TUBERCULOSIS
Item
- Title
- TUBERCULOSIS
- extracted text
-
RF_DIS_5_PART_1_SUDHA
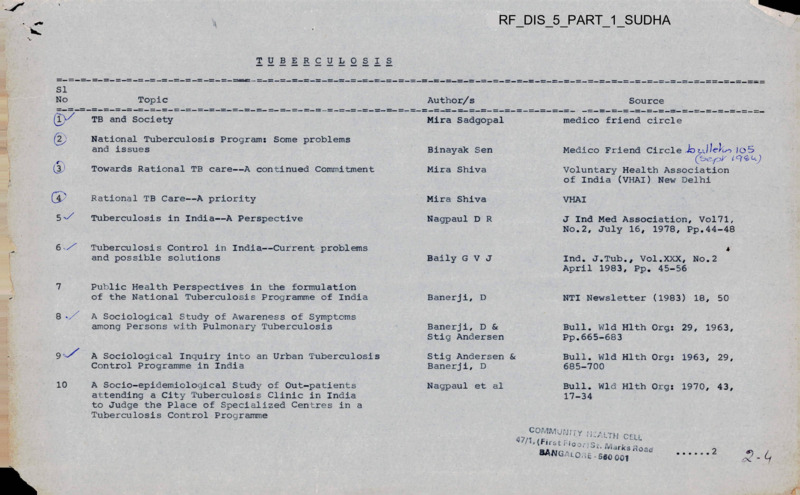
TUBERCULOSIS
SI
No
(2)
(3J
7
8 •
Topic
Author/s
Source
TB and Society
Mira Sadgopal
medico friend circle
National Tuberculosis Program: Some problems
and issues
Binayak Sen
Medico Friend Circle Jo
Towards Rational TB care—A continued Commitment
Mira Shiva
Voluntary Health Association
of India (VHAI) New Delhi
Rational TB Care—A priority
Mira Shiva
VHAI
Tuberculosis in India—A Perspective
Nagpaul D R
J Ind Med Association, Vol71z
No.2, July 16, 1978, Pp.44-48
Tuberculosis Control in India—Current problems
and possible solutions
Baily G V J
Ind. J.Tub., Vol.XXX, No.2
April 1983, Pp. 45-56
Public Health Perspectives in the formulation
of the National Tuberculosis Programme of India
Banerji, D
NTI Newsletter (1983) 18, 50
Banerji, D &
Stig Andersen
Bull. Wld Hlth Org: 29, 1963,
Pp.665-683
A Sociological Study of Awareness of Symptoms
among Persons with Pulmonary Tuberculosis
/O'S
4
9 '■
A Sociological Inquiry into an Urban Tuberculosis
Control Programme in India
Stig Andersen &
Banerji, D
Bull. Wld Hlth Org: 1963, 29,
685-700
10
A Socio-epidemiological Study of Out-patients
attending a City Tuberculosis Clinic in India
to Judge the Place of Specialized Centres in a
Tuberculosis Control Programme
Nagpaul et al
Bull. Wld Hlth Org: 1970, 43,
17-34
COMMuTJj Ty 'h’ALTH CELL
(First Hoar)St. iVtarks Road
BANGALORE - seo ooi
2
2
SI
No v
Topic
Author/s
Source
11
Tuberculosis Situation in India—Epidemiological
Features
Chandrasekhar, P
& Kurthkoti, A G
National Tuberculosis Institute
Bangalore
12
Epidemiological Data of Tuberculosis
Seetha, M A
National Tuberculosis Institute
Bangalore
13
Tuberculosis in a rural population of South India:
a five-year epidemiological study
National Tuberculosis
Institute, Bangalore
Bull. Wld. Hlth. Org: 1974, 51,
473-488
14
Tuberculosis in a Rural Population of South India:
Report on five surveys
Chakraborty et al
Ind. J. Tub., Vol.XXIX, No.3,
July 1982, Pp.153-167
Incidence of sputum positive tuberculosis in
different epidemiological groups during five
year follow up of a rural population in South India
Gothi et al
Ind. J. Tub., Vol.XXV, No.2
April 1978, Pp.83-91
16
Prevalence, incidenceand suspect cases of
tuberculosis in a rural population of South India
Krishna Murthy, W
NTI Newsletter (1982) 19, 75
17
Tuberculosis Mortality rate in a South Indian
Rural Population
Chakraborty et al
Ind. J. Tub., Vol.XXV, No.4,
October 1978, Pp.181-186
18
Distribution of tuberculosis
infection and disease in clusters of rural
households
Nair SS et al
Ind. J. Tub., Vol.XVIII, No.l
Pp. 3-9
Interview as a tool for symptom screening in
pulmonary tuberculosis
Radha Narayan et al
National Tuberculosis Institute,
Bangalore
19
3
3
■s=
SI
No
Author/s
Source
Srikantaramu et al
Ind. J. Pub. Health, Vol.XX,
No.l, Pp>3-8
Symptom Awareness and Action Taking of Persons
with pulmonary tuberculosis in rural communities
surveyed repeatedly to determine the
epidemiology of the disease
Radha Narayan and
N Srikantaramu
Ind. J. Tub., Vol.XXVIII, No.3,
July 1981, Pp.126-130
An operational study of alternative methods of
case finding for tuberculosis control
National Tuberculosis
Institute, Bangalore
Ind. J. Tub. Vol.XXVI, No.l,
January 1979, Pp<26-34
23
Evolution of the National Tuberculosis Programme
Gothi, G D
NTI Newsletter (1981) 18, 22
24 v/
District Tuberculosis Control Programme in
Concept and Outline
Nagpaulj D R
Ind. J. Tub., Vol.XIVf No.4
Pp.186-198
Tuberculosis Control in Primary Health Care
Radha Narayan
J. Com. Dis.14(3):189-191, (1982)
A study of tuberculosis services as a component
of primary health care
Radha Narayan et al
Ind. J. Tub., Vol.XXX, No.2
April 1983, Pp.69-73
Primary Health Care - Evolution in India
Part II : The roots
Radha Narayan
NTI Newsletter (1982) 19, 71
Aneja et al
Ind. J. Tub., Vol.XXVII, No.4
October 1980, Pp.158-166
Topic
rrang"
20
21
25 '
27
28
An Operational Model of the District
Tuberculosis Programme
Feasibility of involvement of the Multi purpose
Workers in case finding in District Tuberculosis
Programme
4
4
SI
No
Topic
29
Training for Multi Purpose Workers in
District Tuberculosis Programme
Author/s
Source
Anej a K S &
Srikantan K
NTI News Letter (1980) 17, 78
30
Case-finding by microscopy
Nagpaul et al
WHO/TB/Techn. Information/68.63
31 \/
Potential Yield of Pulmonary Tuberculosis
Cases by Direct Microscopy of Sputum in a
District of South India
Baily et al
Bull. Wld Hlth Org. 1967, 37,
875-892
32
Tuberculosis—Case finding (summary)
Toman, K (WHO)
Geneva
Tuberculosis Case-finding and
Chemotherapy
33
Priority to sputum positive cases under
NTP—Rationale
Jagota, P &
Anej a K S
National Tuberculosis Institute,
Bangalore
34-^
The BCG Story
Mira Shiva
VHAI
35
Present Status of Immunization against
Tuberculosis (Review Article)
Baily G V J
Ind. J. Tub., Vol.XXVIII, No.3
July 1981, Pp.117-125
6
The efficacy of BCG Vaccination - A brief
Report of the Chingleput BCG trial
Baily G V J
NTI News Letter (1980) 17, 108
37
Chemotherapy in National Tuberculosis Programme
Anej a K S
NTI Newsletter (1982) 19, 58
38
Drug Regimens
National Tuberculosis
Institute, Bangalore
Karnataka State Tuberculosis
Association, 3 Union Street
Bangalore
39
The problem of drug resistance under conditions
of drug chemotherapy
Baily GVJ &
Gothi GD
Proceedings of the 9th Eastern
Region Tuberculosis Conference
& 29th National Conference on
Tuberculosis & Chest Diseases
held in Delhi, Pp.367-371
5
V
5
SI
No
Topic
Author/s
Source
40
Short Course Chemotherapy in National
Tuberculosis Programme
Aneja K S
NTI News Letter (1979) 17, 43
41
Short Course Chemotherapy - Retrospect and
Prospect
Anej a K S
National Tuberculosis Institute,
Bangalore
42
Some Practicable short-course drug
regimens for chemotherapy of tuberculosis
National Tube culosis Institute,
Bangalore
43
Collection and consumption of self-administered
antituberculosis drugs under programme
conditions
Gothi et al
Ind. J. Tub., Vol.XVIII, No.4
October 1971, Pp.107-113
44
Some observations on the drug combination of
INH + Thiacetazone under the conditions of
District Tuberculosis Programme
Gothi et al
Ind J Tub., Vol. XIV, No.1
December 1966, Pp.41—48
45
A concurrent comparison of an unsupervised
self-administered daily regimen and a fully
supervised twice wekly regimen of chemotherapy
in a routine outpatient treatment programme
Baily et al
Ind. J. Tub., Vol.XXI, No.3
July 1974, Pp.152-165
46
VHAI1s Role in TB care
VHAI
VHAI New Delhi
47
Voluntary Agencies and India’s National
Tuberculosis Programme
Debabar Banerji
VHAI New Delhi
48
Tuberculosis Special Issue
Health for the Millions (VHAI)
Vol X No.2, April 1984
6
I
</
1
r
■v
i
6
SI
No
Author/s
Topic
Source
= -=
49
What you should know about Tuberculosis
The Tuberculosis Association of
India, 3 Red Cross Road
New Delhi
50
Beat Tuberculosis
The Tuberculosis Association of
India and the Karnataka State
Tuberculosis Association
51
Diagnosis/ Treatment and Prevention of
Pulmonary Tuberculosis for General
Practitioners
The Tuberculosis Association of
India, 3 Red Cross Road
New Delhi 110001
52
Lectures on Tuberculosis for General
Practitioners
53
Blue Print for Tuberculosis Control in India
54
Planning of Research Studies (some general
considerations)
55
National Tuberculosis Program - Relative merits
of enhancing the efficiency of different
components of the treatment programmes
56
Effect of Treatment Default on Results of
Treatment in Routine Practice in India
Pamra, S P
The Tuberculosis Association of
India, 3 Red Cross Road
New Delhi 110001
-doNair S S
Ind J Tub Vol XVI, No.2,
April 1969, Pp.37-41
Ind. J. Tub., Vol., XXX, No. 1
Banerji, D
Proceedings of the XXth
International Tuberculosis
Conference (1969), Paris:
International Union against
Tuberculosis
J>.s
^0
COMMUNITY hTALTH
CELL
47yl-(^tF,00r)St.1War({3fioad
BAIJGA103E - 560 001
III
medico friend
circle
bulletin
MARCH
TB
I
1985
AND SOCIETY
Preamble
It is the first time in the last eleven years since
our inception that mfc has taken up a single dise
ase entity for discussion at the annual meet.
The disease selected—Tuberculosis'—was particu
larly relevant because of mJany reasons:
i. To begin with there is greater understanding
today of the multifactorial aetiology of the disease
where social factors more than biological are known
to have a significant impact on incidence, preva
lence, spread, diagnosis, m'anagement and control;
ii. Secondly unlike most of the national pro
grammes in India the NTP has developed on crucial
sociological perspectives derived from* relevant
field studies;
iii. In its approach in terms of integration with
general health services, choice of appropriate investi
gative technology, alternatives in chemotherapy and
other aspects it has shown a greater people/patient
sensitivity than most other programmes and a signi
ficant shift from the dependence on the industrial
aspects of medical care;
iv. Inspite of these salient features the case
finding and case holding performance is far from
satisfactory and these have becom'e a matter of great
concern for TB programme organisers and decision
makers,
v. The 1CMR/ICSSR Report while analysing
the drug situation in the country has highlighted the
shocking state of availability of anti-tuberculosis
drugs ('one third of minimal requirement’) when
vitamins, tonics, health restoratives and digestives
are being produced in ‘'wasteful abundance”;
vi. By its inclusion in the 20 point programme
the government has endorsed its relative importance
in the health scene of the country though whether
this step is part of a 'populist rhetoric’ or a nati
onal commitment towards control of the problem,
only time will tell.
It is in this context that the mfc decision to
relook at the whole situation of the TB problem and
its control in India as an exercise for 1984-85 is
significant.
Scope and Focus
The meet of over 110 friends from various
diverse backgrounds (ref mfcb 110 Feb 1985) with
its intensive small and large group discussions
highlighted that the subject was too large and too
important to be tackled in 16 hours of discussion
ano that rather than expecting a meaningful criti
que of NTP to emerge from So diverse a group —
what would really be more realistic would be to
accept the annual meet discussions as the initiating
of a process of critical analysis. This would be
followed up by further study, small group work and
field evaluation through 1985 from which would
hopefully emerge an mfc perspective on the problem.
This sense of realism was forced on the group after
the first session on “Expectations of the Meet” in
which participants were asked to raise issues and
questions for discussion.
Expectations of the Meet
The exercise identified a phenomenal range of
problems far beyond the scope of the meet:
1. Need to understand the organisational
structure and implementation of NTP and the devi
ations from ideal in the actual field situations.
2. Need to identify issues on which we should
put pressure on policy makers.
3. Need to discuss the range of non-pulmonary
tuberculosis and how it is viewed by the NTP.
4. Need to discuss childhood TB and how it is
viewed by NTP.
5. Need to study how NTP actually operates
at the PHC level and what are the components of
the services actually available at the community
(village) level.
6. How do non-allopathic systems view TB as
a problem1?
INSIDE
TB — SEP strategy
2
Towards a relevant
TB Control Programme
3
Subgroup reports on TB
5
AIDAN mfeeting report
7
involve other non health sectors like the education
department etc.?
30. Why is awareness building given such low
priority? Why is there no definite, researched and
evaluated communication strategy integrated into
NTP?
During the discussions at the meet some of
the above expectations were debated in greater detail
and some were not, either due to inadequacy of in
formation or time constraint. We report some of
the key areas of discussion. Decisions for follow
up study or action are given at the relevant places
in brackets. Wherever participants have commit
ted themselves to specific action this is indicated.
Where it is not indicated it means that volunteers
from members/subscribers/readers are welcome to
get involved. We also welcome any information, ,
perspectives, opinions on any of the questions
listed (get in touch with mfc office immediately).
7. How far can TB be considered an occupa
tional health problem because greater susceptibility to it after certain types of occupational ex
posure are well known?
8. Knowledge of cost factors in the range of
alternative regimens of chemotherapy.
9. Data on drug production, distribution and
availability in relation to total estimate of patients
and in the context of recommended drug regimes.
10. Identify genuine constraints in NTP
and false limitations accepted by programme plan
ners.
11. Identify genuine constraints and false limi
tations in TB programmes of voluntary agencies.
12. How far is TB actually integrated with
. general health services? Is there need for greater
integration or greater identity?
13. To develop guidelines for patients who
have already received treatment before — be it
inadequate or inefficient.
14. Role of voluntary agencies in NTP.
15. Role of private practitioners in NTP. Why
are they excluded from the plan?
16. Understanding of the social stigma' associ
ated with the disease and its effect on case finding
or holding and the measures to combat it.
17. The effects of the over emphasis and pres
sures of the family planning programme on PHC
functioning as well as NTP at PHC level.
18. What is the 7th plan policy decisions on
TB programme?
19. TB and its relation to other respiratory
diseases occuring in certain occupational environ
ment.
20. How can NGOs support/complement/supplement NTP of government?
21. What is the method of collection, analysis,
feed back of statistics of NTP from field level?
What is the method of feed back from the centralis
ing agency to the peripheral delivery system?
22. Role of para medicals and community health
workers in NTP.
23. What are the legal rights of industrial
workers vis a vis TB?
24. What are the differences between NTP
performance in different states and regions and
the causes for such difference?
25. What are the present efforts in public
awareness building? What are the available media?
In what way can this be further promoted?
26. What is happening about drug resistance
in NTP?
27. In spite of the more holistic epidemiologi
cal understanding accepted today, why is NTPs
perspective severely clinical and curative?
28. Why/how can TB be seen as a social pro
blem to be tackled by society not as a medical pro
blem to be tackled by the health services only?
TB—a socio-economic-political strategy
From the discussions, it evolved that TB con
trol must be discussed in the context of a radical
reorganisation of society towards a more equitable
and just system* where the smallest and most vulner
able person is central and only this can secure some
stability t0 the health and welfare of the people.
In the strategy to achieve this society, all
interventions particularly those at the grass roots
must be through people’s movements and organisa
tions so that demands and decisions are the peo
ple’s free choice. In this strategy the process of
reflection and conscious action
(ie.f education)
is on all fronts: social, economic, political, cultural,
health and countering myths and superstitions; and
seeks to make the person/group/society self reliant
and confident.
Micro level action is primary but also sharply
limited. It must be linked to the wider reality.
Critical collaboration is necessary with people's
movements and wider political action. However,
there needs to be a high critical awareness of the
daneer of ‘over politicisation’ and a danger of the
sabotage of the people’s freedom by political con
flicts.
Within the context of the above perspective
we as a group endorse the following thought cur
rents, action and demands on the SEP front
1. A demand for the reallocation of resources
in the Union Budget. There should be more money
allocated for health and within the health sector,
the rural-urban bias should be eliminated (There is
need to study the funding of NTP, the cost alloca
tion, for detection, drugs^ and personnel as well as
the rural—urban bias.)
2. Each block and PHC should make it public
t0 the people as to what are the available and allo
cated resources for that area. All these resources
should be channelised for the benefit of all people
in a just manner.
3. Occupational (farming, wood gathering,
wage iabour) and seasonal constraints do not allow
the patient (most often an adult in the working age
29. Why has NTP in its planning not cared to
2
sations. People should be the axis when considering
the TB problem. There should not be an undue em
phasis on extraneous agencies such as doctors or
policy makers. Experts should be made answerable
to the people and crucial decisions should be made
by people. Conscious peoples organisations would
lead to socio-economic changes without
which
general health status or even TB situation would
not improve.
11. mfc members have to emphasise that the
socio economic factor is the most important aspect
in TB and for that matter in other communicable
diseases as well. As an organization we should work
to explode the fallacies accompanying the concept
of TB eg. TB Association of India pamphlet on
‘What should you know about Tuberculosis’ lists
poverty, over crowding, unhygienic living conditions
as legends about TB). mfc members who are already •
involved in organising people should develop a net
work for communication.
12. Nutrition, housing, environment at the
working place and amount of leisure determine resi
stance or susceptibility to TB. This means that only
a fundamental change in the socio economic struc
ture of society will help in the control of TB.
13. Whilst demanding a basic structural change,
we should also demand that existing peripheral
services are more effective. Voluntary agencies
should as far as possible not duplicate the effort of
the government.
In fact the government should be made respon
sible for delivering basic public health services
Whilst doing reformist work at grass roots
we
should ~ work towards basic
change
and contribute towards this change ideologically
and organisationally. Alternatives such as low cost
drug production should also be a simultaneous acti
vity.
14. Land reforms, the minimum wages act
and the right to work should be implemented
strictly. In Kerala these measures have greatly help
ed to reduce incidence of TB
15. To bring about the above mentioned socio
economic changes, a political change aimed towards
socialist society is inevitable.
Marie Tobin, Jansaut
Manish:: G’upte, Bombay
group) to go long distances for treatment regularly.
This reduces access to and availability of TB
treatment. Health services especially those for the
detection and treatment of TB should be handled
by para medicals and should reach the villages if
not the door steps of the people.
4. There should be the least dependence on
International agencies for funding and powerful
individuals in the first world who influence develop
ing countries— India is strongly so influenced.
5. Multinational corporations symbolise the
most centralised economic power and therefore they
should not be encouraged particularly in the drug
industry. However the local government interests
are always linked with that of the MNCs and there
fore just removal of MNCs will not eradicate
inequalities.
6. The profit motives of the drug industry
should be strictly monitored and kept in check by
a relevant drug pricing policy.
7. Doctors should correct their own miscon
ceptions about TB. They should realise that the
germ theory is inadequate to eradicate TB. They
should also get rid of the stigma that they harbour
about TB itself. When doctors harbour such stigma
they perpetuate and legitimise it. The stigma that
the doctor harbours reflects the value system that
most of us inculcate during our education which has
a certain bias. This stigma is particularly , com
mon in our attitudes to the poor, caste problem,
leprosy and TB and we need to fight against it.
8. Health problems cannot be solved by doctors
or government health departments. They can be
solved only by creating people’s organisations.
Health is an indicator of the quality of life and
TB should be seen in this perspective. Enhance
ment of health would therefore be much more
guaranteed if health issues are taken up as a part
of wider people’s movements, ie., trade unions,
rural organisations of the oppressed, feminist
groups etc
9. Health education should be aimed at infor
ming people on their right to be healthy and their
right to prompt, effective, inexpensive and safe
treatment when ill. Health education should also
highlight myths related to TB or illness in general
and show how many of them are used by the elite
classes to perpetuate ignorance.
10. A conscious effort at the grass roots level
is necessary to build decentralised people’s organi-
Towards a relevant TB Control Programme
Many of our members are involved at field
level in community health projects organised by
various non-governmental agencies in which TB con
trol is an itegral part. Based on their own field ex
periences and the discussion on the wider social
issues highlighted in the earlier report certain guide
lines were drawn up at the meet for all who are so
involved. These would help to ensure that their
involvement in the field of TB control would be
based on a clearer focus of the social reality in
which the problem exists. It is also an attempt to
internalise the ideas and positive experiences from
various case studies and projects discussed at the
meet.
mfc’s Bhopal intervention — First Report
A report entitled Medical Relief and Research
in Bhopal—the realities and
recommendations,
was presented by an mfc fact finding team at the
Bhopal convention of People's Science, Democratic
Rights and Environmental Protection Groups on 1718 Feb 1985 is available for sale at Rs. 2-00 each.
If you have not already received a copy write to
the mfc office requesting for copies for sale, pub
licity, lobbying and support.
3
2. The time period of each phase and the spac
ing of the drugs depend on factors such as — a.
accessibility to clinic and health centre;
b. infrastructure available; c. cost? d. availabi
lity of drugs; e. stage of disease—serious and nonserious patients; and f. knowledge of patient com
pliance.
Many regimes taking these factors into account
are already recommended from which a selection can
be made.
3. While the regime is being dispensed it is
essential to ensure: a. psychological reassurance of
the patient; b. maintenance of a satisfactory doctor
patient relationship; and c. tactful information to
the patient to increase his ability to identify toxic
effects.
4. The use of supportive therapy such as cough
mixtures etc., should be done in a rational way
taking care not to overuse/misuse supplementary
medication.
1. Broadly speaking TB control programmes
should ensure the following three crucial features:
(a) A link with socio-economic and developmental
activity
(b) A stress on health education and awareness
building at all levels
(c) A commitment to community participation in the
decision making process and project evaluation.
It was felt that many of us who are working in
the field have already a sufficient rapport with the
community and the above could be integrated pri
marily by sensitising ourselves to these issues
Ensuring the above principles, certain specific
recommendations were made for practical imple
mentation during: A. Case Finding/Case Holding;
. B. Drug Regimes; C. Training of Workers.
A. Case Finding/Case Holding
1. There is need to have a rough estimate of
how many TB patients ought to be in the area and
work towards identifying at least that number.
2. Involve health personnel at all levels in the
programme and also all the cadres of the govern
mental health service be they MPWs, CHWs and
Dais. Local indigenous practitioners and traditional
healers should als0 be involved.
3. School health check ups could be done as
an additional focus for case finding as in leprosy.
School teachers and high school students should be
involved in general awareness building.
4. People’s organisations like organisations of
the rural poor, workers, trade unions and other formal
and informal groups in the community should be
sensitised to the problem and involved.
5. Malnutrition surveys and mantoux testing
could be adjuncts to case finding specially for
childhood. TB.
6. Patients who are on regular treatment or
have been cured should be actively involved.
7. The family of patients should be involved
in a positive way in the programe. Once they are
sensitised to the problem in a positive way (rather
than feeling a fear or social stigma) they can be
helpful in making the community aware and also
bringing patients from other neighbouring families
for treatment.
8. The socio economic difficulties of patients
should be assessed and transportation fare and other
small compensation for wage loss etc., should be
provided.
C. Training of Workers
1. First the present knowledge/myths/perceptjons existing in the particular area should be
studied;
2. The people should be taken into confidence
about the programme envisaged by the team and
their participation in decision making ensured.
3. Grass-root workers at village level to be
involved in the programme should be selected by
the community. The selection should be based
among other things on personal motivation and
stamina.
4. The training of grass root workers or CHVs
should be undertaken in appropriate size of the
group (10-15).
5. The content of the training should include
cause of disease; symptoms|: case holding; side
effects of drugs and their management; and motiva
tion of patients.
6. The training should be theoretical along with
practical field training. The methodology should
include.
a. use of available aids, modifying them to make
them more relevant and meaningful to the local
area; b. involve the patient and get him to talk
about his symptoms/difficulties etc., c. reinforce
the learning by continous on-the-job training; d.
older CHVs to be involved in training newer ones;
e. use simple laymen language and avoid technical
jargon; f. concentrate on training to communicate
effectively with patients and the community.
7. Periodic evaluations of the training pro
gramme should be undertaken eliciting feedback
from the CHVs.
8. Similarly an effective supportive supervision
plan and a system of continuing education in which
problems faced in the field are constantly identi
fied and discussed, should be included.
9. The CHVs should be trained to increase
community awareness of the existing NTP and the
availability of effective treatment as a right so that
B. Drug Regimes
There are several regimes which have been re
commended and are available in the existing litera
ture and also promoted by the NTI. Certain basic
principles to be followed before selecting the ap
propriate regimen are:
1. Technical — an intensive phase of two
bacteriocidal drugs and one bacteriostatic drug
followed by a maintenance phase of a bacteriocidal
and a bacteriostatic drug.
4
problem but as effective educators of their patients
in the preventive/promotive aspects of TB.
CHW training: There was a general feeling that
the existing governmental CHW training programmes
gave low priority and emphasis to TB control. The
lesson plans were limited and not integrated with
the rest of the training but given separately at DTCs
and PHCs.
From the experience of participants who were
involved in health projects in which/ training of
CHWs was being undertaken there emerged the
need t0 include certain innovative methods of train
ing to make the CHWs more effective in the field:
These included:— (i) participation of senior CHWs
in training; (ii) learning through doing;, (iii) decent
ralised and localised training; (iv) participatory
methods; (v) use of locally developed or regionally „
adapted AV aids and s0 on.
The group suggested that we in the mfc should
undertake to:
A. Review all available educational materials
and AV aids on Tuberculosis available from govern
mental and non-governmental sources and check
whether the points included in (1) above are present
and whether the social focus as identified in discus
sions exist.
(Anant Phadke agreed to study the TB Associ
ation Pamphlets for a start).
B. Review all available training manuals of
health workers (CHWs, MPWs, HAs) for the im
portance given, content, and focus of teaching of
tuberculosis.
(Marie D’Souza and Minaxi Shukla agreed to
undertake this exercise).
Based on the above two studies recommendations
can be made to policy makers, programme organi
sers and health educationists in the country.
Narendra Gupta,
Prayas.
demands for more regular drug supply and more
effective government health centre services can be
generated. In the absence of such a commitment
the programme of NGOs will become ends by
themselves duplicating the efforts of government
and supporting their inefficiency. In the long run
since voluntary agencies cannot build up parallel
structures to government health services, the catalyst
nature and the 'awareness of rights’ generation
nature of non-governmental voluntary effort should
be promoted.
Mona Daswani, Bombay
Sub-group Report
Para-professional training and community
awareness in TB
1. The objectives of health education of the
community should be to promote an understanding of
the medico-technological aspects of TB, the socioeconomic-political aspects, the rights and responsi
bilities of the patients and people, the common
beliefs and superstitions and demystification of all
aspects of the TB control programme.
2. The responsibility of providing this educa
tion and awareness is the joint responsibility of
government and non-governmental agencies. However,
it seems that one of the main reasons why health
education has not been given top priority in the
NTP is because of the field reality that the existing
services (even if they are geared up) cannot cope
with the increased demands of TB patients, if
awareness becomes widespread. There seems to be
no other reason why even after decades of NTP,
there is still no rationally formulated and researched
communication strategy. TB Associations have play
ed their role but their efforts seem to lack continuity,
technical competence or creativity and are predomi
nantly urban based.
3. Health education efforts should creatively
and competently involve all sections of the commu
nity not only as recipients of awareness building
efforts but also as promotors of ^further awareness.
While focussing on all sections particular interest
should be taken of policy makers, politicians and
community leaders including the functionaries of the
gram panchayat.
4. Improving the communication skills of all
categories of health workers from doctors all the
way to the community health workers should be an
important part of the strategy. At present this is one
of the most neglected areas in the existing curricula.
5. The science syllabus of schools does not
equip children with practical knowledge of common
diseases in India or for that matter for healthy
Sub-group Report
Tuberculosis in Medical Education
The group focussed upon the problem! of produ
cing a socially useful doctor in connection
with
tuberculosis, and the hurdles in the present medi
cal education system that have to be overcome in
this direction. The group itself was a small one and
represented five medical colleges only.
Preamble
1. The basic structure of present day medical
colleges and medical curriculum, propagates a
certain value system, which is predominantly exploitatory in nature;
2. We believe that propagating the attitudes
currently plaguing the fhedical system is a general
process, which involves the attitudes and practices
of faculty members, the expectations of our families
and society, and the ‘traditional’ role of a doctor
3. That medical education is incomplete in
itself, unless the social dimension of disease is stres-
living. There is considerable scope for incorporating
knowledge about TB in the science teaching of
schools. Schools could also become a focus
of creative involvement of school teachers and
children in health promotion.
6. There are a sizeable section of private
practitioners of non-allopathic systems who should
be involved in awareness building. They should be
involved not only in management of TB as a clinical
5
system into the teaching that unless one's clinical
judgement is backed up by labs, one is practising
'poor medicine'.
In fact, making a confident clinical diagnosis
with limited facilities available, is ‘good medicine’.
7. Emphasis is once again laid out on one
therapeutic regimen (ie., SM/INH/TA) for all TB
patients. The concept of suiting TB treatment to a
particular patient's background is not even
touched upon, eg., A labourer who can at
tend a TB clinic twice a week may be offered a
different treatment regimen compared to another
who can attend daily for SM injections. It is sur
prising that in spite of the fact that much of the
research work on alternative regimens of chemo
therapy emanate from India most of these well ac
cepted findings hardly find a place in medical edu- .
cation in the country.
Limitations of the discussion
We in our group were not able to touch upon
the following topics as regards medical education in
tuberculosis.
1. Research in tuberculosis and research prio
rity identification. Whether research and intervention
of a purely technological nature as is currently
practised by the NTI should be pursued or other
issues regarding socio-economic-political factors be
raised as well. Lack of research in communication
and education strategies which is a major lacunae,
also could not be discussed.
2. Continuing education of doctors about tuber
culosis; whose responsibility it is; and the form of
the continuing education programme. The group sug
gest that in light of the discussion a comprehensive
integrated model of teaching of tuberculosis should
be drawn up which can be tried out within the exis
ting constraints of the medical curriculum in India.
As a preliminary process to this effort a much wider
feed back from members in or of different medical
colleges should be obtained on their own experiences
of TB training in their education. This exercise would
establish a continuing link with the annual meet
theme of 1984 and probably could also be
featured in the Anthology of medical education under
preparatibn.
(Ravi Narayan, Vineet Nayyar, and Srinivas Kashalikar agreed to follow up on this along withf other
♦members).
Vineet Nayyar,
Vellore
fsed upon. It is for this reason, that many of our
senior colleagues (even those from NTI) believe in
purely technical or medical intervention for TB
control.
4. Priority of medical education as it stands
today, is directed towards the question of where is
the lesion? or what is the lesion? rather than how
was it caused and why? Our medical education does
not stimulate an average student to ask and seek
answers to social questions.
5. That trying to produce primary care doctors
in tertiary care centres is a major drawback in
itself.
Specific issues
1. We felt that the topic of TB as a disease is
* dealt with in a fragmented way, and is dealt with by
several departments in a medical college. It is for
this reason that the dynamic nature of TB as a
disease is ill understood, and problems in TB con
trol not even perceived. Some of us even passed
MBBS with the notion that TB meningitis is a dif
ferent disease from pulmonary TB and so on.
2. Specialised departments involved in TB
education cater to their own fields (perhaps a part
of the bigger problem of medical education in a
large set up). Attitudes of the faculty members are
built along the same plane. It is for this reason,
that physicians in the medicine departments absolve
themselves of the responsibility to teach about the
social aspects of TB.
3. Clinical medicine is glorified, while preven
tive aspects are looked down upon. Our system is
disease oriented and not health oriented. We look
at cavities and not at patients!
4. “Germ theory” of causation of disease is
propagated and medical intervention only is stressed
during undergraduate teaching. Even PSM depart
ments which undertake instructions in isociological
aspects of disease, have a narrow view of the dise
ase process. Most recommend medical interventions
as a solution quite like their own colleagues in clini
cal departments. Those that go a step further, preach
'better housing, more ventilation apd more food’
without understanding the deeper social aspect of TB.
Social action U almost never undertaken. Even
development projects which encourage incbme
generation schemes and other such social schemes
suppress a more basic question of unemployment in
society and so on.
5. Clinical teaching overemphasises
that
tuberculosis is a common problem and only classi
cal cases are shown to an undergraduate. This propa
gates the myth that being a common disease, it is
easy to diagnose and manage TB. Realities of TB con
trol are never dealt with or discussed so that an
average medical student at the end of his final year
(never recognizes any problems concerning tuber
culosis.
6. There are dictums laid down by clinicians
who teach that investigations are essential to make
a diagnosis. While this is largely true in places
where facilities are available, it introduces a value
An
Appeal
Thousands of innocent Tamils have been ren
dered homeless and jobless by the recent atrocities
and genocidal acts in Srilanka. Assistance, is parti
cularly required in the fields of food supplies, medi
cal supplies, clothing and so on. A group called
MUST—Medical Unit for the Service of Tamils-—
been formed in January 1985. They have requested
l _ '
1__ 1— 1-x__
A 1
us to put an appeal in- the
bulletin. AH
contribu‘
MUST,
tions and support may please be sent to
144 Choolaimedu High Road, Madras 600094,
India.
a
6
All India Drug Action Network
Report of The All-India Meeting on 30th & 31st Jan. 1985
The Drug Action Forum, Andhra Pradesh
had held a convention on Rational Drug Therapy,
which was attended by about 100 delegates. A spe
cial “Drug Information and communication cell” is
being prepared in the 7th Five Year Plan of Andhra
Pradesh and District Drug Advisory Committees
are being set up to advise the' authorities on the
Drugs-issue.
The AIDAN meeting was planned immediately
after the MFC meet. About a dozen groups from
different parts of the country had sent their repre
sentatives. First half of 30th January was spent in
reporting of what different groups have done during
last 6 months. It was nice to know that things are
moving forward on the Drug-Action front in differ
ent parts of the country. Special mention moist be
made of some of the activities:
J
Other groups in different areas have started
activities on the drug-front and building pressure
for implementing Government’s “Ban-Order” was
seen as an activity that would pick up in coming
days.
People io the Drug Action Movement
The Drug Action Forum of West-Bengal is
quite active. It had organized a protest-March to the
U. S. Consulate at Calcutta against the decision of
the American Congress to allow, under
certain
conditions, the export of those drugs which have
been banned in the U. S. The March was very well
attended. They have brought out a pamphlet in
Bengali with the title—“Are medicines meant for
the people or are people meant for medicines?” This
got a very good response. A calendar to spread this
n.essage has also been prepared and is being sold.
A convention was organized in Calcutta on 20th
January and was attended by 400 delegates represen
ting various organizations working in the people’s
Science and Health movements. The convention
adopted demands like: removal of useless, un
scientific, harmful drugs; ban the banned drugs,
reduce drug-prices, abolish brand names...etc.
. Mira Shiva reported that one political partyCPI-ML (Santosh Rana Group) has taken this ban
order as an action-plan and they had approached
AIDAN for relevant background papers. They have
decided to launch in different cities in India, hunger
strike until death, to pressurize the Government to
implement its own ban-order. This news caused a
lot of flutter and all of us would be keenly interes
ted to know what happens to this action-plan? and
its impact.
Steering Committee Report
Dr. Mira Shiva, the co-ordinator, reported
amongst other things about the recommendations
of the Steering— Committee set up by the National
Drug Development Council. These recommendations
have recommended a smaller span of price-control
on the drugs than what exists today. Only 95 drugs
and their formulations will be under price-control
if these recommendations are accepted. The mark
up for the drugs from this priority list is also sought
to be increased.
The KSSP had organized a campaign on oral
rehydration and irrational anti-diarrhoeals in 600 rural
units of KSSP. The KSSP is planning a state-wide
and then a nation-wide seminar on the drug-industry
•—“A decade after the Hathi Committee.”
This will lead to a rise in prices of all drugs—
both the price-controlled drugs and the decontrolled
drugs. This Steering Committee Report does not say
anything about irrational drug preparations in the
market. Coming a decade after the Hathi Committee
Report, this report is retrograde in character and
all of us must oppose it. It is likely to come before
the Parliament in the coming session.
The Arogya Dakshata Mandal has setup a few
“diarrhoea-centres” in Pune city slum's where slum
dwellers are taught the importance of oral rehydra
tion through demonstration. They are also publi
shing a two-volume book on Rational Drug Therapy.
The Catholic Hospital Association of India
(CHAI) held a two-day workshop on “towards a
people oriented drug policy” during its 41st Annual
National convention from 23rd to 26th November,
1984 at Bangalore. About 500 delegates from dif
ferent parts of the country listened to the different
paper-presentations about drug policy in India and
went back with idea of implementing rational drug
policy at least in their own hospitals.
Mira Shiva had convened an emergency meeting
of the Co-ordination Committee of AIDAN in
Delhi on 26th. November to discuss this report and
to give our response to it in a meeting convened on
29th November by the Ministry of Chemicals and
Fertilizers to discuss the “New Drug Policy.” A
note containing our criticism of these recommenda
tions and our positive suggestions was prepared and
Mira Shiva conveyed this to the officials during the
meeting on 29th November.
The Lok Vidnyan Sanghatana is continuing its
campaign against irrational over-the-counter drugs.
The Bombay unit of LVS has m'ade available plain
aspirin, paracetamol, Chlorpheniramine maleate in
a plastic packet along with a proper label, as an
alternative to Aspro, Anacin, Coldarin etc.
Action-Plan:
1. Action-plan in the coming few months
would concentrate on forcing the Government to
7
•
I
RN.27565/76
mfc bulletin: MARCH 1985
implement its own order banning 18 categories of
drugs. Mira Shiva has prepared a list of brands be
longing to these 18 categories of drugs. This1 list
would be improved upon by rechecking it and ear
marking those brands which sell the largest. This
improved list would be printed in thousands and
made available to doctors and Chemists through
different voluntary organizations and they would be.
requested to stop using, selling these brands.
One specific form of action-plan was suggested
during the discussion—After making available, the
list of brands belonging to those 18 categories of
drugs banned by the Govt, the action-group would
go round the city in a Morcha and would request
. doctors to throw away the samples of medicines
bearing these brands into a ‘'Zoli.” Chemists would
also be requested to throw away some medicines as
a token and to return the rest of their stock to the
drug-companies. This “Zoli” containing these
“banned brands” would be publicly burnt at a pro
minent place in the city.
2. A short summary of A I D A N’s criticism
of the Steering Committee recommendations would
be published and different groups should give ade
quate publicity to this criticism in their respective
areas. These recommendations are quite likely to
be kept before the parliament in the coming session
in the form of a New Drug Policy. It is necessary to
raise our voice at that time and compel the Govern
ment to desist from taking this retrograde step. A
summary of the Steering Committee Recommenda
tions and our criticism of it would be available with
Mira Shiva, Co-ordinator, AIDAN, C-14; Commjunity Centre, S.D.A. New Delhi-110016.
?
3. Court cases:
a) E. P. Forte—
Delhi Science Forum has agreed to launch a
fresh case in the Supreme Court about E. P. forte.
b) Depo-Provera—
Dr. C. L. Zaveri, a gynaecologist from Bombay
has filed a case in Bombay-High Court against the
Drug-Controller of India for not allowing him to
import Inj. Depo Provera. Considering the imiportance
of this case, Wpmen’'S Centre of Bombay and
Medico-Friend-Circle, have with the help of the
Lawyer’s Collective in Bombay, applied in the Bom
bay High-Court to be allowed as co-petitioners on
the side of the Government of India. It may be re
called that the Board of Inquiry set uj> by F. D. A.,
U.S.A, has recently given its verdict ruling out
the use of Depo-Provera as a contraceptive in general
Editorial Committee :
kamala jayarao
anant phadke
padma prakash
ulhas jaju
dhruv mankad
abhay bang
editor: ravi narayan
Regd. No. L/NP/KRNU/202
use. This notorious contraceptive is, however,
sought to be imported in India.
A broad-front of different women’s groups and
Science-groups is being formed to oppose the intro
duction of injectable contraceptives in India. Material
about the hazards of these drugs would be circulated
and a public-campaign would be launched against
its introduction.
Besides these co-ordinated efforts, there would
be local initiatives and its hoped that in 1985, the
Drug—Action—work would strike deeper, wider
roots and would create a much stronger public opi
nion against the irrationalities in the drug-^tuation
in India.
—An ant Phadke, Pune
URGENT
We need urgently contributions and donations
to support mfc’s studies/investigations in Bhopal and
publication of our team's reports for professional
and public awareness (cheques/DDs in favour of
'medico friend circle—Bhopal Fund’)
We are counting on you!
FORM IV
(SeeRule 8)
: Bangalore 560034
1. Place of Publication
2. Periodicity of its
publication
: Monthly
: Thelma Narayan
3. Printer’s Name
(Whether citizen of India?)
: Yes
Address
: 326, V Main I Block
Koramangala
Bangalore 560 034
Thelma Narayan
4. Publisher’s name
Yes
(Whether citizen of India?)
326, V Main I Block
Address
Koramangala
Bangalore 560034
: Ravi Narayan
5. Editor’s Name
Yes
(Whether citizen of India?)
326, V Main I Block
Address
Koramangala
Bangalore 560 034
Medico Friend Circle
6. Name and address of
50 LIC Quarters
individuals who own the
University Road
newspaper and partners
Pune 411 016
or share holders holding
more than one percent
of the total capital.
I, Thelma Narayan, hereby declare that the particulars
given above are true to the best of my knowledge and belief.
THELMA NARAYAN
Signature of Publisher
10-2-1985.
Dated
Views and opinions expressed in the bulletin are those of the authors and not necessarily
of the organisation.
Annual subscription — Inland Rs. 15-00
Foreign ; Sea Mail — US $ 4 for all countries
Air Mail : Asia — US$6; Africa & Europe — US $ 9; Canada & USA — US $ 11
Edited by Ravi Narayan, 326, Vth Main, 1st Block, Koramangala, Bangalore-560034
Printed by Thelma Narayan at Pauline Printing Press, 44, Ulsoor Road, Bangalore-560042
Published by Thelma Narayan for medico friend circle, 326, Vth Main, 1st Block,
Koramangala, Bangalore-560 034
^ 2-
■/
•
$2^
;•
TUBERCULOSIS PROGRAMME REVIEW
INDIA, SEPTEMBER 1992
•X
I
“^1
2
1
TABLE OF CONTENTS
PAGE NO
EXECUTIVE SUMMARY AND RECOMMENDATIONS
INTRODUCTION
LIST OF ABBREVIATIONS
TUBERCULOSIS IN INDIA
ORGANIZATION OF THE PROGRAMME
CASE FINDING AND DIAGNOSIS
TREATMENT
PROGRAMME MANAGEMENT
8.1 CASE NOTIFICATION
8.2 SUPPLIES AND TRANSPORT
8.3 SUPERVISION, MONITORING AND EVALUATION
8.4 EDUCATION AND TRAINING
9. PRIVATE SECTOR
10. RESEARCH
1.
2.
3.
4.
5.
6.
7.
8.
11. SITUATION ANALYSIS
12. RECOMMENDATIONS
3
7
8
9
14
19
22
26
26
27
28
30
31
32
33
36
ANNEXES
1.
2.
3.1
3.2
4.1
4.2
5.1
5.2
6.1
6.2
LIST OF PARTICIPANTS
INSTITUTIONS VISITED AND PERSONS INTERVIEWED
BACKGROUND INFORMATION
MAP OF INDIA
PRESENT TREATMENT PRACTICES
GUIDELINES FOR TREATMENT ORGANIZATION
COORDINATION WITH OTHER PROGRAMMES
VOLUNTARY HEALTH ORGANIZATIONS
EPIDEMIOLOGY REFERENCES
GENERAL REFERENCES
37
38
42
49
51
53
56
58
59
60
I
v>
1^17
1752—
3
TUBERCULOSIS PROGRAMME REVIEW - INDIA, 1992
1.
EXECUTIVE SUMMARY
The Government of India, recognizing the magnitude of the problem of
tuberculosis, the limited progress achieved by previous control activities
and the expected increase in incidence as a consequence of the HIV epidemic
has decided to give priority to tuberculosis control. In support of this
decision the Government requested WHO to carry out a joint programme review
together with other interested parties, A Steering Group was designated to
coordinate the evaluation of the programme, as a first step to formulating a
project for possible external assistance.
The review of the national tuberculosis programme (NTP) of India was
carried out by a team representing the Government of India (GOT), the World
Health Organization and the Swedish International Development Agency (SIDA). '
The purpose of the review was to evaluate present policies and practices,
analyze their adequacy to reduce the tuberculosis problem and recommend
organizational, technical and administrative measures to improve the
programme.
The review team analyzed the available documents including
epidemiological data and reports of previous evaluations of the programme,
discussed with officers of major institutions involved in disease control and
in training, and made field visits in three States (Gujarat, Uttar Pradesh
and Tamil Nadu) to assess the programme at the State, District and peripheral
levels.
The burden of tuberculosis in India is staggering by any measure. More
thaN half of the adult population is infected. About 1.5 million cases are
notified every year and there are probably well over 500 000 tuberculosis
deaths annually. Recent trends show that the programme is not having a
measurable impact on transmission and appears to function far below its
potential.
The Government of India formulated the NTP in 1962. The major objectives
were to prevent tuberculosis through BCG vaccination; to diagnose
tuberculosis cases among symptomatics and provide efficient treatment, giving
priority to sputum positive patients; and to implement these activities as an
integral part of general health services. The District was the basic unit for
the NTP organization.
At present, organization of the general health system has been extended
to reach the community level with primary health services, The tuberculosis
programme is integrated into the general health services, and treatment
services are provided at the levels where medical staff is available.
However, the population growth and the proliferation of public health
services has made many Districts unwieldy for supervision by the tuberculosis
team which is based in a single District Tuberculosis Center. Further,
monitoring and training are mainly under the responsibility of the National
Tuberculosis Institute (NTI), the State TB officers playing only a minor role
in these important areas.
&*
_! '
Human and financial resources are provided by GOI and the States to cover
most of the needs of the programme and current policy is to provide free
diagnosis and-'treatment. Currently available data do not allow analysis of
the adequacy or efficiency with which these resources are applied, but
preliminary indications^ and overall TB programme performance point to the
need for substantial improvements. If the programme is to operate as intended
and begin to make a significant impact on the disease, increased funding will
be necessary, emphasizing the need for improvements in programme
effectiveness and efficiency.
*
4
Th« pieswit
structure St national level requires strengthening
to
lea^erihip in redefining policies, effectively assisting States and
supervising prograaae implenientation, retraining staff involved in TB
activities, administering funds, and procuring supplies. The States, which
provide health services, need also to assume their responsibility in TB
programme management, and will require reorganization and training of the
public and non government health institutions involved in TB control.
There is little coordination between hospitals and primary health
institutions in rural areas, and between the different services providing
tuberculosis care in most urban areas, to ensure the management of
tuberculosis patients until cure.
Improvements in the methods and management of case -finding must take
place. In spite of the recognized priority of bacteriological diagnosis and
cure of sputum positive cases to reduce the problem of tuberculosis, a large
proportion of human and financial resources is currently used to treat cases
diagnosed only on clinical and radiological evidence. This practice is common
both to the NTP and to private practitioners and is reflected in medical
college curricula. Bacteriology is not sufficiently used to confirm medical
diagnosis and criteria for initiating treatment in sputum negative cases are
not well defined. As a result of not identifying correctly smear-positive and
smear-negative cases, and newly diagnosed and previously treated patients,
some patients may be treated with inadequate regimens. Sputum microscopy
examinations are carried out with insufficient standards and microscopy
laboratories are inadequately equipped. A TB laboratory network assuring
equipment, training and quality control is not in place.
Rationalization of treatment is required. There are currently too many
alternative treatment regimens and the conventional regimens are of
unnecessary long duration and low effectiveness. Short course chemotherapy
regimens of higher cost-effectiveness are slowly being implemented but
insufficient priority has been given to ensuring effective treatment of
infectious patients, particularly during the initial intensive phase of
chemotherapy.
The present system of recording and monitoring patient identification an
progress during treatment to ensure health service concentration on achieving
cure of infectious cases is seriously deficient. The present system does hot
allow the systematic evaluation of the results of treatment at health
facility or block level. Neither does the registration systetn permit the use
of cohort analysis of patients to assess cure rate a? the main indicator of
programs efficacy.
Drug supplies are occasionally interrupted by lack of timely funding and
of buffer-stocks-. Additionally; the quality of the drugs supplied is not
controlled. The extensive network of multipurpose health workers (MPHW) has
not been sufficiently utilized at the community level to prevent defaulting
and achieve treatment completion.
The present training system relies mainly on the National Tuberculosis
Institute (NTI) courses. The state-level demonstration and training centres
do not function. District Tuberculosis Centres (DTCs) are not adequately
prepared to provide in-service training for dissemination of policy and
standards. It does not make adequate use of training institutions and NGOs at
the State level to transmit current policies and procedures. The curricula,
at medical colleges do not stress the basic principles of TB control and
there is no systematic continuing education for medical practitioners.
5
In spite of extensive national experience in both operational and basic
TB research, alternative methods to correct the extremely low proportion of
cases diagnosed with bacteriological confirmation and of patients completing
the prescribed treatment and cured have seldom been implemented. The
findings of previous programme evaluations have not always been applied to
improve existing programme procedures, nor has adequate use of the results of
research and programme evaluation b.een made.
Nonetheless, the basic strengths of the India TB programme are
considerable. The objectives on which the programme was established thirty
years ago - integration, decentralization, free services, priority to
treatment of infectious cases - are still valid today. They provide a sound
basis for revitalization of the national TB strategy. In addition, the
tuberculosis control programme can relatively easily build on its strengths:
a well defined structure which provides services within general health care
in an integrated manner; a basic managerial unit at District level with
Central and State Governments providing support for diagnosis and treatment;
experienced training and research Institutions; and, a general health care
system extended to the community through multipurpose health workers. An
updated and strengthened programme can expect to reduce the magnitude of the
problem by about half in each 10-15 years with the consequent savings in
lives, human suffering and more effective use of financial resources. This
will require a political commitment, initial investment and strong
leadership, plus the rapid development of an efficient national model to
serve as training ground and provide operational experience to programme
managers at all levels.
recohh£ndatiohs
1.
The structure of the National Tuberculosis Programme should be
strengthened by 1) establishing an apex policy making authority and an
executive task force with managerial functions to impLement programme
reorganization, and 2) upgrading the central tuberculosis control unit in
the Directorate to provide strong leadership and enhance the efficiency
and effectiveness of the National Tuberculosis Programme.
2.
The quality of patient diagnosis should be improved by 1) using three
smear examinations to detect infectious cases among symptomatics before
deciding on patient treatment, 2) ensuring the quality of microscopy with
adequate equipment, training and quality control, and
3) establishing criteria for diegnosis by radiological and clinical
methods.
3.
National and state tuberculosis programme resources should be directed to
ensuring cure of tuberculosis patients, giving priority to infectious
cases of tuberculosis by 1) adopting short-course chemotherapy, 2)
establishing criteria for treatment completion, cure and discharge from
medical care, and 3) ensuring an uninterrupted supply of drugs of good
quality.
4.
The current NTP system of registration and notification should be revised
to emphasize the cohort analysis of treatment results (completion and
cure, transfers, defaulters, died, treatment failures) as the main
indicator of progr^Jume effectiveness.
5.
Policies should be developed to ensure decentralization of treatment
services closer to the community level to enhance access to care and
patient compliance to recommended therapies.
6.
Pilot projects should be implemented at block level to test the
feasibility and results of different technical and organizational
6
strategies to be adopted by the tuberculosis programme -- i.e., to test
the capacity to implement recomaendjitions 2-5 above.
7.
A medical officer or treatment organizer and a laboratory supervisor,
with the necessary transport, should be added to the existing
administrative structure at the sub-district level (about 500,000
population) to strengthen tuberculosis programme management and to
facilitate decentralization of supervision.
8.
Training materials must be developed to reflect the proposed changes in
programme policies and procedures. The current training infrastructure
will need to broaden the scope of its training capabilities by utilizing
state training facilities, medical colleges, public health institutes and
tuberculosis-oriented voluntary agencies to augment training efforts.
International and national training opportunities should be made
available for the different levels of tuberculosis programme staff.
9.
Operational research must be carried out as an integral part of the
revised tuberculosis programme to evaluate programme performance, improve
delivery of services, problem solving and obtain baseline epidemiologicax
information to measure reduction in the risk of infection.
t
7
INDIA - TUBERCULOSIS PROGRAMME REVIEW 1992
2. INTRODUCTION.
A review of the national tuberculoai* progranae was carried out fro*
9/1/92 to 9/17/92 as a collaborative effort of the Government of Indi* (GOI),
the World Health Organization (WHO) and the Swedish International Development
Agency (SIDA). The purpose of the review was to evaluate present policies
and practices, analyze their adequacy to reduce the tuberculosis problem and
retommend organizational, technical, and administrative measures to improve
the programme.
The assessment included:
1.
2.
3.
4.
An overall description of the current programme achievements and
problems,
An analysis of the tuberculosis burdep, the programme resources and
the programme structure,
Specific discussion of the leading Issues facing the programme and
their underlying causes, and
Recommendations for the next steps to improve the programme.
■
i reviewed information relating to the
At the central level the team
magnitude
or
tne
cuoercuxuaxs
problem
in the country and epidemiological
gnitude of the tuberculosis
trends,
structure, policies, technical norms and procedures
trends, programme
programme structure,
relating to tuberculosis diagnosis and treatment, drug supply and logistics,
supervision, monitoring and evaluation, education and training coordination
with other programmes and research. Meetings were held with the Min stry o
Health, major referral facilities in New Delhi and voluntary organizations.
Following the review at the central level, the review participants
divided into thfee teams to assess tuberculosis control activities at the
State and District levels through facility visits and interviews with
responsible staff in three selected States (Tamil Nadu, Gujarat, and Uttar
Pradesh). Then the teams reconvened in Delhi for discussion of t e rev ew
development of principal recommendations for^
findings, conclusions and (
submission to the Government of India, A draft summary of the conclusions
of Health at the end
and main recommendations was presented to the Secretary
of the review.
is attached in Annex 1, and a list of persons
A list of participants
contacted and Institutions visited as part of the review is in Annex 2.
This document summarizes the findings of the review. Background
information on India can be found in Annex 3.1.
