NUTRITION
Item
- Title
- NUTRITION
- extracted text
-
RF_NUT_3_SUDHA niv-T s \
ST. JOHN'S MEDICAL COLLEGE, BANGALORE
-
.
COMMUNITY HEALTH
Class
Roll No.
Semester
Subject
Date
Examination
A»'C7"Ri i I ON.
47/1,(First Floor)Su M.i<H< ? ••••
*
BANGALORE «
1
i-l'icxj2_<2‘2,.Q.. .2^, .
(
rruo-ek-el
fX-5-fti.
._rta
c-taJJtsL«vcit3 , <<sVi ^o- cJ
6 v^Clctao-s
«=>-/-> r> <-<c .J? (_^.‘ . .
2o<=»<=/’
a
'
pxAe --9.-<^tatt«=34
/taT ^civ<^o.o£Q
7yJs3^ta<oCZ&^|
7
, i-J-'>
rx-^?A7[ix.Q_.. c^RxaxsL-
S’ovTr><e_
^S^JiciAjQ..
,1-.
<ixn_j~jA_C.O-x’=£ z..
<t< . lZ^~^T.
o. ... ...
0--
S7_<^Ci
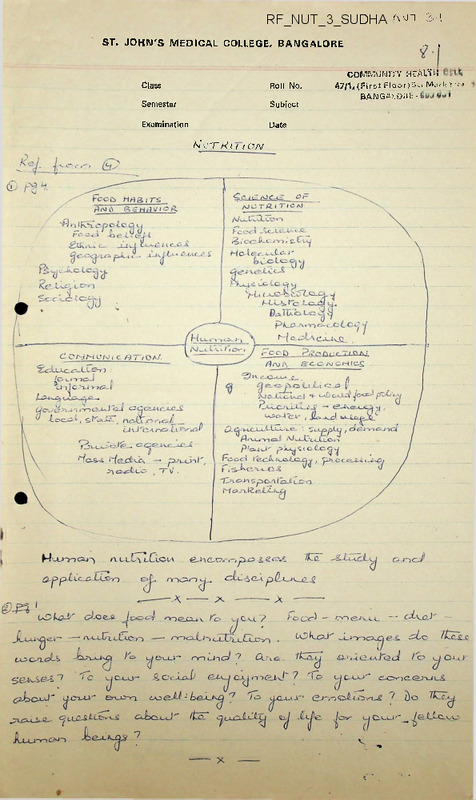
THE DISCIPLINES CONCERNED IJITH NUTRITION
/BIOCHEMISTRY /
/AGRICULTURE /
/PHYSIOLOGY /
/MEDICINE /
/ANIMAL HUSBANDRY /
/NUTRITION /
/ MICROBIOLOGY /
/PUBLIC HEALTH '/
/ECONOMICS /
/ANTHROPOLOGY /
/EDUCATION /
/DEMOGRAPHY /
/ SOCIOLOGY /
ZS „
c- 6
a « £ z
a m c <s
> Z?
*
(Courtesy
o 0
Basic Preventive Medicine by Deodhar Adranwala)w
Co
NO |
3-^-
COMMON,. < .. AL iH CtU
C
47/1, (First. Floor)St. Marks Road
BANGALORE-560 001
,
SO?.T= OBJECTIVES IN THE STUTY OF NUTRITION
At the beginning of any study it is well for the
student to set some specific objectives for himself. These
will not be the same for all individuals because students
begin the study with quite differing backgrounds of
knowledge and experience, and because their professional
interests are likely to vary widely. Moreover, it must be
anticipated that these will, in fact, change as the study
progresses and the student becomes more aware of the field.
Worthwhile goals are not fully achieved within the space
of a few months but should provide the basis for an
ongoing lifetime program of education.
The discussion that
follows will give the student some background for setting up
his own objectives with reference to personal and family
nutrition, and toward a professional career in the health
sciences.
Personal and family nutrition. Regardless of one’s
future professional career, the study of nutrition should first
be directed to onself. Physical and mental health are
essential assets to meet the exciting and sometimes arduous,
requirements of one's life work.
Those who expect to help
other people achieve better health through nutrition must
be enthusiastic and living examples of the benefits of the
application of nutrition knowledge.
Nutrition education applied to the individual also
reaches the family. This is especially important for young
men and women as they establish their own families. Within
the family the wife and mother is the principal decision maker
for the family's food.
She plans the menus, selects the
foods, and prepares them.
Although she makes every effort
to please her husband, her influence also molds many of his
habits.
The food habits of children are formed by the
prevailing attitudes and practices within the home.
Professional opportunities in nutrition.
Professional
people in any discipline related to health are engaged in
activities related to education, prevention, and therapy.
Nutrition education in schools.
Education of the
population holds promise of long-range benefits to the
greatest numbers. Teachers, nurses, nutritionists,
dietitians, home economists, and physicians assume varying
responsibilities for individual and group education.
.. . .2
The elementary and secondary schools afford the single best
opportunity for helping the child to establish attitudes and
practices concerning food selection that will lead him to a
more healthful, productive life.
Nutrition education
must
begin in the kindergarten and continue through the twelfth
grade if it is to achieve maximum effectiveness.
It is
the responsibility of the elementary teacher as well as
teachers of home economics, health, and physical education.
Nutrition programs for the public.
Voluntary and
governmental agencies together with industry are accepting
responsibility for nutrition programs. The researcher in
nutrition and food sciences is equally at home in the labo
ratories of a food company, a university, a hospital, or in
the public health field.
Nutritionists, dietitians, and
home economists, depending upon their education and particular
interests, are the experts who interpret a product for a
company; develop new uses for a food; advise mothers and
children concerning their diets in a clinic; serve- as
consultants to a public health team; supervise food service
in a college dormitory, industrial cafeteria, or hospital;
assist individuals and groups in dietary selection; and teach
in nursing schools, colleges, and universities.
Nutrition and health care.
The concern of today's
health worker is for the maintenance as well as the
restoration of health. Traditionally, health care has
been directed to the patient-that is, the horizontal individual.
Today, health care includes the concept of continuity of care.
The health worker soon learns that there must be concern
for the patient who makes the transition from the hospital
to his home. To implement continuity of care with respect to
nutritional needs, the patient may require counseling in the
proper choice of foods in the market, assistance in planning
for the best use of his food money, and practical suggestions
for food preparation with meaner facilities, or in the face of
physical handicaps.
FPOPLENS AM? REVIEW
1.
2.
What is your understanding of the following terms:
nutrition, malnutrition, foodstuff, nutrient, health, food,
nutritional care, primary prevention?
Industrial and economic developments have been a powerful
factor in the changing of our food habits.
List several
of these which have had an influence on our dietary habits
within your lifetime.
3
Objectives for the student.
To achieve the personal and
professional objectives the student should strive toward the
following behavioral changes.
1.
Shows the proper attitude and convictions relative
to the importance of nutrition in regulating one's own health,
that of the family, and that of individuals of the community.
2.
Knows the kinds of health problems arising from
poor nutrition that exist in his own community, the nation,
and throughout the world.
3.
remonstrates knowledge concerning the science
of nutrition:
a.
Functions, digestion, absorption, and metabolism
of proteins, fats, carbohydrates, minerals, and
vitamins.
b.
c.
The interrelationship of nutrients.
The nutritive requirements of individuals and
the variations that may be imposed by activity,
climate, stage of life cycle, and disease.
4.
Appreciates and understands the meanings that
food has for people and how these are related to economic,
psychologic, and cultural factors.
5.
Interprets the principles of nutrition in the
selection of an adequate diet:
a.
b.
By knowing the food sources of the nutrients.
By applying consumer information to the planning
of meals and the selection of food for quality
and economy.
6.
Uses opportunities for improving nutrition
through the education of individuals.
7.
Counsels people on an individual or group basis
by adapting nutrition information to specific health, socio
economic, and cultural needs.
8.
Knows where to look for reliable sources of
information and how to evaluate publications on food and
nutrition and the claims made through product advertising.
9.
Becomes familiar with agencies concerned with
nutrition and health in order to utilize their services and
contribute to their functioning.
SOURCE: FUNEAMENTALS OF NORMAL NUTRITION
NUTRAL
HISTORY
OF UNDERNBTRITION AND NUTRITIONAL
DEFICIENCY
DISEASE
I Factors influencing undernutrition and
J
nutritional deficiency disease:
'
•
i
i
•
j
j
j
•
AGENT Factors :----------------------------------------- —
Carbohydrates, protein, fat
Fat-soluble vitamins (1,D, and K)
Water-soluble vitamins (thiamin, niacin,
riboflavin,, B,, B
flecin,
pantothenic acid, and ascorbic acid)
Minerals (calcium, phosphorus, sodium,
potassium, chlorine, sulfur, magnesium)
Trace elements (iron, iodine, copper,
cobalt, man.
fluorine)
*
{
j
'j
•
J
j
j
ENVIRON! ■F.1ITAL Factor:
Geographic location (climate, season,
terrain, population density)
Agricultural development
Food processing, storage, distribution,
and preparation
Economic (individual and community)
Social (religion, laws, education,
culture, dietary standards-)
j
[
•
HOST Factors:—-■--------------------------------- —
Habits, customs, mores•
Age, race, sex
|
Nutritional. retirements in various
|
{
|
•
j
|
|
physiologic states (infancy and
early childhood', adolescence,
pregnancy and lactation, old age)
Psychobiologic characteristics
Patholo..ic states (interference with
ingestion, absorption, and utilization:
increased requirements or excretion)
[--------------------------------------------------T"
I
T~
Source of STIMULUS:
interactioru,of factors_______
IRE PATHOGENESIS PERIOD
Natural course of nutritional deficicncy]death
I Defect,
{
J Disability,,
} Chronic
'
state
i
| Illnes s
j short
y------>--------- }or long
jClinically
] manifest
] deficiency
CLINICAL .HCRIZQNJ disease
! Latent deficiency disease:
! evidence apparent,
signs and symptoms indefinite
J and nonspecific
|Potential deficiency disease:
} no clinical evidence^
| low storage of nutrients,
_ } borderline
Unsaturated but
functionally
unimpaired
•Recovery
i-------- ;
|
Saturajti'on:
'
F
]optimal state of j
| • nutrition
'
^"iNTSEACTIOTTSf
“
STIMULU^ and HOST
REACTION OF HOST
PERIOD OF PATHOGENESIS
CO
NVT 3-lf-
r"’=-Vuoooi
47/1,t
<£■
BANG'-^-“
NUTRITION
Nutrition is a dynamic process in which food is consumed and
utilised for growth and repair of the body.
Growth implies increases in physical measures.
Development implies increase of intellectual and emotional
faculties.
Adequate nutrition which is vital for attaining optimum health
This diet
is ensured by providing every individual with a balanced diet.
contains proteins, fats, carbohydrates, minerals, vitamins and water in
proportionate amounts to provide adequate energy for growth and repair of
tissues.
Proteins (derived from the Greek work "protos" meaning to
come first), are complex organic nitrogenous substances containing carbon,
hydrogen, oxygen, nitrogen and sulphur in varying amounts. Some proteins
also contain phosphorus and iron, and occasionally other
elements.
Protein rich foods are milk, meat, fish and eggs from animal sources and
pulses, nuts and beans from vegetable sources.
The recommended daily allowance for the Indian adult is one
gram per kg. of body weight.
This is increased in infancy, adolescence,
pregnancy and lactation..
Lack of protein and vitamin A can cause serious and permanent
defects in children especially.
These range from impaired mental develop
ment and blindness to death.
The reasons for lack of protein in the Indian diet are numerous:
1.
Lack of knowledge of the importance of proteins
2.
Lack of utilisation of locally available proteins
3.
Dietary restrictions
4.
Superstitions and some traditionally harmful customs.
(For example - In some rural areas pregnant women
do not eat green leafy vegetables or drink milk).
5.
Poverty
It was estimated that 10 - 15$ of the people in the world,
or roughly 20$ of the people in the developing countries, did not meet
their energy needs during the decade 1950 - I960, (they were undernourished).
The study was extended to estimate the incidence of protein deficiency as
data became available; this estimate was placed at between 25 and 33$
(Sukhatme 1966)..
What has since become clear is that protein deficiency is for
the most part the indirect, result of inadequate energy intake.
In other
..2
2
words, what diets lack is energy foods to avoid the body katabolizing
(Gopalan 1968).
the protein people do eat.
This finding is the opposite
of what has been reported in various studies of the subject, notably the
study on Protein Gap by the U.N. Committee on Application of Science and
Technology to Development (U.N. 1968) which has formed the basis for
international action.
The finding
that protein deficiency is indirectly caused by
low calorie intake is gradually being confirmed by a number of workers
and is also reflected in the recent writings of F.A.O. (1971).
Based on F.A.O. and W.H.O. Studies (1957 to 1965) and the
recommendation of the I.C.M.R. (1968).
Recommended.
Levels of Nutrient
Intake for the Pre-Social
Child and Adult in India (Approximations only):
% Prot./Cal
Concentration
$ Protein/
Cal Concentration
when NPU relative
to Eggs is 67
Age
Calories
Protein as
Egg in G
*
1-5 years
1,000
12.0
4.8
7.2
Adult Male
2,700
55.0
4.8
7.2
* Defined as average + 20$
Current evidence shows that if a diet has 5$ of its calories from
good quality protein, such as in egg or milk, the individual's needs for
protein will be met regardless of whether he is a pre-school child or an
adult man, provided he eats enough to meet his energy needs.
TABLE
IV
Distribution of households surveyed in India (Maharashtra
State) 1958 by calorie supplies per day per reference man.
CALORIES/per day/per reference man
Upto 1,500
$ Frequency
. 6.8
1,500 - 1,700
9.7
1,700 - 2,100
.14.7
2,100 - 2,500
16.5
2,500 - 2,900
16.6
2,900 - 5,500
12.9
5,500 - 5,700
9.0
5,700 - 4,100
5.5
4,100 - 4,500
5.5
4,500 - and over
5.0
100
by National Sample Survey 862 households.
3
"Since malnutrition (or the lack of a balanced diet) is the
outcome of several factors - social, economic, cultural and psychological
the problem can be solved only by taking action simultaneously at various
levels - individual'family, community, national and international levels.
Other measures to ensure people adequate nutrition are:
1)
Increasing food production
2)
Price control
3)
Prevention of food adulteration
4)
Fortification and enrichment of foods
5.)
Food aditives .
6)
Inventing cheap supplementary foods (e.g. High Protein Foods)
7)
Irradiated Food
8)
Nutrition education, and
9)
Population control
The Government of India is attempting to solve the problem of
malnutrition by implementing the following programmes on a national scale:-
Cro'iVc
1)
Applied Nutrition■Programme
2)
3)
School, Mid-day Meal Programme
National Government Control Programme
4)
Crash Programmes in Nutrition (For 0-3 years)
5)
Vitamin A supplement to facilitate growth and prevent
blindness.
Studies from the United States- and the developing countries
reveal the not surprising fact that as family size increases,
spending for food goes down.
per capita
As a result, corresponding diet inadequacies
and nutritional deficits are common.
FOOD CONSUMPTION PATTERNS BY STUDIES OF F.A.O.
Major Parts of India
Rice, Millets and other Cereals
Moderately High
Pulses, Fats and Oils
Moderate
Milk
Low.
Meat, Fish and Eggs
Very Low
India (Punjab) and Pakistan
Wheat, Rice
High
Milk and Pulses
Moderate ’
Meat, Fish and Eggs
Low
Cereals constitute upto 80$ Calorie Supplies
and upto 70$ Protein Supplies
Pulses constitute upto 10$ Calorie Supplies
and upto 20$ Protein Supplies
Food of Animal Origin constitute upto 4$ Calorie Supplies
Meat, Fish and Milk - 10$ Proteins
4
Malnutrition, especially, protein calorie malnutrition, is
widespread and is to be' feared not only because of its general debilitating
effect but especially because of the irreversible brain damage that
inadequate proteins cause.
Data from 24 countries indicate that the
prevalence of severe PCM (Protein Calorie Malnutrition) ranges from
0.5% to 5% and the prevalence of moderate PCM from 4% to 43%"The human brain reaches 90% of its normal structural develop
ment in the first four years of life.
We now know that during the
critical period of growth, the brain is highly vulnerable to nutritional
deficiences, deficiencies that can cause as much as 25% impairment of
normal mental ability.
Even a deterioration of 10% in the diet is
sufficient to cause a serious handicap to productive life.'.
irreversible brain damage.
This is
What is particularly tragic in all of this is,
that when such mentally deprived children reach adulthood, they are
likely to repeat the whole depressing sequence in their own families.
They perpetuate mental deficiency, not through genetic inheritance, but
simply because as parents they are ill-equipped mentally to understand
and hence to avoid the very nu ritional deprivation in their own children
that they themselves suffered.
In low income countries the high mortality rates among children
in large families and in families with close birth intervals, are in
part due to malnutrition.
The greater the sibling number, the greater
the likelihood of malnutrition among poor families.
Studies of pre
school children in Colombia, for example show that 52% of the children
in families in which there were five or more pre-school children were
seriously malnourished, whereas only 34% of children in families with
only one pre-school child were malnourished»
In Thailand, of the children whose next youngest sibling was
born within 24 months 70% were malnourished; of those in .families
without a younger sibling, only 37%.
Height and weight being affected directly by nutrition showed
variation in children according to family size. Even in high income
countries the children of the poorer families are larger at any given
age when the number of children in the family is small.
For example,
of 2,169 London day-school students, 11.25' years old, children from
one child families were about 3% taller and 17 - 18% heavier than children
from families with five or more children.
The difference in physical growth between children of small
and large families in Great Britain seems to affect mainly the poorer
social classes.
In the higher income classes boys in families with
5 or more children are taller at all ages than boys in small families;
the reverse is true for girls.
In the upper and lower manual working
..5
5
classes children in small families average 3-4% taller than those in large
families at 7 and 11 years of age and 114 to 2.8$ taller at 15 years.
Diet surveys carried out in India have shown that the average
Indian diet is ill-balanced with an excess of Carbohydrates and very little
protective foods like milk, meat, fish, eggs, fruit and leafy vegetables.
The Nutrition Advisory Committee has designed a diet from the
resources available required to give a total caloric value of 2,400.
Such a diet would cost, in I960 Rs.35 per month per adult.
Only 20$ of
our people in India can afford this.
Indian rural economy is not balanced, for while rural earnings
give only Rs.16 per individual per month, the same individual spends
Rs.20 in that month.
Only 70 crores of the total outlay of 361 crores of rupees is
provided for rural hospitals and health care in our 4th Five Year Plan.
The .top priorities of the health tasks are not always properly chosen.
The Green Revolution in India has lulled many into a state of
complacency.
While it is true that great progress has been made in
increasing food production, the increasing population h’s almost nullified
this increase, so that the per capita availability of food is only 446 gms.
(cereals and pulses) per day and a per capita availability of 120 ml. of
milk per day.
Yet India has the largest cattle population in the world -
most of the cattle being of poor quality, yielding little milk and serving
no useful purpose, yet consuming much fodder.
The economic advantages
would be considerable if these animals were permitted to be slaughtered
and much needed meat be made available for consumption and more leather
for foreign trade.
About 1/3 of the people have no objection to eating
beef.
Whereas the proportion of staple cereals and starchy roots in
,the North American diet is estimated to be only 25%, and in the British
diet only 31%, in Latin America it is 54%, in Africa 66%, in the Near
East 71% and in the Far East over 73%.
Conversely, while the proportion
of animals products - milk, meat, eggs and fish - in the typical North
American diet reaches the exceptionally high figure of 40% and in the
British diet can be as high as 27%, the figure for Europe as a whole is
estimated as 21%, for Latin America 17%, for Africa 11%, for the Near East
9% and for the Far East 5%.
In only a few regions of the world are there adequate food
supplies.
These are the United States and Canada,'Australia, New Zealand,
Western Europe, parts of Argentina and parts of South East Asia,
regions have already utilized the means of increasing agricultural
...... 6
These
6
productivity, but only ten centuries in the world today produc i more food
than they consume.
The "dhals" which have a high protein content (vegetarian meat!)
take the place of animals foods in communities where it is consumed
(though in insufficient amounts).
IIowever, the body utilises only 40 - 60%
of the vegetable protein which forms the chief kind of protein (in contrast
to animal protein) that is consumed.
Certain essential amino acids like
Lysine and Methionine are also present in insufficient amounts in this
diet pulses.
According to a National Survev the average daily intake of
calories in India was 1890 calories with a daily protein intake of 53 grams.
Pregnant women, nursing mothers and growing children, ie. ;a
group constituting 60% of the population
*
proteins, vitamins and minerals.
lack adequate calories,
The result of this is seen in the high
incidence of low birth weight babies, still-births and fairly high
morbidity and mortality rates in children.
Health education for adequate nutrition
and balanced diet
needs to be given to all parents, teachers and health personnel.. Many
foods are freely available at reasonable prices and can be used to. supplement
the diet.
These (greens and fruits especially) are often locally
available or easily grown in the kitchen gardens, and found both in cities
or in rural areas.
The C.F.T.R.I. has also developed multipurpose food - which is
a blended flour of groundnuts and Bengal gram.
It is cheap, extremely
nutritious and can be used in a varietv o'7 ways. For children especially,
C.F.T.R.I. has a prepared mixture of wheat, groundnuts, and soya bean or
Bengal gram flour with skimmed milk powder.
More recently, using a machine, C.F.T.R.I. has extracted protein
from leaves and grass.
This process is still in the research stage.
It is interesting to note the view of Dr. P.V. Sukhatme "An insufficient amount of protein in the diet is held to be at the heart
of the problem of persistent and widespread malnutrition in the developing
countries.
However, when one examines the available data, the conclusion
is clear that what diets lack is not protein but energy foods to enable
the body to utilize the protein people actually do eat.
There is no
evidence that the quality and concentration of protein in cereal-legume diets
normally eaten in the developing countries is inadequate to meet protein
needs, provided energy intake is adequate.
essentially a socio-economic problem.
The protein problem is therefore
Production of semi-conventional,
,
cheap,- protein-rich foods using modern technology and distribution of
factory foods so produced through special feeding programmes as recommended
...7
7
by
the international bodies, will be a costly and inefficient method of
solving the problem".
Much can be continued to be said on the subject of nutrition, but
at the present time given the familiar family situation of providing
adequate nutrition two things must be emphasised:
1.
The use of locally available foods like green leafy
vegetables in the diet.
2.
Early recognition of nu ritional deficiencies and their
remedy by sound-dietary practices and use of food
supplements prepared by C.F.T.R.I.
A recent report says "Nearly one million Indian toddlers die
every year because they do not get enough to eat. Although these hapless
toddlers constitute 16.5$ of the population, they account for 40$ of
the total deaths.
One-fifth of the babies born in India never live
beyond the age of five years".
In a paper on Nutrition and Development, Gopalan points out that
apart from the one million small children
who annually fall victim to
malnutrition, many more die of diseases they would have either escaped
or survived if they had been better nourished.
The children would stand
a better chance if they were more sensibly fed from even the available
foodstuffs.
In a countrywide survey, the severely undernourished pre-school
children (17 - 18$
of the number surveyed) were 40$ lighter in weight than
they should be for their age.
About 14$ were 10 - 25$ lighter than normal
and 65$ were 26 - 40$ lighter than they should be.
Only 5$ were the
right weight for their age.
The question of wants also means that the use of resources may
go far beyond what someone from another social background might consider
quite adequate for survival or even for a good life.
It has been
calculated, for instance, that a child born in the United States is likely
to consume in the course of a lifetime 28 times as much as a child in
India.
TABLE
Estimated consumption per head in I960 in various countries
(U.K. = 100)
U.S.A.
Sweden
West Germany
Mexico
Taiwan
Ceylon
India
140
125
86
22
12
9
5
...8
8
Since nutrition is closely bound up with Agriculture, it is imperative
that the problem of malnutrition which is so serious in India be confronted
at "grass-roots" level. Three possible avenues are open:
1.
The growing of food crops to be encouraged, expanded and
2.
The storage, distribution and allotment of food to priority
given positive incentives.
groups (e.g. the vulnerable population) given due attention.
3.
Increased research and exploration of food from a) the sea and
use
b) of the protein containing vegetable foods like
groundnuts and soya bean.
The exact fishing potential of the ocean remains unknown. Indeed
fish farming as a serious, industry is still in its infancy in most parts of
the world.
The Northern Hemisphere is 61% water and provides 98% of the
world's fish supplies.
The Southern Hemisphere is 81% water but is supplies
only 2% of the fish.
The fisheries of the world could yield far more food -
and of a particularly valuable type - being of good protein content.
It is of importance and.interest to look to future trends in food
cultivation for both the rich and the poor countries.
The rich countries, with no greater rate of growth.in food production
but most of it coming from increases in productivity and with only half
the rate of growth in population compared to the developing countries,
improved their pei~ caput availability of food and were able to export
increasing quantities.
As a consequence, trends in the food supplies of the developing
countries have been somewhat more favourable than those in production
but this has taken place at the expense of the trading pattern between
the two groups of countries.
The Far East and Near East, which were
exporters of food before the War, are now importing 6 and 7% respectively
of their supplies.
Africa and Latin America are still exporting but on
a much reduced scale.
This unfavourable development has tended
to increase balance of payment problems and to accentuate the difficulties
resulting from the almost continuous decline since the Korean boom in.
world prices of primary commodities.
The situation is illustrated.by the
example of cereals; the less developed countries (excluding Mainland China)
which exported ten million tons of cereals before the War are now actually
importing nearly 20 million tons, and this largely to maintain their
current unsatisfactory level of diet.
Judged by these trends, the prospects
of stepping up the rates of growth to 3% in total foods and 3.5% in animal
foods over the years 1965 - 2000 seem bleak indeed.
Sine
we cannot take comfort from the past trends, we should
find out what are the possible sources of food supnly, what resources we
9
have and how we can exploit them to meet our future food needs. Never before
the planning of resources use and land use in particular has assumed so much
importance as at present under the heavy pressure of demographic growth.
TABLE
Rate of Growth (1958-63)
Population
Growth
Per Capita Gross
Domestic Product
(per cent per year compound)
Developed Regions
Developing Regions
2.5
Gross National Product is the value of total annual production of
goods and services supplied by all 'normally resident' individuals,
firms and government bodies.
If 'income' is restricted to income
derived from participation in production GNP also equals the annual
sum of their incomes, including net incomes from abroad.
Gross Domestic Product
Equals GNP minus net income from abroad.
COMMUNITY HEALTH CELL
47/1,(First Floor)St. Marks Hoad
' BANGAlOae-560 001
FOOTNOTES TO THS TABLE ON DAILY ALLOWANCES OF NUTRIENTS FOR INDIANS
-f-ColA w
1. Calorie s;
-A MrnYiclf
a)
Calorie allowance for heavy work does not include work under
special conditions like high altitude.
2.
Proteins:
a)
Adult allowance corresponds to 1 gm./kg. of dietary protein
of N.P.U. 65.
b)
Infant allowance during 0-6 months is in terms of milk proteins.
During 7-12 months,part of nrotein intake wil1 be protein in
the formof milk, and supplementary feeding will be derived
from vegetable oroteins.*
' Total daily protein allowance is
calculated from the ideal weight. Protein allowances during
infancy will be:-
0-3 months
3-6 months
6-a months
0-12 months
2-3gm-/:g.
1.2gm./kg.
1.3,gm./kg.
1.5gm./kg.
.
.
■
Allowances for children and alolescents have been computed using
body-weights as obtained in the well-nourished group and
ass'Uning N.P.U. of 50for the dietary proteins.
c)
• Calcium: In the absence of precise information on calcium
requirement of different groups, a range of allowance
has been suggested.
a) Calcium allowance for infants 0-6 months will be for artificially
fed infants. Calcium intake from breast milk will, however,
satisfy the needs of breast-fed infants up to 6 months.
• Iron:
a) This allowance of '30mg. iron is for adult woman during, her
premenopausal period. For the post-menopausal qoman,iron
allowance is the same as for man.
b)
c)
This allowance for preganat woman will be throughout pregnancy.
This allowance is for lactating woman who is not menstruating.
If a woman is lactating and also menstruating, her iron
allowance will be 35 mg./day.
Dietary allowance for Vitamin A is given in terms of retinol
('Vitamin A alcohol) and B-carotene. Either of these is used,
dependin- mon the dietary .source of vitamin. The factor to
be -ised to convert B-carotene to retinol is:
1 ng. of B-carotene
=
0 25 ug. of retinol.
If the diet conta ns both Vitamin A and B-carq.tenes, its-'
content can be expressed as retinol, using the following
formulae.
i)
Retinol content ug. = ug. retinol + ug. B-carotene ^>0.25
if the retinol and B-carotene content of foods are given as
ug. in the food composition tables.
ii) Retinol content, (ug.) = Vitamin A (I.U.) x 0.3 + B-carotene ■
_(I.TJ.) x 0.15 if the Vitamin A and carotene values are given
in terms of International Units.
6,7,3. -Thiamine, Riboflavin and Nicotinic acid;
The daily allowance of these three vitamins are related to
calorie intake.
The basic allowances per 1000 calories are.
Thiamine = 0.5 mg., Riboflavin = 0.55 mg., abd Niacin. = .6.6..mg.
niacin equivalents..
Niacin allowance includes contribution from dietar}’' tryptophan,
60 mg. tryptophan being equal to 1 mg. niacin.
Niacin equivalents in a diet are computed as follows:
Niacin equivalents (mg.) - Niacin content (mg.)
tryptophan content fmg.)
+
"
"6'0 ”
q- Folic Acid:
Dietary allowance of folic acid wil' be in terms of
free folic acid(L. casei activity) present in foods.
a) Folic acid requirements appears to be considerably increased
.durins: pregnancy.
Since the exact requirement is not known,
a range, rather than a single figure, has been suggested for the
daily allowance,of folic acid during pregnancy.
10. Vitamin Bt_q
.
Vitamin B12 is derived entirely from foods-of animal origin.
11. Vitamin D :
Since the exact requirement of Vitamin D is not known, an
arbitrary allowance of 200 I.U./day is made.. This
allowance is in addition to some amount of Vitamin D that
might be derived form exposure to sunlight.
12. Fat:
Since human requirement of fat is not known. no specific
allowance is recommended.
A desirable range for f at in
■ the diet is, however, indicated. Diet should contain at
least 15 gm. fat derived from '..vegetable oils like .sesame,
safflower or groundnut. Itis also desirable that calories
derived from fat in the daily diet sho”ld not exceed 30% of
total calories.
Daily Allowances of Nutrients for Indians
(Recommended b-r tHe Nutrition Exnert group in 1968)
i
Man
Woman
5
9
10
50
100
1
13
15
20
50
100
+2
50 150-300a7
4*
55a
0.4-0.5
20
750
3000
16
19
26
45 a
0.4-0.5
30a 750
3000
Pregnancy
'second half of
pregnancy)
40b 750
3000
lactation '’into
1 year)
30C1150
4600
tfadontary work
Moderate work
Heavy work .
2400
2800 '
3900
fcedentary work
Moderate work
iteavy work
1900
2200
3000
6
8'
3
7
•
/Z)^
■J A<rxZz>
cU'OtfO
'
2cro
I
—
3
4.
&
"7.
l<b
1
11
&
Infants
0-6 months
12.0/ 'g
1 wOmg./kg
2.3-1.3A<?.a
400
1200
300
1200
—
—
• 250
1000
0.6
0.7
3 “
300
400
600
1200
1600
2400
0.3
0.9
ICO
0.3
0.0
1.2
10
17
14
1.8-1.5/kg
’0.5-0.6
1200
17
12
20
0.4-0.5
. 1500
1300
2100
22
33
41
Adole sc- 13-15yrs.boys
girls
. ents
2500
2200
55
50
0.6-0.7
25 .
35
750
3000
1.3
1.1
1.4
1.2
16-15 yrs.boys
girls
3000
2200
. - — 60 ■
50
0.5-0.6
25
35-
’50
3000
1.5
1.1
1.7 . 21
1.2 14__
7-13
Children
"
1 year
2 years .
3years
4-6 years
7-9years
10-^.2 years
100Ag.■
.15-20
32>
^5
02.
30
25
0.2
14 50-50 50-100 ©.5-
2Z.c^=>
COMMON, i ’/ ... .-.uVH C LI
47/1,(First Floor )-A. Marks Road
BANGALORE-560 001
ASSESSMENT OF GROWTH AND NUTRITIONAL STATUS FT INFANCY AND CWLDHOOD
Pattern of growth
In the normal, adequately nourished child, rapid growth takes
place during the first year of life.
In different parts of India
the average birth weight is about 2,700 to 2,900g. Almost all
babies lose weight during..the first 3 to 4 days after birth and
regain- it by 7 to 10: days. After that, the. weight increases, by 25
to 30g a day for the .first 3 months, and thereafter less rapidly
(see table below).
The widely accepted formula that a baby doubles
its birth weight at 5 months and trebles it at I year does not
apply to all babies, and may be misleading. Babies with a lower
birth ’weight may' double their weight at 3 to 4 months and may be
four times their birth weight at 1 year of age. For example, a
baby with a birth weight of 2, 300g may double that at 3 months
and may weigh between 9 and 10kg at one year.
It is better to be
familiar with the weight gain pattern as shown in the table.
The length of a baby at birth is 43 to 50 cm and at 1 year of
age becomes one and a half times as great.
Thereafter it increases
as shown in the table below. The values in the table ape averages and
each child will differ gfrom another to a certain extent,- but as long
as the trend of the growth curve is maintained there is no cause for
concern.
Average weight and height increments during the first five' years
1-2 years
3-5 years
Weight increments per wee's
200g
150g
100g
5b-75g
ne? year
"2.5kg
3.0kg
Age
1st year
2nd year
3rd year
4th year
5th year
Length increments per year
25cm
12crj
9cp
7cn
6cm
Age
0-3 months
4-6 months
7-9 months
9-12 months
Several' Indian studies have' shown that the weight curves of many
children are excellent for the first 3 to 4 mcnths, with the birth
weight doubling by this age, but after this tpe curves tend to flatten.
This is because no, or insufficient, food is given to supplement
the mother's breast milk, which by itself is inadequate forthe baby
from about this age.
Assessment of malnutrition
It has to be remembered that a series oi readings is more
important than a single reading. Any weight ta :en has to be compared
with some reference standard, and by common consent the Harvard
growth c ’rves are used as reference standards. The concept of
centiles sho'Ld be understood before growth can be evaluated and
compared with a reference standard.
It is easier to -nderstand in
relation to height.
£
If 100 children of the same age are lined up from the tallest to
the shortest, the 50th wilt be in the middle and will represent the
median or 50th percentile.
The. tenth from the left will represent
the 10th percentile (90 children wil' be .taller than him) and the
90th from the left, the 90th percentile (only 10 children will be
taller than him). The lower the percentile, the more growth
retardation there is likely to be.
The same criteria can be applied to weight, and this, too, can
be represented as percentile curves. . It is preferable that the
reference standard for comparison should be from the same population
care, being taken to ensure that these children do not suffer from
nutritional constraints or suffer from infections. This, at the
present time, can only be found in the higher socio-economic gpoup
children. Work is already being done on this in different parts of
India and till such time as these norms are available and there is
agreement on y eir use, it is better to use an accepted standard
like the Harvard standard.
• •
Measurement of Growth - Parameters used
1.
Weight:
2.
Height:
3.
Mid-arm circumference:’ An easy and usef-I measurement.
The
middle of the upper arm. is measured while it is hanging relaxed
at the side of the body.
Normally, the arm circumference
increases rapidly from birth to 1 year. Between the 1st and
5th birthdavs, .it rema! ~s fairly constant in well nourished
children and can be used as an age independent method.
4.
Sad and chest measurements: At birth, the head circ nference'is
’ about 2 cm more than the chest circ inference, about 6-9 months
the two meas rements become eq al, after which the chest
circumference be dome's more than the head circumference. The
chest and head ratio is a (good indication of the nutrition of
the child.
5.
Skin folds: .Where skin fold calipers are available, measurement
of .skin .fold thickness is a useful measure of nutritional
status. The common "sites for skin fold measurement’are triceps,
biceps, subscapular, and suprailiac-regions.
GENER Al PR AC.TT bjjlER.S, COjRSE
PSS/ln 11 .
■
,
VlTfll'Ill'l Q
n i ->
jE“ Tr&oJ'rri er)!’’, dcrr-i^f-ol
CUs-td-
Pr&Y'G-.tnI'ferr')
fl. C&^j tA^efov’&J
oP
I,
fWT 3--f-
VEPlCJEl'jC.y
COMMUNITY HEALTH CELL
„
47/1,(First F!oor)St. Marks Road
Xe.KoPHTHfiL.Pllf)
baNc.^ore-wouvI
lfS.&iGr>&,
!$>■
2.. Pre-fe
*~>K'crr->
Cjem)&e>l . —
Ofc>j e.c#yg
*
s
ly.CtmK'ol ,le>kr>ch'»C.6
*
it) improve
'p-r-csTa-rtxr^me.
P- Ps-rfocii o Peio5<S
i)
c^ieA. ZcKe^>5^5>7 .
//) JZ^, P^scJ^oa)
c^nci
.
&>hex&)
B. LL.9t^ oP PocoJly e^reutlpd>/<£
G + P&tKPi ce^Pc~x-> c>P Pao^-S
D.
v^: ce-s.
£. . IPzrffe^/Kiv'&J
u^n'P>
Pcrods.
Vt i^rvtur) Pc^cK'yi Aex>
-r-^lex/’e^-
P . £l<sL<-<.cea/rW>-7csy Z^<s^r<=wvt.<-»7e .
3» rdfi-nohltfL-
It
~c^^a>
JZ^be&u
cwoel
CAAe-rg.
I.
2.
WHO 7Xs
PartGs
3
it.
e
C.
7
9.
o
"
v^i zit
Rm. 7. C-! Cr->
T.6! (J)
)lc>~5
)^7&
"
i&ffi
Oe-H >975
n
2$(JZ)
£?e^/975
h
S.3(I)U^.
^7o
Ao^»ceJ' i , 79^7
//^o-X
McKyHlC
^c^cer
Ip.
II.
12.
^tuK^'her^-i cxxyci
2^-^J
Vai 7o yo/gr4-23©
/ci7’3>.
T-T^p MtA -r lh<>
7& : z^'//5 IH75.
3>t'K T~
27. 2?7-5«4 /97<
7^<aL<^
^ .' 3«>Z-3/e 7972,
7^cp.
rte<A n, 3-7)^ J5 (HUtl)
i3.
fit. V H f) I
HiAl^tl^^na.1 Bl't^-3 ct«e»o o^-yd. Y»7euyi^ 7R .
3chem& —P-ropK^C^t ba C-pjOiXn &}' ^It^cLr-i^ry
by
16.
VtF R /7e^t
c>Mtr»cy
*
z /-axrjily P/cM7rn»» jF^e»yvrw
iz>oee.
*
JB-«^7>e "W P!^-o
'M.F tr?pbvmal'Ryi, MCH tla-Z
SlRGib MPSSiv-R.
7r?<f?
a/
* a/
i^>^^>eb'c\(A)
pde^ eJze^ek. t*->&-S
fke-P'fr9>r inshKu^e. Pb
@
oJoK^cxIly
IniKc^fe- Pse-ld KroJs <&■> PA& kiS<£. &P
dot>££ <as <=<. possible- rnethodlb.-eoAY^oni^<e^Jblondioe-SS> .ie+jmlKnej...fyarrrty&.-A.ue^-t oe £.■?-> c y.
ft) S uami/-?a/Lr> ef ej (l^7c>)
Pootj e
-r crop erf (/7>€zptf-A©©/
cA//<sfv’fi^r? ^//
z?
*
•J-lden.ltSr mlSc-thlCi)
.&.frcrr->
*crCl~Soli^ble^_p>&ptx
€) yj'nOeLin/ P&dely
—p
^ejOTje/^zr, c/ K»9.
de.vslapeeL (Pyp-cj^^jrnCYKXrt^
^t>
”
(jej'l>)
Y<r P daC^ r>oPpfyord^cje. o-<iy
Single- ma.^siYC dose^ianiPfcexd' lySOSoma.1 injury
*
iz.yocKc^ c^f e-rTZ-'.-j /vt&so noK 't-^c-yce^ed
^) £>-t
G Q
/
LJcA/er' d.iSpe-'-isjed o^>d oil So)<-ibl£ prepr” &>
- 3&sf'
c. sPo-re^g. &P v'iP.
Vt'P> p! oy-Y'&^-t O-r-aJly .
&) ^a'kr:A^K<K $■ G ■ ? 7 7o
of
~“ S&rixrr;
m!
ZcrTS-iS
od^erYC- p^e-doc. Is\cl&
e>cct^uced
7
Y-e\^s
erredly o.^d JM.
cjiPlj&^7
esil Soluble,
fnokloienAYK^Ked. e.htld>^r> e Vif" P 5ej» >
**
u
7«CTOyl<y. oFml SeJ^blit. k?ZZ? cnr».^y.
c^eLe- ey^ict
t-~crr"
FH
rneonlPo
,
!&ds
O-^d- Cue-^ sKl!
J) r&rKS-i'^.^.n
A
sj^o’o.
ft erredly cxS tfx. OLrj^lG- eAoSG-— t-e,r&!^' oP Ar,cjcm V/Fti
prC-Kc(?<Pr^^k
2s
ohi/drer') bjho
Goooo/^^ cP VPP p^/m'tPbAc, (few/ <^<srp-<ej)
Zfexc^ eAo^e of /A/2.
>e/feny/ ete&J&Afe .
<S‘S'<% °f d&z>^z ob>&on.b>e.eA. ecn&l
of &/&&& ■>=•«e»dl .
g>, S^r^czTg^g^ M>tprk>.)
P>&t<A SKiA.y
—JPo/olence. of X*®oe><5/S
<xz-?et S/fate
^iCrftpi'C-arAfly T-ectxxeetfi Un’/^u? Z^r^dx-.
dr
coe.r&.
^)
t^p&cK^^A. Locidsrit.
oLt>ir07^
P>
*?
<6
f^jCS forcesek .
0°!^) ^-> ^ub~So.r^p>/G
Sormurry )PPP AsJv’e/S hitjh Par
Pe^tdneA
«X7<51 /A-?ZZ by C^bfen^P 7S^
rfo n^M Ca^^9 of ^Sr>oiKr>^cJa\.cte^
rrterm/l^o
op f'f&ick sfa<Ay chAd'^f
bisf Pep! Ab &/tohACy eJx
£*
oP YiAbmCr^ P Ai> b& efiv'^rj
earjC-G,
(jj -ho-)
TREfJTf^EtiT
J&c-hjr>ieyiA.e- fG-
_ The,
ex. cJ^i'Icl. tS k>e>&p^<^h'‘&a<A. h//#>
u^ue^s-----
xencpInP-’O.lmib. 7h.e. fe>He>L^<>>Cj
p J^-»pY'e>.
■Sy.hI «ar- / / €>Q CsG'li IU\
Pbn cevr»h<^> Ct.K^> /Ofc^l i/ eropvro X. 4?
R&cCYmm') W&feY rtl'Scifol^
Pre~p& Y'eK.K'CYf^
//) C>>!
T^e-eJ^te^k &cheeLu.!c_
—““cAjCcJ^ly crr-> Tjie^pnosis
SC-c-crrtcA. (A<xy
*
/^tor
/» di&cAav’^g. LLneL^-y !/
*>
Ove-s
I
ZZ>./4Jft^r rntSCib/e j It^l
loCfOfDO IU /ail ^ol^tfcmJ.aY'A /
/ac^^° t L>/aii sd^t’r’enn j&
* ■?
^.esrp^oo )
I-yr-
i ,
,
/4>C
OP^>
*
J
tt
/a^aJ>
E^piancJPnr'y VTo/e-S.*
a^~>
2.. l^-perrs
f
.O C>luK&y'> e>P
cmly iP a-tn lM pYepe^o Pe>-y
Gf'l^J&rbtC QreaS
ke^p
io
R. (jtRfBOo lip) sA«tm/«1 4>&-
r>&P
. Lknpi>od tb
nritSctblc pyep&vexPPemo
he^cLy-^P-t'oJf
3. Oral Co-Et/i&K
pre^araKtrrS
a>P V^Ltq*
>?. ?9 »7C.y be
C^k>chtLT&g-X F&r ertl SdM/Tbn® . V,^ P. oCAfo.fi rmo-y A?e.
pla.ce. df -xt/cx? y/ poJrndG'-te.
Q- Oil Coin lions
YtK P- shcrulei-
never foe. ir->jC.cJk A. trf because >^£y
aye. -reloK^rel y tr> elective., lh<2- ri.tcf.mon
^Icro^ly, i£ af cJI, P-rcrm 4A e t^o'jec-Kcsm ^,/f&. .
O bj&c/i^
—'
w «ed
0 "Zp hcjr~ dckf^e. /esi‘en->s.
it) To -r&-p'se.r->> ^>h>
he><Ay ^Tcry^c,.
Ufo-^JiaJ’&ek. Cx^onr^
or csrriiz&i'a^
Vit' P ftiSAopy uiiotle
KcoXrrx^ok' e/ PC-tyi —
Xe^oph&tdrrito.
rrta.y
be- preoipite^feek
Other Pa.c.Kfrs J& b& c.tm^i
I. 7r^eo/r>^er>/^shcruld r^oT b&. e>le.t&ye<£ . rOeltxy P&~ &r<£.r-> c^e. nLexy
aTs)i.^fes <X2. oryr^p
cbe^neyioo o.re >e re-a-o> b!e rrtoy nnoke all lhe
CpUPPe^orje^.
beK^e-O-ra ^r^ht’ <ajoeH bflir}ej.ruz--or> .
ri.. £i^re cc^ndLlt^moe PoJkr^^ To trie^opcmtA. Io a-nlibt'o/it-o—undiejilyiny jeettopthalm70. sAeru/eZ be. Cori^ibLtrteefi e-op\
SoPioJ Circ.Lf.mstoy) cgra Coe. LrtcliccJ^e.
miscible prepr^ rxre especially CrnpcsrtcLriT in Ctxrjeo cf V'crmiK^
It- UneUstlyCriq Ccmdbi^cms need riGCtrcn^9
, P£rfr bluK^lf Or>Al d/SoJeA^
rrle^t i rlakvirai^ -!^f)ba./Mc£, ir>Fe.c.Kcm S. Cnpes/gitrems .
CdNTiZOL.
Pr./£v'£K7'ioiS
C-ot^TRo L.
