MEDICINE ETHICS
Item
- Title
- MEDICINE ETHICS
- extracted text
-
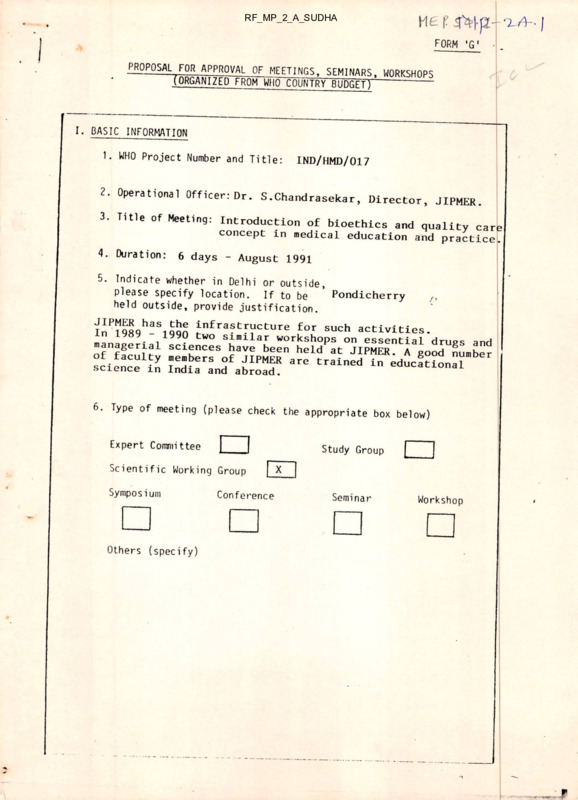
RF_MP_2_A_SUDHA
I
FORM 'G'
PROPOSAL FOR APPROVAL OF MEETINGS. SEMINARS, WORKSHOPS
(ORGANIZED FROM WHO' COUNTRY BUDGET)
~--------
I. BASIC INFORMATION
1. WHO Project Number and Title:
IND/HMD/017
2. Operational OfficerrDr. S.Chandrasekar, Director, JIPMER.
3. Title of Meeting: Introduction of bioethics and quality carl
concept in medical education and practice.
4. Duration:
6 days - August 1991
5. Indicate whether in Delhi or outside,
please specify location. If to be ’ Pondicherry
“
held outside, provide justification.
I^P19S9hTSlS5S jnfra?tF“‘:ture for such activities,
managerial sc?enc:sSL'ie"e“rteUP:t“i™™ntial “T85 S'"1
^ieS
1^
science m India and abroad.
6. Type of meeting (please check the
appropriate box below)
Expert Committee
Study Group
Scientific Working Group
Symposium
Others (specify)
-A
Conference
X
Seminar
Workshop
- 2
II. technical information
A. Justification
u\unv^^kSLOftot'’LPTposed activ,ty
undertaken in the past and tn Hp
l
? sequence of activities
the problem which the sequence of^ctivities
weting, is expected to solve; (c) iustifv whv «
type proposed ,s the nx.st .ppropria(e
St3tJ
udJng the Presort
We
for ooderpraduato^nH^ ln
a new curriculum
University ofPpond-'apUate studies in Medicine
_____
for the
we
workshop (Dec. 3-9) have
on
have already introduce^the171185
rationa]
T“
-- 1- prescribing,
We
undergraduates during thei? int0006^3 into the curriculum fpr
logical sequence to^fJlu. Lnternship training, We feel it
a
use with concept of qualitvScUP lnt5oduction of rational drilig
growing imp^rtanc^of^Jhi^. bi°ethiC3 keeping in
mind
and cost
effective cquality
is occurring and^s'
^nc^n
t
-.i the
medical
sciences that
scientific 8workit exPected to occur- in
r
next decade.
objectives 1, 2 & 3 fRefer15 expocted to dwell at length This
on
5
(Keter appendix I)
Central
th°e"dUcC“depr„fln:ernai1“’f«“^TUJ" De?e-"ber 1989
B. Specific Objectives
tPlease
i 14state
3.Vclearly
■ terms,
2
f the ProPosed nieeting, snow the
ese objectives to the programme area(s), and
identify the expected
-1 outcomes/outputs.
relevanrp nf th
See APPENDIX I
__ i
. . .3
I
3
c- Methods and Approaches to be used
(Please enclose a
copy of the tentative agenda)
See APPENDIX II
1
D.
Proposals for Evaluation and Follow-up
Please indicate: (a) the
me..,.ds of evaluation that you intend
to use during the meeting
to assess its effectiveness; (b) the
methods of evaluation you intend to i
'"'‘■""d to use in order to assess the
long-term impact of the meeting; (c) the’follow “
are .mended to be token end t’eil
d) actions that
------ /;up
(1)
cue time
frame for the
-.J ppreparation and submission of the Report.
Daily evaluation of the various sessions of the workshops.
(2)
Programme evaluation
(3)
Pre and post tests
(4) Outcome analysis is to be done f
to deans of "edxcal colleges seekUg through
li the questionnaires
ethics and quality
'care are included in the areas of bio
finding out the
ex
curricula and
*
---- extent of
f coverage.
...4
- 4
E. Participants/Invitees
(i)
Number of participants from States
(ii)
Number of participants from U.Ts.
(iii)
Number of participants from Ministry/DGHS
(Give designations)
(i v)
Other outside Invitees
16
8
Total Number
F. Technical Staff Support
Resource persons/Guest Lecturers
(Please give names and designations
with justifications)
Technical advisor
Technical staff for preparation
and duplication of course materials
Audiovisual assistants
1
2
2
y—
24
5 -
‘ill. BUDGETARY AND FINANCial
DETAILS
(i)
Total under the Project:
(IT)
For Group Educational Activities:
(iii)
Amount committed so far:
Rs.2,93,500
IV. expenditure sanction
require^ for
T.A. for
{!)
participants
(air/train/others)
(?)
Rs.
NIL
Rs.
NIL
per day for
days.
(4)
NIL
Daily allowance for outside parti. ?ants
□ t the rate of Rs.
(3)
Rs.
O.A. for local participants at the rate
of Rs- Per day for
days.
O.A. for
IQ
(no.) outstation experts
per day for
at the rate of Rs. 4QQ
10
(5)
days
Rs. 40,000
T.A. for 10
____ (no.) outstation experts
(□ir/train/others)
(6)
Rs. 2,00,000
O.A. for 14
(no.) local experts at
the rate of Rs. 200 per day for IQ dayS
Rs_2<LjOOO
(n Xrelar,ai aSS1Stance (Rs'50 Per day)
lease indicate rate of payment)
(H)
(9)
(2 persons for 30 days)
Stat.onery etc. (Please indicate articles
□nd quantity required)
lea/Coffee for
40
Rs. Wa000_
persons daily
10 days
( 10)
Rs. 3,000
Rs.2,500
Any other i tern
Rs1Q4KKL
Payment for technical assist.
Refer F p-4
TOTAL
Rs ._2x91>J0(L
Name, designation and complete address of the nffim t
I mills are to be released bv wiin
O'ficei to whom the
and account number. If any).
t’ nd,“e of the ^nk, its address
Dr. S.Chandrasekar,
J I P M E
Director>
Pondicherry 605 006
India
IM I o ■
ll? llu’
'• ''in.i | ih (.
H'.hii.ih./ri|,c.ra I lunal Or f •< ,.r
APPENDIX
I
B.
(1)
To identify <areas of
_2 ethics and quality
care that need to be
incorporated into medical
----- curricula.
(2)
To identify areas of ethics and
quality care concept
vant to various levels of health care.
(3)
(4)
(5)
rele-
To prepare 1teaching/learning modules relating to
content
areas that are found to be relevant
-- -—to medical educatic n.
To test the Iteaching/learning
—..o
modules developed on (a)
medical students and (b?
c
medical practitioners in order to test
ti'onUSehUlnuSS °f this approach and make r~
necessary modificagained.baSed On the feed back obtained and
--J the experience
To plan strategies for dissemination
of these concepts
through
educational interventions in
India and
other
developing countries.
APPENDIX
C.
II
To realise objectives 1,2 & 3.
(1) Scientific
relatino t°rKin8Jr°Up meeting to deliberate on
issues relating to bioethic:
various
---- 1 - quality
care that are of relevance to medical education and and
practice.
Tentative agenda
Day 1.
Overview of bioethics
Day 2 & 3. Selection of
priority areas for curricula
different levels of health care
Day 4,5 & 6.
(2)
for
Preparation of teaching/learning modules.
To realise objective 4.
Pilot workshops to test the
modules on the 1
and rmedical professionals
tessronals from primary, secondary
health
a care.
Workshop for medical students
Workshop for practitioners
(3)
and
and
tertiary
2 days
2 days - 3 workshops
To realise objective 5.
A 4 day workshop to j
sensitize
medical educators
issues and motivate them
2... to
to iincorporate these into on bioethical
curricula
continuing medical education
a programmes. With 3 educators and
college and 8 colleges
per
per workshop, 5 workshops would
about 40 medical
cover
-- - colleges from all over India.
Time schedule
RF. ••
August 1991
Scientific working group meet
Jan/Feb. 1992
Pilot workshops for medical
students and
practitioners.
1992-1994
(6 monthly)
Series of 5 workshops for medical
educators.
I
MODELS OF DOCTOR - PATIENT’ RELATIONSHIP
A STUDY BASED ON HOSPITAL ORGANIZATION IN INDIA
by
Akhileshwar Lal Srivastava *
Lecturer, Department of Sociology, Banaras Hindu University, ^nranasi-S
The
present
paper
deals with the
± nc
1
•
• *
tional setting and cultural matrix, in which the
doctor and the patient interact. The personality
characteristics of the doctor and expect ition
patterns of the patient provide the several
modes of doctor-patient
-------- relationship.
---------------------- Five
models of doctor-patient relationship are presen
ted in this paper
paper as
as probable
probable hypotheses
hypotheses for
for
empirical verification. In connection with his
research work the author had
— an opportunity
Ito meet doctors and patients both in hospitals
and private clinics. Whatever impressionistic
data thus gathered, the author has used them
in framing the model.
I•
With the rise of new medical values to make
man immortal from the medicinal point of
view, and change in the concept of medical
practice (preventive and promotive aspect), the
doctor-patient relationship has assumed new
dimensions.
The medical profession is a
phenomenon of interactional co-operation and
behaviour.
The doctor-patient relationship
occupies a key position in the functioning of
medical profession. Proper functioning of any
hospital system depends upon the functionally
congruent relations among the doctor and
patient and auxiliary workers.
The concept of doctor-patient relationship
denotes a situation in which the doctor and
patient along with their motivational require
ments interact with each other in a meaningful
way for clinical objectives. This doctor-patient
relationship does not operate in vacuum.
But
it is an end product of various interacting factors,
such as the professional training and competence
of the doctors, the role expectation of the
Patients, socio-psychological characteristic of
__
the doctors and the patients and the last but
not the least important point is the socio-cultural
matrix within which the whole medical system
operates. Keeping in view all these factors, it
may be said that the doctor-patient relationship
is not an individual phenomena but a !sociopsychological phenomena operating ir the
growing complexity of medical profession.
A typology of doctor-patient relationship
with
the....
following specification
may be f’amed
r
ior emPlncal investigation.
(1) Role-performance—It implies over: and
covert influence exercised by the .octor
over the patients in interaction. A cordial,
sympathetic and warm relation with the
patient is informal and a cold impersonal
relation is formal.
(2) Way of dealing—The main variable of
doctor-patient relation is the ‘way of
handling’ the patient, having the degree
of interest as the key variable. If the
doctor keeps his interest confined to the
“ disease and cure aspect ” of the f atient,
- it is specificity oriented relation, tf he is
oriented qualitatively in the whole per
sonal well-being and extra ‘disease-cure ’
syndrome, his relation is diffuseness
oriented.
(3) Organizational bureaucracy—In doctor-pati
ent relationship, several variations are
possible in following the rules an(J regu
lations of bureaucratic structure. If the
doctor follows them rigidly. he is termed
bureaucratic and if he follows them with
flexibility he is non bureaucratic.
The models are based on inc
of the author’**.
u
i
,
.
the nndmgs
findings
Hospital, B.H.U. ”
S
inC author« research work conducted on the te Sir Surider Lal
ussw***
Medical College, B.H.U. for their valuable guidance.
—t------- 2ssor and Head, Department of Sociology,
Of the Department of Preventive and Social Medicine,
29
MODELS OF DOCTOR-PATIENT RELATIONSHIP
DECEMBER, 1971
Typology of Doctor-Patient relationship
(with doctor as Orientation agent)
Performance
Serial
No.
f
Role-Performance
Model
1.
Medico—Technocratic
2.
Magico—Angelic
3.
Angelic—Technocratic
4.
Medico—Particularistic
5.
Medico—Idealistic
Note
+ = Acceptance
Speci
ficity
Diffuse
ness
I
In-
Formal | formal
Bureau
cratic
+
+
+
+
+
NonBureaucratic
+
+
+
+
Organizational
Setting
Socio-cultural
matrix of dealing
+
+
+
+
+
+
- = rejection
D
P = doctor patient relationship
qualities are projected upon his personality.
Such an image is generally accepta ble to the
average Indian who has a tradition of ‘Vaidyas’
and
‘Hakims’. The private practitioner
acquires this image. He is sympathetic and
helping. He enters into informal ?hats with
the patients and shows utmost care for the con
valescence of the patients. Except ; 1 few simpie and convenient rules, he followss, no bureaucratic rules - regulations in his privately
managed clinic.
Model 1— Medico-Technocratic
The doctor is an expert of his branch
of specialization and works instrumen
tally. He adheres to the bureaucratic struc
ture of the hospital and maintains formal rela
tions with patients. His self image is of a
specialist demanding recognition of his skill.
He does not enter into formal conversation
with the patient or pays attention to the pati
ent’s extra-symptomic description. He ruthlessly
advises and maintains a distance from the
patients and auxiliary medical workers.
Model 3—Angelic Technocrat
Of course, he has all the qualities found in
the medico-technocrat except the ‘dealing’
aspect,. Inspite of his ‘expertise’ he maintains
all the cordiality and certain amount of
patience to bear the strains of informality.
Because of his expertise and warmth in hand
ling the patients, he is the most sought for
doctor in Indian cultural matrix.
Model 2—Magico-Angelic
In the doctor-patient relationship in Indian
cultural matrix, a magico-angelic doctor is
viewed with reverence as an ‘angel’ or ‘messiah’
of cure. He is seen as the saviour of life. This
image of the doctor is born out of his interac
tion pattern with the patient. Charismatic
l
2
j
30
VOL. X. KO' 4.
THE INDIAN JOURNAL OF MEDICAL EDUCATION
Model 4—Medico-Particularistic
He is expert and bureaucratic having the
apparent aim of ‘impersonality , he develops
sometimes a soft corner for certain patients.
He: enters with
relations,- may. be due
wnu cathectic
-------------.
particularistic consideration-caste, communi-
X Pus:"IsrZrC'tc?'J,Hism"odel nf
of relation
relation ISis not
not
J-
—------
Sant’with the
d.is
a consistant
the ’doctor, rather it
is a
“ situational
emergent ” relation. For
/. tional emergent
or the weU
being
* r of fhis’ patient, he may deviate irom
from
organizational
.rganizational matrix and medico-ethics.
Model 5—Medico-Idealist
The
variation ux
of D. P-.relation model^l^and
ine vanauuix
of
model 5 is subtle.
- ---- ;
,
distinction is the ‘way of dealing’ with the
rlt.Hnetion
the rules and regulations
‘
11.
JLJ.W ***
wj** -----
y
1
’
«
•
•
«1 I
e'tr m no t nPil C.
informally
in D-P relation, He is
----------— ' sympathetic
r * < r
in relation with the patients but refuses pohtely’ to deviate. He is polite but ‘stern’ in
organization
fouowing rules-regulation Cof- the
* ~y
~
j
•
▼▼
tt
I • 1_ __„1
« w^rlirn-idealist.
^ch'matahim
°a
medico-idealist. ’
The models of relation presented above are
ideal types and by n0 means 1they, exhaust the
typology. We have presented on 1yj a few of
them for empirical testing. It is a conceptual
c
scheme derived out of observatior^, It needs
vigorous testing in various
x------- socio-cultural
■■ K&?
TA- 6
m
*
■
Mr ) rV.'^
•
C-M c '
,
■
.
- 1^(00^
■'
z
.
ORGAN TRANSPLANTATION IN INDIA
Solid organ transplantation is a rapidly evolving discipline
currently involving the heart, lungs, liver, pancreas, intestines
and kidney. However, the Indian experience is confined to Renal
transplantation.
The incidence of end stage renal disease (ESRD)
is 40-60 patients/mi11ion/year. Every year 30,000 patients are
added to this large pool. The logical solution is renal replace
ment therapy which is scarcely available and condensed around the
major cities.
A survey concluded in March 1990 revealed that
approximately 22,000 patients were dialysed in one year for acute
or chronic renal failure in our country.
It is J also estimated
that approximate!y 2000 live donor kidney transplants were done
in 1989 on India.
\
| vW'
''■*
■
.
- '
■
.■M
Renal Transplant Centres:
-
'
'■
■
The major academic institutions, as a matter Of policy accept
only those patients for maintenance dialysis^who have a prospect
of line related transplantation. The obvious reason for this
rationing and denial of life saving maintenance dialysis to this
large pool is grossly inadequate facilities for dialysis and
The
absence of cadaver renal transplant program in the country,
situation is by no means static as the last decade has witnessed
a phenomenal growth with establishment of around 200 centres for
regular dialysis and 30 centres performing renal transplantation.
However, despite this growth, the existing facilities are woeful
ly inadequate for the needs of this vast country.
Cadaver Renal Transplant (CRT) Prograa:
. . • . :j
‘
■
Instead of taking a logistic approach of developing a CRT pro
gram, there has been a trend
__ ‘_____
towards
2
the path of least resistance
ie. ,
the unrelated transplants with the spectrum of i associated
unethical practices.
It is true that CRT in India is beset with
numerous difficulties, such as scarce availability of hospital,
care for the critically ill,
ill
legislative silence-on brain death
criteria and organ donation, inconsistent and unreliable telecommunication and transport facilities and unawareness amongst the
Though
public and professionals regarding organ transplantation,
a tedious task, a viable local CRT program is desperately needed
to meet the growing need of organs and to combat the practice of
unrelated unethical renal transplants.
The * Kidney trade's
1
Recently there has been a lot of press coverage of the kidney
trade. An estimated 2000 or more kidneys taken from live donors
are now sold every year in the country — up from 500 in 1985 and
around 50 in 1983. And while initially it was restricted to
hospitals in the metropolitan cities, it has now moved to smaller
cities.
The 'Kidney business' now has a turnover of Rs 40 crore.
2)
(Contd.
/
'-■
:T
!
-: 2; -
filtruistic Donation:
The concept of Altruistic donation has gained momentum in many of
these centres.
Invariably most of these altruistic donation
is
backed by gratification and financial transection.
Many a
times
the
transection is involving the doctors too.
Lets go into
the
'live related donors'.
The results are very good in this group
and
the financial transections are relatively less.
There
has
been a lot of allegations where the donors have been made 'relat
ed donors'.
There is no agency to check the integrity of
these
related donors.
Un—related Donors;
What do you do for a patient who does not have a suitable related
donor?
Will you refuse treatment for a patient whose
re 1 atives
refuse donation
for various reasons.
These are some
of
the
considerations for those who propagate unrelated donors.
RECOHMENDATIQMS
I
have
a few recommendation to make to this august gathering.
The three major Christian teaching institutions can play a major
role in organising an ethical organ transp1 antation program.
1.
Cadaver Renal Transplant (CRT):
Political pressure must be instituted to have a viable legistalation for cadaver transplantation.
At the moment only the
state Governments of Maharashtra, Tamil Nadu
and Karnataka
have obtained legal clarity on vadaveric organ donation
and
detai 1ing
the
legal procedure for retrieving
organs
from
cadavers.
Despite these efforts, the CRT movement has failed
to gain the desired momentum,
There is an urgent need
for
the
parliament to pass a bill on cadaver organ donation
for
other states to follow.
2.
Concept of Al truism in CRT:
Un 1 ess
the public is made aware of the importance of
organ
donation,
they will never realise the need
for the
same.
Al truism
is a complex phenomenon.
People don't, just
decide
to
be altruis tic« charitable or benevolent.
They must
be
motivated
and guided
by
their
philosophies,
upbringing,
religious & social attitudes and the
immeasurable
contacts
that
effect their perception and determination.
It is here
(Con td.
3)
-:3:-
that media may be enlisted to play a
paramount
role ih
presenting positive attitudes about organ donation.
We must
therefore be over sensitive to opportunities to work with the
media and with the public directly, to inform and educate in
order to disseminate correct and meaningful information.
I here is also a need to evaluate the emotional and other
re
sponses
felt by donor families after a loved one has died.
The death could be traumatic, due to stroke,
primary
brain
tumour
(not metastatised),
or due
to methanol
poisoning
(these
patients can
be dialysed
then organs harvested).
This is a critical and traumatic time in the
life of
the
family and the approach must be psychologically befitting
to
the environment to initiate discussions on organ donation.
This
is a unique area of endeavour, and gentle care and
concern by those of us in the field will inspire and motivate
al truism.
Lack of knowledge or understanding about organ donation,
may
generate fear and mistrust in the minds of families.
In
the
same way , religious attitudes might raise concerns about
the
mor a 1
or religious propriety of invasion of the body of
the
remova1
of part for transp1 antation.
There may be mistrust.
or concern as regards the care or proper respect for a
body
after donation and a lack of confidence that it will not
be
muti1 ated.
There may be understandable
apprehension
that
voluntarily donated organs, perceived to be the act of generosity would somehow be sold for commercial gains,
One of the
most
significant
areas of fear or mistrust is
that organs
might
be removed from a person prematurely before death has
occurred.
People may be superstitious that if they
sign
4
donor card or even talk about the concept while
they are
a1ive, the event of death might in some fashion be preponed.
All these fears and concerns can be alleviated and d i spe11ed
by proper education, & judicious use of audiovisual media and
the written word,
It is imperative for the medical
prof es
sionals
to take up the challenge of educating the public
at
large about the need for organ donation.
To
promote altruism, there is need for advance
planning
to
provide
positive, accurate and informative message so
t ha t
transpl an tation may be better understood
practiced.
Medical
professiona1s engaged in the care of trauma victims
and,
ICU
staff are to be appraised of the need
for
organ
donation,
brain death and care of
such patients.
These
professiona 1s
are the referral source to the organ
procure"
ment team.
(Contd.
4)
-:4:-
3.
What else is the Option?
fill CRf becomes a reality we have to rely upon live donors.
Ethically we are justified to perform transplant on
live
related donors.
But what do we do for those patients who do
not
have a suitable donor?
Is it ethical to deny them
the
option of a live unrelated renal transplant? This needs
to
be discussed
in detailed in appropriate forums within our
hospital infra structure.
I would suggest that each hospital
have a organ donation ethical committee consisting the physician, transplant surgeon, social worker, representatives from
the citizens council and legal profession
to monitor
the
integrity of
these unrelated donors and
avoid financial
transec tions.
It is better to openly do an unrelated organ
transplant
in
excep t i on a1
cases by using a set protocol
mentioned above.
Her r/f • 7
Mr
CHRISTIANS IN MEDICAL EDUCATION
Date s 28^29/2/9 2
MEDICAL COLLEGES AND THEIR ETHICAL RESPONSIBILITIES
Ethics: Science of morals.
Moral
behaviour or code»
Moral behaviour or code is known to all of us. There is
a need, however, for us, a group,to dwell on this responsibility
as Christians, -working in and as part of a Medical College.
In this context of a Medical College, the areas that need
to be looked at carefully are, our ethical resoonsibilities.
A) As Teachers
B) As Managers/part of a working-team of a department
C) As members who are part of the Institution
D) As part of the vast realm of medical professionals in ?
country of numerous medical colleges and varied types of
medical colleges
E) As part of the Society in which we live
As Teachers
n Few boys are incorrigibly idle, and a few are incorrigibly
eager for knowledge, but the great mass are in a state of doubt
and fluctuation, and they come to school for the express
purpose, not of being left to themselves because that could be
done anywhere but that their wavering tastes and propensities
should be decided by the intervention of a master" Syndney Smith.
We are responsible for the finished product of our College.
The child that enters the portals of the Medical College and
the Doctor/Nurse/Allied Health professionals who leaves it.
- The one who enters has his qualifications and has made the
required grade.
- The process of education and training is over.
- He/she makes his/her place in society.
Broadly this may be a) A purely academic career - research, teaching
b) Where the skill acquired is used in the service of the
society
c) Professionalism or commercialising of the training.
.002/
2 z
Each College represented here has its own policies for
selection which are sound and carefully worked out. The
role played by St. John's Medical College in the moulding of
students to face ethical issues is basically in two phases:
Phase I.
Make known what the Institution stands for -
a) Institutional objectives spelt out in the prospectus
b) Ethical values paper included in the Entrance examination
c) The pattern of interview also conveys to the student/
"the ethical stand" of the Institution.
Phase II.
Create an ethos where the students are nurtured in
these ethical values by -
a) Classes on medical ethics/where the principles are taught
b) Providing role models - as teachers/ doctors/ administrators,
nonteaching staff and research staff.
The above steps will provide the student with the basic
foundation in ethics as a subject and the practice of ethics.
This in turn will provide uhe (guidelines in decision making.
I would add the Institution should look to Christ for
example. A Christ-centred life together with the knowledge
of ethics as a subject is the right amalgam.
There are stumbling blocks to the achieving of this goal.
You will be able to list many out of your experience as a
teacher.
As Managers, or Heads of Department
There is a need to constantly remind ourselves about the
stand we take in ethical issues that arise, The one I find
most difficult is to be a good example. Some of the areas
that need to be considered are -
- Using working time for personal errands
- Misuse °f office stationery
- Expecting the 'Helpers' to run errands at home and in the
office
- Overtime wages and compensation for every bit of extra work
o..o 3/
2
3 :
- Fear of the "Workers' Union"' when disciplining is necessary
- Discrepancy in "Management policies" in the various other
departments
- Writing "Confidential reports" on staff who have been irksome.
Do I misuse this hold I have?
and
- Our responsibilities in departmentally acquired infections
injuries.r
constantly supervise the staf£ in
- Need to protect, educate and
the department.
C) As members who are part of the Institution
In a Christian Institution, it is only correct to expect a
Reeling of a common bond with unity of purpose, working for
the common good of the Institution. This may be the case most
of the time but cannot be the case all the time. Few
examples are - Management versus staff issues. Either as individuals or
collectivelyo
~ Protection of the Institution's reputation in the wake of
public criticism.
- Our stand when various categories of staff from other
medical colleges strike work.
- Facilities/ per^cruisites and higher pay scales in corporate
hospitals which lure trained personnel away.
- Mission institutions under the control of the Church/Churchss/
Councils. If there is a resentment do we allL^rw it to grow?
Universities to which, the institution is ai.filiated
The
can pose problems* At times, the University expects
Christian Institutions to be "Lead Institutions" and at
other times laws and rules are laid down which require
major policy changes within the Institution - this may even
at times affect admission policies and the Institutional
objectives. What do we do?
s 4 s
E) Each one of us here belongs to the
in we live.
What is our role as health professionals? Do we have an
ethical responsibility towards -
- Building healthy communities?
- Do we discharge this responsibility as
a) individuals
b) groups of like-minded medical peonle
&
c) through philanthropic groups such as Rotary Club
d) as part of our Church activity
e) any other
Do we consider it as a mandate and find time for it?
Ethical issues in Biomedical Research
There are many facets to this. The guiding principles
are laid down by WHO»
In St. John's Medical College there is procedure for
ethical clearance of a scientific project. The project is
submitted to the’‘Ethical Review Board” comprising of a senior
and a junior representative of the pre and paraclinical
departments; one from the clinical section, a senior research
consultant (one who has had many years of research experience)o
Ethics Consultant, a legal consultant and the Principal of
the College. This committee/board meets, reviews the projeclts
for its ethical clearance and issues a certificate to that
effect. The board has the liberty to reject or modify the
project in order to make it ethically acceptable.
The other areas to be considered in ethics of research,
certain .issues that are not discussed in books. Some of them
are s (1) Authorship of the research outcome and the order
(ii) Interdepartmental research projects are best discussed by
the participating personnel and all issues agreed upon.
(iii) Using of departmental registers, patient’s charts for
analysing data. Bearing in mind the ethics of confidentiality
of patients reports.
■
*
Medical Education. 19X4. .8, 67-70
editorial
Medical ethics and medical education
Declaration of Sydney (1968) on the determination
of death, the Declaration of Oslo (1970) on therapeu
tic abortion, and the Declaration of Hawaii (1977) on
the responsibilities of psychiatrists particularly with
reference to possible misuses of chemotherapy and
invasive brain surgery.
The World Health Organization and in particular
the Council for International Organizations of Medi
cal Science (CIOMS) have long been concerned
about ethical issues in health care and the need for
the integration of medical ethics in medical educa
tion. While in the past the concern has arisen within
the medical profession and has been related either to
the control of medical malpractice or the dilemmas of
clinical medicine (particularly related to new devel
opments) now the pressure is increasingly coming
from the public and the media and relates to a series
of new issues of growing importance.
The first issue relates to the exponential growth in
clinical research and particularly in the trial of new
drugs, and public concern that there should be
adequate control and protection of the rights of
experimental subjects. This issue is particularly
focussed in the developed countries on the ifole of
Research Ethics Committees or Institutional R.eview
Boards in providing ethical review of clinical re
search. and concern at the absence of adequate
controls on pharmaceutical companies and medical
entrepreneurs in developing countries.
The second issue relates to the politic? ; and
economics of health care in a period of world
recession, and the ethical issues to which economic
scarcity has given prominence—namely questions
concerning the ethics of resource allocation. These
arise at several levels; in clinical practice (e.g. in
deciding between patients for renal dialysis or
intensive care when equipment and facilities are
limited), in the management of personnel and re
sources within a health care system (e.g. in shifting
resources from the acute high-technology hospital
Medical ethics, at any rate in the West, has been
traditionally based on the Hippocratic Oath, with its
threefold principles of respect for human life, confi
dentiality in fiduciary relationships and beneficence
(‘the duty to care and do no harm’). For many
doctors and health professionals the Hippocratic
Oath has been a sufficient basis for medical practice
and they do not see the need for new codes or
guidelines. However many developments in the
modern world and contemporary health care have, in
the view of others, made it imperative to clarify these
general principles of medical ethics and consider in
more detail their application in clinical practice and
the larger areas of health care administration in both
developed and developing countries.
Public outrage at the discovery, during the Nurem
berg War Crime Trials, of what had been done by
Nazi doctors in the name of medicine and scientific
research, gave major impetus to the review and
elaboration of medical ethics. The Declaration of
Geneva (1948 amended 1968) attempted to restate
the Hippocratic Oath in modern terms, affirming the
doctor’s duty of respect for human life and service of
humanity, the duty to care regardless of race, sex,
religion or social class; and respect for the secrets of
the patient. The Declaration of Helsinki (1964
revised 1975) sought to further clarify the ethical
principles governing clinical research involving hu
man subjects emphasizing informed consent and
proper scientific research design; and the Declaration
of Tokyo (1975) stressed that medical ethics pre
cluded doctors from participating in torture and
other cruel, inhuman or degrading treatment or
punishment.
Recent developments in bio-medical science and
technology have made it possible to achieve success
ful organ transplants, safe abortions, resuscitation of,
and artificial life support for, those who would
previously have died. This in turn has produced
pressure for further clarification of medical ethics: the
67
■
68
/. Thompson
medicine to primary care or to care of'the elderly and
mentally ill), and in attempts to achieve justice in
health-care at an international level (e.g. in providing
for more adequate staff and resources for developing
countries).
Medical training tends to focus attention on the
clinical relationship of doctor and patient, and much
recent discussion of medical ethics tends to have
concentrated on ethical dilemmas in one-to-one
clinical relationships. The discussion of such issues
tends to be couched in terms of personalist ethics and
individualistic values. This tends to overlook the fact
that doctors also frequently are involved in clinical
research with groups of patients, exercise consider
able power in the management of staff and allocation
of resources within institutions, and may play a
crucial role in determining policy at regional or
national level in their respective countries. The fact is
that personalist and individualistic ethics are in
general inadequate to deal with ethical decision
making at this level. Understanding of institutional
and political ethics with its more universalistic
concerns with justice in health-care and the common
good may be necessary, and these values may in fact
conflict at times with more personal understanding of
patients' rights and professional duties in a clinical
situation.
While there is a growing recognition that medical
education should include medical ethics, the empha
sis in existing courses tends to be either very
traditional (concerned with forensic medicine and
medical etiquette) or at best concerned with ethical
dilemmas of clinical medicine. Little attention is
given to the broader questions involved in medical
research, public health policy and the national and
international allocation of health resources, and yet it
is obvious that most doctors have to address these
questions at some time or other in their professional
life.
Medical Ethics and Medical Education, * a report of
the proceedings of the XIVth Round Table Confer
ence of CIOMS held in Mexico City from 1-3
December 1983, gives evidence that WHO and
CIOMS are attempting to address themselves to these
questions. The first two sessions of the Conference
relate to the ethical review of clinical research,
dealing both with general principles and considering
local applications in several different countries in the
* Medical Ethics and Medical Education. Edited by Z. BANKOWSKI
& J. Corvera Bernadeli.I. Council for International Organiza
tions of Medical Sciences. Geneva. 1981. Pp. 281. Sw. Er. 20.
Americas. The publication also includes the most
helpful Provisional Guidelines for Ethical Review
Procedures for Research Involving Human Subjects.
The third session was devoted to discussion of both
the theoretical importance of medical ethics in
medical education and some interesting practical
examples of courses where the attempt has been
made to integrate medical ethics into the medical
curriculum. The final session was concerned with
the broader ethical and policy questions involved in
the relationship of medical education and govern
ment.
The introductory papers were particularly out
standing. John Ladd, a philosopher, in addressing
ethical issues in human experimentation criticized
Research Ethics Committees (or IRBs) for being
unduly pre-occupied with questions of informed
consent, pointing out that most committees are less
concerned with the ethical issues of protecting patient
dignity and autonomy than protecting themselves
and the institution from legal action. Iriformed
consent as a legal notion pre-supposes an adversarial
relationship between doctor and patient which en
courages defensive responses on the part of both. He
pleads for a disentanglement of moral arid legal
aspects of the subject, greater awareness that ‘bourge
ois’ ideals of freedom are largely inapplicable to
patients who are highly dependent because qf need,
institutionalization or socio-economic circumstances,
and that the real challenge of facilitating patient
autonomy means getting away from legalistic inter
pretations of informed consent.
On the subject of research he pleads for a greater
awareness of the different value-conceptijons or
ideologies underlying those whom he calls ‘enthusi
asts’ and ‘restrictionists’. Both those who consider all
scientific research invariably benefits mankind and
those who are afraid of its Faustian pretentions tend
to argue from absolutist premisses. He argues very
persuasively that both positions need to be qualified
by human compassion and insistence on mainte
nance of the highest standards of scientific research.
He concludes that there are three factors which must
be taken into account in determining the moral
quality of a medical experiment on a human subject:
(a) the balance of risk and benefit for the subject; (b)
the adequacy of the project and its potentiality for
reducing suffering or benefitting future patients; and
(c) the relationship between the experimental subject
and those who stand to benefit from the experi
ment—that is, whether they are remote from him or
■
Editorial
69
•
%
people to whom he is related by some kind of
community of interest.
Robert J. Levine, in discussing the value and
limitations of ethical review committees, makes some
provocative comments as a clinician which must be
of interest to those serving on such committees. He
first points out that the limited research on such
committees in the U.S.A, suggests both that they
have contributed to better protection of the rights and
welfare of human subjects, and also contributed to
the improvement of the quality of research proposals
submitted and the quality of the research done. The
values which such committees attempt to uphold (in
the light of the Declaration of Helsinki and other
directives) are the following: (a) there should be
informed consent; (b) there should be good research
design; (c) there should be competent investigators;
(d) there should be a favourable balance of harms
and benefits; (e) there should be equitable selection
of subjects; and (f) there should be compensation for
research-induced injury. However, he suggests that
ethical review committees are often limited in what
they can do because they lack credibility. This lack of
credibility is related to the fact that many spend too
much time on unimportant details, that there is poor
co-ordination between different committees where
multi-centre trials are involved, there may be incon
sistent criteria determining which projects require
review and which do not. in the absence of standar
dized procedures committees will vary in the quality
of review given, there is no provision for monitoring
research approved, and some committees have diffi
culty in recruiting members who command the
respect of the institution or community they serve.
Francisco Vilardell gives an excellent analysis of
ethical issues in gastroenterology and how these can
be monitored effectively by laying down clear
criteria. The paper is very specific and detailed and is
a model of how ethical review can be developed in
specific clinical areas.
John F. Dunne gives a masterly overview of ethical
review procedures for research involving human
subjects, distinguishing three different kinds of re
search each with its own attendant ethical problems:
(1) detailed studies of a physiological or pathological
process in response to specific interventions, in one or
more individuals; (2) prospective controlled trials of
specific therapeutic regimens in larger groups of
patients; and (3) field studies in which consequences
of prophylactic or therapeutic measures are deter
mined within comparable communities.
In relation to these different kinds of research he
draws attention to several kinds of ethical problems.
First, whether in determining research policies coun
tries will use public funds competently for the general
benefit of society. Second, in developing countries
there are specific problems which arise because of
external sponsorship of research. These include
research projects which are unrelated to the country’s
primary needs, make heavy demands on limited
medical staff and resources, may be in conflict with
local customs and mores, and do not involve long
term commitment to the country or accountability to
its people. Third, developing countries lack the
medical infrastructure in toxicology and pharmacol
ogy to support the regulatory apparatus for monitor
ing new drug developments. Fourth, there is a risk of
exploitation of the underprivileged by sanctioning
research in developing countries that would not be
tolerated in countries with better general levels of
education and health care.
More generally his paper also contains some
excellent observations on the limited usefulness of
the notion of‘informed comment' when dealing with
research involving children, pregnant women, the
mentally ill and when public health measures (e.g.
fluoridation) involve whole communities. These
situations require other safeguards such as proxy
consent, review tribunals, provision for compensa
tion for personal injury and public accountability of
individuals or institutions involved in research.
The succeeding papers were of considerable inter
est in documenting the specific provisions for ethical
review of clinical research in Argentina and Chile,
specifically and more generally in the LatinAmerican Association of National Academies of
Medicine. Two papers of particular interest deal with
difficulties of doing paediatric research in Latin
America with conservative attitudes of parents and
established institutions (Kumate), and research re
lated to fertility control in women (Stoltz) where the
same difficulties apply compounded by the subordi
nate and oppressed condition of many women.
Other papers deal with the teaching of mainly
traditional forensic medicine and medical etiquette in
Venezuela and Brazil, and reveal a debate internal to
North American medical schools, namely between
the teaching of‘bio-ethics’ or ‘clinical medical ethics’.
The development of the Hastings Center and the
Society for Health and Human Values focussed
attention on the need to examine medical ethics in
the wider context of ethical and value questions in
70
1. Thompson
the bio-medical sciences in general. The initiative in
reseat ch had come from theologians and ethicists
rather than doctors. Mark Siegier criticizes this
dttf«lopment and argues for a restriction of medical
ethics to what he calls 'clinical ethics’ and preferably
taught by ethically literate but clinically competent
doctors. Edmund D. Pellegrino, doyen of bio-ethicist . defends the broader view and argues strongly
lor the injection of more training in the humanities
into medical education. In part the debate is about
method and content of medical ethics teaching:
whether it should be theory based or case based,
whether it should be given by philosophers or
clinicians, or in a multi-disciplinary mode, whether it
should be primarily medical or concerned with the
bio-medical sciences in general. In part also the
debate is about the scope of medical ethics: whether it
should be restricted to clinical, doctor-patient rela
tionships or whether it should lake in the ethical
responsibilities of doctor as researcher, hospital
manager, public health planner, policy maker for
health services generally, and international issues as
well.
1 he I nal closing addresses deal with some of these
issue.- but less satisfactorily, perhaps because no one
has really thought through these issues very carefully
just yet. The two Latin-American contributions are
mamly a plea for the independence of medical
schools to be respected, for epidemiological rather
than political criteria to be employed in defining
priorities for developing health services at nations
and regional level, and for realistic partnership ir.
striving to attain the WHO objective ol ' Health for Ab
by the Year 2000. Fitzhugh Mullan's paper is a rathci
smug defence of the U.S. National Health Service
Corps as a means of dealing with the health problciih
of deprived areas by scholarships to medical studcnirequiring them to do compulsory serv ice in deprived
areas following qualification. Why those who car.,
afford to finance their own medical training should
not have to do so is not made clear. Howard 11
Hiatt’s paper is a most useful beginning to
discussion about the need for training of doctors in
health policy and management and the ethical issues
involved al that level.
What this excellent publication lacks is a detailed
discussion of the wider ethical issuei of justice
health care between the developed a id developii.t
countries. What is needed is a WHO 'Brandt Report
which would deal with the ethical and educational
challenges to doctors of the North-Sou th polarizalior.
of wealth and poverty, health and disease, medical
resources and the lack of them.
1. Thompson
Scottish Health Edu|cation Group
Centic.
Health Education
T 1
Woodburn House, Canaan Lane
Edinburgh
^4 lo
Mr-? a-g
Medical Ethics and its Place in
Undergraduate Curriculum
By
Satya Parkash
Dean, Medical Superintendent and Professor of Silvery, Jawaharlal Institue oj
Postgraduate Medical Education and Research, Pondicherry.
‘'Amongst our contemporary experts physicians are
those trained to the highest level of specialised in
competence for this highly needed pursuit"
(/van HUch - 7976)
ABSTRACT
Ethical consideration have a bearing in most disciplines of medical practice
including, research on human beings, therapy on children, mental aberrants, geriatric
patients and similar other gn ups. A 20 hour teaching programme at undergraduate level
and intern level is recommended, which may be incorporated in the existing curriculum.
J
The relationship between a physician and
a patient, in a wider sense, has been a peculiar
have tried to question this distinction (Kass,
■’983). All the same, lack of a strict code can
|
one; of absolute blind faith bordering on
worship to complete mistrust and hostility.
cause havoc with the interests of a sick and
therefore gullible and open to suggestions.
Both the responses are understandable and
i justified. Certain codes weie laid down since
C
:
ancient times which governed relationship,
based on correct perspectives, with a
i view to
proiect the interests of the patients ;as well as
safeguard the legitimate interests
of the
physicians.
Medical people like to describe them
selves as professionals rather than
tradesmen
which per se means professing
to a certain
code of ethics, but
on the other hand traders
l also have a code of ethics
and some gn-ups
Ethics is a much more complicated pro
blem these days with the availability of
assisted life processes, use of cadaver or near
dead and live donors, trials and therapy and
Investigations on human including use of
placebos, question of informed consent when
applied to children or mentally retarded,
euthanasia, medicolegal aspects taking into
account the laws governing the community
and the social structure. Requirements of an
informed consent even for the tried and
accepted
or
surgical
other therapeutic
I
4
1'
52
Indian Journal of Medical Education
measures is not easily spelled out. There is also
a problem of certain drugs which have been
discontinued in some countries, but considering all aspects, may still be useful in some of
the less developed countries where the priori
ties may be different.
Ethics Through the Ages
Ethical codes are as old as medicine. Strict
codes were laid down in ancient Egypt and by
Summarians in about 3000 B. C. Hammurabi's
code in 1200 B. C. laid down severe penalties
for harm following treatment (Thorwald
1952). Sushrutha laid down a moral obliga
tion on the part of surgeons, the patient and
a strict criterion for selection of a candidate,
which may not accord with modern concepts
(Shankaran, 1976). It is recorded that during
the Buddhist period, in India, a public
affirmation of conduct and etiquette was laid
down (Thorwald 1962). Hippocratic Oath is
well known to need any mention and it is
still in vogue in some places, though parts of
its are totally out-moded; some of his
aphorisms have still an eternal message.
However, most of the codes, oaths or affirma
tions were more in the way of ethics laid
down regarding personal relationships between
the physician and his patient and do not have
answers for the problems of to-day.
The modern interest in a suitable code
arose when the world conscience was stirred
by what happened in Nazi Germany and was
the Nuremberg code of 1947. This insisted on
a “voluntary consent” for all experiments
where human beings were involved. World
Medical Association in their meeting at
London in 1949 laid down a code for medi-
Volume XXIV No. 3
cal research. In 1964 W. M. A. adopted’
HELSINKI I declaration governing clidicaj
research and informed consent. In 1975'
"I'
HELSINKI II declaration broadened its scop£
to include , biomedical research involving
human subjects (Bankowski, 1982). Most of
these-'principles were incorporated by th^
I.CM.R. Committee headed by Justice AX
Khanna in 1978 (Satyavathi, 1982; Medappa,*
1980).
Research on Humans
Research on humans is accepted as justified
but is governed by a strict stipulation in the
way of its necessity, because of an inadequajl
animal model, its relevance, peer acceptance
informed consent, rules regarding suspension
of the project if there was any adverse
development or a withdrawal by the volunteef
Informed Consent
This is difficult to define, particularly ii
the context of routine therapy or an operativ
procedure. Warning the patient about all th
possible complications will scare away mpjfe
patients from useful medical aid. Tb&
Supreme Court of Canada in 1980 justified
informing only of special risks of the co^
templated therapeutic procedure (Browi
1984.) On the other hand, a free informt
consent will not absolve the clinicians froi
liability in the case of negligence. Son)
principles would apply to invasive investigl
live procedures. Consent for therapy for tb
benefit of the patient may not pose an ethiefl
problem, but a procedure to benefit soml
other person or purely for research can P
open to objections (Bankowski, 1982.)
September- December 198r
Consent in Children
It is not clear if a guardian can give a
consent for an invasive procedure on a child
which is not of direct benefit to it. What is
more important is whether a child be permitted
to die or come to serious harm, because an
important parent withholds consenbfor a life
saving or a vital procedure.
Research in children is permitted only for
such studies which are exclusively for their
benefit and cannot be done except in that
age group. In older children it should be
possible to obtain their consent apart from
that of their guardian. Similar criteria will
govern mentally unsound patients, patients in
coma, etc. Question may also come up when
research involves less sophisticated com
munities incapable of appreciating the nature
of the trial. No trial can be done on false
pretenses or misrepresentations. Prisoners are
a closed community and a suitable group for
trial, but on the other hand any research based
on financial or other inducement or anyother
considerations or would be not free consent
and thus be illegal (Bankowski, 1982).
Placebos in Therapeutic Trials
Placebos have a place in therapy and also
in double blind trials. However, if their use
results in withholding proved beneficial treat
ment, it is open to objection.
Untried and New Therapeutic
Procedures; Peer Acceptance :
In 1874, Sir John Eric Ericksen opined in
favour of sanctity of the abdomen, chest and
brain from the surgeon’s knife. This was in
i
Medical Ethics...53
spite of the fact that a successful laparatomy
had been done in U.S.A, in 1814 and that
intestinal surgery was performed by Sushrutha
in 600 B.C If such authoritative opinion
had been accepted, there would have been no
progress in medical sciences (Aird, 1961).
Peer acceptance is important but it has to
be remembered that top medical opinion in
early nineteenth century declared Simla as
unsuitable for Europeans because of lack of
oxygen at those heights. Lice in boys’ hair
were considered part of masculinity. Smoking
was considered good for the lungs on medical
grounds and was introduced in public schools
like Eton. Breast feeding was considered an
imposition on women, only a few years ago.
Life Support Systems and
Concept of Death :
Introduction of mechanical respirators in
1950 and cardiac resuscitations in 1950 have
led to a large number of patient being kept
‘alive’ for monihs or years. A patients’
committee in USA recommended defining
death when there was an irreversible cessation
of function of the entire brain, including brain
stem. This has led
to the anomalous
positions such as in the case of Karen Ann
Quinion where higher brain function was lost
but not that of the brain stem (Editorial
Annals of Internal Medicine, 1983). Youngner
and Bartlett (1983) favoured irreversible
upper brain loss, i.e. permanent loss of
consciousness and cognition as the criteria.
Support systems are expensive and relatives
may be unable to afford and may even feel
disturbed at a irrecoverable relative being
kept part alive to a vegetative existence. On
^3
54 Indian Journal of Medical Education
the other hand, in the absence of clear cut
guidelines, the hospital authorities may expose
themselves to charge of murder, if patient is
taken of such systems.
Sanctity of Human Life :
■ •
’^lume XXIV No. 3
trical or other assessment, There must be
substantial safeguards, including a suitable
heavy insurance for such donors.
Robertson (1983) has raised a pertinent
point about loss of human dignity in an
incontinent old person, unable to lool after
himself who becomes a social burden and
source of embarrassment, since he might
expose his body or behave or conduct himself
in someother indecent manner. The family
had built up an image of him through the
years, of a highly revered and respected
symbol in the family. This is lost causing lot
of pain and anguish to all friends and
relatives. Why can one not permit a will for
self deliverance when one is in his senses ?
Social ethos in this context are para
doxical. It is patriotic to kill the enemy in
war but to give him full succour and respect,
if the person is taken as a prisoner. Dozens
die in increasing civic unrest round the world,
but a doubtful default in a patient care even
with an irrecoverable illness may hit head lines
and lead to serious difficulties for the physi
cian. A. numoer of individuals commit suicide
when a political or screen hero is seriously
ill, and this behaviour is accepted socially and
seldom discouraged. Death due to social
A similar case could be made out for
inequalities are common in the poorer coun
patients
born with gross congenital defects
tries, but most societies frown on euthanasia
or
incurable
painful and distressing conditions,
in any circumstances. Sanctity for life extend
such
as
advanced
malignancies. Are support
ing even after death to a cadaver or near
cadaver, has a bearing in obtaining organs systems justified in such cases ? Is it the
like the kidney for transfer as well as utili physician’s job to prolong the act of dying ?
sation of cadaver parts such as cornea, blood,
bone and split skin graft. Most of this Professional Etiquette
material could be of great benefit to the living
This is governed by rules laid down by the
with no harm to anybody, unlike obtaining
Medical Council and this governs -•j—*-■ ■
advertising,
parts from live donors. Most donations,
responsibility of a professional act, copduct
irrespective of what the declaration are for
towards patients and fellow physicians etc.
a consideration, social pressure, emotional
Jurisprudence lays down Jaws regarding
involvement, financial inducements, media
abortion, sex. marriage, professional liability
publicity, hero instinct, etc. Is it ethical to
and they may vary in the same country for
use a major organ from a live donor ? France
different communities. There is also conforbids use of live donors (Holston and
troversy as to how far a professional person
O’Conner, 1966) In India there appears to is liable in his individual capacity and
how
be no law in favour or against such donations far he acts as an agent when he is e
np oyed
and most countries do allow such donations by an agency, such as the government,
in
after a suitable informed consent and psychia- which case the liability mt.v also be of the
September December 1985
Medical Ethics...55
employer and as a consequence he may lay
down constraints on his professional work.
to exposure to it. Olukoya (1983) of the
Logos University of Nigeria found that 88%
Community Programmes Without consent
of ciinical students showed interest in the
subject and recommended inclusion of this
subject as a part of the curriculum. Givner
Community bodies also permit compulsory
drueaing in the way of supplemented foods,
such as iodised salt or flour supplemented with
calcium and enforced innoculations or vacci
nations. Pollution of the environment is
common and is often permitted by the
community. Smoking in public places is a
r classical example and exposes a large number
< of unwilling people to passive smoking, which
I may be more dangerous, even then smoking
by the individual himself. This exposure to
drugs and chemicals is without* any infoimed
or uninformed consent.
Quackery
In 1551, Queen Elizabeth-I could not get
Margaret Kennix, a traditional practitioner,
registered with either of the colleges which
had obtained the royal charter from her
(Simpson,
1962).
An association
with
an
unqualified person was forbidden in the
Hipprocratic Oath, On the other hand in
some countries, particularly the poor countries,
traditional healers have a useful role to play
and this has been well accepted by the WHO.
Also with tne present day highly sophisticated
modern therapy, association with non-rnedical
non-professional personal is inescapable.
Medical Ethics in Undergraduate Curriculum
In view of the complexity and wide range
o the subject, it stands to reason that a suit
able part of tae curriculum should be allotted
and Hynes (1983) found a positive advantage
in outlook of students exposed to medical
ethics for three months Cassidy, Swell and
Stuart (1983) incorporated this subject as a
part of family practice clerkship for the year
IV year students. Thung (1981) emphasized
exposure of medical students to the pleuralistic
morality governing patient’s acceptance of
medical advice in the cognitive and
non-
cognitive fields, in the case of a child patient,
he analysed the role of the child, parent,
doctor and society in acceptance of treatment.
Keller, 1977 recommended a course for
residents consisting of 5 halfdays in I year, 3
days in II year and a day including an
assignment in III year.
The present curriculum allows for two to
three lectures on the legal aspects of the subject
as a part of the forensic medicine curriculum.
The first year students are exposed to 20 hours
course in
community medicine including
sociology. Medical ethics is very akin to the
subject and it is proposed that a 20 hour
programme distributed between first to fifth
year be introduced. Four lectures could be
devoted to the definition of death, informal
consent, etc. and could be part of the PSM
teaching programme in the first year. The
lecture programme for the jurisprudence could
remain unchanged and be covered in 3 to
4 hours of teaching. Department of Pharma
cology could devote one to two hours in
relation to drug trials. Similarly the other
clinical and non-clinical departments could
e
55
Volume XXIV No. 3;
Indian Journal of Medical Education
aspset can be evaluated
as part
devote one to two hours teaching programme
in the ethical aspects pertaining to their
This
specialities. The stress should be on exposure
to the existing problems and taking into
account the accepted norms of the society.
be given suitable assignments during their
evaluation of the subject.
posting in Community Medicine with thfc
PSM department.
REFERENCES
1.
The interns may
Aird, I. The making of a surgeon, London Butterworth, 1961, p. 93.
2. Brown, F.N. Some comments about informed consent. Canadian Journal of Surgery,
27:131-2, 1984.
3.
Bankowski, Z. Ed. Proposed International guidelines for biomedical research involving
human subjects. C1OMS, WHO, Geneva 1982, p. 1-40.
4.
Cassidy, R.C., Swell, D.E. and Stuart, M. Teching biopsycho ethical medicine in
family practice clerkship. Journal of Medical Education, 58 : 778-783, 1983.
5.
Editorial—I he determination of death. Annals of Internal Medicine, 99 : 261-264,
1983.
6.
Givner N. and Hynes, K. An investigation of change in medical students’ ethical
thinking. Medical Education, 17 : 3-7, 1983.
7.
Holston, G.E.W. and C ’Conner, M. Ethics—Medical progress with special reference
to transplantion—A Ciba Foundation Symposium, London, J. & A. Churchill,
1966 pages 1-257.
8.
Illich, I. Limits to medical nemesis—the expropriation of health London, Marion
Boyals, 1976, p. 6.
9.
Kass, L.R. Professing ethically—on the place of ethics in deCning medicine, JAMA,
249 : 1305 1310, 1983
10.
Keller, A.H. Human values of education in the family practice residency. Journal of
Medical Education, 52 : 107 116, 1977,
11.
Olukoya, A.R. Attitude of medical students and medical ethics in their curriculum.
Medical Educaticn. 17 : 83-86, 1983.
i
•S-
12.
o, ta.n Mure |n
Krtmon. C.S. E,h,t,|
287 ; II75-1] 77, 1983.
J3.
Satyavati, G.C. Ethical considerations
in medical research—Paedi tries.
208, 1982.
19 : 201-
14.
Shankaran, P.S. Sushtutha’s contribution to
surgery, Varanasi. Indolog,.dl Book
House. 1976, p. 15-25.
15.
Simpson, R R. Shakespeare and medicine, Edinburgh & London E & S I ' •
1962, pages 69-70.
s
^onaon, t & S Livingston,
16.
Thorwald, J. Science and
secrets or medicine, London, Thomas & Hudson, 1962,
pagee 120, 218-219.
17.
Thung, P.G. Introducing medical students
to ethical issues. Medical Education,
15 : 79-84, 1981.
i
L
18.
»
oi internal Medicine, 99 : 252-258, 1983
5’7
7.
Si
J
S4-11
I
Doctor Patient Relationship —
The Neglected Domain of Medical Education
By
N. Ananthakrishan
Lecturer in Surgery
Jawaharlal Institute of Postgraduate Medical Education and Research, Pondicherry.
J
ABSTRACTS
r.
2
An analysis of the lacunae existing in the field of doctor-patient relationship
during the training period of medical personnel revealed intrestmg facets many of
them amenable to correction with little outlay of man or material. It appeared that
a small shift in emphasis during training along with other miner remeuiai measures
may go a long way in correcting this unhealthy state of affairs. An analysis of the
existing problems has been presented and detailed suggestions made to evolve a
strategy to rectify the same.
Introduction
f
The entire duration of medical training,
undergraduate and postgraduatete is concerned
.1
___________________ 1
mainly. .with the
cognitive
and psychomotor
domains, to the detriment of achieving profiency in what might be the most important
quality expected of the doctor, and perhaps
the one most difficult to master, viz. an ability
to establish rapport with patients and to
communicate with them to the patients
satisfaction.
At the termination of their
training period the end products of medical
education are left to acquire this proficiency
in the affective domain entirely on their own.
This state of affairs is unfortunate, since
S L doctors* work involves not only activity and
| decision making but also communication. It
| cannot be denied that currently there exists a
| profound communication gap between trainee
doctors and patients due to lack of either
ability (physical or mental), understanding or
motivation which leaves the patient some
times bewildered but more often dis-satisfied.
Much of the research on the relations
between cognitive achievement and attitudes
and values shows them to be statistically inde
pendent (Bloom et. al., 1964). This is illus
trated by Mayhew (1958), who reported little
relationship between attitude changes and
growth of knowledge in a college course.
Inspite of research and writings to the
contrary by Tyler (1934, 1951), Furst (1958),
Dressel and others there still persists an
implicit belief that if cognitive objectives are
developed, there will be - corresponding
development of appropriate affective behavi
ours. Jacob (1957) has raised serious questions
about the tenability of this assumption.
82
VOLUME XX JV9. 3
THE INDIAN JOURNAL OF MEDICAL EDUCATION
Bloom et. al. (1964) studied the history of
several major courses at the general education
level of college and found that in the original
confined to
surgical
patients and surgical
trainees.
PROBLEM
statement of objectives there was frequently as
much emphasis given to affective objectives as
to cognitive objectives and even small attempts
were made to secure evidence on the extent to
which students were developing in the
affective behaviour. However, as these courses
were followed, there was a rapid dropping of
the affective objectives and an almost complete
disappearance of efforts at appraisal of
student growth in this domain,
because it is easier to teach and
perhaps
evaluate
cognitive objectives.
In medical college curricula in India also,
institutional objectives often make mention of
the need to develop certain attitudes in
students but little if any effort is paid to this
aspect of their training.
Evaluation material in the affective domain
is rare and is usually connected to some
national educational research project or a
sponsored local research project (Bloom et al,
1964). In the medical curriculum evalua
tion work for effective
objectives are non-
existent.
A study conducted by the author amongst
patients and colleagues, especially those
undergoing training, to identify the extent and
nature of this problem of lack of adequate
rapport and communication between them and
reasons for the general discontent amongst
patients regarding doctors' attitudes to them,
presented interesting facts. The study was
initiated with the idea that if definite lacunae
could be identified, remedial measures might
be possible and could be incorporated in the
training. For obvious reasons of affiliation of
the author the
investigations
were
mainly
a] Patient s Problem
Questioning several patients in the hospital 1
and during outpatient
attendance revealed
I
interesting findings. These problems recounted
by patients and affectiag their faith and trust
in doctors are mentioned below, These have
recounted as far as possible in patient s ownI
words.
i) Ununderstood ‘‘manipulations’’ especially
investigative in “strange” surroundings
with no explanations forthcoming from
the treating doctors.
ii) Unexplained delay in securing definitive
treatment e. g. surgery when compared
to other patients whose turn comes earlier
even though admitted later. This in many
cases due to the necessity for detailed
investigations in the individual case which
are
not conveyed
adequtely to the
patients.
iii) Certain beliefs regarding the lack of
safety of surgery generally based on
superstitions not cleared.
iv Need for surgery as opposed to nonoperative treatment not explained.
v) Fears and anxieties regarding surgery as
a procedure—both endogenous and
i
acquired
as
a
result
of
watching/covercquired
ing with uiiiti patients left to lingtr in
them with the doctors a pparently
unaware of this fact.
vi) No information given after the operative
procedure as to “what was done" and
"7
I —
/o
doctor patient relationship
...
83
19t! 1
SEPTEM BF.R-DECEMBER
naturally, develops certain attitudes in their
,eeted”.
In most
“what is to be exp<
are left in the dark as to
cases they
the surgery is palliative or
whether
L the procedure complete or
curative.
does it require a second stage?
physicians which is lacking here.
Trainee’s problems
A similar study of junior colleagues men
tioning the patients difficulties to them elicited
the following responses.
- 5understand why, if they are feelmg,
wise will, they should go to the
P
i) Language-lack of ability to communi
cate in the “patient, language . Ihis
mainly applies to central government
institutions where doctors from all parts
of the country work.
perhaps missing a day’s earnings.
... „
--for sudden discharge sometimes
viii) Reasons
- not explained especially when symptom^
have not been completely reheved^ Is
ii) A feeling that there is a lack of know
ledge or desire on the patient’s part to
know about their disease. This ,was
intriguing in View of the contradictory
for further investigations as an ou
patient or is it because of incurab e dt
;se or because the pattent is
unfit
opinion expressed by the patients.
iii)
surgery ?
ix)
5
’
i to be
Doctors appear almost always
to be disturbed with
extremely too busy U trivial problems.
aenerally
involved personally.
iv)
not
available
.he..!.-.
dU
8
.ont ro know more about
of patients want to Know
the patients ‘illness .
-t irritant to some patients
xi) An important
educated was
especially those who are
referred to as *a case’ and
in being
never by name.
of the patients’
It is evident that most
lack of communication
| problems stem from, a
This situa'
Ik hgtween them an<*
peculiar to the devempmg
~ tion may
P' -.most patient, are awate
| countries. In the west
know and under.tand what is
| of their right to L--and do not hesitate to
I being done to them
Such an atmosphere ;
I exercise such rights.
Overlapping responsibilities since many
doctors are responsible for the same
patient’s welfare and hence none feels
Lack of time, workload, tiredness.
•.„.l 1 are not available
v ) Patient’s relatives
. short time when the doctors
except for a t——-to relax themselves after a
would like
an inability to
busy day and hence
explain to them.
duration of ppsting in
vi) Extermely short
iJiternship
each discipline during the
of
patients
is
and hence follow up
difficult.
individual
vii) An inability to follow the
uisunai^v
patient from admission to d
. of the -‘patient's
o.
to frequent changing
ward itself leading to
beds”, within the
Zsfer of further responsibility in managment to another doctor.
..
-
-
84 THE INDIAN JOURNAL OF MEDICAL EDUCATION
viii) An absence of any formal training in
patient psychology at any point in the
curriculum.
11
ix) The existence of a communication gap
between faculty/staff/trainees due to
lack of detailed discussion during or
after rounds. Hence, the trainee himself
is left sometimes unconvinced regarding
correctness/advisability of the decided
method of management. The trainees
generally felt that they lack complete
knowledge of the overall plan of
management and hence could not
communicate satisfactorily with patients
even if they desire to do so.
I
x) Lack of material and aids including
facility to recall previous patients to
explain the need for procedures like
colostomy and their compatibility with
normal living to other patients waiting
for such procedures.
fresh entrants. Such facilities already
<exist at JIPMER.
Is
a) The part time services of a clinical
I
psychologist and more important of
medical social workers are rJece-
ssary. These workers should be
available at least one per ward for
one to two hours daily, if possible
during visiting hours. The doctors
will find it easier in some cases to
accept their help in communicating
with patients.
>
B. Ancillary materials-like simple audio
visual aids, health education chiarts,
clinical photographs of patients with
I
external intestinal stomas would enable
the doctor to more effectively convey his
ideas to the patients.
C, Planning-This would involve the follow
ing steps.
i) Inclusion in
It is apparent that many of the problems
mentioned earlier are easily correctable with
little outlay of men or materials. The follow
ing strategy is suggested as a workable model.
DESIGN OF STRATEGY
Extra resources required
•'1
A.
1
Staff:
i) Mandatory—Nil as it mostly involves a
shift in emphasis during training with
existing staff.
ii) Optional—(a) It would be advantage
ous in certain special situations as in
Centra! Government Institutions refer
red to earlier, if language instructions
in the vernacular are available to the
3
VOLUME XX
the curriculum of
the
undergraduate and all other trainees,
instructions in the spoken form of
the regional language, as opposed to
the grammatical, right from the tihie of
admission. Attendance at such classes
should be compulsory and an evaluation
system introduced to increase motivation
for learning. Social workers may help
in this regard. The period of training
would Jasj atleast for a year at not less
than three classes per week. This of
course is a minor problem and exists
only in certain selected institutions.
ii) Impartment of basic training in patient
psychology during the first year nf the
clinical course.
iii) Shifting emphasis during the internship/
resident training period on the lines
SEPTEMBFR-DECEMBER
1901
suggested below
These constitute the
major recommendations and do not
involve extra resources.
Methods and Activities Required for
Implementation
Implementation of the above at various
levels would involve the following steps.
!
I
I
1
it
a) Personal example
by faculty/senior
colleagues. The importance of this
single factor cannot be overstressed and
it perhaps outweights in importance all
the subsequent points.
b) Instituting as far as possible continuity
of management from admission through
the period of hospital stay, operative
h
procedures etc. to discharge and further
to follow up. In practice there is no
allocation of individual responsibility
and several ranks of trainees are
involved in each patient's management
performing tasks allotted to them
according to their position in the
hierarchy
There is no shortage of
personnel in a medical college for
providing individual
attention to
patients, and since all doctors must
pass through the portals of a medical
college, the experiences gained during
their training here is likely to affect a
change in the future behaviour of all
of them.
c) A» an adjunct to the above, overlapping
responsibilities should be avoided and
trainees should be incharge of complete
care with senior colleagues performing
only a supervisory or advisory role.