8
3. LIST OF ABBREVIATIONS
ADGHS
BCG
CHC
DGHS
DHO
DOT
DTC
DTO
DTP
EPI
GH
GNP
GOI
GP
H
ICMR
IMA
IMR
MBTC
MG
MCE
MO
MOH/FW
MPHW
NGO
NRR
NT I
NTP
PHO
PHI
PPD
R
RC
RI
• RS
S
T
TAI
ASSISTANT DIRECTOR GENERAL OF HEALTH SERVICES
BACILLI CALMETTE & GUERIN
COMMUNITY HEALTH CENTRE
DIRECTOR GENERAL OF HEALTH SERVICES
DISTRICT HEALTH (MEDICAL) OFFICER
DIRECTLY OBSERVED TREATMENT
DISTRICT TUBERCULOSIS PROGRAMME
DISTRICT TUBERCULOSIS 'OFFICER
DISTRICT TUBERCULOSIS PROGRAMME
EXPANDED PROGRAMME OF IMMUNIZATION
GENERAL HOSPITAL
GROSS NATIONAL PRODUCT
GOVERNMENT OF INDIA
GENERAL PRACTITIONER
ISONIAZID
INDIAN COUNCIL OF MEDICAL RESEARCH
INDIAN MEDICAL ASSOCIATION
INFANT MORTALITY RATE
MASTER BOOK OF TREATMENT CARDS
MYCROSCOPY CENTRE
MATERNAL AND CHILD HEALTH
MEDICAL OFFICER
MINISTRY OF HEALTH AND FAMILY WELFARE
MULTI-PURPOSE HEALTH WORKER
NON-GOVERNMENTAL ORGANIZATION
NET REPRODUCTIVE RATE
NATIONAL TUBERCULOSIS INSTITUTE
NATIONAL TUBERCULOSIS PROGRAMME
PRIMARY HEALTH CENTRE
PERIPHERAL HEALTH INSTITUTIONS
PURIFIED PROTEIN DERIVATIVE
RIFAMPICIN
REFERAL CENTRE
RISK OF INFECTION
RUPEES
STREPTOMYCIN
SHORT COURSE CHEMOTHERAPY
SWEDISH INTERNATIONAL DEVELOPMENT AGENCY
STATE TUBERCULOSIS OFFICER
STATE TUBERCULOSIS TRAINING AND DEMONSTRATION
CENTRE
THIOACETAZONE
TUBERCULOSIS ASSOCIATION OF INDIA
TRC
TUBERCULOSIS RESEARCH CENTRE
VHAI
VOLUNTARY HEALTH ASSOCIATION OF INDIA
X-RAY CENTRE
see
SIDA
STO
STTDC
xc
KT
9
4. TUBERCULOSIS IN INDIA
Prevalence of Infection- A number of studies over the past 30 years, mainly
in rural Mnithirn India, have shown the prevalence of infection among
children 0-9 y«ari old to b« between 3.IX and 11.2X (Table 1). In the early
1960s, mor® than 50X of tha population 20 years and older was infected with
ft. tuberculosis
most infections occurred before 15 years of age. By the
late 1960s there wa« no evidence of change in this pattern. Since that time,
there is no clear evidence of substantial changes in prevalence of infection
among children beyond that which might have been expected from secular
trends.
Tabic I. India: Prevalence of tuberculosis infection among un-vaccinated
children 0 to 9 years old and estimated annual Risk of Infection (RI)
RI
Year
Location
Source
4.9X
1.0X
1961
Tumkur
NTI
9.6X
2.OX
1969
Tiruvallore
TRC
10. IX
2. IX
1983
Bangalore
NT!
10.4X
2.2X
1984
Dharmapuri
NTI
3. IX
0.6X
1985
Bangalore
NTI
9.OX
1.9X
1989
Kadambatmur
TRC
11.2X
2.3X
1989
Thiruvelangadu
TRC
6.7X
1.4X
1989
North Arcot
TRC
Prevalence of
infection
----- - ------ 1------------------------------------------
Annual risk of infection. The intensity of disease transmission in the
community is beet reflected by the annual Risk of Infection (RI) which
represents the probability of a previously uninfected individual becoming
infected with tuberculosis during a one year period.
RIs calculated from prevalence studies presented in Table 1 range from
0.6X to 2.3X. These data are difficult to interpret because methods vary
among surveys but they qlearly indicate wide variation within limited
geographical areas and provide no clear evidence of a substantial decrease of
the risk of infection over the last 30 years. This stagnant situation is
substantiated by two recently published studies conducted in rupal areas of
Southern India. One showed that the RI decreased from 1.0X in 1961 to 0.61X
in 1985, equivalent to an average decline of 3.2X per year. The other study
showed no decrease in the risk of infection between 1969 and 1984 (RI of 1.7X
in both y^ars). These results would be consistent with a poorly functioning
programme which Would be creatipg chronic cases of tuberculosis and drug
resistance."
Because most adults were infected in their youth, a small decrease of tne
RI would not have any rapid impact on the prevalence of infection in the
adult population. It is safe to estimate that at least 50X of the population
above the age of 20 years is infected and will remain at risk of disease and
death from tuberculosis for their lifetime. A conservative estimate is that,
currently, the RI for India is still between IX and 2X.
Disease prevalence. The Sample Survey of tuberculosis conducted between
1955-58 remains the major source of information used by the NTP to anticipate
10
the tuberculosis situation in the country. The survey showed wide variations
in prevalence of disease among persons aged 5 years or more (sputum-positive
tuberculosis by smear or culture), ranging from a low of 229/100,000 to a
high of 813/100,000. The overall prevalence was 398/100,000.
In 1960-61 and in 1972-73 surveys conducted by NTI showed the prevalence
of radiological disease to be 1900 and 1100 per 100,000 respectively. In
1990, in an area near Madras, the rate was estimated to be 1700/100,000. In
the first of these studies, the prevalence of sputum-positive tuberculosis
was 410/100,000 and in others studies conducted by NTI between 1961 and 1968
in the Bangalore area the prevalence of bacteriologically confirmed
tuberculosis (smear or culture-positive) ranged from 337 to 406/100,000 over
the age of 5 years. About half of these cases (45X to 52Z) were smear
positive. In a number of surveys and studies since that time, there is no
evidence of a significant decrease in TB during the last three decades and
there remains a very wide range of prevalence of TB in India. In the 1972-73
follow up of the 1960-61 study, the prevalence of bacteriologically confirmed
disease was 440/100,000. Two studies conducted in 1989 and 1990 in two are?
near Madras in the population above the age of 15 years found prevalence of
bacteriologically confirmed disease of 1090 and of 430/100,000 (58X and 69X
of confirmed cases were smear-positive).
The only clear exception to this stagnant situation is recent data from
the Tuberculosis Prevention Trial1, in which a 350 000 population of South
India is being followed prospectively. This study indicates a decrease in
prevalence and incidence of both radiologically active and sputum-positive
tuberculosis between 1968 and 1985. Most of the decrease, however, occurred
during the first few years of the study. Data from 1978 to 1985 show
stagnation with a prevalence about 1700/100 000 above the age of 10 years old
(by X-ray or culture) and an incidence of about 450/100 000 over the age of
10 years (X-ray or culture). During th'e same period, 50X of all cases had
bacteriologically confirmed (culture-positive) tuberculosis.
Among the many factors influencing prevalence of disease, the
effectiveness of treatment is important. Poor treatment completion
significantly increases the prevalence of disease. A recent retrospective
cohort study conducted under programme conditions by the Tuberculosis
Research Centre (TRC), Madras, illustrates the potential impact of poor
treatment completion. It showed that among patients on short course
chemotherapy who collected less than 50X, 50% to 79X and SOX or more of their
drugs, 44X, 37X and 21X respectively were still sputum smear-positive after
the end of treatment2.
Low effectiveness of the treatment programme explains much of the
stagnation in disease trends over the last three decades. Further, with the
current treatment completion rate it is probable that chronic and partially
treated patients represent a large proportion of patients diagnosed by the
programme.
Current tuberculosis rates. Age specific incidence rates (NTI, 1974) •
estimates suggest that about 870 000 new smear-positive cases of tuberculosis
may have occurred in 1992. This number is very similar to the 850 000
estimate obtained on the basis of incidence data from the Tuberculosis
Prevention Trial3. If the current average annual risk of infection is 1.7Z,
i
S.P. Tripathy, personal communication, 1992
2
TRC Annual Report, 1990
3
S.P. Tripathy, personal communication, 1992
!
11
1.6 million new cases (all forms) and 714 000 new smear-positive cases o
tuberculosis may occur annually. About a third of the total tuberculosis
burden of India is borne by the urban conglomerations consisting mainly □ f
towns, cities, and their suburbs.
Notifications. Based on the average case notification from districts wirh
existing tuberculosis programmes (with about 83X of the population of the
country), NTI estimated more than l.’S million newly registered cases of
pulmonary tuberculosis in 1991. 21X of them were smear-positive , The trend in
notification, presented in Figure 1, reflects the increase in the number of
districts integrated in the tuberculosis programme from 32Q in 1980 to 337 in
1991, and also an increased proportion of cases not confirmed by smear
examination. The proportion of smear-positive cases has decreased from 25X in
1980 to about 20X in the late eighties. Relapses,, failures"and partially
treated patients are often inappropiately included in these notifications.
Figure 1. India: Notifications of cases
of tuberculosis, 1980-1991
Thousands
1500 Smear-positive
All pulmonary
1200 -
900
600
^QO 4
0
j________ |
i
i______
i -.
i
-i________t________ i _
i
i,
__ I
1980 1981 1982 1983 1984 1985 1986 1987 1988 1989 1990 1991
Year
Extra-pulmonary cases are not reported
Source: NTI, 1992
12
in India occur
Of th. diagnosed cases between 15
S Jen 15 and 40 ykr. old. J thirds of the c.se, are e.tl.at.d to oecnr
anong nales but tuberculosis takes a proportionally ouch larger toll on yo
females than among young males. More than SOX of fema e cases occu
g
age 34.
Mortality
Total mortality due to TB is uncertain but by any estimate poses
a huge economic burden for India. Tuberculosis mortality is estimated by NTI
to have been 69 to 95/100 000 in 1961-68 and 41/100 000 in iS77’81- or °ve
350 000 tuberculosis deaths annually (Table 2).
Data from the Survey of
Cause of Deaths yield a more recent parameter by which to estimate curren
mortality resulting in.400 000 deaths., about 75 000 deaths in the 15-24 age
group, 95’000 in the 25-34 age group and about 160 000 deaths in the 3 '
age group. Using the 1955 Sample Survey estimates of incidence if all cas
wfreSdiagnosed and at the present treatment completion rate of 30X, ther
would belabour 657 000 annual deaths of tuberculosis. A large proportion of
these deaths occur among women and it has been estimated that materna
mortality and tuberculosis claim approximately the same number of lives,
the decade of the 1990's, any of these estimates implyes a staggering
ci..
For
cumulative burden for the disease.
T ab12 .
India: Estimates of probable tuberculosis mortality
Source
& year
Estimated
mortality
per 100 000
Annual deaths
Approximate (1)
cumulative deaths
^1990-2000
41.0
346 000
3 460 000
Causes of deaths survey
92
50.0
422 000
4 220 000
Sample Survey incidence estimates (2)
55-58
■ 77.8
657 000
6 570 000
NT I
77-81
"Styblo model" of incidence with 1.5X RI (2)
4 22'
320 000
92
50.1
432 000
(1)
(2)
Mortality rates from surveys applied to 1992 population structure and
cumulative burden not adjusted for age structure within the decade.
Assuming no improvement from the current treatment completion rate or
30% and assuming 100% coverage of new cases.
Using the number of cases of tuberculosis currently notified by the NTP
the reported completion rate (30X) , a case fatality of 10X among patients who
complete treatment, 48X among smear positive-patients who did not complete
treatment and 24Z among smear-negative patients, it can be estimated that
about 345 000 tuberculosis patients today diagnosed in the programme die.
Almost all of these deaths are preventable. Increasing the treatment
completion rate to only 85X would prevent close to 200 000 deaths annually,
57% decrease in mortality.
. 1
13
Table 3.
India: Number of Tuberculosis deaths which could be expected among
cases officially reported in 1991 at different rates of treatment completion
and potential reduction in mortality.
Completion
rate
30X (current)
40X
70X
85X
Smear
positive
Total
cases
Reduction in mortality
(all cases)
Lives
Percentage
saved
reduction
121 000
1,09 000
71 000
52 000
345 000
309 000
202 000
143 000
Base line
36 000
143 000
197 000
Expected deaths among
10X
41X
57X
* Pulmonary. As extra-pulmonary cases are not reported, they are not
included in this calculation
Cumulative mortality during the decade to the year 2000 will probably
exceed 3.5 million deaths, an enormous burden for society. A large share of
these premature deaths can be avoided with a well-functioning programme.
Given the ages at which deaths from tuberculosis are now occurring and the
low costs for tuberculosis programme inputs in India, it is probable that the
discounted cost per healthy year of life gained as a result of a well
functioning tuberculosis control programme will be well under US $10, making
tuberculosis control one of the highest priority interventions for the State
and central governments.
AIDS and tuberculosis. HIV began to spread in India only in the latter part
of the 1980s and there is no evidence yet that HIV infections are having an
impact on the tuberculosis situation. Only recently HIV testing has become
more common in a few research and academic institutions. A survey conducted
among all newly diagnosed smear-positive tuberculosis patients in 1990 in
Madras found 15 confirmed positive HIV cases among 2165 patients tested
(0.7X). In Vellore, there were 16 confirmed HIV positives among 906 patients
newly diagnosed with pulmonary tuberculosis (1.8X).
In 1992, 12 of 183
(6.3X) tuberculosis patients admitted to a hospital in Bombay were HIVinfected.
In a follow-up study of 220 HIV infected individuals conducted in
Madras, 115 (52X) had radiological evidence of tuberculosis and 34 (15X) were
culture positive. Other studies of HIV-prevalence in the general adult
population have revealed prevalence varying between 0.1X in Calcutta to IX in
Bombay. The AIDS programme estimates that currently there are 750 000
persons infected with HIV in the country and that there will be 5 million in
the year 2000. Assuming half of these people are ’also infected with
tuberculosis, and that the breakdown rate from tuberculosis infection to
disease among dually infected individuals is 10X per year, more than 35 000
HIV-related tuberculosis cases will occur in 1992. There may be as many as
250 000 HIV-related tuberculosis cases annually at the end of tne decade.
Virtually all of these cases will be in addition to the expected incidence.
As important as these cases will be, they will continue to represent only a
fraction of the cumulative cases of tuberculosis during the decade.
Tuberculosis drug resistance, Only a few laboratories can conduct drag
sensitivity testing in India. Although data on drug resistance is scarce and
resistance is not systematically monitored, available information (Table 4)
is cause for concern. The very high rate of secondary resistance to both
rifampicin and isoniazid is particularly serious, with long term implications
as these patients will transmit, a virtually incurable form of disease .within
the community.'
14
Table 4; India: Primary and Acquired’ Drug Resistance in selected areas.
Type of patient
and sample size
S
Failure
81
354
560
50.7
78.8
30.0 65.0
Previously Treated
37
Madras (2)
111
Raichur (2)
Nev cases by history
241
Madras (2)
244
Raichur (2)
324
Delhi (1)
(1) :
(2) :
Delhi Centre (1)
Delhi Suburbs (1)
North Arcot (2)
% Resistance to
H
R
HR
SHR
16.0
33.3
61.5
6.0
9.0
35.0 62.0
11.7 52.7
13.5
17.1
5.4
5.4
8.1
11.7
7.3 12.6
11.0 19.1
18.5
1.6
3.2
0.8
2.0
0.6
0.8
1.2
Ind. J. Tub. Vol.39 No.2 pp 121-124
TRC Annual Report and M. Datta, personal cnnimnntcarion
Conclusions:
The burden of tuberculosis in India is staggering by any measure. About
1.5 million cases are notified every year, more than half of the adult
population is infected, and there are at least 300 000 tuberculosis deaths
annually. Social and economic consequences of tuberculosis for individuals
and for the society are enormous in human suffering, economic loss, and
decreased productivity. Recent trends are discouraging, indicating a
programme which does not have any measurable impact and which appears to
function far below its potential. While further study and improved analysis
are needed to rigorously document the epidemiological situation, it will not
change the broad conclusion that tuberculosis is one of India's most serious
and still neglected health problems.
5. ORGANISATION OF THg PROGRAMME
Hfttivnal Level. The Ministry of Health and Family Welfare (MOH/FW) is
divided into an administrative arm headed by the Secretary of Health and a
technical am headed by the Director General of Health Services (DGHS). The
Secretary of Health is assisted by Additional Secretaries and the DGHS by
Additional DGHSs and several Deputy DGHSs. One of these Deputy DGHS
supervises the NTP as well as several other programmes. The responsible
officer for the TB programme is an Assistant DGHS (TB). The NTP is located
within the technical arm of the MOH/FW and on the administrative side, it is
coordinated by a Joint Secretary who is responsible for its financial and
administrative control.
National Tuberculosis Programme Policies. The long term objective of the NTP
is to reduce tuberculosis in the country to the level where it ceases to be a
public health problem. To accomplish this objective, the NTP focuses on 1)
the BCG vaccination of infants, 2) the detection of the maximum number of
tuberculosis patients among out-patients attending health institutions, and
3) the efficient treatment of identified tuberculosis patients, all as an
integral part of India's general health services.
15
Central Structure of the NT?. The Central Unit of the NTP has a staff of
about 10 people. In addition to the Director, there are two physicians and 6
administrative officers for drug procurement, international assistance,
monitoring of monthly reports, annual planning and coordination with the
National Tuberculosis Institute (NTI)A. Currently, the post of programme
director (Assistant DGHS-TB) and one of the two medical officer posts are
vacant. The level of the programme director is lower than that of other
programme directors (EPI,- Leprosy) and below the level of the director of
NTI. This, plus the fact that two out the three central level posts are
vacant reflect the low priority given to the NTP and show the absence of
strong national leadership. This situation, if maintained, would jeopardize
any attempts to revitalize the programme.
The Central Unit is responsible for drugs forecasting, purchase and
allocation, the annual planning and participation in the discussions of the
MOH/FW with the planning commission to determine the annual and 5-yearly
"plan budget" of the NTP, and for liaison with international agencies (WHO,
SIDA), with NTI, and with state TB programmes. The central unit does not play
any significant role with respect to tuberculosis control technical policy,
training and manual preparation, monitoring and supervision. These
responsibilities have been progressively taken by NTI. NTI management,
however, is virtually independent of the NTP. Additionally, State
Tuberculosis Officers are State employees, and they are not accountable in
practice to the ADGHS (TB).
. NTP budget. The MOH/FW budget is
Is composed of a "non-plan budget" used for
personnel, salaries, hospitals, etc and a "plan budget", allocated by the
’ Planning Commission for future investments or creation of new posts. The
"non-plan budget" is not controlled by the NTP and fluctuates minimally from
year to year. No detailed information could be made available to the review
team about the proportion of the NTP budget corresponding to the "non-plan"
budget nor a breakdown by States of the NTP budget and its trend. The 1992
(March 92 - February 93) plan-budget of the NTP is R 145 million (US$ 5.3
million) of which R 110 million - more than 75X - are used to purchase drugs
and 25 million for other expenses such as X-ray units and films, microscopes,
vehicles, etc. Anti-tuberculosis drug costs are shared on the average on a
50:50 basis between Central and State governments. Within the overall NTP
budget, the Central government also provides anti-tuberculosis drugs to
voluntary organizations, and supplies, equipment, and drugs to the Union
Territories.
Other r^SQurceg. The Swedish International Development Agency (SIDA) has
provided funds through WHO. These funds have been Used to purchase x-ray
units with Odelca cameras, miniature x-ray film rolls, vehicles, anti
tuberculosis drugs and microscopes. Occasionally, District and State
tuberculosis associations provide anti-tuberculosis drugs, materials and
equipment to specific district programmes or local tuberculosis facilities.
National Tuberculosis Institute (NTI).
The National Tuberculosis
Institute (NTI), located in Bangalore, is responsible for training NTP
personnel, monitoring the programme and conducting operational
research studies. Each year, NTI organizes two 10-week courses. In
1991, for example, 166 health professionals were trained. Apart from
training DTC teams, the NTI also provides refresher courses for
persons working for district tuberculosis control programmes and
reorientation/retraining seminars for senior health administrators and
teachers from medical colleges, etc.
Lastly, the NTI collaborates
with the World Health Organzation (WHO) for international.training
efforts.
16
2 State level. India is administratively divided into 25 States and 7 Union
Territories. In the State MOH/FW, the NTP is under the Director of Medical
Services, Health and Family Welfare and the Director of National Programmes.
All States have a State Tuberculosis Officer (STO) , usually assisted by a
staff of 6 to 10. The vast majority of STOs have been trained at the NTI.
In principle, there is a meeting of all STOs at the central level once a
year.
Responsibilities of the Stare Tuberculosis Officer (SlOj. The STO is
responsible for negotiating for the State the amount of drugs provided by the
central government and monitoring drug distribution to the Districts. He is
responsible for the overall supervision of District Tuberculosis Officers
(DTO) and through them of Peripheral Health Institutions (PHI). Lastly, he
should organize and coordinate training activities at the State level, in
conjunction with the State Tuberculosis Training and Demonstration Centres
and with NTI.
State tuberculosis demonstration and training centre (STDTC).. Seventeen
states have training and demonstration centres. These centres were created
in the early sixties to supplement NTI. They have an average staff of 100
people with about 30 professionals. In addition to training, they have
responsibilities in diagnosing and treating patients and have, in some
instances, research activities. In practice, however, the vast majority of
these centres do not have an organized training programme or research
activities and (jperkte solely as District Tuberculosis Centres (DTC).
3, District level. The District is the basic demographic, economic,
administrative and political unit in India, The District is further divided
into Taluks and Community Development Blocks. One District encompasses 1,800
to 2,000 villages, has an average population of about 1.5 million, and a land
Institutions in the District
area of 10,000 square kilometres. Health institutions
generally include:
1.
2.
3.
4.
5.
One district hospital in the headquarters town.
Community Health Centres (CHC).
(CHC). 1Usually one in each Taluk, with
several doctors and specialized services (about 10 CHC per
district).
Primary Health Centres (PHC). In principle, one in each community
development block (about 40 per district).
Varying number of sub-centres (180) , other peripheral health
institutions, dispensaries, maternity and child welfare centres,
employee dispensaries, and private hospitals.
Specialized tuberculosis institutions. ’Tuberculosis clinic, DTC
where the DTC has been implemented, sanatorium (about 100 beds per
district).
100 000 population and one PHC per 30 000 population,
j have about 10 to 15 CHCs and 50 PHCs. The country is
an average district may
network
of
21 805 PHCs and 137 683 sub-centres (Figure 2).
covered by a i._-- With one CHC per
17
Figure 2
ADMINISTRATIVE ORGANIZATION AND HEALTH SERVICES
ORGANIZATIONAL. LEVEL
HEALTH SERVICES
Number
- Average Population
National
Institutes
850 000 000
S tate
Hospitals
25
Sanatoria
34 000 000
State TB Centre (STTDC)
District
District Hospital.
-438
District TB Centre (DTC)
2 000 000
1 500 000
Taluk
Community Health Centre (CHC)
appr. 15 per district
Central Hospital
100 000
CocHgunity Pevelopment. Blok
appr. 40 per district
30 000
40 000
Primary Health Centre (PHC)
Maternal and Child Welfare Centres
Employee and Panchayat Union
Dispensaries
Villages
1800 - 2000 per district
700
Subcentres (each 4-5 villages)
with Multipurpose Health Workers
800
u
18
In addition to these services, it is estimated that there are 330
tuberculosis clinics in operation in urban areas to provide services for the
local residents. Approximately 47,000 hospital beds are available in the
country for the in-patient care of seriously ill tuberculosis patients.
In the district, curative medical services and hospitals are managed by
the District Medical Officer (DMO) and preventive services and primary health
care by the District Public Health Officer. Although the District
Tuberculosis Officer (DTO) works under the authority of the DMO, he has no
formal control or authority over the district hospital and specialized
institutions. Conversely, he controls and supervises tuberculosis activities
in PHIs although these institutions are under the administrative authority of
the District Public Health Officer. This situation means that the DTO cannot
exercise leadership to improve the quality and coordination of tuberculosis
control activities in hospitals and does not have the line of authority
required to properly manage control activities in peripheral institutions.
District Tuberculosis Programme (DTP) . In 1991, District Tuberculosis
Programmes were in existence in 378 districts out of 438 districts in the
country (86X) . In a district, all health institutions which undertake case
finding and treatment for tuberculosis are considered as participating units
of the DTP. These institutions are classified as either DTCs or PHIs. Each
district participating in the DTP has one DIG. Sub centres do not have
medical officers and are not considered as part of the DTP network.
District Tuberculosis Centre. DTCs maintain the patient case registers,
manage the recording and reporting system and are responsible for supervising
the TB activities of the PHIs. The DTCs also serve as referral centres to
PHIs for X-ray examinations, They have X-ray units, microscopes and
vehicles. They receive funds for drugs, gasoline, car maintenance, etc. from
the State, Anti-tuberculosis drugs are. supplied by the national Central Unit
to all districts including those where the NTP has not yet been implemented.
Most DTCs receive additional drugs directly from the State. DTCs have a
staff of 15 to 20 persons including the District Tuberculosis Officer (DTO),
one to three tuberculosis medical officers, one radiology technician, one
laboratory technician, one to five treatment organizers, one statistical
assistant, one pharmacist, and one or two drivers.
Peripheral Health Institutions (PHI). In the District, most CHCs and a
number of PHGs staffed with at least one doctor are selected as PHI to
implement the NTP and conduct diagnosis and treatment of tuberculosis, There
are 3 types of PHIs:
1.
2.
3.
X-ray centres, offering X-ray and microscopy
Microscopy centres, offering microscopy only
Referring centres, preparing sputum smear for or referring patients
to the nearest microscopy centre.
*
No special staff is .posted at PHIs and the Medical Officer in charge is
responsible for tuberculosis activities. In some instances, one of the
health workers of the centre (microscopist, X-ray technician) takes
responsibility for tuberculosis patient management.
Multipurpose Health Workers (MPHW). In all PHIs there are multipurpose
health workers who represent the most peripheral level of health care. The
are usually based in subcentres, in pairs. With respect to tuberculosis, they
are to maintain a list of all patients on treatment, to visit them regularly
and to refer symptomatic patients to the nearest PHI or the DTC. They are
not currently responsible for distributing or administering anti-tuberculosis
drugs.
&
19
Urban tuberculosis control. There are a multiplicity of urban organizations
and institutions involved in tuberculosis control activities, both public and
private. These organizations, however, rarely coordinate their efforts and
often work in isolation and/or overlap activities.
Consequently, areas
and/or population pockets needing tuberculosis services may be overlooked and
manpower and financial resources are not well utilized. Since 1975, city
tuberculosis programmes are to be organized in a similar fashion to DTrs,
with the stipulation that each city programme would be tailored to the
administrative, operational and social conditions of the specific city.
Currently, however, only a few large urban afeas have well-functioning
tuberculpsis programmes. Voluntary organizations and tuberculosis
associations have been able to augment city tuberculosis programmes in many
instances by providing technical and financial support, health education, and
community outreach.
Conclusions:
The NTP has a very weak central structure, which for a long time has not
provided leadership in establishing and updating policy and technical
procedures and assuming programme direction. As a result, programme
procedures have stagnated and the original philosophy of the NTP has not been
fully implemented, or revised to make full use of the development of PHC. The
functions and resources of the State level, in particular training, have not
been developed and properly utilized. In most large urban centers the
coordination of activities among diffrent institutions, under the guidance of
the STO and STDTC, have not yet been implemented. In a similar way, the
curative services (hospitals, etc.) and preventive services (PHIs) are not
coordinated at District level in a single network for TB control, and the
lines of authority of the DTO are not clearly established. The extension of
TB diagnosis and treatment activities to the community through the MPHW has
been sldw, and that valuable human resource is not sufficiently utilized to
enhance access to care and patient compliance to recommended therapies. There
is no technical and policy advisory body to lend credibility and promote
visibility of the programme to government agencies and potential donors and
to provide support to the national team in the preparation and periodic
updating of national policies, technical and administrative procedures, and
•n
monitoring and evaluation of the programme.
6
CASg FINDING AND PIAGNOSIS
Diagnostic services provided by the NTP are free of charge for the
patients. A major stated objective of the NTP is to detect the maximum number
of tuberculosis patients in the community and among outpatients attending
health institutions with symptoms suggestive of tuberculosis, giving priority
to sputum positive patients. According to NTI ‘manuals, the principal approach
of case finding should be routine screening1 by sputum smear examination of
chest symptomatic patients attending health centres, and symptomatic patients
be referred for x-ray only after a negative sputum examination has been
repeated. In practice, however, this policy is not followed.
i
Patients with respiratqry symptoms attending a public outpatient
facility are investigated with chest x-ray and generally one sputum smear
examination. Patients who have to come back a few days after their initial
exams are not routinely requested to bring an overnight sputum sample. Often
diagnostic smears are not done or the results are not recorded on the
treatment card. PHIs without x-ray facilities refer sputum negative patients
to a peripheral x-ray centre or to the DTC. Looking for better care or
because of public transport facilities, which directly link to urban centres,
many patients bypass the microscopy centre and go directly to an x-ray centre
or hospital, adding to their workload and increasing the proportion of cases
diagnosed through x-rays.
20
Most facilities with X-rays diagnose the patients and initiate TB
treatment on radiological evidence, in spite of a negative smear examination.
Very few facilities indicate further sputum examinations, or treat smear
negative tuberculosis suspects with non-specific antibiotics and follow-up
the patient's clinical and radiological evolution prior to initiating anti-TB
therapy, suggesting overdiagnosis based on x-rays. Overall, approximately 20X
of patients diagnosed with tuberculosis have at least one pos1tive smear, a
very low proportion compared to-the expected capacity of~smear examination of
diagnosing 40-60X of all TB cases. The practice of doing generally only’ one
diagnostic- smear examination is probably resulting in infectious cases 1being
treated as noninfectious (with inadequate regimens and supervision) or not
diagnosed at all. Official data published for one state tuberculosis
programme showed that between 1969 and 1987 the total number of tuberculosis
cases almost doubled whereas the proportion of smear positive cases decreased
from 61X to 28X, suggesting that clinical practice is relying less on
bacteriology and further separating from the policies recommended by the NTP.
Gj
Unf ortunatelly, outpatient facilities run by non - govp.mmpnt
organizations (NGOs) generally follow the-same routines. Moreover, NGO
institutions and municipal health facilities were found to charge
registration fees for each visit. In private practice, patients have to pay
for consultations, smear examinations by private laboratories and the
prescribed medication.
It is estimated that up to SOX of tuberculosis patients are identified
and at least partially treated by private practitioners. These patients do
not initially enter the NTP and are not registered. Many patients then move
to the public sector because of the cost of care and drugs. Thus, a large
proportion of patients attending a health, service facility have previously
been seen by a private practitioner.
Due to the high number of PHIs in the district, the maintenance of an
updated cross indexing system at DTC is complex. Patients may not be able to
provide a complete address due to illiteracy or type of dwelling or because
TB has a social stigma and the patient does not want to receive mail from the
DTC or visits from DTC staff. Unless they present an identity card issued by
a public institution, patients previously treated outside the public system
or which are not found in the DTC cross index are diagnosed, registered and
notified as "new" cases. This practice correctly incorporates new cases
initially detected outside the public system, but duplicates notifications if
the patient was detected by a public institution outside the District.
A more serious problem is that the clasification in "new" or "old" bears
no relation to the previous treatment history and is not useful to decide on
patient therapy. If the patient is not found to have been previously indexed
in the DTC, he is considered "new" and is given a regimen for new cases. The
insufficient definition of "new" and previously treated patient leads to the
prescription of wrong regimens. A significant proportion of previously
incompletely treated cases is known to have acquired resistance to isoniazid
and streptomycin. The efficacy of "conventional" chemotherapy for such cases,
who are most likely still symptomatic and smear-positive, is very low.
Laboratory facilities
Most laboratories visited were equipped with monocular, rather than
binocular, microscopes without an (electric light attachment. Some of the
microscopes were in poor condition and the light
~ : source appeared to be
inadequate.' The quality of slides varied and some slides were found to be
uneven <and poorly stained. Acid fast bacilli could not always be found in
smears read as positive. An ocular magnification ratio of five or six was
routinely used rather than the usual 10 ratio. As definitions for data entry
■I
21
are irregular, laboratory registers do not permit determination of the
proportion of new cases, retreatment cases and follow-up examinations. Sputum
smears are not routinely used for monitoring of treatment outcome.
Many laboratory technicians working in peripheral microscopy centres
have been trained for the malaria control programme and are not familiar with
sputum smear examinations. Malaria smears are often given a higher priority
and may constitute a high case load. The number of sputum smears to be read
by one technician per day is usually considerably less than 20 except in
larger institutions such as DTCs and major hospitals. The rate of positive
smears varies between 1 and 10X. These low positivity rates may be partly a
result of poor selection of symptomatics, poor quality of the samples, low
quality microscopes, weak laboratory practices, inadequate training and an
excessively limited exposure to tuberculosis smear slides due to a small
catchment area. The supply of chemicals was adequate and no shortages were
reported. Slides with negative smear results are often reused, as indicated
in the NTI manual, with a risk of false positive results.
Quarterly or semi-annual supervisory visits are made by the DTC team to
assess the performance of the laboratory staff. The supervisors check
usually only all the positive slides, retained at the microscopy centre for
reading. Notes on the supervisory observations made, such as the proportion
of false positive and false negative readings, were not available for
scrutiny. There is no system of quality control through sending slides to the
DTC or to a State reference laboratory. Laboratory staff are often in need of
re-training and staining is of varying quality. Few States have functioning
reference laboratories to train District staff, supervise DTC laboratories,
carry out sistematic quality control of smears and do sputum culture and
sensitivity testing when necessary. In one State it was observed that the
STDTC laboratory had different procedures for smear examination that those
recommended by the NTI manuals and utilized by the DTC laboratories in the
State.
X-ray practices
With very few exceptions, diagnosis in clinical practice is basedI on the
chest x-ray. Even with one negative smear or no.1smear
---- result,. tuberculosis
treatment is initiated if the x-ray appears suggestive of active pulmonary
tuberculosis. The x-rays taken in referral centres are usually kept at these
facilities. The referring PHI only receives a note with the x-ray result.
The standard equipment in most x-ray units is an ODELCA camera with 70 or 100
mm films. In some hospitals, standard size films are used. Chest clinics at
the district level use both small and standard size x-ray films. Most of the
technicians are sufficiently trained and the chest films are of a good,
quality, but complaints were expressed about the quality of the domestic
films.
X-ray centers had well functioning x-ray units and usually sufficient
film to handle the tuberculosis caseload within the centers, although
temporary shortages of x-ray films are commonly experienced by PHIs. 93% of
x-ray machines were in working order at the DTCs as of 1991 (13). Assessment
by an inexperienced reader of the small size x-ray films widely used for
diagnostic x-rays or use of slightly inferior quality films can lead to an
increase in overdiagnosis.
Conclusions:
. The NTP has an infrastructure of microscopy and x-ray centres,
integrated into the primary health care system and staff are available to
perform case finding activities down to the village level of health care
delivery. Major weaknesses of the NTP with regard to case finding are that
usually only one or no sputum smear is obtained before a tuberculosis
diagnosis is made, and that diagnosis is primarily based on the results of a
22
chest x-ray. This practice results in significant underdiagnosis of smear
positive cases by smear examination and in treatment of infectious patients
as smear negative cases with inappropiate regimens, and discourages
monitoring of treatment outcome by sputum smear results. Patients with
respiratory symptoms are often inadequately assessed and treated before the
diagnosis of smear negative tuberculosis is made. The lack of vigorous
procedures for patient management increases the tendency to rely on x-ray
examinations resulting in the overdiagnosis of smear negative tuberculosis.
Inadequate case history and the impractical case registers result in multiple
diagnosis of defaulters and overnotification.
The primary alm Ln case finding should be the identification of sputum
smear positive cases. Before the diagnosis of tuberculosis and decision to
treat are made, the results of at least two sputum smears should be
available. The role of the sputum smear examination in tuberculosis
diagnosis should be greatly emphasized and the role of radiological
examinations should be reconsidered. For differential diagnosis, the ODELCA
cameras and miniature films for diagnostic chest x-rays may be phased out and
replaced with equipment based on the specifications for the WHO Basic
Radiological System, after carefully working out the cost considerations, For
screening of symptomatic attendees in hospitals of large urban areas to
select patients for bacteriology, small size X-rays may be useful.
The NTI laboratory manual should be revised, used for training at State
level and distributed as a reference to the laboratory staff of PHIs. Wall
posters with the basic procedures for microscopy, as were seen in one of the
States visited, ^hould be made available to all peripheral microscopy
centres. Supervision of DTC laboratories should be undertaken by State
reference laboratories. Supervision at State and at District levels should
include a system of quality control whereby samples of positive and negative
smears are systematically Sent to a reference laboratory for confirmation.
Acceptable quality binocular microscopes should be made available. All
diagnostic centre?, including those outside the State health services, must
adhere to uniform programme guidelines.
7. TK^ATMENT
The manuals for the District Tuberculosis Programme (NTI, 1990) include
the current national policies for the treatment of tuberculosis. The
Introduction Manual states that free chemotherapy should be provided to self
referred tuberculosis patients. The highest priority is given to treatment of
sputum positive cases to reduce the transmission of infection in the
community. Five regimens of "conventional chemotherapy" of 12-18 months
duration for all forms of tubetculdsis are recommended. In a phased manner,
two short course regimens of 6-8 months duration are to be provided for
sputum positive cases. Patients are "allowed to collect drugs from the
nearest PHI and are motivated to consume drugs for prescribed duration
regularly".
In Annex 4.1 the regimens found to be most frequently used in the DTP
are presented according to the currently recognized category of patient and
priority given if drugs are available. The categorization used in the
following sections of this report corresponds to that used in the WHO
Guidelines for Treatment of Tuberculosis in NTPs. However, in the India NTP
manuals, the seven recommended regimens do not always refer to the specific
category of tuberculosis patients and the choices of regimens are not
prioritized.
23
Treatment practices,
Patients are mostly treated by "conventional" regimens on an ambulatory
basis and oral drugs are self administered by the patient. In some States
(mostly in the South of the country) the regimen of HT is rarely utilized due
to the reported high frequency of side effects. There, most patients are ,
treated with HE for 18 months or SH twice a week. In some States of the North
where thiacetazone is well tolerated, the drug is not supplied in sufficient
quantity because of shortages in the national market attributed to the low
profit margin on the drug for the pharmaceutical companies.
SCC regimens for pulmonary smear-positive patients are theoretically
implemented in approximately fifty percent of the districts in the country,
but in reality only a minority of patients are treated with SCC so far. SCC
is being implemented slowly, mainly because the expansion of SCC has not been
given high priority in the NTP. The selection of patients eligible for SCC
observed during the review is quite strict, probably because the medical
officers of the DTP have doubts about the ’compliance of patients in selfSCC drugs are often kept at the DTC or
administration of the SCC regimens.
selected PHIs and patients living far away cannot come twice a month for the
drug collections.
The treatment is usually prescribed by a medical officer of the DTC or
PHI, and provided free of charge. Anti-tuberculosis drugs for the recommended
regimens, in particular for SCC, are periodically out of stock, reducing the
motivation of the patient to' regularly attend the institution and
contributing to the prescription of a non standardized regimen. Patients
attending private clinics are required to pay for their medications. They may
go to governmental institutions when they are unable to continue to pay for
treatment, but do so only when they are very sick. In a limited number of
situations, treatment may be supported by voluntary organizations. Often when
there is a shortage of one or more drugs in the health centre, patients are
required to buy the missing drugs. In one State, streptomycin, part of the
"conventional" regimen, was presently missing in most centres visited by the
review team due to a 50X budget reduction from the previous year's budget.
Patients with severe forms of tuberculosis (e.g. meningitis), those with
complications of tuberculosis (e.g. pneumothorax, hemoptysis), those with
tuberculosis complicated by other diseases and failure of an initial regimen
requiring retreatment are hospitalized. Places of hospitalization are
referral hospitals including sanatoria and medical colleges. Seldom are
tuberculosis patients hospitalized in CHCs or district hospitals.
Hospitalized patients frequently receive "conventional" chemotherapy that has
low efficacy for.critically ill and retreatment cases.
Existing hospital
beds for tuberculosis are utilized for advanced disease and not fully
utilized to prevent treatment failure. Hospitalized patients often receive
weak regimens and the beds are therefore not utilized in a cost-effective
manner.
In the DTC, drug collection is done once a month for "conventional'’
therapy and twice a month for SCC regimens. The frequency of drug collections
by the patient is similar during the initial and the intensive phase of
chemotherapy. Streptomycin is administered in the health institution nearest
to the patient home or by a private nurse. Usually the patient dues not see
the medical officer during the follow-up. He may be asked to see the MO if he
has drug side effects. The monitoring of side effects is not systematic and
there is little information regarding the percentage of patients who may have
experienced major side effects.
24
Guidelines for changing regimens during chemotherapy or for prolongation
of the duration of a regimen have not been issued by the NTP, creating
confusion, particularly for MOs in the PHIs. Unnecessarily long conventional
regimens are a burden for the patient, causes an unnecessary workload zzr the
staff, and results in drug wastage. The decision to discharge from treament
is made by the MO on the basis of the treatment card and on the clinical
condition of the patient. Criteria for discharge from chemotherapy are not
clearly specified in the NTP manuals. The patient is permitted to step
SOX of his prescribed regimen. If he
chemotherapy when he has completedI 80X
ne has
nas
he
has
to
continue
the
treatment
for
the
not completed such a course,
duration of time for which he has not collected drugs. Due to the high
incidence of defaulting, most patients receive unnecessarily long regiAe±s.
In addition, the definition of treatment failure is not clearly specizze i*ior
is practice uniform among MOs working in the PHC centres with regards — how
to manage a failure case.
After treatment completion and discharge, the patient is^ instruc-e- ~o
return every 3-6 months for follow-up. This practice is unnecessary an—
results in wasting of effort for both the patient and health staff.
Treatment organization.
Smear examinations are not repeated during conventional chemotherapy, to
confirm that the patient is really sputum negative or to determine sputum
conversion in smear positive patients. For SCC regimens, NTI recommendations
do not require sputum examination at the end of the intensive phase oz
chemotherapy nor are criteria specified for prolongation of the 2 months
initial intensive phase if the patients remain smear-positive. Smear
examination after the initial intensive phase of SCC is required in some
centres partioipating in the Tuberculosis Research Centre operational v—al,
but is done in approximately 20Z of the patients only. The insufficient
monitoring by sputum examination during chemotherapy does not allow for
evaluation of the- outcome of the initial.intensive phase of SCC chemotherapy.
Patients who are still smear-positive at the end of the initial phase should
receive special supervision by the DTP staff because they may not ha\e
be
strictly adhered to the prescribed medications. These patients may st
cured by the same regimen for new cases if the drugs of the initial z. tensive
phase are continued for an extra month and the staff fully supervises the
patient.
National policies require that pulmonary patients be monitored by x-ray
examination after six months and at the end of conventional chemo there., y.
ostThis requirement is not necessary in smear-positive patients and is n:
effective in smear-negative patients. In practice, only a fraction oz
pulmonary cases are followed up by chest x-ray films in the DT^.
Extrapulmon^ry tuberculosis patients are monitored by physical examine. — on
and by appropriate clinical tests.
The decentralization of the treatment of tuberculosis patients z FHIs,
as recommended by the NTP,, is not fully utilized for the administia<--- □ f
SCG regimens. The lack of decentralization results in a high percenuc-tx of
dropouts. A significant percentage of patients diagnosed in DTCs are
defaulting the first drug collection. The treatment card is not openez zior
are the name and address of the identified smear positive cases in tr.e
rommuni ty communicated to the PHI closest to the patient's home to tc
eve
the patient. Name and address of patients under treatment by the DTd
other
institutions are also not routinely communicated to the PHI.
In PHCs, the MO at the beginning of treatment and the pharmacist du:■ring
follow-up should provide patient motivation. At present, the same erztf-: is
made for all categories of patients, without sufficient focus for smea—-
25
• fir
positive cases of TB that are the priority for cure. In DTCs, the DTO and hOs
should provide motivation at the beginning of treatment and the treatment
organizer should do so during the follow-up. Sometimes, in training and
demonstration centres, health education and motivation is provided to small
groups of patients. There is no formal monitoring of the effectiveness of
such practices. There is no special effort to re-motivate patients who are
still smear-positive at the end of the initial phase of SCC, when there is
still a high probability of smear conversion and cure if the drugs are taken
"regularly. ‘Effectiveness of health education practices among the patients and
among the community are seldom evaluated and health education material is
rarely available among patients, family members and health staff. Not enough
emphasis is put on informing thq patient and the health staff about-the
importance of sputum examination.
Follow up of defaulters is not practical because the staff is required
to take action for a large number of patients, without focusing, on those who
remain smear-positive during chemotherapy. The current guidelines recommend
that priority be given- to sputum positive patients, leaving to the DTO the
decision of excluding sputum negative patients from defaulter action.' If home
visits cannot be done, guidelines require that letters be mailed twice: after
three days of defaulting and after 11 days if the patient is still
delinquent. During the review it was found that letters ai^e the most common
action to retrieve defaulters. However, a large number of patients provide
incomplete addresses and therefore reminder letters cannot reach them. In the
PHC, the multipurpose health staff are sometimes asked to retrieve the
patients, but such action is probably not stressed enough by the medical
superintendent and Chief Medical Officer. The village health worker is often
not informed about the TB patient(s) living in the village. The PHC is also
not systematically informed by the DTC about new patients diagnosed and
remaining under treatment by the DTC or hospitals.
The’reasons for defaulting are well identified by the tuberculosis
progranune staff. Among the most important is the fact that the patient loses
interest once he becomes asymptomatic. Disruption of drugs stock," incomplete
provision of the first line drugs for "conventional" and SCC, long waiting
time, inability of the system to adjust to the patient needs, distance of DTC
or hospitals from the patient's home are the other most common reasons for
defaulting. Some patients go to a health institution different from where
they are registered with the hope of receiving better care. This increases
default as well as making it more difficult to retrieve them. The DTC and
other specialized institutions do not use auxiliary staff (HPHW) to retrieve
defaulters and-do not inform PHC of the existence of patients on treatment
from that area.
Among defaulters, approximately 30% to 50% miss cfrug collections before
the fourth month of chemotherapy. 5% of patients default after diagnosis is
made) and before therapy is initiate4. In some instances, the patient is not
informed that he has tuberculosis and should be treated. Lack of motivation
of stafj, weak leadership of the medical officer and little accountability co
the chief medical officer for tuberculosis have been identified by the
supervisory teams as additional reasons for patient defaulting.
In the policies of the NTP there is no target for treatment completion
and cure of pulmonary smear-positive patients. In such patients the fatality
rate is known to be high and irregular chemotherapy leads to drug resistance.
The present policies and practices are insufficient to reduce the spread of
the infection, particularly of drug resistant mycobacteria, and the mortality
due to tuberculosis. The observation of the assessment teams show that the TB
programme objectives are not efficiently prioritized. The existing health
infrastructure and resources available are not fully utilized to sterilize
snlear-positive patients as quickly as possible. In a significant proportion
26
of the sources (of infection diagnosed by the DTP, the chemotherapy is
not
started, and a large percentage of smear -positive patients put under
treatment drop out during chemotherapy.
The decentralization of the programme is not achieved. Guidelines for
patient management are not present at the level of peripheral health
institutions (PHC and CHC for a population of 100.
C00 to 200.000) where most
100.000
of the patients could benefit from the existing health services. Medical
officers working in PHCs and CHCs are generally not trained for the proper
management of the tuberculosis patient. Supervisory visits to PHI from DTC
and chief medical office are not targeted to improve treatment outcomes.
Conclusions:
NTP policies and procedures on treatment do not reflect the WHO
recommended emphasis on short course chemotherapy and patient registration
systems which facilitate the monitoring of completion and cure rates of
patients on anti-tuberculosis treatment. -The tuberculosis programme at the
delivery level does-not adequately emphasize the importance of treatment
completion as the main index for programme evaluation. During the programme
review, the teams observed that DTP practices depart from what should be done
to effectively treat tuberculosis patients. Service delivery focuses on case
finding activities and not on treatment completion and cure. Tuberculosis
staff are not optimally utilized to enhance treatment completion activities.
Additionally, there is no good system to evaluate treatment results. NTP
policies and procedures should be revised to ensure that the most efficacious
and current treatment regimens are recommended, including fewer regimens and
short course regimens where appropriate. . Registration systems should solicit
data to monitor completion and'cure rates, with particular focus on smearpositive tuberculosis patients.
The main goal' of the NTP should be to
ensure that patient completion of anti-tuberculosis
— ---------- ‘ treatment and cure be
reflected in all policies and procedures and that
such be carried out in the
---- ------current integrated health care delivery
'
.system. Guidelines for treatment
organization are attached in Annex 4.2.
8. PROGRAMME MANAGEMENT
8.1 CA3E NOTIFICATION
Tools for programme monitoring are the treatment card, the laboratory
register, the master book of treatment cards (MBTC), the cross index card,
the patient identity card and the report on treatment results. The use of
register books and report forms is in accordance with the NTP guidelines in
DTCs where the statistical assistant is in position and has been trained at
NTI. However, training courses have been rarely.repeated and trained staff
have been transferred to other programmes within the district. The format ef
the treatment registers is not always standard, as they are copied by hand
and not printed, and the content does not include all the‘data required to
analize the results of treatment. The card is sent from the PHI to the DTC
when the patient completes treatment,, <defaults
’ ^ 1__ or
__ dies,
2
so the MBTC is the
only source of data on treatment left at PHI level.
The usefulness of the recording and reporting system does not appear to
e well known at all levels of the system. Consequently, evaluation of
programme outcome and actions are missing, and the evaluation by cohort
^analysis of results of treatment is often not done. Cross checking of
patients registered in the laboratory register, the treatment card, and.
registrations in the MBTC is not operating efficiently. Therefore no action
is taken for smear positive patients registered in the laboratory register
who default from the first drug collection, data on initial defaulters are
not available and the information in the cards and MBTC is not complete.
27
Conclusions:
-. ■
W rhe NTP is cumbersome and
programme, i.e.
The current reporting and recor ing s
does not address the main WH rec°^nsniear
gittve cases of tuberculosis.
Che monitoring of the cure ra e
Jear.p0SItive cases diagnosed and is not
Cohort analysis does not cove
done at the PHI level. The currenC
noclfloatlon should t. r.vlssd "
svstem of registration and
J
recording of essential data,
ra(,haslL th. coll.etlor. and
“bt:srivy3“’ohfi:s^:LTt::it...
s:
effectiveness.
the laboratory register
A printed copy
each PHI implemented to provide
Should L- —
should be kept by
the DTC supervisor.
care . inese
6
at Ipast
least every
every two months by ’ -- -j to assess the
and
check the iSupervisors
—"‘i on the indicators of programme
of the data. Standardized reports
consistency
the end of each quarter and forwarded to
should
be
filled
out
at
performance
from the PHls and forward chem
consolidate
the
reports
the DTC. The DTC will
PHIs should be
TB Office. BTC team supervisory visits to
co the state
prioritized on the basis of performance.
Sh“ld b:h“rd
“.o/ch.
in th.
8.2 SUPPLIES AND TRANSPORT
Anti-tuberculosis dirufcS.
b.7„t£xcht“i d“p6:nlf“
- manufactured or compounded
In principle, 50X of the
the national government
»y
government negotiates with
for druzs based on the capacity of the State c
t--r4Xtir-i on
The amount of drugs needed
the central government^contribution^^
by each state is determined annually by th central^
patients reported the previous year’
are initially scrutinized at the
received fro. dlscrlete. Th“'
the purchase of drugs with che
’ ; negotiates the purchas
long
it must buy from
that Z
20X higher
eii^
hoo8h"e dulces U .he re.p^iU.y
distribution of drugs to t—
;“a".t::Sc.^:d“"cS‘-c irsf
--’r rcl"Tfr;X.“
of the Medical Store Organization.
supply is generally purchased by
The State portion of the anti-TB drug
bids, using allotted State
the District from manufacturers selected in the
Statdrug manufacturer. Monitoring
funds and sent to the District directly by is left to the District. Although
of stock supply, reserve stock, and usa8 s on hand, usage, and drug
the districts send notification of supp_
”it is unclear whether analysis of usage patterns is
projections to the STO, tL
it StTte level. Facilities are likewise unaware of
regularly undertaken at — neighboring facilities or institutions.
drug supplies available in
the needs of antithe DIO
At the district level, the
tne
uiu usually estimates, gs con
sumption. He
consumption.
basis of the previous year'
tuberculosis drugs on the ba3^ °
AyThe central government and the
the central government
receives the drugs purchased direct yy
medtcai officer. In some
medicalhase
officer.
budget allotted by the state through the chief
chi
anti.tuberculosis
State to purchase
situations, the budget obtained from
needs, due to increases in
needs,
dcuga uas sufficient lot only a fraction of
°£e'the
b'p“
:i’;a ye.O. In sc.
drugs costs <.ppcoxl.at.ly 201 ooups d
1£ .ddltlon.l funds wet. necessary,
districts, th. fund. «... S"£“=1“'’
in“0.. Instanc.s, short.g.s ««
'oVertfdVy'u”^?"",'™. S .ssocUlons, mt.rtupt.d .uppiy of so..
28
anti-tuberculosis drugs at district level were noted as being due to late or
incomplete supply by the production laboratories of approved orders or due to
the absence of reserve stocks at the state level. The state does not purchase
or receive drugs directly nor does it maintain a buffer stock.
The rifampicin used by the NTP is not a combination capsule. Fixed dose
combinations of rifampicin with isoniazid, and with isoniazid and
pyrazinamide are however available in the market. The quality of such single
drugs and combination drugs is not currently being monitored by the NTP.
Conclusions:
Ensuring an uninterrupted supply of anti-TB drugs to the tuberculosis
patient should be a key function of the national and State tuberculosis
programmes. Shortfalls in funding and delay of drug supplies from the
pharmaceutical industries can be compensated by 1) closer monitoring of usage
patterns, drug purchase projections and stocks by the STO and 2) establishing
a buffer stock at the State level sufficient to ensure at least a 6 month
supply of uninterrupted drug distribution to the districts. Similarly,
districts and PHIs should maintain internal buffer stocks of three months as
an additional preventive measure. Estimations of the amount p-f buffer stock
should be based on the number of patients reported during the previous year.
In addition, drug quality should be monitored by the National Unit and the
States through a selected scientific institution.
Transport
The non-availability of road worthy vehicles and poor budget allocations
for fuel have been cited as reasons for limiting the number of supervisory
visits by the DTC team to PHIs’. At District level, fuel quotas were clearly
insufficient, in view of the increased number of PHIs to supervise and
distances to cover. As a result, supervision of PHIs is not done with the
frequency required, or several PHIs are supervised in the same trip with
insufficient time allotted to each one. Adequate provision of fuel should be
provided to the DTC for supervision, and transport should be provided to
district supervisors based at subdivisional level to reduce milage and fuel
costs.
8.3 SUfERVISION, MONITORING AND EVALUATION
According to NTP policy, the District Tuberculosis Officer and his team
of laboratory technician, x-ray technician, and treatment officer, etc. are
responsible for the supervision of all personnel within their District
involved in tuberculosis activities. The team is expected to visit each of
their PHIs on a quarterly basis. They are to evaluate diagnostic and
treatment procedures, validate laboratory results, monitor record keeping
activities, check on defaulter actions taken, and monitor anti-tuberculosis
drug supplies and support equipment. In addition to their supervisory
duties, the team is expected to do dn-the-spot training and/or retraining of
staff, collaborate with other disease control programmes on topics of mutual
interest, and offer continuing education to the general public. Supervisory
checklists have been provided by the NTP to guide the supervision of DTCs and
PHIs. At PHI level, Medical Officers have been made responsible for the
supervision of laboratory technicians and multipurpose health workers.
