DOCTORS FORUM
Item
- Title
- DOCTORS FORUM
- extracted text
-
RF_MP_8_SUDHA
Jan. - Mar.
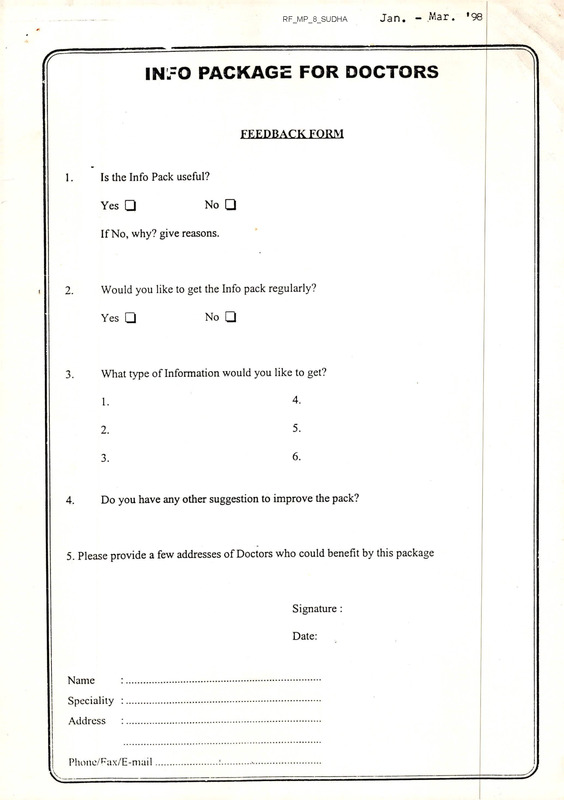
IN-=O PACKAGE FOR DOCTORS
FEEDBACK FORM
1.
Is the Info Pack useful?
Yes
No
If No, why? give reasons.
I
2.
Would you like to get the Info pack regularly?
Yes
3.
4.
No
What type of Information would you like to get?
1.
4.
2.
5.
3.
6.
Do you have any other suggestion to improve the pack?
5. Please provide a few addresses of Doctors who could benefit by this package
Signature :
Date:
Name
Speciality :
Address
Phone/Rix/E-mail
’98
SeptewbeJi, 1997
INTRODUCTION TO DOCTORS FORUM
■ 'J
I
/
’Re idea o(j (jOJi&ting a DOCTORS jyoUUM iit cV<bb4[ is gaiitiitg ivtoutc-ittim siitce
1996.
/
’Re pujtpose o(j de docto/is ^Jo/LUnt is to build up) cut ac.tioe K&twoxfe o(j sociaWy
in iJeahR. Oa/ie to cohte togeden to
conscious Docto/is, wHo a/ie open to new ideas
i
sHaxe ideas and expe/iiences.
'
tybl/r would like to build up and suppo/it a p/io|jessioiial gnoup o(y Docto/is wRo
could dink and act alteJinatiaely to p/ioiride national 4deald Oane, wHe/ie people
a/ie giilen p/iinte impo/itance. Special emphasis would be giiren to de a/iea 05 pneUentiUe
and p/ioivtotiUe Public d^ealtd cane.
Docto/is 2?o/iuivt is planning to take up de (jollowing initiatives.-
❖ 7b provide a platjjOKM. (yon de Doctons to silane tHein Views neganding tHein
pnofression and de bunning Heald issues o(y de countny.
❖
To send rn|jonM.ation Packages (yonDoctons as a pant o(y continuing medical education
especially (yon doctons wonking in nemote aneas.
❖
To debate and discuss about vanious RealtR policies and technologies emenging in
India and pnovide altennate suggestions.
❖
To collabonate witR the existing netwonk like rpD4. O^MDlF, MjJO'. etc. and
wonk togetRen fron a common cause.
In sRont, Doctons ^Jonum is a pnoactive and (jutunistic gnoup feon Doctons wRo could be
in de (yonefynont to take up RealtR issues and (yind solutions to public RealtR pnoblems in
India.
>ls a (yiJist step we a/ie seitdiitg you de (yi/ist [A&O
a pa/it o() cowtiituiug wedicaf. education.
4
DOO-TOlQS as
Kindly (jill in de (jeedbacfe fro/iM. and send you/t cohwents and suggestions.
"Ranking you in anticipation.
QAbl/I ^J/iiends
\
\\
\\
\\
\
73
■J
—
tk /cr-i^l /9/2s/ S rr
Pr'S
t>JcS
P
Co
sPjOljJcJL
______________ s' l i
K■cm
(i
Li'l
c^LiS'O
J
■!
INFO PACKAGE FOR DOCTORS
FEEDBACK FORM
1.
Is the Info Pack useful?
Yes
No
If No, why? give reasons.
2.
Would you like to get the Info pack regularly?
Yes
3.
4.
No
What type of Information would you like to get?
1.
4.
2.
5.
3.
6.
Do you have any other suggestion to improve the pack?
5. Please provide a few addresses of Doctors who could benefit by this package
Signature :
Date:
Name
Speciality
Address
Phone/Fax/E-mai 1
“INFO PACKAGE FOR DOCTORS”
CONTENTS
INTRODUCTION TO DOCTORS FORUM
1.
LEAD ARTICLE:
The Scourge of Hepatitis - B
2.
NEW DRUGS/VACCINES:
WHO Announces Influenza Vaccine Formula - 1996 - 97
3.
LEGISLATION
Important Information for prescribers
4.
WOMEN DOCTORS WING:
Formation of IMA service/Women Doctors Wing
5.
ETHICS
The Doctor’s dilemma - social-Ethical issues related to AIDS.
6.
DECLARATIONS
Declaration of Standing committee of Doctors of the EC
7.
FACTS AND FIGURES
50 facts from the Regional Health Report 1996, WHO - SEARO
8.
BREASTFEEDING NATURE’S WAY
Baby friendly hospitals.
FEEDBACK QUESTIONNAIRE
/
€11}
THE SCOURGE OF HEPATITIS B
The occurrence of Jaundice has been known
for centuries but it is only in this century that
the various causes of jaundice have been
described. The rapid strides in medical
technology have led to elucidation of the
various types of jaundice. Previously we used
to classify jaundice into two categories medical jaundice and surgical jaundice, the
former implying a medical cause for the
jaundice which required no surgical treatment
and the later implying the need for some
surgical intervention for relieving the jaundice.
The commonest cause of medical jaundice is
viral hepatitis. The term has two facets a)
viral implying that it is caused by a virus and
b) hepatitis implying
that there is
inflammation of the liver. Viral hepatitis can
be either acute or chronic. Acute means a
process which is recent and chronic implies
that the hepatitis is more than 6 months
duration. Although a variety of viruses may
cause a hepatitis like illness, five well
characterized hepatotrophic virsuses, A to E,
are the most important causes of acute and
chronic viral hepatitis. These five viruses can
be divided into two major groups. The first
group consists of viruses that are feco-orally
transmitted and don't cause chronic hepatitis
i.e Hepatitis A & E, and the second group
consists of those viruses that are transmitted
through blood and can cause chronic hepatitis
i.e Hepatitis B,C and D.
The hepatitis B virus (HBV) is a DNA virus
that predominantly affects the liver, leading to
inflammation and cell death; in the long term,
some patients develop scarring of the liver
(cirrhosis) and, less frequently, liver cancer.
The spectrum of HBV infection ranges from
acute hepatitis, anicteric hepatitis, fulminant
hepatitis, a hepatitis with a predominantly
cholestatic picture, to chronic liver disease
with minimal acute manifestations. The
danger of HBV lies in the last presentation as
the patient is unaware that he/she is infected
with HBV and may unknowingly transmit it to
others. A few decades later the patient may
develop chronic liver diseases cirrhosis or
hepatocellular carcinoma. HBV shares its
transmission routes with the HIV (the virus
that causes AIDS).
However. <t is one
hundred times as infectious as HIV . Its
potential to cause liver cancer has led to its
recognition as the second most impc riant
carcinogen (cancer-causing agent), after
tobacco. Several hundred million are infected
worldwide and these are the main reservoir of
HBV infection. The predominant moce of
transmission is parenteral i.e by infected
blood transfusions, contaminated syringes
and needles and unsterile instruments used
for surgery, Other nTodes of transmission are
perinatal and sexual. Inapparent parenteral
routes of transmission like use of shared
razors and toothbrushes, and contaminated
needles used for acupuncture, ear-piercing
and tattooing are also known.
An estimated 400 million persons worldwide
are known to be chronic carriers. One in ten
of these is in India, making this country the
second largest pool of the virus. The 40
million - 50 million Indians who carry this
virus form approximately 4% - 5% of the
general population. Various estimates place
the number of infected newborns who Vvill
become carr-iers at 1,50,000 - 4,50,000
annually.
SPECIAL PROBLEMS IN INDIA
The enormity of the problem in In^’a is
indicated by the above available data. Other
factors may compound or aggravate the
situation.
Probably the most important among thes^ is
the HIV. With an estimated 2 million carriers
of the HIV already in this country, Indic is
slated to become the largest pool of HIV in
•the world by the turn of the century. It is well
known that persons immunosuppressed by
HIV infection are more susceptible to other
infections. Since HIV and HBV shjre
transmission routes, high-risk populations will
also be common to the viruses. Data exists to
show a «symbiotic relationship between thqse
viruses ; the effect of HIV
infection
.........
—
on the
progress of HBV infection is not likely to be
favourable, though admittedly data are still
-----
I
lacking.
Coinfection or superinfection by the other
hepatitis viruses (A,C,D,E,G) all of which are
common in India - on a liver already diseased
by HBV can be further detrimental. Data on
such multiple infections with HBV and the C
d D viruses are already available and are a
cause for concern.
The effect of poor nutrition and alcoholism on
HBV liver diseases is not clear yet, though the
latter
is
an
established
liver
toxin.
Administration of antitubercular drugs - many
of which are known to damage the liver - can
also aggravate the condition. It is of course,
common knowledge that tuberculosis is
widespread in this country.
I
-
i
i
l
i
Finally, ignorance and poverty among the
populanon make it difficult to implerhent
barrier habits. It is believed that 30% - 50%
of the blood banks in the country do not
routinely test for the HBV; most of them are
also dependent on paid 'professional' donors
for their supply of blood. This forms a major
source of infection especially amongst the
ignorant who frequent these blood banks to
obtain blood on payment, out of a mistaken
fear among relatives that donating blood is
harmful to physical (including sexual) and
mental well-being. Unfortunately the same
populace is also likely to request blood
transiusion as a 'tonic'.
Preventive Measures
i
The concept of "universal precautions"
requires that all human blood and certain
body fluids be treated as potentially infectious
for HIV, HBV and other blood-bornJ
pathogens, and maximum precautions be
taken at all times when in contact with such
tissue.
Hands should be washed with soap and water
immediately after removal of gloves or other
protective coverings ; if handwashing is not
possible, an appropriate antiseptic cleanser
may be used, and handwashing done as soon
as possible. Any body surface that has come
in contact with potentially infectious material
should be washed with soap and water, or
flushed with water as appropriate.
A particular concern in India is the reuse of
razor blades by haircutters. It is advisable for
the customer to carry his/her own blade:
alternatively, it must be ensured that these
sharps are either disposed off or are
adequately sterilised before reuse.
Disposable / Sterilisable equipment :
All inexpensive equipment and accessories in
use in healthcare settings should ideally be
disposable. When such items are marked as
.sterlisable and reusable, the manufacturers'
guidelines for sterilisation should be adhered
to. Expensive multiple-use items
leg
endoscopes, ventilators, humidifers) should
be thoroughly cleansed mechanically and
sterilised as per the manufacturer's
guidelines, before reuse.
General Measures
Education : The single most important
measure initially is promotion of awareness
and dissemination of information. This should
be addressed both to the general public as
well as to high-risk groups.
Barrier precautions : Among healthcare
workers and emergency care providers
{firemen, ambulance personnel) at all levels,
and especially at the earlier levels in the
hierarchy where contact is more likely (labour
staff, primary healthcare workers, technical
staff, student and staff nurses, medical,
dental and paramedical students , resident
doctors) the use of hand gloves should be
made mandatory at all times when in contact
with biological specimens.
Blood Banking Practices :
Blood banks should be allowed to operate in
this country only if registered with central or
state-level regulatory authorities, who in turn
should enforce a phased replacement of
professional donors by voluntary donors, use
of disposable items for all collection,
transport, resting, storage, and transfusion
purposes, nesting of all collected blood for
HBV/HIV, and preferrably the hepatitis C
virus, use of sensitive third-generation tests
for markers of the above viruses.
In addition to the above measures, medica
professionals should be educated on the
judicious use of transfusion of blood and itc
products.
Vaccination :
Currently fe'e are two types of hepatitis B
vaccines avanaole around the world i.e the
first genera: on plasma derived" inactivated
HBV vaccmes and the second generation
’’genetical!', engineered or recombinant" HBV
vaccines. In the US and in most parts of
Europe the 'ecombinant HBV vaccines have
replaced the plasma derived HBV vaccines.
The plasma derived have been widely used
and have been shown to be safe and effective
but there is an unfounded fear about the
transmission of viruses as these are derived
from the b<ood of a person suffering from
HBV. These vaccines have a long production
cycle, require persons having HBV infection
and hence their supply may be limited. The
level of antibody persistence may vary with
the vaccine and the dose administered.
Recombinant DNA techniques have been used
for expressing hepatitis B surface antigen and
core antigen in prokaryotic cells. These
vaccines are totally synthetic and don't
require the use of blood pr blood products.
The recombinant vaccine, consists of the
purified antigen absorbed onto an adjuvant,
usually alum. Recombinant yeast hepatitis B
vaccines have undergoneextensive evaluation
by clinical trials. The results indicated that
this vaccine is safe, antigenic and free from
side effects (apart from minor local reactions
in a proportion
of recipients).
The
immunogenicity is similar to that of the
plasma-derived vaccine. Recombinant yeast
hepatitis B vaccines are now being used in
many countries. The advantages of the
recombinant vaccine is the unlimited supply,
as no blood products are involved and a
shorter production cycle.
The recombinant vaccine currently available
commercially in India is administered as 20microgram doses (10 micrograms in newborns
and children) at 0, 1 and 6 months. Dose
recommendations for the plasma-derived
vaccines vary from 3 micrograms to 20
micrograms at 0,1, and 2 months or 0, 1 and
6 months. Double the above doses is
recommended for immunocompromised
individuals (e.g in AIDS, and for patients with
chronic kidney failure undergoing dialysis); a
fourth dose is also recommended.
Who should be vaccinated ?
The immediate aim should be to vaccinate
high -risk groups. At the community leve ,this includes healthcare workers, emergency
care providers, and commercial sex workers.
It should be the responsibility of employers to
provide free vaccination to all healthcare
workers and emergency care providers. Such
vaccination should be provided preferably at
entry into training or employment. Catch-up
vaccination of senior personnel should be
done in a phased manner.
At the individual level, patients needinc
multiple transfusions of blood or its products
(haemophiliacs, thalassaemics etc.); those
undergoing elective surgery or dialysis;
newborns of mothers known to harbor HBV ;
sexual partners of HBV carriers and intimate
contacts of patients with acute hepatitis B ;
inmates of institutions (mental homes, old-age
homes, handicapped-persons homes, prisons);
and individuals with high-risk behaviour
(intravenous drug addicts, alcoholics,
homosexuals , promiscuous individuals)
should be recommended vaccination.
All newborns should be vaccinated by
introducing this vaccine into the Expanded
Programme of Immunisation. The World
Health Organisation has recommended that
this be done by the year 1997; over 80
countries have already done so. The Indian
Academy of Pediatrics
----------------and the Indian
Association for Study of the Liver have
endorsed this approach.
Experience in countries in South-East Asia has
shown this results in a remarkable reduction
not only in the HBV carrier rate but also in the
prevalence of liver cancer, within a few years.
\ NEW
I
WHO ANNOUNCES INFLUENZA VACCINE
FORMULA FOR 1996/1997
A new composition of the influenza vaccine for the 1996 - 1997 season has been
/Ljrn
announced by an international experts meeting at the World Health Organization (WHO)
headquarters in Geneva. Scientists are constantly challenged to identify major newly emerging
strains of influenza viruses, so that effective vaccines can be formulated in time, Compared
of the
to last year's recommendations for the vaccine, one c.'
J.- three
2----- influenza vaccine
components has been changed.
Every February, the influenza experts advise the national health authorities and
pharmaceutical companies on the composition of the virus strains that should be used to
produce vaccines for the next influenza season.
Influenza causes epidemics worldwide every year. WHO strongly advises the use of
vaccine as a sound preventive measure against this potentially fatal disease. Special attention
should be paid to vaccinate the elderly, individuals with immunodeficiency, sufferers of
chronic diseases of the heart or lungs as well as diabetes.
adequate. However,
For the adult population one dose of inactivated vaccine should be adequate,
previously unimmunized children in these categories should receive two doses of vaccine,
with an interval between doses of at least four weeks.
"The degree of protection conferred by influenza vaccines varies depending on the age
of
and immune status of the vaccine recipient", explains Dr Daniel Lavanchy, in charge o.
WHO's influenza programme. "We believe that Up to 80 per cent of recipients will^be
circulating
protected against disease when there is a good match between the vaccine and f--**
,~**~2
strains. The severity of illness and the frequency of serious complications is reduced among
the remaining 20 per cent".
The latest formula recommended by WHO is:
n an A/Wuhan/359/95(H3N2)-like strain
n an A/Singapore/6/86(H 1 N1 )-like strain
s a B/Beijing/1 84/93-like strain.
This differs from last year's composition in that the first of these strains replaces an
A/Johannesburg/33/94(H3N2)-like strain.
As in previous years, the specific viruses used in vaccine manufacturing in each country
will need to be approved by the national control authorities.
!
.i
Press Release WHO/IO
Page 2
The WHO programme on influenza surveillance and control was established in 1948
Today, it involves 109 WHO-recognized National Institutes on Influenza in /9 countries, and
threeWHO Collaborating Centres for Reference and Research on Influenza at the Centers for
Disease Control and Prevention (Atlanta, USA), the National Institute for Medical Research
(London, UK), and CSL (Parkville,Australia). This fully operational network help§'WHO to
monitor influenza activity in all regions of the world and ensures that WHO receives
information needed to select the new variants of influenza viruses which will be used
used to
to
produce influenza vaccines for the next influenza season.
There are three main antigenic types of influenza viruses currently circulating among
humans all of which have a remarkable capacity to change their characteristics from year to
year. These are known as A(H1N1), A(H3N2) and B. Vaccines are, therefore, composed of.
two strains of type A and one of type B. With new strains continuously emerging, scientists
and pharmaceutical industry face an annual challenge to produce modified vaccines wpich will
be effective against the latest dominant strains.
Epidemics of influenza were reported between October 1995 and February 1996 in
“
__ j-iA—____ -J A
many countries
in rEurope, ki
North
America,
and Asia. After few rnr>r\rtc
reports in
in (Ir'tmrv
October 1 995,
influenza activity increased in November and reached a peak in December and, n some
countries, in January 1996. By February, influenza had declined in most countries. Influenza
A viruses have been widespread and caused moderate to severe epidemics affecting mainly
children and young adults. European countries and China reported predominantly influenza
most+ —
regions -of
A(H3N2) while influenza A(H1N1) caused epidemics in Canada,
C—--1-. Japan and1 —
the United States of America.
The first outbreaks of influenza A(H3N2) were reported in boarding schools in England
in September and October 1995. The disease spread in the United Kingdom and appearedI in
other European countries during November and December, causing epidemics across most of
Europe (Belarus, Bulgaria, Czech Republic, Denmark, Finland, France, Germany, Greece,
Hungary, Latvia, the Netherlands, Norway; Slovak Republic, Spain, Sweden and the United
Kingdom), Madagascar and the USA. Outbreaks of influenza A(H3N2) started in Beijing
towards the end of December and spread to six provinces in China during January. Isolates
of influenza A(H3N2) virus were also reported in Canada, Europe (Belgium, Ice and.ilreiand,
Italy, Poland, Portugal, the Russian Federation, Switzerland) as well as in Asia (Guam, Hong
Kong, Japan, Singapore) and Oceania (Australia and New Zealand).
Influenza A(H1N1) caused a widespread epidemic in Japan in December 1 995, and was
the predominant virus in North America (Canada and the USA) and parts of Europe (Belgium,
southern France, and Switzerland). These viruses were also detected elsewhere in Asia
(China, Hong Kong, Israel, Thailand) and Europe (Finland, Germany, Italy, Latvia, the
Netherlands, Poland, Romania, the Russian Federation, Sweden and the UK).
Sporadic cases of influenza B have been reported in North America (Canada and the
USA), in Asia (China, Hong Kong, Israel, Japan and Singapore) and in Europe Belarus,
Bulgaria, Finland, France, Germany, Hungary, the Netherlands, Poland, Romania, the Russian
Federation, Sweden, Switzerland and the UK). A few isolates in Oceania (Australia ^nd New
Zealand) have also been reported.
’’The WHO influenza surveillance network together with the influenza vaccine
manufacturers ensure that effective vaccines are available to the public in time to provide
protection against each season's influenza epidemic”, says Dr Nancy J. Cox, Director of the
WHO Collaborating Centre for Reference and Research on Influenza in Atlanta, USA. Ibis
joint endeavour represents a very successful collaboration between the public and private
sectors, in the interests of public health”.
For more information, please contact Valery Abramov, Health Communications and Public Relations,
WHO, Geneva, Tel. (41 22) 791 2543 or Fax (41 22) 791 4858. E-mail abramovv@who.ch.
Le^tSLAVoN < I
IMPORTANT INFORMATION FOR PRESCRIBERS
As per a recent Supreme Court ruling, doctors of modern meo ••
registered under Indian Medical Council Act are permitted to prescriz-■e
ONLY allopathic medicines. Prescription or administration of non-allops:'. •
drugs (such as Ayurvedic, Unani, Siddha or Homoeopathic) shall renze
such doctors liable to prosecution under both civil and criminal
■
resulting in cancellation of registration and/or heavy fine and/or impns; • •
ment. Doctors of modern medicine prescribing non- allopathic dri.-z?
are liable to be considered as "quacks" per se without further evide- ' or argument.
Full text of the Supreme Court judgement and the opinion of law. • • from a leading hm of advocates can be obtained from MIMS by sene r z
a self-addressed, stamped (Ps. 2) envelope of the size of 24 cm x 16 c.m.
