alcoholism
Item
- Title
- alcoholism
- extracted text
-
I.
RF_MH_2_C_SUDHA
n
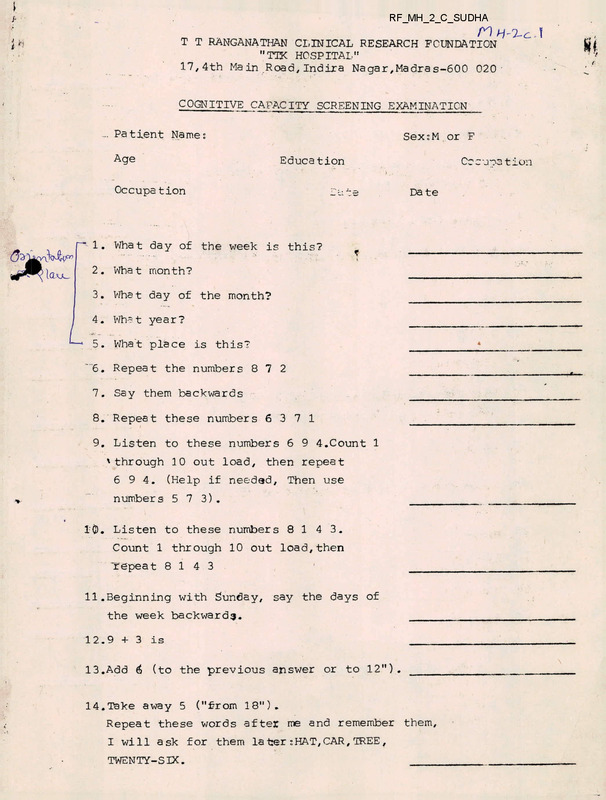
T T RANGANATHAN CLINICAL RESEARCH FOUNDATION
”TTK HOSPITAL”
17,4th Main .Road, Indira Na gar, Madras-600 020
COGNITIVE CAPACITY SCREENING EXAMINATION
**“"^***—*^^“* ■“
“•
*“
**■ ■■
-■
■
IT - ■
1-*■
-‘I-.-.-.
!■ -r LI
--- -
■■! —■U IIIJF -
Patient Name:
Age
|--J—
Sex:M or F
Educa tion
Occupation
~cte
Co c'joa t ion
Da te
1. What day of the week is this?
2. What month?
3. What day of the month?
4. What year?
5. What place is this?
'6. Repeat the numbers 8 7 2
7. Say them backwards
8. Repeat these numbers 6371
9. Listen to these numbers 6 9 4.Count 1
'through 10 out load, then repeat
694. (Help if needed. Then use
numbers 573).
1©. Listen to these numbers 8143.
Count 1 through 10 out load,then
repeat 8143
11.Beginning with Sunday, say the days of
the week backward^.
12.9 + 3 is
13.Add 6 (to the previous answer or to 12").
14.Take away 5 ("from 18”).
Repeat these words after me and remember them,
I will ask for them la ter : HAT, CAR, TREE ,
TWENTY-SIX.
------------------------------------
I
2
15.The opposite of fast is slow.The opposite of up is
16.The opposite of large is
17.The opposite of hard is
18.An orange and a banana are both fruits.Red
and blue are both
19.A penny and a dime are both
<-
20.What were those words? I asked you to remember ? (HAT)
21. (CAR)
22. (TREE)
23. (TWENTY-SIX)
24. Take away 7 from 100, then take away 7 from
what is left and keep goings 100 - 7 is
25. Minus 7
— ./_
26. Minus 7 (write down answers; check correct
subtraction of 7)
27. Minus 7
28. Minus 7
29. Minus 7
30. Minus 7
TOTAL CORRECT (maximum score = 30)
MH - 2-c.
■i k
T T RANGANATHAN CLINICAL RESEARCH FOUNDATION
IV MAINROAD, INDIRA NAGAR. CHENNAI 6QQ 020
V
Daze
■‘
Age:
Name.:
V-'
" ’ * yoan
Xrvte<e^X
AtaZemenZ&
Zntended to ZndZcate
c4-oZZowZng
................ J one
___ .trn. : - '
_ ZnXeZZZ§enee^
7 «P O 1
•f-n A.+ dh/i
/hi
on
Xe^X
anct
Xbexe
cute no
and aZtZtudez, Ttuz 'Zz riot.at
Hw.
abound
the.
nZght ■■and'-^*^ongAlhh^t^'^'<
”
F**
J
x4
tt
I#-<
c.oMe>6ponxl>cng
you <uia not '^unjet guje^M. u
The
1.
TAwe/VaZ^e,
•
I o^Xen geX /ted 4paU oa my n&ch
TJiue/FaC-Aa
Xa be p/toXeed by my
3.
I enjoy many dZ^enent kZndz o^ pZay
and neeneaZZon.
Tjum/
•1'i -"■• •'•
I have neven ^aZnted on ZeZt ZZhe ^aZntZng
Tjuxe/Fotae
I FuLve. UAed. aZc-otioJt. eJUCM^ve^y
TJtue./Fa£-ae.
6.
I uouML ZZhA Zo be. a. muiM
Twa/FaZ^e.
7.
My. pajienZ^ ueJie yenenaZZy nAOzanabZe
Zn maJzZng me obey
r<ue/FoX-ae
8.
I ea^cZy. ,t>&c.oina. ZmpaJtZenZ uZth. peopZe.
Tnu&/FajZ6e.
9.
PecuZZajL .odouJtz (AmeZZA) come to me
aZ Zimez
TAU£./FaZ4A
10.
ThA Zap a^. my hAful PomeZZme^a ^zaZ ZAndeJi
Tkue./FaZde.
11.
My 4.PUZ AomeZZme^ Zea-vez my body
TnuAt FoZza
12.
I do. noZ. aZuayz ZaZZ the. ZJiuth
Tjuia/FclZ^S.
13.
I uAuaZZy. ideZ ZhaZ ZZ^a Za woJithwhZZe.
TJiue./FaZ^e.
,4.
I enjoy dAtecZZve on my^Zeny aZoaZaa
Taua/FoZ^a
15.
I have veny ieut cttuyutAZ^ uZZh membeJiA
oi. my 4amZZy
T^e/FoX^e
4.
■Xj.-
V-.
■• ■••*
16.
I am ZnZejtAoZed Zn the ZoZaoZ ^azhZonz
Zn cZothAZ
TJuZe/FeZoe
17.
I ^qaZ that I have ojtZen been punZched.
ivZthouZ cauze
TJi^e/FaZze
18.
.......... a:.. . bv.;..-
r^ft/Fo&ae
I don't ZZhA to otudy about ZhZnst that
I am uonkZng at
■p.>.? -7
,bWV7
;;
.J.klOQ ■
'■ r*' '
"» • 4 J
T T RANGANATHAN CLINICAL RESEARCH FOUNDATION
IV MAINROAD, INDIRA NAGAR, CHENNAI 600 020
•ci
Vajte.
Age.:
NiMH:
^o^Zow-Cng
£JU^ tntended tq
V**^*6^
jft- ^htttt fUxFoA
tett 0m ZHMA Ojte no
anz>ejiz>. UHUa a atneZe aJtMM. "T"
" and HIM
Lr
<^ne^pondZng ^taJtxment Zz Haue and atouhd "F" z^ Zt Za ^aZ£>e. x<
!#^u. avie not zua£., gaeM>.
Twe./FaZAe
1. I ojften get ned Zpotz on my neck.
The
and
‘
?
2.
I £Zfee Xo be pJULlMia. by my ^apej^coA^
3.
I enjoy many itc^eJient. kindba o± P^o.y
and. JiecjceaiZon.
, v
4,
I have neve^ ^atnted ok iett tthe
5.
I have u^ed ateohot exeAMtvety
6.
I ufoutd ZZke to be a nun^.
TJiueJFa^bA
•1
Tmja/ FcUl^st
tku^/fo^a
Tjuie/Foe^
t
t
7.
My paJientA weJte genAJuatty Aea^onabte
tn mahtng me obey
TJueJFaZ**'
8.
I ea^tty beebme tmpattent bdZth peopte
TJuieJFa^e.
9.
0.
PecuttaA bdouJt^
eome to me
at ttmet
' • ^V''
The top o^' my head AomettmeA ^eeZ tenden
TJvuue/Fat^e
1.
My tout tofnettmet Zeavet my body
TJUie/Fa^e
2.
I do not atway^ tett the. tnuth
' Tau^/Footie.
13.
I UMiaZZy ^eeZ that ZZie Z^> uoAthuhZZe
TJiue/ Fat^e
14.
I enjoy detectZve on my^teny ^tonte^
Tnue/Fdi^e
15.
I have veny ^eu guauJieZa wZth. membeea
04. my ZamZZy
,
TAue/Fat^e
. ., .
TJiue/FatM
16.
I am AjiteneLibtecL 4,n the Zate^t ia^>hZon^
tn etothe^
.... ^.. ■■; ,.Sl.-.
TJdie/Fat^e
17.
1 ^eeZ that I have oiten been pant^hed.
utthout cqf^e
...
TAue/Fat^e
18.
I don't ZZke to ^tudy aPout thtng^ that
I am ubAkZng at
TxMeJFatAe
A
>-
•
1
Page. 2
anyone
19.
I have nevejc been ^Ln Zove
20.
I o^ten have teettngA tthe nuantng.
ttngttng t ok cjiai^ttng
Tnae/PatAe
21.
I am not a^tatcL to hxincLte money
Tnue/PaZ^e
22.
I do not ttlze everyone I know
Tnue/Fat^e
23.
I bn.ood a gjieat deat
TJiue/Fat^e
24.
I am ^onjbled about >5^.x mattejua
TJtue/Fat^e
25.
My com^OAt earner befroJie that o^- othe^
TJtue/Fat^e
26.
I ttke meoJiantoA, (deattng wtth maehtneA,
automobtteA t ete.) magaztneA - poputaK ok
otheouwtAe
TJtue/FatAe
I have had moJte thanmy Abeyta o& thtngA
to wojuty about
TAjue/Fatte
28.
I 4-OJLget Jitght away cjhat peopte Aay to me
Tsiue/FatAe
29.
I dtAtthe havtng peopte abound me
TAJuue/FatAe
30.
1 have a g/ieat deat o-i- Atomath tscoubte
T/iue/Fatte
31.
It doeA not bother me pantteutcuity to
Aee antmatA AuttaK
Tsaie/FatAe
32.
Somettme'^ I put 044 antte. tof> jjulom
bjhat I ^houtd to today
Tnjuue/FatAe
33.
I do not uojut.y about eatehtng dt^eaMA
T/uae/Fat^e
34.
Many peopte exaggeJiate thet^L totoabte to
gatn sympathy
Tnue/Fat^e
35.
I woutd natheuL enjoy the pne^ent than
ptan bon a iutuJie
TJtue/Fat^e
36.
I am not tntejue^ted tn catenae
Tsiue/FatAe
37.
I have no enemtex who Jieatty wtAh to
to hanm to me
Tnae/FatAe
38.
Untmpontant thjeoaghtA ^omettme^ bother
me ^ojl dayA
TJiue/FatAe
39.
Mo^t o^ the ttme I bJt^h I ^ene dead
TJiue/Fat^e
7.
i
40.
I am u^uatty catm and not eoAtty ap^et
TJiue/Fat^e
Page, 3
41.
I g&t angjcy ^om^une^>
42.
1 bJoatcL kcMvzjl uicn them -Co^e Zn a gam&
TJOju^FatAA
43.
Onc^ Zn. a
TKUA/FatcA
44.
I £au,gh, at a (Luity jok&
tn trLoabte, 1 kA&p my moutlt ^tvut
45.
I have vafty
my iJitend^
46.
I navoJL
47.
I am
8.
TJiu&/Fat^a
compa^Ad to
TJUM/FatM
to ptay bjttti cLott^
TJUiA/Fat^a
I am botng tatfej&d about
Taua/Fo^q.
1 get uptet when I have to mahA a
^choJit tntp aiMy It&om home
TAUJ^/Fat4A
49.
I o^te^n
Z4 thtng^ ursJie not /uzat
TKU^/Fat^a
50.
I o^t&n 4^At patn tn the. bach o^ my nech
TAUA/Fat^e.
51.
I can Ataap dUAtng the day bat not at ntght
TJUiA/Fat&i
52.
Somzdxjn&A when I am not. ^eett,ng wett.
I gat annoyed eaAtty
T/J^FattA
53.
I am eattty aiMhened by not^c
TJiuA/Fat^a
54.
My eye *tght t^ a^ good a^ tt haA been
bon. yeanA
TJU/h/Fat^a
55.
Thejuz. t6 vatcy ttttta tova and companton^htb
tn my iamtty
TJiua/FattA
56.
I ttkA adventUHA ^taJitAA bettaJL than
jcomanttc ttanta^
TAUA/FatAA
57.
I thtnh I /fact rnonA tntan^ety than mo^t
paopta do
TMua/FatAo,
58.
I muAt 4top and thtnh. even bAfro*A dotng
AtmptA tathA
TAua/Fat^a
59.
Many oi- my cUiaam^ ojla about -6ex mattoKA
T/LUA/FatM
60.
I hxive. no dZ^CcuMy Zn hoZding ox.
moving my bowtZA
TJlUA/FatAA
61.
A pJitett 04. a KAttgtou^ man can cuka
dtctea^A by putttng ht^ hand, on houA head
T*JUA/Fat4A
62.
I am not otway* prompt
1
TJUJA/FOtAA
&&
•
':
XsnjCY
1;?
■’ ?
c'
-5,
>-■
<y. 4
r r
\5kUA'V
-•_,.’v
JI 1 ?>.
Page 4^r,
63.
.S’O^v. 1 \ muO
I go to tempte on. chunch negutanty
64.
My Ateep
■j y
Tjiua/Fo^c^
^ttiut and di^6tunbed
65.
TJuu^/FaZ^e. >
tndependent and ^nee
TJiu&/FaZ^e.
6n.om ^amtty note
66.
67.
I woutd tthe to tend a ^towen. ganden
Evtt ^ptnttA neven. po^e^ct me
.n^.ci ■
68.
TJLa&/Fa^6&
\ aUJV \
TJUUA/Fa^Q,
i
I o^ten GJtaco the ^tneet to avotd
someone I 4»ee
u -A \ 5^ A
cp-^xH o j»J; .
I get att tfye sympathy I ^houtd
Tjuia/FoZ^
70.
I hav^ JTdA .n^(lti^cutty hotdtng on.
^tanttng my antne
TJLUA/FaZ^Q.
71.
I betteve tf^ tajw enforcement
Tkua/FoZaq.
72.
Once tn a whtte I have bnohen a pnomt^e
Tjuia/Fcu^^
73.
Ontttctm on. Acotdtng hantA me temtbty
Tjluq./ Fcl^ca
74.
My home ttie m a>o ptea^ant a^ that
o^ mo^t peopte
TJUjuz/Fa£4&
75.
I tthed cahoot
TJtue/Fa^e
76.
I ZjJwz pQ^Ji.y v>
69.
\SDA.A -
r^iae/FaC^e
•
Tnue/FatAe
iXjjSJ1; -WCj^ ,
.
77.
I don't betteve that anyone -co ptotttny
agatn^t me
Tnue/Fat^e
78.
I have a habtt o^ counttng untmpontant thtng^
Tjuja/Fcl^q,
79.
I hean thtng^ when I am atone
Tajuuz/FqZ^
80.
I have had ^evenat openatton^ LJhtch
dtd not bene^tt me
TJUjj&/Fa£4e.
81.
SomettmeA I ^eet that. I mact tn^cuie
my^et^. on. someone eZ^>e
TJiu&/FaZ^
82.
I qoa^Cp a
83.
(V/ien I t&avQjl home. I do not wotuty
I toc^jexL
cLoojl
TuL&/Fa£A&
84.
My eondact
abound me
TJiuA/Fat^A
T
-■’r*
at ttme^»
aont^ottexl by the cu^tom^
TJUia/Fat^
> I
| i, 114 .II
'p
'ul U
I.
«
Page 5
85.
I Kave. not Ztvejct tn& Jttgnt ntncL o^
TJiue./Fat^
86.
I Ztne. to coofe
TJiue/FaZ^e
87.
Someone Koa eonUcoZ ovqjl my mZnd
Tsiue/FaZAe
88.
Bad bjoJixLCi eome to my mend and I can't
get Jitd o^ them
TJtue/FaZ^e
89.
Sometimes I enjoy huJuLLng peopZe I Zove
TJiae/FaZ^e
90.
I enjoy ^octaZ gathentng^ Jaat to be
cuttn peopZe
Tnue/FaZ^e
91.
Some pejeeone tn.y to ^teaZ my thought*
and tdea*
TJtue/FaZ^e
92.
At ttmea 1 envy ^cceM^uZ peopZe
Tsuie/FaZAe
93.
I woJLk. unde^ a gjveat deaZ
ten&ton
TJtwe/FaZ^e
94.
The Atght oj^ bZood nettheJt i^itghten^
not make^ me ^ZcJz
Tsuie/FaZ^e
95.
Lu^t i-OJL ptea^ujie o^ten get6 me tnto
tJvoabZe
Tnjue/FaZ^e
96.
I o^ten w^»n I ^enje boJtn o^ opposite ^ec
Ttme/FaZAe
97.
I am on guand wtn peopZe who one
too ^tZendZy
Tnue/FaZ^e
98.
I do not dJiead gotng tnto a /Loom bJheJie
a peopZe have gathered ^addenZy
TJtue/FaZ^e
99.
At tune^ I have enjoyed betng hmit by
someone I Zove
TJiue/FaZ^e
100. I cannot do anything weZZ
Tsuae/FauZAe
CASELETS (CAMP)
The counsellor has to select a campsite. Which ofthe following would you recommend?
1)
a)
b)
The Counsellor was assessing the new camp site. The building was situated on the
outskirts of the town and the atmosphere was peaceful. The newly built building was
bright and airy. Water would be brought in from the town daily and arrangements
had already been finalised.
A voluntary organisation - 'Ladies Club’ is part of an industry. It was run by the wives
of the executives of the industry. The women were interested m conducting a camp ioi the
villagers. The President assured, "We will provide the marriage hall to conduct the camp.
From our fund, we will organise meals for the patients. Our ladies club members can
conduct bhajans in the evenings. One thing we find difficult is to identify and select
patients. We can recommend 10 patients who are husbands of our house maids. The rest
15 you may have to select.
2)
Which of the following organisations will you choose th conduct the camp?
There were two host organisations in the same village. One organisation had a team of
helpful, committed volunteers.
The organisation was known for a lot of welfare
activities in the area - free schools, dispensaries, providing free noon meal to children
under 10 years, running cyclone relief units during natural calamities etc.
The second organisation was involved in organising Micro Credit System for women.
They had experience in conducting medical camps with the help of doctors from the
neighbouring areas. This organisation was never involved in providing free meal to
children or providing free medicine to villagers.
3)
The screening / interviewing is on The camp is to start in a week’s time. Which of the
following patients wouldyou choosefor treatment in the camp?
a)
The patient said he could hear voices who talked to him on and off about what to do or not
to do. Sometimes the voices commanded him not to eat and he skipped lus meals.
b)
The final selection of patients was nearly complete. They could take in only one more
patient. Tlie counsellor had to choose between the thirty five year old agriculture labouier
and the forty year old lorry driver.
Page 2
c)
The patient was from a village about 40 kms. away from the camp site. "It takes only
two hours to come here. I will come everyday for the family programme. It’s no problem/’
assured the wife.
4)
Read thefollowing situations and comment on the appropriateness /inappropriateness of
the treatment staff
a)
It was the first day of the treatment camp. The patients waited expectantly for the doctor
and counsellors to arrive. The counsellor arrived perfectly dressed - wearing a thin nylon
saree with high heal shoes, lip stick and eye shadow, everything perfectly matched. The
patients looked at her in awe.
b)
The treatment team wanted to employ a recovering addict as a counsellor. Tony was a 22
year old addict who was 6 months sober. He was enthusiastic and willing to work hard
even without pay for he wanted to help other addicts.
c)
The day’s programme was to start at 9.00 a.m. ’It's almost 9, Can I ring the bell" asked a
patient. "Let me finish my tea, you can ring the bell in about 15 minutes" said
the counsellor.
One month Regional Training Programme on 'Prevention and Management of Addiction’
from 19 November (Monday) to 13th December (Thursday) 2001
Sponsored By National Institute Of Social Defence, Ministry Of Social Justice &
Empowerment, Government of India, New Delhi
Organised by T T Ranganathan Clinical Research Foundation, Chennai 600 020
TIME TABLE - FROM 19™ NOVEMBER TO 13™ DECEMBER 2001
Date
09.30 -11.15
11.30-1.00
2.00-3.15
3.30-4.45
19.11.2001
(Monday)
Introduction
Welcome Address
About the training
programme (VT)
Sharing by
participants problem of
addiction in their
area, about the
NGO, their
experience in the
field of addiction
(VT)
Disease Concept
of Addiction
(SR)
Activity - case
study
(SR)
20. fl. 2001
(Tuesday)
Basic facts about
alcohol (VT)
A day at TTK Patients
programme (RC)
Classification of
drugs, short-term,
long-term effects
and withdrawal
symptoms(Dr. AR)
Activity - quiz
21.11.2001
(Wednesday)
Building
relationship
(Rachel George)
Personality defects
(R.C.)
Medical
Complications
related to
addiction
(Dr AR)
Psychiatric
complications
related to
addiction
(Dr.Suresh
Kumar)
22.11.2001
(Thursday)
Motivation
techniques
(AJ)
Contd...
Rote play(AJ)
Denial (RC)
Loss and grief
(SR)
23.11.2001
(Friday)
Counselling
Contd
(VT)
Anger and
violence
(Sudha)
Whole person
recovery
(AJ)
24.11.2001
(Saturday)
Art therapy
(Kanakam)
Contd..
Sph ituality and
activity (SR)
Record Keeping
(VT)
WEEK TWO
I
i
Date
09.30 -11.15
26.11.2001
(Monday)
Feelings of family
members and
stamp game
(SHEEBA)
27.11.2001
(Tuesday)
Tl1.30-l.00
2.00-3.15
3.30-4.45
Guidelines and
responses of family
members
(RN)
Co-dependency
(Revathy Thomas)
Structuring
family
Programme
(VT)
Children of
alcoholics
(Rd)
Parenting skills
Contd...
(Ambika Sen)
Problems in
recovery
(Fd)
28.11.2001
(Wednesday)
I Marital counseling
(Dr. Vijay
Nagaswami)
Contd...
About HIV-AIDS
(Dr. Anita Rao)
Harm Reduction
Programme
(Dr.Srivatsan)
29.11.2001
(Thursday)
Causative factors
in addiction
(Dr. Mohan Isaac
Impact of addiction
(Dr. Mohan Isaac)
Pre and post test
counseling
(Dr.Shanthi
Davidar)
Contd...
30.11.2001
(Friday)
Dynamics of
relapse
(Rd)
Dry drunk
symptoms
(A.J)
Methods to stay
sober
(Fd)
Client profiling
(VT)
1.12.2001
(Saturday)
Group therapy
(VT)
Contd....
Self-help group
concept
(Mr.K)
Sharing by AA /
NA members
WEEK 3 (Field Placement)
TTK Hospital
- 7 trainees
After Care Centre
- 5 trainees
Rajaji De-addiction Centre
- 5 trainees
DESH
- 5 trainees
CHES
- 5 trainees
WEEK 4
i Date
09.30 -11.15
11.30-1.00
2.00-3.15
3.30 - 4.45
Presentation on
the field
placement
(Dr.Cherian)
Contd...
Self-esteem
(SM)
Criticism and
activity
(SM)
What works in
treatment
(RC)
Activity
(Tuesday)
Community
approach of
treatment
(Sudha)
Minimum
standards of
care
(S.R.)
! 12.12.2001
(Wednesday)
Assessment
(Kanakam)
Contd...
Visit to YRG Care
13.12.2001
(Thursday)
Prevention
programme Industry and
school
j programme
Contd...
Evaluation
and valedictory
10.12.2001
(Monday)
11.12.2001
i (VT)
i
htfake^armat
Date of intake :
Age
Language of choice
Marital Status
Occupation
Accompanied by
Years of drinking / drug abuse:
Years of excessive drinking / drug abuse:
Present pattern of drinking^drug taking:
Presence of:
Use of other drugs
Psychiatric problem
Denial
: Nil/past use only/presently using
: Nil / Mild / Moderate
: Mild / Moderate / Severe
Physical problems(record specifically):
Prior treatment for addiction i other problems:
Willingness for treatment: Unwilling / half-hearted / willing
Motivating factor for present treatment effort:
Any issue / concerned expressed by client/family:
Impression of intake counsellor :
Action taken
: Admitted / Given later date / referral /denied admission
Category of payment : TTR / B ward / A ward / Company
Address with contact phone number if possible
Signature of Counsellor
'i
INTERNALISING TOOLS
QUIZ
1)
Name the plant source of heroin,
2) What kind of addictive drug is present in cough syrups that are
abused?
3) To which category of drugs does buprenorphine belong? a/
4) The addictive potential of heroin is low-True or False?
5) What is the psycho-active chemical present in ganja?
6) What are the kinds of drugs that come under the category of
Cannabis?
7) Smoking ganja is safe as it comes from a plant - True or False?
8) When is the effect of ganja stronger - when eaten or smoked?
9)
To which category of drugs does LSD belong?
10)
Beer drinkers never become alcoholics - True or False?
11) What kind of drugs can cause synesthesia?
12)
If a drug abuser is eating a lot of sweets what kind of drug could we
have taken?
c<
13) Which category of drugs can cause itchy skin?
iviyz
14)
What is "mainlining"?
15)
Which is the most commonly abuSed drug in India?
16)
What is the percentage of alcohol usually present In beer? G
17)
What is the name of the chemical present in alcoholic beverages?
t rdu-ra V'o
d I
iv /
‘
Page 2
18)
19)
What can cause sudden death due to sniffing?
-
Of which drug is constipation the well known side effect? , I < >
20)
What is the connection between a drug’s short term effects and
withdrawal symptoms?
L-vw-fr
21)
h person can drive safely immediately after drinking three pegs of
whisky True or False?
Can pain killers become drugs of abuse?
23)
if a person regularly takes vitamins and liver supplements, his iiver
will not be affected even if he drinks alcohol heavily - True or
False?
24)
Brown sugar reduces one's appetite - True or False?
>«•
•!
INTERNALISING TOOLS
CASE ANALYSIS
Please point out what is inappropriate in the following examples:
1) "Counsellor: Come in. Sit down. Tell me your name. Where are you from?
Are you married? Has somebody from your family come with you?
2) Client : All the years of married life I have been most unhappy. I hope
this treatment will work.
Counsellor: Don’t worry. Everything will be alright. Just bring him here.
tXvVU
iCJ3) Counsellor: Your daughter-in-law told us that you are not willing to get
your son treated for addiction. What is wrong with you?
4) Counsellor: It is one month since you rejoined vour husband.
Are you happy?
Client : Yes M'am
5. Client: Please advice my wife. She fights with me all the time. After a
days of hard work, I cannot relax. Sometimes I feel I am going mad.
Counsellor: How many years lias it been since you got married?
6) Client : My father still treats me like a kid
Counsellor: He is treating you just the way his father treated him.
That's all. . >
7) Client: I became terribly angry
Counsellor: Come on! Don't tell me you were angry just for a
10 minute delay.
20
A
I ■
;
>3
Page 2
■i
i "•
8) Client: I have been waiting for two hours to see you.
Counsellor: I can’t help it. I was not sitting here simply.
9) Counsellor: This is the third time you have had a relapse.
Why can’t you understand? Can’t you think pr operly?
10) Comment on the appropriateness of the responses listed under each
statement.
Client: That’s it, Madam. I have told you the entire stoiy. Now, you tell
me what I should do. Shall I leave my husband 'or continue to stay with him?
Counsellor:
*
a)
You have been married for six years. Why don’t you try’ and patch up
the maniage?
b)
Sounds like you have two kinds of feelings. There are a few reasons
why you should leave and a few to continue in the marriage.
c)
Your children will be affected. Children from broken families are.
Shouldn’t you think of them? Your parents also may not like it if you get
separated from your husband.
11) Client: Taking medications regularly for a whole year is a big bore
Counsellor:
i) There is no short-cut to that
ii) Shall I take the medicines instead of you then?
iii) A year will go by quickly. Don’t worry
iv) If you can’t spend even 1 minute to take it - you are just lazy
i
t
CASE STUDY
Murugan is a 35 years old fanner. He is married and has two children. He leads a happy
and contended life with his wife and children and lives within Iris earnings. Tire way
Murugan was running his family was taken as an example for the entire village. Every
Saturday, after receiving his weekly wages. Murugan would buy Halwa for his children
and flowers for his wife. His wife too. would wait for him with his favourite dishes. On
festival days and occasions, the entire family would go to a temple and enjoy themselves.
While leading such a happy life, one day one of Murugan's friends came to his house and
enquired about Murugan's health and well-being. Murugan informed him that he was
happy except that for the past two days he was having cold and fever. Immediately, his
friend took out a bottle from his bag and asked Murugan to drink a little from it.
promising that the relieved of his cold. Later, his wife enquired about the foul smell
emanating from him. Only then did he realise that he had taken a drink similar to toddy.
.After a few days, when Murugan was veiy tired - after a hard day in the fields - he
wanted to dnnk and relieve his tiredness. So, he went to a nearby liquor shop and drank.
As days passed, his drinking became a daily habit. He lost interest in eating and also
playing with his children. He stopped giving money to his wife to run the family.
One day when Murugan returned home drunk, his wife was very angry and shouted at
him. She accused him of not eating properly, not giving money regularly and asked him
as to how she could run the household under such circumstances. Thereupon, Murugan
too became angry and started shouting at her and in his anger, broke the water pot. Next
day , he casually enquired about the disappearance of the water pot. Though Murugan
eouldnot remember anything of the incident, his wife was seething with anger.
While Murugan was working in the fields, his thoughts were totally centered around his
dnnk. He was worried as he had no money to buy his next drink. He waswonderingiThe
could sell theold radio set at home and drink with the money raised out of such sale. At
this point of time, one of his friends came to him and commented that for the past few
days, he appeared to be ^eak_andjinheafthy. Murugan, thereon, explained his condition
to his friend stating that if he did not drink, he was not able to sleep well at night or eat
ptoper food and that was the reason for his drinking.
———
fen days later, when Murugan's wife asked for money to buy monthly ration, he did not
have money. The same evening, he borrowed Rs. 150/- from his friend, Kandhan. On his
way back home, Murugan went to a liquor shop and got drunk. He also purchased three
packets-ofbiscuits half ajdtoof Halwa and plenty of flowers for his wife. When he
reached home and gave these to his wife, she was angry as there was not even a grain of
nee at home.
hi the meantime. Murugan s daughter was down with high temperature. They had to take
nm A hospital Murugan offered to bnng an autorickshaw for this purpose and he went
than ti he WaS
£nd
th0Ught Of takm8 just a glass of liquor to relax and
went on'and
« he started drinking, he coukf not^^itlTone aXd it
feSyS^
1 andI promised
dld nOt retum
home
- Thenever
next drink
day’ heagain.
vvent home
with a
t^hngof|uirt and shame
that he
would
The promise
was foi just one day. The next day he drank again.
Around this time, Murugan decided to go to Sabarimalai on a pilgrimage. As part of the
ntuals he was required to abstain from drinking for a period of forty days. Accordingly
startt^XL^inTn^T1"2 alC°h01 f°r the neXt forty days' On the forty &st dav lie
started di inking and that tgo excessively. His wife and children were hurt and angry.'
On seeing his condition, one of his friends - a well wisher asked him why he drankMurugan told him that if he had a wife who could understand his problem, there would
be no need for him to dimk. He told another friend that if he could repay all his debts he
would be able to give up drinking totally.
However
continued drinking. He‘was n°w drinking in the mornings and as
. "Murugan
i
well as iin
.
. -health deteriorated rapidly.
the evenings. —
His
---------- -
Wdlen
st°PPed drinking, the next day his limbs were shaking badly. With great
ifficulty, he abstained from drinking for the next two davs. On the tliird dav he
complained to his wife that he was hearing strange voices and that he was seeing some
huge figures m front of him. His wife got the impressioFthat he had got scared of some
vision and gave him prasadam brought from the temple.
In the meantime, Murugan's landlord gave him Rs.400/- and asked him to buy fertilizer
from the next wllage. When he went to buy the fertilizer, Murugan drank excessively
a fiqu°r sh°p and became unaffiaie_ofjus_^uffoundings. At this stage, someone
lobbed him of his money. When Murugan regained his senses and found that the monev
was missing, he did not know as to what to do. He returned home dejected. He wishes he
were dead and shared this feeling with his wife.
*------
she told him that a camp was being organised at the village for the treatment of
alcoholics. The village officer had also wanted Murugan to avail this opportunitv. Later
Murugan enrolled in the camp and got himself treated.
Identify the symptoms of addiction.
Page 2
A CASE STUDY - Co-Dependency
When Uma and Ashok married, they were both healthy young people Thev
had college degrees, satisfying jobs, close relationships with friends Ld
amily members and enjoyable hobbies. After two years of marriage their first
his jobaHe°m
th3t -time Ash°k 3180 gOt a secant promotion in
his job. He accepted the position of supervisor over a large region of his
company. This promotion brought a considerable pay raise thft enabled him to
purchase a new home for their growing family The unpleasant side of the
a XtiTnDunng
aS ’usn CaIk<
! f°awa
r Ashok
t0 travel
Of town
for several
*
travels
V from
home, out
Ashok
started
drinking
and
gradually switched over to brown sugar .
bilnT611 yearlOf,™rriage’ his brown sugar use steadily increased, and he
Dlfved Xh UP S y ■u^lvement. He seldom visited his close relatives or
Ashokin^Sm
freouentfr
1
«
child™>
and
create
°Ut the noise and normaI
cIutter
cW’d™
Iona hX h h?T ?S rf® consisted of 'S°mg off on business trips', spending
showSiZu tde kome, wben he was
town, shouting and sleeping, nt
h- 1 h
m ^eSt m tke
had become a 'difficult' husband.
and after seven years of marriage, Ashok
friends and hobbies; but she figured that it was ail a passing phase in their life
S 7ri,OllC
Shc rcasoned> Ashok’s work would let up and thev could go
ck to being the happy couple they once were, f inally Uma knew he had a
pioblem, but didn't know what to do. She asked him to stop manv times, but
each tune this only started an argument that led to more problems
J^mg that Ashok was pulling away from her and everything they had once
eld dear, Uma tried hard to make him happy and avoid making him mad. She
X .
faVOnte meals’ kcPt
house clean, switched on the television for
the kids to watch so they would be quiet when he was home, and even
tS,U ™ttjed t0 more fre<luent sex with him. She also assumed responsibilities
that had once been his like paying the bills, going to the bank, etc . Eventually,
her life became focused on keeping Ashok happv so that he wouldn't use
brown sugar.
■
"
Her efforts didn’t work and often he found something to complain about. And
e i n t stop using. In fact, his addiction increased. Uma became even more
determined than ever to bring him back.
-2-
One day while shopping at the supermarket, Uma met her sister, Geetha who
asked how she was doing. They were living in the same city , but had never
met for quite a long time. Whenever Geetha said she would come home, Uma
would give some excuse and prevent her from visiting her. Uma was not
happy to have met her sister. She was afraid she might come to know about
Ashok s problem. How do I avoid her? How do I leave this place? "-She was
so preoccupied that she didn't hear her sister who was enthusiastically talking
to her. Uma quickly left that place to avoid further questioning by her sister
and deluded herself that she had succeeded in hiding their family "secret" from
the rest of the world. Geetha nodded sadly, seeing Uma not the person she
had known earlier.
The fact is Uma s entire personality had changed overtime. She never took any
interest in dressing up neatly or even combing her hair. She always had a
worn out face. She stopped going to the temple because she was convinced
that God had been unjust to her. She stopped lighting a lamp in the pooja
room. She kept it dark as she believed that God had darkened her life.
That niglit when Ashok came home late as usual. Uma got wild and started
shouting and arguing with him. He shouted back and both of them went to bed
without taking dinner. She was unable to sleep and the next morning she got
up with a severe headache. She could not prepare breakfast for the cliildren
and they had to go to school without taking proper food. When the cliildren
complained they were hungry, she shouted at them None of you notice how
I am suffering. As it is, your father is giving me enough problems. Don't pester
me with your minor issues"
After sometime Uma felt sorry for her children and decided that she would not
shout at them any more. ’’ If I don’t cook for them, where will they go?. It is
all because of this man! From now onwards I am going to be indifferent to
him . Let him do whatever he wants to do. I will not shout. Hl not cry. I have
had enough of it . She decided to remain calm but as soon as she saw him, she
got irritated and started shouting. After quarrelling with him, she felt very
depressed, run dowa and weak. She went to bed hardly remembering that
children would come from school hungry and she had to keep something for
them to eat.
are the co dependency behaviour patterns you notice in Vma?
RELAPSE - CASE STUDY
Satish, 25 years old, was working in a departmental stores. He underwent treatment
for ganja addiction and was responding well during the initial 2 months He was
regularly attending NA meetings. His elder brother. Mahesh was very caring and he
would sit with Satish and talk to him in the evenings, drop him at the NA meeting
place and pick him up.
It was the year end and accounts had to be tallied and closed. Satish had to work
overtime and he came horn? only after 9 p.m. This continued for 2 weeks. He used
to say that f ie felt tired, would skip his dinner and go to sleep. When his mother
asked him to eat a little bit, he would shout at her-" Why don't you understand my
problems? I have given up puffing only because you people were constantly
nagging! If you continue to nag like this, ITI start smoking again"
Satish went to the store in a bad mood. His table was filled with papers and was in a
total mess. He could not find the file he was supposed to work on. He shouted at
everyone. When his manager saw Satish, he warned him and insisted that he
should complete the job before 4o'clock Satish got wild and without thinking for a
moment, submitted his resignation and left that place.
e
To him the whole world appeared unjust. ‘Why is everyone behaving like this?
Nobody appreciates what I am doing." When he went home, his mother asked him,"
You have come home so early today. It's only 11 in the morning. Is the store closed
today?" Satish would not answer her. He straightaway went to sieep When he got
up in the evening, Mahesh approached him and wanted him to share his problems.
But Satish did not want to tel! him that he resigned his job. So he shouted at him
also and straightaway went to see one of i n's old 'Triends”
a) What are the warning signs of relapse which you notice in Satish?
b) What are the positive reinforcers which can be strengthened towards achieving
sobriety?
c)
What are the warning sign management plans you would like Satish to make?
A CASE STUDY - Co-Dependency
his job. He accepted the position of supervisor over a large region of his
company. This promotion brought a considerable pay raise that enabled him to
purchase a new home for their growing family The unpleasant side of the
.!°n ™as tha‘.lt cailed for
to travel out of town for several nights
XSf;
A1S travels away from home’ Ashok started drinking and
gradually switched over to brown sugar .
S
After seven years of marriage, his brown sugar use steadily increased, and he
began to give up healthy involvement. He seldom visited his close relatives or
played with his children. Uma and .Ashok now had three young children, and
crit k‘
Y “mplained about the noise and normal clutter chldren
ion
He
consisted of 'going off on business trips', spending
ng hours outside home when he was in town, shouting and sleeping. He
harfT4
6 ^eSt m 016 family and
seven years of marriage, Ashok
had become a 'difficult' husband.
Because Ashok's addiction developed slowly, Uma did not recognize it for
qtule sometime. She rationalized that the longer periods he spent away from
home were part of his job. But it bothered her that he had little time for family,
friends and hobbies; but she figured that it was all a passing phase in their life
together. One day, she reasoned, Ashok's work would let up and thev could go
back to being the happy couple they once were. Finally Uma knew he had a
problem, but didn't know what to do. She asked him to stop manv times, but
each time this only started an argument that led to more problems
Realising that Ashok was pulling away from her and everything they had once
held dear. Uma tried hard to make him happy and avoid making him mad. She
cooked his favorite meals, kept the house clean, switched on the television for
e kids to watch so they would be quiet when he was home, and even
submitted to more frequent sex with him. She also assumed responsibilities
that had once been his like paying the bills, going to the bank, etc . Eventually,
her life became focused on keeping Ashok happy so that he wouldn't use
brown sugar.
Her efforts didn’t work, and often he found something to complain about. And
e didn t stop using’. In fact, his addiction increased. Uma became even more
determined than ever to bring him back.
-2-
One day while shopping at the supermarket, Uma met her sister, Geetha who
asked how she was doing. They were living in the same city , but had never
met for quite a long time. Whenever Geetha said she would come home, Uma
would give some excuse and prevent her from visiting her. Uma was not
happy to have met her sister. She was afraid she might come to know about
Ashok s problem. How do I avoid her? How do I leave this place?"-She was
so preoccupied that she didn’t hear her sister who was enthusiastically talking
to her. Uma quickly left that place to avoid further questioning by her sister
and deluded herself that she had succeeded in hiding their family "secret" from
the rest of the world. Geetha nodded sadly, seeing Uma not the person she
had known earlier.
The fact is Uma's entire personality had changed overtime. She never took any
interest in dressing up neatly or even combing her hair. She always had a
worn out face. She stopped going to the temple because she was convinced
that God had been unjust to her. She stopped lighting a lamp in the pooja
room. She kept it dark as she believed that God had darkened her life.
That night when Ashok came home late as usual. Uma got wild and started
shouting and arguing with him. He shouted back and both of them went to bed
without taking dinner. She was unable to sleep and the next morning she got
up with a severe headache. She could not prepare breakfast for the cliildren
and they had to go to school without taking proper food. When the ciiildren
complained they were hungry, she shouted at them None of you notice how
I am suffering. As it is, your father is giving me enough problems. Don’t pester
me with your minor issues"
After sometime Uma felt sorry for her children and decided that she would not
shout at them any more. ” If I don’t cook for them, where will they go?. It is
all because of this man! From now' onwards I am going to be indifferent to
him . Let him do whatever he wants to do. I will not shout. I’ll not cry. I have
had enough of it". She decided to remain calm but as soon as she saw him, she
got irritated and started shouting. After quarrelling with him. she felt very
depressed, run dowu and weak. She went to bed hardlj7 remembering tliat
children would come from school hungry and she had to keep something for
them to eat.
miat are the co dependency behaviour patterns you notice in Uma?
