NATIONAL HEALTH POLICY - 2001
Item
- Title
- NATIONAL HEALTH POLICY - 2001
- extracted text
-
RF_HP_2_B_SUDHA
4
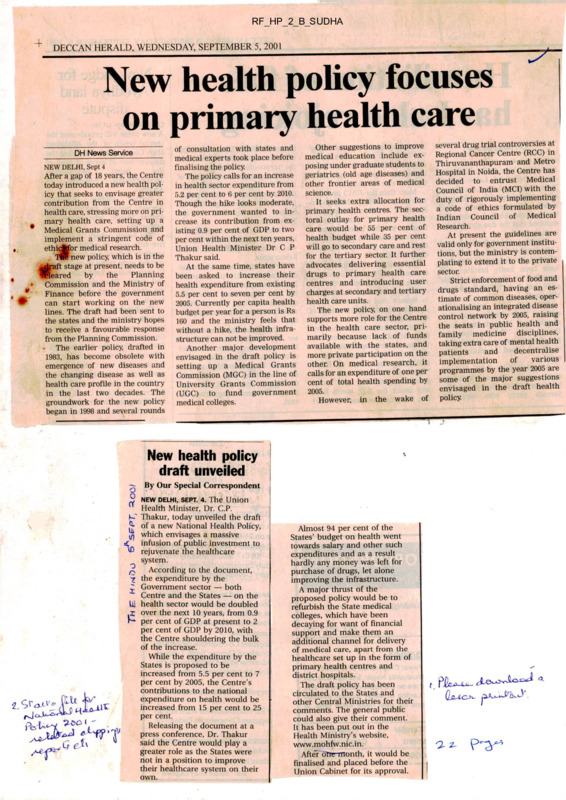
DECCAN HERALD, WEDNESDAY, SEPTEMBER 5, 2001
New health policy focuses
on primary health care
DH News Service
NEW DELHI, Sept 4
After a gap of 18 years, the Centre
today introduced a new health pol
icy that seeks to envisage greater
contribution from the Centre in
health care, stressing more on pri
mary health care, setting up a
* Medical Grants Commission and
implement a stringent code of
ethidfefor medical research.
TW-new policy, which is in the
^iraft stage at present, needs to be
Weared
by
the
Planning
Commission and the Ministry of
Finance before the government
can start working on the new
lines. The draft had been sent to
the states and the ministry hopes
to receive a favourable response
from the Planning Commission.
The earlier policy, drafted in
1983, has become obsolete with
emergence of new diseases and
the changing disease as well as
health care profile in the country
in the last two decades. The
groundwork for the new policy
began in 1998 and several rounds
of consultation with states and
medical experts took place before
finalising the policy.
The policy calls for an increase
in health sector expenditure from
5.2 per cent to 6 per cent by 2010.
Though the hike looks moderate,
the government wanted to in
crease its contribution from ex
isting 0.9 per cent of GDP to two
per cent within the next ten years,
Union Health Minister Dr C P
Thakur said.
At the same time, states have
been asked to increase their
health expenditure from existing
5.5 per cent to seven per cent by
2005. Currently per capita health
budget per year for a person is Rs
160 and the ministry feels that
without a hike, the health infra
structure can not be improved.
Another major development
envisaged in the draft policy is
setting up a Medical Grants
Commission (MGC) in the line of
University Grants Commission
(UGC) to fund government
medical colleges.
several drug trial controversies at
Regional Cancer Centre (RCC) in
Thiruvananthapuram and Metro
Hospital in Noida, the Centre has
decided to entrust Medical
Council of India (MCI) with the
duty of rigorously implementing
a code of ethics formulated by
Indian Council of Medical
Research.
At present the guidelines are
valid only for government institu
tions, but the ministry is contem
plating to extend it to the private
sector.
Strict enforcement of food and
drugs standard, having an es
timate of common diseases, oper
ationalising an integrated disease
control network by 2005, raising
the seats in public health and
family medicine disciplines,
taking extra care of mental health
decentralise
patients
and
of
various
implementation
programmes by the year —
2005I are
of the
major suggestions
some c—--envisaged in the draft health
2005.
However, in the wake of policy.
Other suggestions to improve
medical education include ex
posing under graduate students to
geriatrics (old age diseases) and
other frontier areas of medical
science.
It seeks extra allocation for
primary health centres. The sec
toral outlay for primary health
care would be 55 per cent of
health budget while 35 per cent
will go to secondary care and rest
for the tertiary sector. It further
advocates delivering essential
drugs to primary health care
centres and introducing user
charges at secondary and tertiary
health care units.
The new policy, on one hand
supports more role for the Centre
in the health care sector, pri
marily because lack of funds
available with the states, and
more private participation on the
other. On medical research, it
calls for an expenditure of one per
cent of total health spending by
New health policy
draft unveiled
By Our Special Correspondent
2 NEW DELHI, SEPT. 4. The Union
n Health Minister, Dr. C.P.
k? Thakur, today unveiled the draft
J* of a new National Health Policy,
111
which envisages a massive
infusion of public investment to
£
rejuvenate the healthcare
system.
o According to the document,
o
7 the expenditure by the
" Government sector — both
Centre and the States — on the
U) health sector would be doubled
over the next 10 years, from 0.9
. • per cent of GDP at present to 2
per cent of GDP by 2010, with
the Centre shouldering the bulk
of the increase.
While the expenditure by the
States is proposed to be
increased from 5.5 per cent to 7
per cent by 2005, the Centre’s
contributions to the national
expenditure on health would be
increased from 15 per cent to 25
per cent.
Releasing the document at a
press conference, Dr. Thakur
said the Centre would play a
greater role as the States were
not in a position to improve
their healthcare system on their
own.
£
it
Almost 94 per cent of the
States’ budget on health went
towards salary and other such
expenditures and as a result
hardly any money was left for
purchase of drugs, let alone
improving the infrastructure.
A major thrust of the
proposed policy would be to
refurbish the State medical
colleges, which have been
decaying for want of financial
support and make them an
additional channel for delivery
of medical care, apart from the
healthcare set up in the form of
primary health centres and
district hospitals.
The draft policy has been
circulated to the States and
other Central Ministries for their
comments. The general public
could also give their comment.
It has been put out in the
Health Ministry’s website,
www.mohfw.nic.in.
After dTre-month, it would be
finalised and placed before the
Union Cabinet for its approval.
t
health in India
Subject: health in india
Date: Thu, 06 Sep 2001 11:05:56 -0700
From: iiity <nity68@vsnl.com>
To: amit@corpwalch.org
CC: tnarayan@vsnl.com, sochara@vsnl.com
New health policy will widen inequities
KALPANA JAIN, TIMES NEWS NETWORK
DELHI: The new health policy, revised after a long gap of almost two
decades, will only increase the inequities in provision of health care. The
policy nor only suggests user charges ar rhe district-level hospitals bur
also a system of licentiate medical practitioners to meet the needs of
primary health centres.
Undoubtedly, the policy voices the right concerns on patents, medical
research and education, communicable diseases, ethics and women’s health.
It also seems to be interested in reviving the weakest health care link *
the PHCs, with its suggestion of additional 55 per cent of the current
ouulay for uhem. rhe secondary and rerniary sectors gen only 35 per cenn
and 10 per cent respectively.
But evenas it suggests to revive these sectors, the government does
express its ^n.ot-i-'ty to get nAdic^l doctors to work" the^e. ThereforA, i t
suggests encotiraging th-e practice of licentiate medical practitioners and
training oi paramedical peracanei tc provide health care in difficult
areas. Clearly, cue goverrnuent has different standards of care for the rith
ano che poor.
Moreover, it wants to open more centres, which will require additional
staff as well. As it is, a large part of government money ooes into
salaries. The issue then is how far the additional allocation will he
useful for reviving PECs. It would he worth pointing out that for the
co,CCO PHCs supposed uo be functioning across the country, there is already
a sanctioned strength of 23, GOG doctors.
The PHCs are expected to take the macor disease load while also working at
their prevention. But with the current functioning, the burden spills over
to specialised and super-speciality centres. It is at this level'that the
government proposes a user fee, a suggestion which most likely will push
more into the hands of the private sector.
Source : rhe rimes of India, September 6, 2001
I
1 ofl
9/7/01
4
file: D EMAIL RECEIVED nationalhealthpolic.htm
1
DRAFT NATIONAL HEALTH POLICY - 2001
1. INTRODUCTORY
1.1 A National Health Policy was last formulated in 1983 and since then, there have been
very marked changes in the determinant factors relating to the health sector. Some of the
policy initiatives outlined in the NHP-1983 have yielded results, while in several other
areas, the outcome has not been as expected.
1.2 The NHP-1983 gave a general exposition of the recommended policies required in
the circumstances then prevailing in the health sector. The noteworthy initiatives under
that policy were
A phased, time-bound programme for setting up a well-dispersed network of
comprehensive primary health care sendees, linked with extension and health
education, designed in the context of the ground reality that elementary health
problems can be resolved by the people themselves;
ii. Intermediation through ‘Health volunteers’ having appropriate knowledge, simple
skills and requisite technologies;
in. Establishment of a well-worked out referral system to ensure that patient load at the
higher levels of the hierarchy is not needlessly burdened by those who can be
treated at the decentralized level;
iv. An integrated net-work of evenly spread speciality and super-speciality services;
encouragement of such facilities through private investments for patients who can
pay, so that the draw on the Government’s facilities is limited to those entitled to
free use.
1.
1.3 Government initiatives in the pubic health sector have recorded some noteworthy
successes over time. Smallpox and Guinea Worm Disease have been eradicated from the
country; Polio is on the verge of being eradicated; Leprosy, Kala Azar, and Filariasis can
be expected to be eliminated in the foreseeable future. There has been a substantial drop
in the Total Fertility Rate and Infant Mortality Rate. The success of the initiatives taken
in the public health field are reflected in the progressive improvement of many
demographic / epidemiological / infrastructural indicators over time - (Box-I).
A
Box-1 : Through The Years - 1951-2000Achievements
* i
•
_____
Indftatof
1951
1981
2000
Life Expectancy
36.7
54
64.6(RGI)
Crude Birth Rate
40.8
33.9(SRS)
26.1(99 SRS)
Crude Death Rate
25
12.5(SRS)
8.7(99 SRS)
IMR
146
110
70 (99 SRS)
demographic Changes
9/6/01 4:20 PM
1 of22
■ i t
file: D EMAIL RECEIVED natipnalhe^Jthpolic.hiiTi
1
Epidemiological Shifts
Malaria (cases in million)
75
2.7
: 2.2
Leprosy cases per 10,000
population
38.1
57.3
3.74
>44,887
Eradicated
L,
Small Pox (no of cases)
Guineaworm ( no. of cases)
>39.792
Eradicated
Polio
29709
■ 265
57,363
i 1,63,181
Infrastructure
I__________
SC/PHC/CHC
725
i (99-RHS)
Dispensaries &Hospitals( all)
9209
23,555
! 43,322
(95-96-CBHI)
Beds (Pvt & Public)
117,198
569.495
i 8,70,161
(95-96-CBHI)
Doctors( Allopathy)
61,800
2,68,700
5,03,900
(98-99-MCI)
Nursing Personnel
18,054
1,43,887
7,37,000
(99-INC)
1.4 While noting that the public health initiatives over the years have contributed
significantly to the improvement of these health indicators, it is to be acknowledged that
public health indicators / disease-burden statistics are the outcome of several
*
complementary initiatives under the wider umbrella of the developmental sector,
covering Rural Development, Agriculture, Food Production, Sanitation, Drinking Waiter
Supply, Education, etc. Despite the impressive public health gains as revealed in thej
statistics in Box-I, there is no gainsaying the fact that the morbidity and mortality l|teels • •• •
in the country are still unacceptably high. These unsatisfactory health indices are, in tuifi,
an indication of the limited success of the public health system to meet the preventive
and curative requirements of the general population.
1.5 Out of the communicable diseases, which have persisted over history, incidence of
Malaria has staged a resurgence in the 1980s before stabilising at a fairly high prevalence
level during the 1990s. Over the years, an increasing level of insecticide-resistance has
developed in the malarial vectors in many parts of the country, vvhile the incidence of the
more deadly P-Falciparum Malaria has risen to about 50 percent in the country as a
2 of 22
9/6/01 4:28 PM
file: 7.P /EMAIL RECEIVED nationalhealthpolic.htm
1
whole. In respect of TB, the public health scenario has not shown any significant decline
in the pool of infection amongst the community, and, there has been a distressing trend
in increase of drug resistance in the type of infection prevailing in the country. A new
and extremely virulent communicable disease - HIV/AIDS - has emerged on the health
scene since the declaration of the NHP-1983. As there is no existing therapeutic cure or
vaccine for this infection, the disease constitutes a serious threat, not merely to public
health but to economic development in the country. The common water-borne infections
- Gastroenteritis, Cholera, and some forms of Hepatitis - continue to contribute to a high
level of morbidity in the population, even though the mortality rate may have been
somewhat moderated. The period after the announcement of NHP-83 has also seen an
increase in mortality through ‘life-style’ diseases- diabetes, cancer and cardiovascular
diseases. The increase in life expectancy has increased the requirement for geriatric care.
Similarly, the increasing burden of trauma cases is also a significant public health
problem. The changed circumstances relating to the health sector of the country since
1983 have generated a situation in which it is now necessary to review the field, and to
formulate a new policy framework as the National Health Policy-2001.
1.6 NHP-2001 will attempt to set out a new policy framework for the accelerated
achievement of Public health goals in the socio-economic circumstances currently
prevailing in the country.
2. CURRENT SCENARIO
2.1 FINANCIAL RESOURCES
The public health investment in the country over the years has been comparatively low,
and as a percentage of GDP has declined from 1.3 percent in 1990 to 0.9 percent in 1999.
The aggregate expenditure in the Health sector is 5.2 percent of the GDP. Out of this,
about 20 percent of the aggregate expenditure is public health spending, the balance
being out-of-pocket expenditure. The central budgetary allocation for health over this
period, as a percentage of the total Central Budget, has been stagnant at 1.3 percent,
while that in the States has declined from 7.0 percent to 5.5 percent. The current annual
per capita public health expenditure in the country is no more than Rs. 160. Given these
statistics, it is nd surprise that the reach and quality of public health services has been
below the desirable standard. Under the constitutional structure, public health is the
responsibility of the States. In this framework, it has been the expectation that the
principal contribution for the funding of public health services will be from States’
resources, with some supplementary input from Central resources. In this backdrop, the
contribution of Central resources to the overall public health funding has been limited to
about 15 percent. The fiscal resources of the State Governments are known to be very
inelastic. This itself is reflected in the declining percentage of State resources allocated
to the health sector out of the State Budget. If the decentralized pubic health services in
the country are to improve significantly, there is a need for injection of substantial
resources into the health sector from the Central Government Budget. This approach,
despite the formal Constitutional provision in regard to public health, is a necessity if the
State public health services - a major component of the initiatives in the social sector are not to become entirely moribund. The NHP-2001 has been formulated taking into
consideration these ground realities in regard to the availability of resources.
3 of 22
9/6/01 4:29 PM
file: D EMAIL RECEIVED natjonalhealthpolic.html
1
2.2 EQUITY
2.2.1 In the period when centralized planning was accepted as a key instrument of
development in the country, the attainment of an equitable regional distribution was
considered one of its major objectives. Despite this conscious focus in the development
process, the statistics given in Box-II clearly indicate that attainment of health indices
have been very uneven across the rural - urban divide.
Box II : Differentials in Health Status Among States
Sector
Population
BPL (%)
IMR/
<5iMort-ality
Per 1000
per 1000
(NFHS II)
Live Births
(1999-SRS)
Weight \ MMR/
For AgeLakh
(Annual
% of
Report
Children
Under 3
2000)
years
Leprosy
cases per
10000
popula-tion
Malaria
+ve
Cases in
year
2000 (in
thousands)
(<-2SD)
India
26.1
70
94.9
47
Rural
27.09
75
103.7
49.6
Urban
23.62
44
63.1
38.4
408
3.7
2200
■
Better
Performing
States
Kerala
12.72
14
18.8
27
87
0.9
5.1
Maharastra
25.02
48
58.1
50
135
3.1
138
TN
21.12
52
63.3
37
79
4.1
56
Orissa
47.15
97
104.4
54
498
7.05
483
Bibar
42.60
63
105.1
54
707
11.83
132
i Rajasthan
• 15.28
81
114.9
51
607
0.8
53
i UP
31.15
84
122.5
52
707
4.3
99
I MP
37.43
90
137.6
55
498
3.83
528
Low
Performing
States
Also, the statistics bring out the wide differences between the attainments of health goals
in the better- performing States as compared to the low-performing States. It is clear that
national averages of health indices hide wide disparities in public health facilities and
health standards in different parts of the country. Given a situation in which national
averages in respect of most indices are themselves at unacceptably low levels, the wide
4 of 22
9/6/01 4:29 PM
file: D EMAIL RECEIVED'nationalhealthpolic.htm
1
inter-State disparity implies that, for vulnerable sections of society in several States,
access to public health services is nominal and health standards are grossly inadequate.
Despite a thrust in the NHP-1983 for making good the unmet needs of public health
services by establishing more public health institutions at a decentralized level, a large
gap in facilities still persists. Applying current norms to the population projected for the
year 2000, it is estimated that the shortfall in the number of SCs/PHCs/CHCs is of the
order of 16 percent. However, this shortage is as high as 58 percent when disaggregated
for CHCs only. The NHP-2001 will need to address itself to making good these
deficiencies so as to narrow the gap between the various States, as also the gap across the
rural-urban divide.
2.2.2 Access to, and benefits from, the public health system have been very uneven
between the better-endowed and the more vulnerable sections of society. This is
particularly true for women, children and the socially disadvantaged sections of society.
The statistics given in Box-Ill highlight the handicap suffered in the health sector on
account of socio-economic inequity.
Box-Ill : Differentials in Health status Among Socio-Economic Groups
Infant
Mortality/l 000
Under 5
Mortality/l 000
% Children
70
94.9
47
' Scheduled Castes
83
119.3
53.5
Scheduled Tribes
84.2
126.6
55.9
Other Disadvantaged
I.1
i Others
76
103.1
47.3
61.8
82.6
41.1
Indicator
India
Underweight
' Social Inequity
2.2.3 It is a principal objective of NHP-2001 to evolve a policy structure which reduces
these inequities and allows the disadvantaged sections of society a fairer access to public
health services.
2.3 DELIVERY OF NATIONAL PUBLIC HEALTH PROGRAMMES
2.3.1 It is self-evident that in a country as large as India, which has a wide variety of
socio-economic settings, national health programmes have to be designed with enough
flexibility to permit the State public health administrations to craft their own programme
package according to their needs. Also, the implementation of the national health
programme can only be carried out through the State Governments’ decentralized public
health machinery. Since, for various considerations, the responsibility of the Central
Government in binding additional public health services will continue over a period of
time, the role of the Central Government in designing broad-based public health
initiatives will inevitably continue. Moreover, it has been observed that the technical and
managerial expertise for designing large-span public health programmes exists with the
5 of 22
9/6/01 4:29 PM
file: D EMAIL RECEIVED natipnalhealthpolic.htm
Central Government in a considerable degree; this expertise can be gainfully utilized in
designing national health programmes for implementation in \ arying socio-economic
settings in the states.
2.3.2 Over the last decade or so, the Government has relied upon a ‘vertical’
implementational structure for the major disease control programmes. Through this, the
system has been able to make a substantial dent in reducing the burden of specific
diseases. However, such an organizational structure, which requires independent
manpower for each disease programme, is extremely expensive and difficult to sustain.
Over a long time-range, ‘vertical’ structures may only be affordable for diseases, which
offer a reasonable possibility of elimination or eradication in a foreseeable time-span. In
this background, the NHP-2001 attempts to define the role of the Central Government
and the State Governments in the public health sector of the country'.
2.4 THE STATE OF PUBLIC HEALTH INFRA-STRUCTURE
2.4.1 The delineation of NHP-2001 would be required to be based on an objective
assessment of the quality and efficiency of the existing public health machinery in the
field. It would detract from the quality of the exercise if, while framing a new policy, it
is not acknowledged that the existing public health infrastructure is far from satisfactory.
For the out-door medical facilities in existence, funding is generally insufficient; the
presence of medical and para-medical personnel is often much less than required by the
prescribed norms; the availability of consumables is frequently negligible; the equipment
in many public hospitals is often obsolescent and unusable; and the buildings are in a
dilapidated state. In the in-door treatment facilities, again, the equipment is often
obsolescent; the availability of essential drugs is minimal; the capacity of the facilities is
grossly inadequate, which leads to over-crowding, and consequentially to a steep
deterioration in the quality of the services. As a result of such inadequate public health
facilities, it has been estimated that less than 20 percent of the population seeks the OPD
services and less than 45 percent avails of the facilities for in-door treatment in public
hospitals. This is despite the fact that most of these patients do not have the means to
make out-of-pocket payments for private health services except at the cost of other
essential expenditure for items such as basic nutrition.
2.5 EXTENDING PUBLIC HEALTH SERVICES
2.5.1 While in the country generally there is a shortage of medical manpower, this
shortfall is disproportionately impacted on the less-developed and rural areas. No
incentive system attempted so far, has induced private medical manpower to go to such
areas; and, even in the public health sector it has usually been a losing battle to deploy
medical manpower in such under-served areas. In such a situation, the possibility needs
to be examined for entrusting some limited public health functions to nurses, paramedics
and other personnel from the extended health sector after imparting adequate training to
them.
2.5.2 India has a vast reservoir of practitioners in the Indian Systems of Medicine and
Homoeopathy, who have undergone formal training in their own disciplines. The
possibility of using such practitioners in the implementation of State/Central
Government public health Programmes, in order to increase the reach of basic health
6 of 22
9/6/01 4:29 P.M
file: D EMAIL RECEIVED nationalhealthpolic.htm
care in the country, is addressed in the NHP-2001.
2.6 ROLE OF LOCAL SELF-GOVERNMENT INSTITUTIONS
2.6.1 Some States have adopted a policy of devolving programmes and funds in the
health sector through different levels of the Panchayati Raj Institutions. Generally, the
experience has been a favourable one. The adoption of such an organisational structure
has enabled need-based allocation of resources and closer supervision through the
elected representatives. NHP- 2001 examines the need for a wider adoption of this mode
of delivery of health services, in rural as well as urban areas, in other parts of the
country.
2.7 MEDICAL EDUCATION
2.7.1 Medical Colleges are not evenly spread across various parts of the country. Apart
from the uneven geographical distribution of medical institutions, ,the quality of
education is highly uneven and in several instances even sub-standard. It is a common
perception that the syllabus is excessively theoritical, making it difficult for the fresh
graduate to effectively meet even the primary health care needs of the population. There
is an understandable reluctance on the part of graduate doctors to serve in areas distant
from their native place. NHP-2001 will suggest policy initiatives to rectify these
disparities.
2.7.2 Certain medical discipline, such as, molecular biology and gene-manipulation,
have become relevant in the period after the formulation of the previous National Health
Policy. Also, certain speciality disciplines - Anesthesiology. Radiology and Forensic
Medicines - are currently very scarce, resulting in critical deficiencies in the package of
available public health services. The components of medical research in the recent years
have changed radically. In the foreseeable future such research will rely increasingly on
such new disciplines. It is observed that the current under-graduate medical syllabus
does not cover such emerging subjects. NHP-2001 will make appropriate
recommendations in this regard.
2.8 NEED FOR SPECIALISTS IN ‘PUBLIC HEALTIU AND ‘FAMILY MEDICINE’
2.8.1 In any developing country with inadequate availability of health services, the
requirement of expertise in the areas of‘public health’ and ‘family medicine’ is very
much more than the expertise required for other specialized clinical disciplines. In India,
the situation is that public health expertise is non-existent in the private health sector,
and far short of requirement in the public health sector. Also, the current curriculum in
the graduate / post-graduate courses is outdated and unrelated to contemporary
community needs. In respect of ‘family medicine’, it needs to be noted that the more
talented medical graduates generally seek specialization in clinical disciplines, while the
remaining go into general practice. While the availability of postgraduate educational
facilities is 50 percent of the total number of the qualifying graduates each year, and can
be considered adequate, the distribution of the disciplines in the postgraduate training
facilities is overwhelmingly in favour of clinical specializations. NHP-2001 examines
the need for ensuring adequate availability of personnel with specialization in the ‘public
health’ and ‘family medicine’ disciplines, to discharge the public health responsibilities
in the country.
7 of 22
9/6/01 4:29 PM
file: D EMAIL RECEIVED nationalhealthpolic.hiu.
2.9 URBAN HEALTH
2.9.1 In most urban areas, public health sendees are very meagre. To the extent that such
services exist, there is no uniform organisational structure. The urban population in the
country is presently as high as 30 percent and is likely to go up to around 33 percent by
2010. The bulk of the increase is likely to take place through migration, resulting in
slums without any infrastructure support. Even the meagre public health services
available do not percolate to such unplanned habitations, forcing people to avail of
private health care through out-of-pocket expenditure. The rising vehicle density in large
urban agglomerations has also led to an increased number of serious accidents requiring
treatment in well-equipped trauma centres. NHP-2001 will address itself to the need for
providing this unserved population a minimum standard of health care facilities.
2.10 MENTAL HEALTH
2.10.1 Mental health disorders are actually much more prevalent than are visible on the
surface. While such disorders do not contribute significantly to mortality, they have a
serious bearing on the quality of life of the affected persons and their families. Serious
cases of mental disorder require hospitalization and treatment under trained supervision.
Mental health institutions are perceived to be woefully deficient in physical
infrastructure and trained manpower. NHP-2001 will address itself to these deficiencies
in the public health sector.
2.H INFORMATION, EDUCATION AND COMMUNICATION
2.11.1 A substantial component of primary health care consists of initiatives for
disseminating, to the citizenry, public health-related information. Public health
programmes, particularly, need high visibility at the decentralized level in order to have
any impact. This task is particularly difficult as 35 percent of our country’s population is
illiterate. The present IEC strategy is too fragmented, relies heavily on mass media and
does not address the needs of this segment of the population. It is often felt that the
effectiveness of IEC programmes is difficult to judge; and consequently, it is often
asserted that accountability, in regard to the productive use of such funds, is doubtful.
NHP-2001, while projecting an IEC strategy, will fully address the inherent problems
encountered in any IEC programme designed for improving awareness in order to bring
about behavioural change in the general population.
2.11.2 It is widely accepted that school and college students are the most receptive
targets for imparting information relating to basic principles of preventive health care.
NHP-2001 will attempt to target this group to improve the general level of health
awareness.
2.12 MEDICAL RESEARCH
2.12.1 Over the years, medical research activity in the country has been very limited. In
the Government, such research has been confined to the research institutions under the
Indian Council of Medical Research, and other institutions funded by the States/Central
Government. Research in the private sector has assumed some significance only in the
last decade. In our country, where the aggregate annual health expenditure is of the order
S of 22
9/6/01 4:29 PM
file: D EMAIL RECEIVED nationalhealthpolic.hur
1
of Rs. 80.000 crores, the expenditure in 1998-99 on research, both public and private
sectors, was only of the order of Rs. 1150 crores. It would be reasonable to infer that
with such low research expenditure, it would be virtually impossible to make any
dramatic break-through within the country, by way of new molecules and vaccines; also,
without a minimal back-up of applied and operational research, it would be difficult to
assess whether the health expenditure in the country is being incurred through optimal
applications and appropriate public health strategies. Medical Research in the country
needs to be focused on therapeutic drugs/vaccines for tropical diseases, which are
normally neglected by international pharmaceutical companies on account of limited
profitability potential. The thrust will need to be in the newly-emerging frontier areas of
research based on genetics, genome-based drug and vaccine development, molecular
biology, etc. NHP-2001 will address these inadequacies and spell out a minimal quantum
of expenditure for the coming decade, looking to the national needs and the capacity of
the research institutions to absorb the funds.
2.13 ROLE OF THE PRIVATE SECTOR
2.13.1 Considering the economic restructuring underway in the country, and over the
globe, since the last decade, the changing role of the private sector in providing health
care will also have to be addressed in NHP 2001. Currently, the contribution of private
health care is principally through independent practitioners. Also, the private sector
contributes significantly to secondary-level care and some tertiary care. With the
increasing role of private health care, the need for statutory licensing and monitoring of
minimum standards of diagnostic centres / medical institutions becomes imperative.
NHP-2001 will address the issues regarding the establishment of a regulatory
mechanism to ensure adequate standards of diagnostic centres / medical institutions,
conduct of clinical practice and delivery of medical services.
2.13.2 Currently, non-Govemmental service providers are treating a large number of
patients at the primary level for major diseases. However, the treatment regimens
followed are diverse and not scientifically optimal, leading to an increase in the
incidence of drug resistance. NHP-2001 will address itself to recommending
arrangements, which will eliminate the risks arising from inappropriate treatment.
2.13.3 The increasing spread of information technologt raises the possibility of its
adoption in the health sector. NHP-2001 will examine this possibility.
2.14 ROLE OF THE CIVIL SOCIETY
2.14.1 Historically, the practice has been to implement major national disease control
programmes through the public health machinery of the State/Central Governments. It
has become increasingly apparent that certain components of such programmes cannot
be efficiently implemented merely through government functionaries. A considerable
change in the mode of implementation has come about in the last two decades, with an
increasing involvement of NGOs and other institutions of civil society. It is to be
recognized that widespread debate on various public health issues have, in fact, been
initiated and sustained by NGOs and other members of the civil society. Also, an
increasing contribution is being made by such institutions, in the delivery of different
components of public health services. Certain disease control programmes require close
9 of 22
9/6/01 4:29 PM
file: D EMAIL RECEIVED nationalhe'akhpolic.htir.
1
inter-action with the beneficiaries for regular administration of drugs: periodic carrying
out of the pathological tests; dissemination of information regarding disease control and
other general health information. NHP-2001 will address such issues and suggest policy
instruments for implementation of public health programmes through individuals and
institutions of civil society.
2.15 NATIONAL DISEASE SUR\ EILLANCE NETWORK
2.15.1 The technical network available in the country for disease surveillance is
extremely rudimentary and to the extent that the system exists, it extends only up to the
district level. Disease statistics are not flowing through an integrated network from the
decentralized public health facilities to the State/Central Government health
administration. Such an arrangement only provides belated information, which, at best,
serves a limited statistical purpose. The absence of an efficient disease surveillance
network is a major handicap in providing a prompt and cost effective health care system.
The efficient disease surveillance network set up for Polio and HIV/AIDS has
demonstrated the enormous value of such a public health instrument. Real-time
information of focal outbreaks of common communicable diseases - Malaria, GE,
Cholera and JE - and other seasonal trends of diseases, would enable timely
intervention, resulting in the containment of any possible epidemic. In order to be able to
use an integrated disease surveillance network, for operational purposes, real-time
information is necessary at all levels of the health administration. NHP-2001 would
address itself to this major systemic shortcoming in the administration.
2.16 HEALTH STATISTICS
2.16.1 The absence of a systematic and scientific health statistics data-base is a major
deficiency in the current scenario. The health statistics collected are not the product of a
rigorous methodology. Statistics available from different parts of the country, in respect
of major diseases, are often not obtained in a manner which make aggregation possible,
or meaningful.
2.16.2 Further, absence of proper and systematic documentation of the various financial
resources used in the health sector is another lacunae witnessed in the existing scenario.
This makes it difficult to understand trends and levels of health spending by private and
public providers of health care in the country, and to address related policy issues and
formulate future investment policies.
2.16.3 NHP-2001 will address itself to the programme for putting in place a modem and
scientific health statistics database as well as a system of national health accounts.
2.17 WOMEN'S HEALTH
2.17.1 Social, cultural and economic factors continue to inhibit women from gaining
adequate access to even the existing public health facilities. This handicap does not just
affect women as individuals; it also has an adverse impact on the health, general
well-being and development of the entire family, particularly children. NHP 2001
recognises the catalytic role of empowered women in improving the overall health
standards of the community.
10 of 22
9/6/01 4:29 PM
file: D EMAIL RECEIVED nationalhealthpolic.htm
1
2.18 MEDICAL ETHICS
2.18.1 Professional medical ethics in the health sector is a area, which h not received
much attention in the past. Also, the new frontier areas of research - involving gene
manipulation, organ'human cloning and stem cell research impinge on visceral issues
relating to the sanctity of human life and the moral dilemma of human intervention in the
designing of life forms. Besides these, in the emerging areas of research, there is an
un-charted risk of creating new life forms, which may irreversibly damage the
environment, as it exists today. NHP - 2001 recognises that moral and religious dilemma
of this nature, which was not relevant even two years ago, now pervades mainstream
health sector issues.
2.19 ENFORCEMENT OF QUALITY STANDARDS FOR FOOD AND DRUGS
2.19.1 There is an increasing expectation and need of the citizenry for efficient
enforcement of reasonable quality standards for food and drugs. Recognizing this need,
NHP - 2001 makes an appropriate policy recommendation.
2.20 REGULATION OF STANDARDS IN PARA MEDICAL DISCIPLINES
2.20.1 It has been observed that a large number of training institutions have mushroomed
particularly in the private sector, for several para medical disciplines - Lab Technicians.
Radio Diagnosis Technicians, Physiotherapists, etc. Currently, there is no
regulation/monitoring of the curriculum, or the performance of the practitioners in these
disciplines. NHP-2001 will make recommendations to ensure standardization of training
and monitoring of performance.
2.21 OCCUPATIONAL HEALTH
2.21.1 Work conditions in several sectors of employment in the country are
sub-standard. As a result of this, workers engaged in such activities become particularly
prone to occupation-linked ailments. The long-term risk of chronic morbidity is
particularly marked in the case of child labour. NHP-2001 will address the risk faced by
this particularly vulnerable section of the society.
2.22 PROVIDING MEDICAL FACILITIES TO USERS FROM QA ERSEAS
2.22.1 The secondary and tertiary facilities available in the country are of good quality
and cost-effective compared to international medical facilities. This is true not only of
facilities in the allopathic disciplines, but also to those belonging to the alternative
systems of medicine, particularly Ayurveda. NHP-2001 will assess the possibilities of
encouraging commercial medical services for patients from overseas.
2.23 IMPACT OF GLOBALIZATION ON THE HEALTH SECTOR
2.23.1 There are some apprehensions about the possible adverse impact of economic
globalisation on the health sector. Pharmaceutical drugs and other health services have
always been available in the country at extremely inexpensive prices. India has
established a reputation for itself around the globe for innovative development of
original process patents for the manufacture of a wide-range of drugs and vaccines
within the ambit of the existing patent laws. With the adoption of Trade Related
11 of 22
9'6/01 4:29 PM
file: D EMAIL RECEIVED nationalheakhpolic.htrr
1
Intellectual Property (TRIPS), and the subsequent alignment of domestic patent laws
consistent with the commitments under TRIPS, there will be a significant shift in the
scope of the parameters regulating the manufacture of new drugs/vaccines. Global
experience has shown that the introduction of a TRIPS-consistent patent regime for
drugs in a developing country, would result m an increase in the cost of drugs and
medical services. NHP-2001 will address itself to the future imperatives of health
security in the country, in the post-TRIPS era.
2.24 NON - HEALTH DETERMINANTS
2.24.1 Improved health standards are closely dependent on major non-health
determinants such as safe drinking water supply, basic sanitation, adequate nutrition,
clean environment and primary education, especially of the girl child. NHP-2001 will
not explicitly address itself to the initiatives in these areas, which although crucial, fall
outside the domain of the health sector. However, the attainment of the various targets
set in NHP 2001 assumes a reasonable performance in these allied sectors.
2.25 POPULATION GROWTH AND HEALTH STANDARDS
2.25.1 Efforts made over the years for improving health standards have been neutralized
by the rapid growth of the population. Unless the Population stabilization goals are
achieved, no amount of effort in the other components of the public health sector can
bring about significantly better national health standards. Government has separately
announced the 'National Population Policy - 2000’. The principal common features
covered under the National Population Policy-2000 and NHP-2001, relate to the
prevention and control of communicable diseases; priority to containment of HIV/AIDS
infection; universal immunization of children against all major preventable diseases;
addressing the unmet needs for basic and reproductive health services; and
supplementation of infrastructure. The synchronized implementation of these two
Policies - National Population Policy - 2000 and National Health Policy-2001 - will be
the very cornerstone of any national structural plan to improve the health standards in
the country.
2.26 AL TERNATIVE SYSTEMS OF MEDICINE
2.26.1 Alternative Systems of Medicine - Ayurveda, Unani, Sidha and Homoeopathy provide a significant supplemental contribution to the health care services in the country,
particularly in the underserved, remote and tribal areeas. The main components of
NHP-2001 apply equally to the alternative systems of medicine. However, the policy
features specific to the alternative systems of medicine will be presented as a separate
document.
3. OBJECTIVES
3.1 The main objective of NHP-2001 is to achieve an acceptable standard of good health
amongst the general population of the country. The approach would be to increase access
to the decentralized public health system by establishing new infrastructure in deficient
areas, and by upgrading the infrastructure in the existing institutions. Overriding
importance would be given to ensuring a more equitable access to health services across
the social and geographical expanse of the country. Emphasis will be given to increasing
12 of 22
9/6/01 4:29 PM
file: D EMAIL RECEIVED nationalhealthpolic.htm
1
the aggregate public health investment through a substantially increased contribution by
the Central Government. It is expected that this initiative will strengthen the capacity o?
the public health administration at the State level to render effective service delivery.
The contribution of the private sector in providing health services would be much
enhanced, particularly for the population group, which can afford to pay for services.
Primacy will be given to preventive and first-line curative initiatives at the primary
health level through increased sectoral share of allocation. Emphasis will be laid on
rational use of drugs within the allopathic system. Increased access to tried and tested
systems of traditional medicine will be ensured. Within these broad objectives,
NHP-2001 will endeavour to achieve the time-bound goals mentioned in Box-IV.
