ALCOHOLISM
Item
- Title
- ALCOHOLISM
- extracted text
-
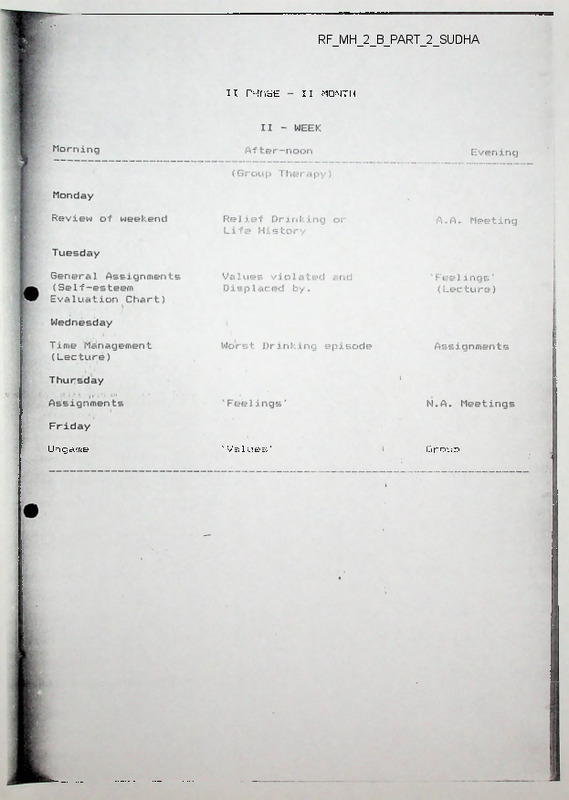
RF_MH_2_B_PART_2_SUDHA
II PHASE
Ungame
'Values'
II MONTH
Group
SEXUALITY
AND
RECOVERY
SEXUALITY
AND
RECOVERY
by
by
Barbara McFarland, Ed.D.
Barbara McFarland, Ed.D.
hzelden
First published November, 1984.
Your reason and your passion are the rudder
and the sails of your seafaring soul.
If either your sails or your rudder be broken,
you can but toss and drift, or else be held at a
standstill in mid-seas.
For reason, ruling alone, is a force confining;
and passion, unattended, is a flame that burns to
its own destruction.
Therefore let your soul exalt your reason to the
height of passion, that it may sing;
Copyright © 1984, Hazelden Foundation.
All rights reserved. No portion of this publication
may be reproduced in any manner without the written
permission of the publisher.
And let it direct your passion with reason, that
your passion may live through its own daily
resurrection, and like the phoenix rise above its
own ashes.
*
Foreword
ISBN: 0-89486-246-4
Printed in the United States of America.
Editor’s Note:
Hazelden Educational Materials offers a variety of information on
chemical dependency and related areas,. Our publications do not
necessarily represent Hazelden or its programs, nor do they official-
In writing this manuscript, I have primarily focused on in
dividuals who are heterosexual. However, in my professional
experience, I have found that gay couples I have treated have
also fallen victim to cultural stereotypes. Despite the fact that
the relationship might consist of two men or two women,
there often is still a dominant, or stereotypically “masculine”
partner and a more passive, stereotypically “feminine” part
ner. All relationships are based on certain expectations which
have been greatly influenced by our beliefs about what is ap
propriately masculine and what is appropriately feminine in
our culture. Gay individuals can still apply the principles and
ideas of this pamphlet to their own recovery.
* Reprinted from The Prophet, by Kahlil Gibran, by permission of
Alfred A. Knopf, Inc. Copyright 1923 by Kahlil Gibran and 1951 by Ad
ministrators C.T.A. of Kahlil Gibran Estate and Mary G. Gibran.
Perhaps another issue that needs to be addressed is that
often people are not in a committed relationship. However,
we do relate to members of the opposite sex most of our
waking day. Stereotypical attitudes can interfere in the
development of positive healthy work relationships, or friend
ships. Therefore, learning about one’s predispositions toward
sexual stereotypes can influence all relationships in a positive
and healthy direction.
Regardless of whether or not one is heterosexual or
homosexual, in a committed relationship or not, rigidly
adhering to one style of relating — dominant or passive — is
detrimental to the relationship and to the personal growth of
the individuals in that relationship.
Introduction
To admit that alcohol or other drugs have made life un
manageable is a beginning — one which is often a major
catalyst in getting a person into treatment. Usually by the
time someone enters treatment his or her life is a shambles, or
close to it. After all, the disease affects every aspect of a per
son’s life: psychological, physical, spiritual, and sexual. Yet,
sexual aspects of recovery are rarely dealt with.
Sex is uncomfortable for most people to discuss unless it is
in the context of a humorous anecdote or an off-color joke J
Consequently, sexual issues in recovery are overlooked com
pletely or only minimally considered as a treatment issue.
Perhaps this is due to an underlying assumption that the topic
should generally be limited to a discussion of sexual activity
or sexual performance, which is considered a private matter
best left alone.'1
Gender Identity
The physical aspect of sex is only one part of sexuality. The
other aspect — the one that is most critical and has a direct
impact on sexual performance — is what we will call “gender
identity.”
Gender identity is the way a person defines him- or herself
as masculine or feminine. There can be a cause and effect
relationship between gender identity and sexual expression.
People who are more accepting of all aspects of their sexuali
ty — their maleness and femaleness — are more able to be
sexually expressive in an intimate relationship.
In order to understand gender identity more clearly, let’s
look at the reentry of the recovering person from treatment
into normal life.' For both men and women, this reorganizational process, integrating sobriety into a life previously con
sumed by alcohol or other drugs, is deeply affected by their
ability to follow standards of sex-appropriate behaviors as
defined by our culture. The underlying assumption is that
such sex-typed behaviors are conducive to personal happiness
and allow men and women to function in the mainstream of
society. As a result of the women’s movement, it has become
increasingly evident that this assumption is wrong. Adhering
to rigid stereotypical behaviors, attitudes, and feelings blocks
personal growth and negatively affects the quality of a per
son’s relationship with self and others.
Stereotyped Roles
Despite the strides the women’s movement has made in
most areas, our culture has continued to perpetuate the vic
timization of both men and womeq by encouraging people to
accept stereotypical role behaviors.('The recovering male is en
couraged, to resume his role as head of household with all the
privileges and headaches inherent in that position.] By virtue
of his place in the labor market, he has the power and con
trol to make major decisions in the household. However, he
also assumes total responsibility for the economic security of
all family members, Given this role expectation, he must be
strong, aggressive, economically productive, and rational at
all times.’ One of the obstacles the recovering man often must
ft •
overcome is the repression of his feelings.
The recovering woman, on the other hand, is encouraged
to return home and resume her nurturing, caretaking, submissive/passive role of wife, mother, daughter, or employee.
The privileges inherent in her role are economic security and a
deep sense of emotional attachment, which are supposed to
give her a sense of purpose and belonging. One of the major
obstacles the recovering woman often must overcome is her
repression of her own internal resources — resources which
help her develop a degree of confidence in her ability to take
care of herself.
The man becomes an emotional cripple dependent on her
nurturance, and the woman maintains a childlike existence,
dependent on his economic power and decision-making skills.
Even lesbian/gay relationships Often take on the
dominant/submissive dynamic&HThis division of labor has
retarded the ability of men to be nurturers and caretakers, as
well as that of women to be decision-makers and bread
winners. As a result, neither gender is able to experience
other aspects of their full potential as human beings.
Even with single persons who are not in a committed rela
tionship, there can be a vague feeling of emptiness. Though a
woman may be working and economically self-sufficient, she
may miss the “status” and “strength” of a male/ The single
man, on the other hand, who has been taught to !be more in
dependent, often tends to look for nurturance in his sexual
encounters with women.
New Choices
There have been changes, but old attitudes die hard. People
are beginning to realize they have a choice. They can in
tegrate many aspects of masculinity/femininity (as defined by
the culture) into their personalities without feeling guilty or
ashamed.
Take, for example, how unusual it was a generation ago
for a man to go grocery shopping, diaper a baby, hug
8
another man, cry in public, cook and sew, or take care of a
sick child. It was quite unusual then for a woman to pursue a
career, pay alimony, be sexually aggressive, choose not to
have children, be athletic, make more money than her spouse,
or give up her children in a divorce.
The cigarette ad that cries “You’ve come a long way baby”
is also making a statement about men’s sex roles. As things
change for women, they will also change for men. This can
be frightening to many people. Adhering to old sexual stereo
types seems comfortable, easier, and much safer. This is
especially true for the recovering person.
Because of the failure each feels in not having lived up to
cultural expectations while using alcohol or other drugs (being
the good wife and mother, perfect daughter or employee, or
the strong, rational husband and father, or productive
employee) recovering people often try desperately to succeed
with these sex-typed expectations. They may cling rigidly to
what they believe will alleviate guilt. Keeping mired in guilt
and trying to make up for past failures only increases the
deep sense of inadequacy. Letting go of these old attitudes is
a beginning of healthy recovery. What makes this letting go
difficult is related to the role alcohol and other drugs played
in the sexuality of the dependent person.
Sex Role Stereotypes and Chemical Dependency
Women have been divided culturally into the Good Girl
type and the Bad Girl type. The Good Girl is the “ideal”
woman — chaste, thoughtful, loving, selfless, kind, generous,
and highly moral. She is a paragon of virtue. The Bad Girl is
the opposite of this saintly creature. She is a tough, pro
miscuous, aggressive, selfish person who thinks and drinks
“like a man.” Women struggle with these bi-polar conflicts,
especially in the area of sexual feelings, since our society has
tended to view the expression of sexual desire as inap
propriate in a female, sometimes even immoral.
In order to maintain the Good Girl image and yet be sex
ually responsive to a partner, many women use alcohol or
other drugs to loosen up, to lower their inhibitions so they
can feel sexier to please their partners more. For the
chemically-dependent woman, this only escalates her disease.
Her drinking gets worse and her self-esteem plummets. She
has become the opposite of what society says she should be.
Having sex while intoxicated helps her deny her true feelings
about her own sexual expression. It’s a great excuse the next
day to look in the mirror and say, “I was too drunk last
night ... I really got carried away . . . oh, well, if I hadn’t
been drinking, I wouldn’t have done that.” She blames the
desire for sexual activity on alcohol or other drugs. That way,
she can still be a “lady” in her own mind. This helps preserve
the female gender identity of Good Girl, at least for a while.
Once into recovery, women are often faced with the dilem
ma of being “good” yet sexual, and must solve it without the
use of alcohol or other drugs. This is a major recovery issue
for women, one that is difficult to discuss because of the
social stigma which has been attached to women who show a
desire for sex. Chemically dependent women have an especial
ly difficult time because of the additional stigma associated
with the disease.
It is interesting that, for a man, the reverse occurs.
Culturally, a “real” man is sexually aggressive and selfassured, not promiscuous but a “playboy” — tough, strong,
and independent. This is the Marlboro Man, James Bond,
Dirty Harry. Culturally, a man who is sensitive, insecure,
emotional, or sexually shy is viewed with disdain. He is
something of an anomaly because of his “feminine”
behavior. What is acceptable for women is not for men.
In order to cope with this image, alcohol or other drugs
can give the man a dose of false courage, the machismo to
“stand tall” and to “bite the bullet.” It lowers his inhibi
tions, too, for different reasons, but the result is the same.
Affects on Sexuality
: Just as there are stages of the disease, there are also stages
of the disease’s effect on individual sexuality. Initially,
chemicals are often used to help a person feel more comfort
able with sex, and more sexually provocative. During the mid
dle stages of chemical dependency, they help the person cope
with conflicting feelings of gender identity and sexual expres
sion. Of course, in the later stages of the disease, sexual pro
wess and conflicting feelings of gender identity become less of
an issue, and the desire to drink or use other drugs becomes
the individual’s primary focus in life.
Alcohol and-other drugs eventually affect physical perfor
mance. For males this might mean difficulty with erection or
premature ejaculation. Many men dread not being good
enough in bed. Because of the stereotypes, most of the
responsibility for sexual initiative and creativity falls on the
man. This pressure can, and often does, lead to impotence.
For a woman, frigidity, shame, or embarrassment might
result from things she did while intoxicated. Because she is
ashamed of and often confused by her sexual feelings, she is
unable to communicate her sexual needs. Her self-hate in
creases, but alcohol or other drugs help her cope. These sex
ual self-images of failure have been embedded in the
chemically dependent person’s mind. Sobriety makes them all
t^ie more a reality.
1 For example, a sexual memory that may haunt a male
might be the painful recollection that during the last several
attempts at sexual intercourse he was unable to achieve an
erection. The ridicule, criticism, or even silence from his part
ner has diminished his self-confidence as a fully functioning,
competent, and desirable sexual partner. Alcohol or other
drugs would numb this fear, but in sobriety he may feel trap
ped unless he is willing to risk again.j (V)
A woman may hold on to the memory of how sexually ag
gressive she was and how her moral values deteriorated dur
ing her drinking or other drug use. These sexual images deep
ly affect her self-esteem. Alcohol or other drugs will numb
her self-hate, but sobriety can keep it alive unless she is will
ing to forgive herself.
In recovery both sexes need to transcend the male/female
stereotypes in order to shed their old rigid sexual images.
Sexual Recovery
■ These painful memories are difficult to shake because there
is nothing to replace them. Cultural pressures and the effects
of alcohol and other drugs on psychological and physical
levels of functioning play havoc with the development of a
healthy gender identity. In part, chemicals are used to help
the person be what culture dictates. This is how they promote
sexual deterioration in the chemically dependent person.
Physical, psychological, and spiritual aspects of recovery
are fairly easy to determine. Physically, abstinence from
mood-altering drugs and adherence to a suitable diet improves
the body. A.A. meetings, therapy, and working the Twelve
Steps of the A.A. program improve the psychological realm;
prayer and meditation improve the spiritual realm. But what
improves the sexual? What benchmarks or goals can in
dividuals look at in order to make strides in their sexual
recovery? Frequent sex is not the answer.
Recovery in the sexual sphere means the recovering person
must go through a process of self-examination. Specifically, a
recovering person can look toward experiencing five stages of
sexual growth. These stages are not rigid and regression is not
unusual.
Being all masculine, drinking or sober, makes a man feel he
has to prove something. While drinking, it can be how much
booze he can tolerate. While sober, it can be how he can
“beat” this problem on his own. All masculine means, “I
can handle anything.” Needing others is a weakness.
Being all feminine, drinking or sober, makes a woman feel
she has to have someone take care of her. While drinking, the
alcohol can keep her helpless and nonfunctional, pulling peo
ple in to take care of her. While sober, she may be getting
sober for everyone else so they’ll take care of her. All
feminine means, “I can’t handle anything without someone
helping me.”
A person can become trapped by personal boundaries of
stereotypical sex-appropriate behavior. These boundaries can
be a safe place to hide. For men, their softer side is denied,
feelings are taboo, and after a period of time, they become
emotionally crippled; their feelings are alien even to them.
This makes it especially difficult to be intimate.
For women, their self-sufficiency is often squelched, and as
a result, their real internal resources are yet to be tested. Be
ing stereotypically feminine keeps a lid on the female’s
strength and ability to master her own fate. Using only half
of one’s potential and abilities causes the other half to
atrophy. As men harden, they become increasingly dependent
on women to nurture them, to be emotional for them; as
women’s strength withers, they become dependent on others
to be taken care of, to be their anchor throughout life.
Breaking Out
STAGE ONE:
Awareness of Self as a Male/Female Person
This stage requires a deep self-analysis of how. the person
defines maleness or femaleness by cultural standards. Before
beginning, one must see how detrimental it is to be either “all
masculine” or “all feminine.”
12
Breaking out of these roles can create problems because the
status quo is being shaken at its very roots. In a stereotypical
relationship, a man reaching out for support can be met with
disdain by the spouse who is fearful her “anchor” is falling
apart. In her eyes, and in his eyes, too, he has to be strong to
take care of her. His move out of his traditional role may be
met with resistance by a spouse who does not want the
balance changed. She fears it means ultimately she must
change.
13
c
The same problem can occur with the recovering female
who asserts herself and wants to become more financially in
dependent by getting a job. The husband may feel threatened,
fearing she won’t need him as much. In his eyes, she has to
need him for economic support; he has to take care of her.
This alters the balance in the relationship and requires the
male to see himself as more than just a paycheck and some
one in charge. In creating a more balanced gender identity,
the recovering person must understand that others may resist
this change and want to keep him or her in what is perceived
as a less threatening position.
Rewards
The rewards for struggling through this major shift in rela
tionship dynamics are immense. With equal, interdependent,
fully functioning partners there are no games or manipula
tions. There is no need to “win” or “lose” when there is
equality. This results in a deep respect for one another’s in
dividuality. The relationship becomes a place to relax, to
share, to let go, and to regroup; a place to feel a deep sense
of belonging and peace.
The recovering person and spouse are used to operating in
extremes. They both need to find a balance in gender identi
ty. Every human being has feminine and masculine traits. Our
culture has taught us to deny the opposite-sex trait. Healthy
sexual recovery requires that people integrate the other side
into their feelings, attitudes, and behaviors.
Can I be both masculine or feminine, depending on the situa
tion?
How do I treat members of the opposite sex?
What do I expect from members of the opposite sex?
As a man, do I view women as “sex” objects?
As a woman, do I view men as “marriage” objects?
Since this is the most critical of the stages, following are
exercises which will help generate some thoughtful answers to
the above questions.
Your Own Stereotypes
On a sheet of paper, write down the first name of a person
of the opposite sex you admire most. List the qualities you
admire (i.e. integrity, kindness, ambition, etc.) in this person.
How stereotypical are the qualities you’ve defined? Ask a
member of the opposite sex what he or she thinks of this list
and your perceptions.
Divide a sheet of paper in half. At the top of one side write
“masculine”; on the other side write “feminine.” List all the
traits that describe you. Share with someone of the opposite
sex who knows you well. Then share with someone of the
same sex who also knows you well. What kind of feedback
have you received about your masculine/feminine self
perceptions?
STAGE TWO:
Self-Examination
Awareness of How Others Perceive You as a
Male/Female Person
In examining your sexual self-awareness, consider these
questions:
How do I feel about myself as a man/woman?
How rigid am I in the expression of my gender?
How stereotypical are my attitudes, behaviors, and feelings?
How easily am I threatened by the unfamiliar?
How fearful am I of letting go?
This stage requires openness and willingness to see how
others perceive you as a man or woman, and how consistent
this is with your own perceptions.
Being able to receive feedback requires the ability to take
criticism. Chemically dependent people sometimes have dif
ficulty with this. Often perfectionistic and their own worst
critics, they typically balk at negative feedback from others.
In order to get in touch with others’ perceptions of your
15
sexuality, you must be willing to accept what may be painful
to hear. This feedback will be the basis for change.
As you work on this stage of sexual recovery, it’s impor
tant to move beyond the safe circles of friendships already
established. It’s imperative to relate to members of your own
sex. A heterosexual man will not usually try to dominate or
control another man. A heterosexual woman will not usually
try to play helpless victim to another woman. Interacting with
members of the same sex forces a person to be more honest
and less manipulative.
In getting feedback about your sexual self, first ask some
one of your own sex how he or she really perceives you.
Questions to consider include:
How do others see me as a man/woman?
How easy is it for members of the opposite sex to relate to
me?
In what ways do I relate to members of the opposite sex, i.e.,
aggressive, dominating, passive, dependent?
How comfortable am I with members of my own sex?
(Women have had much greater difficulty with this because
of the low status ascribed to women in our society.)
STAGE THREE:
Experimentation With Sex Roles
The last three stages are process stages which continue
throughout a person’s life, because, as sexual beings, we are
not static.
This stage involves crossing over the boundaries of stereo
types. Once you have achieved self-awareness and awareness
of others’ perceptions of you, take this information and start
experimenting with new behaviors, attitudes, and feelings.
For example, if you are a man, and you and others
perceive you as too intellectual, rational, and emotionally in
accessible, make a concerted effort to be more open by shar
ing feelings. One way to begin would be to start a daily jour
16
nal in which you record significant events and your reactions
to them. You might also record feelings you remember from
your dreams, and then see how they relate to what is happen
ing in your life.
You can also begin to separate your feelings about what
people do (actions) to you from what people say (words) to
you and decide which has the greater impact. This is another
step in raising awareness of your feelings. Recording these
reflections can be very helpful.
If, as a woman, you and others perceive you as too self
effacing, begin to practice assertiveness. A journal of reflec
tions can also be a powerful tool in raising awareness about
self-effacing behaviors. Therapy and A.A. discussion groups
are powerful springboards for this. Experimentation is pain
ful. During this time you will have to stretch yourself, take
risks, feel uncomfortable with new behaviors. But in riding
these feelings out you will be approaching balanced sexuality.
The key questions to consider during this stage are
How flexible am I?
How willing am I to change?
What sexual defenses have I developed?
What are my fears about my masculine side?
What are my fears about my feminine side?
STAGE FOUR:
Differentiating Between Sexual/Physical Needs
and Sexual/Intimacy Needs
Once you have become more comfortable in expanding
your gender identity, in being more spontaneous and fluid in
the expressions of both your masculine and feminine sides,
sex will take on a new dimension. No longer will sex be mere
ly a means by which you satisfy your physical needs. It will
become a vehicle through which true human intimacy can be
experienced. To someone rigidly fixated in the old sexappropriate behaviors, this intimacy can be terribly frighten
ing and, consequently, avoided.
17
0
The ability to give of oneself to another in the most in
timate of shared experiences requires unconditional self
acceptance as a sexual being. No side of that sexuality can be
repressed.
In sexual expression there is no game. No one should have
to do or be anything that isn’t consistent with the spontaneity
of the shared experience. One reaches out and gives to the
other all of oneself, not just those parts that seem to be ac
ceptable.
The key questions to consider during this stage are
What do I expect from my partner sexually?
Do I communicate verbally what my sexual needs are?
How do I show my affection for my partner outside the
bedroom?
What role does sex play in my relationship with this person?
How do I feel about initiating sex? What are the ways I do
this?
How do I feel about being creative sexually? How do I share
this with my partner?
Quality recovery is based on achieving a balanced lifestyle.
Although sexual aspects of recovery are often minimized, the
recovering person must take responsibility for this part of life
as a sober person. Open discussion of sexual issues, fears,
and doubts is critical to the restoration of healthy sexuality.
CONCLUSION
Integrating a program of recovery for sexual growth and
development only adds to the quality of sobriety for the
recovering person. Reexamination of what is comfortable and
familiar in terms of sexual self-definition is a painful and
often unsettling task. However, ignoring the sexual side of
one’s self inhibits a person from achieving a true sense of
balance in recovery.
STAGE FIVE:
Achieving Sexual Equilibrium
This is the stage of sexual self-actualization. It involves the
ability to be comfortable with oneself as a male or female in
everyday interactions and activities as well as in a sexual rela
tionship. It requires self-acceptance and acceptance by others.
Quality recovery should include the ability to be spon
taneous in the expression of the feminine and masculine sides
of our personalities, and the ability to be intimate by giving
of our sexual selves.
The key question to consider during this stage is this:
How willing am I to continually reevaluate myself as a sexual
human being?
iS
19
directions for
slings are natural
-U hl
They ore to be our friends,
Not our foes.
To be listened to as cues, signals.
To be cherished
As a part of us.
DIRECTIONS
Black stamps — Fear
Purpose: The purpose of THE STAMP GAME is to help players to
better identify, clarify ana discuss feelings.
Orange stamps — Guilt
Green stamps — Embarrassment
Leader: THE STAMP GAME requires that one person act as a
facilitator and not participate in playing the game.
Yellow stamps — Any form of happiness, such as joy,
warmth, love, etc.
Light Brown stamps — Confusion
Because this is an emotionally-charged game, the facilitator
must be a warm, caring person, comfortable with his own
feelings and the feelings of others.
■ Flayers: The game can be played with the facilitator and one
to six players. Groups with up to forty participants can play by
dividing players into groups of five, while the facilitator moves
among the groups. Co-facilitators may assist. (See enclosed
ordering instructions for additional stamps.)
Time Frame: A group of six players will take approximately 60
•to 90 minutes to play the game. Allow 90 minutes if feedback
(see “Extended Play") is utilized. THE STAMP GAME may be
ongoing in that participants may play a portion of the game
during each session. (See "Variations").
White stamps — Any feeling not listed above that player
SWild Card)
wants to identify, e.g., lonely, helpless.
3.
Ask participants to remember what it was like when they
were young children and teenagers growing up in their
fa nily. Then instruct them to pick up stamps which repre
sent the feelings they had as youngsters and adolescents.
4.
Explain that the stamps represent feelings, whether or not
people in their family were aware of them having these
feelings. Participants should select a number of stamps
representing the intensify of each feeling. Example: If a par
ticipant experienced a great deai of anger, he might take
5 to 10 red-anger stamps, compared to feeling a small
amount of fear, where he might take 2 or 3 black-fear
stamps.
Results: Players will be able to relate more honestly to others
when they have learned to express feelings. Players will begin
to respond appropriately to situations when they become
more aware of their reelings. As a result, players will become
increasingly more effective problem solvers.
Let participants know that they may not immediately iden
tity with a particular feeling and they are not required to
pick up any particular stamp color(s).
Setting: Game con be played on a large table or the floor
(more fun).
TO BEGIN:
1.
2.
Players sit in a circle.
Facilitator places stamps in center of circle, in piles accord
ing to cc'or and explains which colors represent what
Red stamps — Any form of anger such as rage, frustration,
irritation, disgust, etc.
Blue stamps — Any form of sadness such as
disappointment, loss, etc.
(This process usually takes approximately 5-8 minutes).
5.
When all group members have selected their stamps, in
struct them to arrange the stamps, in an order beginning
with the feelings expressed the most as a child, to feelings
shown next to the most, to those shown the least. Example:
the person who knows that he hid his anger, yet found it
easier to show sadness might position his blue-sadness
stamp(s) before his red-anger stamp(s). The person who
was afraid and showed that fear will have his black-fear
stamps in front of his orange-guilt stamps if he seldom or
never showed guilt.
There is no one correct way to position stamps; arrange
ment is left up to each player.
-2-
Abbreviated Topics:
2.
Feedback is given only in the form of offering stamps. To
give feedback players (one at a time) take stamps from the
community pile. These stamps represent what feelings they
believe the sharing player has not identified. Participants
place those stamps in front of the player's stamps and brief
ly explain to player their perceptions, e.g. "This is more
anger. I feel that there is more anger with your mom, but it's
too scary to share", or "this is more fear, I don't know what
it's about, I just sense more fear." Instruct group members to"
be as specific as possible, but to limit comments to 2 or 3
sentences. When sharing goes beyond 2 or 3 sentences,
the person giving feedback may be analyzing or intellectualizing, and should be politely asked to stop.
3.
The sharing player listens without verbally responding.
There is no dialogue regarding feedback. While the person
receiving feedback is not responding verbally, he acknow
ledges (agrees and accepts) feedback by picking up new
stamps and bringing them into his pile.
Feedback cannot be rejected.
The player receiving feedback reflects his openness (a will
ingness to reflect and consider feedback) by leaving
stamp(s) in front of pile.
THE STAMP GAME can be used as an integral part of ongoing
individual sessions or groups.
Participant may be asked:
— Pick up stamps that represent feelings you had this week.
— Pick up stamps that represent feelings you had today.
— Pick up stamps that represent feelings you had at school.
— Pick up stamps that represent feelings you had with a
particular person.
_ pick • ’p stamps that represent feelings you would like to
discuss.
Or participants may be asked to associate feelings to specific
si.cations. Pick up stamps that represent how you feit when
(Give example)
Examples:
— When your mom said she was leaving,
■ — When your dad didn't come to see you.
— After you said ‘no’ to your son.
Treatment professionals may suggest that families use THE
STAMP GAME (Abbreviated Topic Section) as a part of family
meetings.
Facilitators are encouraged to use stamps in a variety of situa
tions.
4.
Extended Play:
It is suggested that if facilitator is working with a person or
group over a period of time, clients may play the game more
than once. Often it is played first without the feedback com
ponent. At a later time, feedback can be included.
Feedback can be a vital part of THE STAMP GAME. Let
members know that feedback is optional, not required. Time
and players' familiarity with each other are the key factors in
whether or not this aspect of the game should be included.
1.
Feedback cannot be rejected.
Since the purpose of the game is to assist participants in
identifying and expressing feelings, it is not permissible to
offer feedback which removes a feeling, i.e. removing
player's stamps. Many times participants, in their desire to
protect another from his or her painful feelings, inap
propriately offer yellow-happiness stamps during feed
back. In order to facilitate changing this pattern,
discourage giving yellow stamps during feedback.
5.
When feedback is completed, move to next participant.
6.
Complete this extended version with a self-image or self
reflection exercise.
Feedback is given after each individual has completed
sharing his feelings in adulthood. To give feedback, other
participants reflect on what feelings they think the partici
pant had or presently has that he did not identify or share.
-5-
-6-
htemataalDrag
Carrol Ftep®
Reducing Vulnerability to
HIV/AIDS
In Drug Abusing
Populations
(The Affected, The Afflicted
and Those “At Risk”)
Through A Community Wide
Response
Global Illicit Drug Trends: 2000
Amphetamine Type Stimulants
Drugs of the 21st century?
Following dramatic increases in ATS abuse in early 1990s, markets in
Western Europe and North America are showing encouraging signs of
stabilization or decline
Globally, however, illicit supply and demand are still showing upward trend
In East and Southeast Asia, illicit production, trafficking and abuse are
rising. The region seems to be emerging as a prime source for both ATS
end-products and their chemical precursors. The danger of spread to other
parts of the world remains.
GLOBAL SCENARIO
High-High Risk=HIV
1.
134 countries have reported HIV till 1999
2.
Of these, 114 countries have reported IDU with HIV
Almost all HIV has underlying alcohol or other drug use (UNDCPUNAIDS document: Drug Abuse & HIV/ATDS- a devastating
combination)
Study of 10 million IDUs worldwide shows;
-
IDU is 7-22% of all drug use
1 in 10 IDU has HIV
UNDCP RESPONSE
1.
As a UNAIDS Cosponsor, UNDCP aims to reduce the vulnerability of
young people by carrying out projects that promote a healthy life-style.
2.
Having easy access to health services, developing life skills and being
educated about the health risks that come with drug abuse are the keys to
staying drug free - and free of HIV.
3.
A supportive environment is crucial
The Strategy’
•
Target, reach and bring about behavior change in a critical mass of
vulnerable population
•
.Aim for absolute coverage to reduce vulnerability
•
Reduce vulnerability through behavior change and reduction of risk
taking behavior
•
Bring about behavior change through sustainable innovative
community based, managed processes/ interventions
•
Improve capacities of care givers to bring about behavior change &
to assess coverage
The Challenges
> Create an enabling environment
> Identify, address & ensure appropriate capacity building to change
behavior
> Improve, expand and network available services
> Ensure absolute coverage
> Reach all HIV-IDUs among IDUs and reach all IDUs among Drug
Abusers
> Ensure that a critical mass of IDUs reached, change practices &
reduce vulnerability
> Deal with the family issues & reduce vulnerability
> Target the “at risk” effectively, “Innovative IEC”
NEWS FROM THE REGION
(ASIA - PACIFIC)
•
Only 3 Asian countries have HIV rates over 1% among 15-49 years old Cambodia, Thailand and Myanmar
•
However such low rates conceal huge numbers
•
Sex trade and use of illicit drugs are extensive
•
So is migration and mobility within and across borders.
Myanmar
Population
43 million
Government Figures
25000 HIV infected
World Bank
700 000 HIV infected
Growing sex trade and mounting use of intravenous drugs
Battle
Socio-cultural
Taboo against open discussion of
sexual health
Social stigma attached to
HIV/AIDS disease.
Yunan
•
7% sex workers inject drugs
• Amphetamines use in sex work settings is emerging rapidly in the region.
•
Emerging evidence of the role of other drugs including alcohol as a
Go-factor determining risk.
Northeastern Region - India
7 NE states constitute < 3% India’s total population but have
30% of country’s total IDU population (approx: 200, 000)
Manipur
First case of IIIV detected in 1989
HIV among IDUs > 75% in 1997
Non-injecting wives of male HIV positive IDUs - 45%
(late 1997).
Sentinel Surveillance ANC 1.69%, Blood donors 1.3%
Estimated Drug Users 15-20,000.
Sex Workers 1000
Total Population -1.8 million
The Scenario is comparable to Thailand whose ANC
1998 was 1.53%
& ■
A/"-'
.AC-Vvk. .
^cTiu'i7)fe_S <©£
L'.r:- iuered
Medical Services: v
❖
<•
❖
Doctor visits twice a week
Medications
Psychiatric consultations
Referrals/ testing
Therapeutic services: -
❖ Re-educative lectures
<• Activities
> Art therapy
> Therapeutic Games
> Energiser
❖ Group therapy
•> Individual counselling
❖ Follow up
❖ Home visits
❖ RPP (one month)
❖ Crisis intervention
❖ Family classes
❖ Marital counselling
v Counselling for children with specific problems
❖ HIV pre/ post counsel!ing
Extended services: -
❖
❖
❖
❖
❖
❖
❖
❖
❖
❖
❖
Yoga
Gym
AA / NA / Al-Anon Meetings
Bhajans
Sober Birthday celebrations
Vocational rehabilitation
Special programmes for recovering addicts
Community awareness programme
ACC anniversary celebrations
Celebrations of religious festivals
Programmes for trainees
<C
■
C£aj7£<
Supportive Features: ♦> Staff development programmes
❖ Weekly staff review meeting
Monthly ACC review meeting
❖ Documentation
<♦ Networking with other institutions
❖ Mobilising support groups
COMMUNITY MEETINGS
s programme starts with the community meetings.
used as a methodology to imparl value based thoughts.
RE-EDUCATIVE LECTURES
Disease Aspect
Disease concept
V Denial
J Dry drunk
J Relapse/warning signs
'z Psycho social factors. >
J Children of addicts and family violence
v Over coming grief
V Developmental task
J Powerlessness
J Human needs
J Surrender Vs compliance
J Emotional cost of dependency
J
Personality development
Assertiveness
Anger
Negative I positive feelings
Personality defects
Improving quality of life
J Self esteem
V Value
'C Hurt feelings
J
■/
V
V
v'
Recovery
V Problems in sobriety
V Facing challenge in life
V Building relationship
Medical issues
v'
v'
'■
Medical complications
Smoking
HIV/AIDS
Sexual problems
Coping: skills
✓
v'
v
Work Ethics
Financial Management
Time Management
Stress Management
Communication
•2 ■ reduction to AA
Steps of AA
Making amends
Resentments
Spirituality
Serenity prayer
J Slogans
J
/
/
<
''
' \ c V 'I..''
GROUP THERAPY IjgSiWES
/ Powerlessness
•/ Damages
/ Worst Drinking/ drug taking episode
S Insane And Aggressive behaviour
•/ Positive/ negative qualities
■/ Pleasure Vs pain
■/ Developmental stage
■/ Myths and misconceptions
✓ Tools of recovery
✓ Future risk situations
ACTIVITIES
Art Therapy
''
✓
'z
Problems in sobriety
Group art
Recovery tool box
1-ears
i aside Outside
Beauties in life
Therapeutic activities
Memory game - Ice call
- Anthakshri
- By default
flay modeling
Life skills activities
nmttnication
>
>
>
>
>
Dumb Charades
Guess what’s the good word
Chalk game
Trust walk
Pictionary
Self Esteem
>
>
>
>
>
>
Positive Strokes
Talents time
Tournaments
Self Esteem Envelope
Animals and Good points
Personal skills
Assertiveness
> Debates
Il
MH' '2-L. 3)
•AN
IDEAL ACTION
GENERATE
ENERGY
1.
Mind surrenders to Self
2.
Intellect fixed in Self
3.
Body active
AVOID DISSIPATION
1.
Anxiety for results of the future
2.
Worries of the past
3.
Excitement over the present
CONCENTRATION
Intellect directs mind to chosen action
CONSISTENCY
Intellect directs all actions to chosen ideal
o
CONTROL DESIRE AND EGO
DESIRE
Is the flow of thoughts towards an object or being
for fulfilling an unfulfilment felt within oneself.
MODIFICATIONS OF DESIRE
Desires fulfilled leads to greed (lobha), delusion (moha),
arrogance (mada), envy (matsarya) and fear (bhaya).
Desires interrupted give rise to anger (krodha).
EGO
Arises out of a feeling of :
I am supreme.
I only exist.
I am the doer.
Ego hurt gives rise to anger.
DESIRE/EGO
Causes mental agitations and inefficiency atwork.
INTELLECT
To reach the goals set by you, you need to make the
existing intellect available to you and also to develop
it. The intellect is made available through a process
called introspection. To develop the intellect further
you need to study and reflect upon Vedanta It is
available in the form of a book entitled "Vedanta Treatise".
GOALS TO ACHIEVE
1.
INDEPENDENCE
Examine the life of a plant, an animal and a human
being. The plant is most dependent while the human
is designed to be the least dependent on the world.
But man today is largely dependent upon the amenities
and facilities, the environment and circumstances of the
world You must shed this dependence, become wholly
self-sufficient and thus regain the dignity of a human
being.
2.
3.
HAPPINESS
It is the bliss of self-realisation. It is infinite, absolute
in quality and quantity. Once you enjoy the bliss of
the self within, the greatest joys of the body, mind and
intellect mean nothing to you. These joys are like the
waters entering the ocean.
KNOWLEDGE
Ignorance of Self projects this world. All the knowledges
acquired in this world are in the realm of ignorance
vis-a-vis the absolute knowledge of Self. The
knowledge of Self is pure knowledge compared to the
conditioned knowledges acquired in this world.
4.
LOVE
True love is universal, even, same to one and all. Love
in the purest form is everywhere, nowhere in
particular. It is regardless of caste, creed, colour,
community or country. It has no fixed location. It is
not concentrated in one form, it is realising oneness
with the world.
5.
POWER/STRENGTH
If you are selfish and egocentric in life, your power is
limited. Your actions are poor. Drop your selfishness
and ego, turn selfless you command real power and
strength. You become dynamic.
FUNDAMENTAL VALUES OF LIFE
1.
ACTION
Action is the insignia of life. Inaction is decay, death. ■
The first lesson in personality development is therefore
to be active.
2.
DIRECTION
What are you working for? What is the purpose of your
living? What is the mission of your life? Reflect on
these ideas. Fix an ideal, a goal, a cause for your
living. Let your actions be directed to that ideal.
3.
OBJECTIVITY
Is maintaining an impersonal attitude in life. Opposite
of being involved and entangled in the affairs of the
world. Look at the world as you would a picture on
the wall. Function in the world like an actor on the
stage.
4.
SENSE-CONTROL
Indiscriminate indulgence in sensual pleasures results in
the destruction of your personality. The senses are very
powerful. They distract you from your chosen path and
you lose your goal in life. Your intellect must keep
your senses under perfect control. Be a master and not
a slave to your senses. Besides losing your goal you
ultimately lose the very pleasure of the senses if you,
lack control over them.
5.
DUTIES, NO RIGHTS
The dignity of the human race is founded upon the
principle of obligatory duties, not rights. Develop the
art of giving, not taking. You have no right to claim
anything as yours. Your only right in the world is to
give, serve the society.
6.
CONSISTENCY
Having fixed a goal in life let all your actions flow
towards that particular goal. Keep your priorities clear
and use your sense of proportion and maintain the
consistency of purpose till you achieve the goal that
you have set for your life.
Dear reader,
This manual has been produced as one in a set of four manuals on:
Addiction Rehabilitation Programming; Community Action Against Drugs and
Alcohol; Drug and Alcohol Policy Development; Design, Implementation and
Management of Alcohol and Drug Programmes at the Workplace. The material
is first of all designed for use by the resource centres on drugs and
alcohol, under development in Southern Africa with support from the
Norwegian-funded ILO project RAF/89/MO5/NOR, "Establishment of resource
centres for rehabilitation, workplace initiatives and community action on
drugs and alcohol".
However, we hope that these manuals which are of a
rather universal nature will also be useful to other practitioners
concerned with the reduction of drug and alcohol problems anywhere in the
world.
Please note that this first version of the manuals is presented in
draft form. The manuals have been designed in such a way as to allow easy
additions, adaptations and modifications.
We would like to invite
comments and suggestions on how to improve the content as well as the
presentation of these manuals. Ideas and additional elements, especially
copies of case studies for inclusion, would be most welcome. It is our
intention to collect such comments and feedback for a period of at least
one year and then commence the revision of the manuals. A register of all
those who have received copies of any of the manuals will be maintained
for the purposes of periodic mailings of elements for insertion and
eventual distribution of the revised version.
I take this opportunity to thank you in advance for your interest and
contributions.
Geneva, April 1992.
