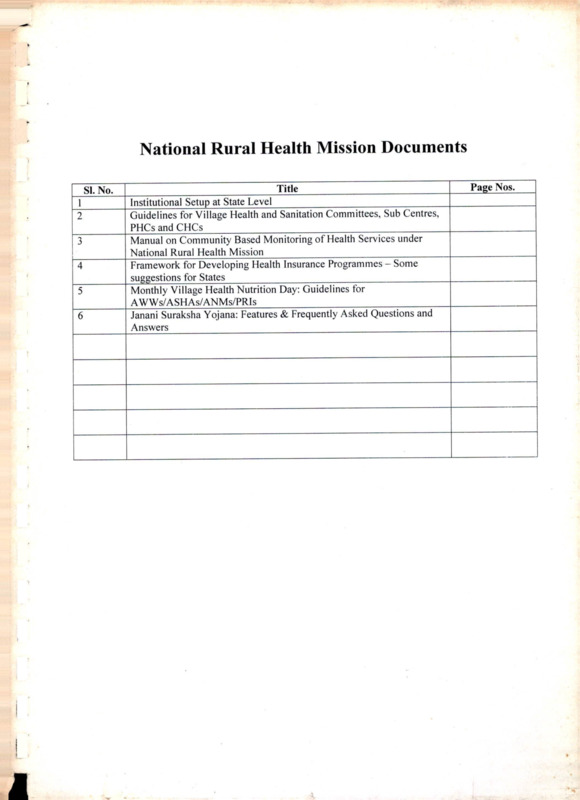
National Rural Health Mission Documents
Item
- Title
-
National Rural Health Mission Documents
- extracted text
-
National Rural Health Mission Documents
SI. No.
j______
2
3
4
5
6
___________________________ Title
_____________________
Institutional Setup at State Level________________________________
Guidelines for Village Health and Sanitation Committees, Sub Centres,
PHCs and CHCs_________________ ___________________________
Manual on Community Based Monitoring of Health Services under
National Rural Health Mission_______
Framework for Developing Health Insurance Programmes - Some
suggestions for States________________________ ________________
Monthly Village Health Nutrition Day: Guidelines for
AWWs/ASHAs/ANMs/PRIs_____________________
Janani Suraksha Yojana: Features & Frequently Asked Questions and
Answers
Page Nos.
National Rural Health Mission: Institutional Setup at State level
State Health Mission and State Health Society
At the National level, the NRHM has a Mission Steering Group (MSG) headed by the
Union Minister for Health & Family Welfare and an Empowered Programme Committee
(EPC) headed by the Union Secretary for Health & FW. The EPC will implement the
Mission under the overall guidance of the MSG.
At the State level, the Mission would function under the overall guidance of the State
Health Mission headed by the Chief Minister of the State. The functions under the
Mission would be carried out through the State Health & Family Welfare Society. The
structures of the Mission and Society and their linkages are mentioned in the following
paragraphs.
State Health Mission
Composition
•
•
Chairperson
Co-Chairperson
Chief Minister
Minister of Health and Family Welfare, State
Government
Principal Secretary/Secretary (Family Welfare)
Convener
Members
•
Ministers in charge of Departments relevant to NRHM such as
AYUSH, Women and Child Development, Medical Education, Public
Health Engineering, Water and Sanitation, Panchayati Raj, Rural
Development, Social Welfare, Urban Development, Planning, Finance,
etc.
•
Nominated public representatives (5 to 10 members) such as MPs,
MLAs, Chairmen, Zila Parishad, urban local bodies (women should be
adequately represented)
•
Official
representatives:
Chief
Secretary/Development
Commissioners and Principal Secretaries/Secretaries in-charge of
relevant departments such as Women and Child Development, Public
Health Engineering, Panchayati Raj, Rural Development, Tribal Welfare,
Urban Development/Affairs, Finance, Planning and Representative,
MoHFW, Gol, Director (Health ServicesJ/Director (AYUSH).
•
Nominated non-official members (5 to 8 members) such as health
experts, representatives of medical associations, NGOs, etc
•
Representatives of Development Partners
Frequency of meetings: At least once in every six months
Ordinary Business: Providing health system oversight, consideration of policy matters
related with health sector (including determinants of good health), review of progress in
implementation of NRHM; inter-sectoral coordination, advocacy measures required to
promote NRHM visibility.
State Health Society
A. Governing Body
•
•
•
•
•
• Chairperson: Chief Secretary/Development Commissioner
Development Commissioner
• Co-Chair :
: Principal/Secretary (Health & Family Welfare)
• Vice-Chair
Officer designated as Mission Director of State Health
• Convener
Mission
Members:
• •
Secretaries of the NRHM related Departments: Health & FW,
Finance, AYUSH, Women and Child Development, Public Health
Engineering, Water and Sanitation, Panchayati Raj, Rural Development,
Tribal/SC Welfare, Urban Affairs and Planning and Programme
Implementation.
• • DHS, Director AYUSH
• • Gol representative(s): MoHFW nominee.
• •
Representatives of Development Partners supporting the NRHM in
the State
• •
Nominated non-official members: Four to six members (Public
Health Professionals, MNGO representatives/ representatives of Medical
Associations)
• •
Regional Directors
Frequency of meetings: At least once in every six months
Ordinary Business of the Governing Body Meeting:
• Approval / endorsement of Annual State Action Plan for the NRHM.
• Consideration of proposals for institutional reforms in the H&FW sector.
• Review of implementation of the Annual Action Plan.
• Inter-sectoral co-ordination: all NRHM related sectors and beyond (e.g.
administrative reforms across the State).
• Status of follow up action on decisions of the State Health Mission.
• Co-ordination with NGOs/Donors/other agencies/organisations.
B. Executive Committee
Principal Secretary/Secretary, FW
1. Chairperson :
Principal Secretary/Secretary, Health/FW (in case of
2. 2. Co-Chair (s) :
separate secretaries in the State)
3. 3. Vice Chair: Director, Health & FW
Executive Director/Mission Director (To be an IAS Officer
4. Convener
of JAG/Selection Grade)
State Programme Managers/Project Directors of National
4. Joint Secretaries:
Disease Control Programme
Members:
1. 1. Director, AYUSH
2. 2. Secretaries / technical officers from NRHM related sectors
3. 3. Executive Secretary, State AIDS Control Society [ for the States
which decide not to merge it with State Health & FW Society].
4. 4. MoHFW, Gol representative.
5. 5. Regional Directors
Frequency of meetings: At least once in every month
Ordinary Business:
•
•
•
•
•
•
Detailed expenditure and implementation review.
Approval of proposals from districts and other implementing agencies/District
Action Plans.
Execution of the approved State Action Plan, including release of funds for
programmes at State level as per Annual Action Plan.
Release of funds to the District Health Societies.
Finalization of working arrangements for intra-sectoral and inter-sectoral co
ordination.
Follow up action on decisions of the Governing Body.
C. Programme Committee for Health & FW Sector
The Executive Committee would ensure execution of integrated NRHM State Action
Plan. However, for administrative convenience, the State may constitute Programme
Committees for the National Programmes for a more focused planning and review of
each activity. Suggested constitution of the Committee is as below:
Chairperson: Director
Member-Secretary: Concerned State Programme Manager
Members: Finance Manager (SPMSU), 2-3 related State Programme Managers and
Consultants
D. State Programme Management Support Unit (SPMSU)
The SPMSU will act as the secretariat to the State Health Mission as well as the State
Society. Headed by an Executive Director/Mission Director, the SPMSU will have
experts in the areas of human resources, BCC, M&E and other technical areas,
recruited from the open market. The SPMSU will provide the technical support to the
State Health Mission through its pool of skilled professionals like MBA, CA, MIS
Specialist and Consultants for RCH and other National Disease Control Programmes.
This technical pool would be accessed by all programmes under NRHM for providing
specific programme support related to logistics, financial management, MIS, tracking of
funds etc.
After sanction of State Action Plan by the Governing Body of State Health Society and
of District Plans by the Executive Committee, funds could be released through joint
signatures of two authorized signatories (viz. State Program Manager/DHS and
Secretary (HFW/Mission Director). The actual release of funds could either be made
by the concerned Programme Management Unit with a copy of the sanction letter to the
SPMSU, or vice-a-versa as per the decided State model. However, the responsibility of
financial management, including tracking of funds, preparation of Utilization Certificates
and audit of the Society, shall be overseen by the SPMSU.
E. Composite Organogram of the State Mission and the State Society
The State Mission and the State Society are inter-linked in terms of a common
secretariat as depicted below:
State Health Mission
Governing Body, State Health Society
<
>
F.
Process of merger of existing societies
After the State Society has been registered, a meeting of the Governing Body of
existing State societies in the health and family welfare sector has to be convened to
adopt the following resolution:
“ Resolved that the
(name of the society) be dissolved with
immediate effect and that all assets and liabilities of the said society shall
stand transferred to the
(name of the State Health Society).
A signed copy of the above resolution has to be then filed with the Registrar of
Societies to complete the process of merger.
Appendices to facilitate creation and functioning of State Society
• Model Memorandum of Association (Appendix-1)
• Model Rules and Regulations (Appendix-ll)
• Generic Bye-laws (Appendix-Ill)
Appendix-1
(Model) MEMORANDUM OF ASSOCIATION
OF
(State name) HEALTH SOCIETY
1. Name of the Society
The Name of the Society shall be “State Health Society, (State
name)” hereinafter referred to as the “Society”.
2. Area of operation
The area of
State of
3.
Location
The Society shall have its office at
in the State of
with liberty for it to establish one or more subordinate
offices or outlets elsewhere in the State, if so required.
4. Objectives
The Society shall serve in an additional managerial and
technical capacity to the Department of Health & Family
Welfare, Government of
for the implementation of
National Rural Health Mission (NRHM) in the State.
5. Scope of functions
To achieve the above objectives, the Society shall direct its
resources towards performance of the following key tasks:
• •
Receive, manage (including disbursement to
implementing agencies e.g. Directorate,
District
Societies, NGOs etc.) and account for the funds
received from the Ministry of Health & Family Welfare,
Government of India.
• •
Manage the
NGO / PPP (public-private
partnership) components of the NRHM in the State,
including execution of contracts, disbursement of funds
and monitoring of performance.
• •
Function as a Resource Centre for the Department
of Health & Family Welfare in policy/situational analysis
and policy development (including development of
operational guidelines and preparation of policy change
proposals for the consideration of Government).
• •
Strengthen the technical / management capacity
of the State Directorate as well as of the Districts
Societies by various means including through
recruitment of individual / institutional experts from the
open market (with total programme management costs
for the State as a whole not exceeding to 6% of the
total programme costs).
• •
Mobilize financial / non-financial resources for
complementing/supplementing the NRHM activities in
the State.
• •
Organize training, meetings, conferences, policy
review studies / surveys, workshops and inter-State
exchange visits etc. for deriving inputs for improving the
implementation of NRHM in the State.
• •
Undertake such other activities for strengthening
NRHM in the State as may be identified from time to
time, including mechanisms for intra and inter-sectoral
convergence of inputs and structures.
operation of the Society shall be whole of the
For performing the above tasks, the Society shall:
• •
Establish and carry out the administration and
management of the Society’s Secretariat, which will
serve as the implementation arm of the Society.
• •
Create administrative, technical and other posts in
the Secretariat of the Society as deemed necessary.
• •
Establish its own compensation package and
employ, retain or dismiss personnel as required.
• •
Establish its own procurement procedures and
employ the same for procurement of goods and
services.
• •
Make rules and bye-laws for the conduct of the
activities of the Society and its Secretariat and add,
rescind or vary them from time to time, as deemed
necessary.
6. First members of the
Governing Body
The names, addresses, occupations and designations of the
First Members of the Governing Body of the Society to whom
by the rules and regulations of the Society, the management of
the affairs of the Society is entrusted as required under section
2 of the Societies Registration Act, 1860 (No. XXI of 1860) are
as follows:
in
Status
Governing
Body______
Chairperson
SI.
No.
Name / Designation
1.
Chief Secretary / Development
Commissioner__________________
Development Commissioner_________ Co-Chair
Principal /Secretary, Health & Family Vice-Chair
Welfare___________________________
Convener
Mission Director of the State Health
Mission________________________
Principal Secretaries / Secretaries Members
for NRHM related Departments:
Finance, AYUSH, Women and Child
Development, Nutrition, Water and
Sanitation, Panchayati Raj, Rural
Development,
Social
/
Tribal
Welfare and Urban Affairs ZDHS
2.
3.
4.
5-7
A copy of the rules of the Society certified to be a correct copy
by three members of the Governing Body is filed along with this
Memorandum of Association.
7.
Declaration
We, the several persons whose names and addresses are
given below having associated ourselves for the purpose
described in this Memorandum of Association do hereby
subscribe our names to this Memorandum of Association and
set our several and respective hands hereunto and form
ourselves into a Society under the Societies Registration Act,
1860 (Act, No. XXI of 1860): this
day of 2005
at
SI.
Name
1
2
3
4
6
7
Dated:
Occupation
address
and
Status in
Society
Signature
Attested
by
Appendix-ll
STATE HEALTH SOCIETY,
(name of State)
THE RULES AND REGULATIONS
SHORT TITLE
1.
These Rules and Regulations shall be called “The Rules and Regulations of
1.1
the State Health Society (State name), 2005”.
These Rules shall come into force with effect from the date of registration of
1.2
the Society by the Registrar of Societies.
DEFINITIONS
2.
2.1
In the interpretation of these Rules and Regulations, the following
expressions shall have the following meaning unless inconsistent with subject or
context:
“Act” means Societies Registration Act, 1860.
“
(abbreviation of State Society)” means the State Health Society,
(State name)1111.
“Central Government” means the Government of India.
“Chairperson” means the Chairperson of the Governing Body of the Society.
“Chief Executive Officer(CEO)” means the chairperson of the Executive
Committee of the Society.
“Executive Committee” means the Executive Committee of the Society.
“Executive Secretary” means the Executive Secretary of the Society.
“Governing Body” means the Governing Body of the Society.
“Member” means the Member of the Society.
“Rules” means these Rules and Regulations registered alongwith the
memorandum of Association & as may be amended by the Governing Body of
the Society from time to time.
“Secretariat” means the Secretariat of the Society.
“State Government” means the Government of
(State name).
“Year” means the financial year of the State Government of.... (State name).
OFFICE
3
Registered office of the Society shall be situated in the premises of
located at
(address where
Society secretariat will be located).
3.1
3.2
The Society may set up its branch offices in the State.
4
MEMBERSHIP
4.1
•
•
•
The following shall be the members of the Society:
First members of the Governing Body.
Additional ex-officio members of the Governing Body.
Member Secretary of the Society, to be appointed under these Rules.
,[1] E.g. State Health Society, Haryana (SHSH), State Health Society, Bihar (SHSB) etc.
•
•
•
•
•
•
Representative(s) of the Government of India.
Representatives of Development Partners supporting the NRHM activities in
the State.
Representatives of NGOs and/or association of NGOs.
Representatives of professionals’ associations (e.g. IMA, FOGSI, IAP etc.).
Representatives of other organisations as may be determined by the
Governing Body from time to time.
Individuals as may be nominated by the Governing Body from time to time.
4.2
The membership of an ex-officio member of the Society and of the Governing
Body shall terminate when he/she ceases to hold the office by virtue of which he/she
was member and his/her successor to the office shall become such member.
4.3
Non official members of the Society will be nominated by the Chairperson in
consultation with other members of the Governing Body. Nominated members shall
hold office for a period of three years from the date of their nomination by the
Chairperson. Such members will be eligible for re-nomination for another period of 3
years.
4.4
The Society shall maintain a roll of members at its registered office and every
member shall sign the roll and state therein his/her rank or occupation and address.
No member shall be entitled to exercise rights and privileges of a member unless
he/she has signed the roll as aforesaid.
4.5
All members of the Governing Body shall cease to be members if they resign,
become of unsound mind, become insolvent or be copvicted of a criminal offence
involving moral turpitude or removal from the post by virtue of which s/he was holding
the membership.
4.6
Resignation of membership shall be tendered to the Governing Body in
person to its Executive Secretary and shall not take effect until it has been accepted
on behalf of the Governing Body by the Chairperson.
4.7
If a member of the Society changes his/her address he/she shall notify his/her
new address to the Executive Secretary who shall thereupon enter his/her new
address in the roll of member. But if a member fails to notify his/her new address the
address in the roll of members shall be deemed to be his/her address.
4.8
Any vacancy in the Society or in the Governing Body shall be filled by the
authority entitled to make such appointment. No act or proceedings of the Society or
of the Governing Body shall be invalid merely by reason of the existence of any
vacancy therein or of any defect in appointment of any of its members.
4-9
INo member of the Governing Body, except the Executive Secretary to be
appointed as per these Rules, shall be entitled to any remuneration.
5
AUTHORITIES OF THE STATE HEALTH SOCIETY
5.1
•
•
•
The following shall be the bodies and authorities of the Society:
Governing Body
Executive Committee
Programme Committees and such other bodies as may be prescribed by the
Governing Body. (Optional)
5.2
GOVERNING BODY
All members of the Society as set out in para 4.1 shall constitute the
Governing Body of the Society.
5.2.1
5.2.2 The first members of the Governing Body of the Society shall be those
mentioned in Clause 6 of the Memorandum of Association. They shall hold office
until a new Governing Body is appointed according to these Rules.
5.2.3
The management of the affairs of the Society shall be entrusted to
Governing Body and the property of the Society shall be vested in the Governing
Body.
5.2.4 The Society may sue or be sued in the name of the Executive Secretary of
the Society or of such other members as shall, in reference to the matter concerned,
be appointed by the Governing Body for the occasion.
PROCEEDINGS OF THE GOVERNING BODY
5.3
5.3.1 The meetings of the Governing Body shall be held at least once in every six
months and at such time and place as the Chairperson shall decide. If the
Chairperson receives a requisition for calling a meeting signed by one-third members
of the Governing Body, the Chairperson shall call such a meeting as soon as may be
reasonably possible and at such place as s/he may deem fit.
5.3.2 At the annual meeting of the Governing Body the following business shall be
brought forward and disposed of:
•
•
•
•
•
•
•
•
•
•
•
•
Income and expenditure account and the balance sheet for the past year.
Annual report of the Society.
Budget for the next year.
Annual Action Plan and research work for the next year.
Appointments for the Executive Committee and the various Committees.
Other business brought forward with the permission of the Chairperson.
5.3.3 Every notice calling meeting of the Governing Body shall state the date, time
and place at which such meeting will be held and shall be served upon every
member of the Governing Body not less than twenty one clear days before the date
appointed for the meeting. Such notice shall be under the hand of the Executive
Secretary and shall be accompanied by an agenda of the business to be placed
before the meeting provided that accidental omission to give such notice to any
member shall not invalidate any resolution passed at such meeting. In the event of
any urgent business the Chairperson may call the meeting of the Governing Body at
clear ten days notice.
5.3.4 The Chairperson shall take the Chair at the meetings of the Governing Body.
In his/her absence, the Co-Chair or in his/her absence, the Vice-Chairperson will
chair the meeting, failing which the Governing Body shall elect one from among the
members present as Chairperson of the meeting.
5.2.5 One third of the members of the Governing Body, including the substitutes
nominated under Rule 5.2.7 present in person, shall form a quorum at every meeting
of the Governing Body.
5.2.6 All disputed questions at the meeting of the Governing Body shall be
determined by votes. Each member of the Governing Body shall have one vote and
in case of any equality of votes the Chairperson shall have a casting vote.
5.2.7 Should any official members be prevented for any reason whatsoever from
attending a meeting of the Governing Body the Chairperson of the Society shall be at
liberty to nominate a substitute to take his place at the meeting of the Governing
Body. Such, substitute shall have all the rights and privileges of a member of the
Governing Body for that meeting only.
5.2.8 Any member desirous of moving any resolution at a meeting of the Governing
Body shall give notice there of in writing to the Executive Secretary of not less than
ten clear days before the day of such meetings.
5.2.9 Any business which it may become necessary for the Governing Body to
perform except such as may be placed before its Annual meeting may be carried out
by circulation among all its members and any resolution so circulated and approved
by majority of the members signing shall be as effectual and binding as if such
resolution had been passed at a meeting of the Governing Body provided that at
least one third members of the Governing Body have recorded their consent of such
resolution.
5.2.10 In the event of any urgent business, the Chairperson of the Society may take
a decision on behalf of the Governing Body. Such a decision shall be reported to the
Governing Body at its next meeting for ratification.
5.2.11 A copy of the minutes of the proceedings of each meeting shall be furnished
to the Governing Body members as soon as possible after completion of the meeting.
5.4
POWERS OF THE GOVERNING BODY
5.4.1 The Governing Body will have full control of the affairs of the Society and will
have authority to exercise and perform all the powers, acts and deeds of the Society
consistent with the aims and objects of the Society.
5.4.2 In particular and without prejudice to the generality of foregoing provision, the
Governing Body may:
• Make, amend, or repeal any bye laws relating to administration and
management of the affairs of the Society subject to the observance of the
provisions contained in the Act.
• Consider the annual budget and the annual action plan, its subsequent
alternations placed before it by the Executive Secretary from time to time and
to pass it with such modifications as the Governing Body may think fit.
•
•
•
•
•
Monitor the financial position of the Society in order to ensure smooth income
flow and to review annual audited accounts.
Accept donations and endowments or give grants upon such terms as it
thinks fit.
Delegate its powers, to the Chairperson, Chief Executive Officer, Executive
Secretary or other authorities of the Society as it may deem fit.
Appoint committees, sub-committees and boards etc. for such purpose and
on such terms as it may deem fit, and to dissolve / remove any of them.
Develop and adopt its own rules and regulations for recruitment and
appointment of experts and administrative / technical staff and set its own
•
•
•
5.5
compensation package for such experts / staff to be recruited from the open
market and/or deputation basis.
Develop and adopt its own procurement procedures for procurement of goods
and services.
•
Authorise the Executive Secretary to execute such contracts on behalf of
the Society as it may deem fit in the conduct of the business of the Society.
Do generally all such acts and things as may be necessary or incidental to
carrying out the objectives of the Society or any of them, provided that
nothing herein contained shall authorize the Governing Body to do any act or
to pass any bye-laws which may be repugnant to the provisions hereof, to the
powers hereby conferred on the Governing Body and other authorities, or
which may be inconsistent with the objectives of the Society.
POWERS AND FUNCTIONS
GOVERNING BODY
OF
THE
CHAIRPERSON
OF
THE
5.5.1 The Chairperson shall have the powers to call for and preside over all
meetings of the Governing Body.
5.5.2 The Chairperson may himself/herself call, or by a requisition in writing signed
by him/her, may require the Executive Secretary to call, a meeting of the Governing
Body at any time and on the receipt of such requisition, the Executive Secretary shall
forthwith call such a meeting.
5.5.3 The Chairperson shall enjoy such powers as may be delegated to him by the
Governing Body.
5.5.4 The Chairperson shall have the authority to review periodically the work and
progress of the Society and to order inquiries into the affairs of the Society and to
pass orders on the recommendations of the reviewing or inquiry Committee.
5.5.5 Nothing in these Rules shall prevent the Chairperson from exercising any or
all the powers of the Governing Body in case of emergencies in furtherance of the
objects of the Society. However, the action taken by the Chairperson on such
occasions shall be reported to the Governing Body subsequently for ratification.
5.6
EXECUTIVE COMMITTEE
5.6.1 The Governing Body will constitute an Executive Committee which will be
responsible for acting for and doing all deeds on behalf of the Governing Body and
for taking all decisions and exercising all the powers, vested in the Governing Body
except those which the Governing Body may specifically specify to be excluded from
the jurisdiction of by the Executive Committee.
5.6.2
The composition of the Executive Committee shall be as follows:
SI.
No.
Name / designation
1
Principal Secretary (HFW)/ Secretary, (FW)
2
3
Principal Secretary (Health)/Secretary (FW)
Director, Health & FW
Programme Managers/Project Directors
4-7
Executive
Status
in
Committee_____
Executive
Chairperson,
Committee.
Co-Chairperson
Vice Chair
of Joint Secretaries
8-10
11
12
13
14
15
National Disease Control Programme
Secretaries/technical officers from NRHM
related sectors
Director, AYUSH
Representative of Development Partners
Representative of Ministry of Health & FW,
Govt of India
Regional Director of Health & FW, Gol
Mission Director/Executive Director of the
Society
Members
Member
Members
Member
Member
Convenor
5.6.3 The Executive Committee may co-opt additional members and/or invite
subject experts to its meetings from time to time.
5.6.4 Meetings of the Executive Committee shall be convened by the Convenor by
giving clear seven days notice in writing alongwith the Agenda specifying the
business to be transacted, the date, time and venue of the meeting.
5.6.5 Meetings of the Executive Committee shall be held at least once a month or
more frequently if necessary.
5.6.6 The minutes of the Executive Committee meetings will be placed before the
Governing Body at its next meeting.
5.6.7 The various Committees constituted by the Governing Body shall submit their
reports to the Executive Committee who shall be empowered to take decisions on
their recommendations.
5.7 SOCIETY SECRETARIAT AND MISSION DIRECTOR/EXECUTIVE DIRECTOR
5.7.1 A Senior Officer of the State Government of the rank of Special
Secretary/Additional Secretary (an IAS Officer of JAG/Selection Grade) shall be
nominated as the Mission Director. Governing Body, with the assistance of the Joint
Secretary and officials such as Director/DG Health Services/Executive Director, will
establish a Secretariat of the Society consisting of technical, financial and
management professionals to serve as the implementation arm of the Society.
5.7.2 The Secretariat shall consist of all such technical / management units put
together and as may be determined by the Governing Body with due regard to the
scope of functions as set out in Article 5 of the Memorandum of Association.
5.7.3 The Executive Committee of the Society will have overall responsibility for
planning and executing the work of the Secretariat, for supervising the work of the
technical/management units of the Secretariat, directing and overseeing
implementation through the Secretariat.
5.8
POWERS AND FUNCTIONS OF THE SECRETARIAT
5.8.1 The Secretariat of the Society shall consist of the Mission Director and Staff
of the Society, including experts and consultants.
5.8.2 As the implementation arm of the Society, the Secretariat will be responsible
for day-to-day management of the Society’s activities. In particular, it will be
responsible for performing all functions of the Society as set out in article 5 of the
MoA.
5.8.3 As a support structure for assisting Department of Health & FW of the State
Government, the Secretariat shall:
• •
cause its experts and staff to be subjected to such operational
arrangements with the Directorate (including seating and reporting
arrangements) as to generate synergies,
• • host external experts within its premises, and
• • provide such logistic support to the officers and staff of the Directorate
and Department of Health & FW of the State Government as may be
determined by the Governing Body.
6
FUNDS OF THE SOCIETY
6.1
6.1
•
•
•
•
The funds of the Society shall consist of the following:
Cash assistance received from the Government of India.
Grants-in-Aid from the State Government.
Grants and donations from trade, industry, institutions and individuals.
Receipts from disposal of assets.
The assets and liabilities of all Societies merged into the Integrated Society
shall be subsumed within the new Society.
7
ACCOUNTS AND AUDIT
The Society shall cause regular accounts to be kept of all its monies and
properties in respect of the affairs of the Society.
7.1
The Executive Committee may cause separate Bank Accounts in respect of
7.2
each scheme or separate ledgers for each scheme under one account. In such an
event, the Governing Body shall prescribe written instructions relating to submission
of Statement of Expenditure (SoE) for each scheme. The separate Accounts of
different Programmes could be audited by different auditors, and submitted to
Programme Units separately. However, the SPMSU will ensure one integrated audit
of the State Health Society.
7.3
The accounts of the Society shall be audited annually by a Chartered
Accountant firm included in the panel of Comptroller and Auditor General of India or
any qualified person appointed by the Government of India/State Government and
any expenditure incurred in connection with such audit shall be payable by the
Society to the Auditors. The Office of the Accountant General of State may also, at its
discretion, audit the accounts of the society.
7.4
The Chartered Accountant or any qualified person appointed by the Govt, of
7.4
India/State Government in connection with the audit of the accounts of the Society
shall have the same rights, privileges and authority in connection with such audit as
the Auditor General of the State has in connection with the audit of Government
accounts and in particular shall have the right to demand the production of books,
accounts, connected vouchers and other necessary documents and papers.
7.5
The report of such audit shall be communicated by the auditor to the Society,
which shall submit a copy of the Audit Report alongwith its observation to the State
Government.
7.6
The Auditor shall also forward a copy of the report to the Chairperson of the
Society and representative(s) of the Government of India on the Governing Board.
8
BANK ACCOUNT
8.1
The account of the Society shall be opened in a nationalised bank approved
by the Executive Committee or in a scheduled commercial bank as may be specified
by the MoHFW, Government of India. All funds shall be paid into the Society’s
account with the appointed bank and shall not be withdrawn except through a
cheque, bill note, other negotiable instruments or through electronic banking (ebanking) procedures signed/electronically authorised by such authorities of the
Society Secretariat as may be determined by the Executive Committee.
8.2
The Society shall switch over to e-banking procedures as and when the
MoHFW, Government of India directs the Society to do so as the principal donor to
the Society.
8.3
The Executive Committee shall authorise the Executive Director (Mission
Director) to operate the accounts of the Society in conjunction with another senior
official as may be decided by the Committee.
9
ANNUAL REPORT
9.1
A draft annual report and the yearly accounts of the Society shall be placed
before the Governing Body at next meeting for consideration and approval. A copy
of the annual report and audited statement of accounts as finally approved by the
Governing Body shall be forwarded within six months of the closure of a financial
year to the Chairperson of the Governing Body and Government of India
representatives on the Governing Body.
10
SUITS AND PROCEEDINGS
10.1 The Society may sue or be sued in the name of Society through its Mission
Director.
10.2 No suit or proceedings shall abate by the reason of any vacancy or change in
the holder of the office of the Chairperson or Executive Secretary or any oofice
bearer authorised in this behalf.
10.3 Every decree or order against the Society in any suit or proceedings shall be
executable against the property of the Society and not against the person or the
property of the Chairperson, Executive Secretary or any office bearer of the Society.
10.4 Nothing in sub-rule 10.3 above shall exempt the Chairperson, Executive
Secretary or office bearer of the Society from any criminal liability or entitle him/her to
claim any contribution from the property of the Society in respect of any fine to be
paid by him/her on conviction by a criminal court.
11
AMENDMENTS
The Society may alter or extend the purpose for which it is established and/or
the Rules of the Society.
11.1
11.2 The proposition for any alteration or extension to the objectives of the Society
and / or the Rules must be circulated to all members of the Governing Body and must
be included in the written agenda of the ensuing meeting of the Governing Body or a
special meeting of the Governing Body.
11.3 No amendments shall be effective unless the proposals in this regard have
been endorsed by 3/5th of the members of the Governing Body provided that such
proposals have been endorsed in writing by the Gol representatives on the
Governing Body either during the meeting of the Governing Body or through a written
communication.
12
DISSOLUTION
12.1
The Governing Body may resolve to dissolve the Society by bringing a
proposal to that effect in a special meeting to be convened for the purpose.
12.2 Upon the dissolution of the Society, all assets of the Society, after the
settlement of all its debts and liabilities, shall stand reverted to the State Government
of Bihar for such purposes as it may deem fit.
13
MISCLELLANEOUS
13.1
CONTRACTS
13.1.1 All contracts and other instruments for and on behalf of the Society shall be
subject to the provisions of the Act, be expressed to be made in the name of the
Society and shall be executed by the persons authorised by the Governing Body.
13.1.2 No contracts for the sale, purchase or supply of any goods and material shall
be made for and on behalf of the Society with any member of the Society or his/her
relative or firm in which such member or his/her relative is a partner or shareholder or
any other partner or shareholder of a firm or a private company in which the said
member is a partner or director.
13.2
COMMON SEAL
13.2.1 The Society shall have a common seal of such make and design as the
Governing Body may approve.
13.3
COMPLIANCE OF STATUTORY REQUIREMENTS
13.3.1 The Society shall register itself with relevant government agencies for the
purpose of complying with the statutory requirements including regulations governing
deduction of tax at source relating to the staff, consultants and experts employed by
it and/or consultancies / contracts awarded by it in the course of performance of its
tasks.
13.4
GOVERNMENT POWER TO REVIEW
13.4.1 Notwithstanding anything to the contrary contained in these Rules, the
Ministry of Health & FW, Government of India, as the principal donor to the Society,
may appoint one or more persons to review the work and progress of the Society and
hold enquiries into the affairs thereof and report thereon, get the accounts of the
society audited by the internal audit parties of the Chief controller of Accounts,
MoHFW, Gol, and issue directions, as deemed appropriate, to the Society.
13.4.2 The Chairperson of the Governing Body shall have the right to nominate one
or more persons to be part of the review / enquiries.
13.4.3 The progress review reports and / or enquiry reports shall be included in the
written agenda of the ensuing meeting of the Governing Body.
We, the undersigned being three of the members of the first Governing Body of the
State Health Society
(State name) certify that the above is a correct copy of the
Rules and Regulations of the said Society.
SI.
No.
1
2
3
Dated :
Name and address
Signature
(Generic) Bye-laws of the State Health Society,
A
Appendix-Ill
(State name)
Procurement Policy and Procedures
Procurement of goods and services to be financed from funds received from Government
of India shall be done as per the procedures recommended by the Government of India.
In all other cases, including where the Gol allows the State a choice, following order of
preference shall be applied for procurement of goods and services:
Procurement of Goods:
A. A. Rate contracts of the DGS&D, failing which,
B. B. Rate contracts of other Gol agencies, failing which,
C. C. Tender procedure as recommended by GOI.
Procurement of services: Procedure as recommended by the GO I.
B
Procedure for release of funds and Financial Powers of the Office Bearers of
the Governing I Executive Committee
I
Classification of Items of Expenditure and Financial powers of the bodies and
office bearers of the Society
(For ensuring smooth flow of funds for the approved plans and activities, it is
necessary that proper delegation of administrative and financial powers is made at
each level. A model delegation is suggested below, which each State/UT may
consider keeping in view their existing systems and procedures and suitably
modify/add for meeting State’s own reguirements and all relevant aspects).
Type of expenditure________ Authority_______ Extent of power
A: Approval of District /City Governing Body / Full powers
Executive
plans.
Committee______
Full powers.
B:
Release of funds for Mission
implementation of plans / Director/DHS*
allocations which have been
approved by Governing Body /
Executive Committee._______
C: Expenditure proposals not covered under categories A and/or B
C-1: Procurement of goods
C-2: Repairs and minor civil
works
Chairperson,
Executive
Committee
Mission Director
More than Rs 5.00 lakh and upto Rs.
10.00 lakh per case.
Upto Rs. 5.00 lakh per case.
C-3: Procurement of services
for specific tasks including
outsourcing
of
support
services for the Directorate.
C-4: Hiring of contractual staff, Chairperson,
including
sanction
of Executive
compensation package.______ Committee
Full powers, provided that the contracts
shall be for a period not exceeding 11
months at a time.
__________
Type of expenditure
Authority_____
Mission Director
Extent of power___________________
Full powers in respect of Clerical /
Class-IV equivalent positions, subject
to compensation package approved by
the Governing / Executive Committee,
provided that the contracts shall be for
a period not exceeding 11 months at a
time.
C-5: Miscellaneous items not Chairperson,
mentioned above such as Executive
hiring of taxis, hiring of Committee
auditors, payments relating to Mission Director
documentation and other dayto-day services, meetings and
workshops, training, purchase
of training material/ books and
magazines, payment of TA/DA
and honoraria to resource
persons and guest speakers
invited
to
meetings
/
workshops, and payment of
TA/DA
allowances
for
contractual staff and/or non
official invitees to Governing
Body /Executive Committee
meetings and/or Government /
Society staff deputed to
meetings outside the State.___________
*as authorized by the State Government.
Upto Rs. 5.00 lakh at a time subject to
a maximum of Rs. 50 lakh per annum.
II
Upto Rs 2.00 lakh at a time, subject to
a maximum of Rs. 25.00 lakh per
annum.
Procedure for release of funds
The Society funds shall be drawn through cheques and/or bank drafts and/or through ebanking instruments as and when the same is introduced.
All cheques shall be signed by two authorised signatories of the Society Secretariat on the
basis of a written authorisation from Executive Committee of the Society in this behalf.
Wherever releases are decided to be made through bank drafts and/or through e-banking,
the authorisation letter to the bank shall be signed by the concerned authorised
signatories.
Wherever, under e-banking procedures, releases are to be made through electronic
authorisation to the bank to issue cheque/draft/account transfer on behalf of the Society,
the electronic authorisation will be executed by the same two authorised functionaries of
the Society Secretariat who have been authorised to sign cheques on the basis of a written
authorisation in this behalf.
III
Review / revision of financial powers
The Executive Committee may review and revise the financial powers of the office bearers
of the bodies of the Society on an annual basis and revise the same, if considered
necessary.
Human Resources Policy and Procedures
C
Recruitment and Appointment
Appointments for the Society can be made only against vacant posts prescribed for the
Society in accordance with the conditions in this regard prescribed by the Govt, of India
from time to time, (such as the overall programme management costs not to exceed 6% of
the total programme costs).
Recruitment would be through either of the following three routes:
•
•
•
Appointments from open market: all such appointments will be on contractual basis
for a fixed tenure.
Appointments on “Deputation” basis : all such appointments will be regulated in
terms of the State Government rules relating to Deputation of its officers / staff.
Individuals recruited and paid for by an outside agency [ e.g. Government of India
and/or Development Partners] but posted to work within the Society Secretariat: all
such persons shall be governed by the terms of employment of the organisation
agency concerned. However, they shall be required to report to the Director /
Executive Secretary as may be decided by the Chairperson, Executive Committee.
All appointments would be temporary and would be made for the contract / deputation
period as determined by the Executive Committee.
Leave rules
Holidays, Casual Leave, Medical Leave: The Society staff and the full time consultants
shall be governed by the State Government rules, in so far as observance of holidays and
grant of casual / medical leave is concerned.
‘ ) shall be entitled to
Leave without pay: The Society staff (including full time consultants)
be sanctioned by the
take leave without pay in exceptional circumstances. This can t:
Executive Secretary after recording the reasons. For the Executive Secretary, this would
have to be endorsed by the Chairperson, Executive Committee.
Training and capability development:
Full time consultants and staff of the Society (including staff on deputation) would be
encouraged to take up skill development courses and even correspondence courses which
further their employment prospects, enhance their skills, and build up Society capabilities.
Travelling I Dearness Allowance (TA/DA) Rules
Travel within State: Travel of Society staff (including those who are employed by the
Society on deputation basis) within the State shall be governed as per the entitlements
given in the table below.
Entitlement for rail
travel_____________
Entitlement for road
travel [1]______ .
Executive
Secretary
and senior officers on
‘deputation’
to
the
Society_____________
2nd AC/AC Chair Car
Taxi
Full
time
consultants
senior
2nd AC / AC Chair
Car
_________
Taxi
Junior
clerical staff
/
3rd AC / AC
Chair________
Bus/Shared
taxi [2]
Per-diem when hotel
is not used________
Per-diem when hotel
is used [3]
Rs. 300/- per day
Rs. 200/- per day
Rs. 1000/- per night [4]
Rs 500/- per night [4]
Rs. 300/- per
day_________
Rs. 500/- per
night [4]
Notes: [1]: The Society shall create a panel of accredited taxi operators through open
tender for hiring the taxis for the travel of Society staff.
[2] : The Executive Secretary can allow the junior staff to use a taxi for undertaking
travel as per an approved itinerary.
[3] : The Society shall identify and negotiate a standard/discounted tariff for its staff/
employees with the State Tourism Corporation, guest houses of PSUs and budget/
hotels in the State.
[4] : Maximum, subject to actuals.
Travel outside the State: Travel outside the State shall be regulated on a case to case
basis in accordance with delegated financial powers as indicated in Section-B above
(Financial Powers, item C-5).
Deduction of Tax at Source: Tax will be deducted at source as per income tax rules and
the Society shall register itself with the relevant authorities in this regard.
*******
National Rural Health Mission: Institutional Setup at the District level
District Health Mission and the District Health Society
On the lines of the State Health Mission, every district will have a ‘District Health Mission’
headed by the Chairperson, Zila Parishad. It will have the District Collector as the Co-Chair
and Chief Medical Officer as the Mission Director.
To support the District Health Mission, every district will have an integrated District Health
Society (DHS) and all the existing societies as vertical support structures for different
national and state health programmes will be merged in the DHS. The DHS will be
responsible for planning and managing all health and family welfare programmes in the
district, both in the rural as well as urban areas. There are two important implications of
this requirement. Firstly, DHS’s planning will have to take note of both treasury and non
treasury sources of funds, even though it may not be handling all sources directly.
