ONE DAY MEETING ON RIGHT TO HEALTH MARCH 15TH 1997
Item
- Title
- ONE DAY MEETING ON RIGHT TO HEALTH MARCH 15TH 1997
- extracted text
-
L
T
10
0
20
30
50
40
60
70
TSO
90
GHI
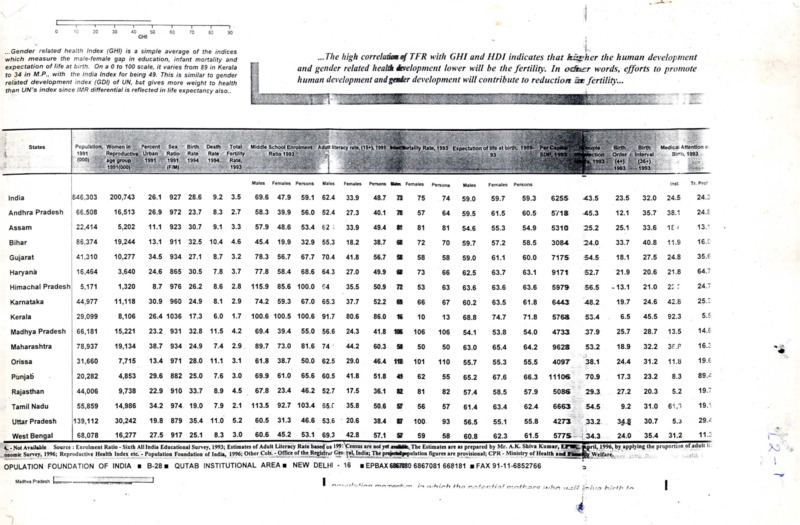
...Gender related health Index (GHI) is a simple average of the indices
which measure the male-female gap in education, infant mortality and
expectation of life at birth. On a 0 to 100 scale, it varies from 89 in Kerala
to 34 in M.P., with the India Index for being 49. This is similar to gender
related development index (GDI) of UN, but gives more weight to health
than UN’s index since IMR differential is reflected in life expectancy also..
I
Percent Sex
Urban Ratio
1991
1991
Birth
Rate
1994
Death
Total
Rate
1994
Fertility
Rate,
sz
. ■izz zz'
/
.
Population, Women In .
1991
Reproductive
(000)
age group
States
...The high correlation of TFR with GHI and HDI indicates that Richer the human development
and gender related health inelopment lower will be the fertility. In odhucr words, efforts to promote
human development andgader development will contribute to reduction an fertility...
Z
■
Middle School Enrolment
■/
,-r’‘
'
'
Adult literacy rate, (15+), 1991
Srs
ectlon
Order
Interval
Medical Attention a
Birth, 1993
. .v.... /7Z:/ZS
Males
Females
Persons
Males
Females
Persons
Females
Persons
Males
Females
Persons
Inst
Tr. Prof
1846,303
200,743
26.1
927
28.6
9.2
3.5
69.6
47.9
59.1
62.4
33.9
48.7
73
75
74
59.0
59.7
59.3
6255
43.5
23.5
32.0
24.5
24.:
Andhra Pradesh
66.508
16,513
26.9
972
23.7
8.3
2.7
58.3
39.9
56.0
52.4
27.3
40.1
71
57
64
59.5
61.5
60.5
5718
45.3
12.1
35.7
38.1
24. E
Assam
22,414
5,202
11.1
923
30.7
9.1
3.3
57.9
48.6
53.4
62
33.9
49.4
St
81
81
54.6
55.3
54.9
5310
25.2
25.1
33.6
18
13/
Bihar
86,374
19,244
13.1
911
32.5
10.4
4.6
45.4
19.9
32.9
55.3
18.2
38.7
62
72
70
59.7
57.2
58.5
3084
24.0
33.7
40.8
11.9
16.C
Gujarat
41,310
10,277
34.5
934
27.1
8.7
3.2
78.3
56.7
67.7
70.4
41.8
56.7
S
58
58
59.0
61.1
60.0
7175
54.5
18.1
27.5
24.8
35.6
Haryana
j 16,464
3,640
24.6
865
30.5
7.8
3.7
77.8
58.4
68.6
64.3
27.0
49.9
fit
73
66
62.5
63.7
63.1
9171
52.7
21.9
20.6
21.8
64.7
5,171
1,320
8.7
976
26.2
8.6
2.8
115.9
85.6 100.0
64
35.5
50.9
n
53
63
63.6
63.6
63.6
5979
56.5
-13.1
21.0
2::
24.7
' 44,977
11,118
30.9
960
24.9
8.1
2.9
74.2
59.3
67.0
65.3
37.7
52.2
61
66
67
60.2
63.5
61.8
6443
48.2
19.7
24.6
42.8
25/
Kerala
29,099
8,106
26.4 1036
17.3
6.0
1.7
100.6 100.5
100.6
91.7
80.6
86.0
16
10
13
68.8
74.7
71.8
5763
53.4
6.5
45.5
92.3
5.5
Madhya Pradesh
66,181
15,221
23.2
931
32.8
11.5
4.2
69.4
39.4
55.0
56.6
24.3
41.8
106
106
106
54.1
53.8
54.0
4733
37.9
25.7
28.7
13.5
14.6
Maharashtra
78,937
19,134
38.7
934
24.9
7.4
2.9
89.7
73.0
81.6
74
44.2
60.3
59
50
50
63.0
65.4
64.2
9623
53.2
18.9
32.2
se.p
16.:
Orissa
31,660
7,715
13.4
971
28.0
11.1
3.1
61.8
38.7
50.0
62.5
29.0
46.4
11B
101
110
55.7
55.3
55.5
4097
38.1
24.4
31.2
11.8
19. e
Punjab
20,282
4,853
29.6
882
25.0
7.6
3.0
69.9
61.0
65.6
60.5
41.8
51.8
45
62
55
65.2
67.6
66.3
11106
70.9
17.3
23.2
8.3
89/
Rajasthan
44,006
9,738
22.9
910
33.7
8.9
4.5
67.8
23.4
46.2
52.7
17.5
36.1
82
81
82
57.4
58.5
57.9
5086
29.3
27.2
20.3
5.2
19.7
Tamil Nadu
55,859
14,986
34.2
974
19.0
7.9
2.1
113.5
92.7 103.4
65. C
35.8
50.6
S’
56
57
61.4
63.4
62.4
6663
54.5
9.2
31.0
61.3
19/
Uttar Pradesh
139,112
30,242
19.8
879
35.4
11.0
5.2
60.5
31.3
53.6
20.6
38.4
87
100
93
56.5
55.1
55.8
4273
33.2
3!t8
30.7
5.3
29/
60.6 45.2 53.1 69.3
8.3 3.0
42.8
16,277
27.5_______________________________________________________________________________________________________________
917 25.1
68,078
57.1 57
West Bengal_________________________
59
61.5
58
62.3
5775 -434.3
60.8
24.0
35.4
31.2
11.3
India
Himachal Pradesh^
Karnataka
46.6
jril, 1996, by applying the proportion of adult Ii
1993; Estimates of Adult Literacy Rate based
not -yet awirfiip The Estimates are as prepared by Mr. A.K. Shiva Kumar,
4. - Not Available Source : Enrolment Ratio - Sixth All India Educational Survey,
...
. 1 on 1991 yensus are
.
£. n
------- j..tr
—uu Index etc. - Population
— r—j-.:-------of
r »_
j:- innx.
r nUfinn figures are provisional;
onomic Survey, 1996;
Reproductive
Health
Foundation
India,
1996; Other r'nic
Cols. -- Offir*
Office nf
of th*
the Rwidr^r
Registrar Gen
Gen ral.
^al, TnrfiaIndia; T>»*
The projededpapulation
provisional; CPR
CPR -- Ministry
Ministry of
of Health
Health and
and TaiMi
OPULATION FOUNDATION OF INDIA ■ B-28 ■ QUTAB INSTITUTIONAL AREA ■ NEW DELHI - 16
Madhva Pradesh
■ EPBAX 68671180 6867081 668181 ■ FAX 91-11-6852766
Welfare.
I
□
J
/I
z-t
m
n-.r'tb.^rc’ '.jt/hn
\rrti
4
hsrfb
I
L.^
Ella, All, Allah, . AUM,
, SHREE, A to Z, That is that
In/TiTUTB of Health 0 ComPARiriVE fflEoicinE. Vogr Therapy
Cehtre
£23, 9th ‘A’ Main Road, 5th Block, Jayanacara
Bangalore, Karnataka, INDIA - 560 041
St: +91-80-6635256; FAX : +91-80-663-5175
Five Doctors & Professor Emeritus Around the World
Studied in Michigan & Bangalore Himalayas have evolved
VACCINES having Lasting'Curative' & 'Instant Relief' Value
1. Psycho-Spiritual % Mind-Space Vaccine, Scientifically &
Philosophically evolved for prevention & cure.
2. Edible Local Fresh & Tender Herbal Vaccines.
3. Dietary combination & MEDICINAL SECRETS OF FOODS observed
over centuries for preventive and lasting cure & relief.
4. AUTO Unit Vaccine, manufactured in one’s own body, at
each moment in blood, fluids, mind, cells etc.,
5. Highly-ground & ELECTRONICALLY CHARGED VACCINES Natural, Inorganic & Organic Chemicals - diluted as Oral
Drops, Tablets, etc., with ‘PUREST" vehicle.
For Every Disease & Symptoms
each time
We can & should aim & wipeout incurability
from Womb to Tomb & Beyond for generations
and correct GENES by Sound Electrons & Hygiene
Essence being brought-out in One World Book in all th e
languages at the same time, updated periodically.