Pf&aFZMrtgs
(rfHo)
- C-e>ul.dL. J^<si^s__ K-k^o^ .rnouLn^ cshyszcK'’<e s
cL^p&r-icLi^->Ci csv-3 S.ezc»M‘J^ aP pf-rcJoicm. Sm'o eecnamc 5i/tia^d
e*-v r<zslc
*.biitPy
&f husno<si cuoe\ per>c^oc-cctl^ ve^>cu'fce^/ ?fec-^no/ensp\c<
*l
Obiecfi ^c P - fe> c-erryLvol blt<->
ccx-t-cogj/y ye /expect
’/V""#,.
d
]ma
flw
o^r-> cL Lik'e-^ (< 5>
?
*
)
73 icnprcsr^
Afeed c rtKc n o ten'll
Ohj^cKv^. S2 -
..
rcicr>-&-
■pv^-v'es.lG-dK C'f'f-) fc.c\!
iii) p!0^3 mo. o-r^ck
faVe-v-
e.en-3
v'i^xmC-o. £ •SfaKm
of- /c^c> 0.1'"
h e. i) P>c-c^^e^>c.y cf >^e Kv>ilcL
>•) (zLt'iS-i'cxry ccjLe^./^
.
•£> ,
&£>£>£. PRo&filf)riME&
P£Kie>P/c.
Xr-?
2^00, aoa
lU
P (jg
oP
•
e7g?,.<7
rz-rrst fsv'dx.mrrs <£.^
££■■)
£>
**
SvCAy
.c/?z7et<«2^r7
<» rx»finr>>^>«k
— ^-rcs^A^h A<g«si//A
PsFf-
))
.
<S
&y
k&.v’ <sks> perwib}^
^y^Zfe»<>7
^cL^CeJ"!«-»">
rdoJ'ively
£.h^e\p.
-c^
*
Pe
FbRT) r/C^T'lO/'f
Y'&h/cle. /^v-
^hcruld. htex'rC. PoUcusCo^ cJ^&^ye^l^rcLoK co ■.
/. Z^^sessst.
/too > vC-o^o,/^ Ccr>v9u/»
*<s^
tx-rf
KA P fa/KfLcofa
*
<3>
™
*
4?>
^oyPu/^A^
2..
Jyle>f rttfuch^n'AK'ayt^ Co pe.'fr.ccxpf'K^ eke>-<.'ly .CcmSMaftlaoa
3.
P&z^&k S^cnj-ldL shffiy> no err^e^oochay&cl'&iioK & <&&> ViPfiod^
if. izzcoroerrot'a. h & &o< bd'fy C>P Pcf ACexKanm C^r-» Co ei^Ct steal Seed&.
1- l~G>-yPPiritik. —
Fo-yP^Cc-Pern ~S fi,Dp
&/ cJUeJaffee! pRrnmek m>Hr.
PH milk ypcroet/c^cJo ^t-<pp^Ce.£^
L>^>
pycr^vc>.r-rin^.^
hcK'^CSiO£jQ !*&&7L. J-ys-rK'^Cn<ok c.g,z2^g<.Zs —
*n
P!esx
Jroc^'T^e^ r-'^eol j 'y/'re> p>^.rr>ix-&o
!<-e^>>oe-l5.
/S>rrt^le>.Kee! -rt'C-&~s.
<so-7«sl CcTjAfeet VI"ce
/!\J^ Vtp'/).
— PrcfJ&.cJ^Im
Gri^t C>!^y>noje\ (l6!
J^ye^^pen^ei^-y — Tmeo.!^ C^n> Stef^
o !X^> JLr'c^
g^y
P-e.^e^yiiRn ezyf_eJl^-^l‘' e.'we.o
<^t&n
!^.&
Ruoil&cH.
^uj>y&o A^KaAawcoA/Jjx 57% GuyereA ^4% ^mih'AQ
C^wdxie^J Lcop Ictiaj 'iOC£3Y-n-&. ^ycriAps)
1-wK'fa'c^Kcrm ef^ rlcmo^pd^j ucon ^luiKt-rrteMe — pi)c>!'
PPcRcpy^&^> • fCo>-ix?<a^v-v«gt co cLCe.^ hy 95?a a!
! Acruv.
!^ot^i
vtht'ei& .
eHy Co ^<2-is>u.
?. Shekel b^. c<b/e^ Fa
>^~s
3. P/l r-'Ce/e)
. McH
Potx^s
y3»e y-e
^es>Kj
/?zyx-> gA^/^gtyy
ixJ&fJCAarS
rruji^oF o.ll
b&-
F^a,
haye.
)F>K Ft
/cttfzy/^y
oP-A^ti
s ^y>ple^>t.cYik^Kor) scFa^xe.
— »<<e^.X&.A>Ze. fioot Zv-u^t'A'>£> Z>-e. p>erpL,tlAn-6oeJf.
'
—
—
1-ea.Fj
fo&- Ctr>CXG^>£.et
VCKvC^^i'e‘£> c>F
^c>
et&rt/p-i
O~^icL ma.$s> rnedU'ez. SkcHpcCh-e
inUcpe^L .j2e&£..eff' pvtuP
PoinF^
L Pocgx.1 ■sesiA-v'ce^o of VrFP J Cok^Pes^z^s.
'
>
v
2. Prt>eFucK'O>~>/SKcrr^j&.JpyR.y2^y^P'^>-> oF
3. OpS-e-iizd ’s^tP^tP'Cir-icJ /TnStfdsZo c/ yOMq
cFHai'^n.
Rich
V>T^p.
Pnimed ^cn^y&e^>
Fe>&P£>
^?®A-3o-Ao
Z^X/fc -
en» •
e>
^ceZ^rv-Lt'
*e->i'
£ce>~7&^>
Z-eVe-x—6-/o<a^»ri
R&o/ e
‘yt«./<e^ok'n
Ghee
plc^h ^cr^-<c-e^>
,
(^ejj(PeKnoi)
^>pCnc\.e.h> 6.ero
/^rz?»y<=<-xj^ _-246 ~H Ci>
z®Z'*
Cc»'
.)
*pAsnpk-
2/7"4»3
- if:^"-2aT>
trilz-
/O -^UUL‘'->
Oxt^a? -35
Rt^pe. /cnnTi^. ho-^3Z
Qc’.hbe^e. — 2/ 7
Vetf. Scrurc&o - & G^Ypf'e^e Pravr)
Gnr&Z-n leo^SOUrcas
P-rne^-i'ciJ/'h }j3-eeJr)/f^-ckb^hj'/Gtolkh)'J5pcs~>cs-e.h
i)Fo)' e>>
PiAult'
Chu'lck
eLitih
ii) £o.y<^<s. piec&o]ycuv'eecC. ,
8 Cevrofcrig.) ckoy
15<x>-/&tz>^y
>•
=
v
/oo <J»
cpsCertS
HPsgjyg
posgs ox--'
mPake.
liver shares.
ii>)
Kf
\C<c/2x^/'g~>r>
lens&o
5uysyo/o»?eo^
CcsTo/fe^oZ C^ ,9^^/ milk.
JS^^-cAve./^ rax^e X/'/O
S<x.ppk^e4- sPeA. be
S&.rii»UL£>
Pmhlrc.
M-eeJfa Probfe-m
TP>cJLjXX .
I mUhcrs-> coses of j&h'ncfaett cLuji k tftfi
E-^Yjim^Ye.^
PoT>e»-/t/ae>e> Ke^e^farncJacec^ c.CL>o&ojyr
So-S©/^,
P>e-t5ch-> o&) eb>lfa<r^(chje^ciesJ)
LOcs^
A^o-wo/a^ 7e^>nifae,<iM, F)7‘t
Qihor .
£S££ X-jcU-ck)
Pr'evaJsnae^
^/j/yrcrp-cA) .
/^e^gxsA. ■
,
J^fe^Y&K'crr-i tAsi fa tlCH r F~P 5ej»v»ceo
Z. h.ojcfa l.u
of VitP tn
f\loj^er>->o.l k^ Aftznto P Z^ro p^>y 7Ckxj'S
oil cmallyy^^M^
/^»euvu>>>e Pcv~
P>e.^&nKi'cm op &h'r~»ckf'>&ss i>j CA;/d»or> (/?7<p)
/97o-7<r
Z9 cL»s^e.>fe/Z©Mjfe{> Tfe 974/j^S^o
S- lt O '^) ~ti
<3^.
Se/Severn o/pe^&s-i <zy
Pe^<
exg - S/'cJ’e. h-lt
*
K-t'Ken^ O-^y'c&TS
cvigl.<y? t>?
I
Urbcx-O
tJe/Ax>e. CJCnfc.es?
C-hilck
Hfbc^i F~.PCenPe
! FP IteaJK Z?ss£
l4cr?pJ'bJ& .
7^7»/y Ff-eymes
Gr®^?^y?ex/
— Sped Pic.
.
, ,
t,
lU ]
LUvlPHtJ ?
cJ^o^z^> Pcn^
.
-a<ey?sei/^cL c^.m^ •
/'t'U ^yee^»>.
_ __ L.___
Gv/B- SAcn^ sAei/A' AZ^r af
.
Afe>g\//A
caJtem •
Pie^~> <2cLla.coJ4ertn o-rtd.
P-rokflje^rm^ esf Viy pi 7^^ -3< /?cJv. <^p>ey>hylmekir pctyon^
^‘vcA./tACx/fcno - ^<ase/tz>e 5ucnvews//2ei?e«a^c/ Su-B^yS
Racef-'eX^ — ii-k ild.
i4^-f,))t~, Pee cn'el^Q
PePCf/^ ~
PROS.
I.
MG'S
13Pr4&LP7D£SH - fiov’*Af-jy^o»7®c
recL
p^t^'oeLi'a
7_9-75 .
r^c^SSj'ys. <Jo«e y7ro^_«w»
»e_^Z&r5
*
-~P)ll 0—6 yr c/->»/eV>-ey> ^/ve^o ZoCjcero/L> _ 77^
*7?
£<xpsulc
—ZL^uoZn.-A?uA^feesi /hvertA&'fa hlMEP. S^Ff'..
— 6‘5%>
cJniltA. fZ^op^l ^-!^i'>^~> fp_&.c
*.ch-ed-
.
^?. Xz/Oo.A/gS/^ — /■'e-r-t'c’cL-ic. m&uooi'rc- ctose prar^'fanx^
5 (pezr 2yx>) „ CsypSct/eo
^.LeJzh !\P. Ytf f^.cx^
Qo !l> 'iacaplygj^y) e^cjg.faJ'e - cx.ctmrt 6/Annua.l^ jby
!e>c>too& cAiM>eo
Cc?XE»n42js(. .
li.-h^r
*.5-r^no
Z?e^
• PHILIPPINES -C-E& U
C^ fZ>'f’crv~i~r)CJZ-^ <5^ ^7c».va^
r>n&.vkeeily
3. y-r
*
pii^P
e.^(ipTL
3 Shre>J'<eefi
0 S. LeJchjfa
ft) P^hh'c. healfP
Pcvfre^JK.cneJ o.c.K-y4V<a^&
Coo^ Tt^ j£jSpec/fve^ie^»o a>/
<f ■ £<- SGLWOaX
- S<4 ck y -
^yoJ^Q/ut^t
^/yQ_.
•
—VtLQko all c/n/lt^Lnt^)
__ capsule
ZLclIcK ID VJT fj 4- I40 ID
l4osp.-^e-cm'ck PtZYX'^i^J
laS^cA
^.£.______________
Per? &YeJiA.Qj&>ct
P^O^i -TO^rMYi e.. (jQc/jyC- Vir-FL^e-!*>&£■ Ceryne^l cl&owtf')
i) Pe-Ve^-) fra>.l
Cc«-rex>o ^0%^
.
.
*
y<Zs^h/kcJrnft
-
v) ffra^olt^o'l'
f/d X- M \f/-
NOT/ZlT/c^!
fZ£.UF)8lLWnOfiJ
&■■ VfenXco.Za.siAJamy'
"
C<e/-?/ne.5 4/7
Pre^o.le^tc.& oP Yi'F P
CJ-iilcA. Ccx.r&
&>
PxscA
chiAt
*
/46> '/z7/c
.^<^s
*
y eu'cpis
- 2.^Z"7t>
^p&^- q%O'7°?6
$/xckAe-^ y >) Dernan&facJ’fcrr’)
beat's
em a. scJccK><
Grt'o^cAe^Hri~^l /&^^eAj2.T£ / G^euZP
eJorfeut
VfrP duef.
P&cxA 3upp/&^>e^>P Car?Stefa
^~O —&Q
3cr&c> iD oFofen>e
.
NuP-r'l'Fcrr-} p-eLmce^Kar^ j
Mc^ch'^e^^
Rjzov'.lfo-------- ------------------------- ----------
E-^tc^ e>? Eeeclesvj Cm ^^ophfl’/cJrrnek .
______gxryta/y^z ■$,_ cff Jit
C~/<^z>>3y%
ckilt)>e+>_____________
On ouaL»?>»»‘a»^....
-.h^M.hthdo^.
.
...C<s-nj. ^€/ia9^ ____
3.
B,^Spo^
Lk._
/e>9
cm cU
Z547/ ...
Ufl
/_ __754.0__ Z/7 « ~2
go
&
£-vp)L.t>nri
I.
iScX'S^. h'r->e. ^Si^-ny&y ,
3..
Gx^evt’cs Pw
public. hjzeJpi p'fdffolfGrn .
J^ Opc^oJ'eormeJ &‘fip^clr>
e&v ■
t)J Ptt'ol a-z^ccesJ <s^pec.f>rvC^i^'&&
yC>>€ v»Je-Qce et^
^~in >eeJ
rnie< &y ViK
^)p> — /?&/ex^>eQ-
! Co&p b&>d-rb
CZM^
VOLUNTARY HEALTH ASSOCIATION OF INDIA
C45 SOUTH EXTENSION PART 2 NEW DELHI-110049
NUTRITIONAl BLINDNESS ANO VITAMIN A
HAI - 240
VITAMIN
AREAS
shaded parts of Map)
Bihar
Bangla Desh
Orissa
FDIET SOURCES
OF VITAMIN A
Andhra Pradesh
Tamil Nadu
Spinach • Carrots
Mango • Papaya
Pepper and Fruit or
Vegetable
Yellow or green on
the inside
EXTENSION PART 2 NEW DELHI-110049
NUTRITIONAL BLINDNESS^Dry Eye or Xerophthaln^) IS PREVENTABLE
TREATMENT
X-0
Night blindness : the child
stumbles in the dark.
Some brown pigmentation may be
seen around the edge of the
cornea.
X-1
The white of the eye is dry.
If in doubt, hold the eye
open for half a minute.
White triangular patches that look
like milk powder or white paint
may or may not be seen on the
outer side of one or both eyes.
(Bitot's spots)
X-2
The cornea is dry.
It looks hazy.
It has lost its shine.
Eyesight is now in danger. Both
eyes are usually in danger at
once.
For rapid effect, give Vitamin A
in watery solution by intramus
cular injection immediately. Also
give some protein-rich food. (3)
X-3
The cornea ulcerates,
the iris prolapses, or the
whole cornea melts
(Keratomalacia)
TOO LATE
Partial sight can be saved tn only
a few.
j
As well as treatment as for X-2
above apply local antibiotics by
injection, atropine eye drops or
ointment, pad and bandage.
X-4
White patches and scars
cause permanent blindness.
TOO LATE
The child is left blind, totally or
partly. Usually both eyes are
affected.
NIL
Only a few
corneal graft.
Green leafy vegetables, eaten
daily,and oral Vitamin A, 200,000
units in oil (as capsules or liquid)
every 3-6 months prevent the
disease. Newborns, until they are
5 Kg. or have doubled their
birthweight, only need quarter of
this dose. (1) (2) (3)
are
suitable for
DOSE
SOURCE
40 Gms or 2 large
spoonfuls daily of
spinach or green leafy
vegetables.
OF
SUPPLY
Seeds are obtainable locally, or by mail, from Pestonjee P Pocha, Seed
Merchants, 1 A Middle Road, Pune, Maharashtra.
Concentrated liquid Vitamin A is obtainable free from the District
Medical Officers in Bengal, Orissa, Bihar, Andhra Pradesh, Tamil Nadu,
Karnataka and Kerala, and commercially from Anglo-Frehch Drug Co.
Eastern Ltd. 28Tardeo Road, Bombay 34 W8. High dose capsules are
obtainable from Seamless Capsules Ltd. Box 2262 Bombay-400002.
■raton ki goli' con
taining Vitamin A
200,000
units
by
mouth, twice yearly,
in oil, as high dose
capsule or concentrated liquid, 2 ml teaspoon
supplied= 200,000 units.
Vitamin A aqueous injection (2 ampoules=200,000 units) is
available from U S Vitamin and Pharmaceutical Corporation
India Ltd. 43 Dr V B Gandhi Marg, Bombay-400001.
200,000 units of aqueous Vitamin A, by
intramuscular injection, immediately, and
not repeated for 3 to 6 months, except
on doctor's order ; combined with rice,
dal and green vegetables daily.
RECORDING OF MASSIVE VITAMIN-A DOSES
Record as immunisation by writing the date given
8
"Zfjo -
AAW'
/<r&
' -HI
L
■
DPT TRIPLE
1^7^-
IT 1 Nfc J
£
or record on the growth or weight chart by writing
a large’A’ opposite the month when it was given.
COMMON SITUATIONS LEADING TO NUTRITIONAL BLINDNESS
POSSIBLE ACTION
PROBLEM
Infection such as measles
whooping cough
diarrhoes
tuberculosis
typhoid
Green leafy vegetables are not available in the village.
Green leafy vegetables are available.
1.
Treat the infection
2.
Do not starve the child (except in early typhoid). Advise or give
extra food, including green leafy vegetables daily. Explain why.
3.
Protect the child for the next 3 to 6 months by giving him 200,000
units of Vitamin A by mouth, in oil. Explain why.
1.
Make seed packets available for starting a small garden of green
leafy vegetables. Use waste water from the house, and protect
the garden from goats and chickens. Start many such gardens.
2.
Give 200,000 units of Vitamin A by mouth, in oil, to prevent dry
eye in the meantime.
1.
An aide or another mother can demonstrate to mothers, how to
feed green leafy vegetables, and how the children like them. Keep
spinach for demonstration.
2.
Teach all staff a simple slogan to teach mothers, such as
greens every day’
3.
Take help of school teachers, village doctors, leading men and
women, and shopkeepers.
But they are not fed to the child.
'eat
PROBLEM
POSSIBLE ACTION
Night blindness only, or conjunctival signs (the white of the eye only is
dry) is present among some children in the community. Village people
will be able to gather for inspection, those who complain of night blind
ness.
Vitamin A in oil (retinol palmitate) given by mouth, in a high does of
200,000 units has been found the most effective treatment. Village women
and schoolteachers or dais can be trained to give all affected children
the Vitamin A, and repeat it every 3 to 6 months. The oral route is
best for slower abserption, and the oil aids absorption from the intestine.
Absorption takes several days.
The central dark cornea is hazy and dry.
Vitamin A is urgently needed in a rapidly absorbed form. High dose
aqueous injection of 200,000 units of Vitamin A is recommended by in
tramuscular injection. This will take effect in a few hours. Use anti
biotic eye ointment to prevent ulceration.
Paramedical staff, village leaders village doctors and village parents do
not, recognise the disease.
Use the eyes of children with night blindness to teach diagnosis and
treatment and prevention. Use posters and coloured Pictures also.
High dose Vitamin A is not available
Use Vitamin A and D capsules each containing 10,000 units of Vitamin
A, until high dose capsules or liquid can be obtained. These capsules
are widely available in chemists shops throughout India.
Also use liquid Paraffin eye drops to lubricate the eyes till the Vitamin
A takes effect.
REFERENCES
(1) Gopalan C (1970) Am. J Clin Nutrition 23 p 35—51
(2) Pereira S et al (1971) Arch Dis Childhood 46 p 525-527
(3) Pereira S et al (1967) Am J Clin Nutrition 20 p 297-304
(4) Pereira S (1975) personal communication
PHYSIOLOGY OF VITAMIN A
INTAKE
ABSORPTION
is from vegetables in
the form of carotene,
or from animal sources
as retinol
is with the help of fat
or oil in the diet, and
of the bile salts, in the
small intestine
STORAGE
TRANSPORT
ACTION
PATHOGENESIS OF VITAMIN A DEFICIENCY
POOR INTAKE
POOR ABSORPTION
POOR STORAGE
NO PROTEIN CARRIER
DAMAGED EYE
refugees
war
poverty
ignorance
dietary customs
famine
crop failure
infections
withholding food in illness
insufficient solid foods
for weaning
feeding programmes
relying on unskimmed
milk containing
no Vitamin A,
diarrhoea
sprue
no fat in the diet
obstruction of the
bile ducts
inadequate stores built
up in the liver, due to
poor intake and absor
ption.
Severe liver cirrhosis
severe protein lack in
the diet as in
kwashiorkor or marasmus
when cornea is already
damaged due to viruses
of smallpox, measles,
or
other
neglected
infections.
When the eyelids can
notclose.
•
IS YOUR CHILD BLIND IN THE DARK?
“Is your child blind in the dark ? Feed him more
green leafy vegetables and give him Vitamin A
twice yearly."
This poster is available at cost from
Voluntary Health Association of India.
It is available in Hindi, Bengali, Oriya, Telugu, Tamil,
Kannada and Malayalam.
It is printed on stiff paper, size 45 cms x 57 cms in
4 colours.
Copies of the above poster and of this brouchre on Vitamin A and Nutritional Blindness are available at
cost plus postage from :
VHAI Community Health Programme.
VOLUNTARY HEALTH ASSOCIATION OF INDIA
C 45 South Extension Patt 2, New Delhi 110049.
Printed with the kind assistance of Christoffel Blindenmission, D614 Bensheim Schoenberg, Nibelungenstr 124, W. Germany.
'Pcfsex’u/wc^ oT Pets&i 2W Z££zJo^t/wj
rh
■
veK‘- °< kr«/e«„^ .
Social Medicine
St. John’? Medical CoJkgK 'S'^
8ANGA t,OR7.560a?<
e.u.u->c
47/1,(First FlodrlSc. Marks Road
BANGAfcQRE - 560 001
QApSU
XjU^-4
4c
.jJayeW;
,^)3ibtc_
-0-s<a4
O'fcU
BANGALORE - 560 001
f• 1 V
ca-Li-
Q
ifefe
^ncUo
>■< A..A_A_
L^jl"
H/:
CaJT'
17-S
112 -2,
IS.7
22-1
H7- 7
21 • 6
/22- 7
t^-
<• f^s
US-1
127'3
2b^
127' 2.
Sif-'SZb-o
/£?’ L
3d-0
133'/
S.7-Z
123-3
/^7>D
!3S ■ <T
>^3'^
Hf-Z' 7
'oP6
D
2S-S
^■1
H>i ' 7
/L^'3
•
33'6
37
/£7 ■ o
^3- o
133-
4-4- S-
^’•2
/^3T- D
^•7
5^-2
/a-T
S "'
JZb-b
COMMUNITY health CELL
«7/1» (First Floor) Si, Marks
BANGALORE - 5uO 001
V7-^'
47/1.
rrvst. Warks
,.560 001
bAMGAlO3‘--suu
MALNUTRITION
Malnutrition has been defined as "a Pathological state r .suiting from
a relative er absolute deficiency or excess if one. or mere es '.ntiaJ
nutrients, this state being clinically manifest:.- ?r d:tzctur nly by bio
chemical, anthropometric nr physio logical tests".
Four forms
malnut 'ition hove been distinguished. (l) Undernutrition s This is the c ndition which results ijhcn insu ’“ici' nt fis eaten ever an extended pericd of time. In extreme cases, it is c.lled
starvation. (2) ( vernut rit ion • This is the pathological : c
resulting
from the consumption of •■xna;sivo quantity of f.: . -wsr -.n c>- ondei ■. nriod
of time.
The high incidence of obesity, atheroma
md diabetes in western
societies is attributed to overtiutritinn. (3) Imr."lance = It is the
pathological state resulting from a dispropert i .n among essential nutrientswith or without the absolute deficiency of any nutrient. (4) Specific
deficiency ' It is the pathological state resulting from a relative cr
absolute lack of an individual nutrient.
Classification of Nutritional Diseasea s
The UHO Expert Committees on Nutrition (1962, 1971) proposed the folio,
ing classification of nutritional diseases s
Nutritional Diseases :
HYPOALIMENTATION s
1.
Prot --.in-calorie Malnutrition (PCM)
(a) Kw-a^qrkor
(b) •'lutritigiu.i marasmus
(c) Severe PCM, Ui,nuaiifj_eci
(d) Moderate PCM, u, ~r,QCipieci
(e) Other PCM.
(f) Malnutrition, unspecific
(g) Nutritional dwarfism
3.
Vitamin deficiency
(a) Vitamin A deficiency
. (b) Thiamine deficiency
(c) Niacin deficiency
(d) Aribcflavinosis
(e) Deficiency of other 0 complex
vitamins
(f) Ascorbic acid deficiency
(g) Vitamin 0 deficiency
(h) Sprue
(i) Vitamin k deficiency
(j) Vitamin
deficiency
2. Mineral deficiency
(a) Iodine
(b) Eluorine
(c) Selenium
(d) Calcium
(c) Others
Co) Essential fatty acid defier
(b) individual amino acid .
defies, riricy
(c) Other stutuo nnd unsptciri-o
HYPERALIMENTATION ;
FOOD TOXICANTS •.
(a) Obesity
(b) Hypervitaminnsis A
(c) Caretenaemia
(d) Hypervitaminos is D
(e) Fluorosis
(f) Other
(a) Lathyrism
(b) Epidemic dropsy
(c) Aflatuxicosis
COMMUNIS •IEALTH CELL
Marks Road
■ . 5 60 001
Diseases of the Bleed end Blood Organs ’
PERNICIOUS AN.iEPlA 8
(a)
Subacute combi sed de : ..aeration
NUTRITIONAL DEFICIENCY .INmEWIA :
(a)
(b)
Iron deficiency anaemias
Other deficiency an-'.r'ias (folic acid, vitamin 3 , vitamin B ,
. . x
12
6
protein)
INDICATORS OF I 'LNL’TR£~1 - L
It will be useful t bear in mind the following "indicators of malNutrition" while assessing he nutritional status
well as evaluation
of nutritional programmes in a community.
(l) Statistical;
(2) Anthror jmotric ?
(a) the mortality in the nge-group
under one year (especially 6-12
months)-
(b) the mortality in ttvu age group
1-4 years.
(c) the ratio :-f deaths of children
Jess than'5 years r.f age to
total deaths.
(3) Clinical;
'(a) the weight of the newborn.
(b) the percentage of newborn
weighing less than 2,500 grams
(c) tho height and .weight of
children aged up to 5 years
(d) the average weight of 7-year
old children entering school.
(e) The index weight/height is
regarded as a simple and
reliable.indicator of tho
nutritional status of preschoo'l
children in a community. An
index of 0.15 has. been used as
a dividing line between well—
nour;~hed and mal-nourishcd
children.
(A) Di.etar.j'. Examination--
(a) the number of cases of mal
(a)
nutrition admitted annually
in hospitals and hca1th centres. (b)
diagnosis pF indivi dual nutrition
al deficiency diseases.
(c) the proportion of pregnant women
with less than 10 g of haemoglobin
per 100 ml of blood in the last
trimester of pregnar;cy«
Intake of calories, proteins
and other nutrients 8
Studies of dietary habits.
Degrees of flalnutrition;
While studying malt.ijhr.tion ininfancy and childhood with special .
reference to kwashiorkor, Ccn>ez(l955) was able to draw up the following
classification by assessing the percentage of underweight in relation to
average
(l) First Degree Malnutrition-
Weight between 85 and 75 per cent of
the theoretical average for the age
(2) Second Degree Malnutrition;
Weight between 75 and 60 per cent of
the theoretical average for the age
(3) Third Degree Walnutrition?
Weight below 60 per cent of
the-th»OTgtj_cal..waKt!rage--fOT the
age.
ST. JOHN'S MEDICAL COLLEGE, BANGALORE
ti eJU-ix
Cflass
Roll No.
Semester
Subject
Examination
Date
4
US o<-( d. 4 <s_cc(LtU
47/1«(Fi;
' 56,0 001
Cu^jclo-^ cc
dzi
i-^-xXZGMy
er^oerrv^ t”?.
(C&
7o. ~ £o. %
GjOws-j ~Pc^>-As^
Itji /- ? cu^-x©.^/ _cSh.
<aS<3J'g_ U.LdmjS'
,|t-uutC^v XeXped
vM-CUd_L«-sai'
<tz/e^d^,y
Ocue^ _ c_ roXto-. .^'S.JUuseJLs
4
2
, '
__ <
,y<J. >>iCwJcLk_Ky
kk. iCLg.
c^p’
C'fecx.v^. _JU4_a_Xvu2L
<S c.'g ifcaji
•*
. ieo-v-j
.jan'gjedka,-
' <aJo-r e' P-vXstcD. <
CJ~ ^ZX2-C^-Q.
e^_iffe ..
* -a e-Col<Lci_u^7
tlSj^ 1^^
^.0^,
-<eo^ "• •
r
•k
C^L-d<dLuXZM. c“ ^<-c
C-3- ~L eycJ©_C£
*M
C
NUTRIT5OM
AMD
PRIMARY HEALTH CARE
'•
aoad
MRS. MANGALAM
TT is said that a man is what he eats. A diet
A sufficient in quantity and adequate in its
rWPition content is the foundation of good
health and well being. It is also an important
factor in raising productivity. Therefore, nutri
tion cannot be separated from health and any
nutrition programme will possess a health com
ponent. One might argue and say that nutrition
will not take place in the absence of an adequate
purchasing power for our people. True, but we
cannot wait until a reasonable standard of living
is achieved. This is because nutrition is the very
basis for achieving an improved economic status.
The objective of nutrition in any Primary Health
Care Programme is not only to prevent malnutri
tion but also to promote positive health.
As correctly said by Dr. David Kerner, if
we all took more care to eat well, to keep our
selves, our homes and our villages clean and to
b^-ire that our children are vaccinated, we could
st^l’most sicknesses before they start.
on the country due to child wastage and de
creased productivity. On an overview of the
determinants of nutritional status, it is clear that
the extent to which a child is well nourished or
malnourished depends directly upon :
(a) His food intake and
(b)
The presence or absence of infectious
disease.
These two in turn depend upon
(a) Nutritional content of food consumed
(b) Presence or absence of non-family feed
ing programmes
(c)
Family’s purchasing power
(d)
Nutrition and health beliefs of mother
(e)
Extent of health care and
(f)
Environmental and social factors.
Mortality Rate in Various Age Groups
Age Group
Rate
Causes
Malnutrition a Serious Public Health Problem
Malnutrition is the biggest problem affecting
public health in any developing country. The
findings of carefully conducted diet and nutrition
surveys carried out under the auspices, of the
Indian Council of Medical Research and the studies
undertaken at the National Institute of Nutrition
have confirmed the existence of widespread
malnutrition among the poorer sections of our
population. Children and women in the produc
tive period appear to be the worst sufferers.
Over 15% of the population in India falls below
the age of 5 years and it is estimated that about
40% of total deaths in India occurs in this group
as compared to a figure of 3—8% in advanced
countries. Apart from causing
ill health,
malnutrition imposes serious economic burden
1st week
51/1000
(i) Low birth weight
P—4 weeks
21/1000
(ii) Starvation
(i) Respiratory
infec
tion
(ii) Low birth weight
1—6 months
27/1000
6—24 months
34/1000
(I) Diarrhoea
(i) Infection
(ii) Diarrhoea and res
piratory
infection
pneumonia
(iii) Delayed
mentation
2—5 years
28/1000
supple
(i) Malnutrition
and
infection forming a
vicious cycle.
Expenditures to overcome or avoid diseases
have commonly been regarded as a form of
WITH BEST
COMPLIMENTS
FROM
AR KO
R.K. K HULL AR <S. CD
C-203. NARAINA INDUSTRIAL AREA PHASE-1. NEW DELHI-110028.
PHONE: 393898
GRAMS MEDISURG
MANUFACTURERS OF :
OPERATION THEATRE EQUIPMENT : Shadowless Lamps,
Suction Pumps, Hydraulic Operation Tables, H.P. Steam
Sterlizers, Bowl Sterilizers, Autoclaves, Hospital Furniture etc.
NUTRITION AND PRIMARY HEALTH CARE
consumption and consumption is often a negative
factor in any national planning. As discussed
above, if children will not live to realise their full
development potential, the cost of child rearing,
education and upbringing invested by society, if
computed, would'probably run into hundreds of
crores of rupees.
Health in Relation to What People Eat
It has long been recognised that nutrition
is but one of the several determinants of optimum
health, though admittedly an important one.
While poverty is an important factor for malnutri1, it is not all due to poverty. There is wideead ignorance about the common foods that
supply the nutrients to promote positive health.
The countrywide survey carried out by ICMR on
18,356 preschool children of six different regions
of India has revealed that in the current dietaries
of preschool children, the major bottleneck is
Food Gap—INADEQUATE FOOD rather than
a particular nutrient gap. Since the mother has
to nurture the foetus her nutrition has a direct
relationship to birth weight of the baby. The
main cause of undernutrition in the mother is
insufficient intake of food within the family. Most
mothers feed their husbands and schoolgoing
children and other family members first, and they
eat whatever is left over.
«
the withholding of foods in an attempt
to take care of diarrhoea.
Energy—Protein deficiencies are
always
accompanied by a lack of minerals and Vitamins
and result in a poor state of health and increased
susceptibility to infection. Simple remedy to
these problems is that the preschool children
should be given more of Energy and Body Build
ing Foods. Vitamin ‘A’ deficiency is frequently
associated with Energy—Protein malnutrition and
is another result of a generally poor diet. The
most serious effect of the lack of Vitamin ‘A’ is
the damage done to the eyes. Night blindness,
the inability to see in dimlight, is an early indica
tion of Vitamin ‘A’ deficiency. A diet lacking
in green leafy vagetables can cause this deficiency.
Therefore, a simple advice on eating more of
greenleafy vegetables daily should be one of the
first attempts in the primary health care
programme.
A diet lacking in dark green leafy vegetables
and other foods rich in iron can cause 'Anaemia'
or make it worse. In children anaemia can come
from not eating foods rich in iron. Therefore, a
diet with dark green leafy vegetables, is the first
step in preventing anaemia.
Acid indigestion and ‘Heart Burn’ often
come from eating too much heavy or greasy food
or from drinking loo much alcohol. Constipation
The primary
deficiency in
children is is often caused by a poor diet, especially, not
“Chronic Starvation”. The term “Marasmus” eating enough fruits, green vegetables or fruits
l^^been widely accepted to describe the energy with natural fibre, or by lack of exercise. Drinking
malnutrition and “Kwashiorkor” to describe more water and eating more fruits and foods with
protein malnutrition. The problems of Marasmus natural fibre like roots and tubers and greens is
and Kwashiorkor start when breast milk becomes better than using laxatives. A goitre is a swelling
insufficient and the baby is offered all kinds of or large mass on the throat that results from
diluted milk due to poor socioeconomic conditions abnormal growth of a gland called the thyroid.
and lack of knowledge of the infant's nutritional Most goiters are caused by lack of iodine in the
requirements.
diet. Also, lack of iodine in a pregnant women’s
diet sometimes causes babies to die, to be born
There are several factors which contribute mentally low and/or deaf. A simple treatment
significantly to ENERGYPROTEIN Malnutrition,
for goitre is use of iodized salt.
which include:—
Most children die from diarrhoea because they
1.
Prolonged nursing at the breast and the do not have enough water in their bodies. With
late introduction of supplementary foods.
good hygiene and good food, most diarrhoea could
be prevented. Headaches that keep coming back
2.
Inappropriate choice of weaning foods.
may be a sign of chronic illness or poor nutrition.
3.
Unhygienic feeding habits which pre Colds and flue are common virus infection that
dispose a child to diarrhoea.
does not need any medicine. Getting enough
4.
The practice of drastic medication and sleep and eating well helps prevents colds.
NUTRITION AND PRIMARY HEALTH CARE
Beri-Beri is common among people whose
nourishment is obtained from highly milled rice.
It is unfortunate, but true, that the introduction
of small rice mills in villages has led to an increas
ing incidence of beri-beri among farming com
munities.
When money is limited it is important to use
it wisely. Men in the rural areas spend often on
alcohol and women buy sweets and other unhygenically prepared foods rather than buying or
preparing nutritious food. Many mothers believe
that some kinds of foods are hot [and others are
cold. Traditional beliefs in food habits are pre
valent among a large majority of the population
who are illiterate and ignorant regarding the
nutritive value of foods. These beliefs profoundly
influence foods eaten.
Health Facilities :
In India 80% of medical professionals have
settled in cities to give medical care to only 19%
of the country’s population. Two-Thirds of the
deaths in developing countries are not attended to
by any medical presonnel and more than half of
the world’s people have no access to medical care.
Generally most of the people who need health
services are neither identified by health personnel
nor do they voluntarily utilise the available
services. Thus the utilisation of health services is
poor in many developing countries. The medical
need is/does/usually not present a complex pro
blem. As discussed earlier many of the recognised
treats to health like diarrhoea, respiratory tract
infections, malnutrition and infections are pre
ventable. Management and prevention of many
of these ailments do not need the services of a
highly qualified doctor.
A Package Program in Primary Health care
through Community Participation :
It is generally agreed that the problem of mal
nutrition can only be solved by educating rural
communities to effectively utilise inexpensive
locally available foods within their economic reach.
Any education in the field of health and nutrition
should be practical and adapted to suit the socio
economic conditions, food habits and local food
resources. For a satisfactory improvement in the
overall health status of preschool children, we
need to have a package program which includes
safe drinking water, environmental sanitation and
control of infection along with proper nurtrition.
Considering the fact that 40% of the total
deaths occur in the firist six years of life and that
80% of such deaths are due to preventable illness
related to malnutrition, the Government, the
International and other Private Welfare Agencies
have initiated supplementary feeding programs in
order to improve the nutritional status of vulner
able groups.
These programs usually have the two-fold pur
pose of teaching better practices in the home
production of highly nutritive foods and their use
and providing some food for children of school
going age and for preschool children and expecting
and lactating mothers. In this connection the
supplementary programmes sponsored by Catholic
Relief Services of United States Catholic Con
ference in India deserve special mention here.
Recognising that education in nutrition is vital for
the success of efforts to improve the health and
well-being of mothers and children, CRS assisted
Maternal and Child Health (MCH) Programmes
to serve as the nucleus for nutrition and health
education in the field of primary health care. The
untrained in India represent a potentially produc
tive and. greatly wasted resource. Through the
MCH Programmes Catholic Relief Services at
tempts to stimulate a desire among the illiterate,
especially, rural mothers to obtain at least a
functional literacy which is related to their health
food habits and environment and which can be
demonstrated to them to be of practical. In view
of the current high toddler mortality rate and in
view of the well known long term implications of
early childhood malnutrition, CRS has recently
launched a nation-wide Nutrition Education Pro
ject in 400 selected MCH Centres. The main
objective of this project is to equip the selected
centres with trained personnel in the field of
.primary health care and nutrition and involve the
local community in the implementation of the
project at the grass roots level. The project is
designed in such a way that it can carry out the
following activities with the support of the existing
Maternal and Child Health centres located in the
selected areas.
(a) Train project personnel
(b) Train local women leaders
(c)
(d)
Education of mothers
Preventive, curative health care
(e)
Provision of nourishing food.
NUTRITION AND PRIMARY HEALTH CARE
The nutrition and health education training
given in the training course will help the local
mothers to appreciate the role of well balanced
and at the same time inexpensive diets in promot
ing food growths and maintaining good health of
infants, children and expectant and nursing
mothers.
The experiences gained over the past years in
executing the Maternal and Child Health Pro
grammes have led to the making of following
recommendations.
.
1.
The participation of the community is
essential for the success of any health
program. It should be considered their
programme rather than anything that a
particular agency or the Government is
doing for them.
2.
The community should be stimulated to
persuade the local dais to recieve the train
ing in scientific methods of antenatal and
confinement care. The large number of
dais available in the villages should be
better equipped for their skilful job.
3. It is absolutely necessary to form village
health committees with whose cooperation
and acceptance the community health
worker is initiated into action and sup
ported in his day-to-day activities and also
watched. A system of cooperative health
insurance or at least a monthly subs
cription from each family can be organised
by the village committee for the mainte
nance of primary health care for the com
munity.
Nutrition and Health Education is a process to
renew and update women and to provide the
necessary insight into today’s health problems for
speedier progress. Like all education, Nutrition
and Health Education is a very slow process but
hopefully it may contribute to a renewal and
regeneration of women/family and society in the
decades to come.
No. 513—International Electric Plaster Saw
The International Electric Plaster Saw is an instrument
which saves valuable minutes in the removal of surgical
plaster. Voltage 220 to 230 for use on AC and DC both.
The circular non rotating blade is arranged to oscillate
through a very small arc, with a balanced high speed
vibration which leaves the instrument poised and steady
in an operator's hand, whether cutting or not whilst
cutting is active against a hard or rigid substance such
as plaster casts including the newer, tougher plastic
kinds, the rapid short stroke movement will not cut
mobile skin or soft tissue under light momentary contact.
Each instrument is supplied with two stainless steel
blades of 1J-" and 2|" diameter which are quickly inter
charged by means of a single screw. This instrument
comes complete in a fitted case.
WE ALSO MANUFACTURE :
Electric Bone Saw (Oscillatory & Rotary Model), Hin^
Prosthesis, S. P. Nails, Sherman Bone Screws, Boni^F
Plates, Kuntscher Nails, Rush Nails, Splints, Watson
Jones Orthopaedic Tables, Harrington Spinal Instru
ments, Balkan Frames, Pneumatic Tourniquets, Artificial
Limbs, Enquiries Appreciated.
International Surgical Works
8-B/U.A. 3, Kartar Niwas,
Jawahar Nagar, Sabzimandi, Delhi-7
Telegrams : "Orthopedic"
Phones : Office 220939, Residence : 220094
[Sole agents for Zimmer (U. K.) and Chr. Diener of
West Germany]
Importers of Pace Makers.
aua
1
t<O4_\
-it\
^c^Lcfubo,
TCe.
fe-Z7 /~-29~/
<^*nz51v<i3,
rvuT 3.16
— 1j!L ' -— Lj C| 2,?,cp
}<
£ fZ y
^n'<sJz' .—pl
r~)
/\Jm_1v.-C'C<xa
('7
3c^X&'
/^=^oJ^-^C<C57<Cc \ — J2tf .3<?-<ctc,4- Z r^rt'
cJ>'
o-cve. <'"
if)
-
rntli^
rk5^oad
-. VJVarU
CO^voorVf^oOO'
- Kl-jo-C L\ ©.- A7<3-V0Cix_lvc-- &A*a£(l\CL>J7-f\,
3
Objectives for the student. To achieve the personal and
professional objectives the student should strive toward the
following behavioral changes.
1. Shows the proper attitude and convictions relative
to the importance of nutrition in regulating one’s own health,
that of the family, and that of individuals of the community.
2. Knows the kinds of health problems arising from
poor nutrition that exist in his own community, the nation,
and throughout the world.
3. Demonstrates knowledge concerning the science
of nutrition:
a. Functions, digestion, absorption, and metabolism
of proteins, fats, carbohydrates, minerals, and
vitamins.
b. The interrelationship of nutrients.
c. The nutritive requirements of individuals and
the variations that may be imposed by activity,
climate, stage of life cycle, and disease.
4. Appreciates and understands the meanings that
food has for people and how these are related to economic,
psychologic, and cultural factors.
5. Interprets the principles of nutrition in the
selection of an adequate diet:
a. By knowing the food sources of the nutrients.
b. By applying consumer information to the planning
of meals and the selection of food for quality
and economy.
6. Uses opportunities for improving nutrition
through the education of individuals.
7. Counsels people on an individual or group basis
by adapting nutrition information to specific health, socio
economic, and cultural needs.
8. Knows where to look for reliable sources of
information and how to evaluate publications on food and
nutrition and the claims made through product advertising.
9. Becomes familiar with agencies concerned with
nutrition and health in order to utilize their services and
contribute to their functioning.
SOURCE: FUNDAMENTALS. OF NORMAL NUTRITION
%2L
OJA^>
'/
'fit
^<sx2L-2<>_i
/(.a-^^prbc. eJL^h ?CH
,
S’—XXA
/4o©-J Q.
OCM_xlA,tu.c
COMMUNITY HEALTH CELL
^7/1,(First FloorjSt. Marks Road
BANGALORE-560 001
PROPHYLAXIS
AGAINST NUTRITIONAL ANAEMIA
AMONG
MOTHERS AND CHILDREN
FAMILY PLANNING PROGRAMME
FOURTH FIVE YEAR PLAN
MATERNAL AND
CHILD HEALTH
Technical Information : MCH No. I
MATERNAL AND CHILD HEALTH
THE CONCERN OF FAMILY PLANNING PROGRAMME
The family planning programme is vitally concerned with promoting the health of
mothers and children. As it advises the couples to limit the size of their family to 2 or 3
children so it takes measures to promote the health of those few children. With this end in
view FP programme has provided funds for schemes for prevention of diseases and promotion
of health among mothers and children. One of them is a scheme for prophylaxis against
nutritional anaemia among mothers and children.
1.
NUTRITIONAL ANAEMIA AMONG MOTHERS AND CHILDREN —
WIDELY PREVALENT
Anaemia is considered to be a major public health problem affecting women of child
bearing age and children in the country. Several research investigations carried out during the
recent past under the auspices of the Indian Council of Medical Research have highlighted the
problem. Nearly 60 per cent of 700 children over six months of age surveyed by the National
Institute of Nutrition, Hyderabad, showed anaemia of some severity. Similarly, incidence 'of
anaemia among women of child-bearing age was found to be 10 per cent, while nearly 50 per
cent of pregnant women showed some degree of anaemia. It has also been reported that
anaemic women have more complaints of vaginal bleeding after insertion of 1UCD.
2.
MATERNAL MORBIDITY AND MORTALITY
Anaemia is reported to be an important cause of maternal mortality; approximately
10 per cent of all maternal deaths are directly due to anaemia. Apart from direct contribution
to maternal death, anaemia aggravates other complications and diseases incidental to pregnancy.