Secondly, its geographical jurisdiction will be greater than those of the Zilla Parishad and
/or Urban Local Bodies (ULBs) in the district2121.
Ensuring Inter-sectoral convergence and integrated planning should be a specific task for
the Governing Body of the DHS. However, the DHS is not meant to take over the
executive functions of the ZP / ULBs and/or the district health administration. On the
contrary, DHS is meant to provide the platform where the three arms of governance - ZP,
ULBs and district health administration and district programme managers of NRHM sectors
get together to decide on health issues of the district and delineate their mutual roles and
responsibilities.
The DHS may also be viewed as an addition to the district administration’s capacity,
particularly for planning, budgeting and budget analysis, development of operational
policy^ proposals, and financial management etc. Because it is a legal entity, the DHS
can set up its own office which has adequate contingent of staff and experts and can
evolve its own rules and procedures for hiring the staff and experts both from the open
market as well as on deputation from the Government.
In other words, the DHS is not an implementing agency; it is a facilitating mechanism for
the district health administration as also the mechanism for joint planning by NRHM related
sectors.
B
Governance structure
B.1
District Health Mission
Chairperson:
Co-Chair:
Vice Chair:
Chairman, Zilla Parishad
District Collector/DM
CEO Zila Parishad
2[2] The 74th Amendment provides for creation of a District Planning Committee to consolidate the plans
prepared by Panchayats and Municipalities in the district and to prepare a draft development plan for the
district as a whole. However, the DPC’s role is limited to planning only and does not include management
functions.
3I-31 At the district level, operational policy will relate to decisions about procedures, priorities etc. which set
the precedent about what management actions are to be followed by the programme managers. For example,
the DHS may be authorised to relocate all or some categories of staff within the district. The DHS will be
required to evolve and approve a procedure to be followed by the programme managers in this regard.
* The State may decide to designate Convenor of the District Health Mission as Mission Director in respect of
the District Health Mission
Convener*:
Members:
B.2
Chief Medical Officer/CDMO/CMHO/Civil Surgeon
MPs, MLAs, MLCs from the district, Chair-persons of the
Standing Committees of the Zilla Parishad, Project Officer
(DRDA), Chair-persons of the Panchayat Samitis and
Hospital Management Societies, District Programme
Managers for health, PHED, ICDS, AYUSH, education,
social welfare, Panchayati Raj, State representative,
representatives of MNGO/SNGO, etc.
District Health Society
The overall governance structure of the Society may be as depicted in Diagram-1 below.
Diagram-1: Governance Structure of the DHS
Governing Body
Chair:
District Collector/DM/CEO Zilla Parishad
Co-Chair:
DDC cum CEO, Zilla Parishad
Chief Executive Officer:
Chief Medical Officer/CDMO/Civil
Surgeon
Members: Project Officer (DRDA), District Programme Managers for
Health, AYUSH, Water and Sanitation [under Total
Sanitation Campaign (TSC)], DPMSU, PHED, ICDS,
education, social welfare, Panchayati Raj, a State
representative, Sub-Divisional Officer, CHC In-charge;
representatives of Medical Association/MNGO/SNGO and
Development Partners
Executive Committee
Chair :
DDC cum CEO Zilla Parishad (CMO in case no
Post of DDC/CEO Zilla Parishad is notified in the
district
CMO/CDMO/CMHO/CS
Co-chair :
Chief Executive
Officer and Convener: District Programme Manager/District
RCH Officer
Members: Superintendent-District Hospital, All District Programme
______ 1_______
DHS Secretariat
District
Programme
Manager**, <
programme
managers
for
projects
sponsored by Development Partners and
support staff
>
Programme
Committees for the
health sector
* Presently, 3 posts at each District level have been sanctioned by Go! in EAG
States. However, in other States also, these may be provided by the States
themselves within 6% of the overall programme costs for the State as a whole.
Till such time these are provided and actually recruited, a Dy. CMO level officer
may be designated as such to function as the District Programme Manager.
c
Role of the District Programme Manager, DHS Secretariat
S/he is seen as the key player not only in setting up and operationalising the DHS
secretariat, but also in arranging managerial and supportive assistance to the district
health administration, including general management and logistic support. It is because of
the twin responsibility that s/he is been made the Convenor of both the Governing Body as
well as the Executive Committee. In the Programme Committees, however, s/he will be a
simple member.
The specific responsibilities of the District Programme Manager, DHS will include, but not
be limited to the following:
A: Management of DHS Secretariat
(a) (a) Facilitate the working of the DHS as per the bye-laws of the
Society.
(b) (b) Organise recruitment of personnel for the DHS.
(c) (c) Maintain records of the Society.
(d) (d) Organise meetings of the Governing Body and Executive
Committee including preparation of agenda notes, circulation of
minutes and compilation of action taken reports etc.
(e) (e) Organise audit of the Society funds and preparation of annual
report of the DHS as required under the Bye-laws.
B: Planning, Monitoring and Evaluation
(a) (a) Create and maintain district resource database for the health sector
including manpower, buildings, equipments and other support
infrastructure.
(b) (b) Assist the Civil Surgeon and district programme managers in
developing the ‘District Work Plan’ based on the National & State goals.
(c) (c) Undertake regular monitoring of initiatives being implemented in the
district and provide regular report and feedback to the Society and
others who are entitles to receive Annual Report of the Society [ District
Collector, Chairperson, Zila Parishad, designated authority State
Government ].
(d) (d) Ensure compilation, analysis & presentation of relevant information
in meaningful formats and assist the Civil Surgeon in making informed
discussions.
(e) (e) Develop strategies/plans to improve the quality of services and
present to the Society for approval.
B: Inventory management, Procurement & Logistics
(a)
(a)
Facilitate preparation of District Logistics Plan for
optimal allocation of resources at each facility.
and compilation of
(b)
(b)
Ensure timely collection
‘demands’ and their timely dispatch.
D
DHS Secretariat
Initially, the Society Secretariat will have a core team of 3 full time persons, consisting of
the following:
•
District Programme Manager (who have been prescribed to be appointed by Gol in
EAG States) or Dy. CMO (in the case of other States, designated as such) since
actual programme implementation will remain with the programme managers under
district
•
Finance / Accounts Manager, and
•
Data Assistant.
Once the Society Secretariat is operationalised (i.e., the above core staff is in place and
the office is set up), the district programme officer posts sponsored under the Centrally
Sponsored Schemes and the contractual staff/consuitants under the various Health
Programmes and bilateral/multi-lateral funding programmes may be brought under the
District Health Secretariat.
Eventually (that is, after integration of the posts sponsored under the Centrally Sponsored
Schemes with the DHS), the DHS will have a number of functional units including technical
officers belonging to State Medical Services posted on deputation to the District Society
Secretariat. This will not only allow the DHS to exercise a choice in the selection of district
programme managers, the tenure issue will also be addressed since all deputation
postings will be for a minimum period of 3 years.
E
Procedure for recruitment and appointment of contractual staff
Recruitment can be facilitated by the State Society as this would allow economies of scale
and save time.
However, offer letters should be issued by the District Society on the basis of a specimen
offer letter (see Appendix-IV, State Society).
The recruitment of the specialists for the hospitals can be similarly organised by the State
Society or the District Society. After recruitment, however, the offer letters should be
issued by the Hospital Management Society.
F
Process of merger of existing societies into integrated District Health Society
After the District Health Society has been registered, a special meeting of the Governing
Body of existing district societies in the health sector has to be convened to adopt the
following resolutions:
Resolved that the
(name of the society) be dissolved with
immediate effect and that all assets and liabilities of the said society shall stand
transferred to the District Health Society, district
(district name).”
A signed copy of the above resolution has to be then filed with the Registrar of Societies to
complete the process of merger.
Appendices to facilitate creation and functioning of Integrated District Societies
• Model Memorandum of Association (Appendix-1)
• Model Rules and Regulations (Appendix-ll)
• Generic Bye-laws (Appendix-Ill)
Appendix-1
(Model) Memorandum of Association for the District Health Society
1. Name of the Society
The Name of the Society shall be “District Health Society,
District
or DHS (district name)”.
2. Area of operation
The area of operation of the Society shall be whole of district
(district name)
3.
Location
The Society shall have its office at the office of Chief Medical
Officer/ Civil Surgeon / Chief Medical and Health Officer /
Chief District Health Officer,
district, situated at
(postal address)
4. Objectives
The Society shall assist district health administration in the
implementation of various health programmes and projects in
the district, with special emphasis on priority sectors like
reproductive and child health, population control, control of
malaria, TB and leprosy and prevention of blindness and
malnutrition etc.
5. Scope of functions
To achieve the above objectives, the Society shall direct its
resources towards performance of the following key tasks:
• •
To act as the nodal forum for all stake holders line departments, PRI and NGOs- to participate in
planning, implementation and monitoring of the various
health and family welfare programmes and projects in
the district.
• •
To receive, manage and account for the funds
received from the State Government (including State
level Societies in the
health sector)
for
implementation of Centrally Sponsored Schemes in the
district.
• •
To strengthen the technical / management
capacity of the District Health Administration through
recruitment of individual / institutional experts from the
open market.
• •
To facilitate preparation of integrated district health
development plans, for health and its various
determinants like sanitation, nutrition and safe drinking
water, etc.
• •
To guide the functions related to ‘Total Sanitation
Campaign’ at the District level.
• •
To mobilise financial and non-financial resources
for complementing/supplementing the health and
family welfare activities in the district.
• •
To assist hospital management societies in the
district.
•
•
To undertake such other activities for
strengthening health and family welfare activities in the
district as may be identified from time to time, including
mechanisms for intra and inter-sectoral convergence of
inputs and structures.
6.
First members of The names, addresses, occupations and designations of the
the
Body
Governing
First Members of the Governing Body of the Society to whom
by the rules and regulations of the Society, the management of
the affairs of the Society is entrusted as required under section
2 of the Societies Registration Act, 1860 (No. XXI of 1860) are
as follows:-
SI.
No.
Name / Designation
1.
2.
District Collector/DM
DDC
Civil Surgeon/Chief Medical Officer
3.
4.
5.
6.
7.
8.
9.
10.
Status in the
Governing
Body________
Chair-person
Co-Chair
Chief
Executive
Officer (CEO)
r
Member
Member
Member
Member
Member
Project Director, DRDA
District Social Welfare Officer
District Programme Officer (ICDS)
District Programme Officer (AYUSH)
District Programme Officer (Primary
Education)
District Programme Officer (Rural Member
Development)
District Programme Manager
Convenor
A copy of the rules of the Society certified to be a correct copy
by three members of the Governing Body is filed along with
this Memorandum of Association.
7.
Declaration
We, the several persons whose names and addresses are
given below having associated ourselves for the purpose
described in this Memorandum of Association do hereby
subscribe our names to this Memorandum of Association and
set our several and respective hands hereunto and form
ourselves into a Society under the Societies Registration Act,
1860 (Act, No.XXI of 1860): this
day of 2005 at
SI.
Name
Occupation
address
1
2
3
4
6
7
8
9
and
Status
Society
in
Signature
Attested
by_____
Appendix-ll
(Model) Rules I Regulations of the District Health Society
1.
SHORT TITLE
1.1
These Rules and Regulations shall be called “The Rules and Regulations of the
District Health Society (District
), 2005”.
1.2
These Rules shall come into force with effect from the date of registration of the
Society by the Registrar of Societies.
2.
DEFINITIONS
2.1
In the interpretation of these Rules and Regulations, the following expressions shall
have the following unless inconsistent with subject or context:
“Act” means Societies Registration Act, 1860.
“Central Government” means the Government of India.
“DHS” means the District Health Society
“Executive Committee” means the Executive Committee as referred to in these
Rules.
“District Programme Manager” means the Programme Manager cum Convenor of
the Society as referred to in these Rules.
“Governing Body” means the Governing Body of the Society as referred to in these
Rules.
“Member” means the Member of the Society as referred to in these Rules.
“Rules” means these Rules and Regulations registered along with the memorandum
of Association & as may be amended by the Governing Body of the Society from
time to time.
“Secretariat” means the Secretariat of the Society as referred to in these Rules.
“State Government” means the Government of
“Year” means the financial year, namely from 1st April of a calendar year to 31st
March of the next calendar year.
3
OFFICE AND JURISDICTION
3.1
F
‘
‘ office of the Society
Registered
shall be situated at the Office of the Civil Surgeon /
Chief Medical Officer / Chief Medical and Health Officer,
District having its
office at
..................
3.2
The jurisdiction of the Society shall be the whole of
4
MEMBERSHIP
4.1
•
•
(district name)
The following shall be the members of the Society:
First members of the Governing Body.
Following additional ex-officio members of the Governing Body:
o Programme Managers / District Officers in charge of national / centrally
sponsored health & FW schemes / programmes and ex-officio office
bearers of the vertical programme / project societies in the health & FW
sector (e.g. District Blindness Control Society, District RCH Society, District
•
•
•
•
•
•
TB Control Society, District Malaria Society etc.), which existed before the
formation of this Society, AYUSH and In-charge of ‘Total Sanitation
Campaign’ in the District.
o Superintendents of District, Sub-Divisional and other hospitals in the
district, including Nagar Nigam hospitals, railway hospitals, ESI hospitals
and other public hospitals in the district.
o Elected representatives (MLAs/MPs) from the district.
District Programme Manager to be appointed under these Rules.
Representatives of Development Partners supporting health and family welfare
activities in the district, if any.
NGO representatives of the vertical programme / project societies in the health &
FW sector (e.g. District Blindness Control Society, District RCH Society, District TB
Control Society, District Malaria Society etc.) which existed before the formation of
this Society.
Local representatives of professionals’ associations (e.g. IMA, FOGSI, IAP etc.).
Representatives of other organisations as may be determined by the Governing
Body from time to time.
Individuals as may be nominated by the Governing Body from time to time.
4.2
The membership of an ex-officio member of the Society and of the Governing Body
shall stand terminated when he/she ceases to hold the office by virtue of which he/she was
member and his/her successor to the office shall become such member.
4.3
Non-official members of the Society will be nominated by the Chair-person with the
approval of the Governing Body. Nominated members shall hold office for a period of
three years from the date of their nomination by the Chair-person. Such members will be
eligible for re-nomination for another period of 3 years.
4.4
The Society shall maintain a roll of members at its registered office and every
member shall sign the roll and state therein his/her rank or occupation and address. No
member shall be entitled to exercise rights and privileges of a member unless he/she has
signed the roll as aforesaid.
4.5
All members of the Governing Body shall cease to be members if they resign,
become of unsound mind, become insolvent or be convicted of a criminal offence involving
moral turpitude or removal from the post by virtue of which s/he was holding the
membership.
4.6
Resignation of membership shall be tendered to the Governing Body in person to
its Executive Secretary and shall not take effect until it has been accepted on behalf of the
Governing Body by the Chairperson.
4.7
If a member of the Society changes his/her address he/she shall notify his/her new
address to the Executive Secretary who shall thereupon enter his/her new address in the
roll of member. But if a member fails to notify his/her new address the address in the roll
of members shall be deemed to be his/her address.
4.8
Any vacancy in the Society or in the Governing Body shall be filled by the authority
entitled to make such appointment. No act or proceedings of the Society or of the
Governing Body shall be invalid merely by reason of the existence of any vacancy therein
or of any defect in appointment of any of its members.
4.9
No member of the Governing Body, except the Executive Secretary to be
appointed as per these Rules, shall be entitled to any remuneration.
5
AUTHORITIES OF THE DHS
5.1
The following shall be the bodies and authorities of the Society:
Governing Body
Executive Committee
Sub-Committees of the Executive Committee, such as Programme Committees
•
•
•
5.2
GOVERNING BODY
5.2.1 All members of the Society as set out in para 4.1 shall constitute the
Governing Body of the Society.
5.2.2 The first members of the Governing Body of the Society shall be those mentioned
in Clause 6 of the Memorandum of Association. They shall hold office until a new
Governing Body is appointed according to these Rules.
5.2.3
The management of the affairs of the Society shall be entrusted to
Governing Body and the property of the Society shall be vested in the Governing
Body.
The Society may sue or be sued in the name of the Executive Secretary of the
Society or of such other members as shall, in reference to the matter concerned,
be appointed by the Governing Body for the occasion.
5.2.4
5.3
PROCEEDINGS OF THE GOVERNING BODY
5.3.1 The meetings of the Governing Body shall be held at least twice a year and at such
time and place as the Chair-person shall decide. If the Chair-person receives a requisition
for calling a meeting signed by one-third members of the Governing Body, the Chair
person shall call such a meeting as soon as may be reasonably possible and at such place
as s/he may deem fit.
5.3.2 Following minimum business shall be brought forward and disposed off in every
meeting of the Governing Body:
•
•
Annual report of the Society relating to last financial year, including (a) income
and expenditure account, (b) balance sheet and (c) audit report.
•
•
Physical and financial progress of the programmes / projects in the current
year.
•
•
Work Plan (including budget) for the next financial year.
•
•
Other business brought forward with the assent of the Chair-person.
5.3.3 Every notice calling meeting of the Governing Body shall state the date, time and
place at which such meeting will be held and shall be served upon every member of the
Governing Body not less than twenty one clear days before the date appointed for the
meeting. Such notice shall be issued by the Executive Secretary of the Society and shall
be accompanied by an agenda of the business to be placed before the meeting provided
that accidental omission to give such notice to any member shall not invalidate any
resolution passed at such meeting. In the event of any urgent business the Chair-person
may call the meeting of the Governing Body at clear ten days notice.
5.3.4 The Chair-person shall Chair the meetings of the Governing Body. In his/her
absence, the Governing Body shall elect one from among the members present as Chair
person of the meeting.
5.3.5 One third of the members of the Governing Body, including the substitutes
nominated under Rule 5.3.7 present in person, shall form a quorum at every meeting of the
Governing Body.
5.3.6 All disputed questions at the meeting of the Governing Body shall be determined by
votes. Each member of the Governing Body shall have one vote and in case of a tie, the
Chair-person shall have a casting vote.
5.3.7 Should any official members be prevented for any reason whatsoever from
attending a meeting of the Governing Body, the Chair-person of the Society shall be at
liberty to nominate a substitute to take his place at the meeting of the Governing Body.
Such, substitute shall have all the rights and privileges of a member of the Governing Body
for that meeting only.
5.3.8 Any member desirous of moving any resolution at a meeting of the Governing Body
shall give notice there of in writing to the Executive Secretary of not less than ten clear
days before the day of such meetings.
5.3.9 Any business which it may become necessary for the Governing Body to perform,
except the agenda prescribed for the full meeting as set out in para 5.3.2 above, may be
carried out by circulation among all its members and any resolution so circulated and
approved by majority of the members signing shall be as effectual and binding as if such
resolution had been passed at a meeting of the Governing Body provided that at least one
third members of the Governing Body have recorded their consent of such resolution.
5.3.10 In the event of any urgent business, the Chair-person of the Society may take a
decision on behalf of the Governing Body. Such a decision shall be reported to the
Governing Body at its next meeting for ratification.
5.3.11 A copy of the minutes of the proceedings of each meeting shall be furnished to the
Governing Body members within 2 weeks after completion of the meeting.
POWERS OF THE GOVERNING BODY
5.4
of tne
the bocieiy
Society ano
and win
will nave
have
5.4.1 The Governing Body will have full control of the affairs or
authority to exercise and perform all the powers, acts and deeds of the Society consistent
with the aims and objects of the Society.
5.4.2 In particular and without prejudice to the generality of foregoing provision, the
Governing Body may:
•
Make, amend, or repeal any bye laws relating to administration and management
of the’affairs of the Society subject to the observance of the provisions contained in
the Act, provided that such amendments are brought to the Governing Body after
obtaining endorsement / approval from the State Government4141.
4[4] This provision is being made to ensure that the DHSs in other districts also benefit from avenues of
improvements identified in a district.
•
•
•
•
•
•
•
•
•
i
i
5.5
Consider the annual budget and the annual action plan, its subsequent alternations
placed before it by the Executive Secretary from time to time and to pass it with
such modifications as the Governing Body may think fit.
Monitor the financial position of the Society in order to ensure smooth income flow
and to review annual audited accounts.
Accept donations and endowments or give grants upon such terms as it thinks fit.
Delegate its powers, other than those of making rules, to the Chair-person,
Executive Secretary or other authorities as it may deem fit.
•
Authorise the Executive Secretary to execute such contracts on behalf of the
Society as it may deem fit in the conduct of the business of the Society.
Appoint committees, sub-Committees and Boards etc. for such purpose and on
such terms as it may deem fit, and to remove any of them.
Recruit administrative / technical staff for the Society secretariat as per the
Operational Manual of the Society.
Procure goods and services in accordance with the procedures laid down in the
Operational Manual of the Society.
Do generally all such other acts and things as may be necessary or incidental to
carrying out the objectives of the Society or any of them, provided that nothing
herein contained shall authorize the Governing Body to do any act or to pass any
bye-laws which may be repugnant to the provisions hereof, to the powers hereby
conferred on the Governing Body and other authorities, or which may be
inconsistent with the objectives of the Society.
POWERS AND FUNCTIONS OF THE CHAIR-PERSON OF THE GOVERNING
BODY
5.5.1
The Chair-person shall have the powers to call for and preside over all meetings of
the Governing Body.
The Chair-person may himself/herself call, or by a requisition in writing signed by
him/her, may require the Executive Secretary to call, a meeting of the Governing Body at
5.5.2
any time and on the receipt of such requisition, the Executive Secretary shall forthwith call
such a meeting.
5.5.3 The Chair-person shall enjoy such powers as may be delegated to him by the
Society and the Governing Body.
5.5.4
The Chair-person shall have the authority to review periodically the work and
progress of the Society and to order inquiries into the affairs of the Society and to pass
orders on the recommendations of the reviewing or inquiry Committee.
5.5.5 Nothing in these Rules shall prevent the Chair-person from exercising any or all the
powers of the Governing Body in case of emergencies in furtherance of the objects of the
Society. However, the action taken by the Chair-person on such occasions shall be
reported to the Governing Body subsequently for ratification.
5.6
EXECUTIVE
Committees)
COMMITTEE
AND
ITS
SUB-COMITTEES
(Programme
5.6.1 The Governing Body will constitute an Executive Committee which will be
responsible for acting for and doing all deeds on behalf of the Governing Body and for
taking all decisions and exercising all the powers, vested in the Governing Body except
those which the Governing Body may specifically specify to be excluded from the
jurisdiction of by the Executive Committee.
5.6.2
The composition of the Executive Committee shall be as follows:
SI.
No.
Name / designation
Status
in
Committee
T”
DDC cum CEO, Zila Parishad
Chairperson
2
3
4
5
6
7
8
9
CMO/CDMO/CMHO/CS
Co-Chair
10
11
12
13
14
Executive
Member
District Programme Managers for health & FW
programmes (6)
Member
Member
Member
Member
District Programme Manager (ICDS)
Chief Executive Officer, Urban Local Body
Member
Member
(Nagar Nigam)
Superintendent(s), District Hospital(s)5l5]
Member
of
the
Member
Member
Member
Member
Manager/District
RCH
Convenor
Representative, Mother NGO for the district
Three Governing body members belonging to
NGOs / charitable hospitals from the district,
by
the
15
nominated
16
Governing Body
District Programme
Chair-person
Officer
5 6 2 Till such time a regular incumbent to the post of District Programme Manager has
been appointed, the District may decide to designate one of the Dy. CMOs to function as
Convenor of the Governing Body / Executive Committee.
5.6.3 The Executive Committee may co-opt additional members and/or invite subject
experts to its meetings from time to time.
5.6.4 Meetings of the Executive Committee shall be convened by the Member Secretary
by giving clear seven days notice in writing along with the Agenda specifying the business
to be transacted, the date, time and venue of the meeting.
5[5] In districts having District Hospital (Male) and District Hospital (Female), Superintendents of both should
be included as members of the Executive Committee.
5.6.5 Meetings of the Executive Committee shall be held at least once every month or
more frequently as necessary.
5.6.6 The minutes of the Executive Committee meetings will be placed before the
Governing Body at its next meeting.
5.6.7 The Executive Committee may appoint one or more programme-committees for the
purpose of day-to-day execution of the various programmes.
5.6.8 The programme committees will submit a monthly performance / progress report to
the Executive Committee which shall incorporate these into the consolidated progress
reports to be placed before the Governing Body.
5.7
SOCIETY SECRETARIAT AND EXECUTIVE SECRETARY
5.6.1 Governing Body, with the assistance of the Executive Secretary, will establish a
Secretariat of the Society consisting of technical, financial and management professionals
to serve as the District Programme Management Support Unit (DPMSU) to assist the
district health administration.
5.6.2 The Secretariat shall consist of such technical / management units as set out in the
Operational Manual prescribed by the State Government.
5.6.3 The district level officers appointed under on-going projects sponsored by
development partners, if any, shall be physically co-located in the Society Secretariat
office6161.
5.8
POWERS AND FUNCTIONS OF THE SECRETARIAT
5.8.1 The Secretariat of the Society shall consist of the Executive Secretary and Staff of
the Society.
5.8.2 The Secretariat will be responsible for day-to-day management of the Society’s
activities. In particular, it will be responsible for performing all functions of the Society as
set out in article 5 of the MoA.
5.8.3 The Secretariat will provide Technical Support to the District Health Mission. It will
also be responsible for financial management of funds of the Society.
5.8.4 The funds sanctioned by the Governing Body/Executive Committee shall be
released by the two authorized signatories and a copy of the sanction order marked to the
DPMSU for financial management of the same.
6
FUNDS OF THE SOCIETY
6.2
6.2
The funds of the Society shall consist of the following:
Grant-in-aid from the State Government and/or State Health Society
•
•
•
• Grants-in-aid from the Central Government, if it decides to give the whole
or part of grants directly to District Society.
•
•
Grants and donations from trade, industry, institutions and individuals.
•
•
Receipts from disposal of assets.
6[6] These include NPSP Medical Officers (WHO), District Programme Managers of the Border District
Cluster Scheme (UNICEF) and District Programme Manager for the nutrition projects of the CARE etc.
•
The assets and liabilities of all Societies merged into the integrated Society
shall be subsumed within the new Society.
7
ACCOUNTS AND AUDIT
The Society shall cause regular accounts to be kept of all its monies and properties
in respect of the affairs of the Society.
7.1
7.2
The Executive Committee may cause separate Bank Accounts in respect of each
scheme or separate ledgers for each scheme under one account. In such an event, the
Governing Body shall prescribe written instructions relating to submission of Statement of
Expenditure (SoE) for each scheme. The separate Accounts of different Programmes
could be audited by different auditors, and submitted to Programme Units separately.
However, the DPMSU will ensure one integrated audit of the District Health Society.
7.3
The accounts of the Society shall be audited annually by a Chartered Accountant
firm included in the panel of Comptroller and Auditor General of India or any qualified
person appointed by the Government of India/State Government and any expenditure
incurred in connection with such audit shall be payable by the Society to the Auditors. The
Office of the Accountant General of State may also, at its discretion, audit the accounts of
the society.
7.4
The Chartered Accountant or any qualified person appointed by the Govt, of
India/State Government in connection with the audit of the accounts of the Society shall
have the same rights, privileges and authority in connection with such audit as the Auditor
General of the State has in connection with the audit of Government accounts and in
particular shall have the right to demand the production of books, accounts, connected
vouchers and other necessary documents and papers.
7.5
The report of such audit shall be communicated by the auditor to the Society, which
shall submit a copy of the Audit Report along with its observation to the State Government.
7.6
The Auditor shall also forward a copy of the report to the following:
•
•
A designated authority of the State Society as may be determined
by its Governing Body / Executive Committee.
8
•
•
•
•
Chair-person of the Governing Body of the Society and State
Government or a designated authority of the State level society.
The District Collector.
BANK ACCOUNT
The account of the Society shall be opened in a nationalised bank approved by the
Executive Committee or in a scheduled commercial bank as may be specified by the
MoHFW, Government of India. All funds shall be paid into the Society’s account with the
appointed bank and shall not be withdrawn except through a cheque, bill note, other
negotiable instruments or through electronic banking (e-banking) procedures
signed/electronically authorised by such authorities of the Society Secretariat as may be
determined by the Executive Committee.
8.1
8.2
The Society shall switch over to e-banking procedures as and when the MoHFW,
Government of India directs the Society to do so as the principal donor to the Society.
9
ANNUAL REPORT:
9.1
A draft annual report and the yearly accounts of the Society shall be placed before
the Governing Body at next meeting for consideration and approval. A copy of the annual
report and audited statement of accounts as finally approved by the Governing Body shall
be forwarded within six months of the closure of a financial year to the following:
District Collector/DM,
Chair-person, Governing Body, and
Designated authority of the State Government.
10
SUITS AND PROCEEDINGS
10.1 The Society may sue or be sued in the name of Society through its Executive
Secretary.
10.2 No suit or proceedings shall abate by the reason of any vacancy or change in the
holder of the office of the Chairperson or Executive Secretary or any office bearer
authorised in this behalf.
10.3 Every decree or order against the Society in any suit or proceedings shall be
executable against the property of the Society and not against the person or the property
of the Chairperson, Executive Secretary or any office bearer of the Society.
10.4
INothing in sub-rule 10.3 above shall exempt the Chairperson, Executive Secretary
or office bearer of the Society from any criminal liability or entitle him/her to claim any
contribution from the property of the Society in respect of any fine to be paid by him/her on
conviction by a criminal court.
11
AMENDMENTS
11.1
The Society may amend these Rules provided that such changes shall not alter the
nature and /or the objectives and/or the purposes for which it has been set up. The
proposals for any amendments shall be carried out only through the following process:
11.1.1
11.1.2
11.1.3
12
Proposals for amendments have been circulated to all members of the
Governing Body and have been duly included in the written agenda of the
ensuing meeting of the Governing Body or a special meeting of the
Governing Body;
The Governing Body has endorsed the proposal at least 3/5th of the
members of the Governing Body; and
The State Government has communicated, in writing, its endorsements to
the Governing Body resolution for the amendment.
DISSOLUTION
12.1
The Governing Body may resolve to dissolve the Society by bringing a proposal to
that effect in a special meeting to be convened for the purpose, provided that the proposal
for dissolution has been duly approved /endorsed through the process prescribed for
amendment as set out in para 11.1 of these Rules.
12.2 The dissolution proceedings shall be made in accordance with the provisions of the
Act as amended from time to time in its application in the State.
12.3 Upon the dissolution of the Society, all assets of the Society, after the settlement of
all its debts and liabilities, shall stand reverted to the State Government for such purposes
as it may deem fit.
13
MISCLELLANEOUS
13.1
CONTRACTS
13.1.1 All contracts and other instruments for and on behalf of the Society shall be subject
to the provisions of the Act, be expressed to be made in the name of the Society and shall
be executed by the persons authorised by the Governing Body.
13.1.2 No contracts for the sale, purchase or supply of any goods and material shall be
made for and on behalf of the Society with any member of the Society or his/her relative or
firm in which such member or his/her relative is a partner or shareholder or any other
partner or shareholder of a firm or a private company in which the said member is a
partner or director.
13.2
COMMON SEAL
13.2.1 The Society shall have a common seal of such make and design as the Governing
Body may approve.
13.3
GOVERNMENT POWER TO REVIEW
13.3.1 Notwithstanding anything to the contrary contained in these Rules, the State
Government and/or Ministry of Health & Family Welfare may appoint one or more persons
to review the work and progress of the Society and hold enquiries into the affairs thereof
and report thereon. The Central Government may also cause the accounts of the Society
to be audited by the internal audit parties of the Chief Controller of Accounts, MoHFW, GOI
or do Management Audit through the Financial Management Group, and issue directions,
as deemed appropriate, to the Society.
13.3.2 The Chair-person of the Governing Body shall have the right to nominate one or
more persons to be part of the review / enquiries.
13.3.3 The progress review reports and / or enquiry reports shall be included in the
written agenda of the ensuing meeting of the Governing Body.
We, the undersigned being three of the members of the first Governing Body of the District
Health Society, certify that the above is a correct copy of the Rules and Regulations of the
said Society.
SI.
No.
7“
2
3
Dated :
Name and address
Signature
Appendix-Ill
(Generic) Bye-laws of the District Health Society
A
Procurement Policy and Procedures
Procurement of goods and services will be organized as per the procedures
recommended by the State Society. Commitments made to multilateral/bilateral donor
agencies with regard to Procurement Procedures under different Projects would be
honoured.
B
Procedure for release of funds
Funds would be ordinarily released from State Health Society to District Health Society
in two tranches. The Society funds shall be drawn through cheques and/or bank drafts
or through e-banking mechanism as and when the same is introduced.
All cheques shall be signed by two authorized signatories comprising of Accounts
Manager and Member-Secretary of the concerned programme committee.
All releases will be made on the basis of a written authorization from the MemberSecretary of the concerned programme committee.
Wherever releases are decided to be made through bank drafts and/or through ebanking, the authorization letter to the bank shall be signed by the concerned authorized
signatories.
Note: Wherever, under e-banking procedures, releases are to be made through
electronic authorization to the bank to issue cheque/draft/account transfer on
behalf of the Society, the electronic authorization will be executed by the same
two authorized functionaries of the Society secretariat who have been authorized
to sign cheques on the basis of a written authorization from the concerned
programme manager and/or consultant and/or Head of concerned Programme
Division and/or Executive Secretary and/or Chief Medical Officer.
C
Financial Powers of the Office Bearers of the Society (Governing Body,
Executive Committees, Programme Committees), Executive Secretary and
District Programme Managers
Type of expenditure_______________ Authority_______
A: Release of funds to Hospitals/ District
hospital societies, block Medical Programme
Officers and other implementing Manager (DHS)/
agencies as per State Government Memberapproved norms and/or proposals Secretary of the
concerned
approved by State Government.
Programme
Extent of power
Full powers.
B:
Release
of
funds
for
implementation of plans / allocations
approved by Governing Body /
Executive Committee, as approved by
the Executive Committee.
Committee
C: Expenditure proposals not covered under categories A and/or B
C-1: Procurement of goods
Chair-person,
Governing Body
C-2: Repairs and minor civil works
Chair-person,
C-3: Procurement of services for Executive
specific tasks including outsourcing of Committee
support services.
C-4:
Miscellaneous
items
not
mentioned above such as hiring of
taxis, hiring of auditors, meetings and
workshops, training, purchase of
training
material/
books
and
magazines,
payment of TA/DA
allowances for contractual staff and/or
non-official invitees to DHS meetings
and/or officials deputed to meetings
outside the district.
Chair-person,
Governing Body
Chair-person,
Executive
Committee_____
MemberSecretaries of the
Programme
Committees
D
Human Resources Policy and Procedures
D-1:
Recruitment and Appointment
More than Rs 2.00 lakh
and upto Rs. 5.00 lakh per
case.__________________
Upto Rs. 2.00 lakh per
case.
Upto Rs. 1.00 lakh at a
time subject to a maximum
of Rs. 10 lakh per annum.
Upto Rs 50,000 at a time,
subject to a maximum of
Rs. 5.00 lakh per annaum.
Upto Rs 5,000/- at a time
subject to a maximum of
Rs. 1.00 lakh per annum.
Recruitment would be through either of the following two routes:
• Appointments from open market: all such appointments will be on contractual
basis for a fixed tenure.
• Appointments on “Deputation” basis: all such appointments will be regulated in
terms of State Government rules relating to Deputation.
Recruitment may either be made by the State Society [ e.g. recruitment of Executive
Secretary from the open market or recruitment of District Programme Managers on
deputation basis] OR by the DHS [e.g. recruitment of support staff for the District
Programme Manager] OR a combination of both a may be determined by the State
Society.
All appointments would be temporary and would be made for the contract / deputation
period as may be determined by the State Government.
D-2: Terms of appointment (applicable to Society staff and Consultants)
The terms of appointment of the staff of the Society shall be regulated in terms of the
guidelines that may be provided by the State Government.
D-3: Compliance of Statutory Requirements:
The Society shall register itself with relevant government agencies for the purpose of
complying with the statutory requirements including regulations governing deduction of
tax at source relating to the staff, consultants and experts employed by it and/or
consultancies / contracts awarded by it in the course of performance of its tasks.
*******
Guidelines for Village Health and Sanitation
Committees, Sub Centres, PHCs and CHCs
Ministry of Health and Family Welfare
Government of India
1
TABLE OF CONTENTS
SUBJECT
PAGE NO
1
Guidelines Regarding Constitution of Village
Health and Sanitation Committees and Utilization
of Untied Grants to these Committees
1-4
2
Guidelines for use of Sub-Centre (SC) Funds
Under NRHM
5-6
3
Guidelines for Utilization of Untied Fund and
Annual Maintenance Grant for Primary Health
Centres (PHCs)
7-10
4
Suggested Guidelines for Implementation of
Indian Public Health Standards (IPHS) in Sub
Centres (SC), Primary Health Centres (PHCs) and
Community Health Centres (CHCs)
11-17
SL.NO.
2
Guidelines Regarding
Constitution of Village
Health and Sanitation
Committees and Utilization of
Untied Grants to these
Committees
1
GUIDELINES REGARDING CONSTITUTION OF VILLAGE HEALTH AND
SANITATION COMMITTEES AND UTILIZATION OF UNTIED GRANTS TO.
------------------------------------ THESE COMMITTEES
The detailed Implementation Framework of the National Rural Health
Mission [NRHM] approved by the Union Cabinet in July, 2006 provides for the
constitution and orientation of all community leaders on Village Sub Centre
Primary Health Centre and Community Health Centre Committees. The NRHM
implementation has been planned within the framework of Panchayti Raj
Institutions [PRIs] at various levels. The Village Health and Sanitation Committee
envisaged under NRHM is also within the overall umbrella of PRI.
Composition of the Village Health & Sanitation Committee
2.
To enable the Village Health & Sanitation Committee to reflect the
aspirations of the local community especially of the poor households and women,
it has been suggested that:
•
At least 50% members on the Village Health & Sanitation Committee should
be women.
.
Every hamlet within a revenue village must be given due representation on
the Village Health and Sanitation Committee to ensure that the needs of the
weaker sections especially Scheduled Castes, Scheduled Tribes, Ot er
Backward Classes are fully reflected in the activities of the committee.
.
A provision of at least 30% representation from the Non-governmental
sector.
3.
•
■ group etc
‘ on these committees etc.
Representation to women’s self-help
undertake
women
’s health activities more
will enable the Committee to i-------effectively.
.
Notwithstanding the above, the overall composition and nomenclature of
the Village Health & Sanitation Committees is left to the State Governments
as long as these committees were within the umbrella of PRIs.
Orientation & Training
Every Village Health & Sanitation Committee after being duly constituted by
the State Governments needs to be oriented and trained to carry out the activities
expected of them.
2
Village Health Fund
Every such committee duly constituted and oriented would be entitled to an
annual untied grant of Rs. 10,000/-, which could be used for any of the following
activities: -
4.
(i)
As a revolving fund from which households could draw in times of need
to be returned in installments thereafter.
(ii)
For any village level public health activity like cleanliness drive,
sanitation drive, school health activities, ICDS, Anganwadi level
activities, household surveys etc.
(iii)
In extraordinary case of a destitute women or very poor household, the
Village Health & Sanitation Committee untied grants could even be used
for health care need of the poor household.
(iv)
The untied grant is a resource for community action at the local level
and shall only be used for community activities that involve and benefit
more than one household.
Nutrition, Education & Sanitation,
Environmental Protection, Public Health Measures shall be key areas
where these funds could be utilized.
(v)
Every village is free to contribute additional grant towards the Village
Health & Sanitation Committee. In villages where the community
contributes financial resources to the Village Health & Sanitation
Committee untied grant of Rs.10,000/-, additional incentive and financial
assistance to the village could be explored. The intention of this untied
grant is to enable local action and to ensure that Public Health activities
at the village level receive priority attention.
Maintenance of Bank Account
The Village Health & Sanitation Committee fund shall be credited to a bank
account, which will be operated with the joint signature of ASHA/Health Link
Worker/Anganwadi Worker along with the President of the Village Health &
Sanitation Committee/Pradhan of the Gram Panchayat. The account maintenance
of this joint account shall be the responsibility of the Village Health & Sanitation
Committee especially the ASHA/AWW [wherever no ASHA]. The Village Health &
Sanitation Committee, the ASHA/AWW shall maintain a register of funds received
and expenditure incurred. The register shall be available for public scrutiny and
shall be inspected from time to time by the ANM/MPW/Gram Panchayat.
3
Accountability
5.
•
Every Village Health & Sanitation Committee needs to maintain updated
Household Survey data to enable need based interventions.
•
Maintain a register where complete details of activities undertaken,
expenditure incurred etc. will be maintained for public scrutiny. This
should be periodically reviewed by the ANM/Sarpanch.
•
The Block level Panchayat Samiti will review the functioning and progress
of activities undertaken by the VHSC.