Box-IV: Goals to be achieved by 2000-2015
• Eradicate Polio and Yaws
2005
• Eliminate Leprosy
2005
• Eliminate Kala Azar
2010
• Eliminate Lymphatic Filariasis
2015
. Achieve Zero level growth of HIV/AIDS
2007
• Reduce Mortality by 50% on account of TB, Malaria
and Other Vector and Water Borne diseases
2010
• Reduce Prevalence of Blindness to 0.5%
2010
. Reduce IMR to 30/1000 And MMR to 100/Lakh
2010
• Improve nutrition and reduce proportion of LBW
Babies from 30% to 10%
2010
Increase utilisation of public health facilities from
current Level of <20 to >75%
2010
• Establish an integrated system of surveillance, National
Health Accounts and Health Statistics.
2005
• Increase health expenditure by Government as a % of
GDP from the existing 0.9 % to 2.0%
2010
• Increase share of Central grants to Constitute at least
25% of total health spending
2010
• Increase State Sector Health spending from 5.5% to 7%
of the budget
2005
2010
Further increase to 8%
4. NHP-2001 - POLIC Y PRESCRIPTIONS
13 of 22
9/6/01 4:29 PM
file: D EMAIL RECEIVED nationalhehlthpolic.hnn
1
4.1 FINANCI AL RESOURCES
The paucity of public health investment is a stark reality. Given the extremely difficult
fiscal position of the State Governments, the Central Government will have to play a key
role in augmenting public health investments. Taking into account the gap in health care
facilities under NHP-2001 it is planned to increase health sector expenditure to 6 percent
of GDP, with 2 percent of GDP being contributed as public health investment, by the
year 2010. The State Governments would also need to increase the commitment to the
health sector. In the first phase, by 2005, they would be expected to increase the
commitment of their resources to 7 percent of the Budget; and. in the second phase, by
2010, to increase it to 8 percent of the Budget. With the stepping up of the public health
investment, the Central Government’s contribution would rise to 25 percent from the
existing 15 percent, by 2010. The provisioning of higher public health investments will
also be contingent upon the increase in absorptive capacity of the public health
administration so as to gainfully utilize the funds.
4.2 EQUITY
4.2.1 To meet the objective of reducing various types of inequities and imbalances inter-regional; across the rural - urban divide; and between economic classes - the most
cost effective method would be to increase the sectoral outlay in the primary health
sector. Such outlets give access to a vast number of individuals, and also facilitate
preventive and early stage curative initiative, which are cost effective. In recognition of
this public health principle, NHP-2001 envisages an increased allocation of 55 percent of
the total public health investment for the primary health sector; the secondary and
tertiary health sectors being targetted for 35 percent and 10 percent respectively.
NHP-2001 projects that the increased aggregate outlays for the primary health sector will
be utilized for strengthening existing facilities and opening additional public health
service outlets, consistent with the norms for such facilities.
4.3 DELIVERY OF NATIONAL PUBLIC HEALTH PROGRAMMES
4.3.1 NHP-2001, envisages a key role for the Central Government in designing national
programmes with the active participation of the State Governments. Also, the Policy
ensures the provisioning of financial resources, in addition to technical support,
monitoring and evaluation at the national level by the Centre. However, to optimize the
utilization of the public health infrastructure at the primary level, NHP-2001 envisages
the gradual convergence of all health programmes under a single field administration.
Vertical programmes for control of major diseases like TB, Malaria and HIV/AIDS
would need to be continued till moderate levels of prevalence are reached. The
integration of the programmes will bring about a desirable optimisation of outcomes
through a convergence of all public health inputs. The policy also envisages that
programme implementation be effected through autonomous bodies at State and district
levels. State Health Departments’ interventions may be limited to the overall monitoring
of the achievement of programme targets and other technical aspects. The relative
distancing of the programme implementation from the State Health Departments will
give the project team greater operational flexibility. Also, the presence of State
Government officials, social activists, private health professionals and MLAs/MPs on
the management boards of the autonomous bodies will facilitate well-informed
14 of22
9/6/01 4:29 PM
file: D -EMAIL RECEIVED nationalhealthpolic.lnni
1
decision-making.
4.4 THE STATE OF PUBLIC HEALTH INFRASTRUCTURE
4.4.1 As has been highlighted in the earlier part of the Policy, the decentralized Public
health sendee outlets have become practically dysfunctional over large parts of the
country. On account of resource constraint, the supply of drugs by the State
Governments is grossly inadequate. The patients at the decentralized level have little use
for diagnostic services, which in any case would still require them to purchase
therapeutic drugs privately. In a situation in which the patient is not getting any
therapeutic drugs, there is little incentive for the potential beneficiaries to seek the
advice of the medical professionals in the public health system. This results in there
being no demand for medical services, and medical professionals, and paramedics often
absent themselves from their place of duty. It is also observed that the functioning of the
public health service outlets in the four Southern States - Kerala, Andhra Pradesh. Tamil
Nadu and Karnataka - is relatively better, because some quantum of drugs is distributed
through the primary health system network, and the patients have a stake in approaching
the Public health facilities. In this backdrop, NHP-2001 envisages the kick-starting of the
revival of the Primary Health System by providing some essential drugs under Central
Government funding through the decentralized health system. It is expected that the
provisioning of essential drugs at the public health service centres will create a demand
for other professional services from the local population, which, in turn, will boost the
general revival of activities in these service centres. In sum, this initiative under
NHP-2001 is launched in the belief that the creation of a beneficiary interest in the
public health system, will ensure a more effective supervision of the public health
personnel, through community monitoring, than has been achieved through the regular
administrative line of control.
4.4.2 Global experience has shown that the quality of public health services, as reflected
in the attainment of improved public health indices, is closely linked to the quantum and
quality of investment through public funding in the primary health sector. Box-V gives
statistics which show clearly that the standards of health are more a function of accurate
targeting of expenditure on the decentralised primary sector (as observed in China and
Sri Lanka), than a function of the aggregate health expenditure.
Box-V: Public Health Spending in select Countries
15 of22
9/6/01 4:29 PM
file: D EMAIL RECEIVED naiionalhealthpolic.lu:::
Indicator
I %Public
%Health
Expenditure to I Expenditure
on Health to
GDP
Total Health
Expenditure
%Population
with income of
<S1 day
Infant
Mortality
Rate/1000
India
44.2
70
5.2
17.3
China
18.5
31
2.7
24.9
Sri Lanka
6.6
16
3
45.4
UK
6
5.8
96.9
USA
7
13.7
44.1
Therefore, NHP-2001, while committing additional aggregate financial resources, places
strong reliance on the strengthening of the primary health structure, with which to attain
improved public health outcomes on an equitable basis. Further, it also recognizes the
practical need for levying reasonable user-charges for certain secondary and tertiary
public health care services, for those who can afford to pay.
4.5 EXTENDING PUBLIC HEALTH SERVICES
4.5.1 NHP-2001 envisages that, in the context of the availability and spread of allopathic
graduates in their jurisdiction, State Governments would consider the need for expanding
the pool of medical practitioners to include a cadre of licentiates of medical practice, as
also practitioners of Indian Systems of Medicine and Homoeopathy. Simple
services/procedures can be provided by such practitioners even outside their disciplines,
as part of the basic primary health services in under-served areas. Also, NHP-2001
envisages that the scope of use of paramedical manpower of allopathic disciplines, in a
prescribed functional area adjunct to their current functions, would also be examined for
meeting simple public health requirements. These extended areas of functioning of
different categories of medical manpower can be permitted, after adequate training and
subject to the monitoring of their performance through professional councils.
4.5.2 NHP-2001 also recognizes the need for States to simplify the recruitment
procedures and rules for contract employment in order to provide trained medical
manpower in under-served areas.
4.6 ROLE OF LOCAL SELF-GOVERNMENT INSTITUTIONS
4.6.1 NHP-2001 lays great emphasis upon the implementation of public health
programmes through local self Government institutions. The structure of the national
disease control programmes will have specific components for implementation through
such entities. The Policy urges all State Governments to consider decentralizing
implementation of the programmes to such Institutions by 2005. In order to achieve this,
financial incentives, over and above the resources allocated for disease control
programmes, will be provided by the Central Government.
16 of 22
9/6/01 4:29 PM
file: D EMAIL RECEIVED nationalhealthpoi
4.7 MEDICAL EDUCATION
4.7.1 In order to ameliorate the problems being faced on account of the uneven spread of
medical colleges in various parts of the country, NHP-2001. envisages the setting up of a
Medical Grants Commission for funding new Government Medical Colleges in different
parts of the country. Also, the Medical Grants Commission is envisaged to fund the
upgradation of the existing Government Medical Colleges of the country, so as to ensure
an improved standard of medical education in the country.
4.7.2 To enable fresh graduates to effectively contribute to the providing of primary
health services. NHP-2001 identifies a significant need to modify the existing
curriculum. A need based, skill-oriented syllabus, with a more significant component of
practical training, would make fresh doctors useful immediately after graduation.
4.7.3 The policy emphasises the need to expose medical students, through the
undergraduate syllabus, to the emerging concerns for geriatric disorders, as also to the
cutting edge disciplines of contemporary medical research. The policy also envisages
that the creation of additional seats for post-graduate courses should reflect the need for
more manpower in the deficient specialities.
4.8 NEED FOR SPECIALISTS IN ‘PUBLIC HEALTH* AND ‘FAMILY MEDICINE/
4.8.1 In order to alleviate the acute shortage of medical personnel with specialization in
‘public health’ and ‘family medicine’ disciplines, NHP-2001 envisages the progressive
implementation of mandatory norms to raise the proportion of postgraduate seats in
these discipline in medical training institutions, to reach a stage wherein 'A th of the seats
are earmarked for these disciplines. It is envisaged that in the sanctioning of
post-graduate seats in future, it shall be insisted upon that a certain reasonable number of
seats be allocated to 'public health’ and 'family medicine’ disciplines. Since, the 'public
health' discipline has an interface with many other developmental sectors, specialization
in Public health may be encouraged not only for medical doctors but also for
non-medical graduates from the allied fields of public health engineering, microbiology
and other natural sciences
4.9 URBAN HEALTH
4.9.1 NHP-2001, envisages the setting up of an organised urban primary health care
structure. Since the physical features of an urban setting are different from those in the
rural areas, the policy envisages the adoption of appropriate population norms for the
urban public health infrastructure. The structure conceived under NHP-2001 is a
two-tiered one: the primary centre is seen as the first-tier, covering a population of one
lakh, with a dispensary providing OPD facility and essential drugs to enable access to all
the national health programmes; and a second-tier of the urban health organisation at the
level of the Government general Hospital, where reference is made from the primary
centre. The Policy envisages that the funding for the urban primary health system will be
jointly home by the local self-Govemment institutions and State and Central
Governments.
17 of22
9/6/01 4:29 PM
file: D EMAIL RECEIVED natipnalheal'thpolic.htm
4.9.2 The National Health Policy also envisages the establishment of fully-equipped
‘hi'b-spoke’ trauma care networks in large urban agglomerations to reduce accident
mortality.
4.10 MI N I AL HEALTH
4.10.1 NHP - 2001 envisages a network of decentralised mental health services for
ameliorating the more common categories of disorders. The programme outline for such
a disease would envisage diagnosis of common disorders by general duty medical staff
and prescription of common therapeutic drugs.
4.10.2 In regard to mental health institutions for in-door treatment of patients, the policy
envisages the upgrading of the physical infrastructure of such institutions at Central
Government expense so as to secure the human rights of this vulnerable segment of
society.
4.11 INFORMATION, EDUCATION AND COMMUNICATION
4.11.1 NHP-2001 envisages an IEC policy, which maximizes the dissemination of
information to those population groups, which cannot be effectively approached through
the mass media only. The focus would therefore, be on inter-personal communication of
information and reliance on folk and other traditional media. The IEC programme would
set specific targets for the association of PRIs/NGOs/Trusts in such activities. The
programme will also have the component of an annual evaluation of the performance of
the non-Govemmental agencies to monitor the impact of the programmes on the targeted
groups. The Central/State Government initiative will also focus on the development of
modules for information dissemination in such population groups who normally, do not
benefit from the more common media forms.
4.11.2. NHP-2001 envisages priority to school health programmes aiming at preventive
health education, regular health check-ups and promotion of health seeking behaviour
among children. The school health programmes can gainfully adopt specially designed
modules in order to disseminate information relating to ‘health’ and ‘family life’. This is
expected to be the most cost-effective intervention as it improves the level of awareness,
not only of the extended family, but the future generation as well.
4.12 MEDICAL RESEARCH
4.12.1 NHP-2001 envisages the increase in Government-funded medical research to a
level of 1 percent of total health spending by 2005; and thereafter, up to 2 percent by
2010. Domestic medical research would be focused on new therapeutic drugs and
vaccines for tropical diseases, such as TB and Malaria, as also the Sub-types of
HIV/AIDS prevalent in the country. Research programmes taken up by the Government
in these priority areas would be conducted in a mission mode. Emphasis would also be
paid to time-bound applied research for developing operational applications. This would
ensure cost effective dissemination of existing / future therapeutic drugs/vaccines in the
general population. Private entrepreneurship will be encouraged in the field of medical
research for new molecules / vaccines.
4.13 ROLE OF THE PRIVATE SECTOR
IS of 22
9/6/01 4:29 PM
file: D EMAIL RECEIVED nationalhealthpohc.htn:
1
4.13.1 NHP-2001 envisages the enactment of suitable legislations for regulating
ninimum infrastructure ar 1 quality standards by 200 . in clinical
establishments/medical institutions; also, statutory gui lines for the conduct oi clinical
practice and delivery of medical services are to be developed over the same period. 1 he
policy also encourages the setting up of private insurance instruments for increasing the
scope of the coverage of the secondary and tertiary sector under private health insurance
packages.
4.13.2 To capitalize on the comparative cost advantage enjoyed by domestic health
facilities in the secondary and tertiary sector, the policy will encourage the supply of
services to patients of foreign origin on payment. The rendering of such services on
payment in foreign exchange will be treated as ‘deemed exports’ and will be made
eligible for all fiscal incentives extended to export earnings.
4.13.3 NHP-2001 envisages the co-option of the non-governmental practitioners in the
national disease control programmes so as to ensure that standard treatment protocols are
followed in their day-to-day practice.
4.13.4 NHP-2001 recognizes the immense potential of use of information technology
applications in the area of tele-medicine in the tertiary health care sector. The use of this
technical aid will greatly enhance the capacity for the professionals to pool their clinical
experience.
4.14 ROLE OF THE CIVIL SOCIETY
4.14.1 NHP-2001 recognizes the significant contribution made by NGOs and other
institutions of the civil society in making available health services to the community. In
order to utilize on an increasing scale, their high motivational skills, NHP-2001
envisages that the disease control programmes should earmark a definite portion of the
budget in respect of identified programme components, to be exclusively implemented
through these institutions.
4.15 NATIONAL DISEASE SURVEILLANCE NETWORK
4.15.1 NHP-2001 envisages the full operationalization of an integrated disease control
network from the lowest rung of public health administration to the Central Government,
by 2005. The programme for setting up this network will include components relating to
installation of data-base handling hardware; IT inter-connectivity between different tiers
of the network; and, in-house training for data collection and interpretation for
undertaking timely and effective response.
4.16 HEALTH STATISTICS
4.16.1 NHP-2001 envisages the completion of baseline estimates for the incidence of the
common diseases - TB, Malaria, Blindness - by 2005. The Policy proposes that
statistical methods be put in place to enable the periodic updating of these baseline
estimates through representative sampling, under an appropriate statistical methodology.
The policy also recognizes the need to establish in a longer time frame, baseline
estimates for : the non-communicable diseases, like CVD, Cancer, Diabetes; accidental
19 of 22
9/6/01 4:29 PM
file: D EMAIL RECEIVED nationalhealihpolic.hu'-
1
injuries; and other communicable diseases, like Hepatitis and JE. NHP-2001 envisages
that, with access to such reliable data on he ir 'idence of various di
es, ’ ' public
health system would move closer to the objective Lf evidence-oased policy making.
4.16.2 In an attempt at consolidating the data base and graduating from a mere
estimation of annual health expenditure, NHP-2001 emphasis on the needs to establish
national health accounts, conforming to the ’source-to-users’ matrix structure. Improved
and comprehensive information through national health accounts and accounting
systems would pave the way for decision makers to focus on relative priorities, keeping
in view the limited financial resources in the health sector.
4.17 WOMENS HEALTH
4.17.1 NHP-2001 envisages the identification of specific programmes targeted at
women’s health. The policy notes that women, along with other under privileged groups
are significantly handicapped due to a disproportionately low access to health care. The
various Policy recommendations of NHP-2001, in regard to the expansion of primary
health sector infrastructure, will facilitate the increased access of women to basic health
care. NHP-2001 commits the highest priority of the Central Government to the funding
of the identified programmes relating to woman’s health. Also, the policy recognizes the
need to review the staffing norms of the public health administration to more
comprehensively meet the specific requirements of women.
4.18 MEDICAL ETHICS
4.18.1 NHP - 2001 envisages that, in order to ensurethat the common patient is not
subjected to irrational or profit-driven medical regimens, a contemporary code of ethics
be notified and rigorously implemented by the Medical Council of India.
4.18.2 NHP - 2001 does not offer any policy prescription at this stage relating to ethics
in the conduct of medical research. By and large medical research within the country is
limited in these frontier disciplines of gene manipulation and stem cell research.
However, the policy recognises that a vigilant watch will have to be kept so that
appropriate guidelines and statutory provisions are put in place when medical research in
the country reaches the stage to make such issues relevant.
4.19 ENFORCEMENT OF QUALITY STANDARDS FOR FOOD AND DRUGS
4.19.1 NHP - 2001 envisages that the food and drug administration will be progressively
strengthened, both in terms of laboratory facilities and technical expertise. Also, the
policy envisages that the standards of food items will be progressively tightened at a
pace which will permit domestic food handling / manufacturing facilities to undertake
the necessary upgradation of technology so as not to be shut out of this production
sector. The policy envisages that, ultimately food standards will be close, if not
equivalent, to codex specifications; and drug standards will be at par with the most
rigorous ones adopted elsewhere.
4.20 REGULATION OF STANDARDS IN PARAMEDICAL DISCIPLINES
4.20.1 NHP-2001 recognises the need for the establishment of statutory professional
20 of 22
9/6/01 4:29 PM
1
file: D EMAIL RECEIVED naiionalhealthpolic.htm
councils for paramedical disciplines to register practitioners, maintain standards of
training, as well as to monitor their performance.
4.21 OCC1 PATIONAL HEALTH
4.21.1 NHP-2001 envisages the periodic screening of the health conditions of the
workers, particularly for high risk health disorders associated with their occupation.
4.22 PROVIDING MEDICAL FACILITIES TO USERS FROM Q\ ERSEAS
4.22.1 NHP-2001 strongly encourages the providing of health services on a commercial
basis to service seekers from overseas. The providers of such services to patients from
overseas will be encouraged by extending to their earnings in foreign exchange, all fiscal
incentives available to other exporters of goods and services.
4.23 IMPACT OF GLOBALISATION ON THE HEALTH SECTOR
4.23.1 NHP-2001 takes into account the serious apprehension expressed by several
health experts, of the possible threat to the health security, in the post TRIPS era, as a
result of a sharp increase in the prices of drugs and vaccines. To protect the citizens of
the country from such a threat, NHP-2001 envisages a national patent regime for the
future which, while being consistent with TRIPS, avails of all opportunities to secure for
the country, under its patent laws, affordable access to the latest medical and other
therapeutic discoveries. The Policy also sets out that the Government will bring to bear
its full influence in all international fora - UN, WHO, WTO. etc. - to secure
commitments on the part of the Nations of the Globe, to lighten the restrictive features of
TRIPS in its application to the health care sector.
5, SUMMATION
5.1 The crafting of a National Health Policy is a rare occasion in public affairs when it
would be legitimate, indeed valuable, to allow our dreams to mingle with our
understanding of ground realities. Based purely on the clinical facts defining the current
status of the health sector, we would have arrived at a certain policy formulation; but,
buoyed by our dreams, we have ventured slightly beyond that in the shape of NHP-2001
which, in fact, defines a vision for the future.
5.2 The health needs of the country are enormous and the financial resources and
managerial capacity available to meet it, even on the most optimistic projections, fall
somewhat short. In this situation, NHP-2001 has had to make hard choices between
various priorities and operational options. NHP-2001 does not claim to be a road-map
for meeting all the health needs of the populace of the country. Further, it has to be
recognized that such health needs are also dynamic as threats in the area of public health
keep changing over time. The Policy, while being holistic, undertakes the necessary risk
of recommending differing emphasis on different policy components. Broadly speaking,
NHP - 2001 focuses on the need for enhanced funding and an organizational
restructuring of the national public health initiatives in order to facilitate more equitable
access to the health facilities. Also, the policy is focused on those diseases which are
principally contributing to the disease burden - TB, Malaria and Blindness from the
category of historical diseases; and HIV/AIDS from the category of‘newly emerging
21 of 22
9/6/01 4:29 PM
1
file: D EMAIL RECEIVED natibnalhealthpolic.hi::’.
diseases’. This is not to say that other items contributing to the disease burden of the
country will be ignored; but only that, resources as also the principal focus of the public
health administration, will recognize certain relatiye priorities.
5.3 One nagging imperative, which has influenced every aspect of NHP-2001. is the
need to ensure that ‘equity’ in the health sector stands as an independent goal. In any
future evaluation of its success or failure, NHP-2001 would like to be measured against
this equity norm, rather than any other aggregated financial norm for the health sector.
Consistent with the primacy given to ‘equity’, a marked emphasis has been provided in
the policy for expanding and improving the primary health facilities, including the new
concept of provisioning of essential drugs through Central funding. The Policy also
commits the Central Government to increased under-writing of the resources for meeting
the minimum health needs of the citizenry. Thus, the Policy attempts to provide
guidance for prioritizing expenditure, thereby, facilitating rational resource allocation.
5.4 NHP-2001 highlights the expected roles of different participating group in the health
sector. Further, it recognizes the fact that, despite all that may be guaranteed by the
Central Government for assisting public health programmes, public health services
would actually need to be delivered by the State administration, NGOs and other
institutions of civil society. The attainment of improved health indices would be
significantly dependent on population stabilisation, as also on complementary efforts
from other areas of the social sectors - like improved drinking water supply, basic
sanitation, minimum nutrition, etc. - to ensure that the exposure of the populace to health
risks is minimized.
Suggestions on the draft policy are welcome. Kindly mail your suggestions to acabopw nb.nic.in within
30 days.
22 of 22
9/6/01 4:29 PM
JI
NATIONAL POLICY FOR THE EMPOWERMENT OF WOMEN
(2001)
Introduction
The principle of gender equality is enshrined in the Indian Constitution in its Preamble,
Fundamental Rights, Fundamental Duties and Directive Principles. The Constitution not only
grants equality to women, but also empowers the State to adopt measures of positive
discrimination in favour of women.
Within the framework of a democratic polity, our laws, development policies, Plans and
programmes have aimed at women’s advancement in different spheres. From the Fifth Five
Year Plan (1974-78) onwards has been a marked shift in the approach to women’s issues from
welfare to development. In recent years, the empowerment of women has been recognized as
the central issue in determining the status of women. The National Commission for Women
was set up by an Act of Parliament in 1990 to safeguard the rights and legal entitlements of
women. The 73rd and 74lh Amendments (1993) to the Constitution of India have provided for
reservation of seats in the local bodies of Panchayats and Municipalities for women, laying a
strong foundation for their participation in decision making at the local levels.
1.3 India has also ratified various international conventions and human rights instruments
committing to secure equal rights of women. Key among them is the ratification of the
Convention on Elimination of All Forms of Discrimination Against Women (CEDAW) in
1993.
1.4 The Mexico Plan of Action (1975), the Nairobi Forward Looking Strategies (1985), the
Beijing Declaration as well as the Platform for Action (1995) and the Outcome Document
adopted by the UNGA Session on Gender Equality and Development & Peace for the 21st
century, titled "Further actions and initiatives to implement the Beijing Declaration and the
Platform for Action” have been unreservedly endorsed by India for appropriate follow up.
1.5 The Policy also takes note of the commitments of the Ninth Five Year Plan and the other
Sectoral Policies relating to empowerment of Women.
1.6 The women’s movement and a wide-spread network of non-Govemment Organisations
which have strong grass-roots presence and deep insight into women’s concerns have
contributed in inspiring initiatives for the empowerment of women.
1.7 However, there still exists a wide gap between the goals enunciated in the Constitution,
legislation, policies, plans, programmes, and related mechanisms on the one hand and the
situational reality of the status of women in India, on the other. 1 his has been analyzed
extensively in the Report of the Committee on the Status of Women in India, "Towards
Equality", 1974 and highlighted in the National Perspective Plan for Women, 1988-2000, the
Shramshakti Report, 1988 and the Platform for Action, Five Years After- An assessment"
t
1.8 Gender disparity manifests itself in various forms, the most obvious being the trend of
continuously declining female ratio in the population in the last few decades. Social
stereotyping and violence at the domestic and societal levels are some of the other
manifestations. Discrimination against girl children, adolescent girls and women persists in
parts of the country.
1.9 The underlying causes of gender inequality are related to social and economic structure,
which is based on informal and formal norms, and practices.
1.10 Consequently, the access of women particularly those belonging to weaker sections
including Scheduled Castes/Scheduled Tribes/ Other backward Classes and minorities,
majority of whom are in the rural areas and in the informal, unorganized sector - to education,
health and productive resources, among others, is inadequate. Therefore, they remain largely,
marginalized, poor and socially excluded.
Goal and Objectives
1.11 The goal of this Policy is to bring about the advancement, development and
empowerment of women. The Policy will be widely disseminated so as to encourage active
participation of all stakeholders for achieving its goals. Specifically, the objectives of this
Policy include
(i) Creating an environment through positive economic and social policies for full
development of women to enable them to realize their full potential
(ii) The de-jure and de-facto enjoyment of all human rights and fundamental freedom by
women on equal basis with men in all spheres - political, economic, social, cultural and civil
(iii) Equal access to participation and decision making of women in social, political and
economic life of the nation
(iv) Equal access to women to health care, quality education at all levels, career and
vocational guidance, employment, equal remuneration, occupational health and safety, social
security and public office etc.
(v) Strengthening legal systems aimed at elimination of all forms of discrimination against
women
(vi) Changing societal attitudes and community practices by active participation and
involvement of both men and women.
(vii) Mainstreaming a gender perspective in the development process.
(viii) Elimination of discrimination and all forms of violence against women and the girl
child; and
(ix) Building and strengthening partnerships with civil society, particularly women’s
organizations.
Policy Prescriptions
Judicial Legal Systems
Legal-judicial system will be made more responsive and gender sensitive to women’s needs,
especially in cases of domestic violence and personal assault. New laws will be enacted and
existing laws reviewed to ensure that justice is quick and the punishment meted out to the
culprits is commensurate with the severity of the offence.
2.2 At the initiative of and with the full participation of all stakeholders including community
and religious leaders, the Policy would aim to encourage changes in personal laws such as
those related to marriage, divorce, maintenance and guardianship so as to eliminate
discrimination against women.
2.3 The evolution of property rights in a patriarchal system has contributed to the subordinate
status of women. The Policy would aim to encourage changes in laws relating to ownership of
property and inheritance by evolving consensus in order to make them gender just.
Decision Making
3.1 Women’s equality in power sharing and active participation in decision making, including
decision making in political process at all levels will be ensured for the achievement of the
goals of empowerment. All measures will be taken to guarantee women equal access to and
full participation in decision making bodies at every level, including the legislative, executive,
judicial, corporate, statutory bodies, as also the advisory Commissions, Committees, Boards,
Trusts etc. Affirmative action such as reservations/quotas, including in higher legislative
bodies, will be considered whenever necessary on a time bound basis. Women-ffiendly
personnel policies will also be drawn up to encourage women to participate effectively in the
developmental process.
Mainstreaming a Gender Perspective in the Development Process
4.1 Policies, programmes and systems will be established to ensure mainstreaming of
women’s perspectives in all developmental processes, as catalysts, participants and recipients.
Wherever there are gaps in policies and programmes, women specific interventions would be
undertaken to bridge these. Coordinating and monitoring mechanisms will also be devised to
assess from time to time the progress of such mainstreaming mechanisms. Women’s issues
and concerns as a result will specially be addressed and reflected in all concerned laws,
sectoral policies, plans and programmes of action.
Economic Empowerment of women
Poverty Eradication
5.1 Since women comprise the majority of the population below the poverty line and are very
often in situations of extreme poverty, given the harsh realities of intra-household and social
discrimination, macro economic policies and poverty eradication programmes will
specifically address the needs and problems of such women. There will be improved
implementation of programmes which are already women oriented with special targets for
women. Steps will be taken for mobilization of poor women and convergence of services, by
offering them a range of economic and social options, along with necessary support measures
to enhance their capabilities
Micro Credit
5.2 In order to enhance women’s access to credit for consumption and production, the
establishment of new, and strengthening of existing micro-credit mechanisms and micro
finance institution will be undertaken so that the outreach of credit is enhanced. Other
supportive measures would be taken to ensure adequate flow of credit through extant financial
institutions and banks, so that all women below poverty line have easy access to credit.
Women and Economy
5.3 Women’s perspectives will be included in designing and implementing macro-economic
and social policies by institutionalizing their participation in such processes. Their
contribution to socio-economic development as producers and workers will be recognized in
the formal and informal sectors (including home based workers) and appropriate policies
relating to employment and to her working conditions will be drawn up. Such measures could
include:
Reinterpretation and redefinition of conventional concepts of work wherever necessary e.g. in
the Census records, to reflect women’s contribution as producers and workers.
Preparation of satellite and national accounts.
Development of appropriate methodologies for undertaking (i) and (ii) above.
Globalization
Globalization has presented new challenges for the realization of the goal of women’s
equality, the gender impact of which has not been systematically evaluated fully. However,
from the micro-level studies that were commissioned by the Department of Women & Child
Development, it is evident that there is a need for re-framing policies for access to
employment and quality of employment. Benefits of the growing global economy have been
unevenly distributed leading to wider economic disparities, the feminization of poverty,
increased gender inequality through often deteriorating working conditions and unsafe
working environment especially in the informal economy and rural areas. Strategies will be
designed to enhance the capacity of women and empower them to meet the negative social
and economic impacts, which may flow from the globalization process.
Women and Agriculture
5.5 In view of the critical role of women in the agriculture and allied sectors, as producers,
concentrated efforts will be made to ensure that benefits of training, extension and various
programmes will reach them in proportion to their numbers. The programmes for training
women in soil conservation, social forestry, dairy development and other occupations allied to
agriculture like horticulture, livestock including small animal husbandry, poultry, fisheries
etc. will be expanded to benefit women workers in the agriculture sector.
Women and Industry
5.6 The important role played by women in electronics, information technology and food
processing and agro industry and textiles has been crucial to the development of these sectors.
They would be given comprehensive support in terms of labour legislation, social security
and other support services to participate in various industrial sectors.
5.7 Women at present cannot work in night shift in factories even if they wish to. Suitable
measures will be taken to enable women to work on the night shift in factories. This will be
acicompanied with support services for security, transportation etc.
Support Services
5.8 The provision of support services for women, like child care facilities, including creches ’
at work places and educational institutions, homes for the aged and the disabled will be
expanded and improved to create an enabling environment and to ensure their full cooperation
in social, political and economic life. Women-friendly personnel policies will also be drawn
up to encourage women to participate effectively in the developmental process.
Social Empowerment of Women
Education
6.1 Equal access to education for women and girls will be ensured. Special measures will be
taken to eliminate discrimination, universalize education, eradicate illiteracy, create a gender
sensitive educational system, increase enrolment and retention rates of girls and improve the
quality of education to facilitate life-long learning as well as development of
occupation/vocation/techmcal skills by women. Reducing the gender gap in secondary and
higher education would be a focus area. Sectoral time targets in existing policies will be
achieved, with a special focus on girls and women, particularly those belonging to weaker
sections including the Scheduled Castes/Scheduled Tribes/Other Backward
Classes/Minorities. Gender sensitive curricula would be developed at all levels of educational
system in order to address sex stereotyping as one of the causes of gender discrimination.
Health
6.2 A holistic approach to women’s health which includes both nutrition and health services
will be adopted and special attention will be given to the needs of women and the girl at all
stages of the life cycle. The reduction of infant mortality and maternal mortality, which are
sensitive indicators of human development, is a priority concern. This policy reiterates the
national demographic goals for Infant Mortality Rate (IMR), Maternal Mortality Rate (MMR)
set out in the National Population Policy 2000. Women should have access to comprehensive,
affordable and quality health care. Measures will be adopted that take into account the
reproductive rights of women to enable them to exercise informed choices, their vulnerability
to sexual and health problems together with endemic, infectious and communicable diseases
such as malaria, TB, and water borne diseases as well as hypertension and cardio-pulmonary
diseases. The social, developmental and health consequences of HIV/AIDS and other sexually
transmitted diseases will be tackled from a gender perspective.
6.3 To effectively meet problems of infant and maternal mortality, and early marriage the
availability of good and accurate data at micro level on deaths, birth and marriages is
required. Strict implementation of registration of births and deaths would be ensured and
registration of marriages would be made compulsory.
6.4 In accordance with the commitment of the National Population Policy (2000) to
population stabilization, this Policy recognizes the critical need of men and women to have
access to safe, effective and affordable methods of family planning of their choice and the
need to suitably address the issues of early marriages and spacing of children. Interventions
such as spread of education, compulsory registration of marriage and special programmes like
BSY should impact on delaying the age of marriage so that by 2010 child marriages are
eliminated.
6.5 Women’s traditional knowledge about health care and nutrition will be recognized
through proper documentation and its use will be encouraged. The use of Indian and
alternative systems of medicine will be enhanced within the framework of overall health
infrastructure available for women.
Nutrition
6.6 In view of the high risk of malnutrition and disease that women face at all the three
critical stages viz., infancy and childhood, adolescent and reproductive phase, focussed
attention would be paid to meeting the nutritional needs of women at all stages of the life
cycle. This is also important in view of the critical link between the health of adolescent girls,
pregnant and lactating women with the health of infant and young children. Special efforts
will be made to tackle the problem of macro and micro nutrient deficiencies especially
amongst pregnant and lactating women as it leads to various diseases and disabilities.
6.7 Intra-household discrimination in nutritional matters vis-a-vis girls and women will be
sought to be ended through appropriate strategies. Widespread use of nutrition education
would be made to address the issues of intra-household imbalances in nutrition and the
special needs of pregnant and lactating women. Women’s participation will also be ensured in
the planning, superintendence and delivery of the system.
Drinking Water and Sanitation
6.8 Special attention will be given to the needs of women in the provision of safe drinking
water, sewage disposal, toilet facilities and sanitation within accessible reach of households,
especially in rural areas and urban slums. Women’s participation will be ensured in the
planning, delivery and maintenance of such services.
Housing and Shelter
6.9 Women’s perspectives will be included in housing policies, planning of housing colonies
and provision of shelter both in rural and urban areas. Special attention will be given for
providing adequate and safe housing and accommodation for women including single women,
heads of households, working women, students, apprentices and trainees.
Environment
6.10 Women will be involved and their perspectives reflected in the policies and programmes
for environment, conservation and restoration. Considering the impact of environmental
factors on their livelihoods, women’s participation will be ensured in the conservation of the
environment and control of environmental degradation. The vast majority of rural women still
depend on the locally available non-commercial sources of energy such as animal dung, crop
waste and fuel wood. In order to ensure the efficient use of these energy resources in an
environmental friendly manner, the Policy will aim at promoting the programmes of nonconventional energy resources. Women will be involved in spreading the use of solar energy,
biogas, smokeless chulahs and other rural application so as to have a visible impact of these
measures in influencing eco system and in changing the life styles of rural women.
Science and Technology
6.11 Programmes will be strengthened to bring about a greater involvement of women in
science and technology. These will include measures to motivate girls to take up science and
technology for higher education and also ensure that development projects with scientific and
technical inputs involve women fully. Efforts to develop a scientific temper and awareness
will also be stepped up. Special measures would be taken for their training in areas where
they have special skills like communication and information technology. Efforts to develop
appropriate technologies suited to women’s needs as well as to reduce their drudgery will be
given a special focus too.
Women in Difficult Circumstances
6.12 In recognition of the diversity of women’s situations and in acknowledgement of the
needs of specially disadvantaged groups, measures and programmes will be undertaken to
provide them with special assistance. These groups include women in extreme poverty,
destitute women, women in conflict situations, women affected by natural calamities, women
in less developed regions, the disabled widows, elderly women, single women in difficult
circumstances, women heading households, those displaced from employment, migrants,
women who are victims of marital violence, deserted women and prostitutes etc.
Violence against women
7.1 All forms of violence against women, physical and mental, whether at domestic or
societal levels, including those arising from customs, traditions or accepted practices shall be
dealt with effectively with a view to eliminate its incidence. Institutions and
mechanisms/schemes for assistance will be created and strengthened for prevention of such
violence , including sexual harassment at work place and customs like dowry; for the
rehabilitation of the victims of violence and for taking effective action against the perpetrators
of such violence. A special emphasis will also be laid on programmes and measures to deal
with trafficking in women and girls.