-------
Mims
I
fL -
!
I
I
F
I
-------- \
a
FORMATION OF IMA SERVICE DOCTOR’S WING
AND IMA WOMEN DOCTORS’ WING.
4
4
4
k
|
I
4
I
t
4
The Central Working Committee at'its meeting held in New Delhi on 2f th-26th
November, 1995, approved the formation of IMA Women Doctors’ Wing and IMA.
Service Doctor s Wing and also accepted in principle the basic structure of the
Constitution of these Wing. It also decided that these Wings will become operative
from the date on which their membership reaches 1,000. This was approved by the
Central Council at its meeting held at Bhubnesawar on 27th-28th December , 1995.
The eligibility conditions and rates of subscription and admission fees of the two Wings
are as under:-
IMA Women Doctor’s Wing
4
a
■
I4
4
4
4
•
4
4
4
■
a
Eligibility : Any Women Life Member of IMA may be enrolled as Life Member of IMA
Women Docotor’s Wing.
Admission Fee: Rs. 30/- per member.
Life Membership Subscription Rs. 450/- per member.
4
■
■
4
4
4
4
4
4
4
A State Wing of Women Doctors’ will be formed on-enrolment of a minimum of 50
members of the Wing.
■
■
IMA Service Doctor’s Wing
■
■
■
■
Eligibility : A Life Member of IMA engaged in any type of service may be admitted as
Life Member of IMA Service Doctor’s Wing.
*
■
■
Admission Fee : Rs. 30/- per member
Life Membership Subscription: Rs. 450/- per member.
A State Wing will be formed on enrollment of a minimum of 50 members of the Wing.
All State and Local Branches Secretaries are requested to start enrollment of members
of these two Wings. Membership Application'forms may be obtained from IMA Head
Quarter.
■
■
4
s
K
■
a
■
■
IMA News
5
■
April, May, June, 1996
■I
I
fTHICS
\
1
The Doctor's Dilemma —
Socio-Ethical Issues Related to AIDS
- - r Him....... mu
............
Whether we like it or not, the pandemic of AIDS
has reached India, and according to postulation, the
epidemic peak with explosive outbreaks of HIV
positivity is yet to occur. In the medical profession
arc we ready to face the challenge ?
The uniqueness of HIV arises mainly out of its
four characteristics.
First, handling a HIV positive patient entails a cer
tain amount ofphysical risk of being contaminated.
Hfr Mcrtir
2. Hov) to confirm the diagnosis? ELISA for HIV
can be false positive, particularly among "Iovj
risk* people.
3. To avoid the risk ofcontamination can a su rgeon or
a gynaecologist routinelyperform preoperat'rve HIV
testing? What happens ifthepatient withhAds con
sent? What to do during an emergency surgery ?
4. Can a doctor refuse to operate or perfo. rm any
invasive procedure on a seropositive patient ?
Second, the long clinical latency means th.it ;uiybodv
could be seropositive without showing any signs and
5. Has a doctor the right to thrust a moraljudgement
symptoms.
on a patient (and his/her behaviour) and then de
Third, because HIV is also sexuallv transmitted, i
cide his/her professional attitudes accordingly?
there is a prevalent attitude of attaching a stigma of j
I 6. Ho-w does a doctor arrange the folia
'ozo up and treat“loose moral" to the infected.
ment
of
HIV
positive/AIDS
cases?
Fourth, as yet there is no cure for AIDS, and all
HIV positive^ have so far been seen eventually to
die due to AIDS or its complications.
8. Except under afev) circumstances a doctor is profes
sionally bound to maintain absolute confidentiality
about a patient and his/her condition. Should it be
follovoed in case ofHIVpositives?
Relating to the AIDS menace, the medical profes- i
sion has to come up with answers to a lot of ques- I
tions not only technical but also social and ethical, j
Let us look into the issues more closely.
However, disclosure may break thefamily and ruin
the patient. Hovo to prevent the social catastrophe
arising out ofdisclosure ?
Should the doctor inform the spouse about the
patient's seropositive status ? Nondisclosure may
spread the disease and may infect the spouse
9. Should a HIV positive denied social and zj•orbing
1. As in other biomedical investigations, a doctor connot '
rights ? What follovos is, if a doctor becomes
ask for HIV testing (e.g. ELISA) without the con- |
seropositive should he/'she be debarredfrom handling
sent ofthe patient - voluntary and Informed. More- ‘
patients ?
over, because of the consequences uj
•
tionassociai/dwithAIDS.pretestcouncellirigisman- ; .10. How to prevent iatrogenic AIDS ? How can a doctor raise the demand individually and collectively da tory. Ge vet; our busy practice, are we prepared/'
ofensuring aseptic procedures in medicalpractice ?
tuned to do this
i
91
39
•
i
7. Hovj to trace the source/route of transmission in a
specific case, in ord^r to preventfurther transmis
sion from the same source ?
The fear of physical risk and social contamina
tion virtually stigmatises a HIV positive into a so
cial outcast. What inevitably follows is discrimination-a HIV positive is denied his/her basic rightsthe right to live (in a community) and work and
what is important in the present context-right to
be treated.
Drug Disease Doctor
f*
I
I
1
Obiter dicta
92
1
•
Absolute quarantine of all HIV positives has been tried in different parts of the world.
But this has failed to contain the epidemic. Testing all persons for HIV is theoretically
possible but logistically impossible in a country like India. Even testing all persons be
longing to so called high risk groups is virtually not possible.
•
Large multi-institutional studies have indicated that the risk of HIV transmission fol
lowing skin puncture from a needle or other sharp object that was contaminated with
blood from a person with documented HIV infection is approximately 0.3%. The risk of
a similar type of exposure to hepatitis B is 20 to 30%.
•
The above mentioned risk, however small becomes a potential threat in Indian condi
tions. In most hospitals and pathological laboratories here, medical personnel draw
blood without wearing gloves and bloc J opill-ge and skin puncture are common
occurences. Anaesthesiologists almost never use gloves. Dentists all over the country
usually perform all outdoor dental procedures without wearing gloves.
•
Nosocomial HIV infection is a reality. In a reported incident in Soviet union 152 neo
nates were infected through use of contaminated syringes and needles. This is of par
ticular concern in the Indian situation Disposable syringes and needles are not only in
short supply in most hospitals, these are often reused after washing or boiling. There is
generally a casual approach to sterilisation procedures except in the operation 'heaters.
(Consider the daily morning activity in the •..•aids when almost all patients have their
blood samples taken.)
•
HIV infected persons have relatively greater number of viruses in their blood during
two stages - the initial post infection viracmic stage and much later during the symp
tomatic stage. During the initial phase of infection lasting tor an average of 2 weeks
(and a maximum of 8 weeks) the HIV infected is seronegetive. What follows is at this
time though the person is ELISA negative, he/she can transmit infection.
•
Ina hospital set up or even in a private clinic, unless spccificallv informed, a doctor may
have no idea as to which of his\her patients belong to the high risk groups. High risk
groups are those who are involved in high risk behaviour (sex workers, clients of sex
workers, intravenous drug users) and the se \ rho are being repeatedly treated with blood
or blood products (haemophilia or thalassaemia pudents).
•
The risk of HIV transmission from an infected doctor to his/her patient is extremely
small. Large multi-institutional studies have put the risk of acquiring HIV infection
from a doctor or a dentist during an exposure prone procedure at 1/1000000, which is
l/10,h the risk that a given unit of screened blood is HIV positive and l/100‘h the risk
of dying from general anaesthesia.
Drug Disease Doctor
39
T he number of HIV infected in this country is
steadily increasing. What happens doctor, if the
next patient in your clinic is HIV positive ?
What happens if the patient declares that he
is HIV positive ? Would you examine the patient
or would you refer him to some other doctor ?
What happens if the patient does not declare
or is himself unaware that he is HIV positive. Is
your system of patient handling such that you
yourself would not be contaminated and would
not transmit the infection to your other patients ?
If you are a professionally active doctor you
can hardly avoid handling a HIV positive. What
is most needed is a predetermined approachscientific, ethical, humane and bold.
The AIDS pandemic has shown its capacity
to evolve and permeate all sectors of society. It is
useless to think that my patients cannot be HIV
positive, as they are all good and respectable
people. Complacency, indifference, denial and
a “business as usual” attitude threaten the
success of the struggle against AIDS.
It is obvious that neither does screening ex
clude all HIV positive nor is screening feasible in
all situations. What is feasible is strict adher
ence to standard procedures of asepsis in
medical practice - irrespective of who your
patients are.This is the only tenable method
of avoiding the transmission to your other
patients. There is no need to shun awav the HIV
positives if you adhere to the nonns of asepsis.
their fight against AIDS. Ultimately in the
end we all have to adapt to the situation of pro
viding optimal health care to the HIV positives
and AIDS patients without discrimination and
with due protection of their rights and dignities.
The quicker we reach the stage the better.
We must remind ourselves of the paradoxi
cal situation that if discrimination persists,
not only will people not volunteer for HIV
testing, but will also hide their HIV sta tus.
Discrimination arises out of misinformation
and ignorance. But that is not all. The relation
between knowledge and behaviour is far more
complex. But knowledge and awareness is the
p ria ma ry pre requisite for behaviour modification.
What follows is that our first task is to know about
HIV and its transmission. Only then can w; take
up the challenge to fight the epidemic.
In the fight against AIDS doctors arc speak
ing in the language of human rights and di >nity.
Measures to.protect human rights will not of
themselves guarantee an effective AIDS
programme, but denial of human rights is clearlv
incompatible with effective AIDS prevendoh and
control.
Today, it is important to realise that
social solidarity has now become
a public health goal, on which
the survival of entire societies
may depend.
— Carballo &. Bayer
r»
,
’I
Today in India, there are media reports oil" and
on of discrimination against HIV positive - in
References
the communit}’ and also in the health care set 1. Harrison i Princifies of Imemal Medicine, 13th edition 1994
ups. But the HIV positives and AIDS patients 2. HIVrisks in the health care organisation,Julie Louise Gerberding,
AIDS 1990, 4 (suppl 1)
are being treated the world over in general hos
3. Glohai AIDS: revolution, pa rudi^tn and solidarity,Jonathan Mann.
pitals, private clinics and in intensive care units.
AIDS 1990, 4 (suppl 1)
Why is the situation different in India ?
4. Social Cultural and Political Aspects, Manuel Carballo and Ronald
B«yer,AIDS 1990,4 (suppl 1)
Such avoidance reaction have occured all over
the world. But many doctors have also engaged 1 Asish Kumar Kundu
Drug Disease Doctor
I
39
93
A
Declaration of Standing Committee of
Doctors of the EC
The Standing Committee of Doctors of the European Community (EC) adopted the following Declaration concern
ing the practice of medicine within the Community at its Plenary Assembly Session held in Nuretnbtirg in
November 1967 (Charter of Nuremburg (original in French)). The text is as published in The Handbook of Policy
Statements 1959-1982, Standing Committee of Doctors of the EC.
1. Every man must be free to choose his doctor. Every man must be guaranteed that whatever a doctor’s ob ligations
vis-a-vis society, whatever he confides to his doctor and to those assisting him will remain secret.
Every man must have a guarantee that the doctor he consults is morally and technically totally independent and that
he has free choice of therapy.
Human life from its beginning and the human person in its integrity, both material and spiritual, mus^e the object
of total respect.
Guarantees of these rights for patients imply a health policy resulting from firm agreement between those responsi
ble to the state and the organised medical profession.
2. The aim common to the health policy of states and medical practice is to protect the health of all its citizens.
It is the duty of states to take all precautions to ensure all social classes - without discrimination - have access to all
the medical care they require. Every man has the right to obtain from the social institutions and the medical corps
the help he needs to preserve, develop or recover his health: he has an obligation to contribute materially and
morally to these objectives.
Economic expansion finds one of its principal human justifications in the advancement of resources allocated to
health; the medical profession intends to do all in its power to increase, at equal costs, the human and social effec
tiveness of medicine.
3. The unusual necessary contact between the doctor and his patient take account of the fact that these two partners
belong to one community, a condition of all health and social policy. But there must be reciprocal confidence
between the patient and his doctor based on the certitude that in his treatment the doctor holds in the highest esteem
and has consciously consecrated all his knowledge to the service of the human person. No matter what hi s method
of practice or remuneration the doctor must have access to the existing resources necessary for medical intervention; he must have free choice of decision bearing in mind the interests of his patient and the concrete possibilities
. offered by the advancements of science and medical techniques.
Doctors must be free to organise their practice together in a manner complying with the technical and sociaf need of
the profession, on condition that moral and technical independence be respected and the personal responsibility of
each practitioner maintained.
4. Whatever is method of practice the medical profession is one. These methods are complementary. They derive
from the same deontology although they may be submitted to different organisation conditions. Respect for moral
laws and for the basic principles of medical practice is assured by independent institutions, emanating from the
medical corps and invested, particularly under the highest judicial processes in the country, with disciplinary and
judicial power.
Every doctor lias a moral obligation to actively parucipate in his professional organisation. Through this organisa
tion he participatcs in the elaboration of the country’s health policy. Members of (he profession can and must fight
for respect of basic principles in the practice of medicine, on condition that the rights of the patient are.safeguarded.
5. Hospital equipment must be within the compass of its specific mission in the service of the whole population. Its
establishment is the result of a planned policy in which the public powers and the organised profession participate,
allocating to public power and private initiative fuller distribution of health establishments. It comprises, a variety
of establishments, graded and co-ordinated among themselves, meeting the task or several tasks given to t: prevention. care, rehabilitation, teaching, research.... The professional independence of the hospital doctor must be
guaranteed by unquestionable criteria of nomination and a statute assuring him stability of function, economic
independence and social protection.
‘Technical progress, the basis of our industrial civilisation and economic expansion which is its fruit have for their
natural end especially thanks to a health policy, to bring about full physical and spiritual development of man. of ail
men’.
[Rowe AJ et al: Philosophy
102
Practice of Medical Lillies. London: British Medical Association 1988. |
Issues in MEDICAL ETHICS
VOL.4 NOJ JUL-SEP 1996
facts
from the
Regional Health Report
10 countries make up the WHO
South-East Asia Region (SEAR)
— Bangladesh, Bhutan, DPR
Korea,
India, Indonesia,
Maldives, Myanmar, Nepal, Sri
Lanka and Thailand.
Population &
Socioeconomic
Situation
About 1.4 billion people live
in the WHO South-East Asia
Region. The 10 Member States
comprise 25% of the world’s
population and only 5% of the
world's land area.
Over the past 15 years the
Region’s population has grown by
367 million and is expected to
increase by another 380 million
during the next 15 years.
Population growth rates of
most SEAR countries have declined
since 1980-85. Three countries Indonesia, Sri Lanka and Thailand
have annual growth rates lower than
the world’s growth rate of 1.57%
(1990-95).
Jw
The number of people living
in urban areas has increased from
almost 229 million in 1980 to 389
million in 1995, and is expected to
reach 460 million by the year 2000
and 641 million by the year 2010.
96
The average annual urban
population growth rate (1990-95)
is highest in Nepal at 7.07% and
lowest in Sri Lanka at 2.20%. The
Region contains four megacities Mumbai, Calcutta and Delhi in
India and Jakarta in Indonesia.
F
In 1995 there were a higher
proportion of children aged 0-14
years living in the SEAR countries
as compared with the rest of the
world; but lower proportions in the
adult (15-64 years) and elders (65
years and more). This trend is likely
to continue until 2010. The number
of elders in the Region is expected
to increase by 10.6 million during
1995-2000, putting a greater
pressure on the health-care and
welfare system.
Most countries showed a
steady GNP growth rate during
1992-94. The gross national product
(GNP) per capita in the Region
ranges from a low of US$170 in
Bhutan to a high of US$2110 in
Thailand (1993). India, Indonesia
and Thailand are included among
twelve major developing economies.
The amounts spent on health differ
among countries. As a percentage
of total income (in terms of GDP),
expenditures range from 2% to 6%
including both government and
private expenditures.
Data on burden of poverty in
1990 were available for six SEAR
countries (Bangladesh, India,
Indonesia, Nepal, Sri Lanka and
Thailand) which represented 95%
of the total SEAR population and
included 507 million people in
poverty - whose income or
expenditure level was below the
amount considered necessary to
afford a minimum, nutritionally
adequate diet plus essential non
food requirements. Poverty is also
widespread in some other SEAR
countries.
'S Literacy rates in 1995 ranged
from 40.9% and 14% for males and
females respectively in Nepal, to
100% for both sexes in DPR Korea.
Nepal, Bangladesh, Bhutan and
India have the lowest female literacy
levels of between 14% apd 38%
respectively. Countries wi(h higher
female literacy tend to have lower
infant mortality.
9
Countries with low fertility
have a higher human deve opment
index (HDI) and gendcrirelated
development index (GDI). Only
one SEAR country (Thailand) has
HDI or GDI above 0.8, putting it in
a higher human development
category. Much progress remains
to be made in gender equality in
almost every country of the Region.
Efforts are to be made so that women
are able to participate in political
decision-making, to increase their
access to professional opportunities,
and improve their earning power.
Births, Deaths
and Life
Expectancy
ire
Since the 1970s, the
birth rates in the Region declined as
crude
a result of population control and
family planning efforts. They now
range from a low of 19.4 in Thailand
to a high of 41.6 in the Maldives.
Thb world average is 25 per 1000
population.
F Women had fewer children in
the past five years than before as
seen from the decline in the total
fertility rate (TER) for the Region.
CA facts from the
Stir Regional Health Report 90
During 1990-95, the TFRs ranged
from 2.10 children in Thailand to
6.80 children in the Maldives per
woman in the reproductive age
group of 15-49.
jfi
Life expectancy at birth
showed an increase for all SEAR
countries. During 1990-95 it was
below 60 in Bangladesh, Bhutan,
Myanmar and Nepal; it was
between 60 and 69 years in India,
Indonesia, Maldives and Thailand
and was 70 years or above in DPR
Korea and Sri Lanka.
K There has been a significant,
steady decline in the crude death
rate in the Region, now ranging
from 5.3 per 1000 population in
DPR Korea to 13.3 in Nepal. These
rates must, however, be viewed
with caution as death registration
systems in most countries remain
inadequate.
The infant mortality rate
(IMR) declined in all countries, but
Bangladesh, Bhutan, India,
Indonesia, Myanmar and Nepal
still have unacceptably high rates
of 70 deaths or above during the
first year of life per 1000 live births.
DPR Korea, Sri Lanka and Thailand
have IMRs below or around 30 per
1000 live births.
Morbidity and
Mortality
Communicable Diseases
F Almost 7 million people in
SEAR countries die each year from
infectious diseases alone. Infectious
diseases are the leading cause of
death worldwide, killing at least
17 million people annually.
F Approximately 1.4 million
children under five die each year
from acute respiratory infections
(ARIs) accounting for more than
30% of deaths in undcr-fivcs.
Pneumonia is the leading cause
taking 90% of this total. Deaths
due to pneumonia could be signi
ficantly reduced by the use of
standard case management as
recommended by WHO ARI
Control Programme.
Tuberculosis still kills more
adults than any other single
infectious disease - an estimated 1.2
million people in the Region will
have died during 1995. 80% of
these deaths are in the most
productive age group 15-59 years,
thus affecting socioeconomic
development of countries. The
most effective way to stop the
spread of tuberculosis is by
curing it and the best curative
method known is directly observed
treatment short course (DOTS).
|F5 TB/HIV co-infection
is
present in many patients - by 2000
it is estimated to increase to
nearly 20% of all TB cases. The
proportion of TB deaths attri
butable to HIV in the Region will
also increase from 2% in 1990 to
14% by 2000.
F The total number of the
leprosy-afflicted in the Region is
more than two-thirds of the global
leprosy cases. Four countries Bangladesh, India, Indonesia and
Myanmar are among the top five
countries accounting for fourfifths of the global case load. Yet
multi-drug therapy (MDT) has
proven so successful that it is
expected to eliminate leprosy as a
public health problem by 2000.
F The Region has achieved a
high level of immunizing children
under one year against the six
immunizable diseases - diphtheria.
pertussis, tetanus, tuberculosis,
poliomyelitis and measles. By the
year 2000, ninety per cent of women
in the child-bearing age will have
been immunized against tetanus.
The Region has demonstrated
dramatic acceleration of polio
eradication activities, particularly
with the implementation of
national immunization da; in seven
SEAR countries. Health experts
are confident that they will be able
to eradicate poliomyelitis through
effective universal immunization
and adequate epidemiological
surveillance.
F A 70% reduction in the
number of reported diphtheria and
whooping cough cases has been
achieved as a result of the 90%
immunization coverage.
39
The total number of measles
deaths in the Regie n has
decreased by about 87% and the
number of reported cases has fal Ion
by about 67% as a result of about
80% immunization coverage.
r4 Five SEAR countries (phular,
DPR Korea, Maldives, Sr Lanka
and Thailand) have achieved the
target of no more than one neonatal
tetanus case per 1000 live births.
IK The pandemic of HIV/AIDS
has spread rapidly during he last
few years in the South-Eapt Asia
Region. It is estimated hat by
the end ofthe century, 8 to 10 million
men, women and children are likely
to become infected wit 1 HIV
accounting for over 25% of the
global cumulative infections. The
spread of AIDS/HIV is particularly
significant in India, Myauniar and
Thailand.
F The total number of curable,
sexually transmitted diseases
(STDs) in the South-Eas Asia
Region were 150 million cases in
1995.
r
Each year, approximately 14
million people are infected With the
hepatitis B virus, and it is est mated
that there are 80 million carriers, i.e.
CA fac*s ^rom the
vV Regional Health Report 90
more than 5% of the total
population.
Diarrhoeal diseases continue
to account for about 25% of underfive mortality in the Region, viz.
over one million children die each
year from diarrhoea. 90% of these
deaths are preventable.
Malaria still dominates the
disease pattern in the Region with
1.2 billion people living in
malarious areas, and at risk. The
overall malaria situation in the
Region has remained static over
the last twelve years - with reported
cases ranging between 2.5 and 3.1
million, and reported deaths
between 5000 and 7500. The
estimated numbers of malaria
cases and deaths are much higher.
The emergence of drug-resistant
malaria and its rapid spread are
posing a major threat to the Region,
and putting severe pressures on
the countries' scarce resources.
Dengue
and
dengue
haemorrhagic fever continues to
persist in several countries - an
estimated 400,000 cases with
8000 deaths were reported in the
Region during 1995. Tetravalent
live attenuated dengue vaccine
has been developed in Thailand,
with support from WHO, and
clinical trials of this vaccine in
children are under way. This is
the first time a developing country
has successfully carried out the
development of a vaccine for
human use.