DOCTOR PATIENT RELATIONSHIP. ... 85
d) Trainees must be encouraged to be the
primary focus of contact with patient—
i.e. all information must be passed on
to the patient through them. This is
extremely important in view of the fact
that they spend the largest duration of
time in the wards with the patient.
e) Institution of detailed discussion on all
patients especially those whose manage
ment is individualised, unusual or
controversial, between faculty and
residents. This must be done atleast
after every admission day or once a
week, preferably outside busy hours.
This will give confidence to the trainee
to communicate with the patient as he
will have the requisite background
knowledge.
f) Institution
of two
different types of
clinical rounds.
i) Teaching/academic conducted du
ring working hours.
ii) Service rounds devoted entirely to
patient management. These should
preferably be held in the evenings
when deadlines do not have to be
met for sending investigations filling
up requisitions etc.
Part of the
service round atleast, should overlap
visiting hours. In the presence of
relatives patients feel freer to
interact with doctors. Undergra
duates posted in the department
should be asked to attend these
service rounds so that they learn by
example.
i
VOLUME XX No. J
JOURNAL OF MEDICAL EDUCATION
86 THE INDIAN
may be learned in a short time and the
g) Provision of aids (charts, materials) to
evidence of learning may be seen at the end of
trainees so that they can be used for
the course. In contrast interests, attitudes and
demonstration to patients.
personality characteristics are assumed to
develop relatively slowly and to be visible in
i
of
facilities
to
recall
certain
h) Provision
appraisal techniques only over long periods of
patients at hospital expense
types of
<
time, stretching perhaps to years (Bloom et al,
(e.g. colostomies) for demonstration to
1964), The only sure guide to success of the
other patients.
plan would be an appreciable change in
patients’ feelings and response over a penpd
i) Trainees should be encouraged to visit
some
of
the
patients
and follow up
of time.
-- > on patients
living nearby. This impresses
An important cause of the lack of healthy
the fact that doctors care for them and
the
need
to
go
for
a
patient
doctor relationship is inadequate
on thetr part
motivation
in the trainees apart from the
follow up.
cooperation
factors
mentioned
earlier. It is suggested here
Departmental and inititutional
that
the
learning
experiences must be of a
needless to say is mandatory.
two way nature in which both trainees and
Evaluation
There are a great many ways
of assessing^
,phisticated
of
people's attitudes, the more so, .
which are known as attitude scales (Oppenheim 1966). A considerable part of the
hesitation in the use of affective measures for
grading purposes stems from the Inadequacy
of the appraisal techniquesand the casewrth
which a student may exploit his ability to
detect the responses which will be rewarded
and the responses which will be penalised
(Bloom et. al. 1964).
However, in the facet of doctor-patient
Interaction, no system of evaluation is required.
Complex abilities in the cognitive domain
teacher are involved in an interactive manner
learning by experience and example rather
than having one present
be
“learned” by the other (Bloom et al, 1964).
Such an atmosphere of personal exampip by
senior staff will go a long way in bringing
about the desired change in attitudes of the
trainees.
It appears that a small stress ‘in emphasis
during the formative period of training can
go a long way in correcting this lacuna in
patient-doctor relationship. Many of the
recommendations here apply to postgraduate
trainees but can be applied with modifications
to suit undergraduates and interns.
SEPTEMBER-DECEMBER
doctor patient relationship.
19^1
references
D. R. and Masia, B. B. : Taxonomy of Educational
1. Bloom, B. S„ Krathwol
r
be
classfication
of Educational goals — Handbook II: Affective
Objectives —
Domain, Longman Group Ltd., London, pp 7, 15, 16. 17, 19. 82, 1964.
or unstable ? Journal of Educational Research,
2. Drcssel, P. L.: Interests—Stable
:
48 : 95-102, 1954.
n
3. Furst, E. J. :
1958.
Constructing Evaluation Instruments, David Me Kay, New York,
4. Jacob, P.E.; Changing Values in College. Harper, New York, 1957.
5. Mayhew. L.B.: -And in Attitude.". Chapter 4 in Paul L. Dressel (EdJ. Evaluation
in Basic College at Michigan State University, Harper, New York, 1958.
«
6. Oppenheim, A. N.: Questionnaire design and attitude measurement. Heinemann.
London, pp. 105, 1966.
7. Tyler, R. W. : Constructing Achievement Tests. Ohio State University Pressa
Columbus, Ohio, 1934.
IJ.
8 Tyler R. W. : “The functions of measurement in improving instruction” Chapter 2
in E^ F. Lindquist (Ed ). Educational Measurement. American Council on
I
Education, Washington DC, 1951.
s
ft
=
I
I
I
I
i
87
health
M E f' S4
CELL
' J
1'
India
_ r
—
f ■
;'X
medico friend Z '
171 circle
kv
172 bulletin
k
■
I
I
mV
mHF
■F , •
May/JUNE 1991
- .
n
*
’
i
I
MEDICAL MALPRACTICE : WHAT IT IS AND HOW TO FIGHT IT
(Report of a Workshop)
Medico Friend Circle (Bombay Group)
The workshop was conducted in three sessions. (1) Irrational and
Unscientific Medical practices: This session discussed the variation
from rational and scientific curative medical care which was harmful
to the recipient. The pre-worksho'p coordination of this session was
done by Dr. Mohan Deshpande. He, along with Dr. Anant Phadke
(Pune) made presentations while Dr. Dhruv Mankad (Nashik) chaired
the session. (2) Negligence In Medical Practice: The pre-workshop
coordination as well as the chairing of the session was done by Dr.
Amar Jesani whereas Dr. Pritam Phatnanl (a well known forensiq",
scientist from Bombay) and Mr. Mihir Desai (advocate, Bombay)
made presentations on the subject. (3) Future Programme : DiscuaZ^
sion, Action and Organisations This session was cpordinated and
chaired by Ms. Annie George.
.
Introduction :
Rapid proliferation of private medical care sector In last two
decadesin ourcountry has brought in its wake the menace of medical
malpractices. Medicine has become a business. 80 % or more of the
health care services are in the private sector which operates in an
unregulated market. Compared to the other business, medicine has
ill^eputation of being more capable of generating what Is called
'Supplier induced demands.' In a way, the malpractices were always
a part of medicine but so far It was belived that they were curbed by
the Internal regulations of the profession or perhaps they were kept
under the lid by people’s apathy and by their blind faith in the noble
character of medical profession.
■ •?
■'
; t }■ . .
V
>• •
• •■ i
This is no longer so. The medical profession's credibility Is
nose-diving. The people have awakened to the reality of malpractices
and they are angry that many In the profession are now behaving as
merchants of death and diseases. However very few have clear idea
of what is malpractice and what to do when victimised by the
malpractice. Hence, the Bombay Group decided to organise this
vorkshopon September 9,1990, Sunday, at ICSSR Seminar Hall, JR
laik Bhavan, Bombay University Campus, Santacruz East, Bombay.
The workshop was attended by sixty two Individuals comprising
of medicos, Social workers, health workers, activists and Journalists.
I. Irrrational and Unscientific Medical Practices : (IUMP) :
IN his presentation, Dr. Mohan Deshpande, Identified five areas
of irrational practices, namely, (1) while actually tregting/investigat-•
Ing patient (2) While diagnosing the ailment (3) concerning the
relationship with the drug industry, (4) concerning other doctors and
(5) miscellaneous. He grouped irrational practices In these areas Into,
three categories, (a) Overt and intentional, wherein the doctor know
ing fully well that what he/she is doing is Irrational, resorts to it for
some other gains (money, prestige, holding on the patient etc.) (b)
non-lntentlonal: Here doctor Is Ignorant of the Irrational nature of his
practice, (use of banned or bannable drugs, anti- cold preparations
having multiple drugs in them etc.) (c) Gray areas: The interphase of
irrational and unethical practices (high rate of caesarian due to
over-cautious approach, use of routine ECG, sonography done on all
pregnant women etc.). He gave numerous examples of Irrational and
unethical practices to support his arguments. He concluded his
arguments by stressing the need to study epidemiology of Irrational
and unethical medical practices.
-
The Invitation letter for the workshop made an attempt to define
medical malpractice. It was suggested that discussing malpractice
was essentially a discussion on a larger aspect of medicine, namely,
the medical practice. The Medical malpractice was, therefore, In Its
broadest meaning, defined as " a variation (it can be graded) from
the normally acceptable, scientific and average standard of medical
practice at a given point of time."
Organisation of Workshop:
A packet of background material was prepared for the par
ticipants. It contained : (1) "Irrational and Unethical Medical Practices"
by Dr. Mohan Deshpande (2) "The Political Economy of Medical
malpractices In India" by Ravi Duggal (3) "Patient’s Right" by Anil
Pilgaokar (MFC Bulletin No : 146, Dec. 1988) (4) "Medicine and Law"
issue of Radical Journal of Health (March 1988), particularly "Medical
Malpractices and Law" by Mihir Desai.
The second presentatiqn was made by Dr. Anant Phadke (Pune).
He concentrated on identifying irrational practices on priority basis
so that a group like MFC can tackle the problem in an effective way.
He suggested three criteria for identification. Firstly, how common is
1
\
■
1
»
p
tho rnalpiaclico? f.H’conrfly, what levol of harm (financial and physi
cal) doos it cause? and Thirdly, Is it amenable to action In short or
medium term (say in a year or two)? He also connected this to the
availability of human power, expertise, resources and time with us.
He recommended four areas for beginning the campaign, (a) Overthe-counter (OTO) drugs (b) Misuse of injections (c) Misuse of in
travenous injections (d) Screening tests for people who have no
clinical symptoms. For the last he gave example of ECG (electrocar
diogram) which is used as screening test for people over 30 yrs. of
ago. I Io argued that such test is giving significantly high false positive
diagnosis of heart ailments. Similarly he mentioned misuse and
wrong use of stress test (to detect heart ailment) and angiography
(where patient is not informed of costly operation needed (if th© test
is positive). Tho also raised hissue that at many places the cardiac
monitor is kept as cosmetic device to fleece the patient as such
hospitals don't have a trained professinal to monitor the cardiac
monitor.
form for procedures should be case specific and must have full
details of the pros and cons of the procedure. The same should be
explained to the patient. (16) The drugs distributed In medical &
diagnostic camps are irrational (17) The doctors cannot refuse to treat
serious (e.g accident) patients (18) For "good" doctors it is not suffient
to follow ethics. They must make their 'passive ethics' into 'active
ethics' and thereby join forces with the people affected to bring about
changes in medical practice.
Dr. Dhruv Mankad, the Chairperson, summarised the discussion
and Identified issues lor discussion in the third session.
II Neglegence In Medical Practice:
Dr. Pritam Phatnanl made a detaile’d and informative presenta
tion. He started with the question of how to define negligence and
then explained the remedies available to the patient.
Negligence is a legal concept and /comps under the law of tort.
When A owes duty of care of B, and there is breach In duty and B
suffers harm, A Is said to be neglegont. ’Ihus there are three basic
ingradients, (a) duty of care to patient (b) dereliction of duty (c)
patient suffers damage directly due to the dereliction of duty. Thus,
legally, if there is no damage, there is no dereliction of duty. For
instance, if hands are not scrubbed and needle, syringe,forceps e
not sterilised before giving Injection, and there is no harm coming
patient due to such 'malpractice' legally, the doctor is not neglcgent.
The presentations wore followed by Intense discussion In which
many participants asked questions and raised new points. The con
tribution of participants is summaraised below:(1) Wliy to restrict only to the allopathy? Is it a Malpractice when
a non-allopathic healer practices allopathy in a village where al
lopathic doctor is not available? (2) Is the use of PAP smear as a
screening test (like the ECG) irrational and harmful? (3) What Is the
role of drug and instrumentation industry in encouraging malprac
tices? (4) How relevent is the text-book knowledge in actual practice?
Is there a need to change syllabus in medical education? (5) There
is a target oriented approach in certain govt, health programmes, eg,
Family Planning. Is such an approach a malpractice? Similarly there
are certain industrial malpractices affecting people's health, e g.
Bhopal gas disaster. Do we include them In our struggle against
malpractices? (G) I here is one doctor (of all systems taken together)
for 800 -900 persons in tho country. However there is overconcentra
tion of them in urban areas. This leads to overuse of medical care in
urban Meas and underuse in rural areas as In tho health care, there
When there is harm sufferred, the aim of civil law is to monetarily
compensate the person who sufferred the harm. Whereas,the aim of
criminal law Is to book the doctor, but in’such case the patient must
prove beyond doubt that a particular doctor committed the crime. In
the Civil case, the onus lies on the patient to prove harm and it's
connection with the negligence. Thus, there is a preponderance of
evidence.
About medical records, he said that there is no specific law in our
country but it is assured that records belong to the doctor (in private
practice) and to the hospital (in case of hospital case). However,
some participants disputed this assumption and argded that it can
bo successfully challenged, using the constitutional rights.
>s supplier induced demand. Further, unhealthy competition in the
urban areas is leading to "crimlnalisation of medicine." Three ex
amples from Bombay were cited. Firstly, murder of a doctor by the
goons of other doctor. Secondly, a cardiac surgeon was slabbed by
goons of another doctor. Thirdly, increasing Investment by builders
and mafias in the nursing homes. (7) Irrational use of medical
technologies in the urban areas whereas the same is not available for
even emergencies in the rural areas. Two examples, first, the sex
determination used for female foeticide but not made available to
women in Bhopal who needed it to delect genetic defects due to gas
effect. Second, cesarian section overused in urban area but not
available to rural women when they really need it. (8) Is the structure
such that malpractice is inevitable ? for instance, It Is difficult to get
rational single ingradient drugs. (9) There is a political aspect of
malpractice, e.g. the doctor colluding in torture in jails, lock-ups etc.
(10) There is no stringent internal regulation of medical profession,
nor thereis regulation of medical care market. Doctors are dependent
on the drug industry for information. Very few subscribe to medical
journals and read them. WTiile drug industry targets doctors, the
instrumentation industry is directly approaching people through
media. (11) Doctors can be educated by other doctors. For this, build
credibility of the MFC in minds of doctors. (12) A mass educational
programme of people on drugs and diagnostic procedures is
needed. (13) 1 he doctor's education should begin with unintentional
irrational practices and alter attaining some success,
embark
an education on intentional practices.
’• m'md standardisation
In health < are, right tn information, (]ir',';lion tho role of institutions
like ICMR in perpetuating malpractices (n.g. Infertility and in - vitro
fertilisation,
NED
FN
injectable
contraceptive
etc),
the
manufacturer's "insert" should not be "jargons" but in simple lan
guage that the patient can understand, and so on. (15) The consent
The concept of reasonable case is related to the qualification and
experience of doctor. Moreover, the doctor is duty bound to keep
pace with advances in medical science. In case of camps (eg. eye
camps, FP camps), if there Is any mishap, tho organisers can be held
responsible. The product liability (in our case, eg. drugs) lies with the
industry. The industry is supposed to Inform the doctor who in turn
is liable to inform patient. Legally, in private practice, tho doctor has
a right to accept/refuse patient on certain grounds but the refusal
should not bo discriminatory based on casto, religion, race etc.
Doctor's 'duty of case’ starts from tho moment tho paliont
accepted as liis/her own by the doctor and not necessarily that fee is
charged. The doctor patient relationship is governed by law of
contract. There are certain features of contract. (1) Both the parties
should be competent to enter contract (2) they should be doing it
willingly (3) the contract has it's dos and don'ts, ie, to do certain things
and not to do others (4) a breach of it is liable for compensation (5)
the contract is about something needed. Once the "duty of care"
starts, tho contract comes into existence. The doctor must take
history, examine patient, carry out tests to diagnosis, reach
provisonal and confirmed diagnosis, treat the patient. If the doctor
does not do any of these, there is breach of duty. The medical record
must contain information on all staled above. In addition.it should
have if any, opinions ol treating doctor, consultants etc. and in case
of death, post maitcm report. I lowevor, wrong diagnosis alone is not
negligence provided, all steps and procedures staled above are
properly followed. At the same time it should be kept in mind that
there is a thin line dividing genuine error of judgement and
negligence.
2
How long are the medical records maintalned/preserved? There
Is no definite law. However, one can file a suit within 3 years from the
date of occurance of negligence or from the date of discovery of
negligence, whichever is later. In case of children, the suit can be filed
3 years after attaining majority, so In the case of children, the medical
records ought to be preserved/malntalned for longer time.
.
medical practice by the profession. (4) malpractices In medical
research (5) Malpractices related to human rights violation (6) target
orientation in health programmes, ’Camp’ approach etc.
Methods for Action : (A) Demand based campaigns (1) right to
Information (2) standardisation of medical facilities and charges (3)
guidelines pertaining to duties of doctors In the case of human rights
violation (eg. torture) (B) Educational Campaigns : (1) Know your
health rights (2) Consumer awareneas (3) to reach out to people
through media, particularly, vernacular press. (C) Individual litigation
: (1 )helping victims of malpractice in fighting suits (2) filing public
Interest litigations.
The doctor cannot treat patient against will, hence, consent Is
essentail. But the consent does not absolve doctor of the charge of
negligence. The consent has six ingredients, all of which must be
fulfilled. (1) the patient must be competent to give consent (l.e. above
18 yrs, mentally sound etc.) (2) It must be free (voluntary) consent
(one cannot use duress, fear of life or death etc) (3) it must be
Informed consent, l.e. the patient must be informed of procedure In
language and words he/she understands. The information must
Include advantages and disadvantages, other alternatives, etc. The
final choice of selecting from alternatives must be that of patient. (4)
It should be Intelligent consent. Thus, it is not sufficient to give
Information, but the doctor must cross-check to find out that the
patient, has properly understood the Information provided. (5) The
consent must be specific, l.e. specific to the procedure undertaken.
If another procedure Is to be done, new consent must be obtained.
(6) It must be expressed consent; i.e. in writing. Normally, for surgical
orocedures (diagnostic or therapeutic) expressed/written consent is
obtained. But for medical examination, giving injections etc. the
consent Is supposed to be implied if patient volunteers to undergo
them.
In the discussion that ensuecj, there was a general agreement on
all except one, namely, to get-involved In individual litigations. The
discussion on this area of disagreement was sharp and heated,
primarily because the Bombay Group is already
already involved In this
method of action. Two viewpoints came to the fore and as it happens
with such strong disagreements’, the workshop could not satisfactorily resolve them.
__________________________________________ a*
a
aa
*
a
a
a
La
. a
«
a
The first position was not ptinciply against undertaking individual
litigation but felt that it should be taken up aftehvards at an ap
propriate time to produce desired effect. In support, this position
advanced following arguments : (1) We are a small group, our first
task is to attracts doctors to our cause. (2) This can be done best by
starding with unintentional irrational practices. (3) Individual litiga
tions would demand lots of time, energy, study and labour. It would
also involve fight against corrupt medical and legal estblishments.
There is also a possibility of threats, goondaism, victimisation etc. (4)
the struggle against malpractices can make an Impact only if we have
a critical mass of doctors to be part of struggle. In order to do so, a
strategy must be worked out. Such a strategy must prioritise tasks
keeping long team Implications.
Dr. Phatnanl explained that In our country the law of medical
negligence is only recently used, and therefore, it was necessary to
select "good" cases to develop the law for taking legal recourse
against Irrational practice, he Identified two ways, (a) When there Is
side effect due to unnecessary/ Irrational medication (i.e. patient Is
harmed), It can be construed as harm due to negligence (b) It pan be
said to be tresspass against the body.
The second position not only thought it appropriate to take up
individual litigations but considered it as a better strategy to attract
commited doctors to the movement. Following arguments were
advanced : (1) Individual litigations also bring out general issues like
right to Information, what regulations for nursing homes/hospltals
etc. (2) Once we educate people on their health rights, we should L»
with them when even one of them wants to take legal action. (3) We
are neither pro - doctor nor anti - doctor. The issue Is that of malprac
tice. Those who are against it are with us, the rest not. (4) We can't
create critical mass by taking "soft" issues, because hose who come
for "soft" issue may desert us when we take up "ha d" Issues. Thus
even those ethical practitioners who don’t stand up £ £gainst malpractices are weaklings arid will ally with the establishnvient. (5) Only a
sharp compaign will polarise the profession, (6) Can we, ethically,
refuse our help to the victims of malpractice ? (7) The best way to
win over reluctant ethical practitioners is to have strong campain
against their harassment and victimisation.
%
The second presentaion was made by advocate Mihir Desai. He
informed that law on medical negligence Is a judge-made law. Thus,
unless more cases are tried till the end, the law can not be properly
developed. He explained that the doctor never guarantees correct
diagnosis/care. But guarantees correct method to reach diagnosis
and to take care.
What is standard care? How Is It measured? It Is time and location
specific. In the developed countries It is only time specific as location
- wise the same standard is demanded. However, perhaps, the
locality rule may apply In India as say for example, the facilities
available in the rural and the urban areas are different.
The Civil law is used to get damages from individual doctors or
the hospitals. Especially when more than one doctors are Involved In
care, the law of vicarious liability is used to sue the hospital. In
criminal law, only individual(s) can be sued because the hospital
can't be jailed. One can go to the medical council when unethical
practice is Involved and there the maximum punishment for the
doctor, if proved guilty, Is deregistration.
The discussion ended without resolving the issue. But it was
agreed that the Bombay Group will continue with Its work on malprac
tices and the same can be reviewed from time to time.
About medical records he agreed that there was no specific law
but argued that one should fall back on constitutional law. Normally
now the court instructs hospital to get the records. But this should be
recognised as patient's right, and if the medical record is withheld
from the patient, It should be considered a criminal offence.
It was also unanimously agreed that MFC should coordinate with
other individuals and organisations to develop effective campaigns
on the issues identified at the workshop.
Ill Future Programme : Discussion Action and Organisation
Report prepared by Amar Jesanl, from the notes of Dhruv
Mankad and Saraswathy Anantaram
The session chairperson, Dr. Annie George, with the help of Dr.
Dhruv Mankad Identified following issues which emerged from the
previous two sessions for discussion.
( Note
7 he workshop background material Is available on
payment of Rs. 20 = 00 to The Coordinator, MFC (Bbiimbay
,Group)
___ r,
310, Prabhu Darshan, 31,S. Sainik Nagar, Amboll, Andherl West,
Bombay - 400058, Tel: 6230227)
Issues for Action : (1) Drugs, particualarly over-(he counter drugs
(2) Screening tests (eg. ECG, Pap smear etc) (3) Self regulation of
3
I
i
COMMUNITY HEALTH CEIX
V Main, I Block
India
)
Editor'# Noto
Malpractices-lntentional or otherwise - in medical care have by
now become a serious public health problem and not confined to
individual clinics or happenings in isolated surgeries. Agressive over
use of drugs and other Interventions, bleeding the patient for money,
rackets of referral, negligence have all acquired qross proportions In
the medical bazaar monopolised by doctors of all hues and degrees;
although it Is heartening to note that there are many who are willing
to stem the rot.
practitioner. (2) Overuse of antibiotics Including higher an
tibiotics (3) Overuse of useless drugs - like tonics etc. (4) Overuse of
steroids and some other select catagories (5) Unnecessary Injection ’
- almost each patient receives and injection or two. (6) 1/V infusions
for any and every occasion - now this is the most popular means of
making quick money - Rs 60 to 100 a bottle within 15 -20 minutes 10 such patients a day and the doctor touches thousand Rs a day
practice. (7) Subjecting patients to unnece^say referral to obliging
consultants and thus carrying more of hysterectomies, tonsillec
tomies, appendicectomies and other procedures. (8) Exhorbilant
fees.
That Bombay MFC group has embarked upon a real fight is quite
evident from the accompanlng article. Bombay Is the commercial
leader and Its practices and malpractices are picked up sooner or
later by professlnals elsewhere and in this sense it is a fitting start in
the right place. While writing this editorial I also feel that it is a duty
for all like minded activists to help the
So here Is a strange situation - JgQolance and yet agression on
the part of the doctor; and ignorance and helplessness of vulnerable
community.
So for the rural situation,- this is my personal opinion - following
line of action should serve well.
‘
cause, so that the group does not experience Isolation.
1. Necessary changes in legislation to accomodate package of
allopathic drugs and procedures in non-allopathic practitioners range
of services - with due training and certificates etc. ; also fixing the
rates of fees for particular services. And ofcourse strict enforcement.
* The Bombay group will no doubt go into the intricasies of
malpractices that are commonplace to Bombay and similar situa
tions. But there Is a rural dimension too. To start with the current
legislation, even if enforced meticulously, can not obviously take care
of the rural situation. The existing legislation generally appears to
protect the right of the patient (only the qualified doctors should
s diagnose, treat etc.) but its original historical purpose was to protect
the interests of the medical profession, (and ‘wood out' the nonprofessionai health care) and this element persists alloast as a sido
effect. This effect would be all more obvious if we imagine the rural
situation. First of all the rural areas are underserved since qualified
doctors'are unwilling to work in rural areas. Majority among them are
non allopathic but would use nothing but allopathic drugs. What do
we make of this situation ? Eulogise this ? Ban this ? Regulate this
?and how ? I think the current legislation can not allow this but law
enforcement is absent from the scene. Secondly, we have to make a
due legal slot for our ANMs, Health Workers etc., if wo are to squarely
face the paucity of services for rur al communities. The law Is nearly
, mute In this ( except tho statement on midwifery services that are
; deleted from medical Intervention )
2. Accomodate health workers (in a minimum essential cur
role) in the legislation- fixing a list of drugs & procedures
.3. Regulation of private clinics/ Nursing homes
4. Community education in select topics of strategic Importance
e.g. l/V infusions, injections, Antibiotics, select clinical conditions
capable of becoming mothers. By involving ANMs as motivators in
(diarhoeas, Pneumonias),services available at PHC etc.
5. Strict Regulations of medical stores - prescription etc.
6. Sample audits of cases/ rcords etc by medical college
staff/Direclorate of Health Services (?)
7. And alleast one institution (RH) in a block that ensures-good
quality medical care to tho community without malpractices &
negligence.
<.
For the average rural general medical practice I would like to mark
out these as problem areas (1) Noldiognisinglhe sickness, or making
a wrong or 'too late' diognosis - all this Is usual with the non-allopathic
THE WILL TO SURVIVE : Aditi Iyer
How Auxiliary Nurse Midwives cope Within The System
t
not bo met, ho started using physical violonco to bully her. Ho was
unemployed, had a drink problem and gambled. Finally, he went on
and married for a second time leaving Sr. Shanti nursing feelings of
vulnerability and anger, a few broken teeth and a stunned sensibility
that she must somehow get on with building her life again. By the
time she applied for the D.Ed course, she was rejected because of
her age (she was over 26 years old at that time), and was declared
as being 'unelogible" because of her declaration of her marital status
In tho necessary forms.
Sr Renu was deserted after 14 years of marriage. Her husband,
a taxi driver in Bombay, had an affair with another woman. When he
left, Sr Renu's whole life changed. Till then, her existance seemed to
revolve exclusively around conjugal and domestic duties. Earlier,
when she wished to teach In a Primary School, the choice was denied
to her by her pregnancy -one In four - and her husband's refusal to
grant her permission. Finally, after 14 years (and four children), with
nothing but a Std 10 education, Sr Renu was thrown to her own
devices. Site heard of nursing and tho ANM's course and though she
knew nothing of what the job Involved, she recognised tire potential
of being economically self sufficient. This was to be a regular job. A
job she needed very badly.......
This was during the mid 1980’8 when an expansion of the health
Infrastructure was accompanied by a shortage of nursing personnel.
Sr Shanti applied and got in as an ANM. Since then, she has managed
to support not only herself and her children but has been able to
contribute substantially to the upgradation of the family land. She
depends on the health services for her livelihood and can't afford to
Sr Shanti was married to her cousin while she was still in school.
This was an arrangement worked out by her fattier who had only a
modest Income coming through cultivating 7 acres. This was
countered by the additional responsibility of building up dowries for
his 5 daughters. However, Sr. Shanti has reason Io rue tier life. I ler
husband soon started making dowry demands and when these could
let it go........
4
The fact that ANM's play a subordinate role within the administra
tive and functional structures of the health services is obvious
enough. The knowledge that empowerment of women is only partial
ly achieved by participation in the labour force is well known. What
makes ANM's like Sr Renu and Sr Shanti more vulnerable is the fact
that their lives are precariously dependent on their jobs.
FORM IV
1.
2.
3.
This article strings together the experiences of a few ANM’s as
they try to cope In a spirit of survival, within a system that empowers
them on the one hand, while creating and justifying their subordina
tion on the other. This Information has been gathered while travelling
through four districts of Maharashtra : Pune, Wardha, Beed and
Ratnagirl.
4.
In the PHO approach to health care, women are viewed as mere
targets - especially those women who are mothers or potentially the
Family Planning and MCH Programmes, the bureaucracy uses Its
women workers to circumscribe the scope of ’motherhood' - the
"idealised state of being for women"! - within those definitions that
are approved by the State.
5.
6.
This creates problems for ANMs.
Sr Renu, who works In a tribal PHO of Pune District, was faced
with some truisms when she set out to explain sterilisations to some
al women. They faced her and said, "you do not want us to have
_ j sons. Alright, give us yours then." Sr Renu was shocked and her
son who was accompanying her was upset on hearing this. Later, she
had a hard time assuring her son , who was already disturbed by the
changes in the family, that she did not intend to send him away.
I.
ANMs live on the edge both within the health services and in the
community as well. The health bureaucracy is quick to penalise their
workers for not fulfilling targets yet take little care to ensure that
adequate supplies and support services reach them. ANMs work
within these constraints, with limited resources, but a determination
to build up legitimacy and respect for themselves.
Sanjeevani Hospital, Dindori,
Nasik.
Periodicity of Publication
Monthly
Printers Name
Sham Ashtekar
Nationality
Indian
Address
Sanjeevani Hospital, Dindori,
Nasik.
Publisher's Name
» Sham Ashtekar
Nationality
Indian
Address
* as above
Editor's Name
Sham Ashtekar & Anita Borkar
Nationality
Indian
Address
.41, Anandvan,
.Yeoleka rMala,
Nashik - 422 005
Names & Addresses of :
Anant Phadke
Individuals who own
50, LIC Quarters
newspaper and partners
Pune 16
or share holders holding
more than 1% of total
capital
• :
Place of Publication
Sham Ashtekar declare that the particulars given above are
true to the best of my knowledge.
Dated : 31-3-1991
Sham Ashtekar
Publisher.
In the face of unrealistic targets, some ANMs are compelled to
show fake cases of Copper T, oral and nirodh. However, not all ANMs
are ready to challenge the necessity and value of having targets In
their work.
, ANMs do curative work in a limited sort of way. Most of the time,
they do not have adequate medicines to last them through to the end
of the year. Given the distances that need to bo nogoclalod Inorder
to reach a dispensary, people look towards the ANM for their supply
of medicines. When stocks of medicines do not suffice and the ANM
Is forced to send patient away, she is charged with being Involved In
their welfare for selfish reasons.
Sr Shanti takes a moderate view as she looks qt problems within
the system. She says, "If targets are removed, some ANMs will work,
some won’t. Targets are needed but the authorities should be less
rigid about it than they are now. The way targets are enforced, the •
pressures it creates, makes ANMs do "khotha kaam". So Instead of
spending so much money on copper-T's all of which may never be
Inserted, the government should concentrate on supplying adequate
meicines and Injections to us."
Sr. Lata, like Sr.Shanti, Is acutely aware of this. In order to ration
stocks, she gives her patients less than to the prescribed dosage - 2
tablets instead of 4 - and takes care never to question the authenticity
of the complaints of her patients. That way, she projects herself as
being a pereon who can be trusted upon when they need her. In cases
here medicines do work, they provide her patients with temporary
Jef. Nobody goes back empty-hended after approaching Sr. Lata
and she is richly rewarded by their respect.
Sr Renu, on the other hand, questions the system within which
she Is being made to function. She slates categorically, "1’11 tell you
the truth. Where I work, people have no demands from us. They work
so hard that they have no time to think, let alone ask for health care.
They have no time to be sick. What they need is a release from
poverty, not family planning!"
Owing to the primacy that is placed on the Family Planning work
over all other activities, many ANMs draw up the link between the two
In their own way. So much so, that their Involvement In deliveries ,
Immunisation, ANC/PNC are perceived as preconditioning factors for
motivation. Sometimes, curative work is also placed within the per
view of family planning.
Family Planning, especially the target approach, has set up the
practise of depersonalised Involvement. This Is particularly apparent
in Wardha and Ratnagirl.
Sr Lata, who works at Wardha, is just one person among several
others vying for targets. The teacher, talathl, gram sevak, the second
Mediclal Officer and compounder have the same interest In seeing
that their targets are completed. This sets up a market situation at
the villae level where the price for an operation is set up according to
the competition prevailing at the moment. For ANMs, this works out
to Rs.200.00 per case as her personal contribution In addition to the
official rale of Rs.130.00. Further, this practise Is fully endorsed by
the authorities at the PHC level who evince more Interest In ensuring
that targets are being completed rather than understanding the
mechanisms that are brought to play In the process.
Sr Anandibal, a veteran In her 50’s has had to use her wits to
survive in the system. Her medicine kit is more Incomplete than
complete. Instead of having to explain her inability to provide
medicines, she has sot up a small private practise in the village, she
purchases vials of basic medicines and administers Injections to her
patients. When It comes to charging them, she forfeits her "fees" from
those who have had operations registered under her name and
charges Rs.4/- from those who haven't done so.
5
X’r. Xiavi Malayan.
Community Health Cell.
326 V Main , 1 Block
Koarmangala.
Banglore- 560 034
^^014/5
Sr Lata, however, is lucky. She pays an average of Rs.100.00 per case. This Is
because of her policy of looking after every need of her subcentre population. By
doing this, she ensures that her family planning work is simplified - and made cheaper
- for her.
MEDICO FRIEND
CIRCLE BULLETIN
For Sr Sulochana, family planning has become the bane of hqr existence. Sr
Sulochana, a Gond woman, took to nursing so as to strengthen the family's economic
position and to protect herself from the marital disharmony that-she was experienc
ing. She imagined that her life would be easy after she started working. Unfortunately
for her, her life has been far from smooth.
w .
Editorial Committee:
Abhay Bang
Anil Patel
Binayak Son
Dhruv Mankad
Dinesh Agarwal
Padma Prakash
Sathyamala
• Vimal Balsubrahmanyan
ShamBorkar
Ashtekar V
Anita
1 (Editors).
When she joined the services, she was taken on as a temporary member of the
staff with a 11 month period of probation and the possibility of being removed from
service without being assigned any reason. Her term ended in December and three
months later she was dismissed without intimating to her the reason.
Sr Sulochana attributes this to the fact that, In the 13 months cT her service, she
was able to complete only one case due largely, to the unfamiltar nature of her job
and its accompanying apprehensions.
For Sr Sulochana, this meant more than losing a job. It meant a loss to her newly
found freedom. She didn't have a union to go to for redressal and so fought her battles
alone. With the help of her neighbours who were lawyers, she filed a case in the high
court but the proceedings, far from questioning the rationale of targets, Implicated
her "non-performance- and begged for reinstatement.
Editorial Office:
c/o Abhivyakti,
41, Anandvan,
Yeoleka’r Mala, Nashik-5.
Since her reinstatement, Sr Sulochana concentrates on surviving within the
system, having been made a victim of it once. She concentrates on family planning
to the virtual exclusion of all other activities. As part of her motivational strategy, Sr
Sulochana promises and conducts follow up services which takes the form of weekly
Injections of B Complex. She does this with her own syringes without always taking
care to sterilise the needles after each prick.
*
Subscrlptlon/CIrculatlon
Equlrles:
Anil Pilgaonkar,
36-B Noshir Bharucha Marg,
Bombay - 400 007
Subscription Rates:
Annual
Inland (Rs.)
a) Individual
30
b) Institutional 50
Asia (US dollars)
6
Other Countries
(US dollars)
11
In spite of creating an effective work record, Sr Sulochana Is still issued 6 monthly
orders. She has yet to complete 6 months of the Step Ladder Course (she doesn’t
get certificate till then). And she can't become permenent till she completes the
course. She has been moving around in cicles Inspite of making a number of
compromises in work. Sr Sulochana angry and alienated from her work and with good
reason. She Is never sure for how long she is going to have her job and the thought ■
of returning home and to her old life scars her Immensely.
Life
XX)
500
75
ANMs In Wardha District have fell the absence of a strong union very strongly.
Suspensions or the threats of suspension have become a recurrent feature In their
careers. They live constantly In a state of tension and wonder when turn might come
next. Some of their colleagues have been brutally raped and murdered.ANMs accuse
the DHO's office of doing nothing to help matters for them. No inquiry. No promise
of support to new recruits who fear their safety. At Ratnagirl, the CEO calls ANMs
"administrative nuisances" and feels that motivation is a bad word In a democracy
that has no discipline. He laments that the country is going to dog?....... ‘
125
Please add Rs. 5 to the outstation
cheques.
Cheques/M.O. to be sent In favour
of :MFC
(Ad. Dr. Anant Phadke, 50, LIC
Colony, University Road, Pune
411 016, India.)
The bureaucracy feels that it Is helping ANMs, but by the attitudes and indif
ference of its officers, no trouble is being taken to find out the odds under which ANMs
are compelled to work. Workers' Unions, like the ones in Beed and Ratnagiri, provide
some solidarity but tend not to look beyond the confines that are drawn up for nursing
within modern medicine. Their victories are transient and their battles are never quite
finished. What needs to be done is to help ANMs look beyond the next hurdle the
next case for family planning or the next immunization camp - and to question the
assumptions that underlie all that they do in the village community
Published by Sham Ashtekar for
MFC and Printed al Impressive
Impressions, Nashlk.
Views and opinions expressed in
the bulletin are those of the
authors and not necessarily of the
organisation.
CORRECTION
The theme for the forth coming Annual Meet ( September 5, 6. 7, th 1991 )at
Bombay is " Private Sector In Health Care : A need for regulation
6
Posted at Nashlk Head Post Office : Postal Registration No. NSM -135
)
INTRODUCTION
There is at the
out on human «
is expected that
of clinical i
volunteers
increase in the
number of
easons.lt 1S being mcreasmgly felt by sclent ists , cl inical
investigators and national health
authorities that the resources of the
country should be utilized for carrying out r-research that would be relevant 1to large numbers of persons living in rural
-.-1 areas in order to deveiop appropriate health
measures for such persons
Th i s wou1d result in
an increase
in the c
r:
epidemiological
and sociological oriented
involving large numbers
of individuals. Further, there is growingresearch
awarethe scient‘fic community that results
not ^ays predictive
predictive of
of what would r ------------- on experimental models are
eventua11y c
‘
occur
in the human and
thata fewweH1 control
controlled
investigations
led
■
on
a
1
imi
ted number
—of human
subjects for a r’
•
*
relatively short duration
---information than a large .number of animal would yield much imore
relevant
experiments carried
longer period of time.
-J
out for a
This awareness
and the fact that in certain
areas of research there
are no animal models at all wou1d 1ead
increasing number of I.
also to
human subjects being involved in
clinical research.
Finally, research on cl ini
■•ical
evaluation of remedies
used in indigenous
systems of medicine and on Plants reputed to possess therapeutic
ties is also increasing,
- properInis factor
together with the conri
for clinicallyV evaluating new drugs developed in national
nuing need
and inst i tut ions
1aborator ies
3nd
would again rretire cHnic fTria^rt^be'00565
:.e country.
tO be Carr'ed out on
subjects
throughout the
CONSIDERATIONS INVOLVED
g
d
g
•d
re
he
rito
ed
In add i t ion to the
increased quantum of medical
research being
undertaken (on human subjects, i
Clinica' investigation- has
also undergone‘ a change in the e!SC?P!
ast decade.
The type of experimental
procedures that a patient is submitted
varied as the complexities of medical
to has become more complex and
research have increased.
ig^s clearly understood that
on huml^ subjects if progress is it is essential to carry out research
to be ma inta i ned and better medical
and therapeutic moda1ities discovered
-.-J for the benefit
— of man.
It
is
equa11y cI ear that such research
on
human
subjects
and
c iated wi th some degree of risk
patients is assoto the individual patients <
The Indian Counc
—
or volunteers.
-------- i
) 1 of Medical
Research (ICMR) feels
that in view of the
increasing
iresearch
----- - ■ — —being
carried out on human subjects and
e
J
• ■ ■y
vail
---- i
the ever
widening complexities of medical
1
research, guidelines
for experimentation on human subjects in the
country are
required to make certain, as
far as poss i b1e:
<—
INDIAN COUNCIL OF MEDICAL RESEARCH
Delhi H9016
Febw&ry 1^80
t
that the rights and welfar
re of human subjects on whom
experiments are carried out
-c are adequately protected;
.^8?
that the risks
t*
to an individual
are outweighed by
potential
benefits to him or to society or by the
importance of the
knowledge to be gained;
■
a
ng
lew
:al
— of
? cts
-1—' nt.
old
hen
any
5
1
ial .
t m
e in
in-
2
3
that informed cconsent is obtained From the individual
by methods that; are appropriate and adequate;
■'sW
that the clinical
iinvestigation on human subjects is
carried out by an investigator
who
ti._ requisite
.
2__
__
- has
.-3 the
background and competence to carry out such research;
and
- that the
investigator has a framework for obtaining
advice, _support and assistance from his peers before
fembarking onya particular clinical research programme.
It is hoped that these guidelines
formulated by the Central Ethi^
in clinidO
the
princi
nine
.
kJ.
ples^ enunciated in the World Medical Association Declaration of Helsinki
(1964) as modified by the 29th World Medical Assembly
< at Tokyo in 1975
and the Nuremberg Code which has clearly laid down thet ten principles to
Committee of the- Council
—---- - would
••—.J assist investigators involved
research to plan their clinical1
research in accordance with
m
- JK-
a
L. —
_t
be kept in mind when conducting research on humans.
It is expected that
the guidelines would protect volunteers and
and patients
patients participating
participating in
clinical
research from being exposed
exposed to
to unjustified
unjustified hazards
hazards and risks
during their involvement in the research project.
These
These would
would also
also pro
;__
tect clinical
i------- ’
■
investigators
and researchers by enabling
them to obtain
support from their peers for the research they intend1 to carry out.
and
ethical committee
and rev ew =j1
ee
i
r
should rmeet at
c 1 i n i ca1 research n
eVery three months
every
by investi
Committee
shouldsearch
aassessproposed
R after approval by the
fall such
nvestl 93tors
all
such
shouldJ the resenr^
investigator and his •u
en committee
•
research be 1n,tia ted and
nis co-mvesti
co- i nvest iqators ...
by
The ethical
human subjects to co/nmTttee should
assess.
research on
voluntary
consent of the individ-' is being obtained;
the experiments are so
designed that
i‘
mean i ngfuI
they 1
’ ■
results that
would yield
could not -be obtained
methods;
by
/ other
the animal rexperiments carried
for clinical
out-support
the need
experimentation;
the ('
”—
experiments
would
-11
unnecessary phjs ica?
avoid al
and injury;
Physical
The Council would,therefore, urge all medical colleges and research
centres involved in clinical research to form ethical committees if they
do not already have a functioning ethical committee at the moment. The
ethical committee should consist of experienced clinicians who have been
Carrying out clinical research and clinical evaluation in the past,
should have on it an expert on drugs and one or two non-medical persons
who could provide guidance to the committee in the matter of ethics and
law.. Wherever possible, a lawyer or a judge should be a member of the
institute ethical committee. It is suggested that the ethical committee
be kept fairly small (5*7 members) but that appropriate expertise avail
able at the centre, in the region or the country be consulted wherever
necessary. The ethical committee at any institute or college should not
hesitate to have on it members from other institutes, if there is need
for such a step.
and mental
manner to
suffering
the c**
—
experiments
have been
the degree c
Planned in a
of" risk to be
manner so that
that <■
determi ned
taken should
by the I
.f
never exceed
prob I em
humanitarian
—’ to be solved
importance of the
by the
INSTITUTIONAL ETHICAL COMMITTEES
The Council feels that clinical research on normal volunteers or
on patients, whether for therapeutic, non-therapeutic or diagnostic purposes, should be undertaken only after an ethical committee of the concerned i ns t i tute or col lege has gone thoroughly into the proposed
research, assessed carefully the balance between
the possible benefit tothe patient/volunteer or to society and the potential risk to the individual participating
in the trial and on the basis of such an assessmen^^
has
approved the project from an ethical ooint of view.
3
experiment-
-Id
’
ty or death;
to
remote
be
iHade and1 <adequate
’
faci1ithe experimental
.
t
—
I
subject
Possfbi1,ti es of
,nJ“ry, disabili-
“ safeguards have
: been taken to
tat ion would |
see that
be
the experimen|Ua' 5f^d persons conducted only by
sc
ientifica|ly
who
*ence,
experience
possess
the
; requisite compeand
Qualities
research;
to carry ou^
the
it wouId L_
be made r
Perfectly clear to
Patient that
he wouId
- J be at ]iberty to the subject or
pe r i men t
to
an end at
br’ng the exany time
- he desires to do so;
the scientist
Prepared to term inate rthe ex the__ reSearch
-Project is
he has probab1 p
’
tne experiment
at any
' stage, if
fo-.u
Se to be Iieve
the good
f
’ in
the l .
exercise of
of him,thatv a conf-'" and care^i1
judgement
requi red
to resul t
experiment i 5 likely
d,Sab,,,ty 1
per imental subject.
or death to
the ex-
i°"-"uad£b°rthe'
3
d
13
td
le
re
re
rt©
ed
' a
Crg
lew
221
of
cts
nt.
old
.her
any
ial.
t in
e in
in-
SJ--
4
The-Council recognizes the fact that it may take time for all the
institutes in the country to form ethTcal committees and for a period of
—ione year the Central Ethical Committee of the .1 ndfarTCouhcTI of Medica 1
Research would undertake to review, on ethical grounds, proposals sub
mitted to the Council, irrespective whether it is submitted for support
of the research proposed or not.
This would be done with a view to
assisting the investigators from the different institutes during the in
terim period when the institutional ethical committees are being formed
at these institutions.
The Council would also, if required to, assist
these institutes to s6t up ethical committees and help in their func
tioning in the early stages.
The Council feels that if the Ethical Committeer is to play a usefu
role and discharge its functions effectively, it must be independent.
SUPPORT OF CLINICAL RESEARCH BY THE COUNCIL
The Council would not consider support for any proposal for
research on human subjects unless the research proposal has been approv
ed by the Ethical Committee of the institute concerned. As has already
been stated, the Council would take on the responsibility of assessing
proposals on ethical considerations for an interim period of one year.
The Council would also carry out this evaluation for proposals that may
be sought to be sent for support to international agencies such as World
Health Organization which does not entertain proposals for research
support unless approved by the Ethical Committee of the institute. This
assistance by the Council would enable investigators in institutes,which
at the moment,do not have institute Ethical Committee to obtain support
from these agencies.
IMPLEMENTATION OF ETHICAL COWITTEE'S GUIDELINES
In addition to its other functions, the Ethical Committee should
monitor the implementation of these guidelines and check whether tha|
principles laid down regarding research on human subjects are beinj
followed and whether the recommendations made by the institute Ethical
Committee about a particular [project are being observed by the investi
gators in charge of the projects.
.
The Council would, of course, retain the right of reviewing at any
time the ethical procedures being observed in any project being support
ed by it.
DRUG TRIALS
The Council would like to make it clear thatxc1inica1 evaluation of
any new drug to be used for prophylactic, diagnostic or therapeutic
purposes should be carried out, only after approval, as is necessary
5
under law, has been received from the'Drugs Controller of India. The
investigator should then formulate the research proposal and submit it______
to the Ethical Committee of the institute. This guiding principle should
be followed irrespective of whether the drug has been developed in this
country or abroad or whether clinical trials with the substance or drug
have been carried out outside India.
Similar principles should be
followed for evaluation of new devices or other similar agents.
CLINICAL TRIALS WITH PLANTS AND INDIGENOUS SYSTEMS OF MEDICINE
The Council would suggest that for clinical evaluation of plants
ing utilized for therapeutic purposes, assessment of treatments being
used
in the traditional
systems of medicine the protocols for such
clin i cal research should again be approved by the Ethical Committee of
the institute. There is no need for clearance to be obtained from the
Drugs Controller of India for such trials of products already in wide
spread use in the traditional systems of medicine today in the country.
INFORMED CONSENT
The question
E
0)
c
of "informed consent" and the best way of obtain ing G
informed consent is one that is difficult and one in which the norms and 5
forms used in other countries are really not fully relevant to the conditions prevailing in this country, Although the procedure of obtaining ip
the signatures of the person giving
<_ ‘
his/her consent cannot zbe dispensed =1
u------------------------------------------------------ .u-------------.. .
with, at the same time, it must. be
emphasized that in the context ofr .L,
the H
conditions prevailing in the country,mere signatures would not ensure
the requirements of informed consent. The Council can only lay down the 0
broad guiding principles that form the basis for obtaining informed con- o
sent and then leave it to individual ethical review committees to
develop their own procedures. These principles are that the proposed J
participants in a clinical research programme should be made aware, by a j
l^rson not in a position to influence the patient such as the treating )
physician but for example, by a social worker, of the fact that a new j
drug or procedure is being evaluated. The patient for a new clinical »
trial should be informed briefly of the potential possible benefits of.
the new treatment as against the existing and the possible side-effects (
or hazards of the new treatment when compared to the existing treatment. [
If it is a randomized double blind trial, the patient should be told
that he would be given either the old treatment or the new. He then
should be informed in clear terms that if he wished to withdraw at any
time from the trial, he could do so and then asked whether, in the cir
cumstances explained to him, he would like to participate in the trial.
The question of any payments to cover his/her expenses in taking part in
the trial should be discussed after his/her agreement to participate in
the trial and not suggested at a time when it could be used as an in
ducement to him to join in the trial.
E
nJ
o
4-»
O
o
<D
E
o
U-l
o
q
ub
co
4->
CO
0)
X)
•H
P
6
7
If the proposed research is not a trial
which would in anyway
directly benefit the subject or the patient, then the benefit that would
accrue to society or to other persons suffering from the disease should
be clearly explained to
the subject, as also the possible hazards to
him,before asking him whether he would like to participate in the trial.
Again, he should clearly be informed that he could withdraw from the
trial any time he would like to.
possession of all his faculties, then, his consent during such a period
should also be obtained before including him as a subject
w
: for the proposed research.
CLINICAL RESEARCH ON PRISONERS, MEDICAL STUDENTS § LABORATORY PERSONNEL
Research on prisoners should never be carried out as it is not only
difficult to obtain informed voluntary consent from prisoners but snducements offered to the prisoner for taking part in the
-.2 trial would
make it unethical to include such persons as subjects in a research
pro
gramme.
Similar considerations also apply, to a lesser extent,
to
c-w-rying out clinical
research on medical students and laboratory ^er■2 fine 1 but
there may be exceptional
occasions when research on stfch
subjects would be perfectly ethical.
The Ethical Committee should juice
each research programme involving such persons with particular reference
to the fact whether the teacher or investigator is in a position to in
fluence the decision of the subject to take part in the research.
CLINICAL RESEARCH ON CHILDREN
Research on children should be carried out only if there is possibility of some direct benefit to the child by taking
part in the clinical trial
or research project,
An experiment on ch iIdren cou1d be
carried out if:
it i s an experiment on the clinical
efficacy of a new
treatment with the immediate aim of curing the child's
it is an experiment on an ill child in order
to find
out more about the condition or disease from which the
child is suffer i ng.
FINANCIAL REIMBURSEMENTS TO PARTICIPANTS TAKING PART IN
CLINICAL RESEARCH PROJECTS
While it is
reasonable to reimburse subjects ana patients for tak
ing part in a trial for the loss in time, leave taken and other expenses
that they may have incurred such as transportat ion expenses, expenses on
food, if the procedure is a long drawn one, or in employment of a parttime helper to look after the children during absence of a housewife
from the house,
this reimbursement
should not be of such magnitude so
as to act as an inducement to the person to join the trial.
The Ethical
Committee of the institute concerned would be the best judge of what
constitutes a
reasonable
reimbursement
in a particular situation as
that would depend,on several factors such as the time required to ce
Jntjn the hospital,
the procedure itself and local factors
such as
A good
i n d i ca t i on
to judge whether an experiment on a child is
ethical
or not
is for the
investigator
to ask himself the question
"Would I do this to my own child?" Voluntary informed consent must be
obtained from the parents or guardian of the child before carrying out
the research project.
CLINICAL RESEARCH ON MENTALLY DEFICIENT PATIENTS
Clinical research on mentally
retarded children or adults is again
a very difficult question and has been the subject of much con t roversy
in the past.
Research on such persons should, again, be carried
I out
bnly if:
existing costs of transportation
‘i etc.
the research on a new treatment could cu re the pat lent;
the clinical research being carried out would add more
information about the condition or disease from which
the patient is suffering.
PUBLICATION OF PAPERS ON CLINICAL RESEARCH IN
THE INDIAN JOURNAL OF MEDICAL RESEARCH
T7
Informed voluntary consent needs to be obtained from the'guardian/
elatives of
the patient before any
research can be conducted on menally deficient patients.
If the patient has intervals when he is in
The official publication of the Indian Council of Medical Research the Indian Journal of Medical Research ~ would review papers submitted
to the journal for publication from an ethical point of view also before
approving such papers for publication. It is expected that in due course
of time, those papers that have been based on clinical
research carried
out only after
approval of the institute Ethical
Committee would be
considered for publication in the Indian Journal of Medical Research.
8
9
CLINICAL RESEARCH SUPPORTED BY AGENCIES OTHER THAN
THE IN DI .AN COUNCIL OF MEDICAL RESEARCH
THE ICMR COMMITTEE TO CONSIDER ETHICAL ASPECTS
OF INVESTIGATIONS- ON HUMAN SUBJECTS
These gu i del i nes have been prepared to assist all investigators in
the country who are involved in carrying out clinical research on hienan
subjects. It is hoped that other agencies in the country supporting
clinical research in India would either incorporate some of these suggestions in their own eyaluation of proposals for support of clinical
research or adopt the guideli
‘‘nes laid down by the Council. The Council
would, from time to time, <organize meetings of all agencies supporting
clinical research in India in an attempt to make uniform the ethical
safeguards that are requiredI of clinical investigators before carrying^
out research on human subjects.
Mr Justice H.R.Khanna,
S-368, Panchsheel Park
New Delhi 110 017
(Cha i rman)
CD w
e 4J
O £4 £4
O O o
_
£1 U-4 CX
CX £ CD
•H £4
(D
w M-4
3
O
4-J
o
rH
Dr Ranjit Roy Chaudhury
Dean and Head
’o
U
Department of Pharmacology
Postgraduate Institute of Medical
Education and Research
Chandigarh 160 012
(X
CD X)
CD £
CT)
o a
Q o
•H
(D 4->
a)
> -H
■p
(J
CT)
£4
<D
Dr S.S.Gothoskar
Drugs Controller of India
Directorate General of Health Services
N i rman Bhawan
New Delhi 110011
£1
cn
a
•H
n 4-J
O
U
<D
CT)
O
a-
•A
a-H
CT) U cu
1
Dr S.Padmavati
A-l/116, Safdarjung Enclave
New Delhi 110 016
U-4 4-J
J
o M :
CT) <_
o
bo CX >>
£l
•H £»
Prof V.Rama 1ingaswami
Di rector-Genera 1
Indian Council of Medical Research
New Delhi 110 016
a £) o
£) O
•H
b0
W I
(V 4-> a) •.
Xi
(1)
*r
-U ’
CT)
(/) > (
Dr B .Sankaran
cn
CT1
Director General of Health Services
N i rman Bhawan
er ctj 1
<u M
M 4-J (
4-’ ~1
£5
<
New Delhi 110 011
<
Dr Badri N .Saxena
Deputy Di rector General
Indian Council of Medical Research
New Delhi 110 016
(Member-Sec re ta ry)
w
0)
W
rC
QJ
(D
_
w
^QJ
Published by the Indian Council of Medical Research, New Delhi 110 029.
<u £ ro
CO
W c£
u
W) 4_)
£5 P
O O
E 30
CTJ CTJ
cr
£
CT
E
CODE OF MEDICAL dETHICS
i -•
■4
h
-
■■
■
•-■
•MM > ■ -•
‘. - "" *’L-
■
c*
T
«■
• r
•
■
‘ (Approved by the Central .Government u/s 33 of the
/•Indian Medical Council-(Act, 1956, - Vide their
letter No. F. 17-64 MPT, dined 23rd October, 197C)
r.
V
3
I-
A ■
i
\
I
’k
KJ©#
i
I•
“" Z :
MBDICAL COUNCIL OF INDIA ~ Aiwin - e - Ghalib Marg“7
Kotla Road
...f
New Dclbi-110002 - \
'
MEDICAL COUNCIL
OF INDIA
CODE OF MEDICAL ETHICS
DECLARATION
Ar the time of registration, each applicant shall be given a copy of me fo!iav.:;:y
declaration by the Registrar concerned and shall read and agree :o abide by the same :
1. I solemnly pledge myself to consecrate m\ lite to the service of humanity.
2. Even under tnreat, I will not use my meJurJ
c::’.tra’>
tiv.' iaw;
of humanity.
S. I will maintain the utmost ic-pcct ior aa.r.av. ide ir.'m »hc t.me of c'r.ceptior.
4.
I will not permit consideration? of religion, iiai.onahty race par-politic: . r
social standing to intervene between my duty and r.y patient.
I will practise my profession with conscience and dignity.
The health of my patient will be my first considerat.on.
I will respect the secrets wiiicl are confided in me.
1 will give to my teachers the respect and gratitude which is tr.eir cue.
I will maintain by all means in my power, the honour and noble traditions of
medical profession.
10. My colleagues will be my brothers.
1 make these promises solemnly, freely and upon nr- honour.
5.
6.
7.
8.
9.
CODE
GENERAL PRINCIPLES
Character of the Physician
The prime object of the medical profession is to render service to humanity;
. -reward of financial gain is a subordinate consideration. Who-so-ever chooses this
profession, assumes the obligation to conduct himself in accord with its ideals. “A
2
physician should be an upright man, instructed in the art of healings.” He must keep
himself pure in character and be diligent in caring for the sick. He should be modest,
sober, patient, prompt to do his whole duty whithout anxiety; pious without going so far
as superstition conducting himself with propriety in his profession and in all the actions
of his life.
2.
The Physician’s Responsibility
The principle objective of the medical profess on is to render service to humanity
with full respect for the dignity of man. Physicians should merit the confidence of
patients entrusted to their care, rendering to each a full measure of sendee and devotion.
Physician should try continuously to improve medical knowledge and skill and should
make available to their patients and colleagues the benefits of their professional attain
ments. The physician should practice methods of healing founffid^on scientific basis
ar.u shouid net associate professionally with anyone who violates this principle. The
honoured ideals of the medical profession imply that the responsibilities of the physician
c.xicnd no: only to individuals but also to society.
Advcrtisieu
Solicitaimn of patients directly or indirectly, by a physician, by groups of
physicians or
mstnuxior.s or organisations is ur.nhical. A physician shall not make
use of 'r aid or permit other;; to make ’..sc of him <or his name) as subject of any form or
ranrer ••• ;d\ertif’.nu
pucr.ciix thiougn lay ch..::r.eis either alone or in conjuctioa
* uh ?t:-..*• w 'ich 'null he of 'Uch a character is to invite attention to him or to ?.i$
.••. ’csmc: .i j)o*iiion. till, qualification, achievements, attainments, specialities, aprointmc.-t.
-ciai:?ns. .lEhaiivr.s or honours and or of such character as would Ordinaniy
r:\ui.
.:s .:cif aggrunuisement nor ihaii he give to any person who-so-ever. whether
;or cor.'.-'ansation or etherv.^c. any approval, recommendation, endorsement, certificate
rerort r statement with respect of any drug, medicine, nosterm remedy, surgical, or
therapeutic article, apparatus or appliance or any commercial product or article wit.i
respect of any property, quality or use thereof or any test demonstration or trial thereof,
for use :n connection with his name, signature, or photograph in any form or manner of
advertising through lay channels nor shall be boast of cases, operations cures or remedies
or permi the publication of report thereof through lay channels. A medical practitioner
is permitted a fprmal announcement in press regarding the following :
(1)
On starting practice.
(2)
On change of type of practice.
(3)
On changing address.
(4)
On temporary absence from duty.
* 5)
On resumption of practice.
(6)
On succeeding to another practice.
3
Payment of Professional Services
The ethical physician, engaged in the practice of medicine, limits the sources of his
income received from professional activities to services rendered to the patient.
Remunerations received for such sendees should be in the form and amount specifically
announced to the patient at the time the service is rendered. It is unethical to enter
into a contract of “no cure no payment”.
-4.
Patent and Copy Rights
A physician may patent surgical instruments, appliances and medicine or copy
right publications methods and procedure. The use of such patents or copyright or
the receipt of remuneration from them which retards or inhibits research or restrict
the benehts derivable therefrom are unethical.
5.
Running an Open Shop (Dispensing of Drugs and Appliances by Physicians)
A physician should not run an open shop for sale of medicine for dispensing pres
criptions prescribed by doctors other than himself or for sale of medical or surgical
appliances. It is not unethical for a physician to prescribe or supply drugs, remedies or
appliances as long as there is no exploitation of the patient.
6.
Rebates and Commission
A physician shall not give, solicit, or receive nor shall he otfer to give, solicit or
receive, any gift gratuity, commission or bonus in consideration of or in return for the
referring, recommending or procuring of any patient tor medical, surgical or other
treatment. A physician shall not directly or by any subterfuge participate in or by a
party to the act of division, transference, assignment, sub-ordination, rebating, spiitting
or refunding of any fee for medical, surgical or other treatment.
The provisions of this para shall apply with equal force to the referring, recom
mending or procuring by a physician or any person, specimen or material for diagnostic, .
or other study or work. Nothing in this section, however, shall prohibit payment of
salaries by a qualified physician to other duly qualified person rendering medical care
under his supervision.
7.
Secret Remedies
The prescriptions or dispensing by a physician of secret medicine or other secret
Temedial agents of which he does not know the composition, or the manufacture or
-promotion of their use is unethical.
8.
. Evasion of Legal Restrictions
The physician will observe the laws of the country in regulating the practice of
medicine and will not assist others to evade such laws. He should be cooperative in
9.
4
observance and enforcement of sanitary laws and regulations in the interest of public
health. A physician should observe the prov .sions of the State Acts like Drugs Act,
Pharmacy Act, Poisonous and Dangerous Drugs Act and such other Acts, Rules,
Regulations made by the Central Govt./State Govts, or local Administrative Bodies for
protection and promotion of public health.
DUTIES OF PHYSICIANS TO*THEIR PATIENTS
Obligations co the Sick
Though a physician is not bound to treat each and every one asking his services
except in emergencies for the sake of human.ty and the noble traditions of the profession.
;.e should not only be ever ready to respond to the calls of the sick and the injured, but
should be mindful of the high character of h:s mission ar.c the responsibility he incurs in
the discharge of his professional duties. In his ministrations, he should never forget
tna.: the health and the lives of those entrusted to his care depend on his skill and
ur.enr.on. A physician should endeavour u add to the comfort of the sick by making his
v.sits a: the hour indicated to the patients.
11-.
Patience Delicacy and Secrecy
Patience and delicacy should charac.enze the physician. Confidences concerning
individual or domestic life entrusted by patients to a physician and defects in the discositicn or character of patients observed during medical attendance should never be
revealed unless their revelation is required
the laws of the State. Sometimes, however,
a physician must determine whether his duty to society requires him to employ know
ledge. obtained through confidences to i.im as a physician, to protect a healthy person
against a communicable disease to which he is about to be exposed. In such instance,
the physician should act as he would desire another to’act toward one of his own family
in like circumstances.
i:.
Prognosis
The physician should neither exaggerate nor minimize the gravity of a patient’s
condition. He should assure himself that the patient, his relatives or his responsible
friends have such knowledge of the patient’s condition as will serve the best interests of
the patient and the family.
12.
The Patient Must not be Neglected
A physician is free to choose whom he will serve. He should, however, respond to
any request for his assistance in an emergency or whenever temperate public opinion
expects the service. Once having undertaken a case, the physician should not neglect
the patient, nor should he withdraw from the case without giving notice to the patient^
13.
I
I
5
his relatives or his responsible friends sufficiently long in advance of his withdrawal to
allow them to secure another medical attendant. No provisionally or fully registered
medical practitioner shall wilfully commit an act of negligence that may deprive bl$
patient or patients from necessary medical care.
DUTIES TO THE PHYSICIAN TO THE PROFESSION AT LARGE
14.
Upholding the Honour of the Profession
A physician is expected to uphold the dignity and honour of his profession.
Membership in Medical Society
For the advancement of his profession, a physician should affiliate with medical
societies and contribute his time, energy ar.d means so that these societies may renreser.i
the ideals of the profession.
15.
16.
Safeguarding the Profession
Every physician should aid in safeguarding the profession against admission to it
of those who arc deficient in moral character or education. Physician should nut employ
in connection with his professional practice ..ny attendant who is neither registered nor
enlisted unccr the .Meuicai Acts in force ami should not permit .such persons to .uicnc.
treat or perform operations upon patients in respect of matters regarding prefessiena.
discretion or skill as it is dangerous to pur’ic health.
Exposure of Unethical Conduct
A physician should expose, without fear or favour, incompetent or corrupt,
dishonest or unethical conduct on the part of members of the profession. Questions of
such conduct should be considered, Srst before proper medical tribunals in executive
sessions or by special or duly appointed committees on ethical relations, provided such
a course is possible and provided also that the law is no: hampered thereby, if doubt
should arise as to the legality of the physian’s conduct, the situation under investigation
may be placed before officers of the law, and the physician investigators may take the
necessary’ steps to enlist the interest of the proper authority.
17
PROFESSIONAL SERVICES OF PHYSICIANS TO EACH OTHER
Dependence of Physicians on each other
There is no rule that a physician should not charge another physician for his service,
should cheerfully and without recompense give his professional services to physicians or
IS.