Over 200 countries registering for training at
Bangalore.
Herambhaha, Ganapa, Brahma
Dr. H.R.B., SADA.A.
TOP_Q Graphics//e:\mallanna\hrb\bro 1 .doc
LS. 3
Forum Interview
Ethics and health
Zbigniew Bankowski
World Health Forum asked Dr Eilif Liisberg to talk to Professor
considerations that have guided the development of medicine
and public hea'tn and about their place in today's society.
Professor Bankowsk. medical ethics has been largely
dominated by the Hippocratic Oath. What were its
basic principles, and are they still valid in modern
society?
In mv opinion the Hippocratic Oath,
although formulated about 2400 years ago,
will be pertinent tor a long time to come. The
Oath itself is a very short statement and
nobody knows who really wrote it; it is probablv based on writings by Hippocrates and
others, so I would prefer to refer to the
writings rather than the Oath alone. The
Hippocratic writings placed certain obli
gations on doctors, such as beneficence,
non-maleficencc, and confidentiality, as well
as some prohibitions — for example, those
against euthanasia - which are still followed
today.
Perhaps at this stage i*. e should define what we mean
by ethics, as this is important for the rest of our dis
cussion.
Ethics is a branch of philosophy dealing with
the distinction between right and wrong, and
Dr Lnsberg. an interna: ?-•= public health consultant,
was previously EdUO' c V.jrid Health Forum His address
is 43 avenue du Lig-?- ’219 Le Lignon, Geneva. Switzer
land
WorldHea’^Forurr • I';.-: ':’ • 199:
the moral consequences ot our actions.
Nearly all philosophical systems include an
ethical component. Wc in CIOMS look at
ethics from this same viewpoint of right and
wrong. Then immediately other questions
arise: right and wrong for whom? where? and
when? Those who support relativism in ethics
say it depends mainly on the circumstances,
11V1 v<x, v/l
.4aviK, ------------------- a moral
whereas
others
hold the view that
ethjca} prindplc has universal value,
In some cultures there is emphasis on the family and
the wider circle beyond the individual. Do the Hippo
cratic writings have a different connotation in different
societies?
Looking at the development of medical ethics
from a historical point of view, we see that
our Western civilization is based on Graeco
Roman and Judeo-Chnstian traditions. Our
so-called Western culture is unified by these
common roots, which for medical ethics are
the Hippocratic writings. Other cultures have
different roots - the Chinese and Hindu
traditions, for example. The limited contacts
between civilizations in the past had little
effect on each ones traditions, culture, and
ethical principles. Recent intercultural debates
about ethical issues immediately bring to light
these differences.
115
f
Forum Interview
Have any of the other ethical principles been codified?
In Chinese medicine, for example?
Not as far as 1 know. 1 am in close contact
with the Chinese medical profession and the)
arc vcrv interested to know how we codify
our ethical guidelines, and are considering
developing ethical principles adeouate for the
needs of their society. For example, the pnnciplcs of informed consent and natural rights
arc valued differently, compared with Western
culture, but this does not mean that China has
no ethical rules - it certainly has!
Do you think it is possible to have a set of basic,
universally accepted principles in ethics?
Mv personal opinion is that, at present,, wc
iot reaay
reads to trv
universal
arc not
uy to
iu develop -a —
JCU.W...?
r— -- ", ’
"IOr
code
of ethics - not -specifically
heakh
or
mediwl
ethics, but
just ethics broadly
medical etnics,
uui jusu
7 -jspeak
ing.
ing It may take centuries to reach such a con
sensus. Still, there are already some pnr
pnnciples
which arc universally recognized. In most
basic principle not to
animal societies it is a basicj>nnciple
till
another of its species. This
is aa biological
mh diiuinvi
> is
.
instinct and, as we are animals, the pnnciple
applies to us too, though it is not accorded the
same importance by all human societies.
\fV 1MV1* «*•
----------------- y
vz
e
,
In the field of ethics, as with any controver
sial issue in society or between different
cultural settings, dialogue must come first
to share ideas and concerns about the
Issues inherent in the Interaction of health
and ethics, and to collaborate In devising
and applying means of resolving them.
I
A great step forward has been the Universal
Declaration of Human Rights which was
developed bv the United Nations after the
Second World War. Human rights are univer
sal in the sense that society accepts them as
such, despite cultural differences in that what
■r Professor Zbigniew
Bankowskl was born in
Warsaw. Poland, in 1925
and is a naturalized Swiss
citizen His medical edu
cation and postgraduate
studies were completed
in Poland where he
x i
acquired his M D and
Ph D at the Faculty ol
Medicine, Lublin He has
held several teaching and
research positions in
experimental pathology in.
the Polish universities o’
Lublm. Lodz and Warsaw
as well as in Pans and Tunis Between 1965 and 1972 he
was responsible for the coordination ol research and trau
ma programmes of the World Health Orgamzation.
Geneva Since 1975 he has been Secretary-General of the
Council for Internationa’ Organizations of Medica
Sciences (ClOMS) Geneva. Switzerland He is the authoof many scientific papers m the fields of radiobiology ano
cancer and numerous articles and reviews dealing wrth
bioethics, drug safety, and medical terminology
is a high pnonty in one society may be less .
important in another. Although it is certainly
feasible to develop a universal code of ethics,
there are substantial differences in values that
are dear to each of us, and we do not like
others to interfere. In the field of edtics, as
with any controversial issue in society or
between different cultural settings, dialogue
must come first to share ideas and concerns
about the issues inherent in the interaction of
health and ethics, and to collaborate in devis
ing and applying means of resolving them.
C1OMS always encourages long debate along
ethical lines before surting to draw up any
normative guidelines.
An economist in Copenhagen once said in the Forum
that there was a contradiction in the doctors’ role to
do their best for individual patients and their social
responsibility to promote the common good (1).
What do you think about this dilemma?
This is a typical example of the conflict that
exists in ethical thinking, between the interests
and rights of the individual and the interests
Wjrit Health Forum • Volume 16 • 19u:
116
\
Ethics and health
and rights of the community. The interests of
individuals do not necessarily coincide with
those of the community - very often the
interests of the community are contrary to
those of the individual. Such conflict exists
and needs to be considered from all points
of new to sec if it is possible to work out a
compromise.
In health ethics, as with any ethical problem,
the first step is to initiate dialogue, to tty to
undersund what others are saying in order to
find a common denominator. I don t agree
with the relativist position that there are dif
ferent ethics: basic ethical principles are the
same for all, but the problem is that it means
different things to different people. If deci
sions about health in the community are
taken bv politicians and others, then the
medical profession has to say forcefully that it
has always been guided by ethical principles.
Medical ethics is at the root of the Hippo
cratic writings, and we in our particular societ)
are obliged to follow this same ethical code.
So you see the doctor as one who defends the rights
of his patients as individuals.
Yes! Doctors have a very special relationship
with their patients: the patient comes to the
doctor in hill confidence that he or she will be
helped; that creates a strong, intimate relation
ship between doctor and patient, whether it is
one person, a family, or a small community
group.
Doctors have sometimes found themselves in
difficult situations, such as assisting in capital
punishment or certifying that a person can tolerate
physical maltreatment or torture.
There is a UN Convention against torture to
which CIOMS contributed: we were
requested by WHO to draw up a code of
ethics for health personnel who might find
themselves involved in torture or maltreat-
mcnt of prisoners. It was a ver}’ controversial
issue and necessitated a long study. CIOMS
evolved six principles which were presented
by WHO to the United Nations; these were
Conflicts in medicine are inevitable when
one cannot satisfy the needs of all who
suffer.
adopted and included in the Convention.
They postulate that physicians and other
health workers are professionally trained
solely to maintain or improve the health of
those for whom they exercise professional
responsibility, and that it is unethical to use
their professional skills to allow any action
that may harm physical or mental health.
Of course, it is easier for physicians to take
a decision in line with their individual
conscience in a democratic society; in a totali
tarian one, a refusal to do what wras asked .
could very’ easily put them in danger. The
Convention came into effect only after twothirds of the Member States of the UN had
signed it but the UN has ven’ little authority
to enforce it. However, it does exist and is
there for anybody to refer to as an inter
national legal instrument.
As for the involvement of medical personnel
in the execution of a death sentence, I should
perhaps mention that the leading organization
for medical ethics is the World Medical
Association. The Association has developed a
very sensitive and well-elaborated declaration
and code of ethics which condemns the par
ticipation of physicians in capital pumshment.
Would you say that the Nuremberg trials of war
criminals after the Second World War were a major
breakthrough for ethical principles?
Certainly, as far as Europe and North
America are concerned. The atrocities which
117
Vko'lC Hsa':^ Forurr. • Volume 16 • 1995
\
(
Forum Interview
were committed shook our consciences. The
Nuremberg trials and the code which was
developed on this occasion with the involve
ment of the medical profession are an
1
VJe should not forget that in our everyday
lives we all have ethical choices — between
what is good and what is wrong.
cxtremelv important milestone. The Nurem
berg Code is the origin of informed consent
and is based on the ethical principle of auton
omy At first it was related only to experi
mental research on human subjects and now,
as vou know, it is integrated into medical
practice. But there is no doubt that this is a
product of our culture: informed consent is
not always applicable in other circumstances.
For example, in Africa a patient expects the
doctor to decide for him, and in Japan the
patient may not be told the results of investigallons or the diagnosis.
Can you explain the origin of the word bioethics ?