Rights of the Girl Child
8.1 All forms of discrimination against the girl child and violation of her rights shall be
eliminated by undertaking strong measures both preventive and punitive within and outside
the family. These would relate specifically to strict enforcement of laws against prenatal sex
selection and the practices of female foeticide, female infanticide, child marriage, child abuse
and child prostitution etc. Removal of discrimination in the treatment of the girl child within
the family and outside and projection of a positive image of the girl child will be actively
fostered. There will be special emphasis on the needs of the girl child and earmarking of
substantial investments in the areas relating to food and nutrition, health and education, and in
vocational education. In implementing programmes for eliminating child labour, there will be
a special focus on girl children.
Mass Media
9.1 Media will be used to portray images consistent with human dignity of girls and women.
The Policy will specifically strive to remove demeaning, degrading and negative conventional
stereotypical images of women and violence against women. Private sector partners and
media networks will be involved at all levels to ensure equal access for women particularly in
the area of information and communication technologies. The media would be encouraged to
develop codes of conduct, professional guidelines and other self regulatory mechanisms to
remove gender stereotypes and promote balanced portrayals of women and men.
Operational Strategies
Action Plans
10.1 All Central and State Ministries will draw up time bound Action Plans for translating the
Policy into a set of concrete actions, through a participatory process of consultation with
Centre/State Departments of Women and Child Development and National /State
Commissions for Women. The Plans will specifically including the following: -
i) Measurable goals to be achieved by 2010.
ii) Identification and commitment of resources.
iii) Responsibilities for implementation of action points.
iv) Structures and mechanisms to ensure efficient monitoring, review and gender impact
assessment of action points and policies.
v) Introduction of a gender perspective in the budgeting process.
10.2 In order to support better planning and programme formulation and adequate allocation
of resources, Gender Development Indices (GDI) will be developed by networking with
specialized agencies. These could be analyzed and studied in depth. Gender auditing and
development of evaluation mechanisms will also be undertaken along side.
10.3 Collection of gender disaggregated data by all primary data collecting agencies of the
Central and State Governments as well as Research and Academic Institutions in the Public
and Private Sectors will be undertaken. Data and information gaps in vital areas reflecting the
status of women will be sought to be filled in by these immediately. All
Ministries/Corporations/Banks and financial institutions etc will be advised to collect, collate,
disseminate and maintain/publish data related to programmes and benefits on a gender
disaggregated basis. This will help in meaningful planning and evaluation of policies.
Institutional Mechanisms
11.1 Institutional mechanisms, to promote the advancement of women, which exist at the
Central and State levels, will be strengthened. These will be through interventions as may be
appropriate and will relate to, among others, provision of adequate resources, training and
advocacy skills to effectively influence macro-policies, legislation, programmes etc. to
achieve the empowerment of women.
11.2 National and State Councils will be formed to oversee the operationalisation of the
Policy on a regular basis. The National Council will be headed by the Prime Minister and the
State Councils by the Chief Ministers and be broad in composition having representatives
from the concerned Departments/Ministries, National and State Commissions for Women,
Social Welfare Boards, representatives of Non-Govemment Organizations, Women’s
Organisations, Corporate Sector, Trade Unions, financing institutions, academics, experts and
social activists etc. These bodies will review the progress made in implementing the Policy
twice a year. The National Development Council will also be informed of the progress of the
programme undertaken under the policy from time to time for advice and comments.
11.3 National and State Resource Centres on women will be established with mandates for
collection and dissemination of information, undertaking research work, conducting surveys,
implementing training and awareness generation programmes, etc. These Centers will link up
with Women’s Studies Centres and other research and academic institutions through suitable
information networking systems.
11.4 While institutions at the district level will be strengthened, at the grass-roots, women will
be helped by Government through its programmes to organize and strengthen into Self-Help
Groups (SHGs) at the Anganwadi/Village/Town level. The women’s groups will be helped to
institutionalize themselves into registered societies and to federate at the Panchyat/Municipal
level. These societies will bring about synergistic implementation of all the social and
economic development programmes by drawing resources made available through
Government and Non-Govemment channels, including banks and financial institutions and by
establishing a close Interface with the Panchayats/ Municipalities.
Resource Management
12.1 Availability of adequate financial, human and market resources to implement the Policy
will be managed by concerned Departments, financial credit institutions and banks, private
sector, civil society and other connected institutions. This process will include:
(a) Assessment of benefits flowing to women and resource allocation to the programmes
relating to them through an exercise of gender budgeting. Appropriate changes in policies will
be made to optimize benefits to women under these schemes;
(b) Adequate resource allocation to develop and promote the policy outlined earlier based on
(a) above by concerned Departments.
(c) Developing synergy between personnel of Health, Rural Development, Education and
Women & Child Development Department at field level and other village level functionaries’
(d) Meeting credit needs by banks and financial credit institutions through suitable policy
initiatives and development of new institutions in coordination with the Department of
Women & Child Development.
-b
12.2 The strategy of Women’s Component Plan adopted in the Ninth Flan of ensuring that not
less than 30% of benefits/funds flow to women from all Ministries and Departments will be
implemented effectively so that the needs and interests of women and girls are addressed by
all concerned sectors. The Department of Women and Child Development being the nodal
Ministry will monitor and review the progress of the implementation of the Component Plan
from time to time, in terms of both quality and quantity in collaboration with the Planning
Commission.
12.3 Efforts will be made to channelize private sector investments too, to support programmes
and projects for advancement of women
Legislation
13.1 The existing legislative structure will be reviewed and additional legislative measures
taken by identified departments to implement the Policy. This will also involve a review of all
existing laws including personal, customary and tribal laws, subordinate legislation, related
rules as well as executive and administrative regulations to eliminate all gender
discriminatory references. The process will be planned over a time period 2000-2003. The
specific measures required would be evolved through a consultation process involving civil
society, National Commission for Women and Department of Women and Child
Development. In appropriate cases the consultation process would be widened to include
other stakeholders too.
13.2 Effective implementation of legislation would be promoted by involving civil society
and community. Appropriate changes in legislation will be undertaken, if necessary.
13.3 In addition, following other specific measures will be taken to implement the legislation
effectively.
(a) Strict enforcement of all relevant legal provisions and speedy redressal of grievances will
be ensured, with a special focus on violence and gender related atrocities.
(b) Measures to prevent and punish sexual harassment at the place of work, protection for
women workers in the organized/ unorganized sector and strict enforcement of relevant laws
such as Equal Remuneration Act and Minimum Wages Act will be undertaken,
(c) Crimes against women, their incidence, prevention, investigation, detection and
prosecution will be regularly reviewed at all Crime Review fora and Conferences at the
Central, State and District levels. Recognised, local, voluntary organizations will be
authorized to lodge Complaints and facilitate registration, investigations and legal
proceedings related to violence and atrocities against girls and women.
(d) Women s Cells in Police Stations, Encourage Women Police Stations Family Courts,
Mahila Courts, Counselling Centers, Legal Aid Centers and Nyaya Panchayats will be
strengthened and expanded to eliminate violence and atrocities against women.
(e) Widespread dissemination of information on all aspects of legal rights, human rights and
(7)
other entitlements of women, through specially designed legal literacy programmes and rights
information programmes will be done.
Gender Sensitization
14.1 Training of personnel of executive, legislative and judicial wings of the State, with a
special focus on policy and programme framers, implementation and development agencies,
law enforcement machinery and the judiciary, as well as non-governmental organizations will
be undertaken. Other measures will include:
(a) Promoting societal awareness to gender issues and women’s human rights.
(b) Review of curriculum and educational materials to include gender education and human
rights issues
(c) Removal of all references derogatory to the dignity of women from all public documents
and legal instruments.
(d) Use of different forms of mass media to communicate social messages relating to
women’s equality and empowerment.
Panchayati Raj Institutions
15.1 The 73 and 7411 Amendments (1993) to the Indian Constitution have served as a
breakthrough towards ensuring equal access and increased participation in political power
structure for women. The PRIs will play a central role in the process of enhancing women’s
participation in public life. The PRIs and the local self Governments will be actively involved
in the implementation and execution of the National Policy for Women at the grassroots level.
Partnership with the voluntary sector organizations
16.1 The involvement of voluntary organizations, associations, federations, trade unions, non
governmental organizations, women’s organizations, as well as institutions dealing with
education, training and research will be ensured in the formulation, implementation,
monitoring and review of all policies and programmes affecting women. Towards this end,
they will be provided with appropriate support related to resources and capacity building and
facilitated to participate actively in .the process of the empowerment of women.
International Cooperation
17.1 The Policy will aim at implementation of international obligations/commitments in all
sectors on empowerment of women such as the Convention on All Forms of Discrimination
Against Women (CEDAW), Convention on the Rights of the Child (CRC), International
Conference on Population and Development (ICPD+5) and other such instruments.
International, regional and sub-regional cooperation towards the empowerment of women will
continue to be encouraged through sharing of experiences, exchange of ideas and technology,
networking with institutions and organizations and through bilateral and multi-lateral
partnerships.
A--,
H p'
August 2301
Draft. Not for citation
Changing the Indian Health System
Current Issues, Future Directions
Rajiv Misra
Rachel Chatterjee
Sujatha Rao
INDIAN COUNCIL FOR RESEARCH ON LNTERNATIONAL ECONOMIC RELATIONS
Core-6A, 4lh Floor, India Habitat Centre, Lodi Road. New Delhi-110 003
rContents
Preface
iii
List of Abbreviations
v
List of Tables, Figures and Annexes
viii
Executive Summary
xv
Chapters
1.
Introduction
1
2.
The Current Health Scenario : An Overview
9
3.
The State Role in Health
42
4.
Economic Growth, Poverty and Health
51
5.
Towards Equity in Health
58
6.
Communicable Diseases
78
7.
Maternal and Child Survival
106
8.
HIV/AIDS
133
9.
Non-Communicable Diseases
144
10.
Private Healthcare in India
161
11.
Health Systems
190
12.
Health Finance
232
13.
External Assistance to the Health Sector
264
14.
Drug Policy and Regulations
283
15.
Indian Systems of Medicine..
296
16.
Health Research : Its Potential in India
312
References
329
ii
Preface
When I accepted this assignment, little did I realize that the exercise
would be so arduous, yet at the same time so rewarding. Never in my long
career has my intellectual stamina been so severely tested. But the
experience was also deeply satisfying, since the study was so timed that
it could make a contribution, however small, to the ongoing exercise of
formulating a new health policy. If this Report helps improve
understanding of health issues, generates awareness and stimulates an
informed debate, our labours will be amply rewarded.
Having worked mainly on global issues since leaving the Health Ministry
in 1994, I was glad to return once again to the national health scene. This
project provided an excellent opportunity to pick up the threads again and
to look at the issues more objectively and in greater depth. Despite some
welcome developments, what I found was deeply disappointing. The
problems that I had left behind seven years back had not only remained
largely unchanged, but had been greatly aggravated, with the health
system becoming even more dysfunctional and iniquitous. The fiscal
situation in the states had deteriorated to such an extent that they
seemed helpless, unable to correct the most glaring inadequacies, even
when there was a sincere desire to do so. On the positive side, there were
some welcome initiatives in the states that could be regarded as the
beginnings of a reform process. There was also a huge improvement in
the availability of data as a result of NSSO 42nd and 52nd rounds, NFHS 1
and 2, and NCAER household surveys. Regrettably though, the NIPFP
initiative in the early nineties to develop national health accounts was not
followed up, so that health finance had become the weakest link in the
database. More important, the new data had been analyzed in depth by
competent researchers, thanks to the collaborative initiatives of donor
agencies and the central government, making available critical inputs to
policymakers. The stage was now set for evidence-based policy
initiatives.
The Report brings out quite unambiguously the gross inadequacy of public
investment in health. It is true that no system can be expected to perform
at the current low levels of funding. However, it is also equally true that
an increase in funding levels by itself is unlikely to produce the desired
results without accompanying systemic changes. As in the case of the
energy sector, increased investment must to go hand in hand with system
reform. This is why we decided that the most appropriate title for the
document would be Changing the Indian Health System: Current
Issues, Future Directions.
I was ably assisted in my endeavours, by the two co-authors, Rachel
Chatterjee (formerly Health Secretary, Andhra Pradesh), and Sujatha Rao
(Joint Secretary in the Ministry of Health and Family Welfare). The former
made a huge contribution because of her intimate knowledge of the health
iii
system at the state level. The latter provided the valuable and
complementary perspective of policymaking and programme management
at the central level. The three of us worked as a team and are jointly
responsible for every word in the document.
This study was conceived by Professor Jeffrey Sachs, Chair of the
Commission on Macroeconomics and Health, and he was instrumental in
arranging the funding support from the Bill and Melinda Gates Foundation
in record time. He has, all through, been the main inspiration for this
work, and has guided it from time to time despite his many commitments.
To Dr. Isher Ahluwalia, Director of ICRIER, goes the credit of giving
concrete shape to his proposal and sponsoring the study by ICRIER. But
for her sustained and ungrudging support, and that of all her colleagues at
ICRIER, this Report could never have been completed on schedule.
Studying any health system is a highly
highly complex
complex task, and
and this is
particularly true for a country as vast and diverse as India. Keeping this is
mind, we commissioned background papers by reputed scholars and
researchers. Despite the very tight schedule, all the contributors were
very understanding of our requirements and compulsions. To all the
contributors, we owe a debt of gratitude.
From the very beginning, we tried to make this a highly participatory
exercise. Consultations were organized with researchers, representatives
of the states, NGOs and public health experts - all of whom contributed
valuable inputs. A steering committee was constituted with representation
from relevant ministries/ departments of the central government, Planning
Commission and multilateral agencies involved with health such as the
WHO, the World Bank, UNDP, UNICEF and UNAIDS. The committee met
regularly and provided valuable guidance to our work. It was the active
support and cooperation of all agencies that enabled us to access
relevant information and data.
Finally, the support and dedication of our staff, Jai Mansukhani, Anidya
Ghosh and Prasanna Ash made it possible to complete the exercise in
such a short time. In particular, the contribution of Jai Mansukhani
deserves a special mention, as he worked tirelessly, with single-minded
devotion, to type out the Report and incorporate the seemingly endless
revisions of the drafts.
(Rajiv L. Misra)
Team Leader, India Health Study, ICRIER
New Delhi, August 16, 2001
iv
List of Abbreviations
1.
2.
AP
HP
3. •MP
4. NE
5. TN
6. UP
7. Lakh
8. Crore
9. Dai
10. Anganwadi
11. Panchayati Raj
Institutions
Andhra Pradesh
Himachal Pradesh
Madhya Pradesh
North Eastern
Tamil Nadu
Uttar Pradesh
Hundred thousand
Ten million
Traditional Birth Attendant
Village level worker in the nutritional and child welfare programmes
Elected local bodies, (Panchayat for group of villages, Panchayat Samiti
for around 1,00,000 population, and Zila Parishad for the district). These
Institutions discharge many responsibilities for local self government
and development in respect of rural areas
1.
2.
All India Institute of Medical Sciences
Aids Prevention and Control
Central Bureau of Health Information
Central Drug Standard Control Organization
Canadian International Development Agency
Commission for Macroeconomic Health
Council of Scientific and Industrial Research
Central Statistical Organization
Drug Controller General
Distnct Chief Health and Medical Officer
Department for International Development
Director General of Health and Medical Services
Director General of Health Service
Delhi Society for Promotion of Rational Use of Drugs
Government of India
Indian Council for Medical Research
Indian Institute of Chemical Technology
Indian Institute of Health Management and Research
Indian Institute of Popular Science
Japanese International Co-operative Agency
Ministry of Health and Family Welfare
Modified Leprosy Eradication Campaign
Medical Relief Societies
National AIDS Control Organization
National Council for Applied Economic Research
National Drug Authority
National Family Health Survey
National Institute od Communicable Diseases
National Institute of Immunology
National Institute of Public Finance and Development
National Malaria Eradication Programme
National Pharmaceutical Pricing Authority
National Sample Survey Organization
Policy and Strategic Planning Unit
Swedish International Development Association
Sample Registration System
Tamil Nadu State Aids Control Society
United States Food and Drug Administration
Voluntary Health Association of India
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
AllMS
APAC
CBHI
CDSCO
CIDA
CMH
CSIR
CSO
DCG
DCH&MO
DFID
DGH&MS
DGHS
DSPRUD
15. GOI
16. ICMR
17. IICT
18. IIHMR
19. UPS
20. JICA
21. MHFW/MOHFW
22. MLEC
23. MRS
24. NACO
25. NCAER
26. NDA
27. NFHS
28. NICD
29. Nil
30. NIPFD
31. NMEP
32. NPPA
33. NSSO/NSS
34. PSPU
35. SIDA
36. SRS
37. TNSACS
38. USFDA
39. VHAI
1.
2.
1.
2.
3.
4.
5.
WHR
WDR
World Health Report
World Development Report
ANC
ANM
APAC
ARI
BIA
Antenatal Care
Auxiliary Nurse Midwife
Aids Prevention and Control
Acute Respiratory Infection
Benefit Incidence Analysis
V
6.
7.
8.
9.
BMI
BOD
BPL
CAM
10. CBR
67.
68.
69.
70.
STD
TBA
TFR
UIP
Body Mass Index
Burden of Diseases
Below Poverty Line
Complementary Alternative Medicine
Child Birth Rate
Central Council of Indian Medicine
Crude Death Rate
Central Government Health Scheme
Community Health Centre
Coronary Heart Disease
Community Health Worker
Child Mortality Rate
Commercial Sex Worker
Cardiovascular Disease
Disability Adjusted Life Years
Directly Observed Treatment, Short-course
Emergency Obstetric Care
Essential Drug List
Enhanced Malaria Control Programme
Emergency Obstetric Care
Global Burden of Disease Study
Gender Development Index
Highly Active Anti-Retroviral Therapy
Human Development Index
Health Maintenance Organization
Human Poverty Index
International Aids Vaccine Initiative
Intravenous Drug User
Iron and Folic Acid
Infant Mortality Rate
Intra Ocular Lenses
Inpatient
Indian Systems of Medicine
Life Expectancy at Birth
Maternal and Child Health
Multi Drug Therapy
Maternal Mortality Rate
Multipurpose Health Worker
National Anti - Malaria Programme
Non Communicable Disease
New Chemical Entity
Novel Drug Delivery System
National Health Policy
National Mental Health Programme
National Mental Health Programme
National TB Programme
Official Development Assistance
Outpatient
Oral Rehydration Salt
Oral Rehydration Therapy
Public Distribution System
P falciparum
Primary Health Centre
Public Private Partnership
Quality Improvement
Quality of Care
Reproductive and Child Health Programme
Rural Medical Practitioners
Revised National TB Control Programme
Reproductive Tract Infection
Short Course Chemotherapy
Sexually Transmitted Diseases
Traditional Birth Attendant
Total Fertility Rate
Universal Immunisation Programme
1.
EME
Established Market Economies
11. CCIM
12. CDR
13. CGHS
14. CHC
15. CHD
16. CHW
17. CMR
18. CMS
19. CVD
20. DALYs
21. DOTS
22. ECO
23. EDL
24. EMCP
25. EOC
26. GBDS
27. GDI
28. HAART
29. HDI
30. HMO
31. HPI
32. IAVI
33. IDU
34. IFA
35. IMR
36. IOL
37. IP
38. ISM
39. LEB
40. MCH
41. MDT
42. MMR
43. MPW
44. NAMP
45. NCD
46. NCE
47. NDDS
48. NHP
49. NMHP
50. NMHP
51. NTP
52. ODA
53. OP
54. ORS
55. ORT
56. PDS
57. Pf
58. PHC
59. PPP
60. QI
61. QOC
62. RCH
63. RMP
64. RNTCP
65. RTI
66. SCC
vi
2.
3.
I.
5.
6.
7.
8.
9.
ESIS
IEC
1PR
MNC
PDS
SC/ST
TOR
TRIPS
Employees State Insurance Scheme
Information, Education, Communication
Intellectual Property Right
Multinational Company
Public Distribution System
Scheduled Caste / Scheduled Tribe
Terms of Reference
Trade Related Aspects of Intellectual Property Rights
vii
tiTables, Figures and Annexes
Page
No.
1
2
Table 1.1
3
Annex 1.1
Studies of the Indian Health System 1999-2000
Commission on Macroeconomics and Health
Reference
Annex 1.2
Proposal for an India Study for CMH
6
Table 2.1
11
Table 2.3
International Comparison of Health Humanpower and Hospital
Beds, 1990-1998
International Comparison of Health Service Utilization and
DALYs Lost per 1000 Population, 1990-1998
India's Share of the World’s Health Problems (in %)
12
Table 2.4
Burden of Disease - India and States
13
Table 2.5
Top 10 Specific Causes of Death in India, 1998
13
Table 2.6
HIV Prevalence in India 1998
17
Table 2.7
Select Goals Under National Health Policy and Achievement
22
Table 2.8
Availability of Health Humanpower in Rural Health Institutions
Health Care Humanpower and Health Facilities in Public and
Private Sector in India
Comparative State Equity Performance for Curative Care
(Income Level)
Health Status Indicators - Comparison between the Poorest
and
Richest Quintiles of the Population, India, 1992-93
Health Outcomes according to Standard of Living, India,
1998-99
23
Table 2.2
Table 2.9
Table 2.10
Table 2.11
Table 2.12
Terms
of
5
11
24
26
26
27
Table 2.13
Outlay for Health in the Central Sector (Actual Expenditure)
31
Figure 2.1
Under-5 Mortality and Crude Birth Rate: A Comparison
10
Figure 2.2
Burden of Disease by Cause - 1998
12
Figure 2.3
Mortality by Causes for India - 1998
(a) Burden of Communicable Diseases India, 1998
(b) Distribution of Burden of Non-Communicable Disease India,
1998
14
Figure 2.5
Projected Population of India
18
Figure 2.6
18
Figure 2.8
Burden of Diseases - 2020
Prevalence of Smoking, Tobacco, and Alcohol Use in India
by Income Quintile 1995-96
Sex Ratio : International Comparisons
20
Figure 2.9
Sex Ratio in India (1990-2001)
21
Figure 2.10
Infant Mortality Rates in India
Share of Public Subsidy for Curative Care Benefiting Income
Groups
22
Figure 2.4
Figure 2.7
Figure 2.11
14
19
25
viii
5
Figure 2.12
Undernutrition in Children in India
30
Figure 2.13
Anemia among Children
30
Figure 2.14
32
Figure 2.15
National Accounts, Public Sector Spending on Health
State-Level Per Capita Public Spending on Health (Rs.), 199596
32
Annex 2.1
Demographic and Health Indicators - India and States
35
Annex 2.2
Health and Demographic Indicators - India and World
36
Annex 2.3
Health Infrastructure of India and its States as on 01.01.1996
37
Annex 2.4
Health Expenditure - India and World
38
Annex 2.5
Demographic Indicators - India and World
39
Annex 2.6
Literacy, Health and Poverty Indicators - India and World
40
Annex 2.7
Population Statistics - India and States
41
Table 5.1
60
Table 5.2
Health Indicators Among SC/ST and Others (Rate per 1000)
Differentials in IMR and Under 5 Mortality - Rural / Urban
Social Group
60
Table 5.3
Nutritional Levels among SC/ST Women
60
Table 5.4
Prevalence of Illness 1990
62
Table 5.5
Rate per 1000 of Treatment during Last 15 days
64
Table 5.6
Rate per 100,000 of Hospitalization
64
Table 5.7
66
Figure 5.4
Percentage Utilization of Treatment in Public
Facilities for OP & IP
Costs of Care - Constant Prices 1986-87 (Rs.)
T reatment/Episode
Per Capita Releases by Center to Select States under National
Disease Control Programmes during 1998-00
Reasons for not Taking Treatment, % by Age and Sex
Share in Utilization of Public and Private Facilities for
Deliveries
Share in Utilization of Public and Private Facilities for
Hospitalization
Outpatient Care by Poverty Groups in Selected States
67
Figure 5.5
Share of Inpatient Days by Poverty Groups in Select States
67
Figure 5.6
Source of Funds for Medical Care
69
Annex 5.1
Distribution of Net Public Sector Subsidies by Level of Care by
Quintile Category - Combined for Rural and Urban
Average Total Expenditure (Rs.) Per Hospitalization by Type of
Hospital for Rural and Urban Areas of 15 Major States
75
84
Table 6.3
Number of Filaria Cases and Disease Rates 1989-2000
Percentage Prevalence of Soil Transmitted Helminths in Pilot
Study Areas 1999-2000
Cases Reporting of Major Diseases - 2000
93
Figure 6.1
Mortality and Morbidity Estimates, 1998
78
Table 5.8
Table 5.9
Figure 5.1
Figure 5.2
Figure 5.3
Annex 5.2
6
Table 6.1
Table 6.2
69
71
63
64
65
77
90
ix
Figure 6.2
Figure 6.3
Figure 6.4
Figure 6.5
Annex 6.1
Annex 6.2
Annex 6.3
Annex 6.4
Annex 6.5
7
8
Trends in Morbidity and Mortality on account of Communicable
Diseases
80
Leading Causes of Mortality and Burden of Disease 1998
80
Number of Cases and Mortality on Account of Malaria - Trends
Evaluation and Completion of Treatment under Conventional,
Short Course Chemotherapy and RNTCP
Malaria Cases in Selected North-Eastern States, 1995-99
Performance of the RNTCP by States (Provisional figures as of
March 2001)
National Tuberculosis Control Programme - Statement
Showing the States and Union Territory-wise Targets and
Achievements with Regard to Sputum
Outcomes of Treatment According to Category of Cases Under
Revised National Tuberculosis Control Programme from 1993
to 1998 (first quarter)
Leprosy Case Detection Treatment and Discharge as on
30.3.2001
81
87
98
101
102
103
105
Table 7.1
Table 7.2
Table 7.3
Causes of Maternal Mortality
Percentage Decline in Infant Mortality and Under-5 Mortality,
1971-98
117
Table 7.4
Nutritional Status by State
Table 7.5
Percentage Distribution of Births by Weight
Table 7.6
Anaemia as a Contributor to Perinatal Mortality
Table 7.7
Health Outcomes by Standard of Living
Table 7.8
Female and Male Health Outcomes and Social Indicators
Table 7.9
Demographic Goals Vs. Current Status
Figure 7.1
TFR, IMR and Under-5 MR by Time Periods
Figure 7.2
Excess Fertility and IMR
Figure 7.3
Framework
Figure 7.4
Causes of MMR
Figure 7.5
Assistance at Delivery
Figure 7.6
IMR of India Vs. Low Income Economies
Figure 7.7
IMR and Under-5 MR
Figure 7.8
Major Causes of Deaths of Infants and Children in India
Figure 7.9
Mother’s Education and IMR
Annex 7.1
Infant Mortality Indicators by Residence, India, 1971-1998
Annex 7.2
Infant and Child Mortality by Background Characteristic, India
Annex 7.3
Annex 7.4
Maternal Care Indicators, India and Major States, 1998-1999
Delivery Characteristics of Live Births, India, 1992-1993 and
1998-1999
119
120
120
120
121
122
107
109
109
1 11
112
117
118
118
121
129
130
131
132
Figure 8.1
Routes of HIV Transmission in India (1986-2001)
110
110
MMR by Select Country
134
x
Figure 8.2
Figure 8.3
Figure 8.4
Figure 8.5
Figure 8.6
9
Table 9.1
Table 9.2
Table 9.3
Table 9.4
Figure 9.1
Annex 9.1
Annex 9.2
10
Table 10.1
Table 10.2
Table 10.3
Table 10.4
Table 10.5
Figure 10.1
Figure 10.2
Figure 10.3
Rationale for Targeted Interventions among High-risk Groups
Trend in Condom Use among CSWs and Trukers in Tamil Nadu
Percentage Who Have Heard about Aids by State
Midlife Mortality due to NCDs in India
Estimated Number of Cases of Selected NCDs in India, 1998
Effect of Treatment of 1000 Patients with AMI
Burden of CVD 1990-2020
Implementation : Operational Components
Assessment of National Capacity : Questions for Situational
Analysis
Growth and Share of Voluntary Hospitals and Beds
Average Charge (Rs.) for Select Services in Private Hospitals
Distribution of Facilities by Availability of Patient Redress
Systems
Distribution of Facilities with Some Consumer Redress
Systems by Frequency of Review
Percentage Share of Private Sector Hospitals,Beds, and
Doctors by Select States
Rural-Urban Distribution of Hospitals / Hospital Beds: Public
and Private Sectors
Percentage of Villages with NGOs, by Select States, 1994
Public and Private Sector Shares in Service Delivery
Figure 10.S
Distribution of Inpatients between Public and Private by State
Average Hospital Charge per Inpatient Day by Public and
Private, by Select States
A Framework for Policy and Action
Physical Standards in the Private Health Sector - Findings of
a Case Study of Rural Maharashtra
Private Practitioners and their Role in the Resurgence of
Malaria in Mumbai : Serving the Affected or Aiding an
Epidemic?
Annex 10.2
Table 11.1
Table 11.2
162
164
170
182
Growth and Share of Private Sector Hospitals and Beds
Share of Private Sector in Outpatient and Inpatient Care
Annex 10.1
145
145
147
150
146
158
160
Early Mortality due to NCDs in India
Figure 10.5
Figure 10.8
135
135
137
138
139
Opportunistic Infections among AIDS Patients
Figure 10.4
Figure 10.7
11
Adult HIV Prevalence
182
163
164
165
167
168
169
170
186
189
189
Infant Mortality Rates, Total Fertility Rates, and Malnutrition in
Major Indian States
Percentage Female Literacy and Percentage Below Poverty
192
193
Line
Table 11.3
Select Indicators Relating to Public Services
Table 11.4
Percentage Covered by ANC and Immunization Services, by
195
196
xi
Standard of Living
Table 11.5
Percentage Covered by ANC and Immunization Services, by
Caste
196
Percentage Not Seeking Care Due to Locational Reasons
197
Table 11.7
Beds Per 10,000 Population in Public Hospitals
198
Table 11.8
Number of Public and Private Hospitalisations per 100,000
Persons
Correlation Coefficients between Llnder-5 Mortality and Per
Capita Health Expenditure
Correlation Coefficients between IMR and Per-Capita Health
Expenditure
Correlation Coefficients between LEB (Female) and Per-Capita
Health Expenditure
Percentage Beds in the Primary, Secondary and Tertiary
Sector
199
Table 11.6
Table 11.9A
Table 11.9B
Table 11.9C
Table 11.10
Table 11.11
201
201
208
209
Table 11.12
Micro-efficiency for Secondary (District) Hospitals
Health Humanpower in Rural Areas - Percentage Shortfall of
ANMs and Doctors
210
Table 11.13
Reported Figures of Immunization, State Data and NFHS 2
221
Table 11.14
Quality Care Indicators for Facility Visits
223
Figure 11.1
191
Figure 11.3
Goals of a Health System
Proportion of In-Patients Below thej Poverty Line That
Borrowed
or
Sold
Assets
for
IPublic
Private
and
Hospitalizations, by State 1995-96
Percentage Vacant Posts in Public Facilities in Rural Areas
213
Annex 11.1
Organogram of the Depa'tment of Health and Family Welfare
227
Annex 11.2
228
Annex 11.3
Proposed Administrative Structure
Public Expenditure on Health - Flow of Funds from Centre to
State
229
Annex 11.4
Flow of funds in Andhra -radesh Health Sector
230
Annex 11.5
Performance Monitoring "ramework
231
Table 12.1
Real Per-Capita Spending on Health (Rs.)
Percentage Share of Salaries and Wages in Total Public
spending on Health
234
Figure 11.2
12
201
Table 12.2
Table 12.3
198
235
236
Table 12.8
Estimates of Total Health Expenditure in India, 1990-91
Percentage of Total Heaiih Expenditure Funded Through
Public/Social Insurance and Direct Government Revenue
Cost Recovery and Health Expenditure by States, 1996
Percentage Distribution of Persons by Income Group,
Employment Status and Main Industry Classification
Percentage Distribution hy Employment and Income
Status
Summary of External Ass stance for Health Sectors (in ‘000 S)
245
Table 12.9
Additional Resource Mob ization Proposals: A Summary
249
Figure 12.1
Share of health in State and Central Budget (in %)
234
Table 12.4
Table 12.5
Table 12.6
Table 12.7
237
237
241
241
xii
Figure 12.2
Annex 12.1
Annex 12.2
Annex 12.3
252
253
Annex 12.10
Property Tax in Municipal Revenues
263
Table 13.1
ODA Received by Selected Countries
264
Table 13.2
Percentage Health to Total ODA - 1990-1996
265
Table 13.3
Project Profiles in Health - 1991-95
265
Table 13.4
Funding During 1970-80
266
Table 13.5
External Assistance by Major Donors in US $/m
268
Table 13.6
List of World Bank Assisted State Health Systems Projects
Percentage of ODA to Central Health and Family Welfare
Budget plans (Rs./Crores)
Budgetary Funding and External Aid for Disease Control
Programmes
List of Externally Funded Projects Under Implementation in
India
268
Annex 12.5
Annex 12.6
Annex 1 2.7
Annex 12.8
Table 13.7
Table 13.8
Annex 13.1
15
251
Annex 1 2.9
Annex 12.4
14
235 ,
Salient Features of Some Insurance Schemes in India
Salient Characteristics of Select NGOs Managed Health
Insurance Schemes
Assessment of Different Methods of Financing Health Care in
India
Employment by Inoustry in Organized and Unorganized
Sectors in
India : 1997
Percentage Distribution of Employed by Socio-Economic
Status under Employment Status, Main Industry Classification
and for Rural - Urban Areas
How Employees are Paid for their Healthcare
Utilization of Health Services and Average Expenditure
Incurred for Treatment as Outpatient and Inpatient
Revenue Receipts of States (Rs. Crore)
Annex 12.3a
13
Per-Capita Real Spending on Health by Selected Major Sta:es
(Rs.)
Trends in Government Expenditure (Revenue and Capital) :
1980-1981 to 1998-1999 (Rs. Lakhs)
Constituents of Primary, Secondary and Tertiary Care Services
254
255
257
258
259
260
261
272
274
279
Figure 14.1
Movement of Price Indices of Drugs and Other Products
289
Figure 14.2
Price Control Regulations
289
Figure 1 5.1
Plan Allocation for Department of ISM & H (Rs. Crores)
Summary of Medical Care, Medical Humanpower and Medical
Education Facilities Available Under Indian Systems of
Medicine and Homeopathy as on 01.04.1999 (Provisional
Figures)
Statewise Number of Registered ISM and Homeopathic
Practioners As on 01.01.1999. (Provisional Figures)
Statewise / Systemwise Number of Hospitals and dispensaries with their Bed
Strength Under Indian Systems of Medicine and Homeopathy Functioning as
on 01.04.1999. (Provisional Figures)
302
Annex 15.1
Annex 15.2
Annex 1 5.3
309
310
311
xiii
16
Table 16.1
Figure 16.1
Figure 16.2
Figure 16.3
Figure 16.4
Figure 16.5
Financial Outlays for ICMR 1997-98 to 2001-02
319
Burden of Diseases and Mortality
World Health: Contrast in Premature Mortality Burden and
Allocation of Health Research Funds (%)
Sources of Funds for Global Health R&D, 1992
312
Indian R&D Expenditure by Objectives, 1996-1997
Central Government Health
R&D
Expenditure
(Constant Prices). Rs. (Million, 1980-1981 Prices).
Significant Research Achievements of Indian
Institutions
313
314
318
in
India
318
Research
326
Achievements of Research Institutions in Diagnostics
“Push” and “Pull" Interventions to Promote the Discovery/
Development of Drugs and Vaccines
ICMR Permanent Institutes/Centers
326
328
Annex 1 6.5
Regional Medical Research Centers
328
Annex 16.6
ICMR Centers for Advanced Research
328
Annex 16.1
Annex 16.2
Annex 16.3
Annex 16.4
xiv
327
Changing the Indian Health System: Current Issues,
Future Directions
Executive Summary
This Report had as its starting point the terms of reference of the WHOappointed Commission for Macroeconomics and Health (CMH). During the CMH
meeting hosted by ICRIER in New Delhi in April 2000, detailed presentations
made by four Indian states clearly brought out the diversity of socioeconomic
conditions, health outcomes and approaches in different parts of the country.
This diversity, together with the quality of research and data available,
suggested that India could make a significant contribution to the CMH exercise.
A team at ICRIER, led by Rajiv Misra, former Secretary Health, Government of
India, prepared the Report with a view to making inputs into the CMH thinking
and contribute to the ongoing debate on the National Health Policy. The Report
thus evolved into a country-specific study with a focus on national issues
relevant to Indian policymakers, while maintaining an international dimension
that addresses the CMH terms of reference. The project was funded by the Bill
and Melinda Gates Foundation.
I.
OK
Introduction
It is increasingly recognized that good health is an important
contributor to productivity and economic growth, but it is, first and
foremost, an end in itself. In a poor country like India, where the
only asset most people have is their bodies, health assumes even
greater significance for their economic status. Good health, and its
natural corollary, defense against illness, is fundamental to every
man and woman and child, not only for their well being, but for their
very survival. If the State exists to safeguard the right of its citizens
to the fundamental prerequisites of survival, this same State must
own up to its responsibility to protect its citizens from illness and
premature mortality.
The Indian State has articulated this responsibility often enough.
Since Independence, the government, ostensibly driven by
socialistic goals, has expressed its intentions to discharge this
responsibility in one Five-Year Plan after the other. Ambitious
systems, programmes and schemes have been drawn up to aUeviate
poverty while promoting the goal of universal healthcare, although
the close linkages between the two have not been fully appreciated.