RT
In India alone, there are an
' estimated 45 million microfilaria
carriers and 19 million people in
the Region are suffering from
filarial diseases, and approximately
500 million people arc at risk.
32 During 1995 there were an
estimated 21,000 cases of Jap
anese encephalitis with 4000
deaths in the Region. In the same
year, the number of meningo
coccal meningitis cases was
estimated to be 20,000 with 5000
deaths.
33 At present, approximately 110
million people in the Region are at
risk of contracting visceral
leishmaniasis (kala-azar). Major
endemic foci have been reported
in border areas between India,
Bangladesh and Nepal. A dramatic
decline in kala-azar cases and
deaths is reported in India since
1994.
No plague cases have been
reported in the recent past from
Bangladesh, Bhutan, DPR Korea
or the Maldives. But natural foci of
plague exist in India, Indonesia,
Myanmar and probably in Nepal.
The reappearance of human
plague in India in 1994 after 27
years caused much concern,
necessitating regular serological
tests of rodents for predictive
surveillance and laboratory
diagnosis of plague in the Region.
Non-communicabie diseases
P5 In India alone, nearly 800,000
persons die from ischaemic heart
disease and more than 600,000
from stroke each year. A health
survey in New Delhi showed that
every tenth person aged 35-64
years suffers from ischaemic
heart disease, and every fourth
person has high blood pressure.
The most common neopl
asms in India are cancers of the
breast, uterine cervix, lip. oral
cavity and pharynx In Thailand,
liver cancer is the most frequent
malignancy among males (8000
new cases every year) and lung
cancer is second in rank
(4700 cases). These two cancers
account for 44% of all new
malignancies in men. In women,
cervical cancer is the most frequent
(5600 cases annually) followed by
liver cancer (3500), breast cancer
(3300) and lung cancer (2600).
These four cancers account for
52% of all malignancies in women.
^7 Diabetes mcllitus has a
prevalence of about 2% in rural
populations, but a prevalence of
3% and more in url an areas
suggests that urbanization and
affluent lifestyles could aggra
vate the risk of disease.
It is estimated that between 4
and 5 million persons ir India are
afflicted by a variety of severe
mental disorders at any given time.
However, facilities an< support
for the care of the afflicted are far
from being sufficient.
Smoking is attribJted to be
one of the main causes of cancers,
cardiovascular diseases and
respiratory ailments. 3very 10
seconds, somewhere in the world,
tobacco causes another death. It
has been established beyond
any doubt, that death rates for
smokers are two-to-three times
higher than for non-smokers of all
ages.
Other causes of Death and
Morbidity
RG
Accidents and injuries
constitute 9 - 10% of the total
mortality in India * with road
accidents accounting for the
maximum number of deaths.
RT
Some 585,000 maternal
deaths occur globally every year.
About 99% of these happen in
developing countries and 235,000
(40% of the total number) in
SEAR countries. A vast majority
of these lives could be saved with
simple available skills and local
technologies. Effective family
!
\
facts from the
Regional Health Report
..
a
planning, good antenatal care and
attendance of a trained midwife
during delivery arc some of the
crucial factors which could
significantly lower maternal
mortality.
£2 Protein-energy malnutrition
and the three micronutrient
deficiencies of iodine, vitamin A
and iron are the main burdens of
undemutrition in the South-East
Asia Region.
^5 The SEAR Region is home
to almost one-third of the
world’s blind persons. Much of
this blindness is avoidable and
curable. Cataract accounts for
nearly 70% of the total blindness
affecting 8 million persons.
Threats to health and
development from deteriorating
environmental conditions affect
everyone. The World Health
Organization ’s Health and
Environment Initiative aims at
mobilizing the national health
authorities to sensitize other
sectors such as environment,
agriculture, and municipalities to
include protection of health and
environment as part of their
development plansif.To address
urban environmentaT issues, the
WHO Healthy Cities Initiative
"strives to promote healthy living
conditions in urban areas with
local governments as key partners.
Health-Care
Infrastructure,
Approaches and
Resources
There are currently 42,774
health centres of various categories
and 164,337 subcentres operating
in SEAR countries providing a
range of outpatient and inpatient
services, and serving as first referral
points. In addition, more than
746.914 outreach sites, managed
by the community with technical
support from health centre staff,
have been established at the
community level in SEAR
countries.
^16 The WHO Regional Office
has successfully assisted Member
States in developing national
drug policies with a focus on the
availability of essential drugs for
primary health care. WHO
collaboration in the Region has
resulted in the establishment of
appropriate national drug
policies and programmes which
focus on the issues of rational
use, availability, accessibility and
affordability of essential drugs
as well as on their quality, safety
and efficacy.
R7 Many questions related to the
balance and relevance of human
resources still remain unresolved.
Newer problems of imbalances in
the types of health personnel and
their geographical distribution
are also emerging, and these need
to be addressed with care and
urgency. Considering the fact
that human resources for health
(HRH) utilizes up to 70% of health
budgets, some of these problems
lead to very costly imbalances. A
significant emerging factor which
contributes to the imbalance of
HRH in the Region is the increased
competition between the public
and private sectors.
The Challenges
Ahead
48 In 1978, health for all (UFA)
by the year 2000 seemed a
reasonably-paced, achievable
proposition. But now. with only
turn of
three years left before the U...
the century, many of the HFA
goals still seem rather distant
for the 10 countries of the SouthEast Asia Regy>n. The challenges
that lie ahead call for political
commitment, community nvolvcment, and a multi-sectoral approach
to health. A combination of these
three factors could well mcan a
healthier future for South-East
Asia.
^9 Sustainability is one of the
major challenges that governments
will have to face as the countries
move into the 21 st century. Muchof
the success of health prog rammes
is due to investment in terms of
financial and human resources by
countries, WHO, other UN (agencies
and bilateral donors, SEAR
countries will have to meet the
challenge of sustaining such
programmes on their own. Only
through vigorous programme
implementation will a significant
disease
impact be made on the cL
—-situation.
8U Population growthi will be
_ •accompanied by rapid
irbanizaL
tion in developing countries. The
urban population in SEAR is
expected to reach 43% of the total
by 2020. Countries will have to pay
serious attention to the needs of
urban infrastructure - sanitation,
safe drinking water, housing and
public transport - as well as to the
increase in demand for health
services. Providing accessible and
acceptable family planning
services will make a significant
contribution to the health of the
population as a whole.
j
•
'
’
zzJsbA World Health Organization
T-L.
p Regional Office for South-East Asia
v Indraprastha Estate, Mahatma Gandhi Marg,
New Delhi 110 002, India
MP
The National Law School - NOVIB Project on the Implementation of SocioEconomic Rights
Status and Implementation of the Right to Health in
the State of Karnataka: A Report
Report prepared by
Padmashree B.S
B.A.LL.B(Hons)
National Law School of India University
H
Towards a definition of the right to health
The conceptualisation of rights of individuals has been predominantly based on
the social and political institutions of the time, throughout history. Changes in
society brought about by the development of liberal humanist ideas and democratic
political practices, led to a gradual conceptualisation of rights for all human beings
Beginning with the magna carta, the Declaration of Independence of the United
States of America (1776) and the Declaration of the Rights of the Man in France
(1789), Libertyjustice, equality and human dignity became the essential attributes
of rights of human beings.
The modem concept of human rights, universal and inalienable, emerged from a
conjunction of moral, legal and political perspectives, defining the rights which must
be possessed by alLhuman beings, equally, embodied in the Universal Declaration
of Human Rights, 1948. The Universal Declaration of Human Rights, has in modern
times, become the primary instrument which defines and protects rights which
must be guaranteed to every human being, one of the most critical aspects of this
conceptualisation of human rights being the capacity of all individuals to assert
these rights.
Therefore, any analysis on implementation of human rights must proceed at two
distinct levels. One, whether the rights are available an possessed by all human
beings. And second, whether the human beings have the actual capacity to assert
these rights which have been theoretically made available to them.
Subsequent to the Universal Declaration of Human Rights, in 1966, the United
Nations adopted two major Covenants, one defining civil and political rights1 and
the other, economic, social and cultural rights2. Both Covenants came into force in
1976. The popular consensus on the division of the two sets of rights is that it is
linked to a political division of the role of state in the society. While civil and political
rights are rights held against eveiyone else, economic and social rights impose
duties on governments.
Although the international human rights system has its own limitations, it
remains a framework—one of the few—within which we may attempt to address the
issues of definition, injustice and abuse of human rights and fundamental freedoms
^he International Covenant on Civil and Politicsl Rights(ICCPR).
international Covenant on Economic, Social and Cultural Rightsf ICESCR).
fit
by governments at the global level. The discussion on human rights also provides a
focus for many of the moral and philosophical dilemmas we face in contemporary
society, and the process of determining norms which can be applied to all human
beings so that they may live with integrity and respect is one which challenges US
today in the face of the disintegration of many social and political institutions.
With this background on human rights, it is essential to locate a framework within
which to view the individual's right to health.
Right to Health in the Universal Declaration of Hu:inn? Rights, 1948
The provision pertaining to right to health is contained in Article 25 of the Universal
Declaration of Human Rights, which states as under.
Article 25
(1) Everyone has the right to a standard of living adequate for the health and well
being of himself and of his family, including food, clothing, housing and medical
care and necessary social services, and the right to security in the event of
unemployment, sickness, disability, widowhood, old age or lack of livelihood in
circumstances beyond his control.
(2) Motherhood and childhood are entitled to special care and assistance. All
children, whether born in or out of wedlock, shall enjoy the same social
protection.
Right to health as in the international Covenant on Economic, Social and
Cultural Rights, 197Q.
The International Covenant on Economic, Social and Cultural rights, in its Article
12, recognises right to health as:
Article 12:
(1) the State Parties to the present Covenant recognise the right of everyone to
the enjoyment of the highest attainable standard of physical and mental
health.
(2) The steps to be taken by the State Parties to the present Covenant to achieve
the full realisation of this right shall include those necessary for:
(a) The provision for the reduction of the stillbirth-rate and of infant
mortality and for the healthy development of the child;
(b) The improvement of all aspects of environmental and industrial hygiene;
(c) The prevention, treatment and control of epidemic, endemic, occupational
and other diseases;
(d) The creation of conditions which would assure to all medical service an 1
medical attention in the event of sickness.
The Wprld Health organisation and Right to health
According to the World Health Organisation, health is a
’state of complete physical, mental and social ivell-being and not merely
the absence of disease or deformity”.
This definition can be said to be the embodiment of the concerns of all human
rights instruments of the century, recognising that health is fundamentally a
function of the every society.
From the foregoing International provisions, and the Who definition, it becomes
possible to define an individual's right to health as his right to a complete physical,
mental and social well-being and not just a right to curative services.
This Right to Health is no doubt a right belonging to the category of social and
economic rights, and therefore, this definition of the World Health Organisation
envisages active participation and responsibility of the state in ensuring that health
is a part of the overall development process of the nation'3
The role of the state in ensuring the right to health
The Declaration of Alma Ata, and various other doctrines that have been built
up by member states through the World Health Organisation and other
international agencies embody a number of fundamental principles for health
development. Among these are :
1. The responsibilities of governments for the health of the people
2. The right and duty of people individually and collectively to participate in the
development of their health;
formulating Strategies for Health for all by the year 2000, World Health
Organisation, Geneva, 1979, Pg.l 1
4 Formulating Strategies for Health for all by the year 2000, World Health
Organisation, Geneva, 1979, Pg. 11
3. The duty of the governments and the health professions to provide the public
with relevant information on health matters so that people can assume
responsibility for their own health;
4. Individual, community and national self-determination and self-reliance in
health matters;
5. The interdependence of individuals, communities and countries based on their
common concern for health;
6.
More equitable distribution of health resources within and among countries,
including their preferential allocation to those in greatest social need so that the
health system adequately covers all the population;
7.
Emphasis on preventive measures well-integrated it curative, rehabilitative and
environmental measures;
8. The pursuit of relevant bio-medical and health services research and the speedy
application of research findings;
9. The application of appropriate technology through well-defined health
programmes integrated into a country wide health system, based on primaiy
health care and incorporating the above concepts;
10. The social orientation of health workers of all categories to serve people and
their technical training to provide people with the service planned for them.
The Alma Ata Declaration, further states that atleast the following should be
included in the primary health care:
Education concerning primary health problems and the methods of preventing
and controlling them;
n
Promotion of food supply and proper nutrition;
ci
An adequate supply of safe water and basic sanitation;
Maternal and child health care, including family planning;
11
Immunisation against the major infectious disease;
[i
Prevention and control of locally endemic diseases;
L!
Appropriate treatment of common diseases and injuries; and ,
II
Provision of essential drugs.
To achieve this goal of Health for all by 2000, the role of the state is crucial in the
context of ensuring basic health standards.
The World Health Organisation Document on 4 Formulating Strategies for health
for all by the year 2OOO*5, lays down certain referral guidelines for formulating
national policies, strategies and plans of action in order to achieve successfully the
goal of Health for All by 2000. A perusal of the same in the light of those adopted by
us in this regard, may shed light on the aspects over-looked and may also help
assessing our present position.
,
To sum up the major points, a national plan of action has to be:
□
A inter-sectoral master plan, including the action to be taken in all sectors
involved, to give effect to the policy. It indicates what has to be done, who has to
do it, during what time frame, and with what resources. It is a framework
leading to more detailed programming, budgeting, implementation and
evaluation.
n
Each country has to develop its health policy as part of overall socio-economic
development policies, in the light of its own problems and possibilities,
particular circumstances, social and economic structures, and political and
administrative mechanisms.
□
Primary health care forms an integral part of the country’s health system, of
which it is the central function and main agent for delivering health care. It is
also an integral part of the overall social and economic development of the
community. For primary health care to succeed, it will require the support of the
rest of the health system and of other social and economic health sectors
concerned.
□
The introduction of strengthening of the development processed needed to attain
health for all, will require unequivocal political commitment. It will most likely
have to be set in motion by political decisions by the government as a whole,
permeating all sectors, at all levels throughout the country and not merely by
the ministry of health or the health sector alone.
□
The overall social goal of health for all has to be broken down into more concrete
social policies aimed at improvement of the quality of life and maximum health
benefits for all. If the gap between the ’haves’ and the ’have nots’ is to be
reduced within and among countries, there will be a need in most countries to
formulate and put into effect concrete measures for equitable distribution of
5 WHO, Geneva, 1979.
resources. In many countries, this wil] imply the preferential allocation Qf health
resources to those in greatest social need as an absolute prioritVi as a step
towards attaining total population coverage.
11
Measures have to be taken to ensure free and enlightened community
participation, so that notwithstanding the overall responsibilities of the
governments for the health of their people, individuals, families, and
communities assume greater responsibility for their own health and welfare,
including self care. This participation is not only desirable, it i$ a social,
economic and technical necessity.
11
In developing health strategies, each country will have to take into account its
cultural and social patterns and its political system.
The W.H.O also recognises that, most countries are dealing with all these
aspects of planning, but not in a systematic and inter-related manner. The initiation
of a more systematic process may start with any of the above-mentioned steps,
subsequently leading to the remaining step being carried out in a systematic and
interrelated manner. Thus, there could be many possible entry points to the country
health programming process.
^7
The National health Policy, 1983
As a signatory of the Alma Ata Declaration in 1978, the Government of India is
committed to taking steps to provide Health For All by 2000 AD. In 1983, the
National Health Policy which aims at achieving this goal by 2000 AD, laid down the
specific goals to be achieved by the year 2000 AD as:
1.
Reduction of infant mortality rate from the present level of 125( in 1978) to
below 60 in 2000 AD.
2. To raise the expectancy of life at birth from the present level of 52 years to 64 tjy
the year 2000AD.
3. To reduce the crude birth rate from the present level of 32 per 100 population to
21 per 1000 by the year 2000 AD.
4. To reduce the crude death rate from the present level of 12 per 1000 population
to 9 by the year 2000 AD.
5. To achieve a net reproduction rate of one by the year 2000AD.
The National Health Policy lays down specific goals to be realised by 1985, 1990 and
2000, such that by the year 2000, the above mentioned could be achieved. In 1983,
this Policy was evolved by the Ministry of Health and Family welfare and approved
by the parliament, and it was sought to be implemented through the sixth and
seventh five year plan and the 20 Point Programme.
According to National Planning, the health sector has been divided into the
following sectors for the purpose of planning:
1. Water Supply and Sanitation
2. Control of Communicable Diseases
3.
Medical Education Training and Research
4. Medical Care, including, hospitals, dispensaries and primary health centres
5.
Public Health Services
6.
Family Planning
7. Indigenous Systems of Medicine
Since the inception of the National health policy,, the Central Government has
evolved various Programmes throughout which the agenda of the policy was sought
to be achieved. The agenda of the health department in each state is basically to
implement the Central Programmes in addition to the State Programmes and
activities in the health sector. Most of these schemes are with the aim to ensure the
availability of adequate infrastructure and medical and para-medical man power
such that goals of health care as envisaged in the national health policy can be
realised.
The Department of Health and Family Welfare Services in the
State of Karnataka and the provision of health services
The main objective of the Department of Health and Family Welfare Services is to
provide comprehensive health care services to the people of the state, by way of
implementation of various national and state health programmes of public health
importance, through its network of various types of Health and Medical Institutions.
Organisational Hierarchy6
The Director of Health and Family Welfare Services is the Head of the
Department, and is responsible to provide the Health Care Services to the
community by way of implementing various National and State Health Programmes
in the state.
The Directorate of Health & Family Welfare Services is located in the State
Head Quarters which has got Director, Health and Family Welfare Services as the
Head of the Department and Co-shared by the Director, Health Education a[id
Training.
Within the state of Karnataka, Primary Health Centres are established at the
rate of one for a population of 30,000 in plain and Maidan areas and 20,000 in the
Hilly and Tribal areas.
By strengthening Primary Health Centres, Health Care
delivery activities in the areas as per the Government of India pattern is adopted.
Primary Health Centres provide Primary Health Care in the areas to the net-work of
sub-centres and other Para Medical Staff. Primary Health care includes preventive
services, Curative Services, Environmental sanitation, Health Education, Family
Welfare Services and recording of vital statistics.
Various National Health
Programmes which are in force from time to time are also implementing through the
network of Primary Health Centres.
Furthermore, one out of every four Primary Health Centres is generally
upgraded into Community Health Centre,
which contain curative services in
addition to preventive services.
6
Status Report) 1990-1995) of the Department of Health and Family Welfare
Services, State of Karnataka.
In addition to Primary Health Centres, Community Health Centres and
District Hospitals, there are General Hospitals and Civil Hospitals in different parts
of the State
Sub-Centres are also established at the rate of one each for a population
block of 5000 in the Plain and Maidan areas and 3000 in hilly, Tribal and
inaccessible and remote areas.
Each Sub-centre is managed by Female Health
Worker who covers comprehensive Health Care activities in the areas allotted with a
due priority to the Maternal and Child Health Care and Family Welfare activities.
She is assisted by a Male Health worker who covers the population of the sub-centre
in the matters relating to Health Care activities, with a priority in the Malaria
Eradication and communicable diseases control programme.
In addition to Community Health Centres and Primary Health Centres, the
Primary Health Units are also providing Curative and Preventive services. Gradually,
these Primary Health Units are upgraded as Primary Health Centres in phased
manner to extend their field activities to cover the area by providing additional
infrastructure.
In the difficult and inaccessible areas, Mobile Dispensaries are also provided
especially in the Forest areas, Tribal areas and remote areas.
Status And Implementation of Right to health in the State of
Karnataka: The Report
The report on the Status and Implementation of Right to health in the State of
Karnataka, as the name itself suggests, consists of two major parts. The first part is
to define and identify what actually are the components of an individual's right to
health, and then, with those defined components of a right to health, an analysis
proceeds as to whether within our state of Karnataka, such a right to health exists.
The definition of a Right to Health
One major setback experienced by the author at the beginning of this report was the
definition of the right to health itself. It was felt that without really understanding
and attempting to define the ambit of an individual's right to health, it is not
possible to analyse the implementation of the right within a meaningful framework.
Therefore, th£ first half of the report completely focuses on attempting to define a
right to health. Starting from the Universal declaration of Human Rights, to the
International Covenant on Economic, Social and Cultural rights, to the Alma Ata
Declaration and the international goal of Health for all by 2000 and the various Who
guidelines for member states, a broader perspective of a right to health as can be
derived from all relevant international instruments has been presented.
With this background, the analysis proceeds to the National Health Policy of 1983 in
order to cull out the components of the right to health which have been recognised
at the governmental level. For a comprehensive understanding of how the National
health Policy envisages as an individual's right to health, the Policy has been
analysed in depth keeping the history of development of a health policy at the
Central level.
The analysis moves on to directive principle of state policy on the duty of the state
towards health and an overview of all the major central and State laws which deal
with the health standards, and the cases decided at the Supreme Court and the
High Court of Karnataka on issues of health.
With the help of all the above, the first part of the report tries to precisely arrive at
what actually constitutes a right' to health, and within what confines this right
should operate.
The implementation of right to health within the State of Karnataka
With the definition of a right to health mainly from the National Health Policy, and
supported by the provisions of other laws and judicial decisions in the first part, the
second part of the report is an analysis of the implementation of this right within
the state of Karnataka.
This part presents the Programmes and Schemes of the State of during the past 20
years and their implementation, with the levels of progress achieved. The main
strength of the report is that the analysis of working of the Department of the health
and Family Welfare Services and the progress in the past twenty years has been
completely supplemented by the State Government Reports of the Department of
Health and family Welfare.
With these statistics on the working and the organisational hierarchy of the
Department of Health and Family Welfare Services, the main focus of the report is
on whether today, is right to health an integral part of our overall developmental
process? If not, what lies ahead to achieve this?
Since this is the main focus of the report, to emphasise the fact that health is an
overall function of the society and cannot be a service provided in isolation, two
clear case studies are presented:
1. The status and problem of street children in Bangalore with an analysis of its
causative factors and a comparison of the reality with the agenda of the
Karnataka State Plan of Action for the Child (which was a plan starting in 1990,
with set objectives to lx? achieved by the year 2000). This is an attempt to
discuss and assess the objective of the state goal in the case of “children in
difficult circumstances* as set out by the state plan in the 1990, and the
position today, to clearly emphasise the link between health and other policies
at the central/ state level. This analysis derives its basis from the work done by
four students of the National Law School on the topic of Street Children in the
past nine months, specifically, street children operating around Cubbon Park
area of Bangalore, where the author of this report was one of them.