■•.’n
.V
......... zV.rs.
CASE STUDY
Arun underwent treatment for his alcoholism. On the day of discharge, he told
everyone he would come again to TTK Hospital only to celebrate his birthday and that
he would definitely not relapse. The counsellor talked to him aboufthe importance of
follow-up, thrTheea to take Esperal and attend AA meetings. Yet, Arun kept insisting
that he did not really need these- 'I am willing to take a bet that I will not relapse’.
Arun came for follow-up only because his wife and counsellor insisted, on it. After two
months, during a follow-up visit, his wife, Usha complained that he ’-Aras getting angry
over minor issues. She was also upset about his impatience. He expected her To
anticipate all his needs like fetching water to drink and fulfil them even if she was very
busy in the kitchen. Arun brushed aside all these issues and said that she was
exaggerating.
At home, Arun was spending many evenings alone in a room. He had very little to
communicate to his family. He did not want to go'out with them - to the temple or even to
their cousin’s wedding. He said,'It is too boring’. He kept on moaning ’Why did these
things happen to me? Nobody appreciates what I am doingr
One area that Arun was very happy with was his job. He went to work reguiariy and feit
good about the appreciation he received. Slowly, he started increasing the working
hours and came home only at 8.00 p.m. When he reached home, he was toq_ tired
and could only eat and sleep The family members were unhappy with Arun for he'rarely
took them out or even speak to them. 'It is better this way*, he said.’ I am bored at home.
After al! I am working only for all of you... Even when I am not drinking, you have
something to complain about1.
He was unwilling to even take the child to the doctor or fetch an electrician when repair
was needed. When Usha requested him, he told her 'I cannot do everything - you run
the house*. Whenever the issue of taking responsibilities at home came up, an
argument would erupt, Arun would threaten to drink and his wife would give in.
Gradually, even taking Esperal became an issue. He would take it if he was in a good
mood. If not, he would brush it aside and^SIk away just to scare his wife. Later, Usha
noticed that he 'was again in touch with his drinking friends. When asked, he said, ’lam
not sitting with them*, i am just talking over the phone. What harm can this cause? You
simply want me to do whatever you tell me to. I won't drink, I know it.’
A month later, Arun came home under the influence of alcohol.
'0.
RELAPSE - CASE STUDY
Satish, 25 years old, was working in a departmental stores. He underwent treatment
for ganja addiction and was responding well during the initial 2 months He was
regularly attending NA meetings. His elder brother. Mahesh 'was very caring and he
would sit with Satish and talk to him in the evenings, drop him at the NA meeting
place and pick him up.
It was the year end and accounts had to be tallied and closed. Satish had to work
overtime and he came home only after 9 p.m. This continued for 2 weeks. He used
to say that he felt tired, would skip his dinner and go to sleep. When his mother
asked him to eat a little bit, he would shout at her-" Why don't you understand my
problems? I have given up puffing only because you people were constantly
nagging! If you continue to nag like this, I'll start smoking again"
Satish went to the store in a bad mood. His table was filled with papers and was in a
total mess. He could not find the file he was supposed to work on. He shouted at
everyone. When his manager saw Satish, he warned him and insisted that he
should complete the job before ^o'clock Satish got wild and without thinking for a
moment, submitted his resignation and left that place.
To him the whole world appeared unjust. ‘Why is everyone behaving like this?
Nobody appreciates what I am doing." When he went home, his mother asked him,"
You have come home so early today. It's only 11 in the morning. Is the store closed
today?" Satish would not answer her. He straightaway went to sleep When he got
up in the evening, Mahesh approached him and wanted him to share his problems.
But Satish did not want to tel! him that he resigned his job. So he shouted at him
also and straightaway went to see one of his old "friends”
a) What are the warning signs of relapse which you notice in Satish?
b) What are the positive reinforcers which can be strengthened towards achieving
sobriety?
c)
What are the warning sign management plans you would like Satish to make?
RELAPSE - CASE STUDY
Satisn, 25 years old, was working in a departmental stores. He underwent treatment
for ganja addiction and was responding well during the initial 2 months He was
regularly attending NA meetings. His eider brother, Mahesh was very caring and he
would sit with Satish and talk to him in the evenings, drop him at the NA meeting
place and pick him up.
It was the year end and accounts had to be tallied and closed. Satish had to work
overtime and he came home only after 9 p.m. This continued for 2 weeks. He used
to say that tie felt tired, would skip his dinner and go to sleep. When his mother
asked him to eat a little bit, he would shout at her-" Why don't you understand my
problems? I have given up puffing only because you people were constantly
nagging! If you continue to nag like this, I'll start smoking again"
Satish went to the store in a bad mood His table was filled with papers and was in a
total mess. He could not find the file he was supposed to work on. He shouted at
everyone. When his manager saw Satish, he warned him and insisted that he
should complete the job before ^o'clock Satish got wild and without thinking for a
moment, submitted his resignation and left that place.
To him the whole world appeared unjust. 'Why is everyone behaving like this?
Nobody appreciates what I am doing." When he went home, his mother asked him,"
You have come home so early today. It's only 11 in the morning. Is the store closed
today?" Satish would not answer her. He straightaway went to sleep When he got
up in the evening, Mahesh approached him and wanted him to share his problems.
But Satish did not want to tel! him that he resigned his job. So he shouted at him
also and straightaway went to see one of i iis old “friends"
a) What are the warning signs of relapse which you notice in Satish?
b) What are the positive reinforcers which can be strengthened towards achieving
sobriety?
c)
What are the warning sign management plans you would like Satish to make?
RELAPSE - CASE STUDY
Satish, 25 years old, was working in a departmental stores. He underwent treatment
for ganja addiction and was responding well during the initial 2 months He was
regularly attending NA meetings. His elder brother, Mahesh was very caring and he
would sit with Satish and talk to him in the evenings, drop him at the NA meeting
place and pick him up.
It was the year end and accounts had to be tallied and closed. Satish had to work
overtime and he came home only after 9 p.m. This continued for 2 weeks. He used
to say that he felt tired, would skip his dinner and go to sleep. When his mother
asked him to eat a little bit, he would shout at her-" Why don't you understand my
problems? I have given up puffing only because you people were constantly
nagging! If you continue to nag like this, I'll start smoking again"
Satish went to the store in a bad mood. His table was filled with papers and was in a
total mess. He could not find the file he was supposed to work on. He shouted at
everyone. When his manager saw Satish, he warned him and insisted that he
should complete the job before 4o'clock Satish got wild and without thinking for a
moment, submitted his resignation and left that place.
To him the whole world appeared unjust. ’Why is everyone behaving like this?
Nobody appreciates what I am doing." When he went home, his mother asked him,"
You have come home so early today. It’s only 11 in the morning. Is the store closed
today?" Satish would not answer her. He straightaway went to sieep When he got
up in the evening, Mahesh approached him and wanted him to share his problems.
But Satish did not want to tel! him that he resigned his job. So he shouted at him
also and straightaway went to see one of his old “friends”
a) What are the warning signs of relapse which you notice in Satish?
b) What are the positive reinforcers which can be strengthened towards achieving
sobriety?
c) What are the warning sign management plans you would like Satish to make?
MH' J-a- 6
CASE STUDY
Senthil, 18 years old, is studying in a technical education institute. His father is working
in a factory as a supervisor. His father takes alcohol on and off.
Senthil learnt to use brown sugar from his fellow friends at the institute. Now he
takes drugs regularly.
One day, Senthil was smoking Ganja on the terrace. The mother was shocked to see
him smoking. But she pacified herself, "he is only smoking cigarettes. He is not
(J? drinking like his father. He must have learnt to smoke fromTiis fricnds. I should not
make an issue of this. I should not tell his father." She called Senthil and advised him to
give up smoking as it causes many illnesses.
As days went by, there were a few more changes in Senthil. Half the time he would not
eat, saying that he was not hungry. Then, Senthil’s mother would make curd rice, and
force him to take food.
One day, there was a letter from his institute stating that he had not paid Ms fees. His
mother had already given money to Senthil to pay his fees. On seeing this letter she was
shocked. She pawned her ear rings and paid Senthifs fees. She apologized on behalf
of her son to the authorities^ saying, "I forgot to give him money for fees". On
reaching home, she shouted at Senthil. He said someone liad stolen theTnoney from his
purse and he was afraid to inform her. Hence he had not paid the fees. The mother felt
that he might be lying. Somehow she wanted to believe that he was telling the truth.
One day, in the market place, Senthil’s mother met one of his friends. He told her
"Senthil spends a lot of time with drug addicts. He is irregular for classes. He has
not written his final exam." Senthil’s mother felt very upset. On going home, she
searched his cupboard. She found cigarettes, match boxes and small packets. She
collected all of them and threw them in the dust bin. When Senthil entered home, she
shouted at him and made him promise in front of God that he would not touch drugs in
future. After that Senthil looked alright for a few days and his mother was not sure
whether he was taking drugs or not.
One day, Senthil’s father received a phone call from the police station. The policeman
said that Senthil had brown sugar in his possession and was, therefore kept in the police
station. On hearing this, Senthil’s father paid money for providing bail and brought
him home. Senthil’s mother blamed his father for the problem of his son. But the
father blamed the mother that she was not capable of bringing up the children. On
bringing back Senthil from the police station, they found him with miming nose and
watery eyes. Senthil was taken to a treatment centre by his parents.
What "enabling behaviour" of the mother do you notice in this case study?
MH'
DEALING WITH DENIAL
Denial is a psychological process that takes place at the unconcious level in an
addict. Denial is a core component of the disease and it gets strenathened as
addiction progresses. During the process, the addict's mind recreates an
illusion so convincingly that he believes it to be the'reality1.
Why does the addict deny his problems?
Normally, no one wants to be categorised and stigmatised as a weak willed
person, morally and mentally inferior to others and subject himself to punishment,
disapproval, rejection and social boycott.
□ The moral stigma and legal barrier associated with addiction, provides the
ground for denial
The enabling behaviour of the people around the addict promotes denial.
□ The addict’s tendency to avoid internal comflicts encourages denial.
As a person’s addiction progresses: conflicts are created. On the one hand., the druo
becomes a ven/ important component of his life - because it produces in him a sense
of well-being and helps him to forget problems. On the other, reality tries to reinforce
the awareness in him that drug use only leads to unmanageable problems. At
this stage, he has two options open to him, reject addiction or reject reality. He takes
the easy route of rejecting reality and the process of denial continues.
There are several types of denial observed amongst the addicts:
SAMPLE DENIAL: Initially, the addict totally denies the existence of the problem of
chemical dependency, «even though the problem is quite ofcMous to others around
him. For example, the addict may say i smoke only occasionally’.
MINIMISING The addict underplays the extent of the problem Here, though he
would superficially agree that he has a problem (with drugs) he would minimize the
extent of damage. ’I give enough money to my wife to run the family and there
are no financial problems as H: is made to appear”.
BLAMING OR PROJECTING. He starts blaming others for his drug use. He
holds them responsible for his own short-comings. For example, he blames his
parents for not caring for him, having no feelings, for him, always nagging hirrf and
that he uses drugs only to forget his worries.
"’
2
RATIONALISING I GIVING EXCUSES. The addict does not admit that the real
problem is his addiction, but goes on giving innumerable excuses, justifications and
alibis for his behaviour. For example, 'I take drugs because it increases my
creativity’.
INTELLECTUALISATION: Here, the addict avoids facing addiction related
problems by dealing with them at a superficial, general, theoretical and intelleotua!
level For instance, he says that he knows the damage that addict;cr: would cause
and he is not so stupid as to allow it to cross the limit/
DIVERTING: At this stage, the addict changes the topic of conversation whenever
it focuses on drug-use or related problems. For example, whenever a well-wisher
points out to him the severe problems faced by him due to excessive drug-use and
suggests approaching a doctor for treatment, he would not allow him to continue,
but would deliberately interrupt and totally divert He would also ensure that the topic
of his drug-use does not come up again.
HOSTILITY: He prevents others broaching the topic of his addiction by getting
angry and aggressive or he avoids it by leaving the place.
SILENCE: Sometimes., the addict deliberately chooses to maintain silence, whatever
be the provocation. He resorts to this method in order to withdraw from reality.
The process of denia'. goes through 3 stages
1. During the First Phase, the addict thinks that he is in total control of himself
and feels independent. Normally he is not prepared to listen to others in the
matter related to addiction. During this phase, his family also minimizes the
extent of the problem. For example, the wife says, "He gives me money to run
the family. The problem is after all not that acute". This sets the stage for his
denial.
2. During the Middle Phase, as addiction progresses, he is no longer able to
function independently. Others around him try to hide the problem in an attempt
to protect the dignity of the family. They pay back his debts, feed him when he
comes home under the influence of drugs. His friends at the office also
protect him by taking over his responsibilities. Such enabling behaviour of others
around him encourages his denial.
3. During the Chronic stage, addiction has progressed to such an extent that others
around him are not able to manage the problems created by his abuse. They
stop covering up. He is unable to handle the situation and faces some crisis or
the other.
What is enabling behaviour?
‘'Enabling” is a therapeutic term which denotes a destructive form of helping. Any act
that helps the addict to continue taking drugs without suffering the consequences of
his inappropriate use of drugs is considered "Enabling Behaviour".
L
3
The Enabler
The Enabler is a person who may be impelled by his own anxiety and shame to
rescue the addict from his problems. He wants to save him from the immediate
crisis, and relieve him of the tension created by the situation. To the enabler, it is
like saving a drowning man. This rescue mission conveys to the addict what the
person really thinks, 'You cannot face your problems without me". Thus, in reality,
the "Enabler" is meeting a need of his own, rather than that of the addict, although
he does not realize it himself. The enabler actually reveals a lack of faith in the
addict’s ability to take care of himself.
This role is normally played by colleagues and friends. The behaviour of these
people conditions the addict to believe that there will always be a protector, who will
come to his rescue, even though these enablers insist they will never again rescue
him. They have always rescued him and the addict knows that they always will.
Such rescue operations are as compulsive to them as drug taking is to the addict.
Victim
The victim is usually the employer, the supervisor or a co-worker. When the
addict fails to perform his job, the "victim" normally completes the work. If the
addict is absent due to taking drugs, the "victim" gets the work done for him.
By the time drugs start interfering with a man's job, he may have been working for
the same company for quite a number of years, and his supervisor or employer, by
now would have become his close friend. Protection of a friend is a perfectly
normal response.
The Victim1 always hopes that this will be the last time that he will be rendering this
sort of a help. But he continues to protect the addict again and again. He
becomes completely dependent on this repeated protection and cover-up by the
victim.
in short, it is this 'Victim" who unknowingly helps the addict to continue with
irresponsible drug use without losing his job.
The Compensator
The key person is normally the wife or parents of the addict This person has
played the role of'compensator' much longer than anybody else. She has to take up
the responsibility to hold the family together in spite of all the problems created by
his addiction. She controls, sacrifices, adjusts but never gives up.
In helping the addict she unconsciously meets a need of her own. She builds her
self-worth on the addict's total dependence on her and continues to protect him from
every crisis.
i
4
When he gets into trouble., her typical response is to minimize it.
"Let us hush this up!"
Let me inform his office that he is taking leave because there is a function at
home!”
These are the ways the compensator minimizes the force and the pain of each
crisis as it develops. While they are trying to be helpful they are actually aiding and
abetting the development of the disease, tvery time they try to rescue an addict,
they are only postponing the necessary treatment.
He will recover only if the above mentioned people learn to break his dependency on
them and make him see the problem which has led to the crisis situation. He will then
find it impossible to deny the problems associated with his use of drugs and it is
the crisis that wili force him to come for help in despair.
The Enablers, the Victims and the Compensators, too, must change their roles, so
that the addicts denial is broken and he realizes the need to take help.
They should realize that.
□ Denial is the result of the social stigma attached to addiction; the addict’s
defence mechanism and the 'enabling behaviour' of the people significant to
him encourage denial.
□
m crisis is an opportunity to break the denial - it need not be threatening. Out of
the crisis, opportunities for intervention develop.
□ The resulting confrontation following a crisis can break through denial and
this will be the first step towards recovery, perhaps even the beginning of
treatment.
The Role of the Counsellor
□
Initially, the goal of the counsellor should be to establish an empathetic
relationship with the addict. Here, the counsellor shall maintain a supportive,
non-threatening climate. The counsellor's emphasis shall also be on the need of
the addict to seek treatment This would, in turn, generate a feeling in the
addict that he is accepted as he is.
□
Once, in treatment, the counsellor should assess the extent of denial and also
the magnitude of the problems caused by it. The addict should be exposed to
re-educative lectures, group therapy sessions and individual counselling. As a
consequence of this process, the denial will start breaking down on its own.
5
5
□
is not broken, confrontation is a technique which can be used.
’Confrontation is the deliberate use of a question or a statement by the counsellor
to induce the patient to face what the counsellor thinks the patient is avoiding.
The counsellor goes in for confrontation after:
a)
b)
C)
Establishing mutual trust.
Showing empathy.
Collecting factual information.
identifying the various discrepancies in the statement made by the addict,
Preparing the family members, if they are to be involved in the process.
Providing focus on the need to change.
d)
e)
f)
However during the orocess of confrontation, the counsellor should not moralize
condemn or
solutions. Confrontation
condemn
or provide
provide solutions.
Confrontation could be carried out .urirgi sndividu^
counselling sessions, group therapy sessions ano moividual sessions witn tne
medical practitioner.
and the counsellor respond
Confrontation may have the following outcome
appropriately.
Outcome
Counsellor's Response
Patient may accept
confrontation
Reinforce positively
Defy confrontation
Maintain empathetic response
Act confused
Ambivalent
hocus on current feelings and
later deal with issues again
Break the relationship
Assure him that help is available and provide
support to family members.
To conclude dealing with denial is the most crucial step in rehabilitation, for
unless denial’ is broken, the chemical dependent will not be motivated to become
actively involved in the recover/effort. By effectively breaking his denial s/otem,
however, the professional can help him not only to deal with his proolem witn drugs,
but also to deal with other life areas.
MH " 2-G. 8
ASSESSMENT
Assessment concerns
^Identifying Hie nature of problem
Severity of problem behaviour
^Understanding conditions that have cansed
^Conditions maintaining the problem behaviour
Assessment helps in
making decision concerning hospitalization
❖ prescribing medications
❖ role of psychotherapy
❖the modiii cation of family patfenis
❖related aspects of treatment
Nature and comprehensiveness of clinical assessment vanes ifom setting to setting
MEDICAL EVALUATON
Data of patient's general physical state and any physical pathology that may have a
bearing on his problem behaviour
;h) Heaxiache
Seizures
PSYCHOLOGICAL ASSESSMENT
Interviewing
Face to face conversation between two people to obtain information on various aspects of
I lie situation
□ simple intake interview
□ structured M.S.E
Psychological tests
Specialized assessment procedures
& The intelligence test
4 P.orschacfi ink blot tests
4 The thematic ^per ception test
2
Direct observation ofbehaviour
Usually confiued to hospital settings - helps to learn about patient's psychological make
up and level of functioning
A Delirium tiomens
Assessrrfent ofgroups
A Focus is on (lie group as a social trystem
Use of interviewing, psychological tests, observing patients
A Concerns determining social roles, communication patterns, aspects of
group’s structure and fimctioinng
Integration ofassessrnent data
Helps to see iJ findings complement each other and whether definitive clinical
piclui e is emerging
if gaps / discrepancies are present, fiuther investigation is needed
O Leads to an agreement on a tentative diagnosis based on which therapeutic goals
arc planned
PROBLEMS ISSUES IN ASSESSMENT
Confidentiality and informed consent
There is implicit or explicit agreement of the professional counselor to keep the
information confidential
I’he loss of confidentiality seriously endangers the very relationship will] the counselor
At limes., information need to be shared with families., ii-lends, relatives or other
personnel for planning the treatment
4 Special cncumslances that warrant disclosure of information
Hatw to self or othei s
Legal authorities require information
CULTORAJ.BIAS
a 'fests arc designed by the western psychologists and standardized based on studies
conducted in (heir own countries
4 Handicap tor persons from oilier backgrounds in taking the tests. Scores may not be a
fair measure of their potential
Using culture specific tests and teste that are standardized in Indian population help
3
LABELLING
® Creates social stigma
May brand a person and limits the opportunities open to him
O counselor needs to be sensitive on these issues, understand the impact of testing upon
die patient and use tests with utmost discretion
THE MENTAL STATUS EXAMINATION
Purpose
A To evaluate quantitatively and qualitatively, a range of mental functions and
behaviors at a specific point in time
A It provides important iidbrmation for diagnosis, assessing the course of the
disorder and response to treatment It is important for psychiatric and
neurological examination. MSE begins when the counselor first meets the
patient
4 Information and observation noted throughout the interview become pari of
the Mental Status Examination - patient's behaviors, thinking and mood
A At an appropriate point in time formal Mental Status Examination is under
taken
A Earlier informal observations about mental state are woven together with the
formal MSE
A The Mental Status Examination must be interpreted along with tlie presenting
history and if necessary with firrther psychological testing, physical
examination and laboratory studies
A Collateral information from families and friends are also valuable to confirm
the diagnosis
KEY FACTORS TO BE CONSIDERED ALONG WITH THE MENTAL STATUS
EXAMINATION
_ It is important to have some understanding of patient's social, cultural and educational
background. It helps the counselor to understand the subtle fluctuations in patient s
mood and other details during MSE
.
_• Patient's familiarity with the language used by counselor for mental status examina.ion
and age of patient are significant factors
- Patient may have difficulty in understanding various components ofMSE, such as
proverbs (used for assessing thinking process), if he does not know the language
4
MAJOR COMPONENTS OF MENTAL STATUS EXAMINATION
Appearance
Motor________
Speech_______
Affect________
Thought-Content
Thought process
Perception
Intellect
Insight
Age, Sex, race, body build, posture, eye contact, dress,
grooming, manner, attentiveness to examiner, distinguishing
features, prominent physical abnormalities, emotional facial
expression, alertness
Retardation, agitation, abnormal movements, gait, catatonia
Rate, Rhythm, volume, amount, articulation, spontaneity_______
Stability, range, appropriateness, intensity, affect, mood
Suicidal ideation, death wishes, homicidal ideation, depressive
cognitions, obsessions, ruminations, phobias, ideas of reference,
paranoid ideation, magical ideation, delusions, over valued ideas
Associations, coherence, logic, stream, clang associations,
perseveration, neologism, blocking, attention
Hallucinations, illusions, depersonalization, derealization,
Deja vu, jamais vu___________________________
_____
Global assessment: average, above average, below average
Awareness of illness
_________ _____
MAJOR UMTrATIONS OF MENTAL STATUS EXAMINATION
4 Subject to interpretative bias
4 Depends on the skill and experience of the counselor
4 Without collateral information and other necessary investigations, reliance on MSE
alone can lead to erroneous conclusions
GLOSSORY
Anxiety
Aphasia
Apraxia
Catatonia
Clang association
Dejavu
Delusion
Depersonalisation
Depressed Cognitions
Dysarfliria
Generalised feelings of fear and apprehension
Inability to communicate by speech, writing or symbols
Inability to complete purposeful movements
Form of schizoplirenia marked by periods of rigidity,
excitement and stupor.
: Speech in which words are repeated based on similarity
of sound without regard to meaning.
: Sense that one is seeing or experiencing something
that has been seen before.
: A false belief; firm belief opposed to reality but
maintained in spite of strong evidence to the contrary.
: Loss of sense of personal identity, often with a feeling
Of being something or someone else.
: Depressive thoughts, of dejection, gloomy ruminations,
feelings of worthlessness, loss of hope and apprehension.
; Difficulty in speech production.
:
.
:
:
5
Echolalia
: Imitative repetition of speech of another person.
Flight of ideas
: Rapid shifting from one topic to another, often with a
common theme.
: Sense perception for which there is no appropriate
external stimulus.
: Thoughts of killing others.
: Ideas/beliefs of an individual that other people are talking
about him, portraying his life on television or otherwise
making reference to him in their activities.
: Misinterpretation of sensory data, false perception.
: Disturbance of associations that render speech vague
and unfocussed.
: Creation of new words; often a mixture of other words.
: Persistent idea or thought which the individual
recognizes as irrational but cannot get rid of
: Presence of delusions of persecution/grandiosity
presence of behaviours characterized by suspiciousness,
envy, extreme jealously and stubbornness
: Excessive continuation of a response or action,
usually verbab
: Irrational fear; the individual may realise its irrationality
but nevertheless be unable to dispel it.
: Psychosis char acterised by breakdown of integrated
personality functioning, withdrawal from reality,
emotional blunting and distortion, and disturbances
in thought and behaviour.
: A delusion dial thoughts are placed in one's mind by
an outside source.
Hallucination
Homicidal ideation
Ideas of reference
Illusion
Loosening of association
Neologism
Obsessions
Paranoid ideation
Perseveration
Phobia
Schizophrenia
Thought insertion
MULTI PHASIC QUESTIONNAIRE (MPQ)
This questionnaire was developed by Dr.Vinodha Moorthy of NIMHANS from the
Minnesota Multiphasic Questionnaire (MMPI), considered to be the mother of all
inventories. It has been adapted to Indian standards and was standardised on Indian
population. The test consits of following scales: anxiety, depression, mania, paranoia,
schizophrenia, psychopathic deviation, hysteria and K-scale. These scales provide a
clinically useful tool in determining Hie nature of condition on each of the clinically
identifiable syndrome for the patient who is examined. The R Scale had been specially
built into the test to check the susceptibility to lying or the tendency to unconscious selfdeception. K Scale score beyond the cut off means "glossing over" or tendency to "Falce
good".
6
WHAT EACH SCALE MEANS :
ANXIETY7
- Free floating
- Inability to concentrate
- Difficulty in making decisions
- Extreme sensitivity
- Discouragement
- Sleep disturbances
- Excessive sweating / palpitations / tremors
- Sustained muscle tension
DEPRESSION
- Gloomy out look
- Loss of hope
- Social withdrawal
- Marked irritability
- Disinterest
- Slowing of thought process
- Obsessional worrying
- Exaggeration of problems
- Indecisiveness
- Negative self image
- Tendency to blame self
- Decreased motor activity
- Fatigue
- Insomnia
- Loss of appetite
- Decreased sex drive
MANIA
- Euphoria
- Elated mood
- Sociability
- Extreme impatience with restraint or criticism
- Short attention span
- Racing of thoughts
- Flight of ideas
- Impulsiveness
Over talkativeness
- Orientation towards action
- Positive self image
- Tendency to blame to others
- Grandiose delusions
- Hyper activity
- Indefatigability
- Decreased need for sleep
- Variable appetite
- Increased sex drive
7
PARANOIA
- Absurd, illogical and changeable paranoid delusions, frequently of persecutory
type
- Sometimes accompanied by hallucinations
- Suspiciousness
- Severe personality disorganization as in schizophrenia may not be present
SCHIZOPHRENIA
- Restricted affect
- Poor insight
- Delusions
- Hallucinations
- Sleep disturbances
- Disorganisation of thought and emotion
- Anxiety and panic
- Frequent loss of orientation to time, place, person
- Withdrawl from reality
PSYCHOPATHIC DEVIATION
- lack of guilt or remorse
inadequate conscience development
- Irresponsible and impulsive behaviour
- Low frustration tolerance
- Rejection of authority / non confirming
- Inability to gain from experience
- Inability to maintain good relationship
- Ability to put up a good front to impress others and exploit others
- Manipulative
HYSTERIA
- Conversion reaction
- High suggestibility
- Dramatic
- Excitable but shallow emotional responsiveness
- Attention seeking
SCALE
- Faking good
- Glossing over
MPQ is usually given when:
- Patient does not ’’settle down” in the programme.
- He presents abnormal/bizarre behaviour.
Understanding of issues in deaddiction is poor (reasons other than cognitive deficit
8
Simple and clear instructions are provided for (he patient on the top of the questionnaire.
He is asked to circle "true" or "false” found against each statement on the sheet. It is
important to establish rapport with the patient before the test (if it happens to be the first
session). The patient should be asked to respond to all items without omitting any. If
specific questions arise about the items of the questionnaire, the counsellor should
respond in a non-committal manner. This test can be both self-administered and also by
the counselor.
SCORING
The Scoring is done with the help of the scoring key. Under each scale certain items are
listed against ’True" and certain items against "False”. If the patient had answered
"True" for a 'True Item" of the particular scale, 1 point is awarded and 0 point for vice
versa. The same method is followed for "False" items also. The total score of " true and
false" items of the particular scale are added and recorded in a table against the cut off
scores of the respective scales. After scoring all the scales, evaluation is done.
INTERPRETATION
If the scores fall above the cut off, the particular scale is considered significant.
Significance of the particular scale means presence of such a condition in the patient
Scores below the cut off is considered as insignificant.
(□□GNTITVE CAPACITY SCREENING EXAMINATION (CCSE)
This test is used as a shortened form of MSE to detect cognitive impairment. It measures
orientation, calculation, attention, serial subtraction, immediate recall, memory and
similarities. This test is less sensitive to delirium or dementia in elderly.
Cognitive Capacity Screening Examination is usually given when:
Patients are screened for selection and camps deaddiction programme.
- Patients are screened for selection to vocational rehabilitation programme.
- Patients manifest poor understanding of issues during the deaddiction programme.
ADMINISTRAHON
Hie patient is instructed to listen carefully and answer the questions. Counsellor calls out
each question and records the answers given by patient discretely on the sheet. This test is
administered by the counselor only and can not be self administered.
SCORING
One point is given for each right answer. Wrong answers are scored zero. Hie total
number of correct responses is the patient's score for the test. The maximum possible
score on this test is 30.
INTTJtPRETATION
A high score (above 22) means above average cognitive understanding. Low score
reveals poor cognitive understanding. Low score are possible with cognitive or when
patient is under influence or during withdrawals (due to lack of concentration and
attention).
2-c-.
'WHAT WORKS' - OUR EXPERIENCE IN THE LAST 20 YEARS
Dr. R R Cherian, Director
Research & Treatment
Services
PRIOR TO TREATMENT - WHAT WORKS
>
Use Recovering patients (sobriety for a minimum period of 2-3 years) as
valuable resources to motivate and offer help to new patients.
>
Screen for psychiatric /medical complications and deal with them appropriately.
>
Spend time with the patient and family to
make them understand the need for professional help
prepare them to go through the process of treatment
-
create hope and conf idence
ensure that their expectation of the outcome is
realistic.
>
Select treatment agency according to patient’s individual needs.
>
Identify an agency which has a good image in the community. Ensure
professionals in the agency having thorough knowledge about addiction and
related issues.
DURING TREATMENT - WHAT WORKS
FOUR ESSENTIAL COMPONENTS OF PRIMARY TREATMENT
-
Medical management
Structured psychological therapy
built in programme to involve family
scheduled follow-up for a minimum period of 2 years.
GOAL CLARITY
❖ focus on ' whole person* recovery - drug free, crime free, gainfully employed
and good relationship with family members.
-v
.
. ... 3
-
TREATMENT PROCESS WHICH FACILITATES RECOVERY
❖ Providing opportunities for fellowship and interaction among patients.
❖ living importance to both group therapy and individual counselling. Using
confrontation method to break denial.
❖ Providing accurate information about the illness, relapse process and recovery.
❖ Initiating patients into recreational activities and help them to enjoy.
❖
Helping the patients to forsee stressful events, high risk situations and develop
coping skills to deal with them.
❖ Introducing AA steps and the concept of AA sponsorship - if possible work
upto 4th step.
❖
Ensuring use of disulfiram for a period of 12 months.
❖
Ensuring support from family members and involving other significant persons
from the community or from the industry.
❖
Helping the patient to strengthen his self-esteem - If he fe^ls valued,
accepted and respected, his motivation will increase.
❖ living special focus to clients with family history of addiction, early onset of
addiction, disruptive social consequences and anti-social personality. Ensuring
additional efforts in counselling
AFTER TREATMENT - WHAT WORKS AND ADDS VALUE
I
I
♦
After care issues to be specif ic and clear - Abstinence and improvements in
every area of his life.
♦
Ensure regular follow-up visits as for other chronic medical problems.
1 year
2 years
5 years
I
I
I
2 fold
5 fold
24 fold - recovery rate
♦
Letters, telephone calls and home visits, to meet this need.
♦
Ensure positive support from and understanding of colleagues and
supervisors in industries.
2
!!•
♦
Work ethics to be taught - regularity in job, punctuality, discipline and
improved interpersonal relationships.
♦
Ensure that the attitude towards the treatment agency is positive and the
staff are seen as role models.
♦
Assess improvements periodically. Collect collateral information regarding
the progress from family members / colleagues from workplace.
♦
Encourage the celebration of birthdays at the centre
♦
Handle relapses immediately so that the vicious cycle is broken.
♦
In case of patient with repeated relapses, look for alternative source of
help - extended care, therapeutic community.
OTHER FACTORS
□
The treatment centre to be airy, bright and comfortable
□
Attitude of staff should be one of care. Staff to work as a team with
understanding and clarity of roles.
a
periodic staff development programme to update the knowledge and skills of
professionals.
a
Ensure methods to retain staff and to minimise turnover
□
Information about patients to be documented in a computer for easy retrieval.
□
Confidentiality about patients to be maintained
3
Al H - X-o-10
4
THE PROCESS OF ADDICTION COUNSELLING
Addiction for obvious reasons has been termed a baffling illness. Helping the
addict overcome this illness, calls for an appropriately planned and skillfully
managed counselling process. In addiction treatment, counselling essentially
offers personal support and guidance to work towards the goal of abstinence from
all mood-changing chemicals and also achieve qualitative life style changes.
The process revolves primarily around the relationship t>etvveen the counsellor
and the client. It is this relationship that leads to growth and change. The
counsellor works ‘^with” the client in and a sense of partnership, and collaboration
prevails. The counsellor functions essentially as an ally or guide who helps the
client change self rather than an expert who ‘fixes” everything the client needs.
The primary goal is to assist the addict in achieving and maintaining abstinence
from addictive chemicals and behaviours. The secondary goal is to help the client
recover from the damage the addiction has caused in his life. That is, the patient
is encouraged to achieve and maintain abstinence and then to develop the
necessary psychosocial skills to continue in recovery as a life long process.
The process of counselling moves through 6 stages from initiation of the
counselling relationship to its termination.
Stage 1 - Developing a therapeutic relationship with the client
The success of any treatment effort, irrespective of the treatment model followed
essentially depends on developing a deeply meaningful relationship with the
client.
Being able to empathise with the client and perceive his life situation from his
angle without being judgemental is extremely crucial. Demonstrating care and
concern for the client and treating him as a human being worthy of respect helps
strengthen the counsellor - client relationship. It is on the basis of this relationship
that any further progress is made and nothing can be achieved without this.
Due to the nature of the illness, one is more likely to encounter a resistant, or even
a hostile client who is grappling with a low self-esteem, low frustration tolerance
and confusion about where he is and where he wants to go. Working with this
client calls for a lot of patience and tolerance.
The first one or two sessions are usually spent on collecting information and
session progresses depending on the pace set by the client. Asking too many
question too soon can be threatening to the client and it is important to be
sensitive to this.
It is a good practice to use the first session to explain the agency’s programs,
treatment goals and howr individual counselling sessions will help. The client can
be encouraged to express concerns about the treatment. Doubts may need to be
clarified and fear set to rest and his motivation and involvement in treatment
heightened.
The client usually uses the first few sessions to size up the counsellor, “Can she
really understand me? How can I tell this stranger all about myself. What if she
does not approve of me?” - are a few unsaid questions that he may bring with
him. By being a good listener and by offering support appropriately the counsellor
is gradually accepted by the client as a knowledgeable yet caring and non-critical
individual.
The client usually discusses non-threatening and non-controversial issues first.
He will probably be willing to talk about his job, family members, childhood etc.
He will provide a lot of facts but desist from discussing the emotional issues
involved. He may slowly progress and discuss his drinking / drug taking in a
superficial manner.
Yet all the while, he is alert to non-verbal and verbal cues from the counsellor.
When the counsellor is perceived as a trustworthy, caring individual the client
will discuss more and more personal and sensitive issues.
By the end oi the first stage, the client feels accepted and comfortable and is
willing to reveal more about himself.
Stage 2 - Exploring problem areas
Addiction affects almost all the life areas - health, education / occupation,
financial status, family relationships. Yet, the addict can be surprisingly ignorant
of these issues. He refrains from self contemplation as it can trigger a lot of
unpleasant feelings.
During counselling sessions, the client is gradually led into discussing each of
these areas. Details about these areas and the impact of drugs on them have to be
focussed. What when, where, with whom, how long as well as how intense the
problem is are questions that need to be dealt with. Certainly the picture that
emerges will be complicated, for if it were not, the client would have coped with
it long ago.
2
4
Talking about these issues in a “safe” environment is often cathartic to the client
who finds relief in it. By getting the counsellor to understand him, the client
understands his own problem in a clearer manner. The more he discusses his life
situations, the clearer the perception becomes - both to the client as well as to the
counsellor. At times, it will be helpful to get the permission of the client to talk to
significant people in his life to explore problem areas. This would give the
counsellor greater clarity about the areas she has to work on.
The counsellor in addition to being an empathetic listener needs to make use of
her skills at this stage.
□ The counsellor needs to be sensitive not just to the thoughts that are expressed
but also to those that are not expressed, help the client focus on them and draw
him out. Probing statements may need to be made to help him express himself
more clearly. These statements / questions can move the therapy process to a
meaningful state.
{iYou discussed a lot about your father but I noticed that you rarely
mentioned your mother's reactions. Can we discuss about it ?
□ Discussions need to help him express his feelings and not just facts. What are
his feelings about the situations and how they are affecting him need to be
clarified. Helping the client get in touch with his feelings is an important part
of Ills recovery that helps him understand himself.
Talking about his debts may provide details about his financial status. But
helping him express his fears, frustrations, sense of loss as well as his hopes
and aspirations take the counselling process to a deeper and more meaningful
level.
□ Talking about the past, revisiting particular events like marriage, child rearing,
illness, conflicts with parents unleash a lot of feelings. The counsellor needs
to be able to stay with the client in this process and deal with it rather than
just reopen the past, listen to it and leave it in the open.
□ Confrontation is a technique that needs to be used sparingly, judiciously afid
carefully. Confrontation needs to be made in a caring maimer when there a
discrepancy between what the client says and the counsellor perceives or
when there is a difference between what he said earlier and actually says
now.
3
'"You perceive your parents of not being supportive. Yet, they nave funded
your education and even your training course which you discontinued
thrice. They have taken you for treatment and I can see that they visit you
daily. Your mother is close to tears whenever she speaks of you. There
seems to be a difference between how you see it and yvhat
what is actually
happening. ”
□ Denial is a part of the disease of addiction. Justification, rationalisation and
blaming are all part of denial. As therapy progresses, denial is slowly resolved
easily in some areas and with resistance in the others. Flexibility to progress
with the client is important. Counsellors need to work with the less
problematic areas first before starting to work on the others.
□ Client may discuss problem areas with clarity but may not link them directly /
indirectly to the problem of addiction. The counsellor’s role lies in helping
him establish these links and see the whole picture rather than view’ it as
fragmental issues. His psychological problems, poor job performance, social
isolation - he may not see the picture as a whole and understand that addiction
has contributed to the deterioration in a big way.
" You said you. had beaten your vrife under the influence on alcohol, l ou
failed to offer support to your wife when your child was seriously ill. For
the past few months, you had not given money for running the household.
Is there a possibility that the separation ofyour wife could have been the
result of these incidents? "
□ Involving family members in this stage is important. Family members are less
confused and can provide details with more clarity. Moreover, just knowing
that his family is also actively participating in treatment will keep his denial
level low.
□ Involving close friends or relatives as part of therapy is often beneficial.
By the second stage, the tendency to blame others for his problems is minimised
and the client is helped to see it as “his problem”. Only when this shift is made,
meaningful problem solving is possible.
By the end of the second stage, the patient has a fairly realistic assessment of his
problem areas. He accepts addiction as “his” problem and is motivated to work on
it.
4
-5
Stage 3 - Goal Setting
Clients often repeat generalised statements like, “IT1 fix everything. Til sort it out.
I am going to be drug free and everything will be alright”. Soon after they
experience relief from the withdrawals and experience a sense of well being,
many clients are over optimistic and see the future as a bed of roses.
To some other clients, life seems bleak and giving up drugs can make life seem
more complicated.
No matter what his expectation of the future, goal setting is the next logical step
in the sequence of events.
Goals, need to be specific, realistic and appropriate. For eg. just saying “Til
pay back the loans” will not work. The client needs to work out a budget
based on his present income, estimated expenditure and amount available to
pay back the loans. Which debtor he will pay first, how much and when, are
details that need to be worked out. Impulsiveness, grandiosity and indiscipline
are traits that can make this part difficult.
Setting goals gives clients a clear sense of purpose and instills a sense of drive
and enthusiasm about the future. Goals also help evaluate one’s progress or
lack of it.
Most of the issues are interrelated and some are more pressing than the others.
Plans need to be made for each area ~ health, family, finances, use of leisure
time, work as well as faith in a higher power.
Plans to maintain abstinence are often the priority. The main issues that need to be
covered include
Having a routine
Identifying high risk places, situations and people where relapse is a
possibility
Coping strategies to deal with each of them.
Methods to handle craving
Need for continued support from counsellor and self help groups
The counsellor as well as the client are active participants in the process. The
counsellor may need to summarise or highlight issues discussed earlier.
5
r
'When discussing the past, w saw that there were short periods in which
you pursued difficult goals vigorousfy, after a while just lost steam and let
them die down. Right nc/w you are full ofplans of what you will do. You
are planning to work full time as well as do an evening course. I am
worried that you. will repeat the same process again. I would rather that
you start off with small manageable activities only and let the other issues
wait till your sobriefy is established”.
Establishing a few short term and long term goals is important. While going to
work regularly may be part of short-tenn goals, getting a promotion may be
the long term goal.
The counsellor needs to brainstorm with the client about all possible options.
Discussions about his future career may include being a sales man, a small
time businessman, teacher or even a computer professional. Evaluating the
different options and weighing the pros and cons is done primarily by the
client with active prodding and stimulating statements made by the counsellor.
For example the patient who is contemplating a shift in his job may need to
consider the work environment familiarity with the job, the challenges involved,
drinking and drug use in the work environment and not just the increase in the
salary.
