MEDICAL ETHICS
Item
- Title
- MEDICAL ETHICS
- extracted text
-
RF_MP_2_PART_2_SUDHA
NUREMBERG DOCTORS’ TRIAL
l0~*14
Informed consent in human experimentation before the
Nuremberg code
;3d°n of,
,on
m°grs^
' has>Sot.
>436,0,■
.
Pnorte^,
hagej b)
« before
Jochen Vollmann, Rolf Winau
qj Muranbog issue of the
‘^comprises seven
in this special
^en, editorials by
^er Leaning and
^ald Acheson, two
■’derljinj’. rKnal views, four news
7>butnp. jps and three book
xias. In addition, we are
/dishing on
//1448-9 the Nuremberg
™ptured: 'adefwm 1947 and the
ed if the Dedaration of Helsinki that
aadavxdfrom it. All the
Svmberg material is
twiable on the BMJ's
impage: hap://
flhe1
COM
?b3e,
rstfc.
pt the History of
“*» Free University
12203 Berlin
, professor
and
The issue of ethics with respect to medical experi
mentation in Germany during the 1930s and 1940s
was crucial at the Nuremberg trials and related
trials of doctors and public health officials. Those
involved in horrible crimes attempted to excuse
themselves by arguing that there were no explicit
rules governing medical research on human
beings in Germany during the period and that
research practices in Germany were not different
from those in allied countries. In this context the
Nuremberg code of 1947 is generally regarded as
the first document to set out ethical regulations in
human experimentation based on informed
consent. New research, however, indicates that
ethical issues of informed consent in guidelines
for human experimentation were recognised as
early as the nineteenth century. These guidelines
shed light on the still contentious issue of when the
concepts of autonomy, informed consent, and
therapeutic and non-therapeutic research first
emerged. This issue assumes renewed importance
in the context of current attempts to assess liabil
ity and responsibility for the abuse of people in
various experiments conducted since the second
world war in the United States, Canada, Russia,
and other nations.
First Prussian directive on informed consent
The introduction of scientific and experimental
methodology into clinical medicine in the nineteenth
century brought with it an increased demand for
experimentation on human subjects, particularly in
bacteriology, immunology, and physiology. This
research was done mainly on patients in hospital, often
without their consent, under an “ethos of science and
medical progress.” As a result of injury to some patients
subjected to non-therapeutic research, however, contro
versy and public debate ensued about the ethics of
human experimentation.1"1
In 1891 the Prussian minister of the interior issued a
directive to all prisons that tuberculin for the treatment
of tuberculosis “must in no case be used against the
patient’s will.’” But the first detailed regulations about
non-therapeutic research in Western medicine came
from the Prussian minister for religious, educational,
and medical affairs in 1900. They were issued after
critical public discussion and political debate on the
Neisser case in the Prussian parliament and set forth the
legal basis of disclosure and unmistakable consent.1 ’ Of
particular interest is the debate within the medical pro
fession and the political circumstances.
The Neisser case
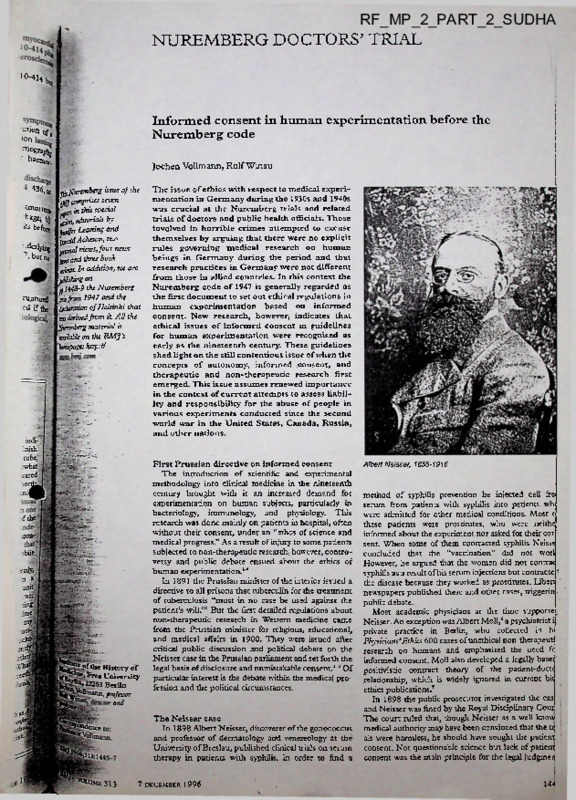
In 1898 Albert Neisser, discoverer of the gonococcus
and professor of dermatology anti venereology at the
University of Breslau, published clinical trials on serum
therapy in patients with syphilis. In order to find a
313
7 DECEMBER 1996
Albert Neisser, 1855-1916
method of syphilis prevention he injected cell fre
serum from patients with syphilis into patients wh
were admitted for other medical conditions. Most <
these patients were prostitutes, who were neithe
informed about the experiment nor asked for their cor
sent. When some of them contracted syphilis Neisse
concluded that the “vaccination” did not worl
However, he argued that the women did not contrac
syphilis as a result of his serum injections but contracte '■
the disease because they worked as prostitutes. Libert
newspapers published these and other cases, triggerin .
public debate.
Most academic physicians at the time supporte.
Neisser. An exception was Albert Moll,‘ a psychiatrist i
private practice in Berlin, who collected in h
Physicians’Ethics 600 cases of unethical non-therapeut
research on humans and emphasised the need f<
informed consent. Moll also developed a legally base<
positivistic contract theory of the patient-doctc
relationship, which is widely ignored in current bit
ethics publications.’
In 1898 the public prosecutor investigated the cas
and Neisser was fined by the Royal Disciplinary Cour
The court ruled that, though Neisser as a well know
medical authority may have been convinced that the u;
als were harmless, he should have sought the patient
consent. Not questionable science but lack of patienj
consent was ±e main principle for the legal judgmen
144
explanation of the possible negative conseqUen fl
the intervention. All research interventions Co«
The Prussian parliament also discussed
As performed only by the medical director or with k 3
eral times and in 1899 asked the government toct. As
her authorisation. In all cases fulfilment of?1*
a result the minister for religious educat onal and requirements as well as all further circumstances^
medical affairs commissioned a detailed repor
case had to be “documented in the medical histo
Scientific Medical Office of Health, wh.ch» Despite all this, however, the directive was not uS
composed of leading German physicians such as Rudolt binding and little is known of its impact °n hu3'l
Virchow. The commission directed its attention to experimentation.
%
beneficence and autonomy. It concluded that a
physician who recognised that an injected serum might
Circular
of
the
Reich
minister
of
the
interior;
;1
cause infection had no right to inject such a serum, n
’
|
any case, both informing the subject and obtauung the guidelines for new therapy and human
-'-JB
subject’s consent were preconditions to experimenta experimentation, 1931
tion. In a handwritten report Emil von Behring argued
Because of criticism of unethical human experin^:
that, particularly with reference to the Neisser case, selt tation in the political press and in parliament as we]j~;
experimentation should always precede experiments on in the context of a political reform of criminal law^l
patients. He personally held that purely scientific Germany, in 1931 the Reich government iSsu® 1
experimentation on human subjects was unethical even detailed “guidelines for new therapy and human expajj
mentation.” The guidelines clearly distinguish^!
if they gave voluntary consent.'
The minister also sought legal advice on the Neisser between therapeutic (“new therapy”) and noify:
case. Lawyers stated that conducting non-therapeutic therapeutic research (“human experimentation”)
research on a subject without consent fulfilled the crite ser out strict precautions.
ria for causing physical injury in criminal law. The
Besides the principles of beneficence and doqS
scientific validity of the experiment did not serve as maleficence, the regulations were based on patient
mitigation. Informed consent was a mandatory precon autonomy and a legal doctrine of informed consent^
dition for any non-therapeutic research. Problems of “New therapy may be applied only if consent or proxji^
coercion, persuasion, and the unequal authority consent has been given in a clear and undebatable man- between doctor and patient were discussed in detail, ner following appropriate information. New therapy®
and the lawyers concluded that respect for rights and may be introduced without consent only if it is urgently^
morality had the same importance for the good of man required and cannot be postponed because of the need'*'
kind as medical and scientific progress. Written to save life or prevent severe damage to health....” In3
documentation and clear responsibility of the medical those cases a written report must clearly outline thea
director for all human experimentation became legal preconditions. But non-therapeutic research was®
doctrine.
“under no circumstances permissible without®
Finally, in 1900 the minister for religious, consent.’”
Written documentation and a clear .
educational, and medical affairs issued a directive to all structure of responsibility for each clinical trial were «
hospitals and clinics.. Medical directors were advised
required. Though an early model of institutional reviewS
that all medical interventions other than for diagnosis, boards was discussed, the official guideline adopted the
healing, and immunisation were excluded under all cir hierarchical model from the directive of 1900, in which;,. cumstances if “the human subject was a minor or not the medical director was responsible for all clinical ■
competent for other reasons” or if the subject had not
research in the institution.
given his or her “unambiguous consent" after a “proper
As later formulated in the Nuremberg code, a careful9
cost-benefit calculation and a detailed research pta'-h
with animal experimentation beforehand were already >
required to minimise risk to human subjects. Some.gB
regulations were even stricter and more detailed than.
those contained in the Nuremberg code and the much
later Declaration of Helsinki. Human experimentation /
on dying patients was absolutely prohibited. Publication . >
of the results of new therapy must respect the patient S'--..
dignity and the mandate of humanity. In academical
teaching every opportunity should be taken td|$
emphasise the special responsibilities of a physician/
undertaking clinical trials. Even further, any exploi^fe
lion of social or economic need in testing new therapies
was rejected.
GOVERNMENT AG I iu.>
Discussion
This paper shows that explicit directives concerned /:<
with the welfare of people subjected to medical
mentation in Germany were in place long before th*
Nuremberg code was devised in 1947.w: Critical pies’ *
reports and debate in parliament forced the Prussia” /
government to issue the first directive concerned with,.
medical experimentation in humans in 1900.
directive was based on medical and legal scientific. .<
reports. A clear distinction was made berwee®,. ■
therapeutic and non-therapeutic research, but regm”-'^
tions were issued only for non-therapeutic .reseat™'
The regulations were based on the principle .
/”
autonomy and represented an early model of
consent. A “proper explanation of the possible neg”” $
Medical experimentation on a metabolic ward of the Kaiserin Auguste Victoria Haus Berlin In
consequences” of the intervention and “unamb'Su.oU. ■'
the 1920s
consent” became the mandatory standard. In ”ddiD .
1446
and do™’and imba'an<:e °f aUth0^' benveen patent’
■
m
’USt u- “ contemFora>'y work." Minors and
incompetent sublets were generally excluded from
?nfn’dl'’7PeUtlC research’ as
could not give valid
informed consent.
We conclude that at the turn of the century informed
consent was already a legal doctrine in medical experi
mentation in Germany, being based on “unambiguous
consent of the subject after “proper” information had
been given by the doctor, including negative conse
quences and side effects. Interestingly, the regulations
were not initiated by doctors or research institutions but
were issued by government authorities. However, it
remains an open question how informed consent was
applied by doctors in research and clinical practice and
how it shaped the individual doctor-patient
relationship.'*’"
The guidelines issued by the Reich government in
1931 regulated therapeutic and non-therapeutic
research in human subjects. Whereas without exception
non-therapeutic research could be performed only with
the subject’s informed consent, therapeutic research
could be performed without explicit consent but only in
a* medical emergency and if it was deemed to be in the
patient’s best interest.
The second part of the Prussian directive of 1900
defined a structure of responsibility in medical
institutions. Because of the hierarchical structure in
German hospitals only the medical director and
physicians authorised by the medical director were
allowed to conduct research on human subjects.
experimentation was the issue of responsibility contro
versial, as all medical directors and professors declared
their personal responsibility. This hierarchical model of
responsibility, also found in the Reich government’s
guidelines of 19 31, differs from the modern concept of
responsibility in clinical research. Under current
concepts the individual researcher is personally respon
sible for his or her actions and ethical issues are assessed
by peers on institutional review boards.
For the first time in history informed consent, the
research process, and explicit clarification of personal
responsibility for the experiment were required to be
included in the medical record. In addition, issues of
written research plans with a risk-benefit assessment,
the need for previous animal experimentation, and
medical self experimentation were raised. Though a
system of public health insurance existed in Germany in
1931 and provided good health care for all citizens,
issues of social justice and the protection of poor people
in medical research were regulated. We question
whether the healthcare system in the United States
would meet these regulations, many patients without
health insurance having no access to regular medical
treatment. In order to obtain medical help these patient
must rely on free experimental treatment in research
institutions without having a choice whether to give free
and autonomous informed consent.
Though present conceptions of informed consent
differ from those in the Prussian directive of 1900 and
the Reich government’s guidelines of 1931, some basic
elements can be identified in postwar regulations” “
together with many ethical issues of human
experimentation.”-” Our primary objective was to show
that the basic concept of informed consent was
developed long before the second world war and before
Nazi crimes in Germany, not on the initiative of the
medical profession or research community but as a legal
doctrine by government authorities. The guidelines of
1031 were not annulled in Nazi Germany, when unethi
cal experiments were performed by German doctors m
concentration camps. Though no other nation seems to
have had such ethically and legally advanced regulations
Key messages
• The Nuremberg code of 1947 is widely regarded
as the first document providing ethical regulations
in human research on the basis of informed
consent
• New research has uncovered ethical issues of
informed consent in human experimentation as
early as the nineteenth century
• Regulations were not initiated by the medical
profession but were issued after critical public dis
cussion and political debate
• Basic elements of the modern legal concept of
informed consent can be found in these early regu
lations
• These early regulations were not binding in the
legal sense and little is known about their actual
impact on clinical research
at the time, these did not prevent crimes against
humanity by part of the German medical profession?"2
We thank Mrs M A Shiftman for help with the English trans
lation and Dr Thomas Lennert (department of paediatrics,
Free University of Berlin) for the photograph of the medical
experiment at the Kaiserin Auguste Victoria Haus.
Funding: Deutsche Forschungsgemeinschaft (German
Research Council; grant Vo 625/1-3).
Conflict of interest: None.
Official Regulations
6
7
8
Germany and Italy. J/I.U.-I
Moll A. Arzthche Elhik. Stuttgart; F.nke. 1902.
Schultz JH. Albert Mods Arctluhe Ethlk. Zurich: Juris, 1986.
Luther E, Thaler B. Das hippokrarische Ethos. Untersuchungen :u Ethos und
Praxis in der deutchen Arzteschaft. Halle (Saale): Wissenschafthchc
Bcitrage der Martin-Luther-Universitat Halle-Wittenberg. 1967
Lambert Schneider, 1949. (English translation: Doctors ofinfamy. The story
tmd Gcistcskrankcn 1933-1945. Reinbeck bei Hamburg: Rowohlt, 1984
Press, 1989.
Totowa: Humana Press, 1991.
York: Oxford University Press, 1986.
of Ethical Problems in Medicine and Biomedical and Behavioral
Research, ed. Making health care decisions. Vol 3. Washington, DC: US
Government Printing Office, 1991.
16 Vollmann J. Das Informed Conseni-Modell als Politikum in der Medium. Pasicntenaufkldrung und Eimsdligung am historischer und medixmethischer
Perspektive. Frankfurt am Main: Suhrkamp (in press).
17 Annas GJ. The changing landscape of human experimentation:
Nuremberg, Helsinki and beyond. Health Matrix J Law Med 1992;2:119-
18 Sass HM. Reichsrundschreiben 1931: pre-Nuremberg German regulations
concerning new therapy and human experimentation. J Med Philos
1983;8:99-111.
19 Beecher HK. Ethics and clinical research. N EnglJ Med 1966374:1354-60.
York: Russell Sage Foundation, 1972.
21 Jones JH. Bad blood: the Tuskegee syphilis experiment. New York Free Press,
.1981.
Washington, DC: Government Printing Office, 1995.
23 Smith R. Time to face up to research misconduct. BMJ 1996312:789-90.
(Accepted 28 October 1996)
The Nuremberg Code (1947)
3.
The experiment should be so designed and-Rl
on the results of animal experimentation and a $9
edge of the natural history of the disease
problem under study that the anticipated
justify the performance of the experiment.
4.
The experiment should be so conducted as t0 •
PERMISSIBLE MEDICAL EXPERIMENTS
The great weight of the evidence before us to effect all unnecessary physical and mental suffering
that certain types of medical experiments on human injury.
beings, when kept within reasonably well-defined 5.
No experiment should be conducted where 4
bounds, conform to the ethics of the medical an a priori reason to believe that death or disjivl
profession generally. The protagonists of the practice injury will occur; except, perhaps, in those einS
ments
where the experimental physicians also s^l
of human experimentation justify their views on the
basis that such experiments yield results for the good subjects.
'afl
The degree of risk to be taken should never etS
of society that are unprocurable by other methods or 6.
means of study. All agree, however, that certain basic that determined by the humanitarian importa^S
principles must be observed in order to satisfy moral, the problem to be solved by the experiment
ethical and legal concepts:
7.
Proper preparations should be made and adeqji
1.
The voluntary consent of the human subject is facilities provided to protect the experimental su$S
absolutely essential. This means that the person against even remote possibilities of injury, disability™!
involved should have legal capacity to give consent; death.
should be so situated as to be able to exercise free
8.
The experiment should be conducted bnjy|a
power of choice, without the intervention of any
scientifically qualified persons. The highest degree^
element of force, fraud, deceit, duress, overreaching,
skill and care should be required through all stages^
or other ulterior form of constraint or coercion; and
should have sufficient knowledge and comprehension the experiment of those who conduct or engage inM
experiment.
M
of the elements of the subject matter involved as to
During the course of the experiment the humi
enable him to make an understanding and enlightened 9.
decision. This latter element requires that before the subject should be at liberty to bring the experiments
acceptance of an affirmative decision by the experi an end if he has reached the physical or mental stag
mental subject there should be made known to him where continuation of the experiment seems to himi
'JS
the nature, duration, and purpose of the experiment; the be impossible.
method and means by which it is to be conducted; all
10.
During the course of the experiment the scientH
inconveniences and hazards reasonably to be expected; in charge must be prepared to terminate dx
and the effects upon his health or person which may experiment at any stage, if he has probable cause#
possibly come from his participation in the experiment. believe, in the exercise of the good faith, superior ski
The duty and responsibility for ascertaining the qual and careful judgment required of him, that a coritinS
ity of the consent rests upon each individual who ini ation of the experiment is likely to result in injury,
tiates, directs, or engages in the experiment. It is a ability, or death to the experimental subject.
.-j
personal duty and responsibility which may not be
delegated to another with impunity.
2.
The experiment should be such as to yield fruitful
results for the good of society, unprocurable by other
Taken from Mitscherlich A, Mielke F. Doctors of m/mnyikj
methods or means of study, and not random and story of the Nazi medical crimes. New York: Schuman, 19^
unnecessary in nature.
xxiii-xxv.
The judgment by the war crimes tribunal at
Nuremberg laid down 10 standards to which
physicians must conform when carrying out experi
ments on human subjects.
J'
Declaration of Helsinki (1964)
Recommendations guiding physicians in biomedical
research involving human subjects
Adopted by the 18th Vfbrld Medical Assembly, Helsinki,
Finland, June 1964, amended by the 29th Ifbrld Medical
Assembly, Tokyo, Japan, October 1975, and the 35th
World Medical Assembly, Venice, Italy, October 1983
INTRODUCTION
It is the mission of the physician to safeguard the
health of the people. His or her knowledge and
conscience are dedicated to the fulfilment of this
mission.
The Declaration of Geneva of the World Medical
Association binds the physician with the words, “The
health of my patient will be my first consideration,”
and the International Code of Medical Ethics declares
that, “A physician shall act only in the patient’s
interest when providing medical care which might
have the effect of weakening the physical and meo
condition of the patient.”
?3
The purpose of biomedical research *nV0,uji
human subjects must be to improve diagnostic, i
peutic and prophylactic procedures and the u° 3
standing of the aetiology and pathogenesis of d*s'jS
In current medical practice most diagnostic,
■
peutic or prophylactic procedures involve
This applies especially to biomedical research. “3
Medical progress is based on research
ultimately must rest in part on experimentation
human subjects. In the field of biomedical rese ■ J
fundamental distinction must be recognised
-J
medical research in which the aim is essentially
tic or therapeutic for a patient, and medical reseat“L,i>
essential object of which is purely scientific and
g
implying direct diagnostic or therapeutic value -U
person subjected to the research.
BMJ VOLUME 313
199?
7 DECEMBER*
caution must be exercised in the conduct of
which may affect the environment, and the
of animals used for research must be
fS&i.
^uSe it is essential that the results of laboratory
Wyjjents be applied to human beings to further
^c knowledge and to help suffering humanity,p^brld Medical Association has prepared the
Jgjing recommendations as a guide to every physibiomedical research involving human subjects.
should be kept under review in the future. It
i^Jbe SIieSSe!1-that
standards as drafted are only
r&je to physicians all over the world. Physicians are
Sdieved from criminal, civil and ethical responsiunder the law of their own countries.
principles
■ Biomedical research involving human subjects
a'jst; conform to generally accepted scientific
-qndples and should be based on adequately
' ^-formed laboratory and animal experimentation
redfin a thorough knowledge of the scientific
-•uature.
■_ fhe design and performance of each experimental
pnxxdure involving human subjects should be clearly
Simulated in an experimental protocol which should
■ be transmitted to a specially appointed independent
committee for consideration, comment and guidance.
3. Biomedical research involving human subjects
should be conducted only by scientifically qualified
persons and under the supervision of a clinically com: peteat medical person. The responsibility for the
' human subject must always rest with a medically
qualified person and never rest on the subject of the
f research, even though the subject has given his or her
| consent.
B i Biomedical research involving human subjects can' not legitimately be carried out unless the importance
of the objective is in proportion to the inherent risk to
..die subject.
! 5. Every biomedical research project involving human
' subjects should be preceded by careful assessment of
-.Predictable risks in comparison with foreseeable benf efiBto the subject or to others. Concern for the inter.-jritt' of the subject must always prevail over the
■ iiat&ests of science and society.
The right of the research subject to safeguard his or
integrity must always be respected. Every precaufeton should be taken to respect the privacy of the subRjjjtand to minimize the impact of the study on the
Kpoject’s physical and mental integrity and on the perft^Sality of the subject.
^.Physicians should abstain from engaging in
^earch projects involving human subjects unless they
^'satisfied ±at the hazards involved are believed to
^Predictable. Physicians should cease any investigajS-jPon if the hazards are found to outweigh the potential
>-Mnefits,
^Publication of the results of his or her research,
Egphysician is obliged to preserve the accuracy of the
Exults. Reports of experimentation not in accordance
Effift 'the principles laid down in this Declaration
fejjjjuld not be accepted for publication.
any research on human beings, each potential
LzJVft must be adequately informed of the aims,
KSShods, anticipated benefits and potential hazards of
BE&study and the discomfort it may entail. He or she
ErK-Uld be informed that he or she is at liberty to
HSfcam from participation in the study and that he or
8 free to withdraw his or her consent to participa
VOLUME 313
7 DECEMBER 1996
tion at any time. The physician should then obtain the
subject’s freely given informed consent, preferably in
writing.
10. When obtaining informed consent for the research
project the physician should be particularly cautious if
the subject is in a dependent relationship to him or her
or may consent under duress. In that case the
informed consent should be obtained by a physician
who is not engaged in the investigation and who is
completely independent of this official relationship.
11.
In case of legal incompetence, informed consent
should be obtained from the legal guardian in accord
ance with national legislation. Where physical or men
tal incapacity makes it impossible to obtain informed
consent, or when the subject is a minor, permission
from the responsible relative replaces that of the sub
ject in accordance with national legislation. Whenever
the minor child is in fact able to give a consent, the
minor’s consent must be obtained in addition to the
consent of the minor’s legal guardian.
12.
The research protocol should always contain a
statement of the ethical considerations involved and
should indicate that the principles enunciated in the
present declaration are complied with.
II. MEDICAL RESEARCH COMBINED WITH PROFESSIONAL
CARE (CLINICAL RESEARCH)
1.
In the treatment of the sick person, the physician
must be free to use a new diagnostic and therapeutic
measure, if in his or her judgement it offers hope of
saving life, re-establishing health or alleviating
suffering.
2.
The potential benefits, hazards and discomfort of a
new method should be weighed against the advantages
of the best current diagnostic and therapeutic
methods.
3.
In any medical study, every patient—including
those of a control group, if any—should be assured of
the best proven diagnostic and therapeutic method.
4.
The refusal of the patient to participate in a study
must never interfere with the physician-patient
relationship.
5.
If the physician considers it essential not to obtain
informed consent, the specific reasons for this
proposal should be stated in the experimental protocol
for transmission to the independent committee (1, 2).
6.
The physician can combine medical research with
professional care, the objective being the acquisition of
new medical knowledge, only to the extent that medi
cal research is justified by its potential diagnostic or
therapeutic value for the patient.
III. NON-THERAPEUTIC BIOMEDICAL RESEARCH INVOLVING
HUMAN SUBJECTS (NON-CLINICAL BIOMEDICAL
RESEARCH)
1.
In the purely scientific application of medical
research carried out on a human being, it is the duty of
the physician to remain the protector of the life and
health of that person on whom biomedical research is
being carried out.
2.
The subjects should be volunteers—either healthy
persons or patients for whom the experimental design
is not related to the patient’s illness.
3.
The investigator or the investigating team should
discontinue the research if in his/her or their judgment
it may, if continued, be harmful to the individual.
4.
In research on man, the interest of science and
society should never take precedence over considera
tions related to the well-being of the subject.
INTERNATIONAL CONFERENCE
HEALTH POLICY : ETHICS & HUMAN VALUES NEW DELHI 1986
Ethics and Human Values in
Medical Education
O. P. Bhatnagar
Prof, of Physiology, Maulana Azad Medical College
New Delhi
In India little attention has so far been paid to the teaching of
“code of ethics and human values’’ to the medical students during their
periods of undergraduate and postgraduate medical education. However
it has been realised that the well trained doctors should be able to meet
the health and allied needs of the community by fulfiling their obligations
and duties towards them. Bhatnagar et al. (1977) have discussed the
competencies in terms of skills, knowledge and attitudes, which the student
may have to learn preferably in a family/community environment, parti
cularly in the rural areas, for becoming a doctor who, in future, is likely to
go in for family medicine/general practice. Such need based rural oriented
training must include the managerial and supervisory skills, basic principles
of research i.e. collection, recording and interpretation of data, and capability-to deliver the comprehensive health care including the preventive,
promotive, curetive, disability—limiting and rehabilitative services, Dr. P.C.
Bhatia, Dean IMA College of General Practitioners, India, (1983) has
drawn a training grogramme including ethical, moral and social aspects of
Family Medicine/General Practice, for postgraduates in these subjects.
While evolving the National Health policies an attempt has been
ipade tc —~^gjde comprehensive health care to ALL, atleast at the Primary
level.
specialist care can be referred to Secondary
or Intermediate Health Care organisations based in or about the district.
Only few selected cases meriting the attention of super-specialists
for Advanced Medical Techology should alone be referred to the tertiary
health care level institutions located in teaching hospitals and Institutes
of National importance. However this system is failing due to our defec
tive Referral services, which are not optimal and criteria-oriented and
because in the opinion of most, in developing countries like India primary
health care to ALL should still be given preference over the costly life
saving demands for few (Bhatnagar et. al., (1982).
The code of Ethics and human values helps guide the National
Health Policy Planners, to examine the priorities and moral validity of
choices available to them. They have to take decisions in terms of Equity,
social Justice, care for all, value of human dignity and life, sociocultural
and religious traditions and moral validity, within the constraints of
availability of Men, Material, Money, Equipment and other resources.
The code of Ethics and human values- commit the medical practi
tioners to certain social values above the selfish ones e.g, of income,
power, and prestige etc. Medical ethics also dedicates the Doctor to the
HIGHER VALUES OF SAVING OF LIVES and the PROTECTION OF
PATIENTS HEALTH—ABOVE ALL MATERIAL AND PERSONAL
CONSIDERATION (RALPH W. TYLER-1952).
[A list of ethical and human values to be learnt by a doctor is given
at the end of this presentation as an appendix.]
It must be realised that moral attitudes and human values are never
inborn. They have always to be learnt consciously in programmes of not
only medical education but also from the education involved in socio
cultural, political and religious activities, Mostly they are developed from
observations and opinions expressed by their seniors, but they can be
consciously developed by motivating the individual to think, feel, actively
participate and often derive satisfaction from a real-life or simulated
situation; thereby developing a relevant desired learning behavioural
pattern/opinion. An occasional feedback from the teacher will facilitate
the development of such a learning.
As these moral attitudes and human values are LINKED WITH
EMOTION, they are relatively vague, impressionistic, and ill-defined and
therefore DIFFICULT TO MEASURE. Yet, some measurement is better
than no measurement, and therefore, changes in behaviours and opinions
are gainfully used to infer the development of a change in attitude (Razler
1973; Bhatnagar 1983)
Before I close, I take this opportunity to thank the organisers of
this International conference on Ethics and human values, for inviting
me to participate and thereby allow me to contribute and to learn from
its proceedings. I hope the free and frank discussions during these deli
berations will be sincerely followed and the results will be fruitful to all.
APPENDIX
List of Ethical and Human Values to be Learnt by a Doctor
The doctor should be able to develop :—
1.
Healthy patient-doctor relationship, with ability to advocate the
patients cause.
2.
Healthy doctor-doctor and doctor-paramedical relationship.
3.
Intrinsic goodness, kindness, understanding, compassion, patience,
politeness, courtesy, helpfulness, trust, personalised attention, good
bedside manners, and moral character.
4.
Excellence in his work, ability to provide advice about genetic
and marriage counselling, health legislation, medicolegal procedures and
family problems after death.
5.
realisation of limitations for referrals.
6.
Respect for national and cultural traditions and for other systems
of medicine.
2
9
?• Ability to rehabilitate vulnerable, handicapped and terminally
ill patients.
Note : Such a list can never be complete, all are welcome to and.
References
1.
Agnes, G. Rezler (1973), The assessment of attitudes, W.H.O.
(1973) Public Health Papers, 52.
2.
Bhatia, P.C. (1983), Residency Training in General Practice,
Family Medicine—A Plan.
3.
Bhatnagar, O.P. et.al. (1977), Health needs of the community—
conclusions of a workshop on medical education. Ind. Jour. Med. Ed.
(1977), 16, 1-5.
4.
Bhatnagar, O.P. et.al. (1977), Duties and obligations of a basic
doctor in relation to health needs of the community. Ind. Jour. Med. Ed.
(1977), 16, 1-9.
5.
Bhatnagar, O.P. et.al. (1977), Suggesting improvements in the
curriculum for the teaching of Physiology and Biochemistry in the fulfil
ment of the duties and obligations of a basic doctor towards the commu
nity—conclusions of a workshop on medical education. Ind. Jour. Med.
Ed. (1977), 16, 1-22.
6.
Bhatnagar, O.P. et.al (1982), Educational consequences of com
prehensive health care—curriculum development tertiary level.
Ind. Jour. Med. (1982), 21, 1-8.
7.
Bhatnagar, O.P. (1983), Evaluation techniques for assessing the
role of social and behavioural sciences in catalysing population change.
Ind. Jour. Med. Ed. (1983), 22, 92-94.
8.
Bryant, John. H. and Bankowski Zbigniew (1984), Health
policy : Ethics and Human Values—An international dialogue—Highlights
of XVIII CIOMS Conference—Athens 1984).
9.
Ralph W. Tyler (1952), Distinctive attributes of education for the
professions. Social work journal of the American Association of Schools
of Social Work—(April 1952).
INTERNATIONAL CONFERENCE
HEALTH POLICY : ETHICS & HUMAN VALUES NEW DELHI 1980
New Trends in Medical Education
Technology Particularly in Relation
to Physiology Teaching
Rai U.C.
Department of Physiology
Lady Hardinge Medical College, New Delhi
Introduction
Medical Education has been a source of concern for many years to
those involved in the training of health personnel. Changes in socio
economic conditions in all parts of the world and more so in India have
been deeply influencing the health status as well as the health needs and
demands of the population but hardly any account has been taken to these
changes and the training of health personnel is still the traditional one as
utilised in the past. It seems reasonable to believe that an educational
programme has more chance of being effective if its goals have been clearly
expressed. Experimental research in this connection indicates that it is
not possible to measure the results obtained from an educational system if
its objectives have not been explicitly defined (Guilbert 1976).
What is required, is to make sure that educational programmes are
made relevant to the health needs of the community. Educational objec
tives must be generated on the basis of data obtained from multiple
sources e.g. Health needs, demands and resources of the society, services
to the patients and to the community, production of health personnel
e.g. practising doctors, teachers and research workers.
After this all the departments in a medical college should develop
the departmental objectives on the basis of which staff members who are
assigned teaching would develop specific intructional objectives. A recent
study suggest that the systematic attempt to write INSTRUCTIONAL/
learning objectives leads to clarification of an instructors goal and provides
the basis for dialogue with colleagues which in turn may lead to further
refinement of one’s objectives. Clear understanding of objectives leads
to better decisions in the teaching and evaluation process (William
etal, 1982).
Educational Technology
Teaching has been defined as a process of helping learners to learn.
As such, it is not merely an art to which one is born but a science that
should be learnt by all future teachers. It is increasingly recognised that
being, for example, a good researcher is no guarantee of being a good
teacher. Awareness is growing that teaching skills are far too important
and there is a need for systematic, conscious preparation of teachers for
their professional tasks (Fulop, 1978).
Most teachers training courses focus attention on the model of
competency based curriculum. Learning objectives are derived from
competencies that a student should acquire. Content and Teaching methods
in turn are dependent upon the learning objectives and evaluation of
students performance (Me Gahie etal, 1978).
Physiology teaching
Methods of teaching physiology fall into the traditional categories
of lectures, tutorials, practicals and demonstration classes. The other
methods are Seminar, Symposium or Group discussions. Some methods
recently introduced are problem based learning; programmed learning or
competency based learning and teaching physiology in the Hospital set up
to make it clinically oriented right from the 1st year curriculum.
Lectures
It is a careful presentation of facts with organised thoughts and ideas
by a qualified person. Lectures continue to be the corner stone of medical
education and efforts should be made to make them more interesting by
the use of audio-visual aids. Moreover, if a students 700 to 1000 lectures
in their preclinical years than a legitimate concern of Medical educators
should be to make lectures efficient for recording by students (Brown 1980).
The advantages of lecture are that they provide upto date and large
amount of material in short time, covers a large group of students and
there is an apparent saving of time and resources.
The major disadvantage is that it keeps the student in passive situa
tion, has low receptivity and offers hardly any opportunity of checking
learning process.
Practicals
Practical play an important role in educational technology because
they help in introducing, developing and reinforcing theoretical concepts
taught in lectures. Traditional Amphibian experiments should be curtailed
to a minimum and more emphasis should be laid on Human Physiology
and Interpretation of graphs and problem solving exercises. These test
the capacity of a student to give a precise, to the point expression of his
thoughts and one exclusive advantage of this system is that its questions
could be framed at leisure by the participation of Faculty in such a way
as to incorporate the type of knowledge it is desired to be inculcated by
the student.
Tutorials
Is a small group activity. These could be usefully utilised by identi
fying students with poor scoring and helping them to take part in dis
cussion. It has distinct advantage of permitting teacher student dialogue
facilitating self evaluation and development of confidence.
Seminar
It is an activity in which group of persons engaged in research or
advanced study meet under the general direction of one or more staff
members for discussion on problems of mutual interest. These are not
utilised in a routine manner for undergraduate teaching. However, every
department arranges a few seminars for the benefit of students. These
are helpful in giving an opportunity to students (all members) to parti
cipate in discussion and to study a subject in depth under an authority.
Disadvantage is constraint of time available to students for preparation of
reports.
New trends—programmed learning
In this instructional workbooks are programmed to help students to
attain a specified level of performance. This is a innovation which has
been tried in certain universities abroad. In this the student uses a
synchronised slide tape equipment or a video tape at his leisure time. This
also enables the student to work at his own pace, facilitates self evaluation
and has been found to be every effective (Alexander etal 1980).
Problem based learning projects into a clinical corelation
This could be introduced in the 1st year curriculum. An important
objective of this project is to show students how their studies in preclinical
courses could help them with the analysis and solution of a clinical problem.
Another aim is to develop student participation in team work. With this
method most students were encouraged to develop their won initiative and
to practice logical sequence of thought required to solve problems.
(Lambie et al 1981). This also helps in interdisciplinary teachings.
Problem based Learning
Learning from problems is regarded as a condition of human ex
perience. Learning occurs naturally in attempts to face the problems
encountered by every person each day—Problem based learning is ideally
suited for student centered and individualised learning. Learning resources
include tape slide programme, video-tapes, audio-tapes, films.
Instructional-media
Role of Audio-visual media in Physiology Teaching. Besides the
role of chalk and Board, overhead and slide projector models and charts,
and interesting recent development has been the application of programmed
audio-visual material for teaching purposes in the class rooms. However,
many faculties of medicine in Europe and USA are experimenting with
different approaches to this method of teaching, in which the student can
proceed at his own pace and which includes various devices to include
active student participation.
In some faculties these studies are carried out in separate booths or
carrels; in others the material with simple battery operated equipment are
taken away by students and worker away from faculty premises; in yet
3
other students in groups of three or four work together on the pro
grammes. The material produced varies from a taped lecture with slides
to a programmed course with defined objectives, which is modified after
a trial with successive student groups until it reaches a predetermined level
of efficacy. Although in most faculties, this system is a innovation and
therefore, difficult to assess in comparison with conventional teaching
practice. However, at the Faculty of Rotterdam Netherlands whole course
of a year has been transferred on to audiotapes with slides and the faculty
had now 3 years experience of this method and found it successful.
In conclusion, there is no doubt that recent educational technology
is an exciting field of development in Medical teaching, if we accept, that
student learning is a major goal of teaching institutes, then we cannot
afford to ignore the most powerful of the senses, the visual channels.
Coloured video tapes
These are very good for self instructional learning or small group
learning. Easy to operate with casettes. Could be used repeatedly. Useful
for programmed instructions/or demonstration of Experiments.
Closed circuit T.V. system
Useful for small and large groups and class rooms. Very efficient
in transmitting an action where only limited persons can participate. Using
a VCR it is possible to record picture or action of an experimental
technique/demonstration and play back for giving revision to those students
who could not follow initially. The limitations are that CC TV is very
costly. Special technical staff is required. Useful for self instruction by
video-tapes.
Evaluation
Out-moded methods of evaluation still in use provide only some
information on the students capacity for memorization but do not assess
the individual’s ability to cope with real problems faced after graduation
(Fulop 1978). Evaluation is a systematic process of determining the extent
to which the pre-determined objectives are achieved. It includes qualita
tive measurement of a student behaviour plus judgements concerning the
desirability of that behaviour. It plays an important role in education.
Helps in selection of students, monitoring of learning process, giving feed
back to students. Determining success or failure of students: .and deter
mining programme effectiveness.
Types of evaluation procedures
(I) Formative (Daignostic)-These are to defect specific strength and
weakness of individual students.
(2) Summative (Certifying)—To determine the overall achievement
of a satisfactory level of competence, usually at the time of
graduation.
4
Methods of evaluation
The conventional old method was to have a written test having essay
types of questions but now it is felt that a mixture of specific essay type
and short structured questions are more meaningful. Multiple choice
questions (MCQ) are very good because they are objective and there is no
element of subjective assessment. Practicals assessment comprises of a
laboratory exercise coupled with some problem solving exercises or inter
pretation of graphs. Along with this there is a oral examination as well
in practically all the medical colleges.
Internal assessment
Continuous assessment of the students throughout the terms forms
the basis of giving internal assessment marks. A percentage is determined
and recorded. This type of assessment has the advantage of being based
on observing the student actually at work throughout their stay in the
department. This type of evaluation is not only fair, but also provides a
feed back to the student and teacher for further improvement. However,
for certification and assessment is also important. These two types of
assessment may carry equal weightage.
Some innovations recommended
(1) PROBLEM BASED LEARNING PROJECTS INTO A CLINICAL
CORELATION IN FIRST YEAR
We would like to emphasize that teaching of physiology should be
clinically oriented as far as possible to make it meaningful and purposeful
for the basic doctors. In view of this exposure of students to health clinics
in OPDS and problem based learning projects into a clinical corelation
course could be introduced in the 1st year curriculum and even during
lectures emphasis should be laid on impressing upon the students as to how
this basic-knowledge of physiology is going to be of value on clinical side.
□
References
1.
Alexander, D.A. & Haldane, J.D. (1980) Medical Education, the
discontinous view point. Medical Education, 14, 16-22.
2.
Brown, G. (1980) Learning from lectures in medicine, University
of Nottingham.
3.
Dowling, M.A.C. (1972) W.H.O. chronicle, 26(1), 3-6.
4.
Fulop, T. (1978) W.H.O. Chronicle, 33(8) : 303-306.
5.
Guilbert, J.J. (1976) Educational handbook. W.H.O. communi
cation.
6.
Lambie, A,T. Una Maclean C.M. and Me. Guive R.J. (1981).
The introduction of problem based learning projects into a clinical corela
tion course in the first year of the edinburgh medical curriculum. Medical
Education, 15,209-215.
7.
Me. Gaghie, W.C. Miller, G.E., Sajid, A.W. and Telder, T.V.
(1978) Competency based curriculum development in medical education
and introduction public Health paper No. 68, World Health Organisation,
8.
16 68-71.
Williams, R.C. and Osborne C.E. (1982) Medical Education,
5
INTERNATIONAL CONFERENCE
HEALTH POLICY : ETHICS & HUMAN VALUES NEW DELHI 1986
A Look at Rural Surgery in
Private Sector in India
Dr. R.R. Tongaonkar, M.S.
Dondaicha, Dist. Dhule 425408
80% population in India is residing in Rural Areas, besides solving
the Health and Medical problems of this population, we need to cater for
their Surgical needs also. This is done by Government Sector through
Primary Health Centres, and Cottage Hospitals but quite a substantial
Surgical work is being done by Private Rural Surgeons.
Let us see the role of these private Surgeons in delivering surgical
care in rural areas, the type of surgical practice in villages and the pro
blems and difficulties faced by the Rural Surgeons.
This paper is based on a Study conducted in an Backward Adivasi
District of Dhule in the State of Maharashtra and analysis of 5769 total
Surgical operations done by the author during 18 years of his work in a
small private Rural Hospital in the town of Dondaicha which is not even
a Taluka place.
From the Statistical Study of the District it was found out that in
1984 total 11724 operations were done in Government Sector out of which
only 3362 were done at peripheral hospitals. In private sector 11652 were
done out of which 2924 were done in Rural Hospitals.
If we compare the individual work done by private General Surgeons
in Dhule City proper with that done by peripheral Private Surgeons it
could be seem that the City Surgeon is doing on an average two hundred
operations per year, while a Peripheral Surgeon is doing more than four
hundred operations per year, double the work than his colleague in City.
This is partly because the rural public is getting surgical facilities at
their door steps as can be seen from the map which shows that the Govern
ment Civil Hospital which undertakes major surgical work is placed at
one corner of the District almost 130 Kms. away from the farthest point
to reach this hospital for free treatment, the patient who is usually
poor, has to first travel by a bullock cart or a hand cart or some times in
hilly areas on hands or bamboos to reach the nearest bus station and then
to spend about Rs. 120/- as fare for himself and his accompanying persons,
at least 2-3 relatives, and almost 2 days having a night halt somewhere,
instead he prefers to pay the nearby peripheral Private Surgeon. That is
why there is lot of work to do for a Private Rural Surgeon.
But the nature of Rural Surgical Practice is entirely different as com
pared to city practice. The patients do not differentiate between a Physi-
cian, a Surgeon or a Gynaecologist so.theretis more, work of consultation
taking major part of the Surgeons time 9 A.M. to 5 P.M. In 18 years
practice there were 75060 O.P.D. patients as compared to only 5769
operations.
Emergencies are much more common in comparison to city practice
and disturb the sleep of the Surgeon almost daily.
As there are no assistants, Registrars or house-surgeons to work
under him even after 18 years of practice, he has to carry out minor proce
dures like circumcisions, suturing CLWS, opening abscesses and what not.
He has to maintain his own Nursing home for which he has to first
find out a building. There are no good buildings and the hospital may
have to be set up in any old building built in kachha mud, but the build
ing can be modified and decorated at least internally using asbestos sheets
or plywood to form false roof and false walls.
As there are no Pathologist the Surgeon has to keep his own Labora
tory and blood Transfusion Service, and a small X-ray machine on which
no special investigations are possible.
There are no facilities for frozen section biopsies.
In abscence of special investigations, clinical judgment is the most
important armamentarium in diagnosis.
Coming to the operation theatre equipment, usually the rural private
surgeon is coming from a poor or middle class family and cannot afford
to have sophisticated equipment at least in the beginning of his career,
even then he has to keep enough stock of all the materials as neither he
can purchase them immediately nor can he borrow from anybody.
Maintenance of costly equipment is a problem and the Surgeon
himself has to repair his own equipment using gadgets like multimeters,
with the help of local technicians.
. Electric supply failure is a‘very common event and a stand by
arrangement for emergency lighting and foot operated suction machine
have to be kept ready and if possible a generator set installed.
Hard water can ruin the electrical heating appliances and instruments.
Ion Exchange water softners can solve the problem.
Oxygen refilling takes months to get the cylinders refilled. Industrial
Oxygen available locally for welding purposes can be used safely.
Anaesthesia is a big problem. Qualified anaesthetists are not available and either wife if medico or some other local doctor has to be trained
for ana'esthesia or some times the Surgeon himself has to induce anaesthe
sia and maintain the patient on Ether bottle. In abscence of Oxygen
supply the only apparatus available is on Oxford of Bellow and some kind
of Ether vaponsor.
2
With all these the Surgeon is now ready for operation, but he has
no qualified staff and nurses, the hospital staff usually consists of his wife,
who should preferably be a medico, and 3-4 unqualified staff trained in
the same hospital.
On the operation table the Rural Surgeon has to handle Surgical
problems from any system and speciality of surgical field. The analytical
data of surgical procedures carried out by author in 18 years shows that
out of 5769 operations 306 were on head and Neck, 601 were of ENT,
1088 of Gastro-Intestinal tract, 534 Urological Procedures, 1423 Ortho
paedic Procedure, 1585 Gynace Procedures and 302 miscellaneous opera
tions.
Thus it can be seen that the Rural Surgeon not only has to under
take general surgical work but also orthopaedic work reducing fractures,
ENT Work knocking out tonsils, gynaec work doing D & Cs and hysterec
tomies and obstetric work conducting difficult deliveries. In fact these
three specialities form almost 65 % of his surgical practice.
But usually he is qualified as a General Surgeon and has no experi
ence of doing these operations and at least in the beginning of his career to
perform any new operations is a night-mare for him.
As a Surgical Registrar the author has removed only one sided tonsil
that too unofficially begging the favour of E.N.T. Registrar and had to
run away leaving the operation half way as the E.N.T. boss came in.
The General Surgeon’s knowledge of gynaec and obstetric operations
is probably limited to whatever he has seen as under graduate sitting in
the operation theatre gallery, but in his practice the Rural Surgeon not
only has to do Caesarean Section but even he has to use the so called
obsolete methods like craniotomy and evisceration which he has never
seen in his student life.
‘
Besides surgery the Rural Surgeon has to admit all cases needing
hospitalisation like unconscious patients, patients with high fevers, convul
sions, status asthmaticus, heart attacks and some times even schizophrenics.
So it is urged that a Rural Surgeon should be specially trained. It is
suggested that after getting basic post -graduate qualification in General
Surgery, the surgeon, if wants to settle in rural areas he should be allowed
to do house-posts for 6 months in Gynaecology and Orthopaedics and
short posts in ENT and anaesthesia. In his basic training more stress
should be given to clinical methods of diagnosis and he should be taught
to handle equipments like X-ray machines and preliminary knowledge of
bio-engineering and repairs and maintenance of these equipments, should
also be given to him. Simpler but useful procedures, may be obsolete, in
fields like anaesthesia and obstetrics should be specially taught to him to
make him jack of all but Master of Surgery.
Besides all these technical and clinical Problems the Rural Surgeon
has to face some social and personal problems, as already said his wife
should be a medico not only because she will help him in his practice
tremendously, but will not get bored in village life with no facilities for
3
entertainment—not even good people to talk with. Children education
is the biggest problem. The Surgeon has no academic life and cannot do
any research, but on the whole the life is calm and quiet, people respect
him all over and in due course of time he earns enough to have a good
livelihood and is probably happier than in his colleagues in big cities.
That is why now more and more surgeons are coming to villages and
settling at peripheral places as can be seen from the map thus delivering
surgical care at the door steps of village people. So also more and more
Government agencies like Primary Health Centres and Cottage Hospitals
are recently being set up improving the medical facilities in rural areas.
That is why now it is rare to see gangrenous hands due to tight plaster un
reduced dislocations with nerve palsies, patients with huge hernia, and
advance breast lesions, intestinal perforations with shock, bladder stones
with recto-vesical fistulae, huge ovarian cysts occupying all the abdominal
cavity sometimes with bleeding gynaec problems brought in almost exsan
guinated state and ruptured uteruses due to obstructed labour, a seen
commonly encountered by the author in the Seventies.
Blind faith is also disappearing fast and now it is rare to see a mori
bund child with branding marks all over abdomen, holy ash applied to
this fore head and a sacred thread tied to his wrist. Even Adivasies now
bring their young-ones not only for emergencies but also for routine
Surgical treatment.
Even then a lot needs to be done to achieve the goal of ‘Health for
all by 2000 AD” especially in rural areas. Government agencies alone
may not be able to fulfil this goal. The private surgeons have a big role to
play in the coming future in achieving this target, therefore it is urged that
more and younger surgeons should come forward and settle in villages
thus serving the masses and helping the nation and the mankind as a
whole.
-V.TAC''LL
Marks Road.
47^.^'"°,
Banqa'0'13 *
0 00A.
INTERNATIONAL CONFERENCE
HEALTH POLICY : ETHICS & HUMAN VALUES NEW DELHI 1986
Under-Development and Poverty
Dr. Mrs. Lalita Rao
Under-development and poverty are corelated, in as much as the
the former is the cause of the latter and vice-versa. Curiously enough
‘Health’ occupies a place of prominance in the phenomenon of underdeve
lopment. Because of the poverty, the people of a country have poor health
status and they cannot effectively contribute in the process of development
of the country. Development means augmenting the goods and services of
a country of which there are acute shortages. In the process of develop
ment, many problems like housing, sanitation, energy, environment, food
production have to be effectively solved. The advanced countries easily
solved these problems and taking advantage of the industrial revolution
achieved faster progress. For these countries population growth did not
pose any problem as did India. Development and prosperity worked as
contraceptives in these advanced countries.
The constitution of India, therefore envisaged establishing in new
social order based on equality, freedom, justice and the dignity of the
individual. It aims at elimination of poverty, ignorance and ill-health and
directs the State to regard the raising of the level of nutrition and the
standard of living of its people and the improvement of public health as
among its primary duties, securing the health and strength of workers,
men and women, specially ensuring that children are given opportunity to
develop in a healthy manner. We, therefore, embarked on economic
planning through the implementation of Five Year Plans. The successive
Five Year Plans have been providing the framework within which the
States may develop their health service infrastructure, facilities for medical
education and so on. During the last three decades and more, considerable
progress has been achieved in the promotion of the health status of our
people. Small pox, which used to take heavy toll, has been eliminated and
plague, is no longer a problem, mortality from cholera and related diseases
has decreased. The mortality rate per thousand of population has been
reduced from 27.4 to 14.8 and the life expectancy at birth has increased
from 32.7 to over 52, according to official statistics.
In spite of such' impressive progress, the demographic and health
picture of the country still constitutes a cause for serious and urgent con
cern. The high rate of population growth continues to have an adverse
effect on the health of the people and the quality of their life. India is
committed to the goal of “Health for All by the year 2000 AD” through
universal provision of comprehensive primary health care services. For
this purpose large inputs are necessary in the health sector and efforts are
being geared up to secure the complete integration of all plans for health
and human development with over-all national socio-economic develop
ment process, specially in the more closely related subjects to health, like
drugs and pharmaceuticals, agriculture and food production, rural develop
ment, education and social welfare, housing, water and supply and sanita
tion, prevention of food adulteration and conservation of the environment.
India’s long-term goals are:— Improved standards of living and a
stable and healthy population. The immediate goals are to reduce poverty
and fertility which are inter-dependent. Therefore, India accords highest
priority to the task of reducing poverty through various programmes.
Improvement in the quality of life of the poor and the weaker sections of
the community are the key elements of the country’s development
programmes and policies. The poorest 40 per cent in India are receiving a
gradual but increasing share of total national income and concentration of
income is declining.
Ever since independence, poverty reduction has been a fundamental
goal of Indian economic and social policy. The sixth Five Year Plan esti
mated that in 1979-80, around 50 per cent of the entire population or nearly
340 million people, lived below poverty line, modestly defined as monthly
per capita expenditure of Rs. 76 in rural, and Rs. 88 in urban areas, accord
ing to Government of India statistics. This gives us an idea of the magni
tude of the task of poverty elimination, which is sought to be tackled by
such national programmes as, the Minimum Needs Programme, National
Rural Employment Programme, subsidising irrigation and rural electricity,
rates, Education and health are two areas which are important not only
from the point of view of investment in human resource development but it
is the first step towards providing some equality of opportunity to the new
borns by seeking to equip them with good health and at least elementary
education. Achievements in these two areas are also crucial from the
point of view of changes in the status of women, which have significant
implications in terms of demographic change, especially fertility reduction.
It is imperative that the active co-operation and involvement of the
people in the various programmes being undertaken by the government to
tackle underdevelopment and eliminate poverty, is ensured, so as to have
speedy results.
(Fiffit flee,.; O;
2
INTERNATIONAL CONFERENCE
HEALTH POLICY : ETHICS & HUMAN VALUES NEW DELHI 1986
Role of Religions for World Peace :
A Baha'i Perspective
Robert J. Kim-Farley, M.D. M.P.H.
National Spiritual Assembly of the Baha’is of India
New Delhi 1 >0001
One of the objectives of this international conference is to identify
and compare the ethical content of selected health policy issues from the
perspectives of different religious settings. The hazards of nuclear war has
become a contemporary health policy issue and many prominent physicians
in the world have worked hard to raise awareness of its importance on the
part of fellow physicians and the public at large. The peoples of the world
increasingly recognize that the release of the destructive power of nuclear
weapons would result in morbidity and mortality of a magnitude never
before imagined. It has been stated that prevention of war, and nuclear
war in particular, could be therefore equated with one of the most,
important public health interventions of our time. The Baha’i Community
is always pleased to participate in conferences organized to examine the
role of religions in health policy and to provide Baha’i perspective.
The topic of the role of religions for world peace is a fundamental
challenge in the world today and cuts across the professional, cultural and
religious levels being discussed in this conference. I would like to take
this opportunity to explore the concept of the world peace, to emphasize
the role of religions in this process, to enumerate the barriers yet remain
ing, and to provide a vision to the remaining steps that must be taken to
achieve a lasting world peace. I will draw from the recently released
message from the World Centre of the Baha’i Faith to the peoples of the
world entitled the Promise of World Peace. This message and topic is very
timely since the United Nations has also declared that this year is the
International Year of Peace.
The Great Peace towards which people of good will throughout the
centuries have inclined their hearts, of which seers and poets for countless
generations have expressed their vision, and for which from age to age the
sacred scriptures of mankind have constantly held the promise, Baha’is
feel is now at long last within the reach of the nations. The writings of
the Baha’i Faith state that world peace is not only possible but inevitable.
However, wo have a choice. Whether peace is to be reached only
after unimaginable horrors precipitated by humanity’s stubborn clinging to
old patterns behaviour, or is to be embraced now by an act of consultative
will, is the choice before all who inhabit the earth.
Baha’u’llah, the Prophet-Founder of the Baha’i Faith, wrote over
one hundred years ago that “the winds of despair are, alas, blowing from
every direction, and the strife that divides and afflicts the human race is
daily increasing. The sign of impending convulsions and chaos can now
be discerned, inasmuch as the prevailing order appears to be lamentable
defective.” Flaws in the prevailing order are conspicious in the inability
of sovereign states organized as United Nations to exercise the spectre of
war the threatened collapse of the international economic order, the
spread of anarchy and terrorism, and the intense suffering which these and
other afflictions are causing to increasing millions.
The Baha’i Faith regards the current world confusion and calamitous
condition to human affairs as a natural phase in an organic process lead
ing ultimately and irresistibly to the unification of the human race in a
single social order who.se boundaries are those of the planet. The human
race, as a distinct, organic unit, has passed through evolutionary stages
analogous to the stages of infancy and childhood in the lives of its indivi
dual members, and is now in the culminating period of its turbulent adole
scence approaching its long-awaited coming of age. Whatever suffering
and turmoil the years immediately ahead may hold, however dark the
immediate circumstances, the Baha’i community believes that humanity can
confront this supreme trial with confidence in its ultimate outcome.
No serious attempt to achieve world peace, however, can ignore the
role of religion. Baha’u’llah has said that ‘‘religion is the greatest of all
means for" the establishment of order in the world and for the peaceful
contentment of all that dwell therein.” An analogy that I particularly
like is that given to us by Arnold Toynbee in this great work on the Study
of History. He states that we can consider religions as the spokes on the
wheel of the chariot of civilization. As the religions come into the world the
wheel moves forward and is the cause of the advancement of civilizations.
Recognition of the oneness of all religions is a fundamental teaching
of the Baha’i Faith. Baha’ is consider that all religions are like chapters
in one book—each chapter dependent and interrelated on the others—and
that the Baha'i Faith, the most recent chapter, is for the purpose of creat
ing world unity. Baha’ is believe that the divisiveness and strife between
religious communities is man made. Far from a fair-minded examination
of the actual utterances of the Founders of the great religions, and of the
social milieus in which they were obliged to carry out their missions, there
is nothing to support the contentions and prejudices deranging the religious
communities of mankind and therefore all human affairs. The teaching
that we should all treat others as we ourselves would wish to be treated, an
ethic variously repeated in all the great religions, lends force to this obser
vation.
Banning nuclear weapons, prohibiting the use of poison gases, or outlawing germ warfare will not remove the root causes of war. However
important such practical measures obviously are as elements of the peace
process, they are in themselves too superficial to exert enduring influence.
Peoples are ingenious enough to invent yet other forms of warfare, and to
use food, raw materials, finance, industrial power, ideology, and terrorism
to subvert one another in an endless quest for supremacy and dominion.
Therefore a genuine universal framework must be adopted. Some of the
barriers to world peace and the role that religions must play to develop
this universal framework are as follows:
F
1.
Racism, one of the most beneful and persistent evils, is a major
barrier to peace. Recognition of the oneness of mankind, implemented by
appropriate legal measures, must be universally upheld if this problem is to
be overcome.
2.
The inordinate disparity between rich and poor, a source of acute
suffering, keeps the world in a state of instability, virtually on the brink of
war. The solution calls for the combined application of spiritual, moral
and practical approaches.
3.
Unbridled nationalism, as distinguished from a sane and legitimate
patriotism, must give way to a wider loyality, to the love of humanity as a
whole. Baha’u’llah has said that “the earth is but one country, and man
kind its citizens.”
4.
Religious strife, throughout history, has been the cause of innumer
able wars and conflicts, a major plight to progress, and is increasingly
abhorent to the people of all faiths and no faith. The challenge facing the
religious leaders of mankind is to contemplate, with hearts filled with the
spirit of compassion and a desire for truth, the plight of humanity, and to
ask themselves whether they cannot, in humility before their Almighty
Creator, submerge their theological differences in a great spirit of mutual
for bearancc that will enable them to work together for the advancement
of human understanding and peace.
5.
The emancipation of women, the achievement of full equality bet
ween the sexes, is one of the most important, though less acknowledged
prerequisites of peace. Only as women are welcomed into full partnership
in all fields of human endeavour will the moral and psychological climate
be created in which international peace can emerge.
6.
The cause of universal education deserve the utmost support. No
nation can achieve success unless education is accorded all its citizens.
Consideration should also be given to teaching the concept of world
citizenship as part of the standard education of every child.
7.
A fundamental lack of communication between peoples seriously
undermines efforts towards world peace. Adopting an international auxi
liary language would go far to resolving this problem and necessitates the
most urgent attention.
Two points bear emphasizing in all these issues. One is that the
abolition of war is not simply a matter of signing treaties and protocols;
it is a complex task requiring a new level of commitment to resolving
issues not customarily associated with the pursuit of peace. The other
point is that the primary challenge in dealing with issues of peace is to
raise the context to the level of principle. There are spiritual principles,
or what some call human values, by which solutions can be found for
every social problem.
The primary question to be resolved is how the present world, with
its entrenched pattern of conflict, can change to a world in which harmony
and co-operation will prevail. World order can be founded only on an
unshakeable consciousness of the oneness of mankind. Acceptance of the
3
1
oneness of mankind is the first fundamental prerequisite for reorganization
and administration of the world as one country, the home of mankind. In
the Baha’i view, recognition of the oneness of mankind “calls for no less
than the resconstruction and the demilitarization of the whole civilized
world—a world organically unified in all the essential aspects of its life, its
political machinery, its spiritual aspiration, its trade and finance, its script
and language, and yet infinite in the diversity of the national characteristics
of its federated units.”
This principle “does not ignore, nor does it may attempt to suppress,
the diversity of ethical origins, of climate, of history, of languages and
tradition, of thought and habit, that differentiate the peoples and nations
of the world. It calls for a wider loyality, for a longer aspiration than any
that has animated the human race. It insists upon the subordination of
national impulses and interests to the imperative claims of a unified world.
It repudiates excessive centralisation on one hand, and disclaims all
attempts at uniformity on the other. Its watchword is unity in diversity.”
Baha’u’llah has written that “the time must come when the impera
tive necessity for the holding of a vast, an all-embracing assemblage of
men will be universally realized. The rulers and kings of the earth must
needs attend it, and, participating in its deliberations, must consider such
ways and means as will lay the foundations of the world’s Great Peace
amongst men.” Concerning the proceedings for this world gathering, the
Baha’i writings state that “they must make the Cause of Peace the object
of general consultation, and seek by every means in their power to esta
blish a Union of the nations of the world. They must conclude a binding
treaty and establish a covenant, the provisions of which shall be sound,
inviolable and definite. They must proclaim it to all the world and obtain
for it the sanction of all the human race. This supreme and noble under
taking—the real source of the peace and well-being of all the world—
should be regarded as sacred by all that dwell on earth. All the forces of
humanity must be mobilized to ensure the stability and permanence of this
Most Great Convenant. In this all-embracing Pact the limits and frontiers
of each and every nation should be clearly fixed, the principles underlying
the relations of governments towards one another definitely laid down, and
all international agreements and obligations ascertained. The fundamental
principle underlying this solemn Pact should be so fixed that if any govern
ment later violate any one of its provisions, all the governments on earth
should arise to reduce it to utter submission, nay the human race as a
whole should resolve, with every power at its disposal, to destroy that
government. Should this greatest of all remedies be applied to the sick
body of the world, it will assuredly recover from its ills and will remain
eternally safe and secure.”
Baha’is around the world appeal to the leaders of all nations and to
their co-religionists of all faiths to seize this opportune moment and take
irreversible steps to convoke this long overdue world meeting. Let men
and women, youth and children everywhere recognize the eternal merit of
this imperative action for all peoples and lift up their voices in willing
assent. Indeed, let it be this generation that inaugurates this glorious
stage in the evolution of social life on the planet.
And yet, as essential as permanent peace among'natiotis is, Baha’u’4
Hah asserts that it is not the ultimate goal of the social development of
humanity which is none other than the unification of all of the peoples of
the world in one universal family. “The well-being of mankind,”
Baha’u’llah wrote, “its peace and security, are unattainable unless and
until its unity is firmly established.” The Baha’is offer their own experience
as an example of a community drawn from many nations, cultures, classes
and creeds, engaged in a wide range of activities serving the spiritual,
social and economic needs of the peoples of many lands. We hold firmly
to the conviction that all human beings have been created “to carry for
ward an ever-advancing civilization” and that the virtues that befit human
dignity are trustworthiness, forbearance, mercy, compassion and lovingkindness towards all peoples.
We convey the anxious plea of our co-religionists everywhere for
peace and unity. We join with all who are the victims of aggression, all
who yearn for an end to conflict and contention, all whose devotion to
principles of peace and world order promotes the ennobling purposes for
which humanity was called into being by an all-loving Creator.
I hope that in some small way these principles of the Baha,i Faith
on the promotion of world peace which I have shared with you today will
contribute to the worthy objectives of this international conference on
ethics and human values in health policy. We must all arise to bring about
world peace and ensure that religion becomes the very source of the unity
of mankind which is the foundation of a lasting peace. The Baha’i
writings state that “the Prophets of God should be regarded as physicians
whose task is to foster the well-being of the world and its peoples, that
through the spirit of oneness, they may heal the sickness of a divided
humanity.” Let me close with the words of Baha’u’liah who emphatically
promises that “these fruitless strifes, these ruinous wars shall pass away,
and the ‘Most Great Peace’ shall come.”
5
INTERNATIONAL CONFERENCE
HEALTH POLICY : ETHICS & HUMAN VALUES NEW DELHI 1986
Challenges Facing Health Care Priorities
in Developing and Underdeveloped
Countries
Dr. Rashid Fulayfil
Undersecretary Ministry of Health Bahrain
Dr. Fawzi Amin
Deputy Chief of Staff Health Centres Directorate
Ministry of Health Bahrain
In the XVIII CIOMS Conference on HEALTH POLICY, ETHICS
AND HUMAN VALUES, we focused on the problems of ethics and
human values resulting from the rapid progress in medical technology. We
deliberated on the ethics of prolonging life with the help of machines; we
focused on the exact meaning and definition of clinical death; and, we dis
cussed the moral aspects of organ transplants and tube pregnancy. These
are questions that are of primary concern to the industrially advanced and
developed nations.
The media, however disseminates with abandonment, information
concerning these issues to developing and underdeveloped nations, thus
proving a potent source for dissonance. In reality, the developing and
underdeveloped countries have different expectations and different value
systems with respect to health care. Consequently, the framework of ethics
as applicable to these countries takes a different shape. Let me pose these
questions to this erudite gathering; and, as I go along, try to identify the
underlying ethical and human values.
Prior to the 1960’s and before the Alma Ata Conference and the
emphasis on primary care, the developing and the underdeveloped coun
tries, in their mistaken zeal to usher in what they believe to be “Hi-tech”
progress, failed to ask themselves two relevant questions:
1.
2.
What is the most cost-effective package of services that is likely
to achieve the most relevant and equitable distribution of health
care?
What is appropriate in this package at this point of time?
Instead of tackling the issues at the grass-root level, the developing
and the underdeveloped countries blindly follow the same path of
secondary and teritary care, neglecting to build an infrastructure based on
preventive medicine. Why? Because the so called elite of the countries,
as well as the politicians who are influenced greatly by the Western media,
in turn influence the policy making in health care.
It is sometimes assumed that health care facilities in developing
countries should be modelled on those found in the more developed coun-
tries and that only a few modifications, mainly those related to climatic
conditions, should be necessary!
Surprisingly this view is held by many experts who participate in
health care projects in developing and underdeveloped countries, but who
lack the insight into the problems involved. In the developing and under
developed countries, some health workers who have become accustomed to
using sophisticated equipment during studies or travels abroad share these
views. Similarly some of the decision makers are tempted to incorporate
sophisticated technology in order to increase prestige whereas in some of
the developed countries the need for this same technology is now beginning
to be questioned.
In the developing and underdeveloped countries, the health planners
are faced with constraints imposed by:
1.
2.
3.
Limitation of financial resources.
Inadequacy of manpower.
Unrealistic expectations of the professionals and the elite.
Of course these three areas are, by no means, water-tight compart
ments; on the contrary, they are closely interlinked. However, it will help
us to appreciate the problems with clarity if we view these areas, one at a
time.
1.
Limitation of Financial Resources
The price paid by the developing and the underdeveloped countries
for imitating the developed countries and allocating their already meagre
resources for the development of secondary care institutions at the neglect
of primary care is considerable.
At the very least, it has left unfulfilled the objectives of developing
primary health care facilities, equipping them with the manpower that is
able to appreciate the real cause of disease and with the ability to commu
nicate with the patient on the same wave length. On the other hand the
imported manpower and the few national professionals who have received
training abroad in highly developed medical technology are frequently more
concerned with secondary and territary care. This attitude naturally proves
a drain on the resources of the countries.
The situation is further compound by the outlook of the policy
makers who are greatly influenced into believing that only that service
which is available in the developed countries is right and will effectively
serve the needs of all people. This thinking, unfortunately, has received
the backing of the elite in the community who may be easily dazzled by the
glamour of “Hi-tech” medical care.
Let me illustrate the dilemma with an almost kindergarden example
Let us suppose a person suddenly fainted in the middle of a street. If this
happened in an underdeveloped country chances are the person is suffering
from starvation. The solution naturally would be to provide food On
the other hand, if the same incident took place in a developed country the
2
chap probably fainted from psychic stress and would need a tranquilizer.
Imagine the absurdity of juxtapositioning the solutions! Yet this is what
we are precisely doing when we blindly follow the path of the developed
countries; and, in the process we drain meagre financial resources by
allocating them to unproductive channels.
The obvious ethical question confronting the planners is one of
identifying priorities for resource allocation. The situation confronting the
policy makers is one of limitless needs to be satisfied by a limited budget.
The questions still arise: Do we channel our resources into avenues that
will ameliorate the health of the majority through emphasing primary care?
Or do we provide the heavy outlay needed for high technology which
is of questionable benefit, even for a minor proportion of the population,
because the manpower needed for such technology is simply not available
in developing and underdeveloped countries?
2.
Inadequacy of Manpower
The reliance of developing and underdeveloped countries on
imported manpower results in a lopsided manpower mix. The truly compe
tent and brilliant are well taken care of in their respective countries and
seldom feel the need to relocate. The developing and underdeveloped
countries thus must offer enormous pay packets to attract so called
“experts”. These are frequently mediocres who can contribute little
toward developing a viable system of health care for the developing and
underdeveloped country. In an attempt to camouflage their inability to
provide the needed expertise, these foreign experts often demand ultra
sophisticated and expensive equipment. Very often, by the time such
technology is purchased and installed at considerale expense, the people
who demand it have left the country, leaving the developing or under
developed country literally “holding the baby”. The fresh batch of
imported experts, for their own survival, naturally must point out how
erroneous are the ways of their predecessors! So the viscious cycle goes on:
Constraints in Budget
Constraints in Manpower
Poor Health Planning
Further Drain on Resources
3.
Unrealistic Expectations of the Elite and Professional
The developing and underdeveloped countries are trapped into
looking at progress through coloured glasses because of the prevalence of
what I would like to call “THE WHITE SYNDROME”. Throughout
these countries, the following currents of thought permeate:
You have a right to call yourself educated and belonging to the top
echelons only if you speak the language of the “White Master”.
Advice coming from the “White Master” is to be taken as ‘gospel
truth’ and blindly implemented.
Anything not done in the country of the “White Master” is not worth
considering.
3
The “WHITE SYNDROME” naturally gives rise to unrealistic
expectations and false value systems.
If we cannot build mammoth secondary and tertiary care hospitals,
fully equipped with the latest that money can buy as advocated by the
propaganda machines of the “White Master”, we are made to feel ashamed
of our health facilities.
Is it ethical to brainwash the policy makers of the developing and
underdeveloped countries into accepting the “WHITE SYNDROME” to
such an extent that the meagre number of the countries’ own professionals
are rendered incapable of functioning without the aid of highly developed
technology?
What is even more distressing is the dissemination of medical miracles
by the media, which more often than not related to a few isolated results
obtained in animal experiments! When the media bombards us with the
message of a breakthrough in medical technology—the promise of restoration
of sight to the blind or morbidity to the lame, you can imagine the anxiety
such misleading information can generate in a country where the basic
problems of malnutrition, poor hygiene and lack of immunization must be
tackled. I leave these ethical issues to you for your pondering and
evaluation.
Admist this scenerio of developing and underdeveloped countries, the
Gulf Countries find themselves in a peculiar situation. We are still deve
lopment with respect to expertise and trained national manpower. How
ever, unlike some of the developing and underdeveloped countries, we have
the financial resources for building secondary and tertiary care hospitals
for the importation of expensive, though perhaps, unstable manpower.
You will get a clearer picture of the existing global scene regarding
problems of health priorities and constraints with respect to developed
developing and underdeveloped countries with the graphic representation
on the following page.
In summary, if the developing and underdeveloped countries wish to
use their limited financial resources to provide health care in relation to
needs, these needs will need to be considered in relationship to:
Allocation of limited resources in relation to these needs.
Inadequacy of manpower, especially in terms of commutation of
labour.
Unrealistic expectations of the elite, professionals and policy makers
regarding the true goals of health care programs.
If we are to be truly successful in providing the health care needs for
the developing and underdeveloped countries, limited resources must be
carefully distributed and monitored to maintain their applicability within the
goals; manpower must be made aware of the needs and goals and in turn
become committed to those needs and goals; and, the expectations of the
elite, professionals and policy makers must insure that the true goals run
parallel with the ethics and human values of the country.
4
c WfJNin' i’.-ALTH
(First Floor) St. Marl
Bangalore - 560 001.
INTERNATIONAL CONFERENCE
HEALTH POLICY : ETHICS & HUMAN VALUES NEW DELHI 1986
To Tell or Not to Tell
Professional practices in the care of the dying
S.K. Jindal1
U.N Jindal2
Departments of the Chest Diseases and Obst. & Gynaecology
Postgraduate Institute of Medical Education
& Research Chandigarh
Abstract
Sixty five responses of postgraduate doctors practising in India to a
questionnaire on their beliefs and practice about telling the truth of inevit
able death to their patients were studied. A majority (69.2%) favoured in
telling the truth. Around 50% of their patients were suspected to be aware
of their fate without being told. 40% of the doctors had had one or more
occasion of feeling sorry later on because of their hiding the truth.
Introduction
Doctors differ in their approach about how much and when to tell
the truth to the patient while caring for the dying. Some doctors have
their own dogmas on this issue while others are guided by circumstances.
Those who believe in telling the truth are usually critical of others who are
evasive and use lies; but they themselves are considered unkind by the
others.
There are few studies on medical perspective in the care of the dying
from our country though in the West it has attracted both the professionals
and the lay.1’2 Issues and ethics while dealing with death in India may
not be the same as in the Western countries in view of wide differences in
social, cultural and religious beliefs. How do the doctors in India deal
with patients facing inevitable and/or impending death ? We undertook a
study with the help of a questionnaire on practicing doctors. One hundred
ex-postgraduate students of the Postgraduate Institute of Medical Educa
tion and Research Chandigarh (PGI, Chandigarh), now practicing in the
field and forty non PGI Alumni, Indian Medical Association members were
sent the questionnaire. Since only three of the 2nd group responded we
excluded them from the final analysis. Sixty five of the PGI alumni res
ponded to the questionnaire.
Results
The responses were grouped into two categories depending upon their
belief in telling the truth about the disease and its outcome to their
patients :
Group I : Those who believed in telling the truth (45 : 69.2:%).
'
Group II : Those who did not believe in telling the truth (20; 30.8 %).
The reasons favoured by those in favour of telling the truth were :
(i) It pacifies the patient who can accept death more peacefully (61.5%);
(ii) it helps in more effective palliative treatment (81.5%); (iii) the patient
can put the family problems like marriages, transfer and division of assests
etc. to order before death (90.8%); (iv) the patient can fulfil the last wishes
(76.9%); (v) it stops their running around to seek treatment from different
sources (93.8 %). Other reasons included economic reasons (i.e. to give
an expenditure versus result ratio to the patient), easier handling by the
family and the patient’s right to know the truth.
Those who were not in favour of telling the truth favoured the
following reasons : (i) it frustrates and angers the patient (86%); (ii) it
makes the family member’s job more difficult (60%); (iii) it is difficult to
tell the hard truth (60%); (iv) the patient may turn to quackery (50.8%).
Group I doctors (90.8%) felt that the truth should be told by the
treating physician only. But 40% of group. II doctors thought that if it
has to be told it should be told by some one else eg. a close friend, relative
or a priest.
About the awareness of the patient without being told 60.8% in
group I and 72.3% in group II thought that over 50% of their patients
knew of their fate.
Only 18.5% had ever felt sorry once or more afterwards about their
decision of informing their patients. But 40.0% had one or more instances
of feeling sorry afterwards when they did not inform the truth. This was
because the patient kept wandering from place to place in search of cure
and spent a lot of money (21.5 %), could not settle worldly affairs (9.2%),
or could not complete the last wishes (9.3 %). Two doctors admitted of
facing official and/or legal problems in view of their not telling the truth.
However, none was ever charged in the court of law.
Discussion
It is generally believed that the knowledge of death takes away the
charm of living. On the other hand, such a knowledge may dispel the
uncertainty and may give the courage to face the situation. In the
Western experience around 50% of the patients are already aware of their
impending death.3’4 In one study on the dying patients over 60% knew
of this fact and none disapproved of open discussion.3 Our results are
similar to these findings. Most of our doctors have preferred a flexible
policy of discussion guided by ‘situation ethics’ i.e. adapting the ethical
standards to the situation. A majority of them would like to discuss the
truth.
Involvement of the family members and the close relatives was
favoured by most of the- doctors. In view of the family structure and
relatively closer ties amongst relatives in Indian set up, this aspect is of
obvious importance.
It may also be worth recalling that 40 % of the doctors had felt sorry
at least once each about their hiding the truth from the patient. The most
important reason here was their failure in giving the patient an opportu
nity to put the worldly affairs in order. This point again needs to be
stressed in our context especially when the head of the family who is often
the sole bread earner of the family and usually the only knowledgeable
person about family assets, debts, loans and other issues, is sick and dying.
Many an official, procedural and legal complications can be avoided if
these things are settled or atleast informed to the kith and kin before
death. The patient also needs to know before hand about the utility of
the expenditure involved in treatment versus the result as the family income
may be meagre. Above all, a doctor is legally obliged to tell the patient
the whole truth and nothing but the truth.
‘The truth’ of course ‘has a broad spectrum with gentleness at one
end and harshness at the other. Patients always appreciate gentle truth.4
References
1. Symposium (1973) ‘Care of the Dying’ Br Med J 1, 29-41.
2. Lamerton R (1973) Care of the Dying. London Priory Press.
3.
Hinton J (1974). Talking with people about to die. Br Med J 3,
25-27.
4.
Thomson WAR (1977). Care of the Dying. In : A dictionary of
medical ethics and practice. John Wright & sons Ltd. Bristol, p. 107-110.
3
INTERNATIONAL CONFERENCE
HEALTH POLICY : ETHICS & HUMAN VALUES NEW DELHI 1986
Euthanasia
Dr. H.N. Sliukla
Introduction
Euthanasia has its origins from a Greek word, the term ‘Eu’
means ‘Well’ and ‘Thanatos’ means death and it literally means an easy
death. It is a form of peaceful or dignified death which is specially
advocated when life become a punishment and dying comes as a pleasure
to a patient, suffering from some incurable disease like cancer with severe
intolerable and uncontrollable excruciating pain, who more often tearfully
pleads to a doctor to relieve his suffering soul from bodily cage. The con
flict is often stated to be between the doctor’s duty to treat to the best of
his ability and patient’s right to be allowed to die quietly and in peace, when
further medical measures appear meddlesome and only prolong suffering.