2. Another analysis on the point is the health and environmental problems caused
by aquaculture ( or Shrimp Farming). Shrimp Farming is presently one of the
most lucrative activities on the coastal areas in Karnataka, Tamil Nadu and
Andhra Pradesh, and is a steady foreign exchange source for the Government.
The work done by the Third Law Reform group of the National Law School
reveals that shrimp farming has severe public health repercussions.
/3
With the above two case studies, the last chapter of the report draws attentior
on the need to re-think health in light of the components of the right to health, the
inter-relation between health and other policy actions, especially in the light of
international developments and national obligations in the form of structural
adjustment programmes, India's obligation to grant process patents to
pharmaceutical products in the Trade-Related Aspects of Intellectual property
Rights and the availability and prices of drugs in the future and issues of equity in
provision of health services with the state of Karnataka and between states in the
country.
We obviously have several achievements to our credit such as reduction in
mortality rates or increase in expectancy of life at birth; the expansion of medical
research and education; the expansion of the health care services including
especially the establishment of the Primary Health Centres; the excellence of our
specialised institutions; the control of communicable diseases like malaria, small
pox, plague and cholera; the provision of MCH services on a larger scale; the family
planning programmes, and the investment of far greater funds than at any time in
the past. These achievements make us proud and give us greater confidence to
think and plan the road ahead.
But there are some greater failures on which the focus has to be shifted in
order to decide our way ahead. It has not so far been possible to integrate health
with overall development. This seems to be the major lacuna in our approach to
health services within the country. That is, we are still far away from the stage when
health could be considered as a major agenda in every policy decision of the
Government. Until and unless we reach this stage, we seem to be creating/
enhancing the health problems of the people on one hand and providing services
through primary, secondary and tertiary care centres on the other hand. This is a
sheer waste of resources.
(Note: A Table of Contents of the final report has been appended to provide for a
better overview.)
Table of Contents
1. Towards a definition of a right to health
a.
Health as a right in the Universal Declaration of Human Rights, 1945.
b.
Health for children as laid down in the Convention on Rights of the Child, 1989.
c.
Health for Women in various International Documents.
d. World Health Organisation's Health For All by 2000
2. Present Policy Pertaining to right to health in India
a.
The Constitution of India.
b.
National Health Policy, 1983.
c.
Outlook of the Sixth and Seventh Five Year Plans.
d.
Health as a right through Judicial Interpretation.
3. Status and implementation of the right in the state of Karnataka
a.
Legislations pertaining to right to health.
b.
Programmes and Schemes of the Government of India and the Government of
Karnataka implemented in our state
Rural Health Component of the Minimum Needs Programme
Medical Development Programme
MCH, Family Welfare and Immunisation programmes
National Leprosy Eradication Programme
National Tuberculosis Control Programme
National Programme for Control of Blindness
National Malaria Eradication Programme
Prevention and Control of other Communicable Diseases
Health Education and Training Programme
Nutrition Programme—Nutrition Education and demonstration
National Goitre Control Programme
Laboratory Services and Vaccine Production Units
Education and Environment Sanitation
Health Education and Training Programme
Curative Services
c.
Institutional Arrangements and the status of medical institutions in our State
d.
Budgetary allocation vis-a vis beneficiaries of health services in the state of
Karnataka
4. Health For all by 2000—a dream or reality?
a.
Strategies suggested by the WHO for a national health plan on health and our
National Health Policy of 1983—a comparison
b.
How far are we from ' Health For AH' as in the National Policy, 1983
I JT
5. Rethinking Health
a. Towards a comprehensive approach on Right to health, with two clear case
studies;
Street Children in Bangalore
The Blue Revolution
b. Conclusions on a right to health in the light of national and international
developments and issues of equity.
Io
A BACKGROUND PAPER FOR WORKSHOP ON SOCIO-ECONOMIC
RIGHTS
A PROJECT OF THE NATIONAL LAW SCHOOL OF INDIA UNDER
SUPPORT FROM NOVIB
AUGUST, 1998
INTRODUCTION
This is a project on implementation of certain social and economic rights. The
rights chosen are of education, health, work and environment. The location for study is
Southern India comprising the four States of Kerala, Karnataka, Tamil Nadu and Andhra
Pradesh. The object of the project is to know the present status of implementation of
these rights in the region and to find out how the level of implementation can be
improved through the processes of law and government. In short, it is a study on social
justice, a study aimed on mechanisms for delivery of social justice particularly to the
poorer sections of society who feel endangered by the policies of economic liberalisation
and structural adjustment.
The project extending to nearly 3 years is part of the extension services of the
National Law School of India University, Bangalore. The first part of the project which
is to conclude by August 1998 consists of four State-wise Task Forces looking at what
has been happening in their respective States during the last five decades and presenting
a Status Report on each of the four Rights in a specially-convened workshop of experts
including Government representatives and NGOs. This paper expects to provide a
proper context to the deliberations, raising issues and concerns relevant to the project in
the various sessions of the workshop.
Are Socio-Economic Rights, Rights at all?
In Law, certain individual needs or interests get recognized as a ‘right’, only
when they cast corresponding duties on those obliged to honour such needs, and when
a mechanism is provided for enforcement of such duties for violation of which certain
remedies are made available to the interest-holder.
According to the above proposition, all needs or interests, however basic it may
appear to be need not be recognized and/or protected by Law. If Law recognizes a need
but does not protect it by way of stipulating duties and providing reliefs if violated, such
need cannot claim to have the status of a legal right. It may be a conditional entitlement
or discretionary benefit which require further legal action to assume the status of a
“right”. To the beneficiary of such entitlements, there is no legal remedy enforceable
through courts and his getting the said benefit depends on the disposition and good sense
of those who command the resources and wield public power. However, once it is
legally protected (legal duties are prescribed and legal sanctions attached jeertain legal
1
F
F
consequences follow to the advantage of the intended beneficiaries. The Government
is obliged to honour the same by creating institutions, allocating resources, providing
equal access and undertaking accountability for its non-performance. This duty on the
part of the Government is a self-imposed one when they agree to extend the services
under a law which they themselves have enacted. Such a legal right can assume still
greater protection in the realm of rights jurisprudence if it is elevated as a Fundamental
Right protected under the Constitution. In such a situation the citizen need not entirely
depend on Government initiative for the fulfilment. There is no further legislation
ordinarily required for accessing Fundamental Right; the Government cannot excuse
itself from honouring such a right on the plea that there are not enough resources
available or they do not form part of their priorities.
Thus, from the citizen’s point of view, a basic need or interest is best protected
if it is a Constitutionally guaranteed Fundamental Right; the second best situation is
when it is part of the statutes and has been articulated in terms of content, conditions of
eligibility, scope of remedies if denied, system of administration for accessing the rights
etc.; the third situation of course less beneficial, is when the need or interest is
acknowledged by policy instruments evolved by the Government with commitments to
progressively implement programmes directed towards its realisation by the
beneficiaries. It is difficult to consider such a promised benefit as a right or even as a
entitlement as its availability is based on purely executive priorities and discretion which
may change with the change of Government or of policies. The worst situation is where
the need or interest remains only in public discourse or political rhetoric awaiting
articulation or attention of policy planners and power-brokers. It is then in the domain
of politics and not of law where political action, rather than legal action, is more
important.
What does the Project/Workshop Seek to Accomplish?
The purpose of the Project on Socio-Economic Rights is to find out where we
stand in respect of the basic need for education, health, employment (work) and clean
environment. There has been international treaties on each of these basic rights. India
ratified most of them and assumed obligations to protect these basic needs of people.
The Constitution of India put them as part of Directive Principles of State Policy and
commanded the State to treat them as “fundamental in the governance of the country”.
The Government at the Centre and in the States have in varying degrees legislated upon
these basic needs promising some benefits and entitlements, the quality and level of
services determined by policies and resources which the Government of the day thought
appropriate. After four decades of planned development, the Government adopted the
policy of liberalisation of the economy which meant that the citizen has to live with
market forces with lesser dependence on Governments. Given the fact that 50% of
India’s humanity are still living below the poverty line, that over 40% of people are still
illiterate, that there is growing unemployment and under-employment particularly among
the youth, that there is not even potable drinking water available to half of rural India,
and that the ecological balance is increasingly disturbed by the so-called development,
2
there is widespread apprehension of the quality of life that Indians will be forced to live
in the coming years. Looking around, people find that the language of rights is used
widely to take care of basic needs of people every where. As if to re-assure them in their
belief, the Supreme Court of India in recent times, by a process of liberal interpretation
of the “Right to Life” under Article-21 declared that the right guaranteed is the right not
for vegetable existence, but a life with dignity. Thus, it was clarified by the Court, that
right to life does include right to education, right to health, right to work and right to a
clean environment.
The people now want to access these rights and ask as to where they should go,
what they can get and how much of it as part of basic human rights. Admittedly, the
theory of socio-economic rights has not developed enough to provide satisfactory nonns
and standards for dispensing judicial reliefs in individual cases. The correlative duties
seem to rest not only in the Government but on individuals themselves and on society
as well. It is this dilemma which this project aims to address by looking at the existing
nature and scope of these rights and inquiring into how they can be enriched by
Governmental or Non-governmental initiatives.
Mechanisms for Enforcement of Socio-Economic Rights
Every right stipulates corresponding duties on others. In the case of basic human
rights, the duties are vested in the State and State agencies. The implementation of duties
and consequent protection of rights are organized both through conventional mechanisms
of Government and through some modem institutional arrangements. Among the
conventional mechanisms are the following:
(a)
The Legislative Assemblies through enabling legislations and appropriation of
budgetary resources;
(b)
The Executive Departments of Government through actual delivery of services
or providing conditions therefor; and
(c)
The Courts through adjudication of disputes thereron.
These are all State institutions which have limitations in respect of access, reach
and remedies. Therefore, in recent times a variety of new mechanisms have been
developed in liberal democracies which play varying roles in protection and promotion
of human rights. Among them are the following:
(a)
The media including a free press through monitoring, reporting and building
public opinion;
(b)
Legal aid and public interest litigation;
(c)
Non-Govemment organizations, trade unions, political parties through mobilising
and lobbying efforts;
3
(d)
Reporting and compliance mechanisms of International Human Rights Law
under United Nations;
(e)
Ombudsman-like watch dog bodies like Lok Ayuktha, Women’s Commission,
SC/ST Commission, Minorities Commission, Back Classes Commission, etc.;
(0
Human Rights Commissions.
With such a range and variety of implementation and supporting mechanisms, no
one can argue that socio-economic rights are not rights because they are not enforced or
enforceable. However, if one considers only judicially enforceable rights arc real rights,
there can be doubt about the status of rights like education, health, employment and
environment.
Courts usually act when violations are complained before it. Socio-economic
rights warrant affirmative action rather than violation on the part of State. When can one
explain that one’s right to health is violated? One’s right to work is violated? It is indeed
difficult to be precise. Ifso, courts cannot act or give remedies. Perhaps, legislaturescan
or governments can provide reliefs. Does it mean that socio-economic rights arc suitable
for enforcement more through legislative and administrative processes, rather than
judicial processes? To be able to articulate the content of socio-economic rights, one
needs inputs from economists, sociologists, political scientists, medical, agricultural and
industrial specialists and a host of other experts apart from lawyers. Then process of
litigation of accessing rights is inadequate to absorb these extraneous inputs for balanced
decision-making of individual entitlements. These difficulties become evident in the
rather convoluted efforts ofthe Supreme Court in reading the right to education in Article
21 dealing with right to personal liberty. Nevertheless, the judiciary did take the struggle
on board and made an honest effort within the parameters of the judicial process to put
education, health, work and environment in the bill of rights.
From the limited experience of litigating these rights in Constitutional Courts on
the basis that they are integral to life and liberty, what have we achieved? Is the position
of the average citizen any way better than what was before in terms of enjoying the so
called rights of education, health, etc.? If citizens continue to knock at the doors of
Supreme Court and High Courts, can they access these rights? What do they complain?
When do they establish violation on the part of the State? What relief should they be
asking? Given the fact that approaching the highest court of the land every time a
violation occurs is not a practical proposition for the majority of Indian humanity, are
there other strategies for better accessing socio-economic rights? If ultimately courts
need to be used, what would a lawyer be seeking to establish in a cause of action? It is
this jurisprudence which this project is aiming to gather and build upon.
UNDP’s Human Development Index has sought to measure the progress in the
realisation of socio-economic rights by evolving certain “indicators” or bench marks for
identifying the core content of these rights. It is questionable whether these indicators
4
can be universally applicable, given the diversities in quality of life and standard of
living. Even if some indicators can help, there are difficulties in gathering acceptable
data and agreeable method of analysis for drawing conclusions. Nonetheless, in the
search for the core content of socio-economic rights, certain ‘indicators' are indeed
useful.
The prevalence of certain human rights postulates or principles such a non
discrimination, the right to information, equity in land holding, democratic participation
in governance, gender equality and parity in economic levels of living are said to be of
assistance in determining the prospects for realisation of socio-economic rights.
Analysis of Government policies, public expenditure patterns, reports of expert
committees and professional bodies as well as agreements entered into between
Governments and international financial institutions should give further material for
drawing conclusions on the realisation of socio-economic rights. A suggestion recently
made in this regard is to seek for every major project involving substantial public
expenditure a “human rights impact statement’’ analysing the nature and extent of
adverse effects of the proposed activity. The story of the Narmada Dam agitation
suggests possibilities in this regard for human rights protection.
The discussion above helps to re-examine the mechanisms and their relevance to
the contemporary situation in India. Poverty, illiteracy, unemployment and disease arc
still the lot of a large number of Indians. For them, all the talk of human rights make
little sense even after 50 years of Democratic Governments. The Constitution proclaims
social justice in eloquent terms. International Human Rights instruments are ratified by
India promising realisation of these rights by every section of Indian humanity. Political
parties swear in the name of social justice. The courts expand the scope of Fundamental
Rights and issue directions to the Governments for making basic rights accessible to all.
Despite all these and more, free compulsory primary education is not available to India’s
100 million children many of whom work in farms and factories. “Health for all’’ is a
distant dream and all types of diseases take their toll regularly. Half of rural India drink
polluted water and succumb to water-borne diseases. There is increasing unemployment
and occasional famine conditions at least in some parts of the country. What does the
future hold out to these millions of citizens? More rights may not mean more justice.
The question is of accessibility, accountability and responsiveness. Can Law, Politics
and Administration provide the answer?
Some Issues for Discussion
1.
Are socio-economic rights merely aspirations to aim at on a future date? Are they
just policies yet to mature into rights?
2.
Does a policy become a right by judicial interpretation or extension of already
existing rights? Is judicial enforceability a condition precedent for legal rights?
3.
From the citizen’s point of view, what difference does it make if education,
5
health, work and environment remain at the level of(a)
policies and declarations,
(b)
laws and regulations, or
(c)
part of Constitutional bill of rights.
4.
How does one know whether a “basic human need” has got the status of a legal
right? With reference to any of the four needs (education, work, health,
environment) please give minimum indicators Which can qualify the said need
to be recognized as a legal right.
5.
What are the constraints in the existing situations which inhibit the availability
of socio-economic rights to all sections of the people? Is it possible to expect the
realisation of the rights in the foreseeable future? What steps are required for the
above purpose?
Dr. N.R. MADHAVA MENON
6
NV °l
Chlormezanone
1/
Drugs
Chlormezanone
on sale in India
hlormezanone, a centrally
I
acting muscle relaxant with
minor anxiolytic properties
has been withdrawn from the French
market in October 1996.
This withdrawal followed a
European pharmaco-vigilance
survey conducted between January
1988 and May 1995, into the
association of chlormezanone with
<oxlc epidermal necrolysis.
Toxic epidermal necrolysis is the
most serious cutaneous drug reaction
and may be fatal. Onset is generally
acute and is characterised by
epidermal necrosis with a minimal
dermal inflammatory process.
The survey identified 153 cases
of toxic epidermal necrolysis. All
these cases occurred during normal
conditions of use.
A Health Education Publication
from the Christian Medical
Association of India
term use in anxiety or insomnia and
for muscle spasm. The BNF then goes
on to state that the clinical efficiency
of chlormazanone as a muscle
relaxant is not well established,
although it is often included in
compound analgesic preparations.
The severity of the drug reac
tions when weighed against
the limited therapeutic value of
the compound could not justify its
continued manufacture and the
product has been withdrawn.
In India, chlormezanone
continues to be available. According
to the Jan-March 97 issue of Drug
Today there are nine preparations
containing chlormezanone available.
These preparations are given in
the table below.
In the British National Formulary,
(BNF) chlormezanone is classified as
an anxiolytic. It is indicated for short
Reference:
Prescrire International
February 1997, Volume 6, no 27 and
Drug Today, Lorina Publications
January-March 1997
Christian
Medical
Assoc ation of
India
Technical consultants
Dr Molly Thomas
Professor and Chief of Clinical
Pharmacology and Adverse
Drug Monitoring Centre
Christian Medical College
and Hospital
Vellore
Mr Alan Cranmer
Consultant Pharmacist
Christian Medical
Association of India
Dr Stanley Macaden
Medical Superintendent
Bangalore Baptist Hospital
Bangalore
Editor
■Ti Ft*!*] I U: 11111 lb
Dicron-C (Kimron)
Diclofenac Sod. 50mg, Paracetamol 325mg,
Chlormezanone lOOmg. -
Dolobak (Brown & Burk)
Paracetamol 450mg, Chlormezanone lOOmg.
Electrogesic (sopd
Diclofenac Sod. 50mg. Acetaminophen 325mg,
Chlormezanone lOOmg.
Ibuflamar-MX ondoco)
Ibuprofen 400mg, Paracetamol 300rng,
Chlormezanone 250mg.
Myospas (Win medicare)
|
fl Wit 11 i I*] 11-:
Chlormezanone lOOmg, Paracetamol 450mg
Ontac Forte (Eider)
Diclofenac Sod. 50mg. Paracetamol 325mg,
Chlormezanone lOOmg.
Powergesic (jenburkt)
Diclofenac Sod. 50mg, Paracetamol 325mg,
Chlormezanone 100mg.
Prestifen-MR (Synthiko)
Ibuprofen 400mg, Acetaminophen 325mg,
Chlormezanone lOOmg.
Systaflam (Systopic)
Chlormezanone lOOmg, Acetaminophen 500mg,
Diclofenac Sod. 50mg.
Drugs Today, Issue no. 13.
Dr Alfred Edwards
Christian Medical
Association of India
All correspondence to:
Communication Centre
Christian Medical
Association of India
Plot No 2,
A-3 Local Shopping Centre
Janakpuri, New Delhi 110 058
0) 559 9991/92/93 or £52 1502
Fax: (011)559 8150
e-mail: cmaidel@giasdlO .vsnl.net.in
Printed at:
New Life Printers Pvt. Ltd.
Mukharji Nagar
Delhi
4
%
Drugs Today
Issue 15
September 1997
An Update on Rational Drug Use
Mefloquine Is now^
available in India bi
recommended on*iiyfor
the
u.v treatment ofcJrudWfc
JJ
resistant malaria.
R
efloquine, a 4 - quinoline
11 / I methanol compound
! V I chemically related to quinine
is now available in India. Marketed
under the trade name Mefliam by
Cipla, it is available as tablets
containing 250mg of mefloquine.
I
Action
Mefloquine is a potent, long acting
blood schizonticide active against
malaria parasites resistant to
chloroquine, sulfonamide/pyrimethamine combinations and other
4 - aminoquinolines. As it is very
slowly eliminated (plasma half life
10 to 40 days), a single weekly dose
of 250mg provides effective
prophylaxis. In uncomplicated
malaria a single dose of 15mg/kg
body weight is usually adequate.
Indications for use
in India
In India mefloquine is recom
mended only as a second line drug
in the treatment of malaria. It
should ideally be used only for the
treatment of chloroquine resistant
malaria and not as a prophylactic
or for the treatment of
uncomplicated malaria.
Mefloquine
use with caution
Neuropsychiatric adverse events
Mefloquine has been available since
1984 and some 16 million doses of
this drug have been taken, often
in combination with sulfadoxine/
pyrimethamine. Despite this
extensive usage, reservations about
using mefloquine, especially as a
prophylactic persist.
This review of the adverse
effects is compiled from western
sources, where mefloquine has been
used for prophylaxis and treatment.
As a result the adverse events
encountered under both treatment
regimens have been documented.
Frequent adverse events
Almost one in every five persons
who takes mefloquine
prophylactically notices some
dizziness, nausea, vomiting,
diarrhoea, or abdominal pain. These
symptoms are generally mild and
resolve without specific treatment,
but may be severe. These events may
be dose dependent. The incidence of
vomiting, which can prejudice the
outcome of treatment, is reported to
be some three times higher among
children given mefloquine at
25mg/kg rather than the more
common dose of 15mg/kg.
Over a ten-year period starting in
1985 more than 1500
neuropsychiatric adverse events,
associated with mefloquine were
reported. The most common were
affective disorders, anx iety
disorders, hallucinations and sleep
disturbances. A few instances of
continued on page 2
F
Adverse events
0 Gastro-intestinal — nausea,
vomiting, diarrhoea or
abdominal pain.
0 Neuropsychiatric — dizziness,
affective disorders, anxiety
disorders, hallucinations and
’ sleep disturbances are common.
Overt psychosis, tcxic
!
encephalopathy and
convulsions have been reported.
0 Cardiovascular — bradycardia
I'
and sinus arrhythmia.
ECG changes, when used with
related anti malarial drugs.
c.
continued from page 1
overt psychosis, toxic
encephalopathy and convulsions
have also been reported. Patients at
highest risk are those with a history
of neurological or psychiatric illness.
One-third of all convulsions
reported occurred in patients with
a personal or family history of
such events.
In the larger doses used for
treating malaria, mefloquine is
associated with a yet higher
incidence of neuropsychiatric events.
Among patients retreated with a
second dose of mefloquine within
one month, the overall incidence of
adverse events has been estimated to
rise some sevenfold and the risk
may also be increased by
concomitant use of quinine. These
adverse events developed more
rapidly among retreated patients.
Three-quarters were noted within
three days; few occurred with a
latency of more than 10 days, and
most had remitted fully within
three weeks.