//
There have indeed been large gains in health status since Independence. Life
expectancy has gone up from 36 years in 1951 to 62 years in 1995. Infant
Mortality Rate is down from 146 in 1951 to 71 in 1997. Crude Birth Rate has
been reduced from 36.9 in 1970 to 26.1 in 1998, and Crude Death Rate from
14.9 to 8.7 in the same period. One of the major reasons for these gains has
been the development of an impressively vast, three-tiered system of rural health
infrastructure, with sub-centres for each 5000 population, PHCs for each 30,000
XV
P P1
C
-tT)
.•_ / .I
L ,A I
population, and CHCs for each 1,00,000 population. Immunization to control
communicable diseases has made a major contribution to these gains; success
stories include small pox eradication, the near elimination of leprosy, and the
extraordinary social mobilization for polio eradication. Improvements in
determinants such as water supply and sanitation have also helped achieve
outcomes. These aggregations, however, mask the wide differentials between
and within states. The health indicators of Kerala are comparable to those of
middle-income countries, while Uttar Pradesh, Madhya Pradesh and Orissa are
almost at the level of Sub-Saharan Africa. There are huge disparities between
urban and rural areas, and between developed and relatively remote areas
inhabited by the marginalized sections of society.
Moreover, the figures regarding achievements present an impressive picture only
when viewed in splendid isolation. First, a comparison of targets and goals
dilutes the gains considerably. The National Health Policy 1983 set some targets
for 1985, 1990 and 2000. A comparison of goals with actual achievements
reveals the real picture: we are nowhere neartargets, except for life expectancy
Crude Death Rate and polio immunization. Second, while India seems to have
performed better than countries with the same level of per capita income, such a
comparison is obviously misleading. With its knowledge base, its administrative
and institutional strengths, and its growth potential, India is capable of much
higher levels of achievement.
It is clear that those health systems that direct their resources and energies
towards the health needs of the poor have a better overall health status. This is a
logical association, since the coor carry the larger burden of disease. But the
facts make a mockery of such logic as they establish the raw deal the poor are
getting from the public healthcare system. A recent NCAER study reveals that
the richest 20% enjoy three times the share of public subsidy for health
compared with the poorest quintile. The poorest 20% of Indians have more than
double the mortality rates, fertility rates and undernutrition levels of the richest
20%. The poor suffer disproportionately more from pre-transition diseases such
as malaria and TB. On an average, they spend 12% of their incomes or
healthcare, as opposed to only 2% spent by the rich. Treatment or hospitalization
for chronic illness often means the liquidation of meagre assets, even permanent
indebtedness. One episode of hospitalization is enough to wipe out all the assets
of the family. It is no wonder then that the number of the poor who did not seek
treatment because of financial reasons increased from 15% to 24% in rural areas
and doubled from 10% to 21% in urban areas in the decade 1986-96.
The obvious question then is Why? If the State has universal healthcare and
poverty alleviation as basic objectives; if there have been gains, however patchy
and inadequate; if there are systems in existence if not actually thriving, why is
the current health scenario so bieak?
The obvious and most impcnant reason is that for a State that promises
universal healthcare through the public health system, India has one of the
lowest health budgets in the wcnc. How is the objective to be met if there are no
xvi
resources to put policy and schemes into actual practice? This gr: ss mismatch
between objectives and resources is at the heart of both tneTnacezuacies and
the inequities of the Indian health system. Higher public health expenditures are
clearly and unequivocally associated with better health outcomes, and thus
productivity, especially in a poor country. Any attempt at unders’.anding the
failures of the health system, and setting these derailed intentions and structures
back on course, would involve, for a start, a much higher priority to the health
sector. This higher priority will then have to be translated into increased
allocation of resources. Otherwise financial risk protection for the pcor, who are
beset by illness as well as the threat of loss of work, will remain wha: it has been
for the last several decades: pious declarations on paper.
The State’s role in health has been so far from its declared intentions that not
only has it failed to provide healthcare to the majority of the popula:ion through
the public sector; it has also countenanced a large and thriving private sector to
grow practically without regulation. In recent times, one point of view has offered
the private sector as the panacea for all ills; another view perceives the private
sector as a negative accompaniment to liberalization and links its growth with
that of inequity. Neither view takes into account two facts: one. that ir the context
of a public health system that does not deliver services to those whc need them,
the private sector has grown to be the main provider of curative healthcare. It
currently dominates both outpatient and inpatient care, and this evicence shows
no significant variations by income group, rural/urban location, gencer, caste or
tribe. Two, the private sector is almost entirely unregulated so that :s costs, its
quality of care and its spatial distnbution are for the large part incomoatible with
national health goals. It is not surprising then that the poor are forced into a
situation where they have to pay for private healthcare they cannot afford. Their
deprivation and vulnerability make the poor ill more easily: and illness makes
them even poorer. There is no dearth of evidence that establishes this nexus. A
recent analysis of the World Bank (India - Raising the Sights: Better Health
Systems for India’s Poor, May 2001) concludes that “the hospitaized Indian
spends more than half of his total annual expenditures on buying healthcare;
more than 40% of hospitalized people borrow money or sell assets to cover
expenses and 35% fall below the poverty line.” The same study also suggests
that out-of-pocket medical costs alone may push 2.2% of the population below
the poverty line in one year.
Given this context, the first task of policymakers is to define realistic goals and
provide the necessary financial resources for their achievement. Besides, the
lack of clarity on the relative roles of the centre and the states has caused the
centre to focus on the day-to-day management of institutions and programmes,
rather than concentrating on its stewardship role. The result is that even the
meagre available resources have not been put to optimal use. Clearly, along with
increased resources, the need of the hour is wide-ranging systemic reforms, both
at the centre and the states. We believe that the reform process mus: begin with
a thorough restructuring of the Ministry of Health and Family Welfare on the lines
indicated in the Appendices of this Report.
xvii
•
II.
The Current Health Scenario: Issues
1. Present Challenges
-XTI '
Communicable Diseases: One of the biggest blots in the current
health scenario is the failure to control communicable diseases,
despite the availability of cost-effective and relatively simple
technologies. These pre-transition communicable and infectious
diseases constitute a major cause of premature death in India: they
kill over 2.5 million children below the age of five and an equal
number of young adults every year. The proportion of total deaths
caused by communicable diseases (including maternity related
conditions and nutritional deficiencies) continues to be unacceptably
high at 42%. (Of the 269 million disability-adjusted life years or
DALYs lost, communicable diseases accounted for 50.3%.) Despite
the global eradication of small pox, and despite expectations that
current efforts will ensure the elimination of leprosy and polio within
the next five years, environmental and social factors impose severe
constraints on the control of two of the communicable diseases that
pose a special threat - malaria and TB. The total number of TB
patients is estimated at 15 million. Moreover, India has been
identified as a hot spot for Multi Drug Resistant (MDR) TB, which is
both difficult and expensive to treat. The resurgence of malaria and
TB in forms difficult to control or treat, along with the exponential
rate of development of HIV/AIDS, have imparted a new sense of
urgency to disease control. Special projects have been launched for
the control of communicable diseases such as malaria, TB and
leprosy with the support of the World Bank and other donors, and
they constitute an appropriate strategic response to the increasing
threat. They have improved performance considerably through
stable funding and programmatic reforms. However, except in the
case of leprosy where the objective of elimination appears
achievable, the coverage in other programmes is still low, and large
uncovered areas have been receiving even less attention than
before. These projects must cover the entire country, and central
funding support must be extendedI to_ 100%, rather than matching
50:50 with the states, as in many cases at present. The
sustainability of these special programmes once external assistance
ceases also needs to be addressed.
TB: India accounts for one-third of global TB, and the largest
number of persons suffering from active TB in the world.
According to available estimates, about 2.2 million persons are
added each year to the existing load of about 15 million active TB
cases. Of these new cases, about 800,000 are infectious, and
about 450,000 die. Most disturbing is that 20% of 15 year olds
are reportedly infected; and among women in the reproductive
age group of 15-44 years, it causes more deaths than all the
xviii
various causes of maternal mortality put together. Added to this
are the facts that every sputum positive case carries the potential
to infect 10-15 individuals in a year, and that TB is the principal
opportunistic infection of HIV. The result is the alarming
possibility that deaths caused by TB can go up to 4 million in the
next decade. At present, the DOTS strategy is implemented under
the aegis of the RNTCP in about 200 districts, covering a
population of 350 million. The programme is supported by about
Rs.746.76 crores of external funding. The results of the RNTCP
are impressive, but nevertheless the future scenario of TB control
appears grim. First, only an estimated 20-25% of TB patients in
the country have been brought under DOTS. The same familiar
reasons crop up as barriers to further expansion and better
performance
low budgets; weak institutional capacity; the
' dangers of MDR exacerbated by unregulated private practitioners
following their disparate, sometimes irrational treatment regimes,
as well as unplanned, unprepared and hasty expansion of the
programme. Multiple systems of TB control - conventional, SCC
and RNTCP - are all being implemented with different financing
mechanisms. And as in other programmes, poor community
support is_a Jilndrance. In addition to all this, the future of TB
control has to be viewed in light of the ominous fact that nearly
two-thirds of opportunistic infection among AIDS patients is TB,
portending a dual epidemic of TB and HIV in the near future.
•
Malaria: The prevalence of malaria was brought down to about
2 million cases by 1984; but in 1994, once again, there were
several focal outbreaks resulting in high mortality. The most
dangerous strain of malaria, caused by the parasite Plasmodium
falciparum (Pf), has been steadily rising to account for almost
half of all malaria cases in 2001. As expected, the disadvantaged
sections are the worst hit: in Andhra Pradesh, the rate of Pf
malaria among tribal groups accounted for 75% of malarial
deaths in the state.
Several reasons have been cited for the failure to reduce malarial
prevalence: parasite resistance to drugs and vector resistance to
insecticides in some high endemic areas, environmental changes
caused by development activities such as irrigation projects, and
rapid urbanization. A three-pronged strategy was drawn up, which is
now being implemented throughout the country under the National
Anti-Malaria Programme (NAMP). The main objective of the strategy
is interrupting the transmission of disease by
> early detection and prompt treatment to reduce the reservoir of
infection;
> reduction of the vector population through selected vector
control using anti-adult and anti-larval measures;
xix
r' enhancement of community based action, such as undertaking
bioenvironmenial control measures and promoting personal
prophylactic measures.
The effectiveness of these efforts is hampered by weak and often
non-functional public health systems, non-availability of required «
manpower, inaccessibility of areas most effected (e.g. tribal areas),
and poor community participation. The removal of these constraints
is a major challenge for the programme.
Maternal and Child Health (MCH): Children below five and women
in the reproductive age group make up 36.2% of the population of
India, and in terms of survival and well being, they also constitute
the most vulnerable group in society. Income levels and social
exclusion only serve to exacerbate this vulnerability: health
indicators
muicdiurb for
iof SC
ou and
ana ST
bi women and children reveal that they are
considerably worse off. As in other aspects of the health sector,
the database so essential for planning and setting of priorities is
not reliable. But the estimates available show that the Maternal
Mortality Rate (MMR) continues to remain at an unacceptable
level - 408 for 1,00,000 live births. The causes for these poor
indicators of maternal health are well documented: the low
socioeconomic status of women, the undernourishment and
anemia rampant among them, the low proportion of institutional
deliveries, and the absence of trained birth attendants in as many
____ as two-thirds of cases. Again, only a revamping of the primary
healthcare
system,
along
with
effective
referrals
for
complications, will help improve antenatal and maternity care.
Simultaneously, a fundamental link - between high mortality on
the one hand and high fertility and age at delivery on the other must be addressed to get a handle on the problem of maternal
f/ZU
survival and health.
•
__
*
_i
i
i
.
The poor status of maternal health is inextricably linked with the
gender disparities that pervade all aspects of life in India. The
results of the 2001 Census seem to indicate that the reported
decline in the sex ratio during the last century has, at last, been
not only arrested but also marginally reversed. But the sex ratio
in the 0-6 age group has worsened, and this is cause for+ serious
concern. Again, the tempo of decline in Infant Mortality Rate
(IMR) and under-5 mortality achieved between 1981 and 1991
has not been sustained. The critical point is that IMR has been
hovering around 72, and under-5 mortality around 95 per 1000
live births, during the last few years. The rate of decline has,
during the last four years, reached a disturbing plateau.
Other Infections: Linked with child survival and health is the
range of water-related or soil-transmitted illnesses. Acute
XX
diarrhea, worm infestations and digestive tract infections become
illnesses to reckon with in view of their debilitating impact on the
immunity system, particularly those of children and of those
already undernourished. In addition to comprehensive health
education - which would promote community hygiene and healthy
living - India needs to make adequate investments in water
supply, sewerage systems and sanitation to reduce the infectious
disease load. Acute Respiratory Infections (ARI) continue to take
a heavy toll, especially among children, despite the availability of
inexpensive and effective anti-microbials, causing almost a
million avoidable deaths every year. This again is due to a
dysfunctional public health system and lack of access to quality
primary and secondary care.
The threat of communicable diseases, as well as perinatal morbidity
and mortality, looms larger because of the poor nutritional status of
a substantial part of the population. Despite a nationwide
programme for nutritional supplementation of pregnant women and
children, NFHS II (1998-99) shows only a slight improvement over
NFHS I (1992-93). The percentage of underweight children has only
reduced from 52% to 47%, and of the severely underweight from
20% to 18%. 74% of children were found to be anemic; the same
study found that 52% women have some anemia, which is a major
cause of maternal mortality.
i ce
The present challenges of communicable diseases and maternal and
child survival show up the weaknesses of the health system. But
even as the system struggles to meet the current demands of
disease control, a new challenge, again a communicable disease, is
emerging in the form of HIV/AIDS, threatening to sharpen existing
problems of resources, health infrastructure and inequities.
2. Emerging Challenges
HIV/AIDS: The threat presented by the rapidly growing HIV/AIDS
infection has not received the priority attention that it deserves,
partly because of the long gestation period between HIV infection
and the development of full-blown AIDS. Also, it is the opportunistic
infections (such as TB) that get noticed; the root cause of morbidity
and mortality often remains undiagnosed. The major route of
transmission in India is sexual contact, but sex as a subject is
weighed down with taboos in a traditional society. The high
prevalence of STDs in India also makes the country particularly
vulnerable to the AIDS threat. In the year 2000, the number of
Indians infected with HIV was estimated at 3.86 million, or roughly a
prevalence rate of 0.7%, quite low when compared to the prevalence
rates of 25% and over in South Africa, Zimbabwe and Botswana. But
the infection in India is no longer confined to high-risk groups or
xxi
only to urban areas and it is spreading rapidly. And since the
epidemic is more than a decade old, mortality due to AIDS is
increasing: in 1999 alone, nearly 300,000 Indians are estimated to
have died of AIDS. As of March 2000, 11,251 cases have been
reported to NACO: 79% are males, 21% female. This is, however,
only a fraction of AIDS morbidity in the country, reflecting the stigma
and
the
ignorance
surrounding
the
infection.
Widespread
discrimination against the infected hinders their access to
healthcare. Similarly, the low income levels of the infected, coupled
with lack of resources in the government funded programme despite the manufacture and availability of the drugs in India at
more affordable prices - preclude the widespread use of highly
active anti-retroviral therapy (HAART). As a result, morbidity and
mortality of those infected continues to be high.
The most important contribution of the National AIDS Control
Programme (NACO) has been sentinel surveillance; it has alsr
heightened awareness regarding blood safety. The Programme has
now begun its second phase, which is to focus on targeted
interventions among high-risk behaviour groups. But awareness
levels are still low or uneven; information, education and
communication (IEC) remain a crucial element. If India is to avoid
the catastrophe that Africa is struggling with, far greater efforts will
have to be made to keep the epidemic at bay. Fortunately, we have
a model in the state of Tamilnadu, which has successfully arrested
the increase in the level of infection by concentrating on high-risk
segments of the population, and by devising innovative mechanisms
for programme implementation. India must act immediately and
vigorously to control the level of HIV infection so that it does not
grow beyond 3% of the population.
3. Future Challenges
As if present and emerging problems do not present enough of a
challenge to a resource-hungry and weak health system, there are
also the challenges of the future for which provisions must be made.
Projections of population increase indicate a changing demographic
profile with profound implications for health
planners and
economists. The next two decades will see a significant increase in
the 15-59 age group; the increase in longevity will almost double the
population of the elderly (> 60 years). As more individuals survive to
middle age, the years of exposure to the risk factors of chronic
disease increase. Non-communicable diseases (NCDs) will gradually
become the dominant contributors to the burden of disease - their
share increasing from an estimated 33% in 1998 to 57% in 2020. In
fact, even at the present stage of health transition, India contributes
substantially to the global burden of NCDs. In 1990, India accounted
for 19% of all deaths, 16% of all NCD deaths and 17% of all CVD
xxii
deaths in tne world. CVD in India alone accounted for around 2.4
million deaths, in contrast to nearly 3.2 million CVD deaths in all the
industrialized countries put together. In addition, recent evidence
suggests that impaired fetal nutrition, reflected in small birth size,
results in programmed susceptibility to adult cardiovascular disease,
diabetes and some cancers. With NCDs positioned as a major public
health challenge, the existing health systems will need to be
reorganized and reoriented to deliver the expanded mandate of
healthcare - involving the prevention, surveillance and management
of chronic diseases along with primary and secondary healthcare.
The emerging burden of NCDs poses a special threat to the poor due
to the often prolonged and expensive treatment required for these
conditions, as well as much greater exposure to risk factors like
tobacco and alcohol.
The management of NCDs is often technology-intensive and
expensive.
Individual as well as societal resources are already
being drained at a disproportionately high level by the tertiary care
management of NCD, drawing scarce resources away from the
unfinished agenda of infectious disease and maternal and child
health. Though NCD epidemics usually originate in the upper
socioeconomic strata, they diffuse across the social spectrum, with
the social gradient ultimately reversing and the poor becoming the
most afflicted.
The exorbitant costs of treating chronic diseases make prevention
the most suitable option for India. Traditionally, public health
approaches to NCD control has consisted of a high-risk strategy,
targeting those with high levels of risk factors and employing
interventions to reduce them, usually with drugs; and a population
strategy that attempts to reduce risk factor levels in the whole
community, usually through lifestyle-related measures. Along with
these approaches, effective low-cost case-management strategies
are required for those who manifest disease. Such technologies are
available, but they await widespread dissemination and application.
Tobacco control is a major public health imperative providing the
largest benefit for NCD prevention. Tobacco-related cancers, CVD
and chronic obstructive airway disease can be effectively prevented
if the tobacco habit is discouraged and overcome among the
population. At present, programmes for NCD control are either non
existent or functioning at a low level in India. The National Cancer
Control Programme involves cancer registries at selected sites and
strengthening of facilities for clinical care (such as radiotherapy).
Pilot Studies for the control of CVD and diabetes have been initiated
but have not had an impact on policy and programme development.
Tobacco control has received greater attention, but it still awaits the
passage of proposed legislation as well as a vigorous public
education campaign.
xxiii
T3ken together, what do the present, emerging and future challenges
imply? To begin with,, they
F
call for the high-priority control of
communicable diseases to avoid the double burden of communicable
and non-communicable diseases. They call for appropriate public
health interventions to control the^j’isk factors of NCDs such as
tobacco and unhealthy lifestyles, emphasize preventive strategies,
and set up arrangements for the early detection and cost-effective
treatment of NCDs at the primary and secondary levels.
4. Finance
The recurring refrain in any discussion of the Indian health system is
finance, a refrain that grows more shrill and urgent because of policy
failures and State neglect. The crux of the problem is abysmally low
public health expenditure — around 0.9% of GDP, below the average
of low-income countries and even Sub-Saharan Africa. Despite the
increasing urgency of problems in the health sector, public health
expenditure as a proportion of total government expenditure has in
fact declined over the years. This has to be seen against a
background of fiscal deficits: the combined fiscal deficits of the
centre and the states are estimated at 10% of GDP. Following a
temporary stabilization in the early nineties, the fiscal situation has
deteriorated, so that government ability to increase investments in
health has been eroded further. Since the states typically account for
about 75% of public health expenditure, their financial health is
crucial for both general development and specific health outlays. But
the combined gross fiscal deficits of the states, which ranged
between 2.4-2.9% between 1993-94 and 1997-98, increased to 4.2%
in 1998-99 and to 4.9% in 1999-2000. Fiscal crises have meant
sharp reductions in the non-salary recurrin^'expendrfure^^ public
health facilities, leading to further deterioration of quality. In
addition, the increase in salary and pension liabilities after the Fifth
Pay Commission has aggravated the resource crunch.
The share of health expenditure in the major states, in the range of
6-7% up to the 1980s, has come down to just over 5% in the 1990s.
This is a significant decline in the proportion of health expenditure to
the total expenditure in the states in over two decades. As far as the
real per capita public spending on health is concerned, the evidence
of 11 states at 1980-81 constant prices shows a steady increase,
though in varying degrees. The sole exception is Uttar Pradesh, the
most populous state; the declining per capita public spending in this
state with very poor health outcomes is indeed a disturbing trend.
Moreover, trends of the real per capita public spending on health of
selected major states, and their distribution among primary,
secondary and tertiary healthcare, show that between the period
1985-86 and 1998-99, per capita public spending increased at the
xxiv
primary and secondary levels by about 50%, while spending levels
increased by more than 100% in the tertiary sector. This has gra •"
: grave
implications for both the equity and efficiency of the health system.
The declared policy was for the State to provide free universal
healthcare to the entire population, but this policy objective has been
totally divorced from the reality on the ground. In fact, India has one
of the highest levels of private financing (87%), with out-of-pocket
expenses estimated to be as high as 84.6%. The highly skewed
pattern of health finance in India is a major contributor to the
• perpetuation of poverty. Indeed, the greatest failure of the Indian
health system is its inability to develop a financing mechanism for
the healthcare of the poor. It is clear then that the foremost objective
of the Indian health finance system is financial risk protection for the
poorer and weaker sections of the population. Access to health
services should depend on individual need, not on ability to pay. The
most efficient way of prdvidmg^Trancial'protection is to pool the risk
between the rich and the poor, the young and the old, and the
employed and the unemployed, to enable cross subsidization. At the
international level, the main instrument used to achieve this
objective is health insurance, but this has remained relatively
undeveloped in India.
That there is a strong case for increasing the share of health in
resource allocation is by now self-evident. But the extent to which
tax revenues can be reallocated to the health sector would depend
not only on political will, but also on the fiscal situation. In a poor
country with a low tax base, mounting debt liabilities, undeniable
security concerns and a legacy of poorly targeted subsidies, we
cannot rest content with merely advocating reallocation of resources
for larger investment in health. Generally speaking, the available tax
resources should be used primarily for provision of public goods, the
healthcare of the poor - particularly those in the informal sector
outside the reach of insurance mechanisms, and for community
financing. To the extent possible, resources should be raised from
dedicated sources to eliminate competition, and to provide stable
and-growing sources of revenue. At the same time, there must be
improvement in the targeting of public subsidies towards the
healthcare of the poor. This implies taking three steps:
•
7?
•
•
Increase allocation for public health and primary and secondary
healthcare, which is better utilized by low-income families.
Utilize user fees at secondary and tertiary levels to reduce the
price advantage of public services, reducing their attractiveness
fo the well off and simultaneously making arrangements for
exemptions of the poor.
Improve the efficiency of public services to encourage their
greater utilization.
xxv
Various options for different categories of the population in different
income groups need to be considered in the course of developing a
framework. As far as the rich are concerned, voluntary private health
insurance deserves government encouragement, but there is no
justification for public subsidies such as the recent tax concessions.
Increased competition would automatically spread the coverage of
voluntary health insurance, leading to improved products and
services. The State’s role is essentially to develop an appropriate
legislative framework, and to appoint a dedicated and independent
regulatory authority that will monitor the insurance sector, and
formulate procedures and regulations to help avoid well-documented
market failures. But even in the absence of voluntary health
insurance, the rich, given their financial resilience, could continue to
depend on out-of-pocket expenses.
The objective for the middle income section is to cover all the
employees in the formal sector via social insurance, primarily
financed by employer and employee contributions. State participation
should at best be nominal. People in the informal sector could join
either voluntary health insurance schemes or community finance
schemes wherever feasible. If none of these options is chosen, they
could continue to rely on out-of-pocket expenses.
Schemes such as ESIS, CGHS, and employer-based schemes
already cover the low-income formal sector, though ESIS and CGHS
have demonstrated deficiencies of coverage and quality, as well as
high administrative costs. ”
These schemes could be replaced by
social insurance, with thej rgovernment playing facilitator and
financier, but not necessarily provider of services."
----- -------- The services for
social insurance could be contracted out; this would enhance
efficiency and reduce costs. The manufacturingj and services sector
would grow with economic growth and industrialization, so that social
insurance could play an increasingly important role. At present,
approximately 10% of the population are covered by social insurance
and employer-based schemes: this can be increased to around 21%
of households, including all income groups, wherever social
insurance is feasible.
An estimated 46.6% of the poor population is in the informal sector,
and they deserve maximum State assistance since they are beyond
the reach of social insurance. The preferred option is Community
Financing Schemes. However, such schemes require strong local
leadership and organizations, capabilities, often provided by NGOs.
Most current schemes do not receive any government support, but
state governments could design a package of incentives that will
encourage NGOs to develop such schemes in designated areas, with
the government contributing a fixed premium for every b’elowxxvi
•
•
•
•
•/ C
’1
\
•
•
Timely release of funds allowing advance preparatory action for
procurement against the next year’s allocation.
Sufficient provision for maintenance of facilities created for the
project.
Identification, training and positioning of the project team before
the project begins, and not shifting them during the project period.
At least one year’s preparatory time for all major projects to
complete formalities such as land acquisition, preparation of
building plans, finalization of technical specifications and
development of training modules.
Improvement of monitoring mechanisms.
Simplification of procurement procedures, avoiding multiple
references to, and approvals from, donor agencies.
Tax on Tobacco: This tax has two main components — the basic
excise duty, a central levy; and additional excise duty in lieu of sales
tax, which is levied and collected by the central government on
behalf of the states. This is a buoyant source of revenue with a
mechanism already in place for the imposition of a cess. The linkage
between tobacco and disease is well established, and taxation
serves the dual purpose of reducing consumption and yielding
resources. There is a strong case for dedicating at least part of the
revenue to preventive and promotive health, particularly to
controlling the risk factors for NCDs.
Even a 15% cess could
contribute at least Rs.1,000 crores to the health sector without
disturbing existing sources of revenue.
Revenues
from
Disinvestment:
The
government's
ambitious
programme of disinvestment in public sector enterprises has had a
slow start because of political pressures, resistance from trade
unions and procedural difficulties.
But the establishment of a
separate ministry for disinvestment, and the successful privatization
of BALCO despite political opposition, augurs well for rapid progress.
The Budget for 2001-02 set a target of Rs.12,000 crores from this
source. Out of this Rs.7,000 crores is earmarked for restructuring
public sector enterprises, and the balance of Rs.5,000 crores for
investment
in
infrastructure
and
social
sectors.
Although
infrastructure is a high priority, there are many other sources to
support it, including the cess on petroleum products and private
investment. It is in this context that we urge earmarking at least
Rs.2,000 crores annually from disinvestment revenue for additional
investment in the health sector.
State Levies:
Levy on Excise: The rationale behind a dedicated levy on tobacco for
health applies equally to a cess on state excise duties, which
predominantly relate to taxes on alcohol consumption. Again, this is
a buoyant source of revenue with an annual yield of about 15,000
xxviii
poverty-line (BPL) family covered by such schemes.
Also, all
donations to genuine community finance organizations should be
exempted from tax. But most of the population would still need health
cover by the State, callingToKa more efficient primary and secondary
healthcare system with a strong referral link. Moreover, even
community financing schemes and access to public primary and
secondary facilities do not provide financial risk protection to the
poor against costs of hospitalization
and
serious
illness.
This requires the setting up of Sickness Funds in each district to
directly reimburse such costs to the public or designated private
facility. On current estimates, a fund to .cover an approximate 300
million BPL population would require Rs.2,500 to Rs.4,000 crores
annually.
The total health spending in 1998-99 is estimated at Rs.161 billion or
Rs.16100 crores. This means the level of public investment will have
to be more than doubled to reach the average of lower middle
income countries, or 2.2% of GDP. The strategy is to develop
dedicated levies that provide a sustained source of finance to
strengthen the health sector and insulate it, at least partially, from
fiscal crises, emergencies and political upheavals.
Central Level:
Reallocation from General Revenues: Considering the tight fiscal
position and the competing claims of different sectors, diverting
significant resources from other sectors to health does not seem
feasible.
But a 50% increase, or roughly an additional Rs.2000
crores, can be made available - partly from General Revenues and
partly by reallocation from other programmes that have failed to
make the desired impact.
Increased External Assistance: From 1990 to 1995, the average
disbursement of external assistance to the health sector has been
216 million dollars or Rs.1000 crores - around Rs.10 per capita.
Considering the Indian context - population size, levels of income
and the burden of disease — the quantum of this assistance is
woefully inadequate.
But despite this, external assistance has
played a key role in directing resources to priority areas. Meanwhile,
in view of a better absorptive capacity, it would not be unrealistic to
expect assistance to increase to at least three times in the coming
years. The resulting yield would mean an additional Rs.2000 crores a
year.
The performance of externally aided schemes could
enhanced by reforms at both conor and recipient levels:
•
Better project preparations involving full
stakeholders.
be greatly
consultation with
xxvii
all
^r™eS ” and a 33% surcharge on existing excise revenue could yield
5,000 crores annually.
Property Taxes.: There are three categories of property-related taxes.
The first one, registration and stamps, is a tax on transfer of
property, and yields an annual Rs.10,000 crores. A 20% surcharge
could yield 2,000 crores annually. The second source is urban
property tax, collected by local bodies. The estimated income, based
on 1997-98 per capita estimates, works out to around 2,300 crores.
This is a rapidly growing source and the present yield would exceed
2,700 crores. A 33% cess could provide Rs.900 crores per year for
Sickness Funds and other healthcare services for the urban poor.
The third source is land revenue, which yields around 1,500 crores a
year; a 33% surcharge could yield 500 crores a year. Property taxes
are currently both low and progressive, and could make a significant
contribution towards the new mechanism of Sickness Funds. These
funds could be created by a suitable cess on both rural and urban
property as well as on their transfers, so that it takes into account
both equity considerations and ease of administration and collection.
The collections could be pooled state-wise, then allocated to district
level societies proportionate to the number of BPL families. The
identified BPL family member would be given free treatment in public
facilities and designated private facilities, and the costs charged
directly to the Fund. These sources of earmarked levies could yield
around 3,500 crores a year, sufficient to support Sickness Funds.
User Fees: This levy cannot be perceived only as a revenue raising
mechanism. It discourages the overuse of public facilities by the
affluent while correcting some distortions in the use of public
facilities. Revenues generated from this source can be used to
improve quality of care, in turn improving the utilization of these
facilities. User fees can also involve the local community in
managing public healthcare facilities, so that a sense of participation
and ownership is fostered. The present yield from this source is
small, but it is capable of considerable expansion, as indicated by
new initiatives in MP and Rajasthan. There are, however, hurdles to
a major expansion, and these include the lack of appropriate
mechanisms to review user charges; the minimal level of cost
recovery caused by low fee structure; the absence of mechanisms to
exempt the poor; and the lack of adequate arrangements to ensure
fund utilization at the point of collection. But again, recent state
initiatives provide lessons that can be applied to overcome these
weaknesses:
•
The income from user fees should be credited to a hospital-based
fund managed at the local level with the authority to review the
charges.
xxix
•
•
•
The income from user fees should be additional to the budget
allocations for the medical facility.
Use of the fund should be exclusively for improvements in the
relevant medical facility by the local fund management committee,
in accordance with state government guidelines.
All BPL families should have identification cards to secure
automatic exemption. Mechanisms should also be in place to
consider the exemption of other indigent families at the discretion
of the local committee.
In sum, while resources must be mobilized to change the health
system through measures such as dedicated taxes, particularly
property taxes, the critical guideline for mobilization is that the
resources must be stable as well as sustainable. Since the object of
the entire exercise is to provide financial risk protection, insurance
as a mechanism must be promoted wherever feasible. So should
community finance, which calls, however, for strong leadership frorr
NGOs and local bodies. What happens then to those who do not
have access to insurance or community finance schemes? It is for
these weaker and disadvantaged sections that mechanisms such as
Sickness Funds are necessary; and most of all, an improved primary
and secondary health system that delivers care to those who need it
most.
5. Health Systems
A. Public:
Our vast rural health infrastructure received substantial financial
support during the 1980s, or the Sixth and Seventh Five Year Plan
periods. But this substantial investment has not yielded optimal
benefits: many institutions are not fully functional as a result of staff
shortage and the lack of drugs and consumables. One of the major
and persistent causes of a malfunctioning healthcare infrastructure in
the rural areas is a critical shortage of key health manpower,
particularly of doctors in public facilities. This is partly due to
inadequate incentives and poor working conditions, and partly
because the posting of doctors in rural areas suffers from a lack of
transparency. The result is that the under-served areas, where even
private sector facilities are not available, are completely deprived of
any healthcare facilities.
The non-availability of key personnel in public health facilities is
often cited as the main reason for under-utilization of public health
facilities. But an analysis of manpower shortage at the primary level
suggests that more than shortfalls of personnel, it is the organization
and management of existing human resources that is the key to
better performance. The lesson is clear: efficiency in the use of
XXX
existing resources should take precedence over mobilizing additional
resources.
The deteriorating environment, the (ack of safe drinking water and
poor nutritional status, all conditions that affect disease burden and
health outcomes, are poverty-related. These health hazards threaten
the growing slum population in cities - as much as 30-50% of the
total urban population. But in the absence of functioning institutional
mechanisms, it is difficult to put the required coordinated and
integrated action into practice. Divisions within the MHFW have also
aggravated compartmentalization . The Ministry is now divided into
three independent departments of health, family welfare and ISM.
Since population control was considered a priority, an independent
department of family planning was created even though public health
and family planning services had to be delivered through the
common rural health infrastructure. The emphasis on family planning
targets transferred the entire rural health portfolio to that
department, divorcing it from other health programmes. The result
was poor utilization; the PHC, in many states, was in the public eye,
only a family planning facility.
An analysis of disparities in health outcomes shows that certain
states in India have consistently worse health outcomes. A crosssectional regression analysis was carried out for 25 states to assess
whether differentials in health service delivery capacity have a
significant association with health outcomes. The analysis was based
on
three
independent
variables,
namely
female
literacy,
immunizations and use of ORT therapy in diarrhea episodes. Since
MCH preventive services are mostly delivered in the public sector, it
was concluded that public sector capacity is considered a relevant
and critical determinant of health outcomes. Jean Dreze and Haris
Gazdar advance the same hypothesis in an analysis of development
experiences in Uttar Pradesh, Kerala and the southern states. The
authors argue that the relevant determinant of the development
status of these states is the reach and functioning of public services,
and support this argument with a comparative picture of select public
services. This reinforces our hypothesis that public health sector
capacity in terms of provisioning of services is a critical determinant
for improved health outcomes.
That access to health services is a key mechanism for better health
outcomes is also indicated by utilization data: states that have high
utilization rates reveal lower mortality rates. NSS data shows that the
percentage of people who did not access healthcare for reasons of
location is higher in the poor performing states. The analysis
indicates a strong association between health outcomes and equity
in the public financing of healthcare. Health outcomes appear to be
strongly associated with higher per capita public health spending,
xxxi
and with higher allocations to the secondary sector. Scarce financial
resources are being inefficiently used, not only in terms of allocative
patterns, but also in the management of fund flow and monitoring.
Several of the problems confronting public health service delivery
call for the reorganization and better management of existing
resources. Access to healthcare is hindered not only by geographic,
social and cost barriers, but also by inherent systemic and structural
weaknesses of the public healthcare system:
•
•
•
•
compartmentalized structures and inadequate definition of roles at
all levels of care; inefficient distribution, use and management of
human resources so that people have to contend with lack of key
personnel, unmotivated staff, absenteeism, long waiting times,
inconvenient clinic hours/outreach, service times, unauthorized
patient charging;
inadequate
planning,
management
and
monitoring
of
services/facilities; displaying insensitivity to local/community
needs; ineffective or non-existent referral systems, resulting in
under-utilization of PHCs, over-utilization of hospital services,
duplication of services and cost-ineffective provision of services;
inadequate systems to enforce accountability and assure quality;
inefficient systems for purchasing drugs, supplies and services,
which fail to ensure quality and value for money;
inadequate attention to health education and public disclosure.
Setting priorities in health sector policy and planning is a matter of
intense debate. International opinion emphasizes the bias in favour
of hospital care and the need to reform health systems in favour of
primary care. Our_analyses suggest that the state must focus on both
primary and secondary sectors simultaneously, linked as they are for
the delivery of basic health services. The focus on secondary care in
the context of referral linkages with the primary sector, and the
welfare objective of insuring the poor against costs of illness, is
considered as essential as the focus on primary care. Most important
is reforming administrative structures to integrate primary and
secondary levels through administrative and technical controls at the
referral hospital level.
The capacity of the public health system to monitor morbidity, and to
respond to changes in disease patterns, is greatly hampered by the
lack of reliable epidemiological data. The current reporting systems
are confined only to public facilities that deal with barely one-fifth of
the illness episodes. Hence the huge under reporting, generating a
sense of complacency. The model developed by the Christian
Medical College, Vellore, and implemented in Kottayam District,
Kerala, needs to be replicated as soon as possible all over the
country to improve the quality of epidemiological data.
xxxii
Another important area that has suffered neglect is public health as a
discipline. Even the highest technical positions in public health,
whether at central or state level, do not require a public health
background; specialized institutions as well
well as faculties of
Preventive and Social (Community) Medicine remain
remain in an equally
sad state of neglect. Unless public health as
as aa field gets the
recognition and importance it deserves, the planning of health
systems will continue to over-emphasize curative services.
The foremost problem in designing an efficient health system is the
top-down approach with negligible community participation and
ownership.