The contribution of anaemia to maternal deaths due to other causes and to maternal morbidity
in general is therefore considerable. Although, it is difficult to give a precise estimate of the
morbidity attributable to nutritional anaemia, broadly speaking, it is known that puerperal
morbidity is 3-4 times greater in patients with Hb levels less than 6-5 g per cent. Genito-urinary
infections are frequent complications of anaemia. Apart from this, when pre-eclampsia, ecla
mpsia, ante-partum haemorrhage, obstructed or difficult labour occurs in an anaemic mother,
the mortality and morbidity due to these complications are further enhanced.
3.
PREMATURE BIRTHS AND PERINATAL MORTALITY
Maternal anaemia also affects the intra-uterine growth of the foetus. In one study,
the average birth-weight of infants born at term in normal pregnancy of a series of 1,000
mothers with Hb levels of not less than 10.5 g per cent was 2.8 kg whereas in mothers with less
than 6.5 g per cent of Hb, the average birth-weight at term was only 2.4 kg. Since 70 per cent of
deaths in the perinatal period occur in infants weighing less than 2.5 kg at birth, the role of
maternal anaemia in perinatal mortality and premature birth is very significant.
4.
CAUSATIVE FACTOR MAINLY NUTRITIONAL
There is considerable evidence on the basis of haemotological studies, biochemical
estimations, therapeutic and prophylactic trials, that iron deficiency is widespread in our
community and the primary causative factor in the great majority of cases of nutritional
anaemia. For example, one study has shown that nearly 95 per cent of all pregnant women
have biochemical evidence of iron deficiency. There are also other studies showing the virtual
absence of any significant iron stores in the Indian population.
There is evidence to suggest that folic acid deficiency also makes a significant contri
bution to the development of nutritional anaemia in pregnancy.
It should be emphasised that anaemia is a late manifestation of nutritional deficiency
Normal persons have reserves of iron, vitamin 'B' and folic acid which they can draw upon in
time of deprivation or physiological stress such as pregnancy and rapid growth. When the
intake of nutrients is inadequate to meet the daily requirements these stores are gradually used
up. Biochemical abnormalities begin to appear even before there is detectable anaemia. 7 he
incidence of anaemia in a community is, therefore, a gross underestimate of the true magnitude
of the problem of nutritional-deficiency. Hence, the importance of prophylactic measures like
routine supplementation with iron and folic acid to prevent the development of overt
anaemia.
2
PLAN OF OPERATION
1.
PROCUREMENT AND SUPPLY OF DRUGS
A provision of Rs. 200 lakhs has been made in the Central sector for the programme.
The drugs are procured by the Department of Family Planning and distributed to the States and
Union Territories on the basis of annual plans. The cost of the drugs thus supplied will be
adjusted as grants to the State Governments/Union Territories. The State FP Officer should
place indents on the Government Medical Stores Depots, Bombay, who would send the supp
lies to the officers at the district level who are responsible for administering the programme.
2.
BENEFICIARIES
Expectant and nursing mothers/acceptors of FP methods, like 1UCD, salpingectomy and
preschool-age children would receive the benefit of the scheme. Before enrolling them on the
prophylaxis programme an estimate of the level of Hb should be done preferably by Sahlis’
method. In situations like rural subcentres where this may not be possible at least an esti
mation by a Talqvest Hb Scale should be done. Women showing a Hb level less than 10g per
cent and preschool-age children showing Hb level less than 8g per cent should be put on active
anti-anaemic treatment straightway. Those women having a Hb level of 10g and above and chil
dren showing Hb level of 8g and above can be put on the prophylaxis programme. All insti
tutions rendering family planning and MCH services like PH centres and their sub-centres,
maternity and children hospitals, maternity homes, urban FWP centres should implement the
programme.
%
3.
DOSAGE
The daily recommended dosage is one tablet containing 0.1 mg folic acid with 60 mg of
ferrous sulphate for children. Pregnant and nursing mothers and family planning acceptors
should receive daily one tablet containing 0.5 mg of folic acid with 180 mg of ferrous sulphate.
The daily administration of the tablets should be continued till the level of Hb attains and is
maintained at a satisfactory level. It is necessary that the estimation of Hb is repeated at 3-4
month intervals. It is estimated that on an average each beneficiary may require adminis
tration of the tablets for a period of six months. The exact period will depend on the pro
gress of the individual beneficiary.
For the sake of convenience the drugs may be issued for a fortnight or for a month at
a time. The auxiliary nurse midwife/Iady health visitor/FP health assistant should check on
the actual use of the tablets by the mothers and children during their routine home visits.
Supply of Drugs
The tablets are supplied in two types and two packings, (i) orange coloured small
tablet containing 0.1 mg folic acid with 60 mg of ferrous sulphate packed in tins of 1,000 tablets
and 5,000 tablets, (ii) a larger grey coloured tablet containing 0.5 mg folic acid with 180 mg
ferrous sulphate also packed in tins of 1,000 and 5,000 tablets. The tablets are sugar coated
and therefore are to be preserved in a dry cool place to avoid absorption of moisture. Folic
acid has a comparatively short shelf-life and care should be taken to use the tablets before the
date of expiry indicated on the tins.
4.
RECORDS
The regular records prescribed by the Health Department—the antenatal card,
the child health card, the follow-up card prescribed for IUCD and sterilisation, should
be maintained in respect of beneficiaries under the programme. These cards should show
records of Hb estimation of the quantity of drugs issued to them. Registers showing the
particulars of beneficiaries and the stock position of iron and folic acid tablets should also be
maintained as per proforma given at Appendix-I.
5.
REPORTS
Monthly reports on the number of beneficiaries and the stock position of the drues
should be sent to their supervising authority from the individual institutions. Consolidated
monthly reports should be sent by the State FP Officer so as to reach the Department of Family
Planning by the 15th of the succeeding month as per the proforma at Appendix-!I,
APPENDIX-I
(A)
REGISTER OF BENEFICIARIES UNDER THE NUTRITIONAL
ANAEMIA PROPHYLAXIS PROGRAMME
of
SI. Card Date
No. No. enrol
ment
(1)
(2)
(3)
(B)
Name
Age
(4)
(5)
CATEGORY
Date of
remo
Mother Child Contraval
ceptor
(7)
(6)
(8)
(9)
Remarks
Initials
(10)
(H)
STOCK REGISTER OF IRON AND FOLIC ACID TABLETS
Date
Receipt
Issue
Balance
Initials
(1)
(2)
(3)
(4)
(5)
5
APPENDIX II
PROPHYLAXIS AGAINST NUTRITIONAL ANAEMIA AMONG MOTHERS
AND CHILDREN
Report for the month ending
197
for the State of
________________ (A) STATEMENT OF BENEFICIARIES______________________
SI.
No.
No. of
No. of
No. of
cases
No. on
cases
cases
Progressive
1st day of enrolled dropped remaining
total for the
at
the month during the during the ofthetheend
year
month
month
month
Category
of
beneficiaries
(3)
(2)
(1)
1.
Mothers
2.
FP Cases
IUCD
Tubectomy
Others
(4)
(5)
(6)
(1)
Remarks
(8)
3. Children (under
6 years of age)
4. Total
(B) POSITION OF RECEIPT AND ISSUE OF THE DRUG
Opening balance
on the first day
of the month
Receipts during
the month
Iss ues during
the month
On hand on the
last day of the
month
Remarks
(1)
(2)
(3)
(4)
(5)
Place.............. Date.................
Signature.............. Designation
COMMON., Y ,,.ALTH C .J,
47/1,(First FloorlSt. Marks ,„,,s
BA&GAlOHE - 560 001
Reprinted from “The Bombay Hospital Journal” Vol. 12, No. 4, October, 1970 pp. 32-35
TREATMENT OF IRON DEFICIENCY ANAEMIA IN GYNAECO
LOGICAL & OBSTETRICAL PATIENTS BY FERRUM
HAUSMANN INTRAMUSCULAR
V. N. Shirodkar, M.D., F.R.C.S., F.R.C.O.G.
*
D. M. Amonkar, M.D., F.R.C.S.,
**
S. L. Shanbhag, M.B.B.S., D.G.O.,\
P. G. Samdani, M.D., D.C.H.l
'T'HE study aims at treatment of anaemia
with a parenteral iron preparation,
Ferrum Hausmann. Each ml. of its solution
contains 50 mg. elemental iron in complex
form (iron polymaltosc in aqueous solution).
The study was carried out on 36 patients of
which 22 cases were treated with intra
venous (l.V.) total dose infusion while the
remaining 14 cases were treated with intra
muscular (I.M.) doses.
In 1963 S. K. Basu, in England, des
cribed the technique of correcting iron
deficiency anaemia by giving the required
amount of iron as a single dose of iron
dextran complex after diluting it with 5
per cent dextrose intravenously.
Since
then this technique is being used more and
more all over the world.
Stools and urine were examined routinely.
Haemoglobin estimation was repeated weekly
and finally at the end of 3 weeks. In a few
patients the haemoglobin was estimated at
the end of 2 months also. Reticulocyte
count was done before starting the therapy
and on the 4th day thereafter.
If the total amount of drug required was
less than 24 ml., 2 ml. was dissolved in a
bottle containing 540 ml. of 5 per cent dext
rose solution. Intravenous infusion was run
at the rate of 40-50 drops per minute for 10
minutes and the rate was reduced then
to 10 drops per minute for 5 minutes and the
patient was watched. If no untoward re
action occurred, the rest of the Ferrum
Hausmann solution was added to the
drip and the rate of infusion increased
gradually to 40-50 drops per minute. The
Material and Method
amount in excess of 24 ml. was added in a
The present study was conducted at St. separate bottle and the drip was continued.
George’s Hospital, Bombay. Patients who This was a necessary precaution to avoid
reaction.
had haemoglobin levels below 9.5 G. per
cent were selected for the study. Age of
In the initial stages of the study, antazoline
the patients in the above study varied 25 mg. was added to the drip, but later on it
between 19 to 40 years. Sixteen patients out was given intramuscularly before infusion
of 36 were gynaecological while 20 cases were was started.
obstetrical of which one case was in recent
Intramuscular injections were given as
puerperium. Two patients were nulliparous, 5 patients primigravidae, 10 between 2 ml. daily by the Z technique.
2nd and 4th gravidae and the remaining 19
Observations
were 5th or more gravidae.
The incidence of anaemia in the different
Before starting iron therapy by l.V. or
I.M. route, all the patients were thoroughly age groups is tabulated below :
examined. The following investigations were Age
No. Percentage
carried out in all the patients in fasting
state, (a) Haemoglobin estimation and R. Between 12-20 years
..
1
2.77
B.C. count (6) Serum Iron (c) Reticulocyte 21-30 years
.. 25
69.25
count (rf) P.C.V. and (e) Serum Proteins. 31-40 years
.. 10
27.7
* Hon. Prof, of Gynaecology and Obstetrics, St. George’s Hospital and Hon. Gynaecologist and Obstetri
cian, Bombay Hospital.
•* Hon. Gynaecologist and Obstetrician, St. George’s Hospital, Bombay.
t Ex. Gyncc. Registrar of St. George’s Hospital, Bombay.
t Ex. Pediatric Registrar, St. George’s Hospital, Bombay.
F’H
F. X. SHIRODKAR, D. M. AMONKAR, S. L. SHANBHAG & P. G. SAMDAM
The average value of the reticulocyte in
The incidence of anaemia was maximum
the beginning of therapy and on 4th day
in 2nd and 3rd decades.
Parity: Anaemia increased with parity was 1.9 per cent and 4.9 per cent res
pectively.
as seen in the following table :
Parity
No. of Cases
Intramuscular Group
Nulliparous
..
2
Hb.
Serum Iron
Primigravidae
..
5
2nd — 4thgravidae
..
10
74 ugm.%
8.2 gm%
Before therapy
5th and above gravidae ..
19
—
9.3gm.%
Duration of Pregnancy: Incidence of anae 1st week
115 ugm.%
11.3 gm.%
mia in relation to duration of pregnancy is 3rd week
55%
37.7%
Percent rise
tabulated below :
Trimester
No. of Cases Percentage
The reticulocyte count in the intra
—
muscular group in the beginning of therapy
1st
and on the 4th day was .9 per cent and 4.5
35
7
2nd
per cent respectively.
65
13
3rd
Anaemia is more evident in the 3rd tri
From the above tables it is evident that in
mester because average foetal requirement of cases treated with intravenous iron, the rise
iron is around 375 mg.
in the haemoglobin level is 18 per cent per
Aetiology : The commonest cause of anae week and the serum iron rise is 86.9 per cent
mia was pregnancy in 30 cases, parasitic after 3 weeks. In cases treated with intra
infestation in 14 cases, menorrhagia in 9 muscular iron the haemoglobin rise was
cases, retained products after abortion or 12.5 per cent per week. The serum iron
normal delivery in 3 cases, cancer in 2 cases was raised by 55 per cent after 3 weeks.
and unknown cause in 2 cases. The com This lower rise in the intramuscular group
monest parasitic infestation found was hook may be due to the fact that these cases had
worms and round worms. In 2 patients E. higher initial haemoglobin levels than those
hystolytica and E. coli were found.
in the intravenous group. The initial hae
Laboratory Findings: The main values of moglobin level of the patients taken for
haemoglobin and serum iron, before and intravenous therapy varied from 2 gms.
after 3 weeks of therapy in the intravenous per cent —9 gms. per cent while in the
and intramuscular group is shown in the series of cases treated with intramuscular
therapy it varied from 6 gm. per cent to
following table :
9 gm. per cent.
Intravenous Group
The initial mean haemoglobin, reticulocyte
Hb.
Serum Iron
count,
serum iron, final haemoglobin, reti
6.9 gm.%
Before therapy
51.9 ugm.%
—
culocyte count and serum iron in both
8.1 gm.%
1st week
10.7 gm.%
97 ugm. %
3rd week
intravenous and intramuscular group is
55%
86.9%
Percent rise
tabulated below along with percentage rises:
Intravenous Group
—
Range of
Haemoglobin
Initial
Hb.
Hb. after
3 weeks
Reticulocyte
Scrum Iron
Before
After
Before
8.2°/. “
.(241%)
increased
4.6%
. «42%)
increased
3.9%
. (387%)
increased
31.1ugm%
2-6gm%
4.7gm%
9.4gm%
(100%)
2.4%
6.1-8gm%
7.6gm%
11.2gm%
(47.3%)
1.9%
8.1-10gm%
9gm%
11.5gm%
(27.7%)
•8%
3 weeks
later
98.4ugm%
(216%)
60.2ugm%
91.5
(52.6%)
64.4ugm%
103 ugm%
(61%)
TREATMENT — GYNAECOLOGICAL & OBSTETRICAL PATIENTS
Intramuscular Group
Reticulocyte
Haemoglobin
Range
Serum Iron
Before
After
Before
After
Before
After 3
weeks.
6-8gm%
7gm%
10.5gm%
(50%)
■95%
66.3ugm%
121.3ugm%
(82.9%)
«.l-9gm%
8.9gm%
11.8gm%
(32.4%)
• 87%
6.3%
(563.1%)
increased
4.1%
(371.3%)
increased
80ugm%
110ugm%
(37.3%)
The analysis shows that the higher the
initial haemoglobin the lower was the
percentage rise in haemoglobin. The patient
having initial haemoglobin between 2 gm. —
6 gm. per cent showed a rise of 100 per cent
after 3 weeks, while those having initial
haemoglobin between 8.1 gm.— 10gm. per
cent showed a rise of 27.7 per cent only.
The rise of the haemoglobin level in cases
treated with intramuscular iron was nearly
the same as in those treated with intra
venous iron and with identical initial hae
moglobin level. The overall weekly rise of
haemoglobin in the intravenous group was
1.26 gm. per cent while in the intramuscular
group it was 0.99 gm. per cent.
Side Effects
The side effects observed during the
therapy are tabulated below :
Intravenous Group
Nature of side effects
Immediate
Irregular
pulse, sweating,
palpitations.
After 2-8 hrs. :— Puffiness
of face, palpitation,
rigors, ringing in ears.
After 24 hrs. :— Mild
loint pains and mild
fever.
No. of
cases
Percentage
1
4.5
1
4.5
5
22.5
Seven out of 22 patients treated with
intravenous iron had reactions. Two cases
out of 7 had reactions of significance whereas
5 patients had mild joint pains and fever after
24 hours. Thus 9 per cent had immediate
reactions and 22.5 percent had reactions
after 24 hours. In one case where imme
diate reaction occurred, the reason could
not be ascertained and the drip was dis
continued. The patient was comfortable
after an antihistamine and hydrocortisone
injection. The same patient was later treated
by the intramuscular route without any
reaction, which suggests that it could have
been a pyrogen reaction. The second patient
who developed puffiness of the face, ringing
of ears and palpitation after 3 hours when
almost half the solution had been admini
stered, had an initial haemoglobin level
of only 1.5 gm. The drip was dis
continued and the patient was given packed
cell transfusion. When the haemoglobin
level came to 6 gm. the drug was given by
intramuscular injection. This patient was
pregnant, the duration being 34 weeks.
None of the Cases treated with intra
muscular iron showed any reactions at all.
A slight brownish discolouration was seen in
a few cases which decreased after 3 weeks
of therapy.
Discussion
The main aim of the present study was to
know the effects and efficacy of intravenous
iron polymaltose therapy and compare it
with intramuscular therapy. The analysis
of the results shows that total dose infusion
increases the haemoglobin in all patients
suffering from iron deficiency anaemia and
the increase was 1.26 gm per cent per week.
In the intramuscular group with similar
haemoglobin levels the rise was nearly
the same.
A 2 months follow-up could not be done
in all the cases because the patients did
not report after 2 months. However, 10
cases out of 22 who were treated by the
intramuscular route showed haemoglobin
rise to about 12 gm. per cent showing
thereby that the maximum rise in haemo
I’. .V. SHIRODKAR, D. M. AMOMCAR, S. L. SHAb'BHAG & P. G. SAMDAJW
globin can be expected after 2 months and
the treatment should be started earlier in
antenatal care.
In hospital practice intravenous therapy
should be favoured because the antenatal
attendance of these patients is very poor
and irregular. Hence the anaemia cannot
be treated on O.P.D. basis by intramuscular
iron. This method of intravenous therapy
would prevent many complications at the
time of labour in severe anaemic patients.
Admission of the patient for anaemia and
treatment with intramuscular iron will in
crease the cost to the hospital, reduce the
number of beds for serious patients and
cause inconvenience to the family. As against
this, in the intravenous therapy, the treat
ment can be completed in a day or two
with definite predictable and faster results
at less cost.
Bonnar (1965) noted a weekly rise of
1.14 gm per cent of haemoglobin in pre
gnant women with an average of 0.16 gm.
per cent of haemoglobin with iron-dextran.
Basu claimed a daily rise of haemoglobin by
1.3 per cent with iron dextran. Motz et al
(1967) observed a rise of .68 per cent per
week in their study of 6 weeks by total
dose infusion of iron dextran complex.
Mehta et al (1968) showed a rise of 2.14 gm.
per cent per week in the first 2 weeks in
gynaec and obstetric patients by iron
dextran total dose infusion.
In our study side effects occurred in 32
per cent out of which 9 per cent had imme
diate and severe reactions of significance
which necessitated withdrawal of the treat
ment. The remaining 23 per cent had very
1.
2.
3.
4.
mild reactions which did not require any
additional specific treatment.
Mehta et al showed systemic reactions in
48.3 per cent of the cases treated by total
dose infusion therapy with iron dextran.
Kamath and Pai noted reactions in 62.69
per cent of the cases by intravenous total
dose iron dextran therapy. Bhat et al
observed systemic reactions in only 16 per
cent of the cases by intravenous iron dextran
therapy.
Conclusion
Total dose infusion therapy with Ferrum
Hausmann intramuscular was found to be
very effective, the average rise of haemo
globin being 1.26 gm. per cent per week.
Side effects were noticed in 32 per cent of
the cases. Of these, in 9 per cent they
were so severe that the treatment by intra
venous route had to be discontinued. The
remaining 23 per cent had mild reactions
which did ript require any special treatment.
Injection of antazoline given before insti
tution of infusion is preferable as a pro
phylaxes. The concentration of the drug in
infusion therapy should preferably be kept
below 5 per cent. Thus intravenous therapy
can be routinely adopted in hospital prac
tice and is quite safe, economical and
effective method of treatment.
In this series, Ferrum Hausmann intra
muscular in total dose infusion therapy
caused fewer bye-effects than reported by
other workers with iron dextran. No side
effects were observed when Ferrum Haus
mann was administered intramuscularly.
REFERENCES
Basu, S. K„ Lancet, 1963, 1, 1430.
Total Dose, diluted and undiluted — National
Conference on Iron Deficiency Anaemia, 1968.
Bonnar, J., Brit. Med. J., 1965, 2, 1030.
Mehta, B. C., Jheweri Kusum and Patel J. C. :
Bhatt. R. V., Joshi S. K., and Patel M. R. :
Total Dose Iron Therapy — National Con
Intravenous use of Iron-Dextran — Five Year
ference on Iron Deficiency Anaemia, 1968.
experience — National Conference of Iron
Deficiency Anaemia, 1968.
Seetamma, J. : Total Dose infusion in Gynae
cological conditions — National Conference on
Kamal, G. R. and Pai, J. R. — Intravenous
Iron Deficiency Anaemia, 1968.
Iron — Dextran in Iron Deficiency Anaemia —
VOLUNTARY
C-K,
HEALTH
Ccrnmunlty Centre, Sirfdarjung
Phone : 652007, 652008
ASSOCIATION
OF INDIA
Development Area,
New Delhi-110016
Telegrams : VOLHEALTH New Delhi-110016
COMMUNITY 'H-ALiH CU.L
47/l,(FirstFloor)St. Marks a°ad
EAtjGAl.03E - 560 001
M-7
ANAEMIA IN PREGNANCY
Anaeinia in pregnancy is a major public health problem in develop
ing countries. While anaemia is directly responsible for 20$ of
maternal deaths, in another 20$ it is a contributing factor.
(Menon, M.K.K. 1967). Besides it is also responsible for the high
incidence of premature and low weight births, thus increasing the
prenatal mortality and morbidity. Studies carried out at the
National Institute of Nutrition, Hyderabad are hij^ilighted below:
Haanoglobin. Surveys:
Hasnoglobin surveys carried out in different parts of the country
indicate that while 15-20$ of women are anaemic at the onset of
pregnancy, the incidence of anaemia (Hb. levels less than 11g$)
increases to 60-70$ in the last trimester. A survey of 1$ 10 women
attending Nlloufer Hospital, Hyderabad indicated that incidence of
anaemia was closely related to parity (Table 1).
The incidence seen in the hospital may in. fact be an underestimate,
since the hospital patients come from a mixed socio-economic group.
In rural population, the incidence of anaemia may be of a much
higher order due to associated infestations and infections.
Etiology;
■Anaemia of pregnancy seen in our population is mainly due to iron
deficiency. However, associated folic acid and B12 deficiencies
also exist.
1. Dietary factors.
The average Indian diet would appear to be adeauate in iron con
tent (20-22ng) for a non-pregnant adult woman. However, various
factors inhibit iron absorption of which phytate is most important
while an absorption of 10$ is essential to meet the iron require
ment of a normal adult. Studies using whole body counter-indicate
that only 3-5$ of dietary iron is absorbed in an apparently normal
healthy individual. The diet is difficient in protein, calcium
and vitamin C. The diet is also deficient in other haemopoietic
factors like folic acid and B12.
The iron needed during pregnancy is of the order of 4-6 mgs of
absorbed iron daily, which cannot be made available through
dietary sources. Since most women do not receive any supplements
during pregnancy, iron deficiency is a common feature.
2. Iron stores and Iron loss.
Most of the population in Asian Countries have very poor iron
stores as indicated by poor bone marrow haemosiderin and low
levels of liver iron. Besides, iron losses through menstruation,
to the extend of l5-3Ctag every cycle, increases the iron require
ment of adult women. Most women enter their first pregnancy with
very little iron reserve.
page 2
3,
Demands of Pregiancy
The net iron loss during pregnancy in Indian wmen is aroun
d
*
350 mg. To meet this additional demand, a -woman needs to absorb
3 mg of additional iron daily. Besides the increased demands
2durirg pregnancy, demands during lactation contribute to reduce
iron stores and worsen the deficiency status. Since many women
have repeated, elosely spaced pregnancies with prolonged periods
of lactation, there is progressive depletion of iron stores with
increasir^ number of pregnancies. This results in high incidence
of anaemia in women with -hi^j-er parities^
4.
Infections and Infestations.
Repeated and chronic infections prevent the utilization of iron
and are additional contributory factors in causing anaemia.
Hookworm infection in some- areas aggregates the situation by
increasing iron loss.
Absorption Studies
Iron absorption
Studies carried out on food iron absorption at the National Inst
itute of Nutrition have indicated that during pregnancy, iron
absorption from food increased from an average of 10% in the
first trimester to 25-30% at term. In addition, iron absorption
was of a much greater order in women in whom the transferrin
saturation was less than 15%. On the basis of these data, iron
requirement during pregnancy has been computed to be around 40 mg
per day. However, the requirement is greater in women who have
very poor iron stores and low haemoglobin levels at the onset of
pregnancy.
Folic acid absorption
There is considerable controversy regarding absorption of folic
acid in pregnancy. It is believed that folic acid deficiency
seen in pregnancy is mainly due to impaired folic absorption and
partly due to increased renal clearance of folate. Transfer of
folate across the placenta to the foetus is also considered as
an additional cause.
Studies carried out on folic acid absorption using tritiated
folic acid in women undergoing therapeutic termination of pre
gnancy in the first and second trimester at the National Insti
tute of Nutrition have indicated that there is no impairment in
the absorption of crystallin folate diring the first and second
trimesters of pregnancy. However, whether this is true of food
folate needs to be investigated. These studies also suggest that
the folate status of the individual influenced the extent of
absorption but this observation needs confirmation.
Serum levels of iron, folic acid and B12.
In spite of normal haemoglobin levels, about 50% of pregnant
women have low levels of serum iron, it being less than 60ug/
10Ctnl in the last trimester. The percentage transferrin saturat
ion is also lew in these women.
page 3
Determination of serum folic acid and B12 levels have indicated
that in about 60% of women, serum folate levels were less than
3ng/ml indicating folate deficiency and that in 25% levels of •
serum B12 were below 100ng/ml in the last trimester.
In a small number of women with severe anaemia, where haemoglobin
levels were less than 8.5 gms, studies on bone marrow indicated
that in 60% of them there was megablastic erythropoiesis. Folate
levels in RBC in these women was below 80ng/ml. There was no
stainable iron in the bone marrow in any of the subjects.
These observations suggest that while in mild and moderate de
grees of anaemia in pregnancy iron deficiency was the major factor,
in the severe forms folate deficiency is clearly present.
Effect of Maternal Anaania on Foetus and Newborn
1. Foetal stores
I The^iron, folate and B12 stores in the levers of infants bom to
. metnors of low socio-economic group was studied. It was observed
' thfit iron stores were only 6o% of the reported figire from wes
tern countries. Similarly, liver stores of folic acid and B12
were far below the reported normal range for newborn in western
countries. The implication of such low stores of these nutrients
is obvious. An infant born with poor' stores of iron, fSlate and
B12 has greater risk of developing anaenia during very early in
fancy. Also, the high incidence of infections and infestations in
early infancy, tended to aggravate and hasten the onset of anaemia.
2. Infancy anaemia
In a recent study it was found that while at birth, haemoglobin
levels of infants bom to mothers
.. unsupplemented
with iron during pregnancy were si mil ar to those bom to iron
supplement mothers, at 3 and 6 months of age, the incidence of
anaemia (Hb. less than 11 gms%) was 45% in infants born to un
supplemented mothers as against 25% in those born to supplemented
mothers. This suggests that supplementation of iron during pre- .
gnancy not only benefited the mothers but also their infants.
3.
Birth weights
As indicated earlier, the incidence of prematurity and low birth
weight were much higher in infants bom to anaemic mothers.
While investigating the iron and folate requirements of pregiant
women, it was observed that infants born to mothers, given su
pplements of folic acid along with iron were heavier by 200 gns
compared to infants bom to mothers receiving iron supplements
alorua. Also the incidence of small-for-date births (weight less
than 2500 gns) was 17% and 37% in infants bom to folate supple
mented and unsupplemented mothers respectively. That such an
improvement in placental efficiency has been shown by increased
weights of placentae in folate supplemented mothers, which also
have a hi^ier DNA and protein content.
Treatment and Prevention of Anaemia
(1)
Blood transfusion
In cases of severe anaemia, during the lasrtrtmester of pregnancy, there is
wttkxxral^ pw^rul
iron. Iq/come tn’a state oTandxta ana cardiac tartare. In such cases, an ini
tial transfusion of packed cells or exchange transfusion needs to be given,
followed by supportive treatment to improve her nutritional status. With the
advent of packed cells or exchange transfusion, maternal mortality rate has
been brought down to a considerable extent.
<2> Parenteral iron therapy
In mild and moderate anaemia, in middle or early pregnancy, in ease
*
whereregularity of intake of oral iron cannot be ensured and in cases who have intolerance for all forms of iron, parenteral iron is the treatment of choice. How
*.
ever, parenteral iron does not have any greater benefit over the-oral iron-as
far as the rate of haemoglobin regeneration is concerned.
(3) Or lai Iron supplements:
Oral iron supplements are useful not only for therapeutic purposes but also for
the prevention of anaemia. Two studies conducted at National Institute of
X Nutrition, Hyderabad using 30 and 60 mgs of elemental iron given dally during
\ the last 12-16 weeks of gestation have indicated that both these levels can, not
\only maintain but also bring about-an increase in haemoglobin levels from the
presupplement levels in about 90-92% of women, tn 3-10% of the women,
haemoglobin levels were still below 11 gms%. Addition of 200-500 pgs of'folic .
ack to the iron supplement resulted in an improvement in RBC folate levels
in txxh the mother and the newborn, but had little of any additional beneficial
influence on haemoglobin levels. The same was true for added Bj2«
Howevbrk as indicated earlier, 200-500 pgs of folic acid was found-to have
beneficial effect on the birth weights of infants to the extent of 200-300 gms and
in reducing the incidense of small-for-date births. While 30-mgs of elemental iron
as supplement daily is adequate to prevent anaemia in pregnancy tn 90% of women,
it has been recommended by a study group in Nutritional anaemia that 60 mgs
of elemental iron with 590 pgs of folic acid should be given as a supplement
daily tn the last 12-16 weeks of pregnancy. This figure has been arrived at on
the basis of (a) the estimated additional needs for iron during pregnansy and
lactation, (b) the extremely poor iron stores, (c) the variability of the levels
of absorption of ingested iron, fld) possible irregularities in supply and intake
and (e) losses that may oegpr due to hookworm infestations.
Anaemia-^reventlon Programme
The Government of India has accepted an anaemia prevention programme and
the proposal hasxbeen included in the Fifth Five Year Plan. Tablets containing
iron and folic acicbare distributed to different MCH and family planning centres'
to cover at least 5^ef pregnant women in their last trimester of pregnancy.
Reference:
Menon, M^K.K, Proc. Soc. India. 2,1,1967.
:5 :
TABLE I
Incidence of anaemia in pregnancy
*(TotalNo. investigated - 1810)
Gestational Overall inciage (weeks) dence (Hb/ll.(Fg%)
7D.(Tg^“
. -Parity
t-td
“ '
aEbve
7rCTgr-7g-.Kg7020.0 (125)
2.0
/16
15.5 (265)
12.5 (140)
16-28
29.2 (974)
23.0(666)
2.2
32.5 (308)
6.0
28-40
41.0(571)
37.0 (371)
3.2
48.5 (200)
8.5
* Sample size
Reproduced from: ICMR Bulletin Vol. 5 No 11 November, 1975
For more copies write to:
Voluntary Health Association of India
C-14 Community Centre
Safflarjung Development Area
New Delhi 110 016
India
VOLUNTARY
C-14,
HEALTH
Community Centre, Safdarjung
Phone : 652007, 652008
ASSOCIATION
Development Area,
OF INDIA
New
Delhi-110016
Telegrams : VOLHEALTH New Delhi-110016
community iy:
alth cell
47/1, (First Floor) 3
t- Marks Road
BANGALORE- 560 001
NUTRITION _IN_ PRE®JANCY_ AND. LACTATION
It has long been recognised that pregnancy and lactation constitute
periods of physiological stress and that the requirements of most
nutri^Ttsr, Increase during these periods. From the nutritional
standpoint, therefore, pregnant and lactating women constitute volnerable segments of the population. During the last two decades
considerable amount of research work has been carried out under
the aegis of the Indian Council of Medical Research on the subject
of nutrition in pregnancy and lactation. Most of these studies have
been carried out at the National Institute of Nutrition, Hyderabad.
These studies have related to increase nutrient requirements, the
effects of maternal nutritional status on the course of pregnancy and
its outcome, and also the inter-relationship between maternal
nutritional status on the one hand and the nutritional status of the
offspring on the other. They have also related to the nutritional
status of nursing mothers and the composition of their breast-milk.
The results of some of these studies are reviewed here.
Ni^HM^^q^uj.rements_during pregT£ncy and_lactation:
Though it is well recognised that requirements of most nutrients in
crease during pregnancy and lactation, there is still some uncer
tainty regarding the quantum of increase. Studies carried out on
Indian subjects have provided some data about the increased calorie
and protein requirements during pregnancy and lactation. The Basal
Metabolic Rate (BMR) of Indian pregnant women was found to be about
7% higher upto 24 weeks of pregnancy and 15% higher subsequently,
as compared to BMR of normal non-pregnant women. Since many
women of poor communities do not curtail their physical activity even
during late stages of pregnancy, the additional daily energy require
ment for Indian women has beeh assessed to be around 100 calories during the first trimester and about 399 calories during late stages
of pregnancy, .
...
n -■
:
.e
'Studies on the basal metabolism of lactating subjects had shown that
during the first six months of lactation, the BMR is generally ele
vated by about 16% over the normal value. Data regarding milk
yield of Indian women have shown that they secrete, on an average,
milk which have a calorie content of about 490. On the basis of
. these data, it has been computed that the additional calerie needs of
lactating Indian women is approximately 569 calories per day.
Nitrogen balance studies in Indian pregnant women have shown that
witii increasing levels of protein in the diet, they show a linear in
crease in retention. The requirements of protein, calculated on
the basis of these studies, showed that they are about 20-40%
higher than that of hen-pregnant subjects. Most of these studies
were carried-otrt-onrnrdernourished subjectsand it is, therefore,
-possible that these apparently high values may be due to their
erstwhile pc^r nutritional status. Li arecenr study-carried-out at
the National Institute of Nutrition, the influence-of gestational
period on nitrogen absorption and utilization were investigated.
It was observed that on an intake of 40g. of protein and 1800 calories per day,
nitrogen retention progressively increased with increasing gestational period
due mainly to decrease^rinary excretion of nitrogen.' These studies indicate
that pregnant women utilize nitrogen more efficiently. Similar studies in
lactating women indicated that they require around 60 g of protein per day to
attain equilibrium. However, retention was found to increase with increasing
intake of protein upto 100 g. per day. As in the case of pregnant women, these
studies were also carried out on undernourished lactating women and this may
have contributed to increase in nitrogen retention upto 100 g. of protein per
day.
Longitudinal studies carried out in.pregnant women regarding the absorption
of iron and calcium showed that in pregnant women belonging to the low in- - ■
come groups', efficiency of absorption of both iron and calcium increased
with advancing gestational period - an observation similar to that made with
respect to protein. Calcium balance studies in lactating women, however,
indicated that all -women studies were in negative calcium balance during
" this period.
'
’
Nutrient^intake_diming pregnancy and Jactation
Diet surveys carried out in different parts of our country have shown .
that the intake of most nutrients by pregnant and lactating women belonging
to the poor socio-economic groups is far below recommended allowances.
In many- in stances, intakes are even lower than the allowances recommended
for non-pregnant subjects. The actual intakes of some of the nutrients have
been indicated in Table.
MEAN NUTRIENT INTAKE OF INDIAN PREGNANT AND LACTATING WOMEN OF
the low
Income groups
Nutrient
Intake ’, '
during
pregnane y_ _
"Lactation
Recommended allowances
Pregnancy Lactation W
Calories--g
*
Protein
Calcium - mg
Iron --mg
VitA-^g
1430
43 "
269 ’
18
'
304.
1860 ~
40
300
18
304'
2500
55
*0
10
40
750
2900
65
1000
30
1150
As can be seen, the intakes of both proteins.and calories are well below recommend
ed allowances, the deficit in calories, however, being of a much greater magnitude
than that in protein. The diets were found-to, be predominantly cereal-based and the
protein mainly of vegetable origin. The diets were found to be deficient in several
vitamins and minerals as well. The major reason for the low intakes has been
found to be the poor purchasing capacity. But an important additional reason is-the
practice of foed taboos and food fads which prevented the intake of certain nutri- tious foods both during pregnancy and laetatien. The fear <»f difficult delivery con
sequent on a large infant also-prevented. s»me- pregnant-women from consuming
adequate amounts. <*f fo«d.
:3 :
As a result, a high proportion of pregnant-women were found to suffer from
signs of nutritional deficiency. Signs of B-complex deficiencies like angular
stomatitis, glossitis, tingling and numbness were found in 30 - 49 percent of
pregnant women, while almost 50 percent of women in the third trimester of
pregnancy v/ere found to have anaemia with levels of haemoglobin below 10 g/400
ml. With increasing parity, the incidence of both anaemia and B-complex de
ficiency signs were found to increase. Biochemical studies on pregnant womenbelonging to the poor income groups have shown activities of the two enzymes transketolase and glutathione reductase in erythrocytes, as lowered, indicat
ing sub-optimal nutritional status with respect to thiamine and riboflavin.
Deficiency of pyridoxine is commonly seen in pregnant women and recent
studies have shown that several cases of angular stomatitis which until now
was considered pathognomonic of riboflavin deficiency, responded not to the
administration of riboflavin, but to pyridoxine. The effects of this unsatis- factory dietary situation of the mother were felt not only on her but on her off
spring as well.
Weight gajn_d_uring_p^egnancy:
The mean gain in body weight during pregnancy in well-nourished women was
found to be around 12 kg. This gain in weight is largely accounted for by the
weight of the foetus, other products of conception and changes in body com
position, particularly accumulation of body fat. In pregnant women of rhe lowsocio-economic group, whose pre-pregnant weight is only around 40 kg., the
net gain in body weight during pregnancy is associated with low birth weights
of the offspring. Studies on the bodv composition of these vo men indicated
that during pregnancy, they gain very little fat which probably accounts for the
relatively low gain in body weight. Further, these studies.have also suggested
that many pregnant women belonging to the poor income groups actually lose
body fat at the expense of fluid accumulation.
Effect_on pregnancy wastage^
while in experimental animals, it has been well demonstrated that severe pro
tein deficiency leads to foetal absorption, similar reliable data on human is
scanty since it is not easy to establish the relationship between maternal
nutritional status and pregnancy wastage. However, in studies both retrospect
ive and prospective, it has been observed that 20 - 30 percent of pregnancies
in women-of low socio-economic group terminated in abortions. This may be
an under-estimate of the real incidence since many abortions which may occur
within the first few days after conception would be missed in such studies.
Birth weights^
Data on birth weights of large numbers of infants from different parts of the
country have indicated that there is a socio-economic gradients with respect
to birth weight. The mean birth weight of infants bom to poor income groups
has been found to be around 2.7 kg. as compared to 3. 2 kg. a tnong infants born
to well-nourished women. The incidence of prematurity has been found to be
around IS-percent, while the incidence of small-for-date births faartfieen found.
to be 10-29 percent in different parts of the country. Studies on perinatalmortality have shown that the rates are considerably higher with small-fordate birth indicating that maternal malnutrition is an important factor which
contributes to a high rate of neonatal mortality in bur country.
Nutritional status of the newborn;_
Assessment of the nutritional status of newborn to under-nourished mother has
bee?, carried out using biochemical parameters like concentration of albumin,
vitamin A, folic acid in circulating as well as nutrient stores of the foetal liver.
Foetuses bom to mothers belonging to the low income groups have considerably
lower amounts of iron, vitamin A, ft lie acid and vitamin B12 in their livers
the values being only about 50 percent of values found in foetuses born to wellnourished mothers. Also, studies on the body composition have indicated that
at all gestational ages, they have lowered amounts of nitrogen and fat as well as
reduced amounts of total body iron and body calcium.
Levels of serum, albumin, vitamin A and folic acid in the cord blood of infants
bom to under-nourished mothers have been found to be lower than that observed in
the cord blood of infants born to well-nourished mothers.
Maternal nutritional status_and placentaljunction:
Since low birth weights are associated with poor maternal nutritmnal status,
studies have been undertaken to assess the influence of maternal malnutrition
of placental function. The mean weight of placentae in women belonging to the
low socio-economic group has been found to be considerably lower than that of
high income group, there being a difference of about 100 g. It has also been
observed that placental weight bears a close correlation with birth weight.
However, since efficiency of placental fnnction and nutrient transfer need not
always depend upon the size, studies have been carried out to determine placental
function.
ft has been established that estio gens and pregnanediol are elaborated by the
placenta and excreted in the urine in increasing amounts as pregnancy advances.
Studies carried out on the urinary excretion of these two hormones have shown
that beyond 28 weeks of pregnancy, -malnourished women excrete considerably
lower amounts as compared to well-nourished subjects. That the lowered
excretion was due to maternal malnutrition was confirmed- by the observation that
nutrient supplements given to mothers of the low income group brought about an
increase in the excretion of estrogens to levels seen in well-nourished women.
This was also associated with an increase in birth weights of their infants.
"
Recent studies on heat stable alkaline phosphatase - an enzyme elaborated by the
placenta, have shown that their levels are significantly higher in women belong
ing to the low income groups as compared to well-nourished women. In
addition, negative correlation was seen to exist between the concentration of the
enzyme at term on the one hand, and at the birth weight of the infant on the other.
The results of some studies have suggested that the higher levels of the enzyme
in malnourished mothers may be due to pre-mature aging and hypoxia-of placental .
cells releasing high amounts ef enzyme into maternal circulation.
Studies on the'chemical composition of placenta have Shown that in placentae of
infants with intrauterine growth retardation, the concentration of nitrogen was
significantly lower as compared to placentae of normal infants, and there was
a reduction in the total number of cells as indicated by the DNA content. Also,
the cell size was reduced as shown by the protein DNA ratio. Levels of heat..stable
alkaline phosphatase were significaltly lower. The concentration of glycogen insuch placentae was significantly lower and the rate of glycogen breakdown signi
ficantly, higher, indicating that there were biochemical differences between placenta, of normal jnfe.nts and_those-of infants withJntmuterine growth retar
dation.
:5:
Anaemia in pregnancy:
As indicated earlier, nutritional anaemia is a major p. Voiem among pregnant
women in our country and results of several surveys n, ve shewn that 10-20
percent of women start their pregnancy with haemogloi :n levels -ess than 10
g. and that with advancing gestation, 50 percent and more of women have
haemoglobin levels below 10 g. Severe anaemia with levels of haemoglobin
belovz 8 g/100 ml are encountered in about 10 - 15 percent of pregnant women
at term. There is also a direct relationship between incidence and severityof anaemia on the one hand and parity on the other. Though the precise con
tribution of the anaemia to maternal mortality is netz known, it is believed
that anaemia accounts for nearly 20 percent of all maternal deaths.
A number of studies have shown that iron deficiency is by fat, the commonest
cause of anaemia, though in many cases, there is concomitant deficiency of
folic acid. Serum folic acid levels have been found to progressively fall with
advancing pregnancy. About 60-70 percent of women have levels below 3 ng/
ml levels considered to indicate difiency, during the third trimester of pre
gnancy. The concentration of folic acid in erythrocytes also fall as pregnancy
advances. Supplements of 300 ug of folic acid daily to such pregnant women
have been found to fully prevent the folate in red cells from falling, indicat
ing that this may be the additional folic acid needs during pregnancy.
A number of controlled studies have indicated that daily supplements of 60 mg
of iron and 500 pg of folic acid given during the last 100 days of pregnancy can
effectively control and prevent pregnancy anaemia.
Effects ofnutrient supplements ^^the_outcome_of pregnancy:
Since it is recognised that maternal malnutrition influences the birth weight
of infants, studies have been undertaken to determine the effects of nutrient
supplements given to undernourished pregnant women on the birth weights of
their infants. Pregnant women were maintained on diets which provided about
2400 calories and either 60 or 80 g. of protein daily, during the last 4-6
weeks of pregnancy. This represented an increase of 500 - 600 C/day and
20 to 40 g. of protein, above that provided by their habitual home diets. Such
women delivered babies whose birth weights were about 300 g. more than
women who did not receive such food supplements. Also, concentrations of
serum albumin both in the mother and in the infant were higher. Maternal
weight gain showed an increase as compared to unsupplemented mothers.
Since t|rere were no differences between those that receive 60 g. protein and
80 g. protein a day, it was concluded that 60 g. of protein was adequate.
That these effects were brought about by an improvement in placental function was supported by an increase in estrogen excretion in the.supplemented
mothers.
Iron_and foHc_acid supplements:
During an investigation done to determine the amounts of iron and folic acid
requirements «f pregnant women, it was-observed that the mean weights of
infants whose mothers had received 300-500 ug. of folic acid daily during
the last 100 days of pregnancy were "ignificantly higher when compared to the
birth weights of infants bom to mothers who had received iron supplements
alone. This suggested that folic acid supplements had a beneficial effect on
birth weights. In a recent investigation, this observation .was confirmed, the
practical significance of winch is obvious.
*son
Studie
j&ctat km
The nutritional status of lactating vzomen is particular] important in develop
ing countries; since wcrren breast feed their infants fcr prolonged period of
time and from the infant's point of view, ’adequacy of m .Ik secretion and the
nutritional quality of the secreted milk. acquires practical significance. As
indicated earlier, lactation is a ported of physiological stress and the
requirement of most nutrients increase.
Dietary intake and nutritional status:
Results of several diet surveys have, however, shown that the dietary intakes
of lactating women, belonging to the poor income groups are far from satis
factory. As in the case of pregnant women, intakes of most nutrients fall
short of recommended allowances, the calorie intake being particularly low.
Intakes of vitamins o.^-‘ - •-■’nerals -are-also inadequate. This is reflected in a
high incidence of frank nutritional deficiency signs - particularly of the
vitamins of B complex group. In spite of these considerations, the-lactation
performance of these subjects seems satisfactory. This observation is^somewhat intriguing, since these mothers do not show-evidence of much loss in
body weight. No.significant differences have been found between mothers in
"the early stages of lactation and those in the later stages with respect to
body weights; also body weights of lactating women with only one infant were
found not to be different from those with several infants. Most mothers
tended to have either a stationery body weight or at most lose about 1-2 kg,
throughout t^e period of lactation, though they, were secreting between 400600
ml of milk daily. There has so for ^cen no satisfactory explanation for this
observation, through results of limited studies have suggested that some of
the lactating women have increased body hydration. Further studies are
obviously needed to determine whether this indicates .an adaptation to low
nutrient intakes, brought about through hormonal changes."
