ASF SEMINAR RIGHT TO HEALTH CARE
Item
- Title
- ASF SEMINAR RIGHT TO HEALTH CARE
- extracted text
-
RF_L_3_A_SUDHA
j) Pedal' c. [4ecJjM-> Q^-f^
Sy£t<om'. T)m-eaj€y‘
_ c
e>p^lcmS
, A
i) Ccnornuu^'ccJn’ooo -
PEOPLE
- De vi^el UJe*<«oe/7
i) Meobaa.^A
/4o5lJJ^ Cq
,4^Aj^O
Asv
V
I4o=uAPm «vo
q.
^-ej'r&naj
/7-tl
/W
Gn
Cbr)£uJU-CLhcyn
hjs - 16-1/ /^jjr 2c>c>l, N H R. C .
~r^a-^
Wo v <
— Prbkcccj
z) A- (bncx^^ pcx-p<4
i-wu4>
r2
on
Pessf
/;
h
/f
I© "T,eetdn
IQ<cc>m l-fc
^)Tke
QrcM- /Probe© '‘
mQrv,
Icctlbej-^,
PeoJtST- lx) fc^jcJq.GL
^nSfc P^cm& A
»5
oil o c.q nnerch
Gvig^? —
t-g> kxLGuU^t Ccire Q<?
CU7
k>
- Hnenkd
BqcJt_£>TrGU)nc3/
b>
l4e4aJjb> G^v-e
JTC, (
rPe-d/ Ccj tas’uranQ-
LJ 0 wi’G^n^c
^CCe^si
—’
C&jY'e • P horyji'ov.
CaTf*
RFMH-fl fs
v
U^Y-e^cAseJ, Pr. /)vo(g .
CEU'npctJdr)
^5
o
*4^ve. l^-cojj-h
PI q h nJ
1^)
h
pnrim^ryy
— Dy.
*9 PeopJk
S’. 0u& Qfpqrcr^l
_pv,
Co Im muirJ
ip Ui<^e^xcJ
i' olc-a.
Atccz^ /» kedK)
y n
CK-|O p'Y OQC^)
(Irovry
SKxMi.
|4<-cjLH>»
UAJve^scJI
lo)
PcJadc l~^ru(y^>
<3 n
|^e_£U_^) Gcir^
'fe»
So^dLc VS.
f-btmah Pi'gtd' - A-cw Cha<+€/7,
l-Mmoun
Pt.
£ e^alb^. oJ
j>a^<-o|
—
KY>cdd-C^ xJ
|e>
— SqrhQ
C^pnopCciof)
l4e_cvLM _
’X
JRb' h> rtenW
ftincU**-.
3
Or^
UJorvie^'t
UJowierj'x
1
tjl^beJ Nefuftvt
■
1^* ^s.
«- Hehah-C„bt lUc.Jv.Vo'mH
Ife) G-S’ha.hJb’S hfn
q
vecJlis h’c-
$ Pepo 'fb
•ao) Repc*'
oy>
C Rt-
3
qpp/Stata
Batik of -My^ge -crn#/
Vz> HeoJU-h Ca-re' SerninQ*-Osp
rR.t
LjculcB
GY)
tleaJjH)
iQ Rl.
^checL-Uj)
O^V-CxI^qI
P*-e^en kk>1^« 1
l\ n-v*-^
lY)eeJ'z
G^Ye- — G»nnpc^,^n
c*>
- p <e>oe
+t> Ut-cJU-h Cq-r-e’ — Is !(_
T-
—
NoJicxnoj
A-C'cCx^
J)i< fir)
CenoJ uJln
5,
Py . Ro X/ i »
C© n $
o-o
Ptvj} 03
Joseph cA
0/Gv. Ay£ I© WojAh
T
2
co
%
5
S
•n
i
2
E
is
£
8
§
B
s
5
0100027
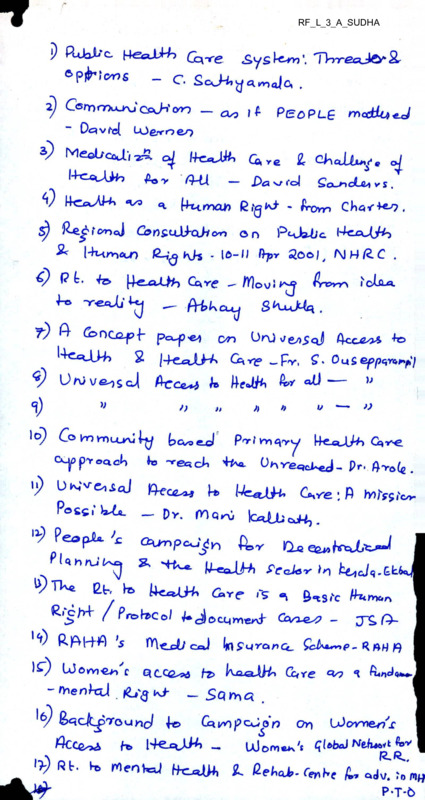
Public Health Care System: Threats and Options
(Concept paper for the mfc annual meet, 2003, draft)
C Sathyamala
The theme for the next Annual Meet, “Public Health Care System: Threats and Options”, is
being proposed at a time when the health care system in India is undergoing a radical
transformation. The massive expansion of the private medical sector, entry7 of private
insurance in medical care, introduction of payment (“user fees”1^1) for medical services in the
government sector are just three such changes we have witnessed in the last decade. The
rapidity with which these changes are taking place leads one to view such developments with
great trepidation. It could well be that in a matter of few years we will have installed the
American model of high-cost, profit-driven, technology intensive, unjust, inequitable health
care system in our country7. This view may perhaps be dismissed as being unnecessarily
alarmist, but there is certainly a general concern that soon health care is going to be out of the
reach of ordinary people.
The growing sense of disquiet many of us are experiencing is beginning to be voiced in
public fora with, surprisingly, the government and its agencies too joining in at the chorus. As
a sign of good "governance”2121, a dual system (one for the rich and one for the poor) is being
proposed to tackle the issue of equity in health care without in any w ay disturbing or altering
the process of disinvestment that has been set into motion. A high-technology based medical
service on par with what is available internationally elsewhere, is to be provided by the
private sector for the small section of the population that can easily meet the costs (and for
the purposes of earning foreign exchange) and a "minimum clinical package courtesy
World Bank (1993)3[31 provided by the government to be availed of by the poor if and when
they can mobilize sufficient resources to meet the direct service charges and the indirect costs
(transport, loss of wages) such care entails.
Concern not withstanding, among the critics there appears to be a tacit acceptance of the
nature of things to come and a tacit agreement as to the near impossibility of stopping or
reversing the relentless march of market forces. Depending upon one's current world view
and analysis, suggestions for ‘improving' the government's national health policy aim at
creating a space for the poor within the framework laid down by the state under the aegis of
the World Bank and Transnational Capital, without challenging the very frame work itself.
While at one level such a strategy7 may be taken to reflect a pragmatism of sorts, increasingly
it is being upheld as the most, and often the only viable alternatives under the given
circumstances. Could this be due to the near absence of a genuine pro-people movement in
the country to articulate the needs and aspirations of the marginalized from their perspective?
Is a different perspective possible? Are there other options which will place people’s need
centre-stage? How should mfc contribute to the development of such a perspective and help
evolve strategies that can translate into concrete demands difficult to coopt and make health
care a justiciable right for all? This should form the focus of the mfc annual meet.
UH why user £^9 The word Tee’ means, a payment made to a professional person or to a professional or
public body in exchange for advice or services (concise Oxford Dictionary, 10th ed). Is the addition of "user’ in
order to camouflage the nature of privatisation of public services?
2l2' There is an entire chapter in one of Susan George’s book (will supply details later) which discusses when
and why the archaic word ‘governance’ was brought back into general usage by the World Bank.
3131 “Investing in Health Care”, World Bank, 1993
It is not sufficient to say that public health is under attack or that the public health care
system is being dismantled. There is need to spell out what exactly is being attacked and what
exactly is being dismantled. And most importantly, how exactly it is going to affect the health
of the poor because, the poor view with indifference (and once-in-a-way, with anger), what
currently exists in the name of public health services. When present, broken down and
vandalized buildings of sub-centres/PHCs in the villages and taluk towns; every cadre of
health personnel from the level of the inadequately trained village health worker to the doctor
at the district head quarters out to exploit their ignorance and capitalize on their misery and
helplessness; corruption from the top to the bottom of the ladder; anti-poor, casteist, sexist
(and in the last decade, communal) attitude of the individual medical personnel especially the
doctors, the 'leaders’ of the medical team; non-availability of medicines/equipment and poor
service in public hospitals, particularly at the district levels; anti-poor, anti-women
aggressions carried out by the department of population control - the poor have borne mute
testimony to what government health services mean at the ground level and are not going to
be impressed very much if they are to be informed that such 'services' are going to be
disbanded.
In any case today even from among the poorer sections of the population, the trend is to
'seek' medical care from the private sector when possible. It is only when there are no
options as in times of serious illnesses when the cost of care is too great, that the compulsion
to utilize government health services arise (which increasingly is turning to be no option at all
w ith the introduction of service charges in the public sector). The irony is that the observation
- people, poor people are spending money on medical care is being seen as a statement of
their '‘willingness" to pay for treatment costs. While this may be more a reflection of an
absence of other options than an exercise of real choice, studies on household expenditure on
health have seldom asked two additional critical questions, how was the money for payment
mobilized in the first place and what was the impact on the household economy as a
consequence of this4'41. Thus, while studies abound on household expenditure on medical
care, equal attention has not been paid to assess, for instance, rural indebtedness due to
disease and treatment costs. How ever one explains the whys of this lacuna, this 'short
sightedness' has worked against the interests of the poor. Studies such as these have
legitimized the notion of payment for ‘services’ and have cleared the way for introducing
"user fees" in public health services. Even here, contrary to the proclaimed objectives, the
introduction of fees is not to generate funds for the resource-poor public sector. The intention
is to wean away from the public sector to the private, that section of the population that is
currently using it but has any surplus at all to spend (if money has to be paid in either case,
why settle for what appears to be ‘second best'?5151). The intractable truth is that with its one
and only goal of‘maximizing profits’ at any cost, the private sector (and monopoly capital)
cannot tolerate any form of competition whatsoever.
We need to understand the move to phase out the state-owned secondary and tertiary’ referral
services in this context as a logical step for removing a major hurdle in the path towards
unfettered private monopoly in curative clinical services. Plans are also afoot to convert the
role of the government from a provider of even basic health services into a mere financier
who will, on behalf of the poor, ‘purchase’ the necessary services from the private sector.
This with an avowed intention of improving quality of care by encouraging competition
4t41 The other important questions are the proportion arid rate of illnesses for which medical care is not sought;
nature of such illnesses; gender, class, caste differentials etc.
5151 In many parts of the country, government hospitals are called dharm or charity hospitals because they did
not charge money
among the private providers, apparently the most effective way of achieving the stated
objective. In reality it could very well be yet another ruse to provide more government
subsidy to the already state-subsidized private sector.
We are situated in a time in history when India has seen more than fifty years of
Independence from direct colonial rule. We are also situated in a time in history when India
has become a seemingly willing subject to the neo-colonial rule under the conditionalities of
the Structural Adjustment Programme. In this period of fifty-five years, an entire generation
of the poor has taken birth and died without having had even the ‘luxury’ of two full meals
every day for the entirety of their life time. In stark contrast to their lives, they have witnessed
the fruits of development built on their labour being reserved for the comfort and enjoyment
of a small section of the population - the upper class and the upper caste. Today, it is no
accident that this very same small section is bartering away the country’s sovereignty’ and
future to buy a place for themselves amongst the global ruling class.
Fifty7 years is a long time to have laid open the true intentions of our country's ruling elite
towards its people. It is not chance but choice that we have millions of people living a life of
chronic starvation when there is food rotting in the godowns. It is not chance but choice that
has created the necessary’ pre-conditions for the dictatorship of transnational capital.
To take an instance, it is not chance but choices made over fifty years that has created a
burgeoning private medical sector over-running the health care system in the country For,
how else does one explain the fact that a private sector which accounted for only 20% of the
health services in the early eighties, is now providing more than 80%? Where did the doctors
currently stocking the private sector come from? Are they not the products of our educational
sy stem and policies and for most part subsidized by the labor of the poor (through indirect
taxes)? Can a critique of medical education be unconnected to a critique of the educational
policy in general? Why are we shocked when we observe the mandalisation and
communalisation of the medical community in utter disregard to the Hippocratic oath? Is not
the dual policy that is being proposed today regarding medical manpower been the norm
rather than an exception since Independence? The training of licentiates in the period
immediately following Independence may have been in keeping with the needs and resource
availability in the country at that time. But choice was made to train a ‘full fledged doctor
matching international standards. Today when we have a surplus of doctors trained to fit
international norms, can we justify the renewed discussion on licentiate course to provide
‘sub-standard’ personnel to take care of the needs of the poor? When we have an optimum
doctor-population ratio6161 why are we opening more and more medical colleges? Why is the
World Bank (1993) which has arrogated to itself the right to set the terms for our country’s
health care system silent regarding the presence of surplus doctors in the country or the fact
that Indian doctors form a substantial portion of the medical community in several western
countries? Why is the national policy (2001 draft) silent on this? Colonial legacy cannot be
the only reason, we have had more than fifty years to over tum it.
The theme for the annual meet should therefore have a historical perspective running through
it. We should re-examine the economic/political considerations and compulsions, that have
shaped the national health policy since Independence and where necessary its links to the
colonial past and ‘heritage’. Only then will the analysis of the new health policy under
Structural Adjustment Programme make sense.
6[6] ■
incidentally, what is the rationale for deciding what is an optimum ratio.
The theme will be incomplete without a discussion on the contribution of non-governmental
organizations (ngo). Historically, the ngo sector, previously called the voluntary' sector, has
contributed in critical ways to the shaping of the national health policy and programmes.
Initially in the role of the service providers, the emphasis was on setting up hospitals,
particularly in rural areas and in training manpower of all levels. Over the years, many such
organizations enlarged their perspective of individual care to include ‘communities' and
experimented with alternate delivery systems by, for instance, training village health workers.
Campaigning for policy changes, highlighting disparities and equity issues, generating critical
data, more often than not from a pro-people (poor, women) perspective, are some of the other
important contributions. However, the last decade has seen the emergence of questionable
priorities largely determined by the agenda of the funders. There has also been a moving
away from working directly with people to Tobbying’ and ‘advocating’ with policy' makers
as the most effective means of bringing about change. Over a period of time, the potential for
supporting people's struggles is being slowly frittered away and the poor are beginning to
view such organizations with cynicism and distrust.
The fact that the disparate ngo sector contains within it a section of the liberal vocal middle
class with little social accountability and no explicit ideology or long-term commitment has
made it a sitting duck for cooption. The dependence on external funding, be it domestic or
foreign, has meant that it is possible to manipulate and pressurize at critical times and shift
their attention from issues of people's livelihood to seeking means to protecting their own.
It is this vulnerability and the accompanying vacillation that makes the ngo sector attractive
to the World Bank (itself an ngo?) and the state who wish to bring into their fold the
dangerous potential for dissent and give it a shape in their own image. A calculated political
act of blurring the lines by clubbing all organizations irrespective of their political leanings
(right, centre or left)7171 under one umbrella term “non-governmental organizations'" was the
first step towards containing dissent, an act which went largely unprotested. However, that it
is still possible to channelize the not inconsiderable energy of the sector into a coherent
political force against oppressive policies has been amply demonstrated by, for instance, the
campaign against hazardous contraceptives, SDSP tests. The move to form a people's Health
Assembly being another such attempt.
MFC is uniquely placed to examine the contribution of the ngo sector to the shaping of
national health policy. Many of its members have been in the forefront at critical junctures in
reaching health care to the poor and the marginalized both in the literal and figurative sense.
With the rich experience and wisdom gained over the past thirty' years of intervention,
experimentation and participating in the political process to influence health policies either at
an individual level or as an organization, the discussion could be very rewarding if we bring
to it our own personal experiences. The strengths of the mfc are its non-sectarian approach
and a potential to critically examine an issue without taking anything as a given. Can we turn
this ability of ours to examine dispassionately, our several attempts at creating an alternate
world view in health care, the successes and failures of our 'projects' and question our own
thinking with the luxury of hind sight?
This decade is going to bring about cataclysmic changes, particularly when the WTO treaty
comes into effect in 2005. The “reforms”81^ that are being ushered in the name of
globalization are already beginning to be experienced with rising unemployment,
retrenchment of workers, and a shift towards insecure, casual labour and poor wages. Added
to this is the impact of privatization of public health care services, rising drug prices and
costs of treatment. These changes are going to have an adverse impact on the health of the
poor and lead to a rise in morbidity and mortality rates in the vulnerable sections of the
population.
Si
SA
commtmacafaon
odoptinq heolth promotion ond sociol oction to the
qlobol imbolonces of the 21st centurq
by PSv/tJ Wome-r
Democracy^ a
prerequisite
for a M EALTHY
SOCIETY
Why participation is essential - and how it
is undermined
he well-being of an individual or commu
nity depends on many factors, local to
global. Above all, it depends on the oppor
tunity of all people to participate as equals in the
decisions that determine their well-being Unfor
tunately, history shows us that equality in collec
tive decision-making—that is to say participatory
democracy—is hard to achieve and sustain.
Despite the spawning of so-called democratic
governments’ in recent
decades, most people
still have little voice in
the policies and deci
sions that shape their
lives. Increasingly, the
rules governing the
fate of the Earth and its
inhabitants are made
by a powerful minority
who dictates the Global
Economy. Thus eco
nomic growth (for the
wealthy) has become
the yardstick of social
progress, or ‘develop
ment,* regardless of
the human and envi
ronmental costs.
And the costs are horrendous! The top-down
‘globalisation’ of policies and trade—through
which the select few profit enormously at the
expense of the many—is creating a widening gap
in wealth, health and quality of life, both between
countries and within them. A complex of world
wide crises—social, economic, ecological and
ethical—is contributing to ill-health and early
death for millions. Increasingly, giant banks and
corporations rule the world, putting the future
well-being and even survival of humanity at risk.
Driven more by hunger for private profit than for
public good—the massive production of consumer
goods far exceeds the basic needs of a healthy and
sustainable society. Indeed, its unregulated
growth compromises ecological balances and
imperils the capacity of the planet for renewal.
Yet in a world where unlimited production and
resultant waste have become a major health
hazard, there are more hungry children than ever
before. According to Worldwatch’s The State of the
World, 1999, the majority of humanity is now
malnourished, half from eating too little and half
from eating too much!
Mahatma Gandhi wisely observed: ‘There is
enough for everyone’s need but not for everyone's
greed.’ Sadly, greed has replaced need as the
driver of our global
spaceship. Despite all
the spiritual guidelines,
social philosophies,
and declarations of
human rights that
Homo sapiens (the
species that calls itself
wise) has evolved
through the ages, the
profiteering ethos of
the market system has
side-tracked our ideals
of compassion and
social justice. Human
ity is running a danger
ous course of increas
ing imbalance. To
further fill the coffers of the rich, our neoliberal
social agenda systematically neglects the basic
needs of the disadvantaged and is rapidly despoil
ing the planet’s ecosystems, which sustain the
intricate web of life.
The dangers—although played down by the mass
media—are colossal and well documented. For
ward-looking ecologists, biologist, and sociologists
sound the warning that our current unjust, unCtrrmjnicaticn as if People lettered
healthy model of economic development is both
humanly and environmentally unsustainable.
Yes, we know that,’ say many of us who believe
in Health for All and a sustainable future. ‘We are
deeply worried.... But what can we do?’
There are no easy answers. The forces shaping
global events are gigantic, and those who accept
them as inevitable so impervious to rational
dissent, that many of us hide our heads in the sand
like ostriches. And so humanity thunders head
long down the path of systemic breakdown—more
polarisation of society, more environmental
deterioration, more neglect of human rights and
needs, more social unrest and violence—as if our
leaders were incapable of thought and our
populations anaesthetised.
What action can we take, then—individually and
collectively—to change things for the better, for
the common good?
The purpose of this background paper
The interrelated crises of our times—the ways that
globalisation, corporate rule, and top-down,
development’ policies undermine democratic
process and endanger world health—are discussed
in other background papers for the People’s
Health Assembly. The purposes of this paper are:
1.
2.
to examine the strategies used by the world s
ruling class to keep the majority of humanity
disempowered and complacent in the face of
the crushing inequalities and hazards it
engenders;
to explore the methods and resources whereby
enough people can become sufficiently aware
and empowered to collectively transform our
current unfair social order into one that is
more equitable, compassionate, health-pro
moting, and sustainable.
TOP.B
o,W,N
MEA5L1KL5 of
SOCIAL CONTROL
Disinformation
With all the technology and sophisticated
1
J means of communication now available,
V
how is it that so many people appear so
unaware that powerful interest groups are under
mining democracy, concentrating power and
wealth, and exploiting both people and the envi
ronment in ways that put the well-being and even
survival of humanity at stake? How can a small
elite minority so successfully manipulate global
politics to its own advantage, and so callously
ignore the enormous human and environmental
costs? How can the engineers of the global
economy so effectively dismiss the emerging risk
of unprecedented social and ecological disaster?
In short, what are the weapons used by the ruling
class to achieve compliance, submission, and social
control of their captive population?
True, riot squads have been increased, prison
populations expanded, and military troops de
ployed to quell civil disobedience. But far more
than tear-gas and rubber bullets, disinformation
has become the modem means of social control
Thanks to the systematic filtering of news by the
mass media, many ‘educated’ people have little
knowledge of the injustices done to disadvantaged
people in the name of economic growth, or of the
resultant perils facing humanity. They are uncon
scious of the fact that the overarching problems
affecting their well-being—growing unemploy
ment, reduced public services, environmental
degradation, renewed diseases of poverty, bigger
budgets for weapons than for health care or
schools, more tax dollars spent to subsidize
wealthy corporations than to assist hungry chil
dren, rising rates of crime, violence, substance
abuse, homelessness, more suicides among teenag
ers—are rooted in the undemocratic concentration
of wealth and power. Despite their personal
hardships, unpaid bills, and falling wages, ordi
nary citizens are schooled to rejoice in the ‘success
ful economy’ (and spend more). They pledge
allegiance to their masters’ flag, praise God for
living in a ‘free world,’ and fail to see (or to admit)
the extent to which the world’s oligarchy (ruling
minority) is undermining democracy and endan
gering our common future. And our textbooks and
TVs keep us strategically misinformed.
-40
People's Health Assentoly
One dollar, one vote: private invest
ment in public elections
One way ‘government by the people’ is
undermined is through the purchase of
public elections by the highest bidders. In
many so-called democracies a growing
number of citizens (in some countries, the
majority) don’t even bother to vote. They
say it makes no difference. Politicians, once
elected, pay little heed to the people’s
wishes. The reason is that wealthy interest
groups have such a powerful political
lobby. Their big campaign donations (bribes?)
help politicians win votes—in exchange for politi
cal favours. The bigger the bribe, the more cam
paign propaganda on TV and mass media. Hence
more votes.
This institution of legal bribery makes it hard for
honest candidates (who put human need before
corporate greed) to get elected. Democratic elec
tions are based on one person, one vote. With the
deep pockets of big business corrupting elections,
results are based on one dollar, one vote. This
makes a mockery of the democratic process.
The erosion of participatory democracy by the
corporate lobby has far-reaching human and
environmental costs. Hence the biggest problems
facing humanity today—poverty, growing in
equality, and the unsustainable plundering of the
planet's ecosystems—continue unresolved.
Sufficient wisdom, scientific knowledge and
resources exist to overcome poverty, inequity,
hunger, global warming and the other crises facing
our planet today. But those with the necessary
wisdom and compassion seldom govern. They
rarely get elected because they refuse to sell their
souls to the company store. Winners of elections
tend to be wheelers and dealers who place short
term gains before the long-term well-being of all.
To correct this unhealthy situation, laws need to be
passed that stop lobbying by corporations and
wealthy interest groups. In some countries, citi
zens’ organisations are working hard to pass such
campaign reforms. But it is hard to get them past
legislators who pad their pockets with corporate
donations. Only when enough citizens become
fully aware of the issues at stake and demand a
public vote to oudaw large campaign donations,
will it be possible for them to elect officials who
place the common good before the interests of
powerful minorities.
But creating such public awareness is an uphill
struggle—precisely because of the power of the
corporate lobby and the deceptive messages of the
mass media. To make headway with campaign
READ AGAIN-With MORE
feeding -the passage
l about the heroes of
XThe revolution. >
reforms, institutionalised disinformation must be
exposed for what it is. To accomplish this, more
honest and empowering forms of education and
information sharing are needed.
Schooling for conformity, not change
It has been said that education is power. That is
why, in societies with a wide gap between the
haves and have-nots, too much education can be
dangerous Therefore, in such societies, schooling
provides less education than indoctrination,
training in obedience, and cultivation of conform
ity. In general, the more stratified the society, the
more authoritarian the schools.
Government schools tend to teach history and
civics in ways that glorify the wars and tyrannies
of those in power, whitewash institutionalised
transgressions, justify unfair laws, and protect the
property and possessions of the ruling class. Such
history is taught as gospel. And woe be to the
conscientious teacher who shares with students
people’s history’ of their corner of the earth.
Conventional schooling is a vehicle of
disinformation and social controL It dictates the
same top-down interpretations of history and
current events, as do the mass media. It white
washes official crimes and aggression. Its purpose
is to instill conformity and compliance, what
Noam Chomsky calls manufacturing consent.’
For example, although the United States has a long
history of land-grabbing, neocolonial aggression
and covert warfare against governments commit
ted to equity, most US citizens take pride in their
‘benevolent, peace-loving nation’. Many believe
they live in a democracy for the people and by the
people, with liberty and justice for all’—even
though millions of children in the US go hungry,
countless poor folks lack health care, prison
populations expand (mainly with destitute blacks),
and welfare cut-backs leave multitudes jobless,
homeless and destitute.
Cbmrunicaticn as if Eteple fettered
-^1
the controlling elite. But to survive they need
listener support.
,-M-UP approaches
gOTT^to communication
j -o see through the institutionalised
I
disinformation, and to mobilise people
Vx* in the quest for a healthier, more equita
ble society, we need alternative methods of
education and information-sharing that are
honest, participatory, and empowering. This
includes learning environments that bring people
together as equals to critically analyse their reality,
plan a strategy for change, and take effective
united action.
Fostering empowering learning methods is urgent
in today's shrinking world, where people’s quality
of life, even in remote communities, is increasingly
dictated by global policies beyond their control.
Alternative media and other means of
people-to-people communication
There have been a number of important initiatives
in the field of alternative media, communication,
and social action for change.
The alternative press. While struggling to stay
alive in recent years, the alternative press (maga
zines, flyers, bulletins, newsletters, progressive
comic books) has provided a more honest, peoplecentred perspective on local, national and global
events. Some of the more widely-circulating
alternative magazines in English (often with
translations into several other languages) include:
The New Internationalist
Z Magazine
Resurgence
The Nation
Third World Resurgence
Covert Action Quarterly
Multinational Monitor
Also, there are many newsletters and periodicals
published by different watchdog groups such as
the International Forum on Globalization, IBFAN,
BankWatch, the National Defense Monitor and
Health Action International, among others. It is
important that we subscribe to and read (and
encourage others to read) these progressive alter
native writings.
Alternative community radio and TV. The role
and potential of these is similar to that of the
alternative press. Stations that do not accept
advertising are less likely to belong to or sell out to
People's Lfealth Asserrbly
Internet Electronic mall and websites have
opened up a whole new sphere of rapid, direct
communication across borders and frontiers. The
Web is, of course, a two-edged sword. The Internet
is currently available to less than 2% of the world’s
people, mostly the more privileged. And Instant
electronic communications facilitate the global
transactions and control linkages of the ruling
class. But at the same time. E-mail and the WorldWide-Web provide a powerful tool for popular
organisations and activists around the globe to
communicate directly, to rally for a common cause
and to organise international solidarity for action.
The potential of such international action was first
demonstrated by the monumental worldwide
outcry, through which non-government organisa
tions (NGOs) and grassroots organisations halted
the passage of the Multilateral Agreement on
Investment (MAI). (The MAI was to have been a
secret treaty among industrialised countries,
giving even more power and control over Third
World Nations.) The primary vehicle of communi
cation for the protest against MAI was through the
Internet.
Mass gatherings for organised resistance against
globalised abuse of power. The turn of the Cen
tury was also a turning point in terms of people s
united resistance against global trade policies
harmful to people and the planet. The huge, wellorchestrated protest of the World Trade Organiza
tion (WTO) summit meeting in Seattle, Washing
ton (now celebrated worldwide as the Battle in
Seattle’) was indeed a breakthrough. It showed us
that when enough socially committed people
from diverse fields unite around a common
concert^ they can have an impact on global
policy making.
The agenda of the WTO summit in Seattle was to
further impose its pro-business, anti-people and
anti-environment trade policies. That agenda was
derailed by one of the largest, most diverse,
international protests in human history. Hundreds
of groups and tens of thousands of people repre
senting NGOs, environmental organisations,
human rights groups, labour unions, women’s
organisations, and many others joined to protest
and barricade the WTO assembly. Activists ar
rived from at least 60 countries. The presence of
so-many grassroots protesters gave courage to
many of the representatives of Third World
countries to oppose the WTO proposals which
would further favor affluent countries and corpo
rations at the expense of the less privileged. In the
end, the assembly fell apart, in part from internal
(^INDIRA 11 TOO THIN- WMX
disaccord. No additional policies were agreed
upon.
DOESH'T BET BNOU6H TO EAT.
^HER PARENTS
/that'* A «OOt> ANSWER . WHO HA* >
( an or ho r ome’wh/ boeent inoiaa,
Perhaps the most important outcome of the Battle
in Seattle was that, despite efforts by the mass
media to denigrate and dismiss the protest, key
issues facing the world’s people were for once
given center stage. It was a watershed event in
terms of grassroots mobilisation for change. But
the activists present agreed that it was just a
beginning.
-------------------
father
IS SICK.
.
( TMME »*
XL
The People s Health Assembly, with its proposed
People’s Charter for Health’ and plans for follow
up action, holds promise of being another signifi
cant step forward in the struggle for a healthier,
more equitable approach to trade, social develop
ment, and participatory democracy. For that
promise to be realised, people and groups from a
wide diversity of concerns and sectors must
become actively involved around our common
concern: the health and well-being of all people
and of the planet we live on.
EDUCATICN
fov
PARTFOTATIOH
ACTION for change
he term Popular Education,’ or Learner
centered education,’ refers to participatory
learning that enables people to take collec
tive action for change. Many community-based
health initiatives have made use of these enabling
methodologies, adapting them to the local circum
stances and customs. Particularly in Latin
America, methods of popular education have been
strongly influenced by the writings and aware
ness-raising praxis’ of Paulo Freire (whose best
known book is Pedagogy ofthe Oppressed}
Education of the oppressed—the method
ology of Paulo Freire
In the mid-1960s the Brazilian educator, Paulo
Freire developed what he called education for
liberation, an approach to adult literacy training,
(which proved so revolutionary that Freire was
jailed and then exiled by the military junta.) With
his methods, non-literate workers and peasants
learned to read and write in record time—because
their learning focused on what concerned them
most: the problems, hopes and frustrations in their
lives. Together they critically examined these
concerns, which were expressed in key words and
provocative pictures. The process involved identi-
ARE in
DEBT
6BT IWU6H
MOT SMOVOH
K rain. 7
HE« MOTHER
DOESN’T
BASA6TFKEO
<
hb a.
SHE HAS
O/AKMMEA
fication and analysis of their most oppressive
problems, reflection on the causes of these, and
(when feasible) taking action to ’change their
world’.
Learning as a two-way or many-way
process
With Freire’s methodology, problem-solving
becomes an open-ended, collective process. Ques
tions are asked to which no one, including the
facilitator have ready answers. The teacher is
learner and the learners, teachers.’ Everyone is
equal and all learn from each other. The contrast
with the typical classroom learning is striking.
In typical schooling, the teacher is a superior
being who knows it all’. He is the owner and
provider of knowledge. He passes down his
knowledge into the heads of his unquestioning
and receptive pupils, as if they were empty pots.
(Freire calls this the banking' approach to learning
because knowledge is simply deposited.)
In education for change, the facilitator is one of
the learning group, an equal. She helps partici
pants analyse and build on their own experiences
and observations. She respects their lives and
ideas, and encourages them to respect and value
one another’s. She helps them reflect on their
shared problems and the causes of these, to gain
confidence in their own abilities and achieve
ments, and to discuss their common concerns
critically and constructively, in a way that may
lead to personal or collective action. Thus, accord
ing to Freire, the learners discover their ability to
‘change their world’. (For this reason Freire calls
this a ‘liberating’ approach to learning).
