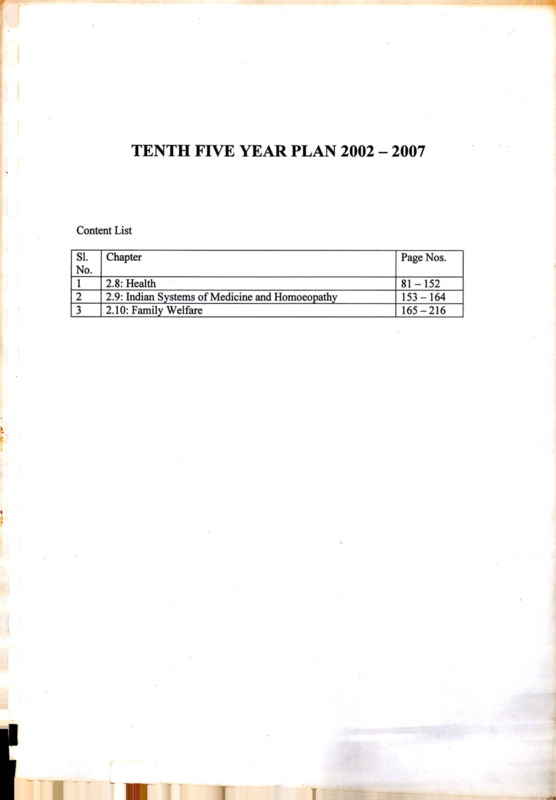
TENTH FIVE YEAR PLAN 2002 - 2007
Item
- Title
- TENTH FIVE YEAR PLAN 2002 - 2007
- extracted text
-
TENTH FIVE YEAR PLAN 2002 - 2007
Content List
SI.
No.
1
2
3
Chapter
Page Nos.
2.8: Health________________________________
2.9: Indian Systems of Medicine and Homoeopathy
2.10: Family Welfare
81-152
153-164
165-216
r
1
CHAPTER 2.8
HEALTH
Introduction
sectors. These institutions are manned by professio
nals and paraprofessionals trained in the medical
colleges in modern medicine and ISM&H and
paraprofessional training institutions. The population
has become aware of the benefits of health related
technologies for prevention, early diagnosis and
effective treatment for a wide variety of illnesses
and accessed available services. Technological
advances and improvement in access to health care
technologies, which were relatively inexpensive and
easy to implement, had resulted in substantial
improvement in health indices of the population and
a steep decline in mortality (Table 2.8.1).
2.8.1
Improvement in the health and nutritional
status of the population has been one of the major
thrust areas for the social development program
mes of the country. This was to be achieved through
improving the access to and utilization of Health,
Family Welfare and Nutrition services with special
focus on under served and under privileged
segments of the population. Over the last five
decades, India has built up a vast health infra
structure and manpower at primary, secondary and
tertiary care in government, voluntary and private
Table 2.8.1: Time Trends (1951-2000) in Health Care
1951
1981
2000
SC/PHC/CHC
725
57,363
1,63,181 (99-RHS)
Dispensaries & Hospitals (all)
9209
23,555
43,322 (95-96-CBHI)
Beds (Pvt. & Public)
117,198
569,495
8,70,161 (95-96-CBHI)
Doctors (Modern System)
61,800
2,68,700
5,03,900 (98-99-MCI)
Nursing Personnel
18,054
1,43,887
7,37,000 (98-99-INC)
75
2.7
2.2
38.1
57.3
3.74
>44,887
Eradicated
Malaria (cases in million)
Leprosy (cases/10,000 population)
Small Pox (no. of cases)
Guineaworm (no. of cases)
Polio (no. of cases)
>39,792
Eradicated
29709
265
Life Expectancy (Years)
36.7
54
64.6 (RGI)
Crude Birth Rate
40.8
33.9 (SRS)
26.1 (99SRS)
Crude Death Rate
25
12.5 (SRS)
8.7 (99 SRS)
IMR
146
110
70 (99 SRS)
Source : National Health Policy - 2002
81
TENTH FIVE YEAR PLAN 2002-07
2.8.2
The extent of access to and utilization of
health care varied substantially between states,
districts and different segments of society; this to a
large extent, is responsible for substantial
differences between states in health indices of the
population.
2.8.3
During the 1990s, the mortality rates
reached a plateau and the country entered an
era of dual disease burden. Communicable
diseases have become more difficult to combat
because of development of insecticide resistant
strains of vectors, antibiotics resistant strains of
bacteria and emergence of HIV infection for which
there is no therapy. Longevity and changing life
style have resulted in the increasing prevalence
of non-communicable diseases. Under nutrition,
micro nutrient deficiencies and associated health
problems coexist with obesity and non-communicable diseases. The existing health system
suffers from inequitable distribution of institutions
and manpower. Even though the country
produces every year over 17,000 doctors in
modern system of medicine and similar number
of ISM&H practitioners and paraprofessionals,
there are huge gaps in critical manpower in
institutions providing primary healthcare,
especially in the remote rural and tribal areas
where health care needs are the greatest. Some
of the factors responsible for the poor functional
status of the system are:
E
mismatch
between
infrastructure;
personnel
and
lack of Continuing Medical Education (CME)
programmes for orientation and skill
upgradation of the personnel;
El
lack of appropriate functional referral system;
E
absence of well established linkages between
different components of the system.
2.8.4
In order to address these problems the
centre and the states have embarked on structural
and functional health sector reforms. However, the
content and quality of reforms are sub-optimal and
the pace of implementation is slow.
2.8.5
As the country undergoes demographic
and epidemiological transition, it is likely that larger
investments in health will be needed even to
maintain the current health status because tackling
resistant infections and non-communicable
diseases will inevitably lead to escalating health care
costs. Last two decades have witnessed explosive
expansion in expensive health care related tech
nologies, broadening diagnostic and therapeutic
avenues. Increasing awareness and rising
expectations to access these have widened the
gap between what is possible and what is affordable
for the individual or the country. Policy makers and
programme managers realise that in order to
address the increasingly complex situation
regarding access to good quality care at affordable
costs, it is essential to build up an integrated health
system with appropriate screening, regulating
access at different levels and efficient referral
linkages. However, both health care providers and
health care seekers still feel more comfortable with
the one to one relationship with each other than
with the health system approach.
2.8.6
Another problem is the popular
perception that curative and preventive care
compete for available resources, with the former
getting preference in funding. Efforts to convince
the public that preventive and curative care are
both part of the entire spectrum of health care
ranging from health promotion, specific
protection, early diagnosis and prompt treatment,
disability limitation and rehabilitation and that to
improve the health status of the population both
are equally essential have not been very
successful. Traditionally health service (both
government and private) was perceived as a
social responsibility albeit a paid one. Growing
commercialisation of health care and medical
education over the last two decades has eroded
this commitment, adversely affecting the quality
of care, trust and the rapport between health care
seekers and providers.
APPROACH DURING THE TENTH PLAN
2.8.7
In view of the importance of health as a
critical input for human development there will be
continued commitment to provide:
82
HEALTH
essential primary health care, emergency life
saving services, services under the National
Disease Control Programmes and the National
Family Welfare Progra-mme totally free of cost
to all individuals and
training, administrative arrangements and
implementation so that they are integral
components of health care; there will be
progressive convergence of funding,
implementation and monitoring of all health and
family welfare programmes under a single field
of administration beginning at and below district
level;
essential health care service to people below
poverty line based on their need and not on
their ability to pay for the services.
2.8.8
Appropriate interventions to ease the
existing funding constraints at all levels of health
system and to promote the complete and timely
utilization of allocated funds will be taken up.
Different models of health care financing at the
individual, family, institution and state level will be
evolved, implemented and evaluated. Models found
most suitable for providing essential health care to
all will be replicated.
E
evolving treatment protocols for the
management of common illnesses and
diseases; promotion of the rational use of
diagnostics and drugs;
The focus during the Tenth Plan will be on
E
reorganisation and restructuring the existing
government health care system including the
ISM&H infrastructure at the primary,
secondary and tertiary care levels with
appro-priate referral linkages. These
institutions will have the responsibility of
taking care of all the health problems
(communicable,
non-communicable
diseases) and deliver reproductive and child
health (RCH) services for people residing in
a well-defined geographic urban and rural
area;
El
development of appropriate two-way referral
systems utilising information technology (IT)
tools to improve communication, consultation
and referral right from primary care to tertiary
care level;
El
building up an efficient and effective logistics
system for the supply of drugs, vaccines and
consumables based on need and utilisation;
improvement in thejuality of care at all levels
and settings by evolving and implementing a
whole range of compre-hensive norms for
service delivery, prescribing minimum
requirements of qualified staff, conditions for
carrying out specialised interventions and a set
of established procedures for quality
assurance;
El
evolving, implementing and monitoring
transparent norms for quality and cost of care
in different health care settings;
El
exploring alternative systems of health care
financing including health insurance so that
essential, need based and affordable health
care is available to all;
improving content and quality of education of
health professionals and para professionals so
that all health personnel have the necessary
knowledge, attitude, skills, programme and
people orientation to effectively take care of
the health problems, and improve the health
status of the people;
skill upgradation of all health care providers
through CME and reorientation and if
necessary redeployment of the existing health
manpower, so that they can take care of the
existing and emerging health problems at
primary, secondary and tertiary care levels;
horizontal integration of all aspects of the
current vertical programmes including supplies,
monitoring,
information
education
communication and motivation (IECM),
research and development to solve major
health problems confronting the country
83
TENTH FIVE YEAR PLAN 2002-07
including basic and clinical research on drugs
needed for the management of emerging
diseases and operational research to improve
efficiency of service delivery;
building up a fully functional, accurate Health
Management Information System (HMIS)
utilising currently available IT tools; this real
time communication link will send data on
births, deaths, diseases, request for drugs,
diagnostics and equipment and status of
ongoing programmes through service channels
within existing infra-structure and manpower
and funding; it will also facilitate decentralized
district based planning, implementation and
monitoring;
social marketing organisation in improving
access to health care;
O
devolution of responsibilities and funds to
panchayati raj institutions (PRIs); besides
participating in area-specific planning and
monitoring, PRIs can help in improving the
accountability of the public health care
providers, sort out problems such as
absenteeism, improve inter-sectoral co
ordination and convergence of services;
E
strengthening programmes for the
prevention, detection and management of
health consequences of the continuing
deterioration of the ecosystems; improving
the linkage between data from ongoing
environmental monitoring and that on health
status of the people residing in the area;
making health impact assessment a part of
environmental impact assess-ment in
developmental projects;
E
improving the safety of the work environment
in organized and unorgani-sed industrial and
agricultural sectors especially among
vulnerable groups of the population;
E
developing capabilities at all levels, for
emergency and disaster prevention and
management;
evolving
appropriate
management systems for emergency, disaster,
accident and trauma care at all levels of health
care;
E
effective implementation of the provisions for
food and drug safety; strengthening the food
and drug administration both at the centre and
in the states;
building up an effective system of disease
surveillance and response at the district, state
and national level as a part of existing health
services;
El
E
E
El
strengthening and sustaining Civil Regi
stration, Sample Registration System;
improving medical certification of death so that
information on specific causes of death
throughout the country are available; use these
data in district based planning and monitoring;
when sustained over the next two decades, this
system will provide valuable insights into inter
district, inter-state, regional variations and time
trends so that district health system could be
modified to cope with the changing disease
burden;
improving the efficiency of the existing health
care system in the government, private and
voluntary sectors and building up appropriate
linkages between them;
mainstreaming ISM&H practitioners, so that in
addition to practising their system of care, they
can help in improving the coverage of the
National Disease Control Programmes and
Family Welfare Programme;
improving inter sectoral coordination;
screening for common nutritional deficiencies
especially in vulnerable groups and initiating
appropriate remedial measures; evolving and
effectively implementing programmes for
improving nutritional status, including
micronutrient nutritional status of the
population.
increasing the involvement of voluntary and
private organisations, self-help groups and
84
HEALTH
HEALTH CARE SYSTEM
2.8.9
E
E
E
E
2.8.12 The government funded primary health care
institutions include:
The Health care system consists of:
the rural, modern medicine primary health care
infrastructure created by the states (Figure
2.8.1) consisting of:
primary, secondary and tertiary care
institutions, manned by medical and
paramedical personnel;
R> Subcentres
R> Primary Health
centres
R> Community
Health centers
medical colleges and paraprofessional training
institutions to train the needed manpower and
give the required academic input;
programme managers managing ongoing
programmes at central, state and district levels;
and
health management information system
consisting of a two-way system of data
collection, collation, analysis and response.
2.8.10 So far the interaction between these
components of the system had been sub-optimal.
In spite of the plethora of primary, secondary and
tertiary care institutions and medical college
hospitals there are no well organised referral
linkages between the primary, secondary and
tertiary care institutions in the same locality. The
programme managers and teachers in medical
colleges do not link with institutions in any of the
three tiers; essential linkages between structure and
function are not in place (Annexure - 2.8.1). Logistics
of supply and HMIS are not operational in most
states. During the Tenth Plan period, efforts will be
made to reorganise health system, build up
essential linkages between different components
of the system so that there will be substantial
improvement in functional status (Annexure - 2.8.2).
137271
22975
2935
(1/4579)
(1/27364)
(1/214000) — rJo
E
subdivisional/Taluk hospitals/speciality hospi
tals (estimated to be about 2000);
E
5435 rural family welfare centres, 871 urban
health posts, 1083 urban family welfare
centres, 550 district post partum centres and
1012 sub-district postpartum centres funded
by the Department of Family Welfare;
Figure 2.8.1 - Growth of Sub-centres, Primary
Health Centres and Community Health Centres
30 -----27-----24 —
21----18-----15
12------
9 —r
6
3 J—
0
rl
I -1
Sub-centres (in
ten thousand)
□ 1985
JI
I
PHCs (in
thousand)
□ 1990
CHCs (in
hundred)
□ 1999
Source: IAMR.2000.
Primary Health Care Services
2.8.11
The primary health care infrastructure
provides the first level of contact between the
population and health care providers. Realising its
importance in the delivery of health services, the
centre, states and several government related
agencies simultaneously started creating primary
health care infrastructure and manpower. This has
resulted in substantial amount of duplication of the
infrastructure and manpower.
85
El
23,028 dispensaries, 2,991 hospitals under the
Dept of ISM&H;
El
urban health services provided by municipali
ties;
E
healths care for central government employees
provided by Central Government Health
Scheme (CGHS);
M
hospitals and dispensaries of railways, defence
and similar large departments providing the
health care to their staff;
El
medical infrastructure of PSUs and large
industries;
TENTH FIVE YEAR PLAN 2002-07
H
Employee’s State Insurance Scheme (ESIS)
hospitals and dispensaries providing health
care to employees of industries;
H
all hospitals - even those providing secondary
or tertiary care also provide primary health care
services to rural and urban population;
IS)
Over three-fourths of the medical practitioners
work in the private sector and majority of them
cater to the primary health care needs of the
population.
2.8.13 The state-wise information regarding
institutions listed under hospitals and dispensaries
in modern system of medicine and ISM&H, rural
primary health care infrastructure as well as post
partum centres is given in Annexure-2.8.3. Health
manpower in government primary health care
institutions is given in Annexure-2.8.4. The vast
infrastructure and manpower catering to the primary
health care needs of the population is not evenly
distributed. The segments of the population whose
health care needs are greatest have very poor
access to health care.
centrally sponsored disease control programmes.
With appropriate skill up gradation these uni
purpose male workers and contractual staff will be
able to perform the task of MMPW in improving the
coverage and quality of all health programmes.
Primary Health Centres (PHCs)
2.8.15 PHC is a referral unit for six sub-centres.
All PHCs provide outpatient services; a majority
have four to six in-patient beds. According to the
norms they have one medical officer, 14 para
medical and other supporting staff. At the national
level there are more than an adequate number of
PHCs and doctors posted at PHCs but their
distribution across states is uneven; there are no
functional PHCs in many remote areas in dire need
of health care.
2.8.16 The number of SCs, PHCs and CHCs in
their own building is shown in Figure 2.8.1a.
Fig 2.8.1a. Construction of Buildings
□ Under
Construction
Sub-Centre
Ml
80
S
°
2.8.14 The Sub-centre(SC) is the most peripheral
health institution available to the rural population.
Even though the sub-centre/population norm at the
national level has been met, there are wide inter
state variations. States with poor health indices do
not have the required number of sub-centres
especially in remote areas. In order to ensure that
lack of funds does not hamper the filling up of
vacancies in the posts of auxiliary nurse midwife
(ANM), the Department of Family Welfare has taken
up funding of sub-centre ANMs (1.37 lakh) from 1st
April 2002. The States will, in return take over the
funding of the staff of the rural family welfare and
post partum centres, who have for the last two
decades functioned as a part of the respective
institutions in the state. There are a large number
of vacancies in the posts of male multi-purpose
workers (MMPW) whose salaries are borne by the
state government (Annexure-2.8.4). Even where
they are present, their contribution to the ongoing
national disease control programmes, disease
surveillance and water quality monitoring is
negligible. There are a large number of male uni
purpose workers with insufficient workload in various
60
□ Rent free
/
Panchayat
buildings
40^
□ Rented
20 k"
0-K—==
Sub
Building
--j
□ Operating
PHCs
CHCs
centres
Govt. Buildings
Source: RHS Bulletin, June 1998-99
2.8.17 Facility Survey undertaken by the
Depart-ment of Family Welfare in 1999 showed
that a majority of the PHCs lack essential
infrastructure and inputs (Figure-2.8.1b). Only 77
per cent had an infant weighing machine, 65 per
cent had a deep freezer, 16 per cent had a
refrigerator, and 60 per cent had an autoclave
and steam sterilizer drum. Less than 20 per cent
had facility for medical termination of pregnancy
(MTP).
2.8.18
Essential drugs for the treatment of
common ailments were not available in a majority
of the PHCs. Only around one-thirds of the PHCs
had stock of iron and folic acid (IFA) tablets, 56
per cent had stocks of contraceptives and 61 per
cent had vaccines. No more than a third of the
PHCs provided delivery care; in them on an
86
HEALTH
Figure-2.8.1b Percentage Distribution of PHCs having all Critical Inputs
10090 n
—
5
I
80 70 I
60
50 —
40 —
30 20 —
'1
I
[^8
io T
o -I-1—
yyX
\
I
X
/z z
□ <20%
I
I
L
■
i
T
/Z ZZZ ZZ Z Z Z
+*
□ 20-39.9%
z
□ 40-59.9%
z
S 60+%
Source: Facility Survey-1999, Deptt. of FW
average of 26 deliveries occurred in the last three
months before the survey. It is obvious, therefore
that PHCs are functioning sub-optimally and are
not providing the expected health and family
welfare services.
than 90 per cent of the CHCs have an out patient
and in patient facilities and operation theatre, only
about one-third had adequate equipments. A
majority of the CHCs do not function as the FRUs
because they either do not have any specialist or
the posted specialists are not from the four specified
specialties.
Community Health Centres/First Referral Units
2.8.19 Community Health Centre(CHC) is the first
referral unit( FRU) for four PHCs offering specialist
care. According to the norms each CHC should have
at least 30 beds, one operation theatre, X-ray
machine, labour room and laboratory facilities and
should be staffed at least by four specialists i.e. a
surgeon, a physician, a gynecologist and a
pediatrician supported by 21 para-medical and other
staff.
Tribal Health
2.8.22 In order to ensure adequate access to
health care services for the tribal population,
20,769 SCs, 3286 PHCs, 541 CHCs, 142
hospitals, 78 mobile clinics and 2305
dispensaries have been established in tribal
areas. In addition, 16845 SCs, 5987 PHCs, 373
CHCs and 2750 dispensaries are located in
2.8.20 The reported gap in the number of
CHCs (about 2000) is more apparent than real.
Currently there are over 2000 functioning subdivisional, taluka and other speciality hospitals
below the district hospital. From the Seventh Plan
onwards, it has been emphasized that these
should be reorganised and brought into the
mainstream, given the status of CHC and the
responsibility of being the referral centre for well
defined PHCs and SCs. Many CHCs/FRUs have
sub-district post partum centers located within
their premises or in the vicinity, but they are not
functioning as a part of CHC.
Experiments for improving access to primary
health care among tribals:
Andhra Pradesh - Committed government
functionaries are running health facilities in
tribal areas
Orissa - Additional central assistance is
provided for mobile health units with a fixed
tour schedule. However, this is expensive
and difficult to replicate.
Karnataka, Maharashtra - NGO have
‘adopted’ and are running PHCs in tribal areas
The success of all these experiments is mainly
due to the commitment of individuals and
credibility of NGOs, which is difficult to replicate.
2.8.21
The Facility Survey carried out by the
Dept, of Family Welfare showed that though more
87
TENTH FIVE YEAR PLAN 2002-07
villages with 20 per cent or more scheduled caste
population. Most of the centrally sponsored
disease control programmes have a focus on the
tribal areas. Under the National Anti Malaria
Programme (NAMP) 100 identified predo
minantly tribal districts in Andhra Pradesh, Bihar,
Gujarat, Madhya Pradesh, Maharashtra, Orissa
and Rajasthan are covered. In spite of all these,
the access to and utilisation of health care remain
suboptimal and health and nutrition indices in the
tribal population continue to be poor
(Table-2.8.2).
Table:2.8.2
Health indices of various social groups
IMR
U5MR
%Under
nutrition
SC
83.0
119.3
53.5
ST
84.2
126.6
55.9
Other disadv
76.0
103.1
47.3
Others
61.8
82.6
41.1
India
70
94.9
47
Source : NHP, 2002
and monitoring. Almost all the states have attempted
introduction of user charges for diagnostic and
therapeutic procedures in government hospitals
from people above the poverty line and use the
funds so generated to improve the quality of care
in the respective institutions.
2.8.24 Some of the ongoing health system
reforms to improve health services include:
H
strengthening and appropriately relocating subcentres/PHCs e.g. Tamil Nadu, Gujarat;
El
merger, restructuring, relocating of taluk, subdivisional and rural hospitals, dispensaries and
block level PHCs; integrating them with the
existing infrastructure to fill the gap in CHCs
e.g. Himachal Pradesh;
E
utilizing funds from Basic Minimum Services
(BT/IS), Additional Central Assistance (ACA),
Pradhan Mantri Gramodaya Yojana (PMGY)
and externally aided projects to fill critical gaps
in manpower and facilities; this is being done
in all states;
E
district-level walk-in-interviews for the
appointment of doctors in PHCs; this had
limited success - e.g. Madhya Pradesh and
Gujarat;
E
use of mobile health clinics; this is very
expensive and had limited success e.g. Orissa,
Maharashtra (for Tribal areas), Delhi (for urban
slums);
E
handing over of PHCs to NGOs - Karnataka,
Orissa; only Karnataka reported success;
E
training MBBS doctors in certain specialties
(obstetrics, anaesthesia, radiology ) in a
teaching institution for three to six months and
posting them to fill the gap in specialists in
FRUs e.g. Tamil Nadu .and West Bengal;
however, professional associations do not
support this because quality of care may be
suboptimal; and
E
improving the logistics of supply of drugs and
consumables - e.g. Tamil Nadu, Orissa.
Health System Reforms at Primary Health Care
Level during Ninth Plan
2.8.23 Faced with the problems of sub-optimal
functioning and difficulties in providing adequate
investments for improving health care facilities in
the public sector, almost all state governments have
initiated health system reforms with public sector
institutions playing lead role. The structural reforms
relate to reorganisation and restructuring of all the
elements of health care so that they function as
integral components of the health system. The
functional reforms are aimed at improving efficiency
by creating a health system with well-defined
hierarchy and functional referral linkages in which
the health personnel would work as a multi
professional team and perform duties according to
their position, skills and level of care. The
community-based link worker who acts as a liaison
between people and health care functionaries and
ensures optimal utilization of available facilities will
provide the last link. The PRIs will participate in
planning programmes and assist in implementation
2.8.25 Several states have obtained external
assistance to augment their own resources so that
the pace of reforms can be accelerated. Funds were
provided under PMGY for improving functional
88
HEALTH
status of rural primary health care institutions. Fifty
per cent of the outlay was to be used for procure
ment of drugs and essential consumables and repair
of essential equipments. The other 50 per cent was
to be used for repair and maintenance of infra
structure in sub-centres, PHCs and CHCs. Under
the RCH Programme, funds are provided for minor
repair and maintenance of buildings, especially for
operation theatres and labour rooms and for
improving water and electric supply. Review of the
health sector reforms during the Ninth Plan period
indicates that on the whole, the content and
coverage are poor; pace of implementation is very
slow and uneven across the states.
Figure-2.8.3- Rural & Urban Distribution
of Hospitals: Public and Private
100
80
□ URBAN
60
40
□ RURAL
20
0
GOVERNMENT
PRIVATE
Source: NCAER-2000
Urban Primary Health Care Services
is aware and has ready access to health care. Data
from SRS, NFHS and other surveys indicate that
health indices of the urban population are better
than those of the rural population (Table-2.8.3).
However, urban migration has resulted in rapid
growth of urban slums; The slum population face
greater health hazards due to over-crowding, poor
sanitation, lack of access to safe drinking water and
environmental pollution. Small scale research
studies have shown that health indices of urban
slum dwellers in some areas are worse than those
of rural population.
2.8.26 Nearly 30 per cent of India’s population
lives in the urban areas. Majority of the hospitals
(Figure-2.8.2 & 2.8.3), doctors and para
professionals are in urban areas. Urban population
Table-2.8.3
Urban/rural health indicators
BPL(%)
IMR U5MR
% Children
Under-nourished
Urban
23.6
44
63.1
38.4
Rural
27.1
75
103.7
49.6
Total
26.1
70
94.9
47.0
2.8.27 Realising that the available infrastructure
is insufficient to meet the health care needs of
growing urban population, the municipalities, state
governments and the central government have tried
to build up urban health care facilities. These urban
health facilities especially the tertiary care
institutions cater to both the urban and rural popula
tion. Unlike the rural health services there have been
no efforts to provide well-planned and organized
primary, secondary and tertiary care services in
geographically delineated urban areas. As a result,
in many areas primary health care facilities are not
available; some of the existing institutions are under
utilised while there is over-crowding in most of the
secondary and tertiary care centres. As there is no
screening and referral system, the available
equipment and expertise in secondary hospitals are
under utilised; inappropriate use of available
diagnostic and therapeutic facilities result in
Source: NFHS-2
Figure: 2.8.2- Rural & Urban
Distribution of Hospital Beds:
Public and Private
100
80
S URBAN
60
40
□ RURAL
20
0
GOVERNMENT
PRIVATE
Source: NCAER-2000
89
TENTH FIVE YEAR PLAN 2002-07
escalating cost of health care without commen
surate health benefits.
2.8.28 The Ninth Plan envisaged the develop
ment of a well structured net work of urban primary
health care institutions providing health and family
welfare services to the population within one to three
km of their dwellings by re-organizing the existing
institutions. In addition to funds provided by
corporations/municipalities, state government and
the central government, externally assisted projects
were taken up to achieve the goal. The Planning
Commission also provided additional central
assistance to some states for undertaking such
restructuring. Though there are several small
success stories, hardly any progress has been
achieved in the overall task of restructuring the
urban primary health care, linked to secondary and
tertiary care and appropriate retraining and
redeployment of personnel. One of the major factors
responsible for the tardy progress is the multiplicity
of agencies funding these institutions.
Role of Panchayati Raj Institutions
2.8.29 According to Article 243 G of the 73rd
Constitutional Amendment Act, states are required
to devolve adequate powers and responsibility to
the PRIs in order to make them effective institutions
of local self government. Funds and personnel have
to be made available to the PRIs for planning and
implementation of schemes pertaining to various
sectors. The PRIs can play a critical role in ensuring
area specific microplanning, monitoring of the
implementation of the national, state level and
district specific programmes, ensuring account
ability and improving inter-sectoral coordination.
However, in many states, there have been no
concrete steps to involve PRIs in the planning and
implementation of state sector or centrally
sponsored schemes.
mainstreamed, reorganised, restructured and
integrated into the three tier rural primary health
care system so that these institutions serve the
population in a well defined area and have appro
priate referral linkages with each other. The village
under each sub-centre, sub-centres under each
PHC, PHCs under each CHC/FRU will be defined
using Geographical information System (GIS)
mapping, taking into account distances, road
linkages and other factors that will improve access.
All sub-district institutions with specialists will be
recategorised as CHC/FRU and all hospitals and
dispensaries without specialists will be merged or
recategorised as PHCs. By the end of Seventh Plan
most of the states have completed setting up
required number of Subcentres and PHCs required
to meet the norms for 1991 population (Figure
2.8.1). As many of them are located in their own
building and cannot be shifted out (Figure 2.8.1a).
Population under each of these primary health care
institutions has grown; but it will be difficult to locate
new institutions to cater to the additional population
in appropriate locations. Therefore the Tenth Plan
goals for primary health care institutions for each
state will be number of the primary health care
institutions required to meet the health care needs
of the 1991 population as per the norms (Annexure
2.8.3). Opening new centers and construction of
new centres will be undertaken only under
exceptional circumstances.
2.8.31
Ninth Plan recommendations regarding
re-organisation of urban primary health care
institutions making them responsible for the health
care of a population living in a defined geographic
area and linking them to existing secondary and
tertiary care institutions will be fully implemented
during the Tenth Plan.
2.8.32 In order to cope with the growing
population/changing needs for health care, the
staffing pattern of both urban and rural primary
health care institutions may be suitably modified
taking into account the population, their health care
needs, the work load, difficulties in delivery of
services and distances to be covered. Most of the
gaps in critical manpower will be met by re
orientation, skill up gradation and redeployment of
the existing manpower. For instance vacancies in
Initiatives during the Tenth Plan
2.8.30 During the Tenth Plan every effort will be
made to implement the recommendations of the
Seventh, Eighth, and Ninth Plan that all hospitals
and dispensaries below district level should be
90
HEALTH
the posts of specialists in FRUs will be reduced by
integrating the staff of the post partum centres with
the FRU staff. As and when required part time or
contractual staff including those provided under the
national disease control programmes and family
welfare programme could be utilised to fill the gaps
in manpower. Release of grants under the centrally
sponsored schemes will be conditional on filling
the vacancies in staff who are critical for improving
performance under the national programmes.
Mismatch between the equipment and personnel
will be corrected by shifting equipment to centres
which have the personnel to operate it or vice versa
2.8.33 Available funds will be utilized to make all
the existing institutions fully functional by providing
needed equipment, consumables, diagnostics and
drugs. In addition to funds from the centre, state,
externally aided projects, locally generated funds
from user charges and donations will be used for
maintenance and repair to ensure optimal functional
status and improve quality of services.
E
strengthen district hospitals so that they can
effectively take care of referrals;
E
strengthen the referral system and rationalize
care at each level to:
2.8.36 During the Tenth Plan priority will be
accorded to the evaluation of the ongoing World
Bank funded secondary health care systems
projects in these seven states regarding:
progress in strengthening of physical infra
structure;
O functional improvement in terms of patient care,
organization of referral linkages between
CHCs, district hospitals and tertiary care
institutions;
2.8.34 The secondary health care infrastructure
at the district hospitals and urban hospitals is
currently also taking care of the primary health care
needs of the population in the city/town in which
they are located. This inevitably leads to over
crowding and under utilisation of the specialized
services. Strengthening secondary health care
services was an identified priority in the Ninth Plan.
In addition to the funds they get from the state plan,
seven states have taken World Bank loans to initiate
projects to build up FRUs/district hospitals. The aim
of these projects is to :
strengthen FRUs to take care of referrals from
PHCs/SCs;
2.8.35 The states have initiated construction
works and procurement of equipments. They have
reported increased availability of ambulances and
drugs, improvement in quality of services following
training to health care providers, reduction in
vacancies and mismatches in health personnel/
infrastructure and improvement in hospital waste
management, disease surveillance and response
systems. All these states have attempted to levy
user charges for diagnostic and therapeutic services
from people above the poverty line. Some states
have been unable to ensure that the collected
charges are retained for use in the same institution
and this problem need be speedily resolved.
H
Secondary Health Care
E
reduce overcrowding at the district and
tertiary care level.
El
improvement in different components of care hospital waste management, disease
surveillance and response, HMIS etc;
E operationlisation of cost recovery through user
charges from people above poverty line while
ensuring that people below the poverty line do
have access to health services free of cost;
E
efforts currently underway to make the
programme sustainable so that it remains fully
functional after project period.
2.8.37 During the Tenth Plan strengthening of the
secondary health system and building up referral
services will be taken up in other states using the
lessons learnt from these seven states.
R>
enable patients to get care near their
residence;
Tertiary Health Care
R>
ensure optimal utilisation of facilities at
PHCs/ CHCs; and
2.8.38 Over the last two decades a majority of
the tertiary care institutions in the governmental
91
TENTH FIVE YEAR PLAN 2002-07
sector have been facing a resource crunch and have
not been able to obtain funds for equipment
maintenance, replacement of obsolete equipments,
supply of consumables and upgrading the
infrastructure to meet the rapidly growing demand
for increasingly complex diagnostic and therapeutic
modalities. There is a need to optimise facilities
available in tertiary care institutions, enhance the
quality of services and strengthen linkages with
secondary care institutions. Overcrowding in tertiary
care hospitals and underutilization of expert care
due to the lack of a two way referral system with
primary and secondary care levels requires
correction. To meet some of the recurring costs and
to improve the quality of services in tertiary health
care institutions the Ninth Plan suggested levying
user charges and establishing pay clinics/pay
cabins.
2.8.39 Some states have provided land, water
and electricity at a lower cost to private entre
preneurs setting up tertiary care/superspeciality
institutions on the condition that they provide
outpatient and inpatient care free of cost for people
below the poverty line. In an effort to augment the
availability of tertiary care, several states (e.g.
Rajasthan and Himachal Pradesh) are trying out
innovative schemes to give greater autonomy to
government institutions, allowing them to generate
resources and utilise them locally. Most states have
not yet fully documented the extent and impact of
their efforts in this direction. Available data suggest
that Kerala, Punjab and Haryana have cost recovery
ratios of around 10 per cent and more than 80 per
cent of the fees for public facility care were paid by
the richest 40 per cent of the population both in the
urban and rural areas. This may be because this
section uses the services more or the quality of care
provided to those who pay may be better than to
those who are exempt from paying. A review of the
existing cost recovery system in states has shown
that:
E
an appropriate institutional framework for
reviewing user charges has not yet been
established;
E
the level of cost recovery is minimal due to the
low structure of fees and inadequate collection
mechanisms;
92
El
mechanisms for identifying and exempting the
poor from user charges are ill defined; and
El
funds collected are not retained at the point of
collection in many states.
2.8.40 During the Tenth Plan, the ongoing efforts
at cost recovery from people above the poverty line
will be encouraged and evaluated; models which
improve the access of all segments of the population
to appropriate care at an affordable cost will be
replicated. One of the major recommendations of
the Ninth Plan was that a Technical Appraisal
Committee should be constituted in all major
government institutions to assess and prioritise the
essential requirements for strengthening and up
grading of facilities keeping in mind the funds
available. Every effort will be made in the Tenth Plan
to implement this recommendation, improve
autonomy and encourage decentralised planning.
Development and Use of Appropriate
Technologies
2.8.41
The development and utilisation of
appropriate technologies for diagnosis and
management of patients is an essential pre-requisite
for an improvement in the quality of health services
without unnecessary escalation in cost of health
care. Realising the need for an in-depth review of
the requirement for supportive and diagnostic
services at primary, secondary and tertiary care a
separate Working Group on this subject was
constituted prior to the formulation of the Ninth Plan.
2.8.42 The Working Group’s recommendations
regarding diagnostic and supportive services
appropriate for the primary and secondary levels
and their maintenance were, to some extent
implemented by some states. Efforts for the
development and testing of inexpensive technolo
gies for weighing, measurement of blood pressure,
haemoglobin (Hb) estimation, hand held data entry
machines to improve HMIS continue to receive
support. Efforts to set up a national mechanism for
the appraisal of the quality of new technologies will
continue.
HEALTH
Public - Private Participation in Health Care
Figure 2.8.5 - Number of Hospital and
Dispensary Beds
2.8.43 The private health sector has played a
significant role in health service delivery right
from the pre-independence days. At the time of
independence public-private participation was in
the form of government doctors being allowed
private practice, an arrangement that continues
even today in majority of states. To cope with the
lack of medical teachers in the 1950s and 1960s
many medical colleges appointed private
practitioners as honorary teachers and honorary
physician in teaching hospital but the number of
such teachers declined with the increasing
availability of full-time paid government teachers.
HOSPITALS
25000
DISPENSARIES
10000 —
5000
0
;—
3
n ,I I
l<H
z
I
Source : CBHI, D/o Health
—■
__
J~~~l
zq
o -U-
z
Source : CBHI, D/o Health
/
z
2.8.45 Available data on infrastructure and
manpower in the hospitals and dispensaries
(excluding PHCs and CHCs) in private and public
sector from both rural and urban area computed
from CBHI reports is shown in Figure 2.8.4 & 2.8.5.
While information on the government sector
institutions is reliable, data on the private sector is
incomplete and is based on information provided
by the state medical councils and state govern
ments. Data from Andhra Pradesh indicate that
there may be massive differences between the data
reported by CBHI and the actual census conducted
by the state government (Figure 2.8.6).
20000
15000
DISPENSARIES BEDS
be taken up and completed on a priority basis
during the Tenth Plan.
Figure 2.8.4 - Number Of Hospitals And
Dispensaries
30000
HOSPITAL BEDS
700000 i
600000 -500000
400000
300000
200000 100000 r
2
z
2.8.44 At present, there is no uniform
nationwide system of registering either
practitioners or institutions providing health care
in the private/voluntary sectors nor is there a
mechanism for obtaining and analyzing
information on health care infrastructure and
manpower in these sectors at the district level.
During the Ninth Plan a Standing Technical
Advisory Committee headed by the Director
General of Health Services was set up and and
the Central Bureau of Health Intelligence (CBHI)
was given the task of compiling data on health
care infrastructure and manpower at all levels in
the private, voluntary, industrial, governmental
and other sectors. So far, very little progress
has been reported in this direction. This task will
Figure 2.8.6 - Number of Hospitals and Beds in
Private Sector
3000
2000
1000
c
0
Andhra Pradesh
t
Reported to CBHI
Census of Hospitals
Private sector Hospitals
Private sector Beds (In ’00)
Source: Census 1993, Director of Health Services and the Andhra
Pradesh Vaidhya Vidhan Parishad
93
TENTH FIVE YEAR PLAN 2002-07
2.8.46 Available data from National Sample
Survey Organisation (NSSO) carried out by
independent investigators and studies funded by
the Department of Health suggest that a majority
of the physicians in both the modern system of
medicine and ISM&H work in the private sector.
The growth and share of private sector hospitals
and beds over the years is shown in Figure 2.8.7.
The growth and share of government sector
hospitals and beds appear low because the CBHI
does not include the PHCs (there are 22975
PHCs; majority have six beds) and CHCs (2985
each with atleast 30 beds) under hospitals and
dispensaries. While there has been a substantial
increase in the number of hospitals under the
private sector during the 1990s, the rise in the
number of beds has been modest. ( Figure 2.8.7)
□ 1974
12000
□ 1979
—I
8000
—
-H
4000 -p
o -Tl=
i
LU
g
F
I
JJ E
£
e
□ 1984
B - TI di i
h ft
i
□ 1988
LU
g
o
120 t100 -
80 60 40
20 0 -
T
hzigMrzLz
-If
z x </Z X
z
□ NO. OF HOSPITALS
X
= NO. OF BEDS IN HOSPITALS
□ NO. OF DOCTORS
SOURCE : M. Uplekar, A. George, 1995 & 1996
outpatient visits and 52 per cent of hospitalisation
at the all-lndia level (Figure 2.8.9), with no
significant variations across income group.
2.8.48 A majority of government and private
sector hospitals and beds are located in urban
areas. Qualified and registered private sector
doctors or private sector institutions are not
readily available in remote rural and tribal areas
because people do not have ability to pay and
there is a lack of social infrastructure. Thus, the
population in these areas where health care
needs are the greatest have very poor access to
Functioning government health services or private
Figure 2.8.7 - Growth anti Share of Private Sector
Hospitals and Beds
16000
Figure 2.8.8 - Number of Hospitals and Beds
in the Pvt. Sector
□ 1996
I HOSPITALS BEDS (In '00)
HOSPITALS
HOSPITALS BEDS (In ’00)
riimrlAr'/ /-\f
Source : Health Information of India and Directory
of □nmilnlr'
Hospitals i.^
in (•-tzlt.
India. CBHI, D/o
Health
facilities. In spite of the abundant supply of
registered physicians in modern system of
medicine and ISM&H, unqualified persons still
provide health care especially to the poorer
segments of the population living in urban slums,
remote rural and tribal areas.
2.8.47 Currently private sector health services
range from those provided by large corporate
hospitals, smaller hospitals/nursing homes to
clinics/ dispensaries run by qualified personnel
and services provided by unqualified
practitioners. A majority of the private sector
hospitals are small establishments with 85 per
cent of them having less than 25 beds with an
average bed strength of 10 beds. Private tertiary
care institutions provi-ding specialty and super
specialty care account for only 1 to 2 per cent of
the total number of institutions while corporate
hospitals constitute less than 1 per cent. There
are wide inter-state differences in the distribution
of private sector hospitals and beds. The private
sector prefers to set up facilities in the more
prosperous districts/ states (Figure 2.8.8). The
private sector accounts for 82 per cent of all
Figure 2.8.9 - Share of Private Sector of
Outpatient & Inpatient Care
90 ------80
-82__ 74....
□ 1985-86
□ 1995-96
70------56
60 -
s
o
CL
50 -
40
40 ----30------
20
10
0 -------
o
OP
SOURCE : NATIONAL SAMPLE SURVEY, 42nd & 52nd ROUND
94
HEALTH
2.8.49 Majority of private sector institutions are
single doctor dispensaries with very little
infrastructure or paramedical support. They
provide symptomatic treatment for common
ailments and because they are conveniently
located and easily accessible, patients from even
below the poverty line utilize them and pay for
their services. These private practitioners do not
have access to updated standard protocols for
the management of common ailments; hence the
quality of care they provide is often sub-optimal.
Some private hospitals have also been found to
be using inappropriate, unnecessary and
expensive diagnostic tests and therapeutic
procedures as well as inappropriate and unethical
treatment practices. Other problems reported in
private sector include use of unqualified service
providers, overuse of diagnostic and therapeutic
measures leading to exorbitant costs. There is
no attempt to screen patients for complications
and refer them to the appropriate level of care,
rationalise drug use or contain the costs of
treatment. These problems have to be addressed
through appropriate interventions, including CME
to update the knowledge and skills of
practitioners, evolving and implementing
standards
for
quality
of
care
and
operationalisation of an appropriate grievance
redressal mechanism.
Figure 2.8.11 - Average Hospital Charge per inpatient
Day by Public and Private Hospitals
350
297
300 4—r-i—269250 —
Public Sector
IX
so -n
Immuni
sation
APL |
BPL
BPL
Antenatal Institutional
care
| deliveries
2.8.51
The average cost of hospital stay per day
in government hospitals is low and there are no
significant inter-state variations in this respect. The
cost of inpatient treatment in the private sector is
much higher (Figure 2.8.11). This has been cited
as the major reason for poorer sections seeking
inpatient care in government institutions. There are
wide inter-state variations in the cost of private
sector inpatient care, ranging from Rs.51 per day
in Himachal Pradesh to Rs. 297 in Tamil Nadu. Part
of the difference might be due to differences in
diagnostic and therapeutic services available in
these hospitals.
APL | BPL /
APL | BPL
Hospitalization
4(
2.8.50 Data from 52nd round of NSSO 199596, National Family Health Survey (NFHS-2) and
a National Council of Applied Economic Research
(NCAER) study shows that there were distinct
patterns for the utilisation of out patient and
inpatient services. A majority of the population
both from below and from above the poverty line,
approached the private sector for outpatient
curative care for minor ailments. However, when
it came to obtaining immunization or antenatal
care, most people, irrespective of their income
status went to government institutions. For
inpatient care for all ailments 60 per cent of the
below poverty line (BPL) families tend to use
government hospitals and while an equal
proportion of above poverty line (APL) families
prefer private hospitals (Figure 2.8.10).
I
APL
2f
sSource
.
.
: NCAER, 2000
40 —
APL I BPL
201
n~T58
0
60 —
0
203
100 —
Private Sector
20 —
1
I 150
80
i
□ PRIVATE I
251
>•200 —
•o
Figure 2.8.10 - Public and Private Sector Shares In Service Delivery
For Those Above and Below Poverty Line. All India, 1995-96
100
□ PUBLIC
Outpatient
(
care
Source: NCAER, 2000
95
TENTH FIVE YEAR PLAN 2002-07
Figure 2.8.12 - Distribution of Inpatients between
Public and Private Hospitals
HP
9,3
ORISSA
89
NORTH-EAST
RAJASTHAN
I
I, ~
MP
UP
52
ALL INDIA
i _
i ‘
KARNATAKA
50
KERALA
TAMILNADU
I
GUJARAT
_____ i
T81
WEST BENGAL
4745
/4
T
I
~~~T____________ _
T
_
........ .
I
I.........
I
I
i
i
wSi
I
...... I .....
T
□ PRIVATE
j.............
py-’',
TZ_ZI—_I__Z
J............. i...........
r;TOMWMR~Z7:.^
BIHAR
□ PUBLIC
._______
wnam
'//.'//M//.
60
80
AP
MAHARASHTRA
PUNJAB
cEMBR
HARYANA
o
20
40
Source: NCAER, 2000
100
Percent
2.8.52 The state-wise distribution of in-patients
in public and private hospitals is given in
Figure 2.8.12. In spite of good government sector
infra-strucure, a majority of patients in Punjab,
Haryana, and Maharashtra went to private hospitals.
In Himachal Pradesh, Rajasthan, West Bengal and
the north eastern states a majority of the patients
seek admission in government hospitals in spite of
inadequacies in infra-structure. In Bihar, poor
government infrastructure might be responsible for
over 60 per cent of patients seeking admission in
private hospitals. Obviously the choice between
public and private sector facilities depends on
several factors including the functional status of
government infrastructure, the price differential
between the public and private sector, the person’s
ability to pay and the preferences of the community.
the coverage of villages by NGOs (Figure-2.8.13).
NGOs providing a variety of services are
relatively few, unevenly distributed across and
within states and have limited area of operation.
