TEACHING AND TRAINING OF DEPARTMENTS IN MEDICAL COLLEGES
Item
- Title
- TEACHING AND TRAINING OF DEPARTMENTS IN MEDICAL COLLEGES
- extracted text
-
RF_MP_8_D_SUDHA
34 The Indian Journal of Medical Education
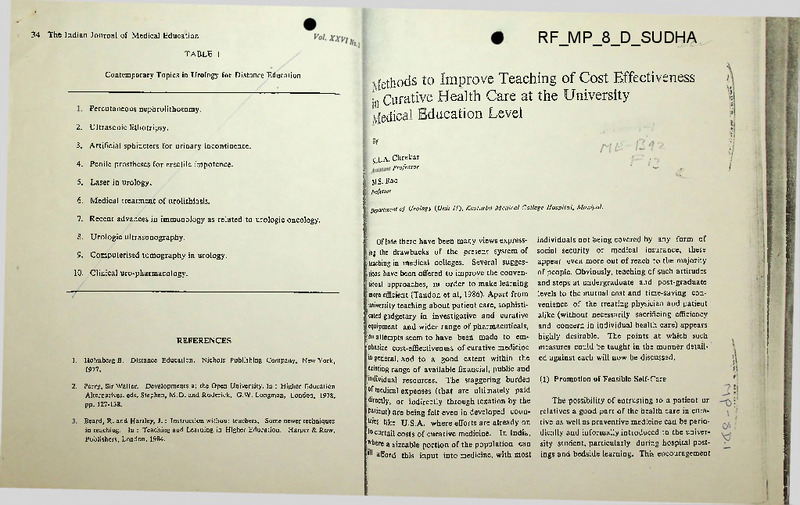
TABLE 1
Contemporary Topics in Urology for Distance Education
Percutaneous nephrolithotomy.
2.
Ultrasonic lithotripsy.
3.
Artificial sphincters for urinary incontinence.
4.
Penile prostheses for erectile impotence.
5.
Laser in urology.
6.
Medical treatment of urolithiasis.
7.
Recent advances in immunology as related to urologic oncology.
8.
Urologic ultrasonography.
9.
Computerised tomography in urology.
10.
Clinical uro-pharmacology.
\fethods to Improve Teaching of Cost Effectiveness
Jn Curative Health Care at the University
yfedical Education Level
*
K.L.A. Chrekar
.
'
Professor
J
M.s. Rao
jrtftssor
REFERENCES
1.
Holmberg B. Distance Education. Nichols Publishing Company, New York,
1977.
2.
Perry, Sir Waller. Developments at the Open University. In : Higher Education
Alternatives, eds. Stephen, M.D. and Roderick, G.W. Longman, London, 1978,
pp. 127-138.
Beard, R. and Hartley, J.: Instruction without teachers. Some newer techniques
in teaching. In : Teaching and Learning in Higher Education. Harper & Row,
Publishers, London, 1984.
Apartment of Urology {Unit 11), Kasturba Medical College Hospital, Manipal.
' Of late there have been many views express: tag the drawbacks of the present system of
; (aching in medical colleges. Several sugges
tions have been offered to improve the conventional approaches, in order to make learning
'more efficient (Tandon et al, 1986). Apart from
university teaching about patient care, sophisti
cated gadgetary in investigative and curative
equipment and wider range of pharmacuticals,
;no attempts seem to have been made to em
phasize cost-effiectiveness of curative medicine
iio general, and to a good extent within the
existing range of available financial, public and
^individual resources. The staggering burden
°f medical expenses (that are ultimately paid
■directly, or indirectly through texation by the
Patient) are being felt even in developed coun
tries like U.S.A, where efforts are already on
to curtail costs of curative medicine. In India,
P'here a sizeable portion of the population can
’H afford this input into medicine, with most
individuals not being covered by any form of
social security or medical insurance, these
appear even more out of reach to the majority
of people. Obviously, teaching of such attitudes
and steps at undergraduate and post-graduate
levels to the mutual cost and time-saving con
venience of the treating physician and patient
alike (without necessarily sacrificing efficiency
and concern in individual health care) appears
highly desirable. The points at which such
measures could be taught in the manner detail
ed against each will now be discussed.
(1) Promotion of Feasible Self-Care
The possibility of entrusting to a patient or
relatives a good part of the health care in cura
tive as well as praventive medicine can be perio
dically and informally introduced to the univer
sity student, particularly during hospital post
ings and bedside learning. This encouragement
36
The Indian Journal of Medical Education
becomes important when facing disabling
or prolonged care problems like paraplegia and
urinary retention, poor control of bowel move
ments etc. after serious injuries to spine,
repeated urethral dilatations for stricture etc.
The patient or attendants could be taught to
pass a catheter up the urethra periodically to
drain the collected bladder urine, self-calibrate
the narrowed urethra in stricture cases, or
remove stool daily by insertion of a gloved
finger up the anus (Rao et al 1986). The
students specially require to be exposed to the
art of patient motivation and counselling rather
than to teaching attitudes under-estimating
the intelligence and willingness of the illiterate
patient group, for instance. Once learnt, the
patient or the attendant can perform these
manovers confidently under home conditions,
thereby cutting down on inpatient costs and
time usually taken up by chronic care nursing
problems alone. This would be far more effi
cient and less expensive on the long run than
indwelling catheter drainage for example.
Cancer, high blood pressure, heart and chest
disease patients could also be selected so that
considerable on us is transferable on an
individual basis to the patient or relatives for
home care.
(2) Promotion of Outpatient Curative Services
The next point at which cost effectiveness
could be taught is at the outpatient levels The
students can be instructed about proper sizingup of an individual patient’s clinical condition
and specific problems, allowing for his/her
selection for outpatient treatment in a sizable
number of cases, and consequent influence of
such attitudes on mutual patient and hospital
V°l-
Methods of Improve Teaching...37
costs, competition for limited hospita] v I
. jnformation from the treatment initially avoidable treatment failures. Short
etc. at such outpatient facility areas.
could be brought to the student’s term antibiotic therapy (e.g. 6 months instead
proportion of major and minor surged ■ '
This will help in bis or her adaption of former 18 months for pulmonary tuber
hernia repairs, circumcision, varico-ele^ culosis, single dose treatment for cystitis in
hydrocele operation, endoscopic pr0C£J? ■ "\us altered facility situations better in
'^■dividual career life. For example, ultra- woman etc.) combining both cost-effectiveness
etc. could then be performed without necesr
rapby at titnes could obviate need for and efficiency should be brought to trainee
ing patient admission (Kaye, 1985).
attention.
*^r radiological contrast studies.
Attention of the student could be w
Optimal utilisation of the available hospital
focussed on the increased number of such c>
If the patient presents to the institution
beds and personnal resources by minimization
multiple disease problems, emphasizing
that can be treated at similar cost with.
of post-treatment time at which point a given
given period than otherwise possible with ( the trainee or student group on priority to
patient could be sent out to be looked after at
conventional method of hospitalization [ iStttly investigate and treat the entity immehome (or as an outpatient), could be high
undergoing the same procedures. Refre£ i,iiely threatening to that individual patient
lighted during bedside posting of students,
course and continuing medical education p becomes important. The message of avoidance
particularly the post-graduates.
grammes could also be effectively used t ^increased costs from further compelled, proimpart this message of choosing patients!; feejed hospitalization for treatment of any
(4) Projection of cost inputs towards patient
ambulatory care thus achieving cost-effect. Fecmplications resulting from wrong priority
care facilities adjusted to individual student
Jtfflsiderations causing delay in timely attention
ness without sacrificing efficiency.
career concerns
|wald then be brought in. Priority of attention
rnr.nj
•
-
pecifl men uc uiuuguu
(3) Cost-Reduction During Invesigation, Trch the vital body system e.
e.g. head thorex over
ment and Hospitalization
wthers in a multiple trauma case is an example
A post-graduate student wishing to start his
own private hospital or joining a new group
>'fsuch teaching.
requires to be given guidelines as to the optimal
Carrying out of as many of the reqoS
investment with cost-effective relevance to his
investigations for a given case at an outpace! Teaching judicious selection and usage o
uu future working enviroment. Many students
level (except
canhas
bealso
inculcs:
'------ ’ for
■ emergencies)
sdniss
an equally important bearing on
Mthougu a wide range cof are under the impression that with progress of
and demonstrated to the students ascou [eon-effectiveness.
t____________ .Although
for treatment of medical sciences and .growth of specialities,
buting to reducing inpatient costs. Diagnes pharmaceuticals areavailable
----tests for a specific disease entity or patr Various ailments, the students require to be cau one will expect prompt increased investment
iMUBj antibiotics
aunuivuvo costs towards the ultimate laudable goal of
should never be a habitual ritual, but sh« ‘honed about drug abuse (e.g. tonics,
cost-ineffective
providing efficient care, at his rapid command
be organised in as logical an order as poS ‘etc.) which in turn can create a tv.™
——
demand. Disillusionment
with the goal to obtain the maximal infon & risky situation for physicians & patients a i e. and affordabiljty
of providing soon
such follows,
services as
is
tion from the minimal number of procei The futility of prolonged antibiotic prop y axis
(preferably arranging the non-invasive (for overuse of combinations of such drugs withbefore the invasive), taking care to avoid tlfiont detection and simultaneous correction of
which are merely confirmatory to that obt» often underlying basic surgically treatable inble by others. Similarly, selection of invest fective disease results in bacterial resistance, as
tions which are economical and feasible ,a consequence of which costlier and a more
given situation and at the same time
----- provi-l
T 10xic compounds are repeatedly and compellingly brought into play for combating such
. JU __ 1....1,....-nj;nnr«nnrresnf an
limited by the slowly expanding resources of any
h
-M:___--------------------- agency. The pinch
public
or private financing
of this problem is being felt even in developed
countries. Therefore the postgraduate student
needs to be informed about rapid, cheep and
easily conducted methods ot investigations but
yet of proven bulk accuracy e.g. dip slide or
38
The Indian Journal of Medical Education
strip test for bacteriurea before resorting to
urine culture (Rao et al, 1984). The latter
facilityin this instance could be reserved for
those few patients in which the rapid testing
is anticipated to be fallacious.
The art of sensing feasibility of acquiring
capital expenditure equipment for one’s own
facility by combining demands with other
professionals or departments could be intro
duced to the post-graduate student at a suit
able point of learning activity (e.g. C.T. scan
or ultrasonography with radiology, laser source
equipment sharing with Ophthalmology etc.).
Both justification for wide range of use and
hence optimal cost-effective utilization of the
Ko/new equipment
attitude.
is reinforced by
(5) ’‘Balanced” follow-up care
I
1
Uie Training and Utilization of Paramedics
ifl Health Services of Bangladesh
The students, during their outpatienl..I
ing, could be exposed to the art of f0||^f
care balancing between “no-concern” or “A By
concern” attitudes in regard to nutn^t
Barua
out-patient visits or frequency of investigftl; p.C.
ll'IIO fellow from Bangladesh.
towards the goal of mutual patient/hov
cost-effectiveness. The students should
B.V. Adkoli
given opportunity to observe consults ' Asitt. Prof, of Educational Technology.
(teaching staff) making use of the dictapfe
telephone or postal correspondence fadfc
B.T.T.C., Jipmer, Pondicherry.
to the maximal mutual convenience and ad<
efficiency of the patients and themselves.
ABSTRACT
REFERENCES
1.
Kaye, K.W. Outpatient urologic Surgery.
Lea & Febiger, U.S.A., 1985.
2.
Rao, M.S., Achrekar, K.L., Manon, C. and Srinivas, V.
Clean, Non-sterile, Araumatic, Intermittent Catheterisation : Suitability under
Indian conditions for Short & Long-term, Urinary Retention Problems Antiseptic
83 : 179 ; 183 ; 1986.
3.
4.
The developing countries like Bangladesh are facing the challenge of providing
need based health services to a large population at a limited cost. Thus develop
ment of appropriate training programmes for different kinds of auxiliary health
personnel assumes great significance in the light of the countries’ commitment to
provide HFA by 2000 AD through primary health care approach. An attempt has
been made to examine the present situation and outline the curriculum of various
paramedical courses which provide basic support to the health care delivery in
Bangladesh.
Ind. J. Surg. 46 : 134-137 ; 1984.
One of the greatest challenges before the developing countries has been to develop cost
effective health services system according to the needs and requirements of the community.
Bangladesh is also committed to the goal of providing Health for All by 2000 A.D. through
Primary Health Care. As rightly emphasized by W.H.O., the development of appropriate
educational strategies has been considered to be the most important factors towards realization
Tandon, S.P., Vaidyanathan. S., Rao, M.S., and Natarajan. V. :
of this ambitious goal.
Rao, M.S., Agarwal. K.C., Vaidyanthan, S., et al Evaluation of a rapid screening
test for detection of bacteriuria in the urological outpatient service.
Application of Mastery concept of Urological Training of M.S. General Surgery
Postgraduate students
Ind. J. Urol. 2 : 76-78 ; 1986.
There is no unique model of training programme for particular health workers in the
developing countries. The approach to the problem should be independently explored by
each country in accordance with the local characteristics, needs and resources. The key word
[he Need for a Rose—(Re-orientation of
Surgical Education)
S.
Ananthakrishnan
Associate Professor of Surgery
hellfiirla/lnstitute of Postgraduate Medical Education and Research, Pondicherry.
ABSTRACT
The current status of undergraduate training in surgery is largely unsatisfactory.
This article analyses the job requirements of undergraduates and the objectives of
surgical training. Lacunae in the existing system are focussed and suggestions are
made for ensuring considerable improvement, without the need for major additional
resources.
The Government of India has rightly appro
ved the need for a reorientation of medical
iucation in this country to make it more
Levant to conditions existing here and thus
hsborn the ROME scheme in 1977. Although
-c primary aim of this scheme was to ensure
stive involvement of the Medical College in
immunity Health problems and in direct
-livery of Health Care Service to the rural
’Pulation, the functioning in practice of the
•jeme has been largely unsatisfactory with
: ’-implied reorientation of medical education
V forthcoming satisfactorily.
The aim of the current presentation is to
- ”nt out certain gross deficiencies as noticed
by the author in the training of the under
graduate in the discipline of surgery and to
suggest remedial measures, within the existing
system keeping in mind the specific objectives
of the ROME scheme.
Task Analysis
An analysis of the job requirements of a
fresh undergraduate on completing bis training
reveals the need for him to function in one of
several roles, viz.
(i)
as a doctor working at the PHC,
(ii)
in private practice,
42
The Indian Journal of Medical Education
(iii)
(vi)
a general duty medical officer in central
or state governments, autonomous or
private undertakings,
Vol. XXVI No. 3 !
(b)
involved in surgical management and
(i)
in taluk or district level hospitals,
(c)
(v)
as a postgraduate student,
(vi)
in teaching institutions and in
(d)
(vii)
other areas (migration abroad etc.).
be an active participant in national
programmes. The list is obviously in
complete and can be improved. /
recognise the nitural anxiety in patients]
and relatives -.-.garding surgical pro-!
cedures and c-.unsel them regarding Current Training Programme
the various indications of surgery,
Keeping in mind the job requirements and
objectives of undergraduate surgical training
to recognise, r»zord and appropriately
enunciated above it is obvious that the current
treat where feasible or refer where
system falls far short of the requirement.
required, Medi-zj-Legal situations met j
within day to cay practice.
Surgical education as at present carried out,
prepares him primarily only to function in a
transient role as a continuum to further post
graduation and does not lay enough stress on
other aspects to enable him to perform satis
factorily in the other roleimentioned earlier.
This lacunae continues to exist side by side
with the recommendations of the Medical
Council of India regarding undergraduate
medical education (MCI, 1977), a document
which in itself is quite vague.
.X
(e)
(f)
/ Objectives
The aim of training in surgery is to ensure
that the fresh graduate is able to :
(a) diagnose, order relevant and feasible
investigations and treat common simple
surgical ailments,
(g)
The Need for a Rose.. 43
Sept.-Dec. 1987
recognise anc refer appropriately
optimum time those surgical ailments]
which requit-, management at spec-1
ialised'centres,
I
to perform baeic and simple surgical
procedures commensurate with his
training and the facilities available e.g.
suturing of wounds, drainage of absces
ses, biopsies, minor operations etc.
I
The lacunae in the current system can be
listed as follows :
recognise that surgical intervention is j
but one aspect and probably a minw
one at that in the management of Pa' I
tients and therefore be aware of th' j
indications, contraindications and liHU'-;
tations of surgery,
(i) over-emphasis on rarer and more major
problems to the detriment of the
common surgical ailments seen at the
OPD,
(ii)
lack of adequate training on the impli
cations of surgery, and on the impor
tance of pre and postoperative manage
ment,
(iii)
total lack of contact with medico-legal
problems during the entire period of
surgical training as this aspect is left to
the department of forensic medicine,
(iv)
total lack of continuous contact, either
to provide first aid in appropriate situa-|
tions, and advise regarding transport j
with the patients or the relatives and
therefore an inability to appreciate the
anxieties and implications of surgery,
(v) minimal contact if at all with emer
gency surgical problems as the entire
duration of surgical posting is spent in
demonstrating ‘cold’ cases and the
students are available with the depart
ment for only a limited time,
(vi) minimal contact with actual operative
surgery. The last two are left generally
to be covered only during the short
interniship period in surgery and are
considered of no consequence to the
undergraduate surgical trainee,
(vii)
a total ignorance in the undergraduate
of the differences in facilities which are
likely to exist between teaching insti
tutions and areas where he may actual
ly have to perform as in PHCs etc.
This is a very important aspect and is
probably partly responsible for the
fresh graduate being reluctant to work
outside major teaching hospitals.
(viii)
complete avoidance of any training in
the effective domain with forms a very
significant part of the Doctor-Patient
relationship in surgery (Ananthakrishnan, 1981).
(ix)
no mention of the ethical implications
patients to major centres if required,
(h)
be aware
of the ethical principle*
44
The Indian Journal of Medical Education
Ko/. XXVI No. 3
of surgery—an area where the under
graduate is left in blissful ignorance.
an exercise is now being undertaken at JIPMER
which falls in the jurisdiction of the Central
University of Pondicherry.
Seasons for the Lacunae
In order to develop proper attitudes it is
necessary that continuous contact is encouraged
The reasons for the existing state of unsatis
between patients and their relatives and stu
factory affairs is obvious. Surgical training to
dents. It is necessary, therefore, to allot more
the undergraduate is at present considered as
responsibility to students, make them more
only the first step in the continuum progressing
active members of the team and encourage
from undergraduation to internship, to resi
them to actively involve themselves in the
dency, to postgraduation and to senior resi
diagnosis, investigations, management and
dency without really preparing him for fulfilling
follow up of patients allotted to them.
job requirements after graduation, were he to
so chose or be forced to do so, keeping in mind
the greater and greater difficulty in getting
Students must also be encouraged either
admission to post-graduate courses. Needless voluntarily or by compulsion if required to
to say an eight week pre-registration internship visit the wards and the casualty beyond work
period cannot compensate for the time lost ing hours to enable them to acquire some
during the entire three clincial years posting in knowledge regarding emergencies which usually
surgery.
tend to arrive after working hours. In the
final year, students allotted to individual units
must work full time with that unit for this
Suggestions for Improvement
purpose as is now being done only for the
department of obstetrics.
Keeping in mind the task analysis of the
fresh graduate and the objectives of training in
surgery it is necessary to completely recast the
curriculum of the undergraduate course in
surgery. However, this expectation is likely to
remain unfulfilled in view of known constraints.
The curriculum should be need based with
greater emphasis on common problems and
practical training rather than theoretical know
ledge. It should also ensure familiarity of the
trainee with facilities existing at the periphery
as opposed to major teaching institutions. Such
Undergraduates must be encouraged to
wash up and thus ‘passively’ assist operative
procedures especially those of a minor nature
like drainage of abscesses removal of lipomas,
cysts, biopsies, hydroceles, hernias etc. Active
involvement in this fashion is more likely to
evolve interest than mere observation as on
lookers.
The ROME scheme demands that a suitable
Sept-Dec. 1987
The Need for a Rose...45
More emphasis is to be paid in training
•me table be worked out by medical colleges
or posting of undergraduate students to Dis- both the undergraduate and the intern in
principles
of operative surgery. Details regard
rict Hospitals, Taluk Hospitals, subdivisional
jvel hospitals and PHCs for not less than 8 ing this have been discussed elsewhere and
will,
therefore,
require no repetition (Ananthareeks. Undergraduates posted in individual
•nits must therefore be encouraged to visit krishnan, 1984). It is necessary at all points
of training to ensure that the undergraduate
?HCs and peripheral hospitals in the vans pro,ided with the ROME scheme along with their understands the relevance of the training pro
:ef?ective surgical specialists. This will give cedure and the need for his active and useful
•hem an idea of the prevalence of actual surgi participation.
cal problems seen at the periphery as opposed
Co teaching hospitals and also give them an
dea regarding facilities likely to be available at
Teaching must be more problem oriented
Che periphery. Seeing consultants perform rather than subject based and appropriate
minor procedures under these conditions is like- efforts must be made to ensure this.
!|y to give them confidence to be able to do so
themselves.
| As is required for the interns in some insti
llations, undergraduates also should be required
to maintain diaries appropriately formulated to
ensure adequate participation on their part in
the activities mentioned earlier.
In conclusion, it appears that considerable
scope exists in improving undergraduate train
ing in the discipline of surgery and much can
be achieved in terms of results with negligible
or minimal additional resources.
46
The Indian Journal of Medical Education
Ko/. XXVI No.
REFERENCES
1. Ananthakrishnan, N. Doctor-Patient relationship—The neglected domain of
medical education. Indian Journal of Medical Education, 20-1-1981.
2. Ananthakrishnan, N. Is training for undergraduate medical students in opera
tive surgery adequate. Indian Journal of Medical Education, 23-1-1984.
3.
Medical Council of India—Recommendations on Undergraduate
Education. Medical Council of India, 1977, page 14.
4.
Rc-orientation of Medical Education (ROME) scheme—Background information,
Ministry of Health and Family Welfare (Department of Health) ME (Policy
Desk), 1977.
Medical
Survey of Existing Conditions in Dental
Departments of Medical Colleges in India
By
J. R. Sofat
Professor & Head of Deptt. of Dentistry,
(Mrs.) R- Sofat
Professor of Gynaecology & Obstetrics,
Dayanand Medical College, Ludhiana.
Dental departments of medical colleges are
in a state of evolution and are being ration
alised. Much has already been done to align
them in their due perspective but a lot yet
remains to be fulfilled. The standard regard
ing the staff members, their qualifications,
basic equipments, 'leds alloted to these depart
ments and teaching schedules differs from
place to place. Ttie Medical Council of India
(MCI) has prescribed some guidelines, but
these are either vague or not followed
uniformly. Since the inspecting teams have
no dental experts the setup of dental depart
ments is ignored altogether.1
Keeping these shortcomings and variations
in mind a survey was planned to assess the
salient features of the dental departments of
all the medical colleges of the country. The
heads of dental departments of all 1C6 medical
colleges were posted self-addressed and
stamped proformas to be filled and returned
to us. Thirty five replies were received in the
first instance. The request was repeated in
the same way to the remaining 71 medical
colleges after a gap of two months. Eighteen
tttore replies were received making a total of
53 replies out of 106 medical colleges i. e. a
50% response, which has been analysed and
reproduced below. Out of 53 responses, 5J
were from the dental departments of medical
colleges and 3 were from dental colleges/dental
wings looking after the dental needs of these
three medical colleges,
1.
TeachingMCI boolet2 recommends
15 days posting of three hours a day in
the department of dentistry in II MBBS,
1st and 3rd term.
The number of medical students
admitted to the 53 medical colleges
ranged from 50 to 200. On analysis of
data it was found that no dental teach
ing was done at one medical college, no
theory classes were taken at another two
medical colleges while in the rest of the
50 medical colleges both theory classes
and clinical demonstrations were taken.
The theory lectures of mostly 60 minutes
duration ranged between 4 to 30 and
these were conducted in 1st Profession
at 1 college, in 2nd Profession at 19
colleges and in 3rd Profession at
“ Volume XXIII No. 3 I
76 The Indian Journal of Medical Education
30 colleges. The clinical demonstration
of mostly 3 hours’ duration ranged
between 10 to 30 and these were con
ducted in 1st Profession at 5 colleges, in
2nd Profession at 29 colleges and in 3rd
Profession at 18 colleges.
2.
Examination in Dentistry :—MCI book
let2 recommends to include dental
diseases in Surgery paper II.
3.
4.
Considering only 50 dental depart
ments of medical colleges, the dental
departments were he'ded by Professors
at 23 places, Associate Professors/
Readers at 18 places Assistant Pro
fessors at 2 places, Lecturers at 6 plaees
and a Registrar at 1 place This showed
that MCI recommendation was flouted
at 9 places. There were 8 dental
surgeons/dental assistant surgeons in 7
medical colleges and obviously they
carried no teaching designations. There
Dental Radiographer :—One each was
available only at four places.
Though the staff recommendation
in dental" departments by MCI is barer
minimal, yet there were only 25 medical I
colleges where staff strength was accord
ing to its directive.
IV.
Sweepers
At least one sweeper was
available at every place, though he was
part-time at many places.
V.
Clerks cum Typists cum Receptionists:One each was available at 23 places
only,
{■/"
VI.
Nurses
24 Nurses were available at
18 places.
VII.
Pharmacists :—One each was available
at 2 places.
VIII,
Ward Boys/Ayas/M.N A.’s/Attendants/
Luscars :—30 of these were available
at 19 places.
One medical college admitting 100
students annually had only one teaching!
staff member with B. D. S. qualifications
and designated as lecturer, while another
medical college with 125 admissions was
headed by a graduate Registrar. Another
two medical colleges admitting 150
students had only two staff members
each with lecturers as heads at both the
places. Another medical college admit
ting 50 students annually had only one
teacher as a Professor.
Medical Interns :—They were posted in
dental departments only at 12 medical
colleges.
Teaching Staff :—MCI booklet recom
mends,3 1 Professor/Associate professor/
Reader, 1 Assistant piofessor/lecturer
and 1 Demonstrator for 100 annual
admissions of medical students.
IH.
Some glaring discrepancies were as I
under :—
On analysis of data, no question on
dental diseases ever appeared in theory
paper of Surgery or any other subject at
22 medical colleges while at 31 medical
colleges only one question or a short
note appeared.
5.
Survey of Existing Conditions 77
September-December 1984
were 36 house-surgeons in 21 medical
colleges only.
Dental Auxiliary StaffMCI booklet’
prescribes four dental technicians and
one store keeper-cum-clerk for 100
annual admissions in M. B, B. S. course.
The analysis of 53 dental depart
ments showed the availability of follow
ing auxiliary dental staff
I.
Dental Technicians :—A total of 61
dental technicians were available at
40 places.
II.
Dental HygienistsA total of 35
dental hygienists were employed at 24
places.
IX.
Chairside Assistants
able at 14 places.
(with 2 dentists) had a single auxiliary
staff in the form of 1 clerk, 1 clerk, 1
chairside assistant, 1 nurse, 1 techni
cian, 1 technician and 1 technician
respectively besides the assistance of a
sweeper at each place.
6.
Dental Casualty Service :—No dental
casualty services existed at 13 places out
of 53. At 34 places, a dentist was called
only when needed. Only at the remain
ing 6 places dental casualty services were
available round the clock on 8-hourIy
staff rotation duty. A dental unit/chair
was available only at 7 places of casualty
service while dental beds were reserved
only at three places in a number of 1, 2
and 2 respectively.
7.
Dental Ward
No beds were available
for dental department at 5 places, while
at other places the bed allotment varied
between 2 and 20 with an average of 6
beds at a place. At 22 places, the beds
were under the independent charge of
heads of dental departments thouah they
did not seem to have sufficient subordi
nate staff, like registrars/house surgeons/
nurses to look after these neds. At other
26 places these dental beds were placed
in the wards of Surgery (14 places),
E. N. T. (6 places), Medical (2 places).
Orthopaedics (I place), Skin (1 place)
and miscellaneous (2 places).
37 were avail
There was hardly a place where
’auxiliary staff was sufficient either
according to the directions of the MCI
or according to the desirability.
Some glaring discrepancies were
as under :—
One place admitting 100 students
annually and with 2 dentists in position
had no auxiliaries whatsoever. The
following places admitting 155 students
(with 5 dentists), 70 students (with 4
dentists), 125 students (with 4 dentists)
120 students (with 3 dentists) 145
students (with 2 dentists), 100 students
(with 2 dentists) and 100 students
8.
Equipment : —
a)
Dental Chairs and units needed in
dental departments were based on
the total number of dentists which
78 The Indian Journal of Medical Education
was 190 including 35 house surgeons
in 50 medical colleges. The number
or dental chairs and units was ade
quate everywhere except at 11 places
where these were deficient.
b)
c)
d)
e)
f)
Dental X-Ray Units:—These were
available at 38 places and there were
no X-Rav Units nt 15 places. At
28 places there was one X-Ray
plant each, at 6 places 2 X-Ray
plants each and at 4 places 3 X-Ray
plants each were avaik-.ble,
Volume XXIII A’o. J
motors, boyie’s apparatus and
amalgamator was available at only
one place each.
9.
Operation. Theatre with General Anaes-j
thesia ;—This facility was available at I
fixed times (mostly once a week) at 34
laces while 19 places had no such
facility.
10.
Post-Graduation :—Post-graduation was
available at 5 medical colleges. Four I
medical colleges had the facility of post
graduation in the specialities of Ortho
dontia, Public
Health
Dentistry,
Operative Dentistry and Oral Surgeryone at each place, while one medical I
college had post-graduation in two I
specialities i. e. Prosthetics and Oral >
Surgery.
Airotors 1—One or more were avail
able at 25 places. At 11 places there
was one airotor each, at 6 places 2
each, at 7 places 3 each and at one
place 6 ol these were available.
Ultrasonic Scalers
One or more
were available at 19 places. At 13
places there was one each, at 3
places 2 each, at 1 place 3, at
another place 4 and still another
place 5 were available.
Dental Laboratories
Dental labo
ratories for prosthetic and maxillo
facial piosthesis work were available
only at 29 places while we bad 67
dental technicians at 40 place out of
53 places. This showed that these
technically qualified people were
being used elsewhere.
Special EquipmentSpecial equip
ment like casting facility was avail
able at three places while cryosur
gery, endobox. diathermy, micro-
11.
Community Dental Clinics :—Community
dental service, either urban or rural,
outside the medical college campus was
available at 15 places out of 53.
12.
Commrnts/Suggcstions of Head of Dental
Departments :—Most of the heads of
dental departments had responded with
following comments/suggestions :—
I.
Present State
Detal departments
are in a bad shape and a lot of
improvement is needed for their
growth and development. Medical
Council of India and Dental Council
of India should be apprised of the
situation and requested for remedial
measures.
September-December
II.
III.
IV.
Survey of Existing Conditions 79
1984
Beds, Casualty and General Anaes
thesia Service :—At least 10 beds
under the head of dental department
and 2 days a week of general anaes
thesia service in the operation theatre
should be available for the dental
department. Adequate junior dental
staff and nursing staff should be pro
vided to look after the admitted
patients and also to look after the
casualty service. A dental unit,chair
should be provided in the casualty
centre.
Regional Repair Workshop :—There is
difficulty in getting the repairs,service
of the equipment. Regional workshops
are suggested at the de,ital/medical
colleges for this purpose.
Dental Specialities Staff and Regional
Ref rral Centres : —Many have
complained of such inadequate staff
that even the treatment of staff
and students of the medical college
could not be carried out satisfactorily
besides the commitment of teaching
and research. Dentul departments
should be uplifted in such a way that
these can have the facilities of all
specialities so that these departments
can render tl e specialised dental ser
vices rather than the present general
dentistry. There should be a minimum
of 5 post-graduates, one each in the
specialities of Oral Surgery, Perio
dontia, Prosthetics, Orthodontia and
Pedodontia/Operative Dentistry for
50 annual M. B. B. S. admissions. If
the number of admissions is more.
these specialists can have their own
sections with an assistant like registrar/
demonstrator and a house surgeon
accordingly. Once all specialists are
there, these deatal departments can
work as regional referral centres for
the patients of the area.
V.
Auxiliary Staff : —At least two dental
technicians, 2 hygienists, 1 radio
grapher. 2 receptionists/typists/chit
clerks, chairside assistants equal to
the number of dentists nnd 1 whole
time sweeper should be there for 50
MBBS admissions.
VI.
Curriculum ;—A uniform pattern is
needed so that medicos are given
adequate knowledge.
VII.
Examination in Dentistry; —For want
of examination in dentistry, attendance
in classes is erratic. Surgery paper
should carry at least one part with
three questions on dental diseases and
the head of dental department should
be the examiner for this part.
VIII.
Finances :—There should be suitable
annual budget for dental departments
for the purchase of equipment, drugs
and materials.
IX.
Post-Graduation
Post-graduation
should be allowed in the speciality
where the conditions laid down by the
authorities can be fulfilled, so that the
teachers in the medical colleges can
persue an active interest in their
specialities.
Survey of Existing Conditions 81
SO The Indian Journal of Medical Education
^^’uhune XXIII No
3
September-December 1984
references
X.
Attitude of Authorities : —Many have
complained of the callous attitude of
the authorities and they must be made
to wake up. The recommendations
of the MCI should be mandatory and
nothing should be left to the local
authorities. The inspection of dental
departments should be carried out by
dental inspectors and not by medical
inspectors who themselves know very'
little about the dental setup.
XI.
All India Annual Meet;—All the
teachers or at least heads of dental
departments must meet at least once
a year so that they can discuss about
their common interests and problems.
An all India body of dental teachers
of medical colleges is desired to be
formed.
XII.
Social and Preventive Measures: —
Social and Preventive dental measures
should be the responsibility of these
dental departments. Fluoridation and
defluoridation of water programme
which is a social health measure
should be got carried out by the heads
of these departments.
Discussion '■—"The basic objective of dental
departments of medical colleges is teaching of
dentistry to MBBS students, research, dental
and maxillofacial treatment of both outdoor
and indoor patients and help in the preven
tion of dental disease. All this is possible
only if we have sufficient staff, auxiliaries,
equipment, accomodation, beds, materials,
cooperation of concerned authorities and pro
per guidelines. Owing to the magnitude of
dental disease in the country, paucity of dental
manpower and urgent need for prevention, it
is all the more important that the dental
departments of medical colleges be well
organized. All clinical specialities have to be
developed so that these departments become
the centres of. referrals. If the graduate
medicos must have the working knowledge of
dentistry the curriculum should be laid down
and students be examined in the subject.
Dentistry should not be isolated as an outside
subject but should be considered as an integral
part of the other body systems. The existing
state of these dental departments is at such a
low ebb that no justice is being done to any
of the objectives of the department. It is high
time a committee of experts from these
departments is formed by the concerned
authorities so that available facilities are
reviewed and suitable recommendations are
made.
Summary :—Existing conditions in dental
departments of 53 medical colleges out of 106
in the country have been surveyed and analysed
in respect of teaching facililies, staff, casualty
service, dental beds, equipment, operation
theatre facilities under G. A., post-graduation
and community dental services. There are
many deficiencies in almost all the categories.
Comments of heads of dental departments
have also been reportad. Most of them feel
strongly about the need to reorganise these
departments.
Acknowledgement:—We are grateful to
heads of dental departments in various
medical colleges who responded to our questionaire. Our thanks are also due to our
Principal, Dr. N. Dube, for all his help,
guidance and permission to conduct this
study.
1.
Sofat, J. R. : Dental Departments of Medical Colleges for Teaching M. B. B. S.,
Indian Journal of Medical Education XXH, No. 3 : 12, 1983.
2.
MCI Booklet : Recommendations on Undergraduate Medical Education; P 17, 23,
April, 1977 corrected upto Feb., 1980,
Volume XXIll No. 1
22 The Indian Journal of Medical Education
TABLE
111
•
Is Trainin^)f Undergraduate Medical Students
in Operative Surgery Adequate ?
Percentages of Correct Responses in Therapeutic Nutrition Statements
Graduate
N=190
Post-graduate
' N = 67
Diploma Holders
N=23
By
N: Ananthakrishnan
Peptic ulcer
59
60
71
Kidney diseases
47
52
67
.■’
Diarrhoea
73
71
Anaemia
62
65
77
Fever
64
76
77
59
Assistant Professor of Surgery
Jawaharlal Institute of Postgraduate Medical Education and Research, Pondicherry.
75
Liver Disease
53
47
Heart Disease
67
71
80
Diabetes
32
32
45
ABSTRACT
The current procedure for practical training of the undergraduate student in
surgery is grossly inadequate. The deficiencies of the existing system have been mentioned:
Clear and concise objectives are suggested as also changes in the existing training
methodology which would ensure better training and a better utilisation of the available
time of without adding to the curriculum eliminating at the same time the impartment
knowledge outside the purview of the MBBS doctor.
: Introduction
TABLE IV
Values Obtained on Chi Squere Test
Graduate and
Post-graduate
Graduate and
diploma holders
Post-graduate
and diploma
holders
n.s
3.161
2.662
Kidney Diseases
n.s
8.143
4.661
Diarrhoea
n.s
n.s
n.s
Anaemia
n.s
5.30*
3.501
Fever
Liver Diseases
3.421
n.s
4.04s
n.s
n.s
2.881
Heart Diseases
n.s
4.3 24
2.182
Diabetes
n.s
3.561
3.561
) Peptic Ulcer
.
Mark Ravitch of Pittsburg, USA, interna( tionally known surgeon, editor, historian and
I linguist is quoted as having stated that when
an editiorial or an article begins with a ques| tion (as this one does), the answer is always no
(Hardy, 1983). The question raised in this
article is very pertinent currently as different
universities tend to adopt widely divergent
approaches to this problem.
.
The Medical Council of India in its recomJ mendations
on
Undergraduate Medical
I Education merely states that the course of
| training in surgery including orthopedics
I should necessarily involve
I
(a) Practical instruction in minor surgical
■ techniques inculding first aid and
(b) A course of practical instruction in
common operative techniques including decom| pression, bandaging, splintings plaster etc.
'
Significant 1 at 0 10% lev I, 2 at 0.20% level,
3 at 0.01% level, 4 at 0 05% level,
The recommendations (MCI, 1977) do
mention that to achieve the above aims the
candidate should have one month clinical
clerkship in the casualty and emergency
services besides outpatient and inpatient train
ing in surgery. No definite guidelines are
available regarding the content of the course of
training in operative surgery of the methods to
be adopted in achieving the objectives of
training in that field.
Existing system
In the absence of any fixed guidelines and
well defined objectives, it is not surprising that
there is a wide variation in teaching the so
called “operative surgery” to underguaduates.
In some universities as in the university of
Madras, the subject assumes great importance
in view of the marked weightage given to
operative surgery in the viva part of the
examination in general surgery for the final
MBBS. Candidates have to undergo a seties of
—q
'
,24 The Indian Journal of Medical Education
Volume XXIII No.
1
'lectures on operative techniques of “Com agreement on the objMR/es and how to achieve
monly” performed surgical procedures in the them.
final year of the undergraduate training. The
It cannot be gainsaid that the aims of the
course usually consists of a series of theoretical
practical training in surgery should include
discussions on the indications, contraindica / (a) a knowledge of resuscitative procedures,
tions and procedures for performing various
first aid, splinting, treatment of abscesses,
surgical operations, supplemented by a short
sutures of wounds etc.
and variable period of observation of actual
operations in the operating rooms. In view of
(b) a familiarity with principles of surgery
the large numbers of students involved and the especially an ability to decide
limited period available for surgery in the final
(i) What to operate-i.e. the simple proced
year, this latter period of observation has
ures which an MBBS graduate can
necessarily to be extremely curtailed in scope,
safely be expected to perform in his day
duration and content. Demonstrations of some
to day practice,
of the operative procedures in cadavers is no
(ii) when to operate as a necessary
longer current primarily due to the shortage of
corollary of the above and
cadavers but also due to difficulty of any
worthwhile operative surgery demonstration on
(iii) most important of all which patients to
preserved bodies.
refer for surgery elsewhere. All these
three factors would imply in addition a
It is not surprising that in view of the above,
knowledge of emergency care, again
student compliance is minimal or nil and
that alone which is within the purview
the course is usually accepted as an unavoida
.--‘r of an MBBS graduate.
ble encumbrance with students taking recourse/-;to memorising a series of operations immedia-' /The course cf training should not include
tely prior to their examination in order to any reference to procedures which would be
satisfy the examiners.
outside the scope of a graduate doctor practis
ing in the usual environment in the country.
The lectures involve large groups of
students without in most cases even the facili
The list therefore should be curtailed to the
ties of Audio-visual aids.
Most of the barest minimum keeping in mind the above
operations described have not been even seen requirements. A list of procedures, knowledge
by the students and the instruments shown are of which could be considered absolutely essen
sometimes archaic and those not commonly tial for undergraduates is given below ;
used.
(a) sutures of wounds, drainage of
abscesses ;
Framing of objectives
Tn view of the lacunae, pointed out above,
it is necessary that strict and observable
guidelines are framed if necesseary by the MCI,
so that students, faculty and examiners are in
(b) tetanus prophylaxis
debridement ;
including wound
(c) venesection and establishment of a safe
and effective l.V. line ;
January-April
(d)
198
tracheostJ^ and emergency care of
obstructed- airway including principles
of airway maintainance in the seriously
ill patients;
(e)
emergency treatment and splinting of
common fractures ;.
(f)
treatment of common perianal condi-,
tions like fissures and piles ;
(g)
recognition of threatened or existing
intracranial hematoma and ? burr hole
exploration ;
(h)
recognition of intraabdominal emergen
cies and the need for referral to .
appropriate centres etc ;
(i)
minor operative procedures like vasec
tomy, circumcision, hydrocelectomy ? .
etc.;
More complicated procedures like herniorr
haphy, gastrjjejunostomy, appendicectomy etc.
which are often taught to the undergraduates
would really be outside their scope.
Is Training of Undergraduate 25
(ii) Training in “practical” surgery should
mainly be in the final year when an
adequate theoretical background would
already be present.
''(iii) There should be no need for formal
lectures with their inherent and well
recognised disadvantages.
(iv) Although the
disadvantages of
cadaveric demonstration are well
known and have been mentioned
earlier there might still be a limited
role for recourse to them for demons
trating procedures like, endotrachea]
intubation, tracheostomy etc.
(v) Finally, the most essential and most I
important part of practical surgical
training would entail a radical '
change in the schedule of undergra- 1
duate posting in surgery.
(a) The students in batches should be posted
full time in the various surgical units as is
being done currently for obstetrics during the
entire period of their final year posting in
A knowledge of the use of common general surgery. This naturally would include i
intruments would ofcourse be part of training out patient and inpatient training with the res
in the relevant procedures,
pective units, attending minor and major operative surgical sessions and also an exposure to
Methodology of training
emergencies with the concerned units on their .
With well defined and clear objectives, the emergency days. This constant exposure for 8
’ framing of a training schedule becomes very weeks would give an adequate opportunity of
much simpler and necessarily becomes more familiarising themselves with most of the ‘
need oriented. The suggested scheme is procedures mentioned earlier on the spot as it
elaborated below :
were, without need for theoretical classes.Since full time posting is already current in the
(i) The disproportionate credit given to
labour ward its adoption for other disciplines
operative surgery in the final MBBS should pose no problems. Since surgical
examination should be dispensed with management is a continuous process, constant
thus eliminating the need to memorise
exposure would ensure optium utilisation of the
and repeat little understood procedures. available period, besides fulfilling the needs of
26 The Indian Journal of Medical Education
Volume XXIII_No±. 1
article, the answer ^Be again as suggested by
“ essential.” practial training. Needless to say,
this would also ensure a sound basis for the Revitch is “no”. The training is certainly
post final examination, pre-registratiop. intern •defective but these deficiencies are largely
correctible if definite objectives are framed and
ship programme. ,
minor changes instituted in the training
To return, therefore, to the title of this programme.
REFERENCES
Hardy J.D. Is (almost) All Cancer Environmental. World J, Surg., 7: 176, 1983.
Medical Council of India—Recommendations on Undergraduate Medical Edu
cation—Adopted by the Medical Council of India, April 197 , page 14.
: jTJHe , ^2-^-.
VOLUME XXII Ho 1
50 THE INDIAN JOURNAL OF MEDICAL EDUCATION
\
What are the financial resources for Health 2000
Low
Income
China
1978
esti
mates
Upper
Middle
Income
Lower
Middle
Income
Higher
Income
z , Hc^-j
Z
■
6"/ -
L
.
•
Education of Undergraduate Medical Students
In Radiology*
By
S. Chawla
39
Number of
Countries
Average annual
300\
per capita income (USS)
1330
Population in
1976 (million)
1
28
28
17
400
300-700
, 1000—2500
3450
930
244
378
79
P. Panag
480
270
And
Principal and Medical Superientendent,
Lady Hardinge Medical College & Associated Hospitals,
New Delhi and Professor of Radiology,
University of Delhi,
Assistant Professor,
GNP in 1976
(5 billion)
220
372
170.6
% GNP allocated
for health,
public sector
0.77
0.78
0.64
Average per
capita health
expenditure
1.2
3.1
4.5
Total health
expenditure
S billion
(public sector)
1.7
2.9
1.1
4.8
2.7
Total estimated
private health
expenditure
$ (billion)
6.8
4.4
19.2
10.8
Total estimated
public+private
health expenditure
(S billion)
8.5
Not
known
5.5
24.0
13.5
Estimated ‘Abso
lute poor' %
45
—
15
8
5
S. Bhardwaj
Associate Professor,
Lady Hardinge Medical College,
New Delhi
ABSTRACT
Source : World Health Forum 1981 Vol. 2 No. 1, Lee M Howard.
Knowledge of radiology is essential for practice of medicine, hence it must
form an integral part of undergraduate training. The students at this level
do not need exposure to the details of specialised radiological techniques.
However, training in underlying piinciplcs, importance, judicious usage and
limitations of radiological procedures is essential. The curriculum content
can be rationalised to ensure coverage of appropriate topics. Integration
of teaching in radiology with pre-clinical, para-clinical and clinical subjects
would be the most effective methods of training. This could be achieved by
including discussions and demonstrations of radiographs and slides etc.
with the body systems taught in these disciplines The faculty from the
department of radfology if and when possible could be directly involved in
these teaching sessions. During the clinical period, attachment of small
groups of students to the department of radiology would be very useful.
The students could observe and participate in the routine procedures being
carried out in the department./
• Based on background paper prepared for a meeting oj the international cemmisshn on Radiological Education
held m Barbados in November, 1982.
52 THE INDIAN JOURNAL OF MEDICAL EDUCATION
The graduate in medicine is not expected to
be a specialist in radiology but he or she is
expected to have some knowledge about the
modalities of imaging so that he can practice
medicine effectively.
In brief, the educational obj.-ctives for
education of undergraduate medical students
in radiology should be as under:-
'GLUME XXII No 2
it would be worthwhile to delete some topics
which are of less practical importance from
various subjects and the time thus saved could
be effectively utilised for giving mote clinical
training, more emphasis on behavioural
sciences, paediatrics medicine and diagnostic
radiologv. How to achieve the objectives laid
down above ?
Probably the best method would be to
The graduates should know the physical integrate radiology with other subjects. •
principles underlying all imaging techniques
In the pre-clinical years, teaching of
including radiologv, ultrasound, CAT and
special
procedures including contrast anatomy and physiology can be supplemented
by appropriate radiographs showing the normal
examinations
skeletal system, card io-vascular system, gastroin
2.
Some understanding of the biological effects
testinal tract, the vascular system and the bron
of radiation, radiation protection and adverse
chial tree etc. Normal movements of the heart
reactions to contrast media and their
can be shown on real time scan and imaging of
management.
organs by radionuclides and perfusion studies.