Health Council of Netherlands has defined Euthanasia ‘A deliberate life
shortening act or deliberate omission of a life lengthening act, in respect
of an incurable patient and in his interest’. This definition includes both
active (life shortening act) and passive (omission) euthanasia. The
‘Declaration of Venice’at the meeting of the World Medical Association
in Oct. 1983, has laid down that ‘Physician may relieve suffering of a
terminally ill patient by withholding the treatment with the consent of the
patient or his immediate family member in case the patient is unable to
express his will’ and ‘The physician may refrain from employing any extra
ordinary means which would prove of no benefit for the patient’.
In the light of above the present article endeavours to stress the role
of Voluntary Passive Euthanasia in the Terminal Care, especially the with
drawing of life sustaining treatment according to wishes of patients suffe
ring from Terminal Illness and withdrawal of life sustaining aids from a
Terminally Injured patient after declaration of brain death. It will be in
public interest for such a measure to be enacted as it would relieve a certain
number of patients from suffering pain and torments which can be avoided.
Good death : Moral and Legal Challanges in Terminal Care
Law and medicine join a common pilgrimage towards protection,
preservation, regulation, care, and all-pervasive welfare of human life.
The Indian Constitution (Article 21) assures that‘No person shall be de
prived of his life by the state except according to the procedure established
by law’. The constitution can guarantee the ‘Security’ or ‘Non-interference’
in the enjoyment of life but no constitution in the world can ever assure
its citizens that their life would remain always free from pain, disease and
physical and mental agony. The right to life protected by Indian Consti
tution has not been judicially held to include ‘Right to die’. The question
is whether a person who has become a mere vegetable mass of protoplasm,
who has worse than animal existence, who has no hope of recovery—
Should he be forced to live ? Should he be not allowed to die peacefully
without suffering from further physical and mental agony ? Cannot
he ask the state that while he has been given right to life, Can’t he be
endowed with a right to die in the event of a terminal illness or terminal
injury ? The death sentence in India has been held to be constitutional
under the very provision which protects the right to life of a person.
Likewise state has legalised the Medical Termination of Pregnancy.
Interaction of law and medicine is notable in cases of abortion. It is now
perfectly legal though may not be perfectly moral or ethical. Man can
choose to give life or death to the helpless unborn child then why should
he not have similar right for his ownself ? The legislation of abortion
means legislation of ‘Death’ of an unborn person. The purpose of abortion
in most cases is to safe guard the health of a pregnant woman or it is for
the convenience of the society and state as a measure of population control
but the voluntary passive euthanasia is for the sake of suffering ‘individual’.
If law can permit ‘killing’ of an unborn child for the sake of ‘others’ Why
should it not allow voluntary passive euthanasia for a willing and suffering
patient.
Role of Voluntary Passive Euthanasia in Terminal Care
Terminal illness or Terminal Injury means any incurable illness or
injury which will in all probabilities result in the expiration of life, regard
less of use or discontinuance of medical or surgical treatment. To day
cancer accounts for 15 per cent of deaths in the world. In U.S. alone more
than 7 million unfortunates are in grip of this dreaded affliction. It is
here that Voluntary Passive Euthanasia becomes relevant. Voluntary
Passive Euthanasia advocates compassion in the preceding stages of
terminal illness. These stages are process of dying which sometimes linger
on for years. When a doctor prolongs the life of a dying patient by days,
weeks, months or by years he merely prolongs his life of suffering. He
simply promotes his vegetable existence or adds to his comatose condition
in the name of preservation of life. No patient wants to put up with
sufferings indefinitely. There is an innate desire in all living beings to
terminate their sufferings as quickly as possible. When the intensity of
suffering is beyond the pale of human indurance the urge to extinguish
life is paramount. Prof. Elizabeth Ross recognises this final state of dying
as a stage of acceptance, the patient is ready to accept loss of his life and
beloved ones.
Withdrawing of Life Sustaining Treatment in Terminal Illness
The life sustaining treatment means all artificial means or measures
of whatever kind administered as medical or surgical treatment designed
solely to sustain life process. In developing nations health expenditure
on the last few months of patient’s lives rises to a crescendo, as might be
expected but the consumer, the patient, often seems to derive little of real
personal value from the money thus spent. Traditionally the medical
ethics has been helped at this point by distinguishing ‘ordinary’ means of
treatment which should be available to all patients, from ‘extra-ordinary’
which should not be employed as they cannot be used without excessive
pain, cost or other inconvenience and which offer no reasonable hope of
benefit.
2
Many people today have a fear that they will be kept alive artificially
in this manner with consequent suffering and distress to them and members
of their family. Since the decision to reject such treatment should be of
patient alone and no one else in case of terminal illness as such provision
of Voluntary Passive Euthanasia in terminal care will enable doctors, in
the interest of compassion and humanity to respond to the patient’s wishes
in suitable cases but it should not provide for mercy killing of any kind.
Declaration for withdrawal of Life Sustaining Treatment
Any person of sound mind shall be entitled to make a declaration
and give powers of Attorney duly executed by such person expressing the
desire that if at any time in future he or she were to suffer from a terminal
illness or terminal injury and be unable to express himself or herself, the
wish embodied in the declaration and power of Attorney regarding with
drawal of life sustaining treatment, shall, if it has been in operation for 30
days and has not been duly revoked in writing be given effect to by his
physician or surgeon and members of his or her family.
Withdrawal of life sustaining aids in patients of Terminal Injury
A person who can be declared dead under the law in U.S.A, and
U.K. is considered to be alive in India. Though this may appear illogical,
it is true because brain death is not legally recognised as death of a person
and our law is silent on the issue of brain death. The main problem
arises in road traffic accident victims who are being maintained on conti
nuous artificial respiration by means of mechanical ventilators after sustain
ing irremediable structural brain damage. In such patients doctors are
not lawfully authorised to switch off the respirator.
Legal recognition of brain death will enable doctors to withdraw life
sustaining aids including the respirator, in patients suffering from terminal
injury the moment brain death is diagnosed, especially in patients who
failed to make any declaration in life time or execute powers of Attorney,
expressing their wish for withdrawal of life sustaining aids in the event of
terminal injury.
Diagnosis of Brain Death in Terminal Injury
The code of practice as agreed by Conference of Royal Medical
Colleges and their Faculties of United Kingdom (1976) has advised the
medical practitioners that before considering the diagnosis of Brain Death
three conditions should be present altogether :—
1.
Patient should be deeply comatose :
(a)
There should be no doubt that this state is due to depressant
drugs.
(b)
Primary Hypothermia as a cause of coma should be excluded.
(c)
Metabolic and endoctrine disturbances that may cause or con
tribute to coma should also be excluded.
3
2
Patient should be maintained on continuous artificial respiration by
means of a mechanical ventilator.
3
There should be no doubt that patient’s condition is due to the irre
mediable structural brain damage for example severe head injury.
Tests for confirmation of brain death
(i)
All brain stem reflexes should be absent.
(a)
(b)
Pupils are fixed and dilated and do not respond to sharp changes
in incident light.
Corneal reflex absent.
(c)
Vestibulo-ocular reflex absent.
(d)
Carinal reflex absent.
(e)
(f)
Gag reflex absent.
No motor response within cranial nerve’s distribution can be
elicited by adequate stimulation of any somatic area.
(g)
Spontaneous respirations—Absent with a normal PaCo., in the
absence of hypothermia.
(h)
The oculo-cephalic reflex or doll’s head eye movements must be
absent.
Other Considerations
(i)
Repetition of Testing—It is customary to repeat the tests to
ensure that there has been no observer’s error.
(ii)
Integrity of Spinal Reflexes—It is well established that the spinal
reflexes may perist after brain death (Ivan Smith 1973).
(iii)
Confirmatory Investigations—It is now widely agreed that E.E.G.
(Electro-encephalography) is not necessary for confirmation of
brain death.
(J)
(iv)
Body Temp.—It is recommended that body temp, should not be
less than 35° C before the diagnostic tests are carried out.
Advantages of Legal Recognition of Brain Death in Terminal Injury
(A) Responsibility of a Doctor : Normally a doctor is not lawfully
authorised to switch off a respirator sustaining the artificial respiration of
a terminally injured patient, lying in a state of coma after sustaining the
irremediable structural brain damage. If a doctor switches off the respi
rator at his own, he will be charged for causing death by an omission.
The recognition of Brain Death legally as death of a person, will save
the doctors from responsibility in such cases of terminal injury.
.
°.rZan transplantation : The recognition of brain death of a
terminally injured person in law will enable to the act legally and correctly
m the field of organ transplantation. After the confirmation of brain
death if a surgeon has to keep on waiting for cardiac arrest to occur before
removing organs for transplantation, a recipient may well receive a
damaged organ and a recipient grafted with a damaged organ will have to
undergo the pain, danger and suffering from two useless operations, namely
one for the insertion of the graft and the second for its subsequent removal.
The most suitable donors for organ transplantation are terminally injured
patients, usually the road traffic accident victims who are being maintained
on continuous artificial (IPPR) respiration by means of mechanical venti
lators after sustaining irremediable structural brain damage. Such people
have been organ donors either in their life times or consent has been
obtained from their relatives. In U.S.A, such patients are also known as
heart beating cadavers. Recognition of brain death as death of such
terminally injured patients will enable doctors to remove the organs from
such decerebrate donors. Normally transplants cannot be lawfully taken
away from a living body if donor can not remain alive without the part
being taken i.e. heart, so for a successful heart transplantation it is to be
removed from a heart beating cadaver only. The most appropriate time
for organ removal is before the vital life support system is withdrawn and
organs are well perfused. Moreover heart has been kept alive and func
tional up to 56 hours after brain death, a duration of time which is long
enough for operative exploration, tissue typing and search for a suitable
recipient.
(C) Economy of Intensive Care Resources : Legal recognition of brain
death as death of a person in case of a terminal injury will help in econo
mising the intensive care unit’s resources in the country, which are being
strained by providing trained man power, intensive care unit beds and
respirator for ventilating these brain dead people who have suffered from
brain death after terminal injuries.
(D) Property Rights : Legal recognition of brain death as death of a
person will have maximum impact in the matter of property rights, negligance claims, insurance, worker’s compensation, probate law and taxes.
A corpse cannot have property. Suppose that X is an old man who
has left Y a large sum in his will. Y himself has suffered from a terminal
injury and is in a state of coma, on artificial respiration at a hospital after
sustaining irremediable structural brain damage. Here doctors are not
lawfully authorised to switch off the respirator so they ask for consent of
relatives but relatives see that Y is kept ‘alive’ on heart-lung machine
because they want X’s money. As soon as X dies the respirator off and
Y is buried. In this example Y is being considered as still alive when X
dies so that his family becomes entitled to property through him. This
dodge will not be successful if Brain Death is legally accepted as death of
a person.
The fact remains although the diagnosis of death is medical, its
definition must be legal. The law protects the living but ceases to protect
the dead (at any rate in the same way) and the line between the two must
be drawn by law. The definition of death presented herein may suit both
medical as well as legal requirements because it does not interfere with the
existing procedure of declaration of death but at the sam; time it includes.
the concept of Brain Death in a terminally injured at the hospital level in
the light of the current knowledge on the subject.
5
Definition of Death
‘A person may be pronounced dead, whether inside or outside a
hospital if based on usual and customary standards of medical practices,
it is determined that the person has an irreversible cessation of cerebral,
cardiac and pulmonary functions or a person inside a hospital only can
be declared dead if having suffered from irreversible structural brain
damage his or her bodily functions cannot be maintained without conti
nuous artificial support, provided the diagnosis of Brain Death in such a
patient is based on diagnostic criteria as agreed by conference of Royal
Medical Colleges and their Faculties of United Kingdom resolved in 1976 .
The above definition of death will be the most appropriate, not only
for declaration of death in a terminally injured patient who has suffered
brain death due is irremediable structural brain damage but will also pave
the way for uniform determination of death in our country.
However it must be emphasised that for declaration of brain death
opinion of two doctors must be obtained out of which one should be the
consultant incharge of the case and the second may be any other doctor, in
case the consultant is not available then his deputy who should have atleast
five years of experience in dealing of such cases after his registration and
none of the doctors who declare the brain death in such a patient should be
the members of transplantation team in case the organ removal has been
planned for transplantation.
Summary and Conclusion
Good medical care includes providing good death in a terminally ill or
terminally injured patient. The dying patient must be considered competent
in terms of capacity for autonomous choice unless proved otherwise. Medi
cal science has now acquired life supporting systems and medications to
extend life artificially for long periods even after loss of brain activities and
control of bodily functions. Many people today have a fear of mind that
they will be kept alive artificially for indefinite periods of time with conse
quent suffering and distress to them and members of their family. The
conflict is often stated to be between doctor’s duty to treat to the best of his
ability and patient’s right to die with dignity, quietly and in peace when
further medical measures prove ineffective and only prolong suffering. Intro
duction of voluntary passive euthanasia in Terminal Care will not only
relieve a certain number of patients from suffering pain and torment which
can be avoided but will also enable the doctors to respond in the interest of
compassion and humanity according to wishes of patients suffering from
terminal illness and terminal injury. In case of a terminally injured patient
who fails to make a declaration or execute powers of Attorney in advance
expressing his wish to withdraw the life supporting treatment legal recogni
tion of brain death will enable doctors to withdraw the life sustaining aid
in a terminally injured patient after the declaration of brain death. Such
a measure legalising brain death as death of a person in the event of termina injury, wil be in public interest, for such a measure to be enacted will
not only protect doctors from needless prosecution and persecution but
but will also have numerous other benefits i.e. It will help in the field of
organ transplantation by permitting removal of organs either with the
consent of their relatives or with their own consent in else the" happened
to be organ donors in their life times, from these terminally injured
patients at a time when they are being sustained on continuous artificial
respiration after suffering from irremediable structural brain damage and
their organs are well perfused; secondly it will help in economising inten
sive care unit’s resources of the country which are being strained by pro
viding trained manpower, beds and respirators for ventilating these heart
beating cadavers, thirdly it will secure a doctor’s right to switch off the
respirator in a terminally injured patient after the confirmation of brain
death in the light of current knowledge on the subject lastly it will help in
the matter of property rights, negligence claims, insurance, worker’s com
pensation, probate law and taxes.
References
1.
Harward (1968) : Report of Ad Hoc Committee of Harward
Medical School to Examine the Definition of Brain Death, Definition of
Irreversible Coma. J. Amer. Med. Asso. 205, 337.
2.
Forrester, A.C. (1976) : Brain Death and donation of cadaver
kidneys Hlth. Bull. (Edinb.) 34, 199.
3.
British Medical Journal (1975) : Brain Death. 1, 356.
4.
Ivan, L.P. (1973) : Spinal Reflexes in cerebral death, Neurology
(M inneap) 23/650.
5.
Jonnett, B. (1975) : The donor doctor’s dilemma, observations on
recognition and management of brain death, J. Med. Ethics. 1, 63.
6.
Lancet (1974) : Brain Damage and Brain Death, 1, 341.
7.
H.C. Churchill-Davidson (1984) : A practice of anaesthesia, 5th
Edn. Lloyd-luke ltd. London, Brain—Death, 759-60.
8.
Mohandas, A. and Chou. S.N. (1971) : Brain death a clinical and
pathological study. J. Neuro. Surg. 35, 211.
9.
Glanville-Williams (1978) : Text Book of Criminal Law, Stevens
and sons. 234-35.
10.
Criteria of Death (1984) : Report of consultation
FIAMC Bio-Medical Ethics Centre Bombay. 20—24.
workshop,
11.
Roger Higgs (1985) : Dying Well : moral challenges in terminal
care, The Practitioner Dec. 1985, Vol. 229, 1073—76.
12.
Journal of Medical Ethics (1983) : ‘Case Conference’ Cutting the
thread and pulling the wool—a request for Euthanasia in general practice,
9, 45—49.
INTERNATIONAL CONFERENCE
HEALTH POLICY : ETHICS & HUMAN VALUES NEW DELHI 1986
Mora! and Ethical Dilemmas in the Care
of Critically ILL Patients
Dr. P.S. Chari, M.S., M.Ch.
Associate Professor of Plastic Surgery
Dr. (Mrs.) Pramila Chari, M.D.
Associate Professor of Anaesthesia
PGIMER, Chandigarh
The knowledge explosion in Science and Technology tends to over
whelm us and we get confused in a maze of technicalities and methods
often forgetting the patient we are treating and who becomes a conglo
merate of signs and symptoms instead of a person. Advances in resuscita
tive technology have enabled anaesthetists to almost indefinitely prolong
the life-supporting systems of critically ill patients who would formerly have
been pronounced as dead after simple traditional measures had failed. The
dilemma lies in the moral and ethical necessity of providing maximal care
for patients who are terminally or irrepairably ill but who have a chance
to survive their present catastrophe (Declaration of Helsinki, 1964). It is
agreed that permanent functional death of the brain stem constitutes brain
death and further artificial support is fruitless and should be withdrawn
(Honorary Secretary, 1976).
In a dilemma one is faced with two alternative choices, neither of
which seems a satisfactory solution to the problem. They arise in situations
of uncertainity and ambiguity when the general principles upon which one
normally relies either offer no help or seem to contradict each other. Such
decisions have to be distinguished from the many important clinical deci
sions which must also be taken by doctors. These decisions may present
as dilemmas but their resolution is dependent solely on the doctor’s know
ledge, experience and intuitive abilities. All these factors are certainly
helpful in a moral dilemma but are insufficient to unravel the moral
conflict, because a different kind of decision has to be made. The more
concerned the profession has become about the formulation of codes of
ethics the more they have become aware of the complexity of the moral
problems. The profession simply provides some generalised statements in
everyday language and leaves it to the good sense and good will of its
practitioners to deal with the ambiguous situations.
The individual conscience is thought of as a kind of inner voice
warning you against wrong doing and creating remorse when the warnings
have been disregarded. Following conscience is the most common way
doctors seek to solve the moral dilemmas they encounter. Peoples’ intui
tions’ about right and wrong often conflict sharply. It seems that con
science is a powerful force in controlling the actions of most individuals;
but although powerful, it may not always be right.
There is confusion about what is useful and advantageous to the
majority and what we feel all men ought to value. Treating every indivi
dual justly usually does benefit society as a whole Respect for the rights
of individuals is a more fundamental moral value than the happiness of the
maioritv. We are still primarily concerned with caring for people and the
art of 'medicine should not be forgotten in the enthusiasm for scientific
precision. Sympathy and understanding are just as important as diagno
stic acumen (Payne 1978). However, in many dilemmas of personal and
social morality the criterion of general happiness is a good corrective to
personal bias and idealistic mounting ot principles.
What we appear to be searching for is a set of absolute or funda
mental values which will clearly and unambiguously inform our choices
and decisions in any given situation. Such a calculus of human rights
cannot and will not be done. Rule following, much of it habitual and
unquestioned, characterizes a high proportion of our daily activities. Our
behaviour is confined within the limits of the socially acceptable, the
legally sanctioned and the routines of personal preference and conviction.
A rule-governed approach to morality becomes a wholly depersonalised
one. What is missing is any consideration of the persons who hold the
principles and the persons to whose circumstances the principles are
applied.
A
It is said that Hipprocrates forbade the administration of remedies to
those who were past hope. This injection we may heed as advice not to
make difficult the final stages when we recognise their finality. None can
relieve us of the responsibility of judging when this moment shall have
come. We should bring to the beside a great hopefulness, a determined
optimism, but is the futility of the struggle is clearly evident, then we
should put aside our remedies as cures, and make the patient easy with
such solation as may offer (Gavey 1950). We are asked to give guidance,
to judge dispassionately upon reasonable probabilities. The fact that many
of our prognosis prove wrong should not detract from a genuine attempt
at a correct forecast. As Osler said “Errors of judgement must occur in
the practice of a art which consists largely in balancing probabilities”.
The question: “should the doctor tell?” is guided in practice by the
circumstances of each case which suggests the line that should be taken. In
general, a guarded prognosis slowly revealed enables a patient to prepare
himself, retaining a hopeful attitude in the background. In these matters
few demand to know the truth and nothing but the truth and even if a
direct question is asked the patient usually welcomes an answer which does
not shut out all hope. The patient senses the true position far more accu
rately than one might imagine and any attempt to soften the blow is wel
comed. There are occasions when it is best never to disclose the true
position, even at the end. The human capacity for self deception is «reat
and this characteristic needs to be promoted occasionally.
Intensive medical care is designed to diagnose, treat and maintain
patients with immediate, acute but potentially reversible life-threatening
impairements. It also aims at prophylactic management to avoid such
catastrophes as cardiac arrest, respiratory arrest, shock, renal failure and
overwhelming sepsis There is a growing beleif that medical and techno
logical capabilities should not necessarily be used simply because they
2
D
.
? there an ethical imperative to preserve all patients in life threatenmg situations including those for whom existence seems only a fiction and
others tor whom it promises to be only severely diminished? On one view,
it is justmcable to moderate the therapy even though earlier death will
occur, when this will result in relief from pain and suffering. Another
Vl5.w, 1S\v at Our training is to preserve life and functions whenever pos
sible . We are not trained to decide who “is better off dead”. The patient
who is alive has an overriding right to life and deserves the maximal pos
sible therapy (Cohen, 1977).
This conflict has implications for the care of those who are not
terminally ill, but who are potentially salvageable with the chance that sur
vival will be accompanied by severe physical or mental impairement or both.
It is these difficult cases concerning the level of salvageability that lead to
the widest divergence of opinion. The problems are complicated by the
fact that it is often not possible to evaluate the likely outcome of intensive
care treatment until the patient has been monitored for some days and
even then, predictions are open to revision in many cases (Cullen et al,
1976, Griner, 1973). It is also to be remembered that there is a moral
difference between “Killing’ and ‘letting-die*. Dying is the final event of a
valuable human being and no one else is morally empowered to initiate and
transact. When a decision has been made that maximal treatment is in
appropriate it is not an acceptable ethical alternative to kill the patient,
but it is permissible to allow the patient to die (Me Cormic, 1974).
Western ethical traditions have reached some general agreement that
it is necessary to use ‘ordinary’ but not ‘extraordinary’ means to support
and comfort patients in such cases (Pope Pius XXI, 1958). By ‘ordinary’
means is meant ‘all medications, treatment and operations which offer a
reasonable hope of benefit for the patient and which can be obtained and
used without excessive expenses, pain or other inconvenience’. ‘Extra
ordinary’ means are those that do not offer such hope or cannot be
obtained or use without those kinds of liabilities. There is a professional
and moral relationship entered into with each patient admitted for intensive
care in which it is understood the patient will receive appropriate care.
Such care cannot be terminated later on the grounds that another patient
with a higher potential for survival needs intensive care without violating
the original obligation to the admitted patient and without violating the
ethical principle that we cannot aid some by harming other (Report of
Clinical Care Committee, 1976).
Survival though important, is not to be bought at any cost and that
to attempt, but fail to achieve, may reduce so-called intensive care manage
ment merely to the level of prolonging the process of dying (Rabkin et al,
1976). It is of primary importance from an ethical perspective to deter
mine whether the right to life is absolute or whether it can ever be over
ridden with justification. Our conclusions will not apply with absolute
finality, like mathematical equations, to all cases as individuals have very
different conceptions of how to exercise their right to the pursuit of happi
ness within the limits of the ethically possible. Reverence for life must be
tempered by restraint and an equal respect for the dignity of death. In the
last analysis, our choice is influenced by the way the personality regards it
destiny and our own conception of death.
3
BIBLIOGRAPHY
I.
A Report of the Clinical Care Committee of the Massachusetts
General Hospital. Optimum Care for Hopelessly Ill Patients. New Engl.
J. Hed. 295:362,364, 1976.
2.
Cohen, C.B.: Ethical Problems of Intensive Care. Anaesthesiology.
47:217-227, 1977.
3.
Cullen, D.J., Ferrara, L.C. and Briggs, B.A.: Survival hospital
charges and follow up results in critically ill patients. New Engl. J. Med.
294:982, 987, 1976.
4.
Declaration of Helsinki. Brit. Med. J. 2: 177, 1964.
5.
Gavey, C.J.: The Management of the ‘Hopeless’ case. Buckston
Browne Prize Essay. E and S. Livingstone, Edinburg, 1950.
6.
Griner, P.F.: Medical intensive care in the teaching hospital:
Costs versus benefits. Ann. Int. Med. 78:581-585, 1973.
7.
Honorary Secretary of the Conference of Royal Medical Colleges
and their Faculties in the U.K. on 11 October, 1976: Diagnosis of Brain
Death. Brit. Med. K. 2:1187-1’118, 1976.
8,
McCormick, R.A.S.J.: To save or let die. The dilemma of
modern medicine. J.A.M.A. 229:172-176, 1974.
Payne, J.P.: Ethical Problems in Clinical Research and Intensive
9.
care. Brit. J. Anaesthesia. 50:413-414, 1978.
10.
Pope Pius XII. Amer. Q. Papal Dec. 4:393, 1958 quoted by
Bishop, V.A.: A Nurse’s view of ethical problems in Intensive Care Clinical
Research. Brit. J. Anaesthesia, 50:515-518, 1978.
11.
Rabkin, MT., Gillerman, G., and Rice, N.R.: Order not to
resuscitate. New Brit. J. Med. 295-364, 1976.
12.
Resolution 613: On the Rights of the Sick and Dying. Parlia
mentary Assembly of the Council of Europe, 1976.
13.
Safar, P. and Grenwick, A.: Critical Care Medicine, Organising
and Staffing Intensive Care Units. V Chest. 59:535-547, 1971.
^Floor) S. V
C?LL
rr
RCad
INTERNATIONAL CONFERENCE
HEALTH POLICY : ETHICS & HUMAN VALUES NEW DELHI 1986
Terminal Care-Ethics and Cultural Aspects
Dr. Rizvi, S.N.A. and Dr. Rajvanshi, P.
Maulana Azad Medical College New Delhi
Mankind is subject to the experience of physical death. The death
is a state or condition with an existence for man beyond the grave, difficult
to describe or quantify. Terminally ill (dying) means that the patient has an
illness has which been accurately diagnosed, and which seems certain to
bring about his death within a relatively short period of time, since the
illness is beyond both cure and palliation. Caring for dying patients and
giving sympathetic support to breaved families are profoundly important
parts of the work of doctors, nurses and other members of the caring
professions. The care of patients during their terminal illness over various
periods of time is a privilege, for they greatly appreciate the visits of the
doctors and realise they are not forgotten. They may be cared for in
hospitals, nursing homes, or family homes and is requires numerous medical
and nursing skills according to the particular illness. Symptoms are treated
so that the patient remains free from pain and in comfort. Much nursing
care is required by some patients, especially those who are paralysed in
various ways.
Guidelines for Delivering Bad News
Every physician derives satisfaction from delivering good news to a
patient; and no physician enjoys delivering bad news. Still, there are rare
occasions when it becomes necessary for the physician to disclose a crippl
ing diagnosis and prognosis to the patient. There are some general guide
lines for delivering bad news as follows:
1.
2.
3.
4.
5.
6.
7.
Keep it simple.
Don't deliver all the news at once. It is good idea to try not to
provide too much information at the first sitting.
Educate the patient gradually and gently regarding the diagnosis.
Wait for questions from the patient.
Ask questions yourself— Valuable clarifications can result from
gentle, and clear questioning.
Do not destroy all hope. “Most people with this form of disease
as chronic renal failure are living longer but are not cured of
their disease” is a useful kind of statement.
Do not say anything that is not true. This would be the crudest
blow of all.
I have the responsibility of caring for many patients with various end
stage renal diseases; this particular diagnosis understandably causes unrest
and anxiety to the patient and family. Various questions require answer
ing at all stages of these illnesses. An explanation about the treatment
and prognosis is given to the family, with the assurance that every thing
will be done to help the patient throughout the illness. The question
whether the patient should be told he or she has end stage renal disease
needs some discussion. Information is given with sympathetic understand
ing of the situation and in the kindest way, in the presence of near relatives
Words are chosen carefully to create faith and confidence, and nothing
shall be said to take away a patient’s hope. I believe we can work profes
sionally in a more helpful way when patients are told about the terminal
illness, and by understanding something about the problems to be solved
they can cooperate usefully.
Emotional Aspects of Death and Dying
In a critically ill and dying patient, palliation and emotional support
are the optimal strategies. A useful approach is to communicate the medi
cal realities to the patient as skillfully, honestly, and clearly as possible and
allow the patient with the help of his or her family to decide upon the
preferred treatment. Health professionals must have the courage and
willingness to acknowledge that the patient’s wishes may take priority over
their own.
Patient-Doctor Communications
Fundamental to the evolution of effective doctor-patient communica
tions is the notion that physicians answer all questions honestly, giving
as much information as is asked by the patient.
Ambiguous or dishonest communication imposes needless emotional
pain on patients and families facing life-threatening illness.
A variety of information inputs that come to the patient:
1.
Direct statements from the physician.
2.
Overheard comments of the physician to others.
3.
4.
Direct statements from others including nurses, ward boys and
technicians.
Statements from family, friends and clergy.
5.
Changes in the medical care routines, procedures, behaviour of
others towards patients and changes in physical location.
6,
Self-diagnosis, including reading
records, charts and books.
of magazines,
newspapers,
It is evident that the dying person is engaged in multiple communi
cations with many people. If the messages are clear the dying person can
make sense out of his experience. But if the messages are confused or
contradictory, the result ts needless apprehension and anxiety Many
patients, once they are aware and acknowledge the untreatable state of
their disease have less pain and discomfort in general and require a minimum of medical supervision.
It is very difficult to answer the questions about the length of time
the patient is likely to live, except when the end is obviously neat and I
explain that all our lives are in the hand of God. I respect the wishes of
2
the family relatives of non-mentioning of the diagnosis and prognosis to
the patient to avoid any upset, although it made more difficult when a
patient realises the gradual deterioration of health without a real explana
tion being given to him. During the final days of the illness, the family
members have to be informed about the time becoming short for the
patient and by that time majority of these patients know about their
condition. Whole family require help at these times to ameliorate the
strains and stresses caused by loss of family member.
Patients who are seriously ill and cannot recover by available recent
mode of therapy and their families, appreciate the frequent visits of the
doctor, who can give much sympathetic help and support to ameliorate the
sorrow and suffering which become more intense as death approaches for
the loved relations. The presence of the doctor who has become a trusted
friend during the illness is a source of solace to them in their grief. A
special, unhurried visit following soon after the patients death to take and
discuss is greatly appreciated by the family and these visits to the breaved
family should continue for a further period of time, until there is an
amelioration of their grief and loneliness.
Community Approach to Psychological Support of Dying Patient
The awareness, tolerance and acceptance of the reality of dying is
difficult for the patient and family. In order to provide emotional, social
and spiritual support, a community-wide effort helps in achieving the
maximum care for the patients comfort and psychosocial support. It is
important to have people involved, whether social workers, trained
volunteers, priests, etc., who can give supportive help to patient and family
members.
Bereavement Follow-up
Bereavement leads to a period of crisis, for the family. The care of
the terminally ill patient and family does not stop when the patient dies.
The members of health team may attend the funeral. Home visits and
telephone contact continues with the family within the first three weeks of
bereavement and subsequently upto approximately one year. Opportunity
for the spouse, parents and children to express their grief and talk about
the illness and death does much to relieve guilt and depression. A
memorial card is sent to the key person on the anniversary of the death.
Role of Clergy Man or Priest
Not all symptoms need medication in a terminally ill patient. Pain
of isolation and inability to attend church and ring with the choir is helped
immensely by the presence of clergy man or priest and with the relatives
and friends at bed side.
Understanding Patient Depression
Frequently observed patient response to life-threatening illness is
depression. It results from:
3
(i)
(ii)
(iii)
(iv)
Prolonged and painful hospitalization and treatment.
Emotional abandonment by family and friends.
The real or imagined insensitivity of hospital personnel.
Depletion of finances due to expensive medical care.
It is not helpful to interrupt this response with false promises of cure
or positive response to treatment. Patients require emotional support.
One can be extremely supportive by sitting with the patient, often in silence,
in an attempt to convey willingness to share this emotionally demanding
period.
The Patient’s Family
The dying patient and his or her family constitute the optimal unit of
health care. It is extremely important for patients to conclude family
relationships in as emotionally satisfying a way as possible. It can be very
distressing for critically ill persons and their families to be separated by
the treatment milieu. Following suggestions are offered to health pro
fessionals:
1. Train family members to participate in treatment.
2.
Encourage them to do such things as continue to cook special
meals for the patient.
3.
Allow unlimited visiting so that the total family,
children, can spend time with the patient.
4.
Provide special social and educational programs for the family
and patient.
including
Continue these programs, adding home visits for the family after the
patient has died.
Despite the importance of care for all troublesome and common
symptoms of terminal patients admitted in hospital (100 cases); it remains
to be said again that good personal relationships and the prevention of
loneliness are of paramount importance in providing high quality terminal
care (Table I).
Pain
Incontinence
Confusion
Nausea
Anorexia
Insomnia
Depression and
anxiety
50%
30%
20%
15%
15%
15%
20%
Dyspnoea
Bed sores
Vomiting
Cough
Dysphagia
17%
>5%
13%
5%
3%
The importance of adequate fluid intake, bowel regulation without
discomfort and the correction of electrolyte imbalance, must be stressed in
the terminal patients as in others. In dealing with all these symptoms the
doctor’s enthusiasm and confidence in his therapy will be, without doubt
4
transmitted to the patient. He should have the same interest in the patient
during this stage of life as in any other. It is stressed that whether patient
is nursed at home, in an institution, or by intermittent hospital admission
and discharge, it is essential to make certain that there is continuity of
care.
The management of terminal illness by the family physician is in
the exploration and development of the doctor/patient relationship where
the feelings of patient and the doctor are fully expressed and understood.
A good relationship is best established when the patient and doctor
acknowledge, either overtly or covertly, their awareness of impending death
and the patient is allowed to test out the relationship without any fear of
the doctor withdrawing.
In hospital, the dying patient receives every attention, constant
medical and nursing care, the advantages of modern palliatives, profusely
planned drug administration for the control of pain and freedom from ne
glect and loneliness. Very little work has been done to estimate the numbers
of patients who die at home compared to those who die in hospital. 90%
of all episodes requiring medical and nursing care attentions are dealt with
in the community, but it is unlikely that a similar percentage rate applies to
death. Once the decision is made, the transfer from hospital to home care
should be effectively planned, so that the home, family and the primary
care doctors and nurses are all prepared.
INTERNATIONAL CONFERENCE
HEALTH POLICY : ETHICS & HUMAN VALUES NEW DELHI 1986
The Right to Live and The Right to Die
Minoo Masani
President, World Federation of the Right to Die Societies
My good friend, Yusuf Meherally, whose useful life was cut short so
cruelly, used to write in every autograph book which was placed before him
by his many young admirers : “Live dangerously”. In my young days I
thought it was a rather good slogan and, by and large, I have tried to live
up to it, and never regretted doing so. The idea of death has never
worried or frightened me right from my young days. I would much rather
be dead than red. What does, however, give me the creeps is the thought
of being crippled and unable to function. I know a great many people
who share this preference for a quick and dignified death to a long and
humiliating existence as a cripple or a vegetable.
At a meeting I addressed on behalf of the Society For the Right To
Die with Dignity, which was the first of its kind in India, I was asked by a
gentleman who believed in karma what advice I would give him. I told
him that, as far as he was concerned, he was altogether entitled to endure
the sufferings to which he had referred as part of the cycle of karma.
Since all we are arguing for was Voluntary Euthanasia, I hoped he would
not mind my exercising my option the other way when the occasion arose,
since I was not convinced of the reality of reincarnation or karma.
Some of my friends find it difficult to accept the thought that, when
they die. it will be their final elimination and nothing will remain of them
at any level of existence. I must confess that to me the idea of absolute
destruction does not hold any terrors, while the idea of going through
Purgatory and then facing whatever came afterwards does not appear to be
particularly restful after a long and busy life on this earth. Why should
one object to being blotted out at the end of this life ? Why should I have
the conceit that I must go on forever ?
All this shows that our perceptions about the matter of life and
death vary greatly and that to deny anyone the right to a different view
from what one holds oneself would be not only dogmatic but stupid. We
all know so little, about these matters, and it is best to keep an open mind,
do the right thing, practice the golden rule, and leave the rest to Provi
dence which, it has been aptly said, “shapes our ends, rough how them
how we will”.
I have always responded warmly to the English poet who wrote :
“I am the master of my fate,
I am the captan of my soul.”
I was therefore greatly touched when Mr. Gopal Mandlik, a well-
known social worker of Poona, ended his own life in 1980 after waiting
two years for the Government of India to amend the Indian Penal Code
and to make it possible for him to do so legally. His only regret was
that his eyes and his kidneys, which he had wished to donate for humane
purpose by deleting Section 309 IPC could no longer be put to use in that
manner. He was a true satyagrahi in the Gandhian sense. Gandhiji
always urged that where one’s conscience held a law to be wrong or immo
ral, the satyagrahi should break the law and take the consequences but not
run away.
Mr. Mandlik’s brave act was one of the factors that led some of us
to establish The Society For the Right To Die with Dignity in May 1981.
Another sad case of someone who was not in a position to imitate
Mr. Mandlik was that of my good friend Norman Thomas, the American
Socialist leader, who was in his old age completely paralysed and pleaded
to be released, but was tormented by being kept alive for many years
because it was not legal in that particular part of the United States to
allow him to die.
When people tell me that public opinion is not ready for an amend
ment of the law which would make Voluntary Euthanasia easier to
practice, under proper conditions and safeguards, I am inclined to wonder.
Public opinion has been described as “a fickle jade” and indeed is very
volatile and changeable. In the middle of the 60s, a well-known lady who
was a champion of birth control in India, pleaded with me not to introduce
a Private Member’s Bill in Parliament for legalising abortion on the ground
that, if I were to do so, it would create such a storm of opposition that
the backlash would injure the cause of contraception. Lo and behold,
four or five years later I found myself a member of a Joint Select Commit
tee of Parliament which recommended to Parliament the legalising of
abortion, and I noted that nobody in the Select Committee and nobody in
Parliament opposed this change in principle. How do we then know what
public opinion is or not in the case of Voluntary Euthanasia unless we first
educate it and then test it ?
That is precisely what our Society has tried to do in the years that
have passed since we took this pioneering step. There has recently been a
great deal of public discussion on this issue.
Much of this is due to a .Bill introduced by Prof. S.S. Varde in the
Maharashtra Legislative Council to provide for immunity and protection
to physicians and surgeons who withdraw life sustaining treatment from
terminally ill patients at their wish. This Bill was ordered to be circulated
by the Council to elicit public opinion and this led to a controversy in the
course of which prominent doctors in Bombay including Dr. Praful
R. Desai, Director, Tata Memorial Centre, Dr. N.H. Keswani, Medical
Director, Jaslok Hospital and Research Centre, Dr. B.N. Colabawala, Dr.
R.R. Soonawala. Dr. K.D. Desai, Dr. F. Soonawala, Dr. J.C.N. Joshipura,
Dr. V. Talwalkar and others have written to the press welcoming the Bill.
The other helpful development is a judgement of a Division Bench of
the Delhi High Court on March 31st 1985, which refused to punish a
young man who attempted to commit suicide despite Section 309 of the
Indian Panel Code which makes such an attempt punishable.
In an outspoken judgement, the Delhi High Court has held that
Section 309 of the IPC is an anachronism unworthy of a humane society
like ours. The High Court went on to observe that many penal offences
were the offshoot of an “unjust” society. ‘,So long as society refuses to
face this reality, its coercive machinery will invoke the provisions like
Section 309 IPC which has no right to remain on the Statute Book”. The
Court said that “the young man (Sanjay Kumar Bhatia) who tried to com
mit suicide because of “over emotionalism” would have escaped human
punishment if he had succeeded in taking his life but was now being houn
ded by the police, because the attempt failed.”
By and large the response to our cause has been encouraging. This
is particularly so in the case of the medical profession, many of whom have
in their own practice faced the “Doctor’s Dilemma”. Most doctors are
humane, compassionate human beings and many of them share Dr. Chris
tian .Barnard’s regret that they are not able to give relief from pain and
distress to those of their patients in whose case they consider it appropriate.
Hundreds of letters have been received by us, many of them extremely
touching, about the sad stories they have to tell and the welcome they have
given to our Society.
Our Society has prepared a draft Declaration and a draft Power of
Attorney which it has issued to members for their use if they so desire.
These documents make clear the wish of a man or woman in sound mind
that, in case he or she is terminally ill and unable to give expression to his
or her wishes, artificial medical treatment should be withdrawn and pain
killing drugs given to him or her. The Power of Attorney would nominate
two persons who would be duly authorised to persuade the doctor and
family to respect the patient’s wish if the occasion does arise. The Power
of Attorney could of course be revoked at any time. Such documents are
widely used in the U.S.A, and in U.K., where the law in regard to the
abetment of suicide is the same as in India. These documents do not
legally bind anyone but are valid documents even under the law as it stands
today and would carry a great deal of moral influence.
Our Society is the 28th of its kind in the world. I was very happy to
hear from my good friend, Arthur Koesler, the well-known writer, who
said in his letter : “I am glad to hear that you are starting EXIT in India.
It will be a long and hard way until charity and commonsense will do
their work.”
The Examiner a Catholic Journal, dealt with this matter in two
issues. In its first issue of August 15, 1981, it naturally came out in opposi
tion. I was glad to see, however, that in the second issue of August 20,
1981, the paper conceded that passive euthanasia may be justified. It
quoted from the declaration on Euthanasia by the Congregation for the
Doctrine of the Faith :
“When inevitable death is imminent inspite of the means used, it is
permitted in conscience to take the decision to refuse forms of treat
ment that would only secure a precarious and burdensome prolonga
tion of life so long as the normal care due to the sick person in
similar cases is not interrupted”.
The most common doubt that is expressed is the fear that any change
in the law to make it more humane would make it easier for unscrupulous
persons to bump off old and sick relatives. This is a genuine fear, but
it relates to mercy killing with which we, as a Society, are not concerned,
and not to Voluntary Euthanasia. The danger of ‘bumping off’ only arises
when ore person can arrange for another person to die. It cannot arise
when a man or woman in sound mind but terminally ill makes his or her
own choice and asks for self-deliverance.
I believe that public opinion can be mobilised within the next few
years when it has been made more aware of the issue. We in the Society
believe in obeying the law, but we would like it to be amended so as to
make it more humane and compassionate.
COMMUNITY HEALTH CELL
47/1. (First Floor, St. Marks Road,
Bangalore - 560 001.
INTERNATIONAL CONFERENCE
HEALTH POLICY : ETHICS & HUMEN VALUES NEW DELHI 1086
Family Planning—A National Priority Social,
Ethical, Cultural and Medical Aspects
Role of the Medical Profession
Dr. Dipak Bhatia F.R.C.S.
Family Planning Foundation, New Delhi
The medical profession over the ages acquired two major roles in
society. The first the more ancient one of ministering to the sick and sorry.
Of providing medication, treatment and relief for illness and injury.
The second role evolved later and gradually. It was that of a mentor
to the society on health matters. It carried out this role by organising
and instituting measures for the prevention of sickness. By advising and
suggesting measures for the promotion of health. This second role less dra
matic and less spectacular has not the glamour associated with the provision
of relief from suffering. But it is perhaps more substantive and important
as it promotes and preserves the weal, welfare and integrity of the society.
The two roles however are not exclusive but mutually supplementary.
It is in the ambit of the second role that the medical profession’s
commitment is invoked to tackle the current population growth and the
health hazards arising thereof.
Let us do a quick review of the estimated momentum of the popula
tion growth since the oneset of the modern era.
It took several thousand year of man’s existence on this planet to
reach the world figures of 500 million by A.D. 1650. It took the next 175
years by A.D. 1825 to double the population to 1,000 million (that is one
billion). 105 years more to again double to 2,000 million or 2 billion)' by
A.D. 1930, and the next 45 years by A.D. 1975 to double again to 4,000
million (4 billion). At this tempo it is estimated that the world population
by the year A.D. 2000 will increase to 7,000 million or 7 billion (Table 1)
TABLE 1
Year
Doubling Time
A.D. 1650
A.D. 1825
. 175 years
A.D. 1930
105 years
A.D.1975
45 years
National Academy of Sciences
U.S.A.
Population
500 million
(J billion)
1,000 million
(1 biUion)
2,000 million
(2 billion)
4,000 million
4 billion)
What are the penalties imposed on human existence and human
health by this runaway population.
The first need of the people is that of food.
The problem is one of food and numbers.
keep pace with the population pace.
Can food production
The pattern of population expansion around the globe is not
uniform. It ranges from zero growth to moderate in the affluent and
developed countries. In the underdeveloped countries it is high. It seems
that poorer the country the higher is the rate of its population growth.
Resulting in the phenomenon that the countries least equipped to increase
their food production are faced with high rise demand for food and
nutrition.
It is estimated that two-thirds of the world’s pre-school children
suffer from one form or other of malnutrition. So does perhaps
one-third of the world’s population. Malnutrition may be one of low
calorie intake or a more serious one of also low intake of proteins and
other essential items. The resulting morbidity is of wide range.
A sensitive indicator of malnutrition in children is the slowing down
of their growth and development. This may also be reflected in their later
years by all round reduced capacity.
Infantile marasmus and kwashiorkar are not uncommon serious
nutritional diseases. These are likely to occur when breast feeding is in
adequate or terminates early due to one or another reason and the supple
mentary food given is deficient in calories and grossly so in proteins and
other essential nutrients. These diseases have high mortality and are likely
to leave permanent scars in the victims.
The classical nutritional diseases of beri-beri and pellagra are still
quite common, Caused by deficiency of thiamine and niacin respectively
in the diet and aggravated by protein deficiency, these may also leave
permanent damages.
Anaemia is another wide-spread manifestation of nutritional defi
ciency occurring in all age groups. It is particularly harmful in mothers
and children.
A number of other malnutrition morbidities like scurvy, rickets,
goitre also occur but much less commonly.
Malnutrition directly contributes to lowered resistance to infections
and inter-current diseases. The penalties on a nation from malnutrition
are the decline in the general health of its population and the impairment
of social and economic developments.
Let us look at our country. At the time of gaining our freedom our
P°pula«AAnriW?S.350 m‘ S T,<?day “ is nearing 800 million and by the
year 2000 likely to cross 1000 million.
With 14 per cent of the world’s population our geographical entity
contains only 1.5 per cent of the world’s arable land.
In the earlier post-independence years we had to import sizeable
quantities of food. Today we are self-efficient. This is, however, a presucarious situation. Apart from the growing demand from an enlarging
population, the vagaries of the weather and climate can tilt the balance.
Our increased food production was achieved by a combination of
inputs. By use of fertilisers and pesticides, by improved variety of seeds,
by better management of land and water resources, by application of new
technology and energy resources.
There is however, a biological limit to what can be produced by these
special essential inputs from the small layer of about 10 to 12 inches of top
soil that covers the earth’s crust. In some parts of the world this limit has
already been exploited.
The population imposes another burden on the land. To meet the
pressure of increasing needs and demands the processes of development
cause diversion of land to other uses. Like for the expanding network of
roadways and rail-tracks, for dams and canals, for the construction of
buildings for habitation, for industries and other institutes. It thus cuts
away land to that extent and diminishes it for food production.
Another problem that the population creates is of deforestation
arising from the mindless cutting of trees to fulfil pressing needs. This
causes erosion of the soil, ecological imbalance and leads to climatic
changes. The sequalae of such disturbances are harish. An example of
such consequences are the recent occurrence of prolonged drought and
widespread famine in Ethiopia.
Poverty is a high breeder of ill-health. The poor denied the resources
and services essential for positive health exist under adverse and insanitary
conditions. Their resistance is reduced and they are easy prey to infections
and diseases.
Poverty is compounded by unemployment. The unemployed para
sitic are not productive. Both poverty and unemployment expand as the
population grows rapidly.
In India the jobless today are estimated at about 50 million.
month another 130,000 new entrants swell their cadres.
Every
Man tends to pollute his surroundings. He does it more at his growing numbers crowd the earth. The environmental deterioration is aggra
vated by the increasing discharge of industrial effluents and toxic by
products of technology onto the soil, the waterways and the atmosphere.
The resultant environmental pollution has both direct and indirect effects
deleterious to health.
The mounting pressure of high population growth imposes other
penalties on the health of the people.
3
Man like other species requires a minimal space dr elbow room in
which be can function and lead a balanced existence. What may be
labelled as his need of essential territorial exclusiveness. If the cordons of
this territory are shrunk or intruded upon it causes his mental and physical
disorientation and deterioration. Much of the social malaise and morbidity
in the cities can be traced to the current fast trend of urban concentrations
of high density.
The application of new health technologies in the developing coun
tries has been comparatively facile. It has dramatically brought down their
death rates. The professional cadres however have not been able to provide
adequate level of individual health care in these regions. The doctor/population ratio there-in is low. So is that of the essential and supportive para
professional cadres. The fast population growth aggravates the deficiency.
The training of these technical manpower groups is slow and time-consum
ing and their production cannot match the population pace. The demands
for health services soon outrun the supply.
High fertility has a direct correlation with the health risks of women
and children. In women besides causing a greater incidence of ill health
associated with pregnancy and childbearing, it makes them more vulnerable
to general health hazards and diseases. It reduces their reproductive effi
ciency and their capacity to give a good start and provide adequate mater
nal care and sustenance to their progeny. This is reflected in the occu
rrence of high fetal loss, more congenital malformations, low birth weights
and raised infant mortality. The surviving children show more signs of
malnutrition, impaired growth and retarded development. The adverse
effects of high parity both in women and children are aggravated if the re
pealed pregnancies occur at short intervals. Uncontrolled and unregulated
parity undoubtedly impose heavy penalties on women and their progeny.
High fertility rates are often associated with high rates of induced
abortions. Often illegal and performed under most unsatisfactory condi
tions, these add to the health hazards of the women.
The communities which continue to have high birth rates show a
profile of a young population and an age distribution of a pyramid with a
wide base. In this pyramid 0-14 years group forms a large cohort. The
need of medical care for this group and the problems of its provision are
more complex and difficult than for other age groups. This puts further
pressure and strain on the medical network and its resources.
In cognition of the changing global pattern of human existence it is
imperative that human fertility is controlled and regulated. The medical
profession must take the prime responsibility to advise family planning as
an essential health measure and propagate contraceptive practices.
Man stands apart from animal life. He is gifted with the power to
think, to formulate, and pursue some enduring values. Amongst them is
his capacity for compassion.
The raison d’etre of the medical profession is to demonstrate the
quality of compassion in operation. It is in the compass of that aura that
4
the profession functions to prevent unnecessary deaths. To the objectives
of reducing pain and suffering. Not for financial rewards, not for economic
gains. But in the fulfilment of the humanistic traditions that inspires the
professional ethos.
The same altruistic grace should move the medical profession to
commit its resources to prevent unnecessary births which but add to the
sprawling numbers condemned to an existence of hunger, want and
degradation.
The atom bomb is man’s brain-child. The population bomb his
biological child. Both a threat to this survival. The first threatening his
dissolution in an instant flash. The second to a slower end by choking up
and dissipation of the earth’s resources essential for his existence.
Man must control both diabolic creations.
profession must be in the vanguard.
In that effort the medical
5
INTERNATIONAL CONFERENCE
HEALTH POLICY : ETHICS & HUMAN VALUES NEW DELHI 1986
Ethical Dilemmas in a Health Policy
Points to Ponder
Dr. Prom Sobti
Medical Officer WHO SEA Region New Delhi
“The enjoyment of the highest attainable standard of health is one of
the fundamental rights of every human being without distinction of race,
religion, political belief, economic or social condition.” This cardinal
principle enshrined in the Constitution of the World Health Organization
has been the guiding light for health planners and administrators the world
over as they have attempted to steer their national health policies in the
turbulent seas of want, hunger and disease.
How successful we have been in achieving this laudable goal, is, of
course, a debatable matter. What, however, is beyond any doubt is the
fact that for vast number of people in the world, health remains an illu
sion, a dream.
What makes the problem more complex is that in an age of conflict
ing demands and limited resources, health unfortunately takes very low
priority. The experience usually has been that when budgetary cuts
become inevitable, the axe falls first on the health sector.
It is largely for the above mentioned reasons that we find ourselves
in a situation where hundreds of millions of people in rural communities
in the developing world have little or no access to health care. On the
other hand, “disease palaces,” as the Director-General of the World Health
Organization, Dr. Halfdan Mahler, once described some ultra-modern
hospitals, consume a sizeable portion of the country’s health budget. We
therefore find ourselves in the uneviable position of spending 80% of health
budgets on 20% of the population, whereas 80% of the population living
in rural areas has to make do with 20 % of the budgetary allocations.
If ever there was an ethical dilemma, this is it.
So, what does one do about it ? How can there be a more equitable
distribution of available health resources ? How can the people be equip
ped to take care of themselves ? All these questions, and many more, have
been raised in the past few years in international conferences as it has
become increasingly obvious that in order to achieve a reasonable standard
of health, the people themselves will h; v: to do something about it.
Health for All
The beginning of this direction was made nearly a decade ago when,
at the World Health Assembly held in 1977, the Member Countries of
WHO adopted the historic resolution setting for themselves the goal of
“Health for All by the year 200.” The following year, WHO and UNICEF
organized the first-ever international conference on Primary Health Care
at Alma-Ata, USSR. It was here that the vehicle through which health
for all could be achieved, primary health care, was identified. Since then
the momentum has grown with countries formulating their national strate
gies and plans of action to achieve the goal. Also, as a result of public
debate on the issue, health has been recognized as an integral part of the
development process. In fact, it is now acknowledged that without health
there can be no development. What has also emerged recently is the under
standing that health is not the responsibility of the health sector alone, and
that in order to achieve common objectives, health development needs to
be a multisectoral effort.
It is, for example, now an accepted fact that health depends on a
number of supportive services, like health education, nutrition, water and
sanitation, just to name a few. This aspect, of health development encom
passing many disciplines was most forcefully emphasized in the Declaration
of Alma-Ata. In spelling out what was meant by primary health care, the
Declaration stated that this included at least: education concerning
prevailing health problems and the methods of preventing and controlling
them: promotion of food supply and proper nutrition; an adequate supply
of safe water and basic sanitation; maternal and child health care,
including family planning; immunization against the major infectious dis
eases; prevention and control of locally endemic diseases; appropriate treat
ment of common diseases and injuries; and provision of essential drugs.
If one examines these eight elements separately, it becomes obvious
that in order to make primary health care available to all would mean
active collaboration and coordination between various departments and
ministries.
Policy-making Problems and Pressures
In order to make any objective assessments or set realistic targets,
it is necessary to keep in mind that health development has to be viewed
in the context of'the prevailing socio-economic conditions. For example,
it is impossible to expect any dramatic improvements in the health status
of the people without a corresponding improvement in the agricultural or
industrial production, literacy rates, status of women, and so on. I am
purposely not going into the area of health statistics, of demographic
profiles or disease patterns, because I wish only to differ some trigger points
for discussion.
What is important to bear in mind is that many developing countries
like ours find themselves in a very real predicament. The predicament of
choice. Not because there are several choices, but because there are very
few. Thus we find that while on the one hand there are millions without
adequate medical care, on the other hand there are thousands of qualified
doctors with nothing to do. Thus we find that whereas production of
drugs is adequate, it never reaches the places it is most needed. Thus we
find that simple, low-cost technologies that arc available and acceptable
to the people are not utilized. Here, it is not so much a matter of inade
quate knowledge as the inability to take the necessary decisions at the
policy-making levels. It is here that political commitment assumes a very
significant role. For without such commitment, most ideas never get
translated into action.
2
Community Involvement
Largely as a result of the movement set in motion by the resolution
setting the goal of health for all and the subsequent actions taken at the
country level, it is now realized that without the involvement of the
community the goal of health for all can never be achieved. An active
and self-reliant people can do a lot for their own health and the health of
their fellow beings as well as prevent, control and treat diseases. But the
real question that needs to be answered is how far do countries want their
people to be self-reliant. This is not merely a rhetorical question, it has
serious political undertones.
Even if one chooses to stay clear of political issues there is no denying
the fact that many factors having a direct bearing on health are largely
influenced by political decisions. To give just one example, one could cite
the per capita expenditure on health. In most developing countries it can
safely be said that expenditure on health is perhaps the lowest, compared
to the other sectors. Here one need not draw comparisons between what
is spent on defence, as compared to health. But the example is important
to keep in mind because of its bearing on policy-making.
Another example in this context is the success achieved in some
developing countries with regard to the provision and training of commu
nity health workers and the steps taken to rationalize the production and
usage of drugs. Though the experience with community health workers
has varied from country to country, the question of essential drugs has
been most interesting. After WHO came out with the list of 200 essential
drugs which an Expert Committee had recommended for use in primary
health care, several countries set about to further refine the list. This was
a political decision, taken at the highest levels as it very directly affected
the interests of the multinational drug companies. But, here again, once
the policy makers were convinced of the merits of the case, they were
willing to take the decisions even though it meant going against well
entrenched vested interests.
Similarly, once a country sets for itself the goal of health for all, the
operative word becomes all. And when a country decides that the way it
will achieve that goal is through primary health care and community
involvement, then it also means that the country is prepared to take care
of the consequent increased demands that will be made on existing health
services.
As any one connected with the health services knows, it is one thing
to create the right awareness and motivate the people to become selfreliant in health care, and quite another to cope with the demands. More
damage is done to the credibility of a service if, having generated the
demand, the health services finds itself incapable of coping. That is why
it is essential to develop the necessary infrastructure before creating a
demand.
These are all factors that have to be carefully examined, keeping in
mind the special needs of the community. In a country as vast and diverse
in its culture as India, no blanket norms can be applied to any situation.
It requires inputs tailor-made to specific needs. And herein lies the biggest
challenge, as well as the opportunity to provide the peop'e with the basics
in health care. It is only then that the cherished goal of health for all will
be achieved.
3
INTERNATIONAL CONFERENCE
HEALTH POLICY : ETHICS & HUMAN VALUES NEW DELHI 1986
Population Explosion and Health Policy—
Ethics and Huamn Values
Dr. K.L. Wig
Emeritus Professor and Former Director of
All India Institute of Medical Sciences
The great importance of population explosion in the formulation of
health policy is recognised by nearly all countries all over the world. The
developing countries, however, consider it of paramount importance.
While the highly developed countries have become somewhat lukewarm
over this problem because they have controlled their populations and their
people are well educated and have attained a high standard of living—the
two important measures for the control of population—the need of such
control for the developing countries and perhaps, most of all for India,
because of its vast population is extremely urgent.
Before dealing with the subject of my address I may quote the defi
nition of the three terms used for the main theme of the Conference.
Dr. Edmund Pellegrino defined as follows the three items, during
his key-note address at a similar Conference in Athens.
—The health policy of a nation or a community is its strategy for
controlling and optimizing the social uses of its medical knowledge
and resources.
—Human values are the guides and justifications people use for
choosing the goals priorities and means that make up that strategy.
—Ethics act as the bridge between health policy and values. Ethics
examines the moral validity of the choices that must be made and
seeks to resolve conflicts between values, which inevitably occur
in making those choices.1"
One of the important factors that determines health policy, therefore,
is to find out what the basic cultural, ideological, ethical and religious
traditions of a nation are, and how they can be harmonised with the health
needs of the nation.1(1
Family planning which is essential for controlling population explo
sion, however, presents one unusual feature. While its urgent need
is acknowledged almost universally, when we go into its methodologies
and the choice of such methodologies—there is hardly any method which
does not evoke controversy. Such controversies are based mostly on
ethical, cultural and religious factors and human values which naturally
show some differences in different nations and various communities, in the
same nation. Legal views and laws on such matters which I think, are
predominantly based on ethics and human values, also differ, to some
extent in different countries. Some objections of course are based on
medical grounds. It is somewhat strange that while the importance of
family planning is acknowledged universally, no other subject which enjoys
such universal acceptance as a basic idea evokes greater conflict with ethics
and human values than family planning when you go into the details of
its working.
The urgent need of family planning needs no emphasis. In India it
should be regarded as number 1 national problem for unless we attain
success in our population control methods, all our planning and other efforts
for improving the economic condition of the population of our country
and improving the lot of poverty stricken millions the majority of whom are
in a state of malnutrition and for achieving the goal of “Health for All”
by the year 2000 AD will go away and may practically come to n.'thing.
Our Government is spending millions on what they call family welfare,
but the question that arises in the minds of those who are unprejudiced
and are willing to listen to the calculations of those who are trained in
such problems, is—are our efforts showing signs of success and are they
likely to bear fruit in time before the situation attains dimensions that will
defy all solutions ?
The birth rate in India in 1984 was 33.8 per thousand and the death
rate 12.5 per thousand. The population growth rate is thus near about
2 per cent. This means that we are adding every year 16 million human
beings to our population. This according to most demographers will mean
that by the year 2000 AD a year by which we are committed to “Health for
All”, we will have a population nearing the mark of 1 billion. It is incom
prehensible that we can provide health for all if the population by that
year attains as high a level as stated above. There is another adverse
effect of this state of affairs that I may point out. Most demographers
point out that a big portion of this population, unlike that in developed
countries, where birth-rate is controlled but longevity has gone up, will be
of younger people of marriageable age. The result of this inbuilt demo
graphic momentum is that even if present family planning efforts <i < ceed
to reduce the growth rate to one per cent by the century end, the
>pulation will eventually stabilise in 2050 at 1250 millions. A delay of 2i> .ears
in reducing the growth rate to one per cent will accelerate the st. bilised
figure to 1.9 billions and of another 20 to 2.6 billion.
To give an idea of the strains placed on the economy by uni died
population growth let us see what the impact of the 136 million popu' tion
added during the seventies decade will mean. The Ministry of Heal i in
a very modest calculation that placed the direct cost of maintainin the
additional population at an average income level of 1000 per ye has
given the estimate of Rs. 13,500 crores as the additional annual r< uirement to cope with this decade’s increase alone. It has been esi i ated
that an additional resource requirement of 11,850,000 quintals of . ood,
180,000,000 metres of cloth, 121,000 schools, 355,000 teachers, 2,3 ,000
homes and 3.8 million jobs for the seventies explosion. Now throui
the
eighties an annual 16 million is being added as opposed to the 14 ir. lion
annual average of the seventies.1
Since 1974, the global population growth rate has declined from 2.03
to 1.67 per cent per year. In the next decade the growth rate will decline
more slowly. However, the annual increase in numbers is expected to
continue and may reach 90 million per year by the year 2000. Ninety
per cent of that increase will occur in developing countries and at that
time 6.1 billion people are expected to inhabit the earth2.
When we come to the various methods employed for family planning,
there is a big range already available, though in a country, like India,
efforts are still going on so far as the research field is concerned to find
a method which may have the widest possible acceptance and may be free
of risk and highly efficacious. So far as the available methods of reason
ably proved efficacy are concerned at one extreme is abstinence and at the
other extreme is medical termination of pregnancy (M.T.P.). Abstinence,
of course, can have no moral or ethical objections. It had the support of
saintly personalities like Mahatma Gandhi. In fact, even some religious
group3 and their leaders which on religious grounds are fundamentally
against all artificial means of family planning are not against it by what is
called natural methods. Some of them have tried to find its modifications
like the rhythm method which has been improved lately by finding the
mucus secretion of cervix which precedes ovulation and which the woman
can be taught to find for herself, and which thus indicates to her the day
of ovulation. However, while such methods may have some practicability
amongst the well educated, closely knit religious communities, it cannot
have much utility for checking the population explosion so far as the vast
mass of 750 millions (out of which 127 million couples are in the reproduc
tive age period), are concerned. In fact, a further improvement may occur
in this method, i.e., science may very soon reveal a method by which the
actual day of ovulation may be found nut by simple tests, yet even then
human nature and instincts as they are it will not make this method
feasible so far as the control of population explosion is concerned. So,
while some communities and religious groups and their leaders are still
advocating it, we may not discuss it further in a limited address.
The methods of family planning and contraception are so numerous
that I cannot discuss the ethical and human values of all of them, but I
may select three items which have evoked or are likely to evoke the maxi
mum controversy on grounds of ethical and human values and their inter
connected legal aspects. They are : (1) Enforcement of a policy of limited
number of children by various types of legislative measures, (2) voluntary
sterilisation and (3) M.T.P. (Medical Termination of Pregnancy).
China by launching a one-child policy claims to have achieved a
spectacular success in their family planning programmes and restriction of
population growth. Some independent observers have confirmed this
claim. Though India was the first country to adopt family planning as
an official programme and can claim some reduction in birth-rate, its
population growth is still maintaining an alarming tempo. Can we, as
also the other democratic developing countries of the world, achieve
success in time to limit our population to such a level that it will not
affect our economic growth and other programmes for prosperity and
removal of poverty ? This raises a highly ethical and legal question for
a conference like this. In such democratic countries, especially in India,
the rights of an individual reign supreme. They cannot be interfered with
except to a limited extent in the event of a war or threat to national secu-
3
ritv even though as is evident from the details that I have given above,
the’jssue"of family planning upon which futureprosperity and stability of
the country depends is of no less importance than the destruction caused
bv an actual war. However, unlike wars-speaking in medical terms it
is not a Question of sudden death but a lingering existence of starvation
and malnutrition for millions. All the same a question arises
Can any
democratic Government impose its will and order that no family can have
more than two children and impose penalties ff this rule is violated ? If
we find at some stage that our present developmental schemes and plans
are not bearing fruit and the deluge in population seems to destroy all
hopes of health, prosperity and well-being of our future generations, can
we have legislation in which the state in this particular matter of number
of children in a family impose its will on the people ?” This would actually
mean that because of an emergency we make the rights of an state or the
nation as a whole supersede the rights of an individual. Individual human
values and rights in practice if not in a written law include right freely to
choose the time of marriage (subject to legal minimal ages); the right to
decide on the number and spacing of children in the family (the right to
contraception) and to decide about one’s own body in relation to this
(sterilisation and abortion, within existing legal constraints)4.
As an alternative to the above type of legislation which would be
repugnant to principle of human rights, can the great legal experts make
some other suggestion which may make people limit their families and thus
ensures progress and prosperity.
Let us, however, hope that the contingency for enacting the above
type of legislation or some similar action will not arise. In facts, at the
1984 United Nations International Conference on Population in Mexico
City there was still some difference of opinion amongst nations over future
policies. For example, while the Vice President of Kenya told the meeting
that the world “cannot wait for the crisis of over-population to right itself
through economic development” the United States delegation presented
an opposing view and gave examples of Hong Kong and South Korea
which though had scarce natural resources had made swift progress by
relying on the creativity of private individuals working within a free
economy. However, the consensus amongst nations was that family
planning is needed to supplement the effort of economic development in
reducing population growth, and almost all developed and developing
fSaTnaertdnfSHed V the Mexico City Conference, family planning as an
health Lf womLdef,Ved°P^nt’ sand acknowledged its contribution to the
neaim or women and children5.
imoos“ble fSf
?f family planning is and how it is almost
to countrv accord ina to°ri!.a- °’5Ject*ons to it which will very from country
apparentHf one goes" hronoT °Wn CU'tUres and traditions wil>
planning at the Mexico Citv TmS^me-°f the recommendations on family
in 1984.
ty International Conference on Population held
Recommendation 25
able information^ education.8 anTaT °f urgency> make universally avaduucation and the means to assist couples and indxvi-
f
duals to achieve their desired number of children. Family Planning infor
mation, education, and means should include all medically approved and
appropriate methods of family planning including natural family planning,
to ensure a voluntary and free choice in accordance with changing individual
and cultural values. Particular attention should be given to those segments
of the population which are most vulnerable and difficult to reach.
Recommendation 30
Governments are urged to ensure that all couples and individuals
have the basic right to decide freely and responsibly the number and spacing
of their children and to have the information, education and means to do so;
couples and individuals in the exercise of this right should take into
account the needs of their living and future children and their responsibili
ties towards the community.
Recommendation 31
Legislation and policies concerning the family and programmes of
incentives and disincentives should be neither coercive nor discriminatory and
should be consistent with internationally recognised human rights as well as
with changing individual and cultural values.
Recommendation 33
Governments that have adopted or intend to adopj fertility policies
are urged to set their own quantitative targets in this area. Countries
implementing family planning programmes should establish programme
targets at the operational level, respecting the basic right of couples and
individuals to decide freely and responsibly the number and spacing of their
children, taking into account the needs of their living and future children
and their responsibilities, exercised freely and without coercion, towards the
community.6
You can see how carefully these recommendations are worded and
how carefully that organisation has avoided objections from any country
on social and ethical grounds. For various countries according to their own
culture may have their own objections. They are giving in every one of
these paragraphs precedence to human rights. But will developing coun
tries attain appreciable success under these conditions.
It is, apparent that while a vast number of countries especially the
developing ones are in favour of family planning, there are objections on
social, human, ethical and legal grounds from Nations and communities in
the same nation and every question concerning the family planning be
comes a complex one. It is for the various learned speakers who will be
taking up various aspects of this subject to throw light on some of the
points that I have raised.
The next item that I may take up is of voluntary sterilisation. In
the beginning there was a lot of opposition to it in many of the well deve
loped countries on certain moral grounds, as the opponents said that it
amounts to mutilation of the human body either in the mart or the woman,
5
i.e., vasectomy in males and tubectomy in females. Moreover, there was
opposition to it because it is irreversible. It is in fact the main method of
irreversible nature—though scientists and surgeons are making efforts to
make the two methods one in males and one in females reversible. Tubec
tomy is being done extensively now through the endoscope (laproscope).
The fact that now tubectomies are being undertaken far more commonly
than vasectomies, though the latter is a much easier operation almost free
from risks only shows the continuing domination of man over woman
which still persists in most countries.
These irreversible operations are open to one great objection and that
is that why should they be resorted .to when reversible methods are easily
available, for if the existing off-springs die due to unforeseen circumstances
the parents become issueless for ever. So, interconnected with the successes
of these operations must be a sustained effort to diminish infant mortality.
In developed countries where reversible methods can be easily followed by
well educated couples, these irreversible methods are no longer favourites.
However, in countries like India where millions and millions of couples in
the reproductive age period exist and cannot be relied upon to use consis
tently the reversible methods, these irreversible methods have remained the
most favourite with administrations. In India it is the most favourite
method with the state governments. This is especially so because it ensures
certainty of results. It is so far done after there have been two children
unless the parents themselves volunteer to get it done earlier. Many state
governments expect some sort of targets from their doctors though they
may not do it openly.
In many of the well developed countries there have been long contro
versies over whether voluntary sterilisation (they never even dream of
forcible sterilisation) should be allowed at all or not. In some countries,
it is still illegal, but generally speaking in most countries a liberal view is
being taken and voluntary sterilisations are either being allowed by law or
at any rate being overlooked, and no prosecutions are done. In India,
however, voluntary sterilisation as I have said is favoured, but there is a
strong public opinion against forcible sterilisation which a democratic
country like India will never allow whatever the needs of the country may
be. This raises, in fact, again the question of individual rights versus the
right of the State to impose its will. However, we should avoid reaching
that stage.
The guidelines protecting voluntarism and ensuring safety should,
however, take priority over more administrative matters.
The most pressing ethical and legal issue today is how to 'ensure that
sterilisation is ‘voluntary’ in the sense that the decision to be sterilised is
one which is informed and unpressurised. (7)
As regards the reversible methods, the main difficulty is whether they
are acceptable and most easily available to our masses of rural population,
quite a lot of whom are not educated enough to understand the utility and
proper applicability of these methods. Out of these methods, the main
controversy lies as regards MTP and certain ramifications of this method
which I will mention later.
to
jle sa^e
avoiding unnecessary objections, it has now been
termed Medical Termination of Pregnancy (MTP) and the word abortion
is hardly ever used. Feelings in certain countries are so strong on this
question that in the last International Population Conference in Mexico,
UbA made the banning of abortion as a measure of population control a
central condition for its population assistance. Moreover, laws for termina
tion of pregnancy raise another ethical question—‘has a foetus a persona
lity . If it has a personality, it naturally has rights.
According to the latest Indian law on medical termination of preg
nancy, such termination has been made permissible under certain condi
tions. The Indian law was enacted in 1971 to protect the women’s rights,
if there was a fear that future physical or mental health of a woman is
imperilled if pregnancy continues. In this connection one out of the various
clauses that allow termination may be quoted :—
1.
If the continuance of the pregnancy would involve a risk to the
life of the pregnant women or of grave injury to her physical or
mental health.
Inclusion of mental health, in fact, makes the attitude of law towards
termination quite liberal but reasonable, for any unwanted pregnancy is
going to have psychological effects on the mother. Explanation of the
above clause states :
“Where any pregnancy occurs as a result of failure of any device or
method used by any married woman or her husband for the purpose
of limiting the number of children, the anguish caused by such unwan
ted pregnancy may be presumed to constitute a grave injury to the
mental health of the pregnant women.’’
This explanation makes the permission liberal indeed and almost any
case who has been making attempts to use cuntraceptives can come under
Though the above law was enacted for a different purpose, it must be
conceded that indirectly it may help population control, as a sizeable
number of patients in whom contraception fails will in all sincerity take
recourse to it. However, it must be acknowledged that MTP as a means
of population control means a failure of contraception either due to care
lessness or due to chance or due to ignorance. We must, however, see the
other side of the picture, also. If it is not made permissible under the law,
the acts of termination will go into the heads of the unqualified persons
which means a very high increase in complications and even fatalities. Such
cases have been quite frequent in many countries including India. That in
itself is a big justification for evolving the present law on medical termina
tion of pregnancy. In fact, in the short run it has been said that a desire
for effective contraception also leads to an increase injaboitions. Because
of this inter-ralationship, contraceptive and abortion services need to be
linked.8
I think there will be no difference of opinion as regards the necessity
of MTP when the future physical health or the life of the mother is in
danger for you have to save one of the two lives and the mother’s life is
no doubt more valuable of the two. Even the most conservative and
religious minded persons will not contest it. However, considerable diffe
rences of opinion arise when we consider the mental health and future
psychological state as a result of an unwanted pregnancy. For a doctor,
however, future mental health is as important as physical health. However,
such a justification does give considerable handle for malpractices.
The opposition to MTP as a means of population control is, however,
understandable. When other effective methods of family planning are
available, why should we destroy a life just because a couple has been
negligent and did not practise the method properly. So, they argue on
ethical grounds that induced abortion should not be included as a method
of population control especially as it destroys a life which legally speaking
has a personality of its own and we have thus, no right to destroy it.
However, the protagonists of MTP who want it to be included as a plan in
family planning argue that as no contraceptive method is infallible, an
unwanted pregnancy should be terminated and, so, I understand certain
countries are very liberal about MTP. They further argue that the popula
tion control for developing countries is a national need which should be
treated as an emergency and must supersede all other considerations.
Moreover, when laws to prevent induced abortions are made more strict it
only leads to the emergence of quacks and secret abortions which increase
manifold the risks to the health and life of the mother. Thus, on this
ticklish question of MTP which involves moral values and religious and
ethical beliefs a consensus of medical and legal opinion is needed as to how
liberal the legislation should be to allow MTP as a legitimate method of
family planning without leading to immorality and sexual promiscuity,
especially at the level of very young age groups. As I have said above, if
it is not liberalised it only leads to abuses and going to quacks. The major
problem, therefore as regards moral and legal issues involved in MTP is
one of proper implementation.
All that I have said above, of course, does not obscure the fact that
the debate over abortion, even in countries where the law has been refor
med, is a passionate one.9
A few related questions may be discussed at this stage. With the
advances in medical sciences, especially ultra-sound examination and
amniocentesis, it is possible in some cases to see if the future child is going
to have physical or mental abnormality. What should be the criteria of
judging which deformity or abnormality, physical or mental, is going to be
so serious that termination of pregnancy is justified. Divergences of
opinion are bound to occur. But it is for medical men and social workers
to devise criteria for allowing MTP in such cases. However, a more serious
problem is arising in this country and may be in some other countries. It
has become possible by the above methods to find out the sex of the future
child. As a theoretical or purely scientific exercise it is interesting but the
knowledge of that to parents is likely to be used for one purpose, especially
in families which have a preponderance of female offsprings. They will
utilise the knowledge for secret termination of pregnancy if the foetus is
found to be a future female child. This means in a way reverting to the
age old highly unethical practice long since prohibited by law of female
8
infanticide. Rather than to take this risk, will it not be better to prohibit
by law the emergence of laboratories which reveal this knowledge to the
parents in early stages of pregnancy.
If induced abortion is to be considered strictly from the moral and
religious angle then certain reversible methods may actually be leading to
the induction of abortion but are not being categorised as such. For
example, MR (Menstrual Regulation) by protaglandins or by an MR
syringe is certainly an abortion in a vast majority of cases. Should it be
allowed even though foetal life at that stage is very early and almost invi
sible. Use of certain drugs may possibly be also an abortion of the foetus
at a very early and almost invisible stage. If a vaccine against protein
carriers of vitamins to the foetus becomes successful that will also be abor
tion at a very early stage of the foetus—only killing it before it become
even recognisable as a foetus. So, if religious and ethical and moral con
siderations prevail there will be objection to such methods also which are
ordinarily regarded as methods of contraception but are really abortions at
a very early stage before the foetus becomes even anatomically visible to
the naked eye.
There are many reversible methods of contraception such as con
doms, pills, insertion of copper T etc., long acting injectables, some herbal
medicines such as gassypol—a Chinese herbal medicine for males—and
coitus interruptus. There are not likely to be any ethical objections to
such methods except by the most conservative and religious groups who do
not want any interference of the natural process, but there can be objec
tions to all such methods on health grounds or on grounds of inadequate
acceptability. We need not discuss that.
An associated question is the question of incentives and disincentives.
There have been not discussions on this question. However, the main
objection which involves ethical values as regards some incentives and
nearly all disincentives is that why should a third or a fourth child suffer
from certain handicaps in comparison to other children who may be even
less bright than him/her, because his/her parents made the mistake of not
falling in line with a policy which was very important from the national
point” of view. Why should the sins of parents be visited on off-springs.
His/her parents may deserve those handicaps but why should the child
suffer who committed no fault ? It is an important objection from the
ethical point of view and, so, there should be no question of disincentives,
thouaht some incentives may be chosen carefully and may help to some
extent in carrying on the family planning programme specially in certain
limited circles like industries etc.
There are two other issues which I cannot/take up in detail, but
which are worth mentioning. One is reducing the infant mortality. In
India it is still shamefully high. It is higher than that of many developing
countries and was 104 per thousand live births in 1984. It is generally
admitted that family planning is acceptable only if the infant mortality is
low and most children which are born have the prospect of living a normal
life The Family Planning Foundation is in the process of investigating in
collaboration with the International Development Research Centre (IDRC),
Ottawa, Canada, whether such a statement is a fact or not so far as Indian
9
conditions are concerned, and also find out the high risk. factors associated
with infant mortality in various areas so that the Government may be
helped to mount an intervention strategy. There can obviously be no
ethical or human objections to it and the lowering of infant mortality will
be welcome to all communities. The second important factor which promotes
family planning is raising the status of women. For quite a number of
extra births take place because the parents want a male child. Moreover,
a woman seems to have in this country only a small place in deciding the
number of children that she should have. The need of raising the status of
women is still felt even in the most developed countries for the opportuni
ties for all types of employment are still less for women than what are
available to males. Governments should formulate and implement con
crete policies which would enhance and raise the status of women.
