4
143.5
35.88
9
352
180.5
36.1
9
349
High Wavys.
12 months i.
Ni Total
N
N
Mean. _N;
1 year to 11/2 years.
- TotalMfAean.
To<g‘?a-LSean.
N
1“/2 years to 2 years«
Tota£leftean. J
Mean.
9
337.5
43.1
9
426
47.3
8
372
46,2
13
574
44.15
4
191.5
47.8?
10
454
45.4
43.29 17
732.5
43.08
15
663.5
44.25
14
574
44.15
44.2
217
43.4
7
309.5
558.5
42.96
9
397.25 44.13
24 1049.5
43.73
12
519.5
5
N
Manallar.
8
282
35.25
14
545
38.93 12
488.5
4o.7
Uppor Manalaar.
3
110.5
36.83
7
272
33.85
7
287
41
6
249
41.5
13
569.5
43.8
9
382
42.4
3
365.5
45.68
6
260.5
43.41
Voniar (l)
(a).
3
101.5
33.83
5
195
39
3
122
40.66
3
125
41.66
2
84.5
42.25
5
211
42.2
4
176.5
44.12
8
349
43.63
Veniar (l)
(b).
5
171
34.2
4
155
38.75
-
-
-
2
83.5
41.75
1
44
44
2
87.5
43.75
7
328
46.85
5
221
44.2
Veniar II.
1
35
35
4
152.5
38.13
7
301.5
43.1
8
339
42.4
1.3
575.
44.2
6
267.5
44.58
12
549.5
45.79 11
493
44.82
Veniar III.
7
24?
35.29
5
199
39.8
10
L
413
41.3
8
346
43.25 10
6
262
43.67
4
182.5
45.63 10
443.5
44.35
36 1271
Group Total:All—India.
ss S3 si r - = n=== ~
35.30 57 2219.5
-
-
-
-
30 . Q 3 p
2320.5
l -
41.43 69 2937.5
-
42.57 67 2948.75 44.01
-
-
-
-
43.1
67 2904
43.34 63 2883
45.76 72 3167
43.98
-
42.1
44.5
43.4
-
-
-
-
~==
Nam© of Estate/
2 years toj2'!/2 years.
Female
N '“tSTSI” Mean<o N "ToTal Mean.
Division.
Cloud Land,
High Wavys.
21/2 years t J 3 years.
3 years to 4 jy•ears •
------ FlSIe—r
Femalo >
“Malej
“Female”
"“Total] Mean. ”n‘ "Total” 'Mean, ~N~ •TStalT Mean. ”1" 1"TotalT Moan.
3
140
46.70
6
270.50 45.10
2
12
575
47.91
13
594.50 45.73
9
446.50 49.61
Manalaar.
6
284
47.33
7
319.5
45.64
8
389
Upper Manalaar
9
415
46.11
8
358.75 44.84 12
557
Veniar I (a).
1
45
45
4
175.5
43.87
2
93.5
(b).
1
50
50
1
46
46
1
Voniar II.
9
430
47,78
3
143
47.67
Veniar III.
6
283
47.17 10
462
46.2
Group Total;-
47 2222
Veniar I
449.5 44.95
All-India.
-
-
4 years
to>
Malo
N ‘ ""ToTaT | *Mean“j
6
sspd.
19-2-1980.
=>
Total
Mean.
626.75 48.20
48.70 16
760.5c 47.50
49.69
16
769.5
48.09 23 1165.5
50.67 20
46/5.7$
36 1758.5 48.84 23
1117.5
48.58 36 1824.4
50.67 47 2310
49.14
500.5
45.5
13
622.5 47.83 23 1098
47.73
15
738
49.2
13
635.5
48.88
46
46
9
425
47.22
6
28 i .1
46.91
4
196
49
3
151.5
50.5
2
97.5
48.75
8
390
48.75
1
50
50
3
146.5
48.83
5
257.5
51.5
48
3
142.5
47,5
17
834.5 49.9
9
439.5
48.83
13
657.5
50.58 22 1032.55 46.93
48.5
5
239
47.8
15
727.25
11
542.15 49.34
8
410.5
51.31
47.27 52 23^9.75 45.57 48 2308.5
48.09 49 2279
46.51
134 6532.2$
45.4
46.6
45.5
44,4
47.50
239
47.80
15 731
453
45.30
21
48.63 12
561.5
46.41
11
46.75
1
50.5
50.5
4
192
10
485
95
10
1043.5
48.48
301.50 50.25
48.74t 105> 5058.
65
48.18 108; I5439.
48.1
46.9
No. of children.
13
973.5
48.67
16
798.5
49.9
50.36 13$
6685.
8
48.82
49.6
I
N
5 years.
43.6
7
89
12.7
9
111.5
12
9 114.25
12.69
13
12.51
12 149.5
1 2.46
17
9
4
164.75 12.67
212.5 |
12.5
15
111
j
8
12.33
33.5
10.44 14
161.5
11.54 12 145.5
12.12 24 300.25
34
11.33
7
76.5
10.92
7
32
11.71
6
72.5
12.08 13 162.5
12.5
28
9.33
5
57
11.4
3
36
12
3
34.5
11.5
2
12.75
2
24
12
1
12
12
88.25
12.61
8
95
11.88 13
159
1 2.24
11.8
8 100.9
12.61
128.5
12.85
6
72
840.25 12.54 67
828
9.74
10.5
10.5
72.5
10.36
—
369.45
10.26
4
47.5
11.87
4
42,5
10.63
7
56v5
11.3
10 118
10
57
653
11.45 56 676.5
12.08 69 843.9
12,23 67
Allilndia.
Male.
N
Total
Mean.
N
Total
Mean.
N
Total
Mean.
N
Total
Mea»»
3
35.5
11.8
6
76
12.7
2
25
12.5
5
65.25
13.05 15 196.25 13.1
High Wavys,
12 152
12.7
Manalaar.
6
Upper Manalaar.
9 118
Veniar I (a).
1
(b).
1
4
2
23
11.5
7
6
72.25 12.04 12
13
12.7
194
12.93
14
103
12.87
6
50.5
12.6g
8
87
12.42
5
12.13 11
12
12
4
48
12.35
53
794.75 12.61
N Total
21
282.5
Moan.
N
Total
Mean.
N
Total
Mean._ N
16
214.95 13.4
6
81
13.5
277.5
13.87
13.95 47
652
13.87
13.88 23
302.5
13.15 15
207.5
13.83 13
187
14.38
8 105
13.12 12 155
12,91
11
144
13.5
13.5
4
12.62
2
25
1 2.5
1
13
13.5
13.5
112
12
1
13
13
2
26.25 13.
3
12.83
4
53.5
13.38
3
39.5
13*17 17 230.75 13.57
9
120
12.43
10 135.5
13.6
5
67
13,4
201
3.4
11
148.25 13.48
I07.25
3.40
3,4
05 1409.15 13.42 108 1491.
55
13.4
Veniar III.
6
13.08 10 124.25
47 604
-
12.85 52
13
562.75
12.74 48
j -
12.8
xsscaa:=ssste»=««scia:5z=»: S£=3SS»SSS:e3'-a:SB33*3S3SSSXSBS = == ess =2 = =s= ====
537
-
13.27 49
13
9 119
13.22
8
12.88
15
639.75 13.05 134 1795.
“
7~
LLjlE...
13.6
14.07 20
13.11
38.5
Moan.
177
502.3
157.75 13.15 36 482.75 13.4
12.83
Total
323.75
127
13.25 12
103
13
13.72 36
216.75 13.54 23
13.77 10
8 106
13
£87.4
315.7
9 124
13.14
50.5
12.29
23
13.45 16
12.61
92
130.5
12.1
12.09
4: years to 5 years.
Female.
Male.
164
13.09 13
72
12.56
12.7
12.1
7
78.5
10
12.73
12.33
145.5
12.66 13
9 115.5
-
8
10
12.92
77.5
Veniar II.
Group Total:-
12.2
12.8
51.25 12.81
115.5
3 years to 4 years.
Female.
Cloud Land.
All-India.
61
12.5
Name of Estate/_ ___________ 2 years to Z^jZ years. ______ _____________ 21/2 years to 3 vears.
Division.
Malo.
Female.
Male.
) Veniar I
9
<\)
48.7
25.5
12.4
0
12 145.5
0 \ to
m -a
5
1 1 .3
i
12.1
12.17
102
w
60.5
109.5
9
6
I
to
5
13 156.25
9
£■
12.3
12.13
10.56
10
Ul
61.5
42.25
0
n1
Ut
Mean.
k;<
Total
'J c
N
Moan .
V<
36
Total
50
I
Group Total:-
N
0\ O
Veniar III,
Mean.
1
to 2_Z.ears.
Fomal e.
N j Total i Mean.
UJ
Veniar I (b).
Veniar II.
Total
Male.
|
N | Total . Clean.
to
Veniar I (a).
N
1V2 years
1 Year to 11/2 Years.
Female5 .
Malo.
Total i Mean.
Total Mean.
N
6-9 months.
io
i-\ ca
r- b.
___ ____________ ____
Upper MaAaiaaar
Moan.
1979.
VO
4
Manalaar.
n n
Cloud Land.
High. Wavys.
Total
9-12 months
-
1
|
N
3-6 mon ths.
HXGIIwavyS GROUP
1
0-3 Months .1
Name of Estate/
Division.
-
CIRCUMFERENCE FOR AGE
1
MID-ARM
78
12
4
56
14
3
46
15.33
13
13
3
40.5
13.5
5
71
14.2
13.33 22
307
13.95
13.41
16
225
14,06
13.81
14
130 1942.5 13.97
13.33 13.11Z3.25
8
:===== ========== = ==t== = ======= =1 = = = ==5
5
_
HEAD CIRCUMFERENCE FOR AGE - HIGHWAVYS GROUP - 1979,
Name of Estate/
Division.
------ --------------------------------------_________________________ _9_~ 12 months.
I
N .Total Mean.I N Total Mean.
N Total , Moan.
N
Cloud Land
4
l4S;5 37.13
9
362
High Wavys
p
183.5 36.7
9
353.5 39.28
40.2
5
12
208
41.6
5
508
42.3
13
1 year to 1]/2 years,
. -Malo
N | Total Mean,
N
■ ■' ■ 7 I
216
43.2
312.5 44.64
9
561.25 43.17 9
403.5 44.83 13
p/2 vears to 2 veors
'©male 7'
Tlale” -----'Mean.
d? 0 a.1
•
389.5 43.28
44.07
573
415.5, 46.2
45.5
182
8
10
367
441
45.88
44.1
682.5 ■ 45.5
14
578
44.46
45.31
6
262
43,66
175.5
43.62
8 '
355
44.3 7
7
321
^5.85
5
215.5 43.1
43.67 12
531
44.25
11
4S5.5 44.14
130.5
45.13
10
441
44.1
45.25 72
3145
43.68
9
4
Manalaar
8
295
556.5 39.75 12
501.3 41.78 24
1051.8 43.82 12
53«
44.67 17
754
44.35 15
Upper Manalaar
3
114.5 38,16
7
2?6
39.42
7
291.5 41.64 . 6
253.5 4-2.25
13
577
44.33
9
386
42.88
8
362.5
Veniar I
(a)
3
104
34.66
5
200
!t0
3
123.5 41.16
3
123
42.66
2
86.5 43.25
5
215
'43
4
Veniar I (b)
5
175
35
4
157
39.25
-
2
84.5 42.25
1
4-4
2
87.5 43.75
Veniar II
1
37
37
4
152
38
7
292
42.71
8
343.5 42.9
13
569.5 43.81
6
262
Veniar III
7
257.5 36.79
5
200.5 40.1
10
414.5 41.45
8
345.5 43.19 10
442.5 44.25
6
269.5 43.25
2257.5 39.61
56
2338.8 4.1.76 69
2984.1
2971.5 44.35 67
Group Total:-
36
1315
Do Illi Study.
-
-
All-India.
-
36.88 14
36.53 57
38.2
-
—
=================; sazssz
-
40.7
L====J======J
to 2;/2 yogjes.
Female.
2 vears
3
139.25 46.42
6
266.5
42.2
-
-
-
_________
— :r./—
Malo
______
‘“KI -TofaKMean.
__Male_
"rot'al “ filean «
Cloud land.
-
44.4
2
94.5
43.25 67
4
2936.4 43.83 63 2850.5
-
-
43.2
-
-
-
-
-
-
-
-
-
-
-
-
43.9
-
-
43
-
- ,
======
------
___
s ,t;o.
-; ~~~
t—=== r- -
=
Male
TofaP" 7-Tffan."
16
744.25 46.3
6
47.25
5
229.5
45.9
15
715.5 47.2
446
44.6
21
1022.75 48.70 16
745
46.56 23
36 1697.5 47.15 23
1102
47.91
611.5 47.03 23
1071.5
46.58 15
12
558
46.54 13
594
6
276
; 46
7
370
45.69 9 422
45.28 8 334.5
46.88
Manalaar,
41.81
12
553.5
46.13
Upper Manaliar.
9
414.5
46.05
8
357.5
44.68 12 550.5
45.87 11
504.5
45.86
Voniar I (a).
1
46
46
4
177
44.3
2
90.5
45.25
1
47
47
Veniar I (b).
1
46
46
1
46
46
1
47
47
2
93
46.5
Veniar II.
9
Jt4l4.2f
46.03 3
139
46.33 4 185.5
46.38
3
134.5
44.83 17
Veniar III.
6
274
45.67 10
450.5
45.05 10 468
46.8
Group Total:-
47 2168
46.12 52 2347.5
45.14 48 2192.5
45.67 49 2238
45.5
44.6
46.3
=====:L=: ; ===s==x==i=====:
-
i
-
45.4
r====A- -sS!*322 531
620.5
47
48.84 20
949.5
47.47
48.48 47 2219.7
47.22
613.5
47.19
36 1745.5
706.25 47.08 13
46.25
4
191.1:
8’
377.5 47.18
1
48.5
48.5
3
l4o
46.88
9
412
45.78 13
623.25
702.5 46.8
11
514.5
46.77
8
385
4681
10E
5293
=si== ==s:
47.2
-T^^^ISan.-
48.25 13
277.5
-
44
112
6
45.67 134' 6343.75 47.34 105 4915.25
-
289.-5
419.5 46.61
5
230
46
15*.
------------------------------- w-
-
======= sass—stss
13
. s/
797
-
45.1
yvitl-L « e
"Male.";
Fomale
Tot"?" ■Mem 7' ’TST" To e SI ■warr;
J .years.,-----
* High Wavys,
All-India.
= E2= ~
~53== S= =5= = U = = = =3 = = SSSSSZ2 =J= Seizes:=U==sU:=== =====
44
-
10
-
i
—
FemaleT*
•max Mean,
Pi
47.87
3
143
47.66
46.66
5
136.5
47.3
22 1039.5
47.25
757.5
47.47
6 39 6571.7
47.27
4^.91
48.15 16
49
47.9
-
47.1
LJ
=
.._
_____
=1=-===
J======= ====== ==== sssssxz.sssass: 1======!==:
-
46.1
-
-
II.
BALANCED DIETS IN TERMS OF STANDARD. CUPS AND SPOONS
The balanced diets for different categories of
people are given in terms of standard cups and spoons in
the following table:
Table-1: Balanced jBiet for Adult Man(Moderate worker)
Approximate
volume in std ’ . Number
cup and std.
spoon.
ft
Food Stuff
I. CEREALS
1. Rice
2. Wheat flour
144
1-3/5
1
50
30
1/5
6 s+d. sp.
125
1-4/5
LOO
0/0
♦ n+edium s’
sized ones
▼5
1/2
12-15■•r a
handful
■ 3.35
II. PULSES
1. Redgram dhal
2. Rlackgram dhal
TTR GREEN LEAFY VEGETABLE
1. Amaranthus
3 bundles
-1
IV. Roots and Tubers
Photato
t
V. OTHER VEGETABLES
Beans
VI. FRUIT
Orange
VII. Milk
VIII. Fats and oils
IX. Sugar & Jaggery
30
-
3 segments.
.^0°
4/5 ■
-
40
2/5
-
1/5
-
4®
-
1 .
Table-II: Balanced Diet for an Adu3>t Women (Moderate
I, CEREAL
230
1. Rice
2. Wheat
1
-4/5
II. PULSES
45
25
-1/5
5 std. sp.
-
125
1-4/5
.3 bundles..
75
1/2
1
75
1/3
12-155or a
handful.
VI. FRUITS - ©range
30
-
3 segments
or a quarter
fruit. ••
VII. Milk
200
4/5
VIII. Fats and Oils
35
1/5
3<J
6 Std. sp. -
■
1. Redgram dhal
2. Blaokgram dhal
III. GRFEN LEAFY VEGETABLE
Amaranth
IV. ROOTS AND TUBERS
Potato
*
V. OTHER .VEGETABLES - Beans
IX. Sugar and Jaggery
Table-III: Additional Allowance for Pregnancy and Laotation
Pregnancy
Food Stuff
Lactation
Qty
(g)
Appx.Vol.
in std.cup.