It must be remembered that the client is the expert about his recovery. It is his
plan for his future rather than the counsellor’s. Objectivity, experience and
knowledge are the counsellors strengths that are offered to assist him in his
effort but it ends there.
Exercises of these sons help develop problem solving skills in the client. Thus
slowly he moves through the processes of effective decision making and learns
self-reliance.
Stage 4 : Maintaining Change
The initial period of abstinence is usually euphoric. Plans that are made in the
safety of the centre may not be just as easy in the real world. Hence, follow-up
visits need to be planned at frequent intervals depending on the need and
accessibility of the treatment centre to facilitate the change process. During the
follow-up visits, adherence to the action plans and progress made need to be
discussed.
His routine including eating and sleeping habits, efforts to maintain sobriety,
mood-status - all may need to be discussed. These sessions are often used to look
back and evaluate recovery.
6
.*
The counsellor is often ihe only cheer-leader in the initial recovery period. The
counsellor needs to he sensitive to progress made and appreciate him for the
efforts he has taken. This strengthens his self-esteem and helps him view the
future optimistically.
Two months of work without absenteeism, no further loans taken, the child
awaiting his arrival, invitation to a relative’s wedding - all these need to be
considered as signs of recovery.
Changes may need to be made if the plans don’t work well enough. The
decision not to do overtime may have to be relaxed for a week if there is
shortage of staff at work. He may be able to attend only 3 N.A. meetings a
week rather than one daily.
The family members also need to be helped to accommodate the changes in
the client. High expectations, casual remarks about the painful past and a
controlling attitude by the family need to be altered.
Clients need help to identify relapse indicators at thought, feeling and
behaviour levels. Bringing these to client’s notice and helping him strengthen
his coping mechanism are important.
-
i(WhGn you met drug using friends, earlier, you would just smile, wave
and move on. Now, you seem to participate in short conversations. You
are also missing out on your gym visits over the past two weeks. You
mentionedjust now, that life is just moving along and isn t interesting. Let
us discuss about what is happening".
Handling relapses is an important issue. Counsellors cannot view the patient s
relapses as a sign of their own failure. The anger and frustration that grows
out of it will limit the counsellor’s ability to help the client.
The main issue is to arrest the relapse and initiate abstinence as soon as possible.
Talking to the client or the family, making house visits, offering medical help 01
motivating him to receive help from the self-help groups helps.
-
Relapse cannot be seen as the client’s complete failure too. It rather indicates
tliat there are areas that need to be changed and that further effort is called for.
Being critical and using “I told you so” statements are not helpful. These only
instigate the patient to be defensive. Rather the counsellor should convert his
guilt and remorse in a constructive manner . Later on, the relapse process the
issues that led to the relapse, and ways to prevent it in the future need to be
discussed.
7
*.
this stage, the counsellor helps the client stay on track, maintain his focus on
the Qoals nudging him on to grow and actively intervene when he is heading in
the wdng diction. When there is a relapse, the counsellor helps the client
providing hope and enthusiasm for his recovery.
Stage 5 - Termination
All tough the preceding stage. Ute councilor i. preparing fte cfenlrio
»
that he is not totally dependent on the counsellor any more. When the counsel
has repeatedly walked him through the process of problem identification, g
SSLhg
client teams toe .Kill, to can be used by temsetf
without the help of the counsellor.
handle issues on his own.
For most clients, termination takes place in 1 or 2 ?'ears of
“
contacts are maintained for a while longer. Keeping in mind to
of the disease, it is necessary to assure the client that heip£s avada
he needs it. It is not uncommon to receive clients even after f
5
after recovery. They may come just to keep in touch, review the piogress
sometimes hasten to take help fearing a relapse.
AU through to five stages, to counseUor’s skill is to primary force; tot keeps
the clientactivelv involved in therapy. In practice, however to chent may n
XSly Process from one stage to to other in a clear cut marmer as outoted
earlier Instead one stage merges into the other and the client may
<
«
U. The sbength of the counsellor to m
chent, helping him stablilise and move forward. This process can be emotion y
aratifring and professionally satisfying but can be frastratmg too. The
Juraeufr’s emotional maturity' to deal with set backs using to support
to
team is of crucial importance.
In Summary
Counselling is a process with two overlapping phases, The tot phase focus ,
building a relationship that is characterised by rapport and trash On
o
this meaningful relationship, the client is helped to explore pioblem areas at the
SuX S feeL level, and identify goals of therapy. Planning implementing
strategies to overcome problems, evaluation and follow-up form the second stag
of counselling.
8
<
V
The process of counselling
Assessment
;
current drug taking history
I => past history of substance abuse
j
including use and abuse of alcohol
=> consequences of substance abuse in
the areas of family relationship,
occupational
and financial
functioning and legal issues
=> information about major medical
problems in the past and present
health status
=> co-existing psychiatric disorders
=> support available
=> previous treatment
Assessment is critical not only before treatment but also as an on going part of
the process. Only by continuously assessing the client's progress and problems,
can the counsellor accomplish the goals of therapy in the time frame available.
Initial sessions
identifying,
focussing
and
prioritizing problems
=> working with the client to develop
a treatment plan that requires the
client’s active participation
=> eliciting client concerns about
problems and solutions
understanding client’s expectations
=> explaining
the
structure
of
treatment including the process
-=> making referrals for critical needs
that have been identified but cannot
be met with in the treatment setting
for
neurological
(treatment
problems etc.)
i
I
I
I
L
9
‘5.
1
Subsequent sessions
The counsellor should help the client to set specific goals - total abstinence as
well as improving the functioning in several areas of life.
I Subsequent sessions
=> strengthen motivation
i
=> identify and enhance the skills,
strengths and resources available to
the client
=> address identified problems
=> monitor changes; to check whether
the accomplishments are consistent
with the treatment plan and the
client’s expectations
=> reinforce the changes made
assess further needs of the client
and if need be referral to other
centres (for example vocational
training)
Maintenance strategies
Continuation of therapy is essential in maintaining abstinence and reinforcing
improvement in the quality of life. The counsellor should continue to provide
support, feed back and assistance in setting goals.
Maintenance strategies
=> educating the client about the
chronic, relapsing nature of
substance abuse disorder.
helping the client tq identify
relapse triggers and methods to deal
with them
=> developing strategies for identifying
and coping with high risk situations
teaching the client on methods to
capitalize the personal strengths
■=> developing a plan for future support
in the form of self help groups,
family support and community
support
10
I
» *•
Ending treatment
Termination of therapy should always be planned in advance.
Ending treatment
provide a sense of hope for
continued change and maintenance
of changes already accomplished
leave the door open for possible
future sessions dealing with the
client’s other problems
elicit commitment from the client to
try to follow-up through on what
has been learnt or achieved
=> review what positive outcomes the
client can expect
review possible problems the client
may encounter
mention the early indicators of
relapse and strategies to deal with
them
11
MH-
PERSONALITY DEFECTS
During drinking days, the patients would have developed certain negative
personality traits. They might have had them even before, but with addiction
these would have become exaggerated.
1.
Selfishness -
Taking care only of one's own comfort and needs, without respecting the feelings
and needs of others.
e g. He would disturb his son who is studying for his exam, to buy him cigarettes.
He watches TV, unmindful of disturbing the children who are sleeping.
He would buy a new shirt for himself, not bothered to get the umbrella which the
wife needs
2.
Dishonesty
Telling half truths and breaking promises are acts of dishonesty, just as lying is.
e.g. The patient would have received bonus or arrears in payments due, but he
would not divulge this information to the family.
He would have taken a loan from his PF to repay the old debts but would tell his
wife, his colleague paid the money.
3.
Resentment
Resentment collected over the years leads to friction, hatred and unjust revenge.
It leads to misery both for the patient and for others around him.
e g The brother-in-law warns about excessive drinking- the patient gets angry at
the brother-in-law.
The supervisor gives a warning letter to the patient - he hates the supervisor for
that.
Since the patient was under the influence of alcohol, the relative did not talk to
him but spoke to his wife. When the relative came to invite him for the wedding in
his family, the patient is angry with the relative.
All these incidents may have taken place years ago, but the patient still carries
these memories and reacts.
■
m'-
-jn-.
2
4.
Jealousy
Sadness at others' good fortune and making fun of their achievements often
springs from jealousy.
e.g. Patient's colleague buys a new two wheeler by saving money - he ridicules
his saving as a miserly act.
Brother-in-Law is a hard worker, takes care of his family, does not drink, smoke
or play cards. He is ridiculed by the patient as that he does not know how to enjoy
life.
The neighbour buys a plot of land by his sheer hard work. The patient teases him
by saying, he is lucky to have brothers-in-law in Dubhai.
5. Procrastination
Putting off, and postponing things that need to be done right away- is a common
trait. (I will do it tomorrow).
e.g. The patient has to buy train tickets for the family to go to an important
'wedding. He will keep postponing till the last minute. He cannot get the tickets,
hence, he would make the family go in the unreserved compartment with lot of
discomfort.
He wiil not pay the electricity bill till the last day . As a result he has to stand in
the long queue for two hours wasting half-a- day's leave, while he could have paid
the same in 10 minutes in the first week.
6. Impulsive behaviour
Making decisions without thinking, taking action without visualising the
consequences.
e.g. Some of the impulsive decisions during recovery are buying things for children
when they do not have sufficient funds or giving loans to friends.
7.
Highly Sensitive
Feeling easily hurt, sensitive and touchy. But not sensitive to others' feelings - he
does not mind hurting others.
e.g. While walking on the road, his brother-in-law would not have noticed his
presence and not said hello. He gets upset. 'He has a good job that is why ne is
behaving in an arrogant manner1, he mutters.
He would have gone for a wedding. A relative would say, '! am glad you have gyen
up alcohol. I want you to stay sober in the future also1 - He gets hurt. 'As thougn, I
am going to go on a binge', he feels.
3
8. Defiance
Not willing to accept any suggestion given by others (without examining the pros &
cons).
e.g. Elder Brother suggests, "you need not take up sales job as you have given up
alcohol recently". Since the suggestion has come from the brother, without even
examining it, he goes ahead and accepts the job.
Wife would suggest, "Don’t go for the friend’s wedding in the night ; instead go in
the morning (to avoid drinking friends)”, but he would go just to spite her.
9. Wishful thinking
Lives in a dream ’world of his own, expects dreams to materialize without proper
action.
e.g. Patient wants to go to Dubhai for a job. Always talks about his dream
without making any practical pian to obtain a job or make money to go to Dubhai.
Action Plan for the Patient
It is important to develop qualities which will help the patient to lead a contented
life and build relationships. ’
Courtesy
being gentle, respecting others
Cheerfulness
seeing beauty in life
Sincerity
genuineness
Kindness
showing care to others
Patience
work towards the goal, without worrying about the results
Gratitude
honest recognition of help received
I’ ■
MH -
GROUP THERAPY TECHNIQUES
Group Therapy has been acclaimed over the years as by far the most effective
method of treatment for addiction. The gains of group therapy are now well
established. Following are a few therapeutic gains that are unique to group
therapy.
Provides an opportunity to share and identify with others who are going
through similar problems. Groups help in developing a sense of belonging.
The spontaneous sharing of older members, of their progress and the changes
they have achieved, instills hope in the new skeptical members.
Helps clients in understanding their own attitudes about chemical dependency
and their defences against giving up chemicals by identifying similar attitudes
and defences in others.
Verbalisation of thoughts and feelings, open feed back from others about
positive and negative behaviour and being a witness to successful conflict
resolution, helps them develop socialization skills.
Teaches members interdependence (in contrast to dependence on chemicals)
and thus build a better social network. This also helps chemical dependents to
work through isolation.
Provides a congenial atmosphere to powerfully confront denial, and assess
high-risk situations. Members utilise the group as a laboratory for developing
new responses and newskills.
Provides an opportunity to formulate realistic goals and plans.
Sharing insights, offering suggestions and support gives an individual the
pleasant feeling of helping another. This altruism aids in strengthening selfesteem.
These gains prove that beyond doubt group therapy can be effective. The task then
for the counsellor is to maximize the gains within the available time frame.
Following are a few basic guidelines that contribute to effective group therapy
sessions.
Size of the group
5 -10 members in a group is termed by Yalom as the 'Acceptable Range’. When
there are less than 5 members, it fails to function as a group; with more, it becomes
unwieldy - both making it less effective.
IN
1
5.
2
Duration of the group meeting
A minimum of one to one and a half hour is needed for the group to settle down and
get to work on an issue. However, if a group stretches beyond 90 minutes, fatigue
sets in and diminishing gains are reported.
Frequency of meetings
Five group meetings a week Is the minimum requirement. On discharge / follow
up, meetings may be held once or twice a week to strengthen changes made and
offer suppoit tluougli the recovery process.
Physical environment
A pleasant quiet room, that ensures privacy is a pre-requisite for group therapy
meetings. The seats should be similar and placed in a circle conveying that all
are equal. Moreover, everybody is visible to the rest of the group; face to face
interaction is made possible and non-verbal behaviour can be easily observed.
Rules and limit setting
At the beginning of the session, the counsellor has to clearly spell out basic rules
like punctuality, regular attendance, staying for the entire session and not leaving
midway, not attending under the influence of drugs. The following norms are a
requisite as they help members function appropriately.
Confidentiality
Any information gained about another group member in the group therapy setting is
to be treated in strict confidence. In short, "What happens in the group, stays within
the group" should be repeatedly stressed.
Listening
Maintaining eye contact, being willing to listen to other person's feelings and
words without interrupting, arc important. Interruptions are not to be made unless
- the member is repetitious.
- the member is rambling without focussing on issues relevant to the topic
of discussion.
- the listener has not understood and wishes to clarify his thoughts.
Using 'I* Statements
'We' and 'they' statements lead to superficial sharing on generalised issues.
You’ statements usually turn into critical, judgemental ones. T statements, on the
other hand, help him speak only for himself and own responsibility for his
feelings, thoughts and behaviour. (Example: "I feel ashamed. I have hurt my
parents").
1/'
3
Open, Honest, Spontaneous sharing
Group therapy offers an unique opportunity for handling issues. It should be
emphasised that to maximise gains, wholehearted participation of the group is
essential. Each member needs to remember that "the more he puts into a group, the
more he will benefit from the experience”.
All participants are considered equal, irrespective of their drmking/drug taking
status, number of days they have stayed at the centre, or nature of the damage.
The counsellor, as a facilitator of the group, need not share any details regarding
herself.
Feedback
Guidelines for giving feedback
Feedback is an essential component of group therapy. The following are a few
guidelines to be discussed with the clients prior to entry into the group:
•
To talk about behaviour one can see.
It should be specific and relevant.
"I notice that you are late by 5-10 minutes everyday. So we are unable
to start the group meeting on time".
•
Feed back should be given caringly and not by hurting or attacking another
member. No judgemental statements should be made.
"1 can see your problems. You continue to have many drug taking friends,
and you have no access to NA. meetings also".
•
Members should avoid sarcasm and condescending remarks while giving a feed
back. No advice is to be given - only responses.
"You want to repay debts to the tune of One lakh in 6 months ?
You must be joking" - Sarcastic remark.
"Listen to me. You cannot handle this. You better ask your wife.Advice.
"Let us plan out various methods and see how best it can be worked out" Proper response.
•
Members should be encouraged to share positive feed back also.
"I am touched by your honest sharing".
■ u
4
Guidelines for receiving feedback
•
Members should spontaneously ask for feed back and openly receive it.
•
Excuses should not be given. Members should avoid defensiveness.
•
Members should learn to acknowledge the value of feed back and express
appreciation.
" I am glad you have helped me see the positive qualities of my brother".
•
Members should think and build upon the feed back given. They should view
feed back as a continuing exploration.
The process of group therapy
Classically the group process can be divided into three phases. The early phase is the
beginning of the group, particularly the first few meetings. The middle phase is the
substance of the group, with the clients coming together, interacting, sharing,
growing and changing in the counsellor’s presence. The last phase is when the client
completes the programme and leaves the group.
The first meeting
Group members are usually very anxious over their first meeting. As in any
relationship, introductions are needed. The counsellor initiates the process by
introducing herself outlining the purpose of the group, and soliciting introduction
from the clients. This can be done in several ways, of which the following is one
example:
"I am glad that every one ofyou could make it. Let's get started.
As you know my name is
I want to tell you why we are here
and what we will be doing in these meetings. Some ofyou know
each other and others do not. One thing that every one has in
common is being dependent on alcohol or drugs. This is going
to be a time to get to know each other, learn about problems
each one is facing, and find new ways to deal with them.
At times we will talk about issues which may be sensitive like
feeling lonely, depressed, problems al home etc. Here you will
discover that you are not alone with these feelings and when
you start sharing you will definitely feel less painful. Members
here will help you minimise your pain."
The introduction sets the tone for the group. In the above example we find the
following messages:
1) A statement of purpose of the group
2) Identification of commonalty. This aids in developing unity in the group.
3) Disclosure of sensitive issues will be explored. It is vital that clients know such
topics will be discussed.
I
i
4) Often they are overwhelmed by their problems and are disillusioned that no
alternatives exist. Group gives them the much needed hope.
♦
Introduction of clients can be done in many ways. When the suggestion is OpOTi
ended i.e. "Let's say our names. Talk something about ourselves," the response may
be either anxiety-ridden silence, or names rattled off in a rapid fashion with no
mention of personal data. Introduction is the chemical dependent’s first step
towards self disclosure. They can be in a state of panic and can have a lot of
anxiety. To get over this initial barrier, the following methods may be followed.
First the group can be divided into pairs and each client asked to introduce himself
to his partner. After this initial contact, they could come back, form a group and
introduce the person each one met. This exercise helps the client take off direct
focus on self. The second method of approach is to request senior members to
introduce themselves first, thereby setting a role model for the new comers. After
the introduction, the next step is to spell out group guidelines. These group
guidelines have been discussed in the earlier part of the chapter.
Extensive clinical observations show how the group evolves and moves through
three stages of growth. In general, a successful group will flow through them. At
times, it may regress to tire previous stage, but it will eventually move into the
later stages.
Each stage is characterised by its own set of feelings and behaviour. Being familiar
with these, will help the counsellor identify' which stage the group is in, so that she
can aid its moving successfully through its developmental stages.
.1
t
Role of the Counsellor
The secret of making group therapy a powerful source for change is an art and a
skill. Here as in a counselling relationship, the basic personality of the counsellor,
her professional training and experience can make a world of difference. The
counsellor has to maintain a relationship characterised by warmth, empathy,
concern, acceptance and genuineness. An effective counsellor will be sensitive and
flexible to the needs of the group and flow with it, all the while making valuable
interventions.
•
Helping members belong
The group therapy situation may be stressful for the new comer. The members
are strangers to each other and look at the counsellor as the unifying force. By
using this "special member" status, the counsellor goes on to create one
physical entry - "a group” from a collection of members with different
experiences and problems.
Being sensitive, accepting and supportive to all members and displaying this
through appropriate verbal and non-verbal behaviour, the counsellor can create
a sense of "oneness” or ’'togetherness”.
Late coming, absenteeism, sub-grouping (two or three members carrying on
interactions while actively excluding others) and "scape goating" (majority of
the group making one member the target of their negative feelings) threaten
cohesiveness. The counsellor should act early and decisively to counteract these
forces.
•
Encouraging ’’Feeling Level” Interaction
Feelings of shame, guilt, resentment and fear are the predominant negative
emotions. Being able to talk about them in a supportive, caring environment to
people who have actually experienced them, is what makes group therapy
effective. Handling anger and resentment means getting to grips with the
underlying hue feelings. Members who are eloquent, may find it easy to share
on a superficial level. By encouraging and emphasising "feeling level"
statements, the counsellor can help them get in touch with their negative
feelings, which they try to run away from. Separating thoughts from feelings
and labeling feelings, helps them explore further and deal with them better.
This exercise stands them in good stead in their future communication patterns
and problem solving efforts.
I
MH-T-ctS
MEDICAL AND PSYCHIATRIC COMPLICATIONS RELATED
TO ADDICTION
Drug abuse has a deleterious effect on specific organs of the body. In addition to this,
the poor eating habits, irregular sleep patterns, poor health care and inordinate delay in
seeking medical help only ser\;e to worsen the situation .
The type of drug abused and the duration influence the :amount of damage caused,
Medical and psychiatric manifestations depend on the following faiictors:
a)
Age: The damage is higher among the veiy young whose bodies arc still in the
process of growing up and in the older age group for obvious reasons.
b)
Nutritional status and living conditions: Tire health damage is more among the
economically weaker sections.
c)
Health condition prior to abuse: The damage is less among individuals whose
physical condition is good when compared to individuals whose health was poor
even before the onset of addiction.
d)
Genetic loading factor: The substance abuser with a genetic pre-disposition or a
family history of specific medical or psychiatric problems is more susceptible to
that particular problem. For example, a family history of schizophemia further
hastens the psychiatric breakdown of a ganja abuser.
Medical and psychiatric complications can be studied under four major heads.
a.
b.
c.
d.
Problems due to intoxication
Problems due to withdrawal
Psychiatric disorders associated with substance abuse
Systemic disorders associated with substance abuse
PROBLEMS DUE TO INTOXIC ATION
Intoxication is a transient condition resulting from recent use of a psycho- active
substance at a sufficiently high dose level. Impaired attention, judgement and
interference with personal functioning can cause any of the four problems.
1.Trauma or other physical injury
a) Mood changes caused by drugs incite negative feelings leading to violence. Street
brawls and gang-fights are often initiated and carried out under the influence of drugs
and alcohol.
0
Driving vehicles or operating machinery under the influence of alcohol / drug cause
accidents and injury. Poor motor coordination and a disregard for safety'
guidelines due to intoxication are the cause of about 50% of our road accidents
and a large number of industrial accidents.
c) Physical injury or death due to crossing railway tracks, falling from high places and
other risky behaviour due to poor judgement of time and space are also commonly
reported.
d) Head injuries are very common. They may cause permanent brain damage. Difficulty
in comprehension and memory or even strokes can follow.
2. Perceptual distortions
Drug intoxication
can maxe
make a person aelinous
delirious and disoriented. Irritability, rapid
uuvAivauuH van
fluctuations in mood and impaired attention may set in. He may hurt himself or others" in
this state.
3. Acute intoxication reaction
Reaction depends on the type of drug abused. Narcotic analgesics can cause apathy,
sedation and psychomotor retardation. Cannabis can cause agitation, suspiciousness,
hallucinations and feelings of depersonalisation. With depressant drugs, vomiting or
convulsions can occur.
Given time, the acute intoxication wears off. If he is agitated, he needs to be watched
carefully as he may harm himself or others.
Forcing him to eat or drink when he is in the stage of intoxication is risky. Food particles
can enter the lungs causing him to choke on it and die. Severe lung infections also can
develop due to aspiration of food into the lungs .
4. Coma anti overdose deaths
The quantity of drug intake is steadily increased due to tolerance. While tolerance
develops to effects like euphoria, the increased drug intake may be too high and produce
respiratory depression, coma and death.
The purity of illegal drugs like heroin can only be guessed. He may use the same
quantity of drug as usual but unknowingly take an overdose if the quality is superior.
IV narcotic abusers are highly prone to over dose deaths of this kind.
Page 2
CombinajolI of alcohol and sleeping pills is particularly dangerous While alcohol is
mXonriZh fClt
Pills teke
to ^t. The user
when the
diml alcohol under the impression that he is not 'high' enough. Later
eping pi s start acting on the brain, the overdose can result in death.
PROBLEMS DUE TO WITHDRAWAL
Sdhl^to^1 SymPtOm! OTfvaiyhig intensity occur as part of withdrawal differing
Xtoms L ± H
? r n°W
th3t the
of Wlthdrawal
symptoms has been blown out of proportion and in realitv is not as painful and
uncomfortable as it was previously made out to be. Offering psychological support and
symptomatic treatment is seem as being most effective.
support and
tefcn toto coT'd bet.reme^ered that the Patie*t’s age and physical condition need to be
accommmed bXdi°ni
“ SCV6re fomi °f ^hdrawal can be
accompanied by medical emergencies and should be handled carefully.
PSYCHIATRIC DISORDERS ASSOCIATED WITH SUBSTANCE ABUSE
Psychoactive substances can induce psychotic disorders either during
or immediately
er eir use, with one or more of the following symptoms:
a) Psychomotor disturbances: The patient may be restless and agitated
or may stay
immobile
b)
t0
Pe°ple’ the p,aCe Wh6re he is “ or
cj Hallucinations: Auditory hallucinations and visual hallucinations are most common
Tactile or olfactory hallucinations though rare, may occur.
d) Persecutory delusions : He may complain that people
are trying to harm him or
plotting against him.
e) Ideas of reference : He may report that others are talking about him and state that he
is being discussed in books or even in the television.
f) Abnormal emotional response ranging from intense fear to ecstasy that has no
iclationship to what is happening in reality'.
Page 3
Cannabis abuse can particularly trigger off neurotic and psychotic disorders. Anxiety,
panic attacks or depression can set in due to cannabis abuse. There has been cases
reported where even a few doses of cannabis has produced a psychiatric breakdown.
Drug induced psychotic states are usually of short duration resolving at least partially
within a month and fully within six months.
SYSTEMIC DISORDERS ASSOCIATED WITH SUBSTANCE ABUSE
L Dermatological complications
i) Septic coetaneous complications:
a) needle tracks can be caused on injection sites
b) tattooing and scaring can occur due to the presence of foreign bodies in the needle
used. Addicts may heat the needle on fire to clean it and carbon deposits can settle on
the needle causing this.
c) abscess formation due to infection can develop on injection sites.
d) cellulitis -infection of the skin which appears as a red inflamed patch can develop.
ii) Other skin problems:
a) Pruritis: Narcotic analgesics can cause itchy skin and scratching can lead to infection.
b) Dermatitis: Inflammation of skin due to infection or allergy also can occur.
c) Acne Rosccia (large boils on the skin) and rhinophyma (red and enlarged nose )
known as brandy nose can be caused due to alcohol abuse.
2. Cardiovascular complications
a)
Endocarditis: Infection of the lining of the heart and the valves can occur among
IVDUs.
b)
Cardiomyopathy: Muscles of the heart are enlarged and cause dysfunction.
c)
Thrombo phlebitis: Repeated infection at same sites causes the development of
thrombus in the veins affecting blood circulation.
Page 4
d)
mbohe phenomena: The presence of air bubbles or thrombus that forms in the
veins can cause embolus to develop. This embolus can move into the blood
stream, lodge itself in any part of the circulatory system and cause problems.
Myocarditis: The muscles of the heart are inflamed and may become permanently
damaged.
f)
SrilSnn„Sit5, hf 1116
^UCed effect On the heart can cause ventricular
fbisT 0r1]hem7hage and sudden ^ath. This is common among IV drag
abusers as well as due to amphetamine and volatile substance abuse.
Pulmonary complications
’’
.i1"’,”8 n'
abn“rs' ""
*>“ -»» I" Mood
am can lodge itself in the lungs and interfere with its functioning.
J°ffa" a*’ ‘“”8 ““s “
b)
norosis which again affects the functioning of the lungs.
C)
Pulmonary oedema: Fluid can collect in the lungs and cause breathlessness
d) Aspiration pneumonia : Due to drug effects the reflexes
may be poor and the food
particles may enter the wrong way causing pneumonia.
e) Pharyngitis, bronchitis, pneumonia and tuberculosis are common infective resoiratorv
stXandnombt™8 abUSerS'
P0OTmedi^’ ^are, poor nutritional
status and pool hygiene increase the nsk of these infections.
4. Hepatic complications
2Z of
Inlake of XohJl n .V
to JXXws
p”,s B “‘J c areOtl"
ci>mmon
n
r W'Cal sisns of
q““ “
’tase“'s« »««■■«
°f 1- cells leading
b) Fatty liver can develop due to alcohol abuse,
This condition is easily reversible if
alcohol intake is discontinued.
c) With continued excessive intake of alcohol, alcoholic cirrhosis can develoo Healthv
liver celIs are replaced by scar tissues and the liver slowlv loses its ability to work
»«m8Jaund,ce. accumuMon of fluid i„ ite akdomen, S.
muX eu
The damage caused is permanent and cannot be reversed.
Page 5
x-lmong IV drug abusers, infections that passed through unclean needles can kill
liver cells leading to post necrotic cirrhosis, (nausea, vomiting and signs of
jaundice)
5. Complications in the reproductive system
The incidence of many kinds of sexually transmitted diseases are common among
drug abusers. Lowering of inhibition, loss of value systems and prostitution for
money to buy drugs are responsible for the casual attitude to sex, increase the risk of
infection.
b) Narcotic analgesic and depressant drugs reduce one's sex drive and cause other sexual
problems as well.
c) Alcohol and cannabis can produce impotency by reducing rhe level of sex hormones.
d) Menstrual abnormality is noted among female drug abusers.
e) Children bom to mothers who abuse drugs and alcohol during their pregnancy usually
have low birth weight and other problems in the physical and mental development.
Newborns can also go into withdrawals soon after birth.
6. Neuromuscular complications
i) Non-infectious neurological problems
a) Cerebro-vascular accidents: The embolus (due to air bubbles or thrombosed
veins) can reach the brain and cause damage. Depending upon the place where this
emboli settles in . the neurological deficits will be mild or severe.
b) Chronic organic brain dysfunction (dementia) : Repeated impact of drugs/alcohol on
the brain cells can cause permanent brain damage. The abuser’s cognitive function is
reduced and new learning becomes difficult.
c) Wemicke-KorsakofFs syndrome: Excessive alcohol intake and associated thiamine
deficiency causes degeneration of the brain cells. Tremors, poor balance and
coordination, involuntary movement of eye balls and loss of memory occur.
d) Neuritis : Tremors, tingling, numbness and pain in extremities develop due to the
damage caused to the nerve fibres.
Page 6
ii) Problems due to Infections
a) Bacterial meningitis: The covering layers of the brain
can be infected by use of
unsterile needles.
b) Abscesses can Tdevelop due to infected needle use and cause degeneration of brain
cells and pus formation.
Drusy alcohol abuse can affect the functioning of the liver badlv Hepatic coma can set
• Following this, all the systems in the
breakdown and
the body
body breakdown
and death
death ensues
ensues
7. Haematopoietic complications
"d"“
a) Sal™o1^Xdir’C,,y
PrO<l"'‘O”
b) Bone marrow depression is common in solvent abusers.
c) Reduction in white blood corpuscles
occurs in ganja abusers and alcoholics causing
reduction in the level of immunitv.
d) Megaloblastic anemia due to folic acid deficiency develops in alcoholics.
d) ®a?^ren“a:
to unsterile needles can spread anywhere in the blood
and lymphatic system and can cause lymph node enlargements.
8. Endocrine system disorders
S) SdXl,”4 “ abU“ ,0'WrS ,he “O'®"™
« fc body cami„g
b) Incidence of diabetes milletus increases among alcoholics.
9. Renal functioning disorders
Nephropathy : Infection of the cells in the kidney can set in and damage it permanently.
10. Gastro-intestinal disorders
effect of the drugs abused.
c“
‘l“' 10 P°” r™1
b) Chronic pancreatitis develop due to damage of the pancreas
c) Cancer due to abuse of alcohol
Page 7
well „ due to fc
in the alcoholic
11. Other complications
a) sharing of needles can lead to spread of HIV, scrum hepatitis, malaria and tetanus.
b) incidence of cancer also increases with abuse. Cannabis addicts are particularly prone
to cancer of the respiratory’ system.
Gout like syndrome due to increase in uric acid level is common among alcoholics.
Drug abuse thus clearly interferes with the functioning of the body. These
complications need to be explained in detail to the drug abuser and the family
members to make them cautious and seek ways to overcome addiction as well as the
medical problems present.
Page 8
biochenucal), can fc. called a
hi(pl’ysloiof“l Psychological or
"Y
iC‘“
*llers ““
physical or m«»ul ftnctiomng of „ tadividnalt
<irass are used
termed ‘drug use’.
““j 'hcir
“y »r my not be legal. When
s, prevent a disease or improve the health condition, it is
ft
or maimer®ta'caus™
^dmgabuse.i An,
“'“S'1'’ ^““y
of'■
!’rOWn 8Ugar and gan-'a have no medical
use at all. To use them, is to
abuse them. From the very outset it is drug abuse.
Omg abuse lead, to dmg addiction with the deretopmen, of
experience the same effect''iXaner'rq1Mitfer "h^h m°re “d
^effective „d
while oto
Of
‘ln“ ‘°
« "»
„„is
^‘p^XiSrdXx^10^' d'p“<fen“
preoccupation wiihX'^ecK of tlTdn^d'’"’'11 ■by era°Iional “d mental
Psychological dependence develops, the
di’" WmtagXe,"te^beX“"o
of the dmg, that i, is able to ftnetion „„™aU; o^fte
sXXX'rTa ±"dX ^t“e “f
'°“y d'P’”<‘m' ™,h'
l1'
'
absence of the drag. IhTSthlaS™T’8
“d
■»*« «»
convulsions, depending on the type of dmTV"1^
miW disc°mfort to
symptoms depends on the physica^ondition of thUSCd' 1JC mtcnsit>’ of withdrawal
amount of drug intake and the duration of abuse
6 USer’
°f
abUSed’ 016
9
i
Symptoms of drug withdrawal tend to be the opposite of the effects produced by the
presence of the drug in the body7. For example, brown sugar intake causes constipation,
while the effect of withdrawal from brown sugar is diarrhea. These withdrawal symptoms
make it difficult for the user to give up drugs. He wants to avoid the unpleasant
withdrawal symptoms; and to avoid them he needs the drug. He is thus forced to continue
the drug use even when he knows that drugs are hurting him.
CLASSIFICATION OF ADDICTIVE DRUGS
Substances that are abused can be studied under seven major categories
Narcotic analgesics
Cannabis
Depressants
Hallucinogens
Stimulants
Volatile solvents
Other drugs of abuse.
Note: For a long time cannabis was classified as a hallucinogen. But since a few effects
like flashbacks do not occur with cannabis a separate category’ was created.
NARCOTIC ANALGESICS
In Greek, the prefix ‘narco5 means to ‘deaden’ or ‘benumb’. ‘Analgesic’ means ‘pain
killing or pain-relieving’. The term ‘narcotic’ medically refers to opium and opium
derivatives or synthetic substitutes that produce opium-like effects.
All narcotic analgesics share the common property of benumbing and thus relieving
pain. As a class, they are painkillers with a high addictive potential. Certain
narcotic analgesics are clinically employed for other actions including suppression
of cough and control of diarrhea.
Drugs belonging to this category can be studied under three broad categoriesnarcotics of natural origin, semi-synthetic narcotics and synthetic narcotics. Drugs
belonging to the first two categories are referred to as opiates while the synthetic
drugs are known as opioids.
Page 2
NARCOTIC xANAI>GESICS
|
Nai
Semi- Synthetic
Synthetic
Poppy Plant
n -I
Opium
___ L
r
Morphine
Codeine
Heroin
Buprenorphine
Pentazocine
(Brown sugar)
Methadone
(Di-acetyl morphine)
(not available in India)
Narcotics of natural origin
The poppy plant, ‘Papaver somniferum' is the source of naturally occurring narcotic
drags. For thousands of years this plant has been widely cultivated for its pleasurable
effects. Today, its cultivation has been restricted bv law.
Opium
The word 'opium' is derived from the Greek word, 'opion' meaning 'poppy juice'. Opium
is obtamed by tapping the milky fluid from the unripe poppy pods. It is a dark brownish
or dark greyish tar-like substance with a musty odour. It is usually sold in the form of
small balls, lumps or bricks.
Routes of Administration
Oral: Opium is primarily taken orally. Tire dried opium is usually boiled in water and the
solution is drunk. Ingestion is a relatively inefficient route of administration and the
effects felt are only mild.
Inhalation: Opium can also be smoked. A special piece of equipment, (sometimes simple
but generally elaborate) is used by opium smokers. It is smoked in the reclining
posture to reduce the feeling of nausea. The infamous 'opium dens' of yesteryears arc
non existent today. Opium is now smoked alone or in groups in their own houses.
Page 3
Morphine
Morphine is the principal alkaloid that is extracted from opium. ( An alkaloid is a type of
organic compound which can be extracted from a plant) About 10-15% of the opium
exudate contains morphine. Morphine is one of the most effective drugs for relief of pain.
It is still used medically.
Route of administration
Injected - subcutaneously, intramuscularly or intravenously. Most morphine addicts use
the intravenous route.
Codeine
Codeine is another alkaloid found in opium, though in a smaller percentage than
morphine (one to two percent).Codeine is used as a cough - suppressant. Cough syrups
containing Codeine are now being abused in man v parts of India.
Route of administration
Oral : Medical preparations of codeine are iusually
“ made
' in combination with other
chemicals and are available in the form of tablets and svrups.
Semi-synthetic narcotics
Heroin/Brown sugar
Heroin belongs to the category of narcotic analgesics and is a semi-svnthetic derivative of
the drug morphine.
Pure heroin is white ciy'stalline powder and it is referred to as ’white sugar’ by the
abusers. When the quality of heroin is poor, its colour is no longer white, but rather
brown, and this inferior quality is referred to as ’brown sugar’.
Routes of administration
Injected: The drug is dissolved in lime and water and injected subcutaneously or
intravenously. Among the intravenous users, an immediate high (rush), described
as akin to an orgasm, is reported. Heroin is rarely snorted.
Page 4
Inhalation. Smoked with tobacco in cigarettes.
Chased: The drug is sprinkled on a silver foil or placed in a bent spoon and heated
from beneath with a match stick or a candle. The thick fumes which arise are
taken in through the mouth with a rolled piece of paper.
18 n0‘taken °r311y- Narcotic analgesics, being alkaline in nature,
aie not absorbed in die acidic medium of the stomach. In the intestine, the heroin
rm
qU1C^y conJu8ale (attach) to other molecules, making absorption difficult. The
little that gets absorbed must pass through the liver before getting into the bloodstream.
The liver quickly destroys the drug thereby drastically reducing its potency. It is
estimated that about 90% of the effect is lost when taken orally.
Synthetic narcotics
r T ,CS are produced on,v in the laboratory. These drugs imitate the
effects of the opiates but are not prepared from opium. Buprenorphine and
pentazocine are the most widely abused synthetic narcotic drugs.
Buprenorphine and pentazocine
Both are synthetic narcotic analgesics which are used as pain killers in a wide variety of
medical conditions.
Buprenorphine (Tidigesic) was initially used to treat the withdrawal symptoms of heroin
addiction as well as in the treatment of cancer. Later, it became a drug of abuse.
Routes of administration
Oral: Administered orally in the form of tablets.
Injected : Subcutaneously, intramuscularly or intravenously. Addicts almost always
inject the drug intravenously.
Metabolism
Distribution
Narcotic analgesics are not absorbed evenly by all the parts of the body. They concentrate
m the tissues especially in the kidneys, liver, skeletal muscle, lungs and spleen. Only
mall amounts of narcotic analgesics cross the blood brain barrier (BBB) but die central
nervous system is so sensitive that even minute amounts are sufficient to cause a
pharmacological effect. Small quantities of the drug cross the placental hairier and fetal
dependency can develop.
Page 5
t
Excretion
" *•
K
A ^11
Short - term effects of narcotic analgesics
When injected, the effects arc immediate and
administration, the effects are felt only gradually. pronounced. With other routes of
The main effects include:
h,meer "d
“felt
drowsiness, sedation, apathy, decreased physical activity
A few other adverse reactions may also appear
vomiting in novice users
dysphoria ( a feeling of unpleasantness)
inability to concentrate
itchy skin
constipation
constriction of pupils (with the exception of synthetic narcotics)
‘After the initial effect wears off there is an increased sensitivity to pain.
usuany
iw.
““w
“
dne Po
System effects
Central Nervous System
Pin point pupils, droopy eye-lids, reduced visual acuity
movements of
S±
“,v,:fla',n
sieep c>cie
«“cuT
fc’body
i, Xa aSZr1'' Sl"P “ m°S'
Page 6
Respiratory System
Respiratory depression due to the effect
on the respiratory centre in the brain .
Cardio-Vascular System
Bradycardia or decrease in the heart rate
Gastro Intestinal tract
C onstipation and poor appetite
Kidneys
^diurXh™^ fo™at,On
t0 U1CreaSed SeCreti°n °f the
(anti-
Long-term effects
aensmal
“"P““
<leVC“”’'
“ *"« ata“.
In addition, the following complications can develop:
-
Serum hepatitis/HRVAIDS caused by use of infected needles
Fetal addiction can Cdevelop.
withdrawal symptoms such
80% of the babies bom to addicted mothers develop
C-Is
birth weights.
Tolerance and dependence
euphoric SeffecKe TokrllcTalso ^evelops^o ^t SatlSfaCtOry ^nalS^ic, sedative and
inducing effects However
constipa'ting effect
’
1 s resPlraloiy_^ePressant and nausea
,erance does not develoP t0 the papillary constricting or
Page 7
As tolerance develops with chronic use, the user gradually increases the dosage to
achieve the desired effect, a dosage plateau is reached where no amount of the drug is
suflicient to produce the intensity of effects desired. The user, however, continues the use
ot the drug to delay withdrawal symptoms.
Powerful physical and psychological dependence develop. Abrupt cessation of the drug
use leads to withdrawal symptoms.
Withdrawal symptoms
Vtth the deprivation of narcotics, the first withdrawal symptoms are usually experienced
s only before the time of the next scheduled dose. The initial symptoms resemble those
of moderately severe bout of influenza. Symptoms such as watetv discharge from eyes
and nose, yawning and perspiration appear about 8 to 12 hours after the last dose
Restlessness, irritability, loss of appetite, goose flesh, tremors, papillary dilation and
yawning also occur. Thereafter the addict may fall into a restless sleep. Withdrawal
symptoms mtens^ and reach their peak between 48 and 72 hours after the last dose.
Nausea and vomiting occur. Stomach cramps and diarrhoea are common. Heart rate and
lood pressure are elevated. Chills alternating with flushing and excessive sweating are
also characteristic symptoms. Excruciating pain in the bones and muscles of the back and
extremities occur, as do muscle spasms and kicking movements. At this time the
individual may develop suicidal tendencies.