Although at CIONS wc arc resisting the
tendency to create new words, bioethics does
seem to have become a generally accepted
term. It was coined in the early 1960s in the
USA when there were many more people
with renal failure than dialysis machines avail
able, so doctors were obliged to take difficult
decisions about allocating treatment. Thus,
bioethics was introduced as a response to the
tremendous scientific and technological devel
opments which created hew situations for
(doctors with regard to their patients.
And health-policy ethics?
Health-policy ethics may be seen as an aspect
of bioethics concerned particularly with the
organization, financing and delivery o ea t
care; it is a concept developed by C1OMS
within the framework of its International
Dialogue on Health Policy, Ethics and Human
Values. Let me tell you how this came about.
In 1983 and 1984 the World Health Assemble
debated whether a spiritual dimension should
be introduced into all health programmes
coordinated bv WHO. There was much dis
cussion involving politics and religion so that
the issues became blurred. 1 discussed it after
wards with Dr Halfdan Mahler, who was at
that time Director-General of WHO, and
suggested that CIONS could take up the sub
ject This was the origin of our programme
of health policy, ethics and human values.
Professor Jack Bry ant was a key collaborator
in initiating dialogue on this programme
internationally.
Nowadays there is a lot of talk about training in
ethics. Looking back to my days in medical school
I remember we were just supposed to imitate the
way our professors and other doctors behaved.
Is it necessary to have special courses?
Several years ago UNESCO and V HO
studied how ethics was being taught in medi
cal schools: it was generally not obligatory in
Europe, more widespread in the USA, and
the developing countries usually followed the
European lead. 1 believe we should sensitize
the students - our future physicians - to all
ethical issues. Many medical schools teach
ethics in an integrated way as cases arise, and
the professors are sensitive to the need to
identify the related ethical question in clinical
situations.
I think that's how we learned but we didn’t know
it was ethics!
Exactly, and that is the best way to teach the
principles, without calling it ethics. The word
itself creates mystery, being heavy with emo
tional overtones. We should not forget that in
our everyday lives we all have ethical choices
— between what is good and what is wrong.
World Health Forum • Volume 16 • 1995
116
<
t
Ethics and health
Human rights and ethics^
fligion, political belief,
Organization, 1946)
-Eveo.o„e ba. .be ngb. ,o a
of himself and of his family, including
,
of uncmploymcnt, sick35X3. old age » o.be. lack of l.volibood in eireunnUnee. beyond
(A„"e"e'2°'j.em 1,
J Deefarenon «f
IMS)
•The Deel.ra.ion of Geneva of .be World
“E^itTrn^
-All research rnvolving human subieers should be condoned in accordance w,.b .hree
CIOMS, 1993)
Ethics is directly related to our behaviour, and
much more should be done to demystify it.
You once said that WHO had introduced a new
principle in health ethics - the equity principle or the
health-for-all strategy, which resulted from the 1978
Alma-Ata Conference. Could you explain its import■ ance?
that health for all is recognized worldwide
and has tremendous influence in both devel
oped and developing countries shows in my
opinion, the exceptional value of the World
Health Organization from an ethical point oi
\new.
Would you say that equity is a major target in health
(
development?
In the revolutionary health-for-all concept,
“air means all human beings. This statement
of equity has a ver}' strong ethical value
behind it: the justice of distribution - mat.is,
health services seen as something good which
should be distributed to everyone. The tact
Certainly on the global level, because it deals
with mankind as a whole. The global
approach for everyone’s benefit is veiy
important, and WHO’s promotion of health
for all has very' strong ethical connotations.
119
• Voljw 16 • 199-
Forvm Interview
L
it
P
I
t
c
s
policy-miking will therefore vary from country to country.
TheCIOMSprogramme^rfonJ cor^er^ce lheld in
1OgUC
o^eS'eS to discuss in an international and intercultural context the ethtcal
Zb raised by health policy-making and policy dectsions.
The
of a na-n or a community isiu
social uses of the availableimed.ca
guides for people when choosmg goal ,T^on
. .
I
c
c
2
that strategy. Etl^ is the link
of the cho; that muSt
I
I
A
5
choices in accordance with accepted norms.
I
A strong recommendation of the At^^^^"CehrionshipabXeen health policy-making.
(
1
1
I
j
i
values across cultural and political lines.
The main means for implementing thh>
national, intercultural conferences with a g
nf intercogences, not
interaction of health policy-making,
WoiJd Health Forum • Volume 16 • 1995
/A-
A
Ethics and health
Do you think that all health ministries now think
in terms of equity when they analyse problems and
prepare their interventions?
It is difficult for me to know this, but it seems
there are wo aspects. One is the development
of guiding principles such as the health-ior-all
strategy-. The other is its implementation.
Policy decision-makers in many countries are
certainly moving in the direction of extending
services to those who have only limited or no
access to existing services. It is obvious y verydifficult to provide health services to all
human beings in the world, and the aims will
vary according to what is feasible and neces
sary for different countries or societies. For
me it is important to sec WHO, as a UN
specialized agency, working steadily to intro
duce equitable policies, following ethical and
moral principles which arc universally recog
nized. This is something which must not be
forgotten.
How do you see WHO's role in the ongoing
development of health ethics?
First of all I think it is important to continue
what was started, namely, to continue to pro
mote health for all - this is a unique role for
^TIO. The Organization is well placed to
convince politicians and to stimulate the politi
cal wdll for translating this commitment into
action. In my opinion WHO is doing this
ver}’ well because there are continually new
developments in global thinking in this field.
Another area is local action. “Think globally,
act. locallyn was the slogan of World Health
Da}’ in 1990 about the environment; I have it
displayed in my office as a reminder of the
importance of different levels in discussion.
Global thinking is health for all; local action
depends on local circumstances, and must be
adapted not only to varying economic,
financial, historical and traditional situations
but also to moral and ethical circumstances.
We are always urging that moral and ethical
aspects should be taken into consideration in
health policy-making, not just in order to
prevent abuses but because wc know from
The fact that health for all is recognized
worldwide and has tremendous influence in
both developed and developing countries
shows the exceptional value ol the World
Health Organization from an ethical point of
view.
experience that some apparently excellent
programmes were not implemented because
society rejected them for moral or ethical
reasons. It is important to discover whv and
try to find another way of presenting the
proposals or make alternative ones. Cultural
differences are central in international work:
we should always keep in mind that people
are different and we must endeavour to
understand them.
I believe CIOMS, with WHO’s cooperation, has
recently evolved a global agenda for bioethics?
Yes, CIOMS s long-term programme on
health policy, ethics and human values
culminated in a conference held at Ixtapa,
Mexico, in April 1994 on “Poverty, Vulner
ability, the Value of Human Life and the
Emergence of Bioethics . The participants
requested CIOMS to draft a declaration on a
global agenda for bioethics for adoption by
the conference (see pages 123-124). Partici
pants in the conference believed the time was
ripe for the establishment of a global agenda
for bioethics, and the Declaration of Ixtapa
constitutes a first step in that direction. The
world needs the moral affirmation and ethical
guidance that such an agenda can bring to the
health sector in all countries, and the partici
pants at Ixtapa and CIOMS welcomed WHO s
role as leader in the pursuit of such a goal.
121
Wo'ld Health Forum • Volume 16 • 1995
Forum Interview
Has the AIDS epidemic influenced the whole debate
on ethics?
No doubt about it. The AIDS epidemic is
stimulating everybody to do as much as pos
sible to sec that ethical values arc respected.
\Xrith a disease for which no adequate treat
ment exists, a diagnosis can be a death
sentence for the patient. It was previously so
with cancer. Now AIDS patients arc in the
same tragic situation. Top politicians arc
aware of the effects of this social problem and
arc looking for solutions which will be as
cthicallv valid in the USA as in Africa. Such
common ground is not easy to find.
Scientific progress in medicine and new devel
opments in therapy and diagnosis will most
likclv continue in the so-called “developed’
countries in Europe and elsewhere; but will
these advances be applicable to the people liv
ing in the developing part of the world - more
than 80% of our population? Often what is
affordable by cenain countries may not suit
others. Take drug treatment for HIV/AIDS
patients, for example. CIOMS was requested
by the Global AIDS Programme to develop
ethical guidelines relevant to the AIDS situ
ation on a global basis. In order to develop the
proper treatment and prevention strategies for
AIDS you need to study the target popu
lations, collect epidemiological information,
and test potential vaccines and drugs. Intercultural differences may mean that
Cultural differences are central in inter
national wort: we should always keep in
. mind that people are different and we must
. endeavour to understand them.
approaches developed in Europe or North
America are not easily acceptable in other
countries, sometimes for political reasons, yet
everything must be done according to ethical
principles.
122
In CIOMS in 1985 wc saw that two aspects
had to be addressed. The first was the formu
lation of ethical guidelines for epidemiological
study: this is when you identify the problem
and how the disease spreads, which is essen
tial basic information. The second was con
cerning research involving human subjects:
experimental vaccine testing, for example. The
U.S. authorities were particularly keen for
CIOMS to develop guidelines which would
be internationally recognized. These two sets
of CIOMS guidelines have been translated
into manv other languages and arc now
widely used (2,3).
I am concerned that although universal rights have
been formulated, less attention is paid to universal
responsibilities
It is true that if you say somebody has rights,
then they also have responsibilities. These
have not been defined up to now, but perhaps
sets of responsibilities of human beings as a
social group should be developed. Certainly
many people are concerned by what is really
needed now for mankind. Fifty years ago the
development of human rights was first priority. That was followed by the rights of differ
ent categories of society - patients, women,
children, etc. - which are good but, at the
same time, there must also be responsibility;
The constitution of many countries specifies
its citizens’ rights and also their responsibil
ities. In my opinion, this practice should be
followed internationally.