Some implement government programmes of the
departments of family welfare and health. Others
run integrated or basic health services
programme or provide special care/ rehabilitation
to people suffering from some specific diseases
e.g., leprosy patients. Health care activities are
also carried out by agencies like the Red Cross,
industrial establishments, Lion’s Club, Helpage
India etc.
2.8.54 Some of the problems faced by NGOs in
delivery of health care include:
El
NGO and Voluntary Sector
limited interaction between the government and
NGOs;
limited financial management, technical and
managerial capacity of the NGO;
2.8.53 Apart from purely private providers of
health care, the NGOs and the voluntary sector
have been providing health care services to the
community. It is estimated that more than 7000
voluntary agencies are involved in health-related
activities. Wide inter-state differentials exists in
96
El
paucity of funds; and
O
delays in transfer of funds from the
government.
HEALTH
Figure-2.8.13 - Percentage of Villages with NGOs, 1994
40
•
o
o
o
0_
34.4
30
21.2
20
10
s 14.
--
j OnI * •>
Fl n:
z z zz
z
6464
____ T7 _
4.7
aii a i
y'
0
z
z
z
10.6
9 7 9.1 8.8
<v
0
<z
26 1.4
PI r~~i
z
0
v-
Jz
SOURCE : AJAY MAHAL, 1999
Ongoing Efforts in Public - Private Collaboration
in Health Care
knowledge and skills through in-service
training;
2.8.55 There have been very few studies
documenting the geographic distribution of
outpatient/in patient
facilities,
existing
collaborations between private sector and public
sector institutions and the role each of them play
in outpatient/ inpatient health care in different
districts/states. The Ninth Plan had recommended
thatthese will be documented and the information
utilised for decentralized district -based planning.
This has not yet been done and may have to be
taken up on a priority basis during the Tenth Plan.
During the Ninth Plan period, the Centre as well
as the states initiated a wide variety of public
private collaborations. Some of the ongoing colla
borations include:
contractual appointment of the health care
personnel and hiring of private practitioners for
providing services in the PHCs have been
attempted in order to fill the gaps. However,
the response has been poor; these practi
tioners need orientation training to fulfill the role
expected of PHC doctors;
O
in most of the states government doctors are
allowed private practice. The doctor benefits
monetarily; patients also gain because they are
being treated by doctors who had updated their
H
part time hiring of general practitioners and
specialists to visit and provide health care in
PHCs/CHCs in under-served areas. Limited
success has been reported in this experiment;
El
state and central governments, PSUs
reimburse cost of medical care provided by
recognized private health care providers/
institutions;
involving NGOs/private sector practitioners in
the national programmes e.g. utilizing the
services of NGOs, and not for profit institutions
in the leprosy eradication programme,
97
TENTH FIVE YEAR PLAN 2002-07
involvement of private practitioners/institutions
in the blindness control programme and the
NGOs in HIV/AIDS control programme;
H
private sector individuals/institutions/industry
e.g. Tata Steel Company provide health care
to the population living in a defined area;
H
private super-specialty, tertiary/secondary care
hospitals are given land, water and electricity
etc. at a concessional rate and permission for
duty-free import of equipment with the under
standing that they will provide in-patient/outpatient services to poor patients free of charge.
The experience in this has been varied; several
problems being reported;
H
private practitioners provide information for
disease surveillance in some districts in Kerala.
2.8.56 The impact of all these on improving
access to and affordability of health care and on
the coverage under disease control programmes
have not yet been evaluated. However, available
information suggest that these schemes succeeded
in places where there were well-defined committed
groups and clear-cut memorandums of under
standing (MOUs) and the MOUs were implemented
properly. During the Tenth Plan attempts will be
made to improve area-specific public-private
collaborations, taking into account the health care
needs of the population, the presence of each of
these sectors, their strengths and weaknesses.
Feasibility of GIS mapping to identify under-served
areas and providing suitable incentives to
encourage private sector to set up health facilities
in such areas will be explored. Monitoring the
implementation of these programmes along with the
PRIs and local leaders will go a long way in ensuring
accountability.
is done, private practi-tioners can play an
important role in increasing the coverage as well
as containing the cost of care.
2.8.58 One essential pre-requisite for improving
the quality of care will be the development of
standard treatment protocols appropriate for each
level of care. The medical colleges and research
institutions should play a key role in preparing these
documents quickly. The existing government
institutions at each level will have to take up the
responsibility of testing these management
protocols and suggest necessary modifications.
These protocols will be made available to all
practitioners through CME programme for skill
upgradation and training. Available IT tools have to
be fully utilised by CME programmes to ensure easy
access to the materials for updating skills and
knowledge. Online consultation services between
paraprofessionals and doctors and among doctors
may improve the quality of services and reduce the
problem of transporting patients to hospitals for
diagnosis and advice regarding management.
Government institutions in the states, which will be
‘model institutions’, will evolve appropriate norms
for the cost of care at different levels of institutions
and monitor both the cost and the quality of care in
their own institutions. The district health officials will
monitor the performance of both public and the
private sector institutions in the district and assist
them in improving the quality of care and containing
cost of care.
2.8.59 During the Tenth Plan appropriate policy
initiatives will be taken to define the role of gover
nment, private and voluntary sectors in meeting the
growing health care needs of the population at an
affordable cost. The public sector will develop
institutional capability at the central, state and local
levels to:
2.8.57 Since private practitioners provide most
of the curative care in the country, it is important
that they are given ready access to updated
proto-cols for the management of common
illnesses and current regimens used in the
national disease control programmes and family
welfare programme. They must be allowed to
have easy access to drugs, devices, and vaccines
provided through the national programmes. If this
98
H
evolve policies and strategies for providing
healthcare and monitor their implementation;
O
increase public-private-voluntary sector
collaborations to meet the health care needs
of the poor and vulnerable segments of
population;
HEALTH
E3
draw up standards for appropriate quality and
cost of care and establish accreditation
systems for individuals/institutions;
mushrooming of health care institutions
particularly in the private sector.
El
monitor and enforce regulations and
contractual obligations;
El
promote excellence and ethics among
professionals, identify and punish professional
misconduct;
E
set up an appropriate and speedy grievance
redressal mechanism.
2.8.61
During 1990s, some initiatives were taken
to address issues relating to quality of care e.g.
inclusion of health sector under the Consumer
Protection Act. Some states have attempted to
provide a legal framework for the functioning of
private health care institutions on the lines of the
Bombay Nursing Home Registration Act 1949.
These legislative measures have so far not been
effectively implemented partly because of the lack
of objective criteria for defining ‘quality of care’ and
the fear that enforcing such regulations may
increase the cost of care.
Quality and Accountability in Health Care
2.8.60 Assessment of the quality of health care
is often thought to be a value judgement but there
are determinants and ingredients of quality, which
can be measured. These include assessment of
infrastructure and manpower, processes such as
diagnosis and treatment or outcome such as case
fatality, disability and patient satisfaction. Health
care quality evaluation includes safety,
effectiveness and timeliness of interventions. It
must also include assessment of the performance
of the system in terms of meeting the changing
needs of the population to stay healthy and learn
to live with illness and disability. In recent years,
there has been increasing public concern over
the quality of health care both because of
increasing awareness of the population and the
Introduction of Quality Control System in
India will:
2.8.62
During the Tenth Plan quality control
concepts and tools will be introduced into every
aspect of health care in order to ensure that:
E
the population and the system benefit from
defined and institutionalised norms, account
ability and responsibility;
E
the Tenth Plan goals are achieved and health
indices of the population improve; and
E
health care is made affordable for individuals
and the country as a whole.
HUMAN RESOURCE DEVELOPMENT FOR
HEALTH
2.8.63 The outcome and impact of any health
programme depends on the competencies and skills
of the personnel who implement it. At the time of
Independence, the country had a population of 300
million. Famine, starvation and epidemics took a
massive toll of human life; infant and maternal
mortality rates were among the highest in the world
and life expectancy was about 33 years. There were
about 50,000 medical graduates and 25,000 nurses
in the modern system of medicine to provide health
care to the population.
E prevent overuse, under-use, abuse
and misuse of facilities;
E improve effectiveness and efficiency;
E help to make positive outcomes more
likely;
E help in effective and responsible use of
resources;
E minimise barriers to appropriate care at
different levels by matching the levels of
care to the level of need;
E bring accountability into the health
system; and
2.8.64 The country then embarked on a massive
expansion of medical and para-professional training
so that the manpower needs for the proposed
expansion of the health system are met . Five
E ensure that optimum use is made of
every rupee invested.
99
smssmwswwwssiii!
TENTH FIVE YEAR PLAN 2002-07
have made rural service compulsory for health
professionals and preference is given for those
opting for rural services in post-graduate courses.
The sustainability and impact of these measures
are yet to be evaluated.
Ninth Plan Priorities for Human Resources
Development for Health
ISI creation of a district data base on requirement,
demand and availability for health manpower
in the government, private and voluntary
sectors;
2.8.65 During the Tenth Plan medical education
will have newer opportunities and challenges. The
country has to train adequate number of health
professionals with appropriate knowledge, skill and
attitude to meet the health care needs of the growing
population and dual disease burden. In this era of
globalization, India with its excellent teachers and
abundant clinical material can become a key player
in medical education. The health care institutions
can transform India into a major medical tourism
destination. Appropriate investment in research and
development and quality control can result in a
massive expansion of the pharmaceutical sector.
The next two decades will show whether the country
has successfully used these opportunities to train
and provide gainful employment to the highly skilled
medical manpower.
ISI periodic updating of information on :
requirement and availability and of
different categories of health manpower;
health manpower production based on the
needs;
El improvement in quality of undergraduate/
postgraduate education;
IE promotion of equitable and appropriate
distribution of health manpower;
IE continuing medical education for knowledge
and skill upgradation;
E appropriate people and programme orienta
tion; and
E continuing multiprofessional education for
promoting team work & intersectoral co
ordination.
Health Manpower Planning
decades later there are 181 medical colleges in the
modern system of medicine and over 400 ISM&H
2.8.66 Unlike health services planning, health
colleges. The country produces over 17,000 doctors
manpower planning in India has not received
in modern system of medicine annually and a similar
adequate attention. Sir Joseph Shore Committee,
number of ISM&H practitioners, nurses/ANMs as
1946 recommended a population-based norm for
well as para professionals. A vast health care
medical (one doctor/population of 1500) and nursing
infrastructure in the government, voluntary and
personnel (one nurse/ population of 500). This was
private sector has been created and
is manned by people trained in the
Figure 2.8.14 - Health Care Provider-population Ratio
country. Personnel costs form a major
12000 -------------------- —n
portion of the investment in health
10000
service delivery. In spite of several
5
to 8000
constraints, Indian health profes
3
o’ 6000
sionals and paraprofessionals have
migrated to other countries and have
4000
gained global recognition for their
2000
x—x—-x—x—x—x—x- X----X X—X- -X- X—X- -X—X
knowledge, skills and commitment.
0 However, it is a matter of concern that
there are huge gaps in critical health
manpower in government institutions
MODERN system
AYURVEDA
that provide health care to the poorer
-Ar- HOMOEOPATHY
—x—ALL
segments of population living in urban
—I—NURSES
AUXILLARY NURSE MIDWIVES
slums, remote rural and tribal areas.
SOURCE : Department of Health, 1995 & 1996
To address this problem, some states
<■
100
HEALTH
subsequently modified taking into account the
changes over the last five decades. The Bajaj
Committee suggested that assessment of health
manpower requirement should be based on multiple
parameters including functionary to population ratio,
inter-professional ratio and manpower-mix. Health
manpower requirements vary from region to region
depending upon stage of epidemiological transition,
the availability of institutions, income-elasticity and
public and private expenditure on health. Available
information on the health care provider-population
ratio over the last two decades is given in Figure
2.8.14.
2.8.67 The Ninth Plan envisaged that health
manpower planning will be based on the district
specific assessment of available manpower and
facilities and the needs and demands of health
services. Fine tuning will be done taking into account
the manpower needed for implementing national
programmes and the manpower requirements in the
voluntary and private sector. In order to realistically
assess the health manpower availability, the CBHI
initiated efforts to obtain reliable and accurate
district-wise data on the number of medical, dental,
ISM&H professionals, nursing and para
professionals and institutions (centre, state, defence
services, railways, private sector or voluntary
sector). There has been very little progress in this
effort; attempts to match the supply of health
manpower with the requirement have not even
begun. During the Tenth Plan, this database will be
created so that decentralised district-based health
manpower planning to meet the needs would
become possible.
is considered and 1:800 if ISM&H doctors are also
taken into account.
2.8.69 There are massive interstate differences
in health indices, health care institutions and health
manpower production. Just four states (Karnataka,
Andhra Pradesh, Tamil Nadu and Maharashtra)
have 81 out of 181 medical colleges. On the other
hand populous states like Bihar and Uttar Pradesh
with poor health indices and large gaps in health
manpower have very few medical colleges. The
medical education curricula have not kept pace with
the changing requirements of the population or skills
required for implementing health and family welfare
programmes. The current system of medical
education does not appear to enable the students
to develop clinical and analytical skills required for
functioning effectively in the primary health care
settings. The number of family physicians with
clinical skills, appropriate people orientation and
commitment to improvement of the health status of
the community appears to be dwindling. There has
been a decline in candidates opting for public health
and paraclinical subjects and increasing competition
for potentially lucrative clinical and diagnostic
specialties. These trends which may have an
adverse impact on public health programmes have
to be reversed.
2.8.70
During the Tenth Plan under graduate and
post graduate training will have to be reoriented to
enable students to become competent professionals
who can effectively implement programmes aimed at
improving the health status of the population. The
curriculum may be periodically reviewed and revised
in keeping with changing health care needs. Several
states have established University of Health Sciences
(UHS) to which all medical colleges, dental colleges,
para professional and nursing colleges are affiliated.
The University ensures uniformity in admission criteria,
curriculum and evaluation system and co-ordinates
activities aimed at improving the quality of education.
During the Tenth Plan all states will be encouraged to
establish a UHS.
Health Manpower Production
2.8.68 As on June 2001, there were 181 medical
colleges out of which 155 (46 of them private) were
recognised and 26 (19 of them private) were
permitted under section 10A of the Indian Medical
Council Act, 1956. A total of 5,39,00 MBBS doctors
were registered with the Medical Council of India
(MCI) till 2000. At the national level, the number of
physicians and specialists available is more than
the estimated requirements. The current doctor
population ratio is 1:1800 if only the modern system
2.8.71
Initially, most medical colleges were
funded either by the central or state government.
Over the last two decades, several private medical
101
-------------------------------- —
GnOV -1 'LO
U8648
< e. ’*• ■ y"
TENTH FIVE YEAR PLAN 2002-07
colleges have been set up. There have been wide
disparities among medical colleges regarding the
adequacy of infrastructure, quality of teaching,
criteria for admission and fee structure. Concerned
about the mushrooming growth and poor quality of
medical colleges, the Indian Medical Council Act
was amended in 1993 making the permission of
the central government mandatory for establishing
a medical college, starting a new or higher course
of study or training and increase in admission
capacity. However, this did not stop the increase in
the number of medical colleges. Judicial intervention
has to some extent, moderated the differences in
the criteria for admission and fee structure between
private and government funded institutions.
2.8.72 Medical educationists feel that over years
there has been a decline in quality of medical
education. This might partly be due to the problems
both teachers and students have in coping with the
explosive expansion in medical knowledge and
technology during the last two decades. The
mushrooming of medical colleges and para
professional institutes with inadequate staff and
infrastructural facilities has also undoubtedly
contributed to the decline in the quality of teaching
and training. Implementation of the of the Ninth Plan
recommendation regarding setting up a commission
on the pattern of University Grants Commission
(UGC) to provide financial assistance to medical
colleges to improve quality of education may help
in arresting the deterioration in quality of medical
education. Implementation of another Ninth Plan
recommendation that inspections by MCI would be
necessary not only for initial recognition but also
for continued recognition as medical colleges and
admission of students, may go a long way in
improving the quality of medical education.
Dental Manpower
2.8.73 At present, there are 142' (113 private)
recognised/approved dental colleges in the country
with 8900 BDS admissions a year. There are 48
institutions with 869 seats providing postgraduate
training. As in the case of medical colleges, there
are regional imbalances in the distribution of dental
colleges. The needs of dental paraprofessionals has
not been assessed and met. During the Tenth Plan
efforts will be made to assess state-wise demand
for dental professionals and district-wise need for
dental paraprofessionals and take steps to meet
the requirements.
Nursing Manpower
2.8.74 Around 7.37 lakh nurses have been regi
stered in the various state nursing councils in the
country; it is estimated that only about 40% are in
active service. About 1.5 lakh nurses are employed
in the government sector. Out of the 654 general
nursing-midwives training schools in the country,
465 are run by private/voluntary organizations /
missionary institutions. Around 20,000 trained
nurses become available annually; the current
production capacity is sufficient for filling up
vacancies in the Government sector. There is a
growing demand for nurses with specialized training,
which has to be met. There are over 4 lakh ANMs
of whom nearly 1.5 lakh work in the~govemment
sector. In some states where there is a shortfall in
required number of ANMs, the ANM training schools
are being reopened in the government sector.
Paramedical Staff
2.8.75 Adequate paraprofessional support is
essential for an efficient and effective functioning
health system. Lack of critical para-professional
manpower, especially laboratory technicians and
male multipurpose workers has been cited as a
major factor responsible for poor performance of
the tuberculosis and malaria control programmes.
The need for different categories of para-medical
persons vary between districts and over time. The
current needs have to be assessed at district level,
and critical gaps filled by skill upgradation and
training of unipurpose workers and laboratory
technicians working under the disease control
programmes.
2.8.76 During the Tenth Plan the changing require
ments for para-professionals will be assessed
preferably at the district level and necessary steps
102
HEALTH
taken to meet the requirement through all available
training channels. Preference should be given to
the 10+2 vocational training courses because
ISI
it would improve career prospects of the
persons trained;
ISl
the problem of trained para professionals not
staying in the place of posting will be reduced
if training is done in the districts after assessing
the need.
2.8.77 The UHS will ensure that appropriate
curricula are evolved and followed. The state
governments will amend the recruitment rules for
these posts so that those who qualify through
vocational courses and open university system
become eligible for the jobs in the government,
voluntary and private sectors. Efforts to set up
paraprofessional council and utilise the UHS to
improve the standard of education and training of
paraprofessionals will continue during the Tenth
Plan period
Continuing Medical Education (CME)
2.8.78 Continuing education and skill upgradation
are essential for all health professionals. Currently,
in-service training courses are being carried out as
a part of all national programmes. CME progra
mmes are being carried out in various institutions,
such as the National Academy of Medical Sciences,
National Board of Examinations, and various
professional bodies and associations. However their
outreach, quality and content are sub-optimal. CME
efforts will receive greater impetus if the proposal
that all medical practitioners have to under go
knowledge and skill up gradation and re-certification
every five years is implemented. Critical thrust areas
such as the ongoing and new national programmes,
rational use of drugs, protocol for management of
common ailments, quality control in clinical practice,
infection control and waste management in health
care settings require focused attention. The National
Academy of Medical Sciences has proposed that
they will hold intramural CME in these topics where
eminent professionals will participate and the
proceedings will be put on the website and made
accessible to all. These efforts will continue to
103
receive support during the Tenth Plan. Open
Universities will be expected to play a major role in
periodically updating the knowledge of various
categories of health personnel in a cost effective
and efficient manner.
Bio-informatics, Telematics and Distance
Education
2.8.79 Information Technology is now one of the
major components of the technological infra
structure for health management. All sub-sectors
dealing with the generation, transmission and
utilisation of demographic and epidemiological data
such as bio-informatics, bio-statistics, HMIS and the
decision support systems (DSS) are finding increas
ing use in health planning and management. The
nationwide network of NICNET provides rapid
reporting mechanism for health information,
MEDLARS Biomedical Informatics Programmes
provides ready access to medical databases to post
graduates and research workers as well as
practising physicians. Planning Commission has
provided additional central assistance to the UHSs
in Karnataka, Andhra Pradesh, Tamil Nadu, Punjab
and Maharashtra for strengthening of libraries and
networking them through IT. This effort has to be
augmented and all medical colleges need to be
brought into the network.
2.8.80 Telemedicine programmes bring experts
together to assist local doctors in the management
of complicated cases. A pilot project on telemedicine
in primary health care is currently ongoing in
Maharashtra. Some of the major hospitals have
taken up online consultation service with other
specialists within the country as well as abroad.
Efforts are underway to link tertiary care institutions
especially in the north-eastern states with major
super-speciality institutions in other regions so that
patients could benefit from tele-consultations.
PREVENTION AND MANAGEMENT OF
COMMUNICABLE DISEASES
2.8.81
The control of communicable diseases
has received priority attention right from indepen
dence. Effective antibiotic therapy for infections and
TENTH FIVE YEAR PLAN 2002-07
diseases, will continue in the Tenth Plan.
Modalities to improve delivery of services
pertaining to these programmes through the
existing health services will be worked out. Efforts
will be made to improve states ownership of the
programmes, participation of the community,
private sector and NGOs. Local accountability
and intersectoral co-ordination will be improved
through the involvement of PRIs. Evaluation and
operational research to rectify problems in
implementation and improving efficiency will
receive attention.
Ninth Plan strategies for improving
communicable disease control
programmes
H Rectification of identified defects in design and
delivery of diseases control programme.
M Filling critical gaps in infrastructure and
manpower.
Bl Making service delivery responsive to user’s
needs.
B Ensuring that health care providers have the
necessary skills and support, including referral
facilities and supplies.
National Vector Borne Disease Control
Programme
B Improving community awareness, participation
/ and effective utilisation of available services.
B Use of PRIs in improving community
participation and monitoring implementation
of programmes.
vaccines for the prevention of infections were the
major factors responsible for the steep decline in
crude death rate from 25.1 in 1951 to 8.7 in 1999.
However, morbidity due to communicable diseases
continues to be high. Deteriorating urban and rural
sanitation, poor liquid and solid waste management
and overcrowding have contributed to the increasing
prevalence of communicable diseases. Treatment
of infections has become more difficult and
expensive because of the emergence of antibiotic
resistance; increasing attention is urgently needed
for prevention of hospital acquired infections
through effective implementation of infection control
measures. Even though health is a state subject,
the central government has provided additional
funds through centrally sponsored schemes for
disease control and this has paid rich dividends.
Smallpox and guinea worm infections have been
eradicated. There has been a substantial reduction
in leprosy and polio cases and elimination of these
two disease is likely to be achieved in the next few
years. However malaria, tuberculosis and HIV
infection have not shown any reduction and require
continued vigorous attempts at containment and
control.
2.8.82 The strategies and programmes initiated
in the Ninth Plan for control of communicable
104
2.8.83 The National Malaria Control Programme,
the first centrally sponsored programme, was
initiated in 1953. The National Anti Malaria Progra
mme currently deals with malaria, filaria, kala-azar,
Japanese encephalitis and dengue. During the Tenth
Plan the programme will be implemented as
National Vector Borne Disease Control Programme.
Malaria
2.8.84 In the early 1950s, malaria was not only a
major cause of morbidity and mortality but also one
of the major constraints in the ongoing
developmental efforts. The National Malaria Control
Programme had spectacular success initially in
bringing down incidence of malaria from 75 million
cases with 0.8 million deaths to 0.1 million cases
Figure 2.8.15 - Total Malaria Cases & Deaths
z
V)
LU
<
u
u
o Z
7y
-r 1400
6 -•
- 1200
5 -
-- 1000
4 -
- 800
LU
3
600
u
2
<§
<
400
x
3
<
CD
Z
X
o
200
0
-------- 1------- 1-------- 1--------1--------1------- 1------- 1------- 1--------1-------- <------- 1------ 1—
o
04 cn
in co
co tn o ■
r- co o oi cn o> o o> ct> o>
oi o 5;
olcoicnocojoaicjooios
V
T—
T—
T—
V
TO
0
t
~ DEATHS3^01^ (ln Million)
-A-
.. ’4~“ MALAR|ACASE (In Million)
Source - NAMP, DEPARTMENT OF HEALTH
* PROVISIONAL
HEALTH
with no death by 1965 even though there was no
well-established health care infrastructure in the
rural areas. However, there was a resurgence of
malaria subsequently. In 1976, over 6.7 million
cases were reported. From 1977, the National
Malaria Eradication Programme started
implementing a modified plan of operation for
control of malaria. In spite of these efforts, the
number of reported cases of malaria have remained
around two million in the 1990s (Figure 2.8.15).
2.8.85 In view of the high incidence of malaria
(particularly of falciparum malaria) and high
mortality, 100 per cent central assistance under the
Strategies for vector control include:
Indoor spraying with appropriate insecticide
in areas where API is over 2
Anti-larval measures Strategies for vector
control in urban areas include:
•" Introduction of medicated mosquito nets
*" Use of larvivorous fishes and biolarvicides
state governments require. The state governments
meet the operational cost, including the salaries.
2.8.86 The percentage distribution of malaria
cases in various states is given in Figure 2.8.16.
The performance during the Ninth Plan period is
shown in Figure 2.8.17. The decline in cases was
not commensurate with the substantial increase in
the funding for the activities. The rising proportion
of P. falciparum malaria, increasing vector resis
tance to insecticides and the growing parasite
resisitance to chloroquin will render malaria
containment and control more difficult in the Tenth
Plan period. The Ninth Plan goal for reduction in
API and morbidity has not been achieved (Figure
2.8.17). The programme review by the Government
of India and the World Bank showed that progress
Ninth Plan strategy
E early diagnosis and prompt treatment
E selective vector control and personal
protection
E prediction, early detection and effective
response to outbreaks
E IEC
Target for 2002
El ABER of over 10 per cent
E API of less than 0.5 per cent
E 25 per cent reduction in morbidity and
mortality due to malaria
NAMP is being provided to the north-eastern states
since 1994. Financial assistance was also obtained
from the World Bank for the Enhanced Malaria
Control Programme (EMCP) to cover 100
predominantly P. falciparum malaria endemic and
tribal-dominated districts in Andhra Pradesh, Bihar/
Jharkhand, Gujarat, Madhya Pradesh/Chattisgarh,
Maharashtra, Orissa and Rajasthan and 19 cities.
The project also has the flexibility to divert resources
to any area in case of malaria outbreak. In other
areas, the NAMP continues to be implemented as
a centrally sponsored scheme on a 50:50 cost
sharing basis between the Centre and states in
urban and rural areas. The central government
provides drugs, insecticides and larvicides and also
technical assistance/guidance as and when the
105
Figure 2.8.16 - Percentage Distribution
of Malaria Cases - 2001
UTTAR OTHERS
PRADESH 7%
S%
CHATTISGARH
13%
RAJASTHAN/f
7%
GUJARAT
4%
JHARKHAND
6%
/\
KARNATAKA
10%
ORISSA’
21%
/
N.E. STATES
15%
Source : NAMP. D/o Health
/ MADHYA
/ PRADESH
9%
MAHARASHTRA
3%
TENTH FIVE YEAR PLAN 2002-07
Kala Azar
Figure 2.8.17 - National Anti Malaria Programme
4.0-------
3.5------3.0—
I
2.5—
2.0--1
2.8.87 Kala azar is endemic in 33 districts of
Bihar, 11 districts of West Bengal and three districts
in Jharkand and sporadic cases have been reported
in Uttar Pradesh. After a reported increase in the
number of cases and deaths due to kala-azar
between 1989-91 period, an intensive programme
for containment of kala azar was launched in 1992.
Ii■I I II I
~-
■
-
1.0 0.5—
S'
o.o-
1996
1997
1999
1998
2000
2001 (P)
□ POSITIVE CASES (in million)
□ P.F. CASES (in million)
□ A.P.I
0 NO OF DEATHS (in 1000)
Source : NAMP, Deptl of Health
in capability building for malaria surveillance and
response at the district level, early detection and
treatment of cases, monitoring drug and insecticide
resistance and insecticide spraying was slow. The
utilisation of funds under the programme has been
sub-optimal (Table 2.8. 4)
Table 2.8.4
NAMP-Outlays and Expenditure
Rs. Lakhs
YEAR
OUTLAY
9TH PLAN
103000.00
1997- 98
20000.00
14276.00
1998- 99
29700.00
16371.00
1999-00
25000.00
17601.00
2000-01
25500.00
18832.00
2001-02
22500.00
23400.00*
Source : Department of Health
EXPD./RE
2.8.88 The strategy for control of infection
includes interruption of transmission through
insectidical spraying with DDT and early diagnosis
and treatment of kala azar cases. The Central
Government provides the insecticides and anti kala
azar drugs while the state governments meet the
expenses involved in the diagnosis and treatment
of cases and insecticide spraying operations. The
number of reported cases and deaths (Table 2.8.5)
have not shown significant decline during the Ninth
Plan period. This is due to inadequate insecticide
spraying operations and poor outreach of diagnostic
and curative services. Increase in drug resistance
to sodium stibogluconate has been reported in the
Muzffarpur and Darbhanga districts of Bihar.
Though sand fly is usually sensitive to DDT, pockets
of insecticide resistance have been reported from
Bihar.
Dengue/Japanese Encephalitis (JE)
2.8.89 Periodic dengue outbreaks occur in many
parts of India, in both rural and urban areas. Mortality
is usually low but may be high in cases of dengue
* Anticipated Expd.
Table 2.8.5
Cases and Deaths due to Kala-Azar
Year
Bihar
West Bengal
Country
Cases
Deaths
Cases
Deaths
Cases
Deaths
1996
25056
674
NA
NA
27049
687
1997
15948
251
1450
3
17429
255
1998
12229
211
1113
6
13577
226
1999
11627
277
1091
6
12869
297
2000 (P)
12039
124
950
8
14239
132
Source: Report of the Working Group on Communicable Diseases for the Tenth Plan. P-Provisional
106
HEALTH
shock syndrome and dengue haemorrhagic fever
(DHF). Diagnostic tests for dengue are not readily
available. Japanese encephalitis outbreaks have
been reported mainly in Andhra Pradesh,
Karnataka, Uttar Pradesh and West Bengal.
Diagnostic tests and case management facilities for
Japanese encephalitis are not readily available in
many parts of the country. In endemic states, efforts
are being made to improve early diagnosis, proper
management and rehabilitation of those with
residual disabilities. Innovative strategies for vector
control are being investigated. The reported total
cases and deaths due to dengue/Japanese
encephalitis during the Ninth Plan are given in
Table 2.8.6.
a feasibility and efficacy study on a mass annual
single dose administration of DEC and albendazole
drugs for the control of filariasis. Kerala has initiated
a pilot project for monitoring and management of
mosquitoes, in three filariasis endemic districts
(Kottayam, Alappuzha and Ernakulam) for the
control of vector-borne diseases. The progress of
such innovative initiatives will be evaluated and, if
found feasible, they will be replicated. The Govern
ment of India is a signatory to the UN resolution to
eliminate lymphatic filariasis by 2020. The National
Health Policy (NHP), 2002 envisages the elimination
of lymphatic filariasis by 2015.
Table 2.8.6
Cases and Deaths due to Japanese
Encephalitis and Dengue/DHF
2.8.92 During the Tenth Plan, the National VectorBorne Disease Control Programme will be
implemented through the existing health care
infrastructure. The programme will focus on:
JE
Tenth Plan Initiatives
DENGUE/DHF
Year
Cases
Deaths
1997
2516
632
1177
36
1998
2120
507
707
18
1999
3428
680
944
17
2000(P)
2313
535
605
7
training of health personnel in the diagnosis of
vector-borne diseases and appropriate
treatment including referral;
Cases Deaths
improving reporting, recording and monitoring
of vector-borne diseases, including cases
treated in the private sector, so that reliable
estimates of the prevalence of vector borne
disease is available;
Source : Department of Health, 2001.
Filariasis
2.8.90 Filariasis is endemic in 19 states/union
territories. Estimates based on surveys by Filariasis
Survey Units suggested that:
about 454 million people (120 million in urban
areas) are living in known endemic areas.
M
monitoring drug and insecticide resistance;
IS)
using standardised protocol for the diagnosis
and management of these diseases;
IS)
involvement of PRIs to:
R>
chalk out the malaria worker’s schedule;
R>
inform the community and the gram sabha
of the spraying operations and seek their
cooperation;
R>
ensure that insecticide spraying is started
well in advance;
R>
identify villages, which are at the risk of
epidemic outbreak;
there are 29 million filariasis cases in the
country and 22 million micro-filaria carriers.
2.8.91
Currently there are 206 filaria control units;
199 filaria clinics; and 27 filaria survey units. A total
of 48 million people in urban areas are being
protected through anti-larval measures. The Indian
Council for Medical Research (ICMR) is conducting
107
TENTH FIVE YEAR PLAN 2002-07
R>
R>
R>
ensure the availability of staff as well as
consumables for diagnosis and drugs for
treatment;
ensure that the malaria worker/male multi
purpose worker identify fever cases, take
blood smears and ensure that the
community follows treatment advice.
ensure that smear positive cases are given
radical treatment and monitor implemen
tation of the programme;
S
improvement in IEC at patient, family and
community levels;
O
involvement of NGOs and the private sector in
diagnosis and treatment of malaria cases;
encourage the pharmaceutical industry,
manufacturers of insecticides and bednets to
produce low cost products for local use; back
up these efforts through IEC and social
marketing.
H
evaluate community acceptance of insecticidetreated bed nets/curtains for personal
protection;
research studies on
vector bionomics and behaviour
R>
bio-environmental methods of vector
control;
R>
screening and development of new antimalarial drugs especially herbal
products;
evaluation of new drugs and insecticides;
S
include malariagenic potential as a parameter
for health impact assessment of developmental
projects.
Goals for Tenth Plan
Malaria:
R>
ABER over 10 per cent
R>
API 1.3 or less
R>
25 per cent reduction in morbidity and
mortality due to malaria by 2007 and 50
percent by 2010 (NHP 2002)
Kala azar
R>
Prevention of deaths due to kala azar
by 2004 with annual reduction of at least
25 per cent
Zero level incidence by 2007 with annual
reduction of at least 20 per cent using
2001 as the base year
Elimination of kala azar by 2010 (NHP
2002)
Revised National Tuberculosis Control
Programme (RNTCP)
2.8.93 Tuberculosis (TB) is a major public
health problem in India, with an estimated 40 per
cent of the population suffering from the infection.
India accounts for nearly one-third of the global
incidence of tuberculosis. The estimated
prevalence of tuberculosis is 1.4 per cent, and
sputum positive TB prevalence is estimated to
be in the range of 4/1000 to 5/1000. A national
sample survey to assess the current
epidemiological situation of tuberculosis in
different zones is currently under way. Some
studies indicate that since 1980s there has been
a progressive increase in primary and acquired
multi-drug resistant cases of tuberculosis.
2.8.94 The aim of the fight against tuberculosis
at the individual level is to cure the disease, to
preserve and quickly restore the individual’s work
capacity, allow the person to be with the family
and maintain their socio-economic status. At the
community level, the aim is to reduce the risk of
infection through effective case finding and
appro-priate management of sputum positive
exploring the cost effectiveness of the use of
remote sensing for mapping the breeding
habitats of mosquitoes and prediction of
densities of vector species, especially in remote
hilly and tribal areas.
108
HEALTH
case. The National Tuberculosis Control
Programme was initiated in 1962 as a centrally
sponsored scheme. The programme was aimed
at early case detection in symptomatic patients
seeking health care, through sputum microscopy
and X-ray and effective domiciliary treatment with
chemotherapy. BCG vaccination at birth for
protection against tuberculosis infection was
incorporated into the immunisation programme.
Introduction of the short course chemotherapy,
which shortened the duration of treatment to nine
months, was begun in selected districts in 1983.
In spite of the availability of effective
chemotherapy, there has not been any decline in
the morbidity or mortality due to TB because of
low case detection, case holding and cure rates.
The programme was reviewed in 1992 and a
Revised National Tuberculosis Control
Programme (RNTCP) was drawn up with
emphasis on:
in the DOTS districts, the proportion of TB
sputum positive cases detected and treatment
completion rates have improved.
an attempt to improve coverage, increased
participation of NGOs and private practitioners is
envisaged. The programme is being closely
monitored.
2.8.96 The performance under RNTCP during
the Ninth Plan is given in Figure 2.8.18. A joint
programme review by the Government of India and
the World Bank in February 2000 showed that there
was improvement in diagnosis, drug supply and
proportion of patients cured in DOTS districts. The
major problems in RNTCP continued to be:
Figure 2.8. 18 - Tuberculosis Detection and
Treatment in India
900000
----------- ------------------ 60
750000
diagnosis through sputum microscopy;
50
1 /I I
600000
450000
S
uninterrupted supply of drugs for short course
chemotherapy;
300000
150000
direct observation of treatment with short
course chemotherapy (DOTS) to improve
compliance; and
systematic monitoring, evaluation and
supervision at all levels.
2.8.95 There were delays in the initiation of the
RNTCP but a rapid scale-up of the programme
began in late 1998. According to programme
reports:
S
El
S
i No. of patients
treated
i
i Smear-positive
patients treated
40
30
20
10
0
i
A— Detection
rate/lakh per
year
0
£ co
1
co
co
cr
(X
1997 | 1998 | 1999
2000
Source: RNTCP, Department of Health
El
poor coverage due to gaps in primary health
care infrastructure and manpower;
IS)
poor quality of sputum examination;
SI
diagnosis not based on evolved criteria;
state and district societies have been formed
and provided with funds.
use of non standard treatment regimens,
especially by private practitioners;
more than 1,50,000 health workers and 1,400
supervisors have been trained.
poor record keeping, lack of follow up care;
diagnostic facilities have been established in
more than 3,000 laboratories.
lack of involvement of health care providers;
poor coordination; and
the coverage of population under the progra
mme increased from 89 million in 1998-99 to
around 365 million in 2000-01.
E
109
patient’s difficulties in compliance with DOTS
regimen.
TENTH FIVE YEAR PLAN 2002-07
2.8.97
It is now recognized that there are inherent
El
problems in ensuring compliance with long-term
drug therapy for any chronic disease. It is essential
that the utility, acceptability and sustainability of the
DOTS strategy is evaluated and if necessary mid
course corrections carried out. Utilisation of funds
has been sub-optimal in the first three years of the
Ninth Plan (Table-2.8.7).
involvement of medical colleges, TB hospitals,
hospitals run by the armed forces, railways,
corporate sector, NGOs and private
practitioners in the pro-gramme;
involvement of PRIs to ensure the availability
of requisite staff;
H
Table 2.8.7
RNTCP- Outlays/Expenditure
quality assurance of sputum microscopy and
quality control of drugs;
(Rs. in Lakhs
provision of sufficient stock of drugs and
ExpdJRE
consumables in the PHCs/CHCs;
YEAR
OUTLAY
9TH PLAN
45000.00
1997-98
9000.00
3131.00
1998- 99
12500.00
6888.00
facilitate referral;
1999- 00
10500.00
8754.00
2000- 01
12500.00
10875.00
2001-02
13600.00
13200.00*
inform the community of time schedule for
availing treatment;
El
evaluation of RNTCP and operational research
to improve performance; and
H
Source: Department of Health
* Anticipated Expd.
research and development efforts to develop
newer drugs to tackle drug resistance, testing
of new generation of TB vaccines;
During the Tenth Plan, the Focus will be on:
O
2.8.98 The NHP envisages a 50 per cent
reduction in mortality due to tuberculosis by 2010.
Goals for the tenth plan are indicated in
Table 2.8.8.
expansion of the RNTCP to cover population
of over 800 million by 2004 and the entire
country by the end of the Tenth Plan;
Table 2.8.8
Goals for the Tenth Plan
INDICATOR
2002
2003
2004
2005
2006
2007
Coverage under RNTCP (Population in Million)
550
650
800
900
1000
1070
Number of patients to be examined (Million)
2.08
2.50
3.04
3.42
3.80
4.07
i
Total Number of patients to be put on treatment under
RNTCP (Million)
0.52
0.61
0.75
0.85
0.94
1.00
New smear positive patients to be put on treatment
under RNTCP (Million)
0.21
0.24
0.29
0.33
0.37
0.40
83
84
>85
>85
>85
>85
Cure rate in new smear positive patients in RNTCP (%)
Source : Department of Health
110
HEALTH
National Leprosy Eradication Programme
(NLEP)
Figure 2.8.19 - Prevalence of Leprosy Cases (1988-2000)
3000
2.8.99 Leprosy has been a major public health
problem in India. In 1984 it was estimated that
there were nearly four million cases of leprosy in
the country, 15 per cent of whom were children.
Recognising that leprosy is a major cause of
disability and the infected persons face social
ostracism, several NGOs and social service/
voluntary agencies had taken up treatment and
rehabilitation of leprosy patients in the pre
Independence period itself. However, the
outreach of these services was very limited. With
the availability of multi-drug therapy (MDT), it
became possible to cure leprosy cases within a
relatively short period of six to 24 months. The
NLEP was launched in 1983 as a 100 per cent
funded centrally sponsored scheme with the goal
of arresting disease transmission and bringing
down the prevalence of leprosy to one in 10,000
by 2000. The strategy adopted to achieve this
was:
S
early detection of leprosy cases through active
community based case detection by trained
health workers;
regular treatment of cases with MDT adminis
tered by leprosy workers in endemic districts
and mobile leprosy treatment units and primary
health care workers in moderate to low
endemic areas/districts;
intensified health education and public
awareness campaigns to remove the social
stigma attached to the disease; and
o
p
------------------------ -------------------------------------------
\
2500 —
2000 —
z
or
LU
1500
s
1000
---------------------------------------
— ---- Xr--------------------------------------------
co
*=
500
0
07
CT>
CT)
<y>
O>
CT)
CT>
O>
CT)
O)
O
YEAR (BY END OF MARCH)
Source: NLEP, Department of Health, 2001
El
preparing for and initiating horizontal integration
of the leprosy programme into primary health
care;
El
strengthening laboratory services in PHCs/
CHCs for detection of leprosy cases;
E
establishing a surveillance system for
monitoring time trends in prevalence of leprosy;
E
providing greater emphasis on disability
prevention and treatment; and
E
implementation of the Modified Leprosy
Elimination Campaign (launched in 1997).
2.8.101 The performance of the NLEP during the
Ninth Plan is shown in Figure 2.8.20. The depart
ment of health has initiated steps for the phased
integration of the vertical programme within the
general health services by training health care
personnel in the detection and management of
leprosy cases, making MDT available at all health
facilities, improving disability and ulcer care and
strengthening of monitoring and supervision.
Figure 2.8.20 - National Leprosy Eradication Programme
appropriate medical rehabilitation and ulcer
care services.
800000
------------------ —-----------------------------------------------------------------
600000 ----
2.8.100 Over the years there has been a sub
stantial decline in the prevalence of leprosy from
57/10,000 in 1981 to 5/10,000 in the year 2000
(Figure 2.8.19). The focus during the Ninth Plan
was on:
aj
E 400000
Z
200000
0
I
1996-97
H
intensifying case detection and MDT coverage
in states with a high prevalence of leprosy and
areas that are difficult to access;
I
0
1997-98
y.
■
1998-99
2000-01
■J
2001-02
□ CASE DETECTION TAR.
□ CASE DETECTION ACH.
□ CASE TREATMENT TAR.
□ CASE DISCHARGE TAR.
□ CASE TREATMENT ACH.
Source : NLEP, Department of Health, 2001
111
1999-00
□ CASE DISCHARGE ACH.
TENTH FIVE YEAR PLAN 2002-07
Outlays and utilisation of funds during the Ninth Plan
period is shown in Table 2.8.9.
Table 2.8.9
NLEP - Outlays and expenditure
(Rs in crore)
YEAR
OUTLAY
EXPD./RE
9TH PLAN
301.00
1997- 98
75.00
79.56
1998-99
79.00
78.03
1999-00
85.00
82.05
2000-01
74.00
73.86
2001-02
75.00
75.00*
Pradesh, Meghalaya, Sikkim, Jammu and Kashmir,
Rajasthan, Manipur and Assam. States that are
close to achieving elimination (1-2/10,000) include
Gujarat, Kerala, Arunachal Pradesh, Lakshadweep.
Leprosy is now endemic mainly in the states of
Bihar, Uttar Pradesh, Orissa, West Bengal, Madhya
Pradesh, Jharkhand and Chattisgarh. These states
account for 64 per cent of the country’s case load,
with Bihar alone contributing 24 per cent.
2.8.104 The Modified Leprosy Elimination
Campaign (MLEC), aimed at the detection of
unidentified cases, was taken up first in Tamil Nadu
in 1997 and then extended to Maharashtra, Orissa,
Gujarat, the Jammu division of Jammu and Kashmir
and Daman and Diu during 1997-98. It was
subsequently extended to all districts during 199899. Performance under MLEC is shown in
Table 2.8.10.
Source: Department of Health, 2001
* Anticipated Expd.
2.8.102 During 1997-98, the duration of treatment
with MDT was reduced from 24 months to 12
months for multi-bacillary patients and from 12
months to six months for pauci-bacillary patients.
Single dose rifampicin, ofloxocin and minocycline
(ROM) treatment for single lesion patients was
introduced. Prior to the initiation of the fixed dose
treatment, treatment was continued until clinical
inactivity. With fixed dose treatment, patients are
released from treatment once the duration of
treatment is completed. Under the programme,
smear examination is optional, it is, therefore,
difficult to determine cure rates and relapse rates.
It is important that surveillance is strengthened so
that relapses are detected early.
2.8.103 As of 2001, the estimated prevalence rate
of leprosy is 4.3 in 10,000. Elimination level (PR <
1/10,000) has been achieved in Nagaland,
Haryana, Punjab, Mizoram, Tripura, Himachal
2.8.105 Some of the evaluation studies indicate
that during the MLEC there was both over diagnosis
and under diagnosis in some districts as the
detection was done by a large number of newlytrained persons. However, this campaign provided
a mechanism for involving the entire health services
and paved the way for the progressive integration
of leprosy care within the health service infra
structure.
2.8.106 The NLEP has been successful in
reducing the number of leprosy cases. However,
this will not result in any immediate decline in the
number of patients who have deformities. There is
a need to give a major thrust to surgical correction
of deformities so that the functional status of
individuals can improve. So far 210 district leprosy
societies were provided funds for conducting
disability/ulcer care management training. Gujarat
Table-2.8.10
Performance under MLEC
Population In Lakhs
Enumerated
Examined
No. of
suspected
cases
8209.67
6448.71
2858267.00
No. of
confirmed
cases
No. of
single
lesion
PR
before
MLEC
PR
after
MLEC
%
increase
in PR
454290.00
53115.00
4.75
10.02
110.95
Source : MLEC 1998-99PR - Prevalence rate/10,000.