It is a proven fact that in development countries that to the extent
to which legislation ensures full and free access for women to education
and to employment on terms and conditions of complete equality with
men, the effect will be to reduce fertility.11
VP
An important point in this connection is raising the age of marriage
of the girls. If that age could be raised from 18 to 21, and sterilisation
could be induced as far as possible after the age of 30 there will be a very
shary fall in the number of births. According to demographers, nearly
half of the births occur before the age of 20 and after the age of 30. There
can be no ethical objections to raising the age of marriage in girls if it is
done on the grounds of improving or saving the health of the young girls.
However, legislation for this purpose is not likely to succeed and will have
ethical and moral objections in addition. It means an interference with
human rights of the individual.
It must be realised that there is no method of contraception which
can have no objections, is absolutely safe and is fully efficacious and uni
versally acceptable. That is why research is going on and on to find a
most acceptable, most efficacious and most harmless method. However,
the problem is so urgent that we cannot wait for the results of such
research. Even when there are some minor objections and flaws on
grounds of health and efficacy, we have to look at such problems from a
different angle, i.e., greatest good of the greatest number and the acute
need of the nation. So occasional small risks have to be taken.
The doctors are, of course, needed for the execution of the various
methods and are key-figures in teaching the public the various techniques
etc. However, they have one greater role to play and that is to mould
public opinion in favour of family planning. Doctors alone cannot achieve
success in family planning. If we want great results, family planning has
to become a people’s programme. Thus, it is necessary to develop exten
sively public opinion in/its favour especially at the grassroot level The
doctors come in close touch with the family and the general practitioner
who is a family physician and almost a family member for most families
can thus be a great factor in developing proper public opinion in favour of
our family planning programme. It must be realised by all of us that
family planning which may be technical easy is socially difficult and
doctors can be a great factor in overcoming that social difficulty Non-
10
fT)
‘
government Voluntary Organisations can also play a very great role in
this direction. In fact, that should be their chief role in addition to help
ing the government in their programmes. Let us hope the combined
efforts of the government, the medical profession and the non-goverment
organisations like the Family Planning Foundation achieve significant suc
cess in the Seventh Plan so that we may succeed in our health for all
programmes by the stipulated year 2000 A.D. and enter the next century
in a prosperous and hopeful vein.
References
1A. Edmund & Pellegrino. Key Note address at Health Policy—Ethics
& Human Values Conference at Athens in 1984. Published in Highlights
of Athens Conference—XVIII CIOMS, Round Table Conference, Athens
1984. Edited by John H. Bryant and Zhijniew Bankowski 1986. page 7,
IB. Robert Veatch.
Some as abovel. Page 11.
1. Address by Shri B. Shankaranand, Minister of Health and Family
Welfare, Government of India, at the Conference of Voluntary Organiza
tions on Promotion of Family Welfare Prgramme.
2.
Mexico City Declaration on Population and Development.
3.
Ganguli, H.C. Sexual Behaviour : A New Perspective in Family
planning—Publication of the Department of Psychology, University of
Delhi, 1984, pages 18 and 109.
4.
Law and Fertility in Europe edited by Maurice Kirk et al—Publi
cation of the European Centre for Research and Documentaion in Social
Sciences and International Union for Scientific Study of Population—1975—
Preface page II.
5.
Malcom Potts—Population and Politics (leading article) BMJ
1984, 289—641.
6.
Ibid.
7.
Law and Planned Parenthood—Edited by John Paxman for Inter
national Planned Parenthood Federation—1980, pages 38 and 59.
8.
Ibid.
9.
Ibid.
10.
Mexico City Declaration on Population and Development.
11.
Trevici, V. Law and Social Status of women—Law and Fertility
in Europe (same as 4) 1975—page 97.
"
0A.
.,s Road,
INTERNATIONAL CONFERENCE
HEALTH POLICY : ETHICS & HUMAN VALUES NEW DELHI 1986
Ethical and Legal Aspects of Family
Planning
Mr. Justice H.R. Khanna
Family Planning Foundation
198-Golf Links, New Delhi.
I deem it a great privilege to have been asked to address this session
of International Conference on Health Policy—Ethics and Human Values.
The topic for this session is family planning—a National Priority. I would
be speaking to you on the ethical and legal aspects.
It was 36 years ago that India became a republic and The Constitu
tion of India came into force to secure, inter alia, to all its citizens social
justice and dignity of individual. Part IV of the Constitution contains
directive principles of state policy, which as mentioned in Art. 37 were
fundamental in the governance of the country and were to be applicable,
as duty of the state, in making laws, clause (f) of Art. 39 Contained in that
part provided that. The state shall direct its policy towards securing that
children are given opportunities and facilities to develop in a healthy
manner and in conditions of freedom and dignity. According to Art. 47
the state shall regard raising of the level of nutrition and standard of
living of its people and the improvement of public health as amongst its
primary duties. These were great objectives, earnesty conceived and nobly
worded, but even though a period of more than three and half decades
has passed since then, the goals visualised by the founding fathers in
these articles have remained elusive and more or less a tantalising illusion.
Not that efforts have not been made towards attainment of those objec
tives. We have had a series of five year plans conceived primarily to
bring about economic regeneration. We have had earnest, well-meaning
persons who have striven in their own way and as best as they could to
banish poverty and raise the living standards. We have made considerable
headway in industry and technology as also in agricultural, dairy and
poultry production. We have built dams and initiated river valley projects.
We have spread network of roads and provided for Quick means of
transport. We have also established a large number of educational
institutions. But despite all these efforts, we still continue to be steeped
in poverty and backwardness and our average standard of living is one of
the lowest in the entire world with one of the lowest per capita income.
If one were asked as to which has been the chief culprit and the main
cause for frustrating and setting at naught all these efforts to raise the
economic level of the people, the finger must pin-point in the direction of
population explosion. The increase in population during the last four
decades has upset all plans and frustrated all efforts to bring about better
ment and amelioration in the living standards of the people. India’s
total population touched figure of 685 millions in the census of 1981.
This represents an increase of 25 % since 1971 when the population was
548 millions. It would be pertinent in this context to mention that India’s
population which was 238 millions in 1901 increased to 361 millions in
1951 and to 685 millions in 1981. Thus in the first half of the present
century, i.e. during the years 1901—1951 India’s population increased by
about 51.5% whereas in the next 30 years from 1951 to 1981 it increased
by 89.8%. The main cause of this increase can be attributed to fall in the
death rate due to better health conditions and more efficient handling of
epidemics. A sample survey revealed that the birth-rate in 1980 was 33.3%
and the death rate was 12.4. The expectation is that the death rate would
decline still further and be brought down to 10 per thousand by 1990.
The increase in world population during the year 1985 was 85 millions
bringing it to a total of 4.9 billions. The population growth rate declined
from 2% in 1970 to 1.7% in 1985. Even at this rate world population
is expected to be 5 billions by middle of 1987 and 6 billions by the end of
the century.
Unless therefore we can devise some measures to control the popu
lation growth, we can take it that all our plans for raising the living
standards would go away and run into rough weather and the problem of
poverty, backwardness and low living standards would haunt us and dog
dur steps for years to come. As it is the average increase per year of the
population of India is more than the total population of Australia. It is
in this context that the question of birth control has assumed tremendous
importance,
So far as the ethical aspect is concerned I would say that it is in
herently immoral to give birth to children if we cannot secure for them
proper food, clothing and shelter and provide them with requisite
education to grow into healthy, self-reliant adult-hood with prospects of
decent standard of living. At the same time it would be unrealistic and
plainly discriminatory to deny to the poor sections of the community the
incident and satisfaction of a normal marital life. Begetting of children
and the continuance of the family line is as such an important objective
and desideratum of married life amongst the poor as amongst the affluent
sections of the community. The difficulty, however, arises because the
growth rate of family members amongst the poorer sections was and
continues to be at a level higher than that of affluent sections who as a
result of education have realised the desirability of restricting the number
of children. It is in this context that some action is called for and some
measures need to be adopted to bring about a state of small families in
regard to poorer section of the community.
At the same time we have to bear in mind that in view of the
consequences of resort to compulsory methods during the period of
emergency the government would be reluctant to enforce compulsivemeasures. Faced with this situation all that we can do is to build a strong
public opinion and create a General awareness of the need for and desir
ability of a small family. It has to be impressed upon every one that
small family is a desideratum not merely because of any altruistic con
sideration or as a part of obligation to the society but much more than
that as a matter of sheet enlightened self-interest of the individual con
cerned and for the benefit and welfare of his own children. Human
nature being what it is, experience tells us that enlightened self interest is
a much more potent motivating factor for an average person.
Coming to the legal aspect I may say that law does not prevent or
impose a ban upon the procreation of children beyond a particular limit.
Law, as was once said by trudeau, has no function in the bed-room of the
married couple. Indeed attempt by law to impose restrictions upon the
number of children might well be construed as an intrusion into the privacy
of individuals’ married life. At the same time law can provide incentives
to couples to restrict the number of children. Such a law has been enacted
in number of countries and it is a perfectly valid piece of legislation.
India adopted family planning as official programme in 1958 as it
recognised that a timely check on population growth would in turn raise
the living standards of the people. During the period of the first two
plans from 1951 to 1961 the emphasis was mainly on research in the
field of motivation, communication, demography, physiology of reproduc
tion and extension of organisations for providing clinical services. Since
then various ideas have been set afloat. The objective of family welfare
in 1978 was to reduce the birth rate to 30 per thousand of population by
the end of 1982-83 from the existing 33 per thousand population. At
present the demographic goal is that the average woman should be replaced
by one daughter and two child family as the normative pattern and to
attain this objective by 1996.
Although section 312 which makes it an offence and provides for
punishment for causing miscarriage, unless it be for the purpose of saving
the life of a woman, still continues to be a part of our panel code, the
parliament enacted in 1971 the medical termination of pregnancy Act.
According to this act notwithstanding anything contained in the Indian
penal code, A Registered Medical Practitioner shall not be guilty of any
offence if any pregnancy of length not exceeding 12 weeks in terminated
by him or where the length or pregnancy exceeds 12 weeks but does not
exceed 20 weeks if two registered medical practitioners are of opinion
formed in good faith that the continuance of the pregnancy would involve
risk to the life of the pregnant woman or of grave injury to her physical
or mental health. Likewise the law relating to abortion has been libera
lised in other countries. In England notable part in this direction was
played by Mrs. Margaret Sanger, while in the United States three Con
necticut women, one of whom was Mrs. Katharine Houghton Hepburn,
mother of the famous Actress Katharine Hepburn, made significant
contribution in starting birth control leagues. Some of the most inte
resting cases relating to birth control and abortion were decided by us
Supreme Court. One of such cases, was Poe vs Ullman decided in 1961.
In this case law relating to ban on clinics for birth control was challenged.
The Supreme Court, however, turned down the request. Justice frank
furter who wrote the majority opinion said that the issue related to a
dead letter and the court could not be umpire to debates concerning
harmless empty shadows. According to him the fear of enforcement of
that law was chimerical or imaginary because provisions of the law had
gone unenforced. Justice Douglas who wrote the minority Judgement in a
Scathing Criticism of the Majority view observed:
“What are these people—Doctor and Patients— to do? Flout the
law and go to prison? Violate the law surreptiticudy and hope they
will not get caught? ... It is not a choice they need have under. . .
our constitutional system.”
3
Soon thereafter clinics started openly working in Connecticut. A
complaint was then filed and the Supreme Court was forced to decide this
issue in 1965 in the case of griswold. This time Justice Douglas was on
the side of the majority. The majority held that the impugned law
trespassed into the zone of marital privacy, a realm of family life which
the state cannot enter without substantial justification. The law was
accordingly struck down. In a subsequent judgement in 1972 the Supteme
Court extended the above principle to the case of single individuals.
Ultimately in a decision given in 1973 in Poe’s case the Supreme Court
held that the right of abortion was not absolute and added a restriction.
All abortions, the Court held, were not legal. A formula was evolved,
according to which in the first three months of pregnancy the right of
privacy prevails and the abortion decision was upto the woman and her
doctor. During the second period of three months the state could regulate
abortion in a way related to maternal health. In other words the state
could require that operation be performed under certain conditions. During
the last stage of pregnancy the court held the state laws could prohibit
abortion except under circumstances in which the life or health of the
mother was in danger.
„
)
One might discern a note of similarity between the view taken by the
the U.S. Supreme Court and that which had been taken earlier in the law
passed by The Indian Parliament in 1971.
Friends, I have been talking to you about the ethical and legal aspects
of family planning, restricting the number of children and about the
permissible limits of resorting to abortion. It would, however, be wrong
to think that the matter has only ethical and legal aspects. More than
anything else it is human problems and relates to some of the most
intimate aspects of human life. This apart the issue has a vital bearing on
the social equilibrium which is bound to get upset and disturbed by
further increase in economic disparities. Unless we can somehow control
the birth rate and introduce planned parenthood with small families the
spectacle of vast areas of slums existing side by side with palatial multi
storied buildings would continue to mar at even a bigger scale the land
scape of all big cities. They would also become focal points of social
tensions. Experience tells us that a few island of richness in vast area of
poverty, a few cases of affluences in a vast desert of penury and privation
generate tensions and give rise to dangerous thoughts which portend ill
for the smooth march forward of the society. Wisdom lies in forestalling
such social convulsion and in taking timely steps to prevents occurrence.
Family planning is one vital step for this purpose.
I think the organisers for asking me to address this August gathering
on a vital issue.
•
INTERNATIONAL CONFERENCE
HEALTH POLICY : ETHICS & HUMAN VALUES NEW DELHI 1986
Health as A Fundamental Human Right
Dr. Pragya Kumar
M.B., B.S.; Ex P.C.M.S., Lady Medical Officer, Panjab University,
Chandigarh-160014.
Dr. Virendra Kumar
LL.M., S.J.D. (Toronto), Professor and Chairman, Department of Laws,
and Dean, Faculty of Law; Panjab University, Chandigarh-160014.
Health as a fundamental human right should be the cornerstone of
any health policy anywhere. This has been recognized assertively in the
Declaration made by the International Conference on Primary Health Care
at Alma-Ata (USSR) in 1978,1 to which India is a signatory. Expressing
the need for urgent action by all governments “to protect and promote the
health of all the people of the world”, in the very first Declaration health
is delineated as “a fundamental human right.”2 Here “health” means not
merely the absence of disease or infirmity, but “a state of complete physical,
mental and social wellbeing.”3 The emphasis on “all” is here to draw our
attention to “the existing gross inequality in the health standard of the
people” not only between developed and developing countries but also
within the same country.4 This means that, so far as health care provision
for bringing about the required health standard in any population is con
cerned, no discrimination is justifiable on any ground whatsoever. It is
“politically, socially and economically unacceptable.”5 An attempt to
realize this very objective is reflected in our resolve to provide “Health for
all by the year 2000 A.D.” which includes provisions of at least a minimum
package of health care services to all segments of the population.6
The signification of projecting health as a fundamental human right
is that it becomes the basic responsibility of the State to protect and pro
mote health of the population under its jurisdiction. According to AlmaAta Declaration such an obligation “can be fulfilled only by the provision
of adequate health and social measures,7 which are “based on practical
scientifically sound and socially acceptable methods and technology made
universally accessible to individuals and families in the community through
their participation.”8
Indeed one of the major preoccupation of the present International
Conference is how to discover and determine our own priorities and strate
gies for “optimising the social uses of medical knowledge and technology,”
consistently with our own “historical, cultural, moral, religious, philosophi
cal perspectives and values systems.”0
Concurrently with the developments at Alma-Ata International
Conference, the Indian Medical Association, the national organization of
the qualified practitioners of modern scientific system of medicine, started
a crusade for the acceptance of health as a fundamental human right,10
and a sound National Health Policy for fulfilling such an objective.11
Eventually, we now do have a National Health Policy of 1982-83,12 envi
saging “an integrated, comprehensive approach towards the future develop
ment of medical education, research and health services” for meeting “the
actual health needs and priorities of the country.”13
Health as a fundamental human right envisages, as stipulated earlier,
two things: one, the notion of health, understood in a comprehensive sense,
involves irreducible minimums of prevention, promotion, curative and
rehabilitation measures, and not just one leaving the others out; two, it is a
right for all irrespective of all other considerations. Keeping in view its
all pervasive nature and also the societal interest involved therein, it
becomes the first and foremost obligation of the State to protect and
promote health as a fundamental right. The question, therefore, now is
how and in what manner this challenge is to be met.
If we just broadly review the work done through successive Five Year
Plans during the past 38 years since independence, we do notice some
measure of success in the realization of health as a fundamental human
right. Thanks to the modern scientific system of medicine, the mortality
rate has declined from 27.4 (1941-51) to an estimated 14 (1980). The life
expectancy at birth has gone up from 32 years (1951) to over 52 (1980).
The infant mortality rate has come down from 135 (1973) to 125 (1978).
Plague, which was a common killer disease, is not heard of now. Smallpox
has been eradicated. Malaria which, prior to 1950, used to take a heavy
toll of about 8 lakh lives, with an incidence of about 7.5 crore cases a year,
has been controlled to a large extent, the incidence having fallen to 24
lakhs and less than 200 deaths in 1980.13"
However, looking at the demographic and health picture of the
country, we find much more still remains to be done on the health count.14
The high rate of population growth, for instance, continues to have an
adverse effect on the health of our people and the quality of their lives.
The mortality rates for women and children are still distressingly high;
almost one-third of the total deaths occur among children below the age
of 5 years; infant mortality is around 125 per thousand live births. The
extent and severity of malnutrition continues to be exceptionally high.
Communicable and non-communicable diseases have still to be brought
under effective control and eradicated. Many eradicable diseases like
Tetanus, Polio, Goitre, Tuberculosis, Blindness, Leprosy, continue to have
a fairly high incidence in the country. A substantial share of diarrhoeal
diseases and other preventive and infectious diseases, especially amongst
infants and children, are caused by lack of safe drinking water, poor
environmental sanitation, poverty and ignorance.
For meeting these challenges within a stipulated period (for instance,
the target of health for all by the year 2000 AD), our National Health
Policy proposes to make “the universal provision for comprehensive
primary health care services.”16 Considering the comprehensive character
of the primary health care, a large variety of inputs flow into health. The
avowed purpose of these inputs is “to secure the overall national socio
economic development process, specially in the more closely health related
sectors.”16 Such sectors may include drugs and pharmaceuticals, agricul
ture and food production, rural development, education and social welfare,
housing, water supply and sanitation, prevention of food adulteration,
maintenance of prescribed standards in the manufacture and sale of drugs
and conservation of environment.16' But, notwithstanding all these efforts
to bring about the socio-economic transformation, “not much headway is
likely to be achieved in improving the health status of the people, unless
success is achieved in securing the small family norms, through voluntary
efforts, and moving towards the goal of population stabilization.” This is
what has been clearly perceived under our National Health Policy.17
Besides, it is also now realistically realized that the goal of population
stabilization is achievable only by substantial augmentation and provision
of primary health care facilities on a universal basis. That there exists a
close and direct nexus between the two is indeed the recurring theme of the
revised 20-Point Programme of our national Government.18
For the realization of comprehensive primary health care on universal
basis, the basic impediment idenitfied in the National Health Policy is the
adoption of the Western model as the basis of our health services. This
model is said to be “inappropriate and irrelevant to the real needs of our
people and the socio-economic conditions obtaining in our country.”19 The
underlying limitations of the western model in the Indian context, as
pointed out in the National Health Policy document, are:20
1.
It has provided benefits to the upper crusts of society, especially
those living in the urban areas.
2.
The proliferation of this approach has been at the cost of pro
viding comprehensive primary health care services to the entire
population.
3.
It has led to neglect of the preventive, promotive, public health
and rehabilitation aspects of health care.
4.
It has tended “to enhance dependency and weaken the commu
nity’s capacity to cope with its problems.”
5.
The education and learning of medical and health personnel in
persuance of this model “has resulted in the development of a
cultural gap between the people and the personnel providing
care.”
6.
It has prevented “individuals and families in establishing a selfreliant community.”
All these limitations, in terms of accepted national health policy,
imply that, somehow or the other we should have the indigenous systems
of medicine (Ayurveda, Unani, Sidha, Yoga, Naturopathy, etc.) in place of
or besides the modern system of medicine as the prime basis of our primary
health care approach, at least for covering the hitherto uncovered vast
segments of our rural population.
so is simply this:21
The rationale and the manner for doing
This resource of indigenous systems has not so far been adequately
utilised. The practitioners of these various Systems enjoy high local
acceptance and respect and consequently exert considerable influence
on health beliefs and practices. It is, therefore, necessary to initiate
organised measures to enable each of these various systems of medi
cine and health care to develop in accordance with its genus. Simul
taneously, planned efforts should be made to . . . integrate their
services (the services of the practitioners of indigenous systems) in
the overall health care delivery system, especially in regard to the
preventive, promotive and public health objectives . . .
A couple of consequences of this suggested shift in our health care
delivery system are now critically examined here.
The first and foremost is that until now in India the benefits of
modern system of medicine as the basis of our health care services has
extended to people who are living in the urbgn areas. But, does this neces
sarily imply that the modern scientific system of medicine is unsuitable for
our village population ? In our submission, it is not the modern scientific
system of medicine which is principally bad, though it is a different matter
that hitherto its beneficial effect is visible only in the urban areas and not in
the rural ones. The real reason is that in urban areas the basic conditions of
sanitation, including the provision of potable water, are met and therefore,
the beneficial effect becomes instantly evident. On the other hand, the bene
ficial effect of the same system is neutralised to a great extent by reason of
the absence of the same supportive conditions.
Another assertion in the National Health Policy document is that
modern system of medicine as the basis of our health care policy creates a
“cultural gap” between the people and the personnel providing health
care: weakens the community’s capacity to cope with its problem, and
robs “individuals and families in establishing a self-reliant community.”
All this seems to indicate that modern medicine is inconsistent with the
indigenous system of medicine and thereby a “cultural gap” and all that is
created. This is entirely a misconceived assumption.22
The modern scientific system of medicine is NOT opposed to indi
genous system of medicine. It should indeed be our proud privilege to
know that the modern system of medicine has evolved from nowhere but
out of our own ancient Ayurvedic System, and it has attained its present
premier position with the help of scientists from all over the world.23 It is
a different matter that, notwithstanding this advancement, we do continue
to have a certain degree of inalienable emotional 'attachment to our indi
genous system of medicine, especially Ayurvedic System, which though for
certain historical reasons could not develop scientifically by maintaining its
original purity and yet, at times, still meets at least some needs of the
people, especially of those residing in remote village and who do not have
access to the modern scientific system. In his editorial, “Need for a
National Health Policy,” Dr. Gouri Pada Dutta has pictured our predica
ment in memorable words:24
The indigenous system as it stands today, is not capable of competing
with modern scientific medicine, but remains as the carcass of a giant,
who had once a magnificent might but now has become only a
monument of pre-historic past. The emotional involvement with
past legacy is blurring the vision . . .
Let the pragmatism be our guide and take over our dogmas, so that
we are able to recognize and say: ‘Scientific development has given to our
national system of medicine an international status for the benefit of whole
mankind.
By implication another often repealed stance in our National Health
Policy document is that modern scientific system of medicine seems to be
suitable only for hospital based and cure-oriented approach. This is also
simply not true. On this count we would like to say and say categorical
ly25 that modern medicine is the only scientific system “which provides
comprehensive, promotive, preventive, creative and rehabilitative services,
and, therefore, is most suited to provide total health care delivery at the
National level.’"28 This is not an assertion of the whims and the fancies
of the practitioners of the modern system of medicine. It is concretely
based upon the fact that it is “through modern scientific system alone that
WHO has succeeded in eradicating small pox from the entire region and is
(now) making efforts for eradication of Malaria and Leprosy. Longevity
has increased; infant and maternal morbidity rates have substantially been
lowered. Epidemics are few and far between.”27 As far as prophylaxis
(i.e., promotive and preventive aspects of medicine for ensuring positive
health) is concerned, modern medicine is the only means by which com
municable diseases and population explosion can be effectively dealt with.28
With prophylaxis, coupled with safe drinking water, “60% of the morbidity
and mortality can be effectively taken care of.”29
There is no gain saying the overwhelming advantages of the modern
scientific system of medicine. But, mind you, it gives us a double-edged
sword, which can make or mar, Its potent medicines, if used with a
qualified and competent knowledge, are indeed a blessing. If used with
half-baked knowledge, catastrophe is only the next door neighbour. Hence,
two things clearly stand out. First, in our national health planning it
should be assumed that our country needs modern scientific system of
medicine for the delivery of health care; secondly, because of their inherent
power to make or mar, allopathic medicines should be administered only
only by persons who are fully qualified to practice the modern scientific
system of medicine, and not by those with half-baked medicinal know
ledge.30
The concept of integrated approach is indeed commendable. Speak
ing functionally, it does not contemplate the concept of “Health Team”
comprising personnel of various grades of skill and competence, each
performing the given task within a co-ordinated action programme.31 But,
if the experience of the working of the Multipurpose Health Workers
Scheme in rural areas is of any index, the integrated approach has proved
elusive. This approach has led to the growth of half-baked doctors enjoy
ing the official status of RMPs (Registered Medical Practitioners), whose
capacity and credentials to “cure” with absolute certainity is anybody’s
Guess.32 It is in this context, that the Indian Medical Association has
5
repeatedly resolved to recommend to the State for banning the use of
potent medicines by the persons who are either not qualified in modern
system of medicine or whose basic orientation is in a system other than the
modern system of medicine.33
There is an explicit statement in the National Health Policy that
there is a “high local acceptance and respect” for the practitioners of
indigenous system of medicine.3'1 It is also stated as a fact that the health
care facilities based on modern system of medicine have hitherto been
made available to the urban elites and not to the rural poors.35 The con
joined consideration of these two statements, especially from the angle of
realization of health as a fundamental human right, prompts us to project
one basic question: From whose point of view are we to access the rele
vance of the indigenous systems of medicine ? If we look at them from the
point of view of the knowledgeable persons who can appreciate and under
stand the difference between the services rendered by qualified men in
modern medicines and the services given by the practitioners of indigenous
systems of medicine, the limitation of the latter would be evident. On the
other hand, if the same is seen from the angle of illiterate or semi-literate
villagers, who have never known anything better than what is being pro
vided to them by the promoters of indigenous systems of medicine, the
experience might be exhilarating. The experience is similar to that of an
old lady, who had collected jungle woods and waited on the road side for
some helping hand. None cared to pay heed to her plea except a man
who happened to be a philosopher. Overwhelmed by his kindness, she
expressed her feelings of deepest gratitude which the philosopher thought
was absolutely unnecessary. Mournfully he mused: ‘Has man fallen so
low that the society has ceased to expect even this much!’
In fact, on the contrary, there is a scientific evidence to show that
there has been no significant cultural resistence to the acceptance of
modern medicine as long as it is available and accessible.36 This can also
be supported in the light of the fact that the number of the patients at the
C.G.H.S. and E.S.I, dispensaries of modern systems of medicine is many
times more than at the similarly situated dispensaries of the indigenous
system.37
Now, if the Government feels satisfied at the expressed satisfaction
of the rural people, it is nothing but a clear manipulation of the ignorant
masses. Is this the commitment of the State to realize health as a funda
mental human right!
Finally, there is an argument in the health policy document that the
western model-based health care delivery system is “inappropriate and
irrelevant to the real needs of our people and the socio-economic condi
tions obtaining in our country.”38 Our response to the argument is simply
this: For the realization of health as a fundamental human right, the
whole problem is to be viewed essentially from the ‘accural of benefit’—
point of view and not from the ‘cost’—angle. We feel firmer in this plea
of ours because the realization of health as a fundamental human right
is the fulfilment of a basic necessity, and it is the minimum obligation on
the part of the State to pursue this social objective which is enshrined in
our Constitution.
e
Moreover, money put in for the promotion of health is an invaluable
investment. It results in the generation of human resources. Isn’t it
strange that, following the lead of developed countries, we in the develop
ing countries do not mind in shelling out millions of dollars for exploring
nuclear energy, oil energy solar energy, wind energy; but start feeling at once
restraint when it comes to the development of ‘human energy’; Realising
the importance of health as a resource generator, Dr. H. Mahler, the
Director General of the World Health Organisation, has pointed out percep
tively that “everybody seems to be overlooking the fact that without human
energy, there would be no kind of progress either socially or economi
cally.’’39 Let us, therefore, structure our national health policy in a
manner which enabled us to realise health as fundamental human right
through the full exploitation of modern scientific system of medicine, which
is comprehensive, preventive, promotive, curative and rehabilitative.
Footnotes
1.
The Alma-Ata International Conference was jointly sponsored by
the World Health Organization and the United Nations Children’s Fund.
This Conference was preceded by a number of national, regional and
international meetings on primary health care, held throughout the world
in 1977 and 1978. The Conference was attended by delegations from 134
governments and by representatives of 67 United Nations organizations,
specialized agencies and non-governmental organizations in official relations
with WHO and UNICEF. See Report of the International Conference on
Primary Health Care (Alma-Ata 1978), published by the World Health
Organization, Geneva, 1978. (hereafter cited as Alma-Ata Conference).
2.
Declaration I. (Emphasis added).
3.
Ibid.
4.
Declaration II. (Alma-Ata Conference).
5.
Ibid.
6.
See the Report of the sub-group on the ‘meaning of health for
all in the background of India’s Health Needs,’ in the Report of Working
Group on Health for All by 2000 A.D., (Government of India. Ministry of
Health and Family Welfare, New Delhi, 1981), para 30, at 50. (Hereafter
referred to Report on Health).
7.
Declaration V. (Alma-Ata Conference).
8.
Declaration VI. (Alma-Ata Conference).
9.
See the circular letter of the Secretary General of the Inter
national Conference on Health Policy—Ethics and Human Values.
10.
See (1978) 71 Journal of Indian Medical Association, No. 3, at 66.
11.
The Indian Medical Association gave a call to observe September
1,
1978, as the “National Health Policy Demands Day” to mobilise a
massive public opinion in the country and to induce the Government to
enuniciate its health policy to meet the total health care of the people.
Id., at 86-88.
12.
A Statement on the “National Health Policy” was laid on the
Table of both the Houses of Parliament on November 2. 1982. The policy
was discussed at length in both the Houses and was approved by the
Raiya Sabha on August 4,1983, and the Lok Sabha on December 22, 1983.
(Hereafter simply referred to National Health Policy).
7
13.
National Health Policy, para 1.2.
13 a. For this estimate, see Report on Health, supra note 6. See also
National Health Policy, para 3.
14.
Id., para 4.
15.
Id., para 5.
16.
Ibid.
16 a. Ibid.
17.
Id., para 6.
18.
Id., para 5.1.
19.
Id., para 4.2.
20.
Ibid.
21.
Id., para 11.
22.
See also for this conclusion author’s IMA Award Winning Paper
of 1980, Pragya Kumar, “Short Term Courses in Medicine: A Necessity or
Political Gimmick.”
33.
See the comments of the Indian Medical Association on the Draft
for Discussion on ‘National Health Policy’ in IMA Document—NHP. 1
(April, 1979), at 13. (Hereafter cited as IMA Document.').
25.
(1978) 71 Journal of Indian Medical Association, No. 3, at 84.
25. See also supra note 22.
26,
IMA Document, op. cit., at 1.
27.
Ibid.
28.
Id., at 4.
29.
Ibid.
30.
See infra note 33.
31.
See National Health Policy, paras 7 and 9.
32.
A report reveals that in the State of Punjab alone there were over
23,000 RMPs in 1979. They are in reality unqualified voids who were
allowed in 1967 by the then Government to get themselves registered by
simply filing an affidavit and thereby becoming entitled to prescribe allo
pathic medicines. See The Tribune, February 16, 1979.
33.
See the Resolution adopted in the Open Session of the 60th All
India Medical Conference held at Hyderabad on January 28-30, 1985,
urging the Government to pass a suitable legislation for banning the
practice of modern system of medicine by persons qualified to do so and
making it a cognizable offence. (1985) 83 Journal of Indian Medical
Association, No. 3, at 92.
34.
National Health Policy, para 11,
35.
See supra note 20.
36.
See D. Banerji, Social and Cultural Functions of Health Services
in India, (Centre for Social Medicine and Community Health, Jawaharlal
Nehru University, New Delhi), cited in Training Capabilities of Primary
Health Centres in India (Technical Report 1), (National Institute of Health
and Family Welfare New Delhi), at 2.
37.
IMA Document, op. cit., at 10.
38.
National Health Policy, para 4.2.
39.
See the Text of Address of Dr. H. Mahler, delivered at WHO
Regional Committee for South East Asia, Thirtieth Session, Bankok,
Thailand, 2-8, August, 1977, in. Final Report and Minutes of the Meeting of
the Thirtieth Session, New Delhi, September, 1977, at 64.
COMML’N/TYH •
y/1. (First floor} £.•’
T’
INTERNATIONAL CONFERENCE
HEALTH POLICY : ETHICS & HUMAN VALUES NEW DELHI 1986
Human Values and Quality of Life
—A Personal Statement
Prem Kirpal
In 1969 while serving as a Senior Specialist at the East-West Centre
at Honululu in the beautiful Island of Hawaii, and also unknown to myself
at the time afflicted with malignant cancer inside my body to be operated
shortly, I wandered at the blueness and vastness of the Pacific Ocean and
the lovely beach of our tiny Earth. From this wander of the beauty of
Nature and some surge of creation inside, I wrote the following poetic
statement on the “Quality of Life”:
I—QUALITY OF LIFE
Life’s quality is comprised of: palatable food to digest well and
enjoy; enough space and scope to contain and express the needs of body
and soul in the full awareness and respect of other bodies and souls; robust
health with abiding element of youthfulness; and, above all, the sheer
love of life-the gift of friendship and love, the sense of wonder and endless
curiosity, the perpetual thirst for giving and receiving, ceaseless strivings
for new creations, and the capacity to accept any outcome in full under
standing and with utmost serenity, cheerfulness and gratitude.
Life is as good as one can live it and it is as big as one can hope,
imagine, aspire and dare 1
Its quality depends a little on luck and chance, but much on what
we value and search and how we go about it with courage, dedication and
faith.
In this way one can never fail, because even failure becomes almost
success when it is preceded by the right quest and effort.
To shoot at the stars and fail is better than a timid and faint-hearted
venture which may satisfy or reward, but cannot thrill and exalt.
The spice of life and its meaning and scope determine its quality in
the depth, breadth and extension of consciousness, from the earthly and
the human to the spiritual, even the cosmic, dimension of man’s percep
tion, experience and vision. There is no limit to life’s quest and quality,
and often we become what we love. Being and becoming arc great gifts of
consciousness and these should be treasured and developed in all ways,
dimensions and potentials of man’s psyche and his cosmos. Remember
always that in Life and its Beyond we are related and joined together to
all Creations and the experience of this Great Harmony is the wonder and
savour of Existence. Give full heed to the vastness of life’s scope and its
endless potentials and be grateful for the wonderful gift of life.
This Statement has been inscribed permanently on the inner wall of
a Public School not far from the river Ganga and the massive machines of
the Bharat Heavy Electric. Hopefully its young readers derive more prac
tical meaning from it than what I have been able to practise. Since 1969
I have written and spoken a great deal on the Quality of Life and Human
Values in the context of education and culture at home and abroad at
several international meetings under the auspices of the United Nations,
but the above Statement of life’s quality abides in both the spirit and con
crete attributes of life’s quality, which is basically reflected in the health of
mind, body and spirit and the inner life of the human psyche.
It is, of course, essential to achieve physical survival and a certain
measure of material well-being before the quality of life is experienced and
treasured in the world of the mind and the spirit. For physical existence
we need food, health, housing, education, work, worship, sex and play.
For man as a spiritual entity we must transcend along the path of
security, freedom, identity, sense of belonging, joy, confidence, love and
creativity. For both being and becoming we must now, in the emerging
planetary order of Mankind, explore, identify and practise human values
upon which will depend the attainment of the quality of life for all, and
not only the privileged few.
From our past of many civilizations, diverse cultures, different reli
gions and conflicting ideologies we are moving towards the unity of
mankind. The formulation of a general statement on human values for
our time could help the shaping of appropriate attitudes, common be
liefs and suitable criteria and content of education for contemporary man.
Such a statement can be based on the following important concerns and
aspects of man, common to all civilizations and culture :
II—HUMAN VALUES
1. Man and his Own Self
In order to take charge of one’s life in an uncertain and fast-chang
ing world, the essentials of personality such as physical and mental health,
right balance and poise of mind, and moral and spiritual qualities of
character should be valued and cultivated. Education and Culture need
to be directed to the enrichment of character and the pursuit of goodness,
wisdom and transcendence. The development of the inner man by the
fullest flowering of man’s potentials and totality of being should be encou
raged in an atmosphere of freedom and security. Man’s care of his own
self calls for measure for measure of austerity, self-discipline, pursuit of
self-knowledge and cultivation of serenity as well as intensity. The luminuous and balanced self ceases to be vulnerable. The power of the inner
self should be directed to love and service of fellow-beings.
2.
Man and his Fellow-man
Man s relationship to Society should be governed by principles of
humanistic morality acceptable to all and reflecting the quality and sensiti
vity of human relations, based upon compassionate love, mutual under
standing and appreciation, and respect for justice and solidarity of
mankind. The invocation to loving one’s neighbour should extend to all
innaoitants of the planet. Such a relationship between man and his fellow
man has to overcome the divisions and barriers of the past and the present
attitudes of superiority and smugness arising from inequalities of wealth,
KnC* knowledge. Man’s common predicament and basic humanity
should be planted firmly in his consciousness and conduct by the fullest
and wisest use of the resources and potentialities of communications. The
exploration and understanding of man’s psyche should strengthen common
humanity.
3.
Man and his habitat
Contemporary man’s habitat extends from his home and local
environment to the entire planet, involving the care and nurture of nature
and ecology from which he derives great benefits. The resources of the
habitat must also be preserved for posterity for which he holds his habitat
in trust. The sense of belonging and gratitude generate loyalty, prudence
and austerity, and in the care and management of the habitat man learns
to live in harmony with others. Narrower loyalities and nationalistic pride
and egocentricity lead to conflict and war. These should give way to
global loyalities.
4.
Man and his work
To a large extent man lives in and for his work, and his mental health
and happiness depend upon the choice of work, its scope for action, ex
pression and initiative, its contribution to his creativity, decision-making,
pursuit of excellence and sense of self-esteem and dedication. While work
affords satisfaction, enjoyment and self-realization, it can also bring obses
sion for success and lust of power. We should avoid such temptation and
work in a spirit of non-attachment and non-violence. Frustrations and
alienations resulting from deprivations of work or its satisfactions warp the
individual and distort society. Socio-economic systems and education
should rectify these.
5.
Man and Art
All men are endowed with artistiq capabilities in varying forms and
measure, and the flowering of these depends upon individual urge and
social receptivity. The manifestations of beauty differ, but its essence and
inspiration are the same. The pursuit of the beautiful strengthens man in
his humanity and elevates his cultural life. In work, education and life we
should recognise and enhance the importance of the arts and the artistic
spirit. Respecting the diversity of art and culture, we can sense and share
in the underlying unity of mankind. The quest of beauty and the joy of
creation reveal life’s meaning and enrich its quality. The artistic nature of
man should be fed and nurtured all through the life span. People should
have the opportunity of appreciating other people’s arts and cultures.
6.
Man and his Technology
Technological advance should be for human welfare and for the
enrichment of man’s humanity. Uncontrolled mechanisation for sheer
power and de-humanisation needs to be checked. By controlling and
regulating technological advance and application of science we can improve
human welfare and quality of life. Appropriate technologies should be
chosen for practical relevance and efficient productivity, and also for their
capacity to humanise life and spread culture. Technology should not be
allowed to undermine or pervert the primacy of the human spirit which is
the source of man’s creations and the abiding values to live by. Technology
must always be subservient to the ends of good life and humanism. As a
significant reflection of man’s relentless curiosity, inventiveness, perfection
of methods and systems and mastery over the external world, technology
projects important human values.
7.
Man and his Ideology
Man cannot live by bread alone. Beyond the materials of economy,
politics, science and industry, his restless mind and probing spirit need
some beliefs to give meaning to life and its goals and purpose. Historical
experience and human choice determine ideologies which are incentives to
action in the present and guides to the making of the future. Ideology „ V
caters to emotional and my; tical elements of man’s consciousness as well
as the quest of truth, faith and humanism. Ideologies are reflected in the
diversities of cultures and choice of life-styles and systems. They can cause
tensions and conflicts and lead to war and destruction. Ideology should
be valued for its ennobling influence, its strength and integrity, its dedica
tion to peace and harmony and its commitment to man’s humanity.
8.
Man and Time : The Stream of past, present and future
In his relationship with time man shares some compulsions and
dreams not only with the fellow-man of his own time in life, but also with
those who have gone before in history and those who have yet to come.
The consciousness in time and the experience of the life-cycles contemplate
the mysteries of life and death and the concept of eternity. Respect for
the past with hope for the future strengthens man’s care of his cultural
heritage and pride in common endeavours and aspirations. Man’s sense of
history is a most precious source and guide to humanistic values, the
understanding of human nature, deep humility and compassion; in the
depressions and elections of the flux of history man recognises his eternal
self and experiences the brotherhood of mankind.
9.
Man and his Cosmos
Man has always pondered about the mystery of existence, the universe
that lies beyond, and the larger scheme of life of which he is only a part.
Imagination, intuition, mysticiam, and religion have all contributed to the
quest of the Cosmos, the ultimate or the larger universe which may be
glimpsed through worship, meditation, knowledge and poetry. Contempo
rary man has greater knowledge of the extent and nature of the universe
than the past generations, and this knowledge brings us close to the life
and unity of our own planet. We can all share in our common predica
ment of the planetary habitat, so small and insignificant in the vastness of
space and time. The Cosmic dimension of life brings us closer to each
other and gives a proper perspective to temporal existence.
4
/
COM.,U.S' !'Y ■;£ V_T 1 CT'.L
47/1. (First floor; St. Marks Read,
§£nfialore - 560 001,
INTERNATIONAL CONFERENCE
HEALTH POLICY : ETHICS & HUMAN VALUES NEW DELHI 1986
Rural Child and Health Development Team
Dr. P. Chandra, MD., DCN., MNAMS.,
Prof. & Head
Department of Paediatrics, Stanley Medical College,
Madras 600 001
The story of Child Health in India is one of needless, avoidable dis
abilities, and missed opportunities. Child Health is not an individual
problem. It is a family and community problem and has to be tackled at
the community basis. 70% of India’s children live in rural areas. The
health needs of the children in our country are entirely different from those
of affluent countries and do not require sophisticated technology. There is
a need to ensure that resources whatever their origin are channeled in to
socially relevant health action-Multisectorial Mass Action for social change.
'A comprehensive National Health Policy has been accepted by the Parlia
ment signifying the political and Government will to Achieve Health For
All by 2000 A.D. The targets to be achieved stresses the importance of
Maternal and Child Health Services. The policy emphasises the preventive,
promotive and Public Health and rehabilitation aspects of health care and
establishment of Primary Health Services, to reach the population in the
remotest areas of the country. Ensuring adequate Nutrition, safe drinking
water supply and improved sanitation for all segments of the population
and Health Education are the other highlights of the Policy Document.
Like any other field of science, Medicine is witnessing a knowledge
explosion in all aspects. Advances in Paediatrics started as a trickle in
fifties, became a rivulet in sixties, a torrent in the seventies and a flood in
the current decade. There is a wide gap between available knowledge and
its availability to the most needy. Obviously we need a break through not
only in science and technology but also in organization, management, edu
cation and motivation. It is in the application of what we know that we
are failing even more than in the discovery of new knowledge. It is a
tremendous challenge for all of us if we wish to meet the Rural Children’s
Cause and Commitment.
The nation has developed a plan for rural services to meet the needs
of Mother and Child Health Care and Family Welfare. The assessment of
available resources, their proper allocation, efficient utilization are
important considerations for providing efficient Health Care Delivery.
Primary Health Care envisages a community based health system which will
emphasise the interdependence of health and development in all ramifica
tions and ensure the equitable distribution of available health resources
leading to accessibility and efficient health care. So optimum mix of
personnel of health and non-health' sectors has to be done for most effi
cient health care services.
In India since our Independence, with the establishment of Primary
Health Centres and Rural Community Development Programme, it was
possible to take modern health development of people living in farflung and
hitherto inaccessible areas. Still the improvement in Health and Nutrition
Status of children is not commensurate with the effort. This has brought
in to question, review of the entire activity of Health Care Delivery with a
view to evolve a strategy more suited to the country’s condition. Health is
not medicine alone. Health development cannot be restricted to the deve
lopment of medical technology alone or devising, ways of applying the
technology. Primary Health Care has to look beyond health sector. It is
time to veer away from the concept of Medical Personnel working in
isolation.
The members to constitute the rural health development team and
their job responsibilities have to be redefined. There should be a vigorous
effort to integrate all agencies like rural development, agriculture, Womens’
Welfare Education, Nbnformal Education and voluntary associations and
departments involved in the challenging task of improving the quality of
children everywhere. There is a need for a fundamental change in the
organisational set up in the block level. In the present changing situation
the Health' Development Team has to co-ordinate various activities to
maximise efforts and accelerate development.
Team is defined as a group of people working together towards a
common goal. Team work is pooling of efforts co-operative working for a
common cause. All group of workers concerned with health development,
promotion, maintenance and recovery of health and prevention of diseasesare members of ‘Health Development Team’. These members have different
qualifications, grades, strength, experience with different types of responsi
bilities varying according to the tasks it has to perform. The challenge of
achieving uniform health development is greatest in the villages. All
sectoral plans and programmes for the social development in the villages
have isolated approaches quite independent of each other with obvious
overlap. It is imperative that if we are serious to achieve meaningful
results within the next decade, within the financial resources, there is no
alternative to the exploitation of available manpower and financial
resources, available with various departments and agencies concerned with
Growth and Development, in the most well planned and co-ordinated
manner. All vertical programmes running virtually independent of each
other with very little co-operation at planning, supervisory and field levels
have to be integrated tota ly and formulate well planned and co-ordinated
practical programmes. Ivan Illick says ‘there is a great deal of medical
capability outside-the medical profession and unlimited opportunities out
side formal institutions’. So the functionaries at the block level who should
be the members of the Health Development Team are to be from all walks
of life.
From (1) Health and Family Welfare
(2) Rural Development
(3) Social Welfare
(4) Education
(5) Non formal Education
(6) Water Su rply and Sanitation
(7) Agriculture
(8) All Voluntary and Philanthropic Institutions
(9) Mass Media.
The objectives of the team will be, all the welfare activities including
health is to be expanded to cover all the population, particularly the
vulnerable, improving the functioning and utilisation within the present
system.
All the concerned team members should be made to
(1)
understand the local maternal and child health problems well to
develop a cost effective health care system.
(2)
Study the problems in implementing existing programmes e.g.
administrative obstacles, female illiteracy and the gap in out reach services.
(3)
Study the conflicts in implementing welfare programmes for
mother and children, (e.g.) deep rooted cultural beliefs.
(4)
Learn how to provide technical education to family members and
local volunteers.
(5)
Learn methods of mobilization of people in the village parti
cularly women for promotion of health.
(6)
Understand importance of documentation of health events,
evaluation and accountability.
Rules and roles for the team members can be so defined as to provide
built-in flexibility, within a clearly defined broad policy framework. Each
block can assign responsibilities and tasks, allocate resources, and set
targets according to the local priorities, health and family welfare needs of
the people, (e.g.) (a) areas where nutrition status is poor nutrition input
must be maximum. In most backward areas female literacy must.have top
priority. Many of the maladies of the present system can be cured at the
village level by a very effective team by involving the family itself. The
goals to be achieved also has to be streamlined, (e.g.) The short term goals
of the team will be, achieving.
(a) 100% Antenatal care
100u'o Natal care
100% immunization coverage
100% Infant follow up.
(b) Training and educating the team in recent advances in child
health care, e.g.) growth monitoring, oral rehydration therapy, breast
feeding, weaning and food supplementation, female literacy and family
spacing.
The overall objectives of education and information with communi
cation programmes of the team is, to educate and mobilise the neediest
sections of the rural population so that, they can themselves initiate actions
to achieve and maintain an acceptable standard of health and family
welfare.
The long term objectives will be-
3
(1)
To inculcate a sense of self reliance and discipline in all segments
of population, so that all four sides of the health square i.e. prevention,
promotion, cure and rehabilitation are effectively handled at the local levels
consistent with development in the field of medicine.
(2)
To improve public health and public health services, to achieve
health for all with expected reduction in mortality and morbidity.
(3)
Universal education and total female literacy.
Training and education of the team and through them the community
is a challenging task. It is on the ability to elevate the standards and
reliance of the community the success can be judged.
Success in one area will turn up problems from an unexpected
direction e.g. once malnutrition and infection is tackled, cardiovascular
degenerative diseases may take an upperhand. The team also should anti
cipate and plan programmes for the future.
This approach will help all to move from knowledge to action.
Tomorrow is too late to help to-day’s children.
INTERNATIONAL CONFERENCE
HEALTH POLICY : ETHICS & HUMAN VALUES NEW DELHI 1986
Man, Medicine and Law: Challenges
of the 21st Century
P.M. Bakshi
Formerly Member, Law Commission of India
1.
Introduction
Bio-medical and technological advances have forced not only a re
definition of some concepts in other disciplines, but also necessitated a
widening of the perspectives of medical science. Science is no longer the
concern of scientists only. It is no longer enough for the man of medicine
to confine himself to the traditional learning of his own discipline.
Whether he likes it or not, he has per force to expand the horizons of
his mind and to take note of the points of view of other disciplines and to
meet the demands of norms flowing from the principles evolved by other
disciplines. Dramatic and frightening progress in knowledge, particularly
in genetics and biology, and radical advances in techniques, especially in
re-constructive surgery and in surgery connected with the process of
reproduction, have raised issues of great consequence to humanity. Some
of these issues are already of pressing interest, such as abortion. A few
others, if not of pressing interest today, are bound to cry for answers
tomorrow. It is only if we start thinking about them today, that the
answers will be ready tomorrow.
It has been said that science often seems to thrust society into
directions which society only partly understands and certainly has not
chosen. This makes the task of social scientists and thinkers on ethical
problems fairly difficut. They must first understand the directions of
science and then offer guidance as to the implications of scientific
advances, and elucidate to the best of their ability the choices open and
the merits and demerits of each such choice. Knowledge must thus come
first, but it has to be followed by wisdom, which a great jurist once des
cribed as the “elder sister of knowledge”.
Both science and ethics have a common origin, as part of the process
of civilisation which distinguished man from apes. In its earliest form,
science was an attempt by man to understand the phenomena of nature
and to exploit the resources of nature for satisfying his instinctive need
for food, shelter and protection. The beginnings of science freed the man
from the drudgery of hunting. Settling down in groups and cultivating
his own food gave man the security and leisure needed for pursuing a
life-style different from that of the ancestors of mankind. This inevit
ably led to the subtler things of life—language, writing; the arts, music,
poetry, religion, ethics and law. In ancient civilisations, scientific thoughts
flourished hand in hand with religion and ethics. Scientific discoveries
were considered revelations. The great writer on the' Indian science of
medicine Charaka was an ascetic. Aryabhata (5th century A-D.) who
propounded the revolutionary theory of rotation of the earth stated that
his knowledge owed itself to the grace of God. Al Biruni, the famous
Arab mathematician, insisted that his experimental work was subject to
the moral principles of Islam. When, in 1543, Vesulius, a physician from
Belgium, published a book on human anatomy based on dissection and
personal observation, he expressed his wonder at the “handiwork of the
Almighty, by which the blood sweats from the right in the left ventricle
through passages that escape human vision”. The feeling of antipathy
between science and religion was a later development, of which Copernicus
and Galileo were the victims.
2.
Nature of the issues
This paper does not seek to present an exhaustive treatment of the
impact, on humanism, of medical advances or a comprehensive catalogue
of the ethical and legal issues arising from such advances. But it seeks
to point out some peculiar features of those issues that are very relevant
to an understanding of their social significance, so as to facilitate the
formulation of a correct approach.
Usually, such issues are seen as presenting a conflict between medical
science and non-medical disciplines. However, this would be taking only
a partial view of the matter. In a sense, science is neutral, because
it does not take sides. The business of science is to discover the fund of
knowledge, to organise it and to present it. What use to make of the
knowledge, and whether to make use of it at all, is a question on which
the scientist, speaking as a scientist, does not claim superiority and would
not claim thp privilege of his speciality. It is in this sense that science
is neutral. When one speaks of a conflict between medicine and other
disciplines, one should not imply that there is an antagonism or antipathy,
as such, between what medicine demands and what society desires or
ought to desire. The truth is, that the conflict really in here is in the conflict
of interests, conflict of demands, conflict of desires and conflict of
approaches between two individual members of society, or between society
and its one or more individual members. For example, if one comes to
questions of life and death and is concerned with the precise issue as to
the determination of the exact moment of death, one finds, on a deep
analysis, that two rival approaches are competing for recognition. It
may be described as a conflict of values. The traditional concept of
sanctity of life and of the peremptory moral obligation of society to maintain that sanctity at any cost, is one of the competing values. Pitted
against this is the emerging movement for “dignity in death” and “the
right to die”. The latter movement has been regarded as an extension of
individualism. It is an extension of the individualistic principles of selfdetermination, autonomy, integrity and self-realisation and the choice to
exercise control over one’s dying as well as oyer one’s living.
3.
The debate about abortion
The conflict of interest between two individual members of society
is illustrated in the debate about abortion. The conflict here is between
the mother and the yet unborn child. Of course, it is a conflict of a
complex character, in which so many moral and scientific concepts or
doctrines are entangled, though very few persons are able to perceive that
the fabric is inter-woven with threads of an infinite variety and number
2
£
a
W
which criss-cross each other. Simply stated, the moral question is this:
Whose desire or interest should prevail? Should the mother’s desire
prevail or should the interest of the unborn human being be given prece
dence? In a more complex form, the questions are really multiple.
Should society recognise any right at all in the unborn? To put it in legal
phraseology, should the zygote, the embryo or the foetus be regarded as
a “human person” and, if so, from what point of time? When does the
right of the embryo to protection begin? At implantation? At the end
of the first trimester? At quickening? At viability? At the moment of
birth? Assuming that the right qf the foetus begins at one or other of
the moments just now referred to, under what circumstances can the right
of the unborn be overridden by the desire of the living and, at what point
during gestation? If both the foetus and tlie pregnant woman have rights,
the one to its survival and other to terminate her pregnancy, who is
competent to adjudicate the conflicting claims, and what are the quali
fications for such a role?
4.
The right to live
The situation of abortion, mentioned abpve, involves a consideration
of the two-fold obligation of the State towards the unborn life. (1) The
obligation to refrain from all interference with unborn life, and (2) the
obligation to prohibit an attack upon unborn life stemming from a private
person. Obviously, any law which permits abortion upto a certain stage
of pregnancy places upborn life at the disposal of society, though this
decision is taken in the name of higher and more paramount demands.
The conflict is seen in a more dramatic form when one comes to the right
to life and the right to die. The right to live is at issue in the unending
debate about the ethical aspects of prolongation of life by artificial means.
In a deeply unconscious individual whose vital functions are maintained
over a prolonged period only by extraordinary means, the question arises
whether a time comes when it is no longer appropriate to continue the
extra-ordinary means of support for the hopelessly unconscious patient.
If man is regarded as being in the image of God (imago clei) then, theoreti
cally, the duty to prolong life has no closing terminus. So long as the
vital functions persist spontaneously or with the aid of artificial process,
“life” survives and must be prolonged to preserve the ‘image”. This is
one aspect of the matter. Apart from this religious aspect, there often
comes to be presented a conflict of interests, though the conflict is not
articulated. The family of the patient very often wants to terminate the
agqnising watch and may urge a discontinuance of extra-ordinary measures
for prolonging life. Those who have an interest in organ transplantation
might press for a new appraisal of what constitutes “death”. The hospital
authorities and society in general have a vested interest in terminating a
costly procedure in a hopeless case. But the presence of these vested
interests raises the possibility of selfish “rationalisation” of the course
which the vested interests wish to adopt. It gives a warning of the need
for a cautious approach. One may also remember that tfle termination
of extra-ordinary care, even for just reasons, with death certain to ensue,
can have a shocking effect on observers.
Some of the problems discussed here arise even out of the existing
canons of medical ethics. The current code of ethics of the Indian Medical
Council, in paragraph 3, provides?—
3
“I will maintain the utmost respect for human life from the time of
conception.”
In paragraph 7 it provides—
. I will respect the secrets that are confided in me.”
5.
Artificial insemination
Some of the techniques evolved by medical science give rise to legal
as well as emotional problems. For example, there are emotional
problems born of artificial insemination, which is now frequently used to
help infertile fathers. Some fathers later resent children born as a result
of A.I.D. Mothers have also been known to develop a romantic in
fatuation for the unknown biological father. The practice is to keep the
donor’s name secret from the parents. But legal problems may arise if
the parents demand, say, a tall or vegetarian donor. There is also the
question of legitimacy of the child born of A.I.D.
6.
Genetic techniques, and IVF
Placed in the social context, any one genetic technique can be
assessed from a number of different angles. The several frames of reference
which apply, say, to a decision on abortion, include exploring it from the
point of view of (i) the parents, who may or may not have a deformed
child, or (ii) society, which may or may not wish to spend money on the
care of children, or (iii) the child yet unborn, whose right to protection
may require to be considered.
In vitro fertilisation is not simply a device to be marvelled at, as an
instance of science fiction turning into science reality. It raises in our
mind serious questions of ethical and social policy; for, genetic technology
has the potential to take human heredity out of the realm of blind faith
or chance into the realm of free will and choice. In the past, nature took
the blame or the credit for genetic inheritance. This responsibility is
increasingly becoming ours, because of expansion of the area of choice.
7.
Coercive genetic and surrogate motherhood
This does not mean that “coercive genetics” (the prescribing of
legal sanctions against the use of genetic techniques) should be readily
resorted to, either to force the weeding out of undesirable genes or to
prohibit the use of new techniques. Excessive intervention by the State
would completely undermine the legitimacy and moral basis of Govern
ment. It is in this context that the most difficult issue is presented by
surrogate motherhood. However morally shocking the practice may be,
a legal prohibition may well remain unenforceable. What matters in
such cases is the social feeling. As has been often pointed out, most new
genetic techniques, once developed, would bring much joy to parents and
cause little discernible harm to society. The State may, therefore, be well
advised to guard itself against the urge to legislate in this field. Improve
ments in genetic technology may well excite the appetite of the State to
interfere by legislation, but the tendency will ha've to be curbed.
4
S. Inchoate rights: the question of privay
The situations so far' discussed concern themselves with legal or
moral rights whose existence is undisputed. Besides these, however,
sometimes there are involved rights which themselves suffer from obscurity,
because of the prevailing uncertainty about their existence and recogni
tion. Here the shadow on a correct appreciation of the ethical issues is
not cast by any scientific advances as such, but arises from the hazy nature
of the very rights themselves, whose existence and precise dimensions have
not yet been demarcated in traditional legal and ethical thinking. Privacy
is an example of such a right.
9.
Privacy and informed consent
Of late, the doctrine of informed consent to medical treatment has
come into prominence. This doctrine initially came to be premised on
the patient’s right of self-determination. This is instanced by the famous
words of Judge Cardozo [Schloendorff v. Society of New York Hospital
(1914) 105 N. E. 26]. The patient’s right to information before consenting
to treatment may also receive support from the principle of the right to
privacy—being the principle of an “inviolate personality” which posits
the individual’s independence, dignity and integrity. It may be mentioned
that of the several facets of this right as explained by Mr. Justice Douglas
[floe v. Wade, (1973) 93 Supreme Court 705], the third deals with the
freedom to care for one’s person and health.
10.
Bio-ethics
All this naturally brings one to the new discipline of bio-ethics.
Broadly, is a discipline dealing with the ethical implications of biological
phenomena as manipulated or encountered by the science of medicine.
It dwells on the frontiers of medicine and ethics, Because it dwells on
the frontiers, it has its own excitement. Sir Ernest Gowers once said that
the crossing of intellectual frontiers is always a thrilling experience, just
as it is a thrilling experience to cross the physical frontiers of one’s own
country.
Bio-ethics is not a totally new subject. In some form or other, the
medical profession has always had something to do with ethical issues.
The celebrated works of Charaka (probably 100 A.D.) on the Indian
system of medicine contain an elaborate code of ethics for physicians.
Amongst the mandates that Code contains, is a direction to the physician
to strive for the relief of the patient with heart and soul. It also directs
the physician not to treat a female patient, unless a male relative is present.
Four goals may be concretely indicated in regard to the discipline
of bio-ethics: (1) identifying the moral issues in a bio-medical context;
(7) developing appropriate strategies for analysing moral problems;
(3) relating moral principles to specific issues; and (4) training a small
group in bio-ethics.
The first two goals imply that the physician is not a primary
decision-maker, but rather one who assists the patient in coming to his
own decision where a moral issue is involved. The physician must learn
5
how to distinguish technical questions of medicine (which are appropriately
his own area of competence) from value dimensions (which are not ex
clusively his own area of competence).
A regards the third goal of bio-ethics (relating moral principles to
specific cases), this will be for the patient, he being primarily the decision
maker. But some ethical issues can still remain for the physician—e.g.
how much information is to be transmitted to the patient about a parti
cular diagnosis.
11.
Conclusion
To conclude, let me quote from Dr. A.S. Duncan’s foreward to
Alastair Campbell's Moral Dilemmas in Medicine: “Curricula have become
so loaded with the very scientific and technical matters which lead to the
dilemmas that little time is left for thought as to the dilemmas, themselves.
As Harold Laski wrote, “expertise sacrifies the insight of common sense
to intensity of experience.” Where human problems are concerned, the
expert fails to see that every judgment, which he makes, not factual in
nature, brings with it a scheme of values which has no special validity
about it.
Reference
1. See George Lobo Current Problems on Medical Ethics (Paul
Publishers, Allahabad 1974) Pages 215-228.
INTERNATIONAL CONFERENCE
HEALTH POLICY : ETHICS & HUMAN VALUES NEW DELHI 1986
Demands of Few vs ^eeds of Many
Dr. V. Parameshvara
President
Indian Medical Association
‘'The right to health is a fundamental right"
W.H.O.
“A state of complete physical and mental and social well-being”
W.H.O.
“Complete freedom from disease and from struggle is almost
incompatible with the process of living”
Rene Dubos
Health is different from pleasure and happiness. As opposed to
health, in happiness there is hierachy. A happy man wants to be happier;
getting one measure of happiness, he desires to get a greater measure of
happiness; getting one kind of happiness, he longs for other kinds of
happiness.
The highest value held out in Indian thought is not happiness or
‘sukha’ because happiness necessarily presupposes its invariable concomit
tant, unhappiness : the two constitute a pair. One cannot be there with
out the other. On the other hand, peace of mind (shanti) is freedon from
all opposites and is therefore, the highest objective. Peace of mind
(shanti) is defined as that, obtaining which, one does not seek to obtain
anything else. It results, when there is no longing and thus no stress.
There are no levels or kinds in peace of mind. A person who is content,
does not aspire for more of it; if he does, he ceases to be content’. Thus
it eliminates rivalry, strife and stress. It is an attitude of mind that is
cultivated, in order to preserve and promote health and to prevent illhealth. Peace of mind is within easy reach and can be attained by a large
majority of people, irrespective of caste, vocation, knowledge of philoso
phical truths and so on.
Health is possible only for mortal beings, for we are born with the
twin inherited and inescapable‘diseases —ageing and mortality’. To lack
health is a misfortune than misdeed. Health is more beauty than virtue,
more an aesthetic than ethical term. One does not condemn some one
for ‘no longer being healthy’. Then, are our goals for attaining health or
prolongation of life ? If we aim at the latter, we go after the diseases that
are the leading causes of death, rather than the leading causes of illhealth. When we tend to evaluate in terms of mortality statistics, we
invariably mean changing one set of fatal illnesses or conditions for
another. Prevention and treatment of causes of ill-health may enable the
prospective or actual victims to live longer.
Modern system of medicine, which is most widely respected of pro
fessions and which has never been more competent technically is in trouble.
Its health is not too well. The reasons are medical care is very costly and
not equitably available. The average doctor sees may more patients than
he should, yet many fewer than would like to be seen. In fact a modern
doctor is overtrained for the job he is doing, yet undertrained for the job
he is expected to do. On the other hand physicians powers and expecta
tions from him have grown enormously, owing to explosion of knowledge
and modes of diagnosis and treatment. His responsibility have grown as
well. All kinds of problems now roll to the doctor’s door from sagging
anatomies to suicide, unwanted childlessness to unwanted pregnancy, marital
maladjustment to learning difficulties, genetic councelling to drug addiction,
from laziness to crimes. It is iromic but not accidental, that the great
technical power of medicine is under confusion about its standards and
goals for guiding its use. When its power was fewer its purpose was
clearer. In fact, medicine was considered the very model of an art in the
past. Today, although fully armed and eager to serve, its targets are no
longer clear. Now health is not the only possible and reasonable goal of
medicine. There are other goals as well Eg. removal of womens breast
because it interferes with her golf swing, performing vasectomy, tubectomy
as family planning for non-medical reasons, artificial insemenisation etc.
Hence happiness is a false goal of medicine.
Without a clearly defined end views, medicine may prove to be only
a set of means, and doctor being reduced to a technician and engineer,
of selling his services on demads. This meands transforming the physicians
into a helper for hire. ‘Endless’ profession is an ‘ended profession’. A
doctor should not be tyrant but neither must he be a servant. Doctor
should remain as a leader and teacher. Public misperception of medicine
is ultimately more dangerous than the doctors misperception of himself.
The community must respect the fact that medicine is an ‘art’ and doctor is
a ‘docere’.
We need to advise better indices of healthiness than mortality and
morbidity statistics. Thus the importance of epidemiological research in
healthiness—about what promotes and what undermines health. Sophis
ticated studies in nutrition, exercise, rest, sleep, relaxation, response to
stress are integral subjects of research. We need to identify and learn
about health sub-groups in the community and to discover what accounts
for their success Eg. change in eating habits, and new treatment for
hypertension has shown a downtrend in death rate from heart attack in
middle age groups. This approach would appear pedestrian in comparision
with the dramatic style of high technology and therapeutics. One has the
highest respect for noble prize winners, for the discovery of chemical
wonder of enzyme structure, but surely he who suggested adding chlorine
to drinking water or invented indoor plumbing system and closed drainage
have contributed more to healthiness of human kind. What is actually
important to note is that major improvements in mortality in Europe
and USA occurred before the massive investment of the last few decades
and before the advance of ‘high technology’ in medicine.
Mortality rates among children, young adults have continued to
improve but not at an enhanced rate and gain in expectation of life at the
age of 65 have been far from dramatic. It spite of enormous scientific
development and availability of drugs and high technology machinery, the
improvement in mortality has been disappointing. Complete eradication
2
of heart disease, cancer and stroke—currently the major mortal disease,
would according to some calculations, extend the average life expectancy
at birth only by approximately six or seven years, and at age 65 by more
than one and a half to two years. Medicine’s contribution to longer life
has nearly reached its natural limits.
There are several countries, where spending on health services is not
below 10 per cent of the gross national product (West Germany,
Netherlands, Sweden, USA). People are now working for a five weeks
year, simply to pay for their health services—less premature death, less
illness and disability, less pain more comfort and support and care when
disability cannot be further ameliorated. There is serious doubt, whether
richer countries of the world have in fact gained any commensurate bene
fits. There is a point at which people want to keep their own money to
spend in their own way. Bulk of the money in health care goes to a
small minority who are seriously ill. There may well be a' limit on what
the healthy are prepared to spend on the unhealthy.
CT scanner is the greatest development in radiology and has enor
mous diagnostic potential but between 1973 and 1977, UK installed 30
brain and 11 body scanners. In USA in the same period, over 760
scanners including 200 body scanners were installed—if each of these
machines did 2000 scanners a year, at average charge of US £300, the
annual cost would be $456 millions. Being excessively impressed with
the technological brilliance of big hospital medicine, mobilizing crusades
and crash programmes against cancer and heart disease, the health poli
ticians speak as if more money, more targeted research, better distribution
of services, more doctors and hospitals, and bigger and better cobalt
machines, lasers, and artificial organs should bring the medical millennium
to every citizen.
Planning must not be vague, unless justified on economic grounds,
increased efficiency or training, new and sophisticated equipments, and big
hospitals can become ‘white elephants’, One approach to the problem
of cost containment is to restrict the supply, both of hospital beds and of
medical man power.
One view is that further preventive efforts may be more cost-effective
than further investment in curative media. Equally important is the fact,
that a section of intelligentia both in and out of medicine, have begun to
wonder aloud, whether and to what extent medicines are doing good.
The countries that appear to spend the most on health services do
not necessarily have the best health. Spread of free or nearly free health
services to vast majority of the population does not seem to have narrowed
relative social class difference in mortality risks. The 13 year increase in
life expectancy from 1950 to 1970 for persons over 25 years old, who are
non-smokers, is also most halved for those smoking more than 25 ciga
rettes a day. We are irrationally suspicious of any attempt to modify
our personal behaviour, even if it kills us.
“A man who has built a fire to warm himself, but continues to fire it,
until it begins to roast him"
Plato
3
Frankly he seeks ingenious devices to measure his discomfort accu
rately and to cool himself down, dazzled by the roaring success of his life,
he fails to see, that the obvious remedy is to put less wood on it. Modern
medicine is often pictured as a stunning breakthough. , Technological
revolution have evidently fostered this image. ‘Technology’ reign as the
primary shaper of medical progress has been strongly challenged, not only
in terms of the financial drain but also in terms of its outcome on the
nation’s health—its excessive use and the possible risks to patients and
societies. Technological revolution has become a controversial issue.
Now it is ‘Technological Problem’. Therefore developed countries have
a lesson to teach the developing countries from their experience—may be
negative rather than positive ‘Don't do it our way’.
The trend towards high technology evidently leads to a disequilibrium
in type and distribution of services provided, with too much emphasis on
acute institutional care and too little on more essential care, for huge
segments of the population. In countries with more limited resources, it
obstructs the development of priority health services, thus possibly contri
buting to a deterioration in the population health. The developing coun
tries should not be mislead by developed countries. Gross attempts to
transfer successful structures from one country to another, can lead to
reactions out of proportions to the often minor adaptations needed to fit
them to the recepient country’s values.
Poverty is the key vector in the developing countries. Poverty creates
illness and illness creates poverty. Health planning is a question of
economic and social planning rather than medical planning. Industrial
development would help a small urban elite. There is relatively high
expenditare on health services in urban areas, concentration of resources,
hospitals and trends towards physicians based security schemes. Usually
training included doctors and specialists, medical education of the curri
culum of more developed countries, heavy expenditure on imported
gadgets and pharmaceuticals, service heirarchially controlled and at the
same time vast majority are denied science based service and spend heavily
on herbal remedies and traditional practitioners.
It is interesting the relatively low priority is given to health compared
to other areas such as ornaments, hotels or air lines in developing countries. Health does not seem to be a priority.
Inadequate investment on the physical and mental well being of the
people can only mean a proportionate decline in the economic develop
ment of the country. Putting greater pressure on its resources.
Pharmaceutical progress eliminated suffering and sadness, has benefitted modern medicine by the saving within the health service itself, saving
from the reduction of loss of working days and savings from the elimina
tion of premature death. For the vast majority of the rural population,
it is now accepted, that basic and generally well established medicines are
what is needed Eg. vaccines and antibiotics.
A case in point is that there are nine million blind persons in India—
3 out of 200 persons and 3 million of them are preventable. 25 lakhs of
children are estimated to go blind every year and 1.25 will need to be
4
'
protected annually with vitamin A—50,000 units costing Rs. 2 per child
with a total cost of Rs. 25 lakhs as against Rs. 25 crores for feeding,
educating and care of the blindand loss in terms of human happiness.
Forty per cent of population are found to suffer some degree of iron defi
ciency anaemia which could be rectified by oral iron therapy, costing hardly
Rs. 2 to 5 per person. Appropriate technology for health and rationing
of services could lead to rational solutions. The need to eliminate waste
and improve cost-effectiveness, and the principle of equal distribution of
service in population.
In many areas of social life, policy and action still continued to be
improved on the basis of prevailing beliefs rather than on informed
appraisal of issues and alternatives. In meeting health needs, technology
must be geared both to the problems to be solved and to local conditions.
It should be scientifically sound, acceptable to those who apply it and to
those for whom it is used and affordable to the nation.
Each country and each society has to decide its own health priorities.
Good information is crucial to good decision making. Their use must
justify the effect involved.
The stock of skill or human capital must be allocated in such a way
as to reduce the cost of any particular treatment.
India has an abundance of men of intellect and aptitude for medical
research, but they should be given all facilities and encouragement. The
declaration of Alma Ata, proclaiming health for all by 2000 AD enjoins
upon research, to gear its efforts to fulfil this goal. The challenges have
to be met by appointing TASK. Forces, comprising groups of experts in
respective medical fields, who should formulate specific targets and time
bound projects in the given fields and identify the priority areas with regard
to their national relevance. IMA will also be happy to associate itself with
this task and 'help the various medical research institutions with a proper
feedback.
srffi: gferr
“May the whole world be healthy and contented”.
References
Concept of Health and Disease—Interdisciplinary Perspectives
—Edited by Arthur L. Caplan; H. Tristram Englhardt, Jr.; James
J. Me Cartney Addison—Wesley Publishing Company—1981.
Economics and Health Policy—Edited by A Griffiths and
Z. Bankowski
—W.H.O. Publication—1980.
INTERNATIONAL CONFERENCE
HEALTH POLICY : ETHICS & HUMAN VALUES NEW DELHI 1986
Identifying Indicators of Quality of
Family Life
As Assessed by Satisfying and Satisfactory
Conditions in Mentally Retarded Children
Dr. S.K. Varma
M.A. D.G.P. DM. & SP. PhD.
Associate Professor of Clinical Psychology Deptt.
of Psychiatry Postgraduate Institute of Medical
Education and Research Chandigarh 160012
“The Constitution of the World Health Organization defines health as
a state of complete physical, mental and social well-being and not merely
the absence of disease or infirmity.”
“The identification and monitoring of indicators of mental health in
all its facets, including subjective well-being and quality of family life, is a
matter of priority in the regional mental health programme of the SEARO,
WHO. [SEARO (1984): Indicators of Mental Health. Report on a
WHO/UN1CEF Inter-country Workshop. SE/Ment/79].
“Mental health refers to the full and harmonious functioning of the
whole personality, that gives satisfaction to self and benefit to the society.”
“One of the related concepts used increasingly in the scientific as well
as in the lay press in recent years has been the concept of Quality of life.
Being somewhat polymorphous, it tends to cover a variety of areas such as
physical and psychological complaints, feeling of well being, personal funtioning and general limitations.”
“It is important to add quantity to years, but it is more important
to add quality to years.”
“Mental health can give quality of life.”
“Quality of life need not be poor in a poor man’s home, nor in a
handicapped person’s home.”
“Qv ty, beauty and virtue lie in the eyes of the beholder.”
“We .mould try to plan with the people and not for them.”
Introduction
In order to add quality to years, it is necessary first to define, describe
and assess the quality of family life. Adding quality to life is perhaps as
important as adding years to life, if not more important Quality of family
life may be defined as the degree of excellence (a) with which the family is
integrated as a unit, acts and together faces life problems and (b) with
which it contributes to the satisfaction and happiness of the individual mem
bers, with benefit to all concerned i.e. those within and outside the family
unit. It refers to the extent to which it accepts the individual contributions
of family members and the extent to which it contributes to their physical,
mental , social and spiritual well being. No doubt, it is a difficult area to
define, as many of the factors may be ill defined inter-related and to some
extent interdependent also. The above operational definition may suffice
till the time a better one is offered and found to be universally applicable
and accepted.
Quality of family life, an expected, would be affected by a number of
significant positive and negative life events.. The actual birth of a mentally
retarted child in the family, its knowledge and related consequences real or
imagined, on the life of family members and atmosphere of the family as a
whole, etc. may be one group of factors that could possibly, adversely affect
the quality of family life. The way of family faces such a situation and
copes with related problems is likely to reflect the quality of family life.
| 'j
There is no dearth of studies on the possible adverse effects of the
knowledge of the presence of mentally retarded child in the family. They
do indicate varied reactions in the families and among its individual mem
bers. The reaction ranges from initial shock and denial to partial or more
or less total acceptance—the last being rather a rare phenomenon. Some
times it may also lead to rejection of the child—physically and/or psycho
logically. This determines as well as determined by the existing quality of
family life.
It is important, therefore, to find out as to what are the possible
indicators of quality of life in such families. This is particularly so, in
view of the increasing studies on the role of parental training to handle and
train such children at home. The indicators so identified, could help in
the evaluation, monitoring, and comparisons of relative effectiveness of
such programmes.
After defining the broader construct of Quality of Family Life, it may
be useful to devide the whole area into a number of measureable specific
constructs which can then be defined and items constructed to measure
them adequately and reliably. Emphasis should be more on practical,
measureable and tangible aspects and relatively less on abstract theoretical ”
constructs that may be difficult to be defined and assessed by the majority
of our population that usually have low literacy rates, low sophistication
levels and are from rural background.
Theoretical Considerations
There are many ways in which the factors can be grouped and the
area divided into relatively mutually independent and homogenous sets of
factors.
A.
BROAD GROUPING OF INDICATORS
The factors contributing to the quality of life in families with men
tally retarded children, may be broadly classified or considered under two
groups:
(a) Those from the points of view of the mental health professionals
—These may be called as satisfactory conditions and would
include such factors as: (i) group cohesiveness in the family,
(ii)
sharing of each others experiences, (iii) helping attitude
towards family members, (iv) understanding and sharing each
other’s problems, (v) absence of conflicts among members e.g.
husband-wife, parents-children, mother-father, among sibs, etc.
(vi) absence of mental illness in the family, (vii) absence of any
severe or chronic physical illness in the family, (viii) positive and
helpful attitude towards the mentally retarded child, etc. These
are indicators as observed/inferred by the professionals, with
certain expectations from such a family.
(b) Those from the points of view of the mentally retarded child:
These may be called as satisfying conditions and would include
such factors as: (i) a sense of belongingness to the family, (ii)
presence of positive attitude towards the family members, (iii)
subjective feelings of physical, psychological and social well
being, (iv) absence of unhappy experiences within the family, etc.
These are all highly subjective factors.
B.
SPECIFIC INDICATORS
(i) Group cohesiveness : In a family, members may have different
interests, roles, statutes, aspirations, value systems, preoccupa
tions, etc. All these are not undesirable aspects, rather they may
add colour, richness and quality to the family life. If inspite of
or in the presence of such diversity of interests and aptitudes,
they can enjoy some degree of group cohesiveness, a sense of
belongingness, togetherness, the quality of the family life would
be increased many times. To the extent it can act as a unit,
taking group decisions, respecting each other’s opinions, interests,
and sensitivities, and stick to those collective decisions or goals,
particularly in facing life problems and in crisis situations, the
family has this desirable quality. Both positive (desirable beha
viours) and negative (undesirable behaviours) aspects of it need
to be rated in order to assess it in a comprehensive manners.