•
The District Mission in its meeting also through its members/block
facilitators supporting ASHA [wherever ASHA’s are in position] elicit
information on the functioning of the VHSC.
•
A data base may be maintained on VHCSs by the DPMUs.
4
Guidelines for use of
Sub-Centre (SC) Funds Under
NRHM
pv-(v’
10184
s\
x
> Vz/
GUIDELINES FOR USE OF SUB-CENTER (SC) FUNDS UNDER NRHM
1. As part of the National Rural Health Mission, it is proposed to provide
each sub center with Rs. 10,000 as an untied fund to facilitate meeting
urgent yet discrete activities that need relatively small sums of money.
2. The fund shall be kept in a joint bank account of the ANM and the
Sarpanch
3. Decisions on activities for which the funds are to be spent will be approved
by the Village Health Committee (VHC) and be administered by the ANM.
In areas where the sub center is not co-terminus with the Gram Panchayat
(GP) and the sub center covers more than one GP, the VHC of the Gram
Panchayat where the SC is located will approve the Action Plan. The
funds can be used for any of the villages, which are covered by the sub
center.
4. Untied Funds will be used only for the common good and not for individual
needs, except in the case of referral and transport in emergency
situations.
5. Suggested areas where Untied Funds may be used include:
•
•
•
•
•
•
•
•
6.
Minor modifications to sub center- curtains to ensure privacy, repair of
taps, installation of bulbs, other minor repairs, which can be done at
the local level
Ad hoc payments for cleaning up sub center, especially after childbirth.
Transport of emergencies to appropriate referral centers
Transport of samples during epidemics.
Purchase of consumables such as bandages in sub center
Purchase of bleaching powder and disinfectants for use in common
areas of the village.
Labour and supplies for environmental sanitation, such as clearing or
larvicidal measures for stagnant water.
Payment/reward to ASHA for certain identified activities
Untied funds shall not be used for any salaries, vehicle purchase, and
recurring expenditures or to meet the expenses of the Gram Panchayat.
6
Guidelines for Utilization of
Untied Fund and Annual
Maintenance Grant for
Primary Health Centres
(PHCs)
7
GUIDELINES FOR UTILIZATION OF UNTIED FUND AND ANNUAL
MAINTENANCE GRANT FOR PRIMARY HEALTH CENTRES (PHCS)
Health sector reforms under the National Rural Health Mission (NRHM)
aims to increase functional, administrative and financial resources and autonomy
to the field units under which every PHC will get Rs. 25,000/- p.a. as untied grant
for local health action. Similarly every PHC will get an Annual Maintenance Grant
of Rs.50,000/- for improvement and maintenance of physical infrastructure.
Provision of water, toilets, their use and their maintenance has to be the
priorities. In addition, every PHC is being strengthened with provision of three
staff nurses as against one at present and provision of two doctors (one male,
one female) and Ayush practitioner.
Necessity of untied fund has been felt mainly due to unavailability of funds
2.
for undertaking any innovative Centre-specific need-based activity, as the
allotment of funds to the States has traditionally been of the nature of tied funds
for implementing a particular activity / scheme and this hardly left any funds with
the public health facilities. This centralized management and schematic in
flexibility in the use of funds allotted to the States, did not provide any scope for
local initiative and flexibility for local action at block and down below level. Also it
has been observed that most of the Primary Health Centres have not been
maintained properly due to lack of steady fund, available locally for
repair/refurbishing of infrastructure and basic facilities.
3.
Since there would be substantial fund flow to the districts to be utilized for
the Centres under NRHM / RCH-II and other programmes, the untied funds
should not duplicate what is / can be taken up under other programmes. Each
activity planned by the Centre should have clear rationale so that the impact of
the untied fund can be distinctively assessed. A separate register be maintained
in the PHC giving sources of funds clearly for various activities.
PHC untied fund shall be kept in the bank account of the concerned Rogi
Kalyan Samitti (RKS)/ Hospital Management Committee (HMC). PHC level
Panchayat Committee/Rogi Kalyan Samiti will have the mandate to undertake
and supervise the work to be undertaken from Annual Maintenance Grant. Both
the funds will be spent and monitored by RKS.
4.
5.
Suggested areas where Untied Fund may be used include:
•
Minor modifications to the Center- curtains to ensure privacy, repair of
taps, installation of bulbs, other minor repairs, which can be done at
the local level
8
•
Patient examination table, delivery table, DP apparatus, hemoglobin
meter, copper-T insertion kit, instruments tray, baby tray, weighing
scales for mothers and for newborn babies, plastic/rubber sheets,
dressing scissors, stethoscopes, buckets, attendance stool,
mackintosh sheet
•
Provision of running water supply
•
Provision of electricity
•
Ad hoc payments for cleaning up the Center, especially after childbirth.
•
Transport of emergencies to appropriate referral centers
•
Transport of samples during epidemics.
•
Purchase of consumables such as bandages in the Center
•
Purchase of bleaching powder and disinfectants for use in common
areas
•
Under the jurisdiction of the Centre.
•
Labour and supplies for environmental sanitation, such as clearing or
•
Larvicidal measures for stagnant water.
•
Payment/reward to ASHA for certain identified activities
•
Repair/operationalising soak pits
6.
The following nature of expenditures should not be incurred out of the
untied fund:
•
Purchase of Office Stationery and equipments, training-related
equipments, Vehicles etc.
•
Engagement of full time or part time staff and payment of
honorarium / incentives / wages of any kind.
•
Purchase of drugs, consumables and furniture.
•
Payments towards inserting advertisements in any Newspaper /
Journal / Magazine and IEC related expenditure.
9
•
Organizing “Swasthya Mela” or giving stalls in any Mela for
ostensible purpose of awareness generation of health schemes /
programmes.
•
Payment of incentives to individuals / groups in cash / kind.
•
Meeting any recurring non-plan expenditure.
•
Taking up any individual based activity except in the case of referral
and transport in emergency situations.
7.
The Centers are not required to take prior approval before implementing
the schemes from the untied funds but shall have to send quarterly SOE and UC.
10
Suggested Guidelines for
Implementation of Indian
Public Health Standards
(IPHS) in Sub-Centres (SC),
Primary Health Centres
(PHCs) and Community Health
Centres (CHCs)
11
SUGGESTED GUIDELINES FOR IMPLEMENTATION OF INDIAN PUBLIC
HEALTH STANDARDS (IPHS) IN SUB-CENTRES (SC), PRIMARY HEALTH
CENTRES (PHC) AND COMMUNITY HEALTH CENTRES (CHC)
Although a large number of Sub-centres, Primary Health Centres and
Community Health Centres have been established to provide comprehensive
promotive, preventive and curative services to the rural people in the country,
most of these institutions, at present are not able to function up to the level
expected of them due to varied reasons. National Rural Health Mission (NRHM),
launched by the Hon’ble Prime Minister on 12 April 2005, envisages to get these
institutions raised to the level of optimum availability of infrastructure, manpower,
logistics etc. to improve the quality of services and the corresponding level of
utilization. Through wide consultation with various stakeholders, Indian Public
Health Standards (IPHS) for these centres have been framed. The key aim of the
Standards is to underpin the delivery of quality services which are fair and
responsive to clients’ needs, which should be provided equitably and which
deliver improvements in health and well being of the population. Each PHC and
CHC, as part of IPHS, is required to set up a Rogi Kalyan Samity / Hospital
Management Committee, which will bring in community control into the
management of public hospitals with a purpose to provide sustainable quality
care with accountability and people’s participation along with total transparency.
To bring these centres to the level of Indian Public Health Standards, is no
doubt, a challenge for most of the States and also may require a detailed
institution specific facility survey to find out the gaps. However, considering the
dynamic process of setting up of the standards and the current manpower
availability, there is a need to bring these centres to IPHS in a phased manner as
the existing institutions are having different level of functional status. Some are at
very rudimentary stage, some are just functioning minimally and the others with
little more input could come up to the level of IPHS. Taking these points into
consideration, a set of guidelines has been framed to enable the States / UTs to
bring these centres gradually to the IPHS level.
National Rural Health Mission (NRHM) envisages a fully functional sub
centre in coordination with the village level functionaries such as Anganwadi
workers, ASHA, and the Village Health and Sanitation Committee. Similarly, all
the PHCs should function as 24-hour PHCs in a gradual manner. NRHM also
envisages a functional 30-bedded rural hospital at the block level providing
emergency obstetric care and neonatal care in the first instance as FRU and
gradually strengthen further to provide other specialists services as per the
details in the IPHS. The guidelines for achieving standards for IPHS centre wise
are as below:
12
Sub-centre:
♦ Conduct a facility survey and identify the gaps.
♦ Ensure that all the existing Sub-centres should be posted with one ANM
immediately. The vacant post may be filled up on contractual basis. There
should be an in-built plan to take care of vacancies arising out of
retirements, long leave, and other emergency situation so that the
services of ANM are available without any interruption.
♦ The appointment of second ANM as envisaged in the IPHS for each Sub
centre is to be made locally on contractual basis as per the demand,
phase wise. The most difficult areas such as hilly and tribal areas may be
given priority.
♦ The services of a Male Health Worker (MPW-M) is also necessary at the
Sub-centre. The states should take steps to fill up the post of these
MPWs (M) in a phased manner. The training capacity in the State for
these MPWs also need to be enhanced.
♦ Utilization of untied fund for strengthening the functioning of Sub-centres.
♦ All the existing Sub-centres buildings should be made environment
friendly, disabled friendly, with a good source of water supply, electricity /
solar power / other alternative energy sources. This can be ensured with
the help of Panchayat and related sectors.
♦ Utilization of Annual Maintenance Grant for strengthening of infrastructure
and basic necessities of the Sub-centres.
♦ The States may declare the names and the number of existing Sub
centres that have been made functional as per the IPHS for the purpose
of showing achievements under NRHM and information to the public.
Primary Health Centre (PHC) - 24 Hours Service Delivery Centre with
emphasis on Institutional Delivery:
NRHM envisages that all the Primary Health Centres (20,000-30,000
population) should function as a 24x7 centre in a phased manner to improve the
institutional deliveries conducted at these centres. The steps that may be needed
are as follows:
13
♦ Conduct an institution specific facility survey and identify the gaps.
♦ In order to make the PHC 24x7 delivery of services, the services of Staff
Nurses are essential. It must be ensured that there should be at least 4
Staff Nurses to perform rotation duties round the clock. In order to
improve the institutional deliveries, appointment of at least three Staff
Nurses may be recruited on contractual basis to fill the gaps. A labour
room with appropriate equipments and drugs with round the clock referral
transport support either managed by the PHC or by the NGOs / CBOs for
referring patients in case of emergency is essential. The States may take
stock of the situation of the training capacity and the facilities available in
the training institutions for turning over the required number of Staff
Nurses.
♦ Appointment of two Medical Officers (MBBS) (preferably one lady MO),
and one AYUSH practitioner, either by relocation or on contractual basis.
All effort should be made, such as contractual appointment or walk-in
interviews, making the District Cadre for Medical Officers and even
appointment of retired MBBS doctors on contractual basis, and other
incentives provided by the State government to see that all the PHCs have
the Medical Officers.
♦ All the existing Primary Health Centres buildings as far as possible should
be made environment friendly, disabled friendly, with a good source of
water supply, electricity / solar power / other alternative energy sources
and telephone. Rain water harvesting should also be promoted in the PHC
building. This can be ensured with the help of Panchayat and related
sectors such as water supply sanitation, horticulture etc. All the proposed
new buildings should have these components in their construction plan.
♦ Utilization of untied fund for strengthening the functioning of PHCs.
♦ Utilization
of Annual Maintenance
infrastructure and basic necessities
Grant
for
strengthening
the
♦ Each PHC must have a Rogi Kalyan Samity and display of the Citizens’
Charter.
♦ Once a specific PHC has achieved the 24x7 / IPHS status, the district
authority / state authority should declare the institution as 24x7 / IPHS.
14
Community Health Centre (CMC) - First Referral Unit (FRU)
Assured Services:
NRHM envisages a 30-bedded fully functional block level rural hospital.
The greatest challenge of bringing these CHCs to FRU / IPHS is the non
availability
of
the
specialists
especially
the
critical
ones
like
obstetric/gynecologist, anesthetist and pediatrician. The following steps may be
taken up:
♦ Conduct an institution specific facility survey and identify the gaps.
♦ The bringing up the CHC to the level of the IPHS may be carried out in
stages. First stage:- It must be ensured that all the CHCs provides 24x7
services with appropriate referral transport service. The basic requirement
for making it 24x7 service delivery, there should be four General Duty
Medical Officers and seven Staff Nurses, one ANM and one LHV along
with other support services and physical facilities. Each CHC must be
certified by the State Government / District Authority that this is
functioning as a 24x7 service delivery.
Second stage:- All the CHCs, declared as 24x7 may be upgraded to First
Referral Units (FRUs). The Minimum requirement of FRUs including
manpower, i.e. gynecologist, anesthetist, pediatrician, and round the clock
services of nurses and general duty officers should be ensured. Blood
storage facility and other supportive services such as laboratory, X-ray,
OT, labour room, laundry, diet, waste management system, referral
transport etc. must be ensured. Each CHC should be clearly demarcated
as FRU. CHCs, as FRU, will provide the 24 Hours delivery services
including normal and assisted deliveries, emergency obstetric care
including surgical intervention like cesarean section and other medical
intervention, newborn care, emergency care of sick children, full range of
family planning services including laparoscopic services, safe abortion
services, treatment of STI/RTI, availability of blood storage unit or effective
linkage facilities with blood banks, and referral transport services.
Third stage (IPHS):- Once the CHCs are qualified for FRU, next step
would be to post adequate number of other specialists and support
manpower as per the IPHS. Once these existing gaps in relation to
manpower, equipments, drugs, supplies and other support services, are
filled up, the CHCs can be declared to have achieved IPHS. The CHCs
declared as IPHS, apart from above mentioned services by FRU, also
must provide the following services:
♦ Care of routine and emergency cases in surgery
15
♦ Care of routine and emergency cases in medicine
♦ Services of a Public Health Manager
♦ Delivery of all
National
Health
Programmes including
communicable and non-communicable diseases and RCH services.
Manpower:
♦ Appointment of specialists may be made on contractual basis. All out
efforts should be made, such as contractual appointment or walk-in
interviews, making the specialist cadre in the State and even appointment
of retired specialists on contractual basis, public private partnership, and
other incentives provided by the State government. Short term training
course on anesthesiology and emergency obstetric care to the existing
serving general duty doctors may also be undertaken, to see that all the
CHCs have requisite manpower depending on the bed occupancy level.
♦ Appointment of Public Health Programme Manager on contractual basis.
♦ Appointment of Eye Surgeon (one for five CHCs) on contractual basis.
♦ Appointment of nine Nurses Midwives / Staff Nurses on contractual basis.
♦ All the existing Community Health Centres buildings as far as possible
should be made environment friendly, disabled friendly, with a good
source of water supply, electricity / solar |5ower / other alternative energy
sources and telephone. Rain water harvesting should also be promoted in
the CHC buildings. This can be ensured with the help of Panchayat and
related sectors such as water supply sanitation, horticulture etc. All the
proposed new buildings should have these components in their
construction plan.
♦ Dislocation of the existing centres for the sake of achieving the Standards
may not be required, unless compulsory due to unavoidable
circumstances. In that case, they could be resettled to an accessible place
where the original client group could easily get the services.
As far as manpower is concerned, optimum strength should be taken into
consideration.
16
Others
♦ Utilization of untied fund for strengthening the functioning of CHCs
♦ Utilization of Annual Maintenance
infrastructure and basic necessities
Grant
for
strengthening
the
♦ Utilization of fund for up-gradation of CHCs to IPHS
Implementation of achieving the Standards should keep into account the
linkage of the referral system right from Sub-centre to Community Health Centres
and to higher up institutions from CHCs.
17
Manual on
Community based Monitoring of Health
services
under
National Rural Health Mission
Drawing from
NRHM Framework of Implementation
Prepared by
Task force on Community Monitoring
Of
Advisory Group on Community Action
Based on the Proposal Sanctioned by Mission Directorate of NRHM,
MoHFW, Government of India
i
*
Contents
Part One - Introduction to Community Monitoring
Preface
3
Introduction to NRHM 4
Community Monitoring in NRHM 9
First Phase of Community Monitoring
13
Implementing the first phase of Community MonitoringlS
Screening Civil Society Organizations for involvement in Community Monitoring 25
Process documentation and review............................................................................. 21
Organisational responsibilities 29
National Secretariat on Community Action - NRHM
29
Organogram...............................................................
31
Budget Break Up for Community Monitoring
32
Block Level.................................................................
32
District Level
33
State Level Budget
34
Part Two - Modules for Training and Facilitation of Workshops
(To be done)
Part Three - Tools for Community Monitoring Activities at different levels
(To be done)
Annexures
Annexure 1 : NRHMSTRATEGIES35
Annexure 2 : MONITORING AND EVALUATION 36
Annexure 3 : COMMUNITY MONITORING FRAMEWORK 38
Annexure 4 : COMPOSITION, ROLESAND RESPONSIBILITIES OF MONITORING
COMMITTEES 40
Annexure 5 : CONCRETE SERVICE GUARANTEES 47
2
Preface
The National Rural Health Mission (NRHM) was launched on the 12th of April 2005 with
the goal of improving the availability of and access to quality health care by people,
especially for those residing in rural areas, the poor, women and children. . In order to
ensure that the services reach those for whom they are meant the NRHM proposes an
intensive accountability framework that includes Community-based Monitoring as one of
its key strategies.
The NRHM Framework for Implementation outlines the composition and broad roles of
monitoring and planning committees at various levels. These outlines were to be
subsequently elaborated for developing the process of community monitoring. The
Advisory Group for Community Action (AGCA) is a standing committee within the
NRHM, constituted to support and advise the MoHFW in the implementation and review
of the NRHM across the country. The AGCA took a lead in initiating discussions with
the MoHFW to develop a detailed proposal on how “Community Monitoring” could be
rolled out in a phased manner across the country. Through a process of discussions and
deliberations the AGCA developed a comprehensive proposal for decentralized
‘Community Monitoring” with the active partnership of the Department and Civil Society
institutions. The proposal was then forwarded Union Ministry of Health and Family
Welfare (MoHFW) for implementation on a national scale. The MoHFW has approved
this first phase of the “ Community Monitoring” proposal and has suggested that the
AGCA for a special Task Group for overseeing the implementation.
The AGCA has established a Task Group for the technical support and oversight in
implementing the project and it is being Chaired by Mr A R Nanda of PFL the convenor
of AGCA. A Secretariat has also been established jointly by Population Foundation of
India and Centre for Health and Social Justice at New Delhi
This Manual is based project proposal that has been approved being presented through
this manual for different stakeholders in the community.
3
Introduction to NRHM
There is an increasing recognition that despite significant improvements in health
parameters like life expectancy at birth of and the reduction of infant mortality there are
large parts of the country where people continue to have very poor access to health care
services and their health status continues to be abysmal. A high proportion of the
population continues to suffer from and die of preventable conditions like maternal
deaths, malaria and tuberculosis. Persistent malnutrition and high levels of anemia
amongst children and women is widespread. Due to the poor status of public health
systems people are also facing poverty and indebtedness from the costs incurred in
seeking health care. Public spending on health in India, especially on preventive and
promotive health is also very low in India. On the other hand the private, out of pocket,
expenditure on health is very high, about three times higher than the public expenditure.
Thus there is an urgency to deal with the multiple health related crisis that the rural poor
in the country are faced with. There is also the need to transform the health system into
an efficient, transparent and accountable system delivering affordable and quality
services.
The National Rural Health Mission has been conceptualized and is being implemented to
bring about these
GOALS
•
•
•
•
•
•
•
Reduction in Infant Mortality Rate (IMR) and Maternal
Mortality Ratio (MMR)
Universal access to public health services such as Women’s
health, child health, water, sanitation & hygiene,
immunization, and Nutrition.
Prevention and control of communicable and noncommunicable diseases, including locally endemic
diseases
Access to integrated comprehensive primary healthcare
Population stabilization, gender and demographic balance.
Revitalize local health traditions and mainstream AYUSH
Promotion of healthy life styles
fundamental changes
in the way health care
services are being
delivered to the rural
poor. The Goal of the
Mission is to improve
the availability of and
access to quality
health care by people,
especially for those
residing in rural areas, the poor, women and children.
4
The Mission seeks to provide universal access to equitable, affordable and quality health
care which is accountable at the same time responsive to the needs of the people,
reduction of child and maternal deaths as well as population stabilization, gender and
demographic balance. In this process, the Mission would help achieve goals set under the
National Health Policy and the Millennium Development Goals.
The Vision of the Mission
•
To provide effective healthcare to rural population throughout the country with
special focus on 18 states, which have weak public health indicators and/or weak
infrastructure.
•
18 special focus states are Arunachal Pradesh, Assam, Bihar, Chattisgarh, Himachal
Pradesh, Jharkhand, Jammu and Kashmir, Manipur , Mizoram, Meghalaya, Madhya
Pradesh, Nagaland, Orissa , Rajasthan, Sikkim, Tripura, Uttaranchal and Uttar
Pradesh.
•
To raise public spending on health from 0.9% GDP to 2-3% of GDP, with improved
arrangement for community financing and risk pooling.
•
To undertake architectural correction of the health system to enable it to effectively
handle increased allocations and promote policies that strengthen public health
management and service delivery in the country.
•
To revitalize local health traditions and mainstream AYUSH into the public health
system.
•
Effective integration of health concerns through decentralized management at
district, with determinants of health like sanitation and hygiene, nutrition, safe
drinking water, gender and social concerns.
•
Address inter State and inter district disparities.
•
Time bound goals and report publicly on progress.
•
To improve access to rural people, especially poor women and children to equitable,
affordable, accountable and effective primary health care.
In order to achieve its goals and objectives the Mission seeks to forge effective
partnerships between the Central State and Local governments. There are flexible
mechanisms built into the Mission so that local needs and priorities can be identified and
addressed and local initiatives promoted. Intersectoral convergence is also seen as a key
strategy of the mission for improving interventions in preventive and promotive health.
The Panchayati Raj institutions and the community have been given key roles in the
management of primary health care programmes as well as infrastructure.
5
Some of the key areas that have been identified for concerted action within the NRHM
framework of action are the following :
•
Well functioning health facilities;
•
Quality and accountability in the delivery of health services;
•
Taking care of the needs of the poor and vulnerable sections of the society and
their empowerment;
•
Prepare for health transition with appropriate health financing;
•
Pro-people public private partnership;
•
Convergence for effectiveness and efficiency.
•
Responsive health system meeting people’s health needs.
The expected outcomes from the Mission are:
1. Reduction of Infant Morality rate to 30/1000 live births by 2012.
2. Reduction of Maternal Mortality to 100/100,000 live births by 2012.
3. Reduction of Total Fertility Rate to 2.1 by 2012.
4. Reduction of Malaria Mortality Rate by 50% up to 2010 and an additional 10% by
2012.
5. Reduction of Kala Azar Mortality Rate by 100% by 2010 and sustaining elimination
until 2012.
6. Reduction of Filaria/Microfilaria Rate by 70% by 2010 by 80% by 2012 and
elimination by 2015.
7. Reduction of Dengue Mortality Rate by 50% by 2010 and sustaining at that level until
2012.
8. Increasing Cataract operations to 46 lakhs until 2012.
9. Reducing Leprosy Prevalence Rate from 1.8 per 10,000 in 2005 to less that 1 per
10,000 thereafter.
10. Maintain 85% cure rate in the Tuberculosis DOTS series through the entire Mission
Period and also sustain planned case detection rate.
11. Upgrading all Community Health Centers to Indian Public Health Standards.
6
12. Increase utilization of First Referral units through increased bed occupancy by
referred cases from less than 20% to over 75%.
13. Engaging 4,00,000 female Accredited Social Health Activists
At the community level it is expected
•
that there will be increased awareness about preventive health including nutrition
•
that there will be a trained worker available at the community level with a drug kit for
common ailments
•
a monthly health day will be organised where services related to maternal and child
health eg. immunization, ante-natal checkups and nutritional services will be
available
Through household and health facility survey
that involve Village Health Teams and discuss
findings locally.
• Through Health Camps that bring a range of
health services to the community and makes
them aware of their entitlements.
• Through “Public Hearings” or Jan Sunawai
oganized periodically where people share their
experience of seeking health care. Such Jan
Sunwais may be organized twice a year, or at
least once a year at PHC, block and district
levels.
• Through training and orientation of village
Health Teams for community action.
• By building team of Community Workers like
Aangan Wadi Sevika , ASHA, School Teacher,
Mahila Samakhya worker, PTA/MTA’ members,
etc.
• By involving group like SHGs, Community
based organizations, MTAs, PTAs, literacy
volunteers, Containing Education Centre
volunteers, etc. who have motivation for
Community action.
• By making local level health functionaries visit
households frequently.
• By making Block and District level Health
Mission teams, including NGOs, organize a
series of activities like health camps, public
hearings, etc.
drugs
generic
How to trigger Community action?
for
common ailments will be
•
at
available
the
Sub-
centre and good hospital
care
will
through
be
assured
availability
of
doctors, drugs and quality
at
services
PHC/CHC
level
•
there will be improved
available
facilities
instutitional
for
deliveries
and the Janani Suraksha
Yojna will also provide
for
opportunities
subsidized hospital care
for
those
below
the
poverty line
Mobile medical units will
ensure
availability
of
7
services to remote underserved areas
•
There will be provision of safe drinking water and household toilets
In order to ensure that these outcomes are achieved and quality and accountable health
services which are responsive and are taking care of the needs of the poor and vulnerable
sections of the society, community ownership and participation in management has been
seen as an important pre-requisite within NRHM. Community monitoring is an important
component for achieving these results.
8
Community Monitoring in NRHM
Introduction to Community Monitoring - The accountability framework proposed in the
NRHM is a three pronged process that includes internal monitoring, periodic surveys and
studies and community based monitoring. Community Monitoring is also seen as an
important aspect of promoting community led action in the field of health. The provision
for Monitoring and Planning Committees has been made at PHC, Block, District and
State levels.
The adoption of a comprehensive framework for community-based
monitoring and planning at various levels under NRHM, places people at the centre of
the process of regularly assessing whether the health needs and rights of the community
are being fulfilled.
The community monitoring process involves a three way partnership between health care
providers and managers ( health system); the community, community based organizations
and NGOs and the Panchayati Raj Institutions. The success of the community monitoring
process will depend upon the ownership of the process by all three parties and a
developmental spirit of ‘fact-finding’ and Teaming lessons for improvement’ rather than
‘fault finding’.
The objectives Community Based Monitoring can be seen as follows:
•
It will provide regular and systematic information about community needs, which will
be used to guide the planning process appropriately
•
It will provide feedback according to the locally developed yardsticks, as well as on
some key indicators.
•
It will provide feedback on the status of fulfillment of entitlements, functioning of
various levels of the Public health system and service providers, identifying gaps,
deficiencies in services and levels of community satisfaction, which can facilitate
corrective action in a framework of accountability.
•
It will enable the community and community-based organisations to become equal
partners in the planning process. It would increase the community sense of
involvement and participation to improve responsive functioning of the public health
9
system. The community should emerge as active subjects rather than passive objects
in the context of the public health system.
•
It can also be used for validating the data collected by the ANM, Anganwadi worker
and other functionaries of the public health system.
Process of Community Monitoring - The exercise of “Community monitoring” involves
drawing in, activating, motivating, capacity building and allowing the community and its
representatives e.g. community based organizations (CBOs), people’s movements,
voluntary organizations and Panchayat representatives , to directly give feedback about
the functioning of public health services, including giving inputs for improved planning
of the same. The community and community-based organisations will monitor demand /
need, coverage, access, quality, effectiveness, behaviour and presence of health care
personnel at service points, possible denial of care and negligence. The monitoring
process will include outreach services, public health facilities and the referral system.
The key institutions for community monitoring as laid out in the Framework of
Implementation are the
•
Village Health and Sanitation Committee
•
The PHC Planning and Monitoring Committee
•
The Block Planning and Monitoring Committee
•
The District Planning and Monitoring Committee and
•
The State Planning and Monitoring Committee
Guidelines regarding the composition, roles and powers of these committees have been
laid out in detail in the Framework of Implementation and are reproduced in Annexure
XX.
The monitoring process will begin with a village report being prepared by the Village
Health and Sanitation Committee after consulting village records ( eg. ASHA records or
ANM records or the Village Health Register) and also conducting interviews and
meetings with potential beneficiaries (like women who are pregnant or have undergone
childbirth in the recent past, or those with small children) to understand the community
members experiences and problems faced as well as assess the extent to which key
10
services are being delivered effectively. The Monitoring committee at each subsequent
level would review and collate the reports coming from the committees dealing with units
immediately below it. For example, Block Committee will receive and review the VHSC
reports while the District committee would receive and review the reports from all Block
committees. However the Monitoring committees would not only rely on reports, but
would also make its own independent observations on selected key parameters. Each
committee would appoint a small team drawn from among its civil society and PRI
representatives who would visit on a quarterly / six monthly basis a small sample of units
(say one facility or two villages) under their purview and directly review the conditions
there. This will enable the committee to not just rely on reports but to also have a first
hand assessment of conditions in their area. For example, the PHC committee
representatives would visit two villages and conduct Group discussions there, in each
trimester selecting different villages by rotation. Similarly the Block committee
representatives would visit one PHC by rotation in each trimester. The monitoring
committees at PHC / Block / District levels will be responsible for making an assessment
of the functioning of the major Health care facility at their respective level (PHC / CHC /
District Hospital).
Sharing of the findings of monitoring committees will not only take place through the
periodic report submitted to the next level of monitoring committee but also through
periodic public sharing . Monitoring committees at PHC, Block and District level will be
involved in six-monthly or annual Jan Samvads or Public hearings at their respective
levels, where committee members would get share the results of their findings and also
get direct feedback of the situation including possible presentation of cases of denial of
health care. Similarly, it is State Planning and Monitoring Committee will conduct an
annual public meeting open to all civil society representatives where the State Mission
report and independent reports will be presented and various aspects of design and
implementation of NRHM in the state, including State specific health schemes, would be
reviewed and discussed enabling corrective action to be taken.
11
A broad outline of the ambit and scope of community monitoring at different levels is
given below in the Table below.
Community
Monitoring
Committee
Village Health
and Sanitation
Committee
Periodicity
of
Monitoring
Quarterly
PHC
Monitoring and
Planning
Committee
Quarterly
Block
Monitoring and
Planning
Committee
Quarterly
District
Monitoring and
Planning
Committee
Quarterly
State
Monitoring and
Planning
Committee
Six Monthly
Activities to be undertaken
a. Reviews Village Health register, Village health
calendar
b. Reviews performance of ANM, MPW, ASHA
c. Reviews communities own experiences as
beneficiaries of services
d. Sends brief three monthly report to PHC
committee________________________________
a. Reviews and collates reports from all VHSCs
b. An NGO / PRI sub team conducts FGDs in three
sample villages under PHC
c. Visit PHC, review records, discuss with RKS
members
d. Send brief three monthly report to Block
committee
a. Reviews and collates reports from all PHCs
b. NGO / PRI sub team visits at least one PHC of the
block, conduct interviews with MO and make
observations
c. Visit CHC and review records, discuss with RKS
members
d. Send brief three monthly report to District
committee__________________________________
a. Reviews and collates reports from all Blocks
b. An NGO / PRI sub team visits at least one CHC of
the District, conducts interviews with Incharge, meets
Block committee members and RKS members,
makes observations c. Visits District hospital and
reviews records, discuss with RKS members
c. Send brief three monthly report to State committee
a. Reviews and collates reports from all Districts
b. An NGO / PRI sub team visits 3 to 5 Districts,
conducts interviews with DHO and District
Committee members, makes observations on DH
c. Sends six monthly report to NRHM / Union Health
Ministry
12
First Phase of Community Monitoring
The outlines of Community Monitoring process provided within the Framework of
Implementation have been developed and elaborated upon by the Advisory Group on
Community Action. The first phase is being seen as a learning phase because no similar
community monitoring activity, either in the health sector or in other social sectors has
been implemented on a country wide scale before. Thus in the first phase the
implementation will be supervised at a national level by a specially constituted
Secretariat and Task Group constituted under the supervision of the Advisory Group. It
has been decided that the first phase will be of eleven months (March 07- Jan 08) and
cover eight states.
Some reasons because of which it would be desirable to start with a learning phase are as
follows:
Learningfrom experiences and mistakes on a smaller scale, then moving to a larger
scale: This is probably the first time in the country that the official health system is
institutionalizing community monitoring of health services on a major scale. There is
scope for many kinds of experiences and even deviation from objectives, so it is thought
to be desirable to try out the process on a smaller scale and make corrections before
moving to a state-wide scale
The need to pool expertise and build an initial critical mass: The number of
organizations with experience in rights-based and accountability oriented work related to
the Health sector may not be very large in many states. Similarly, expertise and
commitment related to this activity within Health departments may also be limited to
begin with. It would be desirable for facilitating agencies both within and outside the
Health department to come together, share expertise, help launch pilots in a few areas,
and analyse experiences, before going to scale at the state level. This would also
strengthen ownership of the process within the Department. Starting directly with a
widely generalized model would demand very extensive involvement of comparatively
few facilitators from day one, they would have to immediately spread themselves thin not allowing much space for initial development of methodologies and building a critical
mass.
13
The process of developing community monitoring is a delicate process that needs to be
handled carefully. Community mobilization experiences in the Health sector show that
the initial response of community representatives is often to assertively point out a whole
range of problems, deficiencies, gaps and even alleged cases of denial of health care
which may be quite difficult for the Health officials to digest and take in the right spirit which could even at times, lead to a virtual breakdown of dialogue. Maintaining the
vitality and authenticity of the process, but not allowing complete polarization which
would disrupt the dialogue and convergence process itself is a delicate task. Starting by
launching the community monitoring process all over the state on a large scale may
conceivably lead to potentially disruptive situations and even demotivation of Health
functionaries - which could be avoided by first working out the process in pilot areas and
building appropriate checks and balances in the methodology before moving to
generalization.
Scale of Implementation of the First Phase - The first phase of the Community
Monitoring component ofNRHM will be implemented in 30 selected districts of 8 states
of the country. These are
# Assam
# Chhattisgarh
# Jharkhand
# Madhya Pradesh
# Maharashtra
# Orissa
# Rajasthan
# Tamil Nadu
In each of these states a number of districts will be selected ( between three and five
depending upon the number of districts in the state) on the basis of regional diversity as
well as the presence of a credible district level NGO/ Civil Society Organisation which
can facilitate the implementation. In each of these districts 3 blocks will be chosen for the
first phase, and from among these three blocks the operational area of 3 PHCs will be
selected. Five villages will be selected for initiating Community Monitoring in each of
the 3 PHC areas. The total numbers of districts, blocks, PHCs and villages is summarised
below
•
For States with 15 to 29 districts: 3 pilot districts to be selected
•
For States with 30 to 39 districts: 4 pilot districts to be selected
14
•
For States with 40 and above districts: 5 pilot districts to be selected
•
This will lead to a total of 30 districts spread across these eight states.
•
In each district, three blocks shall be identified giving a total 90 blocks
•
In each of these blocks, three PHCs shall be identified giving a total 270 PHCs
•
In each PHC area, five revenue villages shall be identified giving total 1350 villages
Needfor involving Civil Society Organisations/ NGOs in the first phase - NGOs or
Civil Society Organisations have been given crucial roles in the NRHM. It is envisaged
that besides providing services in selected areas, they will not be members in institutional
arrangement at all levels, but will also act as resource organizations and provide support
for evaluation, monitoring and social audit. These organizations will have a crucial role
to play in the first phase of Community Monitoring to ensure its success. Although State
health departments would play an extremely important role in developing community
monitoring activities, however the facilitation of Community based monitoring has not
been left to State health departments. Some of the reasons for this are as follows:
It is largely the Health department functionaries themselves who would be monitored;
hence for the monitoring to be robustly independent, it is not sufficient to leave the entire
task of developing the monitoring framework to the Health department alone.
For effective Community monitoring, capacity building of a whole set of actors like
beneficiary representatives, community based organizations (CBOs), people’s
movements, voluntary organizations and Panchayat representatives, who will eventually
do the monitoring ,is imperative. Hence involvement of networks, organizations and
individuals with experience of community mobilization and community based monitoring
to facilitate involvement in the health system of this whole new set of actors is needed.
To facilitate change in the balance ofpower in the Health sector, in favour ofpeople.
The exercise of community monitoring carries meaning only if ordinary people and their
spokespersons in form of both Panchayat representatives and Community based
organizations, gain a degree of authority to identify gaps and correspondingly propose
priorities and influence decision making regarding the Health system.
The kind of capacity required to develop a participatory community monitoring system is
quite different from programme implementation and training usually conducted by the
15
Health department; hence involving voluntary sector agencies with some experience of
accountability building and health rights work would be desirable to help facilitate this
process.
Role of Civil Society Organizations in the First Phase - Civil society organizations i.e.
Community based organizations (CBOs) and Non Governmental Organizations (NGOs)
would have three kinds of roles in the process of Community based monitoring
As members of monitoring committees e.g.
As resource groups for capacity building and facilitation
As agencies helping to carry out independent collection of information.
As members of monitoring committees, social organizations working in close, regular
contact with communities on health related issues, especially from a rights-based
perspective, would be able to present in various monitoring committees the community
concerns, experiences and suggestions regarding improving public health system
functioning.
As resource groups for capacity building and facilitation, NGOs and CBOs will have the
responsibility for overall facilitation of the initial process of committee formation and
capacity building of Community Monitoring committee members about the process of
Community based monitoring including the roles of members, at different levels,
including peripheral committees at PHC and village levels.Based on national model
material, training modules and materials for orientation of Community Monitoring
committee members would be adapted and published at state level and used for this
capacity building process. All three types of members - Panchayat representatives, civil
society organisations and health system functionaries would benefit from such capacity
building.
As agencies helping to carry out collection of information, NGOs and CBOs would
contribute to the collection of information relevant to the monitoring process at all levels
- from the village to state level. In these processes, an element of community
16
mobilisation may be involved. Specific teams would dialogue with communities and
would collect and process community-based information. These teams could be sub
groups drawn from the larger Monitoring committee at specific levels, but could also
include some persons from beyond the Monitoring committee. Formation of such teams
should be encouraged especially at the PHC and Block levels. Each team should include
members from one or more facilitating NGOs and PRI members, and could also include
representatives from among the Health care providers. Such teams should undergo a short
orientation exercise before they undertake the community monitoring exercise.
17
Implementing the first phase of Community Monitoring
The first phase of the Community Monitoring process is being implemented under the
overall supervision of the specially constituted Task Group of the Advisory Group on
Community Action. A National Secretariat has been set up in Delhi through the
collaboration of Population Foundation of India and Centre for Health and Social Justice.
Preparatory Phase - The activities that are to be undertaken during the first phase and the
persons responsible at each level are given in the table below. The preparatory phase will
last from March 07 to June 07.
Activity
Responsibility
Support from
Setting up Task Group___________
Setting up National Secretariat
Contacting State Secretaries in the 8
states________________________
Contacting Civil Society
Organisations in the 8 states______
Preparation of necessary Materials,
Curricula and Modules__________
Meeting with state CSOs and
identifying State Nodal
organization___________________
Meeting with State Health
Secretary and NRHM Directorate
and setting up State Community
Monitoring Mentoring Group
AGCA
AGCA- Task Group
MoHFW
MoHFW. GOI
Task Group
National Secretariat
Task Group
AGCA- Task Group
National Secretariat
AGCA- Task Group
National Secretariat
State Mentoring Group - The State Mentoring group would be formed involving
representatives of the State Health department and state level Health sector voluntary
networks. Based on experience and demonstrated interest, the State Mission Director and
the state designated AGCA members would suggest the names for this mentoring team.
This team would have definite responsibilities to develop community monitoring in the
state during the first phase and beyond, which would be clearly spelt out. This team
would have seven to eleven members, of which at least four to seven would be civil
18
society representatives. In addition, the designated national AGCA members would be
permanent invitees to the State mentoring team.
State Nodal Organisation - One of the State level NGOs with membership in the State
mentoring team would be selected to work as the state nodal NGO during the pilot phase.
This state nodal NGO would work under the direction of the State mentoring team.