When the NTP was operationalized in 1962, the District demographic unit
was designated as the basic unit for the NTP. All NTP activities were
conceived and organized at the District level, In the three intervening
decades, the District has grown in population, and the number of government
health services has grown at least in proportion to the population growth.
i
29
under the
- J, difficult for the DTC
and manage at
It is increasingly
conceived thirty years ago, to teasiory s y
organization <----■
In one District visited, with a populatlo of 4 million,
the District
nf 148level.
Peripheral health institutions have implemented the DTP. The
119 out G-. - • - ■ ■
make 20 visits per month, supervising 2 facilities
centers.
staff
would
have
to
DTC
trip
in
order
to
i
per
This schedule
organizations ,
supervision.
from regular
:
n did q^ke
The assessment team noted that the District Tuberculosis •team
difficult
to
assess,
and thq
visit? to PHIs. The quality of the visits was
o/the visits were difficult to validate, as
frequency and regularity c
scrutiny,
Records were not in
— -3 were not av^rlaoie xoi
supervisory reports
j were noted.
visits
order at facilities
facilities where
where recent supervisory
' l of PHIs
' - decline in the proportion
41X in 1991. In 1987 only 84X
Alarmingly there has been a steady
51X in 1983 to
supervised by the DTC team, from SIX _r_--only 72X ( 60X of
quarterly
reports.. Of these
of functioning DTPs sent
Of- the
60X of DTPs
'
visits
. C
on supervisory
functioning DTPs) gave iinformation
Thus only
45X
of
their
PHIs
.
giving information, they had su;.pervised only
of the
27% of the PHIs have been reportedly supervis
. The quality
supervision istRor-known (5).
used to evaluate record
retrieval activities,
and other equipment. Not
he
supply ui obj ectives_poorly
—r---- fulfilled
but performance
very little wich
time
supervisory
Jullf
111^^
Currently, supervisory visits are Prima^
i patient completion of
treatment.
The National Tuberculosis
■
’• Institute
Institute (NTI) has been resp .
Inforwat
Tnforfflation
ion on
monitoring of the National
Tuberculos
J-grin
e^l
7
8^
National Tuberculosis Programme
at the facilities
^stitutions report
DTP activities is recorded
recorded through
through a system
and periodic reports
NTI.. Peripnerai
Periphera
-1 sent to the NTIDTP. The DTP
case finding and treatment activities o
inclu.sive of data received
prepares quarterly and annual reports 1tuberculcrsis activities.
from the PHIs involved in t---limited
to reView
Programme moditoring
evaluation haS ^^^ptrts
.
moditoring and
and evaluation
The current
and analysis of notification data and regul
cf
for the monitoring of treatment outcome
information system does not provi
indicators and monitoring
Management indicators
or programme outcome indicators.
but- exhibit very little emphasis
finding but exhibit very
on case treatment and cohort an y
'
erculosis hospital beds are not
hpspitalized in the more than
,
Likewise the large number of
registered in the NTI ^formation system
Likewise
r
..c-lvlns
XSX X XL S7X
red
e.s.s of
'
-3 districts out of 438 with DTPs had registration in
In 1991, only 378
place (86.3X). C- .
s on
Of the L-- ■ --.KUK «po„:at;«£ch. ™.198/.In Jepth
out of 12,338 PHIs.
India" (1) showed a
importance of records and reports,
useful for programmme management
of them. Data in the reports was not
- ; records and reports or gave
activities. Supervising officials rarely checke
Reports were very often
guidance regarding their proper maintenance.
.
30
incomp,lete and unreliable. Although on site evaluation of case management: is
reported, it is acknowledged by supervisors that the monthly and quarterly
reports sent to the DTC are not analyzed nor are the sending institutions
given any feedback as to performance as reflected in the written reports.
Conclusions:
There needs to be a clear emphasis placed on supervision if the NTP
programme is going to succeed. Tuberculosis programme personnel need to be
retrained about supervisory methodologies as well as supervisory content
which emphasizes programme performance parameters.
In order to address the
increase in population and health care facilities at the periphery, a medical
officer or treatment organizer and a laboratory supervisor should be added to
the District Tuberculosis team at the sub-divisional level (about 500,000
population) in order to facilitate decentralization of supervision, staff
training, monitoring and evaluation, and management of tuberculosis programme
activities at the level
-1 of
-1 PHIs.
---- To reduce travel time and cost, these staff
should be based in a hospital or X-ray centre and they should be provided
with transportation.
Monitoring of case finding and treatment results has not been
prioritized, is still centralized and is not used at health facilities to
evaluate the quality of programme delivery and implement corrective actions
when necessary. PHIs management staff should be retrained on monitoring and
evaluation methodologies. They should be taught to analyze their own
facilities performance Indicators and to take corrective action promptly.
DTC, State and national staff should analyze the quarterly and annual reports
received and provide feedback to the health facilities on the priority
indicators of programme efficacy.
8.4 EDUCATION AND TRAINING
Since 1962, the National Tuberculosis Institute (NTI) at Bangalore,
India has been the main training institution for tuberculosis programme,
staff. The various members of the District Tuberculosis Center (DTC) team
(medical officers, x-ray technicians, laboratory technicians,
pharmacists/treatment organizers, and statistical assistants) undergo a 10
week training program at the facility, with special emphasis on their areas
of responsibility. The NTI also conducts seminars for state tuberculosis
officers, university faculty, and district medical officers, as well as
refresher courses for DTC staff.
In theory, in addition to NTI, the State Tuberculosis Training and
Demonstration Centers (STTDC) are responsible for training BCG supervisors,
orientation training of health visitors, and training of medical students and
ancillary health care providers on the clinical aspects tuberculosis control.
Continuing education for the private physician is often undertaken with
assistance from the Indian Medical Association and voluntary organizations.
The review teams found, however, that the training given by STTDCs was
neither comprehensive nor consistent with NTI policies and procedures with
regards to diagnosis and treatment recommendations, i.e., x-ray reading,
procedures for procuring and preparing sputum for smear microscopy, treatment
regimen recommendations, etc. Training materials were not available for
scrutiny. Instruction in the STTDC is provided on the basis of observations
of clinical procedures, focusing on clinical aspects rather than programme
operations.
i
31
Since the emphasis on primary health care and the push for integration
of health services, medical officers and MPHWs have, in principle become
part of the tuberculosis control effort. The training and orientation of
these health personnel in NTP policies and procedures varies widely
In some
districts, the DTO and his staff provide systematic, but brief (two-day)
training to medical officers and MPHWs using NTI training materials.
In
other areas, the training has been delegated to Institutes of Public Health
which provide general courses ranging from one year to eighteen months for
health workers and one month for medical officers, where the tuberculosis
content is a component of the course curricula. Medical officers of PHCs are
also expected to train their staff in tuberculosis activities. Many of them
however, have yet to be trained themselves. The majority of medical officers
interviewed in the field stated that they did not carry out any training
activities for their staff.
Since 1962, over 4,800 team personnel or roughly 900 full teams have
been trained by NTI staff. However, as the
tl. number of districts implemented
are
promoted or attain superannuation,
has increased, and as senior personnel
'
‘
not all of the district teams currently have a full complement of trained
only 24% of DTCs had a fully trained team, while 66%
persons. As of 1991,
trained district tuberculosis officer (DTO), 76% had
had the services of a
78% had trained laboratory technicians, 88% had
trained x-ray technicians,
trained treatment organizers, and 59% had trained statistical assistants
(13).
Conclusions:
Training is vital to the successful implementationl of the review team's
Training materials must be developed to reflect
recommendations for the NTP.
------ o
the proposed changes in programme policies and procedures. The needs
nee s for
training of tuberculosis personnel for DTCs, PHIs and other health
institutions exceeds the present training capacity of the NTI The curt
NTP training should be descentralized by utilizing t e ex s
g s
training facilities, medical colleges, public health institutes an
tuberculosis-oriented voluntary agencies to augment training e^°r
.
institutions should receive NTP training materials and train the trainer
courses to maintain standardization of training efforts.
national training opportunities should be made available for the differen
levels of tuberculosis programme staff.
The NTP manuals should be revised to reflect the recommendations of th
Review and standardized educational materials should be developed by NTP for
different categories of personnel involved in tuberculosis control aofivities
(including medical students, general practitioners, etc. in private practic )
and for patient motivation.
9 . PRIVATE SgCTOgl
According to a Study of 102 private doctors practicing in Bombay, 60Z t
70X of patients bypass the public health system and seek care by Private
physicians when they become chest symptomatics (6).
Review team field
observations suggested that the proportion of patients seeking care in the
private sector was slightly lower than evidenced in the Bombay study, bu
still represent about probably half of the new TB cases. Although many of
those patients later move to the public sector, private practicioners have a
major role and their management of TB cases influences also the results of
the NTP. It appears that private physicians do not adhere to any se reg
for TB care. As in the public sector, dependence on x-ray diagnosis was
.
evidenced. Case finding methodology and treatment regimens for tuberculosis
patients vary widely and are usually more costly than regimens recommended by
the NTP. Patients are usually given a prescription and sent to a pharmacy
32
for drug purchase, with very little monitoring of patient compliance.
Defaulter action is rarely taken.
The training of general practitioners is currently not adequate and has
not been updated to incorporate recent advances in knowledge and strategies
of the NTP. The capacity and organization of medical associations (IMA,
Anti-tuberculosis associations) have not been zapped to provide continuing
education and programme awareness to the private sector. Interviewed members
of the Indian Medical Association (IMA) at State and District level showed
strong support for the NTP efforts. IMA members seemed well aware of the
issues and challenges facing tuberculosis control and were'willing to utilize
the organization to promote tuberculosis health education efforts and
distribute educational materials to its members on the topic of TB case
finding and management. The use of health education messages targeted towards
both the private physician and the consumer regarding correct treatment
regimens and the importance of completing treatment should be tested as a
method to standardize care provided by the private sector.
Conclusions:
A large share of the provision of health services in the country,
country,
including tuberculosis diagnosis and treatment, is done by private
practitioners.
’
• They are, however, not currently included in the NTP system,
either for notification of patients or standardization of diagnostic and
treatment procedures. The role of the private sector in the care of the
tuberculosis patient needs to be further clarified by the NTP. If indeed it
is found that a large share of tuberculosis patients seek care in the private
sector, improved training in medical schools and education of private
practicioners must be implemented to ensure proper diagnosis and treatment
and augment cure rates for patients under private care.
10. RESEARCH
India has a long history of tuberculosis research to improve progrAmme
delivery and treatment efficacy, and much of the information and experience
obtained has been applied successfully in other countries. The research
institutions can be utilized to analyze the functioning of the programme and
to test alternatives to improve programme results, in particular organizatit
of treatment delivery to increase the cure rate. To ensure that the studies
provide relevant information for programme improvement, and that this
information is opportune and utilized, this research should be planned and
supported as an integral part of the NTP. fSone operational research projects
have already been discussed before the Review mission,
-Two major
institutions currently involved in TB research are briefly described below.
The Tuberculosis Research Centre (TRC) in Madras was established in
1956, under the joint auspices of the Government of Tamil Nadu, the Indian
Council of Medical Research, the British Medical Research Council and the
World Health Organization, for studying initially the efficacy of domiciliary
chemotherapy, in comparison with conventional sanatorium treatment. The
centre was taken over by the Indian Council of Medical Research in 1965 and
made a permanent research establishment. It established that a wellorganised domiciliary chemotherapy with a daily regimen of isoniazid plus PAS
produced results closely approaching those obtained in sanatorium with the
same regimen; a satellite study established that there was no extra risk to
the close family contacts from the infectious case after the start of
treatment. Subsequently, the Centre investigated various regimens of
chemotherapy in controlled clinical trials, backed up by in-depth laboratory
investigations and solid statistical methodology. Clinical trials of various
regimens of shortcourse chemotherapy that would be suited to Indian
conditions were carried out, and more recently a study on implementation of
33
shortcourse chemotherapy under programme conditions in 18 districts selected
from different parts of the country was initiated. In recent years, a strong
department of immunology and cardiopulmonary function have been added to the
Centre.
Finally, the epidemiological unit that undertook a large trial of
BCG vaccine in South India has now been integrated with the Centre. The
Tuberculosis Research Centre has the capacity for undertaking training
programmes that could complement the efforts of the National Tuberculosis
Institute in Bangalore.
The National Tuberculosis Institute was established in Bangalore in 1960
with the objective of developing a suitable programme for tuberculosis based
on operational research studies, training medical and paramedical workers for
the District Tuberculosis Programme and monitoring the Programme through
periodic reports received from the Districts.
Based on studies on awareness
of symptoms and action taken and on the Madras TRO studies demonstrating the
efficiency of domiciliary chemotherapy, the NTP was evolved and launched at
the NTI..c_In subsequent years, operational studies were undertaken on methods
to improve case - finding, techniques for enhancing patient motivation and
thereby enhance case-holding efficiency, and programme organization.
Concurrently, large-scale field studies were initiated to provide information
on epidemiological indicators such as prevalence and incidence of disease,
fate of newly-diagnosed cases under programme conditions, and on the
prevalence of tuberculous infection and infection with other atypical
mycobacteria. Thereafter, and in view of conflicting reports about the
efficacy of BCG vaccine, the largest BCG trial ever undertaken was launched
in Chingleput, South India, to determine the efficacy of two strains of BCG
vaccine at two different strengths.
Conclusions:
As a step towards the reorganization of India National Tuberculosis
Programme activities, the research potential of the various research
institutions should be evaluated in light of the findings and recommendations
of this review and needs of the NTP for operational research studies.
Operational research to test the feasibility and results of different
technical and organizational strategies to be adopted by the tuberculosis
programme should be an integral part of the revised tuberculosis programme,
H- SITUATION ANALYSIS
Even after three decades of National Programme activities r the
tuberculosis burden on Indian society remains enormous - something on the
order of five million premature deaths in a decade, half of which are among
women, mainly in the reproductive age. This mortality must affect at least
twice that number of Indians with consequent lowered productivity, disability
and perpetuation pf poverty.
Excellence in research, early successes proving
the advantages of some modern treatments, availability of powerful and
effective antibiotics, a well established TB structure at the State level
and, in the last two decades, extensive development of the institutional
structure for primary health care in the rural areas, have not yielded the
progress against the disease which India could have expected. Decline in the
annual risk of infection (and in incidence) has been agonizingly slow in many
areas.
Well over half the population is infected with TB and the risk of
infection is far too high at between 1 and 2X per year. An aging population
structure, increasing HIV prevalence and apparently rising levels of drug
resistance mean that without a reoriented and vitalized public TB control
effort the disease will pose an increasingly serious health and developmental
constraint for several decades to come.
34
The main factors to be addressed in making real progress against TB fall
in four main^categories - organizational, managerial, technical and
developmental. ElemenCs
the present health care system, and many parts of
the current TB control programme provide the basis for implementation of
major improvements. Strengthening
f
and reorientation of policy and program
execution in each of the problem areas offer sound prospects of improvement
in curing TB patients in numbers which will result in 8-10Z annual decline in
the risk of infection and effectively halve the tuberculosis
-- j burden in about
a decade while ensuring much lower disease and infection rates for decades
into the future.
The state TB control programs are well structured and have direct
intervention capabilities at the district level and below in about three
quarters of the country. In contrast, the national TB control programme has
languished with ineffective terms of authority and budgets and an
exceptionally low executive position within the Ministry of Health for such
an important disease. Monitoring, critically examining and adjusting
national policy for effective state performance has consequently atrophied.
In the absence of a strong central Ministry unit, power for TB policie.
has been ceded to the National TB institute (NTI) in Bangalore. The NTI has
had preeminence in training and some_ types of research for TB but now suffers
serious institutional weaknesses. Budget shortfalls, unfocussed direction of
research, training program content which is not replicated at state level and
lack or experience with making and implementing policy have left a gap in
national TB leadership,. The absence of a national policy body for TB at
central level, supported by a strong executive TB unit within the Ministry,
has meant that no irevision
’ ’
of policy has been made in spite of repeated
evaluation showing poor results,, <and’ therefore
'
NTI has not changed or
developed alternative TB Program procedures.
Further, 1the
’
content of their training has stagnated in relation to
recent TB control success elsewhere,
--In the absence of a strong central
program, NTI has been forced to assume program management and standardsetting functions which are inappropriate for a training/research
institution. This is particularly true as NTI does not have the staff and
executive authority to monitor and
__ enforce
------ j compliance of the states with
policy.
Below the State level, TB has been indicated as a priority for
integration into the key health services. I'However, the TB program's
effective cooperation with health service providers
e - ---- at the primary level and
willingness of the providers, under current policies, to devote substantial
attention to TB, remains doubtful at best. The ambivalence resides both in
lack of strong and focussed national program direction and in the absence of
policies responsive to the legitimate interest at the local level for a
clearcut, standard, easy to follow program which is effective for cure.
Strong direction, some decentralization below the district level, training,
increased funding and a comprehensive policy package are needed.
Technical problems confronting the NTP are both historical and the
result of some isolation. There remains traditional emphasis on case-finding
activities when only a minority of discovered cases are being cured.
Technical practices emphasize radiographic methods which are sensitive, but
not specific, rather than concentrating on high-quality microscopy which with
a good quality control system can be both specific and sensitive. Too
frequently, one sputum smear is examined rather than several, leading to
inappropriate treatment of infectious cases. Microscopes are often monocular
and of poor quality, training is uneven and quality assurance systems seldom
function. Protocols for appropriate use of radiography and clinical
diagnostic methods need to be prepared and disseminated.
•
c
35
<
Treatment for diagnosed patients is chosen from too many regimens and
adequate short-course chemotherapy is yet infrequently used and is completed
in only a minority of cases.
Repeated sputum smears during the course of
treatment are not regularly taken to monitor effectiveness of therapy.
Provision of services is often too remote or inconvenient to encourage
patient compliance, and providers lack adequate motivation and training for
patient supervision. Improved treatment protocols, training, adequate
supplies of only SCC drugs, and adaptation of practices to provide some
degree of supervised initial chemotherapy, whenever feasible, are needed.
Recording and reporting procedures do not permit rigorous supervision of
the system as a whole or at the institutional level.
Case definitions are
not adequate.
Criteria for completion of treatment and discharge do not
exist.
Laboratory registers and patient treatment registers do not contain
the information necessary to perform cross checking or to monitor the
performance of states, districts, blocks or individuals providers.
Conversion status of smear positive patients cannot be documented.
Cohort
analysis to ensure and measure program effectiveness cannot be satisfactorily
done with present registry formats and procedures. Therefore, adaptation of
existing TB Program policies and resources to implement and improve recording
and reporting system is required.
;•
■
Developmental constraints include both institutional and financial
issues. Operational research to test and improve on program performance is
not currently an integral part of the TB program. Training materials and
objectives are in need of revision to support a revitalized program and
pedagogical content may need improvement. Medical college curricula need
additions to provide both theoretical and practical exposure to the elements
of TB control as doctors graduating now will continue to see TB throughout
their working careers. Present private medical practitioners need to be
educated about modern treatment and policies of the program. This can be
done through existing NGOs. To do this, strengthening of the NTI, of the
state level training centre, and studies and technical assistance at both the
national and state levels will be needed. Opportunities for overseas
training and experience will accelerate adoption of effective new experience
in TB control elsewhere.
The government has recently decided to increase funding for TB control
and is for now continuing to provide for the treatment of all TB patients
diagnosed in tha public system. The present high number of overdiagnosis and
treatment of patients which now appears to be occurring offer scope for
savings in an improved program. Overall though, financial resources foi? TB
appear to havfe declined in teal t6rms in recent years because of inflation
and rising import costs, despite the government's recognition of the trend
and efforts to counteract it. bforeover, only a fraction of patients tdday
requiring treatment receive it in full.
A strengthened program will require increased resource allocations at
both the central and local levels for drugs, supervision (including
transport), training and operating cost. Given the demonstrated cost
effectiveness of TB control programs compared to other health sector
interventions, revision and expansion of India's TB program with external
financial assistance would appear to be fully justified.
36
12. RECOHKgfrPATIONS
1.
The structure of the National Tuberculosis Programme should be
strengthened by 1) establishing an apex policy making authority and an
executive task force with managerial functions to implement programme
reorganization, and 2) upgrading the central tuberculosis control unit
in the Directorate to provide strong leadership and enhance the
efficiency and effectiveness of the National Tuberculosis Programme
2.
The quality of patient diagnosis should be improved by 1) using three
smear examinations to detect infectious cases among symptomatics before
deciding on patient treatment, 2) ensuring the quality of microscopy
with adequate equipment, training and quality control, and
3) establishing criteria for diagnosis by radiological and clinical
methods.
3.
National and state tuberculosis programme resources should be directed
to ensuring cure of tuberculosis patients, giving priority to infectious
cases of tuberculosis by 1) adopting short-course chemotherapy, 2)
establishing criteria for treatment completion, cure and discharge ftom
medical care, and 3) ensuring an uninterrupted supply of drugs of good
quality.
4.
The current NTP system of registration and notification should be
revised to emphasize the cohort analysis of treatment results
(completion and cure, transfers, defaulters, died, treatment failures)
as the main indicator of vrograqnqe effectiveness.
5.
Policies should be developed to ensure decentralization of treatment
services closer to the community level to enhance access to care and
patient compliance to recommended therapies.
6.
Pilot projects should be implemented at block level to test the
feasibility and results of different technical and organizational
strategies to be adopted by the tuberculosis programme -- i.e., to test
the capacity to implement recommendations 2-5 above.
7.
A medical officer or treatment organizer and a laboratory supervisor,
with the necessary transport, should be added to the existing
administrative structure at the sub-district level (about 500,000
population) to strengthen tuberculosis programme, management and to
facilitate decentralization of supervision.
8.
Training materials must be developed to reflect the proposed changes in
programme policies and procedures. The current training infrastructure
will need to broaden the scope of its training capabilities by utilizing
state training facilities, medical colleges, public health institutes*
and tuberculosis-oriented voluntary agencies to augment training
efforts. International and national training opportunities should be
made available for the different levels of tuberculosis programme- staff.
9.
Operational research must be carried out as an integral part of the
revised tuberculosis programme to evaluate programme performance,
improve delivery of services, problem solving and obtain baseline
epidemiological information to measure reduction in the risk of
infection.
.r>s s'.t-
TUBERCULOSIS PROGRAMME REVIEW
INDIA, SEPTEMBER 1992
*
/
•
V
)
2
TABLE OF CONTENTS
PAGE NO
EXECUTIVE SUMMARY AND RECOMMENDATIONS
INTRODUCTION
2.
LIST OF ABBREVIATIONS
3.
4. TUBERCULOSIS IN INDIA
5. ORGANIZATION OF THE PROGRAMME
6. CASE FINDING AND DIAGNOSIS
7.
TREATMENT
8.
PROGRAMME MANAGEMENT
8.1 CASE NOTIFICATION
8.2 SUPPLIES AND TRANSPORT
8.3 SUPERVISION, MONITORING AND EVALUATION
8.4 EDUCATION AND TRAINING
9. PRIVATE SECTOR
10. RESEARCH
11. SITUATION ANALYSIS
12. RECOMMENDATIONS
1.
3
7
8
9
14
19
22
26
26
27
28
30
31
3.
33
36
*♦
ANNEXES
1.
2.
3.1
3.2
4.1
4.2
5.1
5.2
6.1
6.2
LIST OF PARTICIPANTS
INSTITUTIONS VISITED AND PERSONS INTERVIEWED
BACKGROUND INFORMATION
MAP OF INDIA
PRESENT TREATMENT PRACTICES
GUIDELINES FOR TREATMENT ORGANIZATION
COORDINATION WITH OTHER PROGRAMMES
VOLUNTARY HEALTH ORGANIZATIONS
EPIDEMIOLOGY REFERENCES
GENERAL REFERENCES
37
38
42
49
51
53
56
58
59
60
K
i*
f
17
(752—
3
TUBERCULOSIS PROGRAMME REVIEW
1.
INDIA, 1992
EXECUTIVE SUMMARY
The Government of India, recognizing the magnitude of the problem of
tuberculosis, the limited progress achieved by previous control activities
and the expected increase in incidence as a consequence of the HIV epidemic
has decided to give priority to tuberculosis control. In support of this
decision the Government requested WHO to carry out a joint programme review
together with other interested parties, A Steering Group was designated to
coordinate the evaluation of the programme, as a first step to formulating a
project for possible external assistance.
The review of the national tuberculosis programme (NTP) of India was
carried out by a team representing the Government of India (GOI) , the World
Health Organization and the Swedish International Development Agency (SIDA).
The purpose of the review was to evaluate present policies and practices,
analyze their adequacy to reduce the tuberculosis problem and recommend
organizational, technical and administrative measures to improve the
programme.
The review team analyzed the available documents including
epidemiological data and reports of previous evaluations of the programme,
discussed with officers of major institutions involved in disease control and
in training, and made field visits in three States (Gujarat, Uttar Pradesh
and Tamil Nadu) to assess the programme at the State, District and peripheral
levels.
The burden of tuberculosis in India is staggering by any measure. More
thaN half of the adult population is infected. About 1.5 million cases are
notified every year and there are probably well over 500 000 tuberculosis
deaths annually. Recent trends show that the programme is not having a
measurable impact on transmission and appears to function far below its
potential.
f
The Government of India formulated the NTP in 1962. The major objectives
were to prevent tuberculosis through BCG vaccination; to diagnose
tuberculosis cases among symptomatics and provide efficient treatment, giving
priority to sputum positive patients; and to implement these activities as an
integral part of general health services. The District was the basic unit for
the NTP organization.
1
At present, organization of the general health system has been extended
to reach the community level with primary health services, The tuberculosis
programme is integrated into the general health services, and treatment
services are provided at the levels where medical staff is available.
However, the population growth and the proliferation of public health
services has made many Districts unwieldy for supervision by the tuberculosis
team which is based in a single District Tuberculosis Center. Further,
monitoring and training are mainly under the responsibility of the National
Tuberculosis Institute (NTI), the State TB officers playing only a minor role
in these important areas.
Human and financial resources are provided by GOI and the States to cover
most of the needs of the programme and current policy is to provide free
diagnosis and*-treatment. Currently available data do not allow analysis of
the adequacy or efficiency with which these resources are applied, but
preliminary indications and overall TB programme performance point to the
need for substantial improvements. If the programme is to operate as intended
and begin to make a significant impact on the disease, increased funding will
be necessary, emphasizing the need for improvements in programme
effectiveness and efficiency.
The prosMit
structure at national level requires strengthening
to assusM leadership in redefining policies, effectively assisting States and
supervising programme implementation, retraining staff involved in TB
activities; administering funds, and procuring supplies. The States, which
provide health services, need also to assume their responsibility in TB
programme management, and will require reorganization and training of the
public and non government health institutions involved in TB control.
There is little coordination between hospitals and primary health
institutions in rural areas, and between the different services providing
tuberculosis care in most urban areas, to ensure the management of
tuberculosis patients until cure.
Improvements in the methods and management of case finding must take
place. In spite of the recognized priority of bacteriological diagnosis and
cure of sputum positive cases to reduce the problem of tuberculosis, a large
proportion of human and financial resources is currently used to treat cases
diagnosed only on clinical and radiological evidence. This practice is common
both to the NTP and to private practitioners and is reflected in medical
college curricula. Bacteriology is not sufficiently used to confirm medical
diagnosis and criteria for initiating treatment in sputum negative cases are
not well defined. As a result of not identifying correctly smear-positive and
smear-negative cases, and newly diagnosed and previously treated patients,
some patients may be treated with inadequate regimens. Sputum microscopy
exAiiinations are carried out with insufficient standards and microscopy
laboratories are inadequately equipped. A TB laboratory network assuring
equipment, training and quality control is not in place.
Rationalization of treatment is required. There are currently too many
alternative treatment regimens and the conventional regimens are of
unnecessary long duration and low effectiveness. Short course chemotherapy
regimens of higher cost-effectiveness are slowly being implemented but
insufficient priority has been given to ensuring effective treatment of
infectious patients, particularly during the initial intensive phase of
chemotherapy.
The present system of recording and monitoring patient identification and
progress during treatment to ensure health service concentration on achievir
cure of infectious cases is seriously deficient. The present system does not
allow the systematic evaluation of the results of treatment at health
facility or block level. Neither does the registration systeta permit the use
of cohort analysis of patients to assess pure rate as the main indicator of
progrannifl efficacy.
Drug supplies are occasionally interrupted by lack of timely funding and
of buffer stocks. Additionally, the quality of the drugs supplied is not
controlled. The extensive network of multipurpose health workers (btPHW) has
not been sufficiently utilized at the community level to prevent defaulting
and achieve treatment completion.
The present training system relies mainly on the National Tuberculosis
Institute (NTI) courses. The state-level demonstration and training centres
do not function. District Tuberculosis Centres (DTCs) are not adequately
prepared to provide in-service training for dissemination of policy and
standards. It does not make adequate use of training institutions and NGOs at
the State level to transmit current policies and procedures. The curricula,
at medical colleges do not stress the basic principles of TB control and
there is no systematic continuing education for medical practitioners.
5
In spite of extensive national experience in both operational and basic
TB research, alternative methods to correct the extremely low proportion of
cases diagnosed with bacteriological confirmation and of patients completing
the prescribed treatment and cured have seldom been implemented. The
findings of previous programme evaluations have not always been applied to
improve existing programme procedures, nor has adequate use of the results of
research and programme evaluation been made.
Nonetheless, the basic strengths of the India TB programme are
considerable. The objectives on which the programme was established thirty
years ago - integration, decentralization, free services, priority to
treatment of infectious cases - are still valid today. They provide a sound
basis for revitalization of the national TB strategy. In addition, the
tuberculosis control programme can relatively easily build on its strengths:
a well defined structure which provides services within general health care
in an integrated manner; a basic managerial unit at District level with
Central and State’Governments providing support for diagnosis and treatment;
experienced training and research institutions; and, a general health care
system extended to the community through multipurpose health workers. An
updated and strengthened programme can expect to reduce the magnitude of the
problem by about half in each 10-15 years with the consequent savings in
lives, human suffering and more effective use of financial resources. This
will require a political commitment, initial investment and strong
leadership, plus the rapid development of an efficient national model to
serve as training ground and provide operational experience to programme
managers at all levels.
RECOMMENDATIONS
1.
The structure of the National Tuberculosis Programme should be
strengthened by 1) establishing an apex policy making authority and an
executive task force with managerial functions to implement programme
reorganization, and 2) upgrading the central tuberculosis control unit in
the Directorate to provide strong leadership and enhance the efficiency
and effectiveness of the National Tuberculosis Programme.
2.
The quality of patient diagnosis should be improved by 1) using three
smear examinations to detect infectious cases among symptomatics before
deciding on patient treatment, 2) ensuring the quality of microscopy with
adequate equipment, training and quality control, and
3) establishing criteria for diagnosis by radiological and clinical
methods.
3.
National and state tuberculosis programme resources should be directed to
ensuring cure of tuberculosis patients, giving priority to infectious
cases of tuberculosis by 1) adopting short-course chemotherapy, 2)
establishing criteria for treatment completion, cure and discharge from
medical care, and 3) ensuring an uninterrupted supply of drugs of good
quality.
4.
The current NTP system of registration and notification should be revised
to emphasize the cohort analysis of treatment results (completion and
cure, transfers, defaulters, died, treatment failures) as the main
indicator of programme effectiveness.
5.
Policies should be developed to ensure decentralization of treatment
services closer to the community level to enhance access to care and
patient compliance to recommended therapies.
6.
Pilot projects should be implemented at block level to test the
feasibility and results of different technical and organizational
6
strategies to be adopted by the tuberculosis progrime -- i.e., to test
the capacity to implement recommendations 2-5 above.
7.
A medical officer or treatment organizer and a laboratory supervisor,
with the necessary transport, should be added to the existing
administrative structure at the sub-district level (about 500,000
population) to strengthen tuberculosis programme management and to
facilitate decentralization of supervision.
8.
Training materials must be developed to reflect the proposed changes in
programme policies and procedures. The current training infrastructure
will need to broaden the scope of its training capabilities by utilizing
state training facilities, medical colleges, public health institutes and
tuberculosis-oriented voluntary agencies to augment training efforts.
International and national training opportunities should be made
available for the different levels of tuberculosis programme staff.
9.
Operational research must be carried out as an integral part of the
revised tuberculosis programme to evaluate programme performance, improve
delivery of services, problem solving and obtain baseline epidemiologica.
information to measure reduction in the risk of infection.
*
7
INDIA
TUBERCULOSIS PROGRAMME REVIEW 1992
2, INTRODUCTION.
A review of the national tuberculo.i. program-e was carried out fro.
9/1/92 to 9/17/92 as a collaborative effort of th. Government of India (GOI)
the7World Health Organization (WHO) and the Swedish International Development
Agency (SIDA). The purpose of the review was to evaluate present policies
and practices, analyze their adequacy to reduce the tuberculosis problem and
reioLend organizational, technical, and administrative measures to improve
the programme.
1.
2.
3.
4.
The assessment included.
An overall description of the current programme achievements and
problems,
An analysis of the tuberculosis burdep, the programme resources and
the programme structure,
Specific discussion of the leading issues facing the programme <and
their underlying causes, and
Recommendations for the next steps to improve the programme.
the central level the team reviewed information relating to the
At
magnitude of the tuberculosis problem in the country and epidemiological
ramme structure, policies, technical norms and procedures
trends, programme
'tuberculosis diagnosis and treatment, drug supply and logistics,
relating to
, monitoring and evaluation, education and training coordination
supervision
---, and research. Meetings were held with the Ministry of
with other programmes
Health, major Referral facilities in New Delhi and voluntary organizations.
Following the review at the central level, the review participants
to assess tuberculosis control activities at the
divided into thfee teams
and
District levels through facility visits and interviews with
State
responsible staff in three selected States (Tamil Nadu, Gujarat,, and Uttar
Pradesh). Then the teams reconvened2 l.i
in Delhi for discussion of the review
1 development of principal recommendations for
findings, conclusions and
summary of the conclusions
the Government of India. A draft summary
submission to 1-- -- --and main recommendations was presented to the Secretary of Health
----- at the end
of the review.
A list of participants is attached in Annex 1, and a list of persons
contacted and Institutions visited as part of the review is in Annex 2.
This document summarizes the findings of the review. Background
information on India can be found in Annex 3.1.
8
3. LIST OF ABBREVIATIONS
ADGHS
BCG
CHC
DGHS
DHO
DOT
DTC
DTO
DTP
EPI
GH
GNP
GOI
GP
H
I OMR
IMA
IMR
MBTC
MC
MCH
MO
MOH/FV
MPHV
NGO
NRR
NTI
NTP
PHC
PHI
PPD
R
RC
RI
RS
S
see
SIDA
STO
STTDC
A
T
TAI
TRC
VHAI
XC
ASSISTANT DIRECTOR GENERAL OF HEALTH SERVICES
BACILLI CALMETTE & GUERIN
COMMUNITY HEALTH CENTRE
DIRECTOR GENERAL OF HEALTH SERVICES
DISTRICT HEALTH (MEDICAL) OFFICER
DIRECTLY OBSERVED TREATMENT
DISTRICT TUBERCULOSIS PROGRAMME
DISTRICT TUBERCULOSIS OFFICER
DISTRICT TUBERCULOSIS PROGRAMME
EXPANDED PROGRAMME OF IMMUNIZATION
GENERAL HOSPITAL
GROSS NATIONAL PRODUCT
GOVERNMENT OF INDIA
GENERAL PRACTITIONER
ISONIAZID
INDIAN COUNCIL OF MEDICAL RESEARCH
INDIAN MEDICAL ASSOCIATION
INFANT MORTALITY RATE
MASTER BOOK OF TREATMENT CARDS
MYCROSCOPY CENTRE
MATERNAL AND CHILD HEALTH
MEDICAL OFFICER
MINISTRY OF HEALTH AND FAMILY WELFARE
MULTI-PURPOSE HEALTH WORKER
NON-GOVERNMENTAL ORGANIZATION
NET REPRODUCTIVE RATE
NATIONAL TUBERCULOSIS INSTITUTE
NATIONAL TUBERCULOSIS PROGRAMME
PRIMARY HEALTH CENTRE
PERIPHERAL HEALTH INSTITUTIONS
PURIFIED PROTEIN DERIVATIVE
RIFAMPICIN
REFERAL CENTRE
RISK OF INFECTION
RUPEES
STREPTOMYCIN
SHORT COURSE CHEMOTHERAPY
SWEDISH INTERNATIONAL DEVELOPMENT AGENCY
STATE TUBERCULOSIS OFFICER
STATE TUBERCULOSIS TRAINING AND DEMONSTRATION
CENTRE
THIOACETAZONE
TUBERCULOSIS ASSOCIATION OF INDIA
TUBERCULOSIS RESEARCH CENTRE
VOLUNTARY HEALTH ASSOCIATION OF INDIA
X-RAY CENTRE
9
4. TUBg^CUI/)?IS IN INPIA
Prevalent^ of InfectiQU- a nuaber of studies over the past 30 years, mainly
in rural southern India, have shown the prevalence of infection among
children 0-9 years old to b® between 3.IX and 11.2X (Table 1). In the early
1960s, more than 50X of the population 20 years and older was infected with
y. tuberculos11 and most infections occurred before 15 years of age. By the
late 1960s there waa no evidence of change in this pattern. Since that time,
there is no clear evidence of substantial changes in prevalence of infection
among children beyond that which might have been expected from secular
trends.
Table 1. India: Prevalence of tuberculosis infection among un-vaccipated
children 0 to 9 years old and estimated annual Risk of Infection (RI)
RI
Year
Location
Source
4.9X
1.0X
1961
Tumkur
Nil
9.6X
2. OX
1969
Tiruvallore
TRC
10. IX
2. IX
1983
Bangalore
NTI
10.4X
2.2X
1984
Dharmapuri
NTI
3. IX
0.6X
1985
Bangalore
NTI
9.OX
1.9X
1989
Kadambatmur
TRC
11.2X‘
2.3X
1989
Th i ruv e 1 an g a du
TRC
6.7X
1.4X
1989
North Arcot
TRC
Prevalence of
infection
______________________
Annual risk of infection. The intensity of disease transmission in the
community is best reflected by the annual Risk of Infection (RI) which
represents the probability of a previously uninfected individual becoming
infected with tuberculosis during a one year period.
RIs calculated from prevalence studies presented in Table 1 range from
0.6X to 2.3X. These data are difficult to interpret because methods vary
they clearly
indicate wide variation within limited
among surveys but
.
geographical areas and provide no clear evidence of a substantial decrease of
the risk of infection over the last 30 years. This stagnant situation is
substantiated by two recently published studies conducted in rupal areas of
Southern India. One showed that the RI decreased from 1.0X in 1961 to 0.61X
in 1985, equivalent to an average decline of 3.2X per year. The other study
showed no decrease in the risk of infection between 1969 and 1984 (RI of 1.7X
in both yqars). These results would be consistent with a poorly functioning
programme which Would be creatipg chronic cases of tuberculosis and drug
resistance.
Because most adults were infected in their youth, a small decrease of the
RI would not have any rapid impact on the prevalence of infection in the
adult population. It is safe to estimate that at least SOX of the population
above the age of 20 years is infected and will remain at risk of disease and
death from tuberculosis for their lifetime. A conservative estimate is that,
currently, the RI for India is still between IX and 2X.
Disease prevalence. The Sample Survey of tuberculosis conducted between
1955-58 remains the major source of information used by the NTP to anticipate
10
the tuberculosis situation in the country. The survey showed wide variations
in prevalence of disease among persons aged 5 years or more (sputum-positive
tuberculosis by smear or culture), ranging from a low of 229/100,000 to a
high of 813/100,000. The overall prevalence was 398/100,000.
In 1960-61 and in 1972-73 surveys conducted by NTI showed the prevalence
of radiological disease to be 1900 and 1100 per 100,000 respectively. In
1990, in an area near Madras, the rate was estimated to be 1700/100,000. In
the first of these studies, the prevalence of sputum-positive tuberculosis
was 410/100,000 and in others studies conducted by NTI between 1961 and 1968
in the Bangalore area the prevalence of bacteriologically confirmed
tuberculosis (smear or culture-positive) ranged from 337 to 406/100,000 over
the age of 5 years. About half of these cases (45X to 52X) were smear
positive. In a number of surveys and studies since that time, there is no
evidence of a significant decrease in TB during the last three decades and
there remains a very wide range of prevalence of TB in India. In the 1972-73
follow up of the 1960-61 study, the prevalence of bacteriologically confirmed
disease was 440/100,000. Two studies conducted in 1989 and 1990 in two areas
near Madras in the population above the age of 15 years found prevalence of
bacteriologically confirmed disease of 1090 and of 430/100,000 (58X and 69X
of confirmed cases were smear-positive).
The only clear exception to this stagnant situation is recent data from
the Tuberculosis Prevention Trial1, in which a 350 000 population of South
India is being followed prospectively. This study indicates a decrease in
prevalence and incidence of both radiologically active and sputum-positive
tuberculosis between 1968 and 1985. Most of the decrease, however, occurred
during the first few years of the study. Data from 1978 to 1985 show
stagnation with a prevalence about 1700/100 000 above the age of 10 years old
(by X-ray or culture) and an incidence of about 450/100 000 over the age of
10 years (X-ray or culture). During the same period, 50X of all cases had
bacteriologically confirmed (culture-positive) tuberculosis.
Among the many factors influencing prevalence of disease, the
effectiveness of treatment is important. Poor treatment completion
significantly increases the prevalence of disease. A recent retrospective
cohort study conducted under programme conditions by the Tuberculosis
Research Centre (TRC), Madras, illustrates the potential impact of poor
treatment completion. It showed that among patients on short course
chemotherapy who collected less than SOX, 50X to 79X and 80% or more of their
drugs, 44X, 37X and 21X respectively were still sputum smear-positive after
the end of treatment2.
Low effectiveness of the treatment programme explains much of the
stagnation in disease trends over the last three decades, Further, with the
current treatment completion rate it is probable that chronic and partially
treated patients represent a large proportion of patients diagnosed by the
programme.
Current tuberculosis rates. Age specific incidence rates (NTI, 1974) •
estimates suggest that about 870 000 new smear-positive cases of tuberculosis
may have occurred in 1992. This number is very similar to the 850 000
estimate obtained on the basis of incidence data from the Tuberculosis
Prevention Trial3. If the current average annual risk of infection is 1.7Z,
i
S.P. Tripathy, personal communication, 1992
2
TRC Annual Report, 1990
3
S.P. Tripathy, personal communication, 1992
11
1.6 million new cases (all forms) and 714 000 new smear-positive cases of
tuberculosis may occur annually. About a third of the total tuberculosis
burden of India is borne by the urban c onglomerations consisting mainly of
towns, cities, and their suburbs.
Notifications. Based on the average case notification from districts with
existing tuberculosis programmes (with about 83X of the population of tr.e
country), NTI estimated more than 1.5 million newly registered cases of
pulmonary tuberculosis in 1991, 21X of them were smear-positive. The trend in
notification, presented in Figure 1, reflects the increase in the number of
districts integrated in the tuberculosis programme from 32Q in 1980 to 337 in
1991, and also an increased proportion of cases not confirmed by smear
examination. The proportion of smear-positive cases has decreased from 25X in
1980 to about 20X in the late eighties. Relapsfes, failures and partially
treated patients are often inappropiately included in these notifications.
Figure 1. India: Notifications of cases
of tuberculosis, 1980-1991
Thousands
1500 -
Smear-positive
All pulmonary
1200
900
600
000 4
j________ i
i
i
i r, ?
. i_________t________ i
1
i,
.
i
0
1980 1981 1982 1983 1984 1985 1986 1987 1988 1989 1990 1991
Year
Extra-pulmonary cases are not reported
Source: NTI, 1992
12
Age and sex distribution, The majority of tuberculosis cases in India occur
below the age of 45 years, with about 75% of the diagnosed cases between 15
and 44 years old. Age-specific estimates of incidence from 1974 applied to
the 1992 population, would imply that about 58% of all cases today occur
between 15 and 44 years old. Two thirds of the cases are estimated to occur
Among males but tuberculosis takes a proportionally much larger toll on young
females than among young males. More than 50% of female cases occur before
age 34.
Mortality. Total mortality due to TB is uncertain but by any estimate poses
a huge economic burden for India. Tuberculosis mortality is estimated by NTI
to have been 69 to 95/100 000 in 1961-68 and 41/100 000 in 1977-81, or over
350 000 tuberculosis deaths annually (Table 2). Data from the Survey of
Cause of Deaths yield a more recent parameter by which to estimate current
mortality, resulting in 400 000 deaths, about 75 000 deaths in the 15-24 age
group, 95 000 in the 25-34 age group and about 160 000 deaths in the 35-44
age group. Using the 1955 Sample Survey estimates of incidence, if all cases
were diagnosed and at the present treatment completion rate of 30%, there
would be about 657 000 annual deaths of tuberculosis. A large proportion of
these deaths occur among women and it has been estimated that maternal
mortality and tuberculosis claim approximately the same number of lives, For
the decade of the 1990's, any of these estimates implyes a staggering
cumulative burden for the disease.
Table 2.
India: Estimates of probable tuberculosis mortality
Source
& year
Estimated
mortality
per 100 000
Annual deaths
Approximate (1)
cumulative deaths
1990-2000
41.0
346 000
3 460 000
Causes of deaths survey
92
50.0
422 000
4 220 000
Sample Survey incidence estimates (2)
55-58
77.8
657 000
6 570 000
NTI
77-81
"Styblo model" of incidence with 1.5% RI (2)
92
50.1
432 000
4 320 000
(1)
(2)
Mortality rates from surveys applied to 1992 population structure and
cumulative burden not adjusted for age structure within the decade.
Assuming no improvement from the current treatment completion rate of
30% and assuming 100% coverage of new cases.
Using the number of cases of tuberculosis currently notified by the NTP,
the reported completion rate (30%), a case fatality of 10% among patients who
complete treatment, 48% among smear positive-patients who did not complete
treatment and 24% among smear-negative patients, it can be estimated that
about 345 000 tuberculosis patients today diagnosed in the programme die.
Almost all of these deaths are preventable. Increasing the treatment
completion rate to only 85% would prevent close to 200 000 deaths annually, a
57% decrease in mortality.
13
Table 3.
India: Number of Tuberculosis deaths which could be expected among
cases officially reported in 1991 at different rates of treatment completion
and potential reduction in mortality.
Completion
rate
30X (current)
40X
70X
85X
Smear
positive
Total
cases
Reduction in mortality
(all cases)
Lives
Percentage
saved
reduction
121 000
;09 000
71 000
52 000
345 000
309 000
202 000
143 000
Base line
36 000
143 000
197 000
Expected deaths among
10X
41X
57X
* Pulmonary. As extra-pulmonary cases are not reported, they are not
included in this calculation
Cumulative mortality during the decade to the year 2000 will probably
exceed 3.5 million deaths, an enormous burden for society. A large share of
these premature deaths can be avoided with a well-functioning programme.
Given the ages at which deaths from tuberculosis are now occurring and the
low costs for tuberculosis programme inputs in India, it is probable that the
discounted cost per healthy year of life gained as a result of a well
functioning tuberculosis control programme will be well under US $10, making
tuberculosis control one of the highest priority interventions for the Si_ate
and central governments.
-; and; tuberculosis. HIV began to spread in India only in the latter part
AIDS
of the 1980s and there is no evidence yet that HIV infections are having an
impact on the tuberculosis situation. Only recently HIV testing has become
more common in a few research and academic institutions. A survey conducted
among all newly diagnosed smear-positive tuberculosis patients in 1990 in
Madras found 15 confirmed positive HIV cases among 2165 patients tested
(0.7X).
In Vellore, there were 16 confirmed HIV positives among 906 patients
newly diagnosed with pulmonary tuberculosis (1.8X).
In 1992, 12 of 183
(6.3X) tuberculosis patients admitted to a hospital in Bombay were HIVinfected. In a follow-up study of 220 HIV infected individuals conducted in
Madras, 115 (52X) had radiological evidence of tuberculosis and 34 (15X) were
culture positive. Other studies of HIV-prevalence in the general adult
population have revealed prevalence varying between 0.1X in Calcutta to IX in
Bombay. The AIDS programme estimates that currently there are 750 000
persons infected with HIV in the country and that there will be 5 million in
the year 2000. Assuming half of these people are -also infected with
tuberculosis, and that the breakdown rate from tuberculosis ^nzection uO
disease among dually infected individuals is 10X per year, more than 35 000
HIV-related tuberculosis cases will occur in 1992. There may be as many as
250 000 HIV-related tuberculosis cases annually at the end of the decade.
Virtually all of these cases will be in addition to the expected incidence.
As important as these cases will be, they will continue to represent only a
fraction of the cumulative cases of tuberculosis during the decade.
Tuberculosis drug resistance. Only a few laboratories can conduct drug
sensitivity testing in India. Although data on drug resistance is scarce and
resistance is not systematically monitored, available information (Tcxole 4)
is cause for concern. The very high rate of secondary resistance to bot_h
ri fampic.in and isoniazid is particularly serious, with long term implications
as these patients will transmit a virtually incurable form of disease within
the community.
14
Table 4; India: Primary and Acquired Drug Resistance in selected areas.
Type of patient
and sample size
S
Failure
81
354
560
50.7
78.8
30.0 65.0
Previously Treated
37
Madras (2)
111
Raichur (2)
Nev cases by history
241
Madras (2)
244
Raichur (2)
324
Delhi (1)
(1) :
(2) :
Delhi Centre (1)
Delhi Suburbs (1)
North Arcot (2)
X Resistance to
H
R
HR
SHR
16.0
33.3
61.5
6.0
9.0
35.0 62.0
11.7 52.7
13.5
17.1
5.4
5.4
8.1
11.7
7.3 12.6
11.0 19.1
18.5
1.6
3.2
0.8
2.0
0.6
0.8
1.2
Ind. J. Tub. Vol.39 No.2 pp 121-124
TRC Annual Report and M. Datta, personal communication
Conclusions:
The burden of tuberculosis in India is staggering by any measure. About
1.5 million cases are notified every year, more than half of the adult
population is infected, and there are at least 300 000 tuberculosis deaths
annually. Social and economic consequences of tuberculosis for individuals
and for the society are enormous in human suffering, economic loss, and
decreased productivity. Recent trends are discouraging, indicating a
programme which does not have any measurable impact and which appears to
function far below its potential. While further study and improved analysis
are needed to rigorously document the epidemiological situation, it will not
change the broad conclusion that tuberculosis is one of India's most serious
and still neglected health problems.
5. ORGANIZATION OF THE PROGRAMME
1. National Level. The Ministry of Health and Family Welfare (MOH/FW) is
divided into an administrative arm headed by the Secretary of Health and a
technical arm headed by the Director General of Health Services (DGHS). The
Secretary of Health is assisted by Additional Secretaries and the DGHS by
Additional DGHSs and several Deputy DGHSs. One of these Deputy DGHS
supervises the NTP as well as several other programmes, The responsible
officer for the TB programme is an Assistant DGHS (TB). The NTP is located
within the technical arm of the M0H/FW and on the administrative side, it is
coordinated by a Joint Secretary who is responsible for its financial and
administrative control.
National Tuberculosis Programme Policies. The long term objective of the NTP
is to reduce tuberculosis in the country to the level where it ceases to be a
public health problem. To accomplish this objective, the NTP focuses on 1)
the BCG vaccination of infants, 2) the detection of the maximum number of
tuberculosis patients among out-patients attending health institutions, and
3) the efficient treatment of identified tuberculosis patients, all as an
integral part of India's general health services.
J-
15
Centraj Structure of the NT?. The Central Unit of the NTP has a staff of
about 10 people. In addition to the Director, there are two physicians and 6
administrative officers for drug procurement, international assistance,
monitoring of monthly reports, annual planning and coordination with the
National Tuberculosis Institute (NTI)*. Currently, the post of programme
director (Assistant DGHS-TB) and one of the two medical officer posts are
vacant. The level of the programme director is lower than that of other
programme directors (EPI, Leprosy) and below the level of the director of
NTI. This, plus the fact that two out the three central level posts are
vacant reflect the low priority given to the NTP and show the absence of
strong national leadership. This situation, if maintained, would jeopardize
any attempts to revitalize the programme.
The Central Unit is responsible for drugs forecasting, purchase and
allocation, the annual planning and participation in the discussions of the
MOH/FW with the planning commission to determine the annual and 5-yearly
"plan budget" of the NTP, and for liaison with international agencies (WHO,
SIDA), with NTI, and with state TB programmes. The central unit does not play
any significant role with respect to tuberculosis control technical policy,
training and manual preparation, monitoring and supervision. These
responsibilities have been progressively taken by NTI. NTI management,
however, is virtually independent of the NTP. Additionally, State
Tuberculosis Officers are State employees, and they are not accountable in
practice to the ADGHS (TB).
. NTP budget. The MOH/FW budget is composed of a "non-plan budget" used for
personnel, salaries, hospitals, etc and a "plan budget", allocated by the
Planning Commission for future investments or creation of new posts. The
"non-plan budget" is not controlled by the NTP and fluctuates minimally from
year to year. No detailed information could be made available to the review
team about the proportion of the NTP budget corresponding to the "non-plan"
'
'.The
budget nor a breakdown by States of the NTP budget and* its
trend.
The 1992
R
145
million
(US$
5.3
(March 92 - February 93) plan-budget of the NTP is are
used
to
purchase
drugs
million) of which R 110 million - more than 75X and 25 million for other expenses such as X-ray units and films, microscopes,
vehicles, etc. Anti-tuberculosis drug costs are shared on the average on a
50:50 basis between Central and State governments. Within the overall NTP
budget, the Central government also provides anti-tuberculosis drugs to
voluntary organizations, and supplies, equipment, and drugs to the Union
Territories.
Other resources. The Swedish International Development Agency (SIDA) has
provided funds through WHO. These funds have been Used to purchase x-ray
units with Odelca cameras, miniature x-ray film rolls, vehicles, anti
tuberculosis drugs and microscopes. Occasionally, District and State
tuberculosis associations provide anti-tuberculosis drugs, materials and
equipment to specific district programmes or local tuberculosis facilities.
4
National Tuberculosis Institute (NTI).
The National Tuberculosis
Institute (NTI), located in Bangalore, is responsible for training NTP
personnel, monitoring the programme and conducting operational
research studies. Each year, NTI organizes two 10-week courses. In
1991, for example, 166 health professionals were trained. Apart from
training DTC teams, the NTI also provides refresher courses for
persons working for district tuberculosis control programmes and
reorientation/retraining seminars for senior health administrators and
teachers from medical colleges, etc.
Lastly, the NTI collaborates
with the World Health Organzation (WHO) for international training
efforts.
16
2. State jevej. India is administratively divided into 25 States and 7 Union
Territories. In the State MOH/FW, the NTP is under the Director of Medical
Services, Health and Family Welfare and the Director of National Programmes.
All States have a State Tuberculosis Officer (STO), usually assisted by a
staff of 6 to 10. The vast majority of STOs have been trained at the NTI.
In principle, there is a meeting of all STOs at the central level once a
year.
Responsibilities of the State Tuberculosis Officer (STO). The STO is
responsible for negotiating for the State the amount of drugs provided by the
central government and monitoring drug distribution to the Districts. He is
responsible for the overall supervision of District Tuberculosis Officers
(DTO) and through them of Peripheral Health Institutions (PHI). Lastly, he
should organize and coordinate training activities at the State level, in
conjunction with the State Tuberculosis Training and Demonstration Centres
and with NTI.
