STRATEGIES FOR SOCIAL RELEVANCE
Item
- Title
- STRATEGIES FOR SOCIAL RELEVANCE
- extracted text
-
DISPLAY
□ODD
nnnnJ—------
(MEpfC^L COLLET
8HOR.E
□
WPICAL EDUCATION
faycrt$
Strategies -fa?
"1 SOCIAL RELEVANCE &
COMMUNITY ORIENTATION
(^wldihj On Ja^Iiah
Commiavu
Twiners
& Otke^
( A
^/PW
I
Health
I
w Pwpkzwi
iv^KtwUonS
C.H C. - C.M.A.I. - C H.A.t.
PROJT<T
l9?O-9±9
Cop/
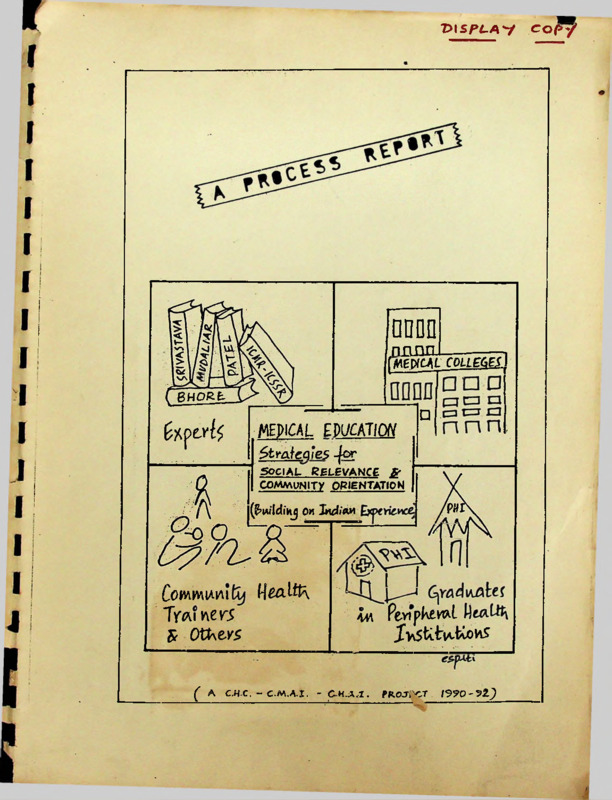
CHC / MEP / 01
Research Project
Strategies for Social Relevance and
Community Orientation in Medical
Education : Building on the Indian
Experience
A PROCESS REPORT
Community Health Cell, Bangalore *
JUNE 1992
Sponsored by : Christian Medical Association of India (CMAI)
Catholic Hospital Association of India (CHAI), Christian
Medical College, Ludhiana (CMC-L),
*Society for Community Health Awareness, Research and Action
No. 326, V Main, I Block, Koramangala, Bangalore - 560 034.
MEDICAL EDUCATION PROJECT 1990-92
June 1992
A PROCESS REPORT
CONTENTS
I. Title
Page
II. Research team and 'supports'
A. Preamble
a) Medical Education reform
b) Some lacunae in the process
1
2
c) Disturbing trends (Diagram A)
3
B. Origins and Scope of the study and its linkages
a) Researchers
b) Sponsors
5
5
c) Other Linkages
d) Scope of Study
5
7
C. Basic premise of the Study
a) Recognising four sectors of innovation
8
b) Need fcr dialogue among sectors
9
c) Faculty development - a neglected issue
9
D. Evolving the objectives
a) The steps in the process
11
b) The original objectives
11
c) The 'Interactive response'
13
d) The Final Objectives
15
E. Methodology
1. Literature Review
16
2. Letters to Medical Colleges
17
3. Letters to Community Health/Development
Trainers
18
4. Survey of graduates with rural experience
19
5. Institutional visits
6. Meetings and Interactive Dialogue
19
21
7. Approaches - Orthodox and Interactive
22
2
2
F. Organisational Dynamics
a) The Research Team
24
b) The Advisory Group
25
c) Peer Group support
25
d) Project time and Process Schedule
28
e) Financial Support
29
G. Responses - Results - Findings
a) Literature Review
b) Medical College survey
30
31
c) Alternative Training Sector - Review
d) Survey of Graduates with PHC experience
41
45
e) Some overall general observations
49
H. The Project Process and outputs
a) Interaction with Individual colleges
54
b) Community Health Trainers Dialogue I and II
57
c) Participation in CMC Network
d) Concurrent Publication - Stimulus for Change
58
59
e) Final Publication
61
f) Towards a collective commitment-Medical Educators
Review Meeting, June 1992
63
I. Challenges for the Future
i) Factors promoting change
65
ii) Obstacles / Barriers to change
67
iii) Task for the future
69
J. SO WHAT - A reflection on the study
I
J
i) Strengths
71
ii) Weaknesses
71
K. In Conclusion
74
L. Acknowledgements
76
M. Reading List (will be prepared at the end of the
manuscript finalisation)
79
LIST
OF
TABLES
Page
I.
II.
Initiatives of the Researchers which
formed the background to the study
6
Graduate Survey Components
20
III. Research Approaches in Study
IV.
V.
VI.
23
Medical College Survey - Respondents
Statewise distribution and source
32
Medical College Strategies - Objectives
and curriculum structure
33
Medical College Strategies - Pre-clinical
Phase
34
VII. Medical College Strategies - Para-Clinical
Phase including Community Medicine
Teaching
Medical
VIII.
34
College Strategies - Clinical Phase 35
Medical College Strategies - Internship
Phase
36
X.
Pace Setter Colleges - Some Features
38
XI.
Pace Setter Colleges - Key Innovative
Strategies
39
IX.
XII. Alternative Training Sector
42
XIII. Alternative Training Sector - Key Ideas
44
XIV.
XV.
XVI.
Graduate Survey I - Skill development/
competence areas
47
Graduate Survey II - Curriculum Structure/
Framework
48
CMC Network Meeting - Areas of Discussions
58
LIST OF DIAGRAMS
A.
Disturbing Trends in Medical Education
4A
B.
Sectors of Innovation/ 'ontribution of
Sectors / The Need for Integration
8A
C.
Medical Colleges and Community Health
Trainers included in Study - a regional
distribution
45
LIST
OF
APPENDICES
A .
CHC-CMAI-CHAI-CMC Network-Project Linkages
1
A2.
CHC-CMAI Project Contract
6
B.
Resource Persons to whom initial project proposal sent
7
C.
Project Announcements in bulletins/journals/press
8
Dj.
Letter to Medical Colleges
9
D2»
Letter to Medical Colleges - II Reminder
10
E.
List of Medical Colleges contacted/responded
12
F.
Letter to IAAME Conference Participants
17
G.
Letter to Corrnnunity Health and Development Trainers
20
H.
List of Community Health and Development Trainers
contacted/responded
23
A. Salient Features of Institutional Visits
24
B. Meetings Linked to Project
25
J.
Medical Colleges included in Project Report
26
K.
Medical College initiatives with college code
28
L.
Project Schedule I
35
ScN.
M.
An overview of financial support for the project
40 & 41
0.
Reports / Publications from Medical Education Project
42
P.
mfc Anthology Handout, 1991
45
G.
Framework of Medical College based workshop on
project determined instruments
46
R.
Health Action Special Issue - June 1991
49
S.
Preliminary Communications from project at IAAME
Annual Conference in Bombay - January 1991 (Abstracts)
50
I.
I
A.
a)
I
I
I
I
I
I
I
I
I
I
I
I
I
I
I
PREAMBLE
Medical Education Reform
Medical Education and its social and community orientation have
been a subject for discussion and dialogue in India especially
since the Bhore Committee Report of 1946. During the last four
decades there has been much rhetoric and many exhortations; a
few concerted attempts by keen medical educators and institu
tions; some progressive recommendations by the Medical Council
of India ( 1 ) and other professional bodies, but little overall
change.
The Srivastava report in 1974 ( 2 ) sums up the problem and the
challenge very effectively when it states :
"Diagnosis of the Problem"
"The stranglehold of the inherited system of medical
education,
the exclusive orientation towards the teaching
hospital,
the irrelevance of the training to the health needs
of the community,
the increasing trend towards specialization and
acquisition of postgraduate degrees,
the lack of incentives and adequate recognition for
work within rural communities
and the attractions of the export market for medical
manpower
are some of the factors which can be identified as
being responsible for the present day aloofness of
medicine from the basic health needs of the people....
"The Challenge Ahead"
The greatest challenge to medical education in our
country is to design a system that is deeply rooted to
the scientific method and yet is profoundly influenced
by the local health problems and by the social, cul
tural and economic settings in which they arise......
We need to train physicians in whom an interest is
generated to work in the community and who have the
qualities for functioning in the community in an
effective manner".
2
2.
The last fifteen years, since the Srivastava Report have
however witnessed a growing spirit of introspection and an
increasing commitment towards serious reorientation of the
curriculum, to suit our own 'needs’ and 'socio-cultural
realities'.
The period since 1975 has been marked by significant develop
ments, of relevance to Medical Education.
At the national level, there have been the National Health
Policy and National Education Policy statements, the opera
tionalization of the Reorientation of Medical Education
(R.O.M.E.) Scheme, the 1982 Recommendations of the Medical
Council of India, and the development of the Health University
concept (3 ).
Within the medical colleges, there have been serious efforts
by a few to evolve community oriented training strategies
based on the MCI guidelines and sometimes going beyond it, but
within the overall stipulated "structure' and framework of
orthodox medical education that has been historically evolved
and is well entrenched. Their efforts have been interesting
but of limited impact due to many factors including inadequate
faculty response and the changing social/value ethos of the
medical college entrants. The absence of the concept of
'autonomy' in the medical education sector in the country,
preventing the development of experimental alternative curri
cula
is also an important factor.
Some medical colleges have been involved in networking around
various new directions including ’epidemiological orientation1,
the ‘alternative *
track concept, and the 'decision based app
roaches to evaluation/innovation' (3 ), Many have been par
ticipating in the annual deliberations of the Indian Association
for the Advancement of Medical Education. The efforts of the
National Teacher Training Centres for medical college teachers
in Pondicherry and PGI-Chandigarh have also been significant (9 ).
Outside the medical college sector, there has been experimenta
tion and reflections on alternatives. Key among these are, the
'Kottayam experiment' ( 6 ), the medico friend circle's 'Antho
logy of ideas' for an alternative (5 ), the JNU plea for a ’New
Public Health' (7 ), the Miraj Manifesto ( 8 ) and others ( 9 ).
A number of innovative community health oriented training pro
grammes for health personnel especially within the voluntary
sector have also developed and are of significance to Medical
and Nursing Education, even though they have evolved in a
separate 'universe'. Similarly outside the health sector, in
the development and informal education sectors there have
emerged a number of 'alternative training' experiments that
have pedagogical innovations relevant to medical education (10).
b) Some Lacunae in the Process
While there is much evidence therefore of the new spirit of
/
-3
3.
introspection and ‘innovation’, which could stimulate change
in the 1990s there are some features of these developments
that are not so healthy and could be considered lacunae
and even going counter to the emerging process. (11)
Firstly, there is not much interaction or dialogue between the
compartmentalised universe of government health services and
training centres, medical colleges - government and private
and voluntary7 agencies and other groups interested in alterna
tive medical education. Even within these compartments there
are divisions and inadequate networking. Groups are therefore
unaware of each others' efforts.
Secondly, there has been inadequate publication of the strengths
and weaknesses of these different initiatives. Even though
there is a growing mass of ‘grey literature’ - reports and
handouts and circulated papers, these are not accessible to
the 'serious' medical educators in India, who are therefore
not aware of the wealth of experience in the country itself.
Thirdly, the innovators within and without the system have not
subjected their own 'innovations' or 'reflections' to any type
of 'objective evaluation' or 'peer group assessment'. In some
instances, where this has been attempted, the results are not
available, fcr others to learn and reflect upon.
Fourthly, in the absence of this awareness of the diversity and
multifaceted experience in the country, there is a tendency
among medical educators to be carried away by 'ideas' and
'expert advice' that have originated in other countries - in
situations of different socio-economic-cultural conditions and
different educational systems. Some of the recommendations and
suggestions are therefore not adequately grounded in local rea
lities and experience.
Fifthly, there has been inadequate attention given to the tradi
tional systems of medicine and healing as well as the prevalent
health culture and folk health practices.
Finally, whatever the focus and orientation of existing medical
education - there are a growing number of young graduates who
have opted for work experience and work commitment to peripheral
health care institutions including those in remote rural and
tribal areas. This is most often without adequate preparation
in their education. Notwithstanding all the rhetoric in recent
years about Primary Health Care little or no effort has been
made to elicit feedback from these pioneers on what could be the
framework of a more relevant education geared to the professional
and emotional challenges.
c)
Disturbing Trends
Simultaneously, the 1980s have also seen the emergence of a large
number of disturbing trends in medical education and health ser
vices development in the country which may have far reaching
,
4
consequences on the concept of social/community orientation of
medical education ( 9 ) .
These include :
i) the growth of capitation fees colleges,
ii) the mushrooming of institutions based on caste and
communal affiliations,
iii) the privatization of health care,
iv) the mushrooming of private high technology diagnostic
centres and the concurrent glorification of high tech
nology through high pressure advertising in the media,
v) the unresolved and probably increasing problem of private
practice among full time teachers of medical colleges,
vi) the increasing ’doctor-drug producer axis' with ’vested
interest in the abundance of ill health1,
vii) the rampant corruption that seems to be accepted as
routine practice and the erosion of norms of medical
ethics without any debate,
viii)
the preoccupation of medical educators with illness care
and the disregard for 'medical education for health".
Taken together they are beginning to have 'an insiduous but
definitive effect on the focus end orientation of health service
development in the country as well as the nature of the manpower
education' investment of the state'. (See Diagram A)
t
5.
B.
ORIGINS AND SCOPE OF THE STUDY AND ITS LINKAGES
ORIGINS
The study arose out of an interaction between different groups,
each one with its own particular interest in health human power
education in general and 'medical education' in particular.
a)
The Researchers
The project coordinators had a long history of interest in
'appropriate medical education' arising out of internship
experiences in a Bangladesh refugee camp (1971) and Andhra
Cyclone Disaster relief camp (1977). The experiences of
'medical care in conditions of acute mass poverty' and
'disaster linked environmental realities' led to a process of
reflection on the relevance of large, high technology, teaching
hospital oriented medical education in preparing doctors for
the challenges of Primary Health Care. This interest led to a
decade of involvement with the community orientation of medical
education in a socially relevant medical college (St. John's,
Bangalore) in South India followed by the development of a
'grassroots' technical resources centre (CHC) to promote
community health action through voluntary effort in South India.
During these years there were many opportunities and initiatives
to reflect on 'appropriate medical education' as outlined in
■ Table I. It was these varied experiences, that led to the
evolution of the project so that the researchers could build on
all the past efforts.
b)
The Sponsors
The sponsors of the study - The Christian Medical Association
of India (CMAI) and The Catholic Hospital Association of India
(CHAI) are membership associations in the voluntary sector which
together network over 2,500 institutions in the country. By
virtue of their commitment to health care particularly focussed
on the 'marginalised and underprivileged' they are interested
greatly in all efforts to produce
more 'socially relevant' and
'community oriented' health professionals in the country. They
were therefore eager to associate and support the project as
soon as it evolved and they were contacted for support. The
detailed background to the evolution of this linkage is outlined
in Appendix A^ and A^.
c)
Other Linkages
The facilitation of the first network meeting of the four Chris
tian Medical Colleges by the CMAI and the invitation to CHC to
provide the 'keynote stimulus' led to an establishment of an
informal linkage between the researchers, the sponsors and the
four medical colleges of the CMC Network, who were all intere
sted in community oriented and community based education and
therefore agreed to participate as an ’interactive peer group' ,
in the evolving study (See Appendix Ap. These colleges, who /
6
I
6.
/
tabu
INITIATIVES
FORMED
OF
THE
THE
i
RESEARCHER’S WHICH
BACKGROUND
TO
THE
,
( 12 )
STUDY
YEAR
INITIATIVE
1972
Refugee Camp Experience
Making Medical Education
Relevant to the needs of
Society - Interns reflections
1973
DTPH Dissertation
Training Doctors for Community
Health Service (Trends in
Undergraduate Medical Education
in India)
1973-83
Community Orientation
of Medical Education
- SJMC, Bangalore
(various experiments)
Moving beyond the Teaching
Hospital
1977
MD - Term Project
(Interactive Evaluation)
The Kottayam Experiment :
Training Programme for
Community Nurses / Health
Supervisors
1982
Year of Travel and
Reflection with Commu
nity Health Action
initiators at the
Grassroots
Notes on a year of Travel and
Reflection in the context of
Social Orientation of Medical
College Educational Experi
mentation
1984
mfc Annual Meeting on
Medical Education Calcutta
Background paper (150 years
of Medical Education :
Rhetoric and Relevance)
Workshop for Rural
Bond Scheme Pioneers
(SJMC/CHAI/CHC)
Report of a Workshop for Rural
Bond Scheme Pioneers
1988
CHC Network - Sub
Committee on Medical
Education
Memorandum to the Health
University Committee of the
Karnataka Government
1989
Supportive stimulus to
Network of Christian
Medical Colleges
Keynote Address : Towards
Greater Social Relevance
Facilitation of first
dialogue of Community
Health Trainers in
India (VHAI)
Report on Proceedings of the
Trainers Dialogue
mfc Anthology - Medical
Education Re-Examined
(Planning Collective
Process)
3 Articles in Anthology inclu
ding Anthology of Ideas Alternative Framework of a
Curriculum (Compilation)
1990-91
PUBLICATIQK/REPORT
. .7
7.
/
were, already involved in innovations/experiments of various
types were interested to hear of the wide ranging efforts in
the 'keynote address' and evinced further interest in the
compilation of Indian experience.
d)
Scope
X.
The present study emerged through an interaction between the
three groups mentioned above, and the scope of the study evolved
as an attempt to explore and document all the 'innovations' and
relevant reflections in India so that a Researched Review Document
would be compiled, which would be practical, relevant, and use to
all those, who wish to explore medical education reform in the
1990's, building on the wealth of Indian experience.
Focussed primarily on the Indian experience and basing itself on
an interactive process which would be multipronged - including
literature review, individual and group discussions, field visits,
questionnaire surveys and other orthodox and alternative appro
aches the project study sought to put together
"a handy reference manual of local innovation,
an anthology of ideas emerging from local experience,
and a resource directory of local Indian expertise"
in community oriented and socially relevant medical
education and health training in India. (11)
After much deliberation the project researchers decided that the
key target group of the project would be "faculty of medicad.
colleges' who in 'groups' wish to reflect and experiment with
alternative/relevant ideas.
Other target groups were also identified during the process and
it was decided that as a 'lobbying for change' process a summary
document of the key findings and conclusions of the study would
also be sent to them as a complementary process in the follow up
of the project.
The researchers and the CHC team had already good contact and
linkages with the 'alternative training sector' and the 'young
graduates in rural centres' due to the nature of CHC work in
past years and this 'network' of linkages was used with great
advantage, for the evolving project.
8.
C.
BASIC
PREMISE
OF
THE
STUDY
The basic premises of this interactive study were that
Recognising Sectors of Innovation
a") There are atleast four sectors of innovation from which stimulus
for reforms in medical education can and have emerged (13 ).
i) The Expert Sector
Starting from the Bhore Committee Report of 1946 till
the recently circulated draft outline of the National
Education Policy for Health Sciences (Bajaj Report 1989) there have been a series of expert committees
in India offering ideas and recommendations of great
relevance to the Indian Situation.
ii) The Medical College Sector
A few medical colleges have made serious efforts to
operationalise some of the expert 'ideas' and reco
mmendations and some have gone further to evolve their
own community oriented training strategies. Much of
this reform is within the framework of 'structure' and
'function' stipulated by MCI.
The 'medical college' sector includes ideas and reco
mmendations put forward by professional associations
at their annual meetings and also covers much of the
materials that has been regularly presented and dis
cussed at the annual meetings of the IAAME.
The 'Expert Sector' and the 'Medical College Sector'
would together constitute what we would like to term
as 'traditional/orthodox expertise '. (Diagram B^ )
iii) *
'Voluntary
Training Sector
Since the 1970's a large number of innovative community
health oriented training programmes for health humanpo
wer has developed especially within the so called
voluntary sector. Many are geared to training or reo
rienting doctors and nurses (produced by the orthodox
system) towards community health oriented work. Many
others train 'lay people' (non-doctor, non-nurse) in
community health work. A large number of 'alternative
training experiments' supplementing these efforts have
also emerged in the development and informal education
sector. While these may appear to have developed in
a 'separate universe' there is growing recognition that
their approaches and methods have great significance
for professional humanpower education in the country (10).
9
DIAGRAM
DIAGRAM
B
CONTRIBUTION
OF SECTORS
m
BBB
|£xPER7S
COMMUNITY
HEALTH
ALTERNATIVE!
MEDICAL
education
EXPERIMENTAL
Parallel
CUR£f CUL.UM
TRAINEES S'
OTHERS
DIAGRAM
GRADUATES
IN
iv) The *
PHC
graduate1 Sector
There are a large number of young graduates of the
existing orthodox medical education system who have
worked in small peripheral rural hospitals, primary
health centres and community health projects and have
had to creatively adapt their own inadequate education
to the 'professional challenges' and 'emotional dema
nds' of community oriented health care. Most of these
'creative tensions' and 'appropriate responses' and
ideas are waiting to be systematically tapped and
explored.
The 'Voluntary training sector' and the 'PHC graduate
sector' would together constitute, what we would like
to term as the ’alternative
*
expertise. (Diagram
)
b) Heed for Dialogue Among Sectors
The second premise of our 'interactive study1 was that while the
above sectors of 'innovation' have, separately and taken together
a lot of interesting ideas to offer to all of us who seek to
reform medical education, there is inadequate documentation and
reporting and inadequate networking and hence this expertise
lies relatively unknown within sectors and between sectors.
Medical college based innovators know little of what each other
aredoing; the voluntary sector trainers have little dialogue
even among themselves; the graduates in the periphery are seldom
contacted for feedback; and therefore there is a 'gross' lack
of awareness of the wealth of experience available in the country
itself. Unless all these ideas, suggestions, experiments and
innovations are available together in some sort of compilation/
publication there is little chance of a cross fertilization of
ideas and for dialogue between the innovators and the enthusiasts
of all the sectors. It is now more than clear that any form of
alternative medical education or experimental parallel curriculum
can emerge only if attempts are made to bring the traditional
orthodox expertise to dialogue with alternative expertise and
evolve an integrated strategy and response to the challenges of
Appropriate Medical Education. (Diagram B^ )
c) Faculty Development - A Neglected Issue
The third premise of our study, which has therefore greatly
determined its focus and scope, particularly in the context of
the 'end products' is that the 'Faculty' of a medical college
are ’the Key to Change’ and that faculty development has been
the single biggest casualty in the Indian Medical Education
Scene. There has been a lot of rhetoric and some lip service
to faculty development but faculty development and training is
at the bottom of the priority list of medical college leadership.
Teaching in a medical college is still not considered an inde
pendent and important enough 'vocation' and tends to be still
relegated to a sort of 'appendage' skill or at best an unavoi
dable task.
>
10
I
10.
If reform in the 1990's has to have relevance, rigour and
collective commitment, then developing a core group of faculty
in every medical college committed professionally to medical
education is an urgent necessity and this study is primarily
oriented to that task.
We have tried to build some 'structure' and a framework towa
rds this 'faculty development process'. The availability of
faculty role models in the institution are crucial for inspiring
students towards more community oriented and socially relevant
vocations in medicine. This task can no longer be ignored.
Cal] it by v.’!:atever name, the need is for a
new treed of physician, who has a broad under
standing of human biology, who is imbued with
the ingredients of rural and peri-urban soci
eties ar.- their way of life, who can communi
cate effectively with the rstient's family
regarding t'r/ nature of the ailment, who car.
address himself to preventive aspects in the
hemes, who will be ar. effective leader of
health workers, and who will use his knowledge
to stimulate other community building programmes.
We need in effect, a social biologist.
Mass
public health and hospital patient care, however
well developed, cannot fill this gap.
Ramal ingaswarr.i,
1968
. .11
11.
'
a)
D.
EVOLVING
THE
OBJECTIVES
\
The Steps in the Process
The objectives of the study based on the premises described in
(C) evolved through an interactive process which consisted of
4 steps.
Step I
A project proposal was drafted in January 1990 and circulated
to the Advisory Committee, Peer group and a group of key
resource persons in the country.
(Appendix B)
Step II
Many ideas, reactions, modifications were suggested by some of
these resource persons and were considered by the researchers.
Step III
At the first meeting of the Advisory Committee in May 1990 all
these suggestions were considered and discussed. A modified
set of objectives, keeping in mind the existing limitations and
constraints available, especially of time framework were evolved.
Step IV
As the project evolved and the field visits and interactions
took place and feedback from respondents and peers came in some
of these objectives got further modified in terms of focus,
priority and significance. This symbolised the interactive
aspect of the action-research.
b)
The Original Objectives
The following were the objectives listed out in the first project
proposal circulated in January 1990 :
I. General Objectives
1. To Document and Review
a. Innovative and alternative experiments in medical
education in India since the 1950s.
b. Alternative Community Health training programmes
in the voluntary health sector.
c. Relevant alternative educational strategies in the
non-health sector.
.
in the context of social relevance and community orient- /
ation of medical education.
/
12
12.
2. To evolve a handy 'resource' book
and some tentative guidelines for social relevance and
community orientation in Medical Education, out of this
cumulative experience, the focus being primarily on
medical educators.
II. Specific Objectives
1. To document descriptively/analytically the recommendations/
key experiments / innovations and 'experiences' in appro
priate medical education in India since the 1950's
(Appendix A).
2. To review the key alternative 'training experiments' in
the 'Health and Non-Health' sectors in India, to determine
issues, perspectives, ideas and 'pedagogical innovation'
relevant to 'appropriate medical education
*
in India.
3. To build an 'Anthology of Ideas' from suggested changes/
reforms/reorientation in Medical Education from
a. a sample of medical graduates who have worked in
peripheral rural hospitals and community health
projects since the 1980's.
b. a sample of Community health project innovators and
community health trainers.
c. innovative medical educators.