New Drug
P. falciparum resistance to chloroquine
?n esistance to chloroquine was first reported in India In 1973. This
1\ was identified In North East India and since then has been
spreading. Unfortunately, the areas where resistance to chloroquine
has been identified have not been mapped, nor has a criteria for
identifying chloroquine resistant malaria been publicised. As a result
second line drugs are often used to treat uncomplicated malaria.
There is a very real danger that Mefloquine will be used indiscriminately
in the treatment of malaria. While it has been recommended that
mefloquine be dispensed only through hospitals our lax supervisory
mechanisms have ensured that it is freely available.
*
Mefloquine is a useful drug but it must be used only when required. In
India the only Indication for the use of mefloquine is severe falciparum
malaria or drug resistant malaria.
Criteria for suspecting drug resistance
The diagnosis of malaria rests on the demonstration of the parasite in
peripheral blood smears.
Both thin and thick blood smears should be examined. The parasitemia
is expressed as the number of parasitised erythrocytes in 100 cells and
then converted to the number of parasitised erythrocytes per microliter.
Drug resistance should be suspected and treatment modified if the
parasitemia does not fall below 25 per cent of the admission value,
48 hours after starting treatment or has not cleared by seven days.
its use during this
period for treating
malaria should be
Adverse effects are:
based on a risk
Transient
dose related
benefit analysis.
dizziness is a
Mefloquine
can
common
increased on retreatment
reasonably
be
complaint among
frequently seen, when
prescribed to protect
patients who
combined with quinine
non- pregnant
have taken
or
chloroquine.
women
of
mefloquine. A
childbearing
single dose of
potential, but pregnancy should
25mg/kg is reported to have caused
be avoided for at least three months
light headedness in each of seven
subsequent to the last dose.
volunteer subjects, and severe
However, in the case of an
incapacity for several days in
unplanned pregnancy, exposure to
four of them.
mefloquine is not regarded as an
Use in pregnancy and nursing
indication for termination.
mothers
There is no evidence that the
WHO currently advises that
small amounts of mefloquine
mefloquine may be given safely
excreted into breast milk constitute
during the second and third
a risk to breast-fed infants.
trimesters of pregnancy both for
Cardiovascular events
prophylaxis and treatment. The
Bradycardia and sinus arrhythmia
organisation recommends that
is estimated to occur in some twoprophylactic use should be avoided
thirds of patients treated with
during the first trimester, and that
Effects on
performance
mefloquine. Administration of
250mg mefloquine weekly for 4
weeks has not been shovVn to induce
changes in either the blood pressure
or the electrocardiogram of
volunteers. However, both
electrocardiographic abnormalities
and convulsions have been reported
when mefloquine is given together
with the related antimalarial
compounds, quinine, quinidine
and chloroquine.
These findings have aroused
concern that mefloquine and other
antimalrials might interact adversely
with cardioactive drugs including
anti-arrhythmic agents and calcium
channel blockers, and possibly with
antihistamines, tricyclic
antidepressants and phenothiazines.
However, cumulative experience has
been reassuring to the extent that
co-medication with such drugs is no
longer contraindicated.
Excerped from:
WHO Druv Information
vol 10, no. 2, 1996
Draff T»aay Issue 15
Drug Resistance
0
Resisfani organisms
Some strains of S. pneumoniae & H. influenzae are now
resistant to commonly used antibiotics.
Regional differences in antibiotic
resistance
The IBIS study has shown that
common invasive S.pneumoniac and
H. Influenzae show significant
resistance to chloramphenicol and
cotrimoxazole.(see below)
Strains with resistance to
I nfections by S. pneumoniae and
I H. influenzae are known to
I cause substantial morbidity and
mortality in infants and children
world wide. There are reports that
suggests that these two bacteriae
cause about 50 per cent of all
ospitalised pneumonia and about ,
20-40 per cent of all pyogenic
meningitis in the community.
The IndiaCLEN Invasive
Bacterial Infection Surveillance (IBIS)
study is an ongoing multicentre
project in India. The study is
conducted in teaching hospitals
from the southern, central and
northern states in India.
Materials and methods
The study is a prospective hospital
based, multicentre surveillance of all
invasive pneumococcal and
H influenzae diseases in six centers
in India. The study was initiated in
October 93 and is currently in
rogress at hospitals in Vellore,
New Delhi, Lucknow, Nagpur,
Madras and Trivandrum.
Microbiology procedures
From all prospectively recruited
patients 5ml or at least 2ml of blood
from children were cultured along
with specimens of other sterile body
fluids as indicated for isolation of
S.pneumoniae or H.influenzae.
Antimicrobial susceptibility testing
Antimicrobial succeptibility testing
for S. Pneumoniae and H. Influenzae
was performed using the disk
diffusion method. The antimicrobials
tested included Penicillin,
Cephotaxime, Cldoramphenicol,
Erythromycin, Cotrimoxazole for
S.pneumonaie and Ampicillin,
Chloramphenicol, Cotrimoxazole and
Cephotaxime for H. Influenzae.
Status of the IBIS Study
A total of 3600 cultures at the six
INCLEN centres have been collected
during the initial two years of IBIS.
The common penumococcal serotype
identified were type 1,4,5,6,16 & 19.
Types 1 to 5; account for more than
25 per cent of infections in India.
IBIS has shown that H. influenzae is
the most common cause of childhood
bacterial meningitis in India causing
30-40 per cent of culture positive
cases and is associated with 20 per
cent mortality. Also interesting to
note is the lack of resistance to
penicillin among the first 157
pneumococcal isolates. However the
data from 1996 (3rd year) shows that
there are a few emerging strains of
pneumococci that show resistance
to penicillin.
Cotrimox.
Delhi
40%
80%
Nagpur
53%
71%
i
s
Vellore
10%
30%
Drugs Today Issue 15
S.pneumoniae
23%
48%
H. influenzae
61%
42%
This variation could possibly be
attributed to the prior use of
antibiotics in these regions.
Excerpted from:
"Epidemiology of infections due to
S.pneumoniae and H. influenzae
in India"
IndiaCLEN Multicentre Study
Invasive Bacterial Infection Surveillance
(IBIS) Study Group
T t is difficult to make a
1 recomendation, on the basis
of the IBIS study, regarding the
drug of choice in Acute
Respiratory Infections (ARI).
The WHO recomendations are
correct but need to be qualified
In ARI when the ch Id is not
very sick, cotrimoxazole
may be given but requires
follow up.
-*■ In ARI when the ch Id is
quite sick, amoxicillin is a
better choice.
-- In a very sick child,requiring
hospitalisation the choice
would be I.V. penic Ilin along
with injection gentamycin.
E
□
Cotrimox.
It is noted that there is a wide
variation in the proportion of
resistant pneumococcal strains from
different centers.
Resistant pneumoccocal strains
Chloro.
Chloro.
L.
Dr Kurien Thomas
Professor of Medicine
CMCollege & Hospital
Vellore 632 004
3
n
Adverse Drug Reaction
A’
Terfenadine
Drugs
A Health Education Publication
from the Christian Medical
Association of India
and other antihistamines may cause arrhythmias.
| n February 1997 the French
I medicines agency decided to
I suspend all preparations of
terfenadine for one year. This
followed an increase in the risk
benefit ratio, based on a French
pharmacovigilance survey showing
new cases of cardiac arrhythmias
Long-established cardiotoxicity
The risk of cardiac arrhythmias such
as torsades de pointes* on terfenadine
was identified in the late 1980s, first
in cases of overdose, then after
concomitant treatment with systemic
ketoconazole. Deaths on terfenadine
have since been reported.
Terfenadine is almost completely
converted by the liver into an active
metabolite. In patients with severe
liver disease or taking drugs
inhibiting the metabolism of
terfenadine, its plasma levels can
increase sufficiently to disturb
ventricular repolarisation and cause
severe arrhythmias. Since 1992,
severe liver failure was a
contraindication to terfenadine
administration, and combining
terfenadine with several enzyme
inhibitors was contraindicated or
advised against. These enzyme
inhibitors included some antifungal
drugs (systemic ketoconazole)
and some macrolide anitibiotics
(erythromycin).
Provisional conclusions
The decision to take terfenadine off
the market was fully justified. This
drug was used for symptomatic
treatment of only mild conditions,
yet carried a risk of life-threatening
adverse effects; in addition, other
antihistamines appear to be safer.
Unfortunately the withdrawal of
terfenadine leaves a number of
problems unsolved.
Astemizole carries the same risk
of cardiac effects as terfenadine, and
is therefore not an acceptable alter
native. Loratadine might also induce
cardiac arrhythmias and sudden
death. Cetirizine seems to be the non
sedative antihistamine with the low
est risk of this type of adverse effect.
An m-depth reassessment of the
risk-benefit ratios of all members of
this class is clearly necessary,
bearing in mind that they are used
for mild conditions.
Recommendations
Pending the results of further
studies, we make the following
recommendations: do not trivialise
the prescription and dispensing the
antihistamines, even if those drugs
are claimed to be 'modern' and 'riskfree'. Follow the recommended
doses and watch out for situations
increasing the risk of overdose
and/or drug interactions (liver
failure, heart failure, polypharmacy
etc.) Bear in mind that the effects of
these drugs have rarely been
studied in children.
Excerpted from:
Prcscrire International
Vol 6, no. 30, August 1997
*Torsades de pointes is a type of ventricular tachycardia characterised by QRS
complexes with cyclical variations in amplitude and duration, oscillating around
the baseline and preceded by QT prolongation. Torsades de pointes usually
induce malaise and syncope, but can sometimes cause ventricular fibrillation
and cardiac arrest .
Drugs
Issue 15
Christian
Medical
Association of
India
Technical consultants
Dr Molly Thomas
Professor and Chief of Clinical
Pharmacology and Adverse
Drug Monitoring Centre
Christian Medical College
and Hospital
Vellore
Mr Alan Cranmer
Consultant Pharmacist
Christian Medical
Association of India
Dr Stanley Macaden
Medical Superintendent
Bangalore Baptist Hospital
Bangalore
i
Editor
Dr Alfred Edwards
Christian Medical
Association of India
Design & Production
Ms Indira Mark
All correspondence to:
Communication Centre
Christian Medical
Association of India
Plot No 2,
A-3 Local Shopping Centre
Janakpuri, New Delhi 110 058
0) 559 9991/92/93 or 552 1502
Fax: (011)559 8150
e-mail: cmaidel@giasdl01 .vsnl.net.in
Printed at:
ASK Advertising Aids (P) Ltd.
New Delhi 110 020
4
ri
>
1
az
Popular Bt nds Rate Low
Our laboratory tested 18 brands - > paracetamol, of which 9 failed — ala thing
for a drug most of us buy without ■ insulting a doctor. What’s more, widely sold
brands like Calpol, Crocin and Metacin . ere found at the bottom of our quality ihart.
O
cc
co
U_l
L-i ittle Bunty was groaning in
pain and fever. It was late in the
night, and his mother was
hesitant to ring up the doctor.
So she decided to give him a
tablet to reduce the fever. The
clock ticked on, but the fever
persisted. Until the next morn
ing, when the doctor changed
the brand.
Maybe, in this Test Report,
Bunty’s mother will find an
answer to her puzzle of that
night.
Many of us may have wondered
why a paracetamol we buy, often
without consulting a doctor,
and whose safety is taken for
granted, works at times, and at
times does not. No wonder, 9
out of the 18 paracetamol
brands we tested failed to meet
the Indian Pharmacopoeia (IP)
specifications.
’
WHAT IS PARACETAMOL ?
Calpol, Crocin, Metacin, etc.
are
familiar
brands,
indispensable in every home.
The generic name of the drug
in these brands is‘paracetamol’.
Paracetamol, in other words,
relieves pain and fever and is
taken also for relief from
headache, toothache, rheumatic
pain, flu, sore throat, earache,
and such others. Paracetamol in
different dosages is recom
mended for infants, children and
adults. For adults it comes in
tablet form, and for children in
both tablet and liquid forms.
Since paracetamol is available
without prescription, drug
quality is a very critical factor.
WHAT WE TESTED
We tested 18 brands of
paracetamol (national and
regional as well as generic
tablets) bought locally from
medical shops in
A h m e d a b a d.
;~
On the basis
of a national
market share
information
and our own
survey, we
went for a
We usually don’t consult a
doctor for minor ailments.
Calpol, a multinational
brand with the largest
market share (see
Appendix III) and
national brands like
Croc in and Metacin
could only get low
ratings, indicating poor
quality control. Their
large market share may
perhaps be attributed to
their large advertising
budgets, and not to
their superior quality.
CONSUMER CONFRONTATION.
4
I
We took up paracetamol for testing because of our
concern for (he safety of a widely-used OTC drug. More
so in the case of bulk drugs. Doctors in their private
practice often dispense drugs to patients. They
generally go in for bulk packs as they arc cheaper
compared to (he branded ones. Hospitals and public
health centres also buy in bulk. While some bulk
products arc of good quality and can be relied upon,
some others are not. Our lest findings supported this.
While
Paracetamol
liom
Manish
Pharmaceutical Works and Jay-Navy
Pharmaceuticals passed, Paracetamol
liom Supharma Laboratories and
Mercury Laboratories failed in some
parameters. We hope that the Food and
Drug Administration (FDA) effectively
monitors the production and sale of these
bulk formulations to prevent substandard
drugs from reaching the patients.
KEY FINDINGS
Out of 18 brands of
paracetamol tested, only 9 met
all the specifications required
by IP. This is disturbing in the
case of an OTC drug whose
“purity, safety and efficacy’’ are
taken for granted.
Pyrigesic, a national brand
from Calcutta with one per cent
market share, topped our quality
ratings with an overall score of
'll per cent. It was moderately
priced at 31 paise per tablet.
Calpol, a brand with the
highest market share of 6.5 per
cent, just met the minimum
requirement of 95 per cent in
assay. It hovered on the
borderline with 95.73 per cent.
National brands like Crocin and
Metacin were found at the
bottom of our overall ratings
table. This is indeed an eyeopener as these three brands
have captured the largest chunk
of the market.
Yet another revelation is that
two local generic products,
Paracetamol
of Manish
Pharmaceutical Works (71%)
and Paracetamol of Jay-Navy
Pharmaceuticals (55%) have
scored over some of the more
popular national brands such
as Crocin (50%)and Metacin
(43%) in terms of quality and
price. They were cheaper at 23
paise and 20 paise
respectively per tablet,
compared to 31 paise of the
branded.
Fifty per cent failure of the
tested brands may speak
volumes about the aspect
of quality control in our
country. Seven of them —
one
national
brand,
Pacimol, and 6 generic
products — failed in the
dissolution test. This is an
important parameter which
simulates the actual release
of the drug in our body.
Four of these generic
products could not meet
the requirements for
uniformity of weight. Two
of them. Paracetamol of
Jay Formulation, Ahmedabad, and Paracetamol of
Infinitive Pharmaceutical,
Disa, also failed in the
disintegration test.
W-
Our study indicates that
the generic products
display
considerable
inconsistency. While two
of them. Paracetamol from
Manish Pharmaceutical
Works and Jay-Navy
Pharmaceuticals, could
reflect a good GMP, the
rest eight could not.
representative selection of both the branded and generic forms of
the drug. (See Appendix II)
Seven of (hem are national brands : Calpol, Crocin, Metacin,
Pyrigesic, Pacimol, Dolo - 650 and Malidens. One local brand.
Demol, was also tested. The rest 10 market samples are generic
paracetamol tablets manufactured in Gujarat, four of which are sold
in bulk (1000 (ablets in a pack).
5
CONSUMIR CONFRONT
All brands were tested against the specifications and
procedures of the Indian Pharmacopoeia (IP). We also
used the US Pharmacopoeia (USP) specifications to
analyse the product’s quality against the benchmark of
international standards.
i
Paracetamol Content or Assay
The only active ingredient in a paracetamol tablet is the
chemical paracetamol. IP standards require that the actual
paracetamol content or assay in a tablet should fall within
the range of 95-105 per cent of the amount claimed on
the label.
Assay value denotes the percentage of actual
paracetamol drug present in the tablet, as against the
quantity claimed on the label. This information is vital in
evaluating the effect of a tablet on a patient. So assay
has the highest weightage in our overall rating.
All brands passed in this test. Surprisingly, Calpol gave
a borderline result of 95.73 per cent in assay, against a
minimum requirement of 95 per cent.
Disintegration
After it is consumed orally, a tablet must break into small
granules in order to release the drug it contains. If it
does not break into smaller pieces, it will not be absorbed
in the circulating blood to effect a cure. The
disintegration test makes sure (hat the tablet breaks
within 15 minutes, as specified in the Pharmacopo&ia.
Two generic products, Paracetamol from Jav
Formulation and Paracetamol from Infinitive
Pharmaceutical, failed in this parameter. They] took as
long as 25 and 40 minutes respectively to break down.
*
I
«
4
This means that if you take
these particular formulations,
they will have a very delayed
effect. The earlier a tablet
breaks, the faster the drug is
available to your body.
For this lest, a disintegration
apparatus which simulates the
process in the body, is used.
'I'liis helps in recording the time
taken by a tablet to disintegrate
(break down).
Among the brands that passed,
a wide range of disintegration
time from a mere 40 seconds to
a long 9 min.45 seconds was
observed. The longest time to
disintegrate was taken by
Pyrigesic (9 min. 45 sec.) of East
India
Pharmaceuticals,
followed by Crocin (5 min. 40
sec.). Metacin, Malidens and
Paracetamol
(Jay-Navy)
disintegrated in just about a
minute and a few seconds.
release of 10.7 percent and 12.5
per cent respectively.
Dissolution is a critical
parameter in determining the
performance and defining the
quality of tablets and capsules.
It measures the release of a drug
into the gastro-intestinal fluid
and is an essential first step in
drug availability to (he body.
Dissolution, therefore, has
been considered an important
parameter in our rating.
Though earlier dissolution was
only a parameter in USP, it has
now been incorporated in the
revised 1996 edition of IP.
Dissolution
Weight
Of the 18 brands tested fur
weight, 14 met the IP standards
of uniformity (95% - 105%). But
four generic paracetamol
produced by Lennecc Reme
dies, Mercury Laboratories,
Jay
Formulation
and
Supharma Laboratories failed
to conform to the standards.
11 brands indicated a good
dissolution percentage. This
test specifies that the paraceta
mol dissolved in a dissolution
medium should not be less than
85 per cent of the labelled
amount in 30 minutes.
Demol gave a marginally lower
standard of 94.75 - 105.03 per
cent in the test. This indicates
that the manufacturer has
chosen to comply with the
lower specifications in IP.
The best dissolution per
centage was given by Pyrigesic
of East India Pharmaceutical
Works (99.5%), followed by
Paracetamol of Supharma
Laboratories (98.6%) and
Manish Pharmaceutical Works
(97.5%), two bulk products. But
Metacin was found to have
only 85.4 per cent which is just
close to the required minimum
of 85 per cent.
Generic Paracetamol from
Infinitive Pharmaceutical and
Jay Formulation performed
poorly with an extremely low
BORDERLINE CASES
From our test findings on both
‘Ampicillin capsules’ and
‘Paracetamol tablets’, it appears
that quite a few manufacturers
comply marginally with the
statutory provisions, merely to
satisfy the minimum legal
requirements. These ‘borderline
cases’ may turn out to be less
effective than (hose with better
quality. They may also lake
more time to bring releif. And.
in turn, the consumer may noi
get good value for his money.
A few brands in the market
A glaring example is Calpol,
which gave a low reading of
only 95.73 per cent in assay,
against a minimum standard of
95 per cent. In dissolution too,
only 89.3 per cent of the drug
could dissolve in 30 minutes,
against a minimum requirement
of 85 per cent. Compare this
with the 99.5 per cent
dissolution rate of Pyrigesic.
Crocin and Malidens also
hovered on the borderline with
a percentage of 96.93 and 96.31
in assay.
Metacin, a widely - used
national brand with only 85.4
per cent dissolution rate and
the bulk Paracetamol from JayNavy with 86.9 per cent were the
other borderline cases in
dissolution. They also gave
borderline results in weight,
along with bulk Paracetamol
from Manish.
iratton
only determines
whether the
tablet breaks
. into granules or
Dissolution
gives
^information on
the actual
releajje of the
drug content
? from the tablet.
A generic product, Parace
tamol (Infinitive) could give
only 96.9 per cent in assay, and
Demol. a local brand, recorded
a lower weight percentage of
94.75 - 105.03 against the
CONSUMER CONFRONTATION
MAU APR
97
6
Paracetamol Tablets :
specification of 95 - 105 per cent.
OVERALL WEIGHTED
BRANDS
VALUE FOR MONEY
We compared the test results of
each paracetamol brand coupled
with its cost per tablet. We wanted
to find out if higher cost provides
better quality. But once more we
found that the costliest brand need
not be the best. (Our test findings
on Ampicillin also confirmed this
- see our Jan-Feb '97 issue). A
generic product. Paracetamol of
Manish Pharmaceutical Works,
coming second in our performance
rating with a creditable score of 71
per cent, also turned out to be
cheaper with 23 paise per tablet.
The cheapest was also a generic
Paracetamol from
Jay-Navy
Pharmaceuticals (20 paise), with
a good rating of 55 per cent.
Pyrigesic which came out of the
test with the best showing of 77
per cent was reasonably rated at
31 paise per tablet along with the
other national brands like Calpol,
Crocin and Metacin. The costliest
tablet
at
49
paise
was
Paracetamol of Shreechem
Laboratories which had failed in
the dissolution test (see Table).
WEIGHTAGES ASSIGNED
A panel of experts from the
pharmacy colleges in Gujarat and
pharmaceutical experts laid down
the final weightages for each
parameter, which helped in rating
and ranking the passing brands :
Valu
Bar chart
50
25
I
75
I
KK
PYRIGESIC
77
East India Pharmaceutical Works, Calcutta
D0L0 - 650
60
Micro Labs Ltd, Hosur (TN)
<
2
X <
5
CQ
MADDENS
51
Nicholas Piramal India Ltd. Pithampur. (MP)
CROCIN
50
Duphar-lnterfran Ltd., Mumbai
METACIN
S
43
Themis Pharmaceutical. Mumbai
CALP0L
38
Burroughs Wellcome, Mumbai
<
o
o
DEM0L
58
Debonair Pharmaceuticals. Ahmedabad
PARACETAMOL (Bulk)
£
5
o
Manish Pharmaceutical Works. Viramgam (Guj)
i
PACIM0L
71
PARACETAMOL (Bulk)
55
Jay-Navy Pharmaceuticals. Ahmedabad
| -.IPCAU^rf
_______________________
HaidSp Plurnuceutic
r______
.