Ctrnrunicaticn as if Pecple ottered
The key difference between typical schooling’ and
education for change' is that the one pushes ideas
into the student's heads, while the other draws
ideas from them. Typical schooling trains students
to conform, comply, and accept the voice of
authority without question. Its objective is to
maintain and enforce the status quo. It is
disempowering. By contrast, education-for-change
is enabling. It helps learners gain ‘critical aware
ness’ by analysing their own observations, draw
ing their own conclusions and taking collective
action to overcome problems. It frees the poor and
oppressed from the idea that they are helpless and
must suffer in silence. It empowers them to build a
better world—hence it is education for transfor
mation’.
examples of
health progranmes
have combatted
ROOT CAUSES of
POOR HEALTH
ommunity-based health programmes in
various countries have brought people
-^together to analyse the root causes of their
health-related problems and to take health into
their own hands' through organised action. In
places where unjust government policies have
worsened the health situation, community health
programmes have joined with popular struggles
for fairer and more representative governments.
The following are a few examples of programmes
where people’s collective ‘struggle for health’ has
led to organised action to correct inequalities,
unfair practices and/or unjust social structures.
£
that the poor often went without. Health workers
helped villagers organise to gain democratic,
community control of the wells. This meant more
water and better health for the poor. And it helped
people gain confidence that through organised
action they could indeed better their situation.
Another example concerns schooling. Villagers
know education is important for health. But most
poor children of school age must work to help
their families survive. So the GK communities
started a unique school, which stresses coopera
tion, not competition. Each day the children able to
attend the school practise teaching each other.
After school these same children teach those
unable to attend school. This process of teaching
one another and working together to meet their
common needs, sews seeds for cooperative action
for change.
Jamkhed, India. For over three decades two
doctors, Mabel and Raj Arole, have worked with
poor village women, including traditional mid
wives. These health facilitators have learned a
wide variety of skills. They bring groups of
women together to discuss and try to resolve
problems. In this way, they have become informal
community leaders and agents of change. They
help people rediscover the value of traditional
forms of healing, while at the same time demysti
fying Western medicine, which they learn to use
carefully in a limited way.
In Jamkhed. women's place relative to men's has
become stronger. Women have found courage to
defend their own rights and health and those of
their children. As a result of the empowerment
and skills-training of women, child mortality has
dropped and the overall health of the community
has improved dramatically.
TOPAY-J
Gonoshasthaya Kendra (GK). GK is a commu
nity health and development programme in
Bangladesh that began during the war for
national independence. Village women, many
of them single mothers (the most marginalised
of all people), have become community health
workers and agents of change. Villagers collec
tively analyse their needs and build on the
knowledge and skills they already have. Re
peatedly health workers have helped villagers
take action to defend their rights.
One example of this is over water rights. In
analysing their needs, families agreed that
access to good water is central to good health.
UNICEF had provided key villages with tube
wells. But rich landholders took control of the
wells and made people pay so much for water
People's Jfealth Assembly
.
SOCIAL
DO
£
farm people leave
)
AWD MO
to c/n
h' rW L
M?1
The Philippines. In this island nation, during the
dictatorship of Fernando Marcus, a network of
community-based health programmes (CBHPs)
evolved to help people deal with extreme poverty
and deplorable health conditions. Village health
workers learned to involve people in what they
called situational analysis. Neighbours would
come together to prioritise the main problems
affecting their health, identify root causes and
work collectively towards solutions.
In these sessions it became clear that inequality—
and the power structures that perpetuate it—
were at the root of ill health. Contributing to the
dismal health situation were: unequal distribution
of farm land (with huge land-holdings by
transnational fruit companies), cut backs in public
services, privatisation of the health system, and
miserable wages paid to factory and farm workers.
The network of community-based programs urged
authorities to improve this unjust situation. When
their requests fell on deaf ears, they organised a
popular demand for healthier social structures.
These included free health services, fairer wages,
redistribution of the land to the peasantry, and
above all else, greater accountability by the gov
ernment to its people.
The fact that the CBHP network was awakening
people to the socio-political causes of the poor so
threatened the dictatorship that scores of health
workers were jailed or killed. But as oppression
grew, so did the movement. The CBHP network
joined with other movements for social change.
Finally, the long process of awareness-raising and
cooperative action paid off. In the massive peace
ful uprising of 1986, thousands of citizens con
fronted the soldiers, putting flowers into the
muzzles of their guns. The soldiers (many of
whom were peasants themselves, acquiesced.
After years of organising and grassroots resistance,
the dictatorship was overthrown. (Unfortunately,
the overall situation has not changed greatly. With
persistent domination by the US government and
multinational corporations, gross inequities
remain and the health of the majority is still
dismal. The struggle for a healthier, more equita
ble society continues.)
Nicaragua. Similar to the
CBHP in the Philippines
under Marcus, in Nicaragua
during the Somoza dictator
ship a network of non-government community health
programmes evolved to fill
the absence of health and
other public services. Grass
roots health workers known
as Brlgadistas de Salud
brought groups of people together to conduct
community diagnoses of problems affecting their
health, and to work together toward solutions. As
in the Philippines, the ruling class considered such
community participation subversive. Scores of
health workers were ’disappeared' by the National
Guard and paramilitary death squads. Many
health workers went underground and eventually
helped form the medical arm of the Frente
Sandinista, the revolutionary force that toppled the
dictatorship.
After the overthrow of Somoza, hundreds of
Brigadistas joined the new health ministry. With
their commitment to strong participation, they
helped to organise and conduct national Jornadas
de Salud’ (Health Days). Their work included
country-wide vaccination, malaria control, and
tuberculosis control campaigns. At the same time,
adult literacy programmes, taught mainly by
school children, drastically increased the nation's
level of literacy.
As a result of this participatory approach, health
statistics greatly improved under the Sandinista
government. Since the Sandinistas were ousted
with the help of the US government, health serv
ices have deteriorated and poverty has increased.
Many health indicators have suffered. But fortu
nately, communities still have the skills and selfdetermination necessary to meet basic health
needs and assist one another in hard times.
Project Piaxtla, in rural Mexico. In the mountains
of western Mexico in the mid-1960s a villager-run
health programme began and gradually grew to
cover a remote area unserved by the health sys
tem. Village health promoters, learning in part by
trial and error, developed dynamic teaching
methods to help people identify their health needs
and work together to overcome them.
Over the years, Piaxtla evolved through three
phases: 1) curative care, 2) preventive measures,
and 3) socio-political action.
It was the third phase that led to the most impres
sive improvements in health. (In two decades,
child mortality dropped by 80%.) Through Com
munity Diagnosis, villagers recognised that a big
david wemer
Cbmrijriicaticri as if Pecple Mattered
cause of hunger and poor health was the unconsti
tutional possession of huge tracts of farmland by a
few powerful landholders, for whom landless
peasants worked for slave wages, 'fhe health
promoters helped the villagers organise, invade
the illegally large holdings, and demand their
constitutional rights. Confrontations resulted, with
occasional violence or police intervention. But
eventually the big landholders and their govern
ment goons gave in. In two decades, poor farmers
reclaimed and distributed 55% of good riverside
land to landless farmers. Local people agree that
their struggle for fairer distribution of land was
the most important factor in lowering child mor
tality. And as elsewhere, people’s organised effort
to improve their situation helped them gain the
self-determination and skills to confront other
obstacles to health.
The practical experience of Project Piaxtla and its
sister programme, PROJIMO, gave birth to Where
There Is No Doctor,’ ‘Helping Health Workers
Learn,’ Disabled Village Children’ and the other
books by David Werner that have contributed to
community-based health and rehabilitation initia
tives worldwide.
nefvyorfeang anol
COMMUNfCATfOMS
amon^.
$ S R tVT S
programmes anol movements
From isolation to united struggle
^n different but parallel ways, each of the com
1 munity initiatives briefly described above
-••developed enabling participatory methods to
help local people learn about their needs, gain self
confidence, and work together to improve their
well-being. Each forged its own approaches to
what we referred to earlier as education for
change.
At first community health initiatives in different
countries tended to work in isolation, often una
ware of each other’s existence. There was little
communication and sometimes antagonism
between them. But in time this changed, partly
due to growing obstacles to health imposed by the
ruling class. (Nothing solidifies friendship like a
common oppressor.) Programmes in the same
country or region began to form networks or
associations to assist and learn from each other. By
joining forces, they were able to form a stronger,
more united movement, especially when confront
ing causes of poor health rooted in institutional
ised injustice and inequity.
National networks in Central America and the
Philippines provided strength in numbers that
gave community health programmes mutual
protection and a stronger hand to overcome
obstacles.
In the 1970s, community-based health pro
grammes in several Central American countries
formed nationwide associations Then in 1982 an
important step forward took place. Village health
workers from CBHPs in the various Central
American countries and Mexico met in Guatemala
to form what became the Regional Committee of
Community Health Promotion.
This Regional Committee has helped to build
solidarity for the health and rights of people
throughout Central America. Solidarity was
particularly important during the wars of libera
tion waged in Central America (and later in
Mexico), when villages were subjected to brutal
and indiscriminate attacks by repressive govern
ments and death squads.
Learning from and helping each other
One of the most positive aspects of networking
among grassroots programmes and movements
has been the cross-fertilisation of experiences,
methods and ideas.
Central America. For example, in the 1970s, the
Regional Committee and Project Piaxtla organised
a series of ‘intercambtos educativus’ or educa
tional interchanges. Community health workers
from different programmes and countries came
together to learn about each other's methods of
confidence-building, community diagnosis, and
organisation for community action.
At one of these Intercambios, representatives from
Guatemala, in a highly participatory manner,
introduced methods of ‘conscientizacidn’ (aware
ness-raising) developed by Paulo Freire, as they
had adapted them to mobilise people around
health-related needs in Guatemala.
<
A
is?
Appropriate planning starts with PEOPLEf
Peqple's Health Assenbly
Likewise the village health promoters of
Piaxtla, in Mexico, introduced to participants a
variety of methods of discovery-based learn
ing, which they had developed over the years
(see below).
Reaching across the Pacific. An early step
towards more global networking took place in
19??, when an educational interchange was
arranged between community health workers
from Central America and the Philippines. A
C
'--- l.\ / /
’A
team of health workers from Nicaragua,
Honduras and Mexico visited a wide range of
community-based health programmess, rural
and urban, in the Philippines. In spite of
erished populations. So the world's nations en
language barriers, the sharing of perspectives and
dorsed the Alma Ata Declaration, which outlined
sense of solidarity that resulted were profound.
a revolutionary strategy called Primary Health
Social and political causes of ill health in the two
Care (PHC), to reach the goal of Health for All by
regions were similar. Both the Philippines and
the Year 2000. The vision of PHC was modeled
Latin America have a history of invasion and
after the successful grassroots community-based
subjugation, first by Spain and then by the United
health programmes in various countries, as well as
States. Transnational corporations and the Interna
the work of barefoot doctors’ in China. It called
tional Financial Institutions have contributed to
for strong community participation in all phases,
polarising the rich and poor. And in both regions,
from planning and implementation to evaluation.
the US has backed tyrannical puppet governments
that obey the wishes of the global marketeers in
Health for No One? We have entered the 21st
exchange for loans and weapons to keep their
century and are still a long way away from 'Health
impoverished populations under control.
for AIL’ If our current global pattern of short
sighted exploitation of people and environment
Participants in the Latin American-Philippine
continue, we will soon be well on the road to
interchange came away with a new understanding
‘Health for No One.' The current paradigm of
of the global forces behind poor health. They
economic development, rather than eliminating
became acutely aware of the need for a worldwide
poverty, has so polarised society that combined
coalition of grassroots groups and movements to
social and ecological deterioration endangers the
gain the collective strength needed to construct a
w'ell-being of all. But sustainable well-being is of
healthier, more equitable, more sustainable global
secondary concern to the dictators of the global
environment.
economy, whose all-consuming objective is
GROWTH AT ALL COST!
It has been said that Primary Health Care failed.
But in truth, it has never been seriously tried.
Because it called for and the full participation of
the underprivileged along with an equitable
RIMARY
economic order, the ruling class considered it
subversive. Even UNICEF—buckling under to
|
| ealth for All? The United Nations estab
accusations by its biggest founder (the US govern
-iJ
-I lished the World Health Organization
ment) that it was becoming ‘too political’—en
|
I (WHO) in 1945 to co-ordinate interna
dorsed a disembowelled version of PHA called
tional policies and actions for health. WHO de
Selective
Primary Health Care. Selective PHC has
fined health as ‘complete physical, mental, and
less to do with a healthier, more equitable social
social well-being, and not merely the absence of
order than with preserving the status quo exist
disease.’
ing wealth and power.
•fho life and death of
Primary Health Care
But in spite of WHO and the United Nations'
declaration of Health as a Human Right, the
poorer half of humanity continued to suffer the
diseases of poverty, with little access to basic
health services. In 1987, WHO and UNICEF
organised a watershed global conference in Alma
Ata, USSR. It was officially recognised that the
Western Medical Model, with its costly doctors in
giant ‘disease palaces,' had failed to reach impov-
The World Bank’s take-over of health planning.
The kiss of death to comprehensive PHC came in
1993 when the World Bank published its World
Development Report, titled ‘Investing in Health.'
The Bank advocates a restructuring of health
systems in line with its neo-liberal free-market
ideology. It recommends a combination of privati
sation, cost-recovery schemes and other measures
that tend to place health care out of reach of the
Cfenminicaticn as if Etecple bettered
poor. To push its new policies down the throat of
poor indebted countries, it requires acceptance of
unhealthy policies as a pre-condition to the grant
ing of bail-out loans.
In the last decade of the 20th century, the World
Bank took over WHO’s role as world leader in
health policy planning. The take-over was pow
ered by money. The World Bank’s budget for
’Health’ is now triple that of WHO’s total budget.
With the World Bank's invasion of health care,
comprehensive PHC has effectively been shelved.
Health care is no longer a human right. You pay
for what you get If you are too poor, hungry and
sick to pay, forget it. The bottom line is business as
usual. Survival of the greediest!
vision is to advance towards a healthy global
community founded on fairer, more equitable
social structures. It strives towards a model of
people-centred development, which is participa
tory, sustainable, and makes sure that all people’s
basic needs are met.
The IPHC is not just a South-South network for
underdeveloped countries, but also includes
grassroots struggles for health and rights among
the growing numbers of poor and disadvantaged
people in the Northern overdeveloped’ countries.
For the last two years the Third World Network
and the IPHC have worked closely together in the
preparations for the People’s Health Assembly.
QwHAT po you SEE HE.RE?)
Cc^ALfTli^NS for tho
health a nJ uell-teirg
HUMANITY
^w'imary Heath Care as envisioned at Alma
I ^ZAta was never given a fair chance,—and
I
globalisation is creating an increasingly
polarised, unhealthy and unsustainable world. —
In response, a number of international networks
and coalitions have been formed. Their goal is to
revitalise comprehensive PHC and to work to
wards a healthier, more equitable, more sustain
able approach to development. Two of these
coalitions, which have both participated in organ
ising the People’s Heath Assembly, are the follow
ing.
MJ
VTethodologies
of
EPUCATipN for CHA
The Third World Health Network (TWHN)
based in Malaysia, was started by the Third World
Network, which has links to the International
Consumers Union. The TWHN consists of progres
sive health care movements and organisations,
mainly in Asia. One important contribution of the
Network has been the collection of a substantial
library of relevant materials, their lobby for
North-South equity and the promotion of net
working between Third World organisations.
The International People s Health Council
(IPHC) is a coalition of grassroots heath pro
grammes, movements and networks. Many of its
members are actively involved in community
work. Like the TWHN, the IPHC is committed to
working for the health and rights of disadvan
taged people—and ultimately, of all people. Its
/
ne of the most rewarding activities of the
IPHCwvas a post-conference workshop
hekf in Cape Town, South Africa, on
Methodologies of Education for Change. Health
educator/from Africa, Central America, Mexico, /
North America, the Philippines and Japan—most
with many years of experienced- facilitated group
activities. Each demonstrated Zome of the innova/
tiye learning and awareness/aising methods they
xlse in their different countjnes. The challenge oj
/ the workshop was to d<
or adapt methods of
education for action to icet the new challenges
of today’s globalised afid polarised world. /
From micro to ma/ro, local to global/ways
of making and uciderstanding the links
The Cape Town Workshop participants agreed
that a global gradroots movement need/ to be
mobilised to he/p rein in the unhealthwand unsus
tainable aspects of globalisation.
/
To do thisyeaming tools, methods, Znd teaching
aids mus/be developed to help ordinary people
see the l/nks between their local p/oblems and
Etecple's Hsalth. Asserrbly
/
s
:1
This emphasis on medically-driven pro
grammes is reflected in the internal organisa
tional structure of many ministries of health
and WHO itself: such arrangements reinforce
the tendency towards vertical technical
approaches and militate against implementa
tion of comprehensive PHC.
□
I
A
Health care continues to be an instrument of
social control.
Overtly unethical behaviour and human
rights violations by health personnel are,
z
unfortunately, not only a disgraceful part of
health history, but persist, particularly in
situations of war and political oppression.
However, health care as an instrument of
social control is much more subtle and
widespread. Central to this is the mystifica
tion by the health professions of the real
causes of illness, which is often attributed to
ill-considered individual behaviour and
natural misfortune, rather than to social
injustice, economic inequality and oppressive
political systems. Examples of such individualised
and conservative approaches range from the
promotion of family planning, in isolation from
social development, as a means of population
control, to oppressive forms of health education
that neglect the social determinants of certain
lifestyle’ factors linked to ill-health.
values
and suggested
acfaon
he vision of the Peoples’
Health Assembly is of an
accessible, affordable, equitably distrib
uted, appropriate and sustainable health system,
based on the principles of comprehensive PHC
and responsive to its users. Mechanisms for
popular participation in the health system should
ensure its accountability and also contribute to the
movement for participatory democracy in society
at large.
In order to achieve such a vision the following
broad types of action are suggested:
Advocate atnationaland international levels for
prioritisation ofand investment in health.
There is accumulating evidence that investment in
the social sectors has not only contributed to social
development but has also often led to economic
Etecple's Health Asserrtoly
icy'
/
da\id w erner
development. The Good Health at Low Cost
examples of Cuba, Sri Lanka, China, Costa Rica
and Kerala State in India demonstrate that a
commitment to broad-based, equitable develop
ment, with investment in women’s education,
health and welfare, has a significant and sustain
able impact on the health and social indicators of
the whole population. To realise the equity essen
tial for a healthy society, evidence suggests that a
strong, organised demand for government respon
siveness and accountability to social needs is
crucial. Recognition of this important challenge
informed the Alma Ata call for stronger commu
nity participation. To achieve and sustain the
political will to meet all people’s basic needs, and
to regulate the activities of the private sector, a
process of participatory democracy—or at least a
well-informed movement of civil society—is
essential: analysts have noted that such political
commitment was achieved in Costa Rica through a
long history of egalitarian principles and democ
racy, in Kerala through agitation by disadvan
taged political groups, and in Cuba and China
through social revolution. ‘Strong’ community
participation is important not only in securing
greater government responsiveness to social
needs, but also to mobilize an active, conscious
and organised population critical to the design,
implementation and sustainability of comprehen
sive health systems.
Good Health a+ Lovy Cost
■ . Wespite the dismal living conditions and health
11 situation in many poor countries, a few poor
states have succeeded in making impressive
strides in improving their people's health. In 1985,
the Rockefeller Foundation sponsored the Good
Health at Low Cost’ study to explore why certain
poor countries with low national incomes managed to
achieve acceptable health statistics. More specifically,
they asked how China, the state of Kerala in India. Sri
Lanka, and Costa Rica attained life expectancies of
65-70 years with GNPs per capita of only USS3001,300.
Upon completing the study, the authors determined
that the increased life expectancies were due to a
reduction in child and infant mortality rates (IMR) in
the four states and were accompanied by declines in
malnutrition and, in some cases, in the incidence of
disease. These remarkable improvements in health
were attributed to four key factors:
co:
co:
co:
co:
political and social commitment to equity (i.e. to
meeting all people s basic needs):
education for all. with an emphasis on the
primary level:
equitable distribution throughout the urban and
rural populations of public health measures and
primary health care:
an assurance of adequate caloric intake at all
levels of society in a manner that does not
replace indigenous agricultural activity.
The importance of factor one. a strong political and
social commitment to equity, cannot be overempha
sised. While the course of action may vary, equitable
access to health services necessitates breaking down
the social and economic barriers that exist between
disadvantaged subgroups and medical services.
Of the four regions investigated. China was the most
exceptional in terms of equality. Whereas in the other
three states, the decline in IMR was largely due to
better social services (improved healdi care coverage,
immunisation, water and sanitation, food subsidies
and education). China’s improvements were rooted
in fairer distribution of land use and food production.
The population was encouraged to become more selfsufficient. rather than to become dependent on
government assistance.
While all four regions developed cooperative,
community-oriented approaches to resolving prob
lems and meeting basic needs, in die 15 years since
the Rockefeller study, China has had the most success
in maintaining Its advances towards ‘good health at
low cost’.
Source: Werner, D. and Sanders, D. (1997) Questioning
the Solution: The Politics ofPrimary Heath Care and
Child Survival. Palo Alto: Health Wrights, p. 115.
Concerted action should be taken to persuade
individual governments to invest in health. WHO
needs to be lobbied to assume a stronger advocacy
role. It should take the lead in analysing and
publicising the negative impact that globalisation
and neoliberal policies are having on vulnerable
groups. It should spearhead moves to limit health
hazards aggravated by globalisation, including
trade in dangerous substances such as tobacco and
narcotics. It needs to strongly assert health as a
Human Right and publicise and promote the
benefits of equitable development and investment
in health. The extent to which WHO and govern
ments play such roles will depend on the extent to
which popular mobilisation around health occurs.
Communities have to be active and organised in
demanding these changes.
Demystify the causes ofill-health and
promote an understanding ofits social
determinants.
Since health'and ‘medicine' have become virtually
synonymous in the popular consciousness, it is impor
tant to communicate the evidence for the fact that illhealth results from unhealthy living and working
conditions, from the failure ofgovernments to provide
health-promoting conditions through policies that
ensuregreater equity. It then becomes obvious that
health problems are the result of structural factors and
political choices and that their solution cannot lie in
health care alone, but requires substantial economic
reform as well as comprehensive and intersectoral health
action. Mechanisms to disseminate this message,
including the use ofthe mass media, must be identified
and exploited.
Advocate andpromote policies and
projects that emphasise intersectoral
action for health.
Government health ministries and international health
agencies need to be pressed to engage as partneis Mth
the sectors, agencies and socialgroups critical to the
achievement ofbetter health. Policy development must
be transparent and inclusive to secure broader under
standing and wider ownership ofhealth policies.
Structures involving the different partners need to be
createdat different levels from local to national, or
within such settings as schools and workplaces. The
priority should be to focus on geographical areas with
the greatest health needs and involve communities and
their representatives at local level. Subgroups with
responsibility for health, within local, provincial or
nationalgovernment (e.g. health committees oflocal
government councils) should bepromoted and should
have links to the above structures. This has occurred in
some ofthe Healthy Cities projects in both industrial
ised and de veloping countries. Currently the Brazilian
law requires differentgroups to discuss the health
policies to be promoted, and includes community and
consumerparticipation.'
The VM-iraliTrtf-im of Ffeelth Chre and the Cballen^ cf Ifealth fcr All
Infersccfora! action fo
traffir accidents
flw the early 1970s, Denmark had the highest rate of
■ child mortality from traffic accidents in Western
I Europe. A pilot study was started in Odense.
Forty-five schools participated in an exercise carried
out with accident specialists, planning officials, the
police, hospitals and road authorities, to identify the
specific road dangers that needed to be addressed. A
network of traffic-free foot and cycle paths were
created as well as a parallel policy of traffic speed
reduction, road narrowing and traffic islands.
Following the success of the pilot study, the Danish
Safe Routes to Schools Programme has been imple
mented in 65 out of 185 proposed localities and the
number of accidents has fallen by 85%. Accidents
can. and must, be avoided. It is the responsibility of
each one of us, but many initiatives can and should
come from local authorities.
Source: Walking and Cycling in the City. WHO. 1998E.
p. 64
A process of engaging the public in a dialogue
about public health problems and in setting goals
for their control can both popularise health issues
and become a rallying-point around which civil
society can mobilise and demand accountability. It
can also create the basis for popular involvement
in implementation of health initiatives.
Actively develop comprehensive, community-based
programmes
Most programmes addressing priority health
problems start from a health care or services
perspective. While curative, personal preventive
/-■'•J
1
if
and caring actions are very important and still
constitute the core of medical care, comprehensive
PHC demands that they be accompanied by
rehabilitative and promotive actions. In address
ing priority health problems comprehensively, by
defining and implementing promotive, preventive,
curative and rehabilitative actions, a set of activi
ties common to a number of health programmes
will be developed as well as a horizontal infra
structure.
The principles of programme development apply
equally to all types of health problems, from
diarrhoea to heart attacks to domestic violence.
After the priority health problems in a community
have been identified, the first step in programme
development is the conducting of a situation
analysis. This should identify the prevalence and
distribution of the problem, its causes, the poten
tial resources to address them,, including commu
nity capacities and strengths that can be mobilised
and actions that can be undertaken to address the
problems. The more effective programmes have
taken the above approach, involving health work
ers, other sectors’ workers and the community in
the three phases of programme development,
namely, assessment of the nature and extent of the
problems, analysis of their multi-level causation
and priority actions to address the identified
causes. Here, partnerships with NGOs with
expertise in various aspects of community devel
opment are crucial.
Clearly, the specific combination of actions making
up a comprehensive programme will vary from
situation to situation. However, there are certain
principles that should inform programme design,
one of which is the deliberate linking of actions
that address determinants operating at different
levels. So, for example, in a nutrition
programme any intervention around
dietary inadequacy (immediate cause)
should also address household food
insecurity (underlying cause). Clearly the
principle of linking curative or rehabilita
tive (feeding), preventive (nutrition
X
education) and promotive actions (improved household food security) should
be applied to health programmes other
than nutrition, together with addressing
basic causes in the political and economic
realm.
1
1
health for the millions, sept-oct. nov-dec 1997
Pscple's Health Assarbly
A Comprehensive Approach to bnjer /Attrition in Zimta&we:
The Children s Supplementary Feeding Programme (CSfP)
— j
I
^he existing community-based popular
infrastructure that had developed during the
war permitted a more rapid and betterorganised implementation of the nutrition pro
gramme than would otherwise have been possible.
Mothers evaluated the children's nutritional status
by measuring and recording their upper arm
circumferences. Those with mid-upper-arm circum
ferences less than 13 ems were included in the
programme. The reasons for this cut-off point were
explained to all parents, both those of children
admitted to the programme, as well as those consid
ered not at risk. They then established locations for
supplementary feeding (which the mothers pre
ferred to be located close to their homes and fields),
and themselves cooked the food and fed the under
weight children.
security. The joint involvement of ministries of
health and agriculture in this project led to the
development of intersectoral Food and Nutrition
Committees at sub-district, district and provincial
levels.
The programme design therefore allowed the
linking of a rehabilitative measure (supplemen
tary feeding) to preventive and promotive
interventions (nutrition education and food
production), thereby displaying the features of a
comprehensive primary health care programme.
This comprehensive approach to child
undernutritiongreatly influenced the manage
ment of this problem within the health sector. It
resulted in a changed approach of health staffto
the dietary management of the sick child and to
nutritional rehabilitation. It also created a com
munity-level infrastructure of feeding points and
The design of the programme was informed, on the
food production plots/child care centres to which
one hand, by an understanding of the most impor
recuperating undernourished children could be
tant factors underlying rural child undernutrition in
sent. Thus the sequenced addressing of immediate
Zimbabwe and. on the other, by knowledge of
(dietary) and underlying causes (household food
rational dietary measures and identification of
insecurity, inadequate young
locally used and cultivable food sources
child
care and inaccessible
(analysis). By deliberately selecting for
health services) by the
use in the programme foods that were
, * Wk
feeding.the communal plots
highly nutritious, traditionally used in
k
and pre-school centres
weaning and commonly cultivated, and
7;
respectively, was made
by reinforcing their value with a very
possible by both careful
specific message in the form of a widely
design based on a prior
distributed poster asserting the impor
analysis and by lite presence
tance of groundnuts and beans in
of a well-organised and
addition to the staple, it was possible to
motivated population.
shift the focus of the intervention from
Intersectoral action and
supplementary feeding towards smallstructures for nutrition and
scale agricultural production pro
$
food security developed
gramme. This was aimed at reinstating
around the project, from the
the cultivation of groundnuts— cultur
bottom-up. and were sup
ally a 'women's crop’— which had been
health for the millions, sept-oct,
ported at higher levels of
largely displaced as a food crop in
rwv-dec 1997
government.
Zimbabwe by the commercialisation of
maize. The provision by the local and the national
government of communal land, agricultural inputs
and extension assistance, together with the policy of
collective production on these groundnut plots,
contributed to improving poor households’ food
In other health programmes - such as the Safe
Motherhood Initiative, the programme for Inte
grated Management of Childhood Illness and
Tuberculosis management (DOTS) - as also in
technical guidelines for the management of com
mon non-communicable diseases, similar mini
mum or core service components can be identified.
Standardising and replicating these core activities
in health facilities is helpful in reinforcing their
practice throughout the health system, but does
not guarantee the implementation of a comprehen-
Source: Sanders in Werner. D & Sanders, D. (1997).
Questioning the Solution: The Politics ofPrimary
Health Care and Child Survival. Palo Alto:
HealthWrights.
sive PHC programme, which must involve other
sectors as well as communities in promotive
actions.
Promote the use and dissemination ofappropriate
health technologies
The use of appropriate health technologies can
have a number of positive effects, which include
spreading health care more widely and increasing
its cost-effectiveness. One of the less obvious, but
The hfadkalizatim cf Itealth Qare and the (Tallaxp of tfealth ficr ALL
very important effects of appropriate technology is
in demystifying health care by giving lower-level
health workers and, through them, community
members better understanding, skills and effective
technologies forhealth care. Thus the medical
professions’ monopoly of knowledge and exper
tise can be challenged. A good example is the use
of homemade cereal gruels, which have been
shown to be very effective in rehydration during
diarrhoea.
Similarly, if certain appropriate health technolo
gies become widely incorporated into standard
health practice, their use can stimulate a critical
approach to the expanding range of Inappropriate,
sophisticated and expensive technologies. A good
example is that of pharmaceuticals. Encourage
ment of the use of a standardised, short list of
inexpensive drugs (essential drugs lists) known by
their own name (generics), not a trade name, can
reduce bad prescribing practices and begin to
undermine the operations of the pharmaceutical
industry. Evidence that such an initiative has
succeeded in challenging the forces that histori
cally have dominated health care has been the
extent of the opposition by the pharmaceutical
industry to WHO’s essential drugs programme.
Increasing the visibility and role ofcommunity
based health workers.
In the early years of the PHC movement an impor
tant and effective role was played by community
health workers (CHWs) in the implementation of
PHC. One of the strongest features of CHWs is
that they are predominantly women who can often
identify and gain access to those households and
individuals with the greatest health needs. In
deed, many of the ‘model’ PHC initiatives relied
extensively on CHWs for their successful opera
tion. Further, the role of CHWs was seen not
merely as a technical one of extending basic health
care to peripheral communities and households: it
was also, importantly, frequently an advocacy and
social mobilising role, enlisting the conscious
involvement of communities and other sectors in
health development.
The conservative economic and political environ
ment of the late 1980s and 1990s has contributed to
Efecple'a Hsalth Assaibly
the demise of many CHWs programmes: policy
makers seldom advocate the retention of this
cadre, and communities are economically unable
to support them.
Given the very positive past experiences of CHW
programmes in diverse situations, and the increas
ing need for community-based workers given the
International health crisis, aggravated in many
countries by the HIV pandemic, it is urgent that
the progressive health movement advocate and
campaign for the reintroduction of this cadre and
look for innovative ways to care for their commu
nities.
Advocate for equity in health andhealth care.
Equity is core to the policy of Health for All. Socio
economic inequalities are growing everywhere, at
a more rapid rate than ever before. Together with
reductions in public health and social services in
many countries, this is leading to growing inequi
ties in health. To advocate equity in health and
health care more successfully amongst interna
tional organisations, governments, donors and
professional organisations, we have to demon
strate the social differentials in access to health
resources and in health outcomes. The progressive
health movement needs to press for the monitor
ing of equity in health through advocacy and
information dissemination.
Promote more appropriate health personnel educa
tion and better management.
The primary health care approach needs much
more strongly to inform the content of health
sciences curricula as well as the learning process
and choice of venues for learning. The aim is to
equip learners with competencies spanning a
broader range than has traditionally been the case.