4. To evolve a set of exploratory guidelines for curriculum
reorientation within the existing MCI recommendations
based on the above 'reviews' and discussions.
5. To formulate a curriculum outline for a year's pre-selec
tion foundation course for potential medical students
which is being contemplated by some medica colleges
basing the community health orientation and sensitization
strategies primarily on educational experiments in the
health and non-health sectors.
(The main goals of such
a course as envisaged at present is intensive community
health orientation and foundation as well as language and
learning skills, necessary for successful medical education
through a reoriented curriculum).
6. To prepare an annotated bibliography/resources inventory
of key books/papers/reports/manuals/studies/pedagogical
innovation and educational aids evolved from the Indian
experience and relevant to 'Appropriate Medical Education'.
7. To supplement the above objectives by the following
additional sub-objectives (if time permits)
a. A short review of Medical Education in Ancient and
Medieval India (Ayurvedic and Unani traditions) to
explore our own cultural roots and identify some
lessons from history.
13
13
b. A pilot survey of student 'ideals' and 'expectations'
in medical education.
c. A pilot survey of 'key policy makers' and 'medical
college administrators' for determining needs, requi
rements and organisational dynamics for pursuing
appropriate Medical Education.
d. A brief overview of 'ideas' and innovative programmes
emerging the world over in order to locate the Indian
experience in a global context.
Ill. The 'interactive response'
The interactive process was quite fruitful. The key ideas/
questions and suggestions that were offered by many peers
who received the first draft proposal were :
a. Whether such an exhaustive review would produce the
results commensurate with the efforts?
b. For whom will the resource book be? Medical Educators?
or policy makers? A focus may be useful.
c. In objective three, the curriculum outline should be
for a one year pre-selection/foundation course for
medical students focussing on
i) community orientation and social relevance
ii) adequate preparation of school leavers for a
community based medical education.
iii) necessary language, terminology and learning
skills.
d. The review of community health training experience should
be in order to formulate the sensitization strategy in the
foundation course and in the medical curriculum itself.
e. Data collection by personal visits to places and (meeting)
people identified through the first three methods of
review is
unavoidable, since one can actually get a
full idea of the experiment only by visiting their sites.
f. To involve the CMC's,a suitable mechanism needs to be
evolved.
g. Meetings no doubt would be needed. They can serve two
purposes
i) Data collection and clarification of issues and
ideas
ii) to facilitate a ferment in the direction taken
by the study.
Meetings aimed at the latter can be thoughtof as following
the study rather than being part of it.
h. It's too ambitious for one year.
Make it two years.
14
14.
/
i) Review of 'ancient medical education1 is useful only if
you have 'tentatively discovered something relevant for
today's scenario.
j) A specific review of the kinds of question papers set,
the kinds of questions asked in the viva should be done.
Examinations rule teaching and the problems of reforming
examination system is a must for any review of any edu
cation in India.
k) Some process must be started to critically review the
textbooks. Even Indian textbooks are lopsided, many
times the rationale of a particular approach is not expl
ained. This is especially true in surgery. The PSM text
book also needs critical review.
1) The questionnaire survey should provide a lot of grassroot
relevant critical information on relevance of medical edu
cation. Irrelevance is being talked about but not docume
nted. This survey should be done very systematically.
m) An opinion survey of practicing physicians and surgeons
etc., in the cities may also yield important information
in documented form.
n) A survey of the knowledge and skill base of fresh graduates
should also be done.
o) Unless there is a specific bearing on medical education how
worthwhile would it be tc revievz non-health development sector
of training in the project review?
p) The goals and objectives are so broad based and comprehensive
that, one wonders whether all these can realistically be
attempted within a year?
q) Different medical colleges may be considering different
strategies in regard to the proposed foundation course. It
may be good to consider the possibility of working on two
or more possible formulations in this regard. For instance,
one medical college may like to devote two or three months
at the beginning of the first M.B.B.S., course after the
students have been selected. Another may prefer a shorter
or longer duration still as a part of the pre-clinical
course. A third group may be considering a pre registration
course of the type that we are thinking about in Miraj. A
fourth group may like to put all their prospective candidates
through such a course for orientation to all the health pro
fessionals. Can different scenarios be evolved indicating
the potential and limitations of each?
The pilot survey of key policy makers and medical college
administrators is a good idea but they are so evanescent
and so short lived in their official roles that one may
not gain much. Perhaps those figures who did play such a
15
15.
role in the past, who had thought a great deal about
the problems under search and who have the
me to
reflect might be more useful.
IV. Final Objectives
The first project advisory committee meeting was held on
12th of May 1990. The committee explored the various
dimensions of the project outline and considered all the
important suggestions and ideas listed earlier and then
decided that the Final objectives of the study would be
1. Document descriptively/analytically - Key recommendations/experiments/innovation/experience in Medical
Education (within Medical College Sector).
2. Review Key Alternative Training Experiments to
Identify issues, Perspectives, Ideas, Pedagogy
relevant to Professional Education.
3. To build Anthology of Ideas from sample of recent
Medical Graduates with Primary/Peripheral Health
Care experience.
Health services and systems of education
must be organised fcr the good of the
people and not to meet the personal needs
of a certain cadre of doctors for material
gain or scientific satisfaction.
Carl Taylor,
1970
.. 16
16.
E.
METHODOLOGY
The final objectives, were then realised by using a multi
pronged data collection methodology that included both
’orthodox1 and 'interactive' approaches.
1.
Literature Review
Identification of key experiments/innovations , experiences
and ideas was done through an extensive literature search
which included the following components.
a) Library Reference
While reference to several professional journals were
made, the key focus was on a detailed search through
the Indian Journal of Medical Education from the late
19601s to date.
Access to the St. John's Medical College Library was
very useful. In addition, a temporary loan of back
issues of the Indian Journal of Medical Education
from the Dept, of Community Medicine at St. John's
Medical College was a major time saving development
and is gratefully acknowledged.
b) Project Announcements in Bulletins and Journals
i)
Several professional bulletins and journals
published by. the 'voluntary' sector, as well
as a few daily newspapers -were contacted for
announcements about the project.
ii) Announcements and or letters to the editor
were carried by the following (See Appendix C)
The Hindu; The Indian Express; Health Action;
mfc bulletin; Health For the Millions; Economic
and Political Weekly; BMJ (Indian Edition).
Letters to the following received nil
response :
Indian Journal of Paediatrics; Indian Journal of
Community Medicine; Indian Journal of Medical
Education; Journal of the Association of Physi
cians in India; Journal of the American Medical
Association (Indian Edition); Indian Journal of
Public Health.
The announcements in bulletins, journals and newspapers
did not get much response. Three announcements got 1
response each, 2 of which were not from medical colleges
Some of the professional journals requested for adver
tisement charges and correspondence to waive this took
time.
>
17
17.
c)
'Online' Search with the National Medical Library was
planned, but not carried out.
d)
Literature Search
Some of the other methods especially library search,
field visits and 'peer' correspondence provided a large
number of references and materials that was beyond our
expectations and to a large extent was the primary
reason for the evolution of Phase II of the project.
e)
From Peers
Some 'peers' provided substantial information and we
would like to particularly record the lists and materials
from Dr. P. Zachariah (CMC-Vellore) , Mr. B.V. Adkoli
(NTTC, JIPMER), FRCH (Bombay), Dr. Abraham Joseph (CMC Vellore), Dr. M.J. Thomas, Consultant Psychiatrist,
Bangalore and Dr. Philip Abraham, Dept, of Forensic
Medicine (SJMC, Bangalore).
2. Letters to Medical Colleges
i) Letters were sent to the Deans/Principals and Professors
of Community Medicine of 125 Medical Colleges in the
country in June - July 1990. (See Appendix
& E).
ii) A reminder was sent to those who did not respond to the
first letter in January 1991. (See Appendix: D2) .
In some cases such as the colleges in Madras and Delhi,
the reminders were hand delivered and personally followed
up by a research assistant and a colleague-researcher.
iii) In addition a letter was distributed to all the parti
cipants of the IAAME annual conference in Hyderabad in
January 1991.(Appendix F).
iv) A second reminder was sent to all the colleges that had
not responded by March 1991.
v) Depending on the replies received from medical college
principals/professors further correspondence was carried
out to determine finer details of ideas and programmes
which were considered relevant for the project.
vi) The letters to medical colleges with two reminders
elicited response from 25 colleges (a 20% response).
Some colleges sent reports and other materials apart
from the letters of reply.
(Appendix e
)
The overall response to the methodology of sending out
letters to colleges has been rather poor in terms of
quantity and also in terms of quality i.e., relevance of
materials received to the overall project objectives.
/
. . 18
18.
While some colleges wrote brief paragraphs on the experi
ments, three just provided annual reports, three sent
'nil' responses. Useful material was received and or
collected from 8 colleges. These probably also represent
the key innovators in the country who have done substantial
work.
(Appendix M).
3. Letters to Community Health/Development Trainers
i) Letters were sent to a select group of Community Health
and Development Trainers in October 1990.(Appendix G
and H).
ii) Reminders were sent in January 1991 to all those did
not respond to the first letter.
iii) Many trainers sent annual reports and training reportsand further details wherever required was elicited
through ongoing correspondence.
iv) Informal discussions were also held with some of the
trainers with whom the CHC team had contact due to
ongoing CHC linkages.
v) The CHC documentation unit already had substantial
material on
a) VHAI Courses,
b) CHAI Courses,
c) SJMC, Fangalore - CHW Courses,
d) SEARCH, Bangalore Courses,
e) INSA, Bangalore, Training Programmes and
f) CHDP, KSSS Programmes.
vi)
Substantial material was received from JNU - Centre
for Social Medicine and Community Health; Deenabandhu
- ACHAN Training Centre; RUHSA, CMC-Vellore; CINI,
Calcutta; Behavioural Science Centre, Ahmedabad and
additionally from SEARCH, Bangalore and VHAI, New Delhi.
Communications and some materials were also received
from individual free lance trainers like Dr. Uma
Sridharan (Bangalore).
In general one could say that the material collected
earlier by CHC and also received from this sector
during the project was very detailed and qualitatively
more relevant, for community oriented medical education
than some of the materials received from the medical
colleges, strengthening one of our earlier mentioned
basic premises that dialogue with the alternative sector .
would be extremely beneficial to the progress of Medical/
Education in the country.
/
19
19.
4. Survey of Medical Graduates with work experience in Peripheral
Rural Hospital and Health Care Projects (14)
i) A preliminary proforma was developed by the researchers
after a group discussion with a few (10) doctors who had
worked in peripheral rural hospitals and were presently
faculty of St. John's Medical College, Bangalore, that
had a rural placement scheme as well as gave preference
in PG and staff selection, to those with rural experience.
ii) The proforma was circulated to the same group and further
developed incorporating their feedback. (Appendix I).
iii) This was pilot tested on 10 postgraduate students who had
oeripheral health care institutional experience and then
finalised.
iv) The pre tested questionnaire was distributed at the post
graduate entrance examination of one college that gives
specific preference to candidates with rural experience
(Examinees were requested to stay back if they qualified
to be in the sample).
v) The questionnaire was distributed to eligible respondents
in another college by one of our advisory committee member
and also at the medico friend circle annual meeting in
Sevagram in September 1990.
vi) Ke explored the possibility of identifying eligible
respondents from three other medical colleges who have a
rural bond scheme and two colleges who have contacts with
rural medical officers. Due to some delays in the
receiving the lists, the survey was ended in June 1991
and responses received by then only were included in the
final report as a pilot study.
(See separate report - 14)
vii) The questionnaire was fairly extensive with 38 different
sub-sections. Table II lists out these components of
medical education on which feedback was elicited.
5. Institutional Visits
i) Visits were made to seven institutions who were identified in
the process of the ongoing project as having programmes of
significance. The field visit opportunities were utilised for
interactions with staff and wherever possible with a group of
interns who had experienced most of the innovative programmes
being studied.
ii) The objectives of the field visits were to observe innovative
programmes wherever feasible and to have informal discussions
with faculty and interns regarding various programmes and
initiatives of the respective institution. This onsite visit
and informal discussion helped us to identify the strengths and
20
20
TABLE II
GRADUATE
SURVEY COMPONENTS
( 14 )
Pre-Clinical
Other Skills___________________
1. Anatomy
2. Physiology
27. Basic Nursing
Procedures
3. Biochemistry/
Biophysics
4. Biostatistics
28. Communication
5. Sociology
6. Psychology
7. Others
29. Management
30. Training of Health
Workers / Other Personnel
31. Any other skills
Para-Clinical
8. Pathology’
9. Microbiology
10. Pharmacology
11. Forensic Medicine
Clinical
32. Internship Training
33. Selection Process
34. Teaching Methodologies
35. Curriculum Structure
12. Medicine
36. Examination System
13. Surgery
37. Any aspects of content/
process environment or
base of teaching
14. Obs. & Gynae
15. Paediatrics
16. PSM/Community Medicine
17. Psychiatry
18. Dermatology
38. Measures to enhance
social/emotional
preparedness for
C.H. Work.
19. Ophthalmology
20. ENT
21. Radiology
22. Anaesthesiology
23. Dentistry
24. Orthopaedics
25. Medical Ethics
26. Others
• 21
21.
weaknesses of various programmes, as they emerge in the
field operation with trainees - a dimension seldom
explored adequately in college annual reports or published
reports.
iii) The institutions were :
a) Christian Medical College, Ludhiana;
b) Christian Medical College, Vellore;
c) Mahatma Gandhi Institute of Medical Sciences, Wardha;
d) St. John's Medical College, Bangalore;
e) King George Medical College, Lucknow;
f) All India Institute of Medical Sciences, New Delhi; and
g) JIPMER, Pondicherry
iv) The visits were linked to other meetings (incidental
opportunity!) and or specially planned in the context of
the project. In two cases it was in response to the
institutional need.
v) Appendix lglists out the salient features of the insti
tutional visits.
vi) Due to a certain degree of inadequate planning, lack of
initial standardization and some logistic, communication
and time schedule problems the field visits though very
meaningful and productive were not of an adequate
'standardised methodology' to allow for inter college
comparisons among the innovators.
vii) However since the research team who visited the college
and observed programmes and interacted with faculty,
interns or students were the same in all colleges and
the method of informal individual and modified focus
group discussion was used, some observations and
conclusions could be drawn from the field visits about
the overall process of medical education reform and many
of the problems and obstacles to change as well as the
diversity of experiences.
viii) All the colleges in the original protocol could net be
visited but the 'seven college field visit1 was a very
relevant experience and definitely gave additional
perspectives that was not possible to get from reports
and correspondence.
6. Meetings and Interactive Dialogue
i) To increase the interactive nature of the project, links
with peers were maintained not only through correspondence
but also through meetings. Some of these were comple
mentary to the project and some organised in the context /
• 22
22.
of the project. Other meetings to which CHC researchers
were invited as participants or resource persons listed
were also utilized to explore ideas and innovations
towards an appropriate medical education.
ii) Some of the meetings helped to clarify issues and ideas
and others just to stimulate further on different aspects
of the challenge.
iii) The key meetings are listed in Appendix
.
iv) From the very beginning it had been decided that the study
would have a strong interactive component and the resear
chers would use every available opportunity for discussion
with peers interested in medical education alternatives.
These would be discussions at individual level as well as
in groups during meetings and dialogues specially called
for the purpose or opportunities utilised at ongoing
meetings/visits related to other topics and occasions.
v) This interactive dimension of the project was emphasised
and operationalised as follows :
a) Many discussions with the Advisory Committee were
not just organisational but interactive in the
context of them being senior peers. Several issues
were raised and explored.
b) Discussions with peers with relevant experience
during visits t'o CHC and/or Bangalore or elsewhere
were held whenever possible.
c) Correspondence with peers and contacts throughout
the study.
d) Three reports were sent out to all our contacts
in November 1990, May 1991 and January 1992. Some
peers responded to ideas and project developments
mentioned in these reports.
7. Approaches - Orthodox and Interactive
As a general policy of the project, and keeping in mind CHC1s
own approach and commitment to networking, the approach to
research was a combination of ‘orthodox1 as well as interactive.
(See Table m ).
While ‘Orthodox1 approaches helped to standardise procedures
and bring in the required rigour the interactive approaches
helped to increase the sense of participation and involvement
among respondents as well as often helped to tap the ‘affective
domain' as much as the cognitive in the data collection process
.. 23
23
Very often we could find out what people felt about things not
only what they thought. Many negative impressions and often
more reflective responses were picked up by this method. Also
different perspectives on the same programme especially from
'organisers' as well as 'participants' were explored. All
this would not easily be possible through ar. objectivised
standardised questionnaire. Since our study was not 'quanti
tative' in its assessment of the situation (not how much?) but
was trying to find out the range of 'what/where/why of medical
education reform'. This combination of methods helped to get
a wider qualitative impression of the diversity of innovations.
Table III
Research
approaches
irt
the
Orthodox / Classical / Established
Study
Interactive
* Literature Review
* Peer Group correspondence
and meetings.
* Letters to Colleges
(with reminders)
* Field visits to colleges
and Group discussions
with faculty/interns
* Letters to Trainers
(with reminders)
* Questionnaire Survey
(Graduates)
* Correspondence with
College respondents and
Community Health Trainers.
"The purpose of medical education is not to produce
Kobe! Prize Winners but to provide doctors for
health services, who will meet the health needs of
the country in which anc for which they are needed."
WHO Regional Committee for South East Asia.
24.
F.
ORGANISATIONAL
DYNAMICS
To operationalise the methodology, five components of the
Organisational dynamics of the project are outlined. These
include :
a. The Research Team
b. The Advisory Group
c. Peer Group Support
d. Project time and process schedule
e. Financial support
The related organisational dynamics were evolved, step by step
as the project took concrete shape. Modifications and changes
were made in response to various constraints and contingencies.
The following are the salient features of each of these orga
nisational components as they evolved during the two year
project, a second year phase II being added to the initial one
year phase I time framework, due to the response and ongoing
dynamics.
a)
The Research Team
There were two primary researchers whose background expe
rience has been outlined earlier.
During the second year Dr. Thelma had to coordinate
another Evaluation Study and Dr. Shirdi Prasad Tekur of
CHC provided additional support as a research associate.
Right through the project we tried to identify suitable
research assistants to join the team on a full-time basis.
Out attempts were unsuccessful because there were very few
research-oriented people interested in medical education
per se, or adequately experienced for this 'interactive
*
sort of project.
The research team therefore tried to involve other members
of the CHC team for specific tasks and various other
contacts were enlisted for short-term assignments (See
Acknowledgements) .
Another problem was that much of the material collected or
compiled was such that it was not possible to delegate its
analysis or assimilation to research assistants. Most of
this had to be done by the primary researchers themselves.
During the second year a request was made for a middle
level staff member from the participating medical colleges
(who would be willing to support the project on a sabattical)
to join the research team. Inspite of some scouting around .
25
25.
/
such a possibility could not be operationalised.
project had to be completed by the primary team.
Thus the entire
The Research team were based in CHC utilising all its facilities
but much of the compilation/analysis was done from a home based
office by the researchers.
b)
The Advisory Group
A small advisory group with 4 resource persons was formed.
included :
These
1) Dr. C.M. Francis - Previously Dean of St. John's Medical
College and Kottayam and Calicut government medical
Colleges and presently Director, St. Martha's Hospital,
Bangalore.
2) Dr. P. Zachariah - Professor of Physiology of CMC-Vellore
and Coordinator of the MMC - Miraj Medical College Project
(when on Sabbatical).
3) Dr. V. Benjamin - Previously Professor, Community Health
and Development Department of CMC-Vellore and presently
Training Consultant to CMAI, New Delhi.
4) Dr. George Joseph - Previously Professor, Centre for
Community Medicine, All India Institute of Medical Sciences,
New Delhi and presently Executive Director, CSI Ministry of
Healing in Madras.
The resource persons were selected for their consistent interest
in the challenges of reorientation of medical education and for
their previous track record in supporting and being part of medi
cal college innovations. They also represented perspectives in
medical education from the different types of experience, viz.,
pre-clinical teaching, community medicine teaching, administra
tion and research. This greatly enhanced the overall planning
of the study.
The advisory committee met formally approximately every quarter
(refer Appendix-L). In addition, since two of the members were
Bangalore based and the two others visited Bangalore fairly
frequently, there were many opportunities for informal inte
raction with the researchers. Some support was also available
through correspondence and in the final phase many of the initial
outputs/reports of the project were intensively reviewed in a
special review meeting in October 1991 and thereafter indivi
dually as the occasion arose.
c)
Peer Group Support
Institutional Linkages - Formal and Informal
The project proposal had envisaged that collaboration and support
from other institutions and associations to widen its scope, as
well as to ensure that it would be of significance and relevance/
• 26
27.
Z
to a larger number of people and initiatives in the 1990's.
It had also been decided to request every collaborating
institution to nominate one of their faculty/staff members
to participate as a peer group member of the study.
This linkage was explored with CMAI, CHAI and VHAI; the three
CMC's - Vellore, Ludhiana and Miraj; St. John's Medical College,
Banoalore and the National Teacher Training Centre, JIPMER,
Pondicherry.
Ultimately as the two year project evolved the following
linkages were established :
1) Formal
i)
CMAI (New Delhi) and CHAI (Secunderabad) co-sponsored
and provided financial support for both Phase I and
Phase II of the project, with CMAI providing the major
share of Phase I support.
ii)
CMC-Ludhiana provided some financial support for
Phase I of the project and offered peer group support
through their Principal, Dr. Alex Zachariah.
iii)
CMC-Vellore, St. John's - Bangalore and Miraj Medical
Centre offered peer group support through their
nominees Dr. Abraham Joseph, Vice Principal and Head
of Department of Community Health, Dr. Prem Pais,
Associate Professor of Medicine and Asst. Medical
Superintendent and Dr. Kalindi Thomas of the Depart
ment of Community Health respectively.
2) Informal
V.’hile these formal linkages were established, the 'inter
active methodologies' of the ongoing project led to the
development of informal links and contacts with some of
the faculty/members of a larger number of institutions
and initiatives. Some previous links already established
by CHC were strengthened including
a) Voluntary Health Association of India, New Delhi
b) Informal evolving network of Community Health
Trainers in India
c) Foundation for Research in Community Health, Bombay
d) medico friend circle (Bombay - Pune)
e) Centre for Social Medicine and Community Health,
(Jawaharlal Nehru University), New Delhi.
f) National Institute of Advanced Studies, Bangalore
28
28
Some new ones also emerged including
i) Network of Christian Medical Colleges
ii) NTTC, JIPMER, Pondicherry
iii) Mahatma Gandhi Institute of Medical Sciences,
Sevagram, Wardha.
iv) King George Medical College, Lucknow.
v) Centre for Medical Educational Technology,
AIIMS, New Delhi.
vi) NHL Municipal Medical College, Ahmedabad
vii) Indian Association for Advancement of Medical
Education
viii) A.P. Health University
ix) Osmania Medical College and Social Paediatric
Unit, Nilufer Hospital.
3) Individual Peer Support
Informal peer group support was also sought from a large
number of people often in their individual capacity as well.
(Appendix—P). A wide circle of contacts was established
through this process.
While the 'individual approach' was probably more fruitful
than the 'institutional approach', at the end of the project
one cannot but feel that the overall interactive process was
not as productive or active as we had initially hoped.
d)
Project -time and Process Schedule
The project time framework can be divided into three phases, as
it evolved since the idea was first conceived in February 1989
by CHC.
A Pre-project phase from February 1989 till March 1990
when the idea evolved into a project proposal and the
sponsors and linkages were identified (See Appendix - L).
Phase I from April 1990 till June 1991 when the objectives
were clarified by an interactive process, and then opera
tionalised through a multidimensional methodology. Data
collection was initiated and completed by June 1991 (See
Appendix - L).
Phase II from July 1991 till June 1992 when the data was
analysed and compiled into a range of definitive outputs.
This phase was also marked by the beginning of a collective
dialogue and lobbying process which will end in the Medical
Educators Review Meeting in June, 1992, the finale of the
Project (See Appendix - L).
/
29
29.
iv) Phase III has not been thought of since CHC, CHAI and
CHAI, the project partners are convinced that any further
commitment to the 'evolution1 of an appropriate medical
education must be based in a specific medical college or
a group of medical colleges and cannot continue to be a
pre occupation or thrust of any of these three organisa
tions any longer. The attempt to bring together Indian
experiences and provide some stimulus for medical educa
tors fits in with the catalyst role of all three orga
nisations, (to stimulate/support a process towards more
relevant health professional education'). Now the
initiative has to be carried further by a medical college
group or a collective/network of colleges. It is hoped
that the June 1992 dialogue will explore this aspect among
other issues discussed in the meeting.
e)
Financial Support
The pre-project phase and the first 3 month's of Phase I were
supported from the resources of the CHC, CMAI, CHAI and
CMC-Ludhiana were partners and co-funded Phase I. Phase II
was co-funded by CHAI and CHAI.
The overall budget of the project was Rs. 4,52,400/-, for the
2 year phase. The detailed break-up of the project grant and
related details is shown in Appendix-N.
Some of the other CMC's were invited to consider the possibility
of co-funding the project but there were organisational/policy
issues that came in the way of a broader consortium of funding
putting a heavier burden on CHAI and CHAI than initially planned.
Their gesture in taking joint responsibility of seeing the
project through was most welcome and is appreciated.
The best way to avoid large scale migration
is to train doctors to work in the conditions
that prevail in their own country.
For most
developing countries this means a curriculum
overwhelmingly geared towards Primary Health
Care in the rural areas.
Earthscan (1978)
I
30
G.
RESPONSES - RESULTS - FINDINGS
The outcome of the study in terms of responses, results and findings
may be discussed under the following subheadings
a) Literature Review
b) Medical College Survey
c) Alternative Training Sector Survey
d) Graduates Survey
e) Some overall general observations/findings
a) LITERATURE REVIEW
i)
The literature review lead to the identification and
compilation of over 750 references on key Indianexperience
in Medical Education which has been arranged into a
bibliography (arranged alphabetically). While the main
source was the Indian Journal of Medical Education, arti
cles from other Indian Journals and articles on Indian
experience in WHO/foreign journals were also identified.