50
1/5
’
Qty
(g)
Appx.Vol.
in std.cup
40
60
1/5
«/5
20
2 std.. sp.
I. CEREALS:
Rice
Wheat
II. PULSES:
■ R-edgram dhal
III. GREEN LEAFY
VEGETABLE
-VI. Milk
V.- Fats & Oils
•VI. Sugar & Ja
ggery
2/5
3/4 .bun-25
dies
125
10
2 std .sp
2/5
©^bundl
es
-
125
. 15
• 1A
/r Ad. sp.
-
20
4 std.sp.
J■
= 3 =
Food Stuff
Qty
(g)
- HL-
i iwi
Table - IV: Balanced Diet for a Child, between the Age
3-6 years (Ref. - 6 years old child)
j32
= (4) _
140
60
3/5
2/5
—
-
30
15
15
6 std. sp.
3 "
3 "
' 75
1-1/5 std.cup
I. CEREALS
ii ;
i
i
I
—__ ——
i
Nd.
i
Appx.Vol* in
std. cup
.
1. Rice
2. Wheat flour
II. PULSES
1. Redgram dhal
2. Blackgram dhal
3. Other grams
III. GREEN LEAFY VEGETABLE:
Amaranth
1^- bundles
IV. ROOTS AND TUBERS
Ebtato
50
2/5
50
2/5 std.sp.
8-10' in no.
5 segments.
"
1 medium size
V. OTHER VEGETABLES
Beans
VI. FRUITS
Orange
56
2/5 std.oup.
VII. Milk
250
1
"
VIII. Fats and Oils
25
7
std.sp.
40
8 std. sp.
IX. Sugar and Jaggery
4
J
!
- 4 -
,
.
Table - V : Balanced Diet. for. a Child Between the Age 1-3 years
(Ref: 3 year old child)
(1)
(2)
(3)
.(4)
I. CEREALS
1. Rice
2. Wheat
90
60
2/5
2/5
-
.25
10
15
5-&td. sp;
2 std.. sp.
3 std.' sp.
—
-
II. PULSES
1. Redgram dhal
2. Blackgram dhal
3. Greengram dhal
.. - -
III. GREEN LEAFY VEGETABLES :
50
4/5 cup
1 bundle
30
2/5 cup
1 small
Beans -
30
2/5 cup
5-7 in no.
FgUITS - Orange
50
1-1/5
5 segments
-
Amaranth
IV. FOOTS APT TUBERS
Potato
V.
VI.
OTHER VEGETABLES
VII. Mi^lk •
300
VIII. Fats and Oils
20
6 std. sp.
30
6 std. sp.
IX. Sugar and Jaggery
ms/18678/*
Fortification Basics
------------------ .
Wheat Flour
Table 1
Per Capita Wheat Comsumption
in Selected Countries
Rationale
Wheat is the most widely produced cereal in the world,
most of which is destined for human consumption; thus,
its contribution to energy intake is significant, particularly
in the Americas and the Middle East (Table 1).
The processing of whole wheat to wheat flour is generally
concentrated in a few large mills . The resulting flour is
used to make bread, biscuits, pasta, and other products.
Because of its widespread geographic distribution,
acceptance, stability, and versatility, wheat flour is a
suitable vehicle for delivering micronutrients to mankind.
Micronutrient Content of Wheat and Wheat Flour
In its natural state, wheat is a good source of vitamins Bi
(thiamine), B2 (riboflavin), niacin, B6 (pyridoxine), E, as
well as iron, and zinc.
Nevertheless, because most of these nutrients are
concentrated in the outer layers of the wheat grain (Figure
1), a significant proportion is lost during the milling
process. For lower extraction rates of flour (i.e. more
refined flour), the loss of vitamins and minerals is greater
Country
Pakistan
Turkey
Syria
Chile
Egypt
Greece
Argentina
Uruguay
Bolivia
South Africa
Peru
Consumption
(g/person/day)
% of Daily
Energy Intake
318
484
490
372
397
371
344
269
159
191
136
45
44
44
42
35
28
28
26
20
18
17
Figure 1
Schematic Diagram of the Wheat Grain
(Figure 2).
Nutrients Generally Added to Wheat Flour
In developed countries, wheat flour is generally fortified
with vitamins Bi, B2, niacin, and iron. In some countries
calcium and folate are also added. Vitamins A and D can
also be added to flour.
The levels of vitamin Bi, niacin, and iron added to wheat
flour is often equivalent to the amount lost in milling, i.e.
these micronutrients are restored and the flour is enriched.
For other micronutrients such as vitamin B2, the amount
added is over and above that lost in milling, i.e. the flour
is fortified.
Fortification rather than enrichment is done when the
overall diet is deficient in particular micronutrients and
restoring the micronutrients lost in milling will not make
good this deficit.
Technology
The technology for fortifying flour is simple. First, a premix
Figure 2
Changes in Micronutrient Content
of Wheat Grain with Milling
Adapted Irom FAO. 1970. Wheat in Human Nutrition and
Thomas. B. 1968. Nutritional - physiological views in
processing cereal products. Vegetables. 15: 360.
Table 2
Example of Premix Composition
Level / '• Product '■
Nutrient ■ (mg/Kg .Form
' Flour) Vitamin Bi 4.45
Vitamin B? 2.65
Niacin
35.62
Iron
30.20
grams/!
Kg
Premix
Thiamine Mononitrate 61.80
Riboflavin
36.90
Nicotinamide
494.70
Reduced Iron
406.60
Dosage: 72 g/ton of flour
Figure 3
Volumetric Feeder for Adding
Micronutrient Premix
MOTOR
HOPPER
Figure 4
Simplified Flow Chart for Flour Milling
of the micronutrients to be added is needed (Table 2).
The advantage of using a premix over that of adding
micronutrients singly is that there is a greater likelihood
of ensuring:
• The correct concentration of micronutrients
• An even distribution of micronutrients
Furthermore, the logistics of adding micronutrients to
flour will be simpler and the quality assurance system
is more likely to be effective.
The fortification process itself is accomplished by
adding the micronutrients through a volumetric feeder
(Figure 3) located towards the end of the milling process.
The most commonly used feeder consists of a rotating
feed screw that is driven by a variable speed motor.
The screw rotates inside a chamber containing the
premix and pushes the premix through an outlet spout. £
The amount of premix added to the flour can be
modified by changing the motor speed. The
concentration of premix added to the flour can be
calculated by weighing the amount of premix deposited
by the feeder in one minute divided by the volume of
flow passing underneath in the same period of time.
The premix can be either fed directly into the flour by
gravity or by air convection using a pneumatic system.
The homogeneity of micronutrients in fortified flour is
largely dependent on the location of the feeder and it
is very important that the mixing of the micronutrients
with the flour is good. In a gravity driven system,
experience has shown that the best site for adding
micronutrients is before the mid point along the screw
conveyor that collects flour from all the mill passages,
just before bulk storage or sacking (Figure 4). If the A
feeder is placed towards the beginning of the screw
conveyor, the amount of flour in the conveyor will be
too little. If, on the other hand, the feeder is located
toward the end of the screw conveyor, the required
homogenisation will not be achieved.
In a pneumatic system feeders can be placed in a
remote centralised location.
The cost of the feeder varies between US$ 2000 and
5000, depending on whether a gravity or pneumatic
system is installed and the quality of the device.
Micronutrient Stability
In foods, the stability of vitamins is more precarious
than that of minerals because vitamins are sensitive
to heat, oxidising and reducing agents, light, and other
kinds of physical and chemical stress.
Vitamins are stable in flour as such, although high
humidity and temperatures together do adversely affect
vitamin A. The use of encapsulated forms of vitamin A
will help to overcome this problem. There is some evidence
of minor losses of other vitamins during flour storage
(Tables 3 and 4).
Most of the vitamin losses ocur during baking, which is
the most common process all wheat flour products go
through. Although baking temperatures are high (over
200°C), the temperature inside the product is significantly
lower, and over 70 percent of the vitamins remain unaltered
(Table 5). Similarly, between 65 and 85 percent of vitamins
remain intact after cooking pastas (Table 6).
Table 5
Nutrient Losses During Typical Bread
Baking
Nutrient
% Loss
during
baking
Vitamin A
Vitamin Bi
Vitamin 62
Niacin
Folic Acid
10-20
15-25
5-10
0-5
20-30
F. Hoffmann - La Roche. Unpublished Data. Basel
Table 3
Nutrient Retention in Flour with 9% Humidity at Room
Temperature
Nutrient
Vitamin A, ID
Vitamin B6, mg
Vitamin E, III
Folic Acid, mg
Vitamin Bi, mg
Level per Kg
Label
Claim
Initial
2 mo
4 mo
6 mo
16,534
4.41
33.07
0.66
6.39
18,078
5.18
35.05
0.82
7.50
18,078
4.85
35.05
0.66
NR
17,681
5.07
35.05
0.77
NR
17,526
4.85
35.05
0.66
7.50
Table 4
Nutrient Retention in Flour with 9% Humidity at 45° C
Nutrient
Vitamin A, IU
Vitamin Be, mg
Vitamin E, IU
Folic Acid, mg
Vitamin Bi. mg
Level per Kg
Label
•■....Claim .
Initial
; 1 mo
.2 mo
3 mo
16,534
4.41
33.07
0.66
6.39
18,078
5.18
35.05
0.82
7.50
16,534
4.85
35.05
0.66
NR
14,175
4.85
35.27
0.57
NR
12,919
4.63
35.49
0.75
NR
NR=Not registered
Cort. W.M., B. Borenstein. B., J.H. Harley. M. Osadca. and J. Scheiner. 1975. Nutrient Stability
of Fortified Cereal Products. 35th IFT Meeting. Chicago. III.
Quality Control
The determination of micronutrients in flour can be done
by simple classical methods (e.g. fluorometric for Bi and
B2 and spectrophotometric for iron) or by faster methods
that require more sophisticated equipment (e.g. HPLC
for vitamin A, folic acid, and niacin and atomic absorption
for iron).
It is important to establish quality control standards for
both commercial premixes and fortified flour.
Legislation
Compulsory fortification of flour is increasing throughout
the world. Currently 14 countries have legislation or
regulations that mandate wheat flour be fortified with
various micronutrients (Table 7). Other countries are
Table 6
Vitamin Losses in Long Durum Wheat
Pasta After Drying and Cooking.
Nutrient
% Loss After
Drying
(759C)
% Loss
. After
Cooking
Vitamin A
Vitamin Bt
Vitamin Ba
Niacin
13
0
5
0
17
32
35
30
E Hoffmann La Roche. 1990. Vitamins and Carotenoids in
Pasta. Basel.
Figure 6
Nutrient Allowance per 100g of Different
Wheat Products
considering this option. The low cost, and simplicity
of the technology has made it one of the most sought
after methods for combating micronutrient malnutrition.
Figure 6, for example, shows the contribution that flour
fortified with vitamins Bl, B2 and niacin, as well as iron,
makes toward meeting the Recommended Dietary
Allowances (RDA) for adult men in the USA.
Table 7
Compulsory Flour Enrichment Worldwide
Code of Federal Regulations. 1973. Enrichment Levels of
Baked Goods. Flour Farina, etc. Title 21.15.525.
Nutrient data: ESHA Research. Food Processor II
NCR. 1989. Recommended Dietary Allowances.
Figure 7
Biochemical Impact of Flour Enrichment
in Newfoundland, Canada
Country
Vitarhin'Bi
,(MgA<g)
"Vitamin Ba
(Mg/Kg)
Canada
Chile
Costa Rica
Dominican Republic
Ecuador
El Salvador
Guatemala
Honduras
Nigeria
Panama
Saudi Arabia
UK
USA
Venezuela
4.4-77
6.30
4.4-5.5
4.45
4.45
4.41
4.0-6.0
4.40
4.5-5.5
4.40
a 6.38
>2.4
6.40
1.50
27-4.8
1.30
2.6-3.3
2.65
7.48
2.65
2.5-3.5
2.60
27-3.3
2.60
>3.96
4.00
2.00
Niacin
(Mg/Kg)
Folic Acid
(Mg/Kg)
■
.
Iron
(Mg/Kg)
(0.4-0.5)
29-43 ■
35-64
30.00
13.00
28.7-36.4
35.2-44.0
29.29
35.62
0.59
58.65
83.58
28.70
35.30
35-40 0.35-0.45 . 55.65
28.70
35.20
28.9-36.7
35.5 - 44.4
2870
35.20
>36.30
>52.91
>16.5
>16.0
44.10
52.90
20.00
20.00
Note: Figures in parenthesis indicate the enrichment is optional
Raunhardt. O. and A. Bowley. 1996. Mandatory Food Enrichment. Nutriview 1.
Aykroyd, WR. el al 1949. Medical Survey of Nutrition in
Newfoundland 1948. The Canadian Med. Assoc. Journal.
60:4
Figure 8
Deaths from Niacin Deficiency in the
U.S.A. Association with Wheat Flour
Enrichment
Miller. D.F. 1955. Enrichments Programs Helping Mother
Nature Along Food Prod. Dev. 12: 4 30-38
#OMNI“
Costs
The cost of fortifying wheat flour is much lower than
generally recognised. For example, the total cost of
adding mandatory nutrients to flour in the USA (i.e. 6.4
mg/Kg Vitamin Bi, 4.0 mg/Kg Vitamin B2, 52.9 mg/Kg
Niacin and 44.1 mg/Kg Iron), is less than one US
Dollar per metric ton of flour. This is about 0.1 percent
of the cost of flour in the shops.
On the other hand, if the cost in the USA is calculated
on a per person per year basis, and average wheat
consumption is 205 g/person/day, the total cost of
fortification is US$ 0.07 per person per year.
In addition to the recurrent costs for the micronutrients,
there are the capital costs for the feeders, which are
not great, and the recurrent costs for quality control.
Impact on Public Health
Figures 7 and 8 show the association between the
introduction of fortification initiatives and the reduction
in vitamin Bi and B2 deficiencies in Canada and niacin
deficiency in USA, respectively.
Iron deficiency anaemia has also decreased in the
USA, Great Britain, Sweden, and Chile and much of
this decline is attributed to food fortification, including
bread, with iron.
Roche'
'ill'll
Fortification Basics
H
Rationale
Sugar is an important source of energy for many people throughout
the world. It is produced in over 100 countries and production
of sugar is increasing, especially in South America (Table 1). Sugar
processing and refining is carried out at only a few mills in sugar
producing countries while sugar refining only is done in some
sugar importing countries. For these reasons, fortifying sugar
with micronutrients is both practical and feasible. In addition,
sugar is eaten by the vast majority of people on a regular basis,
although consumption levels do vary (Table 2); thus, fortification
is an effective means to provide nutrients that are deficient in the
population.
Among the micronutrient deficiencies, vitamin A deficiency is one
of the most widespread, affecting more than 250 million children
throughout the world (Fig. 1). One approach to eliminating this
problem has been the fortification of sugar with vitamin A.
Fortification Criteria
The objective is to ensure that vitamin A needs are met for the
groups at greatest risk of deficiency without resulting in excessive
intakes for individuals having a high sugar intake.
The level of vitamin A to be added is determined by nutritional
requirements and sugar consumption patterns; thus, nationally
representative data disaggregated by socio-economic status and
age groups are needed. Children under 5 years old are most
vulnerable to vitamin A deficiency, and their recommended daily
allowance is 400 pg RE (1,330IU) per day. Pregnant women are
also at high risk of deficiency, and their reccomended daily
allowance is 600 ja.g RE (2,000 IU).
If, for example, the average sugar intake of children under five
years old is 20 grams per day and that for adults in the highest
consuming group is 150 grams per day, 15 pg of vitamin A per
gram of sugar will both satisfy needs and remain below the
maximum acceptable limit.
?ugar
Table 1
Regional and World Sugar Production
('000MT)’
^Region
Central America
S. America
Africa
Asia
Europe
N. America
Oceania
World Total
1988
^1994 1
15,000
13,000
8,000
26,500
31,500
6,500
4,200
104,700
11,500
17,000
7,000
33,300
27,300
7,000
5,800
110,300
1, International Sugar Organization, 1995.
Table 2
Per Capita Sugar Consumption, and
Percent of Daily Energy Intake in Selected
Countries
;CbnsumptIdh'S5t'v»?S.% of dally j
; (cip "r/
n rqy :
.....'■ ./
........ >'■ 'K ... .
17
127
Brazil
14
88
Peru
15
110
Guatemala
12
85
Honduras
5
42
India
5
42
Indonesia
88
Morocco
2
22
Mali
10
80
Egypt
8
31
Zambia
3
17
Cameroon
15
100
South Africa
1. International Sugar Association. 1995.
2. FAO Food Balance Sheets. 1984 - 1986 average.
Technology
Because the quantity of vitamin A being added is so small,
production of an homogeneously fortified product is facilitated
by diluting the retinyl palmitate (the form of vitamin A used in
fortification) in a small amount of sugar to form a premix.