PARACHAMtU.',
Sh^labor^
sm
s
_
PARACETAMOL^
Apollo Pharmaceutic
_________________________________ ____
■
PARACETAMOL^ ie
o
Ptern.aceu
£
5 PARACETAMOL
_ -L—_____ —
!»'■
■/
-'■’M
■
PARACETAMOL' '
''
'
__________________________________
uik).
Vadodara <Gu|)
..
... ..... .
.
PARACETAMOL
_____
■........................................................................................ ............................................................................................................... ................................................................
-
WEIGHTAGES ASSIGNED ►
7
_
■
lannvr Di-nedi.c
Assay - 36% (because it reveals the
actual drug content in the tablet)
Dissolution - 277c (because it
indicates the amount of drug that
reaches the site of action)
Disintegration - 13.57c (because a
drug has to break down before it
dissolves)
Uniformity of weight - 13.57c
(indicates the actual weight of the
tablet)
________
PARACETAMOL
100
Note : Weightages are indicative of the degree of relative importance between the characteristics tested for.
Price - 10% (Although price variation is
small, a 20-50 paise difference becomes
relevant with the varying income-groups in
India)
MAR APR '"7. CONSUMER CONFRONTATION
.
Thus , overall quality in terms of four
parameters is assigned 907c weightaie,
and price is assigned 107 weighlage.
<
I
i
Resu! ' -
Q-’
PRICE OF A TABLET
OF 500 mg
*
E L.
tings
I
Passing
Brands
V-.
I
I I
I
KEY
Borderline
Results
railing
Brands
Failing
Parameters
•JEB
UbMJ.CTITJSTlCS
&
ASSAY LIMIT
95% • 105%
DISINTEGRATION LI H
MAXIMUM 15 Mli.
UNIFORMITY OF WEIGHT
DISSOLUTION LIMIT
85% - 100%
LIMIT 95% -105%
RAISE
WEIGHTED
SCORE (m %)
PERCENTAGE
WEIGHTED
SCORE (in %)
TIME
(Mm./Sec)
WEIGH I ED
SCORE (in %)
PERCENTAGE
WEIGHTED
SCORE (in %)
MINI-MAX
(in %)
WEIGHTED
SCORE (in %)
31
09.7
103.52
30.67
9/45
04.81
99.5
25.87
97.23-102.70
05.56
37
08.1
100.24
18.86
4/25
09.! -
93.3
14.80
97.79-101.35
08.86
30
10.0
96.31
04.75
1/00
12.
95.2
18.20
97.48-103.85
05.51
31
09.7
96.93
06.98
5/40
08.45
94.7
17.28
97.40-102.12
07J18
31
09.7
99.43
15.98
1/30
12.18
85.4
00.70
96.49-102.60
04.48
31
09.7
95.73
02.66
3/00
10.83
89.3
07.67
97.76-102.00
07 51
30
10.0
102.13
25.70
2/35
11. '
91.1
10.85
94.75-105.03
-00.27
23
08.7
101.98
25.13
4/00
09J4
97.5
22.30
04.59
20
10.0
102.42
26.71
1/00
12.61
86.9
03.40
96.58-102.24
~~~~
96.79-104.03
-
977^
02.54
46.2
~
3o"
•
_________________
;
■
99.86
18.3
2/55 .•
__________ ___________________________________________ _____________
; V’-
49
99.97
2/45
38
101.14
2/25
30
96.90
40/0
40
100.90
»-i
18
__
98.86
0/40
100.70
7/15
101.77
25/0
.
- •
2
)
^,.454^
■ ■ I.
. -
'
147
-
i
' l a'
9773-10
I
■-
V
n 10.7
\72.6
—a 90.23-107.50
J
98.6
J
86.99-114.36
-
30
10
HOW THEY RATE
Oul of 18 paracetamol brands
tested, only 9 conlonned to all
the parameters provided by IP.
Quality-wise, Pyrigesic gave an
-■
92.43-107.19
J92.81-107.32
12.5
H___ _
_
36
13.5
excellent performance with a
score of 77 per cent, followed
bv Paracetamol from Vanish
Pharmaceutical Works
).
Quite surprisingly. Crocin
) and Metacin (43‘T ) and
Calpol (38%) came at the
r’d:.
13.5
27
bottom end of the table. These
three nrands, in spite of
adhering
to
the
lower
specifications in IP, might be
below par in therapeutic
effectiveness compared to the
rest.
•h
-.rK <. AikON
H
WARNING !
The major risk with
Paracetamol is poisoning
through overdose,
whether accidental or
intentional. Overdose
causes jaundice, liver
failure and death,
especially in adults who
absorb more than 15 g.
of the drug. Overdosing
can also be cumulative.
It is not recommended
lor those with liver or
kidney problems, or for
heavy drinkers.
It is also possible to take
too much paracetamol
accidentally when you
take different medications
such as cold remedies
and pain killers which
may also contain this
drug.
If symptoms like
diarrhoea, increased
sweating, loss of
appetite, nausea or
vomiting, stomach
cramps or pain, swelling
or tenderness In the
upper abdomen, bloody
or black stools, bloody
or cloudy urine, fever
with or without chills
occur, consult your doctor
immediately.
Anyone who has taken
an overdosage needs
prompt treatment
preferably within 12 hours
for possible recovery,
even though there may
be no visible symptoms.
MANUFACTURERS' VIEWS
Our policy envisages intima
ting the test results to all the
manufacturers, irrespective of
whether their brand has
passed or failed in our tests.
The results are posted to their
Registered Offices under
registered A.I). The manufac
turers receive only the results
of their own product without
any information on its rating
and ranking. They are given a
week from the date of receipt
to respond.
Lennecc Remedies, manufac
turers of generic Paracetamol,
cited disparity in weight “due
to the mistake of the technical
person who is handling the
punching section”. They
assured us of better quality
control in future.
Suphanna Laboratories, which
make generic Paracetamol in
bulk that failed in uniformity of
weight, stated, “We cannot
believe that our tablet does not
comply with uniformity of
weight”. They also clarified
that a “few tablets may lose
weight due to abrasion during
improper transit or bad
handling”.
We stand by our test results.
The testing is conducted
strictly as per IP specification
and the results are double checked before finalising.
Mercury Laboratories (bulk)
and Jay Formulation, whose
generic products failed in
uniformity of weight and
dissolution, and also in
disintegration in the case of the
latter, found our test results al
variance with (heir own.
We stand b\ our test results and
9
MAR-APR
'•»7, CONSUMER
CONFRONTATION
have notified the FDA of our
findings.
Shreechem
Lab oratorio s.
manufacturers of generic
Paracetamol, informed us that
“the products arc manufactured
as per IP specifications and the
additional test carried out by
you is not required”.
Debonair Pharma (Demol)
wrote back to say that “USP 95
is not binding on us because
we are manufacturing as per IP
standard”.
Nicholas Piramal India Ltd
(Malidens), informed us that
“we are not surprised that the
product also meets dissolution
test as specified in the USP
because our specification
already incorporates this test
from the very beginning”,
though “this is not mandatory
with respect to IP specifica
tion”.
We test products against
international standards not to
fail them, but to create
awareness particularly among
the Industry for improvement.
We have been vindicated in our
efforts by the incorporation of
the dissolution parameter in
the revised edition of IP 1996.
East India Pharma, manufac
turers of Pyrigesic and Micro
Labs (Dolo - 650) evinced a
keen interest in our findings
sought
detailed
and
information.
Test reports are for consumers:
No commercial use and
advertising of test results arc
permitted.
Calpol,
Manufacturers of
and
Crocin,
Metacini
Paracetamol
((Manish
Pharma) g
did not
respond.
No reply
• Methodology
was
of calculations
received
(Appendix I)
from the
page 14
manufac
• Names and
turers of
addresses of
these
manufacturers
failed
(Appendix II)
brands.
page 14
Vi/..;
I • Market share
Pacimol
information
( I P C A |I (Appendix III)
Lab), ;
page 14
Parace- [
tamol
Pharma)
(Rajdip
land
ParacetamolfApollo Pharma).
NEED FOR ACTION
Z?ERS proposes to
• circulate its Findings among
doctors, hospitals, government
purchase departments and
professional
concerned
associations;
• issue a Press Release on the
findings to all sections of the
*
media and consumer groups
around the country for wider
dissemination of information;
• initiate legal action under the
CPA against manufacturers of
failing brands;
• demand the recall or4
withdrawal of unsafe products;• seek corrective ads on false
claims.
We have requested the FDA to
initiate suitable action against
the erring manufacturers, and to
improve the monitoring system,
especially with respect to bulk
packings. In response we have
received an assurance from the
Drugs Controller General (India)
(hat (he Directorate proposes
‘To initiate suitable follow-up
measures”.
6
RATIONAL DRUGS
KNOW YOUR DRUGS
ANALGESICS & ANTIPYRETICS
(Continued from the previous issue)
Side-effects
J
Naproxen
Piroxicam
Codeine
Side-effects as for Ibuprofen
Side-effects as for Ibuprofen
Respiratory depression, tolerance,
dependance,
sedation, dizziness, nausea,
Warning
constipation, cough supression, urinary
Aspirin can produce abnormal bleeding tendencies in some
retention.
patients. These may be minor or serious in nature. Alteration (or
9. Morphine
Same as for Codeine
blackening) of stool colour in patients on long-term aspirin- j
10. Pethidine
Same as for Codeine
therapy should be brought to the notice of a doctor immediately. I
11. Pentazocine
Same as for Codeine
Aspirin
not be
children under
rvouniu should
diiuuiunvi
uv used
udvu in
in viiiiujlii
uuutl 12
14 years
VCdia of
Ul age
dUC !'«<%,-»
■■
.
.
...
/
.
12. Buprenorphine :
Same as for Codeine
as it can cause a dangerous condition called Reye s syndrome j
■
..
■
Drug
Interactions
which can be fatal. Ollier drugs could be used instead of this.
1. Aspirin or Acetyl
: Interacts with metoclopramide, an
2. Paracetamol : Prolonged use of this drug or overdose can
Salicylic
Acid
(ASA)
antiemetic drug which potentiates
cause liver damage. Except for this, there
the effect of aspirin.
are no serious side-effects for this drug
2.
Paracetamol
: Cholestyramine, a drug uped in
which is relatively safe for children.
hyperlipidemia causes reduced
: Gastrointestinal discomfort and heartburn, I
3. Ibuprofen
absorption of paracetmol. Meto- c
activation of stomach ulcers, hypersensi
clopromide causes potentiation of
tivity reactions, headache, dizziness and
the effect of paracetamol, j
"
vertigo, pruritus and skin rashes, fluid re
tention, ringing in the ear, blurred vision, Formulations banned
Note : Fixed dose drug combinations in general are to be
comeal deposits, nausea and prolonged
avoided in the rational use of drugs.
bleeding from wounds
4. Indo
1 Fixed dose combinations of vitamins with anti-inflam
: Headache, dizzines, gastro-intestinal ulcers
Methacin
matory agents (such as Ibuprofen) and tranquillisers.
and bleeding, drowsiness and confusion,
2 Fixed dose combinations of atropine, analgesic^ and
depression, syncope, thrombocytopenia,
antipyretics
hypertension, hyperglycemcia, blurred vi
3 Fixed dose combinations of vitamins and analgesics.
sion, corneal deposits,
peripheral
4 Fixed dose combinations of sedatives/hypno^ics/
neuropathy.
5. Diclofenac : Gastrointestinal
anxiolytics with analgesics and antipyretics
Sodium
discomfort and
bleeding, nau
sea, diarrhoea,
hypersensitivity
reactions (such
as angioedema.
asthma, rashes,
headache, dizzi
ness, vertigo,
tinnitus, fluid re
tention. revers
ible acute renal
failure in pa
tients with pre\ ious renal impair
ment and chronic
renal failure.
1. Aspirin or Acetyl
: Gastro-intestinal and skin rea
Salicylic Acid (ASA)
ctions in hypersensitive patients.
/
6.
7.
8.
Health Action • August ’97
35
Recommended dosage schedules
Ibuprofen
: Not to be used in
a. Pregnancy
b. Patients with Acid Peptic dis
ease
: Best avoided in
a. Hypertension
b. Epilepsy
c. Psychiatric disturbance
d. Renal disease
e. lactation
To be avoided in patients with ac
tive peptic ulceration.
: Same as for Ibuprofen
Same as for Ibuprofen
I.
Acetyl Salicylic Acid
:
Adults: 300-900 mg every 4
to 6 hours; ( hildren : not rec
2.
Paracetamol
:
3.
Ibuprofen
4.
5.
Indo Methacin
6.
Naproxen
7.
Piroxicam
8.
Codeine
9.
Morphine
Adults : 500 - 1000 mg, ev 4. Indo Metliacin
ery 6 to 8 hours; children : 13 years - 1/2 tsp every 6-8
hours; 3-7 years - 1 to 2 tsp
every 6-8 hours; 7-12 years 2 tsp every 6-8 hours
Adults : 400 mg, thrice daily 5. Diclofenac Sodium
after food in the initial phase; i
Naproxen
200 mg, twice daily in the
maintenance phase. Children 7. Piroxicam
: 20 mg / kg day in three di 8. Codeine
9. Morphine
vided doses.
10. Pethidine
To be avoided in infants (0-1 year)
25-50 mg, orally, twice daily
11. Pentazocine
Tablets: 25 to 50 mg, thrice
12. Buprenorphine
daily perferably after food;
Injection: deep IM, 50-75 mg These opioid analgesic should be used with caution in patient
once or twice daily for two with a. history of drug abuse
b. decreased respiratory reserve
days; Gel : external applica
c. hypothyriodism
tion at the site of pain.
d. asthma
Tablets : 250 mg, twice daily
e. hepatic impairment
Capsules : 20 mg, daily after
f. Renal dysfunction
food in the initial phase, fol
They should be avoided or used with extreme caution in preg
lowed by 10-20 mg.
Tablets : 10 to 60 mg every 6 nancy and lactation, and in the elderly debilitated patients.
hours (maximum of 200 mg
Contra-indications
per day)
Adults: 8-15 mg im or sc in 1. Acetyl Salcylic Acid
: Not to be used at all in chil
jections 2 mg / min upto JOdren below 12 years.
15 mg by IV; Children : 0.1
2. Paracetamol
Not to be used in hypersensi
mg/kg by injection
tive patients
Adults:25-100mg injection, 3. Ibuprofen & other
25-50 mg IV, Children: 1 mg/
non-opioid analgesics
Active peptic ulcer disease
kg b w by injection
and hypersensitivity are
Oral, 15 to 100 mg / day, in
contraindications.
jection 30-60 mg per dose in Opioid analgesics should be avoided in patients with raised it
jection (may be repeated after tracranial tension or head injury as they will interfere with respi
6 hours); IV injection 30 mg.
ration, pupillary responses etc which are vital for clinical as
Tablets (sublingual): 0.2 mg sessment and diagnosis.
every 6 to 8 hours; injections
0.3 to 0.6 mg or IV (may be Conclusion
repeated after 6 hours)
Useful often as relievers of pain and fever, these drugs are
ommended
)
3.
Diclofenac Sodium
:
:
?
:
11. Pentazocine
:
10. Pethidine
12. Buprenorphine
Special Precautions
1.
Aspirin or Acetyl
Salicylic Acid (ASA)
: Not to be used in
a. Bronchial astma
b. Pregnancy
c. Renal impairment
the mainstay in symptomatic treatment. The fact remains that in
case the symptoms persist inspite oftreatment, the root-cause of
these symptoms should be sought and specific treatment initi
ated.
05
In the next issue
ANTIASTHMATIC DRUGS
d. Hepatic dysfunction
2.
Paracetamol
Not to be used in hepatic dysfunc
tion
Dr MAnthony David, CHD, Catholic Health Association of
India, Secunderabad 500 009
I
36
Health Action • August ’97
-
# .u
..r .'a ■
Mp
S’
I WOMEN'S ISSUES
Women at risk
Quinocrine sterilisation, a pr
i
i
I.
I
i:
i’ •
I
I
r
■■
I:
T
I
actice that defies accepted international norms, continues in India
the trials,
defy accepted
accepted (While all substances that cause such
tinning the
trials, which
which defy
convcnNALINI VISVANATHAN
international norms for the conduct of changes are not
(
tional
scientific
norms
dictate
mat
tney
MOHAN RAO
clinical trials. Indeed, reports indicateuman trials
should be excluded before h
that they arc spreading. It is in this conundertaken.) Kessel also said that
;,c text that the All India Democratic are u------Z^XVER the last several months, the^
while
there is a lack of dataion the long
issue of
or chemical
cncm.ca. sterilisation
swnu^.i <of Women’s Association (AJDWA) and the
’ VJissue
term effects of quinacrinc, the small num
WOL„
ber of insertions minimises exposure.
’ ' that
’ I
aa matter
Mumford, on his par , said
matter of controversy (Frontline, May Nehru University approached the
2,1997). In West Bengal, where Dr. Biral
anti-malarial
drug,
has
vju*.■<•«.*..--» as an •—
Supreme Court with a public interest quinacrinc,
Mullick admits to having sterilised more
over a
been
used
orally
“
in
higher
doses,
' ’ j an immediate - and
c
than
over the
than 10,000
10,000 women
women over
t‘ past two petition^ seeking
longer period of time, on a ' arger popu
enforced
—
ban
on
the
trials.
decades, activists of the Ganatantrik c--------lation"
with
deleterious effects.
IdllVSIB
»>■»•- little ---Mahila Samiti led by Professor Malini
.
.
.
Similar
argument
have been pur forfor
trials
raise
Bhattacharya forced the West Bengal YHE <lulnac"ne "'
als "
,Se aJ host of ward
id by advocates of quinacrinc sterilisa
sterihsaGovernment to
call aa halt
halt to
to the
triX”
i --------tssues regarding
Government
to call
the “tria>o
—
&— - o the safety
i ' of
• the
„ pa,
tion in India also. What thej;e arguments
method of sterilisation, the,
and initiate an enquiry into ~ticular
Dr. Mullick s ticular metnoooi
j ;s ,1,3, reproductive'C causes account
' practice In Bangalore, where the methodology used in assessi..
assessmg
P ------othis,
--- and m ss W tn
small proportic n of deaths
Contraceptive and Health Innovation above all the ethical
eth.cal issues
,ssues «<Kermng
he for o
concerning the
onlyy .
iductivc agcProject (CHIP) of Dr. Pravin Kini and rnals
raised -------around--the amor
g India. Indeed, thfse: causes do
trials that have been raiscu
o.-_/in
world. The sponsors of these trials, which group
Dr. Sita Bhateja hopes to sterilise 25,000
notzz
account
entirely or even argely for the
are said to be going on in 19 Third World not
‘.
women over the next two years (having so
r
.........
..........
. „
a rnnu^uu. countries, arc two U.S. doctors: Dr. Elton high maternall mortality rate in the devel
far sterilised dose to a thousand), a coalidonof health and women’s groups have Kessel and Dr. Stephen Mumford. 1 hey oping countries; the majority of deaths
tion or ncaiu
& . !
arc
by a privatc foundation and occur owing to diseases of poverty, pri
held demonstrations. On May 2,
marily anaemia, undernutrition and
same individuals linked with the
women’s groups held a huge demonstra
infections and lack of access to health care
tion in New Delhi outside the clinic of Federation for American Immigration facilities in the event of complications of
erA_nrini
Dr. J. K. Jain, former member of Reform, a Washington-based group lob- -----’ mor sterilisation
uictiia"'-/. ..----------- r
. .
.
alone thus has an extremely limited role
of the network for
Kessej anJ Mumford responded to a to|
to play in the decline of maternal morralKessel and Mumford responded to a
i-ideed the case, countries
number of arguments put forward by liy
ity-. „
If c...
The Government of India denies
such as Brazil and Indonesi^ (the latter has
7 spoke to the
their critics when they
granting approval to quinacrinc as an
particularly aggressive family planning
Committee for Women, Population and
agent for female sterilisation. In
programme), which have witnessed
Environment
(CWPE)i
based
at
Parliament, in response to questions
remarkable declines in birth rate, should
Massachusetts.
Ashok Mitra, Minister of Hampshire College,
also have experienced declines in vhe
maternal mortality rate. TlJis has not hap-------------? t|iat (|lc tfons unanswered.
World Health Organisation (WHO) had
The argument that quinacrinc was
immended that pending sterilisation pertains to issues of safety.
■ ’ asl-malarial
specifically recoi
used
an anti drug
maintained that risk-benefit — - extensively
further studies, trials with quinacrinc on Kessel
" : as a ste rlising agent it
assessment, the cornerstone of clinical tri- and that therefore
i's'wiihout danger, is eqijially specious.
human populations be stopped. He said:
“Approval for clinical trials of quinacrinc als, “favoured the use of quinacrinc ster Qulnacrine was primarily ised as an amiilisation in populations where maternal itS drug only rill such time
pellets has not been granted to any inves
malarial drug only till such time as better
tigator by the Drug Controller General of mortality was high and contraceptive alternatives such as chlorAtpiine became
India.” He also stated that “no drug man- r
PJ...J_.icc
c/^5n' low." With reference to the
ailable. Further, the extremely high
WHO
ufacturer has been granted licence to 1------ --’s recommendations observing av;
anccr-producing mortality rate: for malaria it that time far
manufacture quinacrinc and the drug is *»•<»»
thatquinacrincmay
cc<
----------- —/
«
i*-'
• i
i ,i
outweighed
the risks due to quinacrinc.
not imported.” Meanwhile, the Indian and thus warranted further studies, he Unlike the case with malaria then, (here
argued that toxicologists maintain that
Council of Medical Research (ICMR), in
arc alternative forms of terminalI contrnpublished statements, condemned the the duration of exposure is the most crit ception today such as ttubcctoiny lor
ical clement when humans arc exposed to
practice.
women and vasectomy for men.
Despite these efforts, some doctors in carcinogenic or mutagenic substances.
Maintaining that stetilisation by the
safe.
the privatc sector and some non-govern Laboratory tests indicate that quinacrinc quinacrinc method was extremely
<
causes mutations or changes in cells.
mental organisations (NGOs) are con-
S zscth;—
I
I
!
.ad.