Other state level activities to be carried out in the preparatory phase are as follows:
Activity
Responsibility
Support from
Selection of districts and blocks for
implementing the project________
Selecting organizations which will
be implementing activities at the
district and block level__________
State level workshop to finalise the
districts and modalities of district
and block level activities_________
State level TOT
State C M Mentoring
Group____________
State C M Mentoring
Group
Task Group - National
Secretariat__________
Task Group - National
Secretariat
State C M Mentoring
Group
Task Group - National
Secretariat
State C M Mentoring
Group____________
State C M Mentoring
Group
Task Group - National
Secretariat__________
Task Group - National
Secretariat
Adapting and translating materials,
curricula and modules for the state
A State level workshop will be organised by the State mentoring team and State Health
Mission involving all stakeholders (State Mission officials, District health officials and
PRI representatives from selected districts, NGO networks and civil society organizations
from these districts) along with NRHM Gol representatives. The activities of the first
phase will be shared and the process would be finalised. Detailed timetable for District
level meetings, formation and orientation of committees could be worked out in this twoday State level workshop.
State level Training of Trainers for the facilitating teams from all pilot districts would
need to be conducted primarily by voluntary sector facilitators in the pilot phase, since
Government officials may not have adequate experience in community monitoring
activities. However State Health department officials would be present and would be
involved in these workshops, enabling them to actively participate in further such
trainings.
19
Outcomes of the Preparatory Phase:
•
National Secretariat has been established
•
State Community monitoring mentoring groups have been established in all eight
states
•
State Nodal Organisation has been established in all eight states
•
State level workshops have been organised in all states
•
State level TOT has been organised in all states
•
Draft of materials, curriculum and modules have been prepared
•
State level adaptation has begun
District level implementation phase - Once the District and block level facilitating
organizations have been trained and selected the key activities will shift to the district and
block levels. The time allocated for these activities is July 07 to December 07 in the first
phase.
The activities at the district and block level will proceed in the following manner:
Getting Ready for Community Montoring - District processes would be facilitated by
NGOs taking responsibility in the first phase districts along with the District health
officials and PRI representatives. A District mentoring team (including representatives of
each of the three groups) to facilitate the Community monitoring process will be put in
place, which would facilitate the orientation activities in this and subsequent stages. In
each district one NGO would need to take responsibility as the District nodal NGO. This
NGO would be assisted by other civil society organisations that would take specific
responsibility in various blocks. The process could start with a District level workshop to
share the concept, identify Blocks and PHCs, involving key district health officials, PRI
members and civil society organisations. Three blocks within the district could be
selected for pilot implementation. Block nodal civil society organisations would take up
responsibility for specific blocks in coordination with the District nodal NGO.
20
There would be a need to conduct a Block level training for at least a four member Block
Community Monitoring facilitation team, including at least two NGO/CBO members.
Preferably half of the Block team should be women. These Block facilitation team
members would be responsible for the subsequent committee formation and orientation
processes. It is anticipated that these activities could be completed in the month of July
07.
VHSC
VHSC
PHC Planning and
Monitoring
Committee
Block Planning and
Monitoring
Committee
VHSC
VHSC
VHSC
PHC Planning and
Monitoring
Committee
PHC Planning and
Monitoring
Committee
Block Planning and
Monitoring
Committee
Block Planning and
Monitoring
Committee
District Planning
and Monitoring
Committee
21
Formation of Committees - During the next four months (Aug. - Nov. 07), there would
be formation of committees at Village, PHC, and Block levels in the selected blocks (in
that order), along with organising primary orientation of their members. Formation of
Community Monitoring committees would start from village committees, then PHC, then
Block, and then District committees. A few members from VHCs would be included in
the PHC committee; similarly a few PHC committee members would be included in the
Block committee. Therefore it would be important to constitute the committees from
village level upwards in such a sequential order. CBOs / NGOs and Panchayat
representatives who have shown leading initiative in organising community monitoring
activities at any level should find representation in the next higher level committees.
Adequate representation of women, Dalits and Adivasis should be ensured in various
committees.
Following committee formation at the peripheral levels, the District level committee
could also be finalised and would become functional by Nov. 07. In the pilot phase, at the
state level a provisional committee could be formed by Dec. 07. This would be given
final shape only after the next phase of ‘Extended implementation’ is completed and at
least half of the Districts of the state have in place Community monitoring committees,
which could send representatives to the State committee.
Community Monitoring - The community and community-based organisations will
monitor demand / need, coverage, access, quality, effectiveness, behaviour and presence
of health care personnel at service points, possible denial of care and negligence. The
monitoring process will include outreach services, public health facilities and the referral
system. The Community Monitoring exercises and collation of information should be
organised village wise, PHC wise, Block-wise, District wise. In this way these exercises
should aggregate information upwards. The monitoring results should also be shared at
the Village level, Block and District level in the appropriate PRI fora. Some of the
frameworks on which Community Monitoring may be done, and which are included
within the NRHM are as follows:
1. Village Health Plan, District Health Plan
TL
2. Entitlements under the Janani Suraksha Yojna
3. Roles and responsibilities of the ASHA
4. Indian Public Health Standards for different facilities like SubCentre, PHC, CHC
5. Concrete Service Guarantees
6. Citizen’s Charter and so on.
Activities that have to be undertaken at the village level for community monitoring have
already been Table x Section y Page z.
PHC and Block level community monitoring exercises would include a public dialogue
(‘Jan Samvad’) or public hearing (‘Jan Sunwai’) process by Dec. 07. Here individual
testimonies and assessments by local CBOs / NGOs would be presented. Individual
testimonies could be identified through the adverse outcome recording process. These
Public dialogues should be moderated / facilitated by the District and Block facilitation
groups in collaboration with Panchayat representatives and CBOs / NGOs working on the
issue of Health rights.
Issues for Monitoring
Mechanism for Monitoring
ANM / ASHA services inch maternal,
infant and child health services at
village level; ASHA activities
Availability of key services at local
health facilities
Selected adverse outcomes like
maternal neonatal death
Denial of health care
Review of documents like - Village
Health register, Village Health
calendar, ANM / MPW records
Group discussion with women
Interviews of ANC/ PNC/
Immunisation beneficiaries
Interview with ASHA and ANM
Interview with those with adverse
outcomes and denial of care
I
Village Health Report Card
PHC Monitoring
•
Staffing, Supplies and services
availability at PHC
• Quality of care at the PHC from
people’s perspective
• Implementation of NHP etc.
Through Observation and Interviews
>
PHC Report
Card
Block
Monitoring
23
Block level Monitoring
•
•
•
•
•
Overview of community outcomes
and experience
Overview of PHC level services
Staffing, Supplies and services
availability at CHC
Quality of care at the CHC from
people’s perspective
Implementation of the National Health
Programmes etc
>
Jan Sanwad/ Jan
Sunwai) Public
dialogue / sharing
District level Monitoring
Overview of community outcomes
and experience blockwise
Overview of CHC level services
Staffing, Supplies and services
Jan Sanwad/ Jan
Sunwai) Public
dialogue / sharing
Health
State level Monitoring
•
•
•
Overview of community outcomes
and experience throughout the state
Overview of status of health care
facilities and the services provided by
them at different levels - PHC, CHC,
DH
All issues of Rural public health
services / NRHM in the state
including State specific health
The Monitoring committee at each level would review and collate the summary reports
coming from the committees dealing with units immediately below it. This enables it to
make an assessment of the situation prevailing in all the units under its purview, and to
24
make a report at its level. For example, the District committee would receive and review
the reports from all Block committees.
However Monitoring committees would not only rely on reports, but would also directly
interact in the field situation and get feedback. Firstly, each committee would appoint a
small sub-team drawn from its NGO and PRI representatives who would visit on a
quarterly / six monthly basis a small sample of units (say one facility or two villages)
under their purview and directly review the conditions there. This enables the committee
to not just rely on reports but to also have a first-hand assessment of conditions in their
area. For example, the PHC committee representatives would visit two villages and
conduct Group discussions there, in each trimester selecting different villages by rotation.
Similarly the Block committee representatives would visit one PHC by rotation in each
trimester.
Secondly, monitoring committees at PHC, Block and District level would be involved in
six-monthly or annual Jan Samvads or Public hearings at their respective levels, where
committee members would get direct feedback of the situation including possible
presentation of cases of denial of health care. Similarly, it is suggested that the State
health mission could conduct an annual public meeting open to all civil society
representatives where the State mission report and independent reports would be
presented and various aspects of design and implementation of NRHM in the state,
including State specific health schemes, would be reviewed and discussed enabling
corrective action to be taken.
Screening Civil Society Organizations for involvement in Community Monitoring
In order to screen civil society organizations for their capacity to partner in community
monitoring activities, and to participate in monitoring committees at various levels, a
simple questionnaire will be used. Such organisations may include Community Based
Organisations (including self-help groups and people’s organisations) as well as NGOs
working at the respective level, with documented activity in the area since at least three
years. In addition to other questions about the organization, the following issues will be
included in the questionnaire.
25
based
Activity Profile
Community
Mobilisation
Women’s
Empowerment
Activities
Rights
Activities
Al - Income Generation
A2 - Environment /
Natural Resource Mgmt
A3 - Education
A4- Health
Cl- Self Help Groups
Level
C2Village
Committees
C3- Federations
C4Community
Leadership training
C5- Work with PRIs
C6 - Village based
organisation
and
mobilisation on specific
issues
level
WlVillage
women’s groups
W2
Women’s
leadership development
and training
W3 - Women and PRI
R1 - Right to Healthcare
R2- Right to Food
to
R3Right
Information
to
R4Right
Employment
R5- Livelihood rights
e.g. rights related to
Forest, Land, Wages,
Displacement
etc.
(specify)
On the basis of their responses to their questionnaire the following screening table will be
used and any organization that has at least one entry in all the four aspects (with brief
report of the activity carried out in that aspect) may be considered as having qualified.
Any organisation with demonstrated experience of monitoring Public services, organising
public dialogues or public hearings should be given priority to participate in the
Community Monitoring committees.
Name
of
CSO
Activity Profile
Al
Community
Mobilisation Activities
A2 A3 A4 Cl
C2 C3 C4 C5
Women’s
Empowerment
Activities
W1 W2 W3
Rights based
Activities
R1
R2 R3
Key considerations while making a selection- To ensure wide participation diverse
group of civil society networks and organizations involved in promotion of Health rights
and monitoring shall be involved at various levels
The process of selecting civil society organisations to be involved in monitoring
committees at all levels could be facilitated by the mentoring team of the respective level,
with guidance from the mentoring team of the higher level. For example, the district
mentoring team could suggest the names of civil society organisations to be involved in
the District monitoring committee, with inputs from the state mentoring team as relevant.
This should be a participatory process including various civil society networks and
26
organisations. It should not be limited to NGOs, and should also definitely involve
Community based organisations and people’s organizations
Civil society involvement in monitoring should not be focussed only on ‘mother NGOs’
which are often deeply involved in implementation and who may not always be the most
objective monitors of work which they themselves are involved in implementing.
Particularly for the Community monitoring process in NRHM, it is imperative that the
idea is not confined to just ‘leave it to mother NGOs’ but rather that organizations with
experience of rights based activities and accountability enforcing activities be given
adequate space and responsibility at all levels.
Process documentation and review
Since the first phase of the Community Monitoring process is a learning phase it will
include process documentation and review as an important component. This will include
the following three distinct stages:
Process Documentation*. To ensure uniformity of recording the activity, each activity of
the project that has been mentioned above will include a documentation procedure. These
documents will be filled in by the responsible agency at different levels and collated at
the state level. The state mentoring team will be responsible for analyzing these
documents and will prepare a review report on the state implementation, reporting what
interventions worked and why and suggesting changes.
Evaluation of the state level intervention'. There will be an independent evaluation of the
different interventions and their impact on different stakeholders by a team of two
experts. The evaluation will include review of the documentation process, interviews
with different stakeholders, including members of the community in a limited number of
locations across each of the 8 states.
T1
State level review workshops'. The third component of the review process will comprise
of an endline workshop with those involved in implementing the pilot phase to review the
process of the pilot in each state.
28
Organisational responsibilities
The entire range activities during the first phase would need to be supported by NRHM
Mission Directorate from the Union Health Ministry level for rapidity of execution, given
the compressed timeframe available. Responsibilities for handling funds and ensuring
activities at various levels may be allocated as follows:
Level
National
State
District
Block and below
Responsibility_______________________________
Overall facilitation by AGCA (in consultation with
NRHM officials). Financial responsibilities and
coordination handled by AGCA secretariat along with
sub-group of AGCA_____ _____________________
State Nodal NGO under guidance of State Mentoring
team (which would include State Mission Director)
District nodal NGO under guidance of District
mentoring team (which would include District Health
Officer)_________________________
Block nodal civil society organisation (in coordination
with District nodal NGO)
National Secretariat on Community Action — NRHM
At the national level, the Task Group of the Advisory Group on Community Action
(AGCA) will be facilitating the entire process of community action in consultation with
the Ministry of Health and Family Welfare. The Population Foundation of India is the
Secretariat for the AGCA. A National Secretariat will be set up under the leadership of
PFI along with Centre for Health and Social Justice at New Delhi. The Secretariat will be
undertaking special facilitation of the community monitoring process at the national level
in consultation with the MOHFW and NRHM Mission. The National Secretariat would
function within the framework formulated by the AGCA for community based
monitoring of programmes under NRHM.
The National Secretariat would have the following role and responsibilities:
• Coordinating activities of the national preparatory phase, which includes
developing tools, model curriculum, workshops, awareness materials and
documentation formats for the programme.
29
• Assist the AGCA members and the state NRHM Directorates and NGO networks
for the state preparatory stage.
• Facilitate process documentation and review of the pilot implementation phase in
consultation with AGCA members.
• Develop a website on community based monitoring of processes and access to
services under NRHM
• Manage the financial responsibility of the pilot programme
• Prepare progress reports, field visits and the national dissemination workshops of
the programme at the national level
• Conduct quarterly review of AGCA for review of the pilot programme.
Staffing - The National Secretariat would be managed by two officers responsible for the
overall programmatic and financial coordination of the programme. The coordinators
would report to the Task Group of AGCA.
30
Organogram
Ministry ofHealth and Family Welfare (Gol)- NRHM
(The pilot project on community based monitoring of health services under NRHM is a
GOI initiative. The fundfor the pilot phase facilitation and implementation would be
given by the NRHM. Supported by the MoHFW, the State health departments have a
central role in developing the Community monitoring framework)
Advisory Group on Community Action (A GCA)
National Secretariat on Community Action- NRHM
State Monitoring and Planning Committee
State Mentoring Team
(At the State level, the State Mentoring team would be formed involving representatives
of the state health department and state level health sector voluntary networks. This team
would have definite responsibilities to develop community monitoring in the state. It will
____________ organize State level workshop with State Health Mission)
State Nodal NGO
(Out of the state mentoring team, one NGO Member will designated as State NodalNGO)
District mentoring Team
(This team will include PRI representatives, district Health Officials and NGO
_____________________________ representatives)_____________________________
District Nodal NGO
The District level and Block level funds in the pilot phase in each state would be given to
designated District nodal NGO to enable a fast start-up and adequate flexibility in the
process)
District Monitoring and Planning Committee
Block nodal civil society organizations
(The District nodal NGO would collaborate with Block nodal civil society organisations
for execution of activities in specific blocks)
Block Community Monitoring Facilitation Team
(Responsible for subsequent committee formation and orientation processes)
Block Monitoring and Planning Committee
PHC Monitoring and Planning Committee
Village Health and Sanitation Committee
31
Budget Break Up for Community Monitoring
Activity Budgets
Block Level
Number of Participants in
Cost per
unit
activity
activity
Level
each unit activity
1 Orientation of members of community monitoring team
20 members per block
15000
1
committee
Block
PHC
15 members per PHC
3 committee.
16500
10 VHC members per
16750
5 village____________
Total_____________
2 Formation of commmunity monitoring Committees
30 participants
(panchayat members,
NGO/ CBO members
3000 per block
and PHC committee
meeting
1
members)
Block
1000 per PHC
meeting
330 people
PHC
1000 per
village for
Villages
Budget
15000
49500
83750
148250
3000
3000
2 preparatory
visits
and 1 meeting
5000
52 facilitators
11000
Total____
slconduction of Jan Samvad / Jan Sunwai in each of the pilot PHCs and blocks
Village
Block
Jan Samvad
PHC
Jan Samvad
18000 per block
Jan Samvad
18000
5 panelists / experts, 10000 per PHC
Jan Samvad
3100 participants
Total
30000
48000
5 panelists / experts,
1 200 participants
Block budget total
207250
32
District Level
Budget- Of one District
Budget
Number of Participants Cost per
unit
in
activity
activity each unit
activity____________
1 [District facilitation, training of trainers_________________
District workshop - one in
125
22,000
each district, one day
participants
Type of Activity
22,000
2 Formation of Community Monitoring committees
District
120
7000 per
participants district
______________________ __________ __________ [meeting
3Orientation of members of Community Monitoring committees
District
1 20 members
23,000
per district
committee
@ Rs.
6000/- for 2
meetings
Training of Block level
4Trainers
5 Facilitation costs for dist. NGO
3
42,000
One middle
level staff
member full
time for 7
months.
7000
23,000
126,000
226000
3 Field staff
full time for
six months
(one in each
block.
226000
6
Budget for each district
7
Budget for each block
3 Blocks
|
207250
Total Budget Allotted for one district (including the Block
[budget)
404,000
621,750
1025,750
33
State Level Budget
Activity
Budget
Total Budget
With 3 districts
Total Budget
Total Budget
With 4 districts With 5 districts
State level workshop(2 days) leads to selection of districts
110000
110000
110000
110000
State Training of trainers (5 days)
187500
187500
187500
187500
State level facilitation by State
nodal NGO
250000
250000
250000
250000
1025,750
3077,250
4103,000
5128,750
36,24,750
46,50,500
56,76,250
District level budget
Including Block Budget
Total Budget
34
Annexure 1 : NRHM STRATEGIES
(a) Core Strategies:
• Train and enhance capacity of Panchayati Raj Institutions (PRIs) to own, control and
manage public health services.
• Promote access to improved healthcare at household level through the female health
activist (ASHA).
• Health Plan for each village through Village Health Committee of the Panchayat.
• Strengthening sub-centre through an untied fund to enable local planning and action
and more Multi Purpose Workers (MPWs).
• Strengthening existing PHCs and CHCs, and provision of 30-50 bedded CHC per
lakh population for improved curative care to a normative standard (Indian Public
Health Standards defining personnel, equipment and management standards).
• Preparation and Implementation of an inter-sectoral District Health Plan prepared by
the District Health Mission, including drinking water, sanitation & hygiene and
nutrition.
• Integrating vertical Health and Family Welfare programmes at National, State,
Block, and District levels.
• Technical Support to National, State and District Health Missions, for Public Health
Management.
• Strengthening capacities for data collection, assessment and review for evidence
based planning, monitoring and supervision.
• Formulation of transparent policies for deployment and career development of
Human Resources for health.
• Developing capacities for preventive health care at all levels for promoting healthy
life styles, reduction in consumption of tobacco and alcohol etc.
• Promoting non-profit sector particularly in under served areas.
(b) Supplementary Strategies:
• Regulation of Private Sector including the informal rural practitioners to ensure
availability of quality service to citizens at reasonable cost.
• Promotion of Public Private Partnerships for achieving public health goals.
• Mainstreaming AYUSH - revitalizing local health traditions.
• Reorienting medical education to support rural health issues including regulation of
Medical care and Medical Ethics.
• Effective and viable risk pooling and social health insurance to provide health
security to the poor by ensuring accessible, affordable, accountable and good quality
hospital care.
35
Annexure 2 : MONITORING AND EVALUATION
•
Health MIS to be developed upto CHC level, and web-enabled for citizen scrutiny
•
Sub-centres to report on performance to Panchayats, Hospitals to Rogi Kalyan
Samitis and District Health Mission to Zila Parishad
•
The District Health Mission to monitor compliance to Citizen’s Charter at CHC level
•
Annual District Reports on People’s Health (to be prepared by Govt/NGO
collaboration)
•
State and National Reports on People’s Health to be tabled in Assemblies, Parliament
•
External evaluation/social audit through professional bodies/NGOs
•
Mid Course reviews and appropriate correction
( NRHM - Mission Document)
Monitoring outcomes of the Mission
Right to health is recognized as inalienable right of all citizens as brought out by the
relevant rulings of the Supreme Court as well as the International Conventions to
which India is a signatory. As rights convey entitlement to the citizens, these rights
are to be incorporated in the monitoring framework of the Mission. Therefore,
providing basic Health services to all the citizens as guaranteed entitlements will be
attempted under the NRHHM.
Preparation of Household specific Health Cards that record information on the
following - record of births and deaths, record of illnesses and disease, record any
expenditure on health care, food availability and water source, means of livelihood,
age profile of family, record of age at marriage, sex ratio of children, available health
facility and providers, food habits, alcohol and tobacco consumption, gender relations
within family, etc, (by ASHA/AWW/Village Health Team).
Preparation of Habitation/Village Health Register on the basis of the household
Health Cards. ( By the Village Health Team)
Periodic Health Facility Survey at SHC, PHC, CHC, District level to see if service
guarantees are being honoured. [By district /Block level Mission Teams/ research and
resource institutions].
Formation of Health Monitoring and Planning Committees at PHC, Block, District
and State levels to ensure regular monitoring of activities at respective levels, along
with facilitating relevant inputs for planning.
Sharing of all data and discussion at habitation/ village level to ensure full
transparency.
Display of agreed service guarantees at health facilities, details of human and
financial resources available to the facility.
Sample household and facility surveys by external research organizations/NGOs.
36
Public reporting of household and health facility findings and its wider dissemination
through public hearings and formal reporting.
(From : NRHM Framework for Implementation)
37
Annexure 3 : COMMUNITY MONITORING FRAMEWORK
124. We have discussed the overall monitoring framework in an earlier section (IV L). The basic
change that NRHM wishes to bring about in the monitoring framework is to involve local
communities in planning and implementing programmes with a framework that allows them to
assess progress against agreed benchmarks. While external institutions will also assess progress,
they will do so on benchmarks that have been agreed with local communities and health
institutions. The intention is to move towards a community based monitoring framework that
allows continuous assessment of planning and implementation of NRHM. Besides the issues
already mentioned earlier on the monitoring framework, the broad principles for community
based monitoring are listed below.
125. Given the overall objective that people should have complete access to rational, appropriate
and effective health care, community based monitoring should preferably fulfill following
objectives:
• It should provide regular and systematic information about community needs, which
would guide related planning
• It should provide feedback according to the locally developed yardsticks for monitoring
as well as key indicators. This would essentially cover the status of entitlements,
functioning of various levels of the Public health system and service providers,
identifying gaps, deficiencies and levels of community satisfaction, which can facilitate
corrective action in a framework of accountability.
• It should enable the community and community-based organisations to become equal
partners in the planning process. It would increase the community sense of involvement
and participation to improve responsive functioning of the public health system. The
community should emerge as active subjects rather than passive objects in the context of
the public health system.
• It could be used for validating the data collected by the ANM, Anganwadi worker and
other functionaries of the public health system.
(i) Ownership of Community monitoring process
• The health department functionaries need to be involved in the preparation and mobilization
phase of the initiative so as to enable ‘ownership’ of the process and outcomes among the
providers and users.
• PRIs, community based organizations and NGOs, along with health department
functionaries should be involved in the preparation and mobilization phase of the initiative so
as to enable ownership of the process and outcomes among the providers and users.
• The government can enable such interactive processes through issuing relevant Government
Orders, and by ensuring effective communication to all levels of public health functionaries
• All the members of any committee that is formed (for example the Village Health
Committee) must have their roles and responsibilities clearly defined and articulated.
(ii) Powers and capacity building
126. The committees that are formed at various levels must have concomitant authority i.e.
they must have the power to initiate action. The capacities of the members of a village level
committee have to be built continuously for them to be able to function effectively. This would
require allocation of resources and capacity building inputs. This process must begin with full and
feady access "to,.information.
’'
>
A
1V
\ 7
■s
38
127. The intent of the newly launched NRHM as mentioned in the core strategy is that it will
promote community ownership and decentralised planning from village to district level. This is
supposed to be through participatory processes, by strengthening evidence based effective
monitoring and evaluation. In order to actually do so it will be imperative that:
• The government should enable such interactive processes by issuing relevant Government
Orders. One example of such orders is the one passed by the Government of Rajasthan for the
formation of Convergence Committees at the district and PHC level. A similar example is the
response of the Gujarat Government to the National Human Rights Commission, wherein
coordination bodies at various levels of the Public Health System are proposed for
operationalising a State level health services monitoring mechanism.
• All the members of any committee that is formed must have their roles and responsibilities
clearly defined and articulated.
• Effective and quality monitoring requires institutional mechanisms at various levels beginning
at the community and going upwards. Adequate investment (time and resources) must be made in
capacity development at various levels.
• Analysis of the collected information must be undertaken at various levels so as to enable
prompt action and corrections. The committees that are formed at various levels must have
concomitant authority i.e. they must have the power to take action.
• The monitoring system must be directly linked to corrective decision making bodies at various
levels. The information and issues emerging from monitoring must be communicated to the
relevant official bodies responsible for taking action (from PHC to state level) so that monitoring
results in prompt, effective and accountable remedial action.
(iv) Further, some overall points to be kept in mind are\
• Effective Community Monitoring would change the status of community members from passive
beneficiaries to active rights holders, enabling them to more effectively access health services.
• We must be realistic in setting indicators and planning activities. Communities need few and
simple indicators for monitoring, and the time devoted by members, especially community
representatives involved in various committees must be utilized optimally.
• Community Monitoring must be seen as an integral part of the Public Health System at all levels
and for all activities, and not as a stand-alone process.
• Panchayati Raj Institutions are not synonymous with the community. For community ownership
and effective monitoring, even if PRI representatives are involved, one still needs to involve user
groups and beneficiaries, and to include Community Based Organisations.
(v) Involvement of the general public by means of regular 'Public dialogue ’ or Public hearing
(Jan Samvad /Jan Sunwai)
128. Most of the public participation in the monitoring process would be mediated by
representatives of the community or community-linked organisations. However, to enable
interested community members to be directly involved in exchange of information, and to improve
transparency and accountability of the health care system, ‘Public dialogues’ (Jan Samvad) or
Public hearings (‘Jan Sunwai’) would be need to organised at regular intervals (once or twice in a
year, depending on the initiative of the local organisations) at PHC, block and district levels (see
section V-I).
What should the community monitor?
129. The community and community-based organisations should monitor demand / need,
coverage, access, quality, effectiveness, behaviour and presence of health care personnel at
service points, possible denial of care and negligence. This should be monitored related to
outreach services, public health facilities and the referral system.
1U134 P'1*’
V *
Annexure 4 : COMPOSITION, ROLES AND RESPONSIBILITIES OF
MONITORING COMMITTEES
Composition of the Village Health committee
This committee would be formed at the level of the revenue village (more than one such villages
may come under a single Gram Panchayat).
Composition: The Village Health Committee would consist of:
• Gram Panchayat members from the village
• ASHA, Anganwadi Sevika, ANM
• SHG leader, the PTA/MTA Secretary, village representative of any Community based
organisation working in the village, user group representative
The chairperson would be the Panchayat member (preferably woman or SC/ST member)
and the convenor would be ASHA; where ASHA not in position it could be the
Anganwadi Sevika of the village.
Some yardsticks for monitoring at the village level
• Village Health Plan
• NRHM indicators translated into Village health indicators
Some roles of the Village Health Committee
Activities
• Create Public Awareness about the essentials of health programmes, with focus on People’s
knowledge of entitlements to enable their involvement in the monitoring.
• Discuss and develop a Village Health Plan based on an assessment of the village situation and
priorities identified by the village community
• Analyse key issues and problems related to village level health and nutrition activities, give
feedback on these to relevant functionaries and officials. Present an annual health report of the
village in the Gram Sabha
• Participatory Rapid Assessment, to ascertain the major health problems and health related issues
in the village. Estimation of the annual expenditure incurred for management of all the
morbidities may also be done. The mapping will also take into account the health resources and
the unhealthy influences within village boundaries. Mapping will be done through participatory
methods with involvement of all strata of people. The health mapping exercise shall provide
quantitative and qualitative data to understand the health profile of the village. These would be
Village information (number of households - caste, religion and income ranking, geographical
distribution, access to drinking water sources, status of household and village sanitation, physical
approach to village, nearest health facility for primary care, emergency obstetric care, transport
system) and the morbidity pattern
• Maintenance of a village health register and health information board/calendar: The health
register and board put up at the most frequented section of the village will have information about
mandated services, along with services actually rendered to all pregnant women, new bom and
infants, people suffering from chronic diseases etc. Similarly dates of visit and activities expected
to be performed during each visits by health functionaries may be displayed and monitored by
means of a Village health calendar. These will be the most important document maintained by the
village community about the exhibition of health status and health care services availability. This
will also serve as the instrument for cross verification and validation of data
• Ensure that the ANM and MPW visit the village on the fixed days and perform the stipulated
activity; oversee the work of village health and nutrition functionaries like ANM, MPW and
AWW
40
• Get a bi-monthly health delivery report from health service providers during their visit to the
village. Discuss the report submitted by ANM and MPW and take appropriate action
• Take into consideration of the problems of the community and the health and nutrition care
providers and suggest mechanisms to solve it.
• Discuss every maternal death or neonatal death that occurs in their village, analyze it and
suggest necessary action to prevent such deaths. Get these deaths registered in the Panchayat.
• Managing the village health fund.
Some tools for monitoring at the village level
• Village Health Register
• Records of the ANM
• Village Health Calendar
• Infant and maternal death audit
• Public dialogue (Jan Samvad)
Powers of the committee
• The convener will sign the attendance registers of the AWWs, Mid-Day meal Sanchalak,
MPWs, and ANMs.
• MPWs and ANMs will submit a bi-monthly village report to the committee along with the
plan for next two months. Format and contents of the bi-monthly reports would be decided
village health committee.
• The committee will receive funds of Rs. 10,000 per year. This fund may be used as per the
discretion of the VHC.
2. PHC Health Monitoring and Planning Committee
Role and Responsibilities of the Committee
• Consolidation of the village health plans and charting out the annual health action plan in order
of priority. The plan should clearly lay down the goals for improvement in health services and
key determinants.
• Presentation of the progress made at the village level, achievements, actions taken and
difficulties faced followed by discussion on the progress of the achievements of the PHC,
concerns and difficulties faced and support received to improve the access to health facilities in
the area of that particular PHC. The discussion could include:
o Sharing of reports of Village Health Committees
o Reports from ANM, MPW about the coverage of health facilities
o Any efforts done at the village level to improve the access to health care services
o Record and analysis of neonatal and maternal deaths.
o Any epidemic occurring in the area and preventive actions taken.
• Ensure that the Charter of citizen’s health rights is disseminated widely and displayed out
side the PHC informing the people about the medicine facilities available at the PHC, timings of
PHC and the facilities available free of cost. A suggestion box can be kept for the health care
facility users to express their views about the facilities. These comments will be read at the
coordination committee meeting to take necessary action.
• Monitoring of the physical resources like, infrastructure, equipments, medicines, water
connection etc at the PHC and inform the concerned government officials to improve it.
• Discuss and develop a PHC Health Plan based on an assessment of the situation and priorities
identified by representatives of village health committees and community based organisations
41
• Share the information about any health awareness programme organized in the PHC’s
jurisdiction, its achievements, follow up actions, difficulties faced etc.
• Coordinate with local CBOs and NGOs to improve the health scenario of the PHC area.
• Review the functioning of Sub-centres operating under jurisdiction of the PHC and taking
appropriate decisions to improve their functioning
• At the end of the meeting brief minutes of the meeting will be developed along with the action
plan emphasizing the actions to be taken by different committee members, which will be shared
at the District level committee. The minutes will also serve as a reference point, while sharing the
progress done between two committee meetings.
• Initiate appropriate action on instances of denial of right to health care reported or brought to
the notice of the committee; initiate an enquiry if required and table report within two months in
the committee. The report may become a part of the performance appraisal of the concerned staff
member. The committee may recommend corrective measures to the next level (block/ district).
The decisions taken in the committee need to be forwarded to higher concerned officials and a
copy to the corresponding health committee of that level who will be responsible to take
necessary decision for action to be taken on the inquiry within a period of three months.
Constitution of the PHC Health committee
The PHC Health committee would function as the health monitoring and planning arm of the
Panchayats coming under the PHC area. It is recommended that the PHC Committee have the
following broad pattern of representation, including members from Panchayats, health care
service providers and civil society:
• 30% members should be representatives of Panchayat Institutions (Panchayat samiti
member from the PHC coverage area; two or more sarpanchs of which at least one is a
woman)
• 20% members should be non-official representatives from the village health
committees, coming from villages under the jurisdiction of the PHC, with annual rotation
to enable representation from all the villages
• 20% members should be representatives from NGOs / CBOs and People’s organizations
working on Community health and health rights in the area covered by the PHC
• 30% members should be representatives of the Health and Nutrition Care providers,
including the Medical Officer - Primary Health Centre and at least one ANM working in
the PHC area
The chairperson of the PHC committee would be one of the Panchayat representatives, preferably
a Panchayat Samiti member belonging to the PHC coverage area. The executive chairperson
would be the Medical officer of the PHC. The secretary of the PHC committee would be one of
the NGO / CBO representatives.
Power of the committee
• Contribute to annual performance appraisal of Medical officer / other functionaries at the PHC.
• Take collective decision about the utilization of the special funds given to PHC (say Rs.25,000)
for the repairs, maintenance of equipments, health education etc and any other aspects, which will
facilitate the improvement of access to health care services. The MO can utilize this fund after the
discussion and approval from the committee.
Some yardsticks for monitoring at the PHC level
• Charter of Citizens Health Rights
42
• EPHS or similar standards for PHC (this would include continuous availability of basic
outpatient services, indoor facility, delivery care, drugs, laboratory investigations and
ambulance facilities)
• PHC Health Plan
Some tools for monitoring at the PHC level
• Village health registers / calendars
• PHC records
• Discussions with and interviews of the PHC committee members
• Public dialogue (Jan Samvad) or Public hearing (Jan Sunwai)
• Quarterly feedback from village Health Committees
• Periodic assessment of the existing structural deficiencies
Block Health Monitoring and Planning Committee
Role and Responsibilities:
• Consolidation of the PHC level health plans and charting out of the annual health action plan for
the block. The plan should clearly lay down the goals for improvement in health services.
• Review of the progress made at the PHC levels, difficulties faced, actions taken and
achievements made, followed by discussion on any further steps required to be taken for further
improvement of health facilities in the block, including the CHC.
• Analysis of records on neonatal and maternal deaths; and the status of other indicators, such as
coverage for immunization and other national programmes.
• Monitoring of the physical resources like, infrastructure, equipments, medicine, water
connection etc at the CHC; similar exercise for the manpower issues of the health facilities that
come under the jurisdiction of the CHC.
• Coordinate with local CBOs and NGOs to improve the health services in the block.
• Review the functioning of Sub-centres and PHCs operating under jurisdiction of the CHC and
taking appropriate decisions to improve their functioning
• Initiate appropriate action on instances of denial of right to health care reported or brought to
the notice of the committee; initiate an enquiry if required and table report within two months in
the committee. The committee may also recommend corrective measures to the district level.
Constitution of the Block committee
It is recommended that the Block Committee have the following broad pattern of representation,
including members from Panchayats, health care service providers and civil society:
• 30% members should be representatives of the Block Panchayat Samiti (Adhyaksha /
Adhyakshika of the Block Panchayat Samiti or members of the Block Panchayat samiti, with at
least one woman)
• 20% members should be non-official representatives from the PHC health committees in the
block, with annual rotation to enable representation from all PHCs over time
• 20% members should be representatives from NGOs / CBOs and People’s organizations
working on Community health and health rights in the block, and involved in facilitating
monitoring of health services
• 20% members should be officials such as the Block Medical Officer, the Block Development
Officer, selected Medical Officers from PHCs of the block
• 10% members should be representatives of the CHC level Rogi Kalyan Samiti
43
The chairperson of the Block committee would be one of the Block Panchayat Samiti
representatives. The executive chairperson would be the Block medical officer. The secretary
would be one of the NGO / CBO representatives.
Yardsticks for monitoring at the Block level
IPHS or similar standards for CHC (this would include continuous availability of
basic outpatient services, indoor facility, community outreach services, referral services,
delivery and antenatal care, drugs, laboratory investigations and ambulance facilities)
(D(D Charter of Citizens Health Rights for CHC
®(D Block Health Plan
Some tools for monitoring at the Block level
€)(D PHC and CHC records
Discussions with and interviews of the CHC RKS members
OG) Report of Public dialogue (Jan Samvad)
®® Quarterly feedback from village and PHC Health Committees
®® Periodic assessment of the existing structural and functional deficiencies
District Health Monitoring and Planning Committee
Role and Responsibility
• Discussion on the reports of the PHC health committees
• Financial reporting and solving blockages in flow of resources if any
• Infrastructure, medicine and health personnel related information and necessary steps
required to correct the discrepancies.
• Progress report of the PHCs emphasising the information on referrals utilisation of the
services, quality of care etc.
• Contribute to development of the District Health Plan, based on an assessment of the
situation and priorities for the district. This would be based on inputs from
representatives of PHC health committees, community based organisations and NGOs.
• Ensuring proper functioning of the Hospital Management Committees.
• Discussion on circulars, decisions or policy level changes done at the state level;
deciding about their relevance for the district situation
of the
denial of health care and ensuring proper
• Taking cognizance of the reported cases c*
--------------------.
redressal.
Constitution of the District committee
It is recommended that the District Committee have the following broad pattern of representation,
including members from Panchayati Raj Institutions, health care service providers and civil
society:
,
• 30% members should be representatives of the Zilla Panshad (esp. convenor and
members of its Health committee)
• 25% members should be district health officials, including the District Health Officer /
Chief Medical Officer and Civil Surgeon or officials of parallel designation, along with
representatives of the District Health planning team including management professionals
• 15% members should be non-official representatives of block committees, with annual
rotation to enable successive representation from all blocks
• 20% members should be representatives from NGOs / CBOs and People’s organizations
working on Health rights and regularly involved in facilitating Community based
monitoring at other levels (PHC/block) in the district
• 10% members should be representatives of Hospital Management Committees in the
district
44
The chairperson of the District committee would be one of the Zilla Parishad representatives,
preferably convenor or member of the Zilla Parishad Health committee. The executive
chairperson would be the CMO / CMHO / DHO or officer of equivalent designation. The
secretary of the PHC committee would be one of the NGO / CBO representatives.
Some yardsticks for monitoring at the District level
• Charters of Citizens Health Rights
• District Action Plan
• NRHM guidelines
• Indian Public Health Standards
Some tools for Monitoring at the District level
®(D Report from the PHC Health committees
®(D Report of the District Mission committee
®(D Public Dialogue (Jan Samvad)
State Health Monitoring and Planning Committee
Role and Responsibilities
®® The main role of the committee is to discuss the programmatic and policy issues
related to access to health care and to suggest necessary changes.
®@ This committee will review and contribute to the development of the State health plan,
including the plan for implementation of NRHM at the state level; the committee will suggest
and review priorities and overall programmatic design of the State health plan.
®@ Key issues arising from various District health committees, which cannot be resolved
at that level (especially relating to budgetary allocations, recruitment policy, programmatic
design etc) would be discussed an appropriate action initiated by the committee. Any
administrative and financial level queries, which need urgent attention, will be discussed.
®® Institute a health rights redressal mechanism at all levels of the health system, which
will take action within a time bound manner. Review summary report of the actions taken in
response to the enquiry reports
®® Operationalising and assessing the progress made in implementing the
recommendations of the NHRC, to actualize the Right to health care at the state level.
®® The committee will take proactive role to share any related information received from
GOI and will also will share achievements at different levels. The copies of relevant
documents will be shared.
Composition ofState Health Monitoring and Planning committee
®G) 30% of total members should be elected representatives, belonging to the State
legislative body (MLAs/MLCs) or Convenors of Health committees of Zilla Parishads of
selected districts (from different regions of the state) by rotation
®(1) 15% would be non-official members of district committees, by rotation from
various districts belonging to different regions of the state
®(D 20% members would be representatives from State health NGO coalitions working
on Health rights, involved in facilitating Community based monitoring
®(D 25% members would belong to State Health Department:
®(D Secretary Health and Family Welfare, Commissioner Health, relevant officials
from Directorate of Health Services (inch NRHM Mission Director) along with Technical
experts from the State Health System Resource Centre / Planning cell
45
0(3) 10% members would be officials belonging to other related departments and
programmes such as Women and Child Development, Water and Sanitation, Rural
development.
0(D The Chairperson would be one of the elected members (MLAs).
0(3) The executive chairperson would be the Secretary Health and Family Welfare.
O(D The secretary would be one of the NGO coalition representatives.
Some yardsticks for monitoring at the State level
• NHRC recommendations and National Action Plan on Right to Health Care; responses
of state health departments and actions to which the State Government has committed
itself
• NRHM state level plan and the State Health Mission guidelines
•IPHS
Tools for monitoring at the State level
O(D Reports of the District Health committees
O(D Periodic assessment reports by various taskforces / State level committees about the
progress made in formulating policies according to IPH Standards, NHRC recommendations
and its implementation status etc.