3. The importance of the judicious usage ofThese will not only enhance their understan
various imaging procedures, when and how ding by visual impact but the students will also
to requisition them, supplying of proper realise the relevance of learning these subjects
clincal history and detailed findings of the for their clinical work.
physical examinations.
In the para-clinical years, especially for
4. He should be able to understand and
subjects
like
pathology,
microbiology
appreciate the report given by the radiolog
radiology
would be
of help.
When
ist and also the inherent limitations of the
pathology of an organ
is being taught
various procedures.
then along with the gross specimens and
There is a dearth of trained radiologists in the histology slides. X-rays of the same part or
the developing countries due to their migration organ, normal as well as the radiographs sho
to affluent countries and the lure of private wing specific changes that the particular
practice. Moreover, most such countries can pathological process causes in the radiographs
not afferd to have diagnostic radiologists in or changes on ultrasound and nuclear imaging
small hospitals and primary health centres. can be shown. This will make the study of
Thus very few radiologists arc available in these pathological processes more interesting as their
countries for the large population attending implication in actual practice can then be
appreciated.
Government and Semi-Government hospitals.
1.
Since the modern system of medicine
depends a great deal on imaging techniques,
Similarly in microbiology, radiological
changes caused by bacterial and viral infections
MAY-AUGUST 1983
EDUCATION OF UNDERGRADUATE MEDICAL STUDENT...53
in various body organs and systems can be
demonstrated.
In forensic medicine, various types of frac
tures, effect of trauma on the heart, lungs, soft
tissues and perforation of the gut etc. can be
shown radiologically, to make the subject come
alive for the students.
In order to achieve this goal, very close
cooperation is required between the faculty of
radiology and pre and para clinical faculties.
The problems which can arise are the length of
time allotted to radiology out of the tight
schedules of the various specialities and the
reluctance of the radiology department to spare
so much time of the faculty.
imaging in isolation without correlating with
actual patients or without emphasis on the
clinical relevance.
Z^ThT students
are also posted
in small
batches to the radiology department during
their clinical posting. This period is found to
be useful for students learning because :i)
They watch and participate in the routine
procedures being carried out in the depar
tment;
ii)
they observe the
procedures;
techniques of special
iii)
they study the x ray films from teaching
files of the department;
In may not be possible to spare a faculty
member from radiology department, each and iv)
see the practical applications of radiation
every time a lecture or practical demonstration
protection measures;
is arranged. However, simple radiographs can
be shown b the teachers of these disciplines v)
understand the value and limitalions of
themselves supplemented by teachers from
radiological procedures and other imaging
radiology department to give a few demons
techniques;
trations of imaging at the end of teaching of
eaeh system before the next part of the vi)
attend the clinco-radiological conferences
curriculum is started.
held by the department;
In the clinical years is India, about 20
lecture demonstrations are given to the final
year students. These do serve some purpose but
the number of students in a class are so large
that not every student can see the lesion or
retain his interest. In our experience, showing
radiographs to undergraduate students is more
effective than projection of slides.
Small batches of students or integration of
imaging in various seminars and in integrated
teaching will be more benificial than teaching
vii)
learn interpretation of routine rediographs
and gross abnormalities of various structures
and organs;
viii)
learn the cost effectiveness of various
procedures as related to the yield of infor
mation. z -
Here, a great deal depends on the faculty of
the radiology department, how much time they
can spare out of their routine work, teaching of
post-graduate students and research, for under-
54 -THE INDIAN JOURNAL OF MEDICAL EDUCATION
graduate teaching. Individual attention is
required, if they want the student to develop
interest in the fascinating world of radiology.
Ability to recognise and interpret radiologi
cal signs and analyse and correlate them with
the clinical findings can only be achieved if
more time is spent near the viewing boxes by
the students supervised by the faculty and
'^^ME XXII ■ No 2
students are encouraged to follow-up their
cases to get the final diagnosis
In our experience, the response of the
students is directly proportional to the enth
usiasm of the faculty. Many undergraduate
students decide to take up radiology as a
speciality after their posting in the radiology
department.
Performance Factors of Attempt and Non-Attempt'
Holding Medical Students — An Indepth
Interrogatory Study (Part-I)
By
H. Saran
A. K Malhotra
W. C. H. Cum Lecturers
R. N. Srivastava
Prof. & Head,
Department of Social and Preventive Medicine,
M.L B. Medical College, Jhansi
Introduction :
The medical science is expanding very fast
and the day is not far off when it will^pbse a
challange to the top level amongst/planners
engaged in the delivery of medical' education.
Recently, it has been observed that the
knowledee in medical science doubles every
7-10 years. It is a bitter truth that the
majority of medical teachers are still untrained,
unab'e to impart ^their full talent, skills and
knowledge to their future on-going generation.
The medical/institutions, in general, are
following the tradational way of teaching/
training m spite of tremendous adancements
made /in the educational methods and
techniques in the past few years (Srivastava
at all, 1982) neglecting the interest of the
medical students (Saran at al?, 1982).
The facts that the medical students are
selected through a tough competitive exami
nation usually with their past brilliant
scholastic performances can not be denied.
Majority of these students experience one or
more failures during the medial career,
However, only a few get through unspotted'
though all reside in the same socio-educational atmosphers, why is it so ? Have the
eminent medical educationists ever thought
about it ? The answer at the most of the
time would be, no. It not only creates a
burden on parents/Governments but also
mental set back amongst the medical students.
A drastic change in the selection method
of medical teachers, initiation of teachers
training programme for medical teachers with
some attractive incentives, adoption of recent
advancements made in the educational
methods/techniques by the medical institu
tions, teaching by and restricting strictly to
the well pre-planned lesson objectives/plans
and provision of due place to the interest/
mental status of the students during teaching/
training may provide some solution. Recently,
Saran at al-*,4,5,6, reported the various per
formance factors of medical students responsi
ble for obtaining different scores m the
Septembtr-December
Dental Departments of Medical CoSgcs
for Teaching M.B.B.S.
By
J. R. Sofat
Professor & Head of Dental Deptl , Dayanand Medical College, Ludhiana
The prevalence of dental disease is very
high in India. Periodontal or gum disease
alone afflicts 90% population. With change in
life style resulting in modern living the occurence of dental caries has risen from 50-70%
in fifties to 60-90% in seventies. The incidence
of oral cancer related to typical Indian habits
with high figures of 40-50% of all diagnosed
cancer as compared to western figures of 1-3%
also poses a serious challenge. It can be
summed dental disease affects approximately
the entire population.
One dentist for 4000 population is the
need as pointed out by Bhore Commission in
I9J5 and one dentist for 80,(00 population
with a mere 9000 dentists in the country is
what we have attained. Since the majority of
dentists are concentrated only in cities, this
ratio will be still worse if one seas only rural
India This number is no doubt far below
need and it is no wonder the ailing public
seeks relief from unqualified practitioners. It
is not practical to reach the target of dentist
population ratio at the existing number of
dental colleges in foreseable future. It is
regretted that Government has not evolved
any specific programme for the promotion of
dental care. There is no mention of such a
programme in the 6th Plan which has the
outlay of Rs, 18,000 crores for the health
care.
The only solution for India is to launch a
massive compaign at community level in pre
ventive dentistry. Despite relatively huge
man power of 1,33,000 dentists in USA there
is a growing realisation that preventive
measures are the only solution to tackle the
problem of dental disease in that country The
limited dental manpower in India will not be
sufficient to treat even a small percentage of
the quantum of existing dental disease. Due
to this magnitude of dental disease, paucity of
dental manpower and urgent need for preven
tion, it is suggested that medical men be given
some dental responsibilities through better
dental teaching at the level of undergraduate
medical education. May be we can incor
porate preventive dentistry with preventive
medicine whose infrastructure is much better.
Dental departments of Medical Colleges are
in a state of evolution. With better under
standing between the Dental Council of India
and the Medical Council of India these dental
department are much better now than ever
before. Since the position of Head of the
Dental Department in medical colleges has
been upgraded to the level of Professor (in
1976) the prestige of the dental profession
has been enhanced. Consequently a sizeable
number of dental experts usefully employed.
These dental experts are performing a notable
role in dental education and research. The
1983
Dental Departments of Med cal- Collegs ...13
dental departmen^k of medical colleges are
being rationalizetSFMuch has already been
Recommendation of M. C. I. to be specific :
done to align them in their due perspective but
a lot yet remains to be fulfilled. The standard
regarding the number of staff members, their
qualifications, basic equipments, beds allotted
to these departments and teaching schedules
from place to place. There are still places
where no teaching designations are given to
staff and dentistry is not taught to MBBS
students. The Medical Council of India has
prescribed some guidelines but these are either
vague or incomplete or not followed uniformly
Since the inspecting teams have no dental
experts the set up of dental departments
is ignored altogether
All recommendations of the Medical
Council of India (M. C. I ) in respect of
dental departments, should be specified for
100 MBBS admissions and should be varied
in proportion to the numbet of admissions.
The minimum recommendations should be
mandatory and nothing should be left to the
discretion.
Teaching : The booklets published by
M. C. 1. contain no mention of the dental
curriculum to be covered during teaching of
M. B. B S. students. The curriculum must
be laid down specifying curriculum. The
following curriculum is suggested :
The following observations need thoughtful
probing and remedial measures at the hands of
the authorities concerned :
(1)
Introduction to dentistry and its
various branches. Aims of teaching
dentistry to M.B.B.S students.
Basic Objective :
(2)
Norms : Anatomy and Histology of
teeth and gums.
Deciduous and
parmanent teeth with their numbers
and dates of eruption and their func
tions.
The dental department is primarily con
cerned with the teaching of dentistry to
MBBS students, the treatment of maxillofacial
and dental outdoor and indoor patients and
conducting research. Teaching dentistry to
medical students is to help the medical teachers
turn out a basic doctor equipped well with
knowledge to treat a patient as a whole in
cluding dental ailments.
This is specially
applicable in remote areas where no dental
expert is available. Besides, the medical
graduates are expected to give first aid dental
treatment in cases of emergencies including
maxillofacial injuries and to decide about the
cases which need referral to the specialist.
Above all, they help the dental profession to
spread out dental health education which is so
important in the’prevention of dental disease.
(3)
Dental Health education :
(a)
Local and systemic ill effects of
diseased teeth.
(b)
Fundamentals of oral hygiene.
(c)
Rules for better dental health.
1 (4) Common
06
dental diseases such as
dental caries, periodontal disease,
malocclusion, oral infections, halitosis,
abnormal growths and non-healing
ulcers due to malposed and sharp
teeth ind ill fitting dental appliances
14 The Indian Journal of Medical Education
Volume XXII No. 3
■ September-December
Dental Department of Medical Colleges ...15
1983
(a) Oral menifestations of systemic recommendatioi^^ar any theory class. This ; units, with the
completement of each that medical teachers in medical colleges except
the tutors, residents, registrars and demons
disease and role of oral diagnos is not the oppertune time for teaching the ■unit of 30-50 beds as :
tician in the overall diagnosis subject and consequently does not serve much
trators must possess the requisite recognised
I
(a) Prof./Associate Prof./Reader. —1
of systemic disease.
postgraduate qualification in their respective
purpose. ■
■
(b) Asstt. Prof./Lecturer.
—1
subjects. But under the heading “Qualifica
(b) Systemic menifestation of oral
tions for Dentistry” on p. 25 the qualifications
Dentistry is like a super-speciality to the
(c) Chief Resident/Tutor/
disease (focal infection).
recommended for the post of Lecturer is only
undergraduate medical student. The student (■
Registrar.
—1
B.D.S. This is a gross anomaly and is not in
(6)
Cysts and abscesses with emphasis on can understand the vast subject in a short time
(d)
Resident/House Officers.
—3 to 4 order. With a large number of dental post
‘no fomentation’ and ‘special drainage only when he is equipped with paraclinical
graduates available in the country now, no
and some clinical knowledge. Hence dentistry
techniques’ in face.
:
It
is
recommended
that
the
dental
departone with mere graduate qualification should
can be taught effectively only in the final year
(7)
Tranmatic injuries to teeth, jaws and of M.B.B S. The best time to teach the subject i ment too should be unit based like all other be promoted beyond a Registrar or a Demons
face and their management. First aid under present circumstances shall be during j cesciplines. There should be two dental units trator, as is done in other departments.
I for 100 admissions and one unit for 50
needed regarding breathing and bleed internship.
B. Non Teaching Posts :
Iadmissions.
ing and the transportation of the
(5)
patient. Special mention of stich'ng at
face.
(8)
(9)
(10)
(11)
(12)
(13)
(14)
Examination in Dentistry :
Examination is a must to make the
Maxillary sinus, oroantral fistula.
students serious towards learning the subject.
In
our examination oriented system, students
Heamorhage from oral cavity includ
do not even attend the dental classes leave
ing post extraction sockets and bleed
aside
being serious. At least one question
ing from gums.
should be compulsarily incorporated in
General Surgery. The M.C.I. booklet “Recom
Stomatitis and Glossitis.
mendations on undergraduate medical edu
Impacted teeth.
cation, April, 1977—corrected upto Feb.
1980” does recommend on page 23 to include
Trigeminal Neuralgias.
dental diseases in Surgery Paper II, but it does
Teeth and jaws during radiotherapy.
not happen in practice.
I
The recommendations of this booklet on
I “Minimum standard requirements....... ” for
|staff in department of dentistry, P. 23 reads
| as :
.
Prof./Assoc. Prof./Reader.
—1
Asstt. Prof./Lecturer.
—1
Demonstrator.
—1
The position of house officers of 3 to 4 as
is available in other specialties is abolished.
I This should be restored. They are all the more
important if dental beds are to be attended
. and dental casuality service is to be run.
Besides, these fresh dental graduates are helped
in getting an over all training.
Exodontia, indication and contrain
STAFF:
dications, innervation of jaws and
technique of giving blook anaesthesia.
A. Teaching Posts :
The qualifications and experience for the
(15)
Routine dental clinic emergencies and »
various positions and promotions should be
their management.
7
The M.C.I. booklet “Minimum standard
exactly the same as in other medical disciplines.
requirements for a medical college for
M C.I. booklet regarding /‘Recommendations
The M. C. I. booklet on ‘'Recommenda 100
admission annually March,
1973 <
tions on undergraduate medical education. revised upto December, 1977” page 20, i on the qualifications required for appointment
persons to the posts of teachers in medical
April 1977, corrected upto Feb. 1980”, P. 17 IX, 2, 3. 4, recommends the staffing pattern
college and attached hospitals for undergrad
recommends 15 days posting of 3 hours a day of departments of Medicine,
Surgery
uate and postgraduate teaching (1982)” states
in the department of dentistry in II M.B.B.S., and their specialities and Obstetrics and
under the head General Page I, serial No. 3,
1st and 3rd term (3rd year). There is no Gynaecology to be organised on the basis of
The M.C.I. booklet “Minimum standard
requirements for a medical college for 100
admissions annually March ]97 —revised
upto Dec. 1977” recommends on page 23,
dental technicians four and store keeper cum
clerk one. This is very vague. The ancillary
staff has got to be specific and classified into
various categories. Besides a store keeper
cum clerk, a sweeper, two dental hygienist, two
dental technicians, there got to be as many
chair side assistants as the number of dental
surgeons sanctioned.
Casuality Dental Services :
The Registrars and house surgeons will
perform rhe casuality dental service round the
clock on 8 hourly duty. Besides there shoe Id
be one dental chair/unit and a dental bed
exclusively for dental casuality services.
Developing Dental Specialities :
The effort should be to develop all clinical
dental specialities. This can be done only
if you reserve one post for each speciality,
16 The Indian Journal of Medical education
the important ones for medical colleges are
Oral Surgery, Periodontia, Prosthetics and
Crown and Bridge work and Orthodontia.
These four specialists can easily be adjusted
in case two dental units are sanctioned.
Inspection :
Inspection of dental department should be
done by a Dental man only and he must take
note of all mandatory recommendations of
M.C.I.
Beds (.Dental Ward) :
There should be a separate dental ward
with atleast 30 beds. Alternatively such a
number of beds should be reserved for dental/
maxillofacial patients in the wards of Surgery,
besides providing a bed and a dental chair/unit
in the Casuality Deptt. M.C.I. booklet on
“Minimum standard requirements fora medical
colleges for 100 admissions annually, March
1973 revised upto Dec. 1977" vide page 11
recommends 300 beds for the department of
Surgery and its specialities but there is no
mention of dental beds, though this booklet
vide page 20, IX, 3 recommends a unit of 30
to 50 beds for all units without mentioning
Dentistry.
Equipment:
The M.C.I. booklets make no mention
of the equipment recommended for dental
departments. The number of chairs and
units should be the same as the number of
working hands including the dental hygienists.
The modern equipment such as airotors,
dental X-Rays, ultrasonic scalers, labaratory
equipment etc. should be provided in adequate
numbers.
Volume XXII No. 3
The list oi^^uipments, instruments and [
materials needed in the dental department .
should be those meant for carrying out oraL
surgery, conservative treatment, periodentali
treatment,
orthodontic
treatment
and
prosthetic treatment particularly related to the
fabrication of maxillofacial and surgical j
prosthesis.
Accomodation :
The M.C I. booklets make no mention of;
accomodation desired for dental department it
should be sufficient to accomodate :
(1)
8 dental units & chairs.
(2)
Patients recovery room with attached'
toilet.
Waiting room with attached toilet.
Office room for Professor with acco
modation for clerical staff.
(5) Office room for Asstt. Prof./Lecturer.
(6) Common staff room.
(7) Store room.
(8) Dental X-Ray room with adjoining
dark room.
(9) Dental Laboratory.
(3)
(4)
Post Graduation in Dentistry :
Clearout guidelines should be laid down if I
postgraduation is to be started in a particular:
speciality of Dentistry. Postgraduation will.
further help in the growth of the department
of dentistry and the profession.
Summary,:
The present state of affairs in dental
departments of medical colleges for teaching
M.B.B S. has been discussed and remedial
measures suggested to streamline these
departments.
Management and Social Science Orientation
of Rural Health Services in India
By
Jagdish C. Bhaia,
Professor
Centre for Population & Health M .napemerit, Indian Institute of Management, Bangalore
Inspite of tremendous advances in medical technology and phenomenal
expansion of health services in our country during the last three decades,
we have not been able to meet the ever growing health needs of our
people, particularly the weaker sections of our society living in the rural
areas. The health and medical care facilities have more often remained II
underutilised due to a combination of several socio-economic, systemic 1I
organisational and management factors. In terms of Alma-Ata declaration,
we are committed to provide health to all our population by the year
2000A D . The role of social sciences and management in the achievement
of this objective has been emphasised by many committees, working groups
as well as the World Health Organisation. It is, therefore, essential that
I training in social sciences and management is included in the curriculum of
I medical students, and short duration training courses organised for the
various categories of medical personnel currently engaged in the planning
and implementation of healtl services. The training load for these tvoes of
training is exceptionally heavy and the need for trainers and teachers in
social aspects of health services and health management in indeed great It
would be helpful if the. University Social
Sciences departments are
encouraged to take interest in the field of health and family welfare and
establish collaborative relationship with the medical colleges and the health
services. The institutional and infrastructural facilities available in the
country for imparting management training are also utterly inadequate.
Available facilities,
thus, need to be strengthened and new health
management training and research capabilities established.
In terms of Alma-Ata declaration, we are committed to provide health
care to all our population by the year 2000. In order to achieve this
objective, the resources allocated to the health sector will not only have to be
augmented, these will have to be efficiently and effectively utilised. During
the last three decades, there has been phenomenal expansion of health services
Role of Specialisation : Medical Students Preferences
By
Prabha Ramalingaswami
Chairman, Centre of Social Medicine and Community Health
Jawaharlal Nehru University, New Delhi,
A. Shyam
Research Investigator, Centre of Social Medicine and Community Health,
Jawaharlal Nehru University, New Delhi,
With the phenomenal growth that has as possible. This was achieved by taking into
taken place in medical science, specialisation account the following :
has become an important feature of medical a. Nature of the Institution :
education. Consequently, there was a sharp
Whether the college was one where post
increase in the facilities available for training
graduate education was imparted or not—
the specialists. Now there is an increasing
and the number of admissions undertaken
realisation among the medical educators that
at the undergraduate level.
primary health care is the need of the day for b. Management:
the large majority of people who belong to the
Some colleges are run by State and Central
rural areas and that comprehensive health care
governments, some by missionary and other
should be readily available. What do the
voluntary organisations and finally some
students think about these issues ? How do
colleges which have started as a private
capitation colleges and later taken over by
they view the specialities ? What are their
government.
preferences ?
In an effort to understand
answers to the above questions I had under
The following colleges have been included
taken a study on the attitudes of medical in this study. These are listed below according
students. I am presenting before you some of to the place of their location and this has been
my findings. The study is still in progress organised in an alphabetical way.
i,
and what I am presenting here is a sort of
TABLE—1
| preliminary communication. Here 1 am
Colleges
No. of Students
I focussing on the students preferences about
1. Alleppey
36
the different specialities and the implication
Benaras
38
2.
of this for comprehensive health care.
3. Cuttack
79
4. Delhi (Lady Hardinge)
46
The Sample :
98
5. Guntur
The sample consisted of 533 final year
6. Hyderabad (Osmania)
37
medical students from ten medical colleges.
7. Ludhiana (C.M.C.)
39
The
criteria
used for
selecting
the
8. Trivandrum
43
medical colleges for this study are (1) that
9. Wardha
62
‘hey should represent different types of medi10. Warangal
55
C*1 colleges in existence and (2) that they
Total No. of Students
533
should have as wide a geographic distribution
Methods ot Data Collection :
The students were administered, in a class
room, a questionaire containing several
sections. The students were assured that there
were no right or wrong answers. They should
write whatever they know. To ensure that
the students take the questionnaire seriously
I explained to the students the purpose of the
study and requested them to come out freely
with their views. After giving the instructions,
myself and my investigator moved among
the students and made sure that the students
understood the questionnaire. We even kept
pens ready to offer those students who said
that they forgot their pens or the ink was over.
Thus every effort was made to assure that we
were interested in the students views. The
students also had taken the questionnair
seriously and answered it as carefully as they
possibly could.
The Questionnaire :
The questionnaire consisted of several
sections. One of the sections is with regard
to ranking of specialities. 19 specialities were
listed. The students were requested to rank
them according to their preference. To avoid
bias the specialities have been listed according
to their alphabetical order. The students
were asked to give first rank to the speciality
which they liked most and according to their
level of preferenee they should rank the others,
the least preferred being given the last rank.
The actual format is given below :
Below are given the various specialities
available for postgraduate work and are
taught at the undergraduate level too. They
were asked to indicate the order of their
preference by putting 1 against the speciality
they preferred most of all, 2 against the second
Pharmacology
most
preferred speciality, and so on. The least
Physiology
preferred
speciality will get 19.
ENT
(Otolarynagology)
Preventive
and Social
Speciality
Rank cf their preference
Medicine
(1 is most preferred, 19
Psychiatry
is least preferred).
Radiology
Anaesthesiology
Surgery
____
Anatomy
Dermatology
Biochemistry
Another section deals with rating of
specialities of medicine, preventive and social
medicine and the speciality they would like to
do their postgraduation on certain adjectives.
They were asked to name the speciality they
would like to do their postgraduation and
then rate it. It was made clear to them that
the speciality should be what they would like
to do and not what they were likely to get
admission.
In another section which deals with their
future plans one of the options indicated is
postgraduation and if the student opts for
JAXUART-JUXE 1980
ROLE OF SPECIALISATION : MEDICAL STUDENT... 43
postgraduation the student was to indicate
the speciality.
Thus there were 3 sections in which the
speciality in which the students like to do
postgraduation comes up in different ways. In
the construction of the questionnaire this was
done deliberately to establish the reliability
of the data.
The data was analysed for the individual
colleges first and later the responses were
pooled together for the total group. On the
ranking of specialities different students gave
different type of rankings. These have been
tabulated and median values worked out. On
the basis of the median values the students
preference for each speciality has been worked
out first for the individual colleges and later
for the total group. Flere I am presenting for
the total group the specialities according to
the ranks worked out by median values.
Medicine
—
1
Surgery
—
2
Paediatrics
—
3
Gynaecology
—
4
Opthalmology
—
5
Orthopaedic Surgery
—
6
7
Pathology
—
E. N. T.
—8
Dermatology
—
Psychiatry
—
10
Anaesthesiology
—
11
9
Radiology
—
12
PSM
-
13
Pharmacology
—
14
Microbiology
—
15
Physiology
—
16
Biochemistry
—
17
Forensic Medicine
—
18
Anatomy
—
19
For the individual colleges there is a slight
variation. In two colleges surgery had been
preferred over medicine, while in another
college the students showed equal preference
for both medicine and surgery. In one college
anatomy ranked 13 (which can also be
understood as this college happens to be exclu
sively for girls). By and large the slight
changes in the order of preferences among the
colleges is of a minor nature.
The most notable feature that has come
out is with regard to the speciality of preven
tive and social medicine. The students rank
it almost at the end of the clinical subjects,
certainly they prefer this to preclinical or para
clinical subjects with the exception of
pathology. In a similar study which was
conducted a few years ago in one of the
medical colleges in New Delhi which I ,
reported in 1971—72 the students then
ranked, this subject at almost last i.e. the 18th
ranked, 19th being anatomy.
The second section where the student had
to name the speciality he would like to do
postgraduation and then rate it on certain
adjectives and the third section in which the
students were requested to indicate their
future plans were also analysed. The corre
lation between the speciality given the first
position in the ranks and the speciality which
the student named for his postgraduation and
-du
Microbiology
Medicine
Opthalmology
Gynaecology
Orthopaedic Surgery
Paediatrics
VOLUME XIX
42 THE INDIAN JOURNAL OF MEDICAL EDUCATION
Forensic
Medicine
Pathology
44 THE INDIAN JOURNAL OF MEDICAL EDUCATION
rated it was very high. It is 0.92 likewise,
the correlation between the speciality given
the first position in the ranks and the speciality
indicated in their future plans also is very very
high. It is 0,931. This only shows that the
students are very clear in their about what
they would like to do.
The most interesting feature of this study
reveals that general medicine stands out the
most preferred speciality and that 99% would
like to do their postgraduation in it. A good
majority of these would like to try for a firm
government job also. Very few students have
shown inclination towards superspecialities.
VOLUME. XIX He. 1
The majority of the students will be happy
to go for general medicine. This poses a great
challenge to the medical educators. How much
of the available knowledge with regard to
different aspects of medical science (which
have made tremendous studies and have
become specialities and super specialities) be
usefully put together in general medicine. In
addition the needs of the country have to be
taken into account so that as comprehehsive a
health care as possible is given to the vast
majority of the people who do not have access
the rudiments of health care at the present
moment.
Acknowledgement :
I want to express my gratitude and deep appreciation to the Deans and Principals of
the Medical Colteges included in this study and the students who had answered the
questionnaire,
Role of Specialization In Comprehensive
Health Care
By
J. S. Bajaj
Professor of Medicine, All-India Institute of Medical Sciences,
Hew Delhi.
PREAMBLE
Deep concern has been repeatedly expressed obout the hiatus between the
advances in technology in the recent years and lack of their application to the solution
of community health problems.
Indeed, it is a paradox of modern times that while
rapid strides are being made in the understanding of the disease processes and possi
ble approaches to the management, there is a'palpable gap in the delivery of health
care even for those diseases where simple and effective remedial measures are readily
available. A ready answer is sometimes provided by those who are involved in policy
planning; it is said that a vast majority of the doctors prefer to stay in towns while
more than 80% of the country's population lives In the rural areas. There has been a
recent appreciation of the fact that our health and man-power plan has been rather
distorted. We have produced a much larger number of doctors and have concentrated
much less on the training of para-professionals, including nurses and other allied
health personnel. This has resulted in a health man-power disequilibrium which has
jeopardised the health care delivery system.
While there is truth in most of these surmises, we should also appreciate
another trend which has emerged in the last two decades. A larger number of medical
graduates are now going in for postgraduate medical education. There are recent
estimates indicating that about 70% of the medical graduates of today are enrolling
for postgraduate degree and diploma courses in the country. It is, indeed, timely to
take cognizance of this trend and give a deep consideration to the role of specialists in
comprehensive health care. It is obvious that unless and until this is done in a rational
manner, and the objectives and training programmes of postgraduate education are
defined in terms of delivery of comprehensive health care, the vast number of specia
lists that are being produced in the country may not be prepared to play a meaningful
role in the existing health care system.
50 THE INDIAN JOURNAL OF MEDICAL EDUCATION
VOLUME XIX JIo. I
JANUART-JUNE 1980
such specialists working in the medical institutions. Finally, the specialists at these institu
tions should be able to seek realistic solutions through need-based research for the
objectives of specialised training.
enunciated.
ROLE OF SPECIALIZATION IN COMPREHENSIVE... 51
Only objectives for training in clinical disciplines will be
Broad Objectives
A specialist in any of the clinical subjects should :
1.
be able to demonstrate comprehensive understanding of the basic sciences related
to the discipline concerned;
2.
be able to practise in the broad discipline of the study as an independent specialist;
3.
be familiar with the current developments in medical sciences as related to the
speciality;
4.
be able to render medical care to the individual and the community, integrating
preventive, promotive, diagnostic, curative and rehabilitative aspects;
5.
be able to plan and conduct educational programmes in the speciality utilizing
modern methods for teaching and evaluation; and
6.
be able to plan and conduct research.
Instructional Objectives
Instructional objectives shall differ from subject to subject and should be planned
keeping in view the needs of the discipline concerned, within the framework of the broad
objectives, already defined. The general recommendations which may serve as a prototype,
are only being enunciated. A specialist in any of the clinical subjects should be able to
1, demonstrate adequate knowledge of applied aspects of structure and fnnctinn nf
human body as related to the practice of the concerned speciality;
Figure 4
community health problems. Figure 4 shows the concept of different levels of health care
and how these should be interlinked. It is obvious that a better definition of coordination
and linkage has still to emerge at the final level of comprehensive health care.
2.
demonstrate comprehensive knowledge of deranged structure and function of
human body,' causes thereof, and of principles underlying the use of drugs and
therapeutic procedures for restoring the deranged structure and function to
normalcy;
3.
demonstrate familiarity with such diagnostic skills and laboratory procedures, as
are relevant to the diagnosis and evaluation of patients under his care and be able
to conduct some of these procedures in case it becomes necessary to do so;
4.
demonstrate comprehensive knowledge of theoretical aspects of the speciality
concerned, including recent advances;
5.
manage adequately routine as well as complicated problems of clinical care in
relation to the' speciality, at the level of a junior consultant;
Training of Specialists For Comprehensive Health Care
It is agreed that the specialist has to perform various functions within the health care
delivery system, and that there has to be an essential support and interlinkage between the
various levels of health care delivery, it becomes imperative that the training of such
specialists should be oriented in this direction. In an earlier communication (Bajaj, 1979a),
essentials of curriculum planning have already been discussed. It is necessary to define the
JANUART-JUNE 1980
52
THE INDIAN JOURNAL OF MEDICAL EDUCATION
ROLE OF. SPECIALIZATION IN COMPREHENSIVE... 53
VOLUME XIX M>.
6.
plan delivery of health care at the community level, including the preventive and)
promotive aspects, with adequate understanding of epidemiology of common
diseases as well as socio-cultural aspects of the community; and
7.
demonstrate familiarity with the principles of medical education, including
definition of objectives, curriculum construction use of learning aids and learning
settings, and methods of evaluation.
Specialization in Family Medicine
While it may be worthwhile to reorientate postgraduate medical education in the
existing specialities so as to make it more meaningful for the delivery of comprehensive
health care, there is also the additional need for developing new postgraduate courses.
own right. It is different from Internal Medicine in the sense that a specialist in Internal
Medicine provsdes care for adult patients suffering from ailments pertaining to medical
specialities. In contrast, a family physician or a general practitioner is involved in providing
: care for all illnesses irrespective of the type and nature of illness or the age-group of the
patient. It is now being increasingly recognized :that an additional period of training
following graduation is likely to improve the quality of health care, provided by a general
practitioner. Furthermore, following a postgraduation in General Practice, a specialist
should be treated at par with the other clinical specialists as far as the emoluments and other
privileges of service are concerned. Finally, a specialist in General Practice with a post- graduate degree in the subject, may be a most appropriate specialist at a primary health
centre as also at the sub district hospital. With the newly emerging operational framework
for the delivery of health care in India, taking into consideration the objective of‘Health for
all by 2000 A D.', there will be increasing job opportunities for such specialists in General
Practice or Family Medicine.
Indeed, the Faculty at the A.I.I.M S has given consideration to this aspect of postx graduate education, although such a course has not yet been initiated at the Institute. Some
. of the objectives cosidered by the Faculty as most appropriate for a posgraduate course in
r. General Practice leading to the award of M.D. degree in this subject include the developx.ment of clinical skills for .the diagnosis and management of common diseases prevaknt in
- the community, the ability to provide timely and appropriate management for various
- medical and surgical emergencies affecting-all age-groups, development of the decisionu making process regarding referral of a patient for a higher level of clinical care,
a development of skills for. identifying common causes of morbidity in the community and
- for imparting preventive and-promotive measures, as well as health education, especially
in the areas of maternal and child health, nutrition and family-planning, and finally,
the ability and confidence.to act as a catalyst of such social chang: as would be conducive
X to. the improvement in the mental and physical health of the individuals and the
"■ community.- Such a-specialization is likely to produce a doctor who would be able to
interact with other para-professionalsand, thus, would constitue an important link in the
health care delivery-team.
The instructional objectives, -.curricular contents as well as the learning settings
» required for specialization-, in General Practice can be further developed and elaborated.
— However, the prime need is to- recognize the importance and the urgency of developing
n such a course at least in a few institutions on an experimental basis.
cEpiloaue :
The role of general practitioner (Figure 5; G. P.) is well recognized. Family Medicine or
General Practice (these should be considered synonimous) is emerging as a speciality in its
figure 6 summarises the role and; place, of specialization in comprehensive health
“ care. It is obvious that there are urgent twin needs for the re-orienttion of postgraduate
a medical education in relation to the existing courres in clinical specialities, as well as for the
development of a new postgraduate course specifically aimed at specialization in General
/
64 THE INDIAN JOURNAL OF MEDICAL EDUCATION
VOLUME XVII Mo. I
in the emplo\of the Board as paid reviewers. reviewed, and necessary changes introduced
Selection of reSiewers could be done on the whenever necessary. Dexterity and innova
basis of qualifications and competence, and tions in medical practice would be known
. their tenure could Derestricted fora limited during evaluation and may be rewarded
period. As in the carespf examinations, peer suitably.
reviewers would not know the names and
Dr.Jacob Fine noted® that a common
particulars of the doctors\reviewed and vice
versa. Substandard performance and defi objection to medical peer review is that an
ciencies, with reference to prescribed standards acceptable method for evaluating a doctor's
in the hospital guidance manuals, if any, performance or expertise cannot be evolved.
could be notified to the doctor concerned, who He says that the prevailing argument is that
is free to challenge them in writing or in patients and problems posed by diseases are
person before the Review Board. AXcritical so widely variant that doctors are bound to
appraisal of the performance and deficiencies react differently. But he is firmly of the
by the Review Board would reveal where opinion that such a contention is not valid
the fault lies, whether in the medical education because the Peer Review Board would lay
system or in the individual performance of\ emphasis on the minimally accepted standards
doctors. This revelation, according to Dr. \of medical care, making due allowance for
Jacob Fine, would cause a distinct improve local or special circumstances in the treatment
ment in the quality of medical care given to given.
patients in hospitals and homes over a period
IK looks that organisation of such a
of years.
National Medical Peer Review Board in India
The Peer Review Board's evaluation, would Be advantageous to the public as well
observes7 Dr. Jacob Fine, should be the as to the doctors, Details and data regarding
criterion for allowing a medical practitioner the medicak care extended to in-patients and
to continue me’dical practice. The Board's out-patients kare already available in the
expert opinion can also be used by courts in records of public hospitals, private hospitals,
settling medical suits for malpractices. Eva and nursing homes. Some of the private
luation data can be computerised fur practitioners maintain records of the patients
advantageous utilisation, such as determina treated by them,\while others do not. It
tion of the impact of the review process on should not be difficult to make proper main
the performance of the individual doctor. tenance of records of patients treated compul
Criteria for evaluation could themselves be sory through an Act. \
REFERENCES
\
1. The Times of India, New Delhi, Saturday, Dec. 16. 1978. P-l, 7.
\
2. Growth of Scientific and Technical Personnel, Technical Manpower, V x\, No. 6,
June, 1970, pp. 1-4.
X
3. Periodical supplements to the Indian Medical Register published in the Gazelle of
tne Government of India (Various issues).
4. Jacob Fine, A Peer Review System for Physicians, The Bulletin of the Atomic Scientists.
V. 33, No. 7, Sep. 1977, p. 39r43.
5. Ibid
6. Ibid
7. Ibid
8. Ibid.
I?
‘Rehabilitation’ - Its Philosophy and Need in Medical Education
By
Dr. R. K. Srivastava
Chief Resident
Shri A. K. Srivastava
Occupational Therapist
Dr. S. C. Goel
Senior Resident
Rehabilitation & Artificial Limb Centre, K. G. Medical College, Lucknow.
“Three decades ago, a great majority of number of disabled veterans which was added
medical profession looked on rehabilitation as to the large and ever growing number of
an extra curricular adjunct activity of medi civilian disabled by disease or accident. To
cine, something dealing with social work and meet the problem of chronic diseases and
vocational training, but something that had disability, there was no solution except to make
little concern with or hold but few implication rehabilitation every doctor's business and
with medicine. The trend has been reversed with this aim in mind rehabilitation medicine
over past 30 years and today majority of was made compulsory during undergraduate
physicians, particularly those who have com training of doctors in Western World and later
pleted their training within recent years, are on as a specific speciality at the post-graduate
now familiar with the aims and procedures of level.
rehabilitation and recognise-that medical
But, on the other hand, the situation is
care cannot be complete until the patient with
tesidual physical disability has been trained quite disappointing in the developing countries
to live and work with what he has left." like India. The fundamental philosophy and
This statement was made in the year 1977, by need of rehabilitation is yet not understood.
Dr. Howard. A Rusk, M. D., Professor, Still there is no training facility for rehabilita
and Chait man of Department of Rehabilita tion medicine even at undergraduate level,
tion Medicine, University Medical Centre, with the result, this branch of medicine is in
continuous process of encroachment by
New-York.
different specialities, which-so-ever has got the
A pretty long time has passed since focal insight of thinking that rehabilitation is ~7
rehabilitation is included as a specific entity imperative fortheir patients only. This state —q
in medical studies in Western countries and the of confusion and conflict, out of ignorance of .
departments of Rehabilitation Medicine led by some and vested interest of others, is slowly
qualified specialists were established as early making this speciality in our country as an
as 1946 (Department of Physical Medicine & abstract painting, which a majority may 'q
Rehabilitation, New York). The need for appreciate but few of them understand. It is
rehabilitation came into sharp focus with the the high time when the authorities responsible
end of World War II which caused a significant for medical education should plan out the
JANUARTjJUNE1978
66 THE INDIAN JOURNAL OF MEDICAL EDUCATION
VOLUME XVII Fo. 1
prospectus of rehabilitation medicine and
institute it immediately as a specific subject
in the basic training course of medical
graduates.
They can be broadly grouped into the blinds,
the deaf and the orthopaedically handicapped.
They constitute only one group of patients,
who need rehabilitation. They need expert
Keeping in view that the need of rehabilita
tion services will rapidly increase in the near
future, on one hand due to rapid development
of basic health services and integration of
medical care in national health programme and
on the other hand, due to increase in number
of disabled by rapid increase in industriali
sation, urbanisation and life expectancy, even
World Health Organisation recommended to
the Government of various countries that every
faculty of medicine must have a Chair of
rehabilitation medicine. It is demand of the
day that Govt, should act on this proposal to
include it at undergraduate level so that young
medicos may opt rehabilitation medicine as
their post - graduate speciality, because, for
efficient utilisation of manpower, the rehabi
litation of disabled should necessarily be left
to full time specialists instead of those w ho
have encroached upon this field due to lack
of such specialists.
multidisciplinary rehabilitation care of various
allied rehabilitation specialities also, like
occupational therapists,
physiotherapists,
speech therapists, psychologists, vocational
counsellors, etc. This can only be provided
in well-equipped rehabilitation centres. But
this above mentioned group of disabled is not
the only group which requires rehabilitation.
The other group of patients requiring' rehabi
litation consists of cases of lung diseases,
traumatic lesions,, arthritis, leprosy cancer,
metabolic diseases, endocrinal disturbances,
cases of chronic illness i.e. patients of all
impariments (disease) which may result in
some functional loss if not taken proper
and timely care, may land up in disability.
These are the cases which a doctor has to treat
mostly in rural areas and sub-urbs. Due to
lack of basic understanding of rehabilitation,
in treating this component of total manage
ment of patient is alltogether neglected
This unintentional neglect of rehabilitation
produces functional loss and ultimately
disability. •
The instillation of philosophy of rehabili
tation and its need and practise in a developing
• country like India must be started from the
very begining of clinical training of doctors,
because tomorrow these medical graduates
will be responsible for the basic health care of
the nation. The awareness of disability and
the need of eliminating, alleviating or reducing
the effect of disability will ultimately reflect
on the physical capacity of the population.
According to World Health Organisation
Policy and Planning for “Disability Prevention
and Rehabilitation,1' 1975, there are about
400 million disabled in the world, which
constitute.about 10% total world population.
The magnitude of this problem is
augmented manifold if we understand that
80% of our patients come from rural areas.
By the time these patients reach the centres,
where rehabilitation facilities are available, it
becomes too late because during that period
the basic impairment with health cf patients
starts manifesting as functional loss or even
lead towards disability. The treating doctor
cannot be blamed for it because, during the
basic training course of a medical student,
rehabilitation medicine is the only subject
which goes untouched,
REHABILITATION’—ITS PHILOSPHY AND NEED...... 67
In a big country like ours, whose 80% of
the population live in rural areas, this aspect
of total health care should be sta.rted from the
very beginning for prevention of disability as
well as minimising and treating its sequeles
This can only be provided by including
rehabilitation ‘ medicine in the medical
curriculum by
teaching our out-going
doctors to pay proper attention for rehabili
tation of these patients. More so, the patient
will also be rehabilitated in his surroundings
to live and work with what he has left.
On the other hand, for those cases like,
blind, deaf and the orthopaedically handi
capped, where specialised rehabilitation care
is needed, it is imperative that rehabilitation
medicine should be recognised as a speciality
in medical curriculum with post—graduate
facility.
Though actual statistics are not available,
but it is estimated that about 4-5 millions of
the blind, 1-1.5 millions of the deaf and 4-5
millions of orthopaedically handicaps exist in
India. This amount to a total of 9-11.5
millions of disabled, who need specialised
multidisciplinary rehabilitation care. They
cannot be deprived of the fundamental rights
of human being. For them all tertiary centres,
medical colleges and medical rehabilitation
centres of the country should have qualified
experts in rehabilitation medicine besides
other members of the rehabilitation team.
These experts must be made responsible
for planning and organisation of rehabilitation
services for this group of patients.
For the existing practising doctors, a well
planned short term refresher course in batches
should be started in the medical colleges and
rehabilitation centres.
These are probably the only ways of
spreading the rehabilitation services to every
patient.
Summary:
The aim of rehabilitation is to train the
patients to live and work with what he is left.
The basic philosophy of rehabilitation
medicine in medical profession was wellrecognised in western world about three
decades back and it was given due impor
tance in the medical curriculum.
The patients, who can be helped by
awareness and understanding of rehabilitation
medicine, are broadly classified into two
groups. Group I includes all the chronic
illnesses, either medical or surgical or
traumatic, which may produce functional loss
and later on disability. For them, there should
be inclusion of rehabilitation medicine at
undergraduate level, so that out—going
medical graduates may treat these patients
with the aim of their total rehabilitation in
the back of the mind.
Group II includes blind, deaf and orthopaedically handicapped. They need intensive
rehabilitation care by specialists. For sue!
patients, post-graduation in rehabilitatioi
medicine should be started. These rehabilita
tion experts should be sent to various tertiarj
centres and medical colleges to plan ant
organise rehabilitation services of nationa
coverage. For existing doctors, there shoult
be provision of refresher courses at all medica
colleges. This may help in spreading threhabilitation services to community level.
68 THE INDIAN JOURNAL OF MEDICAL EDUCATION
VOLUME XVII No. 1
REFE.REN CES
1. Rusk, A Howard : ‘'Rehabilitation Medicine" Fourth Edition, The C.V‘ Mosey
Company, Saint Louis, 1977.
2. W. H. O. Policy and Programme for •'Disability Prevention and Rehabilitation”
S.H.S./75 ; 1.
3. W.H.O. Expert Committee on Medical Rehabilitation Second Report ; W.H.O.
Technical Report Series, No. 4 19, Geneva, 1969.
fin Evaluation of fi Systems Approach To Recall of
Anatomical Knowledge
By
\
Indra Bnargava,
Professor of Ahalomy, Maulana Azad Medical College, New Delhi.
\
ABSTRACT
A system for facilitating recall of anatomical knowledge, and consequent
improvement ik examination performance has been conceived. It was hypothesised
that the usual channels of learning, leading to more confidence and a better perfor
mance in the examination, can be reinforced by increasing motivation, leading to better
learning and more confidence. Performance of this system has been evaluated. It has
been shown that the system has resulted in a significant improvement as shown by
increase in examination scores and significant correlations to confirm this hypothesis.
However, it has been obser\d that the system takes more time and does not prune the
superfluous details. Profilk of the student characteristics as revealed by the
questionnaire is described.
\
Introduction :
\
system was expected to result in a better performance in examination, through better
Top level performers of pre-medical examt-'
nations, constitute a large majority of intake ^learning and increased self confidence. This
system comprised of:
of medical colleges. After entry into the
medical college, the performance of these
1. \Prototype descriptions of different anato
students in preclinical subjects is not consistent
mical structures namely an artery, a
with their past record. This generalisation
vein, a muscle, a nerve, a joint, a move
was aptly confirmed by an analysis of the
ment, an anatomical space, a hollow
performance in Anatomy, of the batch of 180
orgark a solid organ, blood and nerve
students, admitted to Maulana Azad Medical
supply\and lymphatic drainage of an
College, New Delhi, in 1977-78. A probe into
organ. \
the genesis of this academic decline, in form
of small group discussions with students and
2. Procedure lor drawing line diagrams, to
teachers, revealed that learning and recall of
show only essential features, in support
the large magnitude of anatomical facts, was
of prototype descriptions.
the main difficulty with most of the students.
3. Use of a uniformXcolor scheme in thess
Consequently, it was postulated that organisa■ tion of anatomical knowledge in a logical and diagrams for depicting different anatomical
\
systematic manner can be a considerable help structures.
in overcoming this problem.
The knowledge of this system was
Therefore, an organised system for recall transmitted to students by conducting tutorials
of anatomical knowledge was conceived. This of small groups of students. The size of small
DUEL CLINICAL POSTING IN UNDERGRADUATE TRAINING
AN ECONOMICAL, EFFECTIVE AND NEEDBASED APPROACH
by
Dr. H. I. Jhala
Director of Medical Education and Research, Maharashtra Slate, Bombay.
and
Dr. R. B. Bhagwat
Professor of Medicine, Medical College, Aurangabad.
Current pattern of undergraduate postings
for clinical work in the various clinical depart
ments, has certain drawbacks.
1.
2.
Generally students are posted for 3
hours in the wards every morning. He
spends 4 an hour in writing notes and
1 to 14 hours remains engaged in a
bedside clinic. Although he is expected
to spend remaining one hour in examin
ing patients he wastes it.