I RON I LINE,
94
*
I
I
I
Dr. Kessel claimed that there were no
Questions have also been raised about
deaths in the 4() day period following the
the standard cut-oil date ol 4() days after
insertion of quinacrine in 100,000
women. I here arc, however, a number of
sutgery being used to detetmine inoitality rates in the case ofquinacrine sterilisa-
use it as an agent for female .stciilis.it ion is
baseless. Under the Drugsand (’oMm-tii s
Act of India, a new ding is defined io
include “a drug already approved....
problcms with such a facile presentation
of data. Included in this huge number are
lion. Potentially fatal ectopic pregnancy
which is now proposed... with new < laims,
can occur as long as a woman sterilised
namely, indications, dosage form and
presumably the 31,781 women sterilised
with quinacrineis in the reproductiveagc-
route of administration."
1989 and 1992.
group. Fhe use of this cut-off date thus
does not constitute a long enough period
only granted approval for the use of
in Vietnam between
following WHO recommendations the
Vietnamese Government called a halt to
I
to assess the mortality risks associated
with the method.
quinacrine in tablet form, orally for the
VUTHILE Dr. Kessel said that records
W are being maintained and that cases
female sterilisation. It has not received
the trials.
I he New York-based Association for
I
Voluntary
Surgical
Contraception
(AVSC) found serious scientific flaws in
tire Vietnamese study. The data on side
I
effects and failure rates, for instance, were
not derived from the full sample of
women but from much smaller sub-sets
Ihe Drug Controller of India has
arc followed up long enough to establish
mortality rates, Dr. Mumford acknowlcdgcdthattheyhavenoresourcesforfollow
up.
Indeed,
Dr.
Bhuiyan
in
treat ment of malaria, giardiasis and amocbiasis. The drug is thus not approved lor
this approval from any authority any
where in the world, including the U.S.
I
The FDA recently issued a warning on the
Internet where quinacrine was being pro
moted as a method of self-sterilisation.
a The warning noted that the kit advertised
| “uses pellets of quinacrine hydrochloride,
_______
r
< an unapproved drug which can cause
OUINACfllNE PELLETS
t
i
Ii
i !
£j ectopic pregnancies, abnormal pregnan*■ cies and permanent damage to a woman’s
FOR
NON SURGKAL FfMALF STeiHUZAriON
TOBFUStOOV
A OUAltf .CO CLINICIAN ON4.V
^efesjBuui..i?! •
reproductive otgans."
!.-■ ivr! j
Despite the blatantly illegal nature of
this practice, some of India’s leading doc
i ;
i !
tors continue to take part in this dubious
enterprise. At the World Congress of
i i
Gynaecology
and
Obstetrics
in
Copenhagen in August 1997, a special
session on quinacrine sterilisation was
organised by Dr. Kessel. It was chaired by
Dr. J. K. Jain. Prominent doctors from
India making presentations included I )r.
= |
1i
bI
Kini, Dr. Sita Bhateja and Dr. Ajay
•i
Ghosh.
among them. The findings from these
Bangladesh and Dr. Mullick, in pub
varying sub-sets of the study population
lished interviews, admit their failure to
were then extrapolated to the entire sam-
pie. For instance, failure rates were calcu-
follow up cases. Similarly, in Pakistan
where women were, according to a par-
a third of the total
I a ted based on only
(
population. Again it is unclear as to how
ticipant, “picked offstreet corners”, there
independent
institutions of health
research established by the state arc being
were no follow up efforts. It is, therefore,
systematically undermined, it is not sur
I I
the ectopic pregnancy rate was calculat
ed: in one province, two out of nine preg
not surprising that the data presented by
Kessel are met with scepticism.
prising to witness yer another instance of
Third World women being subjected to
I!
nancies were ectopic - a hugely unusual
; i
Biral Mullick, Dr. Ashi Sarin, Dr. Pravin
Qulnacrlne pellets and the equipment for thek insertion.
Kessel
Given
the
globalised,
liberalised
nature of the Indian state today, wherein
government
such experiments. Notwithstanding the
“this troubling finding is not mentioned
in the analysis of ectopic pregnancies.”
approval for quinacrine sterilisation is
“desirable but not essential” since guidelines from
the Food
and
Drug
commitments made at the United
Nations Conference on Population and
Development in Cairo in 1994 to
occurrence. Yet, according to the AVSC,
stated
that
ii
ll
I he AVSC thus maintains that “it is not
Administration (FDA) of the U.S. “per-
enhance women’s health and rcproduc-
possible to conclude that quinacrine pel
lets are a safe and effective non-su rgical
mitted off-label use (that is, the use of
drugs approved for another purpose)
tiverights, theimpunity with which U.S.based NGOs are violating human tights
!|
method of female sterilisation.”
under medical su[ipervision.” The training
in countries ol the South shows up the
II
ety of protocols of dosage, number of
literature for quinacrine sterilisation,
hemever, states thatt one of the advantages
been rendered vulnerable by the incotpo
insertions and adjuvants have been fol
lowed. it is not methodologically legiti-
ofthe method is that it “can be provided
by many types of trained healthi care
tation ol the Indian eumoiny in tin glob
al market. It is ironic indeed that this r
mate to calculate mortality rates from data
obtained by diverse and often unspecified
-----*•— not
— just
:
J--------- ” ’ Indeed
J--- Dr.
workers,
doctors."
Mullick is on record that he has trained
being done in the context of neo liberal
rhetoric on reproductive health rights. F3
methods pooled together. Indeed, it has
“hundreds of health workers” to use
quinacrine for sterilisation.
In addition, given the fact that a vari
been revealed that three known deaths
due to quinacrine sterilisation were not
The
argument
that
approval
for
reported in these findings.. Ibis further
quinacrine for the treatment of other dis-
undermines the credibility of the data.
casts precludes the need for a licence to
I RONTUNF. OCTOBER 3. 1997
I
need to monitor health systems that have
Dr Nd/ini I7n <Uhttl>.ui it a V S. -b.’.-f:!i-tJ itc
hf<ihh rewnher
Dr. Mohan Rao i< on thr
I'aculty oj Social Medicinc. Jawaharlal N'rb'H
(biift rfity. New I hlhi.
MS
I
1
j
J
i
i
.
i
•
i
i t
6.
CLASSIFICATION OF PRACTICES IN NORMAL BIRTH
This chapter classifies the practices common in the conduct of normal childbirth into four
categories, dependent on their usefulness, effectiveness and harmfulness. The classification
reflects the views of thb Technical Working Group on Normal Birth. Arguments for this
classification are not given here; the reader is referred to the preceding chapters, which are the
outcome of the reflection and debates of the Working Group, based on the best currently
available evidence (numbers of chapters between brackets).
CATEGORY A:
6.1
Practices which are Demonstrably Useful and Should be Encouraged
1.
A personal plan determining where and by whom birth will be attended, made
with the woman during pregnancy and made known to her husband/partner and,
if applicable, to the family (1.3).
2.
Risk assessment of pregnancy during prenatal care, reevaluated at each contact
with the health system and at the time of the first contact with the caregiver
during labour, and throughout labour (1.3).
3.
Monitoring the woman’s physical and emotional well-being throughout labour
and delivery, and at the conclusion of the birth process (2.1).
4.
Offering oral fluids during labour and delivery (2.3).
5.
Respecting women’s informed choice of place of birth (2.4).
6.
Providing care in labour and delivery at the most peripheral level where birth is
feasible and safe and where the woman feels safe and confident (2.4, 2.5).
7.
Respecting the right of women to privacy in the birthing place (2.5).
8.
Empathic support by caregivers during labour and birth (2.5).
Care in Normal Birth
WHOIFRHIMSM/9624
J
Page 35
9.
Respecting women’s choice of companions during labour and birth (2.5).
10.
Giving women as much information and explanation as they desire (2.5).
11.
Non-invasive, non-pharmacological methods of pain relief during labour, such
as massage and relaxation techniques (2.6).
12.
Fetal monitoring with intermittent auscultation (2.7).
13.
Single use of disposable materials and appropriate decontamination of
reusable materials throughout labour and delivery (2.8).
14.
Use of gloves in vaginal examination, during delivery of the baby and in
handling the placenta (2.8).
15.
Freedom in position and movement throughout labour (3.2).
16.
Encouragement of non-supine position in labour (3.2, 4.6).
17.
Careful monitoring of the progress of labour, for instance by the use of the
WHO partograph (3.4).
18.
Prophylactic oxytocin in the third stage of labour in women with a risk of
postpartum haemorrhage, or endangered by even a small amount of blood loss
(5.2, 5.4).
19.
Sterility in the cutting of the cord (5.6).
20.
Prevention of hypothermia of the baby (5.6)f
21.
Early skin-to-skin contact between mother and child and support of the initiation
of breast-feeding within 1 hour postpartum in accordance with the WHO
guidelines on breast-feeding (5.6).
22.
Routine examination of the placenta and the membranes (5.7).
J
X
I
4
?
?
*
i
4
!
i
CATEGORY B:
6.2
Practices which are Clearly Harmful or Ineffective and Should be Eliminated
1.
Routine use of enema (2.2).
2.
Routine use of pubic shaving (2.2).
1
3.
Routine intravenous infusion in labour (2.3).
1
4.
Routine prophylactic insenion of intravenous cannula (2.3).
5.
Routine use of the supine position during labour (3.2, 4.6).
6.
Rectal examination (3.3).
<■
I
i
j
j
<
Pa^e 36
Care in Normal Mirth
WIIOIFRHIMSMI96.24
7.
Use of X-ray pelvimetry (3.4).
8.
Administration of oxytocics at any time before delivery in such a way that their
effect cannot be controlled (3.5).
9.
Routine use of lithotomy position with or without stirrups during labour (4.6).
10.
Sustained, directed bearing down efforts (Valsalva manoeuvre) during the second
stage of labour (4.4).
11.
Massaging and stretching the perineum during the second stage of labour (4.7).
12.
Use of oral tablets of ergometrine in the third stage of labour to prevent or
control haemorrhage (5.2, 5.4).
13.
Routine use of parenteral ergometrine in the third stage of labour (5.2).
14.
Routine lavage of the uterus after delivery (5.7).
15.
Routine revision (manual exploration) of the uterus after delivery (5.7).
CATEGORY C:
6.3
Practices for which Insufficient Evidence Exists to Support a C ear
Recommendation and which Should be Used with Caution while Further Research
Clarifies the Issue
1.
Non-pharjnacological methods of pain relief during labour, such as herbs,
immersion in water and nerve stimulation (2.6).
2.
Routine early amniotomy in the first stage of labour (3.5).
3.
Fundal pressure during labour (4.4).
4.
Manoeuvres related to protecting the perineum and the management of the fetal
head at the moment of birth (4.7).
5.
Active manipulation of the fetus at the moment of birth (4.7).
6.
Routine oxytocin, controlled cord traction,, or combination of the two during the
third stage of labour (5.2. 5.3, 5.4).
7.
Early clamping of the umbilical cord (5.5).
8.
Nipple stimulation to increase uterine contractions during the third stagt? of
labour (5.6).
.»
Page 37
Care in Normal Birth
i
WIIOIFRHIMSMI96.24
i
i.
CATEGORY I):
\
i
t
6.4
J
I
Practices which are Frequently Used Inappropriately
1.
Restriction of food and fluids during labour (2.3).
2.
Pain control by systemic agents (2.6).
3.
Pain control by epidural analgesia (2.6).
4.
Electronic fetal monitoring (2.7).
5.
Wearing masks and sterile gowns during labour attendance (2.8).
6.
Repeated or frequent vaginal examinations especially by more than one caregiver
(3.3).
7.
Oxytocin augmentation (3.5).
8.
Routinely moving the labouring woman to a different room at the onset of the
second stage (4.2).
9.
Bladder catheterization (4.3)
10..
Encouraging the woman to push when full dilatation or nearly full dilatation of
the cervix has been diagnosed, before the woman feels the urge to bear down
herself (4.3).
11.
Rigid adherence to a stipulated duration of the second stage of labour, such as
1 hour, if maternal and fetal conditions are good and if there is progress of
labour (4.5).
12.
Operative delivery (4.5).
13.
Liberal or routine use of episiotomy (4.7).
14.
Manual exploration of the uterus after delivery (5.7).
I
2
I
<
J
'3
F\ ?
Miscoiiccptions in Medical Practice
To demonstrate malaria para
site, blood should be drawn
during paroxysms of fever
(sporulation) to parasitize other RBCs.
Some blood merozoites develop intj3 sexual
forms (gametocytes) which restart the man mosquito - man c ycle when ingested by a fe-
male anopheles mosquito.
A notion is prevalent amongst doctors, other
health personnel and general public as well,
that to demonstrate malaria parasite in pe
ripheral blood smear, sample has to be taken
during paroxysm of fever. Doctors and labo
ratory personnel often insist on it and people
take immense trouble at odd hours to arrange
for the same.
This is a misconception. In an infected
Paroxysms of fever coincide with sporu
lation and destruction of RBCs. The cause
of the fever is thought to be related to release of endogenous pyrogens from injured
cells. So it is obvious that when fever has
subsided the released merozoites have already
invaded other RBCs and will be demonstrable
in peripheral blood smear. One nccc not wait
smear at any time of the day irrespective of
for the paroxysm of fever to demonstrate
them. It should be stressed that demonstra
tion of the parasite depends upon the degree
of parasitaemia. When it is scanty , meticu-
the degree of temperature. Let us recall the
lous search is the only option, while in heavy
life cycle of the parasite.
parasitaemia it is easily detected.
person, malaria parasite in its erythrocytic
phase is demonstrable in the peripheral blood
In humans, the sporozoites introduced in
Pcripheral smear may not show the para
the blood stream by an infected anopheles
site at the first instance. Hence it should be
repeated
3 or 4 times at 4-6 hrs interval. Both
rcpi
thick and thin smear should be prepared. It
is needless to point out that the technique of
mosquito develop within 5-12 days into pre
erythrocytic (or tis'sue) schizonts. At the end
of this phase, merozoites produced from tis
sue schizonts arc liberated into the blood
R.B.C. they at first appear as ring shaped
taking blood sam pic and subsequent staining
should be correct. Thick films should be examined for at least 5 minutes (corresponding
to approximately 100 microscopic fields)
trophozoites which later enlarge and assume
while a thin smear must be examined for 15-
an irregular or amoeboid shape. Following
20 minutes before issuing a negative report.
Blood smear should be examined for 2-3 days,
stream. Invading the blood stream, they start
the erythrocytic phase of development. In the
mitotic division of the nucleus, the organism
is known as schizont. After several divisions,
daughter cells (merozoites) fill the corpuscle,
which ruptures and releases them
in case of a negative report.
A. Mitra
67
Drug Disease Doctor O 46
Mp
i-
Quality Health Care
A Crying Consumer Need
N.M. Matheui
«!
>
1*1 e d i c a 1
s e r v i c e s h v e been p rog r ess i v •-> 1 y hecojn ing /nor e and
ma r e
c omp 1 e :< a n d sop h i s t i c a t e d , M i t h t h e r ?< p iL p
ri a ci v a r> c e m e n t s in medical
t e hno 1 og i e s «
With
the
increase
v,
consumer
.1.i.-'\
r.
awareness
and
e xp e c t a t i on s ,
h e a 11
care m a
>:•: 1i a y>• r
e a 1 i z e the
a. n ag
a g e r s ttoda
real
for
need
tot; zil
q u. a 1 i t y
m an ag emen t i n h e a 11;h c r >•? s e r' v i c; es ,
t; o
make
it
e f fee; t i ve ,
econamia al
and
r e 1 e v an t. >• -i e a 11 bi
managers
need
an
e n a.b 1 i n g
system
to ensure that the people associated
w i th
the
del i ve ry
of health care at different levels,
monitor,
evaluate
and account for their own work and, thereby, provide quality care
' to patients on an ongoing basis.
Supreme Court Intervention
The Supreme Court judgment of November 13, 1995 bringing
medical
services
in
the ambit of Consumer Courts was historic
in
many
respects.
It had a great spin-off for the consumer movement,
on
the positive side, and a strained patient-doctor relationship , on
the negative.
I
K-
This
verdict ■ has been
an
affirmation
on
the
doct ors
responsibi 1ities
towards health consumers, suggesting a
greater
need
for transparency in matters of investigations. records
and
charges,
Accountability
has to be established
everywhere,
not
only
in
the private sector but also in the the
public
seeftor.
Even though free medical care remains outside the purview of
CPA
1986,
there are already established precedents to take
care
of
this aspect, as can be seen from the writ petitioni (c> No 796
of
1992
in the matter of Paschim Bangs Khe’c Mazdoor Samity &
Ors •
vs. State of West Bengal, decided on 6-5-1996. In this case,
the
pet i t ioners
filed
a case against the State
run
hospitals
for
ind i f ferente
medical
and callous attitude on the part of
state
author it ies.
They
argued that the patient's
Fundamental
Right
under Art. 21 of the Constitution was at stake. The Supreme Court
agreed
with this view and held that the State had
violated,:;;; the
Right
to
Life
and awarded a compensation of Rs
25000
to
the
petitioners' wife.
The
Court ruled that providing adequate medical
facilities
for
the people is an essential part of the obligations undertaken
by
the government in a welfare state. The medical of fic e rs
empidyed
therein
are
duty-bound
to
extend
medical
ass istance
p reserv i ng hum an life. Failure to do so. amounts to violation
of
Art. 21.
The
mos t
significant aspect of this ru1ing was
the
guide1ines
i ssued
by
the Court to avoid occurrence of
such
incidents
in
future.
These
inc 1uded
upgradation of
PHCs
and
in t e rmediat e
q roups
of
hospitals like the district, sub-division
and
state
hosp itals.
It
directed
that
serious
p a 11en ts
should
be
ot
I
necessarily admitted in hospitals for which a
Central Bed Bureau
must be established besides setting up of of regional casualty or
traumatoldgy
hospitals.
The
State
government
accepted
the
recommendations in August 1995.
Th e
ob 1 i g a t ion
of
to provide
emergency
the State
mach me ry
medical services to the injured to p reserve life had already been
es t ab1ished
in
Pt. Paramand Kat aria vs. Union of India
&
Ors.
1989 (4) SCC 286.
C ross-Pr act ice
Cross-practice
is
in
a
particular
one where a person trained
system of medicine adopts treatment methods of another system, i n
which
he/she
has no training. This is very dangerous
are
and
det r imen ta1
to consumer interests, besides being
and
unethical
illegal,
Safety and quality of care are not guaranteed
this
in
p rocess.
Consumers won a major battle against medical
wh en
malpractices
the
Supreme Court came down heavily on this issue (in
recent
a
judgment. The SC stated that the person who studies one system of
medicine but
practices
another is a quack
and
ch a r1 a t an
and
guilty of medical negligence.
Here
is a case of a Bombay—based Dr Ashwin Patel,
a
registered
homeopath y
who treated a patient, Pramod
with
allopathy
P r a mod Verma,
Verma,
w i th
drugs
for
suspected
viral
fever.
He.
the
patient
two
He. gave
antibiotics y
paracetamol and an injection of: a
sodium
compound
for fever and back pain on 4th July 1992*.
The second
antibiotic
was
for
typhoid, even though there was no confirmation
the
of
disease through investigation, The patient became unconscious and
died in a nursing home ten days later.
Interestingly the National Comm ission did not f i nd anything wrong
with
the way
Dr Patel
handled the
case,
not
even
in
his,
practicing allopathy. The SC overruled the Commission and| awarded
Rs
3 lack compensation plus Rs 30000 as costs to the □ e t, i 11 on e r ,
only because Dr Patel, even when he had exercised r e a son alb 1 e care
and
skill,
had practiced allopathy w i thou t being
in
•a u a I : f i. e d
that
system and therefore, he was gu i 1 ty of n e g 1 i g e n c e
per
se ,
wh i ch
needed
no
other
argument
the
or
proof
to
e s t a b 111 s h
negligence.
The
Court
said negligence has many manifestations
active
or
passiv e,
collateral,
crimi
cont inued,
h a z a rdous, willful or reck less» or negl igence D er s e
1t
31 ,
be
ma y
gross,
p rob 1em
The
of quackery cannot be eliminated by
this
judgment
a 1 one <
Lot more coordinated actions are needed to weed Qut
this
menace. There is yet another big question as what can be
to
b e done
those who practice medicine without any training i n any system?
1
1
H t gh
Another important legal intervention was made by the Bombay
In
Court.
In
a landmark judgment pronounced in January
1996,
the
the
Court
directed that copies of case oapers must be given
to
patients
on
demand
by the hospital/doctor.
These
cannot
be
denied to them in
i n the guise of being con fidentlai
Burgeoning Private Sector
to
be
The
profit
motivated private sector is a serious factor
reckoned with in the health scenario of the country. About 75 per
of
cent
of outpatient care i s handled by this sector. The
cost
this
health
care
invariably i s high.
peop
1
e
p
re
f
e
r
But many
It
sector
because of easier accessibility and better attention,
has been found that private doctors prescribe a larger number
of
and
drugs compared
to government doctors, This has
both
cost
safety implications. Added to this. are the other malpractices
of
unnecessary
hospitalizatiojis,
investigations,
|prolonged
unregulated
vested
with
charges,
ghost
surgeries,
referrals
interests,
monetary
p romotion of particular brands of drugs for
gains and the like.
Intervention by N.H.R.C.
In
an
interesting
Human
Rigfi ts
turn of event,
the
National
Commission
task
of
(NHRC) has recently decided to
take up the
b een
scrutinizing
the functioning of the private sector, having
seriously concerned
over
the mounting
complaints
of
medical
n eg 1igence. The^Commission will examine the various aspects
from
the human-rights angle‘ which include the registration of
priv ate
nursing
homes,4 their
grading on the basis
of
the
facilit i es
available, frequent monitoring of these facilities to ensure that
they
are
maintained, framing of regulations
and
making
their
violations punishable and, finally, shifting of private hospitals
hazards
to
the
from
non-conforming
areas if they pose health
local residents.. It will also investigate whether nursing
homes
employ qualified medical p r ac t11ion e rs and have adequate
mediqal
infrastructure,
blood banking facilities and proper disposal
Qf
hospital wastes, systems.
Only
120 out of the estimated I700 private n u r s i n g homes l n
capital
are registered with the Delhi government, Th e
i ssue
registrati. on
in
of p riv a t e nursing is pending adjudication
Delhi High Court.
;he
of
:he
The
Commission
decided to take the plunge as a
of
the
result
fl led with the Commission on the death
petition filed
old
d e a t h of a 14 year
girl,
who
was admitted in a west Delhi
. th
private*
hospital
complaints of stomach pain, She died on the operation table
scpon
being
after
administered spinal anaesthesia.