46
Annexure 5 : CONCRETE SERVICE GUARANTEES
Concrete Service Guarantees that NRHM will provide:
•
Skilled attendance at all Births
•
Emergency Obstetric care
•
Basic neonatal care for new bom
•
Full coverage of services related to childhood diseases / health conditions
•
Full coverage of services related to maternal diseases / health conditions
•
Full coverage of services related to low vision and blindness due to refractive errors and
cataract.
•
Full coverage for curative and restorative services related to leprosy
•
Full coverage of diagnostic and treatment services for tuberculosis
•
Full coverage of preventive, diagnostic and treatment services for vector home diseases
•
Full coverage for minor injuries / illness (all problems manageable as part of standard
outpatient care upto CHC level)
•
Full coverage of services inpatient treatment of childhood diseases / health conditions
•
Full coverage of services inpatient treatment of maternal diseases / health conditions
including safe abortion care (free for 50% user charges from APL)
•
Full coverage of services for Blindness, life style diseases, hypertension etc.
•
Full coverage for providing secondary care services at Sub-district and District Hospital.
•
Full coverage for meeting unmet needs and spacing and permanent family planning
services.
•
Full coverage of diagnostic and treatment services for RI/STI and counseling for HIV
AIDS services for adolescents.
•
Health education and preventive health measures.
47
1
SB
I
wrw ftw
Framework for developing health insurance
programmes
Some suggestions for States
Ministry of Health & Family Welfare
Government of India
New Delhi
Table of contents
NRHM - The Background
The approach to health insurance for vulnerable groups
3-10
11
Section 1
•
The framework
•
Why health insurance?
•
Pre-requisites for a health insurance programme
•
Organiser of a health insurance programme
•
Communities to be covered
•
Defining the benefit package
•
The premium
•
Empanelling the providers
•
Provider payment
•
Insurer
•
Administration of the programme
•
Monitoring
•
Managing risks
•
Values in health insurance
12-13
14-16
16-17
17-20
20-22
22-24
25-28
29-32
32-33
33-34
34-36
36-37
37
38
Section 2
•
Health insurance programme for BPL families
40-43
•
Health insurance programmes for SHG families
44-46
•
Health insurance programmes where there are no hospitals
47-49
•
Revamping the UHIS
50-52
Appendices
•
Some health insurance terms
•
Some health insurance programmes in the NGO / Government
sector
•
Prices of some common conditions
•
Utilisation rates of some common conditions
•
Provider payment mechanisms
•
Various Insurance Models
54-55
56-59
60-65
66
67-69
BACKGROUND:
The Hon’ble Prime Minister launched the NRHM on 12th April, 2005 throughout
the country with special focus on 18 States, including eight Empowered Action Group
(EAG) States, the North-Eastern States, Jammu & Kashmir and Himachal Pradesh.
The NRHM seeks to provide accessible, affordable and quality health care to the
rural population, especially the vulnerable sections. It also seeks to reduce the Maternal
Mortality Rate (MMR) in the country from 407 to 100 per 1,00,000 live births, Infant
Mortality Rate (IMR) from 60 to 30 per 1000 live births and the Total Fertility Rate (TFR)
from 3.0 to 2.1 within the 7 year period of the Mission.
IMPLEMENTATION FRAMEWORK & PLAN OF ACTION FOR NRHM
The key features in order to achieve the goals of the Mission include making the
public health delivery system fully functional and accountable to the community, human
resources management, community involvement, decentralization, rigorous monitoring &
evaluation against standards, convergence of health and related programmes from
village level upwards, innovations and flexible financing and also interventions for
improving the health indicators.
The Diagrammatic Representation of the 5 Main approaches of NRHM is
illustrated below:
NRHM - 5 MAIN APPROACHES
COMIVI UNITIZE
1. Hospital Management
Committee/ PRIs at all levels
2. Untied grants to community/
PRI Bodies
3. Funds, functions &
functionaries to local
community organizations
4. Decentralized planning,
Village Health &
\
Sanitation
/
x.
Committees ./ /
MONITOR,
PROGRESS AGAINST
STANDARPS
Z/TLEXIBLE FINANCINGNx
1. Setting IPHS Standards
2. Facility Surveys
3. Independent Monitoring
Committees at
Block, District & State
\
levels
,
/1. Untied grants to institutions '
'
2. NGO sector for public
Health goals
3. NGOs as implementors
i
4. Risk Pooling - money
\
follows patient
/
5. More resources for
/,
more reforms
innovation IN
IMPROVED
HUMAN RESOURCE
MANAGEMENT
MANAGEMENT
THROUGH CAPACITY
1. Block & District Health
Office with management skills
2. NGOs in capacity building
3. NHSRC / SHSRC / DRG / BRG
\4. Continuous skill developmenty
support
/
1. More Nurses - local
Resident criteria
2. 24 X 7 emergencies by
Nurses at PHC. AYUSH
\ 3. 24 x 7 medical emergency /
\
at CHC
/
4. Multi skilling
y/
IMPROVING THE PUBLIC HEALTH DELIVERY SYSTEM
Given the status of public health infrastructure in the country, particularly in the
EAG and the North Eastern States, it will not be possible to provide the desired sen/ices
till the infrastructure is sufficiently upgraded. The Mission seeks to establish functional
health facilities in the public domain through revitalization of the^^ing
®
and fresh construction or renovation wherever required. The Mission also seeks to
improve service delivery by putting in place enabling systems at all levels. This solves
simultaneous corrections in manpower planning as well as infrastructure strengthening.
The Mission would provide priority to both these aspects.
A generic Public Health Delivery System envisioned under NRHM from the
Village to the Block Level is illustrated below:
Health Manager
BLOCK LEVEL HEALTH OFFICE
Accountant
Store Keeper
Accredit private
providers for public
health goals
30-40 Villages
/BLOCk\
LEVEL \
HOSPITAL \
Strengthen Ambulance/
transport Services
Ambulance
\
Increase availability of Nurses
Telephone
\
/ Obstetric/Surgical Medical \
Provide Telephones
/
Emergencies 24 X 7
\ Encourage fixed day clinics
'
Round the Clock Services;
X
100,000
Population
100 Villages
CLUSTER OF GPs - PHC LEVEL
.
3 Staff Nurses; 1 LHV for 4-5 SHCs;
/Ambulance/hired vehicle; Fixed Day MCH/lmmunization\
/
Clinics; Telephone; MO i/c; Ayush Doctor;
\
/
Emergencies that can be handled by Nurses - 24 X 7;
\
/
Round the Clock Services; Drugs; TB / Malaria etc, tests
\
5-6 Villages /
GRAM PANCHAYAT- SUB HEALTH CENTRE LEVEL
\
1000
Popu
lation
/ Skill up-gradation of educated RMPs / 2 ANMs, 1 male MPW FOR 5-6 Villages;
Telephone Link; MCH/lmmunization Days; Drugs; MCH Clinic
VILLAGE LEVEL - ASHA, AWW, VH & SC
1 ASHA, AWWs in every village; Village Health Day
Drug Kit, Referral chains
PUBLIC HEALTH INFRASTRUCTURE
The Central Govt, has so far supported only the construction/up gradation of sub
centres. Because of their difficult financial conditions, the States have usuaHy-not
provided sufficient funds for construction / up-gradation of Primary Health Centr
fPHCl/Community Health Centre [CHC]/District Hospitals etc. As a result, heal h
infrastructure is in poor condition in most of the states. NRHM allows
e^®ndl^r®
for construction subject to the condition that it should not be more than 33/o of the total
NRHM outlay in the case of high focus States, and, 25% in the case of non-high focus
States. NRHM also provides for upgradation of District Hospitals.
In the first Cabinet approval, provision had been made for setting up of Indian
Public Health Standards (IPHS) only for Community Health Centres (CHCs)ZPHCs. The
Mission now provides for IPHS at all levels i.e., sub-centres PHC/CHC and district
hospitals.
As per the original Cabinet approval, untied grants were to be made available
only to sub-centres. However, the Mission now proposes provisions for untied funds at
PHC/CHC/district levels.
A provision for funds for taking up innovative schemes at
district/State/Central level has also been made.
Having Rogi Kalyan Samitis for managing health facilities has already been
approved by the Cabinet. Now funds would be released as corpus grants to these
Samitis as 100% grant by GOI during 2006-07, while it would be in the ratio 2:2:6 with
regard to State / Internal / GOI from 11th Plan onwards.
The Mission also seeks to ensure the availability of requisite equipments and
drugs at all the public health care facilities. Procurement of equipments/ drugs would be
progressively decentralized and a road map prepared.
It is proposed to improve outreach activities in un-served and underserved areas
specially inhabited by vulnerable sections through provision of Mobile Medical Units
[MMU] in every district under this proposal. The MMUs would also cover Anganwadi
centres.
IMPROVING AVAILABILITY OF CRITICAL MANPOWER
The issue of availability of critical manpower in the rural areas is proposed to be
addressed through initiatives like introduction of a trained voluntary community Health
Worker (ASHA) in every village of the 18 high focus states, additional ANM at each sub
centre, three staff nurses at the Primary Health Centres (PHC) to make them operational
round the clock and additional specialists and paramedical staff at the Community
Health Centres (CHC). The condition of local residency is proposed to ensure that the
staffs stay at their place of posting. In the North-east, keeping in view the difficulty in
availing services of doctors and specialists, the emphasis is on recruitment, training and
skill upgradation of locally recruited ANMs/nurses/midwives/ para medics.
It is also
proposed to supplement the availability of critical manpower across the States through
contractual appointment/local level engagement of medical and paramedical manpower
upgrading and multi-skilling of the existing medical personnel. Innovations in Public
private participation for service provision, franchising of service providers, licensing and
training of Rural Medical Practitioners (RMP), rationalization of existing manpower are
few of the innovations/options being explored. Stringent monitoring at all levels,
involvement of the PRIs and monitoring by the Rogi Kalyan Samits should ensure
presence of doctors & paramedicals in the rural areas. Besides compulsory posting of
doctors in the rural areas, better cadre management & personnel policies would also
help to improve manpower availability.
CAPACITY BUILDING
In order to provide managerial support, for tracking funds and monitoring
activities under the Mission, provision has been made for setting up Programme
Management Units at the State/District level.
Over 500 professionals have already
been recruited. The successful implementation of the Mission would require health
sector reforms and development of human resources. Capacity building at all levels is a
huge challenge under NRHM. In order to provide technical support to the Mission for
achieving this objective, it is proposed to set up National Health System Resource
Centre [NHSRC] at the Central and State levels (SHSRC) with an annual corpus support
of Rs. 15 crore and Rs. one Crore at the Central and State levels respectively. The
NRHM also emphasizes the setting up of fully functional Block and District level Health
Management systems, as under NRHM 70% of the resources would be utilized at Block
and below Block levels and 20% at the district level. Given the large army of ASHAs,
ANMs, Nurses, Rural Medical Practitioners continuous skill development is needed.
Strengthening nursing institutions, linking medical colleges for providing skill
development support to rural health workers, involving the voluntary sector in skill
development are few key interventions to be taken up.
To make the health facilities more accountable, their control would be gradually
shifted to the PRIs and civil society. The Sub-centres are proposed to be placed
exclusively under the control of the Panchayat. The PHCs and CHCs are also to be
managed by the Panchayat Block Samitis (PBS) and Rogi Kalyan Samitis (RKS).
COMMUNITY HEALTH WORKERS
As per the approval of the Cabinet dated 4.1.2005, one female Accredited Social
Health Activist (ASHA) is to be provided for every village with a population of 1000 (with
provision for relaxation in the eight EAG States, Jammu and Kashmir and Assam) in
each of the high focus states. She would be the link between the community and the
health facility and would be the first port of call for any health related demand. Now
under the Mission, it is proposed to have an ASHA in all the 18 high focus States.
Besides, based on the recommendations of the Committee of Secretaries (COS) in its
meeting’held on 20.10.2005, it is also proposed to support ASHAs in tribal districts of all
the remaining States. In case the other States would like to extend the scheme in
remaining districts as well, it would be possible for them to do so under the RCH II.
ASHA along with Anganwadi workers (AWW) & the Auxiliary Nurse Midwife (ANM), Self
Help Groups & community based organizations, preraks of continuing education centres
through their coordinated action at the village level & through combined organization of
monthly Village Health, Nutrition & Sanitation day at the Anganwadi centres would be
expected to bring about perceptible changes in the health status of the community.
CONVERGENT ACTION ON OTHER DETERMINANTS OF HEALTH
The PRIs and a large range of community based organizations like Self Help
Groups, School, water, health Nutrition & Sanitation Committees, Mahila Samakhya
Groups’, Zila Saksharta Samitis provide an opportunity for seeking local levels
accountability in the delivery of social sector programmes. Schools and Anganwadis
would form the base of these activities. NRHM provides for School Health Check-ups
and School Health Education to be worked out in consultation with the States.
Convergence of programmes would be at the village and facility levels.
Table 2: Specific strategies for specific populations
Type of population
Strategy to be used
Formal sector - employed
Mandatory - Social health insurance
“Unorganised” informal sector
Voluntary - Private health
Subsidy where necessary.
“Organised” informal sector.
Voluntary - Community health insurance.
Subsidy where necessary.
Poor
Social assistance
insurance.
How does one identify the poor? Most states have distributed BPL cards for this
category of the population. However, each state has used its own definition of BPL and
so there is no homogeneity. It is recommended that the government uses the Planning
commission guidelines for identifying the BPL families.
•
The Employees’ State Insurance Scheme (ESIS) provides benefits
for the low paid workers. On the other hand, the Central Government
Health Scheme (CGHS) covers the civil servants and members of
Parliament, judges etc. Most established enterprises either provide
health services for their employees or reimburse medical expenses.
•
The Tribhuvandas Foundation covers dairy farmers who are
members of the local dairy cooperative societies in Anand, Gujarat.
•
Vimo SEWA covers members of the SEWA union and their
dependents in Gujarat.
•
The Student’s Health Home in Kolkata, provides health insurance
cover for all the students in West Bengal.
•
The trader’s association in Palakad district, Kerala are covered under
a health insurance programme that covers their members and
dependents.
•
Karuna Trust provides insurance cover for all the BPL families in T.
Narsipur taluk.
Defining the benefit package?
Once the community is identified, then one can look at their requirements. The possible
benefit packages commonly used in our country are
•
Hospitalisation expenses with or without exclusions. This fits into the insurance
logic, of covering rare but costly events. However, because it is rare, people may
not be keen to have it. They may feel that the insurance scheme will benefit only
a few people. However, this maybe the need of the planners, who would prefer
that the people be protected from high medical costs.
In India, most hospitalization packages are riddled with exclusions, e.g. chronic
illnesses, pre-existing illnesses, TB, HIV etc. This is undesirable and ideally one
should have a package that includes most common illnesses. Many insurance
companies are recognizing this and are providing comprehensive packages now.
Also to limit outflow, many insurance companies usually put an upper limit to the
hospitalization cover e.g. Rs 10,000 per patient per year.
•
OP cover, either as a stand alone package or with hospitalization. This is the
most common demand of the people. This will ensure that they get some benefit
for the premium paid. However, it is difficult to administer and monitor. There is a
great danger that all headaches will land up in the doctor’s clinic, increasing the
cost of health care as well as of the insurance programme. Also it is difficult to
verify each event and release funds. One way out is to have a voucher system,
say 5 vouchers for a family of 5. This will be used for OP care among empanelled
doctors. The doctor has to provide care (consultation and medicines). The doctor
then needs to submit these vouchers at the end of the month and get reimbursed
@ Rs 50 per voucher. Remember that OP cover is costly and increases the
premium by at least 50%.
•
Transport costs for bringing the patient to the hospital. This is usually linked to
hospitalization cover and meets the transport expenses of the patient in coming
to the hospital for treatment. This is a necessity in remote areas where transport
costs are high and form an effective barrier.
One simple way out is to pay the patient a flat rate (e.g. Rs 250 or Rs 500) when
the patient is admitted in the hospital. This can be paid by the hospital and can
be reimbursed by the insurer later.
•
Loss of wages for the patient or attender. If one is insuring BPL families, this
benefit becomes imperative. This is because most BPL households cannot afford
unemployment. A hospitalization episode is a triple burden for them, as they
have to suffer the distress of the illness, to raise money for the treatment and
also undergo a loss of income. To compensate for this, some schemes have
included loss of wages compensation into the benefit package. This is paid
during the hospitalization period, usually @ Rs 50 per patient per day for a
maximum of 15 days.
•
Other products like life insurance, asset insurance, personal accident insurance.
These can be used as a comprehensive package or in various permutations and
combinations. The final choice depends on four factors
The disadvantages are:
•
The insurance company will not be as flexible as desired
•
Changes in the scheme will require necessary clearances at various levels and
will take time
•
The objective of the insurance company is "profits” and not necessarily access to
health care. This conflict of interest may lead to tension between the organizer
and the insurance company
•
The insurance company will of course add to the administrative costs and hence
load the premium
•
Any balance, left over from the premium will be deemed as profits by the
insurance company. On the other hand, if the government is managing the funds
themselves, this money can be used as reserves or carried over to the next year.
Thus the government will have to decide on one way or the other, depending on the
circumstances. If it has the financial and technical capacity, it may be better off
managing the funds on its own. On the other hand, if the above is limited, then it may be
better off seeking the help of insurance companies.
Administration of the scheme
Normally the organizer takes on the insurance function as well as the administration
function of an insurance programme. However, given the wide range of tasks involved, it
is better to outsource this to another body, e.g. a third party administrator (TPA) or a
NGO. This would be better than trying to do everything. The TPA need not be one
registered with the IRDA. It could be any organisation that has the capacity to do the
work. Even a district federation of SHG members, or a district cooperative society (with
adequate technical inputs) can play this role. They need to have accounting skills, social
skills and technical skills. The last maybe lacking even among TPAs. One way out is for
the organiser to provide this support either directly or through existing technical
organisations. In the long run, capacity building of these district bodies will be required.
While short listing a TPA, one must ensure that they are willing to:
4*
Enrol members - The TPA should make the list of insured members and
issue them the necessary insurance cards. These could range from
ordinary cards to smart cards, depending on the availability of funds.
Currently a laminated photo card costs about Rs 10 per card.
4.
Create awareness - Creating awareness is not a one time activity. It
definitely needs to be initiated before the introduction of the health
insurance scheme. It should also continue on a regular basis, even after the
scheme has been implemented. The messages should be simple and
should answer the queries that the people have about health insurance and
their experiences with it.
4.
Monitor the flow of premium funds - The TPA should ensure that the
funds collected reach the end point without leakages. This is an important
task and enhances the credibility of the entire scheme. People will trust an
initiative that has checks and balances. However, one must be wary of
introducing too much bureaucracy also.
Empanel providers - Negotiating with the providers, ensuring that they
accept the prescribed terms and conditions and then empanelling them is
an important task that should be the TPA’s main activity.
4,
Fixing tariffs - once the hospitals have been empanelled the TPA needs
to discuss tariffs with them. This can be done using various ways. One
simple way is to do it on a district basis. Invite the hospitals and classify
them into three broad categories; <25 beds, 25 - 75 beds and 75 - 150
beds. Rarely there may be a fourth category of > 150 beds.
Ask each provider to list out the common conditions that they treat in their
hospitals. Once this list is available, a tariff can be fixed, based on average
costs for each category. This would be a case based tariff. To make things
easier, one could divide the conditions into broad categories like minor
medical admissions, major medical admissions, minor surgical admissions,
major surgical admissions, normal obstetrical admissions, surgical
obstetrical admissions etc. Average tariffs could be fixed for each of these
categories.
■4»
Provide pre-authorisation services — To prevent demand side moral
hazard, one needs to ensure that patients are treated at the appropriate
level. One way is to have a pre-authorisation service that will screen
patients and clear admissions to those patients who require it. This is an
important activity and needs to be performed scrupulously. This is the place
where the TPA interacts with the patients and if it is unsatisfactory, then the
renewal rates may be affected. The main issue to monitor here is the
turnover time between the receipt of application from the provider and the
response.
4
Process claims and reimbursements - The cashless system is the
optimum method of processing claims and reimbursements. In this, the
insured patient goes to the provider and receives care. At discharge, the
patient walks out without paying any money. The bills and necessary
documents111111 are submitted to the TPA who reimburses the hospital. The
TPA then submits the same to the insurer (be it the organizer or the
insurance company) who then reimburses the TPA. However, the TPA and
the provider needs to monitor the amounts closely, so that wherever the
patient has exceeded his / her limits, the balance money is recovered from
the patient at the time of discharge.
Minimise fraud - The TPA should keep a strict tab on fraud and prevent it
wherever and whenever possible. Some of the sources of fraud are -
11[11] Minimum documents could be discharge summary, list of all the medicines prescribed and
investigations performed (with results) and the final bill with detailed breakdown.
abuse of the insurance card by a non-insured, wrong diagnosis, high bills,
false bills, etc.
4.
Develop a management information system - the TPA should develop
the reporting system so that data flows from the field to the organizers. This
includes reports from the premium collectors, to data from the hospitals, to
data from the insurers about claims. Of course other than this, the TPA
should interview patients and community representatives to get feedback
on their perceptions. A mix of quantitative and qualitative data is required.
4,
Provide regular reports to the monitoring committee - for details, see
later
Monitoring the programme
This is an oft neglected element in the implementation of any health insurance
programme. At the maximum, fund position is monitored. But there are many important
indicators that require to be monitored. Some of these are given below:
INDICATOR
DEFINITION
Coverage rate
Number of people enrolled in a defined population
Penetration rate
Number of people enrolled from among the target
population
Distribution rate
Number of people enrolled per distributor
Enrolment trend
Trend over the years
Renewal rate
The number of people who are renewing their
membership
Member satisfaction
The number of members who are satisfied with the
services
Insurance card rate
The number of members with an insurance card
Quality of claims
The number of claims with the proper documents at
the first instance
Utilization rate
The number of members who fell sick and required
care
Claims rate
The number of members who fell sick, and have
claimed insurance benefits for their illness episode
Reimbursement rate
The number of members who have been reimbursed
their claims
Top diseases
The top five disease conditions for which claims are
being made
Top providers
The top five providers from where the maximum
number / amount of claims are being made
Median Medical costs
The median costs of hospital bills
Referral rate
The number of patients who were given pre
Monthly
Annual
+
+
authorisation
+
Quick ratio
The ratio between the liquid assets and the liabilities
Administrative expenses
ratio
The ratio between the administrative expenses and
the total expenses
+
Claims ratio
The ratio between the amount of claims reimbursed
and the amount of premium collected
+
Turn over time for pre The time taken between receipt of pre-authorisation
and the decision conveyed
authorisation
Turn over time for claims The time taken between receipt of claims and
reimbursement
settlement
A monitoring cell (nominated by the organizers) need to meet monthly and look at these
indicators. This monitoring cell can be at the district level (if there is capacity), however,
it definitely has to be at the state level. Action should be taken as soon as any
discrepancy is seen. This is an excellent motivator for the staff as they realise that their
actions are being scrutinised.
Managing risks
Minimising adverse selection, moral hazard, fraud and cost escalation are very important
for the success of any health insurance programme. Some of the measures to achieve
this is given below.
Measures to manage risk
Risk
Adverse selection
•
•
•
•
Have a large unit of enrolment, e.g. a family, a village, a self
help group
Have a definite collection period
Have a definite waiting period
Have a compulsory enrolment as opposed to a voluntary
enrolment
Exclude pre-existing diseases
Have a flat/case-based payment mechanism as opposed to a
fee for service mechanism
Preferably pay the providers a fixed salary - this will minimise
incentives for interventions
Insist on standard treatment guidelines
Insist on medical / chart audits___________________________
Have a referral system or a pre-authorisation system
Introduce co-payments
•
•
•
•
•
•
•
Introduce photo identity cards for the insured
Use social audits to identify fraudulent admissions
Take strict action against fraudulent events
Keep proper registers and records________________________
Try different provider payment mechanisms
Insist on standard treatment guidelines
Insist on generic medicines
•
•
•
•
Supply side moral
hazard
•
•
•
Demand
side
moral hazard
Fraud
Cost escalation
These measures as stand alone methods as well as in combination are powerful tools to
enhance the chances of success.
Values in health insurance
The four values in health insurance - equity, solidarity, risk pooling and community
empowerment have been discussed in the above text. Community empowerment will
take place when the community pays the premium and requests for better quality
services. Risk pooling is enhanced when there is risk sharing between not just the
healthy and the sick, but also between the rich and the poor. Equity is strengthened
when people pay according to their ability and get benefits according to their need. And
this is possible only when people are bonded in solidarity. As it is difficult to promote
solidarity solely through a health insurance mechanism, it is important that health
insurance programmes be piggy backed on existing institutions that have inherent
solidarity e.g. a trade union or a SHG federation.
Conclusions
The above framework is a guideline to help planners develop appropriate health
insurance plans. The main inputs are from the local situation. The final plan will depend
on this. Most of the important elements have been covered in this document. Details like
cost, prevalence etc have been suggested, but ultimately the planner has to use local
and regional data. It is not difficult to access this data, most are available. All it requires
is a little effort to collate the same.
Section 2
Some schemes
In this section, we present a few health insurance schemes that are
‘readymade’ and can be implemented directly in a region or amongst a
specific population. Please note that the theoretical basis for each ‘scheme’
is provided in Section 1.
DECENTRALIZATION
As the indicators of health depend as much on drinking water, nutrition,
sanitation, female literacy, women’s empowerment as they do on functional health
facilities, NRHM seeks to adopt a convergent approach for interventions under the
umbrella of the district plan which seeks to integrate all the related initiatives at the
village, block and district levels. The District Health Action Plan would be the main
instrument for planning, Inter-sectoral convergence, implementation and
monitoring of the activities under the Mission. Rather than funds being allocated to
the states for implementing programmes designed and approved at the GOI level, the
States would be encouraged to prepare their perspective and annual plan which in turn
would be based on the District Plans. Even though village is envisaged as the primary
unit for planning, looking at the extensive capacity building required before it would be in
a position to take up the exercise, the Mission would not insist on the village plans at
least during the first two years. The District Health Mission under the Zilla Parishad
would get the district plan prepared covering health as well as the other determinants of
health. Household and Facility Surveys would define the baseline. Periodic surveys
would thereafter be taken up on an annual basis to track the improvements in the
facilities as well as in the reduction in health indicators. The District Plans would be
collated into a State Plan which would be appraised and approved by the Mission at the
national level. As far as the other determinants of health are concerned, the funds for
them would continue to flow through the existing channels but the District Plan would
clearly bring out the convergent action being taken at the district level. NRHM
recognizes that delegation of financial and administrative powers at various levels would
be necessary for the successful implementation of the decentralized plans.
MAINSTREAMING OF AYUSH
Provision has been made for State specific proposals for mainstreaming AYUSH,
including appointment of AYUSH doctors/paramedics on contractual basis, providing
AYUSH Wings in PHCs and CHCs. As envisaged under NRHM vision and goals, efforts
will be made to integrate AYUSH in primary health delivery.
FLEXIBLE FINANCING
The programmes under the erstwhile Departments of Health and Family Welfare
and Department of AYUSH were not being run in an integrated manner. As a result the
transfer of funds to the states under different budget heads at different points of time
vertically hampered flexibility. It also led to duplication of efforts, and, thereby, wastage
of scarce resources. For improved delivery, the Mission attempts to bring the schemes
of the Ministry of Health & Family Welfare within the overarching umbrella of NRHM as
approved earlier by the Cabinet. Therefore, under the Implementation Framework, from
the Eleventh Plan onwards, it is proposed to have a single budget head for the activities
under the Mission. This would provide the States much needed flexibility to direct the
funds to those areas where they are needed the most. However, a minimum amount
would be earmarked for various disease control programmes to ensure that the national
objectives and commitments are met. The funds under the NRHM budget head would
flow through the integrated health society at the State and the District levels. The norms
under which the funds would be allocated by the Centre to the States and by the States
to districts on the basis of Integrated State/District Health Activity Plans have been
clearly spelt out in the Implementation Framework.
NORMATIVE FRAMEWORK
The District Health Action Plans would be prepared based on a normative
framework. The cost norms have been derived from three sources. First, existing norms
of the schemes brought under the umbrella of the NRHM. Secondly, norms developed
by the NCMH. Thirdly, norms developed and approved as new interventions under
NRHM.
MONITORING AND ACCOUNTABILITY FRAMEWORK
The NRHM Framework is based on a rights based approach. The Framework
proposes accountability at every level through a three pronged process of community
based monitoring, external surveys (SRS, DLHS household surveys by ASHA, facility
surveys in the district level) and stringent internal monitoring. The process of community
involvement of the health institutions itself would enhance accountability and the NRHM
would facilitate this process by wide dissemination of the results.
For effective
monitoring a strong MIS is being put in place.
The Citizen Charter would help the
public to know their rights and entitlements at each facility. The setting up of IPHb at
each level of health delivery system would be instrumental in provision of minimum
service guarantees at those levels.
Monitoring also would be in terms of service
guarantees provided by each facility, utilization of such services by the community
{especially weaker sections} changes in their health seeking behavior, etc. The Facilities
Survey is expected to create a baseline for each health facility and assist in monitoring
annual progress against the baseline in terms of services guaranteed. The MOUs
signed with the States would enable monitoring of progress under NRHM in terms of the
agreed milestones. Independent evaluation would ensure midcourse corrections.
PRO-PEOPLE PARTNERSHIPS WITH THE VOLUNTARY SECTOR
Investments by voluntary Organizations are critical for the success of NRHM.
The Mission provides for partnerships with the voluntary groups/ organisations for
advocacy, building capacity at all levels, monitoring and evaluation of the health sector,
delivery of health services and working together with community organizations. It is
proposed to provide people friendly regulatory framework that promotes ethical practice
through accreditation, standard treatment protocols and training and upgradation of skills
of non-government health providers. 5% of the total NRHM outlay is proposed to be the
resource allocation to voluntary organizations on the basis of approved guidelines &
norms.
REDUCING IMR/MMR/TFR AND THE DISEASE BURDEN
Reproductive and Child Health Programme (RCH-II) was launched in 2005 as a
part of the Mission as the principal vehicle for reducing IMR, MMR and TFR as
envisaged in the original Cabinet Note. Upgradation of Community Health Centres as
First Referral Units (FRUs) for dealing with Emergency Obstetric Care, 24x7 delivery
services at the PHCs, operationalising of Sub-Centres
multi-skilling of doctors,
contractual appointments of MOs and AMOs, training medical officers in Anesthetic
skills, training doctors/ANMs/Nurses as Skilled Birth Attendants (SBA) permitting ANMs
to administer certain drugs in emergency, partnerships with voluntary organizations,
RCH camps accreditation of non profit organizations, I EC activities are the major
interventions in reducing MMR. For reducing neo natal mortality programme for
Integrated Management of Childhood illnesses (IMNCI) is being extended at the
community and facility levels. Activities of ASHAs, Anganwadi workers and ANMs,
preraks of continuing Education Centres and SHG groups at the village level with focus
on both preventive and promotional aspects of health care accelerated immunization
programme, advocacy on age of marriage/ against sex selection, spacing of births,
institutional delivery, breast feeding, meeting unmet demands for contraception, besides
providing a range of RCH services are to have impact on reducing the health indicators.
Efforts are being made to integrate HIV AIDS programme with the RCH at the district
and sub-district levels. Convergence of disease control programmes, integration of
services, combined awareness generation, education and the advocacy at community
and facility levels, taking care of preventive, promotive and curative health care are
expected to bring down IMR/MMR/TFR and the disease burden as stated in the
proposal.
RISK POOLING AND THE POOR
The Mission recognizes that in order to reduce the out of pocket expenditure of
the rural poor, there is an imperative need for setting up effective risk pooling systems as
already envisaged. State specific, community oriented innovative and flexible insurance
policies need to be developed and disseminated. While the first priority of the Mission is
to put the enabling public health infrastructure in place, various innovative models would
be pilot tested to assess their utility.
FINANCING OF NRHM
The National Commission on Macroeconomics and Health (NCMH) has worked
out an additional requirement of non recurring expenditure of Rs. 33811/- crores per
annum and additional recurring expenses of Rs. 41006 crores at current prices for
delivering functional health care in the public domain. This outlay, which would be
shared by the Centre and the States would push the expenditure on Public Health care
to nearly 3% of GDP. As some of the elements included in this computation of fund
requirement relate to activities which are not strictly covered under the NRHM (like
setting up of medical colleges etc) and if allocations to be made on such activities are
excluded, then the additional capital and recurring requirements come to Rs. 30,000
crores and Rs. 36,000 crores per annum respectively over and above the current
allocations. It may, however, be mentioned that with growth in GDP, in order to maintain
the same percentage level of health expenditure vis-a-vis GDP, the expenditure would
have to go up in the same proportion.
Given the absorptive capacities of the States and the time it may take up to build
their capacities, it is projected in the implementation framework that there would be a 30
% annual increase in the central allocation for health till 2007-08, which, thereafter is
envisaged to grow at the rate of 40 %. If the projected funds, become available, the
public health expenditure is likely to reach 2% of the GDP from the current level of 0.9%.
In order to step up the expenditure on public health over the next 5 years, the
states also have to very significantly increase the allocation for the health sector in their
budgets since they contribute almost 4/5th of the current total expenditure. The EFC
has agreed that under the NRHM, 100 % grant be provided to the states during the 10
Plan which could be phased downwards to 85% in the 11 and 75% in the 12 Plan.
The approach to health insurance for vulnerable groups
NRHM is a serious effort to provide quality health care in rural areas that is
accessible, affordable and accountable. The principal thrust of NRHM is to make the
public system fully functional at all levels. Along side the efforts at strengthening the
public system, NRHM also envisages partnerships with non - governmental providers
for public health goals. Health insurance, under the over all NRHM framework is largely
an effort to reduce the distress and duress of households in seeking health care, by
reducing out of pocket expenditures through risk pooling. As NSSO 60 Round data
reveals there are out of pocket expenditures that households incur even when they go
to a public hospital. The effort of the NRHM is primarily to improve the services of the
public hospital but even then there would be out of pocket expenditures. It is on this
count that NRHM strategy for health insurance for vulnerable groups is primarily to
reduce out of pocket burden of poor families when they go to a government hospitaL
This will also improve the utilization of government hospitals. The intent of healt
insurance under NRHM is not to weaken the public system in any manner. It also tries to
address the issue of non availability of services in the public sector in many areas. While
NRHM will make all efforts to make publicly funded health services accessible, there
mav still be a need to seek partnerships with non governmental sectors as service
providers as per mutually agreed standard of services, Procedures and costs. Service
quarantee to the poor households is the prime objective of NRHM and all efforts will be
made to use the instrument of community health insurance to reduce the duress of
households on account of high out of pocket expenditures.
This document is aimed primarily at the government officers who are Planning a
health insurance programme in their state - the Health secretary, the Director of Health
services etc. It gives a step by step approach to introducing health insurance in their
state / districts, within the overall framework of strengthening the public health system
and improving the utilization of services from them. Starting from the rationale for
introducing health insurance, it explores the communities that need to be covered, the
packages that can be offered, the premium that should be collected and finally the
administrative details. While the first section is more generic and gives guidelines for the
framework, the second section is more prescriptive.
Some of the key messages are
•
Be clear why you want to start health insurance
.
Appoint a body that will take the responsibility of organising the health insurance
programme. It may be an independent Health Insurance Corporation, or a cell in
the Dept, of H & FW, or a separate trust, or a NGO.
•
Start with covering ‘organised’ sections of the informal sector first. BPL families
would be another option, but as they are poor, it would not be equitable to make
them pay. We have not tackled the option of involving the formal sector in this
paper.
•
The basic package should be a hospitalisation cover (upto a maximum of Rs
15,000) with no exclusions. For the BPL families, transport and wage loss
compensation could also be included.
•
The premium for this package is about Rs 250 for a family of five. A subsidy of
Rs.150 - 200/- from the NRHM could be admissible with balance coming from
State/beneficiary.
•
An independent body should be appointed to administer the scheme. This could
be a TPA or a NGO with the necessary technical and administrative skills.
•
A monitoring cell should monitor specific indicators to ensure that the programme
is on track.
There is currently a lot of interest in rural health insurance as it is realized that
this is necessary to provide for basic health needs of the poor. Planners and policy
makers in the Centre and States, all are interested in health insurance programmes.
Although there has been a governing body of literature on this subject and several
projects across the country, unfortunately, due to various reasons, including the fact that
it is a new and complex subject, there is very little clarity on how to go about it. This
document presents a framework which highlights some of the main steps and elements
in developing a health insurance programme which will hopefully help in designing
effective health insurance programmes. This document is aimed at the planner at the
state level who wants to start a health insurance programme. However, it can also be
used by district level staff or by national level planners who want to introduce health
insurance schemes for their target group. The emphasis is on the process rather than
on a product.
The document is divided into 2 broad sections. In the first section, each element is taken
and developed in detail, keeping in mind the diversity in our country. This section gives
the rational to choose a particular option for each of the elements. In the second section,
we outline some of the products suited for specific segments of population. This will help
the planner who wants a readymade programme.
Some years ago the Ministry of Finance had started the Universal Health Insurance
Scheme (UHIS) which was to be implemented by Public Sector Insurance Companies.
This had a defined package of inclusions and exclusions, high premium and substantial
subsidy for BPL families. However, this has had poor response for a variety of reasons
- no ownership of States; high premium; many exclusions; criteria about providers;
absence of TPA mechanisms; no marketing. Clearly, all these issues need to be
examined and addressed. Lessons need also to be learnt from many successful but
small social insurance schemes. Costs, and consequently premium and subsidy, need
to be reduced to ensure sustainability while addressing minimum but basic needs.
Health seeking behaviour and savings habit needs to be encouraged but costs of
provision and administration need to be driven down. This requires decentralization of
basic functions and the existence of structures for spread, trust and management. The
State must also share the subsidy burden to impart ownership and accountability.
A meeting of State Health Secretaries had been called on 28 April, 2006 to discuss
these issues. Some reading material was also provided. States have since been
showing interest and taking initiatives. This document is a further steps to facilitate the
work of States.
The Ministry of Health and Family Welfare would like to thank Dr. N. Devadasan of the
Institute of Public Health, Bangalore and Dr. S.P. Goswamy, Consultant (Health
Insurance) for their efforts in putting this volume together.
New Delhi
August 2007
Section 1
The framework
In our country, health insurance is still seen as a financial instrument and the major
perspective is that of the insurance industry. This has various implications, including the
stress on the balance sheet, profit margins and the claims ratio. Products are designed
to enhance these components. In the process, the objectives of health insurance are
totally neglected.
This document has been written from a health systems perspective, rather than a
financial one. The focus is on using health insurance to improve access to health care
and protect households from catastrophic health expenditure.
Yet another focus is on the process of designing and implementing health insurance
plans, rather than just developing a single product. Products are easily developed, but
more important is the need to market and service this product in the Indian context. This
is the challenge that most companies face today.
This entire section is based on the framework that is shown in Figure 1. These are the
elements that are required for developing a health insurance programme.
Risk pooling
Solidarity
Organiser
Why health
insurance 1
Equity
1
Empowerment
Why health insurance?
This is the first question that a planner needs to ask and answer. Why does the planner
want to introduce health insurance at National / state / district / regional level? What is
the need?
•
Is there a problem of access to health care? Is the target population finding it
difficult to access health care (primary or secondary)? Is there a problem of
access because of financial barriers? Are the bills too high and the people too
poor to pay these bills? Health insurance could be a way of removing
financing barriers and improving access to health care.
•
Is there a problem of impoverishment due to medical expenses? The population
is able to pay the bills, but in the process has to borrow or sell their assets to
meet these medical costs. This means that they may be pushed into poverty
because of medical expenses. Health insurance could be a way of providing
financial protection against high medical expenses.
•
Is there a problem of quality of health care? People have the capacity to pay, but
are not getting good quality health care. Health insurance could be a way of
negotiating with the providers for better quality health care.
•
Is there political pressure to start a health insurance programme? Is the Health
Minister wanting to start a health insurance programme? This could be the wrong
reason for starting health insurance in the state, but it could then be used to meet
the above objectives - improving access and financial protection. Especially
since there is high out of pocket payments by individual households in most of
our states.
•
The ACCORD health insurance programme was started because
the tribals did not have financial resources to access hospital
care. They preferred to lie down in their huts and die. After
introducing health insurance, the tribals now pay a small
premium when they are healthy and avail of benefits when they
are sick. They do not have to worry about money at the time of
illness.