112
HEALTH
mobilised experienced surgeons from all over the
country to undertake reconstructive surgery in in
different district hospitals so that patients get
treatment near their residence. The impact and cost
effectiveness of these initiatives need to be
assessed.
2.8.107 The Tenth Plan goal is to eliminate leprosy
as a public health problem by bringing prevalence
to less than 1/10,000. The strategy to achieve this
will focus on:
El
completing horizontal integration of the progra
mme into the general health care system by
2007. The personnel employed under the
NLEP will be transferred to the states during
the Tenth Plan;
E
skill upgradation and redeployment of the over
30,000 leprosy workers and laboratory techni
cians so that existing gaps in male multi-purpose
workers and laboratory technicians in PHC/CHS
are filled and these workers get integrated into
the primary health care system. This will result in
improvement in all health programmes, including
the leprosy pro-gramme;
E
training of the existing personnel in primary
health care institutions in the early detection
and management of leprosy patient; identi
fication and referral of those with
complications;
E
re-constructive surgery to improve functional
status of individuals;
E
inter-sectoral collaboration for rehabilitation of
leprosy patients;
E
increased involvement of PRIs/NGOs in the
detection and management of leprosy patients;
gram sabhas can facilitate house-to-house
surveys by leprosy workers; and
E
the panchayats can inform the community
about institutions where facilities for treatment
are available and facilitate referral.
immemorial. In India, a National STD Control
Programme has been in operation since 1967 but
its outreach and coverage have been poor. There
is no nation-wide surveillance system for STD.
Available data from small-scale studies indicate
that the annual incidence of STD may be about
5 per cent (40 million new cases every year).
Small scale studies have suggested that over the
last three decades, there has been some
increase in sexual promiscuity and perhaps also
in prevalence of STD. However, because of the
availability of effective treatment, the increase, if
any, in the incidence of STD has not resulted in
rising morbidity or mortality rates.
2.8.109 With the advent of HIV infection, in the
late 1970s and early 1980s, there has been a
dramatic change in the situation because there
is no effective drug for the treatment, or vaccine
for protection against, HIV infection. In the early
1980s, the Acquired Immuno-Deficiency
Syndrome (AIDS) was perceived as a rapidly fatal
disease affecting young persons; health sector
took up the challenge of combating and
containing the infection. Over the last two
decades the natural history of the disease has
been documented and it is now realised that HIV
infection has a long, silent phase, and that AIDS
represents the pre-terminal phase of the
infection. Sustained multi-sectoral efforts are
needed to contain the infection, and combat the
adverse consequences on the affected person,
family, community and the country.
2.8.110 The load of HIV infection in the
community depends upon the prevalence of
infection in three groups of population - the highrisk group, the interphase group and the low risk
group. The high risk group (HRG) is a relatively
small group e. g. commercial sex workers,
intravenous (IV) drug users. Soon after the
introduction of infection in the community, there
is a steep rise in prevalence of infection in this
group because they are frequently exposed to
the risk of infection. The inter-phase group
consists mainly of men and women who have
multiple sex partners. They form the link through
National AIDS Control Programme
2.8.108 Sexually transmitted diseases (STD)
have been a global problem since time
113
TENTH FIVE YEAR PLAN 2002-07
which infection spreads to the numerically vast
low risk group of the general population. The
general population (low risk group) acquires HIV
infection mainly from spouses who have multiple
sex partners. The size of the three groups and
the extent of the interphase between them
determines magnitude of the HIV infection in any
country or community; these factors account for
most of the observed differences between
countries in the prevalence of HIV infection
(Figure 2.8.21). Global epidemiological data on
HIV infection indicate that soon after the
introduction of the infection in the community
seropositivity rates are low. In the next phase the
infection spreads to susceptible persons in
vulnerable groups resulting in steep rise in
seropositivity rates. Finally in the third phase the
sero positivity rates plateau when the number of
persons who get infected is similar to the number
who die of HIV infection. The steepness of the
slope and the rapidity with which plateau is
reached are determined by the proportion of
susceptible at-risk persons in the community and
the effective use of prophylactic measures by the
risk groups.
2.8.111 India has the distinction of initiating a
national sero surveillance in 1986 to define the
magnitude and dimension of HIV infection in the
silent phase of the HIV epidemic long before AIDS
cases were reported. Currently, HIV infection in
the general population is seen in all states both
in the urban and rural areas. The apparent
differences between and within states in the
prevalence of HIV infection may, to a large extent,
be due to differences in the type and number of
persons screened. Available data from sentinel
surveillance suggests that over the last two
decades, there has been a slow but progressive
rise in the prevalence of infection in all groups in
all states. The estimated number of HIV infected
person rose from one to two million in 1991, to
3.5 million in 1998 and 3.9 million in 2000. More
than 50 per cent of infected persons are women
and children. Every year, approximately 30,000
deliveries in India occur among sero-positive
women and between 6,000 to 8,000 infants are
peri-natally infected with HIV. At present, the
number of AIDS patients in the country is small.
However, over the next decade, persons who got
infected in the 1980s and 1990s will develop
AIDS, resulting in a steep increase in the number
of AIDS patients.
2.8.112 In spite of the relatively low investment
in and low profile of the National AIDS Control
Programme, the prevalence of HIV infection in
India is relatively low. Some of the projections
made by the National AIDS Control Organisation
(NACO) suggest that HIV infection in India may
reach the plateau by 2010. The UN Population
Division had computed the impact of HIV infection
on longevity in different countries/regions. There
has been a steep fall in longevity in sub Saharan
Africa. In India there has been only a small
reduction in expected improvement in longevity
Figure 2.8.21 Spread of HIV
infection in population
Slow Spread
of HIV
Rapid Spread
of HIV
High Risk
Interphase Group
Source : ICMR Bullettin 1991
114
General pop.
HEALTH
(Figure 2.8.22). The initiation of sero-surveillance
during the silent phase, implementation of a multi
pronged strategy for HIV infection containment
and control, the cultural ethos, relatively low IV
drug use and dedicated work done by committed
professionals are some of the factors responsible
for this. However, because of the one billion plus
population, India is likely to have the largest
number of cases of and deaths due to AIDS.
Capacity building
Awareness generation among all segments
of population through Family Health Aware
ness campaigns;
Focused attention and counselling to
adolescents, sex workers, drug users, mig
rant labourers;
Improvement in the quality of and access to
condoms including social marketing;
2.8.113 A National AIDS Control Programme
(NACP) Phase I was launched in 1992 with World
Bank assistance and was completed in 1999. Phase
II of the programme, with funding from World Bank,
Department for International Development (DFID)
and United States Agency for International
Development (USAID) is currently under way. AIDS
Phase II programme focuses on:
Hospital infection control and waste
management to reduce accidental spread
of infection in health care settings;
Clinical trials on chemotherapy to prevent
mother to child transmission;
•“ Establishment of behavioural surveillance.
E)
El
reducing HIV transmission among the poor and
marginalised high risk group population by
targeted intervention, STD control and condom
promotion;
promotion of IEC, voluntary testing and
counselling;
reducing the spread of HIV among the general
population by reducing blood-borne trans
mission;
80 -r-
E
developing capacity for community-based low
cost care for people living with HIV/AIDs;
Figure 2.8.22 - Life Expectancy at Birth in Different Countries
(without and with AIDS Epidemic)
70-------1=1
flH
60
n i -T
Fl
w 50
-
>40 -
I 30 20
10 0
LJ
j
1
v>
w
g
1 5
!
O
.g
Q
I
<D
E
.£
co
CD
1995-2000
Q.
W
3
•C
Iw
o
I
w
I
O
S
,g
92
1
I
I
i
3
I
O
E
<
.£
4=
£
I! I
s
co
o>
2000-2005
□ With AIDS
115
I
cn
■h
I
O
o
O
.s
E
<
3
co
Q
cn
Source : UN Population Division
</9?>
.£
CO
I
2010-2015
□ Without AIDS
'O’
£
w
.92
i
o
TENTH FIVE YEAR PLAN 2002-07
AIDS Control Programme during the Ninth Plan is
given in Table 2.8.11.
Infrastructure set up by NACO
Modernisation and strengthening of :
Table 2.8.11
AIDS Control Programme - Outlays &
Expenditure (Rs lakh)
Bl 815 blood banks;
Bl 504 STD clinics in district hospitals;
Establishment of:
YEAR
OUTLAY
Bl 40 blood component separation facilities;
9TH PLAN
76000.00
Bl 142 voluntary blood testing centers;
1997- 98
10000.00
12100.00
B 320 sentinel sites for monitoring the time
trends in prevalence of HIV infection;
1998- 99
11100.00
9936.00
B 570 targeted intervention for prevention
and management of HIV infection in high
risk groups;
1999-00
14000.00
13525.00
2000- 01
14500.00
17330.00
2001- 02
21000.00
23500.00*
B low cost community based care for people
living with HIV/AIDS.
Bl
Source: Department of Health
* Anticipated Expd.
strengthening implementation capacity at the
national, state and panchayat level through
appropriate arrangements and increasing
timely access to reliable information;
Bl forging inter-sectoral linkages between public,
private and voluntary sectors.
All these efforts are being monitored.
2.8.114 The recently concluded behavioural
survey and the NFHS-2 (1998-99) have shown that
over two-third of the population knows about HIV
infection. There are considerable urban-rural and
inter-state differences. Awareness about STD was
much lower than that about HIV infection (Figure2.8.23). The outlay and expenditure on National
Figure 2.8.23 - Proportion Of Respondent Who Had Ever
Heard of HIV/AIDS and STD
90
BO70
60
rS
5040
30
20100-
H
I 5HI II& iI = | a
5
S I
s
I
< iwi $m* §I 35 ? = I S I
4
8
I! i
□ HIV/AIDS
2
o
w
o<
2.8.115 During the Tenth Plan, the programme will
be continued with emphasis on:
B
prevention of mother-to-child trans-mission;
B
reduction in blood-borne trans-mission and
accidental infection in health care settings;
B
care of HIV-infected persons/AIDS cases;
B
prevention and management of STD; and
B
improved surveillance to obtain epidemiological
data on time trends in HIV infection.
2.8.116 Monitoring of processes and the impact
of ongoing intervention programmes and sentinel
surveillance (serological, STD/behavioural) to
monitor time trends in the HIV epidemic will receive
adequate attention.
2.8.117 HIV is a multifaceted problem affecting all
segments of society. Until now the department of
health has been the nodal point of interventions not
only for traditional activities of the health sector such
as prevention, detection, counselling and manage
ment, but also for other areas such as legislation,
rehabilitation of infected persons and their families.
During the Tenth Plan it is expected that each
Department will handle HIV infection related issues
in their respective sectors. For instance, the Ministry
of Labour will look after area of prevention of
discrimination at the work place. Voluntary
100
I
I
EXPENDITURE
p
0STD
SOURCE : NACO, Department of Health
116
HEALTH
organisations may be best suited for providing
hospices for AIDS patients who do not have anyone
to look after them and orphanages to take care of
children who have lost their parents due to AIDS. If
each sector takes up the tasks pertaining to that,
the country will be able to look after the needs of
HIV infected persons and their families without any
adverse effect on other programmes.
2.8.118 The Tenth Plan goals for HIV/AIDS
programme are:
inadequate water supply and poor quality of water.
Water borne diseases occur throughout the year
with a seasonal increase in summer, monsoon and
post-monsoon period. Common water-borne
diseases that are of public health importance include
diarrhoeal diseases, cholera, bacillary dysentery,
typhoid fever and viral hepatitis. In children the
prevalence of diarrhoeal disease is higher; severity
and chronicity is also more in children. Over the
last few decades there has been no decline in the
prevalence of water borne diseases though there
has been some decline in mortality associated with
them.
ISI
80 per cent coverage of high risk groups
through targeted interventions;
ISI
90 per cent coverage of schools and colleges
through education programmes;
2.8.121 During the Tenth Plan, efforts will be made
to:
IS
80 per cent awareness among the general
population in rural areas;
H
improve coverage under rational case
management for diarrhoea/dysentery;
ISI
reducing transmission through blood to less
than 1 per cent;
ISI
ISI
establishing of at least one voluntary testing
and counselling centre in every district;
explore the feasibility of monitoring the quality
of water through public health engineering
department and the PRIs;
SI
strengthen the diarrhoeal disease surveillance
programme at the district level to detect and
contain outbreaks;
S
coordinate the efforts of the departments
dealing with urban and rural water supply and
sanitation, municipal corporations and PRIs for
the prevention of water-borne diseases.
IS
scaling up of prevention of mother-to-child
transmission activities up to the district level;
S
achieving zero level increase of HIV /AIDS
prevalue by 2007.
Water Borne Diseases
2.8.119 In the pre-independent era and in the first
decade after independence water supply and
sanitation were two important schemes funded by
the Public Health Department. In view of the
importance of both these components in preventing
water borne and vector borne diseases, allocation
for the two components was nearly 50:50. Subse
quently water supply and sanitation programmes
become the responsibility of rural and urban deve
lopment departments. While water supply received
most of the funds, sanitation and sewage were
under-funded and neglected. This resulted in
environmental deterioration and increase in both
water and vector borne diseases.
Ninth Plan Initiatives
Disease surveillance
2.8.122 Surveillance is the continuing scrutiny of
all aspects of occurrence and spread of diseases
that are pertinent to effective control. So far in India
disease surveillance has been predominantly
focused on communicable diseases. There has
been some small scale research efforts for
establishment of comprehensive communicable
and non communicable disease surveillance but
these have not been opertationalised even on a pilot
basis.
2.8.123 Given the poor environmental sanitation
and the problems in the public health system, it will
not be possible to completely prevent outbreaks of
communicable diseases in the near future. Delays
in recognition and reporting of focal outbreaks and
2.8.120 The contamination of drinking water with
human or animal faeces leads to the spread of
water-borne diseases. The risk of infection is higher
in areas with poor sanitation, poor sewage handling,
117
TENTH FIVE YEAR PLAN 2002-07
absence of a functioning HMIS and disease
surveillance system has been responsible for
delayed recognition and responses resulting in high
morbidity and even mortality in communicable
disease out breaks. In order to prevent these the
Ninth Plan envisaged the establishment of a district
based system for early detection of disease
outbreaks and prompt response for rapid
containment and control through the existing
infrastructure. The necessary back-up laboratory
and epidemiological support was to be provided by
strengthening and optimally utilising the facilities and
expertise available in the national institutions/
medical colleges.
2.8.124 The Department of Health initiated a pilot
project on disease surveillance coordinated by the
National Institute of Communicable Diseases in
1997. Initially the project involved strengthening
laboratories and setting up a disease surveillance
system in 20 districts, and was expanded to cover
100 districts by 2002. Many states have not been
able to utilise the funds released or carry out the
programme as envisaged. The major disease
control programmes continue to have their own
vertical surveillance system; of these, only the polio
surveillance has a good track record. There is as
yet no organised effort to integrate all the ongoing
surveillance under various disease control
programmes into a single programme for disease
surveillance. Common epidemic-prone diseases are
still not being monitored locally and reported to
district officers for analysis and response.
2.8.125 Private sector provides over 75 per cent
of curative care for common illnesses. However,
data from private health providers is not yet included
in any disease surveillance system. In the eighties
ICMR funded a research project in North Arcot
District (NADHI) in Tamil Nadu which private and
government sector practitioners participated. The
Kerala government has replicated this model in
three districts. Kerala has reported that the system
has enabled early detection and containment of
outbreaks of communicable diseases; the state
government proposes to expand this programme
to other districts in the Tenth Plan.
2.8.126 During the Tenth Plan, a comprehensive
review of:
118
H
disease surveillance programmes currently
being implemented in different states, under
different disease control programmes and
under the CSS project on disease surveillance;
H
laboratory facilities available for investigation
of epidemic prone diseases;
O
reporting systems currently in use.
will be carried out. Efforts will be made to integrate
the ongoing programmes for disease surveillance
and develop a comprehensive disease surveillance
programme at the district level. The programme will:
H
strengthen routine data collection at the village
level for selected diseases; monthly reports will
be prepared so that deviation from the normal
pattern could be recognised early;
H
Compile information pertaining to epidemic
prone diseases which are prevalent throughout
the country e.g. diarrhoea, tetanus, diphtheria
will be reported by all; region specific problem
such as malaria, filaria, leptospirosis will be
reported from the endemic areas;
IS)
ensure regular compilation and critical analysis
of data generated at the district level so that
outbreaks are recognised early and
investigated by district health officers and
appropriate timely response is initiated;
El
use modern IT tools to communicate data on
disease incidence on a real time basis,
complete analysis at the state, regional and
national levels and build up a mechanism for
rapid and appropriate response.
Health Management Information System (HMIS)
2.8.127 HMIS is an essential management tool for
effective functioning of the health system. During
the Eighth Plan the Central Bureau of Health
Intelligence and the state Bureaus of Health
Intelligence developed a HMIS system for sending
district-level information on morbidity reported by
the government primary health care institutions
through National Informatics district computer net
work. Though some states responded initially the
system was never fully operationalised in any state.
As a result there is no system through which reliable
data on morbidity in different districts/ states could
HEALTH
be collected and analysed and used for
decentralized district based planning. So far there
has not been any effort to use the currently available
IT tools to build up a comprehensive HMIS and use
it to improve efficiency and functional status of the
health system. During the Tenth Plan efforts will be
made to ensure that effective two way management
information system is built up through out the
country; all the data pertaining to health and family
welfare programmes will be collected, collated and
reported from all districts and utilised to improve
functional status and efficiency of the health system.
Efforts will also be made to build up a fully functional,
accurate HMIS utilizing currently available IT tools;
this real time communication link will send data on
births, deaths, diseases, request for drugs,
diagnostics and equipment and status of ongoing
programmes through service channels within
existing infrastructure and manpower and funding.
It will also facilitate decentralized district based
planning, implementation and monitoring.
India’s share in global health problems
H 17 per cent of the population
H 17 per cent of the total deaths
H 23 per cent of child deaths
H 26 per cent of the childhood vaccine preven
table deaths
H 20 per cent of maternal deaths
(3 68 per cent of leprosy cases
O 30 per cent of tuberculosis cases
H 10 per cent of HIV infected persons
there is a need to obtain data on not only mortality
but morbidity due to chronic illnesses and disabilities
and take them account while formulating public
health programmes. For instance, morbidity due to
mental illnesses is estimated to account for about
15 per cent of the total morbidity but deaths due to
psychiatric illnesses are usually less than 1 per cent
of total deaths even in developed countries.
Disease Burden Estimates
2.8.128 Traditionally policy makers have used
mortality statistics for identifying major public health
problems. In India, reliable age specific mortality
data is available through SRS ; though there are
lacunae in the system for ascertainment of causes
of death, fairly reliable data is available on major
causes of death. In addition to these data, the
country has under taken surveys for estimating the
prevalence of major public health problems such
as morbidity in women and children, nutritional
deficiencies and major communicable diseases.
The estimated share of India in some of the global
health problems is shown in the Text Box . In India
reliable information on overall morbidity is not
available. In the absence of reliable morbidity data,
mortality statistics and available survey data have
formed the basis on which health policy makers and
programme managers evolved public health
programmes and allocated funds. While this might
have been the appropriate option in a situation
where communicable diseases and maternal and
child health problems predominate, appropriate
modification will be required as the country
undergoes demographic and epidemiological
transition and non communicable diseases emerge
as major public health problems. In view of this,
119
2.8.129 The disease burden estimates
measured in terms of Disability Adjusted Life
Years (DALY) which takes into account both
morbidity and mortality as well as the age at
which the problem occurred has been used by
World Health Organi-sation in making global
comparisons with respect to public health
problems and investment in health care. The
estimated disease burden in 1990 due to major
categories of public health problems in the world
and India is shown in Figure 2.8.24. Disease
burden due to four major diseases in different
Figure-2.8. 24- Distribution of Disease Burden in
India and the World
50-------45 -----40-------35 —’
30 —
o
25----Q.
20----.£
15----10-----
s
5 —H
o
1
— ■
—- "O ■g
o
32
I
£ ™
o
I
w
§o £2
ZI
Source: World Development Report 1993
ft
to
£ □
O E
£o
I
World
India
TENTH FIVE YEAR PLAN 2002-07
Table 2.8.12
Burden for four major diseases (millions of DALYs)
Age (years)
Disease and sex
0-4
5-14
15-44
45-59
60+
Total
Male
42.1
4.6
2.8
0.4
0.2
50.2
Female
40.7
4.8
2.8
0.4
0.3
48.9
Male
0.2
10.6
1.6
0.5
0.1
13.1
Female
0.1
9.2
0.9
0.5
0.1
10.9
Male
1.2
3.1
13.4
6.2
2.6
26.5
Female
1.3
3.8
10.9
2.8
1.2
20
Male
0.1
8.1
13.1
25
Female
0.1
**
3.6
**
1.2
3.2
13
17.5
Diarrhea
Worm infection
Tuberculosis
Ischemic heart disease
** Less than 0.05 million
Note : DALY, disability-adjusted life year.
Source : World Development Report 1993
age and sex population computed by WHO is in
Table 2.8.12.The fact that while estimates
regarding mortality are reasonably adequate, the
estimates of morbidity based on the available
data from the developing countries are often
inadequate haas to be kept in mind while
interpreting these global data.
2.8.130 Using the 1990 database ( Figure
2.8.25) and assuming that the trends in
epidemiological transition achieved by other
countries during the previous two decades will
occur in India, the changing pattern of disease
burden for 2020 was also computed by WHO
(Figures 2.8.26). However, data from National
Family Health Survey (NFHS) suggest that during
the 1990s, there has not been any significant
decline in the infant mortality rate and the
maternal mortality rate. Data from SRS does not
show any major change in the age specific
Figure2.8.25 Disease Burden
Figure 2.8.26 Disease Burden
Projections -India 2020
Estimates - India 1990
Injuries
Injuries
15%
19%
T^r*T^r~r\.
Non-
|
Maternal, Child
and
Communicable
56%
Communicable
Non-
29%
Communiable
57%
Source : WHO 1996
Source : WHO 1996
120
Maternal, Child
and
Communicable
24%
HEALTH
mortality rate (Figure 2.8.27) or cause of death.
It would appear that the epidemiological transition
is occurring at the slower pace than projected
for the country. This is perhaps due to persistent
maternal and child health problems and advent
of HIV infection. However, there has been some
increase in the mortality and morbidity due to noncommunicable diseases, accidents and trauma.
There are wide inter-state differences in health
indices, morbidity rates, magnitude and rate of
demographic and epidemiological transition.
Under these conditions, it is important to :
Figure 2.8. 27 Distribution of Deaths (%)
40
35 ”
£ 30 n
■S 25 ~
o 20 ••
5 15 10
5 0 —
0-4
5 to 19
20-45
Age in.years
45-59
60+
J
Source: SRS1997
IS) ascertain and document morbidity and mortality
due to major health problems in different states/
districts;
IS)
evolve appropriate intervention programmes;
IS
invest adequately in well targeted interventions;
IS
implement them effectively by modifying the
health care system, and;
IS
monitor the impact on the morbidity and
mortality.
2.8.131 Such an effort would require a reliable
sustainable database for mortality and morbidity.
While mortality data can be obtained through
strengthening of CRS/SRS and ascertainment of
the cause of death, the data base for morbidity can
come only through a strengthened HMIS supple
mented by the data from disease surveillance.
When sustained, these three systems will, over the
next two decades, provide valuable insights
regarding time trends in morbidity and mortality in
different states/ districts. Development of this data
121
base is critical for evolving appropriate health
policies and strategies, identifying priority areas for
investment of available funds and bringing about
modifications in the existing health system to ensure
equitable, efficient and effective implementation of
the programmes to tackle dual disease burden.
Infection Control and Waste Management in
Health Care Settings
2.8.132 There has been increasing concern over
the incidence of hospital-acquired infections and
accidental infection in health care providers and
waste disposers. One of the major new initiatives
during the Ninth Plan was improvement of infection
control and waste management through appro
priate, affordable technology at all levels of health
care. In November 1998, the Department of Health
has constituted National Hospital Waste Manage
ment Committee under the chairmanship of the
Secretary Health, to coordinate and guide policy
and programme initiatives in the field. A pilot project
was initiated in 11 institutions with assistance from
the department. Hospital infection control and waste
management is also being taken up as a component
of all World Bank-assisted secondary health system
projects. Guidelines on hospital waste management
were prepared and circulated to states and union
territories in November 2000 for their comments.
Some states are providiing funds under the PMGY
for infection control and waste management in
primary health care institutions. During the Tenth
Plan, hospital infection control and waste manage
ment will be incorporated as an essential routine
activity in all health care institutions at all levels of
care.
Horizontal Integration of Vertical Programmes
2.8.133 Initially, when sufficient infrastructure and
manpower were not available for the management
of major health problems, several vertical progra
mmes like the NMEP and NLEP were initiated. Over
the years,the three-tier health care infrastructure
has been established. The Ninth Plan envisaged
that efforts will be made to integrate the existing
vertical programmes at the district level and ensure
that primary health care institutions provide compre-
TENTH FIVE YEAR PLAN 2002-07
hensive health and family welfare services. The
pace of horizontal integration has been very slow
and uneven. During the Ninth Plan, attempts were
made to:
E
integrate the activities related to training and
IEC under different vertical programmes;
E
coordinate the activities for prevention and
management of STD/reproductive tract
infections (RTI) under the RCH and AIDS
control programmes;
E
improve coordination between ongoing HIV
and TB control programmes; and
E
provide leprosy services through the primary
health care infrastructure.
2.8.134 Some states like Orissa and Himachal
Pradesh have formed a single health and family
welfare society at the state and district level for
implementing all health and family welfare
programmes. In some states, middle-level public
health programme managers, who are currently
heading the vertical programmes at the district
level, are being given the additional task of
ensuring coordination and implementation of the
integrated health and family welfare programme
at primary health care institutions in defined
blocks. Their involvement is also expected to
improve data collection, reporting, strengthen
HMIS, improve the supply of essential drugs and
devices at PHCs/CHCs and enable the
operationalisation of disease surveillance and
response mechanism at the district level. The
National Health Policy 2002( NHP2002)
envisages a progressive convergence of all
health and family welfare programmes under a
single field of administration beginning at the
district and below-district levels for funding,
implementation and monitoring. During the Tenth
Plan, efforts will be mainly directed to improving
the pace and coverage of this convergence. The
NHP 2002 envisages manpower in rural/urban
health sytsem should be available for the entire
gamut of public health activities at the
decentralised level, irrespective of whether these
activities relate to national programmes or public
health activities initiated by state/PRI.
122
PREVENTION AND MANAGEMENT OF NONCOMMUNICABLE DISEASES (NCD)
2.8.135 Non-communicable diseases cover a wide
range of heterogeneous conditions affecting
different organs and systems in different age and
socio-economic groups. Over the last two decades,
morbidity and mortality due to cardio-vascular
diseases, mental disorders, cancers and trauma
have been rising due to an increase in:
the number of senior citizens with higher
prevalence of non-communicable diseases;
El
prevalence of non-communicable diseases in
younger people due to life-style changes,
obesity and stress; and
exposure to environmental risk factors and use
of tobacco.
2.8.136 Data from the 52nd round of NSSO
showed that tobacco intake (smoking and non
smoking) and alcohol use are higher in the poorest
20 per cent of the income quintile (Figure 2.8.28)
and hence the prevalence of tobacco-related noncommunicable diseases is likely to be high in this
group. In view of the chronic morbidity and high
cost involved in the management of noncommunicable diseases, attention need be focused
on prevention, early detection and appropriate
management. It is estimated that currently there are
2.5 million cases of cancer in the country and this
Figure 2.8.28 Prevalence of Alcohol and Tobacco
use in India by Income Quintile
T
'=5
1
Richest 20%
I
60%-80%
I
Middle 20%
20%-40%
I-
Poorest 20% f
0
Source:NSSO
1995-96
........
. ..... '
....... <.......... :
. "
'". "... 1
■
I
'
I
I
1
_ ______ L
5
10
15
20
25
Percentage regularly using Substance
□ Smoking
E3 Tobacco (non-smoking)
□ Alcohol
HEALTH
will double over the next two decades. Data on the
prevalence of cardiovascular disease are insufficient
for national level projections. The reported
prevalence of Coronary Heart Disease (CHD) in
urban Kerala is 14 per cent (17 per cent in men
and 10 per cent in women), 7 per cent in rural
Thiruvananthapuram and 3 per cent in rural parts
of North India. Ten per cent of the urban and 5 per
cent of the rural adult population suffer from hyper
tension. The estimated prevalence of rheumatic
heart disease (which constitutes 20 to 30 per cent
of hospital admissions due to all cardio vascular
disease (CVD) in India) is five to seven in 1,000 in
the 5-15 year age group. A recent study carried out
in six cities in India showed an age standardized
prevalence of diabetes and impaired glucose
tolerance in 12.1 per cent and 14.0 percent respec
tively, with no gender difference.
2.8.137 During the Ninth Plan, ongoing progra
mmes for control of non-communicable diseases
included two centrally-sponsored schemes
(National Iodine Deficiency Disorders Control
Programme, discussed in the Chapter on
Nutrition, and the National Programme for the
Control of Blindness discussed in this section)
and one central sector scheme (the National
Cancer Control Programme). During the 1990s,
several pilot projects such as the national mental
health programme, the diabetes control
programme, cardiovascular disease control
programme, prevention of deafness and hearing
impairment, oral health programme and medical
rehabilitation were initiated as central sector pilot
projects. After completion of the pilot phase, these
programmes have been merged with the Central
Institutes dealing with these problems.
2.8.138 The Ninth Plan envisaged the provision
of integrated non-communicable diseases
prevention and control services through the existing
infrastructure. However, the progress on this front
has been very slow. In some states like Kerala
efforts are being made to implement an integrated
non-communicable disease control program at the
primary and secondary care level with emphasis
on prevention, early diagnosis, management and
building up of a suitable referral system. Tertiary
123
care centres are being strengthened to provide
treatment facilities for the management of
complications.
2.8.139 During the Tenth Plan, efforts will be made
to improve preventive, promotive, curative and
rehabilitative services for non-communicable
diseases throughout the country at all levels of care
so as to reduce morbidity and mortality. The major
thrust will be on:
H
a well-structured IEC&M for primary and
secondary prevention of non-communicable
diseases;
El
re-orientation and skill upgradation of health
care providers in diagnosis and management
of non-communicable diseases at different
levels of care;
El
establishment of referral linkages between
primary, secondary and tertiary institutions;
E
production and provision of drugs for treatment
of non-communicable diseases at affordable
costs;
E
development of institutions for rehabilitation of
disabled persons, teaching persons to live with
their disability;
E
development of hospices for care of terminally
ill people who cannot have home-based care;
and
E
creation of an epidemiological database on
non-communicable diseases especially CVDs,
stroke and diabetes.
National Cancer Control Programme (NCCP)
2.8.140 India has one of the lowest rates of cancer
in the world. It is estimated that there are two to 2.5
million cases of cancer in India, with 700,000 new
cases being detected every year. About two-thirds
of the cases are in an advanced stage at the time
of detection and 300,000 to 350,000 cancer patients
die each year. Current projections suggest that the
total cancer burden in India for all sites will double
by 2026 because of increasing longevity, greater
exposure to environmental carcinogens due to
industrialisation, use of fossil fuels, the use of a
wide variety of chemical agents in industry and
agriculture, and the continued use of tobacco.
TENTH FIVE YEAR PLAN 2002-07
2.8.141 The most frequent cancers among Indian
males are those of the mouth/oropharynx,
oesophagus, stomach and the lower respiratory
tract. In women, cancers of the cervix, breast,
mouth/oropharynx and oesophagus are common.
About one-third of cancers are easy to detect and
can readily be cured. Tobacco-related cancers
(especially cancer of oral cavity, lung and cancer
cervix) form more than 50 per cent of the overall
cancer burden in the country. An increase in
tobacco smoking instead of chewing might lead to
a rise in the incidence of lung cancer, which is more
difficult to detect and treat. Changing dietary
patterns (high calorie, high fat intake) and lower
parity may result in increasing incidence of breast
cancer.
early detection of cancer and pain relief was initiated
in 1990-91. The progress in ongoing efforts for
cancer prevention, early detection and management
has been very slow.
2.8.143 The ICMR established a National Cancer
Registry Programme (NCRP) in 1981-82, there are
five population-based urban cancer registries in
Mumbai, Bangalore, Chennai, Bhopal, Delhi and a
rural registry at Barsi in Maharashtra and .six
hospital-based registries at Chandigarh, Dibrugarh,
Thkuvananthapuram, Bangalore, Mumbai and
Chennai. The NCRP provides data on regional
difference and time trends in cancer prevalence so
that appropriate modifications in the ongoing
programmes could be made.
2.8.144 During the Tenth Plan, a major effort will
be to made to sensitise and upgrade the skills of
health care providers in the primary, secondary and
tertiary institutions so that they can take up the
responsibility of:
The objectives of the National Cancer Control
Programme are:
H primary prevention of cancers by health
education through the government and NGOs;
H early detection and diagnosis of cancers
especially cancer cervix, breast and
oropharyngeal cancers;
M developing and strengthening of existing
cancer treatment facilities;
El increasing access to palliative care in the
terminal stage of cancer.
2.8.142 The Cancer Control Programme was
initiated in 1975-76 as a central sector project. It
was renamed as the National Cancer Control
Programme (NCCP) in 1985. The programme
provides funds to 17 Regional Cancer Centres
(RCCs). The RCCs are regional centres for
diagnosis, treatment and follow up of cancer
patients; they undertake surveys of mortality and
morbidity due to cancer, training of medical and
paramedical personnel in cancer care and
preventive measures with emphasis on health
education and research. NCCP provided funds for
the purchase of equipment (cobalt unit,
mammography unit) and for development of
oncology wings in Government Medical Colleges/
voluntary organisations. The District Cancer Control
Programme aimed at promoting health education,
124
El
health education for cancer prevention;
E
early diagnosis and management according to
standard treatment protocols at appropriate
institutions; and
E
referral of cancer patients with complications.
National Programme for Control of Blindness
(NPCB)
2.8.145 Surveys carried out by the ICMR in the
1970s indicated that the prevalence of blindness
is about 1.4 per cent, with cataract accounting
for over 80 per cent of the cases. Most of cataract
blind individuals are in their 60s. They may not
be able to afford surgery and have difficulty in
accessing services, unless these are available
close to their residence. The National Programme
for Control of Blindness was initiated in 1976 with
the objective of providing comprehensive eye
care services at the primary, secondary and
tertiary level and achieving a substantial reduction
in the prevalence of eye disease in general, and
cataract blindness in particular. The progress of
the programme was very slow. A Government of
HEALTH
India-WHO survey in 1986-89 showed that
prevalence of blindness remained unaltered.
Prevalence of blindness was higher than the
national average of 1.4 per cent in eight states
(Andhra
Pradesh,
Madhya
Pradesh,
Maharashtra, Orissa, Rajasthan, Tamil Nadu,
Uttar Pradesh and Jammu and Kashmir).
2.8.146 In 1994, World Bank assistance was
obtained for NPCB in seven of the eight states.
Domestic budgetary support was provided to
implement the project in Jammu and Kashmir. The
major objectives of the programme were:
H
S
to improve the quality of cataract surgery and
clear the backlog of cataract by performing 11
million operations over a seven-year period;
to strengthen the country’s capacity to provide
high volume, high-quality, low-cost eye care
by upgrading the knowledge and skills of eye
care personnel and improving access to
service delivery through government, voluntary
and private sector collaboration; and
to increase eye care coverage among the
underprivileged section of the population
including women, urban slum dwellers and
tribals.
2.8.147 During the Ninth Plan, the programme was
revised to cover the entire country. The performance
during the Ninth Plan is given in Fig. 2.8.29. Outlays
Figure 2.8.29 Blindness Control Programme - All India
5000
o
o
S3
Q 4000
il
Z
55Z) 3000
o
I 2000
z
- CN CN
"n
X•
::: w
S
—
I
1000
0
■
LTd
199697
* upto Dec. 2001
. II
I
1997- 199898
99
19992000
2000- 20012001 2002*
□ CATARACT OPERATIONS TAR.
and expenditure under the NPCB is shown in
Table 2.8.13.
Table 2.8.13
NPCB- Outlays and Expenditures
(Rs. In Lakhs)
YEAR
OUTLAY
9TH PLAN
44800.00
1997- 98
7000.00
5806.00
1998- 99
7500.00
7285.00
1999- 00
8500.00
8373.00
2000- 01
11000.00
10941.00
2001- 02
14000.00
14000.00*
EXPENDITURE
Source : Department of Health
* Anticipated Expd.
2.8.148 The review of the World Bank assisted
project in 2000 showed that even though infra
structure and manpower has been provided,
performance both in fixed facilities and in camps
have been far below the norms. Most of the
district hospitals did not achieve the goal of 700
cataract surgeries/surgeon/year; many mobile
units did not achieve the goal of 1500 cataract
surgery per year. As a result only 8.15 million
cataract surgeries (the target was 11 million)
could be done and cataract prevalence could not
be reduced to 0.3 per cent
2.8.149 The need to restore vision by operating
on one eye in economically blind people has not
been given conscious priority over operating on
the cataract in the second eye. A comparative
assess-ment of extra capsular cataract extract
vs. intra ocular lens insertion in terms of logistics
of implementation, cost of care and complication
rate, when surgery was done at tertiary hospital/
district hospital vs. those done in camps is yet to
be carried out. The quality of care in institutions
and more so in camps had been sub-optimal.
Infections resulting in permanent blindness have
been reported. In view of this NPCB has revised
its strategy, emphasis is now on surgery in fixed
facilities; mobile units will take up only screening
of cases and provide follow up care.
□ CATARACT OPERATIONS ACH.
2.8.150 A pilot survey carried out in 1999 in two
districts showed that there has been a shift in the
Source : Deptt. of Health
™
125
TENTH FIVE YEAR PLAN 2002-07
causes of blindness (Table 2.8.14). The NPCB will
have to be geared up to tackle the backlog of
cataract surgery, glaucoma, corneal blindness as
well as other emerging problems including diabetic
retinopathy (estimated prevalence 20 per cent
among diabetic).
Table 2.8.14
Pilot Survey on causes of blindness (1999)
Percent
Cataract
55.0
Refractive errors
9.8
Corneal blindness
8.0
Glaucoma
3.5
Surgical complication
3.0
Other causes
10.7
2.8.151
to:
ISI
IS)
During the Tenth Plan, attempts will made
clear the backlog of blindness due to cataract
by performing 4.5 million cataract operations
per year. A majority of these will be done in
fixed institutions; and wherever adequate
facilities are available, Intra-Ocular Lens (IOL)
will be used;
improve the utilisation of facilities created in
the government, private and voluntary sector
to cope with the broader spectrum of eye care,
including screening of children for refractive
errors, diabetics for retinopathy and all persons
beyond 35 years for glaucoma;
IS)
develop a system for accreditation of centres
providing eye care;
IS)
improve the quality of care before, during and
after surgery through operationalisation of
standard protocols for management;
monitor quality of care;
IS)
El
modify the ophthalmology curriculum in both
the undergraduate and postgraduate stages
so that the students have the necessary skills
to deal with common ocular problems at all
levels of health care;
E
develop an appropriate continuing medical
education programme to enable practitioners
to deal with emerging ophthalmic problems
effectively.
126
Mental Health
2.8.152 Mental health care has three aspects restoration of health in mentally ill persons, early
identification of persons who are at risk and
appropriate protection and promotion of mental
health in normal persons. It is estimated that 10 to
15 per cent of the population suffers from mental
health problem and the stress of modern life is
resulting in an increasing prevalence of mental
illness. Till about three decades ago, mental health
services consisted mainly of large, centralised
mental hospitals. At the time of independence, there
were 17 mental hospitals accommodating over
8,000 patients. Most of these hospitals had poor
infrastructure and manpower and did not provide
good quality mental health care. A majority of
mentally ill patients did not have access to good
quality psychiatric care and there was no home
based care available for them.
Magnitude of Mental Health Problems
It is estimated that:
E ten million people are affected by serious
mental disorders.
E 20-30 million people have neurosis or
psychosomatic disorders.
E 0.5 and 1 per cent of all children have
mental retardation.
2.8.153 Soon after Independence, efforts were
made to improve the access to mental health
services by increasing the number of mental
hospitals and opening psychiatric units in general
hospitals. Providing psychiatric care through general
hospitals and bringing mental health care out of the
confines of mental hospitals reduced the stigma
associated with treatment of mental illness, removed
legal restrictions on admission and treatment and
facilitated the early detection of associated physical
problems. Most importantly, it ensured that the
family was involved in the care and that on being
discharged the patient went back to the family.
Encouraged by the success in this effort, many
states embarked on the development of district
psychiatric units. Some states like Kerala and Tamil
HEALTH
Nadu have a district psychiatric unit in all districts.
Though others lag behind in this respect, the
concept of mental health care provided as an
integral part of health care system has been
accepted and implemented by all states. Ambulatory
treatment for psychiatric illnesses became accepted
as a norm and effective, relatively inexpensive drugs
for common mental disorders were made available
in tertiary and secondary care institutions.
2.8.154 Currently, 50 per cent of the medical
colleges have a psychiatry department. It is
estimated that there is one psychiatry bed per
30,000 population. There are 20,000 beds in mental
hospitals and 2,000 to 3,000 psychiatric beds in
general and teaching hospitals. Fifty per cent of the
psychiatric beds are occupied by patients
undergoing long term treatment. However, in spite
of all these facilities, even now less than 10 per
cent of the mentally ill persons have access to
appropriate care; prevention of mental illness and
promotion of mental health remain of distant
dreams.
2.8.155 The national mental health programme
was initiated in 1982 with the objective of
improving mental health services at all levels of
health care through early recognition, adequate
treatment and rehabilitation of patients. The
programme also envisaged improvement in the
conditions in existing mental hospitals, effective
implementation of the Mental Health Act, 1987
and adequate manpower development to meet
the growing needs for mental health care. The
Programme did not make much headway in the
Seventh Plan.
2.8.156 During the Eighth Plan, the National
Institute of Mental Health and Neuro Sciences
(NIMHANS) developed and implemented a district
mental health care model in the Bellary district of
Karnataka with the objective of:
El
providing sustainable basic mental health
services to the community and to integrate
these services with health services;
El
early detection and prompt treatment of
patients with mental illness;
127
E
providing domiciliary mental health care and
reducing patient load in mental hospitals;
E
community education to reduce the stigma
attached to mental illness; and
E treatment and rehabilitation of patients with
mental illnesses within their family setting.
2.8.157 Following encouraging results, the progra
mme was expanded during the Ninth Plan to 22
districts in 20 states. It was envisaged that
decentralised district-based training in essential
mental health care will be provided to all health
professionals so that psychiatric care will be
provided in all health care facilities. Attempts were
made to improve early detection of mental illness
in the community, provide ambulatory care at home
and follow up discharged cases. A district mental
health team was to provide referral support and
supervision of the mental health programme.
Simple, accurate records of work done maintained
by the health care providers was to be monitored
by the district team. The progress in these districts
has not yet been evaluated.
2.8.158 During the Tenth Plan, it is expected that
states will progressively improve access to mental
health care services at the primary and secondary
care levels to cover all the districts in a phased
manner. Psychiatry departments in medical colleges
will play a pivotal role in the operationalisation and
monitoring of the programme in the district in which
they are located and synergistic links will be formed
with other ongoing related programmes.
Accident and Trauma Services
2.8.159 Increasing mechanisation in agriculture
and industry, induction of semi-skilled and
unskilled workers in various operations, and rapid
increase in vehicular traffic have resulted in an
increase in morbidity, mortality and disability due
to accident and trauma. Overcrowding, lack of
awareness and poor implementation of essential
safety precautions result in an increasing number
of accidents. The consumption of poisonous
substances accidentally or intentionally is also
on the rise. Technological advances in the last
two decades have made it possible to
TENTH FIVE YEAR PLAN 2002-07
Figure 2.8.30- SCHEMATIC MODULE FOR TRAUMA SERVICES-DELHI
AMBULANCE
<
PERIPHERAL
CENTRES
SATELLITE
TRAUMA CENTRE
>
<
FIRE
SERVICE
POLICE
CENTRAL CONTROLLING
& COORDINATING
AGENCY
OTHER
SAFETY
AGENCIES
TRAUMA SERVICES
AT TERTIARY /APEX
CENTRES
PUBLIC
EDUCATION
▼
RESUSCITATION:
BY PUBLIC AND IN
AMBULANCES WITH
FACILITIES FOR
SPECIALISED CARE
substantially reduce mortality, morbidity and
disability due to accidents, trauma and poisoning.
At present there is no organized comprehensive
trauma care service either at the centre or in the
state. People are unable to benefit from these
advances because of limited access to these
services. During the Ninth Plan facilities for the
management of accident and trauma care have
been strengthened in several hospitals but these
have not been linked into an effective multi
disciplinary trauma care system. A conceptual
model ( Figure 2.8.30) of such a system for Delhi
has been prepared which optimises utilisation of
available facilities and prevents wastage of
scarce resources due to duplication of efforts.The
model includes arrangements for:
DOCUMENTATION
& PERIODICAL
TRAINING AT ALL
LEVELS.
networking among and within institutions for
manpower, materials, communication, training
and research; and
other allied trauma care activities.
2.8.160 Apart from communication networking, the
apex centre would be utilized for human resource
development and creation of a comprehensive
computerized information database on trauma
cases.
2.8.161 During the Tenth Plan efforts will be
made to strengthen primary, secondary and tertiary
care institutions for trauma care through:
El
adequate training to medical and paramedical
personnel;
ISI
for on-site resuscitation of trauma victims;
E
provision of facilities for transport of patients;
El
first aid and transport to the nearest tertiary
care hospital by ambulances with essential
equipment and trained paramedical staff;
E
suitable strengthening of existing emergency
and casualty services; and
E
improving referral linkages.
128
HEALTH
Environment and Health
2.8.162 Environment can affect human health in
many ways. Deficiency of iodine in soil and food
items is the cause of iodine deficiency disorder.
Excessive fluoride in water causes fluorosis.
Environmental degradation may affect air, land and
water. Pollutants may enter the food chain and,
hence, the human body. Rapidly growing population,
urbanization, changing agricultural, industrial and
water resource management, increasing use of
pesticides and fossil fuels have all resulted in a
perceptible deterioration in the quality of
environment and all these have adverse health
consequences. Environmental health would have
to address
E the prevention, detection and management of
the existing deficiencies or excess of certain
elements in the environment;
E
macro environmental contamination of air, land,
water, and food; and
E
disaster management.