5.
Infectious diseases that form the bulk of
cases in general practice remains un
attended to because student works there
for hardly two weeks and gets an oppor
tunity to see only a few diseases.
6.
There is no provision for training in
Minor operation theatre, Family Plann
ing, Nursing, Blood bank immunisation
clinic, O.P.D. laboratory, Occupation
and Physiotherapy departments and in
the casualty departments.
In paediatrics a student works for about
2 months. Considering the place of
In order to prevent the waste of time and
paediatrics in general practice the
utilise it for training in paediatrics and infec
period is inadequate for his training.
tious diseases and to cover the subjects men
3. During vacation half the time is lost. tioned under 6 above the following scheme is
During the remaining half a teacher in introduced for clinical postings in Medical
a whole time set up has to look after College & Hospital, Aurangabad.
additional clinical duties and therefore
A student works at two places every morning,
does not find enough time to teach. In
effect, from the point of view of the 24 hours at one place and 1 hour at another.
student, vacation is wasted although this Longer periods are spent in major discipline
period is counted in terms.
and shorter periods in the ancialliary discipline,
Medicine, Surgery, Obstetrics & Gynaecology.
4. In the operation theatre only a few Paediatrics and Opthalmology are considered
students can actually see an operation. major disciplines and the remaining anci
Others waste their time.
alliary.
THE INDIAN JOURNAL OF MEDICAL EDUCATION
VOL. X.
NO. 4.
DECEMBER, 1971
DUEL CLINICAL POSTING IN UNDERGRADUATE TRAINING
33
KEY TO TABLE No. 1
A and B stand for the two batches of students.
Lab:—O.P.D. lab.
1$: —Infectious Diseases.
VisitVisits to centres of Public Health
interest.
DADentistry, Anaesthesia.
FNFamily Planning & Nursing.
ST
Skin VD & T.B.
BI:—Blood Bank, Immunization clinic.
OR:—Orthopaedics.
OR:—Minor operation Theatre.
PR :—Psychiatry & Radiology
PTOccupation & Physiotherapy.
CMO :—Casualty Medical Officer &
Post Mortem.
It was felt that a single posting of three
In orthopaedics, skin, tuberculosis, ENT,
dentistry, minor operation theatre, O.P.D. months is too long ; hence each posting is of
laboratory etc. the work is chiefly in the early two months. It may be noted that even
hours of the morning. A student works in though full summer vacations are given total
these branches during early hour of the mor periods of effective teaching is not reduced
ning and then goes to the major subject by the (ref. 3 above). No vacation is given in
time the teacher has finished his service ward winter.
round or major operations which are little use
to future general practitioner. A teaching
round or a clinic follow’s.
-du
32
cZ>
A New Approach to Teaching of Acute Medicine and Resuscitation
Techniques to Undergraduate Students & Para Medical Personnel
by
M. T. Bhatia,
Professor of Anaesthesia, Gujarat Cancer & Research Institute,
(MP. Shah Cancer Hospital), Ahmedabad-16
INTRODUCTION
Techniques of Acute Medicine or Resusci
tation have been widely used in restoring car
diac and respiratory function in acute emer
gency patients. Teaching of this aspect of
medicine to undergraduate students and
para medical personnel cannot be over
emphasized.
A new approach in the form of more visual
and practical teaching of resuscitation is advo
cated. It is suggested that the students be
trained in three stages : —
Stage I: In the class room, students may
be-familiarised with physiological aspects by
slides and films.
Stage I:
Teaching in Class Room
Diagnosis of cardiac arrest can be easily
taught by stressing that inability to palpate
the pulse in any major vessels (Radial or caro
tid) may be taken as cardinal sign. Other
signs of cardiac arrest like dilatation of pupil
or absence of respiration can also be stressed
by film or slides. Absence of circulation for
three minutes can lead to permanent brain
damage. This can be easily stressed by des
cribing actual case history with slides of such
patients. Students must be made to realise
that any wastage of time in running after
equipment will be fatal to the patient. Once
cardiac arrest has been ■ diagnosed, treatment
must start immediately.
Stage III: Final training be undertaken by
allowing students to practise resuscitation
techniques on manikin type of foam rubber
dummies.
We have found that visual form of teaching
in the form of slides is the most suitable for class
room teaching. Slides used in teaching use of
resuscitation techniques in local anaesthetic
drug reaction, are shown below (After Cullen,
1961). Role of mouth to mouth respiration in
providing adequate amount of air into the
alveoti by enough expansion of lungs through
clear air way is best taught by showing actual
expansion of lungs on slides along changes in
colour of the patient.
Only full training of medical, dental as well
as nursing staff can ensure proper treatment
by restoring the circulation of oxygenated
blood and solving problems of subsequent
management in acute emergency cases like
Sudden cardiac arrest patients,
Role of External Cardiac message in resto
ring circulation and carrying oxygenated blood
to brain and other vital tissues of the body is
best demonstrated by showing the recording
of pulse and blood pressure after start of
jnassage.
Stage II: Students be made familiar with
techniques
of resuscitation by
actual
demonstration on patients in operation
theatres, Intensive Care and Post-operative
Wards.
304
THE INDIAN JOURNAL OF MEDICAL EDUCATION
1’0/.. XII
X'OS. 3
JULY - DECEMBER, 1973
A NEW APPROACH TO TEACHING OF ACUTE MEDICINE
Stage II: Demonstration of Resuscitation Techniques in operation Theatres and wards
Technique of automatic ventilation is used
daily during anaesthesia in major surgery in
practically all teaching hospitals. Actual
expansion of lungs while giving artificial
ventilation either by mouth to mouth (expired
air ventilation) or with the air viva bag must
be stressed upon students. Actual method of
securing a clear air way can be demonstrated
in the operation theatres or in post-operative
wards. Emphasis should also be given upon
putting the patient on a hard surface and if
the patient is lying on a soft bed then on any
wooden board available in the ward or any
hard material which can be placed under the
patient’s back to carry out effective cardiac
massage and to restore cerebral circulation,
It is also very impressive to show actual
heart control on E.C.G. Monitors in operation
theatres and intensive care wards. Use of
Defibrillator and pace-maker can be easily
taught to students during their study term in
operation theatre and Intensive Care Ward.
Actual use of various vaso-pressor drugs and
their mode of action is routine in most of the
teaching hospitals. Actual demonstration will
lead to better appreciation of role of vaso
pressors in resuscitation.
Stage III: Actual practice of Resuscitation
Techniques on Manikin Dummies
Students can actually practise the techni
ques of resuscitation which they have been
Visual teaching in class room:
Resuscitation of patients having local anaesthetic drug reactions.
305
so far taught on Manikin type of dummy
models having foam rubber structures. These
dummies are being used to teach mouth to
mouth respiration, external cardiac massage,
airway maintenance and also technique of
I.V. injections. Unless students, are made
very familiar with actual resuscitation techni
ques by actual practice on such mankin
models, in actual emergency' they waste lot of
time and effective successful resuscitation is not
achieved by them. This leads to disappoint
ment and loss of faith in resuscitation techni
ques.
If the above schedule of teaching of resusci
tation techniques is followed, better apprecia
tion and effective use will automatically result
in their most common use.
SUMMARY
(1)
Visual teaching of physiological aspects
of acute medicine and resuscitation
techniques in class room is advocated.
(2)
Actual teaching and demonstration of
resuscitation techniques in patients in
operation theatres, Intensive Care Units
and Post Operative Wards is proposed.
(3)
Only actual practice of resuscitation
techniques on Manikin type of foam
rubber dummy models can ensure suffi
cient confidence in students to use these
techniques to effective use during emer
gency treatment.
UNDERGRADUATE clinical curriculum—a reappraisal
Undergraduate Clinical Curriculum—A Reappraisal
By
Dr K. L. Wig*, & Dr J. S. Bajaj|
In planning any course or curriculum for
the under-graduate medical education one
tends to make a basic assumption that the
primary objective of the medical colleges in
this country is to impart a certain type of
scientific education and practical training
to a sufficient number of students which will
enable them to provide adequate medical
care to the people of our country. It has
been repeatedly emphasised that the object
ives of medical education have to be re
oriented to the needs of the country. This
reorientation should be almost a continuous
process. In various world conferences on
medical education only broad outlines for
the duration of the course, content of the
course, methods to impart the necessary
teaching, and the aids to learn the necessary
techniques have been discussed and out
lined. But the major emphasis has always
been that the approach to this problem
should not be rigid. The flexibility of the
approach has been advocated so as to enable
the planners to take into account the
varying needs of the society which are of
fundamental relevance.
Medical education in India has evolved
on a pattern which was first instituted by the
British medical educationists. Only during
the recent years certain distinct voices have
been heard which have tried to focus the
attention of the medical educationists on
the fact that what is eminently suitable for
a medical student in Western countries
need not be necessarily so for a medical
student in India. It is true that in order
to keep up with the rapidly advancing
frontiers of science and also in order to
contribute to the rapid progress of know
ledge, medical students of to-day in this
country should be educated in an atmos
phere of enquiry and research. However,
the basic focus has to be on the production
of a doctor who will be able to deal with the
common medical problems encountered in
the general population and will also be able
to help in advising the public on the social
and preventive aspects of medicine so that
proper help to the community is ensured.
If during the formative years, the emphasis
is placed on research and only a limited
contact with the patients is allowed then
we are strengthening the concept of a
physician as a scholar and investigator
rather than a practitioner and a healer.
It is true that the acquisition of knowledge
and the conduct of research are important
characteristics of a good doctor, but it is
still more true that a humanitarian and
sympathetic relationship with the patients
can often achieve much more than what can
be achieved by the application of pure
knowledge alone.
It has been repeatedly emphasised in
various conferences that the primary aim
of the various medical colleges should be
to produce a basic doctor. Very few have,
however, attempted to define what a basic
doctor means. The result is that the status
quo continues and no sustained attempt is
being made to devise a curriculum which
should aim at producing the basic doctor.
A subgroup of the committee formed by
the Central Government to examine the
under-graduate medical education, in the
light of present day needs and resources,
has attempted to define a basic doctor as
follows:
(a) A basic doctor is one who is well
conversant with the day-to-day
health problems of the rural and
urban communities and who is able
to play an effective role in the
curative and preventive aspects of
• Present Address: 79, Sundar Nagar, New Delhi 11.
t Assistant Professor of Medicine, Ali-India Institute of Medical Sciences, New Delhi 16.
410
411
regional and national health pro development of an attitude of mind. This
blems. He should have the com attitude, when properly applied to a partic
petence to judge which case should ular situation, seeks for itself the proper
be referred to a hospital or a answers. Winslow has outlined this as
specialist. He should be able to follows:
give immediate life-saving aid to
Tn any teaching institution two pro
all acute emergencies. He should cesses are involved: training and education.
have competence in clinical Training is concerned with the cultivation
methods, i.e., history taking, phy of automatic response to external stimuli.
sical examination, diagnosis and We train a dog to heel or we train a plant to
treatment of common conditions. grow in espalier fashion on a wall. We train
(i) He should be capable of constant a child to speak good English. On a
advancement in his knowledge by higher level, we train a medical student to
learning things for himself by recognize the eruption of measles or an
having imbibed the proper spirit engineer to apply mathematical formula for
and learnt the proper techniques determining stress on a beam. Yet educa
for this purpose during his medical tion is something more than a training.
The word means “to lead out”. It implies a
course.
widening of vision, a broadening of thought.
One thing which has to be constantly It is an imaginative and a creative process.
borne in mind is that no curriculum for You cannot, in any sense, educate a dog or a
under-graduate medical education can be plant but you can educate a child’.
static. As the needs and the demands of
Winslow’s definition, applied to medical
the contemporary society change so should
the orientation in a curriculum to those education, raises a question which is of
needs. For example, in countries like the fundamental importance and which the
U.K. and the U.S.A, where the life span educationists must decide. If the major
has been sufficiently prolonged and where objective is to train medical students to
the social and cultural environment is such respond to certain stimuli, to co-operate to
that joint family system is discouraged, comply and to accept what they are told,
care of the old people has assumed im then the procedure be called student
portance. This has led to the development training. However, if the primary aim of
of the speciality of geriatrics and due the Faculty is to provide experiences that
emphasis is being placed on certain aspects will enable the student to understand, to
of geriatric practice in the under-graduate acquire skills, and to develop attitudes that
medical curriculum. For obvious reasons will help him to become an introspective,
geriatrics is not a major problem, at any independent, self-operating learner for a
rate at the present time, in our country. life time, then, education is the objective.
Therefore, to advocate its inclusion in a
After having emphasised that medical
clinical curriculum for the medical students education should be need-oriented, and
in this country would be rather premature after having defined the type of education
and not entirely need-oriented. Examples to be imparted, it is easier to envisage that
of this nature can be multiplied. However, what is needed is to impart broad based
there are certain things which are subtle, medical knowledge with appropriate stress
and less obvious, and, therefore, they go on in the training on the day-to-day problems
creeping into the curriculum at the cost that a basic doctor has to face.
of the total learning experience of the
The basic doctor, however, must have a
medical students.
Education is a living process. It has a proper concept of what the country expects
much wider horizon than is generally appre of him. He must know that comprehensive
ciated. It does not mean imparting a lot medicine is the prime need of our country.
of factual information to the students who This should be clearly defined and properly
in turn try to reciprocate the effort by understood. In broad terms, it implies the
faithfully reproducing it in an examination. utilization of the available medical know
Education is much more than this; it is the ledge for the total care of the patient. It
412 INDIAN JOURNAL OF MEDICAL EDUCATION
VOL. IX, JUNE-JULY 1970
expresses the chief concern for the patient,
rather than his disease. It pleads for the grammes, be it family planning or national
consideration that the human body should malaria eradication. The relevance of social
be regarded as a whole, and not as a com and behavioural sciences becomes signi
bination of various organs and tissues. ficant in the development of the trait of
It tries to undo what fragmentation of community leadership in the future doctor.
scientific knowledge has done. It involves
How can all this be included in the
the consideration of all significant factors already overburdened curriculum? You
that affect the health of a human being. cannot very much increase the duration of
It, therefore, includes the application of the course which is already much longer
preventive measures to individuals and the than any other professional course. The
employment of all practical means for the only way is to evolve a new policy and
early detection of disease. Lee (1961) has rearrange the time allocation of various
succintly defined Comprehensive Medicine subjects, and aim at as much integration of
as ‘An attempt to apply all available know teaching in various subjects as possible.
ledge—be it of Pathology’, Pharmacology, Just addition or subtraction of a few hours
Sociology or Psychology—to the main here or there will not be the answer to the
tenance of health and the diagnosis, treat problem.
ment and rehabilitations of the sicker or the
An impression has gained ground in
disabled patient’. Comprehensive Medicine
is of course ‘good medicine’, but all good almost all the centres in this country and
technical, medical or surgical practice abroad that the number of hours devoted to
a particular subject in the medical teaching
is not necessarily comprehensive.
directly reflect on the importance of the
Some of the important ingredients of this subject and, therefore, on the status of the
concept which, however, are being denied department and of the faculty members who
due recognition at present, are: (1) the work in that department. It is apparent
considerations of emotional and psychiatric that this notion is really not true. A subject
aspects besides the physical factors and (2) may be important for more than one reason;
a continuing care of the patient by an in fact, each medical subject is of con
internist, with or without the help of the siderable importance in its own right.
specialists, so as to enable the patient to However, all the details of all the subjects
achieve an optimal state of health and well
cannot be compressed into the medical
being.
curriculum which has to be taught in a
This brings out the relative importance limited number of years. Therefore, a
of social sciences in the clinical curriculum. co-ordinated effort has to be made by all
This is not a new concept. As early as the faculty members of a particular medical
1847, Virchow observed ‘Medicine is a school to sit together and evolve a pro
social science in its very bone and marrow’. gramme suited to the needs of the country
In his famous book: ‘Disease, Life and Man’, and students, i.e., the future doctors, and not
Virchow wrote, ‘If Medicine is the science to the needs of the departments. In other
of the healthy as well as the ill human words, the curriculum has to be studentbeing, what other science is better suited oriented (need-oriented) and not depart
to propose laws as the basis of the social ment-oriented. This necessitates a great
structure in order to make effective those spirit of accommodation and give and take
which are inherent in man himself? Once on the part of all the faculty members and
Medicine is established as anthropology and more so on the part of the heads of the
once the interests of the privileged no longer various departments.
determine the course of public events, the
The duration of the clinical course in the
physiologist and the practitioner will be medical colleges in India is three years after
counted among the elder statesman who the first M.B. examination which comprises
support the social structure’. The need for of Anatomy, Physiology and Biochemistry.
community leadership is essential for a One year of internship after the final M.B.
physician. This enables him to mobilise examination can also be included in this
effective support for national health pro- which makes it four years. During th?
undergraduate clinical curriculum —a reappraisal
413
For this purpose, however, there should
first one and a half years there is a con be a complete understanding and co
comitant teaching of para-clinical sciences ordination between the various teachers and
like, Pathology, Microbiology, Pharmaco a uniform policy should be evolved at the
logy and Forensic Medicine which leaves commencement of the academic session and
very limited time for training in clinical
the guidelines for various seminars for this
disciplines and the student devotes his type laid down. In case such a teaching
entire time to clinical disciplines only after method cannot be arranged, then the
the second M.B. examination. The social
and preventive medicine is taught all along syllabus should be so planned at the com
in this type of general scheme. It is mencement of clinical and academic sessions
obvious that only broad principles, with that the repetition in teaching is avoided as
far as possible. If the syllabi of clinical
only some essential details, of the main
in the medical colleges arc
disciplines, i.e., General Medicine, General disciplines
reviewed, many common topics will be
Surgery, Pediatrics and Obstetrics and found. The irony is that the teacher of
Gynaecology can be taught in this short one speciality is often completely unmind
period of time.
Before considering each clinical subject ful of the fact that the same subject is also
in some detail, certain general principles being taught by another specialist, some
can be laid down. The clinical subjects times with divergent views and different
should be presented as far as possible in emphasis, to the utter dismay and con
of the students.
an integrated manner and their teaching fusion
Emphasis in the clinical teaching should
should involve the disease process as a be on highlighting the common problems
whole and not as a Medical, Surgical or that are met with in any geographic region.
Obstetrical problem. For example, there Somehow, the interpretation of the words
is hardly any need of arranging three ‘geographic region’ by a specialist is a
lectures on pyelonephritis—one for ‘medical’
narrow one—usually this means the topo
pyelonephritis; another for ‘surgical’ pye graphic area called the hospital. How
lonephritis and still another for pyelitis in
ever, the hospital practice gives an utterly
pregnancy. The essentials for the diagnosis
and principle of management can as well false impression about the relative in
or the prevalence of any disease.
be taught in a seminar in which all the cidence
If a gastroenterologist is interested in the
specialities participate—a horizontal integ problem of ulcerative colitis, many cases of
ration. It will be still more beneficial if this disorder will be referred to him and
the pathologist is also included in this so
then admitted in his wards. As a
that there is a concurrent teaching of are
result, the student may have seen half a
etiology and pathology as well—a vertical
integration. A correlation between the dozen cases of ulcerative colitis during a
three
month posting in that unit, without
clinical presentation and the changes in the
coming across a single case of bacillary
structure and function of various organs can dysentery! The student has learnt all
be achieved by effectively combining the about the place of hydrocortisone retention
clinical teaching with that in applied
pathology. The student who is in-charge enema in the management of ulcerative
colitis, without knowing the dose of sulof a patient in the wards should participate phaguanidine required to manage a case of
in the microbiological examination of
acute bacillary dysentery. The student
specimens obtained from the patient. thus knows all about the immunological
Similarly, in the event of the death of the aspects of ulcerative colitis without knowing
patient, there should be a compulsory
principles of the prevention of acute
attendance at the postmortem examination, the
or chronic infections of the gastrointestinal
in case permission for autopsy has been
obtained. This is the type of approach tract.
Recognition of day-to-day problems of
which is being evolved at the AIIMS.
The quantum of didactic teaching can thus the urban and rural areas and especially,
emergency situation in clinical practice
be diminished appreciably, leaving more should be emphasised and principles of
time for practical training. The student, emergency management of such conditions
moreover, learns the pathological entity as
should be properly taught.
a whole and not in bits here and there.
414
INDIAN JOURNAL OF MEDICAL EDUCATION
As regards the teaching of specialities,
at the under-graduate level, students should
get exposed only to frequently encountered
disorders so as to familiarise them with the
problems which they are likely to come
across during their practice as basic doctors.
This point has been well brought out in a
study conducted by the medical curriculum
committee of the British Medical Asso
ciation. The committee inspected and
analysed the cases seen by a randomly
selected general practitioner over the course
of one year. The results were revealing;
108 of this practitioner’s patients suffered
from haemorrhoids whereas only 3 had
endocarditis; 64 suffered from threadworms
whereas 4 had perforated peptic ulcer;
120 suffered from boils and 2 from rosacea;
among 1023 cases of disorders of the
nervous system, there were 231 cases of
anxiety neurosis. It is certain that any
study conducted on these lines in our
country in a general practitioner’s clinic and
a rural health centre will be as revealing
and striking. In fact, such type of studies
should be undertaken. A study of this
nature is bound to bring out the wide gap
that exists between what a basic doctor
needs to know and what is being taught to
him during his under-graduate days. It is
apparent that you cannot make an under
graduate a specialist in all specialities.
Teaching him the details of various spec
ialities is a waste of effort and time. It is,
therefore, imperative that only the general
principles rather than the minutiae con
cerning the specialities should be dealt with.
The main objective of training in special
subjects is to enable the student to re
cognize such disorders early and give the
necessary immediate treatment if it is an
emergency and to make the necessary re
ferral for further evaluation and management
to the specialist centres. Rare diseases,
details of infrequently used laboratory in
vestigations and operative techniques should
not be incorporated in the syllabus.
General Medicine, General Surgery,
Paediatrics, Obstetrics and Psychiatry should
form the mainstay of the clinical curriculum.
Social and Preventive Medicine should be
taught by all the specialists, in close coll
aboration with the staff of that depart
ment. Ophthalmology, Otorhinolaryngology’,
Dermatology and Venereology and other
VOL. IX, JUNE-JULY 1970
specialities should be taught only to the
extent that a basic doctor needs them in
his day-to-day practice. The review com
mittee of the A.I.I.M.S. (1964) consisting
of eminent educationists of national and
international repute made the following
observations and recommendations in this
context:
‘The Committee consider that such
topics as Otorhinolaryngology, Ophthal
mology, Dermatology and Venereology
and Tuberculosis should be adequately
taught in a series of 12 to 15 lectures
and demonstrations’.
In the field of Ophthalmology, for ex
ample, an argument put forward for teach
ing the subject in great detail, is that
blindness is very common in India. While
this is true, it is also very true that in every
discipline and speciality there are some very
common and serious disorders. Is not
common cold the most common disorder?
Is tuberculosis uncommon in this country?
Is amoebiasis not extremely common? Can
we afford to make the student spend some
weeks in learning each of such common
disorders? Obviously not. In the field of
Ophthalmology, on the other hand, the
student should be made familiar with the
recognition and management of those
disorders which are met with commonly in
general practice. Infections of the eye,
which in one form or the other are a major
cause of blindness, along with malnutrition,
must be adequately taught. Glaucoma, as
an emergency must be recognized and
managed at least for a short while before
arranging for immediate referral to a
specialist centre. Cataract has to be diag
nosed and referred for surgery to an
ophthalmic surgeon. First aid for in
juries of the eye must be taught. However,
it is hardly of any use to spend hours of
lecturing on the surgery of squint or even
cataract, or the management of errors of
refraction, as these have to be undertaken
by a specialist. The ocular manifestations
of systemic disorders should be taught by
the internist, in active collaboration with
the ophthalmologist. What is needed is a
bed-side clinical approach for the recognition
of common as well as serious disorders and
the principles of their management. A
practising doctor should be able to decide
UNDERGRADUATE CLINICAL CURRICULUM—A REAPPRAISAL
whether the effective management can be
done by him or whether the patient needs
referral to a specialist. What is mentioned
about Ophthalmology is equally applicable
to the teaching of Otorhinolaryngology and
other specialities.
Paediatrics, rightly, is assuming increasing
importance. It is estimated that 40 per cent
of the population in India belong to
paediatric age group and 42 per cent of the
patients attending a general hospital are
below the age of 14. Therefore, it has to
be treated as one of the most important
subjects in the medical curriculum. A
sound and adequate knowledge and training
in this speciality is essential for any practi
tioner. In addition to clinical teaching of
the common paediatric disorders, emphasis
has to be placed in the various portions of
the under-graduate curriculum on the teach
ing of nutrition, growth and development,
genetics, immunology and certain social
factors affecting the health of the child.
The special problems pertaining to the new
born and premature infants should form a
part of the teaching and training in
paediatrics. The causes of the behavioural
problems and their management should be
taught in active collaboration with the
Psychiatrist. Preventive health programmes,
immunisation, nutrition school health ser
vices and growth and development should be
taught in association with the department of
preventive and social medicine.
If the theme that the individual patient
as a whole should form the unit of study
is accepted, then, the importance of the
adequate training in psychiatry becomes
obvious. The curriculum in psychiatry
should be spread over the whole of clinical
period. This does not necessarily imply
that the teaching of psychiatry should be
extended or be given more teaching hours.
This only means that there should be a
close integration between psychiatry and
general medicine and the teachers in psy
chiatry should associate themselves with the
teachers in other clinical subjects. The
purpose will be defeated if the psychiatrist
utilises the extra time by increasing the
number of lectures in his subject. What is
necessary is that the psychiatrist should be
present and be actively associated in the
teaching programme when diseases like
415
peptic ulcer, bronchial asthma, thyro
toxicosis, ulcerative colitis, hypertension
etc. are being taught by an internist. The
diseases enumerated above have been
selected from a cross section of subspecial
ities, only to emphasise the fact that a close
integration is necessary in the teaching
programmes. Entities like anxiety neurosis
very often come to the general practitioner
or the internist and collaboration of a
psychiatrist and an internist in this field is
also necessary.
The ideal of the total care will not be
achieved if the students are not acquain
ted with the principles of rehabilitation
medicine. The care of a myocardial in
farction does not become complete by
knowing all about the controversy existing
about the use of anticoagulants in the
management. It extends much beyond
the time the patient is discharged from
the hospital; this area has to be covered
by teaching fundamentals of rehabilitation
medicine.
There has been a lot of thinking re
cently on the content of curriculum and
duration of the teaching in Preventive and
Social Medicine which should actually be
renamed as Community Medicine. This
subject used to be taught only 20 years ago
as ‘Hygiene’ and the teaching comprised
of about 40 lectures (one hour each)—
mainly concerning sanitation and environ
mental hygiene and control of epidemics.
The teaching hours have been increased in
this subject which has been rightly given a
much wider scope, to about 450 in the
total curriculum. In addition three months
are reserved in a rural or urban centre
during the internship period. The crux of
the problem, however, is to know what
results have been achieved by this pro
longed course in this subject during the
last 20 years or so. Is the graduate of to
day more biased towards the preventive
aspects of health problems than his pre
decessor? Has he a better conception of
his duties towards the community and the
role that he should play? So far as one can
judge one cannot say with any degree of
confidence that anything like this is happen
ing. When the student is being imparted
so much training in a subject, very often at
the cost of cutting down his training in
416
INDIAN JOURNAL OF MEDICAL EDUCATION
certain essential subjects like Medicine or
Surgery or Paediatrics etc. without achiev
ing the desired aims, the matter requires
very deep and serious thinking. We con
sider it necessary that if the aims with which
the curriculum of this subject was in
creased are to be achieved, there must be
very close integration of this subject with
other subjects—especially the main clinical
disciplines.
For example, nutrition,
immunisation, growth and development,
preventive aspects of many of the in
fectious diseases, school health services etc.
should be taught along with Paediatrics,
preventive aspects of communicable dis
eases and systemic disorders like cardiovas
cular disorders should be taught along with
the physicians in the wards. The clinicians
must also change their attitude. They
must realise that the teaching of clinical
subjects at present is too much hospitalbased and too little community-oriented.
They must move out frequently to the rural
or urban centres and teach clinical medicine
there laying special emphasis on the
management of such cases and particularly
the emergencies, when they present them
selves in a rural centre. They may occa
sionally along with Preventive and Social
Medicine teachers and interns visit the
homes. They will themselves then learn
what the important problems in the com
munity are and how they are to be tackled
and what stress is to be laid on the various
clinical problems. The obstetrician for
example will learn what problems the young
graduate has to face, if called upon to
deliver a baby in the house. From the
point of view of a young graduate, training
in domiciliary midwifery is more important
than what he learns of this subject in the
hospital. Such examples can be multi
plied for all clinical disciplines. Just in
creasing the number of hours in the subject
of Preventive and Social Medicine will not
bring any dividends unless the teaching
methods are overhauled on the above
mentioned lines.
VOL. IX, JUNE-JULY 1970
An attempt has been made to outline
areas of under-graduate clinical curriculum
where radical changes are needed. It is
bound to provoke differences of opinion.
Such differences in medical education have
existed since antiquity and have served the
purpose of healthy discussion and an
evolution of thinking concerning medical
education.
‘Galen wrote about the nobility con
ferred on the physician by the study of
philosophy. By that he meant that the
physician should possess all the necessary
knowledge of life and its manifestations,
and he estimated that a period of study of
at least eleven years was necessary to attain
this goal. His contemporary and enemy,
Thessaulus, on the other hand, announced
that the medicine of the schools was nothing
but a fraud and.........declared that six
months was all that was necessary to make
an excellent physician’.
—A. Castiglioni (A History of Medicine).
REFERENCES
1. British Medical Association: The Training of
a Doctor: report of the curriculum committee,
London, Butterworth, 1948.
2. Castiglioni, A.: A History of Medicine. ,
Translated from the Italian and Edited by
E. B. Krumbhaar, New York, Alfred A.
Knopf, 1947.
3. Lee, P. V.: Teaching comprehensive medicine
in Medical Education and Medical Care,
Editors C. G. Ships, G. A. Wolf and C.
Jacobsen; Association of American Medical
Colleges, Evanston, Illinois, 1960.
4. Review Committee—All-India Institute of
Medical Sciences, New Delhi, 1964.
5. Virchow, R: Disease Life, and Man. Stanford
University Press, 1958.
6. Winslow, C.. E. A., quoted by Kasey, E. and
McMahan, E: Education as a Living Process
in Health Education in the Hospital, American
Hospital Association, Chicago, 1964.
62 The Indian Journal of Medical Education
Status of Anaesthesia Teaching in Undergraduate
Curriculum : Consultants’ Feedback
By
G.N. Kalla
and
S.O. Ukponmwan
Department of Anaesthesiology, College of Medical Sciences, University of Benin, Benin City [Nigeria).
SUMMARY
The status of undergraduate anaesthesia teaching has changed from none at
all to varying periods of 2 to 16 weeks in one living memory. This questionnaire
study had an overall response rate of 71.92% ; 26.31% being ‘spontaneous response
rate’ and 45.61% ‘provoked response rate.’ It is recommended that (a) anaesthesia
should universally be made an ‘examination subject’ and (b) the duration of anaes
thesia posting in undergraduate curriculum should be increased, 63.41% hospital
consultants have favoured ‘topic teaching’ by holding joint seminars with anaes
thetists to improve quality and standard of undergraduate teaching. 36.58% hospital
consultants have commented that students’ participation must be enhanced to make
them learn resuscitation and certain anaesthesia techniques to combat the shortage
of qualified anaesthetists in developing nations.
deepend in its content, expanded the horizons'
of its scope and watered the roots of its scienti
On 16th October, 1846 William Thomas fic foundations. Needless to say that Anaes
Green Morton gave a successful demonstration thesia teaching has also made considerable
of clinical anaesthesia by using ether on a progress. Nonetheless it is still felt that the
patient in Boston, USA (Atkinson et al 1982). undergraduate medical students are not ade
That made ether anaesthesia popular all over quately exposed to Anaesthesiology. The
in a short time. Since then the practice of attitude of consultants holding teaching
anaesthesia has improved in its standards, responsibilities for undergraduates and the
Introduction
Kof. XXVI No. i
Sept.-Dec. 1987
Status of Anaesthesia T^^hing in...65
jaduated from 10 years to 34 years ago, with happy with the performance of anaesthesia
; mean of 16.63 years and mode of 18 years. department for functioning smoothly inspite of
Jbey have graduated from various universities present shortages and hardships. 36.58 (15)
■a Nigeria (58.53%), United Kingdom (17.07%) commented that students’ participation in the
/India (7.31%), West Germany, (4.87%), Italy, practical aspects of anaesthesia must be im
Hungary, Canada and Egypt (2.43% each) proved. Table 4 lists all the comments.
land one (2 43%) did not state the place Two
.veteran Consultant (4.87%) out of 41, said
Currently, in our institution obviously the
ilbey were not taught anaesthesia in their students are not posted with all the other
(undergraduate curriculum, whereas rest all ; i.e. consultants after they have completed their
139 (95.12%) were taught. All there 39 re- anaesthesia posting.
[collect that anaesthesia teaching was mainly
jin the form of diadectic lectures with demons Discussion
tration of some of the anaesthesia techniques
and equipment. The duration of posting has
A specially designed questionnaire was sent
been stated to vary from 2 weeks to 16 weeks. to our hospital consultant colleagues who have
Table 1 shows the duration of anaesthesia graduated from 10 to 34 years ago from various
posting consultants had and they suggest for Universities of different nations in Africa,
future. The suggested increase in duration Asia, Europe and North America. The status
ranges from 12 weeks to as long as for surgery. of anaesthesia teaching at undergraduate level,
Table 2 depicts the responses for the attendence during one living memory, has evidently
defaulters, end of posting examination con changed from none at all through a varying
sultants had and for the assessment of present period of 2, 4 or 6 weeks to a maximum of 16
students’ acquisition of skill and knowledge. weeks. The overall response rate of 71.92%
Regarding the latter a few (12.19%) did not to our questionnaire, is not excellent. May be
comment, while others (17.07%) stated : I don’t others, who chose not be respond, were either
know, ‘unable to assess’, ‘Not applicable.’ too busy to co-operate, or were not appreciative
12.19% said that the students do not get any of the potentials of this kind of a study.
opportunity to show their knowledge or skill, 26.31% responded spontaneously and quickly,
29.26% felt they did not learn satisfactorily, whereas 45.61% responded after repeated
while 29.26% felt they did learn well.
reminders. Obviously, the responses from the
later group were delayed. It is considered that
26 out of 41 (63.41%) would like to hold the spontaneous response rate’, which is
joint seminars in collaboration with anaesthe normally quick, and provoked response rate,'
tists to improve the quality of undergraduate should be duly recognised in questionnaire
teaching. Table 3 lists the suggested topics studies.
for such joint seminars.
The duration of posting, the content of
19.5% (8) have commented that they are teaching, the attendance by the students and
62
The Indian Journal of Medical Education
Ko/. XXVI No. i
Status of Anaesthesia Teaching in Undergraduate
Curriculum : Consultants’ Feedback
By
G.N. Kalla
and
S.O. Ukponmwan
Department of Anaesthesiology, College of Medical Sciences, University of Benin, Benin City (Nigeria).
SUMMARY
The staius of undergraduate anaesthesia teaching has changed from none at
all to varying periods of 2 to 16 weeks in one living memory. This questionnaire
study had an overall response rate of 71.92% ; 26.31% being ‘spontaneous response
rate’ and 45.61% ‘provoked response rate.’ It is recommended that (a) anaesthesia
should universally be made an ‘examination subject’ and (b) the duration of anaes
thesia posting in undergraduate curriculum should be increased, 63.41% hospital
consultants have favoured ‘topic teaching’ by holding joint seminars with anaes
thetists to improve quality and standard of undergraduate teaching. 36.58% hospital
consultants have commented that students' participation must be enhanced to make
them learn resuscitation and certain anaesthesia techniques to combat the shortage
of qualified anaesthetists in developing nations.
deepend in its content, expanded the horizons'
of its scope and watered the roots of its scienti
On 16th October, 1846 William Thomas fic foundations. Needless to say that Anaes
Green Morton gave a successful demonstration thesia teaching has also made considerable
of clinical anaesthesia by using ether on a progress. Nonetheless it is still felt that the
patient in Boston, USA (Atkinson et al 1982). undergraduate medical students are not ade
That made ether anaesthesia popular all over quately exposed to Anaesthesiology. The
in a short time. Since then the practice of attitude of consultants holding teaching
anaesthesia has improved in its standards, responsibilities for undergraduates and the
’ 1'4,2 - d l j
Introduction
Sept.-Dec. 1987
jaduated from 10 years to 34 years ago, with
; mean of 16.63 years and mode of 18 years.
They have graduated from various universities
a Nigeria (58.53%), United Kingdom (17.07%)
liodia (7.31%), West Germany, (4.87%), Italy,
.Hungary, Canada and Egypt (2.43% each)
land one (2 43%) did not state the place Two
veteran Consultant (4.87%) out of 41, said
jibey were not taught anaesthesia in their
Undergraduate curriculum, whereas rest all ; i.e.
139 (95.12%) were taught. All there 39 re■collect that anaesthesia teaching was mainly
jin the form of diadectic lectures with demons
tration of some of the anaesthesia techniques
land equipment. The duration of posting has
j been stated to vary from 2 weeks to 16 weeks.
liable 1 shows the duration of anaesthesia
] posting consultants had and they suggest for
: future. The suggested increase in duration
ranges from 12 weeks to as long as for surgery.
Table 2 depicts the responses for the attendence
defaulters, end of posting examination con
sultants had and for the assessment of present
students’ acquisition of skill and knowledge.
Regarding the latter a few (12.19%) did not
comment, while others (17.07%) stated : I don’t
know, ‘unable to assess’, ‘Not applicable.’
12.19% said that the students do not get any
opportunity to show their knowledge or skill,
29.26% felt they did not learn satisfactorily,
while 29.26% felt they did learn well.
26 out of 41 (63.41%) would like to hold
joint seminars in collaboration with anaesthe
tists to improve the quality of undergraduate
teaching. Table 3 lists the suggested topics
for such joint seminars.
19.5% (8) have commented that they are
Status of Anaesthesia T^^bing in...65
happy with the performance of anaesthesia
department for functioning smoothly inspite of
present shortages and hardships. 36.58 (15)
commented that students’ participation in the
practical aspects of anaesthesia must be im
proved. Table 4 lists all the comments.
Currently, in our institution obviously the
students are not posted with all the other
consultants after they have completed their
anaesthesia posting.
Discussion
A specially designed questionnaire was sent
to our hospital consultant colleagues who have
graduated from 10 to 34 years ago from various
Universities of different nations in Africa,
Asia, Europe and North America. The status
of anaesthesia teaching at undergraduate level,
during one living memory, has evidently
changed from none at all through a varying
period of 2, 4 or 6 weeks to a maximum of 16
weeks. The overall response rate of 71.92%
to our questionnaire, is not excellent. May be
others, who chose not be respond, were either
too busy to co-operate, or were not appreciative
of the potentials of this kind of a study.
26.31% responded spontaneously and quickly,
whereas 45.61% responded after repeated
reminders. Obviously, the responses from the
later group were delayed. It is considered that
the spontaneous response rate’, which is
normally quick, and provoked response rate,’
should be duly recognised in questionnaire
studies.
The duration of posting, the content of
teaching, the attendance by the students and
,
66
The Indian Journal of Medical Education
the examination all play important role in
achieving a favourable outcome.
Students
always tend to concentrate more on the
‘examination subjects’. For a conscentious
teacher it is imperative to give examination
to his pupils to evaluate how much have they
learnt ? Unless the aim of the teaching is not
really to teach and train the students, but
merely delivering the lecture and that’s all,
not giving examination to students make no
sense at all. Hence, it is felt that anaesthesia
should be made an ‘examination subject’ at par
with other subjects. Even if the attendence is
not made compulsory, students by and large
would attend the teaching programmes of all
the examination subjects’. The content of the
teaching is not solely dependent on the dura
tion of posting. Nonetheless the duration of
posting can have a linear relationship with the
content of the teaching.
All the more when teaching is coupled with
training, the duration of posting becomes
acutely crucial. It is the duration which would
determine the number of chances every student
in a class can get for the practical training.
This questionnaire posed a direct question
to all the hospital consultants, which was :
should the period of anaesthesia posting remain
unchanged from what you had during your
graduation or should it be changed (increased
or decreased) ? Their answers reflect predict
able human behaviour in any society. 63.41%
of them succumbed to the syndrome of ‘Let it
be’ : they said let it remain the same. Not all
of them bad a similar duration of anaesthesia
posting during their graduation. It ranged
from 2 to 16 weeks. 29.26% answered that the
W Vol. XXVI No.3 .
Sept.-Dee. 1987
duration of anaesthesia posting for un<t- !
topic in every department. Time thus saved
graduates should be increased. The suggested I
can be reallocated to the needy departments.
increase ranged from 12 weeks to as long as
Maddison (1978) advocated that ‘topic teaching’
surgery has got. None favoured a decrease
provides horizontal integration in effective
3(7.3%) did not comment on this. In anj. 1
medical education. Criticising further the
society a majority of human beings always tend
existing fragmented approach Maddison quotes
to just follow whatever trend has been set for i
one of his residents who discovered while
them by the ancestors. They, somehow, <|O i
preparing for final graduation examination that
not feel obliged to give a serious thought to I
he had 21 separate lectures and tutorials on
identify the problems, in the face of changed i
thyrotoxicosis. Joint seminars in ‘topic tea
times, and then attempt to solve as well. This |
ching’ can eliminate such wastage of time.
attitude can aptly be described as a syndrome
Another forseeable advantage of joint seminars
of‘Let it be’. It is only a minority of people,
is an improvement in the quality and standard
in any human society, who are thinkers, who ;
of undergraduate teaching by gathering a large
are trend setters, who quite naturally realise the i
pool of upto date information by the concerned
need of the hour. Their opinion should be ■
experts. In the fragmented teaching system
valued more. With this doctrine it is recom
someone can play on dubts by presuming that
mended that the opinion expressed by only
this aspect of the disease should have been
29.26% of respondents, in this study, to 1
covered or would be covered by another
increase the duration of anaesthesia posting for ■!
department ; and so on and on. Eventually
undergraduates should be accepted in principle. .
that aspect may be left out altogether. ‘Topic
The actual extent of increase can then be 1
teaching’ can effectively eliminate this.
decided by the appropriate authorities respon
sible for updating undergraduate curriculum.
Gale et al (1976) reported that improvement
in medical education is largely dependent upon
This may raise'and eye-brow here and there:
the attitudes of clinical teachers towards their
Where to get the additional time from ? Part
own teaching and their students learning.
of the additional time needed for increasing the
Present study highlights the attitude favouring
duration can be made available by simple
‘topic teaching’ in joint seminars among 63 41%
adoption of joint seminars. Certain topics like
hospital consultants. Such sprouting attitudes
shock, care of unconscious, etc. are dealt with
should be immediately harnessed lest they die
by various departments : such as medicine,
off also quickly.
surgery, anaesthesia, obstetrics & gynaecology,
pathology etc. If such a topic, e.g. shock is
Questions regarding acquistion of theo
covered in a joint seminar to be deliberated by
the consultants of all involved departments sim
ultaneously at a time under-one roof, it would
definitely economise the students’ time which
otherwise would have been spent on the same
Status of Anaesthesia Teaching in...67
retical knowledge and practical skill invited
sharply diversent answers. On one extreme the
answers were T dont’t know’, ‘Unable to
asses’, ‘Not applicable’, ‘No opportunity for
students to demonstrate these’. The other
extreme included satisfaction (29.26%) and
dissatisfaction (29.26%).
Some left these
questions unattempted. Some of the responses
‘unable to assess and ‘Not applicable’ were
probably due to the fact that the students are
not posted with those Consultants after com
pleting their anaesthesia posting.
(15) 36.58% have commented that under
graduate student’ participation in the practical
training of resuscitation and some of the
anaesthesia techniques must be enhanced. In
developing nations were qualified anaesthetists
are not available in adequate number the prac
tical training for students becomes very impor
tant. Undergraduates, if well trained in
regional anaesthesia techniques, can at a later
date help a nation improve, to considerable
extent, its health care delivery to masses in
rural areas.
Acknowledgements
Many thanks are due to our colleagues,
without whose co-operation this study could
not have been completed. Trie secretarial
assistance provided by Miss M.N. Ofili is
highly appreciated.
z
TABLE 2
Feedback on some aspects of undergraduate anaesthesia teaching in past and at present
No.=42
Attendance*
(No.)
34
(%) 82.92
Were defaulters
asked to repeat ?*
Had end-of
posting exam.*
5
18
19
12.19
43.90
18
5
20
5
Assessment of knowledge &
skill acquired by present
students during anaesthesia
posting
7
43.90 12.19 46.34 48.78 12.19 17.07
5
12
12.19 29.26
Joint seminars
favoured for
future
11
4
12
26
29.26
63.41 26.82 9.75
These columns have N=39 as 2 consultants were not taught anaesthesia when they were
undergraduate students.
The Indian Journal of Medical Education
70
Vol. XXV1No-3
TABLE 3
TABLE 4
Suggested Topics for Holding Joint Seminars with Anaesthetists
Comments by Hospital Consnltants
SI. No.
Comments
Topics favoured for joint seminar:
1,
1.
Status of Anaesthesia Teaching in...71
Sept.-Dec. 1987
Shock
Anaesthesia department has done very
well inspite of shortages and difficulties
Keep it up.
2.
Care of unconscious patient.
2.
Anaesthesia teaching should be more practical.
3.
Airway management including emergency tracheostomy.
3.
Students’ participation should be increased.
4.
Cardio-pulmonary resuscitation.
4.
Joint seminars should be held for postgraduate students also.
5.
Management of facial trauma, severely
cleft palate, critically ill.
5.
Anaesthesia is the meeting point of all the medical disciplines. Students be
given an opportunity to revise and familiarise with the theory and practice of
anaesthesia and resusciatation before their final examination.
I
injured,, head injury, cleft up and
6.
Dental chair emergencies.
7.
Management of emergencies in paediatric surgery.
This may be the last chance in their life ;
6.
8. .
Facial blocks and problems of ocular surgery.
9.
Drug interactions, management of adverse drug reactions.
10.
Chest radiology.
11.
Obstetric anaesthesia and analgesia.
12.
Effect of anaesthetic agents on various aspects of intermediary metabolism
13.
Community practice and anaesthetic techniques.
Duration of posting in anaesthesia should
be for at least a. month
for every
student.
7.
Less no of students be posted with a consultant anaesthetist to make operation
theatre teaching more effective.
8.
Regional techniques should be emphasised more.
8.
72
The Indian Journal of Medical Education
If Yes (i) were defaulters asked to repeat u>e
XXVI No. 3
.
(ii) failing ta^epeat the posting were defaulters detained from appearing
in Final OTaduation Exam.
Yes/No.
9.
Was there any end-of posting exam. ?
10.
In the light of your specialisation do you think the time devoted to anaesthesia
teaching at undergraduate level should
Yes/No.
Appendix 1
DEPARTMENT OF ANAESTHESIOLOGY COLLEGE OF MEDICAL SCIENCES
UNIVERSITY OF BENIN, BENIN CITY
(a)
Consultants’ feed-back on the status of Anaesthesia teaching at Undergraduate Level
Dear Doctor,
We shall be grateful if you could please complete the following questionnaire as
frankly and truthfully as possibly you can by filling the blank spaces or ticking the
appropriate. Please do not write your name anywhere since the information gathered
will be treated as confidential. Thank you.
1.
Year and place of your medical graduation ?
2.
Year and place of specialisation :
3.
Area of your specialisation :
4.