The
compensat on
iis
s Rs 27 lakh. The prestigious Escorts
claimed
Heart
Institute
has
been sued in another case of a 2 year old girl
for
a 11 e c) e ct
negligence and compensation of Rs 20 crore.
Need for Regulation
CPA
and other health related legislations would do a great
deal
i
to
bring
discipline in this sector. But there has to•
other
be
methods as well to deal with this problem.
Dne
way
is
to
Private
enact/revita 1ize
and
enforce
the
Hosp ital/Nursmg
Homes Act.
Delhi had
an
1956.
in
h ad such
ac t
Hop e fu11y, as per assurance from the Delhi Health Minister,
this
Ac t
will
be revived in the near future.
is
meant
to
future, This Act
regulate private
hospitals
and nursing
homes
by
setting
up
standards for quality, service conditions, personnel, disposal o f
hospital waste, keeping of hospital records and reporting.
/a
- f-' :'s,
The
Bihar Government has already introduced a similar bill.
But
the
NGO hospitals are up in arms aqamst
against the requirement in
the
bill,
for yearly renewal of license to run the
hospical/nursing
home
for
a fee ranging between Rs 10,000 and
I 5 0000
depending
upon the bed
I
strength and location.
Ano the r major initiative towards better quality health iservices
is
the
Delhi
Govt, programme on
promotion
of
rational
d rug
therapy
in its hospitals. This programmes has tried to out
into
practice
a
the
concept of essential drugs. The Govt,
preoared
list
of
essential drugs and asked the hospitals to use
of
8 0 /*
their budgets only for the?? ’'■‘.rugs. The remaining 20 per cent U> 3 '5
left
to1 the discretion or the hospital to meet
th e
specializ e d
needs.
in] t h1s
The
Govt, seems to have met with som^
succ es 5
area.
Doc tors' Responsibi1i t i es
Doctors’
responsibilities
stems
are
from the fact
that
they
dealing with human beings who are sick, and not some
commop i 11 e s
to
be disposed off. The patients are victims of csome
af f 1 lie t i on
needing attention which the doctor is duty-bound to of f e r,
of
professional compulsions and out of pure human concern.
There
are
several measures a conscientious doctor can
make his/her medical practice purposeful and efficient.
■if-
t a Ik e
to
Medical Audit
Medical audit is a method of objective evaluation o f
qua Iit y
of
medicare.
This
is
providers
conducted by
the
service
themselves
(in-house;
medic a1
the treating physicians and
the
administrators)
supervised
by
a peer group.
It
helps
detect
def icienc i es
in
improve
the health care service
provided,
to
a 111tude,
skill
and knowledge of the providers
and
to
ensure
co 11ec t i ve
responsibi 1ity
aud 11
and
accountabi1ity.
Medical
involves
aud 11
at tent
of
structure,
process,
outcome
satisfaction*
economics
and cost. An
effective
aud 11
medica I
system
for
a
ve
a
improving
health
care
facilities,
h
s hou1d
nealth
per formance
4 e 1 a t ea
parameter
and
should cover
heal th
care
1aws/consumer laws and medical ethics.
Rational Drugs
Th e
campaign towards rational drug therapy should
be
subported
and
encouraged
at all levels,
Governments should be
urged
to
adopt policies on essential drugs, similar to that of
the
Delhi
and
Tamil Nadu Governments, States should immediately
come
i mmedlately
out
1 ist of essential drugs,
with list
regional
with suitable regional
variations
1 ist recently re leased by the Central Government.
to the list
Professional Bodies
Formation
of new professional networks
n e tuiork s or joining
with
a 1 ready
existing
associations
like the Medico friend
Circle
or
other
professional bodies should be encouraged among doctors.
CV^A J.
is
also
in
the
process of building up a
Doctors
Forum
for
the
socially conscious and progressive minded doctors).
■*
Continuing Education
A
system
of
con tinuing
education
for
doctors
shou1d
be
s t ream lined
so that they have acc ess to th
latest
advances
in
the medical science which will delink them from the
influences
of
d rug
companies. This process would a 1 so require
developmqnt
of
effective communication materials for these doctors.
-¥
Legal System
The
legal system needs to be t lightened up to
properly
regulate
the services of doctors to urge them to care
for the patients
as
their first
■'
priority. The nursing homes act or other similar ac ts
should L
bej enacted in all the states.
at-
Redressal
Support
Finally9
assistance to the *victims
'
of medical negligence
is of
paramount importance, Generally the gullible
patient is unable to
est ab1i sh
the guilt of the doctor in a court of law,
hence
the
high
failure
rate.
Consumer bodies should
elicit
support
of
medical experts to give evidences in the courts
m support of the
comp 1 ain an ts.
“The
doctor
aims
a drug at
a
disease;
sometimes
somet imes
misses.
The misses are left out of account,
treasured up , reckoned and systematized into a science”
%
it
h i ts ,
the
hits
Sri Aurobindo
Source • VHAI
*
I
.... .1 J. I,
*
.
• >
Non-allopathic doctors form the backbone
of rural health
H. S. Bawaskar
Introduction
Government health service
India is a codrfir} of villages. Most villagers are illiterate,
innocent farmers who are busy round the clock all
through the year. They are unaware of medical facilities
in or around the village till they fall sick. They do not plan
for measures to be taken if and when they are ill, nor do
thex participate in any medical insurance schemes. They
are entirely dependent for medical care on the practitio
ner in or near their village. They call any person giving
drugs and injections ‘Doctor’. When facing him, they are
interested only in getting well and not in the qualification
of the doctor or what ‘-pathy’ he follows.
Civil Hospital This is located at the district
headquarters, is well equipped and has a consultant
physician with ancillary staff. Patients are referred there
from the primary health centre, cottage or rural hospital,
or private nursing homes. The Civil Hospital of Raigadh
District is located at one corner of the district
headquarters at Alibag. Patients prefer to go to Bombay----instead of the Civil Hospital there.
Health pattern in rural areas
Government Health Service
Location
Private health service
Civil Hospital
District
headquarter
Nursing homes
I- -
— ——
Specialists, GPs
Visiting specialists .
Few non-allopaths
Rural hospital or cottage
hospital
Taluka
headquarter
Nursing homes
GPs, surgeon, physician. Few
non-allopalhs
Primary health centre
Pcth
N on-allopaths
Occasional MBBS doctor
Visiting MBBS doctor
I Health visitors Malaria
' workers SEW. SW centre
Village
| Non-allopaths
i Visiting MBBS doctor
1 Visiting health worker?
Kond or wadi | Quacks, mantriks. village
I healer, visiting non-allopath
Villagers usually seek medical help when they are
seriously ill or when illness disallows work. The
common problems one encounters in villages are acute
dysentery, gastroenteritis, malaria, hyperpyrexia,
convulsions, hepatitis, bronchopneumonia, fevers,
infected scabies, conjunctivitis and bites (snake,
scorpion, fox, dog). Of course, one also has to deal with
pregnancies and difficulties in labour.
Due to non-availability of public transport, when a
person falls sick in the dead of night and is seriously ill
(snake bite, scorpion sting, obstructed labour,
eclampsia, acute gastroenteritis...) the patient is placed
in a wicker basket and carried to the nearest
i
■
public
health centre or to a private practitioner at the taluka
headquarters.
H. S. Bawaskar M D. retired as Medical Superintendent of the Rural
Hospital, Poladpur, District Raigadh, Maharashtra. He presently
reside* at Prahhat Colony, Savitri Marg. Mahad, Raigadh 402301
112
The civil hospital should be sited in a centrally located
place, which can easily be approached. As matters s tand,
the consultant at the civil hospital, its medical officers
and others are often busy with their private prac ices.
What little time they do spend at the hospital is often
spent in issuing medical certificates, conducting medical
board examinations and attending to VIPs. __ _
Cottage and rural hospitals These are located at taluka
headquarters and are supposed to possess indoor beds,
staff and radiology and laboratory facilities for
investigations. These machines are often out of order.
Technicians are rarely to be found there. Xray fil ms or
chemicals for developing them are usually out of stock.
The medical superintendent possesses a postgraduate
qualification. Other medical officers are diploma
holders. The nursing staff is inadequate.
The environment in and around the hospital is filthy and
not conducive to health. Bedside lockers are broken, the
mattresses stink, bedsheets soiled and toilets dirty
beyond imagination. Few are willing to get admitted to
these hospitals. The abjectly poor must, perforce seek
help here and lie on these beds. They are made to feel
highly obliged to the staff. The doctors are busy
attending calls in private nursing homes. Soon after they
join the hospital, they start building their own nursing
homes and once these are ready, resign.
Primary health centre This is located at the peth or
large village and is intended to cater to the medical
needs of a population of fifteen to thirty thousand Here
the conditions can only be compared to those in cow
sheds. The centre is spick and span only on the
auspicious day of its inaugural by a VIP. The medical
officer is rarely available. He may visit just for a few
hours to conduct an outpatient clinic. The rest of the
time is spent in private practice or ‘table practice’
(charging patients examined at the centre). When I
stopped this practice, I was harassed by all authorities
Issues in MEDICAL ETHICS
VOL.4 NO.4
OCT-DEC 1996
including the local politician when I compelled these
medical officers to work - as they are supposed to without charging their patients.
These medical officers arc supposed to collect data on
immunisation, ante-natal care and family planning.
Their sincerity and awareness can be judged from the
fact that they claim to have inserted more copper-Ts
than the number received by the centre. The
consequence: population storm.
their trade and diagnose obstructed labour that
necessitates Caesarian section.
Allopathic doctors are unwilling to move to the villages
because of personal or family compulsions. The key fac
tors cited are lack of facilities for the education o their
children and paucity of outlets for recreation.
Non-allopathic doctors This group comprises of those
who have qualifications such as BAM&S, BHMS. DHB.
LCEH, GfAM and those who are registered mpdical
The only person available at the centre all the time is the practitioners (RMP), vaidyas professing ayurveda and
humble servant who informs anyone who calls that the unani practitioners. They include village healers
doctor is not in. Even victims of snake-bites have to (mantriks) and quacks. They reside in the villages,
move from centre to centre, ultimately landing up in a participate in all the activities of the community and are
nursing home.
available to patients round the clock. They are truly
family physicians and villagers repose confidence and
The total absence of’ rational and ethical therapy is trust in them. They treat all acute illnesses with
especially evident in the case of a pregnant primary commonly used allopathic drugs, give intravenous
teacher who was brought to a government dispensary fluids and injections. Their poor understanding
of the
soon after a dog-bite. The person in charge refused to science of modern medicine leads to
grave errors as
administer anti-rabies injections for fear of teratogenic when injecting atropine or digoxin, administering
consequences. The woman died of rabies. It did not corticosteroids and prescribing chloroquin, quinine and
occur to th;s person that ar. abnormal foetus can always' diuretics. Leeches are frequently used.
be identified and terminated but a dead mother cannot
I must refer to retired vaccinators, malaria workers,
be brought to life.
operation theatre assistants, wardboys and compounders
Adivasis. other tribals and all except the most poor shun serving as non-allopathic doctors without any additional
government sen ices.
training. They, prescribe allopathic drugs and give
Government hospitals serve but two purposes: 1. To injections to villagers.
register medico-legal cases -«who are transferred Non-allopathic doctors and allopathic therapy
elsewhere once the first aid has been offered. 2.
Non-allopathic doctors are sincere and eager to learn al
Stepping stones for their doctors who flourish and soon
lopathy. Let me provide some examples. In the v 11 ages
start their own nursing homes in the same area. Sick
where I work, scorpion stings are inot uncommon^ Many
government hospitals and clinics have permitted
victims died of pulmonary oedema. I was able to reduce
allopaths and non-allopathic medical practitioners to
mortality from this complication by using prazosin. I
flourish in rural India.
have travelled throughout this region and have done my
best to spread this knowledge through talks, slides and
Private heailh services
demonstrations
to all doctors, regardless of their back
Allopathic doctors They crowd in district and taluka
ground. I later carried out a postal survey*.
headquarters where multi-storied nursing homes mush
room. Radiology, sonography, endoscopy and cardiac Results of postal survey to assess effects of training on
monitoring are easily available. The staff watching the treatment of victims of scorpion-stings
cardiac monitor may not be able to identify abnormalities ; Reporter Number Total Systemic Treat
Mortality 1
Fatal
on the oscilloscope or use the defibrillator.
cases
involve*
ment 1
’
I
Whilst sophisticated gadgets are freely available, their
usage is questionable. A patient with a renal colic will be
subjected to plain xrays of the abdomen, intravenous
pyelography and sonography. Examination of the urine
will be done only after these have been completed. Xrays
and ECG are carried out on requests by patients and their
families rather then on referral by consultants. Patients
move from doctor to doctor, if one consultant advises
against an investigation demanded by the patient, they
ment
given
• Phvsian
! — MD
7
287
166
Prazosin ;
2
j MD (Ped)
3
67
33
Prazosin ;
4
12
I MBBS
35
2971
251
Prazosin j
5
19
Nonallopath
6
197
79
Prazosin t
2
25
Phwician
2
24
13
Conven
tional
therapy
5
?S
1.2
will go next door to a more obliging doctor.
Surgeons claim that there are few patients in rural areas
for them to operate upon. The\ thus add midwifery to
Issues in MEDICAL ETHICS
VOI..4 NO.4
OCT-DEC 199$
*= consultant not aware of the utility of prazosin
Conventional thcrapy= digoxin, frusemide, atropine,
corticosteroids
113
I found that these non-allopathic doctors were now
d;jgnosing and treating these victims of scorpion stings
effectively with a low mortality whilst a postgraduate
allopathic doctor was unaware of the use of prazosin
reported a high mortality whilst using convention!
tr.erapy.
Tr.e second example is from Gadchiroli.2 Villagers were
--:ned to record the respiratory rate of children with
rronchopneumonia and estimate the severity of the
c-.scase. Excellent results were obtained using
c;-:rimoxazole.
T..e third example is that of an ayurvedic doctor who
was trained in the administration of general anaesthesia,
from 1978 to 1994 he was the only anaesthetist in
Mahad. He provided -excellent anaesthesia for patients
operated upon by seven surgeons in Mahad. Mangaon.
Sr.rivardhan and Poladpur talukas. He was even able to
demonstrate the ideal technique for cardiac resuscitation
tc the cardiologists in the region.
Health care can thus be provided to villagers without a
single allopathic doctor. It will be necessary for the
authorities to help the non-allopathic doctors. Each of
them must be provided training at a functioning civil
hospital where instruction on drugs and their usage
should be imparted. Special care must be taken to
emphasise side effects and complications and caution
them against drugs beyond their competence. They
should also be made to undergo annual training
programmes to update their knowledge. (Such
continuing education is equally necessary for allopathic
cc-ctors.)
Irrational practices
farmers and labourers in villages develop an irrational
faith in the potency of intravenous injections in the
treatment of vat (illnesses such as myalgia and
paresthesiae supposed to result from imbalance of the
four humours). Calcium gluconate is their drug of
choice and is routinely administered by allopathic and
non-allopathic doctors on demand. The consumption of
this drug jumps during the pre-monsoon season and in
October when there is a lot of work to be done on the
farms.
The treatment of tuberculosis also invites criticism. In
many cases a few- injections of streptomycin and tablets
for a few days is all the patient receives. In clinics run
by the government, only patients with positive sputum
are given bactericidal treatment.
nursing home does not have a death on its premises. At
times, lack of transport is used as an excuse by relatives
to take such patients or even the corpse home
Dilemmas consequent to Supreme Court ruling
Confronted with the recent ruling by the Supr<cme Court
disallowing non-allopathic doctors from using
allopathic drugs, I am in a quandry.
Suppose a villager suffers severe anginal pain and the
only medical attendant in his vicinity is a non -allopathic
doctor who has often used nitroglycerine successfully in
such patients, should the doctor be allowed to prescribe
this drug or not? This question becomes even more
relevant when the non-allopathic doctor later learns that
a consultant cardiologist has prescribed the same drug in
the same dose for his patient.
I have taught non-allopathic doctors to treat rhe victims
of scorpion stings with prazosin. Several lives have
been saved thus. Should these doctors now be
disallowed to ;administer this drug in the absence of any
other medical attendant?
Conclusion
The Supreme Court decision needs review if the health
care system in our villages is not to collapse. There is no
dispute over the need to ensure ;adequate
'
training of
non-allopathic doctors with provision for continuing
education programmes and certification. We need to
ensure that the medical practitioner does not deteriorate
into a drug pusher.
Allopathic doctors need to be cautioned against
disparaging their non-allopathic colleagues. We are well
aware of the fact that most Indian medical Colleges are
of low standard. Our journals are 1full of shoddy papers
with little or no ]peer review. The medical profession
consisting of allopathic doctors is no more respectable
or noble, ihe practice of medicine has degenerated into
commerce.
Whilst the allopath demands huge sums from the
patient, the non-allopathic doctor
in the
1
........ ...........
J village
is
content with poultry, lemons, coconuts and clothes from
his patients. As I ponder these facts, it occurs t_
J.
to me that
Mahatma Gandhi would have been greatly saddenedJ at
the sight of the educated in the medical profession
deceiving the illiterates whilst approaching the 21st
century.
References
1.
Patients with severe anaemia are given blood
transfusion without determining the cause or continuing
long-term medication to prevent recurrence.
The unkindest cut of all is when the terminally ill,
brought in gasping, are sent home so that the hospital or
2.
Bawaskar HS: Treatment of envenoming by mesobuthus hamulus
(Indian red scorpion). Transactions of the Roxal Society of
Tropical Medicine and Hygeine 1992:86:459.
Bang A, Bang RA, Talc O ct al: Reduction in pneumonia
mortality and total childhood mortality by means af community
based intervemion trial in Gadchiroli. India.
The Lancet
1990;336:201-206.
114
ksucs in MEDICAL ETHICS VOL.4 NO.4 OCT-DEC 1996
I
I
£
J\[^..2
Jan. - Mar.. *98
INFO PACK FOR DOCTORS
CONTENTS
1.
^Mi-CMopatAic (Doctor ^tni tfie
93adi6onc of, tjUviat JteaUh
2.
Ouality. JteaM, Ccutz:
CL Cxgittg. Coitdiuttex Ateed.
(Lutftai
Sauxce
Jl.S.. Siaiua&kaft
Medical EtfticA, Vel.4 Ate-.4
OU. - tDec. 1996
Alatfiuu-
3. AliAXMiiccpUcit^ in Jltedicat ffuLctice
Vcliuitcvty
CIaacciaticn of Jndia,
(L Mibia
Shag. tDuea&e tDoctcfi
VoUO JV.O-. 3, July 1997
CLawification a/ tJ^acticeA in
JV^uunaL fflvM
4.
5. Watnat at tJlioli
Guinaciinc &teUti&ation, a
practice, that defies accepted
uitwaiatictial nomiiA, contuuicA
in 3ttdia.
Safe Mothe^fwod
Caw in JVewntal tHodti :
a piacticat guide
WJLO, geneva
Natitii ViAuanatfian
Jltofian tfiao
6. Jinouj (lfoivt tD^ug^
frioiittOne, OU. 3t 1997
JtcaCtli Uction V^LW ^.8
Ougiut 1997
(XnatyeAicA <£ (hitipyxetics.
7. JlaHacetamot
CotiAiuneii confrontation
Vol. 17, J\[^. 2,
Marc/l-Clpsdl, 1997
fJfyiirfaH OhaiutA JlatcA Jloiu
8.
Jlle{X#quine : ‘llbc. wM Caution
VrugA Llodaij.
Jaauc 15, - Sept. f97
9.
CAbuane^aiwne
fflaiuted in Ciutcpe
Oji Sate in Jndia
tyxug& flcdag.
jA&ue 13 - t4.eh. *97
cM'0.
•5>OC*. 0-fe
tSlfidA?}
CKz^-j
>-'<C
G.
VU}
csV1.. 'V/^SL, .
\ ^OsyAycV
■ <C'C’^
2t 5'^- S V.kS _ L
Jail. - Mmh. yS
| INTRODUCTION TO DOCTORS FORUM [
^Ducto^,
She idea of forming a ^CS^UIS, SO^JEUM in VSttlS is gaining momentum Aince 1996.
She purpose of the ^Doctors Serum is ta build up, an active network of Aociallg conscious S)actors, who are open ta new ideas in Stealth Care ta come together ta Ahare ideas and
VStSS, would tike ta build up, and Aupport a jp/tafeAAiaaal qitaap, of S)cctanA uiha could thinh
M Care,
(Latte, wAette people one given pxinte impcnand act alteritaiively ta provide rational Stealth
tance. Special emphasis would be gwen to the area of
< psieuentiue and pjiomotiue SluMic Stealth
care.
<
(Doctors Serum is planning ta take up, the following initiatives:
¥
So provide a platfonni fon the S)octons to &hatte thevi views ftegaitding thevi pttofeosion and
the Givaiinty health isAues of the couatia^.
*
Sa Aend Snfounation Sachages fox Slcciotts as a paid a/ cmituiuuity medical edacatum
especially fon fDactons worthing in remote aneas.
*
So dehate and discusA ahout vanious health policies and technologies enteitging id Sadia
and provide alternate Auggestions.
*
Sa collaho*ate with the coasting tietwonh (the SMS, CMSS,, (LSKLS, i£ MS(L and wonh
together fan a common cause.
Sa shont, Stactons Sonant is a pnoactive and futuristic group, fon factors who could he in the
forefront to tahe up health isAues and find Aolutions to puhlic health problems in Sadia.
Enclosed is the S+ALSO, SXKLSIXKJE S,(2Sl S)dCS,(2SiS>. Shis is the oecond pachage we are Aending gau as a part of continuing medical education.
Slindlg fill in the feedbach form and Aend goun comments and AuggestionA. Slease Aend the
addresses of S)vctons who would benefit bg this package.
Shanking gau in anticipation.
Ma. CAaiubta Jlannapvam
Swum. 3\c(i‘iani/ne Office*
fDcctdiA fa'atm,
Valuntaid^ Stealth (ZAAOciaticn of Sadia
Sony SwaAthya iJifiawati
40, SjiAtitxdictiat Cbtea,
Smith of JJS,
JVew. ®Mi - 1W 016
Set: 6518071, 6518072, 6515018, 6962953 SUX: Oil - 6853708
E-Atait: cl)SUU(a)S)ct2uAtdjieLui
\
, v,
7S
/
-
_ ________ _
- Media
 RF_MP_8_SUDHA.pdf
RF_MP_8_SUDHA.pdf
Position: 1808 (6 views)