2.8.163 So far, the major focus of environmental
health has been on the communicable disease
burden due to poor environmental sanitation in
urban and rural areas and methods to tackle these.
These efforts will be intensified during the Tenth
Plan. Emphasis will be laid on
El
establishing cost-effective and environment
friendly technologies for safe, sanitary disposal
of solid waste and waste water;
El
improvement in access to potable drinking
water, especially in urban slums and remote
rural areas;
E
prevention and management of health
consequences of environmental deterio
ration.
2.8.164 Major developmental activities in any field
such as agriculture, industries, urban and rural
development can result in environment changes
which could have adverse health implications. In
the Tenth Plan period, efforts will be made to fully
operationalise the Ninth Plan recommendations
that:
129
E
health impact assessment should become a
part of environmental impact assess-ment of
all large developmental projects; and
E
health care of people involved in these projects
and the prevention and manage-ment of health
consequences of the population living in the
vicinity of the project should be met from the
project budget.
2.8.165 The rapid growth of industry especially in
the small-scale and unorganised sectors is central
to economic development but in the absence of
appropriate technology and environmental safe
guards, these become a major source of air, water
ground and noise pollution. The Central Pollution
Control Board (CPCB) under the Ministry of
Environment and Forests regularly monitors
pollution levels in all major cities and initiates
appropriate remedial measures. In India, the
problem of indoor air pollution due to the combustion
of unprocessed biomass fuels by the urban and rural
poor has to be reduced by providing appropriate
fuel for cooking. Noise pollution is another area of
increasing concern. During the Ninth Plan, the
Biomedical Waste Management and Handling
Rules (1998) and the Municipal Waste Management
and Handling Rules (2000) were notified. A manual
on Municipal Solid Waste Management was
published in May 2000 by the Ministry of Urban
Development. The CPCB has evolved a code of
practice for controlling noise pollution in public
places. Efforts to reduce air pollution, ground water
as well as river water pollution have been taken up.
2.8.166 During the Tenth Plan priority will be
accorded to :
E
monitoring, detection and alleviation of the
macro environmental pollution;
E
creation of national data base on environmental
pollution and related health problems by linking
the existing area specific environmental
monitoring data with data on health status of
the population living in these areas;
E
epidemiological studies on the impact of the
biomass fuel on the health status;
H
health consequences of noise pollution;
MRN
TENTH FIVE YEAR PLAN 2002-07
E
R&D efforts for producing cleaner fuels from
traditional material;
E
monitoring the work environment for detection
and correction of micro environmental pollution;
E
development of biomarkers for long term bio
monitoring designed to detect changes in
aquatic eco systems due to water pollution.
E
monitoring of health status of workers;
E
interventions aimed at prevention, early
detection and effective management of health
problems of workers, including occupational
health problems, with special attention to health
problems in women and children.
Occupational Health
2.8.167 A healthy workforce is an essential pre
requisite for agricultural and industrial development.
Over the last five decades, efforts have been made
to provide health care to workers through schemes
such as ESIS , creation of health care facilities in
industrial towns and arrangement for health care
for workers and their families through existing public
and private health care services. However, both
coverage and quality of care have not been
adequate. There is no attempt to link existing data
from ongoing environmental monitoring at the work
place with the health status of workers and initiate
appropriate interventions. Workers in the agri
cultural and unorganised sectors have not been
covered under specific health care programmes.
The increasing use of mechanisation, induction of
poorly trained workers who operate machines with
which they are not familiar, use of insecticides,
pesticides and chemicals by persons who are
ignorant of the precautions to be taken are resulting
in increasing health hazards to workers in these
sectors. The Ninth Plan had recommended
E
continuous monitoring of the safety of the work
environment and workers’ health status in
industry and agriculture;
E
special attention to the health problems of
vulnerable groups such as women and children
with a focus on the prevention, early detection
and prompt treatment.
2.8.168 Not much progress was achieved during
the Ninth Plan. During the Tenth Plan the focus will
be on:
El
establishment of norms for work environment
in organized, unorganized and agricultural
sectors;
» 130
Drugs - Production, Quality and Supply
2.8.169 Nearly one-third of the health budget at
the centre and in the states is spent on providing
drugs free of cost in all public health facilities.
However, adequate stock of good quality drugs are
not available in many of these institutions, and
health benefit from treatment are sub optimal. Some
of the factors responsible for this include :
E
lack of a uniform essential drug list;
E
poor quality control;
E
problems in the procurement and supply of
drugs;
E
the absence of treatment protocols for common
diseases leading to unnecessary and irrational
drug prescriptions; and
E
poor compliance with the prescribed regimen
due to lack of awareness and counselling.
2.8.170 During the Ninth Plan, several state
governments (e.g. Tamil Nadu, Delhi and Orissa)
have introduced an essential drug programme with
the following components:
E
development of a drug policy;
E
preparation of an essential drug list;
E
establishing a quality control and assurance
system;
[ ’
pooled procurement system and improvement
in logistics of drug supply;
E
improvement in the availability of safe and
effective drugs;
E
preparation of standard treatment guidelines
and dissemination of information; and
HEALTH
providing information about treatment to
patients to improve compliance.
2.8.171 Research and monitoring of all aspects of
drug use including adverse drug reaction were
attempted.
under the Drugs and Cosmetics Act (1940) provide
for good manufacturing practices. During the Tenth
Plan, the regulatory requirements pertaining to
safety, efficacy and quality have to be effectively
implemented by:
El
strengthening the drug control machinery at the
centre and in the states;
El
strengthening quality assurance systems;
cover all states with expanded and strength
ened essential drug programmes;
El
making good manufacturing practices (GMP)
mandatory for pharmaceutical houses; and
adopt an online computer inventory control
programme for the procurement and supply of
drugs; and
E
enforcing stringent quality regulatory processes
for the import of drugs.
2.8.172 During the Tenth Plan efforts will be made
to:
establish a system to monitor cost, quality,
availability and use of drugs.
2.8.173 India has a large pool of technically skilled
manpower and research infrastructure in both
government and private sector laboratories. The
Indian pharmaceutical industry has the ability to
develop and commercialise chemical processes for
manufacturing of a variety of drugs at low cost.
However, financial problems and fragmentation of
capacities makes production of some bulk drugs
uneconomical; this has-prevented Indian industry
from achieving its full potential, both in the domestic
and international market. The existence of nearly
20,000 manu-facturing units and poor quality control
have led to spurious and poor quality drugs reaching
the market. The revised National Drug Policy 2001
had reviewed the situation and suggested remedial
measures.The limit for the situatory foreign direct
investment in the phar-maceutical sector was
increased from 51 per cent to 74 per cent. Several
products reserved for production in the public sector
were de-reserved. Industrial licensing for all bulk
drugs has been abolished except in the case of
those produced by the use of recombinant DNA
technology and bulk drugs requiring in-vivo use of
nucleic acids as the active principles.
2.8.174 The Central Drugs Standard Control
Organisation (CDSCO) under the Drug Controller
General of India is responsible for ensuring the
safety, efficacy and quality of drugs. The provisions
131
2.8.175 Post-marketing surveillance, development
of a self-sustaining and viable adverse drug reaction
(ADR) monitoring and response at the national level
will receive due attention.
2.8.176 Currently, Indian industry is investing
about 5 per cent of turnover on research and
development. These investments may have to be
augmented so that the Indian pharmaceutical
industry achieves its full potential. Parallel efforts
to improve public sector-funded research are also
essential for the development of drugs for the
treatment of public health problems such as
emerging drug resistance, development of newer
contraceptives and vaccines. The private sector
may not be willing to make requisite investments in
these areas because of very low profit margins.
Information, Education, Communication and
Motivation (IEC&M)
2.8.177 An aware and informed population,
actively participating in programmes aimed at
promoting health, preventing illness, accessing
health care at appropriate level is an essential
prerequisite for improvement in health status of the
country. Health education, which is the major tool
for achieving this objective had received a lot of
attention in the 1950s and 1960s. During the
development of various centrally sponsored vertical
programmes for disease control, family welfare
proggramme and state’s efforts to build up state
specific programme, health education efforts got
fragmented. Currently, health education efforts are
mostly limited to information being provided through
TENTH FIVE YEAR PLAN 2002-07
mass media and health functionaries regarding
Family Welfare services and disease control progra
mmes. These efforts have resulted in improved
awareness of the population who accessed these
programmes. However, active participatory health
education aimed at motivating the population on life
style changes and preventive and promotive health
care programmes have not received due attention.
Lack of readily available information at household
and community level on where to go and whom to
access for various health problems continue to
remain a major barrier for seeking appropriate care.
2.8.178 During the Tenth Plan, attempts will be
made to:
E
review existing training programmes on health
promotion/health education and make them
more relevant;
E
integrate the various health education
programmes under different vertical
programmes so that health personnel at each
level of care provide comprehensive I EC to the
population;
E
involve PRIs and NGOs in health promotion/
education and IEC&M; and
E
ensure the involvement of non-formal leaders
in the community in order to make health
promotion/ education/ IEC&M a people’s
movement; and
Public Health
2.8.179 In the pre-lndependence era, India’s
health services had two distinct components:
El
public health services manned mostly by non
health professionals implementing interven
tions aimed at preventing health hazards,
improving environmental sanitation, monitoring
water quality, and prevention of adulteration in
food and drugs; and
medical care services manned by health
professionals and paraprofessionals providing
132
promotive, preventive, curative and rehabili
tative care to individuals.
2.8.180 In the post-independence period, tasks
relating to civic services infrastructure and
environment got transferred to other departments
dealing with urban and rural development,
environment and forests. Medical care also
underwent changes. Specilaists in community
medicine and public health focused on providing
promotive and preventive care for major public
health problems through outreach services. The
clinicians provided institution-based preventive,
promotive, curative and rehabilitative health care
to individuals who came to the health care
institutions.
2.8.181 With increasing knowledge and experi
ence the earlier concept that prevention and curative
care are two sides of the same coin, which mutually
reinforce each other gained wider acceptance. This
led to the re-emergence of the concept of public
health providing comprehensive health care. This
concept was initially developed and implemented
in maternal and child health but soon all other
disciplines including clinical specialities dealing with
non-communicable diseases such as cardiology
adopted this. As a result, public health is today
defined as a discipline aimed at developing a health
system to deliver equitable, appropriate and holistic
care to improve the health status of the individual
and health indices of the country at an affordable
cost.
2.8.182 The newer concepts of public health were
discussed in 1999 and the ‘Calcutta Declaration
1999’ redefined the role of public health. The
declaration stated that as the countries in the
Southeast Asian region are stepping into the new
century with an unfinished agenda of existing health
concerns, amidst new and complex emerging
challenges, there is a need for innovative solutions.
Public health should meet the health needs of the
community and preserve, protect and promote the
health of the people. The declaration emphasized
the need for capacity building in public health as a
multi-disciplinary endeavour to design, develop and
provide health care to meet health needs of the
population.
HEALTH
2.8.183 Taken in this broader perspective, public
health deals with the formulation, implementation
and monitoring of evidence-based health policies,
strategies and programmes. It also attempts to
create a supportive environment for the effective
implementation of such programmes by addressing
critical issues that affect health care including
quality, equity, ethics, environment and globalisa
tion. Every effort has to be made to ensure that
policy makers, programme managers, health care
providers and people themselves internalise and
support this broad concept of public health and
contribute towards attaining the public health goals.
carried out by research institutions, universities,
medical colleges and health service providers.
Biomedical research is currently funded by several
agencies including the ICMR, the Deparments of
Biotechnology, Department of Science and
Technology, the Council of Scientific and Industrial
Research (CSIR) and the concerned ministries.
Basic, clinical and operational research studies
relevant to major health problems have been the
focus of research programmes. In addition, the
private sector has been investing in research, mainly
in the pharmaceutical sector. The national research
efforts have laid the foundation of various health
care programmes in the country and have gained
global recognition. ICMR research studies have also
led to the development of appropriate guidelines
for the implementation of major programmes such
as tubal sterilisation, medical termination of
pregnancy and assisted reproduction. Data from
ICMR surveys on HIV infection, cancer, under
nutrition and blindness have provided the database
for the formulation of national programmes on these
diseases and for monitoring their impact.
Health Systems Research and Bio-medical
Research
2.8.184 India had invested in health system and
biomedical research from as early as 1911 so that
appropriate policies, strategies and programmes to
improve the health status of the population can be
evolved on the basis of data from research studies.
Bio-medical and health systems research is being
Figure 2.8.31 Research Needs
100%
z
x
Biomedical research &
Unavertable with existing interventions
’E
<— development to identify
new interventions
<D
.s
(D
>.
i—
o
E
O
(D
c
o
(D
£Z
O
-C
.£
E
o
O
"o —
o
x
Q
V)
?> (D
cl cd
<D -Q
Q <D
fil.
<D
o
o
o
c
o
(D
(D M- O
tr o Q. E
O
x ■0 o
> ■?=
c o
< E (U Q
Effective coverage
of population
5£
< E
£Z
§ °
3
(D JD
-Q CD
(U C .>
o
X = population coverage with current mix of interventions;
Y = maximum achievable coverage with a mix of available cost-effective interventions
Z = combined efficacy of a mix of all available interventions
Source: Investing in Health Research and Development, WHO, 1996
R&D to reduce cost of
<— existing interventions
(D
O £
-._(!)
<D
.22 (D 0
> X 3=
< 0) (D ,E
Health systems
research
133
cn
c
Y
TENTH FIVE YEAR PLAN 2002-07
National Programmes formulated on the
basis of ICMR’s R&D efforts
H Domiciliary treatment for tuberculosis,
H Short course
tuberculosis,
chemotherapy
for
E) Multi drug therapy for leprosy,
El Oral rehydration therapy for treatment of
diarroheal disease,
El Programme for prevention of blindness
due to Vitamin A deficiency,
El Programmes for antenatal care,
E Management of anaemia in pregnancy.
2.8.185 In India, most of the morbidity and
mor-tality is due to illnesses for which simple,
inexpensive and effective preventive measures
and time-tested cost-effective curative
interventions are available. Therefore, priority has
been given to health systems research for
improving service delivery and coverage as well
as operational research aimed at improving
access to techno-logical advances. Basic and
clinical research leading to development of
products, drugs, vaccines for prevention,
diagnosis and management of illnesses
especially major health problems for which
currently there is no effective cure are
encouraged (Figure 2.8.31).
2.8.186 During the Ninth Plan, the major focus
of research efforts was on basic, applied and
operational research for improving the quality,
coverage, efficiency of health services. The thrust
areas of research included communicable
diseases, improvement of the health and
nutritional status of women and children and
improving contraceptive acceptance and
continuation rates. In commu-nicable diseases,
research has focussed on deve-lopment of
indigenous immuno-diagnostics, improved drug
regimens to combat emerging drug resistance
among microbes, alternative strategies for vector
control to combat increasing insecticide
resistance and testing innovative disease control
strategies through increased community partici134
pation. Studies on the health consequences of
the Bhopal gas disaster (1984) and providing a
database for planning the infrastructure needed
to meet the health care requirements of the
affected population continue. The major research
areas relating to non-communicable diseases
include early detection of cervical cancer in
women and oral cancer in both sexes, anti
tobacco education, lifestyle modification to
reduce the rising morbidity due to hypertension
and cardiovascular diseases, documenting the
health problems associated with lifestyle changes
and increased longevity. Evaluation of the
ongoing mid-day meal programmes in schools,
assessment of changes in the dietary intake and
nutritional status of urban and rural population
over the last two decades, investigating the health
effects of food contaminants and adulterants are
some of the major areas of nutrition research.
2.8.187 During the Tenth Plan, efforts to
generate data on the health impact of the socio
economic, demographic and epidemiological
transition on the health and nutritional status of
the population will continue. Health system
research which will enable the existing systems
to provide appropriate health care using effective,
inexpensive technology for detection and
management of health problems and ensure
equitable, economical, and efficient service
delivery will receive priority. Clinical, and
operational research in both the modern system
of medicine and ISM&H will continue. The major
thrust areas of research in communicable, noncommunicable diseases, nutrition and family
welfare have been indicated in the respective
sections. Other important areas include new drug
development, improved drug delivery system and
harnessing emerging techno-logies in genomics
for diagnosis and management of diseases.
Appropriate bio-safety containment facilities have
to be set up in selected laboratories in order to
facilitate basic research on pathogenic microbes,
storage, handling, cultivation of virulent
pathogens and in-vitro and in-vivo screening of
anti-microbials. Inter-agency collaboration will
ensure optimal utilisation of available resources
and avoid unnecessary duplication of efforts.
HEALTH
Health Care Financing
2.8.188 Since independence, health care has been
recognized as an essential social sector investment.
It was, therefore, initially envisaged that health
services in government institutions will be provided
free of cost to all. During the 1990s, it was
recognized that, given the increasing awareness
and expectations of the people, and the escalating
costs of health care, this policy could not continue.
The Ninth Plan envisaged that major public health
priorities such as essential primary health care,
emergency life saving services, services under the
disease control and family welfare programmes will
be provided free of cost for all. The Ninth Plan
advocated that the Centre and the state
governments should work out appropriate norms
for levying user charges on people above the
poverty line for other services and hospitalisation
and evolve mechanisms for collection and utilisation
of funds. The Planning Commission provided
additional central assistance to the Kerala
government for an experimental model in a district
hospital where different segments of the APL
population pay for health care and the hospital
meets the costs of care of BPL (lowest 20 per cent)
population through a system of cross-subsidisation.
2.8.189 The issue of how much the government
sector, private individuals and the country as a whole
is spending on health care and which segments of
the population are benefiting has been debated
widely during the last decade. As there is no
National Health Accounting system, there is no
information on total government expenditure on
health and categories of people who benefit from
this expenditure. The WHO has estimated that India,
at present, is spending 4.5 per cent of gross
domestic product (GDP) on health, of which 0.9 per
cent is public expenditure. India ranks thirteenth
from the bottom in terms of public spending on
health (World Health Report 2000). The Central
Statistical Organisation (CSO) reported that final
government expenditure on health (which does not
include expenditure on family welfare) for 1998-99
is Rs. 10,588 crore, accounting for 0.6 per cent of
GDP. For the same year the plan and non-plan
expenditure of 26 States and the Central Ministry of
Health and Family Welfare alone comes to Rs.
135
16,771 crore or 0.95 per cent of the GDP. The
Railways, Defence and the Department of Post and
Telegraph have created health care infrastructure and
spend substantial sums on the health care of their
employees and their families. ESIS and PSUs spend
large amounts of government funds on health care.
The expenditure of PRIs and other local bodies on
health is never accounted for as health expenditure
nor is the reimbursement of health care costs by
different departments at the Centre, in the States and
PSUs taken into account while computing public
expenditure on health. It is imperative that a system
of National Health Accounting, reflecting total
government expenditure on health is established.
This will enable periodic review and appropriate policy
decisions regarding modalities for ensuring optimal
utilisation of the current government investment in
the health sector and also future investments to meet
public health needs.
2.8.190 Given India’s size and the fact that health
is a state subject, it is important to examine inter
state differences in spending patterns. While the
central government provides funds to the states
under centrally sponsored schemes based on
uniform norms, per capita expenditure in states vary
depending upon the prevalence of diseases and
utilisation of funds allocated . If these are taken into
account, the central government expenditure does
not show much variation between states (Fig 2.8.32)
Figure 2.8.32 State Level Per Capita Public
Spending on Health (Rs.)
BIHAR
□ Central per capita
MP
UP
□ State per capita
ORISSA
WB
HARYANA
GUJARAT
KARNATAKA
MAHARASHTRA
ASSAM
RAJASTHAN
PUNJAB
KERALA
50
Source: NCAER 2000.
100
150
TENTH FIVE YEAR PLAN 2002-07
2.8.191 There are substantial variations in per
capita expenditure on health by the states. At one
end of the spectrum are states like Bihar, Madhya
Pradesh, Uttar Pradesh and Orissa with low per
capita expenditure, poor access to health care
and poor health indices. At other end are Kerala,
Punjab and Tamil Nadu with high expenditure and
good health indices. However, Rajasthan and
Assam continue to have poor health indices in
spite of relatively higher expenditure (Figure
2.8.32). While funds are, no doubt, needed to
improve health care and health indices,
awareness, equitable distribution and utilisation
of services is equally critical for the improvement
of health indices. Kerala ranks high in two
important dimensions-equitable spending
between income groups and efficiency of the use
of resources.
2.8.192 In all states, patients incur out-of-pocket
expenses to meet the health care cost in public
and privately-funded hospitals. There are
massive differences in private spending on health
care services in public and private facilities
between states. Patients from Kerala and Punjab
spend about four times more on health as
compared to patients from Bihar. The high and
low spending in private and public sector do not
always go hand in hand with each other. In
Rajasthan out of pocket expenditure in private
and government hospitals is almost equal,
because the state has been levying user charges
and providing drugs at cost price to persons
admitted in government hospitals (Figure2.8.33).
It is important that each state undertakes a
detailed analysis of the current situation, identify
critical points where appropriate interventions
would enable the BPL population to utilise
subsidised government health services while
providing affordable health care to other
segments of the population.
2.8.193 The poorer segments of population have
less access to both public and private sector
curative services than the better off sections. The
out-of-pocket expense on both public and private
facilities for the lowest income quintile is about
one-fifth that of the highest quantile population
(Figure2.8.34) suggesting thereby that the richest
quintile utilise both private and public facilities
more than the poorest quintile. The question
whether the amount spent by different segments
of the population results in their receiving the
appropriate care remains unanswered as the
country is yet to evolve and monitor appropriate
treatment protocols and cost of care for specific
illnesses in different settings.
Figure2.8.33 Private Spending on Health Ser vices
at Private and Public Facilities (Rs.) 1995-96
Figure 2.8.34 Out - of Pocket Payments
and Household Income-1995-96
'*
KERALA
PUNJAB
HARYANA
ai
™600 i
c
73 500 ;
UP
MAHARASHTRA
■.PrivateJEacilities
Public Facilities
^400
AP
ALL INDIA
| 300 '
WB
MP
i
i
,= 200
TN
2 100
GUJARAT
ro"
O
o
o_
NORTH EAST
ORISSA
KARNATAKA
FACILITIES
FACILITIES
100
200
Source: Mahal A, et al 2001 ,NSSO, 1995-96
Lb
I
1
BIHAR
RAJASTHAN
0
300
I
o
o
CM
I
i
5?
S
O
CD
Source: NCAER-2000 , NSSO, 1995-96
136
H
HI
$ c£
€ O
Ol
£
HEALTH
Figure 2.8.37. Hospitalisation for major illness is
a cause of indebtedness in all income groups.
With increasing awareness, people are willing to
spend on health care. However, there is, at
present, no mechanisms by which they can pay
a part of their income, throughout their working
life, so that the cost of health care or
hospitalisation can be met without severe
financial crisis. Health insurance in the
government and private sector covers less than
10 per cent of the population, mostly from upper
income group, government or industrial
employees. There is need to explore mechanisms
for providing near-universal coverage of the
population for meeting the cost of hospitalisation
and continuous care for chronic disease.
Figure 2.8.35 Distribution of Total out of Pocket Health Expenditures
as A Proportion of Non-food Expenditures, All India. 1995-96
2
I 15 -|=
8
UJ 10-------
1S
z
i
i
u
5
0
__
3?
3?
o
I
T
ae
o
6?
o
CM
■O
I
a?
o
co
5 oCM
cr
o
co
S
Source: NCAER-2000 .NSSO, 1995-96
2.8.194 Out-of-pocket expenditure is the most
common method of payment for private health care
services. The poorest 20 per cent spent 12 per cent
of the non-food expenditure on health care
and the richest about 14 per cent. (Figure
2.8.35)
2.8.195 The out-of-pocket expenses of the
SC/ST population is higher than the BPL
families perhaps because they have greater
problem in access to health care services
(Figure2.8.36). The urban population spent
larger amount on health care as compared
to their rural counterparts perhaps because
they have ready access to high cost or hitech care.
Figure 2.8.37 Sources of Financing for
Private Expenditures on Hospitalisation
in India by Income Quintile, 1995-96
Richest 20%
60%-80%
Middle 20%
20%-40%
i Poorest 20%
0
10
@ Borrowed
2.8.196 Mechanisms by which different
income groups meet the out-of-pocket
expenses for hospitalisation is shown in
300 —
250 —
200
150 —
100 —
i
£
Cl
<
Z)
(X
Source: NCAER-2000 ,NSSO, 1995-96
40
Sold assets
50
percent
60
Used savings
70
80
90
100
Used Current Income
2.8.197 There are substantial inter-state
differences in the utilisation of public and private
facilities by people below the poverty line. In
Himachal Pradesh, West Bengal and Orissa the
poor predominantly use public facilities. In
contrast, the poor in Bihar and Punjab make very
limited use of public sector in-patient facilities.
The lack of functional government-funded
hospitals in Bihar may be the reason for the poor
going to private hospitals. In Punjab, the
perception regarding convenience, comfort and
quality of care may be the reason why private
sector hospitals are preferred to functional public
sector hospitals. In Orissa, the absence of private
sector facilities in the remote rural and tribal
350
o L-
30
Source: NCAER-2000, NSSO 1995-96
Figure 2.8.36 Out-of Pocket Payments by
Socioeconomic Group.1995-96
50
20
z:
m
cr
z>
137
TENTH FIVE YEAR PLAN 2002-07
continuous care. However, the experience in
developed countries show that health insurance
runs the risk of market failure and cost escalation
because:
Figure 2.8.38 Public And Private Sector of Inpatient
Bed Days by People Below the Pverty Line
WEST BENGAL
ORISSA
RAJASTHAN
HARYANA
El
disproportionately large number of individuals
who get insured are those who expect
significant health expenditure in the future;
E
reduced incentives for individuals to take
precautions against poor health;
E
health care providers tend to give more care
than medically appropriate; and
E
insurance companies have low capital reserves
and incomplete epidemiological information.
MADHYA PRADESH
TAMIL NADU
ALL INDIA
MAHARASHTRA
KERALA
AP
KARNATAKA
UTTAR PRADESH
GUJARAT
NORTH EAST
2.8.200 Attempts by insurance companies to
prevent market failure may have serious health
implications, if it is achieved either by exclusion of
high risk individuals or by escalation of cost of
insurance.
BIHAR
PUNJAB
20
□ PUBLIC SHARE
40
60
80
El PRIVATE SHARE
Source: NCAER-2000 , NSSO. 1995-96
areas might be the reason for the poor using
public sector hospitals (Figure2.8.38).
2.8.198 Health sector reforms during the Tenth
Plan will focus on:
El
addressing the issues of need and equity in
access to health care;
El devising a targeting mechanism by which
people below poverty line have ready access
to subsidised health services to meet essential
health care needs, while those from above the
poverty line pay for the services both in
government and private care facilities.
2.8.199 There is an urgent need to evolve, imple
ment and evaluate an appropriate scheme for health
financing for different income groups. Health finance
options may include health insurance for individuals,
institutions, industries and social insurance for BPL
families. Health insurance has been suggested as
a mechanism for reducing the adverse economic
consequences of hospitalisation and treatment for
chronic ailments requiring expensive and
138
2.8.201 Health insurance can improve access to
good quality health care only if it is able to provide
for health care in institutions with adequate
facilities and skilled personnel at affordable cost.
Some states like Kerala and Delhi are
conceptualising pilot projects where the
government pays the social insurance premium
to meet the hospitalization cost for the poor
admitted in government institutions. During the
Tenth Plan global and Indian experience with
health insurance/health maintenance organi
sations will be reviewed and suitable models
replicated. In order to encourage healthy
lifestyles, a yearly ‘no claim bonus’/adjustment
of the premium could be made on the basis of
previous year’s hospitalisation cost reimbursed
by the insurance scheme.
Financing Health Care in India
2.8.202 The importance of health as a determinant
of human development is well accepted. Health is
high on the agenda of the government and the
people, both of whom are willing to invest for
improving health status. Spiraling costs and rising
demand are putting a severe strain on the health
system, whether government-funded or private.
Health care can absorb a very large quantity of
investments from the government and individuals
and yet leave millions of people, especially the poor
who suffer from a high disease burden, inade
quately covered (Figure 2.8.39) It is also being
increasingly realized that merely investing more in
health is unlikely to improve the health status of the
population. It is essential that policies and strategies
are developed to promote equitable access to
preventive and curative services so that there is an
improvement in health indices ( Figure 2.8.40).
Figure 2.8.39 Unproductive Investment in Health : a Vicious Cycle
Cost escalation
Inadequate
health status
Inequitable, ineffifiien
and poor quality
health services
A.
\
V
Inflation
Inequality of
opportunity
development
Sub-optimal
development
of human
capital
^^X^JVIore
\ poverty
Lower
productivity
and competivity
Source:Fundacion MaxicanaPara La Salud, 1995
Figure 2.8.40 Productive Investment in Health : a virtuous cycle
Equitable, efficient
and high quality ’
health services
Improved
Economic
development
Better health status
V
i Better human
capital
Greater equality
/
of opportunity
Less poverty
Greater productivity
and competivity
Source: Fundacion MaxicanaPara La Salud, 1995
139
TENTH FIVE YEAR PLAN 2002-07
2.8.203 It is essential to quantify the interactions
between the health of the population and
economy, gauge essential potential benefits of
various interventions and ensure adequate
investment in chosen priority sectors.
Concurrently, every effort should be made to
organise and deliver health services equitably
and efficiently. It is important to get adequate data
on disease burden and current modalities of
funding health care in different states. These data
should then be used for:
H
making an enabling policy framework;
El
selecting appropriate strategy;
El
implementing and evaluating packages of
health interventions; and
E
assessing quality of care and its cost
effectiveness.
2.8.204 Health policy research and health system
research at the national level is essential and a
reliable information base is a pre-condition for
effective investment in health care and performance
assessment of the health system.
Health Sector Outlay:
2.8.205 The health sector is funded by the central
and state governments and externally assisted
projects (in both the Centre and the states).
Externally Assisted Projects
2.8.206 Externally-assisted projects can be
classified under the following:
H
assistance to different components of the family
welfare programme;
E
assistance to centrally sponsored schemes of
the disease control programmes;
E
assistance to state governments to strengthen
infrastructure and manpower through bilateral
direct assistance to the states and from funding
agencies like the World Bank routed through
the central government.
140
2.8.207 Externally assisted projects initially
focused on rural primary health care e.g. India
Population Project (IPP I to IV, VI & VII) and later
also covered urban primary health care (IPP V,
VIII). During the 1990s, externally assisted
projects for strengthening secondary care
institutions were taken up in seven states. The
tertiary care institutions have not received much
funding from externally-assisted projects, except
for individual institutions like Sanjay Gandhi
Institute of Medical Education and Research
(from Japan).
2.8.208 Investment from externally assisted
projects was used for strengthening
infrastructure, purchase/re placement of
equipment, meeting the cost of drugs and
consumables and for operationalising health
sector reform. However, it has been reported that
externally assisted projects introduce a project
framework, management structures, parameters
of expenditure, unit costs and institutional
arrangements for monitoring which are very
different from the ones already in place under
national and state level programmes. This
creates distortions and the performance in other
programmes deteriorates. Also, service providers
who have worked in the externally-assisted
projects become de-motivated after the project
is completed because similar parameters of
expenditure may not be sustainable. It has also
been reported that improvement in facilities and
equipment through externally-assisted projects
have not resulted in improved performance. For
example, despite the construction of a large
number of sub-centres and staff quarters,
occupancy remained low and deliveries in these
institutions did not go up. States have not been
able to provide adequate funds for maintenance
of these infrastructure and equipment procured
under the EAPs, so that there has been a
progressive deterioration of these. These aspects
and the issue of sustainability of the projects after
they are completed need be looked into at the
time of deciding areas/schemes for external
assistance in the health sector. The mechanisms
for repayment of loans when the EAR is in the
HEALTH
form of loans is another aspect that has to be
considered before EAPs in health sector are
initiated.
E
vaccine production institutes and special
centres for specific diseases;
State Government:
El
Central Government Health Schemes;
2.8.209 The state governments provide funds for
primary, secondary, tertiary care institutions
(including medical colleges and their associated
hospitals). State governments also receive funds
from centrally sponsored disease control progra
mmes and family welfare programme. Health was
one of the priority sectors for which funds were
provided during the Ninth Plan as additional
central assistance under PMGY. These funds
were to be utilised for meeting the essential
requirements for operationalising rural primary
health care. The ongoing and proposed externally
assisted projects provide additional resources.
The major activities that received funds during
the Ninth Plan were:
restructuring of the health care infrastructure;
re-deployment and skill up gradation of
personnel;
E
development of referral network;
El
improvement in the HMIS;
E
disease control programmes; and
E
development of a disease surveillance and
response system at the district level.
training institution for nurses;
emergency relief measures; and
pilot central sector projects either to
demonstrate the feasibility of disease control
or for working out strategies for health care.
2.8.212 In addition to the domestic budgetary
support, external funds have also been obtained
for several centrally sponsored disease control
programmes.
Zero Based Budgeting-2001
2.8.213 In November-December 2001 the
Planning Commission and the Department of Health
had reviewed all the ongoing Ninth Plan schemes/
programmes and undertaken a zero-based
budgeting exercise. In the Ninth Plan, there were a
total of 91 schemes (22 centrally sponsored
schemes and 69 central sector schemes). Of these
45 are being retained, one is being transferred to
TRe states, 38 are being merged into 14 schemes
and seven are being weeded out. A total of 59
schemes, with a Ninth Plan outlay of Rs. 5,088.19
crore are continuing during the Tenth Plan. The
summary of the zero-based budgeting exercise is
given in Table 2.8.15.
Path Ahead And Goals
2.8.210 Funds provided during the Tenth Plan will
be utilised to improve the existing health care
infrastructure and manpower in the states so that
quality and coverage improves. The state-wise
outlay and expenditure in the Ninth Plan is shown
in Annexure 2.8.5.
2.8.214 Major focus in the Tenth Plan will be to
fully operationalise the structural and functional
health sector reforms initiated in the Ninth Plan
and
improve efficiency of the existing health care
system - in government, private and voluntary
sectors;
Central Sector
2.8.211 Funds from the central sector are being
utilised for supporting:
E
E
improve quality of care at all levels;
mainstream ISM&H practitioners so that in
addition to practising their system of care, they
medical education institutions of excellence;
141
TENTH FIVE YEAR PLAN 2002-07
Table 2. 8.15
Zero Based Budgeting Exercise 2001-Centrally Sponsored Schemes & Central Sector Schemes
Rs. in Crore
Central sector
Centrally sponsiored
Category
No. of
Schemes
Ninth
Ninth Plan
Plan
Anticipated
Outlay Expenditure
No. of
Schemes
Ninth
Plan
Outlay
Ninth Plan
Anticipated
Expenditure
Schemes to be retained
39
995.24
968.39
6
1,984.00
2,055.94
Schemes to be merged
8/24
766.45
850.73
6/14
1,342.50
1,202.59
Schemes to be transferred to the states
1
4.00
1.88
NIL
NIL
NIL
Schemes to be weeded out/dropped
5
22.00
5.69
2
4.00
2.98
Total Ninth Plan schemes
69
1,787.69
1826.69
22
3,330.50
3,261.51
No. of ongoing schemes that will
continue in Tenth Plan
47
1,761.69
1819.12
12
3,326.50
3,258.53
can help in improving coverage and utilization
of national disease control programme and
family welfare programme;
E
develop efficient logistics of supplies of drugs
and diagnostics and promote rational use of
drugs;
E
explore alternative systems of health care
financing so that essential health care based
on needs is available to all at affordable cost.
2.8.215 The National Health Policy (NHP) formu
lated in 1983 - after the Alma Ata declaration articulated the ambition of the country to provide
health care for all based on needs and to rapidly
achieve all round improvement in the health indices
The Ninth Plan recommended a review of
the National Health Policy in view of:
S ongoing demographic transition;
H ongoing epidemiological transition;
M expansion of health care infrastructure;
H changes in health care seeking behaviour;
El availability of newer technologies for
diagnosis and treatment;
E rising expectations of the population, and
escalating cost of health care.
of the population. The NHP (1983) provided a
comprehensive framework for planning, implemen
tation, monitoring of health services and goals to
be achieved by 2000. The Department of Health
has reviewed the performance since 1983 and
formulated the NHP, 2002 so that it provides a
reliable and relevant policy framework for improving
health care and measuring and monitoring the
health care delivery systems and health status of
the population; NHP2002 has laid down the goals
upto 2015.
2.8.216 The NHP 2002 emphasises that any
significant improvement in the quality of health
services and health status of the citizens, would
depend on increased financial and material inputs,
service providers treating their responsibility not as
a commercial activity, but as a service (albeit a paid
one), the citizens demanding improvement in the
quality of services, a responsive health delivery
system, particularly in the public sector, and
improved governance. Recognising that the health
needs of the country are enormous and dynamic
and acknowledging the human and financial
resource constraints, the NHP 2002, attempts to
make choices between various priorities and
focuses on:
expanding and improving primary health care
facilities;
142
HEALTH
NHP2002- Goals to be achieved
Eradicate polio and yaws
2005
Eliminate leprosy
2005
Eliminate kala azar
2010
Eliminate lymphatic filariasis
2015
Achieve zero level growth of HIV/AIDS
2007
Reduce mortality on account of TB, malaria and other vector and water- borne diseases by 50 per cent
2010
Reduce prevalence of blindness to 0.5 per cent
2010
Reduce IMR to 30/1000 and MMR to 100/100,000 live births
2010
Increase utilisation of public health facilities from the current level of <20 per cent to >75 per cent
2010
Establish an integrated system of surveillance, national health accounts and health statistics.
2005
Source: NHP 2002
H
organisational restructuring of the national
public health systems to facilitate more
equitable access to the health care;
El
area-specific programmes to meet the health
needs of women, children, elderly, tribals and
socio-economically under-served sections;
El
programmes for the control of diseases like
TB, malaria, blindness and HIV/AIDS;
E
disaster management plan to cope with natural
and man-made calamities; and
143
H
macro-policy prescriptions for coordination
between government, voluntary, private sector,
NGOs and other institutions of civil society.
2.8.217 It is expected that with effective implemen
tation of the policies and strategies indicated in the
Tenth Plan and NHP 2002 ,the country will achieve
goals set and complete the health and demographic
transition with in the set time frame. The
schemewise outlays of Department of Health for
the Tenth Plan is indicated in Annexure 2.8.6 and
Appendix.
Annexure - 2.8.1
m
z
z
Organisation Chart-1
Current Status of Health Care Infrastructure
m
>
1
State Director
Family Welfare
T]
State Director
Medical Education
State Director
ISM & H
State Director
Health Services
>
o
§
o
i
/
,r
j________ _
District
Family Welfare
Officer
Medical
Colleges & Hospitals
;
I
Medical Colleges
ISM & H
District Health
Officer
J
District j
Hospital I
?
PostPartum
Centre
£
Sub-district
Hospital
ISM & H
Hospital
|
I
Rural
Hospital :
Taluk
Hospital
“x
District
Leprosy
Officer
___ L
District I
Malaria |
Officer |
District
TB
Control
Officer
PHC
\
*
Sub
Center
J
I
ISM & H
I Dispensaries
_____ __ ,
V
■
FRU/
CHC
\
/
'j
I
Leprosy
Worker
x____ .....___ J
TB
Worker
Malaria
Worker
X
District
AIDS
Control
Officer
:
i
V
$
Technician/
Microscopist
f
¥^
J
District
Blindness
Control
Officer
Male
MPW
J
Annexure - 2.8.2
Organisational Chart-ll
Proposed Reorganisation and Linkages
*
State
Director
Medical
Education
State Director
Family Welfare
I L
State
Director
ISM & H
State
Director Health
I'/...J.,.,..,,,;... . .
f
I
Medical Colleges and
Hospitals Modern
medicine
Medical Colleges
and Hospitals
ISM & H
▼
i
V
CMO/District
Hospital Modern
Medicine
District Family
Welfare Officer
& Programme Officer
District Health
Officer &
Programme Officer
■J I-
A
A
(
Sub-centre
145
ANNEXURE - 2.8.3
STATE WISE/SYSTEM WISE NUMBER OF HOSPITALS AND DISPENSARIES UNDER MODERN SYSTEM AND ISM & H
RURAL HEALTH CARE INFRASTRUCTURE
STATES/UTs
Sub centres
Reqd.
1991
In Position
Primary Health Centres
Goal for
the 10th
Plan
Reqd.
1991
In Position
DISPENSARIES
Community Health Centre
Goal For
the 10th
Plan
Reqd.
1991
In Position
Modern System
of Medicine @
ISM&H
Goal For
the 10th
Plan
Dispens
Aries
Beds
Dispens
Aries
@@
i
m
HOSPITALS
Modern System
of Medicine @
Hospi
tals
1
ANDHRA
PRADESH
10242
10568
(326)
1707
1386
321
427
219
208
134
0
1930
2
ARUNACHAL
PRADESH
220
273
(53)
37
65
(28)
9
20
(11)
11
0
46
3
ASSAM
4356
5109
(753)
726
610
116
181
100
81
325
42
409
268
4
BIHAR
11547
10332
1215
1961
1642
319
490
87
403
427
96
831
5
CHHATISGARH
4692
3818
874
704
545
159
176
150
26
6
GOA
138
172
(34)
23
19
4
6
5
1
33
0
7
GUJARAT
6168
7274
(1106)
1028
1001
27
257
242
15
7255
8
HARYANA
2482
2299
183
414
401
13
103
64
39
9
HIMACHAL
973
2069
(1096)
162
302
(140)
40
65
10 JAMMU &
KASHMIR
1176
1700
(524)
196
337
(141)
49
11 JHARKHAND
4278
4462
676
561
115
12 KARNATAKA
6431
8143
(1712)
1072
1676
13 KERALA
4325
5094
(769)
721
14 MADHYA
PRADESH
7430
8835
MAHARASHTRA#10533
3133
Beds
69778
£
ISM&H@@
Hospi
tals
Beds
Urban Family
Welfare Centres
PostPartum
Centres
UFWC Health District Sub
Posts
level
dis
trict
level
22
1249
131
1
15
6
12661
6
260
10
11
30
328
29090
14
1385
42
37
54
115
105
3848
6
245
9289
583
2528
63417
55
2476
113
28
33
55
130
126
454
80
7230
7
850
19
16
13
20
(25)
173
169
1081
63
5463
18
355
89
11
22
53
(4)
610
0
445
67
8202
4
235
12
11
6
169
47
122
(604)
268
249
19
797
1163
642
293
38479
178
8400
87
39
64
944
(223)
180
105
75
53
164
3523
2107
97840
182
4031
22
60
1316
1193
123
329
229
100
256
2
2363
363
18141
47
1810
63
99
47
75
278
28
55
1
4
O)
15
9725
808
1756
1768
(12)
439
351
88
8143
1622
486
3115
78920
160
18618
74
52
69
344
420
(76)
57
69
(12)
14
16
(2)
42
0
10
17
1626
3
75
2
3
1
464
413
51
77
85
(8)
19
13
6
21
0
5
9
1828
0
0
1
3
1
18 MIZORAM
122
346
(224)
20
58
(38)
5
9
(4)
13
130
2
12
1021
0
0
1
2
4
19 NAGALAND
325
302
23
54
46
8
14
9
5
17
68
2
29
1158
0
0
1
1
20 ORISSA
6374
5927
447
1062
1352
(290)
265
157
108
1197
282
1104
273
11980
13
473
10
8
19
60
21
PUNJAB#
2858
2852
6
476
484
(8)
119
105
14
1469
5503
629
220
14921
17
956
23
64
19
35
22
RAJASTHAN
7484
9926
(2442)
1247
1674
(427)
312
263
49
268
134
3689
219
21387
102
1631
61
90
35
100
16 MANIPUR
17
MEGHALAYA
m
z
m
>
>
o
§
o
STATE WISE/SYSTEM WISE NUMBER OF HOSPITALS AND DISPENSARIES UNDER MODERN SYSTEM AND ISM & H
RURAL HEALTH CARE INFRASTRUCTURE
STATES/UTs
Sub centres
Reqd.
1991
In Position
23 SIKKIM
85
24
Primary Health Centres
Goal for
the 10th
Plan
Reqd.
147
(62)
7424
8682
(1258)
25 TRIPURA
579
539
26 UTARANCHAL
1764
27
UTTAR
PRADESH
28
DISPENSARIES
Community Health Centre
HOSPITALS
Modern System
of Medicine @
ISM&H
@@
Modern System
of Medicine @
ISM&H@@
Urban Family
Welfare Centres
UFWC Health District Sub
Posts
level
dis
trict
level
In Position
Goal For
the 10th
Plan
Reqd.
1991
In Position
Goal For
the 10th
Plan
Dispens
Aries
Beds
Dispens
Aries
Hospi
tals
Beds
Hospi
tals
Beds
14
24
(10)
4
2
2
147
0
2
1
300
0
0
1
1237
1436
(199)
309
72
237
512
278
396
408
48780
229
2187
65
40
96
58
38
24
11
13
612
0
96
29
1866
2
30
9
1609
155
265
257
8
66
30
36
20573
18576
1997
3458
3551
865
280
585
1750
5729
2239
735
47278
1843
11496
81
WEST BENGAL# 10356
8126
2230
1726
1262
464
431
99
332
571
0
1153
399
53732
19
1007
111
TAMILNADU
1991
29 ANDAMAN &
NICOBAR
ISLANDS
45
100
(55)
7
18
(11)
2
4
(2)
138
0
7
10
901
0
0
30 CHANDIGARH#
13
13
0
2
0
2
1
1
0
33
0
9
1
500
3
185
31 DADRA & NAGAR
HAVELI
40
36
4
7
6
1
2
1
1
3
6
2
3
115
2
0
32 DAMAN &DIU
12
21
(9)
2
3
(D
1
1
0
28
0
1
3
150
1
5
33 DELHI
190
42
148
32
8
24
8
8
490
0
236
77
19345
17
1322
34
LAKSHADWEEP
7
14
(7)
1
4
(3)
3
(3)
0
0
6
2
70
0
0
35 PONDICHERRY
58
80
(22)
10
39
(29)
4
(D
12
0
21
29
3136
0
0
79
1
25
85
39
930
162
0
0
157
0
0
28
0
0
3
36 CGHS
241
37 CENTRAL
RESEARCH
COUNCILS
38 M/o RAILWAY
36 M/o LABOUR
40 M/o COAL
TOTAL
134108
138044
8181
22349
22928
1714
5587
3077
2562
25911
24803
23028
FIGURES IN BRACKET INDICATE THE SURPLUS INFRASTRUCTURE, SHORTFALL AS ON 31.3.2001;
@ FOR THE PERIOD 1.1.1998: @@ FOR 1.4.1999
# - INFORM=ATinM SSTJrno
NUMBER OF HOMOEOPATHIC HOSPTALS HAVE REDUCED AS UTTAR PRADESH HAS REPORTED REDUCED FIGURES.