Was anaesthesiology taught during your medical training ?
Yes/No.
5.
If Yes, please tick the type you had
(a)
Designation :
theorty classes only, i.e. lectures/seminars/group discussions.
6.
practical demonstrations in the operation thearter i.e. demonstration of
anaesthetic equipment alone/demonstration of conduction of anaesthesia or
parts thereof like endotracheal intubation/demonstration of regional anaes
thetic techniques like spinal or epidural.
Ho^jSjxig was your posting in anaesthesia during your training ?
7.
Was it compulsory to attend anaesthesia posting ?
(b)
Yes/No.
remain the same as you had ?
(b)
be increased ; (if yes then how much, ?
(c)
be decreased,
(if yes then how much, ?
11.
Currently are undergraduate students
anaesthesia posting ?
Yes/No.
12.
While teaching the present undergraduates do you feel that certain topics, like
shocks, cardio-pulmoaary resuscitation care of unconscious patient, drug
interaction, etc, have been well covered during their anaesthesia posting :
13.
Are the undergraduate students able to demonstrate their ability to perform
some basic techniques like setting-up of an intravenous infusion, handling
oxygen therapy equipment and suction apparatus, external cardiac compression,
etc., which have been taught to them during anaesthesia posting ?
14.
Would you have liked to hold seminars for undergraduates in ’collaboration
with anaesthesia department for the benefit of students
Yes/No.
If yes, please specify the topics :
15.
Any other comments on the status of anaesthesia teaching at undergraduate
level ?
posted to you after they have completed
14
The Indian Journal of Medical Education
Vol. XXVI No. 3
REFERENCES
1.
Atkinson, R.S. ; Rushman, G.B., and Lee, J.A. (1982). A synopsis of Anaes
thesia, 9th edn., 3, PSG, Bristol.
2.
Gale, J„ Tomlinson, R.W.S., and Anderson, J. (1976) Changing attitudes of
medical teachers towurds medical education. Medical education, 10, 250-254.
3.
Maddison, DC. (1978). What’s wrong with medical education 7 Medical
education, 12, 97-106.
'jp
/>( tTP ( \
®
Place of Ophthalmology in Undergraduate
Medical Education in India
BY
Dr Lalit P. Agarwal and Dr P. K. Khosla
All-India Institute of Medical Sciences, Nevi Delhi
India is a vast country which is developing
its resources and in spite of this it is an ‘under
developed nation.’ Due to low standard of
I environmental sanitation, poor nutrition,
I diverse social and cultural patterns, illiteracy,
I superstitions, beliefs and taboos, a large
number of diseases both ocular and general
in as many diverse forms are seen. There
is a high incidence of blindness due to in' adequate ophthalmic aid. Ocular diseases
as such are posing big public health hazards
and problems.
This challenge has to be met with all the
resources at our command. Besides the
medical care, a proper orientation of medical
education is desirable.
The medical care of the community in
general should be based towards the needs
] uf the Community which, inter alia, means
I that the medical education itself should be
, orientated according to. this need. To
■ amplify, according to this concept, the
patterns of medical education should be
different in different countries as the rela
tive emphasis on training the undergradu
ates on vocation basis or through the active
process of learning and experiment will
vary from country to country, area to area,
and from time to time within the same
country. It will be influenced by the
pressing needs of the community for
medical service, by economic resources and
by the general state of development of other
sciences and humanities in the country.
It would, therefore, be perhaps advisable
to evolve our own pattern of medical
education rather than follow some set
pattern evolved by other countries whose
problems basically differ from ours. The
Health Survey and Planning Committee
of the Government n.f India IlOAIV lent
support to this line of thinking as it states
that ‘Medical Education should fit in with
the needs of a country, and conditions pre
vailing. For instance, India being more
than 80 per cent rural, the training given to a
doctor should enable him to carry on his
work among the vast masses in the villages’.
One has, therefore, to assess the basic needs
of the community before evolving a pattern
of medical curriculum. This requires na
tion wide and area wide survey of the com
munity needs of the population, a necessity
which is neither realised nor- is this lacuna
being probed by our medical planners. The
differences between what is required and
what is being supplied need to be brought
out and emphasis on the differences needs
to be given in working out the curriculum of
a basic doctor. Unless this is done, a curri
culum sought to be introduced is likely to be
based on inadequate data and theoretical
concepts far removed from practicability
and truth.
Let us briefly analyse these needs in terms
of quantity and quality of the medical per
sonnel in this country. The number of
medical graduates on population basis in
this country is much lower than the re
quirement. It is likely that we will have
one doctor for 6,000 of the population at the
end of the third five-year plan. We will be
hopelessly inadequate in die number of the
specialists in the so called specialities and
this gap is likely to remain for a long time ..
to come. As such, it is obvious that our
medical graduates going out in the commu
nity will have to have a much broader base
and carry a greater load of work both quantitative’*and qualitative—than their counter
parts in the West—if they have to serve
the needs of the community. To face the
situation, therefore, there are two courses.
-■
iG
GUT n’lCvuvax gcau allies 111O1C
broad based in a way that they can tackle the
fundamentals’of various disciplines and ren
PLACE of ophthal^logy in undergraduate MEDICAL EDUCATION IN INDIA
21
der minor services”the community in the an operation.'* Recent World Health Orga
diseases prevalent leading to a greater well nisation figures worked out in conjunction
being of the population, an object to be with Trachoma Control Pilot Project place
cherished by any community; or
the blind population in the neighbourhood
2.
To leave the community bereft of of three million. These figures do not
even basic services in disciplines other than include economically blind or visually
general medicine, general surgery and obs handicapped. Comparing these figures of
2,500 blind persons per million population
tetrics and gynaecology.
with the data in some of the countries of
This leads us to definition of a basic doc the west which are highly industrialised,
tor which would be applicable to this country. the inadequacy of ophthalmic services in
We suggest.that.a_basic doctor is-'one-who this country becomes evident. With the
with proper understandingofthe fundamen: exception of Egypt, India has the highest
tals of medical sciences can apply them to -proportion of blind population. In view of
the “care” of the community he is going to this the Mudaliar Committee says that:
serve’. This concept of a basic doctor is ‘Prevention of blindness is thus a problem
dynamic exhibiting a great range of flexi of great magnitude in this country’. This
bility/ Thus the training and the proficiency can be achieved in the following ways:
of a basic doctor in various branches of the
1. Preventive and Social Medicine per
medical sciences will differ in this country
sonnel should be properly instruc
due to the needs of the community which
ted with regard to the incidence
vary because of the social, cultural and
of these diseases and measures
environmental factors and the resources
necessary for preventing them so
available.
that they can carry out mass
We can have an idea of the basic data for
propaganda regarding the inci
the country in ophthalmology when we
dence and hygienic measures
know that the blind and visually handicapped
necessary for the prevention of
people constitute 3.75 per cent of the
the same.
population. The problems of ophthalmo
2. An intensive ophthalmic. service
logy and their remedies have been spotlight
should be developed throughout
ed by the Mudaliar Committee as well. They
the country, and a separate out
say:
patient section may be utilised
‘The incidence of eye diseases in the
for certain departments like eye.
country is considerably high as compared
to the incidence of similar diseases in foreign
There is a dearth of ophthalmic specia
countries. In some areas the incidence is
as high as 10 per cent ofthe total population’. lists who can take adequate care of these
Trachoma. which is widely prevalent in patients. At present almost 2,700 eye
North India, has probably not been comput practitioners are available in the country
ed in the assessment of the problem as its which works out to one eye doctor for
prevalence rate ranges between 35-78 per 1,70,000 of population, or working out
doctor patient ratio, there is one eye doctor
cent.
for every 17,000 patients as about 10 per cent
Apart from these changes probably due people are affected by eye diseases. .Almost
t ■ malnutrition and refractive errors have a similar number of other medical men,
n at been taken into account. This high not trained ophthalmologists, are working
incidence of eye disease has resulted in an in this field. Thus the inadequacy of
appalling increase in the figures of blindness. ophthalmic aid is glaring. The state of
On a rough estimate the figures of blind affairs is being exploited by quacks, and
ness in India are 2.5.per thousand.of popu even by foreign doctors >vho come here with
lation. The figure does not include partially the pretension of providing ophthalmic
mind population. Thus about one million relief while in effect they use this area as
people arc totally blind, at least double the training and practice ground tor their young
number are-ecbnomically blind and show and inefficient graduates. All these contri
°cular morbidity. These figures exclude bute towards an increase in the rate of
“ases of cataract which can be cured by blindness. It will be desirable to achieve a
• 22 -INDIAN JOURNAL OF MEDICAL EDUCATION
VOL.
target of one eye doctor for every 10,000
"population even which is considered inade
quate in countries like U.K., U.S.A., Japan,
etc., where eye diseases are not as pretalent
as in India.
In spite of the best efforts of the country,
it seems very difficult to provide an adequate
number of specialists and semi-specialists
in the subject. It seems inescapable that
the general practitioner will have to shoulder
a considerable load of this work for a long
time to come. In view of this, the Mudaliar
Committee ‘views with grave concern the
tendency of some of the universities and
Indian Medical Council to reduce the period
of training at the undergraduate level in
this course and in some others the tendency
to abolish the assessment of candidates in
ophthalmology. If this attitude is encourag
ed the ophthalmic services even for minor
ailments will become hopelessly inadequate.
This will adversely affect ocular morbidity
and blindness, thereby increasing the size
of the problem’.
The main causes of blindness are:
(6) Screening for glaucoma and malig,
nant diseases. Screening for
glaucoma is important because
of high incidence of cataract in
this country which presents with
similar symptoms.
OCTOBER 1964
4. A large number of ocular diseases
which are responsible for blind
ness are:
(a) Purulent Ophthalmia,
(b) Small-Pox,
(c)
Trachoma,
(<Z) Corneal Ulcers,
(e) Complications of trachoma which
are many and varied,
(/) Pterygium,
(g~) Glaucoma,
(A) Iridicyclitis,
(i)
Malnutrition,
(j) Genetic disorders,
(A) Myopia, and
(Z) Detachment of retina.
5. Involvement of the eye in large num
ber of general diseases to which the
practitioners and teachers of general
Treatment and operation of eye pati
disciplines are more often than not
ents by quacks which is possible
unmindful. These disorders then
due to lack of trained ophthal
get neglected and inadequately
mic personnel; illiteracy, economic
treated.
Common examples are
backwardness and superstitions.
Small Pox, Typhoid, Tuberculosis,
2. Inadequately trained basic medical
Meningitis, Central Nervous Sys
doctor even for minor eye surgery.
tem disorders, Head injuries, In
These basic doctors are usually
dustrial hazards, Hypertensive
in charge of district hospitals,
states, Liver disorders, haemorrha
tehsil hospitals, rural dispensaries,
gic diseases, infections of nose and
and primary health centres. In
throat, metabolic disorders (dia
spite of their inadequate training
betes and thyroid) kidney disorders,
and lack of knowledge these person
etc.
nel are actively engaged in the minor
and major surgical treatment of eye
Apart from the diseases causing blindness, —.
ailments. They mishandle such there are many others which are quite !
operations resulting in blindness. prevalent as lid inflammations, stye, chala- /
The public whoare unaware of their zion and blepheritis, conjunctivitis of '
professional incompetence in eye various types, corneal ulcers, pterygium, \
surgery gets a false sense of security dacryocystitis, entropion, ectropion, etc.,
in the hands of these doctors lead which could and should be handled by a '
ing to deterioration of ocular con basic doctor.
J
dition and blindness.
We have intentionally not mentioned
3. A general lack of screening procedures ocular conditions associated with systemic
of the population especially:
diseases in which an ophthalmologist is
W Lavk of adequate school medical called for consultation and which should be
service where children can be primarily seen by the internist. In this
seen, screened and treated in country there is a woeful lack of this because
time.
of the absence of orientation of medical
1.
Of OPHTHALMOLOGY IN MTDERGRADUATE MEDICAL EDUCATION IN INDIA
nnel in this section. It i?a sad expe(***’,« see general practitioners treating
rieOCeof SmSl-Pox, Measles, Typhoid,
rv^htheria, etc.,- in which simple ocular
• elike corneal ulcer, iritis, membranous
le**Wctivitis, optic neuritis, etc., have not
been thought of leading to permanent
Sindncss of the patient.
e have also not
mentioned the diseases of pure specialised
interest.
While conducting various eye relief camps
in villages we found that anterior staphyloma
wi» common and we assessed them to be
Juc to past performation of corneal ulcer
which remained either undiagnosed and
untreated or maltreated. Phthisis bulbi was
not uncommonly seen which was believed
to be due to undiagnosed and untreated
iridocyclitis or purulent conjunctivitis with
corneal complications that were inadequately
attended to. Some cases of phthisis bulbi
were seen after small-pox which were under
tire care of medical specialists because they
remained unmindful of ocular lesions.
Blindness due to couching is not uncommon
even today. This is due to the fact that
the public is illiterate and the general
practitioners are unable to appreciate the
dangers of this procedure. These causes of
blindness can only be eradicated if our
general practitioners i.e., Medical Graduates
improperly orientated to theproblems of this
discipline. Blindness from acute glaucomas
I is common as ‘it is often diagnosed and
treated as conjunctivitis. Absolute glau
coma secondary to chronic simple glaucoma
is- quite a common sight in our villages
because our village doctors are unware that
cataract and glaucoma can coexist. They
usually diagnose these cases as immature
senile cataracts rather than chronic simple
glaucomas and ask the patients to wait till
the cataract matures and it always turns into
’bsolute glaucoma. These are only a few
Sr!\nc.cs t0 sP°r-light the inadequacy of
ophthalmic training.
vifW^tr grouP
people may include
calU* y..handicaPped though not economi’ i wk° develop amblyopia since
Childhood. These persons in their adult
me<i;ijC yeJect.'ons at the hands of various
of m
J’ui*rds—thus sometimes' services
comm •' liant y°ung men are lost to the
individuals and in return frustrated young
viuuals are created. We may also
23
correct the misconceptions of some medicos
that ophthalmology is a speciality of surgery;
it is a composite discipline consisting both of
medicine and surgery, more of medicine than
of surgery.
The discipline of ophthalmology has long
since developed an independent and self_
------- status all over the world. „
sufficient
A
general surgeon has hardly any orientation
of this discipline as it has not formed a part
of his training programme. He is as such
not fully conversant with the trends and
progress in the diagnosis, management and
treatment of the diseases relating to these
fields. The teaching of general surgery as
such does not cover the teaching of Ophthal
mology. Due to lack of orientation of the
general surgeon in ophthalmology it is
difficult for him to teach the subject and
more so to assess the candidate. Quite un
like the Western countries the ophthalmic
problems in this country are of much greater
magnitude. The diseases met with as stated
earlier could and should be handled by a
basic doctor.
Let us briefly recapitulate the recommenda
tions of the Indian Medical Council in
this matter. A decade ago the Indian Medi
cal Council recommended the merger of
ophthalmology with surgery at under
graduate level. In spite of its best efforts
tire Indian Medical Council has failed to get
this implemented by a large majority of the
universities which considered these at length
from time to time and were of the opinion
that this procedure is not only undesirable
but positively harmfuL. Some ofthe colleges
and universities which implemented these
recommendations, have after bitter experi
ence returned to or are gradually returning
to the system of assessing it separately.
The Indian Medical Council now have
moved a step towards the implementation of
this recommendation of the Medical Educa
tion Conference by requesting the colleges
under its jurisdiction to institute a compul
sory home examination in Ophthalmology.
Candidates failing in this examination cannot
take the final examination. This is certainly
worse than the separate assessment at final
examination as it gives a veto to the discipline
of ophthalmology io die detriment of the
student.
At the Medical Education Conference,
the conference held the view that ophthalmic
24 INDIAN JOURNAL OF MEDICAL EDUCATION
VOL. IV, OCTOBER 1964
training should be at least for 13 weeks during
the clinical course and that it should prefer
ably be assessed separately.
As far as under-graduate curriculum for
teaching Ophthalmology is concerned, it
should be taught and assessed as a separate
discipline which will be in keeping with the
existing practice in this country and the
recommendations of the Mudaliar Committee
which states as under:
‘The committee considers that at the
under-graduate level the student should be
adequately trained in the subj’ect of ophthal
mology and should be assessed separately with
regard to his fitness in the subject. The
combination of this su^^t with surgery
for assessment must be deprecated. It is
felt that the student should be given at least
50 lecture-demonstrations and should be
posted to the wards and the out-patient
department for a period not less than 13
weeks’. Great stress must be laid on" small
procedures like perimetery and fundus
examination and small surgical procedures
like scraping, syringing and some minor
operations.
In conclusion we wish to draw the atten
tion of the medical educationists to realise the
need and desirability of teaching and assess
ing Ophthalmology as a separate subject.
I
■i
i
I
I
Emphasis on Other
Specialities:
ENDOCRINOLOGY
By
Dr. K. N. GOUR
Professor of Medicine
College of Medical Sciences. Banares Hindu University
Varanasi.
!
The teaching of the subject of
I' Endocrinology has had scant atten1 tion in this
country till very
l recently. About 30 years
ago
students of Medicine could hardly
' see cases of endocrinopathies. The
(Kphysician saw only a few individuals
whom they thought had endocrine
!' .disorders. A great satisfaction was
}| felt by the students if a teacher could
■; demonstrate a case of acromegaly to
l them. But the disease when diagnosed
f was far advanced when nothing could
be done for the patient. He was
b only a scientific curiosity to students.
birth.. There is no doubt that the
development of tho foetus in ule.ro is
much influenced by the maternal
biochemistry of the blood, her nutri
tional state during gestation or by
the diseases which she suffers from
during the period of gestation.
They all may have an important
bearing on the endocrine glands cf
foetus as on any other organ of the
body, In the intrauterine life the
developing foetus is very labile.and
can be influenced even by the minor
alterations on the maternal side,
psychological or somatic.
i
But with the modern development
! of radioactive substances, X-ray
| irradiations, glandular extract thera» pies and radical surgery much can be
i done to help these unfortunate
rvictims to arrest the onward march
I of endocrinopathies.
[ The diagnostic facilities have also
It is further necessary to realise
that if the
serious consequen
ces of endocrinopathies have to bo
prevented the disease has to be
detected promptly and proper and
adequate treatment started- Evon
in a suspected case of endocrinopathy
tho clinical examination and investi
gation have to be carried out in a
great detail because for diagnosis,
especially in early stages, in no other
disoaso detailed clinical examination
and investigations - haematological
biochemical and mdiological - are so
essential-
f increased. The biochemical changes
s which result from
tho various
f. endocrinopathies are better underij stood and with tho additional aid of
| skiagraphy, diagnosis can bo made
| with a fair dogroo of certainty quite
| early.
t It should be remembered, that
j endocrinopathies may start in the
< intrauterine life or may occur after
birth or at varying intervals after
■
Endocrinology
pervades .
and
permeates through tho whole realm
of internal medicine and so the study
of endocrine glands • both physiologi
cal and pathological - is gaining
29ft
Indian Journal of Medical Education
Vo). Ill, April & July, 1964
Endocrinology
considerable importance.
It ’ is
essential therefore that the medjcal
curriculum be so revised as to include
the subject of endocrinology iu the
teaching programme of undergraduate 1. Hormonal disturbances - Mech
student. In the preolinical period
anism of Endocrinopathies due to :
stress should bo laid on teaching of
physiology and about the biochemi
1. Increased or decreased libera
cal changes which can result from
tion of normal hormones.
the various endocrinopathies.
It
needs to be impressed that a signifi
2. Secretion of abnormal hor
cant disturbance can result in the
mones.
body economy by the disorder of one
of the endocrine glands. The endo3. Aberration in hormone con
. crine glands work in harmony with
jugation and degradation.
each other. If one is disordered it
might cause serious disturbances in
4. Inherent abnormality in local
other glands.
tissue responsiveness.
The rapid advancement of biochem
istry and biochemical research has
5. Continued rather than cylicla
added much to our knowledge of
elaboration of hormones.
endocrinopathies.
In the. three clinical years (III* 2. Pituitary Gland :
IV and V years) atleast21 lectures be
Disease of anterior and inter
devoted to this subject, 7 lectures
mediate lobe :
each year. They should preferably
be clinical demonstrations so that the
I. Decreased
ant.
pituitary
student appreciates
the somatic
secretion :
changes
which
may
occur
due' to
endocrinopathies.
The
1. Panhypo-pituitarisin.
biochemical and the haematological
changes resulting from these disor
2. Post pubertal
ders may also be shown at the same
Hypopitui
time along with the radiological
tarism - Simmonds
findings. They must be shown how
disease
the chemical structures of the hor
Sheehan’s
mones can be altered to enhance its
syndrome
activity manifold or to wee.l out the
undesirable aspects of its action. On
3. Frohlich’s syndrome.
the therapeutic side they shou'd be
taught the proper use of hormones
because insufficient and inadequate
4, Laurence
Moon Beidldoses may do no gcod and overdosing
syndrome.
may cause serious harm. Further,
fhe delay in starting the treatment
eg. in the case of cretin, may ham
5. Tumours
of
Pituitary
per the mental development of the
gland.
child.
291
Increased secretion of hor 4.
mones of anterior pitui
tary :
II.
2 Diseases of the Endocrine glands
which should be included in the
teaching programme of the under
graduate students are :
1.
Growth hormone increased
secretion :
(a)
(b)
2.
III.
Giantism.
Acromegaly.
Basophil adenoma-Cushing
syndrome.
Intermediate lobe disease of
Pit. gland-Melanooyte sti 5.
mulating hormone.
IV.
Neurohypophyseal syndrome.
V.
Diabetes Insipidus.
VI.
Excess
of
Anti-diuretic
Hormone - Oedema.
3.
Diseases of Thyroid gland :
A.
B.
Diseases of
Glands :
A.
the
Parathyroid
Hypoparathyroidism.
B.
Pseudohypoparathyroidism.
C.
Hyperparathyroidism
1. Primary Hyperfunetion.
2. Secondary
roidism.
Hyperparathy
Diseases of the Adrenals :
I. A. Hypofunction of the adren
al cortex :
I. Primary adrenal
ciency :
insuffi
(a) Anatomic destruction of
gland :
Hypothyroidism
1. Metastatic invasion
infection.
1.
Cretinism.
2. Haemorrhage.
2.
Myxoedema.
3. Idiopathic atrophy.
Hyperthyroidism
4, Surgical removal.
1. Parenchymatous type.
2. Nodular type
3.
Thyrotoxic heart disease.
4.
Thyrotoxic Myopathy.
5.
Thyrotoxic bone disease.
0.
Thyroiditis.
D.
Tumours
gland.
of
the
or
thyroid
(b) Metabolic failure in hor
mone production :
1, Congenital.
2. Secondary adrenal
sufficiency.
in
3. Atrophy of the gland due
to
lack of trophio
hormone :
(i) Hypopituitarism due
to pituitary disease.
292
Vol. Ill April & July, 1904
Indian Journal of Medical Education
(ii)
1
Suppression of hypothalamic pituitary
axis.
Diseases of Adrenal Medulla :
1. Phaeochromocytoma.
2. Non-functioning tumours
of the medulla.
(o) Addison’s disease :
1. Acute adreno-cortical in
sufficiency.
'_____ 'j
6.
Sex glands - Testes and Ovaries:
2. Adrenal crisis.
1. Male Hypogonadism
3.
Adrenal haemorrhage.
2. Sex hormones in treatment of
carcinoma.
4.
Adrenal insufficiency.
B. Hyperfunction
cortex i
of
adrenal
1. Cushing syndrome.
2. Hyper aldosteronism,
3.
Secondary aldosteronism.
4.
Adrenal virilism.
5.
Aldosterone and Oedema.
6.
Use of adrenal steroids
in clinical practice.
'
Integration of Teaching of Medicine with other
Clinical Disciplines
Dr. S. 8. MISRA
Professor of Medicine
K. G. Medical College, Lucknow, U.P.
3. Female sex Endocrinology :
(i) Gonadotrophic Hormone.
(ii) Ovarian Hormones
(iii) Disorders of Menstrual
functions.
(iv) Sterility.
(v) Recurrent abortions.
(vi) Lactational disorders.
(vii) The menopause.
(viii) Post-menopausal disturb
ance.
Diseases of the Pineal and
mus glands.
Till the early part of the nine
teenth century clinical “Sciences” in
most European Universities .were
taught as Physics; it later on became
clinical medicine which included all
the clinical disciplines. As a relic of
the old days, some universities in
the West still have a professor of
physics. In the second half of the
nineteenth century, surgery grew up
to be a respectable
profession.
Interestingly, it was the physicians
who brought about the separation
of surgery from medicine. A nota
ble exception was Sri Clifford Allbut
who vehemently opposed the move.
Specialities grew in Europe and
America after the second world war.
This specialization has led to a
reaction and now one hoars more
about integration of teaching of
Anatomy and Physiology as well as
the various clinical disciplines as one
discipline for the undergraduates.
It is my firm belief that undergra
duate teaching should be integrated
as one new discipline to give students
a proper perspective of medicine as
a whole. In England, there has been
recently a movement led by Sir
Charles Snow for integration of the
teaching of humanities and social and
biological sciences to give complete
education to the modern man. In
U. 8. A. the Massaohussetts Institute
of Technology has over 100 professors
of humanities and social sciences.
Thus, the world is witnessing a
move for integrated education. We,
as medical educators, should give
integrated education in the clinioal
discipline.
I therefore suggest that the teach
ing of all clinioal disciplines should
be integrated for the undergraduate
student.
After all, he is to be
instructed in the principles of dia
gnosis and treatment, rather than
minute details of obscure or experi
mental drugs, or details of technique
of operations, or the
minutiae
of Biochemistry and Atomic Physics.
With creatipn of chairs in various
specialities,
which is extremely
desirable to give our patients the best
treatment,our post-graduates, the best
teaching in specialities, our bright
Differential Perception of Disease Etiology
And Utilization of Health Services
By
D. N. Kakar
r .f
X'-
Assistant Professor, Commmily Medicine PGI, Chandigarh.
Suksham Chopra
Research Officer, Department of Community Medicine. PGI Chandigarh.
Amrit Malhotra
Lecturer, College of t* ursing, PGI, Chand garh.
ABSTRACT
While more than 67 pcr'eni of India's population lives in the rural areas, threefourths of trained doctors work in the urban areas. Also, while three-fourths of the
incidence of commonly preva'ent diseases is preventible, three-fourths of the health
budget is spent on providing curative services. India has yet to produce a‘basic
doctor’ who could adequately meet her requirements. Numerous studies on the deli
very of health care seivices have revealed that nearly seventy per cent of the healb care
needs of the rural people are met by the indigenous medical practitioners. Despite this
the medical sociologists have not yet paid serious attention to studying these aspects
in different regions. The present study was undertaken to explore people’s
preception about etiology of selected diseases as well as their pattern of utilization
of health services in Haryana. The findings reveals that respondents belonging
to higher orQnon-scheduled castes showed greater recognition of physical causes.
Those belonging to lower classes and scheduled castes tended to recognise supernaturl
causes a great deaf more. Similar pattern emerged in relation to their racognition
of apparent symptoms of these diseases as well as in relation to their
seeking medical attention. An important finding of this study was that a
substantial number of respondents belonging to the lower classes never utilized
the services provided at the health centres. Thus social inequality seemed to have
played an important role in the differential utilization of governmental health services.
The members of the lower classes remained deficient not only in terms of possessing
adequate knowledge about disease etiology but also about seeking therapeutic help in
time. Their life style was indicative of social inequality. In order to remedy this
situation, the study recommended implementation of the newly proffered alternative
model of health care services.
The popultion of India continues to rise
at the enormous rate of about thirteen million
a years According to 1981 census, India
already has about six hundred and eighty
four million people- nearly fifteen per cent
of the total world population-to carve out an
52
THB INDIAN JOURNAL OF MEDICAL EDUCATION
existence in about 2.5 per cent of total land
area of the world. Thus every year more than
two times the population of the Union Territory
of the entire population of Australia is being
added to our country's population One would
be justified to think that if the present rate of
growth continues, in a couple of decades, our
population would be more than one thousand
million. This is a prospect which further
complicates the problem of delivery of health
care services in our country, particularly in
the rural areas. Even today, while more
than seventy six percent of our population
lives in the rural areas, three-fourths of our
doctors, trained in cosmopolitan medicine
work in the urban areas. Moreover, while
three-fourths of the incidence of diseases is
preventible three-fourths of the health budget
is still being spent on providing curative health
sevrices. Besides, it is a matter of common
knowledge that most doctors posted in the
rural areas still spend a 'major part of their
time on curative medicine rather than on
preventive medicine. The country has yet
to produce a ‘basic doc or* who could
adequately meet our requnements.
The
newly
started
‘Community
Health
Volunteers' Scheme' (presently re-designated
as Guides), has yet to prove its worth in the
Indian cultural setting. Very few evalua
tive studies p2 have dealt with the barriers
in its implementation in dfferent parts of
the country. However,
numerous earlier
studies 3-8 done on the delivery of health
care sereices in India have highlighted that
nearly seventy per cent of the health care
needs of the rural people are met by
different types of practitioners of indigenous
systems of medicine who, as yet do not from
an integral part of the centrally-sponsored
health care system. A couple of years back,
VOLUME XX Ao. 3
Boards of Indigenous Medicine in different
States, had registered as many as 2,57,000
practitioners, of which about 93,000 had at
least 4 years of formal training 9 There has
been a great deal of talk about intergration
of modern and indigenous systems of medicine
but no concrete workable proposal has
emerged so far.
The result is that the
existing health centres have failed to cope
with the heavy load of sickness, the bulk of
which is taken care of by these practi
tioners, howsoever dubious some of their
practices may have been. A couple of
decades
back McPhail 10 did a pretty
detailed study of the working of pri
mary health centres in Uttar Pradesh and his
findings were revealing in the sense that he
pointed out that the effective area of coverage
of an average primary health centre in the
State did not exceed a radius of three to four
kilometers. This situation has not changed
even today.
Despite an apparent need to explore these
aspects in much more details, not many
medical sociologists have cared to undertake
systematic studies of the pattern of utilization
of health care services in different parts of
the country, particularly in the rural areas.
A recent study done in a Metropolitan city has
highlighted the wide gap among different
sections of the population in the utilization
of available health services.11 It emphasised
the need to undertake similar studies in other
areas. Durning 1976-80, we did a study of
differential utilizition of health services by
different classes and castes in three villages
of Haryana. These villages were located in
Ambala District and were at a distance of
six to eight kilometers from the main health
centre in the community development. Block
SEPTEMBER-DECEMBER
IS81
DIFFERENTIAL PERCEPTION OF......
53
However, they were all multi-caste villages dents. For conducting interviews, specially
and were roughly comparable in terms of prepared semi-structured interview schedule
eneral demographic and socio-economic was used. This was thoroughly pretested
gharacteristics. The main objectives of this before actual collection of data. On the basics
cstuy were: (i) to explore people's perception of Prasad's 12 classification (which was
about etiology of selected diseases; (ii) to slightly modified by us as we combined Class
understand the extent to which they could IV and Class V), the respondents were
recognise different symptoms of these diseases; classified into four classes. Hower, we also
(iii)
to understand the pattern of utilization attempted data anlysis on the basis of caste.
of health services in relation to class and
PART TWO
caste; and (iv) to identify factors affecting
utilization of health services provided under
People’s doscreption about etiology of selected
the centrally-sponsored health care system.
diseases
The present paper presents certain selected
findings of this study. The paper is divided
It is by now well accepted that most
into five parts; part one deals with metho societies lay dowe their own cultural guide
dology; part two with people's perception lines as to what should be considered as
about etiology of selected diseases; part three disease, who should be approached for the
; with their recognition of disease sysmtoms; purpose of diagnosis and treatment and whet
part four with differential level of utilization her such a state of affairs should be shared
of health services, and part five presents the with persons outside one's immediate family
broad conclusions the study while offering circle.13
In the Indian context, certain
certain recommendations.
earlier studies by Marriott,11 Carstairs15 and
Gould 18 have indicated that the Western
PART ONE
system of medicine has failed to fit fully into
the cultral climate of north India. Certain
1 Methodology
recent studies 17-21 have pinpointed the wide
'
While selecting the villages for our gap that exists between the provision of health
I. detailed investigations we were particular to services and their actual utilization by those
.^select only those villages that were not closely who needed them most. Surprisingly, after
^located to the primary health centre. This years of providing health services as well as
'was done with a view to assess the outreach imparting health education to the rural
of health centre services in these villages. massis, one sees a little change in their perce
KThe selected villages had a total population ption of etiology of commonly prevalent
of 4,826 i.e., about five per cent of the total diseases. This would indeed be enormously
^population of the Development Block. The apparent from the findings of our present
.{interviews were carried out with 480 heads study. Table I reveals how a substantia!
S>f households who represented about 0? per percentage of out respondents attribute such
jSent of the total households in these villages. diseases as marasmus, chicken pox and mea
| Enough care was taken to conduct interviews sles to supernatural causes. (Marasmus to
| it a place and time convenient to the respon- spirit-intrusion (66.7%); Chicken pox and
£
54 THB INDIAN JOURNAL OF MEDICAL EDUCATION
measles to warth of goddess (52.9%). Even
such ailments as cough and cold, typhoid,
skin infections, whooping cough and hook
worm infestations are attributed to supernatu
ral causes by a sizeable number of our
respondents.
(Gough and Cold (23.5%)
Typhoid (22.3%) whooping cough (17.8%)
and hookworm infestation (16 2%). In fact,
there was hardly a disease which was not
attributed by some respondents to supernatu
ral causes. Elsewhere we have dealt with
these aspects in sufficient details.22-23 Inci
dentally, whooping cough and hookworm
infestations were the two diseases which were
also attributed to some ‘unknown causes' by
a substantial number of our respondents.
(whooping cough (40.7%) ; hookworm infe
stations (35.4%)
When we looked at their perception of
etiology of these diseases in relation to the
classes they represented, we found certain
interesting correlations
For instance, we
found a relatively higher recognition of
physical causes in relation to such diseases as
cough and cold, diarrhoea, pneumonia, and
skin infections among the representing Class I
and Class II as compared to those representing
Class III and Glass IV, who tended to attri
bute these diseases more to supernatural
causes. In particular, diseases like Chicken
pox and measles and also marasmus were
largely attributed to supernatural causes.
(Chicken pox and measles (Class III 60 % &
Class IV: 74.1%); Marasmus (Class III: 73 5%
and Class IV: 86.6%).
Table . Similarly,
we looked into the relationship of caste with
their perception about the etiology of these
diseases, we found that a much higher
percentage of respondents representing non
scheduled castes recognized physical causes
of these diseases as compared to their sche
SEPTEMBER-DECEMBER
VOLUME XX No. 3
duled caste counterparts. (Table 3). Thus
on the basis of these findings we are in a
position to conclude that ‘the higher the social
class or caste status, the greater the possibility
of recogition of physical or natural causes
of these diseases’. This would only emphasise
the need to accelerate the pace of all develop
mental programmes that are aimed at bri
nging about a positive
change in the
knowledge and attitudes of the rural masses.
We shall now deal with another important
aspect, namely, recognition of symptoms that
can prompt them to seek medical treatment.
PART THREE
Recognition of symptoms requiring Medical
Intertention
There are no studies in Inida that give us
worthwhile information on differen ial reco
gnition of symptoms of different diseases by
different classes or caste groups. In this
regard, a study done by Koos24 in a developed
country had
proffered some interesting
findings. He gave people a list of symptoms
and asked which ones should be brought
to the attention of a physician. The answer
obtained by him widely varied, depending
upon the social class of the person. To give
just one example, 57 per cent of the upper
class people metioned that ‘loss of appetite'
was a medical problem needing medical
attention; 50 per cent of the middle class
said, it needed medical attention; but only 20
per cent of the lower class (poor or working
people) said ‘loss of appetite' deserved medical
attention Similarly, while 77 per cent of
the upper class mentioned that ‘continued
coughing’ was a symtom needing medical
attention, only 23 per cent of the lower class
people thought it so. Thus he demonstrated
how social class influenced recognition ol
198!
symptoms in a specific cultural setting.
In our study, we made an attempt to ask
our
respondents whether or not they
considered certain apparent symptoms, which
were read out, as indicative of the occu
rrence of a specified disease. We had listed all
symptoms disease-wise and our focus was on
childhood diseases. Our findings revealed that
in this part of the world too, a comparatively
higher percentage of respondents belonging
to Class I and Class II recognized apparent
symptoms of diseases under investigation'
barring, of course, chicken pox, measles and
marasmus, the symptoms of which were reco
gnised, slightly more, by those belonging to
Class III and Glass IV (Table 4). We hardly
need to point out that those belonging to
lower classes tend to suffer more from these
■ ailments. Thus when they respond, to such
questions, they relate them to their individual
I experiences. Obviously, a family’s actual
X disease experience ha? a lot to do with its
I familiarity with the symptoms.
We also made an effort to investigate as
to recognition
of what symptoms would
.■prompt them to seek medical attention. Our
£ findin. s in this regard revealed that when
4 they perceived certain symptoms critically
incapicitating', they hasten to seek medical
attention.
These symptoms included ‘high
fever', persistent vomiting', ‘stiffness of body,
‘cramps of neck and jaw', ‘shortness of breath’,
. and ‘swelling of ankles', Surprisingly, an
I alarming symptom like ‘blood in the stools' was
!
S recognised by only 3.3 per cent of the respon
dents representing Class IV as worthy of
'seeking prompt medical attention. This
■would indicate the extent to which they put
up with such maladies in their poverty envi-
DIFFERENHAL PERCEPTION OF....'.' 55
rontrent. (Table 5'. Even one’s caste status
seemed to do a lot with one’s recognition
of symptom of certain diseases requiring
prompt medical attention. For instance,
our findings would show that respondents
belonging to non-scheduled castes consistently
expressed greater need for medical attention in
the case of practically all listed symptoms with
the exclusion of a specific symtom ‘stiffness of
body.’ (Table 6). All this is indicative of glaring
backwardness of scheduled castes even in
regard to their perception of disease etiology
and seeking therapeutic help.
PART FOUR
Diffarentlal utilization of health services
Normally one would assume that the very
fact that the scheduled caste people suffer
more from commonly prevalent diseases they
would tend to make much greater use of the
governmental health services as offered under
the centrally-sponsored system of health care.
But this is certainly not true of most situa
tions. As would be evident from (Table 7), a
substantial number of our respondents belon
ging to Class III and Class IV mentioned
that despite years of living in the same
environment or surroundings, they never
made use of the services offered by rhe local
health centres. This is not to say that
they did not suffer that much In fact, they
suffered more than their other counterparts
but for the purpose of seeking of therapy,
they relied more on the services of locally
available registered
indigenous medicine
practitioners.
We were also interested in finding out as
to what factors affected their utilization of
governmental health services which were
56 THE INDIAN JOURNAL OF MEDICAL EDUCATION
VOLUME XX Ao. 3
SEPTEMBER-DECEMBER
provided free of cost, After a great deal of consequent, sickness - is indicative of social
probing we, learnt of five specific barriers in, inequality. This is not to say that social
the proper utilization of these health services inequality is a peculiar problem of these
The indentified barriers were: (i) standing for people On the contrary, there is hardly a
a long time in the queue; (ii) prescribed society which can be considered as completely
medicines not given ; (iii) medicines given free from the problem of social in quality.
only for a day; (iv) medicines not effective;
and (v) staff uncooperative. All of these
In sociological literature, one finds a
factors continue to persist in the wake of great deal of overlapping in the use of such
numerous developments in the field of delivery
terms as social inequality, stratification and
of health care for the rural masses. Incide- class. Yet it has been stated fairly clearly
ntallay, a greater number of respondents that the problem of social inequality has
belonging to Class IV seemed concerned
two aspect, a distributive, ajid a relational
about squandering their time while standing
aspect The first refers to . tb,e. ways in
long hours in big queues (78.8%) at the
which different factors such as income,
health centres and, at the same time, not
wealth, occupation,
education,
power,
even getting the prescribed medicine (65.4%).
skill etc., are distributed in. the popu
Even lack of cooperation on the part of the
lation. The second refers to, the ways
health centre staff seemed to have added to
in which individuals differentiated by
their resistance. (Table 8).
these criteria are related to each other
within a system of groups and categories.
PART FIVE
Now even when we look ,iat| the way our
Conclusions and recomendatlons
health services are presently organized, we
It would be apparent from our findings find a certain “dualism", ,fpr, on the one
that social inequality plays an important role hand, there are hospital-oriented services run
in the utilizaition of health serives. There by specialists and super-specialists,>who follow
is little doubt that the members of the lower spohisticated, Western technology, on. the other
classes and scheduled castes remain deficient hand, we find the primary health,centre net
not only in terms of possessing adequate work, primarily looked after by ill-trained
knowlegde about disease etiology but also and ill-equipped paramedical workers who
about seeking therapeutic help in time. even lack, supportive supervision by their
Thus they are placed in an exceedingly disad equally inadequately trained.. supervisors.
vantageous position. Even their counterparts One consequence of this situation is that the
belonging to higher classes or non-scheduled poor whose medical needs are the greatest
castes seemed to have drawn greater benefit are put to maximum deprivation in terms of
from the governmental health services. Thus provision of health services as well as their
the lower social class or scheduled caste status utilization. It would not be an exaggeration
itself acted as a barrier in the proper utili to state that the present pattern of medical
zation of health services. The very life style education, the nature of technology used, the
of these people—poor housing, poor income, pattern of expenditure, and even nature of
poor purchasing power, undemutrition and research being conducted in the health sector
DIFFERENTIAL PERCEPTION OF..-..
1981
indicates one thing and that is that the
governmental health service is still top-down,
elite-oriented, doctor dependent, urban-biased
and centralized with over-emphasis on curative
aspects rather than on preventive aspects. In
order to remedy this situation, a study group
jointly sponsored by the Indian Council of
Social Science Research and the Indian
Council of Medical Research (1981) has
proffered an alternative model of health care
services. This alternative model is claimed
to be strongly rooted in the community, pro
vides adequate, efficient and equitable referral
services, integrates promotive preventive and
curative aspects, and combines the valuable
implementation of the alternative model and
piously hope that it will not meet the fate
of its predecessors.
REFERENCES
1. Boss, A. , Goyal, A. P. ,
Grover, S. R. , Jolly
2.
K G. , Madan, D. Sharma,
P. C. , Singh Chaman.
Kakar, D.j\r.
3 Kakar, D.N. ,
Kumar, V. and
Chhullanl, P,j\r.
4. Kakar, D.N.
5.
Rainke, W. A„
Parkar, R. L.
Alexander, C. A, and Taylor, C.E,
6. Carl, E. Taylor el al.
Kakar, D, .V,
Sriniwas, Murthy, S.K
and Parker, R.
Kakar, D.R,,
Kumar, V.,
Chopra, S.
57
elements in our culture and tradition with the
best elements of the Westm system. It is also
claimed to be more economic and cost-effec
tive. Thus one has simply to wait and see
whether the suggestive alternative model of
health care set vices really succeeds in bringing
about a positive change in the life styles of
the poor, praticularly those belonging to lower
classes and scheduled castes, who have suffered
all these years. By way lof offering our reco
mmendation, we may whole-heartedly support
“An Assessment of the New Rural Health Scheme
and suggestions for imoprovement”.
Demographic Research Center Institute of
Economic Growth, Delhi, May, 1978.
Bare Foot Doctors : Social Science Research
Journal, Nov.-Feb., 1978, Vol. II, No. 3, (135143),
Background, Training and Role of Indigenous
Medicine Practitioners and Mulnpurpse Health
Wokers in a Develpment Block of Haryana,
I.J.M.E. , Vol. XV. No. 2, July-Dec. 1976.
Indigenous and Cosmopolitan Medicine in a
Nor'h Indian Town, G.I.R.H. and F.W. Bulletin
Vol. XVI. No. I, 1981,
The Functioal Analysis of Health Needs and
Services. Asia Publishing House, London 1976.
Doctors for the villages. Asia Publishing House
1978.
People’s Perception for Illness and their use of
Medical Care Services in jPunjab’ I.J.M.E., Vol.
XI, No. 4, Oct-Dec. 1972.
Peponle’s Perception of Childhood Illnesses and
their Therapeutic Practices and Preferences in a
Haryana Village. Indian Paediatrics, Vol. XIV,
No. 8, August. 1977.
SEPTEMBER-DECEMBER
58 THB INDIAN JOURNAL OF MEDICAL EDUCATION
9.
Lulu, Charles
10. McPhail, J. F. B.
11. Tesudian, C. A. K.
12. Parsed, B.G.
13.
Ackerknscht. E.H.
14. Marriot Mckim
15. Carstairs, G. Morris
16. Gould, H.A.
VOLUME XX Jlo. 3
Modern India's Ancient Medicine. Transactions
of tbe New York Academy of Sciences, Series
11,6:46-55, June, 1969.
A study of the Working of Primary Health
Centres in U.P. WHO Regional Office, Docu
ment SEA/RH/14, 1963.
Differential Utilization of Health Services in a
Metropolitan City. Indian Joural of Social work
Vo). LXI, No. 4. Jan 1981.
Journal of Indian Medical Association., 55 198.
1970.
Problems of Primitive Medicine Bulletin of
History of Medicine XI (503-21), 1942.
“Western Medicine io a Village of Northern
India”. In: B.D. Paul, ed.. Health; Culture
and Community, pp. 239-269, New York Russel
Sage Foundation pp 107-134, 1955.
"Medicine and Faith in Rural Rajasthan In:
B.D. Paul, Ed., Health Culture and Community
New York Russel Sage Foundation pp 107-134,
1955.
The Implication of Technological [change for
Folk and Scientific Medicine American Anthro
pologist, Vol. L1X. No. 3, 510, 1957.
17. Hasan, JCA.
The Cultural Frontier of Health in Village India,
Manaktalas: Bombay, 1967.
18. Kakar.DJf.
Folk and Modern Medicine. A North Indian
Case Study, New Asian Publishers New Delhi,
1977.
Tbe Health Centre Doctor and Spirit Medium in
a North Indian village. The Eastern Anthopologist, Vol. XXV, No. 3 1972.
Social and Cultural Foundations of the Health
Services System in India, Inquiry/Supplement
Vol. XXII June, 1975.
19. Kekar.D.N.
20.
Bsnerjte, D
21.
Madan, TJf.
22. Kakar, D.N.
Kumar, V. and
Chopra S.
23. Kakar, DJL
Who Chooses Modern Medicine and Why. Eco
nomic and Political Weekly. 4 (37); 1475-1484,
September, 1969.
Op. Cit.
Op. Clt.
Srinioas Murtep, S.K.
and Parker, RJ.-
24. Koos, E.L.
The Health of Reglonville, New York, Columbia
University Press, pp 33-38, 1954.
1981
DIFFERENTIAL PERCEPTION OF..