Countries Categorized by Degree of
Public Health Importance of Vitamin A
Deficiency
Premix contains:
• Regular sugar.
• Cold water soluble vitamin A palmitate beadlets containing
75,000 pg /g (250,000 lU/g).
• A low peroxide, low in unsaturated fat vegetable oil (e.g.
coconut or peanut), which adheres the vitamin A beadlet to
the sugar crystal (Fig. 2). This prevents the separation of the
vitamin A from the sugar crystal and results in an
homogeneously fortified product, without noticeable changes
in the sugar's organoleptic properties.
WHO XVIIIVACG Meeting. Guatemala. 1996.
Figure 1
Figure 2
Vitamin A Beadlet Adhered to Sugar
Crystal
• An antioxidant blended from natural antioxidants (ascorbyl
palmitate, DL-alpha tocopherol, and lecithin) to prevent the
oil from going rancid. Rancid oil destabilizes vitamin A and
has adverse effects on the sensory characteristics of sugar.
Blending the oil and antioxidant in an inert, oxygen-free
atmosphere, i.e., in the presence of nitrogen gas, prevents
oxidation of the oil.
Premix Composition
'XT;/-.-.-Amount
Sugar
Vitamin A 250 CWS
Peanut oil
Antioxidant
TOTAL
76.35
22.03
2
0.008
100
Units' J-.
Kg
Kg
L
Kg
Kg
.
Figure 3
V-type Mixer and Oil Deposit
Figure 4
Automatic Dosifier and Control Panel
Premix is made by mixing the sugar and vitamin A in a blender
(generally a V-type, Fig. 3), with a spraying device attached to it
that allows the oil-antioxidant mixture to be added during the
mixing operation.
After 10 to 20 minutes of mixing, the premix is packaged in 25
Kg black polyethylene bags covered with polypropylene bags.
This minimizes exposure to light, thereby preventing the destruction
of retinol. This premix is added to sugar in a ratio of 1:1000.
The addition of premix to sugar can be done manually or
automatically. In manual operations, the premix is added into the
centrifuges. This method is not ideal because the accuracy of
the amount of premix added is dependent on the operator. In
automatic operations (Fig. 4), feeders can be placed in different
sites along the production line (Fig. 5). The best site is where the
humidity and temperature are lowest, which would be just before
packaging. This is not always possible because of limitations in
the amount of space available. Fortified sugar is packaged in
polyethylene bags.
Stability of Retinyl Palmitate
An industrially produced encapsulated vitamin A compound that
is dry, solid, and miscible in water, facilitated the development of
fortification technology. Despite its excellent stability, 250-CWS
is still sensitive to air, light, moisture, heat, and acids; thus,
appropriate handling and storage conditions of the premix and
fortified sugar are important.
In the premix and, during the fortification process
Experimental data report retinol losses of between 10 and 20
percent during the processing of fortified sugar, and between 20
and 40 percent during storage after one year. These losses need
to be compensated for by adding the appropriate overage of
premix to sugar during the fortification process.
Retinyl palmitate is susceptible to oxidation in the presence of
sun or artificial light. Packaging premix in bags covered with black
polyethylene bags reduces exposure to light and degradation of
vitamin A.
Retinyl palmitate beadlets resist temperatures of 105 °C for 10
minutes. This is important because the premix is added to sugar
before it passes through the drying turbines, where temperatures
are between 65 and 70 °C.
Figure 5
Possible Points for Premix Addition
In fortified sugar
Stability tests show that fortified sugar packaged for retail sale
in polyethylene bags retains between 50 and 70 percent of the
initial vitamin A level after 3 months of storage (Fig. 6 and 7). Heat
and moisture together are believed to be more detrimental to
retinyl palmitate than either alone (Table 3).
Fortified sugar in foods
Vitamin A in fortified sugar remains stable in foods prepared at
home, although moisture, heat, and acidity do reduce its activity.
When fortified sugar is added to beverages such as lemonade
and orangeade, 60 to 80 percent of the vitamin A remains after
two days.
Vitamin A is sensitive to acids and losses can be expected. Most
of the vitamin A in fortified sugar, however, can be lost in the
manufacturing of soft drinks as a result of using activated charcoal
and diatomaceous earth to eliminate color and impurities; thus,
when non refined sugar is used in manufacturing soft drinks there
is complete destruction of the vitamin. If, however, refined sugar
is used two-thirds of the original retinol level remains.
The stability of vitamin A in baked foods is also good. The retention
of the micronutrient after baking is in the order of 80 to 90 percent.
Micronutrient interactions with vitamin A in sugar are unlikely
because sugar is a pure product with minute quantities of other
compounds.
Quality Control
The vitamin A content of the premix is determined using quantitative
methods, while that for fortified sugar is carried out using both
semiquantitative and quantitative methods.
Quantitative methods include the use of HPLC or
spectrophotometric methods. The HPLC method is based on
the separation of vitamin A (retinol) from other substances that
absorb radiant energy at an equal or similar wavelength to retinol.
Detection of retinol in the HPLC column can be done using UV
light or fluorescence. This method is accurate, does not destroy
retinol, and requires a small amount of sample. However, the
equipment is expensive, highly trained personnel are required,
and few samples can be run at a time, making the analysis
expensive. The spectrophotometric method involves measuring
the absorbance of retinol in sugar after its selective destruction
through exposure to UV light. This method is easy to use, less
expensive than the HPLC method, and results can be obtained
in a much shorter period of time.
The semiquantitative colorimetric method involves adding a
chromogenic reagent to a volume of solubilized sugar to produce
a blue color. The intensity of this blue color is proportional to the
amount of retinol in the sample, measured against a set of
standards. Semiquantitative assays at 1 to 2 hours intervals
during production verify that the fortified sugar contains the
amount of vitamin A that falls within the range stipulated in the
norms. Results are immediate and permit adjustments to the
amount of premix added to sugar.
Costs
The costs of sugar fortification include the capital investments,
i.e. building and equipment costs, and recurrent costs, i.e.
personnel costs, premix and fortified sugar production costs,
as well as-monitoring and evaluation costs. In Guatemala, the
cost of fortifying 1 metric ton of sugar is US$9.51, and the cost
Figure 6
Stability of Vitamin A in Sugar,
Cia. Azucarera La Estrella S.A.
De Gracia. M.S.. FE. Murillo. 1993. Estabilidad de Vitamina
A en aziicar fortificada resumed ejecutivo. INCAPAJ de P.
Figure 7
Stability of Vitamin A in Sugar,
Cia. Azucarera Nacional S.A.
De Gracia. M.S.. F.E. Murillo. 1993. Estabilidad de Vitamina
A en aziicar fortificada resumed ejecutivo. INCAPAJ de P.
Table 3
Stability of Retinol in Fortified Sugar
(% retention in 125 lb. sacs)
is Location Type -‘VsSppJ.Months of Storage •
'j
r,
C
Cold - Humid
90
77
66
Hot-Dry
92
71
63
Temperate - Humid 83
69
43
Hot - Humid
80
62
40
Dary. O.. De Ie6n. L. Conference on XVIIIVACG Meeting,
Guatemala. 1996.
Figure 8
Decrease in % Children with Serum
Retinol Level Below 10 mcg/dL After
Consumption of Fortified Sugar
Arroyave G, Aguilar Jr. Flores M, Guzman Ma. Evaluation of
Sugar Fortification with Vitamin A at the National Level Pan
American Health Organization. Scientific Publication 384
Washington, DC.. 1979.
Figure 9
Effect of Fortified Sugar Consumption
on the Prevalence of Low Retinol
Levels in Human Milk
Arroyave G. Aguilar Jr, Flores M, Guzman Ma. Evaluation of
Sugar Fortification with Vitamin A at the National Level Pan
American Health Organization. Scientific Publication 384
Washington, DC., 1979.
Table 4
Status of Legislation for Sugar
Fortification in Latin America
Countries
Enforcing
Legislation
Countries In Countries with
Process of
Interest (Private'
Legislating : or Official) .' • ■1
Guatemala Nicaragua Brazil
Honduras Ecuador
Dominican Rep
El Salvador
Colombia
Bolivia
per person is US$0.36/year. Given that a kilogram of sugar costs
US$0.45 before fortification, adding vitamin A increases the price
to US$0,459, that is, 2 percent above the original price.
The economic analysis of a program can be presented in different
ways, for example, cost per metric ton, cost per person, cost
per person covered, cost per possible beneficiary, and in terms
of cost-effectiveness. The cost of a sugar fortification program
is inexpensive, especially when compared with the costs of
vitamin A deficiency, and the cost of other interventions.
Legislation
To be successful, a fortification program requires the collaborative
participation between various government sectors, food producers,
private organizations, and international agencies. The strongest
expression of political commitment to eliminate vitamin A deficiency
is legislative action to make a vitamin A fortification program
official. Such legislation shall define the norms for implementing
fortification, including the responsibilities of each sector involved.
The regulations for vitamin A fortification must specify the type
of vitamin A fortificant and the permitted range of retinyl palmitate
in fortified sugar both at the refinery and at the point of sale when
appropriate. The regulations must define the precautions and
food safety conditions to be observed during production,
transportation, storage, and sale of the fortified sugar.
Labeling the bags of fortified sugar at the refinery should be
enforced, especially when unfortified sugar is also produced for
industrial use. Sugar packaged for retail sale should be labeled
in a way that is true and accurate, and provides essential
information specified by the health authorities.
The official creation of a specific committee, for example, a Food
Fortification Committee, with representatives from different sectors
is recommended. The role of this committee would be to monitor
program implementation and analyze the information coming
from the different operating units, and to ensure that the operating
units and those responsible at the points of sale comply with
their responsibilities.
History and Successful Interventions
Guatemala was one of the first countries to implement a sugar
fortification program to ensure an adequate intake by the population
with satisfactory results (Fig. 8 and 9).
Other countries in Latin America are now implementing vitamin
A fortification programs (Table 4). Asian countries are also
considering sugar fortification.
Vitamin A is an essential nutrient and deficiency is associated
with adverse health effects. Sugar fortification presents an
important intervention for improving the vitamin A status of atrisk populations.
Although the current technology is adequate enough, it can still
be improved in order to increase the efficiency of the fortification
program. In existing refineries, space where the dosifiers can be
installed is often limited. Future plant layouts should make
provisions for this limitation.
nsmu
Roche
(0
_
w
Rationale
Oils and fats, along with carbohydrates and proteins are major
components of the human diet. Oils provide energy, fat soluble
vitamins (vitamins A, D, and E), and essential fatty acids that are
required for proper growth and development.
The production of vegetable oils (canola, corn, cottonseed,
coconut, olive, palm, peanut, safflower, soybean, sunflower) is high
throughout the world, and consumption (Table 1) is increasing,
especially among the lower socioeconomic groups. A higher
consumption of vegetable oils over animal fats is preferable because
vegetable oils contain much less saturated fat than animal fats (Figure 1),
and they contain no cholesterol.
Vegetable oils are suitable as vehicles for vitamins A, D, and E
fortification, as the production and refining of the oils is a centralized
process. As vitamins A, D, and E are fat soluble, they can be uniformly
distributed in oil. The stability of vitamin A is greater in oils than in
any other food and oil facilitates the absorption of vitamin A by the
body. Vegetable oils are consumed by almost everyone; thus, it is
possible to improve people’s access to fat soluble vitamins through
fortification.
Hydrogenation converts liquid vegetable oils into solid fats, such
as margarine. The vitamin A and D content in margarine is negligible.
However, fortification with these vitamins can make margarine an
important source of these nutrients, as well as a source of energy.
Fortification with vitamin E may be important where the diet is
high in polyunsaturated fatty acids (PUFA). PUFAs are long chain
fatty acids with more than one double bond, which makes them
susceptible to oxidation. The process of oxidation of fat in oils is the
same as in cells.
• Food oils that are high in triglycerides can contain PUFAs, which
produce hydroperoxyacids on oxidation resulting in a rancid odor
in food.
• At the cellular level, oxidation results in the formation of free
radicals, which have been shown to be associated with cancer
and cardiovascular diseases (CVD); hence antioxidants are
thought to be anticarcinogenic and cardiovascular protective.
Technologies now exist to add water soluble micronutrients
including vitamin C, the B-complex, iron, and calcium to margarine.
Fortification Criteria
Fortification of vegetable oils and their derivatives (margarine,
mayonnaise, etc.) with vitamins A, D, and E is technologically feasible.
Crude vegetable oils are a rich source of vitamin E. Processing crude
oil, however, can result in the loss of this vitamin; the extent of this
loss is dependent on the processing method used. Vitamin E can
be added to refined oil as a nutrient or as an antioxidant. Vitamin E
antioxidants, such as alpha (a) tocopherol, prevent rancidity and
protect other components in the oil susceptible to oxidation, including
vitamin A, but it is not a good fortificant. Alfa tocopheryl acetate, in
contrast, is stable, making it a good fortificant, but it has no antioxidant
activity.
Table 2 shows that the range of vitamin A added to margarine in
a number of countries varies between 3,180 and 45,000 lU/Kg, while
Table 1
Per Capita Vegetable Oil Consumption,
and Percent Daily Energy Intake from
Vegetable Oils in Selected Countries
Country'
■
Argentina
Brazil
Mexico
Costa Rica
Central Africa
Congo
Gambia
India
Indonesia
Philippines
- Consumption : ■
% Energy
.J9./da^bL-. ■ (...Intake
33
’
27
30
35
12
34
31
16
17
12
9
9
11
5
12
7
6
4
Source: FAO.1991. Food Balance Sheets 1984-1986. Rome.
Figure 1
Fatty Acid Content of Different
Vegetable Oils and Animal Fats
Table 2
Mandatory Fortification of Margarine with
Vitamins A&D
Belgium
Brazil
Canada
Chile
Colombia
Denmark
Ecuador
El Salvador
Guatemala
Honduras
India
Indonesia
Malaysia
Mexico
Netherlands
Panama
Peru
Portugal
Singapore
Sweden
Taiwan
Turkey
U.S.A.
UK
22,500 - 27.000
15,000-50.000
> 33,000
30,000
3,180- 7,950
25,200
20,000 - 30,000
15,000
15,000 - 50,000
35,000
> 30.000
25,000 - 35,000
25,000 - 35,000
20,000
> 20,000
20,000
30,000
18,000
> 28,300
S 30,000
> 45,000
20,000
33,000
24,000 - 30,000
2,500 - 3,000
500 - 2,000
2 5,300
3,000
480- 1,200
2,000 - 4,000
1,500
2,500 - 3,500
2,500 - 3,500
2,000
£ 3,000
1,500
3,000
a 2,200
2 3,000
1,000
2,080
2,800 - 3,520
Source: Raunhardt, 0. and A. Bowley. Mandatory Food
Enrichment. Nutriview. Supplement to 1/1996 Issue.
Figure 2
Flow Chart of Fortified Margarine
Manufacturing
Ripened
skim milk
Mixture of Oils/fats
Oily Vitamins
I
■
_______I
t*-------- <-------- 1 Homogenization]
| Emulsification] •
H Rolling I—4 Kneading [—* Margarine
Source: O'Brien, A. and D. Robertson, n.d. Vitamin Fortification
of Foods (Specific Applications). The Technology of Vitamins
in Foods. In Micronutrient Fortification of Foods The
Micronutrient Initiative. Ontario Canada.
Figure 3
Stability of Vitamin A Fortified Soybean
Oil During Storage at 23°C Under
Different Conditions
that for cholecalciferol (vitamin D3) varies between 480 and 5,300
lU/Kg. A 15 g serving (1 tablespoon) of these margarines would
provide between 4 and 51 percent of the recommended daily intake
(RDI; FAO/WHO 1988) for vitamin A, and between 2 and 20 percent
of the RDI for vitamin D for pre-school children.
As a nutrient, it would be appropriate to fortify oil and margarine
with vitamin E at a level of 65 to 190 mg/Kg. The recommended daily
intake for vitamin E increases with intake of PUFA. At a ratio of 0.4
mg a- tocopherol to 1 gm PUFA, there is enough vitamin E in normal
circumstances to counteract the level of PUFA normally being
consumed to prevent oxidation. At a level of 65 to 190 mg/Kg, 1
tablespoon of oil or margarine/day would provide between 15 and
50 percent of the RDI for a child between 1 and 6 years old.
The level of fat soluble vitamins in fortified oils and margarine
depends on consumption patterns and nutritional requirements.
Clearly, before determining the level of nutrient to add to oils and
fats, the use of and consumption patterns for oil by different socio
economic and age groups need to be determined in order to ensure
that the maximum safe level of intake for each nutrient is not exceeded.
Technology
The most common commercial vitamin A and D3 blend used
contains 1,000,000 IU vitamin A palmitate (300,000 mg/g) and
100,000 IU vitamin D3 (2,500 mg/g) in a liquid form, stabilized with
vitamin E (a-tocopherol) or a BHA/BHT mixture. The same vitamin
A/D blend is also available with vitamin E fortificant (vitamin E acetate)
as a custom-made premix.