Narcotic withdrawal is usually not life threatening, although a marked clectrolvte
imbalance caused by excessive vomiting and diarrhoea must be watched.
body1Um 0CCUrS
withdrawa! onIy “ the case of severe infection anywhere in the
CANNABIS
Cannabis drugs arc made from the Indian hemp plant — Cannabis sativa. This plant has
been cultivated for centuries in many parts of Hie world for the tough fiber of the stem
an for its psycho-active properties. When its mind altering properties came to light, the
cultivation of cannabis was banned. Its therapeutic potential and possible medicinal
properties are being studied. As of now, cannabis drugs do not have any medical use.
More than 60 constituents, known as cannabinoids, coccur naturally in and only in the
cannabis plant. The chief psychoactive substancec among them is delta-9-tetrahydrocannabional-commonly referred to as THC.
Page 8
$
4
The main drugs under this category include
Ganja/Marijuana
Ganja is prepared from the dried leaves and flowering tops of the plant. Ganja is
commonly referred to as grass, pot or stuff.
Ganja may range in colour from greyish green to greenish brown and in texture from a
dry. leafy material to a finely divided tea like substance.
Route of administration
Ganja is usually smoked in the form of hand-rolled cigarettes (’joints’ or ’reefers’) or pipes
specially made for this purpose. Ganja is mixed with tobacco and smoked. The
proportion of ganja and tobacco is altered according to the need of the user.
Hashish / Charas
Both male and female forms of the cannabis plant exist. The female plant secretes a
sticky resin which has a high THC concentration. The resinous secretion of the cannabis
plant, which is coUected and dried is known as Hashish / Charas.
Hashish ranges in colour from light brown to almost black and the THC content in
hashish ranges from 5-15%.
Route of administration
a.
Hashish is smoked and sometimes baked with food and eaten.
Hashish Oil
Hashish oil is produced by a process of repeated extraction of the resin of the cannabis
plant to get a high concentration of THC. It is highly potent with a THC concentration
ranging from 20% up to even 60%. Hashish oil is a dark viscous liquid.
Route of administration
a.
It is usually dripped on cigarettes and smoked.
Bhang
This is the least potent of all cannabis drugs. Bhang contains the dried parts of the
plants-leaves and stem. Bhang is brown leafy material with dried twigs.
Page 9
Route of administration
a.
Bhang is usually brewed with tea or milk and drunk.
Metabolism
Distribution
When cannabis drugs are ssmoked, less than 50% of the THC is absorbed and enters the
blood circulation. The effects
---:j are felt within minutes. The effects peak after 10-30
minutes and action ceases after 2-4 hours.
times moie potent when compared to the oral route of administration.
Excretion
After its absolution, THC rapidly leaves the blood and enters the bodv organs. THC
en ers the fat tissues from the blood. From here they pass back to the blood and reaches
the liver to get metabolized. THC is metabolized by the liver into more water soluble
compounds so that it can be excreted. Some of the metabolites (products of metabolism)
which arc produced arc also psychoactive.
Short term effects
The exact effects that cannabis drugs produce cannot be accurately predicted The prior
ac': m
tms
mild euphoria followed by a dreamy state of relaxation
lowering of inhibitions, spontaneous laughter
increased auditory’ and visual acuity (e.g. sound seems louder and clearer, vision
seems brighter and sharper)
sense of smell, touch and taste are often enhanced
^slowlyr °f
perCepti°n °r 'time constant effect' ( time seems to pass more
impaired short-term memory, reduced attention span, poor concentration and disturbed
thought patterns
impairment of ability to perform complex motor tasks
splitting of consciousness that is the user experiences the liigh'. while at the same time
becomes an objective observer of his own intoxication. He may have paranoid
thoughts, and yet simultaneously laugh at them.
Page 10
/
Some usm experience . ■ bad trip. which
fear, anxiety, or even panic. Nausea vomiting and dizziness may oi
’
In addition to the above effects on the central nervous system, the following
effects are
also noticed;
System effects
Cardiovascular system
Tachycardia (increased heart heat) is very prominent. Due to dilation of blood vessels in
th. eonmnctiva, reddening of the eyes can be noticed. There is fail of blood“ X to
Respiratory system
Irritation of the mucosal m<icmbranes lining the respiratory system and broncho
dilation.
Gastro-intestinal system
Increased appetite for sweets.
Long term effects
Pronounced psychological dependence is particularly high among users with
problems.
emotional
Amotivational syndrome: The iuser __
may 2lose all mterest in his work, family etc. He may
become so apathetic that he is not --interested
i
in any goal
oriented activity.
Psychosis: A typical, acute
* psychotic
- ■ episode characterized by confusion, delusion,
hallucinations, disorientation and paranoid symptoms may develop .
’ Fredn^lf-Ttenn C.annabis
may Produce bronchitis, asthma, sinusitis, or chronic
redness oi the eyes because of its irritant effect.
s'":^
•b* prol“8e‘1 u“c"
red““‘i
Children bom to a jmother smoking cannabis during pregnancy may have low birth
weight or mental retardation.
Page 11
Ongoing studies have revealed some evidence to show that cannabis use reduces the
immunity by impairing a component of the white blood cell defense system. It is also
speculated that smoke from cannabis increases the risk of cancer.
Tolerance and dependence
Frequent and regular users of high doses develop tolerance to the drug. To maintain
intensity of effects, users increase their daily dose. Original sensitivity can be restored
with abstinence for several days.
Physical dependence on cannabis develops only in high dose users. Strong psychological
dependence develops with the regular user. User acquires a persistent craving for the drug
which consequently takes on a central role is his life. Even if cannabis is temporarily
unavailable, anxiety or feelings of panic may ensue.
Withdrawal symptoms
Abrupt cessation of cannabis use leads to withdrawal symptoms — sleep disturbances
(sometimes with recurrent nightmares), loss of appetite, irritability, nervousness, anxiety,
sweating and stomach upset. Sometimes chills, increased body temperature and tremors
develop. Withdrawal symptoms usually last for less than a week. Depression or psychotic
symptoms may become prominent.
DEPRESSANTS
Depressants are drugs which depress or slow down the functions of the central nervous
system. The drugs which come under this category include
Sedative-hypnotics
Alcohol
Sedative-hypnotics
Sedative-hypnotics are depressant drugs whose primary effects are calming, sedating or
inducing sleep. Barbiturates like Methaqualone (Mandrax), Secobarbital &
Amylobarbital (Vesparax), and Benzodiazepines like Diazepam (Valiunv Calmpose) and
Lorazepam (Ativan ) are the commonly abused drugs.
Routes of administration
Sedative hypnotics are administered orally in the form of tablets or capsules. They can
also be injected-subcutaneously, intravenously or intramuscularly.
Page 12
Alcohol
ind d
t
Wlth 3 haTsh burning tastc- is the Product of fermentation
Zoholk h
t3 ■° 01 (Cz H; °H) is the ^^ting substance present tn
alcoholic beverages like beer, whisky, mm., brandy, wine, etc. It supplies emptv
calories - calories without any nutritive value whatsoever.
Route of administration
a. Taken orallv.
Metabolism
Distribution
Alcohol is absorbed as soon as it enters the stomach. Unlike other food, alcohol does not
need digestion After ingestion, it is carried to the stomach and small intestines and
thiough the walls ot the stomach gets into the blood stream, from where it is carried to
almost all the organs including the brain.
With alcohol, the rate of absorption is not constant, but depends on various factors like
the speed of drinking, concentration of alcohol taken, the amount of foodstuff in the
stomach, etc.
Intake of 1-2 drinks (1 drink ■= 30 ml. of whisky / brandy) depresses the higher
centres in the brain. Inhibition are thus lowered. The user feels more relaxed and
seems to be able to talk more freely. As more amount of alcohol is consumed, fine
motor coordination is affected, reaction time increases and judgement becomes
poor. This is what makes driving under the influence of alcohol a dangerous
activity. As the alcohol content In the blood continues to increase more and more
centres m the brain are affected. If the user continues to drink, double vision and
oss of balance are evident. When he has had too much of alcohol, he loses
consciousness. This is nature's way of protecting him because if he continues to
drink the respiratory centre in the brain will also shut down.
Excretion
In the liver, alcohol undergoes the process of oxidation whereby it is changed into carbon
dioxide and water and energy' is released. The waste products are excreted through the
lungs and the kidneys.
Page 13
System effects of alcohol abuse
CNS changes
Wemicke-korsakoff syndrome (characterised by disorientation, peripheral nerve damage,
loss of muscular coordination and involuntary; horizontal rapid eye movements)
confabulation (contriving stories to fill in gaps in memory )
Alcohol dementia (disturbances in thought and memory7 cognition)
Other effects
Gastro-intestinal problems include gastritis, peptic ulcer and cancer.
Fatty7 liver, hepatitis and cirrhosis. Also there is an increased likelihood of liver cancer
Pancreatic effects include pancreatitis, diabetes.
Muscle weakness and wasting are commonly seen
Cardio vascular effects of alcohol include damage to the heart muscles
Blood cells (both red and white) and platelets are affected
Kidney problems include diuresis and gout
Sexual dysfunction both in males and females
Short-term effects of depressants
Sedative liApnotics produce effects that are similar to those of alcohol. The main effects
include:
relief from anxiety and tension
euphoria (usually with barbiturates)
lowering of inhibitions
sedation, sleep with larger doses
poor motor coordination ( especially for fine motor tasks)
impaired concentration arid judgement
slurred speech and blurred vision
Nausea, abdominal pain, excitation which may lead to hostile behaviour can occur. Large
doses can cause irregular breathing, weak pulse. Coma and death due to over dose can
occur and occurs with a combination of sedative hypnotics and alcohol.
Long-term effects of depressants
Long term use can produce depression, chronic fatigue, respiratory impairments,
impaired sexual function, decreased attention span, poor memory and judgement.
Chronic sleep problems may develop. Reduced REM sleep due to drug use makes the
quality of sleep so poor that the user does not feel rested on waking up.
Page 14
Tolerance and dependence
-■ .eierance-deX
c'a;?“ deve“>p‘<ie. the desired effect
sX'X";:
level which would ofc™ be
tXffS a"<’“,n' “ '
Physical and ]psychological dependence develop. Craving, anxiety or wen panic is
evident if the user
— is temporarily unable to obtain supply of the drug.
P
Withdrawal symptoms
"■‘“z' sstom!,,il:anxie*
haIl„c1IMtl„„Sa^co“ii:taXZ a8“i<,,''
are usually noticed,
«
temperature, delirium.
bOd''
hallucinogens
« <■'«> ««»~l <° « ■p«yd,edelie:
taind altering)
in India, making it’the least Ibnserf
drugs are listed below.
*
v
Wh„lly Photic
n^01110^1110 drugK are very rarely available
o rugs. The most common hallucinogenic
LSD (Lysergic acid diethylamide)
JSUXspow^' "“""T0-” “is
&“
lysergic acid amide, a chemical found in mo^tg
5^“ .T' 7 &Om
rceamb too! to study
of
ai„8efs7SX nt
’
LSD is a white odourless crystalline material which is soluble in water.
Page 15
Route of administration
LSD is easily absorbed orally and is usually taken in the form of tablets. LSD blotter
papers are also common. Here LSD is dissolved in water and is absorbed in blotting
paper. A piece of this paper is tom off, placed under the tongue and sucked.
PCP (Phencyclidine)
PCP is synthetic drug produced only in clandestine laboratories.
PCP is commonly called 4angel-dust’. PCP in its pure form is a white crystalline powder
that readily dissolves in water
Routes of administration
a.
It is snorted, smoked, eaten and rarely taken intravenously.
Mescaline
Mescaline is derived from a type of cactus and is also produced synthetically. Mescaline
appears as a white or coloured powder.
Route of administration
a.
The oral route of administration is most common.
Psilocybin
Psilocybin is chiefly derived from the ‘psilocybe’ mushroom. The drug can be
synthetically produced with great difficulty. Crude mushroom preparations containing
psilocybin are usually sold as dried mushrooms.
Page 16
Route of administration
This drug is well absorbed orally. The mushrooms itself mav be eaten or dried
powdered and smoked.
’
'
Short-term effects of hallucinogens
The physical effects produced and perceptual
effects created differ from one drug to
another. The main effects include:
Alterations of mood- usually euphoric but sometimes severely depressive.
““or* r™
of “onof
of
Co'o“’
perception or details is increased.
ouy
»■!
'Psuedo hallucinations (‘pseudo’ because the user 1_
knows that the experience is not true
e.g. seeing a myriad of colours or bizarre images).
Synesthesia (melding of two
sensory modalities). User may feel he can see music, hear
colours etc.)
Fee!i8JfOfidXP^OnK1?tiOn’ 10SS of body
loss of sense of reality ( the user
may feel that his body is shrinking or becoming weightless).
Sense of the past, present and future
may be jumbled. Concentration becomes difficult
and attention fluctuates rapidly.
VaT-,m?a‘SJnd eTeTe PreoccuPation with philosophical issues are common. The great
th
he believes that he has discovered are unintelligible or nonsensical
to those not under the influence of LSD.
nonsensical
Hallucmogens are however unpredictable in their effects each time they arc used Acute
panic reactions can also be produced resulting in a ‘bad-trip’. Acute anxiety restlessness
and sleeplessness are common until the effect of the drug wears off.
rest^ssness
Self destructive behaviour
judgement are common.
due to rash decisions and accidents due to impaired
Page 17
Long-term effects
Flashbacks or spontaneous recurrences of an LSD experience can occur without
k=g™r
“ yeaf aft6r LSD U',e' ThS 6XaCt
of this effect is not
mnZmpSVT n!ayuexpenence effect such as intensification of colour, apparent
2w Znm °f 3
4 °bjeCt °r °ther hallucin°genic effects even after abstinence for a
tew monins.
A motivational syndrome: The user becomes very apathetic, is very' passive and shows
no interest in lite.
behaviour. The psychotic episode normally lasts for several hours but in some cases
the psychosis may last for years.
Tolerance and dependence
Psychological dependence develops though the user does not become physically
dependent. Particular withdrawal symptoms are not reported.
STIMULANTS
. imulants are drugs which excite or speed up the central nervous system. The two most
prevalent stimulants are nicotine, found in tobacco products, and caffeine, the active
ingredient m coffee and tea. These however will not be discussed here. The more potent
stimulant drugs will be the focus of attention. They include amphetamines and cocaine.
Amphetamines
.Amphetamines are synthetic drugs produced entirely withini the laboratory’,
.Amphetamines are used in <other
' countries to treat narcolepsy (an uncontrollable tendency
to sleep) and sometimes in weight control .programmes.
Ecstacy
is an amphetamine based
---------j *3
drug currently
eonntripc
;ntly being abused in the develoned
developed countries.
Amphetamines are not abused in India today, even though in the late 70s, they were
being used by
•
Page 18
V
students to ward off sleep, enabling them to study through the night, prior to the
examination
athletes, to mask feelings of fatigue and increase their endurance
Route of administration
a. Oral; Amphetamines are absorbed orally and are taken in the form of tablets
or
capsules.
Cocaine
Cocaine, a potent stimulant of natural origin, is extracted from the leaves of the coca
plant (Etythroxylon coca). It is an odourless, white ciystalline powder, with a bitter
numoing taste.
Cocaine was formerly used in eye, nose and throat surgery because of its ability to
i^norusecfnWff116!!311^ S™u*taneous^ constIict blood vessels and limit bleeding. Now it
Crack
This is made from <cocaine and is widely abused in developed countries like USA.
Cocaine and crack being enormously expensive, are not abused in India as yet.
Routes of administration
Oral. The leaves of the coca plant are sometimes chewed and cocaine, the chief
psycho-motor chemical present is absorbed through the mucous membranes of the
mouth. Very rarely, cocaine is injected for a heightened effect.
b. Snorted: Usually ‘snorted’ or taken in through the nasal passages (like snuff).
Short-term effects of stimulants
b“,hc
“
The main effects include
a heightened feeling of well being, euphoria
a sense of super-abundant energy, increased self-confidence
increased motor and speech activity
suppression of appetite (which is why it is used in diet pills)
an increased wakefulness that masks feelings of fatigue (the reason why amphetamines
are abused by students during examinations)
Page 19
Papillary dilation, dryness of mouth, reduced gastrointestinal activity and urinarv
retention are other effects and increased respiration, heart rate and blood pressure also
present themselves.
Unpleasant effects such as temporary impotence, anxiety or even panic may be noticed.
With large doses, very rapid heart beat, hypertension, headache, profuse sweating, severe
agitation and tremors may occur. Veiy high doses cause rapid, irregular and^shallow
respiration, convulsions and coma.
Long-term effects
Chronic sleep problems, poor
appetite, high
liigh blood
poor appetite,
blood pressure, rapid and uregular heart
beat impotence, mood swings, anxiety and tension states are the long-term effects of
stimulant abuse.
Acts of violence, homicide and suicide rates among stimulant abusers are high.
Sd^umoseks?
;aT^3,Jetarnine Psychosis’, paranoid ideation, hallucinations
Xehm? t I Stfreot?’ped behaviour may develop. A full blown amphetamine
psychotic state closely resembles paranoid schizophrenia.
Snorting of cocaine may result in perforation of the nasal septum.
Tolerance and dependence
btOta myS-Cal and pycholoSicai dependence. Tolerance docs develop to a
01,1,0 p'easu,abie 'ff“B is 'u-k
Withdrawal symptoms
Withdrawal symptoms occur, however the clinical picture does not include
major grossly
observable physiological disruptions. Extreme fatigue, prolonged
but disturbed sleep,
voracious appetite, irritability and moderate to severe depression are the commonly
reported withdrawal symptoms.
VOLATILE SOLVENTS
Keif’S. “ ?S ,‘TSmy
«l parokum derivatives
flu d Tr ? f
F iPOhsh remove,; ether’ Slue’ benzene, vaniish thinner and lighter
i
fk USi o Onn
su^stance abuse is primarily found among younger people who are
les. ta, 18 yeajv of age . Abme of vohiile solvent, is ,li in Lia ta to b.™
reported among the street children.
Page 20
Route of Administration
a.
Inhalation by sniffing the foresaid substances.
Short-term effects
Behavioural effects include euphoria, clouded thinking, slurred speech and staggering
gait. Hallucinations occur in about 50% of the abusers. The effects are about the same as
tor sedative hypnotics and many youngsters who abuse these substance end up dependent
on alcohol or other sedative type drugs.
Sudden death can occur due to sniffing these drugs.
Long-term effects
Long term effects include psychosis and permanent brain damage. Tachycardia with
possible ventricular fibrillation can occur. Damage to the liver, kidneys and’heart is also
possible.
OTHER DRUGS OF ABUSE
Theie are a few other drags of abuse that do not belong to any of the above categories.
Abuse of the following drags has been reported;
Muscle relaxants like carisoprodol, (e.g. carisoma compound). The drug is available in
the form of tablets and abused for its depressant effects that resemble those of
alcohol and other sedative hypnotics.
CNS analgesics like dextropropoxyphene ( e.g. proxyvon) and extropropoxyphene in
combmation with dicyclomine (e.g. spasmoproxywon). Tablets and ampoules are
available. The drag is taken orally or intravenously . The pain relieving effects
are very’pronounced.
These drugs arc ]prescribed usually to relieve pain following accident trauma or
surgery. When its*> use is not carefully monitored by the supervising physician
addiction can develop.
xAntihistamines like chlorpheneramine maleate ( e.g. avil)
Anti-emetic like promethazine ( e.g.phenargan)
Both these categories of drugs are usually abused in combination with narcotic
drugs like heroin or buprenorphine to enhance the effects .
Page 21
e. Anti-depressant drugs like amineptine (e.g. survector)
These drugs are abused for its sedation effects. Prescriptions need to be issued
very carefully to watch out for signs of tolerance. In case of tolerance, most
physicians opt to shift the patient to other category of the anti depressants that do
not produce sedation.
Page 22
r-
-IS*
4
MOTIVATION AND INTERVENTION TECHNIQUES
Addiction is the only disease where the victim does not fully realise the enormity
of his problem. The stigma associated with drug use, the guilt and shame resulting
from inappropriate use and the lack of awareness about the part drugs play in the
problems they face - all these lead to denial of the problem of addiction. In an
attempt to protect the dignity of the family, in most of the cases the family
members also deny the existence of any serious problem. So motivation becomes
one Of the key issues in the treatment of chemically dependent people.
What is motivation?
Motivation’ is creating the desire to change one’s own dysfunctional behaviour
and 'motive' is the energizing condition that directs the individual to achieve the
goal. Motivating the addict to accept help forms the first phase of treatment.
Family intervention
The first person to call for help is generally the parent or wife - the person closest
to the abuser, one who is more worried, afraid and angry than the others. At this
juncture, the family member’s crucial fear will be “How do I bring him to the
treatment centre?” To help the family intervene, the counsellor has to provide
information about addiction. The family member has to understand that addiction
is a disease and that it requires treatment. She has to be shown how the enabling
behaviour of the family has led to the continuation of the problem. She has to see
the role she has unknowingly played in maintaining the process.
Making use of a crisis
She has to be guided to motivate the patient to accept help. What is it that she can
do? Addicted individuals generally come for treatment only when they are left to
face some crisis all by themselves - loss of job, marital dissolution or legal threat.
At this point, most of fliem are open to help, mainly to tide over the crisis. She
has to look for some crisis and make use of it. For instance, the addict would have
suffered severe pain in the stomach, or would have received a letter of warning
from the office. The family can use this crisis to make him see the problem and
accept help.
I
2
Involving others
To make the intervention more effective, as the next step, the other members in
the family for whom the person has regard and respect can be involved.. Their
involvement in the process will increase the motivation of the individual. In this
group it is important to include the addict’s children also. Most often they are the
ones who witness the fights, face the anguish and end up bearing the family’s
pain. Friends, relatives, employers, doctors and others may also be included.
A list of specific, non-judgemental facts relating to the abuse of drugs should be
presented to the patient when he is drug free, particularly, immediately after the
crisis, in a caring manner by these members. The following chart shows the
details to be presented and the manner in which it has to be done.
A Non-Judgmental attitude Avoid looking down on the person or making moral
reflecting care and judgements. The person reporting the data should also be
encouraged to indicate how it makes her feel -such as
concern
embarrassment, fear, unhappiness, etc. 'Alcohol is
destroying your health. When we see your health
deteriorating, it is upsetting for all of us’.
The addict should be made to realise that there are people
who do care for him and are concerned about what is
happening to him.
B Specific details
First hand knowledge of incidents and behaviour as narrated
by significant people should be reported. The change in the
person’s character, behaviour, personality as seen by the
concerned persons can be presented. On any account avoid
gossip or second-hand information. Mohan also told me you
are
taking drugs all the time'. Instead stick to factual
reporting of behaviour and incidents.
Avoid generalisation such as 'You have always given me
problems since your childhood’.
C Plan of action
Decide beforehand as to what type of help you want the
patient to get. If the addict does not accept this, have an
alternative course of action.
D Consequences
What alternatives does the person face if he rejects all forms
of help? Some of the consequences could be highlighted loss of job, mounting debts, marital separation etc. Do not
state conditions that cannot or will not be carried out.
r'
3
There may be addicted individuals who do not respond to any of tlie above stated
motivational / interventional procedures. For them, the emotional acceptance of
the fact will take a very long time. Instead of rejecting the patient or confronting
him with logic and argument, the significant others involved in the process of
intervention, should reassure him that they are always there to help and support
him if he decides to go for treatment.
Professional intervention
Generally after these interventions, the patient comes asking for help. The
counsellor’s most important task during the first interview is to establish a
relationshiP- Her understanding, non-condemning, non-judgmental
attitude, her acceptance of the patient, will in turn, help the latter to accept
himself. Once the person feels accepted, it will be relatively easy for him to
discuss his problems freely, the mere mention of which would have irritated him
earlier.
Alleviating fears
The pattent would already have tried (though unsuccessfully), to stay away from
drugs. He would have experienced problems associated with withdrawal. He will
now be expenencing severe stress, arising out of acute fear - fear of withdrawal
tear about the kind of treatment he is going to be given, fear about others coming
to know about his problem, etc. This addicted individual mav already have taken
£2= Stt r°US CentJ'eS’ 2nd
t0 reCOVer’ Therefore- his acceptance of
treatment will be minimal.
Jgoing to face the physical problems associated with withdrawal?”
What kind of treatment arc they going to give me? - an operation"?
How am I going to face my ‘old friends’ and neighbours"?
It is important that these inner barriers which prevent him from admitting his need
successfu^rAvOgniSe/
discussed with empathy. Open discussion of the
successful recovery of afready treated patients and the feedback from those
h±!0U?
T* may f°;ter additional °Ptimism h*
Patient who has had a
iST-
“■ Wb0 “ d0"““
Focussing on immediate problems
hutiaUy, the patient will focus attention on his immediate problems like loss of
job, separation from wife, etc. At this juncture, it is not at all advisable to tty to
4
make him understand that addiction is his real problem. The most important thing
is to show supportive understanding and give him reassurance that his problems
will be looked into.
When the professional wants to focus his attention on addiction, she can discuss
the obvious physical problems like tremors, loss of appetite, and noticeable
weakness. She should concentrate only on the physical problems which are
obviously seen. Motivation can be increased by using concrete medical records
of the patients if available. Diagnostic tools like blood reports, CT scans, and Xrays with proper explanations from the medical professional will create an
awareness in him about the physical damage caused by his chemical dependency.
Identifying motivable areas
Most of the people addicted to drugs have a ‘motivable area’, which is a
sensitive area that has to be identified by the professional. The person may have
very warm feelings towards his parents, employer or child. These sensitive areas
have to be identified and this can be done by attentive, non - judgmental listening
listening to his verbal and non-verbal communication.
“I have come for treatment mainly because my mother is very much upset and
wonied about my ill health!
“I want to give up drinking because I find that my drinking upsets my daughter. I
will go to any extent to keep her happy”.
These motivable areas can be located by encouraging the patient to talk about his
feelings-the relationships he respects and wants to strengthen.
Assessing motivation
The motivation of a patient can be assessed based on the following factors
>
>
>
>
>
>
Acceptance of his problem with drugs
Understanding the damage caused by addiction
Realizing the need to take an active part in the treatment
Compliance with the terms laid down by the treatment centre
Past history of abstinence
Internal locus of control (a desire to get better for one’s own sake).
However, the motivation has to be strengthened and reinforced, which in turn
will lead to a commitment to recover. This can be done during treatment through
Individual counselling
Group therapy and
Attendance to AA / NA meetings
5
Unwilling patients - Help for their families
We have so far discussed techniques for enhancing the motivation of those
patients who have already come to the treatment centre. On the other hand, there
may be a group of addicted persons who will be unwilling to accept help. 1 such
cases, a family member, usually the wife, or the parent may come to the treatment
centre asking for help. What sort of help can be provided for them?
Encourage them to attend Al-anon meetings
Provide them with reading materials on addiction
Help them to attend family therapy sessions
Help them become aware of their dysfunctional behaviour and make plans
to change.
J t!h / ithe!lutial Usk of motivation is to help the patient accept treatment and it
JhSk “lterventlon t0
t0 treatment. Further, motivation has to be
acW ^d^
81386 °f treatment and WOTked towards ^staining the gains
SKILLS SHARPENING TOOLS
VARIOUS STAGES OF CHANGE AND APPROPRLATE
MOTIVATIONAL STRATEGIES
Prochaska and Diclemente (1984) talked about five stages of motivation - pre
contemplation, contemplation, preparation, action and maintenance.
PRE-CONTEMPLATION - STAGE 1
The client is not yet considering change or is unwilling or unable to change.
Strategies for the clinician
Establish rapport and build trust
Raise doubts or concerns in the client about substance using patterns by
> Exploring the nature of events that brought the client to treatment or the
results of previous treatments.
> Eliciting the client’s perception of the problem
> Offering factual information about the risks of substance use
> Providing feedback about assessment findings
> Helping significant others (relatives, friends, employer) intervene
> Examining discrepancies between the client’s and others’ perception of
the problem behaviour
Express concern and keep the door open ensuring support anytime it is
solicited
. '-i- ric (:
!J;
n
.v;<:
CONTEMPLATION-STAGE 2
The client acknowledges the problem, considers the possibility of change but is
ambivalent and uncertain.
Strategies
in
K
Help the client realise the need for change by
> Eliciting and weighing pros and cons of substance use and change
> Examining the client’s personal values in relation to change
> Emphasising the client’s responsibility for change
H/.V’
i
mods
^rtibrzovj
.
cirite !
to noitq^oieq’giartto bm 8hm>ilc :d;
•
ivon/4rf^d meldoiq s.f|l
<W. j
/. HO TO 8SDAT3 2OOLMZV
ai snrihpifi
meonoo
•iqxa
Elicit self motivational statements of commitment from the client
Elicit ideas regarding the client’s expectations regarding treatment
Summarise self motivational statements
, : r:
PREPARA riON STAGE 3
~
t r
I 3OAT2 The client is committed to and planning to make a change in the near future but
is still
?
gnmbtenti? > w Ion d
v.f| f
Strategies
,50 10| t>oon
- Clarify the^j^wb®^ m4$*ategies^^^
•
Offer alistofo^^M^^^rJfe^^^
If willing, offer expertise and>a4>jp9. j /j^^gnoqatn a’teilo erfi gniaigfidq/i^i <
- Negotiatef&^^
-
gahotaXS <
Help the client enlist family and others’ support
Explore treatment expectancies and the client’s role .^q g'tneiio &rfi •anihorH <
Elicit from client what has worked in the .p^t either for him or fpr others
whom he knows
Assist the client to deal with potential barriers related to entering treatment finances, leave etc.
Have the client openly express to family and significant others his plans to
change
ACTION STAGE 4
Fhe client is actively taking steps to change but has not yet reached a stable
state.
Strategies
-
1
Reinforce the importance of remaining in treatment
Support a realistic view of change through small steps
Acknowledge difficulties experienced by the client in early stages of change
Help the client identify high risk situations and develop appropriate coping
strategies to overcome these.
Assist the client in finding new reinforcers (new non-drug taking friends,
positive relationship with family members) of positive change.
MAINTENANCE ~ STAGE 5
xh io
ot tn&Ho eirh htinnid 'iirft
to ^nn/itr sdl gnholqx'J-- Z
The client has achieved initial goals such as abstinence and is now working to
sustain gains.
Kmstedua to
oifeffnoW i&urjfu
etu-AAt-
"
Acctt'v-e iTXjdThtfcLj <-'•■ V
- --1
^WV)VVT>)
Ovv41
IKc
Ux-cvU-
pTraxt, cji- cwt4
tfKW C i A tv 'T-jJtu- n
•*
fiXockVvlux V)
>-LkjuJ
T^zv-vtq
, v
jj jj
t
u -C-
Itanr^
h’^xA’'
p
C
cXCi-v<(~
)
5
STAGE I - FRE-CONTEMPLATION - NOT YET CONSIDERING CHANGE
OR IS UNWILLING TO CHANGE
Prakash was brought for treatment under pressure by his family members. He met
with a scooter accident the previous day under the influence of drugs and had minor
injuries. The friend who brought him home was concerned as it was the second
accident in two months. Prakash blamed the auto rickshaw driver for the accident.
V/hat strategy would you use to motivate Prakash?
STAGE IU CONTEMPLATION - ACKNOWLEDGES THE PROBLEM,
CONSIDERS THE POSSIBILITY OF CHANGE BUT IS AMBIVALENT
Kumar came with his mother for admission to a treatment centre. He wanted to give
up alcohol but was ambivalent regarding the decision. While interacting with the
counsellor he mentioned that for the sake of his mother he wanted to give up. He
was concerned about situations like attending sales conference where alcohol will be
served and he was expected to keep company with his colleagues.” He said,
“Everybody in the sales side drink and most drink more than I do. After working so
hard all day, only alcohol helps me relax’’. He also mentioned few embarrassing
incidents which happened at home and at work after heavy drinking sprees. But he
was sure that if his friends don’t force him, he would be able to abstain from alcohol
easily.
Kumar wanted to take off from work for one week, get detoxified and join back.
What strategies would you use ro motivate Kumar and deal with his ambivalent
attitude?
STAGE DI PREPARATION - COMMITTED TO AND PLANNING TO MIKE A
CHANGE
Mohan has been abusing brown sugar for the past three years. His friend took
treatment in a centre and was staying sober. Hence, Mohan decided to Join a
treatment programme.
Mohan while talking to the counsellor repeatedly mentioned that he wanted to quit
drugs. He said ’’Once I give up drugs I can easily get a job. Or my parents will
provide me money to start a business. I have to give up drugs. That is all I have to
do". Mohan had many questions to ask - whether the withdrawal would be made
painless with medications ; if he would be 100% fit after taking treatment etc. Mohan
was willing to bring his mother and wanted to be treated without his father’s
knowledge as he would be critical about him.
STAGE TV ACTION - ACTIVELY TAKING STEPS TO CHANGE BUT HAS NOT
YET REACHED A STABLE STATE
Ravi was admitted for treatment in a rehabilitation centre. After four days he was
physically comfortable. He was feeling great that for the first time he has given up
drugs. When Ills brothers came to visit him at the centre, he repeatedly mentioned
6
• i I
that he will never touch drugs again. He said that he has made up his mind and even
if he was discharged immediately, he would stay clean. Even if my friend gives me
ten thousand rupees I will not have drugs. He even went to the point of saying "On
discharge, I will visit my friends and make them come for treatment. I will be with
them, cajole them and make them give up drugs like me". The family members were
very happy about his change of mind.
Wliat strategies would you use to help Ravi be realistic about the change he is
expected to make?
STAGE V MAINTENANCE - HAS ACHIEVED INITIAL GOALS SUCH AS
ABSTINENCE AND IS NOW WORKING TO SUSTAIN GAINS
James had completed his treatment two months ago. His drug using friends no longer
called him and he was happy that he was ’’ clean". Evening hours were a little
boring. He spent his evenings watching television. He was attending work
regularly.
He continued to have a strained relationship with his father and any comment from
his father provoked him. James was clear that he should stay away from drugs. He
had many issues to deal with - poor interpersonal relationship, no friends and no
recreation.
What arc the issues to be dealt to sustain the motivation of James?
I
I
Aju—
(V\x-
QVo 1 cl u
Lc
o 4
0 4
AJ
Km
Ud (-JL
tC i J Pj
cliruuY/kx
MhA
&
SELF-HELP GROUP - ALCOHOLICS ANONYMOUS
Alcoholics AnonymousXAA) is a fellowship of people like us who have one thing in
common - drinking problem. Our common aim is to stop drinking and to stay stopped.
To do this, we regularly meet, talk to and help one another. We help each other to live
the AA way of life. This keeps us sober and also shows us the way to help others.
M No qualification is needed to belong to this fellowship - wanting to stop drinking is
enough.
AA meets its expenses by the money given voluntarily by its members.
X Nothing is collected by AA as fees. No one is compelled to pay anything. If one
cannot afford to pay. one need not and he is still welcome.
M AA does not run any hospitals, clinics, counselling centres etc.
AA does not offer financial help. It does not offer jobs. It also does not help any one
find a job.
What do we mean by anonymous1?
Most members of society do not understand the true nature of a drinking problem.
They feel alcoholism is a sin or a moral weakness. So the}' tend to look down on us.
Tiffs was more so when AA began in the year 1935. Because of tiffs it was decided that
those coming for help would be Anonymous. When one approaches AA for help, he
need not declare his name
need not give his address
need not state where he works
need not disclose his parent’s name or any other particulars.
Even if some particulars arc given, they will not be revealed to any one outside the
fellowship. Thus all members are anonymous. No one outside knows anything about us,
individually.
How do we get in touch?
We can get in touch with recovering alcoholics by attending AA meetings which are
held in different parts of the city. The list of venues can be obtained from the treatment
centre. Those of us who are not in a position to be pail of a group, can keep in touch
with other alcoholics by writing letters or through telephone. Reading and studying
books, periodicals and other literature written by A A members can be of help.
A
What can a new comer expect at a meeting?
All AA groups have regular meetings. Any one who is interested in alcoholism may
attend a meeting. There are no hard and fast rules as to how the meeting should be run.
Each group can have its own way of running the meeting. What is most commonly seen
is described below.
M Those attending the meeting sit on chairs usually in a circle or in rows.
X The meeting begins with the Serenity prayer being said by everyone. After this, the
Twelve steps and Twelve traditions are usually read out.
The person conducting the meeting will ask one of the members to start
speaking. Or he may say that any one is free to speak. Some of these meetings have
only two or three speakers who have been decided upon beforehand.
When a member speaks, he states his first name and then savs he is an alcoholic - for
example, "My name is Ashok, I’m an Alcoholic."
The member will speak only about his own experience. He will usually describe
how alcohol affected his life, how he got out of it and how his life is today.
In other cases, he may merely talk about some problem that is troubling him at the
moment.
M Since he is disclosing his problems to the group, this is called 'SHARING*. The
member, as he speaks, talks of his experience, his expectations or his fears. He
shares this with the group members as one would with a close friend.
X While some one is sharing, no one interrupts. What is shared is totally confidential.
No one talks about it outside.
X When someone has shared his problem, no one gives advice. If one member wants
to help another, he will share about a similar problem he had faced at some time in
the past, and how he coped with it. These automatically serve as
guidelines.
Towards the end of the meeting, a cover or bag or box is passed around. Each
member puts in whatever he would like to contribute. This is usually only a few
rupees. This money is used to pay for the refreshments, to pay rent for the place
where the meeting is held, etc. No one is under any obligation to pay anything.
Usually new comers are not asked to contribute.
& The meeting closes with the Serenity Prayer.
Page 2
What exactly do we gain by attending meetings?
The benefits are many. The meeting is in manv ways the verv heart of AA functioning
There are many alcoholics who do not know even how to read or write- but, merely by
Particularly, just after iwe :have stopped drinking, we are confused about a lot of
things. Many of us take sometime c
even to accept the fact that we are alcoholics. We
take sometime to understand what
i we should do about it. It is here that the meetina
helps. At the meeting, first of all,
not
oniv
1
we see living proof of the fact that life without
alcohol is i ZL
,pQSSlb}e’ but enjoyable and fulfilling. We see so many
examples. If we do just two things when we attend the meeting,
our lives will change
for the better.
I. Sharing
When we share, we must be as honest as we can.
can. It does not matter if one speaks well or
badly. What is important is that the truth should
.-.J be spoken. On certain days we may be
*11’h*PP?I,‘l i” lhe office - to can be shared. On ota days we ma,'
helps ta tm wa* ■
’
’l“"d Sh
"i"g °“r ,l'<’“sllM “i “l»™nces
Sharing
be shared.
□
As we share facts about ourselves in front of others we gradually accept these
facts.
□ When we are confused about what we L
should do, just speaking our minds in the
group will help us to really understand what
----- the problem is. Our will to act is also
strengthened as we share.
II. Listening
XV e can gain almost as much from listening in the meeting as we do in sharing. When we
snS
h°Ut
mtent,?n t0 criticise> bul list6n carefully to understand what the
speaker ts saymg, we can leant a lot. Since AA is full of people like us who are trying
h is quite possible that’s^Ft^Slet^s he hasl^wot^^^^
We can gam a lot of insight into our problems in this way.
The serenity prayer
USUalIy Said thC beSinninS 3114 at the end of most AA meetings. It is believed
that the entire recovery’ programme of AA is contained in the prayer.
Page 3
God Grant us the Serenity
To accept the things we cannot change
Courage to change the things we can
And the wisdom to know the difference
How does this prayer help?
We must first accept the fact that we are alcoholics. There are certain things we can
deal with successfully, but there are certain other things which we just cannot change.
We cannot use mood altering drugs of any nature because that would bring back the
negative attitudes and make the positive sense of self worth disappear. We cannot
change the situations or happenings of the past when alcohol was in full control and
had taken absolute charge. There is no point in clinging to the past and wonying
about things which cannot be changed.
There are several things which we can change. We can correct our past mistakes and
make amends to those we had hurt. We can change our attitude towards our family and
friends. We can change our resentful attitudes and replace them with tolerance
and forgiveness. We can change our entire personality and start practising honesty.
humility7, appreciation, forgiveness, promptness in admitting wrongs, making amends
and rendering service to others. We should not waste our time harping on things which
catmot be changed, but rather direct our time and energy in helpful constructive
activities where satisfactory results are possible.
Each worthy thought put into practice brings us a step nearer to the Higher Power. They
are the stepping stones which we use to slowly progress to greater awareness of His
presence. They are the means by which we make a conscious contact with Him. By
constant practice, we can gain the priceless reward of contented sobriety.
The Serenity Prayer, if internalized, and practiced will give us tremendous power and
strength to manage our problems to lead a meaningful life.
AA Slogans
There arc quite a few AA slogans which if followed, will help us to face life and
manage problems without alcohol.
AA Slogans carry a lot of meaning in our alcohol-free life. They are short and easy to
remember. They mean different things to different people in different situations. They
give a sense of direction - a new way of thinking and acting.
Page 4
A few of these slogans:
One day at a time
We alcoholics are confused and try to live the whole life at once. We keep worrying
about the happenings of the past, and also about what the future holds for us. Our
present becomes a sad state, with hardly anything worthwhile done. We usually forget
that if we have a kilometer to walk, we must take one step at a time; "I will not drink come what may, we experience feelings of confidence and the task becomes much
easier, if we plan it just for today. I will renew this at the start of the day. If I find it
difficult to execute my plan for 24 hours, I will plan just for half-a-day. This can be
renewed at the end of 12 hours. If even that is difficult, I can plan for 1 hour .... If that
is also threatening, for 'just now' - just for this moment.
First things first
For us, to drink is to destroy ourselves. Therefore, staying away from drinks is the first
and the most important thing in our life - anytime, anywhere, under any circumstance.
The first priority for us is to plan each day properly so that we can stay away from
drinking. We can plan to have our daily prayers, attend AA meetings, communicate
with the family members, and so on. We put our plans in writing, and execute them
systematically, keeping in mind the slogan, "Easy Does it."
Let Go Let God
Many of us continue to feel that we can control our drinking by using our will power. A
time has now come when we must let go of such mistaken notions. This slogan enables
us to surrender to God after realising our powerlessness over alcohol. When we have
total faith in a Higher Power, we find that our struggle gets minimised, and our life
takes on a new meaning.
Easy does it
This slogan reminds us that we have not become alcoholics overnight, and
therefore, building up sobriety will also take some time. We simply cannot huny up the
procedure. We have to learn patience, acceptance and tolerance.
If you can’t go through an obstacle, then go around it.
If you can’t solve a problem, accept it.
If you can’t finish today, there will be a tomorrow.
Huny never produced a masterpiece.
Easy does it, but do it!