Milk_ output £
As mentioned earlier, in spite of seemingly inadequate dietary intakes, a
I
great majority of women belonging to the poor income‘groups are able to
breast feed their infants satisfactorily for long periods of time. Serial and
cross sectional studies on breast milk output carried out in different parts
of the country have indicated that milk output was about 600 ml daily during
the rest of the first year and around 100-150 ml during second year. The
use of various substances like garlic, cottonseed and tamarind commonly
used by the rural population to increase the milk yield did not really have
any effect as galactogogues. This may have partly been due to the fact that
the mothers who were studied already had satisfactory levels of milk
secretion. However, when such mothers were provided with diets containing
2900 calories and 60 g„ of protein for a period of 10 days, the milk output
did net show an increase, but the concentration of protein showed a con^iderahle-rcductitm^jieieJieiiig^ometJjicrease^m-the protein content.
Composition of human nnlk:
Extensive studies have been carried out on the chem cal composition of
breast milk secreted by undernourished Indian mothers from different
parts of the country. The results of these studies hivd shown that while the
concentrations of protein and lactose are very similar to those seen in
milks of well •nourished mothers, the concentrations of fat and seme
vitamins are lower. It was observed that the lower concentrations of
vitamins seen in the milk of undernourished mothers could be raised to
normal levels by supplementing such women with the appropriate
vitamin,' indicating that the low concentrations were reflections of low
dietary intakes by the mother. Concentrations of calcium and iron in
breast milk were found to be within normal range. When mothers, were given supplements of these two nutrients, the concentration of these mine
rals in breast milk showed a significant fall. The reason for this fall is,
however, not clear.
It is not uncommon to see mothers who are still breast feeding, to become
pregnant, but continues to nurse the baby. Studies on such women have
indicated that with advancing .pregnancy, there is marked reduction in the
volume of milk, but that there is a considerable increase in the concen
tration of protein and vitamin A. That this is not due to a simple process
of concentration has been show by the observation that the other consti
tuents in milk did not show much changes.
Studies on the effects of duration of lactation on chemical composition have
revealed that the mean concentration of total solids, proteins, vitamin A,
riboflavin and vitamin C were significantly higher in colostrum and early
milk samples as compared to mature milk. Colostrum was also found to
be a rich source of immunoglobulins, especially IgA. The concentration
of all the constituents decreased in mature milk samples with the exception
of thiamine and folic acid both of which tended to show an increase.
Lactation Amenorrhoea:
It has been observed that there is a striking difference with respect to theduration of lactation amenorrhoea between women belonging to the low in
come groups and those be long-in g' to the well-do-do groups. - - While about
20% of urrethers from well-do-do groups resume menstruation within three
months after delivery, this -figure is negligible for the low income group.
By six months, 82 % of well-to-do and only 8% of poor mothers start’their
cycles. By 112 months, the corresponding figures are 100% and 45%. Though
a variety of factors may be responsible for the resumption of menstruation,
the delay in onset of menstruation in twmrien of the poor income groups mayhave a nutritional basis and be the effect of poor-dietary intakes. Alternat
ively, early cessation of lactation in the well-to-do mothers may be res
ponsible for early resumption of menstruation.
The results of these studies clearly indicate that the dietary intakes and
nutritional status of many women be-lougingro the poor income groups in
our country during pregnancy and lactation are - far from satisfactory.
Many women enter pregnancy in an already undernourished state, and the
continuing malnutrition during this period of physiological and nutritional
stress has an adverse effect net only on her, but on her infant. The same
is true cf lactating women too. In view of the recent findings that malnutri
tion during intrauterin growth of the foetus and (iuring early infancy, may
have long lasting effects on subsequent growth - priority should be accorded
to programmes directed towards improvement of the nutritional status of
these vulnerable segments of the population.
=/=/=/=/=/=/=/=/=/
Reproduced from. ICMR Bulletin Vol. 4 No. 6 June 1974
For more copies write to:
Voluntary Health Association of India
C-14 Community Centre
Saftiarjung Development Area
New Delhi 110 016
N\JT 3-xx.
<7^2-
COMMON; iY health cell
4?/1«(First FloorjSt. Marks fload
BANGALORE-560 001
MATERNAL AND CHILD HEALTH
SCHEME FOR PROPHYLAXIS AGAINST BLINDNESS
IN CHILDREN CAUSED BY VITAMIN ‘A’
DEFICIENCY
FAMILY PLANNING PROGRAMME
FOURTH FIVE YEAR PLAN
Technical Information : MCH No. 2
1.
MATERNAL AND CHILD HEALTH—
THE CONCERN OF FAMILY'PLANNING PROGRAMME
The family planning programme is vitally concerned with promoting the health of
mothers and children. While it advises the couples to limit the size of.their family to 2 or 3
children it also takes measures to promote the health of those few.children. With this end in
view, family planning programme has provided funds for schemes for prevention of diseases
and promotion of health among mothers and children. One of them is the scheme for
controlling blindness among children caused by vitamin ’A’ deficiency.
2.
VITAMIN ‘A’ DEFICIENCY AMONG CHILDREN—A PROBLEM
Vitamin 'A’deficiency is widely prevalent in the country, specially amongst the pre
school-age children. Surveys carried in the southern and eastern parts of the country have
revealed that at least 30 to 50 per cent of all childrenin the pre-school agc-group have eye
manifestation as a result of vitamin ’A’ deficiency. The most severe form of vitamin ’A’ defici
ency - keratomalacia - causes softening and necrosis of the cornea of the eye leading to comp
lete blindness. It has been estimated that not less than 12,000 to 14,000 children go blind in
the country every year as a result of keratomalacia. The economics of such malnutrition is
of great significance in view of the large amount of money which has to be invested in the
rehabilitation of these handicapped children in later life.
3.
TRADITIONAL MEASURES FOR CONTROL OF VITAMIN ‘A’ DEFICIENCY
In the past, the control of vitamin ‘A’ deficiency has been linked with the general
improvement of the nutritional status of the population. Nutrition education of mothers
to persuade them to include foods rich in vitamin 'A’ like green leafy vegetables in the diet of
young children has been of some benefit. However, the recent findings that protein malnutri
tion accentuates vitamin‘A’deficiency and that these two deficiencies exist handin hand is
another complicated problem. Both protein-caloric malnutrition and keratomalacia are found
to be common in the southern and eastern parts of India.
Another measure implemented through the health agencies is the distribution of
vitamin ‘A’ and ‘D’ capsules and codliver oil through the Child Welfare Clinics of medical and
health institutions. For such supplementation to show results the child should be given at least
one capsule of vitamin ‘A' and ‘D’ twice a week. Our past experience has shown that it is
difficult in the rural areas to ensure that the mothers administer these capsules regularly to
their children to prevent the development of deficiency of the vitamin. As a result of these
lacunae, no significant impact has been produced on the incidence of keratomalacia in the
4.
A NEW APPROACH
Recent studies have shown that oral administration of a large dose of 2 lakh J. U.of
vitamin ‘A’ in oil every six months can protect children from developing keratomalacia. The
studies have shown that vitamin ’A' given by mouth is readily absorbed and stored in the liver
front where it is gradually released for utilisation in the tissues. Unlike many of the vitamins
vitamin ’A’ is not excreted in the urine and this is an advantage. No toxic manifestations
have been observed in connection with the use of vitamin ‘A’ in the dosage mentioned above.
In the shape of implementation this measure can be equated with prophylactic inoculations.
5.
PLAN OF OPERATION
Rupees forty lakhs have been provided for the scheme in the Fourth Five Year Plan
budget in the Central sector. Supplies of vitamin ‘A’ are procured by the Department of
Family Planning and distributed to the State Health Departments, the cost of the drug being
adjusted as a grant. The State Family Planning Officers who are responsible for the adminis
tration of the programme have to place indents on the Government Medical Stores Depot,
Bombay, for obtaining their supplies. The Medical Stores Depot would send the supplies to
the District Otliccrs concerned.
6.
SELECTION OF AREAS
The Stale Nutrition Officers would select the areas of maximum prevalence of
keratomalacia based on the nutritional status surveys conducted by them. In view of the
limited financial resources the programme for the present would be confined to such areas
identified for this purpose. As far as possible all the children in the age group 1-3 years
should be covered during the first year of the programme. These children should get the
benefit of the programme till they reach five years of age.
AGENCY FOR ADMINISTRATION
7.
The existing maternal and child health and family planning organisations would be
responsible for administration of the programme. In the urban areas the programme should
be administered through the child welfare clinic of the urban family planning centres, general
hospitals, maternity homes, etc. It has to be ensured that there should be no risk of
repeated administration of the drug. Therefore, in such institutions the vitamin ‘A1
should be administered only through the child health clinic and not through the general
out-door department of the institutions.
In the rural areas the programme would be implemented through the primary health
centres and its sub-centres under the supervision of the medical officer. The auxiliary-nursemidwife and the family planning health assistant working in the primary health centre would
have the immediate responsibility for administering the drug to the children. The drug has
to be put into the mouths of the children by the workers themselves.
As coverage of the entire agc-group and avoidance of repeated administration of the
drug are of great importance, it is desirable to fix a specified period for administering the
programme. For example, the primary health centre/ urban MCH centre may decide to
cover all the eligible children during the month of September 1970 and complete the adminis
tration of the drug during the period of one month; the administration of the next dose to
these children as well as new children to be included, would then have to be done in the
month of March 1971 only. Adoption of such a strategy would go towards effective
implementation of the programme and lessen the load on the ANM/FP health assistant who
are multipurpose workers with various other responsibilities. The children could be collected
at the sub-centres or in other suitable places or contacted in the homes according to
convenience.
8.
DOSAGE AND MODE OF ADMINISTRATION
The vitamin ‘A’ preparation supplied has a strength of 1 lakh J.U. of vitamin ‘A’ per
1 ml. The recommended dose is 2 lakhs I.U. of vitamin ‘A’ or 2 ml. of this preparation to
be given by mouth.
The administration should be repeated every six months till the child
is five years of age.
Vitamin‘A’preparation has a relatively short-shelf life of about 15 months. Proper
precaution should be taken about the storage and use of the drug before the date of expiry
indicated on the lable.
9.
HEALTH EDUCATION
The community should be prepared both through individual and group approach on
the problem of vitamin ‘A’ deficiency and the advantages of the prophylactic programme
envisaged.
10.
EVALUATION
The base line survey at the commencement of the programme and repeated surveys
at periodical intervals would be necessary. A small representative sub-sample from each
State would have to be chosen for these surveys. The assistance of the National Institute
of Nutrition, Hyderabad, could be taken in conducting these surveys.
II.
RECORDS
Child health records as prescribed by the State Health Department should be main
tained in respect of the children covered under the programme and the dates of administra
tion of vitamin ‘A’ noted thereon. In addition, a register showing the particulars of the
children covered and the receipt and issue of vitamin ‘A’ supplied should be maintained in
the proforma at Appendix-I.
12.
REPORTS
Monthly reports on the number of children covered and the position regarding the
receipt and issue of the drugs should be furnished by the individual institutions to their
supervising authority. Consolidated monthly reports should be sent by the State Family
Planning Officers so as to reach the Department of Family Planning by the 15th of next
month in the proforma at Appendix-II.
4
<? « 2 •
■TH CELL
Marks Hoad
50 001
APPENDIX I
(A)
REGISTER OF BENEFICIARIES UNDER THE VITAMIN ‘A’
DEFICIENCY PROPHYLAXIS PROGRAMME
Initials
(6)
APPENDIX-11
PROPHYLAXIS AGAINST BLINDNESS IN CHILDREN CAUSED
BY VITAMIN A’ DEFICIENCY
Report for the month ending
197
for the Stale of
(A) STATEMENT OF BENEFICIARIES___________________
Age of children
(year)
Category-
No. covered
during the
month
Progressive
total for
the year
Remarks
1-2
2-3
3-4
4 -5
1) Children given
1st dose
(Total 1-5 years)
2) Children given
2nd dose
1-2
2-3
3—4
______ 4-5_______
(Total 1-5 years)
(B) POSITION REGARDING THE RECEIPT AND ISSUE OF THE DRUG
0 nening
balance on the
1st day of the
month in
millilitres
Receipt during
the month in
millilitres
Issued during
the month in
millilitres
On hand on the
last day of the
month in
millilitres
(1)
Age break-up of children may be given.
1-5 years age group should be given,
place
-........ -Datc
If the break-up is not available then the total children in
Signature
Designation
HEALTH
VOLUNTARY
C-14,
Community
Centre.
Safderjung
OF INDIA
ASSOCIATION
Development Area,
New
Delhi-110016
Telegrams : VOUHEALTH New Delhi-110016
Phone : 652007, 652008
CQMMUN<>¥
LTH Ci It .
47/1,(First Floor jSc. Marks Aoad
BANGALORE-560 001
^B-41
VITAMIN A DEFICIENCY
Kamala S.Jayarao
*
Vitamin A deficiency in pre-school
children is yet one more nutritional
disorder of public health importance
in many developing countries, It contributes to a significant propertion-of preventable blindnesSj a
self-explanatory tragic situation.
Some ophthalmologists in. India believe that the problem of blind
ness due to cataract is seen in a
a greater proportion and hence
demands greater attention than
vitamin A deficiency. However,
in my opinion, such problems should
not be viewed with a statistician’s
mind. Cataract is a disorder of
adulthood whereas' hypovitaminosis
A has its peak between 1 and 10
years of age. Thus young children
become blind before they can see
anything of the world andbecome a
socio-economic burden. It is
hence that vitamin A deficiency
should be looked upon as a public
health problem.
Vitamin A deficiency, like other
nutritional disorders of childhood,
is seen mainly in the poorer classes
and is mostly due-to inadequate
intake of foods rich in vitamin A.
As in the case of PCM (Protein
Calorie Malnutrition), the founda
tions for vitamin A deficiency may
be said to be laid down during
foetal life itself. The intake of
vitamin A by pregnant mothers of
the poorer classes is very low and
their serum vitamin A levels are
also low^-’
They may therefore
be expected to transfer smaller
amounts of the vitamin to the foetus.
The breast milk of such mothers also
has low concentrations of vitamin A.
The levels being not more than 200 /,ug
per 24 hours . The infant thus is not
only born with low stores of vitamin A
but receives low quantities of it during
the immediate post-natal life. In spite
of this, however, ocular signs of Vitamin
A deficiency are rarely seen in the first
6 months of life. One may hence believe
that this amount of vitamin A is probably
adequate during infancy. I say this
because as yet there are no techniques
by which vitamin A requirements can be
reliably assessed.
Beyond 6 months of age the vitamin A
intake drastically falls because
(1)
the breast milk output diminishes
(2)
the infant does not receive any
extra milk (either animal or
formula made)
(3)
the weaning foods being largely
based on cereals contain virtually
no retinol and only small amounts
of B-carotene.
As you are all aware retinol is found
in high concentrations only in animal
foods. Plant foods contain_only carotenes,
of which B-carotene is nutritionally the
most important. The absorption of
B-carotene is not as geodas that of
retinol and its biological availability
is also poor. Hence 1 /vg B-carotene
is equivalent to only 0.25 /ug retinol.
Diet surveys have showed that pre
school children in South India receive
only 300-500 LU. vitamin"A daily,
* National Institute of Nutrition, Hyderabad-500 007
2 :
corneal xerosis (the dry, hazy cornea)
mostly as B-carotene, through
leading to keratomalacia (necrosis of
their diets4’ < jn pre-school
cornea),' the irreversible stage
*
children the incidence of ocular
signs of vitamin A deficiency is
Therapy
quite high. In children of school going age, the incidence is higher
1. Conjunctival xerosis and Bitot's
but the lesions are mainly Bitot’s
spots may be treated with oral prepa
spots and conjunctival xerosis.
rations of vitamin A.- Therapy for at
Below 5 years ,- corneal xerosis
and keratomalacia are more frequent least 4 weeks will ensure fair storage
of the vitamin in the body .
and hence, the condition is of more
serious concern in this age period.
2. Corneal xerosis can progress
The reason for . this age pattern is
not known; this may include factors rapidly to keratomalacia and must be
treated immediately. Since it is
like the severity of the deficiency,
requirements for growth , influence necessary fo raise the serum- vitamin A
levels rapidly, it is not advisable to
of .infections and presence of PCM
start the treatment with oral preparations.
etc. The incidence of vitamin A
deficiency in children with kwashior- Recent studies show that the rise in
serum vitamin A levels is delayed when
• -kor-and marasmus is higher than
oily preparations are injected^. Hence
in children with milder degrees of
it is advocated that children with corneal
ECM.
xerosis and children with kwashiorkor
Ocular manifestations of vitamin A
and vitamin A deficiency be given an
deficiency.
intramuscular injection of a watermiscible preparation of vitamin A,
The first, functional evidence of
immediately on diagnosis and again,
vitamin A deficiency is night blind
48-72 hours later. This may be followed
ness. Being subjective , it is
up with oral therapy; oral therapy
difficult to establish its presence -in should be with oily preparations. Repeated
children, but in most cases, the
parenteral administration is not recommen
mother do notice that the children
ded for fear of inducing acute hyperdo not see well at dusk. The
vitaminosis A.
""
conjunctival lesions include xerosis
and Bitot's spot. In adults and
Prevention
adolescents, Bitot's spots do not
always respond to Vitamin A therapy 1. The ideal way to control and prevent
and hence their association with
vitamin A deficiency wouldbe to provide
vitamin A deficiency has been
the children with foods rich in pre
questioned. But in pre-school
formed vitamin A like eggs,- liver,milk
children they do disappear with
and milk products, butter,ghee, etc.
therapy and are generally indicative However, this being the ideal method,
it may not be expected to take shape
of vitamin A deficiency. The
conjunctival lesions do not interfere in the near future.
/ •
with vision but may be considered
as red signals, indicating the
2. In the present economic circum
stances, the next method would be to
presence of vitamin A deficiency
ensure adequate intakes of B-carotene
-of-sufficiently high degree.
(1200-1600 /ug daily for children,
Blindness due to vitamin A deficiency 3000 /ug for adults and 45.00 y>jg for
pregnant and lactating women). This
is due to corneal involvement-
:,3 :
entails intake of good amounts of
green leaves (beetroot leaves, carrot
leaves, arwt ka sag, methi, hara
dhaniya, sarson, rajagira, palak,
muli ka sag etc.) and fruits (jack
fruit, mango, orange, papita,
tomatoes, etc), This need vigorous
nutrition education to the community.
In certain communities, this may cal
for change in food habits and correc
tion of wrong notions like believing
that fruits cause cough and colds or
greens cause diarrhoea, etc.
The programme has, now been taken
up in Indonesia and Philippines, also.
I may, however, mention here that
not everyone is willing to accept the
efficacy of this programme. Dr.
Pereira from Vellore (Tamil Nadu) has
some reservations regarding this
programme
H However, a group
from West Bengal^ have conducted a
similar study and observed total elimi
nation of night blindness and no new
cases of Bitot's spot. In those'who
already had the latter, the lesion
disappeared in only some children. It
must be remembered here that-in older
children and adults, Bitot's spot may not
disappear despite vigorous vitamin A
therapy. ■ More importantly it must also.
be remembered that this programme is
mainly intended to prevent the develop
ment of serious eye lesions which could
lead to permanent blindness;, this regime
may not totally eliminate vitamin A
deficiency.
In view of the serious nature of the
deficiency, it is necessary that some
public health measures be taken for
prevention rather than rely on the
above two idealistic approaches.
McLaren7 suggested that since the
human liver has a large capacity to
store vitamin A, massive prophy
lactic doses of vitamin A may be
given to control vitamin A deficiency.
Following on this suggestion, the
The aqueous " preparation of massiveNational Institute of Nutrition at
dose vitamin A is made available by
Hyderabad had carried out field
the Family Planning Units of the Union
trials and concluded that oral
Ministry of Health and of the States
administration of 2.00, 000 I. U. of
where the programme is running. It is
vitamin A (as palmitate) every six •
also supplied by the Anglo-French Drug
months during the first. 5 years of ■
Company (Pardon me! I have no vested
life, will considerably reduce the
interest; I am only giving you informa
incidence of ocular signs of vitamin
tion).
A deficiencyg. It was found during
this study that 75-90% of the children
Those of you who are concerned with
are protected from developing any
sign of vitamin A deficiency and also, vitamin A deficiency may also be
no new case of keratomalacia occurred interested to know that there is an
organisation called the Xerophthalmia
during this period. Following the
Club (supported by the Royal Common
recommendation of the Institute, 7
States in India had accepted in
- . wealth Society for the Blind, U.K.).
They
bring out bulletins which give
principle to implement this progra
.information on various programmes
mme. These States are Andhra
the world over, aimed at prevention ,of
Pradesh, Bihar, Karnataka, Kerala,
Orissa, Tamil Nadu .and West Bengal vitamin A deficiency blindness. The
(these cover the southern and eastern Voluntary Health Association of India
has brought out some pamphlets on
regions where vitamin A deficiency
is rampant). The early stages of the this subject, in English as well as
regional
languages, which will be help
trials at Karnataka were followed up
by this Institute and the results .
. ful to the paramedical workers. Those
interested, may write to the following
confirmed the earlier observations”.
: 4 :
addresses:
Xerophthalmia Club
Nuffield Lab of Ophthalmology
Oxford, U.K.
10.
Pereira, S.M. and Begum, A.
(1969). Amer. J. Clin. Nutr. 22:
858.
Voluntary Health Association of India
C14, Community Centre
Safdarjung Development Area
New Delhi-110016.
11.
Pereira, S.M. and Begum A.
(1971). Arch. Childh. 46:525.
12.
Sinha, DP., and Bang, F.B.,j(1976).
Amer, J. Clin. Nutr. 29: 110.
The World Health Chronicle (30: 117,
1976) has an article which touches on
some of the points discussed here.;
Acknowledgement
References
We are grateful for permission to
reproduce this article from Medico
Friend Circle bulletin No..8, Aug.JL976
1.
Shankar, K. (1962). Ind J. Med.
Res. 50:113.
2.
Venkatachalam, P.S. Belavady,
B. and Gbpalan, C. (1962), J.
Pedi.at. 61: 262.
■
Belavady, B. and Gopalan, C, (1969).
Ind J. Med. Res. 47:234.
.
;
3.
4.
Sunderaraj, R., Bsgum, A.,
Jesudian, C., and Pereira, S.M,,
.
(1969)
Ind. J. Med. Res. •57:375..
5.
Rao, N.P., Singh, D. and
Swaminathan, M.C. (1969). Ind.
J, Med Res. 57: 2132.
6..
Srikantia, S. G. (1976). World
Review of Nutrition and Dietetics. •
Vol. 20 (Karger, S., Basle), pp.
185-230.
7.
McLaren, D.S. (1964). Nutr.Rev.
22: 289.
8.
Swaminathan, M. C., Susheela,
T.P. and Thimmayamma, B.V.S.
,(1970) Amer. J.. Clin. Nutr.
23 : 119.
9.
Annual Report (Jan 1872 - Dec.
1972). National Institute,
Hyderabad, 1973, p.102.
5/77-200
(£c<-U.
*T
Tc
f-s——-
<f^-<-.
av<^ <^AAA9C«.k, Ow
*
<JJ>>GtX. G-i^-l-c. <J.
Tlv^Xvn. e-vU-<AA Lii
4~^
j-~
ok«^.t«uW<z
Q. H-,
■U
4-^>
Vu-J- ,^a^c^<jXi-
This reprint comes to you from
EA^AtORE.6XSR°ad
VOLUNTARY HEALTH ASSOCIATION OF INDIA
C-14 Community Centre, SDA, New Delhi 110 016.
Phone : 652007, 652008
Grams : Volhealth
For a detailed catalogue please write to the Publications Officer.
Code N-2
Teaching Nutrition to Mothers
Helen Laugesen
Summary
When planning nutrition education consideration should be given to the.
audience or the people who are to be taught. The correct material, pre
sentation and illustrations can only be prepared when there is knowledge
of the people who will listen to and respond to the teaching. Attention
has to be given to the message which is to be given to the audience. The.
content of the message is only decided after the audience is studied. It
is largely determined by the needs of the audience and by the resources
of the audience. Finally the medium to be used for teaching is important.
The best medium for teaching nutrition is the one most likely to con
vince people. One of the most successful ways of convincing people that
certain food would be good to eat is to give a feeding demonstration.
1.
The audience
1.1
Study who are the people to be taught
Questions such as these below should be asked so that;'
there is good understanding of the people who are to be taught:
Where do they live?
How much do they earn?
How much can they afford to spend on food?
Is their diet good or bad?
What changes if any should they make in their diet?
What are their food customs - things such as hot and cold
% '
food, special diet given to pregnant women and nursing
mothers?
Can they afford to make any changes which we consider
necessary?
1.2. Study which, people most need nutrition education.
Ask who are the people most often malnourished, and who
most often die of malnutrition. These are the children under
five years. One third of children under five suffer from mal
nutrition (1) At least one third of the children who die under
five are malnourished before they die. (2)
1.3. Study the nutrition problems of children under five.
When a baby is five or six months old his mother’s milk
no longer provides enough food.
Many mothers do not give soft foods by the time the child
is six months old. (3)
About half of children under 5 are anaemic. (4)
Increasing numbers of mothers bottle feed their babies.
Bottle fed babies often get diarrhoea and they sometimes
die. (5)
When children are ill many mothers stop giving food and
water.
2.
The message.
2.1. It should be directd at the problems
Teach the remedies for the problems which cause malnu
trition in children under 5. For example, children start to
grow less well at the age of 4 or 5 months. This is because
mother’s milk no longer provides enough food for the chil'd
The remedy is to teach parents that soft foods should be given
to the child from four months of age. As well as this breast
feeding should continue for as long as possible
2.2. The teaching should be appropriate and relevant
People in low income groups cannot afford expensive food.
Foods which are not expensive and are high in calories are
recommended. It is not relevant to advise these mothers to
start giving orange juice when the child is four months old.
It is relevant to tell mother to roast some ragi or maize or
wheat and grind it, then cook it with water and a little gur,
and feed this porridge to the child.
2.3. The message must be clear and easily understood.
It is confusing to tell the mother to give her child 60 grams
of rice a day. It is clear if we tell the mother to give her child
one katori of rice everyday.
It is better to advise normal household foods as much as pos
sible, and avoid special recipes.
2.4. Some basic messages which should be taught.
Rules for child care.
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
Breast feed your child for as long as possible.
Start to feed your young child soft food when he is four
months old.
Feed your young child five or six times a day.
Continue to feed your child when he is ill.
Give your child extra water when he is ill, especially if
he has diarrhoea.
Seek help from the nearest health centre quickly when
your child is ill.
Get your child immunised.
Keep flies off food.
Wash your own and your child’s hands before feeding
him.
Give your child clean water to drink.,
Give your child dark green leafy vegetables to eat daily
(6).
Rules for pregnant women
1.
2.
Eat your normal diet but eat more than usual.
Eat dark green leafy vegetables every day (6).
3.
4.
5.
6.
7.
Visit the health centre in the last three months of preg
nancy.
Protect yourself from tetanus by getting injections of teta
nus toxid.
Prevent anaemia by taking daily iron tablets during pre
gnancy.
At the time of delivery have the help of a trained dai or
ANM who washes her hands before she does an internal
examination.
For delivery have a helper who cuts the cord with an ins
trument which has been washed and help in a flame.
Rules for mothers
4.
5.
Feed your baby breast milk from the first day. Don’t
throw away the first milk.
While breast feeding your child eat your normal diet but
eat more food than usual.
While breast feeding your child eat dark green leafy vege
tables daily (6).
Have no more than two or three children.
Have two or three years space between children.
3.
The medium—how the message is taught
1.
2.
3.
3.1. Demonstration—feeding a child
This is an excellent way of teaching mothers that small
babies really can eat soft foods. Cereal porridge should be pre
pared in the clinic and a number of babies fed this food. This
helps to convince the more sceptical mothers. It is not sufficient
to give a cooking demonstration. Mothers need to see small
babies accepting food.
3.2 Flash card, flip charts or flannel graphs
These are used to repeat the teaching which is given in the
feeding demonstration. Local, people can be trained to this
work. It is not necessary for the busy ANM to do this. In some
places illiterate volunteers have been trained to do this very
well.
3.3. The weight chart and weighing scale.
The worker weighs the child
and writes the weight on
the graph of the weight chart. Both the worker and the mother
can see if the child is healthy or if he is malnurished by study
ing the weight chart. The worker talks to the mother about what
the child is eating. She advises an improved diet. This is a good
opportunity for nutrition education.
4. Nutrition Rules for health workers.
Ensure that staff talk to mothers with respect.
Teach the Rules for child care to every mother.
Have a little soft food ready for giving feeding demons
tration in every clinic. A local volunteer can be trained
to assist with this.
4. Register and care for every malnourished child in your
area, not just the ones who come to clinic.
5. Educate community leaders as well as mothers.
6. Weigh every child and tell his mother how the chiid is
doing.
7 Give every mother a child growth chart and chart the
child’s weight.
8. If weighing is impossible measure the upper arm circum
ference. It should be more than 13.5 centimetres (or 5-1/4
inches).
9. Always look at the lips for anaemia. Explain what is seen
to the mother.
10. Ensure that iron tablets are always available at low cost.
11. Ensure that DPT vaccine is available at lowest possible
cost.
12. Do not advise mothers to stop breast feeding.
13. Do not advise medicines and foods which mothers cannot
afford.
1.
2.
3.
References
1.
2.
3.
4.
5.
6.
Shah, P.M., 1973 Progress report of WHO Aided Project on ’'Domici
liary Treatment of Protein Calorie Malnutrition” at Palgar, page 3.
Shah, P.M. and Udani, P.M., 1969 Ind. Paid. Vol. 6;762.
Studies on Weaning and Supplementary Poods, 1974; page 14, Indian
Council of Medical Research (ICMR).
Gopalan, C. and Raghavan. K.V., 1971 Nurition Atlas of India, page
71, ICMR.
Ghosh, Shanti, 1976. The Feeding and Care of Infants and Young
Children, page 37. UNICEF.
Ibid, see page 37, many dark green leafy vegetables have high quan
tities of calcium, iron, Vitamin A and Vitamin C.
Relevant Health and Nutrition Education*
by J.P. Greaves, Sr.Programme Officer, UNICEF
and
G. Donoso, Regional Nutrition Adviser, WHO
The first point to.make about education - any kind
of education - is that it occurs always in a context.
The
context with which this paper- is concerned is that of rural
India, and the slums of the big cities.
In other words,
with over four fifths of the population.
But the general
content of the paper is applicable to most developing
countries.
The emphasis is on the poorer sections of the
community, and on women and children.
Why?
Because this
is where the need for health and nutrition education is
greatest, where it is most urgent, and where success can
bring .largest returns in terms of improved health and
wellbeing.
The second point to make about education is that
it must be relevant - relevant to the context in which it
is given.
It is necessary to examine the context a little
more closely.
India still has one of the highest infant
and child mortality rates in the world: comparative esti
mates are, for infants below 12 months, 100 to 130 per
1000 live births; for children aged 1 to 4, 45 per 1000
children
in the age group; corresponding figures for
Western Europe or North America are 15 and 1 respectively.
*
Based on a paper prepared for a Workshop on the Role
of Home Science Colleges in Group Feeding Programmes,
New Delhi India; April 1976.
2
The reasons for this are well known: ignorance, often
compounded with superstition about the nature and amounts
of foods to be given to young children, coupled with an
unsanitary environment in which infectious diseases
flourish, both nurtured by poverty.
This leads to a
mutually exacerbating syndrome of malnutrition and disease
especially diarrhoea and respiratory infections, which
commonly ends in death.
Large families, and especially
closely spaced families, further aggravate the problem.
Health and nutrition education must be relevant to
this context.
It must therefore be concerned with the
nature and amounts of foods to be given .to young children,
both in sickness and in health; with simple means of
preventing and coping with infectious disease, and with
the principles and practice of personal and environmental
hygiene.
Above all, it must be directed at correcting an
attitude, a behavioural pattern, which is known to be of
decisive importance in the genesis of malnutrition and
associated infections.
Education in this context should
not be concerned to impart "knowledge" for its own sake;
should not relate to "nutrition" generally; should not be
directed to marginal or non-existent problems
(for example.
undue emphasis on fruit juices where there is no scurvy).
Rather, it should be aimed to effect change in attitude
and behaviour in areas known to be crucial to the develop
ment of malnutrition
in the context in which it occurs.
The messages to be imparted must be based on a sound
knowledge of the local human ecology.
- 3
A vital point to apprehend is that, for the first
two years of life, which is by far the most vulnerable
period, the child is totally dependent on others - usually
its mother -
for what it is given to eat and drink. This
point is so obvious that it deserves to be stressed. There
is a natural tendency to overlook the importance of a fact
so simple.
But this fact is the reason why the problem
of malnutrition in this age group is unique.
There is no
way of circumventing the need - the essential need - to
improve
the understanding and practice of mothers in this
regard.
Older sisters, cousins, aunts are important too;
nor should one forget the father.
Perhaps the person with
the greatest influence is the grandmother.
There are some who believe that economic progress
alone will improve this situation.
They are wrong.
One
does not have to point to the nutritional problems - of a
very different kind - of affluent societies to substantiate
the statement that they are wrong.
There is evidence from
Indian studies that the incidence of malnutrition in
children under 2 is largely independent of the income of
the family.
Some argue, in the jargon of economics, that
improvement in income is a necessary and sufficient condition
for the elimination of malnutrition. But whatever real improve
ments ah increase in income may make to the diet of the
family as a whole, it will have little effect on the child:
below 2 unless the mother’s understanding of the child's
needs is also improved.
Nor is an increase in income
always necessary: a redistribution of the. family's available
food so that the child below 2 gets an amount approaching
its physiological need may make the difference between life
and death to him, but only a marginal difference to the
other family members.
4
To illustrate the relevance of context, one could
turn to a situation in many respects the opposite of the
one with which this paper deals:
Britain in the seventies.
An article discussing what would be appropriate nutrition
education for the mass of people in Britain today, where
the major manifestation of malnutrition is obesity
(especially disturbing in the young), concludes as follows:
"... sensible eating for many people in Britain today
implies an increase in consumption of fruits and vegetables
and of bread (especially wholemeal bread); little change in
consumption of milk, cheese and meat (but avoidance of
their fat), and perhaps increased consumption of fish; and
reduced consumption of fats and oils
(except those rich in
poly-unsaturated fatty acids which might even be increased),
of sugar and sUgar-Cohtaining foods
(such'as cakes, biscuits
and pre-eminently sweets), and of alcoholic drinks. ■ But
above all, sensible eating implies moderate Ratings'
restraint in the quantity, though not in- the Variety, of
foods consumed."
Advice similar to this may-; indeejd~ be appropriate for
affluent India, but the number of people for whom it would
be relevant, while in absolute terms far from negligible,
represents in fact a relatively small proportion of the
total population.
For the mass of the people - the subject
of this paper - quite different messages have to be .conveyed.
Bearing in mind what has been said above about the
preponderant Indian context, the following six groups of
messages have a universal validity:
"*•
.4 s.u4^ ’’3
. <2pO$
- 5 -
z
,
Health and Nutrition Education:
the Six Universal Groups of Messages
1.
Breast feed your child always and as long as possible.
Remember, however, that from 4 months of age onwards
he must receive extra food at least 4 times a day.
Keep in mind that the child depends on you to get
the food he needs.
2.
Feed your child only clean food and clean water,
given with clean hands from clean utensils.
Keep
flies away from food.
3.
Should your child fall ill, seek immediate help from
available services.
If diarrhoea (with or without
vomiting) sets in, give your child immediately and
repeatedly sugared water or weak tea.
Diarrhoea can
kill your baby because he loses more water than you
give him.
4.
Try your best not to reduce his food intake.
Get your child immunized.
Get your child weighed.
Remember that an immunized child, who is growing well,
is a healthy child,
5.
If you are expecting or nursing a child you should
eat more, at least 4 timesa day, with plenty of
dark green or yellow vegetables.
You need more food
to produce a Healthy baby or enough milk.
6.
Two or three healthy children are enough.
Space
your children for your own and for their sake at
intervals of 2 to 3 years.
Remember that today you
can have ybur children when you want.
.
6
The justification for these messages is briefly
as follows:
Message 1
(a) Breast feeding is virtua?.ly universal in
the rural setting but is starting to decline in the slum
areas of the big cities.
The.breast feeding component of
this message will have to be emphasised or not according
to the rural/urban environment.
Recent work has confirmed
that breast feeding does reduce the chances of conception:
this in itself is an important reason for prolonging it.
(b)
A low total calorie intake is at the very
root of child malnutrition.
Inadequately fed nursing
mothers'do not produce enough milk to fulfill the child's
requirements for calories and protein from the 4th month
onwards.
'There is much evidence to show that poor rates
in growth, that eventually lead to' malnutrition/ become
evident 'iri a considerable hurnbei' of children from the 3rd
or 4th month of life.
Supplementary feeding is essential,
and should be done, regi^larly in increasing, amounts from
the 4th month onwards.
The extra amount of food needed
cannot be got into the child in one or two meals: four
times a- day is probably "adequate under village conditions.
(c)
The young child is dependent on its mother
for feeding, as emphasised above.
Message 2
Faecal contamination of food and consequent
diarrhoea axe -nearly always associated with, malnutrition.
This message -aims atef,preventing such contamination.
.Jasw
Message 3
in India.
’■
'
(a) Health services offer only limited coverage
However, even if the services are available.
7
people may not readily make use of them.
The idea of
making use of whatever health services are available
should be a component of nutrition and health education.
(b)
Diarrhoea is inextricably tied to malnutri
tion in children under 2 or 3 years of life. The treatment
and prevention of diarrhoea is very poorly understood by
mothers and very inadequately handled through
traditional
practices and beliefs that emphasise prolonged restriction
of both water and food.
This wrong emphasis enhances the
production of dehydration which is the main killer of the
malnourished baby.
Early oral rehydration can be a most
effective tool in the control of dehydration due to
diarrhoea in the malnourished child.
Prolonged food
restriction is in itself a mechanism in the production of
malnutrition and all efforts should be made for an early
normalization of the diet in the child that is suffering
from diarrhoea.
Message 4
(a)
Infectious diseases such as tuberculosis,
whooping cough, diphtheria and measles are very important
contributory factors in malnutrition.
By promoting immuni
zation, we are ,in fact promoting better nutrition.
(b)
By getting the child weighed at periodic
intervals an early warning that the child.is not progressing
adequately," or that his nutritional condition is deteriora
ting, can be obtained and remedial action initiated.
Message^ 5
(a) Poorly nourished mothers will produce small
babies of lower vitality and insufficient breast milk. Both
factors conspire against good nutrition in the child.
The
- 8 number of meals per day is critical to the total amount of
food intake of mothers, needed to fulfill their calorie
requirements, and four meals per day should be considered
a minimum for the nursing and expectant mother.
(b)
Yellow and green vegetables in the diet of
mothers are especially important where there is a problem
of xerophthalmia.
In such areas the diet of children up
to 5 years of age should also contain a supply of these
vegetables.
Message 6
The more children in the family, the less
food available per head.
This can become critical for
children under 2 or 3 years of age in families that have:
4
or more children.
The last-born is prone to malnutrition
not only as a result of an insufficient diet after birth,. .
but also through his mother'during his intra-uterine develop
ment and growth, J Spacing thechildren will promote a better
nutritional status of the mother which will reflect persis
tently on that of the child she bears,..and nurses.
It is worth noting that none of1the nutritional
components of these messages —.or, for'that matter, of the
ones considered relevant for Britain - makes specific mention
of nutrients as such.
There is no need to talk to people
about protein, riboflavin or A: carotene; but there may be
every need to encourage them to consume, for example, more
dal, curd and drum-stick leaves, and to feed these, appro
priately prepared, to their young children.
It is absurd to
talk about milligrams of this or that vitamin; sensible to
talk about homely.measures of this or that food.
It is
9
doubtful if it is very useful to talk in terms of groups
of foods, as is conventionally done in a number of
"systems":
foods have been classified in 3, 4, 5 or as
many as 9 different "groups", with exhortations about
including examples from every group in each meal.
More
useful to start by observing habitual practice; note what
is good in this, and emphasise it; and then suggest prac
tical and quite specific ways in which practice can be
improved - for example, about age at which semi-solids and
solid foods are introduced, about ways in which foods are
prepared, about frequency of feeding, and about particular
foods that are (or could become) readily available and could
No point in lauding the
be used to supplement the diet.
virtues of eggs if these are beyond the economic means of
those one is attempting to help!
No point in demonstrating
how vegetables and fruits may be conserved with the'aid of
a .pressure cooker and Kilrier jars if these represent wealth
beyond the dreams of avarice!
(These and other examples in
this paper, of inappropriate - i.e. irrelevant - education
are not figments, of' the. imagination:
all have been observed
in the field).
What is being advocated is simply the translation of
the six universal groups of messages into practical and
quite specific advice, relevant to each situation.
"Extra
food", and "dark green or yellow vegetables", means something
different in South India to what it does in North India. Or in
Africa.
What is the local cereal?
oilseeds locally available?.
for youngf children?
What are the pulses or
How .can these best be prepared
How much, and how often, can they be fed?
Which green or yellow vegetables are already available, or
could be grown in.so-called kitchen or community gardens?
10
How should they be prepared and included in the diet? What ■:
are the unusual but often nutritionally valuable food
—
supplements that commonly feature in the diets of tribals,
and consumptidn of which should be encouraged - and perhaps
introduced in larger quantities, at an earlier age than
tradition dictates?
i
What is the local source of water,
and how can it be made more "clean" for drinking?
Given
the economic circumstances of the people, the local avail
ability and price of foods, the nature of food supplements
that may be available (for example,
from a food-for-work .
programme), what is the wisest pattern of food expenditure?
The answers to-such questions’clearly call for home
work on- the part;:of the would-be health and nutrition
educators’ - or, to give it a’more pompous term, research;
Research has been defined'as, firstly, the identification
of a problem, and secondly, the search for a solution.
Relevant problems can only be identified by studying the,
life of the people, not the literature of fellow-workers ;j
Colleges of Home Science, amongst other institutions, are
in principle well equipped for such research. . Research of
this kind is just as intellectually demanding as the more
academic kind, and often very much more useful.
It requires
a certain humility on the' part of the workers-’- they should
not project their own problems
(for example with respect to
hang-ups about breast feeding), but enter sympathetically
into those - recognised or not - of the people.
Such
research must recognise that solutions to problems, if they
are to be effective, must be simple - and simplicity to the
pseudo-sophisticated is suspect.'
It must be concerned not
only with the messages to be conveyed, but equally with the
means by which they are to be communicated.
It requires
persistent monitoring - or follow-up - to e.isure that
relevance is maintained.
And finally it requires a
constant concern for application of its results, and the
recognition that this can
second-hand:
be only fully achieved at
that success can only be realised if local
community workers are trained to deliver the messages, with
the Home Science College or other Training Institutions
acting as an authoritative resource, stimulus and guide.
All those involved should constantly remember that
their objective should be to promote relevant changes in
behaviour, and that success, if it is to endure, will depend
on a conviction by the people that they
themselves".
"have done it
Lao-tzu, a Chinese philosopher, wrote thus
about leadership more than 2500 years ago:
"Of the best leaders
the people only know that they exist:
The next best they love and praise;
the next they fear;
And the next they revile,
When they do not command the people's trust,
Some will lose faith in them.
And then they resort to recriminations!
But of the best, when their task is accomplished,
their work done.
The people all remark, 'We have done it Ourselves!'
*****
What is a nutrient-requirement ? The requirement for
a specific nutrient is defined as the smallest amount
of that nutrient that will ensure a good state of health.
This will however, vary from person to person.
Therefore, nutrient requirements are set down as reco
mmended dietary allowances ( RDA). These levels
are believed to ‘ meet the known nutritional needs of
almost every healthy person. ' By experimental pro
cedures, the highest requirements in a population are
assessed, some further allowances are added and the
RDA for each nutrient is fixed. Thus for many
individuals the RDA will be higher than their actual
requirement. No person need take more than the
suggested RDA. The RDA for various nutrients have
been fixed by international organizations like the
FAO and WHO3 and by various national bodies
including the Indian Council of Medical Research4.
In the process of this search, I came across an
interesting or disturbing feature, depending on how
you wish to perceive it. Many advertisements do not
say what ingredients the preparation contains, leave
alone their quantities. Many inform you that the
preparation is a unique formulation of generous
amounts of vitamins or that it is a vitalizer with
balanced amounts of vitamin ( Incidentally, IDPL is
one of them ). The advertisement merely proclaims
the efficacy of their product in specified condition.
There is one advertisement by a leading company,
which reveals nothing about the formula but claims
that it is good for memory ! It contains nothing but
vitamins Bi, Be and B12. The companies are pro
bably cocksure that the physician will rely more on
their advice than on his own judgement ( and they
are dead right).
I was interested to know how some of the comm
only available vitamin preparations fare when compar
ed to the RDA suggested by the ICMR. Table 1
shows the RDA for some nutrients, for various
physiological groups. For specific reasons, I have
not taken the RDA for infants and children but in
absolute terms these values will be less than those for
adults. In Table II, I have presented the quantities
of various vitamins purported to be present in each
commercial preparation. It is however not the complete
formula of the preparation. 1 have taken only some
important vitamins into consideratoin. The list is by
no means exhaustive. I culled them from some recent
issues of the Journal of the Indian Medical Associa
tion. They are marketed by leading pharmaceutical
companies.
This lack of needed information is one of the
reasons why Table II does not have more preparations
listed. But this is ample for what I have to say.
There is also no reason to believe that those which
escaped inclusion would be any different.
The RDA for any nutrient is the amount which
if taken regularly will ensure that a deficiency state
of that nutrient will not develop. For example if a
sedentary, house-wife takes 1.0 mg riboflavin daily,
she is expected not to develop riboflavin deficiency.