# - INFORMATION FOR THE CURRENT YEAR HAS NOT BEEN RECEIVED. HENCE REPEATED FOR THE LATEST AVAILABLE YEAR.
SOURCE: HEALTH INFORMATION OF INDIA. ISM&H IN INDIA AND D/O FAMILY WELFARE; FIGURES ARE PROVISIONAL
14926 663163 3005
60631
100
150
PostPartum
Centres
1
2
32
87
1
3
72
147
27
55
1
3
10
2
69
28
9
5
3
1083
871
538
1012
>
-i
TENTH FIVE YEAR PLAN 2002-07
Annexure - 2.8.4
Manpower Requirement in Rural Primary Health Care Institutions
Category of manpower
Requirement for
Census 1991
In position as on
30.06.2000
Number
sanctioned
Gap
(2-3)
1
2
3
4
5
22348
3741
6579
18607
22349
25506
29702
3157*
22349
5508
6534
16841
Pharmacist
(1/CHC+1/PHC)
27936
21077
22871
6859
Lab. Technician
(1/CHC+1/PHC)
27936
12709
15865
15227
5587
1768
2137
3819
Nurse Midwife
(7/CHC+1/PHC)
61458
17673
22672
43785
Health Assistant (M)
(1/PHC)
22349
22265
26427
84
Health Assistant (F)
(1/PHC)
22349
19426
22479
2923
Health Worker (M)
134108
73327
87504
60781
Health Worker (F)
(1/SC+1/PHC)
156457
134086
144012
22371
TOTAL
525226
337086
386782
191297
Specialists
(4/CHC)
Doctors at PHCs
(1/PHC)
Block Extension Educator/
Health Educator
(1/PHC)
X-ray Technician/
Radiographer
(1/CHC)
(1/SC)
* indicates surplus and has not been added to Gap
Source RHS Bulletin, June, 2000 (Ministry of Health & FW)
148
HEALTH
Annexure - 2.8.5
Outlay for Health in the States & UnionTerritories
Rs. Lakhs
9th Plan
STATES
1
OUTLAY
HEALTH
1997-98
OUTLAY
HEALTH
1998-99
Act. Expd.
HEALTH
1999-2000
2000-01
2001-02
OUTLAY
HEALTH
Act. Expd.
HEALTH
OUTLAY
HEALTH
OUTLAY
HEALTH
OUTLAY
HEALTH
2
3
4
5
6
7
8
9
ANDHRA PRADESH
63052.00
13937.00
12366.00
20046.00
19865.00
28033.00
27749.95
33223.02
ARUNACHAL PRADESH
33502.00
3149.00
1782.00
3520.00
1814.00
2947.00
2068.93
2476.01
ASSAM
38410.00
6561.00
6223.00
7191.00
6887.00
7741.00
7439.00
12580.00
BIHAR
83200.00
7245.00
4950.00
12177.00
6902.00
12768.00
9891.01
10078.21
GOA
8122.00
1082.00
1032.00
772.00
1069.00
1646.00
1423.00
1649.00
GUJARAT
83225.00
22093.00
17180.00
23550.00
17179.00
25100.00
26000.00
21000.00
HARYANA
35134.00
3882.00
4493.00
5946.00
4126.00
5327.00
5648.00
6595.00
HIMACHAL PRADESH
31765.00
5544.00
6535.00
8965.70
8164.00
10555.00
9685.09
12014.86
J&K
110029.00
7450.00
6989.00
11385.51
8244.00
11974.00
10595.17
11628.32
KARNATAKA
110000.00
18359.00
21914.00
19544.30
22909.00
22774.00
22558.11
26879.60
KERALA
30940.00
6096.00
5828.00
6200.00
7343.00
6400.00
6335.00
5553.00
MADHYAPRADESH
56787.00
9331.00
7031.00
17351.47
14524.00
13524.00
11217.62
13462.62
MAHARASHTRA
91823.00
17391.00
13811.00
22993.00
16224.00
27798.00
30485.85
39128.91
MANIPUR
3600.00
630.00
540.00
809.35
809.00
1080.00
1250.00
1486.00
MEGHALAYA
14000.00
2430.00
1790.00
2430.00
2360.00
3079.00
3300.00
3200.00
MIZORAM
11201.00
1651.00
1651.00
1816.00
1785.00
2286.00
2562.00
2542.00
NAGALAND
10631.00
2506.00
2480.00
2128.00
2022.00
2128.00
1577.00
1283.00
ORISSA
41606.00
4104.00
5198.00
7526.21
7042.00
13208.00
8405.05
14915.16
PUNJAB
51159.00
9938.00
3187.00
16352.00
8374.00
18319.00
19187.00
17465.57
RAJASTHAN
77060.00
13919.00
12339.00
15289.00
10991.00
17262.00
9914.94
12366.30
SIKKIM
8000.00
857.00
757.00
814.00
1914.00
1559.00
1200.00
1373.50
TAMILNADU
78052.00
8909.00
11005.00
11650.93
12843.00
12426.00
12724.42
18084.16
1442.46
1879.18
TRIPURA
8559.00
1371.00
1091.00
1407.92
1448.00
1355.00
UTTARPRADESH
118500.00
17312.00
15609.00
40551.00
10862.00
42816.00
30200.00
37278.00
WESTBENGAL
97864.00
20633.00
3322.00
19286.00
7811.00
23502.00
32176.00
42931.24
TOTAL STATES
UTs
1296221.00
206380.00
169103.00
279702.39
203511.00
315607.00
295035.60
351072.66
A & N ISLANDS
7741.00
1559.00
1831.59
1895.00
2055.29
2000.00
1900.00
1900.00
CHANDIGARH
17065.00
3617.00
3748.90
3548.30
3297.61
3483.00
3717.00
3947.25
D & N HAVELI
514.00
219.00
148.87
252.70
189.82
280.00
217.80
234.80
DAMAN & DIU
887.00
133.00
165.96
173.00
186.91
136.00
150.10
165.00
110140.00
15240.50
12684.15
19700.00
13994.62
27345.00
26642.00
34121.00
LAKSHADWEEP
817.46
233.85
267.78
333.00
323.61
229.03
281.45
211.46
PONDICHERRY
10000.00
1630.00
1546.97
2370.00
1921.30
2720.00
2720.00
3160.54
TOTAL UTs
147164.46
22632.35
20394.22
28272.00
21969.16
36193.03
35628.35
43740.05
GRAND TOTAL
(STATES & UTs)
1443385.46
229012.35
189497.22
307974.39
225480.16
351800.03
330663.95
394812.71
DELHI
CHHATISGARH
6024.66
JHARKHAND
NA
UTTARANCHAL
5972.00
GRAND TOTAL
(STATES & UTs)
Incl 2 states
406809.37
149
TENTH FIVE YEAR PLAN 2002-07
Annexure 2.8.6
Outlays for Department of Health
Rs crores
IX
X Name of the Schemes I Institution
Plan Plan
9th Plan
Allocation
9th Plan
10th Plan
2002-03
Anticipated
Alocation
Expenditure Agreed by PC Outlay
CENTRALLY SPONSORED SCHEMES
Control of communicable Diseases:
1 National Vector Borne Diseases Control Programme
(Malaria, Kala-Azar, Filaria, Dengue and J.E.)
1 &2
1000.00
954.95
1370.00
235.00
3 2 National Leprosy Eradication Programme.
301.00
388.48
255.00
75.00
4 3 National Tuberculosis Control Programme.
450.00
462.73
680.00
115.00
5 4 National AIDS Control Programme including Blood
Safety Measures and National S.T.D. Control Programme
760.00
745.26
1270.00
225.00
2.00
1.29
7 5 Disease Surveillance Programme
25.00
20.32
190.00
10.00
8 6 Hospital Waste Management
2.00
1.79
10.00
5.00
9 7 Assistance to States for Capacity Building (drug Quality)
20.00
29.00
60.00
20.00
10
20.00
1.00
97.00
1.30
5.00
5.00
5.10
0.80
6
National Guinea Worm Eradication Prog.
Strengthening of Drug & Food Administration &
Control Capacity Building
8 Capacity Building for drug & PFA
11
Strengthening of State Drug Analytical Laboratories
12
Strengthening of State Drug Control organisations including
improvement of their information system and strengthening
of enforcement and supporting staff
13
Financial Assistance to the States for Strenghening their
food testing laboratories
5.00
14
Setting up of District Food Inspection Units in the States/
UTs including Management Information System
3.16
Control/Containment of Non-communicable Diseases:
15
9 National Programme for Control of Blindness
448.00
464.79
445.00
86.00
16&17 10 National Cancer Control Programme and Anti-Tobacco Initiative 190.00
198.14
285.00
61.00
18&19 11 National Iodine Deficiency Disorders Control Programme and
Pilot Project on Micronutrients
18.00
14.75
35.00
7.00
20 12 National Mental Health Programme
28.00
20.39
190.00
30.00
21 13 Drug De-addiction Programme including assistance to States
20.00
26.51
33.00
7.00
2.50
4.80
4.80
4924.80
882.10
65.00
12.00
Other Programmes
22 14 UNDP Pilot Initiatives for Community Health
Central Sector Schemes:
Control of Communicable Diseases:
1
2
1
National Institute of Communicable Diseases, Delhi
(ongoing activities including Guineaworm & Yaws Eradication)
23.00
Strengthening of Institute
3.70
1.50
3 2 National Institute of Tuberculosis, Bangalore
22.40
3.69
4 3 Lala Ram Sarup Institute of T.B. and allied diseases,
Mehrauli, Delhi
30.00
3.78
27.60
5 4 Central Leprosy Trainings Research Institute
Chengalpattu (Tamil Nadu) Regional Institute of Training,
Research & Treatment under Leprosy Control Programme:
5.00
3.57
150
10.30
2.00
54.50
10.00
5.50
1.00
..I
HEALTH
Annexure 2.8.6 Contd.
Rs crores
IX
X Name of the Schemes / Institution
Plan Plan
9th Plan
Allocation
9th Plan
10th Plan
2002-03
Anticipated
Alocation
Expenditure Agreed by PC Outlay
6 5 (a) R.L.T.R.I., Aska (Orissa)
2.00
0.56
2.00
0.40
7 6 (b) R.L.T.R.I., Raipur (M.P.)
2.50
0.71
1.00
0.20
8 7 (c) R.L.T.R.I., Gauripur (W.B.)
5.00
4.65
7.00
1.50
9 8 B.C.G. Vaccine Laboratory, Guindy, Chennai
5.00
5.80
19.50
5.00
9 Pasteur Institute of India, Coonoor
5.00
13.10
35.00
7.00
11 10 Central Research Institute, Kasauli
20.00
21.83
10
50.00
5.00
249.80
44.10
Hospitals and Dispansaries:
12 11
Central Government Health Scheme
13 12
Central Institute of Psychiatry, Ranchi
40.00
16.00
8.00
15.00
47.66
17.00
15.21
6.71
80.00
50.00
30.00
20.00
20.00
8.00
7.00
2.70
3.00
3.00
96.36
70.07
3.00
30.00
230.00
150.00
7.00
597.00
6.00
65.00
25.00
1.00
134.70
340.00
382.47
675.00
105.00
175.00
70.00
65.00
162.00
52.05
30.59
200.00
150.00
200.00
25.00
56.00
85.00
49.92
59.50
140.00
380.00
6.00
60.00
25.00
5.00
15.00
38.28
11.28
6.82
50.00
23.00
20.00
10.00
8.00
3.00
35 28 Serologist & Chemical Examiner to the
Government of India, Calcutta
1.25
1.23
2.50
0.50
36 29 National Medical Library, New Delhi
15.00
1.60
0.50
3.90
2.00
60.00
25.12
1.55
0.77
2.78
0.00
80.40
35.00
2.50
1.00
5.00
10.00
120.00
8.00
0.50
0.20
1.00
5.00
24.00
14&15 13
All India Institute of Speech & Hearing Mysore and Pilot Project
16&17 14 All India Institute of Physical Medicine &
Rehabilitation, Mumbai and Pilot Project
18 15 Health Sector Disaster preparedness and Management
19 16 Safdarjung Hospital, New Delhi
20 17
103.00
45.00
Dr. R.M.L. Hospital, New Delhi
21 18 Institute for Human Behaviour & Allied Sciences, Shahdara, Delhi 10.00
Medical Education, Training & Research:
(a) Medical Education:
22-25 19 All India Institute of Medical Sciences & Its Allied
Departments, New Delhi and 3 Pilot Projects
26 20
P.G.I.M.E.R., Chandigarh
27 21
J.I.P.M.E.R., Pondicherry
28 22
Lady Harding Medical College & Smt. S.K.
Hospital, New Delhi
29 23 Kalawati Saran Childrens Hospital, New Delhi
30 24 Indira Gandhi Institute of Health & Medical Sciences
for North East Region at Shilong.
31 25 Kasturba Health Society, Wardha
32 26 V.P. Chest Institute, Delhi
33&34 27 All India Institute of Hygiene & Public Health,
Calcutta and'Pilot Project
37 30
National Academy of Medical Sciences, New Delhi
38 31
National Board of Examinations, New Delhi
39 32
Medical Council of India, New Delhi
40 33 Education Commission of Health Sciences
41 34
N.I.M.H.A.N.S., Bangalore
151
15.00
10.00
TENTH FIVE YEAR PLAN 2002-07
Annexure 2.8.6 Contd.
Rs crores
IX
X Name of the Schemes / Institution
Plan Plan
9th Plan
Allocation
9th Plan
10th Plan
2002-03
Anticipated
Alocation
Expenditure Agreed by PC Outlay
(b) Nursing Education:
42 35 Indian Nursing Councils
43-47 36 Strengthening/adding seats to existing schools of Nursing
48 37 R.A.K. College of Nursing, New Delhi
2.10
0.40
4.50
0.50
8.05
100.00
20.00
3.50
1.53
11.00
3.00
0.25
2.00
0.30
333.37
870.00
110.00
2999.10
414.90
49 38 Lady Reading Health School, New Delhi
(c) Research:
50-55 39 Indian Council of Medical Research,
New Delhi and 5 Pilot Projects
263.00
Other Programmes:
56 40
National Institute of Biological, NOIDA (U.P.)
70.00
63.54
170.90
20.00
57 41
Health Education
6.00
3.97
12.60
2.20
58 42
Health Intelligence (& Health Accounts)
1.25
1.44
8.80
1.90
59 43 Port Health Authority (Including setting up of offices at
8 newly created international airport)
2.00
2.12
9.00
1.60
60 44 Strengthening of D.G.H.S.
3.99
7.87
8.00
2.00
12.00
3.00
61 45 Strengthening of (Deptt. under) Ministry
62 46 Prevention of Food Adulteration
20.00
12.63
83.00
8.00
40.00
23.68
57.00
15.00
361.30
53.70
48 Centrally Sponsored Schemes
110.00
20.00
49 Central Sector Schemes:
11.00
0.50
63&64 47
Central Drug Standard & Control Orgn. and Medical
Store Organisation
NEW INITIATIVES DURING 10TH PLAN
SCHEMES THAT ARE EITHER TRANSFERRED OR DROPPED
65
Rural Health Training Centre, Najafgarh
66
Tejpur Mental Hospital
67
Assistance to Voluntary Organisations
(a) Improvement of Medical Services
4.00
1.78
10.00
1.08
1.00
0.50
0.93
0.42
5118.19
5280.49
(b) Special Health Scheme for rural areas
68
69
Continuing Education of Model Teachers
Training of Medical Officers of C.H.S. Cadre
Total
152
121.00
20.50
9253.00
1550.00
CHAPTER 2.9
INDIAN SYSTEMS OF MEDICINE AND HOMOEOPATHY
INTRODUCTION
lack of quality control and good manufacturing
practices have resulted in the use of spurious
and substandard drugs;
H the quality of training of ISM&H practitioners
has been below par; many ISM&H colleges
lack essential facilities, qualified teachers and
hospitals for practical training; there is no
system of Continuing Medical Education
(CME) for periodic updating of knowledge and
skills;
H the ISM&H practitioners are not involved in
national disease control programmes or family
welfare programme; and
H medicinal plants have been overexploited and,
as a result, the cost of ISM&H drugs has
increased and spurious products are getting
into the market.
H
2.9.1 The umbrella term, Indian systems of
medicine and homoeopathy (ISM&H), includes
Ayurveda, Siddha, Unani, Homoeopathy and
therapies such as Yoga and Naturopathy.
Practitioners of ISM&H catered to all the health care
needs of the people before modern medicine came
to India in the twentieth century. Currently, there
are over 680,000 registered ISM&H practitioners in
the country; most of them work in the private sector.
A major strength of ISM&H system is that it is
accessible, acceptable and affordable.
2.9.2 India also has a vast network of govern
mental ISM&H healthcare institutions. There are
3,000 hospitals with over 60 beds and over 23,000
dispensaries providing primary healthcare. Over
16,000 ISM&H practitioners qualify every year from
405 ISM&H colleges. The Department of ISM&H
supports four research councils and provides
research grants to a number of scientific institutions
and universities for conducting clinical research,
ethno-botanical surveys and pharmacopoeial and
pharmocognostic studies on herbal drugs and
medicinal plants. Pharmocopoeial Committees
constituted by the Department are finalising
standards for single simple formulations and will
shortly take up the task of formulating standards
for compound ISM formulations.
2.9.3 Despite all these efforts, the ISM&H have
not realised their full potential because:
E3 existing ISM&H primary, secondary and
tertiary healthcare institutions lack essential
staff, infrastructure, diagnostic facilities and
drugs;
ISI the potential of ISM&H drugs and therapeutic
modalities has not been fully exploited;
153
2.9.4 The National Health Policy (1983) visualised
an important role for the ISM&H practitioners in the
delivery of health services. In order to give focused
attention to the development and optimal utilisation
of this branch of medicine, a separate Department
for ISM&H was set up in 1995. The Department is
making efforts to ensure that ISM&H practitioners
are brought into the mainstream so that they
provide a complementary system of care along with
practitioners of modern systems of medicine.
2.9.5 Globally, there has been a revival of interest
in a complementary system of healthcare especially
in the prevention and management of chronic
lifestyle-related non-communicable diseases and
diseases for which there are no effective drugs in
the modern system of medicine. India is currently
undergoing demographic and lifestyle transition
which will result in the increasing prevalence of noncommunicable diseases and lifestyle related
disorders. ISM&H, especially ayurveda, yoga and
naturopathy, can play an important role in the
prevention and management of these disorders.
TENTH FIVE YEAR PLAN 2002-07
ISM&H practitioners can undertake the task of
counselling and improving the coverage and
continued use of drugs in national diseases control
programmes and the family welfare programme. If
ISM&H practitioners take up these tasks, they can
enable the country to achieve the health and
demographic goals set for the Tenth Plan.
HEALTH CARE SERVICES
2.9.7 The Ninth Plan aimed at improving the
quality of primary, secondary and tertiary care in
ISM&H, with the Departments of ISM&H in the
centre and the states taking up several initiatives
to improve the quality and coverage of these
services at each level.
Approach during the Tenth Plan
Primary Health Care
2.9.6 The approach during the Tenth Plan will be
to ensure that the ISM&H system achieves its full
potential in providing healthcare by:
E
improving the quality of primary, secondary and
tertiary care;
El
mainstreaming ISM&H institutions and
practitioners with modern systems of medicine
so that people have access to complementary
systems of care;
E
strengthening ISM&H educational institutions
so that students get adequate training, giving
them confidence to practise their system and
participate in national programmes;
E
investing in continuing medical education;
E ensuring the conservation, preservation,
promotion, cultivation, collection and
processing of medicinal plants and herbs
required to meet growing domestic demand for
ISM&H drugs and the export potential;
ISI completing Pharmacopoeia of all the systems
of ISM&H and drawing up a list of essential
drugs and ensuring their availability;
El ensuring quality control of drugs and improving
their availability at an affordable cost;
El
O
2.9.8 ISM&H practitioners provide primary
healthcare to vulnerable sections of the population
especially those living in urban slums and remote
areas. Details of the number of ISM&H hospitals
and dispensaries (as on 1 April 1999) is given in
Annexure 2.9.1. In some states like West Bengal
and Gujarat, ISM&H practitioners alone are posted
in primary health centres (PHCs) in some remote
rural and tribal areas. In Kerala, ISM&H practitioners
provide a complementary system of care in the
PHCs. It is important to ensure that the ISM&H
dispensaries and hospitals are linked with PHC/
urban health care centres so that they can have
ready access to diagnostic and other facilities
available in these institutions and, at the same time,
patients can choose the system for treatment.
Secondary Health Care
2.9.9 A majority of existing ISM&H secondary
hospitals function as separate institutions and do
Infrastructure
Vast infrastructure has been created:
E Hospitals
3005
E Beds
60,681
E Dispensaries 23,028
Problems
investing in research and development (R&D)
for the development of new drugs and
formulations, and patenting them; and
E No organised referral system.
E They provide healthcare only to those who
come to them.
E Each centre is isolated; they are not linked
with other institutions in the area.
undertaking clinical trials of promising drugs
by appropriately strengthening Central
Research Councils and coordinating their
research with other research agencies such
as Indian Council of Medical Research (ICMR),
Delhi.
E No linkage with existing modern system
hospitals - hence they are unable to function
optimally as a complementary system or utilise
the diagnostic facilities available.
154
INDIAN SYSTEMS OF MEDICINE AND HOMOEOPATHY
not have linkages with either primary ISM&H
healthcare institutions or with secondary healthcare
institutions in the modern system of medicine. Very
often these institutions lack adequate diagnostic
facilities, infrastructure and manpower. The Ninth
Plan had envisaged initiation of a pilot project to
test the feasibility and usefulness of posting ISM&H
practitioners in district hospitals. Some states did
attempt to provide ISM&H clinics in district hospitals
but the experience in this area has been limited.
disease control
programmes;
2.9.11 During the Tenth Plan, a major thrust will be
given to mainstream the ISM&H system and utilise
ISM&H practitioners by:
E
E
E
ensuring that ISM&H clinics are located in the
primary, secondary and tertiary care
institutions in modern medicine and financing
ISM&H care through funds provided for these
institutions;
focusing on the use of ISM&H therapeutic
modalities for diseases for which the modern
system does not have effective drugs free of
serious side effects and prevention and
management of lifestyle-related chronic
diseases;
increasing the utilisation of ISM&H practitioners
working in government, voluntary and private
sectors to improve information, education and
communication (IEC) and counselling to
improve utilisation of services under national
family
welfare
E
strengthening tertiary care institutions,
especially those attached to ISM&H colleges
and national institutions, in order to improve
patient care, teaching, training, R&D;
E
establishing effective referral linkages between
primary, secondary and tertiary care
institutions;
E
monitoring how patients are responding to the
efforts in providing complementary system of
healthcare in these hospitals; and
L'l
assessing the pros and cons of providing
complementary system of healthcare and
effecting mid-course corrections.
Tertiary Health Care
2.9.10 All ISM&H colleges, private as well as public,
have attached tertiary care hospitals. In addition,
there are tertiary care and/or speciality centres
attached to national institutes. Private/voluntary
sector institutions also provide tertiary care in
ISM&H. During the Ninth Plan, the Department of
ISM&H provided funds to strengthen many of these
institutions. One Unani speciality clinic was
established in the Ram Manohar Lohia Hospital,
Delhi and one Ayurvedic and one Homoeopathic
unit was established in the Safdarjung Hospital,
Delhi. The Department has also provided funds for
establishing speciality clinics in the National Institute
of Mental Health and Allied Sciences (NIMHANS),
Bangalore. These clinics are reported to have very
good attendance.
and
Development of Human Resources for ISM&H
Table 2.9.1 - Medical Education in ISM&H
Colleges
System
Undergraduate
Postgraduate
Ayurveda
198
53
Unani
39
5
Siddha
2
2
Homoeopathy
166
17
Total
405
77
16,845
821
Admission capacity
Source: Department of ISM & H, 2001
2.9.12 There has been a progressive increase in
the number of practitioners graduating from ISM&H
educational institutions during the last five decades.
Currently there are 405 under graduate and 77 post
graduate colleges in ISM&H (Table 2.9.1). But the
quality of training these colleges impart is poor. A
recent inspection of 160 colleges showed that:
H 44 per cent of them lack the required number
of departments;
ISI 89 per cent do not have the requisite number
of teachers;
El 52 per cent lack required hospital beds;
E
155
79 per cent have less than 60 per cent bed
occupancy;
TENTH FIVE YEAR PLAN 2002-07
postgraduate college in each of the major
states; and
Current Problems in Medical Education
E Students join ISM&H institutions through a
common entrance examination; those who
do not get admission in modern system of
medicine opt for ISM&H colleges.
E The quality of teachers is poor and teaching
aids are in short supply.
E Morale of ISM&H teachers and students is low.
E Present ISM&H syllabus and curriculum are
inadequate. As a result, graduates do not have
the knowledge, skills and confidence to
practice ISM&H therapy.
E
91 per cent do not have adequate diagnostic
equipment; and
E
52 per cent of all colleges have a student/bed
ratio, which is higher than the prescribed ratio
of 1:3.
2.9.13 While a lot of time is spent on teaching
anatomy, physiology and bio-chemistry, not enough
attention is paid to train the students to use ISM&H
diagnostic and therapeutic modalities. As a result,
these students lack confidence, knowledge and
skills in using ISM&H therapeutic modalities and
tend to practise the modern system of medicine in
which they are not trained. Patients, therefore,
do not get the benefit of ISM&H therapy in spite of
accessing ISM&H practitioners.
2.9.14 During the Tenth Plan, states would be
encouraged to:
S
introduce an entrance examination for ISM&H
undergraduate courses with appropriate
eligibility criteria to identify the potential and
interest of students;
El ensure uniformity in the admission system in
undergraduate and postgraduate courses;
El reorient the syllabus keeping in mind the
potential for employment in industry and
ISM&H services being offered through
speciality clinics;
E strengthen existing national centres of
excellence in collaboration with the Depart
ment of ISM&H;
E
strengthen and mainstream at least one college
for each system as a model of undergraduate/
156
E operationalise an appropriate and transparent
accreditation system for educational institutes
through Councils of ISM&H.
Quality Assurance in Education in ISM&H
2.9.15 The Indian Medicines Central Council Act,
1970 was enacted for the constitution of a Central
Council of Indian Medicines, maintenance of a
central register of Ayurveda, Siddha and Unani and
related matters. The Central Council of Indian
Medicine (CCIM) and the Central Council of
Homoeopathy (CCH), constituted in 1970 and 1973
respectively, are responsible for:
E
laying down and maintaining uniform
standards of education for ISM&H courses,
prescribing
standards
of
professional
conduct, etiquette and code of ethics for
practitioners and
E
advising the central government on matters
relating to the recognition of appropriate
qualifications of ISM&H.
They also work in coordination with state-level
board/council to maintain standards in ISM&H
medical institutions. In addition, they maintain
central registers for Indian systems of medicine and
homoeopathy respectively.
2.9.16 A review of the functioning of the Councils
by the Department of ISM&H showed that the
monitoring procedures and schedules are not
adequate. The recommendations of the CCIM and
CCH are often not acted upon. There is no legal
framework and, consequently, no institutional
mechanism available to lay down and enforce
standards relating to yoga and naturopathy. The
standards of education in these two disciplines are,
therefore, poor.
2.9.17 A large number of colleges are being
opened predominantly in the private sector, after
obtaining permission from state governments and
getting affiliated to universities. Between 1995 and
2000, the CCIM permitted setting up of 73 ayurveda
colleges, 11 homoeopathy colleges and three
siddha colleges. This mushrooming of colleges has
adversely affected the quality of ISM&H education.
The problem was discussed in the Central Council
INDIAN SYSTEMS OF MEDICINE AND HOMOEOPATHY
for Health and Family Welfare 1997 and at the first
conference of State Health Ministers in ISM&H in
1997. It was recommended that suitable amend
ments be made to the Indian Medicines Central
Council Act, 1970 and the Homoeopathy Central
Council Act, 1973 to ensure that new colleges
comply with the prescribed guidelines.
2.9.18 During the Tenth Plan, every effort will be
made to reduce the proliferation of substandard
medical colleges and check the deterioration in
standards of teaching. Simultaneously, the
Department of ISM&H will take steps to ensure that
the statutory councils perform the role assigned to
them. Periodic inspection of all established ISM&H
colleges is necessary to ensure that only those
colleges which have the necessary infrastructure,
manpower and facilities are allowed to continue
operating. This is, undoubtedly, a difficult task but
is necessary to improve the standards of ISM&H
education.
excellence providing high quality patient care,
teaching and research. While some of these
institutes are well established and are functioning
effectively, many are in the initial stages of
operationalisation. During the Tenth Plan, these
centres will play a pivotal role in improving
teaching, training, patient care and research
standards.
Continuing Medical Education (CME) in ISM&H
2.9.21 Most of the Registered Practitioners of
ISM&H (Table 2.9.2), are in the private sector; there
is a need to periodically update their knowledge and
Table 2.9.2 - Registered Medical Practitioners in
ISM&H
Ayurveda
4,27,504
Unani
42,445
Siddha
16,599
Paraprofessionals in ISM&H
Naturopathy
2.9.19 Currently there are no arrangements for
providing a degree or diploma in IS&M pharmacy
nor is it included as one of the options in the
general pharmacist course. Similarly, there is no
training for nursing in ISM&H. During the Tenth
Plan these two matters will be taken up, so that
ISM&H practitioners have the necessary support
staff.
Homoeopathy
1,94,147
TOTAL
6,81,124
National Institutes in ISM&H
2.9.20 The Department of ISM&H has set up
national institutes in each of the major
disciplines which are meant to act as centres of
National Institutes Funded by the Central
Government
H National Institute of Ayurveda, Jaipur
KI National Institute of Unani Medicine,
Banglore*
429
Source: Department of ISM&H, 2001
skills through continuing medical education. During
the Ninth Plan period, the Department of ISM&H
started a scheme for re-orientation and in-service
training. The scheme offered one month’s course
for teachers and physicians and a two months’
course for ISM&H practitioners in specialised fields
like ksharasutra, panchakarma therapy, dental
practices and in yoga. The response to this course
has been poor because most practitioners felt that
they cannot leave their practice for an extended
period.
2.9.22 During the Tenth Plan, a major effort will be
made to provide all registered ISM&H practitioners
with updated information about advances in their
respective systems. Government-employed ISM&H
practitioners will be the first to get the benefit of this
in-service training. The training material will be
produced by the national institutes and the state
ISM&H colleges with the help of experts. Optimal
use will be made of advances in information
technology to improve the outreach of the CME
programme so that it does not disrupt their
El National Institute of Homoeopathy, Calcutta
El National Institute of Naturopathy, Pune
Bl. Morarji Desai National Institue of Yoga, New
Delhi
E National Institute of Siddha, Chennai*
Bl Rashtriya Ayurveda Vidyapeeth, New Delhi
* being established
157
TENTH FIVE YEAR PLAN 2002-07
practice.Attempts will also be made to increase the
involvement of ISM&H practitioners in counselling
and improving the utilisation of services under the
national health and family welfare programmes
during the Plan period. The ISM&H practitioners will
play an important role in:
Sustainable Use and Legal Protection of Medicinal
Plants. The Task Force recommended:
El
establishment of medicinal plants conserva
tion areas (MPCA), covering all ecosystems,
forest types and sub types;
El
ex-situ conservation of rare, endangered
medicinal plants may be tried out in established
gardens managed by the Departments of
Agriculture, Horticulture or Forests;
E
health education;
E
drug distribution for national programmes;
E
motivation and counselling in family welfare
programmes;
E
acting as depot holders for selected items such
as condoms and oral rehydration therapy
(ORT) packages;
gene banks created by the Department of
Biotechnology should store the germplasm of
all medicinal plants;
E
establishment of ‘Vanaspati vans' in degraded
forest areas;
E
forest areas rich in medicinal plants should be
identified, management plans formulated and
sustainable harvesting encouraged under the
Joint Forest Management System;
E
technically qualified NGOs must be
encouraged to take up the task of improving
awareness and increasing availability of plant
stock and involved in the promotion of agro
techniques for cultivation of medicinal plants;
E
screening/testing/clinical evaluation of herbal
products to be taken up and completed;
E
E
motivation for immunisation; and
E
improvement in environmental sanitation
through community efforts.
Preservation, Promotion and Cultivation of
Medicinal Plants and Herbs
2.9.23 Over the last two decades there has been a
steady increase in the demand for drugs used in
ISM&H. However, the demand for good quality
medicinal plants and herbs have not been met. The
prices of several plants have increased sharply,
making them unaffordable and some species of
medicinal plants are also reported to be endangered
because of increasing pressure on forests.
E drug testing laboratories for ISM&H products
should be established with qualified staff;
'
establishment of a Traditional Knowledge
Digital Library so that information on medicinal
plants and their use in the country could be
accessed readily; and
E
establishment of a Medicinal Plant Board for
integrated development of the medicinal plants.
2.9.24 The Planning Commission had constituted
a Task Force on the Conservation, Cultivation,
Medicinal Plants
Current Problems
2.9.25 Many of the recommendations of the Task
Force have been implemented. The Medicinal Plant
Board has been established in the Department of
ISM&H to look after all multi-sectoral issues relating
to the development of medicinal plants. The Board
is expected to formalise and organise the marketing
of and trade in medicinal plants, coordinate efforts
of all stakeholders in the sector and improve their
awareness and availability of herbal products.
Twelve state governments have established State
Medicinal Plant Boards. The Ministries of Health
and Family Welfare, Environment and Forest, Rural
Development and Agriculture are promoting the
E The demand for medicinal plants is growing;
the trade in medicinal plants is secretive and
exploitative.
E The profit motive is leading to unsus
tainable practices being employed. As a
result, plant species are in danger of
extinction.
E Quality of ingredients is poor, leading to poor
quality of drugs.
E Cultivation has not been encouraged and
most plants are uprooted from the wild.
158
INDIAN SYSTEMS OF MEDICINE AND HOMOEOPATHY
cultivation of medicinal plants. Agro-techniques are
being standardised for 28 plants identified for fast
track cultivation. States have been requested to
introduce measures to register cultivators and
traders dealing with medicinal plants and to make
the Forest Development Corporation the conduit for
supply of medicinal plants to industry. The proposals
to encourage R&D, support gene banks and support
industry for the identification of export markets and
market segmentation are under consideration.
2.9.26 The Department of ISM&H has initiated a
scheme on a Traditional Knowledge Digital Library.
Around 35,000 formulations described in 14 ancient
texts relating to ayurveda have been entered in this
library and can be accessed by all. This step will
help ready access to traditional practices and
prevent outsiders taking patents on them. The
Department has established a Patent Cell to keep
track of patents concerning ayurveda, siddha and
unani drugs being filed in India and abroad. The
cell will also provide professional and financial
assistance to government and private ISM&H
scientists for filing of patents. An Expert Group has
been constituted for advising the Department with
regard to patenting issues.
ISM&H Industry
2.9.27 The global market in herbal products in
alternative systems of medicine is estimated to be
$62 billion. India’s share in this is very meagre.
Even within the country the share of ISM&H products
is only a modest Rs. 4,200 crore; Ayurvedic drugs
and formulations account for over 80% of the
products (Figure 2.9.1).
Figure 2.0,-1 - torket Share of Drugs of
Difftsrnt Systems of ISM&H
014,27%
\
2.9.28 A survey of the current status of the ISM&H
industry undertaken by the Department of ISM&H
showed that it is divided into the large, medium,
small and very small-scale sectors (Table 2.9.3).
Table 2.9.3 - ISM&H Industry in India
J Rs.4, 200 crore industry (ayurveda accounts for
Rs. 3,500 crore)
7,000 manufacturers of ayurvedic products
Large
( > Rs. 50 crore)
10
<=>
Medium
(Rs. 5-10 crore)
25
<=>
Small
(Rs. 1-5 crore)
965
<»
Very Small (<Rs. 1 crore)
6,000
Source: Deptt of ISM&H 2001
The small-scale sector is not pursuing good
manufacturing practices. Patent proprietary
medicines are being introduced through wide-scale
licensing without checking their efficacy or quality.
These medicines have become expensive. A
number of products claiming to be ayurvedic
medicines use large quantities of synthetic
ingredients as excipients. Classical and shastra
preparations are not getting due importance.
2.9.29 The Department has taken several steps to
ensure good manufacturing practices and quality
control of drugs so that there is increasing
confidence in ISM&H drugs and formulations, as a
result of which their market will expand both within
the country and abroad.
Quality Control of Drugs
2.9.30 There are a large number of ISM&H
pharmacies in the country (Table 2.9.4) and many
of them, especially smaller ones, do not adopt good
/’
Table2.9.4- Licensed Pharmacies in India
H Ayurveda
□Ayurveda □Hc^eopaShy SSicdha O Unani
2 J Unani
462
Siddha
385
Homoeopathy
613
Total
Soorce.: Department of ISM&H, 2001
Source : Department of ISM&H, 2001
159
8,533
9,992
TENTH FIVE YEAR PLAN 2002-07
manufacturing practices. The Department of ISM&H
has finalised and notified good manufacturing
practices for ayurveda, siddha and unani drugs over
the last two years.
2.9.31 Setting up pharmacopoeial standards and
strengthening of the drug control laboratories has
been identified as a priority in the Ninth Plan. The
Pharmacopoeial Laboratory of Indian System of
Medicine (PLIM) and Homoeopathic Pharma
copoeial Laboratory (HPL) at Ghaziabad are the
major ISM&H drug testing laboratories. However,
Central Government’s efforts to strengthen
drug quality control
£3 Pharmacopoeial Laboratory for Indian
Medicines, Ghaziabad and Homoeopathy
Pharmacopoeial Laboratory, Ghaziabad are
being strengthened.
H Appellate laboratories for drug testing and
quality control are being identified.
2.9.32 During the Tenth Plan every effort will be
made to improve the quality control of drugs used
in ISM&H by:
completing all pharmacopoeial work by 2004;
modernising state ISM&H pharmacies;
motivating these pharmacies and the ISM&H
industry to adopt good manufacturing
practices;
strengthening the central and state quality
control laboratories, and exploring the
feasibility of utilising laboratories of the
Central Council for Research in Ayurveda
and Siddha (CCRAS), and chemistry and
biochemistry laboratories of universities/
college departments, as well as existing
drug testing laboratories in the modern
system of medicine, for testing and quality
control of ISM&H drugs;
implementing stringent drug quality control
and strictly enforcing the provisions of the
Drugs and Cosmetics Act (1940) and the
Magic Remedies Prevention Act, 1954; and
® Preparation of drug formularies and
Pharmacopoeias for ayurveda, siddha, unani
and homoeopathy drugs are proceeding
rapidly.
monitoring work relating to testing of survey
samples and statutory samples of ISM&H
drugs.
KI The Department of ISM&H is assessing and
training ISM&H drug industry personnel and
drug inspecting staff in standardisation and
quality control.
Neutraceuticals and Food Supplementation
Products
ensuring quality control is still a major problem
because of lack of adequate number of ISM&H
testing laboratories. In order to address this
problem, the Department has initiated a centrallysponsored programme for strengthening of state
drug testing laboratories and for improving good
manufacturing practices in ISM&H pharmacies.
However, complaints of poor quality of ingredients
or adulteration and substitution of components
used for preparation of ISM&H drugs and lack of
confidence in the safety, efficacy and quality of the
drugs persists. Testing of complex ISM&H drugs
is difficult. Drug testing laboratories at the state level
are either inadequate or non-existent, state
governments are not enforcing the standards laid
down by appropriate licensing and quality control
measures.
160
2.9.33 Food supplements, cosmetics and toiletries
and neutraceuticals are flooding the Indian market.
It has been reported that they have export potential.
These products contain not only plant-based
materials, exotic plant ingredients but also synthetic
chemicals. As these products do not come under
the category of either modern system or ISM&H
drugs, they are not governed either by the Drugs
and Cosmetic Act or the Prevention of Food
Adulteration Act (1986), they enter the market
without any quality control. It is important that these
products are brought under the purview of Drugs
and Cosmetic Act or the Prevention of Food
Adulteration Act through suitable amendments of
these acts and compliance with the Act is monitored
carefully.
INDIAN SYSTEMS OF MEDICINE AND HOMOEOPATHY
Medical Tourism
2.9.34 There has been a resurgence of interest in
traditional medicine in India and abroad, leading to
an increased demand for specialised treatment
available in ISM&H. A number of tourists are visiting
Kerala for panchakarma treatment for rejuvenation,
and for treatment of neuro-muscular and
orthopaedic disorders. Himachal Pradesh has
initiated a scheme on health tourism by offering
panchakarma in good hotels. During the Tenth Plan,
opportunities in this area will be explored and
catered to. At the same time appropriate transparent
quality and cost of care norms will be set up and
monitored to prevent exploitation of the clients.
Research and Development
2.9.35 There are four research councils in ISM&H:
the CCRAS, the Central Council for Research in
Unani Medicines (CCRUM), the Central Council for
Research in Yoga and Naturopathy (CCRYN) and
the Central Council for Research in Homoeopathy
(CCRH). These councils are the apex bodies for
research in the various systems of medicine and
are fully financed by the Government of India. They
initiate, guide, develop and coordinate, basic and
applied research, medico-botanical surveys,
research on cultivation of medicinal plants and
Some of the major problems in R&D
in ISM&H include:
H ISM&H practitioners and researchers need
training in research methodology.
H in spite of growing interest in Indian health
systems, alternate and complementary
medicine, none of the research done by
research councils, industry and academic
institutions has been published in scientific
journals of national and international repute.
El research has not concentrated on areas where
ISM&H has unique advantages such as
prevention and management of lifestylerelated diseases, and diseases for which
drugs are not available in the modern system;
El research work is not carried out in
collaboration with modern hospitals where
abundant clinical material is available.
pharmacognostical studies. These councils also
conduct research programmes aimed at drug
standardisation and clinical trials of new ISM&H
drugs.
2.9.36 During the Tenth Plan the following
measures will be taken to improve R&D:
priority will be accorded for bio-medical
research pertaining to drug development in
specific areas where strength of ISM has
already been established;
importance will be given to research on the
fundamental principles of ISM&H;
emphasis will be laid on research in the
preventive and promotive aspects of ISM
especially lifestyle-related disorders;
medico-historical investigations of ISM&H will
be continued; and
promising and widely accepted practices and
skills of traditional healers in rural and tribal
areas will be identified and evaluated.
Zero Based Budgeting
2.9.37 The Planning Commission had directed all
central ministries/departments to review the ongoing
schemes using the zero-based budgeting
methodology and to ascertain which of the ongoing
schemes require continuation in the Tenth Plan.
The Department of ISM&H also went through this
exercise.
2.9.38 Since the Department started functioning
only in 1995, most of the schemes had been initiated
during the Ninth Plan. A majority of them relate to
strengthening essential central institutions in
medical education, healthcare, drug quality and
research. All these schemes will therefore, continue.
It was found that there were a large number of
small schemes and these were merged into broad
programmes. Some of the centrally sponsored
schemes had been misclassified as central sector
schemes and this error was corrected (Table 2.9.5).
The outlays and expenditure under each of these
during the Ninth Plan is summarised in Annexure
2.9.2.
161
TENTH FIVE YEAR PLAN 2002-07
Table 2.9.5-Summary of Zero Based Budgeting Exercise -2001
Scheme
Centrally Sponsored Schemes
No. of schemes
Ninth Plan outlay
(Rs. Lakh)
Ninth Plan - Sum
of yearly outlays
(Rs. Lakh)
Schemes to be retained
1
51
51
Schemes to be merged
3/8
5,992
8,047
Schemes to be weeded out
1
0
410
6,043
8,508
480
680
Total
4/10
Central Sector Schemes
Schemes to be retained
1
Schemes to be merged
8/34
20,112
27,465
Total
9/35
20,592
28,145
PATH AHEAD AND GOALS SET
2.9.39 During the Tenth Plan the following areas
will receive a major thrust:
mainstreaming the ISM&H system;
utilisation of the services of the ISM&H
practitioners for improving access to health
care and coverage under national
programmes;
improvement in quality of under graduate,
postgraduate education and continuing
medical education of all practitioners, so
that there is improvement in the quality of
care provided by ISM&H practitioners;
monitoring the quality and cost of care at all
levels of health care;
promotion of health tourism especially for
prevention and management of lifestyle
related disorders;
162
implementation of the recommendations of
the Planning Commission’s Task Force on the
Preservation, Promotion and Cultivation of
Medicinal Plants and Herbs;
enforcement of stringent drug quality control
measures and good manufacturing practices
for ISM&H drugs and formulations;
improving the availability of good quality
ISM&H drugs at affordable prices within the
country;
realising fully the export potential for ISM&H
drugs and formulations.
Successful implementation of the above initiativeswill
enable ISM&H system to get its due share in
providing health care for the population, improve
quality and access to health care and enable the
country to achieve the goals set in the National
Population Policy (2000) and National Health Policy
(2002). The schemewise outlays for the Department
of ISM&H is indicated in Annexure 2.9.2 and Appendix.