All the personal communications and unpublished reports
and papers received by the researchers during the phase
of study have also been included.
ii)
Some WHO sources as well as a large number of references
on more recent community/primary health care oriented
innovative experiments in other countries was also
collected. We also identified some key papers on issues
and directions from foreign sources. Just a few key
foreign papers have been included in the bibliography,
though the main focus is on Indian experience.
iii)
40
key titles were also identified and an annotated
bibliography (stimulus for change) was prepared as a
basic collection for a medical education cell of a
medical college.
iv)
A key aspect of the literature review was a thorough
study of what the ’experts' committees have said about
Medical Education and a detailed compilation of reco
mmendations from Bhore (1946) till Draft National
Education Policy for Health Sciences (1989) under
different sub headings/aspects of medical education.
This 'ready reckoner' would help medical colleges to
locate their own organisation and structure and curri
culum framework against the key recommendations of the
expert committee all of whom were focussed on both
social relevance as well as community orientation.
The literature review also identified a large number
of ideas/innovation within medical colleges and within
31.
other sectors of innovation mentioned in ChapterC which \
were not identified by surveys and interactive methods.
All this forms parts of Volume I of the Faculty Resource
Manual which is expected to be a concrete definitive
output of the two year project (See later Chapter H (e)(v).
b) MEDICAL COLLEGE SURVEY
i) 25 colleges responded tc our project related letter (which
included two reminders). Out of the 125 colleges in our
sample this meant a 20% response.
ii) While we cannot conclude that the non-respondents are
necessarily non-innovaters, we could identify only 7
more colleges from the literature review, who had
reported innovative programmes in 'literature' but had
not responded to our letter. This brings the total upto
32 (25.6%).
iii) Table IV shows a statewise distribution of the 'respon
dent' colleges including the sources of identification.
7 colleges, one each from seven states visited by
researchers is also shown.
iv) Recent •guestimates' of the health ministry and planning
commission are that the number of medical colleges as
of 1992 are between 160-170. Most of these are of recent
origin, mostly 'capitation fees' colleges in the states
of Karnataka, Maharashtra and Tamilnadu. Since most are
not recognised by MCI they have not begun to appear in
official statistics. For our survey we restricted our
selves to the 125 which were listed in a guide-publication
on medical colleges for entrants in 1990.
(
)
We did not try to get details of these newer colleges
partly because they were difficult to get through other
sources and partly because of our assumption that they
were too new, and too preoccupied getting established to
initiate experiments or initiatives in social/community
orientation.
v)
Tables v-IX list out key ideas/and innovations that were
identified through the materials sent by medical colleges;
collected during field visits; received from peers; iden
tified through literature search; or already available
with CHC in its pre-project collection.
The ideas are divided into five groups
- General Objectives and Curriculum contents
- Pre-clinical Phase
- Para-clinical Phase including Community
Medicine (PSM) Teaching
- Clinical Phase
- Internship
32
32
TABLE
IV
Medi cal College Survey
(Sample
l
125 j
Respondents - Statewise Distribution and Source
Stat e
ho. in
Sample
Responded
to Survey
From
Litera
ture
Revi ew
Vi sited
Total
(D)
(E)
(B + C)
(A)
(B)
(c)
1.
Andhra
9
2
1
2.
Assam & North
East
4
-
-
3.
Dihar
9
-
-
4.
Gujarat
6
1
1
-
2
5.
Haryana
1
-
1
-
1
6.
Himachal Pradesh
1
-
-
-
-
(1 )*
-
3
-
-
7.
Janimu/Kashmi r
2
-
-
-
-
8.
Karnataka
10
2
-
1
2
9.
Kerala
6
1
-
-
1
10.
Madhya Pradesh
6
-
-
-
-
11. Maharashtra
16
7
2
1
12. Orissa
3
-
-
-
-
-
13. Punjab
*
(1)
9
5
2
1
2
14. Rajasthan
5
1
-
-
1
15. Tamilnadu
13
4
-
1
4
16. Uttar Pradesh
9
1
1
1
2
17. West Bengal
7
-
-
-
-
18. New Delhi
4
2
1
1
3
3
2
-
1
2
125
25
7
7
19.
Other Union
Territories
*
(2)
32
* Osmania Medical College, Hyderabad and LTM Medical College,
Sion, Bombay were visited by the researchers incidentally.
Not included in formal field visits.
33
33.
Totally about 50 strategies/innovations have been
identified which taken together, collectively represent an
evolving framework of an alternative medical curriculum
within the existing MCI determined framework.
It is important to clarify here that since the letter
was an openended survey it helped to get a qualitative
assessment of the range and diversity of innovative
strategies. But what percentage of these respondents
TABLE
V
Medical College Strategies
Objectives and Curriculum Structure - General
1. Defining Institutional Objectives
2. Defining Intermediate (Departmental) and
instructional objectives
3. Development of Medical Education Cell with
adjunct faculty
4. Faculty Training Programmes in medical education
skills
5. Selection Procedures other than academic merit
(Psychological / Social skills / leadership /
value orientation)
6. Curriculum development including
integration,
i)
identification
ii)
of core abilities,
prioritization
iii)
(curriculum planning committees)
identifying
iv)
skills
7. Examination Reforms
objective
i)
examinations
restructuring
ii)
assessment towards HFA/PHC
priorities
8. Faculty/student involvement in Medical Education
feedback/research
9. Tutorial system
10. Student electives
11. Student involvement in Research
12. Regular faculty meeting/facuity-student meetings
curriculum
i)
issues
Social-Societal
ii)
issues
13. Student nurture programme/curricular/extracurricular
14. Rural Bond (Placement) Scheme
15. Continuing Medical Education for alumnus/others
(for further details including colleges involved
refer Appendix J & K)
/
/. -.34
34.
TABLE
VI
Medical College Strategies
Pre-Clinical Phase
1.
2.
Foundation Course for entrants
Community-based orientation programmes
3.
Introduction of New Subjects
i) Behavioural Sciences ii) Ethics
iii) First Aid
iv) Nursing
v) Integrated Growth
and Development
4.
Clinical Orientation in pre-clinical phase
5.
6.
Humanisation of pre-clinical practicals
Samaritan Medicine
7.
Urban-slum based-multi-disciplinary student
programmes
(for further details including colleges involved
refer Appendix J & K)
TABLE
VII
Medical College Strategies
Para-Clinical including Community Medicine Teaching
1. Reorienting Pharmacology Training
i) Rational Therapeutics
ii) Essential Drugs Concept
iii) Clinical Orientation
2. Synchronization of Para-clinical subject
lectures with clinical teaching
3. Involvement in Integrated teaching
i) Para-clinical and clinical subjects
ii) Clinico-Pathological-Social Case Conferences
4. Community based Family Care Programme/Family
Health Advisory Service
5. Community Block Posting (First Clinical Year)
6. Junior Clinical Clerkship
7. Special Training Programmes i) Epidemiology
ii) Biostatistics
iii) Health Education
iv) Clinical Epidemiology
v) Management
vi) Health Economics
35
35
8. Rural/Urban Slum health visits/camps
9. Community Block Posting (2nd Clinical Year)
10. Senior Clinical Clerkship (2nd Clinical Year)
11. Epidemiological / Public Health Projects
(for further details including colleges involved refer
Appendix J & K)
TABLE
VIII
Medical College Strategies
Clinical Phase
1. Integrated Teaching (interdepartmental)
2. General Outpatient Department - GP Training
3. Clinical Clerkship in Primary Clinical Departments
4. Training in
i) Emergency Medicine
ii) Social Paediatrics
iii) Social Obstetrics
iv) Clinical Pharmacology
5. Community visits by Clinical Departments - Camps
and regular clinics in Rural/urban field practice
areas
6. ROME Scheme
7. Interdepartmental Coordinated Clinics in Hospital
Programmes
8. Peripheral Hospital Postings
i) TB
ii) Leprosy
iii) Eye Hospital
iv) Rehabilitation Centres
v) Isolation Hospital/infectious diseases
vi) District / Peripheral Hospitals
(for further details including colleges involved
refer Appendix J & K)
• 36
36
TABLE
IX
Medical College Strategies
Internship Phase
1. Interns orientation programme
2. Community Health postings in Rural/Urban field
practice areas
3. Community based camps/clinics by clinical
departments
4. Posting to Government PHC’s and sub-centres
5. Involvement of interns in special situations
a) Epidemic control
b) Disaster relief
c) Plantations
d) NGOs Health projects
e) Immunization programmes
f) FP motivation
6. Involvement of Interns in Primary Health Care
Training of Health Workers, Dais, Auxiliaries
7. Internship training in specific additional skills
i) Rational Drug Use
ii) Management
iii) Ethics
iv) Health Education
v) Epidemiological Projects
vi) Clinical Research
8. Internship training in special clinics in Hospital
situation - Curative General Practice Unit/GOPD etc.
9. Internship Assessment / Evaluation.
(for further details including colleges involved refer
Appendix J & K)
have actually included these strategies in their present
process could not be estimated since this would need a
check-list survey.
vi) From the survey and literature review we did identify 6
colleges that may be considered fore-runners or pace-setters
in terms of community oriented strategies. They had large
enough number of innovations and a relatively sustained
process of reorientation in their programmes to qualify for
this label.
Table X outlines some of the key characteristics of these
37
37
colleges. It is evident from this table that the reasons
for their sustained commitment to both'quality1 and 'change'
include a combination of predisposing factors which are s
'
X.
a) Established with specific/focussed mandates
b) Smaller number of admissions (50-70)
c) Autonomous or private management
d) Own entrance examinations and selection procedures
e) Adequate teaching hospital beds
f) Rural and urban field practice areas.
vii) Table XI outlines the key innovations that we identified in
each of these pace-setter colleges. These show some similar
thrusts as well as a certain degree of diversity. None of
the colleges, including all the pace-setters had internalised
all the innovations,though CMC-Vellore would probably be the
one college with the maximum number of operational strategies.
From our study determined list St. John's, JIPMER and AIIMS
also had introduced multiple innovations.
viii) Among the larger mainstreamers - i.e., colleges with large
number of admissions and run by government without autonomy
or minority status,a few colleges showed an increasing
openness and involvement in reorientation. From our study
the Municipal Medical College in Ahmedabad (NHLMC); BJ Medical
College, Pune; KMC, Manipal; SVC, Tirupathi; Rangaraya,
Kakinada; TN Medical College, Bombay and Kottayam Medical
College were on the move towards a strategy of change with
NHLMC, Ahmedabad demonstrating a very sustained and planned
commitment to change.
However a word of caution is necessary. With an open-ended
survey it is not completely valid to make intercollege
comparisons and hence these statements reflect a qualitative
judgement - pacesetters being most interested and some of the
mainstreamers mentioned above being increasingly more interested.
ix) An interesting finding was that a significant association like
the Indian Association for the Advancement of Medical Education
was not actively involved in keeping track of these innovations
or initiating processes to document or research the evolving
strategies. Though some of these ideas and innovations were
presented by the colleges at IAAME annual conference and some
even found a place in the recent issues of their somewhat
irregular journal, our overall conclusion was that IAAME and
its journal - the Indian Journal of Medical Education was not
fully in touch with evolving Indian experience.
x)
What was however both an interesting but in a way disconcerting
finding/that most of these pacesetter and mainstreamer colleges
were not aware of each others initiatives. There was little
formal or informal dialogue or networking on medical education
matters, inspite of the presence of an association like IAAME,
y
.. 38
TABLE
X
Pacesetter Colleges
Some Features
SI .
No .
Feature
1 .
Established
2.
Recognised by
MCI
3.
Reason for
For Training
e stablishinent
of women
= Mandate
doctors in
India.
For Training
Medi cal
College
teachers for
India.
4.
Type of
Management
Private
So ciety
(Minority)
J•
University
6.
Seat s
7.
Methods of
Sele ction
Own entrance Own ent raja ce
te s t +
te st .
interviews
Own entrance
te st+Interview
+P sy cho lo gi cal
tests +so cial/
group obser
vation tests.
Entrance
Te st +
interview
Entrance
Test+Test
on Gandhian
thought.
Written Test
Aptitude
and General
awareness
test .
8.
Ho spitals
1492 beds
630 beds
770 beds
501 bods
697 beds
9 .
Field
P racti ce
Areas
SOURCE:
CMC
(Vellore)
Al I MS
(, New Delhi)
SJMC
(Bangalore)
JIPMER
(Pondicherry)
MGIMS
(Sevagram)
191o(LMC)
1942(MBBS)
195b
1963
1956
1969
1 894
1950
1956
1969
195 b
1976
1953
For Training
doctors for
peripheral
rural
hospitals.
By Central
Gove rninent
for Quality
education.
Gandhi
Centenary
project to
promo te
Gandhian
idealism.
For Training
of women
doctors and
nurses and
women health
profe ssional
Central Govt.
(Autonomous)
P rivate
So ci e ty
(. linori ty )
Central Govt,
Private
(Registered
Society)
Private
Trust
( Minority )
Madras
All MS
Bangalore
Madras
Nagpur
Punjab
60
50
60
1053 beds
Rural & Urban
+Mobile Clini cs
(ROME) +
Rural base
Hospital
Rural and
Urban
+
Rural base
Hospital
CBHX - Directory of Medical Education.,
Hural &
Urban +
Mobile
Clini cs
(ROME)
70
Rural & Urban
65
Rural
CMC
(Ludhiana)
50
Rural and
Urban
1986.
00
TABLE
X
Pacesetter Colleges
Some Features
SI .
No .
Fea ture
1 .
Established
2.
Recognised by
MCI
3.
Reason for
For Training
e stabli shinent
of women
= Mandate
doctors in
India•
For Training
Medi cal
College
teachers for
India.
4.
Type of
Management
Private
So ciety
(Minority )
5•
University
6 .
Seat s
7.
Methods of
Sele ction
Own entrance Own entrance
t e s t+
te st •
interviews
Own entrance
te st+Interview
+P sycholo gi cal
tests+social/
group obser
vation tests.
Entrance
Test +
interview
Entrance
Te st+Te st
on Gandhian
thought.
Written Test
Aptitude
and General
awarene s s
test .
8.
Ho spitals
1492 beds
680 beds
770 beds
501 beds
697 beds
9 •
Field
P racti ce
Areas
SOURCEi
CMC
(Vellore)
Al I MS
(New Delhi)
SJMC
(Bangalore)
JIPMER
(Pondicherry)
MGIMS
(Sevagram)
1918(LMC)
1942(MBBS)
195b
1963
1956
1969
189 4
1950
1956
1969
1956
1976
1953
For Training
doctors for
peripheral
rural
hospitals.
By Central
Government
for Quality
education.
Gandhi
1
Centenary
project to
promo te
Gandhian
idealism.
For Training
of women
doctors and
nurses and
women health
professional
Central Govt.
(Autonomous)
P rivate
So ci e ty
(Minor!ty)
Central Govt,
Private
(Registered
Society)
Private
Trust
( Minority )
Madras
All MS
Bangalore
Madras
Nagpur
Punjab
60
50
60
1053 bods
Rural & Urban
+Mobile Clini cs
(ROME) +
Rural base
Hospital
Rural and
Urban
Rural base
Ho spital
CBHI - Directory of Medical Education,
Rural &
Urban +
Mobile
Clini cs
(ROME)
70
Rural & Urban
65
Rural
CMC
(Ludhiana)
50
Rural and
Urban
1986.
w
00
TABLE - XI
KEY INNOVATIVE STRATEGIES IN PACE-SETTER INSTITUTIONS
si,
1T
Common Features
No.
1. Institutional
Ob j e ctive s
2.
3.
U.
Faculty Training
(Pedagogy and
other skills)
Selection
Pro cedure s
Examination
Al I MS
(New Delhi)
SJMC
(Bangalore)
Defined
Defined
Defined
4-
-A-
CMC
(Vellore)
-Psychologi
*
cal Tests
-Interview
-
JIPMER
MGIMS
(Pondicherry) (Sevagram)
—]—
CMC
(Ludhiana)
Defined
Defined
-A-
—j—
4-
-P sy cho lo gi cal
Test;
-Group Obser
vations on
social skills,
values/
motivation.
Knowledge
of
Gandhian
ideology .
-
-
-
—
Restructu
ring towards
hfa/phc
—
Objectivised
Exams(OSCE/
OSPE )
Well
o rganised
CHAD
Centre for
Community
Medicine.
Community
Health
Department.
Community
Me d i c in e
Department.
PSM
Department.
PSM
Department
—
—
5.
Community/PSM
Medicine Dept.
6.
Student-nurture
i programmes
ii )Tutorial
system
4
—
4-
—
7. Rural Bond Scheme
4
—-
4
—
8. Foundation Course
entrant s
-v
-----
—
—
9.
COP/ROP(PreclinicalJ'
A"
—
-V
—
10.
Block Postings
(Community)
CHP I & II
A-
Communi ty
clerkship
CHP - I
-V-
—
4
-4
"A"
si •
No.
Common Features
11.
In ternship
Rural/Community
po sting
12.
Other programmes
SJMC
(bangalore)
CMC
(Vellore)
AIIMS
(New Delhi)
CHAD Hospital
+ Sub centres
Village
Graded i.e.,
based
base Hospital
PHC-Sub Centre centres in
batches of
2
*Clini cal
Epidemiology;
♦Extra ruralperipheral
ho spi tai
po stings;
♦Community
spe ciali st
camps;
♦Internship
As se ssment.
*Family Care
exercises
(Urban);
*Instructional
Obj ective s;
♦Clinical
clerkship.
*Medi cal
Ethics;
JIPMER
MGIMS
(Pondicherry) (Sevagram )
Rural/Urban
po sti ng
♦Interns
Orientation
Pro gramme ;
*Plantation
internship ;*
Rati onal
Drug
♦Community
Training;
Spe ci ali st
♦•Emergency
Camps;
Medi cine
♦Internship
Training;
As sessment ♦
♦Community
♦ Epidemic Spe ciali s t
logical
Camps.
Projects.
CMC
(Ludhiana
PHC/Rural Urban
Slum/
Centres
corporation
centres/
Rural
centre s.
G.O.P.D.
♦Samaritan
Medi cine;
♦Problem
Based
Learning.
41.
a forerunner of its kind when it was first established.
However the recent establishment of the formal consortium
network and the informal CMC network have both been positive
steps in the direction of interactive dialogue for the 1990's.
An equally surprising finding was that while many of them
were aware of the details of experiments in McMaster,
Maastricht, Albuqurque, Dundee, Bersheva, Israel and Suez
Canal Egypt and other community oriented experiments abroad
they knew little about each others initiatives - reinforcing
one of the basic premises of our study that most medical
educators were unaware of the limited but significant Indian
experience.
xi) Our field visits to seven of the respondent colleges and
informal interactive discussions with faculty and interns
led to an identification of key factors stimulating and
sustaining change as well as major obstacles and problems
in evolving experiments particularly towards social relevance
community orientation but these will be listed out later in
the chapter (See Section e).
C. ALTERNATIVE TRAINING SECTOR
-
REVIEWi)
i) Building on a sizable collection of community health training
materials from different training groups in India already
available with the CHC at the beginning of the project, the
letter to health and development trainers led to the iden
tification of many more courses, 1 ideas1 and methodologies,
that are being listed out in a separate report, entitled
’Laying the Foundations’.
ii) Table XII lists out the key programmes included in the
survey or studied through literature survey.
iii) The major contributions of this group of trainers to appro
priate medical education as listed in Table XIII are:
* Experimentation with an alternative philosophy of
education which is more participatory, experiential,
learner centred and action oriented.
* Introduction of a large number of ’small group’
techniques and methodologies in the learning process.
* Strong community orientation in the methods since most
of the training is community based and non-hospital
oriented.
Strong social analysis and exploration of community/
societal responses and initiatives to problem solution.
This is very different from the preoccupation with
42
TABLE
XII
ALTERNATE TRAINING SECTOR - HEALTH
(profile)
si.
No .
1 .
Name/Type of course
*
B
Project
A
CINI - Calcutta
i) MCIl/lCDs/Health/
Development orientation
course
ii) Orientation course in
Community Health.
2.
RUHSA,
3-
Duration
C
6 Days3 Months
6 Months
Target Group
D
i) Middle level
functionaries in
Health & Development
ii) Fresh medical
graduates.
Diploma in Community
Health Management.
15 Months
Institute of Health Management
- Pachod ( Maharashtra)
i) Rural Health Management
0 Weeks
i) NGO-sector NursesDoctors, social
workers,
nutritionists etc.
4.
CMAI - New Delhi
i) Community based Primary
Health Care.
15 Days
i) Project managers
training.
5.
Christian Fellowship Community
Health Centre - Ambilikkai.
i) Diploma course in Health
and Development.
2 Years
i) Young men and
■women •
6.
NIMHANS - Bangalore
i) Training in Mental
Health Care
1-4 Weeks
i) Doctors and
Health Workers
CMC - Vellore
i)
i) Personnel working
in Health and
Development
agencies at middle
and senior level.
>>
N)
oj
31.
No .
Pro je ct
A
Name/Type of Course
*
**
B
Targe t
Group
D
Duration
C
i) Health Workers
(NGO Sector)
7.
St.John's Medical College,
- Bangalore
i) Basic course in Community
Health.
8.
INSA - Bangalore
i) Hural Health and
Development Training
Programme.
i)
10 Weeks +
1 year
supervision/
follow up
9.
VHAI - New Delhi
i ) health Management
(CHPOM)
1 year
10.
JNU (University) - New Delhi
i) Masters in Community Health/
M.Phil / Ph.D
11.
Deenabandhu Training Centre,
-Madras
i) Leadership Course in
Community Health.
3 Months
2 Years
Thread - Orissa
i) Community Health and
Development
i ) Persons in
Development
Projects wanting
to start a CH
Pro gramme
i) Medical/Nursing
Behavioural
Science, Social
wo rk
professionals.
Sponsored
candidate s
from NGOs.
ii) Participatory Training in
Community Bised Health Action.
12.
Health and
Development
Workers at
supervi so ry
levels.
6 Months
i ) Sponsored
NGO
candidate s.
* All these groups also organise short courses and reports of these were also studied )
**The Christian Academy of Medical Sciences has introduced in 1990aJyear postgraduate fellowship
course for doctors working in rural hospitals . This is multidisciplinary and committed to
multi competent skill development.
44.
individual/medical/professional problem solution which
is the current orientation of orthodox medical educa
tion.
* Focus on skill development especially those important
for community based work viz., planning, organisation,
communication, health education, training of health
workers, community diagnosis, participatory management,
evaluation etc.,
* Greater learner centredness with participants of training
programmes involved in planning and giving shape to
learning experiences through feedback,much more actively
than medicos in present day Medical Education.
TABLE
XIII
Alternative Training Sector
(Key
ideas)
Alternative Philosophy/Pedagogy of Education
Participatory/Experiential
Learner Centred/Action Oriented
Small group techniques / methods
Strong
Community
Orientation
Social Analysis
Problem solving - Societal/Community level as well
Focus on skill development
Learning by doing
Participatory Planning/Evaluation
Training in affective aspects as well
(values/motivation/team skills/self
analysis)
Case Studies / Simulation Games
Role models / Learning Exercises
* Exploration of training beyond ‘cognitive aspects' to
include training in 'affective aspects' of work/skills
e.g. value orientation, motivation, self analysis,
group dynamic skills, team work etc..
Evolution of numerous case studies, simulation games,
role models and other interesting problem solving and
situation analysis methods that help participants get
45
45.
MEbICAL COLLEGES
INCLV&EP
IN
ANU
COMMUNITY HEALTH TRAINERS
SWJ>y
i
3-2}
]
Q - Medical Colleges
i
o - ComhwivmUj Rtciltl,/l>€velop>MeHt TyvMh&rs .(jofat- 22.J)
46.
a deeper and more relevant understanding of the
realities in which they have to operate in their
future work.
iv) While much of this experimentation and innovation is
not directly 'translatable' to 'orthodox medical education'
when it is hospital/clinical oriented, these innovations
can be a good stimulus and greatly enrich any process of
shifting focus to community based medical education.
v)
Medical educators experimenting with community orientation
camps, community block postings, community based adhoc or
planned experiential learning and all field based learning
activities beyond the teaching hospital and in health
settings lower down in the pyramid of health care can and
should learn a lot from this experimentation in the
alternative sectors.
vi) Very few medical colleges (probably only SJMC-Eangalore and
CMC-Vellore) had contact and some idea of the evolving
methodologies of this sector. Most others - even the
pace-setters were unaware and therefore untouched by this
wealth of alternative experience.
As mentioned earlier in this section all the ideas and
training strategies identified from the detailed survey
and review of the alternative training sector - both
community health and community development are being
compiled into Volume II of the Faculty Resource Manual
under the title of Laying the Foundation. Apart from
giving a comprehensive overview and listing of resources/
innovations/training methodology from this sector, this
volume of the manual will also make various suggestions
of how this can be introduced into the existing medical
education system as part of foundation courses at diffe
rent phases which are primarily community based and
community oriented.
D.
SURVEY OF GRADUATES WITH PRIMARY HEALTH CARE EXPERIENCE
i)
The pilot survey of graduates of the 1980's was probably
•qualitatively' the most productive method utilised in
the study. Most of the responses from participants in
the pilot survey were serious, offering many constructive
suggestions for improvement in the existing training
programmes and for additional initiatives to make it more
socially relevant and community oriented.
ii) The dialectic tensions faced by these young graduates in
health care service situations for which they were inade
quately prepared by the existing 'medical education'
system led to some 'gut level' and very frank suggestions
which could prove very useful to medical educators. While
.. 47
47.
some institutions like the consortium linked ones are
eliciting feedback from students at different levels
of the course, interns, junior doctors and faculty, this
pilot survey was particularly significant since the
graduates had two years field experiences in the realities
of Primary Health Care - while all the other groups
mentioned above have only experienced the teaching hospital.
iii) For all colleges interested in preparing graduates for
community health / primary health care vocations this
graduate survey feedback will be very relevant. It is
probably the first time that the 'consumers' of medical
education are giving feedback after experiencing clinical/
community work in situations of primary care - a supposed
goal of all medical education in India from the Bhore
report of 1946 to the Bajaj report of 1989.
iv)
A detailed summary of the feedback from 53 respondents in
this pilot survey has been compiled in a companion publi
cation to this report entitled 'Graduate Feedback from
Peripheral Health Care Institutions'.
v) At this juncture we list out a summary of the salient
findings of the survey (15). The focus is on general
aspects and not what has been suggested for each of the
pre-clinical, para-clinical and clinical subjects. Table
Xjlv and XV summarise the main points about skill development
and curriculum structure and framework.