Is
it
possible,
for
instance,
to
conceive
of
bioenvironmental control of vectors, or improvement in sanitation and
hygiene, without the active participation of the people making up the
community? Similarly, the monitoring and supervision of peripheral
health services from state and district headquarters has invariably
failed, underscoring the need for active local involvement.
One of the ways to address this deficiency is decentralization of
authority to local bodies (Panchayati Raj institutions). But the fact is
that decentralization could have conflicting results without sufficient
preparation of local bodies to take on this expanded role. The Kerala
experience indicates that decentralization has to be preceded by a
long period of planning, defining and clarifying responsibilities,
capacity building and advocacy. Capacity building of local bodies as
well as the community is an essential prerequisite to reap the full
benefits of decentralization. It is evident that such devolution
encourages local bodies to consider health as integral to other
development activities, facilitating coordinated action on other
determinants of health such as water and sanitation.
The states provide several examples linking the issue of community
participation with institutional autonomy and delegation of powers to
local committees to raise and use resources for improvements in
medical facilities. The experiences of. Madhya Pradesh and
Rajasthan, for instance, show a marked improvement in the quality of
services, availability of drugs and consumables as well as patient
satisfaction. These are welcome initiatives; but they are yet to be
converted into a comprehensive policy to secure community
participation in all health programmes.
B. Private:
Without in any way underestimating the importance of the public
health system, it must be recognized that the private sector has
grown to be the main provider of curative healthcare. At the all-lndia
level, the private sector currently dominates both outpatient and
inpatient care: 82% of all outpatient visits take place in the private
xxxiii
sector. An important dimension to the utilization of in-patient
,
t care in
Ithe
____________
_ the rich and
public and private health sector is________________
the share between
the poor. Overall for India, the percentage of the poorest quintile
using private sector hospitalization facilities is, at 39%, almost half
that of the richest at 77%. Tertiary care institutions, providing
specialized and super-specialized care in the private sector,
constitute only 1-2% of the total number of private institutions; and
corporate hospitals, which have in recent times gained in visibility
and publicity, actually constitute less than 1%.
The evidence is that the people of India, including the poor, make
considerable use of the private health sector. But at what cost? This
is a crucial dimension of the private health sector in India,
unfortunately under-researched. NSS data reveals that the average
cost of treatment in the private sector for rural inpatients is 2.1 times
higher, and for urban inpatients 2.4 times higher, than in the public
sector during 1995-96. Technology advances are usually associatec
with a decrease in costs, but the reverse holds true for the medical
sector, where technological developments have been capitalintensive, making the provision of healthcare increasingly expensive.
A proliferation of medical equipment and technologies in urban areas
has led to excess capacities, and the consequent unnecessary and
irrational use of these technologies.
I '
In sum, rather than private providers developing into partners with
the State in the achievement of national health goals, the technical
quality of care provided in the private sector is often poor - ranging
from poor infrastructure to inappropriate and unethical treatment
practices, to over-provision of services and exorbitant costs, to
delivery by unqualified providers. Information asymmetry among
users, arising out of a lack of information and an inability to make
sound judgements about available types of healthcare, compounds
the problem. The natural corollary to the concentration of qualified
practitioners and facilities in urban areas, and the limited spread of
the voluntary sector, has been the rise of unqualified, rural medical
practitioners. The estimated one million illegal practitioners are said
to be managing 50-70% of primary consultations, mostly for minor
illnesses, and, in this sense, form the de facto primary curative
healthcare system of rural India. A clear policy promoting private
health facilities in the under-served areas, along with a set of clearly
defined incentives, would correct these imbalances.
Given the extent of private sector dominance in the healthcare
system, any significant improvement in healthcare is inconceivable
without the active involvement and cooperation of the private sector,
particularly the voluntary sector. According to a rough estimate, the
number of voluntary organizations working in healthcare areas is
more than 7000. Despite the lack of comprehensive documentation
xxxiv
on the contribution of NGOs, there is no disputing the fact that NGOs
have the potential to improve access, quality and equity of services,
either through direct provision or through advocacy and other action.
This potential to contribute substantially to public health goals has
not been realized due to several reasons. Their limited size and
spatial distribution is a major cause. That they are missing where
they are most needed hinders effective partnerships with the public
health system. The challenge is to find strategies that will facilitate a
far more substantial participation by NGOs in the health sector,
particularly in backward states and remote areas, and to ensure
systems that will keep such participation accountable and
transparent.
Public-private partnership would make a considerable contribution to
the successful implementation of public health programmes. Also
necessary are continuing medical education, and the active
involvement of professional bodies - to disseminate standard
treatment protocols for diseases such as TB and malaria, to check
the irrational use of drugs, and to regulate unethical practices.
Equally important is the task of developing appropriate independent
mechanisms for the regulation of the private sector - mechanisms
that involve all stakeholders, set up and enforce standards, ensure
quality control, transparency of charges, control unethical practices
and promote accreditation systems. The challenge is to devise
innovative mechanisms that address the acknowledged distortions
and malpractices, yet do not stifle private initiative - so important for
the expansion of healthcare facilities to meet growing demand. The
legislations under consideration in Andhra Pradesh and Karnataka,
and the initiative taken by Maharashtra in developing accreditation
mechanisms, deserve commendation.
-y^
Finally, each state needs to work out the problem of unqualified
practitioners with a view to their eventual elimination. The ban could
be enforced straightaway in well-served areas; in the under-served
areas, they will be gradually eliminated as alternative facilities get
established. In the interim, the registration and training of such
practitioners, limiting the scope of their use of allopathic drugs for
treating minor ailments, needs to be attempted as a temporary
measure.
6. Drug Policy and Regulations
The Indian pharmaceutical industry is already feeling the impact of
globalization, even though the WTO mandated legislation to
recognize product patents is to be brought into force only in the year
2005. The agreement on Trade Related Aspects of Intellectual
Property Rights (TRIPS) came into force with the formation of the
XXXV
World Trade Organization (WTO) in January 1995. TRIPS obliges all
developing countries to make available 20 year patent protection for
novel, non-obvious and useful inventions, whether products or
processes, in all fields of technology including pharmaceuticals.
Violations of TRIPS obligations can lead to trade retaliation or
compensation to affected WTO members. India has so far recognized
only process patents in pharmaceuticals, and legislation for
compliance with WTO obligations is pending passage in Parliament.
As of December 1999, only 16 WTO countries, including India,
continued to exclude pharmaceuticals from product patent protection.
India has no option but to fall in line; but the government should
actively explore ways in which the advantages of the new regime can
be maximized and the disadvantages minimized.
The public policy question will have to be resolved in such a way that
a balance is maintained between the need to keep new drugs
affordable to those who need them, while retaining strong incentives
for the invention of new drugs and the development of new and
better treatments. The selective use of compulsory licensing
provisions for the manufacture of generic substitutes for patented
drugs having major public health significance has to be explored with
international cooperation. So far, the Indian pharmaceutical industry
has paid scant attention to research because of the absence of
product patent protection, and concentrated its energies on
producing generic substitutes for foreign patented and branded
products. But the Intellectual Property Rights Regime (IPR) is set to
change with the introduction of product patents in conformity with
WTO mandated regulations. The Indian pharmaceutical industry
already commands a major advantage over its rivals in the West
since the cost of bringing a new chemical entity into the market is
estimated at $250-500 million in the US, but only $90-100 million in
India. According to a recent study by the Administrative Staff College
of India (The Indian Pharmaceutical Industry, May 2000), “India has
the potential to become the hub of pharmaceutical research.” In
order to harness the resources and skills of the Indian
pharmaceutical industry towards the neglected diseases of the poor,
the government needs to develop an appropriate incentive
framework.
At present, the administration of drugs and pharmaceuticals is
divided between the Ministry of Chemicals and Fertilizers (MCF) that
is responsible for drug policy; and the Ministry of Health and Family
Welfare (MHFW) that sets standards and deals with quality control,
the introduction of new drugs and the enforcement of relevant laws
and regulations. This arrangement prevents the government from
taking a holistic view that includes the interests of both the industry
and the consumer. Often, the policy of one ministry is at cross
purposes with that of the other. As early as 1975, the J. L. Hathi
xxxvi
Committee recognized this dichotomy and suggested that an
independent National Drug Agency be set up to take over al! the
NDa’c*^ulddbfeUnsCtlOnSfPHrfKrmed by the tW0 Ministries. The proposed
imolrt of nb
SuppoJted bV a small cess on the manufacture and
and customs
Q ’ .^.onvenient|y collected along with excise
necessarv Tn mot T tShignif'cant Publ'c sector support would be
in diseases of thL
he pbarmaceutical industry to invest in R&D
National nrlln P HP00rl^UCh 35 TB and malaria' and the Proposed
National Drug Fund could provide one such avenue of support The
current situation is unlikely to improve merely by tinkering with the
existing system. The only option that would make a noticeable
difference is an independent National Drug Authority, supported by
adequate financial resources from the National Drug Fund.
Elsewhere
in the Report, we have recommended greater
decentralization and devolution of powers to the states. However the
indiscriminate licensing of drugs by the states, the poor enforcement
of quality standards, and the open violation of laws regarding sale of
prescription of drugs, compels us to suggest an enlarged role for the
central authority. The proposed NDA, armed by a new law that
provides for more stringent scrutiny before licensing, could weed out
irrational combinations and ensure stricter enforcement. The
National Drug Fund should be used primarily to support the NDA
upgrade public health laboratories, and strengthen the enforcement
machinery. The unauthorized and irrational use of anti-microbials by
unqualified practitioners and registered practitioners of other
systems of medicine, a situation encouraged by the free sale of
prescription drugs across the counter, has been a major factor in the
development of drug-resistant bacteria. Similarly, the proliferation of
over 20,000 manufacturers without the requisite infrastructure to
monitor GMP, and the large-scale manufacture and sale of sub
standard and spurious drugs, pose a major health hazard. Only
stringent laws that are effectively enforced can check these
problems.
7.
Health Research
ndia has great potential and unique capabilities in health research
Its acknowledged strengths in all knowledge-based activities, its
infrastructure and trained manpower, its vast clinical material, rich
bio-diversity, unparalleled heritage of traditional systems of medicine
and a dynamic and technologically capable pharmaceutical industry
all add up to this potential. But only a national health research policy
that creates an incentive environment for both public and private
sectors will help the country realize this potential to the fullest.
Timely enactment of IPR related legislation would bring the present
phase of uncertainty to an end. Next, a substantial increase of public
investment in basic and strategic research is required, with a specific
xxxvii
focus on the neglected diseases of the poor. The international
support for health research has so far been nominal - the estimate is
5% of the total health R&D expenditure in 1992-93. Indian potential
in this area justifies a major increase in external assistance. A
priority should be health policy and systems research, to date a
neglected area excepI^foT-ftre-recent interest shown by the World
Bank and some bilateral donors.
..ef
The lack of available expertise in disciplines such as health
economics, health finance and epidemiology is a major constraint on
health policy and systems research, and special efforts need to be
made to train researchers in these fields. Research capacity should
be strengthened - with the improvement of infrastructure, the
training of scientists, and through new collaborations with institutions
in the North and the South.
In particular, capacity needs to be
developed quickly to undertake clinical trials for new molecules likely
to be introduced for the various communicable diseases. Existing
public sector institutions could produce higher quality of research
with more appropriate management structures. Most important, for
both public and private sectors, is a network of alliances among
academia, research institutions and industry. The utilization of basic
and strategic research outputs by industry to take the process further
toward product development should be the goal of such an alliance.
The ICMR should develop suitable mechanisms to facilitate such an
alliance, and the inter-mediation between research outputs from
academia and research institutions, and the pharmaceutical industry
along the lines of TOR in WHO. It is also essential to establish
institutional mechanisms that will promote interaction between
policymakers and programme managers on the one hand, and
researchers on the other, for setting the research agenda and for
utilization of research outputs.
8. Indian Systems of Medicine (ISM)
The term ISM comprises six different systems - ayurveda, siddha,
unani, yoga, naturopathy and homeopathy - out of which only
ayurveda, siddha and yoga are entirely indigenous. India has a rich
heritage in ancient systems of medicine that make up a veritable
treasure house of knowledge, and these systems can make a
significant contribution to the healthcare of the population. But
despite a vast parallel infrastructure of hospitals, dispensaries and
teaching institutions, and over 6,00,000 registered practitioners, this
v^ J) potential has not been realized. Over 90% of illness episodes are
treated by allopathy. Even registered practitioners of ISM treat
Y>
patients with modern drugs though they are not authorized to do so,
often' with undesirable consequences. The failure to evolve the
synthesized national system recommended by the ICSSR/ICMR
Committee has prevented the use of even proven ISM remedies in
xxxviii
and sustained efforts to prevent the spread of
HIV/AIDS, with focus on IEC and interventions involving high risk
population following the example of Tamilnadu; simultaneously,
arrangements for medical care of AIDS patients through clinical
training in treatment protocols and sensitization of health workers
on HIV/AIDS patients.
• Strengthening of the health system in high malariogenic areas,
particularly tribal regions, for early detection and prompt radical
treatment to reduce the reservoir of infection.
• Development of treatment protocols and regulations for co-opting
the private sector in communicable disease programmes; this
may include continuing medical education and active participation
of professional bodies like the IMA.
2. Facing the Rising Threat of NCDs:
Identification of a menu of core components to provide an
essential package of chronic care with possible extension to an
‘optimal package’
• Integration of these services into various levels of healthcare.
• Development of evidence-based, context-specific and resource
sensitive clinical practice guidelines that can be integrated into
various levels of healthcare to facilitate the use of low-cost, highimpact interventions.
• Modification of the training of healthcare providers of diverse
categories to enhance skills relevant to chronic disease
prevention, surveillance and management.
• Sequential prioritization of ‘essential’ elements for early
implementation and 'optimal' elements for later integration.
• Vigorous efforts to control risk factors by sustained health
education, community participation and legal action with regard
to tobacco and alcohol.
•
3. Reduction of Infant and Maternal Mortality:
•
Targeting of high IMR states first, and within states, high IMR
districts and regions; all CHCs and 24-hour PHCs in high IMR
districts and regions to be fully equipped to handle basic newborn
care and referral.
• Focus on the disadvantaged and poorest groups; trained CHWs
to be located in identified remote regions with a large proportion
of disadvantaged groups such as Scheduled Tribes for the
delivery of essential MCH services.
• Arrangements to effectively screen and identify all high risk
cases, and ensure their deliveries in appropriately equipped
health facilities; in general, promotion of institutional deliveries
by providing appropriate facilities and incentives including
emergency transportation.
xl
public healthcare facilities. Alsp, the vast army of ISM manpower
has rarely been utilized for public health programmes. The failure to
evaluate traditional remedies scientifically has prevented their wider
acceptance in India as well as abroad. What is most important is for
ISM to develop its strengths in providing relief in apparently
incurable chronic ailments such as digestive disorders, asthma and
arthritis. At the same time, ISM needs to popularize preventive
practices such as yoga, which could be an important element in the
strategies being evolved to cope with the threat of NCDs. Some
recent initiatives of the new Department of ISM seem to address
these deficiencies; but on the whole, this area requires priority
attention to explore and realize its full range of possibilities.
9. Conclusion :
The above analysis clearly underscores the need for a quantum
jump in the public investment for health, accompanied by wideranging reforms at every level. This can be achieved only with
strong political will and commitment, which can in turn be generated
only through a strong people’s movement cutting across party
affiliations. The first step is better awareness and the widest
possible dissemination of information on health issues. It is only
vigorous informed debate on health issues — in Parliament, in the
state legislatures, in the media, and in various public forums - that
will eventually grow and gel into a broader people’s movement. It is
in the context of this long and complex process that this Report
seeks to identify, describe and analyze the current issues in Indian
health and the future directions of change.
III.
Future Directions: Summary of Recommendations
1.
Communicable Disease Control:
Acceleration of India’s epidemiological transition by vigorous
public policy to control communicable diseases; malaria control
to focus on those areas with an API above 2; rapid expansion of
DOTS so that the entire country is covered for TB control.
• Substantial increase of central funding without stipulation of
matching contribution by the states.
• The central government to consider a more direct intervention in
actual implementation, if necessary through trained personnel on
contract in weak performing states; in well performing states,
release of block grams against certain clearly defined
deliverables to provide greater flexibility in the implementations
of the programmes.
• Establishment of a comprenensive disease surveillance system in
all districts with central funding for a period of ten years.
•
xxxix
•
•
Strengthening antenatal care by screening every pregnant woman
for anemia, hypertension, diabetes, urinary and reproductive tract
infections, malaria, and TB.
Convergent action at the cutting edge level between health
personnel and anganwadi workers for ensuring full coverage of
child health services.
4. Finance:
•
Public health expenditure to be more than doubled to raise the
level of public investment from the present 0.9% of GDP to at
least the level of the average of lower middle-income countries
(2.2% GDP); additional resources to be mobilized largely through
dedicated levies to avoid competition from other sectors and to
provide increasing and sustainable funding,
• Increase of allocation for public health and primary and
secondary healthcare that is better utilized by low-income
families.
• Differential planning and deployment of budgets in line with the
extent of disease burden, economic backwardness of the
state/region and poverty levels; the government to bear a special
responsibility to ensure good quality care through appropriate
incentives and strengthening of facilities in backward and poorly
developed areas/states, since public sector facilities may be the
only facilities available.
• Utilization of user fees at secondary and tertiary levels to reduce
the
price advantage of public services,
reducing
their
attractiveness to the affluent and simultaneously making
arrangements for exemptions of the poor.
• Setting up of systems of social insurance such as Sickness
Funds to provide financial risk protection to the poor against
serious illness and hospitalization.
• Coverage of employees in the formal sector with social insurance
primarily financed by employer and employee contributions;
social insurance to replace low coverage existing schemes,
especially in the low-income formal sector, with services
contracted out to enhance efficiency and reduce costs.
• Package of incentives to encourage NGOs to develop community
finance schemes in designated areas, with the government
contributing a fixed premium for every BPL family covered by the
scheme.
5. Health Systems:
•
Restructuring of Central Ministry of Health and Family Welfare so
that it withdraws from day-to-day management and concentrates
on its stewardship role by strengthening its planning, analytical
and public health expertise.
xli
Restructuring of the health systems of the states based on three
principles: (i) decentralized authority, responsibility and decision
making; (ii) integration of preventive, pro motive and curative
services; and (iii) local community participation.
• Removal of identified constraints and inadequacies at the primary
healthcare level to improve their efficiency and utilization, and
reducing the load on over-utilized hospital services by providing
essential
drugs,
consumables
and
diagnostics,
making
arrangements for proper maintenance of facilities, and removing
constraints on mobility of health personnel.
• Addressing manpower shortages by an appropriate combination
of incentives, legislative measures, and management reforms:
reservation of PG seats for those candidates in service with a
record of rural service; making rural service compulsory for
admission to PG courses; contractual appointments to fill
vacancies; a transparent transfer policy that requires every
doctor to work in rural areas by rotation for a prescribed period;
preference for foreign training given to doctors with rural service
records; better residential facilities, rural service allowance;
allowing private practice only in under-developed areas where
even private facilities are inadequate.
• Mapping the availability of health facilities in hilly regions and
areas inhabited by tribal populations; the provision of mobile
health teams and community health workers to cover identified
gaps.
• Decentralization and devolution of powers to local authorities
after careful preparation and adequate training.
• Delegation of administrative and financial powers to medical
facilities to be exercised through local committees to promote
efficiency, accountability and mobilization of resources.
• Institutionalization of coordination arrangements at different
levels.
• Involvement of community self help groups and women’s groups
for people’s participation in health programmes.
• Institutional arrangements for regulating the private sector with
the participation of all stakeholders to set and enforce standards,
control unethical practices, and ensure transparency of charges
and non-denial of emergency care.
• Development of capacities for contracting out services to the
private sector; promoting new partnering initiatives with the
private sector for service delivery and management of public
institutions.
• Development of an incentive package for the voluntary sector to
set up facilities in the identified under-served areas.
• Promotion of accreditation networks for identified services
through voluntary organizations/professional bodies.
•
xlii
•
Elimination of unqualified practitioners
beginning with well-served areas.
in
a
phased
manner.
6. Drug Policy and Regulations:
•
•
Creation of an independent
i
National Drug Agency to take over all
drug-related functions, supported by a National Drug Fund
financed by a small cess on the manufacture and import of
pharmaceuticals; institution of a more stringent law to deal with
the proliferation of sub-standard manufacturing units and
irrational fixed dose combinations, poor laboratory facilities, sub
standard and spurious drugs, weak enforcement machinery, and
open violation of law by chemists selling prescription drugs over
the counter.
Selective use of compulsory licensing to produce generic
substitutes for patented drugs of public health significance, and
to provide the necessary incentives and financial support to
pharmaceutical companies for the same.
7. Health Research:
Development of a health research policy to create an incentive
framework to promote research, particularly on the diseases of
the poor.
• Higher investment in development of infrastructure for basic and
strategic research in the public sector, with changes in the
management structures to promote quality research outputs.
• Development of alliances among academia, research institutions
and the pharmaceutical industry to promote the utilization of
research leads by the industry for product development; ICMR to
develop capacities for such inter-mediation on the lines of TDR in
WHO.
• Emphasis on health policy and systems research and reducing
the deficiency of researchers by providing training avenues in
epidemiology, health finance and health economics.
• Creation of an incentive environment for the pharmaceutical
industry to invest in research through tax concessions, pricing
incentives for new molecules, facilitating clinical trials and
regulatory approvals, and supporting promising products for the
neglected diseases of the poor with financial support from the
National Drug Fund.
•
xliii
A
8. Indian Systems of Medicine:
•
•
•
•
•
Development of a national health system incorporating the best of
all systems; including proven remedies of ISM as first drugs of
choice in the public healthcare system.
Encouraging scientific evaluation of traditional remedies.
UtUization of ISM manpower in public health programmes.
Emphasis on the special strengths of ISM in treating chronic
ailments such as digestive disorders, asthma and arthritis.
Popularizing ISM practices such as yoga to prevent and treat
NCDs.
xliv
Health expenditures
Total per
As % of GDP
capita (USS)
Health expenditures by source (%)
Public
Private
Aid flows
Region (N)
N
Established market
economies
25
1675.2
7.73
77.0
23.0
Middle Eastern Crescent
32
189.1
4.27
55.0
42.9
Economies in transition
19
150.3
4.27
72.7
27.3
Latin America and
Caribbean
33
118.1
5.30
54.9
37.4
7.6
Asia and Pacific islands
33
60.2
4.01
40.9
48.1
11.0
Sub-Saharan Africa
47
35.7
4.86
33.4
37.6
28.8
Source: WHO, 1997
2.9
\Ln
'
/
I
I
.5
a
Hp -
6
/-f P-
/
DRAFT NATIONAL HEALTH POLICY
I.
INTRODUCTION
1.
As a consequence of the rapid advances in science and technology, the country's
health system is faced with a range of threats, opportunities, and challenges, for
never before have people, ideas, goods or infections traveled across nations with
such speed. Globally, the increased access to knowledge and information has
profoundly enhanced our capabilities to live healthy and productive lives.
2. Given the modest resources, health gains, over the last fifty years, have been
remarkable for their depth and expanse. The first three decades after Independence
were marked by sustained efforts to control disease, resulting in the eradication of
small pox and plague, the effective containment of malaria, a dramatic reduction in
leprosy and a positive trend towards a drop in fertility and mortality. Due to
expansion in access to water, sanitation, nutrition, better housing and higher
incomes, people are healthier, live longer and a larger number of children survive
their fifth year growing into young adults. These gains were the result of the overall
development in the country but in no small measure, also on account of the
increased investments in expanding access to basic health services in the remotest
corners of this vast country.
Box 1 : Achievements Through The Years - 1951-2000
INDICATOR
DEMOGRAPHIC CHANGES
Life Expectancy
Crude Birth Rate
Crude Death Rate
i IMR
1951
1981
36.7
54
33 9^5^
40 8
25”
J
EPIDEMIOLOGICAL SHIFTS
I 4*| >i <
» .r.c*» pci 10,0(1(1 popu l.il ion
Small Pox (no of cases)
Guineavvorm ( no. of cases)
Polio
INFRASTRUCTURE
SC/PHC/CHC
Dispensaries &TIospitals( all)
I________________ ’________
' Beds (Pvt & Public)
i
, Doctors(AIlopathy)
—
; Nursing Personnel
r _64.6(RGI)
■—I
12.5(SKS)
p
146
Miliaria (cases in million)
2000
75
38 1
>44,887 j
119
26 i(99 SRS) " '
87(99 SRS)2 '
70 (99 SRS)
27
57.3
Eradicated
2.2
3.74
>39,792
Eradicated
......265
29709
—r---------------------725
57,363
9209
23,555
117,198
569,495
61,800
2,68,700
18,054
1,43,887
i
|
1,63,181 (99____ RHS)
43,322
(9596-CBHI)
‘8,70,161 (95__ 96-CBHI)
’ 5,037900’ ’ (98___ 99-MCI)
1
7,37,000 (99INC)
I
3.
4.
The 1983 National Health Policy had advocated a comprehensive approach to
medical education, research and health services that would be relevant to the
country's needs and priorities; involvement of the civil society and inter sectoral
coordination as cornerstones for achieving specific targets related to diseases
• affecting the poor . However, since
then , the health system has become
extiaoidinarily complex, as it seeks to address the demands of a wide variety of pre
and post transition diseases. Due to demographic changes there is a larger
population of the young and the aged entailing, health implications of increasing
vulnerability to sexual infections and demand for chronic and geriatric care.
Children and young adults continue to die prematurely on account of simple, low
cost and easy to treat diseases, namely, diarrhoea, TB, respiratory infections and
maternal causes, as also cancer, cardiovascular diseases, and injuries, which are
expensive and difficult to cure. Corporate hospitals offering state of the art
tieatment coexist with unqualified practitioners dispensing modern drugs for
minor ailments reflecting the wide differentials in the needs, demands and
expectations of health care services among the people.
.
Societal averages hide the diversity that characterises this large country, with
people all at once, living in different time periods. Not only do the poor have higher
evels of mortality compared to the rich, but also suffer disproportionately more on
account of communicable diseases. Due to the gradual decline in the functioning of
public hospitals the poor are being forced to go to the private sector at great
financial risk, the other option being not availing of any treatment al all, making
policies directed to addressing equity central to the achievement of public health’
goals. . Similarly, the lesser-endowed states have worse health outcomes compared
to t le better off, indicating the great amount of unevenness that exists among states
in their ability to provide health care services to their people. The vast differentials
in health status among states is depicted below in Box 2 :
Box 2 : Differentials in Health Status Among States
Indicator
I INDIA
! Rural
Urban
Better
Performing
States
Kerala
Maharastra
J’N'"
Low
Performing
States
Orissa
I Bihar
l Rajasthan
jUP
MP
.. I.
Populati
on BPL
(%)
IMR/
Per 1000
Live
Births
(1999SRS)
70
_ 75^
26.1
27.09
23’62
44
<5Mort
ality
per
1000
(NFHS
H)
94.9
103.7
’63.1
mmr/
Weight For
Age
Children
Under 3 %
<-2SD)
47
49.6
38.4
Lakh
(Annual
Report
2000)
H— 408
Leprosy
cases per
10000
population
Mala-ria
+ve
Cases
2000 (in
'000)
3.7
2200
I
1
I
i
12.72
25.02
~ 21 12
47.15
42.60
15.28
31.15
37.43
’
14
18.8
------------ 1------------------------48
' . 58-i !
52
63.3 '
27
50
37
97
63
81
84
90
54
54
51
52
55
104.4
105.1
114.9
122.5
137.6
. zztji
135
79
O.9
3.1
4.1
498
707
607
707
498
7.05
11.83
0.8
4.3
3.83
5.1
138
56
I
483
132
53
99
528
2
5.
II.
Mindful of the problems and constraints that plagues the health system, but
conscious of the opportunities available for corrective action, the National Health
Policy, 2001 renews its commitment to expeditiously control communicable
diseases, eliminating a few and containing the rest in a time bound manner. The
rapid spread of sexual infections and the emerging epidemic of non-communicable
diseases, particularly among the productive age groups is a matter of concern and
will receive priority attention. The NHP also aims to initiate affirmative action to
protect the poor from further impoverishment or social exclusion on account of ill
health, by formulating policies and action plans directed to addressing inequity.
Based on the need to restrategise and retool for meeting the challenges of an
increasingly technology driven, interdependent world, the Policy will seek to
strengthen research. Finally, it will also facilitate the restructuring of the present
health care system to work together in partnership with all stakeholders, namely,
the civil society, NGOs' and the private sector providers for realizing the goals and
aspirations as articulated in the N1 IP,2()0I.
OBJECTIVES
6.
The main objective of the NHP, 2001 is to achieve a standard of good health that is
acceptable, affordable and sustainable. It will aim to develop a health system that is
appropriate to our needs, has the requisite capacity to effectively reduce disease
burden and arrest any further increase on account of environmental and behavioral
factors. To lend sustainability the rational use of drugs alongside the tried and
tested systems of traditional medicine will be assiduously promoted. As no health
system can sustain the high costs of modern day treatment, advocacy for adopting
healthy lifestyles and preventive health care through community-based strategies
will be our focus.
7.
The most immediate objective of NHP, 2001, will however, be two :1) the overall
reduction in morbidity and the reduction of mortality by over three quarters on
account of communicable diseases, maternal and infectious diseases; and 2) to
improve the functioning of the existing public health system to be assessed in terms
of the utilization, particularly by the poor. To realize the immediate and medium
term objectives the NHP is committed to achieve the following goals during the
period 2001-2015.
Box 3: Goals to be achieved bv 2000-2015
>
>
>
>
>
>
>
>
>
>
Eradicate Polio and Yaws________________________________
2005
Eliminate Kala Azar and Leprosy__________________________
2010
Eliminate Lymphatic Filariasis
2015
Achieve Zero level growth of HIV/AIDS_______________ _____
2010
Reduce Mortality by 50% on account of IB, Malaria and
2010
Other Vector and Water Borne diseases___________________
Reduce Prevalence of Blindness to 0,5%
______________
2010
Reduce IMR to 30/1000 And MMR to 100/LcKh_______________ 2010
Improve nutrition and reduce proportion of LBW Babies from
2010
30% to 10%
_________________________________
Increase utilisation of public health facilities from current
2010
Level of <20 to >75% _____________________________
Establish an integrated system of surveillance. National Health 2005
Accounts and Health Statistics._________________
Increase health expenditure by Government as a % of GDP
from the existing 0,9 % to 2,0%___________________________
Increase share of Central grants to Constitute at least 25% of
total health spending
>
>
III.
2010
2010
8.
Realization of the above goals will be contingent upon the full implementation of
various components of public policy, many of which fall outside the domain of the
health sector. Adequate levels of public health spending, female literacy, universal
access to nutrition, safe water and sanitation, reduction in environmental pollution,
planned urbanisation, macroeconomic policies related to technological self reliance,
mass media and information, reduction in poverty and finally a strong political
support are some of the factors that are outside the health sector but profoundly
influence its ability to fulfill its mandate.
9.
There are ten determinants that have been identified for concerted action and
focused policy attention. These determinants fundamentally impact upon our
ability to achieve the goals. The current status and measures proposed to be taken
under each determinant is detailed below.
fundamentai
DETERMINANTS
1. HEALTH FINANCING
The most fundamental determinant to the achievement of health goals is the
C1?/15101!'!1? °f adeMuate fulKis for publje health. Of the total estimated amount of
4.5% of GDP spent on 1health, government's share is about 20% accounting for 0.9%
of the GDP, the rest being expenditures iincurred’ \
by individual households. India is
one of the 20 lowest public health spenders in the world:
Box-4 :
% Public Health Spending in select Countrics
Indicator
%Populafion
with income of
<$1 day
Infant Mortality
Rate/1000
%Health
Expenditure to
GDP
India
China
Sri Lanka
UK_____
USA
44.2
18.5 •
72
31
16
6
7
5.2
2.7
3
5.8
6.6
13.7
%Public
Expenditure on
Health to Total
Health________
13
24.9
45.4
96.9
44.1
Source : WHR 2000
10. In the past 15 years, health expenditures by government as share of GDP has been
declining from 1.3 in!990 to 0.9% in 1999, while per capita private household
spending has doubled to Rs. 165.The proportion of central budget allocations for
4
health to the total central budget has also been stagnant at about 1.3%, while
declining in the states from about 7% to 5.5% Central share in total health spending
by states is about 15%. Of this 15% about 40% is for disease control programmes,
the rest being for family welfare. There has been a significant shift in resource
allocations within the central health budgets which have shown a decline in the
proportion of the budget earmarked for communicable disease control from 58.7%
during 1986-87 to 47.1 in 2001-2002, the shift being towards non communicable
disease control and Medical Education and Research. Similarly, in the states also
while there has been an increase by about 50% in the allocations for primary and
secondary care, it has doubled for tertiary care. Overall, states spend on an average
about 40% on primary health care, 30% on secondary and about 10% on tertiary
hospitals and medical colleges. With more than three quarters of the money for
salaries and wages, there is little money for procurement of drugs, equipment or
improvement of infrastructure, resulting in the gradual decline in the quality of
services being provided in public facilities.
11.
The amounts ispent by government determines the quality and reach of the public
health system. Low expenditures by government either• mean the partial or the nonimplementation of an activity of public health importance or the deficit being made
up by patients from out of their pocket. Not unexpectedly, the low performing states
spend half of what the better performing states are spending with predictably poor
er health outcomes.
12.
The weak financial health of the states, competing demands, a low political support
and an insufficient understanding of the nexus between poverty and ill health and
the consequent social costs are the main contributory factors for the continued under
funding of the health sector. In view of the criticality of adequate resources the NHP
will seek to :
Double the Health Budgets across the board to constitute at least 2.5% of the
GDP by 2010;
50% of the budgets be earmarked for Primary Health Care and communicable
disease control programmes, 30% for secondary and 10% for tertiary care;
> Increase share of central grants to constitute at least 25% of total state health
spending for the next 10 years till the states fiscal situation improve;
Initiate mechanisms for resource generation for sustaining the investments and
meeting rei til liilg costs al least partially in all institutions such as increased
student fees in all medical colleges and other training institutions or charging
user fees in hospitals for those belonging to a high income level groups , subject
to guidelines;
Provide financial incentives for the non private charitable sector to set up
secondary and tertiary facilities subject to conditions;
> Formulate social insurance packages or establish sickness funds to cover the
hospital expenses of all the poor below a certain income level and thereby
reduce the share of out of pocket expenditures to total health financing.
2.
EQUITY
13.
Benefits arising from the social and economic development of the country have not
been spread in an equitable manner resulting in wide differentials between rural
and urban, men and women, rich and poor. These differentials have a direct impact
5
on the capability of those sections of society who bear the double burden of poverty
and social discrimination, the aged and women, to access public services in
accordance with their needs.
Box 5: Differentials among States
Population BPL %
(Planning Commission,
Government of India)
Rur
Urb
Total
Indicator
IMR Per 100 Live
Births (1999SRS)
Tot
Rur
Urb
Rur
Urb
Tot
Weight For Age % OF
Children Under 3 <2SD (NFHS II)
Tot
Rur
Urb
<5 Mortality per 1000
(NFHS II)
India_______
Better
Performing
States______
Kerala______
Maharashtra
Tamil Nadu
27.09
23.62
26.10
75
44
70
103.7
63.1
94.9
49.6
38.4
47
9.38
23.72
20.55
20.27
26.81
22.1 1
12.72
25.02
21.12
14
58
58
16
31
39
14
48
52
43*
85.5*
105.5
32.7*
60.5*
74.2*
18.8
58.1
63.3
30.6*
57,5*
52.1*
22.9*
45.5*
37.3*
26.9
Low Performing
States________
Orissa________
Bihar_________
Rajasthan_____
UP__________ _
MP
48.01
44.30
13.74
31.22
37.06
42.83
32.91
19.85
30.89
38.44
47,15
42.60
15.28
31.15
37.43
100
64
85
88
96
65
55
97
63
81
84
90
104.8
108.6
120.6
129.5
152.2
102.0
68.3
92.3
85.8
82.9
104,4
105.1
1 14.9
122.5
137.6
55.5
55.1
51.9
53.6
58.44
45.3
66
55
47.4
46.0
42.6
44.3
49.6
36.7
54.4
54.4
5(16
51.7
55.1'
*MFHS I (1992-93)
14. The most reliable form of insurance cover to the poor is a well performing public
health system. However, to address the needs of vulnerable target groups, specific
interventions will be designed such as
•
•
•
•
•
•
providing transportation facilities to the health center, ensuring access to female
providers by earmarking one medical post in all the Community Health
Centers;
training of medical and non medical personnel in geriatric care;
ensuring suitable timings and the regular availability of services, drugs and
medicines needed for diseases suffered by women and the old ,
establishment of health posts in urban slums,
mobile vans with expanded functions and diet for inpatients in the tribal areas.
Regular
monitoring of data covering the vulnerable groups will be
institutionalised.
15. It is estimated that of those poor who receive hospital care, several are pushed
below the poverty line on account of the economic burden of illness. Evidence also
indicates that cost of hospitalisation has increased threefold in the last decade.
Nearly a quarter of the poor are unable to take treatment for lack of money. This
being an unacceptable situation, the NHP will promote social insurance schemes
and encourage states to establish sickness funds for covering the entire cost of
treatment for families below a certain income level.
6
3.