•
The DHAN foundation discovered that the single largest reason
for indebtedness among their SHG women was loans to meet
medical expenses. After starting their health insurance
programme, women no longer have to take a loan when they are
sick, as they are protected by the health insurance programme.
•
With elections looming, the Assam government introduced a
health insurance programme for its citizens. Unfortunately it was
so poorly designed that it did not meet the needs of the people,
especially the poor. Thus a golden opportunity to protect the poor
was lost.
These questions need to be answered based on evidence. The latest NSSO data (60th
round) gives information on the extent of out of pocket (OOP) payments in the states
(Table 1). This could be analysed to understand the extent to which people are facing
barriers to health care, or are becoming indebted. The common dilemma facing policy
makers is “We are providing 'free’ government health services. In such a scenario,
should we introduce health insurance?" The fact is that the ‘free’ government health
services are not meeting the needs of the community. This is why they are using the
private health services and paying out of pocket. Of course, ideally the state and the
central government should make higher budgetary allocations so that the government
spending is doubled and the quality of health care in government health services is
enhanced. This would mean that the government facilities are used and the households
are protected from OOP.
Table 1: Out of pocket payments and indebtedness in some states in India (rural).
High
Middle
Low
Poorest
All India
income
income
income
% of people who do not use
health services
18
% of people who use
government services for OP
24
24
18""
11
30
26
22
18
% of people who use
government services for IP
42^
Average OOP payments made
for OP (Rs)
257
191
237
243
426
Average OOP payments made
for OP in Government facilities
11
9
19
9
12
Average OOP payments made
for OP in private facilities (Rs)
246
163
190
211
377
Average OOP payments made
per hospitalization (Rs)
5695
Average OOP payments made
per
hospitalization
in
Government facilities (Rs)
3,238
2530
2950
3017
6374
Average OOP payments made
per hospitalization in private
facilities (Rs)
7,408
5431
5777
6781
10749
% of people who are indebted
due to OP care
23
21
31
32
20
% of people who are indebted
due to IP care
52
64
65
60
52
Source: NSSO 60th round 2004. Govt, of India.
1(1] Bihar (5%), Jharkhand (13%), Maharashtra (16%), AP (21%), Assam (27%), Kerala (37%), Rajasthan
(44%), Orissa (51%) and HP (68%).
2121 Bihar (14%), Haryana (21%), Maharashtra (29%), Gujarat (31%), Kerala (35%), Karnataka (40%), MP
(58%), Orissa (79%), JK (91%).
But this may not be a feasible option, given the state government’s fiscal situation. So a
health insurance scheme could be an alternative to convert the existing OOP into a risk
pooling mechanism. This would protect the households and improve access to health
services.
From the above table, it is evident that there is a high OOP for both OP as well as
medical reasons. There is not much inter-state variations on the last figure and it is a
clear indication to introduce some financial protection measures like health insurance.
Pre-requisites for health insurance
Given the evidence that there is a need for improving access to health care and
protecting the households, the next main concern is - are there situations conducive for
introducing health insurance? There are some pre-requisites that need to be in place
before one should consider health insurance as an option.
1. There must be a body that will be able to organize the health insurance
programme. This could be the health ministry or the state health department.
More important, it should have the basic capacity to organize the programme.
This includes managerial, administrative, technical and social skills.
o
o
o
o
Managerial skills - to manage the entire programme
Administrative skills - to manage finances and the funds
Technical skills - to understand the complexities of health insurance
Social skills - to understand the community’s needs
2. There must be a network of health care providers (public or private). Without this,
it is not wise to talk about health insurance. Unlike in a tax based system, where
the supply side can always defend the lack of supply by quoting the poor
financial resources, in a health insurance scheme, the organizer cannot use this
excuse.
3. The people must have the capacity to pay the premium. Especially in a
contributory programme where the people are expected to pay the premium.
However, well the programme is designed, if the people cannot afford it, there
will be no takers.
4. There must be some basic data available regarding the demographic profile of
the community, the morbidity rates, the utilization rates, the cost per unit utilized
etc. There is adequate secondary data in our country for this (Census, NCMH,
NSSO etc) and can be used till primary data is collected.
There are many more conditions that need to be satisfied, but at least these need to be
in place before initiating a health insurance programme. The others could be developed
along the course of the programme.
•
In states with scanty provider networks, health insurance
programmes may be difficult to implement, as people will not be
able to access health care even though the programme takes care
of the financial aspects.
•
Most departments of health are busy implementing health care
programmes e.g. RNTCP, RCH, hospitals etc. So there is no time
or capacity to manage a fully fledged health insurance programme
that requires different expertise and skills. To burden these staff
with additional responsibility may not be a feasible option.
•
In some states and regions, the people do not have the capacity to
pay premium. They do not have ready cash because they depend
on a subsistence economy. In such circumstances, the government
needs to pay the premium on their behalf or organize innovative
mechanisms for collecting premium e.g. in kind, etc.
Who will organize the health insurance programme?
This is one of the key elements in any health insurance programme? Who is the
organizer? It could be
•
An autonomous body - “The State Health Insurance Corporation” or
•
The state government’s dept of health or
•
A ministry or a department for its target population, e.g. the Ministry of Textiles
initiated a health insurance programme for the weavers, or
•
A NGO for the community it works with, e.g. RAHA for the tribals, or
•
A hospital for the people living in the catchment area e.g. VHS for the people
living in the outskirts of Chennai, or
•
A cooperative society for its members, e.g. the Mallur dairy cooperative in
Karnataka, or
•
A trade union, a driver’s association etc, e.g. The Palakkad trader’s association’s
health insurance programme.
Basically any group can take the initiative and organize a health insurance programme.
The organizer must meet some criteria to be effective:
1. It must be a credible and trustworthy organization. People must have faith in
the organizer and believe that it is organizing it for their welfare. Which is why
when insurance companies try and introduce health insurance into a community,
there few takers. The classic example being the Universal Health Insurance
Scheme (UHIS). People are wary about such companies. On the other hand,
when it is done through NGOs who have been working with the community for
long periods of time, then they are willing to enroll.
2. This organization must have three basic skills:
■
■
■
It should have technical skills to understand the insurance concepts. Then
it will be able to design a programme that is technically sound. Also this
will help in negotiating with the insurance companies and the providers.
It should have social skills to be able to discuss with the community and
understand their needs.
It should have the administrative capacity to organize the health
insurance programme.
However, in larger organizations e.g. the government, the last two skills may be
outsourced to independent administrators e.g. a third party administrator or a NGO.
The decision to identify the organizer may depend on various factors, e.g. if a state
government wants to do a pilot for a couple of years, then it would be better to identify a
NGO or a CBO who will organize the programme. However, if the state wants to cover
larger populations and for a longer period of time, then an interim body like a “trust”
could be given the responsibility of organizing the health insurance programme. On the
other hand, if the health insurance programme is part of the health department’s drive to
systematically cover its population, then it should develop a “State Health Insurance
Corporation.” This autonomous body should incorporate related departments3131 as its
members and be given the responsibility of steadily covering the entire population under
some form of health insurance.
Figure 2: Potential organizers of health insurance programmes in a state
£
ra
o.
u
.S
/Health \
insurance \
corporation
Q
CD
ra
c
ra
Society/Trust,
?
o
c
x:
o
ra
/ Outsource \
ho NGOsetc/
Short term
vision
Middle term
vision
Long term
vision
3f3] e.g. labour, rural development, panchayat raj, women and child, finance etc as well as representatives
from the community, hospital owner’s association and the insurance companies
This autonomous body has many advantages, one being that it will be an independent
body that will be working for a specific purpose. Secondly it will not have the ‘reputation’
of the existing government departments. And finally being a single purpose unit, it will be
able to achieve universal coverage at a faster rate. Some of its activities could include
governing, organizing and monitoring the scheme, capacity building of the stakeholders,
negotiating with the providers and the insurance companies, However, the ultimate
decision will depend on the vision of the state government and the available capacity. If
the state does not have the techno-managerial capacity, it could try and access the
same from other sources, e.g. academic institutions, NGOs who have experience in
implementing community health insurance programmes, representatives from the
insurance industry, etc. One word of caution here, most of the resource persons from the
insurance industry are used to the “profit” motive, whereas in a state government
sponsored health insurance programme, the motive is improving public health indicators.
So there may be divergent views if one relies solely on the industry inputs.
The Yeshasvini Trust organizes the Yeshasvini Farmer’s Cooperative
Health Scheme. The trust is a combination of Government officers and
doctors. The members of the trust govern this scheme by deciding on
the package, the premium and the target groups, monitor it monthly
and negotiate with the hospitals. Being an independent body, the trust
has the necessary credibility and is not associated with the suspicion
that the Dept of Cooperatives is usually subjected to.
Role of the Health Insurance Corporation
• To provide the oversight for health insurance in the country / state.
•
To explore measures to cover the population in an incremental manner.
•
To ensure that the technical requirements for implementing health
insurance are in place, e.g. legal framework, regulatory framework,
administrative network, monitoring cell, etc.
•
To manage the insurance funds (if it is the insurer) effectively.
•
To provide technical and managerial support to the next level e.g. state /
district.
•
To liaison with the other ministries / departments.
A proposed structure is given in Figure 3
Figure 3: Proposed structure for the Health insurance corporation
Proposed structure
National Health
I
State Health
Insurance Corporation
.. —
State Health
Insurance Corporation
District Health |
Insurance Funds J
State Health
Insurance Corporation
[ District Health
[hInsurance Funds
Which community should be covered under the health insurance programme?
Ideally one should consider the entire population for health insurance. But given the
improbability of doing this in the short to medium term, one should prioritise and select
specific groups. Universal coverage can be done in an incremental way over time. This
can be done either through:
•
•
A population strategy
A geographic strategy
Population strategy
If one looks at other country examples one notices two distinct approaches. The first is a
“formal to informal” approach wherein the government initially covers the formal sector
e.g. civil servants, employees in enterprises, industries and mines etc. This is an easy
way to improve insurance penetration and also gives the government the time to gain
experience. Once the formal sector is covered, then they progress to the informal sector.
The other approach is the “indigent to formal” approach. Here the government initially
covers the poor in their society by paying the premium on their behalf. Once this is done
and they are able to manage this programme, they then move to the formal sector.
There are of course advantages and disadvantages in each and a lot depends on the
political environment.
In the Indian context, one can stratify the society into four broad categories for health
insurance purposes.
1. Employees in the formal sector and their dependents. This includes employees in
large corporate offices, industries, shops, etc.
2. People in the informal sector
a. Who are organized, e.g. farmers, traders, SHGs, etc.
b. Who are unorganized, e.g. vendors, maid servants, landless labourers,
subsistence farmers etc.
3. The indigent e.g. BPL families, destitute, etc.
Of course this is a suggestion and one can decide on different ways to stratify society.
The main advantage of stratifying the population is that one can use appropriate
strategies for each stratum.
For example, the formal sector could be insured using a social health insurance
mechanism. This would be easy as they are organized and can be approached through
their employer. On the other hand, the indigent may be difficult to insure as they have
neither the financial capital to pay premiums nor the social capital of organized groups.
In such instances, it may be better to provide social assistance to this group and insure
them by paying the premium on their behalf. However, the main difficulty in this measure
is to ensure that they are aware of their insurance status. Many such schemes have
shown that it has taken a few years before people are aware about the health insurance
scheme and the benefits that are available.
Existing strata that are “organized” e.g. dairy cooperatives, driver’s associations,
religious organizations, members of self help groups (SHGs), NGO communities, caste
based organizations etc are excellent entry points to introduce health insurance. These
are existing groups and have the advantage of inbuilt solidarity and channels for
communication and premium collection. Estimates suggest that there are about 10 crore
people in the informal sector who are ‘organised’ in groups e.g. traders, drivers, beedi
workers etc.
The unorganized groups are difficult to insure and it is better to cover them at a later
stage.
The community that should be covered depends on the local needs. However, in terms
of ease of coverage, it is easier to cover the informal “organized” sector, the formal
sector, the BPL families and then the informal “unorganized” sector.
Geographical strategy
Yet another approach to covering a population is to have a geographical approach. For
example, one can cover an entire district. This is a feasible option, provided the
organizer is proficient and is capable of designing and managing many insurance
products. This is because the need of the population varies. For example, in a district,
there are different groups of people; farmers, labourers, traders, civil servants, etc. Each
may have different needs and requirements. One scheme will not benefit all. So it will be
necessary to design different schemes for these different groups. This, naturally, is a
difficult task and requires some level of expertise.
1.
The needs of the community. If the community lives in remote villages and
finds it difficult to reach hospitals; a hospitalization package per se will not meet
their needs. One may need to include transport costs also.
2.
The cost of the final package and whether it is affordable for the target
population. Naturally a package that has all the above components will be very
costly and may not be affordable to most communities. So one would have to
prioritise and choose the most relevant benefits - a balance between the
community needs and the technical needs.
3.
The administrative burden in delivering this benefit package. Hospitalization is
a rare event and can be easily administered. On the other hand, OP cover is
more difficult to administer, and requires innovative mechanisms.
4.
Availability of these services. It naturally does not make sense to cover
hospitalization expenses, if there are no reasonable hospitals in the locality.
We propose a stratified benefit package that will meet the needs of varied population
groups.
An
iessential Basic hospitalization cover, with Includes transport Includes loss of
exclusions.
Includes expenses upto Rs wages upto Rs
package (Blue no
maternity. Maximum limit upto Rs 300 per episode of 50 per person
card)
per day for a
15,000 per family per year. hospitalization.
maximum of 10
Patients admissible only in
days in a year.
general wards.
■
An
optimum
package (Silver
card)
Basic hospitalization cover, with
no
exclusions.
Includes
maternity. Maximum limit upto Rs
30,000 per family per year.
Patients admissible in semi
private wards only.
An
enhanced
package (Gold
card)
Basic hospitalization cover, with
no
exclusions.
Includes
maternity. Maximum limit upto Rs
50,000 per family per year.
Patients allowed to use single
rooms.
The upper limits can be changed, depending on the costs of admissions in the region4™
The stratified benefit package can be open to all those who want to subscribe.
One simple way to do it is to visit some of the providers and get a list of admission bills in the past one
year. Sort this by the bill amount from low to high. Find out the figure for the 90th percentile and this could
be the upper limit. This means that the insurance cover will protect 90% of the insured patients. It will be
even more if one introduces cost containment measures (see later). Do not try to cover all 100% as a few
outliers will skew the figure for the rest of the population.
The premium
The premium is the amount that needs to be paid by either the households or the
government to become insured. While of course the premium should be affordable, there
are many other issues that need to be considered while deciding the premium.
Calculating the premium
To calculate the premium, one requires some basic data. While this is usually done by
actuarials in an insurance company, it is desirable that the planners / managers of the
insurance scheme also have some idea about calculating the same. This will ensure that
informed negotiations take place with the companies.
Some of the basic data that is required are:
1. The details of the benefit package.
2. The cost of each unit of the benefit package e.g. average cost of hospitalization,
cost of each episode of transportation etc.
3.
The probability of this event occurring in an individual. This can usually be
obtained from secondary sources e.g. NSSO data etc.
4. The approximate administrative costs.
We use an example to cost the blue card
Cost per
event_____ Probability
306[61
50005[5]
Hospitalisation
_______
30
300
7[7]
Transport______
300
8[8]
30
LoW__________
Premium_______
Admin cost9t9]
Total premium for
1000 individuals
Total premium per
individual______
Premium I
family1*101
Rupees
150000
9000
9000
168000
16800
184800
184.80
211.00
5[5] The median cost of all hospitalizations in the set of providers.
6(6] The probability of hospitalization /1000 individuals; based on NSSO figures. The upper limit has been
calculated, anticipating higher hospitalization rates due to insurance.
7[7] Amount reimbursable per hospitalisation
8[8] Rs 50 per day, for an average hospitalization of 6 days.
9(91 Approximately 10% of the total premium
10[10] 120% of the individual premium
Estimated premiums for the three packages
Premium amount*
Benefit package
(per family of five per year)
Basic
Rs 200*
Rs 150#
Optimum
Rs 400*
Rs 500
Enhanced
Rs 750*
Rs 600
* From actual data and based on a software
# Calculated by an actuarial
There are various other ways of calculating the premium. The above is also called
“community rated” premium and is usually a flat rate for all the members. Income rated
premiums, where the premium increases with the economic status of the individual
(though the package remains constant) is ideal in a social health insurance programme
like ESIS etc. On the other hand, most insurance companies in our country advocate the
risk rated premium. This varies depending on the medical history of the individual. While
it is ideal for individual policies, it is totally inappropriate where one is insuring large
numbers. Mainly because the risks are pooled and so the effect of the high risk is diluted
within the larger pool of low risks. And of course operationally it is impossible and costly
to assess the risks of each and every individual.
Ways of reducing the premium to make it affordable are
•
Reducing the package, so that it costs less. For example one could exclude
treatment of TB, or of family planning operations, or RTI treatment saying that
these are available “free” in the government sector.
•
Reducing administrative costs
•
Enrolling as a family unit
•
At ACCORD, the tribals pay Rs 30 per person per year for a
comprehensive benefit package with a maximum limit of Rs
3000 per patient per year.
•
At DHAN foundation, the premium is Rs 150 for a family and
the benefit package is a comprehensive cover (excluding
deliveries) with a maximum limit of Rs 10,000 per patient per
year.
•
The Yeshasvini scheme covers surgeries for an upper limit of
Rs 2,00,000 per patient per year for a premium of Rs 120 per
person per year.
•
The Universal Health insurance charges Rs 248 for a family of
five and provides cover upto a maximum of Rs 30,000 per
family per year. However, this policy has all the standard
exclusions.
Collecting the premium
While fixing the premium is a technical matter, collecting it depends on the target
population and how close the organizer is with the community. The easiest way to collect
premium is to use existing channels.
•
•
Membership payments - if one is insuring SHG members, then one can use the
existing channels to collect the premium. The same can apply for association
members, union members etc.
Deducting at source - if one is insuring cooperative society members, then one
can instruct the district officer to deduct the premium amount annually from the
member’s dues and send it to the organizer.
In the case of BPL members, the government may want to pay the premium upfront on
behalf of the families. This has the least administrative costs.
In the case of unorganized sectors, e.g. landless labourers, or vendors etc, it may be
very difficult to collect premiums. The only way out is to have a voluntary enrolment
mechanism which is easy enough for the people.
Enrolment unit
While the common unit for enrolment is the individual, this not a good option, as it
promotes adverse selection. On the other hand, it would be better to enrol as large a unit
as possible. If one is enrolling SHG members, then one could say that all the members
of the SHG should enrol. Or if cooperative society members are enrolling, then at least
50% of the society members should enrol for this society to become insured. In the
beginning, this may be difficult, as people may have a lot of scepticism about the
programme. So it may be reasonable to enrol all the family members as one unit. This
way, one can ensure that adverse selection is minimized.
•
JRHIS in Wardha has family as the enrolment unit.
•
Student’s health home has the school as the enrolment unit.
•
SEWA has the individual as the enrolment unit.
Collection periods and waiting periods
There are two possibilities while collecting premium. One is to collect it during a fixed
period. The other is to collect it continuously. The latter is difficult as one has to keep
continuous watch on renewal periods etc. Also it encourages adverse selection as
people will tend to join when a family member is sick. So a fixed collection period (of two
or three months) is more desirable. However, it is necessary to fix this when the
community’s finances is the highest, so that they can use their disposable income to pay
the premium.
Waiting periods are used - again to prevent sick people from joining and using the
benefits immediately. Usually the waiting period is for a month after paying the first
premium. This applies only to those who are joining for the first time or joining after a
break. Obviously, a person who is renewing his insurance on time does not have to wait
any more.
How to empanel the providers?
Providers are an essential element for any health insurance programme. Without this,
one cannot even consider a health insurance programme. So before any organizer
contemplates a health insurance programme, he should review whether there is an
adequate distribution of providers.
The providers could be public or private or NGO providers, could be clinics or hospitals,
could be practitioners of allopathic or AYUSH. The choice depends on the benefit
package. For example, if one is covering OP and IP, then one should empanel a set of
clinics and hospitals. On the other hand, if one is covering only IP, then it makes sense
only to empanel hospitals.
Identifying providers requires a balance between technical capacity and people’s choice.
So ideally one should do it with representatives of the target population. There are two
options:
•
One is a free for all - allow people to choose any hospital, as long as it meets
the minimum criteria, e.g. more than 15 beds, registered with local body etc. The
advantage of this is that the patient has total freedom to choose. However, it is
difficult to monitor many institutions. And worse, one cannot introduce any
quality measures as there is no MoU between the organizer and the hospitals.
•
Empanel according to set criteria - develop a set of criteria and then empanel
the hospitals only if they meet these criteria. It may be advisable to have
reasonably strict criteria, so that quality is assured. Many hospitals may refuse to
cooperate if the criteria are too strict. So one must maintain a balance. The
advantage here is that one can negotiate for quality health care, for cost control
measures and anti-fraud measures. Also the patient should understand that by
empanelling providers their choice may be limited, but they get additional
benefits like cashless service, assured quality and low costs (leading to low
premiums).
It is not necessary to empanel all the providers, rather only those who meet the criteria.
One of the bargaining points for the organizer would be the additional income that the
provider would make if they are empanelled. Hospitals in Gujarat who were empanelled
under the Chiranjeevi scheme had a turnover of a few lakhs every month, just from the
insured patients.
The most important aspect is to purchase care. For this, the government needs to
change its mindset from providing to purchasing health care. Providers in the
government also need to have a change in mindset as they need to compete with the
private sector providers for patients. This could be an excellent opportunity to improve
the health services, both the government as well as the private and make them
accountable to the larger good.
Some suggestions for empanelment are given below:
o
be registered with the local administration
o
be acceptable to the local community
o
have a resident medical officer (allopathic or ayurvedic
homeopathic or sidha or unani) available round the clock
o
have at least 3 nurses (or nursing assistants), one for each shift
o
have facilities to admit at least 10 patients at a time
o
have its own pharmacy or access to an independent pharmacy that
will supply medicines to the patients
o
have its own laboratory or access to an independent laboratory
where investigations will be done on a credit basis for the insured
patients
o
be willing to use generic medicines for the treatment of the insured
patients
o
be willing to follow standard treatment guidelines for the treatment of
the insured patients
o
be willing to provide cashless services to the insured patients
o
not charge any money from the patient. All services (medicines,
investigations and consumables will be supplied by the hospital)
o
accept the tariff rate developed by the insurance organizer
o
maintain necessary records and registers (e.g. IP register, OT
register, Labour room register, pharmacy register, accounts register)
as per the prescribed format
o
allow inspection of its records by prescribed
including medical audits, chart audits etc.
o
be willing to change its treatment practices if some indicators (e.g.
infection rates, Caesarean rates, admission rates, investigation
rates, etc) are found to be higher than average.
o
be willing to submit claims as per the requirements
o
be willing to wait for at least 30 days for reimbursements
o
bear the cost of the fraudulent bills in the event of any fraud or any
wrong billing
or
representatives
Negotiating with the providers
While empanelling providers, the organizers need to negotiate for some benefits. These
include:
•
Development of MIS so that the records of the insured are identified easily.
•
A cashless system for the patient,
•
Cost containment measures like
o Essential drugs
o Generic medicines
o Standard treatment guidelines for common conditions
•
Quality of care measures like
o Medical audits
o Chart reviews
o Appropriate evaluation protocols
•
Special privileges for the insured like
o Different queues
o A special desk for the insured (this may be manned by volunteers or
representatives of the TPA).
o Adhering to the referral system
o Accepting only cases that have a pre-authorisation (unless it is an
emergency)
•
Fixed tariffs and payment systems (see later)
•
Submitting claims in standard formats
Once the terms and conditions are negotiated, it is advisable to have a written Moll with
the providers highlighting what are the responsibilities of each stakeholder. This way,
misunderstandings are reduced to a minimum and the patients benefit the maximum.
Public versus private
This is a major issue in most health insurance schemes started by the states. Should
one empanel only public providers, only private providers or both? The issues for each
are discussed below:
Only public providers (as in Karuna trust).
Plus points
o Government health services are strengthened
o Quality can be easily improved
o Can be used as a tool to motivate government staff
o More benefits at lower costs
•
Minus points
o Choice for the patient is limited
o The insurance plan may appear meaningless as the patient anyway gets
‘free’ or subsidized care at the government hospitals
o Most governments do not have directives on how to use the user fees,
leave along insurance reimbursements. This means that the money
collected will stagnate in bank accounts.
Only private providers (as in most CHIs)
•
Plus points
o More choice for the patients
o Improved access as there are many more providers
o More services will be available for the patient
•
Negative points
o Cost control, anti-fraud measures and quality are difficult to enforce
o Criticism that public money is being used to fuel the private sector
Ideally one should have both public and private providers. But for this certain conditions
need to be in place:
1. The public sector hospitals should be able to receive the insurance
reimbursements. Currently most states permit user fees. So this should be
broadened to include reimbursements. However a few studies and anecdotal
evidence suggests that most of the user fees languish in bank accounts as the
concerned officers are reluctant to spend this money without written instructions.
So if the insurance reimbursements are to be used for the benefit of the patients,
then clear cut guidelines on their use should be developed.
2. The public sector should be allowed to compete with the private sector. This
means that powers be devolved to the district medical officer, so that he / she
can take decisions that will improve the performance of the government
hospitals. This could include incentives for the staff, so that they are motivated to
provide good quality care.
3. The mindset of the government doctors should change from salaried employees
to private practitioners.
Paying the providers
This is a much neglected element in the entire health insurance programme. On the
other hand, it can be a very powerful tool with the organizer to reduce costs. The most
common method currently used to pay providers is “fee for service". For example, a
patient goes to a doctor, gets care and pays the consultation fees, goes to the pharmacy
and pays for her medicines. This means that the patient pays the entire cost of health
care at the time of use. It is a very inefficient manner of paying providers for two
reasons:
•
It places a burden on the patient at the time of illness. And there is no risk
pooling. The entire burden has to be met by the patient.
•
It encourages the doctors to provide more services (whether necessary or not) so
that he can maximize his profits.
There are other efficient payment mechanisms that can be introduced and will help
contain costs. An effective measure is the “payment per case” method. In this a
particular diagnosis is paid a previously decided flat rate, irrespective of the costs
incurred. Thus a delivery could be reimbursed Rs 1000 even if the actual cost of the
treatment is Rs 1200 or Rs 800. This has tremendous administrative benefits, as the
organizer does not have to scrutinize individual bills. Also the incentive for the provider
to prescribe extra services does not exist any more. The only drawback is that it can
compromise quality of care, as providers may actually skimp on relevant treatment to
make profits. This is also called “diagnosis related groups” (DRGs).
Yet another measure is the “capitation" method. Useful when reimbursing OP services,
providers receive payment according to the number of people registered with them, not
for the actual services given. Under-prescription can be countered by introducing
competition between the providers. Thus only those providers who are providing good
quality care will have people registering with them.
A third method is to pay providers a fixed “budget.” The providers have to provide all the
required services within this budget. Useful, if the budget is just right. If budgets are
calculated based on past utilization, there maybe a tendency for over using the budget,
so that the provider gets higher allocation in the subsequent year.
More details are given in the Appendices. It is clear that the organiser requires
considerable technical skills to introduce alternate systems of provider payment.
Who is the insurer?
Who will take the risk of managing the insurance funds, ensuring that it is enough to
meet the needs of the programme? One option is to link up with existing insurance
companies, either private or public. This has many advantages:
•
Management is in professional hands
•
Risk pooling is increased as the funds are merged into the larger pool of “non
life” insurance
•
The organizer is free to manage the programme
•
The company has enough capital reserves to provide buffer, in case the claims
ratio exceeds 100%
•
It is legally acceptable by all concerned
Health insurance programme for BPL families
People living below the poverty line (BPL) have difficulty meeting basic needs like food,
shelter and clothing. Health care for them becomes a luxury and many are not able to
access the health services for want of financial resources. These are the groups who
require protection when they are ill. Unfortunately the current government health
services are not able to meet their requirements, due to various reasons. So one may
need to address their needs on a priority basis.
In their case, one would prefer to use social assistance rather than a traditional health
insurance programme. The basic design is given in Figure 4
Figure 4: Possible design for developing a social assistance programme for BPL
households.
fI
i
Government
BPL HHs
Funds
District
Health Insurance
Fund
/
_ I Providers
Organizer of the programme
The state government or the district government organizes the programme, with the help
of NGOs.
The community
In this case, the community to be insured is the BPL families in a district or the state.
They can easily be identified by the BPL cards. While there may be many objections to
the validity of the BPL cards, if the margin of error is not too much, one can accept it as
an initial identifier. Later, one can refine it with time and experience. The list of BPL
families can be obtained from the Rural Development dept, or from the Panchayat Raj
Dept, or from the Revenue Dept.
The benefit package
In this case, as most of this population will be suffering from communicable diseases, a
low end package will easily meet their needs. So the basic package with hospitalization,
transport cover and loss of wages cover would be the optimal package for them. OP
cover may be considered, but organizing it may be difficult and also expensive.
Hospitalisation cover for all conditions,
maximum of Rs 15,000 per family per year;
upto a
Transport costs of Rs 300 per hospitalisation
episode;
Loss of wages compensation of Rs 50 per patient
per day hospitalised (maximum limit of 10 days).
The premium
The premium as calculated would be about Rs 250 for a family of five. This maybe
unaffordable to many BPL families. So there are two options possible:
4- Totally subsidise the premium
4 Partially subsidise the premium
These two options have various implications. In total subsidy, the government will pay
the premium on behalf of the families to the insurer. So the people are insured at one go.
However, from varied experiences, it is clear that most of such families are not aware of
their insurance status. It takes at least 2-3 years of concerted effort to create
awareness in all the families. Thus this option should be considered only if the
government has the funds to cover the BPL families consecutively for 3 - 5 years. Else
the entire money will be wasted and there will be nothing to show for the effort and
resources spent.
The second option is however a difficult one to implement. The government can
subsidise the premium and collect only an affordable amount from the BPL families.
However, the difficulty is in collecting this premium. As is clear from the UHIS
experience. One way out is to request all the ANMs, the ASHA and the Anganwadi
workers to collect the premiums from the BPL families and pass this to the District
Health Insurance fund. They may be given a performance based incentive for collecting
the premium. However, in such a case, they should be empowered to distribute the
insurance cards to the insured families. A second or third step in distributing these cards
may not be feasible and desirable.
The enrolment unit should be the family, nothing less and the premium (if collected)
should be during a definite collection period. Given the difficult enterprise, waiting
periods may be waived in this instance.
Providers
As the government providers have not been successful in meeting the needs of the BPL
families, it may be necessary to have a combination of public and private providers. The
latter should be empanelled keeping in mind the preferences of the families. The TPA (or
similar local body) should do the empanelling. The criteria for empanelling are given
earlier (Section 1). The providers should be willing to
Provide cashless hospitalization service for the insured card holder
4. Provide all the facilities, including medicines and laboratory investigations at
the hospital
Accept the tariffs and payment mechanisms
Public providers who are empanelled should be willing to accept the insurance
reimbursements. This money may be used partly to finance the essential requirements
in the hospital and partly as an incentive to motivate the staff.
Insurer
In this case, and especially in the early years, the claims ratio will be very low. So it is
better that the government is the insurer. The government transfers funds to a district
health insurance fund who then manages it Any premium collected from the people is
deposited into this fund.
Administration
Independent TPAs could be appointed to manage the scheme. As stated above, they
could be given specific tasks, especially in creating awareness among the BPL families.
Where available, local NGOs could be appointed as the TPAs. Their main roles would
be create awareness, enrol members, issue id cards, maintain lists of members,
empanel providers, negotiate with them for quality services, low cost and administrative
conveniences; process claims and reimbursements and monitor the entire programme.
Further details are given in Section 1.
Indicators to be monitored
The main indicators to be monitored are given above (Section 1). The most important
indicator to be monitored is the utilization rates, especially in the first few years. If
premium is being collected, then coverage rates also need to be monitored. Renewal
rates give an idea about the satisfaction of the programme.
Risk management
As entire populations are insured upfront, adverse selection does not have any role
here. On the other hand, moral hazard may be an important risk to be minimized. Some
of the ways out are:
4- Have a flat/case-based payment mechanism as opposed to a fee for service
mechanism
4- Insist on standard treatment guidelines
■4
Insist on medical / chart audits
4 Have a referral system or a pre-authorisation system
4 Introduce photo identity cards for the insured
4 Use social audits to identify fraudulent admissions
Conclusions
The challenge in this model is to identify the BPL families. While many criticise the
existing BPL cards for their inaccuracy, it could be a good enough starting point. With
time and with specific interventions, the BPL lists could be refined so that false positives
and false negatives are minimised. More important, such schemes should not be
reduced to populist measures, flash in the pans that appear during election times. To be
a sustainable model, such schemes should be functional for at least 3 years with full
subsidy and then with a tapering subsidy over the next five years. This way, the people
will have faith in the scheme and will also get into the habit of purchasing health
insurance.
Health insurance programme for members of SHGs
The author uses SHGs just as an example. The same model can
be used for cooperative societies, for associations, for trade
unions, for beedi worker’s associations etc.
In most southern states, and in some northern states, self help groups (micro credit
groups / micro finance groups) are well established. These are usually formed of women
in low income and middle income strata, who meet once a month to save. Many of these
groups have federated into large district level structures and control crores of rupees.
Evidence, from recent times, indicates clearly that the main reason for taking loans are
medical expenses. So many of them are willing to take the next step of microfinance i.e.
micro health insurance.
Community
The SHG members and their dependents are the eligible members who should be able
to enroll in this HI programme. To reach out to them, it is better to tackle the larger
federations who are well established. For example in Kerala, the government decided to
introduce health insurance through the Kudumbashree - a government sponsored
federation of SHG women. At last count, they had 25 lakh women members.
Organizer of the HI programme
Depending on the state’s interest, the size of membership and vision, the options are:
• The State Health Insurance Corporation
•
A trust / society initiated by the state government for health insurance
•
The district health society
ANGO
•
The Dept of H&FW
The advantages of each are given in Section 1. The last would be the most undesirable
option, as then this activity would be diluted amongst hundred other activities. The
proposed design is given in Figure 5.
Figure 5: Design of a health insurance programme for SHG families
State / District
Body
Insurance
i Premium y ◄ Company^ ►
4*""
TPA ’
y
I
SHG HHs
Care
L
Empanelled
L Providers
The benefit package
This segment of population is categorised as “near poor”, usually above the poverty line.
They have some assets and are able to save, even if only small amounts. More
important, they have access to credit when needed. So in this case the optimum
package (silver card) would be an ideal benefit package for them. This includes
hospitalization cover upto a maximum of Rs 30,000, with no exclusions. The premium
would be between Rs 350 to Rs 400 per family per year, depending on the state.
The premium
The premium as calculated is Rs 400 per family of five. This may seem a high premium
for a low income family. However, given their practice of meeting once every month, the
premium can be collected in monthly instalments and paid at one point in time to the
local collection agent.
While most SHGs identify only the women as members, for the sake of the health
insurance programme, the member and her dependents should be insured. It would
even be better if the entire group could be insured rather than individual families. The
premium could be collected through existing SHG channels - from individual members
to the group, from the group to the cluster; from the cluster to the Block level federation
and from there to the district. The money can be deposited into the District Health
Insurance Fund.
The providers
Where such health insurance programmes are implemented, one must empanel
government as well as private sector providers. This can be done after discussing with
the community and the relevant local district officers. The criteria for empanelment are
given in Section 1.
The providers will be paid on a case base mechanism or a DRG mechanism. Tariffs will
be formulated earlier itself, based on local prices. Later, after conducting costing
exercises, one may arrive at more exact tariffs.
Insurer
If the size of the pool is large, e.g. an entire state, the programme may be able to
manage the funds on its own as a stand alone health insurance fund. However, if it is
small e.g. a district, then it maybe advisable to link up with an insurance company. The
insurer in this case will be a health insurance company. The company could be selected
after floating a tender with the requirements and choosing a company that provides the
lowest premium and also agrees to the conditions laid out.
Administration
The Health Insurance corporation and the insurance company will together decide on a
TPA. This could be an organisation registered with the IRDA or an independent NGO
that has the capacity to manage. The TPA has to have the capacity to service the
programme at the district and sub-district level. The main activities that the TPA should
do are given in Section 1. The indicators that need to be monitored by the Health
Insurance corporation are also given in Section 1.
Risk management
The main risks to be managed here are adverse selection, moral hazard and fraud.
Measures for these are clearly given in Section 1.
Conclusions
As stated earlier, this model can be used for various ‘organised’ groups in the ‘informal
sector’. And depending on the scale of the programme, it could be at the district or state
level. Once this programme has been established, it could be expanded to cover other
groups in the locality. And more important, it could be used to cover groups like landless
labourers, subsistence farmers etc, who normally are out of any formal activities. These
groups could be allowed to join the scheme on a voluntary basis.
OP care in areas where there are no hospitals
In some of the states, especially the northern states and NE states, where hospitals are
not available in the rural areas, a hospitalisation based health insurance may not be
feasible. In these regions, people use the existing “unqualified” medical practitioners as
well as qualified medical practitioners to meet their health care needs. But because of
various reasons, even these practitioners are very costly and people are not able to
access them because of financial barriers. So in such a situation, providing a cover for
OP and transport would be a reasonable option.
Community
The people living in these regions. Where possible, try and use the existing organised
groups e.g. those communities working with NGOs, SHG members, religious groups,
etc.
Since it is a voluntary health insurance, the danger of adverse selection is high. To
minimise this, the family should be enrolled.
Organiser of the health insurance
As a pilot programme, this should be outsourced to a credible NGO in this region. The
NGO should be given the technical inputs and the managerial freedom to cover this
population.
Benefit package
The main benefits would be OP care. Each enrolled family would be given an insurance
card along with 5 pre-printed vouchers. These vouchers can be exchanged at
empanelled providers for health care during the year.
Other than this, the family will also be reimbursed travel costs for one episode of
hospitalisation, up to a maximum limit of Rs 500. This can be obtained from the NGO
organiser who will verify the hospitalisation status and the validity of the insurance card
before reimbursing the money.
Premium
The premium for this package will be about Rs 300 per family (of 5) per year. As most of
these families would be very poor, the government could subsidise the premium by 50%,
paying the NGO directly for each family insured. So the NGO has to collect only Rs 150
from the families.
Providers
As stated earlier, most of these regions will not have hospitals and even qualified
doctors. In such circumstances, one may have to empanel “unqualified” medical
practitioners, or AYUSH practitioners. This should ideally be done in consultation with
the local community, and only credible practitioners who provide some modicum of
quality care should be enrolled. Preference should be given to those practitioners who
live in the villages and are available 24 X 7.
The NGO should reimburse the providers on the basis of the vouchers, Rs 50 for each
voucher. This would limit the unnecessary medication and injectables that is the wont of
such practitioners. The other way of paying the providers is through a capitation system.
The community should be asked to register with a particular practitioner. The NGO pays
the practitioner Rs 50 per patient registered. With this money, the practitioner should
provide OP care to the registered patients. This mechanism has limited tendency for
fraud, the only drawback is that the practitioners may restrict the treatment given.
However, if there is a possibility of competition between the providers, then this will also
be taken care of.
Insurers and the administrators
The NGO becomes the insurer, as it is collecting funds (from the people and the
government) and managing the funds. This may not be acceptable with the IRDA which
does not recognise such stand alone models of health insurance. So other options
should be considered e.g. simplest would be to call it a “Health Fund” rather than a
health insurance programme.
The NGO should reimburse the providers on a monthly basis (if voucher system) or pay
the capitation fees in three monthly advances. They should however monitor the scheme
close|y, especially monitor the extent of fraud. Social audits should be used for
minimising this and the community representatives should be available in the claims
committee. Random checks on claims should also be made, to verify that vouchers are
not being misused by the insured community.
The NGO should also negotiate with the providers for empanelling them and providing
the desired quality of care. It should of course create awareness among the population
about the benefits of health insurance and the possibility of improving their access to
health care.
Risk management
The main risk here is that of moral hazard and fraud. Every headache may land up at the
doctor s clinic for treatment. The people should be informed about the price of abuse. If
they use their vouchers for frivolous conditions, then when they really fall sick, there may
not be any vouchers for their health care. This may reduce moral hazard. Also if people
save vouchers, then it may be carried over for one year. This would be an incentive for
patients not to abuse the system.
Fraud is a potential problem as anybody can borrow their neighbour’s voucher and seek
care. Of course, one can introduce some identification mechanism e.g. a ration card, or
a voter’s id card, or a BPL card etc. But as stated earlier, social audit is more effective.
Responsible members of the community / NGO field staff should verify random claims.
Monitoring
The main indicators to monitor are the coverage rates and the utilisation rates. This will
give an idea about the inflow and outflow and will allow the NGO to plan for the next
financial year.