Yours sincerely,
Jon Wigum Dahl
Project Coordinator,
Vocational Rehabilitation Branch,
International Labour Office,
CH - 1211 Geneva 22,
Switzerland
9
•
Facilitating growth
The counsellor should never forget that her involvement is of prime importance
in shaping the group norms. Too exacting behaviour or being too passive can
both inhibit members. She needs to play her role with confidence and poise.
Basic rules that are set at the start of the group process may sometimes need
further strengthening. The counsellor can draw attention to die norms through
statements, observations, questions and display of appropriate non-verbal
behaviour. For example, to encourage member to member communication, the
following methods can be used:
-
Asking for the other members' reactions
Refusing to answer questions directly
Nodding, smiling, good attending behaviour and verbal reinforcements help
shape positive behaviour. The counsellor choosing not to react to low tone
conversations, late coming etc, will be noticed by members of the group. Not
attending to these can even be seen as non-caring. Unhealthy practices like
frequent interruptions or excessive criticism can grow on quickly and it is the
counsellor's responsibility to guard against them.
The counsellor should encourage feed back. When a member is criticised or
confronted, caring questions like, "How do you feel about what was just said?",
helps that member respond. When many suggestions or comments have been
made in response to one member's sharing, asking him, "What did you find most
helpful? How did you feel to receive so much?", helps members give appropriate
feed back.
The counsellor is a "model setting participant" in many ways. Displaying good
attending behaviour is quickly copied by the members. By giving support and
encouragement, the counsellor invites members to follow suit. The counsellor's
handling of conflicts by permitting expression of negative feelings and working
through them rather than suppressing them, helps members learn to do the same
even in real life situations.
•
Recognising the Group's Power
The primary therapeutic agent in a group is always the interaction between the
members and not die counsellor. As an effective counsellor, she recognises that
the group's power is more than her own and makes the group assume
responsibility to make the interactions. If the counsellor takes the responsibility,
the members would sit back and wait for the counsellor to make the interventions
as if watching a movie.
The counsellor needs to resist the urge to quickly intervene with the right
answers, and should wait for a discussion to follow and allow it to slowly steer to
a conclusion. The group values the decisions that they arrive at and does not look
for quick fix answers from the counsellor even if the solutions are just as, if hot
more effective.
10
Recording
The progress or lack of it among each member in the group and the counsellor's
impressions need to be recorded. This will help the treatment professional to see and
clarify the level of progress and plan further directions of progress. In case a
different counsellor takes over, she will be able to
-
assess the progress of each member
set specific goals for each member
identify- and help him plan to deal with negative factors so that they don't grow
stronger and interfere with the recovery process.
use those facts to give appropriate feedback to members.
Recording is thus extremely useful and clearly necessary. But for the "time-pressed"
counsellor, if recording needs a lot of time, it can become stressful and poor
compliance will result. To prevent this, recording should be structured, and carefully
structured recording will not take more than 10 minutes.
If 5 sessions are held in a week, a weekly recording will suffice. If the session is
once a week, recording can be done immediately. Group therapy initiated changes
may continue in-between these sessions also. Recording helps the counsellor keep
tabs on the issues discussed and maintain continuity between sessions.
The ultimate goal of group therapy is to aid self understanding and initiate change to
the maximum level possible in each and every member of the group. Three factors
contribute to this outcome.
1.
2.
3.
The skill of the counsellor.
The openness of the members who constitute the group
The (genuine) interaction between the members.
Therefore, the skill of the counsellor needs to be sharpened .periodically through
frequent self-assessment, clinical reviews with peers, openness to new techniques
and readiness to explore in directions suggested by group therapy research studies.
Tire counsellor has some control over the second factor also in the sense that through
a display of supportive care and concern, she can facilitate the group to become open
and honest in their sharing. This will lead to genuine "feeling level" interaction and
conflict resolution. To put it plainly, the counsellor even though a catalyst, is the key
player and her skill is of prime importance.
21.12iT3.biuays
i im
i
of sFct Influence
1
I 65.3%
| ACUlt
[ 69.2%
M-’C-P
I
I
I
|
I 1Q
I = . on,
I
I
I Unsuoervised
I 72.1%
I -------I 31.0%
I img inrofiTiauun
| UO.O7U
j
|
j Jobs
I
u.8%
Coping strateges and skills
To deal with a wide rance of dressers likely to be encountered in everyday life, the individual
reouires to acouire a wide range of coping and social skills. They may be cognitive or behavioural
Cogiitive skills- self assurance, cognitive restructuring cognitive detraction, self control etc.
Beha^cral skills - problem solving action throuc^r negotiation / compromise, withdrawal throuc^
*.
leaving^ avddng the dtuation, communication drills, assertiveness, social networking far)g^grt0 in
alternate activities relaxation
Practical performance skins and Survival skiiis ('Ahi ch may be considered :!aberranr in the wider
cun 11 m nuy; —eg. ng nriy run ni y iaai, reacting quickiy, weaii lerii ig physical harm etc. may ba very
•JSP C^’.’OS
9 noninfi efratpfar Th<=i rretinrih/ nf th® dTUG US?HO Child!r6in StUCf^jd hAd '/BP/ DOOT
adatxive cooing skills.
I /'ciaptiver Pro-social (%)
1 coping strategies and skiiis
1 Maj adaptive//inti social (%)
j xjcriPrsi v-sip.r.y Suq;c9>cs
I 88. r
. i31-3
1 Deai'nc with sadness
I 64 1
1 35 9
1 Dealing wim anger
| 65.5
I 59.a
| 34.5
1 ^n ■?
1
- --------- -------------
High Risk Behaviour
One of the major realizations from the study was that d ug use i abuse couid not be viewed in
isaaticri. m ug use iri child'ei ; for med just one of the many elements which cunti ibuted to tneir r.g'i
|
i
|
Delinquency and Criminal behaviour
7S% of the children interviewed had self reported Delinquent behaviour. This included ctcarincj,
rapes and self cirected agression. The delinquent behaviour p^ccfcrrsncntly' occurred in the
context of the peer gang (70.3%) but a significant prooortion of the decant behawour was
solitary.
Age inappropriate sexual behavior
Aoour hair ipr/oi of ihe children who were specifically assessed reported being sexuaiiy active.
ip<4
r«*y fry ermfry* \*4th ry=,-?rc' <=• sicnificsntlv taros nurW*s?,r of children r^QLitarlv Msitsd
crrrvnArnial sex workers
Thgrp
p nexus
street children end locel conmerciaJ sex workers. rrvanv of whom
abused alcohol and drugs. Children frequently acted as pimps or go — betweens in exchange for
money, crugs, sneiter or sexual fawurs.
The SESGJsIly setive children, hy end Jsrcje, reported having sex in intoxicated states and not usng
terrier contraception, despite knowledge of condom use and the potential for HIV and other
infection. Intoxication made them careless or daring. The other attributions for not taking
precautions were that they couiart care less, or that they dd not think it couid nappen to them.
cf beingsexually active[Pearson's correlation coefficient 11.003, cff=1, p= 0.00091] am.
33.40
ff-^sstrsoris
I 1 Had more druq use (71% vs 34%: 02=72.98. df=2: p=0.00001)
j 2. were uiqci i, i 5[iij vs 2»j|,i4j. i=u.*to. p=u.uu5;
’ 3 u?d t?-?
vs'f'G ^eers 'innsi
yre? f=2
7=9
! 4. Had lower education (1(31 vs 3(31: t=3.81: o=O.
* 6. Earned rnore ^Ps.42r20ivsRs 33(31]: t=2.2: p=0.029)
0.000001
KJCMCl dl Dcaiui
r'56%)? 2. Headache (41%): 3 Sfnrnach problems (29%): 4. Feyer and bodyache (28%): 5.
Toothache (27%): 6. Skin problems (26%): 7. Burning sensation while passing urine / sores on
genitaiia (15%); 8. Tinging ana numbness of hands & feet (10%) and 9. Accidental injuries to
iXXjy cd'iCi liD'OS \ tW'/oj.
ThG use of solution was significantly related to occurrence of Tiro1’re
* and
^possible
peripheral neuritis) [Fisher’s Exact Test- p= 0.003]. possible S.T.D.s (Burning sensation while
passnq urine / sores on genitalia) [ Pearson's - 8.4. df=1. p= 0.0002]. stomach problems [
Pearson s —14.6, df= 1, p= O.uuOlj and neadache [ Pearson s—4.5, df= 1, p= 0.03],
qoz.
Deliberate self-harm and self-mutilation
6eif muniauon , specincairy scan n can on and siashingtnemseiveswilh sharp oqects, especially
had an anaesthetic effect.
Some cniicren reported incidents wien other chiicren kiiied themsebes by fiingng tnemseives
Gender and Drug Abuse
Tne data regarcing gri chiicren is much more sketchy. This is partly because most of the
pejj iicipdui'iy organisations in the study' had a greater street preserice amctfig trie ixys. Aso ooys
oUnumbcr grls on the street This is not to detract tan the feet that a significantly large lumber of
gd oh’ld'en fend up r*^
the
rnn<~K5 Af.hich often jnnh irfe mo cr h
*n
Fr^m key informants via? learnt that the of rls stav in their o.m
«ma.ll hws). some of the grls enter into informal "marriages?1
25
with some of the dder tors while ethers are gven shelter bv various adults Almost invariably these
gri criicren are suqect to physical ana sexua abuse. A large proportion are engagea in commercial
&ca vvut k. vvi i«j its wimfiyiy ot ui iwtiiingly. Ti ie use of aicohoi and ini taiai it u uys is. w,i y I iiy i ai i kji ig
rv ri; nf
cvicienr-c. haMnn i m
iobs or establish’no marrieoes and ferries. and seme of the
older hovsdo. Thecirls reportedly have no such choice. Sickness ill health (phyacal and emotional
) are high. Some gris die as a consequence of illegal abortions, most others due to a combination
of pool null ilia i ai id excessive drug use.
Access to resources affects a chilcfs ability to learn drills, change attitudes and perceptions,
decrease some of the stresses.
The chiicren studea had very iittie access to neaitn care education, age appropriate leisure activity.
AJciiiui laliy ti iey were naiui aiiy suspicious of the very structures that the State has erected to take
2
hosr'sjt^i” rathe
**
than having to go to the Juvenile j-iome.
^rrcs^ a? the children ^meve then 90%) h^d been been abused, vidated and evrdc4ed l*w ooheernen
at some time in their short lives and understandably wanted to have nothing to do with the Police.
Vvith respect to Health Services it was quite ciear that tne chiicren:
i.
O ilm utilized ti iw tAibtu ig siaie ii i&tiilieu i icfcuih btiMuei, couiu i id aiiuiu pi iVaile ii kajUc* uait; al iu
Most of th?? can no
ha'jrv’ been dsM^ooedh^ adults for adults rareh? reennnized issues of
chilcten nor dd they accommocfete the valid needs of the chikten. Health and welfare agencies (esp.
Governmental) nave nxea rules ana acmssion criteria which exclude unaccompanied minors from
tiitai
viutsb. t<_zi iiiua ta i n ivuivcun I ciLRd i cui auilMiies ae pJQiiy ui iuca^luoj py i i sai I8u ts-a 11
Childrsn mistrust
values and alien *?
^hsmse^.
dement
vltA^S,
ssrvicss. Addoscsnt childksn tend to reject adjlt
more w’th their Deers, so that it is dfficult for them to submit
themselves to a health care system controlled try adults.
2.
Tlie childen on theii pail rarefy identified health as a maju concern. They often regarded
themselves as invulnerable, focused cn the here and new and not on long term consequences. Their
mor^nalt^tion frcm.tho rest of sccieh-' reinforces the bdiefthst no one cares - the present is s!l they
have to look forward toj
The reluctance to seek helo may also stem from the fear that acfrnittinq to illness miqht make them
afferent rrom peers or cause employers to look for healthier employees,
72.2% of ilie children assessed wanted to stop their drug use but51.S% wanted nothing to do
with establishment structures.
3.
Chiicten also lack informcticn abo< it exiting resources and often pick uo misieadino or erroneous
information. This is a function of what information they trust and who they trust as information
providers. For example 95% of tne chiicren assessed in the Bangalore study had picked up their
iilicii d ugs sdoy u u 11 ii leil peet S. Tl lis is I efiwuied in ii ieii I teip seeking choices.
al icwieuye ai.
jji
*
.-ni vwhm • v zu vt ci’iC viiuCii vii mid vvotii>vM iO Stvp i.i'iCn' di Uy U3C, Scud toCy’ 5’«cid mCVCT tf’iCG tO
Advice and treatment related to Drua Abuse
Avajiaanry
mu FJiJ. pdi us ui u it; utx.ii in yH lei t; cii t; p Ln/uap is im duviue di id u eati I ra ii i tacUtXj’ lO Di uy Abuse.
Oraan’z?t
*ons
(fijnded in laroE? n-ypassjre hv th4? Mnistrv of Social WeKsre).
Access billtv
iviost of these organizations oo net acmit, nor provide care to chiicren. On the other hand, most of
the organizations dealing with children and especially street children are acutely aware of the
Specificity
Furthermore, most of the chug de-addetion centres deal specifically with the treatment of drug abuse
ano some are only centres for detoxification. And going by currently available information, none of
ilie cks-aiiiciion ceiities have u eain ei ii and rei laLiiiitiiui i piogain i fcss iakxed to tile i equi fci i lei its
ios° infwssQr
soyt pnri concentrate their efforts in gettino ha^k onto the streets where they
retaose auicktv.
treatment metea
ca uu ei i cm i hied ii t sui i uui idi igs dui I h laied by adults Will 11iisiCr ies Oi u ug aouse ai io
Referral throuch the r^t.^rnn^nrpi .qudrprns (Juwenile Justice Act)
At ieast in Karnataka and specifically in the citv of Bangalore. cfruq usina chilrten are hardv ever
referred under me provisions or tne juvenile justice Act to ue-aodction centres for treatment.
v vi ufe uctia li ut i : Juvei me rxi i
on frhc. <3TA»=t-=: Affocfrb.v~&/
i icx rfveuidi^'e cit u le lii i k; oi" v.i iiii iy. it it> li ic e/djrn ieiice ui
tn <=£ax/ ojtsde th1? ambit of th
* 3 Gn^^nrrwantai .h Men’!© care
systems. Aid it is these children v.ho are at Greatest risk for drug abuse delinquency and sexual
higi risk oenaviour. Paradoxically, it is this group of children who are in geatest need of
intervention that the organs of tl ie Juvenile Justice Act manage to overlock.
Referral thro roh the !cn Gcy-.'ernrnenta! Systems
It is then left to the N.G.O nehA.ork of chilcken’s agencies'Ahich maintain contact wth the
affected chilcfren and get some of them to care facilities.
Thougi the prodem of street cniicren is net realty nan they nave oy and large been ignored oy
policy i uakers and were fa a faiy iime suusui i ssd ui idd die rubric oi working umfaen ". oiitfa.
welfare and in 1993 introduced a orant-in-aid scheme for N.QOs working with street children.
vvniie most or tnese n.u.U's have an effective street presence the/ are usually CMarw.neimea Dy
rpfprrai
ifoc; tn th#=> H©-ackfchon se
vces
*
in th© reacn.
Netvuork 8c Outreach
A i effective way of L/ypa^i iy these difficulties is to fm ni broad < letv-jm ks 01 oi ganizatiof is offering
different setMces. Erug abuse is a cempfex heterogenous prcbfaii and is the concern of nut only
the specialist in addiction medcine but a'so impinges cn the concerns of a variety of
professionalsv'.orkinci in other areas. Those'Acrkina in the areas of Inroad community
develoomenial work as well as those werkinq wth wemer. and chikfen are likelv to come ud
against a ug acuse reared problems as impedments in tne smooth running or tneir progammes.
Netwjrks prodde tlie pcteitiai fa abroade range of iriterveitiei at lows cost, aixoackn
In addition to lona-standng concerns aver the deleterious health, lead. and pharmacdodcal effects
or sunstance anuse, new urgency now exists for tne oewefopment of effective intervention strateges
it I it« u dt la i laaot i of duquii ed it 111 Hi luusiiuia iuy
'.jf ui uw pciytxi uy n jtf ctv« iuu^» u trj
I'-ri-.-.-3-b5rirc h/r<ral|v r.-ry’j u-p
rnode^t results anH
treatment pains are often lost due to hi<±i rates of relapse.
r: tf.ft!(j i un«s a
dturi ricuiv^ io ucaiiny ii iu\iuuais aftts they nave deveiofjed such an
Prevention strategies: Possible Interventions
to the
*=nt«rn
^6^
^fFrrts
has been concetiualized in terms of suoptv and demand reduction models and as primary,
.ention. tach encompasses a afferent aspect of prevention, ana nas
enforcement aoendes. ceitic'darY with respect to the irterdction of duos bv governmental agencies
;-.rtments. Demana reductioTi efforts, on the otner hand, are conceptuajized as
Supply Reduction
The NDPS Act which regulates Drug Policy in India has a number of defects. To Start with it
drects its attention to the lesser of tne harms. All ever the world, as in Inda, there are
say lifica; illy mm e deaths associated with tl le use of aicohtjj ai id tobacco than tliet e ai e illegal
drug users. Yet the NDPS ".ct focuses cs«clusivety on the illegal efrugs.
..r-vrf.H/--’ '> '
. .r.!
-h .Ter "H-,-? r; imr.i-v-
r-rirv-i'H'nJ r
ir-v? £ho USO CSstflblijOn cLn.d rTSn.’jfect’jrC? Of
j<- eAT1*' 5'??tion. i o to n^ke
ileoal cfruos especially ilScit narcotics
*? rv unr-rtk’d-?. Failinc that to certain dug use by increasing the social econcmic and opportunity
tc
costs of usng ixiying and selling illicit dugs. in effect, this ensures limited availability at sewereiy
Leoa ocntrcss used to Gupprcus die u^.;i of selected drugs produce unai'iLicipcitcd
igrcicd)
the acidtional costs of ociicing this subterranean economy falls on the tax payer.
2.
F
Legal markets in analogous substances (legal dugs) are protected.
i ; ■. -u.. v
i;.i uvu-'i e is ii Mue li'njie iikeiy.
'"i
•“ r c r - c’cc
•/
• • r.r -
irp rv»rs»r5f'--c< - h •ftafpvw-w onr! i&riji-stfirjn X^-r^JS
nv '< • c’ fc-nocrs ana costs of process ng ana pro^ctrcicn are escalated.
fi.-c. r.< . r ,• .-'I 'i
nr- !r >rqr rJ Qf scien^!^r
S? <Ch < leoal
i!!eoa!
classification. Recreational it. : :d - alia iiiq d ugs need to be rationally classified accordng to their
addeuve potential and icncj term neam rratc in such a dassfi cation, cigardtes are the most harmful
c.; li’ic Ltcau of ij r..i;
if. '• cs id ii"rii <-i';dicy to cause laigte in ham not oily to the user
?:«ccoc':> e^’caticria’ ryocran" of modest trooortions and some restrictions on smoking
In G
li. s^iificant reductions in alcohol related liver
“.G- :.i.
cfrtaK ctstns nav- ?? -r,' ~ r ■ ■ -
r.-... limiting
siity ana controlling price to favour
,c
’H 91.T‘tl 'deS'A^SCh
31 H
' ’
A'A.:; : A. cucfthe infon-naUondscrirrination
••. *:i -■• "c r,-;
passive recipients or factual
Lisi SAk-c.' L'.-c'7.jr,73 invoke
■'
■ ’ ■ a~
■’.... and
Chapter in Textbook: Curriculum for IAS Staff College
Children with a Substance Abuse Problem
Vivek Senegal, Assistant Professor of Psychiatry,
wi ivicnidi J Jgm.LL .
> nt and juvenile < ' •».
iot ii'
u>o uie longer-range
r.r.v NimdrnmA()■,i jS> violent crimes
unemoiwment. 'those problems carry costs in lost proiictivitv. '
...enmyui me ooncis mat i iuu society luyetii^. zxivaxmiiu >*MMy
'
'
'■
i ■ ? fr-n
- -Mid a
mi tne social cost due to alcohol abuse in
Karnataka conservatively estimated the cost due to reduced industrial productivity caused by aicohai related
-<--—*--4 ---------- 1
to
approximaiely Rs. 691 crores per year (Senegal, 1988).
' ‘r=dwith cfriin ahnssrt<M„.,nr>nt is that while many effective strategies exist
ThecM?-
iiiu aoainence, long term maintenance oi ausunenue ^-.avuiang t elapse is a greatei w^all
challenge.
A Crit;c-i
Art '
'
'
-i
Transition
'.->1 starts vtaretta mater tncus is m ctpvpinnng seif-identity, a nhf'spwhich is
marked by cframatic cnanges ana re-adustments. This results in nav stresses and anxieties, wtnich
characteristically increases vulnerability to peer pressure. This is also a stage for practicing new roles. From
early childiood, youngsters practice adut rdes, throu^i pretend play. During adolescence this drifts to actual
behaviour. After 10 years of age the pre-adolescent beg ns experimenting with a range of new "adult"
behaviours, and for many child-on, regardess of culture and throuc^iout the world, cigarettes, alcohol and
other d-ugs have become a normal part of coming of age.
The social task of adolescence is increasing autonomy from parents and a ccrrespondng increase in reliance
on peers for validation and drection. Conformity to the peer g-oup increases rapidy during pre and early
adolescence when it peaks and then gadualiy declines. Adolescents typically assess themselves and their
behaviours through the reactions of their peers; acceptance by peers is critically important and more than
at any ether age, rejection can be devastating.
This is also the final stage of intellectual development. There is a shift from concrete operational thinking to
formal cperaionai or abstract thinking which is much more fiexibie. Vvhiie'on the one hand this sophisticated
reasoning capability allows the adolescent to think hypothetically and deal with proposition and theory, this
also invariably results in tensions and confrontations with authority figures and institutions. Adolescents are
able to begn que^ioning rules that had previously been taken for granted and this is also a period when
alternative life styles are considered or experienced.
Risk taking increases during adolescence. Exploring any new behaviour, naturally involves risk taking but
adolescents also appear to engage in risk taking just for the exhilaration of the dare. Adolescents also want
to impress their peers but are not yei. adept at assessing risks. They frequently assume that if they engage
in any behaviour several times without negative consequences the perceived risk goes down.
There is also thetenctency to exaggerate based cn imredate experience, which allows risksto be minimized.
Adolescents have a sense of ‘invulnerability’ - an attitude that "it went happen to me”. Since adolescent
tnougrt is mere anchored in the here and now/ than is adur thougnt, they are iess concerned with the far off
future Given their immedate time orientation, tine immedate gratification of need, for example the satisfying
and pleasurable short term effects of smoking may outweigh the potential longer-term negative health
consequences.
Aso some risks may seem more immedate than others. The risk of losng status with peers, being rejected
or ridculed or thoucht immature or inexperienced may seem more dangerous or aversive than the possible
risks of taking a drink or accepting the offer to take some ether dug.
Adolescent Drug Abuse :
Is defined as the frequent use of alcohol or other dugs during the teenage years or the use of dcohd ar other
dugs in a manner that is associated with problems cr dysfunction. This definition reflects the recognition that
a relatively large number of teenagers try alcchd and other dugs without becoming involved in the frequent
use of those substances or developing dug related problems.
Because of the rapid changes they are ©periendng adolescents are at risk for developing sdcstance abuse
more quickly than are adults. The initiation of subdance use and early stages of abuse have their root in
adolescence althouch the patterns that are characteristic of adult substance abusers are relatively rare in
adolescents. The precise point along the use/abuse continuum at which use becomes abuse is arbitrary.
Criteria for substance abuse involve a) a pathologcal pattern of use, b) impairment of functioning in work and
social relationships, c) physical and emotional deficits.
To wait to intervene until this point with the adolescent would be irresponsible. There is no widely accepted
consensus as to when substance becomes abuse, and for chilcten and adolescents - especially young
adolescents - any degree of substance use is frequently viewed as abuse.
The substance use progression
Drug use follows a rather predctahle developmental progresson, beginning with experimentation and
recreational use of alcohol and cigarettes. Subsequently the indvidual may then progress to use of marijuana
and other illicit substances like opiates.
LAtring eiperimentation and recreational use; substances are associated with etphoria and pleasure aid are
not perceived to cause bad things to happen. With more regular use, tolerance and need for the substance
develops, and the indvidual becomes preoccupied with substances and may bcgn using them every day.
Often at this stage multiple substances are used. Functioning begnsto decline and the reason for using the
substance shifts: indead of using the subdance for pleasure, the indvidual now uses the subdance to prevent
negative feelings. Thus, a major element in subdance use is the prevention of the negative experiences of
the withd-awal symptoms, either physiclog cal or condtioned, as the indvidual associates relief of
improvement with use. Both psychological and physical dependence may follow the dage of regular use.
Attempts to dsccntinue use at this point results in symptoms of an abdinence synd-ome.
The fact that there is this sequence does nd necessarily mean that there is a causal relationship, however,
and use of subdances at one dage does not mean an indvidual will necessarily prog-ess beyond that date.
in feet, most people use alcohol and ocher subdances without ever developing compulsive habits and ioss of
control. Experimentation with subdances has become so prevalent and normative that one recent dudy
suggests that adolescents who experiment with subdances may actually be psychologcally healthier
compared with either individuals who have ne.er experimented or indiiduals who abuse subdances! They
may be more curious and more prone to exploration and adventure.
lAforld wide, the risk for subdance use (legal and illicit) peaks between 18 and 22 years of age, with the
exception of cocaine use, and risk fw use of subdances, excludng cocaine and prescription psychoactive
subdances, appears to decline after age 25 years. The reasons for this decline in young adulthood may be
that conventional adult rdes in marriage, family, and career are being assumed during this dage, and these
roles are incompatible with deviant behaviour. The geated risk thd an indvidual will develop long-lading or
lifelong patterns of abuse occurs fa those indiiduals who begn using subdances before the age of 15 years.
Risk Factors for Adolescent Drug Abuse
It is dfficult to ascertain, which risk factors a combination of risk factors are mod virulent, which are
modfiable, and which are specific to dug abuse rather than generic contributors to adolescent problem
behavia. Current knowledge about the risk factors fa <±ug abuse does not prairie a formula fa pre.entiai,
but it does point to potential targets for prevention intervention.
These risk factors can be roucjily civided into two categories. First are broad societal and cultural factors,
which provide the legal and narrative opectaticns for behaviour. The second g'cup includes factors that lie
within indvduald and their interpersonal environments. The principal interpersonal environments in childen's
lives are families; school, classrooms and peer groups.
Cox'exfua/ Factors
Indviduals and g'cups ®dst within a social context: the values and structure of their society. For example,
daifts in cultural norms in the legal definitions of certain behaviour^ and in economic factors have been
shown to be associated with changes in dug-using behaviours and in the prevalence of dug abuse.
i.
Laws am norms favorable toward nehavior. Research on the effects of laws on alcohol consurrption has
focused on the three interventions by law. (d) taxation, (b) laws stating to whom alcohol may be sold, and (c)
laws regardng how alcohol is to be sold.
Acohd consumption is affected by price, specifically the amount of tax placed on alcohol at purchase.
Increase in taxes on alcohol lead to immediate and sharp decreases in liquor consumption and cirrhosis
mortality. Sudes examining the relationship of minimum dinking age and adolescent dinking and diving
have generally shown that lowering the dinking age increases teen dinking and diving and teen traffic
fatalities; and raising it decreases teen diving while intoxicated (DATs) and deaths.
Studes of restriction on how alcohol is sold have shewn that allowing patrons to purchase dstilled spirits by
the dink increased the consumption of distilled spirits and the frequency of alcohol-related car accidents.
Legal restrictions on the purchase of alcohol and norms unfavorable toward alcohol use clearly are associated
with a lower prevalence of alcohol abuse. Caiversely, laws and norms that express greater tolerance fa- the
use of alcchol are associated with a g-cater prevalence of alcohol abuse. Sim'lar relationships exist between
norms regardng legal dugs and the prevalence of illegal dug abuse.
2.
Availability. The availability of dugs is dependent in part on the laws and norms of society, Nevertheless,
availability is a separable factor, whether or not particular substances are legal, their availability may vary
and is associated with use. Vvi len alcohd is more available; the pevalence of ci inking the amount of alcohol
consumed, and the heavy use of alcohol all increase . Wth regard to illegal dugs; measures of dug
availability were sgificanfiy related to the use of cigarettes, alcohd, marijuana, aid other illegal dugs, even
after contrdling for the amount of money available to the subjects. Availability of dugs affected subdance
use indrectty amona junior hicti schod youths.
3.
Exireiiieecaiom'c derivation. Indcators of socioeconomic dsadvantage, such as poverty, overcrowing
and poor housing have been shewn to be associated with an increased risk of childhood conduct problems
and delinquency. However, research on social class and drug use has not always confirmed papular
stereotypes. A slidit posti'C correlation between parental education and high school seniors' marijuana use
has been reported. Parertal occupational prestige and education were positively related to teenage drinking.
Whereas there appears to be a negative relationship between socioeconomic status and delinquency, a
similar relationship has not been found fa the use of d ugs by adolescents. Only wiien poverty is extreme and
occurs in conjunction with childhood behavior problems has it been shown to increase risk for later alcoholism
and efrug problems.
4.
Neichborfiooddisorganization. Neighborhoods with hicfi population density lack of natural surveillance of
public place, high residential mobility, physical deterioration, low levels of attachment to neighborhood and
higi rates of adult crime also have i'ligli rates of juvenile crime, and illegal dug trafficking. Community
economic level and community dsorder-crim’nal subculture was significantly related to officially recorded
delinquency.
When neighborhoods undergo rapid peculation changes criminalization rates increase. Neighborhood
dsorganization has been hypothesized to contribute to deterioration in the ability of families to transmit
pt osocial values io child et i.
Individual and Irter.personal Factors
Certain characterises of indviduals and of their personal environments are associated with a greater rid<
of adolescent chug abuse.
1.
Physiological factors. Fhysiofogcaily medated tempera rental traits like Sensation seeking and low harm
avoidance predets eariy-onset aicchoism. Poor impulse control in chikhood predets frequent marijuana use
at an early age .
Researchers have sought to assess the independent contribution of genetic factors to the development of
alcoholism through twin and adoption studes. Anong males, similar twins are more than twice as likely as
dssimilar twins to be concordant for alcoholism.
Eariy-onset alcoholism that is associated with impulsivily and aggression apparaitly has a partial foundation
in indvidual phyddcgcal characteristics.
Genetic vulnerability may influence Early onset drug and alcohol abuse
2.
Family attitudes. Families affect children's drug use behavior in a number of ways. Beyond the genetic
transm’sscn of a propensity to alcoholism in males, family modeling of dug using behavior and parental
aitiiudes towards cliilci « i s d ug use are fan iiy influences related specifically to li ie risk of alcohol a id other
*ug
d
abuse. Foo pa/onting practices, ■
lOvds of ccnftct in the fan
*aly
end a lew1 dog
*co
of bond ng between
children and parents appear to increase risk for adolescent problem behavior generally includng the ahi i^p
of alcohol and other dugs
Parental and sibling alcohdism and illegal (tug use increase the risk of alcoholism and dug abuse in childen.
Parental dug use is associated with early initiation of use in adolescents, and with frequency of marijuana
use. Similar findngs have reported for adolescent dinking habits.
Childen who are highly prosccial and assertive generally come from authoritative families. Parenta'
ncndrectivEness or permissiveness seemsto contributeto higher levels of dug use. Common characteristics
of families with adolescent dug abusers include negative communication patterns (criticism blaming lack
of praise), inconsistent and unclear behavioral limits, and unrealistic parental expectations of childen.
Tne evidence suggests an independent contribution of family interactions to adolescent dug use, separate
from the effects of parenta) dug use. Studes have found that parental dug use in a rewardng family
structure cnly slic^tly prenreted frequent marijuana use but in an unrewardng context, there was a clear
association between levels of dug use by parents and their childen.
tn surrmary. the risk cf drug abuse appears to be increased by family management practices characterized
by unciear expectations for behavior, poor monitoring of behavior, few and inconsistent rewards for positive
behavior, and excessively severe and inconsistent punishment for unwaried behavior.
3.
Family conflict. Athou^t childen from homes broken by marital dsccrd are at hicfier risk of detnquency
and dug use, there does nd appear to be a drect independent contribution of "broken hemes" to delinquent
behavior, conflict among family members appears more important in the credction of delinquency than does
family structure per se. Parental conflict is associaedwith antisocial behavior in childen even when the home
is urbroke i and thet even in samples in wiiich ail Itomes are broken, the extent of family conflict is associated
with the likelihood of antisocial behavior in the childen. Use of heroin and other illegal dugs has been
dren^y associated with parental marital dscord.
In summery, children raised in families high in conflict appear at risk for both delinquency and rfiegaf drug
use
4.
Lon hor ding to family. Parent-child interactions characterized by lack of closeness and lack of maternal
invehement in activities with cfslden appear to be related to initiation of dug use. Conversely, positive family'
relationd»ps-i movement and attachment-appea- to d scourage youths’ initiation into dug use. Adolescents'
reports of parental trust, warmth, and involvement explained small portions of the variance in the extent of
tobacco, alcohol and marijuana use.
Bonding to famtiy may inhibit drug involvement curing adolescence in a manner similar to the way in which
(Qiiiiy bonding ifihibtte deHnquenzy.
5.
Esriy andbahavicrs. The cye^er the variety, frecjjency, and seriousiess of childhood
antisocial behavior, the more likely antisocial behavior is to persist into adulthood.
Children characterized by withdrawal responses to new stimuli. bidodcai irregularity, slow adaptability to
change, frequent negative mood expressions, and nigh intensity of positive and negative expressions of
affect noteoflen become icyulai useis d alcoixd, idjaccq andman§uana in adulthood than "easy chldien,
6.
Academic failure. Failure in school has been identified as a precfctor of adolescent cfrug ahi isa Poor
school performance has been found to predict frequency and levels of use of illegal chugs. In contrast
outstandng performance in scnooi reduced the likelihood' frequent, crug use.
7i ie available evidence suggests that social ac^ustri>ant is more imperial«. than academic performance in the
early scltoc» in predicting latc« drug abuse, early aitisoclal behavior in school may predict Ldh academe
failure in later classes, and later drug abuse Academic failure in fate eferrertary gade may exacerbate the
effects of early antisocial behavior or cortribcte independently to drug abuse.
i.
Lav degree of commitment to school. The use of hallucinogens, cocaine, heroin, stimulants, sedative, or
non-medcally prescribed tranquilizers is si^pificantiy louver anongstuefents who expect to attend coiegethan
among those who do not plan to go on to college.
Factors such as hav much students like school, time spent cn homework and perception of the relevance
of course work are also related to levels of drug use. There appears to be a negative relationship btfween
cormdtment to education and frequent drug use amongjunior and senior high school students.
8.
Poor rejection in elementary classes. Low acceptance by peeisseeiris to put an adolescent'at hsk for
*
school problems and crim’nality, which are also risk fact factors for substance abuse.
Traits of the child that hawe been associated with peer rejection agyesdveness shyness andWthd-araf-hawe
been examned fortheir relationship to chug use. Found that children who had been shy in first grade reported
lav levels of involvement in drug use. whereas those who had been agcressive or had shown a combination
of agg-essivenesswirn shyness in first trade had the hipest levels of use. Chlicrood traits relevant to peer
i ejecuui h-sociai iiillilition, isoiaiimi ii oni peers, andaggression against peer-wete net significantly associated
with adolescent drug use stage. However, agg-ession against peers during adolescence was associated with
stage of use, and teenagers who were Jess socially inhibited and less isdated from peer were likely to be at
a more advanced stage of use.
The link between oeer refection and subsequent dug use may not be a simple one. Shyness, to isolating a
cmid from ms or ner peers, may protect the child against crug use by eliminating one source at influence to
u&e, G uy-usii ig peen s>. Ayy essivei
qi the other hand, though resulting for some chilcfreni in exclusion
from g'cups of conventional poors, may be associated with acceptance by other aggressive a, .d perhaps
9.
Association with (tug-using peers. Peer use of substances has consistently been found to be among the
strongest predictors of substance use among youth. Youths who dd not d'ink alcohol reported fewer school
friends who d ank thai i dd those who d ank, friends' use of alcohol and marijuana was related io a youth’s
10.
Alienation and rebelliousness. Alienation from the dominant values of society, lav religiosity. and
rebelliousness. have been shown to be positively related to drug use and delinquent behavior...interpersonal
alienation measured at age 7 predated frequent marijuana use at age 18. Hgn tolerance of deviance, a
strong need for independence, have all been linked with d ug use. All these qualities would appear to
*11 zyfyfLcfes
cffuo use.
also has showi a rdationshio b*rbA i,eon dnjci us€? initiation and
specific attitudes and beliefs reaardna drugs. Initiation into use of any substance is preceded by values
favorable to it use
12. Early onset cf drug use. Early cutset of dug use predets subsequent misuse of drugs. IVIskkss of alcohol
appear to begn drinking at an earlier age than do users. The earlier the onset of any drug use^ihe geater
the involvement in ether druo use andthe creater the freauenev of use. Earlier initiation into ch in use also
increases the probability of eienave and persistent involvement in the use of more dangerous duos and the
involvement in deviant activities such as crime and selling dugs. Conversely, a later age cf onset of dug use
has been shown to pi evict lowtei d ug involvement and a greater probability of dscontinuatiori of use.
Drugs of Abuse
1. Cigarette Smoking
Aithoucp many people smoke because they believe cigarettes calm their nerves, smoKihg releases
epinephrine, a hormone which creates pi lysiological stress in the smoker, rather than relaxaiidfr Ti ie use of
tobacco is addetivo. Most users develop tolerance fa- nicotine and need greater amounts lo.p oduce a
jjegrsd efect Snmkem
dT'^callv and psychdodcally dependent and will suffer "'thdawal
<vmftcms inducing: chanoes in hod
*
temperature^ head rate, dgestion. muscle tone, and appetite.
Psychdag c;
headaches; fatigue
-e lifetime'
'
*
uu © oiiii
’
arid U,
3 A'c-hot
' ._■ ■ -im r&yu iui.yuu uepenctence. It is ,.■;■>! by cr-cl ingestion aid the duration
'
EliiyiA'ud
...'
K is the liquid rtstilled product of fermented fruits; grains and
, Antiseptics ana tor its sedative action.
tiaie potential tor arouse, me puwaae euects it can nave are intoxication, Sensory alteration,
Anxiety reduction
‘'>e%< ,
,
■
’
'
' .tegering Odor of aicohoi on breath, Loss of coord nation,
Siuired
...J pupil's
audtory hallicingtirris. Conluscn dsorientaticn. loss of motor nenre control. Convulsons. shock. Resdratcrv
depression and possible death are other effects of misuse.
Aicohoi is aoused due to its potential to aid relaxation, enhance sociability and g\e a relatively cheap ‘higf.
But aicoi id is a depessaiit ti lat cfeci eases ii le responses of the central nei vous system. As little as two beers
or drinkscan impair coordination and thinking.
In addticn Aicohoi is often used by substance abusers to enhance the effects of other dugs. Alcohol
continues to be the most frequently abused subdance among young people.
On younger (tinkers the developmental process may be slowed, resulting in physical and mental gowth
problems. Acohoi users tend to dspiay impulsiveness, immaturity, pleasure - seeking behaviors, in some
cases, the user may have experience memory loss; liver damage, cai'dovascular problems, and death.
4. Inhalants
Inhalants refer to substances that are siiffed or huffed to gw the user an immedate head rush or hidi.
They include a dve'se crew cf chemicals thet are found in consumer products such as aerosols and cleaning
solvents. inhalants are chiefly abused as they give a cheap and quick Hgi .inhalant use can cause a numoer
. of physical ai id emotional problems, and even one-time use can result in death.
Using inhalants even one time can put a child at risk for sudden death, suffocation, visual hallucinations and
severe meed swings or numbness and tinging of the hands and feet.
Prolonged use can reeJt in headache, muscle weakness, abdominal pain, decrease or loss of sense of smell,
nausea and nosebleeds, hepatitis vident behaviors irregular heartbeat, liver, lung and kichey impairment.
irreversible brain damage, nemous system damage, dangerous chemical imbalances in the body, and
involuntary passing of urine and feces
i agnhwia—sd'Am
*
’ gases can significantly limit available oyvoen in the air. causing breathing to stop;
2.
suffocation—tvoicallv seen with inhalant users who use bags;
3.
choking on '/emit;
4.
car ercss utn tavicrs n i pcxei itialiy uai igeious seiin igs, arid
includ ng permanent brain damage, loss of muscle control, and dedrnotion of the heart, blond, kichey, liver,
and bone marrow.
ivfore than I.OCO afferent products are commonly abused, Many youngsters start because they feei these
substances can’t hurt them, because of peer pressure, or because of low self-esteem Chee hooked, these
victims find it a tcugr habit to break.