Fortification of vegetable oil
Oil fortification consists of adding appropriate amounts of vitamin
A and D3 concentrate to clarified, degassed oil at 45-50°C. The
solubility of commercially available vitamin A and D3 blends in
vegetable oils is excellent.
To ensure that the vitamins are uniformly distributed, mixing takes
place in vertical tanks that contain turbines or propeller agitators.
Edible antioxidants (BHA and/or BHT) or natural antioxidants (e.g. atocopherol or ascorbyl palmitate) may be added to protect both the
vitamin A and the oil; the stability of vitamin A in the oil depends
greatly on the stability of the oil itself. Vitamin A oxidizes faster and
loses its activity in the presence of oxidized oils.
To maintain vitamin A activity, fortified oil needs to be packaged
in light-protected, sealed containers. Replacing the container
headspace with inert gas will help retain the stability of both the oil
and vitamin A prior to the container being opened, but this is not
usually a practical solution and adding an adequate micronutrient
overage may be considered as an alternative.
The production and fortification of margarine is carried out in a
batch or continuous process. The vitamin A and D3 blend is
premeasured according to the batch size of the margarine tanks
and mixed with warm oil, in a ratio of 1:5, until a uniform solution is
obtained. This premix is then incorporated into the margarine before
the emulsifying process (Figure 2). B-Carotene is also added to
margarine (15 to 20 g/ton of a 30% oily suspension) before the
emulsification step to enhance the color as well as to contribute to
the vitamin A content of the product. B-Carotene converts to vitamin
A at a mean level of 555 lU/mg; thus, providing an additional 2,498
to 3,330 IU of vitamin A per kilogram, at the above mentioned level.
Stability of Micronutrients
Source: Favaro. R., J. Ferreira, I. Desai, and J. Dutra de
Oliveira. 1991. Studies on Fortification of Refined Soybean
Oil with All-trans Retinyl Palmitate in Brazil: Stability During
Cooking and Storage. J. Food Comp. Anal. 4: 237-244.
Stability of vitamin A in storage
Studies conducted in Brazil showed that the stability of vitamin
A, in fortified soybean oil stored at room temperature (23°C), depends
on the presence of oxygen and light (Figure 3). The stability of vitamin
A in oil, stored in sealed cans, is excellent after 9 months. However,
if the oil is stored in open containers, where it is exposed to both
oxygen and light, the vitamin A becomes unstable after 6 months
and just under 50 percent of the initial vitamin A remains after 9
months. Stability studies in India showed almost 100 percent retention
of vitamin A in fortified soybean oil after 5 months of storage in sealed
cans.
Vitamin A added to margarine is quite stable during the
manufacturing process and during storage at home. Table 3 shows
that there were minimal losses of vitamin A in margarine after 6
months of storage at 5°C (refrigeration conditions). When the same
margarine was stored at 23°C, more than 85 percent of the initial
vitamin A was retained after the same period of time.
Stability of vitamin A during cooking
The stability of vitamin A in fortified soybean oil added to plain
rice or kidney beans during cooking is good (Table 4). Boiling rice
and pressure cooking kidney beans did not destroy the vitamin.
Frying, however, can destroy vitamin A. The amount lost depends
on the number of times the same oil is used for frying foods (Figure
4). After the initial frying about 65 percent of the original vitamin A
remained, after 4 repeated fryings less than 40 percent of the original
levels of vitamin A was retained, and after 12 consecutive fryings
most of the vitamin A was lost. Thus, how oil is used at the household
level needs to be considered in determining whether oil can be a
good vehicle for vitamin A.
Vitamin A losses in margarine occur under extreme conditions.
Heating it to 160°C, 180°C, or 200°C for one-half hour results in
average vitamin A losses of 20, 35, and 50 percent, respectively.
Vitamin A, however, survives the baking process in biscuits, cakes,
and breads prepared with vitamin A fortified margarine; between 80
and 100 percent of the added vitamin remains.
Table 3
Retention of Vitamin A
in Commercial Margarine
Brand
A
B
C
D
E
' initial’’:
Level (IU)
13*900’
14,200
13,500
12,300
12,400
After 6 Month Storage at
,.23’C.
14,700
13,600
13,400
12,700
12,400
11.500
12,100
12,300
12,100
10.900
Source: Bauernfeind. J.C. 1978. The Technology of
Vitamin A. Hoffmann-La Roche. Basel. Switzerland.
Table 4
Stability of Vitamin A in Soybean Oil
During Cooking
Food
Type of
cooking
’ Amount of
Recovery
Vitamin A (pg/g)
(%) •
Before cooking Alter cooking -
White rice Boiled
Kidney
Boiled
beans
Kidney
Pressure
beans
cooked
330
180
330
150
100
83
120
120
100
Source: Favaro. R., J. Ferreira. I. Desai, and J Dutra de
Oliveira. 1991 Studies on Fortification of Refined Soybean
Oil with Atl-trans Retinyl Palmitate in Brazil: Stability During
Cooking and Storage. J. Food Comp. Anal. 4: 237-244.
Figure 4
Stability of Vitamin A in Fortified
Soybean Oil After Repeated Fryings
of Potatoes at 117-170°C.
Stability of vitamin D3
The stability of Vitamin D3 is similar to that of vitamin A; little or
no loss is experienced during processing or storage.
Stability of vitamin E
Vitamin E losses occur during prolonged heating, such as frying.
Furthermore, the production of hydroperoxides during frying
accelerates the degradation of vitamin E.
Acceptability of Fortified Margarine and Oils
Fortifying margarine with vitamins A, D, and E does not alter its
flavor, making it an excellent carrier for these micronutrients. Foods
made with fortified soybean oil including mayonnaise, fried beans,
cooked rice, fried potatoes, soup, wheat tortillas, and fried meat
showed excellent acceptability among consumers, who were not
able to distinguish between products prepared with either vitamin
A fortified or unfortified oil.
Studies in humans have shown that the bioavailability of vitamin
A in cooked foods, made with fortified soybean oil, is good (Figure 5).
Quality Control
Determination of vitamins A, D, and E in oil and margarine is done
by HPLC. This method is based on the separation of the specific
vitamins from other substances that absorb radiant energy at an
equal or similar wavelength to the specific vitamin. It is accurate,
but the equipment is expensive and highly trained personnel are
required.
Measuring the amount of micronutrients to add, and the process
of their addition to oil or margarine, requires careful attention to
ensure that the final fortified product is both homogeneous and
standardized.
Source- Favaro. R.. J. Ferreira. I. Desai, and J. Dulra de
Oliveira 1991. Studies on Fortification of Relined Soybean
Oil with All-trans Retinyl Palmitate in Brazil: Stability During
Cooking and Storage J. Food Comp. Anal. 4: 237-244.
Figure 5
Serum Retinol levels in Humans After
Ingestion of Cooked and Uncooked
Fortified Oil with Vi'tamin A
Source: Dutra de Oliveira. J.E.. I. Desai. R.M.D. Favaro. and
J.E Ferreira 1994. Effect of Heat Treatment During Cooking
on the Biological Value of Vitamin A Fortified Soybean Oil in
Human. Int. J. Food Sci. Nutr. 45: 203-207.
Figure 6
Distribution According to Year of
Appearance of Xerophthalmia in 72
Patients Admitted to the Rigshospital,
Copenhagen from 1912 to 1919
Source- Bloch. C. E. 1931. Effects of Deficiency in Vitamins
in Infancy. Am. J. Diseases of Children. 42: 271.
Table 5
Vitamin A Deficiency in Newfoundland
in 1944 and 1948
1943.
Number of subjects
312
342
Percent of subjects with
serum vitamin A < 20 ng/dl
serum vitamin A < 30 ng/dl
48
74
2
18
Mean serum vitamin A (y.g/dl)
22
Source: Aykroyd. W.R. et al. 1949. Medical Resurvey of
Nutrition in Newfoundland 1948 Murray Printing Company.
11-12.
Costs
The cost of fortification includes capital costs, such as blending
equipment (tanks, propellers, or agitators), and recurrent costs
including those for the premix, personnel, and monitoring and
evaluation.
If margarine is fortified to provide 30,000 IU of vitamin A/Kg, the
cost of the fortificant would be in the order of USS 0.0020/Kg when
a vitamin A/D3 blend is used. The cost of vitamin A alone is around
USS 0.0017/Kg of product. These estimates do not take in account
the cost of new equipment and training of staff, which are one-time
costs and are likely to be small, as well as the cost of quality control.
Legislation
To ensure that a fortification program is successful, an
interdisciplinary task force with experts from the different, appropriate
sectors should be set up. The sectors include the vegetable oil
industry and trade organizations, nutrition institutes, universities, the
Ministry of Health, regulatory institutions, consumer associations,
and donors.
A fortification plan should specify the type of micronutrients and
levels to be added based on the consumption patterns of oil by
different socioeconomic and age groups. It must also define
precautions and food safety conditions to be observed during
production, transportation, storage, and sale of the products.
History and Successful Interventions
The prevalence of xerophthalmia in Denmark declined drastically
in 1918 and disappeared in 1919 (Figure 6) following the introduction
of butter rationing (which made butter available at a low price and
diminished consumption of non-enriched margarine) at the end of
1917. Xerophthalmia reappeared in 1920 when butter rationing was
discontinued; thus, eliminating access to an important source of
natural vitamin A. Such observations on the curative effects of milk
fat, but not of margarine, eventually led to the enrichment of margarine
with vitamin A.
A successful intervention with vitamin A fortified margarine (45
IU vitamin A/g margarine) initiated in Newfoundland in 1944-45, led
to a marked improvement in the vitamin A status, as shown by
biochemical measurements made in a sample of the population
(Table 5).
Countries Categorized by Degree of
Public Health Importance of Vitamin A
Deficiency
■ Severe: subcfinical
■ Moderate: suDciinical
No data: problem likely
Problem under control
Source: WHO XVIIIVACG Meeting. Guatemala. 1996.
Thirty years ago, Pakistan agreed to fortify processed oil products
with vitamin A at a level of 33,000 lU/kg. Enforcement and monitoring
has been weak as reflected in the levels of vitamin A in vegetable
ghee, which were on average 15,000 lU/kg. With an average vegetable
ghee consumption of 30 g/person/day, the ghee would provide about
30,24, and 15 percent of the RDI for infants, children, and pregnant
women, respectively.
In the Philippines, a collaborative effort between the public and
private sectors resulted in the "Star" brand margarine being fortified
with vitamin A. “Star" margarine is fortified at a level of 25 jig RE/g
(83 IU), and provides 95 percent of the RDI for children 1 to 10 years
old when 15 grams/day (1 tablespoon) is consumed. Other countries
fortifying margarine with vitamins A and D are presented in Table 2.
Sweden fortifies canola oil used in food aid programs with 15 mg
vitamin A/g oil. Canada has adopted an even higher level of 22.5
mg vitamin A/g canola oil used in food aid programs.
nsnn
OMNI Sr
Roche
£
•
Fortification Basics
Principles of Assay Procedures
Micronutrients added to foods are analyzed using various
procedures depending on their nature and properties. Some
micronutrients can be detected using relatively simple
colorimetric methods. Where resources are available, more
sophisticated methods such as high pressure liquid
chromatography (HPLC) (Fig. 1), which separates the compound
of interest in a pre-treated food sample, followed by
spectrophotometric or fluorometric detection can also be used.
Before starting a program for micronutrient analyses, some
essential elements need to be put in place:
•
•
•
•
A quality assurance system must be set up to ensure that
the manufactured food is safe, unadulterated, properly
labeled, and meets all the company's specifications and
government regulations (Table 1).
Food samples must be representative and selected at
random, with an adequate and reproducible sampling
procedure.
Personnel must be trained in the assay method(s), that
should have been previously identified or set-up.
Equipment required must be available on-site in working
condition.
Vitamin A assays
Vitamin A is one of the most unstable micronutrients.
Industrially produced vitamin A, like retinyl palmitate, is more
stable than naturally occurring vitamin A, although it remains
sensitive to air, light, moisture, heat, and acid conditions.
Vitamin A levels have been determined using colorimetric
and spectrophotometric methods for a long time. Currently,
HPLC is the method of choice (Table 2). The use of HPLC is
preferred when samples have a significant amount of interfering
substances such as other vitamins, minerals, proteins, and
carbohydrates.
Semi-quantitative method
Colorimetric method
The colorimetric method involves adding a chromogenic
reagent to a volume of solubilized fortified food sample. The
reagent reacts with retinol to produce a blue color, whose
intensity is proportional to the amount of retinol in the sample.
The intensity of the blue color is measured against a set of
known standards (Fig. 2). The formed blue color is very unstable
and necessitates a fast and skillful worker. Because this assay
method is inexpensive, and does not need sophisticated
equipment, it is used in many countries.
Quantitative method
Spectrophotometric method
The sample is irradiated with UV light and its absorbance
is measured. The absorbance is proportional to the vitamin A
content in the sample. The spectrophotometric method can
be used to monitor vitamin A levels in fortified products at the
production level.
Figure 1
HPLC Equipment
Table 1
Developing a Quality Assurance System
-An effective quality assurance system includes: •'
,
• Ingredient inspection and control- testing all ingredients
against reference standards.
• Manufacturing control • identifying quality criteria and
chemical, microbiological, and physical hazards;
establishing and monitoring the critical control points
involved in manufacturing fortified food.
• Distribution control- ensuring that the fortified food is
unadulterated, properly labeled, and packaged to
minimize micronutrient losses.
Table 2
Vitamin A Assays and their Advantages
and Limitations
Assay,
' Advantages
. Limitations.
Colorimetric Simple
Rapid
Inexpensive
Semi - quantitative
Sample pretreatment
Not applicable for field
SpectraSensitive
photometric Rapid
Inexpensive
Needs UV apparatus
Sample pretreatment
Not applicable for field
HPLC
Expensive
Training of personnel
Sample pretreatment
Not applicable for field
Reliable
High resolution
No interferences
Accurate
Table 5
List of Suppliers for Laboratory
Equipment, Chemicals, and Fortificants
Aldrich
P.O. Box 355
Milwaukee, Wl
53201-9358
Te1:(414) 2733852 Chemicals,
Fax:(414) 2734979 Glassware,
Lab. equipment
Tel:(049) 621 600
BASF
6700 Ludwiglhafen- Fax:(049)622525
Rhein
Ludwigfhafen,
Germany
Fortificants,
Premixes
Beckman
Tel:(714) 871 4848 Spectrophotometer.
Fax(714)521 3700 Chromatography
Instruments. Inc.
equipment
2500 Harbor Blvd.
Fullerton, CA 92634
Fisher Scientific
711 Forbes Ave.
Pittsburgh. PA
15219-4785
Tel.(412) 490 8300 Chemicals
Fax:(201)379 7638 Glassware
F. HoffmannLa Roche Ltd.
CH-4002, Basel
Switzerland
Tel:(061) 688 1111 Fortilicants.
Fax:(061)691 9600 Premixes
Millipore Intertech
P.O. Box 10
Marlborough, MA
01752
Tel:(508) 624 8400 Centrifuge,
Fax:(508)624 8630 Filtration devices
NISTa
Bldg. 202. Room
204
Gaithersburg, MO
20899
Tel:(301) 975 6776 Standards.
Fax:(301) 948 3730 Reference materials
Tel:(203) 762 1000 AAS instrument,
Perkin Elmer
Fax:(203)7626000 Chromatography
761 Main Ave.
equipment
Norwalk, CT 068590012
Sarstedt
Tel:(704) 465 4000 Biological assays
Fax:(704)465 4003
P.O. Box 468
Newton, NC 286580468
Sigma Chemical Co. Tel:(314) 771 5750 Chemicals,
Fax:(314)7715757 Test kits
P.O. Box 14508
St. Louis. MO
63178-9916
VARIANb
Tel:(408) 734 5370 Spectrophotometer,
220 Humboldt Court Fax:(408)744 0261 Chromatography
equipment
Sunnyvale, CA
94089
Tel:(45) 3 527 3527 Iodine spot test kits
UNICEF Supply
Division
Fax:(45) 3 526 9421
UNICEF Plads, Free
port
DK-2100,
Copenhagen
Denmark
a National Institute ol Standards and Technology
6 Parts and supplies center
Modification of the original table by Dary, O.. G. Arroyave. H.
Flores. F.A.C.S. Campos. M.H.C.B. Lins. 1996. Sugar Fortification
with Vitamin A. Part 3. Analytical methods for the control and
evaluation of sugar fortification of vitamin A. USAID/INCAP
AOMNISr
personnel to optimize operating parameters. AAS can also be
used to simultaneously determine the content of other minerals,
including, calcium, copper, magnesium, manganese, and zinc!
The advantages and limitations of iron assays are shown
in Table 3.