TABLE
XIV
Graduate Survey Summary I
Heed for Skill Development/lncreased Competence
in the following areas
a) Basic Nursing Procedures
b) Emergency Medicine
c) Minor Surgical Procedure
a) Obstetrics
e) Local Anaesthesia
f) Running a simple laboratory and Pharmacy
g) Basic Management Skills
h) Basic Communication Skills
i) Assessing Community Health Needs and
evolving simple strategies
j) Training Health Workers
Source(15)
. 48
TABLE
XV
Graduate Survey Summary
II
Feedback on Curriculum Structure/Framework
(8 Key Issues)
a) Introduce integrated teaching focussing on common
problems/clinical applications
b) Reduce unnecessary detail in theory
c) Reduce Pre-Clinical phase to 1 year
d) Teach Sociology/Psychology/Nursing Procedures in
6 months gained from pre-clinical reduction
e) Increase responsibility and decision making
capacity in ward work
f) Long and short postings - stress importance of
both
g) Final MBBS / Internship postings in hospital
pathology laboratory / pharmacy / records
department / blood bank / accounts section
h) Final MBBS / Internship - involvement in training
of health workers.
) The Examination system came under intensive review in the
feedback. The Weaknesses of the present examination system
were felt to be that it was subjective, unreliable, outdated
irrelevant to actual practice and sometimes unethical and
even corrupt. The Challenge was to reorient and restructure
examinations to :
- Assess basic knowledge/skills
- Focus on Approach to Diagnosis and Treatment
- Focus on Common Problems
- Evolve continuous assessment process
- Increase use of multiple choice questions
- Increase short case discussions
) Many interesting suggestions of a more general nature also
came in. These included lectures on principles, advantages,
limitations of other systems of medicine / reflection on
ethics and health practices of different religions / sharing
of experiences with undergraduates by those who have worked
in peripheral health institutions (PHI's) / visits of
49.
specialists to PHI1 si / internship postings to PHI *s /
career guidance cell and preparation or orientation of
graduates opting for rural services.
From the above summary it. is evident that such a structured inte
raction and data collection process from medical graduates who are
performing the functions intended in the objective of undergraduate
medical education is a useful guide to curriculum development. We
found it a particularly useful and satisfying aspect of this study.
However one must mention at.this stage that graduates in small
peripheral rural hospitals form only part of the Primary Health
Care Samples. Other subgroups include Primary Health Centre Doctors,
General Practitioners, Community Health Project Based Doctors and
so on. A larger sample survey involving all these subgroups would
give a more comprehensive feedback for curriculum development.
E.
SOME OVERALL GENERAL OBSERVATIONS
In the previous sections we have outlined the main findings
derived from three sectors viz., the professional sector
(medical colleges), the.-al ternative training sector (health
and development trainers) and the feedback from graduates
with peripheral health.care institution experience. This was
apart from the review.of expert committee prescriptions and
identification of innovations through the literature review.
In a previous chapter, we had mentioned the additional dimension
of interactive dialogue,that was added to the methodology. This
included dialogue with interns, faculty members and peers on
medical education innovation.While this was introduced at every
opportunity, the field:visits to seven medical colleges pro
vided much scope for this dimension. This interaction was
particularly significant,because it gave us a 'real life' feel,
about some of the ongoing innovations and also gave us feedback,
that was 'affective' in nature,supplementing the 'cognitive'
feedback mostly available in published and unpublished reports
about innovations and strategies.
Some overall general observations,that can be made about
strategies for reorientation of medical education,based on the
above process, and particularly among the pacesetters (defined
in Section B) since we visited all six of them, are as follows :
i) Reorientation of medical education towards social and
community relevance is on the periphery of the agenda of
most medical colleges - even the pace-setters and the
innovative mainstreamers because of the established
traditions and ongoing demands of orthodox medical
education.
50
50
ii) Where change is taking place the institutions are caught
in the horns of a dilemm^being socially relevant as well
as being professionally excellent. Since this excellence
is most often defined in high technology and specialisa
tion terms, it means in practice that the students are
trained in a tertiary care environment of the teaching
hospital, with increasing levels of exposure to 'primary
health care situations outside the teaching hospitals.
The glamour of the former far outweighs the challenging
stimulus of the latter.
iii) The value systems of staff and students are changing over
the years keeping in line with the materialist and consu
merist values of the wider 'class society' of which they
are part. Stress on academic merit in competitive entrance
examinations of the pace-setter institution ensures that
majority of the students are still 'middle class' with
elite, urban oriented professional goals. Quality edu
cation, a sign of the pacesetters also ensures an advantage
in the competition of the market economy; both national and
international, affecting career choices.
iv) The culture of 'medical education institutions' is severely
'elite urban middle class' and the observed similarities of
dress, cultural aspirations, hostel life, personal needs
among students in all the seven colleges we visited was
most striking. We will need more than a 'Mandal Commission'
if the culture has to change to prepare them for life among
the larger masses that form the 'Bharat' of this country.
Even if selection procedures change towards a focus on
students with disadvantaged caste and class background the
dominating culture of medical education is more likely to
give them urban aspirations rather than build on and sti
mulate in them a longing for the rural life.
v) Many interns who spoke very encouragingly about the
different Innovations in their college, giving both positive
and some critical feedback were however quite clear about
'large urban specialist hospital' aspirations in their
future vocation. The effect of the reorienting efforts
were not going to affect career choices. All one could
conclude was that the reorientation had made them sensitive
to 'needs' and 'situations' which would modify their atti
tudes and make them more humane and sensitive to patient
needs even in the tertiary care vocations of their choice.
The 'culture' and ‘aspirations' of the faculty are even
more severely elite urban middle class than the students,
and since most of them have never had exposure to the
realities of 'Bharat' except through the news and TV media,
their ability to pass on this 'sensitivity towards wider
social realities' or enthuse the students towards community
oriented vocations were limited. While many institutions
we visited had increasing faculty exposure (other than
community medicine department faculty) to the realities
outside the teaching hospital this was still not on a very/
continuous or sustained basis to make an impact. The
/
51
51.
teaching of other departments.
vii) Faculty enthusiasm for high technology advances in
medicine, the super specialist ethos of medical care and
keeping up with the'western model' aspiration were high.
Hence the few faculty of community medicine departments
and the fewer faculty of other departments involved in
strategies towards social/community relevance were margi
nal to the dominant culture and in terms of attitudinal
change were working against a strongly established tradition.
Even among the innovaters their knowledge of western comm
unity oriented models and the aspirations for WHO assignments
also reflected a fallout of the same tradition. Many of the
younger faculty of community medicine departments were there
fore not sc enthusiastic about 'community based health action'
and 'community based training initiatives' but were caught up
with the 'public health specialization' aspirations towards
health management operations research, epidemiology (espe
cially clinical) health planning, health economics and so
on.
Demystification of health knowledge, training of health
workers and auxiliaries, health education and low cost
communication efforts, exploring the peoples local health
culture and traditions etc were low priority, again reflecting
the dominant culture.
viii) A reassuring finding was that the Medical Council of India
regulation was not the 'bogey' it is sometimes made out to
be. Most of the innovaters were trying out experiments
that seemed to fit in within the wide margins of experi
mentation that is already available within the existing
framework. Where major changes were made, such as block
community postings and changes in pattern of internship,
there seemed to be little problem with MCI or university
regulations. This was even less so if the college faculty
were themselves senior in the university faculty heirarchy
in their own specializations.
The two major constraints: were the division into pre, para
and clinical phases and the consequent phasing of the exami
nations; and the compartmentalization that this framework
caused.
However, it is more than obvious that for the present atleast,
if these two components of the framework were accepted as
'basic structure', there was no other major obstacle to
innovation other than established tradition and 'resistant
attitude' to change within college faculty mostly,and college
management sometimes. Infact a careful reading of the 1981
MCI curriculum guideline will indicate a large amount of
stimulus and freedom to innovate and operationalise change.
Out study of the guideline has convinced us that even the
52
52.
’pace-setters’ are still not utilising the 'stimulus'
and the freedom adequately. In a paradoxical sort of
way MCI is still ahead of most of us.
ix) Committed deans/principals and professors of community
medicine and 'critical masses' of enthusiastic faculty
were seeming to be getting over these above mentioned
internal college constraints without much difficulty
in most cases,proving that there were no structural
constraints but only attitudinal ones.
In this context,however we also found that varying
enthusiasm and commitment of the leadership of insti
tutions, and the leadership of PSM departments,al so contri
buted to phases of growth and phases of 'statusquo' or
routinization,affecting the enthusiasm of faculty and the
challenging stimulus to students. Some institutions were
not aware of innovations in their own institutions during
earlier phaseswhich we picked up through literature review.
x) The 'inspirational' and facilitatory role of community
medicine departments was well established as a major
criteria for change. The morale of the faculty and their
development as 'innovators' and inspirers of change seemed
very crucial. It seemed very important therefore to be
very selective in faculty selection for this department.
The attitudes of the interns,seemed directly proportional
to the morale of the faculty. If the faculty were enthu
siastic, outgoing, field work oriented and committed the
interns were picking up the infection. If they were
arm chair community specialists, cynical and not very
enthusiastic about community based work,the interns were
picking up the 'cynicism' and 'double standards'. The
demands on community medicine department faculty,in terms
of time, wide range of knowledge and multidisciplinary
skills are increasing day by day. Faculty who aspired for
the more limited framework and security of a paraclinical,
preventive and social medicine department,are increasingly
proving to be mismatched with the demands of an active,
clinical but community oriented/community based department
of community medicine.
Also the increasing challenge of 'converting' colleagues
from all the other departments from marginal interest in
social/community orientation to co-workers and partners
in mutually planned and organised initiatives is a major
challenge requiring an 'interactive' and 'communication'
skill of a different order. Improper faculty selection,
and even worse inadequate staff development and training,
can hamper these processes with long term consequences.
xi) Involvement of the faculty of all departments in the process
of reorientation was a great stimulus for both success,
as well asfibaintaining the continuity of change. Where
'
'critical masses' of faculty enthusiasts (beyond community/
53
53
medicine department teams) were available, initiatives,
experimentation and reflective dialogue were getting
well established. Where most of the reorientation was
seen as the primary responsibility of one department, or
was being projected as having to support one departments
training programme, or being introduced as statutory
rules of the institution - the significance of the
reorientation attempt or the enthusiasm of the faculty
was being negatively affected. Projection of programmes
as the colleges' programmes and the collective responsi
bility of faculty, as socially relevant and community
oriented medical educators, was resulting in a more
positive image and greater sustained enthusiasm.
xii) The use of faculty and student feedback (pre, para and
clinical students, interns and senior house officers)
was only gradually gaining ground, even among the
pacesetters. However this was still adhoc or research
project oriented and not a regular part of the planning
cycle. There seemed still a major lacunae in 'consumer
involvement' in medical education, notwithstanding the
fact that the 'consumer experience' within medical
college would include only 'medical college ethos' and
'teaching hospital practices' and not bring in the wider
societal/consumer needs or perspectives. Our study to
elicit feedback from medical graduates who have actually
worked out in peripheral secondary and primary health
care (living out as it were the stated objectives of
medical education in India) is therefore a first step.
While what has been said and collated is very useful,
we wish to emphasise that this too should become a
regular feature of the curriculum planning cycle, with
institutions involving alumni (who specifically live
out institutional stated goals) in the planning process.
.54
54.
H.
THE
PROJECT
PROCESS
AND
OUTPUTS
\
The project proposal and process initiated by CHC in April 1989
was basically motivated by a desire to initiate a "process seeking
collective commitment to appropriate medical education". Phase I
was focussed on a data collection, literature review and intera
ctive dialogue. Phase II was utilized for analysis/compilation of
findings as well as to initiate various steps for collective
reflection, networking, collaboration.
Therefore given the goals and objectives of the project, the output/
outcome cannot only be looked at in terms of the final publication/s
and reports but must also be understood in the totality of all the
complementary and supplementary activities that were undertaken as
part of a process of reflection, dialogue and building collective
commitment to a socially relevant medical education system during
the two years.
In this context we would like to outline four types of 'interactions'
that have emerged from the project already as part of the evolving
process and then focus on the final publication, reporting and
nature of the terminal dialogue planned as endpoint of the project
which ends in June 1992.
a) Interactions with Individual Colleges
The project led to the establishment of a credibility for the
researchers in the context of their interest and commitment
to the evolution of appropriate medical education strategies.
An important interaction of the project, therefore has been
the evolving role of the researchers as non-institutional
based resource persons for many medical college based initi
atives in the project years.
Five colleges - the four CMC's and JIPMER, Pondicherry (espe
cially through the NTTC) have begun to regularly involve the
primary researchers in some aspects of their development of
medical education innovations/initiatives.
The major events/developments falling into this category of
interactions is listed below and give an indication of the
nature and diversity of this output.
CMC - VELLORE
* Workshop on Curriculum Planning for a community based
training programme for undergraduate Medical Education
specifically for Community Medicine (CMC-V / MGR Health
University / WHO)
(January 1990)*
**
* Response to syllabus of Hospital Administration Course
as well as recent fellowship course (April 1991)
<
* Visit to COP for pre-clinical medical students and
students of allied health courses. (January 1991)
I
/
/ •• 55
55.
* Keynote address to DCHM-RUHSA Alumni Meeting and Edu
cational Council Meeting. (July 1991)
* Background materials for 'foundation course' for medical
students going into community oriented MBBS Programme,
being explored by CMC-V with Madras Christian College.
* Request for feedback/observations on CHAD after visit*
.
**
SJMC - BAKGALORE
* Discussion with junior staff who have completed rural
bond scheme to appreciate possible nature of feedback
and evolve framework of graduate survey proforma. (July
1990)
* Discussion with Medical Education Cell related faculty
of St. John's.
(January 1991)
* Participation as resource person in Group Observation
Tests during college entrance selections procedures in
July 1990 and 1991 respectively.
Late Dr. H.J. Mehta Oration on : Rebuilding Pre-clinical
Medical foundations as part of Alumni Association Jubilee
Celebrations.
(December 1991)
* Interaction and background note to SJMC study on "Basic
Skill requirement for doctors working in peripheral health
care institutions" for Consortium meeting in May 1992.
(March 1991)
CMC - LCTDHIAKA
* Request from Principal for use of mfc Anthology of ideas
and related papers as basis for proposed experimental
curriculum and request for CHC team and CHC contacts to
support CMC-L faculty in the process (there has been a
constant interaction through correspondence since then).
* Feedback and suggestions for proposed MPH type course
being considered by CMC-Ludhiana.
* Planning a 3 day Workshop/Consultation for CMC-Ludhiana
faculty to clarify their own objectives and evolve an
action plan. Due to unavoidable circumstances this could
not actually take place. (However the plan drafted for
the purpose has been modified in Appendix Q to be used
as a framework for post project interactions with colleges).
* Feedback on CMC-L Project - on Child Survival through a
slum health and development project.
56
56
MMC - MI RAJ
* Response to Miraj Manifesto and related papers and three
questions in detail :
a) What is the need to start a new medical college
institution for appropriate medical education?
b) Why should that be in the voluntary/christian
sector?
c) Should the efforts be to produce
i) an appropriate medical graduate or
ii) to take the present medical graduate and
give them 'appropriate1 PG training.
* Visit to Bombay to orient CMC-M lawyers about community
oriented medical education in the context of their writ
petition in the Bombay High Court to get state government
to give permission to start a community oriented medical
college which will emphasise primary’ health care and
problem based learning.
JIPMER - PQKDICHERRY
* Participation in formulation of questionnaire for ICMR
sponsored research project on "The Place of Primary Health
Care in Medical Education in India".
* Suggestions for WHO sponsored national workshop on Medical
Ethics in Medical Education.
* Invitation to participate in NTTC Meeting/workshop on
Management Training in Medical Education *
**
* Involvement as resource person in WHO sponsored workshop
for Training core faculty in Disaster Preparedness. (August
1991)
This 'output' and involvement has been mutually supportive, pro
viding the researchers with a lot ofopportunities for dialogue,
discussion, clarification as well as for learning and growth.
At the same time it was also an opportunity to share ideas and
perspectives that would be a 'stimulus' for the medical college
initiatives themselves.
(We could not respond to some of the requests but these have
been included to emphasise the diversity)
.57
57
b)
The Cocanunity Health Trainers Dialogue
CHC had facilitated the first dialogue among Community Health
Trainers in India in October 1988 at the request of the
Voluntary Health Association of India. Since it was the first
'coming together' of a large number of training groups, with
different backgrounds and perspectives, but with a common
commitment to Community Health the meeting focussed mainly on
sharing training experiences and identifying issues and proce
sses significant to networking. Some of the suggestions at
the meeting, including bringing out a directory of trainers
and training programmes was followed up by VHAI, New Delhi.
However for various reasons no further common action towards
sustained networking emerged.
At the suggestion of the Principal of St. John's, Bangalore
during the March 1990 meetinf of the CMC Network, we in CHC
initiated a process to organise another dialogue of Community
Health and Development Trainers. This was to collectively
reflect and respond to the draft National Education Policy for
Health Sciences (Bajaj Report), which had been circulated by
the government to medical colleges, prior to approval and
announcement. While this was not directly linked to the
'Medical Education Project objectives, it gradually became a
'supplementary initiative
*
since exploring the relevance of
the pedagogical innovations of the alternative health and
development training sector to medical education was an
objective of the project.
Our evolving links with the trainers through the letter - survey
of ideas, one of the methods used in the project, built up a
linkage and a common trust. The response to the Trainers
Dialogue on the National Education Policy for Health Sciences
held in October 1991 was very enthusiastic and encouraging.
The statement of 'shared concern and evolving collectivity *
that emerged at the end of this meeting of 28 health and deve
lopment trainers and the 'Proceedings1 have been circulated
to all concerned.
This meeting and document, and the five background papers that
were prepared in the pre-dialogue participatory planning process
provided much support and stimulus to the medical education
project itself and provided a certain cross fertilization of
ideas and perspectives. While the 'review of training metho
dologies' relevant to medical education could not be discussed
at this dialogue (even though it was part of the initial
objectives of the dialogue) the opportunity for informal inte
raction and building up interest in the idea was immense.
Networking among trainers was discussed and some plans for a
third dialogue around the theme of 'Training Methodologies' in
October - November 1992 were initiated.
The Medical Education Project did give the researchers adequate
58
58
opportunity to support and promote the networking of trainers
in India and just like the mutually supportive and interactive
processes with the CMC Network, a similar mutually supportive
process can be said to have taken place with the evolving
Network of Community Health and Development Trainers - this
being another but complementary output of the project.
c)
Participation in the Network of Christian Medical Colleges
The seriousness and regularity of the meetings of this network
is an important development. While the project team would net
claim any responsibility in the evolving dynamics of this group,
the fact remains that it has been a great opportunity to the
project researchers providing a regular forum for sharing and
dialogue. There has been a growing complementarity with the
network and the project which has links with all partners in
the network could also be seen as a common commitment.
Table XII lists out the main areas covered by the Network
meeting during the last four years.
The researchers provided a stimulus to the first meeting through
a keynote address by providing lessons from history; overview of
recent developments and listing out challenges for the network
of colleges to consider as they evolve. In subsequent meetings
however their role has been catalytic raising ideas and sharing
experiences based on grass roots, non institutionalised community
experiences as well as emphasising social/societal relevance.
Having moved beyond the medical college base in 1984 as a
conscious step towards the development of CHC and its objectives,
it has been a very welcome development tc come back full circle
and relink with institutional efforts in a spirit of partnership
and dialogue.
d)
Concurrent Publication - Stimulus for Change
An additional feature of the project was that rather than the
usual focus on the final report or terminal publication,bringing
together the process and findings of the research study, the
project tried to produce a continuous output of 'stimulus' to
the interacting and participating respondents and peer linkages.
From the 28 publications listed in Appendix - O of the report,
18 appeared and werecirculated as part of ongoing/concurrent
stimulus from the project.
i) In the pre project phase mentioned earlier three articles
>
contributed to the mfc anthology - Medical Education
/
Re-Examined were circulated to a select group of medical / ••59
59
TABLE
CMC
NETWORK
-
XVI
MEETINGS
Areas Covered in Discussion
July 1989
Lessons from History;
Overview of recent developments and challenges before
the Network (part of keynote);
Interpretative histories of each participating insti
tution and their initiatives in Medical Education;
Exploring Roles and Challenges;
Rediscovering original commitments/objectives.
March 1990
What is Christian about Christian Medical Education;
WTiat are the values/principles important tc such
colleges;
What are the implications for our colleges being
'minority community1 educational institutions;
Relationship between training and needs of member
churches.
March 1991
Ethics in Health Care;
Ethics in Clinical Practice;
Ethics in Organ Transplantation;
AIDS - implications for Christian health workers;
Formation of teachers.
February 1992
Ethics and the Doctor;
Medical College and their ethical responsibilities;
Ethics in the University teaching hospital;
Clinical ethics;
Brain death and organ transplantation;
Equitable distribution of resources;
Towards a curriculum on Medical ethics;
Decision making in ethics;
Teaching of medical ethics;
A Whitefield document - joint statement on ethics.
. .60
60.
educators to build up interest in the larger project as
well as stimulate collective commitment to appropriate
medical education. (Appendix - 0)
ii) The project proposals for Phase I and II and three
mid-term reports of November 1990, July 1991 and December
1992 were circulated to all concerned to keep them informed
of the evolving processes and responses.
iii)
4 background papers, a collective statement and a detailed
proceedings of the Community Health Trainers Dialogue on
’Education Policy for Health Sciences' was another group
of related publications drawing inspiration from the
project.
iv) A special issue of Health Action - the monthly magazine of
Health Accessories for All Trust (HAFA of CHAI, Secunderabad)
on Medical Education was planned and edited by us as part
of the concurrent communication strategy. The June 1991
issue entitled Medical Education ; Where Does it Lead brought
together not only a detailed cover story by one of the rese
archers on Training of Doctors of India (which included
subsections like the need for a 'new1 doctor; prescriptions
for change; how many doctors? the problems and challenges
before us; Innovations and initiatives within the system;
exploring new linkages; medical education and society-issues)
but also many contributions about ideas and issues identified
by the ongoing experiment. These included reflections by
medical students on a community based experiential learning
initiative at St. John's Medical College; unusual 'travel
elective' by a CMC-Vellore final year medico (S. Prabir);
reflections by a young doctor couple on the challenges of
community health vis a vis their medical education at
CMC-Vellore (Roopa & N. Devadasan); a report on Samaritan
Medicine from CMC-Ludhiana (Dr. Alex Zachariah); an article
on the history of medical education in India (Dr. C.M.Francis) ;
a note on the challenges of Continuing Education from
CMC-Vellore (Dr. Sara Verghese); an article on Medical
Ethics, Medical malpractice and patients rights by the
convenor of medico friend circle (Anil Pilgaonkar) ; a jour
nalists view of an alternative project - the Kottayam experi
ment (Anil Aggarwal); the significant declaration of the
World Conference on Medical Education of the World Federation
of Medical Education at Edinburgh in August 1988 and a
newspaper collage that represented the state of Medical
Education today.
(Appendix - R)
This issue was sent to all the medical colleges in India
of the different systems - Allopathic, Ayurvedic, Unani and
Homoeopathic, as well as to all the nursing, dental, pharmacy, veterinary science and physiotherapy colleges in the
country (totally 626). It was also posted out to all our
respondents and peers who had participated in the project
by June 1991. Because of the journalistic-semi-professional
style of this magazine, the communication effect and the
>
contribution to lobbying would have been significant.
/
61
61
v) Three meetings provided the researchers an opportunity
to present detailed papers on various aspects of the
project scope and evolving perspectives.
a) The keynote address Towards Greater Social Relevance
at the first CMC Network meeting in the pre-project
phase -was an opportunity to bring together all that
the CHC researchers already knew about medical edu
cation at the beginning of the project process.
b) The presentation on An Alternative Vision of Educa
tion for Decentralised Health Care at the workshop
on Towards a Decentralised Health Care : A fresh look
at the National Health Policy, organised in September
1990 by the National Institute of Advanced Studies was
an occasion to bring together primarily the ideas and
contributions from the emerging alternative training
sector.
c) The Late Dr. H.J. Mehta Oration at the Jubilee Cele
bration of the St. John's Medical College Alumni
Association was an opportunity to weave together all
that the project had discovered about Rebuilding
Pre-clinical Medical Foundation which became the focus
of the oration.
vi) Finally the 30th Annual Conference of the Indian Association
for the Advancement of Medical Education at LTM Medical
College, Sion, Bombay ir. January 1992 on the theme of
Research in Education for Health Sciences was a very good
opportunity for the presentation of two preliminary commu
nications by the researchers from the project - the first
an overview of the scope and objectives and premises of the
study and the second a preliminary report of the graduate
survey. These papers were distributed to all the parti
cipants and the conference opportunity was also used to
try7 out a 'self evaluation' score sheet on knowledge of
medical education innovation. (Appendix - S)
The concurrent communication strategy therefore consisted
of a special issue of magazine on Medical Education and
17 technical and process-linked articles and reports sent
to all the contacts of the medical education project •
e)
Final Publication
The plan for the final publications of the project process and
findings has been discussed at a review meeting of the Advisory’
Committee in October 1991 and has gone through several modificati ons.
X^^The main thrust and probably the primary purpose of the study
62
62
was to prepare a reference file/manual for use by 'medical
college faculty* interested in exploring 'strategies for social
relevance and community orientation'. However as the process
evolved it was felt that the key findings and perspectives
arising out of the project would have to be communicated to
decision makers, policy makers and opinion leaders motivating
them to lobby for change. So 'demand creation' and 'system
development' would have to go hand in hand.
x.
As of April 1992, the project final report was planned to consist
of a 'resource manual' as well as 5-6 other complementary publi
cations.
i) The Key to Change - the summary report of the 2 year project
will include process experience of the project, why, who, how,
where, when, what of the project, acknowledgements, key
findings and perspectives, tasks for the future and descri
ptive directory of available resources.
ii) Step by Step - Towards appropriate medical education
A compilation of CHC reflections and initiatives on medical
education before the project began. This arose out of a
suggestion by the Advisory Committee at its first meeting.