Page 5
Live and Let Live
Every one has the right to make his own choices. We have a right to have our own
opinions, but at the same time, we also have an obligation to tolerate the opinions of
others. We have a right to give expression to our emotions; this automatically implies
that we have to tolerate the inadequacies if any, of others. This slogan really helps us
to get along with others who may be totally different from us. This guides us to
concentrate on our own life instead of getting obsessed with others.
Think...Think...Think
Many of our problems arise because we do not think well before we act. How often we
say. If only I had thought!". To maintain sobriety, instead of rushing into action, we
should analyse and think over each and every situation.
And once again, Think!" because - the habit of thinking makes the difference beween
thoughtfulness and thoughtlessness; peace and conflict; dryness and sobriety. Think it
over.
In short Alcoholics Anonymous’ meetings help us realise that we are not "suffering
alone. There are many people around us who experience the same or similar
problems. Sharing our problems with fellow sufferers lessens our burdens and also
gives us clarity as to how we can manage our problems. They had successfully^
done it, and therefore, we can also do it - a real hope based on the practical experiences
of others.
Page 6
Mh- io. 19-
lnternalising tools
CASELETS
Read each of the <case lets and suggest the course of intervention that the
should follow or the issues which havTto
counsellor
---------- > be dealt in counselling sessions:
mourns away and he had to clear about 10 pacers Roth Tn^r>h ,„zt k-
parent, were v«y cnttfltlem of hi. pMsilg
esmiiM„? „P '
‘”h ,,,uph “<l
attend N.A.
3' vXoewas^X^ld 7n7tdsl^afiVeyea7ld 8On' He had lost
• .
j v
father remarried when he was 7 He had a hmthpr
Ossa
4.
It is a month since Ahmed was discharged To celebrate
tXZm ^ed l^el^hS ma
1
d^
«*„3nd “
wo:.dbcfim^t":x"Xa^
5' S XcZS„“TThw“pa?er SM,M He “mp,ai”e‘l
pm"XStaConcenm,‘“
/
6.
Rajiv appeared to be uncomfortable and hesitantly told the counsellor he had a
personal problem to talk about. Slowly, he said he was unhappy about his sexual
performance even though it was nearly three months since he gave up drinking.
7.
Abdul was jubilant about his recovery. He talked of all the improvements he had
made in the six months of sobriety. He had asked his brother for a loan to start a
part time business and his brother had agreed. Abdul was happy that with the
money from the business as well as his salary he could buy a house quickly.
8. Prem had got his first job which involved marketing home appliances two months
ago. Things were fairly okay until the manager expressed displeasure about his sales
targets. Prem was upset and wanted to give up his job.
9.
Jacob was complaining about his mother. He said she was trying to control him
all the time and that they had arguments everyday about - where he went and
how he spent his time and money. He said that she had too many expectations and
that the situation was unbearable.
10. Rahim was meeting his counsellor after New Year Day. It was ten months after
treatment and the first major celebration after discharge. He said that he had a
craving but he did not try’ drugs.
Page 2
MH' 2-0-1 &
T T RANGANATHAN CLINICAL RESEARCH FOUNDATION
"TTK HOSPITAL"
17,1V KAIN ROAD, INDIRA NAGAR,.’MADRAS-600 020
REGIONAL COURSE ON "PREVENTION OF DRUG ABUSE AND ALCOHOLISM"
SPONSORED BY NATIONAL INSTITUTE OF SOCIAL DEFENCE, MINISTRY OF
WELFARE, GOVERNMENT OF INDIA, NEW DELHI.
PSYCHIATRIC PROBLEMS ASSOCIATED WITH ADDICTION
Alcohol intoxication is characterised by maladaptive behaviour
like impaired judgement, belligerence etc. Signs of intoxication
include ataxia, nystagmus, slurred speech, flushing of the face,
irritability and impaired attention, disinhibition of sexual or
aggressive impulses and mood lability.
Alc-ohol - Idiosyp^ra<t jc Intoxica 11 on
This condition is also known as pathological intoxication and is
characterized by the sudden onset of marked behavioural changes
after the consumption of a small amount of alcohol. The person is
confused, disoriented and has visual hallucinations, illusions
and transitory delusions. There is greatly increased psychomotor
activity, impulsive aggressive behaviour or depression with
suicidal ideation. This generally lasts for a few hours, terminates
in a prolonged period of sleep and the person is unable to recall
the episode.
Alcohol Hallucinosis
These are visual or auditory hallucinations usually beginning
within 48 hours of cessation of drinking. This may last for
several weeks or months without any other signs of alcohol with
drawal or delirium. Sometimes, it may be accompanied by delusions
but the sensorium vrill be clear.
• .2.
2
Alcohol Withdrawal Delirium (DT)
It generally follows the cessation of prolonged heavy drinking.
Within hours of cessation, the patient has tremors, hyper reflexia,
sweating, fever, tachycardia, hypertension, general malaise ano
nausea o4 vomiting. Ma jor motor seizures may occur. Patients may
vivid nightmares and.
have transient hallucinations, illusions or
disturbed sleep. In addition to this, there is a severe distu.rbance in sensorium manifested by disorientation and clouding of
consciousness and fluctuating levels of psychomotor activity
ranging from hyper excitability to lethargy . Delusions and
agitated behaviour are commonly present.
Alcoholic Encephalopathy (WernjlckeJs_syndrpme)and
Alcohol Amnestic Disorder
(Korsoko.ff 's syndrome)
Alcoholic encephalopathy is a neurological disease manifested by
ataxia, ophthalmoplegia
c' nfusion. This can either
spontaneously clear in a few days or weeks or can progress into
an irreversible
alcohol amnestic disorder in which the patient has
short term memory loss in the presence of a clear sensorium.
The early acute stage of Wernicke’s syndrome responds rapidly to
large doses of parental thiamine, as it is believed to he caused
a pre-disposing
by thiamine deficiency. •Therefore, malnutrition is
factor and heavy alcohol consumption also produces a malabsorption
syndrome..
Dementia associated with alcohol ^huse
There is impairment in social or occupational functioning which
persists at least
least 33 weeks,
weeks after
after cessation of prolonged alcohol use.
Other complications of slcobolism such es c®r«bellar signs,
pher^l neuropathy or
cirrhosis may be present. It is nob 5
known whether dementia is a primary effect of alcohol or
✓3.
3
metabolites on the brain or an indirect consequence of malnutri
tion, frequent head injury and liver disease.
Excessive use of psycho active substances be it alcohol, ganja
or heroin is generally associated with psychiatric problems or
even underlying personality disorders. In most cases it is diffi
cult to ascertain whether the psychiatric condition preceded or
followed the substance abuse. However whether it is a primary
problem or secondary to addiction, it is very clear that such
problems have to be identified and treated with medications, as
otherwise it will affect the recovery of the addict.
Given below are few of the problems that may co-exist with addic
tion.
I)Depression - Depression is ^he commonest psychiatric problems
associated with addiction. The patient seems dull and shows little
or no interest in interacting with others, in eating and in-
personal appearance. There will also be fatigue, feeling of
worthlessness, guilt, morbid thoughts, poor concentration^ poor
appetite, psychomotor retardation, insomnia or hypersomnia end
suicidal thoughts.
Sometimes there may be reactive depression in which the symptoms
are less severe.
This is the result of a conflicting environment
or situation. In such patients anxiety and depression co-exist.
The patient will have to take anti-depressant drugs for 3-6 months
depending on the severity of bis problems, If suicidal thoughts
are present, it will be advisable to shift the patient to ahospital where 24 hours close supervision is possible.
. .4.
4
iDAnxiety Disorders
Anxiety is a diffuse, highly unpleasant often
or more body
va gue feeling of apprehension, accompanied by one
sensations - eg. an empty feeling in the pit of the stomach,
perspiration, headache.
tightness in the chest, pounding heart.
restlessness etc.
and intense periods of
Panic disorder is a spontaneous, episodic
less than an hour.
anxiety usually lasting for
often associated with the use of
Both these disorders are more
cannabis than with other drugs.
Mild anti depressant / anti-anxiety agents, use of relaxation
therapy and counselling on trigger factors, help.
IlDManic Depressive Psychosis -
Only 1-2% of all addicts may have
bipolar disorders shov;ing episodes of
mania and depression.
the manic phase, there is a euphoric
mood, with excessive
During
spending, talking, gambling, grandiosity and aecreaaea sleep,
Dur ing the
depressive phase psychomotor retardation, depression,
will be seen.
feeling of hopelessness/ suicidal ideas
Psychia tr ic Consultations
and continued use of ’ medications are
extremely important.
IV)Paranoid Disorders -
The dominant symptoms in
is a delusion that does not have an
delusional disorder
identifiable or genic basis,
to the delusion and his
The patient1 s effect is appropriate
deteriorates minimally over a
remains
intact
or
per sona1ity
of time. Other signs and symptoms o£ tn»ght
prolonged period
delusion is a paranoid
disorder are minimal. The most common
delusion in addicts.
..5,
5
V) Other Psychiatric Disorders - Sometimes addicts may also have
schizophrenic feature or schizo-affective disorders. These patients
may he primarily psychotic with secondary addiction.
Both the above categories reruires prolonged medical help and
have to be on anti psychotics under the supervision of a
Psychia tr ist
Regional Training Programme on Prevention and Management of Addiction”
SPONSORED BY
NATIONAL INSTITUTE OF SOCIAL DEFENCE, MINISTRY OF SOCIAL
JUSTICE & EMPOWERMENT, GOVERNMENT OF INDIA, NEW7 DELHI
PARENTING SKILLS
The problems of children that they face today are created by all of us
The problem is ' An Adult’, never the child itself
In short-term many schemes of alleviating the condition of children enhancing and
enriching the physical quality of their life can be suggested and worked out - But in the
long run what will truly help the child is only through
(
+ educating the adult about the needs and problems of the child
sensitizing them to their responsibility towards children
+ strengthening the fabric of family life
Let us understand that
+ behind ill-health of the child is ignorance, apathy or indifference of the adult mother
rather, care giver or doctor.
Behind poor education of the child is lethargy, non-commitment of the adult teacher.
educational authority.
+ Behind child labour is an insensitive exploitative adult and the poverty situation of
the parents.
Behind child exploitation - battering, sexual abuse, drugs, alcoholism etc.
Behind desertion and deprivation of the child is an irresponsible parent.
In whichever direction of children’s problems one turns - there is an adult who like little
sponges have the tremendous capacity to absorb the entire gamut of their environment
“"y toeS”W "P
” ’h" S™’
“”y “pre8S whi“
Children exist in large numbers in our country
Some say this over population is a burden.
We musr realise it is a reality and that we will have to convert this vast human resource
mio a Strength.
If the process does not start now - we will have on hand, large numbers of children
growing up as frustrated youth, lacking vitality and strength of purpose, with untapped
potential, expressing aggressiveness in every sphere of their life and action, steeped in
uncertainty doubt, hesitation, restlessness. The role of NGO’s and their community
based programmes must have
4- the will to deliver and the strength to resist the temptation to tackle the problems at a
superficial and cosmetic level.
4- Networking and sharing of ideas, resources, strengths and infrastructure to avoid
duplication and optimise service.
The courage to take up issues and sustain their expressed commitments.
Children
1
Children are more than the object of their parent’s attention and love, they are also a
biological and social necessity.
The human species perpetuates itself through children.
Cultural, religious and national groups transmit their values and traditions through
children.
Families maintain their lineage through children and
Individuals pass on their genetic and social heritage through children.
The ultimate value of children is the continuity of humanity'.
Early childhood is the foundation on which children build their lives. Ii is not just a
preparation for adolescence and adulthood. It is important in itself.
Children develop at different rates and in different ways emotionally, intellectually,
morally, socially, physically and spiritually. All are important and each is interwoven
with others.
All children have abilities which can (and should) be identified and promoted. What
children can do (rather than what they cannot do) is the starting point of their learning.
Page 2
Voung children learn from eventhing that happens to them and around them: thev do
not separate their learning into different subjects or disciplines for children, their
experience is their learning.
Play and conversation are the main ways by which young children learn about
Sf th
TPe°ple 3nd thC W°rld afOUnd theme' Childrei1 wh0
encouraged to
think for themselves are more likely to act independently.
“fco,h" c“‘r" “‘l wt,h
“c of
Parents
then multiple responsibilities. One aspect of life affected by these trends is the inability
ch^e^' L <
i
C^Id rcarms environment m Ae context of widespread
changes m tlie social fabrtc of families, neighbourhoods and communities.
Adding to this concern is increased recognition of families major influence on young
children s social, emotional and cognitive development.
^ ^“nseqnence of these changes, among all those concerned with the development of
children and families, there is an increased demand for high quality, community based
of
S??1CtS-1fS 3 compIimentarf’ rather than alternate strategy the direct provision
oi high quality child care programmes.
Educators have long acknowledged the significant influence of the family on the care and
evetopment of the child and the tremendous cultural and familial differences in parentchdd patterns of interaction. A major new objective for professional educators would be
St
r
® th1ei"seJves “* training Parents and future parents in family care and
child development skills.
’
Recognition of the family as the child’s primary socialising agent has been accompanied
»r^PT°dlC Cal S f°I monitonng parental performance and for recommendations for
providing parents with child rearing information and guidance.
Page 3
Any parenting programme must therefore understand that
1.
All parents want the best for their children
2.
Parents are in a position to be the best observer of their children and
consequently, are best able to provide for the physical and psychological needs of
their children.
3.
Children need to be exposed to certain environn^ntal experiences / interactions
for optimal development to take place and an understanding of the principles of
child development will help parents to provide these experiences, find methods to
enhance learning if they know how to and why they are important.
4.
There is no one way to rear children each culture has developed their own
methods of parenting. We can enrich our knowledge and expand the life
experiences of children by combining the strengths of differing cultures.
5.
Child rearing practices are embedded in the culture and grounded in cultural
patterns and beliefs and determine / effect style and quality of care giving and to a
large extent, the behaviours and expectations surroundings a child’s birth and
infancy. They also influence childhood, adolescence and the way these children
parent as adults.
6.
The importance of community involvement is vital in all steps of the process
building on what exists already within a community and creating partnerships to
help sustain efforts.
Bonding awareness
Right from day one, a bond is being formed between parent and child. Every contact /
loss of contact leaves on unbelievably deep impact on the relationship. Few parents seem
to know or appreciate just how important they are in the lives of children. How much
more a child wants from them emotionally and spiritually rather than the materialism which the parents are so busy supplying in increasing abundance.
The parents must realise
They are the go - between for their baby /toddler / child and his environment.
They are providers of stimulation to catch his interest:
of responses to his attempts to communicate; and
of physical care, so that his skill of attention and concentration develops
Page 4
COTLuni^elT
Wh° keep him Safe and Umit his environment so he can feel in
They help him achieve what he sets out to do
“he ka™,o
,o
u-
Tn nil
»—-" ~
Children have 3 vital needs
Love / care
(or)
Relationship
Loving and caring relationships can relieve even the most |
extreme levels of stress
j __________ __
Without it the child’s growth cannot be stimulated both
physically and mentally
A stable relationship gives emotional security
Self-esteem
(or)
They must learn to trust themselvies and develop a feeling of
competence and a desire to try
Sense of self
Learn to accept their failures and short comings and vet have
an expectation of success
Communication
(
Children communicate well before they talk
We need to listen and watch and demonstrate our
interest in their words and messages
Encourage language development and expression
Children need to talk - therefore, we need to give
them the opportunities
Children learn to speak by listening to people around
Parent education is a woman’s empowerment programme
”pa!S”'8 0’ “eEducating the parents in their irreplaceable role as “mother” and “father” . ' '
and educating
need
Y reCOgniZC’
and SUpport thcm ”that rolc ~ has bcco^
n
iiuvvl.
'TeS?f W.°meij’S uPIiftment> be they in the direction of social freedom, economic
pportumty, political awareness and / or spiritual awakening, at this point in civilization,
need to stress her non-duplicable, non-transferable role as mother.
Page 5
1
Women’s issues that focus on the inferior /oppressed role in society that the women have
today must include motherhood education and counselling initiatives.
Society and family must
appreciate her significant role in the continuance and enhancement of family life
and perpetuation of the future generation as also respect her individual needs as a
Human Being.
Help her through the frustrations of the loss of her freedom and the physical and
mental strain of being “on demand” 24 hours.
Educate her, in pre-natal and post-natal, in child care so that she has the primary
care giver can provide the much needed stimulation so vital for the healthy
growth and development of the child.
Support her in her endeavours to care for her child and spend as much time with
her child if she is employed.
Stress the ■vital role and responsibility of the Father in the social and emotional
development of the child rather than his largely prevalent role as economic care
giver.
TRUE PARENTING = MOTHERING + FATHERING
Page 6
MH' 2-0- X3
j
ON PREVENTION AND MANAGEMENT OF DRUG ABUSE
AND HIV-AroS"
SPONSORED BY
NATIONAL INSTITUTE OF SOCIAL DEFENCE MINISTRY OF SOCIAL JUSTICE A EMPOWERMENT,
GOVERNMENT OF MtNA, NEW DELHI
REGIOHALTRAIW^^
HARM MINIMISATION - TTK EXPERIENCE
INTRODUCTION
Injecting drug users are at high risk for infection with the human immuno deficiency virus
(HIV). A number of ongoing studies are seeking to identify the specific mode of
transmission and risk factors for progression to AIDS in intravenous drug taking
populations. The primary mode of HIV transmission between intravenous drug users is
parenteral, through the sharing of contaminated needles and syringes (Des Jarlais et
al, 1988). While HIV infection among drug users is mainly transmitted through needle
syringe sharing, the fact remains that it is primarily a sexually transmitted virus. There is
a possibility that drug users as a potential pool of infection can act as a bridge of
infectivity.
Fundamentally, the consequences of HIV infection are the same in people with a history
of injecting drug use as in any of other so called risk groups. There are, however, a few
important differences which should be noted down. Kaposi's Sacoma (KS) is much
more common in people who have apparently acquired the condition sexually rather
than by inoculation. Bacterial infections are generally more common in injecting drug
users than other people with HIV infection. This is particularly true of skin infections,
bacterial pneumonia and tuberculoses (TB). Abscesses and cellulitis are obviously
commonly seen in people who inject drugs. TB is found with increased frequency
amongst injecting drug users regardless of their HIV status. The patient with HIV
infection is however much more likely to develop clinical manifestations from TB than the
seronegative patient.
Incidence of IV drug use & HIV/AIDS In India
In India, heroin addiction is about two decades old and the estimated number of heroin
users stands at 3 million. Over the past few years buprenorphine abuse is increasing
among heroin users. In Manipur, HIV sero positivity among intravenous drug users shot
up from 0%in 1989 to 50% within six months. Now it is around 80%.
In Chennai the ethnic crisis at Srilanka paved the way for increased availability and
usage of heroin in 80’s. Shortages in mid 80s resulted in the users looking for
alternatives. Injecting buprenorphine had become one of the alternatives. Mostly
nitrazepam, diazepam, and dextropropoxyphene were abused.
In 1991, after the
assassination of Rajiv Gandhi by Srilankan terrorists, there was a heavy crackdown on
the Srilankan militants living in Tamilnadu resulting in an acute shortage of heroin.
Brown sugar users shifted to injecting buprenorphine. Thus, there was a sudden
increase in IV drug users.
•A’
t
I
The city of Chennai is currently estimated to have about 10,000 to 15,000 IDU’s mostly
located in ten different pockets. Kodambakkam is one of the major pockets. The drug of
choice is brown sugar and/or cocktails of pharmaceutical preparations like diazepam
phenaramme maleate, promethazine with buprenorphine. A few are known to inject
dextropropoxifine.
J
The HIV status among IDUs has gone up from 20% in 1999 to about 30% now. The
drug users are known to widely share injecting equipment, paraphernalia and also drugs
W are also known to indulge in drinking and high risk sexual activity. Hence the
threat of HIV spreading from the IDU population to the general population looks
imminent and dangerous. It is estimated that only 15% of IV drug users get any medical
assistance. Their general health, productivity and hence economic status are very much
compromised. Criminality has increased mainly to sustain their drug taking habit and
hence increased incidence of arrests and convictions.
The current situation of AIDS looming large in the society with about 30% of IVD
users being HIV positive and part of the society. It is therefore imperative that we
address this alarming situation effectively.
Some of the intervention methods available are - long-term in-patient care with total
abstinence as a goal, in other countries, methadone is provided on a day to day basis
to prevent the use of drugs. Others take a deterrent approach in which the threat of
imprisonment or other penalties are used to motivate behavioural change; and still
others use a model of individual education in which information is presented about HIV,
249$,and ways to avoid becoming infected or transmitting the virus to others. The
hitherto available models of treatment were unable to address this problem effectively
due to high relapse rates and limitation with regard to availability of services.
Obviously, the best way of avoiding the transmission of HIV through injecting drug use
is to avoid using illicit drugs, or at least to avoid injecting illicit drugs. This is certainly
the traditional approach of the health care services to illicit drug use. It does, however,
ha^e2° be reco9n’sed that many drug users do not wish to discontinue their drug usage
and the advent of HIV infection and AIDS has, to some extent, shifted the emphasis of
drug usage from abstinence to harm minimization - to reduce and minimize the harm
posed by continued drug use.
What is harm minimization
Harm reduction is a new paradigm now emerging in the field of addiction. This strategy
recognizes that people always have and always will use drugs and. therefore, attempts
to minimize the potential hazards associated with drug use rather than the use itself.
A set of strategies that encourage substance users and service providers to reduce the
harm done to drug users, their family members and communities by their licit and illicit
drug use. Harm reduction is designed to reduce destructive behaviours associated with
drug abuse and related problems. By this approach, attempts are made to reduce
t
adverse health, social and economic consequences of drug use without necessarily
eliminating drug use. Through this approach, some patients achieve stable abstinence
after treatment, many reduce consumption and there is over all improvement in
functioning i.e. physical health, occupational functioning and psychological state.
The most effective way of getting people to minimize the harmful effects of their drug use
is to provide user friendly services which attract them into contact and empower them to
change their behaviour toward a suitable intermediate objective. This means services
which are easily accessible, confidential, informal, and relevant (focus is not on
abstinence, but reducing the harm). Practitioners of harm reduction programme are
open minded and have a non judgmental attitude towards alternative methods of
reducing the harm caused by IV use.
Some of the harm minimization methods are
methadone maintenance programme (not available in India)
providing buprenorphine sublingual tablets
providing needles and syringes
Harm Minimization Project - Outreach Centre
The goals of the project:
1. Contacting as many drug users as possible from the community of Kodambakkam.
2. To help the addicts stop usage of street drugs and resort to sublingual
use of drugs.
The Objectives
❖
Minimization of the spread of infections like HIV by altering needle sharing behaviour
and teaching safer methods.
❖ Creating awareness about HIV-AIDS.
❖ Helping the addicts resort to a change in behaviour focusing on improving the quality
of their lives.
❖ Motivating the drug addicts to get into a “total abstinence" oriented programme over
a period of time.
Location and target population
IV drug users living in Kodambakkam area (geographical proximity- within 3 to 5 kms
radius)
Principles
❖ Treating the user with respect and dignity.
❖ Providing services with care, concern and empathy.
❖ Involving user in decisions relating to services/ programme choice.
Stipulated behaviour at the centre
❖ No physical or verbal violence of any kind on the premises.
❖ No use of drugs/ alcohol on the premises.
Programme and Activities
□
Substitution therapy
□
Providing sublingual Buprenorphine dispensed under the supervision of a doctor
and a nurse.
Medical help
A The medical practitioner makes the diagnosis.
a Provides appropriate guidance for drug and health related problems.
a Medicines are given for other infections (of chest, stomach, etc.)
a Nutrition supplements are provided.
a Dressing of wounds and abscesses.
a Providing condom/ bleach.
Psychological support
Group therapy sessions
Information, advice and guidance on
□
0
□
HIV/AIDS, hepatitis, blood borne infections.
Safe drugs use, safer injecting practices and ways to reduce health risks.
Safe sexual practices.
Related health issues.
Nutrition and exercise.
Strengthening self esteem.
Developing positive values.
Improving quality of life.
□
Options available to lead abstinent life
□
□
0
0
□
JI
Individual counselling and family counselling
Energisers / activities aimed to build trust, to breakdown barriers
and create a friendly environment.
Referral Services through networking
Madras Corporation
Offers diagnostic investigation for tuberculosis
Reach / Act
Provides tuberculosis medications.
YRG Care Centre, T.Nagar
HIWAIDS testing and counselling.
CHES, Kodambakkam
HIV/AIDS testing and care for clients and their families.
Other Services
During working hours of the centre, telephone services are offered to help drug users
communicate to the staff regarding their problems.
NA meetings are held once a week at the centre to enable drug users to know about NA
as an option.
The community workers visit the clients' home on a regular basis to establish rapport
and to motivate.
Socializing - festivals are celebrated at the centre to teach them alternate ways of
having fun.
Recreational facilities - carom, chess etc.
Providing additional support towards abstinence.
a
Special group therapy sessions.
a
Treatment at the TTK hospital and the After Care Centre.
TTK out reach centre situated at Kodambakkam has been functioning for the past 22
months servicing about 340 IDUs within a radius of about 6-8 kms. About 150 IDUs are
in touch with the centre and there is a substantial change in their drug usage pattern,
change in life style, change in high risk behaviour for the better. There is a substantial
decrease in crime rate and arrests. There is a significant improvement in the general
health of the clients. About 60% of them have become productive.
I
Factors responsible for compliance with programme leading to life style changes
□
Clients selected from a nearby community which
ensures easy accessibility to services (8.00 a.m. to 7.00 p.m.)
□ Choice of services from abstinence to harm reduction
□ Availability of buprenorphine which helps in cutting down IV use
□
□
Other related health issues are also addressed
0
Availability of recreational facilities -Carom, Chess and magazines
Availability of counselling services for individual and family
MH-
PREVENTION ANOMANAQEMENT OF DRUG ABUSE
AND HW-AIDS"
SPONSORED BY
NATIONAL INSTITUTE OF SOCIAL DEFENCE MINISTRY OF SOCIAL JUSTICE & EMPOWERMENT,
GOVERNMENT OF INDIA, NEW DELHI
HARM MINIMISATION - TTK EXPERIENCE
INTRODUCTION
Injecting drug users are at high risk for infection with the human Immuno deficiency virus
(HIV). A number of ongoing studies are seeking to identify the specific mode of
transmission and risk factors for progression to AIDS in intravenous drug taking
populations. The primary mode of HIV transmission between intravenous drug users is
parenteral, through the sharing of contaminated needles and syringes (Des Jarlais et
al, 1988). While HIV infection among drug users is mainly transmitted through needle
syringe sharing, the feet remains that it is primarily a sexually transmitted virus. There is
a possibility that drug users as a potential pool of infection can act as a bridge of
infectivity.
Fundamentally, the consequences of HIV infection are the same in people with a history
of injecting drug use as in any of other so called risk groups. There are, however, a few
important differences which should be nbted down. Kaposi’s Sacoma (KS) is much
more common in people who have apparently acquired the condition sexually rather
than by inoculation. Bacterial infections are generally more common In injecting drug
users than other people with HIV infection. This is particularly true of skin infections,
bacterial pneumonia and tuberculoses (TB). Abscesses and cellulitis are obviously
commonly seen in people who inject drugs. TB is found with increased frequency
amongst injecting drug users regardless of their HIV status. The patient with HIV
infection is however much more likely to develop clinical manifestations from TB than the
sera negative patient.
Incidence of IV drug use & HIV /AIDS In India
In India, heroin addiction is about two decades old and the estimated number of heroin
users stands at 3 million. Over the past few years buprenorphine abuse is increasing
among heroin users. In Manipur, HIV sera positivity among intravenous drug users shot
up from 0%in 1989 to 50% within six months. Now it is around 80%.
In Chennai the ethnic crisis at Srilanka paved the way for increased availability and
usage of heroin in 80’s. Shortages in mid 80s resulted in the users looking for
alternatives. Injecting buprenorphine had become one of the alternatives. Mostly
nitrazepam, diazepam, and dextropropoxyphene were abused.
In 1991, after the
assassination of Rajiv Gandhi by Srilankan terrorists, there was a heavy crackdown on
the Srilankan militants living in Tamilnadu resulting in an acute shortage of heroin.
Brown sugar users shifted to injecting buprenorphine. Thus, there was a sudden
increase in IV drug users.
- Q-S
1
The city of Chennai is currently estimated to have about 10,000 to 15,000 IDU’s mostly
located in ten different pockets. Kodambakkam is one of the major pockets. The druq of
choice is brown sugar and/or cocktails of pharmaceutical preparations like diazepam
phenaramme maleate, promethazine with buprenorphine. A few are known to inject
dextropropoxifine.
J
The HIV status among IDUs has gone up from 20% in 1999 to about 30% now. The
drug users are known to widely share injecting equipment, paraphernalia and also drugs
They are also known to indulge in drinking and high risk sexual activity. Hence the
threat of HIV spreading from the IDU population to the general population looks
imminent and dangerous. It is estimated that only 15% of IV drug users get any medical
assistance. Their general health, productivity and hence economic status are very much
compromised. Criminality has increased mainly to sustain their drug taking habit and
hence increased incidence of arrests and convictions.
The current situation of AIDS looming large in the society with about 30% of IVD
users being HIV positive and part of the society. It is therefore Imperative that we
address this alarming situation effectively.
Some of the intervention methods available are — long-term in-patient care with total
abstinence as a goal. In other countries, methadone is provided on a day to day basis
to prevent the use of drugs. Others take a deterrent approach in which the threat of
imprisonment or other penalties are used to motivate behavioural change; and still
others use a model of individual education in which information is presented about HIV,
AIDS and ways to avoid becoming infected or transmitting the virus to others. The
hitherto available models of treatment were unable to address this problem effectively
due to high relapse rates and limitation with regard to availability of services.
Obviously, the best way of avoiding the transmission of HIV through injecting drug use
is to avoid using illicit drugs, or at least to avoid injecting illicit drugs. This is certainly
the traditional approach of the health care services to illicit drug use. It does, however,
have to be recognised that many drug users do not wish to discontinue their drug usage
and the advent of HIV infection and AIDS has, to some extent, shifted the emphasis of
drug usage from abstinence to harm minimization - to reduce and minimize the harm
posed by continued drug use.
What is harm minimization
Harm reduction is a new paradigm now emerging in the field of addiction. This strategy
recognizes that people always have and always will use drugs and. therefore, attempts
to minimize the potential hazards associated with drug use rather than the use itself.
A set of strategies that encourage substance users and service providers to reduce the
harm done to drug users, their family members and communities by their licit and illicit
drug use. Harm reduction is designed to reduce destructive behaviours associated with
drug abuse and related problems. By this approach, attempts are made to reduce
adverse health, social and economic consequences of drug use without necessarily
eliminating drug use. Through this approach, some patients achieve stable abstinence
after treatment, many reduce consumption and there is over all improvement in
functioning i.e. physical health, occupational functioning and psychological state.
The most effective way of getting people to minimize the harmful effects of their drug use
is to provide user friendly services which attract them into contact and empower them to
change their behaviour toward a suitable intermediate objective. This means services
which are easily accessible, confidential, informal, and relevant (focus is not on
abstinence, but reducing the harm). Practitioners of harm reduction programme are
open minded and have a non judgmental attitude towards alternative methods of
reducing the harm caused by IV use.
Some of the harm minimization methods are
-
methadone maintenance programme (not available in India)
providing buprenorphine sublingual tablets
providing needles and syringes
Harm Minimization Project - Outreach Centre
The goals of the project:
1. Contacting as many drug users as possible from the community of Kodambakkam.
2. To help the addicts stop usage of street drugs and resort to sublingual
use of drugs.
The Objectives
❖
Minimization of the spread of infections like HIV by altering needle sharing behaviour
and teaching safer methods.
❖ Creating awareness about HIV-AIDS.
❖
^Hh
❖
Motivating the drug addicts to get into a “total abstinence" oriented programme over
a period of time.
Edicts resort to a change in behaviour focusing on improving the quality
Location and target population
IV drug users living in Kodambakkam area (geographical proximity- within 3 to 5 kms
radius)
Principles
❖ Treating the user with respect and dignity.
❖ Providing services with care, concern and empathy.
❖ Involving user in decisions relating to services/ programme choice.
Stipulated behaviour at the centre
❖ No physical or verbal violence of any kind on the premises.
❖ No use of drugs/ alcohol on the premises.
Programme and Activities
□
Substitution therapy
0
Providing sublingual Buprenorphine dispensed under the supervision of a doctor
and a nurse.
Medical help
The medical practitioner makes the diagnosis.
Provides appropriate guidance for drug and health related problems.
a Medicines are given for other infections (of chest, stomach, etc.)
a Nutrition supplements are provided.
a Dressing of wounds and abscesses.
4b Providing condom/ bleach.
a
a
Psychological support
Group therapy sessions
Information, advice and guidance on
0
□
□
0
□
0
□
□
□
HIV/AIDS, hepatitis, blood borne infections.
Safe drugs use, safer injecting practices and ways to reduce health risks.
Safe sexual practices.
Related health issues.
Nutrition and exercise.
Strengthening self esteem.
Developing positive values.
Improving quality of life.
Options available to lead abstinent life
Individual counselling and family counselling
Energisers / activities aimed to build trust, to breakdown barriers
and create a friendly environment.
Referral Services through networking
Madras Corporation
Offers diagnostic investigation for tuberculosis
Reach / Act
Provides tuberculosis medications.
YRG Care Centre, T.Nagar
HIV/AIDS testing and counselling.
CHES, Kodambakkam
HIV/AIDS testing and care for clients and their families.
Other Services
During working hours of the centre, telephone services are offered to help drug users
communicate to the staff regarding their problems.
NA meetings are held once a week at the centre to enable drug users to know about NA
as an option.
The community workers visit the clients’ home on a regular basis to establish rapport
and to motivate.
Socializing - festivals are celebrated at the centre to teach them alternate ways of
having fun.
Recreational facilities - carom, chess etc.
Providing additional support towards abstinence.
a
Special group therapy sessions.
a
Treatment at the TTK hospital and the After Care Centre.
TTK out reach centre situated at Kodambakkam has been functioning for the past 22
months servicing about 340 IDUs within a radius of about 6-8 kms. About 150 IDUs are
in touch with the centre and there is a substantial change in their drug usage pattern,
change in life style, change in high risk behaviour for the better. There is a substantial
decrease in crime rate and arrests. There is a significant improvement in the general
health of the clients. About 60% of them have become productive.
Factors responsible for compliance with programmeteading to life style changes
□
Clients selected from a nearby community which
ensures easy accessibility to services (8.00 a m. to 7.00 p.m.)
□ Choice of services from abstinence to harm reduction
□ Availability of buprenorphine which helps in cutting down IV use
□
Other related health issues are also addressed
0
Availability of counselling services for individual and family
□
Availability of recreational facilities -Carom, Chess and magazines
nh -
PREVENTION AND MANAGEMENT OF DRUG ABUSE
AND HIV-AIDS"
SPONSORED BY
NATIONAL INSTITUTE OF SOCIAL DEFENCE MINISTRY OF SOCIAL JUSTICE A EMPOWERMENT,
GOVERNMENT OF INDIA, NEW DELHI
HARM MINIMISATION - TTK EXPERIENCE
INTRODUCTION
Injecting drug users are at high risk for infection with the human Immuno deficiency virus
(HIV). A number of ongoing studies are seeking to identify the specific mode of
transmission and risk factors for progression to AIDS in intravenous drug taking
populations. The primary mode of HIV transmission between intravenous drug users is
parenteral, through the sharing of contaminated needles and syringes (Des Jarlais et
al, 1988). While HIV infection among drug users is mainly transmitted through needle
syringe sharing, the fact remains that it is primarily a sexually transmitted virus. There is
a possibility that drug users as a potential pool of infection can act as a bridge of
infectivity.
Fundamentally, the consequences of HIV infection are the same in people with a history
of injecting drug use as in any of other so called risk groups. There are, however, a few
important differences which should be noted down. Kaposi's Sacoma (KS) is much
more common in people who have apparently acquired the condition sexually rather
than by inoculation. Bacteriat infections are generally more common in injecting drug
users than other people with HIV infection. This is particularly true of skin infections,
bacterial pneumonia and tuberculoses (TB). Abscesses and cellulitis are obviously
commonly seen in people who inject drugs. TB is found with increased frequency
amongst injecting drug users regardless of their HIV status. The patient with HIV
infection is however much more likely to develop clinical manifestations from TB than the
sera negative patient.
Incidence of IV drug use & HIV/AIDS in India
In India, heroin addiction is about two decades old and the estimated number of heroin
users stands at 3 million. Over the past few years buprenorphine abuse Is increasing
among heroin users. In Manipur, HIV sera positivity among intravenous drug users shot
up from 0%in 1989 to 50% within six months. Now It is around 80%.
In Chennai the ethnic crisis at Sriianka paved the way for increased availability and
usage of heroin in 80’s. Shortages in mid 80s resulted in the users looking for
alternatives. Injecting buprenorphine had become one of the alternatives. Mostly
nitrazepam, diazepam, and dextropropoxyphene were abused.
In 1991, after the
assassination of Rajiv Gandhi by Srilankan terrorists, there was a heavy crackdown on
the Srilankan militants living in Tamllnadu resulting in an acute shortage of heroin.
Brown sugar users shifted to injecting buprenorphine. Thus, there was a sudden
increase in IV drug users.
V
1
tCh^Ta' T cur,re?tly,estimated to have about 10,000 to 15,000 IDU’s mostly
cated in ten different pockets. Kodambakkam is one of the major pockets. The drug of
choice is brown sugar and/or cocktails of pharmaceutical preparations like diazepam
phenaramme maleate, promethazine with buprenorphine. A few are known to inject
dextropropoxifine.
J
The HIV status among IDUs has gone up from 20% in 1999 to about 30% now. The
drug users are known to widely share injecting equipment, paraphernalia and also drugs.
They are also known to indulge in drinking and high risk sexual activity. Hence the
threat of HIV spreading from the IDU population to the general population looks
imminent and dangerous. It is estimated that only 15% of IV drug users get any medical
assistance. Their general health, productivity and hence economic status are very much
compromised. Criminality has increased mainly to sustain their drug taking habit and
hence increased incidence of arrests and convictions.
The current situation of AIDS looming large in the society with about 30% of IVD
users being HIV positive and part of the society. It is therefore imperative that we
address this alarming situation effectively.
Some of the intervention methods available are - long-term in-patient care with total
abstinence as a goal. In other countries, methadone is provided on a day to day basis
to prevent the use of drugs. Others take a deterrent approach in which the threat of
imprisonment or other penalties are used to motivate behavioural change; and still
others use a model of individual education in which information is presented about HIV
3;?Srfand ways t0 avoid becoming infected or transmitting the virus to others. The
hitherto available models of treatment were unable to address this problem effectively
due to high relapse rates and limitation with regard to availability of services.
Obviously the best way of avoiding the transmission of HIV through injecting drug use
is to avoid using illicit drugs, or at least to avoid injecting illicit drugs. This is certainly
the traditional approach of the health care services to illicit drug use. It does, however,
ke rec°gn^ ^at many drug users do not wish to discontinue their drug usage
and the advent of HIV infection and AIDS has, to some extent, shifted the emphasis of
drug usage from abstinence to harm minimization - to reduce and minimize the harm
posed by continued drug use.
What is harm minimization
Harm reduction is a new paradigm now emerging in the field of addiction. This strategy
recognizes that people always have and always will use drugs and. therefore, attempts
to minimize the potential hazards associated with drug use rather than the use itself.
A set of strategies that encourage substance users and service providers to reduce the
harm done to drug users, their family members and communities by their licit and illicit
drug use. Harm reduction is designed to reduce destructive behaviours associated with
drug abuse and related problems. By this approach, attempts are made to reduce
i
3.
adverse health, social and economic consequences of drug use without necessarily
ehminatmg drug use. Through this approach, some patients achieve stable abstinence
after treatment many reduce consumption and there is over all improvement in
functioning i.e. physical health, occupational functioning and psychological state.
The most effective way of getting people to minimize the harmful effects of their drug use
is to provide user friendly services which attract them into contact and empower them to
change their behaviour toward a suitable intermediate objective. This means services
which are easily accessible, confidential, informal, and relevant (focus is not on
abstinence, but reducing the harm). Practitioners of harm reduction programme are
open minded and have a non judgmental attitude towards alternative methods of
reducing the harm caused by IV use.
Some of the harm minimization methods are
methadone maintenance programme (not available in India;
providing buprenorphine sublingual tablets
providing needles and syringes
Harm Minimization Project - Outreach Centre
The goals of the project.
1. Contacting as many drug users as possible from the community of Kodambakkam.
stop usage of street drugs and resort to sublingual
The Objectives
❖
Minimization of the spread of infections like HIV by altering needle sharing behaviour
and teaching safer methods.
♦> Creating awareness about HIV-AIDS.
❖ Helping the addicts resort to a change in behaviour focusing on improving the quality
of their lives.
❖ Motivating the drug addicts to get into a 'total abstinence” oriented programme over
a period of time.
Location and target population
radkisf
*n Koclamt)akicarn’area (Geographical proximity- within 3 to 5 kms
wi •
ito
Principles
❖ Treating the user with respect and dignity.
❖ Providing services with care, concern and empathy.
❖ Involving user in decisions relating to services/ programme choice.
Stipulated behaviour at the centre
❖ No physical or verbal violence of any kind on the premises.
❖ No use of drugs/ alcohol on the premises.
Programme and Activities
□
Substitution therapy
a
Providing sublingual Buprenorphine dispensed under the supervision of a doctor
and a nurse.
Medical help
4 The medical practitioner makes the diagnosis.
4 Provides appropriate guidance for drug and health related problems.
a Medicines are given for other infections (of chest, stomach, etc.)
4 Nutrition supplements are provided.
a Dressing of wounds and abscesses.
a Providing condom/ bleach.
Psychological support
Group therapy sessions
Information, advice and guidance on
□
□
□
0
□
□
□
0
0
HIV/AIDS, hepatitis, blood borne infections.
Safe drugs use, safer injecting practices and ways to reduce health risks.
Safe sexual practices.
Related health issues.
Nutrition and exercise.
Strengthening self esteem.
Developing positive values.
Improving quality of life.
Options available to lead abstinent life
I
Individual counselling and family counselling
Energisers! activities aimed to build trust, to breakdown barriers
and create a friendly environment.