KESTRUCTURMG the eubuc health delivery system
16.
health are‘Stactoe ^nZ'^aUreL'’fee^°f
fP,nsion of P"”Mry
institutions were established at every five thirty IndV" .POPU!atlOn norms' heaIth
providing at each level the technical ™
th°USand P°Pnlation,
performed. Yet, in large parts of m?
aPP10Pnate for the functions to be
infrastructure remained unrealized on -- C0.Unftry' °Ptlmal utilization of this
under funding and the thin spread faCC°Unt ° a set of multiple factors such as,
vacancies of critical staff; absenteeism duTto XrT^™-1
irregular supply of inputs- and an .m 1
suPervision; inadequate and
hospitals, inadequate investment ovp1^01^1^ environment- In the case of public
the quality of care due to overcrowdingT° ° hme reSuIted in the ’owenng of
personnel, obsolescent equipment and the 10^ Wait' °Vei’WOrked and underPmd
view of these factors, there KXene 7 7 7
°f eSS6ntlaI drUgS' In
health facilities Less than
" Steady decllne In the utilization of public
lheM developmfnis
being incurred for Irea.^n,
»1 hospitalization is catastrophic resulting7
T Th' CUmUlaliVe M »“ °f
m
r
UfoCXdebtXZ
ePi”de
major S
“—re and .he
At appropriate levels' establishm , t
' neCeSSary on contractual basis;
mechanisms for efficient and
anSPaient and administratively simple
management;
L PIocuiement of inputs and logistics
.m".Kforf“l"“l‘th “"sitoto " 0'"' “! “* “iS,inS facili,r
exercise
enabte^XtXbv^T,’nd
■’"J
S“h “
rational sitting „1 fadlHles, aimed to ensure'XulTacces's’toth'e
" m°re
l2Zs°^MoXTpS
irained practitioners of Indian S„sL ’. < . !
'n‘enS‘Ve USC °f “re
training and competency levels the na ° ,Medlclne- BX upgrading
the
pgrading the
competency levels, the paramedical
be
yet
anolher^oplion
can I
or substitute the medical doctor i
the PHC s located
r
------- ininremote
areas; .
doctor in
In view of the overall i
thT
Statesuto dePloy specialists at the CHC's
in accordance with e GOI guidelines, the states will be free to consider
other options, such
Lraimng m aLth^siXy ^"'7’
mOnth
rigorous training iWhich are the skills required to addresfm'" Zb’diTin rU^'
correct imbalances^aTO^fcXto™™^’”1?8'’ “d proSramme strategies to
Will be provided funds by the center for meef^ °!m‘nS StateS' disthcts and areas
costs ol critica, gaps for sa«aet„„lv impiemern.ng S^fo8
7
accordance with the technical guidelines. The center will also intensify its
monitoring to ensure proper and timely utilisation of these funds. Incentives will
also be extended to personnel working in these hardship areas to motivate them to
achieve the goals in a time bound manner.
19. Policies will also be constituted to strengthen the health infrastructure in rural areas
by expanding the State Health Systems Projects to cover all the states, but
appropriately modified to ensure that investments are for the strengthening of the
primary and community health centers, which are used more and have greater
le evance to the poor. Besides, center will also provide financial support for filling
critical infrastructure gaps in public hospitals at district level besides providing
financial and non financial incentives to charitable and non profit organisations to
motivate them to set up facilities in underserved areas.
20. Given the growing complexities in
administering modern day hospitals,
piofessional managers will be inducted to improve the functioning of hospitals,
This measure 1will also free the critically required medical manpower from routine
administrative work and
----- attend
------- 1
patient care. Delegation of financial and
administrative powers and imparting ian overall sense of accountability will be
8ra^ually converting hospitals into autonomous entities under Trust
Managements. The principal objective of these
measures would be to improve
efficiency, reduce costs and improve the utilisation of these public facilities by the
poor. Therefore, performance indicators will be aimed at evaluating not only
quality of the outcomes but also utilization.
7
8
Box 6 •’ Milestones for System Strengthening
Ensure filling up of critical gaps, of resources; p^rsonn^l
pr.onty programmes by rationalizing existing norms and
and administrative
administrative systems
systems j
/
> Develop managerial and technical capacity in the State and District Health =
Societies to gradually take over functions being performed at the center and state !
levels and for developing District Health Planl based
--------- on local epidemiology for !
securing central grants ;
Intensify monitoring at center, state and district level by increased use of IT and i
trained personnel dedicated to the task of concurrent evaluation ;
Establish in all Districts, Disease Surveillance Units to be centrally funded for the (
next ten years ;
Review norms to facilitate re ■ locationing of facilities and redeployment of 1
personnel for ensuring access, efficiency
and°close superv'isi'on
;
FriraT-»z-l
------- ----------- .
> Develop performance indicators and incentives for enforcing the referral system
-
>
,E,'7'tr™l„Tr'S i5HC’/”d
«eds
~
4.
H“P"als h"e
'
P»”«” •"<<
“-"-"ieasons
lo meet loci i
Earmark one out of the four posts of doctor in the CHC for womenIntegrate health education and early screening of diabetes cancer
cardiovascular disease, mental health and eye care in the primary health
'
care j
system by appropriate training to health functionaries and provisioning of
an^ drugs ;
°
ROLE OF THE CENTER AND THE STATES
21
> continue to be directly involved with the implementation of disease control
p:rogrammes by enhancing assistance to all low performing states and districts
stiengthen and speed up the epidemiological transition ;
Monitor the centrally funded programmes in the low performing states in a
mission mode ;
5
Ui a
- Gradually decentralise many of its current responsibilities and functions to
sta es and mstmmons havmg the requisite capability. To such states /
institutions, center will provide assistance to strengthen managerial and
XaniCaLCaPaCltland thereafter release bulk funds on a per capita bafis, further
releases being subject to achieving certain outcomes •
> Redirect its energies and capacity to focus on providing leadership in settine
echnical standards and the strict enforcement of quality; ensuring universal
cess to health care; containing costs through medical audit and olher policy
instruments; enforcing compliance to regulations regarding the private secto^
drugs, prevention of food adulteration; implementation of insmance
programmes for the poor and eligible target groups; closely monitoring and
eeping a strict vigilance through a well knit surveillance system to ensure no
resmgence of diseases that have been controlled; development of health
s anstics, advocacy and motivation of NGOs'; and social mobilisation for health
thiough health education campaigns etc.
9
.
5.
The center will also actively consider either making the CGHS and MSD into
professionally managed concerns with appropriate managerial autonomy or
close them down altogether and look at other options;
> The states will likewise be motivated to devolve their functions and funds to
district levels. Hospital Trust Committees and locally elected bodies in similar
fashion. The priority attention at the center and state levels will be to improve
the overall governance regarding health programmes;
The Districts will be administrative units for health programmes while the
villages will be the units for health action. Every village will have Village
Health, Nutrition and Population Committees consisting of 6-10 members,
trained to discharge health functions and ensuring every home with access to
sanitation, safe water and health facilities. They will also be trained to do simple
tests such as a urine test, taking blood pressure, dispensary medicines for
treating minor ailments, particularly, traditional medicines and those modern
medicines, which have no side effects and referral. States will be encouraged to
ecentrahse several health related duties and responsibilities to the locally
elected bodies along with a reasonable budget;
PRIVATE SECTOR
The pnvate sector is the dominant provider of health services with a substantial
share of 80/o outpatient treatment and 55% of inpatient care. Rising incomes and
demand for improved care stimulated the growth of the private sector. However,
due to the absence of a regulatory environment, the spread has been uneven, quality
inTcostly5 miXed/ ran8e °f SerV’CeS narrovv with a hlgh propensity for over diagnosis
For harnessing the available potential the NHP will seek to involve the private sector
in the implementation of all national programmes and also in,providing good
quality health services to the people, subject to fair pricing and an accountability to
patient satisfaction. Financial incentives will be extended to the non profit charitable
institutions willing to set up hospitals, medical or dental colleges in the poorer states
and poorer regions as identified by the government but subject to free care to the
poor through referral by public health institutions. Regulations to ensure adherence
o standards and quality will be formulated on priority. Finally, the requisite
capacity for monitoring the enforcement of regulations will be developed at the
private hospitals
AU aUtOn°mOUS b°dy wil1 be established for accreditation of
Partnering with the private sector will be encouraged, particularly for providing
support services in all hospitals such as security, laundry, sanitation maintenance
laboratory
.a^aeory support,
support including
including fee
fee per service contracts for specialized services
Govemment will also extend financial assistance and encourage establishment of
consumer forums and enforce a patient charter in all hospitals, public and private.
6.
HUMAN RESOURCE DEVELOPMENT - FOR A BALANCED MIX
22. The present health system is highly skewed in favor of medically trained doctors to
e neai exclusion of other paramedical and non-medical disciplines The
unbalanced mix of skills and the virtual non availability of some of the sorely
required manpower and specialists such as pediatricians, anesthetists^^
ophthalmologists, surgeons, epidemiologists, entomologists, microbiologists'
nurses, laboiatory technicians, ophthalmic assistants etc. in the low performing
10
states is one of the reasons for their low achievement. Besides, quality of training
and standards m instruction have also been affected due to obsolescent equipment
run down facilities for want of capital investment and the policy of permitting
teaching faculty to do private practice.
23. The NHP will aim to
restore teaching standards and ensure quality. For this, reform in the
examination and evaluation systems will be initiated;
A corpus for providing interest free loans to government medical colleges for
improving the infrastructure and procurement of equipment will be set up- States will be encouraged to establish Universities of Health Sciences for better
integration and standardization of training quality;
High priority will be accorded to increasing the number of nursing colleges and
giadually phasing out / or drastically upgrading the old ANM schools to meet
the emerging challenges and requirements;
Curriculum will be suitably restructuredI to allow for the development of the
community health stream and the clinical stream. This will be an important
step. Bifurcating the doctors at the graduate level, will enable a more efficient
deployment of personnel. Those taking up community medicine will be posted
m the PHC/CHCs' and later as
managers in charge of public health
programmes, while those specialising in clinical disciplines will
work in
hospitals and medical colleges. Such development of a cadre of Public Health
oriented doctors and nurses is required to meet the challenges of the dual
burden of disease, where containment of non communicable diseases will have
to rest on community based strategies with focus on prevention and behavioral
change.
The 10+2 vocational stream will be integrated to the production of required
"“J11ber of lab°™tory technicians ophthalmic assistants and other para medical
>
In recognition of the extreme importance of public health to the country the
three premier public health institutions, namely AIIHPH , NICD and NIHFW
will be made autonomous and upgraded into Institutes of Excellence. Action
will also be taken to encourage states to strengthen existing infrastructure to
upgrade public health training.
B°X 7 :
IgPorlant Initiatives for Improving Training and Medical Education
Establish an Autonomous Medical Grants Commission provided ^thTco7^h^d “
telchmJs^d d lnbaStrUCtUre of government medical colleges and adherence to
teaching standards and giving accreditation to colleges ;
> Ban private practice by teaching faculty and provide incentives ;
!nefpISerCdrr‘CUJUnl tO SUit the health needS Of the COUntry and Introduce credits for
integrated medicine;
I
> Identify scarce disciplines and provide incentives to attract students •
> Gradually make all medical colleges autonomous institutions with Government
EstabHsh^ Ti gT^ SUb,eCt t0 meeting ‘aid d°Wn S0Cla' obiectives and standards;
E^abhsh a National Exammation to be cleared for obtaining a license to practice and
provide for mandatory exammation every five years for renewal of license> Encourage private investment in the establishment of medical colleges and nursing
school subject to equitable distnbution of these colleges for ensurmg a mom
balanced growth of medical infrastructure, tight control on quality and fees to be
cnargecl;
> Dev?loP a ?adre of Public Health specialists
11
legal provisions
° removin8 discretionary powers of
state and
and central
central governments
governments
state
> Enforce
E„fo,„ a. j,„!<.‘ .K.,
h,
f
K do twq>
rural service at the PHC and C'-~
CHC to be ehgible for PG degree. This shall be a
conditionality in the case of all students who
- ...j get tuition waivers, fellowships or
subsidized education.
7.
IMPACT OF GLOBALIZATION
India is a substantial contributor
to the global disease burden,
reversed.
which needs to be
B°X8:
Popul
ation TB
Cases
17
Problems (in %)
Poverty
Leprosy
cases
Total
Deaths
Child
Deaths
36
17
Mat
ernal
Deaths
23
20
j
Persons
TB
with
Cases
HIV
14
I 30
arrangements. ThXroS^
Lepr
osy
cases
68
t0 changes in global
markets have to be responded in a suitable nr, d
7 °f
Particil?ants and
nnU
minimize losses. Import Agreem^^::" 2 ™SnSniiZ<i
impact upon and influence India's abilitv
SPS' and GATS' wi]l
prices; food and nutrition security and snf u ■
e.SSentlal drugs at affordable
border movement of consumers and " .^.y' qUa “y of Pharmaceuticals; and cross
deplete critically required -ourcesld ^enX^i™;^^
with new order as XLue^below appiOpnate safcguards and strategies for coping
Box - 9
.................
TRIPS
from the NEDL;
P^t.t.oners m the public and private sector to prescribe drugs (
>
I
I
!
by strengthening supervision fof wh.ch^FDA to be^TbM a'ld enforcin8 cJuality standards j
prescription and by licensed pharmacists will be enforced
'
Guidellnes regarding sale by ’
SPS
>
I
fety |
I >
I >
I >
!X6Xree"“”s
-n8
sacrificing
Strengthen
a„d
b,parlmen|s
levels to work i
at central and state
—• in partnerships with private industry, consumer
organisations etc.
groups. International [
12
GATS
Develop an Action Plan with the objective of ensuring no depletion of critically required <
expertise and personnel from the public sector on account or migration to private facilities or I
abroad; maximising the comparative advantage India has in skilled human resources; and !
earning!- 6X151108 ,netlultles d° not "’iden "'WIe at the same time increase foreign exchange I
i >
Accord high priority to quickly upgrade and improve quality and standards of medical
education and paramedical training;
■
Establish quality assurance mechanisms and standards of care;
|
Expand the number of institutions, particularly nursing;
j z- Encourage investment, including from the public sector, to establish high quality care
hospitals and medical colleges and nursing schools etc. at designated areas for attracting
!...... j<
-------!orc’,811
^ome an^ establishing centers abroad.
8.
RESEARCH
For various reasons, research on tropical diseases that are of most concern to us has
attracted a low priority, globally. Besides, combined with the imperative need to reduce
risks that arise• from imbalanced dependence on
< external knowledge, there is an urgent
need to invest on promoting indigenous resea
research by having a National Health Research
1 obey. The salient features of such policy will be to encourage the development of
undamental research in areas relevant to health and develop over time a critical mass of
scientists engaged in futuristic areas such as biotechnology, genomics based drug
development, optimal utilization of molecular biologic developments for diagnosis,
therapy and prevention etc. Establishment of appropriate infrastructure and microbial
containment facilities, gene and tissue banks etc. will be pursued. Optimal utilization for
Information Technology will be given high priority. Greater collaboration between
esearch Institutions on areas of national priority will be encouraged and a system of
dissemination of research results set up under a National Research Forum. Most
importantly, financial incentives will be provided to encourage research devoted to
HIV/AIDS, MDR TB and other drug and pesticide resistance under the malaria
programme.
IV.
POPULATION STABILIZATION
Hie elective implementation of population
population control
control policies
help reduce
reduce disease
disease
policies will
will help
burden, improve quality of life and general health of the people. In the context of
decreasing future burden of non communicable diseases which are expensive to treat,
the reduction of low birth weight babies by improving the nutritional status of the
mother and spacing of pregnancies is critical as, recent findings suggest that impaired
foetal nutrition results in susceptibility to adult cardiovascular disease, diabetes and
some cancers. Besides, propagation of safe sex also has the double benefit of reducing
disease transmission on account of HIV/AIDS in the general community. In view of
these linkages to health status, population control measures will be integrated with the
promotion and delivery of health services by the private and public sector.
13
SETOP rSXRING °F THE ADMINISTRATIVE
SETUI FOR COORDINATED IMPLEMENTATION
has” bee’n dividTd’11 diS“b“,i°n in 'he heal,h J'P”lments at the state and district levels
z-E-Sir—F-""—='=~3
■constitute the departments and directorates
primary health care involving far rr8
] f
and Programmes pertaining to
under one head and hosnital
aCtlVlties lmplemented at CHC and below
another
P
lces' manpower planning and regulatory aspects under
VI
legislation
and enact 7eg eSoX Zbl b 1 enK''"CntS
a"d
Mi°" “>
herein. parSXXT to X
7“ ‘"T'’11'’” lh»«
been incorporated
Sector. cLXXjbX-"
'b'
ReS“'a'iOT »'
VII
NEW STRUCTURES
•» "’"■’age new co....... L „„
Intersectoral
t
>■
Surveillance Units, Coordination Committees for
nuXo,:lc ;
viua^Regoiators
“’■*
AU,°n'°va,er
m°US vr
U",,s!ani,a
a"d 'I"s“™nee
and Sickness Funds AnlhorSX
14
NATIONAL HEALTH POLICY - BACKGROUND PAPER FOR DISCUSSION
Objectives
The main objective of the NHP-2001 is to achieve an acceptable standard
of good health amongst the general population of the country.
The approach
would be by increasing to the access the decentralised public health system by
establishing new infrastructure in deficient areas, and by upgrading the
infrastructure in the existing institutions. A central objective would be to ensure
more equitable access to health services across the expanse of the country.
Emphasis will be given to increasing the public health investment through
substantially increased contribution by the Central Government. The contribution
of the private and NGO sector in providing health services would be much more,
particularly for the group which can afford to pay for services. Increased sectoral
share of allocation will be provided for preventive and curative initiatives at the
primary health level.
Emphasis will be laid on use of rational drugs within the
aiiopathic system, appropriately supplemented with tried and tested systems of
traditional medicine. Within these broad objectives, NHP-2001 will endeavour to
achieve the iime-bound goals mentioned in Box-1.
Fundamental Determinants which impact on the goals of Health Policy
Financial Resources
A progressiva increase in the public health spending of which a substantial
part has to come in from the Central Government is a key factor is achieving the
public health goals set in the NHP 2001.
It is noticed that the proportion of
Central Government budgetary allocation for Health of the total budget remains
stagnant at 1.3 per cent. In the States this proportion progressively declined from
7.00 to 5.5%. The Central share in total Health spending of States is about 15%.
The poor financial health of State Governments and their inability to spend
adequate resources for social infrastructure like health has contributed to overall
decline in public spending on health care infrastructure in the country. Taking
1
I ’
.. r'- •;
;v‘
this into consideration, it is planned to increase health sector expenditure to 5.0/o
of GDP with 2.0% of GDP being appropriated to public health investment by the
year 2010. The States should not only try to arrest the declining trend in public
health expenditure but should restore it to 7% by 2005 and progressively
•iuu,
increase it to 8% by 2010.
.7 ::
The, provisioning of higher public health investment will also be dependent
■upon the increased absorptive capacity of health administration to gainfully utilise
the funds in the States. In order to ensure that the access to primary health care
is maximised, at least 55% of the public health investment should be
appropriated to primary health care, the remaining going to secondary health
care (33%) and the balance to tertiary health care. The Central grants in tot'
health care spending by the States should also be increased from the present
;i ,.15% to 25% by 2010.
I,-.
Equity
While inadequate resource allocation led to sub-optimal performance in
public health in the country as a whole, there are wide variations in performance
between better performing and lower performing States, between rural and urban
: .-i it
..1.
. i.
rich and poor and men and women. These differentia’s impact
areas, between
L .
directly on those sections of the society who bear the double burden of poverty
. and social discrimination. Box 2 shows the differentials in health status aero
■
States.
• •(
To ensure equity in allocation of resources and to minimise the
•0-
differentials in health status, the following measures are proposed:
kt;. J
.SCii.:-
.1 ’ ’
•
i.
Increased public spending on health at the grass roots level to strengthen
...r,
the primary health care system
2
ii.
Special needs of socially vulnerable sections like Scheduled Tribes,
nomadic communities, urban slum dwellers, need targetted programmes
for improving their health status.
iii.
There should be provision for social security for poor and vulnerable
sections who lose their life's savings in attending to care and support of
t
members of their families. NHP 2001 will promote social insurance
schemes and encourage States to establish a sickness fund for covering
the cobt of treatment for families below a certain income level.
iv.
Strengthening the public health delivery system: The serious gaps in
infrastructure act as a big determinant in delivering health care to people
living in rural and remote areas in the country. Increased commitment of
resources for primary health care is of prime necessity in strengthening
the delivery system. Shortage of doctors in primary health care institutions
can be met by organising a cadre of Licentiates of Medical Practitioners
(LMPs) and more intensive use of trained practitioners of Indian system of
medicine. The States should liberalize the process of recruitment and
encourage trained professionals to be employed on contractual basis
through simplified administrative procedures.
v.
A big disincentive for people in the rural areas to access primary health
care is the absence of drugs and other consumables in many of these
.i
centres. Drugs and consumables are important components of public
health-care delivery system. To set this right, NHP'2001 would commit
financial resources from the Central Government for funding of the drug
and equipment costs of primary health care centres through a simplified
procedure. The procurement procedure for these drugs and consumables
should be as simple and decentralised as possible. ' '
vi.
There are impediments in the flow of resources' from the Central
Government to programmes operated at the field level like the national
3
disease control programmes. There should be a proper arrangement to
streamline resource-flow to priority programmes. Formation of Health
Societies at the State and district level wold facilitate direct transfer of
funds from the Central Government to the operating
units at the field
level without the usual budgetary constraints.
The Society model
which has initially been experimented in some States has proved to be an
effective delivery system for implementation of targetted public health
programmes and should be adopted by all the States at the State and
district level.
Role of States
States have the primary constitutional responsibility to provide health care
to its people. However, the health care delivery system in many States remain
largely centralised at the Departmental level inspite of the strong and effective
presence of institutions of local self-government at village, block and district
levels. Decentralised management of health institutions especially those at the
primary level through Panchayati Raj institutions is strongly advocated in the
NHP 2001. Flow of Central funds to States for public health programmes Should
be effectively linked to the performance of the States in the area of
decentralisation of programme management to the PRIs.
Decentralisation of programme management should also be reinforced by
convergence of all vertical public health programmes at district level and below.
This will lead to economy of scale and avoid duplication of effort on areas like
IEC, training, etc.
The health care functionaries at the field level now operate under various
Departmental authorities with control at the State level. There is need to bring in
convergence in their work even though it may not be possible to bring them
under one administrative umbrella Personnel like Anganwadi workers, ANMs,
4
male health v/orkers, link volunteers, etc. can be brought on a common platform
for effective delivery of health care at the primary level.
States should also accord priority to school health programmes aiming at
preventive health education, regular health check-ups and promotion of health
seeking behaviour among school children. Investment of resources in school
health programmes would have a long term impact on the general health status
of the people may reduce the requirement of public health spending substantially.
The States should actively involve the private sector in public health
programmes. Medical practitioners in the private sector can be effective
implementers of national programmes for reduction/control of communicable
diseases, spreading awareness about non-communicable diseases and promote
healthy life styles among the people. NGOs and community-based organisations
should find an increasingly important role in the public health programmes for
1 social mobilisation through health education campaigns.
The States should also try to bring in effective linkages with other social
sectors like education, water supply, sanitation and nutrition which are also
contributory factors to improving the general health status of the community.
Convergence of socially-relevant programmes in these sectors with the health
sector would bring in greater effectiveness in implementation.
Private Sector
Private sector is'the dominant provider of health care services with a
substantial share of 80 per cent in outpatient treatment and 55% in inpatient
care. But due to the absence of a regulatory environment, the quality of service
suffered leading to lack of accountability among the private sector health care
providers. NKR 2001 envisages a strong and effective regulatory mechanism for
private sector health care institutions and diagnostic facilities by enactment of a
statute. The law will spell out the minimum statutory requirement for setting up a
5
health
care institution and establish
qualitative
standards
to
bring
in
accountability. With this effective controi. tertiary heatth care can large.y be iett to
the pnvate sector. With proper financial Incentives, the private sector can be
helped ,n channelising the resources to priority areas
of clinical care and
management at the tertiary level.
Human Resource Development
As m other areas, there is serious regional imbalance in availability of
qualified medical practitioners and nursing and para-medical personnel across
the country. NHP 2001 envisages financial support to under-served States in th
country for providing medical education through establishment of medical/dental
colleges, nursing colleges and other health care institutions. The Central
Government should be able to provide adequate resources to these States for
promoting centres of medical education.
The present educational system iis heavily accented towards clinical care
at the expense of public health. INHP
-------2001 will try to give primacy to public health
in medical education. Adequate incentives
----- > will be provided for young medical
aspirants to choose public health as a
career. The experience in other countries,
especially in the developed world
snows that public health needs qualified
managers arid not merely clinicians There is therefore a strong case to open
public health to non-medical professionals which will substantially improve the
quality of the public health cadre
-------- iin the country.
Even in postgraduate medical education, there is wide disparity across
discrphnes which led to neglect of public health-related specialities. The Policy
would actwely try to bong down this disparity and give greater encouragement for
postgraduate medical education in public health-related subjects.
6
.1
Npn*<fctermjnant issues
Research:
Biomedical research in India has not kept pace with fundamental
and applied research in other scientific and technological fields. The Policy will
aim at encouraging development of fundamental research in areas relevant to
health. There should be investments in futuristic areas like biotechnology,
genomic-based drug development, molecular biology, etc. Research in vaccines
and therapeutic drugs for important diseases like HIV/AIDS, cancer, MDR TB,
would be actively promoted by the Government. The Indian Council of Medical
Research will play an increasingly vital role in promoting biomedical research and
transfer of technology to the manufacturing sector. The country should also
develop technical competence in the area of Patent Regimes and in filing
Product Patents for inventions. The scientific institutions should gather adequate
expertise in patents and in understanding the global implications of a patent
regime.
Disease Surveillance and Response: Even though vast sums of money have
been spent on control ot communicable diseases, they continue to take their toll
through outbreaks in various parts of the country. In most’cS? these cases, lives
could be saved if the response were to be quick and effective. In the absence of
a proper surveillance and reporting system, valuable lives are lost in outbreaks of
1-1;
even curable diseases like malaria, GE, cholera, JE, etc. Building an effective
surveillance system was accorded a very low priority in the country till recently.
The surveillance system on polio and HIV/AIDS have demonstrated
that the
Centre and the States can build an effective response to control of diseases by
getting critical and timely information. NHP 2o8'l would strive to build an
integrated disease surveillance system for the entire country initially for
communicable
diseases which will
later be
communicable
diseases
effective
also.
An
expanded to
networking
include
of public
non-
health
laboratories with health care institutions to provide results of samples is an
important component of an effective surveillance system.
7
The country also does not have a proper national health accounts which
acts as a handicap in planning and management of public health programmes.
Development of a proper health management information system would lead to
establishment of a reliable national health accounts which will be one of the
priorities of NHP 2001.
Information, Education and Communication:
Public health programmes
need strong visibility. In a country with around 35% illiterate population, effective
communication of public health-related issues is a big challenge. The NHP 2001
would strive to develop a national IEC strategy for health communication, health
educational programmes, specially tailor-made to rural and illiterate populace. A
the national health programmes should have a very strong component of IEC
which should be implemented not only through Governmental media tiut through
NGOs and community-based organisations. Promotion of a healthy life style is
incumbent upon provision of health messages targetted at different groups like
women, students, youth, migrant workers, etc.
Population Stabilisation: The Population Policy 2000 has certain immediate,
mid-term and long term objectives. The long term objective is to achieve a stable
population by 2045. The Policy sets certain socio-demographic goals for 2010
which are also relevant to the National Health Policy - 2001. Prevention and
control of communicable diseases, containing the spread of HIV/AIDS, universal
immunisation of children against all preventable diseases, addressing the unmet
need
for
basic,
reproductive
and
other
health
services,
supplies
and
infrastructure are goals which run like a common thread in both the Policies The
objective of NHP 2001 to achieve an acceptable standard of good health among
the general population of the country can be attained through these socio
demographic goals set in the Population Policy. Improving the general health
status of the populace in our country will in itself be a contributory factor to faster
population stabilisation.
8
Box |: Goals to be achieved by 2(XX)-2O15
>fo
>
>
>
>
>
Eradicate Polio and Yaws
------------- ----------- -—
Eliminate Kala Azar and Leprosy------------------------ -----Eliminate Lymphatic Filariasis------ ;---------- ;------ - ------- -Achieve Zero level growth of HIV/AIDS---------- --------Reduce Mortality by 50% on account of TB,
Malaria and Other Vector and Water Borne
diseases____________________ _______ _ _______ _—
> Reduce Prevalence of Blindness to 0.5%----------------> jReduceTMR to 30/1000 And MMR to 100/La_kh-------> Improve nutrition and reduce proportion of LBW
Rabies from 30% to 10%
_—--- -------> Increase utilisation of public health facilities.from
current Level of <20 to >75%------------- -------------------> Establish an integrated system of surveillance.
National Health Accounts end Health Statistics.-----> Increase health expenditure by Govemjment as a
% of GDP from the existing 0.9 % to 2.0%
> Increase share of Central grants to Constitute at
,2005
2010
2015
2010
2010
2010
2010
2010
2010
2005■
2010
2010
least 25% of total health spending--------------------------
■ J ■
I
’zT
■
Box 2 : Differentials in Health Status Among States
Indicator
Populat
ion
BPL
(%)
INDIA
Rural
Urban
Better
Performing
States_____
26.1
27.09
I
23.62
........... !
MMIV
IMR/
<5Mo
Weight
Leprosy
Lakh
Per
rtality For Age
cases per
per
1000
Children (Annual
10000
Report
Live
1000
Under 3
populati
2000)
Births (NFH
% <on
(1999SO)
2SD)
SRS)
70
94.9
_47_
408
'■ ..........
3.7
.
75
■ _1°3 J ' 49.6
’ 44“
' 63.f ; 38.4
J
12-72 '
25.02 :
21.12 i
14
4B
52
Low
Performing
States______ [
Orissa
Bihar
Rajasthan
UP
MP
;
47,15 ■
4260 i
I 15.28 !
i 31.15 i
97
63
81
84
i
90
!
37.43
2200
‘
!
i____ i
Kerala
’
Maharastra i
TN
"Mala
ria +ve
Cases
2000 (in
'000)
■ 18.8 i
' 58.1 j
; 63.3 :
kJ
j 104.4 I
i 105.1 !
i 114.9 !
i 122.5 i
i 137.6 ;
Io -
27
50
I
i
37
87
135
79
119
’ll
4.1
5.1
138
56
i
i
54
54
51’
52
55
I
i
498
707
607
707
498
7.05
11.83
0.8
_4.3 _
3.83
483
132
53
99
528
J
I
Box 3 : Achievements Throngh The Years -1951-2000
INDICATOR
1951
DEMOGllAPHIC CHANGES
Life Expectancy
__________
. 36,7
Crude Birth Rate
i 40.8
Crude Death Rate _______ _
25
pMR
146
1981
1
7000
54___ 64.6(RGI)
■
26.1(99 SRS)
8.7(99 SRS) '
70 (99 SRS)
33.9(SRS)
12.5(SRS)
119
I_________
| EPIDEMIOLOGICAL SHIFTS
j Malaria (cases in million)
Leprosy
cases
per
10,000
population__________________
Small Pox (no of cases)
27.
57.3
>4-4,887
Eradicated
>39,792
I
T
I
2<?709
I
Guineaworm ( no, of cases)
Polio__
INFRASTRUCrURE '
T
SC/PHC/CHC
725
57^63
Disf>ens.iries <fcHospitals( all)
9209
23,555
117,198
569,495
Beds (Pvi & Public)
I
75
38.1
22
3.74
Eradicated
265
1,63,181
(99-KJrIS)
43322
(95-96-CBHI) j
8,70,161
[
(95-96-CBHI) ;
Doctors^ Allopathy)
61,800
Nursing Personnel
18,054
2,68,700
1,43^87
i
5,03,900
(98-99-MCI) !
7,37,000
(99-INQ
/I-
i
|
■ ■ ®
.
gox-^:
% fubtic Heatth Spending In select Countries
Indicator
%Population
with Income
of <$1 day
India
China
Sri Lanka
UK_____
USA
44.2
18.5
6.6
Infant
Mortality
Rate/1000
%Health
Expenditure
to GDP
I
72
31
16
6
7
Source: WHR 2000
-/2 -
52
2.7
3
5.8
13.7
%Publfc
Expenditure
on Health to
Total Health
13
24,9
45.4
96.9
44.1
1
Campaign on Access to Essential Medicines
A National Convention, jointly organised by the Jana Swasthya Abhiyan (Campaign for Peoples
Health) and the Federation of Medical Representatives of India (FMRAI) was held in New Delhi on
14th June, 2001. The Convention was addressed by leading public health experts, academics, leaders
of trade unions, women's organisations, farmer's organisations, peoples' science organisations, as
well as representatives from FMRAI and JSA. The Convention adopted the attached Charter on
Access to Essential Medicines. It also resolved to launch a nationwide campaign based on the
charter, the salient targets of which would be:
•
Setting up campaign committees in all States of the country
•
Carry out mass demonstrative actions in State and District centres across the country in the
form of rallies, convention, and other protest actions.
•
Collect 10 million signatures supporting the Charter by September 2001.
•
Organise a mass protest rally in New Delhi in November 2001.
Peoples Charter for
Access to Essential Medicines
1. No privatisation of the public healthcare system.
2. More per capita budgetary expenditure on healthcare.
3.
Increase the number of National Diseases Eradication Programmes and enhanced budgetary
support to each programme.
4. Revitalise public sector drug companies.
5. Develop a public distribution system for cheaper essential drugs.
6. Formulate a rational drug under the aegis of the Health Ministry.
7. Ensure production and availability of all drugs in the national Essential Drug List.
8. Control import of bulk drugs and finished formulations and rationalise duties on imports.
Restrict import keeping in view the needs of domestic producers.
9.
All drugs should be assessed periodically, in order to ban hazardous and irrational drugs.
10. Formulate a new Drug Prices Control Order to bring all drugs under price control and to reduce
prices of essential drugs.
11. No change in the fundamentals of the Indian Patents Act, 1970, that allow domestic manufacture
of patented drugs to counter monopoly, high prices and imports.
12. Utilisation of third party licensing by big companies to evade taxes, reduce employment and
utilise cheap labour should be stopped.
13. Uniform tax structure for all drugs, maximum retail price should be inclusive of all taxes.
14. Strengthen quality control mechanisms to stop proliferation of spurious and sub-standard drugs.
15. Enquire into corrupt practices by drug companies involving tax and duty evasion.
16. All government purchases should be made through a central procurement system, based on the
list of essential drugs.
17. No Foreign Direct Investment (FDI) be allowed in the pharmaceutical sector, except where
there is clear indication that such investment will be accompanied by transfer of technology not
available in the country.
1
Explanatory note on Peoples Charter
for Access to Essential Medicines
Withdrawal of the Government from Health Care
A series of policy changes by the government - including some that are on the anvil - will have a
direct effect on access to medical care in the country. The Insurance Regulatory Authority Act, for
example, is designed to facilitate the introduction of private health insurance, and also to allow
entry to MNCs in the health sector. It, moreover, allows the government to legitimise its withdrawal
from investing in health care.
Public expenditure on health care has been a major casualty of the process of economic
liberalisation and structural adjustment policies. Central allocation to State governments for health
has declined, thereby forcing many States to procure loans from lending agencies such as the World
Bank. Such loans are invariably associated with conditionalities that are directed at a transformation
of the public health system. Such a transformation is sought to be achieved through mecahisms such
as introduction of user charges, purchase of medicines through global tenders, farming out of
primary health care centres to NGOs -- in others words, mechanisms for privatisation of the public
health infrastructure and delivery system.
In many States we already witness the shift of administrative responsibilities in health care delivery
to NGOs and other private organisation, thus minimising the role of elected representatives. This
will further facilitate the privatisation of the health infrastructure. Implementation of such
prescriptions, put forward by the World Bank, has led to utter chaos in the public health
infrastructure in countries in S.America and Africa — a fact that is admitted to even by the World
Bank.
Investment by the government on health care (less than two percent of the budget) in India is one of
the lowest in the world. Per capita investment in health is only Rs.57 a year and 87% of health care
costs are paid for privately. Notwithstanding this the government has not only reduced expenditure
on disease eradication programmes, it has also reduced the number of programmes covered. We see
today a resurgence of communicable diseases, and while old diseases like tuberculosis, malaria,
kalaazar flourish anew, newer diseases have started manifesting themselves — including the
looming threat of an AIDS epidemic. What is urgently required is not a cutback on existing
programmes but a major expansion of disease control programmes.
Abandonment of Price Controls
While access to drugs constitutes only a part of measures required to confront a major public health
crisis, it is still a necessary part. Recent policies that have been announced by the government are
poised to further cut access to essential medicines, especially for the poor. In the recent budget the
government has announced its intention to slash the number of drugs under price control. Moreover,
such changes are being mooted not by the Ministry of Health or even the Ministry of Chemicals, but
by the Finance Ministry.
The move to further reduce the span of price control is directed at improving the health of the
industry and not the Indian people. Since the introduction of the first comprehensive drug policy in
1978, all subsequent policies have pandered to the needs of the industry. While the 1978 policy had
343 drugs under price control, this was reduced to 166 in 1987 and further to just 73 in 1994.
Profitability allowed in controlled categories was increased in this period from 40-75% in 1978, to
75-100% in 1987 and finally to 150% in 1994. It is now proposed that just 15-20 drugs will be kept
under price control — thereby virtually making the whole policy of price control redundant. We
already have a situation where the prices of essential drugs like anti-TB, anti-leprotics.
cardiovascular drugs, etc. are rising at a significantly higher rate than the rate of inflation, and the
situation can only worsen as price control is further relaxed. Many drug companies are known to
openly flout the existing DPCO by not submitting cost-data to the National Pharmaceutical Pricing
2
Authority (NPPA). The pharmaceutical industry has openly expressed its displeasure over the
NPPA (constituted about 5 years ago) and the new pricing policy might decide to scrap the NPPA.