* 260 THE INDIAN JOURNAL OF MEDICAL EDUCATION
VOLUME XX Ao. 3
TABLE-II
Class and Perception of
Class I No: 100
Diseases
SEPTEMBER-DECEMBER
Etiology of Selected Diseases
Class 11 N: 110
Phy
Sup
Both
DNK
Total
Phy Sup
0.0
100.0
83.7
13.6
0.0
DIFFEREN FIAL PERCEPTION OF...... 61
1981
Class IV No: 120
Class III No: 150
Both DNK
Total
Phy
Sup
Both
DNK
Total
Phy
Sup
Both
DNK
Total
100.0
65.4
28.0
2.6
4.0
100.0
47.6
46.7
5.8
9.9
100.0
1
Cough and cold
95.0
3.0
2.0
2
Chicken Pox and
Measles
58.0
27.0
13.0
2.0
100.0
33.6
43.7
18.2
4.5
100.0
10.6
60.0
21.4
8.0
100.0
10.0
74.1
6.7
9.2
100.0
3
Diarrhoea
93.0
3.0
4.0
0.0
100.0
79.1
1.8
7.3
1.8
100.0
66.7
13.5
7.2
1.6
100.0
41.7
26.7
24.1
7.5
100.0
4
Typhoid
69.0
16.0
11.0
4.0
100.0
58.1
19.1
16.4
6.4
100.0
50.0
26.6
16.6
9.8
100.0
47.5
25.0
25.9
1.6
100.0
5
Tetanus Neonatorum 68.0
0.0
17.0
15.0
100.0
56.3
5.5
15.5
22.7
100.0
43.0
8.6
18.6
29.5
100.0
39.1
15.0
7.6 38 3
100.00
6
Pneumonia
78.0
4.0
7.0
11.0
100.0
63.6
20.0
10.9
5.5
100.0
63.3
13.3
7.4
16.0
100.0
16.0
41.6
12.5
30.9
100.0
7
Mesasmus
28.0
42.0
3.0
3.0
100.0
6.4
56.3
7.5
12.8
100.0
0.0
73.5
13.0
13.5
100.0
0.0
86.6
2.8
10.6
100.0
8
Hook Worm
Infections
62.0
5.0
2.0
31.0
100.0
50.0
5.4
3.7
40.9
100.0
26.7
17.3
16.0
40.0
100.0
19.2
34.1
18.4
28.3
100.0
9
Skin Infections
75.0
8.0
7.0
10.0
100.0
61.8
10.9
10.0
17.3
100.0
56.6
20.0
13.4
10.0
100.0
26.6
33.3
20.9
19.2
100.0
10
Whooping Cough
54.0
0.0
18.0
28.0
100.0
36.3
7.2
23.7
31.8
100.0
13.3
20.0
19.3
43.4
100.0
0.0
39.1
13.3
47.6
100.0
2.7
DIFFERENTIAL PERCEPTION OF... .. 63
SEPTEMBER-DECEMBER 1981
TABLE — IV
Class and Recognition of Symptoms of Selacted Diseases
Diseases
1
2
3
4
5
Symptoms
Class II
No. 100
Class III
No. 150
Clars IV
No. 120
50.0
Cough and
1
Running nose
87.0
63.6
54.5
Cold
2
Redness of eye
42.0
40.9
10.9
3.3
3
Fever
33.0
29.1
10.0
8.3
4
Nasal Blockage
55.0
25.4
20.0
16.6
83.3
Chicken Pox
1
Rash on the body
65.0
68.1
72.7
and Measles
2
Body-ache
30.0
46.3
50.0
56.6
3
High Fever
60.0
68.1
73.3
87.5
4
Redness of eye
25 0
29.1
36.3
41.6
10.0
Diarrhoea
Typhoid
1
Sunken Eyes
28.0
20.0
12.0
2
Diy Mouth
38 0
25.4
13.3
8.3
3
Loose watery motion
85.0
77.2
72.7
56.6
4
Urine Frequency less 42.0
36 3
16.3
12.5
1
2
3
4
High Fever
Vomiting
Weakness
Loose Motion
40.0
46.0
13.6
10.0
20.0
20.0
10.9
3.3
8.3
6.6
5.0
—
51.0
52.0
28.0
25.0
Tetanus
1
Body-ache
42.0
25.4
16.3
6.3
Neonatorum
2
Stiffness of body
65.0
51.8
43.6
30.0
3
High Fever
15.0
10.2
6.6
—
4
Cramps in Nack
65.0
61.8
59.1
56.6
and Jaw
I
Class I
No. 110
64 THB INDIAN JOURNAL OF MEDICAL EDUCATION
Diseases
6
7
8
9
Symptoms
Class II
No. 100
Class HI
No. 150
Clars IV
No. 120
DIFFERENTIAL PERCEPTION OF.......
1H81
65
Whooping
1
Dry cough
52.0
40.9
22.7
Cough
2
Fever
45.0
25.4
6.6
16.G
—
TABLE 5
3
Thick Spuium
26.0
10.9
—
—
Need for Medical Attention in Relation to Class and Recognition of Symptoms
4
Shortness of Breath
65 0
52.7
43.6
30 0
62.0
59 1
73.3
87.5
Marasmus
1
Loss of weight
2
Size of Head
Increased
15.0
22.7
54.5
70.8
3
Weakness
35.0
36.3
72.7
75.0
4
Bones of Chest
Prominent
5.0
13.6
. 46.6
56.6
High Fever
72.0
59.1
43.6
37.5
2
Cold/cough
58.0
45.5
29 1
20 8
3
Breathing Problems
32.0
22.7
13.3
8.3
4
Bubbling sound
in the chest
51.0
40.9
Itching
68.0
59.1
46.6
37.5
Irritability
48.0
36.3
25.4
83
Pneumonia
1
Skin Infections 1
2
10
Class I
No. 110
SEPTEMBER-DECEMBER
VOLUME XX No. 3
10.0
-
No. Symptoms Needing
Medical Attention
Class I
No. 100
Class II
No. 110
Class III
No. 150
Class IV
No. 120
62.5
1
High Fever
75 0
68 1
66 6
2
Persistent coughing
40.0
25.4
16.6
66
3
Persistent Body-ache
45 0
36.3
25-3
•
4
Redness in the Eye and
watery discharge
18.0
13.6
5.3
12.5
2.5
|
5
Appearance of Rash
on the Body
75.0
66.3
63.3
54.1
6
t 7
Persistent Vomiting
87.0
77.2
70.0
•66.6
Cramps of Neck & Jaw
88.0
80.0
63.3
56.6
Thick Sputum
35.0
22.7
12.0
0.0
Shortness of Breath
42.0
26.6
10.0
6.6
I
£
1
8
9
I 10
Irritibility
38.0
30.0
18.0
8.3
Patches on the skin
75.0
59.1
36.6
16.2
3
Redness on body
32.0
25 4
10.0
—
' 11
| 12
Paleness of the face
65.0
46.3
32.0
10.0
4
Patches on skin
51.0
45.5
13.3
-
j 13
Swelling of Ankle
55.0
30.0
16.0
12.5
72.0
56.3
51.6
40.0
31.7
18.0
12.5
Infections
2
Weakness
18.0
13.6
—
37.5
_
16
Blood in the stools
78.0
45.0
40.0
53.3
Pale Complexion
n 14
| 15
56.3
1
Stiffness of body
Hookwork
22.7
12.0
3.3
3
Swelling of Ankle
25.0
12.2
—
__
4
Blood in stool
20.0
13.6
83
3.3
Loss of weight
§ 5
TABLE-7
Class-Wise Differential Utilization of Health Services
Utilization
of Health
Services
Social
Class I
No. %
Class II
No. %
Class III
No. %
Always
Sometimes
Never
28 (28.0'
57 (57.0)
15 (15.0)
26 (23.6)
64 (58.2)
20 (18.2)
27 (18.0)
58 (38.6)
65 (43.4)
16
29
75
Total
100
(20.8)
110
(22.9)
150
<31.3)
120
(25.0)
Class IV
No. %
(13.3)
(24.2)
(62.5)
Total
No. %
97 (20.2
208 (43.3)
175 (36.5)
480
(100.0)
TABLE—8
Factors Affecting Utilization of Governmental Health Services
Reasons
1
2
3
4
5
Standing for long time
in the queue
Medicines are prescrbed
but not given
Medicines given only
for one or two days
Prescribed medicine
not effective
Staff Uncooperative
Class I
No. = 72
24
Class 1
No. = 84
(30.0)
20
(23.8)
Class III
No. = 123
78
(63.4)
Class IV
No. = 104
82
(78.8)
25
(34.7)
34
(40.0)
58
(47.1)
68
(65.4)
45
(62.5)
50
(59.5)
70
(58.5)
62
(57.6)
50
12
(69.5)
(16.4)
54
30
(64.2)
(35.7)
35
52
(28.4)
(42.2)
62
(24.3)
(57.6)
r
s
m
o
z
o
1
184 THE INDIAN JOURNAL OF MEDICAL EDUCATION
VIII.
VOLUME XVU1 No. 2
6.
should be sustained by integrated, functional and mutually supportive referral
systems, leading to the progressive improvement of comprehensive health care
for all, and giving priority to those most in need ;
7.
relies, at local and referral levels, on health workers, including physicians, nurses,
midwives, auxiliaries and community workers as applicable, as well as traditional
practitioners as needed, suitably trained socially and technically to work as a
health team and to respond to the expressed health needs of the community.
All governments should formulate national policies, strategies and plans of action to
launch and sustain primary health care as part of a comprehensive national health
system and in co-ordination with other sectors. To this end, it will be necessary to
exercise political will, to mobilize the country's resources and to use available
external resources rationally.
Education Beyond The Classroom
An Experiment in Medical Education.
Health Surveys in Ladakh in Summer of 1977
By
Suraj P. Gupta
Assll. Professor of Medicine,
Department of Medicine
AU India Institute of Medical Sciences, New Delhi,
Daniel Taylor-Ide
Director
Woodlands Institute
Cherry Grove, West Virginia, U, S. A.
Carl E. Taylor
XI.
All countries should cooperate in a spirit of partnership and service to ensure
primary health care for all people since the attainment of health by people in any
one country directly concerns and benefits every other country. In this context the
joint WHO/IJNICEF report on primary health care constitutes a solid basis for the
further development and operation of primary health care throughout the world.
X.
An'acceptable level of health for all people of the world by the year 2000 can be
attained through a fuller and better use of the world’s resources, a considerable part
of which is now spent on armaments and military conflicts. A genuine policy of
independence, peace, detente and disarmament could well be devoted to peaceful
aims and in particular to the acceleration of social and economic development of
which primary health care as an essential part, should be allotted its proper share.
Professor and Chairman
The Johns Hopkins University
School of Hygiene and Public Health
Baltimore, Maryland, U. S. A.
Summary
A dramatic impact was made on the orientation of Indian and American
students In a medical expedition organized as a formal course on Health Care
in the Himalayas. In addition to intensive learning the students were able to
collect data that provide the first information on villages in ladakh on which
little health information bad previously been available. Two clinical condi
tions which especially merit more detailed research are the high prevalence of
adult anemia and systemic arterial hypertension in villages near Leh.
Despite increasing attention in recent years
to community medicine, medical education in
India has remained conventional and didactic
rather than experimental and innovative.
Medical instruction still presents the large
medical college hospital as the desired norm
of health care so that graduates will really be
only suitable to practice medicine in hospitals.
Their preparation proves to be inadequate if
they have to work without these faci
lities. Because this is all they know they e .ter
practice believing that inferior health care is
being given to the masses of India's popula
tion if such medical facilities cannot .be made
available for all the common problems of
some 80% of the people.
This paper describes a course that was
designed to expose medical students to the
reality of medical needs in some of the most
remote valleys and difficult medical situations
in India. A medical expedition to ladakh
was designed as a formal course of medical
instruction. The emphasis was both on
understanding the health situation in these
remote valleys and also on developing appro
priate ways of thinking about the delivery of
health services to people in isolated medical
situations.
186 THE INDIAN JOURNAL OF MEDICAL EDUCATION
This course on Health Care in the
Himalayas was developed jointly by four
institutions : All India Institute of Medical
Sciences, New Delhi, The Srinagar Medical
College, Srinagar, and from the U. S. A , The
Woodlands Institute of West Virginia, and
the Johns Hopkins University, Department
of International Health. The expedition
included 29 medical students and house
officers—12 from India and 17 from U. S. A.
and 4 faculty members.
Ladakh is the largest district in India and
one of the most isolated. The geography is
extcme, with precipitous mountain passes,
vast areas of rocky soil, inadequate wood and
water for tolerable habitation, and harsh
climatic conditions. The average altitude for
settlements is 11,000 feet. The district has
two major divisons. Villages around Kargil
are primarily Balti and Muslim. Villages
around Leh are mainly Buddhist and are
strongly influenced by Tibetan culture.
Modern health facilities are few and have
hardly reached the main towns let alone the
villages. Our expedition did surveys in
6 villages in the valley north of Leh and 2
villages south of Kargil.
It must be stressed that this medical
expedition was a formal programme of
medical education. Its primary focus was to
study the health condi ions of the village
people. In actuality the greatest impact on
the students, resulted as specific findings on
health conditions in Ladakh were uncovered
and discussed. This lead to detailed discussion
of comparative patterns of health care, as the
needs of these remote Himalayan villages were
juxtaposed wi'h the more familiar health
needs of urban India and North America.
Medical conditions in the remote areas
were entirely new to American studentsand
’VOLUME XVH1 M,. 2
very different even for the Indian students.
The support facilities that students took for
granted were not present whil s care patterns
that they did not expect were available.
Obviously facilities such as hospitals, consul
tation options, laboratory facilities, and
technological aids were totally non-existent
outside of Kargil and Leh and were nr'nimal
even there. More difficult to adjust to was
the absence of indirect supporting services —
sanitation, education and health consciousness,
rapid transportation, privacy, and electricity,
An unexpected attitude was that local inhabi
tants were often not as concerned about their
illnesses and health as were urban patients we
were accustomed to treating. This acceptance
of ill health caused many people to feel that
they were healthy when we would have
defined them as sick. Moibidity is, after all,
a matter of perception.
Obviously, the diseases encountered were
different from those in the U. S. A. but also
produced some surprises for the Indian
students. T his was exciting. Because of our
limited field facilities accepted diagnostic
procedures and treatment routines had to be
simplified in dealing with these new diseases,
This caused much discussion about the quality
of health care and the ethics both of simplified
expedition procedures and of resource intensive
hospital procedures.
The totally different ecological and anthro
pological conditions encountered emphasized
the importance of a holistic understanding of
medicine. Within a hospital's walls the doctor
is in control. But in the village and home our
relationship with patients and their families
thrust us into an awareness of dependence
upon family priorities, cultural requirements,
environmental
consequences,
political
JULTIDECEMBER A
EDUCATION
BEYOND THE CLASSROOM... 187
1
determinants, economic constraints
and
tradition.Understanding the whole picture was
impossible since information was less available
than in moi e developed parts of India or the
U.S.A. However, because the situation was so
different from the pictures we were used to, the
Ladakh experiences revealed new dimensions
to the health picture that expedition members
had not seen before and this influenced their
perceptions as they returned to more familiar
conditions.
During the survey activities students
rotated through three programes : a household
survey of morbidity and health care practices,
a survey of village leaders and indigenous
practitioners to define attitudes toward health,
disease, and treatment, and an expedition
clinic where we treated patients. These three
different investigative approaches revealed
very different understanding of the health of
Ladakh District.
In addition, there was a regular pro
gramme of seminars every day that covered
both clinical subjects and issues of health care.
These provided
oppotunity
for
intensive
discussion of the often unsettling experiences
that students had as they found that many of
their preconceptions of the doctor's role and
contribution did not fit the basic realities of
massive need. The facul y members from
India and the U. S. had to be constantly
available for personal counselling to guide
students through the difficult adjustments in
their personal values and ethical orientation
that were both traumatic and eventually
extremely enlightening. The exchanges bet
ween students were especially instructive and
produced mutual learning and friendships.
METHODOLOGY OF DATA GATHERING :
1. Household Surveys
Our major data collection effort was to
conduct household surveys in selected villages
The data were then corroberated by clinical
findings. As detailed maps and census infor
mation were not available, we used rough area
sampling by dividing sketch maps of the
villages into sectors equal to the number of the
field teams. Each team then randomly moved
from house to house in their sector. An effort
was made to survey between 20 and 25 houses
or roughly 10% sample that had been calcu
lated as being necessary to give representa'ive
data.
Survey teams generally consisted of an
interpreter familiar with local language and
culture, a clinical year student to -conduct the
clinical examination and a basic sciences
student for the general demographic, ecologi
cal and anthropological information. Survey
forms were extremely simple (see appendix).
2. Special Studies :
Separate teams carried out the following
special investigations.
(a) Anemia : during the clinical surveys,
a high prevalence of anemia with spanning of
the finger nails was observed. Records were
reviewed to get an estimate of prevalence.
Blood smears were examined whenever people
agreed for a finger prick.
An intensive effort was made to find hook
worm. Stool specimens were collected from
patients having anemia in special household
visits and abo from school children. In the
Leh area most of the households have a latrine
called chagra which is really a room filled
from a hole in the house roof. Once or twice
a year the compost is collected and spread on
188 THE INDIAN JOURNAL OF MEDICAL EDUCATION
fields. By removing part of the wall of the
chagra, we collected the most recent stools for
hookworm analysis from families with a great
deal of anemia.
VOLUME XVI112
a risk of malnutrition, and 13.5 to 16 ems indi
cated adequately nourished.
(d)
Anthropological Observations :
(b) Hypertension : most
clinicians
in a separate team made a particular effort to
Ladakh spoke of a high incidence of hyper identify all indigenous practitioners, especially
tension and thought it was probably associated Amchis. In addition, some Lamas and oracle
with high salt intake resulting from their healers were identified. In-depth interviews
strong tradition of drinking upto 50 cups a were conducted to study their preparations and
day of salted buttered tea. A senior medical practices.
student went from house to house to get blood
pressures from a sample of adults Recordings
were made resting and sitting. A diastolic
pressure over 90 mm kg was considered
diagnostic of hypertension.
(e)
Availability of
Medicines :
Surveys
of all shops and other possible sources of
western and indigenous medicines were carried
out. Attempts were made to determine
patterns of use and cost.
(c) Nutritional
Surveys
of Children :
a nutrition team (two Indian students and one Results of Household Surveys :
American student) conducted a house to
house survey. Data were collected regarding
1.
Eye Diseases : From households in
a child's age, order of birth, age when breast six villages in the Leh area a total of 250
feeding was stopped and age when supple persons were examined. The following cases
mentary weaning food was first introduced. were seen : active trachoma in 3, cataract
Each child (under 5 years) was examined in 9, pterygium in 7, conjuctivitis in 7, squint
clinically for any sigrs of nutritional defi in 4, and plhisis bulbi in 1 (total of 31 cases),
ciencies, and the mid-arm circumference and
body weight were recorded. The degree of
2.
Chronic Pulmonary Diseases:
malnutrition was assessed in two ways, first,
From six villages near Leh, 422 individuals
earh child's age and weight were plotted on a
were examined. Chronic bronchitis with
standardized growth chart using Harvard
emphysema was found in 24, a prevalence
Standards weight-for-age tables (Jelliffe,
1966). Group I (mild malnutrition) was rate of almost 6%. Of these 62% gave a
defined to be when body weight was below history of smoking, however no information
70% to 90% of expected body weight. Group was obtained about usual smoking patterns in
the communities.
II (moderate malnutrition) was between 60%
to 70%. Group III (severe) was when it was
3. Rheumatic Heart Disease : Among the
below 60% of expected weight.
422 persons examined 2 were found with heart
A second technique was by means of mid murmurs, which were presumably results of
arm circumferences according to UNICEF rheumatic heart disease
standards (1975). Measurements ranging
between 9.9 and 12.5 ems were taken to be
4.
Otitis Media : Significantly different
severe malnutrition; 12.5 to 13.5 cm. indicated rates of otitis media were observed among )he
EDUCATION BEYOND THE CLASSROOM 189
JULnDECEMB1^979
children of six villages.
Gund
Khalsi
Thiksey
Shey
Chuchod
Stok
Special Studies:
14%
10%
8%
7%
8%
6%
1. Anemia and Hookworm :
Special
surveys were done of non-clinic patients to
look for clinical signs of anemia, including
spooning of finger nails.
(a)
5. Poliomyelitis
Residuals :
Careful
screening of over 400 patients with detailed
examination was done on all cases of
neurological residual damage to get evidence
on whether poliomyelitis immunization is
indicated in a remote population such as this,
No case of residual paralysis from poliomy
elitis was seen but six other chronic neurologi
cal conditions were found including two
cases of stroke
Demographic and Ecological Information :
1. Infant Mortality Rate : An estimated
infant mortality
was calculated from
the pregnancy histories of mothers interviewed
in household surveys in five villages near Leh.
A total of 448 births had occured to 99
mothers, with an average of 3.5 live births
per woman. Of these, 76 children died before
one year of age. The infant mortality rate
was therefore 170 per 1000 live births. This
is considerably above the All-India figure of
120 per 1000 live births, but it differs , in
methodology since it represents the lifetime
experience of present mothers and not current
levels.
2. Family Planning :
Questions were
asked in all household surveys about family
planning. Twenty percent of women in Leh
villages said they knew about family planning
but only 4% said they were using a method.
Women reported that their family size was
four to five children. Prolonged lactation of
about two years may have been related to
relatively long inter-pregnancy intervals.
Anemia Table I.
In all villages the distribution between
males and females was about equal.
(b)
Stool Survey : Table II.
No case with hookworm infestation
was detected amongst 38 stool samples which
were carefully examined.
(c)
Blood Examination : Peripheral smear
examination revealed microcytic and hypoch
romic anemia in most of(28) subjects examined
with anemia.
(d)
Diets : No major nutritional defi
ciencies were apparent. Abundent use of
especially crude barley called Sattoo, was the
dominant feature of diets.
2.
Hypertension: Table III.
Forty-six persons had casual recordings of
blood pressure taken in household surveys in
Thiksey and Chuchod villages.
Cases of
hypertension (Diastolic pressure >90 mmHg)
were found in 13 or 28%. The average age
of patients was 44 years with a markedly
higher prevalence among Buddhist 50% as
compared with Muslims 21%.
3.
Nutritional Status of Children.
Four villages in the Leh area having 49
children were surveyed for malnutrition.
Weight-for-Age :
36% Normal’
33% Grade I Malnutrition
22% Grade II Malnutrition
9% Grade III Malnutrition
190 THE INDIAN JOURNAL OF MEDICAL EDUCATION
Arm Circumference
.
:
:
36% Normal
'11% Risk of Malnutrition
23% Malnourished
The x2 association between the two mea
surements was positive with p= <0.01. No
relationship between weaning practices and
nutritional status was found. Weaning tended
to start at one year of age and was completed
by two years. Weaning food was mainly crude
barley flour—Sattoo.
4.
Anthropological Data
(a) Preference for Practitioners : Table IV
Amchis practice very simple medical care.
They rely heavily on herbal medicines which
are inexpensive. Many of them use cautery
to treat any kind of pain. They are readily
accessible and greatly respected particularly
in the Buddhist communities.
•Discussion :
The villages of Ladakh have had no
previous studies of their health problems.
These health surveys were initially planned as
an educational exercise for a group of Indian
and American medical students. For all of
the students it was their first exposure to such
a field survey. It was rather surprising that
even though the conditions were extremely
rigorous the data collected by these relatively
inexperienced and uninitiated students under
guidance still yielded information which
seemed to have importance in defining health
problems in an area about which little is
known.
Two major clinical problems of high pre
valence noted in the villages of Leh were
anemia and hypertension. More than a quarter
of persons examined in these villages had
VOLUME XVIII JVo. 2
JULriDECEMBER 1979
EDUCATION BEYOND THE CLASSROOM... 191
Pallor and spooning of the finger nails was
especially marked in young adults including
males. The lack of the clinical symptoms was
very surprising because the average altitude
of the villages was over 11 000 feet. Such a
prevalence of iron deficiency anemia in
villages in the plains of India is generally
considered to be due to hookworm infestation
But in these villages intensive efforts to identify
hookworm ova were all negative and local
physicians working there also have not been
able to find hookworm in Leh or Kargil
hospitals in spite of continuous search. Dietary
conditions are generally fair.
Reports from Northern Japan (Sasaki, 1964)
indicate that a population withan extremely
high prevalence of hypertension was found to
have a very high salt intake (mean sodium
chloride excretion ± 27 gms per day as
compared to Southern Japan (mean sodium
excretion ± 15 gms per day). Another inte
resting observation in this context is of Shaper
et al (1969), who found that among Kenyans
who added no salt to their food blood preasure
did not increase with age.
To define the etiology of anemia in these
villages several hypotheses need to be ^tested,
especially the possibility that some nutritional
factor is interfering with iron absorption. The
local consumption of heavily salted and
buttered tea is remarkable. Dislcr et al (1975)
reported that when tea was taken with meals
the absorption of iron from biosynthetically
labelled rice or bread was reduced from about
12% to 2% The Concentration of phytates
and phosphates in food is also known to
reduce iron absorption. Nutritional anemia
and tea consumption are both common in
India but their relationship has not been
studied. Evidence from a WHO collaborative
study (Sood et al, 1975) on nutritional anemia
showed that pregnant women receiving large
doses of iron do not show the expected rise in
hemoglobin.
An additional area of concern relates to
the delivery of health services. In recent
years the government has made intensive
efforts to expand health services in these
mountainous areas and an increasing number
of villages now have health centres staffed by
physicians. However, the village people seem
to consider these centres to be relatively
ineffectual and not particularly designed to
meet their needs. Physicians tend to sit in
their clinics waiting for patients to come.
Only a few take the initiative to take health
The second observation of significance and
potential research interest is that in the same
predominantly Buddhist villages a high pre
valence of hypertension was found. The
hypothesis which needs to be tested here
specifically is that this may be related to an
extremely high daily salt intake from 50 or
services to the people in their homes. A change
in physician orientation is an immediate and
urgent need, and the medical curriculum
which determines physicians' perceptions of
their responsibilities should be redesigned
accordingly. A crucial observation is that
thus far there has been too much stress on
providing physicians and not enough on pre
paring other members of health team. Many
of these villages can be better reached by well
trained health workers then by physicians. The
potentials of using community health workers
are particularly great.
Other findings on household surveys and
clinical surveys quantified disease patterns
which reveal a heavy burden of illness.
Finally, in view of limited re'ources, in the
Buddhist villages around Leh it seems espe
cially important to work out better colloboration with the Amchis or “Tibetan doctor".
There are one to two Amchis per village and
they are greatly respected, probably more
respected than the physicians posted in the
same villages
Their methods could be
greatly improved by simple and practical
training. Since they have excellent rapport
with their patients the present programme for
providing training and help to this group
should be strongly supported.
TABLE
I
Results of Anemia Survey
Village
Thiksey and Shey (primarily Buddhist)
Chuchod and Stok
(across the Indus from the
above two villages with Chuchod
having a mixed Muslim-Buddhist
population)
Gund Khalsi and Panikar
No. of pa'ients
with severe anemia
( <7 Gms%)
Average age
43
11 (23%)
28
52
5 (9%)
' 33
49
8(16%)
27
No. of Patient5
with anemia
(y«)
JOLTiUECEMEEH 1D7S
TABLE
LADA^i SERVEY QUESTIONNAIRE ON ENVIRONMENT AND
II
ANTHROPOLOGY
Date :
Results of Stool Survey for Parasitic Infestation
No. of Stool samples examined
Hookworm
Ascaris
Thiksey-Shey High School
30
0
2
Chuchod
5
0
0
Specimens from Chagras
3
3
3
Village
EDUCATION BEYOND THE CLASSROOM
VOLUME XV 111 #•. 2
192 THE INDIAN JOURNAL OP MEDICAL EDUCATION
Time :
Time to fill out form :
1
Head of Household
Village :2. Group No.
4. Occupation :5. Ethnic & Religious Group :
6. Language :
7. Who are the local practitioners in the village ?
TABLE
III
a.
Results of Hypertension Survey
No. of subjects with high
blood pressure
Female
Female_______ Male
No of subjects examined
Age Groups
Male
----- --------------------------------20—29 yrs
U
0
7
5
0
2
12
6
3
1
40-49 yrs
50—59 yrs
4
5
2
2
2
2
2
1
7
6
30—39 yrs
60+
yrs
27___________ 19_________
Totol
8.
b.
What type of diseases do they treat
c.
How much do they charge ?
What are the 2 main disease of the village :
(1)__________________ a.
What causes it ?
b
How is it treated ?
c.
How prevented ?
d.
IV
Preference for Practitioners
Preference for Practitioner
Amchi
Both Amchi & Doctor
Lamas
_________
(2)-
.................. -
Who treats it ?
What drugs are kept in your house ?----------------------------------
9.
_—-------- —
--------------- -------- ■
Water Supply :
10.
TABLE
_
What system of medicine does each use ?_
a
What is source & how far away is drinking water ?
b
What is source & how far is washing water ?
c.
What do you store ^drinking waler in & where ?
d.
e.
Where do you defecate and urinate ?
— ...
Where is (d) in relation to water source ?--------------------------------- ---------------------
.
_________ ____
Primarily Buddhist Villages
(Shey, Thiksey, Stok and
K.halsi)
N=380
Primarily Muslim
Villages (Chuchod,
Paniker)
N = 310
50%
11%
a.
When are supplements introduced (child’s age) ?
26%
77%
b.
What supplements are used ? ____________________________________________
11%
Cf
24%___________
Weaning:
11.
—
When is weaning complete (taken off breast) ?
—
VOLUME XVIII Ko. 2
194 THE INDIAN JOURNAL OF MEDICAL EDUCATION
jULTIDECEMBEH 1979
EDUCATION BEYOND THE CLASSROOM
no
LADAKH ^RVEY QUESTIONNAIRE ON CLINICAL CONDITIONS
12.
13.
Family Planning :
a.
b.
What is desired family size ?_
Are there any ways to prevent having children ?
Date :
c.
Have you used any of these ways ?-----------------------------------------------------------------
Time :
Pregnancy History :
Categories
Time to fill out :
Education
(1) Head of House :
(2) Mother 1
Sex
Age is or would
be if died
If dead, age at death
Head of Household :
Village :3. Living in house :
Cold :
5.
_____
Daughters
a.
Cough
Productive/Dry
b.
c.
Hemoptysis J-/—
Dyspnea
Duration
d.
Fever +/—
e.
f.
Smoking
Weight loss
(2) Mother 2
a.
Joint pains (migratory)
b.
Palpitations +/—
c.
Chest pains
e.
Nature
___
Precordial/lateral wall
-----------------
(4) Others living in house :----------------------------------------------------------------------
(if wide age gap, ask about intervening pregnancies)
._________________ ____
Ear discharge 4-/—Duration
a.
------ ------------------------
_______ __________________
Sore throat,
Chronic Suppurative Otitis Media :
7.
----------
___________________
Nature
Duration
d. Pedal oedema
sons :
Duration
Rheumatic Heart Disease :
6.
(in birth order)
(in birth order)
_____________
4. Number present :
_________ __________
-------------------------------------------------------
Sons :
I.
2.
b
Deafness or hearing impairment
0. Eye :
a.
Sore eyes
b.
Watering or discharge from eyes
c.
Visual impairment or loss
_
___________________________________________
_—---------_ __________________________
___________
196 THE INDIAN JOURNAL OP MEDICAL EDUCATION
VOLUME XVIU Ho.
b.
Duration
c.
Are soaps or detergents used
d.
Itching, redness, oozing, scaling
10.
_
_ _____________________________________________
Neurological conditions and Poliomyelitis :
a. Weakness of limbs or limping
b.
Sensory changes-----------------------------------------------------------------------------------------
c.
Traumatic or congenital conditions
d.
Consciousness
We wish to acknowledge with thanks
the generous help received from various
ministries—Ministries of Health and Family
Welfare, Education
& Social
Welfare,
Finance, and External Affairs—for sponsoring
and approving the trip. We are particularly
grateful to Professor V. Ramalingaswami,
then director of All India Institute of Medical
Sciences whose help was indispensable. We
are indebted to Professor Nasir, the principal
12.
Caries :
--------------------------------------------------------------------
Obstetrical History :
13.
a. Age at marriage :
b. Still births •
c.
d.
_
_________________________________________
How cord tied and with what
Who managed delivery------------------ -------------------------------------------------------------
Remarks :
197
of Srinagar Medical College who shared his
knowledge of health conditions in Ladakh
and arranged for three Ladakhi interns to join
the group. We are thankful to various officials
in Jammu & Kashmir State Secretariat and
Ministry of Health for their help. We owe
our special thanks to the District Commissioner
and his staff for all their help and keen
interest in the pioject.
REFERENCES:
________
1,
Jelliffc, D.B. The astcssment of the nutritional status of the community. Wld
Hlth Org Mon Ser, 1966, No. 53.
Examination of systems with positive history in above questions :
11.
EDUCATION BEYOND THE CLASSROOM...
Acknowledgements :
a. Site of sorea
14.
JULTIDECEMBER 197)
Skin:
9.
2.
Arm Circumference—Measure of Nutritional Status,
UNICEF, November, 1975.
3.
Dister, P. B., Lynch, S. R , Charltm, R. W., Torrance, J. D., Bothwell, T. H.,
Walker, R. B., and Mayet, F. The effect of tea on iron absorption. Gut, 16,
193-200, 1975.
4.
Sasaki. N. The relationship of salt Intake to hypertension in the Japanese.
Geriatics, 19,735-744 1964,
5.
Shaper, A G., Leonard. P. J., Jones K.W., Jones, M. Environmental effects on
the body build, blood pie.sure and blood chemistry of nomadic warriors serving
in the army in Kenya. East Afr Med J., 46, 282-89, 1969.
Kathmandu, Nepal ;
Teaching Statistics to the Medical Undergraduates—
Some Facts find Considerations.
By
R. N., Srivasiava
Professor and Head,
B. L. Verma
Statistician cum Lecturer,
Arun Kumar
Reader,
Department of Social and Preventive Medicine, M.L.B, Medical College, Jhaust.
Introduction :
Of late, need of basic concepts of statistics
has widely been recognized in almost all
disciplines of human life. In the field of
medicine/health, the understanding of the
subject, especially in health planning, adminis
tration, clinical practice and research, etc.,
has been thought to be inevitably essential for
proper appreciation of the problem faced. In
view of this, the inclusion of the subject in the
curriculum of the undergraduate medical
teaching, though, was accepted quite some
time back, yet, no considerable attention seems
to have been paid towards the promotion of
its teaching and the subject is still not treated
at par with other courses of medical science.
In U. K., the Royal Commission on
Medical Education (1965—68)1 examined this
subject and emphasised that, at undergraduate
level, the subject of statistics be taught
because of two broad reasons ; firstly the
subject is an integral part of the logic of
scientific method and can be used to interpret
the observations made in the investigation ;
and secondly, the subject
consist of
numerous techniques for studying the varia
tion, association, relationship between the
variables and other different characteristics of
the distributions and includes many methodo
logies which may be applied in the asseesement
of efficiency of new drugs, development of new
vaccines, etc.
In India, in the recent years, such thought
has been devoted to the contents of teaching
of Preventive and Social Medicine and various
seminars, workshops and conferences were
also held in this regard. At every such
occasion, the contents of statistics have always
been the matter of discussion. Teachers of
Preventive and Social Medicine at the Medical
Education Conference2, held in November
1955, recommended the statistical content of
medical undergraduate
curriculum for
Preventive and Social Medicine. In 1965, the
National Institute of Health Administration
and Education, convened a conference3 on
Teaching of Preventive and Social Medicine
in relation to the Health Needs of the country,
which emphasized a close link between the
teachers of Preventive and Social Medicine
and other specialities, including statistics, in the
teaching and training of undergraduate
medical students. A seminar, sponsored by
USAID (1966)4, held in Trivandrum, con
cluded that the importance of statistics in
medical curriculum is not fully recognized by
the profession, in general, and by the students
JULriDECEMBER 1978
TEACHING STATISTICS TO THE MEDICAL...
in particular. This seminar emphasized the
integrated teaching of statislics with other
subjects. More recently in June 1970, a two
week seminar on Teaching of Biostatistics in
Medical Colleges of India was organised by
the National Instituteof Health Administration
and Education (NIHAE, 1970)5. After a
detailed review of the present situation, it was
brought out that the statistical background
being given presently to the medical under
graduates, fell short of the requirement, both
in terms of coverage and depth, and that the
subject had not yet received due recognition
in the medical institutions. It was recom
mended that the teaching of statistics needs to
be strengthened at the undergraduate level.
In view of the existing short falls in the
teaching of statistics to the medical under
graduates and keeping in mind the recom
mendations of various seminars, conferences
etc., made in recent times, attempts were made
to study the present status of the teaching
of the subject in different medical colleges of
India
Method of Assessment
To review the present status, a question
naire, relevant to the purpose of the study was
developed and sent to 99 medical colleges of
India. However, replies could be recieved
from 42 (42.42%) medical colleges only. The
questionnaire, besides seeking basic informa
tion such as, institution's name, name of the
department responsible for teaching of statistics,
yearly load of admission of students and
number of the persons involved in the teaching
of the subject, along with their qualifications
and designation, also included curriculum
contents, topics covered, number of teaching
hours allotted for the subject (both theory and
practicals) and statistician's (or any other
persons teaching statistics) views to promote
114
the teaching of the subject at undergraduate
level. Some findings of the study are reported
here.
OBSERVATIONS AND DISCUSSION :
Department Responsible for the
of Statistics and Staff Position:
Teaching
In all 42 medical colleges, Department of
Social and Preventive Medicine was found to
be responsible for the teaching of statistics.
However, in 17 (40.47%) medical colleges, the
subject was being taught by the teachers
belonging to .the disciplines other than statistics.
It was revealing that in 12 out of 20
(46.15%)
medical colleges, which were
having the postgraduate degree (M.D.)
and/or diploma (D.P.H.) courses, there
was no statistician in the department.
Only one post of statistician, not higher
than the status of a lecturer, was seen in
these medical colleges to teach the subject, to
deal with the research work and also to render
assistance to other departments on research
problems. In reply to the question a whether
single statistician is sufficient in the depart
ments respendents from 20 (47.62%) medical
colleges (respondents were Statisticians/Professors of Preventive and Social Medicine)
respendent in negative and suggested consideincrease rable in the staff in the subject.
Curriculum Contents and Teaching Methods ;
In 1970, a seminar on Teaching of
statistics in Medical Colleges3 held at the
National Institute of Health Administration —*
and Education, recommended the topics which —
need be covered in the teaching of statistics at
the undergraduate level. Besides emphasizing
the teaching of the subject, in both paraclinical and clinical years, the seminars had ‘
also pointed out that introductory topics such
as definition, need of the subject in medical
science, methods of data collection, presenta-
115 THB INDIAN JOURNAL OF MEDICAL EDUCATION
lion of data, central tendency and dispersion
should be covered up within 8 one-hour
lectures and 9 two-hours practicals. However,
rest of other topics, such as elementary ideas on
probability, correlation
and
regression,
sampling techniques, vital statistics ■ and
demography, important indicators of health
and International Classification of Diseases, etc.
should be discussed with the help of the
problem oriented practicals within 12 one-hour
lectures and 7 two-hours practicals.
In the present study, it was observed that
teaching of the subject was divided into two
parts mainly lectures and practicals, schedule
of teaching of the subject differed from one
institution to other in respect of year of
teaching, teaching hours allotted, and curri
culum contents. Introductory topics, like
definition, methods of data collection, tabular
and graphic representation, central tendency,
dispersion and rates of vital events were
covered by all medical colleges. Topics like
correlation and regression, probability, techni
ques of sampling, tests of significance and
demography were covered by only a few
(19.05%) medical colleges. However, topics
like, determination Lof sample size, analysis of
variance, design of experiment and Inter
national Classification of Diseases, etc. were
not covered by any of these medical colleges.
Time allotted for the teaching of statistics
also varied from one medical college to other.
In some medical colleges, there were less
than 5 lectures on the subject. However, in
some institutions, there was a provision of more
than 35 lectures during the entire M. B B. S.
course. On an average, 22 hours of teaching
on the subject was found during the entire
course of M.B.B.S.—an average of 14 hours
for lectures and 8 hours for practicals. In 10
(23.80%) medical colleges, there was no pro
VOLUME XVII Sc. 2
vision of practical work. Here, it may be
pointed out that 1 : 2 ratio of lecture hours to
practical w’ork on the subject had been
recommended from time to time.
Questions on Statisties in the Assessment of
Students :
Questions on statistics at different exami
nations (like day to day, terminals and
professionals) on the subject of Social and
Preventive Medicine/Community Medicine
may create interest amongst students to devomenetetime to the study of the subject. However,
in reply to the question whether at least one
complete question on statistics in theory and
in practical, separately, is being asked in the
professional examination, only 9 (21.42%)
medical colleges responded in, affirmative. In
the rest 33 (78.57%) medical colleges, students
were assessed in statistics on the basis of day
to day/monthly tests or class practicals only.
No specific marks were allotted for the
assessment of students in statistics in any of
the medical colleges studied.
Satisfaction with the Teaching of Statistics :
It was observed that respondents of 18
(42.85%) medical colleges were not satisfied
with the teaching of the subject in their
departments. For this they brought forwaid
various reasons listed in Table I. It was
interesting to note that respondents of 6 out of
16 (38.10%) medical colleges, where the post
of statistician was lying vacant for the last few
years and the subject was being taught by the
teachers belonging to the fields other than
statistics, showed their satisfaction with the
teaching of the subject. It could have been
probably due to the unawareness of the
respondents with the proper curriculum
contents of subject to be covered at the
undergraduate level.
TEACHING STATISTICS TO THE MEDICAL... 116
JULrfDECEMBER 1978
It was also observed that scarcity of
relevant books, Jack of mathematical back
ground of students, negligible contribution of
statistical questions in the examinations were
probably the main reasons for the students to
neglect the subject. Rao and Marwah (1971)6
have also emphasized on the contribution of
statistical questions in the examination and
need of teaching of the subject with the help
of problem oriented practicals to strengthen
its teaching at undergraduate level.
TABLE I
Showing reasons for dissatisfaction with the teaching of Statistics
Reasons
Number of
respondents
Percentage*
to the total
respondents
Lack of staff and qualified teachers on the subject.
8
Syllabus is not well defined.
3
7.14 ■ •
Non-coverage of course, i.e. insufficient number
of teaching hours are provided to teach the
subject.
5
11.90'
Paucity of students’interest as they think that the x
subject will be of no use for them in their
professional career.
9
21.43
Negligible contribution of statistical questions in the
student’s examination and in view of this the
students do not take interest in the subject.
. 3
19.05
problem oriented
5
11.90
4
9 52
Not much
practicals.
emphasis
on
Other reasons.
19.05' . ,
■
♦Percentage based on multiple replies.
Suggestions to Improve the teaching of the subject:
In order to improve the teaching of statistics, the respon lents were also requested to
suggest the ways Their suggestions in this regard are summarised in Table II.
VOLUME XVII He. 2
117 THE INDIAN JOURNAL OF MEDICAL EDUCATION
JULriDECEMBER 1978
Showing Suggestions made by Respondents to Improve the
Teaching of Statistics
Suggestions
Number of
Respondents
Percentage*
to the total
Respondents
Statistics section under the department of
Preventive and Social Medicine should be
strengthened in respect of the staff and mechanical
facilities.
9
21.42
There should be a separate statistical unit in each
medical college, consisting of at leas', one Associate
Professor, one Lecturer and two Statistical
Assistants, with appropriate mechanical facilities.
12
28.57
There should be a provision of uniform syllabus
of the subject in all medical colleges.
16
38.14
Every department should have separate cell of
statistics in each medical college.
5
11.90
Medical Record Section of the hospital should
function under the control of statistics unit in
order to obtain sufficient data on medical and
health statistics, so that problem oriented practi
cals may be given to the students.
4
9.52
Appropriate weightage to statistical questions
should be given during the student's assessment
21
30.00
Discipline of M.B.B.S, in addition to Social and
Preventive Medicine, should also emphasize the
role of the subject in medical science.
3
7.14
Relevant books on the subject should be made
available.
6
14.29
In nutshell, it may be concluded that the
teaching of statistics falls far below the satis
factory level. There is great disparity in
respect of both, topics covered and total
teaching hours allotted to the subject. In
many medical colleges, presently, the teaching
of the subject is being done without
statisticians. In the assessment of the students,
during the entire course of M. B. B. S., there
are hardly any questions on statistics. Provision
of only one statistician in the Department of
Preventive and Social Medicine was seen in
the medical colleges to look after the teaching
and research work in the institution. In most
of the medical colleges, even some important
topics of the subject were not covered. In
view of these lacunae, it is recommended
that : «
1.
2.
Other suggestions.
TEACHING STATISTICS TO THE MEDICAL... 118
Conclusions and Recommendations :
TABLE II
3
‘Percentage based on multiple suggestions.
7.14
There should be a separate and indepen
dent unit of statistics in every medical
college, consisting of at least one
Associate Professor/Reader, one Lecturer
and two Statistical Assistants to deal
with the teaching of the subject at
undergraduate and postgraduate levels,
to promote research activities in the
institution and to help the medical
personnel
on
statistically
related
research problems. This unit should
function in close collaboration with the
Preventive and Social Medicine Depart
ment and should own responsibility of
research activities going on in the entire
institution.
Statistical cell in every
medical
institution should be strengthened in
respect of mechanical/electronic facilities
so that the teaching as well as research
activities may be improved, both quanti
tatively and qualitatively.
3.
At least one question on statistics in
theory and one in practical should be
asked in the professional university
examination so that the interest of the
student towards the study of the subject
may be created.
4.
At the begining of the teaching of
statistics, teachers should emphasize on
the role of the subject in medical
science and its advantages to the doctors
in their future professional life so that
they may realize the significance of the
subject.
5.
Only qualified statisticians,
having
postgraduate degree in statistics (and
not in mathematics/economics
with
statistics) and orientation/experience in
biostatistics should be appointed in
medical colleges.
6.
For orientation of statisticians already in
service, different short duration refresher
/orientation courses should be organised
by leading institutions, having compe
tence of modern teaching techniques
and research methodologies.
7.
Medical Record Section of the associated
hospitals of each medical college should
function under the control of the
statistics unit so that the difficulty of
problem oriented practicals could be
overcome.
3.
The relevant books and other related
literature on the subject should be made
available.
9,
The teachers of the subject from differen
medical colleges and other institution
119
THB INDIAN JOURNAL OF MEDICAL EDUCATION
in the country and abroad should get
together from time to time, to exchange
their views on teaching material and
experience, and to discuss the promotion
of new teaching techniques.
10.
An uniform course contents of the
VOLUME XVI! Ho. 2
subject should be ftillowed by all the
A recommended
medical colleges,
undergraduate course contents of the
subject and number of teaching hours
required for specific topics at this level
have been shown in Table III.
J ULTI DECEMBER 1978
1.
Report of the Royal Commission on Medical Education 1965-68 ; Her Majesty’s
Stationery office. U. K., 1968.
2.
Proceedings of the Medical Education Conference, Ministry of-Health, Govern
ment of India, New Delhi, 1958.
3.
Report and Recommendations of the Conference on the Teaching of Preventive
and Social Medicine in relation to the Health Needs of the country, National
Institute of Health Administration and Education, 1968.
4.
USAID Seminar, 1966, quoted in Report and Recommendations on Teaching of
Biostatistics in Medical Colleges. National Institute of Health Administration
and Education. Tech. Rep. Ab. 11, 1973.
5.
Report and Recommendations on Teaching of Biostatistics in Medical Colleges :
National Institute of Health Administration and Education, Tech. Rep. No. 11,
1973.
TABLE Ill
Showing Recommended Undergraduate Course Contents of Statistics and
Teaching Hours Required for Specific Topics
Number of teaching hours required
Theory
r actical/
Demonstration
Introduction, definition, need of the subject
in medical science.
2
—
Methods of data collection, tabular and
graphic representation of data.
2
2
Central tendency, dispersion, Kurtosis and
skewness.
3
4
Elementry ideas on probability
1
j
Bionomial, Poison and Normal distributions.
3
2
Recommended course contents
TEACHING STATISTICS TO THE MEDICAL... 120
REFERENCES
6.
Rao, N. S. N., and Marwah, S,M.: Biostatistics Section in a Medical College,
Jour. Ind. Med. Acioc., 57, 8, 308, 1971.
Correlation and regression
2
4 •
Determination of sample size
2
i!
Sampling techniques, their applications,
advantages of sampling, sampling and non
sampling errors.