(ii) Sharing of experiences'. Other things remaining the same, a
family that shares each others experiences may be said to have
higher or better quality of life. Sharing of experiences may be
both for positive or happy as well as for unhappy experiences.
The extent may vary in different members but the overall rating
is done rather than a separate one for each member, for it is
quality of family life and not of the individual members that is
judged. It is expected that by sharing such experiences, happi
ness increases and/or unhappiness decreases within the family.
(iii)
Helping attitudes among family members: Presence of cooperation
and helping attitude among family members also contributes
towards quality of family life. The extent to which it is present
without exception in a family, it is rated here. Helping attitudes
have to be mutual and does not include one sided dependence
upon one or more family members. This is inspite of any handi
cap or, disability in any one member and emphasis is on coming
forward to volunteer help rather than waiting for being asked
and taking a long time to decide. Anticipation of each other’s
need helps.
(iv)
Understanding and sharing each other's problems'. In a family
with high quality of life, it is expected that the members not only
understand, and appreciate each other’s problems and difficul
ties but also share them. As its direct or indirect result the felt
burden or, problems may be decreased. It is considered as a
desirable quality and may be present in all families to varying
levels. Even if one is not able to share it, the understanding and
awareness helps in the international processes within the family
and decreases the felt burden in the family.
(v)
Absence of conflicts/quarrels among family members'. The presence
of inter-familial and intrafamilial conflicts are likely to lower the
quality of family life, whatsoever be the reason and whosoever
may be at fault. It is because of this reason that the absence of
conflicts/quarrels among family members are considered as one
of the contributory factors to the quality of the family life. This
however, is different from the conflict of interests—individuals’
and families’.
(vi)
Absence of severe mental illness in the family. There are many
ways in which the presence of a mentally ill person may reflect
or, add to the problems or conflicts in the family. In reactive
mental illnesses, such conflicts may lead on to the precipitation
of a mental illness, and may add to them. Attitudes of other
members of the family may be adversely affected by the know
ledge of a mentally ill person in the family. It may be perceived
by some members as on added burden on and increased respon
sibilities for them. Thus it may not be the presence of mental
illness in the family as such but the reactions of individual
members of the family which may lead to a reduction in the
quality of family life. Absence of mental illness by it self may not 4“)
add to the quality of life. On the other hand, any predisposition to r
mental illness may be dormant because of healthy interpersonal
relations and emotional support system within the family itself.
In such a case, the absence of mental illness in the family could
be called as an indicator of quality of family life.
On the other hand, any predisposition to mental illness may be
dormant because of healthy interpersonal relations and emotional
support system within the family itself. In such a case, the
absence of mental illness in the family could be called as an
indicator of quality of family life.
(vii)
4
Absence of serious physical illness in the family. Absence of
physical illness, to the extent it is a result of the mental health
status and well being of members of the family, may reflect the
quality of family life. Physical illness may be a result of
malnutrition (which may itself be due to faulty or, unhealthy
food habits, knowledge, practice, customs, etc.), personality
disorders, drug and alcohol dependence, indisciplined life as such
and other related factors, which may lower the quality of family
life. It is not implied here that in a quality home or family,
nobody would ever fall sick.
(viii)
Positive and helpful attitude towards the mentally retarded child:
In a family with a mentally retarded child, it is very'important
to study the attitudes of the other members of the family towards
the mentally retarded child. The attitude towards mental
retardation itself may not be negative or harmful, so long as it
is an abstract concept and distant possibility but having aware
ness of this handicap in one’s family and apprehensions about
its real or imagined effects on the life of other members, may
adversely affect the quality of family life. It is important to
know in such cases how the family perceives this and how it
copes with this, in order to correctly assess the quality of family
life in such a family.
(ix)
A sense of belongingness to the family: The quality of family life
may also be judged how the mentally retarded child perceived
and feels about being in that family. Does he feel accepted,
understood, or, pitied ignored or rejected and denied most
privileges given to other family members ? His own sense of
belongingness to the family may be a good indicator of the
quality of family life. It is as important to know how he relates
to and feels about it as it is how he is treated by others in the
family, if not more important.
(x)
Presence of positive attitudes towards the family members:
Belongingness may not always be a direct result of good treat
ment in the family. It may, on the other hand, be present even
if the person may be maltreated as it reflects his feelings and
attitudes and not the family members. The belongingness may be
absent, yet the mentally retarded child may have positive attitudes
towards some of the family members if not towards all. This in
itself may indicate high quality of family life. He may not feel
one, or see eye to eye with other members of the family, may
have poor sense of belongingness after knowing their negative
attitudes towards himself, but all the same, unreasonable as it
may sound to others, may have nothing but good fellow feelings.
Intelligence, fortunately, is no bar to good fellow feelings and
positive attitudes. He may unwillingly blame himself for not
being able to come to other’s expectations.
Ixi) Subjective feelings ofphysical, psychological and social well-being:
v ' Quality of family life is indicated by the extent to which each
individual member, in spite of his own health status, feels wanted
accepted, and has satisfying feelings of own physical, psychologi
cal and social existence in the family. This may be purely a
subjective feelings, but its presence is important. It is implied here
that this feeling may be at times independent of the actual,
5
objective health, mental or social status. One may still be zea
lous, discontended and ill at ease with himself and with others,
inspite of a high status with all the powers of decision making
in the family. Being at peace with oneself and with others is a
positive attribute.
(xii) Absence of unhappy experiences in the family: Unhappy inter
personal interactions within the family, may be quite bitter and
longlasting, at times at least. Some of these may be particularly
severe and always pricking the mind of mentally retarded child.
He may become fearful, apprehensive and withdrawn. Such
unhappy experiences are unlikely to contribute to the quality of
family life. It is not necessary that these experiences may always
remain unresolved or, that their absence would necessarily lead
to high quality of family life. But on the whole, and other
things remaining the same, it is desirable if there are no such
unhappy experiences that may come in the way of enjoying the
life experiences in future. To that extent their absence may be
considered as contributing to the quality of family life.
The Problems in Measurement
These are only some of the indicators of quality of family life in
families with a mentally retarted child. There may be many others that
need to be identified and some of these described above may not be
mutually independent. They may be contributing to the totality of the
concept of quality of family life in different proportions. In fact, it may
come out that the quality of family life is not a unitary concept but there
are a group of independent factors that need to be considered. These and
other issues can be explored, studied and measured reliably only through
systematic experimentation. No amount of armchair speculation alone
would be able to provide a satisfactory answer to these.
A Rating scale or questionnaire can be prepared to measure this
quality of family life. The items have to be simple, brief, and easily under
stood by majority of our population which is rural, low in literacy/illiterate
and unsophisticated in the use of such instruments.
Such a measuring tool is likely to be influenced by certain response
biases. For example, there might be a tendency to agree (Yea Saying) or,
tendency to give a socially desirable response in place of a true one, or to
choose a particular response category (e.g.) the first response alternative,
the middle most replies or the avoidance of extreme categories, etc.).
There is a need to look into these possible sources of biases in the question
naire, before putting them up for reliability, validity or normative studies.
The questions may be put in simple, brief language, that avoids
difficult words and are not to complicated too long. The “underlining
test” can be tried in order to find out the “difficult words”. Some of the
items may be put in negative form, but with care that it may not become
complicated and confusing for the subjects. If three response categories
are to be effectively utilized, it may be more useful if five response cate
gories are actually used. The tool may be administered under “standard
instructions” and “foke good” response instructions, in order to find out
possible effect of social desirability response set. For this, correlation of the
items and of the tool with the lie on Social Desirability Scale may also
be calculated. These are some of the steps that are necessary particularly
for such a scale which is likely to be effected by such response biases.
Test-retest and inter-rater reliabilities need to be established. The
interval for retest need not be very long and may be as short as day, as
there are no right or, wrong responses or any likely lerrning or memory
effect. Split half reliabilities may also be established.
Factor analysis can also be done or elementary linkage analysis to
see the clustering. In addition, the responses may be validated against
external criterion like, subjective well being of individual members in ex
treme families that could be easily identified. Families in which the
mentally retarted children have emotional problems may be compared with
those where mentally retarted children are relatively free from it. For
validational purposes, degree of mental retardation, socio-economic status
of the families, etc. need also be considered. The quality of Family Life
Scale or Questionnaire thus constructed should also show low/insignificant
co-relations with such personality factors like neuroticism, psychoticism,
paranoid, depressive, anxiety and other such pathological states.
BIBLIOGRAPHY
1.
Blan, T.H, (1977) Quality of life, social indicators and criteria of
change, Professional Psychology, 8, 464-473.
2.
Campbell, A. (1976) Subjective measures of well being, Amer.
Psychol. 31, 117-124.
3.
Dupuy, H.J. (1970) Development of rationale, substantive,
derivative and conceptual relevance of the General Well Being Schedule^
Unpublished Working Paper.
4.
Fazio, A.F. (1977) A concurrent validational study of NCHS
General Well Being Schedule, Series 2 Number 73 US Dept, of Health,
Education and Welfare.
5.
Flanagan, J.C. (1982) Measurent of quality of life: Current State
of the Art. Archives of Physical Medicine and Rehabilitation, 63, 56-59.
6.
Nagpal, R. and Sell, H. (1985) Subjective well being, SEARO
Regional Health Papers No. 7. WHO, SEARO, New Delhi.
7.
National Mental Health Programme for India (1982) DGHS,
New Delhi.
8.
SEARO (1984) Indicators of Mental Health. Report on a WHO/
UNICEF Inter-Country Workshop. SE/Ment/79.
9.
Sharma, S.D. (1985) Poverty, health and quality of life. Presi
dential Address, 37th Annual Conference of Indian Psychiatric Society,
Visakhapatnam.
10.
Verma, S.K. Dubey, B.L. and Gupta, D. (1983) PGI General
Well being Scale -some correlates. Indian Journal of Clinical Psychology,
10, 299-304.
11.
WHO (1981) Development of Indicators of Monitoring progress
health for all. Health for All Series No. 4.
<
7
INTERNATIONAL CONFERENCE
HEALTH POLICY : ETHICS & HUMAN VALUES NEW DELHI 1986
Health Problems of the Aged Persons
and Their Place in
Drawing up Health Policy in Our Country
Dr. R.M. Kasliwal
M.D., F.R.C.P. (Lond.)
F.N.A., F.A.M.S., F.C.C.P., F.I.M.S.A.
Emeritus Professor in Medicine
S.M.S. Medical College, Jaipur
President, AGE CARE, India
All over the World the people are living longer and this is specially
seen in the developed countries where the group of elderly from 60 years
of age onwards is increasing. This may range from I/7th to l/6th of the
population which means that every 6th or 7th person belongs to this
category of elderly. It is normal for them to live up to the age of 70 or
75 and lead a useful life. With the introduction and development of
geriatric medicine for treatment and management of aged and specially its
preventive aspect, this age group is rapidly advancing and it is not unusual
to see persons of 80 years or above in a healthy state.
Of course the problems of these aged persons cover a wide range
from medical and health to social, familial, financial and maladjustment
problems and these are to be tackled with sympathy and patience. Large
sum of money is required to be spent on the care of the aged and it is said
that for the care and management of an average elderly patient about 21
to 3 times the amount of money is required as compared to an average
younger patient and the average stay of the elderly in hospital is also pro
portionately much more. In the developed countries all these problems of
the elderly are well recognised and they are being treated and managed by
qualified physicians in Geriatric Medicine and in institutions which have
geriatric medicine wards. In U. K. alone there are at present about 270
departments of Geriatric Medicine and each providing a district service
which includes not only treatment of acute illness but rehabilitation of
persons with disabilities. Of course each institutional service may vary in
various units depending on resources and other allied factors. Besides
training and education of medical officers and medical students in medical
and health problems of the aged, even the members of the health team
such as nurses, social workers and paramedical staff are also trained in
health problems of the aged. Even the general public is made aware of
the problem of the aged so as to receive their cooperation.
The aim is to provide service and tackle problems of the elderly to
enable them to live as long as is possible in an optimum state of health in
their homes, preferably with their families if possible.
In India so far no concerted efforts have been made to tackle the
medical and health problems of the aged by a specialised group of doctors
trained in Geriatric Medicine and hence it has not been possible to give
proper attention and care to the varied problems of aged. Even the
general public has very little awarness of it.
Only during the last few years a few voluntary agencies are taking
interest in the problems of the aged and one or two medical societies have
also started working for solving the health problems of the aged. A Sym
posium on “Hormones and Aging” was recently conducted under the
auspices of Geriatric Society of India at the All India Institute of Medical
Sciences and even this prestigious Medical Institute of our country has no
separate department of Geriatric Medicine and no separate out patient
department for treatment of the old as far as my information goes. Such a
state of affairs exist all over India and the health problems of the aged'have
received no particular attention.
The problems of the aged are manifold and cover a wide range from
medical and health to social, familial and financial and other allied factors
affecting the aged but in this lecture of mine I shall largely dwelve upon
health and social problems.
The health problems may be multifactorial and multidimensional.
It is not unusual for an elderly to suffer from more than one disease. In
fact in many cases they may be suffering from 2 or 3 diseases or more and
more than one system may be involved. Not only that, but even the symp
tomatology and presentation of the disease may be slightly different, for
instance in some acute illness, there may be absence of fever and in some
cases of myocardial infarction there may be absence of chest pain. Multi
ple pathology is the rule rather than the exception with an elderly and
quiet, a typical presentation of illness is commonly seen in and elderly.
Even the prognosis in some of these cases in difficult to assess. Hence it
is very important that there must be proper training of a medical student
at an undergraduate level and a doctor at a postgraduate level under a
competent specialist of geriatric medicine.
There are very few diseases which are solely confined to aged people.
Polymyalgia rheumatica2 is one such disease. Diseases like Parkinsonism
occurs more often in elderly but may effect comparatively at early age also
and here the aetiology may be different.
Every system may thus be affected but the presentation of the disease
may be slightly modified or altered due to poor reserve capacity, increasing
immobility or unsteadiness, Mental incompetence and impaired haemosta
sis. Incontinence of urine and/or faeces is another factor which needs
investigation. Psychological factors and specially mental depression lead
ing on to senile dementia may play an important part in the health pro
blem of the elderly. Relationship of various hormones in health, disease
and aging is now increasingly established and should therefore be thorou
ghly investigated and tackled.
Hence the complete evaluation of the elderly patient by a competent
doctor trained in geriatric medicine is essential and his various systems
2
should be thoroughly examined with sympathy and patience and the doctor
may also interrogate the close relations of the patient’s family. While
investigating the patient, and assessment of the economic and social
circumstances is an important part of evaluation.3
In India, the joint family system which existed from olden times, is
now slowly crumbling down and there is need to emphasise it if possible
or find an effective alternative system of rehabilitation of the elderly.
By the turn of this century, this increasing population of the elderly
may account for 1/1 Oth to l/7th of the total population which means we
may have about 10 to 12 crores of people above the age of 55 years on
wards in our country by the year 2000.
If therefore the Alma Ata declaration of W.H.O. “Health for all
by year 2000” is to be achieved, this large section of our population has
to be looked after. It is time that necessary step are to be taken now in
starting to tackle the multifarious health problems of the aged. Some of
these steps may be mentioned as under.
(1)
Geriatric Medicine must be recognised as a separate discipline
and a subspecially of medicine which eventually may be put in the same
category as Paediatric Medicine as an independent Medicine discipline at it
gradually develops.
(2)
Teaching of Geriatric Medicine both at the undergraduate and
postgraduate levels be started in every major medical teaching institution.
(3)
Special geriatric medicine wards are to be opened in every major
hospital in the century and in every medical teaching.
(4)
Besides imparting training to undergraduate in the subject of
geriatric medicine, 9 months to one year’s diploma course may also be
started for doctors in geriatric medicine and M.D. in geriatric medicine
may also be started in some postgraduate medical teaching institution
under qualified specialists in geriatric medicine.
(5)
To start with effective steps to be taken initially for the training
of doctors in this subject; along with members of health .team like nurses,
paramedical staff and even social workers.
(6)
Some senior physicians to be deputed to Western countries like
U.K., U.S.A., Soviet Union etc. to familiarise and get acquainted with the
progress made in the teaching of the subject and the kind of health care
and management given to old patients.
(7)
A centre of Gerontology for research work in the problem of
aging be set up in our country also specially in two or three postgraduate
medical institutions of which perhaps one may be set up in Delhi immedia
tely in the A.I.I.M.S. with cooperation of I.C.M.R.
(8)
One or two separate hospitals for geriatric patients if not possible
3
at present may be conceived in the long run and specially one may be
established in Delhi.
(9)
Since voluntary agencies will be playing an increasing role in the
tackling of non-medical problems, social and other factors affecting the
aged and their role is very important in giving comfort and security to the
aged, their cooperation is most essential and they should be given proper
recognition together with education and guidance in starting short training
courses regarding the problems of the aged.
The general public should also be made aware of the problems of the
aged in order to secure their understanding and cooperation.
Hence, in the end one may sum up that in drawing up the health
policy of our country, this increasingly large section of our population and
their problems—specially their health problems must be tackled properly,
effectively and in a scientific manner.
Then alone we shall be able to cover all the sections of our popula
tion regarding their health problems and this will be one more positive
step towards achieving the W.H.O. goal of Health for All by the year
2000.
Last of all one may summarise that in this limited time it has not
been possible to give detailed information of various health problems except
that an attempt has been made to highlight the significance of this subject
as, so far, no attempt has been made in our country to tackle these pro
blems methodically, systematically and scientifically. It is therefore time
to emphasize that problem and tackle it in a systematic matter as is
done in the developed countries of the West.
References
(1) Keith Andrews, J.C. Brocklehurst: A profile of Creative Reha
bilitation Units; Journal of the Royal College of Physicians, London, Vol.
19, No. 4, Oct., 1985.
(2) William Ferguson Anderson : Advances in Education, “Geriatric
Medicine, by W.F. Anderson & T.G. .luge, 1974.
(3) William R. Hizzard : Leading the Health Care Team for the
Elderly; Harrison’s Principles of Internal Medicine”, 10th Ed.
)
INTERNATIONAL CONFERENCE
HEALTH POLICY : ETHICS & HUMAN VALUES NEW DELHI 1986
Care of Infants and Women
(Including Hereditary Diseases)
Dr. K. Indirabai
Introduction
Inspite of advances made in medical technology and the enormous
amount of money spent on health care, 80-85 % of the under-priviledged
and vulnerable section of our population which includes infants and women
still do not have access to basic health services.
Many families which are often large, exists in a state of partial
starvation; and the mothers usually consume about 1600 calories/ day and
produce low birth weight babies who contribute to the high perinatal and
infant mortality rates.
In addition, the high incidence of intrauterine, neonatal, and post
natal malnutrition leads not only to high infant mortality rates but also to
poor physical growth, premature senility, and low life expectancy among
those who survive beyond infancy. It had adverse effects on mental
development that result in reduced mental and physical potential and
impose a serious handicap on economic development in all fields, particu
larly in agriculture and industry. This cycle of events also cripple the
social and cultural advancement of the communities.
, Poor nutrition, lack of sanitation, poor hygiene, and inadequate
immunizations result in high incidence of communicable diseases like
gastro-enteritis, respiratory-infections, tuberculosis, measles, whooping
cough, diphtheria, polio myelitis and other bacterial, viral, and parasitic
infections and thus ill health continues to be the way of life in such
families.
Seventy to 80% of the inhabitants in the under-privileged communi
ties are illiterate because of the poor educational facilities.
Due to population growth the services rendered are getting diluted
and IMR continues to be very high i.e., 114/1000 L.B.
Care of Infants
Every child born has a right to live and lead a healthy life.
If we go by the statement of James P. Grant (1), the Executive
Director of UNICEF, on the state of world’s children, it looks that we may
not be able to achieve Health for All and reduce our infant mortality
rate (IMR) to less than 60/1000 by 2000 A.D. as per Alma-Ata Declara
tion.
The challenge of reducing the high IMR in our country is not the
only problem but" it is also a question of survival that these infants face
entering the world.
The medical profession including pediatricians has major role to
play, apart from other agencies.
The highly ambitious 7th Five Year Plan has been launched under
the stewardship of our dynamic; action oriented Honorable Prime Minister
Shri Rajiv Gandhi. This plan distinguished itself from the earlier ones in
several respects. An accountability has been introduced by setting targets
on reduction of maternal and childhood mortality, low birth-weight
prevalence and achieving 85-100% coverage for immunisation. Separate
allocations have been made for the first time for the care of new born and
for creation of the first national Institute of Maternal and Child Health.
The government of India has rightly considered the influence of
mortality on birth rates and it has planned to decrease the Infant
Mortality Rate from the current 114 to 87/1000, and PNMR from 60-80 to
40 by the end of the Plan.
Here comes our most important role i.e. if we assure the survival of
the existing children by taking proper care, the parents will certainly limit
their families.
The problem of reducing IMR is complex and an effective and sus
tained decline can only be achieved by a multi-pronged approach aimed at
resolving social, ecological, educational, public health and environmental
problems. As has been shown by the experience of Kerala, female literacy,
spacing of births and easy access to health facilities, whether Government
or non-Government, are the main determinants of Infant Mortality Rate.
The extremely high and unchanging maternal, perinatal and neo
natal mortality rates are not surprising. The antenatal clinics and delivery
rooms remain overcrowded, understaffed and inadequately or poorly
equipped.
A newborn is considered a mere appendage of the mother and inspite
of the recommendations of the Central Health Council, it has not been
given the status of a hospital bed. The training and education in perinato
logy and neonatology of the primary health care workers, nursing and med
ical undergraduate and postgraduate students is not only inadequate but ig
nores essentials such as ‘at risk approach’ resuscitation of the new born
and so forth. The poorly provided or equipped facilities for primary, secon
dary and tertiary contributes to poor knowledge and acquisition of skills by
health professionals.
The government of India has indeed recognised these problems and
constituted a task force to define the minimum needs for quality oriented
perinatal and neonatal care in terms of physical space, man-power,
equipment, education and training at various levels of health care, and we
fondly hope that they will be implemented soon without further delay.
2
It is true that it may not be possible to create new programmes due
to financial constraints, but the existing National Integrated Child Deve
lopment Services and post partum programmes can be effectively modified
or expanded to include perinatal and neonatal care. The post partum
programme is hospital and urban based and the ICDS a community based
programme. Both the programmes deal with parturient mother and ICDS
has a strong component of child care beyond 6 months. Strengthening of
these programmes with manpower, material, supplies and structural faci
lities for improving and providing neonatal care will certainly make this a
very efficient and effective family welfare programme and it is necessary
to integrate the services of the Obstetricians so that together we can
improve not only the survival but also the quality of life of mother and
her off-spring.
The urgency of controlling preventable infectious diseases, and
malnutrition has already been realized by the Government and an extension
of the ICDS programme to 3000 blocks was dedicated with its emphasis on
growth monitoring, inclusion of measels immunization in Expanded
Programme of Immunization (EPI) and with the adoption of strategies such
as universalization of immunization. Oral rehydration for controlling
deaths due to diarrhoea and looking into the possibility of the treatment
of acute respiratory infections by primary health care workers,, all are steps
in the right direction.
The plan of universalisation of immunization is a good strategy for
covering the gap that exists today between the actual immunisation
coverage and the goals to be achieved by the end of the decade.
Immunization has to be provided continuously and can succeed only
if the community becomes aware of it and seeks immunisation. While
one can with efforts achieve 100% coverage for a population by mass
programmes, the entire strategy may fail if continuity and surveillance of
diseases is not maintained.
Care of Women
“The cumulative result of poverty, under-nutrition and neglect
which girls suffer right from birth is reflected in their poor adult today
size, which in turn influences high maternal mortality, low birth weight
and’ poor nutritional status of their infants. The relative neglect of the
female child is evident from the greater prevalence of growth retardation
even in the infancy among girls than in boys. . .”.
The greatest of those difficulties is the fact that the majority of the
developing world’s women have to large a share of responsibility for family
well-being and too small a share in the decisions which affect it.
For whether we are talking about breast-feeding or weaning, oral
rehydration therapy or immunization, regular growth checking or frequent
handwashing, it is obvious that the mother stands right at the centre of
this programme.
Hence it is our responsibility to protect and improve the lives of
women.
Many millions of the world’s women are permanently in
health.
poor
The cause is not usually a specific illness. It is rather the general
‘maternal depletion’ caused by too much work and too little food com
bined with too many pregnancies to close together.
Family spacing : Leaving at least two years between one pregnancy
and the next can reduce the risk of an infant’s death by 50% or more.
But it is also the most important way, of maintaining the health of those
whose bodies are depleted by the heavy nutritional stresses of almost
continuous pregnancy’ child-bearing, and breast-feeding. In most deve
loping countries, ‘maternal causes’ are the leading cause of death for
women between the ages of 25 and 35. In other words, more than a
thousand young mothers are now dying everyday—and many of those
‘maternal deaths’ are the result of too many births too close together.
Female education : The education of the mother has been found to
be perhaps the most important social determinant and also is a powerful
force for improving the lives of mothers themselves.
Food supplements : A relatively small amount of extra food each
day, for at-risk pregnant woman, has been shown to reduce the incidence
of low birth-weight which is “universally and in all population groups, the
single most important determinant of the chances of the new born to
survive and to experience healthy growth and development.” Similarly,
extra food for breast-feeding women can mean more successful and longer
lactation.
Hereditary Diseases
Hereditary diseases have grown into hundreds and are being dis
covered at an ever-increasing rate and majority of them are due to inborn
errors of metabolism i.e. Albinism, Phenyl Ketonuria. Wilson’s disease,
etc.
At this juncture, genetic counselling comes into the picture. Genetic
counselling is a process of communication dealing with the human
problems associated with the awareness or risk of awareness of a genetic
disorder in a family. The first step in genetic counselling is to make
certain that the diagnosis is correct. Those who receive it can be divided
into a majority who are unaware of their risks and a minority who request
genetic information and counselling. The latter most commonly are couples
whose first child has just been born with a birth defect or medical problem.
Others seek information prior to marriage or before having children
because of medical problems of their relatives.
The challenge for the physician is to recognise which birth defects
and medical problems are hereditary and to offer genetic information to all
families, not just to those who request it.
Parents may assume, that a problem can’t be hereditary if no other
relatives are affected. This issue has to be discussed in great detail and it
is necessary to impress upon the couple that a child with hereditary dis
order can be born to healthy parents with no affected relatives.
INTERNATIONAL CONFERENCE
HEALTH POLICY : ETHICS & HUMAN VALUES NEW DELHI 1985
Leprosy Eradication Programme in India
—an Over-view
Dr. C.K. Rao
Deputy Director General of Health Services (LEP)
Nirman Bhavan. New Delhi,
Leprosy is foremost public health problem in India with far-reaching
social implications. It is estimated that of the 12 million cases in the
world, India accounts for nearly 4 million. 20% of the cases occur in
children; and nearly 15 to 20% suffer from disabilities. About 20% of the
cases are infectious.
Case load
The first survey for leprosy in the country was made as part of British
Imperial Census in the year 1971-72. The extent of the disease was subse
quently reviewed by the British Leprosy Commission in 1890-91. The
prevalence rate of leprosy during the period prior to 1950 was essentially
obtained as part of the decennial population census. However, there are
reasons to believe that the disease was grossly under estimated. Only advan
ced forms of cases were included in the census and not all cases were
reported because of social stigma attached to the disease. Further patients
with minor symptoms were not recognised. The estimated number of
leprosy patients in 1951 was 1.3 million while in 1981 the figure was 3.9
millions. There has been a consistant increase in the estimated cases over
the years accounted Tor by an increase in the population as also extension
of surveys to newer areas.
Considerable inter-state variations occur in the prevalence rate of
leprosy in the various States and UTs. The greatest case load of leprosy
falls on the Eastern belt of the country comprising Andhta Pradesh, Tamil
Nadu, Orissa and West Bengal; these States sharing almost 53% of the
estimated case load.
National Leprosy Eradication Programme
The National Leprosy Eradication Programme made its beginning in
1955 as a Centrally Aided Scheme with its focus primarily on rural areas
of high and moderate endemicity. In the low endemic States the expecta
tion was that leposy services can be provided through existing health care
facilities. In the beginning the programme did not have clearly defined
operational objectives. Only the problem was identified and inputs pro
vided for its strengthening. Thus for nearly two decades it remained an
input-oriented programme. This was due to several factors:
absence of any primary preventive measures (vaccine) and noncultivability of leprosy bacilli;
(ti) non-availability of potent drqgs for quick and complete cure;
(i)
(iii) isolation of all the cases was not feasible as benefits were not
commensurate with costs involved; and
(iv) the population was not fully cooperative due to social stigma
attached to the disease.
It was only in 1976 that the programme was made performance
oriented, giving each State targets by the Government of India for detec
tion of new cases, for cases to be brought under treatment and also the
number of patients to be discharged after disease was arrested.
Strategy
The main strategy of the programme is to control the disease through
reduction in the quantum of infection in the population, reduction of
infective sources and thus breaking the chain of disease transmission.
Four basic activities were envisaged viz;
(i) Survey and case detection;
(ii)
Registration of cases for treatment;
(iii)
Provision of continous treatment with sulphones to all cases;
and
(iv)
Education of the patients, their families and the community at
large about leprosy.
Recently with the discovery of a number of highly effective bacterici
dal drugs, substantial reduction in disease incidence in the near future,
appear feasible. The Government of India in 1982 decided to introduce
Multi Drug Treatment to cover all the cases in a phased manner, starting
with districts where endemicity of the disease was more than 10 per 1000
population. It is expected that with the necessary provision of infrastruc
ture required for MDT, it would be possible to cover all the endemic
districts within the next 10 years.
Infrastructure
The programme extends to rural as well as urban areas. Anti leprosy
activites fan out from leprosy control units and Survey Education and
Treatment Centres in the rural areas and from urban leprosy centres to
the urban population. The total coverage extends to nearly 43 crores
people. Important administrative measures have been undertaken follow
ing recommendations of the Swaminathan Committee to make leprosy
eradication a time-bound programme by the turn of the century. A
National Leprosy Eradication Commission functions under the Chairman
ship of the Union Minister for Health & F.W. with several Chief Ministers
from States and UTs as its members for laying down policies and provide
guidance. The National Leprosy Eradication Board under the Chairman
ship of Union Health Secretary reviews periodically the implementation of
the activities related to the programme.
Training of personnel
National Leprosy Eradication Programme is a vertical programme
2
and therefore, has its own requirements of trained personnel at various
levels. Forty three Leprosy Training Centres function in the country for
training of Para Medical Workers, Non-Medical Supervisors, Physiothera
pists, Laboratory Technicians, Medical Officers, etc. working for the
programme.
Expenditure
Leprosy is recognised as a high priority area for assistance by the
Government of India and forms a part of 20-point programme. The con
cern of the Govt, of India and its political commitment for leprosy eradi
cation are borne out by the fact that there has been nearly a two-fold rise
in the financial outlay for the programme—from Rs. 202.30 million in
1974-79 to Rs. 412.00 million in 1980-85 and Rs. 650.00 million in 1985-90.
Health Education
There is no doubt that a change in the image of leprosy in the minds
of people would in itself be a great factor in promoting anti leprosy activi
ties. For this reason lack of awareness on scientific facts about its causa
tion, complete curability of leposy and to dispel prevalent prejudices and
misconceptions about the disease form the main thrust of health education
campaign as an integral part of the programme.
Rehabilitation
Facilities for vocational and social rehabilitation of deformed cured
leprosy patients have been created and are operated by several philan
thropic organisations/individuals. Medical rehabilitation of the .deformed
patients is supported under the programme through 75 Reconstructive
Surgery Units and Leprosy Rehabilitation Promotion Units. Plans are
underway for stimulating vocational rehabilitation of patients in their
homes/communities.
Voluntary Organisations
The voluntary organisation had been playing a poineering role in
leprosy work in India eversince the first known leprosy asylum was establi
shed in Calcutta in the early 19th century. Over 100 organisations are
involved in various activities pertaining to control of leprosy in India,
including training of personnel, education and research in addition to case
detection, treatment and rehabilitation. The Government of India have a
scheme for financial assistance to these organisations.
Case detection and treatment
The recorded evidence indicate that the performance of the National
Leprosy Control Programme during the last three decades of its existence
has been commendable. There were estimated 3.95 million cases of leprosy
in India in 1981 out of which 2.58 million were reported to have been
detected by December, 1980. Recently there has been a remarkable in
crease in case detection during the 6th plan period accounting for 41.5%
of total case detection so far.
As on 31.3.85 i.e. at the end of 6th plan period, 3.27 million leprosy
cases were on records and 3.05 million of them under dapsone treatment.
Over 95% of the cases are receiving the drugs in their houses. The number
3
of leprosy cases discharged due to cure or death from the inception of the
programme stood at 1.93 million. At the end of December, 1985,3.33
million cases were on record with 3.09 million receiving treatment. During
the 9 month period between April and December, 1985, 0.31 million more
cases have been discharged making the total number of cases discharged
since inception as 2.21 millions.
Multi drug Treatment (MDT) has been introduced in a phased
manner since 1982 is selected districts of high endemicity. Currently, 15
of these districts with a population of 37.0 million and having 0.328 mil
lion cases are under MDT for periods varying from 3 months to 3 years.
The multi drug therapy covered only the multi bacillary cases until June,
1984. Thereafter both multi bacillary and pauci bacillary cases have been
brought under MDT. Available information on 6 of the districts where
MDT activities have been in progress for more than 2 years are summari
sed hereunder. Twenty two per cent of the 83,300 new cases detected are
multi bacillary. Childhood leprosy accounts for 8% in the multi bacillary
group and 20% in pauci bacillary cases. The deformity rates in the new
multi bacillary cases and pauci bacillary cases were 20.8% and 6.5% res
pectively. More than 90% of all cases put under MDT are taking treat
ment regularly. Drug reactions were observed in 4% of multi bacillary
cases and only 0.5% of pauci bacillary type. The reactions were mostly
mild. Over 80 per cent of the multi bacillary cases who received the
prescribed course have been declared cured.
Monitoring and evaluation
The progress of activities under the programme is monitored through
periodic reports from districts to States and States send them to the Cent
ral headquarters of the programme in the Directorate General of Health
Services. The National Leprosy Eradication Commission meets periodi
cally to formulate policies after review. National Leprosy Eradication
Board meets twice a year to evaluate the implementation of the pro
gramme. Similar Committees constituted at the State level are also func
tioning to monitor the programme activities in the States.
An independent evaluation of the programme has been under taken
for the first time jointly'by the Government of India and WHO between
17th and 28th February, 1986. The report is under preparation.
INTERNATIONAL CONFERENCE
HEALTH POLICY : ETHICS & HUMAN VALUES NEW DELHI 1986
An Analysis of Twenty Three Thousand
Laparoscopies
Dr. (Mrs.) Elizabeth lypc
Director & Professor of Obsterics & Gynaecology,
Medical College, Kottayam, Kerala
Endoscopy was started at Medical College hospital Kottayam from
1981. Both diagnostic as well as operative laparoscopy are being done.
All diagnostic laparoscopies are done in the hospital where as majority of
the laparoscopic sterilization are done in camps arranged at the Primary
Health Centres, Taluk Head Quarters and District hospitals.
Laparoscopic sterilization in camps
—19,822
Laparoscopic sterilization at Medical College,
Hospital
—2,850
Diagnostic laparoscopy at Medical College Hospital
— 450
23,112
Technique of Laparoscopy
All the cases in this series was done by the single puncture technique.
under local anaesthesia with premedication. Pneumoperitoneum was
created in all cases using air, since cautery is not used in any one. Mini
mum air is introduced before the introduction of trocar and supplemented
if necessary through the laparoscope Sterilization is done in all cases by
Falope ring application.
Diagnostic laparoscopy was done for
1.
Investigation of Infertility
2.
Primary amenorrhoea
3.
Suspected ectopic
4.
Suspected adnexal masses.
5.
Evaluation of the tube for recanalisation following sterilization.
In cases of infertility laparoscopy was done along with Hysterosal
pingography Chromotubetion was done in all cases.
Analysis of infertility
Total number of cases
Tubal block
Peritubal adhesion
Endometriosis
Fibroid Uterus
Polycystic ovaries
Congenital abnormalities
—325
— 24
— 32
— 46
— 42
r- 4
— 12
In majority of cases laparoscopy and H.S.S. were tallying. In five
cases where laparoscopy showed blocked tubes, tubes were found to be
patent on HSS. which was proved at laparotomy later. Peritubal adhesions
are visible very clearly especially adhesion with minimal endometriosis.
The incidence of endometriosis is in the increase. Among Primary amenorrhoea case—23
Congenital abnormalities of various types were seen.
Absence of Uterus—in six}
Various stages of the development of Mullerian ducts could be seen.
Laparoscopy was done in 5 cases of suspected ectopic and confirmed
in three.
Small ovarian tumours which could not be diagnosed otherwise were
diagnosed in 5 cases.
Complications : encountered during laparoscopy were either due to
premedication and anaesthesia or due to laparoscopy itself.
Respiratory arrest occurred in four—all of them were revived.
Skin rushes occurred due to Pethidine in 15 cases.
There was no reaction to localanaesthesia since sensitivity to xylocaine was tested before the procedure.
Creation of pneumo peritoneum was difficult due to obesity in two
cases. Parietal emphysema occurred in 123 cases and in two of the cases
of laparoscopic Sterilization it was difficult to visualise the tubes due to
the large parietal emphysema. Omental emphysema occurred in 7 cases.
During application of Falope rings tearing of tubes occurred in 202
case. In 16 others separate rings had to be applied at the cut end which
was outside the ring. Haematoma of the broad ligament by the tongs of
the ring applicater occurred in 2 cases in the initial series. Perforation of.
the uterus by the uterine sound is the most common complication during
the procedure since the uterus in our series is manipulated by the sound to
view the tubes, ovaries and fouch of Doughas. Perforation occurred in 512
cases but in all cases the bleeding from the site of perforation stopped
immediately after withdrawal of the sound and did not require laparotomy
in any one. Omental herniation with withdrawal of trocar was prevent in
26 and omentum was immediately pushed back and wound sutured only in
one case introperitoneal haemerrhage took place from the site of introduc
tion of the scope that is at the umbilicus and she was operated upon next
day and bleeding controlled. There were no cases of death is the series.
Failure of laproscopic, sterilization in our series is less than 1 in 1000.
That is 19 cases out of 22,672 sterilization. In 10, cases re-laparoscopic
sterilization was done with M.T.P. Minilap. with M.T.P. in 5 and four
cases went to term and delivered. On relaparoscopy and minilap., the
failure in most of the cases was found to be due to slipping of the falope
ring so that the whole lumen was not occluded. In two the rings were
absent on one of the tubes.
Patients have come back also requesting for recanalisation operation
on death of one of their children since majority are done after two delive
ries. Recanalisation was done in three and two of them have give to
term and delivered one had normal labour and the other a caesarean sec
tion.
With the popularisation of laparoscopic sterilization the number of
multiparas—four and above have almost become a rarity and our maternal
mortality from complications of multiparity has reduced tremendously.
Diagnostic laparoscopy has given an opportunity to make a clear pre-operative evaluation of infertility cases with the facility of planning the opera
tion. It has also made it easy for diagnosis of endometriosis and P.T.D.
without laparotomy and also for evaluation of past operative cases.
3
INTERNATIONAL CONFERENCE
HEALTH POLICY : ETHICS & HUMAN VALUES NEW DELHI 1986
Tuberculosis-Yesterday, To-Day &
To-Morrow
Is Control Possible by 2000 AD
Under Existing Health Policy?
Dr. B.B. Surpal, MD, DTCD, MBA
Incharge Clinical Section,
New Delhi Tuberculosis Centre,
Jawahar Lal Nehru Marg, New Delhi-110002.
Tuberculosis is a specific communicable disease caused by a tiny
germ, tubercle bacillus. Among its victims were Kamla Nehru, Subhash
Chander Bose and Govind Vallabh Pant. Inspite of the fact that highly
effective vaccine and drugs have deen available for more than 30 years,
making TB a preventable and curable disease, the total number of cases
of tuberculosis has increased in India (Table I). It is believed that in our
country, 50°/o of the world tuberculosis population resides1’2. At present,
TB still remains the scandal of a disease3 which continues to be a major
community health hazard in our country, next most dangerous after
malaria4.
National Tuberculosis Control Programme (NTCP)
NTCP was launched in 1962 as an organised effort to bring under
control the problem of tuberculosis in the entire country, with the following
operational objectives :—
(i)
To vaccinate with BCG a majority of the eligibles (if possible
more than 70% in the community, in an efficient manner).
(ii)
To .detect maximumnumber of TB patients amongst out-patients
attending health institutions with symptoms and to treat effici
ently; in doing so, give priority to sputum positive TB patients.
(iii)
To undertake the above activities from all the health institutions
as an integral part of the general health services5.
Dr. piot, a WHO Medical Officer in 1962 defined tuberculosis
control as the reduction over a span of years of the problem of tuber
culosis as expressed by the prevalence of the disease. A reasonable target
for control, he said, might be a 50% reduction in the prevalence of excretors of tubercle bacilli over a period of 20 years8. However, according
to WHO, tuberculosis ‘control’ is achieved when the prevalence of natural
reactors to standard tuberculin among children in the 14 years age group is
less than one per cent7. In India, it is more than 30 per cent8. “Our
ultimate objective is the conquest of tuberculosis if not eradication by the
end of the 5th plan period”, declared Dr. K. N. Rao in 1966, the then
Director-General of Health Services, Government of India9.
NTCP & DTCP : Shortfalls During 1962—82
The District Tuberculosis Control Programme (DTCP) was evolved
by the National Tuberculosis Institute, Bangalore in 1962 to be the basic
uuit of NTCP10. Applying the National Survey findings, the different
areas of an average district contain TB patients as detailed in Table II.
Estimates of the overall level of success and shortfall have been made
by different workers. It was reported by Banerjee11 that after more
than 10 years of work (1962—72) less than 25% of TB patients were
brought within the purview of the NTCP; more than 75 % of the patients
continued to suffer and spread the disease in the community. While
reviewing the achievements of DTCP in 1974 in a symposium on NTCP12
the programme efficiency was reported at 30% and shortfall of 70%.
If the average shortfall was 70% in 1974, it had gone upto in 82% 198213
mid 92% in 1983.14
The three main components of the tuberculosis treatment programme
are case-finding, case-holding and chemotherapy, and their efficiencies at
the moment are estimated to be app. 33 %, 35 % and 75 % respectively14.
From this follows that less than 8 % of the tuberculosis patients in the
community are being successfully treated (Table IV).
Quarterly progress report of the DTCP for the period ending
December, 1980 issued by the Director-General of Health Services, Govern
ment of India, New Delhi showed a disturbing feature that Peripheral
Health Institutions contributed only 35.9 % of the total infectious cases
instead of the expected 80 %ls. .
A study on tuberculosis, conducted for a period of 20 years in New
Delhi Tuberculosis Centre, (1962-82) did not reveal any appreciable change
in respect of any important epidemiological index16. These findings
have also been confirmed by studies from other parts of the country. In
another study conducted in a pediatric hospital in Delhi during 1983, out
of 175 consecutive children suffering from tuberculosis 86.3% did not
have any BCG scar, and the vaccination was not effective in the rest 13.7%
woh had BCG scar : it meant a 100% failure of the BCG vaccination
programme)17.
Extent of TB Problem in the Country 1961—81
It is obvious from Table I (column C & D) that if the population
of India increased from about 439.23 million in 1961 to over 685.18 million
in 1981, the number of radiological disease and infectious disease patients
has also increased proportionately. Whereas, in 1961 about 368960 Indians
used to die of TB every year, now the number is more than 575560. It
meant that on an average, over forty , eight thousand patients died of TB
every month in India in 1981.
Situation in 1986
At present, with an app. population of 765.81 million people, India
is likely to have a total of 14.55 million TB patients including 3.06 million
infectious to their fellow citizens. In addition, TB is likely to claim the
lives of more than 640,000 Indians every year, 53,000 every month, 13,000
every week, 1700 every day, 70 every hour and more than one Indian
every minute. Death from tuberculosis brings shame to our society and
to the-community of nations (Styblo) (18).
The direct and indirect cost of TB affecting 6.8 million persons was
calculated to be over Rs. 20,000/- million in 1966 by Dr. K. N. Rao, the
then Director-General of Health Services, Government of India. With
rising cost of living, and the projected number of TB patients approxima
ting 20 million in the year 2001, the lose to the nation is going to be
colossal.
Whether we take Dr. Piot or W.H.O.’s criteria, our NTCP & DTCP
have failed on all operational objectives. What to say of conquering TB
by 1978 as declared by Dr. Rao, a former Director-General of Health
Services, we have not been able to make in 1986, even a dent in the enemy
territory, inspite of the fact that we have highly effective drugs and BCG
vaccine, and over 110,478 health institutions, including 13,276 for TB
control work (Table III). Tuberculosis population is increasing in our
country. Why this whittling down of achievements ? Why this shortfall ?
It appears that National Tuberculosis Control Programme is a pro
gramme managed by people who have nothing to do, but watch other
people who are doing nothing. National Tuberculosis Control Programme
or District Tuberculosis Control Programme is dangerous in untrained
hands and waste in over-trained hands.
Problem Likely in the Year 2001 AD
It appears that if no adequate and effective control measures are
taken, then, in the year 2001 AD, India may have nearly twenty million
TB patients out of which over 4.21 million would be spreading infection
to their fellow Indians. Not only this, nearly 0.88 million are likely to
die every year from 2001 AD onwards, more than seventy-three thousand
every month (Table I Column E).
Around 1660, the preacher John Bunyan wrote in one of his moral
fables : “The Captain of all these Men of Death that came against him
to take him away, was the Consumption, for it was that that brought him
down to the Grave” (19). If efficient, energetic control measures are not
taken, year 2001 AD may see the return of “The Captain of all these Men
of Death”.
Shortfalls on Other Fronts
TB Patient : Mr. Laskar said there were more than 10 million
persons suffering from TB in the country and the Government did not have
sufficient resources to provide clinical facility to all of them (State Minister
for Health, Lok Sabha Questions, Indian Express, 2nd December, 1981).
State’s Live-stock : Five per cent of the cattle in the state’s live stock
farms are infected with tuberculosis and that similar condition prevail in
live stock farms across the country (Director of Animal Husbandry, West
Bengal). In the case of West Bengal a Calcutta newspaper alleged that
3
70 per cent of the cattle in state farms died from TB.
October, 1984).
(Indian Express, 1st
Tuberculosis Leading to Suicide Attempt : On December 13, Mr.
Justice Sachar collectively quashed 119 cases of attempted suicide pending
in the criminal courts—some of them for years—and directed the Adminis
tration and the Police not to prosecute such victims in the future.
There is sound common sense in the judicial decision. For instance,
one of the cases narrated by Mr. Justice Sachar had to do with a young
man who suffered from an acute case of tuberculosis and was subject to
fits and periods of acute depression. The worst thing such a man would
need is a year in prison where he might infect other inmates, as well as
have a greater reason for attempting suicide once again (The Editorial,
The Hindustan Times Weekly, 29th December, 1985).
7000 from PM's Fund for TB Patients : New Delhi, January 30 (UNI)
Ram Dulare of Purani Jhushi in Allahabad district has been given Rs.
1000 from the Prime Minister’s relief fund for treatment of tuberculosis.
The amount was sanctioned on the recommendation of Mr. Ram Pujan
Patel Congress® member of Parliament from Phulpur of Allahabad
(Indian Express, 31st January, 1986).
Dole to Chronic TB Patients : If each chronic TB patient is to be
given Rs. 1000/- from Prime Minister’s relief fund the total amount
required will be Rs. 3,639 million for 1986 and Rs. 5000 million for 2000
AD at the current rates (Table VI).
Economic Factor : Cost of Treatment : Approximate cost of treating
one TB patient with Conventional Therapy is Rs. 250/- and with Short
Course Chemotherapy is Rs. 1050/-. Treatment of one chronic patient
costs Rs. 3250/- with a Daily Regimen and Rs. 2500/- with an Intermittent
Regimen (Table VII a).
From this one can calculate the cost of treating all new TB patients
(Table VU b), which will be Rs. 3635 million with Conventional Therapy
and Rs. 15267 million with SCC for 1986. For 2000 AD the cost at
current rates is likely to be Rs. 5000 million and Rs. 21000 million res
pectively.
App. cost of treating failure patients is given in (Table VIII c). The
cost comes to Rs. 11797 million and Rs. 9075 million with Daily Regimen
and Intermittent Regimen respectively for 1986. Do we have all this
money ?
Conclusion
The goal of “Health for all by the year 2000 AD” must be seen parti
cularly in the light of the unsatisfactory health situation prevailing in
India at present.
But, surely a nation that can put a satellite into orbit or buy mirage
fighter planes, each at a cost of Rs. 25 crores can also get its NTCP to
work properly and efficiently.
4
TABLE—I
Tuberculosis in India : 1961—2001
A
Index
Column
S. No.
1.
2.
3.
4.
5.
6.
B
Rate**
Total Population**
Prevalence of infectious cases
of pulmonary-tuberculosis
Prevalence of non-infectious
cases of P.I. (X-ray Disease)
Prevalence of TB infection
but no disease
Annual mortality
Annual incidence of new
infectious cases
C
D
E
1961
1981
2001
(In
(In (Projected)
million) million)
(In
million)
439.23
685.18
0.4%
1.75
2.74
4.21
1.5%
6.58
10.27
15.78
36%
1.084%
158.12
0.36
246.66
0.57
378.90
0.88
0.13%
0.57
0.89
1.36
1052.50
*Source : Health Statistics of India (1984), CBHI DG; of HS, GOI,
New Delhi.
**Source : Assistant Director General of Health Services (TB) Government
of India, New Delhi.
TABLE—II
Average Indian District*
(1961 Census)
10,000 sq. kilometers
1.5 million
41 per thousand
18 per thousand
23 per thousand
Total area
Population
Birth rate
Death rate
Growth rate
Number Population
District HO Town
Taluk Towns
Villages
Total
1
10
1,800
% Age
X-ray positive TB
of total
patients
popula---------------------------- —
tion
Sputum+ve Sputum've
60 000
(4%)
20,000x10 (14%)
700x 1,800 (82%)
1,500,000 (100%)
200
650
4,150
5,000
700
2,600
16,000
19,300
*Source ’ DTP Manual, The National Tuberculosis Institute, Bangalore,
‘ 1974.
5
TABLE—III .
Total Health Facilities Available (as on 1-1-1984)’
(a) Total Hospitals
7181
(b)
Total Hospital Beds (Bed Strength ranging from 1 to
over 700)
500628
(a) Dispensaries
21780
(b) Total Dispensary Beds
35742
(a) Primary Health Centres
7210
(b) Sub Centres
74307
Total Health Institutions
110478
1(a) + 2(a) + 3(a) & (b).
1.
2.
3.
Resources Available for Control of TB in India (as on 1.1.1984)**
Institutions rendering anti-TB services
(a) District TB Centres
(b) Implemented Rural Health Centres (Estimate numbers)
(c)
Other TB Clinics
(d)
TB Demonstration & Training Centres
Number of Sanatoria
Beds, available
Total Institutions
l(a+b+c+d)+2
1.
2.
3.
354
12390
330
17
185
45154
13276
* Source : Health Statistics of India (1984), DGHS, Government of India
New Delhi.
** Source : Assistant Director General of Health Services (TB), Government
of India, New Delhi.
TABLE—IV
Estimation of Overall Level of Success Under NTCP/DTCP
Component
Present Estimats of Level of
Efficiencies (%)
No of Successes
per 100 cases
30%
35%
75%
8%
30
10.5
8
Case-finding
Case-holding
Chemotherapy
Over all Success
TABLE—V
Cost of Tuberculosis*
Year
1966
1981
2001
*Dr. K. N. Rao (1966)
DGHS, GOI.
**At the Existing Prices.
No. of Patients
Cost in Rs.
6.8 Million
13.01 Million
20.00 Million
20000 Million
400000 Million**
??
TABLE—VI
Dole to Chronic and Failure Patients
(25 % of the Total Patients is Lower Estimate)
Year
Total Patients
(in Million)
Failure Pts.
(in Million)
Dole in Rs.
(Million)
1986
2001
14.54
20.00
3.63
5.00
3630
5000
TABLE—VII
(a) App. Cost of Treating one TB Patient
Treatment
(in Months)
Regimen
Conventional Therapy
2SHT/10HT
Short-course Therapy
2HRZ/7HR
Treatment of Chronic Patient
6HRZE/12HRE
6HRZE/12 H2R,E2
Cost/Patient
Rs.
12
250/-
9
1050/-
18
18
3250/2500/-
(b) App. Treatment Cost of all New Cases
Year
1986
2001
_____
Total PTS
(Million)
Coventional
Therapy
(Rs. 250/pt)
(Million)-
Short Course
Therapy
(Rs. 1050/pt)
(Million)
14.54
20.00
3635
5000*
15267
21000*
*At the Exisling Prices.
(c) App. Treatment Cost of Failure Cases
(25 % of the Total Patients)
Year
Total PTS.
(Million)
Daily
Regimen
(3240/pt)
Intermittant
Regimen
(Rs. 2484/pt)
1986
2001
3.63
5.00
11797 M*
16200 M**
9075 M*
12420 M**
•Million.
**At the Existing Prices.
□
References
1.
Singh, M.M. (1980); Presidential Address, 35th National Con
ference on Tub. & Chest Diseases, Bombay, p. 2
2.
Kamath, R.N. (1985); Information on INABUTOL, Themis
Chemical Ltd. Bombay p. 1
7
3.
Rouillon, A. (1982); Bull. Int. Un. Ag. 57, p. 200.
4.
Barua, B.N.M. (1977); Tuberculosis in India, CHEB, DGHS,
New Delhi, p. 16.
5.
District Tuberculosis Programme Manual 1974); National
Tuberculosis Institute, Bangalore, p. 1,5.
6.
Piot, M. (1962); Proceedings of the 18th Tuberculosis and
Chest Diseases Workers’ Conference, Bangalore, p. 143.
7.
WHO (1960); Tech. Rep. Ser. 195.
8.
Text-book of Tuberculosis (1981) Vikas Publishing House Pvt.
Ltd. New Delhi, p. 47, 48.
9.
Rao, K.N. (1966); Ind. J. Tub. XIII, p. 87, 88.
10.
Piot, M. (1962); Ind. J. Tub. IX, p. 151.
11.
Banerjee, D. (1981); Textbook of Tuberculosis, p. 530.
12.
Symposium on NTCP (1974); Ind. J. Tub. XXI, p. 112.
13.
Health Statistics of India (1982); DGHS, Govt, of India, p. 59.
14.
Radhakrishan, S. (1983); Ind. J. Tub. XXX, p. 3.
Sivaraman, S. (1982); Ind. J. Tub. XXX, p. 82.
15.
16.
Mathur, G.P. (1982): Personal Communication, New Delhi
Tuberculosis Centre, New Delhi.
17.
Kohli, M. (1983); Thesis for the Degree of Doctor of Medicine
(Paediatrics), Uni. of Delhi, p. 33, 36.
CDMMtHl i'Y HEALTH CELL
47/1. First Hoor) St. Marks Road,
Bangalore - EGO 001.
8
INTERNATIONAL CONFERENCE
HEALTH POLICY : ETHICS & HUMAN VALUES NEW DELHI 1986
Child Care-National Health Policy
Dr. P. Chandra, MD., DCH., MNAMS.,
Prof. & Head
Department of Paediatrics, Stanley Medical College,
Madras 600 001
•
Children of today will be the adults of tomorrow. Any efforts today
for improvement of not only early child health but also child life in general
will thus be considered as investment for future. Childhood is the breeding
time for the future leaders of the country in different walks of life Viz.
Industry, Education, Social Services, Politics, Administration, Military and
Civil Services. Any investment on services for the young generation has
a dfect impact on long term economic and social development. Health
is art inter-related subject and this involves many other disciplines. The
declaration of ALMA ATA by WHO is considered to be the MAGNA
CARTA of health development. This understood the role of Primary
Health Care as the key to the attainment of the goal.
India is a signatory to achieve Health for all. The National Health
Policy had been approved by both houses of parliament signifying the
political will for the implementation of the policy.
The targets set to be achieved reveal the vital role of Maternal and
Child Health in Health Services.
The Existing Picture of Child Health
The child health problems of India and other developing countries
are similar to the problems seen in 19th Century Europe and U.S.A. In
the West, dramatic changes have taken place in child health as a result of
early and continued efforts of Paediatricians combined with those of
immunologists, pioneers in public health and nutritionists resulting in very
marked reduction in childhood mortality and morbidity. In India with
successive 5 year plans, a significant improvement in the health status of
the people have been achieved, like eradication of small pox and plague
and prevention of many other epidemic diseases. Inspite of these various
mentionable achievements health care services particularly child health ser
vices continue to suffer from several deficiencies. There are serious loca
tional and quantitative imbalances in services provided to various sections
of the population.
The number of deaths in infants and among the children under the
age of five is the most commonly used indicator of child health status
within any country and a good gauge of the country’s stage of social
development. The risk of dying before adolescence is about 1 in 40 in the
developed world, [n India it is 1 in 3 or 4; 50% Of total deaths occur
in children below five years. Further study of mortality reveals that about
1 '3rd of all deaths occur in the first year of life, nearly a fifth of all deaths
occur in the first month and about l/10th of all deaths occur in the first
week of life. For every fatal outcome there are many episodes of disease
and ill health.
Beneath this trend is a complex of attendant factors like maternal
malnutrition, foetal under development, inadequate natal care, improper
infant feeding and weaning practices, malnutrition like vitamin A defi
ciency, Iron deficiency, Protein—energy deficiency, preventable conditions
like diarrhoeal dehydration, infections like tetanus, whooping cough,
measles and ignorance about growth failure. The health problems are
ingrained with poverty, ignorance and inertia of life style of the community
that, in order to make any change for the better, it should involve a
change in life styles, feeding and living habits of the community. The
profile of child health problems should form the “SHEET ANCHOR”
of health services strategy including a health manpower development
policy.
Objectives and Imaginative Approach to Child Care
The fundamental concept in child care must be intrinsically different
from adult care. The problems and solutions in providing health care for
village people are intrinsically different from traditional medical practice.
The unthinking tendency to transpose primary care as practised in
hospital, out-patient department or physician’s private office to rural
centres has not met the need of the community. How best can we defend
and protect human life as soon as it begins in the human womb upto the
time it reaches addescence ? Every child born in our country must have
the opportunity to realise in full his capacity for material, intellectual
and spiritual growth. The techniques involved in reducing the problem of
children have not been fully worked out. A mention in the constitution
a plank of policy and a place in planning is not sufficient. Development
of the very young ought to be the paramount national concern. The
health policy has to define the most appropriate pattern of services for
children.
Status of Child Health Care in National Health Policy
The national health policy specifies clearly the goals to be reached
for health and family welfare programmes. Improvement in vital health
indicators like perinatal mortality, infant mortality, preschool mortality
has been stressed establishing accountability. The policy lays stress on the
preventive, promotive, public health and rehabilitative aspects of health
care and establishment of Primary Health Care Services to reach the
population in the remotest areas of the country. Ensuring adequate nutri
tion, safe drinking water supply and improved sanitation for all segments
of the population and health education are the other high lights of the
policy document. The seventh five years plan is largely guided by the
national health policy. The importance of delivery of Maternal Child
Health Services had been emphasised in the policy and plan. Improving
child health has been deliberated in several committees. The translation
and application of recommendations are far from satisfactory. In planning
for implementation of a new pattern of health care it is necessary to
recognise the inter relatedness of a number of interlocked components. If
any of these elements are missing than the whole system may not work.
Programme that are likely to have maximal impact in childhood mortality
and morbidity have been spelt out—The achievements in child health care
are meagre as drops in the ocean. While the 7th plan has been explicit in
spelling out targets, it has not provided details of strategies or programmes
by which these targets would be achieved. In this communication, policy
and programmes will be reviewed and suggest where actions and alterations
are required.
Medical Education
The medical education system and health care delivery system have each
gone their own separate ways. The greatest need is a system of education
oriented towards the promotion of community health and primary health
care. The pivotal place that child health should occupy in any health
plan is so blindingly obvious that most decision makers in health planning
have failed to see it. The recommendation on undergraduate paediatric
education of the Medical Education Conference convened jointly by the
Government of India and Rockfellor Foundation in 1955 were accepted by
Medical Council of India (MCI) only in 1966. Medical Council of India
recommended undergraduate assessment of this discipline only in the
year 1976.
20 years after Medical Council of India’s recommendations, majority
of country’s Medical Colleges are not providing the required 3| months
undergraduate Paediatric Training. Paediatrics is assessed independently
only in three Universities of this country. Majority of Universities are
not assessing undergraduates in Paediatrics at the final professional level,
contrary to the 1976 recommendations of the Medical Council of India.
The discipline of Paediatrics has been neglected inspite of political will,
support of International Agencies like WHO and UNICEF and commend
able efforts of Paediatric Educationists. The inadequate knowledge of
Paediatrics possessed by a great majority of those in private practice,
doctors in non-teaching hospitals and Primary Health Centres is mainly
due to defective undergraduate training. Offering good and comprehen
sive Paediatric Services to India’s large child population will depend mainly
on the quality of undergraduate training in Paediatrics. There is an urgent
need for total implementation of Medical Council of India recommenda
tions on undergraduate paediatrics education and to make it a totally
independent discipline at the undergraduate level.
Continuing Medical Education—An Urgent Need
The character and nature of medical practices have radically changed
in the last few decades and is constantly changing. A major objective of'
medical education today must be to train the student to continue to be a
student and to equip him to imbibe and effectively utilize relevant new
knowledge. The teacher must keep continuously abreast of the fast mov
ing frontiers of knowledge in this field. In the last few years a child
survival and development revolution has begun with low cost inventions
like oral rehydration therapy, universal immunisation growth monitoring
breast feeding, proper weaning and food supplementation, female literacy
and family spacing. How many physicians in practice
aware of these
advances ? It is a great challenge to disseminate latest knowledge without
delay and which is rapidly changing to each and every practising physician.
3
There is not even sufficient awareness of the enormity of these new
challenges.
A pattern of undergraduate and continuing Medical Education has to
be evolved in the country which will adequately meet the new needs
generated by the rapid advances in Medical Sciences. Just as in some
countries like U.S.A. Programmes of re-training and re-licensing after
assessment for physicians to practice has to be seriously considered and
introduced without delay. The present trend of Medical Education being
—once for all phenomenon—must be changed. Medical faculties can make
a valuable contribution to the development of Primary Health Care by
providing instruction for field workers and monitoring progress.
Nursing Education and its Relevance to Child Care
The term Nursing Personnel includes all persons who carry out
nursing functions like general nurses, public health nurses, nursing tutors,
auxiliary nurse and midwife and others. The curriculum content prescribed
by Indian Nursing Council is accepted by all nursing schools and is un
satisfactory and very inadequate in Paediatric Training. The development
of Nursing Profession is no less important to the care of children than
the development of medical profession. Nurses have a major part in
improving health of the children and have the greatest potential to expand
further and raise the standard of health. There is an universal problem
of shortage of nursing faculty. Starting of private nursing schools are in
greater need than medical schools. Continuing Education Course in
Paediatric Care and community health care is essential for professional
growth and to enhance job performance. Nurses profession has to be
accorded its rightful status and recognised for the valuable role it can play
in achieving the marked reduction of childhood mortality and morbidity.
In the light of forgoing discussion the training of pharmacists and other
paramedicals also needs change.
Drugs and Pharmaceuticals in Child Care
The drug policy speaks mainly of self-reliance and abundance of
drugs to meet our health needs and do not lay emphasis on the pattern of
drug production. It is more important to see what drugs are produced
and for whom ? There is, however, production of costly drugs for the
rich and cheaper drugs required by the poor people are not adequately
available, (e.g.) Phenobarbitone, Dapsone and INH. There is also
vaccines shortage. Irrational marketing of drugs and continuous avail
ability of some spurious harmful and dangerous drugs are hazardous. The
pattern of drug production of the country should be closely oriented to the
disease pattern and details have to be spelt. Urgent steps are needed to
improve the efficiency of public sector. The need for an effective quality
control machinery does not require any emphasis. It is necessary to amend
the drug policy suitably.
Care of Children Above Six Years
The children above this age group form nearly 20% of the popula
tion. There is a vagueness and lack of clarity about the welfare both in
plan and policy. All programmes are limited to the school health services.
4
Many more children in this age group are out of school than in the
chools. It is therefore important to realise the special problems of these
children. Promoting uninterrupted growth and development in them an
important aspect of human resources development. Growth retardation
in girls aged 10-15 years lead to low pregravid weight and short stature
leading to obstetric complications and cause low birth weight. It is there
fore important that their needs on health care be stressed in national health
plan and separate provisions are to be made for it.
Health Insurance and Mobilisation of Resources to Improve Child Health
The primary responsibility of providing health services to the people
is that of the Government. It is extremely doubtful that the present
patterns of resource allocations can establish a minimum health organisa
tion considered absolutely essential to meet the basic health needs of the
community. If the community share some of the cost, it will maximise
the efforts. The availability of free medicine should be restricted only
to National Health Programmes, e.g., Leprosy and to the vulnerable
population. This will improve community participation in health activity
and facilitate reattendance. Charging nominal rates for investigations to
out patient and indoor patients and diet is practicable. It is essential that
a definite and a discrete order is issued without delay.
Intersectoral Co-ordination and Child Care
Attainment of nationwide goals, specially social objectives is possible
only through sustained national will and co-ordinated efforts by all related
sectors. Health development is both a cause as well as a result of social
and economic development. Efforts at achieving co-ordination and
establishing linkage have to cover Integrated Rural development, education,
social welfare, agriculture, industry, transport, etc. to ensure protected
water supply, environmental sanitation and hygiene, nutrition, MCH., and
Family Welfare. A highly co-ordinated and integrated approach involving
all sectors is possible only by sustained political will and support given
both at centres and states throughout.
Conclusion
The country is preparing to enter the next century with hopes of a
prosperous nation using up dated technological advances and developments
in different fields. If these hopes are to be realised child health needs top
priority, as children are country’s most potential resources. The problem
of reducing childhood morbidity and mortality is complex. An effective
sustained decline can only be achieved by a multipronged approach aimed
at social, ecological, educational, public health and environmental
problems. If a dent is to be made on maternal and childhood mortality
the Government should without delay and reservations implement the
recommendations as these are highly specific and need based.
5
INTERNATIONAL CONFERENCE
HEALTH POLICY : ETHICS & HUMAN VALUES NEW DELHI 1986
Teaching of Human and Moral Values in
Postgraduate Medical Education
S. Vaidyanathan, M.S, Meh, MAMS (Urology), Ph.D.
G.C. Malakondiah, M.S.
T.P. Mahapatra, M.S. M.ch
S.P. Tandon, M.S.
Department of Urology, Postgraduate Institute of
Medical Education and Research,
Chandigarh 160012
A postgraduate medical student after completing his training is likely
to work as a clinician, a medical teacher, a medical administrator and/or
a medical researcher. During his professional career, he is likely to face
many situations where he will have to take decisions not only on scientific
basis but also on human and moral principles. His acts should reflect
upon his character as a man of virtue and not as an a moral being. Inten
tionally or unintentionally he may speak ill of a professional colleague, be
unkind to an anxious patient suffering from advanced cancer, recommend
purchases from a particular firm which gives his gifts, select a student
belonging to his region, award low marks to a student whom he does not
like or steal ideas for research from a junior colleague. Although the
present system of medical education imparts good theoretical and practical
knowledge on scientific medicine, there is no formal and very little informal
education on human and moral values during post-graduate medical
training. Emphasis is being placed on learning operative acumen e.g.
how to do prostatectomy but little importance is given to humanistic
treatment of a poor old patient or the moral aspects involved in decision
making of various real-life situations such as patient management, medical
education (student selection, examination, etc.) medical administration and
medical research.
The moral components are :
(i)
Attitude : It is not simply an ability or a piece of knowledge.
It is “regarding other people as equals”, “thinking that other
people’s interest count”, “taking notice of other people’s wants
and needs”. Attitudes are detected and verified by the way in
which a person thinks in his everyday, practical living, and to
some extent by the way in which he acts. On the cognitive
side, it is a belief—the belief that other people have equal rights
with onself. This can be tested by certain question or observa
tions :
Does he make some effort to find out what other people’s
wants and feelings actually are ?
Does he listen to other’s opinions and allow them to have
their say ?
(c) How does he actually treat people belonging to a different
ethnic origin/different region/different religion ?
(a)
(b)
(ii)
Ability to know what other people are feeling, in particular
situations. This may be described further as “awareness of
other people’s feelings”, or “the ability to understand what
other people’s interest are”, “knowledge of other’s desires,
emotions, etc.”. This is concerned with awareness of the
feelings of people with whom one actually comes into contact in
one’s everyday life! it also includes being able to predict the
feelings of those whom he has never met. This can be tested
as follows :
Can the student give a reasonally good account of the
feelings of the patient who is to undergo extirpative surgery
e.g. total amputation of penis for penile carcinoma?
(b)
Can he understand the feelings of the patient’s wife and
children when a diagnosis of advanced cancer of urinary
bladder is made?
(c)
Is he interested in other people’s feelings and behaviour?
Has he as a teacher, made any attempt to understand the
feelings of his students? Has he as an administrator made
any attempt to understand the feelings of his subordinates?
(a)
(iii)
Actual knowledge of certain ‘hard’ facts—Knowledge of rules
of the social system in general, knowledge of social conventions
and social expectations.
(iv)
Know-how to translate his moral decision into effective action.
It is a kind of adep’tness rather than a cognitive mastery of facts.
This can be tested by :
(a) Is he capable of playing the roles of a leader and a follower,
of issuing and obeying instructions?
(b) Can he behave efficiently in social situations involving people
of various age groups, and different ethnic origins?
(c)
Can he behave well in formal contexts as well as in less
formal contexts?
(v)
Mode of thought'. Ability to face up to a moral situation and to
consider that situation primarily in terms of other people’s
interests. A person with appropriate attitude, ability to
discern other people’s feelings, and knowledge of ‘hard’ facts
will make a prescriptive moral decision dictated by other people’s
interests. Dimensions of this complex moral component are
(a)
right reasons. Not everybody makes, or even thinks he
ought to make, his moral decision on the basis of other people’s
interests. Other modes of thought are regrettably common.
Amongst these are: desire to please the boss, uncritical tendency
to obey rules, a tendency to do what is most expedient for
oneself, etc. The person with a high degree of this moral com
ponent will always consider other people’s interests, and think
in this mode rather than in others, (b) Sincerity of decision.
There are people who may pay lip-service to a certain mode of
moral thinking but who do not sincerely commit themselves in
making these judgements.
questions :
This can be tested by the following
(a) Does he think that moral values are ‘just a matter of taste’
or does he believe that there are right and wrong answers
to moral questions?
(b)
Do his principles include not only avoiding bad actions,
but doing good ones (actively and positively helping other).
(vi)
Action or Behaviour: When a person has reached a rational
moral decision, he must have the motivation and resolution to
translate that decision into action. There are all sorts of reasons
why people fail to bring their abilities to bear on moral situa
tions, or fail to translate their moral decisions into action.
They may be forgetful, incompetent, lazy, frightened, tired
cowardly, etc. A person should have sufficient sentiment or
love for other people: this is atleast one kind of motivation
which should enable him both to think and act rationally in the
moral sphere. A person should also have good habits, or a
settled disposition to think and act in a rational manner. A
person must possess independence of judgement, the ability to
think and act autonomously as opposed simply to following
other people like sheep. A person must be reflective or thought
ful enough not to be carried away by particular situations, and
not to be forgetful of other people.
Teaching of moral and human values
The spirit of the medical college and its teachers thus becomes the
basic factor in developing moral values. There can be little contribution
to moral and spiritual values from a college which resorts too easily to
arbitrary authority; from an institution in which the chief mainspring of
effort is rivalry; from an institution which fails to exhibit complete honesty;
from a college in which each seeks only to satisfy his own selfish aims;
from a college laden with intolerance, fear and suspicion. Only a medical
college served by a faculty whose members are themselves sensitive and
responsive to moral values; a college with a broad, humane, and flexible
curriculum; a college steeped in a philosophy which commands respect
for the personality of each teacher can hope for success. Medical colleges
that exemplify moral values are better than lesson which preach them.
Human and moral values can be taught while discussing each
patient’s clinical problem. The teacher should be a ‘role-model’ in
exhibiting human values while treating a patient. He should observe the
students'in the out-patient clinics, in the wards, and in the operation
theatre, record resident-patient encounter and discuss it with the concerned
resident later emphasising the need to adopt and practise humanistic
approach and moral values. For example, the urology resident is often
taught how to do urethral dilatation i.e. he should fellow aseptic principles,
there should be no urethral bleeding, etc. Seldom is it emphasised that he
should alleviate the anxiety of the patient before performing dilation,
make an attempt to understand the feelings of the patient’s family as
regards patient’s illness, check whether adequate urethral mucosal anes
thesia has been produced before actually performing dilation. Not
infrequently it may be witnesses that the doctor scolds the patient when he
complains of pain. Thus the human values should be integrated with the
teaching and practice of clinical medicine. Often it may be observed that
the teacher as well as the post-graduate student is kind to a VIP patient but
forgets such human values while attending to a poor and illiterate patient.
The moral components mentioned above can be taught in the medical
college during case discussion, structured lectures, informal coffee-club
discussions, departmental seminars, interdisciplinary seminars and intensive
workshops. At a national level, bibliography development, national
workshops and national conferences on teaching of human and moral
values can be organised.
Evaluation
Assessment of teaching of moral values, student’s learning and
student’s behaviour in this regard should be periodically evaluated.
Preferably, considerable weightage should be given to the above listed moral
components in internal assessment of non-scholastic abilities. Self—
assessment by the post-graduate students is the best method of evaluation
to infuse motivation and self-analysis. He may be encouraged to record
atleast one patient management every fortnight describing how he adopted
human and moral principles. The teachers should act as facilitators of
learning and directors of individually-prescribed instructional programmes.
They should give immediate, positive feed-back to the student appreciating
his good performance and encouraging him to make up his shortcoming if
any. Peer assessment, and evaluation of recorded audiotapes of resident
patient encounter may also be useful. In the beginning, all groups may
express some antagonism or unwillingness to admit to living by moral
values. However, the teachers as role models, will be able to secure
student’s full participation in such programs. When the students are enco
uraged to think harder about these abstract ideas and given a little help
with the terminology, they would quickly become adapt at analysing the
moral issues involved in patient care, and in his professional career.
In conclusion, moral education involves both comprehension and
apprehension, neither can be imposed. It Is wholly open-ended, recognis
ing that genuine morality requires free personal acceptance of values of
that is, the goal is not the heteronomy of the slave, but the autonomy of
the free man.
References
1.
Bull, N.J. Moral Education London, Routeledge and Kegan Paul,
1973.
2.
Educational policies Commission. Moral and spiritual values in
the public schools. National Educational Associations, Washington,
1951. ■
3.
Jewell, M.D. Teaching Medical Ethics. Br Med. J. 289: 364-365,
1984.
4.
Veatch, R.M. and Gaylin, W. Teaching Medical Ethics: An
Experimental Program. J. Med. Educ. 47: 779-785, 1972.
5.
Wilson, J. Moral Education and the curriculum Pergamon Press
London, 1969.
4
i
3~LL
Moor, St-Marks Road,
Bangalore - 560 001.
INTERNATIONAL CONFERENCE
HEALTH POLICY : ETHICS & HUMAN VALUES NEW DELHI 1986
Artificial Insemination-Surrogate Parenthood
Ethical, Moral, Legal Aspects
Dr. J.V. Bhatt, M.D.
Human mind is conditioned by a large number of factors. What
is legal or illegal, what is ethical or unethical, what is good or bad, what
is moral or immoral, what is sinful or otherwise are all determined by an
individuals upbringing, his immediate social and cultural environment,
his religious background and a host of such other factors. All of us tend
to develop, what in transactional analysis are called “Scripts” resulting
from Parent-Adult-Child interactions, within ourselves, and with the
surroundings. Rapid scientific advances which are both as a result of and
which result in information explosion are producing a positive feedback
effect. We do not know where this accelerating cycle will lead us to.
Any organism, organisation or system needs a strong and sensitive negative
feedback component to maintain it in a state of homeostasis or equili
brium. Even if it is a forward moving accelerating system, it requires
inbuilt mechanisms to check its progress and to absorb the shocks. It is
also essential that all parts of the system move at the same speed, to
maintain the integrity of this system. Most individuals are quick to accept
newer techniques if they lead to monetory gains to them. Even an illite
rate farmer in India readily accepts hybrid seeds, chemical fertilisers,
pesticides, and newer methods of farming if he is convinced that he will
get bigger financial returns. In fact at the back of his mind he has been
looking for such inputs. Such inputs have in fact come up as a result of
such a need. Most of us will also accept, though a little less readily,
newer options in the field of health. In my field of rural health programme
I find that the rural farmer accepts much more readily newer techniques
which look after his animals than those which improve the health of his
children. If the social system is slow in accepting newer health techniques,
the legal system is still slower in accepting the facts if life as it were. If
the legal system is slow, religious system is practically static. What may
be acceptable socially and legally may still be considered intolerable from
a religious point of view.
A.I.D. and surrogate parenting are problems, where medical science
has advanced very rapidly. To-day it is possible for a woman to conceive
without any sexual relationship with a man. The sperm could come
from her husband or from any other man who may be miles away from
her, or may be dead since long. It is now possible to collect the ovum
(egg) from a woman, get it fertilised outside in vitro, get it embedded in
the uterus of some,other woman. Time is not far when it will be possible
to produce an entire new individual by cloning from a single cell of any
one of us. A sexual reproduction from a single cell was the earliest form
of reproduction. With cloning the cycle will be complete.
Law in most countries has not yet taken cognizance of all these
developments. An AID child is still illegitimate in many civilised countries
of the world. As is found in most instances those who want to do things
legitimately face problems. One of the report states that in 30% of
couples it is found on detailed examination that the father could not be
the genetic father of the child in the family. Women seem to be finding
their own means of attaining pregnancy. It has been rightly said that
the results of AID can also be obtained by adultry. Seeing newspaper
reports about surrogate parenting, physicians are approached by aspiring
couples to help them out of their predicament. In India and also in many
other countries, producing at least one or two children is not only an
instinctual necessity or a socio-economic need but also a status symbol.
A married couple is under great social pressure to conceive soon after
marriage. A sterile woman is not only looked down upon but is con
sidered inauspicious. This makes it obligatory to conceive by hook or
by crook. Any scientific advance in the field of human reproduction is
therefore not only appreciated but also demanded by the community.
Such advances are eagerly looked forward to, and heartily welcomed by
those in need.
Oxford dictionary defines Surrogate as “Substitute” or “deputy”.
The phrase surrogate parent would therefore mean a substitute parent.
Surrogate father would be one who substitutes for the father or deputised
to be the father. 12% of all married couples are faced with the problem
of sterility. While some of them can be helped by simple means, most
of them would have problems, where at least one of the partners is not in
a position to produce the required gamete (sperm or ovum). In such
cases it would be essential to obtain the gamete from a third party. In
case of such a problem with the male partner, the biotechnical part is
restricted to obtaining the gamete from a suitable feriile male and intro
ducing it it into the fertile female. In case of inability of the female
partner to produce the ovum, it is possible to obtain it from another
female, and after fertilisation in vitro with the male partners sperm,
implant it into the uterus of the female partner, after suitable preparation.