These effects can last 15 to 45 minutes after sniffing.
The products usually abused are erdnarv household products. The problem is that substanceswhich can be
safelv used for legitimate ptrposes, can be problematic in the hands of an inhalant abuser. Glues/adhesives.
nail polish remover, marking pens, paint thinner, spray paint, butane iignter fluid, gasoline, propane gas,
typewriie> ccrrec'tiottfiuid[craz&i] household cleaners^ cooking sp ays deodoi ai is, have ali teem epoi i.ed
Unusual breath ocw- or chemical ndnr on clothing slurred or cisoriented speech drunk dazed, or dzzy
appearance sims of paid or other products where thev wouldn’t normailv be. such as on the face or fincers
red or runny eyes or nose, spots anchor sores around tne mouth, nausea ana/or loss of appetite. Chronic
iti'iiaiai it ateseis nay taxilibit sucji syiiiptoms as anxiety, excitability, iiritability, oi i estlessness.
Inhalant abusers also may te seen constantly smelling clothing deeves or rags,
or sitting with a pen or
5.
Marijuana or Cannabis
iviarijuana is a widely usea illicit crug ana tends to be tne first iilegai crug teens use.
me u lysiuai eilucis ui 11 ai ijUai la use, paliivuial iy Of i cfeveiopii ig aJdesUei is, cai i be acute as b'tu ijuana 11 ay
of . .
.’j L’O.’ ... . . .J-'j C2L
ootbl:;
---
■Short-i-prn-, ejects of1 is ng marijuana inch ide sleepiness. difficulty keeoina track of time, inreired or reduced
short-term memory, reduced ability to perform tasks requiring concentration and coordnation, increased
heart rate, potential cardac dangers for those with preexisting heart dsease
bloodshot eyes dry mouth and throat, deereased social inhibitions, and rarely paranoia, hallucinations
The Long-term effects of using marijuana are an enhanced cancer risk, decrease in testosterone levels for
men; also lower sperm counts and dfficufty having chilcken; increase in tedoderone levels for women, ate
increased risk of infertility: d mini died or extinguished sexual pleasure
osychdogcal dependence requiring more of the drug to get the same effect
Marijuana blocks tne messages going to the brain and alters perceptions and emotions, vision, fearing and
coordnation.
Cannabis nr ft/briii iann rnrrnricac the dn<=d no leaves and flowerinri foos of the hemo plant while Hadiish
consists of resinous secretions of the cannabis plant
o. Narcotics
ivai cuties ai eug» vji id 11 lave been u aJiiu lalry used 1nedcii laiiy to i uiieve petit i. Most ufti'iei 11 i lave a high
can c?' 'Ste
*
shalc
A? hraatlino. c* sarrn''/ skin and can ooteritialk/ result in convulsions coma. andrxjssiWe
death
A characteristic withcrawai Syndrome is manifest in watery eyes, runny nose, yawning cramps, loss of
appetite, irritability, nausea, tremois, panic, chills, srveating.
The outward indications of possible misuse consist of scars (tracks) caused by injectiais, constricted (pin
point) pupils loss of appetite, watery eyes and nose, cout^i, nausea, lethargy and efrowsness. The
paraphernalia required for admi nitration like silver foil, syringes, bent spoons, needes, etc. may be found.
The tyoes of narcotics which are commonly in use are synthetic. semi synthetic derivatives of opium
Morphine or Petnidene (used as analgesics) which have a high potential for dependence ana are usually
found hi anpouies fm injection. Heroin a white crystalline pcwifei and a derivative of morphine and its
th«*/
qjHprf rn strict xXriiance nvver users
SAAtched to ckinkino Couch m’Mtures containirKi Cocfeine
:'s semi svntbetic analocue of Opium) or iniectinq Buprenorphine l“Tidaesic’1 which is a synthetic opioid.
o. uepi essanis
These have a hich ortential for abuse end the development of tolerance. Thev produce State of intoxication
srriiar to war or aiconoi. Comtxnea witn aicohoi, they increase the effects and multiply the risks
T*
j.Jus>dUc tsifeuit
*
«! t:
ibM y ciiti ctiiu i. c? txiwiy i wjuuiiu i a id ii itUrtGatioi i. Sfl fcui fcii i rju its cause Gait iTteSS
’'/??•/ 'zrgo dsccc r.22y 22222 rcspirstcr/ depression, 20.222, deoth. Msv.horn
of obusors may show
*
•.
.
?
/ •=■— of O’- srclose include : Shallow restoration, clamnrw skin, dieted pupils: Weak and radd pulse.
...
•••....
•
- •
■,
- '
•
.
g
coma, oeath.
There is a characteristic withdrawal syndrome comprising : Aixiety, insomnia. muscle tremors, loss of
A-brurt 22
*222222
of .ho dri:22 or rcdj2cd dcccs mov cause ccnvjksons, delirium and d-?2th
■■ elevens o~
r.o-i :q~-
to alcohol intoxication (without odor of alcohol on breath):
Staonsrina stumblina lack of ccorcfnation. burred speech: Fallinq asleeo while at work cifficultv
cenrraiing; miareci pupns
Drug Abuse amongst Street Children in Bangalore
Magnitude of the Krooiem
<rj m uinicitni uunbtiiuiw
11 mi gu laiiztsd p.yjuiatitA 1 in must urban centre^ ui u it; wot id. There ai e major
diriOLiiiiCS ii‘t ti’yirty iU C42n.it I smIG ■.< iO iivii'i bCi Gt' Sti'CCv Gi'iild>‘Gi”i cuiG tl“iC i t C
*f
,
.-- ■
jr ........
?/ ............ ...
h'lmCiC'
.........J.,:;..., ,.!....
Ui vafnOviit-iCG ti‘iC^f
..-.F cO.Wed t»/ POT
find place in the national census, educational cr hedth cfata. This problem is further ccmpcunded ty the fact
that they are also a hiciiiy mobile population.
A very roucf estimate would place the number of street children in the city of Bangalore at around 80,003.
rixxit 3-Z ci liK'j'en land up at tire Bus Statics i alone, every day, i laving run away iron 11 ics i ts. Scs i t; ui lilci«i
live with that parents in urban dums
An Action Research Pforrcnmo nin !?,' the Bangalore Forum for Street end Wcrlting Child'en and- th®
htetiona! Institute <Mental Health and
'n esciences (1997-98) looted at the d'atus. of d ug at> is? amcncist
th s Str sei Child en of Bai igalore and the impact of a brief intervention . Some of the data gathered from a
study of 32 i children are dscussed below.
exclusive pre
rand for criminal acts. Most are male, their peer relationships, g'ouplife
ofv.hde famiieswho Sve on the streets while
31 Chiicren who remain in contact v.
Hies but because of pcwertv, cr.ercrow.dng or sexual and
i he NIMH— Forum Stud/ sb dlariu fr
* ,r ' ■■ w
*id
: war id
the childen interviewed stayed exclusvelv on the streets.
of street I'vno
•/.<■ cm md 35 % of al!
,■ -i-xzi as thev landed no on to the
is! s- .•
ich a nrocee5: b
*/ itsncriir'-* py--:■■■-■
r* ~y <s--:>'nn lr: ottp no inipen t?f toe*ys.-». ‘-p-'ch
many vounq people have been art of home n -. some time: vorkinn henring abandoned or sick. 8v
adolescence they have also
t.
to many ctugs, especially those essly available cr associated with
v»u k - 1. sduihe,! yuc.^ peirci, cannabis, tobacco and alcohol *n a niiieu where social and peer influence are
to rbeam ntay tv- sc;n«- <,.f the fiinohis«\«ri by drun use.
: ■
= r '•■■■;
..
■
■ ' ‘
Stress Model
•!O. 1993). The mode! proooses that increased risk for <±uq use is a
-
—n or tne level or percevea personal ( as)stress, tne image that crugs have in that particular corrrrunity
aiiuSUUMJIUIC oim ti>w paueived ei leuis ui tileiiluviijjai ui"paiiiuuia viuga. Ti io i isk is ueui eeccd by pobuve
R».slf frir Or?
ifo=> =
9) sfre.?,? ■+■
of Dr/jr? /Drun Fffect
*
Attachmerts
Coping Strategies
*
Resources
Sresa. 11 id e ww e 11 fcu ly ieveaa of sii ess u iat ti its children faced .
to ass'st in the period of acfustment.
!n the Bangalore children. Family dsrucrion due to Parental death. Abandonment and conflicts with
stepparents were commonly seen.
Mcratim from rural areas to cities
Physical and sexual assault and exploitation vwe also particularly
common.
?«»
craw?
«$■ pf i*
Ar chiHrpn on ths frosts th?5 sMsrwdsN
^countsred 'or© for nvxe
persist o.ier time and cannot be easily resolved as they relate in most part to their deprived
socioeconomic environment.
rindng accommodation / sanewhere to sieepv enough to eat / cioihes to wear, families demanding money,
unneaitiTy living envircrin lenis, avoiding violence and sexual abuse or coping witn expiotatioi’i oy police and
Survival becomes the all-consurring daily task. Drug use wras often reported by the children as a v®y to
attempt to escaoe from this chronic conflict.
3] Life transitions
Gtre^ children need to be coriinually adapting to new situations - moving between communities/ cities with
dsruntion in peer relationshios and the need to adust with a new croup of peers. Drugs are used to facilitate
acceptance among the new' peers and deal vuth the dscomfort associated with the transition.
'ktil Gi iSTigCs Gi SOGsCSGCil «C©
-tj
For msny strcst chifcksn there is little? time to grsdusfy ccmo-ete the dex^oenx^ntd tmfes of
The
factors which ha«? propelled them on to the streets have forced them to adapt to adult roles while still in the
process of growth and development. Use of chugs as an attempt to cope with their stressful lives can further
impeoe tnar aewaepment and this is most cramaicaiy seen in tnar inability to engage in forma operational
ii lii iking oi pi ug ess beyond ii ie conci eus iiiii mil ig of ycuriga child en.
"normal" in a society or subculture and haw that society reinforces that belief. They include
ij Mice: Vwiereincomes ere cw, tne cneapest drugs tenato be consumed Amongst street chisren therefore
ii ii idiai ils. sow i as lypaM litsl Cui i uuuui i liuiu ( Sm’uiiu 1
p6ti'oi, yuus wi itCi I aft? ci leap cu iu easily available
tcryd to use? slcohcl. Bccsus- slcchd is rdst-k/sly higher priced and perhaps mor© dfficult fcr chilcken to
access its >’se is limited amonci the s*?rv vouno. Cannabis aoain is used bv older adolescents and coioid
crugs like heroin Cbrom sugar") or Bucrenorohine are rarely encountered. This is a peculiar pattern as these
(tugs are reiaiiveiy popular in the ocner indan cities and is probably due to tne fact that opioid drug abuse
trven arricmg adults in the reyoi'i is lew. A reason for this could be tliat Bai igalcre is not o 1 the usual shipment
2] Availability
Availability is to a laroe extent culturally determined
Of the licit ckuos falcohol. tobacco) the community
decides which should be controlled and how. But when it comes to illicit drugs availability is determined by
tne supply of that crug and the leva of mglance of drug enforcement agencies. Tne attractive profits
assoUiaitAJ wiu’i me SUppiy Of ihiuii SUbsiai ices ui rSUi ©S ii leii COIl'd! idii ig supply. i i io ii a.k- is so vesbi. u lai ai ly
f-u ttiA authorities 'Pr*es cxer time and isverv sjpnsitive tn bc^h local and infernation a!
entities. Such valance and the very fact of the illicit nature of certain drugs contributes to the problems
experienced oy tne crug user, i ne illicit nature or these crugs makes the user a criminal, margnaiises nim
Wid<111 i< ie suuitn.y eu iu i equii «s u’ i© usm iu use i uoi u di astic 11 fc?di is to acquire; ule di ug. i i lis is uiitn i d ie
*?n
T^
sejain th«
*e
thos© druos for v^ihich th#?r© sr© no formal controls cm thoir ©vsilAbilitv in dfffersnt
comm initi es such as caffeine andtradtional dues such as betel nut. To these can new be added the unusual
suDstances (at least in tne indan context) wicn are usea ror intoxicant purposes like the freely available
*=-^r;r>rTin.n$:
nr
f.-r -jo in i
r.fenx/ <aih.ridhjres anoear to condone dua use which in the wider commun'tw
would be considered deviant. Use of certain duqs seem to be a normative oattern amona ar cuds of street
cniiden.
La uy usii ig crind ei i wfei t? scj h iicai iuy nue iikw’y to perceive drug taking css Lm lencial, ksbb iikcs’y to consider
drug use qs vXa'vgui cus ernd h«d q
liiiCQTith^ Seif ger c# ug using poor g oup. ourp. iSingy*, ciltl'iCXJC/1
chilcfr’en. which was determined more hv neer influences.
ug uso
Drug experience
utjS veto y if i Mich p lyoiOiOylCeu dOiiOTiS. A pcu iiGUicd’ Ci uy iS n r> c iiKciy CO ijc uScO 11 inc SuujeCuvO
in the Banpakre stuck, almost all the 281 childen assessed for positive drug s<pectancies repealed beneficial
experiences fdlowing inhalant use.
Beoeficial effects of takino “Solution”
' Percentage
r?8 2
Tfro
an in<-ere«ting
rhf=norn?non of WOnression of dfUO USA. Most of the
smaller children (around 10-11 vears) start off wth tobacco use and Vvhen they are a little older
m.T'' cracxiare to use of innarants. tsy me time they are 13 years ad me use of innarants tapers off
wfuy use
Frequency!%)
Aiacnrnsiits (to farriiy, work and peer group)
Dctcicd by cij cXpOSui'tb to Opportunities cti'id influences Vrithin the y OUp
s seen to perform well in that crew through learninq the necessary skills (e.g. ack-pocketing)
r oung people who a^aop strong anaenmenrs io fanny ana'' or scnca^/vcrK are less iikeiy to develop
that thw receive from th^r families are less attractive and
than those i? cm their neers. In these circumstances, when their oeers are using dugs or
c :r;=•
c: :c pro- r~' g anftuoes, tney tnemsaves are more than Skeiy to take up sirriiar orug using behaviours.
usei >. .'■l..e’Ti less tirue at ha rje. c*i'iQ
had sy lificantly less ackjtt attachn ^nts tiian non-using
L’.Y.’.'h.?;-.. Another fcctor which dgv.ficantly predicted dug use v^s the nature of the child's job.
,•
v
worked in ' meuoen ised jobs (e.g ragpicking) were more likely to he using drugs than
chiiden working under the drect supervsion of an adult.
>dep£ndency,
COND HAND LIFE
Other titles that will interest you. ..
Today's Gift
Today's Gift is our first daily meditation book
written with the family in mind. A collection of
readings written specifically to help us, as
individuals, deal with our family concerns, Today's
Gift is an excellent companion for those of us
involved in A.A., Al-Anon, Alateen, Adult Children
of Alcoholics, and other self-help groups. Today's
Gift will inspire discussion among family members
— child and adult alike, and help us all to pause,
regain a sense of balance, and recognize the riches
we have within and around us. (400 pp.)
Order No. 1031
Victims No More
by Thomas R. McCabe. Ph.D.
Those who love a problem drinker need not
remain passive, helpless victims. They can begin to
understand how they may be unconsciously
perpetuating the drinking problem. And they can
learn how to be instruments for constructive
change. Written especially for spouses apd children
of problem drinkers. Victims No More offers real
hope for a new way of life. (104 pp.) •
Order No. 1112
zelden.
Educational Materials
Pleasant Valley Road
Box 176
Center City, MN 55012-0176
(800) 328-9000
(800) 328-0500
(800) 257-0070
(612) 257-4010
(Toll Free U.S. Only)
(Toll Free
r“ Film and
Video Orders
U.S. Only)
(Toll Free MN Only)
(AK & Outside U.S.)
Order No. 5450
ISBN: 0-89486-317<
Stephanie Abbott
As you make these outward and inward changes in things
you do have power over, you will feel much more comfortable
about surrender to lack of power over someone else, even if
that person is greatly loved by you, and is getting very sick.
In spite of all your good intentions and insight, you may
still find yourself devoting time each day to circular thinking,
or yet one more attempt to control the uncontrollable. Pay
attention to the pain it gives you because its message is, you
need more help. Many have found a spiritual counselor is a
helpful guide. Health professionals who understand alcohol
ism have helped many. You deserve as many allies as you can
find to help you on your journey.
About the pamphlet:
Codependency is a normal reaction to alcoholism. This
pamphlet is written for those who are in a relationship with
an alcoholic, and whose behavior is geared toward controlling
or changing the alcoholic’s behavior.
About the author:
Stephanie Abbott is director of Family Counseling at
Brighton Hospital, Brighton, MI, and president of the Na
tional Foundation for Alcoholism CommunicationsrShe
writes a regular column for Alcoholism/the national maga
zine.
11
may have to repeat it several times. Next, follow with what
ever aids you in switching these thoughts. It may be strenuous
exercise, an Al-Anon meeting, or talking it out with a friend.
Other helpful devices include reading Al-Anon or other
literature written for family members. It may help to immerse
yourself in mental work, something challenging that absorbs
all your attention. Others do better with physical chores.
Remember to be gentle with yourself, and that all growth and
change means a certain amount of temporary dislocation.
These are immediate first aid tactics for obsessive thoughts
and actions, or feelings of anxiety and helplessness. They all
work by breaking the cyclical patterns and giving you a sense
of control.
A woman with many alcoholic relatives looks at her recov
ery program like this: “1 decided to look at it like a project. 1
was so overwhelmed with problems, most of them belonging
to other people, that for me the easiest way was to deliber
ately be my own helper. I slowly improved my life by asking
myself every day what a caring friend would recommend.
Today I enjoy most days and accomplish a lot because I think
about what I need for the first time. I can allow myself to get
help from other people.”
For the longer view, think about how you would live your
life if you were not involved with an addicted person. What
would you be thinking about if you were not thinking about
this person and the problem? There lies the clue for what you
could be doing with your life, and it deserves careful thought.
Al-Anon suggests we “act as if,” and to live our way into
healthy thinking. While you are at work on attitudes, examine
what ideas are upsetting, such as the belief that anyone can
control someone else’s drinking. You can behave as though
you did not secretly believe you had enormous power over
others. The new behavior — putting challenge, pleasure, and
accomplishment into your life — will make it more rewarding
to continue the efforts with your emotional growth.
10
CODEPENDENCY,
A SECOND HAND LIFE
STEPHANIE ABBOTT
zelden
First published August, 1985.
Copyright © 1985, Hazelden Foundation.
All rights reserved. No portion of this publication
may be reproduced in any manner without the written
permission of the publisher.
ISBN: 0-89486-317-7
Printed in the United States of America.
Editor’s Note:
Hazelden Educational Materials offers a variety of infor
mation on chemical dependency and related areas. Our
publications do not necessarily represent Hazelden or its
programs, nor do they officially speak for any Twelve Step
organization.
This sounds like a very large job, and it is. But it is to be
done slowly, in small steps, and at your own pace. There are
many people who have gone ahead of you, and they can be
there for you as a sponsor, a counselor, or in their writing.
Use all those resources when you need them.
You will discover change brings anxiety and that is normal.
The fear will diminish as you get used to new patterns in your
life. It’s important to be gentle and nonblaming with yourself.
Remember, your goal was good and reasonable — to help
someone else and to feel better yourself. The problem was
that it didn’t work. You are now beginning a process that will
work and it will be accomplished in small steps, a day at a
time.
You begin with the basic philosophy of allowing the alco
holic the right to be wrong, the right to hurt, and the right to
get well or not. You will begin today to concentrate on your
own thinking, behavior, and needs.
Remember, when you begin to become obsessed about
anything, your thoughts circling around and around, it is
simply a process you’ve used to solve a problem, but it
doesn’t work. Whether you are scheming about methods to
control someone else, rehearsing what you will say next time,
or going over painful events from your past, you are wasting
valuable time. You could be productive instead, by doing
something that feels better, or organizing your own day. Be
aware also, that though it may feel to you that the alcoholic is
the source of your feelings, actually you generate them your
self by your own thoughts and actions. When you notice your
feelings come from you and are not put in you by another
person, you begin to take charge of yourself. This will do a
great deal to lessen your feelings of helplessness. Then you
can begin to change nonproductive bad moods.
For example, when feelings of panic take hold, it helps to
remember that every mood passes. This one will too. Switch
these thoughts by a firm message to yourself to stop it. You
9
stronger than the pain of the current situation. On the emo
tional level, you may even believe you can’t survive without
the alcoholic in your life.
What You Can Do
The Truth Shall Make Ye Free — but first it shall make
ye miserable. — proverb
It’s hard to let go. We hang onto habits, relationships, and
defenses long after they stop being good for us. It’s natural to
ignore what we know, hoping that if we don’t notice it, we
won’t lose what we thought we had. But as Freud com
mented, “Much is Won if we succeed in transforming hysteri
cal misery into common unhappiness.” It is very sad to face
the reality of our powerlessness over someone else and the
uselessness of obsessive behavior, but it will release us from
hysterical misery!
The First Step, as Al-Anon states, is to admit the situation
to yourself: you are powerless over alcohol and your life is
unmanageable. Your thinking and feelings have become
obsessive. The alcoholism is not the problem you can solve;
your anxiety and fear are. Your misery and what to do about
it is the problem that lies before you. The chemically depen
dent person needs help, but so do you.
To admit powerlessness is to surrender to a new way of
looking at your life. Many people equate surrender with
defeat and humiliation. They are like the alcoholic who
chooses death over admitting the self-destructiveness of his or
her life-style.
Yet those who have made the choice to let go of a drug or
another person have found that surrender was liberation. You
can’t stand guard over someone else without losing your own
freedom.
You can make a decision for acceptance, and live through
that pain until it is finished, rather than staying in pain for a
lifetime. Today you can decide to learn how to feel better, by
changing your own thinking and actions.
8
IN OTHER WORDS
In an effort to avoid awkward repetition I have used the
words chemically dependent, alcoholic, and addict inter
changeably. What I have to say applies to anyone in a rela
tionship with someone who uses mood-altering chemicals in a
harmful way. For that matter, it extends to people involved
with someone who uses food, gambling, sex, or work to avoid
feelings and relationships.
If you are in a relationship with an alcoholic, this pamphlet
was written for you. If you have had a normal reaction to
living with alcoholism, then you are familiar with the feelings
of helplessness and confusion, and you have spent time
obsessively trying to solve the problem. Perhaps by now you
are exhausted and depressed, wondering what’s wrong with
you that you can’t make things better. Or perhaps you now
understand that addiction to chemicals is a disease, and the
alcoholic needs special help you can’t give, yet you can’t seem
to stop the “helping” behavior you know is useless.
You know it is useless because you have tried everything
you can think of to change that person’s behavior and noth
ing works for very long. You may know it is useless because
your Al-Anon group tells you it is, or your counselor has
pointed out that nothing you do changes anything.
A wife tells of her efforts: “I hid his bottles, and looked
for the ones he had hidden. I spent hours putting water in the
vodka, and marking levels of alcohol on the bottles. Looking
back, I can see how pointless it all was, but it seemed impor
tant at the time. I used to pace the floor crying, my mind so
blank I couldn’t think. I rehearsed what I would say to him,
and imagined what he would answer. I was sure if I could
plan the right words, I could reach him.”
The reason nothing you do works is because chemical
dependency is powerful. Addiction to mood-changing drugs,
including alcohol, makes people self-centeivd, and the only
thing that gets their attention for very long is a threat to their
well-being. People go into treatment and get well only when
they begin to feel threatened by what will happen to them if
they continue drinking or using. That is why it is so impor
tant that you do not solve the problems or prevent the crises
that drinking causes others.
problem solving. If you were freed from the fears that lead to
obsession, you would have the serenity in which you could
identify choices and options. What, for example, would you
be thinking about if you were not thinking about the alco
holic in your life? What would you be feeling if you were not
using activity to block your emotions?
I f. you did not have a compulsion to play counselor to the
alcoholic, if you stopped helping and watching, what would
you be doing with your life?
A grown daughter looks back on her adult years with her
alcoholic mother: “My sisters got as far away as they could
but I got stuck. I still spend too much of my time checking
on her, thinking about her, and helping her solve her prob
lems. It’s kept me from ever having much of a life of my
own. In a way, I guess I’m living hers.”
Obsessive thinking and behavior serve to block out anxiety,
which may feel overwhelming. This may be a fear of aban
donment, of being alone and unsupported. These fears may
have a traumatic origin. Perhaps you had an alcoholic parent.
If you were raised in an alcoholic home it’s very likely neither
parent gave you focused attention. Your chemically dependent
parent was unable to be emotionally close, or to put your
needs first. Your other parent was usually too absorbed in the
problems created by the chemical dependency to have energies
for you, either. vou may have felt emotionally abandoned.
Now, in your adulthood, these fears of still another abandon
ment can be so intense you will do anything to avoid that
terrible feeling, even to living in a toxic, chaotic environment.
This is a very normal and natural reaction, but you stay in
pain to avoid pain. To survive you will do whatever “works,”
even if it means walling off your feelings by compulsively
focusing on something outside yourself.
Other people may think it is remarkable that you'will cling
to a painful, abusive relationship. That is because they can’t
understand your terror of being aldne.ahd abandoned is far
2
7
POWERLESSNESS AND OBSESSIVE THINKING
You may question yourself, analyzing your behavior, past
and present, as to how it might affect the alcoholic. Living
this way can be a form of addiction. Addiction has been
described as an experience that blocks our awareness, fills
time and occupies attention, and has an overwhelmingly
compulsive quality. It also is a relationship to an activity that
harms the person and affects self-respect. You may decide this
thinking and behavior, revolving around another person, is
indeed addictive.
There are other kinds of obsessive preoccupation. A spouse
may become overly involved with work and begin to use it as
the only source of good feelings. Or the spouse’s energies may
switch to the children, so there will be the kind of emotional
involvement more appropriate to a marriage, plus an engulf
ing kind of control.
A teenager may obsess about collections or sports to block
out negative feelings, or use compulsive achievement as the
connection with life. If you can’t get good feelings from
relationships, you may work all the harder to feel good about
accomplishments.
Why Obsession?
Obsession does serve a purpose. It gives an illusion of
power and control over life. Some people even experience
worry as an accomplishment of a task, and have a worry
quota, whether the problems are large or small. Obsession
gives a sense of movement, though there is no change, so that
it is an “action” that fills the day, whether it is scheming,
actively rescuing the chemically dependent person, or block
ing out awareness by endless, pointless tasks.
From the fear of loss of control and the feeling of omnipo
tence comes compulsive behavior, which helps you feel you
are doing something, and covers the feelings of helplessness.
Obsessive thinking may allow you to blame all your prob
lems on The Problem, which releases you from the effort to
solve them. In this way, it blocks out solutions and creative
6
Powerlessness
If you are the parent, child, or spouse of an addict, you
may find it extremely difficult to admit complete powerless
ness over the behavior of that person. You have spent a great
deal of energy trying to deny that feeling. You may have
covered debts, lied and covered up for the alcoholic, or spent
many hours counseling that person. This behavior helps you
feel better temporarily. It’s normal to tidy up the alcoholic, to
pretend to outsiders that nothing is wrong, or to cover up to
the employer.
It just doesn’t work. As long as you deny your powerless
ness you will continue to rescue the alcoholic from crises. As
long as you rescue the alcoholic from consequences of drink
ing, that person will drink. It’s as simple as that.
If we look at what it means to be powerless, we understand
it means to be completely unable to change or control. In
Alcoholics Anonymous, the First Step is to admit powerless
ness over alcohol. In Al-Anon, the First Step is the same —
you have no power over the alcohol within someone else.
It is very natural when you are under stress to try to control
what is happening. It has been shown in lab animals that a
feeling of control over the environment reduces stress. Those
animals with choice and some power have less pathology, and
fewer negative chemical changes. If the researcher induces
stress but gives the animal no opportunity for control, and no
way to predict events, eventually it will have problems with
eating and sleeping, which are symptoms of depression and
anxiety.
High stress, lack of predictability, and powerlessness are all
part of the environment for the family living with a chemi
cally dependent person. To avoid depression and anxiety, the
family tries to deny reality with efforts to control the drinking
and behavior of the alcoholic. To admit the truth, that the
traumatic events can’t be controlled or completely avoided, is
to admit powerlessness and feel the depression.
3
For example, you may find you spend hours counseling the
alcoholic; you explore the behavior, you lecture and explain.
You may begin to feel like a cassette player forever set to
’’play.” Somehow none of these conversations do any good,
but you feel better temporarily because you have avoided that
feeling of powerlessnness.
Unfortunately, these efforts at control on your part do
accomplish something. They give the addict the idea that
there is no need to change anything, because the family
member will take the responsibility for the lecture, the for
giveness, and whatever is necessary to avoid disaster.
When the family is still struggling for control of the situa
tion, the alcoholic is firmly in control of the family. As long
as you are trying to get good feelings from the relationship,
which is actually impossible as long as the person is using
chemicals, you will walk on eggs to minimize problems. For
example, you may agree to anything to avoid a fight, or take
on all the chores rather than see them undone. This gives all
the power in the relationship to the alcoholic. When you stop
trying to control, and let the natural consequences of the
disease occur, you can no longer be manipulated.
A father commented, “We couldn’t bear to face the truth
about our daughter’s addiction. She kept the house in an
uproar but we kept trying. We bribed her not to drink, we let
her break rules we wouldn’t tolerate the other children break
ing. Finally, we had to admit to ourselves that nothing we
could think of would work. We gave her the choice of treat
ment or leaving home. It was very hard to do. But in admit
ting powerlessness over her condition we gained the strength
to do it.”
As the spouse or parent, you may feel the drinking or drug
taking is rebellion, as though the person were “getting drunk
at you.” You may feel loss of self-respect because you believe
somehow you should be able to control that person’s defi
ance. As long as you believe this, you will feel as though you
have lost a contest every time the addiction manifests itself.
If you grew up with an alcoholic parent and now have an
addicted spouse or child, you respond with behavior you
learned in the past, behavior you used for survival. You may
feel a drive to change others, to control and fix for the
“good” of other people. If you had an alcoholic parent and
now find yourself married to an alcoholic, you may have
unconsciously repeated the original family conflict in order to
give it a happier ending this time. There may be despair and
depression when you discover that your goal of changing the
past by doing it differently in the present can’t work.
If you are a fairly typical adult child of an alcoholic, you
will deny your powerlessness and try to solve all the problems
by yourself. It has been said that children of alcoholics are
seen in all the best self-help bookstores.
Again, power lies in accepting powerlessness. When you
stop exhausting yourself with useless attempts to change
someone else, when you stop blaming yourself for not achiev
ing what no one could achieve, you are free to look at other
options. As Al-Anon literature states, living with alcoholism
is too much for most of us.
4
5
Obsessive Thinking
You may find you spend hours each day, or lie awake at
night, worrying about your situation. This may take the form
of fantasies in which drinking becomes physically impossible
for the alcoholic, or you may scheme about techniques to
avoid drinking situations. Or you may rehearse your lecture to
the addict. You may torture yourself worrying where that
person is, and with whom. You are afraid the addict will get
killed on the highway and yet you are afraid he or she won’t.
You may go over and over the past, reminding yourself of the
pain. Or you may project horrors into the future, as if you
could solve problems before they happen. You may be quite
aware this sort of thinking does you no good and wish you
could stop it.
MH - 2-L.I3
RAF / 89 / M05 / NOR
MANUAL ON COMMUNITY ACTION
AGAINST DRUGS AND ALCOHOL
(First Version)
by Samioullah Lauthan
in collaboration with the
Vocational Rehabilitation Branch
International Labour Office
Geneva
International Labour Office Geneva
MH - 2-4= . 13
RAF / 89 / M05 / NOR
MANUAL ON COMMUNITY ACTION
AGAINST DRUGS AND ALCOHOL
(First Version)
by Samioullah Lauthan
in collaboration with the
Vocational Rehabilitation Branch
International Labour Office
Geneva
International Labour Office Geneva
t
TABLE OF CONTENTS
Page
INTRODUCTION................................................................................................ 1
The Community Action Committee...............................................................2
Understanding the high risk groups............................................................ 4
PART I: PLANNING AND IMPLEMENTING A COMMUNITY BASED
PROGRAMME
Taking the initiative....................................................... ..............................-9
Factors to consider..................................................................................... 9
Needs assessment...................................................................................... 10
Substance abuse indicators................................................................ 10
Social anthropology............................................................................. 12
Epidemiological survey....................................................................... 13
Assessing existing programmes and services.............................................. 13
Interpreting assessment data...................................................................... 14
Community mobilisation - the need for linkages................................................. 14
Constraints in community mobilisation......................................................... 15
Training and manpower development............................................................... 16
Prevention approaches
.............................................................. 17
Basic definitions.................................................................................. 2)
Signs and symptoms of drug abuse..................................................... 21
The nature of denial........................... ................................................ -21
The nature of negative peer pressure.................................................. 22
Decision - making skills to resist negative peer pressure....................... 23
Development of material resources............................................................. 25
Setting goals and objectives... ................................................................... 26
Implementing and monitoring activities........................................................ 27
Evaluating the process and results..................... '...................... ...... ............28
page
PART II. THE ROLE OF GOVERNMENT AGENCIES,
NONGOVERNMENTAL ORGANISATIONS AND OTHER
COMMUNITY GROUPS
Primary health care services.................................. ...................................... 33
Parents’ groups........................................................................................... 33
School programmes.....................................................................................36
Religious groups.......................................................................................... 40
The police and customs service.................................................................... 41
The media................................................................................ ...... .............43
The business community.............................................................................. 45
Service clubs............................................................................................... 47
The Community Action Committee and the high - risk groups.......................... 47
Bibliography....................... .......................................................... ?...... ............. 90
Annexes
I.
II.
Basic structure of Community Action........................................... ........... ......... 52
Some basic facts about drugs........................................ .......... ........................... 53
PREFACE
This set of manuals is a response to the need to introduce measures against drug and
alcohol abuse in developing countries. In those countries a large number of programmes
must be started quickly with limited resources. Lacking well-established programming
practices of their own, their planners and service providers must study the work and ideas
of others; they must analyse what that work means for their own cultures and adapt it to
their needs. These publications are designed to help them in their task.
The four manuals are described briefly below.
“Manual on addiction rehabilitation programming” by Fred Zackon.
This volume is intended for the staff of addiction rehabilitation programmes. It is designed to
be used by all service staff, although it is mainly a tool for programme leaders. The text
provides a guide for the development of model programmes based on the author’s
Reference Design. It describes the key issues and actions for building such programmes.
Most of the approaches described have already gained wide acceptance in the field of
addiction rehabilitation. Some attention is given to administrative issues, but the primary
focus is on client services. The context is integrated and all the elements derive from a
unified perspective, which means that staff must operate as a team with a common
understanding and purpose.
“Manual on community action against drugs and alcohol" by Sam Lauthan.
Those who live in communities where drug and alcohol abuse occurs must feel concerned
at the situation and be aware of the dangers of allowing it to deteriorate further. Community
action to combat substance abuse means that individuals and groups must work together to
find social responses to the problem and to provide healthy alternatives to alcohol and
drugs. All segments of the community must be motivated to develop a total commitment to
the task of protecting vulnerable groups and individuals from the dangers of substance
abuse.
The manual provides guidelines on forming local associations of the widest possible
variety of expertise and good will as the best way to develop the multidisciplinary approach
which is necessary to tackle this complex problem. It describes a step-by-step methodology
to be followed in planning and implementing a community-based demand reduction
-iii-
programme. It also gives a brief introduction to the role of government agencies and
nongovernmental organisations in the fight against drug abuse. The manual includes some
basic information about substance abuse generally, as people involved in community
action need to be well informed about the realities of the situation in order to tackle their
work with confidence and competence.
“Manual on drug and alcohol policy development’ by Ragnar Waahlberg.
The social effects of substance abuse are well known and clearly documented. For
example, there is no doubt that a high level of alcohol consumption in a country correlates
with a high level of social and health problems, with violence and criminality.
This manual is designed to help decision makers formulate a national policy on alcohol
and drugs and to develop a preventive strategy. The aim of a national policy on alcohol
should be to restrict the damage caused by excessive consumption, and the aim of a drug
policy should be a drug-free society. The manual includes chapters on reducing the supply
of alcohol with the objective of preventing excessive drinking, and on preventing people
from ever beginning to use illicit drugs. The focus is on prevention, rather than cure, as the
foundation of a national strategy. It offers a step-by-step guide to drawing up a policy and
creating the instruments needed for implementation.
“Manual on the design, implementation and management of alcohol and drug programmes
at the workplace” by Sverre Fauske.
The aim of this volume is to help managers, union leaders, occupational health
professionals and social workers to design and implement programmes on the prevention
of drug and alcohol abuse at the workplace. It is also intended for local resource personnel
to help them in their collaboration with government, management, union representatives
and consultants on alcohol-and drug-related problems at the workplace.
Concern for the welfare of people at work is central to the activities of the International
Labour Organisation. This concern includes taking measures to combat substance abuse.
ILO involvement in this field is based on the agreement of governments, employers and
workers that workplace initiatives are an effective means of preventing and reducing
alcohol and drug abuse. The scale of the problem should not be underestimated, as drugrelated issues affecting workers have become a serious concern in many countries. The
costs to industry and the community have been estimated in billion dollar terms; they
-iv-
involve lower productivity, absenteeism, accidents and staff replacements as well as
sickness and accident insurance claims. In human terms the costs to individual workers
and their families are also great if they lose their jobs as a result of drug and alcohol abuse.
The focus of this manual is on prevention rather than cure. It distinguishes between primary
prevention (awareness), secondary prevention (assistance) and tertiary prevention
(rehabilitation), and provides guidelines and suggestions for those responsible for
introducing workplace programmes.
The title page of all four volumes indicates that the publication is the first version of the
manual. The manuals are designed in such a way that they can easily be adapted in the
light of experience with their use and the second edition will incorporate new developments
in the field. The ILO encourages and welcomes the ideas of all those who use this material.
Readers are invited to submit their comments and suggestions for the second edition to The
Vocational Rehabilitation Branch, International Labour Office, CH-1211 Geneva 22,
Switzerland.
1
INTRODUCTION
Substance abuse is an extremely complex problem which affects every part of the world
today. In the search for solutions it is necessary to take account of the medical,
psychological, social and legal dimensions of the question as well as the economic
aspects. Abuse of drugs and alcohol occurs on a large scale in the industrialised countries
and has become a real threat to developing nations in recent decades. Most of the
countries of Southern Africa have serious problems with alcohol, cannabis and
methaqualone (mandrax), and some of these countries have begun to experience cases of
heroin and cocaine trafficking.
Those who live in communities where drug and alcohol abuse occurs must feel concerned
at the situation and aware of the dangers of allowing it to deteriorate further. The quality of
life of all members of the community is threatened when substance abuse is rife and every
individual suffers the consequences of inaction. Communities in many countries are
already facing natural disasters such as drought, which are compounded by economic
disasters such as inflation and unemployment; such communities cannot afford to ignore
the issue of drug abuse and cannot allow their precarious economic situation to be eroded
further by the social disasters of drug addiction and alcoholism.
Community action to combat substance abuse means that individuals and groups must
work together to find social responses to the problem and to provide healthy alternatives to
alcohol and drugs. Young people in particular need facilities for physical exercise and
recreation, stimulation for their creative talents and mental abilities, and an environment
which provides aesthetic satisfaction. Their spiritual needs also must not be overlooked in
the effort to provide a positive outlet for the energy and enthusiasm typical of the young.
Young people and workers are statistically most at risk of falling into dependency, but there
is no social group which is free of the threat of substance abuse.
All segments of the community must be motivated to develop a total commitment to the task
2
of protecting vulnerable groups and individuals from the dangers of alcohol and drug
abuse. A large number of people can give assistance in this effort . They include
psychiatrists, doctors, primary health care workers, psychologists, anthropologists,
sociologists, school administrators, teachers, the business community, labour leaders, trade
unionists, police and customs officers, youth club leaders, religious leaders, social workers
and parents. Professional groups and private individuals can all participate in community
action if they can spare a few hours every week or every month to work on an advisory
board or as resource persons on a Community Action Committee. Forming an association
of the widest possible variety of talent, expertise and good will is the best way to develop
the integrated, multidisciplinary approach which is necessary to tackle such a complex
problem.
The Community Action Committee
Prevention activities at grassroots level are the responsibility of local Community Action
Committees.
In order to set up a Committee the project takes the initiative by making a simple survey of
existing resources in the local community, concentrating on potential human resources. A
list is then drawn up of the local organisations whose members could make a valuable
contribution to prevention activities. The list is long: it includes professional bodies and
associations such as the police and customs authorities, the educational system, primary
health care services, the media and the local business community, as well as voluntary
clubs and organisations such as amateur sports clubs, youth groups and parent-teacher
associations. Nongovernmental organisations involved in charity work and religious
bodies can also play a vital role in preventing substance abuse in the community.