State tuberculosis demonstration and training centre (STDTC). Seventeen
states have training and demonstration centres. These centres were created
in the early sixties to supplement NTI. They have an average staff of 100
people with about 30 professionals. In addition to training, they have
responsibilities in diagnosing and treating patients and have, in some
instances, research activities. In practice, however, the vast majority of
these centres do not have an organized training programme or research
activities and aperkte solely as District Tuberculosis Centres (DTC).
3. District levej. The District is the basic demographic, economic,
administrative and political unit in India, The District is further divided
into Taluks and Community Development Blocks. One District encompasses 1,800
to 2,000 villages, has an average population of about 1.5 million^ and a land
area of 10,000 square kilometres. Health institutions in the District
generally include:
1.
2.
3.
4.
5.
One district hospital in the headquarters town.
Community Health Centres (CHC). Usually one in each Taluk, with
several doctors and specialized services (about 10 CHC per
district).
Primary Health Centres (PHC). In principle, one in each community
development block (about 40 per district).
Varying number of sub-centres (180), other peripheral health
institutions, dispensaries, maternity and child welfare centres,
employee dispensaries, and private hospitals.
Specialized tuberculosis institutions. ’Tuberculosis clinic, DTC
where the DTC has been implemented, sanatorium (about 100 beds per
district).
With one CHC per 100 000 population and one PHC per 30 000 population,
.
CQUntry £s
an average district may have abbut 10 to 15 CHCs and 50 PHCs.
21
805---PHCs and 137 683 sub-centres (Figure 2).
covered by a inetwork of
_ ----
17
Figure 2
ADMINISTRATIVE ORGANIZATION AND HEALTH SERVICES
ORGANIZATIONAL LEVEL
HEALTH SERVICES
Number
- Average Population
National
Institutes
850 000 000
State
Hospitals
25
Sanatoria
34 000 000
State TB Centre (STTDC)
District
District Hospital
438
District TB Centre (DTC)
2 000 000
1 500 000
Taluk
Community Health Centre (CHC)
appr. 15 per district
Central Hospital
100 000
CoTOunlty Development.Blok
appr. 40 per district
30 000
40 000
villages
1800 - 2000 per district
700
800
Primary Health Centre (PHC)
Maternal and Child Welfare Centres
Employee and Panchayat Union
Dispensaries
Subcentres (each 4-5 villages)
with Multipurpose Health Workers
18
In addition to these services, it is estimated that there are 330
tuberculosis clinics in operation in urban areas to provide services for the
local residents. Approximately 47,000 hospital beds are available in the
country for the in-patient care of seriously ill tuberculosis patients.
In the district, curative medical services and hospitals are managed by
the District Medical Officer (DMO) and preventive services and primary health
care by the District Public Health Officer. Although the District
Tuberculosis Officer (DTO) works under the authority of the DMO, he has no
formal control or authority over the district hospital and specialized
institutions. Conversely, he controls and supervises tuberculosis activities
in PHIs although these institutions are under the administrative authority of
the District Public Health Officer. This situation means that the DTO cannot
exercise leadership to improve the quality and coordination of tuberculosis
control activities in hospitals and does not have the line of authority
required to properly manage control activities in peripheral institutions.
District Tuberculosis Programme (DTP). In 1991, District Tuberculosis
Programmes were in existence in 378 districts out of 438 districts in the
country (86X) . In a district, all health institutions which undertake case
finding and treatment for tuberculosis are considered as participating units
of the DTP. These institutions are classified as either DTCs or PHIs. Each
district participating in the DTP has one DTC. Sub centres do not have
medical officers and are not considered as part of the DTP network.
District Tuberculosis Centre. DTCs maintain the patient case registers,
manage the recording and reporting system and are responsible for supervising
the TB activities of the PHIs. The DTCs also serve as referral centres to
PHIs for X-ray examinations. They have X-ray units, microscopes and
vehicles. They receive funds for drugs, gasoline, car maintenance, etc. from
the State. Anti-tuberculosis drugs are supplied by the national Central Unit
to all districts including those where the NTP has not yet been implemented.
Most DTCs receive additional drugs directly from the State. DTCs have a
staff of 15 to 20 persons including the District Tuberculosis Officer (DTO),
one to three tuberculosis medical officers, one radiology technician, one
laboratory technician, one to five treatment organizers, one statistical
assistant, one pharmacist, and one or two drivers.
Peripheral Health Institutions (PHI). In the District, most CHCs and a
number of PHCs staffed with at least one doctor are selected as PHI to
implement the NTP and conduct diagnosis and treatment of tuberculosis, There
are 3 types of PHIs:
1.
2.
3.
X-ray centres, offering X-ray and microscopy
Microscopy centres, offering microscopy only
Referring centres, preparing sputum smear for or referring patients
to the nearest microscopy centre.
No special staff is posted at PHIs and the Medical Officer in charge is
responsible for tuberculosis activities, In some instances, one of the
health workers of the centre (microscopist, X-ray technician) takes
responsibility for tuberculosis patient management.
z
Multipurpose Health Workers (MPHW). In all PHIs there are multipurpose
health workers who represent the most peripheral level of health care. The
are usually based in subcentres, in pairs. With respect to tuberculosis, they
are to maintain a list of all patients on treatment, to visit them regularly
and to refer symptomatic patients to the nearest PHI or the DTC. They are
not currently responsible for distributing or administering anti-tuberculosis
drugs.
19
Urban tuberculosis control. There are a multiplicity of urban organizations
and institutions involved in tuberculosis control activities, both public and
private. These organizations, however, rarely coordinate their efforts and
often work in isolation and/or overlap activities.
Consequently, areas
and/or population pockets needing tuberculosis services may be overlooked and
manpower and financial resources are not well utilized. Since 1975, city
tuberculosis programmes are to be organized in a similar fashion to DTPs,
with the stipulation that each city programme would be tailored to the
administrative, operational and social conditions of the specific city.
Currently, however, only a few large urban a£eas have well*functioning
tuberculpsis programmes. Voluntary organizations and tuberculosis
associations have been able to augment city tuberculosis programmes in many
instances by providing technical and financial support, health education, and
community outreach.
Conclusions:
t
The NTP has a very weak central structure, which for a long time has not
provided leadership in establishing and updating policy and technical
procedures and assuming programme direction. As a result, programme
procedures have stagnated and the original philosophy of the NTP has not been
fully implemented, or revised to make full use of the development of PHd. The
functions and resources of the State level, in particular training, have not
been developed and properly utilized. In most large urban centers the
coordination of activities among diffrent institutions, under the guidance of
the STO and STDTC, have not yet been implemented. In a similar way, the
curative services (hospitals, etc.) and preventive services (PHIs) are not
coordinated at District level in a single network for TB control, and the
lines of authority of the DTO are not clearly established. The extension of
TB diagnosis and treatment activities to the community through the MPHW has
been slow, and that valuable human resource is not sufficiently utilized to
enhance access to care £nd patient compliance to recommended therapies. There
is no technical and policy advisory body to lend credibility and promote
visibility of the programme to government agencies and potential donors and
to provide support to the national team in the preparation and periodic
updating of national policies, technical and administrative procedures, and
monitoring and evaluation of the programme.
6
CASg FINDING AND DIAGNOSIS
Diagnostic services provided by the NTP are free of charge for the
patients. A major stated objective of the NTP is to detect the maximum number
of tuberculosis patients in the conmunity and among outpatifents attending
health institutions with symptoms suggestive of tuberculosis, giving priority
to sputum positive patients. According to NT I manuals, the principal approach
of case finding should be routine screening by sputum smear examination of
chest symptomatic patients attending health centres, and symptomatic patients
be referred for x-ray only after a negative sputum examination has been
repeated. In practice, however, this policy is not followed.
Patients with respiratqry symptoms attending a public outpatient
facility are investigated with chest x-ray and generally one sputum smear
examination. Patients who have to come back a few days after their initial
exams are not routinely requested to bring an overnight sputum sample. Often
diagnostic smears are not done or the results are not recorded on the
treatment card. PHIs without x-ray facilities refer sputum negative patients
to a peripheral x-ray centre or to the DTC. Looking for better care or
because of public transport facilities, which directly link to urban centres,
many patients bypass the microscopy centre and go directly to an x-ray centre
or hospital, adding to their workload and increasing the proportion of cases
diagnosed through x-rays.
20
Most facilities with X-rays diagnose the patients and initiate TB
treatment on radiological evidence, in spite of a negative smear examination.
Very few facilities indicate further sputum examinations, or treat smear
negative tuberculosis suspects with non-specific antibiotics and follow-up
the patient's clinical and radiological evolution prior to initiating anti-TB
therapy, suggesting overdiagnosis based on x-rays. Overall, approximately 20X
of patients diagnosed with tuberculosis have atleast^pnepositive smear, a
very low proportion compared-to the-expected capacity of smear examination of
diagnosing 40-60% of all TB cases. The practice of doing generally only one
diagnostic smear examination is probably resulting in infectious cases being
treated as noninfectious (with inadequate regimens and supervision) or not
diagnosed at all. Official data published for one state tuberculosis
programme showed that between 1969 and 1987 the total number of tuberculosis
cases almost doubled whereas the proportion of smear positive cases decreased
from 61% to 28%, suggesting that clinical practice is relying less on
bacteriology and further separating from the policies recommended by the NTP.
Unfortunatelly, outpatient facilities run by non-government
organizations (NGOs) generally follow the-same routines. Moreover, NGO
institutions and municipal health facilities were found to charge
registration fees for each visit. In private practice, patients have to pay
for consultations, smear examinations by private laboratories and the
prescribed medication.
It is estimated that up to 50% of tuberculosis patients are identified
and at least partially treated by private practitioners. These patients do
not initially enter the NTP and are not registered. Many patients then move
to the public sector because of the cost of care and drugs. Thus, a large
proportion of patients attending a health service facility have previously
been seen by a private practitioner.
i
Due to the high number of PHIs in the district, the maintenance of an
updated cross indexing system at DTC is complex. Patients may not be able to
provide a complete address due to illiteracy or type of dwelling or because
TB has a social stigma and the patient does not want to receive mail from the
DTC or visits from DTC staff. Unless they present an identity card issued by
a public institution, patients previously treated outside the public system
or which are not found in the DTC cross index are diagnosed, registered and
notified as "new" cases. This practice correctly incorporates new cases
initially detected outside the public system, but duplicates notifications if
the patient was detected by a public institution outside the District.
A more serious problem is that the clasification in "new" or "old" bears
no relation to the previous treatment history and is not useful to decide on
patient therapy. If the patient is not found to have been previously indexed
in the DTC, he is considered "new" and is given a regimen for new cases. The
insufficient definition of "new" and previously treated patient leads to the
prescription of wrong regimens. A significant proportion of previously
incompletely treated cases is known to have acquired resistance to isoniazid
and streptomycin. The efficacy of "conventional" chemotherapy for such cases,
who are most likely still symptomatic and smear-positive, is very low.
Laboratory facXljtleg
Most laboratories visited were equipped with monocular, rather than
binocular, microscopes without an electric light attachment. Some of the
microscopes were in poor condition and the light source appeared to be
inadequate.' The quality of slides varied and some slides were found to be
uneven and poorly stained. Acid fast bacilli could not always be found in
smears read as positive. An ocular magnification ratio of five or six was
routinely used rather than the usual 10 ratio. As definitions for data entry
21
are irregular, laboratory registers do not permit determination of the
proportion of new cases, retreatment cases and follow-up examinations. Sputum
smears are not routinely used for monitoring of treatment outcome.
Many laboratory technicians working in peripheral microscopy centres
have been trained for the malaria control programme and are not familiar with
sputum smear examinations. Malaria smears are often given a higher priority
and may constitute a high case load. The number of sputum smears to be read
by one technician per day is usually considerably less than 20 except in
larger institutions such as DTCs and major hospitals. The rate of positive
smears varies between 1 and 10%. These low positivity rates may be partly a
result of poor selection of symptomatica, poor quality of the samples, low
quality microscopes, weak laboratory practices, inadequate training and an
excessively limited exposure to tuberculosis smear slides due to a small
catchment area. The supply of chemicals was adequate and no shortages were
reported. Slides with negative smear results are often reused, as indicated
in the NTI manual, with a risk of false positive results.
i
Quarterly or semi-annual supervisory visits are made by the DTC team to
assess the performance of the laboratory staff. The supervisors check
usually only all the positive slides, retained at the microscopy centre for
reading. Notes on the supervisory observations made, such as the proportion
of false positive and false negative readings, were not available for
scrutiny. There is no system of quality control through sending slides to the
DTC or to a State reference laboratory. Laboratory staff are often in need of
re-training and staining is of varying quality. Few States have functioning
reference laboratories to train District staff, supervise DTC laboratories,
carry out sistematic quality control of smears and do sputum culture and
sensitivity testing when necessary. In one State it was observed that the
STDTC laboratory had different procedures for smear examination that those
recommended by the NTI manuals and utilized by the DTC laboratories in the
State.
X-ray practices
With very few exceptions, diagnosis in clinical practice is based on the
chest x-ray. Even with one negative smear or no smear result, tuberculosis
treatment is initiated if the x-ray appears suggestive of active pulmonay
tuberculosis. The x-rays taken in referral centres are usually kept at these
facilities. The referring PHI only receives a note with the x-ray result.
The standard equipment in most x-ray units is an ODELCA camera with 70 or 1
mm films. In some hospitals, standard size films are used. Chest clinics at
the district level use both small and standard size x-ray films. Most of the
technicians are sufficiently trained and the chest films are of a good
quality, but complaints were expressed about the quality of the domestic ,
films. X-ray centers had well functioning x-ray units and usually sufficient
film to handle the tuberculosis caseload within the centers, although
temporary shortages of x-ray films are commonly experienced by PHIs. 93% of
x-ray machines were in working order at the DTCs as of 1991 (13). Assessment
by an inexperienced reader of the small size x-ray films widely used for
diagnostic x-rays or use of slightly inferior quality films can lead to an
increase in overdiagnosis.
Conclusions:
The NTP has an infrastructure of microscopy and x-ray centres,
integrated into the primary health care system and staff are available to
perform case finding activities down to the village level of health care
delivery. Major weaknesses of the NTP with regard to case finding are that
usually only one or no sputum smear is obtained before a tuberculosis
diagnosis is made, and that diagnosis is primarily based on the results of a
22
chest x-ray. This practice results in significant underdiagnosis of smear
positive cases by smear examination and in treatment of infectious patients
as smear negative cases with inappropiate regimens, and discourages
monitoring of treatment outcome by sputum smear results. Patients with
respiratory symptoms are often inadequately assessed and treated before the
diagnosis of smear negative tuberculosis is made. The lack of vigorous
procedures for patient management increases the tendency to rely on x-ray
examinations resulting in the overdiagnosis of smear negative tuberculosis.
Inadequate case history and the impractical case registers result in multiple
diagnosis of defaulters and overnotification.
The primary aim Ln case finding should be the identification of sputum
smear positive cases. Before the diagnosis of tuberculosis and decision to
treat are made, the results of at least two sputum smears should be
available. The role of the sputum smear examination in tuberculosis
diagnosis should be greatly emphasized and the role of radiological
examinations should be reconsidered. For differential diagnosis, the ODELCA
cameras and miniature films for diagnostic chest x-rays may be phased out and
replaced with equipment based on the specifications for the WHO Basic
Radiological System, after carefully working out the cost con»iderations. For
screening of symptomatic attendees in hospitals of large urban areas to
select patients for bacteriology, small size X-rays may be useful.
The NTI laboratory manual should be revised, used for training at State
level and distributed as a reference to the laboratory staff of PHIs. Wall
posters with the basic procedures for microscopy, as were seen in one of the
States visited, $hould be made available to all peripheral microscopy
centres. Supervision of DTC laboratories should be undertaken by State
reference laboratories. Supervision at State and at District levels should
include a system of quality control whereby samples of positive and negative
smears are systematically Sent to a reference laboratory for confirmation.
Acceptable quality binocular microscopes should be made available. All
diagnostic centre?, including those outside the State health services, must
adhere to uniform programme guidelines.
7. TREATMENT
The manuals for the District Tuberculosis Programme (NTI, 1990) include
the current national policies for the treatment of tuberculosis. The
Introduction Manual states that free chemotherapy should be provided to self
referred tuberculosis patients. The highest priority is given to treatment of
sputum positive cases to reduce the transmission of infection in the
comniunity. Five regimens of "conventional chemotherapy" of 12-18 months
duration for all forms of tubetculdsis are recommended. In a phased manner,
two short course regimens of 6-8 months duration are to be provided for
sputum positive cases. Patients are "allowed to collect drugs from the
nearest PHI and are motivated to consume drugs for prescribed duration
regularly".
In Annex 4.1 the regimens found to be most frequently used in the DTP
are presented according to the currently recognized category of patient and
priority given if drugs are available. The categorization used in the
following sections of this report corresponds to that used in the WHO
Guidelines for Treatment of Tuberculosis in NTPs. However, in the India NTP
manuals, the seven recommended regimens do not always refer to the specific
category of tuberculosis patients' and the choices of regimens are not
prioritized.
23
Treatment practices,
Patients are mostly treated by "conventional" regimens on an ambulatory
basis and oral drugs are self administered by the patient. In some States
(mostly in the South of the country) the regimen of HT is rarely utilized due
to the reported high frequency of side effects. There, most patients are
treated with HE for 18 months or SH twice a week. In some States of the North
where thiacetazone is well tolerated, the drug is not supplied in sufficient
quantity because of shortages in the national market attributed to the low
profit margin on the drug for the pharmaceutical companies.
SCC regimens for pulmonary smear-positive patients are theoretically
implemented in approximately fifty percent of the districts in the country,
but in reality only a minority of patients are treated with SCC so far. SCC
is being implemented slowly, mainly because the expansion of SCC has not been
given high priority in the NTP. The selection of patients eligible for SCC
observed during the review is quite strict, probably because the medical
officers of the DTP have doubts about the -compliance of patients in selfadminis tration of the SCC regimens. SCC drugs are often kept at the DTC or
selected PHIs and patients living far away cannot come twice a month for the
drug collections.
The treatment is usually prescribed by a medical officer of the DTC or
PHI, and provided free of charge. Anti-tuberculosis drugs for the recommended
regimens, in particular for SCC, are periodically out of stock, reducing the
motivation of the patient to regularly attend the institution and
contributing to the prescription of a non standardized regimen. Patients
attending private clinics are required to pay for their medications. They may
go to governmental institutions when they are unable to continue to pay for
treatment, but do so only when they are very sick. In a limited number of
situations, treatment may be supported by voluntary organizations. Often when
there is a shortage of one or more drugs in the health centre, patients are
required to buy the missing drugs. In one State, streptomycin, part of the
"conventional" regimen, was presently missing in most centres visited by the
review team due to a 50Z budget reduction from the previous year's budget.
Patients with severe forms of tuberculosis (e.g. meningitis), those with
complications of tuberculosis (e.g. pneumothorax, hemoptysis), those with
tuberculosis complicated by other diseases and failure of an initial regimen
requiring retreatment are hospitalized. Places of hospitalization are
referral hospitals including sanatoria and medical colleges. Seldom are
tuberculosis patients hospitalized in CHCs or district hospitals.
Hospitalized patients frequently receive "conventional" chemotherapy that has
low efficacy for.critically ill and retreatment cases.
Existing hospital
beds for tuberculosis are utilized for advanced disease and not fully
utilized to prevent treatment failure. Hospitalized patients often receive
weak regimens and the beds are therefore not utilized in a cost-effective
manner.
In the DTC, drug collection is done once a month for "conventional"
therapy and twice a month for SCC regimens. The frequency of drug collections
by the patient is similar during the initial and the intensive phase of
chemotherapy. Streptomycin is administered in the health institution nearest
to the patient home or by a private nurse. Usually the patient do.es not see
the medical officer during the follow-up. He may be asked to see the MO if he
has drug side effects. The monitoring of side effects is not systematic and
there is little information regarding the percentage of patients who may have
experienced major side effects.
24
Guidelines for changing regimens during chemotherapy or for prolcr.gation
of the duration of a regimen have not been issued by the NTP, creating
confusion, particularly for MOs in the PHIs. Unnecessarily long conventional
regimens are a burden for the patient, causes an unnecessary workload fcr the
staff, and results in drug wastage. The decision to discharge from treatment
is made by the MO on the basis of the treatment card and on the clinical
condition of the patient. Criteria for discharge from chemotherapy are r:t
clearly specified in the NTP manuals. The patient is permitted to stop
chemotherapy when he has completed SOX of his prescribed regimen. If he has
not completed such a course, he has to continue the treatment for the
duration of time for which he has not collected drugs. Due to the high
incidence of defaulting, most patients receive unnecessarily long regiAelts.
ft or
In addition, the definition of treatment failure is not clearly specif!
is practice uniform among MOs working in the PHC centres with regards rr how
to manage a failure case.
After treatment completion and discharge, the patient is^instructed
return every 3-6 months for follow-up. This practice is unnecessary and
results in wasting of effort for both the patient and health staff.
Treatment organization,
Smear examinations are not repeated during conventional chemotherapy, to
confirm that the patient is really sputum negative or to determine spurum
conversion in smear positive patients. For SCC regimens, NTI recommendations
do not require sputum examination at the end of the intensive phase of
chemotherapy nor are criteria specified for prolongation of the 2 months
initial intensive phase if the patients remain smear-positive. Smear
examination after the initial intensive phase of SCC is required in some
centres participating in the Tuberculosis Research Centre operational trial,
but is done in approximately 20X of the patients only. The insufficient
monitoring by sputum examination during chemotherapy does not allow for
evaluation of the outcome of the initial intensive phase of SCC chemotherapy.
Patients who are still smear-positive at the end of the initial phase should
receive special supervision by the DTP staff because they may not have
strictly adhered to the prescribed medications. These patients may st ill be
cured by the same regimen for new cases if the drugs of the initial i tz-ns ive
phase are continued for an extra month and the staff fully supervises the
patient.
National policies require that pulmonary patients be monitored by x-ray
examination after six months and at the end of conventional chemothajzry.
This requirement is not necessary in smear-positive patients and is net costeffective in smear-negative patients. In practice, only a fraction of
pulmonary cases are followed up by chest x-ray films in the DTf.
Extrapulmon^ry tuberculosis patients are monitored by physical examination
and by appropriate clinical tests.
The decentralization of the treatment of tuberculosis patients tz FHIs,
as recommended by the NTP, is not fully utilized for the administration of
SCO regimens. The lack of decentralization results in a high percentage of
dropouts. A significant percentage of patients diagnosed in DTCs are
defaulting the first drug collection. The treatment card is not opened nor
are the name and address of the identified smear positive cases in the
community communicated to the PHI closest to the patient's home to retrieve
the patient. Name and address of pa'ti'ents under treatment by the DTC :r other
institutions are also not routinely communicated to the PHI.
In PHCs, the MO at the beginning of treatment and the pharmacist curing
follow-up should provide patient motivation. At present, the same efzcrt is
made for all categories of patients, without sufficient focus for smear-
25
rWpositive cases of TB that are the priority for cure. In DTCs, the DTO and MOs
should provide motivation at the beginning of treatment and the treatment
organizer should do so during the follow-up. Sometimes, in training and
demonstration centres, health education and motivation is provided to small
groups of patients. There is no formal monitoring of the effectiveness of
such practices. There is no special effort to re-motivate patients who are
still smear-positive at the end of the initial phase of SCC, when there is
still a high probability of smear conversion and cure if the drugs are taken
regularly. Effectiveness of health education practices among the patients and
among the community are seldom evaluated and health education material is
rarely available among patients, family members and health staff. Not enough
emphasis is put on informing the patient and the health staff about the
importance of sputum examination.
Follow up of defaulters is not practical because the staff is required
to take action for a large number of patients, without focusing on those who
remain smea^:-positive during chemotherapy. The current guidelines recommend
that priority be given to sputum positive patients, leaving to the DTO the
decision of excluding sputum negative patients from defaulter action. If home
visits cannot be done, guidelines require that letters be mailed twice: after
three days of defaulting and after 11 days if the patient is still
delinquent. During the review it was found that letters at'e the most common
action to retrieve defaulters. However, a large number of patients provide
incomplete addresses and therefore reminder letters cannot reach them. In the
PHC, the multipurpose health staff are sometimes asked to retrieve the
patients, but such action is probably not stressed enough by the medical
superintendent and Chief Medical Officer. The village health worker is often
not informed about the TB patient(s) living in the village. The PHC is also
not systematically informed by the DTC about new patients diagnosed and
remaining under treatment by the DTC or hospitals.
The reasons for defaulting are well identified by the tuberculosis
programme staff. Among the most important is the fact that the patient loses
interest once he becomes asymptomatic. Disruption of drugs stock, incomplete
provision of the first line drugs for "conventional" and SCC, long waiting
time, inability of the system to adjust to the patient needs, distance of DTC
or hospitals from the patient's home are the other most common reasons for
defaulting. Some patients go to a health institution different from where
they are registered with the hope of receiving better care. This increases
default as well as making it more difficult to retrieve them. The DTC and
other specialized institutions do not use auxiliary staff (MPHW) to retrieve
defaulters and do not inform PHC of the existence of patients on treatment
from that area.
Amqng defaulters, approximately 30X to 50Z miss drug collections before
the fourth month of cnemptherapy. 5Z of patients default afteD diagnosis is
made and before therapy is initiate^. In some instances, the patient is not
informed that he has tuberculosis and should be treated. Lack of motivation
of staffl, weak leadership of the medic#! officer and little accountability to
the chief medical officer for tuberculosis have been identified by the
supervisory teams as additional reasons for patient defaulting.
In the policies of the NTP there is no target for treatment completion
and cure of pulmonary smear-positive patients. In such patients the fatality
rate is known to be high and irregular chemotherapy leads to drug resistance.
The present policies and practices are insufficient to reduce the spread of
the infection, particularly of drug resistant mycobacteria, and the mortality
due to tuberculosis. The observation of the assessment teams show that the 13
programme objectives are not efficiently prioritized. The existing health
infrastructure and resources available are not fully utilized to sterilize
smear-positive patients as quickly as possible. In a significant proportion
26
of the sources of infection diagnosed by the DTP, the chemotherapy is not
started, and a large percentage of smear-positive patients put under
treatment drop out during chemotherapy.
The decentralization of the programme is not achieved. Guidelines for
patient management are not present at the level of peripheral health
institutions (PHC and CHC for a population of 100.COO to 200.000) where most
of the patients could benefit from the existing health services. Medical
officers working in PHCs and CHCs are generally not trained for the proper
management of the tuberculosis patient. Supervisory visits to PHI from DTC
and chief medical office are not targeted to improve treatment outcomes.
Conclusions:
NTP policies and procedures on treatment do not reflect the WHO
recommended emphasis on short course chemotherapy and patient registration
systems which facilitate the monitoring of completion and cure rates of
patients on anti-tuberculosis treatment. -The tuberculosis programme at the
delivery level does not adequately emphasize the importance of treatment
completion as the main index for programme evaluation. During the programme
review, the teams observed that DTP practices depart from what should be done
to effectively treat tuberculosis patients. Service delivery focuses on case
finding activities and not on treatment completion and cure. Tuberculosis
staff are not optimally utilized to enhance treatment completion activities.
Additionally, there is no good system to evaluate treatment results. NTP
policies and procedures should be revised to ensure that the most efficacious
and current treatment regimens are recommended, including fewer regimens and
short course regimens where appropriate. Registration systems should solicit
data to monitor completion and cure rates, with particular focus on smear
positive tuberculosis patients.
The main goal of the NTP should be to
ensure that patient completion of anti-tuberculosis treatment and cure be
reflected in all policies and procedures and that such be carried out in the
current integrated health care delivery system. Guidelines for treatment
organization are attached in Annex 4.2.
8
PROGRAMME MANAGEMENT
8.1 CASE NOTIFICATION
Tools for programme monitoring are the treatment card, the laboratory
register, the master book of treatment cards (MBTC), the cross index card,
the patient identity card and the report on treatment results. The use of
register books and report forms is in accordance with the NTP guidelines in
DTCs where the statistical assistant is in position and has been trained at
NTI. However, training courses have been rarely.repeated and trained staff
have been transferred to other programmes within the district. The format of
the treatment registers is not always standard, as they are copied by hand
and not printed, and the content does not include all the data required to
analize the results of treatment. The card is sent from the PHI to the DTC
when the patient completes treatment, defaults or dies, so the MBTC is the
only source of data on treatment left at PHI level.
The usefulness of the recording and reporting system does not appear to
be well known at all levels of the system. Consequently, evaluation of
programme outcome and actions are missing, and the evaluation by cohort
analysis of results of treatment is often not done. Cross checking of
patients registered in the laboratory register, the treatment card, and.
registrations in the MBTC is not operating efficiently. Therefore no action
is taken for smear positive patients registered in the laboratory register
who default from the first drug collection, data on initial defaulters are
not available and the information in the cards and MBTC is not complete.
27
Conclusions:
The current reporting and recording system for the NTP is cumbersome and
does not address the main WHO recommended objective of the programme, i.e.
the monitoring of the cure rate among smear-positive cases of tuberculosis.
Cohort analysis does not cover all smear-positive cases diagnosed and is not
done at the PHI level. The current NTP system of registration and
notification should be revised to facilitate recording of essential data,
such as previous history of TB treatment, and emphasize the collection and
cohort analysis of treatment results as the main indicator of programme
effectiveness.
A printed copy of the laboratory register and patient register books
Should be made available to each PHI implemented to provide tuberculosis
care. These registers should be kept by a PHI staff trained in record Keeping
and should be supervised at least every two months by the DTC supervisor.
Supervisors should cross check the records in the registers to assess the
consistency of the data. Standardized reports on the indicators of programme
performance should be filled out at the end of each quarter and forwarded to
the DTC. The DTC will consolidate the reports from the PHIs and forward them
to the state TB Office. DTC team supervisory visits to PHIs should be
prioritized on the basis of performance.
8.2 SUPPLIES AND TRANSPORT.
Anti-tuberculosis drugg
r
Anti-tuberculosis drugs used by the NTP are manufactured or compounded
by pharmaceutical companies within the country. In principle, 50X of the
anti-tuberculosis drugs for the NTP are purchased by the national government
and 50X by the States. The national government negotiates with the states
its financial contribution for drugs based on the capacity of the State to
complement the central government contribution. The amount of drugs needed
by each state is determined annually by the central unit from the number of
patients reported the previous year, the population, and the requests
received from districts. These requests are initially scrutinized at the
state level. The central unit negotiates the purchase of drugs with the
pharmaceutical industry but it must buy from semi-public corporations as long
as the drug price is no more that 20X higher than the price of private
companies. The distribution of drugs to the districts is the responsibility
of the Medical Store Organization.
The State portion of the anti-TB drug supply is generally purchased by
the District from manufacturers selected in State bids, using allotted State
funds and sent to the District directly by the drug manufacturer. Monitoring
of stock supply, reserve stock, and usage is left to the District. Al chough
the districts send notification of supplies on hand, usage, and drug
projections to the STO, it is unclear whether analysis of usage patterns is
regularly undertaken at the State level. Facilities are likewise unaware of
drug supplies available in neighboring facilities or institutions
institutions..
At the district level, the DTO usually estimates the needs of anti
tuberculosis drugs on the basis of the previous year's consumption. He
receives the drugs purchased directly by the central government and the
budget allotted by the state through the chief medical officer. In some^
situations, the budget obtained from the State to purchase anti-tuberculosis
drugs was sufficient for only a fraction of the needs, due to increases in
drugs costs (approximately 20X compared to the previous year). In some
districts, the funds were sufficient, and if additional funds were necessary,
they could be requested from the state. In some instances, shortages *rere
corrected by using funds from TB associations, Interrupted supply of some
28
anti-tuberculosis drugs at district level were noted as being due to late or
incomplete supply by the production laboratories of approved orders or due to
the absence of reserve stocks at the state level. The state does not purchase
or receive drugs directly nor does it maintain a buffer stock.
The rifampicin used by the NTP is not a combination capsule. Fixed dose
combinations of rifampicin with isoniazid, and with isoniazid and
pyrazinamide are however available in the market. The quality of such single
drugs and combination drugs is not currently being monitored by the NTP.
Conclusions:
Ensuring an uninterrupted supply of anti-TB drugs to the tuberculosis
patient should be a key function of the national and State tuberculosis
programmes. Shortfalls in funding and delay of drug supplies from the
pharmaceutical industries can be compensated by 1) closer monitoring of usage
patterns, drug purchase projections and stocks by the STO and 2) establishing
a buffer stock at the State level sufficient to ensure at least a 6 month
supply of uninterrupted drug distribution to the districts. Similarly,
districts and PHIs should maintain internal buffer stocks of three months as
an additional preventive measure. Estimations of the amount of buffer stock
should be based on the number of patients reported during the previous year.
In addition, drug quality should be monitored by the National Unit and the
States through a selected scientific institution.
Transport
The non-availability of road worthy vehicles and poor budget allocations
for fuel have been cited as reasons for limiting the number of supervisory
visits by the DTC team to PHIs. At District level, fuel quotas were clearly
insufficient, in view of the increased number of PHIs to supervise and
distances to cover. As a result, supervision of PHIs is not done with the
frequency required, or several PHIs are supervised in the same trip with
insufficient time allotted to each one. Adequate provision of fuel should be
provided to the DTC for supervision, and transport should be provided to
district supervisors based at subdivisional level to reduce milage and fuel
costs.
8.3 SUPERVISION, MONITORING AND EVALUATION
According to NTP policy, the District Tuberculosis Officer and his team
of laboratory technician, x-ray technician, and treatment officer, etc. are
responsible for the supervision of all personnel within their District
involved in tuberculosis activities. The team is expected to visit each of
their PHIs on a quarterly basis. They are to evaluate diagnostic and
treatment procedures, validate laboratory results, monitor record keeping
activities, check on defaulter actions taken, and monitor anti-tuberculosis
drug supplies and support equipment.
In addition to their supervisory
duties, the team is expected to do on-the-spot training and/or retraining of
staff, collaborate with other disease control programmes on topics of mutual
interest, and offer continuing education to the general public. Supervisory
checklists have been provided by the NTP to guide the supervision of DTCs and
PHIs. At PHI level, Medical Officers have been made responsible for the
supervision of laboratory technicians and multipurpose health workers.
When the NTP was operationalized in 1962, the District demographic unit
was designated as the basic unit for the NTP. All NTP activities were
In the three intervening
conceived and organized at the District level.
decades, the District has grown in population, and the number of government
health services has grown at least in proportion to the population growth.
29
r is increasingly difficult for the DTC team to operate under the
organization conceived thirty years ago, to feasibly supervise and manage at
the District level. In one District visited, with a population of 4 million,
119 out of 148 Peripheral health institutions have implemented the DTP. The
DTC staff would have to make 20 visits per month, supervising 2 facilities
per trip in order to provide quarterly coverage for its implemented centers.
This schedule of activities does not include the general hospitals, voluntary
organizations, etc. which also treat tuberculosis patients and should benefit
from regular supervision.
The assessment team noted that the District Tuberculosis team did q^ke
visits to PHIs. The quality of the visits was difficult to assess, and th§
frequency and regularity of the visits were difficult to validate, as
supervisory reports were not available for scrutiny. Records were not in
order at facilities where recent supervisory visits were noted.
Alarmingly, there has been a steady decline in the proportion of PHIs
supervised by the DTC team, from 51% in 1983 to 41% in 1991. In 1987 only 84%
of functioning DTPs sent quarterly reports. Of these only 72% ( 60% of
functioning DTPs) gave information on supervisory visits, Of the 60% of DTPs
giving information, they had supervised only 45% of their PHIs.. Thus only
27% of the PHIs have been reportedly supervised, The quality of the
supervision is riot known (5).
Currently, supervisory visits are primarily used to evaluate record
maintenance, laboratory performance,, assess defaulter retrieval activities,
and monitor the supply of anti-tuberculosis drugs and other equipment. Not
only are the supervisory objectives poorly fullfilled, but very little time
is devoted to the evaluation and supervision of programme performance with
regard to the accuracy of case-finding and to patient completion of
treatment.
The National Tuberculosis Institute (NTI) has been responsible for the
monitoring of the National Tuberculosis Programme since 1978.
Information on
DTP activities is recorded through a system of records kept at the facilities
and periodic reports sent to the NTI.- Peripheral health institutions report
2treatment
_____
- * ’
s- to the TX
'rn. The DTP
case r finding and
activities
on a monthly ’basis
DTP.
quarterly
and
annual
reports
for
the
NTI,
inclusive
of
data
received
prepares <
from the PHIs involved in tuberculosis activities.
Programme
Prograisme moditoring and evaluation has been largely limited to review
and analysis of notification data and regularity of reports. The current
information system does not provide for the monitoring of treatment outcome
or prngramrae outcome indicators. Management indicators and monitoring
procedures focyis attention on case finding but exhibit very little emphasis
on case treatment and cohort analysis. Additionally, patients who are
hospitalized in the more than 40,000 tuberculosis hospital beds are not
registered in the NTI information system. Likewise, the large number of
patients receiving initial care through tHe private sector are not registered
with NTI.
Consequently, it is estimated that less than 57% of all cases of
identified tuberculosis are registered with the NTI (1).
In 1991, only 378 districts out of 438 with DTPs had registration in
place (86.3%). Of those with DTPs, only 278 out of 378 sent reports (74%).
Of the DTPs which reported to the NT I, they only received reports from 8502
out of 12,338 PHIs. Results from the 1987 "In Depth study on the NTP of
India" (1) showed a general lack of awareness among tuberculosis staff of the
importance of records and reports. Very few officers have readily made use
of them. Data in the reports was not useful for programmme management
activities. Supervising officials rarely checked records and reports or gave
guidance regarding their proper maintenance. Reports were very often
30
incomplete and unreliable. Although on site evaluation of case management is
reported, it is acknowledged by supervisors that the monthly and quarterly
reports sent to the DTC are not analyzed nor are the sending institutions
given any feedback as to performance as reflected in the written reports.
Conclusions:
There needs to be a clear emphasis placed on supervision if the NTP
programme is going to succeed. Tuberculosis programme personnel need to be
retrained about supervisory methodologies as well as supervisory content
which emphasizes programme performance parameters.
In order to address the
increase in population and health care facilities at the periphery, a medical
officer or treatment organizer and a laboratory supervisor should be added to
the District Tuberculosis team at the sub-divisional level (about 500,000
population) in order to facilitate decentralization of supervision, staff
training, monitoring and evaluation, and management of tuberculosis programme
activities at the level of PHIs. To reduce travel time and cost, these staff
should be based in a hospital or X-ray centre and they should be provided
with transportation.
Monitoring of case finding and treatment results has not been
prioritized, is still centralized and is not used at health facilities to
evaluate the quality of programme delivery and implement corrective actions
when necessary. PHIs management staff should be retrained on monitoring and
evaluation methodologies. They should be taught to analyze their own
facilities performance indicators and to take corrective action promptly.
DTC, State and national staff should analyze the quarterly and annual reports
received and provide feedback to the health facilities on the priority
indicators of programme efficacy.
8.4 EDUCATION AND TRAINING
Since 1962, the National Tuberculosis Institute (NTI) at Bangalore,
India has been the main training institution for tuberculosis programme
staff. The various members of the District Tuberculosis Center (DTC) team
(medical officers, x-ray technicians, laboratory technicians,
pharmacists/treatment organizers, and statistical assistants) undergo a 10
week training program at the facility, with special emphasis on their areas
of responsibility. The NTI also conducts seminars for state tuberculosis
officers, university faculty, and district medical officers, as well as
refresher courses for DTC staff.
In theory, in addition to NTI, the State Tuberculosis Training and
Demonstration Centers (STTDC) are responsible for training BCG supervisors,
orientation training of health visitors, and training of medical students and
ancillary health care providers on the clinical aspects tuberculosis control.
Continuing education for the private physician is often undertaken with
assistance from the Indian Medical Association and voluntary organizations.
The review teams found, however, that the training given by STTDCs was
neither comprehensive nor consistent with NTI policies and procedures with
regards to diagnosis and treatment recommendations, i.e., x-ray reading,
procedures for procuring and preparing sputum for smear microscopy, treatment
regimen recommendations, etc. Training materials were not available for
scrutiny. Instruction in the STTDC is provided on the basis of observations
of clinical procedures, focusing on clinical aspects rather than programme
operations.
•
4
*^4
31
Since the emphasis on pri^ heaUh^axe
, become
effort. r ^1^ - ^1^^ o
these health personnel in NTP policies and
(^:day)
districts the DTO and his staff provide systematic, but briet two uay;
sxs «r “Ti
e»
«Pb„
tb.
tp-n
which provide general < month for medical officers, where the tuberculosis
health workers and one J “h. “our.e cnrrleuU. H«ai=al
»»
content is a component
train their staff in tuberculosis activities. Many of the ,
also expected to t’ b« trained themselves- The majority e£ medical
however,
haveInyet
lpt.rvl.ued
the field stated that they did not carry out any tr.lnms
activities for their staff.
roughly 900 full teams have
Since 1962, over 4,800 team personnel or
districts implemented
been trained by NTI staff. However, as the number of
<
l or attain superannuation,
has increased, and as senior personnel are promoted
full complement of trained
all of the district teams
persons, i—
S.L.d
dLtrldC
officer <DT0 . 7« bad
trained district
had tne servi
_ ,
trained laboratory technicians, 88- had
trained x-ray technicians, 78% bad
organizers, and 59% had trained statistical assistants
trained treatment
(13).
Conclusions:
. ,
,
to the successful implementation of the review team s
Training is
Training materials
materials must
must Lbe developed to reflect
recommendations for the Nir.
6
nrncedures
and procedures The needs for
ch. propca cb.n8.. In pr«8r™« policies
pnllol.^.nd^roc.dure.^
training of tubetculosis personne training rcapacity
*nAritv of the NTI. The current
i nct-i riitI ans exceeds the present training capacity of the NTI.
NTP training should be descentralized by utilizing the ex st ng s a
SfX
..dfP.l e.U.Ees. P“•b?%
’' • h
health
““ht institutes
S “TffX.
and
Tb.s.
gencies to augment
nltlonll^rainin^opportunities should be made available for the different
levels of tuberculosis programme staff.
recommendations of the
The NTP manuals should be revised to reflect t e
should
be developed by NTP for
Review, and standardized educational materials
tuberculosis control activities
different categories of personnel involved in
etc. in private practice)
(including medical students, general practitioners,
and for patient motivation.
9. PRIVATg SECTOR
70l
Xelans
X”.PndT..h i. by private
A t.eo.e ^“XrroFplt’lents’Srhln-”.^^ th.
major role and their management of TB cases inf
„
the NTP
It appears that private physicians do not adh
seC re&imen
uas
patients vary widely and are usually more costly
the NTP. Patients are usually given a prescript
pharmacy
*-
32
for drug purchase, with very little monitoring of patient compliance.
Defaulter action is rarely taken.
The training of general practitioners is currently not adequate and has
not been updated to incorporate recent advances in knowledge and strategies
of the NTP. The capacity and organization of uedical associations (IMA,
Anti-tuberculosis associations) have not been tapped to provide continuing
education and programme awareness to the private sector. Interviewed members
of the Indian Medical Association (IMA) at State and District level showed
strong support for the NTP efforts.
IMA members seemed well aware of the
issues and challenges facing tuberculosis control and were willing to utilize
the organization to promote tuberculosis health education efforts and
distribute educational materials to its members on the topic of TB case
finding and management. The use of health education messages targeted towards
both the private physician and the consumer regarding correct treatment
regimens and the importance of completing treatment should be tested as a
method to standardize care provided by the private sector.
Conclusions:
A large share of the provision of health services in the country,
including tuberculosis diagnosis and treatment, is done by private
practitioners. They are, however, not currently included in the NTP system,
either for notification of patients or standardization of diagnostic and
treatment procedures. The role of the private sector in the care of the
tuberculosis patient needs to be further clarified by the NTP.
If indeed it
is found that a large share of tuberculosis patients seek care in the private
sector, improved training in medical schools and education of private
practicioners must be implemented to ensure proper diagnosis and treatment
and augment cure rates for patients under private care.
10. RESEARCH
India has a long history of tuberculosis research to improve programme
delivery and treatment efficacy, and much of the information and experience
obtained has been applied successfully in other countries. The research
institutions can be utilized to analyze the functioning of the programme and
to test alternatives to improve programme results, in particular organization
of treatment delivery to increase the cure rate. To ensure that the studiei
provide relevant information for programme improvement, and that this
information is opportune and utilized, this research should be planned and
supported as an integral part of the NTP. Sone operational research projects
have already been discussed before the Review nission. Two major
institutions currently involved in TB research are briefly described below.
The Tuberculosis Research Centre (TRC) in Madras was established in
1956, under the joint auspices of the Government of Tamil Nadu, the Indian
Council of Medical Research, the British Medical Research Council and the
World Health Organization, for studying initially the efficacy of domiciliary
chemotherapy, in comparison with conventional sanatorium treatment. The
centre was taken over by the Indian Council of Medical Research in 1965 and
made a permanent research establishment.
It established that a wellorganised domiciliary chemotherapy with a daily regimen of isoniazid plus PAS
produced results closely approaching those obtained in sanatorium with the
same regimen;
a satellite study established that there was no extra risk to
the close family contacts from the infectious case after the start of
treatment.
Subsequently, the Centre investigated various regimens of
chemotherapy in controlled clinical trials, backed up by in-depth laboratory
investigations and solid statistical methodology. Clinical trials of various
regimens of shortcourse chemotherapy that would be suited to Indian
conditions were carried out, and more recently a study on implementation of
33
shortcourse chemotherapy under programme conditions in 18 districts selected
from different parts of the country was initiated. In recent years, a strong
department of immunology and cardiopulmonary function have been added to the
Centre.
Finally, the epidemiological unit that undertook a large trial of
BCG vaccine in South India has now been integrated with the Centre. The
Tuberculosis Research Centre has the capacity for undertaking training
programmes that could complement the efforts of the National Tuberculosis
Institute in Bangalore.
The National Tuberculosis Institute was established in Bangalore in 1960
with the objective of developing a suitable programme for tuberculosis based
on operational research studies, training medical and paramedical workers for
the District Tuberculosis Programme and monitoring the Programme through
periodic reports received from the Districts.
Based on studies on awareness
of symptoms and action taken and on the Madras TRO studies demonstrating the
efficiency of domiciliary chemotherapy, the NTP was evolved and lauhdhed at
the NTI.
In subsequent years, operational studies were undertaken on methods
to improve case-finding, techniques for enhancing patient motivation and
thereby enhance case-holding efficiency, and programme organization.
Concurrently, large-scale field studies were initiated to provide information
on epidemiological indicators such as prevalence and incidence of disease,
fate of newly-diagnosed cases under programme conditions, and on the
prevalence of tuberculous infection and infection with other atypical
mycobacteria. Thereafter, and in view of conflicting reports about the
efficacy of BCG vaccine, the largest BCG trial ever undertaken was launched
in Chingleput, South India, to determine the efficacy of two strains of BCG
vaccine at two different strengths.
Conclusions:
As a step towards the reorganization of India National Tuberculosis
Programme activities, the research potential of the various research
institutions should be evaluated in light of the findings and recommendations
of this review and needs of the NTP for operational research studies.
Operational research to test the feasibility and results of different
technical and organizational strategies to be adopted by the tuberculosis
programme should be an integral part of the revised tuberculosis programme.
11. situation ANALYSIS
Even after three decades of National Programme activities, the
tuberculosis burden on Indian society remains enormous - something on the
order of five million premature deaths in a decade, half of which are among
women, mainly in the reproductive age. This mortality must affect at least
twice that number of Indians with consequent lowered productivity, disability
and perpetuation of poverty. Excellence in research, early successes proving
the advantages of some modem treatments, availability of powerful and
effective antibiotics, a well established TB structure at the State level
and, in the last two decades, extensive development of the institutional
structure for primary health care in the rural areas, have not yielded the
progress against the disease which India could have expected. Decline in the
annual risk of infection (and in incidence) has been agonizingly slow in many
areas. Well over half the population is infected with TB and the risk of
infection is far too high at between 1 and 2% per year. An aging population
structure, increasing HIV prevalence and apparently rising levels of drug
resistance mean that without a reoriented and vitalized public TB control
effort the disease will pose an increasingly serious health and developmental
constraint for several decades to come.
34
The main factors to be addressed in making real progress against TB fall
in four main categories - organizational, managerial, technical and
developmental. Elements of the present health care system, and many parts of
the current TB control programme provide the basis for implementation of
major improvements. Strengthening and reorientation of policy and program
execution in each of the problem areas offer sound prospects of improvement
in curing TB patients in numbers which will result in 8-10% annual decline in
the risk of infection and effectively halve the tuberculosis burden in about
a decade while ensuring much lower disease and infection rates for decades
into the future.
The state TB control programs are well structured and have direct
intervention capabilities at the district level and below in about three
quarters of the country. In contrast, the national TB control programme has
languished with ineffective terms of authority and budgets and an
exceptionally low executive position within the Ministry of Health for such
an important disease. Monitoring, critically examining and adjusting
national policy for effective state performance has consequently atrophied.
In the absence of a strong central Ministry unit, power for TB policies
has been ceded to the National TB institute (NTI) in Bangalore. The NTI has
had preeminence in training and some types of research for TB but now suffers
serious institutional weaknesses. Budget shortfalls, unfocussed direction of
research, training program content which is not replicated at state level and
lack of experience with making and implementing policy have left a gap in
national TB leadership. The absence of a national policy body for TB at
central level, supported by a strong executive TB unit within the Ministry,
has meant that no revision of policy has been made in spite of repeated
evaluation showing poor results, and therefore NTI has not changed or
developed alternative TB Program procedures.
Further, the content of their training has stagnated in relation to
recent TB control success elsewhere.
In the absence of a strong central
program, NTI has been forced to assume program management and standard
setting functions which are inappropriate for a training/research
institution. This is particularly true as NTI does not have the staff and
executive authority to monitor and enforce compliance of the states with
policy.
Below the State level, TB has been indicated as a priority for
integration into the key health services. However, the TB program' s
effective cooperation with health service providers at the primary level and
willingness of the providers, under current policies, to devote substantial
attention to TB, remains doubtful at best. The ambivalence resides both in
lack of strong and focussed national program direction and in the absence of
policies responsive to the legitimate interest at the local level for a
clearcut, standard, easy to follow program which is effective for cure.
Strong direction, some decentralization below the district level, training,
increased funding and a comprehensive policy package are needed.
Technical problems confronting the NTP are both historical and the
result of some isolation. There remains traditional emphasis on case-finding
activities when only a minority of discovered cases are being cured.
Technical practices emphasize radiographic methods which are sensitive, but
not specific, rather than concentrating on high-quality microscopy which with
a good quality control system can be both specific and sensitive. Too
frequently, one sputum smear is examined rather than several, leading to
inappropriate treatment of infectious cases. Microscopes are often monocular
and of poor quality, training is uneven and quality assurance systems seldom
function. Protocols for appropriate use of radiography and clinical
diagnostic methods need to be prepared and disseminated.
*
35
Treatment for diagnosed patients is chosen from too many regimens and
adequate short-course chemotherapy is yet infrequently used and is completed
in only a minority of cases. Repeated sputum smears during the course of
treatment are not regularly taken to monitor effectiveness of therapy.
Provision of services is often too remote or inconvenient to encourage
patient compliance, and providers lack adequate motivation and training for
patient supervision. Improved treatment protocols, training, adequate
supplies of only SCC drugs, and adaptation of practices to provide some
degree of supervised initial chemotherapy, whenever feasible, are needed.
i
f
Recording and reporting procedures do not permit rigorous supervision of
the system as a whole or at the institutional level.
Case definitions are
not adequate.
Criteria for completion of treatment and discharge do not
exist.
Laboratory registers and patient treatment registers do not contain
the information necessary to perform cross checking or to monitor the
performance of states, districts, blocks or Individuals providers.
Conversion status of smear positive patients cannot be documented.
Cohort.
analysis to ensure and measure program effectiveness cannot be satisfactorily
done with present registry formats and procedures. Therefore, adaptation of
existing TB Program policies and resources to implement and improve recording
and reporting system is required.
Developmental constraints include both institutional and financial
issues. Operational research to test and improve on program performance is
Training materials and
not currently an integral part of the TB program,
revitalized
program and
objectives are in need of revision to support a
pedagogical content may need improvement. Medical college curricula need
additions to provide both theoretical and practical exposure to the elements
of TB control as doctors graduating now will continue to see TB throughout
their workifig careers. Present private medical practitioners need to be
educated about modern treatment and policies of the program. This can be
done through existing NGOs. To do this, strengthening of the NTI, of the
state level training centre, and studies and technical assistance at both the
national and state levels will be needed. Opportunities for overseas
training and experience will accelerate adoption of effective new experience
in TB control elsewhere.
The
The government
government has
has recently
recently decided
decided to increase funding for TB control
and is for now continuing to provide for the treatment of all TB patients
Hl *
• ’ . The present high number of overdiagnosis and
diagnosed in the public
system.
treatment of patients which now appears to be occurring offer scope
though,. financial resources fo? TB
savings in an improved program. Overall
<
appear to hav6 declined in real terms in recent years because of inflation
and rising import costs, dedpite the government's recognition of the trend
and efforts to counteract it. Moreover, only a fraction of patients tdday
requiring treatment receive it in full.
A strengthened program will require increased resource allocations at
both the central and local levels for drugs, supervision (including
transport), training and operating cost. Given the demonstrated cost
effectiveness of TB control programs compared to other health sector
interventions, revision and expansion of India's TB program with external
financial assistance would appear to be fully justified.
r
A V
36
t
12. RECOMMENDATIONS
1.
The structure of the National Tuberculosis Programme should be
strengthened by 1) establishing an apex policy making authority and an
executive task force with managerial functions to implement programme
reorganization, and 2) upgrading the central tuberculosis control unit
in the Directorate to provide strong leadership and enhance the
efficiency and effectiveness of the National Tuberculosis Programme.
2.
The quality of patient diagnosis should be improved by 1) using three
smear examinations to detect infectious cases among symptomatics before
deciding on patient treatment, 2) ensuring the quality of microscopy
with adequate equipment, training and quality control, and
3) establishing criteria for diagnosis by radiological and clinical
methods.
3.
National and state tuberculosis programme resources should be directed
to ensuring cure of tuberculosis patients, giving priority to infectious
cases of tuberculosis by 1) adopting short-course chemotherapy, 2)
establishing criteria for treatment completion, cure and discharge from
medical care, and 3) ensuring an uninterrupted supply of drugs of good
quality.
4.
The current NTP system of registration and notification should be
revised to emphasize the cohort analysis of treatment results
(completion and cure, transfers, defaulters, died, treatment failures)
as the main indicator of programme effectiveness.
5.
Policies should be developed to ensure decentralization of treatment
3617/1063 closer to the community level to enhance access to care and
patient compliance to recommended therapies.
6.
Pilot projects should be implemented at block level to test the
feasibility and results of different technical and organizational
strategies to be adopted by the tuberculosis programme -- i.e., to test
the capacity to implement recommendations 2-5 above.
7.
A medical officer or treatment organizer and a laboratory supervisor,
with the necessary transport, should be added to the existing
administrative structure at the sub-district level (about 500,000
population) to strengthen tuberculosis programme, management and to
facilitate decentralization of supervision.
8.
Training materials must be developed to reflect the proposed changes in
programme policies and procedures. The current training infrastructure
will need to broaden the scope of its training capabilities by utilizing
state training facilities, medical colleges, public health institutes
and tuberculosis-oriented voluntary agencies to augment training
efforts. International and national training opportunities should be
made available for the different levels of tuberculosis programme staff.