In those cases where the female partner is not in a position to embed a
fertilised ovum (either her own or of another female) it is possible to
embed the ovum in the uterus of a suitable female for its growth and
development. All of the above alternatives are not only possible but are
likely to be generally available shortly.
In case both the partners are not producing gametes, inspite of
medical interventions and where other alternatives also do not yield any
results adoption is the only alternative. The parents of the adopted child
would be substitute parents for that child. Adoption has been practiced
since long. It is a well established custom. There are no ethical or moral
issues, except when a child is sold for adoption or is purchased with an
idea of subsequently using it for immoral or commercial purposes or
for labour. Legal procedures for adoption are well established, but like
all legal matters there will always be some loop holes lacunae. Inter
pretation of legal phraseology may also sometimes lead to some problems,
but by and large the issue can be said to be as settled as any other legal
matter. Other matters like AID, IVE, ET and hire-a-womb are matters
with which law has not been able to keep pace with generally.
There are five or six characters in this drama.
2
1.
The doctor. The medical man or the medical team would be well
advised to take the following precautions.
(a) Take valid written consent of husband, wife and donor, for the
procedures.
(b) Try to keep the identity of the donor a well guarded secret.
(c)
Carefully select the donor to closely match the partner he or
she is to substitute with the same blood group and without any
bad genetic traits or transmissible diseases.
(d)
If possible get a psychologists opinion about the couple’s
mental stability to accept the off-spring.
2.
The father. He should be fully explained the procedure and be
asked to remain present during AID, if possible. It is also possible to
mix the semen of an oligospermic husband with that of the donor in order
to give a chance to his sperm to fertilise the ovum. This combination
procedure is known as AIC and can also be tried in suitable cases. For
birth registration father’s name should be left blank.
3.
The mother. In case of AID the mother is very keen to be
pregnant. So also in case of IVF and ET from another woman. There
should be an unwritten pact that this matter will not be brought up during
any domestic quarrels.
4.
The child-. In some countries or in some states of some countries
such a child would be considered illegitimate. It is better.to legally adopt
the child as early as is legally possible. From medical point of view it is
better if the child is informed, when it grows up, about its origin so that
there is no confusion in medical history about genetic disorders.
5.
The donor: He or she should give accurate and correct history
about illnesses suffered and family history. They should not make
attempts to find the outcome of their donation.
6.
Uterine mother: In case of uterine mother it is better to find one
who does not do this for money. It is better if she has two or three
children—boys and girls, so she is not tempted to keep the child. Preg
nancy even under best of circumstances can sometimes lead to mortality
or morbidity. She should be explained about this. She should be fully
instructed against consumption of alcohol, smoking and taking drugs
which may be harmful to the foetus. The period for which she ™ill be
required to nurse the baby should be explained.
AID is already available as a eugenic measure. There is an attempt
to produce a race of supermen by using sperms of intellectual giants. There
is also demand from unmarried women to get pregnant through AID.
Once it is possible to do IVF the day is not far when it would be possible
AID: Artificial Insemination by Donor semen
IVF: In Vitro Fertilisation
ET : Embryo Transfer
§
to alter the genes prior to fertilisation by genetic engineering. Once a
desired type of individual is produced he/she can be replicated by cloning.
Though sexual reproduction by normal sexual intercourse is unlikely to
lose its popularity for a long time for obvious reasons, some day in future
it will be possible to totally separate the procreational and recreational
aspects of sex. Whether this will be of benefit to mankind or not time
alone will tell. Science keeps on producing deadliest weapons of destruc
tion and also newer means of production and reproduction. At-a micro
level they can be of use but at a macro level their usefulness is ques
tionable. Science, morals, ethic, religion and good sense will have to by
synthesised, if a Frankenstein is not to let loose.
COM?
.i
.
■
..
47/1. (First floor, St. Merits Road,
Bangalore - 560 001.
4
INTERNATIONAL CONFERENCE
HEALTH POLICY : ETHICS & HUMAN VALUES NEW DELHI 1986
Health for all by 2000 A.D.Measures to Implement
Dr. M. Arulpitchai Narayanan
Private Practitioner
Dr. T. Muthusamy, MD. DCH
Private Practitioner
Dr. A. Namasivayam, MD. PHD. MNAMS
Prof, and Head Dept, of Physiology,
Post Graduate Institute of Basis Medical Sciences,
University of Madras, Taramani, Madras 600 113
The World Health Organisation and the Government of India are
keen on providing “Health for all by 2000 AD” utilizing all the available
resources, manpower and funds.
At present all the efforts of the Government is mediated through
Government agencies only. Only a very few non-Governmental agencies
and voluntary bodies take active part in the implementation of Govern
ment Health Policies.
The primary defect in this system is the dilution factor. The idea
and the motivation with which the existing policies were framed, get
diluted as it percolates through the hierarchy of administrative machinery
and practically very little reaches the common public who are at the
receiving end. In addition number of social and-political evils contribute
all their might to dilute this further.
It is a known fact that three fourth of our trained medical people
live in urban areas and three fourth of the Indian population live in rural
areas. Thirty eight years after independence, we are not able to provide
safe drinking water to all our people and how are we going to solve
the problem of providing health for all by 2000 AD ?
A radical change in the approach is required and the mere fact that
our health policy has not benefitted the masses indicate the necessity of
taking on war footing in solving this problem.
Implementation of Governmental Health policies is a slow process
and the Government employees deal only with papers, rules and regula
tions which involve least quantities of logic and rationals. Motivated
local voluntary agencies can solve a lot of these drawbacks, of the admi
nistrative machinery, provided REAL conscientious supervision over the
activities of these organisations can be established.
This point has been well brought out in the speech delivered by Dr.
Sathianathan at the 1985 National Workshop of Health Services Research
in which he said “one of the remarkable features of Private practice is that
even though Government facilities are chronically short of drugs and other
supplies in most of the places, the private sector invariably manages to
purvey basic medicaments even in remote areas’
It is a common know
ledge that if a particular drug is not available in the Government Hospital
the nearby pharmacy will definetly have plenty of stock of that particular
drug.
The main aim and the objective of this paper is not to criticize the
working of the Governmental Institutions but to evaluate a method by
which the health of the Indian population can be substantially improved
by 2000 AD.
The main impediment towards this is the lack of DATA. We actually
do not know what we lack or suffer from. Only when we know the defi
ciency, it can be corrected. Hence the major proposal of this paper is to
emphasise the baseline data collection from the entire population of this
subcontinent in the next 5—10 years. Only when the basic health records
of the population is available for analysis we will know what we lack and
suitable remedial measures can be initiated.
How to Collect Health Data
Collection of general health data and socio economic status can be
entrusted to Government field workers, health visitors and local voluntary
agencies and educational institutions.
For example in Tamil Nadu all the Taluk headquarters has atleast
one college of higher education where students from the neighbouring
village come for learning. If these students are motivated and made to
understand the importance of this health data, reliable data can be collected
from the students native village.
Regarding the common illness disease and nutritional deficiencies in
a particular region, the necessary data can be collected by the medical
practitioners working in these regions who are again to be educated to
understand the significance and necessity of such data. As pointed out by
Dr. Sehgal (1985) the importance of Record keeping should be emphasised
for Rural doctors and when these records are kept properly are valuable
tools in obtaining disease statistics in a region.
On similar lines private laboratories and hospitals IMA, and the
voluntary agencies receiving Government grants should also be involved
in this data collecting work.
Keeping records on health problems of people can easily be solved
if Government introduces health cards similar to ration cards. These
heaith card system is already in vogue in number of Western countries
and it is high time Government of India takes some steps towards initia
ting the card system.
Similar health card systems are in use certain voluntary agencies like
V.H.S. Madras, and with many of the urban private practitioners. Some
of the special departments of Government hospitals maintain their own
card system. But what is needed is such a practice should be adopted by
all the medical people and institutions so that data collection becomes
relatively easy.
No doubt these data collection, storage and retrieval needs consi
derable investment in time and money. Proper motivation of the people
and physicians and incentive for both the group may atleast solve the
problem to certain extent. In larger institutions computerisation may be
essential to store and retrieve data and the money invested in this is defi
nitely not a waste.
The functioning of this data collection network is ultimately depends
upon how efficiently the working is supervised and managed; again dedi
cated supervisory and supporting staff are essential.
Role of Doctors in Data Collection
Once upon a time the medical profession and the medical men and
women were available for service at all time. This continues even today
in remote rural areas but most of the medical professionals in Urban and
suburban regions are far from service oriented. Motivating these people
in this mass data collection process is rather difficult. Reorientation courses
along with refresher courses to motivate the medical people in participa
ting the mass data collection is essential. The local medical association
can do a lot in this respect and these bodies should be encouraged and a
scheme should be organized regionwise so that all the necessary data will
be collected by medical professionals. An incentive scheme may also be
introduced to encourage the medical personnel to actively participate in
this programme.
Role of Hospitals in Data Collection
Though it is a routine practice now to maintain the case records by
the record section in major hospitals the input seems to be defective.
The information fed to the Record section is spurious at many instances.
It has come to the notice of the authors some time back, that cases diag
nosed as Rabies have been cured and discharged as per the records.
Education regarding the necessity for sincerity should be emphasized to
avoid misrepresentation of data.
Similarly the most of the records never show the real cause of
death in hospital patients, because regular postmortem is not
the rule for hospital patients.
Postmortem should be made compulsory in all the hospital
deaths and proper postmortem records should be maintained
along with suitable specimens for future analysis in cases where
the diagnosis is doubtful.
Very few hospitals conduct regular mortality case discussion
3
which should be made compulsory where in all the concerned
medical personnel should participate. Mortality due to negli
gence can be minimized by this techniqe.
Similarly local clinical and Research society meetings must be
made compulsory for all the hospital medical personnel.
Data Through Drug Stores
Data collection through Drug stores and pharmacies can also help
in assessing the health status of the local population. Hence the pharma
cists should also be educated in the significance of record keeping. To cite
an example if the consumption of antihypertensive drug is more in a
particular region the cause must be investigated in depth and such a study
may show some interesting data on the etiology of hypertension.
Stringent drug rules and their strict enforcement will save thousands
of people from the malady of spurious drugs and promote positive health.
Role of Statistician and Computer
These base line health data and the illness data collected by various
sources should be meaningfully analysed by competent, dedicated experts
in statistics to be of any future use. Since India is a vast country, the
quantum of data collected will be astronomical and it is impossible to
analyze them without the help of computers, i.e. suggested to have minor
computer centres at district level linked to a major computer centre at state
level which in its turn is linked to the master computer at National level.
Data fed into any of the peripheral should reach the Master computer unit
in a day to be really useful. The.result of these statistical analysis should
be fed back to the concerned people who are responsible for collection of
data to show various correlations and inference obtained in a simple non
technical manner, which will stimulate the morale of these tail enders and
others to collect more reliable data enthusiastically. Cross checks should
also be made to minimize the entry of wrong or spurious data and severe
deterents should be instituted to those who feed false data.
Some Special Aspects to be Considered
Special attention and care should be given to the health of children
and when education becomes compulsory, health education in schools will
go a long way in improving the health of the nation. Though health
education is available in schools of Urban area, schools themselves are non
existant in many of the Rural areas. Further health education to girls
should be given special emphasis since a previous study in Kerala has
shown that educated mothers have smaller families than uneducated
mothers. Similarly a health educated mother will propagate the value of
health to her future generations better than the males.
Since India is rapidly progressing in Industrialization proper health
care should be given to industrial workers and their family to protect them
from known occupational hazards. Pollution from industries should also
be borne in mind and the rules enforced strictly will go a long way in.
health of people of industrial belts.
4
Practically no official data is available on alcoholism and drug
addiction in India. Since prohibition has been lifted in most of the states
in India, and drug peddling has also come to the surface, data on these
areas are absolutely necessary for proper planning the course of future
action.
Lack of data or its availability and lack of proper analysis of data
has lead to the failure to understand the magnitude of certain conditions
like :
(a)
Incidence of Leptospirosis and Malaria in India.
(b)
Incidence of Silicosis in quarry workers.
(c)
Correlation between nutritional status and prevalance of diseases.
Finally the authors personally feel that it is the high time to reorient
the entire medical and para medical education towards positive health
approach if we are really serious about Health for all by 2000 AD. Nutri
tion and social and preventive medicine should be the major components
of Undergraduate as well as Post-graduate medical education which are
being given step motherly treatment in our present curriculum.
Based on the data collected and analysed, proper planning should be
initiated in consultation with local bodies to eradicate diseases and to
promote positive health.
5
INTERNATIONAL CONFERENCE
HEALTH POLICY : ETHICS & HUMAN VALUES NEW DELHI 1986
Rural Child and Health Development Team
Dr. P. Chandra, MD., DCN., MNAMS.,
Prof. & Head
Department of Paediatrics, Stanley Medical College,
Madras 600 001
The story of Child Health in India is one of needless, avoidable dis
abilities, and missed opportunities. Child Health is not an individual
problem. It is a family and community problem and has to be tackled at
the community basis. 70% of India’s children live in rural areas. The
health needs of the children in our country are entirely different from those
of affluent countries and do not require sophisticated technology. There is
a need to ensure that resources whatever their origin are channeled in to
socially relevant health action-Multisectorial Mass Action for social change.
A comprehensive National Health Policy has been accepted by the Parlia
ment signifying the political and Government will to Achieve Health For
All by 2000 A.D. The targets to be achieved stresses the importance of
Maternal and Child Health Services. The policy emphasises the preventive,
promotive and Public Health and rehabilitation aspects of health care and
establishment of Primary Health Services, to reach the population in the
remotest areas of the country. Ensuring adequate Nutrition, safe drinking
water supply and improved sanitation for all segments of the population
and Health Education are the other highlights of the Policy Document.
Like any other field of science, Medicine is witnessing a knowledge
explosion in all aspects. Advances in Paediatrics started as a trickle in
fifties, became a rivulet in sixties, a torrent in the seventies and a flood in
the current decade. There is a wide gap between available knowledge and
its availability to the most needy. Obviously we need a break through not
only in science and technology but also in organization, management, edu
cation and motivation. It is in the application of what we know that we
are failing even more than in the discovery of new knowledge. It is a
tremendous challenge for all of us if we wish to meet the Rural Children’s
Cause and Commitment.
The nation has developed a plan for rural services to meet the needs
of Mother and Child Health Care and Family Welfare. The assessment of
available resources, their proper allocation, efficient utilization are
important considerations for providing efficient Health Care Delivery.
Primary Health Care envisages a community based health system which will
emphasise the interdependence of health and development in all ramifica
tions and ensure the equitable distribution of available health resources
leading to accessibility and efficient health care. So optimum mix of
personnel of health and non-health sectors has to be done for most effi
cient health care services.
In India since our Independence, with the establishment of Primary
Health Centres and Rural Community Development Programme, it was
possible to take modern health development of people living in farflung and
hitherto inaccessible areas. Still the improvement in Health and Nutrition
Status of children is not commensurate with the effort. This has brought
in to question, review of the entire activity of Health Care Delivery with a
view to evolve a strategy more suited to the country’s condition. Health is
not medicine alone. Health development cannot be restricted to the deve
lopment of medical technology alone or devising, ways of applying the
technology. Primary Health Care has to look beyond health sector. It is
time to veer away from the concept of Medical Personnel working in
isolation.
The members to constitute the rural health development team and
their job responsibilities have to be redefined. There should be a vigorous
effort to integrate all agencies like rural development, agriculture, Womens’
Welfare Education, Nonformal Education and voluntary associations and
departments involved in the challenging task of improving the quality of
children everywhere. There is a need for a fundamental change in the
organisational set up in the block level. In the present changing situation
the Health Development Team has to co-ordinate various activities to
maximise efforts and accelerate development.
Team is defined as a group of people working together towards a
common goal. Team work is pooling of efforts co-operative working for a
common cause. All group of workers concerned with health development,
promotion, maintenance and recovery of health and prevention of diseases?
are members of ‘Health Development Team’. These members have different
qualifications, grades, strength, experience with different types of responsi
bilities varying according to the tasks it has to perform. The challenge of
achieving uniform health development is greatest in the villages. All
sectoral plans and programmes for the social development in the villages
have isolated approaches quite independent of each other with obvious
overlap. It is imperative that if we are serious to achieve meaningful
results within the next decade, within the financial resources, there is no
alternative to the exploitation of available manpower and financial
resources, available wjth various departments and agencies concerned with
Growth and Development, in the most well planned and co-ordinated
manner. All vertical programmes running virtually independent of each
other with very little co-operation at planning, supervisory and field levels
have to be integrated tota ly and formulate well planned and co-ordinated
practical programmes, (van Illick says ‘there is a great deal of medical
capability outside the medical profession and unlimited opportunities out
side formal institutions’. So the functionaries at the block level who should
be the members of the Health Development Team are to be from all walks
of life.
From (1) Health and Family Welfare
(2)
Rural Development
(3)
Social Welfare
(4)
Education
(5)
Non formal Education
(6)
Water Suiply and Sanitation
(7)
Agriculture
(8)
All Voluntary and Philanthropic Institutions
(9)
Mass Media.
The objectives of the team will be, all the welfare activities including
health is to be expanded to cover all the population, particularly the
vulnerable, improving the functioning and utilisation within the present
system.
All the concerned team members should be made to
(1)
understand the local maternal and child health problems well to
develop a cost effective health care system.
(2)
Study the problems in implementing existing programmes e.g.
administrative obstacles, female illiteracy and the gap in out reach services.
(3)
Study the conflicts in implementing welfare programmes for
mother and children, (e.g.) deep rooted cultural beliefs.
(4)
Learn how to provide technical education to family members and
local volunteers.
(5)
Learn methods of mobilization of people in the village parti
cularly women for promotion of health.
(6)
Understand importance of documentation of health events,
evaluation and accountability.
Rules and roles for the team members can be so defined as to provide
built-in flexibility, within a clearly defined broad policy framework. Each
block can assign responsibilities and tasks, allocate resources, and set
targets according to the local priorities, health and family welfare needs of
the people, (e.g.) (a) areas where nutrition status is poor nutrition input
must be maximum. In most backward areas female literacy must have top
priority. Many of the maladies of the present system can be cured at the
village level by a very effective team by involving the family itself. The
goals to be achieved also has to be streamlined, (e.g.) The short term goals
of the team will be, achieving.
(a) 100% Antenatal care
100% Natal care
100% immunization coverage
100% Infant follow up.
(b) Training and educating the team in recent advances in child
health care, e.g.) growth monitoring, oral rehydration therapy, breast
feeding, weaning and food supplementation, female literacy and family
spacing.
The overall objectives of education and information with communi
cation programmes of the team is, to educate and mobilise the neediest
sections of the rural population so that, they can themselves initiate actions
to achieve and maintain an acceptable standard of health and family
welfare.
The long term objectives will be3
(1)
To inculcate a sense of self reliance and discipline in all segments
of population, so that all four sides of the health square i.e. prevention,
promotion, cure and rehabilitation are effectively handled at the local levels
consistent with development in the field of medicine.
(2)
To improve public health and public health services, to achieve
health for all with expected reduction in mortality and morbidity.
(3)
Universal education and total female literacy.
Training and education of the team and through them the community
is a challenging task. It is on the ability to elevate the standards and
reliance of the community the success can be judged.
Success in one area will turn up problems from an unexpected
direction e.g. once malnutrition and infection is tackled, cardiovascular
degenerative diseases may take an upperhand. The team also should anti
cipate and plan programmes for the future.
This approach will help all to move from knowledge to action.
Tomorrow is too late to help to-day’s children.
I
COM.M ’Sir? Hn.ris-LL
47/1.
rloor) St. Marks Roadp
Bangalore - 560 001.
INTERNATIONAL CONFERENCE
HEALTH POLICY : ETHICS & HUMAN VALUES NEW DELHI 1986
Population Explosion and Health Policy—
Ethics and Huamn Values
Dr. K.L. Wig
Emeritus Professor and Former Director of
All India Institute of Medical Sciences
The great importance of\ copulation explosion in the formulation of
health policy is recognised by nearly all countries all over the world. The
developing countries, however, consider it of paramount importance.
While the highly developed countries have become somewhat lukewarm
over this problem because they have controlled their populations and their
people are well educated and have attained a high standard of living—the
two important measures for the control of population—the need of such
control for the developing countries and perhaps, most of all for India,
because of its vast population is extremely urgent.
Before dealing with the subject of my address I may quote the defi
nition of the three terms used for the main theme of the Conference.
Dr. Edmund Pellegrino defined as follows the three items, during
his key-note address at a similar Conference in Athens.
—The health policy of a nation or a community is its strategy for
controlling and optimizing the social uses of its medical knowledge
and resources.
—Human values are the guides and justifications people use for
choosing the goals priorities and means that make up that strategy.
—Ethics act as the bridge between health policy and values. Ethics
examines the moral validity of the choices that must be made and
seeks to resolve conflicts between values, which inevitably occur
in making those choices.1"
One of the important factors that determines health policy, therefore,
is to find out what the basic cultural, ideological, ethical and religious
traditions of a nation are, and how they can be harmonised with the health
needs of the nation.16
Family planning which is essential for controlling population explo
sion, however, presents one unusual feature. While its urgent need
is acknowledged almost universally, when we go into its methodologies
and the choice of such methodologies—there is hardly any method which
does not evoke controversy. Such controversies are based mostly on
ethical, cultural and religious factors and human values which naturally
show some differences in different nations and various communities, in the
same nation. Legal views and laws on such matters which I think, are
predominantly based on ethics and human values, also differ, to some
extent in different countries. Some objections of course are based on
medical grounds. It is somewhat strange that while the importance of
family planning is acknowledged universally, no other subject which enjoys
such universal acceptance as a basic idea evokes greater conflict with ethics
and human values than family planning when you go into the details of
its working.
The urgent need of family planning needs no emphasis. In India it
should be regarded as number 1 national problem for unless we attain
success in our population control methods, all our planning and other efforts
for improving the economic condition of the population of our country
and improving the lot of poverty stricken millions the majority of whom are
in a state of malnutrition and for achieving the goal of “Health for All”
by the year 2000 AD will go away and may practically come to nothing.
Our Government is spending millions on what they call family welfare,
but the question that arises in the minds of those who are unprejudiced
and are willing to listen to the calculations of those who are trained in
such problems, is—are our efforts showing signs of success and are they
likely to bear fruit in time before the situation attains dimensions that will
defy all solutions ?
The birth rate in India in 1984 was 33.8 per thousand and the death
rate 12.5 per thousand. The population growth rate is thus near about
2 per cent. This means that we arc adding every year 16 million human
beings to our population. This according to most demographers will mean
that by the year 2000 AD a year by which we are committed to “Health for
AH”, we will have a population nearing the mark of 1 billion. It is incom
prehensible that we can provide health for all if the population by that
year attains as high a level as stated above. There is another adverse
effect of this state of affairs that I may point out. Most demographers
point out that a big portion of this population, unlike that in developed
countries, where birth-rate is controlled but longevity has gone up, will be
of younger people of marriageable age. The result of this inbuilt demo
graphic momentum is that even if present family planning efforts succeed
to reduce the growth rate to one per cent by the century end, the popula
tion will eventually stabilise in 2050 at 1250 millions. A delay of 20 years
in reducing the growth rate to one per cent will accelerate the stabilised
figure to 1.9 billions and of another 20 to 2.6 billion.
To give an idea of the strains placed on the economy by unbridled
population growth let us see what the impact of the 136 million population
added during the seventies decade will mean. The Ministry of Health in
a very modest calculation that placed the direct cost of maintaining the
additional population at an average income level of 1000 per year has
given the estimate of Rs. 13,500 crores as the additional annual require
ment to cope with this decade’s increase alone. It has been estimated
that an additional resource requirement of 11,850,000 quintals of food,
180,000,000 metres of cloth, 121,000 schools, 355,000 teachers, 2,390,000
homes and 3.8 million jobs for the seventies explosion. Now through the
eighties an annual 16 million is being added as opposed to the 14 million
annual average of the seventies.1
Since 1974, the global population growth rate has declined from 2.03
2
to 1.67 per cent per year. In the next decade the growth rate will decline
more slowly. However, the annual increase in numbers is expected to
continue and may reach 90 million per year by the year 2000. Ninety
per cent of that increase will occur in developing countries and at that
time 6.1 billion people are expected to inhabit the earth2.
When we come to the various methods employed for family planning,
there is a big range already available, though in a country, like India,
efforts are still going on so far as the research field is concerned to find
a method which may have the widest possible acceptance and may be free
of risk and highly efficacious. So far as the available methods of reason
ably proved efficacy are concerned at one extreme is abstinence and at the
other extreme is medical termination of pregnancy (M.T.P.). Abstinence,
of course, can have no moral or ethical objections. It had the support of
saintly personalities like Mahatma Gandhi. In fact, even some religious
group3 and their leaders which on religious grounds are fundamentally
against all artificial means of family planning are not against it by what is
called natural methods. Some of them have tried to find its modifications
like the rhythm method which has been improved lately by finding the
mucus secretion of cervix which precedes ovulation and which the woman
can be taught to find for herself, and which thus indicates to her the day
of ovulation. However, while such methods may have some practicability
amongst the well educated, closely knit religious communities, it cannot
have much utility for checking the population explosion so far as the vast
mass of 750 millions (out of which 127 million couples are in the reproduc
tive age period), are concerned. In fact, a further improvement may occur
in this method, i.e., science may very soon reveal a method by which the
actual day of ovulation may be found nut by simple tests, yet even then
human nature and instincts as they are it-will not make this method
feasible so far as the control of population explosion is concerned. So,
while some communities and religious groups and their leaders are still
advocating it. we may not discuss it further in a limited address.
The methods of family planning and contraception are so numerous
that I cannot discuss the ethical and human values of all of them, but I
may select three items which have evoked or are likely to evoke the maxi
mum controversy on grounds of ethical and human values and their inter
connected legal aspects. They are : (1) Enforcement of a policy of limited
number of children by various types of legislative measures, (2) voluntary
sterilisation and (3) M.T.P. (Medical Termination of Pregnancy).
China by launching a one-child policy claims to have achieved a
spectacular success in their family planning programmes and restriction of
copulation growth. Some independent observers have confirmed this
claim. Though India was the first country to adopt family planning as
an official programme and can claim some reduction in birth-rate, its
population growth is still maintaining an alarming tempo. Can we, as
also the other democratic developing countries of the world, achieve
success in time to limit our population to such a level that it will not
affect our economic growth and other programmes for prosperity and
removal of poverty ? This raises a highly ethical and legal question for
a conference like this. In such democratic countries, especially in India,
the riahts of an individual reign supreme. They cannot be interfered with
except to a limited extent in the event of a war or threat to national secu-
rity, even though as is evident from the details that I have given above,
the issue of family planning upon which future prosperity and stability of
the country depends is of no less importance than the destruction caused
by an actual war. However, unlike wars—speaking in medical terms it
is not a question of sudden death but a lingering existence of starvation
and malnutrition for millions. All the same a question arises, “Can any
democratic Government impose its will and order that no family can have
more than two children and impose penalties if this rule is violated ?” If
we find at some stage that our present developmental schemes and plans
are not bearing fruit and the deluge in population seems to destroy all
hopes of health, prosperity and well-being of our future generations, can
we have legislation in which the state in this particular matter of number
of children in a family impose its will on the people ?” This would actually
mean that because of an emergency we make the rights of an state or the
nation as a whole supersede the rights of an individual. Individual human
values and rights in practice if not in a written law include right freely to
choose the time of marriage (subject to legal minimal ages); the right to
decide on the number and spacing of children in the family (the right to
contraception) and to decide about one’s own body in relation to this
(sterilisation and abortion, within existing legal constraints)4.
As an alternative to the above type of legislation which would be
repugnant to principle of human rights, can the great legal experts make
some other suggestion which may make people limit their families and thus
ensures progress and prosperity.
Let us, however, hope that the contingency for enacting the above
type of legislation or some similar action will not arise. In facts, at the
1984 United Nations International Conference on Population in Mexico
City there was still some difference of opinion amongst nations over future
policies. For example, while the Vice President of Kenya told the meeting
that the world “cannot wait for the crisis of over-population to right itself
through economic development” the United States delegation presented
an opposing view and gave examples of Hong Kong and South Korea
which though had scarce natural resources had made swift progress by
relying on the creativity of private individuals working within a free
economy. However, the consensus amongst nations was that family
planning is needed to supplement the effort of economic development in
reducing population growth, and almost all developed and developing
countries endorsed at the Mexico City Conference, family planning as an
integral part of development, and acknowledged its contribution to the
health of women and children5.
How difficult the question of family planning is and how it is almost
impossible to meet the social objections to it'which will very from country
to country according to their own cultures and traditions will become
apparent if one goes through some of the recommendations on family
planning at the Mexico City International Conference on Population held
in 1984.
Recommendation 25
Governments should, as a matter of urgency, make universally avail
able information, education and the means to assist couples and indivi-
duals to achieve their desired number of children. Family Planning infor
mation, education, and means should include all medically approved and
appropriate methods of family planning including natural family planning,
to ensure a voluntary and free choice in accordance with changing individual
and cultural values. Particular attention should be given to those segments
of the population which are most vulnerable and difficult to reach.
Recommendation 30
Governments are urged to ensure that all couples and individuals
have the basic right to decide freely and responsibly the number and spacing
of their children and to have the information, education and means to do so;
couples and individuals in the exercise of this right should take into
account the needs of their living and future children and their responsibili
ties towards the community.
A
Recommendation 31
<
Legislation and policies concerning the family and programmes of
incentives and disincentives should be neither coercive nor discriminatory and
should be consistent with internationally recognised human rights as well as
with changing individual and cultural values.
Recommendation 33
Governments that have adopted or intend to adopt fertility policies
are urged to set their own quantitative targets in this area. Countries
implementing family planning programmes should establish programme
targets at the operational level, respecting the basic right of couples and
individuals to decide freely and responsibly the number and spacing of their
children, taking into account the needs of their living and future children
and their responsibilities, exercised freely and without coercion, towards the
community.6
<. )
k.
You can see how carefully these recommendations are worded and
how carefully that organisation has avoided objections from any country
on social and ethical grounds. For various countries according to their own
culture may have their own objections. They are giving in every one of
these paragraphs precedence to human rights. But will developing coun
tries attain appreciable success under these conditions.
It is, apparent that while a vast number of countries especially the
developing ones are in favour of family planning, there are objections on
social, human, ethical and legal grounds from Nations and communities in
the same nation and every question concerning the family planning be
comes a complex one. It is for the various learned speakers who will be
taking up various aspects of this subject to throw light on some of the
points that I have raised.
The next item that I may take up is of voluntary sterilisation. In
the beginning there was a lot of opposition to it in many of the well deve
loped countries on certain moral grounds, as the opponents said that it
amounts to mutilation of the human body either in the man or the woman,
5
i e vasectomy in males and tubectomy in females Moreover, there was
opposition to it because it is irreversible. It is in fact the mam method of
irreversible nature-though scientists and surgeons are making efforts to
make the two methods one in males and one in females reversible. Tubec
tomy is being done extensively now through the endoscope (laproscope).
The fact that now tubectomies are being undertaken far more commonly
than vasectomies, though the latter is a much easier operation almost free
from risks only shows the continuing domination of man over woman
which still persists in most countries.
These irreversible operations are'open to one great objection and that
is that why should they be resorted to when reversible methods are easily
available, for if the existing off-springs die due to unforeseen circumstances
the parents become issueless for ever. So, interconnected with the successes
of these operations must be a sustained effort to diminish infant mortality.
In developed countries where reversible methods can be easily followed by
well educated couples, these irreversible methods are no longer favourites,
However, in countries like India where millions and millions of couples in
the reproductive age period exist and cannot be relied upon to use consis
tently the reversible methods, these irreversible methods have remained the
most favourite with administrations. In India it is the most favourite
method with the state governments. This is especially so because it ensures
certainty of results. It is so far done after there have been two children
unless the parents themselves volunteer to get it done earlier. Many state
governments expect some sort of targets from their doctors though they
may not do it openly.
In many of the well developed countries there have been long contro
versies over whether voluntary sterilisation (they never even dream of
forcible sterilisation) should be allowed at all or not. In some countries,
it is still illegal, but generally speaking in most countries a liberal view is
being taken and voluntary sterilisations are either being allowed by law or
at any rate being overlooked, and no prosecutions are done. In India,
however, voluntary sterilisation as I have said is favoured, but there is a
strong public opinion against forcible sterilisation which a democratic
country like India will never allow whatever the needs of the country may
be. This raises, in fact, again the question of individual rights versus the
right of the State to impose its will. However, we should avoid reaching
that stage.
5
The guidelines protecting voluntarism and ensuring safety should,
however, take priority over more administrative matters.
steri 11^1^7?
Iegal issue today is how t0 insure that
iksa n'.u'vS.'n,he decisi“w be
*
.sxs "Si S’o.”“ulty “
?'y
ouite a lot of whom
‘ , 10 our masses of rural population,
proper applicability of these methods “ouf^f0 Xte^T? ‘7
controversy
lies as regards
main
which
I will mention
later MTP
TP d
ain ramifications of this method
6
'
Sak®
avoiding unnecessary objections, it has now been
termed Medical Termination of Pregnancy (MTP) and the word abortion
is hardly ever used. Feelings in certain countries are so strong on this
question that in the last International Population Conference in Mexico,
USA made the banning of abortion as a measure of population control a
central condition for its population assistance. Moreover, laws for termina
tion of pregnancy raise another ethical question—‘has a foetus a persona
lity . If it has a personality, it naturally has rights.
According to the latest Indian law on medical termination of preg
nancy, such termination has been made permissible under certain condi
tions. The Indian law was enacted in 1971 to protect the women’s rights,
if there was a fear that future physical or mental health of a woman is
imperilled if pregnancy continues. In this connection one out of the various
clauses that allow termination may be quoted :—
1.
If the continuance of the pregnancy would involve a risk to the
life of the pregnant women or of grave injury to her physical or
mental health.
Inclusion of mental health, in fact, makes the attitude of law towards
termination quite liberal but reasonable,- for any unwanted pregnancy is
going to have psychological effects on the mother. Explanation of the
above clause states :
“Where any pregnancy occurs as a result of failure of any device or
method used by any married woman or her husband for the purpose
of limiting the number of children, the anguish caused by such unwan
ted pregnancy may be presumed to constitute a grave injury to the
mental health of the pregnant women.”
This explanation makes the permission liberal indeed and almost any
case who has been making attempts to use cuntraceptives can come under
Though the above law was enacted for a different purpose, it must be
conceded that indirectly it may help population control, as a sizeable
number of patients in whom contraception fails will in all sincerity take
recourse to it. However, it must be acknowledged that MTP as a means
of population control means a failure of contraception either due to care
lessness or due to chance or due to ignorance. We must, however, see the
other side of the picture, also. If it is not made permissible under the law,
the acts of termination will go into the heads of the unqualified persons
which means a very high increase in complications and even fatalities. Such
cases have been quite frequent in many countries including India. That in
itself is a big justification for evolving the present law on medical termina
tion of pregnancy. In fact, in the short run it has been said that a desire
for effective contraception also leads to an increase injabortions. Because
of this inter-ralationship, contraceptive and abortion services need to be
linked.8
I think there will be no difference of opinion as regards the necessity
of MTP when the future physical health or the life of the mother is in
7
danger for you have to save one of the two lives and the mother’s life is
no doubt more valuable of the two. Even the most conservative and
religious minded persons will not contest it. However, considerable diffe
rences of opinion arise when we consider the mental health and future
psychological state as a result of an unwanted pregnancy. For a doctor,
however, future mental health is as important as physical health. However,
such a justification does give considerable handle for malpractices.
The opposition to MTP as a means of population control is, however,
understandable. When other effective methods of family planning are
available, why should we destroy a life just because a couple has been
negligent and did not practise the method properly. So, they argue on
ethical grounds that induced abortion should not be included as a method
of population control especially as it destroys a life which legally speaking
has a personality of its own and we have thus, no right to destroy it.
However, the protagonists of MTP who want it to be included as a plan in
family planning argue that as no contraceptive method is infallible, an
unwanted pregnancy should be terminated and, so, I understand certain
countries are very liberal about MTP. They further argue that the popula
tion control for developing countries is a national need which should be
treated as an emergency and must supersede all other considerations.
Moreover, when laws to prevent induced abortions are made more strict it
only leads to the emergence of quacks and secret abortions which increase
manifold the risks to the health and life of the mother. Thus, on this
ticklish question of MTP which involves moral values and religious and
ethical beliefs a consensus of medical and legal opinion is needed as to how
liberal the legislation should be to allow MTP as a legitimate method of
family planning without leading to immorality and sexual promiscuity,
especially at the level of very young age groups. As I have said above, if
it is not liberalised it only leads to abuses and going to quacks. The major
problem, therefore as regards moral and legal issues involved in MTP is
one of proper implementation.
All that I have said above, of course, does not obscure the fact that
the debate over abortion, even in countries where the law has been refor
med, is a passionate one.9
A few related questions may be discussed at this stage. With the
advances in medical sciences, especially ultra-sound examination and
amniocentesis, it is possible in some cases to see if the future child is going
to have physical or mental abnormality. What should be the criteria of
judging which deformity or abnormality, physical or mental, is going to be
so serious that termination of pregnancy is justified. Divergences of
opinion are bound to occur. But it is for medical men and social workers
to devise criteria for allowing MTP in such cases. However, a more serious
problem is arising in this country and may be in some other countries. It
has become possible by the above methods to find out the sex of the future
child. As a theoretical or purely scientific exercise it is interesting but the
knowledge of that to parents is likely to be used for one purpose, especially
in families which have a preponderance of female offsprings. They wifi
utilise the knowledge for secret termination of pregnancy if 'the foetus is
found to be a future female child. This means in a wav reverting to the
age old highly unethical practice long since prohibited by law of female
8
infanticide. Rather than to take this risk, will it not be better to prohibit
oy law the emergence of laboratories which reveal this knowledge to the
parents in early stages of pregnancy.
If induced abortion is to be considered strictly from the moral and
religious angle then certain reversible methods may actually be leading to
the induction of abortion but are not being categorised as such. For
example, MR (Menstrual Regulation) by protaglandins or by an MR
syringe is certainly an abortion in a vast majority of cases. Should it be
allowed even though foetal life at that stage is very early and almost invi
sible. Use of certain drugs may possibly be also an abortion of the foetus
at a very early and almost invisible stage. If a vaccine against protein
carriers of vitamins to the foetus becomes successful that will also be abor
tion at a very early stage of the foetus—only killing it before it become
even recognisable as a foetus. So, if religious and ethical and moral con
siderations prevail there will be objection to such methods also which are
ordinarily regarded as methods of contraception but are really abortions at
a very early stage before the foetus becomes even anatomically visible to
the naked eye.
There are many reversible methods of contraception such as con
doms, pills, insertion of copper T etc., long acting injectables, some herbal
medicines such as gassypol—a Chinese herbal medicine for males—and
coitus interruptus. There are not likely to be any ethical objections to
such methods except by the most conservative and religious groups who do
not want any interference of the natural process, but there can be objec
tions to all such methods on health grounds or on grounds of inadequate
acceptability. We need not discuss that.
An associated question is the question of incentives and disincentives.
There have been not discussions on this question. However, the main
objection which involves ethical values as regards some incentives and
nearly all disincentives is that why should a third or a fourth child suffer
from certain handicaps in comparison to other children who may be even
less bright than him/her, because his/her parents made the mistake of not
falling in line with a policy which was very important from the national
point'of view. Why should the sins of parents be visited on off-springs.
His/her parents may deserve those handicaps but why should the child
suffer who committed no fault ? It is an important objection from the
ethical point of view and, so, there should be no question of disincentives,
thought some incentives may be chosen carefully and may help to some
extent in carrying on the family planning programme specially in certain
limited circles like industries etc.
There are two other issues which I cannot/take up in detail, but
which are worth mentioning. One is reducing the infant mortality. In
India it is still shamefully high. It is higher than that of many developing
countries and was 104 per thousand live births in 1984. It is generally
admitted that family planning is acceptable only if the infant mortality is
low and most children which are born have the prospect of living a normal
life The Family Planning Foundation is in the process of investigating in
collaboration with the International Development Research Centre (IDRC),
Ottawa Canada, whether such a statement is a fact or not so far as Indian
9
conditions are concerned, and also find out the high risk factors associated
with infant mortality in various areas so that the Government may be
helped to mount an intervention strategy. There can obviously be no
ethical or human objections to it and the lowering of infant mortality will
be welcome to all communities. The second important factor which promotes
family planning is raising the status of women. For quite a number of
extra births take place because the parents want a male child. Moreover,
a woman seems to have in this country only a small place in deciding the
number of children that she should have. The need of raising the status of
women is still felt even in the most developed countries for the opportuni
ties for all types of employment are still less for women than what are
available to males. Governments should formulate and implement con
crete policies which would enhance and raise the status of women.10
It is a proven fact that in development countries that to the extent
to which legislation ensures full and free access for women to education
and to employment on terms and conditions of complete equality with
men, the effect will be to reduce fertility.11
An important point in this connection is raising the age of marriage
of the girls. If that age could be raised from 18 to 21, and sterilisation
could be induced as far as possible after the age of 30 there will be a very
shary fall in the number of births. According to demographers, nearly
half of the births occur before the age of 20 and after the age of 30. There
can be no ethical objections to raising the age of marriage in girls if it is
done on the grounds of improving or saving the health of the young girls.
However, legislation for this purpose is not likely to succeed and will have
ethical and moral objections in addition. It means an interference with
human rights of the individual.
It must be realised that there is no method of contraception which
can have no objections, is absolutely safe and is fully efficacious and uni
versally acceptable. That is why research is going on and on to find a
most acceptable, most efficacious and most harmless method. However,
the problem is so urgent that we cannot wait for the results of such
research. Even when there are some minor objections and flaws on
grounds of health and efficacy, we have to look at such problems from a
different angle, i.e., greatest good of the greatest number and the acute
need of the nation. So occasional small risks have to be taken.
The doctors are, of course, needed for the execution of the various
methods and are key-figures in teaching the public the various techniques
etc. However, they have one greater role to play and that is to mould
public opinion in favour of family planning. Doctors alone cannot achieve
success in family planning. If we want great results, family planning has
to become a people’s programme. Thus, it is necessary to develop exten
sively public opinion in/its favour especially at the grassroot level. The
doctors come in close touch with the family and the general practitioner
who is a family physician and almost a family member for most families
can thus be a great factor in developing proper public opinion in favour of
our family planning programme. It must be realised by all of us that
family planning which may be technical easy is socially difficult and
doctors can be a great factor in overcoming that social difficulty. Non
10
government Voluntary Organisations can also play a very great role in
this direction. In fact, that should be their chief role in addition to help
ing the government in their programmes. Let us hope the combined
efforts of the government, the medical profession and the non-goverment
organisations like the Family Planning Foundation achieve significant suc
cess in the Seventh Plan so that we may succeed in our health for all
programmes by the stipulated year 2000 A.D. and enter the next century
in a prosperous and hopeful vein.
References
1A. Edmund & Pellegrino. Key Note address at Health Policy—Ethics
& Human Values Conference at Athens in 1984. Published in Highlights
of Athens Conference—XVIII CIOMS, Round Table Conference, Athens
1984. Edited by John H. Bryant and Zhijniew Bankowski 1986. page 7,
IB. Robert Veatch.
Some as above!. Page 11.
1. Address by Shri B. Shankaranand, Minister of Health and Family
Welfare, Government of "India, at the Conference of Voluntary Organiza
tions on Promotion of Family Welfare Prgramme.
2.
Mexico City Declaration on Population and Development.
3.
Ganguli, H.C. Sexual Behaviour : A New Perspective in Family
planning—Publication of the Department of Psychology, University of
Delhi, 1984, pages 18 and 109.
4.
Law and Fertility in Europe edited by Maurice Kirk et al—Publi
cation of the European Centre for Research and Documentaion in Social
Sciences and International Union for Scientific Study of Population—1975*—
Preface page II.
5.
Malcom Potts—Population and Politics (leading article) BMJ
1984, 289-641.
6.
Ibid.
7.
Law and Planned Parenthood—Edited by John Paxman for Inter
national Planned Parenthood Federation—1980, pages 38 and 59.
8.
Ibid.
9.
Ibid.
Mexico City Declaration on Population and Development.
10.
11.
Trevici, V. Law and Social Status of women—Law and Fertility
in Europe (same as 4) 1975—page 97.
INTERNATIONAL CONFERENCE
HEALTH POLICY : ETHICS & HUMAN VALUES NEW DELHI 1986
A Look at Rural Surgery in
Private Sector in India
Dr. R.R. Tongaonkar, M.S.
Dondaicha, Dist. Dhule 425408
80% population in India is residing in Rural Areas, besides solving
the Health and Medical problems of this population, we need to cater for
their Surgical needs also. This is done by Government Sector through
Primary Health Centres, and Cottage Hospitals but quite a substantial
Surgical work is being done by Private Rural Surgeons.
Let us see the role of these private Surgeons in delivering surgical
care in rural areas, the type of surgical practice in villages and the pro
blems and difficulties faced by the Rural Surgeons.
This paper is based on a Study conducted in an Backward Adivasi
District of Dhule in the State of Maharashtra and analysis of 5769 total
Surgical operations done by the author during 18 years of his work in a
small private Rural Hospital in the town of Dondaicha which is not even
a Taluka place.
From the Statistical Study of the District it was found out that in
1984 total 11724 operations were done in Government Sector out of which
only 3362 were done at peripheral hospitals. In private sector 11652 were
done out of which 2924 were done in Rural Hospitals.
If we compare the individual work done by private General Surgeons
in Dhule City proper with that done by peripheral Private Surgeons it
could be seem that the City Surgeon is doing on an average two hundred
operations per year, while a Peripheral Surgeon is doing more than four
hundred operations per year, double the work than his colleague in City.
This is partly because the rural public is getting surgical facilities at
their door steps as can be seen from the map which shows that the Govern
ment Civil Hospital which undertakes major surgical work is placed at
one corner of the District almost 130 Kms. away from the farthest point
to reach this hospital for free treatment, the patient who is usually
poor, has to first travel by a bullock cart or a hand cart or some times in
hilly areas on hands or bamboos to reach the nearest bus station and then
to spend about Rs. 120/- as fare for himself and his accompanying persons,
at least 2-3 relatives, and almost 2 days having a night halt somewhere,
instead he prefers to pay the nearby peripheral Private Surgeon. That is
why there is lot of work to do for a Private Rural Surgeon.
But the nature of Rural Surgical Practice is entirely different as com
pared to city practice. The patients do not differentiate between a Physi-
cian, a Surgeon or a Gynaecologist so there is more work of consultation
taking major part of the Surgeons time 9 A.M. to 5 P.M. In 18 years
practice there were 75060 O.P.D. patients as compared to only 5769
operations.
Emergencies are much more common in comparison to city practice
and disturb the sleep of the Surgeon almost daily.
As there are no assistants, Registrars or house-surgeons to work
under him even after 18 years of practice, he has to carry out minor proce
dures like circumcisions, suturing CLWS, opening abscesses and what not.
He has to maintain his own Nursing home for which he has to first
find out a building. There are no good buildings and the hospital may
have to be set up in any old building built in kachha mud, but the build
ing can be modified and decorated at least internally using asbestos sheets
or plywood to form false roof and false walls.
As there are no Pathologist the Surgeon has to keep his own Labora
tory and blood Transfusion Service, and a small X-ray machine on which
no special investigations are possible.
There are no facilities for frozen section biopsies.
In abscence of special investigations, clinical judgment is the most
important armamentarium in diagnosis.
Coming to the operation theatre equipment, usually the rural private
surgeon is coming from a poor or middle class family and cannot afford
to have sophisticated equipment at least in the beginning of his career,
even then he has to keep enough stock of all the materials as neither he
can purchase them immediately nor can he borrow from anybody.
Maintenance of costly equipment is a problem and the Surgeon
himself has to repair his own equipment using gadgets like multimeters,
with the help of local technicians.
Electric supply failure is a very common event and a stand by
arrangement for emergency lighting and foot operated suction machine
have to be kept ready and if possible a generator set installed.
Hard water can ruin the electrical heating appliances and instruments.
Ion Exchange water softners can solve the problem.
Oxygen refilling takes months to get the cylinders refilled. Industrial
Oxygen available locally for welding purposes can be used safely.
Anaesthesia is a big problem. Qualified anaesthetists are not avail
able and either wife if medico or some other local doctor has to be trained
for anaesthesia or some times the Surgeon himself has to induce anaesthe
sia and maintain the patient on Ether bottle. In abscence of Oxygen
supply the only apparatus available is on Oxford of Bellow and some kind
of Ether vaporisor.
2
With all these the Surgeon is now ready for operation, but he has
no qualified staff and nurses, the hospital staff usually consists of his wife,
who should preferably be a medico, and 3-4 unqualified staff trained in
the same hospital.
tlie operation table the Rural Surgeon has to handle Surgical
problems from any system and speciality of surgical field. The analytical
data of surgical procedures carried out by author in 18 years shows that
out °f 5769 °Perati.ons 306 were on head and Neck, 601 were of ENT,
1088 of Gastro-Intestinal tract, 534 Urological Procedures, 1423 Orthopaedic Procedure, 1585 Gynace Procedures and 302 miscellaneous opera
tions.
9
Thus it can be seen that the Rural Surgeon not only has to under
take general surgical work but also orthopaedic work reducing fractures,
ENT Work knocking out tonsils, gynaec work doing D & Cs and hysterectomies and obstetric work conducting difficult deliveries. In fact these
three specialities form almost 65 % of his surgical practice.
But usually he is qualified as a General Surgeon and has no experi
ence of doing these operations and at least in the beginning of his career to
perform any new operations is a night-mare for him.
As a Surgical Registrar the author has removed only one sided tonsil
that too unofficially begging the favour of E.N.T. Registrar and had to
run away leaving the operation half way as the E.N.T. boss came in.
The General Surgeon’s knowledge of gynaec and obstetric operations
is probably limited to whatever he has seen as under graduate sitting in
the operation theatre gallery, but in his practice the Rural Surgeon not
only has to do Caesarean Section but even he has to use the so called
obsolete methods like craniotomy and evisceration which he has never
seen in his student life.
Besides surgery the Rural Surgeon has to admit all cases needing
hospitalisation like unconscious patients, patients with high fevers, convul
sions, status asthmaticus, heart attacks and some times even schizophrenics.
So it is urged that a Rural Surgeon should be specially trained. It is
suggested that after getting basic post -graduate qualification in General
Surgery, the surgeon, if wants to settle in rural areas he should be allowed
to do house-posts for 6 months in Gynaecology and Orthopaedics and
short posts in ENT and anaesthesia. In his basic training more stress
should be given to clinical methods of diagnosis and he should be taught
to handle equipments like X-ray machines and preliminary knowledge of
bio-engineering and repairs and maintenance of these equipments, should
also be given to him. Simpler but useful procedures, may be obsolete, in
fields like anaesthesia and obstetrics should be specially taught to him to
make him jack of all but Master of Surgery.
Besides all these technical and clinical Problems the Rural Surgeon
has to face some social and personal problems, as already said his wife
should be a medico not only because she will help him in his practice
tremendously, but will not get bored in village life with no facilities for
3
entertainment—not even good people to talk with. Children education
is the biggest problem. The Surgeon has no academic life and cannot do
any research, but on the whole the life is calm and quiet, people respect
him all over and in due course of time he earns enough to have a good
livelihood and is probably happier than in his colleagues in big cities.
That is why now more and more surgeons are coming to villages and
settling at peripheral places as can be seen from the map thus delivering
surgical care at the door steps of village people. So also more and more
Government agencies like Primary Health Centres and Cottage Hospitals
are recently being set up improving the medical facilities in rural areas.
That is why now it is rare to see gangrenous hands due to tight plaster un
reduced dislocations with nerve palsies, patients with huge hernia, and
advance breast lesions, intestinal perforations with shock, bladder stones
with recto-vesical fistulae, huge ovarian cysts occupying all the abdominal
cavity sometimes with bleeding gynaec problems brought in almost exsan
guinated state and ruptured uterusis due to obstructed labour, a seen
commonly encountered by the author in the Seventies.
Blind faith is also disappearing fast and now it is rare to see a mori
bund child with branding marks all over abdomen, hdy ash applied to
this fore head and a' sacred thread tied to his wrist. Even Adivasies now
bring their*?yotmg.agnes not only for emergencies but also for routine
Surgical trefffmenf.
' ** '
’
Even then a lot needs to be done to achievff-the goal'll ^Health for
all by 2000 AD” especially in rural areas. Government agencie? ftlbfie- •
may not be able to fulfil this goal. The private surgeons have a big role to
play in the coming future in achieving this target, therefore it is urged that
more and younger surgeons should come forward and settle in villages
thus serving the masses and helping the nation and the mankind as a
whole.
„
SO: JAMA. 1997 Sep 10; 278(10): 851-7
____This source is Available in S.J.M.C Library
____Call Number; From: 1918+
LA: ENGLISH
AB: OBJECTIVE: To provide clinical guidelines -for primary care physicians who
are dealing with domestic abuse and who have both the abused woman and her
partner as patients. PARTICIPANTS: A 15-member expert panel with members having
experience in family practice, gynecology, emergency medicine, medical ethics,
nursing, psychology, law, and social work; an 11-member consulting group with
members representing medicine, consumers, police, psychology, social work, and
nursing; and participants from focus groups including 48 previously abused
women and 10 previously abusive men. Members of the expert panel and the
consulting group were recruited by the research team. Focus group members were
recruited through the agencies from which they were receiving services.
EVIDENCE: Available research information, and opinions of the expert panel, the
consulting group, and the focus group participants. CONSENSUS PROCESS: Scoring
of 144 clinical scenarios was performed by the expert panel using a modified
Delphi technique involving 4 iterations. Scenarios were rated in terms of best
practice for primary care physicians dealing with suspected and confirmed cases
of physical abuse. Consulting group members and focus group participants then
commented on the panel's results. Final guidelines were approved by the panel
and the consulting group, with comments reserved in the guidelines for
information from focus group participants . CONCLUSIONS: It is not a conflict of
interest for the physician to deal with abuse of the female partner when both
partners are patients,,Both patients have a right to autonomy, confidentiality,
honesty, and quality care. Patients should be dealt with independently, thereby
facilitating assessment of the magnitude and severity of the victim's injuries.
Physicians should not discuss the possibility of domestic abuse with the male
partner without the prior consent of the abused female partner. Joint
counseling is generally inadvisable and should be attempted only when the
violence has ended, provided both partners give independent consent and the
physician has adequate training and skills to deal with the situation without
escalating the violence. If the physician feels unable to deal effectively with
either patient because of the dual relationship, referral to another qualified
physician is preferred.
10 of 30
TI: Detention of persistently nonadherent patients with tuberculosis [see
commentsJ
AU: Oscherwitz-T; Tulsky-JP; Roger-S; Sciortino-S; Alpers-A; Royce-S; Lo-B
AD: Program in Medical Ethics, University of California, San Francisco, USA.
SO: JAMA. 1997 Sep 10; 278(10): 843-6
____This source is Available in S.J.M.C Library
____Call Number: From: 1918+
LA: ENGLISH
AB: CONTEXT: Patients with tuberculosis (TB) who are persistently nonadherent
to treatment present a public heal th risk. In 1993, California created a new
civil detention process and allowed detention of noninfectious but persistently
nonadherent patients. OBJECTIVES: To determine (1) which patients TB
controllers attempt to detain, (2) how often and where patients are detained,
and (3) how many of these patients complete TB treatment. DESIGN: Case series
with cross-sectional comparison to other adult TB patients in the study
counties. SETTING; Twelve California counties with the largest number of new TB
cases reported in 1994. SUBJECTS: All patients whom TB controllers sought to
detain during 1994 and 1995 because of persistent nonadherence to treatment.
DATA SOURCES: Public health records, interviews with county TB officials, and
Reports of Verified Cases of Tuberculosis to the California Tuberculosis
Control Branch. RESULTS: Tuberculosis controllers sought the civil detention or
arrest of 67 patients during the study period (1.3% of adult TB patients with
the same disease sites). Forty-six percent of these patients were homeless, 81%
had drug or alcohol abuse, and 28% had mental illness. Tuberculosis controllers
*2-1
sought civil detention of 15 patients. Fourteen patients were detained (median
length o-f detention, 14.5 days). Tuberculosis controllers sought to arrest 62
patients during the'study period. Fifty-three patients were arrested (median
time in jail, S3 days). In 10 cases, both civil and criminal detention were
attempted. We analyzed completion of therapy after excluding patients who were
not detained or who died or moved. Overall, 41 (347.) of the remaining 4?
detained patients completed therapy. Of the . patients who completed therapy,
only 17 were detained until treatment was completed. Compared with other TB
patients in these counties, detained patients had 4 times the proportion lost
to follow-up and half the proportion completing therapy within 12 months.
CONCLUSION: Further improvements in the care of persistently nonadherent
patients may require more psychosocial services, appropriate facilities for
civil detention, and detaining patients long enough to assure completion of
treatment.
11 of 30
TI: Managed care in obstetrics.
AU: Devoe-LD
AD: Department of Obstetrics and Gynecology, BAA 700, Medical College of
Geargia, Augusta 30912, USA.
SO: Curr—Opin-Obstet-Gynecol. 1997 Aug; 9(4): 258-61
____this source is not Available in S.J.M.C.Library
LA: ENGLISH
AB: Managed care has marched relentlessly through all fields of obstetric care:
individual and group practices, proprietary hospitals and academic medical
centers, and public health systems. Emphasis on cost containment while
preserving high quality has driven the redesign of healthcare delivery. A
number of models for providing effective and less expensive obstetric care are
now being examined in the USA and abroad. Increased market penetration by
managed care will also exert profound and possibly harmful effects on
traditional academic teaching institutions. These organizations must adapt to
this new environment or face the erosion of physician support and training
bases. Ultimately, significant moral and ethical dilemmas will arise'when
patients' best interests for care are being continually brought into conflict
with the physician's need to earn a living.
12 of 30
TI: Unethical trials of interventions to reduce perinatal transmission of the
human immunodeficiency virus in developing countries [see comments!
AU: Lurie-P; Wplfe-SM
AD: Public Citizen's Health Research Group, Washington, DC 20009, USA.
SO: N-Engl-J-Med. 1997 Sep IS; 337(12): 853-6
___ This source is Available in S.J.M.C Library
___ Call Number: From: 1945+
LA: ENGLISH
TI: The ethics of clinical research- in the Third World [editorial; comment!
AU: Angel1-M
SO: N-Engl-J-Med. 1997 Sep 18; 337(12): 847-9
This source is Available in S.J.M.C Library
___ Call Number: From: 1945+
LA: ENGLISH
14
TI: [Public health in transition—a social science perspective!
AU: Kuhn-H
AD: Wissenschaftszentrum Berlin fur Sozialforschunq.
SO: Gesundheitswesen. 1997 Apr; 59(4): 213-6
____ this source is not Available in S.J.M.C.Library
LA: GERMAN; NON-ENGLISH
of 30
TI: CEthics and economic imperatives in the distribution of care]
AU: Rorive-G
AD: Service de Nephrologie-Hypertension, Universite de Liege.
SO: Rev-Med-Liege. 1997 Jun; 52(6): 412-6
____ this source is not Available in S.J■M.0.Library
LA: FRENCH; NON-ENGLISH
16 of 30
TI: Ethical, social, and legal issues surrounding studies of susceptible
populations and individuals.
AU: Soskolne-CL
AD: Department of Public Health Sciences, University of Alberta, Edmonton,
Canada. Colin.soskolneSualberta.ca
SO: Environ-Health-Perspect. 1997 Jun; 105 Suppl 4: 837-41
____ this source is not Available in S.J.M.C.Library
LA: ENGLISH
AB: Calls for professional accountability have resulted in the development of
ethics guidelines by numerous specialty and subspecialty groups of scientists.
Indeed, guidelines among some health professions now address vulnerable and
dependent groups: but these are silent on issues related to biomarkers. In
parallel, attention has been drawn to human rights concerns associated with
attempts to detect hypersusceptible workers, especially in democratic
countries. Despite this, concern for vulnerable populations grows as advances
in biomarker technology make the identification of genetic predisposition and
susceptibility markers of both exposure and outcome more attainable. In this
article, the principles derived from the ethical theory of utilitarianism
provide the basis for principle-based ethical analysis. In addition, the four
principles of biomedical ethics—respect for autonomy, beneficence,
nonmaleficence, and social justice—are considered for biomarker studies. The
need for a context in which ethical analysis is conducted and from which
prevailing social values are shown to drive decisions of an ethical nature is
emphasized; these include statutory regulation and law. Because biomarker
studies can result in more harm than good, special precautions to inform
research participants prior to any involvement in the use of biomarkers are
needed. In addition, safeguards to maintain the privacy of data derived from
biomarker studies must be developed and implemented prior to the application of
these new technologies. Guidelines must be expanded to incorporate ethical,
social, and legal considerations surrounding the introduction of new
technologies for studying susceptible populations and individuals who may be
vulnerable to environmental exposures.
17 of 30
TI: Can data collection during the grieving process be justifiable?
AU: Robertson-J; Jay-J; Welch-S
AD: Division of Public Health and Primary Health Care, University of Oxford.
SO: Br-J-Nurs. 1997 Jul 10-23; 6(13): 759-64
____ this source is not Available in S.J.M.C■Library
LA: ENGLISH
AB: Research has shown that there are a number of competing theories regarding
the use of bereaved people for research purposes. One view emphasizes their
vulnerability, weakness and inability to take part in decision-making. Another
is that there is an infringement of rights if people are denied the freedom of
choice to take part in research. This article considers issues concerned with
data collection from recently bereaved relatives who were at some stage of the
grieving process. The participants were interviewed as part of the OXMIS study
which aimed to identify the incidence of myocardial infarction in Oxfordshire.
A total of 142 interviews took place (59 home visits and 83 telephone
interviews). Of the cases not interviewed, sufficient information was gained in
947. from other sources to fulfil the required criteria. The perceived benefit
2-3
or apparent risk of vulnerable groups participating in research is discussed in
light of the study results.
IS of 30
An ethical dilemma in rabies immunisation.
John-TJ
Christian Medical College, Vellore, India.
Vaccine. 1997 Spring; 15 Suppl: S12-5
this source is not Available in S.J,M.C.Library
LA: ENGLISH
AS: Rabies continues to be an important public heal th problem in India and many
other developing countries. In India, annually some 700,000 persons are given
post-exposure vaccine prophylaxis using Semple (sheep brain) vaccine. It is
manufactured by government institutions and given free to the public. It is
presumed to be cheap, although the actual cost of production may not be low.
However, it is not a safe vaccine as it causes demyelinating central or
peripheral nervous system side-effects in 1/3000-7000 persons vaccinated; this
adverse reaction is occasionally fatal. Cell culture rabies vaccines are also
available in India; unlike the Semple vaccine they are safe and can be used for
pre-exposure vaccination, but they are more expensive. The dilemma is whether
it is ethically acceptable to continue to use the Semple vaccine in humans
while safer products are available. What is urgently needed is a decision tree
which would enable economical use of cell culture vaccines together with the
backing of professional bodies in medical practice, who will declare that cost
is not the only factor in choosing a rabies vaccine—safety is also of paramount
importance. We must also strive to reduce the cost of cell culture vaccines.
TI:
AU:
AD:
SO:
19 of 30
TI’: ^Linking of individual data. Methods of linkage!
AU: Rumeau-Rouquette-C
AD: Unite 149 de 1'INSERM, Paris.
SO: Rev-Epidemiol-Sante-Publique. 1997 Jun; 45(3): 248-56
____ this source is not Available in S,J.M.C.Library
LA: FRENCH; NON—ENGLISH
AB: This paper gives an overview of linking methods of personal data computed
in different files as registers and administrative or medical records.
Epidemiological and demographic examples are studied, then the successive steps
of record linkage are described definition and choice of identifiants,
searching and comparing pairs of records to determine whether they should be
linked. A special mention is made to probability matching and methods
optimizing the matching procedures. The discussion envisages the advantages of
record 1 inkage:better use of health statistics, new types of epidemiologic
studies. The ethical problems and the need for evaluation are also discussed.
20 of 30
TI: Invited commentary: on the role of ethics committees in epidemiology
professional societies.
AU: Coughlin-SS
AD: Department of Biostatistics and Epidemiology, Tulane University School of
Public Health and Tropical Medicine, New Orleans, LA, USA.
SO: Am-J-Epidemiol. 1997 Aug 1; 146(3): 209-13
____This source is Available only few issues in S.J.M.C. Library
LA: ENGLISH
21
TI: Ethical review is needed for public health studies Cletter!
AU: Al lander—E
SO: Public-Health-Rep. 1997 Jul-Aug; 112(4): 266
____This source is Available only few issues in S.J.M.C. Library
Call Number: From:1949-1984
LA: ENGLISH
2-4
of 30
22 of 30
TI: CThe reduction of mother—child transmission of HIV infection in developing
countries: potential intervention strategies, obstacles to implementation and
perspectives. The Reduction of Mother-Child Transmission of HIV Infection in
Africa Group!
AU: Meda-N; Msellati-P; Welffens-Ekra-C; Cartoux-M; Leroy-V; Van-de-F’erre-F;
Salamon-R
AD: Centre Muraz, Organisation de coordination et de cooperation pour la lutte
contre les grandes endemies (OCCGE), Burkina Faso.
SO: Sante. 1997 Mar-Apr; 7(2): 115-25
____ this source is not Available in S.J.M.C.Library
LA: FRENCH; NON-ENGLISH
AB: Mother to child transmission (MCT) of Human Immunodeficiency Virus (HIV) is
the main cause of the spread of the HIV epidemic in the pediatric population.
It is estimated that to date, three million children worldwide have been
infected by HIV. The epidemic burden in developing countries is dramatic.
Ninety-five percent of the world's HIV-infected women are living in developing
countries. In industrialized countries, antiretroviral treatment of pregnant
women and newborns with azidothymidine (AZT, ACTG 076 regimen) and discouraging
breast feeding by HIV-infected mothers are effectively reducing MCT of HIV.
However, there are three major obstacles to the systematic application of these
strategies in developing countries: (a) difficulties in implementing the
complex AZT administration and its corollary the avoidance of breast feeding;
(b) the complexity of the logistics of the ACTG 076 regimen; (c) cost. Indeed,
in developing countries the socioeconomic situation of the populations are
precarious and health structures and services are underdeveloped. In addition,
the anxiety and the reluctance of general population in the face of the HIV
problem and the high prevalence of maternal anemia reduce the acceptability and
safety of AZT treatment for pregnant women in developing regions. Only
interventions that are applicable, acceptable, safe, affordable, of low cost
and integrated into health system will be able to reduce HIV MCT. We now know
that MCT occurs mostly during the perinatal period and the maternal viral load
in blood, in cervical secretions and in breast milk appears to be the main
determinant of transmission. Maternal vitamin A deficiency may also favor MCT
of HIV. It is however possible that this association is confounded by the
relationship between advanced maternal HIV disease (a known risk factor for
transmission) and vitamin A deficiency. In spite of these uncertainties
concerning determinants of MCT of.HIV, several interventions have been
designed. The first involves treating the mother with antiretroviral drugs for
the perinatal period. The second is vaginal disinfection by application of
virucidal antiseptics during the perinatal period. The third is to give .vitamin
A supplements to pregnant women and children. Finally, passive immunotherapy
with anti-HIV antibodies applied to pregnant women and/or new born, may be
beneficial. The feasibility, safety and efficacy of these potential
interventions have not yet been demonstrated in developing countries. In view
of the dramatic spread of HIV infection in these countries, the evaluation of
these interventions is of utmost priority. These trials are necessary because
of the publi c heal th emergency but should be performed in strict respect of
human rights and medical ethics.
23 of 30
Maintenance of professional privilege as exits in France.
Gromb-S
University of Medicine of Bordeaux, Public Health Department, France.
Med-Law. 1997; 16(2): 395-404
this source is not Available in S.J.M.C.Library
LA: ENGLISH
TI:
AU:
AD:
SO:
24 of
TI: Epilepsy and the law-medical records.
AU: Mallon-L
AD: NSW Medical Defence Union, Australia.
SO: Med-Law. 1997; 16(2): 245-52
this source is not Available in S.J.M.C.Library
LA: ENGLISH
AB: This paper reviews the need to keep medical records and concludes that
Section 126 of the New South Wales Medical Practice Act, 1992, requires such
provision to. comply with adequate "professional conduct". This was above and
beyond other possible mandatory maintenance of appropriate records, such as may
be covered by the notifiable diseases provisions of the Public Health Act.
Ethical codes of conduct imposed further obligations to maintain appropriate
records, and legal defence against claims of misconduct or negligence required
documented evidence to refute false accusations. The emphasis of records has
changed with greater need to stipulate risk exposure associated with proposed
treatments and advice provided for such things as necessary follow-up. It was
further shown that appointment diaries, extra file entries and indications of
any failed attendance and resultant subsequent actions were all part of
adequate record-keeping. Finally, the paper reviews ownership of medical
records and refers to the New South Wales case of Ms Breen, in which it was
found that ownership of records, as at the printing of this paper, resided with
the doctor.
25 of 30
TI: Registered nurses' knowledge and compliance with regulations relating to
the administration of ward recordable medications.
AU: Gill-BI; Bligh-JA
AD: Division of Public Health, Faculty of Health, University of Western Sydney,
Macarthur, Campbelltown, New South Wales, Australia.
SD: Int-J-Nurs-Pract. 1995 Nov; 1(1): 43-51
LA: ENGLISH
AB: An anonymous questionnaire assessing nurses' knowledge, attitude and
compliance with legally mandated regulations relating to the administration of
ward recordable drugs was administered by mail to a random sample of nurses
registered in New South Wales, Australia. Sixty-four per cent of subjects (n =
318) responded. Both seif-reported and col league-reported compliance rates were
less than 50%. A highly significant relationship was evident between knowledge
and attitude, knowledge and reported compliance; and attitude and reported
compliance. Factors that may influence non-compliance are discussed and the
legal, ethical and policy implications of the findings are briefly explored.
26 of 30
TI: Ethical dilemmas in current planning for polio eradication [see comments]
AU: Taylor-CE; Cutts-F; Taylor-ME
AD: Department of International Health, Johns Hopkins School of Hygiene and
Public Health, Baltimore, MD 21205, USA.
SO: Am-J-Public-Health. 1997 Jun; 87(6): 922-5
____This source is Available only few issues in S.J.M.C. Library
Call Number: From: 1942-1991
LA: ENGLISH
AB: Intensification of polio eradication efforts worldwide raises concerns
about costs and benefits for poor countries. A major argument for global
funding is the high benefit-cost ratio of eradication; however, financial
benefits are greatest for rich countries. By contrast, the greatest costs are
borne by poor countries; the Pan American Health Organization- has estimated
that host countries bore 80% of costs for polio eradication in the Americas.
The 1988 World Health Assembly resolution setting up the Polio Eradication
Initiative carried the proviso that program s should strengthen health
infrastructures. Drastic cuts in donor funding for health make this commitment
even more important. Two international evaluations have reported both positive
and negative effects of polio and Expanded Programme on Immunization programs
on the functioning and sustainability of primary health care. Negative effects
were greatest in poor countries with many other diseases of public heal th
importance. If poor countries are expected to divert funds from their own
urgent priorities, donors should make solid commitments to long-term support
for sustainable health development.
27 of 30
TI: Comment: ethical dilemmas in worldwide polio eradication programs [comment]
AU: Sutter-RW; Cochi-SL
AD: National Immunization Program, Centers for Disease Control and Prevention,
Atlanta, Ga, USA.
SO: Am-J-Public-Health. 1997 Jun; 87(6): 913-6
___ This source is Available only few issues in S.J.M.C. Library
Call Number: From: 1942-1991
LA: ENGLISH
28 of 30
TI: Ethics in public heal th practice: a survey of publ ic heal th nurses in
southern Louisiana.
AU: Folmar-J; Coughlin-SS; Bessinger—R; Sacknoff-D
AD: Department of Health Systems Management, University School of Public Health
and Tropical Medicine, New Orleans, Louisiana, USA.
SO: Public-Health—Nurs. 1997 Jun; i.4.(3): 156-60
____this source is not Available in S.J.M.C.Library
LA: ENGLISH
AB: The present study was designed to help learn more about the ethical
interests and concerns of public health nurses employed in state and local
health departments. Self-administered postal questionnaires were mailed to 41
public heal th nurses employed at health units in Region I of the Louisiana
Office of Public Health. Basic demographic information was obtained along with
information about the workers' previous instruction or training in ethics and
the nature of ethical conflicts encountered in their public heal th practice.
Only 387, (15 of 39) of the surveyed nurses had had formal instruction in
ethics. Even fewer (7.37.) had received continuing education on ethics. Most of
the nurses felt confident in their ability to recognize an ethical conflict or
dilemma in the workplace; fewer felt confident in their ability to resolve an
ethical conflict or dilemma. A high proportion of the nurses agreed that there
is a need for continuing education courses on ethics for public heal th workers.
Nurses who had received formal ethics instruction were more likely to feel
confident in their ability to recognize an ethical conflict in their public
heal th practice. Continuing education programs on ethics are needed that are
designed to meet the specific needs of front-line public health workers.
29 of 30
TI: Confidentiality and the acquired immune deficiency syndrome (AIDS): an
analysis of the legal and professional issues.
AU: Hayter-M
AD: Department of Community and Primary Care Nursing, University of Sheffield,
England.
SO; J—Adv—Nurs. 1997 Jun; 25(6): 1162-6
____ this source is not Available in S.J.M.C.Library
LA: ENGLISH
AB: Confidentiality is one of the most significant concepts in health care and
nursing practice, particularly in the arena of HIV infection and AIDS. The
implications for individuals of deliberate or accidental disclosure of their
HIV status can and does have far reaching effects. This paper will explore the
concept of confidentiality by discussing the legal and professional issue of
confidentiality and AIDS. The nature of the law and guidance by professional
bodies allow exceptions to the respect of confidentiality in certain
situations. AIDS and the need for confidentiality often is in conflict when
public health considerations are deemed to be involved. The law is poorly
developed in this area and often professional guidance is less than clear.
30 of 30
TI : Duration and adequacy of dialysis. Overview: the science is easy, the ethi
is diff icul t.
AU: KjelIstrand-CM
AD: Department of Public Health Services, Bowman Gray School of Medicine,
Winston-Salem, North Carolina 27157-.1063, USA.
SO: ASAIO-J. 1997 May-Jun; 43(3): 220-4
____this source is not Available in S.J.M.C.Library
LA: ENGLISH
AB: Because of physiologic, technical, and practical limits, short dialysis is
probably associated with higher mortality when, compared with longer dialysis,
even when dialysis efficiency is maintained with a proportionately higher
clearance. The optimal dialysis efficiency measured as KT/V (or better
expressed as mean standardized urea clearance in ml/min> for hemodialysis,
remains unknown, but it is not unreasonable to assume that either a KT/V of 3
or a mean standardized urea clearance of 30 ml/min is optimal, and certainly
better than the presently used KT/V of 1.2 to 1.8. To achieve KT/Vs on this
order, a 70 kg patient will need at least 7 hours of dialysis 3 times per week
This gives rise to an ethical problem: Should one give many patients short
dialysis, or fewer patients longer dialysis? This is a question to which no
easy ethical solution can be found.
PC-SPIRS 3.40
MEDLINE (R) 1998/01-1998/10
MEDLINE (R) 1998/01-1998/10 usage is subject to the terms and conditions of the
Subscription and License Agreement and the applicable Copyright and
intellectual property protection as dictated by the appropriate laws of your
country and/or by International Convention.
1 of 52
TI: US health journal editors' opinions and policies on research in race,
ethnicity, and health.
AU: Bennett-T; Bhopal-R
AD: Department of Maternal and Child Health, School of Public Heal th,
University of North Carolina at Chapel Hill 27599-7400, USA.
SO: J-Natl-Med-Assoc. 1998 Jul; 90(7): 401-8
____ this source is not Available in S.J.M.C.Library
LA: ENGLISH
AB: Health research on race and ethnicity has been criticized for lacking rigor
in conceptualization, terminology, and analysis. Scientific journals' editorial
processes help determine research quality. This survey assessed editors'
awareness of current debates, attitudes toward recent recommendations, and
involvement in developing editorial policies. Twenty-nine editors of health
journals with impact factors of > or = 1 (based on citation ratings) were sent
a questionnaire including four key problems identified in research literature
and recommendations from federal agencies; 23 (79%) responded. Seven editors
relevant policies. Two had read the federal directive on racial and ethnic
classification; one was aware of its current review. Most perceived the four
key problems as uncommon. The majority agreed with Public Health Service
recommendations on race and ethnicity research, except for analyzing effects of
racism. Approximately 20% had discussed issues with co-editors, editorial
boards, or reviewers. About 40% saw further discussion as beneficial; four
planned to draft guidelines. Editors' potential for helping resolve problems in
race/ethnicity research is not being realized. Greater participation would be
beneficial to public heal th research and practice.
2
of 52
TI: Public health ethics and clinical freedom.
AU: Newdick-C
AD: University of Reading, UK.
SO: J-Contemp-Health-Law-Policy. 1998 Spring; 14(2): 335-64
____ this source is not Available in S.J-M.C.Library
LA: ENGLISH
»
' ■
■
3 of 52
TI: Can ethical management and managed care coexist?
AU: Friedman-LH; Savage-GT
AD: Department of Public Health at Oregon State University, Corvallis, USA.
SO: Health-Care-Manage-Rev. 1998 Spring; 23(2): 56-62
____ this source is not Available in S.J.M.C.Library
LA: ENGLISH
AB: The growth of for—profit managed care organizations raises serious ethical
questions for managers in these settings, such as whether contemporary business
ethics are most appropriate for health care organizations or how the principles
of biomedical ethics can be integrated into profit-seeking firms. A model is
proposed that seeks to consolidate both business ethics and biomedical ethics
into a form that is useful to health service managers.
4 of 52
TI: EEthical issues' regarding individual data collection and utilization in
community health care programs!
AU: Nakamura-Y; Gjima—T; Kurosawa-M; Kikuchi,-S; Inaba-Y; Niino-N; Nakamura—K
PC-SP1RS 3.40
MEDLINE (R) 1998/01-1998/10
MEDLINE (R) 1998/01-1998/10 usage is subject to the terms and conditions of the
Subscription and License Agreement and the applicable Copyright and
intellectual property protection as dictated by the appropriate laws o-f your
country and/or by International Convention.
1 o-f 52
TI: US health journal editors' opinions and policies on research in race,
ethnicity, and health.
AU: Bennett-T; Bhopal-R
AD: Department of Maternal and Child Health, School of Public Health,
University of North Carolina at Chapel Hill 27599-7400, USA.
SO: J-Natl-Med-Assoc. 1998 Jul; 90(7): 401-8
this source is not Available in S■J.M■C.Library
LA: ENGLISH
AB: Health research on race and ethnicity has been criticized for lacking rigor
in conceptualization, terminology, and analysis. Scientific journals' editorial
processes help determine research quality. This survey assessed editors'
awareness of current debates, attitudes toward recent recommendations, and
involvement in developing editorial policies. Twenty-nine editors of health
journals with impact factors of > or = 1 (based on citation ratings) were sent
a questionnaire including four key problems identified in research literature
and recommendations from federal agencies; 23 (797.) responded. Seven editors
relevant policies. Two had read the federal directive on racial and ethnic
classification; one was aware of its current review. Most perceived the four
key problems as uncommon. The majority agreed with Pu b1i c Heal th Service
recommendations on race and ethnicity research, except for analyzing effects of
racism. Approximately 207. had discussed issues with co-editors, editorial
boards, or reviewers. About 407. saw further discussion as beneficial; four
planned to draft guidelines. Editors' potential for helping resolve problems in
race/ethnicity research is not being realized. Greater participation would be
beneficial to public health research and practice.