I
I
6
his dependants if they’ are in his vicinity.
•
beis.”:.' •
19. cCompensation for Expenses
. A physician should consider it as a pleasure and privilege to render grataitiousp^’SIC,ans “d the>r immediate family dependants. When a physician is.
..called from a distance to attend or advice another physician or his dependants reim
bursement should however be made for travelling and other incidental expenses. ’
duties of physician in consultation
—0.. Consultation should be Encouraged
In case of serious illness, especially in doubtful
or difficult conditions the physician
should request consultation.
21.
Consultation for Patient’s Benefit
In every consultation, the benefit to tne patient is c: first imncnance. All nhvsicians
SsponSie'Irienl
Sn°Ulii
ofhi^Hyor
Punctuality in Consultation
Ltinost punctuality should be observed by a physician in
meeting for consultation.
23.
Conduct in Consultation
In consultations, no j----- ■ rivalry or envy should be indulged in. All due
josinccreity.
respect should be observed towards the physician ir.char.’ge of the case and no statement
o> remark be made, which would impair the confidence ireposed in him. For this purpose
no discussion should be carried on in the presence of the patient or his rep^sent'ative^
24.
Statement to Patient after Consultation
nHee'31 ^,lstaterae::ts°f^eca5e t0 lhe patient or his representatives should take
place m toe presence of all tne physicians consulting, except as othenvise aareed' the
announcement of tne opinion to the patient or his relations or friends shall rest” with the
medical attendant.
(b» Differences of opinion should not be divulged unnecessarily but when there is
an irreconcilable difference of opinion the circumstances should be frankly and imoardaily explained to the patient or his friends. It would be open to them to seek furLr
advice should they so desire.
’
25.
Treatment after Consultation
No decision should restrain the attending physician front making such subsequent
I
I
7
r
variations m the treatment as any unexpected change may require bu- -t the n. .
consultation reasons for the variations should be stated. The same pri’vileoe" with its
of 1b T’ i°nSS t0
consult“t whm sen‘ for in atremersency duringAe absence
' nL r I"2 phyS,'C,an- The attending Physician may prescribe at any time for the
patient, the consultant only in case of emergency.
Y
“
26.
Consultant not to take Charge of the Case
When a physician has been called as a consultant, none but the rar-st and
exceptional c.rcumstances would justify that consultant taking charge ofth- cas^ most
He
must not do so merely on the solicitation of the patient or friends.
Patients Referred to Specialists
When a patient is referred to a:specialist
■ ■■ -by the attending physician, a smteir.er.: c.’
the case should be given to the specialist, who should
commanicatv hi\ epinior. :r.
writing m a closed cover direct to the attending physician.
27.
DUTIES OF PHYSICIAN IN CASES OF INTERFERENCE
28.
Appointment of Substitute
Whenever a physician requests another physician to attend his Datienu du-in- b,
t.mporary absence from h.s practice, professional courtesy requires th- acc-ntanc- ■
such appomtment >f consistent with his other dut.es. The phvsicL a-tin"- ml ^r
-•
an appomtment should give the utmost consideration to the interests ai-l r--
ne aoser.t p.iys.cian.
ins return.
All such patients should be restored to inc care c <h-'i-t-- u.... u.u. u.i?..
29.
Visiting another Physician’s Case
A physician called to visit a patient who has recentlv been tinder the care ofar-iher
ph.vs.dan in the same ihness. should not take char- of. nor prescrih- ft 2 J
except in a case of emergency when he should communicate to th- fo-mer
Pai!L’r‘’
circumstances under which the natient was
j
" l0‘mer exPIalning tne
SO as to give him an option of being present. The medka! offit shin Id
upon the diagnosis or the treatment that has been adopt'd.
30.
’n
S’
Engagement for an Obstetric Case
If . a physician agrees to attend a woman during her confinement, he must do so.
1
8
Inability to do so on an excuse of any other engagement is not tenable except when he
is already engaged on a similar or other serious case. When a physician who has been
engaged to attend an obstetric case is absent and another is sent for and delivery
accomolished, the acting physician is entitled to his professional fees, but should secure
the.patient's consent to resign on the arrival of the physician engaged.
DUTIES OF PHYSICIAN TO THE PUBLIC
Physicians as Citizens
PJy.sicians. as good Citizens, possessed of special training should advise concerning
eudh of tne community wherein they dwell. They should bear their part in
enforcing Lite laws of the community and "’in-sustaining tne institutions that advance the
nterests of humanity. They should operate especially with the proper authorities in the
cumin: irai.on of • ar.itnr :aws and regulations.
31.
l
!
!
i
t
Public Health
Physicians, espccia; those engaged in public health, work, should enlighten the
public conceding quare: ne regulations and measures for the prevention of epidemic
. At ail times the physician should notify the constituted public
ar.a c'.'imiHir.:
• •nte vu . c"/.n*.u:ucar! ’ disease under his care, in accordance
.'..-.’.it:: .•.•.itnori
.jo .r.c regulations of the henith authorities. Wb.cn an epidemic
vitr. th lawcmn must certmuc •.is labour without regard to the risk to his
• re*.
•;
52.
•AT.
C..ith.
'V.amncisis
.'hysiJans ‘houid recognize and promote the practice of pharmacy as a profession
a:: ci nouid recognise *.b: cooperation of the pharmacist in education of the public
concerning the practice of ethical and scientific medicine.
DISCIPLINARY action
i
j
1.
The Medical Council of India desires to bring to the notice of the registered
medical practioners the following statement upon offences and form of professional
misconduct, which may be brought before the appropriate Medical Council for discipli
nary action in view of the authority coferred upon the Medical Council of India and/or
State Medical Councils as provided under Indian Medical Council Act, 1956, or State
Medical Councils Acts as may be subsequently amended.
2. *The appropriate .Medical Council may award such punishment as deemed necessary
-or may direct the removal altogether or for a specified period from the Register, the name
I
L
9
of any registered practioner who has been convicted of any such oiTence as implies in
the opinion of the Medical Council of India and/or State Medical Councils, a defect of
character or who after an enquiry’ at which opportunity has been given to such registerec
practitioner to be heard in person or by pleader, has been held by the appropriate
Medical Council to have been guilty of serious professional misconduct. The appropriate
Medical Council may also direct that any name so removed shall be restored.
3.
It must be clearly understood that the instances of offences and of professiona
misconduct which are given do not constitute and are not intended to constitute a
complete list of the infamous acts which may be punished by erasure from the Register
and that by issuing this notice the Medical Council of India and or State Medina:
Coun^jJ^are in no way precluded from considering and dealing with any form o.
professional misconduct on the part of a regi’stered practitioner. Circumstance- ma;
and do arise from time to time ir. relation to which there may occur Question - c.
professional misconduct which do not come witnin any of tnese categories. Every car:
should be taken that the code is not \io:ated in iettcr or spirit. In such instance ; as m a;
others, the Medical Council of India and or State Medical Councils have to consider an
decide upon tne facts brought before t.tc Medical Council of India and or State Mod:cn
Councils.
LIST
Adultery or Improper Conduct or Association with a Patient
Any medical practitioner, who abuses, his profesaiona! position by com r.'.r.ting ;:ny
adultery or improper conduct with a patient or by maintaining an improper a -• cc; .:or
with a patient, is liable for disciplinary action as provided under the Indian ;Uc-;uai
Council Act, 1956 and/or State Medical Council Acts, as may be subsequently umenued.
1.
Conviction by Court of Law for offences involving moral turptituJe.
Professional Certificates, Reports and other Documents
Registered practioners are in certain cases bound by law to give, or may from time
be called upon or requested to give certificates, notification, reports and other documents
of kindred character signed by them in their professional capacity for subsequent use in
the courts of justice or for administrative purposes etc.
3.
(i). Such documents include among other certificates, notifications reports—
(a) Under the acts relating to birth, death or disposal of the dead.
(b) Under the Acts relating to Lunacy and Mental Deficiency and the rules
made thereunder.
(c) Under the Caccination Acts and the regulations made thereunder.
10
(d) Under the factory Acts and the regulations made thereunder.
(e) Under the Education Acts.
(f) Under the Public Health Acts and the order made thereunder.
(g) Under the Workmen’s Compensation Act.
(h) Under the Acts and order relating to the notification of infectious diseases.
(i) Under the Employee’s State Insurance Act.
(j) In connection with sick benefit insurance and friendly societies.
(k) Under the Merchant Shipping Act.
(l) For procuring the issuing of passports.
(m) For excusing attendance in courts of Justice, in public services, in public
offices or in ordinary employments.
(n! In connection with rural and Military matters.
«o‘ In connection with matters under the control of Ministry of the pensions.
(ii) Any registered practioner who shall be shown to have signed or given under
his name and authority and such certificate, notification, report or document of a kind
red character which is untrue, misleading or improper relating to the several matters
above rnccifud or otherwise, is liable to have Ids name erased from the Register.
fiii.' \ Registered medical practitioner shall maintain a Register of Medical
'crtificairs giving :uii detaiis of ccruficatcs issueu. When issuing a medical certificate
. ■••ays •ntcr the indentification marks of the patient and keep a copy of the certificate.
not emit to note down the signature or thumb-mark, address and identification
marks .. the patient on the medical certificates or report.
Contravening the provision of the Drugs Act and regulations made thereunder.
5.
Seiling Schedule poison to the public under the cover of his own qualification
e.\cept to his patient.
6.
Performing or enabling unqualified person to perform an abortion or any illegal
■operation for which there is no medical, surgical or psychological indication.
A physician should not issue certificates of efficiency in modem medicine to
7.
■unqualified or non-medical person.
(Note: The foregoing does not apply so as to restrict the proper training and
instruction of bonafied students, legitimate employees of doctors, midwives,
dispensers, surgical attendants, or skilled mechanical and technical assistants under
the personal supervision of physicians).
I
11
8.
A physician should not contribute to the lay press articles and give interviews
regarding diseases and treatments which may have the effect of advertising himself
or soliciting practice ; but it is open to him to write to the lay press under his own name
on matters of public health hygienic living or to deliver public lectures, give talks on the
radio broadcast for the same purpose and send announcement of the same to thelay press.
9.
An institution run by a physician for a particular purpose such as a maternity
home, a sanatorium, a house for the crippled or the blind, etc. may be advertised in the
lay press, but such advertisements should not contain anything more than the name of
the institution, type of patients admitted, facilities offered and the residential fees.
Name of either the superintendent or the doctor attending should not appear in the
advertisement.
10. it is improper for a physician to use an unusually large signboard and write on it
anything other than his name, qualifications obtained from a University or a statutory
body, titles and name of his speciality. The name should be the contents of his
prescription papers. It is improper to affix a sigh-board on a chemist’s shop or in places
where he docs not reside or work.
11. Do not disclose the secrets of a patient that have been learnt in the exercise of
your profession. Those may be disclosed or.lv in a Court of Law under orders of the
presiding jugde.
12. Refusing on religious grounds alone to give assistance in our conduct of sterility,
birth control, craniotomies on living children, and therapeutic abortions when there is.
medical indication; unless the medical practioner feels himself herself incompetent
to do so.
13. Before performing an operation in wriiting the consent from the husband or wife.
• parent or guardian in the case of a minor, or the pati'ent himself as the case may be.
In an operation which may result in sterility the consent of both husband and wife
is needed.
14. Do not publish photographs or case reports of your patients in any medical or
other journal in a manner by which their identity could be made out without their
permission. Should the identity be not disclosed his consent is not needed.
15. If you are running a nursing home and if you employ assisunts to help you, the
ultimate reponsibility rests on you.
16.
No physician must exhibit publically the scale of fees. But there is not objection.
12
ir
io the same being put in the physicians' consulting or waiting room.
i
No physician shall use tents or agents for procuring patients.
,v:i .... t .-:r -
‘
•>
•
'*
18.' Do not claim to be a specialist unless you have put in a good few years of study
-and experience or a special qualification in that branch. Once you say you are one, do
net undertake work outside year speciality even for your friends.
Ferm of Certificate- Recommearfc^ for Lc^’ c or Extension of Communication of Leave
I
Signature of apniicar.t
or thumb impression..
Tc be filled a bv the <pi:cant in the presence cf the Government
•‘•ie.i.ea; Mitroaivt. or Medical Practior.er.
............................. alte- careful examination
L
of the case hereby that
whose signature is given
u-Kwe is suffering rem
and I consider that a period
cf absence from duty cf
J
“J
with effect from
3 absolute y necessary for the restoration of his health.
Date
^ole
Signature of Medical Attendant
The nature and probable duration of the illness should also be specified.
This certificate must be accompained by a brief resume of the case giving
the nature of the filnesz. its symptoms, causes and duration.
I
(Approved by the Central Govemn.-.-tt u > 33 tm) of the Indian Medical Council
Act, 1956, vide their letter No. E. 17-4.'64-MPT, dated 23-10-70)
f
ISSUES
SOME
Has a patient the
right to
RAISED
be delivered from incurable
suffering?
■Si-
If a person has a right to life has he not also a right
to take away his own life?
-Si
Abortion, though once considered
to
be
a criminal act
is now often considered to be a benevolent and obligatory
act. Should we not go along with the times?
*
ls it wrong to find out and eliminate a retarded foetus?
-Si-
If test tube baby is a breakthrough in medical technology,
why impose restrictions?
*
Is it wrong to attempt to create super-humans through
genetic engineering?
Is it ethical to sell or
-X'
buy organs?
What is our priority - to prolong life of a few or improve
the quality of life of
the masses?
M£f-S4 IJ'
IS MODERN MEDICAL TECHNOLOGY
A CHALLENGE
Copies are available at :
i.
EMFI Office,
Montauban Christian Guest House,
Ettines Road,
Ootacamund-643 001,
The Nilgiris,
Tamil Nadu,
South India
2.
Christian Fellowship Hospital,
Oddanchatram-624 619,
Anna District,
Tamil Nadu,
South India.
3.
International Christian Medical &
Dental Association,
157, Waterloo Road,
London BEI 8XN,
UNITED KINGDOM.
TO CHRISTIAN ETHICS?
Dr. A. K. THARIEN
*
Dr. A. K. THARIEN MBBS. DLO., Z.O.M.S., (Vienna) M.A.M.S.,
F.A.C.S. is a founder - member of the Christian Fellowship
Hospital Oddanchatram, Tamil Nadu, INDIA.
E. M. F. I.
PUBLICATIONS
'Far & Near'
Quarterly free.
VOICE-Journal of EMFI
Two issues in a year
Rs. 15/- doctors
Rs. 10/- students
Rs. 25/- overseas
BOOKLET
Series
A current concern book
Rs. 2. 00
Medical Evangelism
Dr. R. K. Nghakliana
Published by
EMFI
March 1989
CURRENT CONCERNS Series
Printed at
Cosmo Printers
395, Cross-cut Road
Coimbatore-641 012
The only strategy is love
Dr. K. N. Nambudripad
Rs. 1.00
Called to be a witness
Dr. K. Thirumalai
Rs. 1. 00
f
values are gradually being pushed aside or
getting eliminated. Love is the foundation
of Christian ethics. Loving our God with
all our heart, soul and mind and loving our
neighbour as ourselves, are the two found
ations for our ethical practice. Only a code
of ethics based on the Bible and sound
Christian principles, can lead our society to
lasting happiness, harmony and peace.
In recent years Medical Science and
Technology have made great strides of
of technological
progress. The growth
medicine raises some moral and ethical
problems. Our understanding of ethical
■ principles should lead us to find a rational
basis for our medical practice.
CHRISTIAN MEDICAL ETHICS
Christian medical ethics deals with human
behaviour, relationships, biological issues of
health, religious ideals, culture, decisions
regarding when to treat and when to withhold
treatment, dying and death. Christian medical
ethics has now become complex, as it has
medical, legal, theological, moral, social and
2U
personal aspects. Medical and biological
advances in knowledge and technique further
pose new dilemmas in decision making. Many
time honoured principles are being openly
questioned or flouted. New legislative mea
sures are under consideration, if not already
in existence, particularly in areas like organ
transplant, management of human fertility and
infertility, use of drugs to alter brain function,
genetic engineering to change human genetic
stock, euthanasia, amniocentesis, termination
of pregnancy etc.
LET ME SHARE SOME PRACTICAL STEPS
1.
Doctors should serve and care for their
patients in love based on Christian
motivation.
2.
Deliberate attempt to end or shorten life,
whether by ommission or commission is
wrong and should not be done.
3.
The church should proclaim the way of
righteousness and truth, against taking
innocent lives, and provide compas
sionate, care.
4.
Education of medical personnel and
people with moral and spiritual values
should be done, which may lead to
sound legislation.
5.
Bring in Christ's principle of love as
the motive and mainspring.
THREE DIMENSIONS OF A PERSON
A person may be viewed, biologically,
socially and spiritually.
a)
Biological
We have a physical form to our body and
keeping the body healthy is a biological
activity. Health is therefore our right and we
need to safe-guard it. A doctor's duty is to
preserve and promote health in all its aspects,
physical, mental and spiritual.
CONCLUSION
Man is a social being. He lives in
relationship with another. The most import
ant relationship is between husband and
Views and ideas and even concepts
of ethics are fast changing in the context
of the progress of science and technology.
The traditional institutions in our society,
which protect human life and spiritual
2
19
b)
Social
society. So they resigned from their busy
clinical work and offered their lives to start a
centre for children with special needs. An
apparent traumatic experience became the
rallying point for a new mission and for
Christian compassion.
OUR GUIDING
PRINCIPLE
Ever since the time of Hipocrates in the
fifth century BC the medical profession has
been guided by the concept of the worth of
each individual human life, which was recently
reaffirmed by the Geneva code in 1948, which
states, "I will show the utmost respect for
human life from the time of conception".
Suffering is evil, and we should take every
step to mitigate or relieve it, but suffering
has also meaning and purpose.
Hitler had a utilitarian philosophy of
life. Any person who had a utilitarian value,
he preserved, and others he eliminated. But
as Christians we respect the unique value of
human life. Man is made in the image of God
(Gen 1:27) This gives human life a unique
dignity and value (Gen 9:6), (Ps 8:4-8).
The death of Christ on the cross demonstrates
the depth of God's love for mankind. His
creation. Life should be cherished, supported
and cared.
18
wife, each being incomplete without the other.
Out of this partnership, come the children;
then there is the extended family of relatives,
friends and the larger community. Maladjust
ment in relationships or breakdown of relation
ships will affect healthy living.
c)
Spiritual
Man as a whole person, is responsible to
God, as, life is a gift of God. We are cons
cious of the sanctity of human life, because
of this relationship with a living God. Human
being created in the image of God has a worth
and is unique. Unless we maintain this right
relationship with our Greater, we are likely to
wonder about our purpose of existence and
lack a sense of direction in our life. Not being
clear about this may lead to frustration in life
and all the consequences of conflict and
confusion in one's life resulting in ill-health.
If we have a biological, social and
spiritual dimension for our life, our conduct
and behaviour would emerge from this net
work of relationships. How we think and
behave are largely the reflections of our
convictions. As people with convictions, we
are constantly faced with the Biblical under
standing of issues at stake. Let us look at
some of them.
3
The liberalised law of medical termination
of pregnancy Act of 1971, permits termination
of pregnancy on the grounds of danger to the
physical or mental health of the mother or in
the event of failure of a family planning
Let me share with you the experience of
two of my friends who faced the issue of
caring for children with disability. One was
a hospital Chaplain. When a child with disa
bility was born to him, he asked God why this
happened to him, but he could not get an
immediate answer. He loved that child but the
child could not adequately respond to his
love in the normal way. This helped the
pastor to realise how God loves us inspite of
us not being responsive to His love. The other
was a colleague of mine and a highly qualified
Paediatrician. When a child with disability
was born to him and his doctor wife, they
did their very best to sustain her life. The
child became critically ill immediately after
birth, needing exchange blood transfusions.
Though their colleagues questioned the
wisdom of taking such an extreme step for
such a child, they choose to have the exchange
transfusions. The child recovered and subse
quently brought a new purpose to their life
before she finally died at 4 months of age.
Through this the parents realised that God
had a purpose in bringing her to their home.
This experience was an act of God to make
them aware of the need of caring for many
neglected, children with disability in our
4
17
I.
THE DILEMMA OF ABORTION
The debate on abortion is an open ended
issue for most of us. It is a highly emotional
subject as it touches the mysteries of human
sexuality and reproduction. Pro-abortionists
emphasize the rights of the mother, especially
her right to choose. Whereas the Pro-life
advocates, emphasize the right of the unborn
child and his or her right to live. What is not
usually considered in the abortion issue is the
sovereignity of God and sanctity of human life.
"When we debate the rights and wrongs
of induced abortion", wrote Dr. Garetts Jones,
"We are debating a problem of human rela
tionship much broader and more significant
than that of a woman with an unwanted
foetus. Life starts at conception and it is a
continuous process. This developing human
being requires protection from society through
out his life".
measure. This means that almost any one can
demand abortion legally and get it done before
twenty weeks of gestation. Then there are
others who on humanitarian grounds justify
an abortion because of an unplanned
pregnancy, extreme financial or social stress
due to pregnancy, the stigma of a pregnancy
out of wedlock, (unmarried girl, adultery,
incest, rape) and if, the unborn baby is
diagnosed as physically or mentally defective.
of this is that every citizen has also a right to
lay down his own life. When I showed this
news item to Dr. John Wilkinson, a British
medical doctor and a theologian, he reminded
me that according to Christian concept.
Almighty God is the giver and sustainer of
life and He alone has the right to withdraw
breath from life. Life is not a right, but a gift
of God and so we have no right to take away
a human life, even one's own, as it is a divine
prerogative. The famous Arthur's trial of 1981,
where Dr. Arthur had prescribed an overdose
of codeine to a baby born with Downs synd
rome with the object of hastening his death,
can be considered here. Dr. Arthur was char
ged with murder. Many eminent withnesses
were tried.
Most of them justified the
procedure. Finally the court acquitted
Dr. Arthur as his motive was compassion.
There is a strong arguement that if a foetus is
found to be abnormal and severely handi
capped it should be sought out and eliminated
before birth, as such children are socially
valueless. Do not the physically handicapped
and mentally retarded have as much right to
life like others, and get the needed care and
treatment?
16
I
As Christians, our convictions are to be
based on Biblical guidelines. Our view of the
status of the fertilised ovum will largely deter
mine our attitude to abortion. Pro-abortion
campaigners plead that medically and legally
the embryo and foetus are parts of the
mother's body, so she has the right to decide
its'destiny. There are others like the late
Dr. Francis Schaeffer and Dr. Everett Koop
(Surgeon General of U.S.A.) who argue that
though the embryo is carried within the
mothers body, the foetus is a person in the
making with all potentials to grow and
develop. The growing body has a genotypic
distinction from the mother and is "already a
human life, not merely a potential human"
(Pope Pius XII). The Psalmist in the Bible
says "You knit me together in my mothers
womb" (Psalm 139:13) obviously referring to
God as the orginator of every life. Arch
Bishop Ramsay of Canterbury considers the
unborn baby to be reverenced as the embryo
of a life capable of coming to reflect the
Glory of God.
venience. The essence of a Christian approach
to a dying patient is to give ourselves in loving
care to meet his need. A Christian doctor
sees his patients not merely as a biological
4
unit but as a person before God with family
and social connections.
One may want to argue for freedom of
decision or exception to this general rule.
But every exception has to be rigorously and
specifically examined (eg. a serious threat to
the life of the mother or a completely
malformed child as to be incapable of inde
pendent survival). In no case should termina
tion of pregnancy be resorted to as an easy
method of family planning.
One of the great achievements of recent
medical technology is the use of artificial life
support systems which can keep a patient
alive by special means, like artificial feeding,
dialysis, controlled respiration, pump circula
tion etc. But in some cases it may be so
dehumanising, painful, hazardous or costly
that other consideration outweigh the aim to
conserve life.
II.
Recently new knowledge has been
acquired about genetic science, like D. N A.
genetic engineering,
invitro fertilisation
(I.V.F.), Embryo transfer (E.T), amniocentesis.
I.V.F. has found a revolutionary solution to
the human dilemma of infertility by non
human technological means.
The question arises, how long to sustain
life artificially? A patient might say "I do not
want a vegetative existence by drips, drugs
and machines. I want to die with dignity and
I have a right to die when I choose". Some
time ago, there was a judgement in the
Bombay High Court in which two judges
acquitted a man accused of attemped suicide.
They said that according to Indian constitu
tion any citizen has the right to life. Corollary
6
15
RECENT GENETIC DISCOVERIES AND
EMBRYO EXPERIMENTS
IV.
a)
EUTHANASIA
In 1954 Watson and Crick published, the
now famous discovery on the structure of
"deoxy ribo nucleic acid". This has paved
the way for invitro fertilisation and manipula
tion of the genes.
True meaning of euthanasia, is, the
deliberate bringing about of gentle and easy
death, making the patient's last days as com
fortable as possible to ensure a calm and
peaceful death, within context of relieving
incurable suffering in terminal illness or disa
bility. It is voluntary when requested by the
patient; involuntary when resorted to by
those attending on the person. It may be
passive when death is hastened by the delibe
rate withdrawal of effective therapy or
nourishment.
Euthanasia request may come out of
depression and confusion, or out of a feeling
of worthlessness or due to persuasion of
interested
parties with ulterior motives.
Though one may not prolong the act of dying
in a case of irreversal death and thereby
increase suffering, respect for the person of
the patient and concern for the family should
lead us to use our resources as best as we
can to promote life. We should oppose all
attempts for the elimination of human life or
the manipulation of it to suit personal con-
14
Genetic Engineering
The fertilised ovum is grown in culture.
The cells thus formed are then separated into
individual cells which with further culture can
form new individuals, identical genetically to
all others. This can be stored frozen for further
development. Thus a women could give birth
to her twin sister if these cells are used at a
later period.
I
*
By the selection of genes and it's mani
pulation one can choose sex, complexion,
height and other such features of the foetus.
Corrective gene therapy can also be done.
It is also possible to produce allophenes
between species like men and monkey hybrids.
Thus it is reasonable to speculate that, it
should be possible to create novel mutants or
entirely new species. If man, with his scien
tific curiosity and weak human nature, is given
the knowledge and power of a creator, can
one predict where it will lead him to. He may
T
tresspass into regions outside the laws of
God. So it will be necessary to guard against
potential abuses and avoid human vivisection
b)
c)
Organs may be donated after death by
diving wills' or consent of next of kin. When
an organ is required from a living donor, the
age of the donor and his ability to understand
the nature of the procedure, it's complications
and risks are crucial issues. There have been
many instances in countries like India, where
organ selling was done for monetary gain,
organs procured by using coercive methods,
or by giving false or inadequate information.
The recepient should also be given informa
tion about the risks involved, especially, if the
procedure is a high risk one or of an experi
mental nature.
In vitro Fertilization
The procedure of invitro fertilization
(I.V.F.) raises the question of the status
of the fertilized ovum before God,whether
in the womb or in the test tube. The fertiliza
tion of an ovum outside the uterus is a great
break-trough in medical science and an alter
nate means of conception for many infertile
woman. But some argue that laboratory
production of human beings is no longer
human procreation as it amounts to degrada
tion of parenthood and deprives procreation
of its human involvement and love. I.V.F.
might undermine values which biological
parenthood give to marriage. But it is argued
by scientists that I.V.F. is a dramatic extension
of the sort of interference found in delivery,
by ceaserean section or in hormonal induction
of labour.
Consent for organ donation
d)
I
Resources
In these experiments there are a few
surplus fertilised embryos which are kept
frozen for future use or are used for further
experiments for researchers to study genetic
The question should be raised in situations
where there are limited resources, whether it
is justifiable to spend enormous amount of
money, time and energy for prolonging the life
span of a few, temporarily, while thousands
are denied even the elementary and basic
health needs which might cost very little.
Offering a patient extended life without
reasonable quality of life seems to be cruel.
8
13
♦
a)
Organ Procurement
A major obstacle yet to be overcome
is the inadequate supply of donor organs, and
the supply and demand imbalance is increa
singly widening. Till artificial organs are
designed, an ethical problem will be, establi
shing a fair and effective policy of allocation
so that the available organs are used as justly
as possible.
b)
a.
v
Determination of Death
The viability and suitability of certain
organs depend on the time lapsed after death,
and, hence the tendency is to remove the
organ from the donor as early as possible. This
leads to the question of the criteria for death.
The traditional legal view of determining death
used to be the absence of heart beat and
spontaneous respiration. With the advent of
recent life supporting systems, neurological
death is now considered to be the criteria for
death. It would be advisable that brain death
should be certified by a physician who is not
a participant in any phase of the transplant
procedure.
12
I
r
and developmental abnormalities, intricacies of
tissue and cell differentiation etc., or to be ulti
mately destroyed. Can we treat the fertilised
ovum as a lump of jelly or blop of tissue which
can be destroyed, like a tumour or tonsil? Is it
right to use human materials for experiments
and if so how far? At present the proposed
law in the U. K., does not permit embryo
experiments beyond 14 days (which is the
implantation stage). Then the question is
raised, do human embryos have any right at
all? If they have rights, at what stage? Can
such embryos be the material possession of
the donors when they do not intend becoming
the parents. The fundamental issue is whether
or not respect should be shown to human
embryo in view of the potential for full
humanness. If embryos are produced with the
expressed purpose of providing scientific
information, that information has already taken
precedence over the significance of human
existence.
In the West, ovum is fertilised from sperm
of unknown parents and children are born
without identity of biological parents. (This
is now changing, as donors have to record
their identity). A child conceived in a test
3
tube can have as many as five parents; the
egg donor, the sperm donor, the surrogate
mother, (who bears the child,) and the couple
who raise the child. The potential emotional
and psychological ramifications of this could
be deep and disturbing.
The Anglican Church of Australia disap
proved experiments like cloning, genetic
engineering, artificial placenta, surrogate
motherhood, human-animal hybrids and
embryo
freezing. Organisations like the
Order of Christian unity (London) are seeking
to outlaw 'womb leasing' and 'Ovum donation,
to, eliminate legal problems, human tragedies
and to uphold the sanctity of human life. It is
now accepted that no human being is to be
treated as property, as in the days of slavery.
Every one has an inviolable status as regards
life and liberty. It is recognised that every
human being has the right not to be used as
a means to the needs and interests of others
c)
after amniocentesis, revealed that the vast
majority of the babies aborted were females.
This is a small pointer to the way this proce
dure is being used. It is used for determination
of sex giving a chance for the parents to
choose which baby they should keep. This
attitude to females can have devastating
effects on our social structure.
t
III.
I
Amniocentesis
The study of amniotic fluid gives a lot of
information including the sex of the foetus and
of possible malformations of the unborn baby.
A study of abortions conducted in Bombay
10
The real indications for amniocentesis
when ethically used may be for providing
therapeutic support for the unborn baby
(eg. hydrops foetlis) or for diagnostic purpose
to anticipate the special measures needed to
assist the baby at birth. (Respiratory
Distress Syndrome) The decision to resort to
amniocentesis must not be with the bias to
resort to abortion if needed.
$
ORGAN
TRANSPLANTATION
Organ transplantation is another break
through in medical technology, overcoming
many technical barriers like vascular anasto
mosis, immunological rejection problems and
so forth. The process is one of high cost,
prolonged hospitalisation intensive medical
care and follow-up.
11
■
):
MF F ^4' 16
TVth General Meeting of the Faculties of
Colleges/Cont re s
Group Discussion I
ETHICAL RESPONSIBILITY
ethical responsibility
*As a group, identify the major areas of
in your Institution.
Group A;
What are the important ethical issues that you encounter in the
Institution's Administration? Name fpu£ main areas and how
in your opinion can they be tackled.
Group Bs
What are the four main ethical problems you encounter at the
departmental/Unit level?
How do you deal with them?
Could you highlight ethical problems occuring within teaching
faculty; and between teaching and non-teaching staff of your
section?
Group Cs
Kindly list the ethical problems encountered at interdepartmental level. Which are the three main/common ones
and how are these issues dealt with?
HER
DECISICN MAKING STRATEGY FCR CLINICAL ETHICAL PROBLEMS
IN MEDICINE:
BY DR* G-D. RAVINDRAN.MD^DNBE
Department of Medicine
Decision making lies at the very heart of the. art and
science of health care. Medical education and training aims to
train physicians to make decision. As physicians we are constantly
making decision. We make decisions when we listen to a patient Ts
storyi examine the patient, order a test of a treatment.. Nene
these decisions are easy because as Osler says that ’medicine is a
science of uncertainty and. an art of probability’. Nevertheless
physicians generally reach a clinical decision and feel reasonably
comfortable about it.
Many times we prescribe even waen diagnosis are not certain.
Many clinical decisions are made in face of uncertainity i.e. on
the basis of a diagnosis and anticipated, results, which are
probabilities not certainities • To aid in decision making process
decision trees are constructed. A decision tree can help to
1) point out background information
2/ explore need for more diagnostic work up
3) expose the consequence of treatment
When the diagnosis is uncertain or the treatment has risks
f of the patient, a decision tree has to be applied. To apply the
method of decision trees to a clinical problem, the physician^ has
to enumerate the possible consequence of decision, estimate the
probability of each possible outcome and assess desirability or
utility of each outcome.
In recent years decision analysis has been increasingly
advocated as a means of solving complicated clinical problems.
These problems tend to involve numerous variables that must be
carefully weighed before a solution can be proposed. Ihe
rationale for using this method is that it is logically constructed
and mathematically based and will provide a major objective
answers to many clinical questions.
Historically the professional ideal of the physician-patient
relationship held that physician directed care and made.decision
about the treatment. Thu patients role was te comply witn the
doctors orders. Although this paterenalistic approach often
took “account of the patients general preference and attitudes
towards treatment, it gave a minimal role to the patient m.
decision making. When faced with what appeared to be a patient
irrat cnal choice or preference, physicians were encouraged by
this ap-OrOach to overlook or overide them as not being in the
true interests of the patient.
This attitude is changing and it is replaced by a concept of
shared decision in which both the patient and physician have to ,
make an active and essential contribution. Physicians bring them
medical knowledge and patient bring their belifs and conviction,
to make a shared decision.
When there are clinical problems which arise out of a decision
tree it can be solved by mounting clinical studies or search of.
medical literature. But this method cannot be used when physicians
have a difficulty in facing clinical ethical oedsion.
: 2 :
eg* 1) Should we write Qo Net Resuscitate (DNR) on patient
with bilateral strokes and pneumonia?
2) Should we treat a patient with entric perforation
.
who refuses surgery or antibiotics, because of his religicus belifs •
3) Person on ventilator due to C.P. poisoning whose
relatives are not bothered about the patient and the patient is
not get ting 1- medicines as nobody is bringing any medicine and the
ward stocks are exhausted and clinically patient appears brain dead?
These types of question provoke physician discomfort for
several reasons
1 Life & death decision that provoke deepest human emotion.
2 Education & Training has not prepared them to approach the
pr oblems ana lytic a lly.
3) Fear of criminal or civil charges.
With ail these quandpies is it possible to develop a systematic
approach to clinica 1 ethical decision that may to some extent .
improve their ability/reach a reasonable, legal and morally
defensible decision in th^se difficult situations. Any method
that is evolved should take into account, all relevant factors. '
Any method that is evolved should gurantee for the physician
that all relevant considerations are taken into account and that
none is overlooked while reaching an ethical dec-ision.
MARK SIEGL3R has described a method takes into account all the above
mentioned factors •
To make a clinical ethical decision the following factors have
to be taken into consideration they are
1) Medical indications
2) Patient preference
3) Quality of life
4) External factors
Medical indications:
. 0
Ibis is the first and most recognisible part of decision making
process. A physician should examine the patient ano a diagnosis
should be made
Physician should consider all the therapeutic
modalities and the finally recommend the best option available
to the patient.
.
.
,
It does not mean that he will place aT-l the options before
patient^ and then ask the patient to choose. Certain authors like
Ingelfinger characterise this type of approach as. a malpractice
or sheirking of physician responsibility. Hence.it is a primary
duty of the physician to sort cut the possibilities, weigh the
pros and cons and ther,recommend a course of action. Until, this
step is completed we cannot advance in the process of clinical
ethical decision making.
PATIENT PRSFERSCE:
After the physician has recommended the best possible
treatment, patient has the preorgative to accept or reject the
treatment depending upon their personal choice and belifs* If
the patient is not competent then the family members or designated
persons should make the decision.
I
I
I
: 3 :
■
. .................... ■
■
•
■
,
The wishes of family ^members are taken into consideration
because it is felt that they would know the intentions of the
patient better than others. Semetimes it may be difficult to
judgo whether the request made by the family member might have
been that of the patient, If the family members derive some
benefit from choosing this modality.
.
■
i
When the patients refuse recommended treatment then physician should
judge about the competency of the patient in making this decision.
If the patientsi are incompetent the family members should be
consulted.
Cnee a patient makes a choice it has to be respected
sometimes physicians do not accept these decisions (due to the fear
of legal problems) and then it leads to prolonged legal struggles
and unsavory incidents
In US courts hava always upheld the right of patient to make decision
starting from Karen Ann case to the latest Nancy curzan case, tne
right of the patient to make decision is paramount, ccurts have
also taken pams to protect the rights ot
p^ienrs. In
xn the
Cnu Nancy
of patients.
Curzon case, in the first trial the wishes of the.parents
the parents was 1not
accepted as the court felt that there was no sufficient evidence
to show the patient would have, refused treatment. Chly in the
subsequent trial and with fresh evidence court accepted the wishes
of the parents.
In the USA about 10% ofx the patients ...
make
living,.wi(ll.
--J aa living
will. In
shown
that
70%
of
patients
with
a recent study it has been s-—
. chronic
2-_
7 ..
“i
incurable diseases have indicated their preference for D.fcj.R.
and
of
cardiac
for not using life supporting system in the event
arrest•
mvSL vx
u—the
— Patients and physicians choices coincide
Most
of the times
— -j instances
when the medical inoications are grim
But there are some
and in~which the patients are unable to make a choice, ^hone of
■cnera^ljb offer
u^vh much
improvement and patient m incompetent)
the therapies
other
factors
come
into play they are quality of life and
Two <
external factors.
QUALITY CF life:
is
meanin.g/ambigcus•. It is
Although it is frequently used the meanin.g/ambigcus
a subjective evaluation by an cnlccker about a patients subjective
’• ~
whdre a
experience of personal" life.
It is used in a setting whejre
patient is unable to make a evaluation cr is unable to express it.
The standard which is almost always applied by someone other then
the person who is living the life that is being assessedI for its
’ i value on sone collection of
worth represents an attempt to put.a
It is
features of human experience. -"L
\ based on more of subjective k
feelings and less on objective facts, In routine practice
physicians do not place much weight on quality of, life!
consideration except those that are expressed as the. patients own
preference.
preference* However quality eflife considerations will tend to
be invoked in clinical tcircumstances in which both medical
indications a e limited and patient preferences are not kn own.
These are- 1 Untreatable or terminal illness
2 Patients having brain damage
3) Neonates
4) When there are no code decisions
• ...4A
I
1 '
* ..IW
h
■
: 4 :
EXTSRNAhL MS ICRS:
_..„1 factors
_j
refer to
t o any consideration in a case that
External
yie Ids alburden
--------- or_ benifit. to seme party other than the specific
being made. This takes m account
patient for whom the decision is being,made.
the wishes of the family, costs of medical care, allocation of
medical resources and well being cf the society.
Although almost any clinical decision will, involve some
external factors such as these, the question arises as to whether the
physician should ever consider these effects and allow them to
influence the clinical ethical decision making process.. When, if
ever is It ethically permissible to weigh the patients interest
against that of the society? In general external factors do.net
and should not be accounted for great weight in routine clinical
- ethical decision making.
In the US courts have not taken into consideration the quality
of life no-r other external factors like costs. In a celebrated
case of Baby I- the courts did not take into considerstion. ths
quality of life,in the case of Nancy Curzon, the courts did not
take into account the costs of treatment. Hence most of. the
clinical decisions can be made by physician and patient interaction
Why de patient make seemingly irrational choice? When we
analyse th^ causes for irrational decision making
Ihey are
Bias towards present and near, future
It is rational to prefer a restoration of function now rather
than later and it preferable that a loss cf function occurs as far
in the future as possible so as to minimise the period cf
disability or loss of one’s life be as far as possible atleast
ehile it remains a life worth living. It becomes irrelevant,to
refuse to undergo* a painful experience, now if by undergoing .it
one can avoid a much worse experience in the future. This is
known as a bias to present.and near future. People commonly
give a disproportionate weight to securing benefits and avoiding
harm in the near future as opposed to the mere distant future.
It wont happen to me. Some patients will irrationally deny the
possibility that an untoward nvent could happen to them, they also
have maoical illusory belifs about their vulnerability to harm or
simply have a different way of viewing the medical problems.
FEAR OF PAIN:
Patient may delay cr ncr even ecnsider a partieular trea
fcr the fear cf the percived nature of
cf the experience although they
may acknowledge that the treatment dearly is in their best
interests.
FRAMING EFfH^T;
The way a question is framed may provoke a negative response.
eg. prognosis, patients tend to accept the concept of gams m re
I erne tim^s what t he patient wants to do do ;s~ncf>t mak,e_s^nse._ho_±he
physicians..^ Patient may decline the ccurse^of tre|tment because
which physician believes it to be ineffective , ys
hPHVSioU„ have to
S^times the fallu?e.to P»sua<l« ’
3
ch01f
«v b? ‘’Jr^W^f^theNensequ^
-Te phystl.^
w"t exempt to
of harmful effect of the
ch cice •
IM e P rzv.
p - 7- /3 -
CLINICAL 3THICS
/A
Clinical ethical work up outline.
I
Medical Facts: Using the problem oriented medical work up
II
Human values and issues
III
Practical General Ethical Fundamentals
IV
Identify the major conflicting values
V
Decision making
How does medical ethics contribute to patient care?
Clinical ethics is intrinsic to the work of the physician and
the practice of medicine. The. centra
central1. focus of clinical
c * *
etpics
. •
x
“ i i
Clinical ethics
is individual patient-physician
decision
making.
seeks a right and good healing decision for the particular
Patieht. Clinical ethics is often enmeshed in factual uncertain
nity. This is because it is often conducted in an emotionally
charged situation or in emergency circumstances- It is a fact
that medicine and ethics are inseparably linked because the
identification of conflicting values, a necessary step for* ethics,
depends on the medical context or facts. IIn this short paper I
will present the approach used in the clinical ethical work up
of a patient.
’
A' '
‘
......................... ‘
I.
'•
:
'
MEDICAL facts
Identify all significant medical factors and their likely
consequences. Without these facts a critical understanding of
how a case raises moral issues is impossible® If the prognosis
is ambiguous because of improper/incomplete medical work upi
moral issues arising may be impossible to resolve.
II. HUMAN FACTCRS
These arise in each case: Patient’s ace, attitudes,
occupation, family situation, behavioural history indicating
attitudes and values, . ;religicus beleifs and so On. Human
factors often express values that come into conflict with
medical management and give rise to ethical dilemma, eg. The
family wants to know the prognosis of the patient, which the
Physicians are uncertain of.
hi, prachcal general ethical fundamentals
III
(i)
Preservation of life.
/alleviation of suffering.
Injuction that physician "first do not harm”
(Primum non nocere)
Respect for autonomy: Patient alone or their legal
serrogates have the right to control what happens to
them.
c
.......
Concept of social justice: An effort has to be made
to ensure that medical resources are allocated fairly.
Benficence.: act of benefiting patients.
Ncnmaleficence: refrain from harm
Disclosure: Providing adequate and truthful informa
tion for competent patients to make medical decisions.
2
Informed consent*
Brain Death and Organ Transplantation.
Witholding and withdrawing life support.
The vital concept of prcpcrti onate treatment: At least a
reasonable chance.^
benefits to the patient
which outweighs the burdens attendent to the treatment.
Benefits#and Burdens: The reasonable possibility of return
to cognitive and sapient life as distinguished from
biological vegetative existence eg. Instructions for
"Code” versus "No Code"
Effective communication with patients and families: Some
physicians communicate better than others.
Early determination and ongoing review of individual
quality of life values versus Quality of Life Years* The
former is essential in evaluating patients, the latter
is highly controversial*
III (ii)
Policy Guidelines in Hospital Departments
Criteria f or admission to ICU
Policy guidelines for ventilatory care
Policy guidelines for dialysis
“No Code”
Assessment of Organ System Failure
III (iii)
Ethics in EU
In the ICU ethical principl s may be more difficult due
to environmental social and economic, pressures* Commonly
used principles are Beneficence, Nonmaleficence and
Autonomy, Remember principles that may conflict: eg.
Beneficence Vs Autonomy. If the patients human values
(interests and wishes), medical work up and ethical
issues were defined before admission to IGU by the
Patient their surrogates and the primary physician,
many of the most ethically difficult IGU situations
could be avoided. Primary care physicians are in a
particularly good position to inform the patient and
family about the .consequences -of the critical illness,
life support measures and to get their response in order
to help them to prepare durable powers of attorney or
living wills.
III
Criteria for Advanced Ljie Support
Young patient
Previously healthy
(iv)
Strong constituion
„ Disease potential ielf limited.
Criteria f cr No Adva nd ed Lif e Supp ort
Elderly
Long standing illness
Terminal Disease
Emaciated chronically ill: eg. these do badly with
ventilatory care - "Can never be weaned off the
ventilator"
IV
V
the major gcnflicting values and set priorities fcr
DECISICN MAKIN3
: 3 :
Standard academic tests can evaluate students and physicians
ability to think clearly and critically about an ethical
delemcna. Observation is the only way to evaluate Harnan values
eg. whether the patient is treated with respect.
k clinical
ethical work up provides the physician,with a meaningful
experience and search for the best medical knowledge available,
address of, sensitive issues and how they are dealt with by
“problem solving skills” . Cases may be very simple or
c omplicated •
CASE ILW5TRATICN
48 yr male non smoker diagnosed Severe Pulmonary Fibrosis with
Pneumonia and Respiratory Failure. Two years before the
bronchoscopy was negative. He was advised an open lung biopsy
but refused. This patient takes 3 months to improve marginally
and is discharged on oxygen at home. He has copious sputtjm
2-3 cups per day white and frothy and a diagnosis of Alveolar
Proteinosis is considered. But patient is medically unfit for
bronchoalveolar lavage because of profound hypoxia. He is
readmitted after 3 days because oxygen supplies areerratic
at home. The patient is in profound respiratory failure.
Human factorss
- Financial, Cxygen machine costs t Rs.60,000, tc be raised.
Hospital stay four months cost - Rs.50,000. Wife asked family
tohelo financially and many conflicts consequently arose*
The Chest Conference raises the issue that the patient may have
fungal infection of the lung and it shculd be treated. ,
Amphotericin B is started. Patient deteriorated and died.
Postmortum true cut needle lung biopsy taken.
Re p oyt: Bronchclar Alveolar Carcinoma. The wife is informed
of this report she is deeply bereaved by the loss of her
husband but expressed relief of profound guilt she was
experiencing because she had resufed the open lung biopsy two
years before.
was reassured. Throughout the management
of this patient his wife and her mother was. treated medically
(control of hypertension/ and soc■al/financial conflicts
addressed. The patient during his illness went through,
episode of severe situational depression. This
----- case
------ illustraticn mainly the conflicts arising from human factors ano some
ethical issues. Autonomy of the patient to refuse tests.
Disclosure * Patient asked to be told the complete implica tions
of the diagnosis. As we did not have the means to confirm the
diagnosis we gave the presum^diagnosis and treated for this
diagnosis namely pulmonary fibrosis with steroids which failed
and then immunosuppression using azothioprine which is.the
recommended treatment in steroid fail pulmonary fibrosis, This
was reasonable treatment for, this presumed diagnosis. The
Patiert consulted other specialists but showed ho wish to leave
illness.
cur care» This is a frequent consequence,of severe illne
protracted course and when the diagnosis is not confirmed1. (In
During
the last two ,weeks
this case by an open lung biopsy). D-4of the patients stay in the hospital the wife was supported by
adequate explanations to her many questions and for the
economical consequences and difficulties she was experiencing
Imminent death was explained to the wife 1-2.weeks befcrd the
patient’s demise and the necessary support given during this
interview.
TA--1
ETHICS IN THE UNIVERSITY TEACHING HOSPITAL
DR. PREM PAIS, MD
DEPT. OF MEDICINE
JOHN
’
S
MEDICAL COLLEGE & HOSPITAL
ST.
deqis ions
The ethical factor is constantly present in all actions and
facility
especially
a
teaching
one
and
a
Christian
one at
in a hea1th care
and
s
should
evolve
a
written
code
of
ethics
and
moral
that.
Al 1 hospitals
Ethical
values
and
codes
must
be
communicated
have an ethical committee,
Despite this, problems will
constantly
to all staf f in a meaningful way.
rules,
crop up
which
are
not
adequately
covered
in
any
formalised
set
of
up
common
Fortunately such problems can usually be satisfactorily solved with
sense and humane reasoning, against a moral background.
Ethics in a university teaching hospital has 3 dimensions:
- Secular ethics which are followed by all health care institutions.
eg- - care of patients, cure or amelioration of disease
- training students to become competent professionals
moral
Organisation with any religious offiliation have additional
as
considerations eg.
instilling
in students and staff
moral
as well
i n health care
secular
professional
values and codes, social
justice
in
administration.
to a specif ic
of an institution belonging
Specific considerations
teaching
on human
would
be
the
Catholic
Church
’
s
religion.
A prime example
procreat i on.
Remember that a teaching hospital plays the following roles:
- service to patients
of_ medical
and paramedical personnel
- education l
----research
be
now
may
points
as a general background, a few specific
With this
considered.
.
the
Spi r i tua 1
Aspect of Hol iist
s tzziic
c Care ; Christian hopitals must not forget
i
ns
t
i
tut
ions
Mos
t
spiritual
aspect of 1the person who is their patient,
have a chaplaincy service but often the chaplains are not as effective as
they could have been.
tens ion
- adequate training is essentialI for hospital work is not just an ex
in
SJMC&H
has
been
running
a
formal
3
months
course
of
parish duties.
---- ..
Pastoral Health Care for the last 3 years.,
team,
integral
part of
the medical
the chaplains
must form an
i
bridge
between
them
and
patients
and
interacting with doctors and forming a
that
has
been
much
neglected.
relatives.
This is an area t--- --
management
is
The Financial Crunch & Social Justice: Stringent financial
inevitable if we are to make our institutions economically self-supporting,
management
bus iness
But we must not allow ourselves to become schools of
turning out entrepreneurs rather than professionals.
The right message should go out:
- that our institutions have to be self-supporting
- that this can be done justly, humanely and morally
- that students and patients are looked at individually and their
needs and resources considered.
2
that we remain committed to equitable distribution of hea1 th
that
not
"only the rich and the privelaged have access
to the
(Illich).
are so
system"
Conta i n i ng Costs : How can we contain costs without
sacrif icing
"Scademi c
med ic ine "?
- Drugs - Using generic and low cost drugs where possibl e and resorting
to
bulk purchase.
teaching our graduates to prescribe rationally and a 1 ways
consider the costs involved.
Rout i ne
InvestigationsThe routine battery of tests ordered
i
mos t
teaching hospitals add up to a considerable sum and most of them do ot add
much
to diagnosis or therapeutics.
Still it is felt that in a
teach i ng
instituion a certain amrtjount of over-investigation is inevitable.
Where is
the line to be drawn?
Capi ta1 Intens i ve Equipment :The cost of high tech medical equipment
is
astronomical.
The cost of single such item could provide
primary health
care to a village for 1-2 years,
Nevertheless, we strive for excellence in
all fields, and it is our duty to do so.
It is the institutions moral
and
ethical duty
- to carry out a cost analysis to be sure the hospital can
afford to buy and run the equipment.
- to plan an approach for patients neediiig use of the
equipment but unable to pay for it.
|
- when there are competing demands for finite resources to
choose
the
item which will
benefit
the
greater
number
of
peop1e.
T each i ng Mater ia1 : the Genera 1 Ward Pat ient Conventionally the general(ward
patient
is the teaching material for our students.
It is the price t
be
paid
for
not being able to afford a private room.
Our students
get
the
wrong message for the patient is not "teaching material" but is the teacher
to
the
profession.
Medical
teachers and faculty have a key
rol
in
impressing this fact on the students.
The patient has a right to refuse to
be examined
but will often agree if he is treated
respectfully
res pectf u11y and
his
consent obtained after proper explanation.
Do Some Mora 1 Va1ues Deny Learning Opportunities to Students:The catholic Church has strong beliefs in the field of human procreation,
Catholic
hospitals do not carry ouf* IMF, abortions and many birth con ro 1
11
procedures.
Does this deny the learning of certain skill by students?
does, but that is not in any way a valid reason for changing these beliefs.
These beliefs & teachings have evolved for valid and considered
reasons
which are above purely professional or technical considerations.
the
paper attempts to show that for a Christian Teaching Hospital
This
dimension has to be considered even in mundane, every day
thin gE .
eth i ca1
Secu1 ar institutions may find themselves uncomfortable at this fact but for
us morals and ethics have to be the basis for all decisions.
<2
r
C
■
THE WHITEFIELD STATEMENT
1
r?
i
Having discussed the role of Med’ical Ethics in the curriculum of Medical
Colleges and being aware of a growing culture of violence in our country,
we the members of the four Christian Medical Colleges/Centres, tkB
together with the Christian Medical Association of India and the Catholic
Hospital Association of India have deliberated on certain issues involving
violation to human life and wish to express as follows:
!• Abortion
Ihe Medical Termination' of Pregnancy Act was passed in 197^ with
the intention of helping married wonen with repeated pregnancies•
However, it is noted that it has led to a great increase in
abortions, totalling over 11 million annually, three fourths of
which are done for unwed pregnant girls# We reiterate that it is
most unethical to terminate human life from conception onwards and
we decry the practice of abortion#
2. Newer Contraceptives
The health of many women in our country is greatly jeopardized by newer
anti-pregnancy vaccines, hormonal implants, dangerous drugs such as
RU 436# All these experimentations are carried out without any informed
consent and many have “surrptiously11 progressed to field services#
All this human experimentation, leading to dangerous & yet unknmm
consequences, must s top forthwith.
3. Prenatal Sex selection
The use of ultrasound and amniocentesis in pregnancy has invariably
led to female foeticide. We condemn very strongly this violation
against female children and we wish to promote whole heartedly the
value of equality in both the sexes and the need to protect young
innocent lives#
4# IVF Techniques
Many IVE techniques being practised not always ethically, have resulted
in hundreds of live embriyos frozen in the laboratories. This poses
an enormous human problem which must be discussed and guidelines
should be issued#
# Handicaoued children
The practices of infanticide and neglect of handicapped children is
contrary to all norms of natural justice. We must spearhead a
movement for special care of these children and-provide facilities
for their treatment and welfare, including adequate job opportunities.
*
■
"
————————
/
6# .Euthanasia
The fabric of scant respect for human life is manifest at its terminal
I
stage, when doctors are being enticed to actively promote euthanasia.
The introduction of Euthanasia Bills in seme States in India will only
3
lead to debasement of the health profession as seen in seme Western
Countries, where doctors and nurses have taken upon themselves the
onus to terminate lives# We must emphasize the cherished values
incorporated in the Hippocratic Oath and relentlessly expose and
fl
■ '-'$p
oppose such practiced#
■' I
"■
Doctors and health professionals should be true guardian of human life#
It is upto us to provide this leadership through the network of Christian
Hospitals and other Institutions, to oppose vigorously the present
“culture of death” prevailing around us and to restore a sense of well
being and protection of all human -life frem the moment oc conception
to its. natural end.
.
•
< ■
<11/ hr—-)
< LMu L
•
'
****************************
i
1
I ■
MEDICAL
HUBRIS
A REPLY TO IVAN ILLICH
I
Jp • • •■
E
nF-
Ei:-
DAVID F.HORROBIN
K'-- ■-
K&.
I
I ■
b.
B-
II
Ek-. ■
I;
B
E'
1
!
■
!i
Sii CEZSgkZ“d NEW YORK .9,8
6-
Br
E ■'
I.
’
-
87
’ i
i L Proposals for Change
I
1
if.
1i
'The medical establishment has become a major threat to health.’ In
spite of all my criticisms of his work, in spite of all his exaggerations
and inaccuracies, I still feel that Illich’s first sentence is right. He is
wrong about the current seriousness of the threat; he is wrong in extra
polating so glibly to the whole world from the countries of his own
experience, he is wrong in his estimate of the contributions medicine
has made. But he is right in his assessment that things are beginning to
go badly awry and that action is required if they are not to get very
much worse in the near future.
So I agree that the main thrust of description of the state of medicine
and its relationship with society is not too tar wrong. His description of
the syndrome is reasonably accurate but his refusal to recognize that
most of the critical material he has assembled comes from medical
sources and that much of the work has already been done by doctors
themselves is totally misleading. Ulich is not such a lonely prophet as he
imagines himself to be. He does not have a monopoly of insight. Joseph
Conrad wrote a book ‘The Secret Agent’ which was first published in
1907. In it the Professor says to Comrade Ossipon with regard to the
views of a third revolutionary ‘And so Michaelis dreams of a world like
a beautiful and cheery hospital.’ Ossipon replies, ‘Michaelis may not be
so far wrong. In two hundred years doctors will rule the world. Science
reigns already. It reigns in the shade maybe — but it reigns. And all
science must culminate at last in the science of healing - not the weak,
but the strong. Mankind wants to live — to live.’ Many doctors here share
Illich’s concerns but there is little doubt that they are ignored by many
of their colleagues or that their plaints fall on many deaf ears.
But while Ulich is not too far out in his descriptions of what is now
and what things might become, he is hopelessly wrong in his under
standing of the pathogenesis of the situation. Despite his claims to be an
historian, he seems to have little feel for history. Despite his concern
for the individual, he seems to have little understanding of how ordinary
people operate. Despite his repeated desire that the earch should be a
place in which Everyman should live, he consistently wants his Everyman
to be a Hero.
Ulich has a view of the operations of the medical profession which is
very close to tl
.sion that John Kenneth Galbraith has of the function
ing of the modern large corporation. Galbraith sees the corporation as
deciding not what the public needs but what the corporation wants to___
supply. It has enough influence then cynically to manipulate public
desires so that people feel a great hunger for this object which the cor
poration supplies. In a way almost exactly predicted by the corporation,
the supplies are made available. The corporation makes a profit, it rein
forces its power and influence and poor individuals in society are trapped
ever more deeply in the machinations of the new industrial state.
According to Ulich modern medicine operates like the modern corpor
ation. It has decided that it wants to supply perfect health for everyone.
It has cynically set about persuading people that that is what they want,
and having created the desire, it has made arrangements to supply it.
To me this seems to be a completely false interpretation. As far as
1 can see health has always been a major concern of traditional societies.
At no time in the past has the great majority of individuals felt able to
cope with pain, disease and death in a sturdily independent way. Most
people have always felt bewildered in the face of these trials and have
always been willing to put themselves in the hands of healers and priests
who have offered remedies and religions to enable man to cope. In many
traditional societies the role of the healer priest is all pervading and
crippling. So many rules must be adhered to, so many rituals followed
if an individual is to remain healthy that sturdy independence is often
non-existent. For thousands of years the healer priests have been as
powerful as, or sometimes more powerful than, rulers in the communities
they ‘served’.
One thing limited their influence. That was their near total lack of
success in treating disease and preventing death. Certainly some primitive
remedies worked. Certainly healer priests, like many modern doctors,
were willing to exploit for propaganda a spontaneous return to health
which had nothing to do with their machinations. Certainly by means
of mystifying language and impressive ritual many were persuaded that
the healing was more successful than it really was. But never and nowhere
were traditional healer priests consistently able to point to regular major
successes in man’s battle with disease.
Medicine had inherited the role of the healer priests. It is obviously
heir to the healers of traditional societies but the 20th century collapse
of much organized religion has led in addition to many people looking
to doctors for advice and comfort which they previously received from
their priests. It has therefore obtained a double influence. But much
more than that, although it is less successful than it and the public think
it is, it can point to a long series of spectacular and consistent miracles.
t
■■I
J
1
nI
86
I
D*
KJ
" 5 p
89
88
i I
I
K
s
The conquestsof-puikrand-smaHpox^-theremovalofparental fearthat—
their children will die of pneumonia or diphtheria or tuberculosis before
they reach adulthood and many other successes are unequivocal and
readily demonstrable. Because of the traditional desire of the sick to
put themselves in the hands of others, because of the obvious power of
modern medicine, society has willingly accorded to doctors an influence
and a power which they have never had before. But the profession has
acquired this power in a fit of absentmindedness. On the whole it has
not deliberately sought it, and it does not know what to do with it. Far
from using it in a heroic and Promethean manner, it has bumbled along
making decisions of enormous significance without realising what it is
doing. In some ways this is far more dangerous than a cold and deliberate
bid for power would have been.
Finally, Illich is tragically wrong about solutions and perhaps even
uninterested in them. In some ways it seems that the last thing he wants
is for medicine to be reformed effectively either as a result of internal
or external influence. Instead he wants doctors to behave in a ridiculous
and arrogant fashion in order to horrify people so much that the whole
structure of industrial society, including medicine, is brought crashing
down. Hence his solutions are unrealistic or trivial, quite impossible to
achieve in any democratically organized society, yet incompatible with
all but the most benevolent (and therefore non-existent) totalitarian
regimes. Some of his remedies, as in the case with his ideas on pain and
his desire to abolish all control of both doctors and quacks, seem likely
to intensify rather than to ameliorate the very problems he discerns.
While complaining all the while about the use of mystifying language
by doctors, he and his disciples consistently write and talk in ways which
are often nearly incomprehensible. Sir Karl Popper’s remarks about the
philosophers of the Frankfurt school seem to fit Illich and his friends.
They are in ‘a tradition which accepts that something is profound when
it cannot readily be understood and that the sign of a man who has had
a university education is that he can write and speak in a manner which
is both impressive and incomprehensible ’.
Some tentative suggestions
!
My basic philosophy of the way to bring about political change at any
level in any society consists of two propositions. The first is that we must
start from where we are and we cannot do that unless we can see our
present position with a reasonable degree of realism. The second is that,
without any exceptions at all, the consequences of any proposed change
are always different from those that the proposers predict. The gap
between expected and actual consequences becomes greater the greater
the degree of change proposed. Since almost invariably the consequences
are less favourable than expected, the greater the degree of sudden change,
the greater is the shortfall between hope and reality.
At the moment I think that both Illich and the medical profession
have an imperfect grasp of reality. Many doctors do not realize how
serious the situation is and only partly understand the origins of those
defects in the system which they do perceive. Illich has a better but
exaggerated perception of the current situation but has almost no insight
into its origins. He has performed a service by taking the writings of
some concerned doctors and setting them out in such explosive and in
flammatory language that the ideas must command some attention. It
is up to the doctors, infuriated by Illich’s rhetoric, not to condemn him
unthinkingly but to consider seriously his thesis, to admit where he is
right and then to set about doing something about it.
If a large enough number of doctors does become sufficiently roused
to make a realistic assessment of the state of medicine, what is the best
way of generating change? Illich’s answer is essentially to remove most
controls and to allow the public to decide what it wants. He does not
believe that the profession will ever be able to make the decisions to
move medicine towards what he sees as a more favourable state. I think
he is totally wrong. The thirst for miraculous health is such that lay
opinion is likely to be captured by effective publicists anxious to acquire
more and more power. The last state will be worse than the first with a
public dominated more than ever by health concerns and unable to make
any rational assessments of the irrational complaints of competing healers.
My own belief is that most doctors are neither particularly humane
nor particularly perceptive of the needs of society in general or of patients
in particular. But one of the strengths of medicine is that it has repeatedly
produced great healers who have seen the necessity for reform and who
have dragged along their colleagues, grumbling and complaining furiously,
but nevertheless ultimately being willing to change. Often the great men
have been successful simply because they have pointed to the ideals of
the Hippocratic Oath and have shamed their colleagues into agreement.
The agreement has not come from the heart but the hypocritical head.
However as C.D. Darlington has noted when speaking of the early Christ
ians, ‘Within the community, they established a stern uniformity of con
duct, a deference to their own rules. Now although such public deference
must always engender private hypocrisy, it is in practice the only weapon
invented by man for raising the conduct of a heterogeneous society above
the average genetic and instinctive level’. Because of their claims to be
possessors of high ideals no matter how hypocritical such claims may be,
if doctors are to retain public respect they will always be vulnerable to
I
I
i
ft’
fj-
i
those who demonstrate that the medical profession is not acting in the__
interests of society. Ultimately, if the idealists are persistent enough,
they will always be able to force doctors to act hypocritically and
grumbling and groaning, to surrender personal privilege and wealth in
the interests of humane medical practice.
I therefore think that because of its supposed ethical basis the medical
profession is vulnerable to enlightened pressure. But if it is to be fully
successful such pressure should come from within and should be well
informed. Ignorant outside pressure will always be angrily resisted.
Medicine is in a serious state and is in need of reform. But reform is
likely to be effective only if the proposals are based on realistic inform
ation about the current situation and about its origins. I therefore think
that such reform can be effected only by doctors themselves, by doctors
sensitive to the criticism of laymen such as Illich. But doctors should
not be under any illusions. There is a serious breakdown in the relation
ship between medicine and the public and unless doctors move to do
something realistic about changing their behaviour themselves, heavyhanded attempts at reform will come from outside. Because of the
vulnerability of lay opinion to all that is worst in medicine, the end
result is likely to be much worse than before. Precisely contrary to what
Illich hopes, there will be more bureaucracy, more waste, more meaning
less control and the public will be even more firmly in the grip of those
who want to remove its independence and control its destiny.
Simply in order to demonstrate that my approach to medicine is
basically positive I shall conclude by presenting very briefly some possible
solutions. These can be given in outline only here and I would not wish
them to be regarded as more than tentative suggestions. There are four
main issues which must be faced.
1. Is there too much or too little science in medicine?
2. Is there to much or too little technology in medicine?
3. Is there too much or too little administration?
4. Is it appropriate that a profession which claims to be a vocation and
to offer a most important service to the community should also be
the best rewarded financially?