*»*«««*
INDIAN SYSTEMS OF MEDICINE AND HOMOEOPATHY
Annexure-2.9.1
HOSPITALS AND DISPENSARIES UNDER INDIAN SYSTEMS OF MEDICINE AND HOMOEOPATHY
SI. Name of
No.StatesAJTs
1. ANDHRA
PRADESH
2. ARUNCHAL
PRADESH
AYURVEDA
UNANI
HOMOEOPATHY
OTHERS
Dipensaries Hospitals Beds Dispensaries Hospitals Beds Dispensaries Hospitals Beds Dispensaries Hospitals Beds
1437
8
444
207
7
390
286
6
280
0
1
135
3. ASSAM#
4. BIHAR#
5
DELHI#
6 GOA
7
GUJARAT
8
HAR7ANA
9
HIMACHAL
PRADESH
10 J&K#
11 KARNATAKA
12 KERALA
13 MADHYA
PRADESH
14 MAHARA
-SHTRA#
4
1
15
1
329
522
122
59
539
414
1064
2
9
9
6
45
6
16
130
871
771
245
1745
840
330
1
128
19
20
3
1
10
247
561
759#
2105
1
124
109
34
25
6132
2561#
1160
171
45
1#
56
2
11
200
202
1
60
463
73
11713
23
10
1400
41
4
4
414
311
15 MANIPUR
75
181
95
56
34
20
14
2
25
2754
202
0
0
0
4
0
0
0
10
0
0
1
0
0
1
0
2
25
0
50
0
1
0
25
3
1
3
105
100
190
9
730
25
72
12
1480
1440
590
25
11
9#
0
1
18
1#
0
10
586
30
0
77
5505
0
0
0
1
10
2
0
0
0
0
0
2
0
221
0
0
65
0
0
0
0
0
22
0
1716
0
0
527
489
3486
8
11
90
323
771
1179
9
35
79
5
270
10
30
713#
4
1
1671
267
10
9911
6
1
54
148#
136
1186
9
5
1
2
503
105
121
1
41
66
1378
254
3
215
2
110
899
14
682
7
4
1
1
1
25
30 DAMAN & DIU
1
1
1
1
150
29 D & N HAVELI
5
1
2
1
34
41
5
105
0
0
0
0
0
8
5
4
12836
0
2
0
487
16 MEGHALAYA
17 MIZORAM
1
18 NAGALAND
19 ORISSA
20 PUNJAB#
21 RAJASTHAN
22 SIKKIM
23 TAMILNADU
24 TRIPURA
25 UTTAR
PRADESH#
26 WEST
BENGAL#
27 A & N ISLANDS
28 CHANDIGARH#
33 CGHS
34 CENTRAL
RESEARCH
COUNCILS
35 M/O RAILWAY
36 M/O LABOUR
37 M/O COAL
TOTAL
31
32
38
129
28
14416
1
20
25
475
9
8
12
265
150
185
160
3
1
36
150
20
399$
0
0
0
0
1
0
0
0
0
0
2
0
10
0
0
0
0
0
85
0
0
0
254
0
0
0
2660
124
25
1
2258
5
6
5
1
0
0
0
65
0
3
1
339
0
0
5
31 LAKSHADWEEP 4
32 PONDICHERRY 12
40313
970
196
4872
7155
1‘
297
Source : Department of ISM&H, 1999
Note : Institutions Functional as on 1.4.1999; - = Nil Information
# = Information for the current year has not been received. Hence repeated for the latest available year. * = Information regarding Yoga
Hospitals in Delhi is under clarification. $ = Figures as on 1.4.98 @ = No. of beds reported nil is under clarification.
Figures are provisional
163
TENTH FIVE YEAR PLAN 2002-07
Annexure-2.9.2
TENTH PLAN OUTLAYS - DEPARTMENT OF ISM&H
(Rs. In Lakhs)
9th Plan
10th Plan
2002-03
Ninth Plan Sum of YearOutlay
wise Outlay
Anticipated
Expenditure
Outlay
Outlay
Centrally sponsored schemes
1
Development of Institutions
2920.00
4020.00
4279.48
11750.00
1950.00
2
Hospitals and dispensaries
490.00
402.00
73.72
4900.00
750.00
3
Information, Education and
Communication (IEC)
4
Drugs Quality Control
51.00
51.00
0.00
1200.00
300.00
2582.00
3700.00
3146.55
4540.00
875.00
Central Sector
1
Strengthening of Deptt. of ISM&H
1650.00
2129.00
1964.61
2250.00
515.00
2
Educational Institutions
5282.00
6693.00
4990.65
11650.00
2615.00
3
4
Statutory Institutions
176.00
169.00
147.00
265.00
15.00
Research Councils (intra
and extra mural research)
8391.00
10777.00
10661.94
13600.00
2520.00
5
Hospitals and dispensaries
71.00
292.00
314.80
2244.00
276.00
6
Medicinal Plants
1765.00
3420.00
2215.56
10700.00
2516.00
7
Strengthening of Pharmacopoeial
Laboratories
1082.00
1150.00
365.50
2650.00
567.00
8
Information, Education and
Communication (IEC)
480.00
680.00
839.28
1700.00
300.00
9
Other Programes and Schemes
1595.00
2960.00
226.52
New Initiatives during the 10th plan
8550.00
1501.00
1801.00
10
26635.00
36443.00
29225.61
77500.00
15000.00
Grand Total
164
CHAPTER2.10
FAMILY WELFARE
Introduction
2.10.1
India is the second most populous country
in the world, sustaining 16.7 per cent of the world
population on 2.4 per cent of the world’s surface
area. Realising that high population growth is
inevitable during the initial phases of demographic
transition and the urgent need to accelerate the
pace of the transition, India became the first country
to formulate a National Family Planning Programme
in 1952. The objective of the policy was “reducing
birth rate to the extent necessary to stabilise the
population at a level consistent with requirement of
national economy”. The First Five-Year Plan stated
that “the main appeal for family planning is based
on considerations of health and welfare of the family.
Family limitation or spacing of children is necessary
and desirable in order to secure better health for
the mother and better care and upbringing of
children. Measures directed to this end should,
therefore, form part of the public health progra
mme”. This statement preceded the International
Conference on Population and Development (ICPD)
1994 by four decades.
2.10.2 The focus of India’s health services right
from the early 1950s has been health care for
women and children and provision of contraceptive
services. Successive Five- Year Plans have been
providing the policy framework and funding for the
planned development of nation wide health care
infrastructure and manpower. The centrally spon
sored and 100 per cent centrally funded Family
Welfare Programme provides the states the
additional infrastructure, manpower and consum
ables needed for improving the health status of
women and children and to meet all the felt needs
for fertility regulation.
2.10.3 Technological advances and the improved
quality and coverage of health care resulted in a
rapid fall in the crude death rate (CDR) from 25.1 in
1951 to 9.8 in 1991. In contrast, the reduction in
crude birth rate (CBR) has been less steep,
declining from 40.8 in 1951 to 29.5 in 1991. As a
result, the annual exponential population growth rate
has been over 2 per cent in the 1971-1991 period.
The pace of demographic transition in India has
been relatively slow but steady. The 1991 Census
The NDC Sub-Committee on Population recommended that there should be a
paradigm shift in the Family Welfare Programme and the focus should be on:
E3 Decentralised area-specific planning based on need assessment.
Bl Emphasis on improved access and quality of services to women and children.
M Providing special assistance to poorly performing states/districts to minimise the differences in
performance.
El Creation of district-level databases on quality, coverage and impact indicators for monitoring the
programme.
The International Conference on Population and Development (ICPD) at Cairo in 1994 advocated a similar
approach.
A convergence between national (NDC Sub-Committee) and international (ICPD) efforts improved funding
of Family Welfare Programme during the Ninth Plan period.
165
TENTH FIVE YEAR PLAN 2002-07
showed that the population growth rate fell below 2
per cent after three decades. In order to give a new
thrust to efforts to achieve a more rapid decline in
birth rate, death rate and population growth rate,
the National Development Council (NDC) set up a
Sub-Committee on Population (1992) and endorsed
its recommendations in 1993.
2.10.4 During the Ninth Plan period, the Depart
ment of Family Welfare implemented the recom
mendations of the NDC Sub Committee. Centrallydefined method specific targets for family planning
were abolished. The emphasis shifted to decentra
lised planning at the district level, based on
assessment of community needs and implemen
tation of programmes aimed at fulfilment of these
needs. State specific goals for process and impact
parameters for maternal and child health and
contraceptive care were worked out and used for
monitoring progress. Efforts were made to improve
the quality and content of services through training
to upgrade skills for all personnel and building up a
referral network. A massive pulse polio campaign
was taken up to eliminate polio. The Department
of Family Welfare set up a consultative committee
to suggest appropriate restructuring of infrastructure
funded by the states and the centre and revise
norms for re-imbursement by the centre and has
started implementing the recommendations of the
Committee. Monitoring and evaluation has become
a part of the programme and the data is used for
mid-course corrections. The Department has drawn
up the National Population Policy 2000(NPP 2000),
which aims at achieving replacement level of fertility
by 2010. A National Commission on Population was
constituted in May 2000, in line with the recom
mendations of the NPP 2000.
2.10.5 Currently some of the major areas of
concern include:
community health centres (CHCs); lack of
referral services;
S slow decline in mortality during the 1990s; the
goals set for mortality and fertility in the Ninth
Plan will not be achieved;
Ml there has been no decline in the maternal
mortality ratios over the last three decades,
while neonatal and infant mortality rates have
plateaued during the 1990s;
M the routine service coverage has declined,
perhaps because of the emphasis on campaign
mode operations for individual components of
the programme;
M in spite of the emphasis on training to improve
skills for the delivery of integrated reproductive
and child health (RCH) services, the progress
in in-service training has been very slow and
the anticipated improvement in the content and
quality of care has not taken place;
M evaluation studies have shown that the
coverage under immunisation is not universal
even in the best performing states while
coverage rates are very low in states like Bihar;
elimination of polio is yet to be achieved;
M) the logistics of drug supply has improved in
some states but remains poor in populous
states;
decentralised district-based planning, moni
toring and mid-course correction utilising the
locally generated service data and Civil Regis
tration has not yet been operationalised.
Approach during the Tenth Plan
3.10.6 During the Tenth Plan, the paradigm shift,
which began in the Ninth Plan, will be fully opera
tionalised. The shift was from:
M demographic targets to focussing on enabling
couples to achieve their reproductive goals;
the massive inter-state differences in fertility
and mortality;fertility and mortality rates are
high in the most populous states, where nearly
half the country’s population lives;
Bl method specific contraceptive targets to
meeting all the unmet needs for contraception
to reduce unwanted pregnancies;
gaps in infrastructure, manpower and equip
ment and mismatch between infrastructure and
manpower in primary health centres (PHCs)/
M numerous vertical programmes for family plan
ning and maternal and child health to integrated
health care for women and children;
166
FAMILY WELFARE
S centrally defined targets to community need
assessment and decentralised area specific
microplanning and implementation of program
for health care for women and children, to
reduce infant mortality and reduce high desired
fertility;
2.10.9 If the reproductive goals of families are
fully met the country will be able to achieve the
National Population Policy goal of replacement level
of fertility by 2010. The medium and long term goals
will be to continue this process to accelerate the
pace of demographic transition and achieve
population stabilisation by 2045. Early population
stabilisation will enable the country to achieve its
developmental goal of improving the economic
status and quality of life of the citizens.
B quantitative coverage to emphasis on quality
and content of care;
ISl predominantly women centred programmes to
meeting the health care needs of the family
with emphasis on involvement of men in
planned parenthood;
2.10.10 Reductions in fertility, mortality and popu
lation growth rate will be major objectives during
the Tenth Plan. Three of the 11 monitorable targets
for the Tenth Plan and beyond are:
El supply driven service delivery to need and
demand driven service; improved logistics for
ensuring adequate and timely supplies to meet
the needs;
E reduction in IMR to 45 per 1,000 live births by
2007 and 28 per 1,000 live births by 2012;
El service provision based on providers’ percep
tion to addressing choices and conveniences
of the couples.
E reduction in maternal mortality ratio to 2 per
1,000 live births by 2007 and 1 per 1,000 live
births by 2012; and
2.10.7 The population growth rate continues to be
high due to:
E reduction in decadal growth rate of the
population between 2001-2011 to 16.2.
H the large size of the population in the repro
ductive age-group (accounting for an estimated
60 per cent of the total population growth);
Population Projections
2.10.11 The Technical Group on Population
Projections under the Chairmanship of the Registrar
General, India (RGI) constituted by the Planning
Commission in 1996 had made population
projections up to the year 2016 based on the results
M higher fertility due to the unmet need for contra
ception (contributing to around 20 per cent of
population growth); and
ISJ high wanted fertility due to the
prevailing high Infant Mortality Rate
(IMR) and other socio-economic
reasons (estimated contribution of
about 20 per cent to population growth).
FsguraXK’J Age-ciistrijution'&f ’©piilatiore
14W
noo
2.10.8 The Tenth Plan will fully opera
tionalise efforts to:
100:1
H |=l H 3::3:
SCO
E assess and meet the unmet needs for
contraception;
I
■aoa
4ffl
E achieve reduction in the high desired
level of fertility through programmes for
reduction in IMR and maternal mortality
ratio (MMR); and
E enable families to achieve their
reproductive goals.
200
0
B5-
i&§*
^-15 Yrs.
Saursn: Teebncal GroMFan
167
iwm-wtta
B1
Yrs.
2ii^
5S.5SYrs.
■jP.GSj
2011
SMS
® ^'J Yrs.
TENTH FIVE YEAR PLAN 2002-07
of 1991 Census. The projections for different age
groups are shown in Figure 2.10.1. It then estimated
the probable year by which the replacement level
(Total Fertility Rate) of 2.1 will be achieved by
different states if the recent pace of decline in TFR
observed during 1981-93 continues. The Group
estimated that the country would achieve the
replacement level of fertility by 2026. The most
populous states of Bihar, Madhya Pradesh,
Rajasthan and Uttar Pradesh will achieve the
replacement level of fertility by 2039, 2060, 2048
and after 2100 respectively.
Census 2001
2.10.12 The 2001 Census showed that India's
population was 1.02 billion in 2001,15 million more
than the projections made by the Technical Group
on Population Projections. Comparison of the
projections with the Sample Registration System
(SRS) data indicates that projections regarding both
the birth and death rates were substantially lower.
The decadal growth rate has declined from 23.86
per cent for 1981-91 to 21.34 per cent for 19912001. (Figure2.10.2). Tamil Nadu and Karnataka
have attained replacement level of fertility and
Andhra Pradesh has shown a remarkable fall in
fertility and decadal growth rate during the 1990s.
The decadal growth rate in a majority of the states
has shown a decline. Only Bihar has shown a
substantial increase in the decadal growth rate. The
National Population Policy has set the goal that the
country will achieve the replacement level of fertility
by 2010. If this is achieved, the decade 2001-2011
will witness a very steep decline in decadal growth
rate.
Population Projections for the Tenth Plan
2.10.13 Prior to the formulation of the Tenth Plan
it is not possible to make full scale projections taking
into account the trends during the 1990s as the data
on age and sex distribution of the population from
2001 Census is not yet available. The Department
of Family Welfare made the necessary adjustment
for higher actual population in the base year of 1997
in the projections made by the Technical Group on
Population Projection for the period 1997-2012
(Table 2.10.1).
Interstate Differences
2.10.14 The projected values for the total
population in different regions is shown in the
Figure 2.10.3. There are marked differences
between states in size of the population, projected
population growth rates and the time by which TFR
of 2.1 is likely to be achieved. If the present trend
continues, most of the southern and the western
states are likely to achieve TFR of 2.1 by 2010.
Figure 2.10.2. DeMdal Growth Rate
V
15 '
w
I
%
■jC
£
s I
I
e
£
i
i II
I
&
® 1&81-1991
D 1&91^301
Sourw: Registrar Gen&fae
168
j I
FAMILY WELFARE
Table 2.10.1
Population Projections Adjusted For The 2001 Census Totals
Year
1997
2002
2007
2012
Population (millions)*
951.18
1028.93
1112.86
1196.41
Population (millions)**
965.28
1044.18
1129.35
1214.14
technical Group on Population Projections-1996;
**Adjusted for the 2001 census totals
Source: Deptt of F.W.
Urgent energetic steps to assess and fully meet
the unmet needs for maternal and child health
(MCH) care and contraception through improvement
in availability and access to service are needed in
Rajasthan, Orissa, Uttar Pradesh, Madhya Pradesh
and Bihar (before division) in order to achieve a
Figore 2.10.3 Popylation Projections
zoo
ew
r
II ?•'1
..2W
0
!
!
3—
..... I
k:
j
jg
UP
32001
□ 2C’:6
faster decline in their mortality and fertility rates.
The performance of these states would determine
the year and size of the population at which the
country achieves replacement level of fertility. It
is imperative that special efforts are made during
the next two decades to break the vicious selfperpetuating cycle of poor performance, poor per
capita income, poverty, low literacy and high birth
rate in the populous states so that further
widening of disparities between states in terms
of per capita income and quality of life is
prevented. An Empowered Action Group has
been set up to provide special assistance to these
states. The benefits accrued from such
assistance will depend to a large extent on the
states’ ability to utilize the available funds and
improve services and facilities.
Inter state differences
There are massive inter state differences in
population, population growth rates, time by which
TFR of 2.1 and population stabilisation will be
achieved.
These differences will have a major impact on :
S health and nutritional status.
O education and skill development.
R) appropriate employment
emoluments.
with adequate
K rural - urban and inter state migrations.
t3 social and economic development.
The effort is to provide adequate inputs to improve
performance so that the disparities between states
are narrowed.
169
TENTH FIVE YEAR PLAN 2002-07
Figure 2.10.4 Time Trends in Sex Ratio in India
980
970
I 980
§
950 - ■—
940 '•
1
930--920 ‘ -
.r
9TU —
900
8
§
&1
0
Saurds: RGI
■
a
•
i
i
8
C’smus
Gender Bias
2.10.15 The reported decline in the sex ratio during
the current century has been a cause for concern
(Figure 2.10.4). The factors responsible for this
continued decline are as yet not clearly identified.
However, it is well recognised that the adverse sex
ratio is a reflection of gender disparities. There is
an urgent need to ensure that all sectors collect
and report sex disaggregated data. This will help
in monitoring for evidence of gender disparity.
Continued collection, collation, analysis and
reporting of sex disaggregated data from all social
sectors will also provide a mechanism to monitor
whether girls and women have equal access to
these services.
2.10.16 The census based estimates of sex ratio
in the 0-6 age group show massive inter-state
differences (Figure 2.10.5). In addition, data indicate
that over the last three decades there has been a
decline in the 0-6 sex ratio. (Table 2.10.2) There
had been speculation as to whether female infan
ticide, sex determination tests and selective female
foeticide are, at least in part responsible for this.
The Government of India has enacted a legislation
banning the prenatal sex determination and selec
tive abortion while female infanticide is a cognizable
offence. However, unless there is a change in social
attitudes, these legislations cannot achieve the
desired change. Intensive community education
efforts to combat these practices, especially in
Figure 2.10,5 Sex Ratio 0-< Years fFemales Per 1000 IMafes}
^8
I
»
i
SO
»
il
700
1
i
0
X
I I
•y
MWffl 21X11
SR. .at Brth
S&.irzti. 'Registrar 'G^nerai
SR
India
170
Biilh (Mafeona? Aveffige |
I
FAMILY WELFARE
Table 2.10.2
and Child Development are initiating steps to ensure
that these women get the care they need .
Child sex ratio (Females/1000 Males)
Year
Urban
Rural
Total
1981
931
963
962
1991
935
947
945
2001
903
934
927
Population Projections and their Implications
for the Family Welfare Programme
2.10.19 The projected population of India in the three
major age groups (less than 15, 15-59, 60 years or
above) between 1996 and 2016 are shown in Figure
2.10.6. In the country as a whole, there will be a
Source: RGI
pockets from where female infanticide and foeticide
have been reported, are urgently required.
2.10.17 The National Family Health Survey
clearly brought out the sex differentials in the
neonatal, post neonatal, infant and under five
mortality rates . As there is no biological reason for
the higher mortality among the girl children these
differences are an indication of existing gender
bias in caring for the girl child (Figure 2.10.5a).
- India
PraiectO'd
Figar®
TO
—w
? 6410
»:■
"'
n
2 40 0
200
100
-- ------
~~
. Ki'
n
Piyum S.iO.Sci Ska
2001
lit hitant & Chftd
2011
2S16
OortaMty
120 --------------------------------------100
RO----GO ■ —
Age group <15 years
40 —I
20 —
0 ’•—J
li
■
I.
....
|
FM?
morlalily
• ^FHS-2
Morlddy
■Male
2.10.18 In the reproductive age-groups, the
mortality rates among women are higher than those
among men. The continued high maternal mortality
is one of the major factors responsible for this.
Effective implementation of the RCH programme
is expected to result in a substantial reduction in
maternal mortality. Currently, the longevity at birth
among women is only marginally higher than that
among men. However, the difference in life
expectancy between men and women will
progressively increase over the next decade. Once
the reproductive age group is crossed, the mortality
rates among women are lower. Women will
outnumber men in the over-60 age- group.
Departments of Health, Family Welfare and Women
171
There will be no increase in numbers. Focus will
be to improve:
IS quality and coverage of health and nutrition
services and achieve improvement in
health and nutritional status
IS improve access to education & skill
development
marginal decline in less than 15 years of age
population (352.7 million to 350.4 million), even though
in poorly performing states there will be continued
increase in the number of children requiring care. The
health care infrastructure will, therefore, not be under
pressure to provide care to an ever increasing number
of children. They will be able to concentrate on:
M improving quality of care;
M improving on antenatal, intra natal and neonatal
care aimed at reducing neonatal morbidity and
mortality;
TENTH FIVE YEAR PLAN 2002-07
Hi improving coverage for immunisation against
vaccine preventable diseases;
S promoting inter sectoral coordination especially
with the ICDS programme so that there is an
improvement in health and nutritional status;
and
K improving coverage and quality of health care
to vulnerable and underserved adolescents.
2.10.20 The economic challenge is to provide
needed funds so that these children have access
to nutrition, education and skill development. The
challenge faced by the health sector is to achieve
reduction in morbidity and mortality rates in infancy
and childhood, to improve nutritional status and
eliminate ill effects of the gender bias.
quality of these services. The Family Welfare
Programme has to cater to a wider spectrum of
health care needs of this population- including
maternal and child health (MCH) care, contraceptive
care, management of gynaecological problems; the
quality of services also needs to be improved.
2.10.22 There will be a substantial increase in the
population more than 60 years (62.3 million to 112.9
million) in the next two decades. Increasing
numbers of the population beyond 60 years would
necessitate provisions for the management of some
of the major health problems in this age group,
including early detection and management of
cancers.
Evolution of India’s Family Welfare Programme
Age group 15-59 years
Basic premises of the Family Welfare
Programme are:
The challenge is the massive increase in the
number of people in this age group. They will:
K acceptance of Family Welfare services
is voluntary;
H need wider spectrum of services :
maternal and child health services
H Family Welfare programme will provide:
contraceptive care
gynaecological problems
integrated MCH and family planning
services;
RTI /STD management
effective IEC to improve awareness;
easy and convenient access to
Family Welfare services free of
cost.
E>3 expect better quality of services
H expect fulfillment of their felt needs for
MCH/family planning care.
Opportunity is that if their felt needs are met
through effective implementation of RCH
programme, it is possible to accelerate
demographic transition and achieve rapid
population stabilisation.
The 1950s
2.10.21 There will be a massive increase of
population in the 15-59 age group (from 519 million
to 800 million). The RCH care has to provide the
needed services for this rapidly growing clientele.
The population in this age group is more literate
and has greater access to information. These
people will, therefore, have greater awareness and
expectation regarding both access to a wide
spectrum of health care related services and the
172
2.10.23 At the time of Independence, health care
services were predominantly urban, hospital
based and curative. General practitioners well
versed in maternal and child health and
paediatricians and obstetricians provided health
care to women and children. While they did
provide comprehensive, integrated, good quality
services, technology for detection and
management of health problems was limited and
out reach of services was poor. The majority of
the population, especially those belonging to the
poorer sections and those residing in rural areas,
did not have access to health care, as a result of
FAMILY WELFARE
which morbidity and morality rates among them
were quite high. Many women died while seeking
illegal induced abortion to get rid of unwanted
pregnancy because they did not have access to
contraceptive care. Conceptions that were too
early, too close, too many and too late and lack
of antenatal care to detect and treat problems in
pregnancy resulted in high maternal and infant
mortality rates. Antenatal, intrapartum, postnatal
and contraceptive care was not readily available
to women who required these services
desperately.
these available to people, effective programmes for
delivery of identified priority services were drawn
up by professionals and implemented through the
limited health care infrastructure available in rural
areas and supplemented by camps. The family
planning and the immunisation programmes were
among the earliest of such programmes. Subse
quently, several other vertical programmes were
added to the Family Welfare Programme. In an
attempt to improve outreach, the camp approach
was adopted for providing care to pregnant women
and children and improving access to immunisation.
However, these efforts did not result in any marked
improvement in the health status of these vulnerable
groups because the care was not available when
needed and there were no referral services.
2.10.24 Obstetricians, who were daily witnessing
maternal morbidity and mortality associated with
high parity, were willing to persuade their patients
who had completed their families to undergo
surgical sterilisation. The fact that the technique
was simple, safe and effective and could be done
soon after delivery under local anaesthesia
accounted for the popularity of postpartum tubal
sterilisation. The safety, simplicity and efficacy of
vasectomy was also well recognised. For couples
who had completed their family, sterilisation of one
partner resulted in the reduction of maternal morbi
dity and mortality associated with high parity. To
some extent, this was responsible for the decline in
maternal mortality rates in urban areas during the
1950s. However, these measures had no impact
on the mortality or fertility or the population growth
rate of the country as a whole because of poor
outreach, especially in rural areas. Thus, in the
1950s, good quality integrated maternal and child
health care, and family planning services were
available to those who were aware, had access and
could afford the services of physicians. There were
efforts to improve coverage and extend the services
to rural areas as a part of the block development
programme. However, resource and manpower
constraints were responsible for the slow progress
on this front.
2.10.26 The 1961 census showed a rising decadal
population growth rate due to declining death rates
and unchanged birth rates.The health infrastructure
is still predominantly urban-based. During the
1960s, sterilisation remained the focus of the
National Family Planning Programme. Efforts were
made to popularise vasectomy and to provide
services in rural areas through camps. Tubectomy
services, however, remained predominantly in urban
hospitals. Moving health education out of hospitals
into the community through the extension education
approach was attempted to improve awareness and
increase acceptance of family planning methods.
Lippe’s loop provided the first reliable birth spacing
method for women in India. Following encouraging
response in urban clinics, attempts were made to
provide this spacing method to the rural population
through camps. However, without the infrastructure
to provide follow up services, the device fell into
disrepute. It became obvious that it will not be
possible to achieve any improvement in maternal
and child health indices or reduce birth rates without
substantial investment into infrastructure and
manpower to provide the needed follow up services.
The 1960s
1970s
2.10.25 In the 1960s, safe, effective vaccines for
the prevention of six childhood diseases and
effective contraceptives for birth spacing such as
Lippe’s loop became available. In order to make
2.10.27 The 1970s witnessed many initiatives to
improve the health and nutritional status of women
and children. The Massive Dose Vitamin A
programme, the National Anaemia Prophylaxis
173
TENTH FIVE YEAR PLAN 2002-07
Programme and food supplementation to pregnant
and lactating women and pre-school children
through the Integrated Child Development Services
(ICDS) programme were major initiatives to tackle
micronutrient deficiencies and under-nutrition and
its adverse consequences in women and children.
With the improvement in primary health care
infrastructure, access to health care improved.
of post partum centres was expanded to improve
access to family welfare services. In 1983 the
National Health Policy was formulated and provided
comprehensive framework for planning, implemen
tation and monitoring of health care services. The
Universal Immunisation Programme (UIP), started
in 30 districts in 1986, was extended to cover 448
districts by the end of the Seventh Plan.
2.10.28 The 1971 Census showed that population
explosion was no longer a potential threat but a
major problem that needed to be tackled energeti
cally. The Government gave top priority to the family
planning programme and provided substantial funds
for several new initiatives. Sterilisation, especially
vasectomy services were made widely available.
Intra-uterine devices (IUD) and condoms were
made available through the PHCs. The hospital
based postpartum programme provided contra
ceptive care to women coming for delivery. The
Medical Termination of Pregnancy (MTP) Act, 1972,
enabled women with unwanted pregnancy to seek
and obtain safe abortion services.
The 1990s
2.10.29 Increasing concern about the rapidly grow
ing population led to the National Family Planning
Programme being included as a priority sector
programme during the Fifth Plan. The massive
sterilisation drive of 1976 did result in eight million
persons undergoing sterilisation, but this did not
have any perceptible impact on the birth rate, as
the cases were not appropriately chosen. There
was a steep fall in acceptance in the very next year.
In 1978, the Expanded Programme of Immunisation
was initiated to improve coverage for the six vaccine
preventable diseases. In 1979, the Programme was
renamed as the National Family Welfare Progra
mme and increasing integration of family planning
services with those of maternal and child health and
nutrition was attempted.
The 1980s
2.10.30 The major thrust during the 1980s was to
operationalise the WHO’s Alma Ata declaration of
health for all by 2000 A.D. (1978) by establishing a
net-work of centres in urban and rural areas to
provide essential primary health care. The network
174
2.10.31 The 1991 Census showed that India was
entering the opportunity window in demographic
transition, when larger proportion of the population
is in the age group of 20-40 years, when it will be
possible to achieve a rapid decline in fertility and
mortality. The report of the NDC Sub Committee
on Population gave a new thrust and dynamism to
the family welfare programme. During the Eighth
Plan, efforts were made under the Child Survival
and Safe Motherhood initiative and the Social Safety
Net programme to improve the access to maternal
and child health services. In view of the massive
inter-state and intra-state differences in access to
services and health indices, the Department of
Family Welfare abolished the practice of setting
centrally defined, method-specific targets for
contraception. It was replaced by decentralised
area-specific need assessment (community needs
assessment approach), planning and implementing
programmes aimed at fulfilling these needs.
2.10.32 In 1997, the Department of Family
Welfare initiated the Reproductive and Child
Health (RCH) programme aimed at providing
integrated health and family welfare services to
meet health care needs of women and children.
The components of the comprehensive RCH care
is indicated in the Text Box. The essential
components recommended for nationwide
implementation at all levels include:
Bl prevention and management of unwanted
pregnancy;
Bl services to promote safe motherhood;
B services to promote child survival; and
SB) prevention and treatment of RTI and sexually
transmitted infection (STI).
FAMILY WELFARE
B universal registration of births and deaths,
marriages and pregnancies;
Components of comprehensive RCH Care:
M Effective maternal and child health care.
B universal access to information/counselling and
services for fertility regulation and
contraception with a wide basket of choices;
Bl Increased access to contraceptive care.
Bl Safe management of unwanted preg
nancies.
B to reduce the IMR to below 30 per 1,000 live
births and a sharp reduction in the incidence
of low birth weight (below 2.5 kg.);
Bl Nutritional services to vulnerable groups.
B Prevention and treatment of RTIZ STD.
B Reproductive health services for adole
scents.
B universal immunisation of children against
vaccine preventable diseases;
B Prevention and treatment of gynaeco
logical problems.
B promote delayed marriage for girls, not earlier
than the age of 18 and preferably after 20
years;
B Screening and treatment of cancers, espe
cially uterine, cervical and breast cancer.
B achieve 80 per cent institutional deliveries and
increase the percentage of deliveries
conducted by trained persons to 100 per cent;
These services are available in secondary and
tertiary care centres in the country.
B containing of STD;
Efforts are being made to improve the content,
quality and coverage of care
B reduction in MMR to less than 100 per 100,000
live births;
2.10.33 Efforts were made to provide adequate
inputs to improve the availability and access to RCH
services and to improve the programme’s
performance especially in states/districts with poor
health indices. Attempts to reduce disparities
between states/districts and achieve incremental
improvement in the indices by replication of the
strategies adopted by better performing districts
were encouraged.
National Population Policy
2.10.34 The immediate objective of the National
Population Policy is to meet all the unmet needs
for contraception and health care for women and
children. The medium-term objective is to bring the
TFR to replacement level (TFR of 2.1) by 2010 and,
the long-term objective is to achieve population
stabilisation by 2045.
2.10.35 The Policy has set the following goals for
2010:
B universalisation of primary education and
reduction in the drop-out rates at the primary
and secondary levels to below 20 per cent for
both boys and girls.
2.10.36 Several states/districts have demonstra
ted that the steep reduction in mortality and
fertility envisaged in the National Population
Policy are technically feasible within the existing
infrastructure and manpower. All efforts are being
made to provide essential supplies, improve
efficiency and ensure accountability - especially
in the states where performance is currently suboptimal - so that there is incremental
improvement in performance. An Empowered
Action Group attached to the Ministry of Health
and Family Welfare has been constituted in 2001
to facilitate capacity building in poorly performing
states/districts so that they attain the goals set
in the Policy. If all these efforts are vigorously
pursued it is possible that the ambitious goals
set for 2007/2010 may be achieved.
National Commission on Population
universal access to quality contraceptive
services in order to lower the TFR to 2.1 by
adopting the small family norm;
2.10.37 The National Commission on Population
was constituted on 11 May 2000 under the
175
TENTH FIVE YEAR PLAN 2002-07
chairmanship of the Prime Minister. The Deputy
Chairman of the Planning Commission is the vice
chairman. The Commission has the mandate to:
El
E
E
Rgutc-MJ Source of
review, monitor and give direction for the
implementation of the National Population
Policy with the view of achieving the goals it
has set;
4^3
promote synergy between health, educational,
environmental
and
developmental
programmes so as to hasten population
stabilization;
1
immun^ahm
0 Put’Ifc Secfer
E
2.10.38 The
lessons
learnt from
the
implementation of family welfare programmes in the
last five decades are:
E
The governmental network provides most of
the maternal and child health and contraceptive
care services; (Figure 2.10.7)
E
adequate financial inputs and health
infrastructure are essential prerequisites for the
success of the programme;
El
providing efficient and effective integrated
maternal and child health and contraceptive
care helps in building up rapport with the
families;
= 176
□ PrivalE-
El Other
I EC and motivation activities are powerful tools
for promoting the small family norm;
E develop a vigorous people’s programme to
support this national effort.
Lessons Learnt in Five Decades
OflrrtraicBplim, Any MiC. RHS feist Del., RUS
NFHS-2
' HFHS-2
promote inter-sectoral coordination in
planning and implementation of the
programmes through different agencies at
the Centre and in the states; and
A Strategic Support Group consisting of secretaries
of concerned sectoral ministries has been
constituted as a standing advisory group to the
Commission. Nine working groups were constituted
to look into specific aspects of implementation of
the programmes aimed at achieving the targets set
in the National Population Policy. NCP has allocated
funds for action plans drawn up by district
magistrates in poorly performing districts to
implement programmes aimed at accelerating the
pace decline in fertility.
& FP Care
the people are conservative but responsible
and mature and though their response may be
slow, it is rational and sustained.
REVIEW OF PERFORMANCE OF THE FAMILY
WELFARE PROGRAMME DURING NINTH PLAN
2.10.39 The decentralised planning and initiatives
taken up under the RCH programme during the
Ninth Plan were expected to lead to substantial
improvement in the coverage and quality of servi
ces. In order to achieve this, the Department of
Family Welfare was given additional outlay to enable
it to provide adequate financial inputs to the states.
Goals for the Ninth Plan were projected on the basis
of these newer initiatives and additional inputs
provided. Goals set for the Ninth Plan, current status
regarding these are in Annexure 2.10.1
2.10.40 A review of the performance during the
Ninth Plan suggests that the health systems in the
states needed more time to adapt to decentralised
planning and implementation of components of the
RCH programme. In an attempt to improve
coverage under specific components of the RCH
programme, some states embarked on campaign
mode operations which took their toll on routine
services. Efforts to eliminate polio by the end of
2000 through the massive pulse polio campaign also
FAMILY WELFARE
had some adverse effect on routine service delivery.
As a result, it is unlikely that Ninth Plan goals for
CBR, couple protection rate, MMR and IMR will be
achieved.
2.10.41 Independent surveys have shown that
several states have achieved goals set for some
aspect of the RCH programme during the Ninth
Plan, demonstrating that these can be achieved
within the existing infrastructure, manpower and
inputs.
El Andhra Pradesh, Punjab, West Bengal and
Maharashtra have shown substantial decline
in birth rates and the latter three states are likely
to achieve replacement level of fertility, ahead
of the projections.
E
Punjab has achieved couple protection rate and
use of spacing methods far ahead of all other
states.
E Tamil Nadu and Andhra Pradesh have
achieved significant reduction in home
deliveries.
E
Kerala, Maharashtra, Punjab and Tamil Nadu
improved immunisation coverage.
E
Tamil Nadu and Andhra Pradesh had achieved
improvement in coverage and quality of
antenatal care.
2.10.42 During the Tenth Plan, the pace of imple
mentation of the programme will be accelerated
through streamlining of infrastructure; focus will be
on improving quality, coverage and efficiency of
services so that all the felt needs for family welfare
services are fully met. Special attention will be paid
to improving access to good quality services to the
under-served population living in urban slums,
remote rural and tribal areas.
PREVENTION OF UNWANTED PREGNANCY
2.10.43 Efforts to improve the availability of contra
ceptive care during the 1970s and 1980s resulted
in a steep rise in couple protection rates. However,
there was no commensurate fall in the birth rate.
Service reports on couple protection rate and SRS
estimates of CBR indicate that there has been a
steady decline in the latter during the 1990s in spite
of the fact that the rise in couple protection rate
during the decade has been very slow (Figure
2.10.8). This may be because earlier there was over
reporting of contraceptive acceptance or there has
been an improvement in the quality of services
during nineties and appropriate contraceptives are
being provided at the appropriate time.
2.10.44 There are massive inter-state differences
in couple protection rate and CBR. In states like
Bihar, the couple protection rate is low and birth
rate is high. In Punjab, couple protection rate is
high. Kerala, Tamil Nadu and Andhra Pradesh have
achieved substantially lower CBR even while couple
protection rate was lower than that of Punjab.
(Figure 2.10.9). Age and parity at the time of
accepting contraception as well as continuation
?
L; «
:i•' SW'
....
!
... .......... s»i
...
-
a—
1—
—
'
___ _J
%
I
i
I
. .
a
■
1
i
I
i
€ r F LC1M
=
177
I
I
-» i f3“Th BATB
i
»
I
1
j
8
TENTH FIVE YEAR PLAN 2002-07
Fhgum 2...1 &J
In CPR Ani! Birth R.ate
70
4G
X
10
0
I
5r.
2ZZ1 JPR 131 ^20G1 j
Source ; SRSf Depll of F.W
..... B^th Rate W&S
rates of spacing methods are critical factors that
influence the relationship between couple protection
rate and CBR. The high acceptance of tubectomy
in younger women with two or three children in Tamil
Nadu and Kerala and the higher use of spacing
methods even among older women with three or
more children in Punjab may account for the
differences in the couple protection rate and CBR
between these states.
2.10.45 Over the years there has been a fall in
birth rate in all the states and among all segments
of population, but the rate of reduction in the birth
rate is higher in some states. Data from 2001
Census and SRS 2000 indicate that:
2.10.46 Data from service reports during the Ninth
Plan period indicate that there has been a decline
in acceptors of all types of contraception in the initial
years of the Plan, as compared to the level of
acceptance in 1994-95. Subsequently, from 199899 the decline has been reversed except in the case
of IUD (Figure 2.10.10).
Figure 2.10.10 Acceptors of Family
Methods-all fritfia
25
A •
15
f
IS
...................
>1
El eleven states/Union Territories with 11.3
per cent of the population have CBR of
below 20;
El twelve states/Union Territories with 38.6 per
cent of the population have CBR between 20
and 25;
M
seven states with 14.4. per cent of the
population have CBR between 25 and 30;
E five states with 35.7 per centjjf the population
have CBR of more thanZ30~~per~'1,000
population.
There is an urgent need to meet all the needs for
contraception in the populous states with high birth
rate.
--------------““
I
_______ |
0 -----
3
i
A
I I
— SierilisatiDfi
Source: DepU. nf- F.W
CC users
s O
-W'. . IUD
OP Users
2.10.47 The NFHS 1 and 2 provided nation-wide
data on contraceptive prevalence in 1992-93 and
1998-99. Data from the survey (Figure 2.10.11)
indicate that contrary to the performance figures
available from the service reports of the
Department of Family Welfare, there has been a
substantial increase in the sterilisation and oral
contraceptive acceptance in the country. Only
178
FAMILY WELFARE
JO !' Ce h'S
2.10.48 The data from in-built independent sur
veys and coverage evaluations within the National
Family Welfare Programme have been reassuring
in that their findings show that there has been no
deterioration in the contraceptive prevalence in the
1990s. However, the coverage figures under service
reporting for spacing methods, antenatal care and
immunisation are still substantially higher than the
coverage reported by evaluations. This over
reporting needs to be corrected so that service
reporting provides a reliable indication of progress
achieved in the programme. The narrowing of the
gap in coverage figures between the service and
evaluation reports can be used as a new indicator
for the quality in programme monitoring.
br
T IT
i '<»
"1 1
•w
h >-
i
r; •
I
O'
I '‘
— ,4.... J
.»£•
Unmet Need for Contraception
IUD and vasectomy use has shown a decline.
The improvement in couple protection rate
explains the steady decline in the CBR during
the 1990s reported by the SRS. The differences
in couple protection rate data from service reports
of the Department of Family Welfare and NFHS
may partly be due to:
El
a reduction in the earlier over reporting which
was done in an attempt to show that targets
have been met; and
El
incomplete reporting due to changes in service
reporting formats during the current period.
Unmst-
2.10.49 NFHS 1 and 2 (Figure 2.10.12) clearly
indicate that there is still substantial unmet need for
both terminal methods and spacing methods in all
states (Figure 2.10.13). There are inter-state
differences in the magnitude of unmet need for
contraception. It is imperative that all the unmet needs
are fully met within the Tenth Plan period and a
substantial reduction in unwanted pregnancy is
achieved. Making a balanced presentation of
advantages and disadvantages of methods, improving
counselling, quality of services and follow up care will
enable couples to make appropriate choices regarding
contraception, increase couple protection rates and
continuation rates and enable the country to achieve
the goal of replacement level of fertility by 2010.
ngjurc 2.10.13 Unmert Mse-ci for ramify Piartning
fer
x<.
25
20
i
IS:
J 10 —
I
I-
M,.,
r
5
0
fl
n
n i
I
i
o
_
W
Urniir^
Merzes
1
□ NFHS1
Saircsih^H®
Wl'Ha*1 oi 1HWWSJ
179
U»eii
____ _ ____________
TENTH FIVE YEAR PLAN 2002-07
Figure 2/0/4 Contrfoulion ©f Birtns a* Orcsr of Three-and
Above all B rths
40
\
I 2* s’
§
i
Monitoring Birth Order
2.10.50 Monitoring reported birth order is an
easy method of observing the progress towards
achievement of replacement level of fertility.
Currently, birth order of three or more account
for nearly half of all births. There are massive
inter-state and inter-district differences in the
contribution of different birth orders (Table?. 10.3
and Figure 2.10.14). Based on this information,
district-specific differential strategies can be
evolved to improve contraceptive prevalence
rates, increase inter-birth intervals and reduce
higher order of births.
Table 2.10.3
Inter-districtvariations
(Birth order three or more as percentage
of total births)
i 1i IHI j
majority of the women complete their families
during their early 20s. In the current Indian
milieu of stable marriages, sterilisation is the
most appropriate method of contraception for
such couples. There are substantial
differences between states and between
districts in proportion of eligible couples who
have adopted terminal
methods of
contraception (Table 2.10.4). The 1990s saw
some increase in the per centage of currently
sterilised persons in all states except Punjab.
However, the per centage of women under
going sterilisation is very low in Assam, Bihar
and Uttar Pradesh. (Figure 2.10.15). A majority
of women in these states opt for sterilisation
after bearing three or more children. Improving
access to safe, good quality tubectomy/
vasectomy services through RCH camps in
CHCs/PHCs may be the most viable and
sustainable strategy for meeting the unmet
need for sterilisation in these states.
No of districts
<20%
27
20-40%
165
>40%
313
Table 2.10.4
Inter-district variations in the percentage
of eligible couple sterilised
No, of districts
Source: RHS (Rapid Household survey 1998)
Terminal Methods of Contraception
2.10.51 Sterilisation has been the most widely
used method of contraception in all states.
Currently, age at marriage is very low and a
180
>50
75
40-49
101
30-39
106
<30
223
Source: RHS 1998-99
FAMILY WELFARE
Figure- 2.. 10.15 Percgrrts/ge al Coupes Cwmnlly SlerlFis&d
---|
I
n
3
'I
rt—
n rt
31'
S
f . ■ ..-C yyvw -Zv-f'/z/ 'I
w'z-■
*3
a
i
2
5’
I | zr
i t i
i
I
Il Iif
s
§ a
I
&
a
3
I f
1
l
Emerging Needs for Spacing Methods
2.10.52 Data from NFHS clearly shows that in
spite of the low use of spacing methods, the mean
inter-birth interval is about 30 months. (Figure
2.10.16) This is because of universal prolonged
breast-feeding. Exclusive breast feeding during the
first six months offers substantial protection against
pregnancy. However, once supplements are intro
duced to breast-fed infants, the contraceptive effect
of lactation wanes. The introduction of appropriate
contraception at this time will ensure adequate
spacing between births and prevent deterioration
in maternal and infant nutrition due to too early
advent of the next pregnancy. Data from NFHS 2
Births
has also shown that there is an emerging need for
contraception before first birth. (Figure 2.10.17)
This has to be fully met during the Tenth Plan.
Gender-Bias And Acceptance of
Contraception
2.10.53 Data from NFHS showed that the prefe
rence for a son influenced the acceptance of
permanent as well as temporary methods of contra
ception (Figures 2.10.18-19). It is important that
appropriate steps are taken by all concerned sectors
to minimise and eliminate gender-bias which
reduces contraceptive acceptance among those
with girl children.
f igurs 2.1(1.1 ? fetenlpun for
of’ Fanidv Pljm^nq
Birth foStswai
-
I
33
I
2»3
■i..
'3^
•■c
&
Q.
s»
Si^rosdMFHS
□ NFHSd
DNFHS-2
181
1
2
J
4»
TENTH FIVE YEAR PLAN 2002-07
a. TMr W.
w—
.. •—
r—
m—
Kj..-.
1"30 f—-<
?•
SS.-
SW
10
0
1
I
m-4
w -
i
2 9ar»
0k
1 San
1^®
Lhs&vp aoy malate mnUrad
Men’s Participation in Planned Parenthood
2.10.54 Men play an important role in determining
education and employment status, age at marriage,
family formation pattern, access to and utilisation
of health and family welfare services for women and
children. Their active co-operation is essential for
the prevention and control of STI/RTI. In condom
users, consistent and correct use is an essential
pre-requisite for prevention of STI as well as
pregnancy. Vasectomy was the most widely used
terminal method of contraception in the 1960s and
1970s but since then there has been a steep decline
in its use (Figure 2.10.20 ). It is essential that efforts
to re-popularise vasectomy are intensified. Ample
data exists to show that vasectomy is safer than
tubectomy. Every effort will be made to repopularise
vasectomy by improving access to vasectomy
services. These services (conventional or no
scalpel) will be made readily available to all at
convenient times as an outpatient procedure in all
primary, secondary and tertiary care institutions.