2
of 52
TI: Public health ethics and clinical freedom.
AU: Newdick-C
AD: University of Reading, UK.
SO: J-Contemp-Health-Law-Policy. 1998 Spring; 14(2): 335-64
____ this source is not Available in S.J.M.C.Library
LA: ENGLISH
3 of 52
TI: Can ethical management and managed care coexist?
AU: Friedman-LH; Savage-GT
AD: Department of Public Health at Oregon State University, Corvallis, USA.
SO: Health-Care-Manage-Rev . 1998 Spring; 23(2): 56-62
____ this source is not Available in S.J.M.C.Library
LA: ENGLISH
AB: The growth of for—profit managed care organizations raises serious ethical
questions for managers in these settings, such as whether contemporary business
ethics are most appropriate for health care organizations or how the principles
of biomedical ethics can be integrated into profit-seeking firms. A model is
proposed that seeks to consolidate both business ethics and biomedical ethics
into a form that is useful to health service managers.
4 of 52
TI: CEthical issues' regarding individual data collection and utilization in
community health care programs!
AU: Nakamura-Y; Ojima-T; Kurosawa-M; Kikuchi-S; Inaba-Y; Niino-N; Nakamura-K
AD: Department of Public Health, Jichi Medical School.
SO: Nippon-Koshu-Eisei-Zasshi. 1998 Mar; 45(3): 231-61
this source is not Available in S.J.M.C■Library
LA: JAPANESE; NON-ENGLISH
AB: To understand the nature of ethical issues in community-based health care
programs, we conducted a mail survey of subjects who were public health nurses
employed by municipal governments. The questionnaire consisted of questions
about data collection, usage, disclosure, and educational experience. In 1996
we received 536 completed questionnaires which were then analyzed. Regarding
who should input data into computers, the number of those who considered that
municipal offices other than public heal th nurses would be the most appropriate
for the input of examination data was the largest, followed by those who felt
that contracting out was best. Many of the public heal th nurses considered that
they needed to obtain informed consent for collection, usage and disclosure of
sensitive items, such as data on HIV infection. The number of those considering
that they could not disclose results of examinations to other community-based
specialists in health and welfare without the subject's agreement was very
high. In health examination programs, the public heal th nurses requested
information on date of birth and occupations, but there was some hesitation in
requesting the latter information. Although about a half of subjects responded
that they did not require data concerning the first sexual intercourse in
cervical cancer screening, 90 percent asked breast feeding history in breast
cancer screening. Approximately 90 percent gave results of the examination to
participants personally through personal communication or mail. Of the
respondents, 40 percent reported having had educational courses on ethics while
the others did not. There were some responses that reminded us of the
unsatisfactory level of understanding about ethical issues, which underlined
the need to emphasize importance, of including this in educational curricula.
5 of 52
TI: Physicians disciplined for sex-related offenses [see comments]
AU: Dehlendorf-CE; Wolfe-SM
AD: Public Citizen's Health Research Group, Washington, DC 20009, USA.
SO: JAMA. 1998 Jun 17; 279(23): 1883-8
____This source is Available in S.J.M.C Library
Call Number: From: 1918+
LA: ENGLISH
AB: CONTEXT: Physicians who abuse their patients sexually cause immense harm,
and, therefore, the discipline of physicians who commit any sex-related
offenses is an important public heal th issue that should be examined.
OBJECTIVES: To determine the frequency and severity of discipline against
physicians who commit sex-related offenses and to describe the characteristics
of these physicians. DESIGN AND SETTING: Analysis of sex-related orders from a
national database of disciplinary orders taken by state medical boards and
federal agencies. SUBJECTS: A total of 761 physicians disciplined for
sex-related offenses from 1981 through 1996. MAIN OUTCOME MEASURES: Rate and
severity of discipline over time for sex-related offenses and specialty, age,
and board certification status of disciplined physicians. RESULTS: The number
of physicians disciplined per year for sex-related offenses increased from 42
in 1989 to 147 in 1996, and the proportion of all disciplinary orders that were
sex related increased from 2.17. in 1989 to 4.47. in 1996 (P<.001 for trend).
Discipline for sex-related offenses was significantly more severe (P<.001> than
for non-sex-related offenses, with 71.97, of sex-related orders involving
revocation, surrender, or suspension of medical license. Of 761 physicians
disciplined, the offenses committed by 567 (757.) involved patients, including
sexual intercourse, rape, sexual molestation, and sexual favors for drugs. As
of March 1997, 216 physicians (39.97.) disciplined for sex-related offenses
between 1981 and 1994 were licensed to practice. Compared with all physicians,
physicians disciplined for sex-related offenses were more likely to practice in
the specialties of psychiatry, child psychiatry, obstetrics and gynecology, and
family and general practice (all P<.001) than in other specialties and were
older than the national physician population, but were no different in terms of
board certification status. CONCLUSIONS: Discipline against physicians for
sex-related offenses is increasing over time and is relatively severe, although
few physicians are disciplined for sexual offenses each year. In addition, a
substantial proportion of physicians disciplined for these offenses are allowed
to either continue to practice or return to practice.
6 of 52
TIs The ethics of compulsory removal under section 47 of the 1949 National
Assistance Act.
AU: Hobson-SJ
ADs School of Epidemiology and Public Health, University of Manchester.
SO: J-Med-Ethics. 1999 Feb; 24(1): 39-43
____ this source is not Available in S.J■M.C■Library
LA: ENGLISH
AB: Orders for removal under Section 47 of the 1949 National Assistance Act are
little discussed. However, they involve severe infringements of the civil
liberties of those affected. It is argued that all previously presented
justifications for the use of these orders fail. Repeal of the act is called
for. The Law Commission has drafted alternative legislation, but this has not
been enacted. Until this occurs local authorities, the Faculty of Public Heal th
Medicine and individual public heal th physicians should refuse to be involved
in its use.
7 of 52
TI: Dealing with research misconduct in the United Kingdom. An editor's
response to fraudsters.
AU: Farthing-MJ
AD: Digestive Diseases Research Centre, St. Bartholomew's and The Royal London
School of Medicine and Dentistry, London, El 2AD.
SD: BMJ. 1999 Jun 6; 316(7146): 1729-31
____This source is Available in S.J.M.C Library
___ Call Number: From 1914+
LA: ENGLISH
9 of 52
TI: The need for a national body for research misconduct. Nothing less will
reassure the public Ceditorial!
AU: Smith-R
SO: BMJ. 1999 Jun 6; 316(7146): 1696-7
___ This source is Available in S.J.M.C Library
____Call Number: From 1914+
LA: ENGLISH
9 of 52
TI: C125th anniversary of Revista Medica de Chile!
AU: Reyes-Budelovsky-H
SO: Rev-Med-Chil. 1997 Jul; 125(7): 759-60
____ this source is not Available in S.J.M.C.Library
LA: SPANISH; NON-ENGLISH
AB: The first issue of Revista Medica de Chile was printed in July, 1972. Since
then, it has been published monthly, interrupted only for a few months during a
Chilean civil war (1991). This medical journal has been devoted mainly to
clinical topics in internal medicine, but currently it includes an increasing
proportion of research papers in other biomedical and preclinical subjects.
This journal is included in the most important international indexes of
biomedical publications. Most issues cover also medical education, public
health, the ethics of clinical and experimental research, medical
administration and the history of medicine. The evolution of medicine in Chile
along 125 years is clearly reflected in the contents of this journal. Revista
Medica de Chile is one of the oldest medical journals in the world,
3
particularly among those published in Spanish, and a top ranking biomedical
publication in Chile.
10 of 52
TI: Human research beyond the medical model: legal and ethical issues.
AU: Dickens-BM
AD: Faculty of Law, University of Toronto, Canada.
SO: Med-Law. 1997; 16(4): 687-703
____ this source is not Available in S.J.M.C.Library
LA: ENGLISH
AB: Advances in medical health depend on non-medical, as well as medical
research. When research involves human participants, it raises legal and
ethical concerns that have come to be approached by reference to codes of
research ethics. Many of these are centered on physician-patient relationships
and the pursuit of medical science. This article considers a number of issues
that arise from research that follows non-medical models of research, and
applications of rules of ethical medical research outside physician-patient
settings. In particular, it addresses health research in the social sciences,
the exclusion of women as participants in medical research, studies that depend
on incomplete disclosure of information to prospective participants and their
deception, and public health research based on groups and communities rather
than participants as individuals.
11 of 52
TI: Cultural feasibility studies in preparation for clinical trials to reduce
maternal—infant HIV transmission in Haiti.
AU: Coreil-J; Losikoff-P; Pincu-R; Mayard-G; Ruff-AJ; Hausler—HP; Desormeau-J;
Davis—H; Boulos—R; Halsey-NA
AD: College of Public Health, University of South Florida, Tampa 33612, USA.
SO: AIDS-Educ-Prev . 1998 Feb; 10(1): 46-62
____ this source is not Available in S.J.M.C.Library
LA: ENGLISH
AB: A cultural feasibility study is defined as one that investigates scientific
as well as ethical, behavioral, and social issues in the design of clinical
trials. The value of such a broadly defined assessment is illustrated through
the presentation of two case studies conducted to prepare for clinical trials
to reduce maternal-infant HIV transmission on Cite Soleil, Haiti. The first
study addressed issues surrounding a trial of breast-feeding and exclusive
bottle-feeding among HIV seropositive mothers. The second study focused on the
implementation of a double-blind trial of HIV immune globulin and standard
immune globulin to be administered to infants of seropositive mothers shortly
after birth. Both cases used focus group interviews with mothers and in-depth
interviews with key informants to investigate AIDS-related beliefs,
acceptability of trial participation, risks to subjects, and community
reactions and repercussions to the trial. Findings point to the difficulties
posed by attempts to conduct trial involving complex research designs in
socially disadvantaged populations. Recommendations highlight the need to
consider the community-wide impact of a trial, and the need to undertake
extensive educational preparation of participants to ensure informed consent
and adherence to protocols.
12
of 52
13
of
TI: Human rights, not enough [letter!
AU: Dwyer—J
SO: Hastings-Cent-Rep . 1998 Jan-Feb; 28(1): 6
____this source is not Available in S.J.M.C.Library
LA: ENGLISH
T.I: Ethical dilemmas in polio eradication . Hyder responds.
AU: Hyder-AA
AD: School of Public Health, Johns Hopkins University, Baltimore, HD 21205,
USA.
SO; Am—J-Public—Heal th. 1998 Jan; 88(1): 131-2
____This source is Available only few issues in S.J.M.C. Library
___ Call Number: From: 1942-1991
LA: ENGLISH
14 of 52
TI: [The ethical problem of the health-environment relationship!
AU: Comba-P
AD: Laboratorio di Igiene Ambientale, Istituto Superiors di Sanita, Roma.
SO: Ann—1st—Super-Sanita. 1997; 33(2): 279-84
____ this source is not Available in S.J.M.C■Library
LA: ITALIAN; NON-ENGLISH
AB: The need for a specific ethical evaluation in environmental health has been
emphasized in recent years, with special reference to the conduction of
research in environmental epidemiology, and to the subsequent implementation of
public health action. Deontologic aspects that have been extensively debated
include the duties of investigators towards study subjects, conflicts of
interest, and rules to respect when dealing with institutions and with society
at large. Epistemologic issues concern the explicitation of underlying values
that influence choices in the stages of priority setting and study design.
Finally, moral value is relevant whenever decision making takes place. In this
frame it is recommended to refer to the core values of the public health
movement, and to apply them to new, emerging problems.
15 of 52
TI: The debate over maternal-fetal HIV transmission prevention trials in
Africa, Asia, and the Caribbean: racist exploitation or exploitation of racism?
AU: Bayer—R
AD: Columbia University School of Public Health, New York, NY 10032, USA.
SO: Am-J-Public-Health, 1998 Apr; 88(4): 567-70'
____This source is Available only few issues in S.J.M.C. Library
Call Number: From: 1942-1991
LA: ENGLISH
16 of 52
TI: Human rights and materna1-fetal HIV transmission prevention trials in
Africa.
AU: Annas-GJ; Grodin-MA
AD: Health Law Department, Boston University School of Public Health,
Massachusetts 02118, USA.
SO: Am-J-Public-Heaith. 1998 Apr; 88(4): 560-3
____This source is Available only few issues in S.J.M.C. Library
___ Call Number: From: 1942-1991
LA: ENGLISH
AB: The human rights issues raised by the conduct of maternal-fetal human
immunodeficiency virus transmission trials in Africa are not unique to either
acquired immunodeficiency syndrome or Africa, but public discussion of these
trials presents an opportunity for the United States and other wealthy nations
to take the rights and welfare of impoverished populations seriously. The
central issue at stake when developed countries perform research on subjects in
developing countries is exploitation. The only way to prevent exploitation of a
research population is to insist not only that informed consent be obtained but
also that, should an intervention be proven beneficial, the intervention will
be delivered to the impoverished population. Human rights are universal and
cannot be compromised solely on the basis of beliefs or practices of any one
country or group. The challenge to the developed countries is to implement
programs to improve the health of the people in developing countries both by
improving public health infrastructure and by delivering effective drugs and
vaccines to the people.
17 of 52
TI: Immunization -for prevention and treatment of cocaine abuse: legal and
ethical implications.
AU: Cohen-PJ
AD: Medications Development Division, National Institute on Drug Abuse,
National Institutes o-f Health, Rockville, MD, USA.
SO: Drug-Alcohol-Depend . 1997 Dec 15; 48(3): 167-74
this source is not Available in S. J.M.C.Library
LA: ENGLISH
AB: A cocaine vaccine, currently under investigation by several laboratories,
would be an innovative and exciting means o-f treating and preventing cocaine
addiction. However, an approved vaccine will raise at least two major areas o-f
concern. (1) Loss of privacy: cocaine antibodies might be used as a marker to
identify, penalize, and stigmatize vaccinated individuals. (2) Selection for
vaccination: should immunization be voluntary or compelled: should immunization
be restricted to addicts, to those at risk of addiction, or should it be
universal; should immunization be used in children? I propose to analogize
cocaine addiction to an infectious disease which poses a major public health
problem. This approach can provide an ethical and legal foundation on which we
may begin to formulate a societal approach to the use of the cocaine vaccine.
IS of 52
TI: Snyder v. American Association of Blood Banks: a re-examination of
liability for medical practice guideline promulgators.
AU: Noble-A; Brennan-TA; Hyams-AL
AD: Department of Health Policy & Management, Harvard School of Public Heal th,
Boston. MA 02115, USA.
SO: J-Eval-Clin-Pract. 1998 Feb; 4(1): 49-62
____this source is not Available in S.J.M.C.Library
LA: ENGLISH
AB: Medical practice guidelines are playing an increasingly important role in
both the medical and the legal context. As tools for the health practitioner,
it is thought that medical practice guidelines may contribute to an increase in
the quality of patient care and cost-effectiveness. In the legal setting,
guidelines may improve the functioning of the medical malpractice system by
creating more rational, predictable standards of care. The development and
promulgation of medical practice guidelines, while increasing, are still
evolving. A number of concerns, especially in the areas of physician autonomy,
physician control, and ethics, as well as efficacy, need to be resolved. The
use of such guidelines as the legal standard of care in malpractice cases
evokes similar concerns, along with fears that the use of guidelines at trial
may either lower the standard of care, or, conversely, raise the standard of
care to levels that are difficult to meet. Adding to this controversy is the
recent case of Snyder v. American Association of Blood Banks (1996), in which
the New Jersey Supreme Court upheld a jury finding that the American
Association of Blood Banks (AABB) was liable to a plaintiff who contracted AIDS
from an HIV-tainted transfusion, for negligent failure to adopt guidelines
requiring blood testing for surrogate markers. This opinion is significant as
the first to find a duty of care running from a medical guideline promulgator
to a third person, the injured patient. The opinion is examined in depth and
within the context of other relevant case law. The impact the opinion will have
is difficult to gauge., The somewhat unique facts of the case, as well as the
court's unusually stinging critique of the defendant, AABB, and its motivations
informing its response to the concerns about blood contamination, may limit its
value as precedent. However, precedent does exist in analogous non-medical
cases for promulgator liability.‘The pros and cons of promulgator liability are
weighed. While closer regulation of guideline development and promulgation or
promulgator immunity may be warranted, it is premature to consider either
seriously until the impact of the Snyder opinion can be appreciated.
6
19 of 52
TIs CEthics, bioethics and medical sciences]
AU: Fontaine-M
AD: Institut oceanographique, Paris.
SD: Bui1-Acad-Natl-Med. 1997 Oct; 181(7): 1477-85; discussion 1485-6
____ this source is not Available in S.J.M.C.Library
LA: FRENCH; NON-ENGLISH
AB: The aim of bioethics is to define a wise conduct for humans with regard to
their environments, whether living or inanimate. However, owing to their
diversity, bioethics can only deal with general problems such as biodiversity.
Within the framework of bioethics as a whole, different sectorial bioethics
must therefore exist to deal with problems specific to certain environments,
for example the Oceans and Seas, the Forests. General bioethics and sectorial
bioethics have an important contribution to make to medical sciences but
official regulations should be proposed only after an attentive investigation
has been made. For instance, the preservation of an apparently threatened
biodiversity or the revival of a seriously damaged biodiversity must be the
subject of a thorough preliminary scientific study and, if legislative
decisions are taken, a very careful scientific control of their consequences
must be carried out. One example is given: the decree on the protection of
Larids and its impact, with regard to an abusive proliteration of certain gull
populations having varied effects on public heal th. Sectorial bioethics can
also have obvious consequences on medical sciences. Thus various harmful
attacks on coral reefs (contrary to the concepts of thalassoethics) can lead to
the death of corals and the appearance of ciguatera. Thalassoethics, by
inciting pollution control, should help to improve the conditions of
thalassotherapy. Forest ethics, particularly concerning management, can reduce
the greenhouse effect and its consequences on health, as well as protecting
plant and animal species inhabiting the ecosystem and bringing new chemical
bodies to inspire original pharmacological research. Thus the links between
general or sectorial bioethics and medical sciences must always be very close.
20 of 52
TI: Videos, photographs, and patient consent.
AU: Hood-CA; Hope-T; Dcve-P
AD: Ethox, Division of Public Health and Primary Care Institute of Health Care
Sciences, Headington, Oxford.
SO: BMJ . 1998 Mar 28; 316(7136): 1009-11
____This source is Available in S.J.M.C Library
____Call Number: From 1914 +
LA: ENGLISH
21 of 52
TI: Why Australia needs minimum standards of deliberation for public heal th.
AU: Gaughwin-MD
AD: Department of Public Health, University of Adelaide, SA.
mgaughwifimedicine.adelaide.edu.au
SO: Med-J-Aust. 1998 Mar 2; 168(5): 228-9
____This source is Available in S.J.M.C Library
____Call Number: From: 1966+
LA: ENGLISH
22 of 52
TI: Projection of molecular epidemiology in medicine.
AU: Schulte-PA
AD: National Institute for Occupational Safety and Health Cincinnati, Ohio,
USA.
SO: Gac-Med-Mex. 1997; 133 Suppl 1: 155-9
____ this source is not Available in S.J.M.C.Library
LA: ENGLISH
AB: Molecular epidemiology is a term to describe the incorporation of molecular
and other types of biomarkers into epidemiology. Molecular epidemiology uses
the same paradigm as traditional epidemiology but the former represents the
opportunity to use the enhances resolving power of molecular biology and
contemporary biochemical science to assess exposure disease relationships.
There are three types of biomarkers that can be used in this regard: They
include markers of exposure, effect and susceptibility. These markers can be
used as dependent and independent variables in most epidemiologic study
designs. Critical in their use is that they are validated and field tested.
This requires extensive collaboration between laboratory and public heal th
scientist. Special attention also needs or be paid to the interpretation and
communication of biomarker data and the ethical issues attendant to their use.
23 of 52
TI: The Dublin Principles of cooperation among the beverage alcohol industry,
governments, scientific researchers, and the public health community.
AU: Hannum-H
AD: Fletcher School of Law and Diplomacy, Tufts University, USA.
SO:'Alcohol-Alcohol. 1997 Nov-Dec; 32(6): 641-8
____ this source is not Available in S.J.M.C.Library
LA: ENGLISH
AB: A 3-day Meeting held in Dublin, Ireland on 26-28 May 1997 was organized by
the National College of Industrial Relations of Ireland and the US-based
International Center for Alcohol Policies. During this Meeting, the 24
participants representing the beverage alcohol industry, governmental
organizations and the scientific and public heal th communities discussed
cooperation among all those concerned with alcohol consumption and its effects.
These discussions led to the formulation of the 'Dublin Principles of
Cooperation'. This special article describes these Principles and comments on
them.
24 of 52
TI: The Dublin Principles of cooperation among the beverage alcohol industry,
governments, scientific researchers, and the public health community.
AU: Hannum—H
AD: Fletcher School of Law and Diplomacy, Tufts University, USA.
SO: Alcohol-Alcohol. 1997 Nov-Dec; 32(6): 639-40
>this source is not Available in S.J■M,C.Library
LA: ENGLISH
25 of 52
TI: EWhich graft for which patient? and when? II. Organ supply and allocation!
AU: Noury—D; Claquin-J; Romano-P
AD: Praticien hospitalier d'anesthesie-reanimation , 1'EfG Interregion Quest
CHRU Pontchai1lou, Rennes.
SO: Rev-Prat. 1997 Nov 15; 47(18 Spec No): 822-7
____this source is not Available in S.J.M.C.Library
LA: FRENCH; NON-ENGLISH
AB: Despite progress realised in transplantation and organ procurement, there
is an increasing gap between the number of patients on the national waiting
list and the number of harvested organs. As a result, the appropriate organs
must be matched with the appropriate patient, with two constraints: equity and
efficacy. In a context of lack' of -organs, another public health problematic is
to conciliate both the interests of a given patient and the interests of those
on the waiting lists. In 1996, the French secretary of state for health
instituted a public consultation committee chaired by the vice-president of the
Comite consultatif national d'ethique, Counsellor Jean Michaud, to study organ
allocation rules and to plan recommendations for the future. Using, as a
starting point, the allocation rules initiated in the past by France Transplant
and transiently applied by 1'Etablissement francais des Greffes, the committee
conducted a large audition of health care professionals concerned with
transplantation, individuals qualified in ethics, laws, sociology or ethnology,
■3
politicians and a sample representation of the population. A new corpus of
allocation rules and procedures was then defined according to the committee
recommendations and the advice of all medico-surgical transplantation teams,
and published as a ministerial order in the Journal official de la Republique
francaise in november 1996. It specifies shared principles and organ by organ
specific allocation rules.
26 of 52
TI: CThe ethics of public health service!
AU: Diener-V
AD: Gesundheitsdepartement Kanton Zurich.
SO: Schweiz—Rundsch-Med-Prax . 1997 Dec 17; 86(51-52): 2012-5
____ this source is not Available in S.J.M■C■Library
LA: GERMAN; NON-ENGLISH
27 of 52
TI: Global disparities in health and human rights: a critical commentary.
AU: Benatar-SR
AD: Department of Medicine, University of Cape Town, Observatory, South Africa.
SO: Am-J-Public—Heal th. 1998 Feb; 83(2): 295-300
____This source is Available only few issues in S.J.M.C. Library
____Call Number: From: 1942-1991
LA: ENGLISH
AB: Widening disparities in health and human rights at a global level represent
the dark side of progress associated with escalation of economic and military
exploitation and exponential population growth in the 20th century. Even the
most basic universal human rights cannot be achieved for all under these
circumstances. The goal of improved population health will be similarly elusive
while medical care is commodified and exploited for commercial gain in the
marketplace. Recognition of the powerful forces that polarize our world and
commitment to reversing them are essential for the achievement of human rights
for all, for the improvement of public health, and for the peaceful progress
required to protect the "rational self-interest" of the most privileged people
on earth against the escalation of war, disease, and other destructive forces
arising from widespread poverty and ecological degradation.
28 of 52
TI: Fifty years after the Nuremberg Nazi Doctors' Trial: reviewing how the laws
of the Third Reich applied to individuals with oral clefts.
AU: Wyszynski-DF
AD: Department of Epidemiology, The Johns Hopkins School of Public Health,
Baltimore, Md 21205, USA.
SO: Plast-Reconstr-Surg. 1998 Feb; 101(2): 519-27
____This source is Available only few issues in S.J.M.C. Library
Call Number: From:1962+
LA: ENGLISH
AB: The Nazi Doctors' Trial, held in the city of Nuremberg 50 years ago, is a
landmark in the history of medicine and science. For the first time, the
horrors inflicted by a group of German scientists on innocent victims became
widely known. Most of the defendants received sentences that ranged from
relatively short imprisonment to death. The Trial also provided elements to
develop standards for permissible medical experimentation, known as the
Nuremberg Code. The atrocities judged in the Nazi Doctors' Trial, however, were
not isolated. They were part of an overall eugenic system that encouraged
euthanasia, compulsory steri1ization, and. selective marriages based on "genetic
health” and "racial hygiene." Individuals with oral clefts were considered
subject to these laws and suffered their consequences . This paper describes the
main features of the Trial, reviews the state of knowledge on oral clefts in
the 1930s and 1940s, presents how the laws of the Third Reich impacted the
lives of individuals with oral clefts, and speculates on the implications of
past and present eugenic policies in the future of humankind.
29 of 52
TI: [Evaluation of quality of life: a clinical challenge!
AU: Brioul-M
AD: Fondation John Bost, La Force.
SO: Sante-Publique . 1997 Sep; 9(3): 315-28
____ this source is not Available in S■J■M.C■Library
LA: FRENCH; NON-ENGLISH
AB: The possibility to estimate QUALITY OF LIFE opens new perspectives in the
appraising of therapeutic results. The author suggests a scale based on a
critical study of the previously known medical and psychiatric tools and some
original concepts which make it useful in the field of public health. The
estimate obtained with scale takes into account both subjective and objective
data. The results bring to light the possibilities to integrate the "SIQUAV”
scale (and its "DIONYSOS" application program) as complementary means for
clinical reflexion and action. After a survey of the significant data obtained
through the assessment and validation study (which show in all cases the
importance of psychic life, relationships and social esteem), the article
covers some problems relating to QUALITY OF LIFE in the context of public
heal th and to its relationship with the meaning and ethics of therapeutic
practices.
30 of 52
TI: Uncertainty in xenotransplantation: individual benefit versus collective
risk [see comments!
AU: Bach-FH; Fishman-JA; Daniels-N; Proimos-J; Anderson-B; Carpenter-CB;
Forrow-L; Robson-SC; Fineberg-HV
AD: Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA
02215, USA. fbachSbidmc.harvard.edu
SO: Nat-Med. 1998 Feb; 4(2): 141-4
____ this source is not Available in S■J■M.C.Library
LA: ENGLISH
31 of 52
TI: Government responses to HIV/AIDS in Africa: what have we learnt?
AU: Abdool—Karim—Q; Tarantola-D; As—Sy—E; Mcodie—R
AD: Southern African HIV/AIDS International Training and Research Programme,
c/o Medical Research Council, Pretoria, South Africa.
SO: AIDS. 1997; 11 Suppl B: S143-9
____ this source is not Available in S.J,M.C.Library
LA: ENGLISH
AB: While we should not lose sight of the development of vaccines and cures,
more immediate priorities include the implementation of effective STD control.
The syndromic management approach developed in Zimbabwe to overcome laboratory
constraints is a cost-effective way of managing STD. Of urgency is the
integration of STD services into primary health-care services, appropriate
training of staff, adequate provision and control over drugs and condoms, and
incorporation of traditional healers and community-based education on STD. A
second area of priority is the strengthening of the interaction between
prevention, care and support activities, which act in synergy. Effective
prevention and care require easy access to testing facilities with pre- and
post-test counselling, appropriate structures and services to provide
affordable and sustained care and support to those found to be infected with
HIV, provision of drugs for the treatment of opportunistic infections, and the
creation of a social environment and a legislation which protect against any
form of discrimination the rights of people living with HIV, their sexual
partners and their families.
32 of 52
TI: To tell the truth: ethical and practical issues in disclosing medical
mistakes to patients [see comments!
AU: Wu-AW; Cavanaugh-TA; McPhee-SJ; Lo-B; Micco-GP
AD: Department of Health Policy and Management School of Hygiene and Public
Health. Johns Hopkins University, Baltimore, Md. , USA.
SO: J-Gen-Intern-Med. 1997 Dec; 12(12): 770-5
____ this source is not Available in S.J.M.C.Library
LA: ENGLISH
33 of 52
TI: Qn the use of causal criteria.
AU: Weed-DL
AD: Preventive Oncology Branch, National Cancer Institute, Bethesda, MD 20892,
USA.
SO: Int-J-Epidemiol . 1997 Dec; 26(6): 1137-41
____This source is Available only few issues in S.J.M.C. Library
LA: ENGLISH
AB: BACKGROUND: Two recent accounts of the use of causal criteria make opposite
claims: that criteria should be used more often to avoid bias in assessments of
weak associations and, in direct contrast, that criteria are scientifically
invalid. METHODS: A recent review of the current practice of causal inference
in epidemiology, as well as some more theoretical concerns, reveals errors in
the two claims. RESULTS: In practice, epidemiologists often use the criteria of
consistency, strength, dose-response, and biological plausibility, but not
often temporality, when judging weak associations. These criteria are used for
causal assessments as well as for making public health recommendations. In
theory, causal criteria can be used to either refute or predict causal effects.
CONCLUSION: Research on causal inference methodology should be encouraged,
including research on underlying theory, methodology, and additional systematic
descriptions of how causal inference is practised. Specific research questions
include: to what extent can consensus be achieved on definitions and
accompanying rules of inference for criteria, the relationship of meta-analysis
to the criterion of consistency, and the interrelationships of criteria such as
consistency, strength of association, and biological plausibility.
34 of 52
TI: Cardiac xenotransplantation.
AU: DiSesa-VJ
AD: Department of Cardiothoracic Surgery, Allegheny University Hospital, MCP,
Philadelphia, Pennsylvania 19129, USA. disesa@auhs.edu
SD: Ann-Thorac-Surg. 1997 Dec; 64(6): 185S-65
____This source is Available in S.J.M.C Library
____Call Number: From: 1968+
LA: ENGLISH
AB: Heart failure is an important medical and public heal th problem. Although
medical therapy is effective for many people, the only definitive therapy is
heart transplantation, which is limited severely by the number of donors.
Mechanical devices presently are used as "bridges" to transplantation . Their
widespread use may solve the donor shortage problem, but at present, mechanical
devices are limited by problems related to blood clotting, power supply, and
foreign body infection. Cardiac xenotransplantation using animal donors is a
potential biologic solution to the donor organ shortage. The immune response,
consisting of hyperacute rejection, acute vascular rejection, and cellular
rejection, currently prevents clinical xenotransplantation. Advances in the
solution of these problems have been made using conventional immunosuppressive
drugs and newer agents whose use is based on an understanding of important
steps in xenoimmunity. The most exciting approaches use tools of molecular
biology to create genetically engineered donors and to induce states of donor
and recipient bone marrow chimerism and tolerance in xenogeneic organ
recipients. The successful future strategy may use a combination of a
genetically engineered donor and a chimeric recipient with or without
nonspecific immunosuppressive drugs.
35 of 52
TIs EBrain death and organ transplantation: ethical dilemmas for nursing?!
AU: Windels-Buhr—D
AD: Universitatsklinikum Benjamin Franklin, FU Berlin.
SO: Pflege. 1997 Jun; 10(3): 144-50
____ this source is not Available in S.J.M.C.Library
LA: GERMAN; NON-ENGLISH
AB: According to the WHO Program, nurses should be active in public health care
as equal members of a multiprofessional team. This position requires competent
professional action, which also implies moral competence, especially
necessitated by the coming paradigmatic changes caused by shifts in the
previous and current boundaries of the paradigm human being. One reason for
this shift are the greater medical technical possibilities. The medical
definition of brain death as the death of a human being per se is one example
of the altered boundary and its consequences. Must future components of the
nursing metaparadigm be changed because of this? To what extent is nursing
ethically obligated to integrate changes in social values into its
metaparadigm, ethics and objectives? The nursing metaparadigm, Henderson's
definition of nursing, the ICN's Basic Code of Ethics, and the nursing model
according to Roper, Logan & Tierney were used as the basis in the analysis of
the subject matter and problems. Furthermore, philosophical viewpoints of Jonas
& Harris will be included to clarify the deontological and teleological aspects
of standard ethics. Finally, conclusions are drawn about the intra- and
interprofessional ethical discourse about brain death and organ transplantation
among nursing professionals.
36 of 52
TI: Doctoring: University of California, Los Angeles.
AU: Wilkes-MS; Usatine-R; Slavin-S; Hoffman-JR
AD: Division of General Internal Medicine and Health Services Research, UCLA
School of Medicine 90095-1722, USA.
SO: Acad—Med. 1993 Jan; 73(1): 32-40
____This source is Available in S.J.M.C Library
LA: ENGLISH
AB: The Doctoring curriculum at the University of California, Los Angeles, UCLA
School of Medicine covers all four years of medical school. Its goal is to
train physicians to give care that is compassionate, humanistic, high-quality,
and evidence-based through a longitudinal, interdisciplinary curriculum with
integration of learning experiences within and between years and with more
emphasis on certain topics that had been previously neglected (e.g., advanced
physical diagnosis, nutrition, public health, ethics). The curriculum operates
alongside the traditional one, but strong attempts are made to link the two
curricula. The authors describe the gradual introduction of the Doctoring
curriculum, the sometimes formidable barriers that were encountered and in some
cases still exist (e.g., some faculty and student resistance, need to find
funds, faculty recruitment and retention). Active, interested faculty are
essential, and intensive faculty development is needed. A detailed description
of each year's courses- and teaching approaches is given. Year one focuses on
interpersonal communication, the medical interview, human development and
behavior, and the role of the community in health care; year two, on clinical
reasoning, physical diagnosis skills, population medicine, and ethics; year
three, on clinical problem solving, health services, professionalization
issues, and prevention; and year four (which is elective), on medical education
and leadership. The methods of evaluating students, faculty, and the curriculum
itself are described and assessed. The authors conclude with a review of plans,
prospects, and ongoing problems.
37
TI: Physician assisted suicide and the Supreme Court: putting the
constitutional claim to rest.
AU: Mariner-WK
of 52
AD: School of Public Health, Boston University, School of Public Health, MA
02118-2394, USA.
SO: Am—J-Public-Health. 1997 Dec; 87(12): 2058-62
____This source is Available only few issues in S.J.M.C. Library
Call Number: From: 1942-1991
LA: ENGLISH
AB: Like the debate about many controversial questions of ethics and medical
care in America, public debate about physician assisted suicide became focused
on questions of constitutional law. On June 26, 1997, the United States Supreme
Court unanimously rejected any constitutional right of terminally ill patients
to physician assisted suicide. An analysis of the Court's reasoning reveals
that its decisions resolved only a narrow constitutional question that affects
relatively few people—mentally competent, terminally ill patients who wish to
hasten their imminent deaths by having a physician prescribe medication that
they intend to use to commit suicide. Although suicide is not a crime, states
remain free to prohibit assisted suicide. One consequence of the Court's
decisions may be renewed debate on state laws. A more productive result would
be to address the broader public heal th concerns that gave rise to support for
physician assisted suicide—inadequate care for the terminally ill and
prevention of suicide.
38 of 52
TI: Undercover careseekers: simulated clients in the study of health provider
behavior in developing countries.
AU: Madden-JM; Quick-JD; Ross-Degnan-D; Kafle-KK
AD: Harvard School of Public Health, Boston, MA, USA.
SO: Soc-Sci-Med. 1997 Nov; 45(10): 1465-82
____ this source is not Available in S.J.M.C.Library
LA: ENGLISH
AB: The simulated client method (SCM) has been used for over 20 years to study
health care provider behavior in a first-hand way while minimizing observation
bias. In developing countries, it has proven useful in the study of physicians,
drug retailers, and family planning services. In SCM, research assistants with
fictitious case scenarios (or with stable conditions or a genuine interest in
the services) visit providers and request their assistance. Providers are not
aware that these clients are involved in research. Simulated clients later
report on the events of their visit and these data are analyzed. This paper
reviews 23 developing country studies of physician, drug retail, and family
planning services in order to draw conclusions about (1) the advantages and
limitations of the methods; (2) considerations for design and implementation of
a simulated client study; (3) validity and reliability; and (4) ethical
concerns. Examples are also drawn from industrialized countries, related
methodologies, and non-health fields to illustrate the issues surrounding SCM.
Based on this review, we conclude that the information gathered through the use
of simulated clients is unique and valuable for managers, intervention planners
and evaluators, social scientist, regulators, and others. Areas that need to be
explored in future work with this method include: ways to ensure data validity
and reliability; research on additional types of providers and health care
needs; and adaptation of the technique for routine use.
39 of 52
TI: A proposal for the establishment of scientific criteria for health claims
for functional foods.
AU: Clydesdale-FM
AD: Department of Food Science, Chenoweth Laboratory, University of
Massachusetts, Amherst 01003, USA.
SO: Nutr-Rev. 1997 Dec; 55(12): 413-22
This source is Available only few issues in S.J.M.C. Library
Call Number: From: 1946-1922
LA: ENGLISH
AB: Functional foods are defined and used differently in different nations.
Health claims for these foods influence consumer behavior and potentially
affect public heal th. In an increasingly global economy, health claims for
functional foods should meet internationally agreed upon scientific criteria.
The concept of health claims as it exists internationally is discussed, and
suggestions to assist consumers, government, industry, and academia in deciding
on a scientific and ethical basis for international agreement on health claims
for functional foods are offered.
40 of 52
TI: Observational epidemiology is the preferred means of evaluating effects of
behavioral and lifestyle modification.
AU: Stampfer—M
AD: Harvard School of Public Health, Boston, MA 02115, USA.
SO: Control-Clin-Trials. 199?’Dec; 18(6)s 494-9; discussion 514-6
____ this source is not Available in S.J.M.C.Library
LA: ENGLISH
AB: In evaluating the health effects of behavioral change, randomized trials
have the clear advantage of being able to provide unbiased and unconfounded
estimates. However, in practice, many difficulties loom that limit the utility
of trials. These include the inability to assess adverse behavior (except
indirectly), the often unrealistic requirement for very prolonged
adherence—perhaps for decades—to the randomized assignment, the requirement
for huge numbers for precise estimates of effect (as opposed to simply a
"significant result"), and the ethical problem of giving a placebo when an
efficacious agent is available. We must be alert to feasible opportunities to
test behavioral changes in clinical trials, but the many limitations mean that
we will continue to rely on well-conducted, large-scale observational studies
for most of our evidence on the effects of behavioral change.
41 of 52
TI: The study of untreated syphilis in the negro male [see comments]
AU: Brawley-OW
AD: Office of Special Populations Research, National Cancer Institute,
Bethesda, MD 20892, USA.
SO: Int-J-Radiat-Oncol-Biol-Phys. 1998 Jan 1; 40(1): 5-8
____ this source is not Available in S.J.M.C.Library
LA: ENGLISH
AB: PURPOSE: The participation of minorities in clinical studies is the subject
of much discussion and has even become the subject of Federal law. The project
known as the Tuskegee Syphilis Study and officially titled "The Tuskegee Study
of Untreated Syphilis in the Negro Male," is one of the great debacles of
American medicine and a national shame. Despite the fact that its existence is
well known, many do not know the historical facts of the study nor the context
of the study. My purpose here is to recount the facts of the study and its
historical context. METHODS: The history recounted here is taken from documents
gathered during a U.S. Senate investigation of the study, original papers
located in National Library of Medicine, and books about the trial. RESULTS:
The trial began in 1931 as a survey of the natural history of untreated
tertiary syphilis in Black men. This study enrolled 399 men with syphilis and
201 uninfected men to serve as controls. All were at least 25 years old at
enrollment. The men were told they were in a study, but never educated about
the implications. Later, men were not informed that there was a treatment for
effective treatment for their disease—a treatment that was being withheld from
them. This trial continued till 1972. CONCLUSION: Many of the issues that led
to the study and caused it to continue for 40 years still exist. The lessons of
the Public Health Study of Untreated Syphilis in the Untreated Negro include
the dangers of paternalism, arrogance, blind loyalty, and misuse of science.
"Those who do not appreciate history are condemned to repeat it" (Alfred North
Whitehead).
42 of
TI: Defining goals and conditions -for a sustainable world.
AU: Cairns-J Jr
AD: Department of Biology, Virginia Polytechnic Institute andState University,
Blacksburg, VA 24061 USA.
SO: Environ-Health-Perspect. 1997 Nov; 105(11): 1164-70
____ this source is not Available in S.J.M.C.Library
LA: ENGLISH
AB: Sustainable development is being approached component by
component—socioeconomic, sustainable agriculture, transportation , -forestry,
energy use, cities, and the like—but, leaving a habitable planet -for -future
generations will require the development o-f a widely shared paradigm. Further,
the paradigm should be ecological -from a scientific point of view. This
development will be facilitated by a discussion of goals and those conditions
necessary to meet them. The presently shared paradigm is that economic growth
is the cure for all of society's problems, such as poverty, overpopulation,
environmental degradation, and the increasing gap between rich and poor. A
paradigm shift from growth to sustainability might result either from suffering
painful consequences of continuing to follow out-moded paradigms or by
discussing what sort of ecosystems will be available to future generations. The
purpose of this paper is to help initiate such a discussion.
43
TI: Ethical challenges posed by clinical progress in AIDS.
AU: Bayer-R; Stryker-J
AD: Columbia University School of Public Heal th, New York City , NY, USA.
SO: Am-J-Public-Health. 1997 Oct; 87(10): 1599-602
____This source is Available only few issues in S.J.M.C. Library
Call Number: From: 1942-1991
LA: ENGLISH
of 52
44 of 52
TI: Ethics of xenotransplantation : animal issues, consent, and likely
transformation of transplant ethics.
AU: Daar-AS
AD: Department of Surgery, College of Medicine, Sultan Qaboos University,
Muscat, Sultanate of Oman.
SO:. World-J-Surg. 1997 Nov-Dec; 21(9): 975-82
____This source is Available in S.J.M.C Library
____Call Number: From: 1977+
LA: ENGLISH
AB: The shortage of organs, breakthroughs in research, involvement of
biotechnology companies, absence of ethically more acceptable alternatives, and
a vaguely perceived "time to put man on the moon" feeling have contributed to
the current reawakening of interest in xenotransplantation. The focus of
ethical attention has changed from the moral correctness of using animals for
research/therapy to an increasingly appreciated danger of the establishment and
spread of xenozoonoses in recipients, their contacts, and the general public.
The United Kingdom has established an embargo on clinical trials and has set up
a national regulatory authority to oversee and coordinate the development of
research, establish guidelines, and decide on when trials can proceed. In the
United States, on the other hand, the overall attitude is to "proceed with
caution," and the Food and Drug Administration has approved a number of
xenotransplant studies. The Public Health Service guidelines on reducing
infection risk are still evolving and are likely to end up being more cautions
than they are currently. There are a number of reasons for not using subhuman
primates for xenotransplantation, including their closeness to humans, the
likelihood of passing on infections, their depletability (gorillas,
chimpanzees), their slow breeding, and the expense of breeding them under
specified-pathogen free conditions. The pig, although domesticated and
familiar, is too distant to evoke the same feelings we have for primates, has
the correct-size organs, is probably less likely to pass on infections, breeds
rapidly, and is not endangered; moreover, millions of them are eaten every
year. Although drawing ethical conclusions is difficult, at this stage of
knowledge and debate it seems acceptable to manipulate pigs genetically and to
proceed to using their organs for xenotransplantation trials when infection
control measures and the scientific base justify it. The question of informed
consent is likely to be a vexing one. It might end up more of a binding legal
contract than consent as we understand it now. Xenotransplantation is also
unlikely to cost less than, or significantly alleviate the shortage of,
cadaveric organs in the short term. The international dimension of the risk of
infection is becoming obvious, but there has so far been no effort to convene
an international forum to agree on universally acceptable guidelines.
45 of 52
TI: Methodological issues in the use of biological markers in cancer
epidemiology: cohort studies.
AU: Hunter-DJ
AD: Harvard School of Public Health, Department of Epidemiology, Boston, MA
02115, USA.
SO: IARC-Sci—Publ. 1997(142): 39-46
____this source is not Available in S.J,M.C,Library
LA: ENGLISH
AB: In this chapter we summarize the major strengths and weaknesses of cohort
studies; consider how these characteristics influence the use of biomarkers in
cohort studies; briefly reView considerations of statistical power, design and
the influence of measurement error in cohort studies; and discuss some of the
emerging ethical considerations that relate to the use-of biomarkers in
prospective studies.
46
of 52
47
of 52
TI: Synergy, antagonism, and scientific process [editorial!
AU: Hook-GE; Lucier-GW
SO: Environ-Health-Perspect . 1997 Aug; 105(8): 784
____this source is not Available in S■J,M■C.Library
LA: ENGLISH
TI; Human rights, ethics and the Krever inquiry [editorial!
AU: Hoey-J
SO: CMAJ. 1997 Nov 1; 157(9): 1231
____this source is not Available in S.J.M.C.Librar y
LA: ENGLISH
48 of 52
TI: Notifying patients exposed to blood products associated with
Creutzfeldt-Jakob disease: integrating science, legal duties and ethical
mandates [see comments!
AU: Caulfield—T; Dossetor J; Boshkov-L; Hannon—J; Sawyer—D; Robertson—G
AD: Health Law Institute, Faculty of Law, University of Alberta, Edmonton.
SO: CMAJ. 1997 Nov 15; 157(10): 1389-92
____this source is not Available in S.J.M.C.Library
LA: ENGLISH
AB: The issue of notifying people who have been exposed to blood products that
have been associated with Creutzfeldt-Jakob disease (CJD) has arisen at a time
when the Canadian blood system is under intense scrutiny. As a result, the
Canadian Red Cross Society issued a recommendation to health care institutions
that recipients of CJD-associated blood products be identified, notified and
counselled. Although Canadian jurisprudence in the realm of informed consent
may support a policy of individual notification, a review of the scientific
evidence and the applicable ethical principles arguably favours a policy of a
more general public notification. Indeed, situations such as this require a
unique approach to the formation of legal and ethical duties, one that
(6
effectively integrates all relevant factors. As such, the authors argue that
individual notification is currently not justified.. Nevertheless, if a system
of general notification is implemented (e.g., through a series of public health
announcements), it should provide, for people who wish to know, the
opportunity to find out whether they were given CJD-associated products.
49 of 52
TIs Equal treatment: bestowed or earned? [comment!
AU: Soskolne-CL
AD: Department of Public Heal th Sciences, University of Alberta, Edmonton,
Canada.
SO: Ann-Epidemiol. 1997 Oct; 7(7): 434-6
this source is not Available in 5.J.M.C.Library
LA: ENGLISH
AB: PURPOSE: While the complaint against non-industry employed epidemiologists
for holding their industry-based colleagues to a higher level of scrutiny is
accurate, this paper shows that there is a sound basis for such treatment. It
also shows, however, that a shift towards ongoing vigilance is needed on the
part of all epidemiologists to guard against such bias. METHODS: The proposed
shift is made possible through the recent incorporation in ethics guidelines of
principles that indeed identify the impropriety of any such bias. RESULTS: In
the same guidelines, there are principles that require scientific impartiality.
Industry-based epidemiologists, by the condition of their employment, may find
the avoidance of partiality to the corporate interest more problematic than do
non-industry based epidemiologists to their respective sponsors. It is in light
of past examples of partiality among industry-based epidemiologists that other
epidemiologists may be biased against them. CONCLUSIONS: This paper concludes
with the realization that both groups of epidemiologists have the challenge of
correcting the biases inculcated over many years. Trust needs to be established
between industry and non-industry-based epidemiologists through greater
acceptance on the part of the latter and exemplary conduct on the part of the
former to overcome past practice records.
50 of 52
TI: Unintended consequences and professional ethics: criminalization of alcohol
and tobacco use by youth and young adults.
AU: Wolfson-M; Hourigan-M
AD: Division of Epidemiology, School of Public Health, University of Minnesota,
Minneapolis 55454, USA.
SO: Addiction. 1997 Sep; 92(9): 1159-64
____ this source is not Available in 5 . J . M. C., Library
LA: ENGLISH
AB: This paper describes how widespread legal changes appear to have affected
law enforcement practices concerning youth tobacco and alcohol use in the
United States. We argue that the threat of criminalization was seldom addressed
in scientific and public policy discussions of the drinking age, and only
sporadically addressed in discussions of measures to regulate youth access to
tobacco. We argue that unintended consequences are an important ethical issue
for professionals involved in advocating, developing, implementing and
evaluating public policy concerning substance abuse.
51 of 52
TI: Confidentiality, disseminated regulation and ethico-legal liabilities in
research with hidden populations of illicit drug users.
AU: Fitzgerald-JL ; Hamilton-M
AD: Department of Public Health and Community Medicine, University of
Melbourne, Parkville, Victoria, Australia, johnfitzfiariel.ucs.unimelb.edu.au
SO: Addiction. 1997 Sep; 92(9): 1099-107
____ this source is not Available in S. J M ■ C . Library
LA: ENGLISH
AB: An assurance of confidentiality is at the core of trusting relationships in
outreach, ethnographic research and patient/c1ient encounters. In the past,
centralized State health care services have provided assurances of
confidentiality to those engaged in health-related research either through
common law or by statute. However, unless specific confidentiality legislation
is in place, no assurances of confidentiality can now be made to research
subjects involved in either longitudinal, interview-based or ethnographic
research. The consequences of this situation become more serious given the
recent emergence of the use of peer and community outreach. A significant
problem with the outreach model is the failure to provide adequate legal and
ethical support for those in cutreach roles. Additionally, unless research
subjects can be granted assurances of confidentiality, they will not engage in
research for fear of later prosecution. At this time when outreach models are
the modus operandi, the lack of a fundamental commitment to sustain
confidentiality may seriously undermine further research. This paper will draw
on the experiences of some Australian qualitative research and will review some
of the ethical and legal liabilities for research that arise when an assurance
of confidentiality cannot be given to those participating in research.
52 of 52
TI: Legal history of emergency medicine from medieval common law to the AIDS
epidemic.
AU: Curran-WJ
AD: Department of Health Policy and Management, School of Public Heal th,
Harvard University, Boston, MA, USA.
SO: Am—J—Emerg-Med. 1997 Nov; 15(7): 658-70
____ this source is not Available in S.J.M.C.Library
LA: ENGLISH
AB: The early development of legal obligation in emergency medicine is traced
through medieval English common law to the first stages of American law after
Independence. An identifiable set of legal principles in the nineteenth and
early twentieth centuries is described. The movement away from an absence of
legal and ethical duties to answer any emergencies, or to offer any emergency
services in hospitals, toward a growing demand for access to emergency services
in the middle decades of the twentieth century is reviewed. The enactment of
Good Samaritan Laws is described, along with other federal and state law
reforms. In the modern era, there has been a substantial legal and ethical
change to a requirement of extensive duties to operate open-admission emergency
services in virtually all acute-care hospitals. The AIDS epidemic is utilized
as a case example of expanded legal and ethical duties to.offer emergency care
in a nondiscriminatory manner to all patients presenting at hospital emergency
departments.
PC-SPIRS 3.40
MEDLINE (R) 1998/11-1998/12
MEDLINE (R> 1998/11-1998/12 usage is subject to the terms and conditions of the
Subscription and License Agreement and the applicable Copyright and
intellectual property protection as dictated by the appropriate laws of your
country and/or by International Convention.
1 of 14
TI: EPublic health work is improvement without impairment!
AU: Wall-S; Weinehall-L
AD: Institutionen for epidemiclogi och folkhalsovetenskap, Umea universitet.
SO: Lakartidningen. 1998 Sep 2; 95(36): 3807-8, 3811
____ this source is not Available in 5.J.M.C.Library
LA: SWEDISH; NON-ENBLISH
AB: Strategies for community intervention, their evaluation and social
patterning are discussed in the article. Theories and methods are called for to
enable better assessment of social inequalities in health outcome variables and
processes in public heal th endeavours. With this is a starting point some
methodological and ethical issues relating to preventive programmes and their
evaluation are identified.
2 of 14
TI: Develop and strengthen public heal th law.
AU: L'hirondel-A; Yach-D
AD: Policy Action Coordination Team, World Health Organisation, Geneva.
50: World-Health—Stat—Q. 1998; 51(1): 79-87
____ this source is not Available in S.J■M■C.Library
LA: ENGLISH
AB: The rule of law consists of one of the key requirements to implement policy
reforms. The new global health policy, "Health for All in the 21st Century",
indicates the role of public heal th law to attain its values and objectives.
This article studies the status retained to secure both international and
national law in the new policy, and identifies two initiatives to be undertaken
by WHO to develop and strengthen public heal th law. The usefulness and
efficiency of international law depend on national capacities to implement law.
Thus, this article concludes that the Organization should adopt international
legal instruments and that it should, simultaneously, assist Member States to
build institutional and human capacity in public health law. However, these
initiatives require that all Member States confirm political determination to
link economic and social reforms with legislative reforms.
3 of 14
TI: Health for all: analyzing health status and determinants.
AU: Lerer—LB; Lopez-AD; Kjel 1strom-T; Yach-D
AD: Programme on Substance Abuse, World Health Organization, Geneva.
SO: World-Health-Stat-Q . 1998; 51(1): 7-20
____ this source is not Available in S.J.M.C■Library
LA: ENGLISH
AB: An analysis of health status and determinants is presented as a basis for
health for all renewal and in order to provide a model linking the health for
all vision with strategy and action. Equity and gender, at the core of health
for all, directly concern health status and the distribution of health
determinants. The role of the various transitions (demographic,
epidemiological, health risk and technological) is described, the need to
strengthen the link between data and decision-making for health is explained,
and the range of health determinants-—macroeconomic, demographic/nutritional,
environmental, tobacco and alcohol and their implications for policy—is
outlined.
4 of 14
The beast inside.
AU: Klotzko-AJ
AD: Institute of Medical Ethics, Edinburgh.
SO: Nurs—Times. 1998 Aug 5-11; 94(31): 34—5
this source is not Available in S . J■M■C.Library
LA: ENGLISH
5
TI: Physicians as double agents: maintaining trust in an era of multiple
accountabilities.
AU: Shortell-SM; Waters-TM; Clarke-KW; Budetti-PP
AD: School o-F Publ ic Health, Division o-F Health Policy and Management,
University o-F California, Berkeley 94720-7360, USA.
shortell@uc1ink4.Berkeley.edu
SO: JAMA. 1999 Sep 23-30; 280(12): 1102-8
____This source is Available in S.J.M.C Library
___ Call Number: From: 1918+
LA: ENGLISH
of 14
6 of 14
TI: Health reform in America: the mystery of the missing moral momentum.
AU: Brown-LD
AD: Division of Health Policy and Management, Columbia School of Public Heal th,
New York City, USA.
SO: Camb-0-Healthe—Ethics. 1998 Summer; 7(3): 239-46
____this source is not Available in S,J,M.C.Library
LA: ENGLISH
7 of .14
TI: Presentation: Epidemiology and public heal th: is a new paradigm needed or a
new ethic? [see comments]
AU: Gori-GB
AD: The Health Policy Center, Bethesda, Maryland 20816-1016, USA.
SO: J-Clin-Epidemiol. 1998 Aug; 51(8): 637-41
____This source is Available only few issues in S.J.M.C. Library
____Call Number: From: 1994+
LA: ENGLISH
AB: Public heal th militancy has been increasingly frustrated by what many
perceive as the marginally fertile studies of risk factors operating at the
individual level, whose causal underpinnings are often and inevitably weakened
in multifactorial situations. As a remedy, leading advocates propose a
refocusing of epidemiology and pub1i c heal th on socioeconomic, cultural, and
political studies, and on broad interventions at population level. This new
"paradigm" would be aided by a relaxation of evidentiary standards of
causality, away from scientific criteria and more toward dialectic (rhetorical)
precepts derived in a humanistic and sociologic tradition. It is countered here
that such proposals would further reduce the objectivity and thus likely weaken
rather than strengthen epidemiology and the justification of public health
action. Instead, a realistic appraisal finds that multifactorial epidemiology
raises warning signals of varying influence, and that the usefulness of
epidemiology and public hea1th could be enhanced by conceiving of methods to
score the relative strength and priority of such warnings.
8
of 14
TI: American Association of Public Health Dentistry. Code of ethics and
standards of professional conduct.
SO: J—Public—Health-Dent. 1998; 58 Suppl 1: 123-4
this source is not Available in S.J.M.C■Library
LA: ENGLISH
9 of 14
TI : Dental public health competencies.
SO: J-Public-Health—Dent. 1998; 58 Suppl 1: 121-2
____ this source is not Available in S.J.M.C.Library
LA: ENGLISH
10
of 14
11
of 14
TI: Preamble to the competency statements -for dental public health.
SO: J-Public-Hea1th-Dent. 1998; 58 Suppl 1: 119-20
____ this source is not Available in S.J,M.C.Library
LA: ENGLISH
TI: HIV testing of infants: privacy and public hea1th.
AU: Etzioni-A
AD: George Washington University, USA.
SO: Health-Aff-MilIwood. 1998 Jui-Aug; 17(4): 170-83
____ this source is not Available in S. J.M.C.Library
LA: ENGLISH
12 of 14
TI: [Basic medical competence: a neglected educational goal in medical
education?!
AU: Perleth-M
AD: Abteilung Epidemiolcgie und Sozialmedizin, Medizinische Hochschule
Hannover. perlethSepi.mh-hannover.de
SO: Med-Klin. 1998 Jun 15; 93(6): 381-7
this source is not Available in 8.J.M.C.Library
LA: GERMAN; NON-ENGLISH
AB: This paper analyses some recent proposals of how to change undergraduate
medical education in Germany and in other countries. This leads to the
formulation of a set of fundamental clinical competencies, which are defined as
skills that enable physicians to react to challenges pertaining to their work.
in a professional way. These fundamental clinical competencies comprise
knowledge, skills and attitudes. With regard to the actual performance of the
German system of undergraduate medical education, deficits are depicted in the
following areas: psychosocial and communicative competencies including advice
and provision of information to patients, primary care, public heal th, ethics
and clinical epidemiology/evidence-based medicine. For each of these areas, a
proposal for change is provided.
13 of 14
TI: Balancing the quality of consent.
AU: Hansson-MO
AD: Department of Public Heal th and Caring Sciences, Academic Hospital,
Uppsala, Sweden.
SO: J-Med-Ethics. 1998 Jun; 24(3): 182-7
____ this source is not Available in S■J■M■C.Library
LA: ENGLISH
AB: The rule that one must obtain informed consent is well established in
medical ethics and an intrinsic part of clinical practice and of research in
biomedicine. However, there is a tendency that the rule today is being applied
too rigidly and with too little sensitivity to the values that are at stake in
connection with different kinds of research protocols. It is here argued that
the quality of consent needs to be balanced against variables such as degree of
confidentiality and importance of values at stake,, in order to be ethically
acceptable. Appropriate information and consent procedures should be adjusted
accordingly. Three levels are suggested, ranging from extensively informed
consent with both written and oral information, through informed refusal with
only a limited amount of information given to, at the other end of the scale,
just making relevant information available.
14 of 14
TI: EEvolution of medical responsibility and code of ethicsJ
AU: Glorion-B
AD: Conseil national de 1'Ordre des Medecins, Paris.
SO: Bui1-Acad-Natl-Med. 1998; 182(3): 553-8
____ this source is not Available in S.J.M■C.Library
LA: FRENCH; NON-ENGLISH
AB: The evolution of the medical responsibility cannot escape from the
determining influence of the scientific progress, but it is also significantly
influenced by sociological and psychological factors that often are more
difficult to analyse. If the ethical rules express the physicians' obligations
in legal terms, it perfectly determines the spirit which must drive every
physician thus revealing his sense of responsibility. This concept of the
medical responsibility distinguishes and differentiates itself from the penalty
responsibility and from the compensation responsibility which only takes place
in the context of the compensation for a harm caused. The acquisition of the
prime sense of the responsibility is a product of a background dominated by the
experience, the example, the conscience. The expression of the medical
responsibility is most of all personal, but more and more fits in with the
public heal th issues and becomes a collective responsibility. Finally in order
to meet the more and more accurate specialists' demands, the physician's
responsibility which must remain within the boundaries of his competence must
be fulfilled in the frame of a team. This dimension imposes on him new
regulations that affect the quality of the relationship between the various
contributors. An evolution of the responsibility thus grows according to the
progress and within the adapted scope of ethics.
Ethics in Medical Education
Dr. C. M. Francis,
formerly with St. John's
Medical College, is
Consultant to Community
Health Cell, fiangalore.
Dr. C. M. Francis
“Education is not for
knowing more but for
behaving differently"
- Ruskin
edical ethics is a neglected
subject. Medical educators had
been paying insufficient attention to
loping the student’s capability
to face ethical dilemmas. But, in
recent times, many medical schools
abroad have instituted courses in
medical ethics.
Many of the ills of the present day
medical profession can be traced to
the lack of doctors’ ability to properly
tackle ethical problems in their prac
tices. Practically nothing is being
done to equip the medical students
to practice ethically.
Most medical colleges do not
have medical ethics in their curricu
lum. Even in the very few (they can
be counted on the fingers) which
have, the teaching/learning of medi
cal ethics is not a ’required’ subject.
_What do doctors (after graduai^P) think about the need for train
ing in medical ethics? 90% of the
respondents to a survey wanted
training in medical ethics during
undergraduate medical education.
84.5% admitted that they did not
have any training at all.
Ethics depends on the values of
the profession and society. Among
the important values in medicine
are respect for human life and
love and compassion. Charaka
Samhjta (6th century B.C.) states:
“He who practices, not for money
or for caprice but out of compassion
for living beings is the best among all
physicians. Hard is it to find a
conferor of religious blessings com
parable to the physician who snaps
M
the snares of death for his patients.
The physician who regards compas
sion for living beings, as the highest
religion, fulfills his mission and ob
tains the highest happiness".
Learning Medical Ethics
Thompson in an editorial in the
'Medical Education has pleaded for
the integration of medical ethics in
medical education. The World Health
Organisation (WHO) and the Coun
cil for International Organisation of
Medical Science and others have
emphasised the same need.
Can ethics be 'taught' or is it
'caught'? It is important that 'ethics’
is learned. The principles and prac
tice of medical ethics can be learned
in a variety of ways and situations: in
the classrooms, during bedside
teaching and ward-rounds besides
from the examples set by by the
faculty and the institution. A role
model is very important. The teacher
shows how the ethical principles are
applied to a particular patient. The
student is helped to identify the
ethical problems, with respect to the
patient, the family and the commu
nity.
The way the institution functions
can have a marked impact on the
student. If the institution as a whole,
acts responsibly, gives respect to the
patients (and others) and observes
the ethical code of conduct in pro
viding service, training or research,
the student would imbibe these
values. Thus the philosophy and
practice of the medical college play
an important role in shaping an
ethically sound doctor. The objec
tives must be clear. They must be
reinforced by ethical actions at every
level; management, administration,
faculty and other staff.
A Pro-patient Approach
rSifeg-
We tend to consider
patients as
‘teaching material’:
in fact, they are
technical teachers.
1
.
------------------------ --------------------------------------
If we realise this fact, we will give
greater respect to our patients. Il is
unfortunate that there is no 'home
visiting’ in the training of medical
students. It is getting out of fashion!
We want the patients, whatever be
their condition, to come to the clinic
or hospital. Home visiting could have
added to the values.
Ethics in Selection of Students
What determines the quality of a
doctor? It is very difficult to alter the
personality traits of a student when
he/she enters the medical college at
the age of say, of 17 or 18. If positive
traits and qualities are present, it is
easier to nurture and strengthen
them.
There are a few medical colleges
which take the process of selection
very seriously, like St. John’s Medical
College, Bangalore and Christian
Medical College, Vellore. In St. John’s,
the process consists of an entrance
test; in which one paper is on values,
a 2-day group observation, a psycho
logical test and the usual short
interview.
Most of the medical colleges
(especially the Government Medical
Colleges) go by the academic grades
at the common entrance test. A cadre
of students who are intellectually
narrow cannot be expected to beHealth (orlhc Millions • July-August 1996 -3
b.
Patient Preference
The patient accepts or rejects the.
recommended procedure. The
decision of the patient must be
respected. If the doctor feels that
a particular procedure Is essen
tial in an emergency, the doctor
must try to convince the patient
of its essential nature.
c.
d.
come sensible doctors. Worse still is
the situation of ‘capitation fee’ col
leges. When admission is decided
by money power, one cannot ex
pect the medical graduates to cul
tivate the desired ethical values.
Principles of Medical Ethics
The major principles of medical
ethics are:
Beneficence
All medical interventions must be for
the good of the patient (and family
and society).
Non-maleficence
Cause no harm. Where harm might
occur, it must be minimal and the
benefit must outweigh the harm.
Autonomy
TYaditionaily, we had accepted the
ethics of trust. But in recent times,
due to western influence, it is giving
way to the ethics of rights. Patient
has the right to control what hap
pens to him or her.
Informed Consent
Patients’ consent is necessary for all
procedures. The consent has to be
informed and voluntary. The infor
mation must be complete and ad
equate for the patient to make a
considered decision.
Justice
There is need for distributive justice.
There is also a need to allocate
resources fairly and evenly. Equity
4 • Health for the Millions • July-August 1996
has to be assured and this has to be
done with quality.
Allied Factors
Questions of benefit or burden to
other parties (family, relative^
needs consideration. Of late, tlW
cost of medical care has risen
exorbitantly. Medical care can
ruin families, even when the
benefit to the patient is marginal
or doubtful.
Community Health
While it is important to think of the
individual patient, there is a need to
consider the diagnosis and manage
ment of community’s illnesses and
health problems. Thus, there is inter
dependability of society and medi
cine.
Quality of Life
It is important to consider the
quality of life after the procedure
which may be subjective. It has
to be determined by the con
cerned person and not by a third
person.
Ethical Issues Before the Profes
sion
Clinical Ethics
1.
The practice of medicine, with re
spect to the patient-doctor relation
ship, has certain goals:
The doctor-patient relationship is in
the nature of an implied contract.
The doctor has a duty of care in
♦ deciding whether to accept the
patient for treatment;
♦ Preservation of life (prolongation
of life).
♦ Cure of the disease.
♦ Relief of suffering (and symp
toms).
♦ Care of the person.
♦ Promotion of health and preven
tion of disease.
♦ Restoration of function and reha
bilitation.
To make a ethical decision in a
clinical situation, at least four factors
must be considered:
a.
Medical Indication
Make a proper diagnosis. Con
sider alternative therapeutic mo
dalities. Weigh their relative ad
vantages and disadvantages,
short-term and long-term. Inform
the patient of the available op
tions, recommend the best.
Negligence
♦ deciding in diagnosis and man
agement; and
♦ administering the treatment. "
If there is breach of duty, the
doctor is negligent. If harm is caused
to the person, damages can be
awarded against the doctor. “In the
case of a medical man, negligence
means failure to act in accordance
with the standards of reasonably
competent medical man at that
time".
A negligent doctor could be sued
in a court of law ordisciplinary action
taken against him/her by (he Medical
Council. Under the Consumer Protec
tion Act, 1986, the consumer courts
can order compensation to the com
plainant "who hires any services fora
consideration which has been paid or
promised... and includes beneficiary
- ofsuch services... ”
"The physician who sets about to
treat a disease, without knowing
-anything about it, is to be punished
even if he is a qualified physician; if
he does not give proper treatment,
he is to be punished more severely;
and if by his treatment, the vital
functions ofthe patient are impaired,
he must be punished most severely".
2.
every consideration for confiden
tiality and privacy.
refuse participation in any re
search or projects.
•» expect reasonable continuity of
care.
♦ examine and receive explanation
of his bill.
♦ know the hospital rules applying
to his/her conduct as a patient.
♦ access to medical records
♦
♦
Confidentiality
Every patient has a right to privacy.
Matters confined to the doctor in the
course of professional relationship is
confidential. This is upheld in all
oaths and declarations (Hippocratic
oath; Geneva declaration etc.). Con
fidentiality has to be observed with
^bpecl to medical records also.
Information may be given to a
third party only under the following
circumstances:
6.
Abortion
The Medical Termination of Preg
nancy Act, 1971 permits ending of
pregnancy for therapeutic, eugenic
and personal considerations. Most of
the codes of conduct and declara
tions are opposed to it.
"/ will maintain the utmost re
spect for human life, from the time
of conception" (World Medical Asso
ciation, Geneva, 1948). -
♦
Notifiable diseases (to the health
authority).
7.
♦
Risk to public safety (under de
fined circumstances).
♦
Disclosure ordered by the court
or required by law.
Society, in general, is pro-male. Pre
natal sex determination is done
most often with the intention of
rejecting the female foetus. Though
this is banned, selective female
3.
Irrational Drug Therapy
Drugs must be used for proper
indications. They must be effective,
have good benefit - risk ratio and
should be of good quality. Banned,
hazardous and useless drugs should
^ot be used.
Female Foeticide and Infanti
cide
foeticide continues.
8.
Assisted Reproductive Tech
nologies
There is a biological, cultural and
social urge to have children. What
should the doctor do when there is
infertility? Disturbed function must
be treated. Often no particular cause
can be found.
One answer to not
having own children is
adoption. But it is not
popular in India,
though very popular in
western countries,
where there are not
enough children for
adoption.
There are many new technologies
of reproduction such as artificial
insemination by husband or by a
donor; in-vitro fertilisation and em
bryo transfer, gamete intra-fallopian
transfer and surrogacy. Each one
brings in its own ethical problems.
" Prescriptions
Irrational prescriptions can occur in
a variety of ways, such as extrava
gant, unnecessarily and expensive,
incorrect and multiple (too many
drugs prescribed, often in combina
tions). -
5.
Patients’ Bill of Rights
(abridged)
A patient has the right to:
♦ considerate and respectful care.
♦ obtain from his physician com
plete information concerning di
agnosis, treatment and progno
sis.
♦ refuse treatment to the extent
permitted by law.
Health tor the Millions • July-Angusl 1996 -5
9.
The Terminally III
The doctor has to face the problem
of managing the terminally ill and
the dying. It is very important to deal
with them with competence and
compassion. Many of them have
symptoms such as intense pain and
respiratory distress. Relief of these
symptoms is important. Relief of
pain may produce ethical issues,
when large amounts of potent anal
gesics may have to be administered,
these may have side effects of de
pressing respiration. But if the pri
mary aim is relief of pain and there
was no intention of shortening life,
the procedure is ethically accept
able.
Often heroic efforts are made
to preserve or prolong life. But,
when there is no reasonable hope
of any benefit to the patient, there
is no need to resort to extra
ordinary measures to preserve
life. It may not be prolonging life
but prolonging death.
More and more doctors tend to
decide not to resuscitate patients
admitted to the intensive care units,
when death is the most likely out
come to avoid suffering and wastage
of resources.
10.
Living Will
The living will gives the preference of
the person at the time of making it.
It does not give the wish at the time
when the patient is seriously ill. It is
not legal in India.
There is considerable controversy
on the issue of euthanasia, whether
passive or active. Both of them raise
ethical issues.
II.
Suicide
Expensive and complicated tech
niques are introduced without prop
erly conducting controlled trials.
"It is surely a great criticism of our
profession that we have not
organised a critical summary...of all
the relevant randomized controlled
trials".
John Kenneth Galbraith (the noted
Economist and former US Ambassa
dor to India), has said that large
corporations often say that they
meet the needs and demands of the
people. But what they really do is to
create a demand for what they want
to supply. Public desires are manipu
lated. A similar thing often happens
with newer medical technologies equipment, procedures or drugs.
Many ethical questions arise
when doctors use technologies
which are not beneficial to the
patient or when better and less
costly technologies exist.
13.
Health Policy
Doctors often shy away from health
policies, leaving them to administra
tors, bureaucrats and politicians. This
is totally wrong. Health policy de
fines the strategies for the health of
the people. It depends on the value
systems and therefore raises many
ethical questions.
Health policy should ensure a
minimum acceptable level of health
care forall. It should lead to equity
with quality. While a purely medical
response is inadequate, the medical
professionals, individually and col
lectively, must address the issues of
health care. The doctors will have to
make ethical choices and advise the
people and the policy makers on
required improvements.
When a person fails to find meaning
in his or her life or has muddled it
(often financial problems), he/she
may attempt suicide. It often arises
from despair, which may be tempo
rary. Attempted suicide is punish
able in law. Attempt at suicide is
often a call for help.
Large sections of our people live in
deplorable conditions where healthy
living is not possible. About 200
millions are destitutes. This is nega
tion of health. Health care in an
unjust society is unjust.
12.
15.
Technology
There is a sudden spurt in the growth
of costly medical technology,
whether diagnostic or therapeutic.
6 • Healthfcrthe Millions • July-August 1996
14.
Distributive Justice
Human Experimentation and
Research
The various codes of conduct have
stated the conditions under which
human experimentation and research
can be carried out ethically. It is im-_portant to have an Ethics Committee
or Ethical Review Board, whose clear
ance must be obtained for the project.-'
These can be constituted with repre
sentatives of the medical teachers
(other than the researchers), research
consultant (preferably a social scien
tist), ethics consultant and a legal
consultant. If desired, the Medical
and Nursing Superintendents and the
Spiritual Advisor or Counsellor could
also be included.
16.
Emerging Diseases
The medical students must get the
capability to deal with emerging
disease or the newer manifestations
of older diseases. The student must
‘learn to learn’. One such disea^h
with many ethical issues is AIDS.
Many of the earlier graduates have
not seen such cases. They are un
able to comprehend the seriousness
of HIV infection and the ethical
problems arising from them. Con
tinuing education, including ways to
tackle the ethical issues, is a must.
17.
Genetics
With the study of the human ge
nome and genetic engineering, a list
of ethical issues arise. We do not
know how to tackle them.
“The world that we have
made as a result of th^
level of thinking that
have done so far, creates
problems we cannot
solve at the level we
created them”.
wP
- Albert Einstein
----- -----Note: A curriculum co.uering the above
mentioned issues in medical ethics is being
followed at St. John’s Medical College, Ban
galore. The duration is 15 hours in pre-clinical
years and 15 hours in clinical years. The
faculty consists of clinicians who are ethically
literate and practicing; ethicists; sociologists
etc. The judicious mingling of faculty (rained
in different disciplines brings in different view
points which stimulates the moral reasoning
and ethical judgement in medical students
and practicing doctors.
WORLD AFFAIRS
A code of ethics
HE major source of information
ciples which governments could
about drugs is the pharmaceutical
adapt to their national situation.
industry, and much of that informa
However, as Dr. .!• e Collier, editor
tion takes the form of promotion.
of
Drug
and
Therapeutics
Controlling excessive and misleading
Dulleiin, and Robin Fox, editor of
promotion of drugs is therefore a
The Lancet, said in an article in
key measure in improving their ra
(The Lancet, April, 1993), “these
tional use. Clinical pharmacologist
clear and straightforward criteria
Dr. Andrew Ilerxheimer, coordina
have been much neglected.”
tor of the International Society of
The following are the key
Drug Bulletins which links nearly 50
elements of the WHO’s ethical cri
bulletins worldwide that provide in
teria:
dependent and comparative informa
* Promotion should be reliable, ac
tion on drugs, describes drug pro curate, truthful, informative, balanc
motion as “the truth, the half-truth ed, up-to-date, capable of substanti
and nothing like the truth.”
ation and in good taste. It should not
The industry spends about twice contain misleading or unverifiable
much on promoting its products statements or omissions likely to in
it does on research. Canadian duce medically-unjustifiable drug
physician Dr. Joel Lexchin says that,
use or to give rise to undue risks.
in developing countries at least,
★ The word “safe” should only be
promotional expenditure is 20-30 used if properly qualified.
per cent of sales (Pharmaceutical * Promotional material should not
Promotion, in the Third World).
be designed so as to disguise its real
Since 19S1 the International Fed nature.
eration of Pharmaceutical Manufac * Financial or material benefits
turers Associations (IFPMA) has had should not be offered to or sought
a voluntary code of practice to cover by health care practitioners to influ
marketing and promotion. Most na ence them to prescribe drugs.
tional industry associations have * Scientific and educational activit
similar
voluntary
codes. ies should not be deliberately used
Herxheimer, who conducted a sur for promotional purposes.
vey on the effectiveness of the vol * Drug advertisements should not
untary code in the United Kingdom, be directed at children.
describes these codes as “much more * Advertisements should usually
show than substance. Codes are in contain, among others, the name(s)
terpreted rather literally. The spirit of the active ingredient(s) using
of the code is usually disregarded. either international non-proprietary
Enforcement doesn’t exist. There names or the approved generic name
are no sanctions. The same compan of the drug; the brand name; the
ies repeat their transgressions again dosage form or regimen; the contentagain.”
of active ingredient(s) for each dos
The latest study to document this age form or regimen; rhe name of
problem has been carried out by the other ingredients known to cause
Office of Technology Assessment problems; approved therapeutic
(OTA) of the United States Con uses; side effects and major adverse
gress. It found the label and package drug reactions; precautions, contra
inserts for at least half of a sample of indications and warnings;, major in
241 products sold by U.S.-based teractions; the name and address of.
companies in four countries — Bra the manufacturer or the distributor.
zil, Kenya, Panama and Thailand — * Prescribers and dispensers should
failed to provide sufficient informa be provided with complete and
tion for doctors to use the drugs unbiased information for each prod
safely and effectively. The report uct.
concluded that relying on informa * The main part of the remuner
tion from manufacturers could lead ation of medical representatives
to “serious or life-threatening medi should not be directly related to the
cal problems or, at best, ineffective volume of sales they generate
treatment” (Drug Labelling in De ★ Post-marketing scientific studies
veloping Countries.)
and surveillance should not be mis
In 1988, the WHO published its used as a disguised form of promo
Ethical Criteria for Medicinal Drug tion. ■
Promotion to provide general prin
Courtesy: Panos llriefine
T
Haroon Habib
in Dhaka
i Hossain Mohammad Ershad, now
facing jail term on charges of corrup
tion and misuse of power, took upon
himself as Bangladesh ’s President was
gramme — the National Drug Policy
(NDP). Introduced in 1982, soon after
he captured power in a coup, the pol
icy banned 1,666 “useless, ineffective
or harmful drugs” and selected 250 es
sential medicines for the country.
While many at home and abroad wel
comed it as most forward-looking, a
section of multinationals and the coun
try’s drug manufacturers criticised it as
too radical and grossly arbitrary.
Ershad relentlessly enforced the pol
icy during the nine years of his rule.
He clamped strict controls to keep the
• prices of drugs within the purchasing
capacity of the people and stopped the
production of drugs under third party
licence. Framed in the light of the
World Health Organisation’s (WHO)
concept of essential drugs, the policy
was acclaimed all over the world. More
than a hundred countries followed the
Bangladesh model.