There is accumulating evidence that problemoriented and practice-based approaches result in
more relevant learning, and in the acquisition of
problem-solving skills, both necessary attributes
for the successful development of the PHC ap
proach. If health workers are to contribute to a
health system that enables people to assume more
responsibility for their own health through an
emphasis on preventive and promotive measures
Table: Key indicators for monitoring equity in health and health care
Indicator categories
Indicators measuring differences between population groups
Health determinants
indicators
Prevalence and level of poverty
Income distrivution
Educational levels
Adequate sanitation and safe water coverage
Health status indicators
Under 5-year child mortality rate
Prevalence of child stunting
[Recommended additional indicators: maternal mortality ratio; life expectancy
at birth; incidence/prevalence of relevant infectious diseases; infant mortality
rate and 1-4 year old mortality rate expressed separately]
Health care resource
allocation indicators
Per capita distribution of qualified personnel in selected categories
Per capita distribution of service facilities at primary, secondary, tertiary and
quaternary levels
Per capita distribution of total health expenditures on personnel and supplies,
as well as facilities
| Health care utilisation
; indicators
!
I
I
Immunisation coverage
Antenatal care coverage
% of births attended by a qualified attendant
Current use of contraception, percentage
_________
|
Source: World Health Organization (1998). Final report ofmeeting on policy-orientated monitoring ofequity in health
and health care. 29 September-3 October 1997. Geneva: WHO. page ii.
integrated with curative and rehabilitative meas
ures, then their training must expose them to good
practice at district level and to the social issues at
community level. There is also an urgent need for
teaching staff in the health sciences to upgrade
their skills to carry out such a reorientation of the
curricula.
The above suggestions for education reform apply
equally to all categories of health personnel, as
well as to undergraduate and post-graduate
training. It has long been acknowledged that
nurses play a pivotal role in the PHC team; in
addition, they constitute the largest category of
health personnel in many countries. Endorsement
of such educational reforms and their fuller
implementation and promotion by the nursing
leadership within individual countries is critically
important for progress towards Health for All.
In most countries, health education institutions
have not carried out curriculum reform along the
lines described above. Although there are indica
tions that some have embarked or will embark on
such a course, there will probably still be a signifi
cant delay before sufficient ‘new’ graduates are
available to work in and transform the health
system. Clearly, if the implementation of compre
hensive PHC is to be achieved during the next
decades, the process of curriculum reform in the
educational institutions needs to be accelerated
and accompanied by a massive programme of
capacity development of personnel already work
ing in the health system. In short, the current
Health for All imperative demands the rapid
expansion of continuing education activities in
most countries. Some of this in-service learning
should take place in multi-disciplinary teams to
promote better teamwork.
Similarly, education in PHC needs to involve
personnel from other health-related sectors as well
as community members: capacity development for
these constituencies has generally been neglected
and has weakened the growth of both community
participation and intersectoral involvement in
health development.
Health personnel management also needs to be
greatly strengthened through the development of
incentives, appropriate regulations and improved
support and supervision. The technocratisation of
health care that has been a feature of the past
decade has resulted in increasing inequities in
service provision and reduced accountability of
service providers. The progressive health move
ment needs to lobby strongly for greater invest
ment in human resources for health, since people
are the key to more appropriate and accountable
health services.
He NMimliTAt-im of Italth Gare and the Challercp cf Ifealth fix All
aspects of community development is crucial.
The engagement of communities in health
development needs to be pursued with much
more commitment and focus. The identifica
tion of well-functioning organs of people’s
organisations , whether or not they are pres
ently active in the health sector, needs to be
urgently pursued to make the necessary
alliances that can multiply our efforts.
CONCLUSIONS
38
It is clear that progress towards Health for All
has been uneven and is increasingly compro
mised. Gains already achieved are under
threat from a complex and accelerating process
of globalisation and neoliberal economic
policies, which are negatively impacting on
the livelihoods and health of an increasing
percentage of the world’s population and the
large majority in developing countries. Al
though the global PHC initiative has been
successful in disseminating a number of
effective technologies and programmes, which
have reduced substantially the impact of
certain (mostly infectious) diseases, its
intersectoral focus and social mobilising roles
- which are the keys to its sustainability - have
been neglected, not only in the discourse but
also in implementation.
3S
Government health ministries need to be
pressed to enter into partnerships with other
sectors, agencies and communities to develop
intersectoral policies that address the determi
nants of inequities and ill-health. The policy
development process needs to be inclusive,
dynamic, transparent and supported by
legislation and financial commitments.
8?
The time is long overdue for more forcefully
translating policies into actions. The main
actions should centre around the development
of well-managed and comprehensive pro
grammes involving communities, the health
sector and other sectors. The process needs to
be structured in well-managed district sys
tems, which need to be considerably strength
ened, particularly to effectively reach the
household, community and primary levels.
Here, PCH centres and their personnel have to
focus onthe reinstatement of community
health worker schemes.
38
38
The successful implementation of decentral
ised health systems will require targeted
investment in infrastructure, personnel,
management and information systems. A key
primaiy step is a new capacity development of
district personnel through training on the job
practice and health systems research. Such
human resources development must be prac
tice-based, problem and community oriented
and come after we reorient, educational
institutions and professional bodies.
Clearly, the implementation and sustenance of
comprehensive PHC requires inputs and skills
that demand resources, expertise and experi
ence not sufficiently present in the health
sector in many countries. Here partnerships
with NGOs and their expertise in various
People's Hsalth Asserrbly
®
In promoting the above move from policy to
action, WHO needs to be pressed to play a
much bolder role in: advocating equity and
legislation needed for its achievement; point
ing out the dangers of globalisation poses to
health; stressing the importance of partner
ships between the health sector and other
sectors; integrating its own internal structures
and activities to ensure that comprehensive
PHC programmes are developed; entering into
partnerships with and influencing other
multilateral and bilateral agencies and donors,
as well as NGOs and professional bodies,
towards a common Alma Ata rooted vision of
PHC; and advocating for major needed
investments in health, especially in human
resource development, without which Health
for All will remain a mere statement of intent.
Suggested reading list
Sanders. D. (1985). The Struggle for Health. Hampshire,
UK: Macmilliian Education.
Sanders, D. (2000) Primary Health Care 21 - Every
body’s Business’ in Primaiy Health Care 21 - Every
body’s Business: An international meeting to celebrate
20 years after Alma Ata. Geneva: WHO.
Werner, D. and Sanders, D. (1997) Questioning the
Solution: The Politics of Primary Heath Care and Child
Survival. Palo Alto: Heal th Wrights, p.115.
World Bank (1994) Better Health in Africa: Experience
and Lessons Learned. Washington DC: World Bank.
DavidSancfersh?ks more than 20 years experience
working in the health sector in Southern Africa particu
larly in Zimbabwe and South Africa and has been
actively involved in the development of health policy
and services with both the Southern African liberation
movements and with the newly independent govern
ments of Zimbabwe and South Africa. David Sanders
has since April 1993 been Director and Professor of a
new Public Health Programme at the University of the
Western Cape, South Africa, which provides practiceoriented education and undertakes research in public
health and primary health care. David Sanders is author
of "The Struggle for Health: Medicine and the Politics of
Underdevelopment" and co-author of “Questioning the
Solution: the Politics of Primary Health Care and Child
Survival'’ and has researched and written in the areas of
political economy of health, structural adjustment, child
nutrition and health personnel education.
HEALTH AS A HUMAN RIGHT
Health is a reflection of a society’s commitment to equity and justice.
Health and human rights should prevail over economic and political
concerns.
This Charter calls on people of the world to:
• Support all attempts to implement the right to health.
• Demand that governments and international organisations
reformulate, implement and enforce policies and practices which
respect the right to health.
• Build broad-based popular movements to pressure governments to
Incorporate health and human rights into national constitutions and
legislation.
• Fight the exploitation of people's health needs for purposes of profit
TACKLING THE BROADER DETERMINANTS OF HEALTH
Economic challenges
The economy has a profound influence on people’s health. Economic
policies that prioritise equity, health and social well-being can improve
the health of the people as well as the economy.
Political, financial, agricultural and industrial policies which respond
primarily to capitalist needs, imposed by national governments and
international organisations, alienate people from their lives and
livelihoods. The processes of economic globalisation and liberalisation
have Increased inequalities between and within nations.
Many countries of the world and especially the most powerful ones are
using their resources, including economic sanctions and military
interventions, to consolidate and expand their positions, with
devastating effects on people’s lives.
This Charter calls on people of the world to:
• Demand transformation of the World Trade Organisation and the
global trading system so that it ceases to violate social, environmental,
economic and health rights of people and begins to discriminate
positively in favour of countries of the South. In order to protect public
health, such transformation must include intellectual property regimes
such as patents and the Trade Related aspects of Intellectual Property
Rights (TRIPS) agreement.
• Demand the cancellation of Third World debt.
• Demand radical transformation of the World Bank and International
Monetary Fund so that these institutions reflect and actively promote
the rights and interests of developing countries.
• Demand effective regulation to ensure that TNCs do not have
negative effects on people’s health, exploit their workforce, degrade
the environment or impinge on national sovereignty.
• Ensure that governments implement agricultural policies attuned to
people’s needs and not to the demands of the market, thereby
guaranteeing food security and equitable access to food.
• Demand that national governments act to protect public health rights
in intellectual property laws.
•
•
•
Demand the control and taxation of speculative international capital
flows.
Insist that all economic policies be subject to health, equity, gender
and environmental impact assessments and include enforceable
regulatory measures to ensure compliance.
Challenge growth-centred economic theories and replace them with
alternatives that create humane and sustainable societies. Economic
theories should recognise environmental constraints, the fundamental
importance of equity and health, and the contribution of unpaid labour,
especially the unrecognised work of women.
Social and political challenges
Comprehensive social policies have positive effects on people's lives
and livelihoods. Economic globalisation and privatisation have
profoundly disrupted communities, families and cultures. Women are
essential to sustaining the social fabric of societies everywhere, yet
their basic needs are often ignored or denied, and their rights and
persons violated.
Public institutions have been undermined and weakened. Many of their
responsibilities have been transferred to the private sector, particularly
corporations, or to other national and international institutions, which
are rarely accountable to the people. Furthermore, the power of political
parties and trade unions has been severely curtailed, while conservative
and fundamentalist forces are on the rise. Participatory democracy in
political organisations and civic structures should thrive. There is an
urgent need to foster and ensure transparency and accountability.
This Charter calls on people of the world to:
• Demand and support the development and implementation of
comprehensive social policies with full participation of people.
• Ensure that all women and all men have equal rights to work,
livelihoods, to freedom of expression, to political participation, to
exercise religious choice, to education and to freedom from violence.
• Pressure governments to introduce and enforce legislation to protect
and promote the physical, mental and spiritual health and human
rights of marginalised groups.
• Demand that education and health are placed at the top of the political
agenda. This calls for free and compulsory quality education for all
children and adults, particularly girl children and women, and for
quality early childhood education and care.
• Demand that the activities of public institutions, such as child care
services, food distribution systems, and housing provisions, benefit
the health of individuals and communities.
• Condemn and seek the reversal of any policies, which result in the
forced displacement of people from their lands, homes or jobs.
• Oppose fundamentalist forces that threaten the rights and liberties of
individuals, particularly the lives of women, children and minorities.
• Oppose sex tourism and the global traffic of women and children.
o
Environmental challenges
Water and air pollution, rapid climate change, ozone layer depletion,
nuclear energy and waste, toxic chemicals and pesticides, loss of
biodiversity, deforestation and soil erosion have far-reaching effects on
people's health. The root causes of this destruction include the
unsustainable exploitation of natural resources, the absence of a long
term holistic vision, the spread of individualistic and profit-maximising
behaviours, and over-consumption by the rich. This destruction must be
confronted and reversed immediately and effectively.
This Charter calls on people of the world to:
• Hold transnational and national corporations, public institutions and
the military accountable fortheir destructive and hazardous activities
that impact on the environment and people’s health.
• Demand that all development projects be evaluated against health
and environmental criteria and that caution and restraint be applied
whenever technologies or policies pose potential threats to health and
the environment (the precautionary principle).
• Demand that governments rapidly commit themselves to reductions of
greenhouse gases from their own territories far stricter than those set
out in the international climate change agreement, without resorting to
hazardous or inappropriate technologies and practices.
• Oppose the shifting of hazardous industries and toxic and radioactive
waste to poorer countries and marginalised communities and
encourage solutions that minimise waste production.
• Reduce over-consumption and non-sustainable lifestyles - both in the
North and the South. Pressure wealthy industrialised countries to
reduce their consumption and pollution by 90 per cent.
• Demand measures to ensure occupational health and safety, including
worker-centred monitoring of working conditions.
• Demand measures to prevent accidents and injuries in the workplace,
the community and in homes.
• Reject patents on life and oppose bio-piracy of traditional and
indigenous knowledge and resources.
• Develop people-centred, community-based indicators of
environmental and social progress, and to press for the development
and adoption of regular audits that measure environmental
degradation and the health status of the population.
War, violence, conflict and natural disasters
War, violence, conflict and natural disasters devastate communities and
destroy human dignity. They have a severe impact on the physical and
mental health of their members, especially women and children.
Increased arms procurement and an aggressive and corrupt
international arms trade undermine social, political and economic
stability and the allocation of resources to the social sector.
This Charter calls on people of the world to:
• Support campaigns and movements for peace and disarmament.
• Support campaigns against aggression, and the research, production,
testing and use of weapons of mass destruction and other arms,
including all types of landmines.
• Support people's initiatives to achieve a just and lasting peace,
especially in countries with experiences of civil war and genocide.
• Condemn the use of child soldiers, and the abuse and rape, torture
and killing of women and children.
Demand the end of occupation as one of the most destructive tools to
human dignity.
• Oppose the militarisation of humanitarian relief interventions.
• Demand the radical transformation of the UN Security Council so that
it functions democratically.
• Demand that the United Nations and individual states end all kinds of
sanctions used as an instrument of aggression which can damage the
health of civilian populations.
• Encourage independent, people-based initiatives to declare
neighbourhoods, communities and cities areas of peace and zones
free of weapons.
• Support actions and campaigns for the prevention and reduction of
aggressive and violent behaviour, especially in men, and the fostering
of peaceful coexistence.
• Support actions and campaigns for the prevention of natural disasters
and the reduction of subsequent human suffering.
•
A PEOPLE-CENTERED HEALTH SECTOR
This Charter calls for the provision of universal and comprehensive
primary health care, irrespective of people's ability to pay. Health
services must be democratic and accountable with sufficient resources
to achieve this.
This Charter calls on people of the world to:
• Oppose international and national policies that privatise health care
and turn it into a commodity.
• Demand that governments promote, finance and provide
comprehensive Primary Health Care as the most effective way of
addressing health problems and organising public health services so
as to ensure free and universal access.
• Pressure governments to adopt, implement and enforce national
health and drugs policies.
• Demand that governments oppose the privatisation of public health
services and ensure effective regulation of the private medical sector,
including charitable and NGO medical services.
• Demand a radical transformation of the World Health Organization
(WHO) so that it responds to health challenges in a manner which
benefits the poor, avoids vertical approaches, ensures intersectoral
work, involves people’s organisations in the World Health Assembly,
and ensures independence from corporate interests.
• Promote, support and engage in actions that encourage people’s
power and control in decision-making in health at all levels, including
patient and consumer rights.
• Support, recognise and promote traditional and holistic healing
systems and practitioners and their integration into Primary Health
Care.
• Demand changes in the training of health personnel so that they
become more problem-oriented and practice-based, understand better
the impact of global issues in their communities, and are encouraged
to work with and respect the community and its diversities.
• Demystify medical and health technologies (including medicines) and
demand that they be subordinated to the health needs of the people.
• Demand that research in health, including genetic research and the
development of medicines and reproductive technologies, is carried
•
out in a participatory, needs-based manner by accountable
institutions. It should be people- and public health-oriented, respecting
universal ethical principles.
Support people’s rights to reproductive and sexual self-determination
and oppose all coercive measures in population and family planning
policies. This support includes the right to the full range of safe and
effective methods of fertility regulation.
PEOPLE'S PARTICIPATION FOR A HEALTHY WORLD
Strong people's organisations and movements are fundamental to more
democratic, transparent and accountable decision-making processes. It
Is essential that people's civil, political, economic, social and cultural
rights are ensured. While governments have the primary responsibility
for promoting a more equitable approach to health and human rights, a
wide range of civil society groups and movements, and the media have
an Important role to play in ensuring people's power and control In
policy development and in the monitoring of its implementation.
This Charter calls on people of the world to:
• Build and strengthen people’s organisations to create a basis for
analysis and action.
• Promote, support and engage in actions that encourage people’s
involvement in decision-making in public services at all levels
• Demand that people’s organisations be represented in local, national
and international fora that are relevant to health.
• Support local initiatives towards participatory democracy through the
establishment of people-centred solidarity networks across the world.
Amendment
• After the endorsement of the PCH on December 8, 2000, it was called
to the attention of the drafting group that action points number 1 and 2
under Economic challenges could be interpreted as supporting the
social clause proposed by WTO, which actually serves to strengthen
the WTO and its neoliberal agenda. Given that this countervails the
PHA demands for change of the WTO and the global trading system,
the two paragraphs were merged and amended.
•
The section of War, Violence and Conflict has been amended to
include natural disasters. A new action point, number 5 in this version,
was added to demand the end of occupation. Furthermore, action
point number 7, now number 8, was amended to read to end all kinds
of sanctions. An additional action point number 11 was added
concerning natural disasters.
Quick Feedback: Has this information been useful?
4
la
—-
a
I
'I
REGIONAL CONSULTATION
on
I
■
PUBLIC HEALTH
& HUMAN RIGHTS
SBr
a
10-11 April, 2001. New Delhi
REPORT & RECOMMENDATIONS
Organised by
National Human Rights Commission
li. colkUxjfatiun with
• ! Hr.ihh X I .iinily Welfare
< m>i eminent of India
U
ih; Ih ildi Organization
South I .ist Asia
Krgton.il Office
1si
Justice J.S. Verma
Chairperson
(I ormer Chief Justice of India)
Foreword
The World Health Organization, in its Constitution declares that
‘the enjoyment of the highest attainable standard of health is one of
the fundamental rights of every human being’ and it also says that
‘health is a state of complete physical, mental and social well being
and not merely the absence of disease or infirmity’. The Nobel Peace
Laureate, Elie Wiesel has observed that ‘one cannot, one must not.
approach public health today without looking into the human rights
component’. The International Covenant on Economic, Social and Cultural
Rights also recognizes ‘the enjoyment of the highest attainable standard
of health’ as the right of every human being. Thus, right to health
of the highest attainable standards, is a basic human right with universal
recognition. It must, therefore, be treated as a State responsibility with
the obligation to ensure its due respect.
In India, the national Constitution recognizes the State obligation
in clear terms in Article 47 which provides that the raising of the level
of nutrition and the improvement of public health are among the primary
duties of the State. This is a Directive Principle of State Policy contained
in Part IV of the Constitution which lays down the principles fundamental
in the governance of the country and obligates the State to apply them
in making laws. Another directive principle in Article 48A imposes the
duty to protect and improve the environment and to safeguard the
forests and wild life in the country, which too is related to improvement
vii
of public health. Both these articles in Part IV of the Constitution have
been judicially interpreted to expand the meaning and scope of ‘right
to life' guaranteed as a fundamental right in Article 21 of the Indian
Constitution. Thus, in India the national Constitution elevates the ‘right
to health of the highest attainable standards’ to a guaranteed fundamental
right which is enforceable by virtue of the constitutional remedy under
Article 32 of the Constitution.
The National Human Rights Commission, therefore, naturally considers
it of prime importance that the needed emphasis on improvement of
public health is given by all agencies to fulfill the promise held out
in the directive principles in keeping with the State obligation in a republican
democracy.
In April 2000, the Commission constituted a Core Advisory Group
on Health, comprising of experts in the field, with the object of preparing
a plan of action for systemic improvements in the health delivery
systems in the country. The first Chairperson of the Core Group was
the late Prof. V. Ramalingaswamy, who is now succeeded by Prof. N.H.
Antia. The Convenor of the Core Group is Prof. K. Srinath Reddy.
The Commission is grateful to all the members of the Core Group for
their invaluable contribution to the Commission’s efforts in this direction.
Pursuant to this programme, and in keeping with its broad objective
to give greater practical meaning to the right to health care, the Commission
organized two major Consultations on “Maternal Anaemia’ in April 2000,
and on Human Rights and HIV/AIDS’ in November 2000. Continuing
in this direction, the Commission organized a Regional Consultation
on ‘Public Health and Human Rights’ in April 2001 with a view to
bringing the policy makers, public health experts, legal professionals,
human rights activists and others together to deliberate on issues like
Nutritional Deficiencies, Access to Health Care and Tobacco Control.
The rationale behind the exercise was to evolve practical recommendations
for improving the current facilities.
viii
These exercises were performed by the Commission in collaboration
with the Ministry of Health and Family Welfare, Department of Women
and Child Development (Ministry of Human Resource Development),
UNICEF, UNAIDS, WHO, Lawyers Collective and NACO for whose
contribution the Commission is grateful.
The linkage between human rights and human development is
recognized and so is the significance of public health. The primary
targets for the year 2015 of the World Bank also include public health
issues such as improvement of reproductive health of women, reduction
in infant and maternal mortality rates etc. There is a felt need for
genuine partnerships between the government, community, NGOs,
medical and legal professions with points of entry at policy making,
norm setting, professional associations, service delivery area, research
and education. The goal of linking health and human rights is to contribute
to advancing human well being beyond what could be achieved through
an isolated health or human rights based approach.
It is my fervent hope that the recommendations of the Regional
Consultation on Public Health and Human Rights would be given serious
consideration and acted upon by the policy makers, planners and others
to make ‘health for all’, a reality.
(J.S. Verma )
Dated: 21 June 2002
Place: New Delhi
ix
EXECUTIVE SUMMARY
1. Human rights and public health are powerful and modern
approaches with intrinsic connections, which share the common objective
of protecting the health and the well being of all individuals. The Calcutta
Declaration adopted at the Regional Public Health Conference in 1999
had, in its agenda for action, recommended using a rights approach
to health. Upholding human rights and the dignity of all human beings
and adoption of an intergenerational approach are important prerequisites
for improving public health and ensuring sustainable development.
2. The National Human Rights Commission of India, in collaboration
with India's Ministry of Health and the World Health Organization, organised
the Regional Consultation on Public Health and Human Rights
in New Delhi on 10-11 April 2001. The objective was to advocate the
importance of adopting a synergistic approach to public health and
human rights. The Consultation also sought to identify avenues of action
conforming to human rights principles to advance public health objective
in three priority areas, viz., access to health care, nutrition and tobacco
control.
3. The initiative brought together experts in public health, nutrition,
law and human rights, and representatives of NGOs and international
organisations. Keynote presentations by experts were followed by intense
deliberations in working groups to identify key strategies and initiatives.
Two panels of experts discussed the regional perspective and partnerships.
4. Governments have the obligation to respect, protect and fulfil
human rights. They have a responsibility for their people's health, which
could be fulfilled only through providing adequate health and social
measures. Public health officials have dual responsibilities of protecting
and promoting public health, and respecting, protecting and fulfilling
human rights.
1
5. For developing countries, realisation of human rights, as they
apply to health, is a matter of 'progressive realisation' of making
steady progress towards a goal. The services should be scientifically
sound and conform tq public health "best practice". The implications
of the right to enjoy the benefits of scientific progress for health
issues have been at the core of recent concerns on access to drugs
for the developing world, and vaccine development.
6. The 1978 Alma-Ata Declaration called on nations to ensure
essential primary health care availability. The World Health Assembly,
in 1998, stressed the will to promote health by addressing its basic
determinants and prerequisites. Arbitrary restrictive measures that fail
to consider other valid alternatives are abusive of human rights principles
and in contradiction with public health 'best practice'. Discrimination
in health systems, and unsound human development policies and
programmes exacerbate disparities in health. Equal treatment within
societies and within health care settings should be the norm.
7. The major determinants of health lie outside the health system.
Human rights provide a useful tool for advancing public health goals,
and a framework for analysis and research into complex health problems’
A systematic human rights analysis using an analytical and action-oriented
framework, with indicators reflecting compliance with health promotion
and human rights principles, could guide evidence-based health policy
and programme development.
8. Health and development in various parts of India have progressed
unevenly. Health care expenditure is the second most common cause
of rural indebtedness. The health infrastructure needs to be reviewed,
recast and revitalised to ensure its convergence with existing primary
health care priorities. Multi-faceted development efforts can improve
the health situation.
9. Nutrition is a cornerstone that influences and defines people's
2
health. In the South East Asian (SEA) Region, 40% of under-five children
were underweight and out of this 43% stunted, 30% had a low birth
weight, 23% of the population had Iodine Deficiency Disorders. 1.3
million persons had clinical Vitamin A deficiency, and two-thirds of pregnant
women had iron-deficiency anaemia. Among the priority areas for action
are growth monitoring/promotion, nutrition surveillance, promotion/
support of breast-feeding, food security and safety net, and anaemia
prevention and control strategy.
10.
Governments have a responsibility to create enabling conditions
to help individuals make informed choice and to change the vulnerability
pattern by enacting legislation and putting in place appropriate enforcement
and redressal mechanisms. An Anti-tobacco Bill has been introduced
in the Indian Parliament in March 2001 that seeks to protect the rights
to information. Child health would be protected by the prohibition
on sale to minors.
11.
The Royal Thai Government's comprehensive anti-tobacco
package focuses on provision of health education and public information.
The media had helped shape several key health policies. A civil group
had petitioned for a National Health Insurance Act. Sri Lanka effected
a reduction of child mortality to 0.9% in 1999. Its government is working
on appropriate solutions to the new challenges of tobacco control,
environmental issues, drug abuse and Sexually Transmitted Diseases.
Nepal has 747 health posts besides 197 Public Health Centres (PHCs)
and health centres. Female smokers form a third of its hospital out
patients.
12.
Application of the new synergy of Public Health and Human
rights requires additional efforts to create consultative mechanisms, as
well as education, training and research in health and human rights.
Capacity should be enhanced for inter-disciplinary learning and research
on linkages between public health and human rights at national and
regional levels. Purposeful public health action calls for capacity building
3
•»
and development of partnerships among legal and public health institutions/
professionals, relevant government agencies, health NGOs, other sectors
of civil society and representatives of the people. Such networks in
SEA countries will serve national and regional public health needs.
13.
State Public Health Regulatory Authorities and a National
Public Health Advisory Body should be established in India to regulate
public health practices and monitor the implementation of public health
programmes. For dependable delivery of essential health care, the primary,
secondary and tertiary systems should be effectively linked. People's
empowerment makes all the difference in health outcomes. To promote
participation of the people in the development of health care systems,
decentralization of authority in health care systems and structural adjustment
should be facilitated through Panchayati Raj and other local institutions.
should disseminate correct information related to the effects of tobacco
consumption. Assistance for smoking cessation should be integrated
into health care services.
17.
Health and human rights experts have a collective
responsibility to conceptualise and carry forward these agenda for
a better and healthier society. The Human Rights Commissions in South
East Asian countries are uniquely placed to make a significant difference
to the quality of health and health care in the region.
14.
Measures suggested for health personnel include
standardization and quality-assurance in their training, restructuring of
their undergraduate education to make it more public health oriented,
and a continuing medical education programme with emphasis on public
health, and rational use of drugs and diagnostics. To ensure availability
of quality essential drugs, good manufacturing practices must be enforced
and a price control policy evolved with the prices linked to purchasing
capacity of the population.
15.
For effective implementation of the National Nutrition Policy,
the National Policies of Action on Nutrition and Child and the Infant
Milk Substitutes Act should be monitored. Steps should be taken to
minimise loss of procured or stored food-grains.
16.
A comprehensive national Tobacco Policy should be evolved,
and a multi-sectoral national level nodal agency established for tobacco
control. All states should take steps for passing resolutions for adopting
provisions relating to control of all other tobacco products (other than
cigarettes). Information Education Communication (IEC) programmes
4
5
BACKGROUND AND RATIONALE
The goal of extending the benefits of sustainable health over an
expanding life span, to all members of the human family, is the cardinal
uTb H th ,CkhCa'tfh- The Decla«tion of Human Rights eloquently
upholds the nght to life as an inalienable entitlement of all human beings
As the mutually nurturing relationship between health and development
becomes increasingly clear, protection of health (as an essential requirement
tor enabling human beings to develop to their full potential) becomes
integral to the mandate of human rights. Such a shared vision and
shared mission pave the way for a natural alliance between the advocates
of public health and the defenders of human rights. Purposeful partnership
between the two groups, catalysed by a conjoint consultation, would
be very productive for public health.
The National Human Rights Commission (NHRC) of India, under
he Chairmanship of Jus. ice J.S. Verma, has accorded a pivotal position
to the promotion of public health in its plan of action. It has constituted
a Core Group on Public Health to assist the Commission with technical
advice on matters related to health. Prof. V. Ramalingaswami (National
rofessor of Medicine) chairs this group, of which Prof. K. Srinath Reddy
(All India Institute of Medical Sciences) is the Convenor. The NHRC
has, in Collaboration with other organisations (including UN agencies),
organised two i ational workshops on anemia and HIV-AIDS, to consider
issues related ij their control in the context of human rights.
In order to extend the discussion to a broad range of issues relating
1 XrT3" ri9htS’ NHRC Pr°POSeS tO COnVene a consultation,
m April 2001, on Public Health and Human Rights'. The consultation
would involve interaction between health scientists, health activists, jurists,
policy makers and representatives from other sections of the civil society.’
e envisaged end products of the consultation are recommendations
6
for prioritised action in each of the major areas of concern. These
recommendations would be then considered by the NHRC for directing
the relevant national agencies to initiate the desired action and implement
the proposed strategies for advancing public health towards the desired
goals.
The NHRC is organizing this consultation, in partnership with the
Ministry of Health and Family Welfare (Govt, of India) and World Health
Organization (SEARO). By aligning interests and pooling resources,
such a partnership will provide synchrony of effort and synergy of effect
in promoting public health in India and the South East Asia Region.
For the purpose of this Consultation, National Human Rights
Commission, Ministry of Health and Family Welfare and World Health
Organization have identified three areas of public health concern: (1)
Nutritional Deficiencies, (2) Access to health care (including emergency
medical care) and (3) Tobacco Control. Recommendations, generated
at the Consultation, would help provide the NHRC with a framework
for advocacy and action to advance public health goals in these areas,
through relevant administrative, legislative and executive measures.
For these reasons, a partnership between the NHRC (India), Ministry
of Health and Family Welfare (Government of India) and WHO (SEARO)
would provide a confluence of common interests and cumulatively contribute
in the advancement of essential public health goals in India (and other
SEAR countries). The consultation, in turn, will provide a platform for
establishing partnerships between various stakeholder groups for follow
up action and advocacy.
In this context, one of the follow-up measures proposed, to consolidate
and continue the efforts initiated at the consultation, would be to establish
partnerships between public health institutions/groups and the national
law institutes in India (located at Bangalore, Bhopal, Hyderabad and
Kolkata). Through collaborative arrangements between each nationa1
7
*
law institute and one or more public health group, focused work would
be carried out on selected areas of health evaluated in the context
of human rights. For example, one of the law institutes may take up
continued work on nutrition and human rights, in partnership with one
or more public health groups who have expertise and interest in that
area. Others would take up the prime responsibility for providing legal
leadership in other specific areas of health. Such collaborative work,
linking multiple legal and public health institutions, would provide a
filip to the growth of Public Health Law as an academic discipline apart
from facilitating informed advocacy on public health as a human rights
concern.
PARTICIPANTS PROFILE
The Participants would include:
(a)
(b)
(c)
(d)
(e)
(f)
OBJECTIVES OF THE CONSULTATION
1.
2.
3
To identify avenues of actibn which can advance short, medium
and long-term objectives of public health in three prioritised
areas of concern for further advocacy, by the NHRC, for
implementation by the various agencies concerned. The areas
to be covered by this Consultation will be (1) Nutritional Deficiencies,
(2) Access to health care (including emergency medical care)
and (3) Tobacco Control.
To establish partnership between public health experts, jurists
and community representatives (including health NGOs) to pursue
informed advocacy for pubic health action in the context of
human rights.
To create mechanisms for future collaboration between academic
institutions/departments of law and public health experts to
periodically produce well researched position papers on major
public health issues from the perspective of law and human
rights, thereby promoting the growth of Public Health Law both
as an academic discipline and as a pathway for public health
action.
8
(s)
Public Health experts and health scientists.
Legal experts (drawn from national law institutes as Well as from
the Judiciary and the Bar)
Representatives of health NGOs.
Representatives of the community (drawn from various sections
of the civil society, including consumer groups).
Policymakers (drawn from the legislative and executive branches,
from the national and provisional levels)
Representatives of NHRC, MOHFW and WHO (SEARO).
Observers from other UN Agencies (UNDP, UNICEF, UNAIDS.
FAO, ILO, UNESCO, UNIFEM).
WHO (SEARO) will consider the feasibility of supporting the participation
of neighbouring countries who are members of WHO (South East Asian
Region).
Main Content Areas
(1)
(2)
(3)
Nutritional Deficiencies,
Access to health care (including emergency medical care) and
Tobacco Control.
In each of these areas, the Consultation would focus on identifying
specific activities wOhich are desirable but are currently lacking or deficient.