3
2
Tests of significance—t, F, Z and X2 tests
3
3
Vital and health statistics—definition, uses
and sources.
1
As a part of field
practice
Rates of vital events—measures of mortality,
morbidity, fertility, population growth and
population estimation.
2
4
Demography, introduction and uses of life
table, expectation of life.
2 .
1
International classification of diseases and
medical certification of death.
1
As a part of field
practice
Total teaching hours required for the
subject during entire M. B. B. S. course.
27
25
Teaching of Occupational Health in the Undergraduate
Medical Curriculum
by
R. N. Srivastava, m.d. (hOns)., o.p.h., d.i.h.. f.i.p.h.a.
Reader in the Department of Social and Preventive Medicine, MLX Medical College, Allahabad.
curriculum and the teaching and training also
need a dynamic adjustment with the changing
The necessity of developing “ need-based ” needs. It is also true for the subject of
oriented medical education has been recognized occupational health.
throughout the world. The aim should be to
prepare the medical graduate in such a way The field of Occupational Health
that they are fully equipped to meet the social
Occupational health in its modern concept
and health needs of the country, practising is concerned not only with the health of the
medicine at individual, family or community industrial workers but with the health of all
level. The contents of the curriculum and so those who are gainfully employed outside
also the health facilities for their practical their own homes such as in public offices, large
training should thus be determined by the shops, building trades, transport-land, sea and
social and health needs of the country.
air, agriculture, plantation, mines and so on.
In India, medical education should aim
The Joint ILO/WHO Committee on Occu
to equip the young graduates so as to enable pational Health (1950) adopted the following
them to solve the national health needs under definition:
existing social conditions with the limited
resources available. The medical education , “ Occupational Health should aim at: the
thus needs recasting in our context. However, promotion and maintenance of the highest
the objectives of medical education need degree of physical, mental and social well-being
of workers in all occupations; the prevention
precise definition before recasting is effected.
among workers of departure from health
The Medical Education Committee (Govt. caused by their working conditions; the pro
of India, 1969) was appointed by the Govern tection of the workers in their employment
ment of India to examine the question of from risk resulting from factors adverse to
undergraduate medical education in the light health; the placing and maintenance of the
of national needs and resources. Among the workers in an occupational environment adapt
terms of reference of this Committee was also ed to his physiological and psychological equip
“ to consider the development of medical ment, and, to summarize, the adaptation of
curriculum in relation to national require work to man and of each man to his job
ments, the need for uniformity of syllabus,
Thus the field of occupational health envis
apportioning of time between didactic and
practical teaching, selection of entrants to ages health promotion, disease and accident
medical colleges, reciprocity between various prevention, and protection of workers from
medical institutions and Universities and hazards in whatever occupations they are.
domiciliary restrictions in the matter of medi The Undergraduate Medical Curriculum
cal admission. The Committee (loc.cit) has
From times again it has been emphasized
since submitted its report which provides a
that the basis of undergraduate medical
guidline for developing the syllabus and the curriculum should aim to produce the ‘ basic
curriculum.
doctor’, “an intelligent educated and thinking
Social and health needs of a country are man who has reached the stage of voca
pever static. The undergraduate medical tional training which will enable him to
Introduction:
42
THE INDIAN JOURNAL OF MEDICAL EDUCATION
VOL. XIII I/OS. 1 S’ 2
acquire more readily the necessary addition cept in the undergraduate medical teaching,
al knowledge for whichever branch cf keeping in view the essential requirement of
medicine his inclination and potential establishing a firm foundation on which a
ability dictates. (Lane, 1960). There can ‘ basic doctor ’ is to be trained to meet the
not be two opinions on the (already over country’s .social and health needs.
crowded undergraduate medical curriculum.
The problem is to know how far occupational The Contents of the Curriculum
The teaching of occupational health need
health should feature in such a course.
The ultimate aim of medicine is to raise the to be integrated with the teaching of other
level of health of the pconle. The medicine subjects from the very beginning of the under
graduate
medical curriculum. The contents
today needs to be comprehensive in its
approach. This necessitates study of “ total may be spread over the Pre-clinical, Paraclinical
and
the Clinical periods.
man ” in his “ total environment ” which
Pre-clinical: In the pre-clinical period,
also includes the most important component
“occupation”. The curriculum designed to five lectures may be introduced with emphasis
train the “basic doctor” in our set up may on the following subjects:—
have the following few essentials;
1. Role of occupation in man’s life in
1.
The teaching should be integrated with
cluding economics of man.
teaching in other subjects;
■ 2. Work physiology and 'occupational
psychology,
2.
Occupational health need not be
3. Functional
anatomy-anthropometryemphasized as a speciality at the under
graduate level;
static as well as dynamic.
4.
Occupational environment as a compo
3.
The teaching should enable the student
nent of total environment and its effect
to understand the effect of work envi
on health.
ronment on the health of people and
also on occupational and non-occupa5.
Introduction to Ergonomics.
tional diseases;
Para-clinical: At the para-clinical stage, six
4. The training should acquaint the stu lectures may be given with emphasis on the
dents with the common occupational following subjects :
diseases;
1. The principles of preventive medicine
as are applicable in the field of occu
5. Opportunity should be provided to
emphasize the role of rehabilitation in
pational health.
every day practice ;
2.
The genesis of occupational diseases as
viewed in the epidemiologic triad of
6. Due emphasis is needed on the occu
pational history of the patients so that
agent, host and environment.
the students get interested to see
3.
Basic principles of occupational hygiene
occupational health in its right pers
or hygiene at the place of employment.
pective and
4.
Introduction to occupational health
7. The teaching and training need to be
. programme, its contents and benefits.
practical and available occupational
5.
Existing labour legislations in the
health facilities like the employees
country.
State Insurance Scheme need to be
6.
Labour welfare programmes.
freely utilized for training purposes.
A couple of visits to places of employ
Field visits to some places of employment
ment like a factory or a big office like a factory or an office etc. may be
establishment may make the teaching arranged at the'para-clinical level.
more interesting.
Clinical: Five lectures in the clinical years
Thus certain amount of instructions, in may be given covering the following subjects :
oscupational health are essential specially in a
1. Importance of occupational history in
fast industrializing country like ours. There
clinical practice.
is need to introduce occupational health con
JAffUART-JUNE 1074
2
3.
4.
5.
TEACHING OF OCCUPATIONAL HEALTH
Some important and commonly occurring
occupational diseases, their diagnosis,
prevention and treatment.
Accidents at the places of employment,
their prevention and treatment.
Basic principles of industrial toxicology.
Existing occupational Health Pro
gramme in the state and the country.
Visits to existing occupational health services
like E.S.I. may be arranged at this stage.
As mentioned earlier the teaching is to be
developed in an integrated manner. Although
it is recommended (WHO, 1957) that the
teaching is to be best done by a qualified
professor of occupational medicine yet in our
present set up it is felt that teachers in the
department of Social and Preventive Medicine
may develop the teaching in collaboration
with teachers from the departments of
Anatomy, Physiology, Pharmacology, Medi
cine and Surgery including those from the
sub-specialities like dermatology, ophthalmo
logy, otorhinology, orthopaedic surgery etc.
This requires that atleast one teacher in the
department of Social and Preventive Medicine
should be trained (or atleast oriented) in the
field of occupational health. The National
Institute of Occupational Health, at Ahmedabad and the Section of Physiological and
industrial hygiene of the All India Institute of
Hygiene and public Health, Calcutta can
43
develop a programme for training or orientation-of teachers from the departments of Social
and Preventive Medicine. This may form the
basis for future development of teaching of
the subject at the undergraduate level.
Summary
To summarize, in spite of overcrowded
undergraduate medical curriculum, certain
amount of instructions in occupational health
arc essential specially in a fast industrializing
country like ours. Details are to be avoided
but there is need to introduce occupational
health concept keeping in view the essential
requirements in the training of a ‘basic
doctor’. The teaching and the training need to
be integrated with other subjects from the very
beginning of the undergraduate curriculum
and may be phased at three levels viz. preclinical, para-clinical and clinical. In the
present set up, it is felt that the teaching and
training may be developed by teachers from
the departments of Social and Preventive
Medicine. A programme of training of
teachers from the departments of Social and
Preventive Medicine at the National Institute
of Occupational Health and/or at the All
India Institute of Hygiene and Public Flealth,
Calcutta for the purpose may be started to
provide basis for future development of the
teaching and training in occupational-health
at the undergraduate level in the medical
colleges in India.
GOVERNMENT OF INDIA (1969)
“ Report of the Medical Education Committee ”
Govt, of India, Ministry of Health, Family Planning,
Works Housing and U D. (Directorate General of
Health Services) New Delhi.
LANE, R.E. (1960)
The teaching of Occupational Health “ Modem
Trend in Occupational Health”. Edited by Schilling,
R.S.F. Bufferworth and Co (Publishers) Ltd., London
pp. 306-309.
WORLD HEALTH
ORGANIZATION (1950)
Report of the Joint ILO/WHO Commitee on Occu
pational Health, Unpublished Document WHO/acc.
Heallh/2, p.3 (quoted in Wld. Hlth. Org. Techn. Rep.
Ser. 135, 1957 p.4) Geneva.
WORLD HEALTH
Joint
ILO/WHO Committee on Occupational
Health, Wld. Hlth. Org. Techfclep. Ser. 135 Geneva,
ORGANIZATION (19S7)
“The Teaching of Nutrition to the Undergraduate Medical Students
with Reference to Community Needs ”
by
A. R. Shah, M.D.,D.PED, *
Assistant Professor of Pediatrics, B. J. Medical College & Civil Hospital, Ahmedabad-16.
' Xutrition adequacy is important in the life of an individual from the time of gestation to the time of
acceptance of full responsibility as a socially functioning adult. The knowledge of nutrition is most
important to the medical students. Xulrition and its various aspects are discussed. Xulrition is taught
at 'present at various stages without recognition and adequate consideration. Xow it is time for con
sideration of planning for leaching of nutrition, e.g., when to leach, who should leach, how and what
should be taught.
There are now many advances and researches
concerning
medical
science and allied
branches. The expanded horizon of research
has resulted in various disciplines like bioen.
gineering, biochemistry, histochemistry, immu
nochemistry, cenetics, nuclear medicine and
various other branches which were not named
or heard of before a few decades. All these
researches are mainly carried out in developed
countries. It is very difficult for us even to
imitate them at the present contest. Unfor
tunately at the present moment our medical
students are only interested and .excited with
laboratory techniques, various machines and
sophisticated appliances and they are apathetic
to the actual needs of the community. Probably
the fault does not lie with the students but with
their educators who have failed to infuse them
with real needs of the community. The rural
population is 80% and most of the population
is undernourished and inadequatedly looked
after. Nutritional adequacy is important
in the life of an individual from the time
of gestation to the time of acceptance of
full responsibility as a socially -functioning
adult.
Malnutrition
'■
I
Low capacity to work
I
Low income
I
—---------------------------- Inadequate diet.
The needs of the community are enorm
ous. Our population is suffering at all risk
periods ; e.g.,
(1)
Low average birth weight (2. 8 Kg).
(2)
High infant morbidity & mortality
(80-120). Ten times higher than western
countries.
(3)
1-4- year mortality: 30-50 times higher
than western countries.
(4)
10 per cent of total world population
suffer from malnutrition.
(5)
20 per cent of world population (700
million) suffer from iron deficiency suffi
cient to alter productive capacity.
(G) Most of the patients suffering from diseases
are malnourished as undernutrition and
infection act synergistically.
302
THE INDIAN JOURNAL OF MEDICAL EDUCATION
At present there are 5128 Primary Health
Centers in our country and 106 medical colleges.
It is expected that there will be 1/3500 doctors/
population ratio. Now as it stands there is no
scarcity of doctors but we want better trained
doctors who understand the needs of the com
munity. z\t present doctors are excited at
murmur in the heart and knows many details of
S.T. Depresion or gastro-jejunostomy opera
tion, but they are apathetic to nutritional pro
blems and social needs. So the main objective
should be that he should be familiar with needs
of community. However it is not possible to
teach him all the facts and knowledge of nutri
tion as other branches. But he should be
motivated to self learning and should have
deep insight into nutritional problems.
At present in the medical colleges, there is
no seperate subject of nutrition. It is taught
inadequately by everybody and hence it is
neglected by all. Calories, nutritional require
ments etc., are taught in physiology, medicine,
P.S.M. & Pediatrics without much of practical
involvements. It is a common finding that a
doctor is found prescribing only vitamins for
growth failure to a child without analysing the
proteins and calories intake. Hence it is
desired that there should be a nutrition board
in the medical college who would advise, direct
and plan the nutrition teaching to medical
students. The subject of nutrition should not be
seperated but it should be taught adequately at
all levels and by all people—whosoever is
concerned with the patient. Everybody should
VOL. XII. NOS. 3 & 4
be concerned with nutrition and nobody should
be indifferent to it. The nutrition board
should consist of representatives from Preven
tive & Social Medicine, Pediatrician, Physician,
Dietician, Physiologist, Obstetrician, Surgeon.
The objectives of the nutrition teaching should be:—
He should have the knowledge of local
availability of food, its production and dis
tribution.
(2) He should have knowledge of local
customs, beliefs, superstitions about food,
and food habits of community.
(3) He should have knowledge of nutritional
needs at various periods and plann
ing of locally available food under phy
siological and pathological conditions.
(4) He should have knowledge of function,
digestion, absorption and metabolism of
various food stuffs.
(5) He should identify' and treat various
nutritional disorders.
(6) He should be in a position to conduct
various health activities, both promo
tional and preventive.
(7) He should be co-operative with collea
gues, voluntary and government organisa
tions in upbringing nutritional status of
the community.
(8) He should be in a position to train the
paramedical staff.
o
(1)
A Medical Student can be taught in following way
Pre-clinical
Social Anatomy
Family size
Structure of community
Classification, Socially, economically
Social Ecology
Religions
Taboos
Customs
Habits
Diet and
family survey
Clinical
Social Pathology
Poverty
Ignorance
Illiteracy
Unemployment
Food Habits
M.C.H. Centers
Well baby clinic
Family Planning Center
Clinico Social conference
Nutrition surveys
Internship
School Health Clinic
M.C.H. Center
Applied Nutrition
Projects
fjjULY health advisory service—A training EXERCISE FOR MEDICAL STUDENT
Family Health Advisory Service—A Training Exercise for
Medical Student in Family Medicine
From 1963-1967
BY
Col. T. D. Chablani
Former Professor of Preventive and Social Medicine, All-India Institute of Medical
Sciences, Neto Delhi
The vital point of contact between the
public and the medical profession is the
family doctor, the practitioner of family
medicine, the key to the kind of medical
care of the future.
In the medical institutions, however, there
is generally less exposure of the student, in
the practice of the art and science of family
medicine as medical curriculum is not
tuned to the impact of socio-cultural changes
in the family setting.
The last two decades have witnessed the
gradual erosion of the privileged. The
upper ‘class’ enjoyed the material wealth
when the ‘masses’ were denied their very
existence. This vast difference between
the ‘class’ and the 'mass’ is being gradually
bridged, as the mass is movingupwards with
their educational, cultural and intellectual
pursuits. With greater awareness in the
mass of their rights and privileges in the
democratic pattern of society, a sense of
discontentment, based on greater social and
economic justice, is taking place.
A good number of working women are
mothers with children under 10 years of
age. This newly found freedom to work
makes many of them to be dissatisfied with a
career of wifehood and motherhood. Home
making, being a dull glamourless career
when compared with remunerative and
prestige-giving occupations has weakened
the family relationship.
The progressive population increase has
brought to the front the complexities of
psychological and mental health problems
which had hitherto been eclipsed with
physical health problems.
Urbanisation has affected healthy family
life and has brought changes in the social set
206
up. The lower income group of migrant!
are exposed to greater dangers due to thru
shift from safer rural environment to that
of industrial setting and become a prey i<>
diseases arising from stress and strain.
unhygienic environment and malnutrition
The tempo of industrial revolution lu>
gained momentum during the past tw>
decades. The use of modern mechanise,!
process is denying self-satisfaction anil
fulfilment of personality because of thr
mechanical and mass production technique!
In short the modern society has given
the average man and woman a sense of <lncontentment and emotional problems lead
ing to behavioural drift and loss of socustability.
Since health of the people
depends upon biosocial environment under
which they live and work and since in even
illness it is the personality as a whole that
reacts to environmental aspects, it is impor
tant to help people to adjust to the changing
way of life imposed by the social changes i»
relation to socio-cultural factors both i»
health and disease.
To meet these challenges and expectation!
of the community which concern physicianwe have to recognise that the hazards ta
health are greater today from the soew
rather than biological environment.
Medical profession has therefore 10
integrate with sociology and work in W*
with other specialists viz., sociology
psychologist and nutritionist. _Max‘in“^
understanding is to be created in the "V
of the student in terms of social and be
vioural factors. It is this understandiw
which would help the future physician
help the society.
The present-day training of undergm
ates based mostly on bedside teaching
hospital, fails to provide orientation
jjto the concepts that:
‘
Patients have families.
-(J) Family is the unit for both dcvelop/>;
mental and social growth.
(c) Family survives within their socioeconomic structure and in this
cultural and religious tics predo■Wminatc.
(ii) Family lives in a house; in a physical
'asBp structure.
(j) Individual reacts on society and society
"jiT'
reacts on individual’s behaviour.
The student needs to visualise compre
hensive medical care and how it is applied
t9society as a whole, as well as, given opporttmity.to learn family, group and community
Care, which constitutes his laboratory.
Thisessentially means organizing the teachfajprogramme for providing direct experitnce.. The programme has therefore to be
realistic in the sense that it is based on the
Ktual background of the social, economic
ndCultural setting of the community and
finally to pinpoint, how a physician can
tat-contribute in that setting taking into
tocount the needs of the family and the
COfllhiUnity.
Unconformity with this principle, in 1963,
wjDepartment of Preventive and Social
Mediae organised Family Health Advisory
Sttvicc for senior clinical students purely
•^teaching exercise to provide opportuniffS *^rect exPer'cncc >n dealing with the
SjMIffproblems of ‘Family’.
i r, (VMe the broad and general objective of
.
Health Advisory Service is to train
the practice of family medicine,
^•pecific objectives arc:
W to win and
E§; confidence.
sustain
families’
get an integrated picture of the past
present health and disease
conditions of the families.
SaMKjgct an insight into the main health
Ml Pt^lems and needs of the family.
^^^B&deyelop an appreciation of the
MBilfclnterplay of the various biophysi' ,
cal, socio-cultural and psycholoJ^HKfetoal factors which affect the family
health and disease.
207
diagnose and manage common
disorders for which patients do
not seek treatment.
(/) to maintain regular follow- up on the
treatment and advice given with
a view to ensure full rehabilitation.
(g) to guide families towards better health
by laying more emphasis on pro
motion of health and prevention
of disease rather than traditional
cure.
(e) to
In the absence of the field practice area
in the form of an Urban Health centre, the
campus of the All-India Institute of Medical
Sciences has been selected as the venue for
the training exercise for senior clinical
students. The families of Class III and
Class IV staff belonging to lower and middle
socio-economic status and residing inside
campus formed the nucleus for the exercise.
These families arc entitled to medical
care from the health insurance scheme
(Employee’s Health Service) under the
administrative control of Medical Super
intendent.
(a) Each student is allotted three families:
(i) Family needing advice on
infant and toddler care.
(ii) Family needing advice on
family planning.
(i’ll) Family with a member suffer
ing from long term illness.
(6) Students arc provided with 3 family
folders, instructed to record both medical
and social data in respect of their three
families and maintain follow up action for
one year. Each family folder contains
14 proformas covering the following fields:
(i) Demographic aspects.
(ii) Immunity status.
(iff) Environmental conditions.
(iz>) Socio-economic status.
(v) Dietary habits.
(tii) Social customs and habits.
(vii) Interpersonal
relationship and
adjustment.
(viii) Physical examination of infants
children for milestones.
(ix) Morbidity pattern in the family.
208
INDIAN JOURNAL OF MEDICAL EDUCATION
(.v) Summary of health needs of family.
(xt) Recommendations by senior clini
cal students, for future course
of action.
VOL. VIII, JULY, 1969
fyffl-Y HEALTH ADVISORY SERVICE—-A TRAINING EXERCISE FOR MEDICAL STUDENT
.'Special emphasis is given to specific pronew batch of students on the 15th JUnc
in the family with a chronically
In the interval between 15th May to 15th
jjfettient, the family needing family plan
June, the families are visited by paramedical
ning
advice, or family in need of advice on
personnel to maintain continuity in the
care of the infant and the toddler.
F.H.A.S. exercise.
Students also participate in special pro
Students come to the Department at 2.00
genies undertaken as a teaching exercise
p.m. and orientation session lasts for an hour
at which following aspects are dealt with:
: (a) Survey on nutritional status of child(a) Review of problems encountered at
their previous visit to the families
ren.
(J) Survey on physical defects in children.
(6) Discussion on practical problems.
(c)
Discussion on teaching material rele t(c) Distribution of multipurpose food to
the undernourished and follow up
vant to the practice of fatnilt
for improvement in health.
medicine in the form of cyclostyle!
notes.
(<l) Sanitation drives.
(d)
Quiz or test.
(«) Film shows and exhibition in connec.-sfe- tion with problems of national
(e)
Practical demonstration on vaccitu
importance organised by the
tion/inoculation techniques.
tjB department.
Subsequently students go to the field a*
In this exercise, student visualises com
visit their respective families. One-thirprehensive and integrated approach in solv
of their visits are supervised at a time.
ing health problems in the family as a unit
During their visit to the allotted familm
Of Service.
each student:
When a student needs help, especially
(a) Collects information as per proforma
ffhen facing a resistant family, the staff,
in the family folder.
JCUgraduate and, para-medical personnel
(i) Studies the impact of social, econnm»
2nd community leaders involved from the
and environmental factors in i»
CUnpus community, extend a helping hand
family.
m tickling difficult situations.
(c)
Deals with problem encountered M
All the F.H.A.S. (Family Health Advisory
him.
Service) records are scrutinized by the staff
(d)
Summarises lessons learnt and
ttd mistakes made by students are pointed
suggestion from which others al*
Wt and rectified.
benefit.
AQ problems are discussed by the Pro(e)
Gives therapy for minor illness.
•Uta at weekly staff meetings to make every(/) Distributes M.P.F. (multipuff^
Jg^rsant with the nature of problems
food) on payment for sclcf’
undernourished children
indicated.
(g) Motivates the family towards bri'11
health.
The student is also provided with a
doctor's bag which contains common drugs
like A.P.C., Fersolate, Multivitamin tablets,
dressings and bandages for use in consul
tation with postgraduate and staff members
attached to each batch.
The department has been allotted Family
Health Advisory Service room in the out
patient block where all the procedures for the
family health care are attended e.g. immuni
sation procedures, height and weight meas
urements and health education media.
Three community leaders have also been
selected and involved in the training exercise.
The F.H.A.S. (Family Health Advisory
Service) session starts on 15th June every
year. 45 students of the 7th and 8th semes
ter arc attached to the Department of Pre
ventive and Social Medicine. They are
divided into 4 batches. Each batch attends
the department for one afternoon a week for
this exercise.
The staff member of the rank of Assistant
Professor, one postgraduate student, one
Medico-social worker and one Public Health
Nurse are attached to each batch.
At the first session the staff member in
charge of the batch explains the objectives
and the working schedule of the Family
Health Advisory Service in detail.
At the second session, the Medico-social
worker and Public Health Nurse explains
the art of interviewing the family. The
students are then introduced to their respec
tive families by the respective medico-social
worker accompanied by community leaders.
Subsequently students follow their families
by weekly visits or more often when neces
sary.
The student then reports to the
The fourteen proformas included in the (Employee Health Service clinic)F.H.A.S. folder are explained at the sub of the members of the three families'»
sequent session in detail by the staff to their to him attend the dispensary on that e»
respective batch for relevant entries and examines the patient for the ailme
interpretation.
discusses the total home backgroun
The session ends on 15th May every year. patient with Medical Officer in c
The family folders collected from students the E.H.S. before treatment is Pr
are kept back in the department for check iDunng the subsequent visits to the
ing all details prior to handing over to the h e same patient is followed by the
.
J
209
encountered in the families, and to study
the impact of socio-economic factors in
health and disease patterns. Such meet
ings are attended by the community leaders
as well. This ensures better co-ordination
of all activities and integration at all levels
by the staff in F.H.A.S. exercise.
At the end of one year, final assessment
on each student’s performance is done.
Questions are based on practical aspects
concerning comprehensive medical care
as applied to community in the practice of
family medicine. The marks obtained are
taken into account towards day-to-day class
assessment.
The Family Health Advisory Service
Programme outlined above is an attempt at
preparation of senior clinical student as a
family clinician and for the community.
REFERENCES
Quinn, R. W., Zeidberg, L. D. and Christie,
A., ‘A teaching programme based on
comprehensive care for the family’, J.
Med. Educ. 35: 142, 1960.
2.
Family Physician (Editorial), J.A.M.A. 175:
1964.
3.
Chablani, T. D., ‘Practice of Community
Medicine, Community Diagnosis and
Community Therapy’. Med. Ed. Bulle
tin, W.H.O. (SEARO) Vol. X, May 1965,
page 7-14.
4. Chablani, T. D., ‘Provision of Compre
hensive Medical Care by Primary Health
Centres in Rural areas’. Med. Ed. Bulle
tin, W.H.O. (SEARO) Vol. XI, No. 1,
March, 1966, page 12-17.
1.
- &>c-, I fg<5
: SJ/'lZ /V©4 2.#, AJc 2 -3
NUTRITION EDUCATION OF MEDICAL STUBCNTS
- A TOOL OF REORIENTING MEDICAL EDUCATION
OBJECTIVES OagKEACHING PRO
GRAM IN NUTRmON
important subject for health pro
The Govt, of India launched the fessionals, our medical colleges do
Reorientation of Medical Educa not offer adequate training in nu
tion Scheme(ROME) in 1977 with trition.1 It has been observed that
the specific objectives of exposing medical graduates in India have
medical students to rural environ very low profiles of knowledge about
ment. The quality of medical care therapeutic nutrition and dietet
provided in a community is directly ics?-5
related to the knowledge and skills
of health manpower in dealing with The present paper presents an in
common health problems existing novative approach developed by
Dept, of Community Medicine,
in a community.
Nutrition is an important medical Mahatma Gandhi Institute of
science. A physician is expected to Medical Sciences, Sevagram, in
have an adequate knowledge of nu teaching nutrition to medical stu
trition and to make recommenda dents and reorienting their atti
tions for specific...foods.4 While tude towards health care.
nutrition has become such an
disorders and nutritional assesment
of commnity.
i) to reorient medical education by b) Nutrition Survey: The stu
exposing medical students to rural dents cany out diet survey of the
environment.
individuals in their families by
ii) to impart practical knowledgeweighment of raw foods over 3
of nutrition to medical students.
consecutive days. All the individu
iii) to increase the proficiency ofals in the families are assessed for
medical students in tackling vari nutritional status by using various
ous nutritional problems in pres indicators. At the same time the
ent socio-cultural set up.
students study the ecological and
iv) to inculcate epidemiological socio-cultural characteristics of the
principles in undergraduate medi family and the infant feeding and
cal teaching.
child care practices. The whole ac
v) to serve the community through tivity is supervised by faculty
student's active participation.
members of Community Medicine
Department.
METHODOLOGY:
c) Case discussion: The student
Every year a village is adopted by are taught about nutritional disor
the Dept, of Community Medicine, ders by demonstrating various
which serves as a field practice nutritional deficiency diseases
area for new entrants. In the first observed during the survey.
semester the newly admitted medi d) Group discussions: The stu
cal students stay in this village for dents are encouraged to sit in groups
15 days, when each student is to discuss various aspects in which
alotted 4-5 number of families. The they calculate the dietary intake by
nutrition education of medical using food composition tables,
students which is mainly carried correlate the dietary intake with
out during this stay, has following nutritional deficiency and plan out
components:
intervention strategies.
a) Introductory Lectures: In these e) Nutritional Monitoring: In the
(3 lectures) the students are taught subsequent monthly visits the stu
about types of foods, nutrients and dents monitor the nutritional status
their requirements, nutritional and give appropriate nutritional ad-
8
9
M.B. KHAMGOANKAR*. S. RAMKRISHNAN“, K.K. GHULIANI**’,
G.V.S.MURTHY*—
•Lecturer. “Lecturer, Social Paidlatrics. “’Prof. &Head, ““Reader
Department of Community Medicine.
Mahatma Gandhi Institute of Medical Sciences, Sevagram. Wardha
ABSTRACT
The paper presents an innovative approach of teaching nutrition to
medical students^which is based on the concept of exposing medical stu
dents to the rural environment. Tne medical students become more ef
ficient in therapeutic and applied nutrition practices and get a better
understanding of the present socio-cultural set up.
INTRODUCTION
vices.
DISCUSSION:
~
To increase the output of medical
personnel, teaching has to be rele
PROGRAMME EVALUATION:
The evaluation of this teaching vant to existing health problems in
programme is a ongoing and regu a commnity. Nutritional diseases
lar process which is carried out in form the main bulk of patients in
subsequent village visits. The as Indian conditions, where the phy
sessment of the programme is done sician is expected to detect and
manage them.
in the following ways:i) Assessment of the students:- Teaching of nutrition to the medi
The evaluation of the impact on the cal students can be started in the
students is done at regular inter first year. The method of teaching
vals, the students are assessed for nutrition as presented in this paper,
their clinical ability to detect nutri plays a major role in increasing the
tional deficiencies, their ability to proficiency of medical students in
carry out nutritional interventions therapeutic and applied nutrition
in most scientific way and by as as they become well-versed with
sessing their awareness about the food composition tables food ex
feeding and dietary practices in change lists during diet survey.
rural field practice area. This is This proficiency they achieve by
done by giving them practical exer ,the process of self learning during
diet surveys. At the same time it
cises to be done in the field.
ii) Assessment of impact on coinu helps in increasing the clinical
nity: As mentioned earlier, the stu acumen of medical students in de
dents serve the comunity in this tecting nutritional disorders.
process of self learning, the impact Because of exposure to the rural
on the community served is as environment, the medical students
sessed by six monthly surveys of get a better understanding of the
the community to assess the change present socio-cultural aspects and
in feeding practices, dietary intake develops the habit of managing the
the nutritional status. This data is problems with the current socio
compared with the baseline data economic constraints rather than a
bookish approach.
collected initially.
10
Analysing and interpreting the re
sults, correlating the findings helps
in inculcating epidemiological prin
ciples. The active participation of
medical students in growth moni
toring and nutrition education helps
the community in achieving better
health status. Such an activity is,
therefore, recommended for other
faculties of Community Medicine/
Preventive & Social Medicine in
other institutes.
REFERENCES:
1.
Devadas R.P. Integrated role of nutri
tion in medicine. Promotion of health and
family planning and prevention of illness.
Ind. Jr Nutr and Dietect 13; 355: 1976
2.
Jelifle D.B. the assessment of the
nutritional status of the Community. WHO,
Geneva; 1966.
3.
Manju Lata, Ramesh Puri, Physi
cian's nutritional knowledge beliefs and
practices. Ind Jr Med Edu 22: 14-17;
1982.
4.
Margaret, G.Phillips. The nutrition
knowledge of medical students. J Med
Educ 46: 86; 1971.
5.
Ramesh Puri, Manju Handa, Praveen
Chawla. Physicians and Nutrition-their
knowledge profile. Ind Jr Med Edu 23:1619; 1984.
' OLUME XX.il No. 2
5.' ’ All the candidates should be assessed
independently by . all the examiners
individually and effort should be made
•
that questions of a uniform standard be
asked from the trainees.
6.
If there is a significant difference of
assessment of the candidate between the
examiners, then the candidate can be
jointly assessed by a panel of examiners
before a final verdict is given. Despite all
efforts, assessment can never be wholly
■objective but efforts can be made to
reduce the variables and to cover as' wide
■ a range of (opics as possible to truly
evaluate a candidate.
Clinical Thrust in Teaching Biostatistics to
Medical Undergraduates
<'
•
"
A Indrayan
„
-4
H\
. .
Reader in Biostatistics
and
A.K. Sarha
,
.
:
(W*
. .
•
.
Demonstrator
Department 'of Preventive &' Social Medicine
University -College of Medical Sciences, New Delhi
ABSTRACT
Biostatistics is among the lowest rated subjects taught to medical undergraduates.
Most of it is attributable to lack of clinical orientation of the subject. It thus fails to
' meet the professional need of medical students. Realizing that course curriculum is the
single most important item determining teaching, we propose a biostatistics
curriculum based exclusively cn the clinical aspects. Content and structure of the
■ teaching is also mentioned. We indicate how so much of clinical work is inherently
statistical and exploit this to suggest teaching of statistical concepts in a manner that
the subject is seen as a means .to achieve better clinical ability.
Reaction of medical students to the subject
of biostatistics has been expressed, by such
adverse remarks as to leraance (at best) to (more
commonly) active dislike9, neither interesting
nor helpful13, and least interesting*. It has also
received ratings ranging from dislike to
abhorance3. In view of such reactions, the
teachers have made attempts to discover and
utilize any aids to facilitate their task as educa
tors. Some improvement in teaching has been
reported by such devices as defining precise
objectives2 and using timely articles as teach
ing aid11. Experiments like that of self inst
ruction11
and of
independent
study
programme6 have also been conducted with
varying degree of success. However, to meet
the challenge of teaching the subject in a
clinically televant and interesting manner11,
and to relate it closely, forcefully and convin
cingly to the students laboratory and clinical
interests9, further introspection on the content
and method of teaching biostatistics is
needed.
Course curriculum could be identified as a
single most important item determining teach
ing of a subject. .Various curricula have been
suggested on biostatistics x,’,10,12, including
one10 in collaboration with W H.O. AU of
them emphasize on statistics as applied to
63 the Indian journal of medical education
medical research and suffer from statistical
overtones. There is a need of a curriculum
which lays stress on the utility of statistical
concepts in the day to day activities of a
clinician — in forwarding most plausible
diagnosis, in assessing the prognosis, and in
deciding on the most fruitful course of mana
gement.
Besides the needs directly related to clini
cal work, utility of statistics is recognized also
as a basic tool to scientific methods 7,15.
Statistics thus is important to methods in
clinical sciences as well. Since the barrier of
antipathies of clinicians to any form numeri
cal values0 is now broken, the way is clear
for statistical inroads. The fear that the
invasion’ could make statistics master rather
than a tool10 is unfounded since statistics can
never be regarded as a substitute for the
rationale thinking of clinicians
Lot of clinic 1 work is inherently stitistical.
T he present communiealtion exploits this to
suggest a curriculum that brings basic statisti
cal concepts as a means to serve specific
clinical needs. Besides the clinical, the curricu
lum endeavours to meet rhe criteria of being
oi iented to scientific issues as well8. It also
attempts to provide the required meat of clini
cal material to the gravy to statistical
procedures’. The suggested curriculum may
n-’t be comprehensive from the statistics view
point but would be relevant to the needs of the
profession. It is restricted to the concepts
appropriate for undergraduates only. The
curriculum and the content and structure of
teaching is given below.
VOLUME XXII No 2
beings. Each patient presents himself with
unique features yet he is to be managed on the
basis of the experience gained on others.
Besides the biological variability of the
subjects, physicians may diff.-r on diagnosis,
prognosis and/or management of a case.
Laboratory and instrument may also cause
variation. On the top of this, enormous
amount of information, generally needed on a
subject, is hardly ever available in full. Concep
tual, recording and communication variabilities
further confound the uncertainties in clinical
practice. An objective way to evaluate uncerta
inty is by computing probability. In clinical
practice, tne probability needed is generally
conditional — for example, of abdominal
tuberculosis when complaints of pain in
abdomen, constipation and vomitting aie
reported. Such'probabilities should ideally be
based on records of large number of similar
cases seen in the past. In the absence of such
records, they may be based on experience also.
I. Clinical uncertainties and their measurement
For independent events like hypertention
and diabetes, the joint probability of the two
occuring together in a person is the product
of the individual probabilities. A clinician is
rarely interested in such probabilities but he is
interested in the probability of survival when
two (or more) such independent diseases, are
simultaneously present in a case Rules ars
available by which probabilities of such and
other 'complicated’, including dependent,
events could be calculated. For mutually
exclusive events like prognostic categories, the
probability of a person going into 'evere or
critical state is the sum of the probabilities of
these two categories.
inter—and intra- individual variations are
among the most outstanding features of human
The process of diagnosis is an excerci e in
classification wherein the probability of disease
MA Y-AUGUST1983
given signs-symptoms-investigations gets due
consideration. Additional information, as [and
when available, may substantially alter the
probabilities and
thus the
diagnosis.
Probabilities have similar role in assessing
prognosis and in choosing treatment also.
Medicine is increasingly becoming objective
by relying more on quantitative varibles.
Clinical significance of these measurements is
assessed against their reference values.
CLINICAL THRUST IN TEACHING 69
mean in healthy subjects. In case of height and
weight of children, median is used as normals.
Mean in meh cases could lack representa
tiveness due to possibility of substantially low
values even in healthy children. The normal'
haemoglobin level of 15 g% is that volua
around which levels of most of the healthy
people lie. This • is an example of mode.
Depending upon the type of distribution and
purpose, either mean or median or mode could
be used as point normal.
2. The reference values
Variability of the observations give rise to
a scatter in the form of a ‘distribution’. The
common types are the classical bell shaped
Gaussian as of body temerature, right skewed
as of systolic blood pressure, and left skewed
as of haemoglobin level. Most such distribu
tions lend themselves to mathematical theoriz
ing so that the probability of, say, systelic
level > 140 mmHg in a healthy person can be
calculated. Clinically more important is the
probability of a person being healthy when
systolic level > 140 mmHg. (Baye’s) Rule
exists by which such inverse probability could
be calculated.
It is a general practice that clinical signifi
cance of a measurement is assessed by the
magnitude of it ‘s deviations from the ‘normal’.
The term normal indeed has different meaning
in different contexts but let us consider it to be
that value which is generally present in healthy
subjects. This normal could be a single value
or a range depending upon that the variability
is low or high.
Point normal geneially is the central value
measured by either mean, median or mode.
Normal body tvIUjcrature of 98 6, F is the
When the variability of the observations in
healthy subjects is high, clinical interest is
served better by normal range, viz. 70-100 mg
per 100 ml of blood for fasting sugar level.'
Such normal range is generally obtained with’
the help of a measure of variability called'
standard deviation (SD). Variability is the;
difference of observations from: one another
but, to have a common base, we find deviation’
from a central value namely the mean. These'
deviations are ‘standardized’ by squaring to get
rid of the negative sign of some deviations by
computing mean of these squared deviations,
and then by taking the square root to get back
the original scale.
Realizing that some people in any popu
lation may have exceptionally high or low
levels yet be perfectly healthy, we find our
selves willing to exclude certain small fraction
of the healthy population with extreme values
from the range of normality. It is arbitrary
convention to exclude 5% (generally 2.5% on
extreme’) observations so that (middle)
of
the healthy people are included. For measure
ments with Gaussian distribution, such normal
range is obtained by mean ± 2SD limits.
70 THE INDIAN JOURNAL OF MEDICAL EDUCATION
3.. Errors in clinical decisions
In accepting m-an ± 2SD type limits as
normal range, a 5% risk of wrongly classifying
a healthy person as sick is already admitted.
Differential evidence provided by a value of
I0J mg for fasting sugar level against 10 . mg
is sometimes not fully appreciated because
both happen to be within normal limits. Thus,
indiscriminate use of normal limits ignore the
distribution aspects. In some cases, tbe
borderline values within normal limits overlap
with the levels present in sick subjects (e.g.
intra-occular pressure of 24 mmHg.) .Thus,
there is also a risk of sick person being catego
rized as healthy. Clinical relevance of normals
in assessing future risks and needs, of treatment
can certainly be questioned. A pregnant woman
with haemoglobin level of 13 g% could still
be advised to take heamatinics while a non
pregnant woman need not be so advised. The
normals are only a guideline and aid to
objectivity-clinician remains the best judge.
Despite all possible care and despite
decisions’ being based on appropriate pro
babilities, there is always some likelihood of
the decision being wrong. An actual case of
cancer can be missed and a case: of benign
tumour could be diagnosed as cancer. Similar
errors are possible at prognosis and treatment
stages also. Each type of error could be
serious. Missing cancer has obvious serious
implications so. has unwarranted cancer
diagnosis of a benign tumour—thejlatter could
mean unnecessary ■ psychological' and physical
trauma to the person and wastage of treat
ment inputs.
VOLUME XXII H6 2
Tbe outstanding cause of errors in clinical
decisions is the lack of perfection’ in the
medical toolsl These tools for diagnosis, eg,
patient’s history, physical' examination,
laboratory and other investigations.
It is a big help to know predictivity of
each tool. Positive predictivity .is the ability
to correctly, classify a positive case, This is
very high for positive. paraTte slide to. diagnose
malaria but is low for positive serological test
to diagnose syphilis. Negative predictivity is
the ability to rightly exclude negaiive cases.
This is low for negative malaria' parasite slide
but it is high for negative oral glucose’ tdlerance test to exclude diabetes.Tools with high
predictivity, singly or in combination,"should
be used to minimize the probability df error:
The other possible sources of error are
insufficient experience of handling each type
of patients, inadequate records; unwarranted
extrapolation; and host of conceptual, recording/storing, analytical and communication
errors. Merely being alert on these sources
would help minimize the errors.
. A satisfaction from the above ’ mentioned
curriculum is that basic statistical concepts
like that of probability, distribution, mean,
median, mode and SD, and Type I arid TI
errors have been covered. It is hoped that
teaching biostatistics in the manner suggested
above will go a long way in building up a
solid foundation for quantitative and scientific
thinking in the future clinician.
MAf-AUGUST 1983
CLINICAL THRUST IN TEACHING 71
REFERENCES
1. Abu-Zeid H.A H , Choi. N. W. aod Nelson N. A. A proposeci program for introdu
cing epidemiology and biostatistics early in medical curriculum. Can J Hub Hlth
1975 ; 66 : -188-92.
2. Clark M , Clayton D. G. and Donaldson (J. J. Teaching epidemiology and statistics
to medical students—I he Leicester experience. Jnt. J'fcpidemiol 1980: 9 ; 179-85.
3. Colton f. An inventory of biosta.tistics teaching in American and Canadian medical
schools J Med hdu 1975 ; 50 : .596-604.
4, Donnan S. P B. British medical undergraduates in 1975—A student survey in 1975
compared with 1966. Med Ldn 1975 ! 50 : 41-347.
5. Feinstain A. R. On teaching statistics to medical students. Clin Pharmacol Ther
1975 ; 18 : 121-26.
6. Hobel J R. and Morton R. P. Teaching experience with an Independent Study
Programme in epidemiology and biostatistics hit J Epidemiol 1979 ! 8 : 177-79.
7. LevinS G. Understanding and using statistics in nuclear medicine, J Nucl Med
1979 ; 20 : 550-58.
8. Lilienfeld A. M. More statistics in medical education (letter) /v Engl J Med 1979 !
300 : 204-05.
• . ,
9
Lowe C. !<* On the teaching of statistics to medical students. Lancet 16 3 ! 1 :
985:87.
10. Lowe C. R. (ed). Health statistics and medical students—A guide for teachers. A
handbook sponsored by the W. H.
and Government of rakistan, 1980 : 41-43.
11. Mulvihill M.N., Wallman G. and Blum S.A seven-year retrospective view of a course
in epidemiology and biostatistics, J Med Edu 1980; 53 : 457-60.
12. Report of a committee of the American Statistical Association Subsection on Teaching
of Statistics in Health Sciences-Proposal for a core curriculum in medical biostatis
tics. Clin Pharmacol Ther 1975; 18: 127-31.
13. Royal Commission on medical bducation, 1965-68, London H.M, Strtionery Office,
1968.
14. Robinson H., Burke R. and Stahl S. Self instruction teaching of biostatistics for
medical students. J Cumm Hlth 1976 ; 1 : 249-55,
15. World Health Organization Internationally acceptable minimum standards of medical
education (Tech Kep Series no 239); 1962.
16. Wright l.S. Statistics—
Master or tool ? NX State J Med. 1980 ; 80 : 605-07.
, \)<s\ 2.ZL., /Xjo 2 ,
;
PP U
■{:
XCL
Teaching of Communicable Diseases at
Medical College, Aurangabad :
A Review and Plan of Action
POPULATION PROBLEM AMD PHYSICIANS
By
Baride, J.P.
And
Sathe, P.V.
SOCIETY
Department of Preventive and Social Medicine, Medical College, Aurangabad.
PROFESSIONAL
associations
phtsiciw,su«eons.
paediatrician
OBST.& GYNAEC.
S.P.M. TEACHERS
demographer
STATISTICIAN
healthI EDUCATORS
I
COMMUNITY
LEADERS ,
MANAGERS
U/G
INTERNS &
\
\
P/G
MEDICAL
STUDENTS &
ALLIED HEALTH
PROFESSIONALS
STUDENTS 4
ALLIED HEALTH
PROFESSIONALS
INPUT
SOCIAL
SCIENTISTS
MEDICAL EDUCATION
PROGRAMME/ PROCESS
I
I
FACILITIES
|MEH,MATERIAL, FUNDS
WITH
RELEVANT,NEED-BASED
TASK-ORIENTED
________ <
KNOWLEDGE
OUTPUT > SKILLS i ATTITUDES
--------- TO BECOME
EFFICIENT DOCTORS
FAMILY COUNSELLORS,
EDUCATORS. PLANNERS,
MOTIVATORS &
RESEARCH WORKERS
ALONG c QUALITIES OF
MANAGEMENT & LEADERSHIP
MEDICAL EDUCATION SYSTEM AND PHYSICIANS
FIGURE 4
UNDERGRADUATES
INTERNS
POST-GRADUATES, i
PARAMEDICAL PERSONNEL
The objectives of teaching undergraduate students about communicable diseases at
Medical College, Aurangabad, have been stated and the importance of this aspect in total
syllabus of Preventive and Social Medicine has been underlined. The various phases
through which the teaching of communicable diseases has gone through over the last
fifteen years have been outlined. A feedback has enabled changes to be made to make
teaching more effective. For meeting the objectives stated, a plan of action has been
drawn up and has been presented.