9.
Operational research must be carried out as an integral part of the
revised tuberculosis programme to evaluate programme performance,
improve delivery of services, problem solving and obtain baseline
epidemiological information to measure reduction in the risk of
infection.
I
1
f
I . ■
■■
■
•
f
-
!l
■■■ '
Xa ' ■
i? .? '■•.< ■?'. ■
■■
■•
"
■
•■'■
■"••i-- •
•■
-
: ?•
i*
->
■
iW----
x • s ■■
Xxat |iqnfx
< <<XX'
JX !J . XX:/
Y>a
'0,s:
.Di'S S’3
ihYV"W'"' ■YV?■■'" '<■
feB
'
S
i! I
■ .Xm.^.^X -xX^: ■
jv •■ : ■
Oa . . aa a
I '
•
d
■
'WC -xY SN
WL<^x:x ..A'-
»■ Kg .r.a®l»£5:rrtK. '
XaBi:
LCTTX
'a . - :
t^J^33.K<X|r
/ X
.f
qx
SX<
a
'-ax
r< I 3 ....XL
fcffiX 3'X .3i2m2Sb
ax.:, .i
lifts
i
3
^XXaxa: .:
,
X:xaxa;-^X--■ATlOflij
1 ft 3
1
--:WiOtOwOlx™1
•
t. - _,yW
fcaaai
xxx x'
tf5’. i-
•
■.•'■■•*•.
■• '
• .
>
•
. -
' 'x — • ; <
' *«■-'
VcliirtarY
blL-lth
ASS’.N'BAK.n
■.-•» > '-
aXrf:i'
;-< i-r
a V-■'- X siaaasMfi
■.
-ft'.
X »I XlaAYXaX -3.
X
/
:.:ft ft.
ft
.ft.ft ......
V YIx'RY.Yaa
:x
^DIRECTORATE^' GENERAL OF HEALTH SERVICES
:
KOTlA ROAD,. TEMPLE LANE
a- a-X
Ife.ft - ';
. ■
ft-.
:
■
-a.
x-xaa
:
1 lx
IxftX'-. a:x;33xxa x ? < ;a .x :xa.aa:aa''; t'a a
•^aaaa- .a-Xx' ft-axa..' 'aXa-:.|-<a.a?::L,;ft-.
fexaa :ft..aft4a':a-.; ■ v/iB ' aaX3 ;' ' " a' rfTax, X -: .v -'■■■>- '• a: a .X
- - - -'■ «■ -
-a-*-*— •
-a '
by
Dr. B. N. M. Barm
Adviscr-in-Tubcrculos:.*
Government of India
Directorate General of Health ?rrvires
New Dcllii-1 1001 1.
I
f* •
1 ■■
I
/ CENTRAL HEALTH EDUCATION BUREAU,
TUBERCULOSIS
IN
INDIA
i
c f L...
India
H
X. ■ ' :X..
a< 3a a ' X; X x. ib^.ioc-xY-l; ct lII‘
XXxa3xX'
■■■-Xa*a
’- ■ *?xa
;i •;- •-tRa
“.-'a- x■ ..-; • ■ .
■■.■■ N< t.■ Q;;qxiW'i
fiax-Xj;
I
.: c:-'--.cn c/
CENTRAL HEALTH EDUCATION BUREAU
DIRECTORATE GENERAL OF HE AZ TH SERVICES
MINISTRY OF HEALTH & FAMILY WELFARE
GOVERNMENT OF ‘iNT ZA
NEW DELHI
,
... '
?)
/
CONTENTS
Pages
(i)
(iii)
Foreword
Introduction
Chapter I
The Problem
1
Chapter II
Early Attempts
5
Chapter III
Tuberculosis Association of India
9
Chapter IV
Bhorc Committee’s Assessment
14
and Recommendations
Chapter V
Position at the time of Independence
16
Chapter VI
First Five Year Plan
18
Chapter VII
Second Five Year Plan
21
Chapter VIII
Third Five Year Plan
23
Chapter IX
Fourth Five Year Plan
26
Chapter X
Fifth Five Year Plan
29
Chapter XI
National Tuberculosis Programme
31
Chapter XII
District Tuberculosis Programme
33
Chapter XIII
Present Status of the Programme
36
Chapter XIV
Research
39
Chapter XV
Health Education
51
Chapter XVI
Some Important Tuberculosis
Institutions
53
vr M
______ _i
cccS'i^
□ !'. No I
FOREWORD
Ibis book is a comprehensive presentation of the facts
about development of tuberculosis movement in the countrv
and the details of the various aspects of
the I'lilx-rculosis
Control Programme.
The activities taken up by the Government in the various
plan periods, the concept and organisation of the National
1 uberculosis Programme and the various
various significant
sign
research
studies
conducted in India- ----that-----have
contributed
.
- •—
•• -■ ..x..kv».1 new knowledge
in tHie field of tuberculosis control and have formed the basis
of our community
(
wide I uberculosis Control Programme, also
have been highlighted.
Tuberculosis is a major public health problem in the
,CL)inilr1''
tools for
the cases, effective medicine for their treatment and BCG ivaccination
‘
for’ protection
and.. children are ......................
available
beei/ |/iu«iut-d
provided
rof infants
I
.
... and have i/v\.u
ircely m the National Tuberculosis Control Programme.
It
is only with the concerted efforts of the Government, the volun
tary organisations and the community that the programme can
succeed and the problem of tuberculosis can be tackled.
i
I
’I
I hojx? the readers will find this book interesting and
iu having an insight• ■lo ••the problem
useful in
bL... „and’ the efforts
being made lo deal with it under the National1 Tuhert ulosis
Programme.
New Delhi
28-1-77.
.1
!
}
1A.
Dr. I’. P. (JOEL
Director General of Health Services
—li
’J!
Vr
•\cccs- ion
CaH No
INTRODUCTION
•!
j!
Tuberculosis has been known to mankind since the dawn
of history.
From the mummified bodies, engravings and
paintings in Egypt, scriptures and literatures from Babvlonia
and China, literatures from the ancient civilisations of Greece,
Persia and Macedonia and the Vedas and other Sanskrit lite
ratures of India, it is evident that these ancient civilisations
knew tulx?rculosis as a health hazard even 4000 to 5000 vears
before the birth of Christ.
A hymn is consecrated to the cure
of ‘Yakshma’ in Rig Veda which' is dated as about 2000 B.C.
Charak and Susruta in 600 B.C. referred to tuberculosis as very
difficult to cure.
Hipprocratcs (460-377 B.C.), the father of
modern medicine opined that attention to the tul>crculosis
patients was a waste of time and that they were a burden
to the State.
However, till about the beginning of the 19th centurv,
nothing much was known about the cause or cure of the
disease. I uberculosis was known as
white
as consumption,
plague, Kings evil and phthisis.
It
It was
was mostly considered
as an incurable disease.
I
5
From the beginning of the 19ih century, new knowledge
st.iitcd to gather.
Laennee, himself a consumptive, invented
stcthescopc in 1819 and described ‘auscultation' by use of the
stcthcscopc.
\ illemin in 1868 demonstrated that tuberculosis
had to be due to a specific agent, but it was Robert Koch
who made the epoch making discovery of the tubercle bacillus
m 1882.
X-rays were discovered in 1895 bv Prof, Roentgen
which became available for clinical use in 1904.
Von Perquet
in 1907 described i?itra dermal tuberculin skin test. Calmette
and Gucrine in 1922 discovered BCG vaccine which is now
extensively used as a protective measure.
However, specific treatment for tuberculosis bv drugs that
could kdl or inhibit the tubercle bacilli was not known 'till the
new eta of chemotherapy in tuberculosis began in 1944, with
the discovery of Streptomycin bv Bugie and Walksman. ' This
was followed by discovery of other potent anti-TB drugs like
codnirn\rOl |Sal!cyl,.c acicI ky Lehmann in
1946 and isonicotmic acid hydrazide by Grunberg et al in 1951.
Several
very potent anti-TB drugs became available by about the
V r "j I
cs ion !
—JI
I No
Jl
(>■'■)
middle of the present century and thus effective treatment
of lulx'iculosis Ix’cume possible revolutionising the whole con
cept of treatment and care of the tuberculosis.
CHAPTER I
1 iiljcrc ulosis is a peculiar disease in the sense that it is
of a chronic nature, the causative germ is more or less ubiquitous and casih infects most of
the |>eople and vet a few
(
suffer from the disease,
Symptoms may simulate many other
diseases. Diagnosis of a case irequires sjx?cial techniques and
treatment of a
patient
requires special1
c__ o..
drugs
for
a
long duration,
Like any other infectious disease,
tubcrculosis also comes in
bi cipidemics but unlike other diseases, the
secular epidemic curve in tuberculosis lasts for decades if not
centuries.
THE PROBLEM
Tibercllosis in
India began io
io engage
engage atlen-ion
at ten'ion as a
public health problem fromi the carls scars
'cars of thi
ihi ■ ccnturs'.
nn \?l?;^‘rcPardcy Lukis-,thc then Directoi General
of
Indian Medical Services pointed
out to the Goscrnmcnt of
India that I ubcrculosis was fast
spreading and it called for
concerted countrywide control measures.
Houe\cr, we have the knowledge and the means to detect
tuberculosis cases and to treat them effectively. It is possible to
cine a patient of tuberculosis. It is also possible
possible to prevent
spread of the disease and to protect the uninfected from in
fection by I B germs. Tuberculosis control programmes have,
therefore been organised in all parts of the world and many
(cxelopcd countries have been able to bring down the problem
considerably.
1
Thu.EOefcrA‘nScs .o/janit?rL°flicials of I’Klia iin Jthe North
and in the South in 1912 and 1911
... 1 expressed the need tor pro
per investigation about the spread of tuberculosis
in urban
areas and from there to the rural areas.
As a result, the Government of India
appointed
Dr.
Lankaster in 1911 to make an <enquiry into the
Tuberculosis
problem in the country.
After his
enquiry during 1911-lii,
he came to the conclusion that the
prevalence of tuljcrculosis
was alarmingly high in rhe c,.
country, that dining the preceding
forty years even in areas that
were roi»Url
considered'
lat weir
CJC,J ns vjj-rrjjj S()jp
the population has become considerably infected In tuber
culosis and that with development of c'
commerce and industry
and establishment of communication, the prevalence was in
‘-j prevalence
creasing m the towns and cities and spreading to the village.
In India as in other countries, fight against tuberculosis
has been a vers- long battle. Several eminent scientists, philanthiopists, private individuals, non-official organisations apart
irom the government have contributed largelv in the battle
against tuberculosis in India.
Several important studies in the field of tuberculosis cpidcmiology.
and1 treatment have been undertaken in
y- control
. - .....
India, the
t
findings of which have been widely acclaimed all
over the world.
Based on these findings,, a scientifically sound
and operationally
feasible
feasible tuberculosis
tuberculosis
control programme
which is within our resources
i..........
has been evolved and is being
implemented in our countrv.
J^'e'cr apart from a general impression as
as was formed
0} Dr Lankaster after his investigation and that of
k.. many other
specialists working in the field of tuberculosis,
t the exact size
and extent of the problem of tuberculosis in India
--ii 55 <1 s not
knonn as reliable
reliable statistics
statistics were not available.
I he purpose of this book is to give an idea of the nature
and magnitude of the problem of tuberculosis in the countrv
and to review the work done so far for tackling the problem.
The main methods bv which
the size and extent
the problem of tuberculosis' could be ascertained
a rc: —
(1) Deaths from tuberculosis.
T> --
i.
L
- -1
-1
f
.
7
. r
_
of
(2) rhpeVrenCe °f thC dlS€aSC
PatiC”ts suffering from
the disease as ascertained by morbidity survevs.
(3) Infection rate i.e., persons who have been infected
!
I
prey^tSS:.^
2—7 DGHS/ND/77
,ikcI>' tO fal1 a
L
v
I
I
vr
* Acoos- Um ;
•i
—__ i
jCbl! No
. t- \ ***
■p
II!
I,
i
.1 :
•I '
ft
\\
-■
j
9
o
Deaths from Tuberculosis
.Morbidity Surveys
No reliable information about deaths from tuberculosis
was available as vital statistical information even in towns and
cities was not complete.
Mostly information about deaths
from various diseases had to come from inexperienced Govern
ment officials, who in their turn relied on the neighbours or
relations of the. deceased.
Causes of death ■were grouped
under a few broad groups like fevers, dvsentcrv and diarrhoea,
icspiratory diseases and other causes, and tuberculosis could
have been included in any of these broad groups according
to the predominant symptom which the patient presented.
In the earlier part only small studies limited to small p''-'-*
population
y;1 groups in different areas were undertaken by diflerent
workers.
P
" ’
Dr. Benjamin
in 1938 found 2.6%. to be the pre
valence rate~ ''
ofc t-kcr-d;-:.;
tuberculosis ir. the suburbs of .Madras.
Dr.
Lal in 191-1 calculated a morbidity of 7% in A Vest Bengal. Dr.
Sikand and Dr. Raj Narain in 1952 found 1.8%., Dr?
Dr. Phillip
Phillip
in Madras in 1952 found 2.5% and Dr. Hertzlx.-rg in Trivan
drum found 1.8%) tto* be -the
1 i morbiditv
’ ‘
rate for tuberculosis Dr
Sikand
, . and Dr. Rai
r’J Narain
X’ :-1, 111 1W2 indicated 1.36% to be the
niorbidity rate of tuberculosis among displaced persons in
Faridabad.
*' ’
;
I,nI. Madanapalle,
a survey by Dr. Frimodt-Moller
showed a morbidity of 1.6%,
/t, in the (own and 0.12% in the
adjoining villages . in JI?919.
.. . During 19j2-j‘», an X-ray survey
of
die
Government
of
India
empiovees iin Delhi showed a mori .
?
.c- “I hc Sample Survey 111
bitIny.t off).// %.
in 1955 in a small populanon in Ambur in South India
— showed
------ .d a morbidity of 1/1%,.
J
Sir Leonard Rodgers in an investigation estimated that
9% of those classified as dying of fever died of tuberculosis. A
similar analysis of the figures for Cossipore near Calcutta
showed a mortality (from tuberculosis) of 2.68 per thousand.
Of the total deaths. 7.9% were due to tulxnculosis. /\t about
the time of the First World War, Sir Leonard Rodgers analys
ed the post-mortem figures for Calcutta for over 22 veais
and found that no fewer than 17% of the total deaths had
been due to tuberculosis. Since at about that time (1911 —
1921), the crude mortality was 47 per 1000, the tuberculosis
niorbidity could l>e computed at eight jx?r 1000.
Vital statis
tical information from cities collected by Dr. Lankastcr for
his book Tuberculosis in India (1920) showed that tulxuculosis deaths in Calcutta were 2.1; Bombay, 2.83; Madras.
2.5; and Ahmcdabad 5.9 per thousand in 1919. He thought
that actual rate was 4 per thousand or more in most cities.
However, most often these were under-estimates because in a
large number of cases, the cause of death as tuberculosis could
not be established.
• 1 •.
J
All these small r.".
:
.survey
ga\c an impression (hat millions
would be suffering from thc^dixjase in
in both urban and rural
areas and it was felt ncccssarv co have a precise estimate of
tiie morbidity of the disease in the country as a whole.
<],,1.inIJ'C|(r-1-‘q":iI| .S;,ln,’le S,;ne' "
;is' therefore, comluctec!
was,
duiing 19.m-o8 which showed a morbidity of )W to
v'
X-rav cases and 0.-1% bacleriologfcally confirmed ca^s arnf tlms
Prudence was found to be uniform in cities, towns and villages
li e findings of this Survey, which for the first time gave rdiiem nFCHinOrC u CSS PrCt,SC i,,fonilatiou ‘‘^ut the size and ex
tent of the pioblem, on the has:, of which a National policv
for control of tuberculosis in the countrv could be built h is
m
"CXt Cil:,P:".
Subsequent survevs in
clht (I960), Tunikur (1960) znd Bangalore (1961-68) have
also confirmed the findings of the National Sample Survey.'
Frimodt-Moller (1949) and Me. Dougal (1950) estimated
TB deaths in India as 263 and 200 per 100,000 w’ith rigorus
control measures applied to the study population.
FrimodtMoller reported death from tuberculosis to be 64.1/100.000
in 1952 and 21.1 in 1955.
Recent estimate of the longitudi
nal ssurvey of the National TB Institute (1968) is 100 per
100,000 ill
l.i an area Avhere no control measures have been applied.
All these findings give an idea that the death rate due to
tuberculosis was very high some decades back and continues
to be high even now, though it is progressively going down ’
in recent years.
I
Tuberculin Test
Some information about the prevalence of infprH™ .
be obtained from the various tube^ulin 1"“ sune^X^d
severa1 areas in Bengal MadrasA^am andDBihGai11showed0thc
I
»-2% in ,illaS™^'7|<6%,';n'S',
ȣ
I
Vr
.cocsion
4
I
la years of age and in a jsuburb
’
of Madras he found a positive
reaction• ...
in 41.2^.
xi._ ' below 15’ 'ears of age and 69.8% above 15
xcars. Br.
]
Lal in 1944 in Bengal found infection rale to be
ns high as 88% in urban
areas and 32% in rural areas.
Tali No
!
Tuberculin ttesting
‘
conducted in connection with the mass
ECG Campaign in t
in t ie earlier phase of the programme showed
m feet ion rate to be in the
/ .......e lan"c of I
in 0-6 vears agc-group
in the 7-15
'ears age-group, 63% in the 15-24 aoC-rot p
and 83% in the re group above 25 years.
The averatFeZ
culoT
ab°l,t'5<o.
^omn
«Z0.
Contrary to our belief that ‘tuberguIoms was a major problem in
than m the villages, the tuberculin (he cities and towns rather
testwas
results
campaign showed that infection rate
i..... of the mass BCG
niorc or less of the
. ------ ’ indicated that
pci haps equally prevalent in both
tn ban and rural areas. This
both
of
rh
.
v
r3 PrcJu,nP,i(”i "’as later confirmed
by the findings
c National Sample Survey.
ti
Estimated size of the [iroblem
■XS- ‘s,.^ xvn;-a*nd
mated that a^itZZTlninh''J ol|,strv;ilj<,,is it can be esticonsists of reactors to
' P(’P‘l,niion erf the cotmtrv
fection bv tK b?ci ,)C'C
:'Ppmcmlv
because of ilt.
lx-' about nine tnimon nC14 / ? r:"C °f :S%
dumld
tuberculosis disease and - bom , J
S tadiologicallv active
'"•o million, are infeaiL Z '
° tl,c,n.
:|bout
sputum and most of them have sv^ JuljclcIc h-’cilh in theii
bom tuberculosis Ls e
■,
'
l!' ’T'
T',C
1
'W-W population pe, year
1,1(1 P<r
I
CHAPTER H
early attempts
^™d™cueL,-!-:iinCrCaSi,lg a"'arcness Of the ^-ons.
ness (
■ ■’
be made
present centurv.
-s not Itnoum and
<? ‘»« P-blem
ment measures were vet known m
J r .effective
treattreatment had been <raii)in<r
i/-*" Plofcss,onOpen air
"as mainlv for eark* case”
Liirk^ "i
V?Sl but l,HS
vanced cases.
With vlrv ’ limii/d i
C bC C °‘,C for ‘'k1'
hospitals in India for inlwr i
:,cco,nniOclaHon
in
take advanced cases nF , ubci7,los,s- “ "’as not possible to
’he beds for a long tiincl,|ndCin^thc^r’l’”15- |Vh°
octl,l,v
long (inic and in
disease*.
n
1,1 L,,c cnd ,n,ght succumb to the
Attention \
..
; l
"as gradually
diverted
lulwiciilosis clispcnsaHcs 'for
to establishment
of
.
.
. I
Of sorirri.Il,-----'CalITnt °f. lh<? ^‘^rcuious
Promote^hcah^edti^
i,Kl assotiali
°ns mainlv
( tiles ‘’and
associations
irtainlv to
-........i about the
"■i—.... “J
....
A. (Jpia Air Sanatory
I. Private Enterprise
Most of the early clforts t
(to pruvjce treatment for (ubcrCU1OS1S were made bv philanthrop
societies and individuals
>” compassionate grounds.
It Jic
!
"Jis realised also that isolaion
o,lCCli7 Ca5CS Of “'^'culosis
"as a form of prevenOther forms of prevention
- vet.
In several' instaniTs, it"ere not in the public
"as
}
the discovery of
ivl kh led t '‘"I0"8'
PC0Ple
■ u ca t io n a I i n s t i t u t i o nof
s
^.v<.l 'with
starting anc-tuberculosis
ionaeTjhb'd.individuals wh^SX
1'^1''05'5 work was
> had the misfortune
-...... the experience of
‘l-n
1
l[^ ProblS'» iromThe begTnnit^o" the
Noonan ST - '
Christian Missions: The
first cfor isolation
open-air sanatorium
and treatment
founded in 1906 in Tilaunia, of tu here til os is patients was
near Ajmer, by
a
Christian
f
cST
I
Vr !
i- .
i
jAcCCS- 13
iCali No
,1
I
6
7
Mission.
It was intended mainly for girls from schools and
orphanages connected with this mission in North India. An
institution in Almora in the Himalayas for tuberculous women
was also started by a Christian Mission in 1908 and about
the same time a small sanatorium for women and girls at
Pendra Road in the Central Provinces (now Madhya Pradesh)
was also started.
connection with the
first one opened was in
Bombay in
In Madras, the King
Bombav Anti-Tuberculosis League.
Edward Memorial
Institute (now called the 7 uberculosis
Institute) was established in 1917 by the efforts of the late
Dr. P. S. Chandrasckara Aiyar.
In South India. Dr. Louisa Hart, a Missionary working
in Madanapallc was treating a number of tuberculosis patients
in temporary buildings in her general hospital for a number
of years. .After the Union Mission Tulxnculosis Sanatorium
was founded in Madanapallc in 1912. this sanatorium
took
over the patients of Dr. Hart and had them transferred to
the permanent buildings at Arogyavaram in 1915.
(f) Anti-Tuberculosis Leagues:
r\ number of ami-tuber
culosis societies were formed in Bombay, Lucknow and Ajmer
about the time of the First ’World ’War. The main object of
these societies was educative propaganda about the causes and
prevention of tuberculosis.
C. Prevention and Health Education
(d) The Bengal Tuberculosis Association:
(ii)
Through the
inspiration and pioneering efforts of some Missionary groups
in Bengal, the Tuberculosis Association of Bengal was estab
lished in Calcutta in 1929.
'Phis organisation carried out
fairly extensive propaganda in favour of concerned action
against tuberculosis.
(//) Private Societies: The first Sanatorium outside Chris
tian auspices was opened in 1909 ar Dharampore in Simla
Hills, due to the benefactions of some Bombay philanihropists,
mainly Parsis. and under the management of the Consumptives
Homes Socictv of Bombav.
In spite of die growing attention paid to the tulxnculosis
problem, by 1935 there were only about fi.000 beds available
in the whole of India, which then
included what arc now
Bangladesh and Pakistan, for the treatment of tubcrc ulosi*
patients.
II. Under Government Supervision
I he first sanatorium started under Government supervision
was the King Edward Sanatorium at Bhowali. Uttar Pradesh
opened in 1912, with money collected in that province
in
memory of King Edward VII.
(tii') Tuberculosis Association of India: .As a result of
public opinion gathering strength demanding action to deal
with the increasing menace of tuberculosis, the first concerted
effort was made through the organisation of the King George
V Thanksgiving Fund in 1929. With the funds raised by
this organisation, the Tul)crctilosis .Association
of India was
established in February, 1939. Its organisation
and activities
o
arc discussed in the next chapter.
III. Individual Effort
r\n instance of a sanatorium established bv a private indi
vidual is one which was opened in 1912 bv Dr. R. B. Billimoria in Poona and which two years later moved to its present
site in Panchgani, Maharashtra State.
Other sanatoria started about this time were the “Turner"
Sanatorium in Bombay—Dr. Turner was Medical
Officer of
Health, Bombay—and a Sanatorium at Deolai
built from a
bequest by a private individual. Seth Bhagwandas Narotamclas.
(iv) Methods of Treatment in early stages:
The main
line of
treatment
''c .......
““er.: advocated was open air and dry climate and
good food.
Patients who were not too sick to move about
were usually advised to go to a dry climate and take plentv
of exericse for improving their a ppetite; feeding or (overfeeding
of patients was the general rule.
B. Tuberculosis Dispensaries
L
T he opening of tuberculosis dispensaries on the
lines
of Sir Robert Phillip, which had a large part in the campaign
against the disease in the West, started somewhat later. The'
Tuberculin was extensively used between the years 1910
and 1920.
Sodium Morrhuatc which was being advocated
for leprosy was also extensively used in India for tuberculosis.
j
Ii
Vt- :-|j
:cc<-ior
al. No
8
I rom 1925 onwards SantK'iysin and other gold preparations
came into vogue,
Artificial pneumothorax was introduced
in 1921 bv Dr. Johannes Gravesen of Denmark who was
associated with the Union Mission Tuberculosis Sanatorium,
hoiacoscopy and cauterisation of adhesions were started in
the same Institution in 1931 and gradually these operations
became very popular. Thoracoplasty in its modern form, how
ever, came to be increasingly used since 1932 in some of the
institutions. Lung-resection for tuberculosis was started for the
hist time in India in 1918.
CHAP TER III
TUBERCULOSIS ASSOCIATION OF INDIA
At
stage, it
it was
v
____ ’ that all infectious tuber
At that
that stage,
assumed
culosis
...s patients would need hospitalisation.
hospitalisation, as hospitalisation
uas the onIv recognised form of: treatment.
Hospitalisation
alone
•• one of
of all
all infectious
infectious patients would have cost about Rs.
•>bU crores,
crores, in
in addition
addition to the enormous capital outlav in
volved in
in the
the construction of buildings for hospitals ’ and
sanatoria, vet it was realised that this could touch onlv a frinoe
ot the problem.
\ new vision and an entirclv new stratc^v
was called for.
n-
?
■
i
J
In 1937, Lady Linlithgow, wife of the then Vwerov of
India, after an appraisal of the Tuberculosis problem in India
issued an appeal for funds to establish an anti-tufxnculosis
association in India. I he Association was to consist of a ccntial body supponed by provincial and State organisations as
affiliates of the Central body. In response to her appeal, a
sum of Rs. 85 lakhs was collected. After returning 95% to
States and provinces for maintenance of- clinics
-..... -.» and where
possible of sanatoria and after-care settlements, the balante
was retained for the Tuberculosis Association
this was added direct donations and the ----- ) of India. To
corpus of the King
t-icorge Thanksgiving Fund and the nihcTc'u'lo’is
----- -—> Association
C
c
..................................
of India was established iin ..................
Delhi under the Societies Rcgistration Act of I860 on 23 February, 1939.
The main activities of the Association arc
below:
snrninari'icd
New DclJii TB Centre
Fo sene as a model institution for •organised home treatnient of tuberculosis, the Association established
’ " ‘
with the
help of Government of India, the New Delhi TB Clinic in
19-10. Simultaneously, a few voluntary Care and After-care
Committees were formed to assist the New Delhi TB CH me
1 B C'linir- Xt-'IC lin/rrnJr>,l
H 1
—
•
I'llC
New
n™
C1,n,c
upgraded in 11951
as aJ '-rTraining
&
Demon-
-Delhi
WHOnanrUNICFr
|hC11’ °f ,thc
ot India.
An.;
1 .U,i>IJCEF- Subsequently, the activities of the
S one o’f’th/
mf ian.lfoId. and tod“V this Centre is reputed
as one of the most efficient institutions in the country.
TB Sanatorium at Kasauli
Kasaub
AsA%iatio" established a sanatorn.m
at
linlithoSimla Hills. The sanatorium known as Ladv
Emlithgow Sanatorium had 250 beds and was one of the
premier TB sanatoria in the country
country For
For want of enough
paying patients, this institutioni was closed down recentIv.
i
Mi
Vr " r I
—
—i !
cccs-ior;|
10
11
TB Directory
Research
rtiinT11? AssoS,at,0.n collected information regardinotuber
on
thC COt'",1,y
Publisl1^ the first direc.m
dins was revised periodically and the list
re X T T',liS,'Cd in,
rhis is
‘locu;nen(t t'n
espect of information about the facilities available in tuber
culosis institutions in the country.
'all No
The institutions of the Association have also undertaken
several research projects approved bv the Indian Council of
Mccical Research pertaining to tuberculosis.
The Ministry
of Health also had provided grants to the Association to carry
out surveys in urban and rural areas of Delhi by its institutions.
TB Hospital at Delhi
The Association has a Research Committee, un
On the
the re
commendations of this Committee, a research program*-’'•'
been instituted to find out if the period of treatment of’tuber
culosis could be shortened. /\ preliminarv report of this sttidv
was presented recently to the International Tuberculous
onriibcrculoxjs ((.(>))fcrcnce at Mexico.
Rin.™ lh|C do,1:lti(,!,s f,°"' '■> Mhi philanthropist.
Lain
Kn>n a.up Khanna and grants from the Government of India
the Association established the Lala Ramsarup TB Hospital 'at
N53 “ir'is o " "r" I ■'10(i
"I"th St:"tcd Pf»i'ctioning from
I
faH
P > °f "C g™d h(>sP‘t:ils in the country with all
acilmes including thoracic surgery.
Conference
Other Ser\ ices
A regular programme of the Association calculated io
. bring together those working in the aiiii-tulx-rculo>is livid
and to involve tuberculosis workers in the ami uibci c iilo.i.
mosement is the organisation annually of a confcrcmof
tuberculosis and chest diseases workers Irom dilk-rem pmi.
of the country. Fhis conference deals with various aspects of
tuberculosis control work and useful discussions arc held.
Apart from establishment of institutions and
compilation
of Directory, the Association
bad undertaken
services. The y
_____
___
TuI.erculo^ H^iu.gehr^^rT'
Hermitage at
rained by the Association
ioi’ n\e y
}cais
cni's with
'vith Government of
India grants and treated
0VC
''
rcfl,
K
cc
TB patients» upto
upto
March 1955. Th..
Thereafter, the hospital
,
1 was handed over to the
•State Government.
With a giant received from the former Viccrov’s
.poses I-und the Association selected 1-1 sanatoria ill >< War Purover India
■•'"<1 treated over -150 Tuberculosis ex-senSn
o’,
Health Education
of 1J- hl,A
has Ixtcn carrying out regular programme
heahh cducatmn acltvmcs smcc its inception: These ine s a. dO:K ‘ i,'Sl 1
'
;illd distribution of pamph
lets and posters on various aspects of tuberculosis
control
pares'and"^'?'^1’01' :idvcrti™lls- ctc- The Association ptetPh,- P-,
,
”,tcs PIOPa,?;i"da material to its affiliates and
the latter bring these out in regional languages.
-nf...
E\SanatorillIn) in Dharampur, Himachal Pradesh
for ne- lv B
Home'Society
nP<">tained this Sanatorium
of'fi^^ia? ‘ZT;"
C“P-es
deaIsTwilhSdittT:,ti°n ''aS alS° hroi,Rht ollt a blue print which
second
1 echnical Committee
■H
r!lc Tuberculosis Association
of India
established
a
1 echnical Committee in 19-18. T*
I his Committee consists of reputed Tuberculosis workers drawn
..i from various parts of India
to advise the Association on matters
--------s relating to control of
tuberculosis.
:.,S,pCCtS °f tl,l>crculosis control.
Tbc
edition of this blue print has been brought out recetitlv.
Journal
sis in'Teplmber
TH
°f ^clo
the different asnccts o7 /S| ‘S 3 lclu.allerlV .iournal devoted to
bo'u-d rr. • . aspccts of tuberculosis control. Its
editorial
boaid consists of well-known tuberculosis specialists.
I
f'
■fti
■i- ■ Mi
V r :•
---------- -
12
■ I
13
:ccs-iorj
Textbook
ii: No |il
not, of '^le^Ck'on'TX^Xs^1^’
-------- -I
International contacts
was thc pnbhca1 his book deals
s- lha't atXXon to most of'the de ' lPIOb!C,US
eMio^XXr^XooXn X,—X
iion
1
■
J. :
h1
i
■
t
"e^nd
textbook on lubcrculosis is‘now under prepara.
Training of workers
Delhi1 Tl/'cenue' fnl 'il”£ions ‘)f ‘he Association like
Linlithgow Sanatorium
Xew
Regional Organisation1" The TiibttiVe| n,.cn!ijer of thc
■'
hosted the IX Cot e." nee of d, b"Culos,s. Association of India
with its 29th Xationa L.r
gl<’"
Xcw
-‘h-ng.
Diseases in J 74
Confetente on Tuberculosis .<• CheM
thc U<lv
paSX't!
s^tXcoXrx-Xr
1 tiiMt-!a'ni,nS^
“Xlh^
'■ishors. The Association plaved’ -i
of TB Health
the Indian Universities to insrir * i-11/1 1OC 1,1 Pcrsii;,(li”g
culosis.
CS l° ,nsutu^ diploma courses in tuber
rhe Icchnical Committee has been
XS '?|lhe tC;'dli',g Of “dxncuX reviewing cpiestions
at various stages of
dations fromuX’to'tbnc'?5
m:,ki"S '’"'Pnrtant
t rcGominenA Hi I iated Associa t ions
adiliatid' toXXulXdXXClI'°SiS ' AsSOCPi:“iOnS
,.Tll^c,'ci^osis
- - • -. i
ai v
Most of
carrv outAdunational activities.
committees and refresher
O'g:""Se <o"fc>ences. -■
refreshed ernes'"
<;"c
maintain certain Xe
TB i‘hnanXr
TB d”,ic’ TB '“horaton,
etc. 7 hey also <
O1 C financial assistance to indigent TB
patients.
..V-M
!r
I
ci 13U j(_ t
•Seal Sale Campaign
1 he Association
OctoiX'^aXteXX
•”
;;”E,ax . .. .. «»*
-0 Januarv, the Republic Dav
dent of’ India' and
in
taries.
During the. I3‘ t 9? “ by Governors or other digni:
on'the ?,r|’ 1,St SPeC'al PloS™nme has
helped focus attention
SC"C'
rated an appreciable amouXoSXXn "
uueicsc in the programme.
»S.s~ral3 “';h?clpS’b;'£ aS
■fi
r
Since its i
has been T? k? IatC -of L!,c I,1Lcr,lI’tional
culosis. 1. I>» maintained
n..„,..i„ed cordial
Associations all over thc world. J
organised the XIV \ational Conference in New Delhi inIt 19??'
• Its representatives
J‘nS participated in most of thc i •
international conferences after
1947.
i
I
ip
■
.7
■ I
V r ■■
I
i
15
Acccs-iou i
-------- (J
CHAPTER
Cal! No ;i
---------- ;<
i
1 i
i''
I'
pi!
JI',
'r'!
'
1■
'll
: I'
•
bhore
(d) Development of facilities
for training of tuberculosis
workers was considered i
very urgent.
/r
COMMITTEE’S ASSESSMENT
RECOMMENDATIONS
AND
1 he Government
I
“J.
Bhore Committee”
try and .. ........................
mcs.
I.
On the basis of data then available the Bhore Committee
estimated that there
cou.^ easily be about 2.5 million active
ca.s.S?
tuberculosis
everr
;ve“rnl Tl
"'',0,n PC,h:,pS about 0 ;'
million
------ 1 were dying
'tai. rhe recommendations of this
Committee were in t;cn
line with the*
anti-tul>erculo.sis measures
carried out in AVestcrn countries even
t..
wv
though
there were certain modifications
—.3 to suit Indian conditions.
1
he
Committee’s
” ’ A'ire:
recommendations bi icily
I
(^) I-Stablishment
fi
°f •~Pb clinics, one for cverv district
town.
-’ m V?’;a3S'7C ■'hc pa, t do,’>iciliary service
had to play
' turerculos.s control. Thev also reco ,
. •>} nr
mended serv.ces cc mobile clinics to cover the rur’ai
areas.
tuberculosis to advice <
tuberculosis work in the coordinate and further anticountry as a whole,
(g) Encouragement of
non-official efforts to
supplement
government work.
One of the first
iniplement the Bhore
to the creation of a ■
Directorate-General < ;
■ts Adviser. The oilier
dually.
i
i
(b) Establishment of TB hosnimk u i
usual standard of .me bed .XT ana nl Tb'?'? i"'C
recommended 2.17 500 beds -k thn
• •
cl<-«dh but
ment. These were to be establ bed ■n""u.,u refiuirehospitals seconds unit h^iS^an’d cfis'tHcP’
nnm|tCr hf0SP‘^ls- dlnce provision of such a headrn d dr °>f bcds "Culcl take many rears thev , large
rccommended that in the first five years, 9
---'
■ -y, sh()iiJ(J
1
00 hcds
be prov.ded for eve-v 10 million popuhrliom' '
<C) or'aSia?! co°lon7?r b,CUlab,« =>«' establishment
.'-J
cial organisations interested'in"s^^ 'if31 non’oflihelp in this venture and
c
"elfare shoilid
a substantial part cE rt ^2°T."1”6'1' should meet
rous grants
P
eXPendlt^ through gene- .
H
“ S'?™?, “J"';?"
f” <z. '■“*w73 1,1j l^lc DircctoHe ihh
Heahh Services with an expert in
af'S
y.';;
>>;
ta«,.
and 1«
1
i
V. M
Q'/
.1 At'-S’
So^
0’
i
i I
* 'T
v r r.
17
:s 'io*
No :
;i ■:
h
jl
I'1 li
ih !:
ill
B
Th!I
•
sniii
? .i■ i1
d
■
.
i
|
■
.
i;;-1
V’’
: III
■ B
<S■
i
CHAPTER I’
POSITION AT THE TIME OF INDEPENDENCE
i
With the attainment of Independence in 1917, the
National Government naturally devoted considerable thought
and funds lor social welfare in India and gave high priority
a> tuberculosis as it happened to be the most serious public
leal th problem in the country, next only to Malaria. This
.ddo coincided with the increasing interest which the interaarional organisations like the World Health Organisation, the
TNTCEF and the International Tuberculosis Campaign were
■piking in tuberculosis as a world problem. However, the
tvents that followed Indcjxmdencc made the tuberculosis pro
blem even more serious and difficult than were visualised by
■Lie Bhorc Committee. Partition of India brought in as its
izrennath a large number of displaced persons to
India.
W<>*t of them had to live in crowded areas with extremely poor
iv'penic conditions. There was also the problem of mali.u:rition. These accentuated the already bad tuberculosis pro
Hem in the country.
Though the urgency of taking up a large scale control
neasure for such a big and serious problem was fully realised,
i: was not possible for the government to immediately implenent all the recommendations of the Bhore Committee, because
f:r providing even the minimum requirements suggested m
ria: report, a substantially large sum was necessary.
The
lumber of beds available at that time for tuberculosis patients
ii India was only about 6,000 and the number of clinics about
85 whereas the estimated number of patients was about 2.5
Trillion. It was estimated that for controlling the problem of
ttberculosis of such a magnitude, India would require some 3,000
to 4.000 TB clinics and some five lakh beds according to the
uiuM standards obtaining in the Western countries at that
tme. The cost of these was estimated to be over 5,000 million
Tepees. It was obvious that from the point of view of men,
micerial and resources, introduction of such a programme was
inpossible within a reasonable period of time. Attention was.
tferefore, directed towards prevention. Since BCG had pro
ve! to be efficacious in the prevention of tuberculosis in many
of the Western countries and could be applied quickly, easily
ard at a comparatively low cost, the chief method chosen foi
prevention of the disease was BCG vaccination. It was plann
ed that the vulnerable population should be protected by BCG
vaccination within a period of 10 to 12 years and in the mean
time resources and knowledge should be mobilised to adopt
other measures for effective control of tuberculosis.
BCG vaccination was started as a pilot project at first
in 1948 in Madanappalle in South India and thereafter it was
extended as a school vaccination programme in all the States
during 1949 to 1951 with the help of the International Tuber
culosis Campaign. At the same time, the Government of India
set up a BCG Production Laboratory at Guindy, Madras in
1948 for production of BCG and tuberculin for the country’s
programme.
I
About the same time arrangements were made to establish
with the help of the World Health Organisation and the
UNICEF, TB Training & Demonstration Centres at Delhi.
Patna and Trivandrum to serve as model for TB clinics and
also as Centres for training of personnel for the country’s TB
control programme. A number of fellowships for tuberculo
sis workers for training abroad were also given.
I
£
3—7 DGHS/ND/77
•: w
l
—-
:H
11; bi
f. V r
ll'r
I
19
,cocs- io
:all No
be introduced very quickly and because provision of: a very
large number of beds required for treatment of TB (cases as
recommended by the Bhore Committee was found impractic
able due to paucity of funds. The discovery of new anti-bac
terial drugs for treatment of tuberculosis and their effective
ness m domiciliary service provided further justification for
giving top priority to the establishment of TB clinics Fiftv
five new clinics could be established in the First Plan but it
was noted that most of the clinics in the country were not run
satisfactorily.
Majority of the clinics did not have adequate
diagnostic facilities nor did they have adequate staff to carrv
out an effective domiciliary service.
This fact was taken note
of while recommendations were made for the Second Five Yc-ir
Plan.
CHAPTER VI
FIRST FIVE YEAR PLAN
,c«plcd b, .he
Coi!X“ “"„S
(i) Expansion of BCG vaccination on
a mass-scale.
(ii) Establishment of TB clinics and
expansion of domiciliary services.
(Hi) Establishment of more Training &
Centres.
Demonstration
■
(iv) Provision of beds for isolation
and treatment of those
I B patients living in crowded and unhygienic areas.
r
I. I
-J
■ •
I
al,*1
I
ffl
(') Rehabilitation of ex-patients,
(vi) Research.
Ind’nt dCalth|'Si 3 PalC sub.ictt’ tllc National Government
....... .. ,'1"-»'
r-
«
I
^amh^'of'awdne'diX^-'^the
215mfflionBTO\aS
tubercu,in tests and
t'
Priority was given to establishment of TB clinics brrnne^
- s-
■
It was suggested that about 10,000 beds should be provid
ed for tuberculosis in the First Five Year Plan specially for isola
tion of infective patients living in crowded and u nhygicnic
’ ’
homes in cities and towns.
/About 5,000 beds were added
.I1™!? ,the Vlan in lllc various States against the target Lf
10,000” but
mostl)-'added
and
... these
,e were
^vere mostly
added “inn'cxis'ting
existing sauaiorh
sanatoria and
hospitals. In addition, two r
special
hospitals for tuberculosis
‘
children were established during the first Plan period,
period one in
i I onrn ii I « •
TA 11* ... 1 . i
•
•
Msrr 2SjV.
0.’1 *aU 11
I?c,hl n.'!cl
other
in
the South at
the UMT Sanatorium, Madanapalle. The three training; ccnties for tuberculosis at Delhi, Patna and Trivandrum ° Avcrc
completed. Establishment of work centres for rehabilitation
of ex-FB patients was also contemplated but no progress
could be made.
Investigations on use of newly available
anti-bacterial
drugs for treatment of tuberculosis were undertaken at Madanapalle Sanatorium, Kasauli Sanatorium
.w..i and also in other institutions under the Indian Council of Medical Research
important research during the First Plan
“^“’
Plan ’ was\he^
was the communitv
tuberculosis control p.„b..
MacburnnlJ
bX ■
TB Sanatorium in
Aladanapalle where
Madanapalle
■where methods of TB
IB control including isolation
of infective cases and BCG vaccination were introduced in a
rural community around Madanapalle.
luial
main laPdmarks in respect of research that were of
TI^C™r%TCe f°r subsecluent development of a National
Tubercn ns Pr°&ramme Yereu the start of the National Sample
luberculosis Survey and the establishment of the Chemo
therapy Research Centre at Madras by the end of the First
Five ^ear Plan in 1956. Till then, though it was realised thTt
• 20
:cs- inn.I
! No I':
(I
■r
i
"as established
•— im
Council anft .e S”110"’ thc British ^operation of
Medical "Research
this Project w s m d" Cn' °f AIadra^ The n:
main object of
chemothemnv •
dctci™ne the .
efficiency of domiciliary
connected with' 'n"
llosPil?d t;<
ul
treatment and cd
other problems
objective wts to Ca1,no P*iticnts- -J
in their homes
domiciliaty^hX^
’
W-opna.e drug reglmensThe other
-•» specially
’
liu.
I
J
t
I
i
I
I'f
r
I
SECOND FIVE EEAR PLAN
The Priorities in the Sernnd m
Plan
<oume?ed'VhtheF^^
difficulties'and pfif‘'iis the
cn"■ere taken note of and steps were "aken'to^tily
the States except BCG^vaccinadon 0
iniplcmenlcd so|el' by
As a result, TBclin.cs we?^?c v M hrH06^""* :lnC' 1CSca,ch
ment and staff and TB beds were added’mo rIP™P7 Cquipand sanatoria that were not iLh? r • r niostly 111 hospitals
ed areas.
areas. One of the inmor mu / "lfeCt,\e CaScS in CIO"dPlan was.
m thc Second
was, therrTn^
therefore. to JLinrf t an«c? ,1,ndc
of lhe
the TB
TB cuntro
schemes as national to undertake certain of
L°^:\
,nn
i
C
and
thc
Central
Government
to give a subsidy to ti.e
s\7;;‘Z;ermn"ntsCfor
tation.
—«
their impleificn-
I •"
Ji;
i
CHAPTER VH
The target set for BCG
vaccination i l,lc Stcontl ’’'•m
"’as tocompkte
complete the
the “imd
r
million youn
2 people.
peoolemass
F„vaccination
’
‘i “ Programme IO cover 170
young
»,’«P;„S?d by £ S““te “
As a result of expansion 91
n iir
n?1Cnt 10 tlle S,ri'c'91.77,■ million
a/.5 million BCGexpansion,
vaccinations
ll0,1r 'ubcrcidin tests and
vaccinations wc;\.
flan period. Ncw„ build
g and
,,d plam
il^r ‘ 7™'? in thc
holding
of freeze dried BCG vaccinf were a
t'‘F
Laboratory and some
freeze
dried
r
e
.
ava,1;lb|
e at thc BCG
some freeze dried
°n an experimental basis.
accine was manufactured
1” the Second r;
ull uthe Government
1 Jan,
of India agreed to
blish y| X 'ay a,Kl 'abo'-’ato
1'5 l.0 li’c newly estaoiishcd or upgradecI-TB-'di^i^^'""
f *
lor expansion of domiciliary
treatment service
ISO 7 B clinics. As lhe target was-> to establish and upgrade
against this target, 80
^ta^shed, of which
-‘ n>cu’ TB clinics were
-- 60
60 were equipped
with funds provided
the Government of India.
tratmn
°f establishment of 10 TB Trainim
tiatton Centres in association
;
& Demonswith
--1 the Medical" . Colleges in
d-fferent States was fixed
Demonstration Centres could However, three
Training &
only be establishedJ at Nagpur,
Madras and Hyderabad.
•
Vr"| 'u'l
Vr
I
■ b ‘
22
'•;
cccsion
i
Second'pl TB is.o,3tion beds
established <dining
’ ’
‘"r pe,K’tl fo>- "hich mere
the
Sl‘bs,C'-v of Rs- 1.250 per bedthe Government of India"
------ 1 gave
a snh • i
all No II
x.
in the
Hl patients and their farnih- „ } k
i
.. .
training of TH and ev
third five year plan
s,S‘° "n" ,"p■'» ”I».'™sr
.1.” sKdiir"™‘
The Third Five Year Plan from 1961-66
continued for
two more years in 1967-68 and 1968-69 till was
the
start of the
Fourth Five Year Plan in 1969-70.
F
i
I
fci
•' f
Pallewas further" xpanded und'1”1''
ogl ;"’""c in ’
c- oMccIic | Rcsc.I.ch
;'-Pi<es of the fndia,Afadanan Counns increased from 50 (Kin , <?
studv population
sllI<ly was exjianded to'include
’ H>°rand tbc s‘
. 5C<,PC nf the
a communitv bv reneated
C CCt ° ^^‘’ciliiary tieatincnt
lhcj‘- contacts and per S ^an,,nat’<>ns of the
- patients and
communitv.
P
(51,1'ey.s of the Population
in (hat
x<
■ I'-'
CHAPTER VIII
In 1962 the
Health Survey and IPlanning
”
Coni in it ice
(Mudaliar Committee) reassessed the
problem
of
tuberculosis
and recommended measures essential
to deal with it. This
committee recommended that . BCG
----- vaccination should be
should I inriS!nCC,/
do,ni
cil'aiy treatment foi
doimcdiaiy
tuberculosis
siioulci be further c
'
expanded
and niolnle X-rays for rural areas
Should be provided. The Commute,
- ......... lee recommended one TB
clinic for each one million population.
• one lakh additional TB
(A.D.I’.H.‘ ^bbicach'siate"'1 ''' fl'"1 time State TB Ofliccr
v-canS S, aSaW?:I'": .. . BCC
onstration Centres a d T <
r 1 U!n,CS’ 1 ra,,1,”g
»cmtheir expansion provided for^X netC 1 .lcrcfo,fc continued and
of mobi e X-ravPclin c w r-.L
^,C
cslabl^hnient
to the needs of the vast n• i b
pUp "lth a.vic^Jo catering
areas since most of the TP
'• °^.PalIcnts Bving in the rural
J'l’c studies
conducted
bv the Ci.
pachas showed that
the
Chemotherapy (■
Centre.
results
of home
B cl rugs» aas carried e- • i anti
the
Centre
'in
"
itb
as ^‘c results of sanatorium
mere as good
■'
n
""\
n
trc
a'"'cnt
and
bcf|
good dict did
1,01 play anv} niajor role in the
Kst or
tuberculosis.
i»eat men t of
sigiiilicant
blishmcnt of tiie'xationa?
t'‘''t-' ■Sc“,"d 1’,an
m 1959. This
This was n-,?
ru'-,e’eulosis Institute was tlic cMaBangalore
I"
ft
meame and1?"
culo?s n
‘O
siubsenn.,:?^^5
S p,obIcni is late and^"''''' 'ike
l,lc staff required m
l‘Re^uSH"hmuHb^1^c^li-"itC rhi" a Shoit pcli-!
Inc!ia
C rcwt"«s are
0[ t,le-'e two institutions are discussed in
a
I
I
"1 the strategv and concent of \’
r°£lutc :l major change
me bv cvolvintr
1 1 • NatlonaI Tuberculosis ITogrameulosis. On the basis of'ih’^T T
P,o«' """"e
timerSurvey that the prevalence of "'i
°f the Aalion;11 S-”"pic
both rural and urban areas in T'lclpU °S1S "as almost equal in
tial to plan a nrno-m
c
India, it was considered essentreatment
countrv’s population it
n" ""a areas "here S0%
the
the National Tuberci os.\ T°peratlon 'Search conducted bv
1 uberculoSls Institute proved the feasibilitv of
f
i
24
25
establishment of five
five more
r...
Training &
State
- .-.^3
of personnel. As atrainsr thk
m - atJ State level
e'e for
^or Lraming
during the Plan period
Thus
WC1C estabI1'5hcd
Training & DemonSion Thus, the total
‘otal.
of State
Centres came to 15.
-II No ;
i
J
'•accinat.on programme ,vas also
at the ^me of inccp2vasJ0 cover the cn'7*
health service to be nhM , ' PP10Priate agency of
thethereafter
general
i
;“TPS sttg;.
Against the tarset (
ni«, five rvere de;TToped“nadbl;nh?h"tOf 25.raob;ic X'rav cliwere developed anTin
such clinics was no iXer considered
‘he nted lor
was no 1
TB control concept
for
rural
areas
inc
^1C Dlstr,ct
concept for rural
Tuberculosis Institute.
CV°lved bX lhc National
fixedA HrowevSrperi!oHtvhvaent Of 5’00° TB is°Iation bed^ "’as
However, priority
TB CentresTrough
tTch bt^'o'f .? CStab,ist-eOt of District
--L ■ , ,n
, ,
,
lk of lbc patients could l>e tre u
ed
rather
. ...
. - than to establishment of isolation beds A total of
1,571 beds were only established during the Han period
Prop^aSr:'£t^l^;;T^),;v^>|en.cnt:.tion of th, scheme
to be able to the
S™.
su^mTy
I:
I
r
i
hi- 1
I
:fe
.
ih
hi
h
iI
TB Control
test was'fn B?G vacc,,lallon without nrrl-01"0 U1 thc- Third
Third
Has found to be safe nnj •
,l,t P’dinimary tubercnlm
"as tntrotluced and v,c
S"”plc’ tiircct
llbcrculm
group of 0-1-f vears v
k
11 u:is ^toiled to the vaccination
starting with the matmii't^hn Vac^i,latio,> "as -- younger age
also introduced
tntions in urban areas
and other maternity instia"d 55.9 million BCG race n'? °f 957 ,niHion
tubcrculin tests
Period from 1961—68.
S "'crc Performed during
f the
a
is
Hj!
(I) Establishment of reirionni ortranisalionsT
m
-P’cment, supervise and assess the work of
To^hl'disguide
their acti cities six rc^ic
1 f'*
^itid to coordinate
proposed for the FcXh„ c?”t1r“.2'Sc..otisb'a'|y
established in he T
PI
' ° °f 1,,csc "e,=
the Southern dtri^
n/hinxISClf',;i ^'galore for
the Northern districts
C"' ncli" for s0'”c "f
W ^“^Third SvearTl
i
i ist *
ThC ’"h051 importa,1t cvent
for supply of and TR A 1 "thc start of a scbemc
as toPfi5 dinics Ln bvSS I**3'0 TB dinics as
domiciliary treatment
Oroa'?lsat,ons for
Governments and 15 I'P /r
Undcr lilc Slatc
Nations took advant Je^f"^"T V01untar>' Or?a-
•1 '
■ I
course of the Third C Xd "VS w^e;T dUn”~ tht
managerial e
J;"
centre for the cnUrc’
i
f.
u! !
< ■
P
tees- IO
p—
I
CHAP TER IX
’.ill No
r
i
fourth five year plan
i
■!
Fourth
Plan ^it ’r" Scl!cnlcs of 'he Third Plan
"cre continued.
1*'However
continued. However
’
i*- -■ •
.
’
umci v/
ous
in spite
of •ill
thc mrT'
014 dur‘ng' 'he previI
,Plans that in
s
pnc
of
all
the guidance
by the
'he Central
Mmel ,v^■P^^^’o! the’X'umne
"■eminent, i
States was poor. It v-'wi\
develop the
U.
,
entire .i'C.q.l,.,rcd
-••e Goxernmcnt
take the .■ecponsibil.tv
■
of beaHnth
"C"tr°f IncIia sho"<d
Ktanmlc in .'he Fo'u’r'th p'lanbearing
period the
‘dl T °f tllC en‘ire
rB Control Programme
Programme iin P,;
: A t,lc schemes
Centrallv Vm . ■?,I
, C '■O,'rl1' 1>1:m
/ponsored
schemes
‘•■nice. This liieinr
n
schemes T-'
wnh lopw
Central assisGovernment’ of ImI ■
•
in 'he
the picxious Plans, the
1)l's"h- TH Cc.Iues’Zr'i ■ CSt:UCSi'’ die
establishment of
isolation beds I,,
iv bearing a portion
Plan ,!'CCllrr.rin" a"cl
'
purring expenditure.1'
of t ’ -K (,OV' I ninont of India
• in thc Fourth
bcarmg tl1t (,,tirc
ni‘"a
undertook the
ofestabiishmenrandni^P0""6"^
cut and N^intenancc of
mstnutions and of
M-rcd for the programme. anti-TB drugs and BCG
'* vaccine rc-
f
!
i
Se
■' I
I iH
ir
p
V
u
I1' 'i-' •;
1
f
I
I
''■r
i
B .i
hi i
3“0-
■
T
i 'kuu^.-
At the end Of the Third Plan, theic were still two nr.ior
States vtr... Madhsa Pradesh and Assam not having a traini m
& Demonstration Centre. For the other smaller States like
Nagaland. Tripura. Manipur, etc., and the Union Territories
it was not considered necessary to have separate Trainin" fk
Demonstration Centres as they could take advantage of "the
Training & Demonstration Centres of the adjacent St iles
A
target for establishment of iwo Training Jk Demonstration
Ccntics at Assam and Madhya Pradesh was therefore fixed.