The social worker attached to the national drug prevention project contacts all the local
associations identified by the survey and invites them to a seminar or a public meeting in
order to discuss the situation and the possibilities for action. The objective of this
preliminary meeting or meetings is to establish a consensus on the need for action, before
any specific steps are taken to initiate activities. Once such a consensus is clearly
established the social worker invites the associations which have demonstrated their
interest and concern to nominate one of their members to serve on the Community Action
Committee. When the Committee is formed it should elect a Chairman and hold regular
meetings every month or so. The project coordinator should be appointed Secretary of the
3
Committee.
From this point on the active involvement of the national project is gradually phased out;
the project remains in the background, concerned only to maintain the motivation of
Committee members and advise them as requested. The basic structure of the community
action component of a national drug and alcohol prevention project is illustrated in the
organigram in Annex I.
The function of the Community Action Committee is partly to give advice to the local
population on drug-related matters, partly to serve as an information channel between the
local community and the national centre, and partly to mobilise funds and other resources
for prevention activities. Committee members themselves are often actively involved in
lecturing to school-children and youth groups on the dangers of drugs and alcohol, or in
fund-raising for campaign work. The Committee acts independently because activities
undertaken at local level are not usually funded by the national resource centre. This
arrangement gives committee members both responsibility and authority, as they are not
merely carrying out proposals made at national level. The element of independence is
motivating for committee members, who give their time voluntarily.
The basis of community action is networking through informal social contacts. Committee
members can intervene on behalf of recovering addicts by helping them find employment
and assistance when needed. They can also give professional advice on practical matters,
such as handling money and finding a home, or personal matters such as health problems
and mental stress. These activities are more concerned with secondary prevention than
primary prevention, which is aimed at the whole population rather than particular
individuals. This point indicates the importance of the work of the committee members, who
are aware of local needs of all kinds and who are in a position to respond to them.
Community action work must have a target. The target may be quantifiable and relatively
easy to measure (e.g. a reduction in the number of drug- or alcohol-related accidents
during the year), or it may be qualitative, relying largely on people’s impressions and
informed opinions for assessment (e.g. an improvement in the quality of life in the locality).
The ultimate target of community action is to involve the local population at all levels in
raising awareness of the dangers of drugs and alcohol and thus to strengthen the general
level of resistance to the attraction and temptation of dependency-creating substances.
4
Understanding the high-risk groups
During the past twenty years an enormous amount of literature has been published on the
question of substance abuse and the reasons why people fall into dependency and
addiction. However, researchers have not yet reached a comprehensive understanding of
the phenomenon in spite of advances in biophysiology and pharmacology.
In a country where drug abuse is common any young person or adult may be considered
at risk, but some are at greater risk than others because drug problems are not distributed
uniformly over social groups. Adolescents are at high risk, even if they live in so-called
“safe” areas, because of the stresses caused by the personal development which takes
place during adolescence. During this period the healthy young person will learn to:
develop self-confidence;
take the initiative;
explore, experiment and take risks;
discover personal aptitudes and come to terms with weaknesses;
develop an independent identity;
work towards emotional and social maturity;
assume some economic independence;
become physically mature.
During this difficult phase young people lose the protection afforded by childhood before
they gain the experience and maturity of adulthood. In addition to this it must not be
forgotten that adolescents have to respond to the stresses of their environment at the same
time as they are working towards their own personal development. The environmental
stresses include:
increasingly complex relations with other people;
problems related to sexuality;
the disappearance of the extended family;
finding a job or starting a training course;
negative peer pressure;
new technology;
the population explosion.
5
In addition to the above, those adolescents and young adults who live in high-risk areas
often have to cope with a particularly difficult situation in the family and community. They
probably experience economic hardship and may have psychological problems. They also
lack facilities for leisure-time occupations.
There are only two possible responses to the many types of stress listed above; fight or
flight. It is a tragedy that so many adolescents and young adults have chosen the latter
course, through drug taking and heavy drinking. However, not ALL young people in highrisk areas use drugs, and not ALL young people in low-risk areas refuse drugs. We must
therefore be very cautious when using expressions such as “high risk” and “low risk’’.
Programmes and activities designed to combat substance abuse in all areas must develop
different approaches aimed at non-users, experimenters, occasional users, regular users
and addicts.
Non-users must be encouraged to continue to refuse drugs and helped to resist peer
pressure to experiment. Experimenters must be informed that although drug users may
appear to function normally they run the risk of becoming addicted, taking an overdose or
being arrested. Occasional users are the most difficult group to convince because they
derive pleasure from drugs but do not suffer from withdrawal symptoms and are not yet
dependent. For the same reason regular users are difficult to reach, although they may
realise that they are already developing tolerance and increasing their intake of the drug.
Alcoholics, drug addicts and poly-drug abusers need to be motivated to seek treatment,
even if they have made previous unsuccessful attempts to stop drinking or taking drugs.
Treatment must be followed by after-care and rehabilitation services, preferably at
community level.
The expression “high-risk" group does not refer only to adolescents living in an
environment where drug-taking and drinking are common. Other high-risk groups are
retired people who drink to help themselves to cope with loneliness and boredom, and
business and professional people in stressful jobs. The adult children of alcoholics are
also considered to be at risk because they grew up in an environment where alcohol was
always present. Also at high risk are people who live in urban slums because very often
the production and sale of home-made alcohol is their main source of income. This group
should be the target of special programmes designed to tackle the multiple problems of
slum dwellers; such programmes should include field workers and peer leaders with whom
the slum dwellers can identify. Youth clubs and other youth movements should be involved
6
in the planning and implementation of these programmes, which need to help young
people develop the necessary coping skills to grow up and lead a drug-free life in a highrisk environment.
Working in high-risk areas or with high-risk groups is a tough job requiring sustained effort
and almost unlimited patience. Field workers and programme initiators must bear in mind
that modifying the immediate environment of adolescents and young adults will take years,
and that readjusting social trends and lifestyles will take decades. Such long-term goals
are realisable if field workers and members of community action groups are genuinely
motivated and are determined to start NOW.
The present manual is designed to help all those interested in community action to plan
and implement their activities. It is intended for government officials, policy makers,
programme planners, primary health care personnel, educators, voluntary social workers,
religious groups and youth club leaders; in fact it can be useful to any individual or group
wishing to contribute to the fight against drug and alcohol abuse.
The manual consists of two parts.
Part I describes a step-by-step methodology to be followed in planning and implementing a
community-based demand reduction programme. It deals systematically with the different
steps involved in mobilising the community and in designing, implementing and evaluating
the programme.
Part II gives a brief introduction to the role of government agencies and nongovernmental
organisations (NGOs) in the fight against drug abuse. It then lists a number of activities that
can be undertaken by the main community organisations and institutions, including primary
health care services, parents' groups and womens' organisations, schools, religious
groups, the police and customs services, the media, the business community and service
clubs. The organisations mentioned and activities listed are not exhaustive. Programme
planners are expected to add to the suggestions and to try out new ideas. Besides
adapting the proposed activities to the local situation, programme planners and policy
makers must have the courage to initiate and innovate.
The manual also includes some basic information about important aspects of the problem
7
of substance abuse. People involved in community action need to be well informed about
the realities of the situation in order to tackle their work with confidence and competence.
In-depth knowledge about intervention skills can only be provided through intensive
training courses and workshops, which should be organised with the help of local and
foreign experts. It may be possible to organise some technical cooperation activities in this
field with the assistance of international agencies interested in combating substance
abuse. The international community is continuously calling for global, international,
regional and national cooperation to reduce both the supply and demand for dependency
forming substances. In this context it goes without saying that cooperation must first
become a reality at the local community level.
PART I
PLANNING AND IMPLEMENTING A COMMUNITY-BASED PROGRAMME
9
Taking the initiative
During the last few years governments in developing countries have begun to show real
concern about the problems and dimensions of substance abuse. There is now a clear
understanding of the need to revise legislation, to strengthen and update agencies and to
improve services. New measures and appropriate strategies also have to be developed.
Until very recently most resources have been directed towards supply reduction through
suppressing the production, distribution and sale of illicit drugs. However, worldwide
experience and research shows that demand reduction strategies are equally important in
the fight against substance abuse and that there is a need for the further development of
demand reduction strategies through a wider variety of prevention, treatment and
rehabilitation approaches.
Factors to consider
Before designing programmes and setting objectives it is important to consider the factors
which influence the policy and organisation of demand reduction programmes:
the political structures in place and the political processes involved;
the dynamics of decision making by government agencies:
the traditional methods of problem solving and decision making;
the interactions between leadership and power groups within the community;
the availability of financial and human resources at community level;
the feasibility of international assistance in terms of finance and training.
In spite of the urgent need for action and the pressure to respond quickly, it is necessary to
take the time to plan a step-by-step approach and to avoid hasty decisions and mistakes.
Decision makers and service providers have a duty to plan carefully and to pay attention to
all the elements involved in a community-based programme. There are eight essential
steps in the planning process:
needs assessment;
community mobilisation;
10
training and manpower development;
development of material resources;
setting goals and objectives;
defining activities to meet the objectives;
implementing and monitoring activities;
evaluating the process and results.
/
' ■-----
Needs assessment
In order to tackle even a simple problem effectively it is necessary to have a clear
understanding of its causes and consequences. When the issue is as complex as the
problem of substance abuse it is clear that a thorough assessment of the situation is
essential. There are three main reasons why needs assessment must be carried out
adequately:
to enable policy makers and programme planners to make a rational and effective
use of assets, particularly in developing countries where financial resources
are very limited;
to provide clear facts in order to convince government officials, policy makers,
community leaders and funding agents of the urgent need for community action;
to establish priorities for the action plan.
A scientific survey is the most reliable way of collecting data, but it is also the most
expensive method. However, there are a number of alternative approaches, and a lack of
resources and expertise should not prevent programme planners in developing nations
from making an assessment of the nature and extent of substance abuse in their country.
Information available from three main sources can be helpful until the necessary funds and
expertise are available for large-scale surveys; the information sources are substance
abuse indicators, social anthropology and the informed opinions of community leaders.
Substance abuse indicators
These are quantitative and verifiable data which can be obtained from police records and
the health services. They provide information on the following important aspects of the
problem:
11
the drugs which are used in the community;
the demographic characteristics of the drug users;
the number of known drug smugglers, dealers and users;
the number of seizures including illicit alcohol and prescription drugs;
the purity of the illegal drugs seized, which indicates the closeness of the
offender to the producer or smuggler of the drugs;
variations in the market price of drugs, which indicates the availability of drugs
on the streets;
the number of drug-related deaths by overdose, suicide, homicide, work accidents
and traffic accidents;
the number of alcohol- and drug-related crimes of violence and theft, compared
with the number of cases not related to substance abuse;
the percentage of admissions to hospitals, treatment centres and prisons which
are related to substance abuse;
the number of known traffickers.
These data, collected over a number of years, indicate trends in drug trafficking and some
of its consequences. However, it must be noted that experience in the industrialised
countries seems to indicate that the “known’ addicts probably represent only about ten per
cent of the real number of addicts in a given community at a given time. In developing
countries the known cases may represent a still lower proportion of the total number of
addicts in view of the stronger social stigma attached to drug addiction in many parts of the
world.
In order to ensure that police and health service records are as accurate as possible it is
advisable to update and standardise the files on a regular basis. This work could be
undertaken by social scientists or social workers with experience in the field of substance
abuse who should collaborate closely with the data collection and record keeping sections
of the police and prison departments and health services. Data recorders may need to
follow a basic in-service course on principles of case work and counselling to develop their
awareness of the delicate and sensitive psychosocial factors involved in the data collection
process, particularly in regard to substance abuse.
12
Social anthropology
Substance abuse is not only a question of figures and statistics. One of the most important
aspects for programme planners is the need for information on the beliefs, traditions, values
and practices of socio-cultural and ethnic groups within the community.
Social anthropology provides policy makers with a good insight into the sub-culture of drug
abuse. Through detailed case histories a wealth of information can be gathered about the
knowledge, beliefs and values, attitudes and behaviour patterns that characterise drug
abusers in their specific socio-cultural context. Social anthropology is a simple method of
collecting information by involving the human resources which already exist in the
community to be studied. According to Walters (1980) the types of information that can be
obtained by “street anthropologists" are the following:
types of drugs used;
age and circumstance of first drug taking;
routes of administration;
economics of drug use;
drug effects;
relationship of setting to perceived effects;
physical and social benefits and risks;
adverse reactions and treatment histories;
criminal justice cases.
Informed opinions
In every community there are individuals whose professional or social role puts them in a
position to provide an informed opinion on the nature and extent of substance abuse.
These natural information-providers include:
local doctors;
mental health specialists;
primary health care workers;
school teachers;
youth leaders;
police officers;
13
lawyers;
family counsellors;
probation officers;
bankers;
shop keepers;
taxi drivers;
caf6 and bar owners;
community elders.
Data may be collected by interview. Generally, a questionnaire is used to cover the basic
information required but this should be complemented by an unstructured interview in
which the respondent talks spontaneously about the problem. Aspects of the drug scene
which were previously unsuspected by prevention workers may come to light In this way.
Epidemiological survey
An epidemiological survey is the best method for measuring the nature and extent of
substance abuse in a given locality, but it is also the most expensive of the methods
discussed here. Programme promoters will need the collaboration of the local university
survey team and I or experts from the private sector and outside consultants. Considerable
expertise is required to choose a good sampling method and to design a questionnaire
which will be appropriate for the educational level of the population and the socio-cultural
context. If the necessary funds are available the epidemiological survey should be
repeated at regular intervals to show trends in the prevalence and incidence of substance
abuse in the locality.
Alternative data collection methods include self-administered mail questionnaires, groupadministered questionnaires and telephone interviews, although the latter are not
appropriate for the rural areas of developing countries.
Assessing existing programmes and services
After collecting all the available data on the nature and extent of substance abuse in the
community, programme planners need to assess the existing programmes and services
and the human and material resources available for community action.
14
The following factors should be taken into consideration:
the number of government agencies and nongovernmental organisations offering
prevention and treatment services;
the types of activity arranged and the approaches adopted towards prevention,
treatment and rehabilitation;
the socio-demographic characteristics of the various target groups being reached;
the communication network and collaboration between the agencies and
organisations working in the field;
the facilities and equipment available, including teaching materials and transport.
Interpreting assessment data
The findings of the data-collecting effort must be interpreted with caution. It is important to
complement the indicators of drug abuse obtained from addiction registers, health service
records and seizure statistics with reliable data from other sources. Assessment studies
sometimes produce conflicting results, which again emphasises the need for alternative
interpretations. The methodology and findings of the assessment should be formally
reported in a document to be circulated for comment and specialists in social measurement
techniques should be asked to assist in interpreting the data collected.
In summary, needs assessment is a complex undertaking. In order to achieve the best
possible result the national substance abuse resource centre will need the help and
support of experts to design, initiate and evaluate programmes and to undertake research
studies on issues specific to local conditions.
Community mobilisation - the need for linkages
Substance abuse is a community concern that requires a community response. The
problem must be faced in the home, in night clubs and tourist resorts, in public parks and
playgrounds, in schools and youth clubs, at social gatherings and at work.
Substance abusers and the families of substance abusers need the support of government
services. At the same time nongovernmental organisations must be encouraged to work in
15
the field of prevention, treatment and rehabilitation. The various organisations engaged in
combating drugs and alcohol should, however, avoid a duplication of services.
Nongovernmental organisations should aim to supplement government assistance by
filling gaps in the services offered. They can often respond to local needs more effectively
than public services owing to certain special characteristics:
they can act quickly because of their informal structure and independent status;
their voluntary nature means that they are less restricted by financial constraints
than either the public or the private sector;
they are close to the community and can reach specific target groups:
their members are genuine field workers and the local population can identify
with them;
their leaders usually have influence and prestige , and can successfully press for
action or solicit support.
There are three major preparatory steps for involving the community in action to combat
substance abuse. The first step is to reach a consensus on the need for action by
approaching the various community groups individually and contacting leaders in order to
discuss the situation and to share ideas for action programmes. The second step is to
enlist potential volunteers to serve on the Community Action Committee. It should be
stressed that expert knowledge is NOT a requirement for this work; a genuine commitment
to winning the fight against substance abuse is the most important quality that an individual
needs to make a difference to the drug scene in the local community. The third essential
step is to make sure that the aims and objectives of the resource centre are clearly
understood by all the individuals and groups participating in the work.
Constraints in community mobilisation
Several factors might make it difficult at first to interest the general public in drug- and
alcohol-prevention activities, the first problem being that drug-taking is not always seen as
an issue of concern. Certain drugs and alcohol have traditionally been a part of the local
way of life in the majority of communities and although addiction is clearly unhealthy it is
frequently seen as a personal problem rather than a social problem. The resource centre
may have to counter this view by making the general public aware of the dimensions of the
problem and the real costs of addiction, both in terms of economic loss and in terms of
damage to the quality of life.
16
A second difficulty which is frequently encountered is that access to women, adolescents
and social drop-outs may be difficult for religious or political reasons. The personality of
those who voice community needs and organise programme activities may be decisive in
reaching certain target groups. Community action workers need to have credibility and to
be accepted by social groups who are marginalised from the mainstream of community life.
Political and financial interests in the profits to be made from dependency-creating
substances are extremely powerful. Activities related to combating drug and alcohol abuse
may have to face lobbies or other pressures from those who sanction the abuse of these
substances.
Other difficulties faced in mobilising community resources have to do with the personality of
the individuals involved in the work. Programme promoters, educators and trainers who
themselves use substances which create dependency will not have the necessary
credibility in the eyes of the community.
Involvement in community action requires a lot of time and energy, and above all it requires
sustained commitment and enthusiasm. Promoters must therefore guard against the
danger of “burn-out" by delegating responsibility. A second-line community action group
will need to be developed as activities progress.
There is often a tendency to fight against other people instead of fighting against the
problem and conflicts will inevitably arise between individuals serving in community action
programmes, and possibly also between nongovernmental organisations and service
providers. In all circumstances the interests of alcoholics and drug addicts and their
families must be given priority over self-interest and petty jealousies. Individuals and
groups must have the humility to accept the fact that they will not go far alone and that they
need a strong coalition of well-intentioned partners. Above all they must be ready to share
experience, expertise and resources and be willing to learn from their own mistakes and
those of others.
Training and manpower development
Community educators and field workers are the agents of change whose work is
indispensable in a community-based prevention programme. We have already stressed in
17
this manual that it is not necessary to be a specialist or expert to start such a programme
and that people who are genuinely motivated can make a real difference to the situation in
their community if they have some basic knowledge about substance abuse. Information
on the following subjects is necessary for field workers and other potential resource
persons working in primary prevention programmes: prevention approaches; basic
definitions of the terminology of substance abuse; signs and symptoms of drug use and
abuse; the nature of denial; the nature of negative peer pressure; and decision-making
skills to resist negative peer pressure. In addition, field workers should have some
knowledge of the types of drugs used in the community, the modes of use, their effects and
withdrawal symptoms. Some basic facts on drugs are provided in Annex II to this manual.
The following sections present general information on the other six topics listed above.
Prevention approaches
There is now increasing awareness among drug control agencies that too little emphasis
has been placed on strategies to reduce the demand for drugs. Until very recently the effort
to control substance abuse focused largely on reducing supply by suppressing the
production and distribution of illicit substances, but it is now accepted that supply reduction
must be balanced by demand reduction, which means preventing people from starting to
use dependency-creating substances, or preventing them from continuing to use these
substances indefinitely.
ri Preventive measures can be applied at three levels. The first is primary prevention, which
II aims at controlling or reducing the incidence of substance abuse by preventing
experimentation or delaying the age at which young people begin to drink alcohol.
Secondary prevention attempts to reduce the prevalence of substance abuse by early
diagnosis and by providing counselling and treatment for drug users to encourage them to
return to a drug-free lifestyle. Tertiary prevention aims to prevent recovering addicts from
relapsing through the provision of rehabilitation and social reintegration programmes.
The four main approaches to primary prevention are through drug education and
information, alternative activities, values clarification, and social skills.
Drug education and information campaigns are widely used in many countries. The main
strategies are the provision of objective information and the use of scare tactics. Factual
information is provided about the different types of drugs of abuse, the modes of
18
administration, the effects on health, and the economic and social consequences of abuse.
This type of campaign has often been criticised because it may arouse the curiosity of non
users if too much stress is laid upon the euphoric effects of the drugs. On the other hand
the objective and scientific information provided can demolish myths and misconceptions
about alcohol and drug abuse. For example, there is new scientific evidence that cannabis,
which is usually believed to be harmless, can damage the brain, the respiratory organs and
the reproductive system. Scientific information can also help to raise awareness of the real
dangers of needle-sharing and casual sex in the spread of AIDS. Information campaigns
should not be limited to giving facts about drugs but should also lay stress on the benefits
of a drug-free lifestyle.
The scare approach is very commonly used by parents. It may discourage youngsters who
have never experimented with drugs but it does not work with adolescents who have
experienced euphoria induced by a drug. Young people who are at particularly high risk
very often do not care about the long-term consequences of drug abuse and are only
concerned with immediate gratification. They may be using drugs themselves or have
friends who are regular users but who suffer no apparent consequences. It is pointless to
tell such adolescents that their first experiment with drugs or alcohol will make them ill, as
their experience has already shown them that this is not the case. The young people will
then not be interested in hearing what these teachers have to say about drug-taking
because they will believe that they know nothing about the subject.
Young people need to explore their environment, experiment with life and test their limits.
Therefore they should have creative and meaningful experiences which fulfil these needs
and provide an outlet for their energy. Recreational centres must provide activities that
serve some of the functions of drinking or drug-taking; excitement, challenge, relaxation,
and relief from frustration, alienation, discrimination, pain, sickness and boredom. Such
activities are more important when children are left to themselves outside school hours
because both parents are working; it is particularly important to provide occupation for
children during the school holidays. The activities which satisfy the needs of adolescents
include; physical exercise such as swimming, running and climbing; organised sport which
fosters the discipline of obeying rules; games which develop the team spirit and
sportsmanship in accepting defeat and frustration without resort to alcohol or drugs; hiking
in aesthetically satisfying surroundings; camping and sharing tasks and responsibilities;
undertaking voluntary social work; learning to appreciate art; learning to relax in a healthy
way; acquiring the discipline of good eating habits and diet; and learning about counselling
19
techniques.
/ The values clarification approach is based on the assumption that choices are influenced
by values and that people who abuse drugs have not developed a dear set of moral or
spiritual values. This approach relies heavily on inculcating good behavioural norms and
moral values in young children. It is assumed that children who have been taught not to lie
to their parents and teachers will be able to express their feelings freely irrespective of peer
pressure. They are also expected to be able to resist the pressures of advertising for
alcohol. The values clarification approach is an effective prevention tool for young children
and adolescents who have not yet experimented with drugs. It is less effective for
occasional or regular users, who are enjoying the “pleasure phase" of drug taking. In
addition, the approach is not effective with people who are already dependent on drugs
because the whole world of the addict revolves around the drug, which has priority over
everything else in life.
The social skills approach is based on the assumption that most new drug users are
encouraged to experiment by an actual user. Experience has also shown that hard-core
addicts who have experienced severe withdrawal symptoms rarely induce non-users to try.
The main culprits in spreading drug use are casual and occasional users who seem to be
enjoying life. Therefore the social skills (or interpersonal) approach aims to provide non
users with coping skills to resist external pressure to use drugs. The following skills form
the basis of this approach:
interpersonal communication;
increasing feelings of self-worth and self-esteem;
resisting peer pressure;
problem solving and decision making;
analysing and resisting advertising for alcohol;
assertiveness and stress management;
controlling anger and frustration;
distinguishing between positive and negative persuasion.
Substance abuse is a complex problem and no single approach used in isolation will be
successful in preventing it. Community educators should determine which combination of
approaches would best suit the needs of the individual or group in question.
20
Basic definitions
The following terms are very frequently used in discussions on substance abuse.
Drug: any natural or synthetic substance which, when taken into a living organism, may
modify its functions.
Use: use of a substance implies that the individual is in control, not compromising physical
health or damaging family life, social activities or work abilities.
Misuse: misuse refers to a non-medical or inappropriate use of psychoactive drugs.
Abuse: abuse of a substance refers to a pathological pattern of use causing impairment in
social or occupational functioning. The duration of abuse is at least one month.
Tolerance: tolerance is a state in which markedly increased amounts of the substance are
required to achieve the desired effect.
Dependence: abuse leads to dependence, which is characterised by a compulsion to take
the drug on a continuous or regular basis in order to experience its mental effects or to
avoid the discomfort resulting from its absence. There are two types of dependence:
physical dependence, which is a state triggered by the abrupt cessation of a drug which
has produced an adaptive physiological state, and psychological dependence, which is
characterised by an emotional drive to continue taking a drug whose effects are felt to be
necessary to maintain a sense of well-being.
Withdrawal syndrome: withdrawal or abstinence syndrome is characterised by the stressful
symptoms resulting from sudden deprivation of a drug that is habitually used. Symptoms
may be mild and not always clinically evident (cocaine, cannabis), or very marked
(opiates), or even life threatening (barbiturates).
21
Signs and symptoms of drug use and abuse
Field workers and educators engaged in a public awareness campaign are constantly
asked to describe the signs and symptoms of drug use. Great caution is required in
answering this question and people must be constantly warned about the danger of
jumping to hasty conclusions at the first possible signs demonstrated by their children,
students, friends and relatives. It must be stressed that the symptoms which are listed
below are NOT proof of drug taking; they are no more than indications that a person MAY
be using drugs. Even if several of the symptoms appear at the same time it may mean no
more than that the individual in question is passing through a period of emotional or
psychological stress.
With all the reservations mentioned above, the following are some of the signs and
symptoms that may be associated with drug use and abuse:
sudden mood changes;
unexplained irritability or aggression;
loss of interest in hobbies, sports or studies;
frequent lies and subterfuges;
bouts of drowsiness or sleepiness;
loss of interest in physical appearance;
unpunctuality and absenteeism;
borrowing money;
“losing" money or valuables;
lack of respect for authority;
unusual smells on the body or clothes;
stains or marks on the skin or clothes;
approval of the drug culture.
The nature of denial
Programme initiators and field workers must be prepared to face a barrier which is very
often a stronger deterrent that any threat that traffickers can make. This is DENIAL. Denial
must be faced at the level of users , families, the community and the state.
22
USERS deny having a drug problem even after they realise that they have started to
develop tolerance or have already become dependent. FAMILIES deny that one of their
members has a drug problem because the honour and good reputation of the family is at
stake. Unfortunately, many families give higher priority to protecting their reputation than to
protecting the lives of their members. The COMMUNITY denies that there are abusers and
traffickers in its midst, or will only admit that there is a problem in the big cities and the
slums. The STATE denies that the problem is serious in spite of an increasing number of
arrests and cases of overdose. If the problem is acknowledged the authorities fear that hey
will be held responsible for causing it or for allowing the situation to deteriorate.
Users, families, the community and the state, by denying the reality of the problem, tend to
put the blame on the product, the media, neighbouring countries, etc., thus reinforcing the
belief that the only possible strategy in the fight against drug abuse is supply reduction. In
the meantime all the victims of substance abuse continue to suffer physically, morally and
economically.
When substance abuse reaches epidemic proportions the responses are inadequate and
inappropriate because they have not been prepared realistically. Hasty solutions are
sought and very often only a single aspect of this complex problem is addressed. It
frequently happens that foreign models and approaches are “imported” and adopted
without proper consideration of the economic and socio-cultural context in which they are
to be applied.
The nature of negative peer pressure
The negative influence of peers is very often associated with drug abuse, particularly
among adolescents. Parents of young delinquents or drug abusers are well aware of a
terrible force against which they feel helpless but which they are unable to understand.
When the issue of substance abuse occurs, the attitude of uninformed parents is first to
deny the existence of the problem, then to moralise, plead, threaten, scold and evoke the
family honour and reputation. They then try to arrange for treatment, but frequently end by
23
cutting themselves off from their child when nothing works. In response to the same
situation the peer group provides approval, a sense of intimacy, and prestige when the
inexperienced drug taker moves from legal to illegal hard drugs. In cases where parents
might tend to over-protect their children and take all their decisions for them, the peer
group encourages young drug users to decide for themselves about their lifestyle. The
peer group also provides a strong sense of belonging. All members of the group have
similar values and behaviour patterns; they have their own symbols, ways of dress, music
and dance, which together amount to a sub-culture within the larger community.
For all the reasons above peer pressure, which may appear irrational to parents, exerts a
strong influence on young drug users or abusers. The same applies to adults who fall into
drug use, because it must not be forgotten that peer pressure is relevant to all age groups.
It fulfils, although negatively, some of the basic psychological and social needs of the
individual.
Under such real pressure from their peers it is not hard to understand why drug users
disobey or desert their families to move into the drug culture. While they are still in the
euphoric stage they do this in order to gain more pleasure, and when they have started to
experience withdrawal symptoms they do not hear the pleas of their family or see their
distress because they have reached the point where the next dose has priority over
everything else.
Decision-making skills to resist negative peer pressure
Decision making is quite a difficult process. Certain skills are required for a person to be
able to make the right decision in a difficult situation. Some decisions require a long
period of reflection and deliberation. They might include choosing a career or starting a
family. Other situations demand a quick decision. For example, a person driving a car has
to decide in a flash of a second what action to take in an emergency, and at the same time
be as sure as possible that the decision is correct.
Resolving to resist negative peer pressure to use drugs is very difficult, because, apart from
24
the physical and psychological attraction of drugs, the peer group uses rejection strategies
against someone who tries to refuse drugs. For example, they might be called a coward or
a baby. In a slightly different situation the peer group might exert pressure on reluctant
members by providing assurance against the dangers and consequences of risk-taking
behaviour.
Without denying that it is quite difficult to resist negative peer pressure, it is still possible to
avoid problems by adopting the procedure below:
1.
Identify and define the activity that is being proposed by thinking about the
following questions:
is this proposed activity legal?
if it is legal, is it moral? (e.g. truancy)
is it dangerous to the self or others?
will adults be present where this activity is to take place?
would parents approve if they knew of this activity?
does it correspond to the family's cultural values?
2.
Devise a plan of action based on the answers to the questions above.
3.
Evaluate the possible outcomes of the plan. Try to anticipate the likely
consequences of the chosen course of action and assess their advantages
and disadvantages. Re-examine values and emotions which might
have become distorted by the impact of advertising and other media images.
Emotional reactions interfere with the decision-making process and can prevent
a person from making an objective and rational choice. Balance the short-term
pleasure against the real risk factors associated with drug use.
4.
When the evaluation exercise is finished the next step is to act upon the strategy
which has been consciously and deliberately chosen. This means finding strong
arguments to resist negative peer pressure or to counteract any other type of
difficulty.
5.
Whether the final outcome of the decision was positive or negative, rt is possible to
learn a lesson for the future. When a similar situation arises again it will be much
25
easier to deal with.
To help memorise the different steps of the decision-making process described above, they
can be described as the IDEAL method.
I dentify the nature of the activity, situation or problem.
D evise a plan.
E valuate the possible outcomes of the plan.
A ct upon the chosen strategy.
L earn from past mistakes to avoid future problems.
The previous sections presented some very basic and general information for people
working in community-based prevention of substance abuse. For further knowledge and
training in specific intervention skills intensive training courses need to be organised with
the help of local and international experts. Priority should be given to developing skills in
the principles of social work, case work (individual counselling), family counselling, group
counselling, rehabilitation and aftercare (relapse prevention), assessment of drug
dependents, short-term and long-term management of drug-dependent persons, and
treatment approaches.
Development of material resources
Members of the Community Action Committee will need to make an assessment of the
material resources available for a public awareness campaign. They have to know what
teaching aids and audio-visual equipment can be reserved for their use, and then they
have to develop or buy any other material which is found to be necessary. Materials
developed in other countries, such as documentaries, posters or TV spots, will need to be
adapted for the local community. Even after they have been adapted they will have to be
pre-tested on the target audience before they are put into general use. Pre-testing consists
of assessing the reactions of a target audience to a particular approach, message or
material, which will then be modified accordingly.
A pre-test can also be used to determine the background knowledge, attitudes and
perceptions of participants at the beginning of a training course or seminar. A post-test
questionnaire is then administered after the course to measure the impact it has made.
26
Setting goals and objectives
Having gathered all the necessary information on the nature and extent of substance abuse
and the existing programmes and services, the next step for the members of the Community
Action Committee is to develop complementary programmes. These new programmes
should have specific objectives designed to attain the major goal of community action
against substance abuse. The major goal is to reduce the demand for alcohol and other
drugs and to provide help to those already affected by alcoholism and drug abuse. The
smaller and more specific objectives are usually determined by the gaps that have been
discovered between the existing programmes and services, the material resources
available in the community and the real needs which have been identified.
Specific objectives must respect the following criteria. They must be:
limited in time (they must state when various aspects of the programme are to be
accomplished);
qualifiable (they must be clear and precise, not vague and ambiguous);
measurable (they must help determine the success or failure of the programme);
realistic (they must not be utopic or unreasonable).
An example of a specific objective might be as follows:
To reduce by March 1993 (time) the number of arrests of young people between 15-24
(quality) for possession of illicit drugs in the community of
(measurable and realistic).
by 25 per cent
Defining activities to meet the objectives
This is usually done by reversing the observations made during assessment. For example;
Observation
No parent groups
Activity proposed
Set up ten parent groups by organising
talks and film shows to sensitise parents.
27
Lack of resource persons
Increase number of resource persons
by organising short training courses and
seminars for primary health care staff,
social workers, teachers, police officers.
Deficient mass media coverage
Improve contacts with the media through
meetings, submitting articles to the press
and by using a multi-media approach
(magazines, posters, TV, radio, theatre).
Having defined the activities which will meet the specific objectives the Committee will have
to calculate the human and material resources required to organise these activities. It may
be necessary to raise funds by holding a campaign on an appropriate occasion such as the
local carnival.
Implementing and monitoring activities
The resource centre may start to implement its prevention, treatment and rehabilitation
programmes as soon as it has a full-time staff including a national project coordinator, a
centre manager, a job placement officer, one or two trained counsellors and a secretary.
The full-time staff will, of course, need the support of a pool of professionals and voluntary
social workers at two important levels of the structure of the centre, i.e. the Advisory Board
and the Community Action Committee. Another vital aspect is the link with the network of
government ministries and agencies and nongovernmental organisations. The
responsibilities of each agency and organisation must be clearly defined and rationally
delegated in order to facilitate the monitoring of the activities.
Monitoring is a day-to-day evaluation of activities during the implementation of a
programme or project. It depends on the establishment of a communications network
which functions horizontally between government agencies and nongovernmental.
organisations and vertically between the local population and the policy makers and
programme planners.
In order to monitor tasks each member of the Committee should be responsible for
28
monitoring the implementation of the activities specific to each group or organisation
involved. Regular meetings of the Community Action Committee should be held every
month or every three months so that each organisation may report on its past activities, the
problems it has encountered and the progress achieved in present activities, and its plans
for future activities. At these meetings the responsibilities to be assigned to each
nongovernmental agency or service can be discussed and agreed.
Members of the Committee, who are usually very busy people, should make a point of
being present at every meeting and of studying the agenda carefully in advance.
If possible, a full-time coordinator should be appointed for the proper monitoring of
activities which are intra- or inter-nongovernmental organisation.
Detailed record keeping is not only important for good management and service delivery,
but can also help projects and programmes to learn from their mistakes. It is even more
important if it has been decided to replicate a particular model which was developed by a
different programme, perhaps in a different country, or conversely, if another programme
displays interest in replicating this model. Such detailed day-to-day record keeping can
probably best be organised in the form of a diary.
In order to benefit from the close monitoring of activities members of the team and
managers of specific programmes must remain open to feedback and feel able to
contemplate different approaches.
Efforts must be constantly sustained to foster, develop and strengthen the community
network. A multidisciplinary and integrated approach can be encouraged by including a
cross-section of the community in the implementation of every programme.
Evaluating the process and results
A major difficulty in organising the fight against drug abuse is that no objective evaluation
has ever been carried out on hundreds of programmes all over the world. The result is that
many nongovernmental organisations or government services continue to offer activities
which are popular and successful but have neglected to improve their less successful
approaches. A large number of organisations have ceased their activities in the prevention
of alcohol and drug dependence, simply because they have not evaluated the programmes
29
they started in order to detect and correct their weaknesses. Evaluation does not mean
only deriving satisfaction from the successful parts of a programme; it also means
discovering shortcomings in planning and implementation. Substance abuse programmes
need to be evaluated and revised constantly because of the changing pattern of drug use
and the occasional appearance of new drugs on the market.
A proper evaluation exercise provides the following benefits for programme planners:
factual data which permit the formulation of more realistic objectives and
strategies:
better identification of the needs of target audiences and high risk groups;
better understanding of conditions in the field and the needs of field workers
on the part of policy makers and funding agents.
Precise information adds to the credibility of a programme and justifies further funding and
expansion of activities. It also ensures that maximum use is made of existing services and
resources. Further, the testing of strategies, approaches and audio-visual materials results
in a more rational use of human and financial resources.
The two most important aspects of evaluation are process evaluation (efficiency) and
outcome evaluation (effectiveness).
Process evaluation is usually an assessment of the efficiency of the methodology and
procedures used during a campaign. It helps to identify barriers and obstacles that block
service delivery and also brings to light factors that may have been overlooked or unknown
to the initiators of the project at the planning stage.
The factors to be assessed in a process evaluation are as follows:
punctuality and assiduity of programme operators and field workers;
number of operators actually participating in the activity compared with the number
planned;
experience and training required of personnel;
time actually spent on specific activities compared with the time estimated;
money spent compared with budget provision;
reasons why funds voted were not utilised;
30
approaches which proved to be appropriate for the target audience;
number of posters, stickers, pamphlets and handouts distributed;
number of talks, film shows and exhibitions organised;
dynamics of successful collaboration between nongovernmental organisations
and other agencies.
Outcome evaluation aims to measure the effectiveness of the programme and the impact it
has made on the target audience. It indicates whether the programme has reached its
objectives and the extent to which the different community groups have changed their
beliefs, attitudes and behaviour.
An outcome evaluation should not be made immediately after a programme has finished
because the desired results may not be observable for some time. However, too long a
delay may mean that the impact the programme has made is beginning to be forgotten. It
is for programme planners to decide on the best moment to carry out the evaluation in their
own particular context.
The factors to be assessed in an outcome evaluation are as follows:
the extent to which target groups developed an understanding of their role in
prevention;
the way in which the activity or programme was received by the community;
the number of persons it reached;
the number of people who have requested the services offered by the programme;
the number of enquiries made about the programme;
the extent to which young people can demonstrate the skills they have learned
in problem solving, decision making and drug resistance;
the extent to which high risk groups have developed self-esteem and assertiveness;
the advantages derived by members of the community in terms of school, family,
social rehabilitation, health recovery and economic progress.
Factors to be assessed after a certain lapse of time include:
the number of arrests connected with alcohol and drugs;
31
the number of hospital admissions and accidents connected with substance abuse;
increases in personal income as a result of improved attendance at work;
money saved by firms operating an Employee Assistance Programme by a
reduction in the number of working hours lost through absenteeism and
poor time keeping.
Individual programmes should be evaluated in the light of their specific objectives. It is
useful for planners to know which were the most popular and least popular activities in the
programme so that the least popular functions can be re-examined. A successful activity
should also be re-evaluated periodically because the situation in the field changes
constantly. Findings from programme evaluation coupled with any new epidemiological
findings should help planners decide whether to re-invest in a programme, adjust it or
discontinue it in favour of some other prevention initiative.
PART 11
THE ROLE OF GOVERNMENT AGENCIES
NONGOVERNMENTAL ORGANISATIONS
AND OTHER COMMUNITY GROUPS
33
Primary health care services
Primary health care staff are responsible for bringing health services to the community,
particularly in rural areas. Medical personnel and social workers, together with traditional
healers, represent a very important network through which prevention, treatment and
rehabilitation programmes can be channelled. Their presence is fully accepted by the
community, which gives them a major advantage in drug- and alcohol prevention activities.
In the routine of their daily work they deal with patients suffering illness or accidents as a
result of substance abuse; they treat the victims of traffic accidents, those injured at work,
people involved in fights and other forms of violence, attempted suicides and overdose
cases. Health personnel are thus very familiar with the consequences of substance abuse
and are usually willing to take part in prevention work.