It was thought that such a compilation would help to put
the basic premises of the study in perspective.
iii) Building on rural experience : Feedback from the Periphery
A detailed report and compilation of feedback from graduate
doctors with peripheral health care experience collected
through an exploratory survey.
iv) A to Z of Medical Education in India
A bibliography and a directory of innovations, ideas and
recommendations. A decision will be taken after the
compilation is completed whether this will be a joint
publication or separate one?
v) A Faculty Resource Manual
A resource manual in a loose leaf file format w’ill be the
key end product of the project. It will bring together
information on all the strategies for community orientation
and social relevance identified from the review of Indian
experiences and the surveys. It will incorporate all the
ideas classified into 6-7 subsections which include
- Lessons from History and Culture;
- Exhorting Chage : from Bhore to draft NEPHS;
- Situation Analysis;
- Exploring Community Orientation in Medical College;
- Setting the pace for the 1990s;
/
63
- Exploring Nev; Horizons;
- Medicine and Society - Linkages
X
vi) Laying the Foundation
i) A collation of philosophy, objectives, pedagogy,
learning experiences of 10 community health and
development training centres in India.
ii) Suggested applications of above in the evolution
of foundation courses/community based learning
experience in medical college.
Since these experiments are built on an 'alternative
framework1, translating or extrapolation from them into
the irecical curriculum framework is
time consuming
though a creative task that will need to go through a
more rigorous process before it is completed. An outline
of this report will therefore emerge by the end of the
study but the task will be completed only by the next
Trainers Dialogue scheduled for November-December 1992.
All these reports are expected to be ready for distribution and
dialogue by June 1992.
f)
Towards a Collective Commitment - The Medical Educators Review
Meeting - June 1992
Since Phase II of the project ends in June 1992, the process
towards a meeting of medical educators from the CMC’s and half
a cozen other colleges in the country, identified by the project
has been initiated. The objectives of this meeting are :
1. To consider the findings/output of the CHC/CMAI/CHAI Medical
Education Project especially the Faculty Resource Manual and
discuss possible follow up within institutions.
2. To share institutional plans/initiatives in Medical Education
reform for the 1990's.
3. To explore the formation of an informal study group of
concerned individuals to carry on collective reflection
on key issues.
4. To build up a collective response to the mfc Anthology of
ideas which has been submitted by CMC-L to Punjab University
as a plan for an 'alternative track'.
The institutions involved apart from CHC, CMAI, CHAI and the
4 CMC's (the original partners of the project) are JIPMER,
Pondicherry; CMET-AIIMS, New Delhi; MGIMS, Sevagram; NHL
Municipal Medical College, Ahmedabad; Government Medical
College, Bangalore; Foundation for Research in Community
Health, Bombay; Voluntary Health Association of India, New
Delhi; WHC-SEARO; KSSP-Kerala; King George Medical College,
/
\ Lucknow and a few others.
/
64
A preparatory process has already begun with an opinion survey
among the participants on
i) Key changes to be introduced into Medical Education System.
ii) Innovations/experiments currently in practice w’hich will
help this reorientation.
iii) Critical reflections on different aspects of the mfc
Alternative Curriculum Framework.
This meeting, will symbolise a sort of 'end point' for this
two years exploratory and interactive project and will be a
good indication of the level of collective commitment that has
been stimulated by the medical education project.
. .65
65
I.
CHALLENGES
FOR
THE
FUTURE
X
Our study on 'Strategies for Social Relevance and Community
Orientation in Medical Education"- exploring Indian experience,
led us to identify a large number of ideas, experiments, inno
vations and prescriptions that could stimulate the 'content' of
change in the 1990's and which we are bringing together in the
Faculty Resource Manual, Primarily, and also in the complemen
tary publications,that are in the process of being completed.
Our field visits and interaction with peers, faculty, interns,
junior doctors, postgraduates, principals, policy makers,
academics, activists and a host of colleagues and associates
from various backgrounds have all led us to conclude that there
is an extreme dissatisfaction with all aspects of medical edu
cation - the content, the focus, the methodology, the process
and the need for action is urgently felt.
What is also evident that this action has to be part of a
multipronged effort at different levels of the system : at
policy making;at human resources planning; at administration;
governance; and organisation of medical education; at social
control of medical education; at health care service delivery
and a host of other levels as well. Curriculum change - both
content and methodology has to be an integral part of this
effort and with-in the context of the broader framework of change.
While our efforts in the study were to locate the content and
framework of the 'curriculum change' in the context of the larger
social reality, we consciously avoided getting too distracted
by the pursuit of a broader situation analysis.
In terms of the more focussed objective we set ourselves, we
would like to list out 10 factors that will promote and sustain
change and 12 factors that will act as blocks or barriers to
change within medical colleges in the 1990's. These are not in
any order of priority because all along our data collection was
purposely qualitative (interactive) and not quantitative except
for the graduate survey.
We are suggesting that all these factors both positive and negative,
are crucial. The challenge for medical college leadership for the
1990's is to promote and sustain the positive factors and counter
or minimise the negative factors.
FACTORS PROMOTING CHANGE
1. The foremost factor is, an institutional mandate and charism
towards social relevance and community orientation. This
means a management commitment to primary health care,
peripheral rural hospital service, general practice and or
community health.
The availability of defined Institutional Objectives in the
context of the mandate.
66
66
The evolution of Instructional and Department level inter
mediate objectives,keeping institutional objectives and
institutional mandate in context.
4. The presence of a critical mass of enthusiastic faculty in
a formal linkage to a medical education cell, unit, or
department which collectivises effort as well as establi
shes a continuity in the process of change.
5. The presence of a planned process of Faculty Development
and enrichment towards their role as 'medical educators'
and 'inspirers' and facilitators of change - i.e., creation
of faculty role models who are 'professionally competent',
'socially relevant', 'community oriented' and 'educationally
alive'.
6. Availability of or development of field practice areas and
health sex-vice linkages beyond the teaching hospital, where
viable, efficient and realistic community health and deve
lopment service activity is an integral part of ground
realities i.e., availability of a teaching community. Side
by side, while building the teaching community there is need
for promoting greater and greater linkages of all departments
with the teaching community - through programmes evolved by
voluntarism and creative choice and not through centralised
edicts.
7. Development of an institutional policy of staff training and
promotion in all departments which promotes/stimulates/operationalises staff experience, involvement and expertise in
service, training and research efforts, in health care,
beyond the existing teaching hospital focus and tertiary care
orientation of medical colleges.
8. A conscious value orientation and cultural transformation in
institutional ethos, management practice, staff and student
values and aspirations with increasing institutional commit
ment to social justice issues and societal/national needs.
This has to be brought about, through informal processes of
discussion, dialogue and staff/management precept i.e.,
focussing on the needs of 'Bharat rather than the elitist
aspirations of India' and the new market economy.
9. A commitment to networking and dialogue with a wide range of
groups, enthusiasts, 'experimenters' and 'innovators' within
the formal medical college system and outside of it, so that
academic environment of the medical college is allowed to be
stimulated and cross fertilised by the evolving wealth of
Indian grassroots experience i.e., towards a Medical college
without walls in its true philosophical sense.
10. A commitment to concurrent reflective, evaluation of the
change processes - (all the introduced changes, experiments
initiatives) through regular faculty and student feedback
and evaluation. This would also include regular feedback
67
67.
from all the 'consumers of medical education' especially
those who are 'living out' professionally the aspirations
of Indian medical education - the basic doctor goal.
OBSTACLES / BARRIERS TO CHANGE
The key obstacles and barriers to changes in the Medical Educa
tion system at medical college level which we would like to
highlight are :
1.
Mental Disorientation
A confusion in medical college leadership thinking about
the change process - primarily between the pursuit of
technical excellence for the sake of professional satis
faction versus the pursuit of technical excellence for
the state of social relevance.
2.
Nystagmus
Absence of clearly defined institutional and instructional
objectives leading to a continous shift in focus between
primary health care orientation and tertiary health care
orientation in efforts.
3.
Optic Atrophy
Continuing 'cultural colonialism' manifesting in the belief
system that 'what is west is best', resulting in the pursuit
of some ill defined International MBBS standard. In pract
ice it means that community needs, socially relevant issues,
local health culture and tradition and local grassroots
innovation are outside the field of vision of medical college
faculty.
4.
Aneasia
Promotion of individual professionalism in career advance
ment rather than collective institutional team work resulting
in weak individual responses to reform or unidepartmental
process.
5.
Cancer
Inadequate management planning including financial resource
management leading to an initially insidious and later
rapidly growing entry of market economy policies in private
practice policy, cost of services, prescribing and techno
logy policy in the institution.
6.
Mania-Depressive Psychosis
Planning for change far outweighing implementation of
change, leading to increasing rhetoric and simultaneous
growth in faculty cynicism or dissatisfaction. The
I
I
68
68
institution then passes through manic phases 'followed
by depression.
7. A topia - Allergy
Absence of viable and effective linkages between colleges
and 'teaching community' and health care delivery systems
beyond teaching hospital resulting in adhoc, irregular,
ill planned community exposure programmes that cause
'allergy' rather than excitement for students - in the
context of future choice of vocations.
8. Atherosclerosis
Bureaucratization and routinization of efforts so that
changes become statutory and imposed promoting an athero
sclerosis of creativity. This is also symbolised by the
absence of active feedback from students, faculty and
community to modify programmes and keep them responsive
to change.
9. Schizophrenia
The growing dichotomy between community medicine and
clinical medicine is a serious obstacle caused atleast
partially by the creation of separate preventive and
social medicine departments and forcing a rural orientation
mandate on their faculty. This has meant that while one
department pushes towards the health care challenges of
'Interior India'the rest of the departments feel psycholo
gically free to push towards the 'East Coast of USA'. This
growing dichotomy produces schizophrenia responses in
students and faculty alike.
For PSM Departments to be promoters of change rather than
obstacles - staff selection for this multidisciplinary,
skill oriented and multi-situational responsive department
must be very carefully done and PSM faculty will have to
grow into inspirers and facilitators of change rather
than 'individualistic' administrators of teaching commu
nities.
10. Craft Rejection
Caution is required in the planning and evolution of
community oriented experiments and innovations. Care must
be taken to ensure that after having learnt over forty
years, the problems of transplanting western high technology
hospital model transplants, we do not now rush into
unquestioningly accepting 'community oriented education
models that have been developed in different cultures,
health care systems and educational systems. This will
prevent costly and painful graft rejections at a later
date.
/
• 69
69.
11.
Autism
The danger of too much rhetoric and too little active
promotion of change by managements; or of discontinuous
experiments waxing and waning in intensity leads to
faculty withdrawal by the change process. Such an
autistic
response is not an uncommon feature of many
institutions including those with histories of pioneering
efforts in the past.
12. Senile Dementia
Finally the most important barrier to change is either a
commitment to status quo or an defensive response to
critical reflection and evaluation; a rationalisation of
inadequacies and a lack of openness to criticism and new
ideas setting in a senile dementia in the institution.
To reiterate the health of the medical education reorientation
effort towards social/community orientation will depend primarily
on the clinical acumen of medical college leadership in keeping
away the pathologies of :
i)
iii)
v)
vii)
ix)
xi)
mental disorientation
optia atrophy
cancer
atopia - allergy
schizophrenia
autism
ii) nystagmus
iv) anemia
vi) manic-depressive psychosis
viii) atherosclerosis
x) graft rejection
xii) senile dementia
described above from setting into the college system.
TASKS
FOR
THE
FUTURE
At the end of the study 5 key tasks come to mind in the light
of our efforts and findings.
1. Task to inform
We hope that the outputs of our study particularly the
faculty resource manual will help the process of faculty
commitment to change, by putting them in touch with the
‘inspirational stimulus' of Indian experience. All efforts
must be made to reach the multi-sectoral publication to 'all'
concerned with change in the 1990's.
2. Task to buiid further
There is need to stimulate a process within some institutions
atleast to initiate a well planned faculty enrichment/
development process towards a commitment to an alternative
experimental parallel curriculum. To start with these may
be within the existing constraints but efforts could be
initiated towards an alternative framework ultimately.
/
70
70
This task will need institutional commitment to a medical
education cell/unit or department that moves beyond
educational technology to context/process of change
as well.
3. Task to Share
The ongoing networks and fora including the CMC Network,
the consortium of medical educators and the older IAAME
need to be nudged towards a greater collective commitment,
sharing and networking process. There is need to widen
these network and fora and open them to all who are
interested and committed to change. These networks also
need to be made more open to pulling in inspiration from
the diverse sectors of experience, identified by the study.
4. Task -to Integrate
A carefully planned workshop should be organised between
the medical college sector and the voluntary training
sector to help in injecting and adapting the techniques
and insights of the letter into the thinking and methods
of the former ultimately working towards a mutually inte
ractive commitment in efforts and goals, groups with
strategic links with both sectors and commitment to cross
fertilization will have to facilitate this.
5. Task to Critically Reflect, Collectivity
All changes, innovations and experiments introduced should
be subject to critical feedback by staff, students, interns,
graduates in peripheral health care institutions, community
health project initiators, general practitioners and health
activists. This needs to move from adhoc events and research
projects to an integral part of the 'planning cycle1 within
institutions.
6. Task to Change
Finally the most urgent task is the commitment all our
energies and efforts to change itself, not for changes
sake but because the urgent health needs of our people
and our constitutional commitments towards their amelio
ration can wait no longer.
The process towards increasing social relevance and community
orientation in all our efforts will probably be the most
challenging professional tasks of the 1990's.
71
J.
SO
WHAT?
-
A REFLECTION
As we reach the end of Phase II of the project one cannot help
looking back to the nearly 30 months of a project related process
and reflect on the experience and explore some of tasks ahead,
beyond June 1992.
a) Strengths
i) Building on Multi Sectoral Indian Experiences
The first strength of the project has been a conscious
effort to build on experience from four widely divergent
sectors and attempt to study them methodically and
through orthodox and interactive approaches.
ii) Linking ongoing network in dialogue
The second strength of the project has been a planned
process to build linkages and initiate dialogue towards
an 'alternative medical education network1 with a host
of organisations, institutions and individuals e.g.,
the four CMC1s (an evolving network); the community
health and development trainers (also an evolving
network); the consortium network; groups like medico
friend circle; Foundation for Research in Community Health,
Kerala Sastra Sahitya Parishad and other issue raising
and lobbying groups; and the three coordinating agencies
of health related voluntary agencies - CMAI, CHAI and
VHAI.
The Trainers Dialogue (October 1991) and the Medical
Educators Dialogue (June 1992) are symbolic of this
process.
iii)Integrating diversity of ideas into a Faculty Resource
Manual
Keeping in mind the diversity of ideas and experiences
and even issues and viewpoints on medical education of
the different sectors of expertise the researchers have
tried to put together in a somewhat integrated fashion
a document/s that can stimulate further dialogue among
the sectors and can primarily put 'medical college
faculty' in touch with the wealth of Indian experience.
Groups of faculty committed to change can evolve a
reflection/process using the project outputs as stimulus
to their efforts.
b)
Weaknesses
i) Unrealistic Planning
In the context of the large 'canvas' and the multiplicity
of methods and initiatives,the planning of the research
team was rather unrealistic,putting a heavy burden on
72
72.
the primary researchers and the CHC team. Though the
provision for part-time research assistants was made and
some attempts to induct CHC contacts into this function
was tried out - the 'specialist' nature of the tasks and
the need to have some background about the context and
'structure' and 'situation' of medical education made it
very difficult to identify suitable research assistants
or associates. Though the advisory committee provided
good support, the peer-group linkages did not prove to
be that effective. Efforts to induct a 'medical college
faculty member' as a researcher with CHC on a sabattical
from his institution also did not prove fruitful. In
retrospect we feel a project of this nature should have
made provisions for atleast two full time research assi
stants with the requisite background and experience in
medical college teaching.
ii) From individual enthusiasm to collective action - Can
CHC foster a larger response?
Our project experience, has been that, at meetings and
in correspondence many peers, whether medical college
based, or outside the system, are enthusiastic about
the need for change in medical education and are willing
to discuss and explore new ideas. However translating
these ideas into concrete action within the existing
structure and framework is not easy especially for
individual enthusiasts. There is urgent need for a
critical masses of enthusiasts in each instituticn. This
is not easy to build up and even less easy to sustain and
a group like CHC can do little to facilitate a more
concerted process - except by facilitating
reference
publications and 'stimulus' of the type provided by the
two year process. Is more possible?
iii) Individual linkages to collective institutionalised
Linkages
- Will the process take off?
Much of the dynamics of the project has been the result
of CHC team's established personal linkages with a wide
variety of people in all the sectors of experience. These
have evolved particularly since its catalyst open-ended
facilitation work from 1984“have been built on further
during the project. Many of these persons are today in
positions of influence in decision making but the situation
is fluid and often these positions are shortlived and
incumbents change frequently, not necessarily continuing
the work initiated by their predecessors.
One of the key discoveries of this project has been that
even medical colleges, that are known for innovations,
reported in literature in earlier phases by enthusiastic
faculty members, seem to be blissfully unaware of their
own institutional contributions. Even less is known
about the experience of other institutions. There is a
73
73.
a problem of continuity and of collectivity typical
of the Indian scene.
iv) Finally for the project not to lapse into a nice
publication and meet the fate of many such efforts it
is important that we translate the end products of all the
project dynamics into the active planning/homework process
of atleast one institution in the country as soon as
possible so that :project related 'ideas' can be tested
out through praxis in the real-life situation of an actual
alternative experiment. As the project reaches thephase II
milestone we wonder whether this will actually take place.
As action researchers we are keen that the possibility of
this practical examination begins as soon as possible.
..74
74
K.
IK
COKCLUSICK
The Community Health Cell (the functional unit of the Society
for Community Health Awareness, Research and Action) initiated
the project entitled 'Strategies for Social Relevance and
Community Orientation in Medical Education - Building on the
Indian Experience1 in April 1990 with two primary goals :
The first one was to put together a handy reference
manual of local innovation, an anthology of ideas
emerging from local experience and a resource dire
ctory of local expertise in socially oriented medical
education in India.
The second one was to use the research project as a
means tc 'initiating a process seeking collective
commitment to appropriate medical education'
The first goal was pursued by a multi-pronged methodology of
literature review, letters and questionnaire surveys, institu
tional visits along with individual and group discussions which
attempted to pull together the multifaceted and multi-dimensional
experience in India and produce a set of documents that build on
the totality of the generated experiences.
The second goal was pursued by an active communication strategy,
peer group reviews and dialogue, planned meetings, opporutnistic
use of ongoing network meetings and an active correspondence.V.
V.rnile the first goal is reaching completion through a series of
project publications the second goal can be said to have been
initiated only partially, in that so many people have been
informed, involved and stimulated to think about the issues of
medical education reform.
We hope the definitive output of goal one will itself become an
instrument for goal two and take the 'initiated process' to its
logical end.
As 'action oriented' researchers we are very glad that interaction,
participation, collaboration and flexibility were the hallmarks
of the evolving experience and we along with our two chief spon
sors the CMAI and CHAI would strongly hope that this modest project
output ’painted on the broad canvas of multisectoral Indian
expertise' will be a stimulus as well as an instrument for change
towards Educational strategies for the 'new type of Health Pro
fessionals' so urgently needed to lead and give direction to the
primary health care services in the country. Moving beyond the
'philosophic rhetoric' that abounds in medical education circles
we hope that our efforts will prove meaningful and relevant to
all those (particularly faculty of medical colleges) who wish
to be involved in initiatives towards an 'appropriate medical
education' so that in the 1990's they could help to produce the
doctor' the country has been waiting for all these decades
/
75
75.
- the Social Physician of the Shore Report (1946)
and the Mudaliar report (1961);
- the Basic doctor of the Patel report (1970);
- the family/community oriented general practi
tioners with social responsibility of the
Srivastava Report (1975);
- the community oriented physician for compre
hensive health care1 of the ICSSR-ICMR Health
for All report (1981); and
- the'Community Physician* of the recent draft
National Educational Policy for Health Sciences.
Building on the diversity of Indian resources/experiences integrated
by the project, we hope the 'project1 will be a meaningful contri
bution to health humanpower development for HEA-2000 particularly
the above type of doctors.
. .76
76.
L.
ACKKCWLEDGEMEgTS
This project was a conscious effort to evolve a participatory
ano interactive research process so that the final output/s
reflected as far as possible, as large a canvas of Indian
experience and as wide a cross section of committed opinion
on the subject. In this context we would like to acknowledge
the support and participation of all those who responded to
the processes initiated by the study, and express our special
thanks to :
to the sponsors of the study viz., the CMAI and CHAI
and CMC-Ludhiana - Dr. Daleep Mukarji, Fr. John
Vattamattom, and Dr. Victor Choudhrie in particular.
* to the advisory committee of the Project : Dr. C.M.
Francis, Dr. V. Benjamin, Dr. George Joseph and
Dr. P. Zachariah.
* to the leadership and peers from the supporting
medical colleges, CMC-Vellore, SJMC-Bangalore, Miraj
Medical Centre-Miraj and CMC-Ludhiana especially
Dr. Benjamin Pullimood, Dr. B. Moses, Dr. Abraham
Joseph of CMC-Vellore, Fr. Percival Fernandez,
Dr. Alfred Mascarenhas, Dr. Prem Pais, Dr. G.D.
Ravindran and Dr. S. Pruthvish of SJMC-Bangalore,
Dr. Cherian Thomas of Miraj Medical Centre and
Dr. Alex Zachariah of CMC-Ludhiana.
* to all the medical college peers who responded to the
letter survey especially Dr. D.K. Srinivasa and
Mr. B.V. Adkoli of NTTC-JIPMER, Drs. S.C. Gupta and
Kuro. S.N. Wahab (Nagpur Medical College); Dr. Mrs.
D.D. Pandit (TN Medical College - Bombay); Dr. R. Venkatarama Raju (Rangaraya Medical College - Kakinada);
Prof. R. Gopalakrishnan (PSG-Coimbatore) ; Dr. K.J.
Nanavati (Municipal Medical College - Ahmedabad);
Dr. S.B. Dixit (Goa Medical College - Goa); Dr. K.J.
Mathew (Medical College - Kottayam); Dr. Reddy (LTM
College - Sion, Bombay); Dr. Archana Parulkar (Grant
Medical College - Bombay); Prof. R.D. Bansal (Lady
Hardinge Medical College - New Delhi); Dr. P. Koteshwara Rao (S.V. Medical College - Tirupati); and
Dr. Mrs. Rayate (V.M. Medical College - Sholapur).
* to all the medical college faculty who interacted with
the researchers during the institutional visits espe
cially Dr. M.L. Sharma (Pharmacology), Dr. Guliani (Com
munity Medicine) of MGIMS - Sevagram; Dr. Siddarth Das
(Medicine); Dr. Vinita Das (OBG), Dr. Sushma Pandey (OBG),
Dr. R.C. Ahuja (Medicine) of KG Medical College - Lucknow;
Dr. Asha (OBG), Dr. Shashindran (Pharmacology), Dr. Ananthakrishnan (Surgery), Dr. Sethuraman (Medicine),
Dr. K.R. Narayanan (PSM) of JIPMER-Pondicherry; Dr. P.S.
Sundar Rao, Dr. Molly Thomas and CHAD staff of CMC-Vellore
77
77
Dr. Prema Zachariah, Dr. B. Cowan (Medicine), Dr. M. Verma
Dr. Saha (Anatomy), Dr. Natu (Pharmacology) and other
faculty involved in evolving alternative medical curriculum
at CMC-Ludhiana; and the faculty members of the Medical
Education Cell at SJMC-Bangalore; and the adjunct faculty
of CMET of AIIMS-New Delhi; and also Drs. Narasimha Reddy
of Osmania Medical College and Dr. Ajit Kumar of Nilufer
Hospital, Secunderabad.
to all the interns of the institutions visited who inte
racted with the researchers and added a 'consumer per
spective' to the study especially Ganesh Srinivasan,
Vaibhav Bhandari and Partha Pradhan of MGIMS-Sevagram;
N.S. Bharath, Teresa Augustine, Suma B. and M.J. Vijayakumari of JIPMER-Pondicherry; Sanjeev Dayal and the
students council of 1990 of CMC-Ludhiana; and Ashish
Mahendra, Anju Goyal, S. Mukherjee of KG Medical College
- Lucknow and the interns of CMC-Vellore.
* to all the junior staff of St. John's Medical College who
having completed their rural bond scheme provided the
stimulus and framework ofor the graduate survey including
G.D. Ravindran, George D'Souza, Edward Jude, A. Mohan,
Titus Augustine, Sheila Augustine, Mario Vaz, Kenneth
D'Cruz, Ray Jude, Carlton Tavares, Hans Cyril Mathew,
Dominic Misquith, Davies C.M., Vincent Sahayaraj and
Jennifer George.
★ to the 53 respondents of the graduate survey who cannot
be named individually because of the process of confi
dential ity.
* to all our medico friend circle peers who sustained our
interest in medical education since 1984 and provided
some additional stimulus at the beginning of the study
especially Dhruv Mankad, Amar Jesani, Anant Phadke,
Padma Prakash, Sujit Das, S. Prabir, Rajesh Mehta, Anil
Pilgaokar, Ulhas Jajoor, Abhay Bang and S.P. Kalantri.
* to all the community health and development trainers who
responded to our letter survey and or participated in the
Trainers Dialogue in October 1991 including Prof. D. Banerji
(JNU), Dr. Amla Rama Rao and Dr. P.C. Bhatnagar (VHAI),
Dr. K. Pappu (CINI), Ms. Sujatha de Magry (INSA),
Dr. Rajaratnam Abel (RUHSA), Mr. Satish Samuel (SEARCH),
Vijaya Sherry Chand (Behavioural Science Centre), Margaret
and Desmond D'Abreo (ex DEED1s/ANITRA), Prem and Hari John
(Deenabandhu/ACHAN) , Jeyaraman (ambilikkai), Uma Sridharan
(THREAD), Sebastian Poomattom (ex CHAI).
to all our peers and other resource persons not mentioned
earlier including : Prof. V. Ramalingaswami (AIIMS/ICMR/WHO),
Dr. Palitha Abeykoon (WHO-SEARO), Dr. N.H. Antia (FRCH Bombay), Prof. Ashok Sahni (ISHA — Bangalore), Dr. P.V.