Regarding supply of BCG vaccine, it was detided that
“^th^BCC APU,TChi'SC °r BCG V:ictil,c'
etc.,
om the BCG A accinc Laboratory will be paid bv the Govern.
rn^R^r13 l°
Statcs- ‘So f;ir «',s supply of anti-TB drills
atilns'for'd rU". 51:110
‘"‘(I vohmtarv o.gamvoluntary orgatii•taT5 n •
'arV.trCa,mc,,t of TB p:iticnts is emteeined
it nas decided to continue free supply
r----- ’
*r these
’
* drugs bv the
of
Government of India as hitherto.
were established
niear.tirne. BCG vaccination
‘ expanded through other agenties like
i
•ZS& -feR
ra
for want of ]paying tpatients and
suggested to the Spates that in I resources. It was. therefore,
any area without TB beds if
there was a TB hospital 01 V’UP,01111.1.11 run ky a voluntary
?Lga.?.LSainfJ" y iLhinua radius of 250 miles, thev 'should
reserve beds in such voluntary organisations instead of cstablishing new Ibeds and the Government of India
_t
r
.
........... .
'■'*•
Avas
was prepared to
pay the cost of reservation within the stipulated
1 pattern of
assistance to State Governments.
During the course of the Fourth
Plan. 114 more TB
Trn’CS- 'VCJC a<I(,cd as against the target of’ 160
two
Il'a''1'n33.Oc",’on':r:i'i<’'> C
Centres
were The
eslablish’entres as
r targetled
•
'•ourtb Plan so that l>;h he end'Tn d^"S thc coi>rse
1 >e chstnets of the country would t •
’C 1 hm PcHod- all
Cenmei wl. ^Ifor
TA
J7;! .J
,7° f’r l,'«e
27
'Hnnber of beds as
ns ;adjunct to
cases of District TB Progra in
■eel essential. There
here scvcwas no TB bed at all
A.
target of
““"S:.!?f£° T“ ‘“'"ta,;
’>«is as additional TB tvard"
r 0 ■“‘‘V50'4
bed was available. In th‘e X."J1 ‘h°SPitals
l«»>« -I .h. po'p”.,™
voluntary1 or^anis^tio0 H1*™' °f thc TB bccI^
? oi0anisations were at rhn .
1
I
I
I i i 11 i *» %................. .............
•
•
*
freeze-dried per''''1 5G'cnic r°' cxp:tnsion of production of
I’roductonoff^riid
'’
',1C Foilllh F'an.
vaccine BCT
was taken Uup
vaccine
Which was onlv nlmm"
n
T0'10 in the RCG Laboratory
- about 30 :n^onl^I1iv0io^ PvT^d'^ th^Pl"'
ed^and'onR'‘f91"^
tllC -nhc p^r^ I v "tom"
tnilbon dSet vS-d VaCCinC "'V “SCd
A [otaI of ('°
BCC v.. C.lcct \accination.s were performed in Plan ncriod
supplied to’lthenSta"ebsCrtUli'1
ab°Ut Rs' 45 ,nilIion "ere
ii
f
28
:csio
j.
to more than SOcT'tb ciinics^tui' bvS'ti33<;nli111^'1 "eie sl'PPlicci
than SOO^TB clinics
about GO TB clinics run by vohmr'6 S nte Governn,cl'ts and
tun by voluntary organisations for free
supply to the
TB! <-s
-------patients on domiciliary treatment.
I No
!
I
I
In the
Trial, which
regular project in
,
BCG in the prevention of tubcrculosisrin "the circunlt'3'1’0
prevailing in ci
included initial
about 3,67,000 "as completed by Mard^ lJ;! ” COn,P,I5il’g
CHAPTER A’
FIFTH FIVE YEAR PLAN
The Fifth Five Year Plan which started from 197-1 would
continue till 1979. During the Fifth Five Year Plan, it has
been decided to continue the schemes for supply of anti-TB
drugs to State TB clinics as well as to voluntary TB clinics
and supply of BCG vaccine and tuberculin to the States as
Centrally sponsored schemes with 100% Central assistance So
far as establishment of District TB Centres and Isolation beds
are concerned, these are included in the State sector for which
funds arc being provided in the State budget.
The piovision
for the different schemes
under the
National FB Control Programme for the Fifth Plan
.1 arc:
Ih
I.
Centrally sponsored schemes
(i)
i
Supply of anti-TB drugs to
State TB Clinics
Rs. 575 lakhs
(ii) Supply of anti-TB drugs to
voluntary organisation-run
TB clinics
Rs. 100 lakhs
(iii) Supply of BCG vaccine to
States
Rs. 150 lakhs
II. State schemes
(i)
i
I
I-
•I
Establishment of District
TB Centres
(ii) Establishment of TB
Isolation Beds
(ni) Equipment for State/
District TB Centres
T(trgrt
75 Centres
Rs. 335 lakh,
3500 beds
Rs. 506.60,
75 sets
Rs. 90.00.
With the establishment of 284
the end of F
'
districts were to be provided with
each, taking- into con^^°'ld-ed
J Distnct
Centre in
in
created in the nteanri J
tTh,e.:ne'.\dist.ricts ^at were
the meantime. So far, the United Nations5CWldren’s
V r q;
___ J
30
'S-ior
Fund was «
equipment and vehicle^
for these District f GcTLaboratory
S-rIn thc Kifth l’lan UNICEF aid
’> not available, It is. thcicforc, necessary for the States rr>
establish and cqurp the 75 Centres during the course of ti e
Fifth Plan.
i
No |
Ji
75 district I B’Fw\aer\VdfeCFifH fpi esta,blis,lrncnts of these
cover thc entire country by District TH‘V’ S 1O"ld cnable 115 [o
of the Plan period.
'
J Sl1 lct 7 Jj 1 rogranmie by the end
»c.ites5in "hel-iX ph^’01’
i
tO
of Rs. 50 lakh" h2been provit;«rl x"' VC:"S
The Tuberculosis Programme of thc c.
....... ’has been
country
evolved takng into consideration the following facts:
(a) I hat thc nine million or so cases of active tuberculosis
in the country are evenly distributed in the towns and
villages, that is, 82% of the cases arc in the villages
where no special facility for tuberculosis exists.
(d) That
i nac the
inc programme for tuberculosis control must cover
the entire country, be well within the available re
sources m men, money and material and provide size
able benefit to thc community in thc foreseeable future.
s1""
>-l <* * I>1 UL. I I t
1
Jr0C?cd by thc Govern-
,
also being procured centrally for
supply to District TB Centres.
es. BCG vaccine is^being supplied
I
\
f
f
fc
i’
•
NATIONAL TUBERCULOSIS PROGRAMME
(c) That domiciliary tieatmenL is most suited for treat
ment of tuberculosis and institutional treatment bccomes nccessary only for a small percentage of problem
cases.
cidZ
for freeze-drying of vaccine and
^'N'/quipntetit
automatic scaling of ampoules,
raton5 i^KX^
co,^ labo:
freeze-dried BCG can h/f fi l ’ Jf inquired, production of
itself.
° Can be furthcr enhanced in the Fifth Plan
t
CHAPTER XI
(b) That thc :pool of infcctors arc- ---thc sputum positive
cases itotalling
‘
o about
’
two million in the country, most
of whom have also
...oj symptoms and therefore have a
felt need for taking action, ami in fact, are alreadv
seeking relief for their
-suffering from the general
hospitals, health centres and dispensaries in their
areas.
mal work. These persons arc I ■
nS .t,lc course of their norvised bv the ex stin' Bf r , betng tra.ned and will be superthe school-aV’XP To tZ'tl " 'V,H ?"li"Ue t0 c“ver
BCG vaccine, production of eeze hieddim ,siccjuiicincnt
T ■
, of
^d to 60 million dn^
.1
7
,s '^'ug cnhanc-
r
I
I
I’rintat v I-e th ettt es
I,’
"■<» kers of theIn each' P M r > . i
5 bc ,,g 0,^«’Hscd in thc Fifth Plan
H^e AXAIs/bhwF^
‘•’Ic1
C'’
!,lc. Periphery
be lhentb^lte’d^’d^ncs'Z- :“i7'
I:
!
to '>c established by the
I
h-
e
i.
gramme of the District' I B Progratnnt'es ‘''.p '01111" >' service prowards in existing General and ml ’ f 1^Se.,nc Io JC ;,dded
I
I
2
(e) That bv organising tuberculosis control on a communitv
basis through thc existing health facilities which proMdes a permanent programme and is easy of implemen
tation, it is possible to bring under treatment a lai'"
proportion of the infectious cases in communitv 7
a reasonably short period of time.
(f) 1 hat BCG vaccination is an
ventive measure and can
the general health sen h
clive an'l
>.d with
•' .cgular features.
(S) That tuberculosis is
• Me infectious disease njf
ubiquitous distribm’.
and about half i.he total population of thc
; is infected by tub- ■ulosis gcims
that const!” .
ac main source of future patients for
I-
32
3?
Ii
several decades. High birth
bIc population every year rate adds to the susceptineeding a regular BCG
vaccination Programme'all
p**~
the
—
- time. Therefore, the
programme has
'--s got to be
-----ac countrywide,
of
nature and should
---- 1 be integrated with -- a permanent
service.
1 general health
Hie fundamentals of
•ii
(0 Prevention of dcvel
disease ”“"S
(ii) Detection and
iious cases as
non-infcctious.
J
'■
'r
(
™ I'e""J"”" -’“d
f
fee ?.-*r
as large a number of infec3 VICW to rendering them
■
Xation° I ■'Tuberculoses Pro^mm/’h "V"’ el,,P'’asis
■
sh
in the
t'on of District TB pro^rauune h
ha,S,b,ecn 0,1 the
organisaand staffed District Tn ' "nlc
establishing-a inlly
ff ,,■ equipped
and de
>on activities in the r. X r
trcalment ;an d, BCG \ac<Nnafacilities.
tm,,c district through the
-3 existing health
CHAPTER XII
DISTRICT TUBERCULOSIS
PROGRzlMME
Ax Average district in India Inc n
i •
1.5 million. It is divided into abnni t P°PuI‘ition of about
headquarter town in each of which the ? UkS
a taluk
the district headquarter There -.m -.h^ .
St•1S &enerallv
are grouped into 20 blocks each nrovb?
• 1°° Vlllafics "hich
th Centre. In addition to the I’rinnn^Elenbh c""113177 Hcal‘
are another about 30 small hospitals } rlk
h CentrES- there
having about 50 health institutions ‘ each X'l'53''',5'
llu,s
a qualified medical officer.
''
under the charge of
district of whotn'Tbout^OOOmr ffifceC ~(,’0(,b . Patic,1's !"
a
are the ones that are sources of
-0US-. Thcsc 5.000 cases
also have symptoms. They arc ffivrn '°n- ‘'•lt In0St of "honi
TB control programme both' witli ' Prlority ,n the district
of symptoms and 'sterilizi^o-' the infecti™"' t0 Provldin8 W^cf
"'hich new cases (i.e., diseases inrirl^n
5 P°0,' Thc latc at
to the pool'of cases can be'estimated m h^
CVCry ycar
one-fourth of the prevalence "XI n I
b°Ut one-t{"'-d to
12o0 to 1500 infectious cases are added’"if3"5 that about
every year and similar number of cases e tt C iP°01 °f 5-000
from the disease, thus keeoin" the ■ r • ther cI,e or rccover
constant at about 5.000 cases’ On" CCtl0U? P00.1 more or less
basis of the drugs consumed „ > > r°U8h cst"natc, on the
drugs in any district wheie Distri^TB1”?Vided, f°r anti-TB
Has not been organised it is psrim
i
^onlro^ ITogramme
t0 200 cases could be under active "treatmen 1"°'
W°
!
I
i
f
t
I
control programmes are:
di«s;
«
{
tre establishedXt^LCd?s7HLPheSdamnle' tilC District TB
Censonnel trained in the concent nF'ldquarter and faffed bv perproblem of tuberculosis at the CtioXaTT^ aPProach to ‘the
functions as a referral centre for rhe
Tuberculosis Institute,
headquarter of thp
>
the entire district and as the
the pro-r^nA
Iyanagenal team r
responsible for organising
case-finding maitdv
district’ The actual activity of
anti-TB d?ug treaimeXI’n d” e^mination and
Ilin
r ■
I
fig
i
“S'”!
-- o where the district
Patient °n the 2 • ? °rganise the P"
programme.
Thus, each
jn the periphery is offered the
—e diagnostic as well as
7 DGHS/ND/77
i
34
35
; i.Tt'
—
went"vhLh^'ien^Z^mini^ "'hf°,C Pe,i°d °f his Ueatfacility near his home Cn " 7 °f o,;e/cai- »> d>e health
niamtaincd at the Disnict TB Cemre andl\n7'
PatiCnt iS
for the patients receivinoand only neatment cards
respective peripheral heahh instkudons.'0 maintalned in the
No
i
country, it was tried as pilot project in some districts and it
was found that such a coverage is possible without much additional inputs.
• • 3CP ,vacSi.nation also forms an integr al part of the arti
v.ttes of the District TB Control Progranmte. For this a BCG
team is posted in each district TB programme for svstematic
and regular coverage of the susceptible population in he en
tire district. The s.x technicians of the {earn cover the school
children in all the schools and the pre-school and non-sd oo
going children from house to house. For newborn and in an
vaccination, the staff of the existing maternity and other heakh
institutions and the peripheral health workers are trained to
build up a permanent organisation for this purpose.
pick up about
S.’% «f .be iaSWWWg
...\a centres.
TB Beds
i
SSSR s
™.
/XS KX'eJLS'S'SS
’
tysis, spontaneous pneumothorax etc nr fnr z->e
i
!■
Centre" nCCSSair
ln'estloatlFOIb send them to the District TB
:2iX=E=S/--~:
£K^“S=S3Z
i
do and thXfCarC mifrosc°py centre for sputum examinaXiination
1 tO thC nCarCSt X-ra>' faciIitX f°‘- ^-rav
li
^;VB“p,ttcci'hfor Patic’Z;
dZ IndPare rherpfn0 are rCSiSt
1
a
nt
t0
the
^
‘
^dard
-TB
resistant to the standard'
required to be treated with
----- 1 or for those who do not have
- Kt
State TB Centres
I
.L
not rmJlY aC“Vlty
thc D7l ict TB Control Programme docs
nh . ? ! 5 , ,cl'-case. the "O'kload enormously in aim of the pcrinnr hcak!1 lnstltutlons since in actual practice, the workload
\ ndnirn016 tran th?-e °r r°Ur sPutum examinations per dav
A minimum of recording and reporting is provided for to make
■t easy and snnple If a District TB Cenme alX with its 50
moie peupheral health institutions can diaomose and out
under treatment about 1500 sputum positive cases per ve£
such a programme is hkely to reduce the problem or tuberculo
sis. Prior to recommending this progiammc for the entire
I- '
L
■!
I
inonsTradoirCentiT^One^
' T
.
arc otherwise known as
as State
State TB
TB Training
Training &
De- -- One such Centre
model District TB'conti'ol ■The
TB”Ccn^e
i-luding an urban pi^i^Z” "
located for
and •e-odentm on'of■X”’ pi"p0SC.S- !l undertakes training
TB COn'
trol programme of tlie Xmin’”0 t'af^X "
and re-orientation training coupes for
personnel, private
J
W •« J — J
•
«
TB Centres also for
PIallned to be developed as State
Control Programme of the StatT'
nionit°cing of the TB
1
i,
I
1
37
i
No j
C H J P T E p XIII
I
pklsent status OF THE PROGRAMME
I
The Progress (of" the different schemes of the National
f b Control Programme
- are briefly discussed below:
i
!-
rao TO atak,,,, ,„c
...
country
are District Centres
to
'
Each off these
Centres is staffed with~ a team
nfn
'CSC ’^Dist^i
Dlstli« TB
National TB Institute lb' '..V P?™
nn
el
personnel trained at; the
About
bc«» Pro'idcd bv the’UNICEF or t'0"' 250 of
°f these
‘,ICSC ’1b:lvc
uuth full set of X-ray and laboratory the Government of India
Each District TB Centre n„
on ---------' equipments and vehicles
Centrei on an average has about 25 periiibcial health institutions
part.cipatmg i„ the programmed mid
i™,'™231’”
i
f. 7
»!
ta"3„rdls° i"
~ >™ia
otoS
Training & Demonstration Centres
There
tres, which
^ar\mg stages of development.
these centres
...... ........
are having training activity for i
sonnel medical o
college students,
> private practitioners, etc.
apart fiom conducting
certain epidemiological studies. A brief
note on the activities of
some of these centres is given towards the end.
I of a District Pro-
n^-On,'i,^out n districts in the country that
-- -mic.
the
covered bv regular
Distnct InTb
" remaming districts not
not vet
liogramme.
oijmnise TB control r—
. . . it is ipossible
~*•-'*C to
programme
••••’_ effort, osince the
TB clinics as the nucleus
of“t'he with a 1little
District TB Centre1 already
exist and trained personnel
ot can be casilv trained ;,k ;,arc
llul)I1cither
,, , , available ii” the State
at National TB Institute. riic main
case-find"» organise
-.................
....... through the
institutions of a district °
existing peripheral health
I
Regional TB Organisations
senjone She" No^h 1?rSan'Satio,?s arc functioning at preand the otiiei in X So r in'
,thC
Dclhi ™ Centre
lasts Institute, Bann-alore
Thev
^atl0naI Tubercuible for assisting thr <d-,r . -1 hese organisations are responsProgrammes in° their
TB Control
paramedical personnel bmh n th n; br,efiT5 medical and
Peripheral institution and fkr
PCG Programme
guidance.
Th“'«»
have been posted in or integrated
-90 te:1Ills
These teams are mostly coverin' hi °IStriCtJ® Centl«
Bar.
school age children bv
o cbddien in schools and the pre253 miKion persins have ^en
tOtal of
million have been vaccinated sincZ the"
and about 195
paign. On an average about 1" m'lr lr!cePtI0n °f the camare offered vaccination per vear tyhich^n"
“
Cbildren
per ;ear, nhich, however, includes only
Supply of Drugs to State TB Clinics
®J-trlCt TB Ccntr« a"^
and for Pro'''dmg expert advice and
this Sem^’there a?e moTe than^OO TB
■
‘I h •'
■IJ!
j
vtli' i
TB Beds
The total number of TB beds available in the country
today is about 41,500. A little less than
a third of these
beds are run by voluntary organisations and the
rest are under
control of State Governments,, other governmental agencies.
municipalities, etc.
District TB Centres
°<
about a in ill ion new borns and infants below one year of
age. Trr a ini ng
- of ,paramedical
-...... 1 personnel of the rural hr-ibh
----- L___ i i.and
serv.ee for newborn
ai.K^ infant
TC3111 varein.,;^
vaccination iis in
Production of freeze dried BCG vaccine H1
in
Production Laboratory is being expanded. our BCG Vaccine
f
19G4‘
UnC'er
domiciliary treatment of Tn .
t ° TB chn,cs undertaking
ard anti-TB drims directly bwh? r '3'
be‘ng s,1PPh'cd stand
ver 7,00,000 TB paSs are P5?°Vefrnment of India. A little
hary treatment at anv nr.’
c estimated to be under domicithese 300 TB clinics7
th‘s scherne through
tn’ct TB Centres.
d b°Ut 5000 sub-centres of the DisDis-
i
38
XCS-iOil!
I
---------
Suptfy Of Drugs to Voluntary Organisations
bvG^tkT
ill No I. I
in
I
f
cost
to enable them
There are about
' I
5
j
«>PPHed9£e M'St
■■
i ’
In this Chapter, an attempt is made to summarize thc
findings of some of the important research studies conducted
m India, on the basis of which our National Tuberculosis
Programme has been developed. Readers may also find thc
answers to some of thc questions that normallv come to their
mind in respect of thc present concept of tuberculosis control,
home treatment of tuberculosis, thc role of food and rest in
tieatment, risk if any, from a patient under treatment at home
to his contacts, protective value of BCG, whether tulxnculosis
in our country is increasing or decreasing etc., from thc sum
mary of findings of these studies.
Supply of BCG Varcine
V=der this sch^e BCG vaccine is supplied free to the
States for use bv BCG
M.C.E. institmions. etc., teams and other TB, Paediatric or
berculn for ciagnc<>tic participating in the programme. Tu0 iIS-a s.° sl,PP1»ed to certain TB,
paedii_iric and other mkr
medical institutions.
Trainiz^ of Key Personnel
•pi-
n■
k■
$
*S carried out mainlv at t’
I"n 7.-ri«
InStc'tUtC at
a^.rict TJo -F
lejnis
national tuberculosis survey
mechcLl person! from difle/enT^at’es’
courses for ruj
°C / uJ£Ulct IB Programmes. Apart
from tiese.•-dn rdd ^anv
A1^ ' B Cen‘re Pcrson,leI have also
been trained
■
Adtn.mstrattve Medical Officers of
States,
MedicalTeachers
Offic'en of
fro- vartus eSeS’-Di?triCt HeaIth Officcrs>
cipated in the tenting conducte^r^gubdy5'every yean
L
also ^e^o1;6 rSnabroM thTB. ^^‘-annues have
Colotnb.- Plan, etc, in ittSrctlCs
WH0/
■ 11
Hr,-
UlL.
RESEARCH
Lx THE field of research in Tuberculosis, India is in •
the forefront today. Many of our research findings have
contributed to the world knowledge about tuberculosis and
its control and have been useful in evolving a sound pro
gramme for control of tuberculosis in India and in many
other developing countries.
I ■’l.
I
I
CHAPTER XIV
r
°f cPulm°nary Tul’crculosis, one of the most imP01tMt forms from epidemiological and public health points
and vil) A ari0Ut tyPes Of P°Pulation in selected cities, towns
and villages in the States of West Bengal, Bihar, UP Delhi
KemH6’ Andhra hradesh, Mysore, Madras, MaharashJra and
were
TC
by -thc SUrvcy- About tlllcc 1:>kh persons
ere exam ned in six cities, 30 towns and 151 villan-cs The
die stMivir llded
SU"Cy "CrC choscn in :1«°'-dancc with
application
?rlnC,Ples so that 'he findings may be of general
lork
Th’ S‘X lnstItutl0ns wcre entrusted with the survey
Patna J, n
?T
Tubercul°sis Centres in New Delhi,
nf wa’ .H)derabad and Trivandrum, the All India Institute
MisSleT t and! PubliC Health’ Calcutta
'he Union
J> adp
pbcrculosts Sanatorium, Madanapalle in
Andhra
“•esn. lhe entire population excluding children under
I
!
I
■10
41
-b
M
areas selected for (SUrvc)' " subjec ted
fferin f,,’‘n‘:uuic radiograph
o nr
the thsease on'tl e b - ' 'T SUSpecled
be
the basis off X’ray "cre subjected
to ftirth
furdler hactcriological tests.
1
The main findings of this National
'■ J,,p-;'|ence rate for ‘active' and
chiertowm'a^dHlk’g'?
'
Surxey were:
pCrrVAAO
,'00017 aCt,Ve’ tll!"'rrh^ d-'rr“J P°Pulation in
the dliferent zones.
cases for 1,000
2 to 8.
gencrallyhf rat
theh"
<-'s in- -cities,
t-'CS’'• t0"ns and
villages were
same order.
T Prevalence rr.;c
vaieso were lower fhr females
males, specially in
. i age-groups above 35 years. than for
vate showed a continuous
increase with
5' JncS\ShlahPrCValCnCC
-
61H •
the cities
P'ing in /ttcAn'hou^'h^ompm0'!06 a,nonS Persons
nouses indicated the possil ’hi" ‘°c t,losc in Pwca
«mtary conditions. P
C C'rCCt of «onomi^ and
A large majority of the ‘nrrim’
i <
rases had moderately advanced diCscafe°b:'bly
S
f to» =3
33 „„
cases,
««•«.. bei„g pncri “ita '7,1,;
cilic!this
v pei-
The f
survey also shoxved
city where? ithe prevalence (of' tuberculosis 'iiiay £ T? in
.......a
four or fixe
high as
Poorest in the popuialm ofen Hvig'i^
1<?I> ln-'anitary conditions.
COMPAWSON
„UME
SANAtorium tr£atment
OF HOME AND
16o newly diagnosed and previously untreated sput-nn
posi ive patients of pulmonary tuberculosis from poor sec o
of the commumty m Madras City were randomly treated •
sanatonum or home with the same chemotherapy :.c IXH
-00 mg. and 1 AS 10 gm. in two divided doses per day p-1(i
ents of the home series were given weekly suppls of'diuns
to be administered by themselves at home with monthly sum
vision of them progress at the clinic and were visited at iXe
by a Health Visitor every fortnight. The patients in the
. sanatonum series had bed rest, good accommodation, 'balanced
diet and nursing care. Thus, this was a
'
Dn,ancccl
comparison of treat
ment of patients in best sanatorium <conditions with those
in usual day-to-day home conditions of the poor sections of
the community.
11?
-At the end of one ’year, ----86% of the patients treated at
home converted to sputum negative and remained
lologically quiescent) as against 92% in the .....
Sam-J so (bactcrsanatorium patients. Improvement in X-ray and closure of cavity
’
‘were also of
tne same order in both thc groups.
i
I
Follow-up: .After one vear, the sanatorium i
patients ro
turned
• • •homes and the
-J tto their
patients of Both the scries
were closely followed tip for another
four• years u.
------ ----to study
the long-term results. Considering the overall relapse
f
e rate
of the fl
disease in the
two groups, it>vcio
■ .'
___
waslull
found
that seven
se ven per
cent ot
< " the
' patients
in home series
. -- and
—— ten
—i pz
per cent patients
in sanatorium series had bacteriological
re
laps. over a fourrelapse
year period of follow-up.
It was thus conclusively proved that effect of treatment
do.
bX-at 110mC 15 ?S-S°OtI aS Of
in an „ h
tion both m respect of immediate recovery and subseauent
p evention of ielap.se and that good food, nursing cue and
bed rest, etc., do not play any useful role in the treatment of
uberculosis. Domiciliary treatment has the added advantage
of not causing any dislocation in the family during the period
of the patients treatment for tuberculosis.
<- period
therajiv'cemre, Madras^-.T'a01 b)' p'S T,'b««ilosis Chemo
~
■fe.
F■
F
■
sanatorium treatme’t
^tlOlicd ™ntparison of home'
another four years to study rhe 'eai and subs«li'ently for
-n these two groups.
thc Mergence of relapse cases
TB ATTACK RATE AMONG CLOSE FAMILY CONTACTS
rnnvT^iS StUdy W>as PIanned bY tbe Tuberculosis Chemothe
rapy Centre to determine the relative risks for contacts of
patients treated at home and in the sanatorium
f
I
1
—j 'H j
v- ■
42
^1
n_o -^6 close family contacts of patients treated in homes and
272 similar contacts of patients treated in sanatorium ivcrc
intensively followed up by X-ray and bacteriological exami
nation for live years. In each family, there was just one
infectious case and the contacts in the two series were similar
in all other aspects. Effect of isolation of the index cases
could be best studied by comparing attack rate in the two
series in the first year when the index case of the sanatorium
series was isolated in the hospital.
ill Is I '
•i
!
■ .1
Ii! ■
H'!
’"I
ill
Lib
ri:
r
J
p'
■-m
•- - I •
v<
• 4
■
1 .--t !
ii
kI
were interviewed at random by social investigators for symp
toms. Only such symptoms that were associated with Pulmo
nary tuberculosis were taken into consideration. Of these,
pain in chest, haemoptysis or combination of these four symp
toms were analysed statistically. 79% of die experimental
group and 83% of the control group were satisfactorily interviewed.
In the first year, 4.9% of the contacts in home scries deve
loped tuberculosis compared with 7.6% of the contacts of
sanatorium patients. Over the whole period of five years, 9.8%
of the contacts of patients treated at home developed tuber
culosis as against 14.4% of the contacts of patients treated in
sanatorium. There was no difference in the attack rate in
the two groups even when the initially tuberculin negatives
and initially tuberculin positives were analysed separately.
Cough was found to be the most important single symp
tom. G9% of the sputum positives and 46% of the X-ray
positives had this symptom against only 9% of the normals.
An interesting observation of the study was that the majo
nty of cases in contacts occurred in children below five years
and were detected within three months of diagnosis of the
index case and there was suggestive evidence that m most
of them the infection occurred before the index case was
diagnosed.
Analysis of the material also showed that 95% of the
bacteriologically positive cases were aware about their symp‘’•"p
toms, 72% experienced awareness and wcrc
were worried about
their sypintoms and 52% of them actually took action at the
existing health facilities under pressure of their symptoms.
From this study, it can be concluded that there is no
special risk to the contacts of patients treated at home with
effective chcmothcrapv, the main risk to them bcin"- before
treatment has begun.
n
This study showed that half the infectious patients in a
community arc already knocking at the doors of the existing
health service under pressure of their symptoms and if adc°quate facilities arc provided, another one-fourth will immedi
ately report to these health institutions. Thus, about a half
to three-fourth of the infectious cases can be dealt with in a
short period at the existing peripheral health institutions.
Effective treatment of an infectious patient, whether at
home or in a sanatorium, rapidly kills the tubercle bacilli and
makes the patient non-infectious in a short time. The purpose
of isolation is therefore best achieved by putting the patient
on treatment immediately after diagnosis and ensurino- regu
lar introduction of the medicine prescribed.
Sociological Study of Awareness of Symptoms Among Per
sons With Pulmonary Tuberculosis
I
43
/\bout 2,000 persons having evidence of inactive, prob
ably active and active tuberculosis disease in their X-ravs
^hosc sputum results were also
available (experimental
gioups) ^ere age/sex matched with an equal number of
persons with normal X-ray (control group) in 34 villages and
tour towns in Ttimkur district in Karnataka. These persons
I
69% of the sputum positives, 52% of the X-ray positives,
29% of the inactivcs and 15% of the controls had at least
one of the above mentioned four symptoms.
DISTRICT TB PROGRAMME PILOT PROJECT, ANANTAPUR
The District TB Control Programme was formulated by
the National IB Institute on the basis of their knowledge
gained from various case finding, treatment and methodological
alternatives tried in Tumkur and Bangalore districts in £96061 and was implemented as a pilot project in Anantapur dis- *
trict of Andhra Pradesh to study the feasibility of the District
TB Control Programme in 1961.
The district had a population
j
of about 1.5 million. One
District TB Centre equipped withi an X-ray unit was cstablished
-’.^d at Anantapur town. There wcrc 14 Primary Health
/
st
45
■14
II
!
a
'4
Centres, ten health units
rural dispensaries
units anti
and ;>u
30 rural
dispensaries. Mcdic d
doctors ucre available3 in
in almost
almost all
health
all health centres.
centres. Al.crcs
cJ’Cc, .".T10 P10vldetl ‘P 1PHCs
dispensaries. Sputum
HCs and other dispensaries.
ca c-finding was organised with co operation of al! these iiwti
co ected PU‘U'll1 SPCC,mcns of al1 Peis°”s "ith cough were
collected in all these centres throughout the sear ' The
spmmn smears were examined in the centres ha% umvot
smeux to
nOt 1’av?"S nnv microscopes sent their
■“cab to the insutut.ons with microscopes, functioning as
microscopy centres.
In this iway, sputa from 17,000 symptomatics were examined and 1370 <
e/J smear positive cases were found in one year.
I his comes to about 80*
0 per cent of the total estimated infec(ions cases. Ti..
The workload involved in each institution was
collection
of only
•
»,--» . •/ t'vo sputum smears per working dav Ir wnc
?- nlorr. that
°f tl,C ssputum
PutlI1>’ P^itive
positive ca?eS had o 4
for. more than two weeks.
—
All the diagnosed patients were given ambulatorv domi
hii?s trT>UnCnt V tbc PccriPhcral institutions nearest to their
ones The regularity of treatment was better when patients
"ere treated at centres nearest tt> their residence
?
It was ffound easily feasible and useful to or-anise such
case
finding
pherM hr'-,hh
S- and tlcatmcnt programme through the perimethodhof rH "4U‘Ut,ons "? an average Indian district. This
method
incthod of
of case finding and treatment was found to be much
cheaper than orthodox method by X-rav much easier m im. I
rnent and had the virtue of bei^g avaiitZ as a re~X
gramme throughout the year.
o
P* -
I
•'I
i ;
h
>
A
FINE YEAR r-'
”——
S™.
’.V. t,F. KI’IDEMIOLOGY GF TCBERCLLOSIS IX
A RURAL I’OI’ULATIOnTn
--------------------- SOUTH INDIA
This longitudinal study tvas carried out bv the National
monan-UtX In?tlt.Ute
ob?crve the nat«ral historv of pulmonary tuberculosis under the existing socio-economi- enndi
Snal TBa Pa
COntro1 —X under he
Aational TB Programme could be introduced
randnmlv
he'Nationa'i
of G5'000 - Bangalore district S
un-eved four dl?”
Pr0Slalnme
not introduced was
“c c 1
f an average interval of 11 rears over a
tcii,
X^ anL—^^"5 19GI’68 by rePeafed' tuberculi*
ra) ana sputum examination.
The salient findings of the survev are:
(1) I'he prevalence rate of infection was about 30%. It
showed a steady dec Tease specially in the age-group
0—24 years.
(2) The average annual incidence of infection (rate of new
infection by tuberculosis even year among uninfacted) was about one per cent. During the study period,
the incidence rates showed a decline from 1.63% to
0.8% for all ages combined.
(3) Prevalence rate of disease in the study population
gradually decreased from 406 cases per 100,000 popu
lation in die first survey to 337 cases in the third
survey but slightlv rose to 39:5 cases in the fourth
survey probably due to drought in the study twea.
For the 1younger age-group of 5 to 34 years, how
ever, the rales
rates showed a continuous decrease during
the entile study period.
(4) .Annual incidence rates of disease also showed a down
ward trend as in case of prevalence, being 132 cases
per 100.000 population between first and second sur'cys. 99 between second and third and 103 between
third and fourth surveys. The younger age-group
below .‘55 years showed
a steady downward trend
during the entire study period.
(5) Prevalence and
incidence rates of the disease in
creased with age and female cases were much less
(one-third of prevalence cases and half of incidence
cases) than in males.
(6) Of the 126 cases found at the first survey and followed
up lor five ]years,,
‘ ' 49.2% died, “ 32.5% were cured
and 8.3%, continued to
— remain
..i sputum positive at the
end of five years, In the incidence cases (new cases
detected bv survev)
however, there was a sizable
natural cure of 52.4% and 14.3% died. In the pre
valence cases (cases available at any given time) foll
owed up for the same period the death rate was
16.9%.
(7) Primary drug
in five years.
resistance did
not show any increase
r
■. I
46
hi
I
J
The study showed a gradual natural downward trend in
the picvalencc and incidence of the disease, specially in the
younger age-group.
1
DELHI TUBERCULOSIS SURVEY
i■ Ti •
/inroh^NeW Delhi TubcrcuIosis Centre conducted a suney
UJb,__/0\ in Delhi to study the epidemiology of tuberculosis
m an urban population with a TB control programme in
operation. A randomly selected population of nearly 30,000
was under surveillance in one of the most congested locali
ties of Delhi. z\ reasonably good domiciliary service for detec
tion and treatment of tuberculosis cases was available in the
area for the last more than 30 years. Four surveys were
of^^d 0Ut at an 1"ntcrva^
30 months during the period
■.
-I-
c1
The following were the important findings:—
if
(1) The prevalence of total active cases which was 1720
per bundled thousand population in the first survev
in 1962 came down to 880 in the fourth survey in
1970. Total bacillary cases came down from 400 per
hundred thousand population in 1962 to 210 in 1970.
Thus, picvalencc of active cases of tuberculosis was
reduced by about half.
J,
■
■
■
.'
Si1;
I
■
i
Fj
i !!
i
1
ip
ii'
1
;!■
(2) The prevalence rale increased with age. There was,
however, no difference in the prevalence rate among
males and females upto 35
"7 years
{___ of age though after
35 years there was a "steep rise in the disease
’
-2 ;amongst
males.
This w*as perhaps
because
these survevs
covered an urban population.
(3) The incidence rate of bacillary cases was about 90 per
hundred thousand population per vear and that of
total active cases 340 per year. The incidence rate
did not show any downward trend.
The study showed that iin an urban population with a
reasonably good domicilary/ senice
<
programme, there is a
reduction in the
(T prevalence
2____ L
rate of tuberculosis in a reason
ably short period of time.
i-'
I
47
1
I
MADANAPALLE TUBERCULOSIS RESEARCH PROJECT
The project was started in 1950 and comprised Madanapalle town and about 200 villages within a radius of 10 miles
with a population of 50,000. This population increased to
about 90,000 by the end of the study period. Seven surveys
were conducted in the population above five years of age with
tuberculin, X-ray and sputum examination during the period
from 1950 to 1965. Case finding, treatment, both domiciliary
and institutional, and BCG vaccination were provided to this
entire population.
. i
S
I
t
I
The following are the salient findings of the survey:
(1) The number of bacillary cases
eases which was 410 per
100,000 population at the time of the first survey in
1950-51 came down to 320 in 1957-58 and was further
reduced to 110 per 100,000 population in 1964-65.
-
,.V
b
(2) The number of cases in the male population was two
to three times more than in the female population.
(3) The prevalence rate of infectious cases increased with
age, the number of cases in males being much more
than in the females specially above 20 years of age.
(4) The incidence rate of fresh tuberculosis cases was
found to be 34 per 100,000 population and the inci
dence rate of active and
inactive but abacillary
(sputum negative)) cases was found to be 207 per
100,000 population.
i
(5) The death rate which -was about 250 per 100,000
population in 1949 in Madanapalle town came down
to about 64.1 in 1951-53 and further reduced only
to 21.1 per 100,000 population in the period 195455, thus showing a definte reduction in death rate
in the study area.
The findings of this project showed that -with a reasonably
good TB control programme in rural areas providing faci
lities of case findings, treatment and BCG vaccination, the death
rate goes down steeply and the rate of prevalence of infec
tious "cases can be reduced substantially in a reasonable period
. of time.
L
I
H
!!
I!
ri
1-
48
49
STUDY ON DIRECT BCG VACCINATION BY THE NATIONAL
TUBERCULOSIS INSTITUTE
Direct BCG vaccination is a safe procedure as it does not
' ger to the reactors
cause any unusual inconvenience or dang
and the acceptability of the programme is also not affected
in any way.
Till 1964, the conventional procedure in BCG vaccina
tion programme was to do a preliminary tuberculin test and
offer BCG only to the tuberculin negatives. This invoked two
visits to each area and other technical and operational com
plications. Offering direct BCG vaccination would simplify the
procedure and speed up coverage of the young population.
This study was, therefore, taken up by the National Tuber
culosis Institute to see if direct vaccination was safe, effective
and acceptable.
This
Tliis study
studv was
was undertaken to assess the protective value
of BCG vaccination against tuberculosis in Indian population
as a part of the Madanapalle Research Project starting from
1950.
First study: A rural population of 1891 was randomly
divided into four groups: (1) tuberculin tested and vaccinated.
(2) tested but not vaccinated, (3) not tested but vaccinated and
(4) not tested, not vaccinated and these groups were followed up
with periodical examination, tuberculin tests and X-ray for 90
days.
A total of about 21,500 persons were tested with tuber
culin. About 10,000 were found to be tuberculin positive
reactors and 11,500 non-rcactors. The non-rcactors were ran
domly divided into two groups. BCG was given to 5,069 and
5,808 were left as unvaccinated. Both the vaccinated and
control groups were followed up by periodical tuberculin test,
X-rav and sputum examination till 1967.
Results showed that local reaction at the site of vaccina
tion and regional lesion at the lymph nodes in both the tuber
culin non-rcactors and reactors was of the same order. Theje
was no evidence of existing tuberculosis disease being exacer
bated or foci of tuberculosis flaring up.
The findings of the study can be summarized as follows:
Second study:
1186 persons were both simultaneously
tuberculin tested and BCG vaccinated and were followed up
for local reaction for a month.
Local .reactions were found to be of the same order in
both the reactors and non-rcactors as in the first study.
Third study showed that local reactions after direct vacci
nation in one village did not affect the acceptability of direct
vaccination in neighbouring villages.
STUDY OF NEW DELHI TB CENTRE
In a similar study conducted by the New Delhi TB Centre
among primary school children also, it was found that direct
vaccination of reactors was innocuous.
II
MADANAPALLE BCG TRIAL
' In the first five years after vaccination, BCG was respon
sible for reduction of incidence of tuberculosis in the vacci
nated population to the extent of 60% compared to that in
the control group.
In the next five years, the reduction in incidence of tuber
culosis attributable to BCG vaccination was 56.5%.
But if the cases found within the first 1 to 11 years of
the trial that could have acquired the infection before entry
into the trial are excluded, the reduction in cases attributable
to BCG vaccination was 71.4%.
After another four years’ follow up in 1968, it was found
that in 14 years, BCG vaccination was responsible for 24%
reduction of active cases and 33% reduction of bacillary (in
fectious) cases in the vaccinated group.
Thus, it was observed that the vaccination was most effec
tive in the earlier period but gradually became less effective
in the later period because of possible waning effect of vacci
nation. The suggestion was that BCG should be used mainly
shortly before the population to be protected is exposed to
5—7 DGHS/ND/77
I
r
■
r
!
if
4- r
. ui;•L
. cl
‘
■
S4
• -'I’
■’!■
!■!
:i'
i
-
.
-xi''.;
50
SkSi'SI1“'“ n’”
CHAPTERxv
s®
’:-J-
iji
|hi
II
il
11"
1 tl
i I’
■W
fWk
k
health education
Health Education has a
hilcSnitch isP known’ today
march towards a healthiei n *_ jv of nlany of the diseases
"bout the etiology (causes and spread) o
knowleclgc t0 the
that afflict mankind, c°mrau"°nd best remains as much a
neoplc in a language they m
■ •
achieved m medical
Piem as a challenge
rhe ^“ acquired in dtagnosts
^d VSt^kwoiXes imve to be brought^ the nouce^
Sln«
.urfy popula.,™ os d.= M
“
small and as the other stu^csinhs^ir^°lt> a large scale BCG
protection from yet) goo
°cnlion Trial is being con-
SiodiXX iX«t«
I''1™"1”
tectivc value of BCG in Indian context.
.
Tnbertulods co.ul»uo “
“c ^.SlE.'« »
““ p'°-
!
buted in towns and villages m n
disease thrives on low
in the villages. TH being a co?1,r11
|iLionS| overcrowding, in
living standards, poor housi in_
ting and late detection
sanitation and nudnutrition L.ue repo
of tubcr
tubcr-.
-£££?£ra!lh”' *•*
The management of
dJ-ug^? which are remarkably
during the iast three clccn 'V bCG vaccination offers a high
effective, have been ^P'^^Xculosis. Domiciliary treatment
level of protection againstI
;)i|
ihcir doorstcps. 1 he
with potent drugs is
Nilti(,nal Tuberculosis Contiol
fundamentals that go\ ci i
prevention of development o
Programme (NTCP) alc\'rCPnot infected, and (n) detection
tuberculosis among those numbcr o£ infcctiOus cases as possible
■;. "'L
■t
<•i1
I ■-
a
it
’’■HI
:...•
■' -,;
second vaccination may
infection with tubercle bacilli and a efTect of the fust vaccibe necessary before substantial waning
nation takes place.
Other BCG trials in the world have shownl various levels
Danish School chi'dren (^8e’
of protection c.g., 96% in
*.
•
x
__
.k
A
__
82%"in Norlir American In^1^n5
in Chicago in-
I
'
The,e can be
campaign, so that factois s
tn'\r)read the disease arc o\Gr
and neglect winch C(Jntl'lbl"
a vital role in arousing
come. Health ed.uca^
£ lieeded to imbibe a positive
consciousness in the Pe P
htahh not only as freedom horn
attitude towards health z. - ^al well.being. Much of the sucdisease but as a sta u
°
£ TB patients depends on then
cess of the do^^Vav S be made aware of early signs and
co-operation, reopic
i
f
(
I
52
symptoms of tuberculosis, and on suspicion, conic forward for an
CHAPTER A’P7
k-
examination.
Role of Health 'Workers
The success of the domiciliary treatment depends, to a
Zei-vi'^selVa7mhiistZ.'^ ot druf
t3kPe prompt measures w urn. they' h. I
i.Ape-
Sd%S an urb. n -a or working, for a general
s
tors that promote "’’Xhcdisease They need also to be well^edlKhTducation skills and techniques to prove to be
effective communicators.
The multipurpose
strengthening
country and extension of case h din
hcallh
s"n’icc"Pan ckmenurv'scicniiiic knowledge of various aspects o(
senices, an cicmciua .
ni.nv;(icd to the health workers. A
wssrxn “.«b' ....... . -
“•
deal with individuals and gioups.
The workers has to have the support of ditferent inedia
to make his message effective. At present, very little inputs
Mng mU In produdus «l..C«?;.l
ail'aspects of the tuberculosis control programme.
fVith a view to meet the growing needs of educational ma
terials. the Central and State level Health Education Bureaux
are engaged in production of ‘proto-type materials, for use both
bv health workers and the lav public. With the growing literacy
level in the countrv, printed materials and other communica
tion channels like films and television hold great, potential and
—would prove highly useful to health workers in functioning
effectively.
some impoktant
National Tuberculosis Institlie,
Tuberculosis Institute '''as
The National for
the following three obp-ctisc1959 at Bangalore
■ ■ through research a pracucal, compre(i) To .............
formulate
tu
V.itv feasible
hensive and1 economically
feas Ituberculosis tpiy;
a. vell
gramme that could be applied equally
as urban parts of tlm countiy.
(ii> to .rain mrftal and
.fXX ™!ii
„ io the prograiome .o«Wo og »
effectively supervise and maintain
1 °
(iii) To undertake continuing resemeh 1,1 ““'j' l10 „lclhod
simple method
evolve the programme and outline a simp
for its assessment.
Though the objectives appear
sight, in reality they meant exterBiveejmlumol^.c.
and community behaviouia
j
concepts and aporientation of the old idcas^ Completch 1K
1
bC“aK“?b“S?lnSu...« -Uh raSa,d » M-p—
the tuberculosis problem in the countiy.
The Institute is
the Central Government
s„to.. The «al
y
GCTcraf of"
Senior scientist-' 13>
"„thrf. 1. ha. MlI”"”1"3 >nd
port facilities.
Activities of the Institute
The Institute undertakes:
<»
ESS
i
55
54
!
ot mathematical cpidemetric models
ob
servations revealing the tune-trend o ubuc dosts,
extent of infection with atypica m'cobacteria . no
Simpler and more practical methods of epidemiological
j
research.
i
!
f
t
I
I
11
i
f
!! :
I
1
(ii) Operational studies that have brought out the varpng
case-loads and case-yields inTespect of ca efindi g. tica
mtnt and BCG vaccination activities, the cost factoi.
simultaneous smallpox and BCG vaccination as p
as direct BCG vaccination, sputum microscopy a d its
operational implications, efficiency and effectnin of
the programme, etc.
(iii) Sociological and behavioural studies thtowing
the awareness of symptoms, action taking Muan fca
tion of suffering, acceptability of the prodded f. cilurc.
and the drug regimens, reasons for drug default ant
response to defaulter actions, fate of cases treated un
der the programme, etc.
(iv) Bacteriological studies centered on the Zichl-Neelscn
technique "of sputum microscopy, fluorescence microscopv, culture, cost of examinations, etc.
An animal house is under construction which will
open up research possibilities in the field of disease
caused by atypical mycobacteria.
(v) BCG studies concerned with the quality of vaccine,
technique of vaccination, assessment of the LCG vacci
nation campaign, etc.
(vi) Miscellaneous research connected
with radiological
equipment, technique of radiography, training methods
and the results achieved through programme training,
PERT-CPM of programme implementation, monitor
ing and assessment of the programme, etc.
...le has full scale involveApart from research, the Institute
as well as tubercument in training of the programme workers
\.—
’ ” i as well as other
* losis workers of other categories, from India
countries. This activity comprises the following national as well
as international training courses.
(i) Two national courses each of 13 weeks’ duration every
year for training of tuberculosis control teams in the
programme management. Each team comprises a me-
dtol
btonTon-
BCG non-medical tean>Reader.
statistical assistant. Tbe par p
(ii) TwO national.
rear for training of
dcputed by
WHQ £rom
rhe nurses arc debt .1.0 WHO. 1,™
some developing countlies.
;sors
(iii) Two
yeariubercidosis and social and prevcnt.se inedicinc.
i..-of t.
tubcrculosis
workers,
etc.
senior
ncl of State Tubcr(iv) One course every year for the person
culosis Centres.
. •
ttxhcFF sponsored international
fv'i
(v) The participants of UMLLi spongy
' ' training
• •
. -course
-........ r* ffor
r
paediatric teachers.
tvil The participants of the WHO sponsored international
( 0 training course for general epidennologists.
; of the WHO/Japan international
(vii) The participants
epidemiology/and control of tubcrculosts.
training on
’ ; from other countries visiting the
(viii) Tuberculous workers
WHO
fellowship.
institute on
Besides regular Uai.ning
serersl me-
ScS%XleT”~or“.:«» ’-i
paring for diplomas or degrees.
Achievements
—
rormulation of District Tuberculoses Prosranune: ^^
the District Tuberculosis Progranune (DT )sas o.m
the country.
*
i-
56
57 •
Research: In thv field of research, the Institute has already
conducted over 130 studies on pulmonarv tuberculosis, com
munity suffering and behaviour, BCG vaccine and the cost as
pect as well as utilisation of the provided services by the people,
efficiency of the senices, monitoring and assessment of pro. gramme objectives. Over 140 technical repons and papers have
since been published in national and international journals
and periodicals. Besides, technical innovations in the form of
a portable vaccination kit, a daylight X-rav film loading and
developing box, electric and electronic circuitary in X-ray units
and simple staining techniques have been developed. The DTP
work manuals evolved by the Institute arc in great demand in
the country as well as outside.
The supply of BCG vaccine and tuberculin dilutions be
gan in Fcbruaiv, 1949. Subsequently, the laboratory was shi tec
to its own building near the King institute and large-scale
duction of BCG vaccine and tuberculin dilutions was take
up Apart from meeting the full requirement of the countiy s
nrnss BCG programme, the laboratory
gicals to many of its neighbouring countries. It is the woilrt 3
largest BCG producing centre.
Training: In the 33 national training courses conducted
---- <o far, 433 tul>crculosis control teams have been trained, compris
ing 527 medical officers, 524 laboratory technicians, 466 statis
tical assistants as well as 107 foreign programme workers. In
the 13 training courses conducted for public health nurses 65
have been trained. The 12 seminars have attracted 230 part#
cipants so far. The training effort is generally considerably
ahead of the programme needs, after taking care of the turn
over due to retirement, etc., and the wastage.
Miscellaneous: The Institute faculty has functioned as
WHO advisers in several countries of the world, as visiting
professors on international training courses, as members on
several national and international technical committees and as
participants in the international conferences, in order to present
research papers.
BCG Vaccine Laboratory, Guindy, Madras
The Government of India felt the necessity to sponsor a
nation-wide BCG Vaccination Programme in 1948, and, to
achieve this object, Madras was chosen to house a BCG Vaccine
Laboratory, as a building constructed bv the Government of
India for the production of Yellow Fever Vaccine was available
m the King Institute Campus. At the request of the Govern
ment of India, the WHO sent Dr. Poul Lind, a Danish BCG
Expert, with all essential equipment to start the Vaccine Pro
duction Centre, and in August, 1948 the Laboratory was opened
by the then Union Health Minister, the late Rajkumari Amrit
Kaur
I
As the life of the liquid BCG Vaccine is limited and the
vaccine has to be protected from heat and ligh<wepaiation of freeze dried BCG Vaccine, which is hex. s ..b
and which can be kept for longer periods was acu eh Mt. V nh
this object a freeze-drying plant capable °f PrePa °
in
ampoules of freeze-dried vaccine in one shd
,
the year 1957. Three
Three more
more plants each capable o dmng IMO
ampoules at a time were added in Notembcr, l.( .
After netting satisfactory results from the experiments <m
the prep irition of freeze-dried vaccine, it was planned to g
i.ito' laXscT production of freeze-dried vaccine to replace
liquid vaccine in the entire programme, f
conditioned accommodation was provided, a csting and qua
lity control section was added and the required equipment
nrocurcd The production of frcczc-dricd BCG \sas cnhanc .o
to about ■> million doses and was supplied for use in the mas,
campaign in 1969.
In the Fourth Plan “Expansion of the BCG Vaccine Labo
ratory for enhancement of production of fteeze-dned bCG c
cine” was taken up as a plan scheme. A large number of techn <
and non technical"staff Ls addecL equipment was procured nd
an independent testing and quality contio LXion'd
inn- and certifying the vaccine was established at the nation.
Institute of Communicable Diseases in Delhi. The prochiction
was enhanced to 30 million doses by the end of the„ ioi> 1
Plan and liquid vaccine was entirely replaced b\ freeze-dried
wecine in the whole programme. Tuberculin dilutions veie
also prepared and supplied for diagnostic use in the country.
The WHO and UNICEF have been taking active >nlcicst in
the expansion of the laboratory so as to develop tins ^orat°U
as a rcHonal laborator}' for supply of freeze-dried BCG to th
her countries of the "region. The WHO hasi been providing
several consultants and fellowships. The UNICEF have oeen
r:
•
59
58
i
-lotherapy for the same PCI‘0^.”°t11°"]-v/o\laph\T^
reutic response in terms of osera 1 ra« o
,n th(. likelillOod
rivity closure and spucum cons
[ollow.up. Further;f relapse m a subsequent
«• 1
greater in close
riorc. the risk of contracting
th^n in those of
limilv contacts of patmnts e.i e^^ th£ mniu risk to the
oatients treated in sanaton
.
t bvforc treatment had
•ontacts was from the ,1.nfeC?°“i..^‘howed that the traditionally
regun. Thus, these studies c\ear\>sphn°.''„^elv prolonged bed-eld virtues of sanatorium trea
.
nursing and isola
test. good diet, good a.ry accomm°“-c’1U“ctJlalc cbt,no
tion, were rcmarkablv ^‘"'I’^p^^udies conducted by sevetherapy was administered. Contr°
' t anv advantage either
tai other investigators did not demon ^t^an)
of sanatorium treatment o'er c
ambulatorv chemo
ambulation. As a result of these find mgs a,
ui|)crculosis
therapv has become the accep
p •
clcvcloping
control programme in India ana
countlies of the world.
supplying equipment and necessary spare parts, etc.T ^’2. au °'
malic ampoule sealing machine procured by the UN1C • was
installed in the Laboratory in 1973.
In the Fifth Plan, the target is to double the present pro‘duction of the laboratory and further expand it if necessan.
A large part of the vaccine will be supplied in small packings
of 20 doses for use by rural health workers and institutions^ For
this, a semi-industrial type freeze drier with a capacity of b.lUU
ampoules per run has been procured by the
°j
India and has been installed in the Laboratory. The vv HO and
the UNICEF have been assisting with experts, equipments and
material. The Laboratory is also participating in the quality
control and assav of BCG vaccine produced in diflcrcnt Labo
ratories in the world under WHO auspices.