Iodine assays
Qualitative method
Spot tests
Spot tests can be used in qualitative determinations of
iodine in salt. Qualitative iodine tests indicate only the presence
or absence, not the amount, of iodine in salt (Fig. 5). Spot tests
are specific to the form of iodine in salt. In the case of samples
fortified with iodide, salt iodide is oxidized with an acidic
solution to liberate free iodine which then turns starch blue.
Salt fortified with iodate is analyzed with iodate spot tests
where iodate in salt oxidizes an iodide reagent in the presence
of hydrogen ions to form free iodine which turns starch blue.
Quantitative methods
Titration method
Like spot tests, titration procedures also are specific to the
form of iodine in salt. In samples fortified with iodate, addition
of an acidic solution liberates free iodine from salt iodate. Free
iodine is then titrated with thiosulfate and the amount of
thiosulfate used is proportional to the amount of iodine in salt.
In salt fortified with iodide, bromine oxidizes iodide ions to free
iodine, which is titrated with thiosulfate solution. It is a fairly
simple and rapid technique compared with the liquid
chromatography method. However, it requires personnel with
good laboratory skills.
Liquid chromatographic method
Iodine can be quantitatively determined using liquid
chromatography (LC). The sample is pretreated by passing
it through a membrane filter to remove protein and other
insoluble materials. Iodide in the filtrate is separated by ion
pair liquid chromatography and detected electrochemically
at 0 to 50 mV. It is a quick and sensitive method ideal for
analyzing a large number of samples. However, it is an
expensive method and requires skilled personnel to perform
the analyses.
The advantages and limitations of iodine assays are
presented in Table 4.
References
For details on any of the methods above, please refer to:
1. AACC. 1994. Approved methods of the American
Association of Cereal Chemists. Eighth edition. American
Association of Cereal Chemists, Inc. Minnesota, USA.
2. AOAC. 1993. Methods of analysis for nutrition labeling.
Edited by D.M. Sullivan and D.E. Carpenter. Association
of Official Analytical Chemists International, Arlington,
Virginia, USA.
3. Dustin, J.P. and Ecoffey, J.P. 1978. A field test for detecting
iodine-enriched salt. Bulletin of the World Health
Organization. 56(4):657-658.
Roche
Skinfolds
Anthropometric Assessment (Cont.)
Use Harpenden calipers. If other types of caliper are used
the standards for these calipers must be used as calipers with
different pressures and area of cross section at jaws give
different results.
The standard measurements are:
1.
Biceps: over the mid-point of the muscle belly with the arm
resting supinated on the subject's thigh.
2.
Triceps: over the mid-point of the muscle belly, mid-way between
the olecranon and the tip of the acromion, with the upper arm
hanging vertically (Edwards, Hammond, Healy, Tanner and Whitehouse,
1955 , Brit.J.Nutr. volume 9, p.155, 1955.)
5. Subscapular: just below the tip of the inferior angle of the
scapula, at an angle of about 45 to the vertical.
4. Suprailiac: just above the iliac crest in the mid-axillary line.
At these four sites, the skinfold is pinched up firmly between the
thumb and forefinger and pulled away slightly from the underlying
tissues before applying the calipers for the measurement.
If only a single measurement is taken, the triceps skinfold is
the most useful.
If several measurements are made an estimate of
total body fat can be made from the total of four skinfolds (Durnin
and Bahaman. Br.J.Nutr. 1967, vol.21, p.681).
The differences in fat percentages become progressively smaller
for each 5 cm. difference in skinfold as the skinfolds increase in
size.
Percentages of fat corresponding to the total value of
skinfolds at four sites (biceps, triceps, subscapular
and suprailiac)
Total
skinfold
(mm)
___ Fat
Men
(% body weight) ___________
Women
Boys
Girls
15
20
25
50
35
40
45
50
55
60
65
70
75
80
85
90
95
5.5
9.0
11.5
13-5
15.5
17.0
18.5
20.0
21.0
22.0
25.0
24.0
25.0
26.0
26.5
27.5
28.0
15.5
18.5
21.0
25.0
24.5
26.0
27.5
29.0
30.0
31.0
32.5
33.5
34-0
35.0
56.0
36.5
9-0
12.5
15.5
17.5
19.5
21.5
25.0
24.0
25.5
26.5
27.5
28.5
29.5
12.5
16.0
19.0
21.5
23-5
25.0
27.0
28.5
29.5
30.5
52.0
33.0
34.0
—
-
-
-
(Rounding off in the percentages of fat accounts for the differences
between adioinin-p- values not be-ins' uniform)
The following measurements of triceps skinfold thickness are those
which can be considered as including the ran.'.e of "normal" values for
French-Canadian schoolchildren measured in 1970.
Lower limit
3rd percentile
6
7
8
9
10
11
12
13
14
15
16
Upper limit
97th percentile
Boys
Girls
Boys
Girls
5.6
5-5
5.4
5.3
5-3
5-4
5.5
5.6
5.5
5.3
5.1
6.4
6.1
6.3
6.5
6.7
6.8
6.9
7.0
7.3
7.9
8.5
12.6
11.9
12.9
14.5
16.4
18.0
19.0
19.8
19.8
19.0
18.0
15.0
16.0
17.5
19.5
21.0
21.5
22.0
22.3
22.8
23.3
23.8
Read from grapsh of Jenicek and Demirjan, Amer. J. Clin. Nutr.
1972, 25, 576.
L
Robson et al (Amer. J. Clin. Nutr. 1971, 24, 864) have found that
Black children in Dominica have much thinner triceps skinfolds than
London White schoolchildren although the su^fficapular measurements of the
two groups are the same. A racial difference in triceps skinfolds has
therefore been suggested and would certainly explain the very high
proportion of West Indian Black children with thin triceps values.
However, American Black and White children show no differences in their
response in triceps or subscapular skinfolds to changes in weight, and
this suggests that the differences in West Indian children's subcutaneous
layer of fat may be determined by environmental rather than ethnic
factors.
Differences in other skinfolds have been found e.g. subscapular
skin thickness is different in French-Canadian and London children but
the triceps measurements are approximately equal.
Changes in skinfold thickness have been observed over the years
e.g. secular changes in triceps measurements have been very marked in
Canadian children with an increase from 6 to 10mm average in boys'
values in the last 17 years. Nutritional factors rather than genetic
control therefore may be more important.
Most London and Canadian children are weaned early onto diets
containing very high quantities of protein and energy. This will produce
faster growth rates with an increased likelihood of childhood obesity.
Many young obese adults were obese in childhood and have an excessive
number of fat cells in their bodies. This excess, which is probably
determined in the first six to 24 months of life, "programmes" the body
for life-long obesity and perhaps an earlier death. Present values for
skinfold measurements although "normal" may not be "ideal", and we cannot
be certain of the significance of thin triceps skinfold measurements in
community surveys. Sequential changes in an individual's measurements
will be significant, however, and the finding of a low percentage of
body weight as fat means that a subject's energy reserves are limited.
W.P.T. James
Skinfolds
Anthropometric Assessment (Cont.)
/F
Use Harpenden calipers. If other types of caliper are used
the standards for these calipers must be used as calipers with
different pressures and area of cross section at jaws give
different results.
The standard measurements ares
1.
Biceps: over the mid-point of the muscle belly with the arm
resting supinated on the subject's thigh.
2.
Triceps: over the mid-point of the muscle belly, mid-way between
the olecranon and the tip of the acromion, with the upper arm
hanging vertically (Edwards, Hammond, Healy, Tanner and Whitehouse,
1955 , Brit.J.Nutr. volume 9, p.133, 1955.)
5. Subscapular; just below the tip of the inferior angle of the
scapula, at an angle of about 45 to the vertical.
4. Suprailiac; just above the iliac crest in the mid-axillary line.
At these four sites, the skinfold is pinched up firmly between the
thumb and forefinger and pulled away slightly from the underlying
tissues before applying the calipers for the measurement.
If only a single measurement is taken, the triceps skinfold is
the most useful.
If several measurements are made an estimate of
total body fat can be made from the total of four skinfolds (Dumin
and Rahaman. Br.J.Nutr. 1967, vol.21, p.681).
The differences in fat percentages become progressively smaller
for each 5 cm. difference in skinfold as the skinfolds increase in
size.
Percentages of fat corresponding to the total value of
skinfolds at four sites (biceps, triceps, subscapular
and suprailiac)
Total
skinfold
(mm)
___ Fat
Men
(% body weight) ___________
Women
Boys
Girls
15
20
25
30
35
40
45
50
55
60
65
70
75
80
85
90
95
5.5
9.0
11.5
13.5
15.5
17.0
I8.5
20.0
21.0
22.0
25.O
24.0
25.0
26.0
26.5
27.5
28.0
15.5
I8.5
21.0
23.0
24.5
26.0
27.5
29.0
30.0
31.0
32.5
33.5
34.0
35.0
36.0
36.5
9.0
12.5
15.5
17-5
19.5
21.5
23.0
24.0
25.5
26.5
27.5
28.5
29.5
12.5
16.0
19.0
21.5
23.5
25.0
27.0
28.5
29.5
30.5
32.0
33.0
34.0
—
-
-
(Rounding off in the percentages of fat accounts for the differences
between adjoining values not bein'’ ’ *>" Ov*"''
The following measurements of triceps skinfold thickness are those
which can be considered as including the range of "normal" values for
French-Canadian schoolchildren measured in 1970.
Lower limit
3rd percentile
6
7
8
9
10
11
12
13
14
15
16
Upper limit
97th percentile
Boys
Girls
Boys
Girls
5.6
5.5
5.4
5-3
5-3
5-4
5-5
5.6
5.5
5.3
5.1
6.4
6.1
6.3
6.5
6.7
6.8
6.9
7.0
7.3
7-9
8.5
12.6
11.9
12.9
14.5
16.4
18.0
19.0
19.8
19.8
19.0
18.0
15.0
16.0
17.5
19.5
21.0
21.5
22.0
22.3
22.8
23-3
23.8
Read from grapsh of Jenicek and Demirjan, Amer. J. Clin. Nutr,
1972,, 25, 576.
L
Robson et al (Amer. J. Clin. Nutr. 1971, 24, 864) have found that
Black children in Dominica have much thinner triceps skinfolds than
London White schoolchildren although the subscapular measurements of the
two groups are the same. A racial difference in triceps skinfolds has
therefore been suggested and would certainly explain the very high
proportion of West Indian Black children with thin triceps values.
However, American Black and White children chow no differences in their
response in triceps or subscapular skinfolds to changes in weight, and
this suggests that the differences in Vest Indian children's subcutaneous
layer of fat may be determined by environmental rather than ethnic
factors.
Differences in other skinfolds have been found e.g. subscapular
skin thickness is different in French-Canadian and London children but
the triceps measurements are approximately equal.
Changes in skinfold thickness have been observed over the years
e.g. secular changes in triceps measurements have been very marked in
Canadian children with an increase from 6 to 10mm average in boys'
values in the last 17 years. Nutritional factors rather than genetic
control therefore may be more important.
Most London and Canadian children are weaned early onto diets
containing very high quantities of protein and energy. This will produce
faster growth rates with an increased likelihood of childhood obesity.
Many young obese adults were obese in childhood and have an excessive
number of fat cells in their bodies. This excess, which is probably
determined in the first six to 24 months of life, "programmes" the body
for life-long obesity and perhaps an earlier death. Present values for
skinfold measurements although "normal" may not be "ideal", and we cannot
be certain of the significance of thin triceps skinfold measurements in
community surveys. Sequential changes in an individual's measurements
will be significant, however, and the finding of a low percentage of
body weight as fat means that a subject's energy reserves are limited.
W.P.T. James
COMMUNITY HEALTH CELL
«7/1,(First FloorlSt. Marks Road
BANGALORE- 560 001
Assessment of Protein-energy Malnutrition (PEN)
a)
Biochemical tests
Changes in the body's composition in malnutrition are most readily
assessed in general terms by anthropometric techniques which measure the mass
of tissue in the body or arm etc. Many biochemical tests are indirect
measures of the processes which are in progress during the course of
developing malnutrition. Biochemical tests may therefore be more sensitive
to recent dietary experience and may revert rapidly towards normal when a
malnourished child has only just started to recover.
Tests can be categorised into measurements on i) blood and ii) urine.
Blood tests are not always acceptable in population studies but provide the
opportunity for other useful tests eg. Hb.
Blood tests
1.
Circulating proteins of liver origin
a)
b)
c)
d)
e)
Albumin: insensitive but important when low
Transferrin: studied only in severe PEM
Lipoproteins: no more sensitive than albumin
Thyroxine binding pre-albumin: preliminary studies only
Pseudocholinesterase and other liver enzymes: insensitive
Liver-produced proteins are particularly sensitive to a fall in the
dietary protein intake but the concentration in the blood depends not just
on the rate of synthesis but also on the breakdown rate of each protein.
The breakdown rate of albumin adjusts as the synthesis rate falls thus
minimising the effect of the reduced intake of protein. Transferrin does
not show this phenomenon - nor probably does T.B.P.A. but little wprk on
this protein so far. Both proteins may prove more sensitive than albumin
which is often near normal in marasmus. Transferrin and T.B.P.A. show
greater falls than albumin in kwashiorkor but their levels have not been
reported in marasmus. Both tests are time consuming and expensive.
Lipoproteins behave rather like albumin: although both are rather insensitive
any fall is important. At albumin levels below 3.0 gm/100 ml a whole range
of other disorders of hormonal and amino acid concentration are evident and
reflect impaired hepatic function.
Albumin is the simplest and most useful blood test for PEM but is still
of no value in demonstrating the extent of growth failure or wasting in
marasmic children.
2.
Indices of recent absorption: urea, cholesterol.
3.
Amino acid levels a) valine reduced particularly in kwashiorkor
b)
c)
alanine low in starvation states eg. marasmui
but too variable. Tends to rise in protein
deficiency.
Non-essential amino acids
Ratio essential amino acids
. Low in
kwashiorkor, normal in marasmus. Likely to
change within 2-3 days of altering the diet.
- 2 Urinary tests
1. Creatinine excretion. Creatinine is spontaneously formed by the
cyclization of creatine phosphate (C.P.) present as a high-energy compound
in muscle. Creatinine is excreted unchanged in theirine, the rate reflecting
the mass of C.P. in the body. Since the concentration of C.P. is constant
in muscle, its exclusive site, the excretion rate of creatinine reflects
muscle mass. Creatinine excretion is, however, somewhat variable, and in field
studies accurate urine collections for long times are impracticable. Three
hour collections have been tried - coefficient of variation 25%; 24 hour
collections - 10% coefficient. Most meaningful method is to express the
creatinine in terms of the child's height in cm. since this will indicate
the amount of muscle that a child has for his size. Muscle mass in Kg =
creatinine excretion in mgm. 4 50- Creatinine is theoretically one of the
best indices of malnutrition since it- does reflect the extent of muscle
atrophy - a key feature of the whole spectrum of PEM from kwashiorkor to
marasmus. Creatinine excretion is increased for a short time during stress
eg. trauma or infection.
2.
Urinary tests indicating recent dietary intake.
a)
Total Urinary N
b)
3.
N-
% falls on a low protein diet
c)
-■.—
mg creatinine
d)
Urinary SO^/creatinine: ? reflects intake of S-amino acids.
Limited usefulness;.
suitable for single urine but limited usefulness. ■
°
a) Urinary Hydroxyproline 24 hr excretion: reflects the rate of
growth and related to the turnover of collagen. Increased
excretion in infection; not easy to measure.
b) Hydroxyproline index (OHPs x body wt)
creatinine
Disadvantage of two variables each of which may affect index.
Useful for single urine. Index age dependent and thought to
reflect growth.
.
ifay J
crve
Significance of biochemical values
Serum albumin
Deficit
< 2.8
At risk
2.8 - 3.5
Amino acid ratio
> 3.0
2.0 - 3.0
< 2.0
Other index
< 2
-
> 2
Urea N/creatinine
< 10
Acceptable
> 3.5
> 10
Serum albumin is the most commonly used biochemical index but it reflects
the extent of liver synthesis which appears well maintained in starvation
states and the index.although simpler is less sensitive than the T.B.P.A. and
transferrin blood concentrations. Urinary creatinine is the biochemical test
of choice for showing the extent of the nutritional deficit but it is impracti
cable to obtain an accurate estimate of muscle mass by this technique.
W.P.T. James,
February, 1973
#
rrv?ich> IC*
NJ'J'T-'H
visit the centre only during the meal limings. But provision of
nutrition too has been an objective of the programme. Infant
Mortality Rate (IMR) has declined from 110 in 1981 to 58 per
thousand live birth in 2004. Similarly, under-5 mortality has
declined from 161 in 1983 to 87 in 2003 Various surveys have
revealed that there has been significant impact of the scheme.
Many non-monetary benefits like insurance, incentives,
preference in other jobs (teachers) have been given to the
AWW and AWH. There is certainly a scope of enhancing the
honorarium offered to these grass root workers.