As I said earlier, 1.0 is the highest level and most
can afford to live on lesser amounts. The situations
which are under discussion now, are considered to be
deficiency states of mild or moderate degree. The
individual might have depleted levels of the nutrient
and may need higher amounts than the RDA. What
Recommended Daily Allowances*
Table-I
Thiamine
( B| ) mg
Riboflavin
( B, ) mg
N cotinic acid
mg
Man :
Sedentary
Moderate
Heavy work
Vitamin B.9
mcg
1.3
L5
2.2
16
19
26
—
1.4
—
0.1
0.1
0.1
1
1
1
1.0
1.1
1.5
1.0
1.2
1.7
13
15
20
—
2.0
—
0.1
0.1
0.1
1
1
1
1.1-1.3
1.1-1.5
1.2-1.4
1.2-1.7
14-17
14-21
1.6
1.8
0.1
0.1
0.5-1
0.5-1
1.2-1.7
1.4-1.9
1.2-1.9
1.4-2.1
1---22
18-25
2.5
2.5
0.15-0.3
0.15
1.5
1.5
Adolescents :
13-15 yrs
16-18 yrs
Piegnancy
( Sec md half)
L-ctation
Folic acid
mg
1.4
2.0
Woman :
Sedentary
Moderate
Heavy work
Pyridoxinef
( B6 ) mg
- Taken from reference 4
t Taken from RDA of Food and Nutrition Board, U.S.A. 1968.
should this higher level be ? For acute and severe
stales like beri-beri or keratomalacia text-books
prescribe doses, empirically arrived at and found to
bring quick relief. These are usually much higher
than what would be required even for that degree of
amelioration.
Table 111 shows the prescribed thera
peutic doses, as obtained from various standard books
on nutrition and medicine.
For chronic, moderate deficiency states or for
situations where vitamins are prescribed empirically,
we may assume that levels much lower than the
therapeutic doses and slightly higher than the RDA
should be enough. Let us be generous and double
the RDA, remembering that the patient does receive
a certain amount from his diet too. With this
information I would like you to critically compare
Table JI with Tables 1 and III.
Much of the time drugs are not prescribed
according to any therapeutic schedule.
They are
usually prescribed as ‘ 1 dose or 1 tablet, three times
a day '. Items No. 1-4 in Table II are close to the
RDA with respect to vitamins Bi and B2. Given as
Table-11
per the above mentioned schedule they supply 2-4
times the RDA, and it was argued above that double
the RDA should be enough in moderate or doubtful
deficiency states. We must also remember that when
a diet is considered to be low in a nutrient, it is not
totally lacking in that nutrient. The average diets of
the low socio-economic groups provide 0.5 to 0.8 mg
each of Bi and Ba. Items 7-9 provide about 5-25
times the RDA in a single dose. If even such pre
parations are prescribed thrice a day, the intake
would be 15-75 times the RDA. Item 8 in a single
dose supplies thiamine in a quantity prescribed for
the whole day in beri-beri 1 Moreover in beri-beri
it is not necessary to prescribe very large amounts of
other vitamins. Thus preparations like 8 and 9 are
not necessary at all.
An argument may be put forward that since
water-soluble vitamins are harmless compounds there
is no necessity to raise a hue and cry about the
dosages prescribed.
This is no doubt true but,
‘ such practice is economically wasteful and in some
instances, causes financial hardship
Composition of some multivitamin and haematinic preparations available in India.
Vitamin Bi mg
Vitamin B- mg
Vitamin Be mg
Niacin mg
Vitamin B,_, mcg
Folic acid mg
Vitamin C mg
Iron
( Type of salt ) mg
Capsule
Cap.
1
0.5
0.6
4
2
1
2
50
Sulp.
150
timed
release
Vit. A. l.U.
Vitamin D. LU.
3
5 ml.
4
5 ml.
5
Cap.
6
Cap.
7
Cap.
1.0
0.75
0.15
7
0.45
1.6
0.8
0.8
4.0
2.5
3.0
1.0
0.5
30.0
5.0
5
10
10
s
100
5
F.A.C
185
Gluco.
35
1
10
s
1
50
Sulp.
200
250
90
200
Sulp.
41
8
Cap.
50
25
10
100
5
0.5
300
25000
1000
9
Cap.
20
5
2.5
100
5
1.0
100
10000
1000
Table-11 (Coatd)
10
5 ml
Vitamin Bi mg
Vitamin B- mg
Vitamin B,; mg
Niacin mg
Vitamin B,.j mcg
Folic acid mg
Vitamin C mg
Iron (Type of salt)
mg
Vitamin A
Vitamin D
11
Cap.
12
Cap.
13
Cap.
14
5 ml.
15
5 ml.
16
Cap.
17
3. mll.M.
100
io
25
*1
Z.
Colloidal
oxide
JOO
OS
2.0
200
Fuma
rate
350
15
2
150
Fuma
rate
350
50
2.5
100
Fuma
rate
300
7
1.75
15
2
Colloi
dal ox.
500
Fuma
rate
125
25
Fuma
rate
250
18
5ml. I.M
100
27.5
25
1000
500
It must also be remembered that water-soluble
vitamins cannot be stored in large amounts unlike
the fat-soluble ones. This of course is one of the
factors underlying their low toxicity. ‘ In prescribing
thiamine it should be remembered that the healthy
human body contains only about 25 mg of the
vitamin. Furthermore, it has no means of storing
any excess taken in the diet; the excess is lost rapidly
in the urine.
The human body is certainly an
effective machine for dissolving thiamine pills and
transferring the solution to the urinal ’B.
Moreover
it has been shown, atleast for riboflavin that intestinal
absorption is limited by saturability and that higher
the dose, smaller the fraction absorbed. This is no
case in favour of parenteral administration either,
because higher the amount in circulation greater the
excretion in urine.
Thus, most of the ‘ high-potency ’ or ‘ Forte ’
preparations of multivitamins are a sheer economic
waste. It is a drain on the patients’ purse and the
onus is on the doctor because he is. making the
patient buy a specific preparation.
If bought by
goverment or public sector dispensaries, it is a
national waste. If preparations with smaller and yet
adequate quantities were bought, for the same money
more tablets could be purchased and a greater number
of patients benefitted. Manufacture of such ‘ highpotency ’ preparations must also use up an unnecessary
amount of the scarce foreign exchange resources,
since quite a few, and probably all vitamins (raw
materials ) are imported.
Thus it is not proper if one merely prescribes
B-complex tablets and avoids brand name because he
is a ‘ conscientious objector ’ to brand names. As long
as there is no uniformity in the dosage employed in
various preparations, it is necessary to know which
brand supplies or claims to supply requisite quantities
of vitamins. Also, there is no need to blindly follow
Table-Ill
Suggested doses of vitamins for single, acute and
severe deficiency
Condition
Vitamin
Dose (Oral)
Beri-Beri
B]
10-25 mg bid
or tds
5-10 mg
5-10 mg
5-10 mg
Riboflavin deficiency B3
Megaloblastic anaemia Folic acid
Bi3
Megaloblastic antemia
Folic acid
of pregnancy
Corneal xerosis
Vitamin A
Bitot’s spots
Vitamin
D
Rickets
10 mg
5000-10,000 I.U
1000-5000 I.U.
the ' one t.d.s. ’ schedule. How much and how
frequently, should be decided on the merits of the case.
I also wish to draw your attention to one or
two additional points. There is a widely held belief
that a combination of vitamins Bi Ba and B12 is
good for neuropathies and other nervous disorders.
I don’t think this is based on any solid therapeutic
evidence. The reason the three are combined, I think
is because each one has been shown to be effective
in a specific disorder of the nervous system. Hence
the triad is used as a short-gun therapy, indiscrimina
tely. In fact, the brand names of certain such prepa
rations incorporate Greek terms like 1 encephalo ’,
‘ neuro ’ etc. The manufacturers of one preparation
even claimi ts efficacy in improving memory.
‘ It (thiamine ) may be given, though without
expectation of dramatic results, in cases of nutritional
neuropathy. There is no reliable evidence that it is
useful in any other disorder of the nervous system.
The prescription of synthetic thiamine, either alone or
in combination with other vitamins, as a general tonic
or appetiser, is supported by no scientific evidence
and is now discredited. ’5
‘ Vitamin therapy is often given to patients with
polyneuropathy, although it is clear that polyneuro
pathy is not due to deficiency of vitamin Bi, B12 or
any other known vitamin. Such treatment has a
placebo value and probably no other, but is not to
be decried... .’B.
For reasons mentioned right at the beginning
I too do not decry the use of the combination as
I do the dosage in such preparations. Items 17 and
18 in Table-II are two classical examples. Both are
meant for parenteral use, another characteristic of
this triple combination, probably because of the
presence of vitamin Biz. The conventional prescri
ption by physicians for parenteral B-complex is ‘ 2 ml
M.
I.
once a day or once on alternate days ’.
Assuming the patient receives 6 ml in a week, he is
given 600 mcg to 2 mg of vitamin B x 2 ! What a
collossal waste considering that vitamin Biz is an
expensive substance. The prescribed dose even for
pernicious anaemia is 2 mg weekly, even those who
may argue that unlike the other B-complex vitamins,
vitamin Biz is stored to a certain extent in the body
may note that with each 1 ml goes 20-33 mg thiamine.
Many of the oral preparation too contain unnece
ssarily high amounts of B,». The RDA for this
vitamin is 1.0 mcg and in pregnancy and lactation, 1.5
mcg. Even conceding that a majority of the popu
lation cannot afford animal foods and hence many
may suffer from vitamin Bt ,. deficiency, I see no.
reason why any preparation should contain more
than 2 mcg. and at the most 5 mcg vitamin B12 .
This criteria is met by only 7 of the 16 oral prepa
rations listed. If the preparations are haematinics
combined with iron, they have to be prescribed three
times a day. In which case the preparation should not
contain more than 2 mcg B12 . Items 10-13, 15 and
16 must be very expensive and those who really
suffer from B12 deficiency can ill—afford then. 1 also
wish you to note that mixed haemanitics-iron prepa
ration containing vitamins and minerals, are condemed
by authorities in the field of anaemia. “ Recovery
of the patient with uncomplicated iron-deficiency
anaemia is not helped by vitamin supplements or
minerals’7. In our experience vitamin B12 and folic
acid are not needed till haemoglobin levels come upto
II gms. % or more.
Let us now consider the vitamin A content of
these preparations. The prescribed dose of vitamin A
for corneal xerosis and Bitot’s spots is 1500-3000 iug
( 5000-10,000 LU). daily8-9.
The RDA during
lactation, the maximum suggested for any group, is
3500 LU. Notice the vitamin A content of items 7
and 9. Who needs 25,000 I.U. vitamin A daily?
Severe cases of deficiency like keratomalacia are not
to be treated with oral preparations9,10. Those who
really develop xerosis can never afford a pharma
ceutical like 7 or 9, whose price is further raised due
to presence of other nutrients. Imagine to what
extent the price can be reduced simply by bringing
down the vitamin A content, even to 5000 I.U.,
which itself is a high amount.
Then, there is the practice of adding glycero
phosphates to liquid, multivitamin preparations. I do
not know of what therapeutic value these compounds
are. They are not mentioned in any standard text
book of pharmacology and therapeutics. As far as
I know (see any pharmacopoea) they only form basic
ingredients of syrups, possibly for flavour. However,
a widespread misunderstanding is that they are
‘ energy givers ’ or ‘ tonics ’. Some brand names
carry a prefix or suffix of ‘phospho’ and the advertise
ment says ‘energy givers’, ‘ vitalizer ' etc. This in my
opinion is a fraud perpetuated by the drug companies
and worse still, an unpardonable ignorance on the
part of the doctor. The vitamins atleast, despite the
excess and the wastage, do some good. I see no
nutritive or therapeutic value for the glycerophos
phates. Their presence is needed for syrup preparation
but its name should not be included in the brand
name and no claims should be made for its therape
utic efficacies.
One of the nutrients commonly added to multi
vitamin preparations is iron. Witness that out of the
16 listed items, only 4 do not contain iron. It is
well-known that ferrous compounds arc better absor
bed than the ferric, and it is heartening to note that
most arc ferrous salts. A preplexing form is the
colloidal iron oxide (items 10 and 14) which finds
no mention in any book on pharmacology or iron
metabolism. Since it is a colloidal preparation I doubt
if the iron in it is easilly available to the body.
Of the various ferrous salts, ferrous sulphate is
the least expensive and should be the treatment of
choice, yet only 3 preparations contain it. It is said
that contrary to popular thinking and claims,
gastrointestinal intolerance to iron preparations depends
on the total amount of elemental iron in the gut and
on psychological factors;
it is not a function of
the form in which iron is administered.1,7 Thus claims
made for compounds other than ferrous sulphate,
of increased tolerance or decreased toxicity, are not
genuine.
Also, sustained - release ( timed-release )
compounds (no. 2 ) take the compound beyond the
duodenum and proximal jejunum and thus reduce
iron absorption. Therefore it is wasteful to prescribe
such preparations.
The RDA for iron ranges from 20-40 mg per day
depending on age, sex, physiological state etc. This
of course is for food iron and for free inorganic
salts would be less. The therapeutic dose, on the
other hand, is 60 mg elemental iron, thrice a day.
Ferrous sulphate, fumarate and gluconate contain 20%.
33% and 12% elemental iron respectively. Items
11-13 and 16 are probably meant for iron deficiency
anaemia. Prescribed twice a day they supply 250-350
rag elemental iron which is higher than the thera
peutic dose.
Thus taken, 13 supplies 150 mcg
vitamin B12. On the other hand, no. 7 supplies only
8 mg elemental iron per capsule. One may argue
that this may be used as for prophylaxis and not
treatment. Have a second look and tell me the
situation where in an individual is grossly deficient
in every vitamin one can think of and is yet not
deficient in iron ? This is a pure commercial gimmick
to claim haematinic value for the preparation. As
early as 1936 Strauss said “ shot-gun therapy is to be
deplored for a number of reasons. Most mixtures of
substances fail to contain enough of any one ingredient
to give maximal effects. The patient must pay not
only for the material he needs but also for the nonessentials ” (cited from ref. 1).
One can go on endlessly in this manner.
My
intention in writing this is to bring to the notice of
MFC members the fact that all multivitamin and
haematinic preparations are not same.
There is no uniformity in dosage employed.
There is no authority to lay down criteria for
There is no authority to check whether the
claimed doses are actually present.
4. Doctors prescribe these preparations with total
ignorance of or indilference to principles of
nutrition and therapeutics.
5. High-potency preparations should be available
separately for single vitamins.
Multivitamins
need not contain amounts much higher than
RDA. They are economically wasteful.
6. The false claims made for improvement of
unspecified and unproven conditions are perpetua
ted due to the ignorance or compliance of the
doctors.
7. Most of the companies have foreign collaboration.
Most of the raw ingredients ate to be imported.
Could this be one of the reasons for the high
dosages employed ?
I rm sure you will find asking yourself many
more such questions.
1.
2.
3.
References
1.
2.
The Pharmacological Basis of Therapeutics. (L. S. Goodman
and A. Gilman, cds.). Fourth cdn. MacMillan Co.,
London. 1970.
Nutrition Atlas of India ( C. Gopalan and K. V. Raghavan
cds.) National Institute of Nutrition, Hyderabad, 1971.
3.
Energy and Protein Requirements. WHO Tech. Rep. ser.
No. 522, 1973; Requirements of vitamin A. Thiamine,
Riboflavine and Niacin. WHO Tech. Rep. scr. No. 362,
1967, WHO Geneva.
4.
Dietary Allowances for Indians (C. Gopalan, B. S. N. Rao)
Indian Council of Med. Research, Spl. Rep. Scr. No. 60, 1968.
5.
D. Davidson, R. Passmore, J. F. Brock and A. S. Truswell.
( 1975 ). Human Nutrition and Dietetics, Sixth edn. Churchill
Livingstone, Edinburg and London.
6.
W. G. Bradley (1975).
Practitioner 215: 452.
7.
T. H. Bothwell and C. A. Finch ( 1962) Iron Metabolism.
Little, Brown Co., Boston.
8.
S. G. Srikantia ( 1975) Human vitamin A deficiency. Wld.
Rev. Nutr. Diet. 20: 184.
Reddy, V. ( 1969) vitamin A deficiency in children. Indian
J. Med. Res. Suppl. to vol. 57, p. 54.
M. F. C. Bulletin 8, August, 1976.
9.
10.
The treatment of polyneuropathy.
Reprinted from :
Medico Friend Circle Bulletin, November, 1976
Published monthly from 21 Nirman Society, Vadodara-390 005
COMMUNITY I-"
(Firs,tHv
' BANGAlcme
r
? 1 r I r a t 1, i- :'
o_F
'.th cat
.Vlufk
F 0 0 .3 3
IL INDIA Hani’is still a basic shortage of food a<-onf several
-.-lotion
groups which 11
merely on subsistence rations, .is a result, eye the energy
needs of such .. . -,-laticn groups are no- net with, let alone th; t» ■■. ..i;
nut of
other nutrients like prole ins# Vitfiminv and minerals. A tronc-.iour 'ffert
'o
be made to meet the ovr.ntitative and qualitative' requirements of for •.
ON THE AGRICULTURAL front, the development of th-' . ig vi siding variety's of
cereal crops have justifiably raised .our ho-?s. Al?--• i th-this " agri tuii.ur 1
revolution" efforts 1■ »-.-e to be made to .-n?’v the best ; >ssible nee of available
food resources. Concurrently efforts must 1. ".Iso r--.de- io augr-en c’-- -.uppliej;
■of protective foods .uch as milk, eggs, pulse--, ver. tables
frits. These
efforts will no dou’-r. ,-ake time. However, the -.-alls: ‘ive d -fici " i? tn average
Indian diet needs to
rectified as quickly .- - possible. It is ’■ r? that
'fortification' offer.-" an approach worth the t-'lal.
CEREALS, .-l-CH FORK ■’ .= staple fco. in Inii- - nd constitute ne •! • 60-90<of
the diet are deficient ir several nutrient-., t.o n. be improved in nut itiobal
quality by fortification. Other foods like hj- ’-'C-en-ited-’oils, in: -t *<
canned fruits and vegetables, supplement?r/ r-ottin Ispncentratc-s -:ide fro-oilseeds meals have t' undergo commercifsiv}-------e.’sing ba "ore reaching the
consumer. Nutrients '/rich are present in lin-'-ocessed. fw’s mighv get destroyed
during processing. Therefore,.these -nutrients have t-c be added bsd$ to the fooig
in a synthetic fora. Thus 'fortification' ?nd 'enrichment' of foods can be ;n
effective ap-roach for providing a more wholesome and balanced diet.
'FORTIFICATION CT ENRICHMENT' OF ?OC:.J
THE FOOD FORTIFICATION committee of t--,o Indian.Council of Medical Research has
given the following! definition of ■'fortification’ cn-' 'enrichment'.
"FORTIFICATION OF A foodstuff denotes the ad£raion trj a ."--nd of one ,omere
dietary essentials'in amounts wh ch make the
content great”’ t'- bat
found in that particular food in its natural stat-', by fortification also meant
the addition of one or more dietary essential +-’ a food which.the latt'.i- Jo-.--’
not contain in its natural st<tv.
GN'THE OTHER hand the ter’ ERTIP'R-IEIIT is used to signify th.? addition of
dietary essentials to aifon i to restore the ictal content of th..- former to
t'- level..-’, obtaining in the fo'd in its natural (unprocessed). ;3tate’A
F0RTI7TC IT- ON O' FOOD;'- IN PRACTICE
RICE
"'TEN tRAW RICE is n.'. lied to get polished, white rice, most jof the :. r-.-ienAs
present in the - :rrn and the oi’tw? layer of the 'r-vn, especial iyhe IP-Vi train,
Thiamine, are removed along with tho husk. A process was developed in the
united state"- whereby lice grains were enriched by soaking: them in .-> solution
rich in thiamine coat. Th.:.-- latter prevents less of vitamins during the sphsuquent
washing of rice. Thi;: enriched rice 'premix' was mixed with c 'i. ,ry nfllisbed
rice so that th:- vitamins -were' present in the final mixture in
:nt. ^quul to
what was present in the ■> -irinal unpolished rice. This 'enriched', ricu was
used in the phil'.i ippine,? in 1947-50, and the incideho-j of bori-i.v ci a -di.ce’.se
caused by the definiepey of thiamine- was reported to ha •; deersirni'-icantly
as a., result.
THE IMTRCDUC H-1N OF 'pr-.mix' ir ovr country,/bower, involves
r. 1 problems,
The mixing of 'premix' with unfortified rice would have to k-;,- •lone nt c?--tain
centr.-lizid places from wher • istrilution of the enriched vin. will have to be
carried out. Most fara'-rs produce; the Crc-r- and consume it rig'- t off the fields.
Thus enricb.r--.-nt of rice invol-os -nany logistic problems and . ■ .'.ionul
difficultly-. and therefor!, my not be fea.qi^l--- at present in our country.
ON THE OTHER hand, Parboiling of rice is ■ ■ tr=6itional T-r-a-”’ico ir India. The
paddy is steep'd in Wat'.-r, .-.teamed, dried and then dehusked. The nut,ri :-nts
which are present mhinlv in the rice gsr-. and the ou-’-er Ic.yor of h grain get
diffused insi-ln the grain durinr parboiling. In this t--'.rboilcd ric' oven if
..milled Ir-.ter, loss of nutrients ir. pi’ev'nted to a cnnsi-L-.-rab-l - -xtont. However,
parboiling as is done by the '■rad'o may oft on ir-pt'-t in unplor.o.int od-vr,
flavour and. appearanc to the rice- due. to for ■■nV’Vi. n- oc-•.•in ■ du-'-ng
parboiling. Therefore-. the raw polished rice,
*
which.is ’ j
.ic. 1 tv superior
though nutritionally inferior to the parboiled rice, ic often preferred.
Attempts have, however, been made by the central 'oo-’ 'Tecbnolorical Research
Institute in Mysore and Jadayapur Univ sit;,-, CalcuV?'. to ’?'■■■ lop m improved.
method of parboiling or rice. This improved method ipn : tn
■ ooiiirr
increasingly no-ulai' ' ith many mill .owner.’. Tino 1;
: • <.-o • . ■
"?.i-i'ng
parboiled rice wit C-. rusier acceptability
~. {no’-- . ‘0
nt
of India have placed restrictions on the xxter. r- of poll ...nV ■ •..-.< to s
certain, extent this prc-.-int:-. th. cnmplotrtr-'-l of nu-ri-'.-s
th? rice.
For the present, parhailing soems" to be a mor practical 1 solution tlr:r •.■ reduc
tion of an enri ched pr-nix in India, at least •-•it’’> regard to Vce-.
WHEAT (ATTA) MAIDA (r
ined flour) and Bread.
DUEIH5 '» SECO® wo: 1- war ■ :-he United Kn-n dem undertook to■fern.’-' and enrich
several foodstuffs. All flour,was milled to 85 percent 'extraction only, ’.rlr.ch
left enough thiamine (vitamin B.) in tha flour and the addition of synthetic
thiamine was' uhnecdsoery. Since' wheat flour is deficient in calcium, calcium
carbonate (Chalk) was added at the rate of 592 g. of calcium carbonate to
280 lbs. of wheat flour. The practice of enriching wheat flour wit1- vitamins
and minerals has continued in the post war years also.
THE UNITED STATES have strict legislation on ortificatic • and < i.■ ichment of
foods. Rigorous standards have been laid down fo- the' levels of nutrients
to be added to -'arious foodstuffs.' Almost all refined flour in America is
fortified with thiamine, riboflavin, niacin, iron and sometimes with calcium
also.
IN INDIA, WHEAT is: consumed mainly as whole wheat -'lour (almost 100$ extraction)
which has' adequate amonn s of the B-vitamins. However, it is'-lacking in
calcium and therefore the sub-committee -on- Food Fortification of the Indian
Council of Medical Research recommended in 1955 that wheat flour can. be
enriched with calcium carbonate.
THERE IS AN increasing ■ trend towards consumption'of bread in urban communities
in India today. Bread is made from maid a or re'ineej. flour witch is pf>or in
the B-Vitamins compared -to the wheat flour. Thu' there is n- ; ssity for a
judicious enrichment of the flour used in the b* nd. industry. The establishment
of several modern hackeries is a/first step towards improvi ,-• the nutritional
quality of bread. Those bakeries have been set ip at Bombay, Calcutta, Delhi
Hyderabad, Madras, Ahmedabad and Cochin with th - help of monz-friendly foreign
governments. The bread prepared in these bakeri ■:.' is fortified with vitamin A,
B-complex, iron and the amino acid lysine, nutr' -ts in which refined wheat
flour is usually poor.
IN FEBRUARY 1970, the government of India launc ;d a programme’ in Bombay for
fortification of atta with vit-amines and mineral.; arid for- increasing the protein
content by adnixtug^d ’nth echb^e groundnut flou-. A Corufent^^sd vitaiainmineral mixture containing.viri'ain A, 'Riwoflavin, niacin, thi:i->ine, calcium and..
iron salts, is prepared in a •pharmaceutical facte—’' and mixed in a selected
flour mill with edible groundnut flour containin'- 45-50$ protein. This "master
premix" is distributed to other flour mills in 41 citv for blending with atta
at a level of 5 percent. This' programme. is pl.ann'” ’ tn he cztended to the
metropolitian areas of Delhi and Calcutta at a later date.
HYDROGENATED FATE AND oils: Fortification of margarine with vitamins A andD is compulsory in several countries (the U.S. and Europe) Co'noumptio'n of ■
"Vanaspati" (hydrogenated fat) is-becoming popular in India and vanaspati is
replacing ghee (clarified butter), and vegetable oils in many preparations. ■
•Fortification of vanasp-ati with vitamin A Jias bean made compulsory (700
International Units .of Vitamin A per ounce- of v-annspati) by the government
and many manufacturers add vitamin D in addition.
MILK
\SEVERAL COUNTRIES TN the west are cn-riching milk with vita-.in D*.
This is
essential because of paucity of sunlight in those countries during the long
winter month. In Indian substantial1 amount of vitamin D i : synthesized in
our skin when sunlight direct or reflected falls on it. Th rc-forn iilk does
not\appear to require-to-be fortified with vi"•v'd.n D in our country.
SKIMMED MILK PONDER is used in the feeding of children -.nd pr-rn- ■=. and
nursing women in many countries. Sincb 'skimmed i?ilv powde- is -nor in vitamin
A which is hadlv needed by these segments of the peculation nar- -nnui-,-cfurors
fortify’ skimmed milk powder with synthetic vi' w'in
SEVERAL PROPRIETARY INFANT foods based ‘on milk are fort if i-■’ i.ith vitr.-qn A,
D, Bg, C ahd iron and some with vitamin B.. ? •.->■ ■■■ . Spray dried. ri’!> powders
are deficient in vitamin Bg (pyridoxine) which is lost during the processing,
and addition of pyridoxine to spray, dried milk powders is carried out as a
routing procedure.:
COMMON-SALT: IN the Sub-himalayan regions of India, goitre a di'orders caused
by insufficient intake o
* iodine is’ver" wid - .-"read. Th.. incidence of goitre
has been ■ reduced to a' great extent’-in the Un ' :d States -.ad Latin American
countries by the distribution of -iodized salt to the popvlatiorr in
■> goitre
region's. In'India a pilot project for distribu'■on of iodised salt has been
undertaken in the endemic areas. The salt consumed in India is usually not
. the fro# flowing table salt but the crystalline, impure variety. Potcnsiusi
iodate has been found to be more stable than, n^tassium iodid- and is added to
the salt' supplied in these areas. Carefully controlled studies carried out
so.far .have shown that th? consumption of iodised salt in these goitrous
areas has brought down the incidence of goitre.
PROBLEMS ENCOUNTERED' IN FOOD FORTIFICATION
FOR ANY FOOD fortification programme launched on a nationwide- scale, or even
at g/regional level, to be successful:several factorr. .'jed
be considered.
*THBR' HAS TO be a centralized; agency which takes ear.; of fho t rhnology
involved in the fortification.
*THE~vehiCLE OR the food item which is- fortified must bo such that it reaches
the maximum number of consumers. Salt tea and: bread are instances in point,
*THE NUTRIENT ADDED must bo in stable form to withstand subsequent loss due
to storage under varying conditions of humility and temperature.
*THE FORTIFIED FOOD must not be radically different in appearance shape,
colour and taste to the food people are used1 to. This is v- ry important from
the-view point of gaining popular response from the average co? sumer.
♦LAST BUT NOT least, .the cost of the fortified article of food should not be
any different from the-unfortified food.
JUDGED BY ALL these criteria, fortification"of salt and bre-vl appears to have
caught up. Recently, the National Institute of Nutrition has carried out
extensive researches on the possibility of fortifying common, salt with
calcium and iron. The results have been.encouraging and based on these
investigations, fortification of salt with-calcium and iron will bp taken
.up on a national scale in the near future.
IN ACCEPTING FORTIFICATION as a national policy certain other considerations
should not be lost sight of undeveloping countries with expanding-populationsi
the reliance has perforce to bo placed mainly on an adequate supply,especially
of protective foods, to meet the nutritional needs of the population. Also
in considering the quantities and. kinds of nutrients to be- used in fortifying
different foodstuffs, it is useful to take into account the nutritional
deficiencies of the total diet of the population rathern than of any single
foodstuff alone. Fortification should not also be indiscriminate, as use of
nutrients in quantities more than what is needed will only be a waste and may
add tp the cost of the final product which a population subsisting on marginal
income can ill afford to bear.
'. ;
i/!:'iitnmiiiii ■!
.
ktt T)-'
•
i
COMMUNITY HEALTH CELL
47/1, (First Floor) St. Marks .load
BANG.i.tU .c
out
COMMON; rv
■
GOVERNMENT CF KARNATAKA
'
BA^GAiOre.5
DIRECTORATE OF HEALTH AND FAMILY WELFARE SERVICES, BANGALORE
HEALTH AND FAMILY WELFARE COrdFOrilENrS AVAILABLE FREE FOR HEALTH CARE DELIVERY THROUGH VOLUNTARY ORANISATIONS
*
SI
Beneficiaries
PYogrames
Methodology
Objective
No.
1
Role of the voluntary
Renarks
organisations
.3
2
4
6
5
7
NUTRITION PROPHYLAXIS PROGRAMMES
I.
Iron and Folic acid
Expectant and Nursing
tablets for mothers .
(Iron~60ng; Folic
acid 0.5 ng.)
nothers,
wonon Family
Welfare acceptors.
1 tabldt to each of
Prophylaxis against
these wonon daily for Nutritional Anaenia
100 days.
Voluntary organisations
1. Monthly quota.
can’ distribute these
to be distri
drugs to the beneficia
ries.
buted cnee in
• a nonth.
List
of beneficiaries
to be maintained
in prescribed,
fern.
2. To be obtained
fron D.H. & F.W:0./
P .H .C ./Sub-centre.
2.
Iron and Folic acid
tablets for children
(iron-20 ng Folic
Children below 12
years of age School
going and pe-school.
1 tablet daily for
100 days
do
do
do
do
acid 0’.1 ng)
3-
Vitanin ’A’
concentr
ated Sol.2 lakhs units
strenght.
AH children fron
Once in 6 nonths
For preventions of
1 to 4 years.
in the form of
night blindness,
taken up in the
capsule or liquid.
Keratonalacia and
rural area at pre
other conplications
due to Vitanin 'A
*
deficiency.
1. This programs is
sent .
2. To be obtained
fron P Ji ZJ. or
sub-centre.
. .Contd/2-
1WNISATI0N EROGTiJJi'ES
D .P .T.
to 3 years.
and 3 doses at an
interval of 4 to 8
weeks with a booster
dose 18 to 24 months
1. Vaccine to be
Prevention of
Completion of 3 doses.
Diphtheria,
Tetanus, per
tussis (whoo
Voluntary organisations
can organise immunise-
stored in re
frigerator at to
tion campaign in the
of 4°c "to 10°c.
ping cough)
rural area and slums in 2. To be obtained f
the urban areas and
D.H.& F.W.0./P.:
later.
carry out the immunisa
tions •
2.
D & T
All children between 3-8
years.
Two doses at an in
terval of 4 "to 8 weeks
(Primary Vaccination
Prevention of
Completion of 2 doses
Diphtheria and
or one booster dose
Tetanus.
Voluntary Oranisations
i.e. no DPT previously
given) Booster dose in
can organise immunisa
tion campaigns in the
case of previous DPT
rural areas and slums
after an interval of
in urban areas and
carry out the immuni
one year.
do
sations •
3.
T.T.
Antenatal cases
In case of antenatals
3 doses-starting 1st
dose at 16-20 weeks,
Prevention of
Tetanus
2nd dose at 20-24 ■
Voluntary organisations
can t ake up as a part of
MCH Service and immunise
do
anatenatals.
weeks & 3rd dose at
36-38 weeks.
*
4
B .C .G. Vaccination
3 months to 19 years
Earliest at the age
of 3 months •
Prevention of
Voluntary organisations 1. Vaccine to be S'!
Tuberculosis
can arrange mass immuniin regrigeratorsation programmes with" 2. Vaccine availaM
the assistance of Dist>
Dist. T. Centre
T .B. Centres.
..,Contd/3-
5. Snailpox Vaccine
Prinary only
At the age of 3-9 nonths
To prevent snailpox
Voluntary oranisa-
1. Vaccine to be
tions o.-n take up
stored in refri
geration.
2. Vaccine aval Tab! e
as part of MCH
services and con
duct Prinary
Vaccinations.
L. Polio Oral Vaccine
All children 3 to
Start at 3rd north and
To prevent Polio
9 nonths
3 doses at an interval
of 4 to 8 weeks with
cyclitis
do
at the FHC
1 . Vaccine to bo stored
at - 20°c.
a booster dose at 18 to
Likely to be available
during next financial
24 nonths.
year.
■ ,.MILY WELFARE PROGRAMMES
1
Sterilisation
Couples with two
children and above
Vasectony, Tubectony
Pcrnanent nethod
for Uniting the
fanily.
1. Voluntary Organisations can organise
sterilisation amps with the assistance
of local Prinary Health Centro/iJrban
Fanily Welfare Centre.
Loop
Couples with one or
two children.
Loop insertion
For spacing the
children Tenporary
2. Motivate eligible couples for undergoing
nethod of Fanily
sterilisation, IUD insertion at the
nearest Prinary Health Centre or hospital.
Hanning.
They can act as depot holderns for distri
bution of contraceptives.
They can ensure
follow up services by the staff by closely
associating with Prinary Health Centre/
Urban Contres and the Connunity.
. MLrodh
Newly carried couples, 6picces or nore at- a tine
depending on usage. Distri
and couples with one
child.
bution once a nonth.
For spacing the
children Tenporary
nethod of Fanily
planning.
3. They can establish Urban Fanily Welfare
Centres in areas left uncovered by
Governnent institutions after approval
by Governnent.
100% assistance will, be
provided by Govt.
....Contd/4-
: 4 :
Oral Illis
Couples with one or two
Oral pills-first 3 cycles to
For spacing the
4. Volutary organisations having their own
children.
be distributed directly under
childrcn-T emporary method of
hospital, approved by Government for
conducting tubectony operation can main
the supervision of doctor and
when there is no untoward
effect, pills my be distri-
tain sterilisation beds for which bed
Fa.rjily ELanning.
maintainence charges will be paid ley
ted by non-nedical porsonollc
Beneficiaries to be examined
Government as per rules.
5.
6
by a doctor once in
months
or earlier whenever indicated.
Medical Termi-'
Pregnant woman upto 20
Medical institutions
nation of Preg
weeks where pregnancy
is unwanted.
or Government) recognised
health of the
under M .T .P. Act can taken up
beneficiaries aS
this programme.
a welfare measure.
nancy.
(Private
Private Practitioners recommended by
Local Indian Medical Association and
approved by Government can take up
To safeguard the
vasectomy operations and IUD insertion:
The beneficiaries eligible for compensa
tion amount.
The Private Practitioners
are eligible for service charges at the
prescribed rate fixed by Government
provided the services are rendered free
to the community.
They can also take v<
distribution of contraceptives includin
oral pill s.
6. Nursing hones run by private practitior.
and voluntary organisations, satisfying
all the conditions as per M.T.F. Act
and recognised by Government can take up
M .T .P. Services.
(1)
Iron Folic- acid, tablets, D.F.T. Vaccine, Dipthcria and Tetanus, Vaccine, Tetanus Toxoid,
B.G-.G. Vaccine Contraceptives are available
and
D.6.G. Vaccine,
Small-pox Vaccine;
free:
(i) depending on the availability of stock with Government.
(ii) depending on refrigerator facilities availabln with the organisation.
(iii) provided the services are rendered free to community.
............. Contd/5-
(2)
All
the supplies made have to be accounted.
Subsequent supplies will be made, after the previous supply is properly
accounted.
(3)
List of beneficiaries under nutritional prophylaxis,
immunisation prograrme, family welfare programme have to be
maintained in the prescribed registers and ferns.
(4)
Monthly statistical data in the prescribed forms have to be furnished to the concerned Primary Health Centres/Urban
Family Welfare Contres within the due dates.
(5)
Apart from the assistance already approved by State and Central Government, no other monetary assistance will be
be'given to the honorary staff/organisation.
(6)
For -further details the nearest Primary Health Centre/Urban Family Welfare Centre/the District Health and Family Welfare
Officer/City Family Welfare Bureaux may kindly be
contacted.
Dr. J.S. Snksena
Director
Directorate of Health & Family Welfare Services
Ananda Rao Circle
■
Bangalore - 560009 •'
*
BANG
Injurious effect of food may he due to different causes and gives use
■mptoms of Acute Gastro-Enteritis.
I-
Chemical :
a)
Antimony in Enamel wore in contact wiath fmits/acids dissolves out
b)
Zinc from galvanised articles.
c)
As from harmful colouring matter.
d)
Pb (lead) from soldered utensils
e)
insecticides in food grainsf)
Commercial acids used in manufacture of Bees.
II.
Parasites or their Cysts like Tape-worm Cysts
III.
Bacteria : 1. Salmonella Group causing Salmonellosis or Acute Gastro
Enteritis e.g. a) Enteritidis
8 .
from .
b) S'.- Typhimurium Q Ducks, eggs & partially cooked meats
e.g. Sausages.
These organism are nonsporing and Thermolabile. . The symptoms appear after
about 8 hours as severe pain, vomiting, diarrhoea and collapse.
B. Morgani and Proteus
Bact. Flexner!
B. Goli
Stapphylococcus which may contaminate Food, Milk, Milk
Products Cakes, etc., due to Staphylococci from the skin,
nose or throat or from the cow's udder if- some; lesion is
present' This is usually due'.to an Exotoxin which'
multiplies in the food/milk before ingestion and sometimes
known as Toxin Type, or poisoning.
6.
Cl. Botulinum giving rise to Botulism. It produces a. potent
toxin and contaminates, fruits and vegetables. Canned and .
pickled foods are sometimes the source as Cl. Botulinum is an
anaerobic sporing organism. Svmptoms mat be immediate or
delayed after 12-24 hours and are very serious like nervous
disorders or vision and dysphagia to be.differentiated
from Belladonna poisoning. Paralytic iteus may occur and
then failure of the heart and .respiration.
2.
3.
4.
5.
IF.
Pood poisoning may be also caused by poisonous fungi e.g. toadstools
mistaken for mushrooms.
Investigations to be carried out in an outbreak of food poisoning.
Source of infection. Food, -milk, cakes etc. to be determined. Food sample.,
of suspected food' to be taken and examined -bacteriologioally also aerobic and
anaerobic cultures to be made and examined. Stop further consumption of
suspected food and sale of the same food/milk.
2.
Note time interval. When F.P. is -caused by living Infective Bacilli the
incubation period is longer since time for the Bacilli to multiply.and
cause sign. If symptoms anpear rapidly, it is due to be preformed Toxin
the food e.g., tinned foods.
3.
Agglutination, tests may be positive with known culture.
4.
Examination of Vomit/Faeces an, the acute' stage for Bacteria.
1.
Prevention of Food Poisoning .
1.
2.
3.
4.
5.
6.
7.
Promnt refrigeration of sliced meats, pastries, .custards and cream fillings
to prevent any staphylocci from multiplying.
Exclusion from food handling of persons' suffering from pyogenic infections
of the hand cr skin.
Education of food handlers, cook ate, in hygienic standards in preparation,
and. storage.
Extermination of Rodents from kitchens and stores.
Prevention of human carriers e.g. in Salmonella infection's.
Food should- be covered. Left overs avoided.
Proper canning and Preservative methods of. food.
■FOOP-BOBNE diseases
9. Undulant fever
10; Worm infestations, eg, round worms,
thread worms, .tz-iohandua spiralis etc.
11. Leptospira haenorrhagica .
12.
Poliomyelitis
13.
Lathyrism.
14.
Epideaio dropsy.
15.
Ergotism
1. Diarrhoea
3. Typhoid
4. Paratyphoid
5. Cholera
6. Food poisoning
7. ’Tuberculosis ■
8. Brucellosis
Food, allor.vy : occurs among sot.-’; persons due to acquired or inherent, .dissynchhraoy. Usually the allergic manifestations eg. gastrointestinal upsetj^us-ticuria
or asthma are due to protein in the food and. therefore foodstuffs which cause.
allergy are mostly fish, eggs,- prawn, milk, cheese etc.
Fool sanitation :
1.
Milk hazard.
food may serve ns a vehicle in transmission of diseases.
excellent food and ideal culture medium.
Dirty milk.-a_.2ia.jor health
Warm surrounding favour : growth of Bacteria. In Urban areas, where the-.milk is
pooled from various sources before distribution. Contaminated milk samples from
a single source may-contaminate the complete stock of milk.
■1. Those due to salmonellae organism
■ 2. Those due to. shigellas organism
TxiofJs due to staphylocci o’rganism
4, Those ■due to streptocci eg.- sore-.
throat, scarlet fever.
■5. Diphtheria
6. Tuberculosis
7. Poliomyelitis
8. .Undulant. fave:
Sources of milk borne diseases
Dirty udders of cow
Dirty fingers of milker - ...
Dirty utensils and bottles
. Flies
Droplet infection from Milkman etc.
.
Milk sanitation
1.
2.
Animal should be clear, and healthy as certified by vefernary doctor.
Dairy farm to be clean. 3. Milker free- from illness eg. open T.B.,
typhoid, sorethroad or staphylococci eg. boils and abscesses + clothing,
personal cleanliness and naild. 4.Utensils - for storage and transportation
clean + sterilized. 5- Pasteurization - destroys most’organisms. Does notdestroy spore forming organisms.
Meat and fish -
uncovered, and left meat.
Sanitation
Growth of
. 3. Oysters - typhoid
4. Infection, due to fingers and flies •••
•A
■
.1, Animals
.4. Proper storage
?. Inspection of cu-^meat & Ti'sh ’
Corr~ci preservatior
3.
Rapid transportation.
6. Adequate cooking
1. gangrene causing organisms
3.
worm infestations
Fruits and veg-?tables
,
If eaten raw - poor culture media
It Choebic dysentry; , 2» Worm infestations - round worms +.-thread worms.
proper washing preferably in’the KMNO . Steaming if necessary.
Droppings of rats and mice - leptospi-Je haemcrrhagica.
Prevention of dietary infections.
1. Choice of-food--fresh, 'free- from infestations
2.
Storeage and transport + Preservation,.'cool dry place protected from-’rodents.
3.
Kitchen staff - strict hygienic practices free from illness-and infections.
4.
Water - Boiled
.
7. Use of <?f-'ective pesticides.
'5- Sanitary conditions
work place + utensils. 8. Row to use onlv npnrov _J
6.
Health education
’ ch.endc.- Is for >-reserving or
x ap'-ndfi
,
ROSS.
otci'
si h
LTUTE UNIT OF
bwAL HEALTH
Ulcal CWlH
*>
*£-540034,.
■
DJPT OF PRJVENTIV'l AND SOCIAL MEDICINE, ST JOHN'S NODICAL
COLLEGE, BANGALORE
SCHEDULE FOR DIET SURVEY
47.1C°^lJ2‘7y ‘■’-•Ai.TH CELL
Village!
Family No.!
Name of Hoad of family!
/‘-(First FI0Or)St. Marks Road
^GALORE - 660 001
Address!
GENERAL INFORMATION S
Type of Family! Single/Joint
List of Family Members
No.
!
:
Relationship
Name
i
Age
1.
2.
3.
..
i
!
5.
!
Caste !
Religion »
Total Monthly Income
:
Monthly Expenditure opt
U) Milk
(b)
Fruits
(□)
Groceries
(d)
Rent
(e; Others
EATING HABITS :
Vegetarian or Nor-vegetarian
What do you eat
?
.
Morning
Noon
After-noon
Night
Other times
What
foods do you specially like? dislike? why?
How often do you consume the following foods?
'
Education-!
JEccupat^on
:2 :
food
Everyday
J
'
i
Occasionally
j
Never
Milk ’ ’
Fruits
Leafy vegetables
E09S
Meat/Fish
Any food modifications for certain groups within the family ?
(a)
Infants, pre-school children
(b)
Elderly
(c)
Pregnancy
(d)
Illness
FOODS CONSUMED :
Average daily
Items in Ozs./games
Intake
12
Item
4
3
5
6 ■
7
Per
i
Family
(days)
__________ I
Cereals
Per
Consump
tion unit
s
............................................ .. .................................................
Wheat
........
Rice
............................................................. ■■
□□war
.
Ba j ra
Other (state)
.....................................................
Pulses 5
A that
brad
Moong
...................
Masur
..........
Other
............................................ .. .........................................
........................
(state)
Milk and its Products
s
Milk
.................................................................. .. ...................
Dahi
................... ...............................................................
Other
. .............................................. ..
Fats and oils
Chee
Da Ida
Oils
Others
..
’
..............................................................................
...............................................
..3
3
3 :
Vegetables 3
Leafy 3 (Names)
Root 3
(names)
1.
2.
3v
(names)
1.
2.
3.
Fruitss
(names)
2.
.......................................................................................................................
Meat
Fish
Eggs
................................................................................
...
Sugai^Gur
Beverages
1.
Tea
2.
Coffee
3.
Others.....
...........................................
.................. ................................. .. ..............
Miscellaneous
1. Betel nuts
2. Betel leaves
3» Tobacco
.............................................................
Others
METHODS OF COOKING 3
1.
Rice
.................................
2.
Roti
........................................................................................
3. Dhal
4.
................................................................
Vegetables
..
Co you have s
1.
Vegetable garden
2. Fruit trees
3.
Chicken
4.
Cattle
..................................................
..................................................................
.