Science in medicine
*
■
91
90
With ‘love’ being the only possible exception, ‘science’ is the word currently
most misused in the English language. It ought to be a criminal offence
punishable by at least seven years course-work in political science or social
science, to use it without some definition. In the current context 1 mean
by science the attempt, using reasonably reliable methodology, to ascertain
the truth about situations in medicine. I am fully aware that any pedantic
4
J
philosopher — which I sometimes am when wearing another hat — can
shoot that definition full of holes. I am also aware that anyone wearing
an average man full of common sense hat will understand very well what
I mean. The role of science in medicine is to attempt to get at the truth.
When defined in this way it is difficult to see how anyone could object
to scientific medicine.
But the fact is that many do object to scientific medicine. In the
minds of many average men full of common sense there is a strangely
illogical antithesis between a warm and humane approach and a cold,
scientific one. 1 personally find it somewhat difficult to understand why
falsehood and ignorance should be warm, while truth and knowledge
should be cold. They seem to me to be very nearly independently variable
qualities. However I happen to beUeve that what we want in medicine
is not less science but more and so I had better explain a little further
what 1 mean.
We do not know whether most of the things which we do to patients
are better for the welfare of that patient than if we had done nothing
at all. And on the whole we most of us prefer to remain warmly ignorant
rather than coldly knowledgeable about the situation. It is I think obvious
to anyone who looks at medical practice with anything like a critical eye
that many of the things which are done to patients either have no
influence on the outcome of the illness or may increase discomfort and
hasten death. Much money would be saved and many patients would be
better off if less medicine were practised. But which bits of medicine
should be discarded? The only way to find out is by an effectively
designed controlled trial in which the consequences of no treatment are
compared to those of treatment. If more such well designed studies
were performed, I have little doubt that many currently used treatments
would be dropped and many proposed treatments, after careful trial in
a limited number of centres, would never be widely introduced.
Unfortunately it is often difficult to persuade doctors — and in my
experience much more difficult still to persuade most laymen — that to
have a patient untreated may lead to an outcome more favourable than
that resulting from any current treatment. The problem arises because
of the illusion that in an untreated patient nothing is being done. Man’s
body is the product of hundreds of millions of years of refining evolution.
Its survival depends on the ability of bodily control mechanisms to main
tain the constancy of the physico-chemical features of the body fluids
within which the cells are bathed. The potency of these mechanisms is
extraordinary. It is only their superb effectiveness which prevents us from
being continually surprised not that we get ill but that we ever remain
well. In illness these internal control systems fight heroically against the
I
93
92
ft1
j*
s
9r
agents which would upset their equilibrium. With any disease a massive
effort is therefore continuously being made to counter the disturbing
forces. Any human intervention will alter the balance of power in this
struggle between disturbance and equilibrium. It is just as likely to hinder
the equilibrating forces as the disturbing ones and it is therefore by no
means self evident that any treatment is better than none. Yet while
most people, both medical and lay, can see the validity of this argument,
most also have great difficulty in overcoming their emotional conviction
that to do something must always be better than to do nothing. It is
this warm emotional conviction which has done more than anything
else to encourage the introduction into medicine of damaging and in
effective methods of diagnosis and treatment. Only more and better
science will perform the humane function of eliminating the errors
encouraged by warm emotion.
Technology in medicine
Technology is a word misused almost as much as science and so again.
I must begin by attempting to define what I mean. In this context what
I mean by technology is simply the application of a technique to a
situation, without any critical consideration of whether the outcome is
likely to be favourable or not. And while there is too little science in
medicine in the sense in which I have used the word there is unequivo
cally too much technology. There is a certain type of doctor who is
very impressed by techniques particularly when they involve electronics,
computers and oscilloscopes: such doctors love flashing lights, rolls of
chart paper and pale green lines on screens. So mesmerised are they by
the complexity and cost of the equipment that for the most part they
do not even begin to entertain the possibibty that the expenditure of
large sums of money on such wonders might fail to benefit patients.And
so expensive and complicated techniques are introduced without any
properly controlled trials. Since the desire to have such techniques avail
able in one’s own hospital or unit seems highly infectious, once one has
been acquired they tend to proliferate hugely at enormous cost and
with no real benefit - or at the very least before anyone can be reason
ably sure that any real benefits will accrue to the patients. Techniques
should be subjected to controlled trials at least as rigorous as those which
new drugs must undergo. Only if the outcomes of such trials are favour
able should the techniques come into common use. This very simple
device of the application of more rigorous scientific standards would
stop at the outset the introduction of much useless new technology. But
if such a reform comes about it will have to be pushed by doctors since
laymen seem appallingly vulnerable to the megalomaniac intentions of
those members of the medical profession who are obsessed by the ideas
-tha-t any in-rtev-Mion is good and, that there is a strong positive correlation
between the effectiveness of a technique and its cost.
Administration of medicine
One of the greatest paradoxes of the organisation of any modern pro
fession or government department is that while most people instinctively
understand what is required of an effective administrative machine, the
administration machines actually constructed seem specifically designed
to be both very costly and highly ineffective. An administrative structure
whose function is to serve the public should be so constructed that the
maximum number of decisions affecting individuals are made in the
shortest possible time by other individuals in whom the public has con
fidence. Yet most administrative reforms seem to succeed in ensuring
that members of the public almost never meet fact to face in the first
instance with a courteous and competent person who has authority to
make real decisions. Furthermore, the decision making process is so
dominated by complex committee structures and tiers of organisation
that even trivial questions may take months or years to sort out. The
aim seems to be to set out a procedure which takes care of every possible
circumstance and as far as possible eliminates individual error by elimin
ating individual responsibility. The result to the individual member of
the public is a faceless and inhuman monster with which it is impossible
to argue or fight. This leads to an apathy and a despair about the place
of any individual in a modern bureaucratic state.
Medicine is no exception to this general picture. In all countries,
irrespective of whether medicine is state or privately financed, the numbers
of people with no technical role as health professionals but with purely
administrative duties have increased. It is unfortunately true that the
increases have been most dramatic in countries with state controlled
systems and that the resulting administrative patterns have become laby
rinthine and self defeating. It would be foolish to deny that changes in
the pattern of administration have made some things better. But most
of these things have been better for the professionals than for the public.
There is an alarming tendency for improvements to be made purely for
the benefits of administrators and to be in the interests of neither doctors
nor patients. If our altruism has not been stirred by administrative mon
strosities which obviously make things more difficult for the patients it
is just possible that self interest may rouse the profession when the
monstrosities make things more difficult for the doctors as well.
It is very easy to be uselessly generalised in one’s comments on this
situation so 1 shall try to be more specific.
I
i
95
94
1. It has several times been noted that the best administrators are
those busy and competent people who hate administration. They are—
the ones who will make efficient decisions with the minimum of waffle
and bumbling because they cannot afford to waste their time in unpro
ductive ways. This means that as far as possible power should be in
the hands of those people, whether lay or professional, who have no
time to waste because their main function in life is not administrative.
It also means that we should cease the ridiculous practice of defining
promotion in a professional group as an opportunity to become an
administrator. Once anyone becomes a full time administrator, no
matter what their training, they cease to feel the same pressures to get
things done quickly and effectively and they become infected by the
administrative disease. As few decisions as possible should be in the
hands of those whose function is purely administrative.
2. Attempts must be made to keep every medical institution as small
as it is possible to be. The supposed increases in efficiency which come
with centralisation and size have almost all proved either to be illusions
or to have been gained by paying a price which ought to have been
recognized as unacceptable. A good example is the closure of small
hospitals in communities and the increasing centralisation of facilities
in monster institutions. This has arisen because of a failure to recognize
the extraordinarily simple fact that patients are in hospital for very
different reasons. A surprising number are in hospital not because of
any technical services which the hospital can provide but because, for
reasons which have nothing to do with medicine, it is not possible for
them to receive the minimal nursing care which in a well run 19th
century middle class household they would normally have received at
home. Tins sort of patient can readily be housed in an institution which
essentially provides hotel facilities with no resident medical staff, no
complex laboratory or radiological facilities, few professionals of any
kind, but many people, often with no training at all, who are interested
in looking after people. This sort of ‘cottage hospital’ is excellent for
what it aims to do. It is cheap to run, it is usually close to the commun
ity it serves and it is often capable of generating a huge amount of
community loyalty which is a major asset in helping to make it a
humane place in which either to work or to be a patient. Above the
cottage hospital should be another type of hospital whose function is
to provide relatively simple technical services for those who are acutely
ill. This requires simple operating theatres, radiological and laboratory
facilities, resident medical staff and good trained nurses. Again because
there are no facilities which most of the patients in hospital will never
use, the institution can be kept small and can retain a good deal of
community loyalty. Finally there should be specialist hospitals in big
-dt-ies whicIrJwill_take_Qnly that tiny fraction of patients who can be
cared for neither at home nor in the other types of hospital. Only in
these units would the full range of complex techniques be available.
Only these hospitals would cost to run per bed what many of our big
general hospitals, most of whose patients could be in simpler institutions,
cost today. The effect of this type of structure would be to return most
hospital facilities and hospital patients to their own communities and
to reduce costs sharply since the complex facilities instead of being
provided for everyone in hospital would be used only for those who
strictly needed them.
3. We must assess much more carefully the levels of training actually
required to enable people to do jobs effectively. The greater parts of
most courses for most health professionals cannot be justified either on
grounds of technical or general education. All that most courses do is
to delay the emergence from childhood to adulthood on the part of
the students, to reduce the number of years a person can spend in pro
ductive work and to increase the distance between the haughty qualified
professional and the poor bewildered patient.
In essence all I am doing is stressing that Schumacher’s slogan ‘Small
is Beautiful’ applies to things other than economics. Doctors, with their
long traditions as independent individuals, able to take their own decis
ions, must resist vigorously attempts to make them cogs in a supposedly
smooth running administrative machine.
Medicine and money
One of the most interesting features of Medical Nemesis is Illich’s con
sistent refusal to make the most of the attitudes of doctors towards
money. This is partly because he feels that the personal accumulation of
wealth by doctors has an impact on the factors with which he is con
cerned which is relatively trivial. But it is also partly Machiavellian. Illich
quite specifically and quite deliberately says that he does not want to
control medical racketeering. Such obviously anti-social behaviour con
stantly reminds the public that their gods have feet of clay and seriously
limits the power of the profession. If all doctors were humane and not
particularly rich their power as a profession would be enormously in
creased.
I am antiquated and hypocritical enough to believe that a profession
which is as satisfying as medicine, a profession which continually makes
public pronouncements about caring, should not be, as it is in most
countries, a certain road to wealth and security. There is something
offensive in the fact that doctors are on the whole extremely rich by
97
96
»■
J
V
J
any standards other than those of their immediate peer group. If Illich
really wants to rouse the public against medicine, I personally believe
he is being far too Machiavellian and that his strategy will fail. It is
going to be very difficult to persuade laymen that doctors are as lack
ing in miraculous powers and even in competence as they in fact are.
It will be much easier to arouse anger by pointing out the discrepancy
between the high ideals which doctors often profess and their personal
life styles.
But if Illich does not attack the groin in this way, others certainly
will. Doctors must be made to realise the extent of their insensitivity
on this issue and must stop being so greedy before it is too late. I am
not optimistic of their ability to see that this really is an issue which
could bring the whole pack of cards tumbling, and that if doctors do
not reform themselves, someone from outside will most definitely do
so. It should not prove impossible for professional bodies to set reason
able standards of fees and payments and to police these relatively simply.
Unless something like this is done, the bureaucratic government machinery
to carry it out will certainly be imposed in almost every country.
ACTIONS AT VARIOUS LEVELS
I
In all countries, while doctors are progressively losing to laymen their
rights to make decisions they still have a good deal of power to regulate
their own affairs. Possible reforms are legion and each country will have
to devise its own. But I do not want to duck the issue of attempting to
make specific recommendations concerning desirable changes. As 1 have
stressed I believe that real improvements in the way we run a demo
cratic society come from making small piecemeal changes in things which
are obviously wrong and not from devising grand theoretical strategies
for total revolutions whether bloodless or not. If the attitude of doctors
is such that they are fully prepared to recognise problems and are eager
to make effective changes, no matter how small those changes may be,
the whole attitude of the profession towards the public and the public
towards the profession will undergo a transformation.
I envisage changes being made at four main levels, of the individual
doctor, of the organisation of the profession, of the relationship between
government and medicine and medicine-related industries and of the
medical school which is at least partly responsible for the face which
medicine will bear in the future.
f*
Individual doctors
<
arrogant they are or being aware are unconcerned. I am not sure how
their attitudes can be changed, perhaps by a confrontation with an articulately angry patient, perhaps by an effective novel and perhaps not---at all. It may be that fundamental change in the area will require a
change in the sorts of people who are admitted to medical school. But
one can always hope that with maturity will come an ability to treat
as equals patients who do not happen to have specialised knowledge
but who, because the illness is happening to them, deserve a full and
unpatronising explanation of what is happening and what the alter
natives are.
One very practical thing which in most countries would change the
attitudes of people to doctors overnight would be a change of heart on
home visits. I have recently moved from a country where home visits
are a major, though declining, part of medical practice, to a continent
where home visits are almost unknown. In Britain much of the residual
affection which is attached to doctors depends on an experience with
a competent and humane individual who came to see a sick person in
his own home. In North America much of the growing resentment
against doctors is related to their near total refusal to leave their offices
to see any sick person. When two people have to meet, who travels to
see whom is a statement about a number of things, but in part about
who at that moment is the more important. In North America the view
in the profession is near universal that the doctor is always the more
important, that the doctor should waste as little time as possible in
traffic jams, that there are no circumstances in which the patient is
more important than the doctor and that therefore it should always be
the patient who makes the journey, no matter how sick he may be. This
surely is hubris of the worst possible sort and together with doctors’
wealth may well be the issue which could bring nemesis. If they are not
to be destroyed, if they are to retain their proud traditions of humanity
and concern, doctors must change their attitudes to home visiting.
Sometimes doctors may be more important and sometimes the patients
must travel. But sometimes, and especially with the old and the very
young, it is the doctor who should make the journey. Even if the direct
clinical results may sometimes be scanty, even if the patient is not so
ill as was imagined, home visits are very frequently gains for both doctor
and patient. In my opinion one of the touchstones of the real motives
of any doctor should be the attitude to home visiting. I feel uncomfort
ably sure that in North America at least most doctors would be found
to be something less than pure gold.
I
■
I’!
'1
i)
♦■J
The arrogance of some doctors faced with their patients is almost un
believable. Yet alarming numbers of doctors are either unaware of how
i'ai
1!
t I
jV
98
The profession
The professional bodies in each country are in a position to make
decisions and recommendations which can be enormously influential in
changing professional attitudes for better or for worse. Unfortunately
such influential decisions are rarely made by men and women who know
what they are doing and who are fully aware of the enormous conse
quences. Decisions which later turn out to be of seminal significance
are frequently made by incompetent small men with small concerns,
only interested in balancing the personal power games in the organisation
concerned. As a result medicine has drifted disastrously with few attempts
at leadership and far sighted thought. It is certainly not hubris, but a
total lack of it which has been the problem in many cases.
One major positive contribution which professional bodies could make
is to stop assuming that anything which improves the personal financial
position of their individual members is necessarily in the interests of
the profession as a whole. What is good for General Motors is not always
good for America and what is good for individual doctors is not always
good for medicine in relation to society. If doctors as a group set out
scales of fees and remuneration which were not legally binding but made
publicly available and therefore carried a good degree of moral weight,
and if those fees were such that doctors were adequately remunerated
but not at a level which consistently made them the richest group in a
nation, then, as Illicit fears, the profession would gain enormously in
respect and in its ability to influence the future direction of medical
care systems. But if medicine consistently behaves as a purely self-seeking,
money grabbing profession then sooner or later it will be recognized as
such and treated accordingly.
Professional bodies should also be much more prepared to get involved
in making hard hitting recommendations, as fully as possible based on
hard science, as to the real values of treatments and diagnostic procedures.
These should concentrate on demonstrating which techniques are useful,
which are not and which are ones where more evidence is required. Some
effort should be made to channel some research funds into effective
testing of this type and some pressures should be devised to ensure that
individual doctors at least take note of the research findings. The pressures
should always be moral and never absolute since expert recommendations
may sometimes and perhaps often be wrong but as far as possible doctors
should be discouraged from using techniques or drugs whose value is
uncertain or harmful. The profession must become less obsessed with
technology and with innovation for innovation’s sake and must try much
harder to prevent fashionable and irresponsible misuse.
99
Governments and medicine
Since even in countries where medicine is basically privately financed,____
much of the cash flowing into medicine ultimately comes from govern
ment or is dependent upon government decisions, and decisions made by
government can be enormously influential in determining which way
medicine will go.
On the whole and this is perhaps a hopelessly optimistic concept,
government should operate on the ideas that small is beautiful, that
centralisation is very frequently inefficient, that administrative reforms
should never lead to an increase in the number of administrators relative
to those of technical and professional staff and that costly high tech
nology innovations should be fully evaluated scientifically. Clearly it
would be silly in a book of this type to make specific suggestions for
specific national situations. All I want to suggest are principles which
should guide those who are trying to influence the relationships between
medicine and government.
One interesting way in which governments could influence things
would be to change patent laws in an imaginative manner. At the mom
ent drug safety regulations and patent laws are such that it is impossible
for a drug in most countries to enjoy more than a few years of patent
protection while it is on sale to the public. Patent protection is given
equally to drugs which are genuinely much better than existing ones
and to those which are no better or even worse. Since the period for
which patent protection operates is so short, it is frequently the market
ing skill of the company rather than the real effectiveness of the drug
which determines whether or not a product is a commercial success. I
suggest that while the basic patent laws should operate as at present,
patent protection should be withdrawn from any compound which is
not unequivocally better in some clearly defined way than existing
compounds, before the new compound is marketed. This would sharply
reduce the number of competing products and the incentives to market
effectively drugs which have little therapeutic advantage. Simultaneously,
drugs which genuinely do provide an advance should be given perhaps
30 years full patent protection, not from the date of the original patent
o
but from the date at which the relevant regulating body (such as the
Food and Drug Administration in the United States) gave permission
for the drug to be marketed. This would reduce the often unseemly
haste to market a drug before it has been fully tested, haste which often
stems from the knowledge that patent protected time is running out
because it is dated from the time of filing of the original patent. It
would also enormously increase the rewards offered to genuine innovation
and would reduce the current drug company emphasis on the need to
i
101
100
r
——ir —
I
■
V
market relatively ineffective products.
Medical schools
It is one of the illusions of both laymen and doctors that individuals
are admitted to the medical profession at the time they receive their
MD degree or its equivalent. The nature of the course followed and
the examinations set are supposed to determine whether people will
become doctors or not. This is an illusion because in most countries
the failure rates of students going through medical school are now
extremely low. For the most part people are selected to become doctors
at the time they enter medical school.
Another illusion is that the quality of a doctor five years after gradu
ation is related to the content of the courses that the doctor took during
medical school and to the skill with which these courses were taught. It
is my prejudice that this too is a fantasy. These factors may perhaps
be important in the first year or two after graduation but by five years
their influence has almost disappeared and thereafter it is non-existent.
What then is it which determines what sort of doctor a person be
comes? Only two factors are of any real significance. The first is what
sort of person enters the medical school. I do not believe that intelligence
and personality traits can be much altered by education after the age of
20. The second is whether the philosophy of the medical school empha
sizes teaching or learning as the key educational process. This is becom
ing almost an anachronistic consideration since those which used to
emphasise learning have almost all been transformed into teaching orient
ated schools.
It is obvious to anyone who can see beyond the end of his nose that
no matter how complete and valid are the facts taught in a medical
school, those facts will be partly unknown to and partly forgotten by
even the best students within a week of graduation, will themselves partly
cease to be facts within a very short time and within 20 years of grad
uation will be of little value. After graduation, although occasional
‘refresher’ courses may be helpful, especially to morale, the only way in
which a doctor is effectively able to keep up to date is if he personally
seeks out selectively the information of value to him from a vast morass
which is available. One might have thought therefore that a major aim
of a medical school would be to help a student to prepare for a life time
of this sort of study, of learning for oneself. In the great majority of
the medical schools of the world nothing remotely like this happens. All
day, every day, students are fed ephemeral facts by techniques, ranging
from the traditional lecture to the modern computer, which will usually
not be available to them in their lifetime of practice. Virtually no sustained
effort is made to offer a different approach in which the student is set
objectives and then largely left to find and to learn the relevant material
by himself. Lip service to the concept may be paid during a brief elec-—
tive or project course but compared to the sustained weight of teaching
the impact is trivial. The end result is a doctor whose education has
most effectively atrophied the only characteristics which would enable
him to remain competent throughout a lifetime.
Can anything be done to improve the education system? I have serious
doubts because the schools are now so permeated by experts whose
raison d’etre is the provision of teaching rather than the creation of
opportunities for learning that the problems of generating change are
likely to prove unsuperable. The sort of change I would like to see would
be for a medical school to set out for its students the objectives of the
course and then to leave its students to tackle these objectives themselves.
Formal courses would be provided for those who wanted them but they
would be drastically reduced and positive efforts would be made to
ensure that no student imagined those courses to be compulsory. Stud
ents learn in many different ways and they should be given the oppor
tunity to use the ways most appropriate for them. For some lectures
are ideal, for others (myself included) there is nothing like a good book,
for others learning is impossible without a practical experience. Few if
any medical schools allow this diversity to be expressed. Everyone is
forced into the common mode of following time consuming courses
and time available for learning is almost non-existent.
As to assessment I regret to say - or rather am pleased to say - that
I regard examinations as essential goads and guides for most students.
Examinations have innumerable faults: in this they are like democracy.
Both examinations and democracy can appear to be extremely unattract
ive ways of doing things until one looks at the alternatives. All alternative
methods of assessment are less fair to someone, whether teachers, students
or patients, than humanely conducted examinations. It does no one any
harm to be forced to make a reasonably realistic assessment of his own
abilities using a technique which incorporates the minimum of purely
personal bias.
In short the only curricular reforms I would like to see are the intro
duction of clearly stated objectives which are not dependent upon the
personal whims of a single teacher, a drastic reduction in formal tuition
with an emphasis on forcing the student to find things for himself, and
a reasonable emphasis on examinations as a method of assessment. I
think that students emerging from such a system would be rather less
like shell-shocked morons than some of those who now emerge from
our medical schools with the grandiose title of ‘Doctor’.
W-^o
8
105<r0
102
J
i
|
But I have no illusions that any revision of medical education of this
sort would have any substantial reforming effect on the profession. The
Medical Schools would still continue to choose the students with the
very best grades for entry. And all over the world these grades are now
very good indeed and most would agree that medical students, when
assessed by conventional standards are the cleverest of all students in
most universities. There has been a dramatic change in the last twenty
years. Before that medical students were certainly not the brightest of
students: their stereotype was that of the cheerful games playing oaf
rather than the studious intellectual with straight As.
Most medical educators pride themselves on the quality of their stud
ents. In my opinion this pride is largely misplaced. The students have
succeeded in distorting the pattern of medical education. Instead of try
ing to decide just what knowledge and skills most doctors need - and
coming to the blinding realisation of the obvious, that on the whole the
practice of medicine requires a very modest intelligence — educators have
allowed the intellectual abilities of their students to determine the nature
of the education offered. As a result all concerned, students particularly,
and to a lesser extent teachers and laymen have been dazzled by the idea
that competent medical practice requires great intelligence. It has become
impossible for someone of moderate intelligence to become a doctor. Yet
the great majority of jobs in medicine do require only moderate intelli
gence and this disparity between the intelligence available and the intelli
gence required becomes a major source of distress and unrest. It leads to
pressure for the creation of more and more unnecessary high powered
posts and to the demeaning of those necessary types of work which should
make up the greater part of medical practice. It also leads to very clever
doctors believing that their rewards are not commensurate with their
intelligence and hence to an increasing lust for material reward.
The idea that medicine is a vocation seems to be disappearing from
our medical schools. Students want to get into medical school because
that is the ultimate accolade for smart city-bred kids and their parents:
they want to get into medical school because that is a certain route to
wealth: and only very rarely do they want to get into medical school for
those old fashioned vocational reasons. It is therefore not surprising that
we are increasingly breeding a profession whose major concerns are
academic empire building on the one hand, and the rapid accumulation
of wealth on the other.
The bright students who go to medical school are not even particularly
interesting. Their concerns tend to be narrow, their lust to get into medi
cal school at all costs all consuming. Since coming to North America I
have learned that a high proportion of students who want to get into
103
medical school will stop at nothing at all in order to achieve their ends.
Whatever the ability may be, it is inconceivable that those who will be
have like this in order to get into medical school will ever make doctors
who in any sensible meaning of the word could be described as ‘good .
I am therefore very gloomy about the current state of medical educat
ion. I see a cadre of narrowly intellectual, not very pleasant people, enter
ing medical school and being herded through it in a way which is calculated
to suppress any wider concerns they may have and to create a corps of
brilliant morons, incapable of relating to their patients in any sensible
way in spite of receiving more formal courses in sociology and psychology
than ever before. Professor Stuart Sutherland of Sussex University in
England recently wrote a book called ‘Breakdown’ in which he recounts
in some detail his own breakdown and his encounters with those who
profess to understand the working of the mind. In the end Sutherland
concludes that most students would learn more about psychology and
sociology by reading great novels than by going through any of the courses
now available. This conclusion would perhaps be unremarkable if Sutherland
were not himself one of the world’s leading psychologists. Unfortunately
I do not see many medical students reading great novels and their ability
to relate to people in a sane and helpful way seems to be almost inversely
proportional to their theoretical knowledge of psychology and sociology.
Is there any hope at all for medical education and therefore for medi
cine? The people now going through medical school seem to me to be
more likely than ever to create Illich’s nightmare world in which insanely
applied medical power dominates individuals to a greater and greater
extent. I have little optimism that any reform of the educational process
itself will lead to much improvement given the present types of student
entering medical school. As I see it the only hope is to change sharply
the characteristics of the people entering medical school. In Machiavellian
terms this seems to me to be a possibility because the number of people
governing the choice of medical students in each medical school is very
small. If only one or two of these people begin to adopt radically different
ideas about who should be admitted to medical school they may well be
able to exert an influence out of all proportion to their numbers on the
future development of medicine. If change is to be a possibility it seems
more feasible to change the sort of people entering medical school than
to change those who are already in it. The change will take place slowly
but it will be much more profound than any other sort of reform.
I suggest that the first point to be recognized is that while medicine o
requires a moderate degree of intelligence it does not require superb
intelligence. Most posts in medical practice can be more than adequately
carried out by ordinarily able people. The available pool of adequate
104
II1
F
-
competence is enormously greater than the one which is now being
tapped. For most of these posts an ability to get on with people in a
reasonably sensible way, a determination to resist the wilder forms of
academic idiocy, are much more important than very high intelligence.
It therefore follows that what we should be looking for in medicine are
moderately intelligent well-balanced people who want to be doctors not
to prove their high academic ability, not to become rich but to fulfil
what they feel as a vocation.
How are these people to be found? There is little doubt that at the
age of 18 or 22 it is much easier to make a reliable assessment of acade
mic ability than of personal qualities. The difficulties of making reliable
assessments of people on the basis of a 30 minute interview have been
emphasised again and again. Faced with these difficulties and obsessed
with a desire to be fair to the candidates, medical schools have opted
for the only route which offers any hope of any objectivity: they have
selected those with the best academic records without for one moment
asking whether in doing this they may be cheating not the candidates
but the patients who will be treated by these super-intelligent doctors. It
is at least arguable that medicine might in the long run be better served
by deliberately and objectively selecting those with moderate academic
records rather than those with the best. I am certainly not saying that
no highly intelligent people are needed in medicine. Some certainly are
required but this need could be met by taking far fewer into medical
school than at present.
One way of being much more certain about personal qualities is to
defer the selection process until much later, perhaps until the age of
thirty after several years have been spent in jobs unrelated to medicine.
What I would like to see is a sharp change in emphasis whereby at least
half those selected for medical school are aged thirty or more and have
had considerable experience of life outside the narrow confines of the
medical profession. At this stage it is much easier to make a reasonably
reliable assessment of personality and to select people who, while having
more than adequate intelligence, have a genuine vocation and want to
do medicine for reasons other than lust for academic power or a rich life.
What would be the advantages of recruiting a substantial number of
medical students at this much later stage? The first, and by far the most
important, would be to bring into medicine a group of people with a
broad range of experience of life outside the medical profession. These
people would bring to medicine perspectives quite different from those
of the present doctors who on the whole have appallingly little experience
of or interest in life outside medicin^. They would have opinions of
their own and would be far more resistant to attempts by their teachers
105
to mould their opinions.
The second advantage would be that it would be possible for those
governing medical school admissions, without losing any objective assessrhent of academic ability, to use other criteria as well. By 30 most people—
have given some indication of their true worth in non-academic terms
and it would be realistically possible to choose people whose common
sense, moderate and equable approach to life would enable them to
handle effectively the great majority of jobs in medicine.
Thirdly admission at around age 30 would ensure that most of those
admitted were neither academic empire builders nor interested in riches.
With rare exceptions the megalomaniac academics have to start much •
earlier than that - and are fully aware that they have to do so - if they
are to realise their ambitions. Those who at 30 are prepared to commit
themselves to being students for four or five years are almost equally
unlikely to be motivated purely by lust for gold. Such entrants would
come into medicine with a healthily diverse group of motives and would
bring to it aims which are rarely seen with the present method of recruit
ing.
There are two obvious apparent disadvantages, that these entrants
would on the whole have a decade less of life to give to medicine and
that they would require substantial rethinking of the courses in most
medical schools. Both disadvantages are largely illusory. In most Western
countries there is by any sensible standard no overall shortage of doctors.
There are serious problems of distribution both in terms of geography
and speciality with some regions and some speciahties having a substantial
excess and some a substantial deficiency of doctors. I submit that these
problems of distribution are at least in part a consequence of our recruit
ment of the city-bred super-intelligent into the profession. As we choose
such people more and more exclusively I predict that no matter what
the overall numbers going into medicine, the problems of distribution
will become progressively worse. 1 suggest that people of moderate intelli
gence, entering medicine a decade later after a much wider experience of
life, are in contrast much more likely to solve the problems of distribution.
It may well be worth accepting the missing decade in order to correct the
distribution problem which with our present type of medical student is
likely to prove insuperable.
The second disadvantage, that the medical school curriculum would
have to be substantially rethought in order to meet the needs and demands
of those more mature students is one which I personally do not see as a
disadvantage at all. If it produced deep thought about the fundamental
philosophy of medical education as opposed to the trivia of curriculum
development it could do nothing but good.
1
106
a
■I
■J
Index
MEDICAL HUBRIS OR MEDICAL NEMESIS
k
-
.•
f
1
Illich believes that the present state of medicine is disastrous because of
its ia.tro.genic impact, on individuals and soriety. He sees that state as_____
having arisen from an overweening pride and lust for power, a longing
to make decisions and perform miracles which should be the prerogative
of the gods. This hubris is the cause of the present impending nemesis.
I also believe that the present condition of medicine in its relation to
society is seriously defective. I do not think that the situation is as bad
as Illich would have us believe, but it is certainly bad enough. All trends
suggest that things will degenerate progressively and that Illich’s faulty
description of the present may not be far wrong as a true account of
the future.
But I disagree strongly with Illich’s understanding of the causes of our
present disarray. Doctors have acquired an empire in a fit of absent
mindedness. They have inherited the positions of both traditional healers
and traditional priests. But the potential power is much greater because
in spite of the weaknesses doctors can offer miracles which are consistent
rather than capricious. When coupled with the desire of most people for
health and long life, it is obvious that the influence of the profession is
potentially far too great. That influence has been acquired because it
has been and is being thrust upon doctors. With rare exceptions doctors
have not actively sought it. Because of the real power of doctors they
have repeatedly made decisions whose impace on society is incalculable.
They have unleashed forces which it may not be possible to control. But
on the whole these decisions have been made by small men with small
concerns, shuffling papers while sitting bored around a table in some
dingy committee room. Doctors have not realised that they have been
making decisions which should be made by the gods. Because of the
medical profession’s ignorance and narrow concerns it has not been guilty
of hubris.
I personally would have been happier had hubris been one of doctors’
sins. The gods are not going to intervene in the organisation of medicine
and so whether we like it or not doctors have to make the decisions. It
is time the medical profession became aware of what it is doing. Conscious
hubris, a knowing involvement in decisions which will affect the structure
of society in the deepest possible way is what is required. If doctors
abdicate their responsibilities in a headlong rush to become Everyman,
Illich’s prophesies will come true. It may well be too late but some at
this hour must still try to snatch the fire from heaven.
J
Administration 93f
Age 25f, 3 7
Aid, medical 77
Alcohol 25, 54, 61
Allende 24
Anaemia
aplastic 23
pernicious 11
Anaesthesia 54, 56, 61
Antibiotics 36
Appendicitis 10,14
Arthritis 1 0
Aspirin 62
Autonomy 34f
Bacon, Francis 75
Barnard, Christian 3 1
Bicycles 36
Books 36
Bottle feeding 26
Breast feeding 26
Britain 23, 97
Dependence
on drugs 22f
on medicine 20f
Deprofessionalization 71 f
Descartes 55, 60
Developing countries 22f, 37, 42,
77
Diabetes 1 0, 1 3
Diagnosis 65, 68
Dialysis 32
Diphtheria 12, 88
Disease 64f, 76f
infectious 1 Of
Drug companies 24
Drugs 22f, 73, 84
Electroencephalogram 78
Environmental medicine 46
Europe 20, 43
Exercise 25
French revolution 64
Cancer 10, 13, 14
cervical 27, 28
Cardiac catheterization 27
Cardiomyopathy 27
China 21
Chloramphenicol 23
Chloromycetin 23
Chorion carcinoma 13
Compassion 68
Consumer products 35
Controlled trials 91 f
Coronary care units 31
Cost of medicine 20f
Culture 48f, 54f, 87
Darlington, C.D., 89
Death 5Of, 74f
Galbraith, J.K. 87
Goldsmith 35
Gonorrhoea 1 2
Haemophilia 11,72
Health economics 36, 39
Health professionals 44
Heart disease 10, 11, 13, 14, 28, 67,
70, 73
Hip dislocation 28
Hippocratic oath 89
Hiroshima 57
Hodgkin’s disease 1 3
Holmes, Oliver Wendell 56
Hookworm 25
Hypertension 11, 1 3, 28, 67
9
■i
107
E'Z Kc. c cs’P'f
tsf"
o
A BIBLIOGRAPHY ON MEDICAL ETHICS
(Specially prepared tor the Annual Meet o-F the Medico Friend Circle
Sevagram, Wardha,
December 27 to 29,
1995.
COMMUNITY HEALTH CELL
SOCIETY FOR COMMUNITY HEALTH AWARENESS RESEARCH AND ACTION
LIBRARY AND DOCUMENTATION UNIT
367, 1st Main 1st Block, Koramangala,
Bangalore - 560 034.
"Sukarthah Sarvabutanam
Matah Sarvah Pravarthayah
Sukham ca na vina dharmat
Thasmad dharmaparo bhavet."
Vegbhata in Astanga Hridaya.
(All activities o-F man are directed to the end o-F attaining
never achived without
happiness,
whereas
happiness
1s
righteousness.
It is
the
bounden
duty
ot
man
to be
righteous in his action.)
Prepared by:
S.John.
<
MEDICAL ETHICS IN HEALTH CARE
1 . BOOKS
1 .1
AMNESTY INTERNATIONAL. Ethica 1 codes and dec I arations
relevant to the HeaI th
Professions. Ed. 2
(Compilation o-f selected ethical texts)
Author, U.K.
1985.
1.2
BARU, Rama V
and NANDA, Priya. Tradinq o-F organs :
Need for a comprehensive policy
(Health Action Series
VHAI , New Delhi.
1993. 15p.
5)
1.3
International1 conference on hea1 th policy
BHATLA, P.C. Comp Internationa
gthics and human values — Proceedings
IMA House, New Delhi.
1986.
1.4
ELLOS (William J).Ethical Practice in CIinic a 1 Med icine.
Routledge, New York.
1990.
pl 90.
1.5
FRANCIS, C. M. Med ical Ethics
Jaypee Brothers, New De 1 hi.
1993.
pl 90
1.6
LOBO, George.
Current problems in Medical Ethics
Saint Paul Society, Allahabad . 1974 .
p240.
1.7.
MEDICAL COUNCIL OF INDIA.
MCI, New Delhi.
pl 2.
1.8
THARIEN, A. K. Ethical issues in the progress Q-f
med ic a 1 sciences and tec hno1oqy,
VHAI, Mew Delhi.
1995.
44p.
2.
Code o-f Medic a 1 Ethics.
PERIODICALS
2. 1
AGARWAL j, A. K. On o r q a n transplatation Eletter; commont 3.
Natl Med J India 9o1. 6 No.5
1993,
Sep-Oct.
p247-8.
2.2
AMALORPAVANTHAN, J and GEORGE. T.
On organ transpl antat ion C1et ter; comment 3.
Natl Med J India. Vol. 6 No.5
1993 Sep-Oct.
2.3
ANT IA , N.H Misuse o-f Med icine
FRCH Newsletter Vol. 5 No.12 1990, Dec
p247 .
p13-15.
2.4
ANTONY, K. R.
Violence in medical care and hea1th services
Health Action Vol. 3 No.12
1990, Dec .
pl3-15.
2.5
ARUNABH and MADAN, SanJ ay.
the c hanging trend.
Health Action Vol. 2 No.10
(.f)
Doc tor - Patient relationship:
1989,
Oct .
p45—46.
2.6
ARY A, T.V. Ki dney on sale £ 1etter see commen t 3.
J Assoc Physicians India Vol. 37 No.3
1989, Mar.
p24 1 .
2.7
BADRI NATH. Nitho 1d i ng BCG—is i t ei thical?" C1etter c ommen t 3.
Indian J Public Health. Vol.
Vol . 33 No.2 1989, Apr-Jun.
p86-8.
2.8
BAL. A. Medical Counci1s: F
Fai1ure to enforce code of ethics
Health for the Millions Vol.
.. 18 No.6 1992 Dec. pl 1-14
2.9
BASU, Tulsi.
L<=<V'j and Ethics i n Rel ation to Cour t-in ter vent ion
Journa1 of the Vivekananda Institute of Medical Science.
Vol. 18
No.l
1995 .
1995.
p55-56.
2.10
BAX I, Upendra. Lavj and ethics in an era of ex p1od ing sc i ence.
Legal Perspectives No.18
1990. pl -6.
2.11
BHATIA, R. S. I ridigennus medic ines--an ethic a 1 codification
called for C1etter 3.
J Assoc Physicians India Vol. 37 No.10
1989, □ ct .
p675.
2.12
BRANDT, Allan. M. Pol io. Politics, Public i ty and duplication:
Ethica1
Aspec ts of deve1 opmen t of sa1k vaccine.
Radical Journal of Health Vol. II No.
3
No.3
1987, Dec .
p63—69
(Reprinted: Internal Journal
J ourna1 of Health Service
Vol . 8 No. 2 1978).
2.13
CAREY, Norman H. Ethics, Money and the human genome.
BMJ - Indian Edition Vol. 8 No.4
1992, June.
p301-302.
2.14
CHAUDHARY, 8. K. Unethical experimental stud i es on humans
C1etter 1,
J Indian Med Assoc Vol. 92 No.7; 1994 Jul.
p241-2.
2.15
CHRISTIAN MEDICAL JOURNAL OF INDIA - Feature.
Deci si on — Mak i n g
i n clinical ethical problems
CMJI Vol. 7 No. 1. 1992, Jan-Mar.
p32-33.
2.16
CHRISTIAN MEDICAL JOURNAL OF INDIA
Medic ine and Ethics
CMJI Vol. 7 No.2.
1992, A p r - J u n e .
Feature .
pl0-11.
2.17
CURRAN, W.J. American personal-injury 1 awlyers at Bhopa1
Ethics and pub1ic po1icy in mass disaster.
New Eng J Med, Vol. 313 No.17.
1985, Oct 24.
pl 068-70.
2.18
De SOUZA, Eustace.
Ethics,
The 1esson f rom India .
Health Action Vol. 8
No.5.
Euthanasia and abortion:
1995., May.
P33-35.
2.19
De SOUZA, E. J.Ethica 1 and Legal issues and Aids.
J IMA - Special Issues on Aids 1993-94. P26-27.
2.20
DESHPANDE < Mohan) .Irrationa 1 and Unethim 1
FRCH Newsletter Vo1.5 No.4. 1991, Jul-Aug
Medical Practices.
p3 and pS.
2.21
DUGGAL, Ravi and JESSANI, Amar.
Medica 1 Ethics : Awai ting -a_ patients , movemen t.
Health for the Millions Vol. 18 Nos 1 & 2.
1992,
Feb-Apr.
p55-57
2.22
DUTTA,
Gouri Pada.
J IMA
Vol. 92 No.7.
2.23
EK8AL, B. Surqica1 dec i sion making ~ Who bene f its ?
Health Action Vol. 3 No.12.
1990, Dec.
pll-12.
2.24
GOVIND, Babu K. Unethical advertisements C1etter comment J »
J Assoc Physici ans India. Vol. 35 No.5. 1989, May. p353.
2.25
GROVER, N. K. Medical Liabi1i ty
- Li tiqations and Def ensi ve
Medic ine.
J I MA Vol. 92 No.6. 1994, JJne.
pl84-185.
2.26
GROVER, N. K. Consumer Protection Ac t and medical profession,
J Indian Med Assoc. Vol. 90 No.10. 1992, Oct. p277-9.
2.27
GULATI, S. K. Spare parts medicine,
foil OW-LI p
Eeditorial 3.
J Indian Med Assoc.
Vol . 90 No.7.
2.28
Ethics in Medical Profession.
1994, July.
p214-215.
HUNT, Morton. Patients' Rights.
Health Action Vol. 3
No.12. Dec
med ic a 1
ethics—its
1992 July.
1990.
P167-9.
p21-23.
2.29
KUMAR. P.D.Teaching ethics in the India con tex t E1et ter 3,
J Assoc Physicians India Vol. 39 No.12. 1991, Dec. p972-3.
2.30
KUMARASWAMI, T. M. Consumer Protec tion ac t and the
Medica1 Profession.
J I MA
Vol. 93 No.3. 1995, Mar .
pl 12
and pl04.
2.31
MADAN,
Soc ia1
T. M. Dying wi th Diqni t.
Science Medicine Vol.35 No.4.
1992.
p425—432.
2.32
MANI , M. K The trade in human o r q a n s Eeditorial 3,
Nat 1 Med J India Vol . 5 No. 1 . 1992, Jan-Feb. p2-4.
2.33 .
MANI, M. K. Advertising in medic ine
Natl Med J India. Vol. 8 No.2. 1995,
C news 3,
Mar-Apr
p82-3.
2.34 .
MATHEWS, Jolly. Medical confidentiality and AIDS,
Law and Medicine Vol. 1 No.1. 1995. p60-72.
2.35
MATHEW, P.D
MedicaI Neg 1iqence and the Law.
Legal News and Views Vol.7 No.9. 1993, sept.
2.36
MEDICAL COUNCIL OF INDIA.
Code of Medica1
MCI, New Delhi. 1970.
12p.
2.37
MEHDI, Mahboob.
Torture
A Medical Model •
T o r t u r e :?
Health for the Millions Vol. 18 No
.3.
No.
3. 1993,
p286—291.
Ethics.
June.
plS-19.
2.38
MEHTA, P. J. Doc tors and Consumers.
Vol 40'No.10.
J Assoc Physicians India
1992,
Oc± p6491
2.39
MENON (N.R Madava)
Law, Ethics and HIV.
Law and Medicine Vol.1 No.. 1 1995 (Book Review).
2.40.
MOOSA. A. Ethics o-f ma Inutri tion researc h in c hi 1d ren
Lancet Vol. 2 No.8554,
1987, Aug 8. p338-9.
2.41
MUTALIK. S.
Advertising, pharmaceutical industry,
derma to 1ogy E1etter; comment J.
Int J Dermatol. Vol. 31 No.2.
1992, Feb. p!44 .
2.42
PANDYA, S. K. The Maharashtra Medica 1 Counci 1 .
Natl Med J India
Vol. 6 No.2. 1993, Mar-Apr. p89-90.
2.43
PANJWANI, D. D. et al.
T he ethica1 practice of med ic i ne
in ind ia Eletter!.
J Assoc Physicians India Vol. 34 No.12. 1986, Dec .
p895-6.
2.44
PATEL, J. C. The gi -f ts and trinkets to doc tors : cur ren t
prac t ices in India and g1obaI trends in pharmaceutica1 industry.
Indian J Med Sc i. Vol. 48 No.l
1994, Jan. p20-30.
2.45
PILGAOKAR, Anil. Medical ethics,
pat i en ts rights.
Health Action Vol. 4 No.6. 1991 ,
med ica1
J un .
(1 Etter) .
and
ma 1 practice and
P19-21 .
2.46
PRASAD, P. Revisiting med i c a 1 ethics (ed i tori al).
J Indian Med Assoc.
Vol. 85 No.9.
1987, Sept.
p257-8.
2.47
RAMU, M. Med ico-Lega1 emergene ies in Med ica 1 Frac tice:
Some random thoughts.
Health Action Vol. 2 No.5. 1989,
May.
p22 and 27.
2.48
RANJAN, P.S.
T he doc tor's Duty o-f Con -f i den t i a I i ty .
Law and Medicine Vol. 1 No.1 1995. p40-44.
2.49
RAY, I.
Medi c a 1 examination, certification and i n -formed
consent.
J Indian Med Assoc Vol . 91 No.11; 1993 Nov. p293-4.
2.50
REDDY, K. C. Shou1d paid organ donation be banned in India?
To buy or let die C see commen ts J.
Natl Med J India.
Vol. 6 No.
No. 3
1993, May. 137-9.
2.51
ROHDEL, Jan E. Ethical
Ethica1 Perspectives on Popu1 at ion
and Fami1y Planning in India.
p20-22.
CMJI Vol. 8 No.2. 1993,
Apr-Jun.
2.52
SHAH, Vimal. Hospi tai -f au 1 ted on right to in -forma t ion ,
Health Action Vol. 3 No.12. 1990, Dec.
pl7-18.
2.53.
SAHU,
M.
Med i c a 1 Ethics
( 1et ter) .
Cs)
e}Ti_|Ujes
ejjejeio
/jaeqqe pue saseasyp aqowojd
oqM
asoqq
tsaseasyp
^aeqqe
pue
a-f-yj
aqowoud
oqw
asoqy sueraTsAqd
40 sadAq DMq aue ajaqj.
oj-T I
•0B-9Zd
•Daa-ade
'£-2'QN III IQA qqieaH ^o. puunop [eaypey
s uo y 4 e y aosse { euoyssapjd Aq 4 uama4 e4 g
:uoyqeue[aag pue sapoa {eayq4 3 sqqby3 uewny
‘ BB6I
'B172d ‘2661 q-OQ-^dag
£661
' Q * on 9 'IOA ‘eypui
• £ 4 uawwoa i uaq 4a { 3 uo y 4 e4 e { da uea 4 ueb_i□ "uq
* 1766 1
P
PO|J
’ P
‘3
TI^n
'6^6
'B-GB£^ 'aon ‘1/661 •II*QN 26 •{OA aossy pajj ueypuj p
1Z2-G2 JaqwaAO^ * yqfaQ mon 1 asno|-| yn { a
n4 j
o4; "40 sasea
aj
jn
jo
lTt soq 4 3 pue s a y q4 3 [ eay payj Tio doqs^JOM y
yi-J
N II ’* 3 'P ‘ HBOS
'06-ZBT^
sansa t
"Ainp
learq^a
Uu
'2-Ttz2^
' inp
e
' a jed
appap oq
'0I-9d
T9‘Z
_£
09'2
-aossy pa|.j ueTpuj p
•r'QN 26 ' I op,
* saba { {oa aaj- (jot 4^4 idea yo 6<at as j
I e ay paw To uopesi { e y a jawwoj
•'I
j_ ‘H6NIS
•65'2
*6'ON 6B
u
Asajcis
‘ V66T
'B6-G6O
'ue|j 8861 'tz'on '2 ' IOA Ml lean J-o
* Assea
AJ04 anpojyuy TTy :soyqi3 {eaypaij
' 172-02^
Z9'
- aossy papj up pu j
'• q d j e a s a j Ie a y paw u I
ud t u t d q
’1 "NWHIHS
‘ 166 T
suepi s Aqd
uoT^eanpa
' IOA
'29 *Z
leujnop pppey
■tJieXeg ‘H9NIS
S5‘2
-unp ‘3661 *£'on BI "{OA suoyiiyN aqq joj- qqiean
qq { eaq A4 y unwwoa lTt sanss t { eayq43 ' S ‘NttBOAtfAIS
ZG'2
I£d
oq^
•aaa *0661 '21'ON £ " IQA uorqaij cp lean
laeqayw •S3X1IM Pue weT-jiw ‘NWWHOHHS
95'2
•4QQ ‘'6861 'S'on ST'loo suoynyij aqq joj- qq{E?aH
'auyaypaw uaepaw j-o sanbyqyja awog '>1 'd ‘IH13S
GG'2
st
'6V^
•s
-qaj
‘6661
' 2' qn ZB'IOA oossy pa|j ueypu{ p
■ [Japan {eayqqaun >p j * yy^yys
VS'2
3.
3.1
UNPUBLISHED PAPERS
(AVAILABLE AT CHC)
CHRISTIAN MEDICAL COLLEGE.
Med ica1 Colleges and Their Ethical Responsibi1ities.
1992.
3.2
DHANWADE, Subodh. Formation cf Teac hers in Chr i sti an
Med ic a 1 Col 1ege.
(Paper presented at the CMC, Ve11 ore,
CMC, Lud hi ana, S t. John' s Med ic a 1 Co11ege, Mi ra j Medica1
Cen tre. )
3.3
FRANCIS, C . M . Con -f 1 i c ts and Confluence
ethics in India.
3.4
FRANCIS,
C.
M.
Health Po 11'cy of
3.5
FRANCIS,
C.
N.
HIV ,
3.6
PAIS, P r em. Ethics i n the Un i veri sty Teaching Hospita1 .
SJMCH,
Ancient and Modern medical
the church in
India
Ethics.
p30-34
Law and E thic s.
Bangalore.
Pondic herry Declaration on Heal th Rights and Responsibi1ities
and Patients R i g h t s and Responsibilites.
Workshop on "Medicine, Media and Consumer Education" held in
Pondicherry
December 1-4, 1993.
Organised by the Educators -For
Quality Update o-f Indian Physicians with the support of Inter
national Organisation of Consumers Unions.
3.3
RAVINDRAN, G. D.Dec i s i on mating stateqy -for clinical
ethical
problems
i n med i c i n e.
SJMC ,
Banga1 ore.
Note:i)This bibliography does not include any artic1e
from Medical Ethics*and MFC Bulletin
whic h
are already background papers for the meeting.
Newsletter of the Forum for Fedical Ethics.
ii) If you are interested in any of these papers (section 2 and 3)
and are unable to access them from the sources mentioned,
please write to CHC - Library and Documentation Unit. We
will supply them at cost - for photocopying and postage.
C.H.C., Bangalore.
ST. JOHN'S MEDICAL COLLEGE HOSPITAL
©
55 307 24
BANGALORE - 560034
Telegrams : SAINJOHNS
Date.?.|.?l.?.».....
Ref.
J) U-A, /I
41^^
T^C^nxxuv^y
SFXI*<)
0VX
4x^6vvm^^
Z^t
7
t
rfo
/
<s.r4F /Oz VQ
I
^7 —
AHe L
^'e/uufex1^
f.
KJ
a-7
Report on WHO sponsored Regional Workshop on Medical Ethics
on
Medical
30th,
1996.
WHO, SEARO, sponsored a 5 day regional workshop
The
Ethics
in
Paticipants
Lanka,
came
Thailand
Institutions
from
and
from
Lanka
Sri
Kandy,
June
Bangladesh,
Nepal, India,
Indonesia.
26
India
was
by
represented
AIIMS (Dr. L.M. Nath), KMC, Manipal
Sri
Bhutan,
3
(Dr. R.P. Pai )
and St. John's National Academy of Health Sciences (Dr.Prem Fais)
only
one
fact
was
emphasized in the country report for India (copy enclosed).
The
Of
all the Institution represented St. John's was the
which
workshop
Ethics
systematically
taught
the
subject.
This
itself concerned the philosophy and theory
of
Medical
was interesting and thought provoking.
There
is
a
another
on
as
the
and
follow
proposal
to
teaching
medical
up the present
ethics.
Prem Pais
Professor of Medicine
and
Vice Principal
^C-ceAve-ol
with
St. John's has been proposed
venue, tentatively in January 1997.
by the WHO.
workshop
The workshop will be
funded
IS
MEDICAL TECHHOLOGY - ETHICAL ISSUES
- Anil Pilgaokar «
context that ethical facets of Medical Practice become very
important.
"Technology" (described as the science of industrial
arts" - Consise Oxford Dictionary) by its very genesis lends
itself to commercial exploitation.
It is m this light that
.
ethical issues of medical technology become of paramount importance
It
but alas this is a neglected subject in the medical circles.,
felt
that
it
woAld
is with this at the back of the mind that we felt that it would
be of pertinence that there is at least some sort of debate cn
discussion on the subject and hence this paper.
must be
.
clarified at the outset that we are alive to the rather dismd
prospects of putting before you a comprehensive paper before
you but then that is neither our claim nor our aim to co so..
There are limitations of data and more importantly our own.limi
tations which prevent us from taking any firm position(s).m
respect of many topics covered in the paper, but then it is cpu*
hope that vigourous (rigourous) deliberations at the MFC rnee ing
would be helpful in (a) clarifying the grey areas on the one
hand and (b) taking up some position(s) in respect of many aspects
discussed in the paper; (which primarily is concerned with
raising some questions for discussion) .
Admittedly medical technology isj a broad term and it would be
concerned with...
the
purposeless to dwelve on every technology -----practice of medicine; for that _
matter
injections
_____ - even commonplace
__ as
_
'technology, and it would be quite pointless
could be concieved
ethical
aspects of injections here. Rather it is
to discuss the (----intention to restrict oursrIves to newer sophisticated apcb
In very crude terms, for the
or pervasive medical technologies.
technologies.
- -- ignore
■
■ --j "first generation
purpose of this paper we shall
the
______
technologies” (to burrow the current 'in* expression) like say
X-ray machines and devote the discussion to "higher generation
technologies” like CAT-scan or PET-scan.
Grouping/Catagorization of Technologies^2
In our surrvey
surrvey of literature
literature we
we have not come across any grouping
or catagorization
catagorization of
of the
the various
technologies harnessed in
\---medical practi'ee’ but for the purposes of uhis paper it is
important to device one and so even at 'the
:,.- risk of being cnallenged
resorted
to
the
following
classification?
we have :
—
(i) Fuiction replacement medical technologies eg.. Heart-Lung
dialysis units; cardiac pace-makers etc.
machines or say renal
i,
(ii) Investigational-aid medical technologies like CAT-scan;
sonography; echo-cardiography; and its sub-class (ii-a)
(ii-a)
"Investigational-aid extendable (in some cases) to curative
medical technologies like .some endoscopic instruments.
(iii) "Control technologies" like contraceptives, vaccines, and
artificial life-support technologies, and of course ger.etic
engineering and sex_preselection technologies.
Each as a class would have its own ethical considerations in
* “
‘ '
» A priori, the above
addition to general ethical2 considerations,
need
for
increasing
stringency in
classification suggests a
ethical considerations with each class of the medical technology.
Whereas the benifit? risk as also the costs benefit evaluations
vis-a-vis respective populations must form a base for assessing
the relevence (in ethical terms) in all the three classes of
technologies but it is evident that in the first class, the
. .2 ..
2
ethical considerations would mainly relate to 'operational' part
i.e. use; mis—use; denial of use as also the fees for services
etc. The ethical questions in this class mostly relate to the
individual patient and the institution (investigating centre)
policies. In the next class (ii), the ethical questions - all
ethical questions relevent to the previous class are indeed
pertinent but in addition, because of the enormous costs of
some of the instruments involved ethical considerations in
National priorities also must form important facets as many of
the instruments lock up and siphon significant monetory
resources, and thereby quite often affect (adversely) other
medical facilities by depriving funds for these.
In the last
class, even more wider questions relating to demographic,
individual rights vs rights of societies, right (?) to manipulate
human systems and forms etc. could figure-r
(i)
Function replacement technologiesAdmittedly most of
these technologies are indeed 'life-saving' in critical
conditions. But when the question such as whose life?
become appearent (as in many cases in our setting do).then
ethical issues do arise and these need to be debated in
full measure. We shall take just two illustrations to
initiate the debate.
(a) It is well-known that in a renal dialysis unit
priority for dialysis service is given to acute cases
rather than chronic renal failures. Again there is a
long waiting list for routine dialysis of chronic renal
failure patients (who have to be placed in a queue system
because of the paucity of dialysis units.
Even so when
needed dialysis (Jaslog Hospital) he got precedence
over others. With all regards for the noble man, the
question of whether life of other citizen is worth anyless
needs to be taken up.
Again, the dialysis serves as a temparory respite until
the organ teransplant arrangements are available, and.
it is at this juncture that further ethical issues arise
Should kindney of a young person be transferedto older
person? The obvious answer is No.
Yet one finds that
kindney from a young woman (16) being transplanted on
to MGR - knowing that the leader was close to his grave.
The "organ trade" racket with the conivance of the medical
profession has been highlighted in lay press and yet the
ethical questions have not been raised in relevant
bodies.
It must be conceled that the examples quoted above/ are
not strictly ethical issues of medical technology,
rather they are issues related to 'medical practice'.
All the same these are so intimately connected with the
technology usage that the mention mede here would not
be totally out of place.
Cardiac pace - makers are fairly widely used in
(b)
'
► And for harnessing this technology
our country.
Intensive Cardiac Care Units (ICCU) are essential.
The usefulness of these units is widely known and
acknowledged. What is not generally appreciated is
that in our settings is that a proliferation of.such
units could actually impede the quality of service
(medical service) in other faculties of the hospital/
institution. A bed in ICCU could cost (to the institution)
..30.
3
some 100 times more than the bed in say a general ward
(of a public hospital). With relative crunches on the
budget of the hospital, the pinch for resources is felt
by other facilities. Any keen observer, who has obser\
the "progress" of some of our premier public hospital
in last two decades, could not have failed to notice
that with the advent of super-specialities (like ICCU,
Artificial Kindly Units and the like), there is a steady
degradation in the facilities in other departments. 8o
we have a situation where the best of the facilities
would be available in these highly specialized units and
at the same time there would be acute dearth’of common
requirements like cotton, lint and linen in the general
wards of the same hospital.
Even at the cost of increasing the length of the paper
let us labour over this point a little more. It would
not require statistical figures to state that the
incedence of tuberculosis in the city of Bombay far, far
exceeds that of CVDs.
Dr. Amar Jesani ( Economic &
Political Weekly,Sept.24z 1988) has pointed out that the
deaths due to TB in the city have increased over the years
thus emphasising the increased requirement of hospital
beds for TB in the city, but these have in fact been
reduced by Bombay Municipal Corporation (paucity of funds)
in the only hospital for tuberculosis in the city of
Bombay; whereas there is a spurt in the ICCU beds in the
city.
(And mind you the ICCU beds cost some 100 times
more)
The number of
beds in the city(in both public
(— ICCU --and private hospitals together) are some 30 to 35% that
of the beds in the TB hospital.
Is this due to class biases ? CVD is a rich man’s diseIs it ’ethical’
ases and TB is a poor man’s diseases»,
At
the
cost of TB beds ?
to permit spurt in ICCU beds ?.
~
(ii)
Investigationa1—aid medical technolociess— In this group
there are technologies that ‘affordable’ only to insti
tutions as for example CAT-scan instrument and there the
ones like sonography (ultrasound) which can be found with
individuals too. What is peculiar, atleast as far as
Bombay is considered is that none of the public hospitals
have these as of today.
And this brings out two possible
reasons for this viz (a) the aquisition of these instru
ments is primarily for ’marketing' reasons — marketing of
‘image’ of the institution and(b) the law of diminishing
returns impedes the aquisition of these instruments in
public hospital i.e. the additional benefit in investi
gations with the aquisition of these instruments is not
commensurate with the hugh cost of aquisition, operation
and maintenance of the instrument.
It is true that public hospitals have little access to
recovery of costs from the patients (even when these have
resorted to collecting partial fees from the patients (in
Maharashtra) .
-.But in private hospitals fees are
levied for services, it would be unthinkable to operate;
these instruments (CAT-scan) if these are to be used solely
used in well selected cases only. This is because the
capital investment (around Rs.30 lacs) and allocation for
operation and maintenance (another Rs.30 lacs) would work
out in annual interest of Rs.10 to 12 lacs, which would
have to be acrued from the patients, (i.e.Rs.1 lac per
month). And considering that the time required for ’proce
ssing’ a patient is 2 hrs and an 8 hr working period. it
.4
I
4
would mean to break even this Rs» 1 lac would have. to
be recovered from 120 patients or Rs.833/- per patient.
The question that one iieeds to consider is that would
there be 120 truely well selected cases for such scan,
in a month, every month, every year ? If the answer is
NO then it follows that patients who do not require such
an investigation would also be enlisted for such investi
gation - which seems to be the case indeed, How does
this stand on ethical grounds ? How does onei ensure that
such trend is checked ? reversed ? Could there be a
well laid down norms for selecting cases ? Could there
be an audit of such investigations ? Who would conduct
such an audit ? These and many other questions will need
to be answered.
Sonography > Ultrasound technology $ This has been the
domain of obstetricians and many obstetricians perhaps
aquire this instrument for 'image' purposes. The.pre
mise that the technology is ’safe' (is it conclusively
proved ?) has led to rampant ill-use or mis-use. Wides
pread (though unconfirmed) reports have indicated that
this technology is used to detect pregnancy when cheaper,
more accurate and non-invasive pregnancy tests are freely
available.
One reason behind this is to enable to charge
fees (ususally exhorbitant) for the investigation. How
ethical is this ? What does one do to prevent this ?
What are the situations when use of this technology is
rational ? Can there be an audit?
(iii)
Control technologies 2- These are perhaps the most
’impactful* and controversial technologies, and ethical
as also philosophical must be discussed.,
Contraceptives technology s There has been a shift:, in
technology (ies) ’progressing’ !,user-safety" to "contraeeptive duration of action” (from condoms & diapharms to
’implants’); there is a shift from "user-control”
(condoms & diaphrams) to "doctor-control” (implants).
The shift has been from birth control to population
control.
Is this ethical ?
In the case of doctor-control (and therefore state
control) contraceptive if there is a contraception
failure should it not merit compensation ? Is consent
necessary ? imminent ? Is it sought to ?
The question also arises of ’doctored' results of field
trials ? Should there be a third party audit of the
field trials, particularly since there is an obsession
to pushing these technologies.
Vaccines s These technologies being a part of Preventive
Medicine are state mediated and at general population
level some questions need to be raised.
Is consent a
necessary pre-requisit before vaccination ? In the event
of vaccine failure should the patient not be compensated ?
Can vaccination be forced in epidemics ?
Sex-preselection / selective foeticide s Sex-determination
and selective foeticide and Sex-preselection technologies
. . .5
5
are the ones which have discriminitory and demographic
upset potential of the worst kind and yet these techno
logies are vigourously persued. In extremely small
number of cases where a particular sex foetus could
jeopardize the life of the pregnant woman can.these be
justified if at all.
Even so there are no laid down
ethical codes in respect of these at allo. Apart from
catering to individual passion for a particular sex of
spring, scientific ego of achieving control over life
processes, and a political handle to manipulate sex
composition of a population, these technologies.have
little to offer to mankind. The basic premise in medical
research is to improve the quality of human sustenence.
These technologies have very little to offer in that
direction (except perhaps cases mentioned above.)
But
they do have an enormously large adverse potential.
Should such technologies be allowed to be harnessed in
the country ? Should not the medical comunity decrey
these technologies on ethical grounds ?
Genetic Engineering s These technologies can have extre
mely widespread manifestations and carry with them dich
otomous repurcussions.
It is with this at the back of
mind that there needs to be an extensive debate on the
merits and demerits of these technologies to work out a
rigid code of procedures.
The justifiable purpose of genetic engineering (we are.
restricting ourselves only to medical aspects of genetic
engineering only) can be to rectify genetic aberrations
(note the avoidence of the word abnormality) which.can
have disasterous or agonizing consequence and nothing
mor e.
as things stand today the commonly per sued
However as
(and commonly percieved) goal of the technology is.to
rectify genetic abnormalities and improve the quality
( of genes ? ). Just what is abnormal? What is impro
vement in quality of genes ? On this there is no final
word. What is more it is unlikely that there could be
any final word on this. Allow us to elaborate this
further.
Genetic aberration's like Down’s syndrome; inborn errors
of metabolism., juvenile diabetes (?) can have disas
terous consequences and genetic rectification could
possibly avoid these con-sequences and perhaps this
But say,
technology could have credence in these areas
if a person has six fingers on his/her hand, there is no
reason to label him/her as ABNORMAL just because he/she
does not conform to the commonly percieved ^frame of
reference, since
s
. there
----- is no physiological/physical agony
;
This line of argument can be
or distress emanating,
ridiculous
but
effective extent thus.,
extended to :---------
____1 fair skin is normal to certain
Blond hair, blue eyes and
a
dark
skinned, dark eyed and black haired
populations and
population
would be ABNORMAL would genetic
person in this
___
_____
jerts
like
to
engineering experts
to ’’ improve1 (?) this individual
to fair skin, blue eyed and blond haired person.. Decades
.6
6
earlier an ‘engineer’ attempted to do a similar exercise;
his name was Hitler and his goal was called Fascism..
Can genetic engineeriiig lead to camouflaged-Fascism ?
What are the ethical and philosophical positions one
takes on genetic engineering ?
Life support technologies employed in lengthing ’vegitative' forms of human (inhuman) existence s Prolonging
‘life’ with total disregard to QUALITY of life is not
uncommon these days Is this ethical ? Is it ethical to
perpetuate incapacitation ? VTiat is the position one
takes on this issue ?