As a matter of routine, then, primary health care personnel intervene in crisis situations and
provide short-term treatment for alcohol- and drug-abusers. On the basis of their
knowledge and experience they can become first-choice educators for primary prevention
programmes. They simply need some additional training in intervention techniques and
the possibility of improving and updating their knowledge of new drugs coming onto the
market and new modes of use and abuse. It should be noted in this connection that
methaqualone (mandrax) smuggling is fast becoming a real threat in many African
countries, and doctors need to be very aware of the risks of over-prescribing for their
patients. Pharmacists and health educators should work to raise public consciousness of
the real dangers of using prescription drugs for non-medical purposes.
Primary health care workers are also ideally placed to start or pursue the collection of
epidemiological data for research purposes and to help policy makers and programme
planners design accurate and relevant campaigns based upon local realities. Finally,
primary health care professionals need to participate in the development of a pool of
trainers and resource persons to support the programmes. Once prevention activities have
gained the necessary momentum specific courses for the training of trainers will have to be
developed with expert help.
Parents’ groups
Members of all kinds of organisation, both formal and informal, have one thing in common parenthood. Parents have the most significant role to play in any programme for the
34
prevention of substance abuse and the treatment and rehabilitation of addicts.
It is not easy for parents of adolescents today to help their children cope with even the
normal stresses of growing up, not to mention possible drug problems. Adolescents are
living in a world of high technology and sophisticated mass communication, where rapid
change undermines the security of familiar things. Parents who have not kept pace may
complain about the behaviour and lifestyle of their children and point out that they were
adolescents too, and that they did not react as their children are reacting. It is certainly a
fact that today’s parents were adolescents before their children, but not like them. They did
not grow up in the same psycho-social environment. The adolescents of the 1950s and
60s were not exposed to the millions of images that are penetrating our homes today, often
glamourising the drug-subculture of western countries. Pop music, videos, pornographic
magazines and other cheap publications have saturated the market and invaded our public
places. It is hardly possible to ignore their presence.
Today's parents have a duty to assume the new roles they are called upon to play. They
must not rely entirely on the schools for their children’s psycho-social development, and
they must make sure that they have the information they need to protect their children from
the use and abuse of drugs.
When people rely too heavily on the educational system to guide their children they forget
that the mother and father are the child’s first two teachers in any society. In many
developing countries, where the extended family is still common, children can benefit from
the presence of more than just two “teachers" in their infancy. However, this important
cultural advantage is fast disappearing and even the nuclear family is threatened as fathers
move to big cities to find work and children are left alone with their mother for long periods.
Sometimes whole families move to slums on the outskirts of big cities, where the children
are exposed to a high-risk environment.
Parents today can no longer be contented with feeding and clothing their children and
leaving them to grow up without supervision or guidance. It is their duty to give protection
from the negative influences that surround their children on all sides, notably peer pressure
and advertising. Parents must understand that prevention of substance abuse is not a
question of supply reduction alone. While police and customs officers are doing their best
to suppress production, smuggling, distribution and consumption of illicit drugs, parents
need to set up or join existing community groups to form a strong coalition to reduce the
35
demand for drugs and alcohol. Instead of always relying entirely on the government and
waiting for things to happen, parents must come out of the shadows and make things
happen by acting NOW.
Sometimes people who desire to serve their community take no action to set up a parents’
group because they have no meeting place. This is not really a problem at all, as many
national nongovernmental organisations all over the world started with regular meetings of
a small group of 15 - 20 people in the homes of interested neighbours, on a rotation basis.
Such groups can also make good use of under-utilised classrooms after school hours if
they can make appropriate arrangements with the local education authority.
Parents' groups can work to protect young people from substance abuse by:
seeing that a responsible adult is always present during youth activities;
offering only soft drinks to their children and their children’s friends;
setting clear standards of behaviour for their children and insisting that they be
home at a reasonable time in the evening;
avoiding the use of tranquillisers and pain killers when their children are sick;
teaching healthy eating habits from the very beginning. Children who understand
that abuse of food, notably sugar, salt and fat can be harmful to health are likely to
refuse illicit drugs when they are told of the harm they cause, even in small amounts;
helping children to develop self-discipline, self-esteem and decision-making skills;
encouraging children to learn to defend themselves and solve their own problems,
by not being over-protective;
developing an attitude which is not threatening or blaming when talking to children;
getting to know the families of their children’s friends.
In order to promote the growth of parents’ organisations the members of the original group
might undertake to bring along one more parent to the next meeting. Parents’ groups
should contact any women’s organisations in their area because women as wives, mothers
and sisters are transmitters of positive lifestyles and cultural values. Sometimes they are
also the victims of an alcoholic father, husband, brother or son. Parents’ groups and
women’s organisations can make a formidable team when they work together and all the
possibilities for collaboration should be explored.
Parents who are anxious to protect their children from substance abuse need to know the
36
signs and symptoms to watch for so that they can take immediate action to prevent further
drug taking if their child begins to experiment with illicit substances. The commonest signs
ana symptoms of drug taking have already been presented in Part I of this manual.
Parents’ groups and women’s organisations can help adolescents become aware of the
dangers that surround them so that they are better able to protect themselves. For
example, they might organise a lecture or discussion on guarding against the persuasive
effect of alcohol advertisements. The main advertising technique is to associate the
product with the kind of users that adolescents would like to be. They show alcohol being
consumed by rich people, successful people, attractive and healthy people.
Advertisements show people having fun and enjoying themselves while drinking; they do
not show the misery and despair caused by alcohol.
Other activities which might be organised by parents’ groups and women's organisations
could concentrate on the dangers of substance abuse and teenage pregnancy. Films,
lectures and discussions should stress that the body of a young teenage girl is often not
fully grown and not reproductively mature, and that a high proportion of teenage
pregnancies end in miscarriage or still birth. They should emphasise the dangers of
abortion and the risks of trying to conceal a pregnancy. The effects of alcohol and drugs on
the unborn child can be devastating and no dependency-creating substances at all should
be used during pregnancy. There is a particularly serious risk of damage to the foetus
during the early weeks of pregnancy among girls and women who continue to drink or take
drugs , not knowing yet that they are pregnant.
Parents’ groups and women’s organisations can organise talks, film shows and exhibitions
on the role of all the members of the family of a substance abuser during treatment, and
even more particularly during rehabilitation and social reintegration. They should lay stress
on the dangers of relapse after treatment and work to promote relapse prevention
strategies. Finally, in order to gain the best publicity for their cause these groups might
seek the active support of the First Lady, either at local level or at national level.
School programmes
Debate on whether schools should provide drug education for their pupils has continued
37
for decades. School administrators, teachers and parents have shown considerable
reluctance to introduce discussion of substance abuse into the school timetable, arguing
that there are no drug users among school students. This is an example of the denial
response which was discussed in Part I of the manual. In many countries the educational
community still refuses to accept that at least a few of their students may have started to
experiment with drugs.
Educators and parents must realise that alcohol is available everywhere and that children
are bound to come into contact with heavy drinkers. If other drugs, such as cannabis,
amphetamines, opiates and cocaine are fairly easily available in the community, then
sooner or later young people will come into contact with them as well, and possibly with
drug abusers who will induce them to experiment. It is therefore essential that young
people learn about drugs from people who really care for them, not from addicts. Parents
can give guidance in the home, teachers can give drug education at school and religious
leaders can discuss the top^c at their meeting place. This is infinitely better than for such
education to take place in the streets and bars where the “teachers' are drug-abusing
peers, dealers and pushers.
A drug education programme given in a school in no way compromises the reputation of
that school. Quite the reverse is true, because it adds to the credibility of the school and
demonstrates that the administrators and teaching staff have a real sense of civic
responsibility as well as having the best interests of their pupils at heart.
Even if there are known cases of students using or abusing drugs, this does not necessarily
mean that they have experimented with drugs on school premises. They interact with many
youths who are not at school, and they may well be using drugs outside class hours and
away from the school setting.
School children and students are a captive audience for anti-drug and alcohol campaigns;
programme planners can take advantage of the fact that they do not have to attract young
people to attend meetings and discussions because they are already on the spot. Schools
may choose to offer drug education as an extra-curricula activity or to integrate it into the
regular timetable. In countries which have arranged drug education on an extra-curricula
basis the results have not been very encouraging. This seems to be because the initiative
was not supported by teachers who argued that their duties did not include such subjects or
by parents and students because there were no examination credits attached to the
38
classes. Other countries have therefore chosen to integrate drug education in the existing
school curricula. Below we give an example of an integrated approach to prevention
education through the school curriculum.
General science
Nutrition (abuse of sugar, salt and fats)
Medicines - need to read instructions carefully and avoid
improper use
Stress and stress management - physical exercise, aerobics
and relaxation
Effects of drugs on the development of adolescents
Language and
communication
skills
Role playing of peer pressure situations, focusing both on
negative pressure and the decision-making skills needed
to resist it
Essay writing on personal experience of peer pressure
Vocabulary work on the terminology of drug abuse
Oral expression work on advertising and pro-drug messages,
poems and songs
Study of local newspapers for reports on arrests, seizures
and overdose cases
Mathematics
Calculating the alcohol content of drinks
Statistical surveys and data collection
Ratios, percentages, bar charts, pie charts
Art
Art for persuasion
Posters for cigarettes and alcohol
Designing posters for a healthy lifestyle
Art competitions for anti-drug posters and slogans
Sponsoring by local firms for mass reproduction of
the winning posters.
Teacher training courses should begin to include modules on drug education in order to
help the teachers of the future with this aspect of their work in schools. In the meantime the
education authorities should organise in-service courses, seminars and workshops with the
support of health care personnel, police officers and social worters. These professionals
39
may also be invited to the schools as guest speakers to complement the work of the
teachers on specific topics related to substance abuse and to make the curriculum more
effective.
Tasks to be undertaken by schools
Draw up and circulate a clear policy prohibiting illicit drugs, alcohol and
the improper use of prescription drugs on school premises, at school-sponsored
functions and while students are representing the school. All students, parents
and staff should receive a copy of the policy document, which must specify
the penalties following any violation of the rules.
Establish a solid school - family partnership.
Introduce drug education classes into the existing curriculum.
Invite professionals working in the field of drug abuse as guest speakers.
Invite voluntary workers and interested parents as guest speakers and discussion
leaders.
Emphasise the role of physical education and sport in developing a healthy
lifestyle.
Make a file of newspaper cuttings on the national and local drug problem; discuss
the content of these articles with students in class.
Hold discussions, film shows and seminars for students and parents.
Organise fund-raising activities to support anti-drug programmes (a fun run,
sales of stickers or T-shirts).
Refer high risk students to counselling services.
Organise health-promotion activities such as athletics meetings and hikes.
Set up anti-drug clubs using student leaders as positive role models.
Establish a correspondence network with other anti-drug clubs, nationally or locally.
Organise recreational activities and healthy occupations during school holidays.
Strengthen the parent - teacher association and motivate the members to act
as a bridge between the family and the school.
Set up a school advisory board with representatives from the school administration,
the parent - teacher association, the student council, the police, the media, local
nongovernmental organisations, the medical profession, youth organisations and
religious bodies.
40
Religious groups
It is well known that the three fundamental elements governing drug abuse are the agent
(the drug), the host (the user or abuser) and the context (the socio-cultural environment).
The religious beliefs and traditions of a society, its cultural and moral values determine the
ways in which that society reacts to drugs, the importance it attaches to substance abuse
and the attitudes it displays towards users and abusers. The heads of religious bodies and
the leaders of socio-cultural organisations play a very significant role in demand reduction
by reinforcing the teachings and principles of religion.
Like the school community, the religious community can benefit from the presence of a
captive audience. Religious leaders can address their regular congregation without the
need to invest a great deal of time and energy in persuading the public to attend the
meeting. It may be said that members of a church congregation are unlikely to be abusing
drugs or alcohol, but they could well be unaware that their own children are experimenting
with drugs if they do not know the signs and symptoms of drug abuse.
Another very important mission of religious leaders is to stress the distinction between the
sinner and the sin. Non-users of alcohol and drugs sometimes tend to condemn the
individuals who fall into addiction rather than attack the cause of their distress. Medicine
aims to destroy the disease and save the patient, and prevention strategies aim to destroy
the drug culture and save the victims.
Tasks to be undertaken by religious bodies and socio-cultural organisations
Promote and strengthen traditional customs and beliefs.
Publicise and support anti- drug and alcohol activities.
Make drug education publications available on the bookshelves.
Include subjects related to drug and alcohol abuse in the training of
religious leaders. They should have some knowledge of tolerance and
dependence, signs and symptoms of abuse, withdrawal syndrome, the
causes and consequences of abuse, prevention, treatment and rehabilitation
approaches, causes of relapse and prevention of relapse, individual, group
and family counselling.
Refer substance abusers to treatment and counselling services.
Remind members of the congregation of the importance of spiritual values.
41
Invite members of the congregation to take part in an outreach programme
attached to the place of worship. There is an urgent need to contact the
ever-increasing numbers of young people who are leaving their families
and drifting into the big cities where they no longer have the support
of their parents and the extended family. With some training volunteers can
develop a caring attitude towards abusers and relapsed addicts who no longer
attend religious meetings and refer them for professional care.
The police and customs services
Law enforcement officers have a vital role in preventing substance abuse. The four main
objectives of penal laws have been identified as the defence of public security, the
punishment of the offender, the deterrent effect of making an example to discourage others,
and the subsequent rehabilitation of the offender. The fourth objective is quite frequently
forgotten even though failure to rehabilitate an offender is the main cause of recidivism and
the perpetuation of the wrong. Further, many offenders cannot logically be rehabilitated or
reintegrated into society because they were never integrated into the mainstream of
community life.
There are three main groups of offenders in the world of drug abuse. They are:
drug dealers who are selling drugs for profit and who do not use drugs themselves;
drug dealers who are themselves addicted and who are dealing mainly in order
to ensure their own supplies; they are arrested frequently;
drug addicts who have resorted to crime in order to pay for their drugs; they are
usually arrested while committing a crime or while purchasing drugs.
There is a consensus on the need to imprison the non-addicted, profit-seeking dealers or
smugglers and to seize their assets. However, it can be very difficult to make a moral
distinction between addicted dealers, who are often exploited by the big dealer, and
addicted consumers who get involved in theft, violence and prostitution in order to buy
drugs. It is not easy to decide how far they are responsible for their actions in the light of
the various contributing factors that lead to experimentation, tolerance and dependence.
The legislation of Washington DC defines an addict as “ a person who habitually uses any
habit-forming narcotic drugs so as to endanger the public morals, health, safety or welfare,
42
or who is so far addicted to the use of such habit-forming narcotic drugs as to have lost the
power of self-control with reference to his addiction".
Canadian legislation describes an addict as “a person suffering from a disorder or
disability of mind as evidenced by his being so given over to the use of alcohol or drugs
that he is unable to control himself or is incapable of managing his affairs or endangers
himself or others".
These definitions imply a recognition that counselling and rehabilitation services need to
be introduced in prisons. Outside prison, for high-risk groups and the community at large
police officers, customs officials and prison wardens can act as educators, social workers,
allies and friends who care for the welfare of the community.
Tasks to be undertaken by law enforcement officers
Give talks on the importance of rules, discipline, law and authority.
Disseminate information on the law regarding the production, processing,
trafficking, possession and consumption of illicit drugs.
Seek information from the community about the following questions:
the extent to which existing legal provisions are applied in practice;
the reasons why the law is not applied;
the need for new legal provisions to counteract new techniques and strategies
adopted by drug dealers.
Develop more positive attitudes towards prisoners and ex-prisoners.
Set up a pre-release scheme to prepare prisoners for social insertion or reinsertion;
the staff of the resource centre should collaborate in this scheme, which would
have the major objectives of preparing prisoners to face life without resorting
to drugs and alcohol, and of preparing prisoners' families to adopt a caring and
supportive attitude towards the released prisoner in order to prevent relapse.
Introduce drug education into the training curriculum for law enforcement officers.
Update and extend data collection to include etiological and epidemiological
factors of substance abuse.
Make prisoners aware of the dangers and modes of HIV transmission and the
risks of promiscuity in prisons.
Encourage police officers to specialise in drug prevention activities.
43
The media
Radio, television and the press are basic tools for spreading a message quickly, although
the mass media are generally conditioned by whether an event is “newsworthy". Heroin,
cocaine, and crack are considered newsworthy and so are overdose cases involving young
people, but alcohol, tobacco and psychotropic pills have no news value, nor do recovering
addicts and their problems during rehabilitation.
However, it must not be forgotten that the media have helped to raise public awareness of
a drug problem in many countries where its existence was denied or was not accorded
any importance. Once the population is conscious of the problem and the need for action
the role of the media is to support and supplement the efforts of government agencies and
nongovernmental organisations to reduce the demand for drugs through prevention,
treatment and rehabilitation programmes.
Although media messages are considered to be impersonal and receive little feedback
from the target audience, they can still be used to support and reinforce community
activities by announcing functions and events in advance and by reporting them as they
happen. Good media coverage is important for several reasons. It can:
build public support for the goals of the resource centre or a prevention programme;
inject enthusiasm into field workers;
create a snowball effect if the event is newsworthy;
strengthen the legitimacy of the resource centre or the work of the Community
Action Committee in the public view;
put the spotlight on the resource centre so that the opinions of the staff will
be known in the area.
A press release is a cheap means of providing reporters with basic information on any
event organised by the resource centre or a nongovernmental organisation. A press
release usually answers questions beginning with WH:
WHO is organising the event or function? WHAT is being organised? WHERE is it taking
place? WHEN is it scheduled? WHY is it being organised?
44
General strategies in the development of media contacts
Establish personal contacts with editors of newspapers and directors of TV and
radio stations.
Make sure that each member of the Community Action Committee is in touch with
at least one journalist and keeps this journalist informed of prevention activities.
Be impartial and do not neglect “minor" media.
Involve journalists in workshops and training courses on substance abuse. This will
improve their understanding of the complexity of the problem and may encourage
them to adopt a less sensational and more positive approach in their reporting.
Choose knowledgeable people to give interviews in order to build up the
programme’s credibility.
Involve well-known and respected public figures in the publicity in order to attract
attention.
Avoid glamourising the drug culture.
Avoid mentioning the euphoric effects of drugs in short press articles or TV spots
which do not allow for a clear explanation of the dangers of repeated use.
Include people with first-hand knowledge of the drug culture in coverage of
prevention work.
Prepare and distribute media kits with background information on the strategies
being implemented and the responsible agencies.
Prepare material for the publishing or broadcasting in the form which the media
request.
See that the messages to be publicised are accurate and well presented.
Avoid copying the style of communication used in other countries and make sure
that the message is intelligible to the local population.
Respect deadlines.
Send unsolicited material to local newspapers, radio and TV stations.
Include the name and phone number of a contact person working in prevention
who will give further information to the media.
Send a word of thanks to producers, editors and reporters.
In working with the press it is useful to negotiate with editors who run regular editorials on
specific issues, or a letters-to-the-editor feature, or a special weekly column to raise public
awareness of important questions. The articles that are submitted to the press should be
very carefully written by experienced people so that they are accurate and credible. This is
45
a means of avoiding mis-reporting. Newspapers and journals are, of course, primarily a
source of information and should be used as such by prevention programmes. A collection
should be systematically built up of articles and data on alcohol- or drug-related crimes and
accidents, cases of suicide and overdose, and violent incidents connected with substance
abuse.
In working with radio and TV stations it is important that messages should be positive and
that they should emphasise the solution rather than the problem. It is wise to take
advantage of the live quality of these media by organising talk shows and encouraging
direct phone calls from listeners and viewers. Invite addicts and recovered addicts to
appear on the show with their families and friends to give first-hand accounts of the
experience of addiction. Social workers, health staff and law enforcement officers should
also be invited to talk about their work in the prevention of substance abuse. After a talk or
documentary film it is interesting to arrange a discussion session and a panel of experts
might be invited from time to time to take part in this. When the prevention project itself
prepares short radio or TV spots for submission they must be in conformity with the
standard time slots allotted by the media.
Multi-media activities can also make an impact on public awareness and sympathy.
Exhibitions, puppet shows and the theatre can attract a lot of attention. Involve popular
singers in anti-drug concerts and invite well known athletes and sports personalities to
drug- and alcohol-free discos, carnivals, sports meetings and fund-raising activities.
Finally, as an annual event a prevention project could organise a Drug Awareness Week
using a multi-media approach and culminating in a major event on June 26, which is the
International Day against Drug Abuse and Illicit Trafficking.
The business community
In countries where human expertise is limited and financial resources are scarce, the
business community has a major role to play in supporting prevention, treatment and
rehabilitation programmes. Both in the industrialised parts of the world and in the
developing countries private sector firms and agencies working against substance abuse
are moving towards mutual support and assistance. All over the world business firms and
46
companies sponsor drug prevention campaigns and promote healthy activities.
Substance abuse does not affect the abusers and their families alone; it also affects their
employers, the community and the whole nation. This is why Employee Assistance
Programmes and other workplace initiatives are an important component of prevention
strategies. The Community Task Force needs to draw the attention of employers to the
consequences of substance abuse among the workforce, and to make them aware that it
can occur at all levels of the hierarchy from top managers to handymen. The following
consequences are a direct result of substance abuse at the workplace:
sickness causes increased medical costs;
absenteeism and bad timekeeping reduce output;
accidents result in injury, disability or death;
accidents also damage machines and equipment;
there are supervision problems because discipline is not maintained;
bad labour relations cause disputes;
crimes such as pilfering and embezzlement increase because addicts
need money to buy their drugs;
addicts start pushing drugs at the workplace in order to maintain their own supplies;
deadlines are missed and business is lost because of impaired judgment;
trainees fail to benefit from courses because they cannot learn;
time is wasted during working hours because dependents cannot concentrate.
As a result of all the above factors, the quality of service declines, production is sub
standard, resources are wasted and public confidence is lost.
Apart from the negative effects of substance abuse which are obvious in the workplace
there can also be consequences for the physical and social environment. Public health
may be endangered and criminality is likely to rise when there is a problem of substance
abuse among workers. For example, poor quality products may cause illness or injury to
consumers. Drug abusing workers in the transport sector could cause fatal accidents to
innocent members of the public, and workers responsible for essential services could
cause a serious decline in the quality of life of the community if these services broke down.
47
Tasks to be undertaken by private firms
Support public awareness campaigns by providing transport, refreshments, etc.
during seminars and training courses. .
Provide training and employment opportunities to youths who are at risk of
substance abuse and to recovering addicts.
Sponsor pamphlets, stickers, posters, T-shirts, etc. which can be marked with a
logo to identify the donating firm.
Sponsor large-scale coverage of drug-free concerts, sports and recreational
activities.
Invite prevention workers to talk to employees about problems of substance abuse.
Send managers and supervisors on training courses for the prevention of
substance abuse at the workplace.
Refer employees who are abusing drugs or alcohol for treatment and grant
them paid leave until they are able to resume work.
Pay for time on radio and TV for anti-drug spots and programmes.
Note: See the companion manual on workplace programmes for more information on the
role of the business community in the prevention of drug and alcohol problems.
Service clubs
Clubs such as the Rotary Club, the Lions Club and Round Table can undertake or sponsor
the same type of activities as the business community. Members of these clubs are usually
people who are well known locally and have many contacts in the community. Such clubs
can put the expertise of their members at the disposal of the Community Task Force to
stimulate the multi-disciplinary approach which is necessary for combating the drug
problem. They can also sponsor study tours to help field workers improve their knowledge
and skills, and last but not least, they can undertake fund-raising on a large scale to finance
programmes for prevention, treatment and rehabilitation.
The Community Action Committee and the high-risk groups
The introduction to this manual includes a section on understanding the high-risk groups,
notably young people. Members of the Community Action Committee need to be aware of
48
the various risk factors which might predispose certain individuals or groups towards
substance abuse. The three types of factors involved are individual risk factors,
psychological risk factors and environmental risk factors. It may be difficult to make a clear
distinction between them and in any case they tend to operate together so that a person
might be influenced by all three types at the same time. Nevertheless, it is useful to think
about them in isolation and the lists below may be helpful in this.
Individual risk factors
Age:
Increasing evidence is emerging that certain individuals may be
genetically predisposed to develop addiction.
Certain drugs are abused more by young people than older people
Sex:
and vice versa.
Generally, men use alcohol and drugs more than women do.
Genetics:
Personality:
The “non-conformist” type might be at higher risk than the conventional type.
Poor communication and problem-solving skills are common among
addicts. Lack of religious belief is also associated with substance abuse.
Psychological risk factors
Lack of interest in achievement
Rebellion, alienation and early anti-social behaviour
Lack of empathy with others
Sensation-seeking behaviour
Need for immediate gratification
Risk-taking behaviour
Lack of self-confidence and self-esteem
Psychological stress
Affectional deprivation
Feelings of unworthiness
Environmental risk factors
Easy availability of drugs
Alcoholism or drug addiction among family members
Social expectation of drug use
49
Perceptions of the drug culture
Unemployment
Discrimination
Lack of parental control
Broken home
Low educational level
Occupations which involve contact with alcohol ( e.g.catering industry)
Negative peer pressure
Extreme poverty in the midst of affluence
Influence of the media and advertising
Lack of enforcement of drinking laws.
Primary prevention is aimed at the whole population but the Community Action Committee
can still organise activities with the high-risk groups particularly in mind. Below are some
examples of such activities.
Work closely with leaders of youth clubs and train volunteers as peer counsellors.
Organise recreational activities and social events which will interest young people.
Launch awareness campaigns to inform the at-risk groups about the services which
are available in the community.
Organise drug free / alcohol free parties.
Organise recreational activities for the lonely, the sick and the old.
Run sustained information campaigns aimed at reducing casual sex, to combat
the increasing threat of AIDS.
Help young people to improve their coping skills (communication, problem
solving, stress management).
Provide accurate information about the so-called “soft” drugs.
See that the social and psychological needs of young people are met in the
local community.
50
Bibliography
Atkins, C.; Beschner, G. Ethnography: Research tool for policy makers in the drug and
alcohol fields. Rockville, Maryland, NIDA, 1980.
Bell, C. S.; Battjes. Prevention research: Deterring drug abuse among children and
adolescents. Rockville, Maryland, 1985.
Dupont, R. L. Stopping alcohol and other drug use before it starts: The future of prevention.
A report by the committee on the future of alcohol and prevention of other drug use.
The Institute for Behaviour and Health, Inc. US Department of Health and Human
Services, Rockville, Maryland, 1989.
Ebie, J. C.; Tongue, E. J. Handbook of the African training courses on drug dependence.
Lausanne, Switzerland, ICAA, 1988.
Edwards, G.; Arif, A. Drug problems in the sociocultural context: A basis for policies and
programme planning. Geneva, WHO, 1980.
Errecart, M. T.; Person Jr. P. H.; Kotler, M.; Gallardo M.; Me Bride, L. K. Illicit drug abuse:
Early detection, monitoring and measurement in a multicultural setting. 1988.
Glynn, T. J.; Leukefeld, C. D.; Ludford, J. P. Preventing adolescent drug abuse: Intervention
strategies. Rockville, Maryland, NIDA, 1983.
Hiebert, R. E. What every journalist should know about the drug abuse crisis. Washington
D. C., VOA. 1987.
Jones, C. L.; Battjes, R. J. Etiology of drug abuse: Implications for prevention. Rockville.
Maryland, NIDA, 1985.
Nowlis, H. Drugs demystified. UNESCO, 1975.
Schaefer, W. D. Maryland's drug and alcohol abuse control plan, Baltimore, Maryland,
1989.
51
Shaffer, D.; Philips, I.; Enzer, N. B. Prevention of mental disorders, alcohol and other drug
use in children and adolescents. Rockville, Maryland, OSAP, 1989.
Shahandeh, B. Rehabilitation approaches to drug and alcohol dependence. Geneva, ILO,
1985.
Veatchlll, C. L; 0 Neal, J. A. Prevention perspective. Washington D. C., AASADAD &. NPN,
1989.
Vicary, J. R.; Resnik, H. Preventing drug abuse in the workplace.
NIDA, 1982.
Rockville, Maryland,
Walters, M. W. Ethnography: A research tool for policy makers in the drug and alcohol
fields. Rockville, Maryland, NIDA, 1980.
52
ANNEX I
Basic structure of Community Action
53
ANNEX II
Some basic facts about drugs
DRUG
1. OPIATES
• Opium
• Morphine
• Heroin
• Pethidine
• Codeine
• Methadone
MEDICAL USE
MODE
OF USE
Analgesic
- Smoking
- Oral/IM/IV
- IM/IV
- Oral
- Oral/IV
EFFECTS
WITHDRAWAL
SYMPTOMS
Depressant
Analgesic
Antitussive
Euphoria
Sedation
Nausea
Vomiting
Constipation
Respiratory
depression
Common Cold-like
symptoms:
- Rhinorrhoea
- Goose flesh
- Feeling hot
and cold
- Abdominal
cramps
- Diarrhoea
- Restlessness
Pains yawning Bone
Muscle
Joint
II. ALCOHOL
(Ethanol)
Solvent/
disinfectant
Oral
Depressant
Sedative/anxiety
relief in small dose
Depression ataxia in
larger dose
Tremors of hands,
tongue and body.
Anxiety, Insomnia
Most severe,
Delirium Tremens
III.SEDATIVE/
HYPNOTICS
• Benzodiazepine
• Barbiturate
"Sleeping pills"
Oral
Sedatives: calm,
anxiety and
restlessness.
Hypnotics: Induce
drowsiness and
sleep
Insomnia
Anxiety
Statu epilepticus
Tremors
Anorexia
Abdominal cramp
Irritability
Smoking
Depressant in low
dose.
Hallucinogen in
high dose.
Apathy.
Psychosis
Amotivational
Syndrome
- Oral
- Smoking
States of altered
perceptions as
illusions,
hallucinations
and delusions
IV.CANNABIS
• Marijuana
• Hashish
• Gandia
(active agent:
9 - tetrahydro
cannabinoid THC)
V. HALLUCINO
GENS
• LSD
(Lysergic
Acid
Zethyamide)
• Moscaline
•PCP
(Phencyclidine)
Treatment of
glaucoma in a few
countries
(e.g. Jamaica)
- IM/IV
!
1
,
54
DRUG
1. Amphetamines
Dexedrine
Benzedrine
Methylampheta
mine (Ice)
Ephederine
MEDICAL USE
Appetite
suppressant
MODE
OF USE
EFFECTS
Oral
Euphoria, increased
alertness,
wakefulness,
appetite
suppression,
decreased fatigue.
Schizophenia - like
psychosis
WITHDRAWAL
SYMPTOMS
II. Cocaine (an
alkaloid extracted
from the leaves of
i
the coca plant)
I
Crack
-
-Smoking
- Snorting
-1/V
Euphoria, increased
alertness
Insomnia, lethargy
fatigue; Aches and
pains; Nausea and
vomiting, loss of
weight
Paranoid psychosis
III. Khat
The khat leaves
from the schrub
catha edulus.
Active principle:
cathirone
-
Chewing
Euphoria, increased
alertness,
decreased fatigue,
appetite
suppressant
Fatigue, lethargy,
decreased alertness
IV.Cola Nuts
-
Chewing
Euphoria,
decreased fatigue
V. Nicotine
-
Smoking
Decreased fatigue
Oral
Increased alertness.
Decreased fatigue
Inhaling
Skin problems
around
mouth and nostrils
Respiratory
infections
Vl.Caffeine
Vll.Solvents
-
Anti-Liquor Movements In India
When thousands of men give up liquor under the
inspiring influence of women social activists
Bharat Dogra
Pictures on this page and cover depict
the Pather anti-liquor movement.
Father - A Village Which Defeated the
Liquor Contractor
Rather village of Saharanpur district has emerged as a
major symbol of the anti-liquor movement in India. For nearly
three months the people of this village, assisted by Disha, a
voluntary organisation carried out a grim struggle for the
removal of the liquor vend from this village. Nearly fifty
persons of this and surrounding villages, including
(“Yrticularly the women activists of Disha, were injured in the
police repression unleashed on the movement. Such was the
moral force behind the movement that despite this repression
the movement continued till the government finally agreed to
remove the liquor vend from this village.
The determination of the people in the face of severe
repression won widespread admiration in neighbouring
villages and Disha started getting requests to help other
villages to get rid of their liquor shops
The liquor vend at Father had at one time become the
number one problem of the people of this village The
location of the vend was such that it attracted truck-drivers
and tipplers from several surrounding villages as well. Soon
it become a meeting place of several anti-social elements.
.Qrunk people at all times of t‘ day and night created havoc
the marketplace and even ventured into some of the
nearby homes. They frequently entered into violent brawls
with villagers. On one occasion a communal riot was barely
averted when they even entered a religious place.
Within the village the easy availability of liquor led to a big
increase in the consumption of liquor. Even several children
who tried to imitate elders got addicted to liquor and went to
1
the extent of stealing grains and utensils from their owr
houses to buy liquor. Women were the worst affected. It was
difficult for them to walk near the liquor vend but they had tc
come to the market and the bus stand located quite close tc
the liquor vend. There were several cases of harassment anc
attempted molestation. Domestic violence increased greatly
in the village. One drunk person from a neighbouring village
threw acid on a woman.
Disha had been working in this village for several years
particularly to mobilise women and it had set up a Mahila
Jagriti Sangh or women's awakening committee in th:l
village. As the liquor vend increasingly became the number
one problem for villagers, this question was invariably
discussed at Disha's meetings in the village. Initially Disha
was unsure how far it can get involved in an anti-liquor
movement which could affect some of its other work, but once
the villagers, particularly women - expressed their
determination to oppose the liquor vend, Disha felt it was its
duty to support the village women and this involvement went
on increasing as the liquor mafia proved very difficult to
dislodge.
Initially when the villagers had met the DM and other
officials, they appeared sympathetic and said that this liquor
contract will be renewed. But these proved to be false
assurance and the administration appeared increasingly to
take trie side of the liquor contractor. Therefore the village.
decided to sit on an indefinite dharna in front of the liquor
vend.
Seeing a big crowd approaching the liquor shop on March
31, 1993 the contractor fled, but the real battle was to get the
contract cancelled officially and so the dharna (sit-in)
continued.
2
Days passed into weeks and the weeks into months, but
the administration chose to turn a blind eye to the mounting
resentment in the village. Many villagers, particular women,
were beginning to endure a lot of hardships at the dharna
and had to forego their livelihood work. Frequently they were
harassed by goons of the liquor mafia, who even threatened
to kidnap women activists and their children.
Finally the people decided to march to Saharanpur city to
meet the authorities. It was here that the police unleashed a
brutal lathi charge on the protest march of the anti-liquor
Movement.
Mahfooz, a physically handicapped participant in the
movement was beaten so badly that it took three months toi
him to recover from his serious injuries. Several women
activists had to the hospitalised for several days.
However the news of this repression spread far and wide
and the administration and political leaders came under
pressure to withdraw the liquor vend. As soon as the news
of the cancellation of the liquor contract reached the village,
people hugged each other and women cried with happiness.
A halwai (sweet seller) distributed all the sweets stocked in
his shop. People rushed to temples and mosques to offer
thanksgiving prayers.
A In the course of this agitation Such a moral force was
L/eated that many habitual drinkers took a pledge to give up
liquor. What is more many of those gains have been
sustained. During a recent visit to this village, this writer met
several people who gratefully recalled the movement which
rid the village of its biggest problem. Several villagers
testified that the consumption of liquor is now only about 10%
to 20% of what is was before the movement. As a result of
this saving, several kutcha houses and shops have been
3
converted into pucca structures; the village and in particular
the market wears a new prosperous look.
Mahfooz, who was injured so badly in the movement,
says, "If the contractor dares to come again I'll again
participate in the movement to oust the liquor vend."
Anti-Liquor Movements in Bndia
According to World Health Report 1997 (brought out by
the WHO), the use of alcohol, illicit drugs and other psycho
active substances causes at least 1,23,000 deaths annually^
Alcohol is also implicated in a range of social problems
including crime, violence (particularly against women and
children), marital breakdown and major losses in industrial
productivity. Both acute and chronic effects of alcohol on
blood pressure have been noted. The cost of alcohol related
harm is estimated to account for 2 to 3% of GNP in many
European countries. About 120 million people are dependent
on alcohol.
In addition the functioning of several distilleries is
associated with high pollution risks.
Keeping in view the enormous social and health costs of
alcohol addiction, de-addiction can obviously make an
important contribution to human welfare. However, mostly th’ ,
issue is considered at an individual level - and it generally
takes an individual a lot of effort with medical help and family
support to overcome the addiction.
However in India several social movements against
alcoholism have led to the surprising result that thousands of
persons have given up the consumption of liquor under the
strong motivation of movements of social reform and change.
4
In some parts of Mahasamund district of Madhya Pradesh,
during the last 15 years an inspiring effort has been made for
the release of bonded labourers and their rehabilitation by
providing satisfactory livelihood opportunities to them.
Social activists who played a leading role in this campaign
stressed from the outset that unless simultaneous efforts to
fight the menace of alcoholism are made, the economic gains
of released bonded labourers (RBLs) will be lost very soon.
Shashi Sail, a leading woman activist of this region says,
' In the villages women were very willing to participate in this
movement against liquor as they are frequently the worst
victims of alcohol abuse. We encouraged women to form
special squads who drove liquor contractors and traders from
villages."
Mukti Niketan (MN), the leading voluntary organisation in
the release and rehabilitation effort, successfully combined
this with an anti-liquor movement. As the released bonded
labourers were highly motivated for starting a new life, they
were also more responsive to receiving the message against
liquor. As MN had been clearly working at several levels to
rescue them from exploitation and create new livelihood
opportunities, its moral authority to speak against alcohol
_abuse was accepted by the RBLs in large numbers and they
<.• Jgreed to give up the consumption of liquor.
Rajam Tanti a grassroot social activist of MN who has
been involved in several struggles against liquor, says, "Both
aspects of the effort were equally important - the fact that
people were receptive to the message against liquor and the
fact that a sustained effort was continued to keep away the
liquor sellers from villages."
5
As a result several hundred habitual drinkers have been
able to give up the consumption of liquor in this region.
Earlier de-addiction of liquor addicts as a result of a social
movement had taken place on an even larger scale among
the iron ore miners of Dalli Rajhara. Infact the trade union of
iron-ore miners and released bonded labourers both are
closely related to each other.
The iron-ore miners under the leadership of a legendary
trade unionist and social reformer Shankar Guha Niyogi had
won significant economic gains around 1977-78. Initially this
appeared to cause an increase in liquor consumption but
Niyogi soon mobilised the trade union to check this disturbing
trend. He sat on a protest fast against the sale and
consumption of liquor which had a high moral impact on
workers.
Niyogi did not treat the anti-alcoholism as a relatively
insignificant activity of the union. In the initial stage it became
a major concern of leading CMSS activists. Through
repeated assertions a climate was created in which the tribal
members felt that the consumption of liquor was a betrayal of
the union that fought for them. Once this feeling was
generated, the task of weaning the tribals away from alcohol
was not difficult since traditionally they attached a great deal
of importance to honouring trust and loyalty.
It was realised that some constructive work had to b<Q
found to occupy their leisure hours or else the idle mind
would inevitably be driven back to the liquor shop. Hence
various workers were assigned specific tasks such as
keeping a watch on the workers who were more prone to the
various vices. Others were asked to supervise the
construction of schools and a hospital and the numerous
other activities of the union.
6
The punishment given to offenders was quite unique.
Initially an offender would be asked to pay a fine ranging from
Rs 50 to Rs 100. However, behind his back, the money was
returned to his wife. Soon this secret leaked out and the
offenders became smug and careless. The union then
reverted to imposing genuine fines.
Another interesting aspect of this experiment was that the
addict's own family members were effectively used to rid him
of his deadly habit. TheJ' were persuaded to report all
violations of the union's regulation by the addict and
-^continuously protest against the consumption of liquor by
'nim. Helped by the changed climate in the labour colonies the
wives and even grown-up children could now wage their own
individual battles against an alcoholic husband or father.
The overall result of this sustained campaign against
liquor has been that a large number of miners have given up
drinking altogether while the few who continue to drink have
significantly reduced their intake. It is difficult to cite precise
statistics as no studies have been made of this unique
experiment, but in her own simplistic way Sonaribai, a tribal
woman said, "If previously we consumed one rupee's worth
of liquor now we consume four annas worth."
Rajendra Sail, Director of Mukti Niketan who saw the
movement at Dalli Rajhara and later helped to replicate it in
parts of Mahasamund district says, "The anti-liquor
movement had been a very important part of our struggle.
1'he poor and oppressed people have understood how liquor
is used to keep them in a state of helplessness. As this
awareness has grown, so have their feelings against liquor."
Published By : Bharat Dogra,
C-27, Raksha Kunj, Paschim Vihar, New Delhi-110063 Tel.: 5575303
Composed At: Sharma Computers, 4/5 Moti Nagar, New Delhi-110015
Printed By : Kulshreshtha Printers, 11 Tyagi Vihar, Nangloi, Delhi
7
HoghBy Relevant
Media and Book Efforts b,
Madhu and Bharat Dogra
C-27, Raksha Kunj, Paschim Vihar, New Delhi-110063
Tel. No. 5575303
1.