Priority would be accorded to activities where substantial health benefits
are expected to accrue in a relatively short time frame, through specific
legislative/executive measures. The recommendations would have to
be framed in a manner that would enable NHRC to seek their
implementation through clearly indicated actions to be undertaken by
the concerned agencies. The consultation does not aim to produce
state of the art public health reviews but instead will focus on producing
a clearly stated agenda of action which the NHRC can catalyse through
its intervention.
9
Process
PROCEEDINGS
-The above objectives can only be achieved, if adequate preparatory
work is performed to generate a preliminary consensus, among stakeholder
groups, on prioritized areas for action in each of the content areas
listed above. The main multi-disciplinary consultation would provide
INAUGURAL SESSION
an opportunity for critical appraisal of these suggestions and convergence
on key recommendations to be forwarded to the NHRC (to accomplish
objective 1). The consultation would also provide an opportunity to
The Regional Consultation commenced with the ceremonial lighting
of the lamp by Nitin Singh, a Class IV student of Kendriya Vidyalaya,
partnerships, which will advance advocacy and follow-up action (to
accomplish objectives 2 and 3).
The preparatory work would be performed by Planning Group
comprising of Ms S Jalaja (Joint Secretary, NHRC), Dr. Srinivas Tata
(Deputy Secretary, Ministry of Health and Family Welfare) Dr. Tej Walia
(World Health Organization) and Prof. KS Reddy (Convenor, NHRC’s
Core Group on Public Health and Human Rights). The Planning Group
would identify key resource persons in each of the main content areas
listed above. They would be requested to provide suggestions of specific
legislative/executive actions, which will advance public health objectives
in that area. A structured formal would be provided by the secretariat
so that the nature of the action, its rationale and expected benefits
as well as relevance to human rights are succinctly described and the
implementing agencies are clearly identified. Each suggestion by the
resource persons would be provided utilizing such a proforma, which
does not exceed one page.
The Planning Group would screen the suggestions received from
various resource persons, in each in the areas, and shortlist them for
further discussion in the main consultation. Three working groups for
the conference would be established, prior to the conference.
The Consultation would consist of an initial plenary addressing
the broad theme, working group discussions to evolve recommendations
in their assigned areas and a final plenary to consider the working
group reports. There would also be small group meetings to identify
the opportunities for partnership and mechanisms for follow-up action.
10
Delhi.
Mr. N. Gopalaswamy, Secretary General of the National Human
Rights Commission (NHRC) of India welcomed the delegates. The logo
of the NHRC features the famous words of an ancient Indian seer,
sarue bhauantu sukhinah' (let everybody be happy). He said that the
subsequent words, 'sarue santu nirarnayah' (let everybody be free of
disease) were also important and needed to be followed. He mentioned
about the efforts taken by the NHRC in this regard by bringing together
experts in the areas of health and human rights to review the status
and suggest strategic direction and agenda for future action. Two Consultations
had been held earlier which had come forth with meaningful measures
on 'maternal anaemia' and 'HIV/AIDS'.
Dr. Palitha Abeykoon, Director, Health Technology and
Phamaceuticals at the South East Asia Regional Office of the World
Health Organization (WHO) conveyed the appreciation of his Regional
Director for the initiative taken by the NHRC in organising the series
of consultations relating to health and human rights and addressing
some of the most pressing health issues. The Human Rights Commissons
in South East Asia, he said, were uniquely placed to make a significant
difference to the quality of health and health care in the countries of
the Region.
The Calcutta Declaration adopted by the Regional Public Health
Conference organised by the WHO in Calcutta in November 1999 had
identified some key areas in its agenda for action. One of these was
11
ACCESS TO HEALTH CARE
i. Recommendation: Since lack of opportunities for participation
of the people in the development of health care systems is a human
rights violation - the consultation recommends that NHRC facilitate
decentralization of authority in health care systems of the country,
through Panchayati Raj and other local institutions, by devolution
of appropriate financial, administrative and supervisory powers.
Action to be taken: In all national health related programmes
such as those under the Ministries, Department of Health & Family
Welfare, Women and Child Development and Social Justice and
Empowerment, emphasis should be on primary health care with
community participation. Enlisted NGOs, with proven involvement
and commitment in this area, may be appropriately involved in
facilitating this process.
Implementation Steps: Each of the concerned Ministries/departments
to develop and report indicators for progressive decentralization
(from a minimum level to the most desirable level).
2. Recommendation: Since the absence of an adequate quantity
of reasonable-quality health care personnel at the primary and secondary
level health care facilities, resulting in lack of access to basic health
care, is a human rights violation the consultation recommends that
NHRC facilitate standardization and quality-assurance in the training
of the various cadres of health care personnel.
(a) Action to be taken: Restructure undergraduate education for
medical, dental, nursing and rehabilitation professionals to make
the training more public health oriented with regard to knowledge,
motivation and skills.
Implementation Steps: The Ministry of Health (GOI), through
the relevant Councils - Medical Council of India, Dental Council
54
of India, Indian Nursing Council and Rehabilitation Council of Indiato develop plans of action (with curricular content), within one year.
(b) Action to be taken: Develop a programme for continuing
medical education of health care providers with special focus on
primary health centre personnel. This should particularly place emphasis
on the knowledge and skills relevant to public health, and rational
use of drugs and diagnostics.
Implementation Steps: The Ministry of Health (GOI), through
the relevant Councils, develop a plan of action within one year.
3. Recommendation: Since any lack/inadequacy of access to health
care at the various levels for the lower and middle socio-economic
strata of the country would be a human rights violation - the
Consultation recommends that NHRC facilitate strengthening and
effective linkages of the primary, secondary and tertiary levels of
the health care delivery system for dependable and assured delivery
of essential health care services (acute as well as chronic).
Action to be taken: The Ministries of health and Family Welfare
at the Centre and States should develop state-specific plans for
strengthening the health care delivery systems at all three levels
with effective linkages and referral systems.
Implementation Steps: The Planning Commission should
coordinate the development of these plans with the Central and
State Governments and seek their submission within one year.
4. Recommendation: Since the provision of emergency medical care
for trauma related emergencies as well as medical, surgical and
obstetric emergencies is a minimum requirement of a Welfare state,
the Consultation recommends that NHRC should constitute an Expert
Group/Task Force to identify the requirements of Essential Emergency
Health Care and recommend appropriate models and guidelines;
these can then be, forwarded to the Central and State governments
55
of India to:
i) Expand equitable access to essential medicines and ensure mechanisms
to make available vital HIV-related and other essential drugs to
all persons who need them, on a non-discriminatory basis.
for their review and implementation.
Action to be taken: NHRC to constitute the Expert Group and
then forward the recommendations to the Central and State
governments for necessary action.
ii) Refrain from taking measures which would deny or limit equal
access to all persons to preventive, curative or palliative pharmaceuticals
or medical technologies used to treat diseases of public health importance
(such as HIV/AIDS or the most common opportunistic infections
that accompany them).
Implementation Steps: NHRC to constitute an Expert Group and
facilitate its meetings to enable submission of report in 6 months.
5. Recommendation: Since irrational or unethical medical practice,
leading to exploitation of or injury to the citizen, is a human rights
violation- the Consultation recommends that NHRC facilitate the
regulation of irrational or unethical medical practice in the public
and private health care sectors of the country, through the development
of guidelines for use of drugs, diagnostics and therapeutic procedures,
with a regulatory framework for monitoring and enforcement.
Action to be taken: Clinical practice guidelines are to be developed
for common diseases/disorders and clinical procedures. The Ministry
of Health & Family Welfare, Govt, of India should coordinate their
development and widespread dissemination among the health
professionals to the country with the help of premier medical institutions
and professional associations and relevant professional Councils (such
as Medical and Dental Councils).
•>
Implementation Steps: The Ministry of Health and Family Welfare,
Government of India should complete this process within one year,
with a provision for review of the guidelines every three years (or
earlier if needed).
6. Recommendation: The Government of India should put in place
an updated National Drug Policy to ensure “an adequate and reliable
supply of safe, cost-effective drugs of acceptable quality to all citizens
of India and the rational use of drugs by prescribers, dispensers
and consumers.
(a) Action to be taken: NHRC should call upon the Government
56
!
iii) Adopt legislation or other measures to safeguard access to such
preventive, curative or palliative pharmaceuticals or medical technologies
free from any limitations by third parties; adopt all appropriate positive
measures to the maximum of the resources allocated for this purpose,
so as to promote effective access to such preventive, curative or
palliative pharmaceuticals or medical technologies; increase access
to medicines, in accordance with the health needs of the people
(especially those who can least afford the costs); act constructively
to strengthen pharmaceutical policies and practices, including those
applicable to generic drugs and intellectual property regimes, in
order to further promote innovation and the development of domestic
industries consistent with national law.
The government needs to take measures such as compulsory licensing
or parallel importation to increase access to life saving drugs at
affordable prices to overcome hazards to public health and nutrition
caused by HIV/AIDS and other diseases. The availability of lowcost generic drugs needs to be expanded with guarantees of their
quality.
iv) To ensure availability of essential drugs at affordable prices for
HIV/AIDS and other diseases of public health importance, the NHRC
should issue a notice to the Government of India calling upon it
to identify the various areas of government action and the measures
taken / proposed especially in relation to TRIPS.
57
Implementation Steps: The Ministry of Health & Family Welfare
and D/0 Chemicals, Government of India to report on action taken
within 3 months.
(b) Action to be taken: Ensure quality of drugs produced and
marketed for use by the people, by defining minimum standards
of quality and enforcing good manufacturing practices (GMP), with
strong mechanisms for monitoring and regulation through national
and state drug control authorities.
Implementation Steps: The Ministry of Health and Family Welfare,
through Drug Controller General of India and State Drug Control
Authorities to develop protocols for testing and monitoring, on an
ongoing basis.
NUTRITIONAL DEFICIENCIES
1. Recommendation: The Consultation considered that it is essential
to provide access to iodised salt, for all sections of population, on
a sustained and affordable basis. Therefore, there is an urgent need
to monitor the distribution and quality of iodised salt throughout
the country.
Action to be taken: i) The Consultation recommends that NHRC
should direct the Central government to clearly spell out its policy
summarizing the current public health evidence as well as its present
administrative position. The government should come up with a
status paper on this.
ii) Surveys should be conducted on the availability of iodised salt,
quality of iodisation and the prevalence of iodine Deficiency Disorders.
The results should be obtained within one year and remedial actions
be taken to plug the gaps.
Implementing Agencies: NHRC to take up the matter with the
Government of India (Department of Health and Salt Commissioner’s
Office).
2. Recommendation: The Infant Milk Substitutes Act had been enacted
to promote breast feeding and to stop unethical practices of selling
infant milk substitutes. The Consultation felt that despite the enactment
of the Act,’ some infant food manufacturers are still resorting to
promotion of infant milk substitutes in illegal ways through sponsoring
of events, etc.
Action to be taken: The Consultation recommends that a review
be undertaken of the implementation of the IMS Act, with specific
reference to violations and a report be submitted, within 6 months,
of the remedial action taken.
Implementing Agencies: The Government of India, through the
58
59
Department of Women and Child Development.
3.
4.
Recommendation: Right to food availability for all sections of the
community, particularly those who are socially/economically
underprivileged, should be ensured especially in a situation of adequate
food reserves. Loss of food grains/cereals due to faulty storage or
other reasons is unacceptable.
the barriers in effective implementation.
Implementing Agencies: The Department of Women & Child
Development should report to NHRC on this, within two months.
6. Recommendation: The proposed Public Health Regulatory Authorities
should monitor the effective Implementation of the National Nutrition
Policy and the National Policies of Action on Nutrition and Child.
Action to be taken: The Ministry of Agriculture, government of
India to take measures to ensure food availability in coordination
with other concerned Ministries such as Rural Development &
Employment. It should also detail the plan of action for Food Corporation
of India to monitor and reduce wastages in storage or transport.
Implementing Agencies: Till such a time that the proposed Authorities
are established, the Department of Women and Child Development
should annually report to the NHRC about the implementation,
utilizing criteria developed by experts.
Implementing Agencies: The Government of India, through the
Ministry of Agriculture
7. Recommendation: The Consultation suggested that NHRC initiate
an overview, by the Ministry of Law and Justice, of the level of
compliance with the following international covenants to which India
is a signatory:
Recommendation: The Consultation recommends that media
guidelines should incorporate the following:
-
The Practice of breast-feeding should be protected and promoted
-
Adverse effects of child marriage and adolescent pregnancy should
be publicized.
Convention on the Rights of the Child (CRC)
Conventions on the Elimination of All Forms of Discrimination
Against Women (CEDAW)
SAARC Declaration on the Girl Child
Citizens should be provided information related to the right to
nutrition and provision of relevant services
Action to be taken: Guidelines to be declared by the relevant
Ministries within 6 months.
Implementing Agencies: Government of India through the Ministries/
Departments of Health and Family Welfare, Women and Child
Development and Information & Broadcasting.
5. Recommendation: The Implementation of the recommendations
of the NHRC sponsored workshop on Maternal Anaemia (April
2000) should be reviewed to evaluate the progress made and identify
60
61
L_ -3^- 6
The Right to Health Care
Moving from idea to reality
- Abhay Shukla, CEHAT
"Should medicine ever fulfil its great ends, it must enter into the larger political and social
life of our time; it must indicate the barriers which obstruct the normal completion of the life
cycle and remove them. Should it ever come to pass, Medicine, whatever it may then be, will
become the common good of all. "
- ^olf Virchow, c. 1850
Background: Inequity in health and access to health care
India is known to have poor health indicators in the global context, even in comparison with
many other developing countries. However, we also bear the dubious distinction of being
among the more inequitous countries of the world, as far as health status of the poor
compared to the rich is concerned. This underscores the fact that there is a tremendous burden
of unnecessary morbidity and mortality, which is borne almost entirely by the poor. Some
striking facts in this regard are • Infant mortality among the economically lowest 20% of the population is 109, which is
25 times the IMR among the top 20% population of the country.
• Under-five mortality among the economic bottom 20% of the population (bottom
quintile) is 155, which is not only unacceptably high but is also 2.8 times the U5MR of
the top 20% (top quintile).
• Child mortality (l-5yrs age) among children from the ’Low standard of living index’
group is 3.9 times that for those from the 'High standard of living index' group according
to recent NFHS data (UPS, 2002). Every year, 2 million children under the age of five
years die in India, of largely preventable causes and mostly among the poor. If the entire
country were to achieve a better level of child health, for example the child mortality
levels of Kerala, then 16 lakh deaths of under-five children would be avoided every year.
This amounts to 4380 avoidable deaths every day, which translates into three avoidable
child deaths every minute
• Tribals, who account for only 8% of India's population, bear the burden of 60% of
malarial deaths in the country.
Such gross inequalities are of course morally unacceptable and are a serious social and
economic issue. In addition, such a situation may also be considered a gross violation of the
rights of the deprived sections of society. This becomes even more serious when viewed in
the context of gross disparities in access to health care • The richest quintile of the population, despite overall better health status, is six times
more likely to access hospitalisation than the poorest quintile. This actually means that the
poor are unable to afford and access hospitalisation in a large proportion of illness
episodes, even when it is required
• The richest quintile have three times higher level of coverage for measles immunization
compared to the poorest quintile. Similarly, a mother from the richest 20% of the
population is 3.6 times more likely to receive antenatal care from a medically trained
person, compared to a mother from the poorest 20%. The delivery of the richer mother is
over six times more likely to be attended by a medically trained person than the delivery
of the poor mother.
• As high of 82% of outpatient care is accessed from the private sector, met almost entirely
by out-of-pocket expenses, which is again often unaffordable for the poor.
1
•
•
About three-fourths of spending on health is made by households and only one-fourth by
the government. This often pushes the already vulnerable poor into indebtedness, and in
over 40% of hospitalisation episodes, the costs are met by either sale of assets or taking
loans.
The per capita public health expenditure in India is abysmally low, below $5 annually.
India has one of the most privatized health systems in the world (only five countries on
the globe are worse off in this respect), effectively denying the poor access to even basic
health care.
The gist of these sample facts is that the existing system of‘leave it to the market’ effectively
means *leave health care for the rich and leave the poor to fendfor themselves9.
One implication that emerges from the above discussion is that the problem of large-scale ill
health in India should not be seen as primarily a technical-medical issue. The key
requirement is not newer medical technologies, more sophisticated vaccines or diagnostic
techniques. The fact that the prosperous sections of the population enjoy a reasonably good
health status implies that the technical means to achieve good health do broadly exist in our
country today (though there is definitely a need to better adapt these to our country’s
conditions and traditions, and certain improved techniques might help in specific contexts).
In fact, for the vast majority, the key barriers to good health are not the lack oftechnology
but poverty and health system inequity. Poverty, a manifestation of social inequity, leads to
large sections of the population being denied adequate nutrition, clean drinking water and
sanitation, basic education, good quality housing and a healthy local environment, which are
all prerequisites for health. At the same time, we have a highly inequitable health system
which denies quality health care to all those who cannot afford it (the fact that even those
who can afford it do not always get rational care is another important, but somewhat separate
issue!). In this paper, which is primarily addressed to those working in the health sector, we
will focus on the critical health system issues, with a rights-based approach. Let us see how
we can view this entire situation from a rights based perspective.
The Right to Health Care as a component of the Right to Health
Looking at the issue of health under the equity lens, it becomes obvious that the massive
burden of morbidity and mortality suffered by the deprived majority is not just an unfortunate
accident. It constitutes the daily denial ofa healthy life, to crores ofpeople, because ofdeep
structural injustice, within and beyond the health sector. This denial needs to be addressed in
a rights based framework, by systematically establishing the right of every citizen of this
country, to a healthy life. More specifically, health care can no longer be viewed as just a
technical issue to be left to the experts and bureaucrats, an issue of charity to be dealt with by
benevolent service delivering institutions, or a commodity to be sold by private doctors and
hospitals. The role of all these actors needs to be redefined and recast in a framework where
every person, including the most marginalized, is assured of basic health care and can
demand and access this as a right.
It is clear that achieving a decent standard of health for all requires a range of far reaching
social, economic, environmental and health system changes. There is a need to bring about
broad transformations both within and beyond the health care sector, which would ensure an
adequate standard of health for all. In other words, to promote the Right to Health requires
action on two related fronts (WHO, 2002):
2
Promoting the Right to underlying determinants of health
This involves working for the right to ‘the underlying determinants of health, such as access
to safe and potable water and adequate sanitation, an adequate supply of safe food, nutrition
and housing, healthy occupational and environmental conditions, and access,to health-related
education and information, including on sexual and reproductive health’ (WHO, 2002).
Agencies engaged in the health sector cannot deal with most of these issues on their own,
though they need to highlight the need for better services and conditions, and can advocate
for improvements in these areas in a rights based framework. Organisations working in the
health sector should support and ally with other agencies working directly in these areas, to
help bring about relevant improvements.
Promoting the Right to Health Care
Given the gross inequities in access to health care and inadequate state of health services
today, one important component of promoting the Right to Health would be to ensure access
to appropriate and good quality health care for all. This would involve.reorganisation,
reorientation and redistribution of health care resources on a societal scale. The responsibility
oftaking forward this issue seems to lie primarily with agencies working in the health sector,
though efforts in this direction would surely be supported by a broad spectrum of society.
In the remaining portion of this paper, we will focus on the process of establishing the Right
to health care as a imminent task, to be taken up by organisations in the health sector within
the broader context of Right to Health outlined above.
The justification for establishing the Right to Health Care
We may view the justification for this right at three levels - constitutional-legal, social-
economic and as a human right issue.
The constitutional and legal justification
, ,.
The right to life is recognised as a fundamental right in the constitution (Article 21) and this
right has been quoted in various judgements as a basis for preventing avoidable disease
producing conditions and to protect health and life. The directive principles of the Indian
constitution include article 47, which specifies the duty of the state in this regard.
47 Duty of the state to raise the level of nutrition and the standard of living and to improve
health:- The state shall regard the raising of the level of nutrition and the standard of living
of its people and the improvement of public health as among its primary duties ...
In an important judgement (Paschim Banga Khet Mazdoor Samity and others v. State of
West Bengal and another, 1996), the Supreme Court of India ruled that In a welfare state the primary duty of the Government is to secure the wdfere _of the. people
Providing adequate medical facilities for the people is an essential part of the obligations
undertaken by the Government in a welfare state. ... Article 21 imposes an obhgation on he
State to safeguard the right to life of every person. ... The Government hospitals runi by the
State and the medical officers employed therein are duty bound to extend medical ass stanre for
preserving human life. Failure on the part of a Government hospital to provide timely medical
treatment to a person in need of such treatment results in a violation of his right to life
guaranteed under Article 21. (emphasis added)
3
Similarly in the cases Bondhua Mukti Morcha v. Union of India and others, 1982
concerning bonded workers, the Supreme Court gave orders interpreting Article 21 as
mandating the right to medical facilities for the workers.
Basic social services are now being recognised as
; fundamental rights with the 93rd
amendment in the constitution accepting Educationi as a fundamental right. Despite the
controversy and problems regarding the actual provisions of the Bill, it is now being accepted
that essential social services like education can be enshrined in the fundamental rights of the
Constitution. This forms an appropriate context to establish the right to health care as a
constitutionally recognised fundamental right.
The social and economic justification
It is now widelyj recognised that besides being a basic human right, provision of adequate
health care to a population is one of the essential preconditions for sustained and equitable
economic growth. The proponents of ’economic growth above all' may do well to heed the
words of the Nobel Laureate economist Amartya Sen:
'Among the different forms of intervention that can contribute to the provision of social
security7, the role of health care deserves forceful emphasis ... A well developed system of
public health is an essential contribution to the fulfilment of social security objectives.
... we have every reason to pay full attention to the importance of human capabilities also as
instruments for economic and social performance. ... Basic education, good health and other
human attainments are not only directly valuable ... these capabilities can also help in
generating economic success of a more standard kind ... (from India: Economic
Development and Social Opportunity by Jean Dreze and Amartya Sen)
The human rights justification
The right to basic health care is recognised internationally as a human right and India is a
signatory to the International Covenant on Economic, Social and Cultural Rights which states
in its Article 12 -
The States Parties to the present Covenant recognise the right of everyone to the enjoyment
of the highest attainable standard of physical and mental health... The steps to be
taken...shall include those necessary for ...The creation of conditions which would assure
to all medical service and medical attention in the event of sickness.
Reference can be made to other similar international conventions, wherein the Government of
India has committed itself to providing various services and conditions related to the right to
health, e.g. the Alma Ata declaration of ‘Health for all by 2000’. The National Human Rights
Commission has also concerned itself with the issue of 'Public health and human rights' with
one of the areas of discussion being 'Access to health care'. The time has come to begin
asking as to how these human rights related commitments and concerns will be translated into
action in a realistic, time-bound and accountable framework.
Health Rights - people's response to Globalisation-Liberalisation-Privatisation
The negative impact of Globalisation-Liberalisation-Privatisation policies on various social
sector services, especially since the early 1990s has been widely experienced. With the
growing withdrawal of the state from the social sector and encouragement to the private
medical sector, raising the issue of health rights has become extremely relevant today. The
ongoing abdication of basic obligations by the Public Health system needs to be countered by
a strong movement to establish Health rights. Only a determined effort to establish these
4
rights can roll back the trend of weakening the Public health system, and can provide a
framework for rejuvenation of this system with increased accountability.
The core content of the Right to Health Care in the first phase
Moving towards establishing the Right to Health Care is likely to be a process with various
phases. First let us see what could be the core content of this right in the first phase, which
could be achieved in the short to medium term.
Right to a set of basic public health services
In the context of the goal of ’Health for All’ and various Health Policy documents, an entire
range of health care services are supposed to be provided to all from village level to tertiary
hospital level. As of today these services are hardly being provided adequately, regularly or
of the required quality. Components of the public health system to be ensured in a rights
based framework include:
1. Adequate physical infrastructure at various levels
2. Adequate skilled humanpower in all health care facilities
3. Availability of the complete range of specific services appropriate to the level
4 Availability of all basic medications and supplies (also see below)
The expected infrastructure and services need to be clearly identified and displayed at various
levels and converted into an enforceable right, with appropriate mechanisms to functionalise
this. For example, in a justiciable framework, basic medical services especially at Primary
and Secondary levels cannot be refused to anyone - for example a PHC cannot express
inability to perform a normal delivery or a Rural hospital cannot refuse to perform an
emergency caesarean section. In case the requisite service such as a normal delivery is not
provided by the public health facility when required, one approach could be to allow the
patient to take recourse to a private hospital and receive free care, for which the hospital
would receive time-bound reimbursement of costs incurred, at standard rates. This would
firstly constitute a strong pressure on the public health system to perform better and deliver
all services, and secondly, would ensure that the patient receives the requisite care when
required, without incurring personal expenses. This could form one of the steps towards
accessing the right to health care.
Similarly the state has an explicit obligation to maintain public health through a set of
preventive and promotive services and measures. These of course include coverage by
immunisation, antenatal care, and prevention, detection and treatment of various
communicable diseases. However, it should also encompass the operation of epidemiological
stations for each defined population unit (say a block), organizing multi-level surveillance
and providing a set of integrated preventive services to all communities and individuals.
In summary, the movement to establish the Right to Health Care aims to substantially
strengthen, reorient and make accountable the Public Health System. The public has to
come back centre-stage in the Public Health System!
Right to emergency medical care and care based on minimum standards from
private medical services
Although the right to health care is not a fundamental right in India today, the right to lite
is. In keeping with this ‘Emergency Medical Care’ in situations where it is lifesaving, is the
right of every citizen. No doctor or hospital, including those in the private sector, can refuse
minimum essential first aid and medical care to a citizen in times of emergency, irrespective
of the person’s ability to pay for it. The Supreme Court judgement quoted above (Paschim
5
Banga Khet Mazdoor Samity and others v. State of West Bengal and another, 1996), directly
relates to this right and clear norms for emergency care need to be laid down if this right is to
be effectively implemented. As a parallel, we can look at the constitutional amendments
enacted in South Africa, wherein the Right to Emergency Medical care has been made a
fundamental right.
At the same time there is an urgent need for a comprehensive legislation to regulate
qualification of doctors, required infrastructure, investigation and treatment procedures
especially in the private medical sector. Standard guidelines for investigations, therapy and
surgical decision making need to be adopted and followed, combined with legal restrictions
on common medical malpractices. Maintaining complete patient records, notification of
specific diseases and observing a ceiling on fees also needs to be observed by the private
medical sector. The Govt, of Maharashtra is in the process of enacting a modified act to
address many of these issues, and the National Health Policy 2002 stipulates the enactment of
suitable regulations for regulation of minimum standards in the private medical sector in the
entire country by the year 2003. This would include statutory guidelines for the conduct of
clinical practice and delivery of medical services. There is a need to shape such social
regulation of this large medical sector within the larger, integrated framework of Right to
health care.
Right to essential drugs at affordable cost
Attaining this right would consist of two components:
1. Availability of certain basic medications free of cost through the public health system
(see above)
2 A National Essential Drug Policy ensuring the production and availability of an entire
range of essential drugs at affordable prices
The Union as well as state Governments need to publish comprehensive lists of essential
drugs for their areas. A ceiling on the prices of these drugs must be decided and scrupulously
adhered to, with production quotas and a strict ban on irrational combinations and
unnecessary additives to these drugs.
Right to patient information and redressal
The entire range of treatment and diagnosis related information should be made available
to every patient in either private or public medical facility. Every patient has a right to
information regarding staff qualifications, fees and facilities for any medical centre even
before they decide to take treatment from the centre. Information about the likely risks and
side effects of all major procedures can be made available in a standard format to patients.
Information regarding various public health services which people have a right to demand at
all levels should be displayed and disseminated. This should include information about
complaint mechanisms and for redressal of illegal charging by public health personnel.
Superseding the CPA, a much more patient-friendly grievance redressal mechanism needs
to be made functional, with technical guidance and legal support being made available to all
those who approach this system. This would provide an effective check on various forms of
malpractice. In case the services mandated under this right are not given by a particular
facility, the complainant need not take recourse to lengthy legal procedures. Rather, the
grievance redressal mechanism with participation of consumer and community
representatives should be empowered to take prompt, effective and exemplary action.
Right to monitoring and accountability mechanisms
Keeping in mind the devolution of powers to the Panchayati Raj system, we need to
propose an effective system of people's monitoring of public health services which would be
6
organised at the village, block and district levels. Community monitoring of health services
would significantly increase the accountability of these services and will lead to greater
people's involvement in the process of implementing them The Union Ministry of Health and
Family Welfare, with support from WHO, has implemented an innovative pilot project for
'Empowering the rural poor for better health' in six talukas of the country. Taking this and
various other experiments into account, a basic framework for such monitoring needs to be
developed.
Health rights related to various vulnerable sections of the
population and in special situations
It is obvious that the establishment of any system of rights is relevant only if it benefits the
most vulnerable or deprived sections of the population, and addresses the needs of people
facing situations where their basic rights are likely to be denied. All the above types of
provisions need to be implemented keeping in view some of the following key rights (an
illustrative, not exhaustive list):
• Women’s Right to Health Care, including provision of services related to both
reproductive and non-reproductive health problems specific to women, and appropriate
general health services for women;
• Children’s Right to Health Care, with a focus on nutritional supplementation, control of
infectious diseases in childhood and reduction in infant and child mortality;
• Health Rights of HIV-AIDS affected persons, including facilities for detection,
counselling, non-discriminatory treatment and access to anti-retroviral drugs;
• Right to Mental health care, with a focus on strengthening primary mental health care,
non-discriminatory quality treatment and community based rehabilitation systems;
• Right to Health Care for unorganised workers, who lack effective health care coverage
and face a range of occupational hazards, with a clear liability on employers;
• Right to Health Care for urban deprived communities, including putting in place Urban
primary health care systems and effective referral mechanisms;
• Health rights in conflict situations, where due to communal or other forms of violence
persons from particular communities may be denied access to basic health services or may be
discriminated against;
• Health rights of communities facing displacement or involuntary resettlement, depriving
them of their customary environment and livelihood, and placing them in often hostile new
surroundings which may include threats to health and poorer access to health care
This list may be further expanded to include the elderly, disabled persons, migrants and other
categories of vulnerable people. Any system of health rights would need to explicitly address
the special health needs of such groups, which would require provision of special services
and forms of protection against discrimination.
Ways ahead - building a campaign on the Right to health care
Some of the possible areas of activity of a broad coalition like Jan Swasthya Abhiyan, which
could develop a campaign on the issue of Right to Health Care, are suggested below.
Involving diverse social sectors in a dialogue on the Right to Health Care
While some health activists and groups have mooted the concept of the Right to Health Care,
it is an idea, which is yet to be widely discussed and accepted in our country. One of the key
tasks in the immediate future is to generate discussion at the broadest possible level about this
right. Groups to be involved in such a debate include health policy makers, medical and
7
public health academics, private medical professionals, people's organisations, women’s
groups, organisations representing or working with various vulnerable groups, various
segments of the NGO sector including both health related and non-health NGOs and trade
unions of health care personnel. It is obvious that the viewpoints of various social groups and
actors may be greatly divergent on this issue. However, the very process of discussing and
debating the issue gives it a primary legitimacy, which then needs to be built upon. This
becomes a basis for generating a continuously widening consensus about the basic
justification, content and implementation model for the Right to Health Care.
Analysing international experience on the Right to Health Care
There is valuable international experience available about mandating the Right to Health or
Health Care. These experiences need to be collated, and analysed with the Indian context in
mind. Especially legislation and provisions made in developing countries are of value in this
respect.
Cuba with a socialist constitution accords the right to health to its citizens, according it a
status equivalent to civil and political rights.
South Africa, after the overthrow of apartheid, in Article 27 of its constitution has specified
certain provisions relevant to this right. This includes mandating the right to access to health
care services, specifying that the state must take reasonable legislative measures to achieve
realisation of this right, and declaring that no one may be refused emergency medical
treatment. From another end, we have a new system of Universal health care access in
Thailand whose features need to be studied and discussed as relevant to the Indian context.
Similarly, there has been an entire process of developing the concept of right to health and
health care in the international human rights discourse. Various United Nations health rights
instruments refer to health related rights. The UN International Covenant on Economic,
Social and Cultural Rights (ICESCR), UN Convention on Rights of the Child (CRC) and the
UN Convention on the Elimination of All Forms of Discrimination Against Women
(CEDAW) are some such significant conventions, in which India is a signatory.
Given this background, one of the critical tasks ahead of us is to make an in-depth study of
these experiences and utilise this for developing the judicial form and implementation-related
content of the Right to Health Care in the Indian situation.
Organizing regional public hearings on the Right to Health Care
One way of developing such a consensus and mobilising various social organisations is to
organise regional public hearings, on the issue of Right to Health Care. The NHRC could be a
partner or ‘mediator’ for such public hearings, which could involve presentation of cases of
Denial of health care. With the involvement of State Public health officials and policy makers
in such hearings, the stage could be set for addressing the core issues, demanding
accountability and putting in place monitoring mechanisms to ensure basic health rights.