But the policy is now at a cross
roads. Certain influential Ministers of
the Begum Khaleda Zia Government
believe it has opened the market to
spurious medicines. Particularly critical
of it is Finance Minister M. Saifur
Rahman who favours jits scrapping on
the plea that all controls on the phar
maceutical industry should go, when
the country is pursuing the free-mar
ket mechanism.
z
According to zSaifur Rahman, the'
policy destroyed the only blue chip in
dustry
of the
count y.
“The
shortsightedness of some egomaniacs is
responsible for' this debacle,” he says.
out Health and Family Welfare Minis
ter. Chowdhury Kama! Ibne Yusuf is
not in full agreement. He feels the pol
icy needed to be reviewed and the
opinion of leaders of the industry had
to be taken into account.
Salman F. Rahman, a leading indus- trialist,- says - the policy ■ was nothing
more than guidelines for drag registra
tion. “Even its positive aspects were
undermined as it was implemented
without discussion with all concerned.
The policy thus lost its credibility.”
The process of scrapping the policy
started in 1992 following the assump
tion of office of the elected government
of Prime Minister Khaleda Zia. With.
Frontline. June 17. 1994
From: SHUBHA@cedban.ilban.emet.in
Organization: CED, BAngalore
To: sochara@blr.vsnl.net.in
Date:
Sat,
~ 27 Jun 1998 17:52:20+5.30
Subject:
Welcome to il-nuke
Priority: normal
Dear Thelma,
Thanks for everything!
Pl. see the message below and substitute il-med-ethics for il-nuke. more later. If you need
anymore help pl. write back.
shubha
------ Forwarded Message Follows-------
sffe
W'
Date sent: Tue, 23 Jun 1998 13:47:26 +0530
cedban.ilban.emet.inlshubha
To:
Majordomo@ilbom.emet.in
From:
Welcome to il-nuke
Subject:
Send reply to: Majordomo@ilbom.emet.in
Welcome to the il-nuke mailing list!
Please save this message for future reference. Thank you.
If you ever want to remove yourself from this mailing list, you can send mail to
<Majordomo@ilbom.emet.in> with the following command in the body of your email
message:
unsubscribe il-nuke shubha@cedban.ilban.emet.in
Here's the general information for the list you've subscribed to, in case you don't already
have it:
Dear Friends,
Welcome to the IndiaLink Anti-Nuclear Mailing list.
1. Subscription to this mailing list is FREE. All you need is an e-mail address.
2. The name of the list is:
il-nuke@ilbom.emet.in
3. Subsequent to the Pokhran Nuclear Tests by India the debate on nuclear issues has
begun in dead earnest and many individuals and organisations have felt the need to
express their viewpoint widely
topic here is an opportunity.
and forcefully. If you have something to say on this
The purpose is to provide a forum for discusions on views and queries that subscribers
may have.
4.
******** How to Subscribe **********
To subscribe to this mailing list send an e-mail addressed to:
Majordomo@ilbom.emet.in
Leave the Subject: field blank and in the body of the message type:
subscribe il-nuke your-e-mail-address
5.
*********** How t0 post material to the list *************
You will be notified by e-mail once you are included as a subscriber to this list. After
this you can directly post your material to this list by sending e-mail to:
il-nuke@ilbom.emet.in
6.
*********** How to Un-subscribe / sign-off ******************
If you ever want to remove yourself from this mailing list, you can send mail to
"Majordomo@ilbom.emet.in" with the following command in the body of your email
message:
unsubscribe il-nuke your-e-mail-address
Example if you had subscribed to this list as: xyz@youmet.org
then you will send the following msg to: majordomo@ilbom.emet.in
unsubscribe il-nuke xyz@youmet.org
This will un-subscribe / remove your name from this list.
In case of difficulty please send e-mail to: owner-il-nuke@ilbom.emet.in
IMPORTANT NOTE: Please DO NOT send "unsubscribe" messages to the list itself.
This will NOT unsubscribe you. Instead everyone else on the list will be forced to read
your request to be unsubscribed.
With regards,
Aspi B. Mistry
IndiaLink
Mumbai.
Reproductive human cloning :
ETHICAL ISSUES
June 1998
I.
BACKGROUND
In 1993, Federico Mayor, Director-General of UNESCO, created the
International Bioethics Committee (IBC), which is interdisciplinary and multicultural
in nature. The IBC is the only body within the United Nations system to carry out
bioethical reflection on research in biology and genetics and their applications, and is a
unique forum for debate and for the elaboration by UNESCO of standard-setting
instruments in this area.
Indeed, the IBC was entrusted by the Director-General to draw up an
international instrument on the human genome. In December 1996, after four years of
intensive work, the Legal Commission of the IBC approved a revised preliminary
draft, which was finalized in July 1997 by a Committee of Governmental Experts. The
Universal Declaration on the Human Genome and Human Rights was adopted by
the 29th Session of the General Conference of UNESCO, on 11 November 1997.
On 24 February 1997, the Director-General of UNESCO expressed his position
on the debate unleashed by the successful cloning of an adult sheep, ruling out the
application of this technology to humans. On 28 February, Federico Mayor issued the
following statement:
“The cloning of an adult sheep using DNA from an udder - successfully
accomplished by a team of scientists from the experimental farm of the Roslin
Institute of Edinburgh, (UK) - represents a decisive technological step forward
for biology. From a scientific standpoint cloning was already practised at
other levels of animal experimentation.
Bovine embryos have been commonly cloned for several years, notably
in view of selecting the most profitable cross-breeds, but this event opens new
perspectives. But it also raises many questions and fears regarding the possible
application of this technology to humans. We must safeguard human kind’s
infinite diversity, our biological and cultural unicity.
I applaud this scientific and technological achievement which will have
a considerable impact on biology, especially on embryology and genetics. It
will help alleviate and even prevent human suffering. Nevertheless, beyond
scientific knowledge and technological possibility, ethics must draw the divide
between the possible and the acceptable.”
Consequently, he requested the International Bioethics Committee to inform
him of the extent to which the future declaration on the human genome rules out
human cloning and any use of this technology which might undermine the dignity and
identity of each human being.
THE INTERNATIONAL DEBATE
All members of the IBC were consulted by correspondence on this issue. On
14 May 1997, a meeting was convened at UNESCO on “Animal Biotechnology,
Cloning and Transgenic Technology”. The participants stressed the necessary
distinctions between human reproductive cloning aimed at the birth of an individual
and non-reproductive human cloning techniques for research, diagnostic or therapeutic
purposes. Since these latter techniques do not aim at the reproduction of an individual,
only the former was examined from an ethical perspective.
IL
-2-
A consensus emerged that reproductive cloning of human beings should not be
permitted. Besides safety considerations, three main ethical arguments were voiced.
Reproductive cloning:
•
•
•
undermines genetic indeterminability (by intervening on the “genetic
lottery”);
overrates the biological/genetic link (although some participants felt that
the arguments against reproductive cloning fell precisely into the trap of
this overrated biological/genetic link);
could instrumentalize human beings, thus reducing them to the level of
tools, and consequently would be contrary to human dignity.
A number of countries had already adopted legislation covering this issue and,
since February 1997, several national bioethics committees or other bodies have
expressed their views.
This issue was also raised at the “Denver Summit of the Eight” in June 1997
and the final communique states:
“Human Cloning
47.
We agree on the need for appropriate domestic measures and close
international cooperation to prohibit the use of somatic cell nuclear transfer to
create a child.”
More recently, the Vllth Latin American Summit of Heads of State and
Government on “Democracy and Ethics”, which was held in Isla Margarita
(Venezuela) in November 1997, in supporting UNESCO’s Universal Declaration on
the Human Genome and Human Rights, affirmed its opposition to the utilization of
practices contrary to human dignity, such as reproductive cloning of human beings.
Likewise, several intergovernmental organizations, such as the Council of
Europe05 (Additional Protocol to the Convention on Human Rights and Biomedicine of
the Council of Europe of 12 January 1998), the European Parliament05 (Resolution on
Cloning of 12 March 1997), the European Union - particularly through its Group of
Advisers on the Ethical Implications of Biotechnology05 (Opinion N°9 of 28 May 1997
on ‘Ethical Aspects of Cloning Techniques’) - and the World Health Organization (see
below) have taken a similar stand on this subject.
It should be noted that the World Health Assembly, at its 50th Session on
14 May 1997, adopted a resolution affirming that:
“The use of cloning for the replication of human individuals is ethically
unacceptable and contrary to human integrity and morality.”
A subsequent meeting on “Human cloning - The global response” was
organized by the World Health Organization, on 24 October 1997. Its aim was to
review the different positions - legal, cultural and religious - concerning the possible
application of cloning techniques to the human being in view of a report on this subject
for the 51st Session of the World Health Assembly in May 1998.
(1)
Information can be obtained from: Council of Europe, B.P. 6341 R6 - 67075 STRASBOURG Cedex, France.
(2)
Information can be obtained from: European Parliament, avenue de 1’Europe, B.P. 1024 - 67070
Strasbourg Cedex, France.
(3)
Information can be obtained from:-European Commission, Rue de la Loi 200 - 1049 Brussels, Belgium.
-3-
More recently, a draft resolution on “Ethical, scientific and social implications
of cloning in human health” - which makes specific reference to UNESCO’s Universal
Declaration on the Human Genome and Human Rights -, adopted by the 101st Session
of the Executive Board of WHO, will be presented to the 51st Session of the World
Health Assembly in May 1998. It states in particular that:
“... cloning by means of somatic cell nuclear transfer for the replication of
human individuals is both ethically and biomedically unacceptable and
contrary to human dignity and integrity.”
As for international non-governmental organizations, the World Medical
Association, by a Resolution of May 1997, “calls on ... researchers to abstain
voluntarily from participating in the cloning of human beings”. A Recommendation
adopted by the International Federation of Gynecology and Obstetrics.(FIGO) in July
1997 states that “cloning to produce a human individual... is unacceptable”.
Religious authorities have also taken a stand on this issue: to mention just a
few, the Church of Scotland, the Holy See, a group of Muslim theologians.
A report on “Cloning animals and humans”, presented to the 1997 General
Assembly of the Church of Scotland, said:
“The Church of Scotland has already stated that to clone human beings would
be ethically unacceptable as a matter of principle. On principle, to replicate
any human technologically is a violation of the basic dignity and uniqueness of
each human being ... It is not the same as twinning. There is a world of
difference ethically between choosing to clone from a known existing
individual and the unpredictable occurrence of twins of unknown nature in the
womb. The nature of cloning is that of an instrumental use of both the clone
and the one cloned as means to an end, for someone else’s benefit. This
represents unacceptable human abuse, and a potential for exploitation which
should be outlawed worldwide.”
In a document entitled “Reflections on Cloning”, published in July 1997, the
Pontifical Academy for Life stated:
“Human cloning belongs to the eugenics project and is thus subject to all the
ethical and juridical observations that have amply condemned it. ... At the level
of human rights, the possibility of human cloning represents a violation of the
two fundamental principles on which all human rights are based: the principle
of equality among human beings and the principle of non-discrimination.”
During a meeting on 14-17 June 1997 in Casablanca, Morocco - organized
jointly by the Islamic Organization for Medical Sciences, the WHO Regional Office
for the Eastern Mediterranean, the Islamic Educational, Scientific and Cultural
Organization and the Fiqh Academy of the Organization of Islamic Conference - more
than 60 doctors of Islamic law expressed their total opposition to human cloning. This
ban also aims to prevent developing countries from becoming a laboratory for possible
experimentation in this field. In particular, it states that:
“Ordinary human cloning, in which the nucleus of a living somatic cell from an
individual is placed into the cytoplasm of an egg devoid of its nucleus, is not to
be permitted.”
-4REPRODUCTIVE CLONING AND THE UNIVERSAL DECLARATION
At its 29th Session, on 11 November 1997, the General Conference of
UNESCO adopted, unanimously and by acclamation, the Universal Declaration on
the Human Genome and Human Rights, the first universal instrument in the field of
biology. The General Conference matched the Universal Declaration with a resolution
on its implementation, which commits States to taking appropriate measures to
promote the principles set out in the Declaration.
III.
The Declaration, which aims above all to protect human rights from possible
infringements arising from research on the human genome and their applications,
specifically mentions the issue under consideration in its Section C, entitled “Research
on the Human Genome”.
In this section, Article 10 contains one of the cornerstones of the Declaration
when it affirms the primacy of respect for human rights over research in biology,
genetics and medicine. It is inadmissible for such research and research applications to
pursue goals which are contrary to human rights, fundamental freedoms and the
dignity of both individuals and groups of individuals, in particular certain populations
or minorities, or for the manner in which they are conducted to be at variance with
human rights, fundamental freedoms and human dignity.
As a result of the primacy of respect for human rights, Article 11 states that:
“Practices which are contrary to human dignity, such as reproductive cloning of
human beings, shall not be permitted.”
Article 11 further draws attention to the responsibility of States and competent
international organizations in that respect and to the need for co-operation among
them. It should be noted that in this sense the Universal Declaration concurs with
paragraph 11 of the Declaration of the World Conference on Human Rights of 25 June
1993, which, with regard to advancement in biomedical and the life sciences, explicitly
calls upon States to co-operate in order “to ensure that human rights and dignity are
fully respected”.
IV.
CONCLUSION
The Universal Declaration on the Human Genome and Human Rights is a
landmark instrument - the first in the field of genetics within the United Nations
system. One of the issue it addresses is that of human cloning, which - with the
adoption of this Declaration - the international community has now identified as a
practice “contrary to human dignity”.
What exactly does this text set out to do and why is UNESCO promoting the
promulgation of guidelines that seek to prohibit the application of a revolutionary
scientific development?
The answer to this question is that UNESCO is committed to ensuring that, like
all other forms of knowledge, science effectively serves the cause of human progress
and that the Declaration is concerned with making science accord with ethics in the
new Promethean age we are now entering.
-5-
The Universal Declaration on the Human Genome and Human Rights begins by
affirming the fundamental unity of all the members of the human family beyond their
genetic diversity. Individuals can never be reduced to their genetic material. Because
of their freedom of judgement and of choice, human beings transcend their genetic
condition. This means that science is not the arbitrator of what constitutes human
value or a valuable human life.
It is vital to stress this fundamental principle which cannot accommodate the
reproductive cloning of human beings - a technique which denies the uniqueness which
is our birthright. That uniqueness is at the heart of our identity; it is the core of our
existence. Its value is absolute and cannot be relinquished.
Although it does not have binding force, this Declaration represents a moral
commitment of all Member States of UNESCO to adhere to a coherent set of ethical
principles in the field of genetics. It is now for these Member States, in co-operation
with the scientific community, to translate the principles set out in the Declaration into
national legislation and regulations - a process already under way in a number of
countries, particularly in Eastern Europe.
At the turn of the century, solutions to the most acute world problems require a
strong science and technology component. At the same time, these problems have an
essential ethical dimension. This is why UNESCO gives the highest priority to its
ethical mandate. This is why it tries to reconcile scientific freedom and the defence of
human rights in the field of human genetics - a field that presents us with challenges
and opportunities in equal measure.
Legislation/views on human cloning at national level'
ARGENTINA
By a decree of 7 March 1997, the President of Argentina declared that all cloning experiments in
connection with human beings should be prohibited and requested the Ministry of Health and
Social Action to prepare a draft bill in this respect. The draft bill, dated 17 April 1997, states in
its Article 1 that ‘experiments concerning cloning of human cells in order to generate human
beings are hereby prohibited’.
BULGARIA
On 3 April 1997, the Bulgarian Academy of Sciences, the Bulgarian National Academy of
Medicine and the National Agricultural Academy organized a Conference on Human Cloning.
The Conference pointed out that the scientific research in this field should be pursued under
strict conformance with adequate requirements (biological, medical, social, psychological,
legal), reflected in widely accepted legal norms.
CANADA
The Bill C-47 (First reading, 14 June 1996), respecting human reproductive technologies and
commercial transactions relating to human reproduction - cited also as the Human Reproductive
and Genetic Technologies Act - states that ‘no person shall knowingly ... manipulate an ovum,
zygote or embryo for the purpose of producing a zygote or embryo that contains the same
genetic information as a living or deceased human being or a zygote, embryo or foetus, or
implant in a woman a zygote or embryo so produced’.
CHILE
In a Declaration on human cloning of 22 April 1997, the Commission of Ethics, Culture and
History of the Faculty of Medicine of the University of Chile, in referring explicitly to the
Universal Declaration on the Human Genome and Human Rights drawn up by UNESCO,
expressed its opposition to all biomedical research concerning human cloning, even with a
medical purpose.
CHINA
In May 1997, the Chinese Academy of Sciences banned research on human cloning.
DENMARK
Under Act 503 on a Scientific Ethical Committee System and the Handling of Biomedical
Research Projects of 1992, research on cloning (production of genetically identical individuals)
is forbidden. Act 460 on Medically Assisted Procreation of 1997 complements this position by
affirming that treatment may not be initiated in areas where a research ban already exists under
the 1992 Act.
FRANCE
At the request of President Chirac, the Consultative National Ethics Committee for Health and
Life Sciences (CCNE), in its Opinion N° 54 of 22 April 1997, deemed necessary to oppose by
all possible means the development of practices leading to the identical reproduction of a human
being and to research which might lead to this end, recourse to cloning being a serious
infringement on the dignity of the human person.
GERMANY
Under the Federal Embryo Protection Act of 1990, the creation of an embryo genetically
identical to another embryo, foetus or any living or dead person is an offence.
INDIA
In December 1997, the Indian Council of Medical Research issued a Consultative Document on
Ethical Guidelines on Biomedical Research Involving Human Subjects. The section dealing
with genetics states that cloning through nuclear transplantation ‘definitely should be forbidden
by law’.
ITALY
By a decree of 5 March 1997, the Minister of Health prohibited all form of experimentation and
intervention aiming, even indirectly, at human or animal cloning. For its part, on 21 March
1997, the National Bioethics Committee (CNB) expressed its opposition to human cloning,
considered as an infringement on the uniqueness of each human being and of his or her dignity.
Document compiled by the Bioethics Unit of UNESCO.
JAPAN
In May 1997, the Ministry of Health and Welfare and the Ministry of Education, Science,
Culture and Sports set up advisory committees to discuss the issue of human cloning. In January
1998, the Council for Science and Technology, chaired by the Prime Minister, set up another
committee on cloning, expected to report by May 1998 on the appropriateness of introducing
legislation to ban reproductive human cloning
NEW
ZEALAND
The Human Assisted Reproductive Technology Act, which came into force on 1 January 1997,
establishes a legal framework for restrictions and controls on assisted reproductive technology
and creates a Human Assisted Reproductive Technology Authority. Cloning is one of the
forbidden activities which cannot, under any circumstance, be authorized.
NORWAY
Law 56 of 1994 on the medical use of biotechnology implicitly prohibits embryo cloning.
PORTUGAL
On 1st April 1997, the National Council of Ethics for the Life Sciences states that ‘the cloning of
human beings, because of the problems it raises concerning the human dignity, the equilibrium
of the human species and life in society, is ethically unacceptable and must be prohibited’.
RUSSIAN
FEDERATION
On 12 January 1998, the Russian Institute of Molecular Genetics Research called for a law
banning human cloning.
SLOVAKIA
The Health Care Law of 1994 implicitly prohibits embryo cloning.
SPAIN
Law 35/1988 concerning medically assisted reproduction, in Chapter VI, Article 20, deems that
the creation of identical human beings by cloning, or any other technology for race selection
purposes, is a serious infringement on human rights, with criminal sanctions.
SWEDEN
Law 115 of March 1991 implicitly prohibits embryo and ovocyte cloning with criminal sanctions.
SWITZERLAND
The Federal Constitution implicitly prohibits embryo cloning (amendment of 13 August 1982).
If adopted, the Federal Bill on Medically Assisted Procreation of 1997 will explicitly prohibit
embryo and ovocyte cloning with criminal sanctions.
TUNISIA
At the request of the Minister of Health, the National Medical Ethics Committee examined the
issue of cloning. Following initial discussions, the Technical Section of the Committee
concluded that any technology of human cloning should be banned. It deems this technology to
be an infringement on all references in the field of human reproduction and on the dignity of the
human species and an open door to all drifts.
UNITED
KINGDOM
In the United Kingdom a ban on human cloning had been proposed in 1984 in the Warnock
Report, the basic Committee of Enquiry into Human Fertilisation and Embryology. Following
that recommendation, the Human Fertilisation and Embryology Act of 1990 provided for just
such a ban on human cloning. Research involving the use of human embryos is strictly
controlled under the terms of this Act, which would require a licence to be issued by the Human
Fertilisation and Embryology Authority. In May 1997, the Human Genetics Advisory
Commission (HGAC) decided to explore ways of holding a public consultation exercise on the
implications of developments in cloning. More recently, in January 1998, a consultation
document, entitled ‘Cloning Issues in Reproduction, Science and Medicine’ was published by
the HGAC and the Human Fertilisation and Embryology Authority (HFEA). In addition, the
Royal Society issued, in January 1998, a statement on cloning. In this statement, entitled
‘Whither cloning?’, the Council of the Royal Society ‘with respect to human cloning, supports
the view that reproductive cloning of humans to term by nuclear substitution is morally and
ethically unacceptable and believe it should be prohibited’.
UNITED STATES
OFAMERICA
On 24 February 1997, President Clinton requested the National Bioethics Advisory Commission
to examine the legal and ethical issues associated with the use of the new cloning technology.
The Commission, in its Report of June 1997, concluded that ‘at this time it is morally
unacceptable for anyone in the public or private sector, whether in a research or clinical setting,
to attempt to create a child using somatic cell nuclear transfer cloning’. On 9 June 1997,
President Clinton proposed to the Congress a Cloning Prohibition Act of 1997. In January 1998,
the American Society for Reproductive Medicine (ASRM) presented a draft bill banning over a
certain period the cloning of living or dead human beings.
June 1998
WORKSHOP ON ETHICS IN CLINICAL RESEARCH IN DEVELOPING COUNTRIES.
Ethics in Overseas-funded Research in Developing Countries.
T Jacob John, Vellore, India.
Summary
A wider discussion among non-tradional-ethicists on the validity, applicability and above all
the consistent use (or problems thereof) of the widely acclaimed basic principles of ethics in clinical
practice and research is timely and essential. This personal viewpoint paper presents some of the less
recognised issues covering the spectrum of first principles to day-to-day activities.
The main issues include a tension between ethics as we understand and cultural values in some
regions of the world, and arising partly from it a very much stunted health care, public health and
research efforts, the conceptualisation of autonomy, the difficulties in realising informed (truly)
consent (truly voluntary), and the vulnerability and injustice suffered by people of poor backgrounds
when seeking health care in the scientific medical system. We need orders of magnitude more of
research to solve innumerable problems and we need to apply time tested basic principles of public
health, if we take justice and nonmalficence seriously. If there is a feeling that ethics apply only to
acts of commission, we must examine the failure of ethical understanding of the gross and grotesque
attitude of non-action.
Background.
As the world is going through rapid changes, and as most if not all transactions are at least in
part driven by profit motive, the tendency or opportunity for exploitation of the less informed or the
less powerful is becoming almost universal. Therefore, in order to ensure that transactions remain
fair and just to the participating subjects in clinical research and to service recipients in clinical
practice, strict adherence to ethical principles are essential everywhere.
Whenever a system, be it health care, clinical research, public health or social support, is
brought into play to cope with the problems of people with HIV or acquired immune deficiency
syndrome (AIDS), its deficiencies become apparent. Recently, issues about the ethics of clinical
research in developing countries have received much attention due to a debate on clinical trials to
reduce perinatal transmission of human immunodeficiency virus (HIV) (1). I quote from a recent
editorial: "The ethics of American researchers or funders conducting research in resource-poor
environment is challenging beyond words. In the examples at hand, we face an agonizing choice. On
the one hand, by adhering to western standards of medical care we could produce great benefit to the
persons who participate in trials but slower progress for medical science. On the other hand, by
providing less benefit to research participants in developing countries than that which is provided in
developed countries, we are more likely to yield quicker and more relevant answers for the larger
community. Such a dilemma calls for extensive farther public discussion, which must include the
voices of all relevant communities, from American researchers, funders and IRDs (institutional
review boards) to local country researchers, governments, review boards and most essentially
potential research participants and their communities. We can be confident that the ethics of
international research will benefit from so much public attention" (2). (Read 'overseas' for
'American'). Our discussions here are certainly relevant and timely.
to
U-e
■'
The main issues.
In all that I have understood, 'everyone' (mostly western colleagues and a handful of
compatriots with whom these issues have been discussed) accepts that the current stated principles of
ethics in medical research, namely autonomy, beneficence, nonmalficence and justice are universally
true and valid. The absolute need for informed consent by participants derives directly from the
principle of autonomy. Its fundamental basis is the supremacy of the individual, a concept which
itself has its roots in the so-called western culture, deriving from the Judeo-Christian understanding
of humans in relationships. While I do not personally question its validity, I do question whether this
basis, and its derivations have been rubbed against the touchstones of other philosophies or belief
systems of oriental, Asian, African and native peoples of the New World. I do recall a recent
incident in which an English youngster was given corporal punishment in Singapore for an act of
vandalism and the consternation it created in the west. That illustrated the differences in the relative
value given in some cultures to the individual versus the group. I have often wondered but not
investigated if the basic assumptions of fundamental individual rights, upon which modem medical
ethics are founded, will always be in accordance with the Sharia laws. I have a suspicion that many
professionals in poor countries may consider that strict adherence to ethics in medicine is not possible
due to ideological and practical reasons. The necessary process of crosschecking the validity of the ’
basics of medical ethics is perhaps not appropriate for us to undertake, but we might make a point
here that a broader dialogue with other points of view may be essential if we are to address them in
medical research (and much more importantly in clinical practice) in developing countries with
diverse social, cultural, religious and economic backgrounds. At the very least, such a dialogue will
be essential for us to ensure that the basic ethical principles (perceived to be 'western' in origin) will
be accepted and applied in diverse environments. .
Modem medicine (clinical practice and clinical research) itself is a product of the so-called
western culture. Those who practice it are necessarily educated in its basics (in science and
objectivity, and its need to question and experiment on any and every tenet), even though they
themselves may have different belief systems that do not fully accommodate these elements. I
personally believe that there is tension between the two belief systems in many societies, which is not
properly examined, articulated or reconciled, and to that extent, modem medicine remains alien to
many a local culture; if not alien, at least not fully integrated with, or absorbed within, the local
culture. (I also attribute this unrecognised difficulty as one of the causes of the unsatisfactory health
care systems in many developing countries, and not merely a lack of funds. If cost was the main
impediment to health care, we should have seen the growth of primary health care up to the limits of
affordability, which is not the case in many societies, particularly India). The medical personnel learn
to accept the tension by compartmentalisation, so that it does not impair performance. The human
subjects of research, on the other hand, may not understand the very nature of research, nor live by
the belief system out of which the ethical tenets have arisen. We may believe in the value of always
speaking the truth. There may be people who believe that in communications truth is less important
than what is pleasant or appropriate. We may believe that all are equal. There may be people who do
not believe so. We believe in direct cause and effect. There may be people who do not believe in
cause and effect, but may attribute events to divine decisions or actions or to immutable (except by
the divine) destiny (such as fatalism). Even in the western (and other) Christian circles, and in other
religions as well, some felt HIV/AIDS to be God's punishment on sinners and felt justified to
abandon those whom 'God had condemned' (3). We believe that truth is verifiable; others may
believe that truth is what you believe and verification is superfluous. We may accept questioning
widely, but others may consider it inappropriate and disrespectful of what is respected and sacred.
As a successful medical researcher in India, I am struck by the extreme paucity of research by peers,
aimed at solving the local and glaring problems in health care and public health, and also by the
extreme neglect of even the very basic primary health care and public health by successive elected
governments. The explanation is more likely the cultural belief system and not an inhuman
callousness.
It is in the concept of autonomy, perhaps, that there may be the biggest problem with
universal applicability, if not validity. To be autonomous, one has to be convinced of the supremacy
of the individual. In many societies, decisions are often made by the elders for the younger ones, or
by the chief for the group or by parents for their offspring. For people brought up in such traditions,
autonomy as we with western (mostly Christian) education or background understand, may be alien
to their thought processes. Therefore, patients everywhere, but more obviously in developing
country backgrounds tend to "relinquish autonomy to professional authority, in the expectation of
competence" (4). In such situations, informed consent, given voluntarily, is difficult, if not virtually
impossible, to obtain.
Many developing countries are in the process of eradication of poliomyelitis. This entails
virtually every child being given multiple doses of oral polio vaccine. A small number of children will
develop paralysis due to the vaccine itself (calculated to be about 50 per year in India alone). It is
called vaccine associated polio. Beneficence and nonmalficence, as well as justice, will demand that
such children who develop this severe adverse reaction directly due to participation in a global
programme, not voluntarily, but by government directive, must be treated free of charge and also
compensated adequately. Certainly in India and probably in many other developing countries as well,
such children, as also others with wild virus induced poliomyelitis (as a result of the error of policy
regarding the number of doses of vaccine to be taken, or in other words defective service), are left to
fend for themselves, with the government accepting no responsibility whatsoever for their treatment
and rehabilitation. Such a situation is virtually untenable in a western society, but in India, there is no
sensitivity to the ethical norms of a medical intervention for the benefit of the many (indeed for the
entire world), but the adverse reaction, of which is suffered by the few. What is interesting, the
programme is heavily funded by several developed countries (if India continues to have polioviruses,
the world cannot eradicate). Moreover, the WHO is directly involved in the reporting and
investigation of children with polio so that its experts know which children have vaccine associated
polio and which have wild virus induced polio due to defective service. The public and the health
care staff who report the children with paralysis are not given (nor do they want) this information. I
depict these to emphasise the lack of ethical urgency or even sensitivity; people (including most
professionals) and the government accept theses with a sense of fatalism.
The clinical trials to define methods of prevention of perinatal HIV transmission raised several
questions in ethics. The ACTG 076 study gave HIV infected pregnant women zidovudine orally
from the second trimester and intravenously during labour. The neonates were given syrup
zidovudine for 6 weeks. These interventions reduced the frequency of HIV transmission in
nonbreast-fed babies by about 66% (from 25 % to 8%) (5). This treatment has now become the
standard treatment in the USA (6). The total drug doses have been costed at over 800 US dollars
which is about twice the per capita annual income of people in several countries (7). Since then at
least 16 randomised clinical trials have been approved for conduct in Africa, Asia and the Caribbean
(8). Most of them are placebo controlled. Some are to investigate shorter courses of zidovudine,
and others use other interventions such as vitamin A or HIV immunoglobulin (8). The acute debate
and division are on the ethics of using a placebo arm in these studies (1,7,9,10). Since the ACTG
076 has become standard treatment in the USA, one argument is that any further studies, especially if
funded by a developed country source, must be controlled with the standard treatment; placebo
control is therefore unethical (9,10). On the opposite side, there is cogent argument to support the
need for placebo controlled trials to find less expensive regimens to reduce perinatal transmission
(11). For one thing, ACTG 076 is not implementable in developing countries. Even if one arm had
ACTG 076 as control (equivalency study), the study will be inconclusive since we can assume that
the arm with any shorter course of treatment would have a higher frequency of transmission than the
control. So then, it would be virtually impossible to assess the reduction in transmission that the short
course would have caused without simultaneously measuring what the risk of the study group was
for such transmission without intervention (11).
Discussion
In many if not most developing countries, sick people do not get a fair deal unless they
purchase health care. Scientific medicine is very expensive. (Therefore, alternate systems remain
popular, which is a positive outcome of an otherwise unhealthy situation). Research to find new
solutions to even urgent or rampant problems is conspicuous by its infrequency. The so-called
tropical diseases are prevalent, not because of tropical climate, but because even the elementary
principles of public health are not applied (12). The general belief is that the root cause of this
"
situation is poverty. I contest that. True, poverty reduces options, but does not remove the option
of elementary preventive public health. Poverty is an alibi the rich nations attribute and the not-sorich countries readily accept and perpetrate, by which they do not have to face the real reasons which
are in the realm of'culture' or the world view of humans in relationships with themselves, with others
and with God (and/or Nature). The 'culture' of the west, with all its tremendous contributions, has
(perhaps) gone wrong in understanding the true nature of humans within Nature, whereas many other
cultures have all along been more correct. 1 suspect that it has also gone too far in pushing the ideal
of individual advancement (indulgence, supremacy) even at the expense of group interests. This is a
form of'paganisation', a deviation from the Judeo-Christian view of humans in relationships. (Am I
my brother's keeper?). In the culture in which I live, salvation (nirvana) is a personal proposition
between you and your god, it is no one else's business, nor are you responsible for anyone else's.
To me this imbalance between the individual's rights and group interests became an acute
problem, facing HIV/AIDS among ordinary people in India, but now within the newly transplanted
mindset of people that it was a gay plague, or a prostitute's problem, or God's punishment on wrong
doers, an instant killer, a hopeless malady and so on. Modern mass media had brought all these well before we saw the very first 'case' (another pejorative term?). My personal guilt is that I introduced "
HIV testing in India, long before AIDS was recognised, but even doctors confused one for the other.
Now they had a tool to detect and reject those with HIV and even today this tragic drama continues
unabated. Strong ethical views made a difference in the west, but the milieu for meaningful ethical
confrontation does not exist in India. Gross injustice is being thrust upon people with HIV/AIDS.
The problem is by and large neglected, not due to inhuman callousness, but due to a different
understanding of humans in relationships.
. . So, what can we conclude? As human rights issues have been internationalised, medical
ethics also needs visibility and wider discussion.
If researcher and subject as well as clinician and client transactions must be brought within the
ambit of ethics, we must help nations to internalise the basic principles.
The subject or client is from a different cultural background than the assumed culture of the
researcher/care giver, while playing that role. Perhaps autonomy needs redefinition. Perhaps the first
in the list of principles must be justice (which may be more easy to understand across cultures) rather
than autonomy. Perhaps, clinical practice must become based on solid ethics before we can address
ethics in research. Perhaps, the absence of research is a more serious ethical problem than previously
recognised.
External funding has been presented as a potential constraint in ethical conduct of research, as
it brings to focus the gross disparities in what is standard care versus what is locally the norm.
External funding is indeed a good thing from ethics point of view because it demands attention on
ethics. To bring in hidden motives in research, the institutional review boards (they must, obviously
exist) must identify all the cast and crew, on stage and backstage, not merely the subject, researcher
and hinder. If an industry will benefit from research, that (not at all a bad thing) must be clearly
identified, so that unseen forces can be made visible. The board must also identify the intended
emotive and substantive benefits of the researcher in order to help them themselves understand
ethical issues more clearly. Since the clinical setting makes it virtually impossible to make the
transactions 'equal', and true autonomy is virtually absent in most situations, informed consent must
be taken more seriously than as a ritual; but justice and nonmalficence must be the first points to
teach and learn. Perfect research need not be the enemy of good and essential research.
Q
References.
1. Bayer R. The debate over maternal-fetal HIV transmission prevention trials in Africa, Asia and the
Caribbean: Racist exploitation or exploitation of racism? Amer J Public Health 1998; 88: 567-570.
2. Faden R, Kass N. Editorial: HIV research, ethics and the developing world. Amer J Public Health
1998; 88: 548-550.
3. John TJ. Sexuality, sin and disease: theological and ethical issues posed by AIDS to the churches.
The Ecumenical Review, 1995; 47: 3734. Sigeriat HE (1960) The special position of the sick; Parsons T (1951) The social system; Kirby
MD (1983) Informed consent. What does it mean? Cited by: Karim QA, Karim SSA, Coovadia HM,
Susser M. Informed consent for HIV testing in a South African hospital. Is it truly informed and truly
voluntary? Amer J Public Health 1998; 88: 637-640.
5. Connor EM, Sperling RS, Gelber R et al. Reduction of maternal-infant transmission of human
immunodeficiency virus type 1 with zidovudine treatment. New Engl J Med. 1994; 331: 1173-1180.
6. US Public Health Task Force on the use of zidovudine to reduce perinatal transmission of human
immunodeficiency virus. Morb Mortal Wkly Rep. 1994; 43: 1-20.
7. Varmus H, Satcher D. Ethical complexities of conducting research in developing countries. New
Engl J Med 1997; 337: 1003-1005.
8. Annas GJ, Grodin MA. Human rights and maternal-fetal HIV transmission prevention trials in
Africa. Amerj Public Health 1998; 88: 560-563.
9. Lurie P, Wolfe SM. Unethical trials of interventions to reduce perinatal transmission of human
immunodeficiency virus in developing countries. New Engl J Med 1997; 337: 853-856.
10. Angell M. The ethics of clinical research in the third world. New Engl J Med. 1997; 337; 847849.
11. Karim SSA. Placebo controls in HIV perinatal transmission trials: A South African's viewpoint.
AmerJ Public Health 1998; 88: 564-566.
12. John TJ. An Indian point of view (On Tropical Diseases) Lancet 1997; 349: Sill, 31-32.
orders in the operating room, published by the American Society of
Anesthesiologists and the American College of Surgeons are used to provide a
perioperative DNR order management approach consistent with the Joint Statement
on Resuscitative Interventions. PRINCIPAL FINDINGS AND CONCLUSIONS: The
dominant principle is that of the patient's right to self determination. This
right can be exercised either directly by the patient, or through an
appropriate alternate, or in the form of an advance directive. DNR orders are
not incompatible with subsequent surgical care in an operating room. It is
wrong to suspend automatically DNR orders in the perioperative period. It is
wrong to continue DNR orders automatically in the perioperative period. It is
wrong to make assumptions about the meaning of an individual DNR order. An
appropriate approach to the perioperative management of pre-existing DNR orders
is one based on "required reconsideration." All anaesthetists must be aware of
their responsibilities in managing patients with DNR orders in place.
MESH: Ethics,-Medical; Patient-Advocacy
MESH: *Operating-Rooms; *ResuscitationTG: Human
PT: JOURNAL-ARTICLE
AN: 96437273
UD: 9702
21 of 27
Marked in Search: #5
TI: Recommended guidelines for reviewing, reporting, and conducting research on
in-hospital resuscitation: the in-hospital "Utstein style". American Heart
Association.
AU: Cummins-RO; Chamberlain-D; Hazinski-MF; Nadkarni-V; Kloeck-W; Kramer-E;
Becker-L; Robertson-C; Koster-R; Zaritsky-A; Bossaert-L; Ornato-JP; Callanan-V;
Allen-M; Steen-P; Connolly-B; Sanders-A; Idris-A; Cobbe-S
AD: Emergency Cardiac Care Committee, American Heart Association, Dallas, Tx
75231-4596, USA. docrocSu.Washington.edu
SO: Ann-Emerg-Med. 1997 May; 29(5): 650-79
This source is Available only few issues in S.J.M.C. Library
ISSN: 0196-0644
PY: 1997
LA: ENGLISH
CP: UNITED-STATES
MESH: Decision-Trees; Ethics,-Medical; Life-Support-Care ;
Medical-Records-standards; Outcome-and-Process-Assessment-Health-Care;
Resuscitation-methods; Resuscitation-standards; Resuscitation-Orders
MESH: ^Hospitals—; *Inpatients-; *ResuscitationTG: Human
PT: GUIDELINE; JOURNAL-ARTICLE; PRACTICE-GUIDELINE; REVIEW; REVIEW,-TUTORIAL
AN: 972S4979
UD: 9707
SB: AIM
22 of 27
Marked in Search: #5
TI: Research with cognitively impaired subjects. Unfinished business in the
regulation of human research [see comments]
CM: Comment in: Arch Gen Psychiatry 1997 Feb;54(2 ):117-20. Comment in: Arch
Gen Psychiatry 1997 Feb;54(2 ):121-3
AU: Bonnie-RJ
AD: Institute of Law, Psychiatry, and Public Policy, University of Virginia,
Charlottesvi1le, USA.
SO: Arch-Gen—Psychiatry. 1997 Feb; 54(2): 105-11
This source is Available in S.J.M.C Library
Call Number: From; 1959+
ISSN: 0003-990X
PY: 1997
LA: ENGLISH
CP: UNITED-STATES
AB: In 1979, the National Commission -for the Protection o-f Human Subjects o-f
Biomedical and Behavioral Research issued an important report that addressed
the difficult ethical issues arising in research involving subjects with mental
disabilities. However, because of■irreconcilable conflicts between the
scientific community and rights-oriented advocacy groups, the federal
government never issued the special regulations pertaining to these issues that
had been envisioned by the National Commission. Because these important ethical
issues have not yet been adequately addressed by policy-making bodies,
protection of cognitively impaired subjects depends too heavily on the diverse
ethical sensitivities of individual investigators and on ad hoc responses of
particular institutional review boards. Researchers should support a credible
and authoritative process for reexamining and resolving ethical issues relating
to research with cognitively impaired subjects. This can be accomplished
without leading to the stalemate that doomed the National Commission's
proposals. The challenge is to forge a consensus on ethical guidelines and
safeguards that will most reasonably accommodate the goals of protecting the
dignity and well-being of research subjects while avoiding undue impediments to
valuable scientific inquiry.
MESH: Human-Experimentation; Informed-Consent; Mental-Disorders-psychology ;
Patient-Advocacy; Research—Design-standards; United—States
MESH: KEthics,-Medical; *Mental-Competency ; *Mental-Disorders
TG: Human; Support,-Non-U.S.-Gov't
PT: JOURNAL-ARTICLE; REVIEW; REVIEW,-TUTORIAL
AN: 97192684
UD: 9705
SB: AIM
23 of 27
Marked ip Search: #7
TI: CEthical guidelines for scientific research in human individuals supported
by FAPESP. Bioethics Group and Population Research]
TO: Diretrizes eticas para pesquisas em grupos humanos financiadas pela FAPESP.
Grupo de Bioetica e Pesquisa Populacional .
SO: Rev-Assoc-Med-Bras. 1996 Jul-Sep; 42(3): 167-8
this source is not Available in S.J.M.C.Library
ISSN: 0104-4230
~
PY: 1996
LA: PORTUGUESE; NON-ENGLISH
CP: BRAZIL
AB: Ethical guidelines were developed for research projects involving human
groups in biomedical and human sciences areas. The text is divided into four
parts: premises, principles, procedures and recommendations. The granting
agency will institute an Ethical Review Board to mediate ethical conflicts
identified in the research project. It is intended for the guidelines to be
reviewed in 3 to 4 years.
MESH: English-Abstract; Research-Support
MESH: ^Ethics,-Medical; ^Guidelines-; *Human-Experimentation;
^Research-standards
TG: Human; Support,-Non-U.S.-Gov't
PT: JOURNAL-ARTICLE
AN: 97284284
UD: 9709
24 of 27
Marked in Search: #7
TI: Medical and scientific uses of human tissue Ceditoriall
AU: O'Neill-O
SO: J-Med-Ethics. 1996 Feb; 22(1): 5-7
this source is not Available in S. J.M.C.Library
ISSN: 0306-6800
PY: 1996
LA: ENGLISH
CP: ENGLAND
AB: Inevitably a policy-oriented report on issues as complex and as rapidly
chanaino as the medical and scientific uses of human tissue can achieve neither
philosophical purity nor regulatory completeness. The council's strategy has
been to begin with robust ethical principles, for which sound philosophical
arguments can be given, which will (it is hoped) command widespread support.
The council went on to argue for guidelines of sufficient, but not vapid,
generality which could be of practical use to the various medical
intermediaries, professional and regulatory bodies and research ethics
committees which will carry out the tasks of detailed regulation and of making
decisions that affect uses of human tissue. The council's hope is that the
recommendations of the report can be absorbed into regulatory and professional
practice, and where needed into government policy. If they can, the increasing
diversity of uses of human tissues need lead neither to overt nor to covert
'commercialisation of the human body', but will also not put unnecessary
restrictions on advances in research and medical practice.
MESH: Biological-Specimen-Banks-economics;
Biological-Specimen-Banks-legislation-and-jurisprudence; Cadaver—;
Great-Britain ; Tissue-Culture; Tissue-Donors
MESH: *Biological-Specimen-Banks; ^Ethics,-Medical; KHuman-Rights
TG: Human
PT: EDITORIAL
AN: 97086524
UD: 9705
25 of 27
Marked in Search: #7
Ethical issues in genetic research: disclosure and informed consent.
Reilly-PR; Boshar—MF; Holtzman-SH
Shriver Center for Mental Retardation, Waltham, Massachusetts 02154, USA.
Nat-Genet. 1997 Jan; 15(1): 16-20
this source is not Available in S■J.M.C.Library
ISSN: 1061-4036
PY: 1997
LA: ENGLISH
CP: UNITED-STATES
AB: As research to correlate genetic status with predisposition to disease has
accelerated, so has the concern that participation in such studies creates the
risk of genetic discrimination and emotional distress. There is a need to
broaden disclosure during the consent process to ensure that potential subjects
understand these risks and other issues and to address them in the consent
form. We describe the broad approach that we have taken in regard to disclosure
and consent in gene mapping studies.
MESH: Adult-; Child-; Chromosome-Mapping; Genetics,-Medical-legislation-andjurisprudence; Guidelines-; Prejudice-; Research-legislation-and-jurisprudence ;
United-States
MESH: ^Ethics,-Medical; ^Genetics,-Medical; * Informed-Consent; ^Research-;
*Truth-DiscInsure
TG: Human
PT: JOURNAL-ARTICLE
AN: 97141913
UD: 9704
TI:
AU:
AD:
SO:
26 of 27
Marked in Search: #7
TI: The Helsinki Declaration, research quidelines and regulations: present and
■future editorial aspects Ceditoriall
AU: Dale-Q; Salo-M
SO: Acta-Anaesthesiol-Scand. 1996 Aug; 40(7): 771-2
This source is Available only -few issues in S.J.M.C. Library
Call Number: From: 1971-1978 & 19S5
ISSN: 0001-5172
PY: 1996
LA: ENGLISH
CP: DENMARK
MESH: GuidelinesMESH: ^Ethics,-Medical; *Human-Experimentation
TG: Human
PT: JOURNAL-ARTICLE
AN: 97028547
LID: 9703
27 of 27
Marked in Search: #7
TI: Ethical clinical practice of functional brain imaging. Society of Nuclear
Medicine Brain Imaging Council.
SO: J—Nucl-Med. 1996 Jul; 37(7): 1256-9
this source is not Available in 5.J.M.C.Library
ISSN: 0161-5505
PY: 1996
LA: ENGLISH
CP: UNITED-STATES
AB: The development and evolution of functional brain imaging technology and
their broad application to a wide range of neurological and psychiatric
disorders have led to their scientifically sound use in specific clinical
situations. In addition, there is a growing diversity of empirical new
applications where there is little previous research or clinical experience.
Therefore, a committee of the Brain Imaging Council of the Society of Nuclear
Medicine was formed to address the need for specific quidelines regarding scan
interpretation and reporting. This committee considered the wide range of
current and potential uses of PET and SPECT, including its growing role in
forensics. A set of basic guidelines for the reporting and interpretation of
brain imaging studies applicable to all clinical situations, including
forensics, was formulated. These quidelines were composed in a manner sensitive
to the need for standards that are scientifically defensible now, and which
will continue to be valid as the field evolves. It is the intent of the
committee and its summary document to positively influence the clinical use of
brain SPECT and PET by offering guidance concerning the elements essential to a
complete and useful clinical report, defining standards to differentiate
well-established clinical applications from research uses and providing a
framework in which to consider the appropriateness of functional brain imaging
used in the forensic arena.
MESH: Nuclear—Medicine-legis1ation-and-jurisprudence; Societies,-Medical
MESH: tBrain-radionuc 1 ide-imaging; lEthics,-Medical;
^Tomography,-Emission-Computed; ^Tomography,-Emission-Computed,-Single-Photon
TG: Human
PT: GUIDELINE; JOURNAL-ARTICLE; PRACTICE-GUIDELINE
AN: 96268163
UD: 9702
Si IverPlatter 5.11
MEDLINE (R) 10/97-12/97
MEDLINE <R) 10/97-12/97 usage is subject to the terms and conditions of the
Subscription and License Agreement and the applicable Copyright and
intellectual property protection as dictated by the appropriate laws of your
country and/or by International Convention.
1 of 9
Marked in Search: #9
TI: Ethics in environmental epidemiology.
AU: Rossignol-AM
AD: Department of Public Health, Oregon State University, Corvallis 97330—6406,
USA.
SO: Epidemiology. 1997 Sep; 8(5): 599-601
this source is not Available in S. J .M.C.Library
ISSN: 1044-3983
PY: 1997
LA: ENGLISH
CP: UNITED-STATES
MESH: ResearchMESH: *Environmental-Health; ^Epidemiology-; ^Ethics,-Medical;
^Practice-Guidelines
TG: Human
PT: MEETING-REPORT
AN: 97417017
UD: 9712
2 of 9
Marked in Search: #9
TI: Guidelines for managing domestic abuse when male and female partners are
patients of the same physician. The Delphi Panel and the Consulting Group.
AU: Ferris-LE; Norton-PG; Dunn-EV; Gort-EH; Degani-N
AD: Department of Public Health Sciences, Faculty of Medicine, University of
Toronto, Ontario, Canada.
SO: JAMA. 1997 Sep 10; 278(10): 851-7
This source is Available in S.J.M.C Library
Call Number: From: 1918+
ISSN: 0098-7484
PY: 1997
LA: ENGLISH
CP: UNITED-STATES
AB: OBJECTIVE: To provide clinical guidelines for primary care physicians who
are dealing with domestic abuse and who have both the abused woman and her
partner as patients. PARTICIPANTS: A 15-member expert panel with members having
experience in family practice, gynecology, emergency medicine, medical ethics,
nursing, psychology, law, and social work; an 11-member consulting group with
members representing medicine, consumers, police, psychology, social work, and
nursing; and participants from focus groups including 48 previously abused
women and 10 previously abusive men. Members of the expert panel and the
consulting group were recruited by the research team. Focus group members were
recruited through the agencies from which they were receiving services.
EVIDENCE: Available research information, and opinions of the expert panel, the
consulting group, and the focus group participants. CONSENSUS PROCESS: Scoring
of 144 clinical scenarios was performed by the expert panel using a modified
Delphi technique involving 4 iterations. Scenarios were rated in terms of best
practice for primary care physicians dealing with suspected and confirmed cases
of physical abuse. Consulting group members and focus group participants then
commented on the panel's results. Final quidelines were approved by the panel
and the consulting group, with comments reserved in the guidelines for
information from focus group participants. CONCLUSIONS: It is not a conflict of
interest for the physician to deal with abuse of the female partner when both
partners are patients. Both patients have a right to autonomy, confidentiality,
honesty, and quality care. Patients should be dealt with independently, thereby
facilitating assessment of the magnitude and severity of the victim's injuries.
Physicians should not discuss the possibility of domestic abuse with the male
partner without the prior consent of the abused female partner. Joint
counseling is generally inadvisable and should be attempted only when the
violence has ended, provided both partners give independent consent and the
physician has adequate training and skills to deal with the situation without
escalating the violence. If the physician feels unable to deal effectively with
either patient because of the dual relationship, referral to another qualified
physician is preferred.
MESH: Confidentiality-; Referral-and-Consultation; United-States
MESH: *Domestic-Violence-prevention-and-control ; *Family-Practice
TG: Female; Human; Male; Support,-Non-U.S.-Gov't
PT: CONSENSUS-DEVELOPMENT-CONFERENCE; GUIDELINE; JOURNAL-ARTICLE;
PRACTICE-GUIDELINE; REVIEW
AN: 97438220
UD: 9711
SB: AIM
3 of 9
Marked in Search: #9
Compensation for subjects of medical research: the moral rights of patients
the power of research ethics committees.
Guest—S
University College, London.
J-Med-Ethics. 1997 Jun; 23(3'): 181-5
this source is not Available in S.J■M.C.Library
ISSN: 0306-6800
PYs 1997
LA: ENGLISH
CP: ENGLAND
AB: Awareness of the morally significant distinction between research and
innovative therapy reveals serious gaps in the legal provision for compensation
in the UK for injured subjects of medical research. Major problems are
limitations inherent in negligence actions and a culture that emphasises
indemnifying researchers before compensating victims. Medical research morally
requires compensation on a no-fault basis even where there is proper consent on
the part of the research subject. In particular, for drug research, there is
insufficient provision in the current patient quidelines of the Association of
the British Pharmaceutical Industry, since they make "no legal commitment" to
paying compensation for injury to patient subjects. There is a need for the
provision of both adequate insurance and contractual arrangements for making
payments. The solution is for Local Research Ethics Committees (LRECs) to make
use of their power to withhold approval of medical research where compensation
is not legally enforceable.
MESH: EnglandMESH: *C1inical-Trials-1egislation-and-jurisprudence;
tEthics-Committees-1eqislation-and-jurisprudence; ^Human-Experimentation ;
* Insurance,-Liability-legis1ation-and-jurisprudence; *MoralsTG: Human
PT: JOURNAL-ARTICLE
AN: 97364041
UD: 9710
TI:
and
AU:
AD:
SO:
4 of 9
Marked in Search: #9
TI: Implications of managed care for health systems, clinicians, and patients.
AU: Fairfield-G; Hunter-DJ; Mechanic-D; Rosleff-F
AD: Nuffield Institute for Health, University of Leeds.
SO: BMJ. 1997 Jun 28; 314(7098): 1895-8
ISSN: 0959-8138
PY: 1997
LA: ENGLISH
CP: ENGLAND
AB: The rhetoric and realities of managed care are easily confused. The rapid
growth of managed care in the United States has had many implications for
patients, doctors, employers, state and federal programmes, the health
insurance industry, major medical institutions, medical research, and
vulnerable patient populations. It has restricted patients' choice of doctors
and limited access to specialists, reduced the professional autonomy and
earnings of doctors, shifted power from the. non-profit to the for—profit
sectors and from hospitals and doctors to private corporations. It has also
raised issues about the future structuring and financing of medical education
and research and about practice ethics. However, managed care has also accorded
greater prominence to the assessment of patient satisfaction, profiling and
monitoring of doctors' work, the use of clinical guidelines and quality
assurance procedures and indicated the potential to improve the integration and
outcome of care.
MESH: Choice-Behavior; Great-Britain; Health-Care-Costs;
Health-Maintenance-Organizations; Managed-Care-Programs-economics;
Managed-Care-Programs-legislation-and-jurisprudence;
Managed—Care-Programs-organization-and-administration; Practice-Guidelines;
duality-of-Health-Care; State-Medicine-economics;
State-Medicine-organization-and-administration
MESH: *Managed-Care-Programs; ^State-Medicine
TG: Human
PT: JOURNAL-ARTICLE
AN: 97367435
UD: 9710
SB: AIM
5 of 9
Marked in Search: #10
TI: Emergency physicians and sexual involvement with patients: an Ontario
survey.
AU: Ovens-HJ; Permaul-Woods-JA
AD: Division of Emergency Services, Mount Sinai Hospital, Toronto, Ont.
SO: CMAJ. 1997 Sep 15; 157(6): 663-9
this source is not Available in S.J.M.C.Library
ISSN: 0820-3946
PY: 1997
LA: ENGLISH
CP: CANADA
AB: OBJECTIVE: To describe Ontario emergency physicians' knowledge of
colleagues' sexual involvement with patients and former patients, their own
personal experience of such involvement, and their attitudes toward pastvisit
relationships. DESIGN: Mailed survey. SETTING: Ontario. PARTICIPANTS: Emergency
physicians practising in Ontario. RESULTS: Of 974 eligible mailed surveys, 599
(61.5%) were returned. Of these respondents, 52 (8.7%) reported being aware of
a colleague in emergency practice who had been sexually involved with a patient
or former patient. When describing their own behaviour, 37 respondents (6.2%)
reported sexual involvement with a former patient. However, of this group, only
9 (25.0%) had met the patient in an emergency department. Thus, of the total
number of respondents, only 1.5% (9/599) reported sexual involvement arising
out of an emergency department visit. Most respondents (82.4%) agreed that it
is inappropriate behaviour to ask a patient for a date after an emergency
assessment and before the patient's departure, and 66.4% felt that it is
inappropriate to contact the patient after discharge. However, only 10.6%
believed it to be unacceptable to request a social meeting a-fter encountering a
patient previously cared -for in the emergency department in a nonprofessional
setting. Most respondents <96.5%) did not believe that sexual involvement could
ever be therapeutic -for the patient. However, onl,y 66% felt that it was always
an abuse of power and 62.4% supported sero tolerance of all sexual involvement
between physicians and patient^. CONCLUSIONS: Vague regulatory quidelines
currently in place have failed to dispel confusion regarding what is acceptable
social behaviour for physicians providing emergency care. Our results support
the need for clarification, and suggest a basis for quidelines that would be
acceptable to the emergency medical community: that an emergency visit should
not form the basis for the initiation of personal or sexual relationships, yet
neither should it preclude their development in nonmedical settings.
MESH: Adult—; Attitude—of-Health-Personnel; Ethics,-Medical; Middle-Age;
Ontario—; GluestionnairesMESH: ^Emergency-Medicine; *F'hysician-Patient-Rel ations; *Sex-Behavior
TG: Female; Human; Male; Support,-Non-U.S.-Gov't
PT: JOURNAL-ARTICLE
AN: 97452762
UD: 9712
SB: AIM
6 of 9
Marked in Search: #10
TI: Ethical, social, and legal issues surrounding studies of susceptible
populations and individuals.
AU: Soskolne-CL
AD: Department of Public Health Sciences, University of Alberta, Edmonton,
Canada. colin.soskolneSualberta.ca
SO: Environ-Health-Perspect. 1997 Jun; 105 Suppl 4: 837-41
this source is not Available in S.J.M.C.Library
ISSN: 0091-6765
’ ~ ~
PY: 1997
LA: ENGLISH
CP: UNITED-STATES
AB: Calls for professional accountability have resulted in the development of
ethics quidelines by numerous specialty and subspecialty groups of scientists.
Indeed, quidelines among some health professions now address vulnerable and
dependent groups: but these are silent on issues related to biomarkers. In
parallel, attention has been drawn to human rights concerns associated with
attempts to detect hypersusceptible workers, especially in democratic
countries. Despite this, concern for vulnerable populations grows as advances
in biomarker technology make the identification of genetic predisposition and
susceptibility markers of both exposure and outcome more attainable. In this
article, the principles derived from the ethical theory of utilitarianism
provide the basis for principle-based ethical analysis. In addition, the four
principles of biomedical ethics—respect for autonomy, beneficence,
nonmaleficence, stnd social justice—are considered for biomarker studies. The
need for a context in which ethical analysis is conducted and from which
prevailing social values are shown to drive decisions of an ethical nature is
emphasized; these include statutory regulation and law. Because biomarker
studies can result in more harm than good, special precautions to inform
research participants prior to any involvement in the use of biomarkers are
needed. In addition, safeguards to maintain the privacy of data derived from
biomarker studies must be developed and implemented prior to the application of
these new technologies. Guidelines must be expanded to incorporate ethical,
social, and legal considerations surrounding the introduction of new
technologies for studying susceptible populations and individuals who may be
vulnerable to environmental exposures.
MESH: Biological-Markers
MESH: ^Environmental-Monitoring; *Ethics~;
Wccupationa1-Heal th-legislation-and-jurisprudence
TG: Human
PT: JOURNAL-ARTICLE; REVIEW; REVIEW,-TUTORIAL
RN: O
NM: Biological-Markers
AN: 97399442
UD: 9711
7 of 9
Marked in Search: #10
TI: In-formed consent. Explicit guidance is required on valid exemptions for
need for ethical review I letter!
AU: Woodcock-T; Norman-J
SO: BMJ. 1997 Jul 26; 315(7102): 250
ISSN: 0959-8138
PY: 1997
LA: ENGLISH
CP: ENGLAND
MESH: Clinical-Trials; Ethics,-Medical ; Practice-Guidelines
MESH: *Ethics-Commi ttees; *Informed-Consent
TG: Human
PT: LETTER
AN: 97397223
UD: 9711
SB: AIM
8 of 9
Marked in Search: #10
Proposed quidelines for speakers discussing medications and other products.
Daniel-CR-3rd ; Elewski-BE; Scher—RK
University of Mississippi Medical Center, Jackson, USA.
Cutis. 1997 May; 59(5): 271-2
This source is Available in S.J.M.C Library
Call Number: From:1971, 1995+
SB: AIM
TI:
AU:
AD:
SO:
SilverPlatter 3.11
MEDLINE (R) 1/98-9/98
MEDLINE (R) 1/98-9/98 usage is subject to the terms and conditions of the
Subscription and License Agreement and the applicable Copyright and
intellectual property protection as dictated by the appropriate laws of your
country and/or by International Convention.
1 of 8
Marked in Search: #8
TI: Research ethics. NIH examines standards for consent [news]
AU: Marshall-E
SO: Science. 1998 Jun 12; 280(5370): 1688
This source is Available only few issues in S.J.M.C. Library
Call Number: From: 1937-1989
ISSN: 0036-8075
PY: 1998
LA: ENGLISH
CP: UNITED-STATES
MESH: Clinical-Trials-standards; Guidelines-; Human-Experimentation;
Research—standards; United-States
MESH: ^Bioethics-; ^Informed-Consent; KMental-Competency;
*National-Institute-of-Mentai-Health-U .S.-standards;
♦National-Institutes-of-Health-U .S.-standards;
*Professional-Staff-Committees-standards
TG: Human
PT: NEWS
AN: 98314401
UD: 9809
2 of 8
Marked in Search: #8
TI: Critical ethical issues in clinical trials with xenotransplants.
AU: Vanderpool-HY
AD: Institute for the Medical Humanities, University of Texas Medical Branch,
Galveston 77555-13122, USA.
SO: Lancet. 1998 May 2; 351(9112): 1347-50
This source is Available in S.J.M.C Library
Call Number: From: 1930+
ISSN: 0140-6736
PY: 1998
LA: ENGLISH
CP: ENGLAND
MESH: Guidelines-; Informed-Consent; Patient-Advocacy
MESH: KClinical-Trials; ^Ethics,-Medical; ^Transplantation,-Heterologous
TG: Human
PT: JOURNAL-ARTICLE
AN: 98305965
UD: 9809
SB: AIM
3 of 8
Marked in Search: #8
TI: Ethical debate. Too drunk to care?
AU: Cressey-DM; Rigter-H; Rees-G; Walsh-P
AD: Anaesthetic Department, Royal Hallamshire Hosptial, Sheffield, S10 2JF.
D.M.CresseySSheffield.ac.uk
SO: BMJ. 1998 May 16; 316(7143): 1515-7
ISSN: 0959-8138
PY: 1998
LA: ENGLISH
CP: ENGLAND
MESH: Clinical-Competence; Emergencies-; Morals-; Practice-Guidelines:
Professional-Practice; Risk-Assessment
MESH: *Alcohol-Drinking ; KEthics,-Medical; *Physician-Impairment
TG: Human
PT: JOURNAL-ARTICLE
AN: 98248391
UD: 9808
SB: AIM
4 of 8
Marked in Search: #8
TI: Implementation of guidelines for No-CF'R orders by a general medicine unit
in a teaching hospital Esee comments!
CM: Comment in: Aust N Z J Med 1997 Aug;27(4):369-70
AU: Lowe-J; Kerridge-I
AD: General Medicine Unit, John Hunter Hospital, Newcastle, NSW.
SO: Aust-N-Z-J-Med. 1997 Aug; 27(4): 379-83
This source is Available only few issues in S.J.M.C. Library
Call Number: From: 1980-1987
ISSN: 0004-8291
PY: 1997
LA: ENGLISH
CP: AUSTRALIA
AB: BACKGROUND: No-cardiopulmonary resuscitation (CPR) orders are frequently
used to limit the use of cardiopulmonary resuscitation in patients who die in
hospital. International research has consistently highlighted major
deficiencies in the formulation, documentation and communication of such
orders. There has been little Australian research into No-CPR orders and the
impact of clinical quidelines. AIMS: This audit aimed to examine compliance
with published guidelines for Np-CPR orders previously developed by the
hospital Clinical Ethics Committee. METHODS: The notes of all patients who died
while under the care of the General Medicine Unit during June-December 1994
were reviewed to evaluate the use of No-CPR orders. Adherence to hospital
No-CPR quidelines was evaluated as well as the principal diagnosis, age, level
of care and competence of patients to state their wishes. RESULTS: A No-CPR
order was documented in 61% (n = 40) of the 66 patients who died during this
period. Of these patients 807. were judged to be incompetent and were unable to
be involved in decisions not to resuscitate. There was substantial compliance
with the guidelines
SiIverPlatter 3.11
MEDLINE (R) 1/98-9/98
MEDLINE (R) 1/98-9/98 usage is subject to the terms and conditions of the
Subscription and License Agreement and the applicable Copyright and
intellectual property protection as dictated by the appropriate laws of your
country and/or by International Convention.
1 o-f 6
Marked in Search: #3
TI: Ethical practice in managed care: a dose o-f realism.
AU: Ha11-MA; Berenson-RA
AD: Wake Forest University School o-f Medicine, Winston-Salem, North Carolina
27157-1063, USA.
SO: Ann-Intern-Med. 1998 Mar 1; 128(5): 395-402
This source is Available in S.J.M.C Library
Call Number: From: 1972+
ISSN: 0003-4819
PY: 1998
LA: ENGLISH
CP: UNITED-STATES
AB: This article examines the ethics o-f medical practice under managed care
from a pragmatic perspective that gives physicians more useful guidance than do
existing ethical statements. The article begins with a framework for
constructing a realistic set of ethical principles, namely, that medical ethics
derives from physicians' role as healers; that ethical statements are primarily
aspirational, not regulatory; and that preserving patient trust is the primary
objective. The following concrete ethical quidelines are presented: Financial
incentives should influence physicians to maximise the health of the group of
patients under their care; physicians should not enter into incentive
arrangements that they are embarrassed to describe accurately to their
patients; physicians should treat each patient impartially without regard to
source of payment, consistent with the physician's own treatment style; if
physicians depart frbm this ideal, they should inform their patients honestly;
and it is desirable, although not mandatory, to differentiate medical treatment
recommendations from insurance coverage decisions by clearly assigning
authority over these different roles and by physicians advocating for
recommended treatment that is not covered.
MESH: Health-Care-Rationing; Patient-Advocacy; Physician-Patient-Relaticns;
Physician's-Role; Reimbursement,-Incentive
,
MESH: KEthics,-Medical; *Managed-Care-Programs
TG: Human
PT: JOURNAL-ARTICLE; REVIEW; REVIEW,-TUTORIAL
AN: 98138825
UD: 9805
SB: AIM
2 of 6
Marked in Search: #3
Ethical and institutional review board issues.
Skolnick-BE
Department of Neurology, Pennsylvania Hospital, Philadelphia 19107, USA.
Adv-Neurol. 1998; 76: 253-62
this source is serial publication, available only few issues in
S.J.M.C.Library
Call Number: From:1973-1988
ISSN: 0091-3952
PY: 1998
LA: ENGLISH
CP: UNITED-STATES
TI:
AU:
AD:
SO:
AB: IRBs provide an important role in the protection of research
subjects/patients. Research investigators have an inherent potential conflict
o-f interest as health care professionals; as physicians, they are dedicated to
promoting the welfare of individual patients, whereas as researchers, they seek
knowledge that can be generalized and is applicable to persons other than the
individual patient under study. The second goal may be in conflict with the
first. IRBs have the paramount responsibility of protecting the rights and
welfare of human research subjects. Although the IRB system is not perfect,
conscientious IRBs reassure the public that the rights and welfare of human
subjects are seriously considered by people who do not have a vested interest
in the outcome of the research. By exercising their responsibilities, IRBs
promote the protection of human subjects. IRB approval provides a significant
affirmation of the scientific and ethical qualities of research, and therefore
offers important validation to research and research investigators. IRBs,
acting in accordance with the guiding principles of the Belmont Report and
within the regulatory guidelines of 45.CFR.46, are intended to provide balance
between society's interest in advancing scientific knowledge and the mandate to
protect the rights and welfare of human subjects.
MESH: Anticonvulsants-adverse-effects; Helsinki-Declaration; Informed-Consent
MESH: *Anticonvulsants-therapeutic-use; *Clinical-Trials-standards;
KEthics,-Medical; fcProfessional-Staff-Committees-trends
TG: Human
PT: JOURNAL-ARTICLE; REVIEW; REVIEW,-TUTORIAL
RN: 0
NM: Anticonvulsants
AN: 98072764
UD: 9804
3 of 6
Marked in Search: #3
TI: Ethics group drafts guidelines
SiIverPlatter 3.11
MEDLINE (R) 1/98-9/98
MEDLINE (R) 1/98-9/98 usage is subject to the terms and conditions of the
Subscription and License Agreement and the applicable Copyright and
intellectual property protection as dictated by the appropriate laws o-f your
country and/or by International Convention.
1 of 4
Marked in Search: #3
TI: Ethics group drafts quidelines for control of genetic material and
information [news!
AU: Stephenson-J
SO: JAMA. 1998 Jan 21; 279(3): 184
This source is Available in S.J.M.C Library
Call Number: From; 1918+
ISSN: 0098-7484
PY: 1998
LA: ENGLISH
CP: UNITED-STATES
MESH: KEthics-; *Genome,-Human; KGuidelines-; *Human-Genome-Project
TG: Human
PT: NEWS
AN: 98099561
UD: 9803
SB: AIM
2 of 4
Marked in Search:. #3
TI: Genetic testing for cancer risk: how to reconcile the conflicts.
AU: Kodish-E; Wiesner-GL; Mehlman-M; Murray-T
AD: Department of Pediatrics, Center for Biomedical Ethics, Case Western
Reserve University School of Medicine, Cleveland, OH, USA.
SO: JAMA. 1998 Jan 21; 279(3): 179-81'
This source is Available in S.J.M.C Library
Call Number: From: 1918+
ISSN: 0098-7484
PY: 1998
LA: ENGLISH
CP: UNITED-STATES
MESH: Breast-Neoplasms-diagnosis; Breast-Neoplasms-genetics;
Genetic-Screening-economics; Genetic-Screening-psychology;
Heterozygote-Detection; Medical-Oncology-standards;
National-Institutes-of-Health-U.S. ; Neoplasms-diagnosis; Risk-Factors;
Societies,-Medical; United-States
MESH: KEthics,-Medical; *Genetic-Screening-standards; fcNeoplasms-genetics;
*Practice-Guidelines
TG: Human; Support,-Non-U.S.-Gov't
PT: JOURNAL-ARTICLE
AN: 98099559
UD: 9803
SB: AIM
3 of 4
Marked in Search: #3
TI: Indian guidelines allow limited gene screening [news]
AU: Jayaraman-KS
SO: Nature. 1998 Jan 8; 391(6663): 115
This source is Available only few issues in S.J.M.C. Library
Call Number: From: 1956-1993
ISSN: 0023-0836
PY: 1998
LA: ENGLISH
CP: ENGLAND
MESH: Fetus-; India-; Research-standards
MESH: tEthics,-Medical; ^Genetic-Screening; ftGuidelinesTG: Animal; Human
PT: NEWS
AN: 98089028
UD: 9803
4 of 4
Marked in Search: #3
Synopsis of a practical guide: guidelines for ethics committees.
Mulvey-B
Nova Southeastern University, Fort Lauderdale, Florida, USA.
J-Fla-Med-Assoc. 1997 Nov; 84(8): 506-9
this source is not Available in S.J.M■C.Library
ISSN: 0015-4148
PY: 1997
LA: ENGLISH
CP: UNITED-STATES
MESH: Bioethics-; Education,-Continuing; Ethics-Committees-orqanization-andadministration; Ethics,-Medical-education; Organizational-Culture;
Organizational-Innovation ; Organizational-Obj ectives; Organizational-Pol icy;
Policy-Making
MESH: ^Ethics-Committees; HcEthics,-Medical ; KGuidelinesTG: Human
PT; JOURNAL-ARTICLE
AN: 98064614
UD: 9803
TI:
AU:
AD:
SO:
SilverPlatter 3.11
MEDLINE (R) 1/97-9/97
MEDLINE (R) 1/97-9/97 usage is subject to the terms and conditions of the
Subscription and License Agreement and the applicable Copyright and
intellectual property protection as dictated by the appropriate laws o-f your
country and/or by International Convention.
1 of 27
Marked in Search: #5
TI: The rationale and ethics of medication-free research in schizophrenia [see
comments!
CM: Comment in: Arch Gen Psychiatry 1997 May;54(5 ):412-3, Comment in: Arch
Gen Psychiatry 1997 May;54(5 ):415-6
AU: Carpenter—WT Jr; Schooler—NR; Kane-JM
AD: Department of Psychiatry, University of Maryland School of Medicine,
Baltimore, USA.
SO: Arch-Gen-Psychiatry. 1997 May; 54(5): 401-7
This source is Available in S.J.M.C Library
Call Number: From: 1959+
ISSN: 0003-990X
PY: 1997
LA: ENGLISH
CP: UNITED-STATES
AB: Schizophrenia research is receiving intense scrutiny from an ethical
perspective. Medication-free protocols present a most vexing dilemma in that
they greatly enhance the opportunity for advancing knowledge but also raise the
prospect of withholding known effective treatment. In this article, we discuss
the purpose of medication-free protocols in new drug development and
nontreatment research. Potential benefits and risks associated with drug
discontinuation are evaluated, and methods for minimizing risk and increasing
benefits are proposed as quidelines for the protection of individual subjects.
The complex problem of informed consent also is addressed. Medication-free
research in schizophrenia is difficult, but it can be conducted relatively,
safely with freely consenting, competent subjects. Assurance that studies meet
this standard is required. We believe that such investigations can meet high
standards of ethics and subject protection, and that a radical revision of
procedures for research review and implementation is not indicated.
MESH: Acute-Disease; Clinical-Protocols-standards; Clinical-Trials-standards;
Informed-Consent; Patient-Selection; Risk-Assessment;
Schizophrenia-drug-therapy ; Schizophrenia-therapy; Schizophrenic-Psychology
MESH: *Antipsychotic-Agents-therapeutic-use; ^Ethics,-Medical;
jResearch-Design-standards; *SchizophreniaTG: Human; Support,-U.S.-Gov't,-P.H.S.
PT: JOURNAL-ARTICLE; REVIEW; REVIEW,-TUTORIAL
CN: MH40279MHNIMH; MH35996MHNIMH; MH45156MHNIMH
RN: 0
NM: Antipsychotic-Agents
AN: 97296623
UD: 9708
SB: AIM
2 of 27
Marked in Search: #5
TI: Ethical policy guidelines development for general hospital nurses.
AU: Commons-L; Baldwin-S
AD: Department of Nursing, Faculty of Health and Human Sciences Edith Cowan
University, Bunbury, Western Australia.
SO: Int-J-Nurs-Stud. 1997 Feb; 34(1): 1-8
this source is not Available in S.J.M.C,Library
ISSN: 0020-7489
' PY: 1997
LA: ENGLISH
CP: ENGLAND
AB: The purpose of this position paper is to examine ethical situations
involving nurses, and provide suggestions about how to work through ethical
problems they may encounter. Ethics in the nursing profession is ubiquitous.
Nurses need to be aware of the provided codes so any ambiguity regarding
ethical dilemmas can be resolved. Ethical situations which call for such
judgements include: equity, confidentiality, honesty and justice. Resolution of
such situations requires consistent education to ensure full awareness of
societal values which are projected through the care of clients. This will aid
in the provision of quality care and ensure that a holistic approach is
achieved to maintain high standards of care.
MESH: Clinical-Competence; Confidentiality-; Guidelines-; Health-Status;
Patient-Advocacy; Quality-of-Health-Care; Social-Values
MESH: ^Ethics,-Nursing; *Nursing-Care-standards; *Nursing-Staff,-Hospital
TG: Human; Support,-Non-U.S.-Gov't
PT: JOURNAL-ARTICLE
AN: 97207879
UD: 9708
SB: NURSING
3 of 27
Marked in Search: #5
TI: Recommended guidelines for reviewing, reporting, and conducting research on
in-hospital resuscitation: the in-hospital ‘Utstein style': a statement for
healthcare professionals from the American Heart Association, the European
Resuscitation Council, the Heart and Stroke Foundation of Canada, the
Australian Resuscitation Council, and the Resuscitation Councils of Southern
Africa.
AU: Cummins-RO; Chamberlain-D; Hazinski-MF; Nadkarni-V; Kloeck—W; Kramer—E;
Becker-L; Robertson-C; Koster-R; Zaritsky-A; Bossaert-L; Ornato-JP; Callanan-V;
Allen-M; Steen-P; Connolly-B; Sanders-A; Idris-A; Cobbe-S
SO: Circulation. 1997 Apr 15; 95(8): 2213-39
This source is Available in S.J.M.C Library
Call Number: From: 1950+
ISSN: 0009-7322
PY: 1997
LA: ENGLISH
CP: UNITED-STATES
MESH: Adolescence-; Adult-; Aged-; Aged,-80-and-over;
Cardiopulmonary-Resuscitation-methods ; Cardiopulmonary-Resuscitation-standards ;
Child-; Chi Id,-Preschool; Comorbidity-; Data-Collection-methods;
Data-Collection-standards ; Demography-; Emergency-Medical-Services-methods;
Emergency-Service,-Hospital-standards; Ethics,-Medical; Evaluation-Studies;
Follow-Up-Studies; Forms-and-Records-Control; Health-Services-Research-methods ;
Heart-Arrest—epidemiology ; Infant-; Infant,-Newborn; Middle-Age;
□utcome-and-Process-Assessment-Health-Care-standards ; Resuscitation-methods;
Severity-of-I 1Iness-Index
MESH: *Emergency-Medical-Services-standards;
fcHealth-Services-Research-standards; *Heart-Arrest-therapy ;
*Hospitai-Administration-standards; ^Medical-Records-standards;
*Quality-Assurance ,-Health-Care-standards; *Resuscitaticn-standards
TG: Female; Human; Male; Support,-Non-U.S.-Gov' t
PT: GUIDELINE; JOURNAL-ARTICLE; PRACTICE-GUIDELINE
AN: 97278960
UD: 9707
SB: AIM
4 of 27
Marked in Search: #
TI: Medical Council of India on hysterectomy in the mentally retarded [news!
AU: Pandya-SK
SO: Natl-Med—J-India. 1997 Jan-Feb; 10(1): 36
This source is Available in S.J.M.C Library
Call Number: From: 1988+
ISSN: 0970-258X
PY: 1997
LA: ENGLISH
CP: INDIA
MESH: Ethics,-Medical; India-; Practice-Guidelines
MESH: ^Hysterectomy-; ^Mental-Retardation
TG: Female; Human
PT: NEWS
AN: 97222711
UD: 9707
5 of 27
Marked in Search: #'
TI: Guidelines for placement of percutaneous endoscopic gastrostomy tube
[letter]
AU: Stewart-JA
SO: Lancet. 1997 Mar 29; 349(9056): 958
This source is Available in S.J.M.C Library
Call Number: From: 1930+
ISSN: 0140-6736
PY: 1997
LA: ENGLISH
CP: ENGLAND
MESH: Algorithms-; Practice-Guidelines; Duality-of-Life
MESH: ^Enteral—Nutrition; KEthics,-Medical; ^Gastrostomy-;
* Intubation,-Gastrointestinal
TG: Human
PT: LETTER
AN: 97247148
UD: 9707
SB: AIM
6 of 27
Marked in Search: #!