Because of social obligations?
Exactl}’. This is the social aspect of ethics: it is
about relations with other people. There is
nowadays a strong trend to look at everything
from the ethical point of view because
increased mass media exposure brings us all
closer to each other. Previously individuals
just considered their families, then their
villages, and then their countries, but now we
V>:'2 Hea'^ Forum • Volume 16 • 1995
Worlc
Ethics and health
t global igenda to' bloMUs:
. Bionics in .ho heahh
”lhe Declantlm el IMP"
shonld lx gnkM by .he following goner* accepted
hoe! of ho* ..e ,Mf lx =
' Q KX”»' i-1-1’ <o'Jl “ '"d““d ” ,l’c Dic,“ °
&htenfeeS.hoUldbeo«ocb«,effxient.CeeSSibk,.ffo.d«M^
and individuals s
. yhTXeipio. of
»
^Ta?^
XXXXSXXXX bo appiied across ah ^re,
. Effort should be made .o pronro.e and ^^“X^Xerging
national and international capacities for
•
^sterns may be practised that threaten
SKik ■he p™* of equity * non-discrindnaonx
. Efforts should be made .o devebp
"5 ”?eXXXS“K»ndemu»d.»gof d,e causes »d eireumsunces of
principles, acknowledging t
biXd^
bilateral and multilateral links between
their counterparts in developing countries.
(continued overleaf)
____________
123
VMd Health Four • Volume 16 • 1996
Forum Interview
t HIM WM lorbioMIcs: SWW blU» Declbrbl'bb bllOBDb (cohlmbb)
t
i
1
Human rights bodies
Such rights can be divided
I
1
l
into the foDowing categories:
1
I
<
_ gnceE"’
concerned with liberry, secunty, and private life.
,nd‘“lme nsl"s
i
Development banks
health, environment, poverty, and education.
i
Internationa! organizations
. Intergovernmental organizations engaged
tion to bioethical issues in
^]veinent of all concerned, including scientific
Emphasis needs to be placed on the full mvo vemento^
of
and lay organizations, in discusswns o
hou]d be sensitized to pressing
■ESSSS.s===sssxsst.
particularly in developing countries.
Source: BuUem of the World Health Organization, 1994,72:998-999.
■World Health Forum • Volume 16 • 1995
12*
Ethics and health
are all aware of what is happening all over
,hc world. And so ethics is now a main issue
in political debate. The aim of CIONS in the
10 years of its health policy, ethics and human
values programme was to sensitize health
nolicv-makers to the ethical issues. 1 he
I Jirector-General of WHO is convinced of
the imponance of ethics, and now some
Member States are saying that VTdO should
be more involved in this field and that its role
should be established at the highest level. To
me it is a measure of progress that we arc ab c
to bring health policy-makers from different
countries together to d.scuss eth.cal tssues for
a frank exchange of views.
WHO certainly has moral authority.
\cs and that raises an interesting point: the
moral authorin- comes from the fact that
.
as a public-health-oriented orgamzation, is devoted to helping the public at large,
which is an extremely ethical role. People
sometimes ask me why ethical issues need to
be discussed at all, because WHO’s role in
helping poor countries is by definition ethica .
This is certainly true, and because of its moral
authority the role of WHO in promoting dia-
If you say somebody has rights, then they
also have responsibilities.
loguc on the global agenda for bioethics is
crucial. The importance of intercultural
debate among like-minded people cannot be
emphasized enough. Dialogue, and yet more
dialogue, is the way forvs ard. ■
References
1 Mooney G. Conflicting ethics m health care World
heallh foru'T- 1987.8 516-517
Ethics and epidemiology international guidelines
Geneva CIOMS. 1991
3 International ethical guidelines for piomedica.'
research involving human subjects. Geneva. CIOMb
1993
125
Foru'r' • VolU^lC • 1995
L2
Point of View
1
Graham Evans
Health and security
in the global village
With the ecological stability of the world under threat, no country can
stand alone National security should no longer be viewed in a purely
military light but rather as a matter demanding cooperation between all
countries on a broad range of vital issues, not least those related to
health and the environment
Even political system has, or claims to
have, a final arbiter, namely a government,
which settles disputes and allocates
resources; this is the defining characteristic
of politics within the state. In international
politics, however, there is no single
government to regularize relationships
between the panicipating states.
Consequently, the concepts of self-help and
self-defence enjoy a much more legitimate
status than they do within the state; and
power becomes the ultimate arbiter.
Health care: in whose interest?
Formerly, health care was only a peripheral
matter among the concerns of politicians.
The author is Lecturer in International Relations,
Department of Political Theory and Government,
University of Wales, Swansea SA2 8PP, Wales
4ea
Fo’d-n
VO
14
1993
During the nineteenth century it was
introduced not for humanitarian reasons but
because industrialists realized that healthy
workers were more cost-effective than
unhealthy ones.
In general, health was considered important
only to the extent that it touched on matters
of national importance. In domestic politics,
health care provision became a function of a
particular ideological orientation and its
ability to impact on the political process,
whereas in world politics it has always been
intimately associated with the fabric of
security challenges to the state. In both
contexts, the spur was provided by
pragmatism, not idealism.
The issue of global health, like that of the
environment, has become more prominent
on the political stage as the dictates of
interdependence among states have imposed
themselves.
133
]
I
7
I
Point of View
Health practitioners and political scientists
now basically agree on the desirability of
removing inequities in health care,
particularlv in the context of North South
relations. S'et unless the questions of health
begin to impinge directly on states'
on a solid economic base. Security has thus
been regarded as an end-product of a
particular kind of policy-making, usually
involving arms races.
Security: the broad view
The health-for-all goals are bound
to remain beyond reach until
political will has been summoned
up, especially in the developed
countries.
conceptions of national interests, particularly
security, they arc likely to remain
unresolved. The health-for-all goals arc
bound to remain beyond reach until political
will has been summoned up, especially in
the developed countries. Success is only
likely to come if there is a clear recognition
that the security and prosperity of the
developed world arc at stake.
On its own, moralistic pressure cannot
be expected to bring about a transfer of
resources from the military to the health
sector. Even the so-called peace dividend
that many people expected after recent
events in eastern Europe and the former
Soviet Union has failed to materialize.
The potential dangers perceived by states
militate against change in this direction.
Yet expenditure on health care should now
be seen as a contribution to security rather
than as an alternative to it.
Security has always been the central element
. in international affairs, and the principal
instruments for achieving it have been
military and diplomatic. The ability to resist,
deter or overcome an opponent has
depended on visible military capability built
134
In the world of the 1990s, however, security
is no longer just an end-product resulting
from a perceived capacity for retaliation but
is a process reflecting a much wider view of
threat than that traditionally recognized by
governments of nation states.
Of course, the nuclear menace still exists,
but if we shift our focus from states to
peoples and from independence to
interdependence the nature ol the security
issue begins to look diflerent. People
cvervwhere face mam hazards, among them
AIDS, drugs, pollution, starvation,
population growth and environmental
degradation, which fail to appear in
traditional analyses. Military power has not
become unimportant, but its dominance at
the centre of things has been challenged.
Nature does not recognize international
boundaries, and the emphasis now is on the
connectedness and interdependence of
things. Thus, parallelling developments in
social medicine, the new strategic approach
is to embrace the whole picture rather than
isolated parts.
Security , as defined in 1982 by the Palme
Commission on Disarmament and Security,
requires physical and ecdiibmft well-being,
human rights, civil and political liberties,
a sustainable environment, and a programme
of social justice seeking the transfer of
resources from the North to the South. In
the field of strategic or peace studies, threat
assessment exercises, which previouslyfocused primarily on economic and military
capability, now also cover the larger
ecological and environmental dangers that
V.o'Id
Vo
14
1993
\
INDIAN SOCIETY OF HEALTH ADMINISTRATORS, (ISHA), BANGALORE
in Collaboration with
NATIONAL LAW SCHOOL OF INDIA UNIVERSITY, BANGALORE
One Day Meeting on RIGHT TO HEALTH - March 15, 1997
Venue: Committee Room:Di rector’s Office Building, NIMHANS
Health for All and the National Health Programmes: Major Issues
I.
Issues identified in National Health Policy for HFA.
Status of the population (around 1983).
Hea7 th
1 .
The high rate of population growth continues to have an
adverse effect on the health of our people and quality of their
lives.
Mortality rates for women and children below the age of five
2.
years, are very high.
3.
High infant mortality, around 129 per 100 live births.
4.
Extent and severity of malnutrition continuing to be high.
5.
Communicable diseases yet to be effectively brought
leprosy, TB continuing to show high incidence.
control
6.
under
Blindness continuing to show high incidence.
Only 31% of rural population had access to potable water
7.
supply and 0.5% to basic sanitation.
8.
High incidence of diarrhoeal disease, other preventive and
infectious diseases specially among infants and children, lack of
safe drinking water, poor environmental sanitation, poverty and
ignorance are among the major contributory causes of high
incidence of diseases and mortality.
II.
Health Systems and Manpower issues.
1.
The existing situation has been largely engendered by the
almost wholesale adopting of health manpower development policies
and establishment of curative centres based on western models,
which are appropriate and irrelevant to the real needs of our
people and the socio-economic conditions in the country.
2.