Chalapathi Rao (AP Health University), Prof. P. Ramachandran
(ICOR-Bombay), Dr. Siddarth Ramji (Indian Academy of Pae/
78
78.
diatrics), Valli Seshan (SCI), Dr. M.J. Thomas, Dr. Paresh
Kumar (Dept, of Sociology - Mysore University), Dr.G.Gururaj
(NIMHANS).
* to short term research assistants : Raphael Udayakumar,
S.J. Chancer and Dr. William Fullinfaw.
* to CHC team particularly M. Kumar, S. John, V.N. Nagaraja
Rao, M.S. Nagarajan, Xavier Anthony and C. James for
excellent office and secretarial support.
SECTION - B
APPENDIX - A1
CHC-GMAI-CMAI-CMC NETWORK PROJECT LINKAGES
The link up of CHC and CMAI and CHAI to give substantial
attention to Medical Education as an area of
*
interactive
health policy research evolved somewhat accidently.
♦ CMAI facilitated a meeting of the four Christian medical
colleges in the country in August 1989 (for the first
time in the history of those colleges themselves) and
invited the Coordinator of CHC to deliver the keynote
address.
The address entitled 'Towards Greater Social
Relevance 1 (CMAI Journal, Vol. VI, April-June 1991, No.2)
gave a bird's eye view of the history and development of
medical education in the country as well as the ongoing
search for relevance.
It also listed out five possible
challenges and tasks before the CMC Network, these being
to j
a)
"take stock of the achievements and initiatives of the
member colleges and their alumni and explore together
the strengths and weaknesses of these achievements and
initiative s".
b)
"move beyond the 'Christian *
experience
and learn from
the experience of all those initiatives and groups
that share a similar conmitment to patient care,
quality medical education and community health.
c)
"build a new ethos of collaboration and cooperation
amongst themselves and go beyond the histories of
competition and comparisons, by reaffirming their
shared value system and commitment".
d)
"resist the disturbing trends of politicisation and
commercialization, of medicine by continuing to
teach good quality, clinical rational medicine and
exemplifying it in their day to day institutional
practice, while at the same time searching for
alternatives and exploring new dimensions in health
care *
.
e)
"seriously explore and experiment with alternatives
in medical education as well as other health manpower
training strategies to produce professionals with
social vision, community orientation, technical
competence and emotional preparedness to serve the
needy and underprivileges in the most disadvantaged
areas of the country".
2
2
* At this meeting the CMC's shared their own plans for the
future which included the Miraj Medical Centre's
evolving project of a community based medical college
(the Miraj manifesto); CMC-Ludhiana's efforts at
evolving an 'alternative track' or 'experimental parallel
curriculum'; and CMC-Vellore's efforts at evolving a
community oriented medical education which was being
considered by the MGR Health University in Tamilnadu as
the prototype for all the Tamilnadu medical colleges.
♦ A few weeks after the meeting RN of CHC wrote to Daleep
Mukarji (General Secretary of CMAI ) on 27.9.1989
"After a long time it has been quite a stimulus to find
lots of people questioning the existing system of
Medical Education and willing to consider exploring
alternatives.
I am exploring the possibility of making
Medical Education one of the main focus of our next
year's plans.
With the three CMC's talking about changes,
with many new initiatives all over the country including
the one in the North East which you mentioned; the new
MCI bill in parliament and the possibilities of an
alternative track - I think a time has come to take a
rigorous stock of all that has been attempted by various
Medical Colleges in the last few decades in the area of
'alternative programmes' or micro level nitty, gritty of
innovations.
In addition all of us community health
trainers have in our own courses experimented with
alternative pedagogy as well as explored Health and
Development in innovative ways quite different from
orthodox perspectives in ongoing Medical Education.
All
these need to be documented creatively and made available
to the innovators of 1990’s as reference material • ••••
may be such an assignment would also be further stimulus
to the CMC Network you have initiated
.
*
* In his prompt reply Daleep Mukarji mentioned
"I was excited about the possibility of you and your CHC
team taking up Medical Education as a serious focus in
the years ahead
..... I believe we are at a critical
juncture in Medical Education in India and we can see
the different forces or pressures involved we need to
contribute to the debate and the process that can
influence MCI, the universities, some colleges etc., into
new directions and experimental models.
We also have our
own pressures with various churches wanting to start
medical schools I"..
*...... We also need to identify and record the actual
Indian experiences in innovative approaches to Medical
3
2
Education (and the education of other health professionals).
This could be relevant alternatives developed byGGovernment ,
NGC or others".
There was some further correspondence in the matter and in
February1990 CMAI circulated the following memo on the
study.to CMC-Vellore, CMG-Ludhiana, Medical Centre-Miraj
and St.John•s-Bangalore.
Extracts from letter No.GS/Nd/9O/36O
dated
February,
1990
"Dear Colleagues,
Sub:
CMAT Sponsored Study : Strategies for
Social Relevance & Community Orientation
in Medical Education.
It is our desire to facilitate a process by which the CHC
team will interact with senior staff and faculty in the
respective institutions of Vellore, Miraj and Ludhiana and
assist them and us in various aspects of medical education
in the context of Indian needs and problems.
The
researchers come with special interest and background in
this area.
I believe they would be an asset both to CMAI
and to our 3 major institutions.
It is proposed that this
project begins 1st April 1990 and will continue till March
1991.
Further details of the project are enclosed in the
background paper with this letter.
It is our desire that this be timely a participatory.
process in which both for the planning and coordination
out of the study our institutions and thqir staff are
involved.
Amongst specific outcomes that the researchers can prepare
to help us will be the following:
a)
A handy reference manual of local innovations in health
and medical education.
b)
An anthology of ideas emerging from local experience in
health and medical education.
c)
Resources directory of local expertise in
socially oriented medical education in India.
With the above it is hoped that they will also respond
to the specific needs and issues of our institutions as
they plan their medical education changes and other
techings or medical training programme.
4
I would like to take the opportunity of asking you to
take this up with the institutions and your colleagues
and let us hope that something can be worked out.
I
believe the CHC team would be able to help all of us and
through us other in India in this search for a more need
orientation in medical education within what is possible
for India".
* Some correspondence had also been initiated with CHAI,
Secunderabad and its sponsorship of the project was
confirmed by the Executive Director in May 1991 in his
letter to General Secretary of CMAI (3rd May 1991)
"At the very outset let me commit myself and assure you
of our cooperation in all these joint ventures
All the proposals are agreeable to us and the amount
will be made available in due course of time
.....................
Wishing you every success and assure you of our
cooperation always".
* The four colleges which supported the project in
addition to CMAI and CHAI
also expressed the scope of
the linkages in the following waysi
i) This letter is an SOS to you and all the team
members of the CHC to help CMC Ludhiana in this
hour of need.
In a short time we have to write a
detailed curriculum which we believe must be
community based and not just community oriented and
could use recent advances in educational technology
such as problem based learning, small group
tutorials and so on
......
It is too late to
start the experimental curriculum this year and if
we go all out from now on and with the help of
original thinkers like you and your team
I/ndhi ana could take off in starting with ten
additional students on an experimental curriculum
from 1991.
The needs of the hour is 'collective
.
*
action
Our faculty must get in touch with you
and your team as soon as possible.
(letter from
Principal, CMC Ludhiana to CHC on 19.1.1990).
ii) After discussions with the concerned persons, we
have designated Dr. Prem Pais to be the contact
person from St.John's to liaison with....(the)
project•
It is not possible for St.John's to make any
financial contribution but we will be extending
our cooperation in this project.
(letter from
Principal, S.J.M.C. Bangalore to CMAI, July 18,
1990, No.3/CMAl/5^^9/90).
5
A5
5iii ) "We would be happy to take part in the project
pertaining to general objectives A1 and specific
objectives B1 to document descript!vely/analytically the
recommendations/key experiments innovations and
experiments in appropriate medical education in India ...
Our commitments in the project would be limited to
providing the service of either the Principal or one of
the Vice-Principals as a peer group member of the project.
Unfortunately we are unable to contribute much in terms
of money in this project".
(letter from Principal, CMCVellore to CHC on 28.J.1990).
iv) I will be interested to know of further developments (in
the project).
Our own medical college project is still
on the anvil and your work will have a bearing on our
project.
(letter from Director, MMC-Miraj to CHC on
25.6.1990).
6
a6
6.
APPENDIX - A2
CHC ~ CHAI - PROJECT CONTRACT
Extracts from CMAI General Secretary's communication to CHC
of 11th April 1990 (GS/ND/90/1452).
The Medical Education Project
"CMAI accepts your project to review 'Strategies for Social
Relevance and Community Orientation in Medical Education
*
and
seeks to have you both associated with us from 1.4.1990 for
one year to undertake this assignment.
We look forward to
this process and are happy to invite CMC-Ludhiana, Miraj
Medical Centre, CMC-Vellore and St.John's Bangalore.
We
appreciate that CHAI will also be supportive and involved....
To be more specifics
I
I
methodology and budget.
a)
CMAI agrees with the aims, outlines,
b)
CMAI accepts the formation of the Advisory group and the
peer group and leaves this to you.
c)
CMAI requests three monthly progress reports.
The progress
can be shared with others (CHAI, the institutes and your
groups as above).
d)
CMAI would like to review progress, budget and participa
tion from others about Oct/Nov 1990
...............
e)
CMAI expects CHC to be responsible for accounts, reports
and progress.
f)
CMAI looks forward to joint publication, sharing and use of
the review material for wider circulation in India and
elsewhere•••••••".
7
7.
APPENDIX - B
RESOURCE PERSONS WITH WHOM THE PROJECT PROPOSAL WAS SHARED
AS PART OF INTERACTIVE PROCESS
PROJECT ADVISORS
Dr.
Dr.
Dr.
Dr.
PROJECT SPONSORS
C.M. Francis
*
George Joseph
V. Benjamin
P. Zachariah
*
Dr. Daleep S. Mukarji (CMAl)
Fr. John Vattamattom (CHAI)
Dr. Victor Choudhrie (CMC-Ludhiana)
PEERS
Dr. Benjamin Pullimood (Christian Medical College-Vellore)
Dr. Booshanam Moses (Christian Medical College - Vellore)
Dr. Alex Zachariah
(Christian Medical College - Ludhiana)
Dr. Abraham Joseph
(Christian Medical College - Vellore) ♦
Dr. Cherian Thomas
(Miraj Medical Centre - Miraj)
Dr. Kalindi Thomas
(Miraj Medical Centre - Miraj)
Dr. Alfred Mascarenhas (St.John's Medical College-Bangalore)
Fr. Percival Fernandes (St.John’s Medical Co liege-Bangalore)
(st.John's Medical College-Bangalore)
*
Dr. Prem Pais -
-
Dr. M.J. Thomas
- (Ex -St.John’s Medical College-Bangalore)
*
-
Dr. Dhruv Mankad - (Medico Friend Circle )*
Dr. Anant Phadke - (Medico Friend Circle)
*
Dr. Amar Jesani
- (Medico Friend Circle)
*
Prof. V. Ramalingaswami
(All India Institute of Medical *
Sciences - New Delhi )
Prof. S.K. Lal
Dr. Sujit K. Das (Medico Friend Circle/All India Drug Action ♦
Network)
Dr. D.K. Srinivasa (National Teacher Training Centre-Pondicherry)
*
Mr. B.V. Adkoli (National Teacher Training Centre-Pondicherry)
♦Sent written responses / suggestions.
. .8
APPENDIX
Medical education
Sir, - Medical education and its
social and community orientation
has been a subject for discussion in
India since Independence and con
cern about the inadequacy of local
efforts has been voiced in this news
paper as well.
There are definitive signs that the
1990s will see a greater commitment
to concrete initiatives for change,
since in the late 1970s and 1980s
there has been a growth of initia
tives,
recommendations,
micro
level experiments towards a more
appropriate
medical
education.
These have been by medical college
teachers, professional associations,
health and social activist organisa
tions, community health trainers in
the voluntary sector and medical
educationists and policy makers.
However, they have been inade
quately documented.
We have just started a project to
-
collate and study the key experi
ences and experiments and evolve a
reference manual of local innova
tion, a resource directory'of local
expertise and an anthology of re
levant ideas emerging from all these
experiences. We request all readers
. of this newspaper to keep us in
' touch with relevant experiments and
I ideas that have emerged in the
Indian milieu. All correspondence
may be sent to at this address: C/o
Medical Education Project, Com
munity Health Cell, 47/1, St. Mark’s
Road, Bangalore-1.
Dr. Ravi Narayan &
Dr. Thelma Narayan
Community Health Cell,
l 47/1, St. Mark’s Road,
Bangalore-1.
Source $
Indian Express
30th May 1990
Innovations in Medical Education
Over the last few decades there have been many
recommendations by expen committees and professional
groups on medical education and its community orien
tation. It is also believed that there have been a growing
number of serious attempts by some medical college
teachers and community health trainers in the NGO/
voluntary sector to experiment and initiate concrete
changes.
‘Community Health Cell’ have initiated a project to
bring together a reference manual of local innovation, a
resource directory’ of local expertise and an anthology- of
ideas on this important theme. Those who are interested
and concerned about medical education and who have
initiated micro-level change and who would like to
share their experience, are requested to get in touch
with Dr. Ravi Narayan, Medical Education Project,
Community Health Cell, 47/1, St. Marks Road,
Bangalore - 560 001.
C
Announcement
Medical Education and its social
and community orientation has been
a subject for dialogue and discussion
in India since Independence. Though
the situation at the level of integrated
practice is still far from the desired
goal, the last few decades have seen
many recommendations and some
experiments and innovations towards
a more appropriate training for
medical/health personnel. These
have been by government policy
makers, medical college teachers,
professional associations and health
and social activist organisations.
Many training experiments in the
voluntary sector also have experience
relevant to professional education.
The Community Health Cell has
just initiated a project to bring
together this process into a reference
manual of innovations in India, a
resource directory of expertise and
an anthology of ideas. The project
seeks to interact with those who are
interested or have experience
through correspondence, field visits,
focus group discussion and peer
group review.
If you or your project have
something to share on this theme,
please write immediately sending
reports, case studies, articles or other
relevant material to the following
address:
Ravi & Thelma Narayan
Medical Education Project
Community Health Cell
47/1, St. Mark’s Road /
Bangalore-560 001
Source s
Sources British Medical Journal
(Indian Edition) Vol.6
No. 8, October 1990
30 • Health Action
August 1990
9
9
APPENDIX
-
Dj
4?/1,
Mark’s Road,
St.
(First
HEALTH
COMMUNITY
Ref. No.
CHC
CELL
Floor)
Bangalore - 560 001,
Phone
: 212 313(p.p)
81:90
Date
s
Dear
Sub
Medical Education and its
Orientation - a Project.
Education and
Medical
Social
its
and
Social
and
Conununity
Community Orientation has been a
subject for discussion and dialogue in India since Independence.
Over
the last few decades there has been a gradual growth of committed
introspection and initiatives/recom.iendations towards a more Appropriate
Medical Education.
These liave been by different groups including
Government Policy Makers, Medical College Teachers, Professional Asso
ciations and Health and Social Activist Organisations.
In addition,
innovative training experiments in the voluntary health sector as well
as the non-health sector are of increasing relevance to professional
education.
The 1990s have seen a series of new initiatives and plains towards an
appropriate curriculum.
Simultaneously there have been disturbing
trends in the medical education and the health sector as well.
The project proposes to study the spectrum of key experiences developed
during the last few decades, focussing primarily on all that is signi
ficant for social relevance and community orientation of Medical Education.
The Primary
purpose
of
this project is
a.) A
reference manual
b) A
resource directory
c)
An
anthologx'
in
medical
of local
of ideas
to bring together
i
innovation
of local
expertise;
emerging from all
and
those interested
education.
If your college as a whole or any of the departments have experimented
or innovated with any aspect of medical education, please send us details
to be included in the anthology/directory.
Any publications or evalua
tions
of
the
also be very welcome.
efforts will
The one year project will adopt orthodox approaches like literature search
and questionnaires, and interactive approaches like field visits, focus
group discussions and peer group review to bring together this experience.
We
shall
keep you informed
participatory
about
the process as
soon as
we
get your
response.
The materials/coiamunications
may be
sent
to
;
Medical Education Project,
Community Health Cell,
47/1, St. Mark's Road,
Bangalore - 5^0 001.
With best wishes and
looking forward to
Yours
a prompt
reply in the
matter,
sincerely,
THELMA NARAYAN
RAVI N Al-AYAN
MD DTPh DIH
MBBS MSc(Epid)
CO-ORDINATORS
10
APPENDIX
- D2/a
Bnd REMINDER
STRATEGIES FOR GREATER COMMUNITY ORIENTATION AND
SOCIAL RELEVANCE IN MEDICAL EDUCATION
(A Compilation)
COMMUNITY HEALTH CELL
(A Health Policy Research Group)
No. 326, V Main, I Block
Koramangala, Bangalore-560034
To
The Principals and Professors
of Medical colleges and all
.Medical Educators.
ATTENTION
Participation Requested
(1)
Over the last few decades there has been a gradual growth of committed
introspection and initiatives/recommendations towards a more Appropriate
Medical Education for India.
(2)
These have been by different groups including Government Policy Makers,
Medical College Teachers, Professional Associations and Health/Social Activist
organisations. In addition, innovative training experiments in the Voluntary
health/development sector are of increasing relevance to professional educa
tion.
(3)
The 1990s have seen a series of new initiatives and plans towards an appro
priate curriculum. Simultaneously there have been disturbing trends in the
medical education and health sector as well.
(4)
The project is studying the spectrum of key experiences focussing primarily
on all that is significant for social relevance and community orientation
of Medical Education.
(5)
It is bringing together: a reference manual of local innovation; a resource
directory of local expertise; and an anthology of ideas.
If your college as a whole or any of the departments have experimented
or innovated with any aspect of medical education, please send us details
to be included in the anthology/directory. Any publications or evaluations
of the efforts will also be very welcome. The areas of experience focussed
upon are enclosed in the Appendix (Refer Bl-15)
(6)
(7)
(8)
Letters have been sent out in July 1990 and January 1991 about this project.
About 25 colleges have responded so far. We believe there is much more
relevant experience , still to be reported.
Please respond promptly - LATEST BY 1ST MAY 1991. The materials/communications may be sent to the researchers at the above address.
With Best Wishes,
Yours sincerely
rJ
cun
Ravi Narayan MD, DTPH, DIH Thelma Narayan MBBS, MSc (Epid)
FOR NOTICE BOARD
..11
11
APPENDIX - D„/n
______ ___________ *»/ -d
Medical Education Project
(A)
The final report/manual (Tentative Framework as on 1.3.91)
1. Lessons from History and Tradition
2.
3.
Exhorting change-key Policy Recommendations
Situational Analysis
*4.
5.
6.
Exploring Reorientation (Medical College experiences)
Setting the pace for 1990s (Key developments)
Building on Rural experience (Graduate Survey)
7.
8.
Laying the Foundations (NGO training experience)
Exploring New Hori sons
9.
Medical Education and Society
10. Resources for change
11. Reflecting on the process
12. The key to change - key findings and tasks for the future.
(B)
NOTE : The medical college experience in Section 4 will be compiled under
the following sub-sections:
1.
Institutional Objectives
2.
Instructional Objectives
3.
4.
Selection/Admission Criteria
Curriculum Framework
5.
6.
7.
Training base
PSM/CM Department
Pre-clinical Reform
8.
9.
Para-clinical Reform
Clinical Reform
10. Selection/Reorientation of Teachers
11. Pedagogical Reform
12. Examination Reform
13. Internship
14. Rural Bond
15. Other Initiative
(If you would like your college or department experience to be included,
please send details/reports/papers by 1st May '91)
FOR NOTICE BOARD
. .12
12
APPENDIX - E
LIST OF MEDICAL COLLEGES
(to which letters were sent)
ANDHRA PRADESH
1• Andhra Medical College, Vishakapatnam.
2. Gandhi Medical College, Hyderabad.
3.
Guntur Medical College,
Guntur.
k, Kakatiya Medical College, Varangal.
5. Kumool Medical College, Kurnool.
*6. Osmania Medical College, Hyderabad.
*7. Rangaraya Medical College,
Kakinada.
8. Sidhartha Medical College,
*9•
Vijayawada.
Sri Venkateshwara Medical College, Tirupathi.
ASSAM / NORTH EAST
10.
Assam Medical College, Dibrugarh .
11.
Gauhati Medical College,
Gauhati.
12.
Silchar Medical College,
Silchar.
BIHAR
13- A.N.Magadh Medical College,
Gaya.
14.
Bhagalpur Medical College, Bhagalpur.
15.
Darbhanga Medical College, Leheriasarai.
16.
M.G.M. Medical College, Jamshedpur.
17.
Nalanda Medical College, Patna.
18.
Patna Medical College, Patna.
19• Rajendra Medical College, Ranchi.
20. Patliputra Medical College, Dhanbad.
21.
Sri Krishna Medical College, Muzaffarpur.
GUJARAT
*22. B.J. Medical College, Ahmedabad.
23. Government Medical College,
Surat.
♦24. Medical College, Baroda.
13
13
25.
*26.
27.
Shri . M.P.Shah Medical College, Jamnagar.
Smt. N.H.L. Municipal Medical College, Ahmedabad.
Seth K.M.School of Postgraduate Medicine and
Research, Ahmedabad.
HARYANA
*28. Medical College Rohtak.
HIMACHAL PRADESH
29.
Indira Gandhi Medical College,
Simla.
JAMMU & KASHMIR
30.
Government Medical College, Jammu.
31.
Government Medical College,
Srinagar.
KARNATAKA
J2. Bangalore Medical College,
Bangalore.
33. Dr. B .R . Ambedkar Medical College, Bangalore.
34. Government Medical College, Bellary.
*
35
Government Medical College, Mysore.
36.
J.J.M. Medical College,
37.
Jawaharlal Nehru Medical College,
38.
Karnataka Medical College, Hubli.
Davangere.
Belgaum.
*39. Kasturba Medical College, Manipal.
40.
Kempegowda Institute of Medical Sciences, Bangalore.
41.
M.R. Medical College,
42.
M.S. Ramaiah Medical College, Bangalore.
*43.
Gulbarga.
St. John's Medical College,
Bangalore.
44.
Al-Ameen Medical College, Bijapur.
45.
BLDEA's Medical College, Bijapur.
46.
Kasturba Medical College, Mangalore.
47.
J.S.S. Medical College, Mysore.
14
14
KERALA
*48. Medical College,
Kottayam.
49.
Shri Chitra Tirunal Institute for Medical Sciences and
Technology,
Trivandrum.
50.
Medical College,
Calicut.
51.
Medical College,
Trivandrum.
52.
Medical College,
Mulankunnathukava.
53.
T.D. Medical College, Alleppy.
MADHYA PRADESH
54.
Gajraja Medical College,
55-
Gandhi Medical College, Bhopal.
56.
Government Medical College, Jabalpur.
57.
M.G.M. Medical College, Indore.
58.
Pt. Jawaharlal Nehru Memorial Medical College, Raipur.
59.
Shyam Shah Medical College, Rewa.
Gwalior.
MAHARASHTRA
*60. Armed Forces Medical College, Pune.
*61. B.J. Medical College, Pune.
62.
Government Medical College,
*63.
Government Medical College, Nagpur.
64.
*65.
Sangli.
Government Medical College, Aurangabad.
Grant Medical College,
Bombay
66. Indira Gandhi Medical College, Nagpur.
67. Krishna Institute of Medical Sciences,
Satna.
*68. Lokmanya Tilak Municipal Medical College, Bombay.
*69.
70.
*71.
Mahatma Gandhi Institute of Medical Sciences, Wardha.
Seth G.S. Medical College, Bombay.
Ramanand Tirth Rural Medical College, Ambajogi.
72. Dr. Panjabrao Deshmukh Memorial Medical College, Amravati.
*73. Topiwala National Medical College, Bombay.
*74. Dr. V.M. Medical College,
Sholapur.
15
15
75 • Rural Medical College, Ahmednagar.
76o Regional Medical College, Imphal.
ORISSA
77.
Maharaja K.C. Gajpati Medical College, Berhampur.
78.
Sriram Chander Bhanj Medical College,
79.
Veer Surendra Sai Medical College,
Cuttack.
Sambalpur.
PUNJAB
*80. Christian Medical College, Ludhiana.
*81. Dayanand Medical College, Ludhiana.
82.
Government Medical College, Patiala.
83^
Guru Gobind Singh Medical College, Faridkot.
84.
Medical College, Amritsar.
RAJASTHAN
*85. Jawaharlal Nehru Medical College, Ajmer.
86.
Ravindra Nath Tagore Medical College, Udaipur.
87.
Dr.
88.
Sardar Patel Medical College, Bikaner.
89.
S.M.S. Medical College, Jaipur.
Sampuma Naud Medical College, Jodhpur.
TAMILNADU
90.
Chengalpattu Medical College,
*91• Christian Medical College,
Chengalpattu.
Vellore.
92.
Coimbatore Medical College, Coimbatore.
93.
Madras Medical College,
Madras.
94.
Madurai Medical College,
Madurai.
95•
Government Kilpauk Medical College, Madras.
960
Stanley Medical College, Madras.
97.
Thanjavur Medical College, Thanjavur.
98.
Tirunelveli Medical College, Tirunelveli.
99.
Rajah Muthiah Medical College, Annamalainagar.
*100. PSC Institute of Medical Sciences and Research,
Coimbato re.
16
16
Salem.
101.
Salem Medical College,
102.
Sri Rauiachandra Medical College & Research Institute,
Madras.
UTTAR PRADESH
10J. B.R.D.
104.
Medical College,
Gorakhpur.
G.S.V.M. Medical College, Kanpur.
* 105. Institute of Medical Sciences,
Varanasi.
106. Jawaharlal Nehru Medical College, Aligarh.
*
107. King George’s Medical College, Lucknow.
* 108. L.L.R.M. Medical College, Meerut.
109.
Maharani Laxmi Bai Medical College, Jhansi.
110.
Motilal Nehru Medical College, Allahabad.
111.
S.N. Medical College, Agra.
VEST BENGAL
112.
Bankura Sammilani Medical College, Bankura.