Summary
After independence the government of India took many
initiatives to ensure food security for the country. National
nutritional programmes were a firm step in that direction.
Ministry of Social Welfare runs the ICDS programme. Balwadi
nutrition programme and special nutrition programme
Ministry of Health and Family Welfare runs the programmes
for prophylaxis against nutritional anaemia, vitamin A
prophylaxis programme and the iodine deficiency disorders
control programme. The mid day meal programme is run by
the Ministry of Education. The programmes have achieved
improvement in the nutritional status of the children, pregnant
and lactating women. More specifically the ICDS programme
that has a strong nutritional component can be termed as a
successful programme.
Study Exercises
Long Question : What are the objectives of the ICDS scheme?
Discuss rhe benefits offered to various vulnerable groups under
Rajul K Gupta
Assessment of Nutritional
Individuals and Communities
Status
of
Alms of Assessment of Nutritional Status
The assessment of nutritional status is carried out with the
following aims :
• To map out distribution and geography of nutritional
disorders
• To identify high risk groups with respect to nutritional
vulnerability
• To assess various epidemiological factors for nutritional
deficiencies
• Make recommendations to rectify shortcomings leading to
nutritional deficiencies
• To project lor financial allocations and budget for food
the scheme.
Short Notes : (1) Mid day meal programme (2) Anganwadi
worker (3) Iodized salt (4) Services under National Nutritional
Anaemia Prophylaxis Programme (5) Supplementary Nutrition
under ICDS
MCQs
I
Mid day meal programme offers (a) Half of daily protein
and one third of calorie requirement (b) Half of daily
protein and half of calorie requirement (c) One third daily
protein and half of calorie requirement (d) One third of
daily protein and one third of calorie requirement.
2.
To a child under 3 years of age, ICDS provides . (a) 300
Kcal energy and 8-10 g protein (b) 300 Kcal energy and
16-20 g protein (c) 500 Kcal energy and 8-10 g protein
(d) 500 Kcal energy and 16-20 g protein.
3.
In rural areas, the administrative unit for the location
of ICDS Project is (a) Gram Panchayat (b) Community
Development Blocks (c) District head quarter (d) Primary’
Health Centre.
4.
Which of the following is not run by the Ministry of
Health and Family Welfare (a) Prophylaxis against
nutritional anaemia (b) Vitamin A prophylaxis programme
(c) Iodine Deficiency Disorders Control programme
(d) ICDS Programme
5 Which of these is not carried out at the Anganwadi centre
(a) Supplementary nutrition (b) Non-formal pre-school
education (C) Immunization ^d) Nutrition and Health
Education.
Answers : (1) a; (2) a, (3) a; (4) b; (5) c.
materials at a large administrative level e.g. at the national
level.
Various methods are available for the assessment of nutritional
status. These are enumerated in Box ■ I. These can be further
sub-classified into direct and indirect methods of nutritional
status assessment
Direct Assessment of Nutritional Status
The lean 'direct assessment' refers to methods in which
individuals or communities are investigated directly. The
various methods that are available for the direct assessment
are summarized in Box - 2.
Box - 2 : Direct Assessment of Nutritional Status
Clinical signs
disease process. Biochemical changes, on the other hand can
be expected to take place prior to clinical manifestations. Hence
tests that can be conducted on easily accessible body fluids
(blood and urine), can help to detect disease at a sub-clinical
level even in a community setting.
Table -1: Signs ‘strongly suggestive’ of dietary deficiency
or excess
Deficiency Sign
Suggested nutrient
abnormality
Laboratory Tests
• Biochemical
• Haematological
• Parasitological
Pale conjunctiva
Iron
Bitot’s spots
Vitamin A
Biophysical Methods________________________
Angular stomatitis
Riboflavin
Anthropometry
Spongy, bleeding gums
Vitamin C
Bilateral edema (young children)
PEM
Thyroid enlargement
Iodine
Assessment ol Nutritional Status using Clinical Signs :
Clinical examination is a widely practiced direct method to
assess the nutritional status of individuals and communities.
Assessment of clinical signs is based on the examination lor
changes believed to be related to Inadequate or excessive
nutritional intake, that can be observed in superficial tissues
(skin. eyes, hair, mouth) or in organs close to the surface
(thyroid, skull).
Caution with Clinical Examination : The cheapness and
the relatively easy organization of clinical examination
for nutritional assessment, might sometimes lead to the
assumption that the method is simple, can be quickly mastered
by a beginner, and yield results that are quick to interpret. But
this is not the case. This method has got its own limitations.
advantages and disadvantages. Expertise is required to select
it as a valid method in a given situation, to conduct it and to
interpret the results obtained.
Classification of Clinical Signs : Based on their importance
with regard to suggesting a nutritional etiology the clinical
signs can be classified into three groups (I) :
Croup 1 - Potentially Nutritionally Significant (Signs
‘strongly suggestive’ of dietary deficiency or excess) :
Some signs are strongly suggestive of a particular nutritional
deficiency or excess e.g. Bitot's spots (Vitamin A), Flag sign
(PEM). A list of these is summarized in Table - 1.
Croup 2 - Signs that are ofprobable nutritional significance
: There are some signs that are of uncertain nutritional
significance. These have to be appreciated and interpreted in
correlation with the case. e.g. Xanthomata eye might indicate
high blood cholesterol. Corneal scar (previous infection, trauma,
malnutrition, avitaminosis A). Fissure tongue, recession of
gums, transverse ridging of nails, etc.
Bilateral epiphyseal enlargement Vitamin D
of wrists
Sign ofExcess
Suggested nutrient
abnormality
Mottled enamel
Fluoride
Denial caries
Sugar
Available laboratory tests : Three groups of laboratory tests
are available, namely, haematological tests, parasitological
tests and biochemical tests. The haematological tests include
the commonly done hemoglobin estimation, parasitological
tests would include stool examination for intestinal parasites
and biochemical tests include many tests like the urine
examination for albumin, sugar, etc. Advanced biochemical
test are taken up for vitamin, minerals and enzyme estimations
as well, that indicate nutritional status. Normal range of some
of these tests is given in Table - 2.
Assessment of Nutritional Status through Anthropometry :
Nutritional anthropometry is the measurement of human body
at various ages and levels of nutritional status. It is based on
the principle that appropriate measurements should reflect
any morphological variation occurring due to a significant
functional physiological change. For example, a low Fat Fold
Thickness reflects a shift in energy balance. The advantages
of anthropometry are that it is simple, quick to do. easy to
reproduce and objective. In some cases it identifies even
subclinical changes resulting from nutritional variations.
Common Methods of Anthropometry : The common
anthropometric methods should be quick, simple and easy to
reproduce. Minimum training should be required to conduct
the measurement. The commonly used methods are : Height;
Crown-heel length and standing height; body weight, mid
upper arm circumference: and fat fold thickness. Head and
chest circumference are measured for children under five years
of age.
Croup 3 ■ Signs that have no nutritional significance :
These signs are not nutritionally significant but required to
be differentiated from other nutritionally relevant signs, e.g.
pterygium (an insignificant sign) is to be differentiated from
Bitot's spots, geographic longue, pyorrhea.
Assessment of Nutritional Status using Biochemical and Body Weight : Body weight is the commonest and simplest
Laboratory Methods : We have seen previously that clinical anthropometric measure used for the evaluation of nutritional
signs are often non specific and develop rather late in thtj, status. It is a reflection of total body mass comprising of all
body constituents. Il is measured for both children and adults.
Definite body weight standards are available to us. Body weight
is an indicator of ‘current’ nutritional status of the individual.
as weight fluctuates with nutrition. Unlike height which is
irreversible, it reflects the nutrition state of the present day.
It is therefore a useful indicator for acute disorders. Small
illnesses like childhood diarrhoea is also good enough to alter
the weight, it is thus a sensitive indicator.
affected by long standing nutritional deprivation. A short or
retarded height is thus indicative of chronic food insufficiency
over a longer duration, unlike a reduced weight which indicates
a short term nutritional deprivation or infection.
Box - 3 : Precautions while measuring weight
Use the right balance. Avoid bathroom scales.
Weight must be taken in minimum clothing.
Measurement of Weight The ideal weighing instrument is the
lever actuated balance or a beam balance. The balance must
have a least count of not more than 100g. Balances using a
‘spring* are not advisable as the spring loses its tension due
to prolonged use and an error is inevitable. Commonly used
bathroom scales are based on the ‘spring’ principle, thus they
must be best avoided for scientific work. The balance which
is in .use must be calibrated frequently for best results. The
precautions to be taken while measuring weight are given in
the Box - 3.
Height : Height is an indicator of the linear growth of the
individual. It is widely accepted that height is determined
genetically. Environmental factors, most importantly nutrition
and morbidity determine the extent to which the genetic
potential will be harnessed, to achieve the maximum possible
height. Growth retardation resulting from any environmental
factors like infections, malnutrition, etc. result in a retarded
height, resulting in stunting (or short stature). Height is
Remove shoes before weight is recorded.
The zero-error must be checked and corrected before using
a machine.
It is advisable to record weight in the morning (in basal
conditions)
These precautions must be applicable in a standardized
manner for all subjects (within a study group)
Measurement ofHeight: In young children, height is referred to
as length or Crown-heel length in young children who cannot
stand with ease (say up to 2 years of age). An infantometer
is use to measure their recumbent ‘length* (in lying position).
In adults and older children, the height is measured using a
vertical measuring rod. the Anthropometric rod.
The subject should remove his shoes and stand erect. He must
keep his heels together and toes apart. He must look straight.
Table - 2 : Normal range of some biochemical rests (2)
Nutrient
Normal (Acceptable)
Low (Medium risk)
Deficient (high risk)
Albumin (g/100ml)
for age 6-17 yrs
Serum levels
>3.5
2.8-3.4
<2.8
Vitamin A (/ig/dl)
Serum levels
>30
20-30
<20
Vitamin D (ng/ml)
Serum levels
of 25-Hydroxy
cholecalciferol
>10
05-10
<5
Vitamin E
Ratio of serum
vitamin/total lipids
>0.8
Vitamin K
'PIVKAS accumulation
Test
If PIVKAS accumulates
Prothrombin time
Thiamin
Delayed
Urinary thiamin
100;z.g/24 hrs or 65/ig/g
creatinine
Riboflavin
Urinary Riboflavin
80/<g/g creatinine
Niacin
2-Pyridone to Nl-methyl
nicotinamide ratio
Vitamin Bo
Vitamin B(i urinary
excretion
1 tod
<1
<20/zg/g creatinine
<0.5mg/day
Pyridoxic acid excretion
Folic Acid
Serum folate (ng/ml)
>6.0
3.0-5.9
<3
RBC Folate (ng/ml)
>160
140-159
<140
Vitamin Bp
Serum B,, (pg/ml)
Ascorbic acid
Plasma (mg/dl)
<80
>15
08/15/09
’ PIVKAS: Protein Induced by Vitamin K Absence. •• Prothrombin time is a functional test
785
<8
given level are taken into account in this method. Effectively
the difference between receipt (of food various sources) and
expenditure over a given period of time gives the food consumed
by population. The consumption per capita/day is worked out
The method : Weigh the raw food before cooking. It is
preferable to weigh the food again after cooking A conversion
factor is arrived at. For example let's assume that the weight
of raw rice is 100 g. The weight of cooked rice becomes 400g.
Thus a conversion factor of 100/400 or ’/> is arrived at. in other
words 1 g cooked rice represents 1/4 g of raw rice. Or if a person
eats 400g cooked rice it is equivalent to 100g of raw rice. The
nutrient contents of raw rice are extracted from standard Food
Composition Tables The same process is employed to estimate
the nutrient contents of all food preparations.
Food consumed by population
Mid yr pop x 365
These figures are used for various types of planning and
budgeting, natnelyplans for agriculture, fertilizers, productions,
imports and Public Distribution System (PDS). The method
has got certain demerits, it is a gross method. Secondly the
consumption of rich and poor is equated and averaged out
when this method is used. It gives the consumption pattern but
doesn't include purchasing power of the individual.
ideally both, raw and cooked foods must be weighed. But if
it is not possible to weigh the cooked foods an approximate
conversion factor can be taken. Obviously this will lead to
some degree of error. Another alternative is to measure the
volumes of raw and cooked foods and subject them to weight
conversions. In practice measuring volumes of cooked portions
actually eaten by the individuals is easier than weighing the
portions eaten. The volumes can be converted into weights
and subsequently into nutrients, through standard tables The
merits of this method are that it accounts for-ijie non edible
parrs of food as well. The wastage is also taken into account.
This method is more accurate than the inventory method. The
demerit is that it is a very' cumbersome, time consuming and
tedious process as it involves weighing of all foods.
Inventory Method As mentioned earlier the inventory method
is carried out at an institutional level, on a homogenous group
as present in a hostel, jail, mess, army barrack, orphanage etc
It is essentially done from books Amounts of various food
stuffs available as per records are taken into consideration. The
balance of various food items is again checked al ter a reference
point of say 7 days (one week).
Individual consumption / day =
Stocks ar beginning of week - Stocks at end of week
Mo. of individuals x No. of days
The Merits are that it is fast, much easier, less cumbersome and
faster than the weighment methods. It is also (airly accurate, it
may not indicate an accurate individual food consumption but
is«fairly satisfactory for the purposes of planning.
The Demerits are that it-doesn'r account for wastage. Secondly,
it gives only the mean individual consumption but actual
individual consumption is not reflected. Thirdly, the estimates
are as good as the»food records made available. Lastly, the
results will be affected if the subjects are eating some food
stuff obtained from any source other than the common kitchen
under question.
Weighment Method : In this method the foods are actually
weighed using a grocer's balance. Both raw and cooked food
are weighed. In community surveys (at a family level), the raw
food is weighed rather than the cooked food, since weighing
cooked food is not acceptable to the families. In an institution
however, the cooked food can also be weighed, since cooking is
carried out at a central kitchen, while using weighment method
at a family level the following points are important.
1.
Convince the housewife of the need of the survey for the
benefit of the family
2.
Avoid holidays/fares/festivals/feasts as the dietary practice
of these days does not reflect the actual dietary practices.
3.
It should be carried out for 3 to 7 days consecutively.
4.
At least two visits a day for lunch and dinner have to be
made.
5.
Two investigators should be available - one talks and
weighs and the other records observations.
6.
Any pets, breast fed children, guests etc. should be
considered.
24 hour Recall (or Questionnaire) Method : The 24 recall
(questionnaire) method is a relatively easy method based on
the recall capabilities of the individual over a period of the past
24 hours. Since it is a short term retrospective method it is
more prone to errors.
i\ set of cups and ladles standardized for volume are used. The
Tiou'sewile is asked about the types of food items prepared at the
time of breakfast, lunch and dinner. The raw ingredients used
for cooking each meal are noted. The cups are exhibited to the
Housewife. The cooked food items are noted in terms of these
cups. The intake of each food item by the specific individual in
the family is also assessed by using these cups.
The method is fairly accurate. It take lesser time than the
weighment method. However, the disadvantage is that the
method is based on recall capability of the respondent so there
is a likelihood of 'inaccurate recall' and error in derivation of
nutrients. A fair degree of cooperation is to be sought from the
respondent. The process is a cumbersome.
Food Frequency Questionnaire (FFQ) Method: Food frequency
questionnaire (FFQ) method is based on the principle as to how
frequently an item is consumed over a period of time. It is an
epidemiological technique used to study the meal patterns and
dietary habits of people. It can be used to assess the specific
dietary intakes during pregnancy, lactation, etc. It can even be
conducted through post. For example a FFQ may read "In one
week how often do you consume the following items...."
Item
Frequency (Consumption Per Week)
Meat
1
2
3
4.....
GLV
1
2
3
4.....
Sprouts
I
2
3
4......
This filled up questionnaire is then analysed, using pre-decided
values of for nutrients for different food items.
788
The Indian Academy of Paediatrics (IAP) classification on the
other hand puts the degree of malnutrition into four grades
(Table - 4). This classification is used by the 1CDS in India.
Table - 4 : Indian
Classification
Academy of Paediatrics
(IAP)
TirWe-dtGrades of obesity based on BMI (WHO, 1998) (3)
BMI
< 18.5
Risk of co
morbidities
Classification
Underweight
Low
Healrhy/normal weight
rXverage
Weight/Age (%) of normal
25-29.9
Pre-obese (Overweight)
Mildly increased
Normal
> 80%
30-34.9
Obesity Class 1
Moderate
1 Grade
70-80%
35 - 39.9
1 Obesity Class 11
Severe
11 Grade
00-70%
> 40
Obesity Class III
Very severe
11! Grade
50-60%
IV Grade
<50%
18.5-24.9
Malnutrition grade
Weightfor height: The weight for height classification doesn't
take age into consideration. Weight is also related to height
Many a times age is not known. Weight for height is an age
independent parameter. It is a good prognostic indicator of
severe PEM and an index of current nutritional status. Weight
for height of less than 80% of normal is considered to indicate
wasting in preschool children.