Mother Earth NFS-lndia - Journal for a happier
world - now in a new attractive format.
i .
Four issues in a year - Annual subscription Rs. 250 " "
- your subcrption cheque should be in the name of
I
NFS-lndia
2.
Community Libraries - A carefully selected set of 1
100 Hindi books and booklets available for only
.
Rs.1000/-. A great way to start a small library in a
village or a slum.
3.
Press - Clipping Service on 45 subjects development, environment, social welfare and other
■
highly relevant issues - available in Hindi and I or
English.
4.
Encyclopedia of Environment, Development I
and Welfare - Price Rs. 300 only + 70 other books
and booklets by Bharat Dogra in English and
Hindi.
5.
Supply Of articles particularly for small newspapers
We will be happy to send you details and
catalogues of all these efforts.
5/'
I
PROGRESSIVE SYMPTOMS OF ALCOHOLISM
FOR THE PROBLEM DRINKER
at Center City, Minnesota
Business Office: 34 1 North Dale. St. Paul. Minnesota
By Permission of Yale Center
Studies
An act of Irimken br&ftaiity
Alcoholism aorf
dependence on his
wife for money
brought out the worst
in Chandrakeshavalu.
He beat his wife to
death with an iron rod
in front of his children
and fled, but was
caught within hours
Inspector K Manjunath Rai and
right: Chandrakeshavalu
ut for the swift action
of the police, a mur
derer would have got
away
with
his makes
crime
forever.
What
the cold-blooded murder all the
more tragic is that it took place
before the innocent eyes of the
couple’s 12-year-old son and seven
year-old daughter at 4.30 am, on
October 17,2001.
Chandrakeshavalu (42), who
worked as a waiter in the Air
Force
Officers’
Mess
in
Kammagondanahalli, Jalahalli
West, terrorised, brutalised and
bashed his wife for money for his
alcohol. His wife Balnagamma
(34), bought sarees from cities and
sold them in rural areas, for a liv
ing.
Steeped
in
alcohol
Chandrakeshavalu stopped going
to work and became dependent on
B
hil wife and harassed her whenev
er she refused to pay for his
drinks.
The two went to bed after a
quarrel on that fateful night. But
Chandrakeshavalu woke up and
took her to task, around 4.30 am,
much to the helplessness of
Mahesh and Laxmi, their two chil
dren.
All
it
took
for
Chandrakeshavalu to put an end to
his wife’s resistance, was an iron
rod. He hit her so hard on the head
that she was silenced forever. The
sight of the blood-stained face of a
dead Balnagamma spoke volumes
of her husband’s act of brutality.
All this happened with much
screaming. Enough to alert the
neighbours that something seri
1
13 3) 03.
ous
had
occurred.
Chandrakeshavalu he fled with a
few clothes and the iron rod and
ran. Shankar, a neighbour, lodged
a complaint with Gangamma Gudi
police station around 6.15 am.
Gangamma Gudi Police Station
Inspector K Manjunath Rai and
his men took up the case. “Our
immediate challenge was to pre
vent him from leaving the State. If
that had happened, he could have
escaped forever,” says Rai. The fact
that it was not easy to get any
transport in a forest area, during
the wee hours, dawned on Rai.
Investigation was launched and
questioning of people began., In
the process, the police stumbled on
the key informer (whose identity
the police refused to divulge), who
told them that Chandrakeshavalu
had already reached the railway
station and was about to board a
train for Kurnool district, Andhra
Pradesh. He was apprehended on
the platform within 24 hours of
the incident. Not only did he con
fess to the crime but also told the
investigating officers that he had
hid the iron rod and the blood
stained clothes in an old shed in
the Air Force forest area while
escaping. Police later recovered
both items from the spot.
The 8th Additional Chief
Metropolitan
Magistrate’s
(ACMM) Court transferred the
case to City Sessions Court which
in turn transferred it to Bangalore
City Fast Track Court No 1. The
Court after taking the account of
the witnesses, including the two
children of the deceased, pro
nounced life sentence (14 years
imprisonment)
to
Chandrakeshavalu on December,
24, 2002. The verdict was given by
Judge Gopalkrishna and Y R
Jagadish was the public prosecu
tor
The children are being looked
after by. their grandparents
(Balnagamma’s parents), while
Chandrakeshavalu is serving his
life sentence in Parrappan
Agrahar jail. His period of appeal
ing to a higher court is over. The
case file was closed within 14
months.
Gaihlot Mohammed Javed
for smooth & glowing skin
U“VEDICA’
Herbal Body and Face Wash Powder
An effective substitute for soap.
. Reduces pimples
_
. Reduces wrinkles
" 1 .'
• Improves skin complexion
VEDICA
HERBAL HAIR WASH POWDER
• Prevents dandruff
« Promotes hairgrowth
• Keeps hair smooth & silky
Vedic Bio-Labs Pvt. Ltd.
Ph.: 6785646, 98450 72403
Consumers Day Discount Sale
SIEMENS Digital Hearing Aids
On March 13,14 & IS, 2003
WHISPER Hearing Aids (P)Ltd
10.10/13, 25th MalnJOth cross,
4 T Blk, | opp.Bunny Bakery |
Jaygnagar, Bangalore-560 041
1
1
|
6640571
® ’ 6634754
Digital Hearing Aid Rs. 8990/ onwards
Yofr Child Develop
Strong Values
A strong value system can give
your child the courage to say "No"
rather than listen to friends.
A Good Role Model
or Example
Your habits and attitudes may
strongly influence your child's
ideas about alcohol, tobacco, and
other drugs.
Help Your Child Deal
With Peer Pressure
A child who has been taught to be
gentle and loving may need your
"permission" to say "No" to
negative peer pressure.
Make Family Rules
It's helpful when you make specific
family rules about your child
not using alcohol or other drugs or
smoking cigarettes. And it's
helpful to tell your child the punish
ment for using them.
N0UFES»at^
The World Health Organization has identified ten life skills essential for every
individual to develop - These skills are even more important for adolescents to
develop to promote optimum health. They provide a guideline to enable Friendly
Advisors to integrate within the curricula.
1. Problem Solving
Every individual faces problems. The facilitation of solving problems is important. This can be
even undertaken during the games period through games, puzzles apart from academic
mathematics!
2. Decision Making
It is important to delegate some of the routine classroom responsibilities to the students.
Forming them into groups enables the group to take responsibilitiesfor the task/ project being
assigned.
3. Critical thinking
Every change brings in positive and negative consequences. Discuss non-threatening,
impersonal situations first in terms of pros and cons. {Ground Rule: there is no “wrong or
Right answer. Permit students to voice their opinions.} Debates help with critical thinking.
4 . Creative thinking
Opportunitiesfor story writing, art and the SVPWperiod are also avenues to develop creative
thinking
5. Communication Skills
Using verbal and non-verbal communication, practicing of assertive skills is important for
adolescents. Education on the changes an adolescent is going through helps them introspect
on the effective communication processes they need to develop.
6. Interpersonal Relations
Begin with peer relationship building through teams. Introduce teacher guides or Friendly
advisorsfor every team. Work on projects together. Being a liaison between parents and
children 'may be needed.
7. Empathy
Can be done through fun. E.g.: draw a funny picture depicting another person in your class.
After students have drawn it ,ask them to rub off that person’s names and instead write their
own. Then discuss how they felt when drawing some-body else and how they felt when they
found out it was they!
8 . Self Awareness
Read more about Maslows Hierarchy of Needs and Johari’s Window. A teacher once asked
students to write something good about a student on each day of the class. This was displayed
for the named student of the day to read. Several students learnt to value themselves more after
an exercise like this. A Friendly Advisor is very influential in helping students to get to know
themselves.
9. Management of Stress
Stress is part of life and its management within the school enables students to cope with stress
in a healthy manner. Yoga, games, counseling, dramatics, music and peer support helps
address stress. {Tip: Stresses need to be address; they just don’t disappear}
10.Management of Emotions
Awareness of the influence of hormones {“chemicals ”} on mood swings enables adolescents to
cope with their emotions. Further, talking about how to address "anger" constructively {e.g.:
move awayfrom whatever is making you angry; or beat up a cushion instead; or control speaking
when you are aware that you are angry} helps. Anger is a normal emotion that needs constructive
ways ofexpression.
Prepared by INSA/India, May 2001
6# a
INSA'W
\l
I s
quicklist
With Your Child
About Alcohol and
Other Drugs
You can help change ideas your
child may have that "everybody
drinks, smokes, or uses other
drugs."
To Really Listen
to Your Child
Your child is more likely to talk
with you'when you give verbal
and nonverbal cues that show you
are listening.
Your Child Feel Good
About Himself or
Herself
Your child will feel good when
you praise efforts, as well as
accomplishments, and when you
correct by criticizing the action
rather than the child.
Healthy, Creative
Activities
Hobbies, school events, and other
activities may prevent your
child from using alcohol, tobacco,
or other drugs out of boredom.
With Other Parents
You can join other parents in sup
port groups that will reinforce
the guidance you provide at home.
What To Do If You
Suspect a Problem
You can learn to recognize the
telltale signs of alcohol, tobacco,
and other drug use and get help.
OSAP
10 Steps to help your
child say “NO”
MINISTRY OF SOCIAL JUSTICE AND EMPOWERMENT
GOVERNMENT OF INDIA
MANUAL
ON
MINIMUM STANDARDS OF SERVICES
FOR THE PROGRAMMES UNDER THE
SCHEME FOR PREVENTION OF ALCOHOLISM AND
SUBSTANCE(DRUGS)ABUSE
Prepared by
T T Ranganathan Clinical Research Foundation
IV Main Road, Indira Nagar, Chennai 600 020
ACKNOWLEDGEMENT
I owe many people a great deal of gratitude for their support in making this
project of setting quality standards in the field of addiction a reality.
I owe many people a great deal of gratitude for their support in making this project of
setting quality standards in the field of addiction a reality.
My first thanks goes to Ms. Asha Das, Secretary, Ministry of Social Justice
& Empowerment, Government of India, New Delhi for initiating the process of
developing a Manual on Minimum Standards of Services in the field of alcohol
and drug abuse prevention and entrusting our organisation with the assignment. I
am also grateful to Mr. Dharmendra Deo, Joint Secretary in the Ministry for his
continuous support and guidance to the project.
I am thankful to my team at the TTK Hospital comprising Ms. Lakshmi Sankaran,
Dr. Raymol R Cherian, Ms. V. Thirumagal and Dr. Anita Rao for interacting with me,
providing me support and helping me in the preparation of the Manual.
I am appreciative of the efforts and the guidance of the entire team of Resource
Persons (Dr. Rajesh Kumar, Fr. Joe Perreira, Mr. C.G. Chandra, Dr. Pratima Murthy, Mr.
Vijayan Pavamani, Mr. N.S. Manaklao, Dr. A. Jayanta Kumar, Mr. Kanitkar, Dr. Dewakar
and others) present at New Delhi to discuss every component of the draft Manual and
advise on the feasibility for implementation.
I am grateful to Mr. Anand Bordia, National Project Manager, UNDCP and Mr.
Mukhtiar Singh, National Project Co-ordinator, ILO for their appreciation and support for
the initiative.
I am grateful to the members of FINGODAP for providing constructive criticism
during the conference to improve the document and also for their wholehearted
acceptance to implement the Minimum Standards of Services.
I am obliged to Mr. A. Goswami, Desk Officer, Ministry of Social Justice &
Empowerment, Government of India, New Delhi for his ongoing interaction with me
regarding the scheme, continually motivating me to improve, refine and extend my
thinking.
Shanthi Ranganathan
Honorary Secretary
T T Ranganathan Clinical Research Foundation
TTK Hospital
Chennai
FOREWORD
With the mandate for coordinating alcohol/drug demand reduction strategy of the
Government of India, the Ministry of Social Justice & Empowerment, for the last 15
years, has been implementing wide range of community based programmes, through the
voluntary sector, for prevention of alcoholism/drug abuse and treatment/rehabilitation of
addicts. From a modest beginning of 7 centres in 1985-86, we have now 480 centres,
spread all over the country, under the programme
“Scheme for Prevention of
Alcoholism and Substance (Drugs) Abuse”. The budgetary allocation has multiplied
manifold to reach Rs. 22.00 crores.
The community based organisations associated with the programmes have been
engaged in a wide variety of innovative, need based, localized interventions, adapted to
the felt needs of the community in general and the target groups in particular. The
experience gained over these years through counselling, awareness programmes,
treatment through institutionalised as well as camp-based programmes and rehabilitation
of addicts etc. have made available to us a vast repertoire
of knowledge, expertise and
success stories on all aspects of demand reduction. Training programmes meant for the
service providers on the principles and practices of care and protection in substance abuse
rehabilitation have, over the years, set certain minimum standards of services amongst the
rehabilitation professionals.
However, considering the size of the country, the wide variety of socio-cultural
settings, varying degrees of capacities amongst the implementing agencies, there has
been a long felt need to identify the best practices in delivery of services and codify them
into a set of guidelines which could be uniformly applied to all the implementing
agencies as minimum standards.
T.T.Ranganathan Clinical Research Foundation [TTK Hospital], Chennai, with
their pioneering work and vast experience in the field was entrusted with the
responsibility to tabulate and assess best practices and evolve common minimum
guidelines which can be used as minimum standards and practices. They were requested
to prepare a Manual in consultation with the Ministry, the Voluntary Sector and the
experts with experience and knowledge in the field.
This Manual on Minimum Standards of Services for the programmes under the
Scheme for Prevention of Alcoholism and Substance (Drugs) Abuse is a result of this
effort. With “Whole Person Recovery” as the avowed objective, the Manual defines the
essential components involved in alcohol and drug demand reduction programmes under
the Scheme, the minimum infrastructural requirements for each component, the nature
and quality of services, the activities involved in delivery of different services, the inputs
and the anticipated outputs for each of the activity, the mandatory records to be
maintained etc. It has also laid down the framework of networking and linkages between
the services and institutions to ensure holistic interventions and optimum utilisation of
resources. Besides standardising the experiences into practices, it would also ensure an
objective performance based evaluation of the programmes
The Manual has defined a code of ethics for the service providers along with
rights and duties of the clients. This is intended to ensure a positive, empathetic and
caring environment within the institutions.
This Manual, if implemented sincerely by the partners, the Government and
NGOs, is expected to usher in a new era of quality-based services through voluntary
organisations in the social sector. It would also pave the way for continuous review and
refinement
in
standards through new experiences
and
increasing maturity in
implementation of programmes.
Asha Das
Secretary
Ministry of Social Justice & Empowerment
August 6, 2001
CONTENTS
Chapter 1 - Introduction
Chapter 2 - About the Scheme
Chapter 3 - Drug Awareness and Counselling Centres
Chapter 4 - Treatment-cum-rehabilitation centres
Chapter 5 - De-addiction camps
Chapter 6
- Workplace alcohol I drug prevention programme
Chapter 7
- Code of Ethics for Staff
Chapter 8
- Rights and Duties of the Clients
Chapter 9
-Services of Volunteers in drug abuse prevention programmes
Annexures 1-19
CHAPTER 1
INTRODUCTION
• ‘Quality is never an accident. It is always the result of careful planning, teamwork
and a commitment to excellence’.
When drug addiction surfaced as a problem in India in the 1980s, many voluntary
organisations initiated programmes to deal with addiction. In the absence of documented
literature on the nature of services to be offered, each centre developed its own
programme based on its understanding and the resources available. Gradually others
also followed suit. While there were only 36 centres in the year 1987, 480 Centres are
functioning today. The beneficiaries have also increased from 12000 patients in 1987 to
about three lakhs in the recent years.
This tremendous growth in the availability of services has been made possible with
the active support and financial assistance from the Ministry of Social Justice &
Empowerment, Government of India under the Scheme for Prevention of Alcoholism and
Substance (Drugs) Abuse.
While the availability of services has increased, in the absence of specific criteria to
implement services or maintain quality, programmes are still being developed and
implemented in an unplanned, haphazard manner. It is now time to look beyond just the
number of programmes conducted or clients served, and focus on the quality of service
delivery. Work in this field cannot be justified on the basis that we are responding to a
felt need but we also need to ensure that we respond in a manner that is efficient and
effective.
It has become imperative to design a framework, which will help organisations to
develop their programmes and ensure that these programmes maintain an acceptable
standard in service delivery. This manual on 'Minimum Standards of Services’ provides
such a framework.
The Ministry substantially funds the following services: ■
■
■
■
Drug awareness and counselling centres
Treatment-cum-rehabilitation centres
De-addiction camps
Workplace drug prevention programmes
This manual presents specific criteria and defines the minimum standards of care
that should be maintained. The manual addresses issues relating to four major areas:
■
■
■
*
The facilities or resources that are essential
The variety of programmes and frequency with which these will be offered
The specific roles and responsibilities of the staff
The clients’ rights and the code of ethics for the staff
Information related to minimum standards needed for each of these has been
presented in simple language with easy to follow instructions. The formats of records
that need to be maintained have also been provided in the Annexure to facilitate
necessary documentation.
Implementing the 'Minimum Standards of Services' strategy shall bring with it many
benefits.
■
The expectations of the Ministry are clearly perceived without ambiguity, facilitating
adequate level of service delivery.
■
Assessment and evaluation of programmes to ensure financial assistance is based
on objective criteria rather than on subjective issues.
■
NGOs can structure their programmes to ensure effective service delivery.
■
NGOs can review their services and make appropriate changes.
■
It helps staff to work in a focused manner and improve teamwork.
■
Ensures optimum utilisation of resources through networking and convergence.
■
Efforts in this direction can also provide valuable information to support research
studies, assess adequacy of services provided, and plan appropriate staff training
programmes where necessary.
Implementing the minimum standards of service benefits the funding agencies, the
NGOs and the clientele they serve. It helps them to work in a coordinated manner and
use the limited resources available in the most effective way.
CHAPTER 2
ABOUT THE SCHEME
The government believes in addressing the problem of substance abuse in its
totality. This includes creating awareness, early identification, treatment and
rehabilitation and sustained follow-up care. Further, the Government is of the considered
view that substance abuse is a psycho social medical problem which can be best
addressed through community based interventions. Hence, special emphasis has been
given for involving and mobilising the community.
Under the Scheme for Prevention of Alcoholism and Substance (Drugs) Abuse,
the non-govemmental organisations have been entrusted with the responsibility for
delivery of services and the Ministry bears substantial financial responsibility (90% of the
prescribed grant amount).
The Aims And Objectives of the Scheme for Prevention of Alcoholism and
Substance Abuse are:
•
To support activities of non-govemmental organisations, working in the areas of
prevention of addiction and rehabilitation of addicts.
•
To create awareness and educating the people about the ill effects of alcoholism
and substance abuse on the individual, the family and society at large.
•
To develop culture-specific models for the prevention of addiction and treatment
and rehabilitation of addicts.
•
To evolve and provide a whole range of community based services for
the
identification, motivation, detoxification, counselling, after care and rehabilitation
of addicts.
•
To promote community participation and public cooperation in the reduction of
demand for dependence-producing substances.
•
To promote collective initiatives and self-help endeavours among individuals and
groups vulnerable to addiction and considered at risk.
•
To establish appropriate linkages between voluntary agencies working in the field
of addiction and government organisations.
The following legal entities are eligible for assistance under the Scheme:
1.
A society registered under the Societies' Registration Act, 1860 (XXI of 1860) or
any relevant Act of the State Governments I Union Territory or under any State
law relating to registration of charitable societies.
2. A registered public Trust
3. A Company established under Section 25 of the Companies Act, 1956
4. An organisation / institution fully funded or managed by Government or a local
body
9
5.
An organisation or institution which has been approved by the Ministry of Social
Justice and Empowerment.
The eligible organisations as defined above should also:
a)
b)
c)
d)
e)
Have a properly constituted managing body with its powers, duties and
responsibilities clearly defined and laid down in writing.
Have resources, facilities and experience for undertaking the programme.
Not be run for the financial profit of any individual or a body of individuals.
Have existed at least for a period of three years.
Be of a sound financial position.
For financial assistance under the Scheme, an Organisation / Institution, should
apply in the prescribed proformae as revised from time to time, along with the relevant
documents, to the Ministry of Social Justice and Empowerment, Government of India,
New Delhi, along with the recommendation of the State Government IUT Administration.
Grant is generally released in two instalments representing two halves of the
financial year.
The quantum of assistance is not more than 90% of the grant amount. In case of
the seven North Eastern States, Sikkim and J & K, the quantum of assistance will be
95% of the total admissible expenditure. The balance of the approved expenditure shall
have to be borne by the implementing agency out of its own resources. The
Universities, Schools of Social Work and such other institutions of higher learning will be
eligible for 100% reimbursement of approved expenditure.
The Scheme has the following components for financial support:
1)
2)
3)
4)
5)
6)
7)
8)
9)
10)
Awareness and Preventive Education
Drug Awareness and Counselling Centres
Treatment-cum-Rehabilitation Centres
Workplace Prevention Programmes
Deaddiction Camps
NGO Forum for Drug Abuse Prevention
innovative Interventions to Strengthen Community Based Rehabilitation
Technical Exchange & Manpower Development
Surveys, Studies, Evaluation and Research
Any other activity considered suitable to meet the objectives of the Scheme.
The Manual has laid down the standards for the major programmes funded by the
Scheme. In addition, the Manual prescribes a "Code of Ethics for Staff’ simultaneous
with the “Rights and Duties of the Clients". A chapter has also been included on the role
of volunteers in drug prevention programmes.
10
CHAPTER 3
DRUG AWARENESS AND COUNSELLING CENTRES
Drug awareness and counselling centres function as outpatient units and offer the
following services:
□ Awareness building in the community
□ Assessing and motivating clients to take help
□ Referral services
□ Follow-up services
The centres are staffed by counsellors I social workers / psychologists I sociologists /
recovering addicts (with two years of sobriety).
□ Activities for awareness building in the community
• Awareness programmes should address specific target groups
(vulnerable and at risk groups) in the neighbourhood, in educational
institutions, industries, slums and social welfare organisations with the
purpose of sensitising the community about the impact of addiction and
the need to take professional help to treat addiction.
• Most importantly, the awareness programmes should start at school level
addressing adolescent group and continue with college students. Parents
/ teachers should undergo training to develop skills to understand the
psychology of the youth and to help them keep away from substances.
Specifically the high-risk groups like children of alcoholics, street children,
and school dropouts should be addressed.
• The awareness programmes should be appropriate to the local culture
and in local language. Utilization of audio visual aids like OHPs, slides
and films and employing innovative methods like street plays, puppet
shows, seminars, group discussions are to be included.
• The key persons in the community, like panchayat leaders, school/college
principals/teachers/lecturers, men holding position of respect and
credibility should be involved in the programmes.
Minimum activities
Records to be maintained
Two awareness programmes a month
based on the needs of the community /
target group with the active involvement of
key persons from the community.
Awareness
programme
register
(Annexure 1) to be maintained by the
project-in-charge
containing
the
following.
•
Details of programmes conducted
with feedback from 5 people (who
participated in the programme) for
each programme.
One article relating to prevention, treatment
and rehabilitation services on alcoholism
/drug abuse to appear in daily newspaper,
magazine or mass media (television, radio)
once in six months.
Copy of the article published I details
of the programme telecast /
broadcast.
External evaluation of the awareness
programme by a professional in the field of
addiction once a year with assistance from
FINGODAP members.
Evaluation report
□
Activities for assessment and motivation
•
Assessment of addiction through personal interviews (with clients and family
members) and through use of standardized tests
•
Providing counselling services to motivate the addict to enter treatment
•
Delivering services according to a schedule I timetable to offer individual counselling,
group therapy and family counselling for the patients and their families on a regular
basis.
Minimum activities
Records to be maintained
Intake form to be completed on the very first day Intake Form (Annexure 2), which has
of meeting the client.
demographic details, addiction history
and prior medical history to be filled by
counsellor.
Providing counselling every time he visits the
centre until he is motivated to take help from a
government hospital or a nearby treatment cum - rehabilitation centre.
Case history form (Annexure 3),
which
covers
family,
marital,
occupational and financial history with
counselling notes to be maintained by
the counsellor.
Case history to be completed within a week /
four sessions with the client.
Meeting family members / support persons
within 4 sessions.
Objectives and content of each of the services Therapy Manual (Annexure 4) to be
provided (counselling, group therapy, family prepared by the project-in-charge.
counselling, follow-up) to be described.
12
□ Activities related to referral services and follow-up
•
Identification of both government and non-governmental agencies, working in the
field of addiction and networking with them on a regular basis.
*
Referring clients after motivation to other centres for detoxification / treatment.
•
If referred to the government hospitals, maintaining regular contact with the client
during detoxification and providing follow-up services on completion of detoxification
to facilitate rehabilitation.
Minimum activities
Records to be maintained
Directory
Networking
with
government
and
non-governmental Network
organisations working in the field of addiction and allied sectors (Annexure 5) containing all
relevant information to be
for referral purposes.
maintained by project- incharge.
If a client is referred to a government organisation, one visit to be
made by the counsellor every week until discharge (if the
Government organisation is located in the same district as the
NGO) and in other cases, contact to be maintained in the manner
considered feasible e.g. by letter, by telephone and / or fortnightly
visits.
Case
history
form
(Annexure 3) to include visits
to government hospitals to be
recorded by the counsellor.
Organise a minimum of two group meetings every week for Group therapy record form
6)
to
be
clients who have undergone detoxification (mainly for clients who (Annexure
maintained by the counsellor.
are living in the same geographical area as the NGO).
On completion of detoxification, follow-up is to be maintained as Follow-up card (Annexure
7), which has details of
under:
counselling notes, home visits
For clients who are livinq in the same qeoqraphical area as the and letters written to be
maintained by the counsellor.
NGO
One counselling session every week during the
first three months
One session every month from the third month till
he completes one year.
o One session every two months for one more year
till he achieves two years of sobriety.
o Initiating the client to self-help groups wherever
available. If not available, encouragement to be
given to form self-help groups.
o
o
13
1 For clients who do not live in the same geographical area as the
NGO
o one counselling session with individual / family (if
possible) every one / two months for the first one year.
o one counselling session with individual / family (if
possible) every three months for the second year of
sobriety.
The sessions can be held either at the community or at the
premises of the NGO.
Failure to report for follow-up visits for two months to be followed
up with two letters and one home visit for the patient and one
letter to the family / significant person.
Drinking / drug taking history and improvements made to be
recorded.
Whole person recovery to be assessed twice a year and
recorded.
Maintaining letter of endorsement from clients for receiving free
counselling services
o
Follow -up- card (Annexure
7) with details of whole
person recovery to be
maintained by the counsellor.
Endorsement
letter
(Annexure 8) from each(
patient to be maintained by
the project-in-charge.
at the time of referral or
at the time of follow-up on completion of 3
months from clients referred to government
organizations
Cum
Explaining to the client and his family members about the Declaration
treatment and the medicines provided and its consequences and indemnity Bond (Annexure
getting a declaration-cum-lndemnity before treatment.
9) to be maintained by the
Project-in-charge.
Half-yearly report with details of patients to be maintained
To be maintained by Project
in-charge in format prescribed
from time to time for reporting
to the funding agency.
□ The physical aspects of the centre
•
•
•
•
•
•
•
The centre should be preferably located in a reasonably quiet locality with
adequate space.
Name of the centre (with complete address) and sponsoring agency to be
displayed prominently.
Rights of the clients shall be prominently displayed in the premises of the Centre
for information of the clients, the family members and the visitors.
The Centre should be properly ventilated, well lit and maintained in a clean
manner.
It should have toilet facilities, drinking water facilities and telephone facility.
The centre should be easily accessible through public conveyance.
The following facilities should be available:
J reception, enquiry / registration counter I waiting space with seating
arrangements for a minimum 5 persons
J cubicles I rooms for providing individual counselling, group therapy and
family counselling.
/ space to store records of patients to ensure confidentiality and a system of
easy retrieval
•
•
•
Addiction related educational material such as posters to be prominently
displayed at strategic points.
Information pamphlets, handouts and other educational materials in the
vernacular to be made freely available to the public. It is desirable if the Ministry
provides the materials.
Overhead projector to be available for creating awareness. It is desirable if the
Ministry provides it.
□ Job description of staff
1.
Project in charge-cum-senior counsellor
•
•
Coordinating and managing the counselling centre
Taking care of administrative responsibilities of the centre - attendance, allocation of
job and maintenance of discipline.
Preparing Half yearly / Annual report and application forms for grant purposes.
Liaisoning with government and non-governmental organisations working in the field
of addiction.
Checking whether the records are maintained properly.
Supervising and providing guidance to counsellors
Organising case discussions
Organising training programmes for counsellors
Responsibilities as a Project In charge
•
•
•
•
•
•
Responsibilities as a senior counsellor
•
•
•
•
•
•
•
•
Assessing problem areas of clients
Collecting case history both from the client and significant persons
Visiting governmental and non-governmental agencies to support the client in
treatment.
Conducting group therapy for clients
Providing counselling for clients and their family members
Providing follow-up counselling
Maintaining individual case records of patients seen
Conducting awareness programmes
2.
Counsellors / Social workers / Community workers
•
•
Motivating the client to take help
Assessing problem areas of clients
15
•
•
•
•
•
•
•
Collecting case history both from the client and significant persons
Visiting governmental and non-governmental agencies to support the client in
treatment and escorting him for admission to other organisations.
Conducting group therapy for clients
Providing counselling for clients and their family members
Providing follow-up counselling
Conducting awareness programmes
Maintaining records
□ Training requirements of project in charge / counselling staff
•
»
•
•
•
3.
Orientation of one-month duration to be provided to new staff on counselling,
conducting group and family therapy and on maintenance of patients' records.
Updating and training through refresher courses to be provided to existing staff at
least twice a year - to attend one training conducted by Regional Resource Training
Centre by each staff.
Professionals from other counselling centres to be encouraged to visit the centre
once a year and share their experiences. Similarly, staff to visit other counselling
centres once a year and learn from their experiences.
Case discussions to be conducted once a week to ensure quality of service delivery.
Project in charge to be provided orientation of maintenance of accounts and other
records.
Accountant-cum-clerk
As an Accountant
•
•
•
•
Writing main account I petty cash account and preparing monthly expenditure
statement
Disbursement of cash for salaries and incidental expenditure.
Assisting the Chartered Accountants in preparing Balance Sheet and liaisoning with
project coordinator regarding funds
Maintaining asset register
As a clerk
•
•
•
•
•
Receiving phone calls and playing the role of a receptionist
Maintaining attendance, leave letters
Maintaining records for telephone calls, stationery and electricity.
Getting stationery and cleaning items for the centre
Attending to the work of the centre at post office, bank and also purchases of various
items.
16
CHAPTER 4
TREATMENT-CUM- REHABILITATION CENTRES
The Treatment-cum- Rehabilitation centres are mandated to provide the following
services:
□
□
□
□
□
□
Preventive Education and Awareness building
Assessing and motivating the clients to take help
Detoxification and medical care
Psychological therapy
Vocational rehabilitation
After-care / follow-up
The Treatment-cum-Rehabilitation Centres aim to enable the addicts to achieve total
abstinence and improve the quality of their lives by helping them to :
o
o
o
o
o
identify areas of necessary change and taking action.
become aware of risk factors for relapse and develop positive coping
skills
strengthen inter-personal relationships
develop healthy work ethics
sustain their recovery through follow-up services
As prescribed by the grant-in-aid scheme, both medical and psychological services
are provided on an in-patient basis. The after care / follow-up services are provided on
an out-patient basis. Medical care is provided by physician I psychiatrist and nurses.
Psychological care is provided by social worker, psychologist, sociologist or a recovering
person with a minimum of two years of sobriety.
□
Activities for Awareness Building and Assessment and Motivation of
clients
As described in Chapter 3 for similar activities.
□ Activities related to detoxification and medical care
•
Detoxification services are to be provided to make the withdrawal period safe and
comfortable.
•
Treatment is to be provided for other related medical and psychiatric disorders
(diabetes / hypertension / depression, suicidal thoughts etc.). Services of other
specialists, hospitals and testing laboratories should be utilized, where necessary, to
ensure appropriate care.
17
•
Medical care is to be provided during the follow-up as well.
Minimum activities
Records to be maintained
Prescribing medicines to minimize withdrawal symptoms Medical
manual,
which
and to deal with related medical and psychiatric describes protocols (based on
problems.
research or in keeping with
accepted
practice)
for
prescribing medicines to be
maintained by the Medical
Officer.
Medical
case
sheet
(Annexure 10) to be filled by
Providing essential medicines for detoxification and medical officer / nurse.
withdrawal related emergencies free of cost.
Medical history to be obtained on the day of admission.
Medical complaints of patients, prescription of medicines
/ reasons for change of medicines to be recorded by the
medical officer.
In case of any untoward incident like fits, delirium or
accident, the patient to be monitored on an half hourly
basis till he gets back to normalcy.
pressure
chart
For hypertensive patients, blood pressure to be checked Blood
(Annexure
10)
to
be
everyday till discharge
maintained by the nurse.
Temperature to be recorded for patients running Temperature chart (Annexure
temperature, until normal temperature is recorded for a 10) to be maintained by the
nurse.
minimum of two days.
Medicines essential for detoxification and withdrawal Stock Register (Annexure 11)
related emergencies to be made available at all times to be maintained and checked
and to be checked for quantity and availability once a by the nurse once a month.
month.
In case of any medical/ psychiatric problem beyond the
scope of the detoxification centre referral should be
made within 2 days. Violent patients need to be
assessed and transferred if necessary to department of
psychiatry.
Medical
case
sheet
(Annexure 10) - the need for
referral
and
medical
/
psychiatric problems exhibited
by the client to be recorded by
the physician.
> Availability of essential equipment like ECG machine, Oxygen cylinder, suction
apparatus, BP apparatus, weighing machine and urine sugar testing material is
desirable.
> Availability of an ambulance with a driver is desirable to admit patient to the
hospital in case of emergencies.
Activities for psychological services
•
Assessing the problems related to addiction and motivating the addict to participate
actively in the treatment.
•
Providing psychosocial treatment for the total recovery of the addict through
individual counselling, group therapy, re-education and yoga. Treatment plan to
include exposure to self - help I support groups and introduction to other recovering
addicts.
•
Providing psychological care to families and support persons of the addict.
Standards on programme structure
Minimum activities
Records to be maintained
A schedule / timetable to be developed and followed.
Therapy manual (Annexure 4)
to be prepared and maintained by
Rules that need to be adhered to by the clients to be the senior counsellor.
prepared - e.g. waking time, recreation time.
Issues that warrant disciplinary actions - e.g. missing
sessions, trying to abuse drugs inside the centre and
the disciplinary measures that can be taken to be laid
down.
Patients to complete treatment within the prescribed Case History Form (Annexure
period. Drop out or extension of treatment beyond the 3) to be maintained by the nurse /
one month period to be recorded with reasons.
counsellor.
19
Standards on counselling
Minimum activities
Records to be maintained
Record of patient’s attendance to psychological therapy Attendance Register (Annexure
sessions.
12) to be maintained by the
counsellor.
Case history to be completed within two weeks through Case history form
counselling sessions with client and family members.
(Annexure 3) to be completed by
the counsellor.
During the one-month programme, a minimum of 8
counselling sessions to be provided. Each session to
last for at least half-an-hour to forty-five minutes and
main issues recorded in brief.
Issues such as HIV positive status, extra marital affairs,
legal problems, marital separation, gambling or
traumatic childhood experiences to be handled with
extra effort and care.
Treatment plans to be specifically recorded keeping in Case history form
mind the whole person recovery.
(Annexure 3) to be completed by
the counsellor.
Standards on re-educative lectures
Minimum activities
Three educative sessions to be conducted each week.
Records to be maintained
Therapy
Manual
(Annexure 4) to
be
The contents of the re-education lectures to be documented maintained by the senior
and standardized and followed to ensure uniformity.
counsellor
Basic issues such as disease concept, addiction related
damage, relapse, overcoming personality defects, methods to
stay sober, self-help / support groups principles and HIVAIDS to be covered.
Assertiveness, decision making and problem solving skills to
enable them to withstand pressure to be taught.
20
Standards on group therapy
Minimum activities
Records to be
maintained
5 sessions per week and each session to be conducted for at Therapy
Manual
least one hour.
(Annexure 4) to be
maintained by the senior
Each group to have a maximum of 15 and a minimum of 5 counsellor.
clients.
Groups to be divided based on languages the patient speaks
comfortably
Issues related to damage due to addiction, symptoms of
addiction, powerlessness and unmanageability, breakdown of
values and character defects to be discussed.
Observation of individual patient during the group therapy Group therapy record
sessions to be recorded once a week.
(Annexure 6) to be
maintained
by
the
counsellor conducting the
group therapy session.
Standards for the family programme
The addiction treatment centre should have programmes for the family members
including significant persons. The goals of the programme are to help them understand
addiction as a disease and in turn develop a caring attitude towards the addict. Another
goal is to help them deal with their negative emotions and improve their quality of lives.
Minimum activities
Records to be
maintained
history
form
Four counselling sessions for family members to be provided Case
(either individual or combined sessions) whenever possible. (Annexure 3) to be
maintained
by
the
Through the sessions, to help the family members to counsellor.
achieve personal recovery by becoming aware of their
enabling behaviour, negative traits and develop methods to
deal with their feelings of shame, guilt, anger and
resentment.
Therapy
Manual
One educative session to be conducted each week.
(Annexure 4) to be
The contents of the re-education lectures to be recorded and maintained by the senior
counsellor.
followed to ensure uniformity.
■ Basic issues such as the objectives of the treatment
programme, medications given, the disease process,
relapse, recovery, impact of addiction on the family to be
provided.
In the absence of family members / support persons,
this service need not be insisted upon.
Other Issues related to psychological services
Minimum activities
Records to be
maintained
Identity card with registration number to be given to the Identity card (Annexure
patient at the time of discharge.
13) to be issued by the
counsellor.
Discharge to be made by the counsellor in consultation with
the doctor / project director.
A letter of endorsement from the patient that he received Letter of Endorsement
free treatment
signed (Annexure 8) by
the patient maintained by
the counsellor.
Explaining to the client and his family members about the Declaration
Cumtreatment and the medicines provided and their Indemnity (Annexure 9)
consequences and getting a declaration-cum-indemnity.
A manual which provides information about the vision of the
organisation, members of the society, facilities and functions
of the centre to be available and updated every year.
Organisation chart to be included.
Administrative
manual
(Annexure 14) to be
prepared by the project-incharge.
Half-yearly report with details of patients to be maintained
To be maintained by
Project-in-charge in the
format prescribed from
time to time for reporting to
the funding agency.
□ Activities related to Vocational Rehabilitation
Recovering addict to be given a vision for resettling in the society. A list of vocational
options to be provided to the patient.
22
•
Culturally relevant vocational training to be considered utilising local resources and
the marketability of the products wherever possible - e.g. candle making, tailoring,
carpentry and mat weaving.
•
Identification and networking with government recognised vocational centres to refer
recovering clients for training.
•
An employee who has been dismissed due to addiction can be helped to get back to
his prior employment by liaison with the employer.
Minimum activities
Records to be maintained
Education, skills and prior work experience Assessment Form (Annexure 15) to be
of patient to be assessed before initiating maintained by the vocational instructor.
him into vocational training.
Maintenance of a directory and networking Networking directory for specialised
with specialised services - vocational services (Annexure 16) to be maintained
training, job placement
by the project-in-charge.
□ After - care / follow-up and rehabilitation services
After- care and rehabilitation are essential components of addiction treatment. The
outcome of therapy depends largely on the effectiveness of the follow-up efforts towards
the patient's re-integration into the community to attain whole person recovery.
Rehabilitation through vocational training to facilitate income generation can be part of
the services by the Addiction Treatment Centre. After care I follow-up services are
provided on an outpatient basis.
□ Activities for aftercare and rehabilitation of the patients and family
•
A clearly defined after care programme (counselling, relapse prevention programme,
self-help programme, reaching out to patients through home visits) to be made
available with focus on the whole person recovery of the individual.
•
Procedures to be clearly laid out to address relapse issues (in both detoxification and
counselling services)
•
After- care plans of alternative methods for patients who have not recovered have to
be explored and support to their family members to be ensured.
23
Minimum activities
Records to be
maintained
Patient to be prepared for discharge with focus on short-term Case History (Annexure
and long-term goals - e.g. developing work ethics, improving 3) - recovery plans to be
inter-personal relationships and financial management.
recorded
by
the
counsellor.
Regular follow-up services to be provided on completion of Follow-up
card
treatment for clients who are living in the same geographical (Annexure 7) which has
area as the NGO. The sessions can be held either at the details of counselling
community or at the premises of the NGO.
notes, home visits and
letters written to be
- One counselling session every fifteen days during the first maintained
by
the
three months
counsellor.