Investigator
COMMUNITY HEALTH CELL
W
47/1, (First Floor)
Marks .load
NUTRITIONAL ASSESSMENT OF UNuEH FIVE§AMGAtOf'‘fc'5“v001
fVu T
Child's Names
FACE
Mother's Name:Occupation:
Father's Name:
Occupation:
Address:
Date:
Age:
Pale conjunctiva
Bitot's
Xerosis conjunctive
•
cornea
muddy wrinkled conjunctiva
keratomalaciaangular palpebritis
night blindness
photophobia
skin fold over triceps
Birth order:
IMMUNISATION
B.C.G.
Smallpox
Polio
D.P.T.
T.A.B.
Mx test & result
standing ht.
Sitting ht.
Weight
Birth wt.
Bicristal dia.
Head
Chest
Arm
Petichiae,
pellagrous dermatitis
Pigmentation of
knuckles, fingers
toes
Mosaic dermatitis, flaky paint
Scrotal and vulval dermatitis
Musculoskele tai
L^i-S
angular stomatitis.
angular scars
cheilosis
TONGUE
red and raw
oedema
magenta
atrophy papillae
TEETH
mottled enamel
caries
GUMS
GLANDS
spongy - bleeding
thyroid
parotid
xerosis
phrynoderma
SKIN
NAILS . koilonchia - fingers/toes
HAIR
sparse, thin.....
lack of lustre
dyspigmentation
flag sign
'easy pluckability
G.I.T. liver
S(soft) F(firm)
H(hard) (mid. clav.
line below costal
margin)
Muscle wasting .
Craniotabes,
bossing F & P bones
Epiphyseal enlargement
Beading of ribs
Persistence anterior
fontanelles
Bow legs, deformities
C.N.S.
Tingling extremities
Burning feet
Tender calf muscles
Glove, stocking
anaesthesia
Loss of ankle/knee jerks
spleen
2 5-
c,v„s.
Cardiomegaly
Tachycardia
ANY OTHERS
INVESTIGATIONS - Hb%
GENERAL DIET SURVEY
Food Available
Daily consumption
Av.amount/membe r
Rice_________________ __ ______ _________________
Wheat_______________________________ ___________
Ragi________________________ ;______________
Maize
_____
Proteins
____________
Fats___________________________________________
Ve£.
Oils '_________________________________________
Butter
;__________________________
Ghee
__________ _________ ___________ _______
Milk
Dial
Meat_________ _ ____________________________
Eggs_____________________
Fish;
Fruits
Coconut
_____
Any special consideration for under 5
eJ&XLzs
COMMUNITY HEALTH CELL
<7/1.(First FioorJGt. Marks noad
BANGALORE - 5(>0 001
AGRICULTURAL LABOURER'S BASIC MEAL.
PREPARED BY
MISS.T.PADMASINI ASURI.
MISS.TARA IYYAKKU.
OFFICE OF THE REGIONAL HOME ECONOMIST, BANGALORE
IN TRORUCT I U N
The AgricuTtural Labourers normally get their wages,
either by daily or weekly payment.
This inhibits their bulk
purchases and invariably they do not marage their money in
order that they may have adequate food essential for their
maintenance of health, throughout the month.
These agri
cultural labourers whese money income is low, have to learn
to use cheaper substitutes and millets in their diet.
The
f
Menu suggested is only a model one, as it depends upon the
taste and food habit of the people.
However, an attempt has
been made to plan a basic diet for the landless labourers wh»
could get the esseivtial-jnuti^ient^''fcverr^hough^ the diet may
not be so balanced as per the ICMR itandardsbeing a constraint these labourers and their families sheuld be
educated to use different millets and rot try for cereals like
rice or wheat which are of prohibitive prices.
This is an
attempt to see that the nutrients are made available at a lower
cost for landless labouers.
MENU No, 1 (For Lunch & Dinner)
Jowar Roti
Horsegram Curry
Amaranthus - groundnut dry vegetable
Ingredients
Quantity
1 owar
Horsegram
Groundnut
Leafy vegetables
Onion '
Oil
Jaggery
Season ir.gs
400 g
.50 g
10 g
70 g
50 g
Protein EalojLig^C^Qteae_.Cos±,
58.6g
2000
4106 ug Pa. 1.46
NOTE: in place of field beans, any other wholck_graa.
MENU
H .(Foy. Lunch and Dinner)
Jowar Hoti
Fieldbcan - amaranthus curry
Groundnut - Onion chutney
Ingred ients
low ar
Field bean
Groundnuts
Leafy vegetables
Onion Oil
■J aggery
Season ings
Man tit y
400 g
30 g
20 g
70 g
50 g
30 3
20 g
Protein
Cost
Rs. 1.40
■Calorics
Carotene
’
Hl"
-MENU
Lunch
~1!inner
Jowqr Roti
Bengalgram boiledOn ion-tamarind sausc
Ingrod iepts .
.. ., .
Bajra
low ar
.
................
Bengalgram
Gr oun.dn ut
Leafy vegetables
Jaggery
P ot ato
Season ings
Bajra.Roti. .
Lo,afy vegetables with
potato.
. On ion-tamarind sauce.
.. . -fejrtity, ■■
Protein, ■ -
200 g
200. g. .
50 g
10 g
■70 g
■ 30. g.
20 g .
50 g
50.7 g
. -.
-
Cost
Rs. 1.44 .
-?Ual-oricsj?«ortex>g
2110
.
.
. -.
4287 ug
• •-■ •
MENU No. IV(For Lunch
I?Inner)
Jowar Hoti
Field bean onion curry
Leafy vegetable - Bengalgramdhal pugath
Ingredients
Quantity
Protein
Calroes
Carotene
J owar
Field boan
Groundnuts
Leafy vegetables
Onion
Oil
J aggery
.-Seasonings
400 g
30fcg
PO g
70 g
50 g
30 g
26 g
57.7 g
2C1<>
4070 ug
Cost
Rs.l. 45
—
MENU NO.V (For.Lunch ft Pinner)
Wheat Roti
Leafy-vegetable horsegram curry
Potato-onion vegetable with groundnuts.
Ingred ien ts
Quantity
Wheat
Horsegram
Groundnuts
Leafy vegetables
400 g
50 g
10 g
70 g
.30 g
20 g
Jaggery
SolSBr Ings
Seasonings
50 g
protein
65.4 g
Post
Rs. 1.40
Calories
Carot epe
1950
4034 pg
KBJU No. Vi
Dinner
Lynch
J owar Roti
Field bean - leafy vegetable dry
vegetable.
Wheat chapathy
Groundnut curry
Ingredients
Quantity
Protein
Calories
Carotene
Wheat
J owar
Field bean
Groundnuts
Leafy vegetables
On ion
Oil
Jaggery
Season ings
200 g
200 g
30 g
20 g
70 g
50 g
30 g
20 g
64.5 g
2000
40C0 PS
Cost
Rs. 1.41
■
MENU
NO. VII
Binrer
lunch
■Jjgieat Roti
vegetable )
J?ieldbean curry )
Bajra Roti
Horsegram chutney
Ingrad ients
Quantjt y
Wheat
Baj ra
Field, beah
Horsegram
Leafy vegetables
Onion.
Oil
Jaggery
Seas or1 Ing's
200 g
200 g
30 g
20 g
70 g
50 g
30 g
20 g
Protoin
Calories
Caroten e
61.0 g
1950
4012 /•«?
I
Cost
Ps.1.40
n
MENU VIII
Dinner
Lunch
Ragi balls
Horsegram leafy vegetables
Curry
Jowar Roti
Groundnut onion chutney
Ingred icnts
Quantit y
Protein
Calories
Carotene
Ragi
J owar
Horsegram
Groundnuts
Leafy vegetables
On ion
Oil
Jaggexy
■Seasonings
200 g
200 g
30 g
20 g
70 g
50 g
30 g
20 g
50.0g
2018
4063 |ug
Rs. 1. 44
MENU NO, IxCffor Lunch # Dinner')
Ragi balls
Fieldbean - onion curry
.Amaranth - groundnuts dry vegetable
Ingredients
Quantity
Protein
Ragi
Field beans
Groundnuts
Leafy vegetables
Onion
Oil
<T aggory
Seasonings
400 g
50 g
10 g
70 g
50 g
30 g
20 g
47.1 g
Cost
Rs. 1.48
Calories .Carotene
1981
403 2 pig
Io
,.y? liable
M ethod
■Juan tit y
AmaranthMS
Groundr uts
fill
fin ion
Curry leaves
Mustard
Blackgram dhal
Water
70g/l cup chopped
20g/6 std.sp.
10g/3 std.sp.
half of a medium
sized one/50 g
a sprig
i std.sp.
i std. sp.
6 std. «.sp./30 ml.
1. Cipan & chop amajarrthus
2.Roast groundnuts, remove
skin and
coarsely
(a peanut grinder can be
used)
3.Chop onion and green
chillies.
4. Prepare seasonings with
on in on, green chillies,
blackgramdhal an^1 mustard
and curry leaves.
5. Add chopped amaranthus,
water and cook till done.
6.Add salt ard stir.
7. Add groundnut powder and
mix well.
2/5 std.cup
Volume of the product
Number of serving
Protein • Calories Calcium Iron Carotene Vlt.. R1 Vit.B2 Vit. C Cost
(g)
(mg)
(mg)
(ug)
(mg)
(mg)
(mg)
(Ps)
3. ffi
8.0
254
312
19
3872
0.24
0.24
72
33
vegetable
2.
(ingredients
■Altar &n thus
Bheld beans
Onion
l.Soak field ’
cd water
cook in double tn? vo.ujjae of
(includ ing tr£,soaking
.3/1
Curry leaves
Blackgram dhal
Croon chillies
Salt
Water
Oil
of a medium.
sized one
k sprig .
5 i std.sp.
2
i std.sp.
1/5 std.cup
10g/3 std.sp.
water)This takes .gJXkit 20-30
miputes.
2.Clean and cut a®ananthus.
3.prepare seasonings with,,
onion, greer chillies; 'slack
gram dhal, mustard and cuTT,y
leaves.
4.To thia add the chopped
amaranthus and the remaining
water and
for- app.roxi=^
fflatcly 10 -minuc-os..
5.
Add the cooked gram to this
and continue cooking-till the
preparation is dry.
Volume of the preparation
Number of servings -
- 4/5 cup
Cne
Nutritive value ^and, cost nor serving:
Protein Calories Calcium-Iron..Garoiene Vit.Bl Vit.B2 Wit. O' Cost
(g)
(mg)
(mg).
Xug£
(mg)
(mg)—-(mg).. (Ps)
10.0
361
2S4
18.0
3864
C.l
O.?2
72
3.
~l-r ound n pt. On lor. phutnayr
Ingred ients--------- Quant it y
Groundnuts
Onion
■Green chillies
Salt
Tamarind
Jaggery
Oil
Water
20g30g/i of a
small
4
i std.sp.
5 g
5 g
li st.sp./5g
15ml/3 std.sp.
Method
1. Roast groundnuts
2. Chop onion and green chillies
3. Grind all the ingredients,
except oil to a fine paste
4. Add. oil to the ground paste and
mix well.
Volume of the product
- 1/5 std.cup
Number of servings - one
Nutritive value and cost per serving:
Protein Calories Calcium Iron Carotene Vit.Bl Vit.B2 Vit.O Cost
(g)
(mg)
(mg)
(a,.)
(mg)
(mg)
(mg)
(Ps)
5.2
174
30
C.22
0.04
-
26
4^^010 gram - .Pniop Currr^.
,£lgntity
-.-field beans
'Onion
Red chillies
Coriander seeds
Fenugreek seeds
Bengalgram dhal
Tamarind
1041
Water
50g
t of ,a small
sized onion/30g
5 g ‘
10g/5 std.sp.
2g/f std.sp.
10g/2 std.sp.
10g/cnc amla
size
20 g
750 ml.
$gS&2d
1.Soak fieldheans p?SiWight in
thrice its voliVte of water.
2.
Cock it till soft(approximately
20-30 minutes)
3.Roast bengalgram dhal, coriander
seeds, fenugreek and red. chllktes
4.Grind this masala using 100 ml.
of water to fine paste.
5.Soak tamarind in 100 ml. of
water and prepare tamarind
extract.
6.Slice onion
7.Prepare seasonings using onien
and muste.rd in oil
8.
Add tamarind extract to them
and allow to boil for a few mor®.
minutes.
9.To this add the ground masala,
cooked field beans and salt and
allowed to boil for 10-<L5 minutes
10.Removed from the fire.
Total - volume
- 2-2/5 std.cnp
Number of serving - one
Protein Calories Calcium Iroir-Carotene Vit.Bl Vit.B2 Vit.C
(g)
(mg)
(mg)
(mg)
(mg)
(mg)
12.5
368
■
44
l./t
-
0705"------ 3__
Cost
(ps)
33
5. AfflaraHtjh.us - Oniftp Cuitry
.SlgredJ^tg
.Quantity
Am ar asr an thus
*70&/l cup
Method
1.Clean and chop amaranthus
2.Slice onion
(chopp ed) ■
3.Soak tamarind in 50 ml.
T of a small
of water
onion 30^
ft.Prepare season irgs using
S g
mustard and curry leaves
t std.sp.
i std.sp.
5.To this, add the cut
amaranthus, onion and water
T std•sp.
and boil for approximately
10g/3 std.sp
5 £
IQminutes.
150 ml./3/5 std.cup 6. Add tamarind juice, salt and
1 std.sp.
chillie powder and bring it
to boil for few minutes.
7. Add jaggery powder to this
and remove from the fire.
(This is optional)
On ion
Tamarind
Ghillie powder
Mustard
Blackgramdhal
Oil
1aggery
Water
Salt
one std. cup
Total volume of the product
Number of servings - one
Nutritive value and cost per serving;
Protein Calories Calcium iron Career e Vii^Bl Vit J32
.s'
*
2
' 152 ’
'
*
288' 18.56
3664
0.04
0.20
0-o^t
72
30
6- M2^e££^Sl_^Us.8.1i
Ingredients
Quafltity
Field beans
On ion
Green chillies
Oil
Water
Salt
1. Soak field bdans overnight in
thrice the voli me of water
2. Cock it till soft.
3. Add salt and mix
0 g
150 ml.
4. Prepare seasonings with oni'Ti and
i std. s p.
green chillies in oil. g
5. Add the cooked grams to the
seasonings and mix well.
Method
30 g
20 g-
Total volume of the product
- 2/5 std.cup
dumber of servings - One
Nutritive value anj cost per seryine;
Protein Calories Calcium Iron Carotene Vit.Sl Vit. P>2 VictC Cost
(Ps)
(mg)
(mg)
(mg)
(ug) • (mg)
(g)
(mg)
7.5
194
18
0.8
0.16
NSTE: ]h place of fieldbeans either bengalgram
can be used.
0.05
-
or hers eg ram
18
7. Amaran’t'h,
jnsredients
Quantity
Amaranthus
Field beans
Green chillies
Mustard
Blackgram dhal
Gurry leaves
Oil
Salt
Wared
70 g
3o g
2-3
i std.sp.
& sprig
j> sprig
1S£5x7t’istd - crap
'4 std.sp.
1 std . cup
Gram - Curry
Method
1,Soak field beans overnight and
cook in thrice the volume of
waterXineluding the soaking
water) This takes about
20-30 minutes.
2.Mash the conked gram and
keep aside
3.Prepare seasonings with green
chillies, blackgram dhal,
mustard and curry leaves in oil.
3. Add the cut amaranthus,' salt
and any remaining water ard
till done.
5.Add the mashed■gram and
stir well.
6.
Allow to simmer for a few
■'minutes and remove from the
‘fire.
Volume of the product
Number of serving
- If std.cup
on e
Nutritive value and cost per serving;
Protein Calories Calcium Iron Carotene
(g)
(mg)
(mg)
(jig)
10.3
361
296 .
18.7
3864
(mg)
0.10
Vlt~.B2 Vlt^C Cost
(mg.)
(mg) (ps)
0.25
69
' 30
HERSEGRAM - GREENS QURRT
Ingredients
.tit r
Horsegra®
Leafy vegetabtija.^ *
70 g
Tamarind
5 g
Coriander seeds
2 std.sp.
l?ed chillies
2
Blackgram dhal
1 std.sp.
Mustard
i std.sp.
Curry leaves
a sprig
Oil
10 g/15 ml.
Salt
1 std.sp.
Water
1 std.cup
Method
l.Soak horsegram ov- might ir thrice
the volume of water ard cook till
soft in the soaking water
2. Soak tamarind ir 50 ml. of water ard
extract the juice.
3.Fry coriander seeds, red chillies
and black gram dhal ir t std. spoon
of oil ar;d grind.them to a fine
paste.
4. Cut leafy vegetables and add this'
to the frying par with the seaso^t
Ings.
5.Cook the leafy vegetables a little
longer.
6. Add the tamarind juice and bring it
to toil ard add salt to this.
7.To this add ground masala and
cooked gram.
8. Boil for 5-7 minutes.
Total volume of the product - 4/5 std.cup
9.4
218
371
20.3
3885
0.15
0.28
69
NOTE:- In placeof horsegram other whole grams car also be used.
30
HORSEGRAM - Curr
Tngred ients
Quantity
^Method
56- g
l.Soak horsegram evemJLght and cook
Horsegram
3 g
in thrice the volume of^frater-^ir
-^
*
Tamarind
2
std
.
sp.
eluding the soaking water.
Coriander seeds
2
2. Soak tamarind in 50 ml. of water}
Red chillies
■£• std. sp. and prepare tamarind juice.
Mustard
£ std. sp.3.Fry coriander seeds and chillies
Blackgramdhal
a sprig
. in £ std.spoon of oil and grind
Curry leaves
!• g/15 ml.
them to a fine paste.
Oil
■| std . sp. 4. Prepare seasoning's with blackgram
Salt
1 std.cup
dhal, mustard and curry leaves.
Water
5. Add tamarind juice, bring it to
boil and add salt.
■ 6.To this add ground masala'and .
cooked' gram.
7.Boil for 5-7 minutes.'
letal volume of the product - 3/5 std.cup
Nutritive value, and cost, per serving.;
Protein Calories Caleium Iron Carotene
6.6 g
187
J.3 mg
2.3 mg 21 ug
Cost
2ft ps.
NOTE; in place of horsegrams, other wholegrams can-tIso be used.
CM ION
Ingredients
Quant it y
Onion
< Tamarind
Coriander seeds
• Red chillies
’ Mustard
Blackgramdhal
Curry leaves
Oil
Salt
Water
50 g
3.g
2 std.sp.
2
■£ std. sp.
i std.sp.
a sprig
10g/16 ml.
i std.sp.
1 std.cup
CURRY
Method
1.Saak tamarind in 50 ml. of water and
prepare tamarind juice.
2.F:fy coriand er • seed s and chillies in
std.sp. of oil and grind them to a
fine paste.
3. Chop onion and'fry till golden
brown.
4. Add blackgram dhal, mustard and
curry leaves and prepare seasonings.
5. To this add the tamarind juice
bring it to boil and add salt.
6. Add ground masala to this.
7. Boil for 5-7 minutes.
Total volume of the product - 2/5 std.cup
Nutritive value and cost per serving
Protein
Calories
Cost
115
20
COMMUNITY HCAtTH CELL
•vOa
47/1,(First ’ iuo: M
II.
BALANCED DIETS IN TERMS OF STANDARD CUPS AND SPOONS
The balanced diets for different categories ofpeople are given in terms of standard cups and spoons in
the following table:
Table-1: Balanced Diet for Adult Man(Moderate worker)
Qty
(c)
Approximate
volume in std.
cup and std.
Number
I. CEREALS
1. Rice
2. Wheat flour
335
140
1-3/5
1
30
1/5
6 std. sp.
125
1-4/5
100 !
3/5
2 medium
sized ones
75
1/2
12-15 or a
handful
II. PULSES
1. Redgram dhal
2. Blackgram dhal
HI. GREEN LEAFY VEGETABLE
1. Amaranthus' '
. 3 bundles
IV. Roots and Tubers
Pj^otato
V. OTHER VEGETABLES
Beans
VI. FRUIT
Orange'
30
3 segments.
VII. Milk
200
4/5
VIII. Fats and oils
40
2/5
40
1/5
IX. Sugar & Jaggery
2
= 2 =
Table-II: Balanced Diet for an Adult Women (Moderate-Worker)
_____
_-_==-=.=_
I, CEREAL
1. Rice
2. Wheat
1
230
120
-4/5
II. PULSES
1. Redgram dhal
2, Blackgram d; al
45
25
-1/5
5 std. sp.
125
1-4/5
III. GREEN LEAFY ' -'GET ABLE
Amaranth
3 bundles.
IV. ROOTS AND TUBERS
Fbtato
75
V. OTHER VEGETABLES - Beans
1/2
1
1/2
12-15-/or a
handful.
1
75
VI. FRUITS - Orange
30
VII. Milk
200
4/5
VIII. Fats and Oils
35
1/5
30
6 Std. sp. -
IX. Sugar and Jaggery
3 segments
or a quarter
fruit.
Table-Ill: Additional Al--jwance for Pregnancy and Lactation
Lactation
Pregnancy
Food Stuff
Qty
(g)
Appx.Vol. „ Nd.
in std.cu P.
Qty
(g)
Appx.Vol.
in std.cup
40
60
1/5
2/5
20
2 std.sp.
' ’
I. CEREALS:
Rice
Wheat
i/5
50
-
II. PULSES:
Redgram dhal
III. GREEN LEAFY
VEGETABLE
VI. Milk
V. Fats & Oils
VI. Surer 8 T-'-
2/5
25
125
'
i
3/4 buin-25
dies
■
: 125
15
2/5
3/4bundles
1/2
4 std.sp.
= 3 =
Table - IV: Balanced Diet for a Child between the Age
3-6 years (Ref. - 6 year s old child)
Food Stuff
Qty
(g)
Appx.Vol.in
std. cup
No.
(1)
(2)
(3)
- (-L-
140
60
3/5
2/5
-
.30
15
15
6 std. sp.
3 "
3 "
75
1-1/5 std.cup
I. CEREALS
1. Rice
2. Wheat flour
II. PULSES
1. Redgram dhal
2. Blackgram ahal
3. Other grams
III. GREEN LEAFY VEGETABLE:
Amaranth
!-•£ bundles
IV. SPOTS AND TUBERS
Potato
!!
50
2/5
50
2/5 std.sp.
8-10 in no.
5 segments.
1 medium size
V. OTHER VEGETABLES
Beans
VI. FRUITS
Orange
50
2/5 std.cup.
VII. Milk
250
1
n
VIII. Fats and Oils
25
7
std.sp.
40
8 std. sp.
IX.. Sugar and Jaggery
4
= 4 =
Table - w : Balanced Diet for a Child Between the. Age 1-3 years
==_==_=s|==_=r=_==--=GlS?li=^.^fi.S=-c^UL4yLiifD--=_—^==_==_=_==_
(!' '
"
(2)
' (3)’ " "(4) "
I. CEREALS
1. Rice
2. Wheat
90
60
2/5
2/5
-
25
10
15
5 std.sp.
2 std.sp.
3 std.sp.
-
50
4/5 cup
1 bundle
30
2/5 cup
1 small
30
2/5 cup
5-7 in no.
II. PULSES
1. Redgran dhal
2. Blackgram dhal
3. Greengram dhal
III. GREEN LEAFY VEGETABLES:
Amaranth
IV. ROOTS AND TUBERS
Potato
V. OTHER VEGETA!LES
Beans VI. FRUITS - Orange
50
VII. Milk
300
VIII. Fats and Oils
20
6 std.sp.
30
6 std. sp.
IX. Sugar and Jaggery
ms/18578/*
5 segments
1-1/5
-
’Odfc- 5“00°
0p.w9'
A balanced diet is one that contains the nutrients necessary to main-'-
■ tain good head th. in the right proportions.
In planning, a diet the following points must be take:, into
...
consideration.
1) Total calorie value
2)
Proportion of P.F. CHO. Min, Vit a: .d H^O
Calories must provide the energy to maintain B.’-i’. plus extra
energy required Varies
3)
Age
4)
Sex
5)
Occupation & condition
, pregnancy
a)
b)
sickness
c)
convalescent
’Average adult -72 c/hr.
72 x 24 - 1728/Day
Sedentary 800 r- 900 C
Light (■'drk (Prof. Business) 900 - 1400 C
Moderate work (Mechanic) 14 - 1800 C
Heavy Idbourers/Atheletes 1800 C
BietvP; - varies
2 Veg. P -j- animal ■
.
-£• -1/3 calories (45 - 50 gms)
Fat
CHO'
Bulk. (Normal adult 400 - 500'gms)
’ ICMR recommends the' daily allowance of Protein'as follows:
■
.
■
■
•
.
p/ims
fi Light or sedentary work 2400
2800
Men 55 kg./120 lbs. . jj Moderate work .
3600
jj Very hard- wonk
55
55
55
2000
2300
300
45
45
45
100
110
jj Sedentary work
jj Moderate work.
Women 45 kg./lOO lbs' 5 Very hard work
0 Pregnancy
) Lactation
ITBMS
RICE
(milled)
RICE
(parboiled)
RAGI
MAIZE
Prot
eins
gms
Fats
Cho
gms
Cals
val
ue
Ca
gms
6.8
.5
78.2
345
10 .160 3ii
6
4
*
7.3
nil.
kheat
11.8
WHEAT FLOUR 12.1
RED gram
22.3
BENGAL GRAM 20.8
BLACK GRAM
24
GREEN GRAM
24.5
AGATHI
8.4
BEANS
4
CABBAGE
1.8
CORIANDER
3.3
BEETROOT
1.7
CARROTS
.9
ONIONS
1.2
POTATO
1.6
RADDISH
.7
SHEET POTATO 1.2
YAM
1.4
DOUBLE BEANS 8.3
BRINJALS
1.4
CAULIFLOWER
2.6
CUCUMBER
.4
DRUMSTICKS
2.5
KNOL-KOL
1.1
GOOSE-BERRIES 0.5
TOMATOES
1.-9
COCONUTS
6.8
GROUNDNUTS
26.7
1.1
BANANA
LIME
1.5
EGG
13.3
MUTTON
18.5
SHARK
21.6
BUTTER
0
OIL
0
CONS MILK
3.2
BUFFALO MILK 4.3
BREAD
7.8
CURE
0
SUGAR
0
JAGGARY ■
.4
BUTTERMILK
4.3
.4
1.3
3.6
1.5
1.7
1.7
6
*
5
1.4
1.2
1.4
.5
.1
. .6
.1
.2
0
.1
.1
.1
.3
•3
.4
.1
.1
.2
.1
.1
62.3
40.1
.1
1
13-3
13.3
.4
81
100
4.1
8.8
.7
100
0
.1
8.8
P
Fe
'Fit.
A
I.U.
Thi
ami
ne
mgs
Ribo Nico
fla tinio
vin acid
mgs
0
.09
'.03
1.9
Vit.'C
mgs
0
348
0
.21
79
.9 143 4
0
.09 3.8
72
328
344 283 17.4 70 ..42
.1
0
1.166.2 '342
io:'328 2 1502 ,.42
.1
0
1.4
71.2 346 . 41 306 4.9 108 ,.45
.12 5
0
48 423 11.5 49 •.49
69.4 341
.29 4.3
0
57.6 355
73 304 5.8 220 ..45
0
.51 2.6
.59.8 372. . 56 331 9.1 216 ..48
. 18 2.4
1
59.6 347
154 385 9.1 64 •.42
0
.57 2.
59.9 351
0
75 405 8.5 83 ..72
.15 ■ 2.4
7.8
169
93 1130 80 3.9 9000 ,.21
.09 1.2
46
6.3
.1
1 ' ,
397 83 25.5 9230 ..03
99
' 4.6
.8 2000 ..06 ■ .03 • .4
27
39 44
124
48
7.5
.06
.8
184 62 18.5 31530
x35
8.8
200 55 1 ... " 0 .04 .09
43
88
.4
TZ
10.6
80 30 212 3.50 .04 .02
.6
47
11
180 50 '.7
0 .08 .01
49
11
.4
22.6
10 40 .7
40 .1
97
.01 1.2
17
50 22 .4
.5
3.4
17
5 .06 .02
1J
28.2 120
20 50 .8
10 .08 .04
.7
24 x
26
111
60 20 1.3
130 .07 0
0
.7
40 140 2.3
12.3
85
220 0
0
0
22
18 47 .9
24
124 .04 .11
4
12
.9
4
30
1
33 57 1.5
51 .04 .1
' 56
10 25 1.5
2.5
0 .03 .01
13
.2
7
26
30 110 5.3
3.7
.2
184 .05 .07
120
3-8
20 35 .4
27
36 .05 • 09
.5
85
58
50 20 1.2
13-7
600
15 5.3 ’ .01 .02
3.6
20 36 1.8
320 .07 .01
23
.4
31
661
400 210 2.7
0 .08 .06
.6
80.4
7
50 390 1.6
20.3
549
0
63 .9 .3 :14.1
10 30 .25
24.7
104
6
124 .04 .17
.3
90 20 .3
0 0
10.9
0
0
26
69
0
60 220 2.1 :1200 1000 .3
.1
173
0
0
115 150 —
194
0
31 .18 .27 6.8
0
90
0
0
143 175 1.3
0 2.5
0
6
0
0 0
:2500
0
0
729
0
0
0
900
0
0 0
0
0
0
0
0
150
4.4
67
149 96 .2
.1
15
.05 .18
210 130 .2
118
5.1
160
.1
.04 .1
3
11 0 1.1
0
0
51.9
*07
245
0
.7
0
900
0
0 900 900
900. 0
0
0
o
100
398
0
0
0
0
0
0
0
.08 .04 11
280
.02 - 0
95
383
1
0
4
*
118
210
0
.2 160
0 . 0
5.1
.1
3
C. . MUNiTY HEALTH CELL
,
-,:,oor)St. Marks Road
C.'.E-5COOO1
balanced diets for adult man
Moderate work
Sedendary work
Heavy work
vegetarian I N onve getarian 1 Vegetarian > Nonvegetarian; Vegetarian i Nonvegetarian
Cereals
Pulses
Green leafy vegetables
Other vegetables
Roots and tubers
Fruits
Milk
Fats and oils
Meat and fish
Egg
Sugar and jaggery
Groundnuts
*An additional
KG1661976
1
i
(gm)
:
(go)
400
70
100
75
75
30
200.
35
—
!
400
:
I
100
75
75
30
100
40
30
30
30
30
~
’
'
■
!
i
I
i
(gm)
(gm)
475
80
125
75
100
30
. 200
40
—
40
475
65
125
75
■100
30
100
40
30
30
40
i
i
:
(gm)
(gm)
!
1
1
!
■
650
80
125
100
100
30
200
50
1
!
!
|
:
>
■
1
55
*
50
:
i
■
!
30 gm. of fats and oils can be included in the diet in place of groundnuts.
650
65
125
100
100
30
100
50
30
30 .
55
*
50
■
BALANCED DIETS FOR ADULT WOMEN
Additional allowances
Moderate work
Heavy work
______ during___________
Veget- ;Non-vego- jVeget- Non-vegc— ■ Veget iNon-vege- ; Pregnancy | Lactation
"arian • tarian
arian tarian
arian i tarian
!
(gm)
(gm)
■ (gm)
(gm)
(gm)
I (gm) I (gm)
; (grn)
. ....
—1 — —. —- •-*■
~~ — — I —
. — —
■’ - —..... —■ .... .
—- —
: 300 ; 300
350
■ 350
50 •
100
i 475 j 475
—
. 60 ; 45
i 70
10
i 70
55
55
! 125
. 125 i 125
. 125
125
■ 125
25
25
i _
: 100
75 ' 75
■ 75
i 130
75
—
I 100
50 ! 50
i 100
75
75
I
.50
! I 30
’ 30
:
30
• 30 i 30
125
■ 200 , 100
■ 200
100
i 200
j 125
' 1
I 100
i
45
30
i
40
■ 40
35
; 35
15
•! 30
! 40
: 50
1
20
i 30
i
30
■ 40
10
’ —
. —
—
1 —
! 30
,
■
30
i 50
1 —
. 1 —
—
! 30
30
50
| 40
*
; 40
*
■ 1 • -
Sedendary work ■
—- — — — — —
Cereals
Pulses
Green leafy vegetables
Other vegetables
Roots and tubers
Fruits
Milk
Pats and oils
Sugar and jaggery
Meat and fish
Eggs
Ground nuts
*An additional 25 gin. of fats and oils can bo included in the diet in place of groundnuts
K01661976
BALANCED DIETS FOR CHILDREN
School children
Pre-school Children
4-6 years
1-3 years
Veget
arian
(gm)
Cereals
Pulses
Green leafy vegetables
Other vegetables J
Roots and tubers J
Fruits
Milk
Fats and oils
Meat and fish
5
Eggs
5
Sugar and jaggery
KG1661976
150
50
50
Non-vege~| •Veget
tarian
1 arian
(gm)
! (gm)
150
40
50
1 200
'60
75
7-9 years
Non-vegetarian
(gm)
200
50
75
Veget- | Non-vege-
|
10-12 years
ai’isn
(gm)
tarian
(gm)
Veget- | Non-vege
arian 1 tarian
(gm)
(gm)
250
70
75
250
60
75
1 320
70
100
320
60
100
.75
30
30
50
50
50
50
75
50
.300
20
50
200
20
50
250
25
50
200
25
50
250
30
50
200
30
50
250
35
30
-
30
-
30
40
40
50
30
50
-
30
1
50-
1
i
50
200
35
-A
.0
1_ !°_ _
BALANCED DIETS FOR ADOLESCENT BOYS AND GIRLS
BOYS
15-15 years
Jifegetar:Lan
(gm)
Cereals
Pulses
Green leafy vegetables
Other vegetables
Roots and tubers
Fruits
Milk
Fats and oils
Meat and fish
Eggs
Sugar and jaggery
Groundnuts
i
430
70
100
75
75
30
250
35
—
-
i 50
(Non-vegetarian
i
(gm)
|
1
i
1
430
50
100
75
75
30
150
40
30
30
50
GIRL s
1
16-18 years
13-18 years
i Vegetarian ;Nonvegetarian i Vegetarian i Nonvegetarian
'
(gm)
(gm)
i
(gm)
;
(gm)
450
70
100
75
100
30
250
45
1
■
40
*
50
1
;
i
i
!
1
;
350
50
100
75
100
30
150
50
30
50
40
*
50
1
i
i
!
1
1
1
i
|
*An additional JO gm of fats and oils can be included in the diet in place of groundnuts.
KG-,661976
350
70
150
75
75 '
30
250
35
—
30
i
!
i
I
!
;
•
350
50
150
75
75
30
150
40
30
30
30
adultrat ion
of
foods
Adulteration of foods consists of a large number of
practices -mixing, substitution, abstraction, concealing the
quality, putting up decomposed foods for salej misbranding or
giving false labels and addition of poisons. Some forms of
adulteration are injurious to health, e.g. adulteration of
mustard oil with argemone oil. But for th? most part, food
adulteration has an economic rather than a sanitary significance,
e.g. addition of water to milk.
Food adulteration practices vary from one part of the
coun-ry to another, and from time to time-. Our knowledge about the
curreht practices of food adulteration is meagre. The types of
adulteration commonly found in various foodstuffs in India are as
follov/s :
(1) Milk: Perhaps no other food is subjected to such frequent
adulteration as milk. Addition of water, removal of cream, and
addition of starch, paper pulp and skim-mi..k powder are the
common types of milk adulteration
(2)
GheS: Ghee is adulterated with vanaspathi and animal fats
such a* pig's fat.
Ih order to improve the flavour of adulterated
ghee, tributyrin is added. The Government of India have not
succeeded in enforcing the colouring of vegetable ghee.
(3)
Cereals: Rice and wheat are mixed with stones, sand, grit and
mud to increase bulk
(4)
Flours: Wheat flour is mixed with soap stone (talc) powder
and chalk powder. Bengal gram (Besan) flour is adulterated with
lathyrus flour.
Maida is adulterated with singhada flour.
(5)
Pulses: Pulses are adulterated with lathyrus» Chemical
substances such as metanil yellow are added to old stocks of pulses
to"improve the colour and appearance.
(6)
Edible oils: Admixture of cheaper *
oil
and mineral oils is
commonly practised. Dyes are also added t 1 improve the appearance.
Argemone oil is another intentional adulterant.
(
(7)
Tea and Coffee: Tea leaves are adulterated with exhausted old
tea leaves and dust, black gram husk, saw dust and cashew husk.
Coffe-e powder is adulterated with roasted dates, tamarind seeds,
husk powder, added colour and chicory without declaration.
(8)
Honey: Honey is adulterated with sugar or jaggery and
boiled with empty beehives. The list is endless
Food Standards:
■ (1) Codex Alimentarius: This is a collection of
international food standards prepared by the Codex ZJLimentarius
Commission, which is the principal organ of the Joint FAO/WHO
Food Standards Programme. The food standards in India are based on
the international codex alimentarius (2) P~A Standards:’ Under the
prevention of Food Adulteration Act (1954) rules have been framed.
These are revised from time to time by an -.Xpert body called the
"Central Committee for Food Standards". Any food that does not
confirm to the minimum standards is said t.) be adulterate: .
3
The use of foot4 additives is subiected to government ’
regulation throughout the world.
In Indial two reoulations, viz.
n4?3e?reXentloPuof F?or’ Adulteration Act and the Fru?t Products
Order govern the rules anr regulations of food additives. Any
fooc that contains fooc1 acY'itives that arc not ocrmitted is
considered adulterated; if the permissible- limit exceeds, then
also the food is considered adulterated; The nature and quantity
of the ac’c-itive shall be clearly printer1 on the lable to be
affixed to the container. Whenever, any extraneous colouring
matter has been added to any article- of fox’, the words 'Artificially
Coloured' shall be written on the label. At the international
level, food standards arc fixed by the codex alimentarius
commission.
FOOD FOFTIFICATION
The 8th Joint FAO/WHO Expert Committee on Nutrition
(1971)
defined fortification as "the process whereby nutrients are
added to foods to maintain or improve the quality of the diet of a
group, a community or a population". On the other hand, the word
enrichment is used to signify the addition of dietary essentials
to a food to restore the total content of the former. The
following are some examples: (1) Milk: Milk is fortified by the
addition of vitamins A and D (2) Wheat flour:
In February 1970,
the Government of India launched a programme in Bombay for
fortification of atta with vitamins and minerals, and for■increasing
the protein content by admixture with edible groundnut flour.
This programme is planned to be extended to other cities at a later
date.
(3) Edible oils: Fortification of "vanaspathi" (hydrogenated
fat) with vitamin A has been made compulsory (2,500 i.u. of vitamin
A and 175 i.u. vitamin D per LOO g of vanaspathi) by the Government of
India.
(4) Common salt: Common salt is fortified with potassium
iodate and supplied in areas where goitre is endemic.
Fortification
of common salt with calcium and iron is being considered to be taken
up on a national scale in India(5) Synthetic amino acids:
Addition of synthetic amino acids to foods offers great possibilities
for the future, e.g., lysine to wheat flour. (6) Sugar: fortified
with vitamin A is being used in some countries for the prevention
of nutritional blindness.
Fortification and enrichment have made
tremendous contributions to 'the public health in improving the •
nutritional standards of the people and in correcting specific
deficiency states.
SOURCE: FREVENTIVE & SOCIAL MEFICINE
/l/2/1980/
*
ms
3-4<>
COMMUNITY HEALTH CELL.
47/1,(First FloorJSt. Marks Hoad
BANGAlOKE ■ 5iiu 001
. o
(J‘
THS PFWHTTjGK CF'FOOM
ADULTEPATia’ ACT, 1954
(Act 37 of 1Q54)
This Act to make nroirisi on for the prevention of adulteration
of food was enacted by the Indian Parliament in 1954
*
It extends to the
whole of India except the State of Jammu & Kashmir and supersedes all
Food Laws that were passed by individual States in their own territories.
It came into force in May, 1955.
An attempt.has been made under this Act to make the provisions
uniform, broadbased and more deterrant and to remove some of the lacunae
that were found in the existing Food Laws and Pye-laws of the different
States and local bodies.
Sane of the important Sections are summarised below
Section 2. Definitions
(l)
adulterated -
"Adulterated"- an article of food shall, be deemed to be
(a) if the article sold by a vendor is not of the nature, substance or
quality demanded by the purchaser and is to his prejudice, or is not of the
nature, substance or quality which it purports or is represented to be;
(b) if the article contains any other substance which affects, or if the
article is so processed as to affect injuriously the nature, substance
or quality thereof;
(c)
if any inferior or cheaper substance has been substituted wholly or in
part for the article so as to affect injuriously the nature, substance
•r quality thereof;
(d)
if any constituent of the article has been substituted wholly or in part
abstracted so as to affect injuriously the nature, substance or quality
thereof;
(e)
if the article had been prepared, packed or kept under insanitary
conditions whereby it has become contaminated or injurious to health;
(f)
if the article consists wholly or in part of any filthy putrid, disgusting-,
rotten, decomposed or diseased animal or vegetable substance or is
infested or is otherwise unfit for human consumption;
(g)
(h)
if the article is obtained from a diseased animal;
if the article contains any noisonous or other ingredient which renders
it injurious to health;
■ (i) if the container of the article is composed, whether wholly or in part,
of any poisonous or deleterious substance which renders its contents
injurious to health;
(j)
if any colouring matter other than that prescribed in respect thereof
and in amounts not within the prescribed limits of variability is
present in the article;
(k)
if the article contains any prohibited preservative or nermitted
preservative in excess of the nrescribed limits;
(1)
if the quality or purity of the article falls b^low the prescribed
standard or its constituents are present in quantities which are in
excess of the nrescribed limits of variability.
. ......... 2/-
(V)
"Food" moans any article used as food or dfirik for human
consumption other than drugs and water and includes;
(a) any article which ordinarily enters into, or is used in the composition
or preparation of human food, and
(b) any flavouring matter or condiments.
(IX)
"Misbranded"- an article of food.'shall be deemed to be misbranded -
(a) if it is an imitation of, or is a substitut? for, or resembles in a'manner
likely to deceive, another article r>.° food -.-ndo’- the name of which it is
said, and is not plainly and conspicuously libelled so ar. to indicate its
true character:,
(b) if it is falsely stated to be the product c1' any place or country;
(c)
(d)
(e)
if it is sold by a name which belongs to another article of food;
if it is so coloured, flavoured or coated, r owdered or polished that the
fact that the article is damaged is concealed or if the article is made
to appear better or of greater value than it really is;
ifalse claims are made for it upon the label or other;
(f)
if, when sold in packages which have been sealed or prepared by or. at the
instance of the manufacturer or .producer and which bear his name and
address, the contents of each package are not conspicuously and correctly
stated on the outside thereof within the limits of variability prescribed
under this Act;
(g)
if the package containing it, or the label on the package bears any
statement, design or device regarding the ingredients or the substances
contained therein, which is false or misl’a.-’i-ng in any material particular;
or if the package is otherwise deceptive with;respect to its contents;
(h)
if the package containing it. or the label on the package bear the name of
a fictitious individual or comnany as the manufacturer, or producer of the
article;
•
(i)
if it purports’to be, or is represented as being, for special dietary uses,
unless its label bears such information as may be prescribed, concerning
its vitamin, mineral, or other dietary nroo'-rti-s in orJer sufficiently
to inform its purchaser as to its value for such uses;
(j)
if it contains any artificial flavouring, a -t?finial colouring or
chemical preservative, without a’declarator r label stating that fact
or in contravention of the .requirements of ;his Act or rules made
thereunder.
(k)
if it is not labelled in accordance with the requirements of this Act
or rules made thereunder.
Section 3. The Central Govt, to constitute a Central’"ommittee for
Food Standards withD.G;H.S. ex-o^icio as Chairman and Director of Central
Food Laboratory, ex-officio member and the foil nwing members nominated by the
Central GAvemment-twt' exports, one representative each of th: Central
Ministries of Fdod and Agriculture, Commerce and. Industry, Railways and
Defence, two representatives from Union Territories, two" representatives «f
industry and commerce. Besides these, each State nominates one representative
and the Indian Council of Medical Research nominates a representative of
the medical profession.
Section 4. Th. Central Gpvt. to establish a. Central Food
Laboratory, and after consultation with the Central Ccximiittne make rules
regarding the functions of the Central Food Jal oratory. The object «f these
two sections is to bring about uniformity of Food Standards throughout the
country and to maintain a satisfactory standard of laboratory practices in
the different State.-.
....3/.
: 3 :
Prohibition of certain articles of foot1 into India.
Section
any adulterated food ;
any misbranded food ;
any article of food for the import of which a licence is;.
prescribed, except in accordance vrith the conditi ons of the
licence; and
(iv)
any article ,«f food in contravention of any other provision of
this Act or 'of any rule made thereunder.
(i)
(ii)
(iii)
Section 7. Prohibition of manufacturej sale, etc.., of certain
articles of food. No person shall himself or by any person on his behalf
manufacture for sale, or store, sell or distribute -
any adulterated food ;
anv misbranded food ;
any article of food for the sale of which a licence is prescribed,
except in accordance, with the conditions of the licence ;
(iv)
any article of food the sale of which is for the time being
prohibited by the Food (Health) Authority in the interest of
public health ; or
(v)
any article of food in contravention of any other provision of this
this Act or any rule made thereunder.
(i)
(ii)
(iii)
Section 8. The Central or State Govt, to appoint Public Analysis
and define their jurisdiction.
Section 9. The Central or State Govt, to appoint Food Inspectors
who shall be deemed to be public servants within the meaning of the section
21 I.P.O. thereby having definite rights and responsibilities.
Section 1C. (l) A food inspector shall have power
(a)
to take samples of anv article of -food.
to send such samnle for analysis to the public analysts.
with the previous approval of the health officer having
jurisdiction in the local area concerned, or with the
previous approval of the Food (Health) Authority, t* prohibit
the sale of any arti.?’■.-! of -bed in the interest of public health.
(£) Any food inspector may' enter and inspect any place where any
articl 1 of food is manufactured, stored or exnosed for. sale and
take .samplers of such articles of <p.
*d I for analysis.
r
(4) A foqd inspector may seize and carry aw'-v or keep in safe custody
•f the vendor with a bond, if any article intended for food.
appears to be adulterated or misbranded..
(6) Any materi.'1 apparently of a kind which may be employed for
purpose of adulteration may be.seized by the food inspector and
if necessary, a sample submitted, for .analysis to a nublic analyst.
(7) Where the food inspector takes any ac+ion under clause (a; of
sub-section 1), sub-section (2), sub-section ( j.) .or sub-section
(6), he shall call one or pen p>- sons •*0 '-e present at tho
time when such acti- n is taken and take bls or their signatures.