Research What are (should be) the priorities in research for
developing technologies ? Who takes the decisions ? Whose
needs (what needs) are given importance 7 These are the crucial
questions that need to be answered. The situation existing today
is not one where ‘independent’ medical scientists engaged them
selves in research and lead to discoveries. Today he or she is
either employed directly by commercial corporation or if not is
his research effort is heavily financed ( and therefore contro
lled) by commercial corporations (for profits) in the name of
’service to humanity’. The commercial priorities invariably
leed to secrecy, unethical conduct of research (witness the
contraceptive research) and ‘doctored results’ and when scien
tific expertise and commercial power combine (as it is today)
all this become ever so easy and free from challenge.
If there are strict laid down norms for drug research, why can
their not be similar rigidity of conditions in research for
developing technologies ? The question of consent in research
& in practice is a virtual farce.
Ethics of research and prac
tice is evident by its absence. Use of technologies to serve
defence medicine - whether right or otherwise - can be a matter
of debate in United States but in India (today) does it have any
place ?
Fears s
There can be no conclusions to a paper of this sort only
FEARS. When one overviews the situations one distinctly gets
the impression that the entire persuit is one of concentration
of power, centralization of power - Medical Power; Contraceptive
technology is shifting from end-user control to doctor-institution
control. High priced instruments are phasing investigation patho
logy from individual doctor to institution.
Function replacement
technology vulnerably chains the patient to medical establishment.
Artificial Life Support systems virtually confines the patient to
institutions with _very little else. Through selective foeticide
and sex-preselection technology, medical establishment aquires a
manipulative potential and this is further compounded with the
emergence and proliferation of genetic engineering.
We have had
political leaders controlling populations, we have had religious
leaders controlling populations. Will the Medical man > Commerce
man combine also jump into the arena ?
NOTE
2
We appeal to your generosity and pardon us for stretching
the point to ridiculous extent but believe us the inteninten
tion is only to provoke discussion.
—0O0--
*
r/
PERSONAL VIEW
Greed and the medical profession
Ralph Crawshaw
■*
X^Xrganised medicine is not giving
I
1 proper attention to the disturbing
presence in the profession of a uni
versal human trait: greed. Perhaps doctors’
greed is less of a problem in Britain where an
estimated 70% of the doctors are generalists,
and reimbursement in the main is controlled
by the national health system. Not so in the
United States where 70% of doctors are
specialists and an open health care market
allows doctors to charge “reasonable and
customary” fees. This is interpreted by some
as “all the traffic will bear.”
Despite considerable evidence at the other
end of the generosity scale that 64% of US
postulated by the editoc of
Dr
every medical action, an ethic of greed
George Lundberg. Heuristically he divides
changes our elemental belief that the buyer is
the profession into four categories along a always responsible. With an ethic if greed
continuum of reimbursement, starting with
doctors cease to base their motivation on
altruistic missionaries, moving to profes
compassion and caring to become merchants
sionals, then business people, and finally
selling medical services to the highest bidder.
money grubbers. The professional and busi
Given these reasons for concern the first
ness people form the vast majority under the and essential action for the profession is to
curve. The money grubbers, the greedy undertake an open discussion of the problem.
ones, occupy about 3-5% of the area. Three The consequences of continued side stepping
per cent seems a fair beginning for consider- by the profession of the problem of its greedy
ing those within the profession for whom
members is loss of authority, autonomy, and
“greed has become too dominant an ethic.”
honour. The erosion of the profession’s
Some still ask, “What is the importance of
position of respect with the public is <
the problem; greed among human beings is Further erosion will aggravate a 1 clear.
I the
as common as fleas among dogs?” For the
medical profession greed presents three
fundamental problems.
Firstly, greed compromises quality of care.
An egregious example is in the case of
a doctor in the US whose yearly income
exceeds 84m. Literally busloads of patients
from nursing homes arrive at this doctor’s
office and without a sham of a physical
examination undergo a surgical procedure
doctors give away considerable amounts of
with the postoperative care left entirely to a
problems which now diminish tjie deliyery' of
free service there is no end of opinion,
nurse.
health care while blurring the moral goal of
verging on explicit protest, from patients,
Secondly, greed limits access to care for
the profession.
their families, insurance operators, legis
poor patients. The income of specialty stars
Without question doctors should earn in
lators, and the general public that doctors are
raises insurance premiums for all insured
a greedy lot. In my opinion, which I discover patients. As the premiums go up increasing comes which genuinely reflect the training,
time, effort, and trust that goes with their
I must leave my native land to voice, it
numbers of citizens with marginal incomes
care of the sick. It is malignantly counter
behoves the medical profession to address
are forced to forgo insurance coverage; their productive for soaring medical reimburse
any problem vexing its relationship with access to health care evaporates.
ment to diminish the stature of the vast
the public. Doctors’ greed is just such a
Examples of greed can be found in all majority of doctors.
troubling problem.
specialties. Imagine a hospital in a small city
It is imperative for the medical profession
The profession is aware that greed best
considering opening a service for coronary to open its published journals and collegial
describes how some of its members place
bypass operations. To secure a thoracic forums to a candid appraisal of the existence
profit before patient wellbeing. Before
surgeon the hospital board is prepared to of greed in its ranks. There is no need, in fact
addressing the 1991 annual meeting of the
offer a base assured
income beginning
... £11
- at
-is danger of exaggeration and mindless
Federation of State Medical Boards of the
81-25m a j u.. ln.C’ Uding
' „
offife SUPP°«- regulation, for the discussion to be taken up
United States I asked the solons of the
Simultaneously, the area suffers from a lack by the media. This is not to imply
profession to indulge me by responding
the
of family practitioners, who, at best, can .
discourse should be secretive but that it
directly to a question. “Do you believe
expect to make 880000 to 8100000 a year should have the serious attention and
the medical profession has a problem with
without any office support.
encouragement of the leaders of organised
greed?” Out of approximately 150, 90%
C
Consider my city of Portland, Oregon. It medicine, including the editors of
raised their hands in assent.
all
has one hospital offering organ transplant
specialty journals, to insure a scholarly and
The US medical profession as a whole
services and two other “non-profit” hospitals objective appraisal. The discussion should
nevertheless seems hesitant to move beyond planning competitive services,
x------ - _——All three strive to determine objectively sane and
acknowledging the greed problem and to
hospi tals expect to offer high if not exorbitant
comment on its scale. The profession has a staff incomes, ultimately to come out of the prudent limits for medical reimbursement,
curious
propensity to avoid the issue*by
<----but not be confrontational, pitting one
existing health insurance pool that makes no doctor against another, one specialty against
relegating possible doctor greed to the status
provision for the health care of the homeless.
of a r ’
’ ’
—
non-problem.
The subject seldom, if An editorial in the local newspaper labels this another. Those that exceed considered limits
ever, appears in professional journals. The health care business at its worst, “greed- should no longer have the tacit approval of
the majority, the 97% who do not let a desire
side stepping is accomplished by labelling
driven nonsense.”
Jim/
____
f
for money determine their service to the
J?CUSed. c?ncern
about
greeda as doctor
Thirdly, the most corrosive effect of greed sick. Clearly, a serious problem with an
bashing and thus beneath the profession’s
and the tacit approval of greed is to the exaggerated and misanthropic human trait,
purview.
profession’s philosophy of service. Where greed, challenges the medical profession to
Little data exist for doctor greed. One
most of us were trained to believe that our
rough approximation of the problem Ia
is service is based solely on trust, with firstly move to higher moral ground in the care of.
the sick.—ralph crawshaw if a professor of
implied in a bell curve for doctors’ incomes
avoiding harm as the ultimate measure of psychiatry m Portland, Oregon
The income ofspecialty stars
raises insurance premiums
fo^ all insured patients.”
((The most corrosive effect of
greed .,<isto the profession*s
philosophy ofservice. ”
<1 ROM BMJ VOL. 306 9 JANUARY 1993, 15 )
SELECTIONS FROM BMJ
vol. 9
MARCH 1993
95
ea'*'r'br'oaia
cat M
'•-660034 ■
EFEh NEWSLETTE
July - Aug 1991
SPECIAL ISSUE ON MEDICAL MALPRACTICE
Vol V No, 4.
MISUSE OF MEDICINE
N.H.Antia
There is no field of human endeavour where misuse of
privileges, authority and funds can be entirely eliminated.
Hence society devises methods for limiting such misuse in the
form of rules, regulations and legal measures even though
enlightened self monitoring and self restraints are ideal. What
differentiates professions from trades is that the former not only
possess special knowledge and skills but also evolve a code of
conduct and ethics to monitor their own members. This is in
order to ensure not only the level of technical competence but
also the obligation to the society which has entrusted them with
responsibility and has placed its trust in them. The medical
profession has enjoyed a uniquely privileged position because of
their technical skill as well as the intensely personal relationship
which develops between a doctor and his patient, whereby the
latter puts his/her entire faith in the doctor who not only cures
but also cares and consoles the patient as well as the family. The
epithet ‘noble’ is symbolic of the love and respect that this
profession has enjoyed over the ages, which is somewhat akin to
that of the priest.
It is unfortunate that there is now a rapid deterioration of
this happy relationship between the profession and society at
large and a degree of suspicion and mistrust pervades this
relationship today. Before we blame the profession as a whole,
let us not forget that there still exists the same relationship
between the family physician and his clientele; only that this
breed is rapidly diminishing as a result of the new, impersonal
and materialistic trends which affect not only this profession but
also the rest of society of which they are an integral part.
The wholesale adoption of the western model by our policy
and decision makers after independence, based on an alien
culture and its science and technology lias shaken the entire
social and economic fabric of our society and distorted age old
values associated with our civilization and its culture. It has
polarized our society with a small, wealthy, elite group
marginalising the vast majority whose life is being increasingly
degraded, as clearly observed by the burgeoning urban slums.
While this western science and technology has given the
knowledge and technology to provide for . the basic needs of
everyone on this planet, yet, because of its very materialistic
nature and lack of a human and moral basis, it is used chiefly as
a tool for aggrandizement and exploitation. Such misuse is not
Dr. N.H.Antia is an eminent plastic surgeon and honorary
Director of both the Foundation for Medical Research and
the Foundation for Research in Community Health.
only restricted to the western nations where it has originated,
but is also rampant in the poor countries, in the hands of those
who have been able to obtain access to this technology. The gross
misuse of such knowledge and technology in the field ofmedicine
is demonstrated by the fact that the most simple, cheap and
efficient aspects ofthe cure and control ofcommunicable diseases
(which still remain the major health problem for the vast
majority of our people, especially the poor) are neglected and
undue emphasis is paid to the most expensive, complex and 'cost
ineffective diseases like cancer, heart-stroke which affectl the
small, affluent sections of our society.-This clearly demonstrates
that the dominant consideration in the import and use of such
science and technology is dictated by the requirements of] the
rich and that of the medical profession rather than the needs of
the vast majority. In the process, medicine is being converted
from a profession to a lucrative trade in human suffering; an drea
where consumer resistance is at its lowest.
The gross overproduction ofdoctors, drugs and sophisticated
medical instillments and that too of the wrong type has ensured
that malpractice has been built into our present health system.
Unfortunately, over the years, this has become an accepted form
of medical practice by both the medical profession as well as the
public. This is further compounded by the absence of any
regulatory measures like public information and education on
health and suing for malpractice, as exist in the USA and many
other western nations.'
In the case of the urban rich this is demonstrated by the
unnecessary, excessive and even dangerous investigations and
medications, inclusive of surgery, and the pressures to imp ose
the latest and most expensive glamour technology imported
from the West regardless of its appropriateness. Also, the patient
or the public isseldom informed of the attendant dangers which
are reported in Western journals, leave aside the far greater
shortcomings in our own limited experience. Due to availability
of easy money, the rich are unwittingly at the greatest peril of
iatrogenic (doctor made) diseases, as is demonstrated by the
mushrooming ‘five star’ urban hospitals with the latest
specialities, the latest scanners and the latest drugs and
operations. Intensive care units are indiscriminately used, even
for terminal care patients, who now have to end their life in stark
aseptic conditions monitored by the latest gadgets, rather than
in an ordinary hospital bed or preferably in the home, surrounded
in their last moments by loving and caring relatives and friends.
Each one of these facilities have their specific limited use, but
when unintelligently or deliberately pushed to their Emits |by
FOR PRIVATE CIRCULATION ONLY
o
those trained as technical robots or for satisfying their monetary
gre^d, these “wonders” of modern science prove to be counter
proc?uctive, if not actually harmful.
Illness:
A Lucrative Business
iTie growing middle class has now been caught in the cleft
stick bet ween providing the latest medical care like renal dialysis,
kidney transplant and coronary bypass surgery for their loved
ones and being pauperized in the bargain. Many search for a
good, old fashioned family doctor, who is now in short supply, or
turn to other cheaper and more acceptable alternative systems
such as Ayurveda and Homeopathy. Without insurance and
adequate financial resources, the thought of illness has become
a source of anxiety and neurosis for this rapidly enlarging
section of our society
/z.... .a common public opinion is tha t patients trust tlieir
physicians technically and personally but not
economically,.... The harshest judgment comes from
some medical economists who bluntly state that the
ethical Ideals of the Hippocratic Oath are out-moded
and mythical...... The doctor-patient relationship is a
commercial transaction that should be regulated by the
rules of the marketplace,..... normal business activities
such as aggressive advertising, paying in advance, and
undertakingpmfit-makingenterprisesthatare unrelated
to direct provision of physicians services are all clearly
legal and good business practice. But, are they ethical?
Are they primarily in tlie spirit of what is best for the
For the vast majority of the poor who live in villages and
urban slums, this poser, an entirely different problem. While the
middle class are their role model they can hardly conceive of
using the private hospital with its specialists or even the nursing
home for their medical needs. And yet they too have been hooked
by the medical profession, albeit by those in the lowest rungs, to
the universal injection as a panacea for all ills. The blunderbuss
therapy of Rs. 20 or more for a so-called ‘cocktail’ injection
consisting of an antibiotic, corticosteroid, vitamin B, antihistaminic and analgesic is now familiar even to most villagers,
leave aside the older ‘heat’ producing injection of calcium
gluconate. The public hospital, whose mal-functioning was so
starkly revealed by Justice Lentin, remains their last resort.
Fear of these institutions now drives them to small, unhygienic
private nursing homes, often after a preliminary visit to the
moneylender. The government Primary Health Centre, which
was designed to serve the preventive, promotive and basic
curative health needs of the 70% of our population that lives in
rural India, has ceased to undertake any of these functions as a
result of its almost total devotion to Family Planning and its
accessories like Immunization and MCH. Shrouded in secrecy,
the PHC is unaccountable to the people for whom it is meant.
patientr________________________
ExcerptedfromthepresidentialaddressbyFrankC.Spencer,(M.D.,FACS,
New York), to the American College of Surgeons, as carried in the ACS
Bulletin, November, 1990.
for Western science, the continuation of the use of this model,
that too in its worst aspects, despite ample experience to the
contrary, can only be ascribed to the selfish and exploitative
nature of those who continue to promote and operate this form
of development.
It is regrettable that this type of medical practice now poses
a threat to the health of our people. The public health colleges
produce doctors who are mostly trained for, and work in, the
private sector. It is inconceivable that any sane politician honestly
believes that private medical colleges, which levy a capitation
fee of several lakhs in declared and undeclared monies, are for
the benefit of the rural masses. The mad rush for securing the
highest marks for admission to government medical colleges, or
paying high capitation fees by the rich, for their children who
cannot get into the former colleges, does not demonstrate love for
the health ofthe people but a clear indication of the extent ofsafe
monetary returns that this profession ensures them. The type of
medical education and even worse, the values inculcated in them
are directly opposed to the health needs ofour people. Permission
to produce 60,000 drugs and formulations (costing Rs.3,600
crores), when the WHO lists only 258, is surely not for the benefit
of the people but that of the pharmaceutical industry and those
who give them licenses on the basis of kickbacks. The
multinationals who control the major drug companies and
increasingly, the medical instrumentation industry, do not come
to India for the health of our people.
What is it that has lead to th is lack of accountability of the
public sector and the exploitative nature of the private one? The
answer lies clearly in the inappropriate Western model that has
been chosen for the development, of this country. While we may
forgive Nehru for being enchanted with the post-war euphoria
1■^ippotratKfiM)
tofll prescribe regum tor tJje goob ot mp patients anorttug to nip
ability art) my fubgnmt an b nrber bo baun to anyone. please no one bill
J prescribe a beablp bmg nor gibe abb ice toliich map cause b& beaib—••
__ Jf 3 teep this oath f/tttftfully. may 3 enfoy my lite art) ptartte m? art,
respcteb by all men art in all times; but if 3 efonue from it or btolate it,
r,iay the reberse be my lot.
The medical profession and the associated health industry
have the unique opportunity to trade in an area where consumer
resistance is at its lowest, as a result of fear and ignorance.
Public ignorance and absence of consumer resistance is
demonstrated by the fact that malpractice insurance premium
of doctors in India is Rs. 100 per annum, while that in the UK
it is over 1200 Pounds sterling, and for certain specialities in the
USA over $ 60,000 per annum. This is not to advocate legal action
as the optimal way for improving the health services, but under
the prevailing conditions of increasing material values and
human greed, public awareness and threat of legal action remain
Excerpt, as contained in “Medical Negligence”, S.Raghavan, The Free
Press Journal, Apr. 13,1980.
2
IRRATIONAL AND UNETHICAL MEDICAL PRACTICES
Mohan Deshpande
In recent years the press has been abundantly covering
hitherto unreported and under reported cases of malpractice in
the medical field. Undoubtedly, these and many more unreported
cases will have to be fought in the legal courts, which in turn, will
hopefully have a deterrent effect on the medical profession. This
will also make people at large aware of their health rights to
some extent.
Much goes under these press reports of overt malpractice
and negligence. This consists of a bulk of irrational medical
practices which are invisible and seldom brought to light owing
largely to ignorance of people and a smart combination oftactics
and the skills the profession possesses collectively. Moreover, to
locate and to identify irrational practices needs quite a good
knowledge of medicine and its practice. Since the effects of these
irrationalities are neither immediate nor severe enough on the
patients, they are rarely complained about. Even if a patient
suspects an irrationality, he/she usually refrains from asking for
clarification. He/she is simply a stupefied victim of so-called
‘faith’.
Usually medical doctors, even those rational in their own
practice, do not come forward to report such irrationalities even
though in private they would express their dissatisfaction about
the increasing commercialization in their profession. Some even
try to protect fellow professionals under the pretext ofprotecting
the medical fraternity. There is also a false notion prevailing
amongst doctors that it is ‘unethical’ to divulge information on
such matters to the ‘lay’ public. There are attempts even to
justify the wide-scale unscientific and irrational practices on
grounds such as, it is beingunfair to isolate the medical profession
to blame leaving untouched the general social atmosphere of
rampant corruption at every level. Some tend to blame the
professional (or business ?) competition or the dog-eat-dog
health bazaar (too many doctors ?) as if these are entirely
extraneous to their profession and thereby justify the so-called
‘survival instinct’.
Irrational practices can be grouped in the following
categories:
A)
B)
C)
D)
E)
life saving purposes and intractable diseases) for
simpler ailments, for quick relief. The doctor also
provides a (false) sense of well-being to the patients.
This attracts more patients to him.
3) Irrational use of antibiotics notwithstanding their
longterm severe effects like tolerance cross-resistance
etc.
4) Using banned or bannable drugs: the profession
cannot absolve itself from its responsibility to update
knowledge of recent research and government/legal
decisions.
5) Using sub-standard drugs for dispensing: Thes e drugs
are usually available in local markets in bulk quantities
produced by various ill-known companies.
6) Prescribing tonics, milk powders, protein powders.
7) Injecting B complex for a variety of ailments vhere
injectable vitamins have no role to play.
8) Using intravenous (I.V.) fluids when not indicated.
Using I. V. calcium gluconate for various non-specific
indications.
9) Use ofanabolic steroids (even injectables) for {growth/
gaining height etc.
10) Using drugs (especially from other ‘palhies) without
proper knowledge of their pharmacology. This applies
not only to heteropat hie practice but also to allopaths
using allopathic drugs which are banned or bannable.
The newer drugs and their information reach doctors
sometimes through unethical and un-scientifip
literature from the drug industry with reports of
contrived trials. There are also wide ranging
empiricisms (e.g. ‘no side effects’) in the use of brand
prescriptions from the Ayurvedic industry.
11) Unnecessary investigations, both invasive and noninvasive.This is not a ‘defensive’ practice. The sole aim
is profit.
12) Unnecessary admissions/surgery.
13) Refusing to treat seriously ill/dying/leprosy/HLV
positive patients/accident victims.
While diagnosing ailments
Usually the following diagnoses are thrown to patients:Weakness, low blood pressure, backache, white discharge
due to weakness, deficiencies, psychosomatic illness etc.
Creating cardiac neurosis: patient is not a heart patient in
reality but is made to believe she/he is.
While actually treating/investigating patients,
While diagnosing the ailment,
Concerning the relationship with the drug industry,
Concerning other doctors,
Miscellaneous.
Concerning drug industry
While actually treating/investigating patients
1)
i)
Injection>practice: irrational or over use of this
2)
mode of drug administration, for profits.
‘Steroid’practice: using steroids (reserved for
2)
Mohan Deshpande is a medical practitioner who is also a
researcher with FRCH, Bombay. The above is a slightly
modified version of the paper presented in the
workshop. 'Medical Malpractice; what it is and how to fight it"
organised by Medico Friend Circle (Bombay Group) in 1991.
3)
Acceptingsamples and gifts from drug industry causing
both overt and unconscious obligation to prescribe.
Accepting and not verifying information coming from
drug industry. One such example is the use of high
potency combination Bl B6 B12 for a variety ofillnesses
ranging from weakness to serious nerve-brain
disorders.
Engaging oneself in false, fabricated research for drug
industry.
Continued onfpage 8
3
EDUCATIONAL INTERVENTION IN MEDICAL MALPRACTICE
Amar Jesani.
The term Medical Malpractice (MM) encompasses a very
broad (perhaps entire) area of inappropriate medical practices.
The Bombay Group of Medico F riend Circle tentatively proposed
a working definition (1990) of MM for its workshop on this topic
as, ‘a variation from the normally acceptable, scientific and
average standard of medical practice at a given point of time’.
There may be many shortcomings in this definition (readers are
invited to suggest their alternatives) but, for the time being it
will serve our purpose, because the subject of this article is to
discuss the strengths and weaknesses ofeducational intervention
intended to bring about appropriate changes in the doctors
medical practice so that it becomes acceptable, rational, scientific
of minimum average standard, ethical and free from possible
negligence.
it is obvious that the prescribing doctors have grossly inadequate
scientific information on what they prescribe .Lastly, the problem
of doctors’ incompetency is a universal one. Even in countries
where the profession is better organized, internally regulated,
and has strong emphasis on continuous education, a significantly
high proportion of doctors are found to be incompetent. For
instance, in the UK, 107, to 15% of independently practicing
doctors are estimated to be incompetent (Smith, 1989). A
Canadian study in 1988, found that in their sample, 15% of
family practitioners and 2%' of specialists, had serious deficiencies
in medical records or care (Smith, 1989). In our country, at least
3/4th, of all practising doctors are independent practitioners
havingno regular continuous medical education. Only a fraction
of them subscribe to standard scientificjournals. The prevalence
of incompetency among them is, of course, anybody’s guess.
Why educational intervention?
Inshort, inspite ofnon-availability of hard data, the doctor’s
ignorance/lack of information on the scientific therapeutics need
no further elaboration. The socially conscious doctors and others
have therefore strongly argued that this ignorance or gap in
information is greatly responsible for many irrational practices
or malpractices by doctors. Due to lack of information, doctors
also fail to critically evaluate information provided by
commercially vested interests like pharmaceutical companies.
As a result, many have suggested that malpractices be classified
under two broad categories; intentional and unintentional. The
former is deliberate MM indulged in with a motive, such as
augmenting one’s income. The latter is supposedly due to
ignorance. A typical argument for the latter is, why should a
private doctor prescribe wrong medicine for tuberculosis when
it is not going to help him to hold the case. That is why
educational intervention is considered useful, particularly to
remedy unintentional MM.
We believe that there is a strong case for advocating
continuous, scientific education of all practicing doctors. How
can one object, in principle, that all doctors must be continuously
educated so that the quality of medical care provided by them
can be of optimum standard? In fact this is a truism universally
accepted as an essential ingredient of medical ethics.
Unfortunately in our country this component of medical ethics
is violated by the profession as it has hardly any effective
mechanism to provide systematic continuous education. As a
result doctors’ reading habits are found to be abysmally
inadequate to do justice to their role in medical care.
There is another compelling reason for advocating
educational intervention. Although there is no systematic study
available on the medical ‘competence’ of Indian doctors, certain
indirect indications show that 'incompetency' among Indian
doctors is shockingly high. For instance, in two studies of
prescription practices of private general practitioners in Bombay
city by Uplekar (1989a, 1989b), for the FRCH, it was found that
a majority of them had grossly inadequate knowledge of drug
treatment for two highly prevalent diseases; leprosy and
tuberculosis.
The structure and practices of the medical profession raise
further doubts. In 1986 we had 7,63,437 qualified doctors of all
systems of medicine. Of them about 42% were allopathic and
58% were non-allopathic. While in the developed countries,
scientific criteria to assess competency of allopathic doctors are
well developed, we have nothing to go by tojudge the competency
of non-allopathic doctors. In fact, we are almost sure that there
will be divergent views about the methodology used to assess the
competency of non-allopathic doctors. Secondly, cross system
therapeutic practices are highly prevalent. It is generally accepted
that a majority of non-allopathic doctors regularly use allopathic
drugs and devices. With the ayurvedic drug industry coming of
age, the use of ayurvedic drugs by allopathic doctors has also
substantially increased. Inthis use ofcross system therapeutics,
Another strong argument advanced for educational
intervention is that individuals in the profession have inflated
egos and are very sensitive to criticism. Positive educational
intervention would help some sensitive and ethical individuals
to see reason and thus to change their behaviour. Also, since
such intervention would not generate extreme negative reaction,
it would help win over some to the cause of rational practice.
After this is accomplished, it is believed that tactics can be used
against those who refuse to ‘shed their ignorance’.
Undisputedly, these arguments are highly logical, clear,
and straightforward. However, these arguments are clinically
too precise to explain the actual reality. It is indeed tempting to
put high prevalence of MM and lack of continuous education into
a one-to-one, direct relationship. But this relationship is highly
complex with many other variables more crucial in determining
the prevalence of MM. The need for continuous education is not
only because the MMs are highly prevalent but that even if it
fails to make a significant dent in the prevalence of MMs it is still
badly needed for many other reasons. The point being emphasized
here is that though educational intervention is necessary, its
mere presence is not a sufficient condition to bring about a
lasting change in the behaviour of doctors.
Amar Jesani is a researcher at FRCH, Bombay. He is also
a non-practising medico, actively involved in the Medico
Friend Circle.
4
Limits of educational intervention.
(c)
In our country some voluntary efforts have been made to
change doctors’ behaviour through education. Most of such
efforts are in the field of drugs and pharmaceuticals. “Dear
Doctor” letters, along with educational material on the rational
use ofdrugs, information about hazardous, banned and bannable
drugs, appeals against the use of drugs such as high dose
estrogen-progesterone (EP), fixed dose combinations and so on
have been circulated amongst doctors. In addition, certain
categories of drugs (anti-diarrhoeals, tonics) have been studied
for their rationality and reports have been compiled and
circulated amongst doctors. These are highly commendable
voluntary efforts and we have been participating in them in
various ways.
However, to what extent do they make a dent in the MMs?
Unfortunately, none of these efforts were adopted for
experimental research by institutes. Most of these reports were
by activists, done with the full conviction that such things ought
to be done, irrespective of the extent of the immediate impact
that they would make. Further, some important attempts were
part of a wider campaign to get a particular drug banned, as the
campaign against the high dose EP drugs. It was not a simple
educational campaign but a definitive campaign to get the drugs
banned on the ground that these are irrational and hazardous.
Thus, there was no scope to wait for the results of the educational
intervention. The ultimate ban on EP drugs was, in fact, brought
about despite the lack of support from the profession!
Most systematic research on improving prescription
practices through educational intervention is done in the
developed countries, particularly in the USA, as the vagaries of
the market in health care has made that country cost-conscious.
But all experimental researches carried out there, on this
subject, are also not scientifically rigorous. In a review of such
services, Soumerai, McLaughlin and Avorn (1989) found that
almost one third of them were inadequately controlled studies.
They found that 85% of the inadequately controlled studies
reported positive findings as compared to 55%' of well controlled
studies. They also found that in several studies, the control
groups showed positive improvement due to the effects of other
factors. (Note: in the control groups there was no educational
intervention).
0
There are seven categories of educat ional approaches used
in various studies reviewed by them. Thev are:
1) Dissemination of printed educational material,
2) Reports ofpatient-specific lists ofprescribed medicines,
3) Group education including conferences, lectures,
seminars, tutorials,
4) Feed back of physician specific prescribing patterns,
5) Reminders at the time of prescribing,
6) One-to-one education,
7)
some may be very costly such as providing one-to-one
education by a visiting physician, and so on.
On scanning through some of the study reports we find that
the method ofproviding doctors with mailed, printed material is
the least effective method whereas the one-to-one education of
the physician by a visiting physician is the most effective
method. Perhaps this is the chief reason why the pharmaceutical
industry uses an army of medical representatives who can
change the doctor’s prescription behaviour through one-to-one
education. In any case, it will be the height of irrationality to
create another army ofvisiting physicians for providing rational
drug education.
Those who propagate the idea of rational prescribing most
often depend on the method of providing doctors with print
material. Studies of this method however, show disappointing
results. At the same time it is found that the provision of pointed
material could create a necessary condition for trying other
methods out. Further, studies using a patient care protocol to
guide doctors at the time of examining and treating patients,
show that the protocol makes a great difference in the behaviour
of those doctors who participate in formulating such a protocol.
That is, a participatory exercise in creating educational ma terial
is more important than in the use of the same educational
material for other doctors.
What influences prescribing behaviour?
When we talk about alternative rational ding information,
it is necessary for us to understand the role of such inform ation,
on the prescribing behaviour of doctors. A rational enquiry into
the prescribing behaviour ofdoctors would reveal a very dominant
phenomenon called ‘the non-pharmacological basis of
therapeutics’, (Avorn et al, 1982). It is this phenomenon which
makes educational intervention, which is chiefly centred around
rational pharmacological information, less effective. Avorn et al
(1982) argue that “irrational drug choices are made frequently,
despite the availability of ample empirical evidence counseling
otherwise”. In a study of doctors they found that “although a vast
majority of practitioners perceived themselves as paying little
attention to drug advertisements and ‘detail men’ (commonly
used term for medical representatives) as compared with papers
in the scientific literature, their beliefs about the effectiveness
of index drugs revealed quite the opposite pattern of influe: ice in
large segments of the sample”.
Thus, in actuality, what a doctor normally does in treating
patients is customary behaviour that is routinised, habitual and
automatic. Such customary beliaviour is fonned with the influence
of history, locality, peer groups and above all, environment and
the system within which medicine is practised.
When sufficient weightage is given to the factors which
actually condition prescribing behaviour of doctors, we find that
the role of simple information dissemination or education is
gi-ossly limited. Kenhouse and Jacoby (1988), in an article
reviewing the subject, argue that the ‘customary behaviour’ of
doctors is likely to change only in the presence of a motivating
trigger. Such information has a useful role only in conditions
which are introduced to change the environment in which
medicine is practised.
On going clinical pharmacy services.
Going through the above list we realize that:
(a) some of them are clearly suitable in the hospital set up and
very difficult to implement in the case of independent
private practitioners,
(b) some are very cumbersome, for instance, providing reminder
at the time of prescribing ma^y need a higlily computerized
set-up,
5
Continued on page 8
COMMUNITY HEALTH
CELL
326. V Main, I Block
Koraniongala
tiangalore-560034
India
PRIVATE HEALTH SECTOR
Regulation and Control
Ravi Duggal
Prevailing Situation.
Auditing of prescriptions of the doctors in relation to the
diagnosis.
Determining a fixed tariff of charges that patients pay to
V
doctors.
vi Providing continuing medical education to all those who
practice medicine. For instance, a 'summer' refresher
course eveiy three to five years should be compulsory for all
practitioners and their license renewal should be dependent
on this.
vii Regulation ofgeographical distribution ofsettingup practice
to correct the urban-rural disparities. (We feel that as of
present there is adequate medical humanpower in the
country and it only needs redistribution.)
viii Annual return of patients treated; some minimum data to
be maintained and filed with an appropriate authority.
iv
The private health sector consisting of general practitioners,
nursing homes and hospitals, employs two thirds of the medical
manpower and is responsible for two thirds of the total
expenditure on health in this country. Despite this there is
hardly any regulation of the practice in this sector of health.
This is indeed surprising, because such activity cannot be
carried out without registration. The medical professional has to
be registered with the Medical Council, which is a statutory body
that last set the standards of medical practice — ‘discipline’ the
professionals, monitor their activities and check any
malpractices. The doctors who decide to set up their own clinics
as well as hospitals, nursing homes, polyclinics etc. have to
register with the respective local body.
b). Nursing homes and hospitals:
Similar to the practitioner, regulations need to made for
setting-up and runningof hospitals and nursing homes. Minimum
quality standard, nurse:doctor ratio, patientmurse ratio, proper
location ofpremises, geographical distribution, fixed reasonable
tariff charges, proper medical records, maintenance, filing of
minimum data returns, properly qualified and adequately trained
peMoimel for jobs assigned, prescription auditing, medical
auditing etc.
The problem with the above is that the controlling bodies
are virtually non-functional. The reason for this is not only lack
of interest but also weak provisions in the various acts. They are
also heavily influenced by the private health sector.
Another agent in the private health sector which needs to
be regulated further is the pharmaceutical industry. As a chemical
industry, this agent is regulated to some extent but as a
participant in the health sector, it operates virtually unregulated.
c). Pharnviceutical industry:
The piiarmaceutical industry must be allowed to manu
i
facture only rational drugs in required amounts with clear
priorities in favour of essential drugs. All irrational and
non-essential and dangerous drugs must be banned.
ii Branding of drugs must be prohibited.
iii There is every reason for a progressive nationalization of
the pharmaceutical industry.
iv The regulatory body for the pharmaceutical industry must
be the Health Ministry and not the Ministry of Chemicals.
The practice of canvassing drugs tlirough pharmaceutical
V
(medical) representatives should be banned.
vi A National Formulary should be evolved with generic drug
names becoming the basis of prescription writing.
vii Continuing pharmacological education of doctors should
be through the Medical Council or other such statutory
body.
In view of the existing health situation and practices,
regulation of those who provide the nation's health care is an
urgent neccessity. Regulation exists in other sectors, so why not
in health? This is especially needed as consumer resistance is at
its lowest in this field and therefore lends easily to malpractice.
How to regulate
a). Medical practitioner’s:
Each medical practitioner is registered with the respective
state Medical Council. Presently, beyond tills registration the
Medical Council does not concern itself with the practitioner,
unless some complaint is made and a prima-facie case is
established. The Medical Council and other related bodies, in
consultation withthe health ministiy, must regulate the following
areas of health practice: (This is only a selective list).
i
ii
iii
d). General regulations:
To prevent unnecessary concentration in urban
especially metropolitan areas, state subsidies, 4oft
loans, must not be given to those wanting to set up
practice, or hospitals and nursing homes in these
areas. Such loans should be restricted to rural
areas and taluka towns.
ii A tax on private medical practice and private hospitals
and nursing homes must be levied. This tax should be the
highest in metropolitan areas and the lowest in rural areas.
Private hospitals should not be allowed to be operated as
Monitoring that only registered practitioners practice
medicine.
Assuring that clinics have minimum standards of
quality by setting standards for the same. (This should
include X-ray, CT scan and pathology laboratories.)
Making maintenance of patient records compulsory and
accessible to patients.
Ravi Duggal is a researcher at FRCH, Bombay. The above
formed a part of a larger note on the private health sector,
presented by FRCH to the Planning Commission in April,'90.
Continued on page 8
6
k
MEDICAL MALPRACTICE AND THE LAW
The issue of medical malpractice is dealt with by the rules
governing medical negligence, which forms a sub-branch of the
law of negligence. These come under the Law of Torts which
offers civil redressal in the form of compensation. “A person is
said to be negligent when s/he acts without due care in regard to
the harmful consequences of her/his action”. A physician surgeon
orother member oft he medical profession, if he has not exercised
reasonable care in the treating of a patient, may be liable to a
negligence suit. While the degree of care to be exercised depends
on the facts of each case, it is generally presumed that the test
is the standard of the ordinary skilled person, exercising and
professing to have that special skill.
Duty of care
Hospital/nursing home liability
Private as well as public hospitals (including charitable
hospitals) are liable for the neghgence of their employees. In a
landmark American case, (Darling vs Charleston Community
Hospital, 1966), the judges held:
“...The present day hospitals, as their manner of operation
plainly demonstrates,do far more than furnish facilities for
treatment. They regularly employ, on a salary basis, a large staff
of physicians, nurses and interns, as well as administrative and
manual workers....certainly the person who avails himself ofthe
hospital facilities expects that the hospitals will act on their own
responsibility”.
Pleadings
Once a doctor accepts a patient, the principle of exercising
reasonable care becomes applicable, whether the doctor accepts
fees or not, and whether the doctor is a private practitioner or
public servant, general practitioner or specialist. A person who
offers medical advice and treatment, impliedly undertakes that
he/she has the requisite skill and knowledge. Such a person owes
to the patient certain duties, of which the following are important:
Duty of care in deciding whether to take in a case.
Duty of care in deciding what treatment to give and in
diagnosis.
c) Duty of care in administering the treatment.
d) Duty of care in answering a question put to him by a
patient when he knows that the patient intends to rely
on his answer.
A breach of any of these duties will support a suit by the patient.
a)
b)
In any suit claiming compensation for negligence, the
plaintiff must plead and prove three things:
The defendant owed a duty of care to the plaintiff
(Exact situation must be mentioned).
ii) The defendant had committed a breach of that duty.
(How such breach was committed must be clearly
stated)
iii) The breach of duty resulted in an injury. (The cause
effect relationship must be definitely brought out.)
i)
As in the above, while the onus to prove guilt lies with the
patient, in some cases, due to a number of reasons ( such as
incomplete information given by a doctor etc.) it becomes difficult
for the patient to provide sufficient proof. In certain of these
cases, when circumstances make it quite obvious that neglige ice,
in fact, has been the cause, the doctrine of lies Ipsa Loquita i the
thing speaks for itself) is applied. This doctrine has been
extensively used in "swab cases" where after an operation an
instrument is left inside the patient's body.
Forms of medical negligence
Medical negligence may assume a variety of forms. These
include:
a) negligent diagnosis,
b) negligence in operation,
c) failure to listen to a patient's complaint,
d) negligent administration of a wrong drug,
e) negligent exposure of the patient to risk of infection,
0 negligence in advice about the risk of an operation or
negligent failure to warn the patient of such risks',
g) negligence in post-operative care,
h) inadequate supervision or inadequate staff in the
nursing home.
Damages
Damages are classified as special andgeneral. Special
damages include pain and suffering, loss of expectation of life,
loss of amenities and the injury itself. General damages refer to
pecuniary loss, such as loss of earnings, legal expenses, loss of
pension rights, loss of marriage prospects, and loss of
opportunities for gainful employment.
Conclusion
At present, litigation in case of medical malpractice is not
widely prevalent. But the trend is catching on, especially in
urban areas. While litigation in itself, may not serve to wipe out
malpractice, the threat of legal recourse can certainly create
conditions compelling accountability on the part of the medical
profession. Needless to say, the extent of utilization of legal
recourse would be pre-determined by its accessibility as well as
the extent, to which demystified information reaches the masses.
*The article above has been compiled from the following:
-Mathew, P.D., Bakshi P.M., "Medical Negligence", Legal
education series, No. 21, Indian Social Institute, New Delhi,
1986.
-Desai, Mihir, "Medical Malpractice and Law", in the Radical
Journal of Health ,Vol.II, No. 4, March 1986.
[Editor]
7
NEW ARRIVALS
BOOKS
1. Government of India,"Diamonds Fox Grants of Central Govt. 1988-89",
GOI, New Delhi, 1989, pp. 153.
2 All India Drug Action Network, “A Rational Drug Policy: Problems, Per
spective, Recommendations", VHAI, New Delhi, 1986, pp. 157.
3 Baker Selwyn J. (Dr.). "Design and Analysis of Iron Supplementation
Trials”, Nutrition Foundation, USA, 1984, pp. 34.
4 Demaeyer E.M., “Preventing and controlling Iron Deficiency Anemia
through Primary Health Care, A Guide", WHO, Geneva, 1989, pp. 58.
5 Nofziger Margaret, "The Fertility Question", The Book Publishing Com
pany, Summertown, 1982, pp. 104.
6 Burton J.L, “Aids to Postgraduate Medicine", 1st edition, Churchill
Livingstone, New York, 1988, pp. 263.
7 Nath Uma Ram, "Smoking Third World Alert”, Oxford University PreJs,
New Delhi, 1986, pp. 292.
8 Society for Participatory Research in Asia, “The Takeover". SPRA, New
Delhi, pp.32.
9 Rubenson Brigitta, “What is AIDS? Manual for Health Workers", Christian
Medical Commission, Switzerland, 1989, pp.28.
10 Wilson Sir John, "Disability Prevention: The Global Challenge", Oxford
University Press, Oxford, 1983, pp. 107.
REPRINTS
1 Kerala Shastra Sahitya Parishad (K.S.S.P.), .“Need for a peoples drug",
PP- 8Anderson Roy M„ "Modern Vaccines: Immunization and Herd Immunity",
Lancet, 1990, pp. 641-645.
3 Hall A.J., "Modern Vaccines: practice in developing countries”, Lancet,
1990, pp. 774-777.
4 Bannerji D., “Crisis in the medical profession in India", EPW, 1989, pp.
1091-2215.
5 Medico Friend Circle (MFC), "Effect of Bhopal gas leak in women’s
reproductive health", pp. 6.
6 ShivakumarM.S., "Voluntary agencies and planned development". 1985,
pp. 31-32.
7 Lancet, “Potential value of serology for diagnosis of extra-pulmonary
tuberculosis”, 1990, pp. 641-644.
8 Panchamukhi, "Economics of health and nutrition; A review of policy
oriented thinking....’’, 1989, pp. 1-89.
9 British Pharmacopoeia, "Vitamin A", 1988, pp. 596-598.
10 KSSP, "Mortality, morbidity, and disability in Kerala; Resultsfrom a rural
health survey", 1987, pp. 1-4.
2
Continued from page 3
Continued from page 5
Concerning other doctors
In conclusion one can say that MMs exist not simply
because there is a dearth ofeasily available rational and scientific
literature but often inspite of it. The fight against MMs therefore,
cannot be just an educational effort but must address to more
fundamental factors which decisively shape the environment in
which medicine is practised.
Accepting / offering ‘cuts’ (percentages) for referring /
treating / investigating patients.
Miscellaneous
1)
2)
3)
4)
Giving false certificates,falsification of reports e.g.
pathology, post mortem etc.
Advertising
Not preparing case papers records, not making them
available to the patients.
Overcharging: There is no standard/prescribed price
for medical care nor are there stipulated rules and
regulations for monitoring. There are no grades given
to dispensaries/nursing homes.The price of health
care is guided by such factors as professional
competition, crowding of doctors in a locality, patient's
income and living standard, needs and greeds of
doctors etc.
There is a minuscule section of doctors who are guided by
ethics and rationale against the dominant market forces which
usually control the attitude of doctors. It is necessary today to
widen this circle of conscious,ethically motivated doctors and
thus reverse the tide which threatens to wash away the noble
principles on which this profession is supposed to be based. •
The British Connection
About two-thirds of the world drug sales a re controlled
by big trans-national drug companies in West Germany
(Hoechst, Bayer), Switzerla nd (Hoffman, La Roc he, CibaGeigy, Sandoz), and USA (Merck, Pfizer, etc), all with
subsidiaries in the U.K.
Source: Prescription for Change, Virginia Beardshaw, as carried in HAl's
Guide to Rational Health Projects, pg.74
References:
1
Avom Jerry, Chen Milton, Hartley Robert; ‘Scientific vs commercial sources of influence on
the prescribing behaviour of physicians' in The American Journal of Medicine, Vol.73, July
1982, pp. 3 to 8.
Kenhouse David E., Jacoby Itzhak,: When does information change practitioner's behaviour'
2
in International Journal of Technology Assessment in Health Care. Vd.4,No.1,1988, pp. 27-33.
Medico Friend Cirde (Bombay Group): Medical Malpractice; what it is and how to fight it’.
3
Report of a workshop in Medico Friend Circle Bulletin. May-June 1991.
Smith Richard, Profile of the GMC: Dealing with sickness andincompetence; successes and
4
failures.'in the British Medical Journal 298,1695-8 (24 June, 1989).
Soumerai Stephen, McLaughlin Thomas, Avorn Jerry, ‘Improving drug prescribing in private
5
care; a critical analysis of the experimental literature' in The Milbank Quarterly, Vol. 67, No.2,
1989. pp. 268-317.
Uplekar Mukund (1989 a), Prescribing behaviour of private G.P's of Bombay in treatment of
6
pulmonary tuberculosis', Bombay, FRCH, (unpublished).
7 Uplekar Mukund, (1989b), ‘Private doctors and public health: the care of leprosy in Bombay’,
Bombay, FRCH, (unpublished).
Continued from page 6
iii
iv
v
trusts or societies which give them cover for tax relief. They
should be treated as corporate bodies. Hospitals operating
‘research centers’ must be audited and their tax reliefs
questioned.
A social audit of the health sector must be an ongoing
activity of a statutory body which should be created for this
purpose.
A tax on the international migration of doctors.
Embargo on private practice ofthose receivingstate financed
medical education by part training at civil/rural hospitals
or PH Os. This should be combined with a long term change
of relocating medical colleges at the district centers.
9
Edited by Nagmani Rao. with secretarial assistance from Sunita Kesavan and produced by the Foundation for Research in Community Health.
84-A, R.G. Thadani Marg. Worli. Bombay 400 018. Registered under the Bombay Public Trust Act. Primed at Printext Offset. Pune 30.
AMNESTY INTERNATIONAL
MEDICAL POLICY
In the past few years, Amnesty International
medical groups have discussed a number of
questions which are relevant to the organiz
ation’s work. These include:
• medical aspects of torture and its sequelae,
and involvement of health professionals
in torture.
• the abuse of psychiatry for political
purposes.
• forcible feeding during hunger-strikes.
• floggings and amputations.
• medical involvement in the death penalty.
• international codes of medical ethics for
health professionals.
• prison medicine.
• psychological effects of “disappearance”
on families.
The views of medical groups have helped
to shape Amnesty International policy in
these areas and have contributed, in turn,
to major Amnesty International campaigns
against the death penalty and “disappear
ances”.
CARE FOR REFUGEES
Victims of torture and those who are forced,
for reasons of conscience, to flee their oM
country frequently need medical help for
problems arising from their experiences.
Amnesty International doctors can play a
valuable role in this field either by treating
the refugees themselves or by referring the
patient to another sympathetic doctor. A
number of Amnesty International doctors
have played a part in the rehabilitation of
former torture victims.
FOR FURTHER DETAILS CONTACT:
Amnesty International, International Secretariat, 1 Easton Street, London
WC1X 8DJ, United Kingdom.
Telephone: 01-833 1771
Telegrams: Amnesty London WC1
Telex: 28502
INTERNATIONAL RECOGNITION
Amnesty International’s work is based on the United Nations.
Universal Declaration of Human Rights. The organization has ford®
relations with the United Nations (ECOSOC), UNESCO, the Council
of Europe, and the Organization of American States.
On the occasion of the 30th anniversary of the Universal Declaration
of Human Rights, Amnesty International was awarded the United Nations
Human Rights Prize for “outstanding achievements in the field of human rights”.
Amnesty International received the Nobel Peace Prize in 1977 for its contribu
tion to “securing the ground for freedom, for justice, and thereby also for peace
in the world”.
In recognition of the medical work of Amnesty International, the Council of
Europe awarded the organization the European Human Rights Prize in 1983.
I
Amnesty
International
Doctors
& Health
Workers for
Human Rights
Thousands of people are in prison
because of their beliefs. Many are
held without charge or trial. Tor
ture and the death penalty are
widespread. In many countries
men, women and children have
“disappeared” after being taken
into official custody. Still others
have been put to death without
any pretence of legality: selected
and killed by governments and their agents.
These abuses—taking place in countries with widely
differing ideologies—demand an international response.
Founded in 1961, the Amnesty International movement,
comprising members from all walks of life around the
world, is working to expose and halt these violations of
fundamental human rights—and to help the victims and
their families. Doctors and other health workers are play
ing a vital role in this worldwide effort.
A MEDICAL PROGRAM FOR
HUMAN RIGHTS
Health professionals working as members of Amnesty
International focus particularly on prisoners with serious
health concerns whose cases have been taken up under
the organization’s mandate (see box). Many of the
prisoners are suffering as a result of torture, ill-treatment
in custody or appalling prison conditions. Many of them
will continue to suffer, physically and mentally, long
after their release.
The need for medical attention is vital. Prompt action,
supported by doctors in other countries simultaneously
sending letters of concern in specific cases where prisoners
are known to be in need of medical care, can save lives.
There are now more than 4,000 doctors in nearly 30
countries involved in the work, ranging from letter writ
ing campaigns to the care and rehabilitation of torture
victims.
OUR MANDATE
Amnesty International’s medical program is part of its
contribution to the international protection of human
rights. Its activities are focused strictly on prisoners:
• It seeks the release of prisoners of conscience. These are
people detained anywhere for their beliefs, colour, sex,
ethnic origin, language or religion, who have not used or
advocated violence.
• It works for fair and prompt trials for all political
prisoners and on l^ialf of such pe^Ie detained without
charge or trial.
• It opposes the death penalty and torture or other cruel,
inhuman or degrading treatment or punishment of all
prisoners without reservation.
Through its network of members and supporters Amnesty
International takes up individual cases, mobilizes public
opinion and seeks improved standards for the treatment of
prisoners.
You can add to the campaign: you can become a sub
scriber, join a local group, send in a donation and inquire
about the growing medical program which needs support
from the medical profession for special interventions on
behalf of prisoners and their families.
DIRECT ASSISTANCE
The clinical cons^fcnces of toi^fce can be severe.
Amnesty Internatiomu doctors hav^een able to provide
practical and invaluable assistance to people who have
suffered unbearable physical and mental pain and the
stress of isolation and exile. Using their professional
skills to counteract the work of the torturers, these
doctors have been able to improve the health of a number
of former detainees. One such victim was a 38-year-old
woman who had suffered temporary paralysis as a result
of beatings sustained in police detention. “You have
given me a new life”, she wrote to doctors in Copenhagen
after they had restored her ability to walk.
WHAT IS HUMAN RIGHTS
MEDICAL WORK?
Members of Amnesty International medical groups and
other health professionals who participate in the move
ment’s activities are involved in a range of activities.
They make appeals on behalf of prisoners of conscience
who need medical attention. Appeals are sent as well on
behalf of members of the medical profession who are
detained solely because of their beliefs or origins. The
work also includes promoting professional and public
awareness about human rights. Refugees who have fled,
often with their families, from political persecution are
given medical and psychiatric care by doctors and other
specialists working voluntarily with Amnesty Interna
tional. This direct experience enables the medical groups
to contribute to the organization’s policy on medical
questions and professional ethics related to the care of
prisoners.
A LIFE-SAVING OPERATION
At the International Secretariat of Amnesty International
careful research is carried out into the cases of prisoners
needing attention. The secretariat’s medical office
relays requests for urgent appeals to a worldwide net
work of doctors and other health workers. They are
asked to send letters or telegrams in cases where:
• prisoners of conscience are suffering from serious
medical problems.
• medical or paramedical professionals are illegally
detained or threatened with torture.
• provision of health service in places of detention is
absent or inadequate or is abused as punishment.
• amputations or other cruel, inhuman or degrading
treatment is inflicted with the help of doctors.
• doctors are involved in executions.
)6o
INTERNATIONAL CONFERENCE
HEALTH POLICY : ETHICS & HUMAN VALUES NEW DELHI 1986
Artificial Insemination-Surrogate Parenthood
Ethical, Moral, Legal Aspects
Dr. J.V. Bhatt, M.D.
Human mind is conditioned by a large number of factors. What
is legal or illegal, what is ethical or unethical, what is good or bad, what
is moral or immoral, what is sinful or otherwise are all determined by an
individuals upbringing, his immediate social and cultural environment,
his religious background and a host of such other factors. All of us tend
to develop, what in transactional analysis are called “Scripts” resulting
from Parent-Adult-Child interactions, within ourselves, and with the
surroundings. Rapid scientific advances which are both as a result of and
which result in information explosion are producing a positive feedback
effect. We do not know where this accelerating cycle will lead us to.
Any organism, organisation or system needs a strong and sensitive negative
feedback component to maintain it in a state of homeostasis or equili
brium. Even if it is a forward moving accelerating system, it requires
inbuilt mechanisms to check its progress and to absorb the shocks. It is
also essential that all parts of the system move at the same speed, to
maintain the integrity of this system. Most individuals are quick to accept
newer techniques if they lead to monetory gains to them. Even an illite
rate farmer in India readily accepts hybrid seeds, chemical fertilisers,
pesticides, and newer methods of farming if he is convinced that he will
get bigger financial returns. In fact at the back of his mind he has been
looking for such inputs. Such inputs have in fact come up as a result of
such a need. Most of us will also accept, though a little less readily,
newer options in the field of health. In my field of rural health programme
I find that the rural farmer accepts much more readily newer techniques
which look after his animals than those which improve the health of his
children. If the social system is slow in accepting newer health techniques,
the legal system is still slower in accepting the facts if life as it were. If
the legal system is slow, religious system is practically static. What may
be acceptable socially and legally may still be considered intolerable from
a religious point of view.
A.I.D. and surrogate parenting are problems, where medical science
has advanced very rapidly. To-day it is possible for a woman to conceive
without any sexual relationship with a man. The sperm could come
from her husband or from any other man who may be miles away from
her, or may be dead since long. It is now possible to collect the ovum
(egg) from a woman, get it fertilised outside in vitro, get it embedded in
the uterus of some other woman. Time is not far when it will be possible
to produce an entire new individual by cloning from a single cell of any
one of us. A sexual reproduction from a single cell was the earliest form
of reproduction. With cloning the cycle will be complete.
Law in most countries has not yet taken cognizance of all these
developments. An AID child is still illegitimate in many civilised countries
1
of the world. As is found in most instances those who want to do things
legitimately face problems. One of the report states that in 30% of
couples it is found on detailed examination that the father could not be
the genetic father of the child in the family. Women seem to be finding
their own means of attaining pregnancy. It has been rightly said that
the results of AID can also be obtained by adultry. Seeing newspaper
reports about surrogate parenting, physicians are approached by aspiring
couples to help them out of their predicament. In India and also in many
other countries, producing at least one or two children is not only an
instinctual necessity or a socio-economic need but also a status symbol.
A married couple is under great social pressure to conceive soon after
marriage. A sterile woman is not only looked down upon but is con
sidered inauspicious. This makes it obligatory to conceive by hook or
by crook. Any scientific advance in the field of human reproduction is
therefore not only appreciated but also demanded by the community.
Such advances are eagerly looked forward to, and heartily welcomed by
those in need.
Oxford dictionary defines Surrogate as “Substitute” or “deputy”.
The phrase surrogate parent would therefore mean a substitute parent.
Surrogate father would be one who substitutes for the father or deputised
to be the father. 12% of all married couples are faced with the problem
of sterility. While some of them can be helped by simple means, most
of them would have problems, where at least one of the partners is not in
a position to produce the required gamete (sperm or ovum). In such
cases it would be essential to obtain the gamete from a third party, in
case of such a problem with the male partner, the biotechnical part is
restricted to obtaining the gamete from a suitable feriile male and intro
ducing it it into the fertile female. In case of inability of the female
partner to produce the ovum, it is possible to obtain it from another
female, and after fertilisation in vitro with the male partners sperm,
implant it into the uterus of the female partner, after suitable preparation.
In those cases where the female partner is not in a position to embed a
fertilised ovum (either her own or of another female) it is possible to
embed the ovum in the uterus of a suitable female for its growth and
development. All of the above alternatives are not only possible but are
likely to be generally available shortly.
In case both the partners are not producing gametes, inspite of
medical interventions and where other alternatives also do not yield any
results adoption is the only alternative. The parents of the adopted child
would be substitute parents for that child. Adoption has been practiced
since long. It is a well established custom. There are no ethical or moral
issues, except when a child is sold for adoption or is purchased with an
idea of subsequently using it for immoral or commercial purposes or
for labour. Legal procedures for adoption are well established, but like
all. legal matters there will always be some loop holes lacunae. Inter
pretation of legal phraseology may also sometimes lead to some problems,
but by and large the issue can be said to be as settled as any other legal
matter. Other matters like AID, IVE, ET and hire-a-womb are matters
with which law has not been able to keep pace with generally.
There are five or six characters in this drama.
2
1. The doctor. The medical man or the medical team would be well
advised to take the following precautions.
(a) v Take valid written consent of husband, wife and donor, for the
procedures.
(b) Try to keep the identity of the donor a well guarded secret.
(c) Carefully select the donor to closely match the partner he or
she is to substitute with the same blood group and without any
bad genetic traits or transmissible diseases.
(d) If possible get a psychologists opinion about the couple’s
mental stability to accept the off-spring.
2. The father. He should be fully explained the procedure and be
asked to remain present during AID, if possible. It is also possible to
mix the semen of an oligospermic husband with that of the donor in order
to give a chance to his sperm to fertilise the ovum. This combination
procedure is known as AIC and can also be tried in suitable cases, For
birth registration father’s name should be left blank.
3. The mother. In case of AID the mother is very keen to be
pregnant. So also in case of IVF and ET from another woman. There
should be an unwritten pact that this matter will not be brought up during
any domestic quarrels.
4. The child'. In some countries or in some states of some countries
such a child would be considered illegitimate. It is better to legally adopt
the child as early as is legally possible. From medical point of view it is
better if the child is informed, when it grows up, about its origin so that
there is no confusion in medical history about genetic disorders.
5. The donor. He or she should give accurate and correct history
about illnesses suffered and family history. They should not make
attempts to find the outcome of their donation.
6. Uterine mother. In case of uterine mother it is better to find one
who does not do this for money. It is better if she has two or three
children—boys and girls, so she is not tempted to keep the child. Preg
nancy even under best of circumstances can sometimes lead to mortality
or morbidity. She should be explained about this. She . should be ffilly
instructed against consumption of alcohol, smoking and taking drugs
which may be harmful to the foetus. The period for which she wifi be
required to nurse the baby should be explained.
AID is already available as a eugenic measure. There is an attempt
to produce a race of supermen by using sperms of intellectual giants. There
is also demand from unmarried women to get pregnant through AID.
Once it is possible to do IVF the day is not far when it would be possible
AID: Artificial Insemination by Donor semen
IVF: In Vitro Fertilisation
FT : Embryo Transfer
to alter the genes prior to fertilisation by genetic engineering. Once a
desired type of individual is produced he/she can be replicated by cloning.
Though sexual reproduction by normal sexual intercourse is unlikely to
lose its popularity for a long time for obvious reasons, some day in future
it will be possible to totally separate the procreational and recreational
aspects of sex. Whether this will be of benefit to mankind or not time
alone will tell. Science keeps on producing deadliest weapons of destruc
tion and also newer means of production and reproduction. At a micro
level they can be of use but at a macro level their usefulness is ques
tionable. Science, morals, ethic, religion and good sense will have to by
synthesised, if a Frankenstein is not to let loose.
c-w.yj
>7
"■ k.’<-.rV.s Road,
47/1.
• i/OV
Banaalore - ■ •
INTERNATIONAL CONFERENCE
HEALTH POLICY : ETHICS & HUMAN VALUES NEW DELHI 1986
Demands of Few vs Needs of Many
Dr. V. Paramesh vara
President
Indian Medical Association
“The right to health is a fundamental right”
W.H.O.
“A state of complete physical and mental and social well-being”
W.H.O.
“Complete freedom from disease andfrom struggle is almost
incompatible with the process of living”
Rene Dubos
Health is different from pleasure and happiness. As opposed to
health, in happiness there is hierachy. A happy man wants to be happier;
getting one measure of happiness, he desires to get a greater measure of
happiness; getting one kind of happiness, he longs for other kinds of
happiness.
The highest value held out in Indian thought is not happiness or
‘sukha’ because happiness necessarily presupposes its invariable concomit
tant, unhappiness : the two constitute a pair. One cannot be there with
out the other. On the other hand, peace of mind (shanti) is freedon from
all opposites and is therefore, the highest objective. Peace of mind
(shanti) is defined as that, obtaining which, one does not seek to obtain
anything else. It results, when there is no longing and thus no stress.
There are no levels or kinds in peace of mind. A person who is content,
does not.aspire for more of it; if he does, he ceases to be content’. Thus
it eliminates rivalry, strife and stress. It is an attitude of mind that is
cultivated, in order to preserve and promote health and to prevent illhealth. Peace of mind is within easy reach and can be attained by a large
majority of people, irrespective of caste, vocation, knowledge of philoso
phical truths and so on.
Health is possible only for mortal beings, for we are born with the
twin inherited and inescapable‘diseases —ageing and mortality’. To lack
health is a misfortune than misdeed. Health is more beauty than virtue,
more an aesthetic than ethical term. One does not condemn some one
for ‘no longer being healthy’. Then, are our goals for attaining health or
prolongation of life ? If we aim at the latter, we go after the diseases that
are the leading causes of death, rather than the leading causes of illhealth. When we tend to evaluate in terms of mortality statistics, we
invariably mean changing one set of fatal illnesses or conditions for
another. Prevention and treatment of causes of ill-health may enable the
prospective or actual victims to live longer.
Modern system of medicine, which is most widely respected of pro
fessions and which has never been more competent technically is in trouble.
1
Its health is not too well. The reasons are medical care is very costly and
not equitably available. The average doctor sees may more patients than
he should, yet many fewer than would like to be seen. In fact a modern
doctor is overtrained for the job he is doing, yet undertrained for the job
he is expected to do. On the other hand physicians powers and expecta
tions from him have grown enormously, owing to explosion of knowledge
and modes of diagnosis and treatment. His responsibility have grown as
well. All kinds of problems now roll to the doctor’s door from sagging
anatomies to suicide, unwanted childlessness to unwanted pregnancy, marital
maladjustment to learning difficulties, genetic councelling to drug addiction,
from laziness to crimes. It is iromic but not accidental, that the great
technical power of medicine is under confusion about its standards and
goals for guiding its use. When its power was fewer its purpose was
clearer. In fact, medicine was considered the very model of an art in the
past. Today, although fully armed and eager to serve, its targets are no
longer clear. Now health is not the only possible and reasonable goal of
medicine. There are other goals as well Eg. removal of womens breast
because it interferes with her golf swing, performing vasectomy, tubectomy
as family planning for non-medical reasons, artificial insemenisation etc.
Hence happiness is a false goal of medicine.
Without a clearly defined end views, medicine may prove to be only
a set of means, and doctor being reduced to a technician and engineer,
of selling his services on demads. This meands transforming the physicians
into a helper for hire. ‘Endless’ profession is an ‘ended profession’. A
doctor should not be tyrant but neither must he be a servant. Doctor
should remain as a leader and teacher. Public misperception of medicine
is ultimately more dangerous than the doctors misperception of himself.
The community must respect the fact that medicine is an ‘art’ and doctor is
a ‘docere’.
We need to advise better indices of healthiness than mortality and
morbidity statistics. Thus the importance of epidemiological research in
healthiness—about what promotes and what undermines health. Sophis
ticated studies in nutrition, exercise, rest, sleep, relaxation, response to
stress are integral subjects of research. We need to identify and learn
about health sub-groups in the community and to discover what accounts
for their success Eg. change in eating habits, and new treatment for
hypertension has shown a downtrend in death rate from heart attack in
middle age groups. This approach would appear pedestrian in comparision
with the dramatic style of high technology and therapeutics. One has the
highest respect for noble prize winners, for the discovery of chemical
wonder of enzyme structure, but surely he who suggested adding chlorine
to drinking water or invented indoor plumbing system and closed drainage
have contributed more to healthiness of human kind. What is actually
important to note is that major improvements in mortality in Europe
and USA occurred before the massive investment of the last few decades
and before the advance of ‘high technology’ in medicine.
Mortality rates among children, young adults have continued to
improve but not at an enhanced rate and gain in expectation of life at the
age of 65 have been far from dramatic. It spite of enormous scientific
development and availability of drugs and high technology machinery, the
improvement in mortality has been disappointing. Complete eradication
2
of heart disease, cancer and stroke—currently the major mortal disease,
would according to some calculations, extend the average life expectancy
at birth only by approximately six or seven years, and at age 65 by more
than one and a half to two years. Medicine’s contribution to longer life
has nearly reached its natural limits.
There are several countries, where spending on health services is not
below 10 per cent of the gross national product (West Germany,
Netherlands, Sweden, USA). People are now working for a five weeks
year, simply to pay for their health services—less premature death, less
illness and disability, less pain more comfort and support and care when
disability cannot be further ameliorated. There is serious doubt, whether
richer countries of the world have in fact gained any commensurate bene
fits. There is a point at which people want to keep their own money to
spend in their own way. Bulk of the money in health care goes to a
small minority who are seriously ill. There may well be a limit on what
the healthy are prepared to spend on the unhealthy.
CT scanner is the greatest development in radiology and has enor
mous diagnostic potential but between 1973 and 1977, UK installed 30
brain and 11 body scanners. In USA in the same period, over 760
scanners including 200 body scanners were installed—if each of these
machines did 2000 scanners a year, at average charge of US £300, the
annual cost would be $456 millions. Being excessively impressed with
the technological brilliance of big hospital medicine, mobilizing crusades
and crash programmes against cancer and heart disease, the health poli
ticians speak as if more money, more targeted research, better distribution
of services, more doctors and hospitals, and bigger and better cobalt
machines, lasers, and artificial organs should bring the medical millennium
to every citizen.