The hospitais-based disease and cure-oriented approach
towards establishment of medical services, had provided benefits
to the upper crusts of society, specially those residing in the
urban areas, at tho cost of providing comprehensive primary
health care services to the entire population whether residing in
urban or rural areas.
1
3.
High emphasis on curative approach has led to neglect of the
preventive, promotive, public health, and rehabilitative aspects
of health care.
4.
Instead of improving awareness and building up selfreliance, the existing approach has tended to enhance dependency
and weaken the community capacity to cope with problems.
5.
Prevailing policies in education and training of medical and
health personnel have resulted in a cultural gap between the
people and personnel providing care.
6.
The various health programmes have failed to involve
individuals and families in establishing a self-reliant .
community. This is in view of the fact that the ultimate goal of
achieving a satisfactory health status for all our people cannot
be secured without involving the community in identification of
health needs and priorities and in implementation of the national
health programmes.
III. Medical Education
Keeping in view the above issues, the National Health Policy
called for the:
i.
Review of the entire basis and approach towards medical
education in the light of national needs and
priorities, and a restructuring to produce personnel of
required professional and social skills and competence,
motivated to achieve results, within existing
constraints.
ii.
A National Medical Education Policy which
a.
sets out changes in curricular contents and
training programme of medical and health personnel
at all levels.
b.
Takes into account the need for establishing the
extremely essential inter-re 1 ations between
functionaries of various grades.
c.
pro v1des guidelines for production of health
personnel on the basis of realistically assessed
manpower requirements.
d.
seeks to resolve existing sharp
imbalances in their availability.
e.
ensures that personnel at all levels are socially
motivated towards the rendering of community
health services.
i
2
regional
Immediate Priorities
IV.
The National Health Policy identified the following priority
areas to be urgently attended to:
i.
Nutrition; Raising the nutritional level of al 1
segments of population, on a time-bound bases, using
every possible strategy.
ii.
Prevention of food
quality of drugs.
adulterati on
and
mai ntenance
of
provision of facilities
i i i. Water supply and sanitation
together with health education for effective use
towards health and sustainability.
iv.
Environmental protection
v.
Immunization Programme
of target population.
vi .
Maternal and Child Health Services: to provide and
ensure utilization of all necessary preventive and
promotive services nearest to the door-steps of the
people, particularly anti-natal, intra-natal and post
natal care.
achieve cent-percent coverage
vii. School Health Programme to reach al 1
chi 1dren.
school
going
viii. Occupational Health Services to ensure outreach of
services to prevent and treat occupational hazards not
only in organized but also unorganized sector such as
agriculture.
i
ix.
Health Education: Vital for success of every scheme and
programme.
x.
Management information system for appropriate decision
making and programme planning.
xi.
Medical Industry - to ensure adequate availability of
life-saving and essential drugs and vaccines produced
within the ^country at affordable prices even for the
poor, using available technological and manufacturing
capability. *To bcvw
vaa cAxA/oy*
-to i'y^vXjz.
X i i. Health Insurance: to enable health for all, in all the
above dimensions to become an affordable proposition.
xiii. Health legislation
xiv. Medical research: with the basic objective of
transition of available know-how into, simple, low
cost, easily applicable, acceptable, appropr i ate
3
t
technologies, devices and interventions to suit 1 ocal
condition. thus placing the latest technological
achievements within the reach of health personnel,, even
in the remotest corners of the country, particularly
|
with regard to
a.
b.
c.
d.
e.
xv.
Contraception
' Bli ndness
Leprosy
Tuberculosis
Other communicable diseases
Inter-sectoral co-operation for health
xvi. Monitoring and Review of Progress
In the light of the National Health Policy, the Fami1y
Welfare and Communicable Disease Control Programmes, were sought
to be strengthened, and additional Programmes were act i ve1y
initiated, prominent ones being the Nutrition-related programmes
for women and
children, Anemia
prophylaxis programme and Vitamin
t
A distribution, Immunization Programme,
Programme, National Blindness
Control Programme, and National Goitre Control Programme.
All
these programmes, specifically the Mother and Child Health
Programmes, Family Welfare Programme received a major boost in
made, However,
the decade 1983-93 with significant achievements made.
some- of the programmes such as Malaria Control Programme, T B
Control lagged behind the newer priority programmes.
Subsequently, however, following initiation of the national
reforms and restructuring process and other complex developments,
some of the major issues facing public health and family welfare
in India, affecting the implementation of all the Programmes are
as follows;
Reductions in outlays for health and social sectors (in real
1 .
terms)
2.
Reduced emphasis on health and social sector by the
government (as compared with industrial and other economic growth
sectors)
Inadequate recruitment of personnel at all levels in the
3.
health, system by all State Governments on the plea of financial
tightness.
Specifrca 1 1 y , gross inadequacy of male health
workers, lab technicians at PHCs, health supervisors, male and
female, and health educators is evident. Inadequacy is not merely
due to increased population; large number of vacancies caused by
retirement are not being filled. Almost every public health
programme depends on these critical front-line workers.
4.
In all States, the system of having Medical Officers of PHCs
as the leaders of the health team has, by and large, failed in
achieving community health objectives, with MOs largely confined
to a curative role at the PHCs/HCs. Resultantly, the paramedical
4
workers are unable to look to a leader for technical,
supervisory, and motivational guidance.
gu i dance.
In the present
framework, in every public health programme,
programme, the leadership of
the PHC/MO is critical for effective implementation.
5.
The issue of whether to have a non-medical leadership for
all non-curative/non-surgical aspects of public health and Family
Welfare Programmes, needs to be examined.
It had been suggested
in the late eighties, to have non-medical Community Health
Officers, as officers in- charge of the PHCs and Community Health
Centres, responsible for providing technical and administrative
leadership to all the public health programme manpower, and
getting the curative/surgical assistance of the medical doctors.
V.
Critical National Health Programmes
A.
NATIONAL MALARIA ERADICATION PROGRAMME
i
The NMEP in India after
a spectacular success during the
period 1958-65, due to a combination of setbacks showed a major
resurgence with its peak in 1976.
The annual incidence of cases
and deaths were reducedI from about 75 million cases and one
million deaths prior to 1958, to 0.1 million cases and no death
in 1965, and again with resurgence increased to 6.47 million
cases in 1976. Since then, with modification of strategies, and
fluctuating inputs for implementation of the NMEP, malaria has
•become chronically endemic in India, with epidemics from time to
time in certain pockets. The major problems and issues for
effective malaria control are;
Admi ni strati ve
1.
Low priority given to the Programme by the Health
administrators at National and State levels, specifically in the
contexts of: a) Low priority to health as such , and, b)
Increasing priority to MCH and Family Welfare, AIDS etc.
2.
Gross inadequacy of field personnel
control activities timely, which is the
programme.
to carry out malaria
key to sucess of the
Technical
a.
Mosquito Resistance to Conventional
insecticides.
3.
Relative mosquito resistance to conventional i nsecti ci des
(currently DDT is the only one implicated since it has been
widely used). Resistance would emerge equally rapidly to other
insecticides also.
b.
Emergence of Drug resistant malaria parasite strains
4.
Haphazard, indiscriminate use of anti-ma 1 aria 1s by the
public, private practitioners, etc, has resulted in emergence of
malaria parasite strains resistant to conventional drugs.
Agai n
5
this is due to inadequacy of systematic malaria
treatment activities by the Government machinery.
c.
control
and
Community Participation in the Programme
Since malaria prevention is closely linked to lifestyle and
5.
peop1e’s action, community participation is critical for i ts
success. So far the Health officials at all levels, have been
1 east geared to mobilize community participation for success of
the Programmes.
d.
Lack of follow-up on alternative strategies such as
insectici de-impregnated mosquito bednets
6.
Inspite of promising results with field trials of
insecticide-impregnated mosquito bednets, there has been no
follow-up to assess its potential on a large scale and implement
the same.
e.
Leadership to the Programme at PHC and District level
Effective committed leadership at PHC and District 1 eve 1s,
is critical for malaria control, These two aspects have been the
weak links in NMEP.
Among the above issues, the most critical ones are ;
B.
a.
Gross inadequacy of paramedical and field health staff,
specifically lab technicians and male health workers.
b.
Leadership factors at PHC and District levels.
NATIONAL TUBERCULOSIS CONTROL PROGRAMME (NTCP)
This programme, which did not gain due priority so far, has
become critical due to emergence of HIV infection and AIDS, The
critical issues facing the TB control programme are;
TB is a silent killer
Being a chronic disease it does not cause epidemic cases or
1 .
deaths. Hence it does not catch the attention of the media and
administrators, consequently very low priority to this programme.
A major, shift in strategy
2.
There has been a major shift in the strategy of India’s TB
programme, under the aegis of international agencies, just when a
widespread awareness of the strategies of the original NTCP had
gained momentum. Worldwide, there have been major changes in
perceptions about TB treatment, particularly in the context of
the developed countries’ response to the HIV-TB linkage. As a
result, together with considerable World Bank funding for TB
Control, there has been a statergic shift, from domiciliary, self
administered treatment, to DOTS - a system of supervised
6
contact. Although i ts
chemotherapy by person to person contact.
was
not
studied,
it gained wide
effectiveness in
i n India
strategy
inabandoning
the
former
resulting
acceptance,
effectiveness
and
cost
benefits
DOTS has
a 1 together . Lately, the c . .
~ -----------been called into question by series of studies.
b.
Problem of Diagnosis at periphery
2.
Diagnosis at the periphery requiires sputum examination by
of being “dirty",
microscopy. Culturally sputum has a connotation
c~.
Besides
traditionally,
doctors
compared with blood examination.