Wasting and Stunting : In the Waterlow classification weight
for height and height for age are used to classify children as
normal, wasted, stunted and wasted and stunted. Children
with low weight for height are considered as wasted and those
with low height are ‘Stunted’ (Table - 5)
I'he guidelines have been revised and made more stringent
lately for Asians, considering the fact that Asians (esp.
South East Asians including Indians) are more susceptible to
metabolic syndrome. These are summarized in Table - 7.
Table - 7: Grades of obesity for Asians (5)
BMI
< 18.5
Classification
Underweight
Risk of co-morbidities
Low
Normal weight
Increasing but acceptable
23 -27 5
Pre-obese
Increased
>27.5
Obese
High
18.5-23
Dietary Assessment for Nutritional Status
Weight for
height
Height
for age
Normal
Nonna!
1 Nonna!
Nonna!
Low
Normal
Wasted
Acute malnutrition
Normal
Low
Stunted
Nutritional dwarf
Low
Low
Wasted and Acute on Chronic
malnutrition
stunted
A nutritional survey is never complete without a diet survey.
We may be able to find out that there is a nutritional deficit
through clinical, laboratory or anthropometric methods, but
in order to find out if this nutritional deficiency is because of
diet and which particular diet/nutrient, we have to invariably
resort to a diet survey. It is thus an integral part of nutritional
survey. A diet survey objectively defines importance of diet in
various health state and disease (2). Diet survey is nothing but
the scientific assessment of food consumption, and using this
data lor various purposes including assessment of nutritional
status.
Body Mass Index (BM!) .Body Mass Index (BM1) is the ratio of
weight in Kg to square of height in metre
Methods : Various methods are there to undertake diet
surveys. These are appropriate in different settings (6) and are
summarized in the Box - 4.
Table - 5 :
classification
Wasting
BM
and
Stunting
Nutritional
status
-
Waterlow
Interpretation
Mass (Kg)
Height (tn)'
It gives an indication of the nutritional status, esp. obesity.
Now-a-days in context of lifestyle diseases. BMI is taken as an
Indicator of risk of cardiovascular diseases as well.
BMI does not measure the body fat but relates well with the
degree of obesity. The categories of obesity as pronounced by
the WHO are depicted in Table - 6. A BMI of 25-30 is considered
as a warning sign and may warrant intervention, especially in
the presence of additional risk factors. A BMI of 30 or higher is
generally considered the point at which some form of treatment
is required. Obesity Class III i.e. BMI >40 or morbid obesity, is
a medical condition that impairs a person's overall health and
therefore requires medical attention.
Box ■ 4 : Methods of Diet survey_____________________
Food balance sheet method
Inventory method___________________________________
Weighment method
24 hr Recall method (Questionnaire method)
Dietary score method________________________________
Food Frequency Questionnaire method
Duplicate sample (chemical analysis) method
Diet Balance Sheet Method : This method is used when
information regarding availability and consumption of food is
required at a macro level like at the global, national, region or
state levels. The total food supplies available and used up at a
body constituents. It is measured tor both children and adults.
Definite body weight standards are available to us. Bodyweight
is an indicator of'current' nutritional status of the individual.
as weight fluctuates with nutrition. Urilike height which is
irreversible, it reflects tire nutrition state of rhe present day.
It is therefore a useful indicator for acute disorders. Small
illnesses like childhood diarrhoea is also good enough to alter
the weight, it is thus a sensitive indicator.
Measurement of Weight: The ideal weighing instrument is the
lever actuated balance or a beam balance. The balance must
have a least count of not more than 100g. Balances using a
'spring' are not advisable as the spring loses its tension due
to prolonged use and an error is inevitable. Commonly used
bathroom scales are based on the spring' principle, thus they
must be best avoided for scientific work. The balance which
is in use must be calibrated frequently for best results. The
precautions to be taken while measuring weight are given in
the Box • 3.
Height : Height is an indicator of the linear growth of the
individual. It is widely accepted that height is determined
genetically. Environmental factors, most importantly nutrition
and morbidity determine the extent to which the genetic
potential will be harnessed, to acnteve*fne maximum possible
height Growth retardation resulting from any; environmental
factors like infections, malnutrition, etc. result in a retarded
height, resulting in stunting (or short stature). Height is
affected by long standing nutritional deprivation. A Short or
retarded height is thus indicative of chronic food insufficiency
over a longer duration, unlike a reduced weight which indicates
a short term nutritional deprivation or infection.
Box - 3 ; Precautions while measuring weight
Use the right balance. Avoid bathroom scales.
Weight must be taken in minimum clothing.
Remove shoes before weight is recorded.
The zero-error must be checked and corrected before using
a machine.
It is advisable to record weight in the morning (in basal
conditions)
These precautions must be applicable in a standardized
manner for all subjects (within a study group)
Measurement ofHeight: In young children, height is referred to
as length or Crown-heel length in young children who cannot
stand with ease (say up to 2 years of age). An infantometer
is use to measure their recumbent 'length' (in lying position).
In adults and older children, the height is measured using a
vertical measuring rod. the Anthropometric rod.
Tile subject should remove his shoes and stand erect. He must
keep his heels together and toes apart. He must look straight.
Table - 2 : Normal range of some biochemical tests (2)
Nutrient
Test
Normal (Acceptable)
Low (Medium risk)
Deficient (high risk)
Albumin (g/100ml)
for age 6-17 yrs
Serum levels
>3.5
2.8-3.4
<2.8
vitamin A (pg/dl)
Serum levels
>30
20-30
<20
Vitamin D (ng/ml)
Serum levels
of 25-Hydroxy
cholecalciferol
>10
05-10
<5
Vitamin E
Ratio of serum
vitamin/total lipids
>0.8
Vitamin K
•PIVKAS accumulation
If PIVKAS accumulates
Prothrombin time
Thiamin
Delayed ••
Urinary thiamin
100/zg/24 hrs or 65;ig/g
creatinine
80/xg/g creatinine
Riboflavin
Urinary Riboflavin
Niacin
2-Pyridone to Nl-methyl
nicotinamide ratio
Vitamin B6
Vitamin B„ urinary
excretion
Folic Acid
Seram folate (ng/ml)
>6.0
3.0-5.9
<3
RBC Folate (ng/ml)
>160
140-159
<140
1 to 4
<1
<20/xg/g creatinine
<0.5mg/day
Pyridoxic acid excretion
Vitamin B,,
Serum B,, (pg/ml)
•Ascorbic acid
Plasma (mg/dl)
<80
>15
08/15/09
• PIVKAS: Protein Induced by Vitamin K Absence. " Prothrombin time is a functional test
• 785 •
<8
He stands against the anthropometric rod kept at his back,
placed perpendicular to the ground. The investigator standing
to the left holds the subject’s chin with his left hand and the
occiput with the right little finger in the Frankfurt horizontal
plane (an imaginary line joining the tragus of the ear to the
eye). The moving head piece of the anthropometric rod is
brought down and placed on the head with little pressure, in the
saggital plane. The reading is taken. Average of three readings
is recorded. The disadvantage of height as a measure of
nutritional status is that it doesn't indicate present nutritional
status of the individual, but indicates only the past history of
a chronic disease.
Mid-Upper Arm Circumference (MUAC) : Mid-upper arm
circumference indicates the muscle development. Since poor
muscle development is seen in PEM. the lower MUAt'ihdtcafiS
poor nutrilion“MUAC correlates well with weight, weight for
heigfir'hnu Clinical signs of malnutrition? It can be used to
calculate the mid arm muscle circumference using a simple
formula, if the value of fat fold at triceps is also estimated
simultaneously. The mid calf circumference can also be used
instead of MUAC.
The mid-upper arm circumference is measured on the non
dominant arm (left arm in case of right handed subjects and
vice-versa) of the subject. The mid point between tile lip of the
acromion (of scapula) and olecranon process of ulna is located
with the arm Hexed at the elbow. It should be marked with a pen.
The arm is now held hanging freely by the side of rhe subject
and a fiberglass tape is placed gently but firmly embracing the
arm without 'squeezing' the soft tissue, at the point marked in
pen. The reading is taken to the nearest millimeter.
interpretation ; The usefulness of MUAC is based on rhe
principle that MUAC remains almost constant between 1 to 5
years of age (increasing only approx 1.5 cm between 1 and
5 years of age). Tlius fair degree of standardization can be
achieved even if the age is not known in a preschool chil<$A
cut off point of 12.5 cm is taken. MUAC of less than 12.5 cm
is taken as low. To make the procedure of measurement even
simpler and usable at the grassroot level. Shakir introduced
a simple tricoloured tape in 1975, called as the Shakir's tape.
The red colour in the tape (which fell in the less than 12.5 cm
zone) marked Danger, yellow or white colour, fell in 12.5-14 cm
zone marked Caution and green colour more than 14.0 cm is
considered as OK or normal.
MUAC can be used as an efficient technique for screening large
population of children for malnutrition. Children thus screened,
can be subjected to further anthropometric measurements
and'Other (Clinical/biochemical) tests for specific nutritional
deficiencies.
physiological, nutritional and health status of the individual.
Anthropometric Measurement ofBody Fat: Fatfold thickness
Anthropometric measurement of body fat can be carried out
at various subcutaneous sites. These sites are commonly
undertaken : Two sites on the trunk namely sub scapular and
supra-iliac and three sites on the extremities namely triceps,
thighs and mid calf. Biceps fat fold is also done. The fat fold
thickness al triceps is the most sensitive (to socioeconomic
changes) and most reliable (indicator of obesity).
Fat fold at triceps is the commonest measure. It is carried
out at the dorsal side at the same mid point where MUAC is
measured. Tiie skin fold is picked up between the thumb and the
forefinger I cm above the midpoint, taking care not to include
the underlying muscle. The tips of the skin fold calipers must
be applied at the mid point at a depth equal to the skin fold.
The skin fold is held gently in the left hand throughout the
measurement. Average of two measurements must be taken.
HeadandchestCircumference -. Head and chest circumferences
are measures used in children. A neonate is born with a bigger
head. The chest grows faster than the head in a normally
nourished child tn the 2'"1 and 3"1 years of life. As a result, the
chest circumference overtakes the head by about 1 year of age.
In a child suffering from PEM, the chest grows at a lower rate
and it remains smaller than tile head even till 2 '/a to 5 years of
age. This indicates a poor slate of nutrition.
Head and chest circumferences are measured using a fiberglass
tape. Head circumference is taken at the supraorbital ridges
of the frontal bone (just above the eyes) in front and the
most protruding point of the occiput in the back. The chest
circumference is taken at the level of the nipples in mid
inspiration.
Classificationof Nutritional Status Based on Anthropometric
Parameters
Weightfor age : There are standard weights laid down for a
particular age. Thus a given child’s weight (for his particular
age), is compared to the 'standard' weight of a 'normal' child.
This standard is taken as per the 50th centile of the Boston
standard. The Gomez classification is one of the commonest
classifications used to classify malnourishmenl into various
grades.
weight for age(%) =4eighl or^Xof same age x 100
The grades as per Gomez classification are given in Table - 3.
The biggest advantage of using the MUAC is that it is easy to
conduct and it is age independent till about 5 years of age.
A modified tape (Shakir's Tape) can be used easily even by a
village health worker.
Body Fat : Body Fat Indicates reserve of energy in the body.
The quantity of fat present subcutaneously at various sites
indicates the gross nutritional status of the person. The
thickness of fat can be correlated to the body content of fat.
Fat distribution in and around the body varies with age. sex.
786
Table ■ 3 : Gomez Classification
Malnutrition grade
Normal
Weight/Age (%) of normal
>90%
Grade 1 (Mild)
75 - 89 %
Grade II (Moderate)
60 - 74 %
Grade III (Severe)
< 60 %
Direct Assessment of Nutritional Status
The term 'direct assessment' refers to methods in which
individuals or communities are investigated directly. The
various methods that are available for the direct assessment
are summarized in Box • 2.
Box - 2 : Direct Assessment of Nutritional Status
Clinical signs.
disease process. Biochemical changes, on the other hand can
be expected to take place prior to clinical manifestations. Hence
tests that can be conducted on easily accessible body fluids
(blood and urine), can help to detect disease at a sub-clinical
level even in a community setting.
Table - / : Signs ‘strongly suggestive’ of dietary deficiency
or excess
Deficiency Sign
Suggested nutrient
abnormality
Laboratory Tests
• Biochemical
• Haematological
• Parasitological'
Pale conjunctiva '
iron
Bitot's spots.
Vitamin A
Biophysical Methods
Angular stomatitis
Riboflavin
Anthropometry '
Spongy, bleeding gums
Vitamin C
Bilateral edema (young children)
PEM
Thyroid enlargement
Iodine
Xssessmeut of Nunitioti.il Stains using Clinic.ii Sittns ■
Clinical examination is a widely practiced direct method to
assess the nutritional status of individuals and communities.
Assessment of clinical signs is based on the examination for
changes believed to be related to inadequate or excessive
nutritional intake, that can be observed in superficial tissues
(skin. eyes. hair, mouth) or in organs close to the surface
(thyroid, skull).
Caution with Clinical Examination : The cheapness and
the relatively easy organization of clinical examination
for nutritional assessment, might sometimes lead to the
assumption that the method is simple, can be quickly mastered
by a beginner, and yield results that are quick to interpret. But
thig is„.not the case This method has got its own limitations.
advantages and disadvantages/Expertise is required to select
it as a valid method in a given situation, to conduct it and to
interpret the results obtained.
Classification of Clinical Signs : Based on their importance
with regard to suggesting a nutritional etiology the clinical
signs can be classified into three groups (I):
Group 1 - Potentially Nutritionally Significant! (Signs
'strongly suggestive' of dietary deficiency or excess) :
Some signs are strongly suggestive of q p^kular nutritional
deficiency or excess e.g. Bitot's spots (Vitamin A), Flag sign
(PEM),' A list of these is summarized in Table ■ I
Group 2 - Signs that are ofprobable nutritional significance
: There are some signs that are of uncertain nutritional
significance These have to be appreciated and interpreted in
correlation with the case. e.g. Xanthomata eye might indicate
high blood cholesterol, Corneal scar (previous infection, trauma.
malnutrition, avitaminosis A), Fissure longue, recession of
gums, transverse ridging of nails, etc.
Bilateral epiphyseal enlargement Vitamin D
of wrists
Sign ofExcess
Suggested nutrient
abnormality
Mottled enamel
Fluoride
Dental caries
Sugar
Available laboratory tests : Three groups of laboratory tests
are available, namely, haematological tests, parasitological
tests and biochemical tests. The haematological tests inchide
the commonly done hemoglobin estimation, parasitological
tests would include stool examination for intestinal parasites
and biochemical tests include many tests like the urine
examination for albumin, sugar, etc, Advanced biochemical
test are taken up for vi'thtnin. minerals and enzyme estimations
as well, that indicate nutritional status. Normal range of some
of these tests is given in Table - 2.
VssesMiu-ni ol Xiitiiiioii.il Status through Anthropometry :
Nutritional anthropometry is the measurement of human body
at various ages and levels of nutritional'status. It is based on
the principle that appropriate measurements should reflect
any morphological variation occurring due to a significant
functional physiological change,* For example, a low Fat Fold
Thickness reflects a shift in energy balance. The advantages
of anthropometry are that it is simple, quick to do, easy to
reproduce and objective. In some cases it identifies even
subdinical changes resulting from nutritional variations.
Group 3 - Signs that have no nutritional significance .
These signs are not nutritionally significant but required to
be differentiated from other nutritionally relevant signs, e.g.
pterygium (an insignificant sign) is to be differentiated from
Bitot's spots, geographic tongue, pyorrhea.
Common Methods of Anthropometry : The common
anthropometric methods should be quick, simple and easy to
reproduce. Minimum training should be required to conduct
the measurement. The commonly used methods are : Height:
Crown-heel length and standing height: body weight, mid
lipper arm circumference; and fat fold thickness. Head and
chest circumference are measured for children under five years
of age.
Assessment of Nutritional Status using Biochemical and
Laboratory .Methods .- We have seen previously that clinical
signs are often non specific and develop rather late in the
Body Weight : Body weight is the commonest and simplest
anthropometric measure used for the evaluation of nutritional
status. It is a reflection of total body mass comprising of all
visit the centre only during the meal timings. But provision of
nutrition too has been an objective of the programme Infant
Mortality Rate (IMR) has declined from 110 in 1981 to 58 per
thousand live birth in 2004. Similarly, under-5 mortality has
declined from 161 in 1983 to 87 in 2003. Various surveys have
revealed that there has been significant impact of the scheme.
Many non monetary benefits like insurance, incentives,
preference in other jobs (teachers) have been given to rhe
AWW and AWH. There is certainly a scope of enhancing the
honorarium offered to these grass root workers.
Summary
After independence the government of India took many
initiatives to ensure food security for the country. National
nutritional programmes were a firm step in that direction.