Discussing detailed proposals to implement the Right to Health Care
One of the crucial issues in furthering this campaign is the development of a model for
implementing this Right. This needs to be done, keeping in mind the specificities of the
Indian health care system, judicial framework (including the fact that Health is a state
subject), socio-economic situation including major class, caste and gender disparities and
recent processes such as the positive and negative lessons of the impending 93
Constitutional amendment. Considerable groundwork and consultation is required to develop
a model, which would take into account legal, operational and human rights considerations
and form the basis for practical implementation of this right.
8
Legal actions towards implementation of the Right to Health Care
Next, there is a need to take appropriate legal action to establish this basic right. Submitting a
National petition on Right to Health Care to the National Human Rights Commission, with
extensively documented cases of denial of health care could be a logical first step. Filing of
specific Pits, focussed on key health rights may also be necessary to exert legal pressure and
to provide leverage to the campaign. Political lobbying for passage of state level legislations,
such as Public Health Acts, may be essential to actually establish legal entitlements, which
can be activated by any ordinary citizen.
Making the Right to Health Care a Fundamental Constitutional Right
Finally, we need to move towards the medium-term objective of establishing Health Care as a
Fundamental Right in the Indian Constitution. This would be a prolonged and challenging
process, and would involve political mobilisation and influencing public and political opinion
on a large scale, besides formulating an appropriate bill based on legal inputs. This would
need to be complemented by State level legislations and effective strengthening of the Public
health system. Putting in place effective monitoring mechanisms, and widespread public
awareness about the entitlements would be essential for this right to become operational in
any meaningful form. One conception of the minimum content of the fundamental right to
health care is outlined in the accompanying box.
Proposed minimum content of the fundamental right to health care
1. Making the right to health care a legally enforceable entitlement by legal enactment
2. A national health policy with a detailedplan and timetablefor realization ofthe core right to health
care
3. Developing essential public health infrastructure required for health care; investing sufficient
resources in health and allocating these funds in a cost-effective andfair manner
Providing
basic health services to all communities andpersons; focusing on equity so as to improve
4.
the health status ofpoor and neglected communities and regions
5. Adopting a comprehensive strategy based on a gender perspective so as to overcome inequalities in
women's access to health facilities
6. Adopting measures to identify, monitor, control andprevent the transmission ofmajor epidemic and
endemic diseases
Making
reproductive health andfamily planning information and services available to all persons
7.
and couples without any form ofcoercion
8. Implementing an essential drug policy
(Adaptedfrom Audrey R. Chapman, The Minimum Core Content of the Right to Health)
While the course and outcome of all our efforts would depend on the much larger political
environment, the slogans of ‘Right to Health’ and ‘Right to Health Care’ should continue to
be the rallying-cry on our banner. Whether we are confronting the State or are trying to
envisage models for the future and shape people’s counter-hegemony, the vision of the Right
to Health and Health Care should form one of the components of our dream for a more just
and humane society.
(This article is an updated version of a note prepared by Dr. Abhay Shukla of CEHA T, for the
Seminar on 'Right to Health Care' organised on 3-4 January 2003 during the Asian Social
Forum at Hyderabad. Several sections of this article are adaptedfrom Abhay's article 'Right
to health care'published in Health Action, May 2001)
9
Annexure
Suggesting a system for Universal access to health care
While trying to achieve these specific rights in the first phase, our overall goal should be to
move towards a system where every citizen has assured access to basic health care,
irrespective of capacity to pay. A number of countries in the world have made provisions in
this direction, ranging from the Canadian system of Universal health care and NHS in Britain
to the Cuban system of health care for every citizen. In the Indian context, while the right to
health care needs to be enshrined in the Constitution as a fundamental right, there is a need to
develop a complementary system of Universal access to health care.
The existing massive private medical sector in India, which commands over three
fourths of the doctors and provides a similar proportion of outpatient care, needs to be
addressed and tackled in any system to provide Universal health care coverage. One possible
scenario to make this right functional could be a system of Universal social health insurance.
The services could be given by a combination of a significantly strengthened and communitymonitored public health system, along with some publicly regulated and financed private
providers, under a single umbrella. The entire system would be based on public financing and
cross-subsidy, with free services to the majority population of rural and urban working people
including vulnerable sections, and affordable premium amounts (which could be integrated
with the taxation system) for higher income groups.
One key aspect would be that this should be a Universal system (not targeted), which
would ensure coverage of the entire population and also retain a strong internal demand for
good quality services. (Of course, certain very affluent sections may choose to pay their share
of taxation / premium and yet opt out and access private providers.) Another issue is that
there should be no fees or nominal fees at the time of actual giving of services. Finally, the
patient should be assured of a range of services with minimum standards, whether given from
the public health system or publicly financed and regulated private providers. The entire
system could be managed in a decentralised manner, with consumer’s monitoring of quality
and accessibility of services.
This entire model would of course imply a significantly higher public expenditure on
health services. However, with decentralised management and a focus on rational therapy, it
has been estimated that it should be possible to organise the most basic elements of such a
system by devoting about 3% of the GNP towards public health care to start with. This
should then be progressively raised to the level of 5% of GNP spent on Public health to give
a full range of services to all. This level of funds could be partly raised by appropriate
taxation of unhealthy industries, reallocations within the health sector (including reorganising
existing schemes like ESI) and ending all subsidisation of the private medical sector. This of
course needs to be combined with changed budgetary priorities and higher overall allocation
for the health sector. Incidentally, the new National Health Policy claims on paper the
intention to more than double the financial allocation for the public health system and bring it
to the level of 2% of the GDP, and to increase utilisation of public health facilities to above
75% by the end of this decade. This admirable yet vague intention needs to be converted into
concrete action by means of strong and sustained pressure from various sections of civil
society, coupled with concrete proposals to functionalise universal access to health care.
In this context, ensuring the Right to Health Care for all is not an unrealistic scenario,
but has become an imperative for a nation, which as the ’world’s largest democracy’ claims to
accord certain basic rights to its citizens, including the right to life in its broadest sense.
10
G
A concept paper on universal access to health and health care.
Fr.S.Ousepparampil
The fifties and the sixties really witnessed a considerable shift towards “Health for
all” especially in the developing countries. In India the Shore Committee
recommended a decentralized Primary Health Care approach to make health
accessible to marginalized and the underprivileged. At the dawn of independence
this was adopted as the basis for India’s health care policy. But the actual
implementation of this policy was beset with major problems and in the process it
became over medicalzed, over westernized, over centralized, and over
professionalized and beaurocratized. The focus of peoples health in peoples hand
was over looked and peoples health ended up in specialists hands. The strength and
resilience of Indian systems of medicine and the social, cultural and economic
factors too were ignored. It goes with out saying that today the public health system
is in disarray characterized by inadequate capacity in the field, organizational
fragmentation and disjointed decision making. Thus we failed to mobilize people to
play a vital role in their own health and health care set up. After 55 years of
independence access to health still remains a cutting edge issue in India. Health is a
function not only of medical care, but of the over all integrated development of the
society - cultural, economic, spiritual, educational, genetic endowment,
environmental exposure, lifestyles, social and political influence, income and
available medical care. And thus health is a multifaceted phenomena.
The setting up of Indian Council of Social Science Research (ICSSR) and Indian
Council of Medical Research in the seventies again kick-started the thinking
process to bring people oriented health care to the fore friend. The report of this
panel is unique in that, it represents the joint deliberations of national experts from
both medical as well as social sciences.
The report clearly demonstrated that health as a component of overall social and
economic development, which in turn is influenced by our own health culture and
practice based on the influence of mind and body interactions. The report
emphasized the need to have an integrated approach to health and medical care and
insisted that the best of the Western and the indigenous systems be integrated. And
this process can provide an accessible, affordable and sustainable health care
systems to this country which is people oriented and decentralized.
The report clearly defines the role that people can play in this set up. The 73rd and
74th aineiidinems
me consuniuon
nas reauy
nave such a
amendments of the
constitution has
really maae
made it possible to have
viable, alternative model today. And health is one of the subjects under the
Panchayat Raj system under section 11 of the schedule and it provides ample
opportunity to inaugurate a nation wide move for universal access to health in the
third millennium.
Today we need to make health and medical care a peoples movement. Tire report
clearly indicates that appropriate health care can be provided to the entire
population at about half the existing expenditure in the combined public and private
sector. We need to harness the locally available human resource and empower
especially the women by demystifying health which has been highly mystified
subject in the hands of the professionals. Today all of us know that what our country
need is a “bottom up, people oriented system, which can provide health care to the
marginalized and the underprivileged people living below the poverty line.
The committee looked at various options of alternative models of health set up
1) The village level
2) Sub-center level.
3) Community health center with a population of 100,000.
4) District level
5) Specialist center.
It is true that in a large subcontinent like ours we certainly need modifications to
meet the varying needs and there should be no hesitation to do this. In all these
effort we do need a well informed health care sector which presupposes education
of the masses and it is here that we envisage a special role for voluntary secotor.
In the ultimate analysis we need to realize and recognize that we need to move
away from counter productive, consumerist, western model and replace it with
people based, participatory model of health and health care facilities as
unprecedented opportunities and challenges face the nation and the world we seek
to improve human health through participation and collaboration.
Universal Access to Health for all
UN and its WHO have done a lot to make the health accessible to all through
different documents and institutions. On the other hand WTO and many of the
pharmaceutical companies are trying to do the opposite to make profit and
exploit the whole world for profit. Poverty and illness are in a vicious circle.
Because of poverty illness come and because of illness poverty increases.
Illness is prevented not mainly by medicine but by nutrition and sanitation.
Global ethics demands availability of health care for all. It is premised on
universally accepted values and norms. There is a common ground apparent in
the process of development of medical systems. That ground is the universal
values and norms shared by all- values of sanctity of humanness, human rights,
and preservation of environment. It is the individual and collective ethics of
responsibility. The global ethics is an ongoing and never-ending process. The
civilized world is held together by the global ethics. From this universal ethics
emerges the rights and duties recognized and operationalised by the
internationally accepted charter like the UN. Declaration. Now all the nations in
the world must individually legitimate, empower, protect and implement these
values and norms with structures and strictures in every aspect of human
medical needs. The final norm is interact, integrate and progress and become
accessible to all by avoiding isolation in the name of specialization. All the
medical systems are good for humanity but not all those who deal with them.
They, many of them, do not respect ethical values and moral norms. What is
needed is metanoia against the prevailing paranoia The present paranoia must
go The global ethics demands availability of health care for all.
Medical Science, and also any science, is the process of knowing the bits and
pieces of the phenomenal world It deals with attaining the manipulative power of
the material world. Atoms are bonded, different kinds of things are bonded. The
Universe is a bond. Some call it ‘field", electric field, magnetic field, gravitational
field, etc. The bonds bind and build. All these bonds and fields postulates are
fragmentary explanations of the observed phenomena. When we put them
together with logic behind it a particular science is born. When legal bit s are
bound together we have legal system. When medical bits are put together we
have medical science.
Integration is a synthesis of the valid elements of the different systems of
medicine into a modern scientific health science, which the people need. All the
systems have valid and invalid elements in them. Therefore, the attempt
required is to put the valid elements together and without adhering to the ego
reinforcing antiquities. The development of a scientific world-view, sharing of the
experiences of private practitioners with scientists and researchers, development
of scientific data for the existing practices, and eradication of quackery in the
non-developed areas are included in integration
There are three groups of Medical systems. 1) Allopathic medical system with a
philosophy of man, 2) Chinese, i yurveda, etc., meeting the medical needs of
man with an equal footing as that of Allopathic medicine with their own
explanations of man. Therefore, these systems are to be called parallel systems
of medicine - parallel to that of allopathic medicine. Hence, we have allopathic
medicine, parallel medicine and alternative medicine. Alternative practices are
interventions for one or the other ailment without a proper philosophy supporting
it. It can get integrated to into allopathic or parallel medicines. These three
groups of medicines can be further integrated into each other. Cross-reference
of patients to different practitioners is easily possible if the integration of medical
systems is a reality. . Integrative medicine is a term loosely used to describe
biomedicine, parallel medicine and alternative medicines used in combination.
Systems of medicine grew up with integration like any other science. This we
have seen already. Now what we need is simple integration and inter-system
integration of medical systems. This is a natural out come based on the very
nature of the development of science. Divisions and analyses are for better
understanding. True learning is in integration. Unless the integration of medical
systems is an on going process universal access to health care is a mirage.
Health care needs coalition and integration of the knowledge of a man with a
single medicine and of the trained medical practitioner. It is a holistic and
interactive approach, not isolative and solipsistic.
1
Universal Access to Health for all
DR. J. OUSEPARMPIL,
Senior Fellow, University Grants Commission,
Dept, of philosophy. University of Poona
drouse@pn2.vsnl.net.in
020- 7171803, 9822256275
In the following two pages I put forward only two points: 1) Medical science grew up
with a process of integration. This is true in the case with any science, physical or social.
2) The world is moving fast towards a global ethics. Human rights demands universal
access to health for all. All the systems of medicine are good but not all that handle
them. A metanoia is the need of the day. Avoid isolation by specialization, integrate
medical systems andfollow human rights, which is part ofglobal ethics.
UN and its WHO have done a lot to make the health accessible to all through different
documents and institutions. On the other hand WTO and many of the pharmaceutical
companies are trying to do the opposite to make profit and exploit the whole world for
profit. Poverty and illness are in a vicious circle. Because of poverty illness comes and
because of illness poverty increases. Illness is prevented not mainly by medicine but by
nutrition and sanitation. Unethical exploitation of resources is the main cause of denying
universal access to health for all.
Global ethics demands availability of health care for all. It is premised on universally
accepted values and norms. There is a common ground apparent in the process of
development of medical systems. That ground is the universal values and norms shared
by all- values of sanctity of humanness, human rights, and preservation of environment. It
is the individual and collective ethics of responsibility. The global ethics is an ongoing
and never-ending process. The civilized world is held together by the global ethics. From
this universal ethics emerges the rights and duties recognized and operationalised by the
internationally accepted charter like the UN. Declaration. Now all the nations in the
world must individually legitimate, empower, protect and implement these values and
norms with structures and strictures in every aspect of human medical needs. The final
norm is interact, integrate and progress and become accessible to all by avoiding isolation
in the name of specialization. All the medical systems are good for humanity but not all
those who deal with them. They, many of them, do not respect ethical values and moral
norms. What is needed is metanoia against the prevailing paranoia. The present paranoia
must go. The global ethics demands availability of health care for all.
Medical Science, and also any science, is the process of knowing the bits and pieces of
the phenomenal world. It deals with attaining the manipulative power of the material
world. Atoms are bonded; different kinds of things are bonded. The Universe is a bond.
Some call it "field”, electric field, magnetic field, gravitational field, etc. The bonds bind
and build. All these bonds and fields postulates are fragmentary explanations of the
2
observed phenomena. When we put them together with the logic behind it a particular
science is bom. When legal bits are bound together we have legal system. When medical
bits are put together we have medical science. Medical science is grouped with different
logic and we have different systems of medicine. This process is never complete unless
we integrate all the different systems of medicine with the same logic.
Integration is a synthesis of the valid elements of the different systems of medicine into a
modern scientific health science, which the people need. All the systems have valid and
invalid elements in them. Therefore, the attempt required is to put the valid elements
together and without adhering to the ego-reinforcing antiquities. The development of a
scientific world-view, sharing of the experiences of private practitioners with scientists
and researchers, development of scientific data for the existing practices, and eradication
of quackery in the non-developed areas are included in integration
There are three groups of medical systems. I) Allopathic medical system with a
philosophy of man, 2) Chinese, Ayurveda, etc., meeting the medical needs of man with
an equal footing as that of allopathic medicine with their own explanations of man.
Therefore, these systems are to be called parallel systems of medicine - parallel to that of
allopathic medicine. Hence, we have allopathic medicine, parallel medicine and
alternative medicine. Alternative practices are interventions for one or the other ailment
without a proper philosophy supporting it. It can get integrated to into allopathic or
parallel medicines. These three groups of medicines can be further integrated into each
other. Cross-reference of patients to different practitioners is easily possible if the
integration of medical systems is a reality. . Integrative medicine is a term loosely used to
describe biomedicine, parallel medicine and alternative medicines used in combination.
Systems of medicine grew up with integration like any other science. This we have seen
already. Now what we need is simple integration and inter-system integration of medical
systems. This is a natural out come based on the very nature of the development of
science. Divisions and analyses are for better understanding. True learning is in
integration. Unless the integration of medical systems is an on going process universal
access to health care is a mirage. Health care needs coalition and integration of the
knowledge of a man with a single medicine and of the trained medical practitioner. It is a
holistic and interactive approach, not isolative and solipsistic.
IO
Community Based Primary Health Care Primary Health Care
approach to reach the unreach
55 years after independence health conditions of majority of Indians are steadily
deteriorating. Widespread malnutrition among children and women is a major health
problem. Lack of clean portable water primitive sanitary conditions and environmental
degradation contribute to nearly 60% illnesses in rural areas. There is growing disparity
between women - men, urban-rural, rich-poor, landowner - landless labors and high caste
- low caste. Unchecked population is detrimental to physical, mental and social health of
people, specially women and children.
There is a need to accept and promote broader definition of health, which is physical,
mental, social and spiritual well being. Health and medical care are different. The
government has wrongly promoted medical care in the name of health. Highly
commercialized and greedy private medical sector is promoting curative care and
medicalizing the society. It is promoting unnecessary and expensive technology. This
commercialization is resulting in erosion of ethics and moral values.
Health and development go together. They are two sides of the same coin. World Health
Assembly promoted Primary Health Care approach to meet universal health needs of all
in the world. The Alma Ata Conference highlights following principles:
•
Health is fundamental right and therefore it should be accessible, available,
affordable and culturally acceptable to all
•
People have right and responsibility to plan and maintain their own health.
•
Health and development are intimately related. Integration with sectors such as
environment, agriculture, education and women’s income generation needs to be
promoted.
•
There is a need to integrate curative services and with promotion, prevention and
rehabilitation.
•
The present curative oriented and technical care needs to be replaced by wholistic
health.
•
No one system is perfect and it has limitations, therefore the best in all system
should be available to the community.
•
Health care personnel should replace hierarchal approach by team approach.
In the early 80s ICS SR and ICMR appointed a committee to suggest alternate strategy
to achieve ‘Health For AH’. This committee provided, some far reaching solutions.
Empowering local communities through knowledge, skill and budget.
1
Decentralization up to block level and provision of integrated graded health services.
Unfortunately, there was no infrastructure or mechanism to bring these ideas in
practice. With the promotion of Panchayati Raaj System (PRS) it may be possible to
decentralize health services and meet the health needs of all. However, PRI has some
problems.
•
Feudal Indian villages with widespread politicization.
•
Low status of women with unbelievable discrimination and violence against
women.
•
Unjust treatment of tribal and low caste people.
•
Rural poverty and lack of basic infrastructure.
The civil society therefore has the challenges of:
•
Bringing health, especially to women and children.
•
The rural masses and marginalized groups like adivasis and city slum dwellers.
•
To bring awareness to these groups about their own health, their rights and
responsibilities.
•
To increase the capacity of local communities to plan and promote their own
health programs.
•
To train and empower the grassroot workers.
•
To monitor the activities of doctors, paramedical workers and others who are
supposed to serve the communities.
•
Integrate different development activities which result in better health.
•
To promote people’s organizations for self-reliant health care.
2
Many non-govemment organizations like Comprehensive Rural Health Project (CRHP)
have promoted primary health care approach to improve health of the people with
varying degrees of success.
Grassroots worker
Variously called as VHW, VHG, CHV,or Animator. The grassroots worker is kingpin
for the Primary Health Care (PHC) approach. She should be a middle aged woman with
standing in the community and who has enough time and social consciousness to serve
the people. As the vulnerable population in the village consists of young women and
children, woman volunteer is essential. She should be chosen by community, especially
community from target group. Illiteracy need not be a hindrance. She should not be
directly paid salary by the organization. Many alternate avenues should be explored to
support her. It is important that she should have adequate financial support, which not
only gives her security but provides her good status in the community.
Training
Initial training of grassroots worker should be of 1-2 weeks, followed by continuous
monthly or fortnightly training for couple of days at a time. Training should be problem
based, participatory and opportunities for group work should be given. The training
should be more in community than in the classroom. Doctors may not be good trainers
therefore preferably a nurse / social worker should be trained as a trainer. Training should
include:
A, Technical
Technical knowledge about child nutrition, immunization, common illnesses, pregnancy,
delivery, common illnesses of women should be included. Similarly they should know
about common drugs and herbal medicine. In addition to technical medical knowledge
she should be provided other skills.
B, Leadership
The grassroots worker is a bridge between health professionals and the people. She is a
spokesperson on behalf of the community. As a leader of community she has different
roles as advocacy, reconciliation and control of health workers. She should be able to
mobilize people for health and development activities. She should be promoting moral
values. Identify malpractices and report to appropriate authorities.
C. Health Worker as a Development Worker
She should identify and promote linkage between development and health e g. agriculture
and nutrition, women’s education and family health, environment and health. She should
be a good communicator. She should be able to coordinate activities of other
functionaries such as Anganwadi worker, TBA, etc.
3
D. Community organizer
The health worker needs support of the community when dealing with many community
health issues e g.
Remove stigma about leprosy, TB and AIDS
(i)
To eliminate harmful practices which are detrimental to health.
(ii)
(iii)
To sensitize community regarding discrimination against women and girl
child.
(iv)
Dealing with sensitive issues like family planning, dowry etc.
Increasing capacity of the communities
Elected women members of Panchayat and the Village Sarpanch / Pradhan together with
other functionaries take responsibility for health. In addition to information on health,
they will be trained to manage their health programs including financial management.
Under PRI they should receive financial support, thus making Primary Health Care
sustainable.
Networking
Health and development are inseparable. The NGOs should be looking for involving
development agencies in health program. There should be interaction between staff
members and community with various agencies, NGOs and Governmental. One should
be on the lookout to identify development agencies who can also incorporate health
program. This kind of an integrated health program has a better chance of success than
one started in isolation. On the other hand it is extremely difficult for hospital
management to start Community Based Primary Health Care (CBPHC) programs. Often
they end up in transferring hospital culture to village communities. It is better for
motivated hospital staff to disassociate from hospital and start a new program, than be
saddled with the institution.
It has been a pleasure to interact and train the members of CHAI in CBPHC all over
India. Many of them have participated in Jamkhed training and have had tremendous
success in promoting primary health care in remote parts of the country. Civil Society
like CHAI have tremendous challenged in bringing equity and justice to meet health
needs of the masses. Due to limitations of time I have confined my remarks to
Community Based Health Care at grassroots level.
Thank you for giving me this opportunity to share my thoughts.
Dr. R. S. Arole
Director
Comprehensive Rural Health Project
Jamkhed
4
c_ - Sfl io
Community Based Primary Health Care Primary Health Care
approach to reach the unreach
55 years after independence health conditions of majority of Indians are steadily
deteriorating. Widespread malnutrition among children and women is a major health
problem. Lack of clean portable water primitive sanitary conditions and environmental
degradation contribute to nearly 60% illnesses in rural areas. There is growing disparity
between women - men, urban-rural, rich-poor, landowner - landless labors and high caste
- low caste. Unchecked population is detrimental to physical, mental and social health of
people, specially women and children.
There is a need to accept and promote broader definition of health, which is physical,
mental, social and spiritual well being. Health and medical care are different. The
government has wrongly promoted medical care in the name of health. Highly
commercialized and greedy private medical sector is promoting curative care and
medicalizing the society. It is promoting unnecessary and expensive technology. This
commercialization is resulting in erosion of ethics and moral values.
Health and development go together. They are two sides of the same coin. World Health
Assembly promoted Primary Health Care approach to meet universal health needs of all
in the world. The Alma Ata Conference highlights following principles:
•
Health is fundamental right and therefore it should be accessible, available,
affordable and culturally acceptable to all
•
People have right and responsibility to plan and maintain their own health.
•
Health and development are intimately related. Integration with sectors such as
environment, agriculture, education and women’s income generation needs to be
promoted.
•
There is a need to integrate curative services and with promotion, prevention and
rehabilitation.
•
The present curative oriented and technical care needs to be replaced by wholistic
health.
•
No one system is perfect and it has limitations, therefore the best in all system
should be available to the community.
•
Health care personnel should replace hierarchal approach by team approach.
In the early 80s ICSSR and ICMR appointed a committee to suggest alternate strategy
to achieve ‘Health For AH’. This committee provided, some far reaching solutions.
Empowering local communities through knowledge, skill and budget.
1
IO
Decentralization up to block level and provision of integrated graded health services.
Unfortunately, there was no infrastructure or mechanism to bring these ideas in
practice. With the promotion of Panchayati Raaj System (PRS) it may be possible to
decentralize health services and meet the health needs of all. However, PRI has some
problems.
•
Feudal Indian villages with widespread politicization.
•
Low status of women with unbelievable discrimination and violence against
women.
•
Unjust treatment of tribal and low caste people.
•
Rural poverty and lack of basic infrastructure.
The civil society therefore has the challenges of:
•
Bringing health, especially to women and children.
•
The rural masses and marginalized groups like adivasis and city slum dwellers.
•
To bring awareness to these groups about their own health, their rights and
responsibilities.
•
To increase the capacity of local communities to plan and promote their own
health programs.
•
To train and empower the grassroot workers.
•
To monitor the activities of doctors, paramedical workers and others who are
supposed to serve the communities.
•
Integrate different development activities which result in better health.
•
To promote people’s organizations for self-reliant health care.
2
Many non-govemment organizations like Comprehensive Rural Health Project (CRHP)
have promoted primary health care approach to improve health of the people with
varying degrees of success.
Grassroots worker
Variously called as VHW, VHG, CHV,or Animator. The grassroots worker is kingpin
for the Primary Health Care (PHC) approach. She should be a middle aged woman with
standing in the community and who has enough time and social consciousness to serve
the people. As the vulnerable population in the village consists of young women and
children, woman volunteer is essential. She should be chosen by community, especially
community from target group. Illiteracy need not be a hindrance. She should not be
directly paid salary by the organization. Many alternate avenues should be explored to
support her. It is important that she should have adequate financial support, which not
only gives her security but provides her good status in the community.
Training:
Initial training of grassroots worker should be of 1-2 weeks, followed by continuous
monthly or fortnightly training for couple of days at a time. Training should be problem
based, participatory and opportunities for group work should be given. The training
should be more in community than in the classroom. Doctors may not be good trainers
therefore preferably a nurse / social worker should be trained as a trainer. Training should
include:
A. Technical
Technical knowledge about child nutrition, immunization, common illnesses, pregnancy,
delivery, common illnesses of women should be included. Similarly they should know
about common drugs and herbal medicine. In addition to technical medical knowledge
she should be provided other skills.
B. Leadership
The grassroots worker is a bridge between health professionals and the people. She is a
spokesperson on behalf of the community. As a leader of community she has different
roles as advocacy, reconciliation and control of health workers. She should be able to
mobilize people for health and development activities. She should be promoting moral
values. Identify malpractices and report to appropriate authorities.
C. Health Worker as a Development Worker
She should identify and promote linkage between development and health e g. agriculture
and nutrition, women’s education and family health, environment and health. She should
be a good communicator. She should be able to coordinate activities of other
functionaries such as Anganwadi worker, TBA, etc.
3
D. Community organizer
The health worker needs support of the community when dealing with many community
health issues e.g.
Remove stigma about leprosy, TB and AIDS.
(i)
(ii)
To eliminate harmful practices which are detrimental to health.
(iii)
To sensitize community regarding discrimination against women and girl
child.
(iv)
Dealing with sensitive issues like family planning, dowry etc.
Increasing capacity of the communities
Elected women members of Panchayat and the Village Sarpanch / Pradhan together with
other functionaries take responsibility for health. In addition to information on health,
they will be trained to manage their health programs including financial management.
Under PRI they should receive financial support, thus making Primary Health Care
sustainable.
Networking
Health and development are inseparable. The NGOs should be looking for involving
development agencies in health program. There should be interaction between staff
members and community with various agencies, NGOs and Governmental. One should
be on the lookout to identify development agencies who can also incorporate health
program. This kind of an integrated health program has a better chance of success than
one started in isolation. On the other hand it is extremely difficult for hospital
management to start Community Based Primary Health Care (CBPHC) programs. Often
they end up in transferring hospital culture to village communities. It is better for
motivated hospital staff to disassociate from hospital and start a new program, than be
saddled with the institution.
It has been a pleasure to interact and train the members of CHAI in CBPHC all over
India. Many of them have participated in Jamkhed training and have had tremendous
success in promoting primary health care in remote parts of the country. Civil Society
like CHAI have tremendous challenged in bringing equity and justice to meet health
needs of the masses. Due to limitations of time I have confined my remarks to
Community Based Health Care at grassroots level.
Thank you for giving me this opportunity to share my thoughts.
Dr. R. S. Arole
Director
Comprehensive Rural Health Project
Jamkhed
4
L -
H
Universal Access to Health Care: A Mission Possible.
(Dr. Mani Kalliath, Community Health CHAI)
la)
Beginning of the Country’s Dream for Health:
At the time of Independence 55 years ago Bhore Committee identified the major
determinants of country’s ill health namely poor nutrition, lack of access to amenities of
water and sanitation, low health awareness and inaccessible health care. Accordingly
independent India proudly launched the country -wide structure of Primary Health Centres
and sub-centres and programs for nutrition and sanitation. By the seventies it was clear that
the developmental efforts were not bearing fruit to the expectations generated by the Freedom
Movement. Frustrated by the slow pace of development of the country and its poor, educated
young men and women including professionals started initiatives in various sectors, moved
by a spirit of idealism. These NGOs (as they came to be called) realized through trial and
error that there needed to be an alternative, community-based approach to development. In
the health sector many notable community based programs developed, most notable among
them being the Jamkhed Project.
b)
Primary Health Care Can Deliver:
Programs like Jamkhed demonstrated in the micro situation (up to a hundred villages) that
they were operating in, that low cost quality health care is practical and possible within the
country's resources. In combination with efforts at tackling the determinants of diseases
namely poverty, lack of basic amenities and unhealthy life sty le, they could demonstrate
remarkable improvement in the health status of people in the micro situation.
The proof of effectiveness of comprehensive of Primary Health Care was established as early
as the Seventies. In this process other important lessons were also highlighted.
Illiterate village women could be empowered and trained to deliver complicated and
quality health care (A village level health care provider is a critical lack in the country, as
majority of village level ailments can be responded to such a provider).
Though health care is important control over other determinants contributed more in
impacting on health status.
A low' cost and quality' health care system is practical and possible within the country is
resources.
People need to be organized to effectively demand their rights for health care and other
facilities as the Public Health System was geared to respond only upwards to the higher
levels of the hierarchy.
c)
The Assault on Primary Health Care:
However these working models and the lessons they brought out could not be replicated
across the country. Over the next two and a half decades the opposite efforts became stronger
namely to debunk and prove that Comprehensive Primary Health Care is impractical, is a
failure and need to be scrapped. The assault on Comprehensive Primary Health Care was
initiated as early as the 80’s internationally when multilateral agencies started promoting
1
‘Selective Primary Health Care.’ Within less than a decade of proclaiming ‘Health for All’
and simultaneously with the adoption of India's first Health Policy’ (which is supportive of
Primary Health Care), The conditions were being set for its failure and eventual scrapping.
The national and state health beaurocracy steadily allowed the PHC to deteriorate, through
changed priorities, inadequate funding, beaurocratic neglect and lack of competence. The
way it was being implemented, the Primary Health Care was doomed to fail for the following
reasons.
•
It is a verticalised system, where the decisions related to Planning and Implementation is
done at the capitals, far away from the locations where the problem exist.
• The system is controlled by techno - beurocrats whose thinking are in the curative mode
and who have scant respect for the potentials of the common people for creating health.
•
It is compartmentalized, and inefficient and does not have sy nergistic effect.
•
It is designed not to elicit community’ participation, but only passive acceptance by an
unquestioning public.
•
It has very’ little service solutions to offer to the multitude of problems affecting the poor.
In the renewed assaults on Primary Health Care, under the Globalization Forces it is being
scrapped without offering alternatives to the country’s poor. The middle class and upper class
have disowned it(Govemment Primary’ Health Care) and now the Government is disowning
it and transferring the responsibility to non accountable ’Societies' What is offered instead
is the ‘Mantra of Privatization’ as is happening in other sectors in the country. The poor are
not being taken into confidence, nor is there a national consensus on these policy shifts
d)
The Health Conditions of the Poor have deteriorated
A brief look at the current Health Indices (NFHS 2) show that:
IMR at 68, Child Mortality Rate at 29 are high. However the same Indices are higher by 22%
and 45% among SCs and STs. Maternal Mortality Rate estimated to be between 437- 570
remain unacceptably high, with 42% of rural women not getting any Ante-natal Care.