.
are inot oriented
-. ----- to diagnosis of TB by simple sputum examination.
c.
Problem of prolonged treatment
3.
Due to need for prolonged treatment, patients tend to
d i sconti nue treatment or take irregular treatment, a situation
which is worsened by poor treatment organization at the
per iphery.
d.
Effective Drugs not available under in the TB programme
4.
Even though highly effective drugs for treatment are
a v a i 1 a b 1 e , they have not been utilized or misused due to cost and
other factors. For a long time, the available drugs under the
programme were of low effectiveness, and required very long of
treatment, which demoralised the patient and the staff. Since the
last eight years, availability of any type of anti-TB drug has
been very poor, particularly under the Programme. This has led to
a through demoralization of staff who are expected to diagnose
cases without the means to treat. Patients are demoralized due to
inability to afford on their own, and lack of drugs in the Govt,
setup.
Lack of effective and continued leadership to this programme
5.
at District Level.
The organization of TB Programme requires effective,
committed leadership and continuity of leadership at the District
level which is a weak link in the system.
Lack of clarity on the epidemiological linkages between HIV
6.
and TB
C.
HIV AND AIDS CONTROL PROGRAMME
HIV - AIDS poses a serious threat to the health of our
country, with serious implications for physical, mental, social
and economic health. The National AIDS Control Organization, WHO
and other agencies have estimated that about 30-40 lakh Indians
are currently HIV positive, which may increase to about one crore
(10 million or 1% of the population) in 2001.
The major issues
are as follows:
related to HIV-AIDS control and management
1 .
Inspite of widespread HIV-AIDS awareness large number of
people of' all social strata are still getting infected.
This raises questions regarding the outreach, i ntens i ty,
content, and nature of the AIDS educational programmes, vi sa-vis their effectiveness.
2.
The issues of stigma and fear related to HIV and AIDS are
causing serious constraints in containing the spread of
disease and in enabling HIV affected individuals and
families adapt to the problem, These issues have not been
tackled in the educational effort.
*2*
By the year 2000 approximately 10 lakh individuals will need
AIDS related inpatient, care. But the total bed capacity in
the Government sector is about six lakhs. A planned approach
to the problem of care; of HIV related illness, is critical,
considering the magnitude of the problem.
D.
FAMILY WELFARE PROGRAMME
a.
Political Commitment
The most critical issue is lack of adequate political
How critical is political
commitment to implement the Programme,
is
evident
from
the tremendous success
commitment for its success
achieved by Tamil Nadu in reducing the birth rate from 31 in 1981
to 24 in 1992, improved from, a ranking of 16th to 3rd in India,
and achieving one of the lowest decadal population growth rates
in India of 21% (next only to Goa and Kerala). All this was
achieved due to political
commitment of successive Chief
Ministers of the State. Family Welfare Programme currently
remains, a women’s Contraception Programme.
1 .
Family planning - perceived as the women’s responsibility
From the top management level of the Programme upto the
2.
peripheral health worker, the basic premise is that family
planning and avoidance of pregnancy/ childbearing, is the need
and responsibility of the womenfolk.
Interventions being
researched, put to field trials, and released for mass
application, are all
methods to be used by women,
and
consequently the massive IEC strategies in operation are also
spreading the message as if Family Welfare means contraception by
women.
Thus a psycho-social climate has been created in India,
that family planning is for the benefit of women and to be
practised by women.
Keeping in view the social psyche, which
treats women as second class beings, the Programme emphasis on
female contraception has created a climate of low priority for
family planning among rural and urban poor population.
This
emphasis has to change. Unless Family Planning is projected as a
need and responsibility of both spouses, as a means to economic
8
development of the family,
conti nue.
b.
the low priority in rural
Delay in mass production and
convenient new contraceptives.
distribution
areas wi11
of safe and
3.
The th ird critical, issue is that safe and convenient
contraception methods recently discovered and cleared for field
use, are not being manufactured in sufficient quantities for not
being distributed through government, PHCs and workers.
Particularly, the newer safe methods such as, Saheli which is
ideal for temporarily contraception by women independent of their
husband’s consent, is neither manufactured in sufficient quantity
nor distributed through Government agencies; similarly also other
contraceptives.
c.
Updating
methods
TEC
to d i ssem i nate
1 atest
safe
cont racept i ve
4.
Fourthly, the IEC strategies and content need to be rapidly
updated, to include the latest developments in contraception
technology (such as Saheli, upgradation of condoms quality in
recent times, etc). The updated IEC content needs to be
communicated down the line upto Health Educator and Health Worker
level, and to the masses through mass media.
5.
Lack of dissemination of scientific and authoritative
ev ide nee concerning safety of newly discovered contraceptive
methods.
Recently engineered contraceptives such as Saheli,
Depoprovera, Nor-plant, Birth Control Vaccine, are proven by
international and national trains to be safe, convenient and
highly advantageous to physical and mental health of women, in
comparison with the risks and burdens of repeat chi 1d-bearing’ and
care. Inspite of clear, scientific evidence available and the
WHOs statements to this effect, GOI and State Governments have
not communicated professionally acceptable (scientific) data to
all their doctors down the line, and to the public at large,
through newspapers, journals of the Ministry, and audio visual
media. As a result, a number of NGOs with hardly any appreciation
of the issues involved, and many with their own hidden agendas,
create adverse publicity for valuable contraceptive methods, thus
virtually throttling .Government’s efforts.
The Governments,
Central and State, should ensure adequate publicity for
scientific information on the benefits, statistically proven
risks as well as precautions, to prevent or neutralise undeserved
adverse publicity.
d.
Lack of IEC emphasis and clarity
temporary contraceptive methods.
on safe and acceptable
IEC efforts, through mass media (TV and radio continue to
emphasize only sterilization operations which are either feared
or rejected by several sections of the population.
Regular IEC
9
on safe and accessible temporary methods which can be practised
by women in their own, is needed, if Family Welfare has to reach
the unreached families so far.
e.
Ensure Availability of contraceptives right upto village
level
6.
There is need to ensure availability of safe and acceptable
contraceptives right upto PHC and health worker level,
appropriately trained to handle the same.
In case of orally
self-administered ones, products like Saheli could be socially
marketed through fair price shops other village shops, bang 1e
sellers in rural areas, and other innovative woman to woman
approaches.
The effort for wide spread availability of all types of
convenient contraceptive methods for rural population, should go
hand in hand with IEC effort.
7.
Need to promote vasectomy to dispel myths, popularize
noscalpel vasectomy, and train adequate doctors in the
procedure
Tubectomy, being an intra-abdominal operation carries far
women, as well as chronic pain and other
risk to health of women,
debilitating complications
comp 1i cat ione for women, causing many women to
hesitate or refuse.
refuse. Vasectomy, which is now modified to a
subcutaneous and safe procedure, should be effectively promoted
and doctors right upto peripheral level trained in the procedure.
more
8.
Need for people-friendly
and follow-up services
Family
Programme
pre-operati ve
The entire family welfare machinery needs to be geared up
for an integrated people-friendly approach in providing Family
Welfare services. This implies adequate prenatal care/preoperative care to correct anemias, make the person fit for
surgery, and post-operative follow-up care for complications.
For effective implementation, these aspects should be monitored
as part of the PHC/District/State Family Welfare performance.
9.
Role of Financial Incentives in Promotion of Sterilizations
Inspite of a number of studies and expert opinions that
incentives are not critical factors in accepting Family Planning,
ISHA’s interactions with eligible couples show that stoppage of
financial incentives for sterilization in some States has been a
• major barrier to Family Welfare Programme in recent years.
Our
interactions in Maharashtra State show that rural women
undergoing tubectomy are now compelled to go for work to the
fields the very day following tubectomy, for economic reasons,
thereby going in for life-long abdominal pain and other
complications.
Thus the image of tubectomy and Family We 1 fare
Programme itself has been tarnished.
10
It needs to be understood that financial incentive is not
the primary factor to induce acceptance of sterilization, but
lack of financial compensation would seriously retard the
programme. Though it is termed as "incentive” in Family Welfare
jargon, in reality it is the compensation for loss of daily
wages.
This is essential for the family food during the period
when the mother has to take rest.
There is urgent need to review the decision on "incentive”,
and to fix a compensation level equal to wages for the period of
rest required.
To avoid misuse of cash by family members,
equivalent in grain and essential commodities could be provided
for.
10.
Target setting and Family Welfare monitoring to be refined
to included the dimension of parity of acceptors.
Decade after decade, planners and experts are emphasizing
the need for quality of target achievements, and not merely
quantity. Since sterilization needs to be accepted after two, or
maximum three children, to achieve a demographic impact.
Mere
target achievement by doing sterilization of couples with four or
more children, does very little for demographic change. Therefore
targets fixed should be linked to parity of acceptors. Similarly
also, monitoring and corrective actions should take into
consideration parity of acceptors.
11
INDIAN SOCIETY OF HEALTH ADMINISTRATORS, (ISHA), BANGALORE
HEALTH FOR ALL: SOME RECOMMENDATIONS TO ACHIEVE THE GOAL
The Indian Society of Health Administrators, chose the theme
of Health for All by 2000 AD for its first annual conference in
1980. Recommendations were made. r
We need' to review how far these
recommendations have been implemented at
- various
.
--- ; 1 eve 1 s .
1 .
The present allocation of financial resources for the health
system being inadequate in absolute and relative terms and in
comparison with other countries, the conference recommended that
1.
The allocation both by the centre
increased substantially forthwith.
ii .