TI: Guidelines for placement of percutaneous endoscopic gastrostomy tube
[letter1
AU: Rosner—F
SO: Lancet. 1997 Mar 29; 349(9056): 958
This source is Available in S.J.M.C Library
Call Number: From: 1930+
ISSN: 0140-6736
PY: 1997
LA: ENGLISH
CP: ENGLAND
MESH: Algorithms-; Practice-Guidelines; Gluality-of-Life
MESH: ^Enteral—Nutrition; KEthics,-Medical; ^Gastrostomy-;
* Intubation,-Gastrointestinal
TG: Human
PT: LETTER
AN: 97247149
UD: 9707
SB: AIM
7 of 27
Marked in Search: #5
TI: Confidentiality and the AMA's new code of ethics: an imprudent formulation?
Cletter!
AU: Komesaroff-PA
SO: Med-J-Aust. 1997 Feb 17; 166(4): 221
This source is Available in S.J.M.C Library
Call Number: From: 1966+
ISSN: 0025-729X
PY: 1997
LA: ENGLISH
CP: AUSTRALIA
MESH: Australia-; Public-Health
MESH: *Confidentiality-; KEthics,-Medical; KPractice-Guidelines;
^Societies,-Medical
TG: Human
PT: LETTER
AN: 97219254
UD: 9706
8 of 27
Marked in Search: #5
TI: Professionalism in health care delivery.
AU: Shapiro-R
SO: Wis-Med-J. 1997 Jan; 96(1): 28-31
this source is not Available in S■J.M.C.Library
ISSN: 0043-6542
PY: 1997
LA: ENGLISH
CP: UNITED-STATES
MESH: Ethics,-Medical; Interprofessional-Relations;
Physician-Patient-Relations; Practice-Guidelines; United-States
MESH: *Delivery-of-Health-Care-trends; ^Professional-Practice
TG: Human
PT: JOURNAL-ARTICLE
AN: 97172728
UD: 9706
9 of 27
Marked in Search: #5
TI: World Medical Association declaration of Helsinki. Recommendations guiding
physicians in biomedical research involving human subjects [see comments]
CM: Comment in: JAMA 1997 Mar 19;277(11 ):922-3
SO: JAMA. 1997 Mar 19; 277(11): 925-6
This source is Available in S.J.M.C Library
Call Number: From: 1918+
ISSN: 0098-7484
PY: 1997
LA: ENGLISH
CP: UNITED-STATES
MESH: Ethics,-Medical; Guidelines-; Informed-Consent
MESH: KEvaluation-Studies; *Helsinki-Declaration ; *Human-Experimentation
TG: Human
PT: JOURNAL-ARTICLE
AN: 97216044
UD: 9706
SB: AIM
10 of 27
Marked in Search: #5
TI: Institutional review board approval and publication of human research
results Csee comments!
CM: Comment in: JAMA 1997 Mar 19;277(11 1:922-3
AU: Amdur—RJ; Biddle-C
AD: Dartmouth-Hitchcock Medical Center, Lebanon, NH 03756, USA.
robert.amdurShitchcock.org
SO: JAMA. 1997 Mar 19; 277(11): 909-14
This source is Available in S.J.M.C Library
Call Number: From: 1918+
ISSN: 0098-7484
PY: 1997
LA: ENGLISH
CP: UNITED-STATES
AB: OBJECTIVE: To determine if journals' instructions for authors require that
manuscripts being considered for publication indicate that studies involving
human subjects had appropriate institutional review board (IRB) approval.
DESIGN: A descriptive study of the ethical guidelines published in the
Instructions for Authors sections of the 102 English-language biomedical
research journals listed in the 1995 Abridged Index Medicus. INTERVENTION:
Literature review. MAIN OUTCOME MEASURE: Policy regarding IRB approval of
studies that involve human subjects. RESULTS: Of the 102 journals surveyed, 48
(477.) require IRB approval of studies involving human subjects as a
prerequisite for publication, and 25 (247.) do not present or refer the author
to any information related to human research ethics. Of the remaining journals,
15 (15%) referred authors to the Uniform Requirements for Manuscripts Submitted
to Biomedical Journals, 3 (3%) to the Declaration of Helsinki, and 10 (107.)
simply indicated that informed consent should be obtained. There was only 1
. medical specialty (anesthesiology) in which all the representative journals
presented the same ethical requirement. In the 48 journals that clearly
required IRB approval of studies, 37 (777.) documented IRB approval with a
statement in the manuscript, 7 (15%) required, a separate signed statement from
the author, and 4 (87.) did not mention a method of documentation. CONCLUSIONS:
The results of this study suggest that about half of the 102 English-language
biomedical research journals listed in the 1995 Abridged Index Medicus do not
publish quidelines indicating that IRB approval of studies involving human
research subjects is a requirement for publication. The manner in which
publication requirements related to ethical standards are presented in
biomedical research journals is extremely variable.
MESH: Documentation-; Ethics,-Medical; Helsinki-Declaration; Informed-Consent;
Special ties,-Medical-standards
MESH: ^Evaluation-Studies; ^Human-Experimentation; ^Periodicals-standards;
*Professional-Staff-Committees; ftPublishing-standards
TG: Human
PT: JOURNAL-ARTICLE
AN: 97216040
UD: 9706
SB: AIM
11 of 27
Marked in Search: #5
TI: Ethical issues in the development and use of guidelines for clinical
practice.
AU: Redman-BK
AD: School of Nursing, University of Connecticut, Storrs, USA.
SO: J-Clin-Ethics. 1996 Fall; 7(3): 251-6
this source is not Available in S.J.M.C■Library
ISSN: 1046-7890
PY: 1996
LA: ENGLISH
CP: UNITED-STATES
. AB: In order to serve the purposes expected o-f them, practice guidelines must
be more than summaries of available research; they must also challenge the
values that are implicit in the way practice questions have been framed and
outcomes have been chosen. The IOM has defined desirable attributes of practice
guidelines, focused on the characteristics of measurement and implementation.
It is also desirable for guidelines to meet certain ethical criteria.
MESH: Anemia,-Sickle-Cell-diagnosis; Anemia,-Sickle-Cel1-therapy ; Counseling-;
Health-Care-Reform-standards; Neoplasms-physiopathology;
Pain,-Intractable-therapy; United-States; United-States-Agency-for-HealthCare-Policy-and-Research
MESH: ♦Ethics,-Medical; ♦Practice-Guidelines-standards
TG: Human
PT: JOURNAL-ARTICLE
AN: 97135659
UD: 9705
12 of 27
Marked in Search: #5
TI: Ethically justified, clinically comprehensive guidelines for percutaneous
endoscopic gastrostomy tube placement.
AU: Rabeneck-L; McCullough-LB; Wray-NP
AD: Department of Veterans Affairs, Houston, Texas, USA.
SO: Lancet. 1997 Feb 15; 349(9050): 496-8
This source is Available in S.J.M.C Library
Call Number: From: 1930+
ISSN: 0140-6736
PY: 1997
LA: ENGLISH
CP: ENGLAND
AB: Guidelines for the placement of percutaneous endoscopic gastrostomy (PEG)
tubes are not available. We developed a decision-making algorithm by
integrating the medical and ethical dimensions of the decision. According to
our algorithm, physicians should not offer PEG tubes to patients with
anorexia-cachexia syndromes. For patients with permanent vegetative states,
physicians should offer and recommend against the procedure. For patients who
have dysphagia without other deficits in quality of life, physicians should
offer and recommend the procedure. For the the remaining patients who have
dysphagia with other deficits in quality of life, the physician's role is to
providei non-directive counselling regarding the short and long-term
consequences of a trial of PEG tube feeding.
MESH: Algorithms-; Counseling-; Decision-Making; Deglutition-Disorders-therapy ;
Gastrostomy-; Practice-Guidelines
MESH: ♦Enteral-Nutrition; ♦Ethics.-Medical
TG: Human
PT: JOURNAL-ARTICLE
AN: 97192999
UD: 9705
SB: AIM
13 of 27
Marked in Search: #5
Public confidence in public health research ethics [comment!
Comment on: Public Health Rep 1997 Jan-Feb;112(1 >:29-32
Mariner—WK
Boston University Schools of Public Health and Medicine, MA, USA.
Public-Health-Rep. 1997 Jan-Feb; 112(1): 33-6
This source is Available only few issues in S.J.M.C. Library
Call Number: From:1949-1984
ISSN: 0033-3549
PY: 1997
TI:
CM:
AU:
AD:
SO:
.LAs ENGLISH
CP: UNITED-STATES
MESH: Human-Experimentation; Informed-Consent
MESH: *Attitude-to-Health; ^Ethics,-Medical; ^Guidelines-;
*Publie-Health-standards ; *Research-standards
TG: Human
PT: COMMENT; JOURNAL—ARTICLE; REVIEW; REVIEW,-TUTORIAL
AN: 97171012
UD: 9705
SB: AIM
14 of 27
Marked in Search: #5
TI: Thinking about a medical school core curriculum for medical ethics and law
[editorial; comment!
CM: Comment on: J Med Ethics 1996 Dec;22(6 );325-6
AU: Gillon-R
SO: J—Med—Ethics. 1996 Dec; 22(6): 323-4
this source is not Available in S.J.M.C.Library
ISSN: 0306-6800
PY: 1996
LA: ENGLISH
CP: ENGLAND
MESH: Great-Britain ; GuidelinesMESH: ^Curriculum-; ^Education,-Medical,-Undergraduate-organization-andadministration ; ^Ethics,-Medical; ^Legislation,-Medical
TG: Human
PT: COMMENT; EDITORIAL
AN: 97120443
UD; 9705
15 of 27
Marked in Search: #5
TI: Torture, ethics and health professionals [editorial!
AU: Ray-I
SO: J-Indian-Med-Assoc . 1996 Jul; 94(7): 250
this source is not Available in S.J.M■C.Library
ISSN: 0019-5847
PY: 1996
LA: ENGLISH
CP: INDIA
MESH: ^Ethics,-Medical ; fcHuman-Rights ; KPractice-Guidelines ; XTortureTG: Human
PT: EDITORIAL
AN: 97171898
UD: 9705
16 of 27
Marked in Search: #5
Physician-operated networks and the new antitrust guidelines■
Kuttner—R
The American Prospect, Cambridge, MA 02138, USA.
N-Engl-J-Med. 1997 Jan 30; 336(5): 386-91
This source is Available in S.J.M.C Library
Call Number: From: 1945+
ISSN: 0028-4793
PY: 1997
LA: ENGLISH
CP: UNITED-STATES
MESH: American-Medical-Association; Community-Networks-economics ;
TI:
AU:
AD:
SO:
Economic-Competition-legislation-and-jurisprudence; Ethics,-Medical;
Fees,-Medical-1egislation-and-j urisprudence;
Hospital—Physician-Joint-Ventures-economics;
Hospitai-Physician-Joint-Ventures-1egislation-and-jurisprudence;
Independent-Practice-Associations-economics;
Preferred-Provider-Organizations-economics;
Pre-Per red-Provider—Organizations- legislation-and-j urisprudence;
Professional-Autonomy; United-States; United-States-Federal-Trade-Commission
MESH: *Antitrust-Laws; ♦Community-Networks-legislation-and-jurisprudence;
*Independent-Practice-Associations-legislation-and-j urisprudence
PT: JOURNAL-ARTICLE
AN: 97163333
UD: 9704
SB: AIM
17 of 27
Marked in Search: #5
TI: Informed consent in human experimentation before the Nuremberg code.
AU: Vollmann-J; Winau-R
AD: Institute of the History of Medicine, Free University of Berlin.
SO: BMJ. 1996 Dec 7; 313(7070): 144S-9
ISSN: 0959-8138
PY: 1996
LA: ENGLISH
CP: ENGLAND
AB: The issue of ethics with respect to medical experimentation in Germany
during the 1930s and 1940s was crucial at the Nuremberg trials and related
trials of doctors and public health officials. Those involved in horrible
crimes attempted to excuse themselves by arguing that there were no explicit
rules governing medical research on human beings in Germany during the period
and that research practices in Germany were not different from those in allied
countries. In this context the Nuremberg code of 1947 is generally regarded as
the first document to set out ethical regulations in human experimentation
based on informed consent. New research, however, indicates that ethical issues
of informed consent in quidelines for human experimentation were recognised as
early as the nineteenth century. These quidelines shed light on the still
contentious issue of when the concepts of autonomy, informed consent, and
therapeutic and non-therapeutic research first emerged. This issue assumes
renewed importance in the context of current attempts to assess liability and
responsibility for the abuse of people in various experiments conducted since
the second world war in the United States, Canada, Russia, and other nations.
MESH: Germany-; Government-; History-of-Medicine ,-20th-Cent.; Patient-Advocacy;
Practice-Guidei ines; War-Crimes-history
MESH: ♦Ethics,-Medical; ♦Human-Experimentation-history; * Informed-Consent;
♦War—Crimes
TG: Human; Support,-Non-U.S.-Gov't
PT: HISTORICAL-ARTICLE; JOURNAL-ARTICLE
AN: 97128675
UD: 9703
SB: AIM
18 of 27
Marked in Search: #5
TI: Eying quidelines I letter!
AU: Wensel-RH; Carter-AO; Walters-D; Beardall-S
SO: Can-Med-Assoc-J. 1996 Dec 15; 155(12): 1666, 1668
this source is not Available in S.J.M.C.Library
ISSN: 0008-4409
PY: 1996
LA: ENGLISH
.CP: CANADA
MESH: Attitude-of-Health-Personriel; Canada-; Ethics,-Medical; JudgmentMESH?' ftPractice-Guidelines-standards; *Quality-of-Health-Care-legislation-andjurisprudence; ^Societies,-Medical
PT: LETTER
AN: 97130567
UD: 9703
SB: AIM
19 of 27
Marked in Search: #5
TI: The changing nature of neonatal ethics in practice.
AU: Kinlaw—K
AD: Center for Ethics in Public Policy and the Professions, School of Medicine,
Emory University, Atlanta, Georgia, USA.
SO: Clin-Perinatol . 1996 Sep; 23(3): 417-28
This source is Available in S.J.M.C Library
Call Number: From: 1976
ISSN: 0095-5108
PY: 1996
LA: ENGLISH
CP: UNITED-STATES
AB: This article overviews the current practice of neonatal care ethics.
Tracing the evolving nature of neonatal care over the last few decades, the
author reviews Rhoden's categories of approaches to neonatal care and raises
questions about the nature of responsibility in neonatal decision making. The
role of the parent or guardian and the importance of communication is explored.
Current neonatal outcome studies are reviewed in considering what "best
interests" means for the newborn. The article concludes by reviewing several
issues raised by current court cases that may point to the future of ethical
decision making in neonatal care.
MESH: Anencephaly-; Brain-Death; Guidelines-; Infant,-Low-Birth-Weight;
Infant/-Newborn; Physician's-Role; Prognosis-; Resuscitation-Orders;
United-States
MESH: tEthics,-Medical; *NeonatologyTG: Human
PT: JOURNAL-ARTICLE; REVIEW; REVIEW,-TUTORIAL
AN: 97038535
UD: 9702
20 of 27
Marked in Search: #5
TI: Do not resuscitate orders in the operating room.
AU: Craig-DB
AD: Department of Anesthesia, University of Manitoba and Health Sciences
Centre, Winnipeg, Manitoba.
SO: Can-J-Anaesth. 1996 Aug; 43(8): 840-51
This source is Available in S.J.M.C Library
Call Number: From: 1966+
ISSN: 0832-610X
PY: 1996
LA: ENGLISH
CP: CANADA
AB: PURPOSE: The background to a current analysis of the management of "do not
resuscitate" (DNR) orders in the operating room is reviewed, with an emphasis
on the current status of resuscitation/DNR issues in Canada. SOURCE: The Joint
Statement on Resuscitative Interventions published by the Canadian Medical
Association and cooperating organizations and the report of the Senate of
Canada Special Committee on Euthanasia and Assisted Suicide are examined for
information relevant to the DNR issue. Guidelines on the management of DNR
Hp-1Pw? 1 rtf 9
Main Identity
From:
To:
Sent*
Subject:
sandhya srinivasan" <sandhya_srinivasan@vsnl.comj<southasianmedicalethics@yahoogroups.com>
Sunday, July
9003 11 77 AM
[southasianmcdicalcthics] "ver donor dies
www.newindpress.com
Thursday July 10 2003 14:24 1ST
1'iSn DELHI: what was uouued as the 25th successful liver transplant, at
Indraprastha Apollo last month turned into a tragedy with the donor's death
nine days after' the surgery. The death of the donor is a rare phenomenon and
rhe 24-year-ola aonor, Subash, died on July 3 and was cremated around 10 am
that day.
.sri sanr., according to Apoiio authorities, is recovering in the TOT of the
hospital.
’’Only six cases of deaths in donations of liver have been reported in the
^^dica! historv. Ther'e is less than 0.1
cent chance of the donor1? death.
tiie veins is transplanted.
"The death in this case can be due to comolications after the suraerv, such as
While the treating surgeon was not available tor comment, A-pollo confirmed
that the donor died in their hospital. ''It was the 25th successful surgery in
uc vciGpcu xil CxIG pUxiuGi'icix y Vcj.liz
Julu x»r AHupuHt SxOuxz
uicuICuj.
uiloCuOjS Ox
indraprasuna apoiio.
The hospital said Subash was a relative of Srikant and an authorisation
nCc xb^i ai'iO uuiici' xawo Oil Oxtail QOHauxOll ill u£lS COuiit£'yz
C116 GOiiOr Cail 06
me first. degree relative, spouse or exception unrelated on r.ne basis of love
and affection and without any'monetary transaction11.
[Non-text portions of tnis message have been removed]
Page i of 3
Cc.
Sent:
Subject:
"bioethics' 'bioeihics@SKLi.edu>
Monday. September 29. 2003 4:48 PM
fsouttasianmedicatethics} Sex Selection for Social Reasons: Rehgiousand Moral
nr
Page 1 of2
Main identity
From:
To:
Cc:
Sent:
Subject:
"bioethics" <bioeihics@aku.edu>
"bioethics" <bioethics@aku.edu>
"amyn.majeedlassi" <amyn.majeedlassi@aku.edu>
Tuesday, September 02, 2003 6:27 PM
[southasianmedicaiethics] Proceedings of 2nd Symposium & Workshop onEthicai Issues in
Health Research
SECOND SYMPOSIUM AND WORKSHOP
ON ETHICAL ISSUES IN HEA.LTH RESEARCH IN DEVELOPING COUNTRIES
Held on: August 14-18, 2003, Aga Khan University, Karachi, Pakistan.
Report, Presentations & Croup Photograph are available on the
'AKU Bioethics Initiatives website
To view the Report, Presentations and Group Photograph please click
here:
htto: /
aku, edu/bicethics/newsandevents, shtrr.
Amvn Laasi, HDSE, DISM, CPISM
Sr. Administrative Staff, Pakistan Bioethics Program,
Aga Khan University, P.O. Box 3500, Stadium Road, Karachi, Pakistan
phone: (9221) 4859-4880 : Cell: 92-333-2286283
Email:
bioethicseaku.edu; amyn.rnajeedlassi0aku.edu
Websi te: www. a ku. edu/bi oethi cs <httr>: //www.aku. edu/bi oethi cs/i ndex .htm>
[Non-lexl. portions o£ this message, have been removed]
Yahoo! Groups Sponsor
ADVERTISEMENT
tO 'jfGSJF dySi’;
T.. .V. S
P ,*S f J
sr *Vr.
\
« Cvw *5,000 7i»cs
i! Free Shipping
to fry it for
todksyf
9/3/03
To unsubscribe from this group, send an email to:
9/3/03
Page 2 of 2
•ihoo! Search Results
http://search.yahoo...p=ETHICS+%2B+HEALTH
Help - Check Email
Personalize
Search Result Found 0 categories and 65 sites for ETHICS + HEALTH
Categories
Web Sites
Web Pages
Yahoo! Site Matches
Related News
Net Events
(i - 20 of 65)
Regional: Countries: Canada: Provinces and Territories: Alberta: Counties and Districts:
Edmonton: Cities: Edmonton: Education: College and University: University of Alberta:
Departments and Programs: Bioethics Centre
Buy Books On
ethics + health
lamazoaroml
□ Health Ethics Centre
Science: Biology: Biomedical Ethics: Institutes
□ Pope John Center for the Study of Ethics in Health Care - a Catholic institute which engages in
research, education, and publication in biomedical ethics.
□ University of Buffalo Center for Clinical Ethics and Humanities in Health Care
Science: Biology: Biomedical Ethics
□ National Consultative Ethics Committee for Health and Life Sciences (France) - contains all the
opinions, recommendations, and reports, in French and English, on ethical problems raised by
progress in the fields of biology, medicine, and health, published since the committee's establishment.
□ Issues in Health Care - discussing issues in medical ethics such as euthanasia, HIV disclosure, and
others.
□ Medical Ethics: Where Do You Draw the Line? - new developments in medicine and health care
raise many ethical questions. Learn about current research and explore your own beliefs about these
a
controversial issues.
Society' and Culture: Religion and Spirituality: Faiths and Practices: Christianity: Denominations and Sects:
Catholic: Education: Organizations
□ Pope John Center for the Study of Ethics in Health Care - a Catholic institute which engages in
research, education, and publication in biomedical ethics.
Arts: Humanities: Medical Humanities
□ University' of Buffalo Center for Clinical Ethics and Humanities in Health Care
Business and Economy: Companies: Health: Software: Medical
□ Doctor's Dilemma. Essentials of Medical Ethics Bioethics - interactive role-playing program that
allows the user to explore his or her own approach to medical ethics.
Regional: Countries: France: Science
□ National Consultative Ethics Committee for Health and Life Sciences (CCNE) - contains all the
of 3
02/12/99 18:17:53
ihoo! Search Results
http://search.yahoo...p=ETHICS+%2B+HEALTH
opinions, recommendations, and reports, in French and English, on ethical problems raised by
progress in the fields of biology, medicine, and health, published since the committee's establishment.
Regional: U.S. States: Massachusetts: Cities: Braintree: Community
□ Pope John Center for the Study of Ethics in Health Care - a Catholic institute which engages in
research, education, and publication in biomedical ethics.
□ Pope John Center for the Study of Ethics in Health Care - a Catholic institute which engages in
research, education, and publication in biomedical ethics.
Regional: U.S, States: New York: Cities: Buffalo: Education: College and University: Public: SUNY
Buffalo: Departments and Programs
□ Center for Clinical Ethics and Humanities in Health Care
Net Events: Health: Chat Rooms
□ Current Events in Health - discuss all current events related to health and fitness such as ethics in
medicine, the latest medical findings and more.
□ Basic Ethics in Experimental Studies - channel #biomedicina. Chat in Spanish.
Health: Health Care: Policy: Journals
□ Journal of Health Politics, Policy and Law - original scholarship on health politics, policy, and law
from areas such as political science, economics, history, sociology, health services research,
philosophy, ethics, and so forth
Government: Law: Health: Organizations
□ American Society of Law, Medicine and Ethics (ASLME)
Health: Procedures and Therapies: Organ Transplants: Xenotransplantation
D Ethics of Xenografting: Transplanting Animal Organs into Humans
Health: Reproductive Health: Abortion
□ Abortion and Reproductive Rights: Medicine, Ethics, and the Law
Health: Reproductive Health: Preimplantation Genetic Diagnosis
□ Ethics and Regulation of PGP in Germany
Next 20 Matches
Categories
Web Sites
Web Pages
advanced search - help
Related News
Net Events
! of 3
02/12/99 18:19:46
fahoo! Search Results
http://search.yahoo...p=ETHICS+%2B+HEALTB
Other Search Engines
Alta Vista - HotBot - Infoseek - DejaNews - Lycos - More-
Yellow Pages - People Search - City Maps - Get Local - Today's Web Events & Chats - Image Surfer - More Yahoos
Copyright © 1994-99 Yahoo! Inc. - Company Information - Help
ft A (Lie PfiLo-^'ci/k ' '
PC-SPIRS 3.40
MEDLINE (R) 1/97-9/97
MEDLINE (R) 1/97-9/97 usage is subject to the terms and conditions o-f the
Subscription and License Agreement and the applicable Copyright and
intellectual property protection as dictated by the appropriate laws of your
country and/or by International Convention.
1 of 57
TI: Moral tensions and obligations of occupational therapy practitioners
providing home care.
AU: Opacich-KJ
AD: University of Illinois, School of Public Heal th, Chicago, USA.
SO: Am-J-Occup-Ther. 1997 Jun; 51(6): 430-5
____This source is Available only few issues in S.J.M.C. Library
LA: ENGLISH
AB: Home care has been valued as a relevant context for the provision of
occupational therapy since the inception of the field. The setting provides
rich opportunities to restore meaningfulness in living for clients whose lives
have been disrupted by illness or untoward events. Additionally the home care
bsetting allows practitioners to exercise professional commitments and to meet
®>thical obligations congruent with the'field of occupational therapy.
Nevertheless, the home care arena is not. exempt from the pressures that pervade
the health care industry. To thrive in the provision of home care, occupational
therapy practitioners must prepare themselves to deal with the philosophic,
economic, and moral challenges inherent in the setting. This article explores
the moral obligations of occupational therapy practitioners who provide home
care. More specifically, it addresses obligations to self, to patients, to
caregivers, to society, to the profession, to fellow health care providers, and
to agencies and payers. Ethical principles associated with each are
highlighted, and issues are raised. Home care practitioners who are attuned to
the moral commitments imbedded in occupational therapy philosophy will most
likely incorporate these tenets into their clinical decisions.
2 of 57
TI: [Quality in public hea1th. Deficits, concepts and political quality key
issues from the ministerial viewpoint!
AU: Ruprecht-TM
AD: Behorde fur Arbeit, Gesundheit und Soziales Hamburg.
|B0: Z-Arztl-FortbiId-Qualitatssich . 1997 Feb; 91(1): 75-91
'this source is not Available in S.J.M.C.Library
LA: GERMAN; NON-ENGLISH
AB: To preserve the quality of the German health care system as well as
continuously optimize it towards the needs stated by ethics and law, an
inter—professional and inter-institutional quality policy is required. It
should be patient-centered, focus on process management and be based on EN
ISO-Standards adapted to the specific needs of health care. The latter could
provide internationally compatible models for quality management and quality
improvement including economic efficiency. The 40 nation Council of Europe's
5th European Conference of Health Ministers in Warsaw as well as the 69th
Conference of German Federal State Health Ministers (GMK) at Cottbus, who
tackled the issue in November 1996, pointed out essential aspects. The GMK
stated a lack of effective general concepts, quality control and patients'
rights protection in Germany. Both conferences demanded equity, social justice
and an active participation of patients in the setting of quality standards and
the conception, functioning and control of health care. This includes
rationalisations by using the limited funds in a most effective way.
3 of 57
TI: Is research into ethnicity and health racist, unsound, or important
science? [see comments!
I
AU: Bhopal-R
AD: Department of Epidemiology and Public Health, University of Newcastle.
rbhopal@sph.unc. edu
SO: BMJ. 1997 Jun 14; 314(7096): 1751-6
___ This source is Available in S.J.M.C Library
___ Call Number: From 1914+
LA: ENGLISH
AB: Much historical research on race, intelligence, and health was racist,
unethical, and ineffective. The concepts of race and ethnicity are difficult to
define but continue to be applied to the study of the health of immigrant and
ethnic minority groups in the hope of advancing understanding of causes of
disease. While a morass of associations has been generated, race and ethnicity
in health research have seldom given fundamental new understanding of disease.
Most such research is "black box epidemiology." Researchers have not overcome
the many conceptual and technical problems of research into ethnicity and
health. By emphasising the negative aspects of the health of ethnic minority
groups, research may have damaged their social standing and deflected attention
from their health priorities. Unless researchers recognise the difficulties
with research into ethnicity and health and correct its weaknesses, 20th
century research in this subject may suffer the same ignominious fate as that
of race science in the 19th century.
4
of 57
TI: Screening and the new genetics Eletter!
AU: Cooper-JD; Franks-AJ
SO: J-Public-Health-Med. 1997 Mar; 19(1): 121
____ this source is not Available in S.J.M.C.Library
LA: ENGLISH
5 of 57
TI: EEpidemiology and public heal th—useful tool or a problem?!
AU: Nordhagen-R; Forde--R
AD: Avdeling for samfunnsmedisin , Statens institutt for folkehelse, Oslo.
SO: Tidsskr-Nor—Laegeforen, 1997May 10; 117(12): 1799-803
____ this source is not Available in S■J.M■0.Library
LA: NORWEGIAN; NON-ENGLISH
6 of 57
TI : Preparing physicians for practice in managed care environments.
AU: Lurie-N
AD: University of Minnesota Schools of Medicine and Public Heal th. Minneapolis,
USA. Iurie001@ma.rbon . tc . umn . edu
SO: Acad-Med. 1996 Oct; 71(10): 1044-9
This source is Available in S.J.M.C Library
LA: ENGLISH
AB: The author first describes the evolution and characteristics of managed
care and its emphasis on the care of populations as well as individuals. She
then reviews managed care's implications for medical education; for example,
managed care physicians must know non-office-based approaches to keeping their
patients healthy. She identifies and defines eight domains of knowledge in
which physicians must be competent for practice in environments dominated by
managed care. These are epidemiologic thinking, human behavior, organizational
behavior, information systems, quality measurement and improvement, health
system financing and delivery, ethics, and systems based care. Teaching
students to practicein managed care environments is a challenge partly because
there are few role models of the new breed of physician among medical school
faculties. The author suggests strategies and attitudes to remedy this
situation (for example, faculty must understand that, managed care is not
homogeneous and that it is not all bad; medical schools should develop "master
teachers” for the rest of the faculty; and interactive CD-ROM-driven
problem-based learning sets could be used). Focusing on training faculty for
the new era and on emphasizing the eight knowledge better physicians, whether
they practice inside or outside managed care.
7 of 57
TIs Law and medicine.
AU: Gostin-LO
AD: Georgetown/Johns Hopkins University Program on Law and Public Health.
Washington, DC, USA.
SD: JAMA. 1997 Jun IB; 277(23): 1866-7
____ This source is Available in S.J.M.C Library
___ Call Number: From: 1918+
LA: ENGLISH
8 of 57
TI: Ethical and legal issues associated with substance abuse by pregnant and
parenting women.
AU: Garcia-S
AD: University of South Florida, Tampa 33620, USA.
SQ: J-Fsychoactive-Drugs. 1997 Jan-Mar; 29(1): 101-11
____ this source is not Available in S.J.M.C.Library
LA: ENGLISH
AB: The many pressing medical, psychological, legal, and ethical problems
associated with substance abuse by pregnant and parenting women present
daunting challenges. One approach is to adopt a legal perspective where the
rights of mothers, fetuses, and children are pitted against one another in
courtrooms and state legislatures. Another approach is to embrace a public
heal th perspective, characterized by treating pregnant and postpartum substance
abusers, protecting at-risk fetuses and children, and strengthening broken
families. Both ethical concepts and legal tenets must be considered to develop
new paradigms designed to help at-risk mothers and children and to protect the
rights claimed by all involved.
9 of 57
TI: Alcohol, the individual and society: what history teaches us.
AU: Room-R
AD: Addiction Research Foundation, Toronto, Canada.
SO: Addiction. 1997 Mar; 92'Suppl 1: S7-11
____ this source is not Available in S.J.M.C.Library
LA: ENGLISH
AB: Drinkers derive both pleasure and pain from drinking, but harm may come
also to others. Through religious or secular rules, societies have sought to
limit these "externalities" of drinking. Societal reactions have primarily
focused on social harms from drinking; policy attention to casualties and
chronic health effects is fairly recent. Drinking behaviour varies greatly
according to the cultural framing of alcohol; societal policies tend to vary
accordingly. Ecological constraints and social norms on preparation and use
meant that alcohol was often available only sporadica1ly in tribal and village
societies. Alcohol production has been increasingly industrialized and
marketing increasingly globalized in the modern era. Now, free trade agreements
and the doctrine of consumer sovereignty increasingly limit the scope of
national alcohol control policies. On the other hand, modern society demands
exacting standards of attention and care incompatible with intoxication, for
instance when driving a car or minding children. Managing the conflict between
these and alcohol's ready availability is seen as a wholly individual rather
than a societal responsibility. Those who fail the task are defined as
alcoholics, and modern states have increasingly provided treatment for them.
While there is a renewed public health concern about the externalities of
drinking, substantial availability reductions have historically often required
the mobilization of strong popular movements of remoralization.
10 of
3
TI: Confidentiality versus disclosure of a patient's infectious status.
AU: Nicol-TE
SO: Sen-Dent. 1997 Jan-Feb; 45(1): 78-80
____ this source is not Available in S.J.M.C.Library
LA: ENGLISH
AB: Patients in health care settings have a legal and moral right to privacy,
which includes confidentiality of all information related to the patient or
gathered by the patient's health care team. Even so, the right to privacy is
not total. Under certain circumstances, that right must yield to a state's
fundamental right to enact laws to promote public health and to ensure public
safety and welfare. Justifiably, dental health care team members are concerned
with their health and with the possibility of being infected by a fatal disease
such as acquired immunodeficiency syndrome (AIDS). The right to know patients'
infectious status is growing with the mortality rate of the disease. However,
as more health care workers learn of a patient's infectious status, that
patient's privacy diminishes. Abiding by laws that enforce doctor-patient
confidentiality while still fulfilling their obligations to their staffs and
related third parties often proves difficult for dentists and physicians. Since
the discovery of AIDS, believed to be caused by the human immunodeficiency
virus (HIV), health care providers have been increasingly conscientious in
maintaining these professional relationships.
11 of 57
TI: Domestic violence identification and referral.
AU: Gibson-Howel1-JC
AD: Department of Periodontics, West Virginia University School of Dentistry,
Morgantown, USA.
SO: J-Dent-Hyg. 1996 Mar-Apr; 70(2)": 74-9
____ this source is not Available in S.J.M.C.Library
LA: ENGLISH
AB: This report reviews the dental, medical, nursing, and public heal th
literature concerning domestic violence prevalence, morbidity, mortality,
education, and legislation. The primary goal of this, report is to increase
awareness of the signs of suspected domestic violence and the importance of
being involved in prevention and early intervention. A second goal of this
report is to increase awareness of domestic violence and to encourage the
dental hygiene community to investigate methods to intervene and prevent this
increasing problem. For dental hygienists, the commitment to learn and to help
others should drive the initiative to address this concern for the well being
of society. Due to the nature of domestic violence and our tendency to avoid
involvement in the personal lives of others, this issue may be difficult for
some people to encounter. It is through professional and continuing education
that we strive to be better informed and equipped to venture effectively into
this arena. Lastly, we are obligated to adhere to the commitment of the Dental
Hygiene Code of Ethics by promoting public public health and safety for all in
the community, the nation, and the world.
12 of 57
TI: Commentary: don't forget the plumber: research in remote Aboriginal
communities [comment)
AU: Miller-P; Rainow-S
AD: Nganampa Health Council, Alice Springs, NT.
SO: Aust-N-Z-J-Public-Health. 1997 Feb; 21(1): 96-7
this source is not Available in S.J.M.C.Library
LA: ENGLISH
13 of 57
TI: Hepatitis C and policy implementation: ethics as a dialogic process for
resource allocation [editorial)
AU: Hepworth-J; Krug—G
SO: Aust-N-Z—J-Public-Health. 1997 Feb; 2.1(1): 4-7
____ this source is not Available in S.J.M.C.Library
LA: ENGLISH
14 of 57
TI: [Genetics and society: ethic and legal implications!
AU: Mattei-JF; Rauch-C
AD: Departement de genetique medicale, Hopital d'Enfants de la Timone,
Marsellie.
SO: Rev-Prat. 1997 Jan 15; 47(2): 182-6
____ this source is not Available in S.J.M.C.Library
LA: FRENCH; NON-ENGLISH
AB: Medical genetics, recently individualised as a full medical specialty,
evidences new problems issued from its natural and historical developments.
Genetics counselling, prenatal and predictive diagnosis may be considered as a
real progress when applied in the strictly medical and individual fields. When
extended to the whole community to answer collective choices, these
technologies can turn into eugenic and standardizing practices. Regarding the
public health and the economic necessity it could be inviting to overpass the
essential values on which are founded our humanity. In that context laws are
required to defend the best use for human being several practices, but only
after an ethical debate in which everyone should participate.
15 of 57
TI: Ethical decision making for children.
AU: Savage-TA
AD: Department of Public Health, Mental Health, and Administrative Nursing,
University of Illinois at Chicago College of Nursing, Illinois, USA.
SO: Crit-Care-Nurs-Clin-North-Am. 1997 Mar; 9(1): 97-105
____ this source is not Available in S„J.M.C.Library
LA: ENGLISH
16 of 57
TI: Positive toxicology screening in newborns: ethical issues in the decision
to legally intervene.
AU: Burns-DL
AD: George Mason University, College of Nursing and Health Science, Fairfax,
VA, USA.
SO: Pediatr-Nurs. 1997 Jan-Feb; 23(1): 73-5; discussion 76-8, 86
____this source is not Available in S.J.M.C.Library
LA: ENGLISH
AB: Perinatal substance abuse causes a host of problems including physical and
psychological impairments to a developing fetus. However, responding to the
needs of pregnant women who use drugs and their children poses an additional
challenge in this already deplorable situation. Foster care, adoption,
criminalization, and reunification are all possibilities as intervention
options in this dilemma. Each of these options prompts additional problems for
mother, child, and provider. What was once uncommon or uncontroversial for
pubIic health nursing is now bringing a new wave of discussions in the health
system and nurses need to be cognizant of the ramifications of delivering care
to perinatal substance abusing mothers and their families. Assessment, .
planning, intervention, and evaluation—the nursing process—emerges as an
invaluable tool.
17 of 57
TI: Communication with the cancer patient in China.
AU: Li-S; Chou-JL
AD: Shanghai Cancer Institute, China.
SO: Ann-N-Y-Acad-Sci. 1997 Feb 20; 809: 243-8
____This source is Available only few issues in S.J.M.C. Library
Call Number: From: 1946-1980
LA: ENGLISH
18 of 57
TI: CManagement of prenatal diagnosis of trisomy 21 for women with increased
risk. An approach of public heal thJ
AU: Manuel-C; Auquier—P; Devictor—B; Simeoni-MC
AD: Laboratoire de Sante publique, Faculte de Medecine, Marseille.
SO: Presse-Med. 1997 Mar 15; 26(8): 373-7
____ this source is not Available in S.J.M■0.Library
LA: FRENCH; NON-ENGLISH
19
of 57
TI: The health of prisoners and the two faces of Benthamism.
AU: Wiener-MJ
SO: Clio-Med. 1995; 34; 44-58
____ this source is not Available in S,J■M■C.Library
LA: ENGLISH
20 of 57
TI: Conflicts of interest: conceptual and normative issues [see comments!
AU: Pritchard-MS
AD: Center for the Study of Ethics in Society, Western Michigan University,
Kalamazoo 49008-3899, USA. pritchardSwmich.edu
SO: Acad-Med. 1996 Dec; 71(12): 1305-13
___ This source is Available in S.J.M.C Library
LA: ENGLISH
AB: Growing university-industry ties, particularly in biomedical areas,
naturally raise concerns about conflicts of interest. Such conflicts are
essentially problems in business and professional ethics. As of the fall of
1995, all institutions seeking funding from either the Public Health Service or
the National Science Foundation have been required to maintain and enforce a
written policy on conflicts of interest. The PHS and the NSF also require the
disclosure of "significant" financial interests that might affect the research.
Although the PHS and NSF requirements may prove helpful, they are not
sufficient for monitoring the full range of serious conflicts of interest that
can arise in university-industry relations. The PHS and the NSF are basically
concerned with potential bias in the design, conduct, and reporting of
research. Their disclosure requirements are restricted to financial
considerations of $10,000 or more. However, bias in research can result, from
conflicts of interest when much less is at stake financially. Furthermore, it
can arise at both individual and institutional levels. This article attempts to
provide a conceptual and normative analysis of conflicts of interest that
better enables us to understand the subtleties that can be involved. This
article is one of three in this issue of Academic Medicine that deal with
issues of conflict of interest in university-industry research relationships.
These articles are discussed in an overview that precedes them.
21 of 57
TI: Ethics issues in academic-industry relationships in the life sciences: the
continuing debate [see comments!
AU: Blumenthal-D
AD: Harvard Medical School, Boston, Massachusetts, USA.
SO: Acad-Med. 1996 Dec; 71(12): 129.1-6
____This source is Available in S.J.M.C Library
LA: ENGLISH
AB: The author reviews in detail the status of academic-industry relationships
(AIRs) in the life sciences from both ethical and empirical perspectives, and
identifies ethical issues that have been resolved and those that must still be
debated. He summarizes by stating that ethical reasoning militates against the
involvement of scientists and universities in those AIRs in which a financial
conflict of interest on the part of life science investigators may affect the
welfare of human subjects and trainees. Even in other types of AIRs, conflicts
6
of interest have effects on professional decision making that could damage the
integrity and productivity of life sciences research, especial ly"'sc'ien'fists'
withholding of data and their redirecting of research in more commercial^ "
directions. These effects could also help undermine -public trust in and suppor
of-university researchers. Balanced against these worrisome effect’s are the—
benefits of AIRs in increasing some investigators' creativity and productivity
in encouraging technology transfer, and thus in promoting economic growth and
public health■ He concludes that more research is needed on the harms and
benefits of AIRs, especially the development of better data on the effects of
withholding data, and also on the economic and health benefits of AIRs and
public attitudes toward issues of. scientific research that involve possible
conflicts of interest. More information on these questions would allow
policymakers to make more realistic estimates of the gains and losses
associated with AIRs. In the meantime, current information suggests that in
general the conflicts of interest created by AIRs are real, consequential, but
tolerable if managed carefully. Until more is known about the effects of AIRs,
it is prudent for universities and faculty to participate at modest levels in
such relationships and to monitor them carefully. This article is one of three
in this issue of Academic Medicine that deal with issues of conflict of
interest in university—industry research relationships. These articles are
discussed in an overview that precedes them.
22 of 57
TI: [Healthy life style. Perspectives of prevention in modern society!
AU: Raspe-H
AD: Institut fur Sozialmedizin, Medizinische Universitat zu Lubeck.
SO: Z—Arztl-Fortbild—Jena. 1997 Jan; 90(8): 741-6
____ this source is not Available in S.J.M■C■Library
LA: GERMAN; NON-ENGLISH
AB: Clinical prevention is defined as the application of all individual
practice contacts of patients and physicians during the screening after risky
habits or living conditions for the following specific consultation (i.e.,
aiming for "free of tobacco") and/or induction of specific interventions (i.e.
medical check-up, health examination, immunization)» Al 1 data available up to
now are demonstrating that the theoretically accessible options for clinical
prevention are realized merely imperfectly by physicians and/or are hardly
accepted by the patients. This may be due to the restricted perception and
clarification of three problem areas; they are separately discussed: 1. The
clinical prevention is also part of a comprehensive "prevention politic" and
needs adequate general conditions. I.e., it is generally unclear, who is
supposed to take care of the health promotion and prevention: the government
with its pu b1i c heal th services, the health insurances, the society of panel
physicians? 2. Clinical prevention is more distant to a strict outcome
orientation than other medical areas. There is a lack of a firm proof of its
individual, epidemiological, cultural, and economical effects - namely the
positive and negative ones. 3. (Clinical) prevention is especially exposed to
ethical tensions. The protection of the patient's (or the client's) autonomy
plays a particular role. If it~is possible 1. to reduce the fear of physicians
and patients for the political implications of clinical and medical prevention
more than in the past, 2. to work out and distribute convincing empirical
proofs of the desired (and undesired) effects of prevention, and 3. to discuss
'the--ethical tensions typical of prevention as well as to reduce them in each
single case, the program of clinical prevention would have a real chance in
Germany. Otherwise it has to be feared that there will only be "Medical
Prevention Weeks".
23 of 57
TI: [Public health surveillance: historical origin, methods, and assessment!
AU: Declich-S; Carter—AO
AD: Laboratorio di Epidemiologia e Biostatistica, Istituto Superiors di Sanita
Roma.
SO: Ann-Ist-Super-Sanita. 1996; 32(3): 317-37
____ this source is not Available in S.J.M.C.Library
LA: ITALIAN; NON-ENGLISH
AB: In the last three decades disease surveillance has grown into a complete
discipline, quite distinct -From epidemiology. This expansion into a separate
scientific area within public heal th has not been accompanied by parallel
growth in the literature about its principles and methods. The development of
the fundamental concepts of surveillance systems provides a basis on which to
build a better understanding of the subject. In addition, the concepts have
practical value as they can be used in designing new systems as well as
understanding or evaluating currently operating systems. This article reviews
the principles of surveillance, beginning with an historical survey of the
roots and evolution of surveillance, and discusses the goals of the public
health survei1 lance. Methods for data collection, data analysis,
interpretation, and dissemination are then presented, together with proposed
procedures for evaluating and improving a surveillance system. Finally, some
points to be considered in establishing a new surveillance system are
presented.
24 of 57
TI; "Socialized medicine," resource allocation and two-tiered health care—the
Danish experience.
AU: Holm-S
AD: Department of Medical Philosophy and Clinical Theory, Faculty of Health
Sciences, University of Copenhagen, Denmark.
SO: J-Med-Philos. 1995 Dec; 20(6); 631-7
____ this source is not Available in S■J.M.C.Library
LA: ENGLISH
AB: This paper describes the present resource allocation. problems in the Danish
tax-based public health care system and' presents an analysis of the two policy
options put forward as a solution to these problems: (1) explicit rationing of
services, and (2) the introduction of two-tiered health care. It is argued-that
a two-tiered system with a private second tier is unlikely to be acceptable and
viable in Denmark, whereas an introduction of a'secofTd'_t'ieij—w±thrn~the public
system may be more acceptable. It is further argued that present implicit
rationing-methods-may be unethical and ought to be replaced by explicit
rationing.
25 of 57
TI: Confidentiality and the AMA's new code of ethics: an imprudent formulation?
Cletterl
AU: Komesaroff-PA
SO: Med-J-Aust. 1997 Feb 17; 166(4): 221
___ This source is Available in S.J.M.C Library
___ Call Number: From: 1966+
LA: ENGLISH
26 of 57
I: The two cultures and the health care revolution. Commerce and
professionalism in medical care [see comments]
AU: McArthur—JH; Moore-FD
AD: Harvard Business School, Boston, MA, USA.
SO: JAMA. 1997 Mar 26; 277(12): 985-9
____This source is Available in S.J.M.C Library
___ Call Number: From: 1918 +
LA: ENGLISH
AB: The current trend toward the invasion of commerce into medical care, an
arena formerly under the exclusive purview of physicians, is seen by the
authors as an epic clash of cultures between commercial and professional
traditions in the United States. Both have contributed to US society for
centuries; both have much to offer in strengthening medical care and reducing
8
costs. At the same time, this invasion by commercialism of an arena formerly
governed by professionalism poses severe hazards to the. care of the sick and
the welfare of communities: the health of the public and the publicHeaFth.
Some of these hazards are briefly listed and reviewed, together with a brief
outline of standards that might be established nationaliy~to abate these
hazards. A national agency in the private sector is proposed, the National
Council on Medical Care, to set standards and provide an approval, mechanism
that would then be the basis for state enforcement through"1icensing. Two*
models for such an initiative are outlined, one based on the National Academy
of Sciences as the initiating force, and the other on an initiative provided by
a consortium of national charitable foundations interested in health policy. In
both cases, wide support from the national foundations would be essential. In
the case of the academy model, some government funds might also be available
without loss of the freedom of a private—sector initiative. Some operational
options for such a national council, its membership, and the conduct of its
affairs are briefly outlined as a basis for further discussion.
TI: Not just for breakfast anymore [news]
AU: Hanson-MJ
SO: Hastings-Cent-Rep. 1997 Jan-Feb; 27(1): 49
____ this source is not Available in S.J.M.C.Library
LA: ENGLISH
28 of 57
TI: QALYS and ethics: a health economist's perspective.
AU: Williams-A
AD: Centre for Health Economics, University of York, UK.
SO: Soc-Sci-Med. 1996 Dec; 43(12): 1795-804
____ this source is not Available in S.J.M.C.Library
LA: ENGLISH
AB: Objectors on ethical grounds to the use of GlALYs in priority-setting in
public health care systems are here categorised as (1) those who reject all
collective priority-setting as unethical; (2) those who accept the need for
collective priority-setting but believe that it is contrary to medical ethics;
(3) those who accept the need for collective priority-setting and do not
believe that it is contrary to medical ethics, but. reject the role of QALYs in
it on other ethical grounds; and (4) those who accept the need for collective
priority-setting in principle, but are unwilling to specify how it should be
done in practice. It is argued that the first two groups of objectors are
simply wrong, if distributive justice is a proper ethical concern in this
context. The third group is of more interest, as this group appears to believe
that QALYs are unethical because it is unethical to regard QALY maximisation as
the sole objective of the health care system. This paper argues that QALYs are
relevant to a much wider range of objectives than QALY maximisation, and that
they can accommodate a wide variety of health dimensions and sources of
valuation. They can also accommodate the differential weighting of benefits
according to who gets them, so they do not commit their users to any particular
notion of distributive justice. What they do commit their users to is the
notion that the health..p.f . people is a central concept in priority-setting, and
that it is desira*ble, for reasons of accountability, to have the bases for such
priority-setting made as precise and.explicit as .possible. The fourth group of
objectors-needs to acknowledge that there is no perfect’system on offer, and
since priority—setting does and will proceed willy-nilly we cannot wait until
there is. It would be more constructive to set up the desiderata that a
priority-setting system should ideally fulfil, and then appraise all feasible
alternatives (including the status quo) even-handedly by those criteria. None
will be perfect, but. this author predicts that QALYs would emerge from such an
appraisal with a significant role to play.
29 of 57
TI: The consequences of knowing: ethical and legal liabilities in illicit drug
research.
AU: Fitzgerald-J; Hamilton-M
AD: Department of Public Heal th ?< Community Medicine, University of Melbourne,
Parkville, Australia.
SO: Soc-Sci-Med. 1996 Dec; 43(11): 1591-600
____ this source is not Available in S.J,M.C■Library
LA: ENGLISH
AB: Ethnographic research into illicit drug use necessarily involves the
researcher being aware of illegal activities. Information about illegal
activities is obtained through the establishment of confidential relationships
with research participants; however there are legal and ethical obligations on
researchers to breach confidential relationships formed in the research
environment. The recent suspension of a research project by an Institutional
Ethics Committee serves to illustrate some of the processes that form the
research process, shape the boundaries to legitimate knowledge and some of the
consequences of knowing about illegal activities.
30 of 57
TI: EEthical issues in public health activity with special emphasis on
nonclinical biomedical study!
AU: Inaba-Y
SO: Nippon—Koshu-Eisei-Zasshi'. 1996 Oct; 43(10): 879-81
____ this source is not Available in S.J.M.C.Library
LA: JAPANESE; NON-ENGLISH
31
of 57
32
of 57
Public confidence in public hea1 th research ethics [comment!
Mariner—WK
Boston University Schools of Public Heal th and Medicine, MA, USA.
Public-Health-Rep. 1997 Jan-Feb; 112(1): 33-6
This source is Available only few issues in S.J.M.C. Library
Call Number: From:1949-1984
LA: ENGLISH
TI:
AU:
AD:
SO:
TI: Ethical awareness in practice.
AU: MacPhail-S
AD: Bioethics Centre, University of Alberta.
SO: AARN-News—Lett .• 1996 Dec; 52(11): 8
____ this source is not Available in S.J.M.C.Library
LA: ENGLISH
33 of 57
TI: ECurrent legislation in public heal th—an example for post-modern social
ethics?!
AU: Rothfuss-J; Adam-H
AD: Abteilung fur Innere Medizin, Medizinische Hochschule Hannover.
SO: Gesundheitswesen . 1996 Oct; 58(10): 505-9
____ this source is not Available in S.J.M.C.Library
LA: GERMAN; NON-ENGLISH
AB: Social ethics of affirmative postmodernists are discussed in relation to
recent German health care legislation. It could be shown that: 1. the health
care legislation 1989 and 1993 only partially fulfills the postmodern cal 1 for
“cultivation of individual responsibility". 2. both laws largely fail to
enforce the principle' of"subsidiarity, and 3. postmodernist thinking is weak on
the—question" of “globa 1 strategies-but strong In the area of individualism and
subjectivity. We conclude that postmodern social ethics are useful to
compensate areas largely neglected by recent German health care legislation,
rather than that the legislation is an example of postmodern social ethics.
IO
34 of 57
TI: Standards of care and ethical concerns in genetic testing and screening.
AU: Parker-LS; Majeske-RA
AD: Department of Human Genetics, University of Pittsburgh, Graduate School of
Public Heal th, PA 15261, USA.
SO: Clin-Obstet-Gynecol . 1996 Dec; 39(4): 873-84
This source is Available in S.J.M.C Library
___ Call Number: From: 1959+
LA: ENGLISH
35 of 57
TI: From genes to public health: the applications of genetic technology in
disease prevention. Genetics Working Group [see comments!
AU: Khoury-MJ
AD: Birth Defects and Genetics Diseases Branch, Centers for Disease Control and
Prevention, Atlanta, GA 30341-3724, USA.
SO: Am-J-F'ubliC-Heaith. 1996 Dec; 86(12): 1717-22
___ This source is Available only few issues in S.J.M.C. Library
___ Call Number: From; 1942-1991
LA: ENGLISH
AB; OBJECTIVES: With advances in the Human Genome Project, the implications of
genetic technology in disease prevention should be assessed. METHODS: The
paradigm suggested in The Future of Public Health—assessment, policy
development, and assurance—was used to examine the continuum from genetic
technology to public hea1 th practice. RESULTS: First, important public hea1 th
functions are to (1) assess the impact of genes and their interactions with
modifiable disease risk factors on the health status of the population and (2)
assess the impact and safety of genetic testing on the population. Second,
given the many implications of genetic testing, the public health community
should participate in policy development related to the timing and use of
genetic testing in disease prevention. Third, whenever appropriate, the public
health community needs to ensure the development of public health genetics
programs (e.g. newborn screening) and evaluate the quality and effectiveness of
the use of genetic testing in disease prevention. CONCLUSIONS: Although most
current genetic tests are not ready for disease prevention, there is an
important role for the public health community in translating genetic
technology into disease prevention.
36
TI: CDC's first 50 years: lessons learned and relearned.
AU: Satcher-D
AD: Centers for Disease Control and Prevention, Atlanta, GA 30333, USA.
SO: Am-J-Public-Health. 1996 Dec; 86(12): 1705-8
____This source is Available only few issues in S.J.M.C. Library
Call Number: From: 1942-1991
LA: ENGLISH
of 57
.
37 of 57
TI: Testing for human immunodeficiency virus infection among tuberculosis
patients in Los Angeles.
AU: Asch-SM; London-AS; Barnes-PF; Gelberg-L
AD: Division of General Internal Medicine, Pacific Center for Health Policy and
Ethics, University of Southern California School of Medicine, Los Angeles, USA.
SO: Am-J-Respir-Crit-Care-Med. 1997 Jan; 155(1): 378-81
____this source is not Available in S.J,M.C.Library
LA: ENGLISH
AB: To investigate patterns of testing for human immunodeficiency virus (HIV)
infection in tuberculosis patients, we obtained data from the tuberculosis
registry and from medical records of 500 tuberculosis patients in Los Angeles
County. Sixty-three percent of tuberculosis patients were tested for HIV
infection, and multivariate logistic regression analysis revealed that the
II
likelihood of testingwas .significantly higher among males, persons between_20
afig~45"yr old/ individuals with_ HJV .risk _fac.tors, and patients treated by
publ ic heal th care providers, A minimum of 12% of the total samplej 77. of
females, 27. of ■ those outside the ages of 20 to 49, 7% of patients without.
recorded HIV risk factors, and 17% of patients treated by private practitioners
were infected with HIV. These results suggest that health care providers,
fparticularly private practitioners, do not follow national recommendations for
urilversal HIV testing,of tuberculosis patients.. Instead, HIV testing “is
*—preferentially performed on patients perceived to be at high risk for HIV
infection. Because HIV seroprevalence is at least 2 to 77. in "low-risk" groups,
failure to test these patients may result in significant missed opportunities
for diagnosis and treatment of HIV coinfection.
38 of 57
TI : Preparation and applications of the International Aquatic Animal Health
Code and Diagnostic Manual for Aquatic Animal Diseases of the Office
International des Epizooties.
AU; Hastein-T
AD: Department of Fish Health, Central Veterinary Laboratory, Oslo, Norway.
SO: Rev—Sci-Tech. 1996 Jun; 15(2): 723-31
____ this source is not Available in S.J.M.C.Library
LA: ENGLISH
AB: The Office International des Epizooties (DIE) has recently prepared an
International Aquatic Animal Health Code, based on the principles set out in
the corresponding DIE International Animal Health Code for terrestrial animals.
The principal aim of the Code and the companion Diagnostic Manual for Aquatic
Animal Diseases is to harmonise health guarantees for international trade in
aquatic animals (fish, molluscs, crustaceans) and aquatic animal products, and
to guide state Veterinary Services and/or other competent authorities in the
preparation of appropriate health certificates. The Aquatic Animal Health Code
and Manual provide detailed information on definitions, notifications, ethics
in connection with certification, import risk analysis and import/export
procedures. By these means, the preparation of international health
certificates can be based on a uniform approach to health control in.aquatic
animal populations, using the standardised methods described in the Diagnostic
Manual. In general, health certification under the Aquatic Animal Health Code
is required only for diseases notifiable to the DIE. In addition to such
notifiable diseases, however, the Code establishes a list of other significant
diseases which need consideration. The? listed diseases are recognised as
serious transmissible diseases of socio-economic and/or public health
importance, in relation to which the international trade of aquatic animals
and their products poses a significant risk of transfer between countries. The
current status of the Code and Manual is described in detail.
39 of 57
TI: Health as a fundamental human right.
AU: Hobdell-MH
AD: Faculty of Dentistry, University of the Western Cape, Cape Town, South
Africa.
SO: Br-Dent-J. 1996 Apr 6; 180(7): 267-70
____This source is Available only few issues in S.J.M.C. Library
___ Call Number: Frcm; 1961-1971
LA: ENGLISH
AB: Access to health care is problematic for many people throughout the world,
and the environments in which they live are often detrimental to their health.
Recognising health as a human right provides a platform from which to argue for
strong public health programmes.
40 of 57
TI: Ethical problems in the relationship between health and work.
AU: Berlinguer-G; Falzi-G; Figa-Talamanca-I
SO: Int-J-Health-Gerv. 1996; 26(1): 147-71
____ this source is not Available in S.J.M.C.Library
LA: ENGLISH
AB: Throughout history, the relationship between employers and workers has been
subject to the equilibrium of power, to legislative norms, to ethical
considerations, and more recently to scientific knowledge. The authors examine
the ethical conflicts that arise from the application of scientific knowledge
to preventive health policies in the workplace. In particular, they discuss the
ethical conflicts in the application of screening practices, in the setting of
"allowable limits" of harmful work exposures, and in the right of workers to be
informed about work hazards. Ethical problems are also created by.conflicting
interests in the protection of the environment, the health of the general
public, and the health of the working population, and by conflicting interests
among workers, and even within the individual worker, as in the case of "fetal
protection" policies. The authors emphasize the positive use of scientific
information and respect for human dignity in resolving these conflicts.
41 of 57
TI: Informed consent in human experimentation before the Nuremberg code.
AU: Vollmann-J; Winau-R
AD: Institute of the History of Medicine, Free University of Berlin.
SO: BMJ. 1996 Dec 7; 313(7070): 1445-9
____This source is Available in S.J.M.C Library
____Call Number: From 1914+
LA: ENGLISH
AB: The issue of ethics with respect to medical experimentation in Germany
during the 1930s and 1940s was crucial at the Nuremberg trials and related
trials of doctors and public heal th officials. Those involved in horrible
crimes attempted to excuse themselves by arguing that there were no explicit
rules governing medical research on human beings in Germany during the period
and that research practices in Germany were not different from those in allied
countries. In this context the Nuremberg code of 1947 is generally regarded as
the first document to set out ethical regulations in human experimentation
based on informed consent. New research, however, indicates that ethical issues
of informed consent in guidelines for human experimentation were recognised as
early as the nineteenth century. These guidelines shed light on the still
contentious issue of when the concepts of autonomy, informed consent, and
therapeutic and non-therapeutic research first emerged. This issue assumes
renewed importance in the context of current attempts to assess liability and
responsibility for the abuse of people in various experiments conducted since
the second world war in the United States, Canada, Russia, and other nations.
42 of 57
TI: Reproductive health and blurred professional boundaries.
AU: Chavkin-W; Breitbart-V
AD: The Center for Population and Family Health, Columbia University School of
Public Health, New York, USA.
SO: Womens-Health-Issues. 1996 Mar-Apr; 6(2): S9-96
____ this source is not Available in S.J.M.C.Library
LA: ENGLISH
AB: We recognize that many of the issues raised are not simple. Our proposal
calls for the same thoughtful deliberation applied in other settings to be
brought to bear on reproductive health care. Some have already tried
alternative approaches. In Albuquerque, New Mexico, a university hospital
neonatologist and the district attorney have collaborated to create an
alternative to sentencing program for women who are arrested for drug-related
crimes and found to be both pregnant and drug addicted. Rather than proceed
with criminal sanctions, these women are offered entry into a drug treatment
program that is geared to families with young children and run by the
pediatrics department. Here, the physician and the district attorney
collaboratively responded in ways congruent with the professional integrity of
13
each. In another example in Portland, Oregon, physicians, drug treatment
providers, and child protective social service representatives cooperatively
defeated a legislative proposal to mandatorily test and report pregnant women
for illicit drug use and, instead, formed a task force to jointly develop state
policy regarding the issue. Drug use, HIV infection, child abuse, and poverty
are all cause for alarm. Yet it is critical that cur frustration about these
difficult problems not be translated into blaming individuals for "deviance,"
or into short-term inadequate responses. In developing policy we should
consider the impact on the legal and ethical rights and obligations of both
patient and physician. For every course, we should evaluate both immediate and
long-term efficacy, the consequences for the doctor—patient relationship, and
the consequences for medical integrity. In the midst of the present regulatory
and fiscal turmoil affecting health care, we urge physicians to be careful and
deliberate in the policies they embrace and the actions they take.
43 of 57
TI: The public hea1 th basis of cancer screening: principles and ethical
aspects.
AU: Miller-AB
AD: Department of Preventive Medicine and Biostatistics, University of Toronto,
Ontario, Canada.
SO: Cancer-Treat-Res. 1996; 86: 1-7
____ this source is not Available in S.J.M.C.Library
LA: ENGLISH
44 of 57
TI: An ethicist's commentary on the case of the veterinarian who will not
utilize the proper regimen for control of roundworms.
AU: Rollin-BE
SO: Can-Vet-J. 1996 Oct; 37(10); 585-6
____ this source is not Available in S.J.M.C.Library
LA: ENGLISH
45 of 57
TI: Model curricula in public health ethics.
AU: Coughlin-SS
AD: Department of Biostaristics and Epidemiology, Tulane University School of
Public Health and Tropical Medicine, New Orleans, Louisiana 70112, USA.
SO: Am-J-Prev-Med, 1996 Jul-Aug; 12(4): 247-51
____ this source is not Available in S.J.M■C.Library
LA: ENGLISH
46 of 57
TI: Remember Tuskegee: public hea1 th student knowledge of the ethical
significance of the Tuskegee Syphilis Study.
AU: Coughlin-SS; Etheredge-GD; Metayer-C; Martin-SA Jr
AD: Department of Biostatistics and Epidemiology, Tulane University School of
Publ ic Heal th, New Orleans, Louisiana,, USA.
SO: Am-J-Prev-Med. 1996 Jul-Aug; 12(4): 242-6
____ this source is not Available in S.J.M.C.Library
LA: ENGLISH
AB: The ethical problems that surrounded the Tuskegee Syphilis Study prompted
widespread public criticism when they first surfaced in 1972; the Tuskegee
Study remains an important case in bioethics. We recently examined public
health student knowledge of the ethical significance of the Tuskegee Study as
part of an ethics curriculum needs assessment at Tulane University. A brief
questionnaire was administered to 236 graduate students currently enrolled in
seven epidemiology courses. Basic demographic information was obtained along
with information about degree program. A series of questions was then asked to
assess student knowledge of bioethics including the ethical significance of the
Tuskegee Study. Only 197. (46 of 236) of the students demonstrated knowledge of
the ethical significance of the Tuskegee Study. Knowledge of the Tuskegee
Study's ethical significance was higher among students who were from the United
States and those who were enrolled in the epidemiology program (P < .05). The
ethical problems that surrounded the Tuskegee Study have rarely been
encountered in public hea1 th. However, this important case stands as an
exemplar of the potential for ethical abuses in human subjects research. Such
cases ought to be highlighted in public health curricula. Medical Subject
Headings (MeSH): blacks, African Americans, educational curriculum,
epidemiology, ethics, public health, racism.
47 of 57
TI: Development of an ISO 9000-compatible occupational health standard—II:
defining the potential benefits and open issues.
AU: Levine-SP; Dyjack-DT
AD: Department of Environmental and Industrial Health, University of Michigan
School of Public Health, Ann Arbor 48109-2029, USA. SLIH@umich.edu
SO: Am-Ind-Hyg-Assoc-J. 1996 Apr; 57(4): 387-91
____This source is Available only few issues in S.J.M.C. Library
Call Number: From: 1970-1975
LA: ENGLISH
AB: The International Organization for Standardization (ISO) is currently
voting on a final draft of ISO 14000 Environmental Standards that follow the
general philosophy of ISO 9000 product quality standards. Should the
international community also consider development of an ISO 9000-14000
compatible occupational safety and health management standard (OS&HMS) or an
environment, safety, and health management standard? The first paper in this
series (Am. Ind. Hyg. Assoc. J. 56:599-609 C19951) introduced this subject,
reviewed the historical precedents, and identified the underlying issues. In
this paper the authors identify some of the potential benefits and most
critical open issues that may affect the viability of an OS&HMS at the national
and international levels. Twelve potential benefits are identified in the major
categories of national and international, and industrial and governmental
benefits; 16 open issues are identified in the major categories of
applications, ethics, cost, and international issues.
48 of 57
TI: Harmonization of clinical practice guidelines for the prevention and
treatment of osteoporosis and osteopenia in Europe: a difficult challenge.
AU: Reginster—JL
AD: Bone and Cartilage Metabolism Unit, University of Liege, Belgium.
SO: Calcif-Tissue—Int. 1996; 59 Suppl 1: S24-9
____ this source is not Available in S.J,M.C,Library
LA: ENGLISH
AB: Europe is a patchwork of various medical cultures and financial resources.
Variations abound with respect to financing, accessibility to public health
systems, health expenditures, drug registration and reimbursement, the
prescription of drugs, and clinical applications, as well as the perception of
osteoporosis itself. However, there are possibilities for the harmonization of
medical services among the various countries within Europe. The European Agency
for the Evaluation of Medicinal Products (EAEMP) is attending to the
centralized or decentralized procedures for the registration of drugs. The
Group for the Respect of Ethics and Excellence in Science (GREES) is
investigating guidelines for drug registration as well as gathering and making
available medical references. The European Foundation for Osteoporosis and Bone
Diseases (EFFO) is increasing awareness of the prevalence of the disease and
the need for prevention and treatment. Finally, the International Federation of
Societies on Skeletal Diseases (IFSSD) is coordinating epidemiologic, clinical,
and social research. There is a need for increased awareness of osteoporosis
throughout Europe. Health authorities are in need of cost/benefit reports
leading to the registration and reimbursement of agents. Primary care
physicians need information about osteoporosis and need to become involved in
the diagnosis and science of the disease. Awareness needs to be generated among
specialists; they need to be educated in the latest techniques for diagnosis
and treatment. Finally, the general population needs to become aware of
osteoporosis and to be encouraged to participate in the prevention and
treatment of this disease. Current screening and detection in Europe is being
done by densitometry. However, other techniques on the horizon include
ultrasound and biochemical markers. Primary prevention, i.e., maximizing peak
bone mass, includes examining the genetics of osteoporosis to determine the
high-risk population and promoting reasonable physical exercise and
dietary/life-style habits (e.g., increased calcium and avoidance of tobacco).
Secondary prevention includes the identification of high-risk groups through
risk factors, biochemical markers, and densitometry and adherence to the World
Health Organization definition of osteopenia-osteoporosis (adapted to financial
concerns by GREES guidelines). Other therapies include hormone replacement
agents (although there are risks for cancer and concerns about durability),
calcium and other inhibitors of bone resorption, physical activity, and vitamin
D prophylaxis in the elderly. Treatment of established or severe osteoporosis
includes drugs upon availability (inhibitors of bone resorption and stimulators
of bone formation), surgery, and experimental approaches.
49 of 57
TI: The American Cancer Society's National Prostate Cancer Detection Project.
AU: Littrup-PJ
AD: Department of Radiology, Wayne State University School of Medicine, HarperHospital , Detroit, Michigan, USA.
SD: Can-J-Oncol. 1994 Nov; 4 Suppl 1: 65-9
____ this source is not Available in S.J.M.C.Library
LA: ENGLISH
AB: As a significant public health problem, prostate cancer meets nearly all
the criteria for screening. While concerns about incomplete natural history,
progression rates and need for better prognostic factors are valid, important
social and public hea1 th issues also need consideration. If future expenditures
for terminal cancer care are minimized via reductions in therapy choices or
coverage, no economic benefit for prostate cancer screening should exist.
Narrowly focused attempts at cost reduction could inappropriately discourage
highest risk groups from participating in early detection programs, thereby
eliminating the greatest potential benefit of screening. The ACS--NPCDP has
demonstrated that early detection of prostate cancer produced distinct stage
migration to earlier, more curable disease through optimized use of DRE, TRUS
and PSA. PSA is the most objective test and detects tumors of significant
biologic potential. Current cost savings are possible with improved public
health education about the appropriateness of early detection in the oldest age
groups or those with significant pre-existing medical conditions. Prostate
cancer control perhaps requires a tailored approach of screening in high risk
groups and more appropriate "case finding" in the lower risk general
population. The initial combination of PSA and DRE represents an ethical and
economical choice for individual patients consulting with informed physicians.
50
of 57
51
TI: Stanton Glantz on snuffing tobacco research ^interview by Thomasine
Kushner1
AU: Glantz-S
SO: Camb-Gl-Heal the—Ethics. 1996 Summer; 5(3): 415-21
of 57
TI: Second, let no harm be done: an American antiimmigration dilemma.
AU: d'Oronzio-JC
AD: Columbia University School of Public Health, New Jersey, USA.
SO: Camb-Q-Healthc-Ethics. 1996 Summer; 5(3): 467-72
____ this source is not Available in S.J.M.C.Library
LA: ENGLISH
____ this source is not Available in S.J.M.C.Library
LA: ENGLISH
52 of 57
TI: Patient access to experimental drugs and AIDS clinical trial designs:
ethical issues.
AU: Schuklenk-U; Hogan-C
AD: Monash University Centre for Human Bioethics, Australia.
SO: Camb-Q-Healthc-Ethics. 1996 Summer; 5(3): 400-9
this source is not Available in S.J.M.C.Library
LA: ENGLISH
53 of 57
TI: Review of the 1995 Food and Drug Administration/National Institutes of
Heal th Public Forum on informed consent in clinical research conducted in
emergency circumstances.
AU: Lamiell-JM; Grabenstein-DD; Vander—Hamm-DG
AD: Clinical Investigation Regulatory Office, U.S. Army Medical Department
Center and School, Fort Sam Houston, TX 78234, USA.
SO: Mil-Med. 1995’Dec; 160(12): 599-603
this source is not Available in S.J.M.C.Library
LA: ENGLISH
AB: We describe some of the deliberations and questions raised by the recent
Food and Drug Administration/National Institutes of Health Forum on Informed
Consent in Clinical Research Conducted in Emergency Circumstances. Consent will
have to be waived in emergency medical research if such research is to be
conducted, because it is virtually impossible to obtain meaningful informed
consent in emergency circumstances. There is clearly a conflict between
research subject autonomy and society's perceived need for answers about
emergency medical care. Who will resolve this dilemma and how it will be
resolved are important questions for modern medicine.
54 of 57
TI: Ethics and public health promotion.
AU: Nilstun-T
AD: Department of Medical Ethics, Lund University, Sweden.
SO: Epidemiol-Prev. 1994 Dec; 18(61): 200-3
____ this source is not Available in S.J.M.C■Library
LA: ENGLISH
AB: As a goal, promotion of public health is .quite uncontroversial. But
attempts to modify people's lifestyles and life conditions in order to realize
this goal bring up a number of ethical conflicts. One such conflict concerns
the balance between autonomy and paternalism in the process of changing human
behaviour. In this paper a model for analysis of such conflicts is presented
and applied to assess anti-smoking policies. The model consists of two
dimensions: the first specifies the relevant ethical principles, the second
specifies the persons involved in or affected by such policies. My conclusion
is that anti-smoking policies cannot be justified by reference to the good of
the person whose right to seifdetermination is limited, but only by reference
to the need to protect others from that person, i.e. prevent them from being
exposed to tobacco smoke.
55 of 57
TI; Some ethical ground rules for BSE and other public health threats [comment!
AU: Hunt-G
SO: Nurs—Ethics. 1996 Sep; 3(3): 263-7
____ this source is not Available in S.J.M.C.Library
LA: ENGLISH
56 of
TI: Bovine spongiform encephalopathy (BSE): the ethics concerning decisions
about whether to continue taking a risk with this disease [see comments]
AU: Dealler-S
SO: Nurs-Ethics. 1996 Sep; 3(3): 259-62
____this source is not Available in S.J.M.C.Library
LA: ENGLISH
57 of 57
TI: Women's health and end-of-life decision'making [comment]
AU: Grodin-MA
AD: Law, Medicine & Ethics Program, Boston University Schools of Medicine and
Public Health, Massachusetts, USA.
SO: Womens-Hea1th-Issues. 1996 ■ Sep-Oct; 6(5): 295-301
____ this source is not Available in S.J.M.0.Library
LA: ENGLISH
PC-SPIRS 3.40
MEDLINE (R) 10/97-12/97
MEDLINE (R) 10/97-12/97 usage is subject to the terms and conditions of the
Subscription and License Agreement and the applicable Copyright and
intellectual property protection as dictated by the appropriate laws of your
country and/or by International Convention.
1 of 30
TI: Palliative medicine and HIV/AIDS.
AU: O'Neill—JF; Alexander-CS
AD: AIDS Bureau, Health Resources and Services Administration, US Public Health
Service, Rockville, Maryland 20857, LISA.
SO: Prim-Care. 1997 Sep; 24(3): 607-15
this source is not Available in S.J.M.C.Library
LA: ENGLISH
AB: This article provides an introduction to the field of palliative medicine
as it applies to the care of HIV/AIDS. Issues of pain management, end-of-life
care, ethics, and bereavement are discussed with the intention of providing the
primary care physician additional resources in the provision of care to
patients with HIV/AIDS.
2 of 30
TI: Medicine and public health, ethics and human rights.
AU: Mann-JM
SO: Hastings-Cent-Rep. 1997 May-Jun; 27(3): 6-13
this source is not Available in S.J.M.C.Library
LA: ENGLISH
AB: There is more to modern health than new scientific discoveries, the
development of new technologies, or emerging or re-emerging diseases. World
events and experiences, such as the AIDS epidemic and the humanitarian
emergencies in Bosnia and Rwanda, have made this evident by creating new
relationships among medicine, public heal th, ethics, and human rights. Each
domain has seeped into the other, making allies of public heal th and human
rights, pressing the need for an ethics of public hea1 th, and revealing the
rights-related responsibilities of physicians and other health care workers.
3 of 30
TI: Why "underpowered" trials are not necessarily-unethical .
AU: Edwards-SJ; Lilford-RJ; Braunholte-D ; Jackson-J
AD: Department of Public Heal th and Epidemiology, University of Birmingham
Medical School, UK.
SO: Lancet. 1997 Sep 13; 350(9080): 804-7
This source is Available in S.J.M.C Library
____Call Number: From: 1930+
LA: ENGLISH
4 of 30
TI: Ethics in environmental epidemiology.
AU: Rossignol-AM
AD: Department of Public Hea1 th, Oregon State University, Corvallis 97330—6406,
USA.
SO: Epidemiology. 1997 Sep; 8(5) s 599-601
____ this source is not Available in S.J■M.C.Library
LA: ENGLISH
5 of
TI: Informed consent in epidemiologic studies involving genetic markers.
AU: Hunter—D; Caporaso-N
AD: Department of Epidemiology, Harvard School of Public Health. Brigham &
Women's Hospital, Boston, MA, USA.
SO: Epidemiology. 1997 Sep; 8(5): 596-9
____ this source is not Available in S■J.M.C.Library
LA: ENGLISH
6
of 30
TI:
AU:
AD:
SO:
Good performance of vaccination by education.
F'eltola-H
Children's Hospital, University of Helsinki, Finland.
Biologicals. 1997 Jun; 25(2): 237-9
this source is not Available in S.J.M.C.Library
LA: ENGLISH
7 of 30
TI: CPublic health safety and transfusion organisation J
AU: Vachey-L
AD: 1'Agence Francaise du Sang, Paris.
SO: Bull-Acad-Natl-Med. 1997 May; 181(5): 853-61
____ this source is not Available in S.J.M.C■Library
LA: FRENCH; NON—ENGLISH
AB: The reform of French blood transfusion, launched in 1993, has established a
control system of blood transfusion public services and blood products. This
reform was implemented in accordance with Ethics regarding the use of products
of human origin; while assuring autosufficiency, it favors a sparing use of
blood products. Product safety is guaranteed firstly by the official blood
transfusion practice guidelines which provide rules for each stage of the
process, and secondly by the performance and quality controls performed prior
to transfusion (registration of products, screening tests) as well as in the
course of the process (quality control and assurance) or after transfusion
(external product control performed by the French agency for drugs "Agence du
Medicament"). The safety of products is based on a series of organisational
measures for blood . transfusion public services: local organization schemes, .
staff qualifications, computerization, implementation of an hemovigilancy
system. It is the control of the whole network which is a guarantee of the
final security for the patients transfused. Time is required to carry out such
a large scale reform, even if much progress has already been made. The level of
safety and quality reached today by French blood transfusion permits a
favorable comparison between France and the other developed countries.'
8 of 30
TI: Professional solidarity versus responsibility for the health of the public:
is a nurses' strike morally defensible?
AU: Tabak-N; Wagner—N
AD: Department of Nursing, School of Health Professions, Tel Aviv University,
Ramat Aviv, Israel.
SO: Nurs-Ethics. 1997 Jul; 4(4): 283-93
____ this source is not Available in S.J.M,0,Library
LA: ENGLISH
AB: The purpose of this article is to deliberate the moral and legal dilemma
entailed in the weapon of the labour strike as a pressure tactic on the Israeli
Finance Ministry regarding job slots, budgets and, in effect, violating the
collective agreement signed by the nurses and impairing patients' treatment, as
opposed to refraining from striking and suffering the heavy burden of work, the
lack of trained personnel, low wages, and the inability to give patients
proper, high quality treatment.
9 of 30
TI: Guidelines for managing domestic abuse when male and female partners are
patients of the same physician. The Delphi Panel and the Consulting Group.
AU: Ferris-LE; Norton-PG; Dunn-EV; Gort-EH; Degani-N
AD: Department of Public Health Sciences, Faculty of Medicine, University of
Toronto, Ontario, Canada.
- Media
 RF_MP_2_PART_2_SUDHA.pdf
RF_MP_2_PART_2_SUDHA.pdf
Position: 422 (28 views)