Referral Services through networking
Madras Corporation
Offers diagnostic investigation for tuberculosis
Reach / Act
Provides tuberculosis medications.
YRG Care Centre, T.Nagar
HIV/AIDS testing and counselling.
CHES, Kodambakkam
HIV/AIDS testing and care for clients and their families.
Other Services
During working hours of the centre, telephone services are offered to help drug users
communicate to the staff regarding their problems.
NA meetings are held once a week at the centre to enable drug users to know about NA
as an option.
The community workers visit the clients' home on a regular basis to establish rapport
and to motivate.
Socializing - festivals are celebrated at the centre to teach them alternate ways of
having fun.
Recreational facilities - carom, chess etc.
Providing additional support towards abstinence.
a
Special group therapy sessions.
a
Treatment at the TTK hospital and the After Care Centre.
TTK out reach centre situated at Kodambakkam has been functioning for the past 22
months servicing about 340 IDUs within a radius of about 6-8 kms. About 150 IDUs are
in touch with the centre and there is a substantial change in their drug usage pattern,
change in life style, change in high risk behaviour for the better. There is a substantial
decrease in crime rate and arrests. There is a significant improvement in the general
health of the clients. About 60% of them have become productive.
Factors responsible for compliance with programme leading to life style changes
□
Clients selected from a nearby community which
ensures easy accessibility to services (8.00 a.m. to 7.00 p.m.)
0
Choice of services from abstinence to harm reduction
□ Availability of buprenorphine which helps in cutting down IV use
0
Other related health issues are also addressed
□
Availability of counselling services for individual and family
□
Availability of recreational facilities -Carom, Chess and magazines
Regional Training Programme on Prevention and Management of Addiction"
SPONSORED BY
NATIONAL INSTITUTE OF SOCIAL DEFENCE, MINISTRY OF SOCIAL
JUSTICE & EMPOWERMENT, GOVERNMENT OF LNDIA, NEW DELHI
ART THERAPY
Art therapy programme
Art
4 Art symbolizes personal cultural aspects of development
It predicts trends in a society
It is personal expression of creative ideas
Artistic work has aesthetic considerations as prime importance. It gives only
satisfaction. It has minimal therapeutic value.
❖
♦
4
Art therapy
4 Person and process is of prime importance
4 Individual feelings, thoughts and attitudes matter very much
4 The client and therapist relate and the whole dynamic process has therapeutic value
Definition
4 Art therapy is a therapeutic procedure using art and other visual media designed to
assist favourable change in personality or living that will outlast the session itself
Reasons why art therapy helps
4
4
4
4
4
4
Visual thinking
Expressing what words cannot
Emotional release
Creating a product
It is possible for everyone to involve in the therapy
Art as a way of knowing others
History of art therapy
4 The term first used over 40 years ago
♦ From prisons - drawing with charcoal on walls
♦ Prom hospitals- drawing on napkins and other available material
4 Practiced now in more than 60 countries around the world
Pagel
Scope of art therapy
♦ The drawing once created is a personal record that can be referred over time
♦ A sequence of drawing can reveal changes in attitudes or relationship over time
♦ It permits fantasy to create something lost or past. (Return back to relationship to
finish unfinished tasks)
♦ Client can safely represent the frightening ideas and after creation can work his fears
♦ Possibility of projecting into future and learning to deal with it.
What art therapy is not
♦ It is not only for people who show interest in art or have natural talent in art
♦ Art therapists are not art teachers. They should have training in psychological
therapies and possibly in ail too
♦ Art therapy is not a form of occupational therapy
Choice of art materials
♦
♦
♦
♦
♦
♦
♦
♦
♦
Crayons
Colour pencils
Water colour
Sketches, markers
Poster colours
Oil colours
Collage
Chalks
Charcoal
Choice of material depends on
♦
♦
♦
♦
Versatility of the medium
Type of client
Stage that has been reached in therapy
Clients in presenting therapeutic problems
Client groups
♦
♦
♦
♦
Individuals
Families
Specific client groups (chemical dependency, Institutionalized, Terminally ill
All people of any developmental range: Children, Adolescents, Adults and old people
Page 3
Techniques
Introduction
♦ Art therapist is both participant and observer of the process of change
♦ Before each session, explanation about session and instructions are clearly given
about materials, boundaries and settings
No direct interpretation or analysis of art work allowed
The client and therapist explore the meaning of drawings
The client should be helped to share how he feels
Reflection and clarification of feelings allowed
The same rules as group therapy apply. Enquiry and questioning as in group therapy
allowed
♦ The therapist can summarize at the end of the session
♦
♦
♦
♦
♦
Few theoritical standpoints
Behaviourist
4
Recognition of order and fonn, acquisition of skill and learning techniques
Freudian
♦ Spontaneous imager}7 released from unconscious-other concepts of psychoanalysis
apply. Client is brought from 4couch’ to the 4easel’
Rogerian
♦ Relationship between client and therapist is important.
♦ Boundaries and settings are clearly explained
4 No judgement/7 praising the work on its aesthetic or technical merit
As used in TTK Hospital
4
Art therapy is used as adjunct therapy
♦ Through art therapy, counsellor accepts and understands patient
♦ Counsellor is warm, empathic and non-judgemental and genuine.
♦ Materials, setting and boundaries are clearly explained.
4 No criticism or evaluation of work based on technical merit or aesthetic value
♦ IvIiiToring, reflecting, questioning, clarification, confronting and bringing insight
4
♦
allowed as and when appropriate in the process of therapy
Summary of session given at the end
Counsellors are trained before conducting sessions
Page 4
Art therapy in groups
Projective art groups
Common frame work to which client relates his personal meaning. Self and group
exploratmn m sharmg of a common theme (e.g. house, tree, person)
P
Group art work
Structured art therapy groups
♦ Includes simple boundary7 rules and some prescribed activities
♦ Boundary rule-paint what you like, but use onty 3 colours
♦ Prescribed activities-choose one crayon and have a non-verbal conversation with the
other person on the same sheet of paper
Art games
Based on rules which define the frame work of that activity
♦ Draw an advertisement for yourself
If outcome is not satisfactory; free to change or add rules by' agreement of
participants
♦ Imagine yourself' as a owner of a department store and depict your personal qualities
Family art therapy
♦
♦
♦
♦
Can observe the entire family unit’s functioning
Portrays dynamics of the family unit
Can understand person’s perception of his/her position within it
Whole family can work together as ‘projective art group’ or ‘group art work’
Art therapy as a tool in diagnostics
Can be used as a tool in assessment'diagnosis
♦ Neurological conditions
♦ Psychiatric conditions
♦ As projective method for testing personality- traits/defects
Page 5
Few web sites
Art therapy on the web
http:/wwyv.sofer.com/arttherapy- (American art therapy association)
http:/vnvw.arttherapy.org - ( British Association of Art therapists)
http:/yvM^>.baat.co.uk- (Australian National Art Therapy Association)
http:/www, anata. synflux. com. att
Regional Training Programme on Prevention and Management of Addiction"
SPONSORED BY
X1TI°NAL IXSIIT,rE OF SOCIAL DEFENCE, MINISTRY OF sort at
JI STICE & EMPOWERMENT, GOVERNMENT OF INDIA, NEW DELHI
FAMILY THERAPY
Die list below summarises the main characteristics of two contrasting models of family
Dominator families
Competitive structures_______
Misuse of power
No equal rights_______
Family secrets
JRigid and compulsive rules
; Rigid gender roles
_No sharing of housework
No joint family activities
LEconomic “burdens” unshared
j No respect for personal privacy
LWin-lose conflict resolution
I No shared decision - making
No shared parenting
______
No support for feelings
-Discipline by violence and shame
Mistakes not admitted
apologies given___________
r No
Ii xProblems
ivuivHis blamed
uidincQ on otn
e
others
Resistance to "outsiders ”
-Loyalty to family based on Uduty
Resistance to change
"
No family unity7
No protection from abusive acts
Conflicts are ignored
Little or no laughter or joy
C hildren unplanned and unwanted
Partnership families
Cooperative structures
j Equitable use of power
Equal rights
Open communication, no secrets
I Flexible rules ___________
Flexible gender roles
_ Housework shared equitably
Planned family activities
| Economic responsibility shared
; Respect for personal privacy
_i Wimwin conflict resolution
__
I Shared decision — making
_j Parenting shared equitably
All feelings are accepted
__ Discipline based on respect and trust
IVEstakes admitted
J Apologies made when needed______
Pgrsonal^responsibility- for problem^"
Openness to7utsiders
—
Loyalty to family based on trust
Openness to change______
i Cohesive family unit
T Members feel safe, protected
j
j Conflicts are resolved immediately
j Family is seen as a source ofjoy
I Children planned and wanted
"wui be
What causes tension in the family
A study conducted by the family life and marriage counselling centre of the New Delhi
Branch of the Family Planning Association of India has enumerated the following causes
as sources of tension in the families in India.
♦ Economic or financial problems
♦ The husband coming home late
♦ The husband s habits like gambling and alcoholism particularly under conditions of
economic hardship
♦ Suspicion on the character of husband / wife
♦ The husband not trusting the wife and lying about where he goes and the wife
eventually coming to know about it all
♦ The husband being without a job and being dependent on other members of the
family
♦ Mother-in-law versus daughter-in-law
treatment of the daughter-in-law
situation,
Mother-in-law’s
indifferent
♦ Sex differentiation in children bom to different daughters-in-law resulting in different
treatment of the daughters-in-law the one giving birth to a male child being preferred
to the one giving birth to a female child
♦ Difference in opinion between husband and wife and the in-laws over upbringing of
children
♦ Infertility as a cause of family tension, particularly in families where one daughter-inlaw has a child and other does not
♦ Different treatment to working and non working daughters-in-law. Difference in
attitude to working women
♦ Indifferent or cold treatment to wife’s parents and other relations
♦ Educated children in the family being unemployed
♦ Property disputes
♦ Lack of mutual acceptance and understanding
Page 2
4
♦ One earning member and various dependents
♦ Discrepancy between needs and resources
♦ Dowiy system and related problems
♦ Lack of proper housing facilities leading to disputes with the neighbours regarding
sharing of common resources
♦ Dominance of one partner over the other
♦ ^tude towards management of finances and the respective role of the two partners
Page 3
4
MH-
REGIONAL TRAINING PROGRAMME ON PREVENTION AND MANAGEMENT OF DRUG ABUSE
AND HIV-AIDS"
SPONSORED BY
NATIONAL INSTITUTE OF SOCIAL DEFENCE MINISTRY OF SOCIAL JUSTICE & EMPOWERMENT,
GOVERNMENT OF INDIA, NEW DELHI
ABOUT HIV /AIDS
AIDS (Acquired Immuno Deficiency Syndrome) has been described as the ’’worst plague
of the century”. Despite intensive research for medical and clinical intervention, there has
been little success; a vaccine or cure for AIDS in the foreseeable future seems
improbable. Under these circumstances, it is evident that the worldwide spread of this
infection can only be controlled by attempting behavioural change through a societal
response comprising of awareness and education strategies.
Today a total of 34.3 million people (1999) are estimated to be infected with Human
Immuno Deficiency Virus (MV) the causative agent of AIDS. HIV infection is on the
increase all over the world. Everyday about 8000 new HTV infections occur. With at least
3.7 million people in India infected with HIX’ and with the infection rapidly spreading,
health personnel in India need to be well aware of the magnitude of problems associated
with the spread of HIX7 / AIDS .
The diagnosis of HIV is very traumatic and the mental trauma for the patient is often as
great (or even greater) than the physical distress. As HIV carries a strong social stigma,
there are social issues that are relevant. Due to the massive and well directed prevention
campaigns, the spread of HIV-AIDS is slower in the industralised countries. On the other
hand, majority of the new infections occur in developing countries like India, Thailand
and Indonesia.
What is HIV?
Our body is like a fortress, with a very efficient defence / immune system. The first line
of defence is the skin, mucus membrane, tears, ear wax etc. They ward off the surface
dangers the body could be exposed to. If the infective agents get under the surface, the
WBC (White Blood Cells) and lymphoid tissues like the tonsils, spleeh, lymphatic
system etc. attempt to fight it If it still persists, then the acquired immunity system
takes over. Antibodies are produced to vanquish that particular infection.
The essential ammunition the WBC system contains is the T4 lymphocyte or helper
T cell. The T4 cells are produced in the spleen and bone marrow of man during the fetal
stage, infancy and childhood. The T4 cells keep circulating in the lymph and blood,
during which they pass through the Thymus gland. The gland acts like a computer and
programmes the T cells to identify
self cells belonging to one’s own body and
foreign cells from foreign bacteria, viruses and other germs.
XG
r.
Mt?-•
:.
•
5
■
2
The T 4 cell not only recognises anything foreign but also gives the command to the rest
of the immune system to go ahead and attack the foreign organisms. But, unfortunately
the Thymus gland stops activity after childhood and the adult body cannot make anymore
programmed T4 cells. So the number of programmed T4 cells in our body is limited to
200-300 billion. The T4 cell lives for 60 to 65 years which is why older people after the
age of 70 are more prone to infections.
The T4 cell has a projection on its wall into which the HIV agent fits like a key fits into a
lock. On impact, the T4 cell unwillingly starts producing viral particles. Thousands of
HTV are produced in one T4 cell and the T4 cell bursts, releasing these viruses which
then go on to attack other T4 cells. As the number of viruses in a person’s body increases,
the number of T4 cells decreases, and slowly but surely, the immune system is destroyed.
Where is HIV found?
HTV is present in all body fluids like blood, semen, vaginal fluid, mother’s milk, sweat,
tears, saliva, urine etc. But only blood, semen, vaginal fluid and mother’s milk are
implicated in the spread of HIV.
How docs HIV spread?
The three routes by which HIV can spread from one person to the other are
1. Infected blood
2. Sexual contact and
3. Infected mother to child
Infected blood
□ Blood transfusion of inf ected blood will definitely result in infecting the recipient. In
India, around 10 to 15% cases of infection are the result of infected blood
transfusions.
□ Use of infected needles, syringes and other skin piercing instruments also pass on the
infection from the infected individual to others. Among IV drug abusers, reuse of
unsterilised, infected needles and syringes by many people is very common.
Sexual contact (through infected semen and vagina! fluid)
In India 70 to 80% of all HIV infections is through the hetero-sexual route. Though all
penetrative sexual activity can lead to infection, the following points are to be noted.
1. If one of the sexual partners has ulcers on the penis or in and around the vagina
due to other sexually transmitted diseases (STDs) eg: syphilis, genital herpes or
genital warts, the HIV spreads more easily.
3
2. Anal sex is the riskiest fr om of penetrative sex because multiple injuries and tears
sfreX^fthTp^S31^311’ Wht,iCh makeS 11 eaSier f°r the 1117 t0
blood
stream of the partner. This is why it spreads fastest among homosexuals.
m0UtVS
penetrative sex>
amount of virus secreted
sLLXT v lvely Iess’SmaU
but stlU
a certain«
of
risk faCt°risaSSOciated
with deep
h S iT ’ n mcr83ses there are bleeding
bleedin8 gums and
and ulcers/
uIcers/ injuries
w8
dSndt WsS Th
From an infected pregnant mother to her child
The IHV passes from the infected mother:
a. during pregnancy through the placenta to the fetus
b. through the mother’s breast milk to the baby
30 to 40% of babies bom to HIV positive mothers are infected Experimentally
tTeX^
I"
8
” Pregn3nt W°men With soms success Preventing
onti!n of h1SS-°n fr°m ”10ther t0 child’ The mother should be told about the facts and the
option of having an abortion can be presented to her.
What happens when a person is exposed to HIV ?
It is important to establish the fact that exposure to the virus mav or may not lead to
infection. Many factors like the route of infection, the quality and quantity of virus and
some as yet unknown factors play a part. But, once infected with HIV, the person carries
the virus in his body throughout his life.
There are four stages in the development of the disease:
Stage 1
Hv-“
Stage 2
ThiVS
^mptomatic sta8e where no symptoms are noticed. Between six and 12
weeks after infection, the body produces antibodies against the virus. This period lasts
from three months to 12 years.
F
Stage 3
Illness associated with
infection may appear. The person may begin to show signs of
ess ike generalised swelling of the lymph nodes particularly at the back of the neck
4
and armpits. Other signs such as weight loss, prolonged diarrhoea, unexplained fever
lasting more than one month and fungal infection in the mouth appear. Breathlessness,
fatigue, night sweats, persistent cough and recurring skin infections may occur.
Stage 4
As the immunity system has totally collapsed he is unable to fight off any infections. So,
any opportunistic infections can set in and become life threatening. Some of the common
infections are:
Lung infections - Pneumonia and TB
Gastro
- Intestinal infections - severe diarrhoea
Brain infections causing severe head aches, fits and dementia
Cancers
- Skin cancer (Kaposi Sarcoma, non Hodskin’s lymphoma and
primary lymphoma of the brain)
The end finally conies in the form of death in about 6 months to two years.
WHO Classification
Since sophisticated methods for counting CD4 cells and carrying out blood tests may not
be available in many developing countries, WHO has listed a few signs that help in the
provisional diagnosis of AIDS in adults. The presence of at least two major sigrts
associated with at least one minor sign can be an indication of AIDS provided other
causes of depleted immunity, like malnutrition have been ruled out.
The major and minor signs are listed below:
Major signs
□ Weight loss greater tlian 10% of body weight
□ Fever for longer than one month, intermittent or continuous
□ Chronic diarrhea for longer than one month, intermittent or constant
Minor signs
□
□
□
□
□
□
Persistent cough for longer than one month
General itchy dermatitis (skin irritation)
Recurrent herpes zoster (shingles)
Oropharyngeal candidiasis (fungus infection in the mouth / throat)
Chronic progressive and disseminated herpes simplex infection
Generalised lymphadenopathy (swelling of lymph glands).
♦
5
Who are at high risk?
Any person who has
Multiple sexual partners
Casual unprotected sex (without using condoms)
Sex with male or female prostitutes
Homosexual encounters and
Intravenous drug users
Persons who receive blood transfusion with untested blood
People needing multiple blood transfusi
sions due to haemophilia, thallasaemia, cancer
etc.
Having sexual partners who are one of the above
How one can prevent infection
etSskk T; mS“V“d ”
10 “ “,e Vin“ “ '“8 “ f
«» body. But
once outstde, the HIV ,s a very weak, ftagfle vi™ which is easily destroyed by:
- Heat through diving or boiling
- Use of chemicals such as acid or household bleach
Prevention of infection through the sexual route by
□
□
□
□
Having sex with only one partner who is faithful
Avoiding pre-marital and extra marital sexual activities
Avoiding unprotected, casual sex
Avoiding having sex under the influence of alcohol / drugs when the power of
discrimination is likely to be impaired
P
□ butafso*^1
COndom®’ TIus gives considerable protection against not onlv HIX’
but also against other sexually transmitted disease like syphilis, gonoirhoea etc.
Prevention of infection through infected blood
□ S"wS ,^w0" u
used.’
h
d
W'’“l fr0'" ‘ votaI^ ^/vohrnbry blood
lh“* “ “ ELISA
should be
□ Use disposable or adequately sterilised needles and syringes
□ ZuM
likC knives’ SCalPels’ needles
dental equipment
hould be sterihsed before use. Razors and blades can be sterilised by boiling in waler
s-0 minutes or keeping them immersed in household bleach for 30 minutel
One cannot get HIV through
♦
6
□
□
□
□
Normal social contact like shaking hands, hugging, sharing plates, cups, glasses, etc.
Using public toilets, swimming pools, public transport like buses, trains, etc.
Food, drinks etc.
Insects, bugs, mosquito bites
a Sneezing, coughing etc.
Play safe
• Practice safer sex. Always insist on the use of condoms, even in the case of oral
sex, no matter how embarrassing this may be. Remember this is, quite literally, a
matter of life and death.
• Insist on using sterilized equipment when you go in for any invasive procedure;
this includes a visit to the dentist and the occasions when you get your ears and
nose pierced. Always use disposable needles when you need to take an injection.
• In case you have to have a blood transfusion, make sure that the blood you receive
has been screened for .AIDS by a reliable blood bank. Or better still, ask such
friends and relatives who have the same blood group as you, to donate blood.
(Experts from Sunday, September 5-11, 1993).
MH-
^6
REGIONAL TRAINING PROGRAMME ON PREVENTION AND MANAGEMENT OF DRUG ABUSE
AND HIV-AIDS”
SPONSORED BY
NATIONAL INSTITUTE OF SOCIAL DEFENCE MINISTRY OF SOCIAL JUSTICE & EMPOWERMENT,
GOVERNMENT OF INDIA, NEW DELHI
ABOUT HIV/AIDS
AIDS (Acquired Immuno Deficiency Syndrome) has been described as the "worst plague
of the century". Despite intensive research for medical and clinical intervention, there has
been little success; a vaccine or cure for AIDS in die foreseeable future seems
improbable. Under these circumstances, it is evident that the worldwide spread of this
infection can only be controlled by attempting behavioural change through a societal
response comprising of awareness and education strategies.
Today a total of 34.3 million people (1999) are estimated to be infected with Human
Immuno Deficiency Virus (HIV) the causative agent of AIDS. HIX7 infection is on the
increase all over the world. Everyday about 8000 new HTV infections occur. With at least
3.7 million people in India infected with HIX’ and with the infection rapidly spreading,
health personnel in India need to be well aware of the magnitude of problems associated
with the spread of HIXZ / AIDS .
The diagnosis of HTV is very traumatic and the mental trauma for the patient is often as
great (or even greater) than the physical distress. As HIV carries a strong social stigma,
there are social issues that are relevant. Due to the massive and well directed prevention
campaigns, the spread of HTV-AIDS is slower in the industralised countries. On the other
hand, majority of the new infections occur in developing countries like India, Thailand
and Indonesia.
What is HIV?
(Dur body is like a fortress, with a very efficient defence / immune system. The first line
of defence is tlie skin, mucus membrane, tears, ear wax etc. They ward off the surface
dangers the body could be exposed to. If the infective agents get under the surface, the
WBC (White Blood Cells) and lymphoid tissues like the tonsils, spleen, lymphatic
system etc. attempt to fight it If it still persists, then the acquired immunity system
takes over. Antibodies are produced to vanquish that particular infection.
The essential ammunition the WBC system contains is the T4 lymphocyte or helper
T cell. The T4 cells are produced in the spleen and bone marrow of man during the fetal
stage, infancy and childhood. The T4 cells keep circulating in the lymph and blood,
during which they pass through the Thymus gland. The gland acts like a computer and
programmes the T cells to identify
self cells belonging to one’s own body and
foreign cells from foreign bacteria, viruses and other germs.
Mil J
.Ui'u'riX , y.-j;
2
The T 4 cell not only recognises anything foreign but also gives the command to the rest
of the immune system to go ahead and attack the foreign organisms. But, unfortunately
the Thymus gland stops activity after childhood and the adult body cannot make anymore
programmed T4 cells. So the number of programmed T4 cells in our body is limited to
200-300 billion. The T4 cell lives for 60 to 65 years which is why older people after the
age of 70 are more prone to infections.
The T4 cell has a projection on its wall into which the HIV agent fits like a key fits into a
lock. On impact, file T4 cell unwillingly starts producing viral particles. Thousands of
HIV are produced in one T4 cell and the T4 cell bursts, releasing these viruses which
then go on to attack other T4 cells. As the number of viruses in a person’s body increases,
the number of T4 cells decreases, and slowly but surely, the immune system is destroyed.
Where is HIV found?
HIV is present in all body fluids like blood, semen, vaginal fluid, mother’s milk, sweat,
tears, saliva, urine etc. But only blood, semen, vaginal fluid and mother’s milk are
implicated in the spread of HIV.
How does HIV spread?
The three routes by which HIV can spread from one person to the other are
1. Infected blood
2. Sexual contact and
3. Infected mother to child
Infected blood
□ Blood transfusion of infected blood will definitely result in infecting the recipient. In
India, around 10 to 15% cases of infection are the result of infected blood
transfusions.
□ Use of infected needles, syringes and other skin piercing instruments also pass on the
infection from the infected individual to others. Among IV drug abusers, reuse of
unsterilised, infected needles and syringes by many people is very common.
Sexual contact (through infected semen and vaginal fluid)
In India 70 to 80% of all HTV infections is through the hetero-sexual route. Though all
penetrative sexual activity can lead to infection, the following points are to be noted.
1. If one of the sexual partners has ulcers on the penis or in and around the vagina
due to other sexually transmitted diseases (STDs) eg: syphilis, genital herpes or
genital warts, the HIV spreads more easily.
t
- 3
2. Anal sex is the riskiest from of penetrative sex because multiple in juries and tears
are caused in the anal wall, which makes it easier for the HTV to enter the blood
stream of the partner. This is why it spreads fastest among homosexuals.
3. Oral sex-when the mouth is used for penetrative sex, the amount of virus secreted
in the saliva is comparatively less, but still there is a certain amount of risk of
infection. Similarly there is a very small risk factor associated with deep kissing
(french kissing). The risk increases if there are bleeding gums and ulcers/ injuries
in the mouth.
From an infected pregnant mother to her child
The IHV passes from the infected mother:
a. during pregnancy through the placenta to the fetus
b. through the mother’s breast milk to the baby
30 to 40% of babies bom to HIV positive mothers are infected. Experimentally,
antiretroviral drugs have been tried in pregnant women with some success in preventing
the transmission from mother to child. The mother should be told about the facts and the
option of having an abortion can be presented to her.
What happens when a person is exposed to HIV ?
It is important to establish the fact that exposure to the virus may or may not lead to
infection. Many factors like the route of infection, the quality and quantity' of virus and
some as yet unknown factors play a part. But, once infected with HIV, the person carries
the virus in his body throughout his life.
There are four stages in the development of the disease:
Stage 1
A healthy person gets infected with HIV. (The infected person remains healthy with no
signs of illness for several years.)
Stage 2
This is an asymptomatic stage where no symptoms are noticed. Between six and 12
weeks afrer infection, the body produces antibodies against the virus. This period lasts
from three months to 12 years.
Stage 3
Illness associated with HIX' infection may appear. The person may begin to show signs of
illness like generalised swelling of the lymph nodes particularly at the back of the neck
4
and armpits. Other signs such as weight loss, prolonged diarrhoea, unexplained fever
lasting more than one month and fungal infection in the mouth appear. Breathlessness,
fatigue, night sweats, persistent cough and recurring skin infections may occur.
Stage 4
As the immunity system has totally collapsed he is unable to fight off any infections. So.
any opportunistic infections can set in and become life threatening. Some of the common
infections are:
Lung infections - Pneumonia and TB
Gastro
- Intestinal infections - severe diarrhoea
Brain infections causing severe head aches, fits and dementia
- Skin cancer (Kaposi Sarcoma, non Hodskin's lymphoma and
Cancers
primary lymphoma of the brain)
The end finally conies in the form of death in about 6 months to two years.
WHO Classification
Since sophisticated methods for counting CD4 cells and carrying out blood tests may not
be available in many developing countries, WHO has listed a few signs that help in the
provisional diagnosis of AIDS in adults. The presence of at least two major signs
associated with at least one minor sign can be an indication of AIDS provided other
causes of depleted immunity, like malnutrition have been ruled out.
The major and minor signs are listed below:
Major signs
□ Weight loss greater than 10% of body weight
□ Fever for longer than one month, intermittent or continuous
□ Chronic diarrhea for longer than one month, intermittent or constant
Minor signs
a
□
□
□
□
□
Persistent cough for longer than one month
General itchy dermatitis (skin irritation)
Recurrent herpes zoster (shingles)
Oropharyngeal candidiasis (fungus infection in the mouth / throat)
Chronic progressive and disseminated herpes simplex infection
Generalised lymphadenopathy (swelling of lymph glands).
5
Who are at high risk?
Any person who has
-
Multiple sexual partners
Casual unprotected sex (without using condoms)
Sex with male or female prostitutes
Homosexual encounters and
Intravenous drug users
Persons who receive blood transfusion with untested blood
People needing multiple blood transfusions due to haemophilia, thallasaemia, cancer
-
Having sexual partners who are one of the above
-
How one can prevent infection
X'SS
'1™ ‘l“ virus “ '“8 “ if« in«ide the body. Bui
once outside, the HIV is a veiy weak, fragile virus which is easily destroyed by:
- Heat through drying or boiling
- Use of chemicals such as acid or household bleach
Prevention of infection through the sexual route by
□ Having sex with only one partner who is faithful
□ Avoiding pre-marital and extra marital sexual activities
a
Avoiding unprotected, casual sex
□ Avoiding having sex under the influence of alcohol / drugs when the power of
discrimination is likely to be impaired
□ Using good quality condoms. This gives considerable protection against not only HIV
but also against other sexually transmitted disease like syphilis, gonorrhoea etc. ’
Prevention of infection through infected blood
□ When blood transfusion is required, blood from a voluntary donor/voluntary blood
bank, which is tested, and has a Libel stating that it is ELISA negative, should be
USvQ.
□ Use disposable or adequately sterilised needles and syringes.
□
.S P‘ercing msttuments like knives, scalpels, needles and dental equipment
should be stenlised before use. Razors and blades can be sterilised bv boiling in water
tor .0 minutes or keeping them immersed in household bleach for 30 minutes
One cannot get HIV through
i
6
□
□
□
□
□
Normal social contact like shaking hands, hugging, sharing plates, cups, glasses, etc.
Using public toilets, swimming pools, public transport like buses, trains, etc.
Food, drinks etc.
Insects, bugs, mosquito bites
Sneezing, coughing etc.
Play safe
• Practice safer sex. Always insist on the use of condoms, even in the case of oral
sex, no matter how embarrassing this may be. Remember this is, quite literally, a
matter of life and death.
Insist on using sterilized equipment when you go in for any invasive procedure;
this includes a visit to the dentist and the occasions when you get your ears and
nose pierced. Always use disposable needles when you need to take an injection.
• In case you have to have a blood transfusion, make sure that the blood you receive
has been screened for .AIDS by a reliable blood bank. Or better still, ask such
friends and relatives who have the same blood group as you, to donate blood.
(Experts from Sunday; September 5-11, 1993).
Regional Training Programme on Prevention and Management of Addiction”
SPONSORED BY
NATIONAL INSTITUTE OF SOCIAL DEFENCE, MINISTRY OF SOCIAL
JUSTICE & EMPOWERMENT, GOVERNMENT OF INDIA, NEW DELHI
CLIENT PROFILING
Addiction treatment centers generally offer a program structure wherein a large part is
group based. Through the lecture sessions and other group-based activities, input about
general aspects of addiction is provided. The client is able to relate to the program,
increasing his insight and strengthening his decision to abstain from drugs and alcohol.
Yet, this by itself is not sufficient. Each client enters therapy with a unique set of
problems as well as strengths. Client profiling which goes on as part of counseling,
ensures that adequate help is provided at the individual level in a way that each client’s
specific needs are recognized and addressed.
Client profiling can be done at three levels:
> at intake, prior to admission
> during the active phase of trea tment
> during the follow-up phase.
The focus at each level is different and aspects covered will also be different.
CLIENT PROFILING DURING INTAKE
As this is the first meeting of the client with the treatment center, it is of crucial
importance. While the general progress of the disease and the damage it causes are
similar, the individual aspects need to be recognized even at this level.
At the intake level, client profiling is necessary to assess
> the severity of addiction
> the problem areas and identify7 drug related damage
> his motivational status and factors that influence it.
Purpose
Client profiling at the intake level serves a variety of purposes.
a)
. Screening clients before admission ensures that only the appropriate kind of
clientele enter the program.
For example, a client with a primary psychiatric problem may need in-patient
psychiatric treatment rather than addiction treatment. Apart from being
unmanageable, his presence can be very unsettling both for the other patients as
well as the staff.
b)
Client profiling ensures that client-treatment matching is made possible. It helps
the professional provide the level of care the client needs to ensure smooth
recovery.
A client in the initial stage of abuse may profit from a few out-patient sessions or
brief intervention therapy rather than a specialized treatment program.
The client with a long history of abuse, multiple drug abuse, previous
unsuccessful treatment efforts and poor family support will possibly profit more
from a long-term after care program rather than a fifteen day primary treatment
program.
c)
On admission, client profiling helps in client-counselor matching. Designating
clients to counselors cannot be randomly done without recognizing individual
needs.
The complexity of the client’s problems, his personality, age, the language he is
comfortable with and social background are issues that should be considered. The
counselor’s level of expertise and style of interaction also need to be taken into
consideration.
A 50-year-old villager will probably relate better to a middle-aged counselor who
speaks his native language rather than to a 22-year-old who speaks his language
with an English accent.
Clients respond differently to different counselors. While some clients may need
firmness and active prodding, others need a lot of patience and support to work on
issues. Client profiling thus helps tire center choose the right kind of counselor for
the client.
d)
By focusing on individual needs and problems, the client and his family are made
to understand the severity of the problem and this ensures their involvement and
cooperation.
e)
The client is helped to see that the program is related to his own special needs and
not a general approach which will see him as just another in the crowd. Profiling
thus helps in enhancing the client’s motivation.
Page 2
At intake, the treatment goals and objectives of the program are explained to the client on
an individual basis. Based on profiling, the different aspects of treatment can be
emphasized to make it more appealing and meaningful to the client. For a client with a
marital problem, the family therapy program and marital counseling are probably going
to be more meaningful. A client who thinks for himself and wants to know more, is likely
to value the lectures and group sessions.
Structure for Intake Session
The following details arc collected both from the client and family members:
> basic details of age, sex, occupation, income, marital status
> a brief history with information about the kinds of drugs abused, years of abuse
> I wblems related to physical health, family, work, finances and a brief assessment
of mental status
> patient’s motivation to take help and the influencing factors.
As the focus of the session is to quickly assess the client and highlight the need for
treatment, the issues are not discussed in detail at this level. For instance, it may be just
sufficient to know that a significant amount of debt exists without details of where and
when the loan was procured.
This structure is of course only an outline and it calls for flexibility from the counselor to
take die client and the family through this. When intake profiling is carried out with
sensitivity and professionalism, it goes a long way in enhancing the quality of treatment.
CLIENT PROFILING DURING TREATMENT
During treatment, information about the past as well as the present is required. The past is
discussed not to trace the cause of addiction but rather to understand the factors that
influenced him. The past events may be unchangeable, but is necessary to understand the
client's present situation in relation to the past.
While discussing the present situation, two aspects need to be considered:
> The variety and intensity of problems the client faces. The problems need to be
identified and assessed to develop an appropriate strategy.
> The resources available to meet the problems. His personality strengths and skills
are the internal resources he can draw on. Support from his family and friends
both at the material and emotional level are external sources of support available.
Page 3
During the treatment program client profiling is done in a more detailed and
comprehensive manner than at the intake. Flexibility and patience are often called for as
the client may provide details in bits and pieces rather than in a focused manner. Each
area of life is discussed in isolation and gradually the fragmented pieces of information
are put together to understand the client in totality. Family’s involvement is necessary as
details are most often forgotten or suppressed by the client either by design or by
oversight.
Structured formats are generally used to make effective client profiling.
The following is an analysis of how information collected can be made use of towards
client profiling.
Family History
Details of Family Constellation
Details of client’s brothers and sisters, their age, education, present occupation and other
details can help the counselor understand his position in the family.
Only male child or the birth order (the eldest or the youngest) or a vast age difference are
factors that can influence the manner in which he is viewed by significant others.
When the client’s education or income is much more or much less than the other siblings,
it is important to think about what made him achieve more or less than the family norm.
This helps to reconstruct the past and understand his position in the family system - the
position assigned to him, the power he enjoyed and the role he played.
Details of Parents
Details about early parental loss or absence of one parent (due to work, illness or poor
involvement) can help one understand the lack of emotional nurturing he experienced as
a child.
Family routines followed, the disciplining process, the emotional ties with family
members as well as the socioeconomic environment at home help one assess the level to
which his needs were recognized and fulfilled during childhood.
Details regarding the family history of addiction, especially of parents, are important due
to the deprivation it brings on all fronts. Alcohol / drug intake may be seen as an
accepted norm. Poor work ethics, financial mismanagement and inappropriate ways of
handling feelings may be seen as acceptable behavior patterns.
Page 4
Being witness to or a victim of physical violence can add further trauma as well as lead
the child to perpetuate the violence in his adulthood.
Childhood and Adolescence History
Presence of behavior problems like rebellion or iunwillingness to conform during the
early years can point to poor limit setting. It can also
- -----alert
--O one to underlying psychiatric
p ooiems mood disorders or even an anti-social personality disorder.
A4justment at school, relationship with peers, academic performance, interest in games
and other activities are details that enable an assessment of liis interests and skills
Information about performance at school (dropping out, poor or excellence), handling of
money and time, the goals he visualized for his future, the issues that he considered as
helpful or detrimental to his growth are important to understand his personality
evelopment. His perception of problems (real, imagined or exaggerated) and his
response to them will reveal a lot about his personality.
Social skills development, problem solving skills, need for achievement, a sense of self
worth, are all well established by adolescence. Events in his adult life may build or alter
this basic structure. In such a situation, recognizing significant events / people who made
this shift is again of importance as the negative aspects fuel the damage caused by
addiction.
I he interpersonal skills and the family ties he developed as an adolescent can point to the
support he enjoys as an adult. Even if addiction in the intermittent years has eroded his
support base, the relationship can be revitalized if it was strong in the pre-morbid years.
On the other hand, conflict ridden or withdrawn style of functioning further aggravated
by addiction, point to the need for social skills training during treatment.
Alcohol / Drug Use History
Information about the age of first use and the perceived need to do so, helps one
understand the process of initiation into drug / alcohol intake. While for some drugs are a
promise of good times, for others they are a crutch to handle negative feelings.
Details of the gradually increasing quantity and frequency of drug / alcohol intake help
one trace the progression of the disease. The client’s perception of his drug use is
different at different stages of his disease. From a pleasurable activity it would have
become a stress-relieving act. Later, he may see it as something that has to be just
endured. This helps the client to understand his gradual loss of control over drug use and
the severity of his addiction.
Page 5
It is necessary to identify the factors that propelled or sanctioned the continuing abuse
and events or people who cautioned against it. These very7 forces will continue to
influence his recovery and thus need to be addressed.
The client s previous efforts at abstinence either through his own efforts or treatment
have to be taken into consideration. The events that motivated, as well as the relapse
triggers, can be identified.
Occupational History
Details of jobs held, reasons for the choice or change of jobs and the satisfaction gained
out of each, provide important and necessary information.
Absenteeism, poor job performance, poor interpersonal relationships with colleagues and
supervisors, impulsiveness or even inability to meet standards expected, could have been
the causes of problems on the job. The link between his addiction and job problems needs
to be understood. Work ethics also need to be discussed to help him change.
In the post-treatment period the client may suffer from memon^ problems, poor judgment
and new learning can be difficult. This needs to be worked on and supportive measures
need to be planned. Postponing major life changes is important.
Clients may not have any marketable vocational skill to find a job. Vocational training
may be called for. Recognition of skills / interests is also part of profiling. This can fuel
hrs ambition to tram himself further and improve his job prospects. For example a
col ege dropout may join a correspondence course so that the lack of a foimal degree will
no longer block his career prospects.
Marital History
Factors that influenced his choice of spouse, the extent to which his expectations were
luliilled and the strength of the relationship need to be discussed.
Understanding his spouse’s perception and reaction to his addiction will help in
assessment of the support he will receive during recovery. A passive, enabling spouse
may tail to be firm enough, while a domineering spouse may be too controlling.
Information about the separation (where applicable) - the duration, the events that led to
it and the reason for getting back - help one understand the dynamics involved.
Page 6
The presence of violence can point to an aggressive personality style or even an
underlying psychiatric problem. Paranoia can further damage the marital relationship. If
aggression or paranoia is present only when he is actively drinking or abusing drugs and
not otherwise, this is seen as drug / alcohol induced effect. If it persists otherwise too.
medication may be needed. He also needs to leam new ways to cope with his feelings and
strengthen his self-esteem, so that he can alter the violence cycle.
His relationship with his children and the aspirations he nurses for them can be used
positively for his recovery.
Divorce or desertion leaves behind grief and unexpressed anger. Providing a supportive
setting to discuss this is important.
If he is still single, it is necessary to discuss his long-term plans. It would be advisable to
postpone any plans for marriage until a year after recovery.
Sexual History
Sexual problems need to be discussed. While alcohol / drug induced damage can cause
nem, the anxieties and myths surrounding them compound the problem.
Pre- and extra-marital relationships can complicate recovery. If a client has entered into
sucn a relationship due to poor judgment and now expresses doubts about the need to
continue with it, a plan of action has to be made to break out of it.
When an excessive sexual urge and inappropriate ways of expression are reported a
psychiatric assessment needs to be made.
Kigh-nsk sexual behavior like multiple partners calls for some input about HIV-AIDS
and testing with due counseling.
Financial Status
Discussing details about his income, the manner in which money is spent, will help in
altering impulsive and grandiose style of handling money. The amount of loans he has
the source, the rate of interest he pays - these are some of the details needed to make a
financial management plan. Budgeting, prioritizing, making monthly payments for loans /
savings are part of the treatment plan.
Page 7
Legal History
The client’s record of arrests and his legal status have to be looked into. Court
appearances called for long after the offence can be stressful during recoveiy. Accidents
due to driving under the influence, street fights or arrests due to anti-social
behavior can be used to help client understand drug-induced behavior.
Social Relationships / Leisure Activities
Loneliness and social withdrawal have to be replaced through meaningful changes.
Otherwise the empty space created when the client quits dings / alcohol will make life
very difficult for him. Participation in leisure activities and maintaining good social
relationships are crucial to recovery.
Revisiting the pre-addiction days and identifying activities, hobbies, people whose
company he enjoyed and attempting to revive those interests and relationships are an
essential part of his recovery. Making amends, even if it is a simple call, letter or a short
visit, may be necessary to review relationships. Handling anxieties and fears related to
relationships is part of therapy.
Religion
Faith in a higher power can be a very supportive source during recoveiy. Prayer routines,
visits to places of worship or some faith in the concept of a higher power, even if it is not
actively pursued, can be used to strengthen his recovery.
Blaming the higher power for all his problems without accepting self-responsibility or a
passive ‘He wih take care of everything’ attitude needs to be altered.
Personality Traits
xAssessing his personality’ strengths and deficits is an important part of patient profiling.