Studies be
I
undertaken to determine the
the optimum
increase, taking into consideration, the
the economic
situationi of the country and the possibilities of
and the states
be
mobilizing funds for health efforts.
2.
Given the fact that the financial resources (inspite
larger mobilization of funds) will continue to be inadequate
the foreseeable future, recommended that
of
in
i.
there should be intensive training programmes for
health personnel at all levels in order to equip them
with
modern
management
techniques
for
better
utilization of funds, and
i i.
priorities must Ibe assigned in the distribution of
funds for those programmes which are more cost
effective in bringing about better health to larger
sections of the people, viz., health education,
nutrition, immunization
immuni zation programmes, eradication and
control programmes and water supply and sanitation.
2
As the country is still lagging behind in the matter
of
production, distribution and proper utilization of drugs
and
pharmaceuticals to ensure the availability of essential drugs at
feasible costs,
recommended that the country identifies low cost effective
drugs essential for primary health care, produces them in bulk
quantities and Iensures proper distribution (with distribution
systems at the periphery)
4.
FFree supply of drugs and services being neither feasible
nor
desi rable,
recommended that the beneficiaries
according to their capacity to pay.
12
be charged for
them,
5.
The judicious development of appropriate
respect to types and numbers being imperative,
manpower
wi th
recommended that steps to be taken to train
i.
one community health volunteer for 1000 population or
for each village, where the population is less than
1000.
ii .
village level worker, as needed depending on the 1 oca 1
conditions, and
iii. other identified health personnel such as multi-purpose
workers, doctors, nurses, pharmacists, dentists,
laboratory technicians and health inspectors, as per
the recommendations of the committees which have
considered these needs.
Since school teacher form a large body of persons who can
6.
influence the young minds for better health,
recommended that
i.
school teachers be given training in health education,
covering all school teachers by 1990.
ii .
the syllabus for training of school teachers (B.Ed, B T
and other similar courses) should have the theory and
practice of health education, and
iii . The school curriculum for the age groups 10 to 15 years
should include "Health Education in effective manner".
7.
Health being multisectoral and there is
coordination of all programmes of primary health care,
need
for
recommended that the departments of health at the center and
the States should coordinate the activities of all implementing
departments, such as Industry, Agriculture, Education and Health.
Community participation is essential if primary health care
8.
is to succeed. To ensure the involvement of the community at all
stages of planning, implementation and evaluation,
recommended that health committees
i.
be formed at various levels (Village, Block, district,
State and linked to the National Development Council);
ii.
should include elected representatives of
and various health functionaries, and
13
the
people
iii. at the village and block levels, they should include
local practitioners of medicine, school teachers,
representatives of women’s organizations and leaders of
the local community.
91Voluntary agencies have an important role to play in primary
health care and in order to ensure their participation,
recommended that
i .
voluntary agencies
their efforts;
ii.
they be involved in health activities
sector from the planning stages; and
be
i denti f i ed
and encouraged
in
any
area
in
or
i i i. their activities be fully co-ordinated with government
activities and a machinery be devised to ensure coordi nati on, to avoid duplication.
10.
'The planning for primary health care needs proper recording
and complication
and macro levels. Though a
- of data at the micro _..J
machinery exists, in order to ensure that the compilation is
sat i sfactory,
recommended that the forms of reporting and the mechanics of
record keeping be reviewed so that the forms can be simplified
and the information is utilized as needed.
1 1 .
Primary health care needs are dynamic and changing. In order
to respond to these needs,
recommended that there be research and development wings in
each state,
i.
to monitor these
adequately, and
ii .
to develop appropriate technologies, making use of the
local resources and talents to the maximum extent
possible.
needs
and
to
respond
to
them
12. As it is essential to ensure protection of the environment
which is threatened-by the industrialization and other factors,
recommended that
i.
effective legislation be enacted,
ii .
suitable machinery be devised to effectively implement
the legislation.
14
HEALTH INDICATORS AND INFRASTRUCTURE CHANGES IN INDIA
Year
1997
1946
1 .
Population Served
2.
Health manpower
(population per unit)
342 million
970 million
a.
Doctors
1:6,300
1:2,680
b.
Nurses
1:43,000
1:4,500
c.
Health Visitors
1:4,00,000
1:30,000
d.
Mi dwi ves
1:60,000
e.
Trained Dais
Ni 1
5.64 lakh
trained since
1974
0.24
0.59
3.
Beds available/
1000 population
4.
Health and Family
Welfare Indicators
Year
1946
1993
a.
Crude Death Rate
44
9
b.
Crude Birth Rate
46(1941 )
28.3
c.
Infant Mortality Rate
(per 1000 lives birth)
162
74
d.
Maternal Mortality Rate
(per 1000 lives birth)
20
4.37
e.
Couple Protection Rate(%)
(NFHS)
nil
f.
Life Expectancy at Birth
32
51
male
58.6
female 59
Sources:
Bhore Committee Report (1946)
1 .
Statement of National Health Policy Government of
2.
(1983)
Health Information India (1988)
3.
SRS 1994 (Provisional figures).
4.
National Family Health Survey, 1992-93
5.
India
INDIAN SOCIETY OF HEALTH ADMINISTRATORS, (ISHA), BANGALORE
**********************************************************************
Right to Health - Notes prepared for the Meeting on
March 15, 1997
1.
World Health Organization:
Geneva, Switzerland.
The World Health Report,
1996,
Infectious diseases are attacking us on multiple fronts.
Together, they represent the world’s leading cause of pre-mature
death. The heaviest burdens of ill-health will continue to fall
on those who live in developing countries, especially those least
able to sustain economic development.
2.
UNICEF. The State of the World’s Children 1995.
An underclass is being created under-educated and unskilled,
economic
standing beneath the broken bottom rungs of social <and
--------------------progress.
The 1994 International Conference on Population and
Development (Cairo Conference) emphasized the need to extend
reproductive health services to women i n all communities, to
raise levels of female education and to accelerate progress
towards gender equality.
3.
World Health Forum, 1987 , Vol . 8, No. 2, pp 190
RIGHTS AND RESPONSIBILITIES OF INDIVIDUALS
Individuals and families function best within a particular
social, economic and environmental context. To the extent that
this framework allows adequate opportunities and resources for
all citizens to make free choices, they have both rights and
obligations in relation to health, with responsibilities to
pursue better health for themselves, their families and the
communities in which they live.
Individuals have the right to:
*
a social,
economic,
phys i cal, emotional and legislative
economi c, physical,
social
environment that is as safe and healthy as it can be made;
*
an education that permits them to make well-judged choices
about their health and the avoidance of health hazards;
1
*
a valued role in society that offers them self-respect and
the respect of others;
*
encouragement and support
*
participate in the making
that affect their health.
in selecting a healthy life-style;
implementation
and
of
policies
Individuals are responsible for:
*
valuing their own health and that of members of their
family; seeking information to make responsible decisions to
preserve and promote health; and adopting a healthy life
style wherever they have a choice to do so;
*
recognizing that they have opportunities to shape their own
lives and those of their families; and power to make choices
as individuals, as consumers and as electors who determine
their own future health and that of fellow citizens;
*
seeking to maintain a purposeful attitude to life, giving
respect, friendship, love and minimal hurt to others; and
pursuing reconciliation in preference to conflict.
4.
World Health Forum,
1984, Vol.5, No 2, pp 131
RIGHT TO LIFE OF HANDICAPPED
Alison Davis
I am 2 8 years old, and suffer from a severe physical
was
born
with
which
is
irreversible.
I
i s
disability
myelomeningocele spina bifida.
I have suffered considerable and prolonged pain from time to
time, and have undergone over 20 operations thus far, some of
Even now my health is at best
them essential to save my life.
uncertain. I am doubly incontinent and confined to a wheelchair
and thus I should have "no worthwhile quality of life".
However, because I was fortunately born in rather more
tolerant times, I was given the chance to defy the odds and live,
which is' now being denied to handicapped newborns. Even so, my
parents/were encouraged to leave me in the hospital and "go home
and have another" and I owe my life to the fact that they refused
to accept the advice of the experts.
2
Despite my disability I went to an ordinary school and then
to university, where I gained an honours degree in sociology. I
now work full-time defending the right to life of handicapped
people.
I have been married eight years to an able-bodied man,
and over the years we have travelled widely in Europe, the Soviet
Union and the United States.
This year we plan to visit the Far
East.
Who could say I have “no worthwhile quality of life"? I am
sure though that no doctor could have predicted when I was 28
days old (and incidentally had received no operation at all) that
despite my physical problems I would lead such a full and happy
life. I do not doubt that they were “acting in good faith" when
they advised my parents to abandon me, but that does not mean
that their advice was correct.
I feel that the medical profession could go a lot further
it has to condemn the constant undermining of the rights of
handicapped people at progressivel
progressivelyy later stages in their lives.
There is nothing magical about the age of 28 days after all. It
is simply the currently accepted boundary of "non-personhood
”non-personhood” for
babies with congenital defects.
than
’
r.
!
to
the
de
facto
Legislation
could
well
lead
decriminalization of the act of killing a handicapped person of
any age, just as it did in Hitler’s Germany, And if it does, woe
betide any handicapped people who are too ill to defend their
right to life by protesting that they are in fact happy. And woe
betide us all, when we get too old to be considered “useful” and
all the friends who could have spoken in our defence have already
been oh so lovi ngl y ' "al 1 owed to die”.
5.