A new Drug Price Control Order, in fact, needs to do quite the opposite of what is being proposed —
increase the span of price controls, so that all essential drugs are put under price control.
Skewed R&D Policy
Almost two years back the Govt, had appointed two committees - one to prepare policy guidelines
towards R&D and the other to review the existing Drug Price Control Order (DPCO). The
committee on R&D, among other recommendations, proposed the setting up of a corpus fund of
Rs. 150 crores for the pharmaceutical industry. In India the private sector had done little R&D for
drug development, while major R&D work has been largely done in public funded institutions like
CSIR laboratories. While the specific mechanisms for setting up the corpus fund are awaited, it is
apprehended that this fund would be created by imposing higher taxes on drugs. Thus the private
sector, in spite of its poor record in R&D, will be allowed another largesse by the government.
Instead it would make much better sense for the government to invest in strengthening public
funded R&D.
Revitalise the Public Sector
Even today there is a large infrastructure for manufacture of drugs in the public sector. Of these, the
production units of Hindustan Antibiotics Ltd. have been rented out to private enterprises, who are
making profit out of it. The Indian Drugs and Pharmaceuticals Ltd. (IDPL), once the largest
company in the pharmaceutical sector in India, has been lying idle since 1996 and the Bureau of
Industrial Finance and Restructuring (BIFR) has recommended that the company be wound up.
HAL and IDPL, in the formative years of the drug industry in India, were the largest manufacturing
units in the country and played a major role in helping the country become self reliant in the area of
production of essential drugs. Moreover these two companies pioneered production of drugs from
the basic stage in the country, and were the first to challenge the monopoly of MNCs. Unfortunately
the same conditions which led to these companies becoming sick still exist — corrupt and inept
management at the highest levels coupled with a lack of direction. Today, faced with a change in
the patent system and a renewed challenge from the Multinational Sector, these public sector units
(IDPL, HAL as well as Bengal Chemical, Bengal Immunity and Smith Stanistreet) still have a
major role to play. Given the will and the vision these public sector units can be revitalised and can
play an important role in making available life saving and essential drugs at cheaper prices.
Public Distribution System
It is estimated that 60-70% of the Indian people have little or no access to medicines, primarily
because they cannot afford such medicines and the public health system is woefully adequate. In
such a situation the government needs to establish a public distribution system for drugs, through
which all essential drugs at subsidised prices (where necessary) should be distributed.
Ensure Rational Drug Use
A large number of hazardous and irrational drugs are sold in the market. Sale of such drugs is not
only a major health hazard, but also deflects scarce resources away from essential medicines. Such
a situation has been made possible because there is no real drug policy in existence — merely a
pricing and licensing policy. Companies, as a consequence, are able to sell these medicines with the
help of their high-pressure unethical marketing. A rational drug policy under the aegis of the Health
Ministry (and not the Industry Ministry) is the first necessary step to remedy this situation. Such a
policy needs to prioritorise drug needs of the country on the basis of a list of essential drugs, ensure
production of quality drugs at cheaper prices and minimise import. The policy should also devise
means to ensure rational drug production and usage.
3
Stop Unethical Promotion
Steps are required to put a check on the unethical promotion of drugs. In spite of repeated
assurances the government is yet to enforce the ‘Criteria of Ethical Promotion of Pharmaceuticals’
prepared by the WHO. In recent years there is a noticeable tendency towards marketing of
expensive new drugs, most of which have little or no advantage over older and cheaper drugs.
These drugs, many of them being imported, are marketed with the help of lucrative inducements
offered to a section of the medical profession and chemists. Therefore a rational drug policy should
include mechanisms to ensure ethical drug promotion and prevent the import of non-essential drugs.
Reverse Import Liberalisation
Following the liberalisation of imports, multinational drug companies are closing down their
production units in the country. They are either importing their products from their parent
companies or getting them manufactured in the small scale sector. This has led to a sharp increase
in imports in the last two years, while closure of large production units has caused unemployment
of thousands of workers. While mergers, acquisitions and brand selling has flourished, there is no
significant investment in the industry. All these have led to increasing unemployment and loss of
job security in the pharmaceutical sector. Liberalised imports have also forced the closure of many
medium scale bulk drug companies who face competition from cheaper imported bulk drugs.
Urgent measures are required to stop unrestricted import of bulk drugs through appropriate duty
structures that favour domestic manufacturers.
Save the Indian Patents Act, 1970
The Indian Patents Act of 1970 was instrumental in helping the country achieve self reliance in the
production of drugs. It helped Indian companies introduce new drugs within 2-3 years of their
introduction in the global market, that too at prices that were one-tenth or less of global prices. It
also encouraged the development of process technologies for a large majority of essential drugs,
principally in public funded institutions. Today the government is poised to change the Indian
Patents Act in order to "honour" its obligations at the WTO. Changes envisaged will reverse most of
the benefits of the earlier Act. It is of vital importance that the new Act retain licensing provisions
that allow domestic manufacturers to manufacture patented drugs if monopolies are created, if
prices are high, or if domestic manufacture is not done by the original patentee. Various other
safegaurds need to be built in to see that all the gains of the 1970 Patents Act are not frittered away.
Today many developing countries, who amended their Patent Acts in accordance with the TRIPS
accord are faced with exorbitant prices for new drugs — a situation that has brought the whole
continent of Africa, reeling under the onslaught of an AIDS epidemic, to the brink of a disaster.
Many of these countries are today prepared to come together and unitedly demand a revision of the
TRIPS accord. The issue has also led to the building of an unparallelled global coalition that is
prepared to question the TRIPS accord. India has, arguably, the most developed pharmaceutical
industry in the developing world. Instead of rushing in to amend its Patents Act in a foolhardy
manner, India needs to provide leadership to the rising tide of discontent all over the globe, against
the TRIPS accord.
Stop Third Party Manufacture
The government allows large companies to get their drugs manufactured in the small scale sector,
even if they have the capacity to manufacture such drugs. This opportunity is being misused by
many large companies, some of whom have even closed down their factories. This facility for "third
party manufacturing" allows big companies to utilise exemptions provided to the small scale sector
and also to reap the benefits of cheap labour costs in the small scale sector. Moreover, such
manufacturing leads to poor quality control and increases the presence of sub-standard and spurious
drugs in the market. Many large companies, however, are content to reap profits as mere traders,
leaving the manufacturing to the large, unorganised and poorly monitored small scale sector.
4
Stop Tax and Duty Evasion, Rationalise Taxes
Unregulated manufacturing also allows large scale defaults in the payments of taxes and duties.
This leads to crores of revenue being lost by the government. While the practice is widely known,
the government has refused to act till date. Because the tax structure varies in among different
states, it too promotes illegal trade in drugs across state borders. Moreover, in the absence of a clear
tax structure, consumers are charged in accordance with the arbitrary whims of retail chemists. This
situation can be remedied by having an uniform tax structure, and by clearly printing the price of
drugs on packages, inclusive of all taxes.
Centralised Drug Procurement
The government is a major purchaser of drugs and if government purchases are co-ordinated it can
provide it with a major bargaining handle to push down drug costs. Such a procedure is in place in
many countries, including many developed countries, and should be introduced in India too.
5
International symposium on
TRIPS and Access to Medicines
An International symposium on TRIPS and access to medicines was organised by the National Working Group
on Patent Laws and Medecins Sans Frontieres (doctors Without Borders) on 4th June. This was followed by a
Working Group Meeting on "Intellectual Property and Access to Drugs'* in New Delhi India, on 5th and 6th
June, 2001. The meeting was held in the background of MSF's ongoing "Access to Essential Medicines"
campaign and the upcoming WTO Ministerial Conference. This working Group, constituted of 25 international
experts, has been set up by MSF to advise it in its campaign.
Background to the Symposium
The widely evocative issue of access to anti-retrovirals, i.e. drugs that are used to treat AIDS patients, has
played a major role in the way the international community today sees the pharmaceutical industry. Treatment
of AIDS with a combination of drugs - called Highly Active Anti-retroviral Treatment (HAART) - has
decreased mortality from AIDS by 84% in developing countries. Unfortunately less than 5% of AIDS infected
people across the globe have access to such treatment currently, because the estimated cost of treatment by
HAART is about $12,000 per person per year. At present rates, Zimbabwe, Uganda and Ivory Coast would
require to spend 265%, 172% and 84% of their respective Gross National Products, just to buy drugs to treat all
their AIDS patients! This issue has been the rallying point of a major global campaign that today is demanding
a closer, critical look at the TRIPS agreement.
Condemnation of the role of pharmaceutical companies reached a crescendo due to the lawsuit brought against
the South African government in Pretoria’s High Court by 39 pharmaceutical companies. The lawsuit targeted a
legislation by South Africa — the Medicines and Related Substances Control Amendment Act, No. 90 of 1997 - which allowed the country access to cheaper anti-AIDS drugs. The 1998 lawsuit was supported by the US
Government, which placed South Africa on the Special 301 Watch List, and the European Union, which wrote
to then Vice President of South Africa, Mbeki, to express its concern about the legislation. This move by the
pharma majors evoked a massive counter-response across the globe, led by MSF. The companies suffered a
major defeat when, in April, 2001 the companies capitulated to mounting anger and disgust over their conduct
and agreed to withdraw the case unconditionally. About two months back Brazil moved a resolution at the UN
Human Rights Commission, which was approved by 52 votes in favor, 0 against and 1 abstention (USA). The
resolution, among other things, called upon States, at the international level, to ensure that “the application of
international agreements is supportive of public health policies which promote broad access to safe, efficient
and affordable preventive, curative or palliative pharmaceuticals and medical technologies...” Today many
national governments in third world countries are backing protests and demonstrations against the WTO in
general and the TRIPS regime in particular.
Countries in Africa, Latin America and Asia, as well as organisations campaigning for access to cheap anti
JDS drugs see India as a potential source of cheap drugs. In March 2001, an Indian company, Cipla,
announced that it would offer the combination of anti-AIDS drugs at a cost of S600 per patient per year, and
later announce that they could bring down costs to $350. Cipla’s offer was matched within weeks by two other
companies, Hetero Drugs and Ranbaxy. These offers are, till date, by far the cheapest that have been made
anywhere in the world. In other words, Indian companies are now offering drugs to treat AIDS at prices that are
one fortieth of global prices! Such a precipitous fall in prices can revolutionise AIDS treatment in developing
countries, and save millions of lives.
The defeat for the 39 pharmaceutical companies in South Africa is not the end of the battle. Every country that
has tried to interpret the TRIPS Agreement in a manner that allows access to cheaper drugs for its people is
faced with a hostile reaction from the US. But it has led to the building of an unprecedented global coalition
against the use of TRIPS to deny the poor access to drugs.
Summary of Deliberations at the Symposium
<
Participants at the symposium expressed concern at the trend in Intellectual Property protection, that is
increasingly skewing the balance of the rights of patent holders and consumers, in favour of the former.
Speakers noted that the TRIPS agreement marks a fundamental shift in this balance, as well as a shift in global
attitudes where private profits are put ahead of social benefits. This is further fueled by dependence of
economies in the developed world on industries that require strong IP protection. Of the 15 most profitable
industries today, 6 are from the pharmaceutical sector and 5 from the IT sector. It was also pointed out that IP
protection allows such industries to create monopolies, not only over production, but also in the control of
knowledge.
The net result of this trend, in the pharmaceutical sector, has been high cost of medicines and the consequent
denial of access to medicines by the income poor across the globe. Further, it has also led to a situation where
medicines required to treat disease that predominantly occur among the poor are not researched at all. Instead
drugs that are being researched are drugs used for "lifestyle" diseases like baldness, impotence, obesity, etc. It
was underlined that while the pharmaceutical industry claims that high prices are explained by the massive
expenditure on R&D, the truth is that drugs they actually research have little relevance to real medical needs.
Moreover, the kind of profits that big pharmaceutical MNCs generate are an indication of profiteering and not
just legitimate profit making.
Speakers at the symposium also stressed on the need to utilise provisions available in the TRIPS agreement to
ensure production of cheap drugs by domestic manufacturers in developing countries. For this, legislations in
developing countries need to have licensing and other provisions that prevent abuse of monopoly positions by
MNCs and also allow imports of drugs from the global market at lower prices. It was also pointed out that the
next few years are going to be crucial, as developed countries challenge laws enacted by developing countries
like Brazil in the WTO dispute settlement mechanism. The resolution in WTO of the complaint made by the US
against Brazil for violation of the TRIPS agreement because the former has included provisions that allow it to
produce cheap ant-AIDS drugs by licensing domestic manufacturers, is being seen as crucial in this context.
Speakers also commented on the adverse effect that TRIPS has on R&D and technology dissemination in
developing countries. It was pointed out that such capabilities, built up in countries like India, Brazil and
Argentine are under serious threat. The need to organise public funded research in these countries was stressed.
Representatives from the Indian Drug Manufacturers Association and the Indian Pharmaceutical alliance spoke
of the need to tailor the Indian Patent ACT - still at the drafting board — to the needs of domestic industry, and
domestic consumers. Speakers also expressed concern that there are already are signs that the Indian
pharmaceutical industry is moving from a position of self reliance and relatively stable prices to a situation of
import dependence and high prices.
Those who spoke at the Symposium include Mr. S.P. Shukla, formerly India’s chief negotiator at GATT;
4s.Ellen 't Hoen, Co-ordinator of MSF's Access campaign; Prof. Prabhat Patnaik and Prof. Ashok
Parthasarathy from JNU; Dr James Orbinski, Director MSF Working Group on Drugs for Neglected Diseases;
Dr. Pushpa M. Bhargava, Founder Director, CCMB; Dr. Nitya Nand, Chairman, NWGPL and Former Director,
Central Drug Research Instt.; Dr. Arun Ghosh, Former Member Planning Commission; and Mr.James Love,
Director, Consumer Project on Technology (USA), Mr.B.K. Keayla, Convenor, NWGPL, Dr. Amit Sen Gupta,
NWGPL, Prof. Fredrick M. Abbott, Florida State University; Prof. Jerome H. Reichnmn, Prof, of Law, Duke
University; Mr.Dinesh Abrol, Co-convenor, NWGPL; Dr. Biswajit Dhar, NWGPL; Dr. Vandana Shiva,
RFSTE; Dr. Gopakumar Nair, Indian Drug Manufacturer's Association; Mr. Dilip G. Shah, Indian
Pharmaceutical Alliance; Dr. D.B.A. Narayana, Director, Dabur Research Foundation; Dr. Graham Dukes,
Universities of Groningen and Oslo; Mr. Balraj Mehta, NWGPL; Dr.Mira Shiva, Co-ordinator All India Drug
Action Network; Dr. N.N. Mehrotra, CDRI; Mr Amitava Guha, Federation of Medical Representatives' Assn,
of India, Dr.Zafar Mirza, Health Action International; Mr.Prabir Purakayastha, Delhi Science Forum; and Ms.
Pascale Boulet, MSF.
^ll^l
t
^--pl^-^-'
^Lxtgy ~e»A JI* •■ \ yo-u-jvx^?-^, jGX^i
a^tAySy
t
gl
{jl-
x<cvKo('
-Aj2
U9 b—<.
J
I
^cjxP CLct^—
3.
r
h__ L
J Cz{tLz
f *P
q_s.jk fl,__
9-*~
^-z<^^ pi-e>^cJp2_-^<-7^LL "^P^)
C/
ZviZjEZ
PoJ>
JS-^JkX^ Z ^-V-----££\
'S-,'~'K3
8
Z^S
-- <^5^
'
----------- A----------------- 2a
Jjv-^epv'
$
L^.
'F*J C ^V^Y;
L4-Sx-*O
“X
°U^-D
■
LAXJUL- -r- ^>vX^nt AsxkJLJtZ'
.^Kxkvx&Ai’\^
Avaigi
J ' Tr f-. I
\ | _0>XM^ <a.*-i < >
•- Lmm
------- A--------------
L
,
JUAj^eAAXO-M-SZ^^O
Ca-^' /
>
*v.
-X. I
1
file: D EMAIL RECEIVED nationalhealthpolic.hr
DRAFT NATIONAL HEALTH POLICY - 2001
1. INTRODUCTORY
1.1 A National Health Policy was last formulated in 1983 and since then, there have been
very marked changes in the determinant factors relating to the health sector. Some of the
policy initiatives outlined in the NHP-1983 have yielded results, while in several other
areas, the outcome has not been as expected.
1.2 The NHP-1983 gave a general exposition of the recommended policies required in
the circumstances then prevailing in the health sector. The noteworthy initiatives under
that policy were
A phased, time-bound programme for setting up a well-dispersed network of
comprehensive primary health care sendees, linked with extension and health
education, designed in the context of the ground reality that elementary health
problems can be resolved by the people themselves;
11. Intermediation through ‘Health volunteers’ having appropriate knowledge, simple
skills and requisite technologies;
111. Establishment of a well-worked out referral system to ensure that patient load at the
higher levels of the hierarchy is not needlessly burdened by those who can be
treated at the decentralized level;
IV. An integrated net-work of evenly spread speciality' and super-speciality services;
encouragement of such facilities through private investments for patients who can
pay, so that the draw on the Government's facilities is limited to those entitled to
free use.
1.
1.3 Government initiatives in the pubic health sector have recorded some noteworthy
successes over time. Smallpox and Guinea Worm Disease have been eradicated from the
country; Polio is on the verge of being eradicated; Leprosy, Kala Azar, and Eilariasis can
be expected to be eliminated in the foreseeable future. There has been a substantial drop
in the Total Fertility Rate and Infant Mortality Rate. The success of the initiatives taken
in the public health field are reflected in the progressive improvement of many
demographic / epidemiological / infrastructural indicators over time - (Box-I).
Box-1 : Through The Years - 1951-2000Achievement$
Indicator
1951
I 1981
I
2000
Demographic Changes
1
1 of 22
..
■ ,
,
54
64.6(RGI)
| 40.8
| 33.9(SRS)
26.1(99 SRS)
Crude Death Rate
25
12J(SRS)
8.7(99 SRS)
IMR
146
110
70 (99 SRS)
• Life Expectancy
36.7
; Crude Birth Rate
__________
9/6/01 4:20 PM
file: D EMA-IL RECEIX'zL nauorialheakhooi
i
Epidemiological Shifts
Malaria (cases in million)
I 75
Leprosy cases per 10,000
population
i 38.1
Small Pox (no of cases)
| >44,887
i 2.2
I “•J
3.74
. ■ Eradicated
Guineaworm ( no. of cases)
j >39792
i Eradicated
Polio
29’09
265
Infrastructure
SC/PHC/CHC
! 725
I
. I 57.363
. 1,63,181
■
(99-RHS)
Dispensaries &Hospitals( all)
j 9209
Beds (Pvt & Public)
i 117,198
1 43.322
! (95-96-CBHI)
509.495
I 8,70,161
(95-96-CBHI)
Doctors(Allopathy)
i 61.SOO
l
i
I
Nursing Personnel
i 2.OS.700
I
! 5,03.900
i (98-99-MC1)
18.054
173.887
! 7.37,000
! (99-INC)
1.4 While noting that the public health initiatives over the years have contributed
J
significantly to the improvement of these health indicators, it is to be acknov iedged that
public health indicators / disease-burden stanstics are the outcome of several
complementary initiatives under the wider umbrella of the developmental sector,
covering Rural Development, Agriculture, Food Production, Sanitation, Drinking Water
Supply, Education, etc. Despite the impressive public health gains as revealed in the
statistics in Box-I, there is no gainsaying the tact that the morbidity and mortality levels
in the country are still unacceptably high. These unsatisfactory health indices are, in turn,
an indication of the limited success of the public health system to meet the preventive
and curative requirements of the general population.
1.5 Out of the communicable diseases, which have persisted over history, incidence of
Malaria has staged a resurgence in the 1980s before stabilising at a fairly high prevalence
level during the 1990s. Over the years, an increasing level of insecticide-resistance has
developed in the malarial vectors in many parts of the country, \< hile the incidence of the
more deadly P-Falciparum Malaria has risen :o about 50 percent in the country as a
2 of 22
9/6/01 4:28 P>
1
file: D EMAIL RECEIVED nationaiheaithpohc.hr
' whole. In respect of TB, the public health scenario has not shown any significant decline
in the pool of infection amongst the community, and, there has been a distressing trend
in increase of drug resistance in the type of infection prevailing in the country. A new
and extremely virulent communicable disease - HIV/AIDS - has emerged on the health
scene since the declaration of the NHP-1983. As there is no existing therapeutic cure or
vaccine for this infection, the disease constitutes a serious threat, not merely to public
health but to economic development in the country. The common water-bome infections
- Gastroenteritis Cholera, and some forms of Hepatitis - continue to contribute to a high
level of morbidity' in the population, even though the mortality rate may have been
somewhat moderated. The period after the announcement of NHP-83 has also seen an
increase in mortality through ‘life-style’ diseases- diabetes, cancer and cardiovascular
diseases. The increase in life expectancy has increased the requirement for geriatric care.
Similarly, the increasing burden of trauma cases is also a significant public health
problem. The changed circumstances relating to the health sector of the country since
1983 have generated a situation in which it is now necessary to review the field, and to
formulate a new policy framework as the National Health Policy-2001.
1.6 NHP-2001 will attempt to set out a new policy framework for the accelerated
' achievement of Public health goals in the socio-economic circumstances currently
prevailing in the country.
2. CVRRENT SCENARIO
2.1 FINANCIAL RESOURCES
The public health investment in the country over the years has been comparatively low,
and as a percentage of GDP has declined from 1.3 percent in 1990 to 0.9 percent in 1999.
The aggregate expenditure in the Health sector is 5.2 percent of the GDP. Out of this,
about 20 percent of the aggregate expenditure is public health spending, the balance
being out-of-pocket expenditure. The central budgetary allocation for health over this
period, as a percentage of the total Central Budget, has been stagnant at 1.3 percent,
while that in the States has declined from 7.0 percent to 5.5 percent. The current annual
per capita public health expenditure in the country is no more than Rs. 160. Given these
statistics, it is no-"surprise that the reach and quality of public health services has been
below the desirable standard. Under the constitutional structure, public health is the
responsibility of the States. In this framework, it has been the expectation that the
principal contribution for the funding of public health services will be from States’
resources, with some supplementary input from Central resources. In this backdrop, the
contribution of Central resources to the overall public health funding has been limited to
about 15 percent. The fiscal resources of the State Governments are known to be very
inelastic. This itself is reflected in the declining percentage of State resources allocated
to the health sector out of the State Budget. If the decentralized pubic health services in
the country are to improve significantly, there is a need for injection of substantial
resources into the health sector from the Central Government Budget. This approach,
despite the formal Constitutional provision in regard to public health, is a necessity if the
State public health services - a major component of the initiatives in the social sector are not to become entirely moribund. The NHP-2001 has been formulated taking into
consideration these ground realities in regard to the availability of resources.
3 of 22
9/6/01 4:29 PX
file: D EMAIL RECEIVED nationalhealthpoiic.h
2.2 EQUITY
2.2.1 In the period when centralized planning was accepted as a key instrument of
development in the country, the attainment of an equitable regional distribution was
considered one of its major objectives. Despite this conscious focus in the development
process, the statistics given in Box-II clearly indicate that attainment of health indices
have been very uneven across the rural - urban divide.
Box II : Differentials in Health Status Among States
Sector
Population i
BPL (%) I
!
IMR/
<5Mort-aiity
Weight
For Age-
Per 1000
per 1000
(NFHS II)
Lakh
% of
(Annual
Children ! Report
Under 3 i 2000)
years
Live Births
(1999-SRS)
MMR/
Leprosy
cases per
10000
popula-tion
Malaria
+ve
Cases in
vear
2000 (in
thousands)
I
(<-2SD)
India
26.1
70
94.9
47
Rural
27.09
75
103.7
49.6
Urban
23.62
44
63.1
38.4
I
I
408
3.7
2200
r
Better
Performing
States
I
Kerala
12.72
14
18.8
27
87
0.9
5.1
Maharastra
25.02
48
58.1
50
135
3.1
138
TN
21.12
52
63.3
37
79
4.1
56
Orissa
47.15
97
104.4
54
498
7.05
483
Bihar
42.60
63
105.1
54
707
11.83
132
Rajasthan
15.28
81
114.9
51
607
0.8
53
UP
31.15
84
122.5
52
707
4.3
99
MP
37.43
90
137.6
55
498
3.83
528
Low
Performing
States
I
iI
Also, the statistics bring out the wide differences between the attainments of health goals
in the better- performing States as compared to the low-performing States. It is clear that
national averages of health indices hide wide disparities in public health facilities and
health standards in different parts of the country. Given a situation in which national
averages in respect of most indices are themselves at unacceptably low levels, the wide
4 of22
9/6/01 4:29 P3
I
file: D EMAIL RECEIVED nanonalhealthpolic.hi
inter-State disparity implies that, for vulnerable sections of society in several States,
access to public health services is nominal and health standards are grossly inadequate.
Despite a thrust in the NHP-1983 for making good the unmet needs of public health
services by establishing more public health institutions at a decentralized level, a large
gap in facilities still persists. Applying current norms to the population projected for the
year 2000, it is estimated that the shortfall in the number of SCs/PHCs/CHCs is of the
order of 16 percent. However, this shortage is as high as 58 percent when disaggregated
for CHCs only. The NHP-2001 will need to address itself to making good these
deficiencies so as to narrow the gap between the various States, as also the gap across the
rural-urban divide.
2.2.2 Access to, and benefits from, the public health system have been very uneven
between the better-endowed and the more vulnerable sections of society. This is
particularly true for women, children and the socially disadvantaged sections of society.
The statistics given in Box-Ill highlight the handicap suffered tn the health sector on
account of socio-economic inequity.
Box-Ill: Differentials in Health status Among Socio-Economic Groups
Infant
Mortality/1000
Under 5
Mortality/1000
% Children
70
94.9
47
Scheduled Castes
83
119.3
53.5
Scheduled Tribes
84.2
126.6
55.9
Other Disadvantaged
76
103.1
47.3
Others
61.8
82.6
41.1
Indicator
India
Vnderweight
i
( Social Inequity
2.2.3 It is a principal objective of NHP-2001 to evolve a policy structure which reduces
these inequities and allows the disadvantaged sections of society a fairer access to public
health sendees.
2.3 DELIVERY OF NATIONAL PUBLIC HEALTH PROGRAMMES
2.3.1 It is self-evident that in a country as large as India, which has a wide variety of
socio-economic settings, national health programmes have to be designed with enough
flexibility to permit the State public health administrations to craft their own programme
package according to their needs. Also, the implementation of the national health
programme can only be carried out through the State Governments’ decentralized public
health machinery. Since, for various considerations, the responsibility of the Central
Government in funding additional public health services will continue over a period of
time, the role of the Central Government in designing broad-based public health
initiatives will inevitably continue. Moreover, it has been observed that the technical and
managerial expertise for designing large-span public health programmes exists with the
5 of 22
9/6/01 4:29 PM
1
file: D EMAIL RECEIVED nanonjihealthooiic.:
Central Government in a considerable degree; this expertise can be gainfully utilized in
designing national health programmes for implementation in varying socio-economic
settings in the states.
2.3.2 Over the last decade or so, the Government has relied upon a ‘vertical’
implementational structure for the major disease control programmes. Through this, the
system has been able to make a substantial dent in reducing the burden of specific
diseases. However, such an organizational structure, which requires independent
manpower for each disease programme, is extremely expensive and difficult to sustain.
Over a long time-range, ‘vertical’ structures may only be affordable for diseases, which
offer a reasonable possibility of elimination or eradication in a foreseeable time-span. In
this background, the NHP-2001 attempts to define the role of the Central Government
and the State Governments in the public health sector of the country.
2,4 THE STATE OF PUBLIC HEALTH INFRASTRUCTURE
2.4.1 The delineation ofNHP-2001 would be required to be based on an objective
assessment of the quality and efficiency of the existing public health machinery in the
field. It would detract from the quality of the exercise if, while framing a new policy, it
is not acknowledged that the existing public healjh infrastructure is far from satisfactory.
For the out-door medical facilities in existence, funding is generally insufficient; the
presence of medical and para-medical personnel is often much less than required b\ the
prescribed norms; the availability of consumables is frequently negligible; the equipment
in many public hospitals is often obsolescent and unusable; and the buildings are in a
dilapidated state. In the in-door treatment facilities, again, the equipment is often
obsolescent; the availability of essential drugs is minimal; the capacity of the facilities is
grossly inadequate, which leads to over-crowding, and consequentially to a steep
deterioration in the quality of the services. As a result of such inadequate public health
facilities, it has been estimated that less than 20 percent of the population seeks the OPD
services and less than 45 percent avails of the facilities for in-door treatment in public
hospitals. This is despite the fact that most of these patients do not have the means to
make out-of-pocket payments for private health services except at the cost of other
essential expenditure for items such as basic nutrition.
2,5 EXTENDING PUBLIC HEALTH SERVICES
2.5.1 While in the country generally there is a shortage of medical manpower, this
shortfall is disproportionately impacted on the less-developed and rural areas. No
incentive system attempted so far, has induced private medical manpower to go to such
areas; and. even in the public health sector it has usually been a losing battle to deploy
medical manpower in such under-served areas. In such a situation, the possibility needs
to be examined for entrusting some limited public health functions to nurses, paramedics
and other personnel from the extended health sector after imparting adequate training to
them.
2.5.2 India has a vast reservoir of practitioners in the Indian Systems of Medicine and
Homoeopathy, who have undergone formal training in their own disciplines. The
possibility of using such practitioners in the implementation of State/Central
Government public health Programmes, in order to increase the reach of basic health
6 of 22
9/6/01 4:29 P\
i
file: D EMAIL RECEIVED nanonalheaiihDoiic.h:
care in the country, is addressed in the NHP-2001.
2.6 ROLE OF LOCAL SELF-GOVERNMENT INSTITUTIONS
2.6.1 Some States have adopted a policy of devolving programmes and funds in the
health sector through different levels of the.Panchayati Raj Institutions. Generally, the
experience has been a favourable one. The adoption of such an organisational structure
has enabled need-based allocation of resources and closer supervision through the
elected representatives. NHP- 2001 examines the need for a wider adoption of this mode
of delivery' of health services, in rural as well as urban areas, in other parts of the
country.
2.7 MEDICAL EDUCATION
2.7.1 Medical Colleges are not evenly spread across various parts of the country. Apart
from the uneven geographical distribution of medical institutions, ,the quality of
education is highly uneven and in several instances even sub-standard. It is a common
perception that the syllabus is excessively theoritical, making it difficult for the fresh
graduate to effectively meet even the primary health care needs of the population. There
is an understandable reluctance on the part of graduate doctors to serve in areas distant
from their native place. NHP-2001 will suggest policy initiatives to rectify these
disparities.
2.7.2 Certain medical discipline, such as, molecular biology and gene-manipulation,
have become relevant in the period after the formulation of the previous National Health
Policy. Also, certain speciality disciplines - Anesthesiology. Radiology and Forensic
Medicines - are currently very scarce, resulting in critical deficiencies in the package of
available public health services. The components of medical research in the recent years
have changed radically. In the foreseeable future such research will rely increasingly on
such new disciplines. It is observed that the current under-graduate medical syllabus
does not cover such emerging subjects. NHP-2001 will make appropriate
recommendations in this regard.
2.8 NEED FOR SPECIALISTS IN ‘PUBLIC HEALTH’ AND ‘FAMILY MEDICINE'
2.8.1 In any developing country with inadequate availability of health services, the
requirement of expertise in the areas of‘public health’ and ‘family medicine’ is very
much more than the expertise required for other specialized clinical disciplines. In India,
the situation is that public health expertise is non-existent in the private health sector,
and far short of requirement in the public health sector. Also, the current curriculum in
the graduate / post-graduate courses is outdated and unrelated to contemporary
community needs. In respect of ‘family medicine’, it needs to be noted that the more
talented medical graduates generally seek specialization in clinical disciplines, while the
remaining go into general practice. While the availability of postgraduate educational
facilities is 50 percent of the total number of the qualifying graduates each year, and can
be considered adequate, the distribution of the disciplines in the postgraduate training
facilities is overwhelmingly in favour of clini cal specializations. NHP-2001 examines
the need for ensuring adequate availability of personnel with specialization in the ‘public
health’ and ‘family medicine’ disciplines, to discharge the public health responsibilities
in the country.
7 of 22
9/6/01 4:29 P.X
file: D EMAIL'RECEIX zD nanonalheakhpoiic.i.
2.9 URBAN HEALTH
2.9.1 In most urban areas, public health sendees are very meagre. To the extent that such
sendees exist, there is no uniform organisational structure. The urban population in the
country is presently as high as 30 percent and is likely to go up to around 33 percent by
2010. The bulk of the increase is likely to take place through migration, resulting in
slums without any infrastructure support. Even the meagre public health sendees
available do not percolate to such unplanned habitations, forcing people to avail of
private health care through out-of-pocket expenditure. The rising vehicle density in large
urban agglomerations has also led to andnereased number of serious accidents requiring
treatment in well-equipped trauma centres. NHP-2001 will address itself to the need for
providing this unserved population a minimum standard of health care facilities.
2.10 MENTAL HEALTH
2.10.1 Mental health disorders are actually much more prevalent than are visible on the
surface. While such disorders do not contribute significantly to mortality, they have a
serious bearing on the quality of life of the affected persons and their families. Serious
cases of mental disorder require hospitalizanon and treatment under trained supervision.
Mental health institutions are perceived to be woefully deficient in physical
infrastructure and trained manpower. NHP-2001 will address itself to these deficiencies
in the public health sector.
2.11 INFORMATION, EDUCATION AND COMMUNICATION
2.11.1 A substantial component of primary health care consists of initiatives for
disseminating, to the citizenry, public health-related information. Public health
programmes, particularly, need high visibility at the decentralized level in order to have
any impact. This task is particularly difficult as 35 percent of our country’s population is
illiterate. The present IEC strategy is too fragmented, relies heavily on mass media and
does not address the needs of this segment of the population. It is often felt that the
effectiveness of IEC programmes is difficult to judge; and consequently, it is often
asserted that accountability, in regard to the productive use of such funds, is doubtful.
NHP-2001, while projecting an IEC strategy, will fully address the inherent problems
encountered in any IEC programme designed for improving awareness in order to bring
about behavioural change in the general population.
2.11.2 It is widely accepted that school and college students are the most receptive
targets for imparting information relating to basic principles of preventive health care.
NHP-2001 will attempt to target this group to improve the general level of health
awareness.
2.12 MEDICAL RESEARCH
2.12.1 Over the years, medical research actinty in the country has been very limited. In
the Government, such research has been confined to the research institutions under the
Indian Council of Medical Research, and other institutions funded by the States/Central
Government. Research in the private sector has assumed some significance only in the
last decade. In our country, where the aggregate annual health expenditure is of the order
Sof22
9/6/01 4:29 P\
1
file: D EMAIL RECEIVED naiionalhealihpolic.h
of Rs. 80.000 crores, the expenditure in 1998-99 on research, both public and private
sectors, was only of the order of Rs. 1150 crores. It would be reasonable to infer that
with such low research expenditure, it would be virtually impossible to make any
dramatic break-through within the country, by way of new molecules and vaccines: also,
without a minimal back-up of applied and operational research, it would be difficult to
assess whether the health expenditure in the country is being incurred through optimal
applications and appropriate public health strategies. Medical Research in the country
needs to be focused on therapeutic drugs/vaccines for tropical diseases, which are
normally neglected by international pharmaceutical companies on account of limited
profitability potential. The thrust will need to be in the newly-emerging frontier areas of
research based on genetics, genome-based drug and vaccine development, molecular
biology, etc. NHP-2001 will address these inadequacies and spell out a minimal quantum
of expenditure for the coming decade, looking to the national needs and the capacity of
the research institutions to absorb the funds.
2.13 ROLE OF THE PRIVATE SECTOR
2.13.1 Considering the economic restructuring underway in the country, and over the
globe, since the last decade, the changing role of the private sector in providing health
care will also have to be addressed in NHP 2001. Currently, the contribution of private
health care is principally through independent practitioners. Also, the private sector
contributes significantly to secondary-level care and some tertiary care. With the
increasing role of private health care, the need for statutory licensing and monitoring of
minimum standards of diagnostic centres / medical institutions becomes imperative."
NHP-2001 will address the issues regarding the establishment of a regulatorymechanism to ensure adequate standards of diagnostic centres / medical institutions,
conduct of clinical practice and delivery of medical services.
2.13.2 Currently, non-Govemmental service providers are treating a large number of
patients at the primary level for major diseases. However, the treatment regimens
followed are diverse and not scientifically optimal, leading to an increase in the
incidence of drug resistance. NHP-2001 will address itself to recommending
arrangements, which will eliminate the risks arising from inappropriate treatment.
2.13.3 The increasing spread of information technologt raises the possibility of its
adoption in the health sector. NHP-2001 will examine this possibility.
2.14 ROLE OF THE CIVIL SOCIETY
2.14.1 Historically, the practice has been to implement major national disease control
programmes through the public health machinery of the State/Central Governments. It
has become increasingly apparent that certain components of such programmes cannot
be efficiently implemented merely through government functionaries. A considerable
change in the mode of implementation has come about in the last two decades, with an
increasing involvement of NGOs and other institutions of civil society. It is to be
recognized that widespread debate on various public health issues have, in fact, been
initiated and sustained by NGOs and other members of the civil society. Also, an
increasing contribution is being made by such institutions, in the delivery of different
components of public health services. Certain disease control programmes require close
9 of 22
9/6/01 4:29 PM
file: D EMAIL RECEIVED r.auonalheakhpolic.h
1
inter-action with the beneficiaries for regular administration of drugs: periodic carrying
out of the pathological tests; dissemination of information regarding disease control and
other general health information. NHP-2001 will address such issues and suggest policy
instruments for implementation of public health programmes through individuals and
institutions of civil society.