Follow up care will be provided to all taking into
account the existing time constraints and the
conveniences of men. Efforts will be made to seek
men’s active participation in improving utilization of
funds provided for emergency transport and
ensuring that women and children reach appropriate
centers where emergency services are available.
Their cooperation will be sought in improving
Figure 2.10.20 Acceptors of Vasectomy
Tubectomy
................................... .......................
e«w_ tutf/rnmn,.
I 3D
—---------- >
_____ , i
n&
■ -* m *
«y,. ■ .
.-W.. I....,
r
k £
! 5 'f
5
¥ B I * S
a.
182
7
| S S # |
«
•^S-EETWr
feturw -
2
FAMILY WELFARE
antenatal, child health and immunization care as
well as compliance with referrals. Over the next
five years efforts will be made to ensure men’s
participation in every facet of planned parenthood
activities.
Tenth Plan Strategy for Meeting the Felt Needs
for Contraception
been any substantial decline in the estimated
number of illegal abortions, reported morbidity due
to illegal abortions or share of illegal abortions as
the cause of maternal mortality. The management
of unwanted pregnancy through early and safe MTP
services as envisaged under the MTP Act is an
important component of the ongoing RCH
programme.
2.10.55 Tenth Plan strategy to meet all the felt
needs for contraception would include:
Figure 2.10 21 Medical Termin-atton
of Pregnancies
7
In all districts
6
E
E
counselling and balanced presentation of the
advantages and disadvantages of all available
methods of contraception to enable the family
to make the right choice;
S
4
5
I
....
1
improve access to good quality contra
ceptive care services in the vicinity of their
residences;
W-
El good follow up care.
II
I
s
H H
J : : I
F.<
In statesldistricts where birth order of three or
more accounts for over 40 per cent of the births:
ensure ready access to tubectomy/vasec-tomy
by sending doctors, if necessary, from CHCs/
district hospitals to PHCs/CHCs on fixed days.
In statesldistricts where birth order of two or
less accounts for over 60 per cent of the births
2.10.57 During the Ninth Plan efforts were made
to:
El
M cater to the demand for MTP;
improve access to safe abortion services by
training physicians in MTP and recognising and
strengthening institutions providing these safe
abortion services; and
meet the unmet needs for spacing methods
on a priority basis and also continue to provide
terminal methods.
H
MANAGEMENT OF UNWANTED PREGNANCY
2.10.56 It is estimated that in 1998, about 9 per
cent of maternal deaths were due to unsafe
abortions. Available service data on MTPs indicate
that following an initial rise in early 1980s, the
number of reported MTP’s hovered around 0.5- 0.7
million in the 1990s(Figure-2. 10.21). The estimated
number of illegal induced abortions in the country
is in the range of four to six million. There has not
183
improve access to family planning services and
reduce the number of unwanted pregnancies;
decentralise registration of institutions to the
district level.
2.10.58 In spite of these efforts, there has not been
any increase in terms of coverage, number of MTPs
reported and reduction in the number of women
suffering adverse health consequences of illegal
induced abortions.
2.10.59 Tenth Plan strategies for reducing
morbidity due to induced abortion include:
TENTH FIVE YEAR PLAN 2002-07
H
reducing the number of pregnancies by fully
meeting the felt but unmet needs for
contraception;
H
improving access to safe MTP services through:
R>
ensuring the availability of MTP services
in all institutions where there is a qualified
gynaecologist and adequate infrastruc
ture;
decentralising registration of MTP clinics
to district level;
simplifying the regulations for reporting of
MTP;
training physicians working in wellequipped institutions in the government,
private and voluntary sector in MTP so that
they also can provide safe abortion
services;
providing manual vacuum aspiration
(MVA) syringes in recognised MTP cen
ters where there is a trained physician but
no vacuum aspiration machine;
using MVA for performing MTP in CMC/
PHC , when a gynaecologist visits the
CHCs/PHCs on a fixed day; and
exploring the feasibility and safety of intro
ducing non-surgical methods of MTP in
medical college hospitals and extending
the service in a phased manner to district
hospitals.
El Ensuring that women do accept appropriate
contraception at the time of MTP to prevent
unwanted pregnancy requiring a repeat
MTP.
MATERNAL HEALTH
2.10.60 The prevailing high rates of maternal
morbidity and mortality have always been a
source of concern, and antenatal and intrapartum
care aimed at reducing these have been
184
components of the National Family Welfare
programme since its inception. Although data
on state/district-specific maternal morbidity/
mortality is not available, available figures from
the SRS and the Survey of Causes of Death
provide sufficient information on mortality rates
and causes of death so that rational programmes
Table 2.10.5
Maternal Mortality Ratio
1992-93
1997
1998
RGI (Sample Registration
Scheme)
NA
408
407
National Family Health
424*
540*
‘Differences are not statistically significant
Source : RGI and NFHS 1& 2
could be evolved to combat major health
problems in women. In the 1990s, the SRS and
the NFHS 1&2 provided independent data to
assess the impact of ongoing programmes on
maternal mortality. During the 1990s, there has
not been any decline in MMR and more than
100,000 women continue to die each year due to
pregnancy-related causes. (Table 2.10.5)
2.10.61 Data from SRS indicate that the major
causes of maternal mortality continue to be
unsafe abortions, antepartum and post-partum
haemorrhage, anaemia, obstructed labour,
hypertensive disorders and post-partum sepsis.
There has been no major change in the causes
of maternal mortality over years(Table 2.10.6).
Table 2.10.6
Causes of maternal death (%)
Haemorrhage
30
Anaemia
19
Sepsis
16
Obstructed labor
10
Abortion
8
Toxemia
8
Others
8
Source: Survey of Causes of Death 1998
FAMILY WELFARE
Deaths due to abortion can be prevented by
increasing access to safe abortion services.
Deaths due to anaemia, obstructed labour,
hypertensive disorders and sepsis can be
prevented by improving the access of essential
obstetric care, universal screening for detection
of obstetric problems, referral and timely
treatment of complications of pregnancy,
promoting institutional delivery and postnatal
care. Emergency obstetric services will help
saving lives of women with haemorrhage during
pregnancy or complications during deliveries. The
Ninth Plan envisaged universal screening of all
pregnant women, identification of women with
health problems, problems during pregnancy and
appropriate management including referral to
centres where appropriate care is available. This,
however, has not been operationalised; highest
priority will be accorded to operationalise this
during the Tenth Plan.
2.10.62 During the Tenth Plan, every effort will be
made to:
ensure 100 per cent registration of preg
nancies, deaths and births so that reliable
state/district-level estimates of MMR are
available on a sustainable basis; and
improve ascertainment of the cause of death
through SRS and hospital records so that it
becomes possible to assess time trends and
changes in causes of maternal mortality.
Figure 2.10..22 .Antenatal Care
t2S
’ip
too
6ft
S ' ±1...
B
si
aM
i !
i
■S&irca
C3 Full
■ -4
J
• -J
I
2.10.63 Under the RCH programmes, efforts were
made to improve the coverage, content and quality
of antenatal care in order to achieve substantial
reduction in maternal and perinatal morbidity and
mortality. Data from the rapid household Survey
(RHS), 1998-1999 indicate that at the national level,
67.2 per cent pregnant women received at least
one check-up but only 10.6 per cent had three
antenatal checkups. Antenatal coverage in popu
lous states with poor health indices such as Uttar
Pradesh, Bihar and Madhya Pradesh are very low
(Figure-2.10.22). Antenatal coverage was good in
almost all districts of Andhra Pradesh, Tamil Nadu
and Kerala. Surprisingly, most districts in Punjab
reported very low coverage. (Figure 2.10.23)
o
Oi
O 4^60^
■ W185
UM'
Antenatal Care
Figure 2.10.23 Distribution gF Districts as Per Three or
More AHC Check-up
•J
ti..
TENTH FIVE YEAR PLAN 2002-07
Antenatal Care
2 1-0 2$ Quni 1y OF Arlenatal
rbrn■
:: 99 i
R Early registration of pregnancy (12-16
weeks).
O Minimum three ante-natal check-ups.
K Screening all pregnant women for major
health, nutritional and obstetric problems.
H Identification of women with health
problems/complications, providing prompt
and effective treatment including referral
wherever required.
LLP
T.
3 FA
H Universal coverage of all pregnant women
with TT immunisation.
am
pregnancy and referral to appropriate facility for
treatment. (Figure 2.10.25)
H Screening for anaemia; providing iron folic
acid tablets for prevention of anemia; pro
viding appropriate treatment for anemia.
2.10.65 The problem of poor screening is aggra
vated by the fact that referral linkages for the
management of problems are also poor in these
states and, as a result, both maternal/perinatal
morbidity and mortality continue to be high.
® Advice on food, nutrition and rest.
H Promotion of institutional delivery/safe
deliveries by trained personnel; advising
institutional delivery for those with health/
obstetric problems.
2.10.64 RHS data clearly indicates that only in 95
districts more than 75 per cent women had three
antenatal visits during pregnancy. In as many as
265 districts, less than 40 per cent of the women
had three antenatal visits (Figure-2.10.24). In Uttar
Pradesh and Bihar, the content and quality of
antenatal care was poor as compared to Haryana
and Tamil Nadu. Universal screening of pregnant
women using appropriate antenatal care is essential
for the detection of problems and risk factors during
2.10.66 Anaemia is a major cause of maternal
mortality in India. The Ninth Plan envisaged univer
sal screening for anaemia in pregnant women and
appropriate iron folate treatment. This is yet to be
operationalised. In none of the states screening for
anaemia was included as a component of antenatal
care. RHS data indicated that less than 30 per cent
pregnant women had taken iron folic acid tablets in
267 districts (Figure 2.10.26). During the Tenth
Plan, every effort will be made to fully operationalise
the Ninth Plan strategy for prevention and manage
ment of anaemia.
Fl^u^2.'W„24 three ANC& during pregnancy
Figured. 10.28 Consymptson of IFA
41
E3 fitters
95
%
A
265
IDS
75%
B9
OMore than
©50-75%
□ 30-4G%
J
® Losb than 40%
^HSiSSS-SB
Scarce RHS 1998-^
186
WS!W5MiMa&^^
B L«kk than 30%
109
FAMILY WELFARE
number of ANMs, there is need to strengthen the
existing ANM schools. In states/districts with heavy
work load/difficulty in transport or communication,
additional ANMs may be recruited on a contractual
basis, in order to meet all the unmet needs for
maternal health.
Problems In Antenatal Care
H training of health personnel in antenatal
screening, risk identification and referral
had been very slow;
H inadequate coverage under essential
obstetric care;
E3 poor content and quality of antenatal scre
ening, lack of systematic recording of
findings; poor referral system; referrals
not honoured;
M lack of screening and gatekeeper function
and reverse referrals leading to over crow
ding in hospitals;
S lack of emergency obstetric services-at
CHCs/FRUs.
Tenth Plan Strategy for Improving Maternal
Health
2.10.67 The initiatives taken under the RCH pro
grammes to provide essential obstetric care to all
women will be continued during the Tenth Plan.
Training to upgrade the skills of health care
providers and improve the content and quality of
antenatal care, will be completed expeditiously so
that they follow the protocol for screening all
pregnant women to identify those with problems.
The auxiliary nurse midwife (ANM) is the key person
in the screening of pregnant women and she will
be given the necessary skill up gradation training
and equipment. In order to ensure screening and
two way referrals becomes a standard practice, it
is essential to ensure that findings are recorded in
a standard format in an antenatal card which is
retained by the woman who takes it with her where
ever she gets referred to. For this purpose an
antenatal card was designed and tested in some
states during the Ninth Plan. It is essential that
these cards, with suitable modifications, if
necessary, are made available to all states. The
ANM will work closely with the anganwadi worker
and will conduct maternal and child health clinics in
anganwadis on specified days according to her
advance tour programme. She will be the
gatekeeper whose referrals will be honoured at
PHCs/CHCs. In states where there are inadequate
187
2.10.68 The CHC/FRU is the critical institution
which provides emergency obstetric care and plays
a vital role in the referral system. The reported
gaps in the number of CHCs/FRUs will be filled by
appropriately reorganising the subdivisional
hospitals, post-partum centres and block-level
PHCs. The required number of core specialists will
be posted through appropriate redeployment of the
manpower; wherever adequate number of
specialists are not available, hiring them on a
contractual or part-time basis can also be
considered. In order to strengthen the capability
of CHCs/FRUs in antenatal and intrapartum care,
states can take up training of one of the staff nurses
in CHC so that there is someone who has
specialised in midwifery available to provide care.
Over the next five years, efforts will be made to
improve the Emergency Obstetric Care in all CHCs
in a phased manner, by ensuring that these CHCs
have well equipped operation theatre, access to
banked blood, qualified obstetricians, paedia
tricians and anaesthetists.
2.10.69 In view of the massive differences bet
ween districts in the availability and access to
essential and emergency obstetric services, and in
maternal health indices, the following differential
strategies will be adopted for achieving incremental
improvement in essential and emergency obstetric
care during the Tenth Plan.
In all districts:
awareness generation to ensure universal
screening of pregnant women; identification
of women with problems;
manage/refer women with complications to
appropriate institution for care;
100 per cent coverage for tetanus toxoid (TT)
immunisation;
vssMxsoaim&semfsga
TENTH FIVE YEAR PLAN 2002-07
screening for and treatment of anaemia;
when doctors/specialists will be available to
examine women with problems and provide
treatment/referral.
provide information on:
nearest PHC where women with
problems can seek a doctor’s advice;
nearest FRU with obstetricians and faci
lities where women with obstetric emer
gency can seek admission; and
how to access the emergency transport
system.
In better performing districts focus on:
improvement in universal coverage and
content and quality of antenatal care to enable
very early identification of women with any
antenatal problems;
referral of those with problems to CHC/FRU
for care.
In poorly performing districts, the focus will be
on:
improving coverage for antenatal screening
by an ANM providing antenatal care at least
thrice during pregnancy;
building up a system of RCH camps in PHCs/
CHCs on specific days throughout the year
Delivery Care
2.10.70 During the Ninth Plan, it was envisaged
that efforts will be made to promote institutional
deliveries both in the urban and rural areas. Simul
taneously, in districts where a majority of the
deliveries were taking place at home, efforts were
made to train the traditional birth attendants (TBAs)
through an intensive Dai Training Programme and
to increase the availability of disposable delivery
kits. The available data from the NFHS-1 and 2 and
RHS-1998 suggest that there has been some
improvement in institutional deliveries, especially
in states like Tamil Nadu and Andhra Pradesh
(Figure2.10.27). However, there are a large number
of districts in many states where the situation with
regard to safe deliveries is far from satisfactory.
2.10.71 In states like Kerala, over 90 per cent of
deliveries are in institutions and neonatal mortality
rates are very low.However, neonatal mortality is
high in states like Uttar Pradesh, where the majority
of deliveries occur at home and are conducted by
untrained persons. Efforts to train TBAs and provide
Figures, 10.27.Safe Deliveries
#3
■J
s
‘J
-O
W
0
a
J
I i I
Boyrce NEWS 1 K 2
f I l1 fHo i i% 1t
I
i
I
a
NFHSI
188 =
©
t-
FAMILY WELFARE
Figure 2.10.28 Neonatal ^©rtality and Home Delrverhs
TO
...
h
■ r -B0
4 70
-
I
50 •»
I
s
4 ®_
f 30 • -
- 40 ci
” 30
4 20 z
- W
a
[j TW
8 =
v t 5I
0.
|
fl
I
71
Horn&
Saurrs'.Nn IS 2
them with disposable delivery kits have not resulted
in substantial decline in the maternal morbidity or
neonatal mortality rates. (Figure2.10.28). Data from
NFHS-2 showed that even though there has been
a steep increase in institutional deliveries in Tamil
Nadu and Andhra Pradesh, there has been no
commensurate decline in neonatal mortality,
indicating the need to improve the quality of
intrapartum and neonatal care for those coming for
institutional deliveries.
2.10.72 Women with problems like anaemia,
malpresentations, suspected cephalopelvic
disproportion , hypertensive disorders of
pregnancy and gestational diabetes mellitus
should not deliver at home. Screening all women
during pregnancy to detect those with such
problems and referring them at the appropriate
time to pre-designated institutions for
management and safe delivery will substantially
reduce maternal and perinatal morbidity and
mortality. The mechanism for screening, as well
as referral, will have to be streamlined during the
Tenth Plan period. Easy-to-follow protocols for
referral will have to be developed and made
available to all health care providers. If home
delivery is anticipated in low risk cases, provision
has to be made for aseptic delivery by trained
persons. The TBAs will be trained to recognise
women with complications and those in labour
longer than 12 hours and refer them to hospitals
for delivery. This strategy is expected to result
189
1/1907-98)
in some reduction in maternal and neonatal
deaths and pave the way for good antenatal care
and safe institutional deliveries at a later date.
2.10.73 Unpredictable complications can arise
even during apparently normal labour and rapid
transportatiion of these women to hospital for emer
gency obstetric care is essential. In order to assist
families in arranging transport to centres where
emergency care is provided, the Department of
Family Welfare provided funds which will be
available at the village level. Panchayats, NGOs
and women’s organisations and men in villages will
play an important role in ensuring that optimum use
is made of this fund and timely transport saves life.
In the postpartum period, early detection and
management of infections, support for breast
feeding and nutrition counseling will receive due
attention.
Tenth Plan Strategy to Improve Delivery Care
2.10.74 In view of the massive differences bet
ween states/districts in the proportion of institutional
deliveries (Figures 2.10.29) and neonatal mortality
rates, a differential strategy to achieve incremental
improvement in maternal and neonatal care will be
taken up during Tenth Plan.
In all districts
efforts will be made to identify women with
complications during pregnancy through
TENTH FIVE YEAR PLAN 2002-07
2.10.75 Specific efforts will made to strengthen
FRUs/CHCs/district hospitals to provide emergency
obstetric care for all referred cases. The attempt
will be to:
Figure 2.10.29 Jristhutional Deliv'eries Situation io districts
4B
E
-4I
288
/ 109
provide for funding specialists on contract/parttime basis, if necessary, so that care is
available when needed; and
□ rv’cre th&o 75%
□ 5£J-75%
C 30-49%
tew iw
operationalise adequate number of FRUs/
CHCs by posting specialists in obstetrics,
gynaecology/pediatrics in institutions where
infrastructure is available;
E
improve access to anesthetists and banked
blood.
W LeB'S than
CHILD HEALTH
antenatal check up and refer them to
appropriate institution for safe delivery.
In districts with low institutional delivery,
attempt will be made to:
E
screen all women in the last four weeks of
pregnancy and ensure that those with
complications deliver in institutions;
2.10.76 Infant and under-five mortality rates are
excellent indicators of the health status of children.
In India there is no system for collection and analysis
of data on morbidity during childhood. In the
absence of this, available mortality data and analysis
of causes of death have been utilised for drawing
up priority interventions for improving child health.
Ongoing major intervention programmes in child
health include:
E train TBAs in clean delivery;
E train TBAs to recognise problems that arise
during labour and refer those women to
hospitals;
E essential new born care;
El ensure that referrals are honoured; and
E food and micro-nutrient supplementation
programmes aimed at improving the nutritional
status;
E
build up community support for transport of
women with problems to functional FRUs.
E
/n districts with high institutional delivery,
efforts will be made to:
H
immunization to prevent morbidity and mortality
due to vaccine preventable diseases;
programmes for reducing mortality due to acute
respiratory infection (ARI) and diarrhoea.
2.10.77 Improved access to immunisation,
health care and nutrition programmes have
resulted in substantial decline in IMR between
1950-1990. However, it is a matter of concern
that the decline in perinatal and neonatal mortality
has been very slow (Figure-2.10.30). IMR has
remained unaltered in the1990s. There are
substantial differences between states in
neonatal, infant and under- five mortality
improve the quality of services available;
El address problems and needs of the women in
labour seeking institutional deliveries;
E aim at universal institutional delivery by making
institutions people friendly; and
H
E
perform medical audit for monitoring
progressive improvement in quality of care.
190
FAMILY WELFARE
140
120 r. I
X
1 100 --I
ao
§
60
40 -
20
0 -I
1971
S Infant Martelhy
1W1
1W1
Rtfkaital MortaSty S
rates(Figure-2.10.31). Higher under-five mortality rates
in girls persist, indicating gender bias in child rearing
practices Over the last three decades there has not
been any substantial change in the major causes of
deaths during infancy and childhood.
Inter-Relationship between IMR and CBR
2.10.78 Access to family welfare services and
contraceptive care is a critical determinant of infant
mortality and birth rate. In spite of the fact that health
and contraceptive care are provided by the same
personnel, the decline in these indices do not always
go hand in hand. There are massive inter-state and
intra-state differences in birth rates and IMR. In spite
w
MorteJIty
of a relatively high IMR, states like Tamil Nadu and
Andhra Pradesh have achieved a steep decline in
fertility. In states/districts where fertility has declined
without a commensurate decline in IMR, there
should be a focussed, area-specific situation
analysis and intervention to reduce IMR. For this,
reliable district-specific data on birth rates and IMR
must be available on an annual basis. This can be
achieved only though 100 per cent recording of birth
and death and collation and analysis of this data at
the district level. Such a system would also enable
continuous monitoring of the impact of the
intervention and mid-course corrections. In order
to achieve this, strengthening of the CRS will be
given priority during the Tenth Plan period.
Figure 2.10JI Interstate Oifferentials in Child Mertehty
140
120
100
ao
a©
40
20
a
I
0
I
191
TENTH FIVE YEAR PLAN 2002-07
Child Health Interventions During the Ninth Plan
BMii WgM cf
Rfw X10
2.10.79 Under the RCH programme, comprehen
sive integrated interventions to improve child health
were initiated to address each of the major factors
contributing to high IMR and under five mortality.
r
|
■■
S 2303 --
40
£ TO g WQ
-
Components of child health care include :
Z2JX> 4-
30
11
■\
1........ i
!
i i i
H Essential newborn care
I
1
• Mi
1C
M. Q
Bl Immunisation
Sscfsk Nutrmcn Nwn. tWI
KI Nutrition:
exclusive breast-feeding for six months
2.10.81 Birth weight is influenced by the nutritional
and health status of the mother. There is a good
correlation between birth weights and the body
mass index (BMI) of the mother (Figure-2.10.32).
A significant reduction in birth weight has been
observed in anaemic women and the low birth
weight rate doubles when Hb levels fall below 8
gms/dl. Some factors, which have significant
influence on birth weight, such as the parent’s build,
are not amenable to short term corrective interven
tions. On the other hand, factors like anaemia,
pregnancy induced hypertension and low maternal
weight gain during pregnancy can be corrected and
could result in substantial reduction both in pre-term
births and birth of small for dates neonates. During
the Tenth Plan, efforts will be made to identify
women with these problems by ensuring universal
antenatal screening; provision of appropriate
management including referral services forthose with
problems may result in improvement in birth weight.
timely introduction of complementary
feeding.
detection and management of growth
faltering.
massive dose Vitamin-A supplemen
tation.
iron supplementation, if needed.
K Early detection and appropriate management
of:
acute respiratory infections;
diarrhoea.
other infections.
Essential New Born Care
2.10.80 India has the dubious distinction of having
a very high prevalence of low birth weight. Currently
nation-wide data on birth weight in different states
and districts is not available because a majority of
births occur at home and these infants are not
weighed soon after birth. Estimates based on
available data from institutional deliveries and
smaller community- based studies suggest that
nearly one-third of all Indian infants weigh less than
2.5 kg at birth. There are differences between states
and between economic groups, with incidence of
low birth rate being the highest among the low
income groups. There has hardly been any change
in birth weight trends in the past three decades. A
gender difference has been noted in mean birth
weights, with female infants tending to weigh lesser
than male infants.
192
2.10.82 The experience of states like Kerala,
Pondicherry and Goa have shown that it is possible
to achieve substantial decline in IMR and child
mortality rates without any significant improvement
in birth weight and reduction in the number of infants
born weighing below 2.5 kg.
2.10.83 Available data suggests that only 10 to 15
per cent of all births occur before 37 weeks (pre
term births), about 20 to 25 per cent infants weigh
less than 2.5 kg but are mature and thrive under
normal care even at home. If all the new born babies
weighing below 2.5 kg are considered as being at
risk and are sent to hospitals for care, hospitals will
get over crowded. Studies conducted over the last
three decades have shown that the neo-natal and
»
FAMILY WELFARE
infant mortality rates steeply increase only when
birth weight falls below 2.2 kg or infants are
premature. During the Tenth Plan priority will be
accorded to weighing all neonates at or soon after
birth and ensuring referral of preterm/ <2.2 kg
neonates to the centers where appropriate care
could be provided.
2.10.84 During the last three decades efforts were
made through antenatal care to reduce low birth
weight because:
it is closely linked to infant (especially
neonatal) mortality;
developing countries have the highest rates
of low birth rate;
developing countries cannot afford the
technologies for intensive neonatal care
needed to reduce mortality among infants with
low birth rate.
I3 During the last three decades there has
not been any major reduction in the pro
portion of low birth weight babies.
Operationalisation of New Born Care
2.10.86 Two-thirds of all the neonatal deaths occur
in the first seven days after birth (Table 2.10.7). The
major causes of neonatal deaths are premature
birth, asphyxia and sepsis. (Table 2.10.8). If
neonates requiring care are identified and referred
to an appropriate facility where they can be
effectively treated and it will be possible to achieve
substantial decline in neonatal mortality.
Table 2.10.7
Components of IMR
%
Early neonatal mortality
48
Late neonatal morality
17
Post neonatal mortality
35
Source: SRS ’1996
Table 2.10.8
Causes of neonatal deaths(%)
K In most states there has been substantial
reduction in IMR even though there is no
change in birth weight.
K Reduction in low birth weight is not an
essential prerequisite for reduction in IMR.
2.10.85 During the Tenth Plan every effort will be
made to:
screen pregnant women for under-nutrition
and anaemia and provide appropriate
interventions;
advise at-risk individuals to have delivery in
institutions, which can provide optimal
intrapartum and neonatal care and improve
neonatal survival;
have the anganwadi worker check the birth
weight of babies as soon after delivery as
possible in all home deliveries and refer those
neonates with birth weight less that 2.2 kg to
hospitals where there is a pediatrician
available;
if these interventions are fully operationalised
it will be possible to achieve substantial
reduction in the neonatal mortality rate within
a short period.
Sepsis
52
Asphyxia
20
Prematurity
15
Others
13
Source: RGI
2.10.87 In order to accelerate the decline of IMR,
essential newborn care was included as an
intervention under the RCH programme. Equip
ment for essential newborn care was supplied to
districts; training was provided for medical
officers and other staff at the district hospitals
and medical colleges to improve content, quality
and coverage of essential newborn care.
Operationalisation of newborn care facilities at
the primary health care level was initiated in
collaboration with the National Neo-natology
Forum (NNF). Department of Family Welfare and
the ICMR are funding research studies on the
feasibility and effectiveness of community-based
new born care in reducing neonatal mortality in
settings where access to primary health care
institutions are not adequate. The focus during
193 «
TENTH FIVE YEAR PLAN 2002-07
Figure
Cov®rag^-.AII India
30-!--------------- ---- ------------------------------------------------------------
Figure 2.10.34
Cases of Vaccine
Preventable Diseases
100000
25
25
fi : « : ! i «
. . .. . ........................... . .......
i
B0800
:::
200&D •;---------------- jH-----15
3
8?
g
I
8
- DPT-
■ POLIO‘S
I
!
I
BCG— f|- ’• MEASLES- ■ >- - TT<W>
of F.W.
the Tenth Plan will be to operationalise the
appropriate essential new born care in all settings
so that there is substantial reduction in the early
neonatal mortality both in institutional deliveries
and home deliveries.
Immunisation
2.10.88 The Universal immunization program
which was taken up in 1986 as a National
Technology Mission, became a part of the Child
Survival and Safe Motherhood (CSSM) programme
in 1992 and the RCH programme in 1997. Under
the programme, infants are immunised against
tuberculosis, diphtheria, pertussis, poliomyelitis,
measles and tetanus. Reported immunization
Coverage during the nineties is shown in Figure
2.10.33. The National Health Policy, 1983, set the
goal of universal immunisation against these six
vaccines preventable diseases by 2000 , this has
not been achieved. However, reported cases of
vaccine preventable diseases have declined over
the same period (Figure 2.10.34).
2.10.89 Data from NFH8 indicate that there has
not been any decline in the immunisation coverage
in the 1990s. However, none of the states have
achieved coverage levels of over 80 per cent;
coverage level in states like Bihar, Uttar Pradesh
and Rajasthan were very low (Figure2.10.35). The
drop-out rates between the first, second and third
doses of oral polio vaccine and DPT have been very
high in most states. Lower coverage of around 20
per cent is reported for measles as compared to
= 194
q I—IKwj,
Hue;
Diphtheria
Tetanus
y
Polio
Measles
fnade’KCi 1590:<
Source.'
Depl d F.W
□
-igss;.
other vaccines. One of the main reasons for not
achieving 100 percent routine immunisation, is the
focus on campaign mode programmes in health and
family welfare. The Department of Family Welfare
has now taken up a scheme for strengthening of
routine immunisation. A pilot project on Hepatitis B
immunisation has also been initiated.
2.10.90 The Tenth Plan will concentrate on :
achieving hundred per cent coverage for the
six vaccine preventable diseases;
elimination of polio and neonatal tetanus;
strengthening routine immunisation pro
grammes and discouraging campaign mode
operations which interfere with routine
services;
greater involvement of the private sector;
improving awareness through all channels of
communication;
improving the quality of care, ensuring
injection safety using appropriate, sustainable
technology;
correcting the over-reporting of coverage,
evaluating on-going pilot projects on the
introduction of Hepatitis B vaccine, including
those where the vaccine costs are borne by
the parents;
exploring appropriate sustainable models of
providing newer vaccines without over
burdening the system and programme
including charging actual costs for the newer
vaccines from people above the poverty line;
FAMILY WELFARE
Figure 2.10.35 Children Fully Immunised 1 Percent]
80 70 •
60 -
& 50 '
I 40
30 20 ■
10 ’
0
1
1
©
a...
n 1H u i ?i zs
6
a
«IIs h" iU f»
s £¥
Smr«: NFHS 1S2
expanding on-going polio surveillance to
cover all vaccine preventable diseases in a
phased manner.
Pulse Polio Immunisation
2.10.91 Under the Pulse Polio initiative, launched
in 1995-96, all children under five years of age are
to be administered two doses of oral polio vaccine
in December and January every year until polio is
eliminated. Coverage under the programme has
been reported to be over 90 per cent in all states,
with over 120 million children taking the vaccine
every year. However, it is a matter of concern that
over the last five years coverage under routine
immunisation has not improved. There are sections
of the population who escape both routine immuni
sation and the pulse polio immunisation. As a result,
through there has been a substantial decline in the
number of polio cases, this was not sufficient to
enable the country to achieve zero polio incidence
by 2000.
2.10.92 Confirmed polio cases reported in the
last four years is shown in Table 2.10.9. Uttar
Pradesh and Bihar account for most of the
reported cases. Mop-up immunization is being
undertaken following detection of wild poliovirus,
including areas with clusters of polio compatible
cases and in areas of continued poliovirus
transmission. The sub-national immunisation
days (SNID) and national immunisation days
(NIDs) are being conducted using the combined
fixed posts and house-to-house approach in all
states. Special efforts are being made to achieve
high routine and campaign coverage in under
served communities and remind families about
the need for routine immunisation during the
pulse polio immunisation campaigns.
2.10.93 The medical goal of polio eradication is to
prevent paralytic illness due to polioviruses by the
elimination of wild poliovirus so that children need
not be immunised perpetually. India will probably
achieve zero incidence of polio by 2004. If there
are no more cases over the next three years, the
country will be declared polio free. When this is
achieved, steps will have to be taken to ensure that
the disease does not return, by continuing to ensure
100% coverage under routine immunisation for
another decade.
Table 2.10.9
No of Polio Cases
Year
No. of cases of confirmed polio
1998
1999
2000
2001
1931
Source : Dept, of FW
195
1126
265
268
TENTH FIVE YEAR PLAN 2002-07
2.10.94 The oral polio vaccine contains live
attenuated virus. Recent experiences in Egypt, the
Dominican Republic and Haiti have shown that the
vaccine-derived viruses can become neuro-virulent
and transmissible. Such mutant viruses have
caused outbreaks of polio in areas where there was
a decline in immunisation coverage. Several
countries that have eradicated polio have shifted to
injectable killed polio vaccine after elimination of
the disease. India, along with other South-Asian
countries, may have to consider all these options
and prepare appropriate strategies during the Tenth
Plan.
supply of ORS through the public distribution system
are being taken up in some states. However RHS
data indicate that ORS was used in more than 50
per cent of cases of diarrhoea in only nine districts
(Table 2.10.10). Improving access to and utilisation
of home available fluids/ORS for the effective
management of diarrhoea will receive priority atten
tion during the Tenth Plan as an inexpensive and
effective tool to reduce IMR/under-five mortality.
Table2.10.10
Children with Diarrhoea
(Percentage treated with ORS)
Percent
Infections in Children
2.10.95 Data from NFHS-2 indicates that 30 per
cent of children below three years of age had fever
during the two weeks preceding the survey, 19 per
cent had symptoms of ARI and another 19 per cent
had diarrhoea. About two-thirds of the children who
had symptoms of ARI or diarrhoea were taken to a
health facility or health-care provider. Knowledge
of the appropriate treatment of diarrhoea remains
low.
Diarrheal Disease Control Programme
2.10.96 Diarrhoea is one of the leading causes of
death among children. Most of these deaths are
due to dehydration caused due to frequent passage
of stools and can be prevented by the timely and
adequate replacement of fluids. The Oral rehy
dration programme was started in 1986-87 in order
to prevent such deaths. Health education aimed at
the rapid recognition and appropriate management
of diarrhoea has been a major component of the
CSSM and RCH program.
2.10.97 The use of fluids available at home and
oral rehydration solution (ORS) has resulted in a
substantial decline in the mortality associated with
diarrhoea, from an estimated one million to 1.5
million children every year prior to 1985 to 600,000
to 700,000 deaths in 1996. In order to further imp
rove access to ORS, 150 packets of ORS are
provided as part of the Drug Kit-A, two of which are
supplied to all the sub-centres every year under the
RCH programme. In addition, social marketing and
196
Districts
>50
9
25-49
82
<25
413
Source :RHS 1998-99
Control of Acute Respiratory Infections
2.10.98 Pneumonia accounts for around 30 per
cent of under five deaths in the country. Under the
RCH programme, co-trimoxazole tablets are
supplied to each sub-centre in the country as part
of Drug Kit-A. Mothers and community members
are being informed about the symptoms of ARI,
which would require antibiotic treatment or referral.
Training of health care personnel in the early
diagnosis of ARI and appropriate treatment,
including referral, as envisaged under the RCH
programme has not yet been completed. This will
receive immediate attention during the Tenth Plan
period.
Tenth Plan Strategy for Improving Child Health
2.10.99 In view of the substantial differences in
the IMR and neonatal mortality rates between states
and between districts, a differential strategy will be
adopted during the Tenth Plan. Wherever district
specific data is available from CRS, district-specific
strategy will be adopted. State-specific strategy will
be evolved when such disaggregated data is not
available. In states/districts with a high IMR and
where early neonatal mortality is less than 50 per
cent of the IMR, the focus will initially be on impro
ving post-neonatal mortality. In districts/states
FAMILY WELFARE
where the IMR is relatively low, and early neonatal
mortality accounts for more than 50 per cent of the
IMR, the focus will be on antenatal, intra partum
and neonatal care.
100 per cent registration of births and deaths and
building up the capacity for data analysis. This task
will be taken up on a priority basis during the Tenth
Plan.
2.10.100 The strategy adopted for all districts will
have the following elements:
2.10.102 The country is yet to ensure 100 per cent
registration of births and deaths. Available infor
mation with the RGI’s office indicates that till the
mid 1990s, over 90 per cent of all births and deaths
are registered in states like Kerala, Tamil Nadu,
Delhi, Punjab and Gujarat. Steps have also been
initiated in these states to collect, collate and report
these data at the PHC/district level on a yearly basis.
These data should be used at the district-level for
PHC-based planning of RCH care as well as
evaluation of the coverage and impact. In districts
where vital registration is over 70 per cent, efforts
are being stepped up to ensure that over 90 per
cent of births and deaths are reported so that an
independent data base is available for planning as
well as impact evaluation of PHC-based RCH care.
The goal of 100 per cent registration of births and
deaths is expected to be achieved by the end of
the Tenth Plan.
At Birth
essential new born care.
weighing at birth and referring pre-term
babies and neonates weighing less than 2.2
kg to institutions where a paediatrician is
available.
Nutrition Interventions
H
El
El
E
E
promote exclusive breast-feeding upto six
months.
introduce semi-solid supplements in the sixth
month.
screen all children to identify those with severe
grades of under-nutrition and treat them.
administer massive dose of vitamin A
supplements according to schedule.
administer iron-folate supplements, if needed.
Health Care for Adolescents
Health interventions
E
E
universal immunisation against the six vaccine
preventable diseases.
early detection and management of ARI/
diarrhoea.
Use of District-wise Data Generated by CRS for
Planning and Monitoring the National Family
Welfare Programme
2.10.101 There are huge inter-state and inter-district
variations in the access to health care and health
indices of women and children. During the Tenth
Plan, efforts are being made to rapidly improve the
health indices by increasing the availability and
utilisation of health care facilities. In order to respond
to the changing needs at district level the
Department of Family Welfare has introduced
decentralised district- based planning and pro
gramme implementation, based on district-wise
indicators. The data base needed for this can be
made available in a sustained fashion only through
197
2.10.103 The 1990s witnessed a rapid increase
in the adolescent population, a trend that will
continue over the next two decades. Under the
RCH programme an effort was made to address
Ninth Plan strategy for adolescent health care
E Efforts to educate the girl, her parents and
the community on the need to delay
marriage.
E Programmes for the early detection and
effective management of nutritional
(under-nutrition, anaemia) and health
(infections, menstrual disorders) problems
in adolescent girls.
E Appropriate antenatal care
adolescent pregnant girls.
to high risk
Inter-sectoral coordination between RCH and
KSY programmes is being strengthened in
blocks where ICDS centres have an adolescent
care programme.
TENTH FIVE YEAR PLAN 2002-07
'Women Aged 20-2^ Years who married below age I B
Figure
an -------- ------- ----------------------------------------------------------....
BO
K
I". 7T
lJ. L_J1.
I
-
“
t r-... I
____________ g £ ? * n
40
2-0
!■
id
0
Z
n
L_
I
B.
I
i xI 1I
I f
5
some of the the health care needs of adolescents.
The Department of Women and Child Development
has initiated the Kishori Shakti Yojana (KSY) in
selected blocks. Specialized counselling and IEC
material to be provided through NGOs, is being
prepared. However, coverage under all these
programmes has been very low.
cycle of under-nutrition an ill health. Appropriate
nutrition and health education, for all adolescents,
advocacy for delay in age at marriage, optimum
health and nutrition interventions during pregnancy
in adolescents are some of the inter-sectoral
initiatives to break this vicious cycle.
2.10.104 Data from NFH8 2 indicate that median
age at marriage of girls in India is 16 years and 61
per cent of all girls were married before they were
18 years. The mean age at first birth is 19.2 years.
There are massive inter-state differences in
proportion of girls who got married before 18 years
(Figure2.10.36). Under-nutrition, anaemia and poor
antenatal care lead not only to increased morbidity
in the mother but also to high incidence of low birth
weight and perinatal mortality. Poor child-rearing
practices add to the morbidity and under-nutrition
in infants, thus perpetuating the inter-generational
2.10.105 In view of the high prevalence of teenage
marriages, in depth investigations have been carried
out to document the adverse consequences, of
teenage conception in the Indian setting. Data from
Indian studies indicate that pregnancy in the early
teens before 16 years is associated with an adverse
effect on maternal nutrition, birth weight and survival
of the offspring. The extra nutritional requirements
of pregnancy coming close after the nutritional
requirements for adolescent growth spurt might be
the major factor responsible for the observed poor
nutritional status of girls who conceived before they
are 16 years of age.
Figyre 2.10.37. Effect of Age and Parity on
Ne-Gnatal Mortality
Figures. 10.3B Effect of Age and Parity on
Perinatal Mortality
h
03
1 i(». §
■
Lf ’_____
____________ _
-
|
7
i HEiL
30 ■ -
2’i
j CTk
tn -
&1Dr**r.> ?
^83
tSparr/ ** 5?n;
I iUj
Pi-^r,r?:88g
---
QQ
I iKi
J. >ii-
iiJl
FAMILY WELFARE
Nutrition
FigoFB2„10.3& Effect of Age and Parity an
Infant Mortality
2.10.108 The importance of maternal nutrition in
determining obstetric outcomes and child nutrition
as a determinant of the survival and health of child
ren is well known. The current status and proposed
interventions for improving maternal and child
nutrition are dealt with in the section under Nutrition.
t- 2541 y—«
| 2 C€ 4—
i
g
I
-|—
-
SG -
.AWj a r
16^.19
28.24
29-29
? jk)
RTI and STI
; j’
Prsma 19?^
2.10.106 Lower maternal body weight, lower preg
nancy weight gain, and higher prevalence of anemia
and possibly pregnancy-induced hypertension
among girls who conceived before they were 16
might account for the observed lower mean birth
weight and higher perinatal, neonatal and infant
mortality rate in these groups, both in urban and
rural areas (Figures 2.10.37,38 and 39). The higher
low-birth weight rates, obvious deficiencies in childrearing practices of these young girls, and poor
availability and utilization of health care services,
especially in rural areas, account for the high infant
mortality rates.
2.10.107 Undoubtedly, there is a very urgent
need to create awareness regarding adverse
consequences of early teenage conception and
to mobilize social support for strict implementation
of laws regarding age at marriage. As and when
pregnancies occur in early teenage, these girls
should be considered as a very high-risk group
and provided with adequate nutritional and health
care; their infants should also receive appropriate
health care. The health personnel should be
sensitized to the needs of this very vulnerable
group who are unlikely to seek or utilize available
health care that they urgently require.In addition
to appropriate education to delay age at marriage,
the Tenth Plan will take up nutrition and health
interventions to promote optimum health and
nutrition in adolescent girls. While adolescent
health care will have to be the focus in states
where the age at marriage is increasing, effective
antenatal and intra-partum care will remain the
focus in a majority of the states where teenage
pregnancies are common.
199
2.10.109 It has long been recognised that RTI
and STI are common problems in women in the
reproductive age group. During the last two
decades, there has been resurgence of interest
in the detection and management of RTI/STI.
This is partly because clinicians have access to
accurate tests for aetiological diagnosis and, are
in a position to provide prompt, appropriate treat
ment for many RTIs/STIs and prevent the long
term health consequences of these infections.
The other reasons for the increased focus on RTI/
STI are:
El doctors are seeing a large number of patients
belonging to a wider spectrum of age
(adolescents, women in the reproductive age
group and elderly women), and socio-economic
strata seeking care for RTI;
E with the availability of antibiotics for treatment
of RTI/STI and contraceptives for preventing
pregnancy, there has been an increasing
prevalence of multi-partner sex and an
inevitable increase in RTI/STI;
E
in spite of the increasing availability of specific
tests for diagnosis and efforts to prescribe
appropriate antibiotics, antibiotic resistance is
increasing, leading to poor response to therapy
and recurrence of infection; and
E
available data from research studies suggest
that the risk of transmission of HIV infection is
increased by RTI.
2.10.110 The importance of prevention, early
detection and treatment of RTI/STI is well-recog
nised. Reliable, easy-to-perform tests for accurate
diagnosis are readily available. Most of the
TENTH FIVE YEAR PLAN 2002-07
infections still respond to commonly-used antibiotics
and chemotherapeutic agents. The management
of common lower reproductive tract infection has
been included as a component of RCH care; these
services are to be provided through the existing
primary health care infrastructure. The Department
of Family Welfare has provided the necessary drugs
and funds to fill gaps in laboratory technician in
PHCs/CHCs. However, the training of health care
personnel in RTI diagnosis and management has
been inadequate in most states. The Department
of Family Welfare has coordinated its efforts with
the National AIDS Control Organisation (NACO) so
that the latter provides the input for diagnosis and
management of RTI/STI at the district level and
above.
2.10.111 It is important to recognise that there are
problems in the current programmes for manage
ment of RTI. The Piot and Fransen model of RTI/
STI management graphically sums up the problems
in treatment of RTI. (Figure 2.10.40.). The model
shows that about 40 per cent of women have
RTI/STI at any given time but only 1 per cent
complete full treatment of both partners even under
optimal conditions. It is, therefore, hardly surprising
that in spite of all the current efforts to improve
treatment of RTI/STI patients, gynaecologists and
public health professionals feel that there has not
been any substantial improvement in the situation
over the last decade. However, it is important to
persist with health education, providing ready
access to diagnostic facilities and appropriate
treatment.
Figure 2,10.40 Prablems m
of RTI in Women
Hoi-rransen Model
Treatment
Con-Chance
Treat cmesify
Go Io health uni,
Seek Tr®£S>.n-<er.5
-------------------1
SytwIrniattK
Wamen with RTI
——
Q
Pkrt - UN AIDS
40
BO
P&rr^l
S2
i®
200
Infertility
2.10.112 It is estimated that between 5 and 10
per cent of couples are infertile. While provision of
contraceptive advice and care to all couples in the
reproductive age group is important, it is equally
essential that couples who do not have children
have access to essential clinical examination,
investigation, management and counseling. The
focus at the CHC level will be to identify infertile
couples and undertake clinical examination to
detect the obvious causes of infertility, carry out
preliminary investigations such as sperm count,
diagnostic curettage and tubal patency testing.
Depending upon the findings, the couples may then
be referred to centres with appropriate facilities for
diagnosis and management. By carrying out simple
diagnostic procedures at the primary health care
institutions, it is possible to reduce the number of
couples requiring referral. Initial screening at the
primary health care level and subsequent referral
is a cost-effective method for the management of
infertility both for the health care system and for
those requiring such services.