Addiction brings with it low self-esteem and his strengths can provide a strong support
base for his recovery. Helping him see his positive side (skill as a workman or the care he
shows for his children) enables him look at himself in a positive manner.
Poor frustration tolerance can show up as irritable behavior at home, frequent job changes
on the employment front, and unnecessaiy expenditure. Helping the client see these links
is important.
Page 8
CLNT PROFILING DURING FOLLOW-UP
Based on the individualized treatment plan, recovery goals and activities are listed The
Conclusion
Of?’eaJtae,nt’ help iS needed at the “dividual level. Client profiling helps
in identifying each individual’s unique strengths and addressing his specific problems.
Page 9
MH -
2-^
, 4
mytnornons 94}
Regional Training Programme on Prevention and Management of Addiction**
SPONSORED BY
NATIONAL INSTITUTE OF SOCIAL DEFENCE, MINISTRY OF SOCIAL
JUSTICE & EMPOWERMENT, GOVERNMENT OF INDIA, NEW DELHI
COMMUNITY APPROACH OF TREATMENT & PREVENTION
A group of people
<!
Live in a specific geographical location
Relate to each other
Share a sense of belonging.
Community Based Rehabilitation
Persons with disabilities are helped to develop themselves to their full potential within
their own community
Making use of local resources
Achieving maximum integration into their families / communities
r
Primary Focus
Shift the intervention from costly, specialised institutions to the homes and communities
of the persons.
Advantages of community involvement
Their feeling of oneness constructively utilised
Responsibility of managing alcohol problem shared between the professionals
and the community, leading to ' doing with’ rather than ’doing for*.
Community understands the processes of alcoholism and recovery. Hence is
empathetic and willing to support treated patients in recovery.
Key issues in organising camp programmes
Identifying
points
substance users living in one specific area through multiple
entry
Teachers
Health workers
Clergymen
Animators
Relatives
>
Initiating the process of rehabilitation before the camp
Home detoxification
Dealing with medical problems
Motivating the client and the family to attend the camp programme
Involving a host organization
Requirements of the host organization
Enjoys the trust and respect of the community
Willing to provide the basic infrastructure to run the camp
Willing to provide support to the patients during the follow-up period
Prior to the camp
To identif}- and motivate patients for treatment
To provide accommodation
During the camp
To organise meals for the patients and staff
To mobilise support persons for patients
After the camp
To act as support persons for patients
To get patients for monthly follow-up
To monitor the progress of patients
To provide help when there is a need
Empowering the community
Making use of relatives and friends to support the patients in recovery
Page 2
Maintaining the momentum
Organising regular follow-up programmes
Organising celebration of sobriety birthdays to encourage their efforts
Conducting awareness programmes in the community
Key Findings
With minimal infrastructure quality care can be provided in villages at low cost
Help is available at their doorstep, hence people are willing to accept help
Therapy and treatment procedures are made relevant even to the illiterate villagers, hence
appealing
Disulfiram acts as a powerful support
The entire community gets involved in the process
Prevention Activities in India
Gadchiroli in Maharashtra
Data on impact of alcoholism collected
Collective realisation of a common problem
Common will and organisation to act
Formation of ‘Darumukti Sangathana’ to create awareness on alcoholism mainly by
women
Benefits
Alcohol consumption dramatically reduced in 200 villages
Drawn the attention of public and the government and acknowledged as a public health
problem.
Dubagunta - Andhra Pradesh
Women and children joined together
Resulted in imposition of prohibition for a few months.
Chittoor — Kerala
Priests and nuns were forerunners
Churches took up this issue in Sunday mass
Widows of Vypeen tragedy expressed their solidarity
150 days of agitation - women picketed the shops
Manmathan, a well known Malayalam writer supported the movement
Page 3
In Father Village in Saharanpur in Utter Pradesh
3 months round the clock ‘dhama’ by women
Benefit
Liquor shop was permanently closed
In Naktara Chauraha in Raisen District in Madhya Pradesh
3 day hunger strike by woman
Benefits
The sole shop was shifted to the outskirts of the village
Anti liquor movement spread to other villages — Bansoj, Nara, Barchha,
Digari and Shindi
Some of the salient features of community approach
Women (the victims of alcoholism) spearhead the movement
Mainly the villages have taken up the initiatives rather than cities and the towns
No big organisation / no political parties lead this programme, it is a programme of
ordinary women.
The methods used are ‘dhama5, hunger strike and group activities.
The women have also asked for other control measures like shifting the shop to the
outskirts of the village or reducing the number of outlets
Successful implementation of the programme in one village has a snowballing effect spreading the movement to the neighbouring villages as well.
The role of non-governmental agencies
The non-governmental agencies can play an active role in
helping the villagers to organise rallies and dhamas
organising repeated awareness programmes on the ill effects of alcohol and drugs during
festival times.
Page 4
creating visibility to the programme by publishing articles in local newspapers and
broadcasting programmes in radio.
making the people talk about the problems and solutions whenever there is a death in the
community due to alcohol abuse
making use of community resources like physicians, recovering addicts, local leaders to
organise treatment camps on a periodic basis.
mobilising the support of patients who have given up alcohol and the youngsters who do
not take alcohol.
providing alternative means of livelihood for illicit brewers.
Page 5
MH- ?_e.
Regional Training Programme on Prevention am, Management or Addiction"
SPONSORED BY’
HSKSSSSKSSffS™-®;
record keeping
usually established and
are - the
mcohamsms for their safe keeping; these am'spJX M the outer
J and
Records in a treatment center for addiction are i
maintained by the detoxification / medical
unit, the intake counselor, the client’s counselor
~ and the group counselor. Referrals to
a er caie programs, vocational training etc <
are also recorded. Hence, the entire treatment
Xam” ‘
" '”inla“’g
“ -iourphteZTt’he'
— _.j client’s treatment
the purpose of record keeping
> The
aXx^^XTdXdta:
“r1" “a 'Mm*’"«‘ “» PraWemdata oolleoted frX fc Md^Se f metn"”"'
recorded by her m the prescrihed'XXted“1K“
>
”
*available or has left the organization lhe new slaT
rr
-“’7p'“
«««
’
he “un“lor 18 ”M
help the client with recover using the case recording " a^Sence
>
mcX^XX^oX1-. *"\T °f ‘'LT'"8 ““
work and the ultimate objective Xte
quality of counseling the efficacy of the
reviewed in the lonf’run Th 2^ f
T""”8 iS. 8
S
examine effective and ineffective inrtrv
in addiction treatment.
™c“'“'8
PS6
°f the clients’ the
techniques etc. can be
assessed through systematic maintenance of reeordy31111601
>
“P ““
““
“““ °f “
°Ug l matena, to helP t,le center to
10n’ towards a more scientific approach
h
TYPES OF RECORD KEEPING
IrnraT
tyPTeS Of mamtenance of individual case records - process and summary
record keeping, m process recording, all details including verbal and non-verbal
communication are recorded by the counselor immediately after the session with the
C ®nt ,In.surnmary wording, brief and pertinent points arc recorded and described
suDjcct“Wise.
Summary recording
Collected information is
summarized and brief, with
significant parts in detail
Focus is on the client with
j counselor’s observation of the
| client________
i Information is not presented in
chronological order
Describes the outcome, not the
j steps to accomplish the results
! Less time consuming
Process recording
| Entire information about the client is
i listed
I
-4---------- —_______ __ _______________ _ _________________
! Both sides of the session arc given
! in detail
I
T_
------------- ------------------------------------------- ------------------
I mlormation presented in
i clironological order under specific
areas_____
Steps are explained in detail;
includes verbal and non-verbal cues I
I l ime consuming
I
Counselors at treatment centers usually use summan- recording as an important reference
tn the management of the client. A copy of the summary recording is filed and made
accessible to her when the client visits the center during follow up. The summary
recording highhghts both short-term and long-term plans of the client and significant
information to be worked on, and is crucial in the recover of die addict.
FACTORS TO BE ENSt'RED WHILE RECORDING
>
Uniformity in recording: The staff should be trained iin recording; as a result
uniform record writing methods are used.
Page 2
A'
• I
.Uh
>
Readable and visible: Often, the information given in the case records are not
written legib y and may not highlight the crucial areas to be worked on The
ViS,Mity Of s«cant ^nation fot appwpnTte
ntT^rT
intervention by the relevant professional.
P
>
Description of events, not evaluation: During the collection of information the
ounselor must ensure that she is merely recording information as it is and not
rmdmj ?hemstaffeheVai1d
JUdSmental du™g *e process of
ordrng. The staff should ensure clarity, accuracy and objectivity.
>
^ncS’Tshion' ^8Xene38: The c<>unselOT mU3f «cord information in a clear and
hi«“^b"^Xf?ps m ““ectto8 "onM,iM ab“«»
>
■“«“«“»
As f" “ p?“ible ,he
reme“bered >h»t the records are ihe only backbone of
k d
rnZtotoZ' trea“”5nt 8°alS °f
>
C““ m mM ”d
°f CU^tS’ CaSe reC
°rds Should
records
should be ensured Wlth
with separate room or
brnet for storing. Clients’ records, should not be left unsupervised e g on tables.
ad*te
10 —* - “
OVERCOMING PROBLEMS IN RECORD KEEPING
^en. CCTtor
Often counselors.have clients coming for follow nnnfw
As ““
to
case
>i C
.
,3
long time, taking into account the
Pl>™™ of rofapso ta toe field „f ad(lictta. etoublo
meZ”
of storage of data
including computenzation ofrecords should be given priority.
ciUor ■•hoiAtith;it
U'f Ul-
.
. .!'Uo
‘
.on-»
b
■
•
•:
'
''
•
'•
|
v> nwaaf-on; ■
o, ,jh.v-u
.. ...
"•
'
:
■
■ ■ ■
■
■.
i
'
. ........... ■' '
i
.
■
'
Pige 3
■
(
■
M'vh Retmi:.
'1::
■■
■'
'
■
•
'
•
•
'
•
/;
•
■■
'
.•
...
■
■
.
/■
■
•
’
O
•
■ ■
•
■
■■■
.
and
not
■
'
■
•
ruvi <y>u ibeir
tn the
..
...
-
.
twitted wuh ■. ^pataii. room or
.
use ofc nxt.’n.h
h.;
:
.j
.
..
are th
kj'/',!?
1■ •
■,
I I
■■
■ .-v
ih.<
■■
.
',
■.<:
hhU' '■£i u'
1 -
- '
• J
. :fit
liiu
i.i.'iiit'urii n«o.M<.nuhHi i’he
• ki .
I<
:
/xi
.
**•
iKi’ i>
pic;
.
.
.
r
■
k- -as’/s-'loft'-
■
to n ■'
, -.
■■ ?
. * I.,
••
•"iC- hV!!’. !
atnsiia
_.;;j .:-•<,otfii
.emd
<
Tn bhR
iiUsb ib; sgKwte fo ?.bod*^rn
.?
•■grtiMlotti
Improper maintenance of :recordfc;is4-du^^d-’iifany >fao '6rs. fjiitraincd cqynsciqTS’jwho lack
recoi d’keeping skills;.
record-keeping
skills;, tfcse^Who
those1 wfio lack art understand iig
tig qf
of the- importance of recording;
lack of 4ime;
4im0; lack ”6f ^<$ef facflities
facilities(pnyaw
(pw ?
iofHh&fi.
sof
theth. ffie
Jhe
importance”6f recoftf keeping has ip be emphasized...since adequate data is essential to
back their
'
./
’ v,;
tlieir suCcessfbT
suCcessffil inteivehtion
intervention efforts.
. r;
THE ROLE OF RECORDS
i'G
iiJOOT
iia/Z
j
• U 1 f'. ,i/. - <, ■/
»
it I-' h~- iC
' wm!
'.j’'--
/s/tnoii* ‘tyi
The Rom of RfTorDs
:
■
,j bhiptfe
-y*bm;
The individual case record includes altreatment plan!
/ outlining the goals and objectives
for the client during treatment., They shpuld^Uke pto
educational vocational^ ^an^i psychological, needs^^ef ’ each’^ti^t: life
' in
^^fieht of clieiiiM PfrOgress; need foredification^
The case record, upon termination of the treatment with the patient, includes a discharge
summary in which a final evaluation regarding the progress of the patient towards the
goals and objectives set forth in the initial treatment, plan and the short and long term
goals are recorded.
The Role of Records in Program Evaluation
The data collected as part of the required record keeping and reporting activities is useful
in ongoing program evaluation towards ensuring quality service. This entails analysis of
overall program effectiveness and identification of areas needing refinement. Data such
as the number of clients served, types of services provided, client outcome, follow-up
outcome, and staff utilization etc. can be evaluated based on the records maintained by
the organization.
Benefits For the Counselor
Proper record keeping presents a complete profile of the client in a precise and clear
form; it helps the counselor to render effective and systematic service to the clients; it
facilitates the evaluation of the client’s progress and setbacks before and after availing
the medical and counseling services; and it ensures continuity of work.
Benefits for the Treatment Center
Record keeping helps in the periodic review of data at any point of time; facilitates
supervision and training of the staff; improves the professional skills and techniques of
the counselors and others; evaluates the work of the agency and helps to improve upon
the methods and techniques used therein; and indicates the efficacy of the agency to
donor organizations, board of trustees and the communit)’ at large.
Page 4
, ,
3>O
IM H
Regional Training Program™,
Pr,,^,,,, and M,nagenlMt or Ad(|lcaM1„
SPONSORED BY
ntsTT?r^ ^ITOTE OF SOCIAL defence, MINISTRY OF SOCIM
JUSTICE 4 EMPOWERMENT, GOVERNMENT OF S^W^L^
WHOLE PERSON RECOVERY
°US
re™*
“fe - ““
»
qualitative sobriety. Qualitatiw sobrietv is
Spmtu311)'- This W1U result in
lifestyle changes.
* ’ &lving up chemicals and making qualitative
The strength or weakness of rhe wall d 11111 ofhfeJus>t 3S 3 bnck is the unit of a wall.
S““y Here are a few tips for qualitative, wholistic recoveiy for recovering patients.
1. My life should have a goal
The goal can Ibe anything - saving money for the
son’s education, getting the daughter
married, getting a job.
pm S'™ toTta8
»”W. h «pi« of holding
•
---- J a good job, he has
pur ms son in a free school, as he had no i
money
to
pay
for
the school fees. After
treatment he set a goal for himself.
college.
set fire to the hav stack which
P-w hhn tan „„u,g ta. He
“ 6 0“
"d
t
I™ to gel into the engineing
““ Mur °f ato“- h=
occasion’m a drunken mood, he
K
Page 2
leader called him and asked him to leave the village and stay on the outskirts. After this
incident, he sought help in the camp which was being conducted in his neighbouring
village. It was during the camp, that he realised his mistake. He set a goal for himself - T
should get back to the village and gain the acceptance of the villagers’. He worked
towards achieving his goal.
Now he has completed 5 years of sobriety. He is living happily in his village. In each
camp, he is bringing 3 or 4 patients from his village. In the recent election, he was elected
to the Panchayat Board.
e.g. An eagle’s egg got caught among the eggs of a hen. It was hatched and an eaglet was
bom. It grew with other chicken. One day, the eaglet noticed an eagle flying high in the
sky. It was impressed and wanted to fly high. When he asked the hen, the hen told him,
\\e are different, we cannot fly high*. The eagle accepted this and decided not to
attempt to fly higher than the chicken.
What does the story convey?
All of us are bom to win. Sometimes we programme ourselves to disaster / failure.
Nothing will happen by itself. We have to make it happen. A goal-directed life is a
growth oriented lite.
2. My daily activities should be related to my goal
Just having a goal in life is not sufficient. It is very important to make conscious
efforts on a day to day basis to work towards the goal.
e.g. If my goal is to save money, I should stop travelling by auto and adopt cheaper mode
of transport. If I am keen on strengthening relationship with my son, I should be
prepared to spend more time with him.
e.g.-P T Usha - four hours of exercise both in the morning and evening; and strict diet,
she achieved success only through committed efforts and hard work.
3. I should do my work with interest and involvement
xAny activity will become enjoyable provided we are interested and involved.
e.g. Three men were involved in building a temple. A man asked the first worker.
What are you doing?’ He replied, ‘ Can’t you see what I am doing? I am breaking
Page 2
/
stones. It is my fate and I slog on!’. The second worker said, T have to take care of my
family. Since I have to earn for my family, I am doing this boring work'. The third
man was very enthusiastic and he said, I am fortunate because I have got the opportunity
to build a temple for my Lord’. Same work, but each one had a different perception.
UTiatever we do, when we do it with gusto and enthusiasm, the entire process becomes
enjoyable.
e.g. Cleaning the house for Pongal; Making food for guests.
4. I should act according to my conviction
Once I make the decision to give up drinking, it is very important that I stand bv my
conviction. People may mock, criticise or laugh at me. Relatives may not trust me. ’
e.g. My friends may tease me 'Don’t you have will power?
wife? Is that why you have given up alcohol?’
Are you afraid of your
Whatever be the external environment, I have to decide and go steady on my decision.
5.1 should take responsibility for my growth
In my life I have various roles and responsibilities and I am entirely responsible for my
growth and development.
e.g. I wanted to be on time for my work, but my wife never woke me up.’ ‘I really did
not want to drink, but my wife fo^ot to give Esperal, that is why I drank/Here, lam
not taking responsibility for my actions, I am holding others responsible.
I should take up responsibilities and also hold myself responsible for the consequences of
my actions.
6. Overcome handicaps and limitations
During the course of our life’s journey, we may have to face some hurdles like a steep
slope, a peak, small and huge boulders, and so on. These can be overcome, provided
we are willing to put in effort. We may be required to make a few sacrifices. But once we
achieve our goal, all these will add on to our sense of fulfillment
Page 3
\
I
i
Louis Braille
He was blind from the age of three and in 1818 he went as a foundling to the National
Institute for the Young Blind in Paris. Soon showing marked ability in both science and
music, he became famous. In 1828. Braille began teaching the blind in the institute and
the following year, he conceived the idea of modifying the Barbier “point writing
system, used for coded army messages, to enable the blind to read. Point writing consists
of embossed dots and dashes on cardboard ; the Braille system derived from it, is used
successfully today in a slightly modified form in many countries.
Helen Keller
When nineteen months old. she was stricken with an acute illness that left her deaf and
blind. No method could be found to educate her until the age of seven, when she began
her special education in reading and writing at the Perkins Institute for the Blind. She
quickly learned to read by the Braille system, and write by means of a specially
constructed typewriter. Ten years later, she was able to enter Radcliffe College from
which she graduated with honours in 1904. Keller then served on the Massachusetts
Commission for the Blind. Throughout her life, she worked and raised funds for die
American Foundation for the Blind and traveled and lectured in many countries. She
visited wounded veterans in American hospitals and lectured in Europe on behalf of the
physically handicapped.
Milton was a great poet who wrote the epic Paradise Lost when he was blind.
Demosthenes who was a Greek Orator, had a speech impairment when he was young. He
practiced regularly with pebbles in his mouth and became an outstanding orator.
Wilma Rudolf was a polio victim. By sheer determination, she won a medal in
Olympics.
Sonal Mansi ng h
An accomplished Oddisi dancer, she suffered multiple fractures in a road accident, during
the spring of her career. Senior surgeons and consultants attending on her ruled out the
possibility of her being able to walk, much less dance again. But she would not let the
doctors decide her fate. She endured years of painful physiotherapy, and by sheer grit,
determination and hard work regained strength in her legs. Today she is one of the best
known Oddisi dancers.
Page 4
V
-I
Sudha Chandran
Almost the same history as Sonal Mansingh, only difference being Sudha is a
Bharathanatyam exponent
God has given us the freedom to choose and inner strength to overcome handicaps and
limitations. It isj unwise to blame the past, parents or say it was my fate.
Page 5
MH -
3)
REGIONAL TRAINING PROGRAMME ON PREVENTION AND MANAGEMENT OF DRUG ABUSE
AND HIV-AIDS"
SPONSORED BY
NATIONAL INSTITUTE OF SOCIAL DEFENCE MINISTRY OF SOCIAL JUSTICE & EMPOWERMENT,
GOVERNMENT OF INDIA, NEW DELHI
ISSUES IN PRE AND POST TEST COUNSELLING
What is HIV counselling?
HIV / AIDS counselling is an ongoing dialogue and relationship between patient and
counsellor with the aims of
1) preventing transmission of HIV infection and
2) providing psychosocial support to those already infected.
In order to achieve these objectives, counselling seeks to help infected people make
decisions about their lives, boost their self confidence and improve family and
community relationships and quality of life. HIV / AIDS counselling also provides
support to the families and loved ones of infected people , so that they in turn can
provide encouragement and care for those with HIV infection.
Pre test counselling
Counselling before the test should provide individuals who are considering being
tested, with information on the technical aspects of screening and the possible
personal, medical, social, psychological, and legal implications of being diagnosed as
either HIV-positive or HIV-negative. The information should be given in a manner
that is easy to understand and should be up to date. Testing should be discussed as a
positive act that is linked to changes in risk behaviour.
A decision to be tested should be an informed decision. Informed consent implies
awareness of the possible implications of a test result. In some countries, the law
requires explicit informed consent before testing can take place; in others, implicit
consent is assumed whenever people seek health care. There must be a clear
understanding of the policy on consent in every instance, and anyone considering
being tested should understand the limits and potential consequences of testing.
Testing for HIV infection should be organised in a way that minimizes the possibility'
of the disclosure of information or of discrimination. In screening, the rights of the
individual must also be recognized and respected. Counselling should actively
endorse and encourage those rights, both for those being tested and for those with
access to the records and results. Confidentiality
should be ensured in every instance.
Issues in pre-test counselling
Pre-test counselling should focus on two main topics.
1) The client’s personal history and risk of being or having been exposed to HIV
2) Assessment of the client’s understanding of HIV/AIDS and previous exper ience in
dealing with crisis situations.
Assessment of risk
In assessing the likelihood that the person has been exposed to HIV, the following
aspects of his or her life since about 1980 should be taken into account:
& Frequency and type of sexual behaviour; specific sexual practices, in
particular, high-risk practices such as vaginal and anal intercourse without use
of condoms, unprotected sexual relations with sex workers
Being part of a group with known high prevalence of HIV infection or with
known high-risk life-styles, for example, users of intravenous drugs, male and
female sex workers and their clients, prisoners and homosexual and bisexual
men.
ft. Having received a blood transfusion, organ transplant, or blood or blood
products.
Having been exposed to possibly non sterile invasive procedures, such as
tattooing and scarification.
Assessment of psychosocial factors and knowledge
The following questions should be asked in assessing the need for HIV testing:
□ Why is the test being requested?
a
What particular behaviour or symptoms are of concern to the client?
□ What does the client know about the test and its uses?
□ Has the client considered what to do or how he/she would react if the result is
positive, or if it is negative?
□ What are the client s beliefs and knowledge about HIV transmission and its
relationship to risk behaviour?
□ Wlio could provide (and is currently providing) emotional and social support
a
(family, friends, others)?
Has the client sought testing before and, if so, when, from whom, for what
reason and with what result?
CERTIFICATE COURSE ON COUNSELLING & REHABILITATION OF
SUBSTANCE ABUSERS
Sponsored By Nations! institute Of Socia! Defence, Ministry Of Social Justice &
Empowerment, Government of India, New Delhi
Organised by T T Ranganathan Clinical Research Foundation, Chennai 600 020
IMPACT Or ALCOHOLISM
DR= MOHAN ISSAC
*
*
*
Mortality
Morbidity
Disability - 'DALY, QALY*
Effects on Family'5, industry
Costs of alcoholism
MORTALITY
Pramafi ira HaatKc
Cirrhosis of liver
Strokes, other disorders
Dnarl _ frofRn ar'^iHontc
Suicide
Homicides
MORBIDITY
Various alcohol related physical disorders
Psychiatric disorders associated with alcohol
Cognitive impairment, other neurological disorders
Morbidity foilowing R.T.A.
DiABiUTY
DALY - 'Diability Adjusted Life Years'
Global burden of diseases
Alcoholism - one out of ten
Most disabling and burdensome disorders
HOSPITAL ADMISSIONS (for alcohol related problems)
❖ Psychiatf ic Hospitals
- Growing proportion of admissions for alcoholism
Eg. institute of Mental Health, Madras
No patients with alcoholism
Percentage of admissions for alcohol problems
- 0 1 to 3
996 1997
MOrs than 25%
(Somasundaram, 1985. Paianiappan & Soundararajan, 1994)
1953-1965
1966-1981
Page 2
NIMHANS
1960
1995
Less than 2%
About 25%
Private psychiatric practice
1977
Alcohol dependence constituted only 1%
of private practice (Bagadia, 1977).
1988
J 2% clientele made up of people with
alcohol problems
(Gopalakrishna & Sayee Kumar, 1.988)
■C1 More than 75% of GPs treat alcohol abusers with
a variety of health and family /
social problems (Verma & Malhotora, 1988)
15% of in-patients ii<n General Hospitals have drinking related problems (Babu &
Sengupta 1997).
More than 10% of male PHC attenders
- moderate to heavy drinkers (Molly, 1992)
IMPACT OF ALCOHOLISM
$ Effects on family
Family disruption
Domestic violence 'Wife-beating2
Marital discord, separation, divorce
Neglect / Abuse of children
Psychopathology in other family members:
■A
*
-
Depressive disorder - wife
Conduct disorder
Emotional disorder - children
Effects on family budget
industry - work related impact
-
-
Reduced / Loss of productivity
Absenteeism
Inefficiency
Reduced uptake of training
Lack of skill enhancement
Legal problems
raqe3
ISSUES IN ESTIMATION OF COSTS OF ALCOHOLISM
□ Cost estimation - complex and controversial
□ Costs - difficult to identify and quantify
□ Incomplete / poor - epidemiology base
□ Absence of routine information gathering system
□ Inaccuracy of reporting mechanisms
□ Absence of relevant, reliable and comprehensive database
□ Bias towards underestimation
□ A range of estimates to be made
□ Tentative, conservative, 'Guestimate1
(to be regarded as 'indicative' rather than 'firmly reliable’)
Alcohol produces costly problems of large and diverse extent
□ Policy makers - ill informed about the costs and benefits of manipuiatino
the demand for alcohol
ESTIMATION OF COSTS OF ALCOHOLISM
♦> Direct health care costs
nOspitai ireatment for alcohol related diseases / accidents
Treatmerit and rehabilitation costs within health / social welfare sectors
Sickness insurance
Disability pension
v Other Direct Costs
Insurance coverage for damages due to accident / crime
C: iminal justice interventions — police / courts / prisons
tnforcement of aicohoi related laws, alcohol control
Alcohol education. Research
❖
Indirect Costs Due To Loss Of Productivity
Due to premature death
Due to disability
Dus to sickness absenteeism
inefficiency, reduced uptake of training, iack of skill enhancement
v Value of lost life
In Finland (1990), costs of alcoholism amounted to about 3.5% of the G.N P
/
Page 4
ALCOHOL RELATED PROBLEMS - RESPONSES
v Growing number of treatment centres
Special / additional facilities in existing psychiatric hospitals / units
Centres run by NGOs in India
*
Lcoo u laii v tu t ouO
More than 250 in 1993
❖ Innovative treatment strategies
- 'Camp Approach'(Ranganathan. 1996).
❖ involvement of primary care sector
Training programmes. Manuals (A.I.I.M.S.)
❖ Educational and training materials
- For patients, family members, health workers, counsellors (TTR Foundation)
Community action against alcohol
- Andhra Pradesh, Haryana, Maharashtra
v
‘Jtetatet tnvvlvtri uci st ui
octcic/!
Alcoholics anonymous groups
- in smaller cities and towns
- In local languages
*> Employee assistance programmes (E.A.P.)
I
M H - '2-c - 3.3
^HAB'UTAT'ON OF
;FST,!=,CftTe
^ponSorea ey A/jf/ona/Zn^^fe Of Soc/aZ Defence. Ministry Of Sociai
O^jsedP^sr^nt’ p^srr.ment of India, Naw Dsihi
organised by 1 , Ranganathan dinical Rasaarch Foundation
Chennai 600 020
MAkiTAL iNTERVENTiON
Vijay Nagaswami
What is marriage?
*
physira'3nd seraal
wim the objective of achieving a state of harmony between the vin and the
j SHI
*
0
s
and promoting a sense of emotional and spiritual well being in both partners
through the mutual resolution of unresolved intra-psychio conflicts
and the harmonisation of the b«U.nce between the inW^i ai;ri
environments of both partners.
•—and external
This definition includes ail committed
consenting aduits of either gender
fnonogamous relationships between
-
The Purpos^%¥ Carriage”*
•i.'
'>•
.
■.
< .fW
.ft
:
.J
EnhaTfcement ofWKage
•
Enhancement of identity
*.
-Engendering physical, economic and social security
*
Gratification of sexual, belonging, parenting and intimacy needs
■» -•
-r&.'n ■
!"
■
t
0
Resolution of infra-psychic conflicts carried over from earlier relationships
i3
Companionship and spiritual fulfilment, BUT MOST OF ALL
&
BLENDING THE YIN AND THE YANG
• 4^:
■&' ’
The Location of Marriaue
iSSif
» 9 • » ■
I FAMIL Y &
I FIENDS
B WORK
iB
■ « r
9 • •
.I
lifHBWw
The Anatomy of Marriage
$
LuVh
&
TRUST
RESPECT
IN IIMACY
Marital Dynamics
«
Search for unconditional love - impacts on LOVE
Need for individuation -impacts on TRUST
Playing control games - impacts on RESPECT
Harmonising relationship patterns - impacts on INTIMACY
Manifestations of Pathology
Each holding the other responsible for their respective unresolved conflicts
«
Each viewing their respective extended family as a domain inaccessible to
ths other
or
Inadequate definition of roles - hence competitive relationship
Porh
cAAkinn tn rtariw^
vi < VWiXH IM IV
idontih/
frrvm
th cur rocnar'fn/A
irvsfifjft
iI
i » I 1.B0WI4 IVwVVWVV WVM VVU.IV1 I
iMViimV
incomplete resolution of conflicts
Avrudonrci
IVV VI SVtv'Z iri
Z Ilf
9
i liun
I t
Incongruent expectations of or dependence on community
Overemphasis on child rearing with the children becoming ths principal
means of communication between the partners
ft
Disagreement on child-rearing process
o
InoHaci
irato w««ia>w<
ta+tontinn
nair! fn
cAYiisaliK/
in M'ut
ih;vi :
*w w
j
Seeking intimacy outside of the marital relationship
Breakdown of mutual nurturing
Conflicts regarding source of spiritual awakening
e o, how can ws help ?
Object of intervention
To negotiate a compromise settiement between two warring factions <
NO
To assist a couple in relieving stress?
NO
To save the marriage from divorce?
NO
To empower the couple to make considered cnusces ■.
YES
Couple Empowerment
.
Facilitating the understanding of dynamics in the relationship
o
Providina a framework to view the marriage with
Learning to use the marriage to enhance individuas soentity
*6
Goals of intervention
•
Redefine location of the marriage
-
Each to take responsibility for respective self
•
Enhancing iove. trust, respect and intimacy
.
Redefining relationship template
Types of Intervention
Pre-maritai
IS
Marital - proactive
Marital - reactive (crisis)
£
Pre-divorce
Intervention Setting
•
Individual therapist
¥
Conjoint - two therapists
a
Consensual - two therapists
Group - one or two therapists
*
t
Intervention Techniques
Negotiation
Gos! setting
9
interpretation
Homework assignments
Stages of intervention
stage i
Negotiating the Contract
Stage II
Identifying patterns
s
Stage ill Formulating template
c
Stage iV
Review
Stage I: The Contract
■5
S-3 •’a& r<
» «■/«. •»< r«
a
af
•rk r.-A
VV«t V!«W VS
tn.
VWHUVH
c
Clarify expectations
a
Provide overall formulation
GciinaDic yvaj*
Stage il . Patterns
Need for unconditional love - unstated expectations
individuation needs - fight analysis
s
Control games - defining boundaries
Intimacy needs - relationship patterns
111
•
OwQ6 ih .
•
J UjA
tnn m I »-k4* a
t fit? itMjC
Redefining expectations
Redefining boundaries
a
Re-formatting fights
Refining patterns
Staae iV : Review
w
Review insighte
Review investment
3
Set medium-term goals
Set up periodic reviews
Schedule of intervention
The Contract
r **
' IO
4 4“^* <£3 *•*
r-ia*.•>*.-»
*-> IV V W-'-OS V! !C<
• emplate
2 to 4 sessions
Review
1 session
D
‘
«
1 or 2 sessions
4>4>
CBent-reteted issues
9
i aking responsibility for outcome
Client selection
Recalcitrant spouse
•M
dropping out
I hera.pist-rela.ted issues
3
T" I* <"* ««
tTT (Art z-» *4
’ ! t‘- f < WU LV
4
identifying with one partner
4*—.
iii&ueatv
Serving as conduit
Therapist’s own relationship
Who is the client?
THE MARRiAGE
MH - Xg."32
*
crtihcate course on counsflung 8 REHABILITATION of
Organised by T T ^ng^an
Chennsi BOO 020
MARiTAL INTERVENTION
Vijay Nagaswami
»
What is marriage?
e
P^IP ent-ed
into by two consenting adults
with the objective of achieving a state of harmony between the yin and the
yang
«
©
and promoting a. sense of emotional and spiritual well being in both partners
through the mutual resolution of unresolved intra-psychic conflicts
$
This definition includes
consenting adults of either
mono^nTOus relationships between
The Purpose of Marriage
8
Enhancement of self imaae
.■
“■■■
>!■■"«.:,
Enhancement of identity
•«'.
t■
.£.'
Engendering physical, economic and social security
Gratification of soxual. belonging, parenting and intimacy needs
Resolution of intra-psychic conflicts carrie
d over from earlier relationships
Companionship and spiritual fulfilment, BUT MOST OF ALL
&
BLENDING the yin and the yang
4
The Locehon of Marneae
lIMiii comu^
v.-.-.-. .-.v.v.-; :7rr?7.z .7; tt'ZTTTTTT
11
■-■mNDS^ '
WOkk,
. .. . f n»v.qu/ J
,
:
The Anatomy of Marriage
e
LOVE
&
TRUST
S’
RESPECT
9
IN i IMACY
Marital Dynamics
*
Search for unconditional love - impacts on LOVE
e
Need for individuation -impacts on TRUST
Playing control games - impacts on RESPECT
Harmonising relationship patterns - impacts on INTIMACY
Manifestations of Pathology
Each holding the other responsible for their respective unresolved conflicts
9
Each viewing their respective extended family
a domain inaccessible to
the other
v
inadequate definition of roies - hence competitive relationship
Each seeking to derive their identity from their respective occupation
■3
incomplete resolution of conflicts
Avoidance of confrontation
3
■incongruent expectations of or dependence on community
Overemphasis oh' child-rearing with the children becoming the principal
means of communication between the partners
Disagreement on child-rearing process
9
Inadequate attention paid to sexuality
M
Seeking intimacy outside of the marital relationship
Breakdown of mutual nurturing
9
Conflicts regarding source of spiritual awakening
i*4K*a*
c JK
V,
V<3!1
J*
k-.
O
:
Object of intervention
To negotiate a compromise settlement between two warring factions?
NO
To assist a couple in relieving stress?
NO
To save the marriage from divorce?
NO
To empower the couple to make considereu CHvices :
YES
Couple tmpowerment
•
Facilitating the understanding of dynamics in the relationship
G
Providing a framework to view the marriage with
Learning to use the marriage to enhance individual identity
Goals of intervention
•
Redefine iocation of the marriage
•
Each to take responsibility for respective seif
•
Enhancing love, trust, respect and intimacy
•
Redefining relationship template
Types of Intervention
Pre-maritai
■3
Marital - proactive
Marita! - reactive (crisis)
£
Pre-divorce
Intervention Setting
•
individual therapist
«
Conjoint - two therapists
Consensual - two therapists
*
Group - one or two therapists
intervention Techniques
Negotiation
•sJVCZI OOUr? ty
$
interpretation
Homework assignments
*
stage i
Negotiating the contract
Stage ii
Identifying patterns
Stage il'Formuiating template
©
Stage iV
Keview
Stage i: l he Contract
f IvViUtf Wtst tfittW V! IHiV! VWffUVt!
©
Clarity expectations
a
Provide overail formulation
oet Gtsittiauft? yvcua
Stage ii : Patterns
Need for unconditional love - unstated expectations
©
individuation needs - fight analysis
9
Control games - defining boundaries
Intimacy needs - relationship patterns
C^rAJM/A
til
•
* U**, if
IAA BA i Za4> a
Oiaye ih . f ttw itu
9
Redefining expectations
Redefining boundaries
9
Re-formatting fights
Refining patterns
¥
Stage iV : Review
Review insights
e
Review investment
Set mediurn-term goals
Set up periodic reviews
Schedule of intervention
The Contract 1 or 2 sessions
9
Patterns
4 to S sessions
’ empiate
2 to 4 sessions
Review
1 session
Client-related issues
I aking responsibility for outcome
Client selection
e
Recalcitrant spouse
*
Dropping out
Therapist-related issues
2
The need to mediate
9
identifying with one partner
Serving as conduit
S
Therapist’s own relationship
Who is the client?
THE MARRIAGE
nvt-Zc..S3
*
CERTIFICATE COURSE ON COUNSELLING 8 REHABILITATION OF
S uBS i ANCc ABUSERS
OroanfePrf
ft,/T
o
of India, New
Delhi
OrgonsM by
T’
, Ranganathan
CiMca! Research
Foundation
Chennai 600 020
’
MARITAL INTERVENTION
Vijay Nagaswami
What is marriaae?
•
6mfional' Physical and sexual partnership entered
into by two consenting adults
the objective of achieving a state of harmony between the yin and the
and promoting a sense of emotional and spiritual well being in both partners
0
'through the mutual resolution cf unresolved intra-psychic conflicts
»
hetween the internal and axte™.
This definition includes all committed
monogamous relationships between
consenting adults of either gender
The Purpose of Marriage
Enharicement of self image
*
■■
w...f
■'
W.;-
_ _
-
Enhancement of
i.
Engenctenng physical, economic’-arid social security
>
. .... :
Gratification of sexual, belonging, parenting and intimacy needs
0
Resolution of intra-psychic conflicts carried over from earlier relationships
Companionship and spiritual fulfilment, BUT MOST OF ALL
ft
BLENDING THE YIN AND THE YANG
$
The Location of Marriage
•v.J 4.J. •. T-J.Jy.*.TTw .*2 T.1
I”
!>
I:
I
ilMil
i
j
.
V
J
pill ■^•■*7 .T- ■•. ■ - ■~.r,R,l IW! ‘
Family &
V.
VORK
mm
.........
.......
••
\
The Anatomy of Marriage
©
LOVE
s>
TRUST
RESPECT
o
IN I iMACY
Maritai Dynamics
w
*
e
Search for unconditional love - impacts on LOVE
Need for individuation -impacts on TRUST
Playing control games - impacts on RESPECT
Harmonising relationship patterns - impacts on INTIMACY
i
Manifestations of Pathology
ft
Each holding the other responsible for their respective unresolved conflicts
Each viewing their respective expended family as a domain inaccessible to
the other
inadequate definition of roles - hence competitive relationship
Each seeking to derive their identity from their respective occupation
9
incomplete resolution of conflicts
/Avoidance of confrontation
incongruent expectations of or dependence on community
Overemphasis on child-rearing with the children becoming the principal
means of communication between the partners
Disagreement on child-rearing process
0
Inadequate attention paid to sexuality
Seeking intimacy outside of the marital relationship
Breakdown of mutual nurturing
Conflicts regarding source of spiritual awakening
So, how can w® help ?
Object of intervention
To negotiate a corripi’ornise settlement between two warring sactionsr
NO
To assist a coupie in relieving stress?
MP)
To save the marriage from divorce?
NO
To empower the couple to make considered choices ?
YES
oupte Empowerment
Facilitating the understanding of dynamics in the relationship
Providing a framework to view the marriage with
e
Learning to use the marriage to enhance individual identity
Goals of intervention
Redefine location of the marriage
Each to take responsibility for respective self
Enhancing love, trust, respect and intimacy
Redefining relationship template
Types of Intervention
Pre-marital
a
Mental - proactive
©
Marital - reactive (crisis)
Pre-divorce
Intervention Setting
.
Individual therapist
¥
Conjoint - two therapists
Consensual - two therapists
Group - one or two therapists
intervention Techniques
e
Negotiation
Goal C-Ctt'n^
9
interpretation
Homework assignments
Stages of intervention
s
Stage i
Negotiating the Contract
Stage il
Identifying patterns
e
Stage IIIFormulating template
c
Stage fV
Review
Stage I: i he Contract
Provide overview of intervention
Clarify expectations
a
Provide overall formulation
Set definable goals
Stage ii : Patterns
Need for unconditional love - unstated expectations
9
individuation needs - fight analysis
9
Control games - defining boundaries
Intimacy needs - relationship patterns
Stage II!: The template
9
Redefining expectations
Redefining boundaries
Re-formatting fights
9
Refining patterns
4
Stage iV : Review
Review insights
9
Review investment
Set medium-term goals
Set up periodic reviews
Schedule of intervention
9
3
The Contract
1 or 2 sessions
Patterns
A
! empiate
2 to 4 sessions
Review
1 session
IV
6 sessions
CBent-related issues
I eking responsibility for outcome
Client seiection
e
Recalcitrant spouse
Dropping out
Therapist-related issues
2
Thie needu to mediate
3
identifying with one partner
«
©
Serving as conduit
Therapist’s own relationship
Who is the client?
THE MARRiAGE
H
MH - 2-c^ <+•
CERTIFICATE COURSE ON COUNSELLING & REHABILITATION OF
SUBSTANCE ABUSERS
Sponsored By National institute Of Sociai Defence, Ministry Of Socia! Justice &
Empowerment, Government of India, New Delhi
Organised by T T Ranganathan Clinical Research Foundation, Chennai
CAUSES OF ALCOHOLISM
DR. MOHAN ISSAC
** Multiple, interacting factors
w Different factors are important at different stages
'Bio-psycho-social moder
Biological factors / theories
Genetic factors
* 3-4 fold increase in relatives of alcoholics
* No single major locus
* Twin / adoption studies
* Follow-up of children of alcoholic men
What is transmitted?