Planning must not be vague, unless justified on economic grounds,
increased efficiency or training, new and sophisticated equipments, and big
hospitals can become ‘white elephants’, One approach to the problem
of cost containment is to restrict the supply, both of hospital beds and of
medical man power.
One view is that further preventive efforts may be more cost-effective
than further investment in curative media. Equally important is the fact,
that a section of intelligentia both in and out of medicine, have begun to
wonder aloud, whether and to what extent medicines are doing good.
The countries that appear to spend the most on health services do
not necessarily have the best health. Spread of free or nearly free health
services to vast majority of the population does not seem to have narrowed
relative social class difference in mortality risks. The 13 year increase in
life expectancy from 1950 to 1970 for persons over 25 years old, who are
non-smokers, is also most halved for those smoking more than 25 ciga
rettes a day. We are irrationally suspicious of any attempt to modify
our personal behaviour, even if it kills us.
“J man who has built a fire to warm himselfi but couiiiiues to fire it,
utjtil it begins to roast him"
Plato
3
Frankly he seeks ingenious devices to measure his discomfort accu
rately and to cool himself down, dazzled by the roaring success of his life,
he fails to see, that the obvious remedy is to put less wood on it. Modern
medicine is often pictured as a stunning breakthough. Technological
revolution have evidently fostered this image. ‘Technology’ reign as the
primary shaper of medical progress has been strongly challenged? not only
in terms of the financial drain but also in terms "of its outcome on the
nation’s health—its excessive use and the possible risks to patients and
societies. Technological revolution has become a controversial issue.
Now it is ‘Technological Problem’. Therefore developed countries have
a lesson to teach the developing countries from their experience—may be
negative rather than positive ‘Don't do it our way’.
The trend towards high technology evidently leads to a disequilibrium
in type and distribution of services provided, with too much emphasis on
acute institutional care and too little on more essential care, for huge
segments of the population. In countries with more limited resources, it
obstructs the development of priority health services, thus possibly contri
buting to a deterioration in the population health. The developing coun
tries should not be mislead by developed countries. Gross attempts to
transfer successful structures from one country to another, can lead to
reactions out of proportions to the often minor adaptations needed to fit
them to the recepient country’s values.
*
Poverty is the key vector in the developing countries. Poverty creates
illness and illness creates poverty. Health planning is a question of
economic and social planning rather than medical planning. Industrial
development would help a small urban elite. There is relatively high
expenditare on health services in urban areas, concentration of resources,
hospitals and trends towards physicians based security schemes. Usually
training included doctors and specialists, medical education of the curri
culum of more developed countries, heavy expenditure on imported
gadgets and pharmaceuticals, service heirarchially controlled and at the
same time vast majority are denied science based service and spend heavily
on herbal remedies and traditional practitioners.
It is interesting the relatively low priority is given to health compared
to other areas such as ornaments, hotels or air lines in developing coun
tries. Health does not seem to be a priority.
Inadequate investment on the physical and mental well being of the
people can only mean a proportionate decline in the economic develop
ment of the country. Putting greater pressure on its resources.
Pharmaceutical progress eliminated suffering and sadness, has benefitted modern medicine by the saving within the health service itself, saving
from the reduction of loss of working days and savings from the elimina
tion of premature death. For the vast majority of the rural population,
it is now accepted, that basic and generally well established medicines are
what is needed Eg. vaccines and antibiotics.
A case in point is that there are nine million blind persons in India—
3 out of 200 persons and 3 million of them are preventable. 25 lakhs of
children are estimated to go blind every year and 1.25 will need to be
4
□
protected annually with vitamin A—50,000 units costing Rs. 2 per child
with a total cost of Rs. 25 lakhs as against Rs. 25 crores for feeding,
educating and care of the blindand loss in terms of human happiness.
Forty per cent of population are found to suffer some degree of iron defi
ciency anaemia which could be rectified by oral iron therapy, costing hardly
Rs. 2 to 5 per person. Appropriate technology for health and rationing
of services could lead to rational solutions. The need to eliminate waste
and improve cost-effectiveness, and the principle of equal distribution of
service in population.
I
In many areas of social life, policy and action still continued to be
improved on the basis of prevailing beliefs rather than on informed
appraisal of issues and alternatives. In meeting health needs, technology
must be geared both to the problems to be solved and to local conditions.
It should be scientifically sound, acceptable to those who apply it and to
those for whom it is used and affordable to the nation.
Each country and each society has to decide its own health priorities.
Good information is crucial to good decision making. Their use must
justify the effect involved.
I
The stock of skill or human capital must be allocated in such a way
as to reduce the cost of any particular treatment.
-
India has an abundance of men of intellect and aptitude for medical
research, but they should be given all facilities and encouragement. The
declaration of Alma Ata, proclaiming health for all by 2000 AD enjoins
upon research, to gear its efforts to fulfil this goal. The challenges have
to be met by appointing TASK Forces, comprising groups of experts in
respective medical fields, who should formulate specific targets and time
bound projects in the given fields and identify the priority areas with regard
to their national relevance. IMA will also be happy to associate itself with
this task and help the various medical research institutions with a proper
feedback.
*rt:
“May the whole world be healthy and contented”.
References
i
Concept of Health and Disease—Interdisciplinary Perspectives
—Edited by Arthur L. Caplan; H. Tristram Englhardt, Jr.; James
J. Me Cartney Addison—Wesley Publishing Company—1981.
Economics and Health Policy—Edited by A Griffiths and
Z. Bankowski
—W.H.O. Publication—1980.
5
4.-
3
INTERNATIONAL CONFERENCE
HEALTH POLICY : ETHICS & HUMAN VALUES NEW DELHI 1986
Man, Medicine and Law: Challenges
of the 21st Century
P.M. Bakshi
Formerly Member, Law Commission of India
1. Introduction
Bio-medical and technological advances have forced not only a re
definition of some concepts in other disciplines, but also necessitated a
widening of the perspectives of medical science. Science is no longer the
concern of scientists only. It is no longer enough for the man of medicine
to confine himself to the traditional learning of his own discipline.
Whether he likes it or not, he has per force to expand the horizons of
his mind and to take note of the points of view of other disciplines and to
meet the demands of norms flowing from the principles evolved by other
disciplines. Dramatic and frightening progress in knowledge, particularly
in genetics and biology, and radical advances in techniques, especially in
re-constructive surgery and in surgery connected with the process of
reproduction, have raised issues of great consequence to humanity. Some
of these issues are already of pressing interest, such as abortion. A few
others, if not of pressing interest today, are bound to cry for answers
tomorrow. It is only if we start thinking about them today, that the
answers will be ready tomorrow.
It has been said that science often seems to thrust society into
directions which society only partly understands and certainly has not
chosen. This makes the task of social scientists and thinkers on ethical
problems fairly difficut. They must first understand the directions of
science and then offer guidance as to the implications of scientific
advances, and elucidate to the best of their ability the choices open and
the merits and demerits of each such choice. Knowledge must thus come
first, but it has to be followed by wisdom, which a great jurist once des
cribed as the “elder sister of knowledge”.
Both science and ethics have a common origin, as part of the process
of civilisation which distinguished man from apes. In its earliest form,
science was an attempt by man to understand the phenomena of nature
and to exploit the resources of nature for satisfying his instinctive need
for food, shelter and protection. The beginnings of science freed the man
from the drudgery of hunting. Settling down in groups and cultivating
his own food gave man the security and leisure needed for pursuing a
life—style different from that of the ancestors of mankind. This inevit
ably led to the subtler things of life—language, writing, the arts, music,
poetry, religion, ethics and law. In ancient civilisations, scientific thoughts
flourished hand in hand with religion and ethics. Scientific discoveries
were considered revelations. The great writer on the Indian science of
medicine Charaka was an ascetic. Aryabhata (5th century A-D.) who
propounded the revolutionary theory of rotation of the earth stated that
1
his knowledge owed itself to the grace of God. Al Biruni, the famous
Arab mathematician, insisted that his experimental work was subject to
the moral principles of Islam. When, in 1543, Vesulius, a physician from
Belgium, published a book on human anatomy based on dissection and
personal observation, he expressed his wonder at the “handiwork of the
Almighty, by which the blood sweats from the right in the left ventricle
through passages that escape human vision’’. The feeling of antipathy
between science and religion was a later development, of which Copernicus
and Galileo were the victims.
2. Nature of the issues
This paper does not seek to present an exhaustive treatment of the
impact, on humanism, of medical advances or a comprehensive catalogue
of the ethical and legal issues arising from such advances. But it seeks
to point out some peculiar features of those issues that are very relevant
to an understanding of their social significance, so as to facilitate the
formulation of a correct approach.
Usually, such issues are seen as presenting a conflict between medical
science and non-medical disciplines. However, this would be taking only
a partial view of the matter. In a sense, science is neutral, because
it does not take sides. The business of science is to discover the fund of
knowledge, to organise it and to present it. What use to make of the
knowledge, and whether to make use of it at all, is a question on which
the scientist, speaking as a scientist, does not claim superiority and would
not claim the privilege of his speciality. It is in this sense that science
is neutral. When one speaks of a conflict between medicine and other
disciplines, one should not imply that there is an antagonism or antipathy,
as such, between what medicine demands and what society desires or
ought to desire. The truth is, that the conflict really in here is in the conflict
of interests, conflict of demands, conflict of desires and conflict of
approaches between two individual members of society, or between society
and its one or more individual members. For example, if one comes to
questions of life and death and is concerned with the precise issue as to
the determination of the exact moment of death, one finds, on a deep
analysis, that two rival approaches are competing for recognition. It
may be described as a conflict of values. The traditional concept of
sanctity of life and of the peremptory moral obligation of society to main
tain that sanctity at any cost, is one of the competing values. Pitted
against this is the emerging movement for “dignity in death’’ and “the
right to die”. The latter movement has been regarded as an extension of
individualism. It is an extension of the individualistic principles of selfdetermination, autonomy, integrity and self-realisafion and the choice to
exercise control over one’s dying as well as over one’s living.
3. The debate about abortion
The conflict of interest between two individual members of society
is illustrated in the debate about abortion. The conflict here is between
the mother and the yet unborn child. Of course, jt is a conflict of a
complex character, in which so many moral and scientific concepts or
doctrines are entangled, though very few persons are able to perceive that
the fabric is inter-woven with threads of an infinite variety and number
i
2
which criss-cross each other. Simply stated, the moral question Js this:
Whose desire or interest should prevail? Should the mother’s desire
prevail or should the interest of the unborn human being be given prece
dence? In a more complex form, the questions are really multiple.
Should society recognise any right at all in the unborn? To put it in legal
phraseology, should the zygote, the embryo or the foetus be regarded as
a “human person” and, if so, from what point of time? When does the
right of the embryo to protection begin? At implantation? At the end
of the first trimester? At quickening? At viability? At the moment of
birth? Assuming that the right of the foetus begins at one or other of
the moments just now referred to, under what circumstances can the right
of the unborn be overridden by the desire of the living and, at what point
during gestation? If both the foetus and the pregnant woman have rights,
the one to its survival and other to terminate her pregnancy, who is
competent to adjudicate the conflicting claims, and what are the quali
fications for such a role?
4. The right to live
The situation of abortion, mentioned above, involves a consideration
of the two-fold obligation ofthe State towards the unborn life. (1) The
obligation to refrain from all interference with unborn life, and (2) the
obligation to prohibit an attack upon unborn life stemming from a private
person. Obviously, any law which permits abortion upto a certain stage
of pregnancy places unborn life at the disposal of society, though this
decision is taken in the name of higher and more paramount demands.
The conflict is seen in a more dramatic form when one comes to the right
to life and the right to die. The right to live is at issue in the unending
debate about the ethical aspects of prolongation of life by artificial means.
In a deeply unconscious individual whose vital functions are maintained
over a prolonged period only by extraordinary means, the question arises
whether a time comes when it is no longer appropriate to continue the
extra-ordinary means of support for the hopelessly unconscious patient.
If man is regarded as being in the image of God (imago dei) then, theoreti
cally, the
to prolong life has no closing terminus. So long as the
vital functions persist spontaneously or with the aid of artificial process,
“life” survives and must be prolonged to preserve the ‘image”. This is
one aspect of the matter. Apart from this religious aspect, there often
comes to be presented a conflict of interests, though the conflict is not
articulated. The family of the patient very often wants to terminate the
agonising watch and may urge a discontinuance of extra-ordinary measures
for prolonging life. Those who have an interest in organ ^transplantation
might press for a new appraisal of what constitutes “death”. The hospital
authorities and society in general have a vested interest in terminating a
costly procedure in a hopeless case. But the presence of these vested
interests raises the possibility of selfish “rationalisation” of the course
which the vested interests wish to adopt. It gives a warning of the need
for a cautious approach. One may also remember that the termination
of extra-ordinary care, even for just reasons, with death certain to ensue,
can have a shocking effect on observers.
Some of the problems discussed here arise even out of the existing
canons of medical ethics. The current code of ethics of the Indian Medical
Council, in paragraph 3, provides1—
3
I'
“I will maintain the utmost respect for human life from the time of
conception.”
In paragraph 7 it provides—
. I will respect the secrets that are confided in me.”
5. Artificial insemination
Some of the techniques evolved by medical science give rise to legal
as well as emotional problems. For example, there are emotional
problems born of artificial insemination, which is now frequently used to
help infertile fathers. Some fathers later resent children born as a result
of A.I.D. Mothers have abo been known to develop a romantic in
fatuation for the unknown biological father. The practice is to keep the
donor’s name secret from the parents. But legal problems may arise if
the parents demand, say, a tall or vegetarian donor. There is also the
question of legitimacy of the child born of A.I.D.
6. Genetic techniques, and IVF
Placed in the social context, any one genetic technique can be
assessed from a number of different angles. The several frames of reference
which apply, say, to a decision on abortion, include exploring it from the
point of view of (i) the parents, who may or may not have a deformed
child, or (ii) society, which may or may not wish to spend money on the
care of children, or (iii) the child yet unborn, whose right to protection
may require to be considered.
In vitro fertilisation is not simply a device to be marvelled at, as an
instance of science fiction turning into science reality. It raises in our
mind serious questions of ethical and social policy; for, genetic technology
has the potential to take human heredity out of the realm of blind faith
or chance into the realm of free will and choice. In the past, nature took
the blame or the credit for genetic inheritance. This responsibility is
increasingly becoming ours, because of expansion of the area of choice.
7. Coercive genetic and surrogate motherhood
This does not mean that “coercive genetics” (the prescribing of
legal sanctions against the use of genetic techniques) should be readily
resorted to, either to force the weeding out of undesirable genes or to
prohibit the use of new techniques. Excessive intervention by the State
would completely undermine the legitimacy and moral basis of Govern
ment. It is in this context that the most difficult issue is presented by
surrogate motherhood. However morally shocking the practice may be,
a legal prohibition may well remain unenforceable. What matters in
such cases is the social feeling. As has been often pointed out, most new
genetic techniques, once developed, would bring much joy to parents and
cause little discernible harm to society. The State may, therefore, be well
advised to guard itself against the urge to legislate in this field. Improve
ments in genetic technology may well excite the appetite of the State to
interfere by legislation, but the tendencv will .have to be curbed.
4
I
fl
I
8. Inchoate rights: the question of privay
»•
The situations so far discussed concern themselves with legal or
moral rights whose existence is undisputed. Besides these, however,
sometimes there are involved rights which themselves suffer from obscurity,
because of the prevailing uncertainty about their existence and recogni
tion. Here the shadow on a correct appreciation of the ethical issues is
not cast by any scientific advances as such, but arises from the hazy nature
of the very rights themselves, whose existence and precise dimensions have
not yet been demarcated in traditional legal and ethical thinking. Privacy
is an example of such a right.
9. Privacy and informed consent
Of late, the doctrine of informed consent to medical treatment has
come into prominence. This doctrine initially came to be premised on
the patient’s right of self-determination. This is instanced by the famous
words of Judge Cardozo [Schloendorff v. Society of New York Hospital
(1914) 105 N. E. 26]. The patient’s right to information before consenting
to treatment may also receive support from the principle of the right to
privacy—being the principle of an “inviolate personality” which posits
the individual’s independence, dignity and integrity. It may be mentioned
that of the several facets of this right as explained by Mr. Justice Douglas
[/?£><? v. Wade, (1973) 93 Supreme Court 705], the third deals with the
freedom to care for one’s person and health.
10. Bio-ethics
All this naturally brings one to the new discipline of bio-ethics.
Broadly, is a discipline dealing with the ethical implications of biological
phenomena as manipulated or encountered by the science of medicine.
It dwells on the frontiers of medicine and ethics, Because it dwells on
the frontiers, it has its own excitement. Sir Ernest Gowers once said that
the crossing of intellectual frontiers is always a thrilling experience, just
as it is a thrilling experience to cross the physical frontiers of one’s own
country.
Bio-ethics is not a totally new subject. In some form or other, the
medical profession has always had something to do with ethical issues.
The celebrated works of Charaka (probably 100 A.D.) on the Indian
system of medicine contain an elaborate code of ethics for physicians.
Amongst the mandates that Code contains, is a direction to the physician
to strive for the relief of the patient with heart and soul. It also directs
the physician not to treat a female patient, unless a male relative is present.
Four goals may be concretely indicated in regard to the discipline
of bio-ethics: (1) identifying the moral issues in a bio-medical context;
(2) developing appropriate strategies for analysing moral problems;
(3) relating moral principles to specific issues; and (4) training a small
group in bio-ethics.
The first two goals imply that the physician is not a primary
decision-maker, but rather one who assists the patient in coming to his
own decision where a moral -sue is involved. The physician must learn
5
how to distinguish technical questions of medicine (which are appropriately
his own area of competence) from value dimensions (which are not ex
clusively his own area of competence).
A regards the third goal of bio-ethics (relating moral principles to
specific cases), this will be for the patient, he being primarily the decision
maker. But some ethical issues can still remain for the physician—e.g.
how much information is to be transmitted to the patient about a parti
cular diagnosis.
■
11. Conclusion
To conclude, let me quote from Dr. A.S. Duncan’s foreward to
Alastair Campbeil’s Moral Dilemmas in Medicine'. “Curricula have become
so loaded with the very scientific and technical matters which lead to the
dilemmas that little time is left for thought as to the dilemmas, themselves.
As Harold Laski wrote, “expertise sacrifies the insight of common sense
to intensity of experience.” Where human problems are concerned, the
expert fails to see that every judgment, which he makes, not factual in
nature, brings with it a scheme of values which has no special validity
about it.
Reference
1. See George Lobo Current Problems on Medical Ethics (Paul
Publishers, Allahabad 1974) Pages 215-228.
/gs
4/ / ‘
Bana.a'ore -
6
r
j
f
I
VM|
"7-^' -2- 'jp
INTERNATIONAL CONFERENCE
HEALTH POLICY : ETHICS & HUMAN VALUES NEW DELHI 1986
Teaching of Human and Moral Values in
Postgraduate Medical Education
S. Vaidyanathan, M.S, Meh, MAMS (Urology), Ph.D.
G.C. Malakondiah, M.S.
T.P. Mahapatra, M.S. M.ch
S.P. Tandon, M.S.
Department of Urology, Postgraduate Institute of
Medical Education and Research,
Chandigarh 160012
A postgraduate medical student after completing his training is likely
to work as a clinician, a medical teacher, a medical administrator and/or
a medical researcher. During his professional career, he is likely to face
many situations where he will have to take decisions not only on scientific
basis but also on human and moral principles. His acts should reflect
upon his character as a man of virtue and not as an a moral being. Inten
tionally or unintentionally he may speak ill of a professional colleague, be
unkind to an anxious patient suffering from advanced cancer, recommend
purchases from a particular firm which gives his gifts, select a student
belonging to his region, award low marks to a student whom he does not
like or steal ideas for research from a junior colleague. Although the
present system of medical education imparts good theoretical and practical
knowledge on scientific medicine, there is no formal and very little informal
education on human and moral values during post-graduate medical
training. Emphasis is being placed on learning operative acumen e.g.
how to do prostatectomy but little importance is given to humanistic
treatment of a poor old patient or the moral aspects involved in decision
making of various real-life situations such as patient management, medical
education (student selection, examination, etc.) medical administration and
medical research.
The moral components are :
(i) Attitude : It is not simply an ability or a piece of knowledge.
It is “regarding other people as equals”, “thinking that other
people’s interest count”, “taking notice of other people’s wants
and needs”. Attitudes are detected and verified by the way in
which a person thinks in his everyday, practical living, and to
some extent by the way in which he acts. On the cognitive
side, it is a belief—the belief that other people have equal rights
with onself. This can be tested by certain question or observa
tions :
(a) Does he make some effort to find out what other people’s
wants and feelings actually are?
(b) Does he listen to other’s opinions and allow them to have
their say ?
(c) How does he actually treat people belonging to a different
ethnic origin/different region/different religion ?
1
(ii) Ability to know what other people are feeling, in particular
situations. This may be described further as “awareness of
other people’s feelings”, or “the ability to understand what
other people’s interest are”, “knowledge of other’s desires,
emotions, etc.”. This is concerned with awareness of the
feelings of people with whom one actually comes into contact in
one’s everyday life! it also includes being able to predict the
feelings of those whom he has never met. This can be tested
as follows :
(a) Can the student give a reasonally good account of the
feelings of the patient who is to undergo extirpative surgery
e.g. total amputation of penis for penile carcinoma?
(b) Can he understand the feelings of the patient’s wife and
children when a diagnosis of advanced cancer of urinary
bladder is made?
Is
he interested in other people’s feelings and behaviour?
(c)
Has he as a teacher, made any attempt to understand the
feelings of his students? Has he as an administrator made
any attempt to understand the feelings of his subordinates?
(iii) Actual knowledge of certain ‘hard’ facts—Knowledge of rules
of the social system in general, knowledge of social conventions
and social expectations.
(iv) Know-how to translate his moral decision into effective action.
It is a kind of adeptness rather than a cognitive mastery of facts.
This can be tested by :
(a) Is he capable of playing the roles of a leader and a follower,
of issuing and obeying instructions?
(b) Can he behave efficiently in social situations involving people
of various age groups, and different ethnic origins?
(c) Can he behave well in formal contexts as well as in less
formal contexts?
(v) Mode of thought: Ability to face up to a moral situation and to
consider that situation primarily in terms of other people’s
interests. A person with appropriate attitude, ability to
discern other people’s feelings, and knowledge of ‘hard’ facts
will make a prescriptive moral decision dictated by other people’s
interests. Dimensions of this complex moral component are
(a) right reasons. Not everybody makes, or even thinks he
ought to make, his moral decision on the basis of other people’s
interests. Other modes of thought are regrettably common.
Amongst these are: desire to please the boss, uncritical tendency
to obey rules, a tendency to do what is most expedient for
oneself, etc. The person with a high degree of this moral com
ponent will always consider other people’s interests, and think
in this mode rather than in others, (b) Sincerity of decision.
There are people who may pay lip-service to a certain mode of
moral thinking but who do not sincerely commit themselves in
2
making these judgements.
questions :
This can be tested by the following
(a) Does he think that moral values are ‘just a matter of taste’
or does he believe that there are right and wrong answers
to moral questions?
(b) Do his principles include not only avoiding bad actions,
but doing good ones (actively and positively helping other).
(vi) Action or Behaviour: When a person has reached a rational
moral decision, he must have the motivation and resolution to
translate that decision into action. There are all sorts of reasons
why people fail to bring their abilities to bear on moral situa
tions, or fail to translate their moral decisions into action.
They may be forgetful, incompetent, lazy, frightened, tired
cowardly, etc. A person should have sufficient sentiment or
love for other people: this is atleast one kind of motivation
which should enable him both to think and act rationally in the
moral sphere. A person should also have good habits, or a
settled disposition to think and act in a rational manner. A
person must possess independence of judgement, the ability to
think and act autonomously as opposed simply to following
other people like sheep. A person must be reflective or thought
ful enough not to be carried away by particular situations, and
not to be forgetful of other people.
Teaching of moral and human values
The spirit of the medical college and its teachers thus becomes the
basic factor in developing moral values. There can be little contribution
to moral and spiritual values from a college which resorts too easily to
arbitrary authority; from an institution in which the chief mainspring of
effort is rivalry; from an institution which fails to exhibit complete honesty;
from a college in which each seeks only to satisfy his own selfish aims;
from a college laden with intolerance, fear and suspicion. Only a medical
college served by a faculty whose members are themselves sensitive and
responsive to moral values; a college with a broad, humane, and flexible
curriculum; a college steeped in a philosophy which commands respect
for the personality of each teacher can hope for success. Medical colleges
that exemplify moral values are better than lesson which preach them.
Human and moral values can be taught while discussing each
patient’s clinical problem. The teacher should be a ‘role-model’ in
exhibiting human values while treating a patient. He should observe the
students in the out-patient clinics, in the wards, and in the operation
theatre, record resident-patient encounter and discuss it with the concerned
resident later emphasising the need to adopt and practise humanistic
approach and moral values.
For example, the urology resident is often
taught how to do urethral dilatation i.e. he should fellow aseptic principles,
there should be no urethral bleeding, etc. Seldom is it emphasised that he
should alleviate the anxiety of the patient before performing dilation,
make an attempt to understand the feelings of the patient’s family as
regards patient’s illness, check whether adequate urethral mucosal anes
thesia has been produced before actually performing dilation. Not
3
infrequently it may be witnesses that the doctor scolds the patient when he
complains of pain. Thus the human values should be integrated with the
teaching and practice of clinical medicine. Often it may be observed that
the teacher as well as the post-graduate student is kind to a VIP patient but
forgets such human values while attending to a poor and illiterate patient.
The moral components mentioned above can be taught in the medical
college during case discussion, structured lectures, informal coffee-club
discussions, departmental seminars, interdisciplinary seminars and intensive
workshops. At a national level, bibliography development, national
workshops and national conferences on teaching of human and moral
values can be organised.
Evaluation
Assessment of teaching of moral values, student’s learning and
student’s behaviour in this regard should be periodically evaluated.
Preferably, considerable weightage should be given to the above listed moral
components in internal assessment of non-scholastic abilities. Self—
assessment by the post-graduate students is the best method of evaluation
to infuse motivation and self-analysis. He may be encouraged to record
atleast one patient management every fortnight describing how he adopted
human and moral principles. The teachers should act as facilitators of
learning and directors of individually-prescribed instructional programmes.
They should give immediate, positive feed-back to the student appreciating
his good performance and encouraging him to make up his shortcoming if
any. Peer assessment, and evaluation of recorded audiotapes of resident
patient encounter may also be useful. In the beginning, all groups may
express some antagonism or unwillingness to admit to living by moral
values. However, the teachers as role models, will be able to secure
student’s full participation in such programs. When the students are enco
uraged to think harder about these abstract ideas and given a little help
with the terminology, they would quickly become adapt at analysing the
moral issues involved in patient care, and in his professional career.
In conclusion, moral education involves both comprehension and
apprehension, neither can be imposed. It is wholly open-ended, recognis
ing that genuine morality requires free personal acceptance of values of
that is, the goal is not the heteronomy of the slave, but the autonomy of
the free man.
References
1. Bull, N.J. Moral Education London, Routeledge and Kegan Paul,
1973*
2. Educational policies Commission. Moral and spiritual values in
the public schools. National Educational Associations, Washington,
1951.
3. Jewell, M.D. Teaching Medical Ethics. Br Med. J. 289: 364-365,
1984.
4. Veatch, R.M. and Gaylin, W. Teaching Medical Ethics: An
Experimental Program. J. Med. Educ. 47: 779-785, 1972.
5. Wilson, J. Moral Education and the curriculum Pergamon Press
London, 1969.
4
COM.»iJfSITY HI A . '
47/1, (Fiist f-lcor^ S fv.. ks head,
Bangalore - 660 U01.
Hp-
INTERNATIONAL CONFERENCE
HEALTH POLICY : ETHICS & HUMAN VALUES NEW DELHI 1986
Human Values and Quality of Life
—A Personal Statement
Prem Kirpal
In 1969 while serving as a Senior Specialist at the East-West Centre
at Honululu in the beautiful Island of Hawaii, and also unknown to myself
at the time afflicted with malignant cancer inside my body to be operated
shortly, I wandered at the blueness and vastness of the Pacific Ocean and
the lovely beach of our tiny Earth. From this wander of the beauty of
Nature and some surge of creation inside, I wrote the following poetic
statement on the “Quality of Life’’:
I—QUALITY OF LIFE
Life’s quality is comprised of: palatable food to digest well and
enjoy; enough space and scope to contain and express the needs of body
and soul in the full awareness and respect of other bodies and souls; robust
health with abiding element of youthfulness; and, above all, the sheer
love of life-the gift of friendship and love, the sense of wonder and endless
curiosity, the perpetual thirst for giving and receiving, ceaseless strivings
for new creations, and the capacity to accept any outcome in full under
standing and with utmost serenity, cheerfulness and gratitude.
Life is as good as one can live it and it is as big as one can hope,
imagine, aspire and dare !
Its quality depends a little on luck and chance, but much on what
we value and search and how we go about it with courage, dedication and
faith.
In this way one can never fail, because even failure becomes almost
success when it is preceded by the right quest and effort.
To shoot at the stars and fail is better than a timid and faint-hearted
venture which may satisfy or reward, but cannot thrill and exalt.
The spice of life and its meaning and scope determine its quality in
the depth, breadth and extension of consciousness, from the earthly and
the human to the spiritual, even the cosmic, dimension of man’s percep
tion, experience and vision. There is no limit to life’s quest and quality,
and often we become what we love. Being and becoming are great gifts of
consciousness and these should be treasured and developed in all ways,
dimensions and potentials of man’s psyche and his cosmos. Remember
always that in Life and its Beyond we are related and joined together to
all Creations and the experience of this Great Harmony is the wonder and
savour of Existence. Give full heed to the vastness of life’s scope and its
endless potentials and be grateful for the wonderful gift of life.
1
A-
This Statement has been inscribed permanently on the inner wall of
a Public School not far from the river Ganga and the massive machines of
the Bharat Heavy Electric. Hopefully its young readers derive more prac
tical meaning from it than what I have been able to practise. Since 1969
I have written and spoken a great deal on the Quality of Life and Human
Values in the context of education and culture at home and abroad at
several international meetings under the auspices of the United Nations,
but the above Statement of life’s quality abides in both the spirit and con
crete attributes of life’s quality, which is basically reflected in the health of
mind, body and spirit and the inner life of the human psyche.
It is, of course, essential to achieve physical survival and a certain
measure of material well-being before the quality of life is experienced and
treasured in the world of the mind and the spirit. For physical existence
we need food, health, housing, education, work, worship, sex and play.
For man as a spiritual entity we must transcend along the path of
security, freedom, identity, sense of belonging, joy, confidence, love and
creativity. For both being and becoming we must now, in the emerging
planetary order of Mankind, explore, identify and practise human values
upon which will depend the attainment of the quality of life for all, and
not only the privileged few.
From our past of many civilizations, diverse cultures, different reli
gions and conflicting ideologies we are moving towards the unity of
mankind. The formulation of a general statement on human values for
our time could help the shaping of appropriate attitudes, common be
liefs and suitable criteria and content of education for contemporary man.
Such a statement can be based on the following important concerns and
aspects of man, common to all civilizations and culture :
H—HUMAN VALUES
1. Man and his Own Self
In order to take charge of one’s life in an uncertain and fast-chang
ing world, the essentials of personality such as physical and mental health,
right balance and poise of mind, and moral and spiritual qualities of
character should be valued and cultivated. Education and Culture need
to be directed to the enrichment of character and the pursuit of goodness,
wisdom and transcendence. The development of the inner man by the
fullest flowering of man’s potentials and totality of being should be encou
raged in an atmosphere of freedom and security. Man’s care of his own
self calls for measure for measure of austerity, self-discipline, pursuit of
self-knowledge and cultivation of serenity as well as intensity. The luminuous and balanced self ceases to be vulnerable. The power of the inner
self should be directed to love and service of fellow-beings.
2. Man and his Fellow-man
Man’s relationship to Society should be governed by principles of
humanistic morality acceptable to all and reflecting the quality and sensiti
vity of human relations, based upon compassionate love, mutual under
standing and appreciation, and respect for justice and solidarity of
2
mankind.. The invocation to loving one’s neighbour should extend to all
inhabitants of the planet. Such a relationship between man and his fellow
man has to overcome the divisions and barriers of the past and the present
attitudes of superiority and smugness arising from inequalities of wealth,
power and knowledge. Man’s common predicament and basic humanity
should be planted firmly in his consciousness and conduct by the fullest
and wisest use of the resources and potentialities of communications. The
exploration and understanding of man’s psyche should strengthen common
humanity.
3. Man and his habitat
Contemporary man’s habitat extends from his home and local
environment to the entire planet, involving the care and nurture of nature
and ecology from which he derives great benefits. The resources of the
habitat must also be preserved for posterity for which he holds his habitat
in trust. The sense of belonging and gratitude generate loyalty, prudence
and austerity, and in the care and management of the habitat man learns
to live in harmony with others. Narrower loyalities and nationalistic pride
and egocentricity lead to conflict and war. These should give way to
global loyalities.
4. Man and his work
To a large extent man lives in and for his work, and his mental health
and happiness depend upon the choice of work, its scope for action, ex
pression and initiative, its contribution to his creativity, decision-making,
pursuit of excellence and sense of self-esteem and dedication. While work
affords satisfaction, enjoyment and self-realization, it can also bring obses
sion for success and lust of power. We should avoid such temptation and
work in a spirit of non-attachment and non-violence. Frustrations and
alienations resulting from deprivations of work or its satisfactions warp the
individual and distort society. Socio-economic systems and education
should rectify these.
5. Man and Art
All men are endowed with artistic capabilities in varying forms and
measure, and the flowering of these depends upon individual urge and
social receptivity. The manifestations of beauty differ, but its essence and
inspiration are the same. The pursuit of the beautiful strengthens man in
his humanity and elevates his cultural life. In work, education and life we
should recognise and enhance the importance of the arts and the artistic
spirit. Respecting the diversity of art and culture, we can sense and share
in the underlying unity of mankind. The quest of beauty and the joy of
creation reveal life’s meaning and enrich its quality. The artistic nature of
man should be fed and nurtured all through the life span. People should
have the opportunity of appreciating other people’s arts and cultures.
6. Man and his Technology
Technological advance should be for human welfare and for the
enrichment of man’s humanity. Uncontrolled mechanisation for sheer
power and de-humanisation needs to be checked. By controlling and
3
I
regulating technological advance and application of science we can improve
human welfare and quality of life. Appropriate technologies should be
chosen for practical relevance and efficient productivity, and also for their
capacity to humanise life and spread culture. Technology should not be
allowed to undermine or pervert the primacy of the human spirit which is
the source of man's creations and the abiding values to live by. Technology
must always be subservient to the ends of good life and humanism. As a
significant reflection of man’s relentless curiosity, inventiveness, perfection
of methods and systems and mastery over the external world, technology
projects important human values.
7. Man and his Ideology
Man cannot live by bread alone. Beyond the materials of economy,
politics, science and industry, his restless mind and probing spirit need
some beliefs to give meaning to life and its goals and purpose. Historical
experience and human choice determine ideologies which are incentives to
action in the present and guides to the making of the future. Ideology
caters to emotional and mystical elements of man’s consciousness as well
as the quest of truth, faith and humanism. Ideologies are reflected in the
diversities of cultures and choice of life-styles and systems. They can cause
tensions and conflicts and lead to war and destruction. Ideology should
be valued for its ennobling influence, its strength and integrity, its dedica
tion to peace and harmony and its commitment to man’s humanity.
8. Man and Time : The Stream of past, present and future
In his relationship with time man shares some compulsions and
dreams not only with the fellow-man of his own time in life, but also with
those who have gone before in history and those who have yet to come.
The consciousness in time and the experience of the life-cycles contemplate
the mysteries of life and death and the concept of eternity. Respect for
the past with hope for the future strengthens man’s care of his cultural
heritage and pride in common endeavours and aspirations. Man’s sense of
history is a most precious source and guide to humanistic values, the
understanding of human nature, deep humility and compassion; in the
depressions and elections of the flux of history man recognises his eternal
self and experiences the brotherhood of mankind.
9. Man and his Cosmos
Man has always pondered about the mystery of existence, the universe
that lies beyond, and the larger scheme of life of which he is only a part.
Imagination, intuition, mysticiam, and religion have all contributed to the
quest of the Cosmos, the ultimate or the larger universe which may be
glimpsed through worship, meditation, knowledge and poetry. Contempo
rary man has greater knowledge of the extent and nature of the universe
than the past generations, and this knowledge brings us close to the life
and unity of our own planet. We can all share in our common predica
ment of the planetary habitat, so small and insignificant in the vastness of
space and time. The Cosmic dimension of life brings us closer to each
other and gives a proper perspective to temporal existence.
4
COM jJ^lTYMEALTHCZLL
47/1, (First Floor) St. Marks Read,
Bangalore - 560 COL
INTERNATIONAL CONFERENCE
HEALTH POLICY : ETHICS & HUMAN VALUES NEW DELHI 1986
Ethical and Legal Aspects of Family
Planning
Mr. Justice H.R. Khanna
Family Planning Foundation
198-Golf Links, New Delhi.
I deem it a great privilege to have been asked to address this session
of International Conference on Health Policy—Ethics and Human Values.
The topic for this session is family planning—a National Priority. I would
be speaking to you on the ethical and legal aspects.
It was 36 years ago that India became a republic and The Constitu
tion of India came into force to secure, inter alia, to all its citizens social
justice and dignity of individual. Part IV of the Constitution contains
directive principles of state policy, which as mentioned in Art. 37 were
fundamental in the governance of the country and were to be applicable,
as duty of the state, in making laws, clause (f) of Art. 39 Contained in that
part provided that. The state shall direct its policy towards securing that
children are given opportunities and facilities to develop in a healthy
manner and in conditions of freedom and dignity. According to Art. 47
the state shall regard raising of the level of nutrition and standard of
living of its people and the improvement of public health as amongst its
primary duties. These were great objectives, earnesty conceived and nobly
worded, but even though a period of more than three and half decades
has passed since then, the goals visualised by the founding fathers in
these articles have remained elusive and more or less a tantalising illusion.
Not that efforts have not been made towards attainment of those objec
tives. We have had a series of five year plans conceived primarily to
bring about economic regeneration. We have had earnest, well-meaning
persons who have striven in their own way and as best as they could to
banish poverty and raise the living standards. We have made considerable
headway in industry and technology as also in agricultural, dairy and
poultry production. We have built dams and initiated river valley projects.
We have spread network of roads and provided for Quick means of
transport. We have also established a large number of educational
institutions. But despite all these efforts, we still continue to be steeped
in poverty and backwardness and our average standard of living is one of
the lowest in the entire world with one of the lowest per capita income.
If one were asked as to which has been the chief culprit and the main
cause for frustrating and setting at naught all these efforts to raise the
economic level of the people, the finger must pin-point in the direction of
population explosion. The increase in population during the last four
decades has upset all plans and frustrated all efforts to bring about better
ment and amelioration in the living standards of the people. India’s
total population touched figure of 685 millions in the census of 1981.
This represents an increase of 25% since 1971 when the population was
548 millions. It would be pertinent in this context to mention that India's
population which was 238 millions in 1901 increased to 361 millions in
1
1951 and to 685 millions in 1981. Thus in the first half of the present
century, i.e. during the years 1901—1951 India’s population increased by
about 51.5% whereas in the next 30 years from 1951 to 1981 it increased
by 89.8%. The main cause of this increase can be attributed to fall in the
death rate due to better health conditions and more efficient handling of
epidemics. A sample survey revealed that the birth-rate in 1980 was 33.3%
and the death rate was 12.4. The expectation is that the death rate would
decline still further and be brought down to 10 per thousand by 1990.
The increase in world population during the year 1985 was 85 millions
bringing it to a total of 4.9 billions. The population growth rate declined
from 2% in 1970 to 1.7 % in 1985. Even at this rate world population
is expected to be 5 billions by middle of 1987 and 6 billions by the end of
the century.
Unless therefore we can devise some measures to control the popu
lation growth, we can take it that all our plans for raising the living
standards would go away and run into rough weather and the problem of
poverty, backwardness and low living standards would haunt us and dog
our steps for years to come. As it is the average increase per year of the
population of India is more than the total population of Australia. It is
in this context that the question of birth control has assumed tremendous
importance,
So far as the ethical aspect is concerned I would say that it is in
herently immoral to give birth to children if we cannot secure for them
proper food, clothing and shelter and provide them with requisite
education to grow into healthy, self-reliant adult-hood with prospects of
decent standard of living. At the same time it would be unrealistic and
plainly discriminatory to deny to the poor sections of the community the
incident and satisfaction of a normal marital life. Begetting of children
and the continuance of the family line is as such an important objective
and desideratum of married life amongst the poor as amongst the affluent
sections of the community. The difficulty, however, arises because the
growth rate of family members amongst the poorer sections was and
continues to be at a level higher than that of affluent sections who as a
result of education have realised the desirability of restricting the number
of children. It is in this context that some action is called for and some
measures need to be adopted to bring about a state of small families in
regard to poorer section of the community.
At the same time we have to bear in mind that in view of the
consequences of resort to compulsory methods during the period of
emergency the government would be reluctant to enforce compulsive
measures. Faced with this situation all that we can do is to build a strong
public opinion and create a General awareness of the need for and desir
ability of a small family. It has to be impressed upon every one that
small family is a desideratum not merely because of any altruistic con
sideration or as a part of obligation to the society but much more than
that as a matter of sheet enlightened self-interest of the individual con
cerned and for the benefit and welfare of his own children. Human
nature being what it is, experience tells us that enlightened self interest is
a much more potent motivating factor for an average person.
2
Coming to the legal aspect I may say that law does not prevent or
impose a ban upon the procreation of children beyond a particular limit.
Law, as was once said by trudeau, has no function in the bed-room of the
married couple. Indeed attempt by law to impose restrictions upon the
number of children might well be construed as an intrusion into the privacy
of individuals’ married life. At the same time law can provide incentives
to couples to restrict the number of children. Such a law has been enacted
in number of countries and it is a perfectly valid piece of legislation.
India adopted family planning as official programme in 1958 as it
recognised that a timely check on population growth would in turn raise
the living standards of the people. During the period of the first two
plans from 1951 to 1961 the emphasis was mainly on research in the
field of motivation, communication, demography, physiology of reproduc
tion and extension of organisations for providing clinical services. Since
then various ideas have been set afloat. The objective of family welfare
in 1978 was to reduce the birth rate to 30 per thousand of population by
the end of 1982-83 from the existing 33 per thousand population. At
present the demographic goal is that the average woman should be replaced
by one daughter and two child family as the normative pattern and to
attain this objective by 1996.
Although section 312 which makes it an offence and provides for
punishment for causing miscarriage, unless it be for the purpose of saving
the life of a woman, still continues to be a part of our panel code, the
parliament enacted in 1971 the medical termination of pregnancy Act.
According to this act notwithstanding anything contained in the Indian
penal code, A Registered Medical Practitioner shall not be guilty of any
offence if any pregnancy of length not exceeding 12 weeks in terminated
by him or where the length or pregnancy exceeds 12 weeks but does not
exceed 20 weeks if two registered medical practitioners are of opinion
formed in good faith that the continuance of the pregnancy would involve
risk to the life of the pregnant woman or of grave injury to her physical
or mental health. Likewise the law relating to abortion has been libera
lised in other countries. In England notable part in this direction was
played by Mrs. Margaret Sanger, while in the United States three Con
necticut women, one of whom was Mrs. Katharine Houghton Hepburn,
mother of the famous Actress Katharine Hepburn, made significant
contribution in starting birth control leagues. Some of the most inte
resting cases relating to birth control and abortion were decided by us
Supreme Court. One of such cases, was Poe vs Ullman decided in 1961.
In this case law relating to ban on clinics for birth control was challenged.
The Supreme Court, however, turned down the request. Justice frank
furter who wrote the majority opinion said that the issue related to a
dead letter and the court could not be umpire to debates concerning
harmless empty shadows. According to him the fear of enforcement of
that law was chimerical or imaginary because provisions of the law had
gone unenforced. Justice Douglas who wrote the minority Judgement in a
Scathing Criticism of the Majority view observed:
“What are these people—Doctor and Patients— to do? Flout the
law and go to prison? Violate the law surreptitiously and hope they
will not get caught? ... It is not a choice they need have under. . .
our constitutional system.”
3
I
Soon thereafter clinics started openly working in Connecticut. A
complaint was then filed and the Supreme Court was forced to decide this
issue in 1965 in the case of griswold. This time Justice Douglas was on
the side of the majority. The majority held that the impugned law
trespassed into the zone of marital privacy, a realm of family life which
the state cannot enter without substantial justification. The law was
accordingly struck down. In a subsequent judgement in 1972 the Supreme
Court extended the above principle to the case of single individuals.
Ultimately in a decision given in 1973 in Poe’s case the Supreme Court
held that the right of abortion was not absolute and added a restriction.
All abortions, the Court held, were not legal. A formula was evolved,
according to which in the first three months of pregnancy the right of
privacy prevails and the abortion decision was upto the woman and her
doctor. During the second period of three months the state could regulate
abortion in a way related to maternal health. In other words the state
could require that operation be performed under certain conditions. During
the last stage of pregnancy the court held the state laws could prohibit
abortion except under circumstances in which the life or health of the
mother was in danger.
One might discern a note of similarity between the view taken by the
the U.S. Supreme Court and that which had been taken earlier in the law
passed by The Indian Parliament in 1971.
Friends, I have been talking to you about the ethical and legal aspects
of family planning, restricting the number of children and about the
permissible limits of resorting to abortion. It would, however, be wrong
to think that the matter has only ethical and legal aspects. More than
anything else it is human problems and relates to some of the most
intimate aspects of human life. This apart the issue has a vital bearing on
the social equilibrium which is bound to get upset and disturbed by
further increase in economic disparities. Unless we can somehow control
the birth rate and introduce planned parenthood with small families the
spectacle of vast areas of slums existing side by side with palatial multi
storied buildings would continue to mar at even a bigger scale the land
scape of all big cities. They would also become focal points of social
tensions. Experience tells us that a few island of richness in vast area of
poverty, a few cases of affluences in a vast desert of penury and privation
generate tensions and give rise to dangerous thoughts which portend ill
for the smooth march forward of the society. Wisdom lies in forestalling
such social convulsion and in taking timely steps to prevents occurrence.
Family planning is one vital step for this purpose.
I think the organisers for asking me to address this August gathering
on a vital issue.
4
H
f
or
T.J '-’Tl 1
" 1' .
Marks Road.
8- SC > SOK
i-'ny
• 7- •
INTERNATIONAL CONFERENCE
HEALTH POLICY : ETHICS & HUMAN VALUES NEW DELHI 1986
Ethical Dilemmas in a Health Policy
Points to Ponder
Dr. Prem Sobti
Medical Officer WHO SEA Region New Delhi
“The enjoyment of the highest attainable standard of health is one of
the fundamental rights of every human being without distinction of race,
religion, political belief, economic or social condition.” This cardinal
principle enshrined in the Constitution of the World Health Organization
has been the guiding light for health planners and administrators the world
over as they have attempted to steer their national health policies in the
turbulent seas of want, hunger and disease.
How successful we have been in achieving this laudable goal, is, of
course, a debatable matter. What, however, is beyond any doubt is the
fact that for vast number of people in the world, health remains an illu
sion, a dream.
What makes the problem more complex is that in an age of conflict
ing demands and limited resources, health unfortunately takes very low
priority. The experience usually has been that when budgetary cuts
become inevitable, the axe falls first on the health sector.
It is largely for the above mentioned reasons that we find ourselves
in a situation where hundreds of millions of people in rural communities
in the developing world have little or no access to health care. On the
other hand, “disease palaces,” as the Director-General of the World Health
Organization, Dr. Halfdan Mahler, once described some ultra-modern
hospitals, consume a sizeable portion of the country’s health budget. We
therefore find ourselves in the uneviable position of spending 80% of health
budgets on 20% of the population, whereas 80% of the population living
in rural areas has to make do with 20% of the budgetary allocations".
If ever there was an ethical dilemma, this is it.
So, what does one do about it ? How can there be a more equitable
distribution of available health resources ? How can the people be equip
ped to take care of themselves ? All these questions, and many more, have
been raised in the past few year m international conferences as it has
become increasingly obvious that in ' :<ier to achieve a reasonable standard
of health, the people themselves will m ■ iodo something about it.
Health for All
The beginning of this direction was made nearly a decade ago when,
at the World Health Assembly held in 1977, the Member Countries of
WHO adopted the historic resolution setting for themselves the goal of
“Health for All by the year 200.” The following year, WHO and UNICEF
organized the first-ever international conference on Primary Health Care
1
at Alma-Ata, USSR. It was here that the vehicle through which health
for all could be achieved, primary health care, was identified. Since then
the momentum has grown with countries formulating their national strate
gies and plans of action to achieve the goal. Also, as a result of publi?
debate on the issue, health has been recognized as an integral part of the
development process. In fact, it is now acknowledged that without health
there can be no development. What has also emerged recently is the under
standing that health is not the responsibility of the health sector alone, and
that in order to achieve common objectives, health development needs to
be a multisectoral effort.
It is, for example, now an accepted fact that health depends on a
number of supportive services, like health education, nutrition, water and
sanitation, just to name a few. This aspect, of health development enconipassing many disciplines was most forcefully emphasized in the Declaration
of Alma-Ata. In spelling out what was meant by primary health care, the
Declaration stated that this included at least: education concerning
prevailing health problems and the methods of preventing and controlling
them: promotion of food supply and proper nutrition; an adequate supply
of safe water and basic sanitation; maternal and child health care,
including family planning; immunization against the major infectious dis
eases; prevention and control of locally endemic diseases; appropriate treat
ment of common diseases and injuries; and provision of essential drugs.
If one examines these eight elements separately, it becomes obvious
that in order to make primary health care available to all would mean
active collaboration and coordination between various departments and
ministries.
Policy-making Problems and Pressures
In order to make any objective assessments or set realistic targets,
it is necessary to keep in mind that health development has to be viewed
in the context of the prevailing socio-economic conditions. For example,
it is impossible to expect any dramatic improvements in the health status
of the people without a corresponding improvement in the agricultural or
industrial production, literacy rates, status of women, and so on. I am
purposely not going into the area of health statistics, of demographic
profiles or disease patterns, because I wish only to differ some trigger points
for discussion.
What is important to bear in mind is that many developing countries
like ours find themselves in a very real predicament. The predicament of
choice. Not because there are several choices, but because there are very
few. Thus we find that while on the one hand there are millions without
adequate medical care, on the other hand there are thousands of qualified
doctors with nothing to do. Thus we find that whereas production of
drugs is adequate, it never reaches the places it is most needed. Thus we
find that simple, low-cost technologies that are available and acceptable
to the people are not utilized. Here, it is not so much a matter of inade
quate knowledge as the inability to take the necessary decisions at the
policy-making levels. It is here that political commitment assumes a very
significant role. For without such commitment, most ideas never get
translated into action.
2;
Community Involvement
Largely as a result of the movement set in motion by the resolution
setting the goal of health for all and the subsequent actions taken at the
country level, it is now realized that without the involvement of the
community the goal of health for all can never be achieved. An active
and self-reliant people can do a lot for their own health and the health of
their fellow beings as well as prevent, control and treat diseases. But the
real question that needs to be answered is how far do countries want their
people to be self-reliant. This is not merely a rhetorical question, it has
serious political undertones.
Even if one chooses to stay clear of political issues there is no denying
the fact that many factors having a direct bearing on health are largely
influenced by political decisions. To give just one example, one could cite
the per capita expenditure on health. In most developing countries it can
safely be said that expenditure on health is perhaps the lowest, compared
to the other sectors. Here one need not draw comparisons between what
is spent on defence, as compared to health. But the example is important
to keep in mind because of its bearing on policy-making.
Another example in this context is the success achieved in some
developing countries with regard to the provision and training of commu
nity health workers and the steps taken to rationalize the production and
usage of drugs. Though the experience with community health workers
has varied from country to country, the question of essential drugs has
been most interesting. After WHO came out with the list of 200 essential
drugs which an Expert Committee had recommended for use in primary
health care, several countries set about to further refine the list. This was
a political decision, taken at the highest levels as it very directly affected
the interests of the multinational drug companies. But, here again, once
the policy makers were convinced of the merits of the case, they were
willing to take the decisions even though it meant going against well
entrenched vested interests.
Similarly, once a country sets for itself the goal of health for all, the
operative word becomes all. And when a country decides that the way it
will achieve that goal is through primary health care and community
involvement, then it also means that the country is prepared to take care
of the consequent increased demands that will be made on existing health
services.
As any one connected with the health services knows, it is one thing
to create the right awareness and motivate the people to become selfreliant in health care, and quite another to cope with the demands. More
damage is done to the credibility of a service if, having generated the
demand, the health services finds itself incapable of coping. That is why
it is essential to develop the necessary infrastructure before creating a
demand.
These are all factors that have to be carefully examined, keeping in
mind the special needs of the community. In a country as vast and diverse
in its culture as India, no blanket norms can be applied to any situation.
It requires inputs tailor-made to specific needs. And herein lies the biggest
challenge, as well as the opportunity to provide the peop’e with the basics
in health care. It is only then that the cherished goal of health for all will
be achieved.
3
p- •) ^■^'3
INTERNATIONAL CONFERENCE
HEALTH POLICY : ETHICS & HUMEN VALUES NEW DELHI 1986
Family Planning-A National Priority Social,
Ethical, Cultural and Medical Aspects
Role of the Medical Profession
Dr. Dipak Bhatia F.R.C.S.
Family Planning Foundation, New Delhi
The medical profession over the ages acquired two major roles in
society. The first the more ancient one of ministering to the sick and sorry.
Of providing medication, treatment and relief for illness and injury.
The second role evolved later and gradually. It was that of a mentor
to the society on health matters. It carried out this role by organising
and instituting measures for the prevention of sickness. By advising and
suggesting measures for the promotion of health. This second role less dra
matic and less spectacular has not the glamour associated with the provision
of relief from suffering. But it is perhaps more substantive and important
as it promotes and preserves the weal, welfare and integrity of the society.
The two roles however are not exclusive but mutually supplementary.
It is in the ambit of the second role that the medical profession’s
commitment is invoked to tackle the current population growth and the
health hazards arising thereof.
Let us do a quick review of the estimated momentum of the popula
tion growth since the oneset of the modern era.
It took several thousand year of man’s existence on this planet to
reach the world figures of 500 million by A.D. 1650. It took the next 175
years by A.D. 1825 to double the population to 1,000 million (that is one
billion). 105 years more to again double to 2,000 million or 2 billion) by
A.D. 1930, and the next 45 years by A.D. 1975 to double again to 4,000
million (4 billion). At this tempo it is estimated that the world population
by the year A.D. 2000 will increase to 7,000 million or 7 billion (Table 1)
TABLE 1
Year
Doubling Time
A.D. 1650
A.D. 1825
175 years
A.D. 1930
105 years
A.D. 1975
45 years
Population
500 million
(I billion)
1,000 million
(1 biUion)
2,000 million
(2 billion)
4,000 million
4 billion)
National Academy of Sciences
U.S.A.
1
What are the penalties imposed on human existence and human
health by this runaway population.
The first need of the people is that of food.
The problem is one of food and numbers.
keep pace with the population pace.
Can food production
The pattern of population expansion around the globe is not
uniform. It ranges from zero growth to moderate in the affluent and
developed countries. In the underdeveloped countries it is high. It seems
that poorer the country the higher is the rate of its population growth.
Resulting in the phenomenon that the countries least equipped to increase
their food production are faced with high rise demand for food and
nutrition.
It is estimated that two-thirds of the world’s pre-school children
suffer from one form or other of malnutrition. So does perhaps
one-third of the world’s population. Malnutrition may be one of low
calorie intake or a more serious one of also low intake of proteins and
other essential items. The resulting morbidity is of wide range.
A sensitive indicator of malnutrition in children is the slowing down
of their growth and development. This may also be reflected in their later
years by all round reduced capacity.
Infantile marasmus and kwashiorkar are not uncommon serious
nutritional diseases. These are likely to occur when breast feeding is in
adequate or terminates early due to one or another reason and the supple
mentary food given is deficient in calories and grossly so in proteins and
other essential nutrients. These diseases have high mortality and are likely
to leave permanent scars in the victims.
The classical nutritional diseases of beri-beri and pellagra are still
quite common, Caused by deficiency of thiamine and niacin respectively
in the diet and aggravated by protein deficiency, these may also leave
permanent damages.
Anaemia is another wide-spread manifestation of nutritional defi
ciency occurring in all age groups. It is particularly harmful in mothers
and children.
A number of other malnutrition morbidities like scurvy, rickets,
goitre also occur but much less commonly.
Malnutrition directly contributes to lowered resistance to infections
and inter-current diseases. The penalties on a nation from malnutrition
are the decline in the general health of its population and the impairment
O1»f social and economic developments.
Let us look at our country. At the time of gaining our freedom our
population was 350 million. Today it is nearing 800 million and by the
year 2000 likely to cross 1000 million.
2
With 14 per cent of the world’s population our geographical entity
contains only 1.5 per cent of the world’s arable land.
In the earlier post-independence years we had to import sizeable
quantities of food. Today we are self-efficient. This is, however, a presucarious situation. Apart from the growing demand from an enlarging
population, the vagaries of the weather and climate can tilt the balance.
Our increased food production was achieved by a combination of
inputs. By use of fertilisers and pesticides, by improved variety of seeds,
by better management of land and water resources, by application of new
technology and energy resources.
There is however, a biological limit to what can be produced by these
special essential inputs from the small layer of about 10 to 12 inches of top
soil that covers the earth’s crust. In some parts of the world this limit has
already been exploited.
The population imposes another burden on the land. To meet the
pressure of increasing needs and demands the processes of development
cause diversion of land to other uses. Like for the expanding network of
roadways and rail-tracks, for dams and canals, for the construction of
buildings for habitation, for industries and other institutes. It thus cuts
away land to that extent and diminishes it for food production.
Another problem that the population creates is of deforestation
arising from the mindless cutting of trees to fulfil pressing needs. This
causes erosion of the soil, ecological imbalance and leads to climatic
changes. The sequalae of such disturbances are harish. An example of
such consequences are the recent occurrence of prolonged drought and
widespread famine in Ethiopia.
Poverty is a high breeder of ill-health. The poor denied the resources
and services essential for positive health exist under adverse and insanitary
conditions. Their resistance is reduced and they are easy prey to infections
and diseases.
Poverty is compounded by unemployment. The unemployed para
sitic are not productive. Both poverty and unemployment expand as the
population grows rapidly.
In India the jobless today are estimated at about 50 million.
month another 130,000 new entrants swell their cadres.
Every
Man tends to pollute his surroundings. He does it more at his grow
ing numbers crowd the earth. The environmental deterioration is aggra
vated by the increasing discharge of industrial effluents and toxic by
products of technology onto the soil, the waterways and the atmosphere.
The resultant environmental pollution has both direct and indirect effects
deleterious to health.
The mounting pressure of high population growth imposes other
penalties on the health of the people.
3
Man like other species requires a minimal space or elbow room in
which he can function and lead a balanced existence. What may be
labelled as his need of essential territorial exclusiveness. If the cordons of
this territory are shrunk or intruded upon it causes his mental and physical
disorientation and deterioration. Much of the social malaise and morbidity
in the cities can be traced to the current fast trend of urban concentrations
of high density.
The application of new health technologies in the developing coun
tries has been comparatively facile. It has dramatically brought down their
death rates. The professional cadres however have not been able to provide
adequate level of individual health care in these regions. The doctor/population ratio there-in is low. So is that of the essential and supportive para
professional cadres. The fast population growth aggravates the deficiency.
The training of these technical manpower groups is slow and time-consum
ing and their production cannot match the population pace. The demands
for health services soon outrun the supply.
High fertility has a direct correlation with the health risks of women
and children. In women besides causing a greater incidence of ill health
associated with pregnancy and childbearing, it makes them more vulnerable
to general health hazards and diseases. It reduces their reproductive effi
ciency and their capacity to give a good start and provide adequate mater
nal care and sustenance to their progeny. This is reflected in the occu
rrence of high fetal loss, more congenital malformations, low birth weights
and raised infant mortality. The surviving children show more signs of
malnutrition, impaired growth and retarded development. The adverse
effects of high parity both in women and children are aggravated if the re
peated pregnancies occur at short intervals. Uncontrolled and unregulated
parity undoubtedly impose heavy penalties on women and their progeny.
High fertility rates are often associated with high rates of induced
abortions. Often illegal and performed under most unsatisfactory condi
tions, these add to the health hazards of the women.
The communities which continue to have high birth rates show a
profile of a young population and an age distribution of a pyramid with a
wide base. In this pyramid 0-14 years group forms a large cohort. The
need of medical care for this group and the problems of its provision are
more complex and difficult than for other age groups. This puts further
pressure and strain on the medical network and its resources.
*
In cognition of the changing global pattern of human existence it is
imperative that human fertility is controlled and regulated. The medical
profession must take the prime responsibility to advise family planning as
an essential health measure and propagate contraceptive practices.
r
Man stands apart from animal life. He is gifted with the power to
think, to formulate, and pursue some enduring values. Amongst them is
his capacity for compassion.
"
•
■
••
’
;o..;
The raison d’etre of the medical profession is to demonstrate the
quality of compassion in operation. It is in the compass of that aura that
4
■ -wJ
the profession functions to prevent unnecessary deaths. To the objectives
of reducing pain and suffering. Not for financial rewards, not for economic
gains. But in the fulfilment of the humanistic traditions that inspires the
professional ethos.
The same altruistic grace should move the medical profession to
commit its resources to prevent unnecessary births which but add to the
sprawling numbers condemned to an existence of hunger, want and
degradation.
The atom bomb is man’s brain-child. The population bomb his
biological child. Both a threat to this survival. The first threatening his
dissolution in an instant flash. The second to a slower end by choking up
and dissipation of the earth’s resources essential for his existence.
Man must control both diabolic creations.
profession must be in the vanguard.
In that effort the medical
I
■
5
'I
INTERNATIONAL CONFERENCE
HEALTH POLICY : ETHICS & HUMAN VALUES NEW DELHI 1986
The Right to Live and The Right to Die
Minoo Masani
President, World Federation of the Right to Die Societies
My good friend, Yusuf Meherally, whose useful life was cut short so
cruelly, used to write in every autograph book which was placed before him
by his many young admirers : “Live dangerously”. In my young days I
thought it was a rather good slogan and, by and large, I have tried to live
up to it, and never regretted doing so. The idea of death has never
worried or frightened me right from my young days. I would much rather
be dead than red. What does, however, give me the creeps is the thought
of being crippled and unable to function. I know a great many people
who share this preference for a quick and dignified death to a long and
humiliating existence as a cripple or a vegetable.
At a meeting I addressed on behalf of the Society For the Right To
Die with Dignity, which was the first of its kind in India, I was asked by a
gentleman who believed in karma what advice I would give him. I told
him that, as far as he was concerned, he was altogether entitled to endure
the sufferings to which he had referred as part of the cycle of karma.
Since all we are arguing for was Voluntary Euthanasia, I hoped he would
not mind my exercising my option the other way when the occasion arose,
since I was not convinced of the reality of reincarnation or karma.
Some of my friends find it difficult to accept the thought that, when
they die, it will be their final elimination and nothing will remain of them
at any level of existence. I must confess that to me the idea of absolute
destruction does not hold any terrors, while the idea of going through
Purgatory and then facing whatever came afterwards does not appear to be
particularly restful after a long and busy life on this earth. Why should
one object to being blotted out at the end of this life ? Why should I have
the conceit that I must go on forever ?
All this shows that our perceptions about the matter of life and
death vary greatly and that to deny anyone the right to a different view
from what one holds oneself would be not only dogmatic but stupid. We
all know so little, about these matters, and it is best to keep an open mind,
do the right thing, practice the golden rule, and leave the rest to Provi
dence which, it has been aptly said, “shapes our ends, rough how them
how we will”.
I have always responded warmly to the English poet who wrote :
“I am the master of my fate,
I am the captan of my soul.”
I was therefore greatly touched when Mr. Gopal Mandlik, a well-
1
known social worker of Poona, ended his own life in 1980 after waiting
two years for the Government of India to amend the Indian Penal Code
and to make it possible for him to do so legally. His only regret was
that his eyes and his kidneys, which he had wished to donate for humane
purpose by deleting Section 309 IPC could no longer be put to use in that
manner. He was -a true satyagrahi in the Gandhian sense. Gandhiji
always urged that where one’s conscience held a law to be wrong or immo
ral, the satyagrahi should break the law and take the consequences but not
run away.
Mr. Mandlik’s brave act was one of the factors that led some of us
to establish The Society For the Right To Die with Dignity in May 1981.
Another sad case of someone who was not in a position to imitate
Mr. Mandlik was/that of my good friend Norman Thomas, the American
Socialist leader, who was in his old age completely paralysed and pleaded
to be released, but was tormented by being kept alive for many years
because it was not legal in that particular part of the United States to
allow him to die.
When people tell me that public opinion is not ready for an amend
ment of the law which would make Voluntary Euthanasia easier to
practice, under proper conditions and safeguards, I am inclined to wonder.
Public opinion has been described as “a fickle jade” and indeed is very
volatile and changeable. In the middle of the 60s, a well-known lady who
was a champion of birth control in India, pleaded with me not to introduce
a Private Members Bill in Parliament for legalising abortion on the ground
that, if I were to do so, it would create such a storm of opposition that
the backlash would injure the cause of contraception. Lo and behold,
four or five years later I found myself a member of a Joint Select Commit
tee of Parliament which recommended to Parliament the legalising of
abortion, and I noted that nobody in the Select Committee and nobody in
Parliament opposed this change in principle. How do we then know what
public opinion is or not in the case of Voluntary Euthanasia unless we first
educate it and then test it ?