Ministry of Social Welfare runs the ICDS programme, Balwadi
nutrition programme and special nutrition programme.
Ministry of Health and Family Welfare runs the programmes
for prophylaxis against nutritional anaemia, vitamin A
prophylaxis programme and the iodine deficiency disorders
control programme. The mid day meal programme is run by
the Ministry of Education. The programmes have achieved
improvement in the nutritional status of the children, pregnani
and lactating women. More specifically rhe ICDS programme
that has a strong nutritional component can be termed as a
successful programme.
Study Exercises
Long Question : What are the objectives of the ICDS scheme?
Discuss the benefits offered to various vulnerable groups under
•
' Nutritional Assessment and
Surveillance of a Community
Rajul K Gupta
Assessment of Nutritional
Individuals and Communities
Status
of
Aims of Assessment of Nutritional Status
The assessment of nutritional status is carried out with the
following aims:
• To map out distribution and geography of nutritional
disorders
• To identify high risk groups with respect to nutritional
vulnerability
• To assess various epidemiological factors lot nutritional
deficiencies
• Make recommendations to rectify shortcomings leading to
nutritional deficiencies
• To project for financial allocations and budget for food
the scheme.
Short Notes : (1) Mid day meal programme (2) Anganwadi
worker (3) Iodized salt (4) Services under National Nutritional
Anaemia Prophylaxis Programme (5) Supplementary Nutrition
under ICDS
MCQs
I.
Mid day meal programme offers (a) Half of daily protein
and one third of calorie requirement (b) Half of daily
protein and half of calorie requirement (c) One third daily
protein and half of calorie requirement (d) One third of
daily protein and one third of calorie requirement.
2.
To a child under 3 years of age, ICDS provides : (a) 300
Kcal energy and 8-10 g protein (b) 300 Kcal energy and
16-20 g protein (c) 500 Kcal energy and 8-10 g protein
(d) 500 Kcal energy and 16-20 g protein.
3.
In rural areas, the administrative unit for the location
of ICDS Project is (a) Gram Panchayat (b) Community
Development Blocks (c) District head quarter (d) Primary
Health Centre.
4.
Which of the following is not run by the Ministry of
Health and Family Welfare (a) Prophylaxis against
nutritional anaemia (b) Vitamin A prophylaxis programme
(c) Iodine Deficiency Disorders Control programme
(d) ICDS Programme.
5.
Which of these is not carried out at rhe Anganwadi centre
(a)
Supplementary nutrition (b) Non-formal pre-school
education (c) Immunization (d) Nutrition and Health
Education.
Answers : (1) a; (2) a; (3) a; (4) b> (5) c.
materials at a large administrative level e.g. at the national
level.
Various methods are available for the assessment of nutritional
status. These are enumerated in Box - I. These can be further
sub-classified into direct and indirect methods of nutritional
status assessment.
Box - 1 : ABCD... of Nutritional Status Assessment
Anthropometry
Biochemical & lab methods
Clinical assessment
Diet survey
Ecological studies
Functional assessment
G - - Vital statistics
Nutritional Surveillance
Purpose of surveillance
It is dear from the earlier chapters that the state of nutrition
of an individual or a community depends on a variety of
(unrelated) factors. These could be as diverse as the ’health'
of the crops, state of rainfall, GDR per capita income, efficiency
of the public distribution system, availability of food and the
health state of the community.
Given this dynamic and ever changing state of availability and
use of food, it is vital to keeping a constant watch over all these
factors concerning nutrition, in order to continuously assess
the situation, give an early warning and take appropriate
decisions that will lead to improvement in the nutritional
status of population. This! on-going process of constant
scrutiny of the nutritional situation and factors influencing
them and its application in the public health inierest is termed
as nutritional surveillance. The word was used first in 1074
with respect to drought relief, during a World conference in
nutrition. A nutrition surveillance programme was developed
for the developing countries 1976. The term has been used
extensively by the UNO since 1980. The process of nutritional
surveillance finds the following applications :
a)
It provides inputs for health and development planning
b)
It is useful for programme management and evaluation
c)
It provides timely warning and intervention to prevent
(short term) food consumption crisis and plan for long
term action
Steps : The various steps of nutritional surveillance are :
a)
Identify community/population
b)
Data collection
c)
Data transit
d)
Data processing
e)
Interpretation
f)
Responses and Planning
g)
Improvement
h)
Further implementation
Methodology ol Nut i it ionaI Surveillance: The methodology of
the nutritional surveillance can be outlined through answering
the following basic questions :
• What is the problem? — Define & describe the type of
nutritional problem e.g. malnutrition (acute or chronic),
micronutrient deficiency, etc.
• who is at risk? — Describe the population groups affected
by area, socioeconomic status, biological/physiological
status, etc.
• Why is this population at risk?--Identify the causal factors.
These causes could be immediate (non availability of food.
poor health, etc) or of long standing nature like unequal
resource distribution, poor sanitation and infections.
• Where to get the data from? — Identify the data sources.
These will depend on the purpose for which surveillance
has been undertaken.
Health and development
planning
Data source
Household survey
Data from records
Programme management
and evaluation
Interviews and records
Timely warning and
intervention programme
Rainfall, prices, employment
Health system surveys
Define food supply system. The food can be obtained
mobilizing the existing stores, through national and
international aid, improving the agricultural production.
•
Obtain the data, analyse and provide feedback to decision
makers. Finally, evaluate the nutritional surveillance
system.
N u tritiona I Re ha bi litation
The cases of severe malnutrition are treated in a hospital
setting. Such a treatment no doubt, does make the child
survive; it doesn't guarantee that he will live a life free of
malnutrition and disease in future. Besides only medical.
additional inputs like those of social, physical, psychological
and emotional rehabilitation have to go in. if the child is to live
a life of positive health.
Principle .■ More often than not it is seen that after a short spell
in the hospital, once the child returns back to the original social
milieu, the condition recurs. The child either dies or becomes
extremely vulnerable to subsequent infections, malnutrition.
disease and death. The basic principle of nutritionally
rehabilitating a child is not only to treat his malnutrition and
related acute complications, but to prevent a rectirrence of the
condition.
Methods : The process of rehabilitation is to be dove-tailed
with treatment. It can be undertaken at three levels, depending
on the severity of the condition and the facilities available.
(a) Hospital ; The child is hospitalized in severe cases or when
he has concomitant complications. Special standardized dietary
regimes (intensive feeding with high proteins and energy dense
diets) are required to be instituted and continued for a long
time to come. Systematic education of parents in food selection
and cooking has also to be imparted. The standardized dietary
regimes and specific nutritional education It is initiated in the
hospital but is required to be followed up either at the day care
centre or at home.
(b)
Day Care Centre : A day care facility is an intermediate
arrangement between the hospital and home. Children who are
not required to be admitted to a hospital or those who have
been discharged from the hospital are expected to visit the
day care centre. This centre may be run by a health worker
who is trained in preparation of special feeds for malnourished
children and who could educate the mothers on preparation
of special feeds suitable to the particular child (as discussed
in last paragraph). Any health facility like an anganwadl
centre, sub-centre or a PHC can be used as a day care centre.
The advantage of a day care centre (over hospital) is that it
789
is cheaper; the mother can spend the day at the centre under
supervision of a trained health worker, learn sufficient skills
in specialized feeding and child-craft, in an informal setting,
closest to her home environment and really imbibe it.
of acute malnourishment. This can be achieved through
appropriate measures begun ar the hospital. Subsequently the
child may be managed at a day care centre or at home.
Study Exercises
(c)
Domiciliary : In case the child is not severely affected, after
medical consultation, he can be treated at home. He could also Long Questions .• (1) Enumerate the various methods for
be one who has been weaned off a hospital or a day care set nutritional assessment. Describe any one in detail. (2) What is
up. To maintain health of child it is important that the mother nutritional surveillance? Outline the methodology of nutritional
is trained in handling the 'special' nutritional needs of this surveillance. (3) what are the various anthropometric
techniques available to assess nutritional status of a 5 year
child.
old child? How can weight for age be useful to ascertain
Summary
malnutrition in this child?
Short Notes . (1) Mid Upper Arm Circumference (2) 24 hour
recall method (3) FFQ (4) Using BMI to assess CED in adults
(5) Disadvantages of using clinical signs for nutritional status
assessment
The condition of the body resulting from intake, absorption
and utilization of food and the effect of pathological factors is
termed as nutritional status.
Nutritional status is assessed too map out distribution and
geography of nutritional disorders, identify high risk groups
and to assess various epidemiological factors for responsible
for nutritional deficiencies. It is also an administrative tool
used to allocate budget for food materials at a large scale.
The important methods are anthropometry, biochemical and
laboratory methods, clinical assessment, diet survey, ecological
studies, functional assessment and indirect assessment from
vital statistics data.
MCQs
I.
All can indicate nutritional status except: (a) Fall in weight
(b) Falling hair (C) Failure to gain height (d) Flag sign
2.
All are signs of FEM except (a) Flag sign (b) Unilateral
pedal edema (c) Low weight for age (d) Dermatoses
3.
Stunting is________ weight for height but_________
height forage: (a) Normal; Low (b) Low; Normal (c) Low; Low
(d)
High; low
4.
Acute malnutrition may be indicated by : (a) Stunting
(b) Wasting (c) Stunting and wasting (d) All of the above
5.
Which of these is not true for nutritional surveillance :
(a) It is an ongoing process (b) It can be used as a nutritional
survey technique (c) It is a close scrutiny of events related
to nutritional changes (d) It provides timely warning for
action
Match the following
There are clinical signs that may be 'strongly suggestive' of
dietary deficiency or excess (e.g. Bitot's spots), of probable
significance (eg. corneal scar) and those that are of no
nutritional significance (e.g. pterygium). Clinical signs might
develop rather late and are subjective and non specific.
Biochemical tests on the other hand give objective and
quantitative indication of nutritional status, but these are
costly and instrument intensive.
Anthropometry remains the sheet anchor of nutritional
assessment. Weight, height, head and chest circumference.
MUAC and fat fold thickness are the common anthropometric
parameters used. Many derived parameters like the BMI,
weight for age, weight for height, etc are also used in different
situations.
various methods of diet survey are used to ascertain as to what
an individual or a group of people are eating. This indicates
the deficiency of nutrients in the diet and thus appropriate
measures can be suggested to improve it. The main methods
Food balance sheet method are inventory method, weighment
method, 24 hour recall method (Questionnaire method), dietary
score method, food frequency questionnaire method and
duplicate sample (chemical analysis) method. The inventory
method, weighment method and 24 hour recall method are the
most commonly used dietary survey methods.
Nutritional Surveillance is an on-going process to keep a
constant watch over all the nutrition related factors, in order to
continuously assess the situation, give an early warning and
take appropriate actions.
Age
6.
New born
Suitable anthropometric measure
(a)
MUAC
7-
3 years
(b)
Weight
8.
42 years
(C)
BMI
9.
S years
(d)
Head & chest circumference
10.
I '/a years
(e)
Weight for age
Answers : (I) b; (2) b; (3) a; (4) b: (5) b; (6) b; (7) a; (8) c:
(9)e;(10)d.
References
Jellil’fe DB. jelliffe EFR Community Nutritional Assessment. Oxford University
Press. 1989.
Baniji MS. Rao NR Reddy v. Textbook of Human Nutrition. 2nd ed. Oxford &
IBH Publishing Co Pvt Ltd, New Delhi. 2003.
World Health Organization. 1998. Obesity. Prevention and managing the
global epidemic. Report ol the WHO Consultation on obesity. WHO, Geneva.
4.
Based on lames WPT, ferro-Luizzi. Waterlow JC. Definition of chronic energy
deficiency in adults—Report on working party of the intervention diewr
eneigyconsukation group. Am | Clin Nutr. 42; 969-98!, 1988.
5.
AstrupA. Obesity. In : Human Nutrition. Editors; Getssler C. Powers H.2005,
2.
3.
Nutritional Rehabilitation aims at re-establishing the severely
malnourished child medically, nutritionallyand psychologically
into the family and society. The aim is to prevent a recurrence
• 790
Thiminayamma BVS, Rao R Diet Survey Methods. ICMR. National Institute
of Nutrition. Hyderabad.
Comparative study of Guwahati, Ahmedabad
Sivasish Thakur
GUWAHATI, Jan 3 - A comparative study of underdeveloped belts in the hearts of the cities
of Guwahati and Ahmedabad has shown how the state contributes to creating a structural
violence of deprivations with regard to housing, basic services, citizenship rights, etc.
The study - 'Does Urban Planning Create or Mitigate Conflicts and Violence in Indian Cities?
Findings from Ahmedabad and Guwahati' - conducted by the Centre for Urban Equity, CEPT
University, Ahmedabad, has found many similarities in the perpetuation of
underdevelopment in the two areas of the two different states.
"Some of our case studies within the two cities - Bombay Hotel area in Ahmedabad and hill
settlements in Guwahati - represent this type of local informal actors-led or people-led
housing developments without basic services access and formal status of their housing.
They are prone to evictions any time the state wants to redevelop the area.
In Guwahati, the instrumental state has stepped in to assist capture of the hill settlements'
land for real estate interest or reportedly for ecological protection. These settlements,
therefore, suffer from structural violence in the form of deprivations and insecurity in their
day-to-day life and occasional physical violence in the form of eviction drives," the report
noted.
Noting that the idea of'urban' was on the upsurge and so was the zeal to make cities that
are visually appealing and functionally productive, the report found that the urban
constituency had become more vocal than before and was being wooed by the political class
more than before.
The outcome, it says, is national governments (Centre's) pre-eminent focus and funding of
urban development projects since mid-2000 and the economically-advanced states
projecting their cities as their brand ambassadors, upcoming Amravathi city for Andhra
Pradesh, Ahmedabad and her urban projects such as the BRTS, Riverfront, etc., for Gujarat,
and so on.
This thrust also resulted, for the first time, in major urban development programmes being
introduced in the mission mode by the previous Central Government under the name
Jawaharlal Nehru National Urban Renewal Mission (JNNURM) and Rajiv Awas Yojana (RAY),
both discontinued now. The present government has launched the Atal Mission for
Rejuvenation & Transformation (AMRUT), Pradhan Mantri Awas Yojana - Housing for All
(Urban) (PMAY) and Smart Cities Mission.
The study chose Ahmedabad, the brand ambassador of the Gujarat development model and
Guwahati, the gateway to the Northeast and also a city located in a state that is a site of
ethnic conflicts and conflicts with immigrants from Bangladesh.
"Their specific dynamics have influenced the way urban development programmes have
been implemented, conflicts ensuing on account of the same and tipping of some of the
conflicts into occasional physical violence in the form of eviction drives," it said.
It added that in Guwahati, the hill settlements had been evicted many times and people had
experienced violence from the state. The residents are mostly the tribal communities, who
have been mobilized by an organisation named Krishak Mukti Sangram Samiti (KMSS) for
land rights. Their movement has faced state repression and violence and there have been
instances of counter violence from the hill residents. The most recent incident was in
February 2014 when during a protest demonstration, a hill settler died through selfimmolation.
"The state's neglect in supporting the poor to realize their rights and exclusions has led to
informal settlements' residents making claims for survival rights or claims over their 'life
space' in a subtle manner of organising for demanding water rights, approaching local
politicians for such claims, making demands before elections and so on. There are local
actors, often NGOs and local leaders and CBOs, as in the case of Bombay Hotel area in
Ahmedabad as well as hill settlements in Guwahati, that assist residents to organise for
issues and stake claims,'' it said.
The report noted three types of conflicts in the case of the street vendors' market in
Guwahati - (a) of the vendors with the local State in the form of evictions, (b) of the
vendors with the non-state actors to whom the state has outsourced management of the
markets and (c) among the vendors for vending space.
"NGO and local Welfare Association (WA) intervention mitigated the conflict with the state
by organising the evicted street vendors into a new informal market elsewhere in the city.
But then, the state has once again clamped down and evicted the vendors from this market
which was part of our study, namely Ulubari market," it observed.
The attempt often is to expand the rights but only in certain situations, such as in the KMSS
movement in the hill settlements, it turns into a political movement, which can in turn lead
to occasional counter-violence when the state remains unresponsive to its concerns and
demands.
"In the informal settlements like Bombay Hotel, there is near absence of the welfare state.
Instead, informal non-state actors step in. They draw their power from their links with the
local state apparatus and politicians. They have provided land for housing and water solely
for their own profit and they govern these activities through threat of violence and
occasional violence," it said.
Even ’welfare' interventions for rehabilitation of evicted people are subverted from the
beginning by the local state. The rehabilitation in Ahmedabad in general and the BSUP
housing in Vatvain particular was so badly planned and managed that the Vatvasites are
now replete with various crimes including gender violence, illicit and illegal activities, and
actors engaging in them.
- Media
 RF_NUT_7_SUDHA.pdf
RF_NUT_7_SUDHA.pdf
Position: 396 (30 views)