Community' Studies in tribal areas show' half the w omen dying of maternity related causes die
at home and another 15% die on the way to hospital. 53% of Under 5 children are
malnourished and in low income categories is much higher as also 36% of women are
undernourished, which is higher among disadvantaged groups. 50% of infant deaths and 35%
of under 5 deaths are attributed to Diarrheas and Acute Respiratory Infections. Among adults
TB Malaria and HIV/AIDS have come to occupy epidemic proportions with 15 million TB,
20- 30 million Malaria and 4 million HIV/AIDS positive cases.
Yet only 29% of the population use public medical sector for treatment and even among the
poor households only 34% use the public medical sector. The rest are forced to seek care
from the private providers at exorbitant prices with the result that medical expenses have
become the second most important cause for rural indebtedness.
2
Are the poor aware their Health Rights are being snatched away? (In spite of the
Constitutional guarantees)
How can the country’s majority poor pay for the costly privatized curative care?
Who is responsible for responding to the epidemics of old and new communicable disease
raging among the poor and the burden of wasted lives?
These are a few of the mute questions the poor are asking, but unheard by the centres of
power in health decision making.
II a) The time has come to challenge the myth that Universal Access to Health Care is
not Feasible.
The time has come to challenge this myth that Primary Health Care approach is a failure and
also Universal Access to Health Care is be> ond the means of a developing country such as
India. The successful micro experiments of community health need to be translated across
the country not by creating Jamkhed's across the country, but by spreading the Jamkhed
perspective across the country. What is required is to mobilize people large scale for health,
to create a demand for delivery of public health and related services. It is also necessary for
people to regain competency for tackling health problems they can at their own level.
The beginnings of the process have started in the country. There is a joining of forces of
health and development activists, people oriented resource centres and health care providers,
NGO’s with interest in health and people's networks fighting for their Health Rights. We
shall see later in the paper the emerging coalition for Health.
II b) A theoretical mode! for replicating Primary Health Care at a larger level.
A three tier theoretical model is presented for promoting primary' health care, starting from
the village and going up to the district level.
At the village level:
The village health committee is to be promoted consisting of the Panchayat member or
village leader (heading the committee) the presidents of the women’s groups and youth
groups and the dai’s and traditional healers. The ICDS worker would also need to be a
member.
The committee would have the functions of.
1. Monitoring the health of the village community - especially the various priority segments
2. Ensuring availability7 of village level health care (for common ailments) through a trained
health volunteer. The health volunteers who could be the Dai or any person with aptitude
who has been trained to deliver simple care and to identify serious health problems or
potential health problems. The ICDS worker is also responsible for health of the children
and mothers.
3
I
3. Monitoring the services of the public health functionaries, that is the ICDS worker the sub
- centre ANM’s village duties and any other service provider, Male Health Worker,
where the post exist and private health sector where it exists.
4. Develop a health plan for the village and ensuring all health related information's
available to all village members.
5. The committee would need resources allocated from the village fund to meet minimum
requirement and for emergencies. The community would purchase health care from the
health providers at agreed upon charges and get stripulated public health care services
from the public health functionaries free of cost. The committee would receive
appropriate training’s for these functions where-in the health providers will get more
intensive training to be competent for treating common ailments and monitoring for
serous ailments, (it is posssible for the same committee to be responsible for other
service areas such as Animal Husbandry’ given appropriate training.
Some of the priorities for Training would include the following: Treatment of common ailment
Monitoring for potentially serious diseases.
Village level perspective on health
Duties and functions of sub centre and other government facilities / serv ices at the village
level
At the Mandal Level
The mandal level health committee need to be promoted under the leadership of the mandal
president. It would have representatives of the village health Committees, apex
representatives of people’s organizations such as federated SHGS, farmers Clubs, Youth and
Children’s Clubs (if existing). Other possible members would be the NGO health facilitator,
representative of special needs groups (if existing, such as People living with
HIV/AIDS(PLHA’s) , Differently abled persons etc.. The Primary Health Centre doctor or
representative. The Public Distribution System (PDS) representative and other mandal level
welfare related government bodies would also be represented.
The functions of the mandal level committees would be similar to the village health
committee mentiond but at a higher levels of details and complexity. At this level the health
care provider would be primarily the PHC. One of the key functions of the Committee would
be to ensure full service from the Primary Health Centre, Sub - Centres and other
government bodies and as well as support health related campaigns and awareness programs
of the public bodies with the community.
The Mandal Committee would be allocated a health fund from the Mandal Panchayat
Fund, augmented from local resources, which would be used for implementing Mandal level
health plan. The Mandal level Health Plan priority would emerge from the village plans and
that which cannot be implemented by the village committees. Technical facilitation would be
required to ensure that the plan address determinants of health and is not biomedical
focussed(as is the PHC plan).
4
The Mandal Health Committee requires capacity building for various competencies to play
effective roles among which immediate priorities would include - a broad perspective on
health, skills in developing implementing and monitoring mini-plans, the responsibilities of
the public health systems at the mandal level.
At the level of the District / Taluk.
(As the district appear to be too large a unit Taluk level Committee may be appropriate) The
District/Taluk Health Committee or Health Watch Committee would need to be lead by the
Zilla Parishad President or such appropriate authority and would have representatives from
NGO health networks, reputed public-spirited citizens. The district level officers of Health,
Women and Child Welfare. Government Societies (Such as District Society for HIV, TB
etc...) with a bearing on health would also need to be part of it, as well as private sector in
health care represented by Indian Medical Association, Nursing Home’s Association
representative etc.
The Taluk/District Health Watch Committees would have the functions of
1. Monitoring the Health Status of the people.
2. Monitoring the quality and implementation of health care services both by the public sector
and the private sector.
3. Implementing need based plans emerging from the village plans, which require district
level implementations.
Appropriate capacity building would be required for the district level committee, among
which the priority would be on District level Health Perspective based on determinants of
health, Skills for Planning, Implementation and Monitoring of District/Taluk Health Plans,
Responsibilities of the Public Systems in Health and allied areas at the district level.
III)
Experiences adding credence to such a Democratic Health Structure:
a)
Is the theoretical model presented purely a visionary' one, out of touch with ground
realities? There are macro level experiences lending credence to the effectiveness of
decentralized planning and monitoring of health. The two experiences quoted below
demonstrate the effectiveness of People’s Watch Groups over Health Functionaries, when the
community has been made aw are and mobilized for health. Refer footnotes for a brief sketch
of two programs. Arogya Iyyakkam from Tamil Nadu and Arogya Sathi program functioning
in Maharashtra and Madhya Pradesh.
b)
The Peoples Plan Process or Democratic Decentralization process in Kerala, where
the state government supported building up the structure and process for decentralized
planning is another wonderful example. The three layers of Local Self Government structures
were empowered through capacity building, technical and financial support to develop need
based plans relating to social services, infrastructure development and income generation.
The committees at each level were empowered to develop plans and implement them, within
the grant allocated, with the help of a technical advisory body. This process resulted in
addressing key priorities of the community that determined their health status - such as
environmental sanitation, provisioning of safe water, toilet facilities. These structures also
5
helped to motivate the public health system to function more efficiently and to co-ordinate
better with the non-medical interventions. Where necessary the Local Body had sufficient
financial powers to hire a doctor or supplement the PHC infrastructure or intervene with bio
medical interventions in response to a local epidemic. The People’s Plan Process also resulted
in demystification of health, - as a Lady Panchayat President of Dalit background explained. 1
Health is not just doctors hospitals and medicines. More importantly it has to do with safe
water, sanitation and sufficient food? (CHAI Network Representatives visit to People’s Plan
Process at Vaikom ? Aug 2000)
c)
Experiences of CHAI Network
What are CHAI network’s experiences in promoting access to Health Care by the
Communities?
Almost seven years ago the CHAI leadership set in motion a bold and visionary process,
which was also very timely. This process had three thrusts, which was summarized as 4
Decentralization, Government - NGO Collaboration and Planning from Below'. CHAI had
been promoting for over one and half decades prior to that the process of Community Health.
Its member institutions were encouraged and supported to facilitate in the communities
around them, health promotional activities, complementing the curative work of the
institutions. Some of these institutions even began to work on 4 Right to Health' aspects.
However there was no structure existing in the net work to sustain this process as it was a
direct partnership between CHAI Centre and the institutions and these become isolated
examples not having larger impact. Hence Decentralization of Structures, Roles and
Capacities of the CHAI Network was an immediate priority, on which was to be built up the
other two processes of Government- NGO Collaboration and Planning from Below
(Decentralization Thrust of CHAI- Mani Kalliath, 1998).
Decentralization
Though it was to be a long and laborious process, CHAI network has moved steadily in the
Decentralization path. Decentralisation process has resulted in the formation of:
• 11 Regional Units (a Regional Unit or RU may be confined to one state or may cover
several states especially in North India) have been strengthened and 5- 6 RUs are
functioning effectively, some even as recognised state level Resource Agencies.
• 100 Diocesan Units ( a Diocesan unit or DU usually extends over 2- 3 districts) with
atleast 50% of them being active and 11 'Model Diocesan Units with intensive
developments.
Government-NGO Collaboration:
The Government - NGO collaboration was facilitated through the newly developed program
of4 Promotion of District Health Action Forums'. CHAI network like other Church Bodies
has had an inward looking, approach in networking, wherein networking within Church
Institutions was comfortable, where as there is reluctance to network with NGO's or other
groups. Underlying this reluctance are historical, perspective related, skill related as well as
structure and systems related reasons. Hence developing a structure of DHAF for relating
with Government and NGOs is a very important starting point. CHAI network has now over
three years experience of formal networking and by and large it has been positive.
6
1
Planning from Below
CHAI networks initiative in promoting ‘Planning from Below' at a macro level got
encouragement through its involvement in the Jan Swasthya Abhiyan Networking at the
national level as well as its experiences through DHAF. The more advanced Regional Units
incorporated this strategy in their Regional Plans. As an example the Tamil Nadu Unit
strategized Planning from Below into its three year Diocesan Unit Strengthening Program
presently being implemented. The planning is based on participatory identification and
prioritization of village level health needs, which gets consolidated into a Diocesan Unit level
plan. A drawback in CHAI networks activities has been the poor emphasis on
documentation. As no professionally developed baseline data is available quantify ing impact
of these efforts at people’s health, is difficult. In its future thrust CHAI Network hopes to
build a coordinated national plan of activities, building on the Needs identified at the village
level, with built in Management Information System (MIS).
(Refer for a detailed discussion on the CHAI experiences, the supplementary note on
'Universal Access to Health Care- Potential and Possibilities for CHAI Network )
d)
Jan Swasthiya Abhiyan- the beginning of National Coalition Building.
The Jan Swathya Abhiyan is the first time several types of actors who could contribute to
health have come together in the country. As mentioned earlier it includes health care
provider networks (including CHAI), networks focussed on related issues, health activists
and socially concerned resource groups and a large number of interested NGO s. Its potential
strenghts have been a loose democratic organization, with a representative National Co
ordination Committee and State level Co-ordination Committees, and a transparent sy stem
for sharing information. There is a countrywide or regional focus on a few priorities, in which
a campaign for Health as a Right is one of the priorities. Each participating network
contributes by strengthening their efforts towards the common campaign issues within their
areas of operation. Support can be sought and given to other groups based on each group’s
strength and specialization. JSA had decided to draw public attention to health related issues
during the celebration of National Days this year.
In some states the JSA has been more active, Maharashtra being one example. Recently JSA
related groups have been influential in making the State Health Department to recognize the
need of a "Health Worker for every Village’, though the modalities of ensuring this is yet to
be known. Going beyond the state level in many districts JSA bodies are active providing a
platform for raising health issues.
At the International level JSA is active through the People’s Health Assembly Committee
representing all the regions of the World. JSA has been actively raising issues related to
transparency and accountability' of WHO in relation to World’s Poor, the hijacking of Health
Agenda by the Multinational Corporations through their financial contributions to WHO and
through other private bodies created such as the Global Fund for Health.
As a coalition of various types of networks and groups working with different approaches and
background skills, JSA is yet to establish sufficient confidence and acceptance among the
different constituents. This requires ongoing efforts, sensitivity and mutual respect and a
willingness organizationally to share resources. To some extend testing out relationships
require time and evaluating of how the relationship has strengthened each groups genuine
agendas.
7
IV
Summary :
Universal Access to Health Care is not is not just a possible dream, it is a need whose hour
has long been delayed. With the impact of Globalization forces on the lives and health of the
poor, there is an urgency to make it a reality. The technical elements for its strategy has been
demonstrated by hundreds of 'models’ micro as well as macro level, that were created by
pioneering groups across the country in the last two and a half decades. They have
demonstrated the health creating abilities of ordinary' and illiterate individuals, families,
village communities and even macro groupings. The missing thread running through these
efforts has been the creation of an effective structure/ network for releasing this potential
country wide as well as for channeling and focussing people's demand for Health Rights. The
beginnings of the Health Coalition emerging in the country is a welcome signal.
CHAI Network with its countrywide presence, organisational structure and variety of health
promotional experiences and skills is a major actor in this respect and looking to play an
effective role. Recognising the complementary strenghts of various national level health
actors, CHAI Network is continuing in its effort towards concerted action for 'Universal
Access to Health Care'.
(The author of this paper and its supplementary note 'Universal Access to Health Care - Potential and Possibilities for CHAI Netvtork' is
beholden to the following persons: Fr.Sebastian Ousepparambil, Director CHAI for the inspiration and philosophical frame work of this
paper. Sr.Fatima Associate Director CHAI andformer Secretary CHA T as well as Dr.Sam Roy Liaison Officerfor the insight into Diocesan
Strengthening program in Tamil Nadu. Shri Shaju Joseph DHAF Co-ordinator for the insight into CHATs DHAF experiences).
1. Arogya Iyyakkam’ T.N.
This was an evolution from the people's literacy movement and women’s movement, at the point when
government support was withdrawn. This comprehensive health programme with people's participation is
being implemented roughly in one thousand (1000) villages spread over twenty one (21)blocks of Tamil N adu.
The Programme had the following objectives.
Focus on improving children's nutrition (using weight measurement as an index of change).
Making government health services responsive to people's needs and demands.
Improving the cultural health practices
Putting health on the agenda ofPanchayati Raj Institutions (PRIs)
The key intervention strategies included:
■ Intervening through the 'Pillage Health Worker ’ who is a community representative and whose orientation
on health included a socio-political perspective of the family's health (world view)
■ Maintaining a register of every child, which records vital events, six monthly records of weight and which,
is 'understood and owned by the family ’.
■ Maintaining a village level register of services provided by the public health services (Primary Health
Centers) which is placed in the Gram Sabha ’ meetings for monitoring and follow-up.
■ Promoting and mobilizing a broad-based organizational structure at the village level (which includes the
Panchayat member) for taking responsibilityfor health.
During this short period of implementation Arogya Iyyakam ’ has advocated on issues such as
Resumption of Dai Training ’ by the PHCs
Public hearing on the abusive style offunctioning of the public health functionaries.
2.
Arogya Sathi’
Arogya Sathi ’project functions in four different locations in Maharasthra and Madhya Pradesh.
The objectives that guides these efforts included:
8
■
Developing strategies to make public health care an 'entitlement' for the people (as opposed to the present
notion that it is a set ofservices provided by this welfare state)
■
■
Ensuring sustainability ofcommunity health process.
Developing innovative approaches to training ofArogya Sathis (illiterate Health Workers)
The Strategies for implementing included:
Engaging mass organizations to take up health agendas (as NGO based health programmes were not
sustainable in the long run)
Promoting people based structures (village health committes and Jan Swasthya Samithis, which
includes NGOs) for taking responsibility for health.
Developing pictorial training materials including for assessment of the trainees (even if illiterate) and
campaign materials that demystified health.
The Programme aimed to address issues relating to public sector in health, the private sector in health, the
health/ill health determinants as well as towards promoting people's alternative strategies for health. The
public health sector was challenged to be accountable by monitoring their services (village health calendar)
and through specific issue based campaign. The private sector was challenged to be rational and transparent in
their services through promoting awareness of the people on their exploitation and through signature campaign
with the private professionals. The determinants’ affecting health taken up for campaigning included Anti
Alcohol Campaign ’ and Right to Food Campaign
Within a short period the programme has yielded results in the form ofArogya Sathis being able to handle 60%
health contingencies of the community and considerable savings of the health expenditures of the people.
(These extracts are taken from the presentations at the Asian Social Forum 2003, Hyderabad)
9
C_-
0
People’s Campaign for
Decentralised Planning
and
the Health Sector
in Kerala
Peon
Healt
by B. Ekbal
Assembly
II
l!l
hi
w
I
HH
Rd
1
i
a
i
i
rRlI
f
l|i1
Ii
I
Rii„i
w
m
i
IH a
!
Nadine Gassman, Coordinator, Analytical Process, Fuente de Emprador 28,
Tecamachalco, Estado de Mexico CP 53950, Mexico.
tel: 525-251 0283; fax: 525-251 2518; email: gasmanna@netmex.com
PHA Secretariat, 250A Jalan Air Itam, 10460 Penang, Malaysia.
tel: 604-229 1396; fax: 604-228 6506; email: phasec@pha2000.org; website:
i.pha2000.org or www-sph.health latrobe.eclu.au/pha
0
'4 ; sia
R B
ifI
i
11
lli
In spite of the economic backwardness, Kerala has made remarkable achievements in health almost compa
rable to that of even developed countries. The widely accepted health indicators like crude death rate, infant
mortality rate, and life expectancy evidence this. (Table 1)
Most analysts have seen Kerala’s achievements in health as something of an enigma. Kerala achieved the
health status as par with that of USA spending roughly 10 US $ per capita per year while US spends about
3500 $ per capita per year on health care. The GDP of Kerala is even less than that of the National average.
Kerala’s achievement in health in spite of its economic backwardness and very low health spending has
prompted many analysts to talk about a unique “Kerala Model of Health,” worth emulating by other devel
oping parts of the world
Kerala Model of Health
There are many socio-economic conditions unique to Kerala, which have been postulated to make this health
model possible. Kerala has a highly literate population compared to other Indian states. This especially the
high female literacy, has to be given due credit when we look for explanatory factors. All over, the world
indices such as infant mortality have shown an inverse relationship with female literacy.
It is also to be noted that Kerala has nurtured a political climate wherein the rights of the poor and the under
privileged have been upheld and fought for. This was the result of a fairly long period of struggle for social
reforms exphasising dignity of people who were considered socially ‘inferior’ which later found expression
in secular-democratic movements culminating in nationalist and socialist movements. One common thrust of
all such movements was on education and organisation of the downtrodden people. Hence, as has been
pointed by many social scientists there is a remarkable reduction in the rate of exploitation of the underprivi
leged in Kerala compared to other Indian states.
The agrarian reforms that were implemented in the late 1950s ended the feudal relationship in agriculture and
giving land to the tillers. This improved the social living conditions of the landless poor in the rural areas.
This might have contributed to the alleviation of poverty among the agricultural laborers leading to the
improvement of their health status.
The public distribution system of food through fair-priced rations shops distributed throughout Kerala as
sures minimum food materials at relatively cheap cost to the people. This has assured certain amount of
nutritional status to the poor, warding of poverty related diseases.
Apart from the socio-economic factors outlined above the universally available public health, system in
Kerala has also contributed to the high health status of the people. Kerala has a three-tier system of health
care, the Primary Health Centres (PHC) and the Community Health Centres (CHC), Taluk and District
Hospitals and the Medical Colleges evenly distributed both in the urban and the rural areas. Apart from
Modem Medicine, Ayurveda, Homeopathy, and other alternative systems are also very popular in Kerala.
However, the widely acclaimed Kerala Model of Health has started showing a number of disturbing trends
recently.
Kerala Health from Success to Crisis
Although the mortality is low, the morbidity (those suffering from diseases) is high in Kerala compared to
other Indian states. Though there is a data gap in this regard the NSS (1974) and KSSP (1987) studies
confirmed these observations (Table 2). Hence the Kerala situation was described as ‘Low Mortality High
Morbidity Syndrome” (Panicker and Soman 1985). It can be argued that when the expectancy of life in
creases there can be a corresponding increase in morbidity in terms of the high incidence of diseases like
Cancer, Heart diseases etc. that affect old age people more. However, here also the Kerala situation is pecu
liar in that the infectious diseases like diarrhoea, hepatitis, tuberculosis etc are still prevalent in Kerala.
Moreover, many epidemics that were supposed to have been eliminated from Kerala like Malaria are defi
nitely staging a come back. In addition, diseases like Japanese Encephalitis that was sporadic in Kerala has
appeared in many parts of the state as epidemic apart from the appearance of the modem scourge like AIDS.
B. Ekbal
2
Another disturbing trend is that the Public Health System is getting alienated from the people and only 30%
of the people even from the lower income group seek medical help from the Government hospitals (Table 3).
This is because of the fall in the quality of services at the Government hospitals. Lack of political commit
ment, bureaucratic inefficiency, corruption at various levels, lack of proper planning etc has contributed to
this sorry state of affairs.
This environment of the perceived inefficiency of the Government medical facilities is one of the factors that
provided the impetus for the growth of the private medical care set up in the state. The social milieu of the
state is changing and features of a consumer society are visible in all occupations. This has led to the com
mercialisation and the commodification of health care. Health is no more seen as a right but as a commodity
to be purchased by money. The huge remittance of foreign exchange from gulf countries even to the low and
middle-income group houses further reinforced this attitude. All these tendencies are leading to a virtual
uncontrolled growth of the private medical care facilities in the state.
A comparison of the infrastructure and health manpower development in the private and public sectors
confirms the supremacy of the private sector in the state. The number of beds in the government institutions
grew from around 36000 to 38000 in the 10-year period from 1986 to 1996, whereas in the same period,
beds in private institutions grew from 49000 to 675000. This amounts to nearly 40% growth in the private
sector beds in a period of 10 years as against nearly 5.5% in the Government sector. In the case of doctors
about 5000 doctors work in the government sector whereas double the number work in the private sector
(Table 4). More significantly, private sector has far outpaced the government facilities in the provision of
sophisticated modalities of diagnosis and therapy, such as CT Scans, MRI Scans, Endoscopy Units etc.
Simultaneously, public sector itself is being subjected to internal privatization. Because of the irregular sup
ply of medicines and other materials patients seeking medical care from the government hospitals are forced
to buy them from outside. Also the laboratory facilities are quite inadequate in the government hospitals and
patients have to depend upon the private labs for getting investigations done in time.
The privatisation of medical care is leading to over medicalisation and escalation of the health care cost. The
net result is the marginalisation of the poor and it is roughly estimated that at least 30% of the people in the
state are denied health care or find it extremely difficult to meet the growing health expenditure.
The changing health scenario in Kerala has provoked analysts like the present author to comment that the
Kerala Model of Health Care is slowly drifting towards an American Model ofHealth Care. The hallmarks
of Kerala Model were low cost of health care and its universal accessibility and availability even to the
poorer sections of society. This may be changing to the American Model where in spite of the technological
supremacy 40 million people are denied health care because of privatisation and the escalation of the health
care cost.
In short the important aspects of the present health scenario in Kerala are:
1. The simultaneous presence of the diseases of poverty and the diseases of affluence or life style diseases.
2. The decay of the public health system.
3. The uncontrol led growth of the private sector.
4. Escalation of health care cost.
5. Marginalisation o f poor.
Towards a People’s Health Policy
Toning up of the health care system in the state and making it capable of taking on the burden of provision of
equitable, efficient and good quality health care needs concerted actions from the political parties, social
movements and the professional organisations. Taking into consideration the specific problems of the Kerala
health scenario a People’s Health Policy for Kerala should be formulated. Reinstating the primacy of the
government health services, with its emphasis on primary health care should form the basis of the health
policy for Kerala. There should be some amount of social control and auditing of the private sector.
B. Ekbal
3
Decentralisation and Community Involvement in Health
These objectives can be realised only through an administrative and financial decentralisation of the health
services department, while ensuring community involvement in formulating and implementing health care
programs and reforms. The Panchath Raj now provides the possibility for the people to demand the re
sources to operate a health service in which the people themselves will play the dominant role and of which
they will be the chief beneficiaries. All infrastructure, health manpower development, training, distribution,
and production of drugs and equipment must conform to achieve this, and not in reverse as is at present. Only
thus can a cost effective, human and accountable health service be provided that is funded and operated by
the local bodies with the technical assistance of the health professionals. This system involves the entire
community and especially the women in identifying their health problems. The people can be mobilised to
improve not only the curative care but even more so in health education as well as in the prevention and
control of the diseases that originate in their environment. The people have the greatest interest in improving
the conditions that affect them and their children. This would also be an impetus to the overall improvement
of the community of which they are a part.
The World Health Organisation was advocating Community Involvement in Health(CIH) as a pre-requi
site for solving the health problems of the developing countries (Community Involvement in Health Devel
opment: Challenging Health Services-Report ofa WHO Study Group WHO Geneva - / 991). WHO study
group reports says that “A critical step will be the decentralisation of health services and the corre
sponding strengthening of the local health services that will serve as the basis for CIH** and further
“Structural changes in health systems will be necessary to support the CIH process. These changes
include; decentralisation of planning, management, and budgeting C*
The administration of the Primary Health Centres, Community Health Centres and the Taluk and District
Hosptials are already handed over to the local bodies. Moreover, thanks to the on going Peoples’ Campaign
for Decentralised Planning, there is a tremendous scope for solving the health crisis through which Kerala is
passing. And CIH as advocated by WHO has become an achievable objective in our state.
Panchayath Raj and the Health Sector
The possibilities that are opened up with the financial and administrative decentralisation of the health sector
and the People’s Campaign for Decentralised Planning are the following:
1. The control of infectious diseases and even the prevention, early detection, and management of the life
style diseases can be achieved only by strengthening the primary and secondary level health care facili
ties. With the local bodies in control, this can be achieved with better community involvement.
2. Once the primary and secondary health care facilities are improved through the local bodies, the tertiary
care centers like the medical colleges can entirely concentrate on medical education, research, and terti
ary health care.
3. The problem of resource constraint in health sector can be solved with a more need-based reallocation of
resources and generating local resources through community participation.
4. A better relationship between the health workers, people’s representatives, and the people at large can be
accomplished.
5. Once the public health system is reinforced the poor people who cannot afford the private health services
will be benefited social equity in health care will be re- established.
6. There are provisions in the Panchayath Raj Act which can be invoked for the social control of the private
sector.
An analysis of the experiences of the campaign so far shows that the we are definitely moving in the correct
direction in solving the rural health problems of the state.
Decentralised Planning: Achievements
The concrete achievements realised so far can be summarised as follows:
1. As evidenced by the participation in the Gramasabhas, Development Seminars, Task Forces, Voluntary
Technical Corps, and voluntary contributions both in terms of money and labor power, community participa
tion in local development has become a reality in Kerala. More than anything else the sense of optimism
B. Ekbal
4
generated among the people by the campaign is the greatest achievement of the decentralisation process.
2. It was feared by many that, the health related projects would be confined to building more and more
curative centres. It is true that there is a contradiction in health between the felt and real needs of the people.
While only through a preventive and promotive approach the basic health problems can be solved, there is a
growing demand formore sophisticated curative health facilities from the community. However, the prelimi
nary examination of the health projects show that majority of them are for sanitation, health education and
for improving the primary health care infrastructure in the villages. Of course, there are instances of unreal
istic and inappropriate demands for hospitals. However, the thrust is on prevention and improvement of the
existing health care facilities.
3. With the reallocation of plan funds within the health sector, the problem of financial constraints of the
health sector appears to be solved. Of the 6000, Crores of rupees allotted to the local bodies for the Ninth
Five Year 30% can be spent on social services sectors like health, education, water supply, sanitation etc. Of
this at least 500 crores are available for heath sector. In the first year, the projects were mainly on water
supply and sanitation. Nevertheless, the estimates from the first year projects shows that the local bodies are
likely to spend at least 340 crores exclusively on health and health related projects. It may be interesting to
note that the departmental allocation for Ninth Plan amounts to 310 crores. Thus, the primary and secondary
health care institutions have been given adequate funding for improvement of the services rendered by these
institutions. Once these facilities are better organised, the department can spend the fund allotted to them
exclusively for improving the tertiary care facilities. Over all compared to the Eighth Plan, health funding
has increased from 2.37 to 4.03 percentage of the total plan allocation.
4. A better working partnership is developing between the doctors, the health workers, the Panchayath func
tionaries, and the people in the rural areas. The health workers now feel that with out bureaucratic red-tapism
and the involvement of the higher authorities improvements can be made at the Panchayath level itself. For
the first time in the history of the medical profession, the doctors working at the rural areas have a role in the
planning of the health care set up where they are working. This has given them a sense of participation and
professional satisfaction.
5. The autonomy with in the decentralised set up has offered the local bodies to formulate and implement a
number of imaginative community based health programmes. From organising blood donation camps to
issuing health cards to the people of the Panchayats and conducting health surveys to study the health prob
lems of the local community a number of innovative programmes are being accomplished by the local
bodies.
It was pointed out that the widely acclaimed Kerala Model of Health that can be described as ‘good health at
low cost’ and based on social justice is passing through a period of crisis and if unchecked this may lead to
an American Model of Health based on privatisation and the marginalisation of the disadvantaged. The
Panchayath Raj system rooted in community involvement is poised to change the health scenario in our state
and is likely to conceive a new Decentralised and Participatory Model of Health Care in our state. In case
this becomes a reality then Kerala will bestow another unique model of health care worth emulating not only
by the other Indian states but also by other developing parts of the world.
B. Ekbal
5
TABLE ONE
KERALAM HEALTH STATUS
1996
India
USA
Crude Death Rate
6.3
Infant Mortality Rate 11
Crude Birth Rate
17.7
10
79
29
7
8
17
Male
Female
57.7
58.1
Indicators
Keralam
Life Expectancy
66.8
72.3
73
79
(Sources: 1. Health Services Data Government ofKerala 1996; 2. World Health Report WHO Geneva 1996)
TABLE TWO
KERALAM MORBIDITY
Keralam
NSS 1974
India
Keralam
KSSP 1987
71
83
22
21
206
136
Acute Diseases
Chronic Diseases
Group
Public
One
Two
Three
Four
33
25
16
8
TABLE THREE
UTILISATION OF HEALTH SECTORS
1987
Private
%
43
50
60
66
(Group One - Poorest, Group Four - Richest)
(Source Table 2 to 3 Health and Development in Rural Kerala KP Kannan etal KSSP 1991)
TABLE FOUR
GOVERNMENT AND PRIVATE SECTOR
1995
Private
Government
No of Institutions
No of Beds
No of Doctors
1249
42432
4288
67517
10388
4907
(Source: Report on the Survey ofPrivate Medical Institutions in Kerala 1995 Department of Economics and
Statistics Government ofKerala 1996)
B. Ekbal
6
TABLE FIVE
PLAN ALLOCATION - HEALTH SECTOR
(in Indian Rupees-Crores-10 Million Rupees)
r
EIGHTH FIVE
YEAR PLAN
TOTAL
ALLOCATION
HEALTH
SECTOR
PERCENTAGE |
5460
120
2.2
NINTH FIVE
YEAR
PLAN
ALLOCATION
HEALTH
SECTOR
PERCENTAC
10100
309.4
3.06
TABLE SIX
PLAN ALLOCATION- HEALTH SECTOR
( LOCAL BODIES)
LOCAL BODIES
ALLOCATION
HEALTH
SECTOR
(EXPECTED)
j
HEALTH
SECTOR
TOTAL
TOTAL NINTH
PLAN
ALLOCATION
HEALTH SEC
PERCENTAC
500+309.4
6000 Crores
500 Crores
16100 Crores
5,02;
809.6 Crores
(Source: Planning Board Documents: 1999)
B. Ekbal
7
3^’
The Right to Health Care is a Basic Human Right!
Towards attaining the Right to health care...
The Government of India has been unable to fulfill it’s commitment of ‘ Health for All by 2000
A.D.’ till now. In fact, primary health care services are becoming more and more difficult to obtain
for people living especially in urban slums, villages or remote tribal regions. The condition of
government hospitals is worsening day by day. Nowadays, in most of the Government hospitals there
is inadequate staff, the supply of medicines is insufficient and the infrastructure is also inadequate.
There are very inadequate facilities for safe deliveries or abortions in Govt, hospitals. Given the fact
that women do not even get adequate treatment for minor illnesses such as anaemia, services for
problems such as the health effects of domestic violence remain almost completely unavailable. At the
village level, there is no resident health care provider to treat illnesses or implement preventive
measures. All hospitals are located in big cities, and here too public hospitals are increasingly starved
of funds and facilities. Thus there is lack of availability of government health care services on one
hand and the exorbitant cost of private health services on the other. This often leaves common people
in rural areas with no other option but to resort to treatment from quack doctors who often practice
irrationally. Thus most of the population is being deprived of the basic right to health care, which is
essential for healthy living.
The Indian Constitution has granted the ‘Right to Life’ as a basic human right to every citizen of
India under article 21. In article 47 of the Directive Principles of the Indian Constitution, the
Government’s responsibility concerning public health has also been laid down. Yet the Government is
backtracking from fulfilling this responsibility. This is obvious from the fact that the Governments
proportion of expenditure on public health services has been declining in successive years.