That is precisely what our Society has tried to do in the years that
have passed since we took this pioneering step. There has recently been a
great deal of public discussion on this issue.
Much of this is due to a Bill introduced by Prof. S.S. Varde in the
Maharashtra Legislative Council to provide for immunity and protection
to physicians and surgeons who withdraw life sustaining treatment from
terminally ill patients at their wish. This Bill was ordered to be circulated
by the Council to elicit public opinion and this led to a controversy in the
course of which prominent doctors in Bombay including Dr. Praful
R. Desai, Director, Tata Memorial Centre, Dr. N.H. Keswani, Medical
Director, Jaslok Hospital and Research Centre, Dr. B.N. Colabawala, Dr.
R.R. Soonawala. Dr. K.D. Desai, Dr. F. Soonawala, Dr. J.C.N. Joshipura,
Dr. V. Talwalkar and others have written to the press welcoming the Bill.
The other helpful development is a judgement of a Division Bench of
the Delhi High Court on March 31st 1985, which refused to punish a
young man who attempted to commit suicide despite Section 309 of the
Indian Panel Code which makes such an attempt punishable.
2
In an outspoken judgement, the Delhi High Court has held that
Section 309 of the IPC is an anachronism unworthy of a humane society
like ours. The High Court went on to observe that many penal offences
were the offshoot of an “unjust” society. ‘,So long as society refuses to
face this reality, its coercive machinery will invoke the provisions like
Section 309 IPC which has no right to remain on the Statute Book”. The
Court said that “the young man (Sanjay Kumar Bhatia) who tried to com
mit suicide because of “over emotionalism” would have escaped human
punishment if he had succeeded in taking his life but was now being houn
ded by the police, because the attempt failed.”
By and large the response to our cause has been encouraging. This
is particularly so in the case of the medical profession, many of whom have
in their own practice faced the “Doctor’s Dilemma”. Most doctors are
humane, compassionate human beings and many of them share Dr. Chris
tian Barnard’s regret that they are not able to give relief from pain and
distress to those of their patients in whose case they consider it appropriate.
Hundreds of letters have been received by us, many of them extremely
touching, about the sad stories they have to tell and the welcome they have
given to our Society.
Our Society has prepared a draft Declaration and a draft Power of
Attorney which it has issued to members for their use if they so desire.
These documents make clear the wish of a man or woman in sound mind
that, in case he or she is terminally ill and unable to give expression to his
or her wishes, artificial medical treatment should be withdrawn and pain
killing drugs given to him or her. The Power of Attorney would nominate
two persons who would be duly authorised to persuade the doctor and
family to respect the patient’s wish if the occasion does arise. The Power
of Attorney could of course be revoked at any time. Such documents are
widely used in the U.S.A, and in U.K., where the law in regard to the
abetment of suicide is the same as in India. These documents do not
legally bind anyone but are valid documents even under the law as it stands
today and would carry a great deal of moral influence.
Our Society is the 28th of its kind in the world. I was very happy to
hear from my good friend, Arthur Koesler, the well-known writer, who
said in his letter : “I am glad to hear that you are starting EXIT in India.
It will be a long and hard way until charity and commonsense will do
their work.”
The Examiner a Catholic Journal, dealt with this matter in two
issues. In its first issue of August 15, 1981, it naturally came out in opposi
tion. I was glad to see, however, that in the second issue of August 20,
1981, the paper conceded that passive euthanasia may be justified. It
quoted from the declaration on Euthanasia by the Congregation for the
Doctrine of the Faith :
“When inevitable death is imminent inspite of the means used, it is
permitted in conscience to take the decision to refuse forms of treat
ment that would only secure a precarious and burdensome prolonga
tion of life so long as the normal care due to the sick person in
similar cases is not interrupted”.
3
The most common doubt that is expressed is the fear that any change
in the law to make it more humane would make it easier for unscrupulous
persons to bump off old and sick relatives. This is a genuine fear, but
it relates to mercy killing with which we, as a Society, are not concerned,
and not to Voluntary Euthanasia. The danger of ‘bumping off’ only arises
when ore person can arrange for another person to die. It cannot arise
when a man or woman in sound mind but terminally ill makes his or her
own choice and asks for self-deliverance.
I believe that public opinion can be mobilised within the next few
years when it has been made more aware of the issue. We in the Society
believe in obeying the law, but we would like it to be amended so as to
make it more humane and compassionate.
; ;y.T4C~LL
Hccr. St Marks Road,
47/1. (Fhs' 1 •
Bangalore - 560 001.
4
INTERNATIONAL CONFERENCE
HEALTH POLICY : ETHICS & HUMAN VALUES NEW DELHI 1986
Terminal Care—Ethics and Cultural Aspects
Dr. Rizvi, S.N.A. and Dr. Rajvanshi, P.
Maulana Azad Medical College New Delhi
Mankind is subject to the experience of physical death. The death
is a state or condition with an existence for man beyond the grave, difficult
to describe or quantify. Terminally ill (dying) means that the patient has an
illness has which been accurately diagnosed, and which seems certain to
bring about his death within a relatively short period of time, since the
illness is beyond both cure and palliation. Caring for dying patients and
giving sympathetic support to breaved families are profoundly important
parts of the work of doctors, nurses and other members of the caring
professions. The care of patients during their terminal illness over various
periods of time is a privilege, for they greatly appreciate the visits of the
doctors and realise they are not forgotten. They may be cared for in
hospitals, nursing homes, or family homes and is requires numerous medical
and nursing skills according to the particular illness. Symptoms are treated
so that the patient remains free from pain and in comfort. Much nursing
care is required by some patients, especially those who are paralysed in
various ways.
Guidelines for Delivering Bad News
Every physician derives satisfaction from delivering good news to a
patient; and no physician enjoys delivering bad news. Still, there are rare
occasions when it becomes necessary for the physician to disclose a crippl
ing diagnosis and prognosis to the patient. There are some general guide
lines for delivering bad news as follows:
1. Keep it simple.
2. Don't deliver all the news at once. It is good idea to try not to
provide too much information at the first sitting.
3. Educate the patient gradually and gently regarding the diagnosis.
4. Wait for questions from the patien t.
5. Ask questions yourself—Valuable clarifications can result from
gentle, and clear questioning.
6. Do not destroy all hope. ‘’Most people with this form of disease
as chronic renal failure are living longer but are not cured of
their disease” is a useful kind of statement.
7. Do not say anything that is not true. This would be the crudest
blow of all.
I have the responsibility of caring for many patients with various end
stage renal diseases; this particular diagnosis understandably causes unrest
and anxiety to the patient and family. Various questions require answer
ing at all stages of these illnesses. An explanation about the treatment
and prognosis is given to the family, with the assurance that every thing
will be done to help the patient throughout the illness. The question
1
whether the patient should be told he or she has end stage renal disease
needs some discussion. Information is given with sympathetic understand
ing of the situation and in the kindest way, in the presence of near relatives
Words are chosen carefully to create faith and confidence, and nothing
shall be said to take away a patient’s hope. I believe we can work profes
sionally in a more helpful way when patients are told about the terminal
illness, and by understanding something about the problems to be solved
they can cooperate usefully.
Emotional Aspects of Death and Dying
In a critically ill and dying patient, palliation and emotional support
are the optimal strategies. A useful approach is to communicate the medi
cal realities to the patient as skillfully, honestly, and clearly as possible and
allow the patient with the help of his or her family to decide upon the
preferred treatment. Health professionals must have the courage and
willingness to acknowledge that the patient’s wishes may take priority over
their own.
Patient-Doctor Communications
Fundamental to the evolution of effective doctor-patient communica
tions is the notion that physicians answer all questions honestly, giving
as much information as is asked by the patient.
Ambiguous or dishonest communication imposes needless emotional
pain on patients and families facing life-threatening illness.
A variety of information inputs that come to the patient:
1. Direct statements from the physician.
2. Overheard comments of the physician to others.
3. Direct statements from others including nurses, ward boys and
technicians.
4. Statements from family, friends and clergy.
LL1V IJLlVMlVCll
5. \_yIlcrilgVD
Changes 111
in the
medical Vdl
careV IvUllllVdj
routines, procedures, UVlldV
behaviour of
others towards patients and changes in physical location.
6, Self-diagnosis, including reading of magazines,
records, charts and books.
newspapers,
It is evident that the dying person is engaged in multiple communi
cations with many people. If the messages are clear the dying person can
make sense out of his experience. But if the messages are confused or
contradictory, the result is needless apprehension and anxiety. Many
patients, once they are aware and acknowledge the untreatable state of
their disease, have less pain and discomfort in general and require a mini
mum of medical supervision.
It is very difficult to answer the questions about the length of time
the patient is likely to live, except when the end is obviously neat and I
explain that all our lives are in the hand of God. I respect the wishes of
2
the family relatives of non-mentioning of the diagnosis and prognosis to
the patient to avoid any upset, although it made more difficult when a
patient realises the gradual deterioration of health without a real explana
tion being given to him. During the final days of the illness, the family
members have to be informed about the time becoming short for the
patient and by that time majority of these patients know about their
condition. Whole family require help at these times to ameliorate the
strains and stresses caused by loss of family member.
Patients who are seriously ill and cannot recover by available recent
mode of therapy and their families, appreciate the frequent visits of the
doctor, who can give much sympathetic help and support to ameliorate the
sorrow and suffering which become more intense as death approaches for
the loved relations. The presence of the doctor who has become a trusted
friend during the illness is a source of solace to them in their grief. A
special, unhurried visit following soon after the patients death to take and
discuss is greatly appreciated by the family and these visits to the breaved
family should continue for a further period of time, until there is an
amelioration of their grief and loneliness.
Community Approach to Psychological Support of Dying Patient
The awareness, tolerance and acceptance of the reality of dying is
difficult for the patient and family. In order to provide emotional, social
and spiritual support, a community-wide effort helps in achieving the
maximum care for the patients comfort and psychosocial support. It is
important to have people involved, whether social workers, trained
volunteers, priests, etc., who can give supportive help to patient and family
members.
Bereavement Follow-up
Bereavement leads to a period of crisis, for the family. The care of
the terminally ill patient and family does not stop when the patient dies.
The members of health team may attend the funeral. Home visits and
telephone contact continues with the family within the first three weeks of
bereavement and subsequently upto approximately one year. Opportunity
for the spouse, parents and children to express their grief and talk about
the illness and death does much to relieve guilt and depression. A
memorial card is sent to the key person on the anniversary of the death.
Role of Clergy Man or Priest
Not all symptoms need medication in a terminally ill patient. Pain
of isolation and inability to attend church and ring with the choir is helped
immensely by the presence of clergy man or priest and with the relatives
and friends at bed side.
Understanding Patient Depression
Frequently observed patient response to life-threatening illness is
depression. It results from:
3
(i) Prolonged and painful hospitalization and treatment.
(ii) Emotional abandonment by family and friends.
(iii) The real or imagined insensitivity of hospital personnel.
(iv) Depletion of finances due to expensive medical care.
It is not helpful to interrupt this response with false promises of cure
or positive response to treatment. Patients require emotional support.
One can be extremely supportive by sitting with the patient, often in silence,
in an attempt to convey willingness to share this emotionally demanding
period.
The Patient’s Family
The dying patient and his or her family constitute the optimal unit of
health care. It is extremely important for patients to conclude family
relationships in as emotionally satisfying a way as possible. It can be very
distressing for critically ill persons and their families to be separated by
the treatment milieu. Following suggestions are offered to health pro
fessionals:
1. Train family members to participate in treatment.
2. Encourage them to do such things as continue to cook special
meals for the patient.
3. Allow unlimited visiting so that the total family, including
children, can spend time with the patient.
I
4. Provide special social and educational programs for the family
and patient.
Continue these programs, adding home visits for the family after the
patient has died.
Despite the importance of care for all troublesome and common
symptoms of terminal patients admitted in hospital (100 cases); it remains
to be said again that good personal relationships and the prevention of
loneliness are of paramount importance in providing high quality terminal
care (Table I).
Pain
Incontinence
Confusion
Nausea
Anorexia
Insomnia
Depression and
anxiety
50%
30%
20%
15%
15%
15%
20%
Dyspnoea
Bed sores
Vomiting
Cough
Dysphagia
17%
15%
13%
5%
3%
*s
The importance of adequate fluid intake, bowel regulation without
discomfort and the correction of electrolyte imbalance, must be stressed in
the terminal patients as in others. In dealing with all these symptoms, the
doctor’s enthusiasm and confidence in his therapy will be, without doubt,
1
4
!
■
transmitted to the patient. He should have the same interest in the patient
during this stage of life as in any other. It is stressed that whether patient
is nursed at home, in an institution, or by intermittent hospital admission
and discharge, it is essential to make certain that there is continuity of
care.
The management of terminal illness by the family physician is in
the exploration and development of the doctor/patient relationship where
the feelings of patient and the doctor are fully expressed and understood.
A good relationship is best established when the patient and doctor
acknowledge, either overtly or covertly, their awareness of impending death
and the patient is allowed to test out the relationship without any fear of
the doctor withdrawing.
In hospital, the dying patient receives every attention, constant
medical and nursing care, the advantages of modern palliatives, profusely
planned drug administration for the control of pain and freedom from ne
glect and loneliness. Very little work has been done to estimate the numbers
of patients who die at home compared to those who die in hospital. 90 %
of all episodes requiring medical and nursing care attentions are dealt with
in the community, but it is unlikely that a similar percentage rate applies to
death. Once the decision is made, the transfer from hospital to home care
should be effectively planned, so that the home, family and the primary
care doctors and nurses are all prepared.
■
I'
Bn
5
INTERNATIONAL CONFERENCE
HEALTH POLICY : ETHICS & HUMAN VALUES NEW DELHI 1986
Moral and Ethical Dilemmas in the Care
of Critically ILL Patients
Dr. P.S. Chari, M.S., M.Ch.
Associate Professor of Plastic Surgery
Dr. (Mrs.) Pramila Chari, M D.
Associate Professor of Anaesthesia
PGIMER, Chandigarh
The knowledge explosion in Science and Technology tends to over
whelm us and we get confused in a maze of technicalities and methods
often forgetting the patient we are treating and who becomes a conglo
merate of signs and symptoms instead of a person. Advances in resuscita
tive technology have enabled anaesthetists to almost indefinitely prolong
the life-supporting systems of critically ill patients who would formerly have
been pronounced as dead after simple traditional measures had failed The
dilemma lies in the moral and ethical necessity of providing maximal care
for patients who are terminally or irrepairably ill but who have a chance
to survive their present catastrophe (Declaration of Helsinki, 1964). It is
agreed that permanent functional death of the brain stem constitutes brain
death and further artificial support is fruitless and should be withdrawn
(Honorary Secretary, 1976).
In a dilemma one is faced with two alternative choices, neither of
which seems a satisfactory solution to the problem. They arise in situations
of uncertainity and ambiguity when the general principles upon which one
normally relies either offer no help or seem to contradict each other. Such
decisions have to be distinguished from the many important clinical deci
sions which must also be taken by doctors. These decisions may present
as dilemmas but their resolution is dependent solely on the doctor’s know
ledge experience and intuitive abilities. All these factors are certainly
helpful in a moral dilemma but are insufficient to unravel the moral
conflict because a different kind of decision has to be made. The more
concerned the profession has become about the formulation of codes of
ethics the more they have become aware of the complexity of the moral
problems The profession simply provides some generalised statements m
everyday language and leaves it to the good sense and good will of its
practitioners to deal with the ambiguous situations.
The individual conscience is thought of as a kind ol inner voice
warning you against wrong doing and creating remorse when the warnings
have been disregarded. Following conscience is the most common way
doctors seek to solve the moral dilemmas they encounter. Peoples’ intui
tions’ about right and wrong often conflict sharply. It seems that con
science is a powerful force in controlling the actions of most individuals;
but although powerful, it may not always be right.
There is confusion about what is useful and advantageous to the
majority and what we feel all men ought to value. Treating every indivi-
1
dual justly usually does benefit society as a whole. Respect for the rights
of individuals is a more fundamental moral value than the happiness of the
majority. We are still primarily concerned with caring for people and the
art of medicine should not be forgotten in the enthusiasm for scientific
precision. Sympathy and understanding are just as important as diagno
stic acumen (Payne 1978). However, in many dilemmas of personal and
social morality the criterion of general happiness is a good corrective to
personal bias and idealistic mounting of principles.
What we appear to be searching for is a set of absolute or funda
mental values which will clearly and unambiguously inform our choices
and decisions in any given situation. Such a calculus of human rights
cannot and will not be done. Rule following, much of it habitual and
unquestioned, characterizes a high proportion of our daily activities. Our
behaviour is confined within the limits of the socially acceptable, the
legally sanctioned and the routines of personal preference and conviction.
A rule-governed approach to morality becomes a wholly depersonalised
one. What is missing is any consideration of the persons who hold the
principles and the persons to whose circumstances the principles are
applied.
It is said that Hipprocrates forbade the administration of remedies to
those who* were past hope. This injection we may heed as advice not to
make difficult the final stages when we recognise their finality. None can
relieve us of the responsibility of judging when this moment shall have
come. We should bring to the beside a great hopefulness, a determined
optimism, but is the futility of the struggle is clearly evident, then we
should put aside our remedies as cures, and make the patient easy with
such solation as may offer (Gavey 1950). We are asked to give guidance,
to judge dispassionately upon reasonable probabilities. The fact that many
of our prognosis prove wrong should not detract from a genuine attempt
at a correct forecast. As Osler said “Errors of judgement must occur in
the practice of a art which consists largely in balancing probabilities”.
The question: “should the doctor tell?” is guided in practice by the
circumstances of each case which suggests the line that should be taken. In
general, a guarded prognosis slowly revealed enables a patient to prepare
himself, retaining a hopeful attitude in the background. In these matters
few demand to know the truth and nothing but the truth and even if a
direct question is asked the patient usually welcomes an answer which does
not shut out all hope. The patient senses the true position far more accu
rately than one might imagine and any attempt to soften the blow is wel
comed. There are occasions when it is best never to disclose the true
position, even at the end. The human capacity for self deception is great
and this characteristic needs to be promoted occasionally.
Intensive medical care is designed to diagnose, treat and maintain
patients with immediate, acute but potentially reversible life-threatening
impairements. It also aims at prophylactic management to avoid such
catastrophes as cardiac arrest, respiratory arrest, shock, renal failure, and
overwhelming sepsis. There is a growing beleif that medical and techno
logical capabilities should not necessarily be used simply because they
exist.
2
Is there an ethical imperative to preserve all patients in life threaten
ing situations including those for whom existence seems only a fiction and
others for whom it promises to be only severely diminished? On one view,
it is justificable to moderate the therapy even though earlier death will
occur, when this will result in relief from pain and suffering. Another
view is that ‘our training is to preserve life and functions whenever pos
sible’. We are not trained to decide who “is better off dead”. The patient
who is alive has an overriding right to life and deserves the maximal pos
sible therapy (Cohen, 1977).
This conflict has implications for the care of those who are not
terminally ill, but who are potentially salvageable with the chance that sur
vival will be accompanied by severe physical or mental impairement or both.
It is these difficult cases concerning the level of salvageability that lead to
the widest divergence of opinion. The problems are complicated by the
fact that it is often not possible to evaluate the likely outcome of intensive
care treatment until the patient has been monitored for some days and
even then, predictions are open to revision in many cases (Cullen et al,
1976, Griner, 1973). It is also to be remembered that there is a moral
difference between “Killing’ and ‘letting-die’. Dying is the final event of a
valuable human being and no one else is morally empowered to initiate and
transact. When a decision has been made that maximal treatment is in
appropriate it is not an acceptable ethical alternative to kill the patient,
but it is permissible to allow the patient to die (Me Cormic, 1974).
Western ethical traditions have reached some general agreement that
it is necessary to use ‘ordinary’ but not ‘extraordinary’ means to support
and comfort patients in such cases (Pope Pius XXI, 1958). By ‘ordinary’
means is meant ‘all medications, treatment and operations which offer a
reasonable hope of benefit for the patient and which can be obtained and
used without excessive expenses, pain or other inconvenience’. ‘Extra
ordinary’ means are those that do not offer such hope or cannot be
obtained or use without those kinds of liabilities. There is a professional
and moral relationship entered into with each patient admitted for intensive
care in which it is understood the patient will receive appropriate care.
Such care cannot be terminated later on the grounds that another patient
with a higher potential for survival needs intensive care without violating
the original obligation to the admitted patient and without violating the
ethical principle that we cannot aid some by harming other (Report of
Clinical Care Committee, 1976).
Survival though important, is not to be bought at any cost and that
to attempt, but fail to achieve, may reduce so-called intensive care manage
ment merely to the level of prolonging the process of dying (Rabkin et al,
1976). It is of primary importance from an ethical perspective to deter
mine whether the right to life is absolute or whether it can ever be over
ridden with justification. Our conclusions will not apply with absolute
finality, like mathematical equations, to all cases as individuals have very
different conceptions of how to exercise their right to the pursuit of happi
ness within the limits of the ethically possible. Reverence for life must be
tempered by restraint and an equal respect for the dignity of death. In the
last analysis, our choice is influenced by the way the personality regards it
destiny and our own conception of death.
3
BIBLIOGRAPHY
1. A Report of the Clinical Care Committee of the Massachusetts
General Hospital. Optimum Care for Hopelessly Ill Patients. New Engl.
J. Hed. 295:362,364, 1976.
2. Cohen, C.B.: Ethical Problems of Intensive Care. Anaesthesiology.
47:217-227, 1977.
3. Cullen, D.J., Ferrara, L.C. and Briggs, B.A.: Survival hospital
charges and follow up results in critically ill patients. New Engl. J. Med.
294:982, 987, 1976.
4. Declaration of Helsinki. Brit. Med. J. 2: 177, 1964.
5. Gavey, C.J.: The Management of the ‘Hopeless’ case. Buckston
Browne Prize Essay. E and S. Livingstone, Edinburg, 1950.
6. Griner, P.F.: Medical intensive care in the teaching hospital:
Costs versus benefits. Ann. Int. Med. 78:581-585, 1973.
7. Honorary Secretary of the Conference of Royal Medical Colleges
and their Faculties in the U.K. on 11 October, 1976: Diagnosis of Brain
Death. Brit. Med. K. 2:1187-1118, 1976.
8. McCormick, R.A.S.J.: To save or let die. The dilemma of
modern medicine. J.A.M.A. 229:172-176, 1974.
9. Payne, J'.P.: Ethical Problems in Clinical Research and Intensive
care. Brit. J. Anaesthesia. 50:413-414, 1978.
10. Pope Pius XII. Amer. Q. Papal Dec. 4:393, 1958 quoted by
Bishop, V.A.: A Nurse’s view of ethical problems in Intensive Care Clinical
Research. Brit. I. Anaesthesia, 50:515-518, 1978.
11. Rabkin, MT., Gillerman, G., and Rice, N.R.: Order not to
resuscitate. New Brit. J. Med. 295-364, 1976.
12. Resolution 613: On the Rights of the Sick and Dying. Parlia
mentary Assembly of the Council of Europe, 1976.
13. Safar, P. and Grenwick, A.: Critical Care Medicine, Organising
and Staffing Intensive Care Units. V Chest. 59:535-547, 1971.
S’tU.
r
f /
P
4
:
iiCO.
S:
^BtKSPoaA
'
> - [C
i •> •
INTERNATIONAL CONFERENCE
HEALTH POLICY : ETHICS & HUMAN VALUES NEW DELHI 1986
Euthanasia
Dr. H.N. Shukla
Introduction
Euthanasia has its origins from a Greek word, the term ‘Eu’
means ‘Well’ and ‘Thanatos’ means death and it literally means an easy
death. It is a form of peaceful or dignified death which is specially
advocated when life become a punishment and dying comes as a pleasure
to a patient, suffering from some incurable disease like cancer with severe
intolerable and uncontrollable excruciating pain, who more often tearfully
pleads to a doctor to relieve his suffering soul from bodily cage. The con
flict is often stated to be between the doctor’s duty to treat to the best of
his ability and patient’s right to be allowed to die quietly and in peace, when
further medical measures appear meddlesome and only prolong suffering.
Health Council of Netherlands has defined Euthanasia ‘A deliberate life
shortening act or deliberate omission of a life lengthening act, in respect
of an incurable patient and in his interest’. This definition includes both
active (life shortening act) and passive (omission) euthanasia. The
‘Declaration of Venice’ at the meeting of the World Medical Association
in Oct. 1983, has laid down that ‘Physician may relieve suffering of a
terminally ill patient by withholding the treatment with the consent of the
patient or his immediate family member in case the patient is unable to
express his will’ and ‘The physician may refrain from employing any extra
ordinary means which would prove of no benefit for the patient’.
In the light of above the present article endeavours to stress the role
of Voluntary Passive Euthanasia in the Terminal Care, especially the with
drawing of life sustaining treatment according to wishes of patients suffe
ring from Terminal Illness and withdrawal of life sustaining aids from a
Terminally Injured patient after declaration of brain death. It will be in
public interest for such a measure to be enacted as it would relieve a certain
number of patients from suffering pain and torments which can be avoided.
Good death : Moral and Legal Challanges in Terminal Care
Law and medicine join a common pilgrimage towards protection,
preservation, regulation, care, and all-pervasive welfare of human life.
The Indian Constitution (Article 21) assures that ‘No person shall be de
prived of his life by the state except according to the procedure established
by law’. The constitution can guarantee the ‘Security’ or ‘Non-interference’
in the enjoyment of life but no constitution in the world can ever assure
its citizens that their life would remain always free from pain, disease and
physical and mental agony. The right to life protected by Indian Consti
tution has not been judicially held to include ‘Right to die’. The question
is whether a person who has become a mere vegetable mass of protoplasm,
who has worse than animal existence, who has no hope of recovery—
1
Should he be forced to live ? Should he be not allowed to die peacefully
without suffering from further physical and mental agony ? , Cannot
he ask the state that while he has been given right to life, Can’t he be
endowed with a right to die in the event of a terminal illness or terminal
injury ? The death sentence in India has been held to be constitutional
under the very provision which protects the right to life of a person.
Likewise state has legalised the Medical Termination of Pregnancy.
Interaction of law and medicine is notable in cases of abortion. It is now
perfectly legal though may not be perfectly moral or ethical. Man can
choose to give life or death to the helpless unborn child then why should
he not have similar right for his ownself ? The legislation of abortion
means legislation of ‘Death’ of an unborn person. The purpose of abortion
in most cases is to safe guard the health of a pregnant woman or it is for
the convenience of the society and state as a measure of population control
but the voluntary passive euthanasia is for the sake of suffering ‘individual’.
If law can permit ‘killing’ of an unborn child for the sake of ‘others’ Why
should it not allow voluntary passive euthanasia for a willing and suffering
patient.
Role of Voluntary Passive Euthanasia in Terminal Care
Terminal illness or Terminal Injury means any incurable illness or
injury which will in all probabilities result in the expiration of life, regard
less of use or discontinuance of medical or surgical treatment. To day
cancer accounts for 15 per cent of deaths in the world. In U.S. alone more
than 7 million unfortunates are in grip of this dreaded affliction. It is
here that Voluntary Passive Euthanasia becomes relevant. Voluntary
Passive Euthanasia advocates compassion in the preceding stages of
terminal illness. These stages are process of dying which sometimes linger
on for years. When a doctor prolongs the life of a dying patient by days,
weeks, months or by years he merely prolongs his life of suffering. He
simply promotes his vegetable existence or adds to his comatose condition
in the name of preservation of life. No patient wants to put up with
sufferings indefinitely. There is an innate desire in all living beings to
terminate their sufferings as quickly as possible. When the intensity of
suffering is beyond the pale of human indurance the urge to extinguish
life is paramount. Prof. Elizabeth Ross recognises this final state of dying
as a stage of acceptance, the patient is ready to accept loss of his life and
beloved ones.
Withdrawing of Life Sustaining Treatment in Terminal Illness
The life sustaining treatment means all artificial means or measures
of whatever kind administered as medical or surgical treatment designed
solelv to sustain life process. In developing nations health expenditure
on the last few months of patient’s lives rises to a crescendo, as might be
expected but the consumer, the patient, often seems to derive little of real
personal value from the money thus spent. Traditionally the medical
ethics has been helped at this point by distinguishing ‘ordinary’ means of
treatment which should be available to all patients, from‘extra-ordinary’
which should not be employed as they cannot be used without excessive
pain, cost or other inconvenience and which offer no reasonable hope of
benefit.
2
Many people today have a fear that they will be kept alive artificially
in this manner with consequent suffering and distress to them and members
of their family. Since the decision to reject such treatment should be of
patient alone and no one else in case of terminal illness as such provision
of Voluntary Passive Euthanasia in terminal care will enable doctors, in
the interest of compassion and humanity to respond to the patient’s wishes
in suitable cases but it should not provide for mercy killing of any kind.
Declaration for withdrawal of Life Sustaining Treatment
Any person of sound mind shall be entitled to make a declaration
and give powers of Attorney duly executed by such person expressing the
desire that if at any time in future he or she were to suffer from a terminal
illness or terminal injury and be unable to express himself or herself, the
wish embodied in the declaration and power of Attorney regarding with
drawal of life sustaining treatment, shall, if it has been in operation for 30
days and has not been duly revoked in writing be given effect to by his
physician or surgeon and members of his or her family.
Withdrawal of life sustaining aids in patients of Terminal Injury
A person who can be declared dead under the law in U.S.A, and
U.K. is considered to be alive in India. Though this may appear illogical,
it is true because brain death is not legally recognised as death of a person
and our law is silent on the issue of brain death. The main problem
arises in road traffic accident victims who are being maintained on conti
nuous artificial respiration by means of mechanical ventilators after sustain
ing irremediable structural brain damage. In such patients doctors are
not lawfully authorised to switch off the respirator.
Legal recognition of brain death will enable doctors to withdraw life
sustaining aids including the respirator, in patients suffering from terminal
injury the moment brain death is diagnosed, especially in patients who
failed to make any declaration in life time or execute powers of Attorney,
expressing their wish for withdrawal of life sustaining aids in the event of
terminal injury.
Diagnosis of Brain Death in Terminal Injury
The code of practice as agreed by Conference of Royal Medical
Colleges and their Faculties of United Kingdom (1976) has advised the
medical practitioners that before considering the diagnosis of Brain Death
three conditions should be present altogether :—
1.
Patient should be deeply comatose :
(a) There should be no doubt that this state is due to depressant
drugs.
(b) Primary Hypothermia as a cause of coma should be excluded.
(c) Metabolic and endoctrine disturbances that may cause or con
tribute to coma should also be excluded.
3
2.
Patient should be maintained on continuous artificial respiration by
means of a mechanical ventilator.
3.
There should be no doubt that patient’s condition is due to the irre
mediable structural brain damage for example severe head injury.
Tests for confirmation of brain death
(i) All brain stem reflexes should be absent.
(a) Pupils are fixed and dilated and do not respond to sharp changes
in incident light.
(b) Corneal reflex absent.
(c) Vestibulo-ocular reflex absent.
(d) Carinal reflex absent.
(e) Gag reflex absent.
(f) No motor response within cranial nerve’s distribution can be
elicited by adequate stimulation of any somatic area.
(g) Spontaneous respirations—Absent with a normal PaCo2} in the
absence of hypothermia.
(h) The oculo-cephalic reflex or doll’s head eye movements must be
absent.
Other Considerations
(i) Repetition of Testing—It is customary to repeat the tests to
ensure that there has been no observer’s error.
(ii) Integrity of Spinal Reflexes—It is well established that the spinal
reflexes may perist after brain death (Ivan Smith 1973).
(iii) Confirmatory Investigations—It is now widely agreed that E.E.G.
(Electro-encephalography) is not necessary for confirmation of
brain death.
(iv) Body Temp.—It is recommended that body temp, should not be
less than 35° C before the diagnostic tests are carried out.
Advantages of Legal Recognition of Brain Death in Terminal Injury
(A) Responsibility of a Doctor : Normally a doctor is not lawfully
authorised to switch off a respirator sustaining the artificial respiration of
a terminally injured patient, lying in a state of coma after sustaining the
irremediable structural brain damage. If a doctor switches off the respi
rator at his own, he will be charged for causing death by an omission.
The recognition of Brain Death legally as death of a person, will save
the doctors from responsibility in such cases of terminal injury.
(B) Organ transplantation : The recognition of brain death of a
terminally injured person in law will enable to the act legally and correctly
4
*
in the field of organ transplantation. After the confirmation of brain
death if a surgeon has to keep on waiting for cardiac arrest to occur before
removing organs for transplantation, a recipient may well receive a
damaged organ and a recipient grafted with a damaged organ will have to
undergo the pain, danger and suffering from two useless operations, namely
one for the insertion of the graft and the second for its subsequent removal.
The most suitable donors for organ transplantation are terminally injured
patients, usually the road traffic accident victims who are being maintained
on continuous artificial (IPPR) respiration by means of mechanical venti
lators after sustaining irremediable structural brain damage. Such people
have been organ donors either in their life times or consent has been
obtained from their relatives. In U.S.A, such patients are also known as
heart beating cadavers. Recognition of brain death as death of such
terminally injured patients will enable doctors to remove the organs from
such decerebrate donors. Normally transplants cannot be lawfully taken
away from a living body if donor can not remain alive without the part
being taken i.e. heart, so for a successful heart transplantation it is to be
removed from a heart beating cadaver only. The most appropriate time
for organ removal is before the vital life support system is withdrawn and
organs are well perfused. Moreover heart has been kept alive and func
tional up to 56 hours after brain death, a duration of time which is long
enough for operative exploration, tissue typing and search for a suitable
recipient.
(C) Economy of Intensive Care Resources : Legal recognition of brain
death as death of a person in case of a terminal injury will help in econo
mising the intensive care unit’s resources in the country, which are being
strained by providing trained man power, intensive care unit beds and
respirator for ventilating these brain dead people who have suffered from
brain death after terminal injuries.
(D) Property Rights : Legal recognition of brain death as death of a
person will have maximum impact in the matter of property rights, negligance claims, insurance, worker’s compensation, probate law and taxes.
A corpse cannot have property. Suppose that X is an old man who
has left Y a large sum in his will. Y himself has suffered from a terminal
injury and is in a state of coma, on artificial respiration at a hospital after
sustaining irremediable structural brain damage. Here doctors are not
lawfully authorised to switch off the respirator so they ask for consent of
relatives but relatives see that Y is kept ‘alive’ on heart-lung machine
because they want X’s money. As soon as X dies the respirator off and
Y is buried. In this example Y is being considered as still alive when X
dies so that his family becomes entitled to property through him. This
dodge will not be successful if Brain Death is legally accepted as death of
a person.
The fact remains although the diagnosis of death is medical, its
definition must be legal. The law protects the living but ceases to protect
the dead (at any rate in the same way) and the line between the two must
be drawn by law. The definition of death presented herein may suit both
medical as well as legal requirements because it does not interfere with the
existing procedure of declaration of death but at the sam? time it includes
the concept of Brain Death in a terminally injured at the hospital level in
the light of the current knowledge on the subject.
5
Definition of Death
‘A person may be pronounced dead, whether inside or outside a
hospital if based on usual and customary standards of medical practices,
it is determined that the person has an irreversible cessation of cerebral,
cardiac and pulmonary functions or a person inside a hospital only can
be declared dead if having suffered from irreversible structural brain
damage, his or her bodily functions cannot be maintained without conti
nuous artificial support, provided the diagnosis of Brain Death in such a
patient is based on diagnostic criteria as agreed by conference of Royal
Medical Colleges and their Faculties of United Kingdom resolved in 1976’.
The above definition of death will be the most appropriate, not only
for declaration of death in a terminally injured patient who has suffered
brain death due is irremediable structural brain damage but will also pave
the way for uniform determination of death in our country.
However it must be emphasised that for declaration of brain death
opinion of two doctors must be obtained out of which one should be the
consultant incharge of the case and the second may be any other doctor, in
case the consultant is not available then his deputy who should have atleast
five years of experience in dealing of such cases after his registration and
none of the doctors who declare the brain death in such a patient should be
the members of transplantation team in case the organ removal has been
planned for transplantation.
Summary and Conclusion
Good medical care includes providing good death in a terminally ill or
terminally injured patient. The dying patient must be considered competent
in terms of capacity for autonomous choice unless proved otherwise. Medi
cal science has now acquired life supporting systems and medications to
extend life artificially for long periods even after loss of brain activities and
control of bodily functions. Many people today have a fear of mind that
they will be kept alive artificially for indefinite periods of time with conse
quent suffering and distress to them and members of their family. The
conflict is often stated to be between doctor’s duty to treat to the best of his
ability and patient’s right to die with dignity, quietly and in peace when
further medical measures prove ineffective and only prolong suffering. Intro
duction of voluntary passive euthanasia in Terminal Care will not only
relieve a certain number of patients from suffering pain and torment which
can be avoided but will also enable the doctors to respond in the interest of
compassion and humanity according to wishes of patients suffering from
terminal illness and terminal injury. In case of a terminally injured patient
who fails to make a declaration or execute powers of Attorney in advance
expressing his wish to withdraw the life supporting treatment legal recogni
tion of brain death will enable doctors to withdraw the life sustaining aid
in a terminally injured patient after the declaration of brain death. Such
a measure legalising brain death as death of a person in the event of termi
nal injury, will be in public interest, for such a measure to be enacted will
not only protect doctors from needless prosecution and persecution but
but will also have numerous other benefits i.e. It will help in the field of
organ transplantation by permitting removal of organs either with the
consent of their relatives or with their own consent in case they happened
6
to be organ donors in their life times, from these terminally injured
patients at a time when they are being sustained on continuous artificial
respiration after suffering from irremediable structural brain damage and
their organs are well perfused; secondly it will help in economising inten
sive care unit’s resources of the country which are being strained by pro
viding trained manpower, beds and respirators for ventilating these heart
beating cadavers, thirdly it will secure a doctor’s right to switch off the
respirator in a terminally injured patient after the confirmation of brain
death in the light of current knowledge on the subject lastly it will help in
the matter of property rights, negligence claims, insurance, worker s com
pensation, probate law and taxes.
References
1. Harward (1968) : Report of Ad Hoc Committee of Harward
Medical School to Examine the Definition of Brain Death, Definition of
Irreversible Coma. J. Amer. Med. Asso. 205, 337.
2. Forrestor, A.C. (1976) : Brain Death and donation of cadaver
kidneys Hlth. Bull. (Edinb.) 34, 199.
3. British Medical Journal (1975) : Brain Death. 1, 356.
4. Ivan, L.P. (1973) : Spinal Reflexes in cerebral death, Neurology
(Minneap) 23, 650.
5. Jonnett, B. (1975) : The donor doctor’s dilemma, observations on
recognition and management of brain death, J. Med. Ethics. 1, 63.
6. Lancet (1974) : Brain Damage and Brain Death, 1, 341.
4
7. H.C. Churchill-Davidson (1984) : A practice of anaesthesia, 5th
Edn. Lloyd-luke ltd. London, Brain-Death, 759-60.
8. Mohandas, A. and Chou. S.N. (1971) : Brain death a clinical and
pathological study. J. Neuro. Surg. 35, 211.
9. Glanville-Williams (1978) : Text Book of Criminal Law, Stevens
and sons. 234-35.
10. Criteria of Death (1984) : Report of consultation workshop,
FIAMC Bio-Medical Ethics Centre Bombay. 20—24.
11. Roger Higgs (1985) : Dying Well : moral challenges in terminal
care, The Practitioner Dec. 1985, Vol. 229, 1073 —76.
12. Journal of Medical Ethics (1983) : ‘Case Conference’ Cutting the
thread and pulling the wool—a request for Euthanasia in general practice,
9, 45—49.
7
INTERNATIONAL CONFERENCE
HEALTH POLICY : ETHICS & HUMAN VALUES NEW DELHI 1986
To Tell or Not to Tell
Professional practices in the care of the dying
S.K. Jindal1
U.N Jindal2
Departments of the Chest Diseases and Obst. & Gynaecology
Postgraduate Institute of Medical Education
& Research Chandigarh
Abstract
Sixty five responses of postgraduate doctors practising in India to a
questionnaire on their beliefs and practice about telling the truth of inevit
able death to their patients were studied. A majority (69.2%) favoured in
telling the truth. Around 50% of their patients were suspected to be aware
of their fate without being told. 40% of the doctors had had one or more
occasion of feeling sorry later on because of their hiding the truth.
Introduction
Doctors differ in their approach about how much and when to tell
the truth to the patient while caring for the dying. Some doctors have
their own dogmas on this issue while others are guided by circumstances.
Those who believe in telling the truth are usually critical of others who are
evasive and use lies; but they themselves are considered unkind by the
others.
There are few studies on medical perspective in the care of the dying
from our country though in the West it has attracted both the professionals
and the lay.1’2 Issues and ethics while dealing with death in India may
not be the same as in the Western countries in view of wide differences in
social, cultural and religious beliefs. How do the doctors in India deal
with patients facing inevitable and/or impending death ? We undertook a
study with the help of a questionnaire on practicing doctors. One hundred
ex-postgraduate students of the Postgraduate Institute of Medical Educa
tion and Research Chandigarh (PGI, Chandigarh), now practicing in the
field and forty non PGI Alumni, Indian Medical Association members were
sent the questionnaire. Since only three of the 2nd group responded we
excluded them from the final analysis. Sixty five of the PGI alumni res
ponded to the questionnaire.
Results
The responses were grouped into two categories depending upon their
belief in telling the truth about the disease and its outcome to their
patients :
Group I : Those who believed in telling the truth (45 : 69.2%).
Group II : Those who did not believe in telling the truth (20: 30.8%),,
1
The reasons favoured by those in favour of telling the truth were :
(i) It pacifies the patient who can accept death more peacefully (61.5%);
(ii) it helps in more effective palliative treatment (81.5%); (iii) the patient
can put the family problems like marriages, transfer and division of assests
etc. to order before death (90.8%); (iv) the patient can fulfil the last wishes
(76.9%); (v) it stops their running around to seek treatment from different
sources (93.8%). Other reasons included economic reasons (i.e. to give
an expenditure versus result ratio to the patient), easier handling by the
family and the patient’s right to know the truth.
Those who were not in favour of telling the truth favoured the
following reasons : (i) it frustrates and angers the patient (86%); (ii) it
makes the family member’s job more difficult (60%); (iii) it is difficult to
tell the hard truth (60%); (iv) the patient may turn to quackery (50.8%).
Group I doctors (90.8%) felt that the truth should be told by the
treating physician only. But 40% of group II doctors thought that if it
has to be told it should be told by some one else eg. a close friend, relative
or a priest.
About the awareness of the patient without being told 60.8 % in
group I and 72.3% in group II thought that over 50% of their patients
knew of their fate.
Only 18.5% had ever felt sorry once or more afterwards about their
decision of informing their patients. But 40.0% had one or more instances
of feeling sorry afterwards when they did not inform the truth. This was
because the patient kept wandering from place to place in search of cure
and spent a lot of money (21.5%), could not settle worldly affairs (9.2%),
or could not complete the last wishes (9.3%). Two doctors admitted of
facing official and/or legal problems in view of their not telling the truth.
However, none was ever charged in the court of law.
Discussion
It is generally believed that the knowledge of death takes away the
charm of living. On the other hand, such a knowledge may dispel the
uncertainty and may give the courage to face the situation. In the
Western experience around 50% of the patients are already aware of their
impending death.3’4 In one study on the dying patients over 60% knew
of this fact and none disapproved of open discussion.3 Our results are
similar to these findings. Most of our doctors have preferred a flexible
policy of discussion guided by ‘situation ethics’ i.e. adapting the ethical
standards to the situation. A majority of them would like to discuss the
truth.
Involvement of the family members and the close relatives was
favoured by most of the doctors. In view of the family structure and
relatively closer ties amongst relatives in Indian set up, this aspect is of
obvious importance.
It may also be worth recalling that 40% of the doctors had felt sorry
at least once each about their hiding, the truth from the patient. The most
2-
important reason here was their failure in giving the patient an opportu
nity to put the worldly affairs in order. This point again needs to be
stressed in our context especially when the head of the family who is often
the sole bread earner of the family and usually the only knowledgeable
person about family assets, debts, loans and other issues, is sick and dying.
Many an official, procedural and legal complications can be avoided if
these things are settled or atleast informed to the kith and kin before
death. The patient also needs to know before hand about the utility of
the expenditure involved in treatment versus the result as the family income
may be meagre. Above all, a doctor is legally obliged to tell the patient
the whole truth and nothing but the truth.
‘The truth’ of course ‘has a broad spectrum with gentleness at one
end and harshness at the other. Patients always appreciate gentle truth.4
References
1. Symposium (1973) ‘Care of the Dying’ Br Med J 1, 29-41.
2. Lamerton R (1973) Care of the Dying. London Priory Press.
3. Hinton J (1974). Talking with people about to die. Br Med J 3,
25-27.
4. Thomson WAR (1977). Care of the Dying. In : A dictionary of
medical ethics and practice. John Wright & sons Ltd. Bristol, p. 107-110.
3
@PRR
s
t'j
NIK
PROTECTION
OF
HUMAN SUBJECTS
CODE OF FEDERAL REGULATIONS
45 CFR 46
Revised as off March 8, 1983
J
PHS
HHS
<
rr".-
/A
I?
NATIONAL RESEARCH ACT
PUBLIC LAW 93-348
JULY 12, 1974
INSTITUTIONAL REVIEW BOARDS; ETHICS GUIDANCE PROGRAM
Sec. 212. (a) Part I of title IV of the Public Health Service Act, as
amended by section 103 of this Act, is amended by adding at the end the
following new section:
"INSTITUTIONAL REVIEW BOARDS; ETHICS GUIDANCE PROGRAM
"Sec. 474. (a) The Secretary shall by regulation require that each entity
which applies for a grant or contract under this Act for any project or
program which involves the conduct of biomedical or behavioral research
involving human subjects submit in or with its application for such grant or
contract assurances satisfactory to the Secretary that it has established (in
accordance with regulations which the Secretary shall prescribe) a board (to
be known as an ‘Institutional Review Board’) to review biomedical and
behavioral research involving human subjects conducted at or sponsored by
such entity in order to protect the rights of the human subjects of such
research.
"(b) The Secretary shall establish a program within the Department
under which requests for clarification and guidance with respect to ethical
issues raised in connection with biomedical or behavioral research involving
human subjects are responded to promptly and appropriately.
(b) The Secretary of Health, Education, and Welfare shall within 240
days of the dale of the enactment of this Act promulgate such regulations as
may be required to carry out section 474(a) of the Public Health Service
Act. Such regulations shall apply with respect to applications for grants and
contracts under such Act submitted after promulgation of such regulations.
THE CODE OF FEDERAL REGULATIONS,
45 CFR 46, IMPLEMENTS THESE AMENDMENTS
TO THE PUBLIC HEALTH SERVICE ACT.
salus ubi multi consiliarii
/
.<
>
/A
CODE OF FEDERAL REGULATIONS
TITLE 45
PUBLIC WELFARE
DEPARTMENT OF HEALTH AND HUMAN SERVICES
NATIONAL INSTITUTES OF HEALTH
OFFICE FOR PROTECTION FROM RESEARCH RISKS
/
J
\
PART 46—PROTECTION OF HUMAN SUBJECTS
REVISED AS OF MARCH 8, 1983
/
45 CFR 46
Page 4
PART 46—PROTECTION OF
HUMAN
SUBJECTS
Subpart A—Basic HUS Policy for
Protection of Human Research
Subjects
Sec.
46.101
46.102
To what do these regulations apply?
Definitions.
46.103 Assurances.
46.104 Section reserved.
46.105 Section reserved.
46.106 Section reserved.
46.107 IRB membership.
46.108 IRB functions and operations.
46.109 IRB review of research.
46.110 Expedited review procedures for
certain kinds of research involving no
more than minimal risk, and for minor
changes in approved research.
46.111 Criteria for IRB approval of
"l- research.
5.112 Review by institution.
46.1 13 Suspension or termination of IRB
approval of research.
46.114 Cooperative research.
46.115 IRB records.
46.116 General requirements for informed
. consent.
1
46.117
Rcllvllies Involving leimc*. prcgnunl
women, or human in vitro fertilization.
46.206 General limitations.
46.207 Activities directed toward pregnant
women as subjects.
46.208 Activities directed toward fetuses in
utero as subjects.
46.209 Activities directed toward fetuses ex
utero. including nonviable fetuses, as
subjects.
46.210 Activities involving the dead fetus,
fetal material, or the placenta.
46.21 I Modification or waiver of specific
requirements.
Documentation cf informed
1 1 ’ consent.
46.118 Applications and proposals lacking
definite plans for involvement of human
subjects.
46.119 Research undertaken without the
■ intention of involving human subjects.
46.120 Evaluation and disposition of
applications and proposals.
46.121 Investigational new drug or device
> 30-day delay requirement.
46.122 Use of federal funds.
46.123 Early termination of research
. funding; evaluation of subsequent
applications and proposals.
46.124 Conditions.
Subpart B—Additional Protections
11pertaining to Research,
I, Development, and Related
I, Activities Involving Fetuses,
Pregnant Women, and Human
1 In Vitro Fertilization
I:
Sec.
46.20.1 Applicability.
46.202 Purpose.
46.203 Definitions.
46.204 Ethical Advisory Boards.
46.205 Additional duties of the Institutional
Review Board! in connection with
/
Subpnrt A — Basic 1IIIS Policy for
Protection of Human Rcsenrph
Subjects
Source: 46 FR 8386, January 26, 198 , 48 FR
9269. March 4, 1983.
§ 46.101 To what do these
regulations apply?
(a) Except as provided in
paragraph (b) of this section, this
subpart applies to all research
involving human subjects conducted
by the Department of Health and
Subpart C—Additional Protections
Human Services or funded in whole
Pertaining to Biomedical and
or in part by a Department grant,
Behavioral Research Involving
contract, cooperative agreement or
Prisoners as Subjects
fellowship.
(1) This includes research
Sec.
46.301 Applicability.
conducted by Department employees,
46.302 Purpose.
except each Principal Operating
46.303 Definitions. —
Component head may adopt such
46.304 Composition of Institutional Review
nonsubstantive, procedural
Boards where prisoneis are involved.
modifications as may be appropriate
46.305 Additional duties of the Institutional
Review Boards where prisoners are
from an administrative standpoint.
involved.
(2) It also includes research
46.306 Permitted activities involving
conducted
or funded by the
prisoners.
Department of Health and Human
Services outside the United States,
but in appropriate circumstances, the
Subpart D—Additions! Protections
Secretary may. under paragraph (e) of
for Children Involved as Subjects in
this section waive the applicability of
Research
some or all of the requirements of
these regulations for research of this
Sec.
46.401 To what do these regulations apply?
46.402 Definitions.
46.403 IRB duties.
46.404 Research not involving greater than
minimal risk.
46.405 Research involving greater than
minimal risk but presenting the prospect
of direct benefit to the individual subjects.
46.406 Research involving greater than
minimal risk and no prospect of direct
benefit to individual subjects, but likely to
yield generalizable knowledge about the
subject’s disorder or condition.
46.407 Research not otherwise approvable
which presents an opportunity to
understand, prevent, or alleviate a serious
problem affecting the health or welfare of
children.
46.408 Requirements for permission by
parents or guardians and for assent by
children.
46.409 Wards.
Authority: 5 U.S.C. 301; sec. 474(a). 88
Stat. 352 (42 U.S.C. 289/-3(a)).
iype(b) Research activities in which the
only involvement of human subjects
will be in one or more of the
following categories are exempt from
these regulations unless the research
is covered by other subparts of this
part:
(1) Research conducted in
established pr commonly accepted
educational settings, involving
normal educational practices, such as
(i) research on regular and special
education instructional strategies, or
(ii) research on the effectivenejss of or
the comparison among instructional
techniques, curricula, or classroom
management methods.
(2) Research involving the use of
educational tests (cognitive,
diagnostic, aptitude, achievement), if
45 CFR 46
/
information taken from these sources subjects cannot be identified, directly
or through identifiers linked to the /
is recorded in such a manner that
subjects cannot be identified, directly subjects.
(6) Unless specifically required by
or through identifiers linked to the
statute
(and except to the extent
subjects.
specified in paragraph (i))» research
(3) Research involving survey or
and demonstration projects which
interview procedures, except where
are conducted by or subject to the
all of the following conditions exist:
approval of the Department of
(i) responses are recorded in such a
Health and Human Services, and
manner that the human subjects can
which are designed to study,
be identified, directly or through
evaluate, or otherwise examine: (i)
identifiers linked to the subjects, (ii)
programs under the Social Security
the subject’s responses, if they
Act, or other public benefit or
became known outside the research,
service programs; (ii) procedures for
could reasonably place the subject at
risk of criminal or civil liability or be obtaining benefits or services under
those programs; (iii) possible changes
damaging to the subject’s financial
in or alternatives to those programs
standing or employability, and (iii)
or procedures; or (iv) possible
the research deals with sensitive •
aspects of the subject’s own behavior, changes in methods or levels of
payment for benefits or services
such as illegal conduct, drug use,
under those programs.
sexual behavior, or use of alcohol.
(c) The Secretary has final
All research involving survey or
authority to determine whether a
interview procedures is exempt,
particular activity is covered by these
without exception, when the
regulations.
respondents are elected or appointed
(d) The Secretary may require that
... public officials or candidates for
specific research activities or classes
public office.
of research activities conducted or
(4) Research involving the
observation (including observation by funded by the Department, but not
otherwise covered by these
participants) of public behavior,
regulations, comply with some or all
except where all of the following
of these regulations.
conditions exist: (i) observations are
(e) The Secretary may also waive
recorded in such a manner that the
applicability of these regulations to
human subjects can be identified,
specific research activities or classes
directly or through identifiers linked
of research activities, otherwise
to the subjects, (ii) the observations
covered by these regulations. Notices
recorded about the individual, if they
of these actions will be published in
became known outside the research,
the Federal Register as they occur.
could reasonably place the subject at
(f) No individual may receive
risk of criminal or civil liability or be
Department funding for research
damaging to the subject’s financial
covered by these regulations unless
standing or employability, and (iii)
the individual is affiliated with or
the research deals with sensitive
sponsored by an institution which
aspects of the subject’s own behavior
assumes responsibility for the
such as illegal conduct, drug use,
research under an assurance satisfying
sexual behavior, or use of alcohol.
the requirements of this part, or tne
(5) Research involving the
individual makes other arrangements
collection or study of existing data,
with the Department.
documents, records, pathological
(g) Compliance with these
specimens, or diagnostic specimens,
regulations
will in no way render
if these sources are publicly available
inapplicable
pertinent federal, state,
or if the information is recorded by
or
local
laws
or regulations.
the investigator in such a manner that
Page 5
(h) Each subpart of these
regulations contains a separate
section describing to what the subpart
applies. Research which is covered
by more than one subpart shall
comply with all applicable subparts.
(i) If, following review of
proposed research activities that are
exempt from these regulations under
paragraph (b)(6), the Secretary
determines that a research or
demonstration project presents a
danger to the physical, menial, or ,
emotional well-being of a participant
or subject of the research or
demonstration project, then federal
funds may not be expended for such
a project without the written,
informed consent of each participant
or subject.
§ 46.102 Dennitions.
(a) “Secretary” means the
Secretary of Health and Human
Services and any other officer or
employee of the Department of
Health and Human Services to whom
authority has been delegated.
(b) “Department” or “HHS”
means the Department of Health and
Human Services.
(c) “Institution” means any public
or private entity or agency (including
federal, slate, and other agencies).
(d) “Legally authorized
representative” means an individual
or judicial or other body authorized
under applicable law to consent on
behalf of a prospective subject to the
subject’s participation in the
procedure(s) involved in the research.
(e) “Research” means a
systematic investigation designed to
develop or contribute to generalizable
knowledge. Activities which meet
this definition constitute “research”
for purposes of these regulations,
whether or not they are supported or
funded under a program which is
considered research for other
purposes. For example, some
“demonstration” and “service
programs may include research
activities.
45 CFR 46
Page 6
unpaid consultant. Changes in IRB
§ 46.103 Assurances.
(f) “Human subject” means a
membership
shall be reported to the
(a) Each institution engaged in
living individual about whom an
Secretary.
*
research covered by these regulations
investigator (whether professional or
(4) Written procedures which the
shall provide written assurance
student) conducting research obtains
IRB
will follow (i) for conducting i s
satisfactory to the Secretary that it
(1) data through intervention or
initial
and continuing review of
interaction with the individual, or (2) will comply with the requirements set research and for reporting its findings
forth in these regulations.
identifiable private information.
(b) The Department will conduct or and actions to the investigator and the
“Intervention” includes both
institution; (ii) for determining which
physical procedures by which data are fund research covered by these
projects require review more often
regulations only if the institution has
gathered (for example, venipuncture)
an assurance approved as provided in than annually and which projects
and manipulations of the subject or
this section, and only if the institution need verification from sources other
the subject’s environment that are
than the investigators that no material
has
certified to the Secretary that the
performed for research purposes.
changes have occurred since previous
research has been reviewed and
“Interaction” includes
IRB review; (iii) for insuring prompt
approved
by
an
IRB
provided
for
in
communication or interpersonal
reporting to the IRB of proposed
the
assurance,
and
will
be
subject
to
contact between investigator and
changes in a research activity, and for
continuing
review
by
the
IRB.
This
subject. “Private information”
assurance shall at a minimum include: insuring that changes in approved
includes information about behavior
research, during the period for which
(1) A statement of principles
that occurs in a context in which an
IRB approval has already been given,
governing the institution in the
individual can reasonably expect that
may not be initialed without IRB
discharge of its responsibilities for
no observation or recording is taking
review and approval except where
protecting the rights and welfare of
’'lace, and information which has
human subjects of research conducted necessary to eliminate apparent
,een provided for specific purposes
immediate hazards to the subject; and
at or sponsored by the institution,
by an individual and which the
(iv) for.insuring prompt reporting to
individual can reasonably expect will regardless of source of funding. This
the IRB and to the Secretary* of
may include an appropriate existing
not,be made public (for example, a
unanticipated problems involving
code, declaration, or statement of
medical record). Private information
risks to subjects or others.
ethical principles, or a statement
must be individually identifiable
(c) The assurance shall be executed
formulated by the institution itself.
(i'.e., the identity of the subject is or
. authorized
-L
.....
by
an individual
to act' r^r
for
This requirement does not preempt
may readily be ascertained by the
on
the
institution
and
to
assume
provisions of these regulations
investigator or associated with the
behalf of the institution the
applicable to Department-funded
information) in order for obtaining
obligations imposed by these
the information to constitute researchi research and is not applicable to any
regulations, and shall be filed in such
research in an exempt category listed
involving human subjects.
form and manner as the Secretary
'(g) “Minimal risk” means that the in § 46.101.
may prescribe.
(2) Designation of one or more
. risks of harm anticipated in the
(d) The Secretary will evaluate all
IRBs established in accordance with
proposed research are not greater,
assurances
submitted in accordance
the requirements of this subpart, and
considering probability and
with
these
regulations
through such
for which provisions are made for
magnitude, than those ordinarily
officers
and
employees
of the
encountered in daily life or during the
meeting space and sufficient staff to
Department
and
such
experts
or
support the IRB’s review and
performance of routine physical or
consultants engaged for this purptose
recordkeeping duties.
psychological examinations or tests.
as the Secretary determines to be
(3) A list of the IRB members
' (h) “Certification” means the
appropriate. The Secretary s
identified by name; earned degrees;
official notification by the institution
evaluation, will take into
to the Department in accordance with representative capacity; indications of consideration the adequacy of the
experience such as board
the requirements of this part that a
proposed IRB in light of the
certifications, licenses, etc.,
research project or activity involving
anticipated scope of the institution s
sufficient to describe each member’s
human subjects has been reviewed
chief anticipated contributions to IRB research activities and the types of
and approved by the Institutional
deliberations; and any employment or subject populations likely to be
Review Board (IRB) in accordance
other relationship between each
with the approved assurance on file at
1 Reports should be filed with the Office
member and the institution; for
for Protection from Research Risks. National
HHS. (Certification is required when
Institutes of Health. Department of Health
example: full-time employee, partthe research is funded by the
time employee, member of governing and Human Services. Bethesda. Maryland
Department and not otherwise exempt
20205.
panel or board, stockholder, paid or
in accordance with § 46.101(b)).
a ■
'I i
•
i ■
•. • •
i.- ii-
*
45 CFR 46
—L
Page 7
(b) Except when an expedited
possessing the professional
review
procedure is used (see
competence necessary to review
§
46.110),
review proposed research
specific reseaich activities, the IRB
at
convened
meetings at which a
shall be able to ascertain the
1 ! IRB
majority
of
the
members of' the
acceptability of proposed research in
are present, including at Lleast
—.. one'
terms of institutional commitments
» are
member
whose
primary
concerns
and regulations, applicable law, and
areas.
In
for
in
nonscientific
areas,
in
order
fui
ithe
standards of professional conduct and
research
to
be
approved,
it
shall
practice. The IRB shall therefore
receive the approval of a majority of
include persons knowledgeable in
those members present at the
these areas. J fan IRB regularly
meeting.
reviews research that involves a
(c) Be responsible for reporting to
vulnerable category of subjects,
the
appropriate institutional officials
including but not limited to subjects
covered by other subparts of this part, and the Secretary 1 any serious or
continuing noncompliancp by
the IRB shall include one or more
investigators with the requirements
individualsJwho are primarily
and determinations of the IRB.
concerned with the welfare of these
subjects.
§ 46.109 IRB review of research.
(b) No IRB may consist entirely of
(a) An IRB shall review and have
men or entirely of women, or entirely
authority
to approve, require
of members of one profession.
modifications
in (to secure approval),
(c) Each IRB shall include at least
or
disapprove
all research activities
one member whose primary concerns
covered
by
these
regulations.
are in nonscientific areas; for
(b)
An
IRB
shall
require that
example: lawyers, ethicists, members
information
given
to
subjects as part
of the clergy.
of
informed
consent
is
in accordance
(d) Each IRB shall include at least
with
§
46.1
16.
The
IRB
may require
one member who is not otherwise
affiliated with the institution and who that information, in addition to that
is not part of the immediate family of specifically mentioned in § 46.116,
be given to the subjects when in the
a person who is affiliated with the
§ 46.104 [Reserved]
IRB’s judgment the information
institution.
would meaningfully add to the
(e) No IRB may have a member
§ 46.105 [Reserved]
protection of the rights and welfare of
participating
in
the
IRB
’
s
initial
or
§ 46.106 [Reserved]
subjects.
continuing review of any project in
(c) An IRB shall require
5 46.107 IRB membership.
which the member has a conflicting
documentation
of informed consent or
interest, except to provide
(a) Each IRB shall have al least
may waive documentation in
information requested by the IRB.
five members, with varying
accordance with § 46.1 17.
(0
An
IRB
may,
in
its
discretion,
backgrounds to promote complete and
(d) An IRB shall notify
invite
individuals
with
competence
in
adequate review of research activities
investigators and the institution in
special
areas
to
assist
in
the
review
of
commonly conducted by the
writing of its decision to approve or
complex issues which require
institution. The IRB shall be
disapprove the proposed research
expertise
beyond
or
in
addition
to
that
sufficiently qualified through the
activity, or of modifications required
available on the IRB. These
experience and expertise of its
to secure IRB approval of the
individuals may not vote with the
members, and the diversity of the
research activity. If the IRB decides
IRB.
members’ backgrounds including
to disapprove a research activity, it
consideration of the racial and
shall include in its written notificalioi
§ 46.108 IRB functions and
cultural backgrounds of members and
________ _
operations.
sensitivity to such issues as
• Reports should be filed wiith the Office
In order to fulfill the requirements
for Protection from Research Risks, National
community attitudes, to promote
of these regulations each IRB shall:
Institutes of Health, Department of Health
respect for its advice and counsel in
and Human Services, Bethesda, Mar>land
(a)
Follow
written
procedures
as
safeguarding the rights and welfare of
20205.
provided in § 46.103(b)(4).
human subjects. In addition to
involved, the appropriateness of the
proposed initial and continuing
review procedures in light of the
probable risks, and the size and
complexity of the institution.
(e) On the basis of this evaluation,
the Secretary may approve or
disapprove the assurance, or enter
into negotiations to develop an
approvable one. The Secretary mayx
limit the period during which any
particular approved assurance or class
of approved assurances shall remain
effective or otherwise condition or
restrict approval.
(D Within 60 days after the date of
submission to HHS of an application
or proposal, an institution with an
approved assurance covering the
proposed research shall certify that
the application or proposal has been
reviewed and approved by the IRB.
Other institutions shall certify that the
application or proposal has been
approved by the IRB within 30 days
after receipt of a request for such a
certification from the Department. If
the certification is not submitted
within these lime limits, the
application or proposal may be
returned to the institution.
•p:
45 CFR 46
Pa^e 8
*
■it
••
•
a statement of the reasons for its
decision and give the investigator an
opportunity to respond in person or in
writing.
(e) An IRB shall conduct
continuing review of research covered
by these regulations at intervals
appropriate to the degree of risk, but
not less than once per year, and shall
. have authority to observe or have a
third party observe the consent
process and the research.
■t
proposals which have been approved
under the procedure.
(d) The Secretary may restrict,
suspend, or terminate an institution’s
or IRB’s use of the expedited review
procedure when necessary to protect
the rights or welfare of subjects.
§46.111 Criteria for IRB
approval of research.