Conclusions
This programme should be a pilot to test whether insuring OP services is feasible in poor
rural areas. The programme should be monitored closely to understand what are the
other measures that need to be introduced to make it run successfully.
Using UHIS
The UHIS was launched with much fanfare, but unfortunately was not accepted by the
people due to various reasons. Latest data (Sept 2005) suggests that only 45,118
families have been insured and the claims ratio is about 11%
While we shall not go into the reasons for its failure, we suggest some measures to
make more acceptable to the community.
Organiser of the health insurance plan
The department of health could be the main organiser of the plan. It can take on the
governance of the programme, and outsource the administrative functions to
independent agencies. For example, it could appoint a TPA (or a large NGO) who would
market the product among NGOs, SHG groups etc. This same TPA would administer the
scheme.
There are other possibilities,
•
One is for the State Health Insurance Corporation (or the Trust) to organise the
marketing and servicing of the UHIS; or
•
The other is to identify a NGO with significant presence in the districts and who is
involved in health; or
•
The federation of SHG at the state level, e.g. Kudumbashree (in Kerala).
Community
The community is restricted to BPL families.
Benefit package
The benefit package is the standard UHIS. However, this package would be more
acceptable if maternity was included. The government may have to pay an additional
amount - in the range of Rs 50 per family.
While this package does exclude pre-existing illnesses, if one is insuring in large
numbers, it will not be feasible for all the insured to undergo a medical check up. Thus
this condition will become non-functional. Also many of the conditions that come under
pre-existing illnesses and chronic illnesses like diabetes, hypertension, IHD etc do not
affect BPL families. So one should not be unduly worried by this clause.
The other elements of the package, i.e. personal accident cover and wage loss
compensation cover can remain as it is.
Premium
The premium will be as per the current guidelines. However, one may need to add Rs 50
to the family premium if one has covered maternity also.
Actual premium
Subsidy by Gol
Premium payable
by household
For an individual
Rs 365
Rs 200
Rs 165
For a family of 5
Rs 548
Rs 300
Rs 248
For a family of 7
Rs 730
Rs 400
Rs 330
The family should be the enrolment unit. However, the package is restrictive when it
describes the family of 5 and 7. These restrictions can be waived and anybody in the
family can be insured.
The premium of Rs 248 (or Rs 330) can be collected in its entirety or the state
government can also add to the subsidy. If the state government plans to provide a
100% subsidy, it should recognise two aspects. One is that as the people have not
contributed, they will not be aware of their insurance status. So it is necessary to invest
considerably on insurance education and awareness building. The second is that in the
long run, this may not be sustainable. So it may be desirable in the initial years, till
people become accustomed to the insurance mechanism. Once the demand is created,
the subsidy can be progressively reduced.
The administrator of the scheme will collect the premium from the designated groups
and hand it over to the government health insurance fund. This premium will then be
handed over to the insurance company.
Premium collection will be during a fixed period. And as per the policy, there will be a
waiting period of 30 days.
Kudumbashree is the federation of all government sponsored Self Help
Groups in Kerala. There are about 22 lakh women who are members.
The department of panchayat raj introduced the UHIS through this
organisation. The premium was subsidised by the government of India
(Rs 300), the state government and the local panchayats. The
individual household had to pay only Rs 33
Providers
One must empanel the providers. This is the work of the administrator of the scheme.
The TPA should use the guidelines given in Section 1 and empanel the providers in the
districts and sub-districts.
Payment mechanisms for the providers are clarified in Section 1. The department
through a decentralised District Insurance Fund can reimburse the hospitals directly.
However, the payment should be on a case basis or DRG basis.
Insurers
The four public sector non-life insurance companies are the insurers of the product and
they take the risk. While the insurance company will receive the premium, it will also
distribute 50% of the premium to a designated government account as a rolling fund.
This fund will then be used to settle claims. The insurance company will top up this
amount as and when necessary. At the end of the year, if there is any balance, then it is
transferred back to the insurance company.
Administration
The government needs to appoint a TPA for this scheme. This could be a registered
TPA (as per IRDA guidelines) or it could be a large NGO with significant presence in the
districts. They should be given the responsibility of
•
Creating awareness about the plan
•
Marketing the plan to groups (NGOs who work with BPL / SC / ST families; SHGs with
significant BPL memberships; LAMP societies; employee welfare associations with
significant BPL employees etc).
Issuing identify cards and developing and maintaining enrolment registers
Collecting the premium from the people and depositing the same in the designated
insurance fund
Empanelling hospitals
Developing STGs, tariffs
Developing a referral / pre-authorisation system
Having a desk in some of the important hospitals to receive the insured patients
Processing claims and passing it to the district insurance fund
Tracking reimbursements
Monitoring the programme as per the indicators (Section 1)
Conducting medical / chart audits on a random basis
The TPA / NGO would be paid fees (5% of premiums collected) for administering the
plan. This could be an indirect subsidy of the scheme by the state government.
Risk management
The various measures to reduce risk are
•
•
•
Family as the enrolment unit
Referral / pre-authorisation system
STGs, audits, essential drugs etc.
Appendices
Appendix 1
Some definitions
Adverse selection: It occurs when those who anticipate needing health care choose to
buy insurance more often than others. It is because insurance suppliers lack full
information about the risk of individual insured persons. Adverse selection may result
from the tendency among patients to seek or continue insurance coverage to a greater
extent than healthy people. An example of adverse selection is when only the baby in a
family is insured. This is done because the family knows that the chances of the baby
falling ill are higher. Adverse selection needs to be prevented, else it affects the financial
sustainability of the insurance programme. It can be controlled to a certain degree by
making the insurance mandatory and/or by enlarging the subscription unit, e.g. if the
entire family is insured rather than an individual.
Benefits: Benefits are the sum of money received by an insured or an assignee (e.g. a
hospital) as reimbursement for medical costs incurred due to illness. Benefits may also
be in the form of health services received. These benefits are in lieu of a premium paid
to an insurance provider.
Cap: A limit of the benefit amount that an insurance company will pay. The cap may be
an overall maximum, such as an maximum of Rs 10,000 per patient per year, or may
apply to specific services, such as a cap of Rs 500 per year for outpatient services.
Claim: A request to an insurer by an insured person (or by the provider of a good or
service on behalf of the insured individual) for payment of benefits according to the
terms of an insurance policy.
Exclusions: Specific conditions listed in an insurance or medical care policy that are not
covered by benefit payments. Common exclusions include pre-existing conditions, such
as heart disease, diabetes, hypertension, or asthma which began before the policy was
in effect. Because of exclusions, persons who have a serious condition or disease are
often unable to secure insurance coverage either for a particular disease or in general.
Sometimes conditions are excluded only for a defined period after coverage begins,
such as nine months for pregnancy or one year for illnesses. Exclusions are often
permanent in health insurance coverage for individuals and temporary (e.g., one year)
for small group insurance. They are uncommon in large group plans that are capable of
absorbing extra risk.
Fee-for-service: A method of charging whereby a physician or other practitioner bills
each encounter or service rendered. E.g. separate fees for consultation, medicines,
laboratory, procedures etc. This is the usual method of billing by the majority of India's
private physicians. Under a fee-for-service payment system, expenditures increase not
only if fees go up, but also if charges are made for more units of service or more
expensive services are substituted for less expensive ones. This system contrasts with
salary, per capita, or prepayment systems, where by payments do not change according
to the number of services actually used or if none are used.
Health Insurance: A financial instrument that, in return for payment of a contribution (or
premium), provides members with a guarantee of financial compensation or service on
the occurrence of specified events. The members renounce ownership of their
contributions. These are primarily used to meet the costs of the benefits.
Moral hazard: The tendency of individuals, once insured, to behave in such a way as to
increase the likelihood or size of the risk against which they have insured. Can be
classified into 'supply side Moral Hazard' (when the doctor provides unnecessary care
because the patient is insured) or 'demand side Moral Hazard' (when the patient
demands unnecessary care because he is insured).
Out-of-pocket payments or costs: Costs borne directly by a patient who lacks
insurance benefits; sometimes called direct costs. Unless covered by insurance, they
include patient payments under cost-sharing provisions.
Pre-authorisation Certification: A procedure whereby the insured or his doctor is
required to contact the insurance company before admission to a hospital, and get the
latter’s permission.
Third-Party Administration: Administration of a group insurance plan by some person
or firm other than the insurer or the policyholder.
Underwriting: The process by which an insurer determines whether or not to accept an
insurance application and on what basis/terms it will be accepted.
Appendix 2
Some health insurance products in the government / NGO sector
_
NGOs_____
Community
Organiser
Insurer
Administrator
Provider
Premium
Benefit package
Risk management
ACCORD
Tribals
ACCORD
Royal
Sundaram
Insurance
Company
ACCORD
ACCORD
hospital
Rs 30 per
person
per year
Hospitalisation
expenses upto a
maximum limit of
Rs
3000.
No
exclusions.
Collection period,
Salary
for
providers, essential
medicines
and
STGs
Karuna
SC / ST
population in
T’ Narsipura
taluk
of
Mysore
district
Karuna
Trust
National
Insurance
company
Karuna Trust
Government
hospitals
Rs 20 per
person
per year
Medicine cost @
Rs
50
per
inpatient day.
Collection
Flat rate
Yeshasvini
Members of
the
cooperative
societies
Yeshasvini
trust
Yeshasvini
trust
Family Health
Plan Ltd.
Private
hospitals
Rs
120
per
person
per year
Cover
for
surgeries upto a
maximum of Rs
200,000
per
patient per year.
Collection
period,
Only
surgical
conditions,
Preauthorisation,
Tariffs fixed for
procedures, photo
id card,
RAHA
Tribals
RAHA
RAHA
RAHA
Network
of
"mission"
clinics
and
hospitals
Rs 20 per
person
per year
Unlimited
OP
cover,
Hospitalisation
cover
for
a
maximum of Rs
1250
Collection
period,
Salary
for
providers,
Strict
referral system, co
payments.
JRHIS
Farmers
JRHIS
JRHIS
JRHIS
MG Medical
College
Rs
100
per family
per year.
OP
cover
by
VHWs,
Hospital
cover at medical
college
Family
as;
the
enrolment
unit,
collection
period,
referral system,
Trust
period,
Loss of wages @
Rs
50
per
inpatient day
Community
Organiser
Insurer
Administrator
Provider
Premium
Benefit package
Risk management
DHAN
foundation
Members of
SHG
and
their
dependents
KKVS - the
SHG
federation
KKVS
the SHG
federation
KKVS - the
SHG
federation
6
empanelled
hospitals
150
Rs
a
for
family
Hospitalisation
expenses upto a
maximum of Rs
Some
10,000.
exclusions
Family as the unit,
co-payments,
referral
system,
collection period.
SEWA
Self
employed
women and
their
dependents
SEWA
ICICI
Lombard
SEWA
and
Public
private
hospitals
Rs 85 per
person
per year
Hospitalisation
expenses upto Rs
2000 per patient
per year.
Collection period,
Student’s
Health
Home
Students
SHH
SHH
SHH
SHH
Rs 5 per
student
per year
Unlimited OP and
IP at SHH run
facilities
School
is
the
enrolment
unit,
providers paid fixed
salaries.
Definite
collection
period,
referral system,
VHS
Rural
population
VHS
VHS
VHS
VHS
100
Rs
per
person
per year
Hospitalisation
expenses
upto
maximum limits
Nil
Government
Community
Organiser
Insurer
Administrator
Provider
Premium
Benefit package
Risk management
Universal
Health
Insurance
Scheme
BPL families
?
4
public
sector
insurance
companies
?
Any hospital
Rs 548 for a
family of five
(Rs
300
subsidised
by the Gol.
Hospitalisation
cover
upto
a
maximum limit of
Rs
30,000
per
family per year.
Personal accident
upto Rs 25,000
Loss of wages @
Rs 50 per patient
day.
Family
as
the
enrolment
unit,
waiting period.
Kudumbashree
(proposed)
SHG
members and
their
dependents
who
belong
to
BPL
families.
Kudumbashree
and Govt of
Kerala
ICICI
Lombard
SHGs
Empanelled
hospitals
Rs 399 per
family
per
year, Rs 366
subsidised
by
government
Hospitalisation upto
a maximum of Rs
30,000 per family
per
year.
No
exclusions
Personal accident
upto Rs 100,000
Loss of wages @
Rs 50 per patient
day for a week.
Family
as
enrolment unit.
AP scheme
(proposed)
BPL families
AP
Government
4
public
sector
insurance
companies
ATPA
Empanelled
hospitals
Rs 548 for a
family of five
(Rs
400
subsidised
by
the
Government.
Hospitalisation
expenses
upto
25,000 for surgical
conditions and Rs
75,000 for serious
conditions. But only
for the first three
days for medical
conditions.
Waiting period. Co
payments after 3
days for medical
conditions.
the
Community
Organiser
Insurer
Administrator
Provider
Premium
Benefit package
Risk management
Karnataka
scheme
(proposed)
BPL families
Karnataka
government
public
4
sector
companies
Dept of Health
(for
staff
collection
of
premium).
Any hospitals,
especially
public sector
hospitals.
Rs 548 for a
family
of
five. Rs 300
subsidy from
Gol.
Hospitalisation
cover
upto
a
maximum limit of
Rs 30,000 per
family per year.
Personal accident
upto Rs 25,000
Loss of wages @
Rs 50 per patient
day.
Waiting
period,
family
as
the
enrolment unit.
Assam
scheme
All
Assam
citizens
except
government
servants/
with
those
than
more
Rs. 2 lakh per
annum
income_____
Assam
Government
ICICI
Lombard
?
?
?
Hospitalisation
expenses upto a
maximum of Rs
25,000 for select
disease conditions
e.g. cancer, IHD,
Renal
failure,
stroke etc.
Mandatory cover of
the
entire
population.
Appendix 3
Prices of some common conditions
Minor medical conditions
Name of condition
AP prices maximum (Rs)
AGE
2000
Acute abdominal
pain
2000
Acute asthma
2000
Pleural effusion
2000
Amoebic hepatitis
2000
Amoebic abscess
2000
Typhoid
2000
Heat stroke
2000
Allergic disorders
2000
Acute psychosis
2000
Acute fevers
2000
Seizure disorders
2000
ARI e.g.
Bronchopneumonia,
Bronchiolitis.
2000
NCMH
prices
Local prices
<25
beds
26-75
beds
76-150
beds
Medium medical conditions
Name of condition
AP prices maximum (Rs)
Acute upper Gl
bleed
4000
Acute cholecystitis
with medical
management
4000
CCF
4000
4000
Acute HT
encephalopathy
Cardiac arrhythmias
Acute myocarditis
Status epilepticus
Acute paraplegia
Acute meningitis
Acute encephalitis
Acute Coma
Acute pneumonia
Acute
pneumothorax
Acute nephritis
Diabetic
ketoacidosis
4000
4000
4000
4000
4000
4000
Acute arthritis
4000
Neonatal sepsis
4000
Cerebral malaria
Severe anaemia
2500
4500
4000
4000
H’agic fevers
Hypoglycemic coma
<25
beds
4000
4000
4000
4000
4000
4000
4000
Thyrotoxic crisis
Local prices
NCMH
prices
1000
7000
2400
26-75
beds
76-150
beds
Major Medical conditions
Name of condition
AP prices maximum (Rs)
Acute pancreatitis
8000
AMI
8000
Cardiogenic shock
8000
Cerebro vascular
accidents
8000
Acute respiratory
failure
8000
Acute renal failure
8000
NCMH prices
Local prices
<26
beds
10,000
26-75
beds
76-150
beds
Minor Surgical admissions
Name of condition
Normal delivery
AP prices maximum
(Rs)
1500
Local prices
NCMH
prices
<26
beds
500
Septic abortion
1100
Delivery with APH
4750
Delivery with PPH
3500
Delivery with
Eclampsia
8000
Delivery with
obstruction
2200
Excision biopsy
1200
Closed reduction of
long bones
3500
Minor amputations
1000
Closed reduction of
dislocations
1500
Circumcision
1000
Dilatation of urethra
1000
Hydrocoele
4000
Tonsillectomy
3500
FB removal trachea,
oesophagus
1500
Polypectomy
3500
Cataract
2500
Angiogram
4500
Lumpectomy
4000
Haemorrhoidectomy
4000
Herniarapphe
5000
26-75
beds
76-150
beds
Medium Surgical conditions
Name of condition
AP prices maximum
(Rs)
Hysterectomy
8000
LSCS
7500
Oopherectomy
5500
Gastrectomy
20000
Pyloroplasty
13000
Gl with Vagotomy
7000
Gastro
duodenostomy
13000
Cholecystostomy
9000
Laproscopic Chole
13000
Appendectomy
5500
Intestinal resection
9000
Colectomy
6000
Inguinal hernia
6000
Amputation
7000
Arthrodesis
9000
Open reduction
9000
Fracture neck of
fem u re
12000
Nephrostomy
13000
Uretero-lithotomy
9000
TURP
10000
Thyroidectomy
9000
Tympanoplasty
7000
Laryngotomy
12000
Radical mastectomy
9000
Pacemaker
implantation
10000
Cataract surgery
NCMH
prices
2200
1800
Local prices
<26
beds
26-75
beds
76-150
beds
Major surgical procedures
Name of condition
AP prices maximum (Rs)
Open heart surgery
75000
Closed heart
surgery
45000
NCMH prices
Local prices
Appendix 4
Utilisation rates of some common conditions
Name of condition
Cases per lakh population12[12]
Birth asphyxia
25
Neonatal sepsis
25
LBW
570
ARI
322
Normal delivery
2108
Puerperal sepsis
18
Septic abortion
5
APH
12
PPM
21
Eclampsia
25
Obstructed labour
32
LSCS
92
Severe anemia
248
40
2065
1714
Complicated malaria
Diabetes mellitus (without insulin)
Hypertension
COPD
Major surgeries
1461
2330
438
Accidents
438
IHD (prevalence)
3353
118
Asthma
Stroke
Schizophrenia (without
hospitalisation)
289
Mood disorders
1543
913
Epilepsy
l2tI2] Source: Report of the National Commission on Macro-economics and health.
Note: all the cases in the community will not land up at the hospital. So one will have to reduce the same to
the appropriate level depending on local circumstances, while calculating premium.
Appendix 5
Provider payment mechanisms
13[13]
The manner in which health care providers are paid can significantly affect both the cost
and quality of care, and in these ways helps in optimal use of resources
. Once a
patient has taken the step of contacting the provider, it is thereafter the provider who
determines to a large extent, the demand for his or her own services, and the kind and
quantity of treatment requiredl 5[15]. Thus, the provider payment mechanisms determine
the quantity of services consumed as well as their costs. They are an important
component in the strategic purchasing of health services by insurers, with the other
component being negotiating and contracting with providers so that they agree to
provide health services according to the requirements and conditions of the
insurersl6[16]. Negotiating and contracting have been discussed in another module.
It must be remembered that like any other provider of services, the health provider would
also like to maximize his income. He could do this by attracting more patients, over
treating these patients, increasing the number of visits by the same patients, or by
charging more for his services. The provider payment mechanisms chosen by the
insurer must contain costs, but also give the provider an opportunity to earn a
reasonable income to motivate them to provide quality services. Commonly used
provider payment mechanisms are discussed below.
Fee-for-service
The providers are given a fee for each service, procedure or act provided to a patient. It
provides an incentive to providers to provide health services, and this could be perceived
as leading to better quality. However, this incentive effect could itself lead to
overproduction of health services (supplier-induced demand), a tendency to reduce the
time spent per activity and to encourage repeat visits as they generate fresh fee. It has
been suggested that the overproduction can be counteracted by combining this
mechanism with fixed fee schedules, ceiling budgets, or by co-payments for patients. By
far this is the pre-dominant provider payment mechanism in our country, though it is
also perhaps the most expensive, and has high administrative costs for processing
claims and prevention of fraud.
Daily (per diem) payment
This is a simple and easy to administer method for inpatient treatment, but like the feefor-service method, it has a weak capacity for cost-containment because there is a
similar incentive to expand the length of stay of patients, and/or to increase the number
of admissions. The hospitals also have an incentive to cut down on the inputs to limit
13[,31 Copied from “Empanelling Providers” (Dr Somil Nagpal) in “Training Manual for health insurance
managers.” Institute of Public Health, Bangalore. 2006.
14[141 Carrin G, James C. Reaching universal coverage via social health insurance: key design features in the
SCStX
WHO
>LO, 1994.
16l16’ WHO, Geneva. Community based Health Insurance Schemes in Developing Countries: facts,
problems and perspectives. Discussion paper, 2003.
their costs. Attempts have been made to provide a progressively reducing per diem
payment, which could remove the incentives to prolong the inpatient stay. A ceiling
budget for the hospital could also be used, like that in fee-for-service.
Case payment
This is based on managing the whole case, rather than a single act as in fee-for-service,
and can be used for both ambulatory and inpatient care. The system is easy to
administer, and could be a flat rate system where all types of cases are paid the same
flat rate, or a system where the type of case determines the quantum of payment. An
important example of the latter is the Diagnosis Related Group (DRG) payment method
followed in many countries, where hospitals are paid an all-inclusive flat payment for a
patient’s treatment according to his/her diagnostic group. The system encourages
efficient providers, but the effect could be offset by encouraging increased admissions
and by the “DRG creep”, the tendency to record a more complicated diagnosis if that
qualifies for a higher DRG slab. There could also be an incentive for providers to transfer
the more complicated (and thus more expensive) cases towards other providers,
particularly public providers, rather than managing them.
Capitation
Under the capitation system, providers receive payment according to the number of
people served and cover services for each enrolled member for the entire enrolment
period for a pre-specified sum. There is no incentive to provide excessive health
services, but it could give rise to the opposite problem of potential underproduction.
Further, referral of cases to higher levels of care could affect the potential of this method
in containing costs. Competition amongst providers may also help lessen the problem of
under-production, as providers’ income is dependent on the number and type of people
served and people, once given the choice to select their provider, are likely to enrol with
the providers who provide due care. The administrative costs of this method are very
low, and are especially suited in primary care settings.
Budgets
Budgets are the predominant method of funding the government health system in our
country. As with capitation, there is no link between the quantity and mix of health
services given to the individual patient and the total amount received by providers.
However, if the budget is insufficient or utilized inefficiently, not enough services may be
produced and this results in other providers having to provide the necessary care. Also,
when budgets are not very strict, and as they are often based on historical costs, there is
no incentive for providers to minimize costs, and there is even a perverse incentive to
exceed the budget ceiling as it implies a higher provision in the next year.
Underproduction and waiting lists are thus common where budgets are the sole mode of
financing services.
Salaries
This is where the insurer employs personnel to provide health services and pays these
personnel a salary, unlinked to workload handled. Here again, overproduction is unlikely
but underproduction is, because fixed salaries may not provide sufficient motivation for
sustained good performance. Administrative costs are low, but it may be difficult to
encourage and retain good personnel. Ensuring variable, performance-related factors in
the salary could be an important way of ensuring better quality.
Combinations of these payment mechanisms can also be attempted. For example, the
NHS in the UK uses capitation for paying its general practitioners, but they are also paid
fee-for-service for certain specified activities, bonus payments for certain performance
targets etc. Different mechanisms can also be combined at different levels of care, to
optimize the cost-quality balance.
■.' lb ;4
MONTHH
llEAI.IHf»|tf “ DAY.
wr
-■.■
,j.
t
■f>"
■/
8-
u
^S»
***««***> ,
K
^JW
a\^L^
• IKhmI di
W^U
jl
| oo
ro
jn’Sta wr«j ft?H
(2005-2012)
fltqiiq vi^A
Ministry of Health and Family Welfare
Government of India
■
w
iJ'i
PREFACE
The NRHM guarantees better health outcomes for millions of people in
rural areas, especially those belonging to marginalized and vulnerable
communities. The VHND promises to be an effective platform for
providing first-contact primary health care.
Quite often, programme managers, service providers,community-based
organizations, and PRI representatives do not share a common
understanding about the activities to be undertaken and how these are
to be operationalised while organizing the VHND.This manual provides
information about organizing the VHND in a simple and lucid manner.
It is hoped that this manual will serve the needs of all concerned,
including medical officers, ANMs, MPWs, and ASHAs. A clear
understanding of the relevant procedures and operations will lead to
the effective organization of the VHND, which is an importanttool under
NRHM for the convergence of all activities. I take this opportunity to thank
the Maternal Health Division (GOI) and United Nations Population Fund
(UNFPA) for providing technical support in preparation of this document.
S. Jalaja
Additional Secretary and Mission Director,
NRHM
Ministry of Health & Family Welfare
Date: 26 February 2007
Government of India
ABBREVIATIONS
AD
Auto Disposable
AIDS
Acquired Immunodeficiency Syndrome
ANC
Ante Natal Care
ANM
Auxiliary Nurse Midwife
ASHA
Accredited Social Health Activist
AWC
Anganwadi centre
AWW
Anganwadi Worker
AYUSH
Ayurveda, Yoga & Naturopathy, Unani, Siddha and Homoeopathy
BCC
Behaviour Change Communication
BF
Blood Film
DPMU
District Programme Management Unit
DPT
Diphtheria Pertussis and Tetanus
ECP
Emergency Contraception Pills
ENBC
Essential Newborn Care
GDI
Government of India
HIV
Human Immunodeficiency Virus
IEC
Information, Education and Communication
IFA
Iron Folic Acid
J SY
Janani Suraksha Yojna
LHV
Lady Health Visitor
MCH
Mother and Child Health
MO
Medical Officer
MP
Malarial Parasite
MPW
Multi Purpose Worker
MTP
Medical Termination of Pregnancy
NRHM
National Rural Health Mission
OCP
Oral Contraceptive Pills
OPV
Oral Polio Vaccine
ORS
Oral Rehydration Salt
PHC
Primary Health Centre
PPTCT
Prevention of Parent-to-Child Transmission
PRI
Panchayati Raj Institution
RCH II
Reproductive and Child Health Programme-Phase II
RMP
Rural/Registered Medical Practitioner
RTI
Reproductive Tract Infections
SC
Scheduled Castes
ST
Scheduled Tribes
STI
Sexual Tract Infections
TB
Tuberculosis
TBA
Traditional Birth Attendant
UNFPA
United Nations Population Fund
VCTC
Voluntary Counselling and Testing Centre
VHND
Village Health Nutrition Day
VHSC
Village Health and Sanitation Committee
VVM
Vaccine Vial Monitor
CONTENTS
1.
INTRODUCTION
1
2.
WHY ORGANIZE A MONTHLY HEALTH
2
NUTRITION DAY IN EVERY VILLAGE
3.
CHECKLISTS
5
4.
SERVICE PACKAGE FOR THE VILLAGE HEALTH NUTRITION DAY...
7
ANNEXURES
1.
REQUIREMENTS FOR ORGANIZING VHND
12
2.
PUBLICITY FOR VHND
14
3.
SUPERVISORY ARRANGEMENTS
15
4.
SUPERVISORY CHECKLIST
17
5.
OUTCOMES
18
1
I
I
INTRODUCTION
ill
The VHND is to be organized once every month (preferably on
Wednesdays, and for those villages that have been left out, on any other
day of the same month) at the AWC in the village. This will ensure
uniformity in organizing the VHND.The AWC is identified as the hub for
service provision in the RCH-II, NRHM, and also as a platform for inter
sectoral convergence.VHND is also to be seen as a platform for interfacing
between the community and the health system.
Keeping in view the significance of holding the VHND, the important
steps that need to be taken while organizing the event have been put
together in this manual.The roles of the ANM, ASHA and AWW should be
well defined.The quality of the VHND needs to be improved, and hence
the outcomes should be measured and monitored.
This document will help AWWs, ASHAs and PRI members to understand
their respective roles in providing their services effectively to the
community during the monthly VHND and will also help in educating
them on matters related to health. VHND if organized regularly and
effectively can bring about the much needed behavioural changes in
the community, and can also induce health-seeking behaviour in the
community leading to better health outcomes.
Programme managers at district/block level should ensure availability
of necessary supplies and expendables in adequate quantities during
the VHNDs. Similarly, supportive supervision by Programme Managers
at different levels will result in improved quality of services.
2
— WHYCfefcANIZE
A MONTffl^ HEALTH
NUTRITION DAY
IN EVERY VILLAGE
On the appointed day, ASHAs, AWWs, and others will mobilize the
villagers,especially women and children,to assemble at the nearest AWC.
The ANM and other health personnel should be present on time;
otherwise the villagers will be reluctant to attend the following monthly
VHND. On the VHND, the villagers can interact freely with the health
personnel and obtain basic services and information.They can also learn
about the preventive and promotive aspects of health care, which will
encourage them to seek health care at proper facilities. Since the VHND
will be held at a site very close to their habitation, the villagers will not
have to spend money or time on travel. Health services will be provided
at their doorstep. The VHSC comprising the ASHA, the AWW, the ANM,
and the PRI representatives, if fully involved in organizing the event, can
bring about dramatic changes in the way that people perceive health
and health care practices.
A) SERVICES TO BE PROVIDED:
■ All pregnant women are to be registered.
■
Registered pregnant women are to be given ANC.
b
Dropout pregnant women eligible for ANC are to be tracked and
services are to be provided to them.
Guidelines for AWWs/ASHAs/ANMs/PRIs
H
3
All eligible children below one year are to be given vaccines against
six Vaccine-preventable diseases.
ffl
All dropout children who do not receive vaccines as per the
scheduled doses are to be vaccinated.
M
Vitamin A solution is to be administered, to children.
All children are to be weighed, with the weight being plotted on a
card and managed appropriately in order to combat malnutrition.
■ Anti-TB drugs are to be given to patients of TB.
■ All eligible couples are to be given condoms and OCRs as per their
choice and referrals are to be made for other contraceptive services.
a Supplementary nutrition is to be provided to underweight children.
B) ISSUES TO BE DISCUSSED WITH THE
COMMUNITY:
a Danger signs during pregnancy
a Importance of institutional delivery and where to go for delivery
a
Importance of seeking post-natal care
a Counselling on ENBC
a
Registration for the JSY
a Counselling for better nutrition
■
Exclusive Breastfeeding
a Weaning and complementary feeding
a Care during diarrhoea and home management
a Care during acute respiratory infections
a
Prevention of malaria,TB, and other communicable diseases
a
Prevention of HIV/AIDS
a
Prevention of STIs
a
Importance of safe drinking water
4
Monthly Village Health Nutrition Day
Personal hygiene
H
Household sanitation
a
Education of children
Dangers of sex selection
B
Age at marriage
B
Information on RTIs, STIs, HIV and AIDS
n
Disease outbreak
a
Disaster management
C) IDENTIFICATION OF CASES THAT NEED
SPECIAL ATTENTION:
■
Identify children with disabilities.
■ Identify children with Grade III and Grade IV malnutrition for referral
■
Identify severe cases of anaemia.
■
Identify pregnant women who need hospitalization.
■
Identify cases of malaria,TB, leprosy, and Kala Azar.
■ Identify problems of the old and the destitute.
■
Pay special attention to the SC, ST, the minorities, and the weaker
sections of society.
D) COLLECTION OF DATA:
■ Compile data on the number of children with special needs,
particularly girl children with disabilities.
■ Report outbreaks of disease.
■
Report/audit deaths of children and women.
■ Compile data pertaining to the SCs, the STs, the minorities, and
weaker sections of society that need services.
5
I,.,........... .j.. ..................................... |
It would be useful to have checklists for ASHAs, AWWs, and ANMs to
ensure that all the activities for which they are responsible are planned
properly and carried out effectively, step by step.The following checklists
are to be used by these workers for organizing the VHND.
ASHA
Actions to be taken before the Village Health and Nutrition Day:
■ Visit all households and get to know all the families. Make it a point
to visit all poor households, especially SC/ST families.
Make a list of pregnant women.
Make a list of women who need to come for ANC for first time or for
repeat visits.
Make a list of infants who need immunization, were left out or
dropped-out.
Make a list of children who need care for malnutrition.
Make a list of children who were missed during the pulse polio round.
Make a list of children with special needs, particularly girl children.
Make a list of TB patients who need anti-TB drugs.
U
Coordinate with the AWW and the ANM.
On the day:
■ Ensure that all listed women come for services.
« Ensure that all listed children come for services.
Monthly Village Health Nutrition Day
6
Ensurethat malnourished children comeforconsultation with the ANM.
a
Ensure supplementary nutrition to children with special needs.
■ Ensure that all listed TB patients collect their drugs.
a Assist the ANM and the AWW.
AWW
H
Ensure that the AWC is clean.
a
Ensure availability of clean drinking water during the VHND.
a
Ensure a place with privacy at the AWC for ANC.
a
Keep an adequate number of MCH cards.
a Coordinate activities with the ASHA and the ANM.
ANM
a
Ensure that the VHND is held without fail. Make alternative
arrangements in case the ANM is on leave.
a
Ensure that the supply of vaccines reaches the site well before the
day's activities begin.
a
Ensure that all instruments, drugs, and other materials as listed in
the annexure are in place.
a Carry communication materials.
a
EnsurethatadequatemoneyisavailablefordisbursementtotheASHA.
a
Ensure reporting of the VHND to the MO in charge of the PHC.
a Coordinate with the ASHA and the AWW.
PRIS
a
Ensure that the members of the VHSC are available to support the
sessions.
a
Ensure participation of schoolteachers and PRI members.
a
Ensure availability of clean drinking water, proper sanitation, and
convenient approach to the AWCfor participating in the VHND by all.
7
—surviciZLvckkge
FOR THE VILlXGE HEALTH
NUTRITION DAY
MATERNAL HEALTH
■ Early registration of pregnancies.
■ Focused ANC.
■ Referral for women with signs of complications during pregnancy
and those needing emergency care.
■
Referral for safe abortion to approved MTP centres.
H
Counselling on:
□ Education of girls.
□ Age at marriage.
□ Care during pregnancy.
□ Danger signs during pregnancy.
□ Birth preparedness.
□ Importance of nutrition.
□ Institutional delivery.
□ Identification of referral transport.
□ Availability of funds under the JSY for referral transport.
□ Post-natal care.
□ Breastfeeding and complementary feeding.
□ Care of a newborn.
□ Contraception.
Monthly Village Health Nutrition Day
8
■ Organizing group discussions on maternal deaths, if any, that have
occurred during the previous month in order to identify and analyse
the possible causes.
CHILD HEALTH
Infants up to 1 year:
Registration of new births.
a Counselling for care of newborns and feeding.
■ Complete routine immunization.
a
Immunization for dropout children.
First dose of Vitamin A along with measles vaccine.
H
Weighing.
Children aged 1-3 years:
■
Booster dose of DPT/OPV.
■ Second to fifth dose of Vitamin A.
8
Tablet IFA - (small) to children with clinical anaemia.
Weighing.
a Provision of supplementary food for grades of mild malnutrition
and referral for cases of severe malnutrition.
All children below 5 years:
Tracking and vaccination of missed children by ASHA and AWW.
H
Case management of those suffering from diarrhoea and Acute
Respiratory Infections.
B
Counselling to all mothers on home management and where to go
in even of complications.
B
Organizing ORS depots at the session site.
B
Counselling on nutrition supplementation and balanced diet.
B
Counselling on and management of worm infestations.
Guidelines for AWWs/ASHAs/ANMs/PRIs
9
FAMILY PLANNING
■ Information on use of contraceptives.
■
Distribution - provision of contraceptive counseling and provision
of non-clinic contraceptives such as condoms and OCRs.
■
Information on compensation for loss of wages resulting from
sterilization and insurance scheme for family planning.
REPRODUCTIVE TRACT INFECTIONS AND
SEXIJALLY TRANSMITTED INFECTIONS
■ Counselling on prevention of RTIs and STIs,including HIV/AIDS,and
referral of cases for diagnosis and treatment.
■ Counselling for perimenopausal and post-menopausal problems
s Communication on causation, transmission, and prevention of HIV/
AIDS and distribution of condoms for dual protection.
■
Referral for VCTC and PPTCT services to the appropriate institutions.
SANITATION
a
Identification ofhouseholds for the construction of sanitary latrines
« Guidance on where to go and who to approach for availing of
subsidy for those eligible to get the same under theTotal Sanitation
Campaign.
■ Avoidance of breeding sites for mosquitoes.
■ Mobilization of community action for safe disposal of household
refuse and garbage.
COMMUNICABLE DISEASES
» Group communication activities for raising awareness about signs
and symptoms of leprosy, suspected cases, and referrals.
■ Group communication activities for elimination of breeding sites
for mosquitoes, management of fever cases, i.e. importance of
collection of blood film for MP and presumptive treatment.
Monthly Village Health Nutrition Day
10
■ Awareness generation about symptoms of TB (coughing for more
than three weeks), importance of continued treatment, referral of
symptomatics for sputum examination at the nearest health centre.
e Provision of anti-TB drugs to patients.
B
Reporting of unusual numbers of cases of any disease or disease
outbreak in village.
GENDER
B
Communication activities for prevention of pre-natal sex selection,
illegality of pre-natal sex selection, and special alert for one-
daughter families.
■ Communication on the Prevention of Violence against Women,
Domestic Violence Act, 2006.
B
Age at marriage, especially the importance of raising the age at
marriage for girls.
AYUSH
b
Home remedies for common ailments based on certain common
herbs and medicinal plants like tulsi found in the locality.
a Information related to other AYUSH components, including drugs
for treating conditions like anaemia.
HEALTH PROMOTION
Chronic diseases can be prevented by providing information and
counseling on:
a
Tobacco chewing
a
Healthy lifestyle
B
Proper diet
B
Proper exercise
Guidelines for AWV/s/ASHAs/ANMs/PRIs
77
NUTRITION
Diseases due to nutritional deficiencies can be prevented by
giving information and counseling on:
■
Healthy food habits.
■
Hygienic and correct cooking practices.
■ Checking for anaemia, especially in adolescent girls and pregnant
women; checking, advising, and referring.
■ Weighing of infants and children.
■ Importance of iron supplements, vitamins, and micronutrients
s
Food that can be grown locally.
■
Focus on adolescent pregnant women and infants aged 6 months
to 2 years.
Please see the following annexures for more details:
Annexure 1: Requirements for Organizing VHND
Annexure 2: Publicity for VHND
Annexure 3: Supervisory Arrangements
Annexure 4: Supervisory Checklist
Annexure 5: Outcomes
12
Annexure 1
REQUIREMENTS FOR
ORGANIZING VHND
WHO ARE NEEDED
e
ASHA
AWW
u
PRI member
Helper of AWW
a
Staff to come from outside the village:
□ ANMs
□ Male MPW (if available)
□ ASHA facilitators (if available)
INSTRUMENTS, EQUIPMENT, AND FURNITURE
■
Weighing scale-adult, child
M
Examination table
Bed screen/curtain
B
Haemoglobin metres, kits for urine examination
B
Gloves
B
Slides
Stethoscope and blood pressure instrument
B
Measuring tape
B
Foetoscope
■ Vaccine carrier with ice packs
If these items are not available, their provision could be arranged by using
the untied fund of Rs 10,000/- available with the ANM or with the VHSC.
These items should be kept under the safe custody of the ANM/ AWW/
ASHA as the case may be.
Guidelines for AWWs/ASHAs/ANMs/PRIs
13
SUPPLIES
Supplies such as vaccines, IFA tablets, Vitamin A, condoms, OCRs,
(ECPs), ORS, and Cotrimoxazole
$
Anti-helminthic drug
Chloroquin
B
Anti-TB drugs
n
Paracetamol
B
Stains for fixing BF
■
AD syringes in sufficient quantity
IEC material for communication and counseling
14
Annexure 2
PUBLICITY FOR VHND
PUBLICITY
■
Day and time
Site
■
Key services
KEY COMMUNICATION OBJECTIVE
To make the community, especially women from vulnerable sections and
other stakeholders in the community, aware of service availability right
in the village on fixed days at AWC.
WHOM TO INVOLVE
PRI members
■
SHG members
Teachers and other informal leaders
Schoolchildren
■
All beneficiaries
a
TBAs and other RMPs
MEDIA AND METHODS
■
Wall writings in the local language
■
Hoardings at one or two prominent places in the village
■
Handbills and pamphlets
Resources for publicity activities can be accessed through the untied
funds available with the VHSC or through the sub-centre joint fund.
15
Annexure 3
SUPERVISORY ARRANGEMENTS
SUPERVISION AND MONITORING
The proper organization of the VHND is the most crucial component of
NRHM for guaranteeing service provision at the village level. Hence, at
all programme meetings at the state, district, and block levels, one should
ensure the review of the VHND and the problems encountered should
be addressed promptly and effectively. Each district and block should
maintain a record of the number of VHNDs planned and the number
actually held.The quality of the services offered and available during the
VHND will depend on the quality of the supervision and leadership.The
LHV and the AWW Supervisor should jointly visit the pre-identified
centres as per the roster and submit their joint report, which will be
discussed at the monthly meeting convened by the MO in charge
of the PHC.