*
113
Burdwan Medical College, Burdwan.
1 l4.
Calcutta National Medical College,
115.
Medical College,
116.
North Bengal Medical College, Darjeeling.
117.
Nilratan Sircar Medical College,
118.
R.G. Kar Medical College, Calcutta.
Calcutta.
Calcutta.
Calcutta.
CHANDIGARH
119.
Post Graduate Institute of Medical Education and Research,
Chandi garh„
NEW DELHI
*
120. AU India Institute of Medical Sciences, New Delhi.
* 121. Maulana Azad Medical College, New Delhi.
122. University College of Medical Sciences, New Delhi.
123. Lady Hardinge Medical
College for Women, New Delhi.
OTHERS
* 124.
Goa Medical College, Panaji.
125. Jawaharlal Institute of Postgraduate Medical Education
and Research, Pondicherry.
* Responded to letter.
17
APPENDIX - F
COMMUNITY
HEALTH CELL
No.326, V Main,
I Block,
Koramangala,
Bangalore 560 034.
INDIA
Ref No.CHC.
Date :
Attn : Participants of IAAME Annual Conference, Hyderabad.
January 1991
STRATEGIES FOR GREATER COMMUNITY ORIENTATION AND
SOCIAL RELEVANCE IN MEDICAL EDUCATION
an ongoing p'loje.&t (Mazich '90 - Jane. *97)
A iummany
*
Medical Education
has
a
been
and
subject
social
its
for
and
community
orientation
discussion
and
dialogue
there
have
been
in
India
since Independence.
*
During
the
last
few
decades
committed introspection, recommendations and
towards
evolving
a
more
appropriate
examples
of
new
initiatives
medical
education
responsive to the health needs of the masses in
our
country.
These have been made by different groups including Government
and
Professional
Activist
organisations
Expert Committees, Medical College Teachers
Associations.
*
More recently some Health
have
also
begun
to
offer
alternative strategies.
(1991) entitled
effort.
ments
in
and
'critical
analysis'
and
evolve
circle
anthology
1MedZcal Educatcon : Re-examined1
is one such
The medico
innovative
the
Voluntary Health
development
friend
community health
Many
non-health,
Social
sector
Sector
as
are
also
training
well
of
as
experi
in
the
increasing
relevance to professional medical education.
.18
18
(Appendix-F (Contd.)
Simultaneously,
there
also
have
been
disturbing
medical education and in the health care
Unfortunately, orthodox medical
like
IAAME
or
journals
and
educators
l.J.M.E.
like
trends
forum
a
even
focussed
have
in
a whole.
sector as
inade
quately on these experiements and issues.
A
has
project
spectrum
been
of key
to
initiated
experiences
together
bring
during
developed
decades in both the 'orthodox' and the
the
'alternative'
focussing primarily on all that is significant
the
relevance
social
Education.
who
have
A
over
and
community
orientation of
sample
feedback
from
a
two years
of
work
for
of
recent
experience
health/primary health care situations is also
the
wide
last
two
sectors
enhancing
Medical
graduates
in
community
being
collated
by the project.
The project will shift emphasis from 'traditional, empirical,
expertise' to new sectors of innovation and
have been
so
unrecognised
far
and
will
creativity which
bring
together
the
following :
Z)
*
a ne^eftence manual
local Innovation,
11)
a neiou'tce dlnecto>iy of, local ex.pe'itlie, and
ZZ2)
an anthology of Ideai emerging f^om all thoie who
an.e Inteneited tn medical education and health manpower
training.
The
project will
also
formulate
a
curriculum
a proposed pre selection, community health
tion
course
for medicos,
to introduce in the 1990s.
also
be
relevant
for
which
some
Components
community
based
outline
oriented,
for
founda
like
colleges
would
of
course will
this
teaching
within
the
existing MBBS Courses.
19
19
(Appendix-F(Contd. )
fifteen month
The
project
is
adopting
orthodox
approaches
to research like literature review, letters and questionnaires
as well as
group
Interactive
discussions
and
approaches
like
peer
review
to
bring
together
by
Community
Health
group
field
visits,
focus
a large and varied experience.
The
project
Cell,
is
being
Bangalore,
Research
a
coordinated
professional
Community
Health
with
the
Voluntary
Health
Sector
by
CMAI,
few
collabo
group working
in India and is
the
supposed
CHAI
and
a
Policy
rating medical colleges in the country. An advisory committee
and a peer group are also supportive of the process.
/YOUR PARTICIPATION/CONTRIBUTION IS REQUESTED/
*
IF
VOUR INSTITUTION/DEPARTMENT/CENTRE hat
undentaken
any
expenEjnentatEon/exencdte
■in MedicaE Education towandi
gneaten
communEty onEentation and tocEaE neEevance,
pEeate contact ut EjnmedEateEy wEth copEet
of, nepontt/papent, pubEEthed on unpub tithed.
We ane focuttEng on concnete fEeEd and
cEattnoom expenEence and not adhoc, untetted
tuggetiEont.
RetuEti 0/ ttudEet on nepontt of evaluated
expenE mentt; Repontt
of
changet/nefonmt
Entnoduced En the cunnEcuEum; InnovatEve
appnoachet to tnaEnEng; and Concnete changet
pnopoted even though onZy unden contEdenaiEon
ane aEE weZcome.
*
PROMPT RESPONSE BEFORE FIFTEENTH MARCH 1991
WOULD BE APPRECIATED
FOR
INCLUSION
IN THE PROCESS OF COLLATION.
For all further enquiries and correspondence,
Please contact :
Dr.Ravi Narayan/Dr.Thelma Narayan,
Medical Education Project,
Community Health Cell,
326, V Main Road, I block,
Koramangala,
BANGALORE 560 034.
20
20.
47/1 St. Mark's Road
(First Floor)
COMMUNITY
HEALTH
CELL
Ref No. CHC /81/90
Bangalore-560 001
Phone : 212313 (P.P)
Date :
06.10.1990.
NGO Community Health and
Development Trainers,
Dear
,
Sub
: Medical Education and its Social &
Community Orientation - A Project.
Medical Education and its Social and Community Orientation has
been a subject for discussion, dialogue and experimentation in
India since Independence. Over the last few decades there has
been a gradual growth of committed introspection and initiatives/
recommendations towards a more appropriate Medical Education.
These have been by different groups including government policy
makers, medical college teachers, professional associations and
health and social activist organisations. In addition, innovative
training experiments in the voluntary health sector as well as the
non-health sector are of increasing relevance to professional
education.
The 1980s have seen a series of new initiatives and plans towards
an appropriate curriculum. Simultaneously there have been disturbing
trends in the Medical Education and the health sector as well.
The project proposes to study the spectrum of key experiences
developed during the last few decades, focussing primarily on all
that is significant for social relevance and community orientation
of Medical Education.
The primary purpose of this project is to bring together :
a) A reference manual of local innovation,
b) A resource directory of local expertise, and
c) An anthology of ideas emerging from all those interested
in medical education.
In this context we are particularly keen to study the alternative
Community Health Training and Development Training experience in
the Country and extract whatever is relevant, so that it can be
incorporated into the framework of the alternative curriculum.
We in the NGO sector have had the freedom to plan and organise
our own training orogrammes, concretely basing it on the needs
..21
COMMUNITY HEALTH CELL
21
and dynamics of Community Health as we experience it at the field
level. There was no problem of control or accreditation, central
supervision, history, peer group opposition or ’any of the other
problems that innovators within the system experience. There are
many other features that make the NGO training initiatives significant.
They do not cater to medicos only but are available to all health
action initiators. Many are focussing on development activists
as well. host of us have used participatory, interactive and
community based approaches. Most of us have evolved case studies,
field exercises, simulation games, group exercises and various
other types of programmatic and pedogogical innovation.
We are very keen to review all this. You will be glad to know
that some medical colleges with whom we are in touch are considering
the possibility of a years foundation course in 'Community and
Social Orientation’ for all their entrants so that a substantial
value reorientation can take place even before the medicos move
into the formal course. This foundation course would be autonomous
of the University and would therefore be able to include any innovative
idea/methodology you have developed to help with this value/experience
orientation. There is also a move to radically alter the professional
course itself but this foundation course itself is a very significant
development. We are convinced that the wealth of experience of
alternative health and development trainers will be particularly
relevant to this course.
We therefore earnestly request you to send us information covering
as many of the following areas as possible :
a) Outline and content of your training programme,
b) Objectives and methodology,
c) Methods of selection of candidates and of evaluation both
concurrent and terminal,
d) An outline of innovative exercises, field projects, case
studies, games or other group based and community based
methods which you employ. Even if these were not developed
by you, please send them all the same mentioning the source
or reference,
e) A detailed report of any one complete training programme
in recent years,
f) Any papers you have written on your course,
g) If your team has had any reflections on methodology of
training or evaluated your own methods this would be
welcome,
h) Finally through your training efforts you must have also
developed some perspectives relevant for the modification
of formal medical/nursing/para medical education, please
send us these as well.
We A^ve begun to build resource files on each of the NGO training
centres/courses from the material we have collected over the years.
However we would like your active participation to bring it upto date.
22
COMMUNITY HEALTH CELL
22
All materials included/mentioned in the final project report will
give due credit to source (whether published or unpublished). The
focus of this section will be to make the medical educators,aware
of all the efforts in Community Health training which could be
incorporated into their programmes.
We do not know whether you are aware that a National Education
Policy for Health Sciences has been formulated and is presently
being circulated all over India for comments, suggestions and
modification. Not surprisingly it completely ignores the contribution
and the perspectives of the NGO trainers. The Bajaj Report as it is
called needs our urgent consideration and all of us individually or
in groups should respond to its formulation and send our contribution
in the context of our own experience. If any of you are interested
to get a copy of the draft report, please write to us immediately.
If you send a response to the government on this we would like to
have a copy for record. A joint response would have helped to
ensure that we are not ignored in the future, but this may not be
easy to organise now.
The materials/communication may be sent to Medical Education Project
(Community Health Cell), 326, V Main, Koramangala I Block,
Bangalore - 560 034 (Attn. : Ravi/Thelma Narayan). We would be glad
if it could be sent before the 1st of November '90.
With best wishes and looking forward to your response,
Yours sincerely,
Ravi & Thelma Narayan,
Co-Crdinators.
P.S.
:
We enclose copies of some appendices of our project
outline which will give you an idea of the scope and
focus.
. .23
23
APPENDIX
-
H
Alternative Training Sector
Community Health and Development Trainers Contacted for Study
Stat e
Community Health
Trainer
A. Andhra Pradesh!.
B.
Gujarat
*2.
Development Trainer
—
Catholic Hospital
Association of
India, Secunderabad
CHETNA, Ahmedabad
1.
Behavi oural
Science Centre,
Ahmedabad.
C. Karnataka
3. International Nurses 2.
Service Agency,
*3o
Bangalore
4. st. John’s Medical
4.
College, Bangalore
5. NIMHANS, Bangalore
SEARCH, Bangalore
Indian social
Institute,
Bangalore
Institute for
Cultural Research
and Action,
Bangalore
D. Maharashtra
6. Institute for Rural
Health Management
- Pachod
*7. Comprehensive Rural
Health Project Jamkhed
Trace Team,
Nandurbar
E. New Delhi
Voluntary Health
*6 c Indian Social
Institut e
Association of
India
9. Jawaharlal Nehru
University - Dept.
of Social Medicine
& Community Health
10. Christian Medical
Association of India
F.
Orissa
G. Tamilnadu
Ho West Bengal
5.
8.
*11o Thread
12. Deenabandliu Trai
ning Centre Deenabandhupuram
13. Rural Unit for Health
and Social Affairs,
Karur
*14. Christian Fellowship
Community Health
Centre, Ambilikai
150
Child in Need
Institute, Calcutta
*No response to project letter but CHC Documentation Unit
had material on courses.
..24
24.
1
f
APPENDIX - I-a
SALIENT FEATURES OF INSTITUTIONAL VISITS
Christian Medical College - Ludhiana (February 1990)
1. Discussion with Faculty interested in Medical Education.
"
2. Discussion with Student Council.
1
3. Discussion with PSM Faculty.
j|
|
Mahatma Gandhi Institute of Medical Sciences,
Wardha(Augus t 90)
1o Discussion with some Faculty.
2. Discussion with interns group.
3. Discussion with PSM Professor.
J
I
King George Medical College - Lucknow (October 1990)
1. Discussion with a joint faculty/student group.
Christian Medical College - Vellore
1. Visit to fre-clinical Community Orientation Programme.
2.
|
(December 1990)
Discussion with some faculty.
3« Discussion with interns group.
Jawaharlal Institute of Postgraduate Medical Education and
Research, Pondicherry.
(January 1991~J
1.
Visit to NTTC, Rural field practice area and Urban field
practice area.
2.
Discussion with some faculty interested in Medical Education.
3.
Discussion with interns group.
4. Discussion with PSM faculty.
Ail India Institute of Medical
1.
Sciences, New Delhi(April 1991 )
Discussion with adjunct faculty of Centre for Medical
Education Technology.
St. John's Medical College, Bangalore
1.
Discussion with Junior staff with rural expert.ence(July 90).
2.
Discussion with faculty members of Medical Education Cell
(January 1991)
25
25.
APPENDIX - I-b
MEETINGS LINKED TO PROJECT
Project Related
1. Peers meeting,
Bangalore (July 1990).
2.
Graduates -with Rural Experience (November 199O)„
3.
Community Health Trainers Dialogue - Bangalore(October 1990).
4. Advisory Committee Meetings.
Complementary
1.
CMC Network Meeting
2. CMC Network Meeting
I (August 1989 )
II
(March 1990)
3.
CMC Network Meeting III (March 1991 )
4.
CMC Network Meeting
IV (February 1992)
Other s
1. NIAS Health Policy Workshop (September 1990)
2. IAAME Annual Conference
3.
(January 1992)
Annual Conference of Indian Association of Physiologists
and Pharmacologists (December 1991)
. .26
26
APPENDIX - J
CODE FOR MEDICAL COLLEGES INCLUDED IN PROJECT REPORT
QUsed in Tables}
'Pacesetter1 Colleges
Christian Medical College - Vellore
-
1
All India Institute of Medical Sciences - New Delhi
-
2
St.John’s Medical College - Bangalore
-
3
Jawaharlal Institute of Postgraduate Medical Education
and Research - Pondicherry
-
4
Mahatma Gandhi Institute of Medical Sciences - Sevagram
-
5
Christian Medical College - Ludhiana
-
6
Rangaraya Medical College - Kakinada
-
7
Sri Venkateshwara Medical College - Tirupathi
-
8
Other Colleges
Smt. N.H.L. Municipal Medical College - Ahmedabad
-
9
Baroda Medical College - Baroda
-
10
Rohtak Medical College - Rohtak
-
11
Kasturba Medical College - Manipal
-
12
Kottayam Medical College - Kottayam
-
13
Armed Forces Medical College - Pune
-
14
B,J< Medical College - Pune
-
15
Government Medical College - Nagpur
-
16
Grant Medical College - Bombay
-
17
Lokmanya Tilak Municipal Medical College — Bombay
—
18
Ramanand Tirth Rural Medical College - Ambajogai
-
19
Topiwala National Medical College - Bombay
-
20
Dr. V.M. Medical College - Sholapur
-
21
Dayanand Medical College - Ludhiana
—
22
J.L.N. Medical College - Ajmer
-
23
PSG Institute of Medical Sciences & Research - Coimbatore-
24
Institute of Medical Sciences - Varanasi
-
25
k-ing George Medical College - Lucknow
-
26
Maulana Azad Medical College - New Delhi
-
27
Lady Hardinge Medical College for Women - New Delhi
-
28
27
27
Goa Medical College
- 29
L.L.R.M., Medical College - Meerut
- 30(n)
Thanjavur Medical College - Thanjavur
- 31
Osmania Medical College - Hyderabad
- 32
Government Kilpauk Medical College - Madras
- 33
Others
Consortium
-
Medical Council of India
— 35
28
28.
APPENDIX - K
Medical College Initiatives(with college code)(refer Appendix j)
A o General / Structural / Process
01. Defining Institutional Objectives (1,2,3,5,6,9)
02. Defining intermediate (Departmental and
instructional objectives
(1,2)
03• Development of Medical Education Cell
with adjunct faculty
(2,3,4,6,9,12)
i)
ii)
iii)
Conducting workshops
Evolving objectives;
Developing MCQ banks, etc.
04. Faculty Training/Development
i)
ii)
iii)
iv)
v)
vi)
05.
(1-4,6,9,12,15)
Educational Technology
Problem based learning
Tutor training for PBL
Assessment / Evaluation technique
Research
Self learning methods.
Selection Procedures other than Academic merit (3,1)
i)
ii)
Psychological tests
Group observations on social skills/
values orientation/motivation
iii) Problem solving abilities
iv) Leadership skills.
06• Curriculum development / content
through curriculum planning committee
i)
ii)
iii)
Integration of teaching
Identifying core abilities / skills
Prioritization of topics within departments
(9)
(3.25)
(9)
07. Examination Reform
Objectivised assessment
OSPE / OSCE
ii) Restructuring assessment towards
HFA-PHC
i)
(2 '
(4'
..29
29
08.
Faculty / student involvement in Medical
Education Reform
i)
ii)
iii)
iv)
v)
vi)
Faculty survey - curricular
deffici encie s
Student survey - curricular
defficiencie s
Intern survey - curricular
defficiencie s
Department programme evaluation
students
Department programme evaluation faculty
Self Assessment by faculty
09. Tutorial system for student support
counselling, development
(1,2,4,6)
,1,2)
*
(
)
*
(
(1)
(6)
(6)
(6)
(1.3 )
10.
Students Electives — during clinical years(l,3)
11.
Student involvement in Research
Pre/Para/Clinical phases
( 1 , 3,7 )
12.
Regular Faculty Meeting (inter and intra
departmental) and Faculty-students meetings (9)
13•
Student nurture pro gramme s
Curriculur/cocurricular activities
including NSS/NCC.
14. Rural Bond Scheme
(1-6,7)
(1,3)
Placement in peripheral/rural hospitals
for 2 years post-internship experience.
ii) Preference for RBS candidates in PG
selections.
i)
15• Continuing Medical Education
( 1 ,3 )
Programme for alumni/graduates especially those
in general practice or small peripheral hospitals
and health projects.
B. Pre-clinical phase
16. Foundation Courses for entrants
i)
Community oriented - Gandhian Philosophy
and values course-self help, dignity of
labour, simple living, etc.
Study skills course - Group dynamics,
Educational Objectives, Tests for learning
skills, communication reading skills,
History of Medicine, National Health Policy.
iii) Foundation Course - Group dynamics, Team
concept, linkages between basic sciences and
health care, self directed learning
communication skills, value based education.
ii)
(5)
(21)
(l)
• -3o
30.
17. Community Orientation Programmes (Rural)
1)
ii)
ill)
iv)
v)
vi)
COP - 3 weeks block posting
ROP - 2 weeks rural camp
Social Service Camp - 2 weeks
COTP - 2-3 weeks
Post COP/ROP knowledge attitude evaluation
Involvement of preclinical faculty (nonPSM)
18. Introduction of additional
i)
ii)
iii )
iv )
Behavioural
Ethics
First aid
Nursing
1 )
3)
5)
(24)
(1,3,24)
(1,3)
S
subjects
Sciences
(1,3,24)
(3)
(3 )
(3)
19. Clinical orientation in preclinical phase
i) Implementation of MCI 1982 guidelines
ii) As an adjunct to preclinical teaching
20. Humanization of Physiology/Biochemistry practical^(1,2)
21.
Samaritan Medicine - to make students attentive
listeners, compassionate and skilled in
interpersonal relationships (visiting patients
and their relatives in hospital)
22. Multidisciplinary student teams training in
urban slum setting
(urban equivalent of COP)
(6)
(6 )
C• Para-clinical Phase / Teaching
23. Reorienting pharmacology Training
24.
i) Instructional objectives
ii) Human experiments
iii) Orientation to Rational Drug use and
Essential Drug Concept
iv) Clinical orientation
(15)
(15)
Synchronization of Theory lectures
in Medicine/pharmacology/pathology
(9)
25• Involvement in Integrated Teaching
(1,3,4)
(5)
(8,29)
i) integrated seminars
ii) clinico-pathologlcal-social conferences.
D. Community Medicine
26. Family care programme — community based
1) Family care programme (rural) 1st year
till internship
(5,13,20)
• •31
31 .
ii) Family care practice (Urban) throughout
(2)
studentship
iii) Family Health Advisory Service in 4th year
Three week family study + one week clinico- '2B'
social case review.
27.
Community Block Posting (first clinical year)
CHP-I-block posting in first clinical year
(l)
to be exposed to Epidemiology, Health
planning, health administration and national
health programmes(Health Planning exercises)
ii) Community Diagnosis Camp 2nd clinical level
(24)
i)
28.
i)
29.
12 weeks urban health centre posting.
Special focus training programmes in
i)
ii)
iii)
iv)
v)
vi )
vii)
30.
(2)
Junior clinical clerkship in Community Centre
Epidemiology and statistics
(1,2,3,28)
(through problem oriented teaching methods)
Health Education methods and preparation
of HE aids
(20)
Clinical Epidemiology
(1)
Health Economics
(l)
Managerial skills
(1,4,34)
Integrated Health team
(1,6,34)
Orientation to other systems of medicine
(3)
Rural/urban slum health trips to peripheral centres (7)
(Health Education/minor ailment care/MCH motivation/
referrals).
31-. Community block posting in 2nd clinical year
i)
32.
CHP-II for learning experiences in
epidemiological studies, evaluating national
health and development programmes at
periphery, organising health education.
Senior clinical clerkship in Community Centre
i)
( 1 )
(2)
Posting in rural health centre/sub centre
in second clinical year.
33. Epidemiological/Public Health Research Projects
(13)
for Final M.B.B.S students.
•*32
32.
Ko Clinical Phase / Teaching
34. Integrated. Teaching (inter departmental - coordination )
Medicine synchronised with Pathology and
Pharma co lo gy
ii) PSM/Paediatrics/Obst. and Gyn. integration
iii) Special focus integration courses/seminars
i)
a)
b)
c)
d)
e)
( 9)
(20)
Human reproduction, FP and population
dynamics
Human sexuality and FP
Epidemiology and control of TP, leprosy,
smallpox, preventable blindness.
MCH, FP, and School Health
Integrated leprosy course
(8)
(16)
(29)
(29)
(35)
35• General Out Patient Department for training in
. general practice and primary health care -Run by CM Department - coordinated with Medicine/
Surgery/Paediatrics/Obst. & Gyn.
i) G.O.P.D. Programme
ii) Curative/preventive general practice unit
(CPGP)
36.
(5)
(1O)
Clinical clerkship in Primary Departments
i) Posting in Obs. & Gyn. Department
(all colleges)
ii) Student clerkship in Medicine/surgery
Paediatrics
(1,34)
37.
Training in Emergency care / Medicine
38.
Community visits/programmes by clinical departments
(4)
Field visits by OBG department for family
welfare motivation and services
ii) Specialist camps in field practice areas
(diagnostic and surgical)
i)
39.
(7)
(1,3,5,7)
Reorientation of Medical Education(ROME ) Scheme of GOl(3,13,29)
First year till internship-graded exposure
and responsibilities
ii) Two month posting in 2nd/jrd clinical year
(13)
(29)
Inter departmental coordination in clinics in
Hospital programme itself
(1 1 )
i)
40.
i) Antenatal/postnatal clinics
ii) Under five clinic/well baby clinic
iii) Immunization clinics
iv) Family Welfare Programme
v) Health Education in Hospitals
vi) Hospital extension services to neighbourhood.
• -33
33.
41 . Peripheral Hospital Posting
i) Posting to small peripheral mission hospital
(1)
for a month during vacation in pre final year.
F. Internship
42 . Interns Orientation Programme
i) Integrated orientation programme
(doctor patient relationship , Rationa1 drug
prescriptions and investigations, medical
records, medico legal aspects)
)
(*
ii) Interns Orientation Programme
(Hippocrates Oath, At ti tud es-relation ship
building, Diagnosis and treatment within
re source/knowledge updat e/re search )
(17)
43. Community Health posting in compulsory rotating
internship 3-6 months
i) Three months posting with specific objectives
ii ) 6 months b 2 months GOPD + 2 months PHC +
2 months sub centre
iii) Village based CH clinics in batches of 2
iv) 6 months - CH internship in 2 week units
v) Internship detailed guidelines for posting
(1)
(5)
(j)
(17)
(l,3)
44. Community based camps and clinics with clinical departments
(interns accompany clinicians)
i) Departmental Scheme in coordination with PSM (1,3,5,15)
ii) ROME scheme
(13,29)
iii) Mobile Rural Hospitals scheme
(11)
45• Interns posting experience at Government
Primary Health Centre and sub centre
i) Orientation to functions / organisation
ii) Orientation to work of specific team member.
46. Involvement of Interns in special situations
i)
ii)
iii)
iv)
Epidemic control
Disaster relief
Plantations
Voluntary Health Projects
(3,9)
(9)
(3)
(3)
(3)
47. Involvement of Interns in training of Primary Health
Care workers
(3,13)
. .34
^8. Interns Training in specific skill areas
i)
ii)
iii)
iv)
v)
vi )
Rational Drug concept and essential drug use
Management skills
Ethics
Health Education skills
Epidemiological projects
Clinical research (elective)
4
4
1,3
20)
3)
49. Internship training in special clinics in Hospital
situation
GOPD
{ for general practice
CPGP Unit
Q orientation
ANC/PNC/Family Welfare clinic
Under five clinic/lmmunization clinics
50. Internship Assessment / Evaluation
(11,17)
(12)
(1,3,8)
35.
APPENDIX - L
PROJECT SCHEDULE
- I
(Based on Actual Experience)
Pre-Project phase
>
(February 1989 till March 1990)
February - March 1989
Completion of two additional articles for mfc anthology Medical Education Re-examined
i)
ii)
Recent initiatives towards an alternative;
Anthology of ideas - the framework of an alternative . (Compila ti on) .
April
1989
Meeting with Dr. P. Zachariah at CHC (with CHC contacts) on the
Miraj Manifesto for an Institute of Health Sciences at Miraj
for Appropriate Medical Education.