The objective of teaching the C. D. as seen
Medical education has been viewed by
many as transference of knowledge and the by us are, (1) to impress upon the student the
emphasis has probably been on teaching and important place occupied by C. D. among the
not on learning. Many teachers hold a view that prevantable sickness in our country; (2) to
once a medical student Is equipped with the impart knowledge and give him experience so
necessary knowledge, he should be able to as to be able to be a good diagnostician; (3)
apply this knowledge in his professional career; to be able to practice comprehensive manage
This view, however, is not shared by the others ment of cases; (4) to understand the epidemio
and they feel that the student also ought to be logy and measures for pervention and control "7
demonstrated the application of knowledge. of C. D., in the individual, in the family and in <3
They also feel that actual participation would the community; (5) to be able to play his part
be still better to form clear concepts, attitudes well in the national programmes for control os
and development of the skill of application of eradication of C. D.
knowledge in specific situation. The evolution
Thus it is considered essential to involve the
of teaching porgramme of communicable students in such activities and give them such ~
diseases (C.D.) at Medical Collete, Aurang- practical experience as will enable them to
bad, during the period of last fifteen yeats, to develope proficiency and competence in the
fflake it more elfective, has been reviewed in application of knowledge and practice of
ls paper, and reflects changing concepts skills adopted, and meet the obiectlves
*12 THE INDIAN JOURNAL OF MEDICAL
EDUCATION
^'OL UME XXII NO 2
In the inital days, after the establishment
and also inculcated them
the aspect of
_ of medical college, Aurangabad, the topics of
family care. However, from
the experience of
C. D. were dealt by the department of medicine
students and teachers over
ouu me
in the form of didactic lectures. It was soon
evaluation of students performance in examina
realised that there was too much stress on tions it became clear that there were some
didactic lectures (which made them boring to lacunae in the training and that there was a
the students), and that too related to clinical
scope for betterment of the programme. The
aspects and little if any, the epidemiology, students sometimes did not pay the home visits
prevention and control. Therefore, in addition regularly and enthusiastically. It was difficult
to a formal posting of a fortnight in isolation for the limited staff of the PSM Department
ward, a series of lectures e.g. epidemiology was
to accompany or to supervise the students at
started by Preventive and Social Medicine (PSM
the time of every home visit. An inevitable time
deaprtment, to stress the importance of C. D. lag occurred between diagnosis in the O.P.D.
independently; and medicine department con
or admission of a case in the ward, allotment
tinued with theory lectures and clinics as
to the batch of studnts, actual home visits and
before.
discussion. On some occasions a disparity in
teaching
by physicians and by teachers in PSM
The feedback from time to time from
was
noticed. The students naturally were
undergraduate students revealed, a confusing
difference in emphasis in teaching epidemiology confused by the different approaches.
and clinical aspects during these lectures,
In order to overcome this problem, the
particularly showing an absence of correlation
didactic lectures on epidemiology as well as
in teaching and practical application by both
clinical course and management of C.D. were
the departments. Therefore, PSM department
taken over by PSM Depaitment from the
introduced the home visit programme for fourth
Medicine Department. After a couple of
clinical term students, weekly for four hours
yeary another change introduced was that in
since 1966-67.- The students were allotted addition to home visits, the bedside clinics in
cases of C. D., like tuberculosis, leprosy, infectious disease ward by PSM teachers in
diphtheria, gastroenteritis, etc. selected from fifth clinical term once a week were started.
O.P.D./Urban Health Centre/indoor patients The ward posting and clinics by medicine
and were expected to pay home visit once a department also continued. Thus the major
week in two hours. Following home visit the task in teaching of C.D. was done by PSM
next two hour session in the week was kept department. After working this system for
for discussion on home visit. This was done some years it was realised that the teachers in
with a group of 15-20 students, divided into PSM while teaching C.D. either in didactic
3-4 batches, each batch given a separate case lectures or in clinics did not stress much on
for home visit. It was thought that this training clinical course of disease and management of
would provide an opportunity to students to cases. This was with the presumption that
study the situation in family setting and use the student know and all this while posted in
knowledge and to develop the skills. This infectious disease ward, tubeiculosis or skin
programme did help the students study the and V.D., where actually they spent less time
disease in family set up and social conditions, In Medicine Department the teachers did not
MAY-AUGUSI 198^
give sufficient emphasis to cover all the
diseases and particularly the facets like
chemoprophylaxis,
immunologicals, early
diagnosis, bedside laboratory tests etc. were
not touched to the desired extent by them.
There thus was a division into ‘preventive’
and ‘curative’ clinics with repetition in
teaching and a confusing overlap.
TEACHING OF COMMUNICABLE... 1J
susceptible, to make stain and examine the
nasal smears or throat swab, how to keep
follow up, detect the source thereby, whom to
give and how to give which type of immuno
logical, how to impart health education etc.
In chronic conditions like tuberculosis the
study of epidemiology, assessing the effects of
disease on family, the relevant socio-economic
factors, the difficulties in domicilary treatment
In order to obviate these problems in and how to make the patient regular, or in a
teaching, to make it more interesting and case like leprosy how to achieve isolation
practical, to make the students practice in without hospitalisation, rehabilitation etc. will
realistic setting and to provide opportunity to be demonstrated to them. The role played
use knowledge and skills, some more changes by different organisations in control of
communicable diseases like tuberculosis,
were essential in the teaching of C.D.
malaria, leprosy will be shown through field
visits.
The staff of Urban health Centre, and
Now we have planned a combined coordi
nated endeavour by medicine, paediatrics and Venersal Disease Control Unit attached to the
PSM
department
will be actively involved in
PSM Departments. The students while in
fifth clinical term will be taught about the this field work.
clinical course, early diagnosis, bedside tests,
AU this endevour is with the expectation of
management etc. by the physicians in the increasing the motivation of students towards
posting of stndents in isolation ward, This learning with interest and understanding as
will be immediately followed by demonstration they will have an opportunity to visualise the
of epidemiological techniques and preventive/ practical application of what they are being
control measures with reference to the indi taught. It is felt that this approach of
vidual family and community in all aspects starting with a patient of C.D. in the hospital
by teachers in PSM by taking the students for and going to the family is one way of exposing
home visits to suitable local case. In acute the student. We are also planning to utilize
conditions like diptheria they will be shown the other approach, starting from community
how to examine the contacts, how to detect and going to the patient, simultaneously.
56
The Indian Journal of Medical Education
Vol. XXVI No. $
REFERENCES
1.
Bhatt R.V., Soni J.M. and Patel N.F.
“Performance of women medical graduates from Medical College, Baroda,
1949-74’’.
framing of Epidemiology during Undergraduate
' Medical Education—Need for Reorientation
Medical Education (1976) 10, 293-296.
By
2.
FLYNN C.A. AND GARDNER F. (1969).
“The careers of women graduates from the Royal Free Hospital School of
Medicine, London”.
Bansal, R.D.
professor & Head
British Journal of Medical Education 3, 28.
Bachani, D3.
Robb Smith, A.H.T. (1962).
"The fate of Oxford Medical Women”.
Lancet II, 1158.
4.
Assistant Professor
Department of Preventive and Social Medicine, Lady Hardinge Medical College, New Delhi.
Timbury M.C. and Ratzer M.A. (1969).
Glasgow Medical Women (1951-54).
ABSTRACT
British Medical Journal 11, 372.
Inspite of various national health programmes and new drugs, control of
5.
Whitefield A G.W. (1969).
common communicable disease is negligible in India. The question is whether our
“Women Medical Graduates of the University of Birmingham 1959-63”.
health manpower is suitably trained in Epidemiology so as to be of help in control
British Medical Journal 111, 44.
of these diseases. In light of existing patterns of training in Epidemiology and
lacunae thereof, some suggestions for reorientation of training in Epidemiology are
put-forth.
Introduction
The quality of medical care provided in a
community is directly related to the production
of health manpower which should be fully
equipped with knowledge and skills to provide
appropriate and timely health care to the bene
ficiaries. It has to be planned in view of
health needs of the community and according
to availability of resources and technology.
Unfortunately there has been tendency to over
emphasize use of the most sophisticated techno
logy as the ultimate answer which a country
like India can hardly afford.
Medical teaching and training pattern in
India at undergraduate and postgraduate level
has been a matter of criticism for a long time.
It has been shown that hospital based, cure
oriented approach is a complete failure
(UNICEF/WHO, 1975). Generally speaking,
a medical graduate after passing through six
58' The Indian Journal of Medical Education
Jears of medical education is bewildered and
finds himself gropping amongst a few phar
maceutical names only. He cannot be regarded
as the pioneer of provoding comprehensive
health care to the community in whatever way
he renders his services.
Ko/. Xyl'l au >
does not detail out clinical a^^ects because of
;‘,$ipt.'Dec. 198'7
Training of Epidemiology during Undergraduate....;:*
Lrain-power, human garbage a^0a handful of
two reasons :
1.
Lactising giants. There is no one else to
Name except providers of medical education
As the students are still in para-medical
Lad health care.
phase, it is thought to be untimely and
premature. •
environment and other factors in the
community should be incorporated.
— The teaching should not be based on
high level teachnology alone in investiga
tions and management but also depend
jfhe
‘
Integrated
’
Model
2.
The teachers of Preventive & Social
able on available resources and aids.
As a step towards production of appro
Medicine are usually not associated
priate health manpower, the Reorientation of
with hospitals and thus they are not
Medical Education Scheme has been implemen
In
the
present
situation,
teaching
of
epide
fully equipped with clinical teaching.
Keeping in view these aspects, some pre
ted in medical colleges in India (Govt, of India,
miology particularly of communicable diseases,
In the final clinical phase, the students are
1975). But unless there is a proper under
needs considerable change. A model has been requisites are essential. The teaching should
standing amongst the teachers of medical insti taught and trained solely about clinical picture
framed in this regard keeping in view the emphasize commoner conditions prevalent in
the area. The Department of Community
tutions and until the objectives of the scheme of diseases without mentioning the epidemio
following aspects :
Medicine should be regarded as clinical with an
are taken care of, it is going to be another logical characteristics of the disease. The
infectious disease ward/hospital. There should
refuse in the dustbin of high level policies and teachers of medicine are not reoriented in
programmes.
epidemiological understanding. The outcome
—The teaching should be need-oriented and be provision of minimum facilities in urban
slum and rural areas for proper training and
is, as expected, unorthodox. The student who
competency based.
residing. The duration of training should be
now becomes a medical graduate is filled with
In developing countries where more than
equitably divided in hospital and field situations
symptoms, signs and syndromes without any
three quarters of total morbidity is because of
understanding of epidemiological lay out. Thus
—Prior educational objectives should be with care not to hinder relevant knowledge
infections and malnutrition, there is further
he observes a patient as a single entity and a
identified on which course curriculum being imparted to students.
need and importance of teaching and training
disease as a single episode without bothering
should be designed.
of infectious diseases and nutrition in parti
for its origin and causation, the underlying
cular. Tuberculosis, Malaria, Filarias, Leprosy
Programme in the model
factors and the community implications. The
and Enteric Infections are at the helm of
measures taken are therefore unit-based. The
—Clinical training should be ‘integrated’
morbidity pattern and cause widespread
whole chain of complex events have been in
with right emphasis on individual and
mortality as well (Health Statistics of India,
In this model, the subject of epidemiology
progress for so many years and inspite of the
community orientation.
1981).
extends throughout the para-clinical and clini
fact that new drugs and better technology is
cal phases of undergraduate courses. In the
available the situation of communicable disease
Existing Teaching Methodology
has remained same or worsened. We have not
—The teaching should be comprehensive beginning, an understanding of medical socio
been able to control Malaria, Filariasis, Veneral
with right emphasis on promotive, pre logy and biostatistics should be imparted. In
With minor differences and exceptions aside, Diseases and Tuberculosis as a consequence
ventive and curative aspects of health para-clinical phase, after basic knowledge of
the teaching and training of epidemiology in only of inadequate approach to teaching and
care and rehabilitative aspects wherever microbiology and clinical pharmacology has
majority of institutions is irrational. The practice of Medicine. The resources go waste,
been given, epidemiology should be taught for
needed.
theoretical aspects of epidemiology are taught the basic health needs of the people remain the
4-5 terms in late para-clinical phase and clinical
in and after second phase of M.B., B.S. by the same, the economic stagnation stays and what
phase. General epidemiolgy should correspond
Department of Preventive & Social Medicine, we gain is over-increasing disease load,
—The teaching should not be only hospital with clinical methods in Medicine. Once this
now called Community Medicine. The teaching «$itg£int>urished future population, deteriorating
based but underlying causes, role of is achieved, systemic epidemiology and clinical
. 60
The Indian Journal of Medical Education
picture of a disease should be taught and in
detailed programmes care should be taken to see
that the two pronged teaching corresponds
diseasewise, as far as possible. During ward
training and posting, the teaching should be
integrated in the wards etc. With participation
of faculty members of Departments of Com
munity Medicine and other departments.
Vol. xxviNo 3
64
Community posting of 4-6 months during
internship can be vitally utilised for training in
epidemiology. In the urban areas, small postings, may of week or fortnight duration, in
District Tuberculosis Centre (D.T.C.), Malaria
Centre, Leprosy Unit etc. can be beneficial
besides posting in the infectious disease ward/
During the rural posting of undergraduate hospital. In the rural posting the interns can
students in the final phase, further training by be trained in implementation of various natio
these departments should be undertaken in nal vertical programmes in collaboration with
field conditions with stress on environmental clinical departments and Directorate of Health
and socio-economic factors. The teaching Services. Field studies, Family Health Care
should include :
Programme and seminars and discussions can
be arranged in the area. The interns can be
posted at sub-centres where they can learn
1.
Individual case studies with community administrational and management aspects,
implications.
peoples’ participation and total health care
concepts. In adopted Primary Health Centres
under the Scheme of R.O.M.E. there is wide
2.
Epidemiological studies of prevalent scope of integrated teaching of students and
diseases in the community.
interns. The visiting specialist alongwith the
community physician can discuss the morbi
dity in the area and they can train interns in an
3.
Family study of infectious diseases in integrated manner, the epidemiological con
field practice areas.
cepts of diseases prevalent there.
4.
Assessment of Community Health.
Emphasis should be given to diagnose and
manage a particular disease in rural areas with
minimum laboratory aids and treatment facili
ties (Annexure I).
Vol. XXVI No. 3
The Indian Journal of f^Bical Education
Internship Programme
Researchers have time and again recom
mended team approach. It has been rightly
said that the specialists have to develop an
understanding of and make a commitment to
Community Medicine as fundamental as their
commitment to superior scientific care
(Cherkasky, 1969). The present model envisages
interaction among various disciplines, may as
well have a decisive role on the emphasis and
status Anaesthesiology receives at under
graduate curriculum. Keeping pace with this
the present study was undertaken to find out
I (a) how much the present consultants themi selves were exposed to Anaesthesiology, while
they were undergraduate students ? (b) in the
light of their area of specialisation and the
subsequent years of experience of having inter
action with Anaesthesiology how much time do
they feel should now be devoted to Anaesthe
siology at undergraduate curriculum ? (c) would
they like to have inter-disciplinary approach
by holding joint seminars with Anaesthesiology
to improve the standard of teaching during
undergraduate medical curriculum ? (d) any
other comments on undergraduate anaesthesia
teaching and (e) to make certain recommenda
tions for improvement if deemed necessary.
Method
The undergraduate students are posted for
eight weeks in Anaesthesiology department at
this College. The students are divided into
groups and each is attached to a Consultant
Anaesthesiologist for practical demonstrations
and participation in the administration of
anaesthesia in the operating theatres. The
theoretical aspect is mainly in the form of
diadectic lectures, at times making use of audio
visual aids, by consultants io the department ;
and tutorials by' consultants, senior registrars
or registrars. They are also given opportunity
to attend departmental postgraduate seminars,
journal clubs, case conferences and encouraged
to take part in the discussion that follows.
Anaesthesia, analgesia, resuscitation, and in-
tensive care medicine are the main fields they
cover during their posting. The practicals
include demonstration of various methods of
general anaesthesia, regional analgesia ; practice
of endotracheal intubation and cardiopulmo
nary resuscitation on manikins, setting up of
intra-venous infusion, monitoring of vital signs
in an anaesthetised patient, maintenance of
airway in unconscious patient, and the handling
of anaesthetic equipment. At the end of the
posting they are given an examination, con
sisting of theory, and orals covering the
syllabus. Students who performed poorly are
asked to repeat the posting.
A questionnaire specially designed for this
study was sent to all the Consultants, in the
hospital. The Consultants in our own depart
ment were excluded from the study. They
were informed not to disclose their identity
while filling in the questionnaire. All the
responses obtained were subsequently analysed.
Resnlts
Out of 67 Consultants manning our hospital
5 of us are in the department of Anaesthesio
logy who were not served this questionnaire.
Five were on leave, who could not be served.
Thus 57 questionnaires were served. We bad
a ‘spontaneous response rate’ of 26.31% : 15
responded on their own with-in ten days’
period. Inspite of several reminders after a
three months’ period the total responses
received were 41; giving the ‘provoked response
rate’ of 45.61% and an overall response rate of
71.92%.
By the time of this study the consultants
Sept.-Dec. 1987
Training of Epidemiology during Undergraduate...61
team approach in teaching so as to have a
total concept of the situation. The crux of
the matter is that we have to develop students
intellectually and to cultivate their intrinsic
potentials. The quality and range of know
ledge and skills and attitude towards work of
future medical graduates will largely determine
the health of the community. The teaching
and training should be taken in such a way
that it is not felt as an undeserving punishment
but rather a rewarding experience.
Suggestions
—Development of competencies, educationoal objectives and course curriculum
and evaluation.
—Recognition of Community Medicine as a
clinical subject.
—Establishment/development of infectious
disease ward/hospital and its control with
Community Medicine.
—Establishment of Epidemiological Unit in
teaching hospital.
—Change in examination pattern of Com
munity Medicine after clinical phase.
—Community posting including in rural
areas during uhdergraduate curriculum
and internship.
—Reorientation of staff of Community
Medicine towards infectious diseases.
—Reorientation of staff of internal medi
cine, paediatrics, Obstt. & Gynae. and
others towards epidemiology.
—Specialist courses of postgraduate levels
in epidemiology.
—Establishment of perfect liasion between
Community Medicine and Internal
medicine.
—Provision of better living and teaching
facilities in rural areas including better
communication.
REFERENCES
1.
Cherkasky, Martin : ‘Medical Manpower needs in deprived areas'. J. Medical
Education (1969), 44 : 126-131.
2.
Government of India, Ministry of Health & Family Planning (1975) : Report of
Group on Medical Education and Support Manpower,
3.
Govt, of India, Ministry of Information and Broadcasting : Health Statistics of
India (1981).
4.
Rais Ahmed : ‘Reorieatation in teaching, learning anu evaluation*. J. Higher
Education (1980), 5 : 331-333.
5.
UNICEF/WHO study : Alternate approaches to meeting Basie Health Needs in
Developing Countries ; WHO Geneva, 1975, edited by V. Djukanovic, Epmach.
An Approach to the Teaching of Demography
In Medical Colleges in India
By
G.N. Prabhakara
Lecturer in Preventive and Social Medicine, Bangalore Medical College, Bangalore.
Summary
1972-74 experience of Teaching of Demo
graphy to
medical students at J1PMER,
Pondicherry gave an impetus to continue this
effort to gain experience for future teaching
and training. During 1974-76, an effort was
made at Mysore Medical College to
emphasis, teaching of demography to medical
students. From this experience students and
staff reactions, lacunae in teaching of demo
graphy in Medical College is highlighted.
Areas of application in demography is pointed
out which is the present concern for India and
the World.
Introduction
Demographic approach to study the com
munity is being emphasised sometimes for
flG A.
Fll/nctexmentzxi Fu-noixoA.
analytical purpose or as health indicators.
Linking demographic data and social data
with epidemiological data is a technique for
analysing the interaction between these variables
and the health situation. Demography exposes
characteristics of individual, of family and
features of the environment;
Irregularities in the. demographic indices
are characterised by differences in age structure
between population which in turn makes it
necessary to use different approaches to the
organisation of Medical care in various parts
of the country. Medical Education system has
a link to facilitate a change. (Fig. 1) Thus
in the last few years efforts are being .made to
bring. Medical Education in tune with bur
country’s situation.
JVjecliCai
SEPTEMBER-DECEMBER 1982
Countries like India, which are suffering
from population pressure have come to realise
that a whole’ new set of measures are needed
to change some age old ways of thinking of
habits and tradition.
Recommendations
Recommendation of M.C.I. on Graduate
Medical Education (Sept. 81) recommends—’
During first three terms principles of sociology,
including demography, population dynamics
and elements of biostatistic social factors
related to health and disease, urban and rural
society urbanised impact on health and disease,
community behaviour and ecology...
Recommendation of the Conference on
Medical Education held in 1971 at New Delhi
recommends—’ Every medical college should
have a standing curriculum committee which
should always be active, should incorporate
the desirable changes from time to time
depending on national and community needs.
AN APPROACH TO THE TEACHING ...57
It has to be responsive to social and cultural
changes...
National Seminar on the Physician and
Population change 1979 recommends— ’reorient
to produce competent physician... Social
science and Demography should be included...
Sri Lanka conference on Population and
Development in 1979 points out—population
and development are recoganised almost
universally as different sides of the same coin...
Bucharest represented a milestone in making
Governments consider how population affects
economic and political stability.
Conference on the Teaching of Demo
graphy . in Medical Schools held in Bogota,
Colombia during
1968 recommends—to
coordinate a series of demographic theme and
their interrelationships with health.
Current Picture
Fig. (2) and (3) depicts the current picture
of teaching of demography in Medical collegeswievit ftcTivte
Si>uicLe4
"to the- Cu^AcrTt
fUowpMj. ofc EcUe.oti’oA
TeaeLirt
3)EMo6RfiPH)
TJiaiyttr^
U.G.
P.G
lDeveJ.o|XTitj. I'n'tertexti-)
VOLUME XXI No. 3
58 THE INDIAN JOURNAL OF MEDICAL EDUCATION
Medical science and Statistics have contributed
Biostatistics which is the main area of work
today. Other developing interests are Demo
graphy and Population Dynamics. Fig. (3)
clearly points out starting from teaching of
demography in U.G. course in 2-4 hours to
Faculty indifference and not clear about
objectives.
SEPTEMBER-DECEMBER
AN APPROACH To THE TEACHING ...59
Selected group of teachers were interviewed
to obtain:
—their consideration regarding importance
of teaching of demography in medical
4. VW<
Fig 3 : Teaching of Demography—Current Picture
colleges.
—their applicability.
—additional skills for the teaching of
demography.
(jotWd. in Wkrj. ©j)
Avai-lziAZt
1.
Mainly Lectures 2-4 hours.
n ctotio nA
2.
Subject is taught by P & S M department.
r
r
| OBJECTIVES |> SihietccL
3.
Staff orientation to teaching of demography is inadequate.
4.
Resource persons (in demography) are not readily available.
5.
Library referene insufficient.
6.
Collaborative Research (MedicalScience and Statistics) practically nil.
7.
Faculty interest in curriculum oriented to effective demography teaching—
indifferent and not clear about the objectives.
Objectives and work models followed
Out of many objectives one can formulate
in teaching demography following were taken
into consideration :
1.
To provide a basic educational and
informative guide.
2.
To coordinate a series of demographic
themes and their inter-relationship
such as socio economic implication,
fertility, mortality, migration and
urbanisation, family planning and
tions in development planning and
development of policies and pro
grammes in the country.
Work Model
The aid series prepared by the programmes
of teaching and research in population of the
Pan American Foundation of Associations of
Medical Schools were used in teaching demo
graphy. Before theory, after theory and on
the day of terminal examination—questionnaire
on the demography were given and answers
were collected for analysis.
policies on population.
3.
To make students aware of the help
from demography.
4.
To make the students to understand
the need for an alternative policies,
promotion of demographic considera
Post demography exereise was given to I
clinical year students and answers were
analysed. Here population growth, important
problems of India, factors affecting population
growth were emphasised. At the end of the
course students reaction was obtained through
evaluation slip.
Fig. 5 : Teaching of Demography—Main activities at Mysure Medical College
—Lecture.
—Lecture cum Discussion.
—Discussion primarily with students preparation.
—Field exercises in small group.
—Library studies in small group.
—Syndicate studies.
Reactions from Students
Majority of students reaction were favour
able.
A few were critical for teaching in a
seperate name. They felt that demography
was too elementary for medical students.
A few were of the opinion that demography
was nothing but figures, rates and ratios.
Application of demography in service
planning was appriciated by one and all.
Reactions from Staff
Staff whom we interviewed did not favour a
seperate course in demography to medical
students.
They accepted the relationship between
physician and population change and further
doubted the application of knowledge in the
health planning.
VOLUME XXINo. 3
60 THE INDIAN JOURNAL OF MEDICAL EDUCATION
Teaching with
practical
approach was
welcomed by all.
• The views summeriscd here highlight the
area of misunderstanding among staff and
students in teaching demography to medical
students. Here time factor, discipline respon
sible and applicability are questioned by them
It is specifically pointed out by majority that
Preventive and Social Medicine department
puts show off through incorporation of sub
disciplines in teaching.
Areas of Importance and Future Interest
SEPTEMBER, DECEMBER 1982
the need and
the serviec Community
aspirations in health, fulfilment of community
expectations,
manpower
planning for
our
country, demographic
indices as
Work plan is suggested for an effective
colloboration which can result in a fruitful
outcome (Fig. 6). From time immemorial
it is known that faculty and students play key
role in this regard.
AN APPROACH TO THE TEACHING ...61
determinents of community need
and
services have become the present concept
and scope in teaching of demography in
Medical colleges.
Ag.7 Avia 0£ SauieL Oxi Reipwei, )n
MecLieal
Seienea
I OBJECTIVELY
,------------------------ ------------------------------------- -------------- --
J
ii) Li
til)
lae-nA^ca-tLo-n
R*<z|>oOTCCtLon
u.
CUteru,^
CAJ-wuiLu/oot
Pointed out areas of search and research in
demography (Fig. 7) clearly indicates’the
Conclusion
On the whole, there is a need for :
Three years of trial and approach in teach
ing of demography in medical college clearly
indicates that it is in formative stage. Deve
loping interest in demography are not yet
touched upon. Staff orientation and collo.barative research have greatest importance.
1.
Teaching of demography in the area
of developing interest.
2.
Formulation of pattern of integration
of teaching of demography in medical
colleges.
3.
An approach to the teaching can be
arrived at through workshop or Insti
tution.
4.
Crystalisation of World Meet, Popula
tion Commission Sessions, World
Conferences on Population are needed.
5.
Not to allow exponential growth of
our ability to collect, store and porcess
CefZaio’taXive RwuxaeV
tungsten in the bulb for glowing. Exposing .
characteristics of individul and family directs
The tried experiment is one of gradual
exposure on applied aspect of demography.
Method of teaching was kept flexible for an
active experience in learning.
Faculty sneezed uncertainty and students
appreciated to little extent with a feeling of
load on their curriculum.
62 1 HE INDIAN JOURNAL OF MEDICAL EDUCATION
VOLUME XXI No. y
information far faster than our ability
, to synthesise and interpret it.
say is sustained by human experience, is simply
,
that the greatest number of people will go to
the areas of greatest opertunities and that it
6. Aboptibility of resolutions of leading
w,ll work out over time:
organisations like UNESCO, UNFPA
re to be pointed out from time to
ACKNOWLEDGEMENT:
time.
The author is highly indebted and grateful
Lastly, • the words of Demographer
to the primary stimulation and experience at
Ashish Bose —-“What we are seeing is proof
J1PMER, Pondicherry under the guidance of
that urban misery is a necessary but not
Dr. D.K Srinivasa, now Professor and Head of
sufficient impetus for migration.
the department of Preventive and Social
“The hope of the demographers which they Medicine, Goa Medical College, Panaji, Goa.
REFERENCES
1.
H;alth needs ofsoci.ty : A challenge for Medical Education. 10th C1OMS Round fable
Conference —W.H.O. 1977.
2.
Journal of the United Nations Fund for Population Activities vol.6 No 4 1949.
3.
M.C.L Recommendations on U.G, Medical Education.
4.
Prabhakara G.N. — National Policy on Medical Education. Ind.J.M.Ed. vol XVII No
2 July/Dec 79 pp 198-206.
Prabhakara G.N.— Social Science in Medical Education—The Response of a trial
5.
IndJ.M.Edn. voLXVI No. 1 Jan-June 77 pp 5-10. .
6.
Prabhakara. G.N. — An opproach to the Integrated teaching in Medical colleges in
' India. Ind J.M.Edn. vol XVII No.I-2 Jan-Dec 78 pp 1-6.
7,
Recommendations of the Conference on Medical Education-New Delhi-Septem'; er
1971. .
8.
Recommendations of the National Seminar on ‘The Physician and Population change’
held in India in March 1979 (at Jaipur organised by 1.A.A.M.E,)
9.
Recommendations of the conference on the teaching of demography in Medical
schools in Bogoto, Colombia, June 1968.
- Statistical Indices of family health W.H.O. Technical Report series 587, 1976
10.
111 ‘The Philosophy of Medicine in relation to the population problem,-Lecture by Dr.
Rajam R.V. delivered under the Medical forum (1961-63) Government of India,
Ministry of Health.
12.
The Teaching of demography m Medical schools-series prepared by the
programmes of teaching and research in Population of the Pan • American Federa
tion of Associations of Medical Schools.
13.
UNFPA newsletter vol 8 No 3 March 1982.
14.
UNFPA newsletter vol 7 No 12 Dec 1981.
15.
World population year Number I.J.P.M. vol. XVIII No. 3 July-Sept.' 1974. ’
Performance Factors of Medical Students—
An Interrogatory Study (Part III)
By
M. Saran
M.O.H. Cum Lecturer
And
R.N. Srivastava
Professor and Head
Social & Prevenive Medicine M.L.B. Medical Preventive, College, Jhansi
INTRODUCTION
covered due to various obvious reasons such as
The eminent medical educationists all over continuous absence from the class and non-cothe world have not spared even a little span of operation in the study. The informations on
various period for the critical analysis of the various performance factors were collected on
performance
factors
of
the medical predesigned and pretested proforma.
students which might prove directly or
The medical students were categorised into
indirectly
beneficial
to
the
incoming
future professional colleagues. The medical three groups depending upon the percentage
students, inspite of their best efforts, achieve of average scores obtained in the first profes
a wide range of scores in the examination, sional examination. These scoring groups were
though they are exposed to almost same low with 50-55% marks, average with 55-60%
teaching/training environment
with their marks and high with more than 60% marks.
test
past brilliant scholastic performances in most The analysis was done manually and
was applied to elucidate the significane of
of the cases. Keeping in view the importano
difference wherever possible.
and practical, utility, a study on performance
factors of medical students was carried out with
Though, a large number of performance
the objectives to find out the extent of signifi
factors were taken into account for the purpose
cance of these factors in relation to various
of the study, however, only a few are commu
score grades.
nicated in the present communication as
various other factors have already been repor
MATERIAL AND METHODS :
ed (under publication).
The present investigation was conducted on
paraclinical students (1980-81 batch) under the OBSERVATIONS:
Department of Social and Preventive Medicine,
Various
performance factors such as
M.L.B. Medical College, Jhansi (U.P.) India.
personal habits, addictions, hobbies, mental
Of 98 students, only 69 (70.4%) could be
status, extra curricular activities and monthly
104
THE INDIAN JOURNAL OF MEDICAL EDUCATION
due to rapid urbanization and the attendant
socio-pathology are quite visible in the dense,
crowded cities like Calcutta or Bombay
although we may not have large scale studies
on this aspect. One must be, however, cautious
in adding that all these manifestations of men
tal ill health may not be entirely due to over
population per se but due to its interaction
with other factors like poverty, societal failures,
disease, etc. Thus it may be stated that over
population has been one of the crucial factors
impeding the attainment of social goals in
India. This is an illustrative rather than an
exhaustive discussion.
FOL. XIII NOS. 3 & 4
REFERENCES
1. Draft Fifth Five Year Plan, Vol. I and II.
Planning Commission, Government of
India.
2. Psychologicalperspectives on population, J ames
Fawcett (Ed) Basic Books, N.Y. 1973.
3.
Population crisis-an interdisciplinary perspec
tive, S.T. Reid and D.L. Lyon (Ed) Scott,
Foresman and Company, 1972.
4.
Population in India's development—1947-2000
Asish Bose et al (eds) Vikas Publications,
Delhi, 1974.
Health in the Epidemiological Perspective
GEORGE JOSEPH
Professor and Head, Centre of Community Medicine, All India Institute of Medical Sciences, Ansari Nagar, Netv Delhi.
The factors determining the fertility behaviour, the national and regional differences in the fertility
patterns and the factors responsible, for these differences are dealt with. The correlation between family
size and the health status of the family is illustrated. Infants and pre-school age children are worst hit
in large families particularly with upper respiratory trad infections ; high birth order children suffer mal
nutrition.
The content and scope of Public Health like
society itself has undergone constant change.
As old problems are solved or fade into minor
significance, new ones or those unappreciated
in the past arise to take their place, so much
-so. that Public Health finds it necessary to
redefine its field. From its traditional concern
for dealing with problems of the environment
and pestilential and mass diseases at a time
when these posed as formidable threats to
human existence, it has grown into newer
fields. In this endeavour ‘ Epidemiology ’ was
its principal tool. Soon it was realized that the
perspectives and principles of epidemiology
could be usefully applied far beyond the
disciplines traditional realm of communicable
diseases to the study of multiple determinants
and consequences of chronic diseases and
accidents, to studies of growth and develop
ment, pregnancy outcome and prematurity
and to studies of health relevant behaviour
and the working of health service systems.
Admittedly, Epidemiology has been a late
comer in the field of Population and Family
Planning. As a discipline basically concerned
with problems of health and disease as ‘ mass
phenomena’ it is only justifiable that its
frontiers are now extended to comprehend the
complex problems of population overgrowth
and approaches to solve them. Conceptually,
Public Health’s growing concern about popula
tion problem is most appropriate, timely and
sound as ‘ Health ’ is now being thought of not
in terms of disease or mortality alone but in
terms of the overall well being of the individual
in the society so much so our health strategy
ideally should be geared to promoting higher
Standards of human efficiency and satisfaction.
In this context, let us examine how an
epidemiological approach is not only relevant
but offers, the plausible solutions to population
problems related to health. It may be useful
to identify certain special areas in which
epidemiological principles can be applied with
advantage to population and family planning:
Firstly, it relates to Community Diagnosis of
the population problem itself which will
include:
determination of the extent of the problem
at various levels including pressures on the
social, economic and health systems;
assessment of reproductive
identification of high risk groups;
risks
and
study of the changes in patterns of health
and disease and health behaviour and their
determinants in population groups;
examination of the relationship between
family size and health: relationship between
high infant mortality and foetal wastage to
fertility.
.
(II)
Epidemiological assessment of fertility
control methods under clinical and field trial
situations.
.
(III)
Field studies relating to physiology of
reproduction - study of physiologic variables
in fertility, lactation practices, antecedents and
consequences of foetal wastages, perinatal and
childhood mortality, etc.
.
(IV)
Epidemiology of family planning be
haviour,
106
THE INDIAN JOURNAL OF MEDICAL EDUCATION
.(V) Epidemiology of programme accep
tance including jtudy of impact of health
programmes on Family Planning acceptance.
.
(VI)
Evaluation
Programmes.
of
Family
Planning
Our main objective today is enhancing the
quality of life of people aiming at promotion
of health and human efficiency. Family
Planning is no longer viewed in isolation but
as an integral facet of health care.
This conceptual change helps to bring into
sharper focus the potential benefits accruing
from family planning to all members of the
family, especially to women and children.
This in turn must enhance the acceptance of
family planning and bring down birth rate.
In order to appreciate the favourable influ
ence of family welfare planning on the
physical, mental and emotional health and well
being of the total family, it is essential to
examine carefully the effects on health by
repeated, ill-timed and unplanned births. One
has to consider the complex interrelations
between family planning variables such as
family size, birth order, birth interval, maternal
age and set of dependent variables such as
perinatal and childhood mortality, maternal
morbidity and mortality, the total health of the
members of the family including physical and
intellectual development of children, the inter
play of environmental and socio-economic
factors which influence this association should
not be Jost sight of, but a detailed discussion
on this is beyond the scope of this paper.
It must be remembered that ‘ Health ’ is a
■key variable in population dynamics and family
planning programmes. Morbidity and morta
lity which are epidemiological determinants of
health status are variables which influence
fertility behaviour and in turn are affected by
it. Let us look briefly into the dialectical
nature of this eternal interaction. Perinatal and
childhood mortality, deemed as sensitive
community health indices are shown to be
affected by family planning variables such as
parity and maternal age. It is relevant to
recall that the association between parity and
childhood mortality was recognised nearly two
centuries ago. At a time when I. M. R. in
Great Britain cannot have been less than
200/1000 live births, it was shown by Bland
(1781) that proportion of children surviving
decreased with increasing family size.
VOL. XIII NOS. 3 & 4
Several recent studies have clearly shown
that the risk of still-birth is relatively high for
first births, lowest for the second birth, and
gradually increasing after the fifth or the sixth
birth. Infant deaths especially in the post-neo
natal phase and early childhood mortality
increases steadily with parity. Morris and
Heady (1964), who studied the social and
biological factors associated with infant morta
lity, observed that ‘ social factors act through
and upon biological factors affecting the size
of the family, the spacing of children, the
nutrition of mother and child and opportunities
for infection1 and concluded that parity,
mother’s age, her social class and the region
in which the parent lived exerted largely
influences on still-birth, neonatal and postneonatal mortality rates. The British perinatal
mortality survey (1958) too reported identical
results.
American study, Shah and Abbey (1971)
brought out that risk of both neonatal and
post-neonatal deaths was considerably greater
among infants whose mothers had no prenatal
care as against those whose mothers received
pre-natal care. New Combe (1965) based on a
study undertaken in Canada found that the risk
of infant death was highest for infants born to
mothers under 20 years and dropped to a low
in the maternal age range (25-29 years) and
rose against with age. Indian studies (based
on hospital statistics principally) have shown
family size-and malnutrition of mother and
infant as important factors-associate with
infant mortality. Constant child bearing is not
only an unhealthy burden on the mother but
that large families, malnourished and living
in overcrowded dwelling places were very
susceptible to infection. Bajpai et al (1966)
brought out that risk of perinatal mortality
increases at maternal ages greater than 25
years and sharply after 35 years and that it was
highest in first births, lowest for second and
increased thereafter. It was observed that low
birth weight was another major cause of peri
natal mortality and that 70 per cent of losses
occurred in poorer classes of people. Mehdi
et al (1961) brought out that the principal
biological classes of perinatal death were rela
ted to maternal age and parity. One of the
major recommendations for pre-natal care was
not only to correct the obvious deficiencies but
to maintain optimum nutrition of the mother
and the foetus. Regarding the hazards of
grand multiparity there is documented evi
dence that it carries increased risks of maternal
mortality and obstetric complications such as
7 ULT - DECEMBER 1974
HEALTH IN THE EPIDEMIOLOGICAL PERSPECTIVE
107
pre-eclampsia, eclampsia, placental disorders, natal and infant mortality were high for
uterine
rupture,
mal-presentation
and infants born less than two years after a previous
birth; the mortality rates declined as birth
haemorrhage.
intervals became progressively longer than two
Asa result of general decline in fertility in the year for mortality in the second year of life,
West, there has been significant reduction in the rate was highest for infants born after an
the mortality among grand multiparas treated interval of less than one year.
in modern hospitals; yet the relative riskassociated with multiparity continues to exist Family Health
and morbidity has not declined as much as
There is overwhelming evidence from studies
mortality. Studies have shown that maternal conducted in various settings to illustrate the
mortality in grand multipara remained twice correlation between family size and health
as great as that for all deliveries and I.M.R. status of the family for risk of infection. In
nearly 3 times greater for infants of grand fants and pre-school children are the worst hit
multiparas.
especially with upper respiratory tract infec
tions and gastroenteritis.
Grand multiparity continues to be highly
prevalent in the developing world and morbi
It has been well established that malnutri
dity and mortality associated with it are obvi tion is directly related to the increased strain
ously high. It may be recalled that in India on family resources with each additional child.
the incidence of ‘Improvident maternity’ itself The worst hit are children and women during
is nearly 40 per cent. Though reliable data on pregnancy and lactation. Children below’ 5
mortality experience by parity and age are rare years constitute a major vulnerable segment of
from developing countries, it may only be. fair our population from the nutritional point of
assumption that grand multiparas fare worse in view, 15 percentof India’spopulation as against
these countries compared to the West.
6-8 per cent in advanced countries. It may be
remembered that 40 per cent of our total
Among other health hazards to which multi deaths occur in this age group as against 3-7
para are exposed, two deserve special mention: per cent in advanced countries. It is also a
namely diabetes and cancer cervix. Several matter of concern that the decline in I. M.
studies have indicated that after the age of 40 Rate witnessed in this country has not been
years the incidence of diabetes is higher reflected on the pre-school child mortality rate.
among women than among men and that This apparently acts as a motivating force for
diabetes increased with parity for the women. bringing up large families specially in our
In one study it was pointed out that occurrence society where every surviving child is deemed
of diabetes was equal in unmarried women and a potential asset. Nutritional status of survi
in married women who had no children and ving children is most unsatisfactory. In a
that compared with multipara diabetes was revealing study confined to Pediatric Wards in
about twice as common in women who have S & E. India it was found that 15 per cent of
had three children and six times as common in hospital beds were occupied by frank cases of
those who have had six or more. There have malnutrition (P.C.M. avitaminosis A and
been several reports on the association anaemia).
between multiparity and cancer cervis. It has
been suggested that association with high
Analysis of hospital cases of severe forms of
parity may be due to early marriage in these PCM showed that of these children only 39 per
women. Indian workers, Wahi et al. (69) have cent belonged to birth orders three and below
further corroborated this view.
while 61 per cent belonged to birth orders four
and above. A Study of 1,500 children in Peri
Birth/Pregnancy intervals
urban Hyderabad showed that 32 per cent of
It is well known that pregnancy constitute5 children of birth orders four and above exhi
an intense stress in any woman’s life preying on bited various signs of nutritional deficiencies
her innate resources. An appreciable interval whereas only 17 per cent of children of earlier
between births therefore is generally accepted birth orders (1-3) showed such evidence.
as useful to the health of the mother and the
Another vulnerable segment of population is
child. Khanna study has shown that birth
interval seemed to exert the greatest influence expectant and nursing mothers. At any one
on mortality during the first year of life; neo time in India there would be atleast 5 million
108
THE' INDIAN JOURNAL OF MEDICAL EDUCATION
expectant mothers in their last trimester.
Approximately 25 million pregnancies occur
per year in India. Great majority of the
pregnant women subsist on diets grossly
inadequate in many nutrients both during
pregnancy and lactation. Contributing consi
derably to maternal mortality and morbidity
the relationship between family size and die
tary status deserves particular attention.
Anaemia as an important cause of ill-health
and mortality among women of child bearing
age deserve special mention. Hyderabad
studies have shown that the incidence of severe
anaemia was significantly different between
women having three pregnancies or less and
those with four pregancies or more.
It may in conclusion be observed that there
is clear indication of the impact of family size
on nutritional status. Frequent pregnancies
of women subsisting on marginally adequate
diets impair their health and impose additional
burden on child care. It is also noteworthy
that given the food standards limitation of
family size 3 or less children will significantly
improve the nutritional status of preschool
children and reduce maternal ill-health and
mortality.
A word about the association between intel
ligence and family size would be in place here.
Studies conducted in the West have indicated
progressive decline in intelligence scores with
increasing family size regardless of social
class. It has also been shown that development
of intellect is favoured by the small family
environment. There has also been some indi
cation to suggest high degree of association
between family density and mental retardation.
There is likely to be great emotional invest
ment, warmth and concern on the part of
parents of small families for physical and
mental development of children whereas in
large families in spite of parents’ concern for
their children’s well-being, there is simply less
opportunity for parent-child contact. This
smaller degree of contact in larger families
may be reflected in poorer-slower-development
of verbal ability in these children, a factor
which may affect the children’s performance
on intelligence tests. Investigations have esta
blished that the growth of the intrauterine
Child is significantly retarded in the last seven
weeks, of pregnancy on account of lack of
nutrition to the expectant mother. There is
also evidence that the last six weeks before
birth and first six weeks afterwards are the
VOL. XIII NOS. 3 & 4
period of most rapid and critical brain develop
ment. The magnitude of the problem and
the urgency for critical intervention are obvious
when we recall that approximately 17 percent
of births in India are premature, partly attri
butable to malnutrition.
My endeavour simply has been to broadly
outline the gross implications of the unplanned
family for the total health of the family. There
is overwhelming evidence available today on
the subject, as could render further research on
the subject nugatory. But this knowledge
would
mean little unless it percolates
through all the echelons of the service
hierarchy and thence to the village couples
who need it most. That brings us to the crux
of the problem. Have we today the requisite
machinery to disseminate this message to the
masses ? And, what is more, are we confident
enough to accept this great challenge? If past
performance is a pointer, our failures and
weaknesses both in strategy and implementa
tion are fairly obvious. The images of rural
health in general and family planning services
in particular are far from flattering. It is
worthwhile to recall here a significant state
ment by the Hon. Minister for Health, Dr.
Karan Singh,“ Unfortunately the family plan
ning scheme had been conceived in such a
manner that it had come to mean a scheme that
benefitted only the Government. “Family
Planning”, Hon. Minister suggested, “should
become a mass movement where people are
motivated to ‘demand’ family planning
service”.
Two issues implied in his statement, namely
motivation of the couples to demand family
planning and matching it with adequate health
services based on an epidemiological analysis,
demand special attention. Let it be remem
bered here that ‘demand for service, in our
context’ should be deemed as a late stage in the
process of integrating modern medicine with
our cultural matrix. To render this possible
one should begin with, as Bryant has put it,
creating an awareness; The awareness
‘becomes a concern, then an expectation, then
a demand and the demand grows faster than
the possibilities of response’. It has to be
frankly admitted that we have not progressed
beyond the initial phase in this direction. It is
here that the epidemiological approach would
be of great help.
While considering the family planning be
haviour of the community, the question of
JULY ■ DECEMBER 1974
HEALTH IN THE EPIDEMIOLOGICAL PERSPECTIVE
acceptability of contraceptive methods deserve
our attention. Let us take the question of the
‘ ideal contraceptive—a thing that is so elusive.’
We seem to be sold to the idea especially in
recent times that once we develop a suitable
contraceptive, it may be a panacea for all our
ills in the population front; While we should not
slacken our research efforts in this direction by
any means, one has to be pretty guarded while
making such assumptions. History has taught
us that community acceptance of a certain
health dictum or practice, however beneficial
and attractive it may appear to be, cannot be
taken for granted. The consumer has his own
value of judgement which we often lose sight
of. To quote an example: even a health
practice like smallpox vaccination has not
received universal acceptance even today
among our communities.
109
I had occasion to closely observe the rural
health scene in one of the prosperous districts
of a prestigious state in the country. I was
stunned to learn that M. C. H. services often
exist only on official records. Cut away totally
from social life to which they arc accustomed,
made responsible for one lakh to one-andhalf-lakhs population scattered over 100
villages with primitive communication systems,
and operating on a meagre budget (Rs. 50007000) the medical officers feel unequal to the
demands of the situation.
Today we are committed to giving an added
boost to our family planning efforts making it
the pivot of our health scheme. It remains to
be admitted that while the great struggle to
provide basic services to rural masses continues
relentlessly, the academic community of the
medical college unfortunately, remain passive
onlookers. The prevailing tendency was to
isolate themselves completely from the main
stream of public health services. It may be
pointed out that the corrective lies in a whole
hearted attempt to move out of their
traditional realm to join hands with health
administration in developing health strategies
to suit regional singularities within the overall
framework. It is obvious that a deliberate
and total commitment on the part of the
medical educationists to improve the image of
rural health services should be deemed an
essential pre-requisite to usher in the social
orientation of medical education.
The second crucial issue is the provision of a
basic minimum health care and merging family
planning with it as its core. Drawing inspira
tion from the reports of the Bhore Committee
and the Mudaliar Committee—the Govern
ment have undertaken the major responsibility
for tackling health problems of the country for
which purpose a huge network of service
agencies has been established. The P. H. C.
sub-centre complex has come to stay. But if
it is to act as a powerful instrument for
providing basic integrated health care to the
rural masses it needs to be thoroughly over
hauled. It is generally agreed that the pride
I shall conclude by quoting Rene Saud “The
of place among the basic services should go to place of medicine is in the stream of life and
not on its banks”.
the maternal and child health services.
57.
Future Strategies for Ensuring Effective
Rajaram
^uesl
Implementation of National Programmes
for Family Welfare
60.
Health Economics in Medical Curriculum—
Relevant or Reduntant
M. E, Yeolekar
Community Medicine—The Never Born—
A Story of two Decades
64.
Need for Intrasectorial Planning in
D. Anand
°-.Anpndr
Rajaram
Faculty of Medicine,
Suez Canal University,
Ismailia, (Egypt)
Community Development
71.