Section 11. (l) When a food inspector takes a sample of food for
analysis, he shall
(a)
give notice in writing then and there of his intention to have it so
analysed to the person from whom he has taken the sample :
(>) except in special cases provided by rules under this Act senarate the
sample then and there into three parts and nark and seal or fasten up
each part in such a manner as its nature permits ; and
‘(c) (i) deliver one of the parts to the person from whom the sample was
taken;
.(ii) send another part for analysis to thepublic analyst; and
(iii) retain the' third -part for production in case any legal proceedings are
taken or for analysis by the Director of the Central Wood Laboratory
under sub-section (2) of section 13, as the case may be.
Section 12. A purchaser may have food analvsed by. giving notice to ■ '
the vendor of his intention to have the same analysed; if, on analysis, the
article is found to be adulterated, the fete paid by him for analysis will be
refunded to him and the vendor will be.dealt with according to law.
Section 15. The Central Government or the State Govt. may, by
notification in the Official Gazette, require medical practitioners carrying
on their profession in any local area specified in the notification to report ,
all occurences of food poisoning coming within their cognizance to such officer
as may be. specified in the notification.
Section 16 to 20. Penalties : If any person whether by himself or
by any other person on his behalf (a) contravenes Sec. 5 »r 7, or (b) prevents
a food inspector from taking samples for analysis or (c) obstructs the food
inspector in the discharge of his duties or (d) being a manufacturer has any
material, that can be used for adulteration in his possession or in one of his
premises, or e) uses any report or certificate of a test issued by the Director
of Central Food Laboratory for advertising or (f) gives a false warranty to the
purchaser in, writing in respect of any food seld by him, .he shall bo punishable.
He shall, in addition to the penalty to which he may be liable under
the provisions of section 1, be punishable with imprisonment for a term which
shall not be less than six months but which may extend to six years, and with
fine whiqji shall not bo les-- than one thousand rupees. There are other
provisions also.
If ary person convicted of an offence under this Act commits a like
offence afterwards, it shall be lawful "’or the court before which the second or
subsequent conviction t akes place to c’ane.el the licence and to cause the
offender's name and place of residence, uhe offence and the penalty imposed
to be published at the offender's expense in such newspapers’ or in such other
manner as the court may direct. The expenses of such publication shall bo
deemed to be part of the cost attending the conyieticn and shall be recoverable
on the same manner as a fine.
No court inferior to that of r Presidency Magistrate or a Magistrate
of the first class shall try any offenc-> under ‘he Act.
Section 23. The Central Govt., may after consultation with the
Committee and subject to the conditions of previous publication, make rules:
: 5 s
(a) specifying the articles of food or classes of food for the imnort of which
a licence is reouired and prescribing the form and conditions of such licence
the authority empowered to issue the same and the fees payable therefor;
(b)
defining the standards of quality for, and fixing the limits of variability
permissible in respect of any article of food ;
(c)
laying down special provision for innosing' rigorous control carer the
production, distribution and sale of any article or class of articles of
food and other rules for proper inn’’orientation of the Act.
Section 24. The State Government may also make rules in the same way
as above in matters not falling within the nurview of sect?.on 233-
THE PP’TATEPTION OF FOOD
ADULTERATION RULES, 1955
In exercise, of the powers conferred under the Act, the Central
Government after consultation with the Central Committee of the Food Standards
have made the following rules.
These cover the definitions and standards of quality of various
articles of food as also definite directives regarding the Central Food
Laboratories> Public Analysts and Food Inspectors, packing, sealing and
despatch of samples, conditions for sale and licence, colouring matter and
preservatives, anti-oxidants, emulsifying, stabilising and flavouring agents.
Standards of Quality of food are given be!ow:
The standards of some food items
A.OS Coffee A.0801 (l) Coffee (green, raw or r.nroasted) means the seed of
goffea arabica, Coffee liberica.
Joffea robusta, freed from all
but a small portion of its snermodera by decortication.
(2)
Roasted Coffee means the properly, cl aned green coffee which
has been roasted to a-brown colqui and has developed its
characteristic aroma.
(3)
Ground coffee means the powdered product obtained-from
'roasted coffee1 only and shall bo free frqpi husk.
(4)
Coffee (green, raw or unroasted-), ‘roasted coffho( and
. 'ground coffee' Shall be free from any artificial colouring,
flavouring, facing, extraneous matter or glazing substance and
shall be in sound, dry and frosh condition free from rancid or
obnoxious flavour.
(5)
Coffee (green, raw or unroastad), 'roasted coffee1 and
'ground coffee^ shall confor-. to the following analytical
standards «
o >
(i) Total ash (determined on the sample dried to constant weight
at 100 C), shall 1c feathery white or bluish white in colour and shall be
not less tha.n 3.5 per cent and not more than 5-0 nor cent by we- ght of which
not less than 65 nor cent she’llbet soluble in boiling distilled :ater. The
ash insoluble in hot dilute HC1 shall be not more than O.i per cent.
(ii)
The alkalinity o” the soluble ash no?’ gram., of dried coffee
shall be equivalent to not loss -"-an 3-4 ml. and not more than 4.4 of N/lO
acid.
6A
: 6 :
(iii)
Tho caffeine content, as obtained by standard methods, shall be
not 3ess than 1.0 per cent.
(iv)
The aqueous extract determined by extraction of 2 grams of the
sample direct to constant weight at 100°C with 100 mli of boiling distilled
water for one hour under reflux shall bo not less than 25 per cent and not
more than 32 pc1" cent.
A.11 Milk and Milk Products.
A.11.01 Milk means the normal clean and froch secretion obtained by
complete milkinc: of tho udder of a healthy cow, buffalo, goat or sheep during
the period following at least 72 hours after calving or unt-’l colostrum free
whether such secretion has been processed or not.
The standards prescribed for milk shal1 amply for boiled milk also.
A.11.01.01 Cow milk shall contain not loss than 3-5 per cent of
milk fat, except in Orissa, where it shall be not less than 3 per cont and in
Punjab and PEPSU whore it shall be not less than 4.0 per cent. Tho milk solids
other than milk fat, shall bo not less than 8.5 per cent.
’
.
A.11.01.02 Buffalo milk shall contain not less than 5.0 per cent
of milk fat except in Delhi, Punjab, PBPSTJ, Uttar Pradesh, Bihar, West Bengal,
Assam, Bombay and Saurashtra where it shall not be less than 6 per cent. The
milk solids other than milk fat, shall be not less than 9 per cent.
A.11.01.03 Goat or Sheen milk shall contain not less + han 3.0 per cent
of milk fat except in Madhya Pradesh, Punjab, pEPSU, Bombay, Uttar Pradesh,
and^Travancore-Cochin where it shall bo not loss than 3.5 per cent. The milk
solids other than milk fat, shall, be not i«sn than 9 nor cone.
Where milk, other than skrnmne milk, is sold or offered for sale
without any indication as to whether it is derived from cow, baffalo, goat,
or sheep, the standard prescribed for buffalo milk shall apply.
A.11.02 Skimmed milk, either frosh or reconstitute means milk from
which all or most of the milk fat has boon removed b
* rnchanical or any other
process and includes "separated milk" op "machine si-immnd milk". The milk
solids other than milk fat shall bo not less than 8.5 per cent
*
A.11.03 Butter-milk moans tho product obtained after removal of
butter from curds- by cherning or otherwise,
A. 11.04 Toned milk moans the product prepared by blending milk with
fresh separated milk or with separated milk reconstituted from snray dried
skim milk, powder or by partial abstraction o*" ~at through skimming or
separation of milk.
It shall, contain not less than 3.
*
percent of milk solids other than milk fat.
per cent of milk fat and 8.5
A.11.04.01 Double- Toned Milk moans the product prepared by
blending milk with
(a) fresh separated milk ; or
(b)
separated milk reconstituted from spray dried skip- milk powder;
or
■-7:
(c)
by partial abstraction of fat through skimming or separation
of milk; ant1 containing not less than 1
5
*
per cent of milk fat and 10 per
cent of milk solids other than milk fat.
A.11.06. Dahi or curd - (a) Whole milk dahi or curd means the
product obtained from fresh whole milk either of cow or buffalo by souring.
It shall not contain ary ingredient not found in milk except sucrose and/or
gur.
The standard of nuri.ty of dahi or curd shall be the same as
prescribed for the milk from which it is derived.
A.11.11 Ice-cream shall contain not loss than 36 per cent by weight
of solids and 10 per cent by weight of milk fat except that when the ice-cream
contains fruits or nuts or both, the content of milk fat may be proportionately
reduced but not less than 8.0 per cent by weight. Ice-cream propared from
skimmed milk shall not contain less than 8.5 per cent of milk solids other than
milk-fat.
Mixed Ice Cream should have the same fat content and total solid
contents as prescribed for Ice cream.
A .11.14 Ghee means the pure cilAiified fat derived solely from milk
or from curd or from deshi (cooking) butter or from cream to which no colouring
matter tor preservative has been added?. The standard of quality of ghee produced
in a State or Union territory shall conform to the standards as laid down for
that area. Although the maximum limits of the percentage of (l) free fatty
acid (as. oleic acid) and (2) noistre have been uniformly specified, the
standards for minimum Reichert value and Rutyro-refractometer reading at 4
°C
*
varies from region to region.
A.14 Tea ifcans tea derived exclusively from the leaves, buds and
tender stems of plants of the Camellia genus and thea species. It shall conform
to the following specifications:
(a) Totgl ash determined on tea dried to constant weight at 100°C
- 5i0- to 8.W per cent
(b) Total ash soluble in boiling Distilled Water - Mot less than
40.0 per cent of total ash.'
(d)
Ash insoluble in HC1-Not more- than 1.0 per cent.
(d)
ExtracJ obtained by boiling dry tea. (dried at constant weight
at 100 C) with 100 narts of distilled water for one hour under
reflux - Mot less than 1.3 per cent.
(e)
Alkalinity of soluble ash - Not less than 1.3 per cent and not
more than 2 per cent expressed as K^O
(f)
Crude fibre-Not more than 15 per cent.
any added colouring matter.
It shall not contain
A.17.06 Mustard oil (Sarson-ka-tel) means the oil expressed from
clean and sound mustard seeds, belonging to the compestris, juncea or napus
varieties of Brassica. It shall bo- clear, free from rancidity, suspended or
foreign matter, separated water, added colouring or flavouring"substances or
mineral oil. It shall conform to the following -standards:
(a) Butyro-refactometer reading at 40 C0 -58.0 to 60.5
(b, Saponification --qIuc - 168 to. 176
;c) Iodine value - 96 *
-''10$'
d) Unsanonifiable matter - Not more than 1 .2 per cent
: P :
Free fatty acid as Oleic acid - Fot more than 3.0 per eent.
(e)
Pel 11nr (Turbidity test) by Fver's method (Acetic Acid) - Fot
(f)
more than 26 i 5 0.
The test for argemono oil should be. negative.
A.17.11 Til Oil (Gingdly or-sesame oil) means the oil expressed from
clean and. sound seeds of Til. (S-osamum indicum) 1'ckj brown, wa?tc^ or miked.
It shall be clear, free from rancidity, susp.nd-.fi or other fore?gn-matter,
separated water, added colouring- or flavouring 'substances, or- mineral oil. It
shall conform to the following standards}
(a) Butyro-rnfractcmetor reading at 4
* ’' -58.C to 61.0
(b) Saponification value-188 to 198
(c)
Iodine valuo-105 to 11 J.
(d)
Unsaponifiahle matter - Not more than 1.5 nor c-'nt.
(e)
Free fatty acid as Oleic acid-Not more than 3.0 nor pant.-
(f)
Bellier Test (turbidity temperature - Acetic acid method) Not more than 22°C.
A.19. Vanaspati m-'-ans any refined edible vegetable oil or oils,
subjected to a process of hydrogenation from groundnut oil, cotton seed oil
and sesame oil or mixtures thereof or any other harmless vegetable'oils
allowed by the Government for the purpose’ It shall conform to the standards
specified below:
(i)
It shall not contain any. harmful colouring, flavouring or any
other matter deleterious to health.
*
*
(ii)
No colour shall be added to hydrogenated vegetable oil unless
so authorised by Government, but in no event any colour- resembling the colour
of ghee shall be added.
(iii)
If any flavour is used, it shall bn distinct from that of
ghee in accordance with a list of permissible flavours and in such quantities
as may be prescribed bv Government.
Provided that diacetyl to the extent of not more than 4.6 o.p.m. may
be added to Vanaspati exclusively meant for c-.ohsumption by the Armed Forces.
(iv) It shall not have moisture exceeding 0.25 per cent.
(v)
The molting point as determined by the can-ill ary slip method
shall be from 31 C to 37 G both inclusive.
(vi)
The Putyro-refractemeter reading at 4»°0, shall not be less
(vii)
It shall not have unsanonifiable matter exceeding 1.25 per cent.
than 48.
(viii)
It shall not have free fatty acids (calculated as Oleic acid)
exceeding 0.25 per cent.
(ix)
The product on melting shall be clear in appearance and shall be
free from staleness or rancidity, and pleasant tn tabte and smell.
(x)
It shall contain raw or refined .- same (til) oil not less than
5
per cent by weight, hut sufficient so that when the vanaspati is mixed with
refined groundnut oil
the proportion of 26:8h, the md colour produced by
the Baudouin test shqll .not bo lighter than 2.6 cits in a 1 cm. cell on a
lovibond scale.
... .9/-
(xi)
’A' per gram.
It shall. contain not less than 25 LIT. of synthetic Vitamin
(xii) No anti-oxident, synergist, emulsifier or any other such
substance shall be added to it except with the prior sanction of the
Government.
PART X
PRESERVATIVES
Preservative has been defined as a substance which when added to
food, is capable of inhibiting, retarding or arresting the process of
fermentation, acidification or otho-~ decomposition of food. Preservatives
have been divided into two classes:
(i) Class I preservatives comprise of : Common Salt, Sugar,
Dextrose, Glucose, Wood smoke, spices, Vinegar or acetic acid, Honey, Hons,
Commercial salt petre, and Alcohol or potable snfrits. Addition of Class
I preservatives in any food in any proportion is not restricted.
(ii) Class H Preservatives are : Penzonic acid including salts
thereof, Sulphurous acid including salts thereof, and Nitrites of Sodium
or Potassium in respect of food like ham, pickled meat. Use of more than
one Class II Preservative in or upon a food is prohibited,. Their use has
been restricted to the specified group of foods in concentration not exceeding
the proportions fixed against each. Those foods comprise of Sausage and
sausage meat, Fruits and fruit juices, Cooked nicked meat, Alcoholic and
non-alcoholic wines, Syrups, Sherbets, Dehydrated vegetables, etc.
PART XII
AJT?T_ryjpANTS, Eh^TT STFVtttg AND
STABILISING AGENTS
’Anti-oxidant’ means a substance■which when added to food retards
or prevent oxidative deterioration of food and does not include sugar,
cereal oils, flours, herbs and spices. No anti-oxidant, otb r than lecithin,
ascorbic acid and tocopherol shall be added to any food, but a number of
anti-oxidants have boon specified which may be added to edible oils and fatss
"Emul.sifyi.ng agents" and "Stabilising agents" moan substances
which when added to food are capable of facilitating a uniform dispersion of
oils and fats in aqueous media, vice versa, and or stabilising such emulsions
and do not include the following, namely -
Agar, alginic acid, calcium and sodium alginates, carrageen, edible
gums, dextrin, sorhitol, pectin, sodium and calcium necuate, sodium citrate,
sodium phospha.te, sodium tartrate, calcium lactate, lecithin, gelatin, quillaia
modified starches and hydrolysed protein.
Except in milk and cream, a number 6f specified emulsifying or
stabilising agents are permitted to be used in foods.
Container of an article of food to which any emulsifying and
stabilising agent has been added shal’’ bear a statement of the chemical
nature of such emulsifying and stabilising agents in addition to any trade
name.
...10/-
PART xm
FLAVQriRTFG AGEPTS
The use of coumarin and dihydrocoumarin as flavouring agents in any
article of food is prohibited. Use of Diethylene Glycol monoothyl ether as
a solvent in flavours has boon prohibited.
'///////
COMMUNITY HEALTH CELL
AN ARTICLE? Cn food Adulteration and Poisons 47/1,(First Hoor)^-. Murks noad
BANGALORE-560 001
-------------- =
CONQUEST
OF
DEATH,
INDIAN
STYLE
Author? Sumanta Banerjee
Magazine? ’'Perspective” (Natinal Monthly published in Delhi)
Issue? Plarch 19?8
Editor ? Bhabani San Gupta
Getting used to hygienic living, like drinking unpolluted water
or having unadulterated food,
may have its hazards, especially in a
country like India,
Tha other day, we took along a friend cf ours who has been living
in Europe for the last 10 years, to dine out in a restaurant. While
we woke up quite hale and hearty the rext morning, this friend from
abroad could not gat up from his bed because cf what turned out to be,
after a medical examination, a case of' foodpoisoningl One man’s food
is indeed another man's poiscn, After years of daily consumption of
poison in small doses in the shape of cereals mixed with a variety of
items like wood shavings and stone, pebbles and cooked in adulterated
oil, we Indians have developed a strong stomach that can digest what
in scientific terms is known as "unedible for human beings." But even
a single dose of such stuff could be fatal for an alien uninitiated
to the secrets of modern Indian cooking.
In a sense, therefore, we can claim to be conquering death in stages.
At least in this respect we score a point over the developed nations of
the West.
Our food can be the bane cf the rich nations, who have, grown
soft and flabby all these years on nutritous food preserved carefully <
from any pollution, its ingredients sterilized and checked and re
checked by sanitary experts. We do not need the dreaded bomb to wipe
them away, if there is any war in the future. A taste of our food
would be enough to scare thorn away.
The benefits of immunity through poisoning in doses were known to
Indians long beforo Hahnemann discovered the principles of homoepathy.
If you inoculate- a man with a small quantity of a disease he becomes
immune to a large quantity. Our traders have, taken this lesson to
their hearts and are doing their best to immunize us against all dis
eases of the :.'crlr'J Go to any eating place, and name any germ and you
are sure to pick it up.
May be the first time, ycu may get a bout
of amoebic dysentery or gastro-enteritis which may unnerve you. But
do not worry. You will soon get used to it.
It will become, part of
your daily life. Soon, even larger doses of amoebic germa will fail
to upset you. Thus a time may coma when medical experts will have
to revise their definitions of terms like "fatal".
CONQUEST OF DEATH
page 2
If this seems to be an idle speculation, let us have a look at the.
facts. A recent study by the Institute, of Science, Bombay, revealed
that an urban Indian every day is consuming unwittingly along with
vegetables, fairly sizeable amounts of pesticides like DDT, Landane,
Dieldrin and Endrins,
Potatoes and french beans showed an incidence of
residual pesticides cf over 70-% and carrots over 50#,
Incidentally, 42
of the 63 pnlluted samoles, of vaqctab1'ra_exaisined bv the institute
showed that tho ^amount j? fjoollu ■’ j-.Qnjcns^ mi Jnh _ebqve the recommended hu
man tolerance limits
f HTl
n?> specified by the Ucrld Health Organisa
tion and the Food .end. f,cn.i£j.l.ti;,cajj_nrn=?.Hjsation£ Since even after the
consumption of these highly polluted foodstuff wo are not only living
but kicking away, we are clearly on cur way to conquer, death.
The capital of India - Now Delhi - takes the cake in this respect.
The, morning milk for which the Delhiwalla faithfully queues, up before
government booths has been found to be contaminated (or shall we say
"flavoured” since the presence, of the extraneous element apparently
does not soem.to have any destructive effect, but on the contrary by
increasing our immunity can be said to be beneficilj) to the tune of
over 47% by C0~I rosidues. DDT is also found in mustard, sesame and co
conut oils. A Punjab Agricultural University entomologist is of the
view that tho Jsvnl of DDT in human fat in people from the. Delhi region
could well be the, hi q hgot in the world.
Incidentally;
DDT appears to have emerged into a favourite food for
both mosquitoes and human beings,
judging by recent Indian habits.
Ori
ginally meant to destroy mosquitoes, instead of disappearing, they arethriving under DDT spray. The long-departed friend of our rural homes
- malaria - has come back,. And this time, it is -going to stay put.
Scientists: have discovered a DDT-sesistant strain among the new breed
of mosquitoes, who, like human bejnos, have also developed immunity.
I can well imagine Lira displeasure, of some of the readers who may
feel that I am being facetious about a serious matter. They may point
out that some years ago in Wash Bengal about 3U0 men, women and child
ren developed porelysis cf the lower limbs after having consumed mus
tard oil adulterated with a colourless toxic liquid used in the plas
tic industry. They may add that Anger,ono, which is popularly known
as yellow poppy,
is added to mustard seeds and when consumed, causes
epidemic dropsy, Did dal is polished with metanil yellow, a cheap
soluble colouring substance that makes dais deceptively brighter and
freshlooking, but causes cancer.
CONQUEST OF DEATH
page. 3
But than,
one should look at it from the. point of our leaders who
are running the country. There are too many people and too feu jobs to
go.
In such a situation if soma are rendered disabled through paralysis
or dropsy, isn't it a relief for the overburdened employment market?
While adulterated foods have played their part in crippling healthy
people, the police in the former regime have made an even more decisive
contribution by killing off a sizeable portion of the able-bodied youth
who otherwise would have clamoured for jobs or changes and become a
thorn in the flesh of our administrators.
Besides, those chicken-hearted people who get upset over food adul
teration should also pause to remember how many people, in these days
of shrinking employment opportunities, will be. thrown out in the. streets
if adulteration is put an end to. A number of small-scale and cottage
industry workshops are in operation in different parts of the country
engaged in producing their speciality — artificial adulterants.
not a simple job.
It is
Colours have to be matched. The exact sizes have to
be fixed so that they blend properly with the original. Tastes have to
be determined so that the consumer cannot make out the difference. It
is an all-embracing affair taking care of all human senses.
Isn't this
a challenge to human ingenuity?
An entirely new technology has emerged in response to the needs. We
heard some years ago about a sophisticated machine somewhere in North
India which could chop wood into any size to produce a variety of
"dais" to be. mixed with the real stuff,
In a corner of West Bengal
there is reported to be a factory which manufactures stones cut in
various shapes to be mixed with cereals.
Such being the case,
our leaders, instead of pretending to penalize
the adulterators (in the decade between the
'sixties and the 'seven
ties on an average 4,000 cases anually resulted in short terms of
imprisonment - a sort of ritualistic holiday for the accused traders
who usually come back to business with renewed vigour after the short
interval),
should, in fact, encourage them.
According to one estimate, out of about 5,000 cases of food
poisoning in ona year,
copy EEV
780509
nearly 700 proved fatal!
’iTERHATIONAL FOOD EDUCATION
5 blHo1 LL
BOARD OF DIRECTORS
PRESIDENT
AMERICAN INSTITUTE
OF CHEMICAL ENGINEERS
NEWSLETTER
April 1978
COMMUNITY HEALTH CELL
(First Floor)St. Marksaoad
bangalore. 560001
VICE PRESIDENT
ROBERT W. HARKINS. Ph.D.
AMERICAN INSTITUTE
-OF NUTRITION
SECRETARY-TREASURER
KENNETH MORGAREIDGE. PH.D.
AMERICAN CHEMICAL
SOCIETY
C. O. CHICHESTER. Ph.D.
INSTITUTE OF FOOD
TECHNOLOGISTS
WILBUR S. CLAUS. PH.D.
AMERICAN ASSOCIATION
OF CEREAL CHEMISTS
THOMAS H. FOX
VOLUNTEERS IN
TECHNICAL ASSISTANCE
HUGH POPENOE, PH.D.
AMERICAN SOCIETY
OF AGRONOMY
S. JACK RINI
AMERICAN OIL
CHEMISTS' SOCIETY
HAROLD V. WALTON. PH.D.
AMERICAN SOCIETY OF
/RO2ICULTURAL ENGINEERS
L.l.F.E. NEWSLETTER
HUGH J. ROttRTS, PH.D.
ASSOCIATE EDITOR
ANN L. DYER
FOR
FURTHER INFORMATION
DR. HUGH J ROBERTS
EXECUTIVE DIRECTOR
LEAGUE FOR INTERNATIONAL
FOOD EDUCATION
1126 SIXTEENTH STREET. N.W.
WASHINGTON. D.C. 20036 U.S.A.
TELEPHONE (202' 331-1658
THE OPINIONS EXPRESSED IN
THIS PUBLICATION ARE THOSE
OF THE CONTRIBUTORS AND
EDITORS. THEY ARE NOT TO BE
CONSTRUED AS THE VIEWS OF
THE CONSORTIUM SOCIETIES.
THE L.l.F.E. NEWSLETTER IS
FUNDED BY A CONTRACT
FROM THE AGENCY FOR IN
TERNATIONAL DEVELOPMENT.
UNDERUTILIZED SPECIES OF FISH:
A NEW FOOD SOURCE
Robert C. Baker, Ph.D.
Professor of Food Science
Cornell University
Ithaca, New York 14853 USA
Did you know that each year we waste or "underutilize"
mill ions of tons of fish?
It is estimated that as much as
70$ of the fish in the oceans are underutilized. According
to fishermen, there are many areas in the oceans where only
underutilized species of fish exist. In lakes, it is esti
mated that more than 70% are underutilized.
Known to the
fishing industry as "trash" fish, these fish are frequently
netted, killed, and returned to the water as a pollutant.
Why are these fish underutilized?
Some have tiny, needle
like bones which make them difficult to eat.
Others have
unfortunate names, like sucker, crappie, or cancer fish
Still others are considered too small to be worth the effort
to prepare them. But all of these problems can be overcome.
And on the plus side, these fish contain a high level of good
quality protein. And they are extremely low in fat (1-3$).
And what is more, the fat is unsaturated which is another
plus.
With high quality protein running short in the world, we
cannot afford this kind of waste. Along with others, we at
Cornell have been looking for solutions to this problem of
underutilized fish.
One answer is to debone these fish
mechanically.
We remove the head and entrails, wash the
carcass, and place the cleaned fish between a heavy plastic
belt and a large cyclinder which contains many small holes.
The pressure from the belt forces the flesh, but not the
skin, bones, and fins, through the holes in the cylinder.
This process can also be used on the fish frames which re
main after a larger fish is filleted.
From this dressed
fish, we obtain yields of 50 to 75$ depending upon how well
the job of filleting was done.
The deboner that we use is made in Japan and may be too expensive for peo
ple in some developing countries.
An alternative to the machine process
would be to clean the fish, removing the fins, tail, and scales, and then
grind the rest of the carcass through a manual grinder.
Since fish bones
are soft, they disperse well in the ground product and are not particularly
objectionable; moreover they are a good source of calcium.
Most species of fish have a mild flavor and are not fishy in taste.
The
deboned or minced fish looks very much like coarse ground hamburger except
that it is much lighter in color.
The product has a variety of uses. It
can be substituted for hamburger or used in such traditional dishes as
spaghetti and meat saucq Swedish meat balls, sweet and sour fish, lasagna,
chili, and tacos.
Gourmet chefs can also use the product for such dishes
as Newburg or quenelles. They have told us they find the product excellent
and especially appreciate the fact that it saves them time by not having
to grind fillets.
We have just finished market testing two seafood chowders:
Manhattan
(tomato-based) and New England (milk-based).
In each case, the seafood
used in the chowder contained 65% of seafood products that previously have
been wasted. Sales were excellent.
We have also market tested one-pound frozen blocks of minced fish.
It
was packaged in a cardboard box with a heavy waxed paper overwrap. The
label served a dual purpose. It opened up into a recipe book with fifteen
different recipes for the use of the minced fish.
The product sold well
at 89 cents per pound.
What does all this mean?
I hope it means that in the near future there
will not be such a thing as underutilized fish.
We just cannot afford to
waste this perfectly good food.
INTERNATIONAL NUTRITION:
PROBLEMS, POLICIES, AND STRATEGIES
Problems affecting world food supply and nutritional status, and the impact
thereon of population growth, particularly in third world countries, are
now at the center stage of world concern. Over the past twenty-five years,
numerous policies, plans, and programs have been developed and implemented
by third world countries to deal with these challenges, frequently with in
puts from multinational and bilateral assistance agencies.
This summer
program, to be held at Cambridge Massachusetts, July 17-July 21, 1978, will
be of special value to individuals involved in policy formulation and in
program planning and administration in developing countries, and to others
in academic, governmental, and commercial institutions concerned with in
ternational and third world problems.
For further information, please write to: Max Milner, Associate Director;
International Nutrition Policy and Planning Program Massachusetts Institute
of Technology; Cambridge, Massachusetts 02139 USA
-2-
THE 4-H TRAINING CENTER IN BELIZE
(The following is adapted from "People-Oriented Projects Making Progress
in Belize" by John Dieterly. The article appeared in the Winter 1977 issue
of Sharing Life, published by Heifer Project International (HPI).)
Agricultural development in Belize has as much to do with developing new
attitudes and getting farmer acceptances of new practices as it does with
developing new practices.
For various historical reasons, farming is not
seen as an attractive vocation. Young people usual1y move to the towns to
seek employment; many emigrate to other countries. With 60%of the popula
tion under 21, any agricultural program needs to focus heavily on the young
people.
With the School Farm pilot project, HPI can introduce children to the idea
that farming can be enjoyable. If they like some phase of it, they can
pursue that interest through U-H, which is active in most schools.
Then
they can take the three month course at the 4-H Training Center At present
four to six boys can live at the Center at a time, but a new dormitory is
under construction which will house 20 student^ both male and female. Here
young people come for three months to get practical training with rabbits,
broilers, layers, milk goats, and bees, as well as experience in the grow
ing of vegetables and a basic understanding of the simple mechanics of a
small tractor.
The primary purpose of the Center is to prepare young people for opportuni
ties in agriculture. We do not lecture much. Learning is by doing.
Young
people learn about rabbit diseases by treating sick rabbits.
They learn
how to slaughter chickens by slaughtering chickens.
Each trainee, when
completing the course, should be capable of starting in any of the farming
projects we have at the Center, on the basis of experiences they have had,
not on the basis of notes taken during a lecture.
We cannot train at the Center all the young people who want to come, so we
teach the trainees to teach others.
When visitors come to the Center, we
encourage the trainees to show them around. In this way they learn not
only about chickens, but also about how to tell others about chickens. In
turn, when they return to their villages, they are able to tell others what
they have learned, and the impact of the training program is multiplied.
This has already been illustrated in several instances. A Training Center
graduate may return home, start a broiler project, and soon with his help
two or three other 4-H'ers in the village also start broiler projects.
Another value of the Center is that it is a place 4-H'ers can call their
own. Many were involved in building it and have since watched it grow.
They use its services to get started with agricultural projects, and they
take pride when it is on display to visitors, notably the 10,000 people who
come each year to the National Agricultural Show on which grounds the Cen
ter is located.
Since the Center is also on the main highway only a mile
from Belmopan, it is visible to all who come to the capitol. The attitud
inal impact this makes on youth and adults alike is most significant.
-3-
L.I.F.E. Lines
In response to "Hens and Eggs, Parts I and II" (October and November 1977)
these remarks from Richard Forsythe, Campbell Institute for Food Research,
Camden, New Jersey:
...While I am sure it is just an oversight, one important element seems
to be missing — namely, the male birds.
Obviously one will not have
fertile eggs to set from an all pullet flock. Depending on the types of
birds, one male should be supplied for every 15-20 light breed females
and for every 10-15 heavier type females.
And from Wilmer Dagen, World Neighbors, an offer of additional information:
...Eggs are definitely a good source of protein, if the motivation to sell
■the eggs for badly needed cash is not too great. World Neighbors produced
a filmstrip that has had good reception and is excellent for starting a
discussion on the subject.
Editor's note: "Who Should Eat the Egg" is available in both Philippine
and Guatemalan versions.
Both are in English, have a horizontal format,
come in color, consist of 21 frames, and are available at US $4.00 each
from: World Neighbors; 5116 North Portland Avenue; Oklahoma City, Okla
homa 73112 USA
*
***•»•»
* * ****
#c
-K#
**
#-»#»
«
»
f
*
afc
)f
*
.S«
A year ago we started the L.I.F.E. Lines section of the Newsletter.
It
appears whenever we receive comments, questions, or additional information
from you, the Newsletter readers. We have been pleased with your response
thus far and we hope you will continue to write us. Letters can be sent to:
L.I.F.E. Lines; 1126 Sixteenth Street NW; Washington, DC 20036 USA
LETTER FROM THE EDITOR
On this my last day as Executive Director of L.I.F.E. and Editor of the
Newsletter, I want to take a few moments to express my gratitude to you,
L.I.F.E.'s readers and friends.
Thank you for taking time to write about
something you read in the Newsletter; for providing helpful and overwhelm
ingly favorable input to AID's evaluation of L.I.F.E.'s services; for re
sponding to L.I.F.E.'s requests for help. Through the communication links
between us, I have derived a sense of partnership with you in the struggle
to alleviate malnutrition.
In my acceptance of the position of Technical Director of the Meals for
Millions Foundation in Santa Monica, California, I am not withdrawing from
the battle. Meals for Millions also encourages and supports the poor, the
hungry, and the malnourished in their efforts to improve their own well
being. I look forward to continuing to work with you for development that
honors the dignity of the individual and enhances self-respect.
Hugh J. Roberts
Washington, DC
April 14, 1978
-4-
e
PRESIDENT
GARY F. BENNETT, Ph.D.
AMERICAN INSTITUTE
OF CHEMICAL ENGINEERS
VICE PRESIDENT
ROBERT W. HARKINS, Ph D.
AMERICAN INSTITUTE
SECRETARY-TREASURER
KENNETH MORGAREIDGE. Ph.D.
AMERICAN CHEMICAL
SOCIETY
C. O. CHICHESTER. PH.D.
INSTITUTE OF FOOD
TECHNOLOGISTS
WILBUR S. CLAUS, Ph.D.
AMERICAN ASSOCIATION
OF CEREAL CHEMISTS
THOMAS H. FOX
VOLUNTEERS IN
TECHNICAL ASSISTANCE
HUGH POPENOE, PH.D.
AMERICAN SOCIETY
OF AGRONOMY
S. JACK RINI
AMERICAN OIL
CHEMISTS' SOCIETY
HAROLD V. WALTON. PH.D.
^ERICAN SOCIETY OF
OlCULTURAL ENGINEERS
COMMJN.'.Y i-i.ALTH CELL
NEWSLETTER
17/1.(First Floor)St. Marks 8oati
BANGALORE- 560 001
May
1978
COMMUNITY rl.ALTH CELL
LEAP PROTEIN GAINS RESPECTABILITY47/1.(First FloorlSc. Marks Hoad
BANGALORE-560 001
N. W. Pirie
Rothamsted Experimental Station
Harpenden
Herts, England AL5 2JQ
Recent increases in the cost of energy and of protein-rich
foods and fodders have combined to awaken interest in leaf
protein (LP).
The pressed leaf residue after extraction
contains two to three times as much dry matter as the orig
inal crop so that much less energy is consumed in drying it
to produce winter fodder. The annual yield of LP in Britain
can be 2t/ha; in India, it can be 3 t/ha.
It may not be
economically realistic to strive for such yields, neverthe
less, in similar conditions, a leaf crop that is photosyn
thetically active during most of the year should always outyield a seed crop that becomes inactive while ripening.
This long overdue interest in LP has not yet stimulated a
corresponding interest in the design of efficient extraction
equipment.
l.i.f.e. newsletter
ASSOCIATE EDITOR
ANN L. DYER
FOR
FURTHER INFORMATION
EXECUTIVE DIRECTOR
LEAGUE FOR INTERNATIONAL
FOOD EDUCATION
1 126 SIXTEENTH STREET. N.W.
WASHINGTON. D C. 20036 U S.A
TELEPHONE '202- 331-1658
THE OPINIONS EXPRESSED IN
THIS PUBLICATION ARE THOSE
OF THE CONTRIBUTORS AND
EDITORS. THEY ARE NOT TO BE
CONSTRUED AS THE VIEWS OF
THE CONSORTIUM SOCIETIES.
THE L I F.E NEWSLETTER IS
FUNDED BY A CONTRACT
FROM THE AGENCY FOR IN
TERNATIONAL DEVELOPMENT.
Method of preparation
LP can be coagulated with acid: it is usually coagulated by
sudden heating to 70-80°.
The coagulum is filtered off,
washed, and pressed to a hard, moist cake which can be pre
served with the usual bacteriostatic agents. For prolonged
conservation it is usually dried. It is at this stage that
LP is most often damaged; most of the differences in nutri
tional value that have been observed between preparations
from crops of differing age, and between species, are prob
ably in reality the result of differing conditions of drying
in the rather unsystematic work that has been done so far.
If dried in air, or in an oven, LP becomes hard and nearly
black. The product is more attractive if it is partly dried
and then ground finely before the drying is completed. How
ever it is dried, there is risk of damage through Maillard
reactions if the filter cake is not washed to remove most of
the sugars present in the original leaf extract.
Carotene
and xanthophyll are valuable components of LP whether it is used as a human
or an animal food. As is well known, they are less rapidly destroyed cur
ing storage if the material is made slightly alkaline and is protected from
light and air. Drying should be avoided whenever possible.
Nutritional Value
Experiments on rats, mice, chickens, and pigs show, as would be expected
from the amino acid analyses, that LP is a satisfactory substitute for
fishmeal and is a little better than groundnut or soybean meal. The limit
ing amino acid appears to be methionine. There is some evidence that part
of the methionine in LP is unavailable; more work on the extent to which
this is the result of complex formation during separation and drying is
urgently needed.
Trials in Nigeria and India confirm earlier work in Jamaica on the value
of LP in infant feeding.
Particular emphasis was laid in Nigeria on in
creased alertness as well as the improvement in the physical condition of
malnourished children. In the Indian trial, in six villages, near Coimba
tore, preliminary results show that LP is superior to the usual legume
seeds, and nearly equal to milk.
Composition
When made carefully, for human consumption, from suitable species, LP con
tains 9 to 11% N (nitrogen), i.e., 56 to 68% protein.
When made for use
as animal feed it seldom contains more than 50% because the fiber is usually
less carefully removed by straining the initial extract, and surface dust
is less completely removed from the crop before it is extracted.
Most of
the non-protein material is lipid (20 to 25%) and this is highly unsatu
rated.
Because of the value of the lipid both as an energy source and as
a source of essential fatty acids, it would be unwise to remove chlorophyll
and its breakdown products by solvent extraction.
If pheophorbide forma
tion is prevented, they appear to be harmless. The amount of nucleic acid
depends on the interval between extraction and heat coagulation; there is
little if leaf ribonuclease is given time to act, but 1 or 2% if an extract
from very young leaves is coagulated after a few minutes.
Commercial production
There is work on LP in research institutes in at least 16 countries. There
is commercial interest in five or six but it is difficult to get reliable
information. Material produced commercially in France and Britain is suit
able for animal feeding only.
************************************
onriIafapiotei^:SUeS°fthe
^Sletter have ^0 featured articles
May 1973
Leaf Protein: A New Protein Source for the
Management
of Protein-Calorie Malnutrition in Nigeria
February 197^
Leaf Protein: Update
' S
March 1975
Leaf Protein Child Feeding Trial
We still have a few copies of each of these issues in stock
interested in receiving any of them, please send your requests If you are
to L.I.F.E.
-2-
UNCSTED and The Lund Letter
UNCSTED, the United Nations Conference on Science and Technology for Devel
opment, will take place in 1979- It has three major goals:
—Implementing strategies for the successful use of knowledge and technol
ogy to meet the basic needs of the world’s poor.
Strengthening the technological autonomy of the developing countries.
—Harnessing the potential of science and technology for the solution of
global problems.
The Lund Letter is trying to provide a forum where independent views on the
progress of UNCSTED can be expressed. In the words of its editor,
.. .We believe that the following can be important means by which to im
prove the results of the Conference:
—An.active preparation process, especially in the least developed coun
tries, aiming at identifying those social needs in fulfillment of which
science and technology play a vital role.
—Involvement of broad circles in the preparatory process, not only gov
ernment officials and the established scientific community but also
individual scientists and planners.
—A broadening of the classical definition of science and technology to
embrace the entire process of knowledge production and information dis
semination.
If you are interested in receiving the Lund Letter, please write to:
Research Policy Program; University of Lund; Solvegatan 8; S-223 62 Lund
Sweden
XI INTERNATIONAL CONGRESS OF NUTRITION
The XI International Congress of Nutrition will be held in Rio de Janeiro,
Brazil, August 27-September 1, 1978Promoted by the International Union
of Nutritional Sciences, the Congress has as its main objective to discuss
"The practical utilization of available multisectorial technical and scien
tific knowledge to solve food and nutritional problems."
In addition to the plenary sessions, case studies, symposia, workshops,
poster sessions, and short courses are also scheduled.
Discussions will
be conducted on a multi-disciplinary basis, covering specific problems of
basic and applied nutrition as well as their socio-economic, cultural, and
political implications.
A number of parallel meetings are also scheduled, including those of the
International Society of Parenteral Nutrition, the Latin American Nutrition
Society, the Federation of Asian Nutrition Societies, the International
Vitamin’A Consultative Group the International Nutritional Anemias Consul
tative Group the Nutrition Programmers Forum, and the International Diete
tic Committee.
For further information, please write to:
XI International Congress of
Nutrition; Sociedade Brasileira de Nutricao; Av. Churchill, 9^-6 andar;
20.000 Rio de Janeiro, RJ, Brazil
-3-
L.I.F.E. Lines
On "Whose Milk Shall We Market" (September 1977)> we received two letters.
The first from Mushtaq Ahmad, Federal Chemical and Ceramics Corporation,
Karachi, Pakistan:
...Another vital aspect which has not been given any thought is the rate
of incidence of breast and uterine cancer among the women who are breast
feeding their babies as compared to those who have adopted the method of
bottle feeding. It may be worthwhile to explore and collect statistical
data and find if possible any link between the diseases like breast and
uterine cancer arising out of not feeding the baby on breast milk. Cer
tainly with the advancement of medical science and the fine techniques of
diagnosis and compiling the relative statistical data for these two mal
adies one may find some clue of a basic vital link which may appeal to
the mothers to resort to breastfeeding to avoid contracting such maladies.
and the second,a case history, from Jorge 0. Casale, Institute Nacional de
Tecnologia Industrial, Buenos Aires, Argentina:
...In August 1973> during a visit to the Department of Technical Guidance,
Coordination of Integral Technical Assistance (C.A.T.I.), the Director of
the Zootechnical Division, Dr. Jorge Adibi Roston, told me of their ex
perience in mass media transference of technical information to farmers.
The usual leaflets were found inadequate. Much more useful were the ra
dio and T.V. spot messages.
But their best tool was the inclusion of
disguised technical messages into the plot of the popular radio and T.V.
"serial" theater plays.
These continuing serial programs are extremely
popular. (Inyour Newsletter the Nicaraguan "Pancho Madrigal" program
is mentioned.) Instead of using "spots" among other commercials (people
tend to pay less attention to commercials rather than to the actual play),
they convinced the radio and T.V. operators to include disguised messages
into the plot. People tend to imitate what they see or hear through the
mass media, and this proved to be an excellent asset for C.A.T.I. I
thought it to be a very clever use of the mass media to reach sublim
inally the target population.
In response to the inclusion of The YFC Intensive Unit in "Recent Publica
tions of Interest" (December 1977)> Dudley Hall, Rhodesian YFC Association,
Salisbury, Rhodesia, writes:
...We have been overjoyed at the response to the publicity you have given
YFC and our leaflet. ... People have tried to pay us with an American
check for US$.31. Such checks cannot be accepted here and if they were,
the cost of processing to get payment would be much more than the 31
cents I
Moreover, air mail postage is as much as $3.00 on our booklet.
Hence we are having to post by surface mail which takes weeks to reach
its destination.
if************************************
Do you have a comment on or a question about something you have read in the
Newsletter? Take a moment to let us all know what it is. Please write to:
L.I.F.E. Lines; 1126 16th Street NW; Washington, DC 20036 USA.
-4-
NATIONAL INSTITUTE OF NUTRITION
Indian Council of Medical Research
HYDERABAD - 500 007 : INDIA
Green leafy vegetables are vital for growth and
good health as they contain all important nutrients.
In India a wide range of greens are consumed,, the more
popular ones being Spinach (Palakura), Amaranth (Thotakura), Gogu (Gongura), Fenugreek (Methi), Drumstick
leaves, Mint (Pudina) etc.,
Leafy vegetables are particularly rich in mineral
nutrient, iron. Iron deficiency leads to anaemia, a common
health problem among pregnant and lactating wome^
and also children. Inclusion of greens in daily diet wou®
help prevent anaemia and promote good health.
Green leafy vegetables are also a rich source of
Calcium, B-carotene and Vitamin C. In India nearly
30,000 children under five years of age go blind every
year due to lack of Vitamin A. Carotene in green^)
gets converted in the body to form Vitamin A which
prevents blindness.
To preserve Vitamin C content
in greens, prolonged cooking should be avoided, as this
nutrient, which keeps gums in good condition is lost
on overcooking.
Greens also contain some of the
B-Complex Vitamins. The recommended dietary allowance
of green leafy vegetables for an adult women is lOOg/day,
adult man 40 g/day, preschool children (1-3 yrs) 40g/day,
preschool children (4-6 yrs) 50g/day. And for boys and
girls beyond 10 yrs of age it is 50g/day.
NUTRITIVE VALUE OF SOME OF THE COMMONLY
EATEN GREENS
(100 g. of edible portion)
Nutrients
Calories
Mint
Amaranth
Spinach
Drumstick
leaves
Coriander
leaves
Gogu
45
26
Protein (g)
4.8
4.0
2.0
6.7
3.3
1.7
Calcium (mg)
200
397
73
440
184
1720
^■on (mg)
48
92
44
56
10.9
7.0
5520
5580
6780
6918
2898
Thiamine (mg)
0.05
0.03
0.03
0.06
0.05
0.07
Riboflavin (mg)
0.26
0.30
0.26
0.06
0.06
0.39
Vitamin C (mg)
27.0
99
28
220
135
20.0
Carotene (pg)
15.6
1620
25.5
18.5
2.28
It is generally believed that greens cause diarrhoea
in children. So most mothers abstain from giving this
nutritious food stuff to their children. Several bacteria/
germs/insects and other extraneous matter contaminate
2
3
xgfe}
4
]\9
J]
greens through water and soil. And if not washed properly,
they may cause diarrhoea on consumption. All greens
must be washed thoroughly under running water to eradi
cate such contaminants and prevent diarrhoea.