- One session every month from the third month till he
completes one year.
- One session every two months for one more year till he
achieves two years of sobriety.
Failure to report for visits for two months to be followed up
with two letters and one home visit for the patient and one
letter to the family / significant person.
up
card
Drinking / drug taking history and improvements made to be Follow
(Annexure 7) to be
recorded in every visit.
updated
by
the
Whole person recovery to be assessed twice a year and counsellor.
recorded.
letter
Patients completing one or more years of sobriety to be Congratulatory
(Annexure 17) signed by
encouraged by sending a congratulatory letter.
the counsellor / project-incharge.
Manual
Relapse has to be handled with specific input to increase Therapy
the understanding and coping mechanism of the addict - (Annexure 4).
four counselling sessions.
Directory
Maintenance of a directory and networking with specialised Networking
services - vocational training, job placement, referral to for specialised services
(Annexure 16) to be
half way home / after-care centre.
maintained by the project
in-charge.
24
The physical aspects of the Treatment-cum-Rehabilitation Centre
•
The centre should be located in a reasonably quiet locality with adequate space.
•
Name of the centre with complete address and sponsoring agency to be displayed
prominently.
•
Rights of the clients shall be prominently displayed in the premises of the Centre for
information of the clients, the family members and the visitors.
•
The centre should be properly ventilated, well lit and maintained in a clean manner.
Water to be made available.
<»
Following facilities should be available:
Waiting space with seating arrangements for a minimum 5 persons
Reception I enquiry and registration counters
Cubicles I rooms for consultation for physical examination
Nursing Station with facilities to store drugs, linen, and records of patients
Facilities with privacy for providing individual counselling, conducting group
therapy, re-educative lectures, family classes. They should be airy with
comfortable seating on floor mats/ chairs. Blackboard, chalk and other material to
be provided.
J Recreational facilities such as books for reading, indoor (carrom, chess) I outdoor
games, radio and television.
J
J
/
J
J
•
Mattresses and pillows should be provided for each patient. Bed linen to be changed
at least once a week
•
Each patient to be provided with a locker I storage space to store personal
belongings.
•
There should be one bathroom for ten patients and one toilet for five patients. Open
toilets to be discouraged.
•
Space should be provided to store records of patients to ensure confidentiality and a
system of easy retrieval. Computerisation of case histories to be considered and
implemented.
Addiction related educational material such as posters to be prominently displayed at
strategic points.
Information pamphlets, handouts and other educational materials in the vernacular to
be made freely available to the public.
25
Job responsibilities of staff
1. Project Director
Responsibilities as a Project In charge
•
•
Coordinating and managing the treatment and rehabilitation centre.
Taking care of administrative responsibilities of the centre - appointment of staff,
attendance, allocation of job and disciplinary action.
•
•
•
Preparing Half yearly I Annual report and application forms for grant purposes.
Checking whether the records are maintained properly.
Liaison with governmental and non-governmental organisations working in the field
of addiction.
•
•
•
•
•
•
•
•
•
•
Responsibilities as a senior counsellor
Supervising and providing guidance to counsellors
Organising case discussion
Organising training programmes for counsellors
Assessing.problem areas of clients
Collecting case history both from the client and significant persons
Conducting group therapy for clients
Providing counselling for clients and their family members
Providing follow-up counselling
Maintaining individual case records of patients seen
Conducting awareness programmes
2. Medical Officer / Psychiatrist
•
•
•
•
•
•
Assessing clients with regard to their physical / mental condition and providing
treatment for their medical and psychiatric problems.
Prescribing medication during detoxification, follow up and relapses and handling all
medical emergencies e.g. DT, fits and acute psychotic episodes
Liaison with specialists in psychiatry, internal medicine, neurology, pathology and
biochemistry for referral in case of further treatment.
Maintaining all records of detoxification, emergencies and follow up of patients
Participating in the case discussion with the counsellors to plan the treatment and
recovery of individual patients.
Contributing to awareness building and preventive education programmes.
Training requirement for general physician / psychiatrist
•
Exposure to new trends regarding kinds of drugs abused, medical and psychiatric
problems, new medicines / methodologies available for the treatment of addiction
through participation in training programmes and conferences once a year.
26
3.
•
•
•
•
•
Nurses
Minimal history taking on admission
Dealing with emergencies and assisting the Medical Officer
Giving medication and injections;
Maintaining all registers and records of patients in detoxification (e.g. blood pressure
and urine sugar)
Supervising the functioning of ward boys, sweepers
Training requirement of Nurses
•
•
A mock emergency drill to be carried out once every three months to deal with issues
like breathlessness, acute psychotic episode, convulsions and cardiac arrest. The
medical officer will guide the drill.
New nurses will be given training for a period of one week with information on drug
addiction, about psychiatric problems, effects of psychiatric medicines and day-today management of the centre.
4. Ward boys
•
•
•
•
•
•
Assisting the nurses in the detoxification unit
Attending to the personal hygiene of bed- ridden patients
Escorting the patients to labs or other specialists
Monitoring the visitors and checking patients for possession of drugs
Conducting physical exercises for the patients
Cleaning of the detoxification centre including toilets
5. Counsellors / Social workers / Psychologists I Recovering addicts
•
•
•
•
•
•
Functioning in a team to coordinate activities and receive feedback from other
members of the team.
Counselling to include assessment, motivation, building rapport, counselling families
and significant others and planning treatment strategies from admission to follow-up.
Conducting re-educative classes, family therapy and group therapy.
Recording and documentation of the patient's treatment processes.
Conducting awareness programmes in the community.
Net working with government and non-governmental agencies.
Training requirements of counselling staff
•
•
•
•
Orientation of one-month duration to be provided to new staff on counselling,
conducting group and family therapy.
Updating and training through refresher courses to be provided to existing staff at
least twice a year - to attend one training conducted by Regional Resource Training
Centre by each staff.
Professionals from other addiction treatment centres to be encouraged to visit the
centre once a year and share their experiences. Similarly, staff to visit other
treatment centres once a year and learn from their experiences.
Case discussions to be conducted once a week to ensure quality of service delivery.
27
6.
Yoga/ other therapists
•
•
Conducting physical exercises / yoga for the patients
Conducting meditation and classes on spirituality
7.
Accountant-cum-clerk
As an Accountant
•
•
•
•
Writing main account / petty cash account and preparing monthly expenditure
statement
Disbursement of cash for salaries and incidental expenditure.
Assisting the Chartered Accountants in preparing Balance Sheet and liaison with
project coordinator regarding funds
Maintaining asset register
As a clerk
•
•
<•
•
•
•
Receiving phone calls and playing the role of a receptionist
Maintaining attendance, leave letters
Maintaining records for telephone calls, stationery and electricity.
Getting stationery and cleaning items for the centre
Visiting post office, bank and shops as and when needed
Keeping receipts, bills and disbursing cash.
8.
Sweeper / Peon
•
•
Cleaning the entire centre including bathrooms
Visiting post office, shops, paying electricity, telephone bills as and when needed
28
CHAPTER 5
DE-ADDICTION CAMPS
An organisation running a Treatment-cum-rehabilitation Centre may organise De■ addiction camps in areas prone to drug abuse especially in rural I semi urban areas
where institutional services are either not available or not feasible due to socio-economic
reasons.
□
The camp approach has many benefits:
o Treatment is cost effective because existing facilities available in the
community are made use of.
o Involvement of family / support persons become feasible.
o The local community is involved in organising the camp, hence, they
provide support to the addict in recovery and they also get sensitised to
the impact of addiction.
o Sustained involvement of the community promotes collective initiative
towards prevention of addiction.
□
Activities for conducting de-addiction camps
•
Creating awareness in the community about the problems associated with drinking
and drug addiction and the need for appropriate treatment.
•
Prior to conducting the camp, a local host organisation has to be identified from the
community. The host organisation could be any local organisation (government /
non-govemment / panchayat), providing health care / education I rural upliftment I
micro credit system. The host organisation should have credibility and be trusted by
the community. The host organisation should be involved in providing I facilitating
infrastructure such as accommodation for conducting the camp, organising meals for
the patients and treatment staff, and mobilising local support persons.
•
Involving the community in identification, intervention and providing support during
recovery. Identification of addicts to be done through multiple contacts - formal I
informal leaders, local physicians, community workers, teachers etc.
•
Treatment to include detoxification and psychological therapy for the patients and
therapy for family members for a period of 15 days by conducting a camp at the
community itself.
•
On completion of camp, to provide follow-up care for a minimum period of one year.
•
To sustain the momentum built at the time of the camp, meaningful follow-up
activities to be conducted on an ongoing basis.
29
Minimum activities
Records to be maintained
To involve the community, identification of a host Profile of Host organisation
organisation and sensitizing them about the impact of (Annexure
18)
to
be
addiction and the need for treatment.
maintained by the counsellor.
Two programmes to be organised prior to the camp at
the community.
Identification of patients through community network formal / informal leaders, panchayat leaders, families of
addicts, Youth Associations, teachers, Mahila Mandal
workers, Religious leaders and health workers /
recovering addicts.
List of identified addicts to be
maintained by the counsellor.
List of resource persons with
addresses to be maintained
by the counsellor.
Through personal contact or by distribution of pamphlets,
making people aware of the camp programme.
The selection criteria to be clearly defined and followed- Camp
Manual
to
be
up.
developed and maintained by
the counsellor.
case
sheet
Providing detoxification and dealing with addiction Medical
(Annexure
10)
to
be
related medical complications.
maintained by the medical
officer.
directory
Identification and creating linkages for medical services Network
5)
to
be
to handle emergencies during detoxification, during (Annexure
follow up and relapses through local resources such as maintained by the project-incharge.
physicians, hospitals and primary health centres.
Developing a structured programme for duration of 15 Therapy Manual (Annexure
days with the focus on medical care as well as providing 4) to be maintained by the
project-in-charge.
support to improve the quality of life.
Providing a minimum of 8 re-educative sessions for
patients, 8 group therapy sessions and 4 individual
counselling sessions.
To provide support to the family, conducting five
sessions for families with components of re-educative
sessions, group therapy, and counselling.
To sustain the recovery, conducting one follow-up
meeting at the camp site once in two months for a period
of two years.
Case History Form to be
maintained by the counsellor
(Annexure 3)
Camp
Manual
to
be
maintained by the project-incharge.
Follow-up card
to -be
maintained by the counsellor
(Annexure 7).
30
□ Activities for creating awareness in the community
Formal and informal methods that include community participation such
as dramas, competitions, pantomime shows, street plays and folk media to be
organised depending on the target audience.
Messages to be sensitively designed so as not to arouse any undue scare, curiosity
or experimentation with alcohol and drugs
The language, content and style of message to be culture-specific according to the
target groups to be addressed
Education against alcohol and drug abuse to incorporate contents of socially healthy
alternative life styles
Refer Chapter 3 for minimum activities and records to be maintained.
□ Staff required for conducting a camp
A minimum of three counsellors, one nurse and a ward boy are required for 25
patients.
Physician and other support persons from the campsite to be utilised.
Training requirements of staff
• The treatment staff to be exposed to work in a treatment centre that already
conducts de-addiction camps to observe and understand the camp approach.
• Training to include methods to mobilise and work with the community.
• Specific training on pantomime shows, street plays and folk media to be
included.
31
CHAPTER 6
WORKPLACE ALCOHOL / DRUG PREVENTION PROGRAMME
Addiction, especially addiction to alcohol is a major problem in industries and other
places of work. According to some of the studies conducted, 7-10% of the work force
may have problems related to alcohol I drug use. It creates problems for the employer,
managers, union office bearers and supervisors. Some of the problems faced are
unpredictable absenteeism upsetting production plans, accidents leaving an unpleasant
impact, constant worry over product quality and deteriorating discipline in the
department.
A comprehensive strategy against the spread of alcohol and drug abuse includes
building awareness, training supervisors / managers on the impact of addiction and
offering treatment services. The scheme by the government of India encourages and
gives grants to non-governmental organisations to undertake work place alcohol / drug
prevention programmes in urban areas. The programme is focussed towards promoting
health, maintaining safety and improving work performance.
The Scheme has listed two types of interventions
1.
A 15 or 30 bedded treatment cum rehabilitation centre to be established by the
industry / enterprise. Financial assistance upto 25% of the expenditure for setting up
such a Centre shall be provided by the Ministry. Only an industry with a minimum
strength of 500 workers or a cluster of units wherein 500 people work will be eligible
for assistance. For this component, the services shall be the same as that of 15 / 30
bedded Treatment-cum-Rehabilitation Centre (Chapter 4).
2.
A Treatment cum Rehabilitation Centre (15/30 bedded) run by an NGO taking up
work place alcohol / drug prevention programmes as part of its activities. Additional
funding of 25% of that admissible to a 15 bedded centre to be provided to employ
additional staff such as counsellors I community workers I part time medical officer.
•
To create awareness among the employees about the impact of use and abuse of
alcohol / drugs in relation to the quality of work.
•
To create awareness among the families of employees about the impact of use and
abuse of alcohol / drugs in relation to health, finances and general well being.
•
To educate and change the attitude towards use of alcohol and drugs and promote
healthy leisure time activities and coping skills.
□ Activities related to workplace alcohol / drug prevention programme
32
•
To conduct awareness programmes for the management as well as union office
bearers regarding the impact of addiction and the need to develop a policy.
•
To conduct training programmes for supervisors I managers to identify early phase
addicts through poor job performance, absenteeism etc.
•
To collect data regarding absenteeism, accidents, poor job performance among the
employees and relating them to use and abuse of alcohol.
•
To identify, refer and facilitate treatment of workers with problems of addiction.
Minimum activities
Records to be maintained
To conduct one programme a month on creating
awareness about the impact of addiction and related
issues - lecture, film shows / street plays and puppet show
at the workplace / res;dential areas of employees.
Awareness programme
register to be maintained by
Project-in-charge (Annexure 1).
To conduct one programme every six months for families
of employees on the impact of addiction and related
issues.
To conduct one programme every three months for
supervisors / managers / worker representatives on early
identification / motivation of problem employees and
related issues.
To conduct one programme every six months for
management / union office bearers on the need to have a
policy to deal with addiction and to develop a plan of
action.
To create and organise a meeting of steering committee in
the institution to deal with addiction once in three months
to
be
To help the industries to collect data regarding Questionnaire
absenteeism, accidents and poor quality of work due to the developed based on the
requirement of the industry
use and abuse of alcohol / drugs.
(Model as prescribed by the
ILO).
for
patients
To treat patients referred by industries as and when Register
referred by industries to be
needed.
maintained by the counsellor
(Annexure 19)
33
□ Training requirement of staff
The counsellors or community workers should have undergone at least one week
training in an organisation that conducts such workplace alcohol / drug prevention
programmes.
34
CHAPTER 7
CODE OF ETHICS FOR STAFF
The primary obligation of all staff is to ensure quality of services to the clients. The
relationship between the staff and the client is a special one and it is essential that the
staff have the maturity as well as the ability to handle the responsibilities entrusted to
them.
Every staff member on joining the organisation shall undertake to abide by the
following code of ethics: -
1.
Conduct oneself as a mature individual and a positive role model by not using
alcohol / tobacco / other drugs on the premises.
2.
Respect client by treating him with dignity.
3.
4.
No sexual relationship of any kind with clients or their relatives.
No physical restraint or corporal punishment of any kind to be used to detain or
restrain patients who are in normal physical and mental condition even for acts of
misbehaviour. Only in extreme cases where the client is violent or delirious
or not in a position to take care of himself, physically restraining him is
allowed to ensure protection to the patient from inflicting harm to himself
or others. This should be resorted to with the prior permission of the project in
charge.
5.
No denial of food to any client as a means of punishment or otherwise.
6.
Not to make use of I exploit the client for the benefit of self/staff/organisation.
7.
Recognize the best interest of the client and refer him if necessary to another
agency or a professional for further help.
8.
No photographic, audio, video or other similar identifiable recording is made of
patients without their prior informed consent. If done for research / training, the
purpose has to be explained and consent obtained preferably in writing.
9.
Maintain all client information in the strictest confidence. Information about the
patient or his progress in treatment not to be divulged to any individual or
authority without the patient’s consent.
10.
No discrimination to be made against a HIV-AIDS patient regarding admission or
in providing any other services.
35
CHAPTER 8
RIGHTS AND DUTIES OF THE CLIENTS
Rights of the clients
1.
Services shall be available irrespective of religion, caste, and political belief of all
clients.
2.
Services shall be available irrespective of the particular drug (s) abused (e.g.
alcohol, ganja, brown sugar) or routes of administration (e.g. intravenous).
3.
Services shall be available irrespective of the history of prior treatment.
4.
Services shall be provided with dignity, respect and safety in a supportive drugfree environment.
5.
Exclusion criteria for admission shall be clearly stated e.g. medical complications
/ psychiatric problems.
6.
Expulsion criteria from services shall be clearly defined - e.g. being violent and
abusing drugs I alcohol on the premises.
7.
Clients and their relatives shall be informed of the nature and content of the
treatment as well as the risks and benefits to be expected of treatment. They
would be made aware of conditions and restrictions prescribed in the centre
before admission.
8.
Clients can wear their own clothes in keeping with local customs and traditions.
9.
Clients can have contact with, and visits from, family or support persons while in
treatment with the prior approval of the treatment staff.
10.
The Centre shall maintain confidentiality of information regarding participation in
the programme and of all treatment records except in the case of inspection,
monitoring I evaluation by the funding agency.
11.
Access shall be made available to the project-in-charge or management to air
grievances I register complaints about the treatment or the staff.
12.
Rights of the clients shall be prominently displayed in the premises of the centre
for information of the clients and their family members.
36
Duties & Responsibilities of the Clients and Family members/ Support persons
There can be no absolute rights. Enjoyment of rights and privileges enjoins upon an
individual to fulfil certain duties and responsibilities. Patients and their family members /
support persons shall have to abide by the following guidelines which will help in the
smooth running of the centre and in ensuring them to avail of their rights:
1.
The use and / or possession of alcohol and / or drugs shall be prohibited. Anyone
found to be in possession or use of alcohol I drug shall face disciplinary action as
prescribed by the organisation. Similarly smoking shall be strictly prohibited in the
prescribed areas.
2.
The centre shall have the right to check the belongings of the patient for
possession of alcohol / drugs at the time of admission and at any time during his
stay at the centre.
3.
Violence or using foul language shall be strictly prohibited.
4.
Sexual relationship of any kind with other patients I their family members shall be
strictly forbidden
5.
Gambling in any form and playing cards shall be prohibited.
6.
Borrowing from or lending to (money or any valuables) other patients I family
members shall not be allowed.
7.
Adhering to the rules set by the treatment centre regarding waking up time,
bedtime, meals, therapy programme, for issue of medicines, etc. shall be
mandatory.
8.
Keeping the rooms, kitchen, dining room etc. clean; making beds for oneself,
changing linen; watering the plants etc. shall be other duties of the inmates.
9.
Lights, fans and geysers should be switched off when not in use.
10.
Wastage of water shall be strictly prohibited.
11.
Radio/tape recorder to be used in low volume not inconveniencing other patients.
12.
Family members / support persons shall follow the rules prescribed by the centre
with regard to out-passes and visiting hours.
37
CHAPTER 9
SERVICES OF VOLUNTEERS IN DRUG ABUSE PREVENTION PROGRAMMES
Utility of Volunteers and their Applicability
The problem of addiction is increasing with time and the available resources are
becoming increasingly insufficient to meet the needs. People showing care and concern
are a rich human resource. There is a need to develop committed individuals who are
prepared to provide voluntary services. Mobilising them in Drug Abuse Prevention
Programmes is one of the best ways to enhance the quality of services provided.
Besides, there is no additional cost incurred by the organisation.
People who can be Volunteers:
Z
Z
Z
z
recovering addicts and their family members
retired persons from tiie local area
youth, students and lecturers from colleges
women with some spare time who are committed
Selection and development of Volunteers
Some precepts for developing and managing the services of volunteers call for a
systematic effort. These have been outlined below:
•
Volunteers must be selected carefully. Selecting good role models showing
commitment with personal qualities that addicts or family members can look up to is
important. They should be preferably be non-smokers and teetotallers. If the
volunteers are recovering addicts, they should be sober for a minimum period of one
year.
•
Volunteers need orientation through proper training inputs. Programmes or
procedures instituted to train volunteers could be in consultation with the professional
staff. The qualification, experience and personal qualities of volunteers should be
assessed before assigning them tasks. Some of the areas which could be included in
training are as follows:
❖ The disease concept of addiction and its impact on the different areas of the
individual's life
❖ Some theoretical inputs on human relations and basic communication skills
❖ The various services offered by the organisation e.g. some information about the
characteristics of the community being served, the types of problems
encountered by patients and the role of the volunteer in relation to the
programme, the patients and the community.
❖ A clear delineation of the volunteer’s role emphasizing particular functions and
activities she/he is expected to perform as well as those of the professional staff.-
38
❖ Instructions regarding the necessity for maintaining confidentiality.
•
Volunteers need supervision once they assume their position as part of the
programme’s workforce. They should be assigned a capable staff supervisor who
can help, guide, be supportive and evaluate their work. By providing regular
supervision, the staff could also indicate that the volunteers' efforts are taken
seriously.
•
Volunteers who are recovering patients should work along with a senior staff
member. It is important that no ex-patient is to be treated as a specimen on display
by either the public or the staff.
•
Volunteer’s spirit of service and 'voluntarism' need to be nurtured through
genuine teamwork with the professional staff. It is important that she/he feels
supported and appreciated by the professional staff as a partner deserving respect.
Sharing credit with them is a key means of rewarding volunteers. Ceremonies held in
the community at which volunteers are honoured are ideal for sustaining their
commitment and for stimulating the spirit of service in other community members.
Role of Volunteers
While it is for the concerned organisation to work out the various roles of a volunteer
depending upon the, requirement, the following areas are suggested for the possible
involvement of them.
In the service delivery:
■
Organising / conducting awareness programmes - educating community members,
preparing posters, display materials, etc.
■
Networking with government I non-governmental organisations working in the field of
addiction in the same locality
■
Making visits to the government hospital to meet the patients admitted for
detoxification.
■
Making home visits
■
Initiating the patients to join self-help groups and conducting self-help groups (for
recovering addicts I family members / support persons)
■
Providing social and emotional support to patients
■
Conducting re-educative lectures for patients and family members/ support persons
■
Writing letters on behalf of counsellors
■
Networking with other agencies in getting employment for patients, medical
assistance for related illnesses, legal aid etc.
39
■
«
Maintaining records such as awareness programme register, network directory etc.
Conducting recreational programmes at the centre
■
Organising special programmes during festival times at the centre/ community
■
Helping the Project Director in preparing the various manuals viz. therapy manual,
administrative manual and other documentation work.
In Administration:
■
Maintaining cleanliness of the premises
■
Receptionist activities viz. receiving phone calls, giving information and guiding
patients
■
General secretarial and clerical activities
■
Fund-raising activities
********
41
AWARENESS PROGRAMME REGISTER
Lectures / street play / puppet show / film
1.
2.
3.
4.
5.
6.
Date and month of awareness programme
Locality where the programme was held
Target group and number of participants
Topics handled
Methodology used to impart information
Feedback from a minimum of 5 people including key persons
Articles published / broadcast / telecast
1.
2.
3.
4.
Date and month of publication/broadcast/telecast
Name of publication I TV channel / Radio Station
Title of the article/message/programme
Feedback received, if any.
Yearly evaluation report
1.
2.
3.
Name of the evaluator
Background information about the evaluator
(education, work experience, expertise in the areas of evaluation / addiction)
Feedback given by the evaluator
42
INTAKE FORM
(Assessment, diagnosis, referral, admission and discharge)
Socio-Demographic Information
Name of the patient
Address &
Telephone No
Registration No:
Date of entry
Sex
Religion :
Age :
Caste :
Educational Qualification:
Occupation:
Illiterate
Primary education
Middle
High /Higher Secondary (equiv.)
Graduate
Post graduate
Training (Diploma etc.)
Never employed
Currently unemployed
Part-time employment
Full time employment
Self-employment
Student
House wife
Pensioner
Others
Income
Marital Status :
Living arrangements:
Never married
Married
Widow / widower
Divorced
Separated
Separated / divorced due to drug use
With family
With friends or distant relatives
Living alone
On the street
Referral by:
Self
Friends
Family
Social worker
Physician
Recovered addicts / their family members
Government hospital
Treatment-cum rehabilitation centre(NGO
Through awareness programme
Any other
43
Name of family member I Support person accompanied the patient:
Address
Telephone No:
Drinking / Drug History
Record all details about alcohol / drugs abused:
Drugs
Depressants
Alcohol,
Tranquilizers,
Sedatives / Hypnotics
Narcotic analgesics
Opium,
Heroin / brown sugar,
Morphine, Codeine,
Pentazocine ,
Buprenorphine
Cannabis
Ganja, Charas,
Bhang
Stimulants
Amphetamine,
Cocaine
Hallucinogens
LSD, PCP
Inhalants
Petrol, Glue
Substance not
classified
Cough syrup,
Anti histamine /
Anti depressant /
Anti psychotic /
Anti cholinegic
Age
of
first
use
Years
of
use
Years of
excessive
use
Specific Route of
type of admini
drugs
stration
Frequency
of use in
the last 6
months
F
Quantity
i
used in
the last 6
months
44
If the client is an IV user, frequency of sharing practices: (indicate Never-N,
Rarely-R, Occasionally-O, Frequently-F)
Sharing practices
Needle
Needle and syringe
Paraphernalia
Drugs
Frequency
Date of last drink I drugs taken:
days ago
Diagnosis:
Drug dependence
Alcohol dependence
Alcohol and drug dependence
Prior treatment for addiction:
Year
Place of treatment
Days / months of
sobriety
Other associated psychiatric complications in the past I present:
Depression
Suicidal ideation / attempts
Confusion
Aggressive outbursts
Hallucinations
Paranoia
Physical problems (record specifically):
Impression of counsellor (for counselling centres):
Denial:
Mild I Moderate / Severe
Motivating factor for present treatment efforts:
Willingness for treatment:
Unwilling / ambivalent / willing
Action taken: Yes / No
Describe details:
45
If referred, name of organisation:
Government De-addiction Centre
NGO Treatment-cum-rehabilitation Centre
Treatment for TB
Treatment for HIV-AIDS
Psychiatric treatment centre
Treatment for any other infections
Any other
Details of treatment received:
Hospital visits of counsellors
Date
Details of visits
Name & Signature of Counsellor (with date):
EMB
CASE HISTORY FORM
(to be used prior to detoxification / after treatment)
Medical history and drug taking history are available in Intake / Medical form.
I. Family History
1. Details regarding parents and siblings (provide relevant information)
II. Childhood and adolescent history
2. How would you describe your childhood I teenage years?
3.
Did you experience the following before the age of 15 years?
Situations
Poverty / severe debts
Early parental loss
Extra marital affairs of parents
Broken home / single parenting
Violence
Any other
Present
Absent
46
4.
Childhood / adolescence (before the age of 15 years)
Behaviour problems
Identified
Childhood &
Adolescence
Present
Absent
Running away from home
Frequent physical fights and violence
Destruction of others’ property
Stealing
Scholastic backwardness
Experimenting with drugs / alcohol
Gambling
Any other
III.
5.
Marital History
Details regarding spouse:
Name
Age
Religion / Community
Education
Occupation
Income per month
Other details about spouse (history of addiction in her family, her addiction
history if any, any other significant event in her life and attitude towards
addiction)
6.
Number of years of marriage :
7.
Details regarding previous or subsequent
marriages, if any
Yes
No
8.
Have you been separated from your spouse
due to your addiction?
If yes, period of longest separation
Yes
No
9.
10.
Is patient suspicious of spouse?
Any instance of violence in the family?
If yes, give details
Under the
Influence of
alcohol/drugs
While
abstinent
Yes / No
Yes / No
Yes
- Physical violence directed towards family members
No
47
- Violent incidents with neighbours and outsiders
- Breaking articles at home
- Verbally abusive
11.
Details regarding children
No. of children
12.
Male
Female
Health status of family
Has there been anyone in your family who has suffered from any of these
problems?
Parents & Siblings
Problems
Yes
Relation
-ship
No
Spouse / Children
Don't
know
Yes
Relation
-ship
No
Major depression
Suicide / attempted
suicide
Psychiatric illnesses
Alcohol dependence
Drug dependence
Any other
13.
Family damage as seen by the counsellor
IV.
Sexual history
14.
Record extra marital experiences
(If unmarried, pre marital)
If present,
Mild / Moderate / Severe
Present Absent
N.A
- Age of partner:
- Is it a sustained relationship?
- For how many years have you known each other ?
- What is the living arrangement?
- Any children
Yes
No
Details
Don't
know
48
15.
Have you been involved in any high-risk sexual activities?
Sex with commercial sex workers
16.
Always
Sometimes
Always
Sometimes
Sex with casual acquaintances
Yes
If yes, did you use condoms
17.
No
Yes
If yes, did you use condoms
Never
No
Never
Have you been tested for HIV?
If yes,
Positive/ Negative
Not willing to reveal
Not collected reports
Not applicable
18.
At present do you have any sexual problems?
Yes
No
Reduced libido
Impotency
Excessive sexual urge
Complete abstinence
Any other
V.
Occupational History
19.
At what age did you start working?
20.
How long have you been working?
21.
Have you received any special award, recognition, merit certificates or
promotions in the past?
22
Did you change your job frequently due to addiction?
Yes
No
23.
Did you have any periods of unemployment?
If yes, for how long and for what reasons?
Yes
No
24.
Occupational damage
Yes
25.
Yes
No
Absenteeism
Warning / memos
Suspension order
Dismissal order
Transfer order
Specify nature of current work:
Loss of pay
Accidents on the job
Attend work under the
influence of alcohol /
drugs
No
49
26.
Occupational damage as perceived
by the counsellor
VI.
Financial History
27.
Moderate
Mild
Details of debts to be cleared:
Severe
Amount
Money borrowed from family and friends
Loans from banks
Loans from place of work
Money borrowed from money lenders
Money for redeeming articles from pawn shops
Outstanding debts at various shops
None
28.
Financial damage as perceived by counsellor
VII.
Legal history
29.
Have you driven a vehicle under the influence of
alcohol / drugs?
If so,
Stopped by police
Arrested / fined
Had an accident (major or minor)
30.
Mild Moderate Severe
Yes
No
Yes
No
No. of times
Have you got into trouble with law for the following?
Assault
Possession of drugs
Pushing drugs I sale and production of alcohol
Any other crime
VIII.
Religious beliefs
31.
Are you a
Believer
Non believer
Indifferent
32.
Do you
Always
Pray at home
Visit temple regularly
Go on pilgrimages
Celebrate festivals
Sometimes
Never
50
33.
Counselling notes (with clients and family / significant members):
Session No. with date
34.
Issues dealt with
Record treatment I recovery plans related to the following areas
♦ alcohol I drug free life
♦ physical well being
♦ healthy relationship with family members
♦ crime free
♦ occupational and financial improvements
35.
Case Summary
(To include demographic details, family of origin, alcohol / drug use history,
medical history, occupational history,
financial situation, marital history,
short and long-term goals).
Discharge details (for de-addiction-cum-rehabilitation centres)
Date of discharge
If extended, reasons for extension
Period of extension
In case of drop out
Date
Reasons for drop out :
o
Poverty, hence not able to stay
♦ Lack of family support
♦
Legal problem
♦ Inadequate facilities
♦ Personal / Any other reasons
♦ (lack of motivation)
THERAPY MANUAL
(for drug awareness and counselling centres)
I.
Guidelines to prepare therapy manual
♦ Schedule I timetable for patients
♦ Rules that need to be adhered to by the patients at the counselling centre
♦ List of re-educative topics - relapse prevention, whole person recovery, coping
skills, improving relationships with family etc. to be included.
♦ Content of re-educative topics for patients
♦ Issues to be dealt with in counselling sessions for patients
♦ Group therapy rules, topics for group therapy and role of therapists
♦ List of re-educative topics for family members
♦ Content of re-educative topics for family members
♦
Issues to be dealt with in counselling sessions for family members
♦ Statement of quality parameters
THERAPY MANUAL
(Treatment-cum-rehabilitation centres)
II. In addition to the above
♦ Rules to be adhered to by the patients
♦ Issues that warrant disciplinary action
♦ Disciplinary measures prescribed by the management
♦ Strategies to deal with relapses - re-educative sessions and their content,
issues to be handled in counselling sessions.
52
NETWORK DIRECTORY
(for various referral services)
Name of the organisation
Address
Phone No
Contact person
Government I Non-government:
Services available
Admission procedures
Time and day of admission
Duration of treatment
Kind of treatment provided
Discharge policy
GROUP THERAPY RECORD FORM - WEEKLY
Date
Level and focus of
Sharing
Attendance
1
2
3
4
5
Participation /
response to
others’
sharing
Observation
and
Signature of
Counsellor
53
MB
FOLLOW-UP CARD
Name of the patient
Address
Referral to
Date /month
Reg.No.
Issues dealt in
counselling
Other forms of
communication - letter,
telephone calls etc.
Status of whole person
recovery
Status of whole person recovery - Half yearly assessment
Areas of improvement
Half
yearly
Half
yearly
Half
yearly
Half
yearly
Alcohol / drug free life
Physical well being
Healthy relationship with family
members
Crime free
Occupational and financial
improvements
Regularity in follow-up and
attendance to self-help groups
Home visits
Date and
month
Date of
patient’s last
visit to the
centre
Reasons for
making home
visits
Issues dealt
during the
visits
Response to
the home
visits
54
LETTER OF ENDORSEMENT FOR FREE TREATMENT SERVICES
Name of patient:
Reg. No.
For counselling services
I,
Mr / Ms
of age
residing
at
(address)
.... have received free of cost counselling / treatment services from (date)
for alcohol I drug addiction. I shall also avail of the follow
to
up services to be provided free of charge by the centre.
| Fortreatment-cum-rehabilitation services
I, Mr/Ms
residing
of age
at (address)
have received free treatment from (date)
to
for alcohol I drug addiction.
I received free treatment which included medical care, essential medicines and
counselling
services at the treatment centre. I shall also avail of the follow-up
services to be provided free of charge by the centre.
Signature of the patient
Date:
Signature of support person
55
Project in charge
Name of the Organisation
DECLARATION-CUM-INDEMNITY
Counselling centres and de-addiction-cum-rehabititation centres
(to be signed by the patient)
I
aged
years,
presently
residing
do hereby solemnly declare and state as under:
1. I have voluntarily and of my own accord admitted myself to the
counselling centres/ de-addiction-cum-rehabilitation facility run by
2.
I state that I have been informed about the entire treatment and medication
in detail and that I also fully understood and am aware of the implications
and consequences thereof.
3.
I am aware of the provisions of the various rules, regulations, bye-laws and
guidelines in respect of any act governing such treatment and medication as
also all laws, rules regulations and guidelines, relating to the same including
the narcotic Drugs and psychotropic Substances Act, 1985, and the Drugs
and Cosmetics Act, 1940, and the rules, regulations and bye-laws framed
thereunder as also all guidelines and notifications pertaining to the same.
4.
I declare and confirm that I have taken upon myself the entire responsibility,
liability, risk and consequences as may arise during or after the said
treatment and medication and that I shall not in any manner and at any time
hereafter hold the said treatment facility, the said
and the
said Trustees I members, as also the staff and representatives liable and or
responsible in any manner whatsoever.
5.
I agree and undertake that I shall from time to time and at all times hereafter
render harmless, indemnify and keep indemnified the said counselling
centres/ de-addiction-cum-rehabilitation facility, and the Trustees / members
as also the staff and representatives and all such other persons lawfully
claiming under them, or any of them or their estates and effects against all
suits, actions, proceedings, claims and demands that may be made taken or
adopted against the said counselling centres/ de-addiction-cum-rehabilitation
facility, their Trustees / members, as also the employees, representatives
and others claiming under them by virtue of them having commenced,
carried out and treated and given medication to me and also from and
against any claim or demand made, taken or adopted by any public body
or authority or by person or persons whatsoever for any act, deed, matter or
56
thing done, committed, omitted, caused, contemplated, purported or sought
to be done by me or by anyone whatsoever under my instructions, direction
during the course of and after the completion of treatment and medications
or otherwise however and shall also indemnify and keeping for me /
indemnified the said counselling centres I de-addiction-cum-rehabilitation
facility, and their Trustees I members, as also the staff, representatives and
all persons legally claiming by and from under howsoever and shall also
indemnify from and against all costs, charges, expenses, damages,
penalties or payments that they or any of them may have to suffer or insure
or be put to by virtue of them or any of them having commenced, carried out,
completed / terminated 0: stopped the said treatment and said medication on
me.
6.
I further agree and undertake that this indemnity shall ensure for the benefit
of the said counselling centres/ de-addiction-cum-rehabilitation facility, their
Trustees / members, the said employees, representatives or any of them
and all persons and parties claiming under them or any of them.
7.
I state that I am aware of all the statements and declarations made by me in
the Declaration-cum-indemnity executed by me on
day of
200 and I hereby confirm and ratify the same. I further state
that I am aware of all the statements, declarations and forms executed/filled
in by me and I hereby confirm and ratify the same.
8.
I further agree and undertake that the statements, undertakings and
indemnities herein contained shall remain in full force and effect for all times
to come for the benefit of the said counselling centres/ de-addiction-cumrehabilitation facility, their trustees I members, the said staff, representatives
and such other persons claiming under them or any of them for all times
hereafter.
9.
I am making this declaration solemnly and sincerely without any force,
coercion or undue influence and the full force and effect should be given to
all the statements and declarations made by me herein above.
Solemnly declared at
this
day of
200
Signature
In the presence of:
1)and
Signature
2)
Signature
57
To
Project in charge
Name of the Organisation
DECLARAT10N-CUM-INDEMNITY
Counselling centres and de-addiction-cum-rehabilitation centres
(to be signed by parents / spouse)
We, (1)aged
2)
years and
years both presently residing at
aged
do hereby solemnly declare and state as under:
1. We
are
the
parents
/
spouses
Smt'
I
guardians
aged
of
Shri
years
I
of
presently residing at
2.
Our son / daughter / spouse has voluntarily and of his/her own accord
admitted himself/herself to the Counselling Centres I De-Addiction-cumRehabilitation Centre run by the
and we are aware of the
same and have granted our consent/approval in that behalf.
3.
We state that we have been informed about the entire treatment and
medication in detail and that we are aware of the same and have granted our
consent/approval in that behalf.
4.
We also confirm that the entire details of the said treatment and medication
have been given in full detail to our son/daughter/ward and that he/she has
fully understood the implications and consequences thereof.
5.
We along with our son I daughter I ward are aware of the provisions of the
various rules, regulations, bye-laws and guidelines in respect of and
governing such treatment and medication as also all laws, rules, regulations
and guidelines touching, relating to the same including the Narcotic Drugs
and Psychotropic Substances Act, 1985 and the Drugs and Cosmetics Act,
1940 and the rules, regulations and bye-laws framed thereunder as also all
guidelines and notifications pertaining to the same.
6.
We declare and confirm that we have taken upon ourselves the entire
responsibility, liability, risk and consequences as may arise during or after
the said treatment and medication and that we shall not in any manner and
at any time hereafter hold the said Counselling Centres I De-Addiction- cumRehabilitation Centre and the said Trustees / members, as also the Doctors,
58
employees, staff, servants representatives liable and/or responsible in any
manner whatsoever.
7.
We agree and undertake that we shall from time to time and at all times
hereafter save harmless, indemnify and keep indemnified the said
Counselling Centres I De-Addiction- cum- Rehabilitation Centre and the
Trustee / members as also the Doctors, employees, staff, agents,
representatives, servants and all such other persons lawfully claiming under
them or any of them or their estates and affects against all suits, actions,
proceedings, claims and demands that may be made taken or adopted
against the said Counselling Centres I De-Addiction- cum- Rehabilitation
Centre, the said Trustees / members, as also the Doctors, employees, staff,
agents, representatives, servants and others claiming under them by virtue
of them having commenced, carried out and treated and given medication to
our son/daughter/ward and also from and against any claim or demand
made, taken or adopted by any Public body or authority or by any person or
persons whomsoever for any act, deed matter or thing done, committed,
omitted, caused, contemplated, purported or sought to be done by us or by
anyone whomsoever under our instructions, directions during the course of
and after the completion of treatment and medications or otherwise
howsoever and shall also indemnify and keep informed/indemnified the said
Counselling Centres / De-Addiction- cum-Rehabilitation Centre, and the
Trustees / members, as also the Doctors, employees, staff, servants, agents,
representative and all persons legally claiming by and from under or in trust
for them or any of them may have to suffer or insure or be put to by virtue of
them or any of them having commenced, carried out, completed/terminated
or stopped the said treatment and said medication or our son/daughter/ward.