The Testing and Quality Control Laboratory at the Na
tional Institute of Communicable Diseases is also being fuither
developed.
Tuberculosis Chemotherapy Centre
The Tuberculosis Chemotherapy Centre was established
in Madras in 195G, under the joint auspices of the Indian Coun
cil of Medical Research, the World Health Organisation, the
British Medical Research Council and the Government of Tamil
Nadu as a temporary project to conduct controlled studies de
signed to provide information on domiciliary chemotherapy in
the treatment of pulmonary tuberculosis.
administration of druqs. u
,
• domicilimv condireneral police being.‘■■■P-^b u
Xlministration
tions, it might be possible to organise stij£
intcrvals e.g.,
'dru5’ * feVs ’a -sax “
The Centre has three main divisions: (/) Laboratory Divi
sion consisting of bacteriology and biochemistry sections.
(ii) Statistical Division and a Clinical division consisting of out
patient department, and (hi) Radiographic section and a ascII
organised domiciliary' service. A W.H.O. Senior Medical Officer
acted as the Director of this Centre from 19o6 to ;961. In
1964. the National Director was appointed by the Indian Coun
cil of Medical Research, and the Centre was made a permanent
establishment under the Indian Council of Medical Research.
The AVorld Health Organisation continues -to maintain active
interest in the Centre’s research work and provides expertise
___ and supplies not available in India.
Controlled studies carried out at the Tuberculosis Chemo
therapy Centre have revealed that ambulatory chemotherapy for
tuberculosis, based on a well-organised clinic service for a
year, virtually equals sanatorium treatment with the same che-
hiE?
incc or twice a
*
b
] j _ twirr a ■week
dosage isoniazid given
c!fecti;,e in the treatunder supenision "as for
g rccimcn is inexpensive
mcnt of pulmonarv tulierculo is. h tcginten
and has the advantage that the plns.cian k oi s c
gfsSsiisWsE
Sens wh^h
’
"d towards
60
61
lhe Centre also undertook studies on other chemothera
peutic regimens for treatment of tuberculosis with different
standard and reserve drugs and chemoprophylaxis studies. The
clinical studies were all supported by bacteriological and bio
chemical investigations in depth. Notable among other studies
conducted at the Centre arc studies on metabolism of anti-tuber
culosis drugs, tests for detection of anti-tuberculosis drugs in
urine, biological characteristics of Indian strains of tubercle
bacilli and the comparative studies on different measures of
msitivity of tubercle bacilli to various anti-tuberculosis drugs.
After a preliminarv feasibility study, the BCG trial xxas
started in 1968 in Chinglcput District. Tamil Nadu. A sample
survev showed that this area had
high prevalence on non
specific sensitivity as well as of pulmonary tuberculosis. The
initial examination included complete census, tuberculin tests
with PPI) S and PPD-B. vaccinations with BCG or an injection
with a placebo, examination by X-ray of persons over 1(» xcais
of age and bacteriological examination of 2
specimens of
sputum from jxnsons with X-ray abnormality. Tins phase of
the work was completed bv the end of March 1971, coxering
32 months. Of the 3.66,265 persons registered, 2,82,247 were
vaccinated with BCG or placebo.
Many of the findings of the Centre have received a world
wide acknowledgement and indeed some of them have had a
great impact on the formulation of tuberculosis control pro
grammes in Asia, .Africa, South America and some parts of
Europe. Though the main aim of the studies at this Centre is
to evolve practical and effective methods of treatment for tuber
culosis patients in India, the logical sequence of the investiga
tions undertaken, together with supporting laboratorv inxestigatwns, has resulted in invaluable knowledge of the principles of
chemotherapy. Thu Centre is recognised by the Inter University
Guard for Post-Graduate Study leading to Ph.D. degree in bac
teriology and bio-chemistry.
The training activities of the Centre include lecture de
monstrations to senior medical students, interns and post-gradu
ate medical students from the National Tuberculosis Insti
tute, Bangalore and for the International Course in Tuberculoss. In addition, two I.C.M.R. fellowships arc awaided anrally for training in the methodology of controlled clinical
ils and laboratory methods.
Tuberculosis Prevention Trial
A number of controlled
BCG trials have given very
coiflicting results. Developing countries are dependent to a
very gTxnt extent on BCG vaccination for the control of
tuberculosis, becaun* of l|lc shortfalls in diagnosis and treatmot of tuberculosis. l-bw«.. it has become essential to assess
precisely the value of BCG vacci.uMtinn jn our own context
Tlx Project Tuberculosis Trial was, therefore,1
___
___
::'trted in 1964
uliter the auspices of the ICMR,
the U.S. Public Heann
the HO.
The entire population of the area including the popula
tion examined
initiallv is under continuous
sin keill.nice.
Tuberculous patients diagnosed by the study teams arc Ixiing
treated on domiciliary basis.
Aboht 2A months after the vaccination a random sample
of the vaccinated population was retested with tuberculin and
was also examined for BCG scars.
It was found that 0.4%
and (>.0^ of those vaccinated with the strong and weak doses
of vaccine rvspcctivelv had no scars and 2./% of those injected
with placebo had scars. Among children aged (M l) years and
leading with induration measuring (0-/) mm to the tuberculin
test the mean size of post-vaccinalion allergy was found to be
16.8 mm for the strong vaccine and 12.8 mm for the weak
vaccine. In the same group the mean size of scar was 5.2 mm
for the strong vaccine and 3.4 mm for the weak vaccine.
Other .Activities of the Project
Tuberculin testing of samples of population in certain
aieas of North India' with PPD-S and PPD-B, was done to
as<cs< prevalence of non-specific sensitivity. It has been found
that onlv the hills of the Uttar Pradesh, Kashmir Valley and
Himachal Pradesh have verv much lower prevalence of non
specific sensitivitv. It has been found that thc’Nilgiri hills also
have a iow prevalence of non-specific sensitivity. The study
suggested
that mm-specific sensitivitv was associated
with
altitude and not with the geographical location of the area.
Retesting of random samples of the TB Prevention Trial
population with tuberculin was carried out at 2A years and
€'mr vears after the initial examination. It was observed that
63
62
three months to —A
post-vaccination allergv had waned from
further waning from 2| years to
years and that there was no
4 years.
significance of this waning is not
. The reason for or the
clear.
to have gone
The prevalence of infection does not seem
clown at four years.
BCG in the prevenupn of
A Trial for the ‘•alue of
So far, about 2.;)-.000
Leprosy was started from October, 1973.about 1.73,000 persons
---- registered. and well as suspicious cases c.
of
persons have IIkcu
examined. About 9OTe definite as
leprosy have been diagnosed so far.
tar.
tuberculosis patients
The effect of BCG vaccination on
1..J been studied. Long term
and tuberculin positive children ofhas15 L—
■
months
in patients and
follow-up results over a period c. -: BCG vaccination
over 2A vears in clnlcren have shown th.
of pulmonary tubcrdid not’ increase mortality among Pat*^ );•„ in
* i children or
culosis or among strong reactors o uocrct 1 n i It can safely
bacteriological breakdown rates of st sp< t ca* ; :: that BCG
be concluded that the data studted don°l ......
su o children did
vaccination of patients or strong rca^rblc when
° '
any harm of the kinc considered possible ....... -direct BCG
vaccination was initiated.
Results of the Main Study
tuberculosis only among those
BCG can
wu protect against
Or the total numlxr of
who arc non-rcactors to tubeic llin‘
havc developed
of
tuberculosis
new culture positive cases Ou tu ici
among ibis
that adequate
negatives
a.
“s”'’ so
” ““
be
studied.
protective effect of BCG can
State TB Training Sr Demonstration Centres
New Delhi TB Centre
The Ne’.x Delhi Tub- rc<. .
wJo‘- " ’ known as
is Cenue, originallv
T-hed by “the Tuber- '
G; •
.. Lite
. ■ iai .<of ) t.iiia ;
as I rainiu“ ^7'
country to be upgrade;! from the Goverumcnt of Incaa, the
in 1951 with assistance
AV H.O. and the UNICEF. R«e^ch traini"5^emce to^TB
patients have been the mam f
own domiclliary
clinical sectton, patients
^‘°n?on0o£ about 8 lakhs and also
treatment area coveting a p p
from neighbouring States
patients from other a.ieas
numbers. Care committees have
Svail of the ^rvices in large nun
locaiities in its
SAw •-««—* ““ ““ p“
of patients.
Research in various asPe^
^^fficiency^f dotnicirespect of methods anmng to. impro
o£ l)ie
n
linry management and case Ending
o[
,tleof cp
cpidcfunltions obf the Centre. Sev 1 stud
in
ucc
miology and time trend o
by fhe Centre. Fhe
vaccination, etc., hate
international cooperative
Centre has participa «l n sc'cr
luberculosis and in
studies in respect of van0
■
bv the I.C.M.R.
several other cooperative stud cs
Ccntr(. 0
More than 100 papers based
eP
presented at naiional
national
in medical jour-
sss sw-i
i
TraintnS oi v.riou.
personnel has been one
include students for D.EC.D.
Centre since its >nccP“°nf' Tl'edSC * tgradaute medical students,
course and under-gradu^
^-^.culosis Health Visitors,
Para-medical workers inc‘l
radio<rraphers, laboratory techmnurses, medical social
refresher courses are
cians, BCG_ tcch"‘cl‘'1' ’
The Centre is running three
Oi Mh‘-
S
i
-o
TR Outre is located in this Ccn-
The
..
«d»tol saltoc. and
tie and
Diwctor
“
f
the
Centre.
of '
1•
j ju: Iml’. of
of the
the running expenditure of tl
provided by the Government (
^enciesniikc It-.’ubcrculosis
k.rrninck Association of: India
Association and certain statutory local bod. ‘"gani^uon also contribute toward: •
tutions.
- w Delhi
i;i. Other
• - e TB
insti-
i
65
64
TB Training & Demonstration Centre, BanLady Willingdon
galore
Starting as a Tuberculosis dispensary in 1936, the Lady
WilHn-dont’TB Training K Demonstrat.on Centre, Bangaloie
Ls ungraded to i training and demonstration centre fm
'^Rso^awataka State) in" 196(1 It runs a mode 1 disme
TB programme in the State. It has one mobile X-ray unit
and culture and sensitivity testing facilities.
State Training & Demonstration Centre, Trivandrum
The State Training and Demonstration Centre. Trivand
rum established in 1951, is one of the first three institutions
of-the country run as Training and Demonstration Centres
jointly bv the W.H.O., Government of India and the State
Government. Several WHO experts were associated with this
Centre in the earlv years. The routine activities of the Centre
are case detection, organisation of
domicilian treatm
,
health education and participation in certain epidemiological
studies. The Centre participated m the National Tuberculosis
Sample Survey. It started working on lines of the National TB
Control Programme from 1st of April, 1964. It runs a mo e
district TB
programme apart from arranging training for
various medical and para-medical workers. From 2 April. 196S,
the Training and Demonstration Centre was re-designated as
the State TB Centre for Kerala State to discharge duties and
responsibilities envisaged in the National TB programme.
X. cE e
BCG mh'nicim, and TB heahh vi«»r. and
In .he .eeea.ch and field dnd.e, at .he S-T.L
The N.T.I. has also been undertaking a pilot project of
urban TB programme in the city of Bangaloie.
TB Training & Demonstration Centre, Ahmcdabad
TB Training & Demonstration Centre, Patna
The TB Training & Demonstration Centre. Ahmcdabad
in Gui iri was established in 1961.
Iniually it functioned
in a sm-di building but in 1972 it was shifted to Hs new commodious building.
Tr-iinincr is inven to BCG technicians, health visitors,
sanitary inXctoi^s, public health
medical students,
health nurses,
nurses.
medical officers of the State Government health semce, tuberculosi; medical officers and students of post-graduate courses
courses in
in
The TB Training
Demonstration Centre. Patna was
established in 1951 as a joint venture of the WHO. Govern
ment of India and the State Government of Bihar. In Jub,
1059, the Centre was upgraded as Training L* Demonstration
Centre for the State of Bihar and the Centre established several
sub-centres to undertake the pilot project schemes for domiciliarv treatment within the corporation area of Patna.
I his
Centre has the following sections: Epidemiological Section
comprising X-rav and BCG Section, Laboratory Section, Clini
cal Section. Domiciliary Section and Health Education and
Rehabilitation Scheme.' It has indoor beds a Chest Surgipil
Unit. It runs a model district TB programme m Patna district.
tuberculosis.
model district TB programme for the State.
It runs a
’: and participates m research activities
It has a mobile X-ray unit
workers, etc.
like periodical survey in
L. textile
.
The Centre provides training to under-graduate and post
graduate students of Patna Medical College.
Besides, the
Centre also imparts training to para-medical staff, health visi
tors. laboratory technicians. X-ray technicians, BCG technicians
and nurses.
State TB Training & Demonstration Centre, Agra
The State TB Training & Demonstration Centre, Agra
is meant for the State of Uttar Pradesh having a P°P“lat10^
of 90 million
It started functioning m 1963. It is one or
the la^e Training 8= Demonstration Centres in the coun
try
There are about 21 different sections and during rhe
lalt 13 years, more than 3,00,000 persons have been taken up
' for investigations, diagnosis, treatment and follow-up.
The Centre participated in the National Sample Survey
It has been taking part in different research acti
in 1955-58.
vities in respect of tuberculosis.
I
67
66
Training in Tuberculosis is imparted to medical and para
medical personnel including interns and TB health visitors.
The centre is recognised by the University of Agra for M.D.
in Tuberculosis.
The centre has been participating in chemotherapy trials
and has been conducting non-specific sensitivity and other suiveys in the area. It has contributed several scientific papeis
in manv international and national conferences.
State TB & Demonstration Centie, Patiala
TB and Demonstration Centre. Patiala was
The State
TB Clinic in 1958. It was upgraded to i Trainestablished as a
Demonstration Centre in 1966. It has epidemiological,
in g
1
laboratorv. statistical, radiological, treatment and BCG sections
apart
an out-patient
out-patient depaitment
department and m-door wards. It
apart from
from an
apart
noui
a
, t..... ...
modeJ dlstrict TB proalso has a surgical section. It runs a ---- - .
.. ,
gramme for the State. All necessary facilities being JwaiUMe.
all around, including adjacent
the Centre attracts patients 1from
----- ------States.
Kamla Nehru State TB and Demonstration Centie, Ajmci
The Kamala Nehru State TB and Demonstration Centre.
Ajmer, Rajasthan was established on 1 January, 1964.
It
runs a model district TB programme and has the following
Sections: Statistical section, Treatment section, X-ray section.
Laboratorv section, BCG section and 1 raining section.
I
I
miniature radiographic camps.
Training is imparted1 to TB health visitors. BCG techniand
medical students from ...
medical
...... ..........
cians and also interns a
college. Mobile X-rav and sputum culture and sensitivity
test facilities arc available.
The staff of the centre has contributed several scientific
papers in national conferences.
This
drug trials conducted
This centre
centre has
has participated
participated in
m the
t
72 and
,2 is undertaking
’ --1 :- j a study on the
by the I.C.M.R. in ATS
1969-72
prevalence and incidence of Pulmonary 4^ uberculosis among
mica mine workers of Rajasthan.
The TB Training
Demonstration Centre Srinagar was
n. a TB clinic in 1969. which was later upgraded
to ^Trainin"- L Demonstration Centre for the State of .fam1™
< Kashmir ° Facilities exist for X-rav. domiciliary treatmen
programme, laboratorv services, culture and sensitivity test I
TB controltraprogramme
in thestudents
distnct or
Xr nJctrirt
?tX undertakes
Pin^g of medical
Tram-
Training 5c Demonstration Centre, Cuttack
g
Trainin- is imparted to TB health visitors, medical nterns
sanitan inspectors.
nursing students.
basic health
workers medical practitioners of other systems of medic me
laboratorv technicians, etc., and the Centre organises lericshc
courses also
Under the intensive health scheme of the State
Health Department, the Centre is organismg several mass
The Training 5c Demonstration Centre. Cuttack was devcloped by
bv upgrading the Chest clinic of S.C.B. Medical College
loped
Hospital in Cuttack in Jtily. 1964.
It runs a Tuberculosis
control programme for the Cuttack District and trains medi
cal and para-medical personnel of the State. The following
categories of persons are trained in the centre: Health Visi
tors laboratory technicians, radiographers, under-graduate stu
dents of medical college, house surgeons, post-graduate students
of both diploma and degree courses or TB and Chest diseases
and post-graduate students of other departments like medicine,
social and preventive medicine, pathology’, etc.
It has also
TB beds and a thoracic surgery unit attached to it, and func
tions as a referral hospital for the entire State.
TB Training & Demonstration Centre, Shri Nagar
ina is triven to BCG technicians and other para-medical <.ss .
"ms and basic health workers. It also undertakes onentation
course for medical officers of the State health services.
— -r,
------ - anj certain
Assessment of District TB Programmes
by the Centre.
search activities are also
a— undertaken
----
rc-
Training & Demonstration Centre, Bhopal
______
x I was
The Training & Demonstration Centre^
Bhopal
State"TB Centre for Madhya Pradesh.
established in 1972 as a S---- --
: ■' r
VHAI JLIBRARY
I
DUE DATE SLIP
68
Author:
The Centre is organising a model district TB programme lor
I
<ollro-cs TB health visitors, nurses, bCG technicians, etc.,
•
been° ot’ganised. Additional accommodatton and ^teequ pment fo? developing this Centre into a full-fledged State IB
Centre are under way.
!
''
j
«•
!
■
I
Published by Central Health Education Bureau, Directorate
General of Healthy Scmces,_Kotla Road, New Delhi-110002.
o/
I
%
VHAI LIBRARY
U? l|
1
'X.
!
MGIPCBE—
1
■
s’
I
<78—5,000.
ri •
Class No.:
Title : TTXl^lcccCc’SuS -
Acc. No.: 3A'3C'/
Borrower's Name
Due and Returned
Date
I3 - X->
,
,
'■
1
■'
I
%
Y
I
I
TUBERCULOSIS
IN
INDIA
J( :•
j
■
■
-■
«
Jg»|:
I
W <■
by
Dr. B. N. M. Bar hl
Adviscr-in-Tubcrculr.x,:
Government of India
'
■
Directorate General of Health Services
New Dclhi-110011.
■■" IhjFOF’M’A I 10k 1AWhT-vCJA--wnAilON
B
O®'<
c 1
Vchmt.uv tU.M AUcc^i-. H India . .
-A^a. --F-; CI lU*
■
C- ■• V- T:^- D
Nev. Dclm-iivXCe.
Ir
W' /
A
t'cn c/
A'-'
tM
....
■
.^DIRECTORATE GENERAL OF HEALTH SERVICES
KOTLA ROAD, TEMPLE LANE
NEW DELHI—110002
■
■w '-U '
A
CENTRAL HEALTH EDUCATION BUREAU
■
3
§
i
CENTRAL HEALTH EDUCATION BUREAU ..A
DIRECTORATE GENERAL OF DEA: TH SERVICES
MINISTRY OF HEALTH & FAMILY WELFARE
GOVERNMENT OF INI YA
NEW DELHI
■
1
CONTENTS
Pages
Foreword
(i)
Introduction
(iii)
Chapter I
The Problem
1
Chapter II
Early Attempts
5
Chapter III
Tuberculosis Association of India
9
Chapter IV
Bhore Committee’s Assessment
14
and Recommendations
Chapter V
Position at the time of Independence
16
Chapter VI
First Five Year Plan
18
Chapter VII
Second Five Year Plan
21
Chapter VIII
Third Five Year Plan
23
Chapter IX
Fourth Five Year Plan
26
Chapter X
Fifth Five Year Plan
29
Chapter XI
National Tuberculosis Programme
31
Chapter XII
District Tuberculosis Programme
33
Chapter XIII
Present Status of the Programme
36
Chapter XIV
Research
39
Chapter XV
Health Education
51
Chapter XVI
Some Important Tuberculosis
Institutions
53
j
1
f
1
_____ i
lAcccs-i^^j'
|Cai: Nn
FOREWORD
-
Phis book is a comprehensive presentation of the facts
about development of tuberculosis movement in the countrv
and the details of the various aspects of
the Tulicrculosis
Control Programme.
activities taken up by the Government in the various
plan periods, the concept and organisation of the National
Tuberculosis
significant research
Tuberculosis Programme
Programme1 and
and the
the various
various significant
studies conducted in India that have contributed new knowledge
in the field of tuberculosis control and have formed the basis
of our community wide Tuberculosis
~~
Tuberculosis Control Programme, also
have been highlighted.
Tuberculosis is a major public health problem in the
country, 1 he tools for diagnosis of the cases, effective medicine for their treatment and BCG» vaccination for protection
of infants and children arc
- - available and have been provided
freely in the National I uberculosis Control Programme.
It
is only with the concerted efforts of the Government, the volun
tary organisations and the community that the programme can
succeed and the problem of tuberculosis can be tackled.
I
I hojx? the readers will find this book interesting and
useful in having an insight to the problem and the efforts
being made to deal with it under the National Tuberculosis
Programme.
New Delhi
28-1-77.
I
F
Dr. P. P. GOEL
Director General of Health Services
Vr "
I
lAccesion
(Call No
INTRODUCTION
Tuberculosis has been known to mankind since the dawn
of history.
From the mummified bodies, engravings and
paintings in Egypt, scriptures and literatures from Babvlonia
and China, literatures from the ancient civilisations of Greece,
Persia and Macedonia and the Vedas and other Sanskrit lite
ratures of India, it is evident that these ancient civilisations
knew tuljerculosis as a health hazard even 4000 to 5000 vears
before the birth of Christ. A hymn is consecrated to the cure
of ‘Yakshma’ in Rig Veda which is dated as about 2000 B.C.
Charak and Susruta in 600 B.C. referred to tuberculosis as verv
difficult to cure.
Hipprocrates (460-377 B.C.), the father of
modern medicine opined that attention to the tuberculosis
patients was a waste of time and that they were a burden
to the State.
However, till about the beginning of the 19th century,
nothing much was known about the cause or cure of the
disease. Tuberculosis was known as consumption, white
plague, Kings evil and phthisis.
It was mostly considered
as an incurable disease.
i.
r
From the beginning of the 19th century, new knowledge
started to gather.
Laennec, himself a consumptive, invented
stethcscopc in 1819 and described ‘auscultation’ bv use of the
stcthcscopc.
Villemin in 1868 demonstrated that tuberculosis
Had to be due to a specific agent, but it was Robert Koch
•
C \h5 cpoch makinS discovery of the tubercle bacillus
in lHb£.
X-rays were discovered in 1895 bv Prof. Roentgen
■„llICm^ainC1aVJa,,.ablc for cIinical use in 1904.
\’on Perquet
in J JO/ described uitra dermal tuberculin skin test. Calmette
and Gucrine in 1922 discovered BCG vaccine which is now
extensively used as a protective measure.
However, specific treatment for tuberculosis bv drugs that
could kill or inhibit the tubercle bacilli was not known till the
ew era of chemotherapy in tuberculosis began in 1944, with
w\C Cl1^OvcrJ ?f Streptomycin bv Bugie and Walksman. This
was followed by discovery of other potent anti-TB drugs like
codn^tr^ h
m aKd
Lehmann in 1946 and^sonicotinic acid hydrazide by Grunberg et al in 1951.
Several
very potent anti-TB drugs became available by about the
(iv)
Vr
Acccs ■
:
CaB No
ii
ii i
middle of the jpresent century and thus effective treatment
of tiilierculosis became possible revolutionising
o the whole• con
cept of treatment and care of the tuberculosis.
Tulien ulosis is a peculiar disease in the sense that it is
of a chronic nature, the causative germ is more or less ubiqintous
and easih infects
( " the
'
•
’ - most of
people and vet a few
suffer from the disease.
fSymptoms may simulate many other
diseases. Diagnosis of a case requires
i
special techniques and
treatment of a
patient
requires special1
drugs
for
a
long duration.
Like any other infectious disease,
tubcrculosis also comes in
j
T e
epidemics
but unlike other diseases, the
secular epidemic curve* in tuberculosis lasts for decade?"if
not
centuries.
However, we have the knowledge and the means to detect
tuberculosis cases and to treat them effectively. It is possible to
cine a patient of tuberculosis. It is also possible to prevent
spread of the disease and to protect the uninfected from in
fection by I B germs. Tuberculosis control programmes have,
therefore, been organised in all parts of the world and many
developed countries have been able to bring down the problem
considerably.
1
In India as in other countries, fight against tuberculosis
has been a very long battle. Several eminent scientists, philan
thropists, private individuals, non-official organisations apart
from the government have contributed largclv in the battle
against tuberculosis in India.
'd
CHAPTER I
THE PROBLEM
Tuberculosis in I..d.\.
India began to engage atten hm as a
public health problem from the? carb
years of thi- centurv.
In 1910, Sir Pardey Lukis, the ithen Director-General of
Inuian Medical Services pointed out to t
the Govern men t of
inaia that Tuberculosis was fast spreading and it'called^ for
conceited countrywide control measures.
The conferences of sanitary officials of India in the Xon'i
and in the South in 1912 and 1911 exprosed the need tor pro
pel investigation about the spread of tuberculosis n. ufban
areas and from there to the rural areas.
As a result the Government of India appointed
Dr
nrobleS>Cr- ‘"I 914 tO '"akC
Cll<luiry i"to the Tulxrculosis
problem tn the country.
After his enquire durin- I'U-LIt;
vas^hrnihmk0^0!"61115^" that
Prc':,le,’« <’f ‘^rculosis’
was alarmingly high in the country, that during the preccdin"
oyv years even in areas that were considerecf as
'oif
the population has become considerably infected In tuber
culosis and that with development of commerce and induce
and establishment of communication, the prevalence was in
creasing in the towns and cities and spreading to the villages.
Several important studies in the field of tuberculosis epi
demiology. control and treatment have been undertaken in
India, the findings of which have been widely acclaimed all
over the world.
Based on those findings, a scientifically sound
and operationally
feasible tuberculosis control programme
which is within our resources has been evolved and is being
implemented in our country.
t J101? • a Sen€raI impression as wa< formed
j.La,lkas^r after h,s investigation and that of manv other
and 1 ’t WO1pk11^ in the flcld of tuberculosis, the exact size
and extent of the problem of tuberculosis in India was not
known as reliable statistics were not available.
The purpose of this book is to give an idea of the nature
and magnitude of the problem of tuberculosis in the country
and to review the work done so far for tackling the problem.
The main methods bv which the size and extent
of
the problem of tuberculosis' could be ascertained
arc: —
(1) Deaths from tuberculosis.
(2) Prevalence of the disease i.e. patients sufferin'^ from
the disease as ascertained by morbidity surveys.^
(3) Infection rate i.e., persons who have been infected
by tubercle bacilli and therefore are likelv to fall a
prey to the disease.
• t0 tali a
2—7 DGHS/ND/77
VF |
2
3
f—
’Acccsior
jOH No
Deaths from Tuberculosis
Xo reliable information about deaths from tuberculosis
was available as vital statistical information even in towns and
cities was not complete.
Mostly information about deaths
from various diseases had to come from inexperienced Govern
ment officials, who in their turn relied on the neighbours or
relations of the. deceased.
Causes of death were grouped
under a few broad groups like fevers, dvsenterv and diarrhoea,
icspiratory diseases and other causes, and tuberculosis could
have been included in any of these broad groups according
to the predominant symptom which the patient presented.
Sir Leonard Rodgers in an investigation estimated that
9% of those classified as dying of fever died of tuberculosis. A
similar analysis of the figures for Cossipore near Calcutta
showed a mortality (from tuberculosis) of 2.68 jxn- thousand.
Of the total deaths. 7.9% were due to tuberculosis. z\t about
the time of the First World War, Sir Leonard Rodgers analvsed the post-mortem figures for Calcutta for over 22 veais
and found that no fewer than 17% of the total deaths’ had
been due to tuberculosis. Since at about that lime (1911 —
1921), the crude mortality was 17 per 1000, the tuberculosis
morbidity could l>e computed at eight per 1000.
Vital statis
tical information from cities collected by Dr. Lankaster for
his book Tuberculosis in India (1920) showed that tuber
culosis deaths in Calcutta were 2.1; Bombay, 2.83; Madras.
2.5; and Ahmedabad 5.9 per thousand in 1919. He thought
that actual rate was 4 per thousand or more in most cities.
However, most often these were under-estimates because in a
large number of cases, the cause of death as tuberculosis could
not be established.
Frimodt-Moller (1949) and Me. Dougal (1950) estimated
TB deaths in India as 263 and 200 per 100,000 with rigorus
control measures- tapplied
x
to the study population.
FrimodtMoller reported death from tuberculosis to be 64.1 /100,000
in 1952 and 21.1 in 1955.
o.
Recent estimate of the____
longitudinal survey of the National TB Institute (1968) is 100 per
100,000 in an area where no control measures have been applied.
Alorbidity Surveys
In the earlier part only small studies limited to small population gioups in different areas were undertaken bv different
workers.
r
Dr Benjamin in 1933 found 2.6% to be the nrcvalence
rate of tuberculosis
I ->1 in iou
'J
j?, the suburbs of Madras.
Dr.
Lal in 19-14 calculated a morbidity of 7% in West Bemml Dr
Sikand and Dr Raj Narain in 1952 found 1.8%, Dr" Phillip
in Madras m 1952 found 2.5- and Dr. Hertzber" inTrivam
diiim found l.h‘„ to be the morbidity rate for tuberculosis Dr
Sikand and Dr. Raj N’arain in 1952 indicated 1.36% to be the
moibiditv rate of tuberculosis among
displaced "persons
in
among displaced
persons in
Fandabad.
In Madanapalle, a survey by Dr. Frimodt-Moller
survey by Dr. Frimodt-Moller
snowed a morbidity of 1.6% in the [own and 0.42% in ti e
adjoining villages in 1949.
1949. During
During 1952-53,
1952-53, an
X-ra? sir
an X-rav
bdi tv ofo';?"" TheSlnd,l1 Ce,n?10yccs in Dclhi Sho"-«I a morOKiitt ot 0./ / 0■. The
I he Sample Survey in 1955 hi
in a small nomilanon in Ambur in
m South India showed a morbidity of 1.4%.'
All these small survevs
tu '
•>n impression that millions
would be suffering from the disease
i both urban and rural
------- c in
areas and it was felt neccssarv co have
a precise estimate of
the morbidity of the disease in the country as a whole.
X-rav cases and 0.4% bacteriologfcally confirmed X°s tuur'this
xx
teni
Delhi (1960),
also
p!
<
Tuberculin Test
be o^ed^X’v^
w the country.
All these findings give an idea that the death rate due to
tuberculosis was very high some decades back and continues
to be high even now, though it is progressively going down '
in recent years.
Tumkur^GO)Xd BanX'XeuXf
confirmed the finding ofX XatiotS Sarnie SurX
Tuberculin tesu done by n" WU ,“19^
and 69.9% above that age
V? S
°f
rural South India noted tuberculin positive reaction T l’"
8.^% in vtllages and 11.6% in small towns amongXie und^r
J
if
V r ■’
4
Accesio^l
Cal! No
' li
'
k> years of age and in a suburb of Madras he found a i
positive
reaction in 41 2% below 15 years of age and 69.8% above 15
Dr%Q?J in 19I4 m Bcnoal founcI infection rate to be
high as 88 ;c in urban areas and 32% in rural areas.
RrrTAlberCUl,n teSting conducted in connection with the mass
bLG Campaign in the earlier phase of the programme showed
-nation ramto be in the range of 19% in (j.G ?ears age^
.'ndcXt!1C
'ears a8e-gronp, 63% in the 15-2-1 age-group
a d 83% in the age-group above 25 rears.
The average for
culos?s w\aS ab0Ut
Contlarv to Ol11' belief that 'tuber
than
/n hCa|ra,Or1Pr°b ein T thc dtics and to""s rather
nan in the villages, the tuberculin test results of thc mass BCG
samTXr •°Ued-that infCC,i°n ratC "as ”1°re
l«s of die
tXrcThTs ‘d.TT^' t0"'nS a>nd ViIlageS "hich ■■'dicated that
lUKiculosis disease was perhaps equally prevalent in bnrh
bv^hrV^F11^ ?rC;lS’ ThlS Presu,nPlion was later confirmed
h' thc findings of thc National Sample Survey.
Estimated size of the problem
From thc rrecent
------ studies and observations it can
lx.- cstimated that a little
”11 t°Vcr
t^ci3otaI population of
.......the
e country
consists of reactors to tuberculin
...h.i apparentlv
I,because of 111"
Al
,
inlection by tubercle bacilli,
At /I,,c r‘?fe of 1.8% there should
lx: about nine million persons -having radiologic'dl
‘berculos.s disease ami tibout a quarmr of Tern ev active
abom
about a quarter of them i.e., about
t"o million, arc infectious. c.\cr.-‘-*
’
'
a )out
excreting tubercle bacilli in then
sputum and most of them have
symptoms.
The death rate
i^nnnnllb€rcilIosis is estimated to be about 80 to JOO per
100
Hi .ih)() population per year.
CHAPTER H
EARLY ATTEMPTS
ness 'ofT.I^-r =r!!du.ally increasing awareness of the seriousi e.s of tuberculosis in the countn. attempts also be"nn to
prese'nt centurv "‘in ‘Jh P'’0','""
the
‘>>e
p X.
century.
In the earlier stages, however the mea
sures were not organised and the procress was slow
This was
mainJy because the exact size Ind' nature of the prlbllm
'as not known and no preventive or reallv effective treat
/neasures were yet known to the profession.
Open "dr
treatment had been gaming popularity in the West but this
r
be done for
hospitals in T r
XCr\ hnnted bed accommodation
in
|
ln India for tuberculosis, it was not possible to
ilie l‘lC?‘fnC<?C faSeS °f tllL>ercuIosis patients who miUt occupy
the beds for a long time and in the end might succumb To ihe
disease.
Attention was
"as gradually
gradually diverted
diverted tv, establishment
of
tuberculosis dispensaries for treatment to^
of
t‘
-the tulx-rcuious
and organisation
organisauon of societies and associations nntnlv
-..... -..s niainlv
promote health education about the causes of tuberculosis and
Its prexcntion and to organise care of the sick.
A. Open Air Sanatoria
I. Private Enterprise
lion ° OtheT'f6 CaSCS r°f tuberculosis was a form of prevenn inH
f?rmS of P^'ention were not in the public
ruhz> a]S '•eL
1° SCV€ral ’^stances, it was the discoverv of
Other countries.
I
sh f d the experience of
(/) Christian Missions: The first
open-air sanatorium
for isolation and treatment of
tuberculosis patients was
founded in 1906 in Tilaunia, near
Ajmer, by a Christian
f.
i
I
t
I
Vr
6
Acccs-in
|Cal! No
'e
Mission.
IIt was intended mainly for girls from schools and
orphanages connected with this mission" in North India,.An
institution in Alniora in the Himalavas for tuberculous women
was also started by a Christian Mission ...
in 1908 and about
the same time a small
s
sanatorium for women and girls at
Pendra Road in the- Central
Provinces
2L....... 1 r...(now
Madhya Pradesh)
was also started.
7
first one opened was in
Bombay in
connection with the
Bombay Anti-Tuberculosis League.
In Madras, the King
Edward Memorial Institute (now called the Tuberculosis
Institute) was established in 1917 by the efforts of the late
Dr. P. S. Chandrasekara Aiyar.
C. Pre\'e.\tiox and Health Education
In South India. Dr. Louisa Hart, a Missionarv working
in Madanapalle was treating a number of tuberculosis patients
in temporary buildings in her general hospital for a number
of years. After the Union Mission Tuberculosis Sanatorium
was founded in Madanapalle in 1912. this sanatorium took
over the patients of Dr. Hart and had them transferred to
the permanent buildings at Arogyavaram in 1915.
I
(o') Private Societies: The first Sanatorium outside Chris
tian auspices was opened in 1909 ar Dharampore in Simla
Hills, due to the benefactions of some Bombav. philanthropists,
mainly Parsis. and under the management of the Consumptives
Homes Socictv of Bombav.
II. Under Government Supervision
'I he first sanatorium started under Government super vision
was the King Edward Sanatorium at Bhowali. Uttar Pradesh
opened in 1912. with money collected in that province
in
memory of King Edward VII.
III. Individual Effort
An instance of a sanatorium established bv a private indi
vidual is one which was opened in 1912 bv Dr. R. B. Billiinoria in Poona and which two years later moved to its present
site in Panchgani, Maharashtra State.
Other sanatoria started about this time were the “Turner"
Sanatorium in Bombay—Dr. Turner was Medical Officer of
Health, Bombay—and a Sanatorium at Dcolai built from a
bequest by a private individual, Seth Bhagwandas Narotamdas.
B. Tuberculosis Dispensaries
J
I
J
The opening of tuberculosis dispensaries on the
lines
of Sii Robeit Phillip, which had a large part in the campaiem
against the disease in the A Vest, started somewhat
somewhat later.
later. The'
(z) Anti-Tuberculosis Leagues:
A number of anti-tuberculosis societies were formed in Bombay, Lucknow and Ajmer
about the time of the First World War. The main object ot
these societies was educative propaganda about the causes and
prevention of tuberculosis.
(u) The Bengal Tuberculosis Association:
Through the
inspiration and pioneering efforts of some Missionary groups
in Bengal, the Tuberculosis .Association of Bengal \was
.... estab.
lished in Calcutta in 1929.
This organisation carried out
fairly extensive propaganda in favour of concerned action
against tuberculosis.
In spite of the growing attention paid to the tuberculosis
problem, by 1935 there were only about 6,000 beds available
in the whole of India, which then included what arc now
Bangladesh and Pakistan, for the treatment of tuberculosa
patients.
(iii) Tuberculosis Association of India: As a result of
public opinion gathering strength demanding action to deal
with the increasing menace of tuberculosis, the first concerted
effort iwas made through the organisation of the King George
V Thanksgiving
—Fund
" -1 in 1929. TWith
*T- ’. the
T. funds
L. ’ raised
’ ’ bv
"
u _ ___
• .•
«
this organisation, the Tuberculosis Association of India was
established in February, 1939. Its organisation and activities
are discussed in die next chapter.
(iv) Methods of Treatment in early stages:
The main
line of treatment
advocated
—--------- was < x open air and dry climate and
good food.
Patients who were not too sick to move about
were usually advised to go to a c._
dry climate and take plentv
of exericse for improving their appetite; feeding or overfeeding
of patients was the general rule.
Tuberculin was extensively used between the years 1910
and 1920.
Sodium Morrhuate which was being advocated
for leprosy was also extensivelv used in India for tuberculosis.
—
I
V i- .v'
8
----- 7
|Cai: No
From 1925 onwards ^•nuKrvsin and other gold preparations
came into vogue,
Artificial pneumothorax was introduced
in 1921 bv Dr. Johannes
[
Gravesen of Denmark who
was
associated with the Unioni Mi.
Mission Tuberculosis Sanatorium,
Thoracoscopy and cauterisation of adhesions were started in
the same Institution in 1931 and crraduall
these operations
CHAP TER HI
TUBERCULOSIS ASSOCIATION
OF INDIA
t
c19a/’ Lady LinIithgow, wife cl
;1V1 Viceroy
v..
of, tlie Uthen
of
India, after an appraisal of the Tuberculosis problem i
in
India
issued an appeal for funds to establish aii
anti-tuberculosis
association in India. The Association \\ as to consist
of a central body supported by provincial and State organisations as
amliates of the Central body In
sum of Rs. 85 lakhs was collected. response to her appeal, a
After returning 95% to
States and provinces for i
maintenance of clinics and where
possible of sanatoria and after-care settlements*
, the balance
c\as retained for the Tuberculosis Association
*
’
of India. To
this was added direct donations
and the corpus of the King
George Thanksgiving Fund and uw i uncrciUosis A
the , I ubercuiosis Association
of Indm was established in Delhi under the Societies
23 Fcbruarv
February, 1939.
Rcoistiat on Act of 1860 on 23
lO‘io
At that stage, it was assumed that all infectious tuherulosis patients would need hospitalisation, as
uas the onIv recognised form of treatment, > hospitalisation
one of all infectious patients would have < Hospitalisation
cost about Rs.
crores,
crores, in addition to the enormous capital outlay ininvolved in the construction of buildings for hospitals' and
sanatoria, vet it was realised that this could touch only a fringe
of the problem,
\ new vision and an entirely new strategy
was called for.
The main activities of the Association
arc
below:
summarised
^ew Delhi TB Centre
ser\c as a model institution for "iorganised home
ment” of
tuberculnsis
.1Vi urganiseu nome treat
tuberculosis,, ib,.
the * Association
Association
heln nc -rtuL>clcu,osls
the
established with
the
India, the New Delhi 4'B
a few voluntaiy Care and
Committees were formed
d to
to assist
assist the
the X™
New DeHn
Delhii ’
requirements
patients The New
Delhi TB Clinic i'^nients of patients.
upgraded
in 1951
as a “
stration Centre wTdiTl
eh/of
^hVco
Training & DcmonWHO and UNICEF? Su^entl
Subsequently,
f
’
---- ....J today this Centre is
e country.
a.
TB Sanatorium at Kasauli
In 1941, the Association
established a sanatorium
Kasauli rnear Simla Hills.
at
The sanatorium known as Ladv
Linlithgow Sanatorium had 250
beds and was one of the
premier
TB
e
---------- A1X
L11C <
sanatoria
in the county. For want of enough
paying patients, this institution
i was closed down recently.
ill
r
V r "]!
Acocs-io
Call No
10
r ■
II
TB Directory
Research
enloJhe Association collected information regarding
tuber
on in^TJ^Tb-''1 £he C0U"5,y 3nd Published ‘he first direc
edition XuXd XX1
The mstitutions of the Association have also undertaken
severa1 researcb projects approved bv the Indian Council of
Mectcal Research pertaining to tuberculosis.
The Ministrv
of Health also had provided grants to the Association to carrv
out surveys tn urban and rural areas of Delhi by its institutions
tbC 13St
respect of information about the f cil ties Xb eTI'T"1
CU10S1S institutions in the country.
‘bailable in tuberTB Hospital at Delhi
The Association has a Research Committee. On the re
commendations of this Committee, a research programme has
been instituted to find out if the period of treatment of tuber
culosis could be shortened. A preliminarv report of this studv
was presented recentlv to the International Tuberculo"’\ Con
ference at Mexico.
KbaXml’grXfre.Xe
facilities including thoracTc surg^y?'5 'n
C°UntrV with aI1
Conference
Other Services
Association calculated
the anti-tubcrculoMs
and to involve tuberculosis workers■» iin J.
the anti-tulxrculosis
niovenient is the organisation annually oTa ''conference
of
tuberculosis and chest diseases workers from (liflcrem
part"
of the country. This conference deals with various
aspects of
tuberculosis control• work and
....J useful discussions are held.
of Direct<>1vOn,'|)peStablisl!n’S"t Y
-nst.tut.ons and compilation
of1 institutions
services
The 'ITl AsilOfl‘,.tl(>,l. had
hacl undertaken severa other
rained by ^ e
w±^mitafiC M
was mam-
India grants and' treatedI os”r ^0’XJe'°f
March 1955 ThereiftPr
■State Government
’
Poses^Ftmd11 ThT'x
i
• r, 1 h>cc ff> patients upto
Sp,tal "aS hanr,ctl "'c
'he
X the former V-cetov’s
> War Purover India
Health Education
The Association has been carrying out regular pio-rainntc
of health education activities since its inception' These
lets \,1bf03dC:'St t:llks' I’rcP;lr;ll'O'i and distribution of paraphe s and posters on various aspects of tuberculosis
control
pares and nd"tSTPCr :idvcrtl5ements- etc. The Association pieFi t h-te bri " dteS Pr°PaS;,nd;! materi;d to its affiliates
and
ne latter bring these out in regional languages.
dealsTueithSrhCff3ti°n h3S 3150 bcrOUKht out
bk'e P>int which
second edLra^rH
ra15'”5
tuberculosis control.
The
this blue punt has been brought out recentlv.
Technical Committee
Technical Commkree XX^hi
, eStabIished
Journal
a
puted Tuberculosis workers dra«m ^ Committce consists of
from various parts of India
to advise the Association on matters
—.s relating to control of
tuberculosis.
« i^Sep^mber^q""13^
the diffe?en? aspect0
1
j0,lr'lal °f l ubercuh3 5u.arteily journal devoted to
board cons^«1^r^o^ialS, edit°ri31
v r;-. I
rjAcces-iorij
jCajTNo Jjj
I
i-
12
13
Textbook
tuin’ofTmxtbookAn'-rul'’ "’I AsSOdation
the pubhea'vith all asX of tubltc Jo^s STh" 1970M Thi\ b°°k
Sis that are common to most of the dev ,pr<?bIem5 of tuberculoand Africa have also been d Act
M. .t?"1? c?untries
-Asia
edition of the textbook on T.d
i n. l^ls ^oo^- The second
t.on
textbook on Tuberculosis is’now under preparaTraining of workers
I
tb
^Indian Uni^ities to
r
■
‘r
Association like
I.\„
Xew
played
fhe 1 cchnical Committee has been
nwdic’d '? thC tcathing of tuberculosis reviewing questions
at various stages of
and has been
"“k"'p -p"-™t reconinien-
Affiliated Associations
&
afhliJcT to'l'tL2TuberculflisbCI\ U1O-'S 'Associations "hich ate
them have established d^rrirr Assoc.,at'on <’f India. Most ,,f
cational activities.
Thev OIAnise'rcT :"’d Ca"V 0Ut ec'ucommittees and refresher counes
ManA"?’' ‘""'P5’ 'are
™ ilinstitutions
2stitut.ions like
tIOnS
niamtain certain TB
like TBd'inic^TB''
Tli'c hiic
$°
etc. Thev also o-ive fimnr-ioi
•
C1,nic< t b laboratorv.
J
assistance
to
patients.
°
*
assistance to
indigent TB
*
Seal Sale Campaign
The Association started the
campaign in 1950.
taries.
During the past ->5 veX V^OVernor,s or olhtr dignihelped focus attention on’the tuberculos^0'3 Progranlme has
III
International contacts
Since its (ST..
i
thV Tuberculosis Association of India
has been an affiliate of the International
culosis. It has maintained cordial •1 union Against Tuberrelations with National
Associations
— all cover the world. X
«
U
,?
r
5?
in •x‘ew Oelhi in 1957 insed the XIV \atioinal. Conference
. .
ha\e participated in most of the i. • ------ - Its representatives
international conferences after
1947.
The Association is also :
CA\V1^n!ber of.thc Easte‘"
Regional Organisation. The T,,K
Tuberculos
J1S. Association of India
hosted the IX Conference <nf th‘
“V1.6 Reg1<)n '■> New Delhi alo„o.
with its 29th National Conference
------ ‘ on 1 uberculosis X: Chest
Diseases in 1974.
—
V r A;
I
Acc^sio
(d) Development of fariliriec c
''■o>k«.s
c„sW„'ed
CHAPTER I]'
Cal! No
bhore
COMMITTEE’S ASSESSMENT
RECOMMENDATIONS
15
if
11
I
B
“““
»d r„, effeccire
On the basis of data tthen
’
available, the Bhore Committee
estimated that there could easily
Mses of tuberculosis in lbT
'>0Ut
• —t U—
> million active
country,
million were dying eVen ,e
ar. th.of whom perhaps about 0.5
ie recommendations of this
anti-tuberculosis measures
though there were cer...... The Committee’s
.
dually.',SC1'-
i
(a) Establishment of TB rli»n>- ,
r
town. They emphasised rhe’
C 1for.c.vcry district
Tutercutai,
the DirectoTuberculosis to advice
"ilh a" e-xpert in
tuberculosis work nr the Xm’ry V"d fUr
'h' anri—-*ier
country
a whole.
(g) Encouragement of
government work. non-official efforts 10 supplement
Bhore Committee” to siudv the1 hea’hp0^111^1' known as the
^and suggest plans fo: the developn^f health progX
sx”1?'
of a
-VWS
K
--I of Health
rhC °th« ■eeonm.eXon;1'we^XTTgra'
recommendations
™»d«d xrri„ « „„Ufc
(6) Establishment cT P ,h0JPitals- Ti>ev accepted the
usual standard of
recommended S.h.SOO beds
tZ"1'''1 TB C'Cath but
ment. These were m it
I, e "nnimi'ni requirehospitals, secondar. \lnit hosphalMnd dpr,r,nar>', unit
quarter hospitals Since
nd district head
number of teds
beds wrnld rate many1 ve^r-'Th 3 13186
mended that in the first five vears 900 t
Koprovided
------ _i , .for. <
.ears, 00 beds should
be
e^ery w million population..
[c) Provision of homes f»for incurables and establishment
of after-care colon!cial r
w
helpjn this venture and
part c-c the
'T-M
A^ociet’o^o/
mJ*in".ssd,.
i
V.-.M
.1 Area-
..
"t ...bereule,:,
AND
“ S“c™°i
I
■ ■
'S-
?
17
-
al! No
I! -
I
■
I
■
■ S1’
I
r
!
I
prevention of the disease was BCG vaccination. It was plann
ed that the vulnerable population should be protected by BCG
vaccination within a period of 10 to 12 years and in the'meantime resources and knowledge should be mobilised to adopt
other measures for effective control of tuberculosis.
CHAPTER I'
H____
|:4
B
>■
1
tI
1■
1. -
I
r. ,
! -J
POSITION AT THE TIME OF INDEPENDENCE
With the attainment of Independence in 1947, the
National Government naturally devoted considerable thought
and funds for social welfare in India and gave high priority
zo- tuberculosis as it happened to be the most serious public
wealth problem in the country, next only to Malaria. This
iLo coincided with the increasing interest which the international organisations like the World Health Organisation, the
UNICEF and the International Tuberculosis Campaign were
taking in tuberculosis as a world problem. However, the
events that followed Independence made the tuberculosis pro
blem even more serious and difficult than were visualised bv
the Bhore Committee. Partition of India brought in as its
ifrermath a large number of displaced persons to
India.
Most of them had to live in crowded areas with extremely poor
Hgienic conditions. There was also the problem of
malratrition. These accentuated the already bad tuberculosis proUem in the countr).
I
I
I
BCG vaccination was started as a pilot project at first
in 1948 in Madanappalle in South India and thereafter it was
extended as a school vaccination programme in all the States
during 1949 to 1951 with the help of the International Tuber
culosis Campaign. At the same time, the Government of India
set up a BCG Production Laboratory at Guindy, Madras in
1948 for production of BCG and tuberculin for 'the country's
programme.
About the same time arrangements were made to establish
with the help of the World Health Organisation and the
UNICEF, TB Training &: Demonstration Centres at Delhi.
Patna and Trivandrum to serve as model for TB clinics and
also as Centres for training of personnel for the country’s TB
control programme. A number of fellowships for tuberculo
sis workers for training abroad were also given.
■
Though the urgency of taking up a large scale control
neasure for such a big and serious problem was fully realised,
n was not possible for the government to immediately implenect all the recommendations of the Bhore Committee, because
f:r providing even the minimum requirements suggested in
tiaz report, a substantially large sum was necessary.
The
nnpber of beds available at that time for tuberculosis patients
h India was only about 6,000 and the number of clinics about
8; whereas the estimated number of patients was about 2.5
Trillion. It was estimated that for controlling the problem of
tuberculosis of such a magnitude, India would require some 3,000
tc 4.000 TB clinics and some five lakh beds according to the
uriM standards obtaining in the Western countries at that
tine. The cost of these was estimated to be over 5,000 million
rupees. It was obvious that from the point of view of men,
nnrenal and resources, introduction of such a programme was
impossible within a reasonable period of time. Attention was.
therefore, directed towards prevention. Since BCG had proveijzo be efficacious in the prevention of tuberculosis in manv
of the Western countries and could be applied quickly, easily •
ard at a comparatively low cost, the chief method chosen foi
I
I
I
I
3—7 DGHS/ND/77
j
AilJ» ■ 1 n
■
Vr
.J
Accesi;’f
19
r(Call
----f
No?
CHAPTER VI
S’“"C'™a'" "" ,“"‘l
first five year PLAN
K
In 1951, the First Five Year F'
lan of the Government of
‘sis was given a prominent
of tuberculosis in the
country as a whole was drawn control
no bv ^^b^tilosis
consisting of experts from different nar-rc fchnical Committee
5:"' ”S accepted
“"I””1 by the
ness in domiciliary service nrnvid^d cS %an . 1 leir effective»vi„g iop prforitv
,he rMUi.ho ep \ "TB"d'i“iO"r I"
satisfactorily.
Majoritv of
/-Ii, * . erCjOuntr' Were not run
diagnostic facilities nor did they harc adeonaJ ^' n: adecluate
out an effective domiciliary servile
TWs f 4
Can>'
of .hile recommendations were made for the SeZl'S Y™
(i) Expansion of BCG
vaccinatio.n on a mass-scale.
(ii) Establishment
of TB clinics and
expansion of domiciliary services.
i
i
If
I
I
•
.
F
■
I
.It
. j| i
■i
■
(iii) Establishment
of more Training &
Centres.
Demonstration
<-> r»vi,i0„ o!
•r isolation and iremtn[
crotvded and unhygienic areas.
(V) Rehabilitation of ex-patients.
PB patients living
(vi) Research.
"»r:,?
the State sector.
^^^-tionai C......
Governmcnt
implcm
ill ion
’
'inch Rs. 38.0 million
was in
'
During the First Plan period BCC
■
was expanded on a mass-scale to covTr the "
?
he age of 25, approximatelv 170 millinn
J>°P“iatlon below
Laboratory in Guindv was exnanded
’ 7 he BCG Va«ine
quantity of vaccine necessaU for^h 35 tO P{oduce adequate
The target for BCG vaccTaln n the
and vaccination of a total of 87 millif F
PIan "’as testing
achievement was, however 71 5 m r
PTOns- The a«utd
24.5 million BCG vaccinaSnl
tubercuBn tests and
i
Investigations on use of newly avaiHhU
anti-bacterial
napalle'sanatoFum KasluHSanmo ■"C’e U?dytaken
at 'Mada-
L
and. also 1in
tutions under the Indian Council oTAIedicaFu
" other instiimportant research during the First PI ,n --1 Research,
Research. An
tuberculosis control pro^amme1 bv dm TR
coinmunilv
was the community
Madanapalle where methods nf tr th i • 1Sanatonum in
of infective cases and BCC v J C°ntr01 lncludinS isolation
^Unimportance to^luVse^uem
«th8™;1,
°( tb
b“"“ ■
™g,„g ao„Miary ,re,„mi for Jynjjg, „,ho* to.
st
It was suggested that about 10,000 beds should ho
cd for tuberculosis in the First Five
Pl-.n
• , f provid—
tion of infective patients living ;
1 > ?Pec,ally tor isolahomes in cities aifd towns
About 5 000^
llnh>Sienic
during the Plan in the virinn.