Infants should be served greens only after they
have been cooked, mashed and seived so as to remove
the fibrous part. To retain the nutritive value of greens,
excessive or overcooking must be avoided; also the
water obtained from the greens on cooking must not
be thrown away. Always ensure the vessel in which
greens are cooked is covered with a lid. Do not dry
the leaves in the sun as carotene will be lost. AvokL
frying greens.
w
The nutritive value of greens should not be judged
by its cost which most people wrongly do and discard
them as inferior foodstuff.
For although inexpensive,
greens are highly nutritious and required by all.
Cultivation of green leafy vegetables should be
encouraged so that they may be available all through
the year. Kitchen gardens, roof gardens, school gardens
etc., are ideal for growing green leafy vegetables. Use
of green leaves from trees like drumstick, agathi etc.
helps to obtain them regularly without much effort
if a tree is planted in the backyard.
4
Drumstick Leaves
Amaranth
oooo
Original Article
Indian J Pediatr 1998; 65 : 565-572
Tamil Nadu Nutritional Survey Comparing Children Aged
0-3 Years with the NCHS/CDC Reference Population
Rajaratnam Abel-and V. Sampathkumar
RUHSA Department, Christian Medical College and Hpspital, Tamil Nadu
Abstract: A cross-sectional nutritional survey of children belonging to Tamil Nadu State of India,
aged 0-3 years was conducted on a representative sample of 2039 children. The collected data
was analysed using the recommended indices of height-for-age and weight-for-height based on
standard deviation (SD scores) and cross-classified using the SD scores. The nutritional status of
these children was compared with the NCHS standard. Prevalence of stunting (27.6%), wasting
(9.9%) and simultaneous wasting and stunting 10.7%) was high among the children studied:
(Indian J Pediatr 1998; 65 : 565-572)
Key Words : Nutritional status; Stunting; Wasting.
Protein-energy-malnutrition (PEM) still re
mains a major public health problem in
most of the developing countries, India be
ing one with a high prevalence of PEM.1
PEM among children is known to cause
permanent stunting besides affecting their
mental performance.2
PEM prevails among populations with
poor socio-economic conditions (poverty).
These populations are characterised by low
levels of income, inadequate diets, poor
levels of education, poor environmental
sanitation and housing conditions, large
family size and high prevalence of morbid
ity and clinical signs of undernutrition. In
1979 WHO had launched its strategy and
campaign of health for all by the year
2000? One of the indicators identified by
them to gauge the health progress was the
nutritional status of pre-school children.
Reprint requests : Dr. Rajaratnam Abel, RUH
SA Department Christian Medical College and
Hospital, RUHSA Campus P.O. 632 209, North
Arcot Ambedkar District, Tamil Nadu, India.
Previously prevalence of malnutrition
among pre-school children was assessed
using weight-for-age as criteria. However,
use of weight-for-age criteria alone cannot
distinguish acute from chronic malnutri
tion. In 1976, a Joint FAO/UNICEF/WHO
Expert Committee recommended the use
of height-for-age and weight-for-height as
primary indicators of nutritional status of
children? Besides, Waterlow et al suggested
a method of nutritional classification that
facilitated comparison of results of surveys
carried out in different regions or at differ
ent times and recommended the use of
height-for-age (as an indicator of past mal
nutrition) and weight-for-height (as an in
dicator of the present status)? They also
recommended that nutritional data from
the National Centre for Health Statistics/
Centres for Disease Control (NCHS/CDC)
reference population6 would be most ap
propriate for making international com
parisons. This was subsequently endorsed
by WHO.7
566
RAJARATHNAM ABEL AND V. SAMPATHKUMAR
The present study was carried out to as
sess the nutritional status of children aged
0-3 years in the entire rural Tamilnadu.
MATERIALS AND METHODS
Tamil Nadu (TN) lies in the southern most
part of India. There are 21 districts. The
state is largely dependent on rainfall for re
plenishing its sources of water and there
fore the onset or failure of the monsoon
plays a key role in its economic well being.
The state has a population of 55.6 millions
according to the 1991 census. The sex ratio
is lower with 972 females per 1000 males.
The literacy rate of the state is 63.7%. The
infant mortality rate in 1989 was 68 for the
state as a whole while it was 80 for rural
Tamilnadu.8
Studies of the nutritional status of pre
school children in Tamilnadu done in the
past may be of limited use for any present
planning. In 1976 the prevalence of wast
ing (< 80 per cent weight-for-height) and
stunting (< 90 per cent height-for-age) was
15.1 per cent and 47.6% respectively.9 In an
other study conducted in a drought prone
district of Tamilnadu in 1983, the preva
lence of underweight was 44.6%, of stunt
ing 41.4%, of wasting 11.1% and of simulta
neous wasting and stunting 9.6%.10
In TN, nutrition intervention is being
carried out by the Tamilnadu Integrated
Nutrition Programme (TINP). This was
started in the year 1980 on a pilot basis and
subsequently, in 1982 it was implemented
in 10 districts. More recently the pro
gramme has been extended to all the dis
tricts. While the emphasis in the first two
phases was on direct nutrition intervention
with food supplementation and nutrition
education, in the third phase it is moving
on to a sustainable level through effective
Vol. 65, No. 4,1998
community participation and food security
through income generation schemes espe
cially for women.
It is in the above setting that a cross-sec
tional survey was carried out in 20 districts
of rural Tamilnadu. A multi-stage sam
pling technique was used to select families
from the districts. Initially, one block from
each district was selected using the simple
random method. In the second stage one
revenue village was picked randomly from
each of the selected blocks. A second rev
enue village was randomly selected from
each block to keep as stand-by in case of in
adequate sample size from the first village.
All children under three years of age
from the selected villages were surveyed.
The formula used for calculating the sam
ples size was 2 V PQ = 20% of P. P is 50%
n
which is based on a previous survey. The
sample size obtained was 100 per district.
This gave a total sample size of 2039 for 20
districts. Madras district was excluded
from this study as it was predominantly ur
ban in nature.
The survey was carried out in two
phases by four trained field workers with
sufficient experience in anthropometric
surveys. The first phase included survey in
10 districts from May-June 1992. In the sec
ond phase the remaining 10 districts were
surveyed from December 1992 to January
1993. The two teams were supervised
throughout the survey by one of the au
thors. The children were measured for
weight, height, length and mid-upper arm
circumference (MUAC). Weights were
measured to the nearest 0.1 kg using Salter
Spring Balance Scales. The recumbent
length of children < 2 years of age was
measured to the nearest centimetre using a
portable scale locally manufactured as per
Vol. 65, No. 4,1998
THE TAMIL NADU NUTRITIONAL SURVEY
the WHO standards. The standing height
of older children was measured to the
nearest centimetre. MUAC was measured
with the help of the Zerfas insertion tape to
the nearest millimetre. Measurement tech
niques were standardized according to the
UN manual, "How to weigh and measure
children".11 It was decided that clinical
manifestation would not be studied in this
survey as the total survey was to be com
pleted within a short stipulated period. As
part of quality control the first author vis
ited one of the surveyed districts and vis
ited the houses of sampled children and ex
amined for clinical signs of malnutrition.
The survey team had identified one child
suspected with clinical form of severe mal
nutrition. This was confirmed by the au
thor. Socio-economic information was ob
tained by interviewing the mothers
through a structured interview schedule.
Data was analysed on an IBM Compat
ible PC. A total of 2039 children were sur
veyed. Complete data was available for
2010 children. In the remaining 29 children
data was either incomplete or the height
and weight fell outside the reference stand
ard-6 standard deviations and therefore ex
cluded from further analysis.
The anthropometric standard utilized in
this study was the NCHS standard. Differ
ent classifications used to define malnutri
tion are based on various cut-offs. There
are two main methods that are usually
used to analyse anthropometric data.
(a) Calculating the percentage of the me
dian standard represented by a certain
weight-for-age (W/A), height-for-age (H/
A) or weight-for-height (W/H), and choos
ing the point under which malnutrition
may be regarded as present. A disadvan
tage with the percentage of the median
method is that the cut-off points chosen to
567
define malnutrition are not similar for WA,
HA and HW.
(b) Choose as cut-off point, 2 standard
deviation (SD) units below the median of
reference population. Children who fall be
low this cut-off of W/A, H/A and W/H
are considered to be malnourished for hav
ing some degree of functional disnormality.
The advantage of SD measure is that it is
based on a statistical principle and is the
same for all anthropometric parameters.
For this reason SD measures were used in
this analysis. MUAC was also analysed for
children. Anthropometric analysis was
done with the help of NCHS/CDC
anthropometric package.12
RESULTS
Complete data was available for 2010 chil
dren out of which 1040 were males and 970
were females. The overall level of non re
sponse was less than 1%.
The percentage distribution in the sam
ple population of the main characteristics
surveyed are outlined below. Majority of
the children belonged to the backward
caste (72.7%) and they were followed by
schedule caste (22.4%) and forward caste
(4.5%). The proportion of tribal children
was low with 0.4%. Educational status of
mothers was low with 55.6% of them hav
ing no education, 19.8% with 1-5 years of
schooling, 22.5% with 6-10 years of school
ing and 2.1% with college education.
The occupational pattern of mothers
was as follows : agricultural manual work
40.9%, household work 49.5%, family occu
pation (weaving, pot making, rope mak
ing) 3.5%, white collared 0.3% and other
occupations (beedi making, petty business,
blue collared) 5.8%. The occupational pat
tern of fathers was as follows : farming
568
RAJARATHNAM ABEL AND V. SAMPATHKUMAR
Vol. 65, No. 4,1998
25.4%, agricultural manual work 46.9%, given in 5th month, 17.1% in 6th month,
family occupation (weaving, pot making, 14.2% in 7th month arid 28.1% after 8
rope making, tailoring, fishing) 8.3%, white months. Around 15.5% of the mothers had
collared 5.4%, blue collared 4.0%, petty not started supplementary feeding to their
business 5.6% and others (beedi making, children. Out of these 7.1% of the children
money lender) 4.7%. Regarding size of were below the age of 4 months and 8.4%
family 39.8% of the families surveyed had of the children were above the age of 4
four members, 39.5% had five to six mem months.
Waterlow's cross-classification of heightbers and 20.7% of them had more than
for-age and weight-for-height provides a
seven members.
Over 58.8% of the children were fully complete classification of malnutrition
immunized while 25.3% were in the proc among children in any population. Accord
ess of immunization. These children were ing to this classification four groups of chil
below the age of one year and in different dren can be obtained (Table 1).
The proportion of children who were
stages of immunization. Only 3% of the
children were not immunised and 12.4% normal (H/A, > - 2SD and W/H >-2SD)
were partially immunized. There were was 51.8%, that of stunting (H/A <-2SD
16.9% child deaths among the families of and W/H >2SD) was 27.6%, that of wast
the children surveyed. Similarly, 1.9% of _ ing (H/A > 2SD and W/H < - 2SD) 9.9%
the mothers surveyed had delivered still and that of simultaneous wasting and
birth babies and 3.3% of the mothers had stunting (H/A <- 2SD and W/H <- 2SD)
experienced at least one abortion.
10.7%. Female children were found to have
Only 27.0% of mothers had given colos lower prevalances than male children but it
trum to the children surveyed. Majority of was significant for only wasting (p < 0.05).
the mothers had given sugar water (64.1%)
Prevalences of stunting, wasting arid una= the first feed and others (8.9%) had , derweightby age group are shown in Table
.ven honey and donkey's milk. Children 1 2. Prevalences of severe stunting (5.1%)
who were given supplementary food by and severe underweight (3.0%) were ob
4th month constituted 11.3%, 13.7%.were served in the sample children studied.
Table 1. Distribution of Children According to Normal, Stunted, Wasted and Simultaneously
Wasted and Stunted Based on Waterlow's Cross-classification of Height-for-Age and
Weight-for-Height
Male
No.
%
female
Nj/
%
Normal
521
50.1
520
Stunted
286
27.5
Wasted
118
11.4
Wasted and stunted
114
Total
1039
Total
No.'
%
53.6
1041
51.8
268
27.6
554
27.6
81
8.3
199
9.9
11.0
102
10.5
216
10.7
100.0
971
100.0
2010
100.0
Vol. 65, No. 4,1998
THE TAMIL NADU NUTRITIONAL SURVEY
However, there were no children with se
vere wasting. Prevalences of stunting,
wasting and underweight were at their
lowest among children below six months
but steadily increased reaching the peak
569
between 18-23 months and there on de
clined.
In Table 3 prevalence of malnutrition
based on MUAC is presented. According to
this 6.5% of the children were found to suf-
Table 2. Distribution of Number of Children by SD Scores for Height-for-Age, Weight-for-Height
and Weight-for-Age for the Sample of Tamilnadu Children
Age group
_____________________________
0-5
months
6-11
months
12-17
months
18-23
months
24-29
months
30-35
months
Total
Height-for-Age (SD Score)
-2.00 or more
278
(90.5)
-2.00 to -2.99
20
(6.5)
-3.00 to -3.99
8
(2-6)
-4.00 or less
1
(0.4)
267
(72.0)
80
(21.5)
14
(3.8)
10
(2.7)
221
(59.4)
94
(25.3)
38
(10.2)
19
(5.1)
153
(43.9)
109
(31.2)
53
(15.2)
34
(9.7)
190
(55.1)
86
(24.9)
50
(14.5)
19
(5.5)
139
(52.2)
74
(27.8)
33
(12-4)
20
(7.6)
1248
(62.1)
463
(23.0)
196
(9.8)
103
5.1)
Weight-for-Height (SD score)
-2.00 or more
290
(94.5)
-2.00 to -2.99
15
(4-9)
-3.00 to -3.99
2
(0.6)
-4.00 or less
0
(0.0)
320
(86.3)
48
(12.9)
3
(0.8)
0
(0.0)
268
(72.0)
95
(25.5)
9
(2.5)
0
(0.0)
220
(63.0)
115
(33.0)
14
(4.0)
0
(0.0)
271
(78.5)
71
(20.6)
3
(0.9)
0
(0.0)
230
(86.5)
34
(12.8)
2
(0.7)
0
(0.0)
1599
(79.6)
378
(18.8)
33
(1-6)
0
(0.0)
Weight-for-age (SD score)
-2.00 or more
281
(91.5)
22
-2.00 to -2.99
(7.2)
4
-3.00 to -3.99
(1.3)
0
-4.00 or less
(0.0)
202
(54.4)
118
(31.8)
42
(11.3)
9
(2.5)
160
(43.0)
122
(32.8)
77
(20.7)
13
(3.5).
109
(31.2)
148
(42.4).
80
(22.9)
12
(3.5)
120
(34.8)
130
(37.7)
77
(22.3)
18
(5-2)
96
(36.1)
120
(45.1)
42
(15.8)
8
(3.0)
968
(48.2)
660
(32.8)
322
(16.0)
60
(3.0)
371
372
349
345
266
2010
Total
307
’Figures in parentheses are percentages
570
RAJARATHNAM ABEL AND V. SAMPATHKUMAR
Vol. 65, No. 4,1998
Table 3. Distribution of Children According to MUAC
<12.5
Total
Female
Male
No.
%
No.
■%
No.
%
63
6.1
68
7.0
131
6.5
12.5 -13.5
120
11.5
141
14.5
261
13.0
>13.5
856
82.4
762
78.5
1618
80.5
Total
1039
100.0
971
100.0
2010
100.0
fer from severe muscle wasting and 13.0%
were suffering from moderate muscle
wasting. A higher percentage of female
children were suffering from muscle wast
ing when compared to male children and
this was statistically significant (p < 0.05).
DISCUSSION
This study was carried out in rural
Tamilnadu. Tamilnadu stands second to
Kerala with respect to some of the health
indicators. Birth rate and infant mortality
rate is low when compared to other states
in India. Female literacy has increased con
siderably over the years.8 This could have
increased the utilization of health services
particulary immunization of children
which has a high coverage in the state.
The survey methodology was well ex
ecuted. Data on 2039 children was col
lected, out of which 29 were excluded. The
proportion of males to females did not dif
fer from that estimated for the study popu
lation.
The percentage distribution of socio-demographic factors such as caste, educa
tional qualification of mothers, immuniza
tion coverage, number of child deaths,
number of still births and number of abor
tions of the sample surveyed by us were
similar to the National Family Health Sur
vey carried out in 1992.1’ According to the
National Family Health Survey the per
centage of Schedule caste children was
23.2% (22.4% in the present survey) and
tribal children 0.4% (0.4% in the present
survey). Similarily, 54.9% of the mothers
had no education while in our study it was
55.6%. The proportion of fully immunized
children reported by the National Family
Health Survey was 50.5% while it was
58.8% in the present survey.
According to National Family Health
Survey, the proportion of child deaths was
17.7% and that of still births 2.8%. In the
present survey the proportion of child
deaths was 16.9% and that of still births
1.9%. Mothers who gave colostrum consti
tuted 21.8% in their survey while it was
27.0% in the present survey. Similar find
ings obtained in both the studies indicate
that the sample chosen for this study was
representative of rural Tamilnadu.
The prevalences of stunting, wasting
and simultaneous stunting and wasting
found using the cross-classification of
height-for-age and weight-for-height rec
ommended by Waterlow et al5 were higher
when compared to the reference popula
tion. Female children were found to have
significantly higher weight-for-height
Vol. 65, No. 4,1998
THE TAMIL NADU NUTRITIONAL SURVEY
when compared to male children. This is
surprising as Tamil Nadu has lower sex
ratio and female infanticide is practiced in
some parts of Tamil Nadu.14
Prevalence of stunting and wasting
among children has decreased consider
ably when compared to the prevalences re
ported by earlier studies conducted in the
years 1976’ and 198310 from the same re
gion. This could be attributed to the WHO
compaign of health for all by the year 2000
which underlines improvement of nutri
tional status among children as one of its
goals. Agewise trends indicated a higher
prevalence of stunting, wasting and under
weight among children between the age
group of 18-23 months.
A striking feature was the absence of se
vere wasting (below-4SD) in the sample of
children studied. On the contrary the sam
pled children were found to suffer from se
vere stunting and severe underweight. This
suggests that the present state of nutrition
(as reflected by the values of weight-forheight) is strikingly better than the past nu
trition (as measured by height-for-age). Be
sides weight-for-height responds faster to
intervention programmes than height-for
age which takes a longer period for the in
terventions to get translated. The National
Health Survey13 reported a prevalence Of
46.6% under weight (< - 2SD) while it was
51.8% (Table 3) in the present study.
Although clinical forms of protein-en
ergy-malnutrition were not studied, the
field investigators were on the look out for
children with marasmus and kwashiorkar.
Out of 2039 children the number of cases
with clinical signs of malnutrition was less
than 10 (0.5%). Of these only one was
kwashiorkar and the remaining were
marasmus. This is an indication that the
clinical forms of malnutrition are no more a
571
major problem in this part of India.
Conclusion
Stunting remains a problem among chil
dren of Tamil Nadu. The problem of stunt
ing among children can be addressed by
ensuring food security, good health care
services, better sanitation and also by in
creasing the awareness among mothers on
health and nutritional aspects.
Acknowledgements
We are grateful to Tamil Nadu Integrated Nutrition
Programme (TINP), Government of Tamilnadu for
their help rendered towards this survey.
We are thankful to Dr. P.S.S. Rao, then Professor
and Head of Bio-statistics, Department of Christian
Medical College, Vellore for his guidance in design
ing the study, Dr. Richard, Professor and current
Head of Bio-statistics, Department of Christian Medi
cal College, Vellore for going through the draft and
for statistical suggestions, and Ms. Mercy, Statistician
in RUHSA for help in analysis of data. The authors
also acknowledge the field workers who collected the
data and Ms. V. Mahalakshmi for computerisation.
REFERENCES
Administrative Committee on Coordina
tion-Sub Committee on Nutrition. Over
view of trends in malnutrition. Second Re
port on the World Nutrition Situation. Glo
bal and regional results, Vol. 1. ACC/
SCN, Geneva, 1992; 11.
2. Gopalan C. Stunting significance and im
plications for public health policy. In :
Waterlow JC, ed. Linear Growth Retarda
tion in Less Developed Countries. Nestle
Nutrition Workshop Series. Vol. 14, New
York; Raven Press 1988; 256-2843. World Health Organisation. Global strat
egy for health for all by the year 2000.
Health for All Series, No. 3 WHO, Geneva,
1981; 15-18.
4. WHO Technical report Series. Methodol1.
572
RAJARATHNAM ABEL AND V. SAMPATHKUMAR
ogy of nutritional surveillance : report of
a joint FAO/UNICEF/WHO Expert
Committee, No. 593. WHO, Geneva,
1976; 36.
5. Waterlow JC, Buzina R, Keller W, Lane
JM, Nichaman MZ, Tanner JM. The pres
entation and use of height and weight
data for comparing the nutritional status
of group of children under the age of 10
years. Bull WHO 1977; 55 : 489-498.
6. Food and Nutrition Board. National
Academy of Sciences - National Research
Council. Comparison of body weights
and lengths and heights of groups of chil
dren. Nut Rev 1974; 32 : 284-288.
7. World Health Organisation. Measuring
change in nutritional status. Guidelines for
assessing the nutritional impact of supple
mentary feeding programmes for vulnerable
groups. WHO Geneva, 1983; 21.
8. Bose A. Population of India. 1991 Census
results and methodology. Delhi : B.R. Pub
lishing Corporation, 1991; 54.
9. Anderson MA. Comparison of anthropo
metric measures of nutritional status in
preschool children in five developing
countries. Am J Clin Nutr 1979; 32 : 23392345.
10. Steinhoff MC, Hilder AS, Srilatha
Vol. 65, No. 4,1998
VL, Mukarji D. Prevalence of malnutri
tion in Indian Preschool age children :
a survey of wasting and stunting in
rural Tamilnadu. Bull WHO 1986; 64 :
457-463.
Households survey capability
programme. How to toeigh and measure
children. New York : United Nations
11. National
12.
13.
14.
15.
Department of Technical Cooperation for
Development and Statistical Office, 1986;
14-59.
Jordan MD. The CDC anthropometric
software package. Atlanta, GA : Centres
for Disease Control, 1986; 136.
National Family Health Survey. Population
Research Centre. The Gandhigram Insti
tute of Rural Health and Family Welfare
Trust. Ambathurai R.S. Tamilnadu and
International Institute for Population sci
ences, Bombay, 1994; 174-177.
George S,. Abel R, Miller BD. Female
infanticide in rural South India. Economic
and Political Weekly 1992; 27 :1153-1156.
Administrative Committee on Coordiantion - Sub-Commitee on Nutrition. Wom
en's Nutritional Status. Second report on
the World Nutrtion Situation.Global and re
gional results, Vol. 1. ACC/SCN, Geneva,
1992; 51-57.
BANGLADESH INTEGRATED NUTRITION PROGRAMME
Ministry of Health and Family Welfare
_____ Government of the People's Republic of Bangladesh_____
Monitoring Report, June 1999
Monitoring report for the month of June 1999 presents data on the status of the monitoring indicators of
Community Based Nutrition Component (CBNC) in the programme thanas as of June 30, 1999. This
report was prepared in three sections to show the status of indicators separately for group of first, second
and third phase thanas where CBNC is being implemented in phased manner. Data were collected through
the Monthly Performance Reports (MPR) prepared at the Community Nutrition Centres (CNC) by the
Community Nutrition Promoters (CNP). Information collected in CNCs were compiled to produce
summarized unionwise and thanawise report by CNOs and thana level officials like ATFPO and
Managers of partner NGOs. The report contains information on the status of routine activities at CNC
level like GMP coverage, malnutrition rate among children under two years of age, weighing of women,
supplementary feeding of pregnant and lactating women, Anti-Natal Care (ANC) of pregnant women, birth
weight, nutrition management committee meetings, status of training and use of iodized salt postpartum
Vitamin A supplementation and Iron supplementation. Status of some key monitoring indicators during
Table!: Comparative Status of Some Selected Monitoring Indicators During Last Six Months (First Phase 6 Thanas)
Some Selected Monitoring Indicators
Comparative Status During Last 6 Months (%)
January’99 February
March
April
May
June ‘99
Average
GMP Coverage (<2 Children)
90.76
90.51
90.94
91.25
89.30
89.91
90.45
Severe Malnutrition (<2 Children)
2.43
2.15
2.00
1.80
1.93
1.75
2.01
Weighing of Pregnant Women
92.13
92.6
92.55
92.11
92.07
92.28
92.29
46.99
of CBNC Activities
Coverage by ANC
36.86
42.68
47.93
50.64
50.98
52.85
Coverage by SF (Sev. & GF <2 Children)
90.34
90.29
91.41
90.08
87.86
85.70
89.28
Coverage by SF (Preg. & Lac Women)
94.68
93.58
93.23
93.91
92.87
92.28
93.43
77.53
Households using Iodized Salt
84.88
81.95
73.8
75.98
74.25
74.30
CNP Refresher Training
96.10
73.96
80
93.84
93.99
93.58
88.58
Women Received Vitamin A Capsule
87.01
90.5
87.33
87.77
88.13
89.37
88.35
Women Received Iron Tablet
77.44
79.53
78.59
78.54
76.44
73.86
77.40
Coverage of VNMC Meeting
90.06
90.06
92.97
88.55
90.11
88.68
90.07
last six months in first phase program thanas are presented in table-1.
GMP is considered as one of the key indicators of the successful CBNC. It appears from the above
table that the average GMP coverage was 90.4 % during the last six months. Percentage of severely
malnurished children is also gradually reducing. It may be mentioned here that the percentage of
severe malnutrition was 13.8% at the begining of the implementation of CBNC in April 1997.
Improvement by 16% in the coverage of ANC of pregnant women was observed during last 6 months.
Status of Monitoring Indicators in Second Phase 17 Thanas:
CBNC activities were supposed to start from early 1998 but the implementation was delayed for
more than six months for different reasons like flood and delay in disbursement of funds. Training
and other preparatory activities were completed in March 1998 and opening of the Community
Nutrition Centrs started in April 1998 but all community level activities were disrupted in most of
the thanas due to flood during August-September 1998. Reorganization in the CNCs and to bring
the situation in normal shape took about three months after the flood. From February 1999 the
CBNC activities again started in full swing with the active cooperation of the 6 partner NGOs.
Name of second phase CBNC thanas and some vital statistics along with the names of the partner
NGOs working in those thanas are presented in table-2.
Table- 2 : Some Selected Statistics of Second Phase 17 Thanas
Lactation
Women
Partner
NGO
CARE
Estimated
Population
Household
No. of
CNO
CNP/
CNC
Under 2
Children
Severe Mal
nourished
Pregnant
Women
Norshingdhi Sadar
498,554
86368
34
328
21874
1565
5887
5353
Barisal Sadar
Proshiika
457,624
52719
22
198
12860
713
2573
2894
Chandpur Sadar
BRAC
468,393
61460
31
312
19173
1893
4108
3314
Fatikchari
CARE
428,608
77402
39
359
22607
2819
5342
6063
Kulaura
BRAC
375210
65711
31
340
20334
1010
3745
4068
17008
2357
4594
4211
Name of Thana
CARE
340027
57917
24
216
Goplalgonj Sadar
Proshika
321896
46291
26
240
14484
996
3371
2597
Dumuria
W. Vison
283339
52520
19
189
11109
301
2310
2835
Shibpur
BRAC
262067
52638
18
174
14272
441
3435
2904
Bhanga
Proshika
237164
41856
24
195
10789
758
3850
2568
4426
Madaripur Sadar
Bhedergonj
CARE
228942
44137
21
177
12907
1463
2441
Adamdhighi
BRAC
188145
33213
13
129
6119
67
1476
1833
Teknaf
SHED
168517
27563
22
166
11934
699
3199
3712
Sreepur
BRAC
159586
26987
11
109
6739
81
1509
2198
Dacobe
W.Vishon
158105
27558
18
151
6459
275
1500
1977
Tarail
SARD
152977
29371
16
138
9531
375
2351
1938
CARE
95836
22044
8
74
5525
97
1070
1619
48,24990
805755
377
3495
223724
15910
52761
54510
Tetulia
Total
Monitoring activities at CNC, Union and thana levels were established systematically in second
phase 17 thanas in September 1998. Complete Monthly Performance Reports (MPR) are received
by the central office regularly from November ‘98. Status of monitoring indicators are stated below:
Weighing Coverage of <2 Children and Pregnant Women:
About 250,000 children below two years of age and 52,000 pregnant women in 17 programme thanas
were brought under regular monthly weighing. Overall
Fig. 1 : Weighing Coverage of <2 Children and
coverage of Growth Monitoring and Promotion (GMP) June
Pregnant Women in Second Phase 17 Thanas
(November 199X - June 1999)
1999 was 82.27 per cent which appears to be highest during the
last six months started from January 1999. While looking at the
GMP data by thana, the highest coverage (97.43%) was reported
in Gopalgonj Sadar>thana while the lowest coverage (64.58%)
was reported in Narsingdi Sadar thana. Weighing of pregnant
women is one of the important activity at the CNC to monitor
weight gain during pregnancy. About 86 per cent of the
pregnant women were brought under weighing in the month of
June 1999 which is also highest coverage over a period of last
six months. Highest per cent (95.13) of pregnant women was
in Gopalgonj Sadar thana and lowest per cent(77.56) were
weighed in Chandpur Sadar thana in June 1999. Weighing coverage of <2 children and pregnant women
over a period of last six month from January 1999 is presented in Fig.-1.
Monitoring Report, June 1999
Since weighing of <2 children and pregnant women are the most important indicators considered for
effective CBNC activities at community level, coverage of
weighing of <2 children and pregnant women was reviewed in
case of all partner NGOs. While looking at weighing data by
NGO. it appears that highest coverage exists in the thanas where
Proshika is working. On the other hand lowest coverage observed
in Narsingdi thana where CARE is working. However the
difference in terms of weighing coverage is not very big. Average
GMP coverage of partner NGOs in the month of June 1999 are
BRAC 88.92%. CARE 75.14%, PROSHIKA 95.62%, SARD
73.91%. SHED 84.42% and World Vision 87.42%. Regarding
weighing of pregnant women the highest average coverage
(93.19 %) was found in the thanas where Proshika is working and
the lowest coverage was ( 87.62 %) in Teknaf thana where SHED is working.
Nutritional Status of <2 Children
On the basis of the information obtained through monthly performance reports it was found that the severe
malnutrition among children under two years of age was 11.96 per cent in second phase 17 thanas in
the month of November 1998 and it came down to 5.68 per cent
in June 1999. The percentage of moderate malnurished children
was 35.91 in November 1998 and also decreased by 5.16 per
cent over a period of eight months upto June 1999.
However the percentage of children in the category of mild
malnutrition has increased from 23.12 per cent to 33.99 per cent
over a period of last eight months. Probable reason for increase in
the proportion of mild malnutrition is shifting of the severely and
moderately malnourished children to the mild and normal group.
Percentage of children falling in normal group has also increased
by 6 per cent during the above mentioned reference period.
Highest per cent of severe malnutrition (13. %) exists in Madaripur Sadar thana and lowest ie only 1.0% in
Sreepur thana under Magura District.
Status of Supplementary Feeding
In June 1999, 83.79 per cent of the Severely malnourished/growth faltered children (detected through
GMP) were brought under supplementary feeding in 17 second phase thanas.. Nearly 93 per cent of the
targeted children were brought under supplementary feeding at Tetulia thana which is the highest
coverage of supplementary feeding among all of the thanas in June 1999. The lowest supplementary
feeding coverage (69.50%) was reported at Bhadergonj thana.
Regarding feeding of malnourished pregnant and lactating women, the average coverage rate
was 84.19 per cent in June 1999. Highest feeding coverage (96.48%) of malnourished PLW was
reported in Tetulia and lowest coverage (69.50%) was reported in Bhadergonj thana. Average
feeding coverage in case of malnurished PLW over a period of last eight months starting from
November 1998 was 86.26 in third phase 17 thanas. Coverage of other important indicators in
second phase 17 thanas over a period of last 8 months is shown in table-3.
Monitoring Report. June 1999
Table-3 : Comparative Status of Some Selected Monitoring Indicators During Last Six Months in Second Phase 17 Thanas
Some Selected Monitoring Indicators
of CBNC Activities
Comparative Status During Last 6 Months (%)
January’99 February March
June‘99
Average
GMP Coverage (<2 Children)
72.87
76.61
80.72
81.04
80.41
82.27
78.99
Severe Malnutrition (<2 Children)
11.25
9.28
7.19
6.74
6.56
5.68
7.78
Weighing of Women (Pregnant Women)
75.8
79.68
83.94
82.33
85.05
86.26
82.18
Coverage by ANC (Pregnant Women)
20.01
22.53
27.82
27.11
31.72
32.55
26.96
Coverage by SF (Sev. & GF <2 Children)
82.15
86.09
86.68
85.2
87.07
83.79
85.16
Coverage by SF (Preg. & Lac Women)
81.82
87.73
87.87
86.04
86.31
84.19
85.66
Households using Iodized Salt
57.97
59.38
68.88
70.2
72.37
67.25
66.01
CNP Refresher Training
82.05
86.24
96.5
93.7
99.14
86.91
90.76
69.03
May
April
Women Received Vitamin A Capsul
65.05
63.84
66.78
73.3
75.71
69.49
Women Received Iron Tablet
42.96
57.04
67.03
60.78
69.73
68.87
61.07
Coverage of VNMC Meeting
92.84
90.96
88.66
90.82
87.85
94.38
90.92
Since the contract with the partner NGOs assisting GOB in implementation of CBNC in second phase
17 thanas has expired on 30 June 1999 immediate follow up action is needed to renew the contracts
for running the CBNC without any discontinuation.
Progress of CBNC activities in Third Phase 17 Thanas:
Selection of partner NGO and signing contract with them for assisting Government in implementing
CBNC activities in third phase 17 thanas were completed on March 01,1999. Name of partner
NGOs and thanas assigned to them are : BRAC for Matlab, Sariakandi, Jamalpur Sadar, Srimongal,
Nikli and Shibpur, Madhukhali. CARE for Damudia, Amtoli, Gaurnadi, Monohordi and Bada.
World Vishion for Batiaghata and Rupsha . Proshika for Tungipara. SHED for Chokoria and TMSS
for Sherpur.
Orientation and Training of Core Training Team (CTT) and Thana Trainng Team (TTT) were
completed in May 1999. 1st and 2nd installment of funds to the NGOs were disbursed. Local
committees like Thana Nutrition Management Committee <TNMC), Union Nutrition Management
Committee (UNMC) and Village Nutrition Management Committee (VNMC) were formed.
CNO/CNP selection by involving local committees and through social mobilization by NGOs are
going on. Training of CNO and CNPs were started in phased manner where selection procedure has
been completed. All registrars, forms and equipment were supplied to the NGOs for starting CBNC
in their respective thanas. Some NGOs have already started household profile survey in each
household to collect baseline information and preliminary selection of target beneficiaries.
Report prepared by : Md. Yeakub Patwary, Consultant (Programme & MIS) and Dr. Rowshan Jahan, Deputy Director (Programme &MIS)
Edited by: Mohammad Ayub, Line Director, 7A Paribagh, Dhaka-1000, Phone-862033
>4
ona
A BI-MONTHLY BULLETIN ON PRIMARY HEALTH CARE IN COMMUNITY HEALTH
COMMUNITY HEALTH CELL
326. V Main, I Block
Koramangala
Issue 19th August 1991
NUTRm^OHECK BY
@UA© STUCK
In Fiona Plus issue 4 we published a weight-for-length chart for infants and small children up
to 100 cm in height. This is reproduced in this issue for continuity in checking nutrition.
Weight--for-Length Chart
Length
Mimimum Weight
.Length
Minimum Weight
55 cm
56
57
58
59
60
61
62
63
64
65
66
67
68
69
70
71
72
73
74
3.5 kg
3.7
3.9
4.1
4.4
4.6
4.9
5.2 ■
5.4
5.6
6.0
6.2
6.4
6.7
7.0
7.2
7.5
7.8
8.0
8.2
8.4
8.6
8.8
78 cm
79
80
81
82
83
84
85
86
87
88
89
90
91
92
93
94
95
96
97
98
99
100
9.0 kg
9.2
9.4
9.6
9.8
9.9
10.1
10.2
10.4
10.6
10.8
11.0
11.2
11.4
11.6
11.8
12.0
12.2
12.5
12.8
13.0
13.2
13.5
76
77
A BI-MONTHLY BULLETIN ON PRIMARY HEALTH CARE IN COMMUNITY HEALTH
B Fiona TluT
Issue 19th August 1991
fe Fiona -Plus Focuss
Fionc r'lus
Issue 19th August 1991
STANDING ORDERS FOR PRIMARY HEALTH CARE
Signs & Symptoms
Medicines
Baby below 1 year
Small child 1-3 years
Older Child 4-13 Years
Adult
Suggestions
Abdominal pain without
Belladonna tab
Carry baby in
1/4 tab 3 x /day x 2 days
1/2 tab 3 x /day x 2 days
1/2 tab 4 x /day x 2 days
Hot Water Bottle to abdomin. Send to dr, after 2 days
vomiting
Antacid tab
upright position
1/4 tab 3 x /day x 2 days
1/2 tab 3 x /day x 2 days
1/2 tab 4 x /day x 2 days
Abscess of skin
Warm salt water
Compress 4 x /day
same
Same
Same
Open pus with sterile needle
Anaemia and weakness
Iron with folic acid tab
1/4 tab 2 x /day x 30 days
1/2 tab 2 x /day x 30 days
1/2 tab 2 x /day x 30 days
1 tab 3 x /day x 30 days
Nourishing food. Look for bleeding.
Asthma, short of breath
Aminophyllin tab
1/4 tab 3 x /day x 2 days
1/2 tab 3 x /day x 2 days
' 1/2 tab 3 x /day x 2 days
1 tab 4 x /day x 2 days
Send to doctor after 2 days.
Bleeding after delivery
Ergotamine
1 tab 3 x /day x 2 days
Send to doctor if serious.
Burns
Gentian violet 1%
Apply to possible infected areas.
Same
Same
Same
Send to doctor if serious.
Constipation
Ispaghule (Isapgol)
1/2 tsp 1 x /day
1/2 tab 2 x /day
1/2 tsp 3 x /day
1 tsp 3 x /day
Drink plenty of water.
Cough only
Cough sedative tab
1/4 tab (crushed) 4 x /day
1/2 tab (crushed) 4 x /day
1 tab (sucked) 3 x /day
1 tab (sucked) 4 x /day
Send for Xray after 15 days.
Cough and sputum
Trimethoprim tab
1/4 tab 2 x /day x 5 days
1/2 tab 2 x /day. x 5 da,^^
1 tab
2 tab 2 x /day x 5 days
Send for Xray if blood in sputum.
Cracked heels
Vaseline
Rub with soft stone
Apply after soaking in soapy water.
Cracked lips
B complex tab
1/2 tab daily
1/2 tab 2 x /day
1 tab 2 x /day
1 tab 3 x /day
Nourishing food best.
Cracks between toes
Fungicidal ointment
Keep feet clean
Apply daily
Same
Same
Apply after soaking in soapy water.
Diarrhoea, mild
Furazolidone
1/4 tab (crushed) 3 x /day x 2 dats
1/2 tab (crushed) 3 x day x days
1 tab (crushed) 3 x /day x 2 days
1 tab 4 x /day x 2 days
Report to doctor if stools ^bloody
Diarrhoea, severe
Rehydration (ORS) fluid
Give frequently after each motion.
Give often to stop thirst.
Give 1 cup after each motion
May need 3-4 litres/day
Give until diarrhoea stops.
Ear infection
Tetracycline eye/ear ointment
2 drops into infected ear
Same
Same
Same
Warm ointment before putting in, then lie on other side 20 minutes.
Warm ointment before putting in.
x 5 days
Eye infection
Tetracycline eye/ear
ointment
1 drop in infected eye
1 drop in each eye at birth
Same
Same
Same
Fever only
Paracetomal
1/4 tab (crushed) 2 x /day x 2 days
1/2 tab (crushed) 2 x day x 2 days
1 tab 3 x /day x 2 days
2 tab 3 x /day x 2 days
Send to doctor if drowsy.
Fever and chills
Chloroquine tab
1/2 tab (crushed) daily x 3 days
1 tab daily x 3 days
2 tab daily x 3 days
3 tab daily x 5 days
Take malaria blood slide first.
Headache
Paracetomal
1/4 tab (crushed) 2 x /day x 2 days
1/2 tab (crushed) 2 x day x 2 days
1 tab 3 x /day x 2 days
Aspirin 2 tab 3'X /day
Take aspirin with food.
Haemorrhoids (piles)
Haemorrhoid ointment
Apply as needed after motion
Same
Same
Same
1 tab daily x 8 days
1 tab daily x 8 days
2 tab daily x 8 days
Repeat after 1 month if necessary.
Aspirin 2 tab 3 x /day
Take aspirin with food.
Night blindness
Vitamin A tab
Pain in body
Paracetomal
Pain in joints
Aspirin
Poisoning
Charcoal and milk
Pregnancy
Iron/folic acid tab
Give as much as possible
1/2 tab (crushed) 2 x day x 2 days
1 tab 3 x /day x 2 days
1/4 lab 3 x /day x 2 day^_
1/2 tat^x /day x 2 days_________ 2 tab 3 x /day x 2 days
Same^^
Same
Same
1 tab 3 x /day x 30 days
Calcium tab
Replace haemorrhoids first Sit 15 minutes in hot water.
Menthol balm on joints' useful. Hot water compresses 2 x /day.
Send to doctor immediately.
Tetanus toxoid injections. Repeat medicines monthly
1 tab 2 x /day x 30 days
Round worms
Piperazine tab
2 tab (crushed) at one time
1 tab 2 x /day x 3 days
2 tab 2 x /day x 3 days
2 tab 2 x /day x 4 days
Drink plenty of water,___________________________________________ _
Scabies
Benzyl Benzoate
Apply 1 x daily x 3 days
Same
Same
Same
Wash first with soap and water.
Skin, infected
Gentian violet 1%
Apply to infected area
Same
Same
Same
Wash first with soap and water.
Skin, itching
Chlorpheniramine
1/4 tab 2 x /day x 2 days
1/2 tab 2 x /day x 2 days
1/2 tab 3 x /day x 2 days
1 tab 3 x /day x 2 days
Send to doctor if severe.
Skin, rash, dry
Sulphur ointment 10%
Apply 2 x /day to rash
Same
Same
Same
Cover with bandage.
Skin, rash, wet
Calamine lotion
Apply 2 x /day
Same
Same
Same__________________ __ Leave skin uncovered to dry.
Toothache
Aspirin
1/4 tab as needed
1/4
Oil of cloves
Apply to tooth 3 x /day
Same
tab
3 x /day x 2 days
1/2 tab 3 x /day x 2 days
2 tab 3 x /day x 2 days
Same
Same________________ _
Consult dentist. Brush teeth after each meal.
Urinary burning
Trimethoprim tab
1/4 tab 2 x /day x 5 days
1/2 tab 2 x /day x 5 days
1 tab 2 x /day x 5 days
2 tab 2 x /day x 5 days
Take plenty of water.
Vomiting
Avomine
1/8 tab only as needed
1/4 tab only as needed
1/2 tab as needed
1 tab as needed
Send to doctor if pain in abdomen.
Wounds, fresh, deep
Soap and water
Wash thoroughly.
Control bleeding.
Pressure dressing.
Treat shock.
Treat shock
Give TT and send for stitching
Issue 19th August-1991
■Fiona rlusB
The QUAC (Quaker Arm Cirumference) stick as
described in the Current Medicine Scan of the
Christian Medical and Dental Society (May 1990) is
a very useful way to determine whether an older
child is malnourished or not. It measures whether
the arm circumference of a child is as great as it
should be for a child of a particular height.
The QUAC stick is made from a flat piece of
wood 1 cm thick 4cm wide and 140 cm long,
painted white and marked at the appropriate
places with a black ball-point pen. A coat of clear
varnish protects the markings.
The arm circumference tape is made of paper. A
pattern of 10 tapes with centimeter markings is
-<?rawn on a sheet of standard type writer paper. The
pattern is photo copied and cut into strips 2 cm
wide and 28 cm long. These paper tapes will be as
accruate as the pattern. They provide a check from
being drawn too tight during the measuring proce
dure because they tear easily. Replacement cost is
practically nothing. It is efficient to measure chil
dren ranging from 5-10 years of age and children
taller than 133cm are not included 200 children
can be checked in each hour.
An assistant measures the arm circumference at
the mid-point of the left upper arm of each child.
Another assistant writes this measurement on a
small piece of paper and gives the paper to the
child. The child then goes to the QUAC stick some
distance away and hands its paper to a 3rd
assistant there.
See Table:-
Table-Markings for QUAC Stick
Heights (cm)
Arm Circumferences (cm) I
16.5 I
16.0 I
133
129
125
121
118.5
116
113.5
110
106.5
103
97.5
90
15.5 i
15.0 |
14.75
14.5
14.25
14.0
13.75
13.5
13.25
13.0
i
:
i
1
;
i
|
A.4 Assistant stands the child agains. The QUAC
stick and calls out the marking at his height. This
figures is written on the paper slip underneath the
arm circumference figure. After the measuring
session the two figures on each slip are compared.
18 the first figures (the child’s arm circumference)
is less than the second figure the child is counted
as “malnourished".
The percentage of malnourished children'can thus
be recorded and compared from time to time.
Fiona Plus is a free bi-monthly bulletin on primary health care in community health, being brought out by the
Christian Medical Association of India, the official health agency of the Protestant and Orthodox churches in
---------- India, a related ageny of the National Council of Churches and concerned with the promotion and
maintenance of health of all people, irrespective of caste, colour, creed or community.
Please let us know the name and address of any individual or instition for our mailing list, whom you feel
could be assisted by the receipt of this free bulletin in our efforts to create awareness of primary health care in
community health.
Editor
Managing Editor
Consultant.
Dr. Sukant Singh
Head. Dept. of Community Health, CMAI.
Ms. L.M. Singha
Communications Officer, CMAI.
Dr R. Seaton
Dept. of Community Health
Published by: Dr. D.S. Mukarji, General Secretary, Christian Medical Association of India & Printed at Mayar Printers, New Delhi.
All correspondence may be directed to:
Christian Medical Association of India, Plot No. 2, A-3, Local Shopping Centre, Janakpuri,
New Delhi-110 058. Tel:5552046 Telex:76288 CMAI IN Fax:011-5598150
-
A BI-MONTHLY BULLETIN ON PRIMARY HEALTH CARE IN COMMUNITY HEALTH
- Media
 RF_NUT_3_SUDHA.pdf
RF_NUT_3_SUDHA.pdf
Position: 1566 (7 views)