2.15 NATIONAL DISEASE SURVEILLANCE NETWORK
2.15.1 The technical network available in the country for disease surveillance is
extremely rudimentary and to the extent that the system exists, it extends only up to the
district level. Disease statistics are not flowing through an integrated network from the
decentralized public health facilities to the State/Central Government health
administration. Such an arrangement only provides belated information, which, at best,
serves a limited statistical purpose. The absence of an efficient disease surveillance
network is a major handicap in providing a prompt and cost effective health care system.
The efficient disease surveillance network set up for Polio and HIV/AIDS has
demonstrated the enormous value of such a public health instrument. Real-time
information of focal outbreaks of common communicable diseases - Malaria. GE,
Cholera and JE - and other seasonal trends of diseases, would enable timely
intervention, resulting in the containment of any possible epidemic. In order to be able to
use an integrated disease surveillance network, for operational purposes, real-time
information is necessary at all levels of the health administration. NHP-2001 would
address itself to this major systemic shortcoming in the administration.
2.16 HEALTH STATISTICS
2.16.1 The absence of a systematic and scientific health statistics data-base is a major
deficiency in the current scenario. The health statistics collected are not the product of a
rigorous methodology. Statistics available from different parts of the country, in respect
of major diseases, are often not obtained in a manner which make aggregation possible,
or meaningful.
2.16.2 Further, absence of proper and systematic documentation of the various financial
resources used in the health sector is another lacunae wimessed in the existing scenario.
This makes it difficult to understand trends and levels of health spending by private and
public providers of health care in the country, and to address related policy issues and
formulate future investment policies.
2.16.3 NHP-2001 will address itself to the programme for putting in place a modem and
scientific health statistics database as well as a system of national health accounts.
2.17 WOMEN'S HEALTH
2.17.1 Social, cultural and economic factors continue to inhibit women from gaining
adequate access to even the existing public health facilities. This handicap does not just
affect women as individuals; it also has an adverse impact on the health, general
well-being and development of the entire family, particularly children. NHP 2001
recognises the catalytic role of empowered women in improving the overall health
standards of the community.
10 of 22
9/6/01 4:29 Pi
tile: D EMAIL RECEIVED nationaihealthpoiic.hr:
2.18 MEDICAL ETHICS
2.18.1 Professional medical ethics in the health sector is a. , area, which h. > not received
much attention in the past. Also, the new frontier areas of research - involving gene
manipulation, organ human cloning and stem cell research impinge on visceral issues
relating to the sanctity' of human life and the moral dilemma of human intervention in the
designing of life forms. Besides these, in the emerging areas of research, there is an
un-charted risk of creating new life forms, which may irreversibly damage the
environment, as it exists today. NHP - 2001 recognises that moral and religious dilemma
of this nature, which was not relevant even two years ago, now pervades mainstream
health sector issues.
2.19 ENFORCEMENT OF QUALITY STANDARDS FOR FOOD AND DRUGS
2.19.1 There is an increasing expectation and need of the citizenry for efficient
enforcement of reasonable quality standards for food and drugs. Recognizing this need.
NHP - 2001 makes an appropriate policy recommendation.
2.20 REGULATION OF STANDARDS IN PARA MEDICAL DISCIPLINES
2.20.1 It has been observed that a large number of training institutions have mushroomed
particularly in the private sector, for several para medical disciplines - Lab Technicians.
Radio Diagnosis Technicians, Physiotherapists, etc. Currently, there is no
regulation/monitormg of the curriculum, or the performance of the practitioners in these
disciplines. NHP-2001 will make recommendations to ensure standardization of training
and monitoring of performance.
2.21 OCCUPATIONAL HEALTH
2.21.1 Work conditions in several sectors of employment in the countiy are
sub-standard. As a result of this, workers engaged in such activities become particularly
prone to occupation-linked ailments. The long-term risk of chronic morbidity is
particularly marked in the case of child labour. NHP-2001 will address the risk faced by
this particularly vulnerable section of the society.
2.22 PROVIDING MEDICAL FACILITIES TO USERS FROM OVERSEAS
2.22.1 The secondary and tertiary facilities available in the country are of good quality
and cost-effective compared to international medical facilities. This is true not only of
facilities in the allopathic disciplines, but also to those belonging to the alternative
systems of medicine, particularly Ayurveda. NHP-2001 will assess the possibilities of
encouraging commercial medical services for patients from overseas.
2.23 IMPACT OF GLOBALIZATION ON THE HEALTH SECTOR
2.23.1 There are some apprehensions about the possible adverse impact of economic
globalisation on the health sector. Pharmaceutical drugs and other health services have
always been available in the country at extremely inexpensive prices. India has
established a reputation for itself around the globe for innovative development of
original process patents for the manufacture of a wide-range of drugs and vaccines
within the ambit of the existing patent laws. With the adoption of Trade Related
Il of22
9 6/01 4:29 PM
file:
1
D EMAIL RECEIVED nationalhealmpoiic.htT
T
Intellectual Property (TRIPS), and the subsequent alignment of domestic patent laws
consistent with the commitments under TRIPS, there will be a significant shift in the
scope of the parameters regulating the manufacture of new drugs/vaccines. Global
experience has shown that the introduction of a TRIPS-consistent patent regime for
drugs in a developing country, would result in an increase in the cost of drugs and
medical services. NHP-2001 will address itself to the future imperatives of health
security in the country, in the post-TRIPS era.
2.24 NON - HEALTH DETERMINANTS
2.24.1 Improved health standards are closely dependent on major non-health
determinants such as safe drinking water supply, basic sanitation, adequate nutrition,
clean environment and primary education, especially of the girl child. NHP-2001 will
not explicitly address itself to the initiatives tn these areas, which although crucial, fall
outside the domain of the health sector. However, the attainment of the various targets
set in NHP 2001 assumes a reasonable performance in these allied sectors.
2.25 POPULATION GROWTH AND HEALTH STANDARDS
2.25.1 Efforts made over the years for improxing health standards have been neutralized
by the rapid growth of the population. Unless the Population stabilization goals are
achieved, no amount of effort in the other components of the public health sector can
bring about significantly better national health standards. Government has separately
announced the 'National Population Policy - 2000’. The principal common features
covered under the National Population Poiicy-2000 and NHP-2001, relate to the
prevention and control of communicable diseases; priority to containment of HIV/AIDS
infection; universal immunization of children against all major preventable diseases;
addressing the unmet needs for basic and reproductive health services; and
supplementation of infrastructure. The synchronized implementation of these two
Policies - National Population Policy - 2000 and National Health Policy-2001 - will be
the very comerstone of any national structural plan to improve the health standards in
the country.
2.26 ALTERNATIVE SYSTEMS OF MEDICINE
2.26.1 Alternative Systems of Medicine - Ayurveda, Unani, Sidha and Homoeopathy provide a significant supplemental contribution to the health care services in the country,
particularly in the underserved, remote and tribal areeas. The main components of
NHP-2001 apply equally to the alternative systems of medicine. However, the policy
features specific to the alternative systems of medicine will be presented as a separate
document.
3. OBJECTIVES
3.1 The main objective of NHP-2001 is to achieve an acceptable standard of good health
amongst the general population of the country. The approach would be to increase access
to the decentralized public health system by establishing new infrastructure in deficient
areas, and by upgrading the infrastructure in the existing institutions. Overriding
importance would be given to ensuring a more equitable access to health services across
the social and geographical expanse of the country. Emphasis will be given to increasing
12 of 22
9/6/01 4:29 PM
1
file: D EMAIL RECEIVED nanonalhealthpolic.h:
the aggregate public health investment through a substantially increased contribution by
the Central Government. It is expected that this initiative will strengthen the capacity- of
the public health administration at the State level to render effective service delivery'.
The contribution of the private sector in providing health services would be much
enhanced, particularly for the population group, which can afford to pay for services.
Primacy will be given to preventive and first-line curative initiatives at the primary
health level through increased sectoral share of allocation. Emphasis will be laid on
rational use of drugs within the allopathic system. Increased access to tried and tested
systems of traditional medicine will be ensured. Within these broad objectives.
NHP-2001 will endeavour to achieve the time-bound goals mentioned in Box-IV.
Box-IV: Goals to be achieved by 2000-2015
• Eradicate Polio and Yaws
2005
• Eliminate Leprosy
2005
• Eliminate Kala Azar
2010
• Eliminate Lymphatic Filariasis
2015
• Achieve Zero level growth of HIV/AIDS
I 2007
i
• Reduce Mortality by 50% on account of TB. Malaria
and Other Vector and Water Borne diseases
2010
• Reduce Prevalence of Blindness to 0.5%
2010
. Reduce IMR to 30/1000 And MMR to 100 Lakh
2010
• Improve nutrition and reduce proportion of LBW
Babies from 30% to 10%
2010
• Increase utilisation of public health facilities from
current Level of <20 to >75%
2010
_____
• Establish an integrated system of surveillance. National
Health Accounts and Health Statistics.
2005
• Increase health expenditure by Government as a % of
GDP from the existing 0.9 % to 2.0%
2010
• Increase share of Central grants to Constitute at least
25% of total health spending
2010
• Increase State Sector Health spending from 5.5% to 7%
of the budget
2005
2010
Further increase to 8%
4. NHP-2001 - POLICY PRESCRIPTIONS
13 of 22
9/6/01 4:29 P>
1
file:. D EMAIL RECEIVED nauona’.healmpolic.;
4.1 FINANCIAL RESOURCES
The paucity of public health investment is a stark reality'. Given the extremely difficult
fiscal position of the State Governments, the Central Government will have to play a key
role in augmenting public health investments. Taking into account the gap in health care
facilities under NHP-2001 it is planned to increase health sector expenditure to 6 percent
of GDP, with 2 percent of GDP being contributed as public health investment, by the
year 2010. The State Governments would also need to increase the commitment to the
health sector. In the first phase, by 2005, they would be expected to increase the
commitment of their resources to 7 percent of the Budget; and, in the second phase, by
2010, to increase it to 8 percent of the Budget. With the stepping up of the public health
investment, the Central Government’s contribution would rise to 25 percent from the
existing 15 percent, by 2010. The provisioning of higher public health investments will
also be contingent upon the increase in absorptive capacity of the public health
administration so as to gainfully utilize the funds.
4.2 EQUITY
4.2.1 To meet the objective of reducing various types of inequities and imbalances inter-regional; across the rural - urban divide; and between economic classes - the most
cost effective method would be to increase the sectoral outlay in the primary health
sector. Such outlets give access to a vast number of individuals, and also facilitate
preventive and early stage curative initiative, which are cost effective. In recognition of
this public health principle, NHP-2001 envisages an increased allocation of 55 percent of
the total public health investment for the primary health sector; the secondary and
tertiary health sectors being targetted for 35 percent and 10 percent respectively.
NHP-2001 projects that the increased aggregate outlays for the primary health sector will
be utilized for strengthening existing facilities and opening additional public health
service outlets, consistent with the norms for such facilities.
4.3 DELIVERY OF NATIONAL PUBLIC HEALTH PROGKAM.MES
4.3.1 NHP-2001. envisages a key role for the Central Government in designing national
programmes with the active participation of the State Governments. Also, the Policy
ensures the provisioning of financial resources, in addition to technical support,
monitoring and evaluation at the national level by the Centre. However, to optimize the
utilization of the public health infrastructure at the primary level, NHP-2001 envisages
the gradual convergence of all health programmes under a single field administration.
Vertical programmes for control of major diseases like TB, Malaria and HIV/AIDS
would need to be continued till moderate levels of prevalence are reached. The
integration of the programmes will bring about a desirable optimisation of outcomes
through a convergence of all public health inputs. The policy also envisages that
programme implementation be effected through autonomous bodies at State and district
levels. State Health Departments’ interventions may be limited to the overall monitoring
of the achievement of programme targets and other technical aspects. The relative
distancing of the programme implementation from the State Health Departments will
give the project team greater operational flexibility. Also, the presence of State
Government officials, social activists, private health professionals and MLAs/MPs on
the management boards of the autonomous bodies will facilitate well-informed
14 of 22
9/6. 01 4:29 P'
f i
file: D EMAIL RECEIVED nationalhealthpolic.bi
decision-making.
4.4 THE STATE OF PUBLIC HEALTH INFRASTRUCTURE
4.4.1 As has been highlighted in the earlier part of the Policy, the decentralized Public
health service outlets have become practically dysfunctional over large parts of the
country. On account of resource constraint, the supply of drugs by the State
Governments is grossly inadequate. The patients at the decentralized level have little use
for diagnostic sendees, which in any case would still require them to purchase
therapeutic drugs privately. In a situation in which the patient is not getting any
therapeutic drugs, there is little incentive for the potential beneficiaries to seek the
advice of the medical professionals in the public health system. This results in there
being no demand for medical services, and medical professionals, and paramedics often
absent themselves from their place of duty. It is also observed that the functioning of the
public health service outlets in the four Southern States - Kerala, Andhra Pradesh. Tamil
Nadu and Karnataka - is relatively better, because some quantum of drugs is distributed
through the primary health system network, and the patients have a stake in approaching
the Public health facilities. In this backdrop. NHP-2001 envisages the kick-starting of the
revival of the Primary Health System by providing some essential drugs under Central
Government funding through th; decentralized health system. It is expected that the
provisioning of essential drugs at the public health service centres will create a demand
for other professional services from the local population, which, in turn, will boost the
general revival of activities in these service centres. In sum, this initiative under
NHP-2001 is launched in the belief that the creation of a beneficiary interest in the
public health system, will ensure a more effective supervision of the public health
personnel, through community monitoring, than has been achieved through the regular
administrative line of control.
4.4.2 Global experience has shown that the quality of public health services, as reflected
in the attainment of improved public health indices, is closely linked to the quantum and
quality of investment through public funding in the primary health sector. Box-V gives
statistics which show clearly that the standards of health are more a function of accurate
targeting of expenditure on the decentralised primary sector (as observed in China and
Sri Lanka), than a function of the aggregate health expenditure.
Box-V: Public Health Spending in select Countries
15 of 22
9-6/01 4:29 P'
i-ie: D EMAIL RECEIVED nationalhealrhpolic.f.
i
: %Pubiic
%Health
Exoenditure to Expenditure
GDP
on Health to
Total Health
1 Expenditure
| %Population
with income of
<S1 day
Infant
Mortality
Rate. 1000
India
44.2
70
5.2
17.3
China
18.5
31
2.7
24.9
Sn Lanka
6.6
16
3
45.4
I
5.8
96.9
L
13.7
44.1
Indicator
UK
6
USA
7
1
Therefore, NHP-2001, while committing additional aggregate financial resources, places
strong reliance on the strengthening of the primary health structure, with which to attain
improved public health outcomes on an equitable basis. Further, it also recognizes the
practical need for levying reasonable user-charges for certain secondary and tertiary
public health care services, for those who can afford to pay.
4.5.1 NHP-2001 envisages that, in the context of the availability and spread of allopathic
graduates in their jurisdiction. State Governments would consider the need for expanding
the pool of medical practitioners to include a cadre of licentiates of medical practice, as
also practitioners of Indian Systems of Medicine and Homoeopathy. Simple
services/procedures can be provided by such practitioners even outside their disciplines,
as part of the basic primary health services in under-served areas. Also, NHP-2001
envisages that the scope of use of paramedical manpower of allopathic disciplines, in a
prescribed functional area adjunct to their current functions, would also be examined for
meeting simple public health requirements. These extended areas of functioning ot
different categories of medical manpower can be permitted, after adequate training and
subject to the'monitoring of their performance through professional councils.
4.5.2 NHP-2001 also recognizes the need for States to simplify the recruitment
procedures and rules for contract employment in order to provide trained medical
manpower in under-served areas.
4 6 ROI .F OF LOCAL SELF-GOVERNMENT INSTITUTIONS
4.6.1 NHP-2001 lays great emphasis upon the implementation of public health
programmes through local self Government institutions. The structure of the national
disease control programmes will have specific components for implementation throwgh
such entities. The Policy urges all State Governments to consider decentralizing
implementation of the programmes to such Institutions by 2005. In order to achieve this,
financial incentives, over and above the resources allocated for disease control
programmes, will be provided by the Central Government.
16 of 22
9/6/01 4:29 1
file: D EMAIL RECEA'ED r.a:se::„:h=-ilthpo.
4.7 MEDICAL EDUCATION
4.7.1 In order to ameliorate the problems being faced on account of the uneven spread of
medical colleges in various parts of the country, NHP-2001. envisages the setting up of a
Medical Grants Commission for funding new Government Medical Colleges in different
parts of the country. Also, the Medical Grants Commission is envisaged to fund the
upgradation of the existing Government Medical Colleges of the country, so as to ensure
an improved standard of medical education in the country.
4.7.2 To enable fresh graduates to effectively contribute to the providing of primary
health services. NHP-2001 identifies a significant need to modify the existing
curriculum. A need based, skill-oriented syllabus, with a more significant component of
practical training, would make fresh doctors useful immediately after graduation.
4.7.3 The policy emphasises the need to expose medical students, through the
undergraduate syllabus, to the emerging concerns for geriatric disorders, as also to the
cutting edge disciplines of contemporary medical research. The policy also envisages
that the creation of additional seats for post-graduate courses should reflect the need for
more manpower in the deficient specialities.
4.8 NEED FOR SPECIALISTS IN TUBLIC HEALTH* AND ‘FAMILY MEDICINE'
4.8.1 In order to alleviate the acute shortage of medical personnel with specialization in
‘public health’ and ‘family medicine’ disciplines, NHP-2001 envisages the progressive
implementation of mandatory norms to raise the proportion of postgraduate seats in
these discipline in medical training institutions, to reach a stage wherein % th of the seats
are earmarked for these disciplines. It is envisaged that in the sanctioning of
post-graduate seats in future, it shall be insisted upon that a certain reasonable number of
seats be allocated to 'public health’ and 'family medicine’ disciplines. Since, the 'public
health' discipline has an interface with many other developmental sectors, specialization
in Public health may be encouraged not only for medical doctors but also for
non-medical graduates from the allied fields of public health engineering, microbiology
and other natural sciences.
4.9 URBAN HEALTH
4.9.1 NHP-2001, envisages the setting up of an organised urban primary health care
structure. Since the physical features of an urban setting are different from those in the
rural areas, the policy envisages the adoption of appropriate population norms for the
urban public health infrastructure. The structure conceived under NHP-2001 is a
two-tiered one: the primary centre is seen as the first-tier, covering a population of one
lakh, with a dispensary providing OPD facility and essential drugs to enable access to all
the national health programmes; and a second-tier of the urban health organisation at the
level of the Government general Hospital, where reference is made from the primary
centre. The Policy envisages that the funding for the urban primary health system will be
jointly borne by the local self-Govemment institutions and State and Central
Governments.
17 ot'22
9/6/01 4:29 P?
file: D EMAIL RECEA'ED naiionajheaithpolic.hr
4 9 2 The National Health Policy also envisages the establishment of fully-equipped'
'hub-spoke’ trauma care networks in large urban agglomerations to reduce accident
mortality.
4.10 MENTAL HEALTH
4.10.1 NHP - 2001 envisages a network of decentralised mental health senices tor
ameliorating the more common categories of disorders. The programme outline for such
a disease would envisage diagnosis of common disorders by general dur\ medical sta
and prescription of common therapeutic drugs.
4.10.2 In reaard to mental health institutions for in-door treatment of patients the policy
envisages the upgrading of the physical infrastructure of such institutions at Central
Government expense so as to secure the human rights of this vulnerable segment ot
society.
4.11 information, EDUCATION AND COMMUNICATION
4.11.1 NHP-2001 envisages an IEC policy, which maximizes the disseminanon of
information to those population groups, which cannot be effectively approached through
the mass media only. The focus would therefore, be on inter-personal communication of
information and reliance on folk and other traditional media. The IEC programme wou
set specific taraets for the association of PRIs/NGOs/Trusts in such activities. The
nromamme will also have the component of an annual evaluation of the penormance ot
the non-Govemmental agencies to monitor the impact of the programmes on the targeted
groups The Central/State Government initiative will also focus on the development of
modules for information dissemination in such population groups who normally, do not
benefit from the more common media forms.
4 11.2. NHP-2001 envisages priority to school health programmes aiming at preventive
health education, regular health check-ups and promotion of health seeking behaviour
among children. W school health programmes can gainfully adopt specially designed
modules in order to disseminate information relating to ‘health and familv life . This is
expected to be the most cost-effective intervention as it improves the level ot awareness
not only of the extended family, but the future generation as well.
a 1? MEDICAL RESEARCH
4 p i NHP-7001 envisages the increase in Government-funded medical research to a
level of 1 percent of total health spending by 2005; and thereafter, up to 2 percent by
2010. Domestic medical research would be focused on new therapeutic drugs and
vaccines for tropical diseases, such as TB and Malaria, as also the Sub-types of
HIV/AIDS prevalent in the country. Research programmes taken up by the Government
in these priority areas would be conducted in a mission mode. Emphasis would also be
naid to time-bound applied research for developing operational applications. This would
ensure cost effective dissemination of existing / future therapeutic drugs vaccines m the
general population. Private entrepreneurship will be encouraged in the field of medical
research for new molecules / vaccines.
4.1
ROLE OF THE PRIVATE SECTOR
9/6/01 4:2<'
IS of 22
1
file: D EMAIL RECEIVES r.ancnaiheairhpoiic.ii!
4.13.1 NHP-2001 envisages the enactment of suitable legislations for regulating
minimum infrastructure and quality standards by 200.'. in clinical
esrablishments/medical institutions; also, statutory gui ’ dines for the conduct or clinical
practice and delivery of medical services are to be developed over the same period. The
policy also encourages the setting up of private insurance instruments’for increasing the
scope of the coverage of the secondary and tertiary sector under private health insurance
packages.
4.13.2 To capitalize on the comparative cost advantage enjoyed by domestic health
facilities in the secondary and tertiary sector, the policy will encourage the supply of
sendees to patients of foreign origin on payment. The rendering of such services on
payment in foreign exchange will be treated as ’deemed exports' and will be made
eligible for all fiscal incentives extended to export eamings.
4.13.3 NHP-2001 envisages the co-option of the non-governmental practitioners in the
national disease control programmes so as to ensure that standard treatment protocols are
followed in their day-to-day practice.
4.13.4 NHP-2001 recognizes the immense potential of use of infonnation technology
applications in the area of tele-medicine in die tertiary health care sector. The use of this
technical aid will greatly enhance the capacity- for the professionals to pool their clinical
experience.
4.14 ROLF. OF THE CIVIL SOCIETY
4.14.1 NHP-2001 recognizes the significant contribution made by NGOs and other
institutions of the civil society in making available health services to the community. In
order to utilize on an increasing scale, their high motivational skills. NHP-200’
envisages that the disease control programmes should earmark a definite portion of the
budget in respect of identified programme components, to be exclusively implemented
through these institutions.
4.15 NATIONAL DISEASE SURVEILLANCE NETWORK
4.15.1 NHP-2001 envisages the full operationalization of an integrated disease control
network from the lowest rung of public health administration to the Central Government,
by 2005. The programme for setting up this network will include components relating to
installation of data-base handling hardware: IT inter-connectivity between different tiers
of the network; and, m-house training for data collection and interpretation for
undertaking timely and effective response.
4.16 HEALTH STATISTICS
4.16.1 NHP-2001 envisages the completion of baseline estimates for the incidence of the
common diseases - TB, Malaria, Blindness - by 2005. The Policy proposes that
statistical methods be put in place to enable die periodic updating of these baseline
estimates through representative sampling, under an appropriate statistical methodology.
The policy also recognizes the need to establish in a longer time frame, baseline
estimates for : the non-communicable diseases, like CVD, Cancer, Diabetes; accidental
19 of 22
976/0 1 4:29 P.\
1
file: D EMAIL RECEIVED nationalhealihpoiic.?
injuries; and other communicable diseases, like Hepatitis and JE. NHP-2001 envisages
that, with access to such reliable data on he incidence of various dis -es.'1' public
health system would move closer to the objective of evidence-oased policy making.
4.16.2 In an attempt at consolidating the data base and graduating from a mere
estimation of annual health expenditure, NHP-2001 emphasis on the needs to establish
national health accounts, conforming to the 'source-to-users’ matrix structure. Improved
and comprehensive information through national health accounts and accounting
systems would pave the way for decision makers to focus on relative priorities, keeping
in view the limited financial resources in the health sector.
4.17 WOMENS HEALTH
4.17.1 NHP-2001 envisages the identification of specific programmes targeted at
women’s health. The policy notes that women, along with other under privileged groups
are significantly handicapped due to a disproportionately low access to health care. The
various Policy recommendations of NHP-2001, in regard to the expansion of primary
health sector infrastructure, will facilitate the increased access of women to basic health
care. NHP-2001 commits the highest priority' of the Central Government to the funding
of the identified programmes relating to woman’s health. Also, the policy recognizes the
need to review the staffing norms of the public health administration to more
comprehensively meet the specific requirements of women.
4.18 MEDICAL ETHICS
4.18.1 NHP - 2001 envisages that, in order to ensurethat the common patient is not
subjected to irrational or profit-driven medical regimens, a contemporary code of ethics
be notified and rigorously implemented by the Medical Council of India.
4.18.2 NHP - 2001 does not offer any policy prescription at this stage relating to ethics
in the conduct of medical research. By and large medical research within the country is
limited in these frontier disciplines of gene manipulation and stem cell research.
However, the policy recognises that a vigilant watch will have to be kept so that
appropriate guidelines and stamtory provisions are put in place when medical research in
i
the country reaches the stage to make such issues relevant.
4.19 ENFORCEMENT OF QUALITY STANDARDS FOR FOOD AND DRUGS
4.19.1 NHP - 2001 envisages that the food and drug administration will be progressively
strengthened, both in terms of laboratory facilities and technical expertise. Also", the
policy envisages that the standards of food items will be progressively tightened at a
pace which will permit domestic food handling / manufacturing facilities to undertake
the necessary upgradation of technology so as not to be shut out of this production
sector. The policy envisages that, ultimately food standards will be close, if not
equivalent, to codex specifications; and drug standards will be at par with the most
rigorous ones adopted elsewhere.
4.20 REGULATION OF STANDARDS IN PAR.AMEDICAL DISCIPLINES
4.20.1 NHP-2001 recognises the need for the establishment of statutory professional
20 of 22
9'6 01 4:29 P:
1
tile: D EMAIL RECEIVED natio.nalhealthDolic.i.
V
councils for paramedical disciplines to register practitioners, maintain standards of
training, as well as to monitor their performance.
4.21 OCCI NATIONAL HEALTH
4.21.1 NHP-2001 envisages the periodic screening of the health conditions of the
workers, particularly for high risk health disorders associated with their occupation.
4.22 PROVIDING MEDICAL. FACILITIES TO USERS FROM Q\ ERSEAS
4.22.1 NHP-2001 strongly encourages the providing of health services on a commercial
basis to sendee seekers from overseas. The providers of such sendees to patients from
overseas will be encouraged by extending to their earnings in foreign exchange, all fiscal
incentives available to other exporters of goods and sendees.
4.23 IMPACT OF GLOBALISATION ON THE HEALTH SECTOR
4.23.1 NHP-2001 takes into account the serious apprehension expressed by several
health experts, of the possible threat to the health security, in the post TRIPS era. as a
result of a sharp increase in the prices of drugs and vaccines. To protect the citizens of
the country from such a threat. NHP-2001 envisages a national patent regime for the
future which, while being consistent with TRIPS, avails of all opportunities to secure for
the country, under its patent laws, affordable access to the latest medical and other
therapeutic discoveries. The Policy also sets out that the Government will bring to bear
its full influence in all international fora - UN. WHO, WTO, etc. - to secure
commitments on the part of the Nations of the Globe, to lighten the restrictive features of
TRIPS in its application to the health care sector.
5. Sf MMATIO.N
5.1 The crafting of a National Health Policy is a rare occasion in public affairs when it
would be legitimate, indeed valuable, to allow our dreams to mingle with our
understanding of ground realities. Based purely on the clinical facts defining the current
status of the health sector, we would have arrived at a certain policy formulation: but.
buoyed by our dreams, we have ventured slightly beyond that in the shape of NHP-2001
which, in fact, defines a vision for the future.
5.2 The health needs of the country are enormous and the financial resources and
managerial capacity available to meet it, even on the most optimistic projections, fall
somewhat short. In this situation, NHP-2001 has had to make hard choices between
various priorities and operational options. NHP-2001 does not claim to be a road-map
for meeting all the health needs of the populace of the country. Further, it has to be
recognized that such health needs are also dynamic as threats in the area of public health
keep changing over time. The Policy, while being holistic, undertakes the necessary risk
of recommending differing emphasis on different policy components. Broadly speaking,
NHP - 2001 focuses on the need for enhanced funding and an organizational
restructuring of the national public health initiatives in order to facilitate more equitable
access to the health facilities. Also, the policy is focused on those diseases which are
principally contributing to the disease burden - TB, Malaria and Blindness from the
category of historical diseases: and HIV/AIDS from the category of‘newly emerging
21 ot'22
9/6/01 4:29 P'
1
file: D EMAIL RECEIVED nauonaiiiealthooiic
diseases’. This is not to say that other items contributing to the disease burden of the
country’ will be ignored; but only that, resources as also the principal focus of the public
health administration, will recognize certain relative priorities.
5.3 One nagging imperative, which has influenced every aspect of NHP-2001. is the
need to ensure that ‘equity’ in the health sector stands as an independent goal. In any
future evaluation of its success or failure, XHP-2001 would like to be measured against
this equity norm, rather than any other aggregated financial norm for the health sector.
Consistent with the primacy given to ‘equity’, a marked emphasis has been provided in
the policy for expanding and improving the primary health facilities, including the new
concept of provisioning of essential drugs through Central funding. The Policy also
commits the Central Government to increased under-writing of the resources for meeting
the minimum health needs of the citizenry. Thus, the Policy attempts to provide
guidance for prioritizing expenditure, thereby, facilitating rational resource allocation.
5.4 NHP-2001 highlights the expected roles of different participating group in the health
sector. Further, it recognizes the fact that, despite all that may be guaranteed by the
Central Government for assisting public health programmes, public health services
would actually need to be delivered by the State administration. NGOs and other
institutions of civil society. The attainment of improved health indices would be
significantly dependent on population stabilisation, as also on complementary efforts
from other areas of the social sectors - like improved drinking water supply, basic
sanitation, minimum nutrition, etc. - to ensure that the exposure of the populace to health
risks is minimized.
Suggestions on the draft policy are welcome. Kind> mail your suggestions to aeabon^/ nb.nicJn within
30 da vs.
22 of22
9•6/01 4:29 P'
HEALTH POLICY
In Sickness and in Wealth
A likely switchover to a ‘pay-and-be-treated’ regime can only compound the misery of the poor
By DAVINDER KUMAR
M T'S a 'revamp' of the healthcare system
I one should well be wary of. Free or sub| sidised medicare at public hospitals and
I medical centres could well become a
■ thing of the past as the government
puts the final touches to its National Health
Policy (nhp), 2001. Similar to the strategy
adopted by the food ministry for the Public
Distribution System (pds), those above the
poverty line may now find themselves bra
cketed as "those who can afford to pay" and
be asked "reasonable user charges" to avail
secondary and tertiary healthcare facilities.
The switchover to the 'pay and be treated'
mode in a country which has a sizeable
population living below the poverty line
has understandably caused concern to
those monitoring public health. Says Robert
J. Kim-Farley, the World Health Organisa
tion (who) representative in India: "It must
be ensured that there is total access to
healthcare and that such services arc afford
able. Sometimes the costs of hospitalisation
are so high that it alone can push one below
the poverty line. These points need to be
considered while finalising the policy."
This is just one of the contentious issues
in the draft nhp due to be finalised in a fort
night. Coming as it does after a gap of nea
rly two decades, it has angered several
organisations working in the health sector
who have alleged that it is anti-people, lack
ing in vision and a total 'sell-out' to transna
tional forces eying the huge health market.
Over 1,()()() countrywide
organisations
associated
with healthcare and health 1
policy have come together
under the banner of the Jan
Swasthya Abhiyan (jsa) and
are contesting several points
in the policy. In its critique,
as *
the |sa says: " I he draft intro
duces tne concept of user
tor to occupy the space that
can pay’ and
would be left vacant.”
fees, albeit couched in the Fbe charged
The policy draft does admit
usual sugar-coating of 'those
grave deficiencies in the hea
wiio can pay'. Global experi
user fees.
lth sector and notes how
ence of user fees at any level
only 20 per cent of the pop
shows that they serve only
one purpose—to drive out the poor. While ulation seeks opd sen ices and is forced to
the targeting of primary healthcare is to be turn to private clinics. It also admits the col
welcomed, this should not constitute an
lapse of the primary healthcare system and
argument for legitimisation of the govern acknowledges the poor coverage of
ment's retreat from providing comprehen women’s health and prevention of infant
mortality. Ironically, its prescriptions fail to
sive and quality secondary and tertiary care.
I he draft hints at this possibility in different address the problems or offer solutions.
sections and at encouraging the private secI he draft policy, for instance, admits that
i
66
P
OUTLOOK! December3,2001
Rernernoei
for business
enquiries, please conract
'i
ARHIJI1 RIIAIirKAR
public lieallli investment has been 'compar
atively low' and plans to raise it from 0.9
per cent to 2 per cent of the gdp by 2010.
But experts say it's still well below the wnorecommended share of 5 per cent. "The pol
icy does not admit that public health
investment in India has been abysmally
low. In fact, considered as a percentage of
total health expenditure, it is perhaps the
lowest in the world, making it the most pri
vatised health system in the world," says B.
Ekbal, vice-chancellor of Kerala University
and chairman of the health subcommittee
of the Kerala Sastra Sahithya I’arishad.
I
GlfiEESH G.V.
4MW
•’
^555
“n
i 31
Wi:
IS 5
ft
:
A
■
■
1^1
Rather than OPDs (left) of public hospitals
(above), most have to go to private clinics
What makes this pill even more bitter is
the strong influence of mnc forces in draft
ing the health policy. "Nearly 80 per cent
of the health services in India is already
controlled by the private sector. The policy
provides further space for it without
putting any defined mechanisms of keep
ing a check," says Pune-based community
health expert Anant I’hadke, associated
with the Medico Friend Circle.
I’hadke has a point. The policy calls for
providing incentives to the private sector to
move to the primary healthcare system.
However, the experience in urban centres
Las been discouraging. The incentives in
terms of subsidised land, water, electricity
and duty-free import facility doled out to
high-profile private medical centres and
hospitals in the urban areas has seen little
benefit for the poor. Very few of these hos
pitals conform to the mandatory provision
of free medical care to the population below
the poverty line or the reservation of a cer
tain percentage of their beds for the poor.
■■iHE government is being accused of
I shirking its responsibility of improving
I public health services. The policy has
chopped the earlier much-publicised goal of
universal healthcare. Says Mira Shiva of the
Delhi-based Voluntary Health Association
of India (viiai): "After wrapping up the ms,
the government is trying to wash its hands
of the healthcare services. How can the
healthcare services be left to the private sec
tor when there is absolutely no regulatory
or social control over it? At this rate, profit
ISSUES OF CONTENTION
• Free public health services to be
restricted
• Incentives to private sector to
enter the primary healthcare system
• Universal healthcare goal dropped
• No integration of associated
sectors like food, water or sanitation
• No effective regulatory mechanism
suggested for the private sector
• No clear safeguards to meet
WTO/TRIPS challenges
maximisation; , irrational healthcare, irra
tional use of medical technology will prolif
erate. Entry of large corporations into basic
needs with the backing of the international
trade regime will become a very dangerous
situation for India.”
The health ministry counters this by say
ing that the new policy proposes to regulate
the private sector with the enactment of
suitable legislations by 2(XB and also evolv
ing guidelines for the conduct of clinical
practice and delivery of medical services.
Experts take this with a pinch of salt. Obser
ves Shiva: "Despite all the rules in place,
sex-determination is still so rampant."
The policy is also being criticised for a dif
fused focus. It is being said that the issue of
health has been discussed in isolation with
out even considering the associated and
vital areas of nutrition, food security, water,
sanitation and even population control.
OUTLOOK! December 3. 2001
In fact, the advisory note by the wuo
country team has suggested that "the vision
for health needs to be strengthened". Il has
also touched upon women's health which,
as also pointed out by several Ni;os, has
been dismissed with a vague mention in the
policy. According to the who suggestion,
"the final nhp may more clearly spell out
strategies, interventions and targets for imp
roving maternal health". It has also pointed
out the need to focus on food safely, lack r>f
which results in starvation deaths.
Ravi Duggal, director of ( ehat, a promi
nent Mumbai-based healthcare a < points
to the absence of a focused drug policy in
the nhp. "Ibis a serious anomaly and the
health department must exert its right to
determine the drug policy, especially with
regard to price control over the who list of
300 essential drugs. This is extremely criti
cal in the context of India switching over
to the product patent regime under the
new wio/irips arrangement from 2005.
1 he advantage India has of lowest prices of
drugs in the world will be lost if a drug pol
icy favouring public health concerns is not
put in place before the 2005 deadline."
Interestingly, the policy also has plans to
attract overseas patients for comparatively
low-cost treatment as a means of generating
foreign exchange. To which S. Srinivasan of
Low Cost, an ngo that manufactures lowpriced drugs for the poor, says: "First, let us
manage our staggering health system rather
than look for foreign currency."
Undeterred, the officials at the health
and family wellaie ministry are busy finali
sing the policy. One thing they sa\ with
certainty is that the rns formula will defini
tely make its way to the health sector. ■
67
- Media
 RF_HP_2_B_SUDHA.pdf
RF_HP_2_B_SUDHA.pdf
Position: 1003 (12 views)