(a) In order to approve research
covered by these regulations the IRB
shall determine that all.of the
§46.110 Expedited review
following requirements are satisfied:
procedures for certain kinds of
(1) Risks to subjects are
research involving no more than
minimized: (i) By using procedures
minimal risk, and for minor
which are consistent with sound
changes in approved research.
research design and which do not
(a) The Secretary has established,
unnecessarily expose subjects to risk,
and published in the Federal
and (ii) whenever appropriate, by
Register, a list of categories of
using procedures already being
— J ‘.search that may be reviewed by the performed on the subjects for
iRB.through an expedited review
diagnostic or treatment purposes.
procedure. The list will be amended,
(2) Risks to subjects are reasonable
as appropriate, through periodic
in relation to anticipated benefits, if
republication in the Federal
any. to subjects, and the importance
Register.
of the knowledge that may reasonably
(b1) An IRB may review some or all be expected to result. In evaluating
pf the research appearing on the list
risks and benefits, the IRB should
through an expedited review
consider only those risks and benefits
procedure, if the research involves no that may result from the research (as
more than minimal risk. The IRB may distinguished from risks and benefits
also use the expedited review
of therapies subjects would receive
procedure to review minor changes in even if not participating in the
previously approved research during
research). The 1RB should not
the period for which approval is
consider possible long,-range effects
aulh?rized. Under an expedited
of applying knowledge gained in the
review procedure, the review may be research (for example, the possible
carried out by the IRB chairperson or effects of the research on public
I by one or more experienced reviewers policy) as among those research risks
lesignated by the chairperson from
that fall within the purview of its
among members of the IRB. In
responsibility.
reviewing the research, the reviewers
(3) Selection of subjects is
!may exercise all of the authorities of
equitable. In making this; assessment
tfte^RB except that the reviewers may the
should take into account the
’
not.disapprove the research. A
purposes of the research and the
research activity may be disapproved
setting in which the research will be
only after review in accordance with
conducted.
the, non-expediled procedure set forth
(4) Informed consent will be
• in,§>46.108(b).
sought from each prospective subject
. ('its(c) Each IRB which uses an
or the subject’s legally authorized
expedited review procedure shall
representative, in accordance with,
adopt a method for keeping all
and to the extent required by
members advised of research
§ 46.116.
•
<
I
(5) Informed consent will be
appropriately documented, in
accordance with, and to the extent
required by § 46.117.
(6) Where appropriate, the research
plan makes adequate provision for
monitoring the data collected to
insure the safely of subjects.
(7) Where appropriate, there are
adequate provisions to protect the
privacy of subjects and to maintain
the confidentiality of data.
(b) Where some or all of the
subjects are likely to be vulnerable to
coercion or undue influence, such as
persons with acute or severe physical
or mental illness, or persons who are
economically or educationally
disadvantaged, appropriate additional
safeguards have been included in the
study to protect the rights and welfare
of these subjects.
§ 46.112 Review by institution.
Research covered by these
regulations that has been approved by
an IRB may be subject to further
appropriate review and approvial or
disapproval by officials of the
institution. However, those officials
may not approve the research if it has
not been approved by an IRB.
§46.113 Suspension or
termination of IRB approval of
research.
An IRB shall have authority to
suspend or terminate approval of
research that is not being conducted
in accordance with the IRB’s
requirements or that has been
associated with unexpected serious
harm to subjects. Any suspension or
termination of approval shall include
a statement of the reasons for the
IRB’s action and shall be reported
promptly to the investigator,
appropriate institutional officials, and
the Secretary.1
’ Reports should be filed with the Office
for Protection from Research Risks, National
Institutes of Health, Department of Health
and Human Services, Bethesda, Maryland
20205.
I
r*'. i •.
I
I: -.!•
*
•
Page 9
45 CFR 46
§ 46.114 Cooperative research.
Cooperative research projects are
those projects, normally supported
through grants, contracts, or similar
arrangements, which involve
institutions in addition to the grantee
or prime contractor (such as a
contractor with the grantee, or a
subcontractor with the prime
contractor). In such instances, the
grantee or prime contractor remains
responsible to the Department for
safeguarding the rights and welfare of
human subjects. Also, when
cooperating institutions conduct some
or all of the research involving some
or all of these subjects, each
cooperating institution shall comply
with these regulations as though it
received funds for its participation in
the project directly from the
Department, except that in complying
with these regulations institutions
may use joint review, reliance upon
the review of another qualified IRB,
or similar arrangements aimed at
avoidance of duplication of effort.
§ 46.115 IRB records.
(a) An institution, or where
appropriate an IRB, shall prepare and
maintain adequate documentation of
IRB activities, including the
following:
- (1) Copies of all research proposals
reviewed, scientific evaluations, if
any, that accompany the proposals,
approved sample consent documents,
progress reports submitted by
investigators, and reports of injuries
to subjects.
(2) Minutes of IRB meetings which
shall be in sufficient detail to show
attendance at the meetings; actions
taken by the IRB; the vote on these
actions including the number of
members voting for, against, and
abstaining; the basis for requiring
changes in or disapproving research;
and a written summary of the
discussion of controverted issues and
their resolution.
(3) Records of continuing review
activities.
J
(4) Copies of all correspondence
between the IRB and the
investigators.
(5) A list of IRB members as
required by § 46.103(b)(3).
(6) Written procedures for the IRB
as required by § 46.103(b)(4).
(7) Statements of significant new
findings provided to subjects, as
required by § 46.116(b)(5).
(b) The records required by this
regulation shall be retained for at
least 3 years after completion of the
research, and the records shall be
accessible for inspection and copying
by authorized representatives of the
Department' al reasonable limes and
in a reasonable manner.
§46.116 General requirements
for informed consent.
Except as provided elsewhere in
this or other subparts, no investigator
may involve a human being as a
subject in research covered by these
regulations unless the investigator has
obtained the legally effective
informed consent of the subject or the
subject’s legally authorized
representative. An investigator shall
seek such consent only under
circumstances that provide the
prospective subject or the
representative sufficient opportunity
to consider whether or not to
participate and that minimize the
possibility of coercion or undue
influence. The information that is
given to the subject or the
representative shall be in language
understandable to the subject or the
representative. No informed consent,
whether oral or written, may include
any exculpatory language through
which the subject or the
representative is made to waive or
appear to waive any of the subject’s
legal rights, or releases or appears to
release the investigator, the sponsor,
the institution or its agents from
liability for negligence.
(a) Basic elements of informed
consent. Except as provided in
paragraph (c) or (d) of this section, in
I!
/
seeking informed consent the
following information shall be
provided to each subject:
(1) A stateiqcnt that the study
involves research, an explanation of
the purposes of the research and the
expected duration of the subject’s
participation, a description of the
procedures to be followed, and
identification of any procedures
which are experimental;
(2) A description of any reasonably
foreseeable risks or discomforts to the
subject;
‘
,
(3) A description of any benefits to
the subject or to others which may
reasonably be expected from the
research;
, ,.
(4) A disclosure of appropriate ,
alternative procedures or courses of
treatment, if any, that might be
advantageous to the subject;
(5) A statement describing the ( ,
extent, if any, to which
confidentiality of records identifying
the subject will be maintained;
(6) For research involving more
than minimal risk, an explanation as
to whether any compensation and an
explanation as to'whether any
medical treatments are available if
injury occurs and, if so, what they
consist of, or where further
information may be obtained;
(7) An explanation of whom to
contact for answers to pertinent
questions about the research and
research subjects’ rights, and whom
to contact in the event of a researchrelated injury to the subject; and
(8) A statement that participation is
voluntary, refusal to participate will
involve no penalty or loss of benefits
to which the subject is otherwise
entitled, and the subject may
discontinue participation at any time
without penalty or loss of benefits to
which the subject is otherwise
entitled.
(b) Additional elements of
informed consent. When appropriate,
one or more of the following elements
of information shall also be provided
to each subject:
|
•
i • •’»
45 CFR 46
*
• i
Page 10
>
x
i
6
i
_____________
.
'I '
.
.
adequate opportunity to read it before
which alters, some or all of the
. (1) A statement that the particular
it is signed; or
elements of informed consent set
treatment or procedure may ■involve
(2) A “short form” written
forth
above,
or
waive
the
risks to the subject (or to the embryo
consent document stating that the
requirements to obtain informed
or fetus, if the subject is or may
elements of informed consent
consent provided the 1RB finds and
become pregnant) which are currently
required by § 46.116 have been
documents that:
unforeseeable;
presented orally to the subject or the
(1) The research involves no more
(2) Anticipated circumstances,
subject’s legally authorized
than minimal risk to the subjects;
under which the subject’s
representative. When this method is
(2) The waiver or alteration will
: participation may be terminated by
used, there shall be a witness to the
not adversely affect the rights and
the investigator without regard to the
oral presentation. Also, the 1RB shall
welfare of the subjects;
subject’s consent;
approve a written summary of what is
(3) The research could not
(3) Any additional costs to the
to be said to the subject or the
practicably be carried out without the
% subject that may result from
representative. Only the short form
waiver or alteration; and
participation in the research;
itself is to be signed by the subject or
(4) Whenever appropriate, the
(4) The consequences of a
the representative. However, the
subjects will be provided with
subject’s decision to withdraw from
witness shall sign both the short form
additional pertinent information after
. the research and procedures for
and a copy of the nummary, and the
participation.
orderly termination of participation
person actually obtaining consent
(e) The informed consent
by the subject;
shall sign a copy of the summary. A
are
requirements in these regulations
(5) A statement that significant
copy of the summary shall be given to
not intended to preempt any
\ new findings developed during the
the subject or the representative, in
applicable federal, state, or local laws
•'burse of the research which may
addition to a copy of the “short
which require additional information
elate to the subject’s willingness to
form.”
.
,
to be disclosed in order for informed
(c) An 1RB may waive the
continue participation will be
consent to be legally effective.
requirement for the investigator to
provided to the subject; and
(f) Nothing in these regulations is
! (6) The apptoximate number of
obtain a signed consent form for some
intended to limit the authority of a
or all subjects if it finds either:
subjects involved in the study.
(1) That the only record linking the
‘ (c) An IRB may approve a consent physician to provide emergency
subject and the research would be the
procedure which does not include, or medical care, to the extent the
physician is permitted to do so under
consent document and the principal
which alters, some or all of the
applicable federal, state, or local law.
risk would be potential harm resulting
elements of informed consent set
from a breach of confidentiality. Each
forth above, or waive the requirement
§ 46.117 Documentation of
subject will be asked whether the
id'oblain informed consent provided
informed consent.
subject wants documentation linking
lhe'IRB finds and documents that:
(a) Except as provided in
the subject with the research, and the
'(1) The research or demonstration
paragraph (c) of this section,
subject’s wishes will govern; or
project is to be conducted by or
informed consent shall be
(2) That the research presents no
subject to the approval of state or
documented by the use of a written e more than minimal risk of harm to
local government officials and is
consent form approved by the 1RB
subjects and involves no procedures
designed to study, evaluate, or
for which written consent is normally
and signed by the subject or the
otherwise examine: (i) programs
required outside of the research
subject’s legally authorized
under the Social Security Act, or
C°?necases where the documentation
representative. A copy shall be given
other public benefit or service
requirement is waived, the IRB may
to the person signing the form.
require the investigator to provide
programs; (ii) procedures for
(b) Except as provided in
subjects with a written statement
obtaining benefits or services under
paragraph (c) of this section, the
regarding
the research.
those programs; (iii) possible changes consent form may be either of the
in-or alternatives to those programs
following:
§ 46.118 Applications and
dr procedures; or (iv) possible
(1) A written consent document
proposals lacking definite plans for
changes in methods or levels of
tll
iu
UU
ivj
»..*
________
that embodies the elements of
involvement of human subjects.
payment for benefits or services under
Certain types of applications for
those programs; and
§ 46 (1& This form may be rea(j t0
grants, cooperative agreements, or
. '(2) The research could1 not
or (he subject,s |egally
’ 1 out without the au(horized repres(;nlalive, but in any
practicably be carried
contracts are submitted to the
_
o
Department
with the knowledge that
waiver
or
alteration.
-(dMJ lRBrm'aynapprove
consent event, the investigator shall give
----- 2 aa consent
the representative subjects may be involved within the
procedure which does not include, or either the subject or t
' * : J'
t I'-1 *'!
', lii'd'
’iC;
I
1 V. ’ I! •
L 4.1.1 . <
JllJ?
• |.l? J I
j q
.1
Page L
45 CFR 46
■ i
period of funding, but definite plans
would not normally be set forth in the
application or proposal. These
include activities such as institutional
type grants (including bloc grants)
where selection of specific projects is
lhe institution’s responsibility;
research training grants where lhe
activities involving subjects remain to
be selected; and projects in which
human subjects’ involvement will
depend upon completion of
instruments, prior animal studies, or
purification of compounds. These
applications need not be reviewed by
an IRB before an award may be
made. However, except for research
described in § 46.101(b), no human
subjects may be involved in any
project supported by these awards
until the project has been reviewed
and approved by the IRB, as provided
in these regulations, and certification
submitted to the Department.
5 46.119 Research undertaken
without the intention of involving
human subjects.
In the event research (conducted or
funded by the Department) is
undertaken without the intention of
involving human subjects, but it is
later proposed to use human subjects
in the research, lhe research shall first
be reviewed and approved by an IRB,
as provided in these regulations, a
certification submitted to lhe
Department, and final approval given
to the proposed change by the
Department.
§ 46.120 Evaluation and
disposition of applications and
proposals.
(a) The Secretary will evaluate all
applications and proposals involving
human subjects submitted to the
Department through such officers and
employees of the Department and
such experts and consultants as lhe
Secretary determines to be
appropriate. This evaluation will take
into consideration the risks to (he
subjects, the adequacy of protection
against these risks, the potential
benefits of lhe proposed research to
lhe subjects ami others, and the
importance of the knowledge to be
gained.
(b) On the basis of (his evaluation,
the Secretary may approve or
disapprove the application or
proposal, or enter into negotiations to
develop an approvable one.
§ 46.121 Investigational new drug
or device 30-day delay requirement.
When an institution is required to
prepare or to submit a certification
with an application or proposal under
these regulations, and lhe application
or proposal involves an
investigational new drug (within the
meaning of 21 U.S.C. 355(i) or
357(d)) or a significant risk device (as
defined in 21 CFR 812.3(m)), the
institution shall identify the drug or
device in the certification. The
institution shall also stale whether the
30-day interval required for
investigational new drugs by 21 CFR
312.1(a) and for significant risk
devices by 21 CFR 812.30 has
elapsed, or whether the Food and
Drug Administration has waived that
requirement. If the 30-day interval
has expired, the institution shall state
whether the Food and Drug
Administration has requested that the
sponsor continue to withhold or
restrict the use of lhe drug or device
in human subjects. If the 30-day
interval has not expired, and a waiver
has not been received, the institution
shall send a statement to lhe
Department upon expiration of the
interval. The Department will not
consider a certification acceptable
until the institution has submitted a
statement that the 30-day interval has
elapsed, and the Food and Drug
Administration has not requested it to
limit the use of (he drug or device, or
that the Food and Drug
Administration has waived the 30-day
interval.
§ 46.122 Use of Federal funds.
Federal funds administered by lhe
Department may not be expended for
research involving human subjects
unless the requirement of these
regulations, including all subputts of
these regulations, have been satisfied.
§ 46.123 Enrly tcimli mt ion of
research funding; evaluation'of
subsequent applications and '*• i
proposals.
; •
(a) The Secretary may require that(
Department funding for any project
be terminated or suspended in the
manner prescribed in applicable
program requirements, when the
Secretary finds an institution has
materially failed to comply with the
terms of these regulations.
(b) In making decisions about
funding applications or proposals
covered by these regulations lhe
Secretary may take into account, in
addition to all other eligibility
requirements and program criteria,
factors such as whether lhe applicant'
has been subject to a termination or
suspension under paragraph (a) of this
section and whether lhe applicant of t
lhe person who would direct the' 1 '
scientific and technical aspects of an.
activity has in the judgment of the
Secretary materially failed to
< ’
discharge responsibility for lhe
;
protection of lhe rights and welfare of
human subjects (whether or not
,
Department funds were involved). .
§ 46.124 Conditions.
With respect to any research
project or any class of research
projects the Secretary may iriipose
additional conditions prior to or at the
lime of funding when in the
Secretary’s judgment additional
conditions are necessary for the .«
protection of human subjects, j
Subpart B—Additional Protections
Pertaining to Research
Development, and Related
Activities Involving Fetuses,’
Pregnant Women, and Human in
Vitro Fertilization
:i .»
Source: 40 FR 33528. Aug. 8. 1975. 43 FR
1758. January 11, 1978. 43 FR f ,
51559, November 3. 1978
’’ '•
§ 46.201 Applicability.
(a) The regulations in this subparl
are applicable to all Department.of ■
Health, Education, and Welfare I
: .H.:i
' Page
' I J1' 12
grants and contract supporting
research, development, and related
activities involving: (1) The fetus, (2)
pregnant women, and (3) human in
vitro fertilization.
(b) Nothing in this subpart shall be
construed as indicating that
compliance with the procedures set
forth herein will in any way render
inapplicable pertinent State or local
laws bearing upon activities covered
by this subpart.
(c) The requirements of this
subpart are in addition to those
imposed under the other subparts of
this part.
*
i
§ 46.202 Purpose.
;! It is the purpose of this subpart to
I
provide additional safeguards in
reviewing activities to which this
subpart is applicable to assure that
ey conform to appropriate ethical
standards and relate to important
societal needs.
45 CFR 46
beat and respiration. The Secretary
may from time to time, taking into
account medical advances, publish in
the Federal Register guidelines
to assist in determining whether a
fetus is viable for purposes of this
subpart. If a fetus is viable after
delivery, it is a premature infant.
(e) “Nonviable fetus” means a
fetus ex utero which, although living,
is not viable.
(D “Dead fetus” means a fetus ex
utero which exhibits neither
heartbeat, spontaneous respiratory
activity, spontaneous movement of
voluntary muscles, nor pulsation of
the umbilical cord (if still attached).
(g) ”/n vitro fertilization” means
any fertilization of human ova which
occurs outside the body of a fernale,
either through admixture of donor
human sperm and ova or by any other
(1) Must be submitted to the Board,
or (2) need not be submitted to the
Board. Where the Board so
establishes a class of applications or
proposals which must be submitted,
no application or proposal within the
class may be funded by the
Department or any component thereof
until the application or proposal has
been reviewed by the Board and the
Board has rendered advice as to its
acceptability from an ethical
standpoint.
(d) No application or proposal
involving human in vitro fertilization
may be funded by the Department or
any component thereof until the
application or proposal has been
reviewed by the Ethical Advisory
Board and the Board has rendered
advice as to its acceptability from an
ethical standpoint.
means.
5 46.205 Additional duties of the
Institutional Review Boards in
connection with activities
involving fetuses, pregnant
women, or human in vitro
fertilization.
(a) In addition to the
responsibilities prescribed for
Institutional Review Boards under
Subpart A of this part, the applicant’s
or offeror’s Board shall, with respect
to activities covered by this subpart,
carry out the following additional
§ 46.204 Ethical Advisory
Boards.
(a) One or more Ethical Advisory
§ 46.203 Definitions.
Boards shall be established by the
i As used in this subpart:
Secretary. Members of these board(s)
(a) “Secretary” means the
shall be so selected that the board(s)
Secretary of Health, Education, and
will be competent to deal with
Welfare and any other officer or
medical, legal, social, ethical, and
employee of the Department of
related issues and may include, for
Health, Education, and Welfare to
example, research scientists,
whom authority has been delegated.
physicians, psychologists,
(b) “Pregnancy” encompasses the
sociologists, educators, lawyers, and
period of time from confirmation of
ethicists, as well as representatives of
implantation (through any of the
presumptive signs of pregnancy, such the general public. No board member
may be a regular, full-time employee
as missed menses, or by a medically
of the Department of Health,
acceptable pregnancy test), until
Education, and Welfare.
expulsion or extraction of the fetus.
(b) At the request of the Secretary,
1 (c) “Fetus” means the product of
the
Ethical Advisory Board shall
conception from the time of
render
advice consistent with the
implantation (as evidenced by any of
policies
and requirements of this Part
•! the;presumpiive signs of pregnancy,
as
to
ethical
issues, involving
. such as missed menses, or a
activities
covered
by this subpart,
medically acceptable pregnancy test),
raised
by
individual
applications or
’ until a determination is made,
proposals. In addition, upon request
following explusion or extraction of
by the Secretary, the Board shall
theifetus, that it is viable.
render advice as to classes of
I (d) “Viable” as it pertains to the
applications or proposals and general
fetus means being able, after either
policies, guidelines, and procedures.
spbptaneous or induced delivery, to
(c) A Board may establish, with
survive (given the benefit of available
the approval of the Secretary, classes
medical therapy) to the point of
of applications or proposals which:
independently maintaining heart
I l!
'r1'
:■ J’..'
>
lr
ffh
duties:
(1) Determine that all aspects of
the activity meet the requirements of
this subpart;
(2) Determine that adequate
consideration has been given to the
manner in which potential subjects
will be selected, and adequate
provision has been made by the
applicant or offeror for monitoring
the actual informed consent process
(e.g., through such mechanisms,
when appropriate, as participation by
the Institutional Review Board or
subject advocates in: (i) Overseeing
the actual process by which
individual consents required by this
subpart are secured either by
approving induction of each
individual into the activity or
4
3
<: j-
45 CFR 46
verifying, perhaps through sampling,
that approved procedures for
induction of individuals into the
activity arc being followed, and (ii)
monitoring the progress of the
activity and intervening as necessary
through such steps as visits to the
activity site and continuing evaluation
to determine if any unanticipated
risks have arisen);
(3) Carry out such other
responsibilities as may be assigned by
the Secretary.
(b) No award may be issued until
the applicant or offeror has certified
to the Secretary that the Institutional
Review Board has made the
determinations required under
paragraph (a) of this section and the
.. Secretary has approved these
determinations, as provided in
5 46.120 of Subpart A of this part.
(c) Applicants or offerors seeking
support for activities covered by this
subpart must provide for the
designation of an Institutional Review
Board, subject to approval by the
Secretary, where no such Board has
been established under Subpart A of
this part.
for terminating the pregnancy solely
in the interest of the activity.
(b) No inducements, monetary or
otherwise, may be offered to
terminate pregnancy for purposes of
the activity.
(40 FR 33528. Aug. 8. 1975. as amended at
40 FR 51638. Nov. 6. 1975)
Page 13
i"7
father are legally competent and have
given their informed consent, except
that the father’s consent need not be
seemed if: (1) His Identity or
whereabouts cannot reasonably be
ascertained, (2) he is not reasonably
available, or (3) the pregnancy
resulted from rape.
.
I
§ 46.209 Activities directed
§ 46.207 Activities directed
toward fetuses ex utero,
toward pregnant women as
including nonviable fetuses, as
subjects. subjects.
(a) No pregnant woman may be
(a) Until it has been ascertained
involved as a subject in an activity
whether
or not a fetus ex utero is
covered by this subpart unless: (1)
The purpose of the activity is to meet viable, a fetus ex utero may not be
the health heeds of the mother and the involved as a subject in an activity
fetus will be placed at risk only to the covered by this subpart unless:
(1) There will be no added risk to
minimum extent necessary to meet
the
fetus resulting from the activity,
such needs, or (2) the risk to the fetus
and
the purpose of the activity is the
is minimal.
development
of important biomedical
(b) An activity permitted under
.
knowledge
which
cannot be obtained
paragraph (a) of this section may be
by other means, or
conducted only if the mother and
(2) The purpose of the activity is to
father are legally competent and have
enhance
the possibility of survival of
given their informed consent after
having been fully informed regarding the particular fetus to the point of
viability.
possible impact on the fetus, except
(b) No nonviable fetus may be
that the father’s informed consent
involved
as a subject in an activity
need not be secured if: (1) The
covered
by
this subpart unless:
purpose of the activity is to meet the
(1)
Vital
functions of the fetus will
health needs of the mother; (2) his
§ 46.206 General limitations.
not
be
artificially
maintained,
identity or whereabouts cannot
(a) No activity to which this
(2)
Experimental
activities which
reasonably be ascertained; (3) he is
subpart is applicable may be
of
themselves
would
terminate the
nof reasonably available; or (4) the
undertaken unless:
heartbeat or respiration of the fetus
pregnancy resulted from rape.
(1) Appropriate studies on animals
will not be employed, and
and nonpregnant individuals have
§ 46.208 Activities directed
(3) The purpose of the activity is
been completed;
toward fetuses in utero as
the development of important
(2) Except where the purpose of
subjects.
biomedical knowledge which cannot
the activity is to meet the health
(a) No fetus in utero may be
be obtained by other means.
needs of the mother or the particular
involved as a subject in any activity
(c) In the event the fetus ex utero
fetus, the risk to the fetus is minimal covered by this subpart unless: (1)
is
found to be viable, it may be
and, in all cases, is the least possible The purpose of the activity is to meet
included
as a subject in the activity
risk for achieving the objectives of
the health needs of the particular fetus
only
to
the
extent permitted by and in
the activity.
and the fetus will be placed at risk
accordance
with the requirements of
(3) Individuals engaged in the
only to the minimum extent necessary
other
subparts
of this part.
activity will have no part in: (i) Any
to meet such needs, or (2) the risk to
decisions as to the timing, method,
(d) An activity permitted under
the fetus imposed by the research is
and procedures used to terminate the minimal and the purpose of the
paragraph (a) or (b) <f>f this section
pregnancy, and (ii) determining the
may be conducted only if the mother
activity is the development of
viability of the fetus at the
and
father are legally competent and
important biomedical knowledge
termination of the pregnancy; and
have
given their informed consent,
which cannot be obtained by other
(4) No procedural changes which
means.
• except that the father’s informed
may cause greater than minimal risk
(b) An activity permitted under
consent need not be secured if: (1) his
to the fetus or the pregnant woman
paragraph (a) of this section may be
identity or whereabouts cannot
will be introduced into the procedure conducted only if the mother and
reasonably be ascertained, (2) he is
i
45 CFR 46
JPage 14
b
i
not reasonably available, or (3) the
pregnancy resulted from rape.
§ 46.210 Activities Involving the
• dead fetus, fetal material, or the
> placenta,
,i Activities involving the dead fetus,
mascerated fetal material, or cells,
tissue, or organs excised from a dead
fetus shall be conducted only in
accordance with any applicable Stale
or local laws regarding such
activities.
§46.211 Modification of waiver
of specific requirements.
Upon the request of an applicant or
offeror (with the approval of its
Institutional Review Board), the
Secretary may modify or waive
specific requirements of this subpart,
with the approval of the Ethical
Advisory Board after such
opportunity for public comment as
the Ethical Advisory Board considers
appropriate in the particular instance.
In making such decisions, the
Secretary will consider whether the
risks to the subject are so outweighed
by the sum of the benefit to the
subject and the importance of the
knowledge to be gained as to warrant
such modification or waiver and that
such benefits cannot be gained except
through a modification or waiver.
Any such modifications or waivers
will be published as notices in the
Federal R egister.
barred by applicable State or local
law.
(c) The requirements of this
subpart are in addition to those
imposed under the other subparts of
this part.
requirements in § 46.107 of this part,
an Institutional Review Board,
carrying out responsibilities under
this part with respect to research
covered by this subpart, shal also
meet the following specific
requirements:
§ 46.302 Purpose.
Inasmuch as prisoners may be
under constraints because of their
incarceration which could affect their
ability to make a truly voluntary and
uncoerced decision v/hether or not to
participate as subjects in research, it
is the purpose of this subpart to
provide additional safeguards for the
protection of prisoners involved in
activities to which this subpart is
applicable.
(a) A majority of the Board
(exclusive of prisoner members) shall
have no association with the prison(s)
involved, apart from their
membership on the Board.
§ 46.303 Definitions.
As used in this subpart:
(a) “Secretary” means the
Secretary of Health, Education, and
Welfare and any other officer or
employee of the Department of
Health, Education, and Welfare to
whom authority has been delegated.
(b) “DHEW” means the
Department of Health, Education,
and Welfare.
(c) “Prisoner” means any
individual involuntarily confined or
detained in a penal institution. The
term is intended to encompass
individuals sentenced to such an
institution under a criminal or civil
statute, individuals detained in other
facilities by virtue of statutes or
Subpart C—Additional Protections
commitment
procedures which
( Pertaining to Biomedical and
provide
alternatives
to criminal
■ Behavioral Research Involving
prosecution
or
incarceration
in a
Prisoners as Subjects
penal
institution,
and
individuals
Source: 43 FR 53655, Nov 16. 1978
detained pending arraignment, trial,
§ 46.301 Applicability.
or sentencing.
(a) The regulations in this subpart
(d) “Minimal risk” is the
(are, applicable to all biomedical and
probability and magnitude of physical
behavioral research conducted or
or psychological harm that is
supported by the Department of
normally encountered in the daily
Health, Education, and Welfare
lives, or in the routine medical,
involving prisoners as subjects.
dental, or psychological examination
(b) Nothing in this subpart shall be of healthy persons.
construed as indicating that
§ 46.304 Composition of
compliance with the procedures set
Institutional Review Boards
forth herein will authorize research
where prisoners are involved.
involving prisoners as subjects, to the
In addition to satisfying the
extent such research is limited or
i-
<1.
/
*.
i
r
r
H
(b) At least one member of the
Board shall be a prisoner, or a
prisoner representative with
appropriate background and
experience to serve in that capacity,
except that where a particular
research project is reviewed by more
than one Board only one Board need
satisfy this requirement.
§ 46.305 Additional duties of the
Institutional Review Boards
where prisoners are involved.
(a) In addition to all other
responsibilities prescribed for
Institutional Review Boards under
this part, the Board shall review
research covered by this subpart and
approve such research only if it finds
that:
(1) The research under review
represents one of the categories of
research permissible under
§ 46.306(a)(2);,
(2) Any possible advantages
accruing to the prisoner through his
or her participation in the research,
when compared to the general living
conditions, medical care, quality of
food, amenities and opportunity for
earnings in the prison, are not of such
a magnitude that his or her ability to
weigh the risks of the research against
the value of such advantages in the
limited choice environment of the
prison is impaired;
(3) The risks involved in the
research are commensurate with risks
that would be accepted by
nonprisoner volunteers;
(4) Procedures for the selection of
subjects within the prison are fair to
Page 15
45 CFR 46
all prisoners and immune from
arbitrary intervention by prison
authorities or prisoners. Unless the
principal investigator provides to the
Board justification in writing for
following some other procedures,
control subjects must be selected
randomly from the group of available
prisoners who meet the characteristics
needed for that particular research
project;
• J
(5) The information is presented in
language which is understandable to
the subject population;
(6) Adequate assurance exists that
parole boards will not take into
account a prisoner’s participation in
the research in making decisions
regarding parole, and each prisoner is
clearly informed in advance that
participation in the research will have
no effect on his or her parole; and
Secretary the proposed research
involves solely the following:
(A) Study of the possible causes,
effects, and processes of
incarceration, and of criminal
behavior, provided that the study
presents no more than minimal risk
and no more than inconvenience to
the subjects;
(B) Study of prisons as institutional
structures oT of prisoners as
incarcerated persons, provided that
the study presents no more than
minimal risk and no more than
inconvenience to the subjects;
;Subpart D—Additional Protections
for Children Involved as Subjects in
Research.
Source: 48 FR 9818, March 8, 1983
§46.401 To what do these
regulations apply?
(a) This subpart applies to all
research involving children as
subjects, conducted or supported by
the Department of Health and
Human Services..
(1) This includes research
conducted by Department
employees, except that each head of
an Operating Division of the
Department may adopt.such
nonsubstantive, procedural
modifications as may be appropriate
from an administrative standpoint.
(2) It also includes research
conducted or supported by the
Department of Health and Human
Services outside the United States,
but in appropriate circumstances, tl
Secretary may, under paragraph (e’
(C) Research on conditions
particularly affecting prisoners as a
class (for example, vaccine trials and
other research on hepatitis which is
much more prevalent in prisons than
elsewhere; and research on social and
psychological problems such as
alcoholism, drug addiction and sexual
(7) Where the Board finds there
assaults) provided that the study may
may be a need for follow-up
proceed only after the Secretary has
examination or care of participants
consulted with appropriate experts
after the end of their participation,
including experts in penology
of §46.101 of Subpart A, waive the
adequate provision has been made for
medicine and ethics, and published
applicability of some or all of the
such examination or care, taking into notice, in the F EDERal R EGISTER,
requirements of these regulations f(
account the varying lengths of
of his intent to approve such research;
research of this type.
individual prisoners’ sentences, and
or
(b) Exemptions (1), (2), (5) and
for informing participants of this fact.
.as listed in Subpart A at § 46.101(b
(D) Research on practices, both
(b) The Board shall carry out such
are applicable to this subpart.
innovative and accepted, which have
other duties as may be assigned by
Exemption (4), research involving
the intent and reasonable probability
the Secretary.
the observation of public behavior,
of improving the health or well
(c) The institution shall certify to
listed at §46.101(b), is applicable t(
being of the subject. In cases in
this subpart where the investigator
the Secretary, in such form and
which those studies require the
does not participate in the activitie
manner as the Secretary may require,
assignment of prisoners in a manner
that the duties of the Board under this
being observed. Exemption (3),
consistent with protocols approved by
section have been fulfilled.
research involving survey or
the 1RB to control groups which may
interview procedures, listed at
not benefit from the research, the
§ 46.101(b) does not apply to reseai
§ 46.306 Permitted research
study may proceed only after the
involving prisoners.
covered by this subpart.
Secretary has consulted with
(c) The exceptions, additions, ai
(a) Biomedical or behavioral
appropriate experts, including experts
in penology medicine and ethics, and
research conducted or supported by
provisions for waiver a^ they appt
in paragraphs (c) through (i) of
DHEW may involve prisoners aS
published notice, in the Federal
R EGIS1 ER, of his intent to approve such
§ 46.101 of Subpart A are applical
subjects only if:
research.
to this subpart.
(1) The institution responsible for
the^conduct of the research has
certified to the Secretary that the
Institutional Review Board has
approved the research under § 46.305
of this subpart; and
(2) In the judgment of the
(b) Except as provided in
paragraph (a) of this section,
biomedical or behavioral research
conducted or supported by DHEW
shall not involve prisoners as
subjects.
§46.402 Definitions.
The definitions in §46.102 of
Subpart A shall be applicable to t
subpart as well. In addition, as usi
in this subpart: •
45 CFR 46
^Page 16
• (a) “Children" are persons who
have not attained the legal age for
consent to treatments or procedures
involved in the research, under the
applicable law of the jurisdiction in
which the research will be
conducted.
(b) "Assent" means a child’s
affirmbtive agreement to participate
in research. Mere failure to object
should not, absent affirmative
agreement, be construed as assent.
(c) "Permission" means the
agreement of parent(s) or guardian to
the participation of their child or
ward in research.
(d) "Parent" means a child’s
biological or adoptive parent.
(e) "Guardian" means an
individual who is authorized under
applicable state or local law to
consent on behalf of a child to
general medical care.
§46.403 IRB duties.
In addition to other responsibilities
assigned to IRBs under this part,
each IRB shall review research
covered by this subpart and approve
only research which satisfies the
conditions of all applicable sections
of this subpart.
§46.404 Research not involving
greater than minimal risk.
HHS will conduct or fund
research in which the IRB finds that
no greater than minimal risk to
children is presented, only if the IRB
finds that adequate provisions are
made for soliciting the.assent of the
children and the permission of their
parents or guardians, as set forth in
§ 46.408.
§46.405 Research involving greater
than minimal risk but presenting the
prospect of direct benefit to the
individual subjects.
HUS will conduct or fund
research in which the IRB finds that
more than minimal risk to children is
presented by an intervention or
procedure that holds out the
prospect of direct benefit for the
individual subject, or by a
• i
I'
monitoring procedure that is likely to
contribute to the subject’s well-being
only if the 1KB finds that:
(a) The risk is justified by the
anticipated benefit to the subjects;
(b) The relation of the anticipated
benefit to the risk is at least as
favorable to the subjects as that
presented by available alternative
approaches; and
(c) Adequate provisions are made
for soliciting the assent of the
children and permfssion of their
parents or guardians, as set forth in
§46.408.
§46.406 Rescnrpli involving greater
than minimal risk and no prospect of
direct benefit to individual subjects,
but likely to yield generalizable
knowledge about the subject’s disorder
or condition.
HHS will conduct or fund
research in which the IRB finds that
more than minimal risk to children is
presented by an intervention or
procedure that does not hold out the
prospect of direct benefit for the
individual subject, or by a
monitoring procedure which is not
likely to contribute to the well-being
of the subject, only if the IRB finds
that:
(a) The risk represents a minor
increase over minimal risk;
(b) The intervention or procedure
presents experiences to subjects that
are reasonably commensurate with
those inherent in their actual or
expected medical, dental,
psychological, social, or educational
situations;
(c) The intervention or procedure
is likely to yield generalizable
knowledge about the subjects’
disorder or condition which is of
vital importance for the
understanding or amelioration of the
subjects* disorder or condition; and
(d) Adequate provisions are made
for soliciting assent of the children
and permission of their parents or
guardians, as set foith in § 46.408.
§ 46.407 Research not otherwise
approvable which presents an
opportunity to understand, prevent, or
alleviate a serious problem affecting
the health or welfare of children.
HHS will conduct or fund
research that the IRB does not
believe meets the requirements of
§§ 46.404, 46.405, or 46.406 only if:
(a) The IRB finds that the research
presents a reasonable opportunity to
further the understanding,
prevention, or alleviation ofja serious
problem affecting the health or
welfare of children; and
(b) The Secretary, after
consultation with a panel of experts
in pertinent disciplines (for example:
science, medicine, education, ethics,
law) and following opportunity for
public review and comment, has
determined either: (1) That the
research in fact satisfies the
conditions of § § 46.404, 46.405, or
46.406, as applicable, or (2) the
following:
(i) The research presents a
reasonable opportunity to further the
understanding, prevention, or
alleviation of a serious problem
affecting the health or welfare of
children;
(ii) The research will be conducted
in accordance with sound ethical
principles;(iii) Adequate provisions are made
for soliciting the assent of children
and the permission of their parents or
guardians, as set forth in § 46.408.
§ 46.408 Requirements for
permission by parents or guardians
and for assent by children.
(a) In addition to the
determinations required under other
applicable sections of this subpart,
the IRB shall determine that
adequate provisions are made for
soliciting the assent of the children,
when in the judgment of the IRB the
children are capable of providing
assent. In determining whether
children are capable of assenting, the
IRB shall take into account the ages,
maturity, and psychological state of
the children involved. This judgment
A
Page 17
45 CFR 46
parents, both parents must give their
may be made for all children to be
permission unless one parent is
involved in research under a
particular protocol, or for each child, deceased, unknown, incompetent, or
as the IRB deems appropriate. If the not reasonably available, or when
IRB determines that the capability of only one parent has legal
responsibility for the care and
some or all of the children is so
custody of the child.
limited that they cannot reasonably
(c) In addition to the provisions for
be consulted or that the intervention
waiver contained in § 46.116 of
or procedure involved in the
Subpart A, if the IRB determines that
research holds out a prospect of
direct benefit that is important to the a research protocol is designed for
conditions or for a subject population
health or well-being of the children
and is available only in the context of for which parental or guardian
permission is not a reasonable
the research, the assent of the
children is not a necessary condition requirement to protect the subjects
(for example, neglected or abused
for proceeding with the research.
Even where the IRB determines that children), iLmay waive the consent
the subjects are capable of assenting, requirements in Subpart A of this
part and paragraph (b) of this section,
the IRB may still waive the assent
provided an appropriate mechanism
requirement under circumstances in
for protecting the children who will
which consent may be waived in
participate as subjects in the research
accord with § 46.116 of Subpart A.
is substituted, and provided further
(b) In addition to the
that the waiver is not inconsistent
determinations required under other
with federal.state or local law. The
applicable sections of this subpart,
choice of an appropriate mechanism
the IRB shall determine, in
would depend upon the nature and
accordance with and to the extent
that consent is required by § 46.116 of purpose of the activities described in
the protocol, the risk and anticipated
Subpart A, that adequate provisions
are made for soliciting the permission benefit to the research subjects, and
their age, maturity, status, and
of each child’s parents or guardian.
condition.
Where parental permission is to be
(d) Permission by parents or
obtained, the IRB may find that the
permission of one parent is sufficient guardians shall be documented in
accordance with and to the extent
for research to be conducted under
§§ 46.404 or 46.405. Where research required by § 46.117 of Subpart A.
(e) When the IRB determines that
is covered by § § 46.406 and 46.407
assent
is required, it shall also
and permission is to be obtained from
!
i
determine whether and how assent
must be documented.
§ 46.409 Wards.
(a) Children who are wards of the
state or any other agency, institution,
or entity can be include^ in research
approved under §§ 46.406 or 46.407
only if such research is:
(1) Related to their status as wards;
or
(2) Conducted in schools, camps,
hospitals, institutions, of similar
settings in which the majority of
children involved as subjects are not
wards.
(b) If the research is approved
under paragraph (a) of his section,
the IRB shall require appointment of
an advocate for each child who is a
ward, in addition to any other
individual acting on behalf of the
child as guardian or in loco parentis.
One individual may serve as
advocate for more than one child.
The advocate shall be an individual
who has the background and
experience to act in, and agrees to act
in, the best interests of the child for
the duration of the child’s
participation in the research and who
is not associated in any way (except
in the role as advocate or member of
the IRB) with the research, the
investigator(s), or the guardian
organization.
45 CFR 46
Page 18
;•
NOTICES
< >
Elsewhere in this issue of the
Federal R egister, the Secretary
is amending 45 CFR Part 46 by,
among other things, adding a new
On March 13. 1975. regulations
Subpart B to provide additional
were published in the Federal
protections pertaining to research,
R egister(40 FR 11854) relating to the development, and.related activities
protection of human subjects in
involving fetuses, pregnant women,
research, development, and related
and in vitro fertilization.
activities supported by Department of
Section 46.203(d) of Subpart B
Health. Education, and Welfare
provides inter alia as follows:
grants and contracts. These
The Secretary may from time to time,
regulations are codified at 45 CFR
taking into account medical advances,
publish in the F ederal R egist er
Part 46.
HUMAN SUBJECTS
Minimum Criteria Identifying the
Viable Fetus
* i
I
guidelines to assist in determining whether a
fetus is viable for purposes of this subpart.
This notice is published in
accordance with § 46.203(d). For
purposes of Subpart B, the guide ines
indicating that a fetus other than a
dead fetus within the meaning of
§ 46.203(f) is viable include the
following:
an estimated gestational age of 20 weeks or
more and a body weight of 500 grams or
more.
FEDERAL REGISTER, VOL 40,
AUGUST 8, 1975
Page 19
45 CFR 46
RESEARCH ACTIVITIES WHICH MAY BE REVIEWED
THROUGH EXPEDITED REVIEW PROCEDURES
I
, ,1
i
!
Research activities involving no more than minimal risk and in which th(
of human subjects will be in one or more of the
only involvement c_
(carried out through standard methods) may be
,Ijss '(carried
following categoric
institutional
Review. Board through the expedited r e v i e v/
reviewed by the -procedure authorized in U6.110 of 45 CFR Part 46.
milliliters in an eight-week
(1) Collection of: hair and
period and no more often than
nail clippings, in a
two times per week, from
nondisfiguring manner;
subjects 18 years of age- or
deciduous teeth; and permanent
older and who are in good
teeth if patient care indicates
health and not pregnant.
a need for extraction.
(5) Collection of both
(2) Collection of excreta
supraand subgingival dental
and external secretions
plaque
and calculus, provided
including sweat, uncannulated
the
procedure
is not more
saliva, placenta removed at
invasive than routine
delivery, and amniotic fluid at
prophylactic scaling of the
the time of rupture of the
teeth and the process is
membrane prior to or during
accomplished in accordance with
labor.
accepted prophylactic
(3) Recording of data from
techniques.
subjects 18 years of age or
(6) Voice recordings made
older using noninvasive
for
research purposes such as
procedures routinely employed
investigations
of speech
in clinical practice. This
defects.
includes the use of physical
(7) Moderate exercise, by
sensors that are applied either
healthy
volunteers.
to the surface of the body or
(8)
The
study of existing
at a distance and do not
data,
documents,
records, #
involve input of matter or
pathological
specimens,
or
significant amounts of energy
diagnostic
specimens.
into the subject or an invasion
(9) Research on individual
of the subject’s privacy. It
or group behavior or
also includes such procedures
characteristics of individuals,
as weighing, testing sensory
such as studies of perception,
acuity, electrocardiography,
cognition, game theory, or test
electroencephalography,
development, where the
thermography, detection of
investigator does not
naturally occurring
manipulate
subjects’ behavior
radioactivity, diagnostic
and the research will not
echography, and
involve stress to subjects.
electroretinography . It does
(10) Research on drugs or
not include exposure to
devices
for which an
electromagnetic radiation
investigational
new drug
outside the visible range (for
exemption
or
an
investigationa.
example, x-rays, microwaves).
device exemption is not
(4) Collection of blood
required.
samples by venipuncture, in
amounts not exceeding 450
* U.S. GOVERNMENT PRINTING OFFICE:
J984-2 1-132:4759
source:
46 FR 8392
1/26/81
!
MR'
’Research Ethics Training Curriculum
http://www.fhi.oig//en/topics/ethics/<urriculum/defaulthtm
Wl’.VAV' ■
m Family Hx+ahh
j Search j
A JL&il irtwtttation&i
HOMc|rAHILV rUfiNHING | HIV/AIDS j VOUTH
FB -
•AWA-.
PAODUOTS/SCRVIOCS | PUDLIOATIONS | ABOUT FHI | COUNTAV PROGRAMS | TOPIOS
wx
..w;
•AW—.V.V
iWAW.W
S
WAVAWAW
sx
. awX'aw
••»a:^:
W
:•••
w
*-
f awr B S.
T.tfl i f
.V.W.
no
•« •»: Ws
SfflwWAVAwXjA ?AW
. W.
...........
w?-'
wX< -
AW
’ ^WTO.Ww'
:«•
-AV
W
s 8*r rs n s § 8 nro
w
av sSaw>h
w
"wavav
It
F:‘
.
........ .
aS.
u
WWW
j
•entf-.'M
7*
Family Planning | HIV/AIDS | Services & Products | Publications | About FHI | Countries | Home
Publications Catalog | Books & Reports | Training & Multimedia | Periodicals | Search
Africa & Near East | Asia | Europe & Central Asia | Latin America & Caribbean | North America | All Regions
© Copyright 2001. Family Health International (FHI).
URL: http://www. fhi. org
If you experience problems browsing this page, please send e-mail to Webmaster
of 1
9/20/02 11:01 AM
http://^¥ww.fhi.org/en/topics/e^
Research Ethics Training Curriculum: Self Study, Introduction
-I of3
I
family Htaafoh
^=4^
Searcq j
HOME JrmilLV FLOHHIHG t mv. nio; I YOUTH i rROOUOTJ/ffEnVIOCS i rUDLIOATIONS i ABOUT FHI joOUNTAV PROGRAMS i TOPICS t.
|
Introduction to
Research Ethics
Training Curriculum
How to Use
this Curriculum
Getting Started
Disclaimer:
Some
interactive
features of this
curriculum are
not compatible
with older
browsers.
Older Browsers:
Help
Self Study
Introduction to the Research Ethics Training
Curriculum
It is essential that fundamental ethical principles be included in the
design and implementation of research involving human
participants. Ethical research principles are considered universal,
transcending geographic, cultural, economic, legal and political
boundaries.
Although these principles are universal, the availability of the
resources needed to maintain these principles is not universal, and
the procedures used for the ethical vigilance of research studies
may not be optimal. For instance, no universal principle exists to
monitor how research will be conducted.
Regardless of limitations, ethical research principles must guide
those who plan, conduct and sponsor research that involves human
participants. Human participation in research projects has
contributed to better quality of iife through the development of
diagnostic tools and successful treatments.
This Research Ethics Training Curriculum has been developed for
international researchers who:
• conduct research that includes human
participants
• want to incorporate fundamental ethical
considerations in design and implementation of
their research
The Lotus Flower
The Research Ethics Training Curriculum uses the lotus flower to
symbolize fundamental ethical elements. The lotus flower image
represents "purity and perfection" in some cultures. The ethical
considerations discussed in this curriculum aim for a pure and
perfect research designflthe foundation on which ethical research
study is developed and implemented.
However, each research design will be unique in that it will be:
• specific to the studyOs design and research
outcomes
• important to the local research population
• intrinsic to the local culture
9/20/02 11:03 AM
http://www.fhi.org//ew1»pics//etluqs/cumculuin//iritro.htm
Research Ethics Training Curriculum: Self Study, Introduction
->of3
Because each research design will be unique, a different lotus
flowerNrepresenting the local culture and characteristics of each
research studyfiis shown at the beginning of each section of the
Contents section of the Research Ethics Training Curriculum.
MW.'.WAW.
.wwwwwww
The Research Ethics Training Curriculum offers international
researchers:
• an overview to the development and
philosophy of research ethics
• case studies so that the learner can consider
real-world examples of ethical issues
• materials to assist researchers in designing
studies that respect local regulations, cultures
and expectations
• ancillary reference documents on modem
perspectives that shape the research ethics
field
The researcher sets as a primary goal the protection of research
volunteers while at the same time incorporating ethical
considerations for project design and implementation.
The principles of research ethics have grown out of abuses in the
past. Today a great amount of attention is directed at research that
involves human participants. International research ethics ensure
that research conducted at the local level follows international
expectations and standards. Following such international
expectations validates the time and energy invested by the
researcherAas well as the good will and trust invested by the
participants.
It is essential that local researchers familiarize themselves with the
subject matter in this curriculum. Knowing current attitudes about
research ethics will assist each researcher in aiming for the goal
symbolized by the lotus flowerApurity and perfection in each
research study.
Back
Next
Introduction I Contents I Case Studies I Post Testing I References I Credits
Research Ethics Training Curriculum: Self Study, Introduction
http://^¥ww.fhi.org//en/'topics/ethics/curriculum//mtro.htm
Presenter
Shortcut
Family Planning | HIV/AIDS | Services & Products | Publications | About FHI | Countries | Home
Publications Catalog I Books & Reports | Training & Multimedia I Periodicals | Search
Africa & Near East | Asia | Europe & Central Asia | Latin America & Caribbean | North America | All Regions
© Copyright 2001, Family Health International (FHI).
URLhttp:/Mww.1hi.org
If you experience problems browsing this page, please send e-mail to Webmaster
»f3
9/20/02 11:05 AM
http://^¥ww.fhi.org//ew/topics/ethics/curriculum/>esenters/presintrolitm
Research Ethics Training Curriculum
■1 of 3
f...
i Search
Family Hiaatth
J
home § ratia.v rLANMiric |iiiv.*aio$ J youth j rnoouoTS.’scnvjocs £ ruotioATiOHs J about rm Soouhtav rnocnAMs t topios
.W.-.VZwAwAVAV.V.V.WAV.V/^.V.V.W.V.-S%WAV.V.W.WAr.W.V.W.,.W»W.W..V.'.'.-W.V.VAVAWnV.VAW.VZ.V.^.VAVlWV.VA-AVAV.W.W.VA-AV^
iwpi
How to Use this
Curriculum
Presenter
Getting Started
How to Use This Curriculum
Presenter Tools
Disclaimer:
Some
interactive
features of this
curriculum are
not compatible
with older
browsers.
Older Browsers:
Help
This Research Ethics Training Curriculum is designed to engage the learner. Adult
learning and retention improves when the learner participates actively in the learning
process. The Research Ethics Training Curriculum can be used as either an interactive
self-study program or as a participatory, group training experience, it is expected that
completing this curriculum will take approximately 4 hours. If you are a self-study user
or a first time group presenter, please click your browser’s back button twice and
choose the Self Study option or use the Self Study Shortcut at the bottom left of
this screen. Note that while in the Self Study section, you will find a Presenter Shortcut
link in this same location. We recommend that group presenters work through the
self-study version of the curriculum first, to prepare for the group training. After
completing the seif-study version of the curriculum, group presenters should return to
this point to prepare to lead a training session using the Presenter Tools.
The Presenter Tools contain print and projection tools in Adobe© Acrobat© format,
including:
•
•
•
•
•
•
Color Slides for Online Presentation
Master Slides for Overhead Projection
Presenter Notes
Student Handouts
Case Studies
Evaluations
The Color Slides for Online Presentation section is for presentation on a computer
screen or projection from a computer. If an overhead projector is your only available
projection device, print the Master Slides for Overhead Projection and copy onto
transparencies for presentation.
Use the Presenter Notes section to print speakers notes for yourself, and review them
before presenting. The Presenter Notes section is composed of grayscale summary
slides followed by narrative text. At times, the narrative is followed by a shaded box
labeled Obeamer Note.6 Learner notes contain interactive questions or activities. Ask
the group to call out or write on flip chart paper some answers to the questions asked b•y
the learner notes. This will help your participants retain the key messages.
Use the Student Handouts section to print note-taking handouts for your participants.
Each page displays three slides with space for taking notes during the presentation.
These can be printed in color or grayscale.
The Case Studies section provides 8 reproductive health case studies followed by
thought provoking questions. The case studies help anchor the curriculum to the reality
of designing and implementing research studies. These case studies address
reproductive heaith ethical considerations and are based on actual situations
encountered by researchers at Family Heaith international (FHi).
Five of these case studies are found in the Narrative section of the curriculum; the other
3 case studies are found only in the Case Studies section. You will want to print a copy
for yourself and photocopy the case studies for your participants to have available
9/20/02 11:06 AN'
httpjVwww.fhi.org/'ewtopics/ethics/curriculunk'presenters/presintro.htm
■Research Ethics Training Curriculum
-2 of 3
during the training session.
The Evaluations section includes a Pre-Test, a Post Test, an answer key to the Pre and
Post Test, and the Evaluation form. Please inform your participants that in order to
receive their certificate of completion, they need to fill out the Evaluation form and send it
to FHI at the address provided in the next section.
Note: If you have Microsoft PowerPoint installed on your computer, there Is a fully
functional version of the Color Slide Show with Presenter's Notes in a folder on the CD
directory of the Research Ethics Training Curriculum CD.
Back
W" Next
Introduction I Presenter Tools I Self-Study I References I Credits
9/20/02 11:06 AM
wysiwyg:/Z157/http://^¥ww.fhi.org/'eiv/^/nfp.h^
FHI: Improving Contraceptive Choices and Services
\ Easy Links
Francois | Espafiol | Russian pyrrimC | Arabic
V.V.V.WAVA-.V.VAVAW.WAW.VAVAWAV.V.WAVZ?JWMWAWAWAV.W?AWAW.W.W.WA^
Contraceptive FAQs
.^V.VAV.W•VW/.WW.V/.V.WWMWW.W/.VA• ’
Youth Net Overview
....
Family
Ramiing
What's New
H Search \
Improving Contraceptive Choices and Services
'y
'V-'';;y
For nearly 30 years, FHI has focused on strengthening the
capacity of partners in developing countries to improve
contraceptive choices and services through contraceptive
development, research, education and information programs.
FHI has worked to improve the safety, efficacy, acceptability and correct use of nearly
every contraceptive method currently in use. We conduct studies on contraceptive
methods and their use, the relationship between contraception and sexually
transmitted diseases, health economics, maternal mortality and morbidity, and the
reproductive health needs of special groups, including young adults and refugees.
Current and recent programs:
Older Browsers: Help
• The Contraceptive Technology and Family Planning Research Project, funded
by the U.S. Agency for International Development, includes ongoing research,
technical assistance and educational activities in more than 30 countries each
year.
• Selected projects: Among our many ongoing family planning projects are
efforts in collaboration with the World Association of Giri Guides and Giri
Scouts to improve the health of female adolescent refugees; a multi-center
study on the spermicide nonoxynol-9 (N-9) for the National Institute of Child
Health and Human Development (NICHD); participation in a Cochrane
Collaboration on fertility regulation; evaluation of the UNFPA-supported
adolescent reproductive health program in Jamaica; training of reproductive
health managers and providers in Haiti, and collaboration with the Population
Council on the Frontiers Project.
• Fellowship: An FHI Fellowship in Contraceptive Technology Research brings
outstanding scientists to the United States from developing countries. A year
of advanced study in clinical trials design and implementation is followed by a
fellowship-sponsored research project conducted in the participant's home
country.
• Our recently completed Women's Studies Project (WSP) (1993-1999), funded
by USAID, examined how women's family planning experiences - their
contraceptive use or non-use, pregnancies and childbearing, and experience
with family planning and reproductive health programs - affected women's
lives in 14 countries.
Select key words on the drop-down list and hit "Enter" to launch a search, or click
here to conduct a simple or advanced search using other terms.
Summaries of FHI contraceptive research
Network magazine on family planning and reproductive health.
The FamPlan Glossary: This collection of terminology provides translations in English,
1 <jf2
9/20/02 12:47 PM
FHI: Improving Contraceptive Choices and Services
Wysiwyg://! 574ittp://www fhi.org/en/fp/nfp.html
Spanish and French of reproductive health terms. It was created in order to provide
standardized translations for member organizations of the Population and Health
Materials Working Group (PHMWG). The PHMWG is a group of cooperating
agencies that work with USAID's Office of Population, Health and Nutrition and
produce reproductive health materials for use around the world.
Family Planning | HIV/AIDS | Youth | Services & Products | Publications | About FHI | Countries | Topics | Home
Publications Catalog | Books & Reports | Training & Multimedia | Periodicals | Search
Africa & Near East 1 Asia | Europe & Central Asia | Latin America & Caribbean | North America | All Regions
© Copyright 2002, Family Health International (FHI).
URL http://www.fhi.org
If you experience problems browsing this page, please send e-mail to Webmaster
September 20, 2002
of 2
9/20/02 12:47 PM
wysiwyg://160/http:/7www.fhi.drg/en/aids/ndds.hti^
FHI: International leadership in HIV/AIDS prevention & care
M
j Easy Links
Francais | Espafiol | Russian pycCKttfil Arabic
:>.VAW.W\«VAV.VAW.\WA^\WA\W/.W?.WZA\W.VAJ.W.\WJWAW\WAVAWA-AWA\WAVAWW.WW.V.'.W.W.*".V.V.'. ’
News release: fhi
Recognizes Four
Orqanizaticns for
HIV/AIDS Efforts
K:;
jweMMMWKc ❖: • :• >:<• < ”•»
■H FHtV/AlDS
ivXv.v T
w.’.
XfcVW.'.W.'.SV.W
.v.............. .7.. JwXw*
>.
What’s New
,, yAW.VZ7AVZ/A%V/A.V.W.VA
H Search \
International leadership In HIV/AIDS prevention & care
Since 1986, Family Health International has pioneered ways to
curtail the spread of HIV/AIDS. Many of the HIV prevention "best
practices" in use today have emerged from FHI’s work in more
than 60 countries.
MM
Interventions for HIV prevention
j ;J
FHI’s efforts range from clinical trials of promising HIV/AIDS prevention methods to
managing and supporting prevention and care programs worldwide. These include:
Mato7<
• Behavior Change Interventions (BCIs)
• Blood safety and universal precautions
• Behavioral Surveillance Surveys
• Care and support for families, people with AIDS, and orphans
Older Browsers: Help
• Counseling and testing
• Evaluation and surveillance
•
•
•
•
•
•
•
Policy support
Prevention research
Reproductive health service integration
Sexualiy transmitted infection (STI) management
Technical services
Tools for prevention and care
Tuberculosis prevention and management
FHI’s HIV/AIDS programs
FHI began its AIDS prevention efforts with pilot AIDS prevention programs in West
Africa. FHI’s leadership role in the effort to slow the spread of HIV in the developing
world has continued through our AIDSTECH, AIDSCAP. and HIVNET projects.
Ongoing programs include our IMPACT Project, supported by USAID, and HPTN
Project, supported by NIH.
Where we work
FHI currently conducts HIV/STI prevention and care programs in more than 30
counfries in Africa and Near East, Asia, Eastern Europe, Latin Amenca and the
Caribbean and North America.
Publications
• Workplace HIV/AIDS Programs: An Action Guide for Managers (pdf
952K*)
• HIV/AIDS Prevention and Care in Resource-Constrained Settings: A
Handbook for the Design and Management of Programs
1 of 2
9/20/02 12:49 PM
•FHI: International leadership in HIV/AIDS prevention & care
wysiwygi/VlGOZhttpz/Twww.fhi.org/en/aids/iiaids.litml
This 28-chapter handbook offers state-of-the-art knowledge on
designing and managing HIV/AIDS programs; reducing risk and
vulnerability to HIV infection; strengthening STD management and
services; reducing risk of HIV infection to infants; reducing risk of
parenteral transmission; management and support of people infected
and affected by HIV/AIDS; and prospects for the future. It is intended to
be used by program managers, technical and programmatic field staff;
staff of donor and international partner agencies; health care providers;
and field researchers.
• Strategies for an Expanded and Comprehensive Response (ECR) to a
hiationai HiV/AiDS Epidemic
• FHI/UNAIDS Best Practices in HIV/AIDS Prevention Collection (pdf
11.914K*)
State of the Art Briefs on HIV/AIDS
Supporters and partners
FHI has worked with more than 500 organizations worldwide to support and improve
HIV/AIDS prevention and care programs.
Family Planning | HIV/AIDS | Youth | Services & Products | Publications | About FHI | Countries I Topics | Home
Publications Catalog | Books & Reports | Training & Multimedia | Periodicals | Search
Africa & Near East | Asia | Europe & Central Asia | Latin America & Caribbean | North America | All-Regions
© Copyright 2002, Family Health International (FHI).
URL http://www.fhi.org
If you experience problems browsing this page, please send e-mail to Webmaster
September 20, 2002
.oH
9/20/02 12:49 PM
vvysivvyg://167/http:A\v^v-\fhi.org'/eiVgen/'npr(xlsen'-.html
FHI: Services and Products
Frangais | Espafiol | Russian pycCKWfi | Arabic
j Easy Links
I •
'WSS»
I
What's New
..................................... ■ VA\VA\\W.\V.WZ/A%V.W.V,
... n Search j
Family Health International offers a range of technical services,
publications and other materials focusing on contraceptive
technology, HIV/AIDS and sexually transmitted diseases, and
improving the health and well-being of women of reproductive
Featured service*:
age.
■-w.w.w
Major capabilities and areas of technical expertise
Applied research: FHI’s experience conducting thousands of
research studies in more than 100 countries since 1971
includes biomedical, programmatic and behavioral studies
using a vast array of study methodologies and approaches:
formative research, feasibility assessments, case studies,
clinical trials, situation analyses, longitudinal studies, policy
assessments and meta-analyses of existing data.
Older Browsers: Help
Research capacity building: Through collaborative research
and educational activities, FHI strengthens skills for local
ownership, management and implementation of health
programs. FHI staff provide technical assistance to
investigators around the world in various quantitative and
qualitative data collection techniques, including focus groups,
market analysis, clinical trials, surveys and questionnaires, as
well as operations research and epidemiological, clinical,
biomedical, demographic and economic studies.
Clinical research design
and management
Pharmalink: Web-based
data management
International Clinical
Studies Support Center
Training Presentation
Modufee:::::::::::::::::-;:::::::
Health economics
research
care, capabilities and
service*
FHI puMicotions
Education & training in
reproductive health
Maternal Health Center.
reducing mortality and
HIV prevention programming: FHI designs, manages and
morbidity
evaluates comprehensive programs, providing documented
accountability in both program impact and financial
management. We offer the full range of technical services
neeoeo for effective efforts to control the epidemic, including
behavior change interventions; prevention and management of
sexually transmitted infections: voluntary HIV counseling and
testing, support for people infected and affected by HIV,
preventing mother-to-child transmission of HIV; blood safety;
and evaluation and surveillance. FHI has pioneered programs
to meet the complex needs of mobile populations and to
piovide peer education and other HIV prevention services in
workplaces. We have also expanded efforts to reduce HI V risk
behavior among marginalized groups to reach men who have
sex with men and drug users. Our expertise in participatory strategic planning and
community mobilization has helped create and nurture hundreds of grassroots
prevention and care projects. This broad experience in community-based programs,
which FHI developed by managing more than a thousand interventions in over 60
countries, is now being applied to improve tuberculosis treatment and prevention and
to strengthen blood donor recruitment and retention.
Training and education: FHI strengthens the skills of developing country
researchers, service providers, program managers and health communicators to
ensure the highest quality work in our collaborative projects. Health organizations and
donor agencies provide financial support to us to conduct training and continuing
medical education programs which focus on: contraceptive technology; research
of2
9/20/02 12.51 PM
wysiwyg://167/1ittp://www.fhi.org//ei|'f
'geiv'nprodserv. html
I
FHI: Services and Products
methods; research monitoring; clinical management; data analysis; epidemiology;
clinical skills enhancement; program development; STD/HIV prevention and
treatment; qualitative research: gender-sensitive research and programs; training
materials development; provider counseling; training of trainers; and health
journalism.
Scientific publishing: FHI publishes several periodicals, including Network (circ.
Zb,000 in English, French and Spanish) and IMPACI on HIV (circ. 5,000 in English).
FHI publishes reports, case studies, monographs and training materials on a broad
range of reproductive health topics, including in Arabic, English, French, Portuguese,
Russian and Spanish.
Information dissemination: As part of its public health mandate, FHI is committed to
disseminating research findings and helping developing country counterparts
strengthen their own information dissemination capabilities. FHI works with
organizations to assess communication skills and resources, prepare information
campaigns and materials, strengthen media relations, write and disseminate scientific
papers, produce publications, and plan strategic dissemination.
Maternal health: FHI works to reduce maternal mortality and morbidity. We develop
strategies to improve maternal and neonatal care at all health system levels, and
assist governments and other health organizations to assess their maternal health
needs, plan for solutions and translate their plans into action. FHI designs,
implements and evaluates innovative interventions, and disseminates information on
maternal health to clinicians, consumers, policy-makers and the scientific community.
How to contact us
To learn more about technical services please contact Albert J. Siemens PhD, Chief
Executive Officer, Family Health International, P.O. Box 13950, Research Triangle
Park. NC 27709 USA. Email: services@fhi.org
Family Planning | HIV/AIDS | Youth | Services & Products | Publications | About FHI | Countries | Topics | Home
Publications Catalog j Books & Reports | Training & Muitimedia | Periodicals | Search
Africa & Near East | Asia | Europe & Central Asia | Latin America & Caribbean | North America | All Regions
© Copyright 2002, Family Health International (FHI).
URL: http://www.fhi. org
If you experience problems browsing this page, please send e-mail to Webmaster
September 20, 2002
2 on
9/20/02 12:51 PM
- Media
 RF_MP_2_A_SUDHA.pdf
RF_MP_2_A_SUDHA.pdf
Position: 425 (31 views)