World Health Forum,
Vol 14, 1993, pp 135
RIGHT TO A HEALTHY ENVIRONMENT
People need to have the means to acquire the resources on
which health depends: safe food and water, fuel, and a secure
They need to be protected not only from physical,
shelter.
chemical, and biological hazards, but also from crime and
vi olence, which are encouraged by poverty and the use of drugs,
and from injuries at their place of work. A healthy environment
i s not only a need, it is also a right; the right to live and
work in an environment conducive to physical and mental health is
enshrined in the Universal Declaration of Human Rights. Everyone
shares the responsibility for ensuring that this right is duly
acknowledged.
3
i
I
Everyone also shares responsibility for health and for
passing on to the next generation a world whose resources are not
depleted and whose natural systems are not degraded. There is a
powerful synergy between health, environmental protection, and
sustainable resource use.
Individuals and societies who share
the responsibility for achieving a healthy environment and
managing their resources sustainably become partners in ensuring
that global cycles and systems remain unimpaired.
6.
WHO Chronicle, Vol 38, No 5, 1984
REPRODUCTIVE HEALTH, YOUTH, AND THE LAW
Health cae is the legitimate concern of any nation, with the
right to health said to pertain to individuals and the duty to
provide health care to the State. Legislation is used not only as
a vehicle for expressing this concerni but also as a method for
treating the system of "rights” and "duties".
"duties”. Health
Heal th codes are
often extensions of constitutional statements and are central to
any rational attempt to organize and regulate the various health
care and promotion services.
7.
The Indian Practitioner , Vol. XLII, No 12, December 1989
WORLD MEDICAL ASSOCIATION
ABUSE OF THE ELDERLY
DECLARATION OF HONG KONG ON THE
The elderly have the same
respect as other human beings.
r i ghts
to
care,
we 1fare
and
Physicians whether consulted by an aged person directly, the
nursing home, or the family will see that the patient receives
the best possible care.
8.
The Health Provider’s Guide to Contraception. The Pathfinder
Fund, 1983
Family planning is an essential component of any broad-based
development strategy that seeks to improve the quality of Life
for both individuals and communities, the lives of millions of
mothers and children will be saved (through family planning).
Family planning is the basic human right.
i s a Key Concept in family planning. There is no
Choice is
perfect contraceptive method, and some methods will be more
suitable to a particular client’s needs than others. Clients must
be offered the full range of methods available in the community,
■and health providers must help explain how these methods vary in
convenience, effectiveness, and appropriateness.
4
9.
World Health Forum, Vol 17, No 1, 1996
THE SOCIAL ACTION DIMENSION OF HEALTH DEVELOPMENT
...J social action for health support the
Health promotion and
,health-for-al
lea , UII_,
... 1two ways; by promoting healthy lifestyles
1 goal, in
and community action for health, and by creating conditions that
make it possible to live a healthy life. The first entails
empowering people with the knowledge and skills needed for
healthy living. The second calls for influencing policymakers so
a 1th-supportive public policies and
that they pursue he
L^_l_
Strong
social
support for health action needs to be
programmes.
accelerated
and
maintained. A public that knows its
i n i t i ated,
responsibilities,
supported by political will and
r i ghts and
at
all
levels
of
government,
can make health for all a
awareness
reali ty.
5
ISHA
One Day Symposium on
“Right to Health*, 15th March, 1997
Jointly organized by National Law School of India University
and
Indian Society of Health Administrators
1.
Universal Declaration of Human Rights - Adopted by the
U N on 10th December, 1948.
"Article 25 (1) Every one has the right to a standard of living
adequate for the health and well-being of himself and of his
family including food, clothing, housing and medical care and
necessary social serivices
(2) Motherhood and childhood are entitled to special
care and assistance..... “
2.
International Covention on Economic, Social and
Cultural Rights - Entry into force on 3rd January, 1976
"Article 12 (1) The State Parties to the present Covenant
recognize the right of everyone to the enjoyment of the highest
attainable standard of physical and mental health.
(2) The steps to be taken by the States Parties
to the present Covenant .to achieve the full realization of this
right shall include “"-those necessary for:
(a) The provision for the reduction of the still birth-rate
of infant mortality and for the healthy development of the child;
(b) The improvement of all aspects of environmental and
industrial hygiene;
(c)
The prevention, treatment and control
endemic, occupational and other diseases;
of epidemic,
(d)
The creation of conditions which would assure to all
medical serivce and medical attention in the event of sickness".
3.
The Convention on the Rights of the Child, 1989
"Article 24
(1) State Parties recognize the right of the child
to the enjoyment of the highest attainable standard of health and
to facilities for the treatment of illness and rehabi111tation of
health.
States Parties shall strive to ensure that no child is
deprived of his or her right of access to such health care
services".
ISHA
4.
The Constitution of India, 1948
The State shall in paticular, direct its
"Article 39.
policy towards securing * (e) that the health and strength of
workers and the tender age of women are not abused.... (f) that
children are given opportunities and facilities to develop in a
healthy manner....
"Article
The State shall, within the limits of its economic
"Article 41.
41.
capacity and development, make effective provision for securing
old age,
age,
the right ....to public assistance in cases of .......... old
sickness and disablement....
"Article 47.
The State shall regard the raising of the level of
nutrition and the standard of living of people and the
improvement of public health as among its primary duties and, in
paraticular, the State
shall endeavour to bring about
prohibition of the consumption except for medicine purposes of
intoxicating drinks and of drugs which are injurious to health.
While international treaties on Human Rights do recognize
health as a basic right, the Indian Constitutional text
accomodates this basic need as a Directive Principle of State
Policy
to be realized subject to the economic capacity and
development of the State.
In the last nearly five decades, the
Governments at the Centre and in the States have enacted
a
number of laws and launched a variety of programmes directed
towards the increasing realisation of health services to the
people gnerally, and to women, handicapped, and children in
particular.
A national health policy is promulgated and hundred
of thousands of crores of rupees spent in the delivery of health
services.
The object of the symposium is to examine the evolution
of health from a mere welfare programme to a right which every
citizen can legitimately claim from the Government.
Is it a
legally enforceable right or is it only a policy to become a
_________________________
right sometime
in future? What is the content of right to
Is
the
H
hea1th for all by 2000 A D" a slogan or wishful
health?
thinking only? How far are we from that goal? What are the
programmes now in place at the Central and State levels on the
Who gets
what out of these programmes?
How
health front?
adequate are they and what are the prospects of making themi more
effective?
What are ’the budgetary allocations for health at
Centre and in States and what are the priorities?
Where are we
lacking - in infra-structure, personnel, funds, political will?
What
is
the
view of
the medical
profession
on
righJ^tf^^
health in the context of India.
Should the courts take the
concept as a fundamental right and start directing the government
to enforce it as such?
What will be the impact or consequence?
How does the 1iberalisation/privatisation process affect health
services?
In short, the Symposium expects to gather the considered
views
of
the
profession
(doctors,
nurses,
hoep1ta1
(doctors,
administrators, health policy planners) on the nature, content,
scope and the present reality of the "Right to Health" with a
view to develop a jurisprudence
which hopefully will support
Problems of health in Indian
health as a basic human right,
context have to be borne in mind rather than looking at it in an
abstract or ideal perspective.
INDIAN SOCIETY OF HEALTH ADMINISTRATORS, 9ISHA0, BANGALORE
in collaboration with
SCHOOL
OF INDIA UNIVERSITY, BANGALORE
NATIONAL LAW
One Day Meeting on RIGHT TO HEALTH - March 15, 1997
Venue: Committee Room: Director’s Office Building, NIMHANS
TENTATIVE PROGRAMME
SESSION I-RIGHT TO HEALTH; MAJOR ISSUES
Chairman; Dr. 3.M. Channabasavanna, Director, NIMHANS
A. Dr. N. R. Madhava Menon,
Di rector,
National
Law
□ ui iuu I •
B. Dr Ashok Sahni, ISHA.
SESSION II
RIGHT TO HEALTH: SECTORAL ACHIEVEMENTS
Chai rman: Dr R M Varma, Professor Emeritus, NIMHANS.
Short presentations
A. D r V Para mes hv a r a, Past President, IMA.
B. Dr Chikka Nanjappa, President, Karnataka Medical
Cou n c i 1
C. Mr T V Antony, Former Chief Secretary, Tamil Nadu
D. Dr G V Nagaraj, Addl. Director, Directorate of
Health and Family Welfare Services, Government of
Karnataka
E. Prof N S Ramaswamy, Director, CARTMAN, Bangalore.
Addl . Director (Planning), India
F. Dr P N Halagi, Addl.
Population Centre.
G. Dr H R Basavaraj, Institute of Health Comparative
Medicine.
H. Mrs Krishnakumari Menon
Menon,, President, Karnataka
Parents Association for Mentally Retarded Citizens
SESSION III - RIGHT TO HEALTH; PUBLIC HEALTH ISSUES
Chairman: Dr Madhava Menon, Director, National
School of India University.
Law
A. Dr K Basappa, Prof Preventive and Social Medicine
S. Dr M Narayanapp, Prof Preventive and Social Medicine
C. Dr (Mrs) M K Vasundhra, Prof Preventive and Social
Medicine
(
D. Dr Om Prakash, Consulting Physician, St Martha’s!
Hospital.
\
E. Dr Mohan K Issac,
Addl . Professor of Psychiatry,
Issac, Addl.
NIMHANS.
SESSION IV - SUMMARY OF ISSUES
C ha irman; Dr Mad h av a Me n on,
School of India University.
Di rector,
Nat i onal
Law
Report by Prof. Joga Rao, National Law School of India
Universi ty.
- Media
 RF_L_3_SUDHA.pdf
RF_L_3_SUDHA.pdf
Position: 775 (16 views)