July 1989
The mfc articles and alternative framework sent to CHC
advisors, CMC-Vellore and NTTC-JIPMER, Pondicherry, and others.
August
1989
Keynote address : Towards Greater Social Relevance in Medical
Education, at the first meeting of the Christian Medical
College Network facilitated by CMAI.
September 1989
A detailed CHC response to the
’Miraj Manifesto’.
November 1989
Draft Medical Education Project proposal formulated and sent
to two ’referees’.
January 1990
SOS from CMC-Ludhiana to CHC to assist them in their
initiatives towards an experimental parallel curriculum.
ii) Medical Education Project proposal sent to CMAI sponsorship.
i)
February 1990
i)
Letter from CMAI to CMC•s about project proposal and
i n~i ti ution to support/participate (see Appendix Aj j
ii ) visit to CMC-Ludhiana and interaction with management
faculty and students on proposed initiatives.
iii) Invitation and Medical Education Project proposal sent to
Advisory Coimnittee members.
March 1990
i) Second meeting of the Christian Medical College Network
and sharing of evolving project plans.
ii) Project proposal sent to CHAI for sponsorship.
36
PROJECT SCHEDULE
Phase I I
- II
(April 1990 till June
1991 )
1990
April
1) CMAI sponsorship confirmed (Appendix
ii)
iii)
CMC - Ludhiana sponsorship confirmedo
Literature review initiated.
May 1990
i) First Advisory Committee meeting to finalise objectives
and methodology<>
ii)
Letter to bulletins / journals / press (Appendix C).
July 1990
i) First letter to
ii)
Local
August
iii)
).
'peer' group meeting held on evolving project.
1990
i) Visit to MGIMS,
ii)
125 Medical Colleges sent (Appendix
Discussion with
Sevagram .
’medico friend *
circle
peers.
Meeting with junior faculty of St.John’s Medical CollegeBangalore, who have completed rural bond - to evolve
graduate survey forms (RBS Staff).
September 199°
NIAS National Workshop on ’National Health Policy - Towards a
Decentralised Health Care
.
*
(Paper on ’Educational Perspectives’
presented).
October 1990
i) Letter to Community Health and Development Trainees sent
(Appendix G).
ii) Visit to King George Medical College - Lucknow.
iii)
Project Advisory Committee Meeting.
November 1990
i) Graduate survey proforma evolved in a participatory way
with RBS staff (Appendix l).
ii) pilot testing of proforma.
iii)
First project report sent to all concerned.
December 1990
i) Graduate survey forms distributed at post-graduate
entrance exams at St.John’s Medical College-Bangalore.
•37
31
ii) Request to other institutions/network to identify
potential respondents»
iii)
Visit to CMC-Vellore and RUHSA-Kavanur.
January 1991
i) Discussion -with St.John's Medical Education Cell.
iii)
Letters with enclosures sent to IAAME annual Conference
participants in Hyderabad (Appendix F).
iii)
First reminder sent to all medical
re sponded.
colleges who had not
iv)
Visit to JIPMER - Pondicherry.
v)
mfc-Anthology 'Medical EducationiRe-examined' published
and some lobby work initiated.
February 1gg1
Discussion with A.P. Health University Coordinator.
March 1991
i) Project Advisory Committee.
ii) Third meeting of CMC Network.
(paper on mfc Alternative framework as well as initial
findings of graduate survey presented).
iii)
Discussion with Department of Community Medicine (Osmania
Medical College) and Social Paediatric Unit (Nilufer
Hospital) in Secunderabad.
iv)
Second reminder sent to all medical colleges (Appendix Dg)
*
April 1991
i) Visit to Delhi for discussion with
a) CMAI;
bj WHO-SEARO Medical Education Unit;
c) Prof. V. Ramalingaswami, Professor, Emeritus, AIIMS.
ii) Visit to AIIMS and interaction with CMET adjunct faculty.
iii)
Community Health Trainers Dialogue - background work
initiated including opinion survey.
iv)
Phase II project proposal formulated and sent to CMAI
and CHAI for approval.
v)
Resource in Community Health Trainers training in programme
organised by CSI Ministry of Healing.
May 1991
Second Project report sent all concerned.
June 1991
Special issue of Health Action (monthly magazine of HAFA TrustSecund erabad) on Medical Education facilitated by us.
(Theme 1 Medical Education - Where does it lead?).
-x-x-x38
38.
PHASE - II (July 1991
- June 1992)
July 1991
1) Visit to Bombay to brief lawyer for MMC-Miraj's writ
petition on Comniunity Oriented Medical College application.
ii) Project data analysis and compilation started.
iii)
September 1991
i) Three chapters of Project Manual sent to Advisory Committee
for review.
ii) Response sent to CMC-Ludhiana’s project on Child Survival
through a slum Health and Development Project.
October 1991
i) Project Advisory Committee on review of four initial
chapters•
ii) Community Health Trainers Dialogue on ’National Educational
Policy for Health Sciences'.
November 1991
Advisory Committee review meeting minutes and summary circulated.
December 1991
i) Late Dr. H.J. Mehta Oration at St.John's Medical CollegeBangalore, on the theme 'Rebuilding Preclinical medical
foundation'•
ii )
'Medical Education
*
Seminar at Annual Conference of
Association of Physiologists and Pharmacologists of India,
Bangalore Medical College.
January 199
*
i) Third project report
circulated.
ii) Preliminary conmunications presented at 30th Annual
Conference of IAAME at LT Medical College, Sion, Bombay.
iii)
Visit to Delhi to discuss Medical Education Project follow
up with CMAI, WHO-SEARO, CMET-AllMS,
-Meeting with Prof. V. Ramalingaswami and Dr. Mohan GargCED Til in-i o« (consortium Consultant).
••39
39
February 1992
Fourth meeting of Christian Medical College Network,
Theme t Ethics in Medical Care and Ethics in the medical
curriculum.
March 1992
i) Compilation on basic skills in medical education from
Graduate Survey for SJMC research project.
ii) Preliminary planning process on Medical Education Review
Meeting initiated.
April - June
1992
i) Work on final reports and manual.
ii) Opinion survey of Medical Education review meeting
participants on ‘Medical Education Innovations’ and
•collective response to ntfc alternative curriculum
*
initiated.
iii)
Background papers for Medical Educators Review Meeting.
June 1992
Medical Educators Review Meeting to consider findings and follow
up of project.
CMAI / CHAI sponsored project ends.
. . 4o
40.
APPENDIX
-
M
AN CVEKVIEF OF THE FINANCIAL SUPPORT FOR THE PROJECT
1. Total Project Outlay and Partnership in funds
Phase I
April 1990
to June 1991
Phase II
July 1991
to June 1992
Phase II
Additional
Rs.
Rs.
Rs.
C.M.A.I.
90,000/-
30,000/-
75, 000/-
C.H.A.I.
60, 000/-
60,000/-
75, 000/-
C.N.C.-L
30,000/-
——
—
C.H.C.
32,400/-
—
——
2,12,400/-
90,000/-
1', 50,000/- *
Contributors
TOTAL
* This includes support tofor C.H.T. Dialogue
and Pc. 50,000/- for publications.
her Meeting
..4l
4l
APPEKDIX - N
(Contd.)
2. Break-up of Total Outlay
Head of Account
Phase I
Apr. 90
to
Jun. 91
Phase II
July 91
to
June 92
Total
April 90
to
June 92
Percentage
Rs.
Rs.
Rs.
%
1) Salaries/
Allowances
1 ,26,900/-
45,000/-
1,71,900/-
38.0
2) Travelling
25,050/-
22,500/-
47,550/-
10.5
6,150/-
2,250/-
_l,08,400/-
24.0
-
52,250/-
11.5
-
72,300/-
16.0
4,52,400/-
100.0
3) Meetings
a) Advisory
Committee
b) C.H.T.D. I &
M.E.R.M. I
1,00,000/-
4) Publications
a) Publications
—
50,000/-
b) Media
—
2,250/-
8,100/-
2,250/-
b) Xerox/Report^/
Cyclostyling 7,800/2,400/c) Contingency
4,500/-
5) Administration
a) Postage/
Stationery
6,000/d) Rent
e) Others (CHC
Contr. for
team servi
ces, office
accdn. etc.) 30,000/Total
N.B.
6,750/4,500/-
2,40,000/*
2 ,12,400/-
* Revised mid-Phase I (Refer Document 2 dated 9.1.91 of
the project proposal and budget estimates compilation
of CHC-CMAI—CHAI Medical Education Project)
- All figures are rounded off to the nearest 50.
^2
42 .
APPENDIX - O
REPORTS / PUBLICATIONS / PAPERS ARISING OUT OF THE CHC/CMAl/
CHAI MEDICAL EDUCATION PROJECT APRIL 1990 TILL JUNE 1992.
01.
Strategies for Social Relevance and Community Orientation
in Medical Education s Building on the Indian Experience
(A project proposal ) .
02. Towards Greater Social Relevance in Medical Education a keynote presentation at the first Network of CMC Medical
College in India, March 1991, CMAI Journal, Vol.VI,
April-June 199103. An Alternative Vision of Education for Decentralised
Health Care - paper presented at a Workshop on "Towards a
Decentralised Health Cara 3 A fresh look at the National
Health Policy", organised by the National Institute of
Advanced Studies, Bangalore. (Proceedings of workshop
being published by Wiley & Co»)
04. A brief progress report of th® Project-ljjth November 1990.
05. A brief progress report of th® Project-lst May 1991.
06. Medical Education - where does it lead - special issue of
•Health Action
*
magazine (Vol.IV, No.6, June 1991)
published by HAFA Trust, Health Action, P.B. No.2153,
157/6, Staff Road, Gunro ck Enclave, Secunderabad - 500 003.07. Key components which should form part of an education
policy for Health Sciences in India - collective concerns
from an opinion poll. (Conmnmity Health Trainers DialogueBackground Paper II).
08. Key issues which are important to review in order to
enhance the contribution of Community Health Trainers in
India - collective concerns from an opinion poll (Community Health Trainers Dialogue, Background Paper III).
09• Overcoming Nebulous thinking and action on medical education
in India (Debabar Banerji) (Community Health Trainers
Dialogue - Background Paper IV).
10.
The Bajaj Report - some view points - I
Amla Rama Rao, Rajaratnam Abel, C.M. Francis, Ulhas Jajoo,
George Joseph and M.J. Thomas (Community Health Trainers
Dialogue - Background Paper V)•
11.
The Bajaj Report - some view points - II
Vijaya Sherry Chand^ Thelma Narayan (Community Health
Trainers Dialogue - Background Paper VI)
43
12.
Rebuilding the Foundations » Re-examining preclinical
Medical Education - H.J. Mehta Oration-1991, delivered
by Ravi Narayan at St.John's Medical College in
December 1991•
13.
Medical Education in the *
s
199O
- Towards greater
participation and value orientation - a reflection on
the project, for LINK Newsletter of Asian Community Health
Action Network (submitted in September 1991 )•
1 4 . Education Policy for Health Sciences - A statement of
shared concern and evolving collectivity - a collective
statement from the Community Health Trainers Dialogue,
October 1991«
Proceedings of the Community Health Trainers Dialogue,
October 1991 <>
16. A brief progress report of the Project - 1st January 1992®
1 7Strategies for greater community orientation and social
relevance in Medical Education - Building on the Indian
Experience ’-‘"Ta proliiainary ©ommuni cation) - presented at
the 3°tb Annual Conference of the Indian Association for
the Advancement of Medical Education on the theme
"Research
in Education for Health Sciences’ held at
LTM Medical College, Sion, Bombay, - January 1992.
18.
Curriculum Change » Building on graduate doctor feedback
of peripheral health care experience - an exploratory
survey - (a preliminary communication) - presented at the
30th Annual Conference of the Indian Association for the
Advancement of Medical Education on the theme ’Research
in Education for Health Sciences’ held at LTM Medical
College, Sion, Bombay - January 1992.
19.
The CHC/CMAl/CHAI Medical Education Project - A process
report (April 1990 to May 1992).
20.
Towards an alternative medical education - step by step
(an anthology of CHC papers and initiatives).
IN THE PROCESS OF COMPLETION
21.
The key to change i Reflections on strategies for social
relevance and community orientation in Medical College
(summary of Project findings).
22. Towards curriculum change t Building on graduate doctor
- feedback from peripheral health care experiences - the
final report of an exploratory survey.
44
44
23.
A faculty resource manual on 'Strategies for Community
Orientation and Social Relevance in Medical Education 1
Building on the Indian experience.
24.
Laying the Foundation - towards foundation community
experiences in medical education.
25• A to Z of Medical Education in India .
(A bibliography with some annotations of key materials).
IN ANTICIPATION
26.
Key changes and innovations towards social/community need
based medical education in India - an opinion survey.
27.
The mfc Anthology of ideas - a collective response.
28.
Collective Coaimi tment for Change s Proceedings of a
Medical Education Review Meeting, June 1992.
NOTE? Items 26 and 27 are background
papers arising out of an
opinion survey conducted among
the participants of the Medical
Educators Review Meeting,
June 1992.
..45
FOR NOTICE BOARD
CONTENTS
P1<1 1 ACI-.
Idea ol Anthology
Ihsloricai Overview
IM) Years ol Medical l.ducaiion: Rhetoric und Relevance
Ravi Narayan
I i -lies
I
2.
Pic-requisites Necessary lor Making of the 'Basic Doctor
Dhruv ManLid
23
1
Critique of the l-jcisting Methodology lor Training of
Medical Students
K.J. Nanuviiti and NX'. I'lirulyu
A Noic on the 1 caching ol Community Medicine: A
('ritique and lew Suggestions And I’aicl and Admin Tnlel
Medicine and Society. Socio 1 listory in Preventive and
Social Medicine
I'adma I’rnkuth
Sociology and Ideology in Medical Education.
Anam i'hadke
33
4,
5.
bl
83
Discussions
Ashvm Patel
93
Issues lor group discussion on Medical Education - X
Annual Meet
Admin Palcl
‘J.
Report ol lhe Group discussions: X Annual Meet
Alternatives
KH
Towards a Clinical Syllabus lor Alternative Medical
Education
Anunl I'hadke
Integration ol Traditional and Modern Medicine in
Alternative Medical Curriculum
DhruvMankud
125
12.
Innovative Programmes: Case Studies
141
13.
Anthology ol Ideas
7.
An Alternative Medical Education
8.
10.
11.
C. Sadiyamala
C'unifidcd by Ravi Narayan
A PPEN D IX
<>.
41
107
133
157
UPDATE
14.
IS.
Recent Initiatives towards an Alternative
Medical Education
Ravi Narayan
Ilililogriipliy
Bombay - 400 007.
&
CENTRE FOR EDUCATION AND DOCUMENTATION
3, Suleman Building,
4, Battery Street,
Behind Regal Cinema,
191
Price
Copies Available at
MEDICO FRIEND CIRCLE
34-B Noshir Bharucha Road,
171
Bombay.
Hard Cover
Paper Back
: Rs. 100/: Rs.
35/-
(Sr
46
APPENDIX - Q
MODIFICATIONS FROM ORIGINAL PREPARED FOR CMC - LUDHIANA
(to be used as a framework by any college interested in the
process in the post-project lobbying phase)
A Workshop on ‘Exploring Objectives and Methodology* for
enhancing Community Orientation, Social Relevance, problem
based, learner centred medical education within the existing
framework of the MCI recommended MBBS Curriculum.
- Building on the Indian experienceo
FOR WHOM
For a core team of faculty from any Medical College interested
in a *planning exercise9 on the theme«
BY
Facilitated by Community Health Cell,
Bangalore.
FROM
Resource persons from an informal network of resource persons/
institutions interssted/involved in appropriate medical education.
OBJECTIVES
1.
To outline the relevant objectives of medical education in
India, particularly for the college.
What do we want to do?
2.
To review the existing educational programme at the college
in the context of the above as well as in the context of
the 1982 MCI Curriculum.
What are we doing?
3.
To explore new objectives, roles and programmes in the
context of the Indian experiences particularly from ongoing
experiments and the mfc alternative.
What else can we do?
4.
To assess these possibilities in the ocontext of the r
resources and constraints in the college.
5.
To evolve a plan of action to be operationalised by a
medical education cell and or a core group of faculty of
the college interested in the ‘exercise
.
*
47
(Appendix-Q (contd.)
DRAFT PLAN FOR WORKSHOP
(This is a tentative plan subject to modification / finalisation by the college faculty
team)
Day
First Day
Second Day
Time
Typ® of session
Session I
i) Introduction to
•workshop and
objectives.
ii) Getting to know
each other
iii) Getting to know
*
•instruiisnts
of
change .
Session II
Group Work
Theme
Background
Material
What do we want to do?
i) Defining
What could be the
Objectives
ideal objectives of
ii) Objectives of
Medical Education in
some of the
the Indian context?
Indian
Both general for the
1 innovator'
institution and
colle ge s.
specific to some of
your/other departments.
Session III Five presentations and
discussion
n
n
Modifying and
redefining the above.
Session IV
Discussion
What are we doing?
Reviewing existing
educational programme
of the medical college
Why is it happening
that way?
What is the student
expected to do?
Se ssion V
Study and group -work.
Read the 1982 MCI
guidelines and asses
the college objectives/
actuals in that context
MCI 1982 guidelines.
(Appendix-q(Contd.)
Day
Third Day
Fourth Day
Ti me
Type of session
Theme
Session VI
SWOT Analysis
What else can we do 7
Given the MCI 1982
guidelines what are
tha possibilities and
constraints in the
college.
Session VII
Input session
Learning from each
other
Exploring initiatives
of other institution
(Medical Education
Project check list)
Session VIII
Individual Work
Reflect on a pla of
action for the year
for the college as a
whole and especially
for one ' s own
Department.
Session IX
Group Discussion
A plan of action for
the year for the
college.
Session X
Input Session
What are the resources
available in India?
Session XI
Exploring CHC/CMAl/
CHAI Project manual
and reports
Evolving a plan to use
these resource materials
in an ongoing process of
a formal/informal
medical education cell
of a college.
Session XII
Final Session
Summing up/Feedback from
participants.
Background
Material
Objectives/
reports of
other
institutions.
00
Appendix - R _______________
Vol IV
No 6
June 1991
]
Health
Action
Contents
• Training of Doctors for India
Dr Thelma Narayan................................ 5
xot.
A HAFA NATIONAL MONTHLY
FROM THE HOUSE OF CHAI
o History of Medical I ducation in
India
EDITOR
Dr C M Francis................................... 15
Dr CM Francis
® The Challengesol Continuing
Education
EXECUTIVE EDITOR
Ms Patricia Palaparti
Dr Sara Verghese................................ 17
BUSINESS CONSULTANT
Mr Jose K Chomkara
® Medical Ethics. .Medical malpra
ctice and Patient’s Rights
CIRCULATION MANAGER
Dr Anil Pilgaokar................................ 19
Mr Pulaparthi Ganesh
ART COORDINATION
® Go to the people... learn from
them
Mr Magimai Pragasam
EDITORIAL BOARD
Uday George Zachariah, Ajit Thachil,
Dr Antony KR
Mr Augustine J Veliath
Fr Eowin MJ
Mr George PO
Mr Kumarswamy Reddy
Dr (Sr) Plaoda
Dr Prem Pais
Mr Suresh Maximus
Shireen-rese Andrade and Sean Joy
mathicken ............................................ 23
® A View from the Periphery
Drs Roopa Devadasan and
N Devadasan ....................................... 27
® The Samaritan Medicine
EDITORIAL ADVISORY
COMMITTEE
Dr Alex Zachariah............................... 29
Mr Aiok Mukopadhyay
Dr Cn>ranjeev> K
Dr Daieep S Mukarji
Fr George LoPO Si
Dr George Joseph
Mr Jose Vincent
Dr Paul Neelamkavil
® Health and SocietyReflections on a Final Year
Medico’s Elective
Dr S Prabir...........................................31
Printed and published by Ms Patncia
Palaparti for and on behalf of Health
Accessories for All (HAFA) at Pragati Art
Pnnters. Red Hills. Hyderabad
• Doctors or Health Educators ?
The Kottayam Experiment
Anil Aggarwal.....................................
Editorial and Administrative Offices:
HEALTH ACTION
PB 2153
157/6 Staff Road
Gunrock Enclave
Secunderabad 500 003
T el 848293 848457 841610
• The Edinburgh Declaration...... 35
• Nutrition and Vegetarianism
Bikash Kumar Gosh............................. 36
• A collage that peeps into the state
of Medical Education today...... 37
DELHI OFFICE:
CATHOLIC HOSPITAL ASSOCIATION or INDIA
C8O Centre Astro
*
Race. Gokfchanna
N6W DELHI-110 001 Te< 3’0694
Articles and statements in this publication
do not necessarily reflect the policies and
views of HAFA
Subscription rates from January 1990
Annual Individual
Annual Institution
bfe Membership
Foreign Annual
Foreign bfe
Single Copy:
Rs
60
Rs
80
Rs 1000
USS 50
USS 500
Rs
7
33
Thought for the Month....
The physician turned from the telephone
and said to his wife, “I must hurry to
Mrs. Jones’ boy — he's sick”.
“Is it serious?"
“Yes. I don’t know what’s the matter
with him, but she has a book on what to
do before the doctor comes. So I must
hurry. Whatever it is, she mustn’t do it.”
• Leprosy in India — Role of
modified M.D.T.
Dr B Kameswara Rao......................... 40
• Leprosy in Andhra Pradesh
Dr P Sivaraman................................... 42
• May 31. World No-Tobacco Day
WHO message..................................... 44
Health Action June 1991 • 1
Appendix
S
16
15
CURRICULUM CHANGE : BUILDING ON
GRADUATE DOCTOR FEEDBACK OF
PERIPHERAL HEALTH CARE EXPERIENCE - AN
EXPLORATORY SURVEY.
STRATEGIES FOR GREATER COMMUNITY
ORIENTATION AND SOCIAL RELEVANCE IN
MEDICAL EDUCATION : BUILDING ON THE
INDIAN EXPERIENCE
WARAYZLH RAVL MARAYAWtHtLMA, TCKUR SHRIDI PRASAD.
MARA YAM
THELMA, A
NARAYAN RAVL
(COMMUNITY HEALTH CELL. SOCIETY FOR COMMUNITY
HEALTH AWARENESS.
RESEARCH AND ACTION. BANGALORE 550 034)
(CCA4WJMTY HEALTH CELL SOGETY FOR COMMLWTTY HEALTH
AWARENESS. RESEARCH AND ACTION. BANGALORE - 560 034)
The Indian sxperisneo of kmevstion and reorisrtation
Gf nxxEcal educetica cen be buS tip from a study cf ideas/
'©rpsrisnsnis femsa courcsx
This paper is 3 pceEmsnary report of a questxxmarre
survey of over 50 young graduates doctors. This survey was
R ecommandations of Export Committees
from Shore (1946) to Bajai (1989)
a compoosnt of a fcrger study entitled Strategies for greater
Community Onentation and Social Relevance tn Medical
Education; Bidding on the I no? an Experience undertaken by
(ii)
Experiments with.n medical coheg?i-Z
departments
(iii)
Alternative training experiments in
Community Health Cell
Community Health
There have been some attempts in recent yesrs to
build curriculum change and innovation Shrough feedback of
I Development in the
- voluntary sector.
medical students and interns ixrt this is probably the first
frv)
survey which focuses on graduate {factors who had com' pieted etleasl two years work experience in a peripheral
heaJth care institution in the 1980‘s. They were asked to
Reflections of graduate doctors who have
worked in Primary Health Care/Community
Health Satuations.
reflect on medical education and how R could be made ‘more
The Community Health Cell, a policy research group
supportive and refovari to present day peripheral hospital
in the voluntary seder has just completed an eighteen month
exploratory end interactive study covering all the four sources
practice and community health action'.
The proforma sought ideas and feedback on 26
subjects in Medical Education which included (1) Anatomy *1
(2) Physiology (3) Biochemistry end Biophysics (4) Biosiatistics (5) Behavioural Sciences (6) Others (7) Pdhology (8)
Microbiology (9) Pharmacology (10) Forensic Mec&ane (11)
Medicine (12) Surgery (13) Obs. & Gyn. (14) Petfiafries (15)
PSM (16) Psychiatry (17) Dermatology (18) Ophthsimotogy
(19) ENT (20) Radiology (21) Anesthcstotogy (22) Dentistry
(23) Orthopedics (24) Medical Ethics (25) Other (specify)
(26) Internship.
Feedback was also efidted on few additional skill
areas which included (1) Basic Nursing Procedures (2)
Communication (3) Management and (4) Training of Health
Workers and Personnel and five aspects of Medical Educa
tion which included (1) Selection Process (2) Teaching
Methodology (3) Curriculum Structure/Framework (4) Ex
amination System (5) Other aspects of content, process,
environment and base of teaching.
The respondents were also Ecked to give sugges
tions of methods/ experience that would enhance the soda!/
emctiocal preparedness of graduates for such work.
The am was to bu3d a reference manual on the Indian
experience for faculty of medical colleges exploring innova
tion in the 1990's. This paper is a preliminary report and gives
an overview of the study process and findings.
The study included a communication to all deans/
principals and professors of PSM of 125 medical colleges in
India with two reminders; interactive field visits and discus
sions with stafl/intems of some medical colleges; a question
naire survey of over 50 young graduates with work expen
j once in peripheral health institutions; communication and
I dialogue with health end development trainers in the volunI tary sector; and a comprehensive literature review.
The manual to be ready later this year will include (i)
(ii)
(iii)
Change
-
Key
policy
A situation Analysis
(rv)
Exploring medical college experiences
(v)
Key innovations/experimentsforthe 1990‘s
(vi)
Building on rural experience (graduate
survey)
(vii)
Laying alternative foundation (NGO training
experience)
(vffi)
Exploring new horizons/areas in
medical education
Source :
Souvenir of XXXI Annual Conference
of the Indian Association for
Advancement of Medical Education
- Free Paper Abstract - Page
Nos. 32 & 33.
Exhorting
recommendations
The survey is being analysed presently. This prefimi-
nary communication highBghis^ha key fcxSngs.
Lessons from History and Tradition
fa)
Medical Education and Society (Unkag es)
(x)
Resources and Key to Change
- Media
 2231.pdf
2231.pdf
Position: 3962 (2 views)