During the supervisory visits, special attention should be given to the
following elements:
1.
Women and children from vulnerable communities should come
forward to seek services.
2.
ASHA should be available at the session site and should be engaged
in the tracking of women and children, especially those from
vulnerable communities, for complete coverage.
3.
All resources (human resources and materials) should be in place.
4.
The quality of the services available should be satisfactory.
5.
Issues related to the clients' satisfaction with the services should
be addressed properly and promptly.
6.
BCC methods should be employed.
16
Monthly Village Health Nutrition Day
The holding of the VHND should be discussed at the monthly meetings
convened by the MOs at the PHC level at the executive committee
meetings of the District Health Society, of which the District CMO is the
convener.The DPMUs will monitor it, and will also compile data on it.
17
Annexure 4
SUPERVISORY CHECKLIST
SUPERVISORY CHECKLIST
(to be used by the different cadres of supervisors during visits to the
VHND sites)
1.
General information: Session site, availability of staff, timings
displayed
2.
Cold chain: Vaccine carrier with ice packs, WM's status on vaccine
vials
3.
Availability of essential supplies in adequate quantities
4.
Procedure of vaccination, especially injection safety
5.
Availability of communication and counselling materials
6.
Record review for
a. Women and children from vulnerable communities
b. Immunization for children scheduled to arrive
c. Follow-up activities for ANC
d. Blood films collected for MP
7.
Disposal of AD syringes
8.
Client satisfaction: Exit interviews with some clients about the dates
of repeat visits for immunization, birth preparedness, and the
institution identified for delivery
9.
Disbursement of incentives to ASHA for mobilizing clients to get
immunization
IS
Annexure 5
OUTCOMES
OUTCOMES
The organization of the Village Health and Nutrition Day on a regular
basis as perthe guidelineswill result in the achievement of the following
outcomes:
Hundred per cent coverage with preventive and promotive
interventions, especially for pregnant women, children, and
adolescents
■
Preventive and promotive coverage for the National Disease Control
Programmes
»
Increased awareness about the determinants of health such as
nutrition, sanitation, timely care, etc.
H
Improved knowledge about the services offered under the various
Nutritional Health Programmes
U
Greater emphasis on the community's role in making the health
system responsive to the health needs of the community and in
demanding and ensuring accountability
■
JANANI SURAKSHA YOJA
......................................................................—.......................................... ................................................................................. ........................................ ........................................................................................................................................................... —.......................................................... ..... ..................... -__________________ _ _________________ ________________________________________________________________________________________________________________________________________________________________________■......................................................................................................................................................
WUumvl
FEATURES
&
EQUENTLY ASKED QUESTIONS AND ANSWERS
('•7
Government of India
As in October 2006
......................................................................................................
Government of India
Ministry of Health and Family Welfare
Maternal Health Division I
Nirman Bhavan
New Delhi
JANANI SURAKSHA YOJANA (JSY)
Janani Suraksha Yojana (JSY) is a safe motherhood intervention under the
National Rural Health Mission (NRHM) being implemented with the objective of
reducing maternal and neo-natal mortality by promoting institutional delivery
among the poor pregnant women. The Yojana, launched on 12th April 2005, by
the Hon'ble Prime Minister, is being implemented in all states and UTs with
special focus on low performing states.
2.
JSY is a 100 % centrally sponsored scheme and it integrates cash
assistance with delivery and post-delivery care. The success of the scheme would
be determined by the increase in institutional delivery among the poor families
3.
The Yojana has identified ASHA, the accredited social health activist as an
effective link between the Government and the poor pregnant women in 10 low
performing states, namely the 8 EAG states and Assam and J&K and the
remaining NE States. In other eligible states and UTs, wherever, AWW and TBAs
or ASHA like activist has been engaged in this purpose, she can be associated
with this Yojana for providing the services.
3.1 Role of ASHA or other link health worker associated with JSY would be to:
Identify pregnant woman as a beneficiary of the scheme and report or
facilitate registration for ANC,
Assist the pregnant woman to obtain necessary certifications
wherever necessary,
Provide and / or help the women in receiving at least three ANC
checkups including TT injections, IFA tablets,
|
■
1
ter
cir
Identify a functional Government health centre or an accredited
private health institution for referral and delivery,
Counsel for institutional delivery,
r^;>
Escort the beneficiary women to the pre-determined health center and
stay with her till the woman is discharged.
csr
Arrange to immunize the newborn till the age of 14 weeks,
Inform about the birth or death of the child or mother to the
ANM/MO,
Post natal visit within 7 days of delivery to track mother's health after
delivery and facilitate in obtaining care, wherever necessary,
Counsel for initiation of breastfeeding to the newborn within onehour of delivery and its continuance till 3-6 months and promote family
planning.
Note: Work of the ASHA or any link worker associated with Yojana would be assessed based
on the number of pregnant women she has been able to motivate to deliver in a health
institution and the number of women she has escorted to the health institutions.
4.
Important Features of JSY:
4.1
The scheme focuses on the poor pregnant woman with special
dispensation for states having low institutional delivery rates namely the states of
Uttar Pradesh, Uttaranchal, Bihar, Jharkhand, Madhya Pradesh, Chhattisgarh,
Assam, Rajasthan, Orissa and Jammu and Kashmir. While these states have been
named as Low Performing States (EPS), the remaining states have been named as
High performing States (HPS).
4.2
Tracking Each Pregnancy: Each beneficiary registered under this Yojana
should have a JSY card along with a MCH card. ASHA/AWW/ any other
identified link worker under the overall supervision of the ANM and the MO,
PHC should mandatorily prepare a micro-birth plan. Please see Annexure - I.
This will effectively help in monitoring Antenatal Check-up, and the post
delivery care.
4.3
Eligibility for Cash Assistance:
IPS States
HPS States
IPS & HPS
All pregnant women delivering in Government health
centres like Sub-centre, PHC/CHC/ FRU / general wards
of District and state Hospitals or accredited private
institutions________________ _____________ _________
BPL pregnant women, aged 19 years and above_________
All SC and ST women delivering in a government health
centre like Sub-centre, PHC/CHC/ FRU / general ward of
District and state Hospitals or accredited private
institutions
Note: BPL Certification - This is required in all HPS states. However, where BPL cards have
not yet been issued or have not been updated, 5tates/UTs would formulate a simple criterion
for certification of poor and needy status of the expectant mother's family by empowering the
gram pradhan or ward member.
4.4
Scale of Cash Assistance for Institutional Delivery:
Total
Category _____Rural Area
LPS
HPS
Mother's
Package
1400
700
ASHA's
Package
600
Rs.
2000
700
Urban Area
Mother's ASHA's
Package
Package
200
1000
600
Total
Rs.
1200
600
Note 1: Importantly, such woman in both LPS and HPS states, choosing to deliver in an
accredited private health institution will have to produce a proper BPL or a SC/ST certificate
in order to access JSY benefits. In addition she should carry a referral slip from the
ASHA/ANM/MO and the MCH - Janani Suraksha Yojana (JSY) card.
Note 2: ANM / ASHA / MO should make it dear to the beneficiary that Government is not
responsible for the cost of her delivery. She has to bear cost, while choosing to go to an
accredited private institution for delivery. She only gets her entitled cash.
4.5
While mother will receive her entitled cash, the scheme does not provide
for ASHA package for such pregnant women choosing to deliver in an
accredited private institution.
4.6
Limitations of Cash Assistance for Institutional Delivery:
In IPS States
All births, delivered in a health centre health
Government or Accredited Private
institutions. Refer to para (b).
In HPS States
Upto 2 live births.
4.7
Disbursement of Cash Assistance: As the cash assistance to the mother is
mainly to meet the cost of delivery, it should be disbursed effectively at the
institution itself.
4.7.1 For pregnant women going to a public health institution for delivery,
entire cash entitlement should be disbursed to her in one go, at the health
institution. Considering that some women would access accrediting private
institution for antenatal care, they would require some financial support to get
atleast 3 ANCs including the TT injections. In such cases, atleast three-fourth
(3/4) of the cash assistance under JSY should be paid to the beneficiary in
one go, importantly, at the time of delivery.
4.7.2 To Beneficiary;
The mother and the ASHA (wherever applicable) should get their
entitled money at the heath centre immediately on arrival and registration
a. a.
for delivery.
b. b. Generally the ANM/ ASHA should carry out the entire disbursement
process. However, till ASHA joins, AWW or any identified link worker,
under the guidance of the ANM may also do the disbursement.
4.7.3 At accredited private institution: Disbursement of cash to the mother
should be done through the ANM/ASHA/ Link worker channel and the money
available under JSY should be paid to the beneficiary only and not to any other
person or relative. Also refer to para (e).
J J Should ensure that:
• Such accredited private institution would also be responsible for any
postnatal complication arising out of the cases handled by them.
• • They should not deny their services to any referred targeted expectant
mother.
•
Note: Every month, accredited private health centers would prepare a
statement of JSY - delivery / ANC/ obstetric complication cases handled by
them and. send it to the Medical officer, along with the referral slips for
sample verification by the concerned ANM / ASHA.
4.7.4 In the District / Women's Hospital / State Hospital etc :
•
State / District should allocate sufficient amount of money
(based on the load of deliveries in these institutions) for each of
these institution. This money should be kept in a separate account
under the supervision of the Rogi Kalyan Samity.
•
• The residency of the beneficiary would determine entitlement of
cash benefit in such institutions, to be verified based on the referral
slip from the ANM, carried by the beneficiary.
Format of Referral Slip: State should prepare a format of the referral slip, which
should mainly indicate, identification details of the beneficiary, JSY registration
number in the register of the ANM, reason for referral (including medical
complications), name of ASHA, amount already disbursed, amount due, including
referral transport money (if applicable), amount due to ASHA and to be paid, signature
ofMO/ANM.
•
• It is therefore, essential that all targeted expectant mother should
carry a referral slip from the ANM/MO where she generally resides.
This will, infact, help all such pregnant woman who go to her
mother's place for delivery.
•
Disbursement of money to expectant mother going to her
mother's place for delivery should be done at the place she delivers.
The entitlement of cash should be determined by her referral slip
carried by her and her usual place of residence.
•
4.8
• A voucher scheme may be introduced in such a way that along
with admission slip for delivery, a voucher amounting to mother's
package plus the transport assistance money is given to the
expectant mother and that she should be able to encash the same at
the Hospital's cash counter, at the time of discharge.
Flow of Fund:
i.i. State/ District authorities would advance Rs. 5000/- and Rs.
Rs.10,000/- to each ANM in HPS /IPS States respectively as a
recoupable impressed money from the JSY fund.
ii. ii.
This money could be kept in the joint account of ANM and
Gram Pradhan, as in case of untied fund placed with sub-centers so
that the ANM could 'roll' the entire amount by advancing Rs.1500 to
Rs. 2,500/- to ASHA / AWW per delivery and later she could recoup it
from the PHC or CHC, where JSY fund is parked by the authorities.
Expenditure Monitoring: ASHA / AWW should provide an expenditure statement of
money advanced to her in previous month to the ANM in the monthly meeting held by
ANM.
__
__
iii.iii. There should be a clear authority for ANM to withdraw cash
from this account for advancing it to the ASHA or AWW / any other
health link worker, needed for ready use towards disbursement to the
pregnant and also for arranging the referral transport for escorting the
pregnant women to the institution.
Note: Where an elected body of the Panchayati Raj Institution (PRIs) exists, the State
Covernments/Health society may keep the money in a joint account of the Cram Pradhan and
the ANM (like that of the untied fund). The process of recoupment of fund should be so simple
to be able to disburse the cash to the pregnant women in time.
ASHA Package: This package, as of now, is available in all IPS, NIE States
the tribal districts of all states and UTs. In rural areas it includes the
and in
following three components:
4.9
•
•
Cash assistance for Referral transport to go to the nearest health
centre for delivery. The state will determine the amount of assistance
(should not less than Rs.250/- per delivery) depending on the
topography and the infrastructure available in their state. It would,
however, be the duty of the ASHA and the ANM to organize or
facilitate in organizing referral the transport, in conjunction with gram
pradhan, Gram Sabha etc.
Note: This assistance is over and above the Mother's package.
•
• Cash incentive to ASHA: This should not be less than Rs.200/- per
delivery in lieu of her work relating to facilitating institutional delivery.
Generally, ASHA should get this money after her postnatal visit to the
beneficiary and that the child has been immunized for BCG.
•
•
Transactional cost (Balance out of Rs.600/-) is to be paid to ASHA
in lieu of her stay with the pregnant woman in the health centre for
delivery to meet her cost of boarding and lodging etc.. Therefore, this
payment should be made at the hospital/ heath institution itself.
Note 1: In Urban areas, ASHA package consists of only the incentive for ASHA, for providing
the services, as at para 3.1
Note 2: In case ASHA fails to organize transport for the pregnant woman to go to the health
institution, transport assistance money available within the ASHA's package should be paid to
the pregnant woman at the institution, immediately on arrival and registration for delivery.
Note 3: In case ASHA is yet to join, transport assistance money may be kept with the institution
and a voucher scheme may be introduced for disbursement.
4.10
Payment to ASHA: ASHA should get herFirst payment for the transactional cost at the health
centre on reaching the institution along with the
expectant mother.
S The second payment should be paid after she has
made postnatal visit and the child has been immunized
for BCG.
All payments to ASHA would be done by the ANM only. In this case too, a
voucher scheme be introduced in such a manner that for every pregnant woman
she registers under JSY, ANM would give two vouchers to ASHA, which she
would be able to encash on certification by ANM.
Important: It must be ensured that ASHA gets her second payment within 7 days of the
delivery, as that would be essential to keep her sustained in the system.
4.11
Special Dispensation for LPS states:
Age restriction removed
Restricting benefits of JSY up to 2 births removed. In other words, the
benefits of the scheme are extended to all pregnant women in LPS states
irrespective of birth orders.
J J No need for any marriage or BPL certification provided woman
delivers in Government or accredited private health institution.
Important: The state / UTs would be responsible for instituting an appropriate
monitoring mechanism and ensure that a proper accounting procedure is put in
place for all transactions.
4.12 Subsidizing cost of Caesarean Section or management of Obstetric
complications: Generally PHCs/ FRUs / CHCs etc. would provide emergency
obstetric services free of cost. Where Government specialists are not available in
the Govt's health institution to manage complications or for Caesarean Section,
assistance up to Rs. 1500/- per delivery could be utilized by the health institution
for hiring services of specialists from the private sector. If a specialist is not
available or that the list of empanelled specialist is very few, specialist doctors
working in the other Government set-ups may even be empanelled, provided
his/her services are spare and he/she is willing. In such a situation, the cash
subsidy can be utilized to pay honorarium or for meeting transport cost to bring
the specialist to the health centre. It may however be remembered that a panel
of such doctors from private or Government institutions need to be prepared
beforehand in all such health institutions where such facility would be provided
and the pregnant women are informed of this facility, at time of micro-birth
planning.
Important: State Governments would ensure that this assistance is not misutilized and would
exercise adequate control and monitor expenditure under this component.
4.13 Assistance for Home Delivery: In IPS and HRS States, BPL pregnant
women, aged 19 years and above, preferring to deliver at home is entitled to
cash assistance of Rs. 500/- per delivery. Such cash assistance would be available
only upto 2 live births and the disbursement would be done at the time of
delivery or around 7 days before the delivery by ANM/ASHA/ any other link
worker. The rationale is that beneficiary would be able to use the cash assistance
for her care during delivery or to meet incidental expenses of delivery. It should
be the responsibility of ANM/ASHA, MO PHC to ensure disbursement. It is very
important that the cash is disbursed in time. Importantly, such woman choosing
to deliver at home should have a BPL certificate to access JSY benefits.
5. Compensation Money: If the mother or her husband, of their own will,
undergoes sterilization, immediately after the delivery of the child,
compensation money available under the existing Family welfare scheme should
also be disbursed to the mother at the hospital itself.
6. JSY Benefits in Accredited Private Health Institution: In order to increase
choice of delivery care institutions, at least two willing private institutions per
block should be accredited to provide delivery services. State and the district
authorities should draw up a list of criterion / protocols for such accreditation.
(Please see a model criterion at Annexure-2) Such beneficiaries delivering in these
institutions would get the cash benefits admissible under the JSY.
7. Equip Sub-centers for Normal delivery: For women living in tribal and hilly
districts, it becomes difficult to access PHC/CHCs for maternal care or delivery.
A well-equipped sub-center is a better option for normal delivery. Deliveries
conducted in sub-centers, which are accredited by the state / district authorities
will be considered as institutional delivery and therefore, women delivering in
these centers would be eligible for all cash assistance under JSY.
Important: All States and UTs to undertake a process of accreditation of all such sub-centre
located in Govt, buildings and having proper facility of light, electricity, water, and other
medical requirements of basic obstetric services including drugs, equipments and services of
trained mid-wife for the purpose of conducting normal deliveries in these institutions.
8. Provision of Administrative Expenses: Upto 4 % and 1 % of the fund released
could be utilized towards administrative expenses like monitoring, IEC and office
expenses for implementation of JSY by the district and state authorities
respectively.
9. Essential Strategy: While the scheme would create demand for institutional
delivery, it would be necessary to have adequate number of 24X7 delivery
services centre, doctors, mid-wives, drugs etc. at appropriate places. Mainly, this
will entail
•
Linking each habitation (village or a ward in an urban area) to a functional
health centre- public or accredited private institution where 24X7 delivery
service would be available,
•
Associate an ASHA or a health link worker to each of these functional
health centre,
•
It should be ensured that ASHA keeps track of all expectant mothers and
newborn.
All
expectant
mother
and
newborn
should
avail
ANO
and
immunization services, if not in health centres, atleast on the monthly health
and nutrition day, to be organised in the Anganwadi or sub-centre:
o
o
o
o
o
o
o
o
Each pregnant women is registered and a micro-birth plan is prepared
(please see Annexure-1)
o
Each pregnant woman is tracked for ANC,
o
For each of the expectant mother, a place of delivery is pre-determined at
the time of registration and the expectant mother is informed,
o
A referral centre is identified and expectant mother is informed,
o
ASHA and ANM to ensure that adequate fund is available for disbursement
to expectant mother,
o
ASHA takes adequate steps to organize transport for taking the women to
the pre-determined health institution for delivery.
o
ASHA assures availability of cash for disbursement at the health centre and
she escorts pregnant women to the pre-determined health centre.
10. Possible I EC strategy:
•
To associate NGO and Self Help Groups for popularizing the scheme among
women's group and also for monitoring of the implementation.
To provide wide publicity to the scheme by:
Promoting JSY as a component of total package of services under RCH along with
programmes like Pulse polio programme, Monthly Village Health Day, Health Melas
etc,
Printing and distributing JSY guidelines, pamphlets, notices in local languages at
SC/PHCs/CHCs/ District Hospitals/ DM's and Divisional Commissioner's office and
even in at the accredited Pvt. Nursing Homes, in abundance,
Supporting printing of state's stationery, specially for State's Health Secretary, DMs
/ SDMs/ Block/ PHCZ CHC/ District Hospital, advocating on Institutional Delivery and
cash benefits of JSY,
Facilitate organizing workshops and meetings in villages / blocks - by women's
group, local leaders (PRIs), Opinion Maker, at functional health institutions on
promoting maternal health in general. Institutional Delivery and JSY,
Undertaking wall painting in all sub-centers, PHCs and CHCs, District & State
Hospitals and the accredited private institutions,
Supporting women self help Groups and NGOs for promoting the scheme,
Facilitating woman Panchayat member to take review of Janani Suraksha Yojana (JSY)
11. Establish a grievance redressal cell in each district, under the District
Project Management Unit, mainly to facilitate meeting people's genuine
grievances on J J Eligibility for the scheme,
J J Quantum of cash assistance,
J J Delays in disbursement of the cash assistance,
An officer, supported by an assistant, if necessary, may be made responsible to
supervise the grievance cell. However, proper information about the grievance
cell, giving the officer's name, postal address and his telephone number should
be displayed prominently at all health centers and institutions. If necessary, fund
available under administrative expenses could be utilized for this purpose.
12.
Display of names of JSY beneficiaries: The list of JSY beneficiaries along
with the date of disbursement of cash to her should mandatorily be displayed on
the display board at the sub-center, PHC/CHC/District Hospitals (from where
beneficiaries have got the benefit), being updated regularly on month-to-month
basis. Wherever necessary, display boards may be procured.
13.
Guidelines For urban areas: The state shall prepare detailed guidelines by
stating a simple procedure of implementing the Janani Suraksha Yojana (JSY) in
the urban areas through the Municipalities/local bodies ((where an elected body
exits) and quickly obtain approval of the state Government/SHS. The guidelines
should bring out clearly, the chain of fund flow as well as disbursement of the
benefits to the ultimate beneficiaries. The quantum of grants to be placed at the
disposal of the Municipalities shall be in proportion to the BPL families in the
Municipal area. The district annual plan will also include the plan of the
municipalities in the districts wherever applicable. The Chief medical Officer of
such an authority should be the implementing authority. It must be ensured that
basic objectives and the scale of disbursements are not altered. A copy such
plan along with necessary Government's order should be sent to the GOI.
14. Monitoring:
14.1 Monthly Meeting at Sub-centre Level: For assessing the effectiveness of the
implementation of JSY, monthly meeting of all ASHAs / related health link
workers working under an ANM should be held by the ANM, possibly on a fixed
day (may be on the third Friday) of every month, at the sub-center or at any of
Anganwadi Centres falling under the ANM's area of jurisdiction. If Friday is a
holiday, meeting could be held on following working day.
14.2 Prepare Monthly Work Schedule: In the monthly meeting, the ANM,
besides reviewing the current month's work vis-a-vis envisaged activities, should
prepare a Monthly Work Schedule for each ASHA / village level health worker of
following aspects of the coming month:
Feed back on previous month's schedule -
(a) Number of pregnant women missing ANCs,
(b) No. of cases, ASHA/link worker did not accompany the
pregnant women for Delivery,
(c) Out of the identified beneficiary, number of Home deliveries,
(d) No. of post natal visits missed by ASHA,
(e) Cases referred to Referral Unit (FRU) and review their current
health status,
(f) No. of children missing immunization.
Fixing Next Month's Work Schedule (NMWS): To include
(i)
(ii)
(iii)
(iv)
(v)
(vi)
(vii)
(i)
Names of the identified pregnant women to be registered and to
be taken to the health center/Anganwadi for ANC,
(ii)
Names of the pregnant women to be taken to the health center
for delivery (wherever applicable),
(iii)
Names of the pregnant women with possible complications to
be taken to the health center for check-up and/or delivery,
(iv)
Names of women to be visited (within 7 days ) after their
delivery,
(v)
List of infants / newborn children for routine immunization,
(vi)
To ensure availability of imprest cash,
(Vii)
Check whether referral transport has been organized.
Note 1: While no target needs to be fixed, but for the purpose of monitoring, some
monthly goal of institutional delivery for the village may be kept.
Note 2: A format of monthly work schedule to be filled by the ANM /ASHA incorporating
the physical and financial aspect may be printed.
15.
Reporting: For the purpose of reviewing the progress of implementation
and also for allocating fund to the state, under the RCH-flexi Pool, all States
would provide
• Annual District-wise report as per Annexure IV, reaching MoHFW in
the month of April of the following financial year
• • Quarterly Report as per Annexure V, reaching MoHFW in the month
following the end of the Quarter.
•
However, depending on the requirement of the Ministry, special reports may
also be sought.
Most Important:
16.
16.
Any deviation from the above process will not be
accepted by the Central Government and that such expenditure will not be
treated as legitimate utilization of the fund given under JSY. It may be noted that
all payments before or after seven days of delivery will be treated as illegitimate
subject to audit objection.
Annexure-I
MICRO-BIRTH PLAN FOR JSY BENEFICIARIES
STEP
1
2
Activity
To be undertaken by
Proposed Time
_______Line
Identification
and ANM/ASHA/AWW
or Atleast 20-24
Registration
of any link worker
weeks before the
beneficiary
expected date of
delivery.
Filling up of Maternal and ANM/ASHA/AWW or an Immediately
on
Child card ( In duplicate - equivalent link worker
registration
one each for mother
ASHA/Link worker)
and
(This will form part of the
JSY'S Registration Card).
3
4 l-s':
ANM/ASHA/AWW or an
equivalent link worker
Inform dates of 3 ANC &
TT Injection (s)
Immediately
registration
Identify the health center
for all referral
Identify
Delivery
the
Place
on
of
Inform expected date of
delivery
Provide
the
T*
ANC
immediately on Registration.
ASHA to follow up the ANCs
at the Anganwadi Centres/Subcenter (SC) and ensure that the
beneficiary
attends
the
SC/Anganwadi centre /PHC
for ANC on the indicated
dates
Motivation: ANM should call
the
beneficiary
to
the
Anganwadi/SC to participate
in the Monthly meeting and
explain enhanced cash and
Transport assistance benefits
for Institutional delivery._____
4
Collecting
necessary
/certificates
Wherever
BPL
necessary
or
proofs
ANM/ASHA/AWW or an
link worker
from
Within 2-4 weeks
from Registration
5
6.
Panchayat / local bodies /
Municipalities ____________
Submission
of
the MO, PHC
completed JSY card in the
for
Health
center
the
verification
by
authorized/Medical
officer.
II. Take necessary steps
arranging
toward
making
or
transport
to
the
cash
available
beneficiary to come to the
Health Centre
ANM/ASHA/AWW/link
worker
III. Ensure availability of
fund
to
ANM/Health
worker/ASHA etc._______
Payment of cash benefit /
incentive to the mother
and ASHA
ANM/MO, PHC
ANM/MO, PHC
Atleast 2-4 weeks
before
the
expected date of
delivery
At the institution.
For complicated cases or those requiring cesarean section etc:
Ac -1
Ac -2
Ac -3
Ac -4
Pre-determine a Referral health center By ANM/ASHA/link worker
and intimate the pregnant women
Familiarize the woman with the ANM/ASHA/link worker
referral centre, if necessary carry a
letter of referral from MO PHC
Pre-organize the transport facility in A N M/AS H A/Com m u n i ty
consultation
with
family
members/community leader
Arrange for the medical experts if MO, PHC
the same is not available in the
referred heath center______________
Annexure-II
CRITERIA FOR ACCREDITATION OF 24 HOURS COMPREHENSIVE
EMERGENCY OBSTETRIC CARE
Casualty services
•
A pregnant woman in labour or distress on entering the hospital at any time during
the day or night is directly taken to the obstetric casualty and immediately examined
by a professional with midwifery skills and decision taken within fifteen minutes.
If there are signs or bleeding, convulsions or shock, she should
be immediately attended by the Obstetrician on duty and necessary
treatment to be initiated.
Send the mother to the labour room, ward or operation theatre,
depending on the signs and symptoms.
•
No pregnant woman in labour or distress
should be turned away from the hospital for any reason at any time of the day or
night.
Casualty should be located close to the labour
room and theatre.
•
Casualty to receive advance intimation about
the arrival of the mother and keep the specialist team ready with blood, if needed.
•
Casualty should have the following round the
clock:
An obstetrician
Life saving drugs and IV fluids
Facility for examining the patient (including pv)
List of Officers of Ministry of Health & Family Welfare/ Prog. Deptts.
SI. No.
Name
Designation
1
Dr Anbumani Ramadoss
HIM
2
Smt Panabaka Lakshmi
MOS
_______________________ !
3
Shri Naresh Dayal
Secretary(H&FW)
Shri Raghubir Singh
Shri Deepak Gupta
Ms K Sujatha Rao
Shri S. K. Sinha
AS
AS & FA
AS(DG)
AS&DG(NACO)
ADG(stat)
£
5_
£
7_
8
........ .................................
15
16
Shri B.K. Prasad
Smt Bhavani Thyagrajan
E-mail ID
Extension
No.
Telephone
Fax
N.B.
Room
No
348-A
101
250-A
102
23061647
23061751
23061661
23061157
hfm@alpha.nic.in
N.B.
23061647
23061751
23061661
23061016
23061551
23061157
23061863
23063221
23062432
23061451
23061673
23063809,
23061066
23061334
23061863
23063221
23062432
23061451
23061673
23063809
23061066
23061334
secvhlth@nbnic.in
secyfw@nb.nic.in
Department Address
Secretary, Additional Secretary, ADG
201
150-A
N.B.
305
244-A
N.B.
302
258-A
N.B.
202
254-A
N.B.
308
145-A
N.B.
243-A ____________
435
N.B.
______________ __________
__________
Panabaka@nic.in
as-mohfw@nic.in
asfa@nic.in_______
asdq-mohfw@nic.in
asdq@nacoindia.orq
_
.1 .................................................................................................................................".................... ...........
N.B.
155-A
337
23061723
23061723
JS(BT)
N.B.
343-A
2695/345
23061481
23061481
155-A
147-A
2656/511
2510/304
23061195
23061706
JS(BKP)
isbt@nb.nic.in
17
18
Ms Aradhana Johri_____
Shri K Ramamoorthy
.IS(AJ)
JS(KR)
N.B.
N.B.
19
Shri Amarjeet Sinha
JS(AS)
N.B.
242-A
312
23062157
23061842 aradhana.johrii inic.in
23061706 Kr.i-noorth' inic.in
23062157 amarjeet.sinhai inic.in
JS(VC)
N.B.
147-A
2690/329
23062579
23062579
JS(DP)
N.B.
146-A
307
23062857
23061447
PS to JS(AS)
PS to .IS(DP~
N.B.
25 9-A
20
21
Shri Vineet Choudhary
Shri Debasish Panda
22HSh. N. Satish
N.B,
103-A
159- A
N.B.
148-A
N.B.
158-A
N.B.
157-A
N.B.
157-A
N.B.
160- A ..
__________________ N.B.
_________________
vineetchaudhrv@hotmai
332
23062157
23062157
2630/564
2656/496
2690/442
2630/500
2510/512
2510/512
2669/428
23062857
23061195
23062579
23061447
23061706
23061706
23061723
23061447
23061842
23062579
23061447
23061398
23061398
23061723
,
23
24
25
26
27
28
29
Sh. Deepak Kukreja
Sh. Sanjay Tomar
Sh.______ Sharma
Sh. N.K.. Neelakantan
Sh. S. Ramesh______
Sh. M. K. Saxena
Sh.
. Mahender Rao
PS to JS(AJ)
PA to JS(VC)
PA to JSQ
PS to JS(KR)
PS to JS(KR)
PS to JS(BKP),
30
Shri J. P. S. Chawala
■ccaH
N.B.
145-A
2716/306
23061126
23061126
cca@mohfw.delhi.nic.in
31
Shri Partha Chattopadhyay
CD(Stat)/ CD(M&E)
N.B.
243-A
2641/429
23062699
23062699
cdstat@nb.nic.in
32
Smt Gangamurthy
EA
N.B.
244 B-A
335
23061730
23061730
q.murthv@nic.in
List of Officers of Ministry of Health & Family Welfare/ Prog. Deptts.
SI. Nod
Name
33
34
35
36
37
Dr. I.P. Kaur
Dr M S Jayalakshmi
Dr R N Rai_______
Dr N Namshum
Vacant
38
Dr Tarun Seem
39
40
41
Shri Vinayak M Prasad
Shri Arun Baroka
Smt Aastha S Khatwani
42
43
44
45
46
47
48
49
50
51
52
53
Sliri A P Singh
Shri P K Aggarwal
Shri Parveen Srivastav
Shri Vikram Singh
Shri Ravinder Singh
Shri J.S. Choudhary
Shri K D Maiti
Dr. Vishwa Jeet Ringe
Shri Chaitanya Prasad
Shri 1 lari Ram Joshi
Ms Archana Varma
Shri /Xmardeep Singh
Bhatia___________
Shri J K Trikha
Shri D.R. Sharma
Dr Sangeeta Gopal Saxena
Dr. Sandeep Kumar
Dr Manisha Malhotra
Dr Himanshu Bhushan
Dr P Biswal
Dr Naresh Goel
Shri S K Sikdar
54
55
56
57
58
59
60
61
62
Designation
DC(MH)
DC(RSS)
DC(ID)
DC(Trg)
DC(NGO)
Room Extension
No.
No
2570/416
206-D
N.B.
2547/414
311-D
N.B.
2587/417
407-D
N.B.
2573/316
212-D
N.B.
1st Floor, CGHS
Dispensary, Sect-12,
R.K. Puram, N. Delhi
Department Address
Telephone
Fax
E-mail ID
23062193
23062193
23061281
23062791
26166874
26105456
23061281
23062791
26166874
ip.kaur@nic.in_______
iaYa.ms(a)nb.nic.iri
rnrrai@vahoo.com
n.namshum@vahoo.co
tarun.seemfajnic.in
Dir(NRHM-II/
NGO)
Dir (CHS)
Dir (AB)
Dir(ASK)
N.B.
210-1)
411
.23061360
.............
23061360.
............
N.B.
N.B.
243-B/A
106-D
209-D
331
535
2527/410
23061120
23061033
23064495
Dir(DC)
Dir(NRHM-Fin)
Dir (Stat)
Dir(V&T)
Dir(NCP)
Dir(SSM)
Dir (MH)
Sr. Tech. Dir(NlC)
Dir(IEC)
DS(A&G)
DS(NRHM.1/UH/AP)
DS(NE)
N.B.
N.B.
N.B.
N.B.
N.B.
N.B.
N.B.
N.B.
N.B.
N.B.
N.B.
N.B.
207-D
349-A
518-A
404-D
405-D
401-D
529-A
145-A
204-D
202-D
301-D
520-A
2727/328
2688/549
2777/459
2502/313
2527/424
2501/418
336
23061262
23062205
23061238
23062091
23062108
23061640
23062667
23062146
23061333
23062642
23061656
23063523
23061120 Vinvavak63@hotmail.com
23061033 arunbaroka@vahoo.co.in
23064495 Dirmemhfw@nic.in,dirif@nic.i
23061262 ap.singh@nic.in
23062205 Pk.aggarwal@nb.nic.in
DS(ID & RSS)
DS(lmm.)
AC(CH)
AC(CH-II)
AC(MH-l)
AC(MH-Il)
AC(Imm)
AC(UIP)
AC(RSS)
N.B.
N.B.
N.B.
N.B.
N.B.
N.B.
N.B.
N.B.
N.B.
307-D
2516/509
431-C
2728/423
410-D
505-A
106-D
106-D
452-A
2541/426
2787/315
543
361
2528/420
2557/327
2571/415
2629/314
449
23061669
23062666
23061218
23062677
23063479
23062930
23062728
23016126, 23062728
23062427
23061238
23062091
23062108
23061640
23062667
23062146
23061333
23062642
23061656
23063523
routineindia@rediffmail.co
singhravendra@hotmail.co
dirssm-mohfw@nic.in
dirmh@nb.nic.in
ringe@nic.in
Chattyl 1 l@hotmail.com
hrioshi@nic.in
archanavarma321@gmail.
asbhatia@nic.in
23061669
iktrikhYa@vahoo.co.in
23061218
23062677
23063479
23062930
23062728
sgsaxena@nic.in
acch2 mohfw@nic.in
acmhl-mohfw@nic.in
dr hbhushan@nic.in,bhim
pbiswal@hub.nic.in
drnqoel@vahoo.com
sk.sikdar@nic.in
mily Welfare/fr
List of Officers
SI. No.
63
64
65
66
67
68
Name
Dr Dinesh Baswal
Designation
Department Address
Room
Extension
Telephone
Fax
E-mail ID
No.
2787/315
dinesh126@hotmail.com
AC(Trg)
N.B.
No
505-A
23062930
23062930
N.B.
N.B.
N.B.
N.B.
N.B.
514-D
425-C
105-D
429-C
353-A
458
560
525
2505/468
2595/409
23062391
23063426
23063543
23061255
23061960
23062391 raieshmrt@qmail.com
23063426 kumar.ganga@nic.in
23061730 rakeshiss@qmail.com
Shri Rajeshwar Prasad
JD(BoP)
Shri Ganga Kumar
DD(NRHM)
Sh. Rakesh Maurya
DD(BoP)
Shri Rajesh Bhatia
DD(1D)
Sh. S. K. Gupta
DD(DC)
itsraiesh44@vahoo.co.in
23061960
sanieev.qupta@nic.in,sk
qupta22@vahoo.com
69
Shri K Syama Prasad
Chief Media
N.B.
206-D
2526/447
23061540
cm iec@nb.nic.in
70
Shri Rakesh Bhatia
PO(AV)
N.B.
511-A
2777/465
23061155
poav@nb.nic.in
71
Shri R K Sarkar
Editor (E)
N.B.
409-D
2512/463
23019466, 23062466
72
Shri R S Meena Kalky
Editor (11)
N.B.
524-A
2774/425
23061487
73
Shri Raman Prasad
AVMO
N.B.
353-A
2595/409
23017960, 23061960
74
Ms. Anita Gulati
PPS to Secretary
75
Shri Shiv Basant
JS(AYUSH-I)
76
Shri Verghese Samuel
JS(AYUSH-II)
77
Shri Bala Prasad
Dir (AYUSH)
78
Suit Sangeeta Goyal
Dir (AYUSH)
79
Dr. D.C. Katoch
Deput)' Adviser
(AYUSH)
80
Sh. Sudhir Arora
PS to JS(AYUSH-l)
DEPTT OF AYUSH, RED CROSS BUILDING
225
Red Cross
Building,
New Delhi1
_________
R.No. 220, 2nd Floor,
Red Cross Building,
New Delhi-1
R.No. 220, 2nd Floor,
Red Cross Building,
New Delhi-1
Red Cross
Building,
New Delhi1
206-A
205
Red Cross
Building,
New Delhi1
23715564
23327660
23327187
23731846 jsismh@nic.in
23716704
23359914
23327669
23731755
Red Cross Building,
New Delhi-1
raiusarkar@gmail.com
poiec@nb.nic.in
11
23731025
226
23327187
23327669
verghese.samuel@nic. in
balapasad@,hotmail.com
balaprasad@nic.in
23070994 sangeet-goel@nic.in
23351885,
23731846
23731846
dc.katoch@nic.in
dckatoch@rediffmail.co
m
Welfare/ Prog. Deptts.
SI. No.
Department Address
_______________
Name
Room Extension
No
|
No.
Telephone
E-mail ID
Fax
DTE GENERAL OF HEAL TH SERVICES
23062924 dghs@nb.nic.in,
rakeshsrivastava789@hot
81
Shri R.K. Srivastava
DGHS
N.B.
446-A
601
23061438, 23061063
82
83
Dr M Venkatateswarlu
Prof P 11 Ananthnarayanan
DCG(l)
N.B.
N.B.
667
660
23061806
23063220
_______ dci@nb.nic.in
ddgm@nb.nic.in
84
85
Dr G P S Dhillon
Dr L S Chauhan
DDG(Lep)
DDG(RNTCP)
N.B.
N.B.
342- A
343- B
'A' Wing
341-A
522-C
687
624
23062401
23063226
86
Dr (Mrs) R Jose
N.B.
343-A
599
23061594
87
Dr. P.L. Joshi
DDG(Opth)/
DDG(NCBP)
Dir(NVBDCP)
23062401 ddql@nb.nic.in
23063226 ddqtb@tbindia.orq,ddqtb
________@nb.nic.in____________
23061594 ddqo@nic.in
88
Dr Brij Bhushan
DADG(O)
89
Dr A K Puri
90
Dr D M Thorat
91
Dr P K Srivastava
DADG (Leprosy
Eradication Prg)
DADG (Leprosy
Eradication Prg)
JD(NVBDCP)
92
Dr. Ichhpujani, IDSP
NPO(IDSP)
93
Dr. Jagvir Singh
Coordination Divison
94
Dr B K Tiwari
Adv. (Nutrition)/
Adv.(NlDDCP)
________mail.com_____________
DDG(M)
Leprosy
TB Control Prg
Vector Borne
DC Prg
605
23062366
672
23061109
341-A
632
23061148
N.B.
Vector Borne
DC Prg
NICD
23967745, 23967780
22, Shamnath Marg,
Delhi-110054
453-A/
N.B.
756-A
531-C
N.B.
23061148 dmthrorat@rediffmail.co
_____ m
23967745, 23967780 23918576, pkmalaria@Yahoo.co.in
23968329,
23972884
23935530 idsfir
23934517
22, Shamnath Marg,
Delhi-110054
IDSP Division, 3rd
Floor, 22, NICD,
Shamnath Marg,
DELHI- 110054
NICD, 22 Shamnath
Marg, Delhi-110054
355-A
N.B.
23061109
npo(a>nic.in,ichhpuiani@
hotmail.com
23928700
666
23062113
23928700 idsp coord@nic.in
23062113
advnut@nb.nic.in
- Media
 10184.pdf
10184.pdf
Position: 1129 (11 views)