What can be done in the near future to establish the Right to Health Care?
The year 2003 is the silver jubilee year of the ‘ Health for all’ declaration. On this occasion, Jan
Swasthya Abhiyan is launching a nationwide campaign to establish the Right to health care as a basic
human right. Some of the following activities are being taken up as part of this campaign•
We can document case studies of ‘denial of health care’ in our areas. This process has
already started in Maharashtra. Information is being collected in a specific format with the
help of a questionnaire. The cases where denial of health services has led to the loss of life,
physical damage or severe financial loss of the patient are being emphasised. These case
studies would be presented to the National Human Rights Commission. These case studies
would help us to depict the real status of provision of the primary health services by the
government, would strengthen our demand for improving public health services and would
help us in dialoguing with the public health system.
i
•
On the occasion of completing 25 years of the Alma Ata Declaration, a National
Workshop is bein^ organised by JSA on 5,h September 2003 in Mumbai, for JSA activists
from all over the country. During this workshop, the perspective, issues and campaign
strategy regarding Right to Health care would be discussed in detail, and the cases that have
been documented would be shared. This would be followed by a National Public
Consultation on “Right to Health Care" on 6th September in Mumbai. The Chairman of
NHRC^the Chairperson and Secretary of the Health committee of NHRC and the Health
Secretary, Central Ministry of Health and Family Welfare are being invited to this programme
which will be in the nature of a public hearing. Various public health experts and legal experts
will also speak during this program about the Right to Health Care. Selected case studies ol
denial of right to health care will be presented to the NHRC, and an attempt would be made to
build a social consensus on this issue, so that this can be established as a legal right.
•
A report on “ Status of Health Care in India” is under preparation, which would give an idea
about the availability of health care services, differentials in accessibility to these services,
state of health care financing and issues related to health care services for specific sections of
the population. Well-known public health experts are authoring various chapters of this
report. This report could be released in various State capitals, along with case studies and
other information related to the state. This could be done during the ‘People’s Health
Assembly anniversary’ from la to 8th December 2003 (anniversary of the Kolkata and Dhaka
Health Assemblies) and would also be an occasion to highlight the situation of health services
in each state and the need to establish the Right to Health Care.
•
Filing of a Public Interest Litigation (PIL) to establish the constitutional right to health care
is also under consideration.
These are some of the steps being planned to move towards establishing the Right to health care.
Let us join this campaign and strengthen the movement to achieve health care and health for all!
Jan Swasthya Abhiyan
Let’s all join the fight,
___________________For health as a basic right!
For further details contact: Dr. Ekbal (National Convenor) -ekbal@vsnl.com
Ami t Scngupta (Jt. Convenor) - ctddsffg^^snl .com
T. Sundararaman (Jt. Convenor) - sundar2@ 123india.com
Ihe 1 ma Narayan (Jt. Convenor) - sochara@vsnl.com
Amitava Guha (Jt. Convenor) - finrai@vsnl.net
Abhay Shukla (Jt. Convenor and National Secretariat) -cehatpun@vsnl.com
Vandana Prasad (Member, National Secretariat) - chaukhat@vahoo.com
N.B. Sarojini (Member. National Secretariat) - samsaro@nda.vsnj.net.in
2
Protocol to document cases of
Denial of Right to Health Care
rhe purpose of these case studies is to demonstrate how specific persons have been denied
basic health care that is expected from Public health services. The idea is to capture events where
obvious and major violations have taken place, leading to loss of life, disability, serious health or
economic consequences. We should focus on availability of those services, regarding which the public
health system cannot deny its responsibility. The idea is to document structural deficiencies and not
cases of negligence by individual doctors or staff. However, lack of availability of required medical
staff when required, because of significant understaffing should be documented. The objective is not
to target individual public health care providers, but rather to document the serious structural
deficiencies that exist, which need to be corrected by major strengthening of the public health system.
Some of the major types of cases of this kind are outlined below, however any other similar
cases, which come to the attention of activists, can be documented.
Some types of cases of denial of Right to Health Care
(This is not an exhaustive list but rather outlines certain broad categories with examples)
A. General Emergencies: Cases where a patient with a serious medical problem has been taken to a
Govt, health centre or hospital (PHC / Rural / Cottage / Sub-divisional / District Hospital) and has
been denied the life-saving or stabilising services expected at that facility. The patient may have
unnecessarily been referred to a higher facility, leading to delay in treatment and serious adverse
consequences, including death. Examples may include non-availability of:
• In a PHC - Non-availability of treatment for snakebite or Anti-rabies vaccine; Non-availability
of treatment for a child with pneumonia or severe dehydration due to diarrhea resulting in death
• In a Rural hospital-. Above or Lack of blood transfusion for a bleeding patient due to accident or
bleeding related to pregnancy; Non-availability of emergency drugs leading to serious delay in
treatment and death or disability of the patient
• In a Cottage / Sub-divisional / District Hospital: Above or Non - availability of emergency
surgery leading to death or disability of the patient; non-availability of essential or emergency drugs
B. Women’s health care: Women should receive certain basic health care related to both
reproductive and non-reproductive health problems. Denial may include for example:
• Maternal Health Care: Lack of facility or performance of a normal delivery in a PHC or higher
facility; lack of facilities for necessary cesarean operation in Rural hospital or higher facility;
unavailability of blood transfusion service to a woman before, during or after delivery; lack of
abortion facility leading to septic abortion or other adverse consequences
• Care for burns: A woman reporting with bums in a Rural hospital or higher facility and not
receiving care for bums
C. Major chronic illnesses: Any facility, PHC or above not regularly giving full range of
medication to patients with T.B. leading to deterioration of the patients condition including death;
Sub-divisional hospital or higher facility not treating/admitting a case of AIDS
D. Outbreak of immunisable or other major preventable illness such as measles, cholera, epidemic
hepatitis or malaria - due to failure of basic preventive or public health measures.
E. Mental Illnesses - Patients who have been denied health care for mental illness in a CHC or
higher facility
Some guidelines for activists documenting the case studies.
• At least two case studies should be collected from each district / by each organisation. The
attempt should be to document cases where denial of health care has resulted in significant loss to
the patient, either in physical or financial terms, to strengthen the case for a human rights
violation. Document only those case studies where incidence of denial has taken place in the last 6
months. Collect at least half of the case studies concerning women who have been denied health
care. Any case papers / prescriptions or other relevant documents should be collected as supportive
documents.
• Take oral consent of the person from whom the information will be elicited. Give that person
information about the campaign. Tell him / her that the case study may be presented to NHRC, and
in such case would have relevant implications. Fill the questionnaire only after taking oral consent
from the person.
1
Primary Health Center/ Govt. Hospital Services - Survey Questionnaire
Name of patientAge-
SexAddressDate of interview -
z
.
Details of care received at PHC / Hospital
♦ Location of the PHC / Location and type of Hospital -
♦ Illness / complaints for which PHC / Hospital was visited -
♦ Total Number of visits to PHC / Hospital for this illness -
4 Date of last visit-
1. History of last visit in the patients / attendants words -
(Here we want to collect infonnation regarding the main symptoms of the patient, who gave
care and what kinds of examination, investigation and treatment were given)
1
What were the perceived shortcomings or deficiencies in care? (As perceived by the
•
patient or attendants)
♦ According to patient, was there any adverse outcome because of deficient care? (Death,
disability, continued or chronic health problem, severe financial loss e.g. major loan or
sale of assets)
2. Medical attention received:
♦ Name of the doctor who attended le-you -
If the doctor was not available at that time, then who attended
-
1. Nurse / ANM
2. MPW
3. Pharmacist
4. Any other person, specify
♦
How long after you reached the PHC / Hospital did the Medical Officer / Doctor attend te-
♦
Was examination / treatment / operation delayed or denied because of non-availability of
a nurse, doctor or specialist?
2
♦
In case of an emergency did the doctor immediately attend to the patient? During hospital
stay, regarding conditions that required immediate care, was the doctor available to
immediately attend to the patient?
♦
Were nurses or hospital stafl'available to attend to the patient as and when required?
♦
Do you think that non-availability of any crucial equipment or supply (oxygen,
incubator, anaesthetic equipment, blood, emergency drugs etc.) adversely affected the
quality of care?
♦
Were all the equipments required for the examination and treatment of the patient
available in working condition in the hospital?
Diagnosis- (as told by the doctor)
3. Medicines:
♦
Did you get all the required medicines at the PHC / Hospital?
♦
Did you have to go to any private medical shop to buy some medicines?
♦
If so, which medicines you had to buy from private medical shop?
♦
How much did it cost?
♦
Do you have the prescription?
4. Expenditure:
♦
Case paper / card made - yes/no
♦
Case paper fee / indoor fees charged
3
Did you receive a receipt for the payment made?
♦
Were you charged excess money at the PHC / Hospital (more than specified rates)?
♦
If yes, how much excess was charged?
♦
Did your family have to sell assets (land, cattle, jewelry etc.) or take loans to pay for
o
treatment in the Govt, hospital?
5. Referral:
♦
Was the patient refused admission or referred to another hospital without giving first aid
care?
♦
If the patient was referred, was ambulance or other vehicle made available for the same?
♦
Did the Govt, doctor ask you to avail of any private services (e.g. laboratory services,
Sonography / X ray) while you were admitted in the Govt, hospital?
♦
In case you had to take the patient to a private hospital, which hospital? (name and
address of the hospital)
♦
What was the total expenditure on care at the private hospital / private lab or imaging
centre?
♦
Did your family have to sell any assets (land, cattle, jewelry etc.) or take loans to pay for
the private hospital charges?
4
MEDICAL INSURANCE SCHEME
RAHA’s SELF FINANCING MEDICAL
INSURANCE SCHEME (MIS)
• The Journey of Raighar Ambikapur Health
Association began with the organizing
committee meeting on June 8, 1969 in Holy
Cross Hospital, Kunkuri, Raigarh dist,
Chattishgarh State. The meeting was called
to discuss a proposal for a Health
Association. With the agreement of the
participants RAHA was born.
1
VISION
RAHA envisions a wholesome, sustainable, caring
and
transformed
community
of
people.
MISSION
1.
2.
3.
4.
5.
To build up local leadership through value - based
training.
To work in partnership with people through an integrated
and holistic approach.
To facilitate preventive, promotive, <curative and
rehabilitative health care services.
To promote Alternative System of Medicine.
To collaborate with like-minded individuals, organisations
and government.
HEALTH CARE SERVICES THROUGH RURAL
HEALTH CENTRES
> The Rural Health Centres are established to provide
health care services in the most needy areas. The
services are provided with the understanding of
wholistic health care.
The emphasis is on treating
the person as a whole and not only the disease.
> RHCs are managed by various church related NGOs.
There are certain agreements between RAHA and
RHC.
2
OBJECTIVES
"People’s Health in people’s Hand"
❖
To make medical facilities available in the community itself.
❖
To subsidise the medical care of the members at primary,
and tertiary level.
❖
To encourage people’s participation in health care services
❖
To encourage people to be a caring community and contribute towards
the medical care of their fellow beings through membership fee.
❖
To reduce exploitation from money lenders.
secondary
STRATEGY
A movement of people “I AM MY SISTERS/BROTHERS KEEPER”(Genus :4 .9
)
taking
responsibility
for
each
other.
WHO CAN BECOME A MEMBER
Any person (male orfemale) irrespective of age, caste, colour or creed.
THE MEMBERSHIP FEE
Any person desirous of becoming a member of the scheme shall pay
annually a membership fee in kind or in cash equivalent to 2 kg of rice.
DURATION OF MEMBERSHIP
One year.
3
PRIVILEGES OF MIS MEMBERS ENJOYS
a.
At the Village level: The VHW gives health education and free treatment on the
specified minor sicknesses. For minor ailments they are advised to take home
remedies.
b.
At the Rural Health Centre level: A member enjoys the following privileges:
As Out-Patient Free consultation
Free medicine (pills) upto Rs. 100/- per year
As In-Patient •
Free consultation
•
Fifty percent rebate is given on the total bill
•
A pregnant mother, who is an MIS member if admitted for delivery at the Rural
Health Centre will be expected to pay only Rs.50/- towards the entire cost of
delivery charges.
c.
At the Hospital Level
A contribution to the extent of Rs. 1,250/- is given on the total treatment per year.
Patients contribution towards hospital services is fixed as per the distance.
MEDICAL INSURANCE SCHEME
(MIS)
Achievements:
No. of districts RAHA provides health care services:
4
No. of Rural Heath Centres coordinated by RAHA :
85
Medical insurance members benefited
77,604
No. of health workers trained and activated
2200
No. of TBS trained and activated
2500
No. of Traditional Practitioners trained and activated :
850
4
The trend of MIS Membership from its inception
90000 -tg.
80000
75032
70000
0
56358
60000
50000r
4=
2
37000
40000
1s
30000
20000
10000
10000
2000
0
■
1 g
Ii c
- !
45000
50000
o
E
o
n
I
51000
Q.
50226
'I
I
77604
H 70508
64311
®I
58816
56578
54243 [-1
51496
®
I 1 n ri n
50000
51063 504M
n
45677
!
i
I |
5
s
53933
f .j"-
n [8
!
i s I
■
I*
1931 1932 1983
J
I
I
8I
IF
o
22
53598
■
J
I
-
s
rn f")
EJ ■ r~1 r~I I
Wl
to ua ■ yg' E
1984 1985 198619871988 1939 19901991 1992 19931994 1995 1996 1997 1998 19992000 2001 2002
Year
MEDICAL INSURANCE MANAGEMENT
COMMITTEE
The Medical Insurance Scheme is a people’s movement. From its inception
efforts were made to decentralize the scheme allowing greater participation for
the people. The emphasis is on the role of VHW/Dai at the village level and
the Rural Health Centre as a secondary level of treatment and support. Now it
is considered essential to formally establish Local Committee to administer
the scheme at the local level through Medical Insurance Management
Committee.
PURPOSE OF THE COMMITTEE
The committee is constituted with a purpose of administering the Medical
Insurance Scheme at the beneficiaries level. The committee is an expression
of RAHA’s purpose of empowering the people to manage their own affairs.
5
L- 3
.i y
\\Pc-09\d\Personal\Amita\6th September event\Women_sacces tohealthc-l.doc
Women’s access to health care as a fundamental right
By Sama Team, New Delhi
“Health for all” by the year 2000, a proclamation that has enough potential quite
unfortunately has taken a backseat with disastrous result in terms of women’s lives. At the
outset, it is important to state our position. This will help us better to communicate what we
exactly mean by women \ access to health care as a fundamental right When we talk of
women’s access to health care, we make it clear that it is not only the physical access to
health services that we have in mind. This is not to argue that physical access is unimportant;
but to point out that there is more to it. This broader concept of health (‘the all encompassing
wellbeing’} and the access to it is what we mean, when we speak of health as a fundamental
right
Before, we probe into the matter further we will first locate the hurdles that come in
the way of women’s access to public health services. This can be listed as infra-structural,
attitudinal, social, and economic.
All these obstacles are being looked both from the macro and micro-level
perspectives. Through these dual perspectives we see both the state and the family in
perpetuating the women’s subordination; and the latter falling prey to the norms of
patriarchal, sexist society. To begin with there is sheer lack of adequacy of Primary Health
Centers (PHC) and those existing lack the minimum necessary drugs. Though theoretically
they are supposed to coves 20,000 population, our practical experience reveals something
quite different. A woman had to travel a minimum oflOkm distance; For Tuberculosis (TB)
drugs, which is such an important and common disease people in the tribal belts have to
travel 100-150 km. This becomes all the more problematic for the women who cannot travel
alone due to the existing social taboos. Moreover, having deprived of any kind of economic
resources, travelling such a long distance just for the sake of one’s own medicine becomes
problematic and often loose importance. The paradox lies in the fact that twice the amount
of money in the budget is allocated to family planning, than in the overall health sector.
Even within the health budget, most of the money goes for contraception whereas women’s
primary health needs are not taken care of. This is because women are not thought to have
an existence outside their reproductive functions.
Hence, we not only talk of inadequacy of health facilities but an insensitiveness to
understand women issues in general and health issues in particular. This is so because the
government planners, medical personnel, who are made to ‘treat’ these ‘women’ do not
share the same universe with them and hence often find their complaints as ‘vague ’ and
' fancy story-tellingf Moreover, to talk of women as a ‘group’ often becomes problematic
due to the differential treatment that the so-called deviants (single woman, lesbian, deserted)
received. Here, it would not be out of place to even talk of the differential treatment that
mental-health patients and victims of violence undergo. To this one can always add upon the
existing inequalities rising from caste, class and the low status of women in general. The
women arc hence not in a position to decide both at the macro and the micro-level and there
is no space open to them where they can feel the urge to ask for themselves. Moreover,
patriarchy and the inbuilt gender stereotypes have ingrained in women to shape up
subordinate outlook towards their own health needs.
1
\\Pc-09\d\Personal\Amita\6th September event\Women_sacces tohealthc-l.doc
However, having laid these obstacles we have cleared our vision about whfit is the
reality at stake. We do not think that our Work ends here. As there is no point in analyzing
the world, unless we do not take initiative in changing it.
We would like to lake into consideration the campaign strategy to address such a wide
range of issues. This would mean the need for a multi-pronged campaign at various levels,
right from the grassroots to the highest levels of policy and planning, including the
international arena. On the one hand the government cannot shove of its duty; on the other
hand it must take the views, wants and needs of all those for whom primary health care is to
be provided. Otherwise, this would also lead to another ineffective planning and execution
of it would call for another disastrous result.
Why we are highlighting this is because health is a basic right of the people. And it is
the government that can and should provide it. Therefore, the task that we set ourselves is
not to provide symptomatic treatments to the problem. But it is to try out the difficult path.
That is, to move the government health structure to fulfill the needs of the people. We
further demand that all plans made for the people takes into account socio-economic
condition like class, caste, religion and sexual preferences.
Thus taking a Primary Health Care approach, we demand a broader understanding of
health as the interaction of socio-economic and political factors. This would help us to
address women’s need more holistically; and provide preventive, primitive and curative care
from a gender sensitive point of view. For this to take place, there is an urgent need for the
health movement to make alliances with other movements because health cannot be
segregated from larger issues.
It is important to understand that health is not just about illness and treatment. So
when there is abject poverty, even the best medical infrastructure will not be able ensure that
people would be able to access it, or they would be healthy. In a situation of constant stress
due to overwork and low wages, a person cannot be healthy, in a degraded environment, it is
not possible for a person to remain healthy. When a family is evicted from its habitat to
make way for a development project, (and obviously it is not rehabilitated), can anyone in
that family remain healthy? When a person of a disadvantaged caste or tribe is constantly
subjected to humiliation and violence by the upper castes, we cannot expect him or her to be
healthy. Similarly, when a woman is constantly subjected to subjugation, humiliation and
violence within own family, or she is gang raped and tortured in a communal riot, we cannot
expect her to be healthy. Neither can we expect the healthcare services to take care of her
needs. Therefore, it is important to make linkages of all other issues that affect people’s
lives, with health.
Subsequently, we come to our central point of contestation i.e. it is important to
establish health as a right issue. The government can have millions of excuses for its
inability to provide healthcare - budget constraints, population explosion, Indo-Pak tension,
debt burden and whatever else. As well as to justify its compulsions to follow the guidelines
of international lending agencies, but when it has ratified var.ous international treaties and
covenants that underlie healthcare as a basic right, there is always a space to demand its
fulfillment and question policies that undermine this right.
\\Pc-09\d\Personal\Amita\6th September event\Women sacces tohealthc-1 .doc
By Sama Team
Sama -Resource Group for women and health
New Delhi
2
?
Background to the Campaignion Women’s Access to Health (WAHC)
Women’s Global Network for Reproductive Rights
From 2003 to 2005 the WGNRR Coordination Office will coordinate the Women’s Access to Health
Campaign, in close collaboration with the People’s Health Movement (PHM). The core activities will
be centred around, but not restricted to May 28; International Day of Action for Women’s Health. The
Coordination Office will bring out campaign material to support Network members and other
interested groups and will be engaged in activities, meetings and conferences that are organised
around the campaign. Campaign participants will regularly receive updates. The reports/articles they
send to the Coordination Office will be sent to other participants, in order to stimulate and inform
each other.
The campaign will focus on the specific objectives laid down in the Alma Ata Declaration of 1978
(USSR) for the implementation of Health for All by the Year 2000 and show within that framework
the missing themes vis-a-vis women’s health. We will in this way not just highlight the failure of the
implementation of the Alma Ata Declaration, but also show our solidarity with the concept of primary'
health care which is the larger theme taken up by the People’s Health Movement for the next few
years. At the May 1999 meeting of all health ministers at the World Health Assembly the call of
“Health for All in the Year 2000”, as agreed upon in 1978. was reformulated to “Health for All in the
21st century’ and the targets reset to 2020. What happened to the Alma Ata vision?
The concepts outlined in the Alma Ata Declaration (1978) will form part of the three subsequent Calls
for Action (2003 - 2005). Specific reproductive and sexual health and rights angles will serve to
exemplify and strengthen the demands.
The 3-year campaign slogan will be “Health for All - Health for Women”. The 3-year core demand is
that primary health care be provided for all people and peoples everywhere, taking into account, in
theory and practice, women’s reproductive and sexual health needs. In 2003 the C impaign’s slogan
will be directed at national governments: “Governments Take Responsibility for Women’s Health”.
The slogans for the 2004 and 2005 Calls for Actio.n will be decided upon according to WGNRR
member’s input, since the Network members have indicated their wish to form part of the
developments of campaigns.
Background
“Health for All” is really being pushed back by health sector reforms and privatisation with disastrous
result in terms of women and children’s lives. We therefore need to take up the call for the inclusion
of a focus on women’s health within the framework of primary health care. This is an important
means to reach out to as many people as possible - both rural ana urban and the underprivileged
everywhere who are currently excluded from any care at all.
Since 1993 the World Bank (WB) has taken a greater role in the development and the implementation
of health policies for developing countries, whereas the role of the World Her-1th Organisation (WHO)
has been diminished. Government health policies, with the support of WHO and the WB, have been
redirected to focus on privatisation, cost-effectiveness and the development of public-private
partnerships in the provision of health care. This development has dramatically affected people s
health in poor countries and specifically women’s health. We fine that the under the prevailing
circumstances governments have had little say in protecting the needs and interests of their people
since they are or claim to be dependent on the Bank for loans and hence ‘have to’ agree to the
conditions placed by this institution.
Over the years governments and religious fundamentalists have denied women’s right to make
decisions central to their lives. They have done this by implementing policies that are more in the
interest of private businesses and cost-effectiveness and less in the interest of equity and quality for
all. Religious fundamentalists have been able to influence policy makers with patriarchal attitudes
\\Pc-09\d\Personal\Ainita\6th September event\WGNRR background note.doc
1
related to women’s sexual and reproductive lives. The right to health also eludes many women who
because of deeply internalised subordination and the absence of enabling conditions, fail to claim this
entitlement.
Women’s right to health has to be addressed by comprehensive primary health care systems and
comprehensive social and economic policies all over the world. Our campaign will focus on getting
women’s needs highlighted at all levels of health policymaking and programmes. We join the
People’s Health Movement in their efforts to spread support for the primary health care approach as
widely as possible and to mobilise through the PHM and our combined networks.
What do we plan to do?
According to the Alma Ata some of the fundamental charac'eristics of primary health care include:
•
•
•
•
•
•
Universally accessible health care
Community participation
Affordable and appropriate services
Plans integral to social and economic development
Prevention, promotion and curative care
Inter and multi-sectoral collaboration
The characteristics outlined above show that the Alma Ata Signatories recognized health as a political
issue related to questions of socio-economic justice. The identified need for community participation
and intersectoral cooperation indicates that it was understood that if we were to address not just the
symptoms of ill health but its root causes, a radical change had to be made in the medicalised
approach to health. The Declaration also called on governments to take up their responsibility towards
ensuring that I lealth for All becomes a reality, a demand that needs to be highlighted in these times of
increased privatisation and the shifting of responsibilities away from governments.
We have purposefully chosen to focus on ihe campaign on women’s access to health i.e. not on health
services. Although we find health services very essential, they cannot in and of themselves ensure
women’s health and reproductive and sexual rights. While we wish to address women’s needs for
basic services that include reproductive and sexual rights, we also want to address the ‘enabling
conditions* that are essential for women to enjoy good health. International and national policies that
result in greater poverty of populations and an ever-growing gap between the rich and the poor, as is
currently the case, have a direct impact on women’s possibilities to stay healthy or enjoy their
reproductive and sexual rights.
Under the banner of reproductive and sexual rights there are several issues that interlink with
women’s status - and affect their health detrimentally. For instance women are more likely to be
infected with the HIV virus than men in sexual encounters; pregnant women are more exposed to the
risk of domestic violence; women are less likely to demand and receive health care until they become
seriously ill. Some of the issues the women’s movement has been demanding attention for over the
years are listed below:
Violence against women
Maternal mortality and morbidity
Abortion rights and services
Sexually transmitted diseases
- HIV-AIDS and PHC
Communicable diseases like TB and Malaria
Need for safe and effective, woman friendly contraceptives and policies not driven by
population control
\\Pc-09\d\Personal\Amita\6th September event\WGNRR background note.doc
2
No doubt some aspects of the problems/illnesses mentioned above have received some attention
within what existed as primary health care in many countries. For instance in Argentina and several
other countries up until the mid-1990’s pregnant women did have the possibility to have antenatal
check ups during their pregnancy; a certain amount of maternal and child care was provided for by
health care centres worldwide; free treatment for TB and malaria were offered and programmes were
set up to distribute oral rehydration therapy in case of diarrhoea. Above all in many parts of the world
free contraceptives were provided in the effort to reduce the birth rates, as part of population control
programmes. In fact in the context ot India and Bangladesh the complaint has been that primary
health care centres often may not have antibiotics to offer clients but definitely have hormonal
contraceptives that are highly questionable in terms of their effects on women’s health.
Broadening the Campaign Beyond WGNRR’s Network
We will work with our members to develop the campaign and the related annual Calls for Action. We
propose to broaden the campaign to include other social movements that may not have women’s
health and reproductive and sexual rights as a central focus. We believe that including a wider range
of groups will build solidarity and strengthen our demands of reversing international) health and
other policies that have a negative impact on women’s reproductive and sexual health and rights and
women’s access to health and to health care. In particular we are linking with the People’s Health
Movement (PHM, for more information please visit their website at www.phmovement.org ) and
coordinating a PHM v/orking circle on the issue of women’s access to health.
The Peoples Health Movement (PHM, formerly the Peoples Hesith Assembly, PHA) has come out of
an international initiative that started in 1998. In that year, a group of health activists, doctors, health
and drug action NGOs, public health professionals and academ’cianb came together because of their
deep concern at the deteriorating health situation for the majority of people,'especially in poor
countries. The idea was to elaborate an analysis of health policies :ntemation:xUy and its effects on
people on a national and local, and use such analysis as a starting point for campaigns at all levels, to
demand better health care provisions for the disadvantaged world . ide.
Since June 1999 the coordination office of the WGNRR. is involved in the coordination, first of the
Peoples Health Assembly in December 2000 in Bangladesh, and more recently in international
networking under the umbrella of the PHM. Many activities are being undertaken by grassroots
organizations all over the world.
What we would like to see happen:
We join the People’s Health Movement the next three years in demanding primary health care for all
people everywhere. Within that demand we would like to highlight for the year 2003 that
governmfciits take responsibility for women’s health!
\\Pc-09\d\Personal\Amita\6th September event\WGNRR background note.doc
5
1
I?
RIGHT TO MENTAL HEALTH CARE AND REHABILITATION
A BRIEF NOTE
Center for Advocacy in Mental Health, 36B, Ground Floor, Jaladhara Housing
Society, 583, Narayan Peth, Pune 411 020, Maharashtra.
Tel: 020-4451084 Email: wamhc@vsnl.net
Population in need of mental health care
Epidemiological surveys in India have shown that 1 or 2 persons in a 1000 may be
suffering from a severe mental disorder (SMD) and between 10% - 25% may be
suffering from various kinds of common mental disorders (CMDs), largely
depression. CMDs may also reach a high level of chronicity and disability, requiring
secondary or tertiary level rehabilitative care and treatment. Social and economic
vulnerability increases mental vulnerability. Research in India and elsewhere has
consistently shown that mental illness is caused by social determinants, including
poverty, economic hardships, poor educational, social and cultural status, community
upheavals (diasters, communal violence, migration, war), nutritional, health and
reproductive health status, domestic violence and other types of gendered violence.
The population in need of mental health care at all levels of public health is therefore
large.
NEED TO INTEGRATE MENTAL HEALTH CARE IN RIGHT TO HEALTH
CARE
Persons diagnosed with a mental illness (PMI) continue to be treated with fear and
suspicion, and may be living a life of total dependency, humiliation and loss of human
dignity. Mental illness is a health care issue, and mental health care should find a
meaningful place in all efforts to build a rights perspective in general health care.
Right to mental health care
The right to basic mental health care and rehabilitation in India can be discussed
under 2 heads:
Institutional care
- Primary health care
Institutional care
Government mental hospitals (40 in number), private mental hospitals and
shelters, and Government Hospital Psychiatric Units (GHPUs) provide institution
based, tertiary care for persons with mental illness [PMI], Mental Health law, viz., the
Mental Health Act [MHA, 1987], governs institutionalization for PMI. The MHA
covers the following areas:
1. Legal procedures for institutional admission and discharge of PMI
2. The Mental Health Authorities (Central and State)
3. Basic minimum requirements for institutional psychiatric care
4. Registration, licensing, and Inspection of institutions and
5. Human rights chapter
In the MHA. we have an already existing public health legislation, which can
be strengthened. Institutional care for PMI is also regulated by various PILs, notably
1. Sheila Barse versus Government of India, 1989, on the wrongful confinement
of non-criminal mentally ill within the jails of West Bengal
)
1
2
2
2. Suo moto action by the Supreme Court, 1999, against Government of India, in
the case of the deaths of inmates in the Erwadi Mental health shelter, Tamil
Nadu
High Court petitions (e.g. Sukhri versus Government of Maharashtra) have also
brought policy attention to the plight of PMI within institutional care.
The Human Rights chapter of MHA, with 3 sections, is very inadequate. It has
only a general clause prohibiting cruel and inhuman treatment of PMI. It makes no
reference to the basic right to mental health care and community rehabilitation of
PMI. Because of this large omission in law, MHA has remained an instrument for
forced or the ‘involuntary commitment’ and custodialisation of PMI. The law needs to
be reformed so that it promotes accessible, affordable and good quality community
mental health care and rehabilitation for PMI.
Most mental hospitals spend between 80 to 90% of the scarce resources on staff
salaries. Most of the remaining resources are spent on medicines. Old, dangerous and
obsolete drugs are still being used. Shock treatment without anesthesia is still
practiced in most Indian hospitals and in private institutions. Psychotherapies are not
available. Mental hospital conditions in most public and private hospitals are dismal.
Advocates for the right to basic mental health care within the institutional context
have demanded at least the following:
1. Adequate housing, halfway facilities and rehabilitative care within institutions
2. Basic physical infrastructure, adequate and human living conditions (clothing,
toiletries and grooming, bedding, etc.), a clean, hygienic environment,
adequate and clean water and sanitation facilities, nourishing and adequate
food
3. Adequate and functional medical facilities, emergency medical facilities
(especially in the context of shock treatment), basic health care, including
gynecological care within the institution, and a fully functioning referral
system
4. Clear policy guidelines with respect to psychiatric care and treatment,
including providing standard clinical assessments, risk assessments, rational
drug treatment and an active regulation of the use shock treatment
5. Non-medical, therapeutic and rehabilitative education and care including
psychotherapy, counseling, family therapy, creative healing mediums, life
skills training, etc.
6. Clear institutional rationality and proper rule implementation for interinstitutional transfers of PMI (mental hospitals, prisons and jails, police
custody, beggar’s homes and shelters, remand homes, etc.)
7. RIGHT TO COMMUNITY REHABILITATION of PMI including disability
reduction, protection against stigma, skills development for work and
employment, creation of employment opportunities, wages, pensions and
social security, schemes under right to food and disability benefits.
8. Regard for patient ethics and creation of patient centered services in mental
health
9. Regulation of the private sector
PMI is a special population, unlike other populations needing health care. Among
them, further marginalized are, destitute mentally ill, criminal mentally ill, mentally
ill women and children within custodial institutions (including shelters).
The women’s wards within institutions (jails and mental hospitals) are far more
inhuman than the male wards. Women live in degrading health and reproductive
health conditions, being prone to various types of gynecological morbidities. Little
2)
5
effort is being made to address the mental health care and rehabilitative needs of most
women.
.
.,
.
....
Traumatised and abused destitute children, children with mental disabilities as
well as persons with epilepsy are still being custodialised in the mental hospitals.
Primary health care
The National Mental Health Program (NMHP, 1982) is the guiding policy
document in mental health, which covers aspects of community mental health care.
The policy promises the following salient features:
1. Mental health care at all levels of the existing infrastructure (PHCs, rural and
district hospitals, general hospital psychiatric units and the mental hospital).