Gynaecological Disorders
2.10.113 Women suffer from a variety of
common gynaecological problems including
menstrual dysfunctions at peri-menarchal and
peri-menopausal age. Prolapse uterus of varying
degrees is yet another major problem in parous
women. Facilities for diagnosis of these are
available at district hospitals or tertiary care
centres. During the Tenth Plan period, the CHCs
with a gynaecologist will start providing requisite
diagnostic and curative services. The PHCs and
CHCs will refer women requiring surgery to
district hospitals or tertiary care centres. Cervical
cancer is one of the most common malignancies
in India accounting for over one-third of all
malignancies in women. It can readily be
diagnosed at the PHCs and CHCs. Early
diagnosis of Stage I and Stage II and referral to
places where radiotherapy is available will result
in rapid decline in the morbidity and mortality
associated with cancer cervix in the near future.
FAMILY WELFARE
Access to RCH Services
Logistic Support
2.10.114 Data from research studies and clinical
experience shows that social and economic depri
vation lead to poor health outcomes. Poor health,
in turn, results in deterioration of economic status
partly due to loss of wages and partly due to cost
of health care. Specific efforts have been made
to focus on health and nutrition interventions so
that the vulnerable segments of the population
have better access to health and nutrition
services and the vicious circle of poverty and ill
health is broken. However, in spite of efforts over
the last 50 years, better access to public health
services continues to elude the poor, whose
health care needs are the greatest. While this is
true in all states, RHS data brings out some
interesting inter-state comparisons. The poorest
quintile in Tamil Nadu have better immunisation
coverage rates than the richest quintile in Uttar
Pradesh suggesting that socio-economic barriers
can be overcome through improved awareness
and access (Figures 2.10.41 and 2.10.42).
Ninth Plan strategy
Improve uninterrupted supply of essential drugs,
devices, vaccines and contraceptives, adequate
in quantity and appropriate in quality.
2.10.116 Under the Family Welfare program the
central government procures and supplies drugs,
equipment kits, contraceptives and vaccines to the
states. While the drug kits are supplied at district
level, vaccines and contraceptives are supplied at
the state or regional level. The states have, so far,
not created any specialised or dedicated system
for receiving such supplies, storing them in accep
table conditions and distributing them. As a result,
there are delays, deterioration in the quality and
wastage of drugs. Supplies under the family welfare
programme are to the tune of Rs. 500 crore and it
is estimated that the losses due to deterioration
and inefficiencies may be to the extent of 20 to 30
per cent.
2.10.115 During the Tenth Plan, every effort will
be made to improve access to essential primary
health care, family welfare services and diseases
control programmes totally free of cost. The Centre
and the states are evolving and evaluating various
options for reducing the financial burden of
hospitalisation on the poor.
2.10.117 The Department of Family Welfare, in
collaboration with different external funding
agencies working in different states, has formulated
logistic projects for each of the major states. It
envisaged that a specialised agency will be created
in each state which will manage warehouses at the
regional level for each cluster of five to eight districts.
These warehouses will receive an indent from each
hospital in the area and will ensure delivery of
10.411m mu n isation
Coverage-Tamil Nadu
Figure 2... 10.42 Immunisation
Coverage-Uttar Pradesh
10^
■M-
Ml mm
S
a
h
..
I
<0^
■■
1*
[
u
......
Pea ms I.
hexi
Next
u
b
a
40%
20%
&%
Richest
•Peered
20%
.• J -
® Partial
ilJiI lilt
J!
60^ J
3
a ext
Scwre RUS 9^99
rnid- 20SRill
201
next
Partial
31 Msre
——
Gn Oxy - 30
08648
p0<\
5
TENTH FIVE YEAR PLAN 2002-07
supplies within 15 days through a contracted trans
porter. To ensure efficiency, the state government
agency will be paid only on the basis of a per
centage of supplies it handles. The logistics project
has already been initiated in some states.
2.10.118 During the Tenth Plan, efforts will be
made to ensure that facilities which are being
created , handle all the drugs/vaccine/devices
provided by the central government and state
governments for all health care institutions. The
progress of this programme and the problem
encountered will be monitored and appropriate mid
course corrections initiated.
Private Sector Participation in RCH
2.10.119 Over 80 per cent of the practitioners of
modern medicine and a higher proportion of the
ISM&H practitioners work in the private sector. It is
estimated that while the private sector provides
more than three-fourths of all curative health care
services, its contribution to maternal and child health
and family planning services is less than one-third.
The major limitations in private sector participation
include:
Role of NGOs/Voluntary Organisations in the
Family Welfare Programme
2.10.121 The National Population Policy 2000
envisages increasing role of NGOs/voluntary
organisations in building up awareness about and
advocacy for RCH interventions and also in impro
ving community participation. Until recently, only a
small number of NGOs were getting funding from
the Department of Family Welfare, because a
majority of them did not have adequate technical
knowledge and the skills required. In an attempt to
increase NGOs participation, the Department
involved several well-established NGOs such as the
Family Planning Association of India and Voluntary
Health Association of India in selecting, training,
assisting and monitoring of smaller, field-level NGOs
for carrying out the following functions:
E
advocacy for maternal child health inter
ventions;
E
promotion of small healthy family;
E
improving community participation;
E
counselling and motivating adolescents to
delay the age at marriage, young couples to
delay first pregnancy and couples with two
children to limit their families by the use of
appropriate contraceptive methods;
E
act as a link between the community and health
care providers.
[XJ the focus till now has been mainly on curative
services;
El the quality of services is often variable; and
E) the poorer sections of population cannot afford
to pay for these services.
2.10.120 Under the RCH programme, several
initiatives were taken to improve collaboration
between the public and private sectors in providing
family welfare services to the poorer sections,
especially in the under-served areas. Efforts were
made to increase the involvement of private medical
practitioners in RCH care by providing them orien
tation training and ensuring that they have ready
access to contraceptives, drugs and vaccines free
of cost. These efforts will be augmented during the
Tenth Plan. The private sector has immense
potential for improving the coverage and quality of
RCH services. The challenge is to find ways to
optimally utilise this potential.
202
2.10.122 Currently, the Department of Family
Welfare funds 97 mother NGOs(larger NGOs
looking after smaller ones) covering 412 districts
and over 800 NGOs. These NGOs cover all districts
in ten states. However, states with high fertility and
mortality rates still have a large number of districts
without any NGO presence.The state governments
have also been trying to involve NGOs in providing
services, or by adopting a PHC. The results have
been mixed; these experiments need to be carefully
monitored.
2.10.123 During the Tenth Plan, NGOs will have
a major role in promoting community participation
in the following areas:
FAMILY WELFARE
El gender sensitivity and advocacy regarding
providing adequate care for the girl child;
El
baby-friendly hospital initiatives and promotion
of exclusive breast-feeding for six months;
advocacy for the introduction of semi-solids at
the right time;
E social marketing of contraceptives, ensuring
easy availability of ORS/social marketing of
ORS;
E
sensitising the community regarding the
adverse consequences of sex determination
and sex selective abortions.
2.10.124 The Department of Family Welfare has
also proposed that the NGOs who have adequate
expertise and experience may participate in RCH
service delivery. The interventions undertaken by
the NGOs will be independently assessed at the
end of the project period; funding will be dependent
upon mid-term evaluation based on specific bench
marks. Efforts will be made to improve networking
between the NGOs, state/district administration as
well as PRIs.
2.10.126 The labour force in the organised and
unorganised sector and their families require cover
age in order to achieve rapid improvement in health
and demographic indices. Trade unions can expand
their role to address the health care needs of wor
kers and their families. During the Ninth Plan period,
family welfare projects have been undertaken in the
unorganised and semi-organised sectors in Tamil
Nadu, plantation workers in West Bengal, beedi
workers in Uttar Pradesh, and milk producers in
Gujarat. The lessons learnt from these projects will
be utilisied to improve access to family welfare
services.
2.10.127 During the Tenth Plan, attempts will be
made to enhance the quality and coverage of family
welfare services through the involvement and
participation of the organised and unorganised
sectors of industry, agriculture and labour represen
tatives. The problem-solving approach of the
corporate sector can be used to improve the
operational efficiency of the health care services.
Initiatives to Address the Needs of Under-served
Population
Role of Industries and other Organisations
2.10.125 Governmental efforts alone will not be
sufficient to achieve the desired goals of the family
welfare programme. The organised industrial sector
provides health/family welfare services to about 14
per cent of the country’s population. Industry can
improve acceptance of family welfare services by
educating, motivating workers and improving
access to services. Industries which provide health
care to their personnel and their families can extend
these facilities to the people living in the vicinity of
factories, especially when they are located in under
served semi-urban and rural areas. They may take
up an area-specific approach to improve services
available in a block by adopting it. Smaller industries
could form a cooperative group for providing health
and family welfare services in collaboration with the
government. Managerial and other skills available
in industry can be made available to improve the
efficiency of the government infrastructure. The
marketing skills of industry may be useful in
improving the I EC and motivation activities and in
social marketing.
203
2.10.128 Access to health care is poorer in states
like Uttar Pradesh, Madhya Pradesh, Bihar and
Rajasthan. The Empowered Action Group (EAG)
constituted by the Department of Family Welfare in
2001 reviews the available infrastructure,
performance of the health system and health indices
and suggests steps for improving access to health
care so that there is a rapid decline in fertility and
mortality. During the Tenth Plan, special efforts will
be made to upgrade the capacity of the health
system in these states/districts so that there is rapid
decline in both fertility and mortality. This is an
essential step if the ambitious goals for decline in
fertility and mortality set in the National Population
Policy are to be achieved because these states
contribute to over 50 per cent of the country’s
mortality and fertility.
2.10.129 The tribal population (except in the
north-eastern states) faces immense problems in
accessing essential health care services and have
poor health indices. The Department of Family
Welfare has already initiated several programmes
TENTH FIVE YEAR PLAN 2002-07
focusing on meeting the health care needs of the
tribal population. These will be continued during the
Tenth Plan. Special efforts will be made to address
the health needs through area-specific programmes
and increasing the involvement of NGOs and the
tribal community in all activities.
2.10.130 The urban slum population has been
shown to have poor maternal and child health
indices. In many slums, immunisation coverage is
very low and children are undernourished. The
Department of Family Welfare and the Department
of Health have been investing in improving urban
primary health care infrastructure and ensuring that
they are linked to existing secondary and tertiary
care institutions. The India Population Project (IPP)
V, VIII and Urban RCH Pilot Projects have built up
the capacities of the urban health system in several
cities. Efforts to rationalise urban health care and
improve efficiency so that reproductive care needs
of urban population are fully met within the available
infrastructure will be continued during the Tenth Plan
period.
Strategies for Increasing Efficiency
2.10.131 A vast infrastructure for the delivery of
health and family welfare services has been created
over the last three decades based on uniform
norms for the entire country. Evaluation studies
have shown that they are functioning poorly
because of:
H
mismatch between structure and function;
El
lack of training to health care personnel to
update their knowledge, skills and programme
orientation;
E absence of a proper medical hierarchy with
well-defined functions;
E
lack of first line supervision and mechanism to
bring about accountability;
E absence of a referral system and lack of
functional FRUs.
All the states have initiated health sector reforms
aimed at improving the functional status of the health
system, These are discussed in the chapter on
Health.
204
2.10.132 Under the RCH programme, the Depart
ment of Family Welfare has invested heavily in
training programme managers in managerial
aspects for the effective implementation of the
programme including decentralised district-based
planning, implementation, monitoring and mid
course corrections. Skill upgradation of all cate
gories of health care professionals and para
professionals is envisaged for improving the quality
of screening and management of persons with
complications, including referral as and when
required. It is expected that the training programme
will be completed soon and will promote effective
functioning of the infrastructure and improve
efficiency. These efforts will continue during the
Tenth Plan period.
2.10.133 Though all states have shown some
improvement in access to health care and in
health and demographic indices, the rate of
change has been very slow in some states.
Efforts during the Ninth Plan to provide more
funds to these states to upgrade infrastructure
and manpower, and making schemes more
flexible to enable private and voluntary sector
participation has not been effective in improving
access to services. During the Tenth Plan, efforts
will be made to improve efficiency by undertaking
task analysis, assigning appropriate duties/tasks
to designated functionaries and training them to
act as a multi-professional team. The first link in
such a chain will be the village-based workers
who will liaise between the people and health
functionaries and ensure utilisation of available
facilities. The PRIs will participate in the planning
of programmes and assist in the implementation
and monitoring. The ANM will administer
vaccines, screen infants, children and pregnant
women, identify and refer the at-risk persons to
appropriate institutions. The medical officer at
the PHC will undertake PHC-based planning and
monitoring of the health and family welfare
programmes and provide curative services,
organise and supervise preventive and promotive
health and family welfare-related activities and
develop a viable, functional referral systems. The
specialists in the CHCs will provide appropriate
emergency care and care for referred patients,
FAMILY WELFARE
participate in the development of the CHC-based
RCH programmes, monitor the activities and
initiate mid-course corrections. If this pattern of
functioning is followed, the community, the link
worker and the health functionaries will be
performing the tasks that they are best suited for
and the implementation of the programme will
improve.
Involvement of PRI in Family Welfare
Programme
2.10.134 There are immense differences between
states in the involvement of PRIs in the Family
Welfare Programme. States like Kerala have
embarked on decentralised planning and monitoring
programmes utilising PRIs and have devolved
powers and finances to PRIs. Rajasthan, Andhra
Pradesh and Haryana have implemented their own
models for the involvement of the PRIs in the health
sector. In other states, the involvement is mainly in
planning and monitoring without devolution of power
and finances. In some states, the PRIs have not
yet started participating in the programme. There
is a need to continuously review the situation and
initiate appropriate interventions.
The Ninth Plan envisaged the involvement
of PRIs for:
El
Ensuring inter-sectoral coordination and
community participation in planning,
monitoring and management of the RCH
programme.
Assisting
states in supervising the
functioning of the health care related
personnel including ANM, MMPW and
AWW.
2.10.135 The real challenge of the Family
Welfare Programme lies in effectively delivering
the needed services in the remote and
inaccessible areas where the services provided
by the government machinery are the weakest and
the private sector and NGOs are non-existent.
During the Tenth Plan, it is envisaged that mature
PRIs with intelligent, service-oriented members will
play a key role in making the programme a
people’s programme and improving access to its
services. The health committee of the gram
panchayat can plan locally, identify area-specific
unmet needs for reproductive health services and
ensure that efforts are made to meet them. It can
also be entrusted with the task of monitoring the
attendance and performance of health care
personnel. The PRIs can play a vital role in
programme advocacy and monitoring the
availability, accessibility and quality of services in
government PHCs, NGOs and private practitioners
and the cost of services provided by the latter.
The PRIs will have the advance tour programmes
of the ANM and male multipurpose worker and
lists of nearest functioning PHCs with a doctor,
nearest FRU/CHC with a peadiatrician,
obstetrician, surgeon or physician where persons
with complications and those requiring emergency
care could be referred. They will monitor the
funding of emergency transport provision as well
as dispersal of funds under the Balika Samridhi
Yojana and the Maternity Benefit Scheme. The
active role and supervision of the PRIs is also
crucial for ensuring 100 per cent registration of
births, deaths, marriages and pregnancies at the
village level.
Intersectoral Coordination
2.10.136 Inter-sectoral coordination, especially
between the Departments of Health, Department
of ISM&H, Women and Child Development, Human
Resource Development, Rural Development, Urban
Development, Labour, Railways, Industry and
Agriculture is critical for increasing the coverage of
the Family Welfare Programme and improving
implementation. Some of the areas where inter
sectoral coordination is envisaged during the Tenth
Plan include:
IS Ensuring coordination of activities of
workers of different departments such as
health, family welfare, ICDS, social welfare
and education etc. functioning at the
village, block and district levels.
Improving the acceptance of the Family
Welfare Programme through increased
community participation.
205
TENTH FIVE YEAR PLAN 2002-07
E
E
E
involvement of the extension workers of these
departments in propagating IEC messages
pertaining to reproductive and child health care
to the population with whom they work;
efforts to improve the status of the girl child
and women, improving female literacy and
employment, raising the age at marriage,
generating more income in rural areas,
improving nutritional status of women and
children;
coordination among village-level functionaries
-anganwadi workers, TBAs, Mahila Swasthaya
Sangh, Krishi Vigyan Kendra volunteers and
school teachers - to achieve optimal utilisation
of available services.
2.10.137 Suggested areas of convergence of
services with Department of Education include:
E
inclusion of educational material relating to
health, nutrition and population in the
curriculum for formal and non-formal
education;
E
involvement of all zilla saksharata samitis in
IEC activities pertaining to the RCH
programme;
E
involving school teachers and children in Class
V and above in growth monitoring,
immunisation and related activities in the village
at least once a month as a part of socially useful
productive work.
2.10.138 Convergence of services with the Depart
ment of Women and Child Development include :
El
involvement of anganwadi workers in the
compilation of births and deaths and the
identification of pregnant women;
E
involving anganwadi workers in weighing
babies as soon as possible after delivery and
referring neonates with weight below 2.2 kg to
centres where a paediatrician is available;
IHj
utilising the services of the anganwadi worker
in improving the coverage of Massive Dose
Vitamin A in children when they are 18 months,
24 months, 30 month and 36 months of age
206
and improving the compliance among pregnant
women under iron-folic acid medication;
E
identification of undernourished pregnant and
lactating women and pre-school children to
ensure that they get priority in food
supplementation programmes under the ICDS
and appropriate health care from ANMs and
doctors;
promoting the cultivation of adequate quantities
of green leafy vegetables, herbs and
condiments in coordination with the PRIs and
agricultural extension workers and ensuring
that these are supplied to anganwadis on a
regular basis to improve micro-nutrient content
of food supplements.
2.10.139 The anganwadi worker can assist the
ANM in organising health check ups of women and
children and immunisation in the anganwadi. She
will act as depot holder for iron and folic acids
tablets, ORS, condoms and disposable delivery kits.
She will be provided with a list indicating the nearest
facility to which women and children could be
referred so that she can help in organising emer
gency referral. Intersectoral co-ordination with
Department of Health and Department of ISM & H
are discussed under respective chapters, co
ordination with Department of Women and Child
Development for improving nutritional status are in
the chapter of Food and Nutrition Security.
Research and Development
2.10.140 The ICMR is the nodal research agency
for funding basic, clinical and operational research
in contraception and maternal and child health. In
addition, the Council for Scientific and Industrial
Research (CSIR), Delhi, Department of Biotech
nology (DBT) and the Department of Science and
Technology (DST) fund research pertaining to the
Family Welfare Programme. The National Com
mittee for Research in Human Reproduction under
the Chairmanship of the Secretary, Department of
Family Welfare assists in drawing up priority areas
of research and ensuring that there is no unneces
sary duplication of research activities. Some of the
FAMILY WELFARE
major institutions carrying out research in this area
include the National Institute for Research in Repro
ductive Health, Mumbai, the National Institute of
Nutrition, Hyderabad, the National Institute of
Health and Family Welfare, New Delhi and the
Central Drug Research Institute, Lucknow. The
ICMR undertakes clinical and operational research
studies through a network of Human Reproduction
Research Centres (HRRCs) in medical colleges.
The International Institute of Population Studies,
Mumbai, and a network of 18 Population Research
Centres conduct studies on different aspects of the
Family Welfare Programme and undertake
demographic surveys.
2.10.141 Under the RCH programme the Depart
ment of Family Welfare has constituted an expert
committee for research in reproductive health and
contraceptions under modern system of medicine
and ISM&H to examine and recommend proposals
that require funding. In addition, the Department is
making efforts for the creation and support of an
appropriate institutional mechanism to test and
ensure the quality of products utilised in the
programme.
2.10.142 Priority areas of research during the
Tenth Plan are:
E
diagnosis and management of RTI/STI;
E
development of newer technology for
contraceptive drugs and devices in modern
system of medicines, including immunological
methods for fertility regulation;
O
examining the safety and efficacy of ISM&H
products;
identification and characterisation of genes/
gene products and detailing their functional role
in reproduction and health of women and
children;
E development and testing of new drug delivery
systems for contraceptive steroids;
E
I
safety and efficacy studies on newer
vaso-occlusive methods, spermicides based
on plant products such as neem oil and
saponins and other plant-based substances;
207
innovative methods for improving neonatal care
at the primary health care level, including
assessment of simple methods for the
diagnosis and management of sepsis, asphyxia
and hypothermia in new born babies;
studies on the prevention, detection and
management of infections in children; and
E early detection and management of obstetric
problems.
Demographic/Operational Research
ongoing demographic transition and its
consequences;
E continuation rates and effectiveness of
contraceptives under actual programme
conditions;
El
operational research to provide integrated
delivery of health, nutrition and family welfare
services at the village level through the existing
infrastructure and manpower;
El
testing of the relationship between couple
protection rate and CBR and between the
reduction of IMR and reduction in birth rate in
states in different levels of demographic
transition;
H
improving access to safe abortion services;
Basic and Clinical Research
E
clinical studies on the use of emergency
contraception and non-surgical methods of
MTP;
research aimed at detection, prevention and
management of RTI/STI in different levels of
health care; and
O socio-behavioural research to improve
community participation in increased utilisation
of family welfare services;
Monitoring and Evaluation
2.10.143 The recommendation of NDC Sub
committee on Population for the creation of district-
TENTH FIVE YEAR PLAN 2002-07
level databases on quality, coverage and impact
indicators for monitoring the programme was
implemented during the Ninth Plan period. The
following systems are being used for monitoring and
evaluation of programmes in the Family Welfare
Programme:
M
reports from state and implementation
agencies;
O
Sample Registration System and Population
Census;
H
Rapid Household Surveys;
H
large-scale surveys - NFHS, sample surveys
by the NSSO and area-specific surveys by the
Population Research Centres;
other specific surveys by national and
international agencies.
2.10.144 The Department of Family Welfare has
constituted regional evaluation teams which carry
out regular verifications and validate the data on
the acceptance of various contraceptives. These
evaluation teams can be used to obtain vital data
on failure rates, continuation rates and compli
cations associated with different family planning
methods. RHS data about the progress on progra
mme interventions as well as its impact are being
used to identify district-specific problems and rectify
them. To assess the availability and the utilisation
of facilities in various health institutions, facility
surveys were conducted in 101 districts during
1998-99 and deficiencies found are being brought
to the notice of the states and districts concerned.
The format for monitoring the process and quality
indicators under the RCH programme have been
developed and sent to all the states. These may
be operationalised during the Tenth Plan and the
information generated used for mid-course
corrections.
2.10.145 The substantial investments made in
evaluation during the 1990s have increased
awareness about the need for concurrent impact
evaluation. During the Tenth Plan, efforts will be
made to consolidate the gain by putting in place a
sustainable system of evaluation at the district level
208
in the form of CRS and district surveys. Efforts will
also be made to reduce duplication of efforts through
appropriate intersectoral coordination .
Reorganisation of Family Welfare Infrastructure
2.10.146 When the Family Welfare Programme
was initiated in the early 1970s the infrastructure
for providing maternal and child health and family
planning services was inadequate at the primary
health care level, and sub-optimal in the secondary
and tertiary care levels. In order to quickly improve
the situation, the Department of Family Welfare
created and funded post-partum centres, urban
family welfare centres/ health posts and provided
additional staff to the then existing PHCs (block level
PHC’s). In addition, the ANMs in the sub-centres,
created after the initiation of the Family Welfare
Programme, were also funded by the Department.
The Department of Family Welfare also created
state and district level infrastructure for carrying out
the programmes and set up training institutions for
pre/in-service training of personnel. All these
activities were being funded through Plan funds.
2.10.147 Over the last three decades, there has
been considerable expansion and strengthening of
the health care infrastructure by the State. Family
welfare services are now an integral part of services
provided by primary, secondary and tertiary care
institutions. The staff funded by the Department of
Family Welfare under the scheme of rural family
welfare centres and post partum centres are state
health services personnel functioning as part of the
state infrastructure. In view of this, the Ninth Plan
recommended that their funding should be taken
over by the state department of Health. States will
take over the responsibility of funding staff of post
partum centres and rural family welfare centres from
1st April 2002.
2.10.148 Since ANMs are crucial for increasing the
outreach of the programme, it is important to ensure
that the posts of ANMs are filled and steps taken to
ensure that they are available and perform the
duties they are assigned. One of the major problems
with respect to the ANMs is that while the
Department of Family Welfare funded over 97,000
FAMILY WELFARE
posts, about 40,000 were funded by the state (from
non-Plan). The Ninth Plan recommended that this
dichotomy in funding should be removed and all
the ANMs, as per the norms for the 1991 population
should be funded by the Department of Family
Welfare. This has been done from 1st April 2002.
It is expected that this would ensure that the states
do employ the required number of ANMs, streamline
their functioning and improve the coverage, content
and quality of maternal and child health care.
maternal health, child health and nutrition were
identified as specific schemes. After this, a zero
based budgeting effort was taken up and schemes
were identified for convergence, weeding out and
transfer to the states. The summary of the zero
based budgeting exercise is given in the Table2.10.11. The scheme- wise outlays and anticipated
expenditure during the Ninth Plan are given in
Annexure-2.10.2. Yearwise outlay, R.E., and actual
expenditure for the Ninth Plan is given in Table
Zero Based Budgeting
Path Ahead and Goals Set
2.10.149 In the past, the Family Welfare Pro
gramme has been considered as a single centrally
sponsored scheme. As a result, the heads of funding
were functional viz. Personnel, Services, Supplies,
Transport, Area Development etc. All ongoing
programmes including maternal and child health and
immunisation, received inputs from these functional
heads. In the Ninth Plan, major projects like RCH,
pulse polio immunisation and strengthening of
routine immunisation were added as schemes with
large outlays. The Planning Commission and the
Department of Family Welfare carried out an
exercise to rationalize the schemes. A revised
scheme-wise listing was evolved where, schemes
for strengthening of infrastructure, area
development project, training, research, programme
related activities for contraception, immuninsation,
2.10.150
Reduction in fertility, mortality and
population growth rate are major objectives of the
Tenth Plan. These will be achieved through meeting
all the felt needs for health care of women and
children. The focus will be on improving access to
services to meet the health care needs of women
and children by:
2.10.12.
a decentralised area-specific approach to
planning, implementation and monitoring of the
performance and effective mid-course
corrections;
differential strategy to achieve incremental
improvement in performance in all states/
districts;
special efforts to improve access to and
utilisation of the services in states/districts with
high mortality and/or fertility rates;
Table-2.10.11
Zero Based Budgeting 2001
Outlay for
Ninth Plan
(Rs. crore)
Anticipated
expenditure during
Ninth Plan (Rs. Crore)
3
2,080.00
2,198.00
11/40
7,640.20
7,398.39
Schemes to be weeded out
8
185.85
31.25
Schemes to be retained
43
5,213.95
4,961.33
Total
94
15,120.00
14,588.97
Total No. of schemes to be continued in the Tenth Plan
54
12,854.15
12,359.72
No. of
Schemes
Category
Schemes to be transferred to the states
Schemes to be merged and retained
209
TENTH FIVE YEAR PLAN 2002-07
Table2.10.12
Outlays, RE and expenditure during the Ninth Plan
(Rs in Crores)
Year
B.E.
R.E.
Actual Expenditure
1997-98
1829.35
1829.35
1822.00
1998-99
2489.35
2253.00
2342.75
1999- 2000
2920.00
3120.00
3099.76
2000- 01
3520.00
3200.00
3090.11
2001-02
4210.00
3700.00
3596.63
Total
14968.70
14102.35
13951.25
H filling the critical gaps, especially in CHCs, in
existing infrastructure through appropriate
reorganisation and restructuring of the primary
health care infrastructure;
H ensuring that post of specialists in CHCs do
not remain vacant; upgrading skills and
redeploying existing manpower to fill other
critical gaps;
ISl streamlining the functioning of the primary
health care system in urban and rural areas;
providing good quality integrated RCH services
at the primary, secondary and tertiary care
levels and improving referral services;
El providing adequate supply of essential drugs,
diagnostics and vaccines; improving the
logistics of supply;
El well coordinated activities for delivery of
services by public, private and voluntary
sectors to improve coverage;
E involvement of PRIs in planning, monitoring
and mid-course correction of the programme
at the local level;
El involvement of industry in the organised and
unorganised sectors, agriculture workers and
labour representatives in improving access to
RCH services;
E effective use of social marketing to improve
access to simple over the counter (OTC)
products such as ORT and condoms;
E effective IEC and motivation programmes;
and
E effective inter-sectoral coordination.
210
2.10.151
Tenth Plan envisages reduction in
IMR to 45 /1,000 by 2007 and 28/1,000 by 2012,
reduction in MMR to 2/1000 live births by 2007
and 1/1,000 live births by 2012 and reduction in
decadal growth rate of the population between
2001-2011 to16.2. The steep reduction in
mortality and fertility envisaged are technically
feasible within the existing infrastructure and
manpower as has been demonstrated in several
states/districts. It is imperative that the goals set
are achieved within the time frame as these goals
are essential prerequisites for improving the
quality of life and human development. In view
of the massive differences in the availability and
utilsation of health services and health indices of
the population, a differential strategy is envisaged
so that there is incremental improvement in all
districts. This, in turn, is expected to result in
substantial improvement in state and national
indices and enable the country to achieve the
goals set for the Tenth Plan. Annexure 2.10.1
provides information of present status (as
indicated by NFHS-2 and SRS) of process and
impact indicators, the goals set for these in the
National Health Policy 1983 (for 2000), Ninth Plan
(for 2002), Tenth Plan and National Population
Policy 2000 (for 2010). Statewise goals have
been shown in Annexure 2.10.3. Tenth Plan
scheme wise outlays for Department of Family
Welfare are in Annexure 2.10.2 and Appendix.
I
FAMILY WELFARE
Annexure 2.10.1
Indicator
Present
Status
NHP-1983
Ninth Plan
Tenth Plan
NPP2000
2000
2002
2007
2010
21
24
21
21
2.85*
2.3
2.9
2.3
2.1
46.2 Dept, of
60
51
65
Meet all
needs
Below
200
300
200
Below
100
35
26
Below 60
56
45
below 30
100
100
Target Year
Crude Birth Rate
Goals
25.8
SRS (2000)
Total Fertility Rate
Couple Protection Rate (%)
F.W. (2000)
Maternal Mortality Ratio
540*
Perinatal Mortality Rate
Neo Natal Mortality Rate
Infant Mortality Rate
30-35
43.4*
68
SRS (2000)
Under five Mortality Rate
94.9*
% immunished against 6 VPD (%)
Measles
DPT
Polio
BCG
42*
51*
55*
63*
72*
85
65
Ante-natal care (ANC)
% at least 3 ANC
% received I FA for 3 or 4 months
% received two doses of TT
43.8*
100
90
90
66.8*
95
100
100
100
100
100
Institutional Deliveries (%)
33.6*
35
80
80
Deliveries by trained
health personnel & TBA (%)
42.3*
100
30
(Estimated)
10
47.5*
Deliveries
Prevalence of low birth weight (%)
* Source: NFHS-2
211
45
100
TENTH AVE YEAR PL/kN 2002-07
Annexure 2.10.2
Outlays for Deptt. of Family Welfare
(Rs. in crore)
Ninth Plan
IX
X
Plan Plan
A
1
Name of Scheme
Approved Outlay
Approved
Outlay
Sum of
Annual
Outlay
Ant. Expdt.
Tenth
Plan
Annual
Plan
2002-03
INFRASTRUCTURE MAINTENANCE
6231.90
6654.85
7506.17
12645.64
2303.00
Rural Family Welfare Centres
1500.00
1600.00
1600.36
1809.00
2
1
Sub-Centres
2200.00
2346.00
2344.60
9663.00
3
2
Urban FW Services
250.00
307.00
305.69
580.00
122.00
4
3
Direction & Administration
671.90
541.00
465.25
1100.00
200.00
Post Partum Centres
530.00
560.00
557.94
5
6
7
Village Health Guides Scheme
50.00
40.00
39.70
4
Logistics Improvement
80.00
51.85
4.84
90.00
10.00
5
Contractual Services/ Consultancies
Included
inRCH
1212.64
162.00
Included
in RCH
8
ANM (Part of Sub-Centres)
9
Additional ANMs/PHNs/Lab. Technicians
10
SM Consultant
11
Aneasthetist
12
Other Exp. (State/National level Consultants/
Contingency)
13
Arrears
950.00
1209.00
2187.79
B
INFRASTRUCTURE DEVELOPMENT
1050.00
1202.35
915.76
2412.00
364.20
14
6
Area Projects (IPP Projects)
800.00
820.00
637.79
987.00
74.80
15
7
Social Marketing Area Projects
82.35
6.42
25.00
10.00
16
8
USAID Assisted Area Project
300.00
271.55
400.00
59.40
17
9
Other Externally Aided Infrastructure
Development Projects
Included
inRCH
EC Assisted SIP Project
Included
inRCH
18 10
250.00
Included
inRCH
Included
in RCH
1000.00
220.00
250.65
C
TRANSPORT
378.00
113.00
19
11
Maintainence of vehicle already available
303.00
98.00
20
12
Supply of Mopeds to ANMs
75.00
15.00
D
TRAINING
257.35
301.28
289.29
521.00
99.60
13
Basic Training for ANM/LHVs
150.00
181.40
182.07
350.00
67.00
Maintenance & Strengthening of HFWTCs
40.00
48.06
46.94
70.00
14.00
35.00
37.90
35.76
50.00
10.00
10.00
2.00
21
22 14
150.0
250.50
23
15
Basic Training for MPWs Worker (Male)
24
16
Strenthening of Basic Training schools
25
17
F.W. Training and Res. Centre, Bombay
5.00
5.00
2.53
10.00
1.50
26
18
NIHFW, New Delhi
21.00
21.35
14.52
20.00
3.15
27
19
UPS, Mumbai
10.00
1.70
5.70
212
6.90
6.83
FAMILY WELFARE
Annexure 2.10.2 (Contd/-)
28
20
Assistance to I.M.A.
0.65
0.67
0.64
1.00
0.25
E
RESEARCH
96.00
107.00
96.58
159.50
30.30
21
Population Research Centres
35.00
33.00
22.47
45.00
8.00
30 22
CDRI, Lucknow
8.00
8.00
8.00
12.00
2.30
31
23
ICMR and IRR
53.00
66.00
66.11
100.00
20.00
32
24
Other Research Projects
2.50
0.00
F
CONTRACEPTION
1541.50
1578.70
1458.35
2727.50
483.50
25
Free distribution of contraceptives
460.00
491.30
436.83
1045.00
184.00
33
Conventional Contraceptives
265.00
310.00
286.20
800.00
34
Oral Contraceptives
80.00
78.40
65.66
130.00
35
IUD
115.00
102.90
84.97
115.00
400.00
428.70
407.40
660.00
29
36
New Methods
26
Social marketing of contraceptives
37
Conventional Contraceptives
360.85
339.04
550.00
38
Oral Contraceptives
67.85
68.36
110.00
680.20
653.80
610.26
1002.00
27
Sterilization
115.00
180.50
39
Sterilization Beds
8.60
8.60
8.79
12.00
40
Sterilsation and IUD insertion
600.00
575.00
534.22
900.00
41
Supply /Procurement of Laparascopes
70.00
68.00
66.75
90.00
42
Recanalization
1.60
2.20
0.50
43 28
Testing Facilities
1.30
1.90
1.24
2.50
0.50
Included
in RCH
3.00
2.62
18.00
3.50
3.00
2.62
8.00
29
Role of Men in Planned Parenthood
44
No Scalpel Vasectomy
45
Other Innovative Schemes (Male Participation)
10.00
G
REPRODUCTIVE & CHILD HEALTH
5150.00
4423.30
3753.49
6333.86
1174.20
30
Immunisation
Included
in RCH
Included
in RCH
Included
in RCH
1410.00
226.00
46
Procurement ofVacccines for Routine
Immunisation
47
Cold Chain
850.00
(a) Cold Chain Maintenance
(b) Cold Chain Equipment
48
Surveillance against VPDs
49
Other Vaccines (Hepatitis B)
35.00
200.00
325.00
50
31
Routine Immunisation Strengthening
Included
in RCH
Included
in RCH
Included
in RCH
17.86
10.00
51
32
Pulse Polio
Included
in RCH
Included
in RCH
Included
in RCH
1450.00
400.00
870.00
580.00
240.00
160.00 |
(a) OPV
(b) Operating cost
213
TENTH FIVE YEAR PLAN 2002-07
Annexure 2.10.2 (Contd/-)
33
52
Child Health
Included
in RCH
Included
in RCH
Essential New Born care (Home based
neonatal care)
53
Diarheal Diseases - Prevention/Treatment
54
ARI-Prevention/T reatment
34
55
56
Included
in RCH
Included
in RCH
Included
in RCH
Included
in RCH
Included
in RCH
Included
in RCH
Vitamin-A Programme
35
Adolescent Health
Included
in RCH
Included
in RCH
Included
in RCH
50.00
3.00
36
Maternal Health
Included
in RCH
Included
in RCH
Included
in RCH
1384.00
254.00
Ante-natal care
58
Nutritional Anaemia (Anaemia
Control & De-worming)
59
Home Delivery Care
60
30.00
(a) Community based midwives
30.00
(b) Dais Training
40.00
Dais Kits (Drugs, Kits & Equipments)
(a) Drug Kits/FRU Drugs/PHC Drugs/RTI Drugs
704.00
350.00
10.00
125.00
20.00
(b) MTP/RTI/STI Equipment/Kit/IUD Kit
(c) Equipment for Blood Storage & Lab. Equipment
(d) Needles & Syringes
(e) Neo-Natal Equipment
61
Promoting Institutional Deliveries
(a) 24 Hour Delivery
25.00
(b) Operationalising FRUs for
Emergency Obs. & NN Care
62 37
50.00
MTP Services (Manual Vac. Aspirator for
safe abortion)
Included
in RCH
Included
in RCH
Included
in RCH
4.00
1.20
38
RTI/ STI prevention and management
Included
in RCH
Included
in RCH
Included
in RCH
35.00
2.00
39
Other RCH Interventions and services
Included
in RCH
Included
in RCH
Included
in RCH
730.00
122.00
64
Referral Transport
65
Out reach Services
66
67
RCH Camps
15.00
130.00
MIS
95.00
350.00
40.00
90.00
Expdt. At Headquarters
10.00
Civil Works
68
69
70
71
1.00
20.00
NUTRITION
57
63
20.00
Research (In RCH Activities)
40
NGOs and SCOVA
Included
in RCH
214
Included
in RCH
Included
in RCH
130.00
22.00
FAMILY WELFARE
Annexure 2.10.2 (Concld/-)
41
Training
Included
in RCH
Included
Included
in RCH
328.00
53.00
72
RCH Training
265.00
73
Training of ISM&H
15.00
74
Training of AWW
48.00
75 42
Tribal Projects
Included
in RCH
Included
in RCH
Included
in RCH
76
43
Urban Slums Projects
Included
in RCH
Included
in RCH
Included
in RCH
700.00
5.00
77
44
District Projects
Included
in RCH
Included
in RCH
Included
in RCH
75.00
75.00
Other Projects under RCH
Included
in RCH
Included
in RCH
Included
in RCH
643.25
450.72
318.68
1900.50
355.90
Transferred
from M/o Rural
Development
80.00
80.00
500.00
90.0
170.00
184.80
160.91
489.50
84.70
78 45
H.
OTHER FAMILY WELFARE PROGRAMMES
79 46
Maternity Benefit Scheme
80 47
Information, Education and Communication
Non-RCH
RCH
81
48
Travel of Experts/Conferences /Meetings etc.
16.10
15.35
2.15
7.00
1.50
82
49
International Contribution
6.30
6.99
6.33
9.00
1.70
83
50
Empowered Action Group
30.00
30.00
250.00
50.00
84
51
Community Incentive Scheme
30.00
5.00
300.00
60.00
85
52
Family Welfare Link Health Insurance Plan
0.01
0.01
250.00
50.00
86 53
PolicySeminars
3.00
3.00
20.00
3.00
54
Other Initiatives
75.00
15.00 !
25.00
0.30
22.00
6.00
27125.00
4930.00
87
88
Strengthening of Rural Family Welfare
Centres under National Human
Development Initiative
265.00
0.03
0.03
Included in
Sub-centres
(scheme 2)
20.00
Included in
Sub-centres
(scheme 2)
89
Other Offices under Direction & Administration
28.10
29.60
29.02
90
ISM Institutions
7.00
5.02
1.39
91
Regional Institute of MCH
0.75
0.60
0.31
92
Hindustan Latex Limited
1.90
1.72
0.13
93
Family Welfare Counsellor Scheme
1.00
1.00
0.00
94
School Health Scheme
147.10
42.60
0.40
55
Additional RCH activities in the Tenth Plan
56
Other New Initiatives
GRAND TOTAL
15120.00
215
14968.70
14588.97
Goals for the Tenth Plan
Annexure-2.10.3
SI. Name of State/UT
..No.
Couple Protection Rate
Crude Birth rate
Current Level
Expected Level
(Average of
2007
NFHS.RHS)
By Ster.
Spacing Permanent Spacing
(Modern)___________ (Modern)
INDIA
ro
Cd
Total Fertility Rate
Current Expected
Current Expected
level
Level
level
Level
SRS 2000
2007
SRS 1998
2007
Infant Mortality Rate
Current Expected
level
Level
SRS 2000 2007
Neo Natal Mortality
Rate
Safe Delivery
Current
level
NFHS-2
Expected
Level
2007
Current
level
NFHS-2
Ante Natal Care
(3 ANCs)
Expected Current Expected
Level
level
Level
2007
NFHS-2 2007
35.5
8.0
50.0
15.0
25.8
21
3.2
2.3
68
45
43.4
26
42.3
80
43.8
90
Andhra Pr
57.4
1.4
65.0
10.0
21.3
17
2.4
1.8
65
42
43.8
22
65.2
90
80.1
95
2
Assam
15.1
12.5
35.0
16.9
26.9
22
3.2
2.3
75
50
44.6
30
21.4
55
30.8
80
3
Bihar
20.7
2.2
30.0
10.0
3'1.9
24
4.3
2.8
62
45
46.5
25
23.4
70
17.8
80
4
Chattisgarh
38.0
5.0
45.0
10.0
26.7
22
NA
2.6
79
50
54.9
38
65.9
95
28.1
85
5
Gujarat
44.0
8.8
60.0
21.2
25.2
20
3.0
2.1
62
40
39.6
22
53.5
80
60.2
95
6
Haryana
40.1
12.9
56.3
26.0
26.9
22
3.3
2.2
67
40
34.9
23
42
80
37.4
95
7
Jharkhand
21.0
2.0
30.0
10.0
26.5
22
NA
2.6
70
50
46.5
35
42.4
60
17.8
80
8
Karnataka
52.5
4.8
60.0
12.7
22.0
20
2.4
2.0
57
40
37.1
21
59.1
85
71.4
9
Kerala
50.7
6.3
60.0
10.7
17.9
15
1.8
1.6
14
9
13.8
5
94
100
98.3
95
100
10
Madhya Pr
38.0
5.1
55.0
17.0
31.2
23
3.9
2.6
88
58
54.9
30
29.7
70
28.1
85
11
Maharashtra
51.4
66.0
14.9
20.9
17
2.7
2.1
48
34
32
20
59.4
95
65.4
98
12
Orissa
34.8
55.0
12.9
24.3
21
2.9
2.2
96
68
48.6
35
33.4
70
47.3
90
13
Punjab
31.0
5.1
22.8
55.0
30.0
21.5
18
2.6
2.1
52
35
34.3
15
62.6
90
57
95
14
Rajasthan
37.1
6.2
45.0
15.5
31.2
4.1
2.7
79
50
49.5
30
35.8
70
22.9
80
15
Tamil Nadu
45.8
4.4
60.0
12.0
19.2
22
16
2.0
1.7
51
30
34.8
20
83.8
100
91.4
100
I.
MAJOR STATES
1
16
Uttar Pr
14.9
7.0
35.0
21.0
32.8
24
4.6
2.7
83
58
53.6
35
22.4
75
14.9
80
West Bengal
32.9
13.5
50.0
19.4
20,6
17
2.4
2.1
51
38
31.9
25
44.2
80
57
95
II.
SMALLER STATES
1
Arunachal Pr
18.4
15.0
30.0
20.8
22.3
20
2.8
2.4
44
40
41.8
30
31.9
65
40.5
80
2
Goa
28.6
8.9
45.0
12.4
14.3
12
1.8
1.5
23
9
31.2
20
29.7
75
95.7
100
Himachal Pr
51.5
10.1
65.0
19.6
22.1
20
2.4
2.0
60
35
22.1
15
40.2
80
60.9
85
J& K
30.3
14.1
40.0
18.5
19.6
17
NA
2.0
50
40
40.3
30
23.4
75
66
80
Manipur
12.8
9.8
30.0
15.8
18.3
16
2.4
2.0
23
20
18.6
10
53.9
85
54.4
80
Meghalaya
8.6
8.0
30.0
10.8
28.5
23
4.0
2.6
58
50
50.7
40
20.6
50
31.3
80
7
Mizoram
42.3
10.0
56.8
15.5
16.9
16
NA
2.0
21
19
18.8
12
67.5
90
75.8
90
8
Nagaland
12.3
10.7
30.0
14.1
NA
15
1.5
1.5
NA
32
20.1
15
32.8
60
23 1
85
i 9
Sikkim
I 10
23.9
20.2
31.3
28.5
21.8
17
2.5
2.1
49
45
26.3
20
35.1
60
42.6
85
Tripura
20.0
20.0
30.0
36.4
16.5
16
3.9
2.6
41
35
48.3
60
51
85
. 11
Uttaranchal
30.0
10.0
40.0
18.2
20.2
18
NA
2.0
50
40
53.6
30
22.4
80
19.6
80
I:
III.
UNION TERRITORIES
1
2
A&N Islands
44.7
13.6
50.0
15.0
19.1
15
1.9
23
22
71.3
80
92.3
100
Chandigarh
21 1
35.9
40.0
35.0
17.5
14
2.1
1.9
28
25
I 3
71.2
80
73
85
D&N Haveli
29.7
5.7
35.0
34.9
2.8
58
50
27.6
60
74.6
85
Daman & Diu
44.4
6.3
50.0
23.7
23
16
3.5
4
10.0
10.0
2.5
2.1
48
45
70.6
85
80.7
90
Delhi
28.7
33.6
40.0
30.0
20.3
16
1.6
1.6
32
25
73.7
85
68.2
85
6
Lakshadweep
7.4
4.1
30.0
26.1
20
2.8
2.4
27
25
74.1
85
98.3
100
7
Pondicherry
50.6
6.2
65.0
10.0
10.0
17.8
16
1.8
1.6
23
20
93.4
100
95.8
100
I 5
T
m
m
>
>
o
17
I 3
m
z
29.5
20
§
o
- Media
 8648.pdf
8648.pdf
Position: 3116 (3 views)