8.
We further agree and undertake that this indemnity shall ensure for the
benefit of the said Counselling Centres I De-Addiction-cum-Rehabilitation
Centre, the said Trustees I members, the said employees, staff, agents,
representatives and servants or any of them and all persons and parties
claiming under them or any of them.
9.
We state that we are aware of all the statements and declarations made by
our son/daughter/spouse in the Declaration-cum-lndemnity executed by our
said
son I daughter I spouse on
day or
200
and we hereby confirm and ratify the
same. We further state that we are aware of all the statements, declarations
and forms executed/filled in by our son/daughter/ward and ourselves, and
we hereby confirm and ratify the same.
10.
We further agree and undertake that the statements, undertakings and
indemnities herein contained shall remain in full force and effect for all times
to come for the benefit of the said Counselling Centres I De-Addiction- cumRehabilitation Centre, the said Trustees / members, the said employees,
staff, agents, representatives and such other persons claiming under them or
any of them for all times hereafter.
59
11.
We are making this declaration solemnly and sincerely without any force,
coercion or undue influence and the full force and effect should be given to
all the statements and declarations made by us herein above.
Solemnly declared at
this
day of
200
1)
and
Signature
2)
Signature
In the presence of:
and
1)
Signature
2)
Signature
Acknowledgement
•
The Declaration-cum-lndemnity Bond has been provided by Kripa
Foundation.
60
MEDICAL CASE SHEET
Regn. No.
Date of Registration :
Age:
Name:
aggmi^
Drinking / Drug History (refer Annexure 2)
Previous history
Withdrawal symptoms experienced when the patient stopped
□
□
□
□
□
Alcohol
Drugs
Tremors
Insomnia
Fits
Nausea
Aches / Pains
T remors
Insomnia
Diarrhea
Severe pain
Restlessness
Other psychiatric complications
□
□
□
□
□
□
Depression
Suicidal ideation I attempts
Confusion
Aggressive outbursts
Hallucinations
Paranoid ideas
History of other medical problems in the past
□
□
□
□
□
□
Haematemesis
Jaundice
Abscesses
Bleeding piles
Skin problems
Any other
Chronic health problems
□ Diabetes
□ Liver disorders
□ Epilepsy
□ Respiratory problems - Pulmonary TBI Chronic Bronchitis / Bronchial
asthma
□ Cardiac problems-HBP / IHD / RHD
□ Infections
□ Others
History of previous head injuries, if any
61
Other information
Use of Tobacco products - Smoking I Pan chewing I Others
Knowledge of allergy to specific drugs
Family history of alcoholism / drug abuse / psychiatric illness
Physical condition at the time of admission
Physical examination on the day of admission
Pulse rate
Urine sugar
Blood pressure
Weight
* Tremors
* Jaundice
* Malnutrition
* Lymph nodes
* Loss of body hair
* Clubbing of nails
* Glossitis
* Wasting of muscles * Spider naevi
* Flushed face / excessive sweating * Abscess
* Anemia
* Palmar erythema
* Gynaecomastia
* Pedal Edema
* Injection marks
Record abnormalities, if any, on examination of the following :
Respiratory system
Cardio vascular system
Gastro intestinal system
Nervous system
Medication provided during treatment
Date/
month
Complaints
Medication
Reasons for
continuing / change
of medication
Signed by
physician
Any untoward incident occurred during treatment
If yes, describe the incident
Action taken:
Referral to other organisations
Date of referral:
Need for referral:
Name of the institution where
referral was made
Medical
Psychiatric problems
62
B.P. CHART
Age:
Name:
Reg. No:
Time
Date
B.P.
Pulse
Medication
TEMPERATURE CHART
Name
Month
Diagnosis
Date
Hours
7
F
107
106
105
104
103102
101
100
99
98
97
Pulse :
B.P.
Age
Year
13
19
7
13
19
7
13
19
7
13
19
63
BUI
STOCK REGISTER OF MEDICINES
(pertaining to detoxification and emergency
medical conditions)
Date
Items
Available
stock in No.
Nurse’s signature
—
ATTENDANCE REGISTER
For patients
Name of patient
Date / Present / absent
123456789 10
For family / support person
Name of family member /
support person
Date / Present / absent
123456789 10
IDENTITY CARD
Name of the Organisation and Address
Name of the Patient
Address
Year of Admission
Registration No
64
IHEIE
Administrative Manual - A Manual on the functioning of the organisation
•
•
•
•
•
•
•
•
•
•
•
Vision of the organisation
Milestones in the growth of the organisation
Organisation chart
Functions of the organisation
Registrar of Societies - formalities to be adhered to
Grant application and other relevant material
Contract for renting the premises
Staff details
Staff welfare measures - leave rules, list of holidays
Information about issues like electricity, water, telephone etc.
Code of ethics
Vocational rehabilitation unit- Assessment form of trainees
Reg. No.
Name & Address:
Name of counsellor:
Age:
Education:
Marital status:
Kind of drugs
abused
Years of abuse
Year of treatment
Follow-up
Regularity of follow-up
Regularity for NA / AA
Work experience
Details of any skill training undergone:
Details of past employment if any:
Counsellor's remarks, if any
Reasons for initiation to vocational training:
Period of sobriety
1
EEE3S33E
NETWORKING DIRECTORY - SPECIALISED SERVICES
•
•
•
•
•
Vocational Training Centres
Job placement services
Half way homes / After Care Centres
HIV Rehabilitation Centres
Day Care Centres
Name of the Organisation
Address
Phone No.
Contact person
Services provided
Admission procedure
Charges levied
Any other remarks
CONGRATULATORY LETTER
Dear
Congratulations! You have successfully completed one year without alcohol and
drugs. In addition, you have also made many positive changes in your life after
treatment. All of us here are delighted and send our best wishes for many more
years of sobriety.
Your efforts through follow-up have made it possible for you to stay sober. Your
family members have also extended their support for your recovery. We hope you
will continue these efforts to safeguard your sobriety in the future too.
We would like you to come to the centre and share with the patients who are
currently undergoing treatment. Your experience will provide hope for them and
increase their motivation to recover. This will be a gratifying experience for you.
Do let us know in advance your convenient date so that we can make
arrangements.
Wishing you many more years of sobriety.
With best wishes
Yours sincerely,
COUNSELLOR
66
PROFILE OF THE HOST ORGANISATION
Name of the organisation
Address
Telephone No
Contact person
Year of establishment:
Services provided
Community's perception regarding the
services provided by the organisation
(interview five persons who have
made use of their services)
REGISTER FOR PROVIDING TREATMENT TO PATIENTS
REFERRED BY INDUSTRIES
Name of the patient
Name of the industry
Department where the patient works
Department I individual who referred
the patient
Problems due to addiction in the
area of work
Date of admission
Date of discharge
Type of intervention I treatment provided
Remarks by the counsellor
Date & signature of counsellor
Mental Health Situation In India
Orf
"Since eleven years he is stjjenngjroni menial illness but in these years he never put an\
other physical illness. It is really surprising...not even fever for that mailer... Why does
he live... ? Why doesn 7 he die soon due to some other dreadful illness... ? This is how »’<?
often feel about him " - father of a person with mental illness
Abstract: Mental disorders have profound implications on the health and well being of
not only individuals but also of families and entire communities. The magnitude of the
problem is increasing day by day with the rapid changes in the life style of the present
demanding society. In the process of understanding this paper, we are presenting the
mental health scenario in three levels. Firstly, we are trying to give you the ground
realties behind mental illness. Secondly, we are trying to give you an idea about
available infrastructure and their current situation in terms of human resource, existing
government hospitals and private facilities. Lastly, to acquaint you with the government
initiatives and legislations regarding mental health.
Mental, behavioral and social health problems are an increasing part of
health problems in the world and in India too. Though the burden of illness
resulting from psychiatric and behavioral disorders is enormous; it is grossly
under represented by conventional public health statistics, which lead to focus on
mortality rather than morbidity and dysfunctional. The number of people with
mental illness will increase substantially in the coming decades for following
reasons. First the number of people living in the age groups of risk for certain
illness is increasing because of the changes in the demographic features. Thus
there has been increase in the number of person with mental illness in the age
group of 15- 45 years. Secondly, there has been substantial increase in the'
geriatric population having mental health problems, as the life expectancy is
increasing. Thirdly, overall increase in the rate of depression seen in all age
groups as an effect of changing socio- cultural-economic and political situation.
Mental and behavioral disorders account for 12% of the global burden of
disease. It is estimated that nearly 450 million people suffer from a mental or
behavioral disorders in the world. Nearly 10 % of disability adjusted life years
(DALYs) across all age groups are due to depressive disorders, suicides and
alcohol related problems. Depression ranks third among men and second among
women, yet mental health budgets of most of the countries is less than 1 % of the
'tot'alTiealth expenditure.
The current situation with regard to mental health care is characterized by
(i) very limited mental health care facilities;(ii) grossly inadequate professionals to
provide mental health care; (iii) less than 10% of those needing urgent care are
getting any modern medical care; (iv) families are the current care providers but
with limited support and skills for care; (v) no support schemes for voluntary
organisation; (vi) lack of a regular mechanism for public mental health education;
(vii) limited administrative structure for monitoring the mental health programme
and (viii) limited budget for mental health care as part of the total budget.
Ground realities
1. Demographic characteristics
India is a country with an approximate area of 3287 thousand square
kilometer (UNO, 2001). Its population is 1.081 billion and the sex ratio (men per
hundred women) is 106 (UNO 2004). The literacy rate us 68.4 % for men and
45.4% for women. The proportion of population under the age of 15 years is 32
% and the proportion of population above the age of 60 years is 8%. The life
expectancy at birth is 60.1 years for males and 62 years for females. The healthy
life expectancy at birth is 53 years for males and 54 years for females.
2.
Prevalence:
A majority of the classical psychiatric epidemiological studies in the last four
decades have been population based, focusing on general psychiatric morbidity
in a small to medium population. A conclusion arrived at from these house-tohouse surveys:
o It is estimated that 1 percent of the population suffers from severe mental
disorders
o Ten percent of the population is reported to have common mental
disorders.
® The reports also reveals that 15-20 % (in some studies it is 40 %) of the
people approaching primary health care centers, general hospitals or
private clinics for general health problems requires psychiatric assessment
and evaluation. But most of them are not aware of it. They think and
believe that they have some physical illness, and take various methods of
treatment for relief, often in vain.
If we project this figure in our country, there would be little more than 10 million
population suffering from severe mental illness, and the figures for common
mental disorders will be 10 times to that of severe mental illness.
3. Treatment
Mental health care has always been influenced and determined by contemporary
beliefs, and India is no different. Traditionally, mentally ill people were often
cared in temples and religious institutions, based on the principles that mental
illness is a form of spiritual affliction and could thus be cured by religion.
Superstition with inadequate mental health services in the community makes
people with mental illness to subject to various harmful treatments, they are
subjected to black-magicians, village quacks and witches and physical abuse in
the name of treatment. They are kept outside the margin of the community
meaning chained, locked in the rooms, wandering in the streets, staying for ever
in closed wards of asylums, hospitals, etc.
Stigma and discrimination:
A large section of people with mental illness are still inside their houses
without any treatment, because their family members don’t recognize the illness
4.
or they find it embarrassing to be recognized as family member of mentally ill
who are commonly called as 'mad'. There is a fear that they would be victims of
disgrace and indignity and thereby they loose the status or acceptance they
enjoy in the community. The stigma is so tremendous, people feel ashamed and
deny the illness. Therefore, the first and foremost element that shrouds the realm
of mental illness is stigma attached to it. The very thought of some one in the
family getting mental illness is a big shock and they do not want to believe it.
Due to stigma attached to the families, people with mental illness become
the victims of discrimination and human rights abuse. The discrimination is seen
from the family members and goes right up to the policy makers and state
authorities. The attitude of the public is that, who care what we do for people
with mental illness. People with mental illness have been treated as second-class
citizen with no adequate facilities given either the state or the central
government. As a result they face chronic ill health, and are an economic &
social burden to the community leading to social destitution. Soon families loose
hope and are left to the mercy of others.
5. Legal discrimination:
As per the law, a person with mental illness cannot sign any documents
of sale, purchase, lease or any contract The act is silent on these issues during
the lucid moments/stabilized stage. Family members, mostly brothers, take
undue advantage of this clause to deny the property rights to the person with
mental illness; end up with ensuring the chronic mental illness, so that the socalled sane siblings enjoy the property.
Marriage and Divorce Act also permits legal separation of life partners if
one of them is found to be mentally ill (certified by a psychiatrist). Generally in
rural communities men are permitted to marry for the second time if his first wife
is suffering from any disease like mental illness, epilepsy and etc. On the other
hand if a married man becomes mentally ill, community insists wife to be
caregiver and undergo all the problems. If a family has person with mental
illness, eligible boys and girls getting life partner is almost next to impossible
because of the stigma and is seen as a family illness. There are occasions where
they hide the information and after marriage, problems erupt. It is also common a
close relative getting pressurized to marry such a person.
Poverty and mental illness
Poor people with mental illness are not only vulnerable due to their
condition, but also the vulnerability brought about by poverty, which is a
consequence and to some extent cause of their condition. One of the main
reasons that people find it hard to accept people with mental illness as equal
members of their communities is that they do not see them as capable of
contributing to the household or the community. For decades, researchers have
known that poverty and mental illness are correlated; the lower a person's
socioeconomic status, the greater his or her chances are of having some sort of
mental disorder. Yet determining if one comes first - if being poor renders a
6.
person more susceptible to mental illness, or if mental illness pulls a person into
poverty - is decidedly difficult and the relationship between poverty and mental
health has long been assumed to be interactive.
Available infrastructure and their status
The major changes in mental health scenario began_with the tragedy at
Erwadi, the asylum fire in the Ramanathapuram district of Tamilnadu, it was a
disaster which opened the eyes of policy makers and the general public to attend
to the needs and voices of people with mental illness. During the last 50 years,
the place of mental health as part of the general health has changed to some
extent. From a situation of no organized mental health care at the time of
independence, currently mental health issues are seen as part of the public
agenda in few places all the credit goes to judiciary intervention. I
Regional disparity
The state run health care system in India is striving hard to overcome the
regional disparity between rural and urban. The adequate health services and the
normal health standards in rural areas seem to be much below the average.
Cities and big towns are growing with private health care facilities catering to the
needs of middle class and rich communities. The costs for diagnosis and
treatment are so exorbitant that some get into debt traps. In rural areas hardly
any facilities exist and the attitude of the government health professionals is not
at all patient friendly. When people are losing faith in the government health care
system, we can imagine what will be the fate of mental health care in India. The
budgetary allocation for mental health is very meager, most of it goes to
maintenance of hospitals and a very little portion for treatment.
A.
in paper mental health has been stated as part of primary health care
system. But in reality, primary health centers are not equipped to treat people
with mental illness in their centers. Only few primary health centers (DMHP
programme has been implemented) are providing mental health care and
treatment in the community.
B.
Mental health professionals:
We have limited facilities to train human resource in mental health. The
irony is that all this centers have become centers to export trained people
abroad. Many mental health professionals are immigrating to other developed
countries, where jobs are more lucrative. For instance in 2003 itself, more than
82 psychiatrist sought short term and long term employment in the United
Kingdom in response t the latter’s international recruitment drive.
Undergraduate training in psychiatry is not changing in spite of many
efforts and this continues to be a major barrier to create medical doctors
adequately trained in psychiatry after their basic training.
Some of the government and private medical colleges do not have the
oepartments of psychiatry in its full strengths to train the young medical
graduates in psychiatry,
The inadequacy of mental health human resource is a major barrier in
caring for people with mental illness in the community. Even most of districts
don’t have public sector psychiatrists. Comparatively mental health professionals
are more in the states of Kerala and Tamilnadu. Very few mental health
professionals are based in rural areas, most states allow public sector
psychiatrist to have private clinics.
Availability of mental health professionals for entire country:
Number of psychiatrist per 100, 000 population
Number of psychiatric nurses per 100,000 population
Number of psychologist per 100,000 population
0.2
0.05
0.03
Infrastructures available
Most of the district hospitals are not fully equipped and supplied with
psychiatric medicines to treat people with mental illness; most often they are
referred to multi specialty centers in the capitals/big towns. The medical
professionals view mental health as an alien subject and do not give importance
to either learn or practice in their day to day practice.
C.
There are 42 mental hospitals in the country with the bed availability of
20,893 in the government sector and another 5096 in the private sector hospital
settings to take care of an estimated 1,02,70,165 of people with severe mental
illness and 5,12,51,625 of people with common mental disorders needing
immediate attention.
The psychiatric medicines nave been supplied only in few primary health
centers, community centers anc the district hospitals, amitriptyline, lithium,
chlorpromazine (CPZ),
phenobarbital, phenytoin sodium, haloperidol,
carbamazepine, imipramine and risperidone is made available in few district
hospital. The rates of resperidone (oetter drug than CPZ in terms of side effects)
is cheaper then CPZ. Drugs like CPZ have been purchased in surplus, which
has lesser utility (eg- in Karnataka). Adequate laboratories facilities are lacking in
the district hospitals to find out the serum level for lithium administration. None of
these drugs are routinely distributed by government to the primary health centers
except in some districts, where DMHP is operational.
Child guidance and rehabilitative services are available only in mental
hospitals and in big cities, it is not felt important to cascade down so that the
services are decentralised.
One third of the mental health beds are in the state of Maharastra and
several states do not have mental hospitals. Some mental hospitals have more
than "1000 beds and several still have a large proportion of long stay patients
During the past two decades, many hospitals have been reformed through the
intervention of the voluntary organizations, media, national human rights
commission and judiciary.
Availability psychiatric beds
Total psychiatric beds per 10,000 population
Psychiatric beds in mental hospitals per 10,000 population
Psychiatric beds in general hospitals per 10,000 population
I Psychiatric bedsjn other settings per 10,000 population
0.25
0.2
0.05
0.01___________
The survey of 37 mental hospitals conducted between November 2001
and January 2002 revealed a dismal picture, apart from poor infrastructure, the
most glorious defiencies are in the area of qualified staff. Some mental hospitals
do not have even a single psychiatrist on their permanent roster.
Inadequate
Number
%
25
67.6
SI No
Facilities
1
2
3
4
5
6
7
8
Infrastructure
Adequate
Number
%
12
32.4
Staff
10
27
27
Clinical services including investigations
16
43.2
21
Availability of medicines and treatment modalities
28
75.7
9
24.3
73
56.8
Quality of food
23
62.2
14
37.8
Availability of clothing and linen
15
40.5
22
59.5
Recreational facilities
18
48.6
19
51.4
Vocational rehabilitation facilities
14
37.8
23
62.2
D.
General hospital psychiatry:
It is speculated that the birth of general hospital psychiatry in India was
due to lack of sufficient funds to open more mental hospitals. These new units
needed mobilization of very few resources like a little space in an already
functioning hospitals and few mental health professionals to manage the people
with mental illness. What started, probably as an economic necessity, has now
become a major force in the delivery of health care. A provision for establishment
of inpatients wards for people with mental illness requiring admission has been
provided in the mental health act. It has to be noted that the psychiatric units in
the general hospitals are not well established, and able to take care of psychiatric
problems associated with other illnesses.
E.
Private psychiatry:
it is interesting to note that very large numbers of private psychiatrist have
located themselves in cities which are district headquarters but are not the state
capitals. The reason could be that most state capitals have medical college
departments of psychiatry or some other governmental psychiatric facility and a
private psychiatric facility would be more welcoming in other cities of state where
no such facility exists. It seems that distribution of private psychiatrist in India is
some what related to the position of the states in socioeconomic hierarchy. Thus
a relatively prosperous and educated states of west and south India (Kerala,
Tamilnadu) has highest number of psychiatrist. North zone has proportionately
less number with exception from Punjab and Delhi. States of central and east
zone have the least number of psychiatrists in private practice.
Mental health financing:
The country spends 2.05% of the total health budget on mental health.
The primary sources of mental health financing in descending order are tax
based, out of pocket expenditure by the patient or family, private insurance and
social insurance. Government fund for health services are provided both by the
states and the center. In the 10th five-year plan estimates; mental health
constitutes 2.05% of the total plan outlay for health. The country has disability
act, which has included mental illness as 7th disability, in reality people with
mental illness are not availing any benefits under disability schemes.
F.
Non governmental organization:
NGOs are involved with mental health in the country. They are mainly
involved in advocacy, promotion, prevention, treatment and rehabilitation. NGOs
are involved in counseling, suicide prevention, training of lay counselors, and
provision of rehabilitation programmes through day care, sheltered workshops,
halfway homes, hostels for recovering patients and long term facilities. There are
also self help groups of parents and people with mental illness which has been
recently established. It has to be noted that most of the NGOs have their setups
and outlets in the urban areas catering to the needs of middleclass and upper
economic groups.
G.
Policy and legislation
National Mental Health Programme (NMHP) 1982
The National Mental Health Program is the outcome of the developments
in providing mental health care through different methods as well as the overall
goals of the health care in general. The first concerted efforts to formulate a
national program were held in July 1981. On August 2 1982, a small group of
experts met to consider the revised document and finalize the same. This
document was presented to the central council of health and family welfare and
the committee recommended the NMHP for implementations.
A.
The objectives of the program are:
> To ensure availability and accessibility of minimum mental health care for
all in the foreseeable future, particularly to the most vulnerable and
underprivileged of the population
> To encourage application of mental health knowledge in general health
care and social development.
> To promote community participation in mental health services
development and to stimulate effort towards self -help in the community.
H ie specific approaches suggested for the implementation of the NMHP are:
z- Diffusion of mental health skills to the periphery of the health service
system
> Appropriate appointment of tasks in mental health care.
> Equitable and balanced territorial distribution of resources
> Integration of basic mental health care with general health services
> Linkage to community
Progress of the NMHP:
From the time of the formulation of the NMHP in August 1982, in the last two
decades the following initiatives and activities have been taken up in districts
where the district mental health programme been implemented:
> Sensitization and involvement of state level programme officers
> Workshops for voluntary agencies
> Workshops for mental health professionals namely psychologists,
psychiatric social workers, psychiatric nurses
> Training programmes in public mental health for programme managers > State level workshops for the health directorate personnel, development of
models of integration of mental health into primary healthvinto primary
health care up to the level of district
> Preparation of support materials in the form of manuals, health records for
different types of health personnel and health education materials
> Training program for teachers pf undergraduate psychiatry,
> Initiation of district mental health programme in 28 districts of 22 states
> Expansion of district mental health programme for 100 districts with the
budgetary allocation of 190 corers in the 10th five year plan.
The District Mental Health Programme (DMHP)
The DMHP, which operates as part of the National Mental Health
Programme was launched in 1996-97 in four districts. By 2000 the DMHP was
extended to 22 districts in 20 States and Union Territories and by 2002 the
DMHP further extended to 27 districts in 22 States and Union Territories,
providing for services to over 40 million of the population. In the current 10th plan
period (2003 - 2007) the government has announced the programmes extension
to 100 districts across the states, with a total budget outlay of 200 Core rupees
B.
Barriers to reach the goals set out in the in the 1982 document have been many.
The goals were too ambitious to begin with and sufficient attention was not paid
to all aspects of implementation of NMHP. The first and foremost barrier has
been the lack of funding. Though NMHP came up in 1982 the subsequent three
five years plans did not make adequate funding allocation. Further even the
funds allotted were not fully utilized. It was only in the 9th Five-year plan that a
substantial amount of Rs 28 cores was made available and it is projected in the
10th Five-year plan to be Rs 190 cores.
The critical review of District Mental health programme reveals that
Lack of administrative clarity to utilize the allocated funds, The
programme looked good on paper, but was extremely unrealistic in
its targets, especially considering the available resources of
manpower and funds for its implementation.
b.
The approach was top down and did not take into consideration the
ground realities. The poor functioning of the primary health care in
India in general as well as the poor morale of the health workers
not taken into account. A structure that was attending to given tasks
so inadequately would certainly be unable to absorb new targets of
integration.
c.
The DMHP continues to be the extension of professionals rather
than integration of mental health with primary care
a.
Central Government has sanctioned DMHP in 100 districts in year 2004,
the districts are yet to implement the programme and appoint required mental
health professionals for the programmes. It has to be noted that few districts do
not have psychiatrist and the facilities in the district hospital to support the mobile
team of district mental health programme.
National Health Policy- 2002
The 2002 health policy refers twice to mental health. In its assessment of
the current scenario Section 2.13 states that:
‘Mental health disorders are actually much more prevalent than is
apparent on the surface. While such disorders do not contribute significantly to
mortality, they have a serious bearing on the quality of life of the affected persons
and their families. Sometimes, based on religious faith, mental disorders are
treated as spiritual affliction. This has led to the establishment of unlicensed
mental institutions as an adjunct to religious institutions where reliance is placed
on faith cure. Serious conditions of mental disorder require hospitalisation and
treatment under trained supervision. Mental health institutions are woefully
deficient in physical infrastructure and trained manpower. NHP 2002 will address
itself to these deficiencies in the public health sector’.
C.
Section 4.13 states the policy prescription towards mental health:
'NHP 2002 envisages a network of decentralized mental health services
for ameliorating the more common categories of disorders. The programme
outline for such a disease would involve the diagnosis of common disorders, and
the prescription of common therapeutic drugs, by general duty medical staff.
The proposed National Mental Health Policy outlines the prioritized
agenda for extending within a pragmatic time frame basic mental health care
facilities to all sections of the populations across the country by the year 2020.
D.
Legislations related to mental health:
The Mental Health Act of 1987 and the Persons with Disabilities Act 1995
are the two legislations that are directly applicable to people with mental illness.
The Mental Health Act (MHA). 1987" ••
Mental Health Act is “an act to consolidate and amend tne law relating to
the treatment and care of mentally ill persons, to make better provision with
respect to their properly and affairs and for matters connected therewith or
incidental thereto”. In the Mental Health Act, 1987, a modest attempt has also
been made to bring mental illnesses on par with physical illnesses, thus
reducing the stigma attached to mental illnesses
It is not simply a. cosmetic improvement over the out dated Indian Lunacy
Act 1912, but represents the conclusion of lengthy presentation by the Indian
psychiatric society to the Government of India. This Act came into force in April
1993, as per the Government of India order, even though it is still in hibernation
in some states. The establishment of mental health authorities, both at the center
and state is a welcome step. These authorities are expected to act as friend,
philosopher and guide to the mental health services. Provisions have been made
for establishing separate hospitals for children under the age of 16 years; for
people abusing alcohol and other drugs and for other special groups. Emphasis
on outpatient care has been made to safeguard the human rights of the mentally
ill person. Stringent punishment has also been lead for those who subject the
mentally ill to physical and mental indignity within hospitals.
The notion of care in the community has not been addressed in the
current legislation. No effort has been made to provide after care services for the
discharged patients. There is no thinking over the alternative to hospital care.
Authorities are using the clause of the act leading to many medico-legal
problems, and difficulties for the private nursing homes.
The ground realities of its implementation:
The mental health act has not been implemented in Arunchalpradesh,
Chattisgarah, Utaranchal, Bihar, and Orrisa
State Mental health Authority has not been constituted in Arunchal
pradesh, Chattisgarah, Uttaranchal, Bihar and Orrisa.
Mental health rules have been framed only in Goa, Manipur, Sikkim.
Assam, Chandigarah, Delhi, Gujarath, Madyapradesh, Mizoram, and
Tamilnadu,
The Persons with Disabilities (Equal Opportunities. Protection of Rights and Full
Participation) Act 1995:
PWD act came into force on February 7, 1996. This law is an important
landmark and is a significant step in the direction of ensuring equal opportunities
for people with disabilities and their full participation in the nation building. The
Act provides for both preventive and promotional aspects of rehabilitation like
education, employment and vocational training, job reservation, research and
manpower development, creation of barrier-free environment, rehabilitation of
persons with disability, unemployment allowance tor the disabled, special
insurance scheme for the disabled employees and establishment of homes for
persons with severe disability etc. There are also statutory bodies for
implementing the Act at central and state levels.
Even though it is welcoming, that people with mental illness have been
considered as disabled in the act, the later chapters of the act does not talk about
any provisions to be given or set aside for people with mental illness. The act
does not assure right to treatment and make financial provision for the purchase
of the psychiatric medicines.
While there is much talk about the implementation or lack of implementation
of the Act, there is little understanding about the indicators to measure the level
of implementation. At present, conducting a session on the Act or putting up
posters on the Act, are referred to as ‘advocacy’. A clearly defined set of
indicators for the implementation needs to be worked out. There is also a great
need to come up with strategies to decentralize the implementation of the Act at
the District/Taluk and village level.
The rate of mental illness is increasing cutting across rich/poor, urban/rural.
Though it seems like the states are taking notice of the gravity of the issue and
attempts to address the needs of people with mental illness, let us be clear that,
this lukewarm response is because of the pressure from the judiciary. Health
including mental health is a fundamental right. Millions in India perhaps, don’t
know that it is their right to avail treatment. People with mental illness are crying
"my name is today” Do we hear his/her voice?.
T- M- £■&■!>
NATIONAL CENTRE FOR DRUG ABUSE PREVENTION (NC-DAP)
INTRODUCTION
* The NC-DAP was set up in NISD in September 1998, in lieu of the existing
Bureau of Drug Abuse Prevention to strengthen and provide Technical inputs
to the Government of India’s Programmes on Drug Abuse Prevention.
VISION STATEMENT
•
Empowering Communities for Drug Abuse Prevention
AIMS AND OBJECTIVE
* Raising the competency standards of the functionaries / Raising’ the
competency standards of the functionaries I personnel working in de
addiction centres ztnd other related sectors.
a
Invigorating efforts for preventing or minimizing any anticipated or
consequent harm related to drug abuse in clients and in the community.
a
Standardization of care-in drug abuse prevention.
a
Updating information and creating a database on extent and pattern of
drug abuse and its various interventions at local, regional and international
levels.
| Developing standards of monitoring systems of various interventions.
ACTIVITIES
❖ Capacity building of various levels of functionaries working in the field of Drug
Demand Reduction.
❖ Up-gradation of information and establishment of appropriate database and
monitoring systems.
❖ Development of linkages and networking arrangements in the field of Drug
Demand Reduction at local, regional, national and international levels.
TRAINING INITIATIVES BY NC-DAP
Instituted three month certificate course on De-addiction Counselling &
Rehabilitation and 5 day short-term training courses.
<b Developed 12 short-term training manuals in collaboration with expert NGOs.
Established 3 Regional Resource Training Centres in Collaboration with
UNDCP.
SHORT-TERM TRAINING MANUALS
v VVVv V
> Symptomatic Behaviour & Addictive Personality
> Counselling issues and process
> Rehabilitation & Relapse Prevention - Issues and Modalities
> Prevention and Management of Drug Abuse and HIV / AIDS
> Organisation of Self-help Groups
> Preventive Interventions for High Risk Groups
Patient profiling, recording and documentation
Research, RAS & Monitoring of Trends of Drug Abuse
Programme Management for Families and Codependency of Addicts
Treatment and Rehabilitation of drug addicts in Prisons / correctional settings
Training for Youth Coordination of NYKINSS
Workplace prevention
ACHIEVEMENTS
•
Three month certificate courses on De-addiction Counselling & Rehabilitation
•
21 short-term training courses based on the developed training manuals
FUTURE ACTION PLAN FOR YEAR 2001
The centre intends to organise the following training courses:
1.
6 Three month certificate courses at national and regional level
2.
50 short-term training courses based on the 12 training manuals
3.
courses for Training of Trainers
4.
management Development Programmes for the Management / executive
members of NGOs
5.
orientation on DAMS and subsequent implementation of the activity
WHAT CAN YOU DO?
O Respond promptly in deputing participants for the courses
O Ensure the eligibility criteria of NC-DAP for the participants, are maintained
□ Give regular feedback / suggestions
0 Suggest specific subject / issues to be included in training initiatives
O Cooperate in follow-up activities
ELIGIBILITY CRITERIA
❖ Minimum one to two years experience in the field of Drug Abuse Prevention
and Rehabilitation
❖ Should not have attended any training course organised by this institute
❖ Should be working as Project Director / Officer, Senior Counsellor, Medical
Officer / Doctor and Social Worker having basic knowledge of addiction
rehabilitation.
❖ Participant should be highly motivated towards the cause and likely to stay in
the organisation for a minimum period of one to two years.
❖ Should have good communication skills and able to write, read, speak and
understand English.
❖ Participant should be prepared to stay continuously for full three months
without any absenteeism.
❖ The nominee should be below 50 years of age.
CONTACT US FOR FURTHER INFORMATION:
M. Sunil Kumar, Lecturer
National Center for Drug Abuse Prevention (NC-DAP)
National Institute of Social Defence (NISD)
West Block-1, Wing 7, Ground Floor
R.K. Puram, New Delhi 110 066
Tele/Fax: 011-6173257
E.mail : nc_dap@excite.com & agerawl@bol.net.iji
- * 1 a'J'«■ 1 ^iTMHlUT.iEH
Thirteen Principles of Effective Drug
Addiction Treatment v •
fX f\ ore than two decades of scientific research have yield
fl ▼ ■ ed a set of fundamental
principles that characterize effective
drug abuse treatment.These 13 princi
ples. which are detailed in NIDA'S
new research-based guide. Principles
of Drug Addiction Treatment: A
Researcb-based Guide, are:
1. No single treatment is
appropriate for all individuals.
Matching treatment settings, interven
tions. and services to each patient's
problems and needs is critical.
2. Treatment needs to be read
ily available.Treatment applicants can
be lost if treatment is not immediately
available or readily accessible.
3. Effective treatment attends
to multiple needs of the individual.
not just his or her drug use.Treatment
must address the individual's drug use
and associated medical, psychological.
social, vocational, and legal problems
*i. Treatment needs to be
flexible and to provide ongoing
assessments of patient needs, which
may change during the course of
treatment.
5. Remaining in treatment
for an adequate period of time is
critical for treatment effectiveness.
The time depends on an individual's
needs. For most patients, the threshold
of significant improvement is reached
at about 3 months in treatment.
Additional treatment can produce fur
ther progress. Programs should include
strategies to prevent patients from
leaving treatment prematurely.
6. Individual and/or group
counseling and other behavioral
therapies are critical components
Volume 14, Number 5
NIDA NOTES
of effective treatment for addic
tion. In therapy, patients address
motivation, build skills to resist drug
use. replace drug-using activities
with constructive and rewarding
nondrug-using activities, and
improve problem-solving abilities.
Behavioral therapy also facilitates
interpersonal relationships.
7. Medications are an impor
tant element of treatment for many
patients, especially when combined
with counseling and other behavioral
therapies. Methadone and levo-alphaacetylmethadol (LAA.M) help persons
addicted to opiates stabilize their lives
and reduce their drug use. Naltrexone
is effective for some opiate addicts and
some patients with cooccurring alco
hol dependence. Nicotine patches or
gum. or an oral medication, such as
bupropion, can help persons addicted
to nicotine.
8. Addicted or drug-abusing
individuals with coexisting mental
disorders should have both disor
ders treated in an integrated way.
Because these disorders often occur in
die same individual, patients present
ing tor one condition should be
assessed and treated for the other.
9. Medical detoxification is
only the first stage of addiction
treatment and by itself does little to
change long-term drug use. Medical
detoxification manages the acute phys
ical symptoms of withdrawal. For some
individuals it is a precursor to effective
drug addiction treatment:
10. Treatment does not need
to be voluntary to be effective.
Sanctions or enticements in the fami
ly, employment setting, or criminal
justice system can significantly
increase treatment entry, retention,
and success.
11. Possible drug use during
treatment must be monitored con
tinuously. Monitoring a patient's drug
and alcohol use during treatment, such
as through urinalysis, can help the
patient withstand urges to use drugs.
Such monitoring also can provide
early evidence of drug use so that
treatment can be adjusted.
12. Treatment programs
should provide assessment for
HIV/AIDS, hepatitis B and C,
tuberculosis and other infectious
diseases, and counseling to help
patients modify’ or change behaviors
that place them or others at risk of
infection. Counseling can help
patients avoid high-risk behavior and
help people who are already infected
manage their illness.
13. Recovery from drug addic
tion can be a long-term process and
frequently requires multiple episodes of
treatment. As with other chronic illness
es, relapses to dnig use can occur during
or after successful treatment episodes.
Participation in self-help support pro
grams during and following treatment
often helps maintain abstinence.
Principles of Drug Addiction
Treatment: A Research-based Guide
(NCADI publication BKD347) has been
mailed to NIDA NOTES subscribers in
the U.S. Copies of the booklet can be
obtained from the National
Clearinghouse for Alcohol and Drug
Information, P.O. Box 2345, Rockville,
MD 20847. 1-800-729-6686.The guide
also can be downloaded from NIDA'S
home page at www.drugabuse.gov. CE
15
NIDA NOTES
Editor David Anderson. Editor. Public Information and Liaison Branch. Office ofScience
Policv and Communications
Managing Editor Margi Grady. MasiMax Resources. Inc.
Associate Editor: Barbara Cire, MasiMax Resources. Inc.
Editorial Board: David Anderson, Cochain Editor. Public Information and Liaison Branch.
Office of Science Policy and Communications
Beverly Wvckon Jackson, Cochair Chief. Public Information and Liaison Branch. Office of
Science Policy and Communications
Khursheed Asghar, Ph.D, Chief. Basic Sciences Review Branch. Office of Extramural
Program Review
Roger Brown, Ph.D-, Chief. Behavioral Neurobiology Research Branch. Division of
Neuroscience and Behavioral Research
|.C. Comolli, Public Health Advisor. Center on AIDS and Other Medical Consequences of
David Conrad, Program Analyst Planning and Financial Management Branch. Office of
Planning and Resource Management
Leslie Cooper. Ph.D., R.N., Nurse Epidemiologist, Division of Epidemiology, Services. an<
Prevention Research
Lee Cummings, Special Assistant to the Director, Division of Treatment Research and
Development
Bennett Fletcher, Ph.D., Chief. Services Research Branch, Division of Epidemiology.
Services, and Prevention Research
Robin Mackar, Office of Science Policy and Communications
Wallace Pickworth, Ph.D., Pharmacologist. Intramural Research Program
Vincent Smenglio, Ph.D., Research Psychologist, Center on AIDS and Other Medical
Consequences of Drug Abuse
Frank Vocci, Ph.D., Director, Division of Treatment Research and Development
Cora Lee Wetherington, Ph D., Psychologist. Behavioral Sciences Research Branch.
Division of Neuroscience and Behavioral Research
Staff Writers: Robert Mathias and
Patrick Zickler, MasiMax Resources. Inc.
Contributing Writers: Steven Stocker and
Ravmond Vansco. ROW Sciences. Inc.
Design/Layout: Ken Lostoski.
ROW Sciences. Inc.
NIDA
NATIONAL INSTITUTE
ROW Sciences. Inc., under Contr,
DEPARTMENT OF
HEALTH & HUMAN SERVICES
National Institutes of Health
National Institute on Drug Abuse
6001 Executive Boulevard
Room 5213
Bethesda, MD 20892-9561
Official Business
Penalty for Private Use S300
NTH Publication No. 99-3478
Printed December 1999
NIDA NOTES covers drug abuse research in the areas of treat
ment and prevention, epidemiology, neuroscience, behavioral
science, health services, and AIDS.The publication reports on
research; identifies resources; and promotes communication
among clinicians, researchers, administrators, policymakers, and
the public. Readers are encouraged to identify subject areas they
would like to see highlighted.
:
ON DRUG ABUSE
I
I
j
NIDA NOTES is a publication of the U.S. Government produced
by the National Institute on Drug Abuse. Use of funds for print
ing this periodical has been approved by the Director of the
Office of Management and Budget. Except for material specifical
ly identified as copyrighted, all materials appearing in NIDA
NOTES are in the public domain and may be reproduced with
out permission. Citation of the source is appreciated.
Subscriptions and Changes of Address
To subscribe free to NIDA NOTES, or to change the addre^fck
your current subscription, contact the NIDA NOTES
Subscriptions Department at:
MasiMax Resources, Inc.
1375 Piccard Dr., Suite 360
Rockville, MD 20850
Fax: 240-632-0519 E-mail: nidanotes@masimax.com
Additional Copies
To order additional copies of NIDA NOTES, contact:
National Clearinghouse for Alcohol and Drug Information
P.O. Box 2345
Rockville, MD 20847-2345
Phone: 800-729-6686 or 301-468-2600
TDD number: 800-487-4889
Fax: 301-468-6433 E-mail: info@health.org.
FIRST-CLASS MAIL
POSTAGE AND FEES
PAID
DHHS/NIH
PERMIT NO. G-827
- Media
 _MH_2_B_PART_2_SUDHA.pdf
_MH_2_B_PART_2_SUDHA.pdf
Position: 1383 (8 views)