Individual 'vulnerability*
w Psychological theories / factors
- Psychoanalytic theories
- Behavioural theories (Learning, conditioning)
Alcohol - Reduces tension, effects of psychological pain, feelings of nervousness
- Enhances feelings of power
’ Alcoholic Personality1
- cause or consequence?
i*-
Psycho-social and cultural factors
- Early childhood experiences and learning
- Broken home
- Faulty role models
- Alcoholic father / parents
- Family interactions *
Social pressures a
Demographic variables
aiGuHMi
Affordability, cost factors
Accessibility
Laws related to alcohol use
Social acceptability of use
Peer pressure, peer behaviour
Cultural / social attitudes
Permissive
Abstinent
Ambivalent
J*
CERTIFICATE COURSE ON COUNSELLING & REHABILITATION OF
SUBSTANCE ABUSERS
Sponsored By National institute Of Social Defence, Ministry Of Social Justice &
Empowerment, Government of India, New Delhi
Organised by T T Ranganathan Glinica! Research Foundation, Chennai 600 020
IMPACT OF ALCOHOLISM
DR. MOHAN ISSAC
A
*
A
Mortality
Morbidity
Disability-pALY', QALY’
Effects on Family'5, industry
Costs of alcoholism
MORTALITY
Premature deaths
Cirrhosis of liver
Strokes, other disorders
ROAf! — ♦“’’offin Qr'r-idontc
Suicide
Homicides
MORBiDiTY
Various alcohol related physical disorders
Psychiatric disorders associated with alcohol
Cognitive impairment, other neurological disorders
Morbidity following R.T.A.
DiABlUTY
DALY - DiabiSity Adjusted Life Years'
Global burden of diseases
Alcoholism - one out of ten
Most disabling and burdensome disorders
HOSPiTAL ADMiSSiONS (for aicohoi related problems)
# Psychiatiic Hospitals
- Growing proportion of admissions for alcoholism
t g institute of Mental Health, Madras
1953-1965
1966-1981
No patients with alcoholism
Percentage of admissions for aicohoi problems
- 0 1 to 3
1996 -1997
More than 25%
(Somasundaram, 1985. Paianiappan Soundararajan, 1994)
Page 2
NJMHANS
1980
Less than 2%
About 25%
1995
Private psychiatric practice
1977
Alcohol dependence constituted only 1%
of private practice (Bagadia, 1977).
1988
32% ciienteie made up of people with
alcohol problems
(Gopalakrishna & Sayee kumar, 1988)
More than 75% of GPs treat alcohol abusers with a variety of health and family /
social problems (Verma & Malhotora, 1988).
$ 15% of in-patients in Genera! Hospitals have drinking related problems (Babu &
Sengupta 1997).
m
More than 10% of male PHC attendees
- moderate to heavy drinkers (Moily, 1992)
IMPACT OF ALCOHOLISM
X* Effects on family
Family disruption
Domestic violence 'Wife-beating*
Marital discord, separation, divorce
Neglect / Abuse of children
Psychopathology in other family members.
•*
*
Depressive disorder - wife
Conduct disorder
Emotional disorder - children
Effects on family budget
& industry - work related impact
Reduced / Loss of productivity
Absenteeism
Inefficiency
Reduced uptake of training
Lack of skill enhancement
$ Legal problems
Paqe3
ISSUES IN ESTIMATION OF COSTS OF ALCOHOLISM
□ Cost estimation - complex and controversial
□ Costs - difficult to identify and quantify
□ Incomplete / poor - epidemiology base
□ Absence of routine information gathering system
□ inaccuracy of reporting mechanisms
□ Absence of relevant, reliable and comprehensive database
□ Bias towards underestimation
□ A range of estimates to be made
□ Tentative, conservative, Guestimate’
(to be regarded as 'indicative’ rather than 'firmly reliable’)
Aicohoi produces costly problems of large and diverse extent
□ Policy makers - ill informed about the costs and benefits of manipulating
the demand for alcohol
ESTIMATION OF COSTS OF ALCOHOLISM
❖ Direct health care costs
Hospital treatment for alcohol related diseases / accidents
Treatment and rehabilitation costs within health / social welfare sectors
Sickness insurance
Disability pension
Other Direct Costs
Insurance coverage for damages due to accident / crime
Criminal justice interventions - police / courts / prisons
enforcement of aicohoi related laws, alcohol control
Aicohoi education. Research
❖ Indirect Costs Due To Loss Of Productivity
Due to premature death
Due to disability
Due to sickness absenteeism
Inefficiency, reduced uptake of training, lack of skill enhancement
Value of lost life
In Finland (1990), costs of alcoholism amounted to about 3.5% of the G.N P.
Page 4
ALCOHOL RELATED PROBLEMS - RESPONSES
v Growing number of treatment centres
Special / additional facilities in existing psychiatric hospitals / units
Centres run by NGOs in India
X
Less than 10 in 1986
More than 250 in 1993
❖ Innovative treatment strategies
- 'Camp Approach’ (Ranganathan. 1996).
*;* Involvement of primary care sector
Training programmes.. Manuals (A.IJ.M.S.)
*> Educational and training materials
- For patients, family members, health workers, counsellors (TTR Foundation)
♦> Community action against alcohol
- Andhra Pradesh, Haryana, Maharashtra
O'
❖ Greater involvement of NGO S
Alcoholics anonymous groups
- in smaller cities and towns
- In local ianauaaes
Employee assistance programmes (E.A.P.)
ANGER
Prepared by
T.T.Ranganathan Clinical Research Foundation
17, IV Main Road, Indira Nagar, Madras 600 020
ANGER
Anger is a normal human emotion - to never feel it, is never to
be fully human. Yet, this most common emotion can be the
most destructive too.
Anger can work against the person. Anger fr quently turns
the very atmosphere into an alienating one, which in turn,
prevents the individual from resolving his problem speedily.
In the angry position, he finds himself unable to function
effectively - which infuriates him further. When he fails to
achieve what he wants, he turns critical of himself and of
others. Flis anger spills over and he shows hostility towards
other relationships far removed from the original cause.
Anger is a powerful emotion
that can hurt a person
physically. Getting angry, is
like letting a high voltage
current pass through the
body. People who anger easily
and stay angry, let themselves
in for a list of health problems
- headaches, skin problems,
back-pain, ulcers, and even
heart attacks.
Anger is
frequently the cause not only
behind minor mishaps like
tripping, knocking against
furniture, etc., but also behind
more serious problems like
accidents, fist-fights and even
murders.
Two radically different forms of expres
i of anger are
delineated below. While some people display them to the last
letter, most exhibit different shades between the two extremes.
With the same individual, expression may depend on the
situation or the person, one is relating to.
i)
She does not object to the
unfair treatment meted out
to her. So others see no reason
why they should change. She
either moves away and lives
in loneliness to avoid further
hurt, or continues to hide her
feelings with a gnawing pain.
'Hot Head'
He is well known for his impulsive outbursts, and
frequently goes blind with rage. He freely vents his
feelings and often says things he does not really mean.
His anger hurts people's feelings and consequently
breaks relationships permanently.
Since the aggressive
content is high and his
complaints are not
clearly voiced, he is
met with disapproval,
and actual issues go
unnoticed. Resent
ment towards him
grows and people
move away or simply
write him off and
never
take
him
seriously.
He expends a lot of
energy in his fits of
anger, but achieves practically nothing.
ii)
'All Sweetie'
She keeps her anger, even when realistic, to herself, to
avoid open conflicts. She burns with anger inside; but
struggles to maintain a calm exterior as though nothing
hurts her. In doing so, she ends up as a store-house of
anger and rage.
2
Anger, in both these cases, is
displayed inappropriately vented ineffectively or turned
against oneself. In either case,
nothing is gained through
anger.
We cannot ignore anger or totally eliminate it from our lives.
Anger is neither "good" nor "bad" - it just is. Anger always
exists for a reason and therefore deserves attention.
PRACTICAL GUIDELINES
You can minimise, if not totally eliminate self-defeating anger
and yet deal effectively with people and situations. Here are
a few suggestions that can help. Pickup at least one or two
suggestions which would be relevant, practical and there
fore beneficial to you.
1.
Express your problems and expectations explicitly
Anger sometimes stems from unexpressed problems,
desires and expectations. The mother who is nursing a
bad head ache may simply blow up in anger if the child
makes a request for a special dish. As she has not told
the child about her physical problem, he cannot be
expected to understand her pain and display concern.
3
Her angry outburst
only alienates her
further and she will
not get the treatment
she deserves.
3.
Ask for clarifications
Statements and questions designed to get the other
person to speak his mind are very helpful.
When you are in a
crisis and need help,
ask for it Most people
get to know clearly that
you need help only if
you tell them so. The
attitude of 'they ought
to know7 is not very
practical.
2.
Speak out your problem by stating facts
Being just as curt and grouchy as your colleague has
been, for the past one week, does not help in solving
problems.
By expressing feelings and avoiding accusations, by
being descriptive and not judgemental, one can prevent
anger 'build-up'. Open discussion about the conflict
clears the air and helps speedy resolution.
"I get the impression that you are unhappy with me.
Are you?' - may invite him to speak his mind. Well, that
may get you somewhere.
Raju was invariably furious with his wife
when he left for work. When shouting
and angry lectures did not work, he
decided to tell her specifically what he
expected of her. "When lunch is packed
late, I get tense because I might be late for
work. That's why I shout at you. I
become anxious and drive recklessly. I
feel bad all day because I know I have
hurt you. I would be happy to go for a
simpler meal which can be prepared well
in time." Raju found that this disclosure
worked better than the usual outburst.
4
4.
Develop an assertive* approach
Anger frequently stems from our non-assertive behaviour.
We give in more than what is necessary, invite others to
take advantage of us and subsequently boil with anger!
If a colleague takes leave too often, loading you with an
unfair share of work, you can firmly refuse to 'pitch in.'
Carrying that anger inside and being 'testy and nasty' all
day long, will permanently disrupt the relationship with
the colleague and hurt you also.
*
Effective communication and assertiveness are powerful tools
to avoid / handle anger. Brevi ty has been forced here, as elaborate
discussion on these is beyond the scope of this booklet.
5
5.
Channelise 'anger energy7
basic issue honestly, and thereby let it weaken your
healthy relationships too. Misplaced anger hurts more
and more meaningful relationships just as a single stone
can set off a number of ripples in a pool.
Anger produces a lot of energy. Some physical activity
may help you to let off steam without hurting yourself
or others. For instance, cleaning or tidying up the house
helps get anger out of the system, for a housewife.
Similarly you can think of some constructive activity to
channelise anger.
Prakash, sales executive, resorts to another
method when he feels like 'shaking
them till their teeth rattle7. "I write a
stem letter stating each and every thing
of what I feel. Feeling better after having
let it out of my mind, I leave the letter
aside for a day. By the next day, I usually
cool off enough to think rationally.
Sometimes, I feel it is not worth writing
about and therefore destroy the letter. Or
else, I tone it down, use more courteous
language and send it across. This really
works! I do not ignore anger. At the same
time I act instead of reacting.'7
6.
*
a
d
Recognise 'misplaced anger7
In 80 to 90 percent of the occasions, anger becomes
misplaced. When anger in a situation or relationship is
not handled properly, it is spewed on to the other
areas, leaving behind a trail of damages. The
worker's disappointment in not being considered for an
important assignment, may be earned over as irritability
towards his wife. His wife, in turn, shows her anger
stemming from this uncared-for feeling, on her children.
Your misplaced anger is vented frequently on people
who are on your "can be angry with" list - your family
members and not colleagues, your subordinates but not
the boss. You may punish yourself by failing to handle
6
Stress at workplace is often the cause of anger in the
home-front. Discussing work pressures with family
members helps. Sharing makes them more sensitive to
your problems and you get to enjoy their support too!
7.
I
Check the 'trigger'
When your anger is scrutinised, you may identify a few
specific situations or individuals with whom you anger
easily. Identifying them can be a powerful tool to deal
with your anger. For this purpose, maintaining an 'anger
diary7 for a fortnight or a month, may help. Being sensitive
to anger in its disguises (silence, sulking, banging doors
or avoiding people) is imperative. In the 'anger diary'
note down all events or situations which 'upset7 you.
7
Analysing will bring to light the angry situations and
their associated triggers.
8.
9.
Avoid letting anger 'build up'
Anger,
even when
reasonable, if left far too long,
festers like an unattended
wound, and turns into
resentment, bitterness and
hatred. Past resentments injustice done
by one's
parents,
siblings or
acquaintances - are normally
carried over as an unbearable
load.
Realise the link with hunger
Hunger and anger have much more in common than
the last four letters. When the body is devoid of its
energy, a person is not himself fully. Fatigue can make
a person anger fast.
Trivial things seem major disappointments and slight
disagreements can lead to heated arguments. Discussions,
especially those in which disagreements are anticipated,
are best scheduled after a meal.
Feed him if you want him to stay calm" seems a good
idea.
Forgiving and 'letting go'
has to be done by exercising our will. Seems difficult, but
is there a better option? To let bitterness and resentments
remain, is to permit them eat you from within - a slow
suicide.
10.
Developing a flow chart for handling anger
Devi, a teacher, finds the following steps
helpful in dealing with anger.
Step 1
Am I just upset or am I 'somewhat angry7?
Step 2
Pnya takes a lot of interest in her husband's
work; but all her questions only elicit
curt replies. The reason is only too
simple - wrong timing. After the day's
work, he needs time to switch roles, relax
and talk. With some food and time, he
may unwind and be more pleasant.
If I am angry, is it because of something
which happened now, or, am I carrying it
over from elsewhere?
Step 3
If I am carrying it over from elsewhere, it
is misplaced anger. In that case, let me
tell the person "Give me sometime, I will
8
9
get back to you." Theret I acquire
some time to deal iwith
’ ’ anger. I avoid
unloading it on the next
--- 1 unsuspecting
victim.
Monday mornings, soon
reaching office
after
Day of resuming work following a
tour
Step 4
If it is not misplaced anger, and the cause
of anger is clearly known, let me analyse
and think about it. If necessary, let me
talk it over with somebody I trust.
Gopinath an executive, used the following model, involving
simple analysis, and application. He achieved it in three stages8
Month end (Performance reviews?)
For about 30 to 45 minutes pr eceding
lunch break
For about 30 to 45 minutes after
reaching home
Stage 3
Stage 1
Analysed my anger patterns :
Shouting, screaming at subordinates
Upsetting wife and children for no
specific reason
Stage 2
Took appropriate steps to avoid or deal
with those situations:
Ate regular meals - especially
breakfast (reducing 'prelunch addity)
Went for work an hour earlier during
peak periods to organise myself and
set targets for others
Scheduled meetings involving
disagreements after lunch
Requested family members not to
raise issues for decision as soon as I
reached home.
Reviewed my anger at work and at
home every day, and continued doing
it for a month.
These few steps really worked!
Identified specific situations/periods
during which I felt angry
Using any one of these tools in isolation, or in combination, you
can arrive at a model suited to your needs. With this tool in
hand, you can check your daily progress about how well you
adhere to goals you had set for yourself.
10
11
You may recover from unhealthy anger by sticking to the 'one
day at a time' principle. Set goals for each day and hold on to
them for just '24 hours.'
Anger is wholly yours to change. Assume personal responsibility
for your unhealthy anger patterns and resist the urge to blame
others for your anger.
You may start with family relationships - which are usually
the most influential and the most difficult, and then move on
to other less complicated ones.
Remember
Practical guidelines are available to you to minimise
'anger reactions'
You should develop your own model based on
these guidelines
Even if one or two ideas can work, it could give you
tremendous relief
-
By minimising anger you become healthy and
assertive.
Should anger be allowed to obsess your thinking and ruin
your life?
Should you punish and destroy yourself for what others are
doing?
Exercise your choice.
Handle anger sensibly and
Become a 'BETTER YOU'.
12
COMMUNICATION
A "BETTER YOU" SERIES-4
Prepared by :
T.T. Ranganathan Clinical Research Foundation
17, IV Main Road, Indira Nagar, Madras 600 020
Sponsored by:
Ministry of Welfare, Government of India,
New Delhi 110 001
COMMUNICATION
Your 17 Year Old Can Be Your Best Friend
"Why do little kids grow up as adolescents at all!" Ganesh
thought wearily. He and his seventeen year old son could not
spend a few minutes together without snapping at each other.
"She is a stranger to me now!" Rukmani exclaimed, confused
at her teenage daughter's 'inconsistent' behaviour.
"Where did I go wrong?" Thomas lamented. He had so much
looked forward to a camaraderie' with his son when he grew
up and now this seemed impossible.
"Generation gap!" says the arm chair psychologist.
1 "They don't care for
elders", complain many,
shaking their heads
despondently.
"It's no use" exclaim a
few who find refuge in
avoiding arguments
with the adolescents.
"There is no way out!"
the pessimists give up!
1
"Does it have to end this way?" distraught parents question.
1. "My parents brought me up this way and I grew up right;
why doesn't it work with my son?'
No, not at all! Your adolescent child's difficult behaviour does
not signal his loss of respect for you or all that you stand for.
It only points to the need for communicating better.
WHERE
e
GjaNERArtoN (hftp!
World is no more the same. It has changed a lot. The
whole scene is different now. Take a walk in your home
town - see if anything is the same - the way people dress,
eat or shop. There are a few 'decades' between you and
your adolescent son and that is a lot of time, and
consequently 'a lot of change.'
Ramnath says.
"The way I run my firm is vastly different
from the way my father ran it. During my
father's days, the workers stood around
reverentially.
'Generation gap' is a myth. A term, we take refue in, use
conveniently to deny our contribution to the problem and
convince ourselves that nothing can be done. Generation gap
does not exist - communication gap does, and this gap can be
bridged - if only you really care.
This booklet carries views, opinions and examples of parents
who have trudged up this path. With effort, they tried different
methods of communication and surprisingly enough, these
worked! We invite you to try them and experience a closeness
with your child.
Before you proceed, let us clarify two doubts that may be
foremost in your mind.
2
Now there is union; we exchange views and
involve the workmen in the decisions we
make. Autocratic system is breaking down
everywhere.
3
Illi
\\
' 1// Jip1
2.
I am aware of the enormous changes that
have taken place all over. I know my father's
management will not work today. But at
home, until recently I fought desperately to
keep a rigid hierarchy. No wonder I failed
with my son! The nasty scenes I had with
him every day were proof enough for this".
Smaller children may accept instructions more easily and act
the way you want them to. As they grow up, they do question
your authority and no longer hide their resentments when
parental pressure is used. Punishments which did work well in
the past, now backfire. Trying to cow them down with threats,
may only taunt them to pay you back with the same coin.
"I have been bringing him up this way since he was a
child. So why change now?"
Every adolescent is trying to find his 'bearings' in the adult
world. He is often all at sea - confused about what he should do
or how he should behave. He needs an anchor to hang on to in
this period of turbulence. He needs you.
He is different now. Isn't he? Every adolescent wants you
to recognise that he is big and demands to be treated like
an adult. When he isn't, others have a problem.
Looking back, Joseph says "I was incorrigible
then. I expected my 17 year old son to 'obey'
my orders the same way as he did when he
was a child. I expected him to take up more
and more responsibilities and behave like an
adult, but, persisted in treating him like a
child!"
4
•-
This is a period when crucial decisions are made - decisions
that will mark his future. Only when a strong parent-child
relationship exists, can you influence him to take the right
decisions. He needs to stay emotionally close to you. And, you
need to help him stay this way by communicating well.
Be alter to non-verbal cues
Your adolescent son or daughter may often wear a woe begone
expression, seem withdrawn or start sulking when things are
5
not going their way. These may be invitations to initiate a
conversation.
Normally, we parents get worked up when our son indulges in
long telephone conversations with his friends or when our 17
year old daughter spends hours together in front of a mirror.
These are really minor issues and are best ignored, as arguments
about them will only worsen the situation. We often waste our
energy in handling trivial matters like these, which in turn,
weakens our relationship further. When our focus is on minor
matters, really serious issues are likely to go unnoticed.
"You seem upset about something" - will be a statement
enough to get him to talk about it. It shows your concern and
willingness to help too.
Remember, the teenager today is made to study at the school
level as much as what we parents studied at college level! Over
and above that, consider the kind of competition they are
pushed into in pursuing higher and higher grades or ranks. A
teenager today has one hundred reasons to feel insecure,
anxious, tense and 'highly worked up'.
Listening - First Step to Emotional Closeness
0
Relationships grow with effective communication. Effective
communication takes place only with 'effective listening.'
Good communicators are essentially good listeners.
Listening is much more than just hearing. When you are trying
to listen while reading a newspaper, to your son's report of the
debate in which he participated, you are not doing a good job
of listening. Being mentally set to hear, does not suffice.
Making the other feel it, is important. If you were to approach
Z
6
7
your superior with a suggestion or request and he 'heard' you
while skimming through a few papers how would you like it?
Looking at the person who is speaking, conveys your willingness
to listen and your respect for what he has to say. Eye contact,
appropriate facial expression and a leaning forward posture
will encourage your child to talk.
my son did make interesting conversation. He
knew much more than what I credited him with the recent political crisis, the business takeover by
a tycoon and so on. And until then I thought, my 16
year old cared for nothing more than cricket and
the latest piece of jazz."
Listening helps you to really get to know him - his hopes,
aspirations, interests and friends, in addition to his hurts and
pains.
<1
Only when good listening is established during normal days,
he will turn to you in moments of trouble. When he sees in you
a 'confidant' and is sure of receiving a patient hearing, he will
be willing to lower his defences and air his .feelings and
thoughts.
© V
© X
a®® 0
@ e
®©
® Oh1®
P/i VI
Listening means undivided, focussed and total attention, to
the exclusion of distraction. When you listen really well, you
model the behaviour of your child to follow. If you want him
to take what you say seriously, treat his talk the same way.
Interestingly, listening well is an enjoyable activity and not an
exercise. It tells you more about your child and draws him
closer to you.
Says one parent,
"Understanding the need to spend at least a little
time with my son each day, I forced myself to it. It
was with some misgivings, no doubt. To my surprise.
8
Reacting to feelings and not words
Listening means listening to what is said and also to what
remains unsaid. Feelings are the vital part of messages which
are often hidden. A good listener senses and understands the
feelings behind the words. When the feeling content is ignored,
we unconsciously place blocks and prevent the other from
communicating. Figuratively speaking, we muzzle the other to
stop him from speaking.
Ashish walks in, crest fallen, throw his books in a
comer and makes an announcement.
"I am not going to the Maths Tutorial any more. I
hate the teacher."
Typical responses which block communication will
be:
"Don't throw the books that way"
9
Criticism
'^Without going to school, what are you planning
to do - rear pigs? Ridicule
Mother :
"She reacted badly, because you had
not taken the book?"
"Pick up those books and come and have your
tea!" Order
Child
"And in front of all the students too!"
Mother :
"It was embarrassing."
Child
:
"Some giggled. Arjun made faces. It
was a bad scene. If only I had taken the
book..."
Mother :
"You are just wishing that you had
remembered."
Child
:
"Yes! I guess I need to be more careful.
I meant to take it, but in the morning
rush to school, I just forgot."
"School education is important for you. Without
education you will be nobody..." Advice
Mother :
"With so many things to do in the
morning, you missed out this."
An effective communicator would have probably proceeded
along the following lines:
Child
"I think that hereafter I will get my
things together at night before I go to
sleep! I have always meant to do it, but,
put it off. In future I am going to."
"You have to go to school, if not, I will make you!"
Threat
"You are a bright intelligent boy, you should not
speak like that!" Praise
"Teachers are to be respected, you should not use
terms like these!" Moralise
"You must have done some mischief and got into
trouble!" - Blame
(Seen the facial expression and the act of throwing books as
signs of strong negative emotions)
Mother :
"You are upset about something which
happened in the school!"
Child
"That teacher is stupid!"
:
Mother :
Child
"You seem to be angry with your
teacher!"
Yeah! She insulted me for nothing. I
had just forgotten to take my book and
she took off."'
10
:
Here she has resisted the temptation to use blocks and pressurise
the child into doing what she wanted him to do. By listening
without passing judgements and reflecting the feeling to him,
she helped Ashish. Negative feelings have been ventilated and
the situation has been resolved.
Listening by focussing on the feeling content of the messages
sent, helps the child resolve the problem situation. This may
take a little time; so do not attempt it when you are hard
pressed for time. It would be better to get back to your child
when you have time at your disposal rather than try to rush
11
through in hurry. If the child seems unwilling to discuss it, do
not push. She may get back to you when she does need a
patient ear.
Communicating a need for change
"Why can't you put your books back as soon as you
finish with them?" Shouting with indignation.
Communicating a need for altering unwanted behaviour does
not necessarily lead to hurt feelings. Change can be achieved in
a smooth, non-threatening manner.
With these responses, the desired action might be achieved,
but only with some negative feelings. At times, your child may
decide to pit his prowess against you. In a battle of wits and
power, your child is in a better position to win, for he has all the
time and energy at his disposal.
When the parent disapproves of the child's behaviour
traditionally, solution messages are sent.
Here's what a few parents say:
"Getting him to remove his books from the sofa,
takes atleast half an hour. I am often so tired that I
do it myself."
n
"When I did not give him permission to go to the
party, he told me he was going to the playground
and went to the party anyway."
"My lectures generally fall on deaf ears. Often, he
would be out before I finished."
Descriptive messages which emphasise on feelings and avoid
being judgemental, work well.
"Remove the books from the sofa immediately.
Ordering, Commanding
"If you don't clean up, you will not be allowed to
go the party." Warning, Threatening
"I take a lot of pains to keep the house neat. When books are left
on the sofa, I feel frustrated/'
Ravi told his son, "When the music is played
loudly, I am unable to proceed with my reading."
"There's a place for everything and each should be
in its place." Preaching, Moralising
12
13
When any particular behaviour of your child is hurting you,
frame statements with the following components:
1.
2.
3.
State the problem behaviour
Describe your feelings
State the effect of the behaviour
With these statements, the child's willingness to change, becomes
stronger, as negative evaluation is kept at the minimum.
Compliance is higher.
Expressing feelings openly
Very often we mask our true feelings, twist them out of shape
and express them in a negative manner.
He told this in a clam, even tone. Seeing that his music was
interfering- with his father's work,' his> son willingly toned
down the volume. If he had been ordered to do it, still he might
have done it, but probably not without resentment - "Do I not
have the freedom to even listen to music in this house? The
music was not too loud after all."
When her son arrived at 7 p.m. instead of at 4 p.m.,Sa vithri told
him "I was very anxious. I kept imagining the worst. I was so
worried''. This response elicited a honest "Sorry, I had a
problem" from him. If she had responded in the usual manner
saying "Where have you been? Do you think this is a hostel,
where you can come and go when you please", he would have
sulked and muttered a few unpleasant words.
Vijaya left her lunch box at home. This has happened
thrice this month and she just had a soft drink
during lunch time. Typically, her mother, retorted
in the evening saying, "How can you be so absent
minded? You don't do anything around the house
after all. It is packed and given to you, and you
cannot even remember to take it. If your memory
is that bad, no wonder your test results are poor".
>
In the above mentioned positive responses, the focus is on the
behaviour that is causing the problem and not on the person.
Since the person is not being criticised in an unconditional
manner, he is not forced to defend himself. As the feelings are
correctly described, the other person is not able to criticise in
turn.
14
15
Vijaya felt resentful about the hurting remarks and
walked away muttering "Big deal!"
On the other hand, if Vijaya's mother had expressed
her positive feelings, her response would have
been different. "You must have been hungry all
afternoon. I had taken pains to pack your lunch
and I was disappointed since you could not eat it."
It is Easy to Sound Persuasive
We unconsciously mouth the same destructive responses that
our parents used. We are so familiar with them that we say
them with ease - without a thought of what it is doing to our
relationship. When I was an adolescent, I vowed not to speak
to my children the way my parents did. But here was I, a
parent, now saying the same things in the same tone.
To take a sample - What happened if my children did not come
to have dinner quickly? The old dialogues rolled off my tongue
with ease. "Are you deaf? Why can't you come to dinner on
time? I have so much of work to do later. No body in this house
bothers about my work "
After a lot of thought I changed my responses to sound
positive. "Dinner is ready. The rice is hot. The pappads are
crisp. Come quickly" I cried out in an enthusiastic voice. They
did come - and quickly too. I felt more relaxed. I didn't hurt
anybody for sure. I just made my words more pleasant and
sounded more inviting'.
We are at our best with friends and worst where our children
are concerned. Yet our children and their feelings mean a lot to
us. Things will surely start working well if we treat our
children with the same politeness and respect with which we
treat our friends.
Here, Vijaya gets to feel the positive feelings and
would probably tell herself to make sure that this
is not repeated.
Later on also, Vijaya may forget to take her lunch.
But when she does so, she is going to feel sorry and
atleast the negative feelings will not be there.
To sum up
Children go through tremendous problems during
adolescence. That is the time they need parental help.
They may not ask for it. But the parents must understand.
Relationships are built through good communication.
And, all good communicators are essentially good listeners.
16
17
Good listening means listening not only to spoken words,
but also to the teenager's feelings, emotions, impulses,
interests and aspirations.
While suggesting a change in behaviour or habits, think
and say how the change will benefit the kid. In any case,
make sure that your focus is on the behaviour of the kid
and not on him as a person. ("This behaviour hurts"
instead of "You are hurting")
Think in term of "What it means to him." This ensures
that the communication is persuasive.
Treat your teenage child like your friend. You will find
that the 'your 17 year old' is, indeed, a good friend.
Become a better parent. A BETTER YOU, in fact.
18
EFFECTIVE WAYS TO
CHANGE PEOPLE
f
WITHOUT OFFENDING THEM
i
A ’’BETTER YOU” SERIES - 6
Prepared by:
TT Ranganathan Clinical Research Foundation
17, IV Main Road, Indira Nagar, Madras 600 020
Sponsored by:
Ministry of Welfare, Government of India,
New Delhi 110 001
EFFECTIVE WAYS TO
CHANGE PEOPLE
WITHOUT OFFENDING THEM
"I want him to change. I wish he could see the truth in
what I say.... Will he take it in die right spirit?.. I definitely
don’t want to hurt him. What do I do? How do I
communicate?" - 'This is the problem we quite often face.
More often, unknowingly we ride roughshod over the feelings
of others, getting our own way, finding fault, issuing threats,
criticising a child or an employee in front of others, without
ever considering the hurt to the other man’s pride! Whereas
a few minute’s thought, a considerate word or two, a genuine
understanding of the other person’s attitude would go a
long way in alleviating the sting.
We want to point out ... and not be hated for it.
i'1
We wish to use words that influence and motivate the other
to change.
How do we do this?
#
Describe your feelings - The way it affects YOU
If we intend changing people without arousing resentment,
we must begin with an attitude of respect for and acceptance
of that person. His response totally depends on our attitude.
We normally assume the right to point out others' mistakes;
but never take the initiative to appreciate them when they
deserve it.
When judgements and negative evaluation of behaviour are
made, the other person becomes defensive. Rationalisation
and
counter accusations follow. If others’ feelings are
commented on, they may deny or sound evasive. But when
your own feelings arc described, you leave no ground for
argument or unpleasantness.
If and only if we are appreciative when things go well,
do we have the right to criticise. Appreciation makes a world
of difference in the way our words are received and the
motivation they provide to effect a change.
Sharadha’s husband was away on a business tour.
It was her birthday and she waited in vain for
his telephone call. When he came back, Sharadha
shouted, “You were so busy, that you could not
even make a call.... Is it?-. All you care for is
your business.
Compliment the person if you sincerely have something
to appreciate in him. This will enable him to remain open
to your criticism. Appreciation and Criticism should always
be in the proponion of atleast 2:1.
Relationships that do not enjoy positive strokes will certainly
not respond to negative feed back.
I WANT YOU TO CHANGE - HOW DO I CONVEY
IT?
Words that attempt to bring about a change, most often
sting and offend, not so much because shortcomings and
mistakes are pointed out, but because our choice of words
and their expression are faulty.
We want to ask the other person to change without sounding
offensive or critical. How do we do this?
Here are a few7 valuable tips
2
)
Her husband quickly reacted to her taunt and
said, “Do you know how strenuous it is over
there? You comfortably sit at home and think
only of silly issues like these.”
3
#
Describe situations without lecturing - Be brief
Our attempts to bring about a change often fail because
we take over completely and lecture on what they should
do and how.
A
Orders and directions that our lectures contain, tend to
belittle their ideas and feelings. Just describing what we
see, works.
Instead, Sharadha could have said, “I was very
disappointed. I waited all day for your telephone
-JI.” Through this response, she clearly states
call.
what she feels without finding fault with her
husband. Now her husband is more likely to
reply in a caring manner.
Words like ‘bully’, ‘selfish’, ‘mean’, ‘useless’, ‘slow as a
tortoise’, ‘dirty as a pig’ etc. should definitely be avoided.
When labelling words are iused and judgements arc passed,
the other finds only negative implications. If a change is
to be effected, the other person should be helped
t I to see
your side of the picture and understand how his behaviour
has affected you.
When Senthil, a supervisor, saw his shop floor
in a disarray, he told the workman, “There are
tools.... also an oil spill. Watch out! With your
workman’s shoes on, you will slip”. These words
got the job done.
Senthil just described the situation and effected
a lasting change in the behaviour of his workman.
He says, “I had to say this only once. Since
I got them to see the reason, they do it on
their own now. Today I have the cleanest.shop
floor in the factory - no effort and no ill feelings.”
5
4
Instead, if Senthil had lectured, “Can’t you see
this mess? Didn t your factory’s safety programmes
teach you this? You want someone to point this
out everyday?”, a sullen worker would have done
a half-hearted job and this too with Senthil
monitoring him closely. Since the cleaning was
done to keep Senthil’s mouth shut, the shouting
would have to be repeated every day.
When your neighbour plays music too loudly or c____
dumps
garbage, on the road, the person you should speak to iis
that neighbour - not the others.
•<
Lectures on “Why can’t you do that’ and Don’t you think
you should’, only stop the other person from thinking along
those lines. Since you
nick- un
c^ii.r^rxyou do
do the
the thinking
thinking and
and pick
up solutions,
the other person sees no reason why he should abide by
it.
#
“When my colleague tells me that I should work
faster, I can take that. But when somebody else
reports it to me, I turn red. 'What else did she
say about me., How could she have
go my
thoughts.”
Complaining to others rserves
----- no purpose. It
r is similar
‘ "
to
the act of the foolish man who
lost...s
hismoney
i
y in7. his field,
— ---but looked for it near the street light because it was brighte::r
there.
Express directly
#
Express your views directly to the person concerned.
Express your comments in private
Comments that hurt the most, are those that have been
made in the presence of other people.
When opinions are expressed through others, they take the
form of gossip. They arc given a negative flavour by each
person who reports them. Your words can be twisted out
of shape and turned unrecognisable.
GOSS IP
)
Embarrassed and angry with you for finding fault with him
when others are around, the other person fails to understand
what you are saying. For him, his feeling of being insulted
becomes the prominent issue.
6
7
Akhil says, u“I got into a scrap at school and
my teacher sent a note. My mother was furious
and she just took off. My brother said, 'He thinks
he is too smart. He needs some shaking up.’
My kid sister whispered, 'You refused to lend
me your pen. See! God is punishing you. You
deserve this.’
When criticised in the presence of others, I feel
I am challenged and my self-esteem gets weakened.
When alone, defences are down. I am able to
tackle the issue without having to play up to
the audience.
'X
#
Focus on only one issue at a time
When too many complaints are voiced together, we will
not be taken seriously.
When I entered home, I was feeling very embarrassed
and sorry about the note. After this scene, all
remorse disappeared. I was just waiting to get
even with my brother and sister.”
If I am criticised when I am alone, it makes
things easier - I have only one issue to handle
■ ‘the problem’. With others around, a full set
of forces come
into> play
| ’ - What they might think,
- ---------say and do, and how I should react to them.
8
“Just look at your marks! You have failed this
term also. You just do not bother to listen to
us. You play till 7.00 p.m. every day with your
friends. Your room is always in a mess, and I
have to clean it up every' time. Moreover, you
don’t hear what we say. Yesterday also I saw
you shouting at Grandma. Getting up in the
morning, eating on time - everything is a problem
with you. I have to repeatedly shout at you from
morning till night ” continued Lakshmi. Satish
had stopped listening long back.
9
Focussing on just one issue at a time and expressing it
clearly, is crucial for the message to be effective. When
too many issues are presented at one go, nothing gets registered.
Moreover, when too many
issues are pointed out, one
feels worthless. “How can I
handle all these drawbacks?
With so many things thrown
at me, I feel condemned and
rejected.”
4:
i
Complaints are to be given
in manageable doses. If given
one at a time, the person can
chew on it, think about it and
assimilate it. An overdose can
only turn him off.
#
I
’
Sulking, banging doors, cold stares - none of these work.
Non-verbal messages confuse the other, and he does not
understand where he has gone wrong.
Murali came home late in the evening. When
he entered, he found the whole environment
different. His father did not speak to him at
all. After half an hour, his father literally banged
the door and went off. Murali was confused.
’’What is wrong with Daddy? Why is he behaving
like this? Has something gone wrong in his office"?
- thought Murali.
Instead of sending non-verbal messages^ Murali’s
father could have effectively told him, “Last
evening I told you that you have to be back
home by 7. I am upset because in spite of it,
today you arc late by one hour.”
Express verbally as to what needs to be done
Do not sound apologetic
If we are dissatisfied with what the other person has done,
we have to
.j explicitly state what we feel about it.
Feeling uncomfortable when criticising, we sometimes attempt
to glide the pill. The crux of the issue will then be lost
in the frills.
Ravi’s boss said, “I am impressed with your
qualification and the assignments you have
successfully completed. As somebody much older
to you in age, I feel I can tell you a few things.
Coming to office on time, is something I consider
very important. When I joined work, I used to
come half-an-hour ahead of time and leave only
after my boss did. Punctuality had always been
my strong point. Imagine the model you will
set to your subordinates if you come late. You
are a young man with a career ahead of you.
10
11
So I want you to take care of small issues like
these.”
In each of these, the first set of sutements hurt. Comparisons
offend feelings and deliver a blow to one’s self-esteem. When
a person is told time and again that he is not good enough,
he will dismiss your standards and your words will lose
their value.
Ravi’s boss sat back with a sigh of relief, for
he thought he had conveyed to Ravi the importance
of being punctual.
When Ravi’s friend asked him what the discussion
was all about, he said, “I don’t know why he
called me in. He was reminiscing about the past
and telling me of things he did during his younger
days.”
#
Do not use words like ‘Always’ and ‘Never’
Words like ‘always’ and ‘never’ dilute the power of statements
and lead to a total disregard for your ideas.
Situation:
Apologetic statements like, “I am saying it all for your
sake , or “Don’t get upset about what I am saying” are
not required. J hey take the power off your words.
#
I accidentally broke a cup while washing it.
Criticism:
“You always keep breaking things. You uill never
change, You can never be trusted to do anything
properly.
Avoid comparisons
Many believe that comparing unfavourably with another calls
for a healthy competition. But it doesn’t work. Instead,
it leads to resentment and a total rejection of your views.
Reaction:
“When you are used to my being this way, and since
I am not going to change, why are you wasting
your breath?”
“I have dined so many times at Rajesh’s house. Unlike
you, Rajesh’s wife cooks marvellously well.”
“Curry is burnt and Sambar is too salty.”
Situation:
“Shankar’s handwriting is so neat. Look how untidy
your work is.”
“I lost my pen during the camp.”
Criticism:
“Your handwriting is illegible.”
“You always keep losing things. You can never take
care of your belongings.”
“You have not completed your target. Ganesh is less
experienced than you. Still he has overshot his sales
target. Why don’t you learn from him and improve?”
“I want your sales to increase.”
Reaction:
i
“I lost a pen worth just Rs.2.00. This is the first
pen I have lost. What about the purse that you lost
last month?”
12
13
The statements here do not [pin
’ point particular behaviour,
but rather condemn globally.
John worked out the sum and showed it to his teacher.
“With your kind of brains, you ought to be in a museum,”
remarked the teacher.
‘Always’, completely decries the past. ‘Never’ seems to say
that
... one is bound to stay that way for ever. His reaction
will then be, “True, I might be wrong just now - but there
were dozens of times when I had been right,. He does not
even remember. He is too prejudiced. I will not listen to
him.”
Statements like these are like acid that corrodes. The receiver
only feels embarrassed, ashamed and furious. It does not
help him understand where he has gone wrong. Even when
he does, it does not motivate him to change.
#
So far, we have seen 10 cardinal rules to be followed in
changing people without sounding offensive or critical. They
are
Do not be sarcastic
Sarcastic comments fail to convey messages, but leave in
their wake, hurt feelings.
Dinesh silently finished his dinner of cold chapathis
and left over curry. He said, “What an excellent dinner!
Food is piping hot and absolutely tasty.”
Shantha entered office at 11.00 a.m. “You are very
early. How did you manage that?”, asked her boss.
Describe your feelings - The way it affects
YOU.
2.
Describe situations without lecturing - Be brief.
3.
Express
4.
Express your. comments in private.
5.
Focus on only one issue at a time.
6.
Express verbally as to what needs to be done.
7.
Do not sound apologetic.
8.
Avoid comparisons.
9.
Do not use words like ‘Always’ and ‘Never’.
10.
Do not be sarcastic.
directly.
When we are right, let us try to win people gently and
tactfully to our way or
of tninKmg;
thinking; and when we are wrong
- and that will be surprisingly often, if we are honest with
ourselves - let us permit others to point out our shortcomings.
It pays to listen
'-A
I
14
1.
It pays to listen patiently and with an open mind. Be sincere
about it. Allow him to express his views fully. Suddenly
15
you may be tempted to interrupt. But don’t. If you do
so, he may stop abruptly and there may be quite a number
of things he had wished to point out and you had missed.
Listening helps you to understand new truths - new angles
to your personality which you may hitherto be unaware
of. Convince yourself that his intention is not to find fault
with you, but to help you to change for the better.
If others suggest a change, it does not mean that you are
not valued. It only means that with the change, you will
be valued more.
So far, we have explored methods to criticise others without
offending, and also to listen to criticism and get benefited
by it. Conscious practice of the valuable tips given, could
lead to a turning point in your life. You already possess
hidden assets within yourself that can make your personal
and social interactions meaningful All you need now is
the determination to uncover, use them and become
A BETTER YOU.
16
4
- Media
 RF_MH_2_C_SUDHA.pdf
RF_MH_2_C_SUDHA.pdf
Position: 1566 (7 views)