Appreciation and Fulfilment of Community
Expectation to Ensure Community
Participation
-
Visiting Professor,
i
/-
^33,
z
'll
V ;
It was in early sixties that India as many
other countries in
world were happy to turn a new leaf in the medical education system.
75.
Manpower Planning for Community
Health Needs
K. N. Seneviratne
78.
Preventive Health Care in the Third World ;
B. Sanjeeva Reddy
Role of Psychosocial Variable in the
Acceptance of Family Planning
V/joy K. Varmh
Anil K. Malhotra
92.
Evaluation Techniques for Assessing the
Role of Social and Behavioural Sciences
O. P. Bhatnagar
Book Review
most of the ills related to the preparation of a medical graduate for service in the rural .
areas. Perhaps in that euphoric period it was not realized that we are attempting to
entrust so much to so few with so little. Well, in the eighties now we do have a
85.
Executive Director's Corner
thrid
was added to the medical school with the hope that medical education will get rid of
Health Behaviour.Education Being a task
from Indian Point of View
in Catalysing Population Change
the
Social and
preventive medicine - a newly constituted department with full time faculty members
hind-sight if not the wisdom.
One may ask the question .'did community medicine or its synonims
(social medicine, social and preventive medicine) ever get a chance to be born and
become viable ? What went wrong between the concept as visualized and the
realities observable in most of the medical schools who experimented with the idea
particularly so in the developing countries
The answer to these questions can be obtained by a review of three facets
to the development of the academic aspects of community medicine.
Firstiy. the faculty drawn for community medicine was mostly composed of
those who in the early period came from the field and there-after completed post
graduate studies to qualify as teachers. They were considered out-siders to the
academic world who get rapid promotions because of the vacancies that existed.
Even today the faculty members in this department as one teacher stated 'continue to
be second class citizens’. The ranking is not so much a result of lack of professional
training. It is a part of mental block mostly attitudinal, which accepts the presence
of community medicine departments in medical schools with reservations.
It also needs to be noted that if the early teachers in the subject lacked ■
academic
experience.
competance,
today they are handicapped
with lack of adequate field >
Either of the two situatious prevent optimum growth and professional '
recognition.
Secondly, the facilities given to the departments of community medicine.
Medical faculties concious of standards so as to provide the details of dessecting
tables or microscopes, failed to identify the minimum requirements of a department.^
There are very few medical colleges where the faculty in the early stages were
responsive to the needs for establishing out of the wall field training sites. Intrestingly
enough some of these experiments were successful in those medical schools where
there was
no
separate
department or where a
clinical professor coordinated the
student activities such as in Thailand, Turkey and Colombia. These are.exceptions
but they did provide strength to support the statement that community medicine at the
undergraduate level should be primarily seen as practice of good medicine.
Paradoxically the institutional problems fade into insignificance compared
to the bottle necks faced in dealing with the government controlled health care
programms to establish field training sites. In retrospect, it is the government
health
departments which fostered the ideas
and stimulated
the
universities to
take more active interest in training a basic doctor who could serve the largest
section of the population of their respective countries. But in implementation, the
beurocracy has moved at its own pac.e some-time even contradicting the tacit
acceptance to support the medical faculties community based programme. The
governments in most of the countries have moved with extreme caution in providing
universities the freedom to operate in a community as they do in a hospital. Very few
medical colleges in recent history and specially so after the Alma Ata Conference (1978)
can claim to have carried out any significant research which may have contributed to
innovative approach(es) in primary healthcare.
To
a
large extent, this could be
associated to the governments lack of support to the university programme
On the
other hand where the governments have trusted the medical faculty to undertake
operational research specific to the service needs, the tesk has been successfully
accomplished
One of the most recent examples is the Departmeat of Social and
Preventive Medicine of the University West Indies which has been given the UNICEF
awaid for their contribution to the development of health service in
region (fourteen Carribean territories).
the Carribean
Thirdly the student perception of the role of community mediciae in their
professional development. In most of the para and clinical departments students get
fair mix of learning opportunities of what is taught to them.
In this learning experience,
the teachers are active participants. On the other hand, the teachers in community
medicine act through and with the cooperation of the staff in health centres
Very
often the discussions in the classroom find little evidence in every day work experience.
In such a
situation student is
likely to get an
impression
(and very n turally that
community medicine is the name of a mental concept that is to be talked and discussed
but it is not seen in day to day pjactice for it is not born,
When will the gestation period be over ?
When will the medical faculties
take the step forward to demand their rightful place in providing services and conduc
ting operational research on major health problems seen in their respective regions ?
When will the government health departments accept the medical faculties as equal
partners in a joint venture for service to all by the year 20C0 ? It is only then that the
community medicine wiil be born.
(
n )
Inaugural Session
Opening Remarks*
By
P.N. Wahi
Hony, Executive Director, I.A.A.M.E., New Delhi.
Students and teachers all over the world
Your Excellency; Dr. D.J. Reddy. President
of the Association, Mr. Vice-Chancellor, Dr. are equivocal in expressing their discontent
Sharma, distingushed participants, ladies and with the existing medical educational pattern
gentlemen As Executive Director of the as completely inadequate to train a doctor to
Indian Association for the Advancement of meet the constantly changing needs of the
Medical Education, if is my privelege to society. The changes are a reflection of the
welcome the distinguished guests, members of dynamic revolution of our social structure,
the Association and participants to the XXII especially during the last three decades. Since
Annual Conference of the Association. We are medicine functions as a part of the society, it
very grateful to the Director General of Health must be amnable to change, if it is to
Services, and the Central Institute of Psychiatry, survive. To day, we are launching on a
especially its Director, Dr. Shridhar Shaima realistic programme of seeing hew medical
who has put in considerable efforts to organise education can meet the requirements of a
the holding of the Conference.
developing society
and
how best to
We are very grateful to His Excellency the shape the future of medical education and
Governor for his agreeing to inaugurate the research, so as to be acceptable to a demo
Conference. On behalf of the Association I cratic society in a developing country like
feel happily priveleged to welcome you, Sir, to ours. It is for this reason that we have
the Conference. Advice coming from a leading decided at this.occasion to invite, besides the
personality
like
yourself — involved in medical educationists and health personnel,
education and selection of educationists, res economists, sociologists and experts in popu
ponsible for shaping the destinies of the lation dynamics to participate in the conference
country, would be acceptable to the profession to give a frank appraisal of the structure and
in the much needed reorientation of medical the manner in which the problems that face
education and health service programmes of the society in regard to medical care can be
tackled.
the country to meet the needs of the society.
*XXII Annual Conference on the I.A.A.M.E. Central Institute of Psychiary, Ranchi-29th-31st January, 1983
14
The Indian Journal of Medical Education
Vol. XXVI M,.|
on their capacity to function as an integrated
team, each of its members performing given
tasks within a co-ordinated action programme.
It, therefore, goes on to observe that it is of
•crucial importance that the entire basis and
approach towards medical and health educa
tion, at all levels, is reviewed in terms of
national needs and priorities and the curricular
•and training programmes are re-structured to
produce personnel of various grades of skill
and competence, who are professionally equip
ped and socially motivated to effectively deal
■with day-to-day problems, within the existing
■constraints. It is for experts like the present
■distinguished gathering to translate these expec
tations into an effective system of education
producing the personnel of requisite compe
tence and motivation.
central focus will continue to be elitist
coverage. Unless we are able to supply r.
personnel from our medical colleges who n’ Dr. N. G. GADEKAR ORATION
the service specifications, the imbaW
referred to in the National Health Policy do{
ment as between the rich and the poor on (
one hand and the urban and the rural on(
other would continue. Social justice J By
removal of regional imbalances are as relevi
in the matter of health care as in the econo* Dr. (Mrs.) S. Chawla
field. It is no doubt a challenging task, f
given the rich cultural background and i
high sense of idealism, it is not beyondc
Mr. Chairman, colleagues and friends, I
capabilities to produce the professionally co •deem it a great honour and privilege, to be
petent manpower which would be in tune w ■asked to deliver the first Professor N.G. Gadethe aspirations of the poor and the needy.
kar Oration, at this, the 26th Annual Coniference of the Indian Association for the
I have great pleasure in inaugurating f 'advancement of Medical Education.
Conference and wishing it complete success*
In our country, any system which does not
keep the poor and the country-side in the
the achievement of its objectives.
“Training of a Diagnostic Radiologist”
Since this is the first oration to be delivered
in honour of this great man, it would not be
■out of place, to give a brief sketch of the life
fof Professor Gadekar.
|
great privation and suffering, which caused
permanent damage to his health, he kept up
his own morale and those of fellow officers.
After demobilisation, he joined the J.J. Group
of Hospitals, Bombay. Later, he moved to
Delhi and worked at the erstwhile Irwin Hos
pital. Bombay’s loss was Delhi’s gain as
subsequent events showed. Dr. Gadekar re
organised the Radiology department at Irwin
Hospital, cut out a lot of dead wood and set
an example to the staff of the department by his
hard work and dedication.
Professor Gadekar, born in March, 1904,
■died in March 1986. He graduated from the \
This was the time, after the British left
[University of Bombay in 1929 and soon after India, when a large number of Indian physi
?that, obtained the D.M.R.E. from Cambridge cians and Surgeons were working in an hono
[University.
rary capacity in this hospital. Thus, all these
clinicians came in close contact with him. At
During the Second World War, he joined that time, in the early fifties, radiology as a
■the Army Medical Corps and served as a speciality and radiologist as a specialist in his
Major upto 1945. He was captured, along own right, had not gained wide acceptance in
.with many other British and Indian Officers by the medical profession in India. Professor
the Japanese, at Singapore, and spent a number Gadekar’s analytical approach, his diagnostic
•of years as a prisoner of war. Here aimdst acumen and his keen interest in the follow up
16
The Indian Journal of Medical Education
of his patients, contributed a great deal towards
raising the status of Radiology in Delhi and
subsequently in the country.
In 1956, he joined the newly established
All India Institute of Medical Sciences as the
Professor and Head of the Department of
Radiology. I had the privilege of working
with him there from 1959 to 1962.
In those days, the department was located
in a few small rooms in the nurses hostel, but
the excellent, meticulous and painstaking work,
done by Professor Gadekar earned him a high
reputation amongst his clinical colleagues. He
was the first radiologist in Delhi, to establish
regular interdepartmental meetings, a practice
that is now universal. He was a greatly res
pected and much loved chief in his own depart
ment. He was gentle, friendly and helpful,
totally unselfish and a man of exceptional
integrity. The hospitality of Professor Gadekar
and his gracious and charming wife is legend
and was extended alike to the high and the
low. All of us, who came in contact with him,
are richer by the experience.
The subject, 1 have chosen for the oration
today, is the ‘Training of a diagnostic Radio
logist’. Before I proceed, let us first define
the term ‘Radiologist’. Soon after Roentgen’s
discovery of X-rays in 1895, it was easy to
define a ‘radiologist’. A ‘radiologist’ was a
physician who had special knowledge of the
uses of ionising radiations, both for diagnosis
and for treatment of diseases. As the scienti
fic knowledge inreased and the scope of both
the specialities widened, it became impossible
for one person to be an expert in both the
Vol. XX VI No. I
<^Jan.-Apr,l 198
fields. So, Radio-diagnosis and Radio-therapk
bl m since conventional X-rays,
separated and evolved as distinct s{>ecialiti®inical pr°tbe developing countries will contiThe term Radiologist, was then used, maiij*‘
mainstay of radiology, lor a long
for the diagnostic Radiologist.
i°u= t0 ^ome training in X-ray diagnosis will
Training of Diagnostic Radiologist
17
the training is inadequate in almost all the
Medical Colleges.
Many clinicians still argue that little formal
fiT. to be more comprehensive.
teaching is needed as the clinicians teach
The situation is different now. Many 1
radiology to the undergraduate students on
the newer imaging modalities do not emplf
next point is to assess, how much their ward rounds. There is no doubt that
ionising radiations and thus are not strict^ —,
does a graduate know, when he the clinician acquires considerable knowledge
‘radiology’. Prime examples of these are ult^/”
p0Sl.graduate course ? It is the expeof the radiology of his own speciality, but he
sound which uses sound waves, and magnet^?*^. of mOst teachers of radiology, that very
does not, however, have the radiologist’s
resonance based on magnetism. Both
tbe newly qualified doctors do not experience in teaching the subject. He may
modalities produce images which have to fl ossess even a basic knowledge of the subject. teach them how to recognise various patterns
interpreted. Since the diagnostic radiologis!^^ js due l0 the fact that not enough teaching
of diseases pertaining to his own speciality,
are trained in the art of reading shadows atfor training m radiology is being imparted to but without training them in the analytical
interpreting images, it is easier for them to
undergraduate Medical students. V/e all approach. Tbe students need a well planned
these techniques also. Most of these newj' ree tbat undergraduate medical curriculum radiology course, which should not only
imaging modalities are, actually, being used b‘-s already overloaded and additional burden on introduce them to film interpretation but also
people who were originally using X-rays. Scthe student is undesirable. If it is accepted, that instruct them to choose the safest, cheapest
the term radiologist is usually used instead c'a basjc knowledge of radiology is an essential and the most direct means of arriving at a
an imaging specialist.
£an of tbe training of any physician or Sur
diagnosis. This will be of great help to them
geon, then ways and means can always be in their clinical work after graduation, even if
In developed countries, where the depar£ound> ofimparting this, knowledge.
very few of them will take up the speciality as
ments of Imaging are large, most radiologist'
their career. Those who will take up the
take up only one sub-speciality. Here, tb.. jn most medical colleges in India, a few speciality will benefit if they already have some
conditions are very different. The number Cradiographs showing normal anatomy are basic knowledge of the subject.
radiologist are very few. Often there are on!ahOwn to the students during their Anatomy
one or two radiologists in the department anjectures. During the clinical years, they are
Next, we come to the Selection of Candi
they have to carry out all the imaging invest£Upposed to study the radiographs of their dates. In the past, every aspirant to a post
gations. Therefore, it is essential that a traine'ward patients and thus learn the rudiments of graduate qualification in India, at first tried
radiologist should be given an exposure, thougfajdiology. During the final year, some didactic for admission in one of the major specialities
a limited one, to all the relevant imaging techjectures are taken, the number of which varies like medicine, surgery and their allied subjects.
niques. Later on, depending upon the specififrom one College to another. The quality of Radiology was a last resort, of the unsuccessful
needs of the department, where they will woriteaching and the number of radiographs shown candidates.
they can take refresher courses and furtheand lbe techniques discussed again varies from
training in that particular imaging techniquedne individual teacher to another. During
Now, with the advent of modern imaging
Only a person who knows something about thinternship, there is a very brief exposure of
techniques and the ever-increasing reliance
various imaging modalities, their uses anfthe jnterns to the Radiology department but being placed on investigations and better
limitations, can select or advise regarding th'tbis js agaln optiOnal and insufficient. However,
career prospects, the scene has now completely
most appropriate investigation for a particular
The Indian Journal of Medical Education
changed. More and more students are now
opting for radiology, some of them making it
their first choice. The selection of candidates,
is however mostly not in the hands of the
teachers. The Universities follow a uniform
pattern for admission into various disciplines.
It may be argued that the practice of radiology
•depends a great deal on visual acuity and on
analytical approach, so a good eyesight is
essential and psychological tests for the reason
ing power, mandatory. However, in actual
practice, marks in the examination, either in
the M B.B.S. or in the admission test are
usually the only criterion for selection. Once
the candidate is selected, there are only 2 to
3 years in which the person has to be trained.
It is understood that the trainee will be a
full-time student attached to an academic
•department for the duration of the course.
The training can be divided into four basic
components:
Jan.AprilWl
up a great deal of the time of the trainee. | machines and knew each and every component
the other band, if no exposure is given; of their equipments.
research methodology and review of the wo' ■
literature, the training remains incomplete.!
This is not possible now. With each passing
is my belief that writing a dissertation is uslLear the machines are getting more and more
provided it is kept brief and doesnot el sophisticated and computerised technology has
spending too much time, on the partofixome toplay an important role in imaging.
candidate.
I These machines are now repaired by highly
^qualified engineers usually under annual
1 service contracts. But, it is still necessary to
I know the principles on which these equipments
.
I are based and also how to handle them so as
The practice of diagnostic Rad.ologyj
t break.downs and damage to
based on knowledge of normal anato^
ts. Such training is usual)y
physiology, biochemistry and the paraclio .
d by radiation pbysicists but in depart
subjects of pathology and microbiology <Lents where there are no physicists, the senior
When seeing an image, unless one is ftf*
t
A
• K
...
. . ... Jcadiology teachers have to do this job.
conversant with the normal, the deviation fr®
the normal is not noticed. If deviation!
...
S The third component oi training is expertise
noted then the next question is, is it a varii: ..
. .
„ ,
,
. .
, ’
„ fin diagnosis by imaging techniques
of the normal or is it pathological ? If ifc.
pathological, then what is the pathologl. How much emphasis should be given in the
(ii) Basic Sciences
Adequate knowledge of the basic subjectsl ricu)um t0 the different modalities ? This
related to radiology is thus essential.
|atural)y depends to some extent on the local
(i) Thesis or Dissertation.
(ii) Basic sciences, including physics as
applied to Radiology.
(iii) Diagnostic Radiology
imaging techniques.
Vol. XXVI
and
newer
(iv) Concepts which are specifically appli
cable to diagnostic Radiology.
(i) Thesis or Dissertation
In most Universities a thesis is a pre
requisite forgetting a postgraduate degree.
The thesis subject, if properly researched, takes
[conditions. In India, except for a few upgraded
This can be best achieved by briefly disc(institutions with large and well equipped
sing the anatomy, physiology and pathologykmaging departments, most of the teaching
various systems or organs before their radfhospitals have only conventional radiology
logy is discussed. If it is possible, muliqUipments and ultrasound.
disciplinary seminars and symposia can be h*
on selected subjects. This will be helpfull Therefore, knowledge about modalities like
the post-graduate students of all the speciicomputerised Axial Tomography, Nuclear
ties of that Institution.
[Magnetic resonance and Positron emission
tomography etc. can only be theoretical in
The trainees also need to learn basic radinature. Too much time need not be spent on
logical physics and details of the equipmethese. A brief introduction to the subject,
used in the department. In the past, whlthe basic principles on which these modalities
equipments were simple, many radiologisare based, indications for their use, advantages,
were able to repair minor defects of thtdisadvantages and their limitations is all that
Training of Diagnostic Radiologist
19
is necessary. If it is feasible, the students
should be posted for a fortnight to upgraded
departments of Radiology where they can see
these techniques being used.
Ultrasound is in a different category
altogether. The ultrasound equipment is now
available in most teaching hospitals and is
being used extensively in the country. Ultra
sonography is essentially an operator oriented
modality and improper placement of the
transducer can completely transform the image.
It is a recognised fact that if the operator is not
properly trained, incorrect diagnosis are often
made, bringing the modality into disrepute.
In addition to the formal, theoretical teach
ing of ultrasonography, actual practice and
handling of the equipment must be done by the
trainee. The students should be posted by
rotation to the ultrasound section of the
department, where they can work under the
supervision of a member of the faculty. A
very large number of diseases can be correctly
diagnosed by ultrasound. Therefore, certain
amount of expertise is expected from the
post-graduate.
Diagnostic Radiology which constitutes the
major work of any department, needs a great
deal of time and attention of the trainee. Large
number of conditions have, to be recognised
and correctly diagnosed. , The best method of
learning radiology is to see a large number
of X-ray films, of various lesions, study them,
describe the images and then by process of
elimination, reach the most likely diagnosis.
Before this can be done effectively, a sound and
‘in-depth’ knowledge of various clinical dis-
Fy;-
I
18
' 20
The Indian Journal of Medical Education
ciplines like medicine,- surgery,- pediatrics and
orthopaedics etc is required.
It is the experience of all of us -that despite
the one year’s internship and one year’s house
manship usually the graduate has only super
ficial and perfunctory knowledge of the clinical
subjects.
In the short training period available, it is
not possible to post the students to various
clinical departments for refreshing their
knowledge. Therefore, the trainees should be
encouraged to take detailed history and do the
clinical examination of the patients who are
referred for radiological examinations. If it is .
not practical to do this on all routine cases, at
least all the patients who are referred for
special investigations should be studied in
detail.
All academic departments should have daily
departmental meetings.
At these, all the
positive and interesting X-rays of that day
should be seen by all the faculty members and
the trainees, before the X-rays are despatched
to the various outpatients departments and
wards.
The radiology department should also have
frequent interdepartmental meetings with the
various clinical departments, by rotation. These
meetings would be useful 'not only for the
trainees of all the specialities but also for the
faculty In these, clinical history of the patient
and radiological findings can be correlated. If
the patient has had a biopsy or surgery or an
autopsy has been performed, then combined
clinical, radiological and pathological correla-
W Vol. XXVI No. i Jan.-April 1987
tibn can be obtained. Such free exchanfegist is given only a very rudimentary knowof information between the various specialistedge about radiography and dark room work.
results in better diagnosis and treatment of Jhiese countries have well regulated and well
patients, in addition to inculcating go|pp°’n,ed Schools of radiography where the
practices in the students.
Radiographers are trained under the supervision
bf senior and highly qualified Superintendents.
Trainees should also be encouraged to goMoreover, most of the radiology equipments
the wards for following up their patients ajtre computerised, arid the radiographic expoto get the final diagnosis, if possible. Patbgires are automallca,ly re8ulated- Developing
logy department is another important plaMd
*s a*s0 done automat‘cal'y-
which the trainees should visist frequently, g
great deal is learnt by correlating the radii ,D India’ the position is quite different’
logical findings with the gross morphology
few institutions in the C0UDtry run courses
histology of the resected specimens.
> radiographers. The duration of the course
jnd the curriculum content varies widely from
In the radiology department itself, all tfe Institution t0 aDOther So the trainin8
trainees should be posted to various sections |jf radi0«raphers leaves mucb t0 be deS,red’
rotation. Amongst these sections, the da£here is also a brain drain and many g0od
room is very important. Good radiologVray techniciaDS !eave every year for 8reener
depends to a great extent, on the radiograph™ in oil rich countreis’
techniques and darkroom work. The reputS
tionofa specialist depends upon the accural Thus, the radiologists have to most often
of his diagnosis, this accuracy can only fafn !heir own technicians, hence radiography
achieved, if the X-ray films are of good qualit!pd dark room experience must form an inteThese can only be obtained, if there is careira’ part
tke tra‘n'Dgpositioning of the patient, standard radif’
graphic views are taken and there is meticulo^ 3n order to gain experience of radiography
work in the dark room. Often cardiomegh13 various examinations they should be posted
has been dignosed when X-ray film of the che'° different X‘ray rooms by rotatioD’ Here
is taken in expiration or in supine position (hey sholud see a11 the retluisition forms. Plan
at short focus film distance. Fractures can
“amination and view the wet films before
easily missed or their lack of alignment ovehe patient leaves the department They should
looked unless standard projections are takelrst observe contrast studies !ike barium exami'
Artefacts on the intensifying screens, due[atlons and intravaneous urographies being
careless handling in the dark room can ca!°ne- Later- a certain specified number of
shadows on the X-rays which can be wroog?aminations should be Mrried 0Ut by the
interpreted as pathological lesions.
[ainee himself’ Fluoroscopy, with or without
page intensifier still plays an important role
In most western countries, the trainee radif dia8nostic radiology. It is required for
Training of Diagnostic Radiologist 21
barium studies, for Hystero-Salpingography
and various angiographic studies.
It is now universally accepted that screening
of the Chest for pulmonary lesions is worse
than useless as small lesions can be missed
while the patient gets a false sense of security
that he has no lung disease. Fluroscopy, how
ever, is required for seeing the movements of
the domes of the diaphragm, for cardiac pulsa
tions and for cardiac valve calcification etc.
specially in Institutions where echocardiogra
phy is not available. Fluroscopy is an art. How
to handle the patient in the dark, specially the
young and the infirm, how to allay apprehen
sions and bow to make a diagnosis without
giving too much radiation to the patient and
to the radiologist. These are the various
aspects of fluroscopy which need emphasis.
Interventional Radiology for therapeutic
purposes has recently becomes a very impor
tant part of imaging. Ultrasound and compu
terised ’ Axial Tomography guided biopsy,
drainage of abscesses and various angiogra
phic procedures to' control bleeding from
various sites, are done routinely in some depart
ments. Most of the interventional techniques
require sophisticated imaging equipments and
experience in these procedures and may not be
available in all the departments. But, some
exposure to interventional techniques is neces
sary.
In order to train the postgraduate to
diagnose various lesions, a very large number
of conditions have to be shown. In the limited
period available for training, no single radio
logy department can come across the very
22
The Indian Journal of Medical Education
large variety of X-rays required for training.
Therefore, all teaching departments need -to
have good film libraries. In these, X-ray films,
sets of investigations and fully worked up
cases should be kept. These should have a
brief clinical history, description of the radio
logical findings, possible diagnosis and differen
tial diagnosis written on the covers The best
method would be to have taped audiovisual
lectures which the students can project and see
as well as hear the description. These are
beyond the reach of most teaching depart
ments in the country. So, X-ray films and
slides showing various conditions would serve
the purpose equally well. The trainees should
be encouraged to spend some time every week
for self-study in the film museum.
The emphasis in the training should be
mostly on common ailments. Time and again,
medical educationists have discussed and
bemoaned the fact that undue importance is
being given in the curricula to rare and exotic
•diseases, at the expense of common diseases.
This is applicable to the radiology students
also. Very often, the students rattle off, all
the radiological signs of uncommon diseases
but cannot recognise diseases like mitral
stenosis, ileo-caecal tuberculosis and carcinoma
oesophagus etc. on the X-rays. This tendency
cannot be decried too strongly. The faculty,
more than the students, is to be blamed for
this. Many faculty members hrve their pet
subjects and research projects and these inter
ests very often spill over in their daily work
and teaching. The trainees should be made
fully conversant with all the common as well
as the uncommon radiological manifestations
of diseases which are prevalent in India. After
Jan.Aprll^
Training of Diagnostic Radiologist 23
Some time should also be devoted to the
medicolegal aspects of radiology. In the
Western countries, specially in the United
most of the common diseases when he obj ose a hazard to the patients and to the States of America, medical malpractice suits
a post-graduate qualification, then to my J pub]jc at iarge, in this context, the history of are filed frequently and often unnecessarily.
the purpose of training would be served,| ^-acjiology is extremely important. A great deal These are not common as yet in India. How
any case, all doctors with post-graduate qul was published in the radiological literature ever, with more and more public awareness of
cations are expected to be conversant with|.jo early ninetees about the lives of pioneers its rights and with spread of knowledge, it is
use of the medical library. So, if and jn Radiology and the damage they suffered possible that in the near future, all doctors
faced with an uncommon condition, i ^,y WOrking with various radiation sources. including radiologists will have to prepare them
should be able to refer to the literature’ some of the injuries caused to the hands by selves for medical malpractice suits. Once the
consult a senior colleague. Those of 1handling radiation sources and various malig- patient comes to the radiology department,
trainees who later get absorbed in teadloancies which were caused by ionising radia- then the radiologist is solely incharge of the
Hospitals or in large imaging departments! tions can be emphasised. This will go a long conduct of the examination. If the radiologist
take refresher courses or can get training-way towards ensuring compliance with radia- finds that carrying out of a particular exami
nation is likely to harm the patient due to
the particular modality which they are gejtion safety precautions.
to use.
excessive radiation dose which the examintion
|
It is true, that with modern sophisticated entails, then it is his duty to discuss this
An important part of training is radiation fcX-ray equipments one has to be grossly careless with the referring clinician and then take a
Lto receive that much damage. However, many joint decision. More serious than this is the
tection
\radialogists have to work with simple, low death of the patient during or immediately
Since the radiologists have to spend fpowered equipments, which may not have after a radiological examination. Some side
times in the X-ray departments, they mus^.adequate in-built protection. Moreover, a effects are bound to occur in a few patients
fully conversant with the harmful effecti'rworker in the radiology department in his or with use of contrast media for various special
radiation. It is well known that effects'-tor
01" her
'1Rr life
life time
tim<. is
ic exposed to
tn continuing
mntimimtr subcuK investigations and in interventional techniques.
ionising radiation are both short-term | minima] doses of radiation. Since the effect With the advent of modern non-ionic contrast
long-term, both somatic and genetic. Not irLis
cumulative, radiation can decrease the life media, the incidence of severe and fatal reac
is the radiologists and all the staff of the ra ■span, can cause genetic mutations and many tions has been considerably reduced. However,
logy department but the patients as well as i somatic effects. Various international commis- these are rather expensive and not readily
public at large has to be protected from ex inions on Radiation protection have laid down available in India. The trainee radiologist
sive radiation doses. It should be empbasMhe maximum permissible doses which a radia- must be given a good grounding in the pharma
that the only safe dose of radiation is no raM'on worker can receive per week, per quarter codynamics of all the various contrast media
tion. Since this is not practical, rigid saf^nd annually etc.- These are the maximum used in radiology, their relative advantages and
rules must be followed to keep the dose tt permissible doses but efforts have to be made disadvantages, the various reactions associated
minimum.
:"to keep them much lower. Various ways and with them and how to combat them. In order
• means of achieving this can be taught both to safeguard the radiologist from medicolegal
In my experience of the last three aofhy the medical faculty and by the radiation point of view, patient’s consent to treatment is
half decades of working as a Radiologist, I f Physicist
required. The cons-nt is only valid if the
that people even if they know the facts, tend
!
all, our aim is to train radiologists whoi become complacent and do not in practice
expected to work in India, under IQ1 ^1[ow rigidly the safety requirements. Thus,
conditions. If a trainee can recognise corrl flOt oniy do they harm themselves but also
> VOL XXVI No i
24 The Indian Journal of Medical Education
Apr.ix^
• patient has been made tounderstand the nature
The next point is purchase of equipment
cai] services
between Weveloping
e<Iu’PnieI®ojo„jica
of the examination and consequence of what is Various machines are available, some
and Industrialised societies varied by
proposed. This is normally done before all some sophisticated and some specifically meat^ctor of 40- Even this does not reflect a
surgical procedures in India but usually not for for certain investigations. It is true, th<
-ctUre as most of the services are concenradiological examinations. Ideally, every patient ' usually the purchase of equipment depends ^ed in Urban areas. What we need are good
for intravenous urography or for angiography the budget available but in order to avogeral radiologists who should be able to
or arteriography should give valid consent wasteful expenditure, the radiologist shon§gDOSe with the help of X-rays and ultrabefore the examination is carried out.
have some knowledge about the various typ^nd most of the common diseases. There
of machines and their uses and limitations!'
that equipment appropriate to the needs ■
The various facets of training which I have the hospital should only be purchased.
I
mentioned uptil now are general and would be
applicable to training in most clinical disci
The third item is preparation of a train;
plines. In addition to these, there are certain
specific concepts which have to be kept in mind to be a good leader of the team. Radiologist
have
to normally work with a large numb;
in the training of radiologists. These are,
planning of an imaging department, purchase of paramedical workers whose cooperatin'.
and
devotion
to duty is essential to run k
and maintenance Of equipment, administration
of a department, and lastly quality control of department successfully. The fourth itei®
quality control is very closely related atfe
images. Let us take these, one by one.
interlinked with good team spirit. It shouB
be inculcated in the trainees that in order L
have discipline and high quality precision.
.Planning of an X-ray Department
work in the department, all the staff membt;
have to work in harmony with each oth |
Although these days there are architects
who specialise in planning hospitals, yet in
many parts of the country, a radiologist will
• have to guide the planning of a new depart
ment or renovating of an old department.
Location of the X-ray department in the hos
pital, relation of the darkroom to the X-ray
rooms, radiation protection, construction of
light traps etc. are important considerations in
planning a department. There should be some
didactic lectures of this important subject.
and it is upto the radiologist as the leader
the team to ensure this.
The Aim of Training
In India, as in most developing countrie there is a great dearth of radiologists.
study of manpower, facilities and utilisatioof radiological services was conducted in 1978
It was found that the level of the use i
Training of Diagnostic Radiologist
25
should be well balanced training programmes
which can produce sufficient members of
young, competent radiologists. capable • of
managing small departments alone and
interested in keeping their knowledge up to
date;-'■
Thank you
MAINSTREAMING GENDER IN PRE
SERVICE TRAINING OF HEALTH
PROFESSIONALS
Issues for discussion
Gender mainstreaming
The term ‘mainstream’ is used to indicate
that issues of gender inequality should be
dealt with in every aspect of organisational
structure and programming, rather than as a
separate, add-on activity. In other words,
gender inequalities should be addressed in
the mainstream of organisation and
programming.
* Having a module or a course addressing
gender issues in health may be seen as only
a first step in gender mainstreaming pre
service training of health professionals.
• The goal is to have gender issues addressed
integrally in all aspects and in all topics
included in the training.
• Process of gender mainstreaming
• Content of a ‘gender-mainstreamed’
curriculum
2
PROCESS
• First decisions
- Appropriate group to start with: Medical? (UG or
PG? Specific specialisations in PG?) Public
health? Nursing? Paramedical? Or combinations
of these?
- Factors governing this decision?
PROCESS
• Ground work
- Reviewing literature on education methodologies
and curricular integration efforts on gender and
other topics
- Mapping ongoing initiatives
- Identifying good practice examples
- Informal consultations with potential collaborators
and resource persons
- Developing an understanding of challenges and
constraints
PROCESS -2
Creating an enabling environment at national and
state levels, and within the institution
Long-term goal: Gender perspective becoming
part of the institutional/professional ethos and
culture
Short-term goal: Operationalising gender
mainstreaming of curriculum through: Favourable
attitudes; Formal policy; Adequate resources;
Functioning mechanisms to support (technical and
other), monitor and evaluate
PROCESS -3
• Identifying Change Agents to provide
leadership to and implement the process
• Capacity building for Change Agents
• Outlining a ‘piloting’ or ‘action-research’
process
• Planning for upscaling
CONTENT
Identifying Core Competencies in terms
of knowledge, skills, attitudes and values
that health professionals are expected to
have in order that they are competent to
provide health services/ plan health
programmes/ carry out health research that
integrates a gender (and social?) perspective
CONTENT -2
Carrying out curricular reviews to
identify competencies that are part of the
objectives and included in actual
training, mentioned in objectives but not
adequately addressed in actual training,
and competencies that are not included
even in the objectives
CONTENT -3
Identifying and generating teaching,
learning and assessment methods to fill in
gaps, starting with improving
competencies that are recognised as
needed but inadequately addressed in the
present curriculum
CONTENT -4
Identifying suitable entry points on a
casc-by-case basis for progressive
curricular changes-which topics, in
which years of training, through what
mechanisms (i.e. part of core teaching?
Special projects? Optional modules?)
6
n - 3%
/
Gender And
Medical Education
Sharon Fonn
MBBCh PhD FFCH
Prof. School of Public Health
University of the Witwatersrand
When to intervene?
• How big is the problem?
• How serious is the problem?
• Is there something that can be done?
Determinants
Why gender?
Differences between groups illustrates
what we understand about health
• .The reason for understanding gender
issues is not because women have
some intrinsic value over and above
men
• Rather because this is yet another
area where there are inequalities
Rich vs. poor
Rural vs. urban
Black vs. white
Male vs. female
Absorption
If we ignore gender
a flawed body of medical knowledge
providing students to potentially
incorrect information
preparing students inadequately to
<
deal with the issues that they will face
may result in programmes and
anu policies
that have less impact than they may if
they did take gender into account
breathing
through the skin
eating
affects the way toxins are dealt with in
the body
affects the way we metabolise drugs
Transdermal absorption: sweat
increases the absorption of water
soluble substances and impedes the
absorption of lipid soluble substances
Are we told
men exchange about 50% more air in a
given period than women
• men sweat more
pregnant women exchange 70% more air in
a given period than non pregnant women x
the larger blood flow in men and pregnant
women can deliver greater total amounts of
toxin to the target tissue
.
• men have thicker epidermal layers on
their upper extremities
• dermal hydration is greater for men
and pregnant women
• dermal blood flow is the same for men
and women but greater for pregnant
women
2
7g
In relation to ingestion:
• men have higher gastric acidity
enhancing the absorption of weak
acids and impeding the absorption of
weak bases
• women have increased residence
time in the stomach and intestines
during pregnancy due to lower motility
. for the same levels of alcohol intake
even after correcting for body weight.
women have higher blood alcohol
levels
In relation to metabolism men have a
higher basil metabolic rate and
metabolites can be either less or more
toxic than their parent compound
1
Zjg
is any of this relevant?
.
. The data we do have are usually developed — :
for the average man and we do not know if
exposures (toxins, drugs, etc.) are more
safe or less safe for women
. Women also have been systematically
d'jY/v;
excluded from many drug trials so that the
pharmacokinetics is not known for them
<
• Side effect profiles may be different
• Yet information is presented as finite and
fact
Common knowledge
• TB and leprosy are more common in men
. TB is known to be related to poor social
conditions
• Women make up 70% of the worlds poor
• So how come there are more men infected
with M Tuberculosis than women?
TB
Gender sensitive
research
Before the age of 15 boys and girls have
similar rates - then men begin to outstrip
women
Once infected with the bacillus only some
people become infected
Progression rate from infection to disease in
people aged 10 - 44 is 130% higher in
women than in men
• Yet more men than women are reported as
having TB infection.
• And more women than men die from TB
• Some must be explained by biological
differences
■ Some must be explained by gender
differences
■ Women's access to health services has
been described as more restricted than
men’s - and this could explain why women
are not diagnosed and reported as having
TB
. less access to treatment
• could explain the increased mortality
'ft
•'
■.
... •
Any evidence?
• Equal prevalence of malaria in men
and women in Thailand
• Men access services more
Any evidence?
Rresearch on leprosy has shown that
women are more likely to hide their
condition
Passive case finding, which relies on people
presenting themselves at a health service. identifies more men than women, but dbor
to door surveys find more women
Similar findings have been documented in
relation to leishmaniasis
Non communicable
disease
Traditionally, and still a popular belief, is the
notion that men have heart attacks
Women doing clerical work, married to blue
collar workers with 3 three children had a
higher risk of coronary health disease than
Caucasian male executives
Gender sensitive
research
It has been postulated that because of this belief
• women have not always received optimal treatment
• diagnosis in women takes longer (68 months for
women compared to 9 months in men in one study)
• they are referred later
• have fewer diagnostic tests
’
v
So what?
the example of myocardial infarction
illustrates how inadequate training can
impact on individual and population
health
what was taught to medical students
can prepare them inadequately for
future work
4
7g
Why worry about
gender?
Health programming
• To provide up to date adequate
medical education
• HIV infection is the biggest epidemic
facing medicine, science and society
• To impact on our ability to graduate
professionals who can adequately
treat individuals
• To improve our ability to impact on
population health
■-. ■
• As a sexually transmitted disease the
transmission of HIV is related to the
abilities of individuals to determine if.
when, with whom and how they have
sex
So - in relation to
progammes
In what way does gender play
in HIV?
How to prevent spread?
Women find it difficult to negotiate condom useo
High rates of rape^
Rape in marriage^
indicate how difficult it is for women to control the
sexual encounters
HIV programming must deal with women's
rights to control their own sexual relations
Reinforce the notion of joint responsibility
between individuals for sexual health
Making condom use more likely is one way
that sex could be safer for everyone
Is this approach used at every opportunity?
Antiretroviral treatment
during pregnancy and
childbirth
Z'W
• This has been called PMTCT - preventing
maternal to child transmission
• This terminology presents a missed
opportunity in trying to deal in a more
holistic way with the HIV epidemic
Technically correct
the virus passes from a mother to a
child - only women get pregnant -
: •;
• •
people working in public health are
long past focusing on the technical
aspects, to the exclusion of other
contributing factors, of disease
causation
- .
So what’s in a name?
it implies that the mother alone is
responsible for her child's infection
yet we know that women get infected from
sex with another infected individual
Negotiating when and how to have sex is
difficult for women
It seems apportioning blame here is not
useful or accurate
It is parents who are involved not just
mothers
Cnt.
To leave it to sound like the responsibility of
the mother alone is to compound the
problem
Why blame and shame a woman who is
likely to be devastated about having an ill
child in the first place
She also has less control over the nature of
her sexual encounters?
It also promotes the idea that women alone
are responsible for children.
Is this programming taking gender
issues into account?
• HIV programming must deal with women’s
rights to control their own sexual relations
• Reinforce the notion of joint responsibility
between individuals for sexual health
• No....
Will this help?
This language empowers men as well
as women to take responsibility for
protecting themselves and their
families
Avoids reinforcing blaming and
shaming stereotypes
OK one rhetoric for
another?
/’
There need to be programmatic
changes as well
Note that preventing children being
•>
born with HIV will not impact on the
jgJij
overall epidemic significantly
Need to prevent everyone (as many as
possible) becoming infected
-eg
6
How to prevention
infection?
What programme
changes?
Requires that people, men and
women, of any age take responsibility
for their sexual behaviour and the
consequences of that sexual
behaviour
Including being a parent to their
children irrespective of whether that
child is HIV positive or not.
Offers an opportunity to draw men into the
programme
Men could be invited to attend at least one
antenatal care visit with their partner
They can access information on PTCT
They can receive information on getting
tested and how this will benefit the family in
terms of prevention
Change social norms
a
They can also be part of the antenatal
"Si/V
HIV programming must deal with women's
rights to control their own sexual relations
This may promote them being involved
in the post natal care of their children <?E&Sk
Reinforce the notion of joint responsibility
between individuals for sexual health
Making condom use more likely is one way
that sex could be safer for everyone
Is this approach used at every opportunity?
care of their children
In other words insitutuions in society
begin to challenge a social norm that
women alone care for children
Condoms....
So - in relation to
progammes
How does this relate?
5-10% of pregnant women sero-convert
during the year that the they are pregnant
• Need to normalise condom use
The risk of PTCT goes up to 80% during
sero-conversion
Preventing new or re-infection in women at
any time during pregnancy and
breastfeeding would be an advantage to her
and to the couples' child.
7
So when we teach
Has anyone done this?
/
■ Suzanne Wil iams, Janel Seed and Adelina Mwau The
Develop methods that help to explore how
we relate
Illustrate that we relate in particular ways
that are patterned
Resources for reflecting are required that
enable us to see ourselves in new ways and
to imagine new ways of relating
To achieve this, it is essential that the
training methods include self-reflection.
Oxfam Gender Training Manual.
Hope. A. and Timmel. S. (1984). Training fOT
transformation Volumes 1 2 and 3.
Workshop on Gender, Health and
Development: Facilitator’s Guide, Pan
Ameri
can Heallh Organization (PAHO). Washington D C 1997
A few more
In closing
Fonn sWandHO Geneva
xaba m.1996Health Workers for Change.
WHP/
Varkey SJ. Fonn S. and Ketlhapile M. Health WOfkeFS for
ChOICe. Women's Health Project. Johannesburg. 2001.
KlugmanB. Fonn Sand Tint KS. Reproductive Health for
All. AIDOS Italy and Women's Health Project South Africa. 2001.
Cottingham J. Fonn S. Garcia-Moreno C. Gruskin S. Klugman B. Mwau A.
Rzvura/an s. snow r. xaea m. Transforming Health
Systems: Gender and Rights in
Reproductive Health. 2001. who
• 1 trust 1 have made my point
• If we seriously want to train people to
deal appropriately with the health
problem we face we must include
gender
The challenge to all of
us to is to move from
rhetoric to action, to
change the way we
teach and what we
teach.
9
sgv
Gender and Medical Education
Work so far
&
Strategies of the AMCHSS/SCTIMST
Medical Education
183 Colleges of Modern System (2001)
About half of them established in last 20 years,
a big majority of them in private sector
Produces over 20,000 doctors/year
Nearly 400 Colleges of Indian Systems of
Medicine 5U)d pf Hppieopathy
Produces about 15,000 doctors/year^
Over 80% of all doctors, and over £5% of
modern systems doctors in private-sector
1
AMCHSS/SCTIMST
• Being a national medical and public health
institute,*SCTIMST concerned about medical
education
”• AMCHSS was established in mid-1990s to
strengthen public health
• AMCHSS also has strong component og gender
in its training
• Discussion started in later part of 2001 and
culminated in consultation on Jan 31, 2002.
Project began in 3rd quarter of 2002
National Consultation, Jan 31, 2002 in Mumbai
OBJECTIVES
• Understanding the Needs for Gender Sensitisation
• Critiquing Content and Method of Medical Education
• Developing Long-Tein strategies for Intervention
QUESTIONS EXPLORED
• Is there a need to understand gender in medical
education?
• What is the nature of this need?
• How do we approach this need?
• Whom would we approach?
Issues Raised
RELATED TO MEDICAL PRACTICE
• Women needs are often ignored, though
women’s bodies are sites of exploitation and
malpractice
• Unnecessary/irrational drugs and surgeries,
unethical trials, etc.
• Population control policies target women
• Doctors do not provide information to women,
for informed consent only husband is consulted
or husband’s consent demanded
Issues Raised
RELATED TO MEDICAL PRACTICE
• Even women’s reproductive health issues are
given less importance
• Women’s specific problems and needs in
disease conditions are studied less and are
ignored
• Lack of continuing training and orientation
• Etc.
5
What should be the process of engendering medical
education and practice and other stakeholders & groups?
• Gender sensitive healthcare involves 'unpacking
patients'.
• It means looking at men and women patients and their
specific needs, look at what class backgrounds and
cultural backgrounds they belong to, examining
presumptions and stereotypes that have been
entrenched.
• re‘cbgnisingithfc.ftfdt that patients come from households
and they live in a social environment.
• Gender could be used as an indicator because it
incorporates all kinds of inequities.
W|j(jt should be the process of engendering medical
education and practice and other stakeholders & groups?
• There should be a gender analysis of the
different diseases.
r The medical systemispremised on the
assumption that there is a family, which is able
and willing to carry outthe role of caring.
Women really struggle to fit into this.
perspective because they often do not have this
kind of support.
7
Strategies, Tools and Mechanisms for
Engendering Medicine - General
Research topics related to gender must be given to
students
In student selection for medical schools, gender
sensitivity should be one of the=criteria. This will also
start influencing the school education
Introduction of rights perspective in medical education
with appropriate emphasis on gender
Social science teaching in medicine needs to be
introduced or improved
Identify gender sensitive trainers
Strategies, Tools and Mechanisms
Changes in the curriculum
First priority would be to develop a module for
under-graduate medical students because they
form the large majority of the medical students
To use the existing network of medical colleges
for introducing innovations in medical
curriculum
Existing literature and training modules on
gender should be reviewed and adapted for use
Documentation of local level initiatives in this
field
9
Strategies, Tools and Mechanisms
Changes in the curriculum
• Should we do review of present curriculum to
make recommendations on what should be
removed for being gender biased?
• Thus, critical review of existing textbooks from
gender perspective is essential. Such material
will be useful in training as well as in sensitising
the authors
• For multiplier effect, training of the trainers
and policy makers should be given importance
Strategies, Tools and Mechanisms
Setting in which ME is provided
Changes in the curriculum and teaching would
not be sustainable unless there are structural
changes made in the institutions and actual
practice is re-oriented.
For gender sensitisation, engendered setting is
also required
Gender hierarchies in medicine, and strategies
at institutional level to reduce and eliminate
them and discrimination that goes along with
them
II
The AlWCHSS/SCTIMST Project
• National Consultation
• Designing Training-dlJTrainers’ module
• Training-Of-Trainers
• Training of two or three medical teachtrs of all medical
colleges in six states
• Review of medical Text books
• National seminar
• National Conference of decision makers
- Media
 RF_MP_8_D_SUDHA.pdf
RF_MP_8_D_SUDHA.pdf
Position: 1266 (9 views)