2. Staff training at all levels of medical and community health care
3. Accessible, affordable and available mental health service facilities at all
levels
4. Mental health care for all
5. Community based care
.
6. Conversion of centralized institution based care into community care by
including OPDs, teaching and training programs, extension services in rural
areas, etc.
,
. .
7. Multi-disciplinary staff including psychiatrist, clinical psychologist, social
workers, counselors, vocational therapists and other rehabilitation
professionals.
This promise of the NMHP has remained merely a vision. Only Karnataka had
some show case models in community mental health care until recently, showing the
feasibility of community care. Funding for implementation of the NMHP is not
provided. Following serious human rights violations in recent times, the program is
now being implemented in a few states in the last 2 years, including Maharashtra, as
model programs. Most hospitals in India have not taken the initiative of converting
their institutions into community based institutions. The few posts making up the
multi-disciplinary teams, especially that of the clinical psychologist, are largely not
being filled. Posts required for rehabilitation work have not been created.
Rehabilitation services have not been started at the community level, though good
models are available. Staff training at various levels has not happened. The mental
health care service delivery has therefore remained centralized, being confined to
custodial care within mental hospitals.
It is necessary to advocate strongly for strengthening and implementation of
the NMHP in every state. Maximum human rights violations of mental health
care rights happen within custodial institutions, needing urgent intervention
through law reform, PILs and community mobilisation. The needs of the special
groups, including women and children, must be addressed. -----------------------
3
Establishing ‘Right to Health Care'
Is it a realisti c appro a ch ?
More than 50 years after the Independence of our country; we
have significant gains in the health sector. Some of the noteworthy
gains include the increase in the life expectancy fre-m a
years in 1951 to 64 years in the year 20CX). Infant mortality rate
XrK'nC’*- ^7*00 CO VurrK oe
1 /4
a
•
• \z
F1 O
£ a
1 1 knr
a j
JIlUj
f-
VaVtUI
a-U
nk/>nt *7/ 1 i m
/ ’^
±-l A
2000. In spite of all these gams, today, India is known to have poor
health indicators in the global context, even in comparison with
many other developing countries. Our health system is one of the
vorst in the world as far as health status of the poor compared to
the rich are concerned. There is also vast inequality’ among the
advan^ged and marginalised communities and among various
geographical groups. In other words-a major portion of the avoidable
disease conditions and deaths are borne by the poor and other
marginalised. Following statistics of health status and availability of
health care speaks for themselves;-; i
•
Infant Mortality Rate [IMRf among the economically lowest
20% of the population is 109, which is 2.5 times the IMR among
the top 20% of the population.
•
Child mortality [1-5 years] among children from ‘Low standaid
o’ living Index’ group is 3.9 times more than'of those from the
high living standard group. This shows that majority of 20 lakh
children die under the age of five in India every year, are from
the poorer sections of the society. It is being pointed out that at
least 16 lakhs of these deaths can be avoided even’ year. This
amounts to 4380 avoidable deaths every day
•
Tribals, account for only 8% of the population, b ear the burden
of 60% of the malarial deaths in the country'
•
ire richest 20% of the population, despite their overall better
nealth status, 6 times more likely to access hospitalisation than
poorest 20%
Delivery of the richer mother is over 6 times more likely to be
attended by a medically trained person than the delivery of the
poor mother.
What are the reasons for this inequality?
Government of India has been unable to fulfill its commitment
of ‘Health for All by 2000 AD’ till now. The very7 concept of
Primary Health Cspe rPFICIj which r? presented as the key to
attain an acceptable level of health for all is being totally ignored
over the years. A careful analysis of our health system clearly reveals
t-wo aspccteTvhy such high levels of inequality in health exist in
India.
1. The unsatisfactory indices are an indication of the failure of
public health SA'Stern in meeting the basic preventive and
curative services of the general population. Primary health care
sendees are becoming more and more difficult to obtain for
people especially in urban slums, villages or tribal regions. The
conditions of government hospitals are worsening day by day. At
the village level there is no village health care provider to treat
illness or provide preventive services.
2. Similarly there is a failure in ensuring other determinants of
health including adequate nulntion, clean drinking water and
sanitation, basic 'education, good quality housing and healthy
environment which are all prerequisites for better health.
Besides this the new policy thrust forcing the government to
withdraw from the social sectors and welfare activities is
increasingly threatening the vulnerability of the poorer sections of
the society.
In the health sector, it is an obvious fact that
Government s [both Central and the State] proportion of expenditure
on public licalth is declining in successive years. The public health
expenditure in India is abysmally low at Rs. 21 per person per year
which is among the lowest in the world.
What should be the Christian response?
•
ri
Lookinn ai tlic issue, it can be obseivecl that the massive burden
of dLses and death suffered by the
it; not lust an unfortunate accident. It coru^denial of hcallt life to millions of people,
phnnt' /woik-ins stnong the poor
injustc-t \vi ’
i
— i*u
’■r’trt v
hallh care system will be obliged to ensure foliowms *uet« an
-
\a. i it i
i
’uvh
-wa * - — —
i_
- -
t
—
r
r
, iji «•« i u < ii v
o »•.*
*>
3. ZSiSot .
—>■
-** -
morally
should b’ seen as lhe denial of basic right to life. - neahh system
a
“"‘“S
•»-
to that level and
4 A?laS>^,'sSiC^liCSal> explicit obligation “
the right or person’s life
totally unacceptable. The overall responsibility of p.rform
X henTsvsteni is the in efufable duty of the Government and
all o’-er stake holders including the NGOs, prnate sec ors
pXtanals, ehurehes eK
eemribute and eomplri— to
that effort.
How do we establish the Right to Health?
Health can no longer viewed as just a technic, s
to U
to the -Herts and bureaucrats. Health is a lundamental ! ght ul ich
needs to be established by systematically estabhsmng the right of
1 , c zen of this country to a healthy life. There is a need to bnno
L=
ensure access to appropriate and good qual.ty bas.c health
“"’SSLthe ’Rigbtto Hcllb Csr.’ »
'T
Wlh various phases. A first step towards this diedt is, en
' funcamental right for basic health care ^r
Lh-iah Tidit to life is a constitutional right [under article -IJ,
acc-'ss to basic health care is not explicitly slated as a legal
1 _ right
_ of
ZXuS Xu. care and
of various communicable diseases. Thio of c
,
combined with changed budgetary priorities and a hign.i over a.,
allocation to the health sector.
unrealistic
In this context ensuring Health tor All u no
approach, but a practical possibility which is imperative for tn.
nation to ensure the dignity of every citizen.
Nul,^i Coordu^on Ccnnn.tee
a:
^e.! v’,7/1 apM.c co.-^auon on
o M Care
5d f'j.-J
of Scpfembtv, ^’hcre /Xationul Immcui .[
t Rime
XI hJce Anand ..li be Pma^. It ts ejected that MffiC -
Zlfr'S J» Ji..
jnunifcsto]
to commit
““r
1
Another World is Possible' Health ©are toi all s Posslblell
(A brief report of the ‘Right to Health Care Seminar Asian Social Forum. Hyderabad)
{arranged fey OEhAT (Centre for Enquiry into Health and Allied Themes) in partnership with the-National Centre tor
‘Advocacy Stuaies. Pune and the Glcoal Health Council, U.S.A. The seminar took place under the larger tneme of 'Social
ilnfrestructure Planning and Cooperation. It was a part of the series or events arranged under the aegis of the Jan
jSwasthya Abhiyan The Jan Swasthya Aohiyan is a national level platform of health and social organizations working on
__ ______________
____ _
£>_____________________
3’?
:_____________________________________
_________ ______________________ .. . - _____
uk
. right functional in the existing Legal
'and Constirutional framework, looking at International Experiences regarding Universal Access to Health Care, working
lout an Operational ano Financial framework required to realize it and last but certainly nor the least, Campaign Strategies
■that need to be adopted • v/ere the topics around which presentations and discussions at the seminar were centered. The
fse.minar was attended by about 200 participants.
The Asian Social Fprum- The Asian Social Forum was convened in Hyderabad from 2nd to 7th January 2003. This forum
was aprelude to the World Social Forum, which took place in Brazil in late January. The Forum was a response of the
growing International movement cnriaiiirig the neo-iiberal economic policies and capitalist globalisation being imposed on
Imost countries It was convened in expression of the WSF principle of offering space for free discourse, debate
Hrteracjon in the procs;,: of mutual learning, informed debate, and participatory fcr nulation of alternative models with the
^ort. ano' . ab cy to address i. e challenges of development with justice. About 10,000 people atterxied the Forum and
'gave the slogan 'Another Vvond is Possible!’ The'Rightto Health Care Seminar1 and the various events organized by‘the
Jan Swasthya Abhiyan re-iierateq tn at'Health For All too is possible'.
brne necessif/ to demand the Right to Health Care- Dr. Abhay Shukla, Co-ordinator, SATHI Cell CEHAT facilitated the
• - e dismal he^lUi scenario in India which makes articulating the rightto health care a necessity
li’ndir. .J
/n t . c . xr nea t indicators in the global, context, even tr. comparison with many other developing
Jcoujj.es. . lie per capita puoiic health expenditure in India is abysmal low ai Rs. 21 per-person, among the lowest in the
[world, f-o. xs vasi majuiky the key barriers to good health are not the lack’of technology but poverty and health system
Hnequiry He stated that the objective of this seminar was to serve as platform for academics and activists, to come
(together r.qd pia^ a strategy to redlize universa' a vailability, of bask: health care
’Legal ano Jonsti.
•
-..iA-o'.-fc-cite Rightto Health Care-The theme on the first day of the seminar v-zas'Lega.
[and ^oriSuiuLGi.i. . .u..!^work for the Rightto Health Care.ana relevant International Expe
^-x1 The presenters who
■Talked on me lega< aspects were Jean Dreze (Professor of Economics. Delhi School of-Economics). Colin Gonsalves
^Advocate Supreme Court ana India Centre for Human Rights and Law), John Samuel (Director. National Centre for
.. _. _...i
fAdvocate and activist of a people's organization, Kashtakan Sanghatana)
Ji, /yas re . grated
/ without any specific amendments, the case for basic health care to be provided to all citizens
as the., right .s sTor^. The 'Right to Life' (Article 21) enshrined in the constitution, as well as the directive principles
[regarding Nutrition. Standard of living and Hearth (Article 47), and various Supreme Court Judgments in favour of
emergency and occupational health care, illustrate th is.’ The 93rd amendment in the constitution accepting Education as a
Ifundamental ngr* has strengthened the case of basic social services to be accepted as people's right. The 'nternationai
it on Econon
Social and Cultural Rights in its Article 12 clear!. -ecognlses the right of everyone to the
jenjo,. - nt of the ghost attai’ able standard of physical and mental health and creation of conditions which would assure
to ah mea i service a x medical attention in the event of sickness. The Alma Ata declaration of Health for ail by 2000'
signed in ’< J/8 is yet an other declaration which the government endorses. Even so. it was agreed that adequate financial
allocat'd^ poiit’c?i '"'H awareness of this right among oeople ano strong political mobilization will be required to realize
ithis right
ing a study like the gROgE^study, which had an important part to play in
is dec?ai sd a fu. ’d amenta! ngh.. on the availability an^uL?.za. .of basic health care services at the grass
iroots level, was discussea D. Shrinaih Reddy, National Human. Rights Commission (Health Committee) and Professor of
iCardtoloav Alliv’S, New Delhi spoke on the next day about the active roie of the health committee in NHRC to uphold the
citizen's nghtto health care. Some othernovel experiences at the village level like the communltlsation of law in
Nagaland, where th ? village health committees control the making of ’ ea’th plans as well as their functioning and
financing^ and village teve mon tormg of health care services in Dahapu taluka of Thane district were also related It was
slessee that Rights-a. e toothless v/onders without support of law or finance' Therefore the 'Right to Health Care should
r
oy a^Riyhtto infcrrr.^.ion(
.-.j ob a gallon to ensure me Im pl ememat.on of these rights.
jnt■•c Monitor There is :eed for svc; 3 por^oa,
{international 5vnenences- Sadnana Hail (Director, Global Partnerships Department Global Health Council USA) and Dr
A H M Neuman (Chairperson PHM Bangladesh Circle) spoke about international experiences in providing Universal
(Experiences m four couniries- Costa Rica Canada. S'Outh Africa and Bangladesh were shared. Costa Rica and South
Africa both scend upto 9% of their GDP on health care, in spite of not being rich countries. Costa Rica has the oest health
(outcomes of any country in Latin America. South African health care system faces the formidable challenge of the HIVj-MDS epidemic wy.h air ost ohe in nine persons affected by year 2000 Given the short time span which South Africa had
in which to develop the atidral Health System, it had done good progress. On the other hand the much-acclaim ed
Canadian Hea th System, fa eng skyrocketing costs and plummeting s-af.sfaction levels. Canada has been advised, not
to regress .‘.om tne accumplisnments of tlie Medicare system toward a hybrid privatlzea system. For Bangladesh too
poverty reduciiori and village Health Worker Programs seem to be the most effective tools to improve health and access
to henlth car' mon c--' dravz valuable lessons from the experiences cf these countries.
Operational and Financ al - ramework- Ravi Duggal (Co-ordinator, CEHAT), Dr H. Sudarshan (Chairperson, Task Force
'U 1 Hearth c ■ :<ainataka Gc .: ': ent) and Father Sebastian (Director, Catholic Health Association of India) spoke in this
session
The core content of the Right to Health Care, Organising and Managing the Universal Healthcare System, Projection of
Resource Requirements and Financing the Health Care System through mecnamsms such as Social insurance were
plscusse' Dr H, Sudarshan ic-oke about nis .experiences a$ the chairperson of the Task Force on Health of Karnataka
Government The task orce nas aeraonstrated that Health Sector Reforms can take place if necessary politico' will is
present Co;:uption in rhe heaitn sector has, been identified as-the greatest obstacle for the availability of services to all in
an equitable manner. Tne task force is currently involved in. weeding out corruption. The role of the NGO sector ;n Health,
towards operationalising tne Right to Health Cafe was discussed.
Campa:,
.7 T: jy. The
ch^ad- SarpHni [Convenor, Medico Friend Circle. Women’s Health Activist and Member of
Jawaharlal.. .suXic or Post Graduate Medical Education and Research. Pondicherry)’have ail been active in the People 3
Health Assembly process and represent the Jan Swasthya Abhiyan. They spoke about the campaign strategies that could
jbe employed to realize universal access to Health Care. Dr. Zafarulla Chauobary chaired the session
•-•c • i of the communities is the key to success when we lock at experiences in other campaigns.
and ’The Cupreme CouU case against sex selective abortion1, .twas emphasizes that making alliances with othe
imovements hke the Narmaoa Bachao Andolan is important because health cannot oe segregated from larger
(development issues
i!t wac oroposec! that strengthening the public health system and making it more effective with community basing of health
prc-grai • ^s, could ue 31 effective strategy towards gaining the 'Right to Health Oare'. There should be a health worker in
every whage. who will nelp entitlements of health care services to reach the community. Giving the health worker such a
imeaning ana context will help build a major mobilization of people for this right.
(The need for Political C-omm'tment across the political spectrum. Elect on Manifestoes to carry this programme ana
?'3te :f th ? 'Right to Health Care’ were to be realized were emphasized. Dr. Zafarulla Chaudhury
'be expected in this process. Our strategy to combat would be to invite then' to come with us, failing which the only course
of action would oe to go against them.
'Achon plan for the Future- It is planned to form a group of representatives of organizations and individuals who attended
(the semir ar in order to fc'lov up c" the strategy to realize the 'Right to health Care' Some activities that are tentatively
(I: sing discussed are A study to assess the availability and utilization of basic health services at the grass roots level,
Atting fore viable operationa; and financial mechanisms to make the- right functional, and filing a Public Interest Litigation
-to Oring such a rig. it into reality are among a few activities thought of. Systematic efforts would have to be made to induce
the issue in the election manifestos and generate political will.
{The key ; gredientto achieve health for all Is real political comn'tmentto reach the poor and involve them in the process
bf change- •/-./itrol. . r ils, no major change, is poss.oie. with this, no change is impossible.
I
L-
o-o
A brief report on the Hunger Watch Meet
22nd and 23r<!February 2003, Mumbai
A group of activists from the Jan Swasthya Abhiyan, met on the 22' "and 23’ February 2003 to
form a 'Hunger Watch Alert' in the backdrop of the worsening situation of food security in India.
Reports of drought, crop failure, suicides by farmers, starvation and hunger deaths are pouring in
from various parts of the country. This includes rural areas of Maharashtra like Wada, as well as
metropolises ' ke Mumbai. Jan Swasthya Abhiyan, convened this meeting as a response to high
ie -. is of undernutrition, growing instances of hunge. deaths and go . ..-uiment apathy towards
them The aim was to arrive at a scientific protocol to investigate and document hunger related
mortality Those attending me meeting included Dr. Veena Shatrughna (Deputy Director, National
Institute of Nutrition, Hyderabad). Dr. Vandana Prasad (Paediatrician) Dr Narendra Gupta
(Prayas), Dr.-Sunita Abraham (Christian Medical Association of India) Sarojini (SAMA and
Convenor of MFC), Du. C. S. Kapse (Professor. Department of Forens c Medicine, D. Y. Patil
Medicai College). Dr. Neeraj HateKar (Professor, Department of Econo;-ncs, University of
Mumbai), Sanjay Rooe (Ph. D. student. Department of Economics. University of Mumbai), Dr.
Abhay Shuk.a (Co-ordinator, SATHI Ceil. CEHAT), Dr. Neelangl Nanai (CEHAT), Dr. Amita Pitre
(CEHAT) and Ms Qudstya (CEHAT)
I
Undernutrition in oh’lc en as well as Adults is well documented in various government
publications. "/ s data from NNMB (National Nutrition Monitoring Bureau)'Diet and Nutritional
Status of Tribal Population Report on First Repeat Survey' shoves extremely high prevalence of
malnutrition (92%).. and significant numbers of severely undernourished (20%). This situation of
si’ent hunger hanSy seems to draw any action for relief while incidences of suspected starvation
deaths send the government machinery into action to vehemently dery their occurrence
Therefore it was thought that efforts must be made to systematica I iy 'vestigate and document
starvation deaths, at the same time keeping a focus on a community diagnosis of a starving
popuia:ion and to gain reiief forthe entire community. The occurrence or a starvation death could
be used as an advocacy tool to nignhghtthe omnipresent undernutrition, and a chronically
starved population on the brink of death in case of drought or crop faiiiire
Abhay Shukla presented the experiences of Badvvank Madhya Pradesh and Wada, Maharashtra.
Narendra Gupta presented those of Baran, Rajasthan and Neeraj Hatekarthose of Mumbai
slums. The reports of these studies were circulated. Veena Shatrughns presented the
Verbal Autopsy Forms was an important tool that was discussed. A standardised form available
for the children, ano the WHO form available for adults weie modified to accommodate specific
provisior-s to oragncse me srems of food security forthe community, family and individual and
used in the Badwar; study Also discussed was which would be the best parameters to assess
adult and child r utritior The Body Mass Index (BMl) in adults and the Weight for Age in children,
are the test ava labie parameters for use The group will also be exp o
Mortem findings co diagnose a starvation oeath. The dearth of iin^'nratior egarding his and the
reported facts that forensii. experts nardly ever diagnosed Snarvatcn' as i.he cause of death was
ourpno’Hgi Thio e>gc»ir’ r-onfinnod that yvhilo malnutrition ooulu ho quotoh in mnbiaal ro»cuc*H-» anw
death certrficates ^jvaTbn was a raooo wdra. to be aveieee.
The importart meinedological -ssue mat came up was whether calcu.ation. of three monthly death
rates as was do;.e in Badwanl was a valid tool in assessing death rates. Weekly death rates had
been calculated by the British in case of the Bengal Famine A study should be done to record
seasonal variations and the phenomenon of clustering of deaths and this is a statistically
significant phenom-erm Q^erwise there seemed no problem with ca'culating such death rates.
«
<
i
i
rv* •••'* zx , .
A
i
lci
l
-Fzxr Arf^+;><A azJwaaaa.. rlxzx \ v, z, zx+o zx# 4-aa zxir, ilz>l rzxrx
■■ • ’ i c?-. c (vas mai iu; w icglivc au
•' u ■ -
'.»x ‘►x^x
vciyi no vi u ic vi ui'.i! r?i: hi
ci ic
affected area should be compared with those of middle class children in the same age group
This would bn ng out the d’^erences more sharply than do figures of percentages in the various
categories of ndernutrition
Another stumobng block to prove a starvation death is one has to rely a lot on physical
? nance as rela^ea oy close relations, as anthropometry is out of question An important proxy
indicator would be the weighs o* siblings The Nandurbar study done by the Tribal Research and
Training Institute relied on weights of mother and siblings. This could be an important tool to
decide if the entire community was starving.
Another important issue was that malnutrition, hunger and starvation seem to lie In a continuum.
How is it possible to demarcate one from the other. One important finding that was told here was
i
. \ nersc.
T '.’
13} needs bOO Kcal per day tc- ma.ritain I
at Basa>. Metabolic Rates,
•/. itnout any activity. Therefore such a low intake is also an indication of starvation
ne following indicators may serve to define an adult starving populaiionincreased death rates in the community
no mass disasters epidemics, or other accidents
Nutrition indicator below national or state averages
Otne: criterion of reduced food security like eating unusual foods, crop failures, rain failure,
suicides, indebtedness, very iow incomes, no work
Verbal autoostes should be used in conjunction with the above to assess any starvation deaths
.1
• Increased aeath rates. An exercise must be done to calculate age specific death rates, and
compare this with the national averages to define increased death rates
• To do anthropometry and assess nutrition status of siblings
• Access ICDS records if possible
« Doubling of pe c?' tags grade II and IV of the national average dan be taken as a starving
child population
Verbal autopsies to assess any suspected starvation deaths a statistical exercise may be done
With existing data to find out how much does a mortality increase with irc'easing under nutrition
No sharp cut off points can be seen currently.
It was decided to form a Hunger Watch group, which would go ana investigate any suspected
cases of undemutrioo. and try to diagnose a starving population and do advocacy tor relief
,wv
"i
CLPiripPliGr^ STG.PlT&G.'f
57bpy/cout/^-ne- - Xfuoia^j Exp-£-ib./cakf
(T) £vol/£-
Be.r<.^e.f"^
'DtR logcS.
CObJ5£nf SO S
P Ptp^tO&j2.s(co^S'J^n.ie.&
D'A LZXSue.
\P/
r^e>vE.n K..^T& I
N P-no e>
I fPb & oc.tA-r t o m- s (pm jw| -jSfl)
P^COGUG.
L.e.GnL.lE^a.^c.t-U.'&T
SAc.tpi^fnea.pic.fnJ Pu&i.ic. KeotTw
PpOF£.©S( oNftl. S
Z^A £ve>L.v£.
STR.RTeG y
(Het^LTn cm= campaign
MA
^<£> t-ITi CAL
»
Uj KAT
^orzPoxieMrs
•
LOA/E^e-E
L. E V S5 L~ S
S’Te-FmzG't'')
{CAnnorj PKnt^p♦*>K.^
^~’1
**
(3)
r'ls/fterwoo s
H c> i>i.)
e>C.&C.'f
Lit TP
POLITICAL CAMr-»?r r7E»J7
C»c te.c ■&& Po, Ll r< e.pl
• ~. i. Pfn.of.; /'-zAmi re.STo
s.
Gove.fi.rme.rfT
QPOL.lTlC.PL. FPU.O P-e)
© E- Ig. h Pt L-LELI^E D
_c>A.f &T i TOTio N Al
♦
4^0^O» Ol CJT//(^^euPTLorJ-V
m ft’KjO ATE
t&reejas')
ZJDzo^ACy/
C.o dmr ee. op po & it i om^pl.rts,/e^JPTi v®«)
»WY6LzeMff*JT
LJITU
----- P/iOVlQeR.S
Re.-^5Tpec/si/
iffcp D E=Hr0^ e se^/ZLH^f^;
c,z>rJ P^ors.iT
E^T^\ c.nc.
BASis/Oupixiy
/ B # fH ,s
Ce>r4n^ie^.i P C(
R. FR TiOhSfacJ Exh OE-KfCeD? At66l/£
fD
f%> Nf O
uir^ CownuMw//
MoY£rj£NTs/Ul>;lorj5 '
•
•
&
rt oyeV-teMT
BXK.K
C.^^:.
^jCoMtexT
Of=
Pp«JC»»*»YAT C.AZJ
flND
« ,,\
-^Ct>NS tfMfVUt Wove^-tEi^)
(
54'HcvT 5^)
TfJT£G,x^Tior4/fl Sri
FOCK TXtAO/Ho/MS
C'l-J'n/ ! SoP POfitT
vCA-r? Pfti Gms
ro&g T H C e.
NATIONAL CONSULTATION OF EXPERTS ON THE UNIVERSAL ACCESS TO HEALTH
4 AUGUST 2003
PROGRAMME SCHEDULE
THEME: UNIVERSAL ACCESS TO HEALTH CARE
PRESENTER
MODERATOR
10.00 am to 10.05 am Prayer and lighting of the lamp
Ms. Cecilia Alexander
Dr. R.S. Arole, Dr. N.H. Antia,
Ms. Tracey’ Hayes, Dr. Thelma
Narayan, and Fr. Sebastian
10.05 am to 10.20 am Welcome and introduction to the theme
Fr. Sebastian Ousepparempil,
Director, CHAI
TIME____________
9.00 am to 10.00 am
10.20 am to 10.40 am
10.40 am to 11.00 am
SESSIONS
Registration
Universal Access to Health, Perspectives
Universal Access to Health. Perspectives
11.00 am to 11.10 am Health Watch Group and DHAF
11.10 am to 11.20 am Case Study - CHABIJ regional Unit and
DHAF, RAHA Health Cooperative
Dr. Rajnikant S. Arole, Director,
Institute of Training and
Research in Community Health
and Population.
Dr. N.H. Antia, Director,
Foundation for Research in
Community Health.
Dr. Mani Kaliath. HOD.
Community Health Department,
CHAI
_________________
Sr. Prabha. Director, CHABIJ
Ms. Tracey Hayes. Global Health
Council, New York
c.
I
I?
r
Respected Chair, Distinguished Delegates,
I am thankful to the organizers of this event for giving me an opportunity to share my views. When
we discuss about the Universal Access to Health Care, I strongly feel that we should understand
the national scenario about Health Care. The word health depends on the environments such as
social, economical, cultural and political. In today’s stinking political scenario of our country,
parties and their leaders are struggling for their own existence,
existence, so
so how
how can
can they
they care
care for
for National
National
Health?
The Word health care brings to the center of attention The Medical Profession. Major medical
institutions are under the control of the private sector comparative to the public sector. It has
become a major profit making industry. Now a day a Doctor is created not on the basis of talent
but the capability of his or her "Fathers Money". In the public sector the system of reservation has
also badly hampered the chances of eligible candidates. Finally the product of this industry
remains qualitatively poor and their intentions are not to serve the people only to recover the
money they have invested with profit. Ultimately very less moral or ethical values are left with the
profession as on today.
Due to the development of Science and the influence of western Culture we have lost a very rich
heritage based on a simple and natural life and health care. For. E.g. the food which we are
eating contains fertilizer and pesticides, water we drink is also not natural, and the medicines we
consume are also totally chemical after paying a high cost .In this situation how can we be
expected to have a better health care scenario for the common man.
r
The so called modern medicine is creating more patients and sickness every day. This is high
time to realize the dangers of modern medicine. On this occasion I would like call your attention
to that time before the advent of modern medicine in this country as to how people were treated
and cured with our natural medicines found and developed by the great Sages and Rishis.
Sushrut and Charak were not the product of any medical colleges and Sushrutsamhita and
Charaksamhita are not the research product of any ICMR. Culture of ayurvedic treatment is
derived from great Gurus whose knowledge was transferred from generation to generation. The
institutionalization of traditional knowledge of Health care has created substandard doctors in the
field our Traditional systems of medicine.
Today an Ayurvedic or homeopathic physician after completion of their institutionalized training,
practice with Allopathic medicine about which they have never ever learnt. Why is this
happening? This is because; the knowledge that they have gained through training is not
competent enough to make them good Ayurvedic or Homeopathic doctors. Main reason for this is
that the teaching faculty is not competent to teach the student about the subject.
Principles of Ayurveda can not be taught by a pre defined Syllabus. It can be learnt only by
practice under the guidance of a proper Guru. Any person can learn and practice Ayurveda
provided that he should have self-interest and a proper Guru to teach him.
For better access to health care facilities in our country modern medicine can not contribute to the
majority of the population because of its high cost and availability. I strongly feel that proper
training system to be developed to create good Health Workers based on out traditional
knowledge of Ayurveda , Unani etc. In India lacks of health workers practicing across the country
without any proper training or license to do so.
These so-called health practitioners treat major population of this country because they are easily
accessible to the common man. For e. g. there are so many practitioners of traditional medicine
from West Bengal practicing in other states for treating piles and fistula. Piles and fistula is a
common problem with most of the people. Today in modern medicine a surgery to be conducted
for this purpose costs minimum Rs. 15,000/- + antibiotics. This can not be affordable to the
common man. Here this so called traditional medicine practitioners from Bengal treat such
patients with costs ranging from Rs. 2,000/- to Rs. 3,000/- without hospitalization and antibiotics.
Like this in our country a number of traditional practitioners are successfully practicing for the
treatment of paralysis, arthritis, Asthma, Jaundice etc.. As we are discussing about traditional
practices I would like to mention about a practitioner namely Mr. Rambabu Gaikwad of Akiwad,
Miraj - Sangli, Maharashtra who treats only paralytic patients.
His clinic starts in the morning at 8.00 and continues till 8 in the evening. He just sees the patient
(no physical examination) and gives medicine. He, depending on the condition of the patient fixes
dose of the medicine. His medicine for a fresh paralytic patient is only two packets a day (1 gm of
herbal powder) costing one rupee per packet. Morning when his clinic starts we can see
hundreds of patients already in the Queue from all walks of life. I have personally seen that his
patients are getting cured within a period of two to three months. He does not require any MRI or
other reports. I am sure even a famous Neuro-physician can not treat and cure paralytic patients
with his modern medicine like Mr. Rambabu Gaikwad.
In this vast country we got thousands of traditional medicine practitioners like Mr. Rambabu
Gaikwad. Identify such golden jewels and make such knowledge available to common man,
through this National Access to Health Care can be achieved. For this purpose the Government
along with the NGO’s should come forward with an open mind to promote TM / CAM as per the
program proposed by the United Nations in 2002 -2005.
Modern medicine has got its own limitation as far as the treatment, medicine are concerned. They
do not have a holistic approach. They always depend on the investigation reports for diagnosis. If
the diagnostic report is false or misguided patients get the wrong treatment which can be very
dangerous. In Indian system of medicine we physically and psychologically assess the patient for
diagnosis. Accordingly treatment is given.
Primary educational facilities are to be developed to teach TM / CAM with the help of present
practitioners of Traditional medicine and other alternative therapies. (We propose to start
Ayurvedic Schools to undertake this activity.)
Last 15 -20 years research in the field of Ayurveda, Traditional medicine and Complimentary
alternative medicine I could develop a number of formulation for the treatment of Heart disease,
arthritis, jaundice, spine disorders, sinusitis, obesity etc.. Due to extensive research and studies
with the cardiac patients we could give a new dimension to cardiology in Ayurveda and Indian
system of medicine where we see Heart is a myogenic organ just to manage the function of blood
supply and purification system in the body. In the 50’s and 60’s the western world has given
unwanted importance to heart and especially its problems which has been adapted by the entire
world even though they could not find out any permanent solution except temporary surgical
ones even today which are very risky. Where in our research we see heart problems also as a
functional change due to many reasons which can be corrected by a holistic approach. For this
purpose we introduced a cardiac health substitute “ Cardioflo ™" the benefit of which is being
experienced by thousands of patients. This patent Medicine has been appreciated and tried by
doctors even in European countries but still is not acceptable to Cardiologists in our country even
though they know the benefit of this medicine. This attitude of practitioners of modern medicine is
harmful to Universal Access to Health care for all.
Presently a team of Ayurvedic Doctors are given training to use all these formulae in their
practice. Already we have treated thousands of Heart patients all over India successfully.
Through Dhanvantri Manava Seva Sanstha, a newly formed charitable trust we are planning to
organize free training programs for Ayurvedic Doctors to exchange our knowledge with them.
Through National Association of TM/CAM Practitioners, India we are planning to organize such
practitioners under one roof and conduct training schools for such Doctors. I am of the opinion
that it is good to exchange our knowledge with any group working in this same field.
■
Presented At Hyderabad on 4/8/2003 by
Dr. Antony Joseph
Pune
Tel: (020) 7273110, 7274614
Mobile: 9823072620
- Media
 RF_L_3_A_SUDHA.pdf
RF_L_3_A_SUDHA.pdf
Position: 674 (18 views)