? ’00° bcds were addcd
10,000 but these were mostly added
lhC target of
hospitals. In addition two sneci d i ,c>Is.tinS sanatoria and
children -r^nablhhed'duri^X'S
die North at Mehrnuli in nr.n •
i i C 1 an pcnod, one m
^s ?IT ISanatri;-- -Nadanapahe. The1^ V S°-"
Uth
*• i at
training ccnties for tuberculosis at Delhi Patm nnd t •
F*"
completed. Establishment of ’work centms fo/3^'™
..... am were
rehabilitation
could be made*611
W3S 3 S° ContcniPlat«1 hut
no progress
that
were of
ment
of
a National
Contro Programme were the star of he I’
—e National Sample
»«“ the Chemoat•hsAfori
u —of
Five Year Plan in 1956. T ll^n Fby Lhe end of the First
lill then, though it was realised that
I
-
V r /•
20
Acccs ion
Cail No I
•_________ l1;
the j
’ *
Precise extent, prevalence^
^unities and
and this was P Sig°^anPdicapdinthoerJa'^;^«
"'ere not known
gramme and fix‘”g rational priority"
S a niass control pro<«««■,
CH J P TER VH
SECOND LIVE YEAR
I
The Priorities in the Second
S””1 .-5
“ .*»«A
=^’ ini-n^tF«ieXl^Is the
cn-
-re taken note of and steps X" ^^^Xi
<>tS”
connected with
iosPIta^ treatment and
i ^omici^’arv
objective H-:;1 to
in ^irahomOeshCrTPhrOb!etmS
donticiliary chemotherap)l>PrOPriate (irU° regimenT^°^yr
fci
Ii
the States except BC^ vaccinatfo'0
imPlemen'cd solelv by
As a result, TB^linkNe
esubl
;"'d ,eScaich
ment and staff and TB bed vere a’?,wIlthout,Proper equip,
and sanatoria that were not usefulI for h5 ,m° Y in.hosPi'als
ed areas. One of the imnorranr I
tfective cases in CrowdPlan was, therefore, to undertake
“'’r16
the Sccond
schemes as national programmetml |a‘^Of ‘he TB con['ol
to give a subsidy to the State Cove
16 Cfentr;i1 Government
tation.
f
State Governments for their implcmcn-
1
I
I
1I
II
was to compete Ae^tass v^ccinT"3''011
'!’C Scconc! |,!'ln
n>;Ilion young people. FOr‘ in cnsifvin™™-"1C
C0Vcr 170
states were provided by the Central
i,ct,vlt,cs- tcrtain subAs a result of expansion, 9T7 mili?on ™bCnt i'° the S'ar'c$o/.a million BCG vncr^../:
million tuberculin test* and
^lan
period. New
New buikiin^anTphm^'
n ‘hc Scco,kI
rtan period.
1
'
of freeze dried BCG vaccine
vaccin? were made’
t' 7 I,la,"'f:>eture
Laboratory/ and
freeze
dried
•ava!lab!e « the BCG
and some
jc,
on an exnerimen^t
experimental n..."
basis. 2e dr,ecl 'accme was manufactured
In the Second riun
1
PLAN
m
n
“? and
aim Iaborato
laboratory equipments of
to India agreed t0
bl'Cd or'?'
upgraded TB clinics9fo? eZ
•
'e, ne'vlv cs'a-
treatment stx.j
service. The target was to est"^ °f domiciliary
ISO TB clinics. which^o"51 thlS tal?et’ 80 ^'''T-Bclinics^ere
sstablished/of'
by the Gove:
Government of India!"C CqiIIPPed "ith funds provided
fe r
tratrcm
°f estaWishment cof" 10
‘ ’ TB
- .. & Deinonsyrainmg
fcnt sZS wasaSS.tiOn with the Medicaf1 Colleges in
MadraTandHyd^rabad.
1
However, three
:Training
&
only be established1 at Nagpur,
■
' I
0
V F '-J \
I____ I
•\cccs-ion;;
Cail No ‘jl
22
Sh
Second Plan
cst‘lhlished
<’
the
subside of Rs i o-n
1 . ■ e Omernment of during
India
■ UI *s. 1.2o0 per bed
T --a gave
cemres^co^T
B
in thc ^^nd6PhT y d,^e[ent handicrafts
-e sire anfTat
coinplctCouncil
ion for tile
'i •
■
community.
‘
pc"odlt:d s“rveys of tbc
the
B
l
I
11- ■
I
PT
1 .h™£S,cT,d ou‘" s
("
home
and
Centre,
antigood
(Mudaliar Committe^'reTOesse^the'1'1 J’!31"1'"" Committee
and recommended
recommended neasnrA t
Problem of tuberculosis
Committee recommended
that
BCC
'O
■"ilh it' Threcommended
that
further, intensified,
domiciliary
tr^tment*'"oi'0”tul’e1*'11.
u ,
.....— >
domiciliai
should
exP^
' d'c;,,,d ni°Wle X-ravs for rural" areas
•
‘ ‘ be further
......... ■' ^
should be provided. '
I he Committee recommended one TB
clinic for each one million population.
one lakh additional TB
(A.D.I-'h." TB)' incach'sh-tte."'1
time State TB OfFicer
vaccinadon and eSisht^^^
(ol:
BCC
Of mobile X-ravclim-cs 1V
fo' ^tablishment
to the needs of'the vast maior h. «r P "‘th v Vle"’ t0 catcring
areas since most of the TB' inst'it [ patientj llvlnS 1,1 the rural
hshed so far were located on 1 in , T”5 a'1C C ",ics' etc-> estabthe National Tuberculosis ln«;r
" ?an aicas- •Slninltancously,
tempt at evolving suitable n.rT i i 'VaSt .en^a«"ed_in dieir atcould be integrated with the co S ' '?blcb uiiti-TB measures
jn the rural a?eas wit a vie v to nrnUT' deYc,oPI^nt service
m the periphery.
pioviding tuberculosis services
oi-
ti eat men t of
significant
of tile .second ?I;
ln 1959. This was inn
Tuberculosis Institute
Jawaharlal
o„as,bc
Sepu-mbe
,,,
planned Seta
to serve
n J,6
6 Sc
Ptember, I960,
i methods
SCrve as abes^Pcentre to
evolve
i
Fhls Institute
culosis ennt
control
10
/'
01
'
0
and
control methods best sui>H f
nC 'vork Ol’t tuber
■■'•here tnberculosis
tuberculosis problem
nmhl
is
• Late
,ed t0 and^?
a r------0India
meagre and to train ^he staff -S
and the
to tram the staff required tn ;
le Sources are
Wished br°3rai?.me in the country
country*d The^Tn^
4° ™pi<?n,cnt
tf>e ttiber-1Cnr dle
Government of Ind,;
-v! Institute was esta-
afte/its6 eX°hhmmHTas' abV'T'1’'0 '.vilhin a short P^iod
m the strategy and concent of XSt’ ln!rEduIce a major change
me bv evolvin<r 3 fnnin
.1 National Tuberculosis Prooramculosis. On th°e basis of’^h^T C?"tro1 Programme for tuberSurvey that the prevalence of mbe."55! °f the National Sample
”7„2reil',se5.then made
''m World Health c’
Organisation and the UxJ'c^1’* help of
subsequent Chapmi-0'
THIRD flVE YEAR pLAX
The Third Fire Year Plan f
from 1961-66 was continued for
tuo more years in 1967-68 and IfiiiS-OT
till the start of the
Fouith Five 5 ear Plan in 1969-70.
ed in IQjg'^Th3' Sample Survey started in to-,-
Xr
CHAPTER VIII
both rural and SCXs° in
t ai to plan a programme for
tn
____;S considered essen3"lprrenti°P Cities in theTTI‘"I
, treatment
country’s population hves OoernHn
S0% of thc
the National Tuberculosis TnSit t
icscarch conducted bv
uoerculosis Institute proved the feasibility of
c"-o institutions are discussed in
a
I
L
.
-
B
.....JAcces- ioq
H-•1
}--------Call No J
24
25
Programme aimed
prevention of
Based
, ' and cpc
Xttli,
Operational
j—
...................
Pjoach, a district TB
- 3 control
' and ^ro....
“■puisation
of the District
Tuber7ulosisdirUSSed0
in
°f the National TB Programme^nce !■ntent of District^TB
then has been establishCentres for °rganising
through all the
controli rneasures
Peripheral health facilities
in the
’ district.
Fhc s::.-*
ehanged. It
t«on of the •BCG
JCG i
Phn ^mmc '^s also
- appropriate
a^enev of'T
■’
to cover the newdy add^t h gcncraI
•ition. However, since a barge backlocr nf
dd d youno popunation was still ?vailable
; - • * and neithe^he schoo?TPl;b?C
nor the maternity
and’chiM welfare
tr•
<aikh ^rvice
organised
BCC ;»» tO • )C -a^c to taked
hninunization
the BCG
>«t was found to bc^sa'fe'Tnd
Training
Damonm^tan^ta'^'5^^' °\eS''f fmoit .S'a,e
Train,ng g, De„„„?lr.S„
■ ■*““
°i ».-*»•
=“•
nics, five
such clinics rraa „„ l„„g„ „nsMerrf „"gX“Xr"'L"i?i
TB control
TnterntateTnX'r
I
proposed for [hfronni," pia^nere'teo'ink'0'' <1E ‘i* Sdle"lc
course of the Third Plan period.
tor supply pl SXK,
I'
■
t[’C
proposed for the Fourth pi Cen?rts "'cre originally
established n he Th
PT
fl'-° °f ,hcse ""e
the Southern dritrict nl \ SC‘fJn Bar'.galore for
the Northern districts
'n C"’ De‘hi for some °f
<2>
tb'&ev0;;
These wer"2P
(1) Establishment of regional ornanimtio,^- T
guide
^Plewent, supervise and asset the work ofTothf'dri
group
I
«*>«• ”'SS
A target for establishment of 5 000
TB isolation beds
fixed.
lVaK..?!VeiJ ? establishment
TB
bulk
rf r.ihor
b,S “
f of the
“ patients
1““”“ ™M
could lxbe treatbeds.
PreIimiuao' Euberculin
S™'„’E State, S™»y“X TB
»< S.a.e
J',
l"P~<»■ even.
to”'”' ’ ‘'"'T
as to TB clinics rnn
I
te
clinics as well
donricilian treatment pVtr"?-1” Oroanisations for
Governments and 45 Tr /1
4“ Under the State
an. Anti'-
X,“Si rx^n^tog-'too,, ucre sup-
. ._ t
!
;? V r ofj
27
.?CCS - io it: I
chapter ex
JI No
for want of paying patients and
I resources. It was, therefore.
suggested to the States that in i
anv area without TB beds it
there was a TB nospital or sanatorium
run by a voluntary
organisation within a radius of 250 miles
insteadUldf eVtabreserve beds in such
such voluntary
voluntary corganisations
..
hshing new beds and the Government of India
pay
the cost of «.reservation
wi^n
JV-l
S' thn
-. •
...
11
fourth five y£AR PLAN
I
I.\ the Fourth Plan all
i
were continued. However* it ? scl}eiues of the Third Plan
ous Plans that in spite of all d?' a 0^Servcd d"ring the previ
assistance to State Governments.
!
■J
the
i hi ^
le entire countrv the^Cn\
n °r tl,berculosis con'•■be the raponsibihty of bemdtm °'ynnicn' «f India should
This mca'u,'Ztdwhmv^Sil,0°-. Centra?'^’i?
i
¥“"£ n C'"™ ■“ ‘J”’ “““
Pl!
J
and "on-recurrina e?
a I,o,‘io»
„r
‘
>.
’
.■
Cn'euimeut
of
JndH
hi
the
of bearing tne ™"
,s?" ,dcl“’ok
re^ponFourth
?'
'bese tnstitutions and of ant T t > "C"itt and
a,,(1
enance of
9-ed for the prog/mmne.
TB t,ri'gS and RCG vacHne
■
I
XC ,;Sre"Sv'mX;,''’n'5“r”ra,"V/,“',."r “■
•
!
-is
i
«sL
1711
a
.. ........ -
from the lire ,. ”.Pll'cll‘ls<- °f BCG vaccine, tubcreu in. etc
‘l»‘'
Government of India as hitherto.
P '
H
d,l’gS by thc
.Fhiring thc course of the Fourth
Plan. 114 more TB
clinics were added as aSt
against the target of 160.
The two
Training & Demonstration
^.n Centres as targetted were establishcd and 1571 isolation
ntea-ti^ 'nii Cstal)lishc(I ^nst the target
of 2500. In thc i
mca..tlmc, BCG vaccination programme of The
ountiy was further expanded through
<-f the Fourth Plan so ,^M>vhnlefie^S^fd^‘he' course
Plan
of the ProgJ2nmeslIClAhr’e
g'stnct TB Control
co'"bv ’the
Control Programs:
Centres was. therefore
"i i
t;,rSc'' of 1(50 District TB
therefore, fixed fo:
-- ^or the Fourth Plan.
railway^ nrmnrl
mm
.,
necd for a rIra2i™
■ ■
nI ,’umbcr, °F beds as adjunct to
T’"
pi-Sta,
v-.1 ...
ca,ses °F District TB Program
--cd essential. There u-pr^°■ b"’ ’as no TB bed at all
A \
’eVe;
establishment of 2500 T
or the Fourth Plan,
oeds as additional TB
a> dtaria lmpi,iX “o W
ofddnaS- availabIe- In "•art.
‘be
ot domiciliary service
voluntary organisations
i! ■h' p“™ ■><
«i, £i""£'
s„£
s,“!- ■
A
Cen,„. .. A.a,n
1
!
I
At the end of the Third Plan there were <nll
States v.z., Madhva Pradesh and Assi.m not havini a ?rS
& Demonstration Centre. For the other smaller° States
L
h was3 nd’f IllpU,r2- yaniPt"-. etc., and the Union Tei i hoiies
it uas not considered necessary to have sennrniP tv- ; • Co’
I
,te
freeze-dried BCg'vaedne^vas^ ,cxPansl0.n of production of
Production of freeze?- ed BC '
■ U'’ ”L the Fourth
which was only abomTlni
i'CClne
the BCG Laboratory
to about 30 million doses by^OTs’TA By1^9'70 ]'asf c,1lhanced
period use of linin'/-!
\
^hc end of the Plan
cd and only freeze dried16
16 entire Proorainine was stoppmillion d ect vX ot
USed’
A total of ™
BCG vaccine and tl
i '^re performed in Plan period,
supplied to the State* CU 111 WOrth about Rs. 4.5 million were
I
28
cces-i3i|i
10 more than SOo'TB clinics^ml b^'th^s^r11’^1 "eie slIPPlied
Iz
about 60 TB clinics run icshvrun
vnl.L^
5
Governments and
run by
voluntary a^“
-PPb- to the TB Patients
bon't^^
domiciliary i
TriJ whilh'S’wi th" Sbiiitv Ttud61'-1"0.5^ Pr™'°"
project:
legular project in 1968 was feasibility
mnrin \ study
s5U(^y ln 1^64 and as a
°f BCG in the prevention of rnbn UCi ^°r- assessin? the value
pievention
tuberculosis
i
Prcvajhngjn our
country. of
The
first^hat10
circumstances
included initial examinaiion
^f
«
examination of ?he
about 3.6,,000 "as
was comnlen-H
m,
comprising
completed by Marcli?
■—------- ----------------------------------------------------------------
all No I
CHAPTER X
FIFTH FIVE YEAR PLAN
The Fifth Five Year Plan which started from 1974 would
continue till 19,9. During the Fifth Five Year Plan, it has
oeen decided to continue the schemes for supply of anti-TB
drugs to State TB clinics as well as to voluntary TB clinics
and supply of BCG vaccine and tuberculin to the States as
Centrally sponsored schemes with 100% Central assistance So
far as establishment of District TB Centres and Isolation beds
are concerned, these are included in the State sector for which
funds are being provided in the State budget.
I
■
provision
Vnt- Thei 'Pn
O\iS,On i for the di^erent schemes
uunder the
national 113 Control Programme for the Fifth Plan
a are:
I.
IdiJ
I
Centrally sponsored schemes
Supply of anti-TB drugs to
State TB Clinics
Rs. 575 lakhs
(ii) Supply of anti-TB drugs to
voluntary organisation-run
TB clinics
Rs. 100 lakhs
(i)
i
(iii) Supply of BCG vaccine to
States
II, State schemes
(i)
Establishment of District
TB Centres
(ii) Establishment of TB
Isolation Beds
(ui) Equipment for State/
District TB Centres '
Rs. 150 lakhs
Tctrget
75 Centres
Rs. 335 lakh,
3500 beds
Rs. 506.69,
75 sets
Rs. 90.00.
With the establishment of 284
the end of Fourth Prent-°f 284 Distlict TB Centres “P'O
to be provided
n
was
«tIlnated
thatTB
another
‘75
districtsqvere_t°
wkh
a District
Centre
ench toi •
1 b provided with a
’
created
j “the
I lnt° «™W«adon
the districts that were
_____
“xo/ Lalso
?e new
’-icaiea
m the
t..
tie meanrimp
meantime. So far, the T
United
Nations Children’s
.
Vf •
30
CCS-13^
I No I
___ i
CHAPTER XI
oTs,
NATIONAL TUBERCULOSIS PROGRAMME
.s
“y
Stat^h? XTiRh Plan
i
es^Wi^ed by the
gramme of the District TB"programmes
as wards in existing General and n.i
i
(a) That the nine million or so cases of active tuberculosis
in the country are evenly distributed in the towns and
villages, that is, 82% of the cases arc in the villages
where no special facility for tuberculosis exists.
°
7 Sei?’1Ce pr°‘
to be added
:•
I’limaiv Health Cent -s
"'orkers of the .
In each P H r L
i
5 bc,,lg orS‘"Hscd in the Fifth Plan
'I?;,1'"■
■'» f
vised hv the eXin" BCC f/ClnS) tral'1Cn and "’i11 be superthe school-age moup0 tTuV ,/'''t
cJonli,lue to c°vcr
BCG vaccine0, p'hdtiction of ^ze
°C
cd to 60 million dowc in ,i,
f
,s being enhanc-
The Tuberculosis Programme of the ccountry
wu..ltI, has
’
been
evolved takng into consideration the following facts:
(b) That the pool
of infectors
are the
.
-- —
—~ sputum positive
cases totalling
t~* } ’ about two............
million in the country, most
of whom have also symptoms and therefore have a
felt need for taking action, ami in fact, arc alrcadv
seeking relief for their suffering from the general
hospitals, health centres and dispensaries in their
areas.
(c) That domiciliary treatment is most suited for treat
ment of tuberculosis and institutional treatment be
comes necessary only for a small percentage of problem
c? as cs«
(d)
That the
K
uu programme
pivoidiiHnc for
ioi tuberculosis
tuberculosis control
control must cover
the entire country, be well within the available re
sources in men, money and material and provide size
able benefit to the community in the foreseeable future.
'“s ,“h
(e) That by organising tuberculosis control on a communitv
basis through the existing health facilities which pro
vides a permanent programme and is easy of implemen
tation, it is possible to bring under treatment a lam
proportion of the infectious cases in communitv a reasonably short period of time.
freeze-dried BCG can he’fnrd
f inquired, production of
itself.
Can be fuither enhanced in the Fifth Plan
Anti-TB drugs as usual are 1 ‘
being procured by the GovernTT2" t andr?re beino -ppliecTdi^"J
-2; to t’
“
miniature X-ray films are ap’ ei’ ng Proc;ured the TB clinics.
* S0Ji
I
centrally
for
supply to District TB Centres. BCG Vaccine i
from the BCG A’accine L '
6 is
’ being supplied
Laboratory, Madras. Tuberculin for
surn^Rs1'^1-5 aln- SUpPiled tro^
...
V/ ’ - R,s- L3;? million was utilised
for same Laboratory. A
supply of drugs and •
uShe^n 19^7and
15 lniIlionJ
~n was likely to be
(f) That BCG vaccination is an
ventive measure and can
the general health service . ■
I
K
..
ffective and
..cud with
egular features.
fe) That tuberculosis is a
.•me infectious disease of
ubiquitous distribv' • and about half the total population of the
■ _ __> is infected by tub', ulosis germs
that constif
,ie main
source
---- ------------- of futur patients for
J:
Hi
gvi
32
3---------- -ri
' ’ Jil
pes-iodj
1 No I
I
several decades, High birth
ble population every year r^e adds to the suscepticeding
eedina- a regular BCG
vaccination p*-~
programme all thee time.
programme has
Therefore, the
-as got to be
nature and should be . countrywide, of
-a permanent
integrated with general
service.
health
r
CH APT ER XII
district tuberculosis PROGRAMME
The fundamentals
$
I'I,
>
°f control r.^ammes
programmes ate:
W Prevention of devek
thosCX t
disease among
a*--—5 mux:
and
wno are nnf
C
(n) Detection and treatment of
1
Parge a
a view to
aax .... .. .
I
;e;
objectives, the main
1 rogramme has been
and staffed District ^Tp3'"1116 b>' establishing a fuffv e°au'?n 'C
-loping tuberculo i^sShm
°f th? di^- W
Ax Average district in Indio hne
1.5 million. It is divided into about ten
“ ab°Ut
headquarter town in each of whirl, t , ks w?th a taluk
the district headquarter. There are about
llS generallv
are grouped into 20 blocks each nrnviX t • u IlllaSes "hich
th Centre. In addition to the Prinrarv Hp W ,?nmary Hcalare another about 30 small hospitals * d^ne
entreS’ thcrc
having about 50 health institutions
P
,eS' ctc-’ ‘hus
a qualified medical officer.
’
h Under t,le charge of
distrktVwhom^out^OO^ i^ 2O’°OP Patients
a
are the ones that are sources of Mr'•°US- T"56
also have symptoms. They are o-ivf
• a"d most of "bom
oftoVov^g^f
f
every year and similar number of
d P.the P°o1 of ±000
from the disease, thus keeping the inferrin"
°r rCC0ver
constant at about 5.000 cases On a ™ u P°0 more or less
basis of the druo-s consnmrd \ \ id rou8^ estimate, on the
dr«gs in any district whT d
budget provided for
anti-TB
has not been organised it is pDt‘Stncl: ,TB Contr°l Programme
tO 200 cases could be under actire^eltme^t”0' m°re than 100
t
ft'
9
I
i “ It
■
IS
it
I
tre «tabliS1Cat^heCX°LPhe?dam“e^ 'hC DiStrict TB
> Censonnel trained in the concern ldcluarter .an<l staffed
staffed bv
by perproblem of tuberculosis at the Nnr
aPProach t<to the
functions as a referral centra f^at/onaI Tuberculosis ’
Institute,
beadquarter of the
? 7for the entire district and
as the
programme in th^eS d*^ reSPOnsible ^r organising
case-finding mainly bv emit dlstnct. The actual activity of
anti-TB drug treaLem
.eV.mination and of
50 and odd peHn^rnl t f^^bary basis takei
tuberculosis team^s to orsaX^thT^0”5
"he
Pabent m the periphery fs offered CT1”1116'• ThuS’ each
4-7DGHS/ND/„
7
the duagnosttc as well as
.11 •
I
IM
34
35
cs-ion
tieatment facility throughout the whole nerind
; No
maintained at ^District TB Centre
k*
country, it was tried as pilot project in
i
w r\vj111 some districts and it
was found that such a <coverage is possible without much additional inputs.
eaCh patient is
iT I
• • BCP vaccination also forms an integral part of the acri
vities of the District TB Control Progranmie. PFor this a BCC
team is posted in each district TB programme for systematic
and regular average of the susceptible population in die em
tire district. The six technicians of the team cover the school
children m all the schools and the pre-school and nnn i
going children from house to house. PFor n^ bom and infan
I
i.
vaccination, the staff of the existing maternity and other heahh
institutions and the peripheral health workers are trained o
build up a permanent organisation for this purpose
of .he Intel
TB Beds
.4
b
treatment.
1'“'
i"l<..iSo.in “hTh,” °X"d|JS TO
tfs ,
T-B.,Veds available in the district are used as adjunct
to
the
domiciliary
service
of the Tor
nictriVt
^rn «
ux:u
me. Hospitalisation
is arranged
cmemend
like‘‘s aajunct
tysis, spontaneous pneumothorax etc nr
Jiaeinop-
hSK? "a?™V™
;.y
*£?as X “E“ &
drX ITd^mVh Wfh°
In such an organisation, the peripheral health institutions
£aesina§ndP"—“I-, f-aimPfutUn a^XXpv Z
State TB Centres
patients to the
noc. havina microscopes can refer their
don and t£r
m^roscoPy centrc for sputum examinaexamination efr°ra tO
XraV facility for ^-av
These are otherwise known ; ”
—
One such Centm ™
of 'thVm^or^X^of ?hTcounVCThe Sta?e°TOCe "
five status over a period of one to two years.
P
rC^nt to the standard ^ii-iB
P
Such activity of the District TB Control Programme does
nhA 1<;ai ■ Jn,cr.ease. the rvorkload enormously in an? of the peri
pheral health institutions since in actual practice the workload
A min™0176 £lFan ^ee °r f°Ur Sputum
aminations per d£
A minimum of recording and reporting is provided for to make
it easy and simple. If a District TB Cenfre alona with “s 50
ox more penpheral nealth institutions can diagnose and put
under treatment about 1500 sputum positive cases per ve^
such Prio?Stomme IS I,ked’ tO re>,dUCe the Problem or tuberculosis. Bnoi to recommending this programme for the entire
D?'
Sta£e TB
gamses a model District TB So!
rnnt^i v
• Centre orjn^jng an
located "for d7monsPr°?Iam™e±.Ae
°r.£°"n ^em’Ft'i
re-ori;nSnnofath0en‘ pUrp0Se,S- Xt undertakes training
and
trol progr:X“0nof0fth^coP^ne te:fased in the TB conand re-orientation training courses for generT hSthTerX"
Personnel, private practitjoners, etc
It conducts epidetnioloSIcal and laborator
gramme. These" centre, n
“sentlaJ'fol' the TB control proare jPanned to be developed as State
~~
Centres Xcentres
for
TB C__
r the
assessment
T P;
Programme—of
s”' and monl£oring of the TB
Control
V
."J
I
CCCS-13^
37
ial; No I
CHAPTER XIII
PRESENT status OF THE I’ROGRA.M.ME
I
?HE Progr£Ss (of" the different schemes of the National
b Control Programm<
-ie are briefly discussed below:
?
t-d
about a million new horns and infants below
one year of
age.
_
Training of paramedical1 personnel
r
of the rural'health
service for newborn and infant vaccination is in progress
Production of freeze dried BCG
.
vaccine in our BCG Vaccine
Production Laboratory is being
expanded.
TB Beds
■
The total number of TB 1beds
' available in the country
today is about 41,500. A little less than
1 a third of these
beds are run by voluntary oiganisations ----and the rest are under
control of State Governments, other governmental agencies,
municipalities, etc.
District TB Centres
J
tI’
P-’
There are at v
of which about sob
;?; a0^X743
Co”Sent
iOl,t 600Centres
TBU.Cl,n,cs ii!1 .the country
District
TB Programme in °300
districts
Farh
0I.gailIS"1S District
300 districts.
Centres is staffed with
a tew of
°f 1 le5e District TB
■* a team of
National TB
Bangalore A‘boma£ th. , , Institute,
,bv ---> Bangalore,
been provided
provided
'':>0 of dlcsc h^’e
bv the
the UNICFF
UNICEF nr /i
'vith full
and
1° Govcr,nnent of India
--11 set of
t r X-rav
''
Each District TB Centre on an n-’ e^uipnicnts nnci vehicles,
beral health institutions oartirL
gC
about 25 PcriPabout 2800 patients are PundcrP irr^
the Pro?r‘l^nics and
gramme.
Undci ^^tme^t of a District Pro-
Training & Demonstration Centres
treS^hiceh\rreainPreEent '7 TraininS
.-SET-
I
wards the end.
still have no Tb”clinic^In
111 the cou,ltrv t{1at
covered bv regular District T1h
.dis.tricts not vet
organise TB control nro^L
Pr.0?rai™e, it is possible to
demonstration Gen-
c lcse centres is given to-
Regional TB Organisations
I
t?
si“" ■'»
exist and trained personnel are ,;7i,
' Centre alrcadv
are
cither
available
i
or can be easily tr.Tned at Xationaf C 1,1 lhe St;it^
actnaty of a District TB pX" ‘Jne •3 fIInstitute.
nst,tute- The main
■ng and treatment through T
• is• to
‘0 °
rgan’5e case-find«se-findorganise
mstitutions of a district. °
existing peripheral health
BCG Programme
These hra
'
have been posted in or integrated
nP"0Fa““es- 290 teams
These teams are mos-lv cov^™ rh;u D1S.trictJB Centr« 50 Tar.
school age children Kv
g children in school and the pre253 million persons have h^n
visits- 4 tota> of about
million have^nand about
sent Tone hiX" \ Jth
x? £uncT°n™g at pre-
and the other in the So nh 14 "7hC 4CW Delhi Tp Tentre
losis Institute, Bangalore
These 31 C
4atlonal Tubercu■ble for assisting the s?,4 ■ , e, o''gan‘sations are responsProgramme nSthei,
■" developing District TB Control
parame“ personal
briefin& medical and
peripheral institutions and for nrn DJ?trict TB Centres and
guidance.
tOr PrOT'dmg expert advice and
Supply of Drugs to State TB Clinics
this rchem^there a?e mo™ than^OO TB
Undei
domiciliary treatment nf TR .
k° TB. dinics undertaking
ard anti-TB druo-s directly bv ?h?
arC beino/upplied standover 7,00 000 TB
T ' h Government of India. A little
Hary treatment at aPny XtTf
tO be Under do^
these 300 TB clinic? anH
thls scheme through
ttict TB Centres.
'
d b°Ut a00° sub-centres of the Dis-
paign. On an average about 13 mill * ir!cePtlon °f ^e camare offered vaccinatioS per vear vvh ch h
chiIdren
per }ear, which, however, includes only
f
--
I
:cesion,
:ccs- ’-jn
"--- 1
Vr
38
Supply of Drugs to Voluntary Organisations
-ill No I
I
Under
cost
CHAP TER XIV
RESEARCH
SI
lx the field of research in Tuberculosis, India is in ■
the forefront today.
Many of our research
findings have
contributed to the world knowledge about tuberculosisi and
its control and have been useful in evolving a sound programme for control of tuberculosis in India and in many
other developing countries.
55 TB clinics/TB institution ™
i.. TilCIe are about
that are takhio- advantage of th" b-, voIuntary organisations
patiercs are Ser
St n th'5 “ p"?6 and about 75'°00
at am rime.
' eatmcnt in these clinics under this scheme
In this Chapter, an attempt is made to summarize the
findings of some of the important research studies conducted
m India, on the basis of which our National Tuberculosis
Programme has been developed. Readers may also find the
answers to some of the questions that normallv come to their
mind in respect of the present concept of tuberculosis control
home treatment of tuberculosis, the role of food and rest in
treatment, risk if any, from a patient under treatment at home
to his contacts, protective value of BCG, whether tuberculosis
m our country is increasing or decreasing etc., from the sum
man of findings of these studies.
Supph of BCG Vaccine
Sv -
I
r
,lp.
Ender this scheme BCG vaccine is supplied free to the
Srates for use by BCG
M.C.E. institunons, etc., teams and other TB, Paediatric or
E^rcuLn for ciagncwtic participating in the programme. Tuuse is also supplied to certain TB,
paediicric and other medical institution's.’
it*
S
I
I
■
|
■
I
H
I
■
I
l.<
action is carried out mainly at the Government of
India s Nationii TB I,
’
Institute
at Bangalore.
Bangalore.
So far, about
yiO^dijrrict. 13 Te-oms c _
persomiel torn different States I
5'
■’
io
from these, a
iSd manv AH
ntre Personilei have also
been trained Lzd
_ _
-d many Administrative Medical Officers of
iiers offro^tarffii^n
Medical:eac
Officer,
■ D'StriCt Health Officers,
dpated in the seminars conductedrngX"' evSy yean
cipated
i
■
Training of Key Persomiel
also b^o^nTa^V^th^. TB ^ogrammes have
Golomb: Plan,• etc., in TuSrctdolis lont™!.1^
1
I
national tuberculosis survey
The National Tuberculosis Sample Survev (1955-58) was
CouncTof^'r,T“berculosis Sub-Committee of the Indian
Council of Medical Research. The survey was limited to innomnl’T5 °f fPUlmon‘lM Tuberculosis, one of the most imof vtw vS £r°m cP'cIem>ological and public health points
and villao- a^10u? tIPes of population in selected cities, towns
V!Ua8.es ,*n the States of West Bengal, Bihar, U.P., Delhi
Keral3?’ Andhra P{adesh- Mysore, Madras, Maharashtra and
X exam^nTby the
Ab°Ut three lakh P^ons
ere examined in six cities, 30 towns and 151 villages1 The
the sutislir l1ded- ln \he SUr'vy were chosen in accordance with
application Principles so that the findings may be of general
Xrt
SlX mstltutIons were entrusted with the survev
Patna
K T
J'?berculosis Centres in New Delhi,
nf
Hyderabad and Trivandrum, the All India Institute
Mis£n
Hygiene
leT K and! Public HeaIth’ Calcutta and
the Union
n ,On Tuberculosis Sanatoriam, Madanapalle in
Andhra
‘Pradesh. lhe entire population excluding children under
...
A-;.,-.;.,
40
\cces-i
";!s subje«ed
sufft^radio^api^anl
Sal' >1
'“"S’ »'
Sunq. „.m,
culosis varied'from 13 "to ^’pe?'°^O'' aa'Ve’ tUber'
towns and Hl.ages 17
o
Population VSarS^
y positive c
aieas varied from 2
generalRof the saine order ’ towns
t0"'nS and
a'ld 'il!ages Here
I
41
^X^i^in^" 1OWer
for females
age-groups above 35”years. than for
J- In general, the prevalence
rare showed a continuous
increase with age.
163 newly diagnosed and previously untreated sputum
posiuve parents of pulmonary tuberculosis from poo-- £ o
of the community in Madras City were randomly treated ■
vnn ^IUn\°rpl1?n;eA Wlth the samc chemotherapy ! c IXH
200 mg. and PAS 10 gm. in two divided doses per dly Pati
m LOndn
°mCI Kei,iS were Sivcn weekly supply of’druts
to be administered by themselves at home with monthly super
vismn of their progress at the clinic and were visited7t home
by a Health Visitor every fortnight. The patients in the
. sanatorium series had bed rest, good accommodation, ba In ed
diet and nursing care. Thus, this was a c„..,Fal;.
comparison of treatme nt of patients in best sanatorium conditions
in usual day-to-day home conditions of the 1—j with those
poor sections of
the community.
At the end of one year, 86% of the patients treated at
home converted to sputum negative and remained so (bacteriologically quiescent)\ ‘^/'gmnst 92% in the sanatorium natients. JImprovemcnt in X-ray and closure of cavity were also Jf
the same
order in both the groups.
ne rnde»
X
6‘ ]In. the cities the
& si.";,'js""
.
u
-----
compared to_ those in
------- economic and
A large majority of the ‘active’
7 <
cases had moderately advanced dtase.
probably active’
t™. SCBex
ta 4.. ~
per cent
per-
Hrv
SUr,Ve>' a!so showed t
’nmy^^5
city where the ^enceofXi
r
’
in a
four or fire
ccnt
high as
and
that
these
areas
were
k-.
inhabned by the poorest in the
generally
population, often living
remely insanitary conditions.
”7 in exCOMPARISON
OF HOME AND SANATORIUM TREATMENT
yLfbe, Tuberculosis Chemoa controlledJ companson of home
another3?0"1™ treatmellt for one
.eat and subsequently for
- foese
tO StUd>- the emergence of relapse cases
1-
•
(4
nouses indicated
sanitary conditions.
■
- *■
Follow-up: .After
one year, the sanatorium patients m
turned ow-up:
r ° ,l•hcir
• .After
horn
cs and the patients of both the scries
^ere closely} followed
_9_.owed up
up for
for another four years to studv
eS£tS-. Consideii
ng the overall relapse rate
the i
iong-term :fresults.
Considering
of the disease in the two gI0ups, k
„ao ffound
uu.._ that seven per
it was
patients in home series and ten pc
per cent patients
m sanatorium scries had bacteriological relapsi
>e over a fouryear period of follow-up.
It was thus conclusively proved that effect of treatment
donPahoT at h°me IS taS-S°Od aS of treatmen£ in a institu
non both m respect of immediate recovery and subseauent
prerention of relapse and that good food, nursing c u^ and
bed rest, etc., do not play any useful role in the treatment of
tuberculosis. Domiciliary treatment has the added advantage
of not causing any dislocation in the family during the period
of the patients treatment for tuberculosis.
8
penocl
TB ATTACK RATE AMONG CLOSE FAMILY CONTACTS
ranvTrlmStUdfy T Planned by £he Tuberculosis Chemothe
rapy Centre to determine the relative risks for contacts of
patients treated at home and in the sanatorium
*
F
..
It
.1
42
256 close family contacts of patients treated in homes and
272 similar contacts of patients treated in sanatorium were
intensively followed up by X-ray and bacteriological examination
for five years.
In each family, there was just one
- f
infectious case and the contacts in the two series were similar
in all other aspects. Effect of isolation of the index cases
could be best studied by comparing attack rate in the two
series in the first vear when the index case of the sanatorium
series was isolated in the hospital.
±3
.69°° ?f the sputum positives, 52% of the X-ray positives,
-9% of the inactives and 15% of the controls had at least
one of the above mentioned four symptoms.
An interesting observation of the study was
iiiC majo
was that
that the
ntv of cases in contacts
occurred
in- children
below five years
,
.
,
.
,
----------—
and iuere
••
’
’ within
; • *
detected
three months of diagnosis of the
index case and there was suggestive evidence that m most
of them the infection occurred before the index case was
diagnosed.
Analysis of the material also showed that 95% of the
bacteriologically positive cases were aware about their symp
toms, /2% experienced awareness and were worried about
their sypmtoms and 52% of them actually took action at the
existing health facilities under pressure of their symptoms.
Effective treatment of an infectious patient, whether at
home or in a sanatorium, rapidly kills the tubercle bacilli and
makes the patient non-infectious in a short time. The purpose
of isolation is therefore best achieved by putting the patient
on treatment immediately after diagnosis and ensuring reo-ular introduction of the medicine prescribed.
Sociological Study of Awareness of Symptoms Among Per
sons
fth Pulmonary Tuberculosis
r
'
’
|
iJ
If
were interviewed at random by social
for symp. investigators
--------- o—
toms. Unly
O"1.......
-L symptoms that were associated with Pulmosuch
narv tuberculosis
takeninto
intoconsideration.
consideration. OfOfthese,
-----— were
--pain in chest, haemoptysis or combination of these
fourc symp-----------toms were analysed statistically,
79% of the experimental
group and 83%’ of the control group were satisfactorily inteniewed.
In the first year, 4.9% of the contacts in home series deve
loped tuberculosis compared with 7.6% of the contacts of
sanatorium patients. Over the whole period of five years, 9.8%
of the contacts of patients treated at home developed tuber
culosis as against 14.4% of the contacts of patients treated in
sanatorium. There was no difference in the attack rate in
the two groups even when the initially tuberculin negatives
and initially tuberculin positives were analysed separately.
From this study, it can be concluded that there is no
specuil risk to the contacts of patients treated at home with
effective chemotherapy, the main risk to them being before
treatment has begun.
'-f fell
43
About 2,000 persons having evidence of inactive, prob
ably active and active tuberculosis disease in their X-ravs
whose sputum results were
also
available
(experimental
groups) were age/sex_
i
matched with an equal number of
persons with normal
31.^
—
'T^Y (control group) in 34 villages and
four towns in Tumkur district
district in
m Karnataka. These persons
Cough was found to be the most important single symptom.
69% of the sputum positives and 46% of the X-ray
positives had this symptom against only 9% of the normals.
This study showed that half the infectious patients in a
community are already knocking at the doors of the existing
health service under pressure of their symptoms and if adc°quate facilities are provided, another one-fourth will immedi
ately report to these health institutions. Thus, about a half
to three-fourth of the infectious cases can be dealt with in a
short period at the existing peripheral health institutions.
DISTRICT TB PROGRAMME PILOT PROJECT, ANANTAPUR
The District TB Control Programme was formulated by
the National FB Institute on the basis of their knowledge
gained from various case finding, treatment and methodological
alternatives tried in Tumkur and Bangalore districts in f96061 and was implemented as a pilot project in Anantapur district of Andhra Pradesh to study the feasibility of the District
TB Control Programme in 1961.
*
The district had a jpopulation of about 1.5 million. One
District TB Centre equipped with
‘ ’i an X-ray unit was established at Anantapur town. There were 14 Primary Health
/
7
S3
.
:.EE-
■• •••
-•
-14
-•ccer
E
45
Enlr«-’,ten
health units
30 rural
doctor/
ten ™.
units and
and 30
rural dispensaries.
If !..a
a,b.e T,Alinost aI1 health centres. Medical
Microscopes were provided in PHcfand
•d other dispensaries. Sputum
case-finding was organised with
tutions. Sputum specimens of co-operation of all these instiU
*,’
- - a persons with cough were
collected in iall
” these
centres throughout the vear
The e
sputum smears were exammed in the centres having micK
copes. The centres not ihaving any microscopes sent their
smears to the institutions■ with microscopes, functioning
as
microscopy centres.
I
for more than two weeks
I
P
P°SltlVe Cases had (ouSh
hom2. The reETart of tE h
^VCn ‘-"^ulntorv dominearest to their
a ca^ finEf0Und f aSi'y feasible and uscful to organise such
pi.?iHh7i;s„5,g-
Jl'E YEAR STUDY OF EPIDEMIOLOGY OF ---------JN
A RURAL POPULATION IN SOUTH TVfiERGULOSIS
INd7a
-
Tuberculos/sEns'th'E/ E'tbsEE "he ^tuElh'iE^ Naftional
monary tuberculosis under
w natllr.al history of pul-
'Sis srsa *
if
The salient findings of the survev are:
(1) The prevalence rate of infection was about 30%. It
a stcady decrease specially in the age-group
(-) The average annual incidence of infection (rate of new
infection u..
by tuberculosis
...i :
s every year among uninfactcd) was about one per
}
cent. During the study period,
the incidence rates showed a decline from 1.63% to
0.8% for all ages combined.
(3) Prevalence rate of disease in the study population
gradually decreased from 4065 cases per 100,000 population in tthe first survey to 337 cases in the third
thhd
survey but slightlv' rose tto 393 cases E.
in the fourth
surveyy probably due to drought in the study/ area,
For the younger ;age-group
7
of 5 to 34 ;years, however, the rates showed” a continuous decrease during
the entiie study period.
(4) Annual incidence rates of disease also showed a down
ward trend as in case of prevalence, being 132 cases
per
100.000 population between first and second surv
'
’
.'S " bct;vccn, second and third and 103 between
third and fourth surveys. The younger age-group
below 35 years showed ‘ a steady downward trend
during the entire study period.
■■
r ,x
_______ ________
(:>) Prevalence and
incidence rates of the disease in
creased with age and female cases -were much Ic'S
(one-third of prevalence cases and half of incidence
cases) than in males.
(6) Of the 126 cases found at the first survey and followed
up for five years, 49.2% died, 32.5%> were cured
and 8.3% continued to remain sputum positive at the
end of five years. In the incidence cases (new cases
detected by survey)
however, there was a sizable
natural cure of 52.4% and 14.3% died. In the pre
valence cases (cases available at any given time) follno/ UP fO1 the Same Period the death rate was
16.9%.
(7) Primary drug resistance did
in five years.
not show any increase
i
1
":i‘
a
46
The study showed a gradual natural downward trend in
the prevalence and incidence of the disease, specially in the
younger age-group.
DELHI TUBERCULOSIS SURVEY
i
il
,ioThe ^ew DeUii Tuberculosis Centre conducted a survey
/0) in Delhi to study the epidemiologv of tuberculosis
m an urban population with a TB control programme in
operation. A randomly selected population of nearly 30 000
was under surveillance in one of the most congested locali
ties ot Delhi. A reasonably good domiciliary service for detecuon and treatment of tuberculosis cases was available in the
area tor the last more than 30 years. Four surveys were
carried out at an interval of 30 months during the period
of study.
The following were the important findings:—
(1) The
of total active cases which was 1720
inc prevalence ot
per hundred thousand population in the first survev
in 1962 came down to 880 in the fourth survey in
1970. Total bacillary cases came down from 400 per
hundred thousand population in 1962 to 210 in 1970
Thus, prevalence of active cases of tuberculosis was
reduced by about half.
(2) The prevalence rate increased with age. There was,
however, no difference
in the prevalence rate among
-----males and females upto
i
35 years of age though after
33 vears there was a steep rise in the disease ;amongst
males.
This was perhaps because
these survevs
covered an urban population.
■
(3) The incidence rate of bacillary cases was about 90 per
hundred thousand population per vear and that of
total active cases 340 per year. The incidence rate
did not show any downward trend.
The study showed that in ahn urban population with a
reasonably good
domiciliary
.
,
> sen-ice
’ ‘ programme, there is a
reduction in tthe
’ prevalence
____ T
rate of tuberculosis in a reasonably short period of time.
I
*1
47
madanapalle tuberculosis research project
The project was started in 1950 and comprised Madana
palle town and about 200 villages within a radius of 10 miles
with a population of 50,000. This population increased to
about 90,000 by the end of the study period. Seven surveys
were conducted in the population above five years of age ivith
tuberculin, X-ray and sputum examination during the period
from 1950 to 1965. Case finding, treatment, both domiciliaiy
and institutional, and BCG vaccination were provided to this
entire population.
The following are the salient findings of the survev:
(1) The number of bacillary cases which was 410 per
100.000 population at the time of the first survey in
1950-51 came down to 320 in 1957-58 and was further
reduced to 110 per 100,000 population in 1964-65.
(2) The number of cases in the male populationi was two
three times more than in the female population.
to t'
(3) The prevalence rate of infectious cases> increased with
e’ lnumber
’ - ’
/ cases . in
.. males ’being
J
. aSthe
of
much more
than in the females specially above 20 years of age.
(4) The incidence rate of fresh tuberculosis cases was
found to be 34 per 100,000 population and the inci
inactive but abacillary
dence rate of active and
(sputum negative) cases was found to be 207 per
100,000 population.
(5) The death rate which was about 250 per 100,000
population in 1949 in Madanapalle town came down
to about 64.1 in 1951-53 and further reduced only
to 21.1 per 100,000 population in the period 195455, thus showing a definte reduction in death rate
in the study area.
The findings of this project showed that with a reasonably
good TB control programme in rural areas providing faci
lities of case findings, treatment and BCG vaccination, the death
rate goes down steeply and the rate of prevalence of infec
tious cases can be reduced substantially in a reasonable period
. of time.
J
..J.
r?
i
48
49
STUDY ON DIRECT BCG VACCINATION BY THE NATIONAL
TUBERCULOSIS INSTITUTE
Direct BCG vaccination is a safe procedure as it does not
cause anv unusual inconvenience or danger to the reactors
and the acceptability of the programme is also not affected
in any way.
Till 1964, the conventional procedure in BCG vaccina
tion programme was to do a preliminary tuberculin test and
•offer BCG only to the tuberculin negatives. This involved two
visits to each area and other technical and operational com
plications. Offering direct BCG vaccination would simplify the
procedure and speed up coverage of the young population.
This study was, therefore, taken up by the National Tuber
culosis Institute to see if direct vaccination was safe, effective
and acceptable.
' i
I
I4
I t
' •
First study: A rural population of 1891 was randomly
divided into four groups: (1) tuberculin tested and vaccinated.
(2) tested but not vaccinated, (3) not tested but vaccinated and
(4) not tested, not vaccinated and these groups were followed up
with periodical examination, tuberculin tests and X-ray for 90
days.
Results showed that local reaction at the site of vaccina
tion and regional lesion at the lymph nodes in both the tuber
culin non-reactors and reactors was of the same order. Thc^e
was no evidence of existing tuberculosis disease being exacer
bated or foci of tuberculosis flaring up.
i
MADANAPALLE BCG TRIAL
This study was undertaken to assess the protective value
of BCG vaccination against tuberculosis in Indian population
as a part oFthe
of the ” Madanapalle Research Project starting from
1950.
A. total of about 21,500 persons were tested with tuber
culin
About 10,000 were found to be tuberculin positive
reactors and 11,500 non-reactors. The non-reactors were ran
domly divided into two groups. BCG was given to 5,069 and
5 808 were left as unvaccinated. Both the vaccinated and
control groups were followed up by periodical tuberculin test,
X-rav and sputum examination till 1967.
The findings of the study can be summarized as follows:
In the first five years after vaccination, BCG was respon
sible for reduction of incidence of tuberculosis in the vacci
nated population to the extent of 60% compared to that in
the control group.
Second study:
1186 persons were both simultaneously
1186
tuberculin tested and BCG vaccinated and were followed up
for local reaction for a month.
In the next five years, the reduction in incidence of tuber
culosis attributable to BCG vaccination was 56.5%.
Local ^reactions were found to be of the same order in
both the reactors and non-reactors as in the first study.
But if the cases found within the first 1 to 11 years of
the trial that could have acquired the infection before entry
into the trial are excluded, the reduction in cases attributable
to BCG vaccination was 71.4%.
Third study showed that local reactions after direct vacci
nation in one village did not affect the acceptability of direct
vaccination in neighbouring villages.
After another four years’ follow up in 1968, it was found
that in 14 years, BCG vaccination was responsible for 24%
reduction of active cases and 33% reduction of bacillary (in
fectious) cases in the vaccinated group.
STUDY OF NEW DELHI TB CENTRE
In a similar study conducted by the New Delhi TB Centre
among primary school children also, it was found that direct
vaccination of reactors was innocuous.
r
Thus, it was observed that the vaccination was most effec
tive in the earlier period but gradually became less effective
in the later period because of possible waning effect of vacci
nation. The suggestion was that BCG should be used mainly
shortly before the population to be protected is exposed to
5—7 DGHS/ND/77
I
_ __ 1..... .......
■r
I
J
50
} 'll
infection with tubercle bacilli and a second Yaccination may
be necessary before substantial waning effect of the first
nation takes place.
i i
■
1^
f-
I
I
£
i
I
.
CHAPTER XV
HEALTH EDUCATION
Other BCG trials in the world have shown various levels
of protection e.g., 96% in Danish Scl\°o1
SQo/ in North American Indians (Aionson, IJoo), / /o
English School leavers (B.M.R.C 1963):- ^%chwSn'Ser
fants (Rosenthal, 1961); 31% >" Puero ,R'cna" S' "
etc, 1958); and 36% in seven years and only 14/o m 14. yea
in an American population (Comstock and Palmer, 19 6).
inarch towards a healthiei Indmany of the diseases
about the etiology (causes and p
th}s k7nowiedge to the
that afflict mankind, c?mmii"H;rsnnd best remains as much a
people in a language t ic}
advances achieved in medical
problem as a challenge.
k‘nowhow acquired in diagnosis
sciences, and the techno
notice of the
anonVr“nd: accepted"and ‘adopted bv them to get adequate
kturm, investments on health programmes.
Since the study population of the Madanapalle trial was
small and Is the other studies have shown different levels of
protection from very good to insignificant a large sea e BCG
trial known as Tuberculosis Prevention Trial is beino con
ducted in South India to get precise information about the piotective value of BCG in Indian context.
Tuberculosis continues to be one of,the major public heal*
problems in ou*
are infectous, are evenly distriTB cases of whom 2-a mil ion ar
are
buted in towns and ullag
n,inicable disease thrives on low
in the villages. TB being a con nun
d,sc vcrcrowding. in-
!
rM
The manaSenie^
during the last three decadts Nev. ari
;
n
a high
effective, have been ^“y’k.berciiloiis ‘ DoXcUiary treatment
level of protection against tubercuh□
doo’rsleps Thc
with potent drugs is avadab e
•.(inal Tubcrculosis Control
fundamentals that gover
‘revcntiOn of development of
Programme (Mtr) are.
y 1
infected and (ii) detection
■
11 ■
• »«»!■« “xr
11
11
with a view to rendering them non-infectious.
“ p°”ib"
The<e can be achieved only through a sustained educational
in
IT
come. Health €“uca“°‘ ,
consciousness in the peop
attitude towards hYalth
disease but as a status_ o
1 14 L!
cc::Pl “
-----------------------------■*■
-
M
--n-ff
,
fs needed t0 imbibe a positive
j
freedom from
„al kdlbbeing. Much of the sucpatients depends on then
-de —of early signs and
i
i
52
svmptoms of tuberculosis, and on suspicion, cotne forward for an
|
examination.
OKTV.T TVBERCULOStS ^ST.TUTIOSS
Role of Health Workers
The success of the do^11c\11^Pco^p^
o^the periphecertain extent, also on the ski ai‘
h
opportunities to
ral health workers. As these workers hat eopp
move closely with patients, it shotiId be^em
supervise self-admimstration 0
» ;1
adhere t0
pres
take prompt measures when^thej.^
posted ;p spc.
cribed treatment. The hea“"
WOrkino- for a general agenc\
cialized clinic in an urban, aica
dm£s efficientlv and effecin the rural area, can dischar
knowledge regarding factivelv provided they possess. the ba
“
?evcn.
tors that promote transmissio. oH nte .tm
I
i
effective communicators.
health worker’s scheme also calls for
The multipurpose
.
of Basic Health
the con\Pcle”C.?,
strengthening the sskill
— and educate
the communities on preWorkers and A.N.Ms. to -3 of health services. With the orgaventive and promotive aspects
nized development of t-b-rc
country t— —
right upto the .eman]
scientific knowledge of various aspects o(
services, an elementary
has Vo scl
be^.....
provided to the health workers. A
the programme has
has to I 1 ,
’ ■ trained and equipped to
peripheral worker has to be properh
deal with individuals and groups.
i
have the support of different media
The workers has
h^e tt t H n[ verv
inputs
to make his message;
educational materials for use by
are being made in pro
o
puhlic There is, therefore,
rrAPeatrneed°rof“eTeloping suitable educational materials on
a"d “-Sd 2™.“S=
F:
z..
i
1w
I O’
aifaspccts of the tuberculosis control programme.
With a view to meet the growing needs of educational ma
terials the Central and State level Health Education Bul;eaux
are engaged in production of ‘proto-type materials, fot use both
bv health workers and the lav public. With the growing literacs
leUl in the country, printed materials and other commumcation channels like films and television hold great potential and
would prove highly useful to health workers tn functioning
effectively.
w
SOME IM*’
TUBERCULOSIS INSTITUTE, BANGALORE
National
THF. National Tuberculosis
1959 at Bangalore fot the
i
(i) To formulate through. icstuberculosis
hensive
gramme
as urban parts of the country.
,
pio-
(ii) To train medical and
could
h“‘" 21 Sd””b”wi“
“
-nd .ednn,.,., .« Pro,e ■» b=
“
I
CHAPTER A'1'7
for its assessment.
Though the objectives aPP^
sight, in rcalitv they meant extcnsiv
p
complete re-
the tuberculosis problem in the country
The Institute is
Director' GcnCTa? of Health
the Central Government un
.
j qqq. Senior scientists 13,
Services The
strengthdc^s^ of^^^
R
full.
d«a
»d ...»
port facilities.
Activities of the Institute
The Institute undertakes:
(i) Epidemiologicalthat have X"
meters regarding pim alence a
q£ .
STSenU^“Aing time periods, formulation
........................................
55
a
54
BCG non-medrcal team leader, X:ra,
by
statistical assistant. The p t p
WHQ fi.om
State Governments and s0™e“^s developing countries of the Reo
1 rnnKM each of 4 "ceks duration every
of mathematical cpidemetric models
°h
servations revealing the time-trend of
extent of infection with atypical im cobacteria an1
simpler and more practical methods of epidemiological
research.
that have brought out the \arying
’’ —. treat-
I
I!
il-
I
w
?■ :
i;
«!
ment and BCG vaccination activ
t.-.- ’ities, the cost factor.
simultaneous smallpox and BCG vaccination as well
as direct BCG vaccination, sputum mlc;'osc°P2>■ and its
and effectivity
of
operational implications, efficiency a..the programme, etc.
(iii) Sociological and behavioural studies throwing lightt on
action taking,
the awareness of symptoms, a-----... quantifica.
tion of suffering, acceptability of the provided L cilit cs
default and
and the drug regimens, reasons for drug defaul
response to defaulter actions, fate of cases tteated
der the programme, etc.
(iv) Bacteriolofrical studies centered on the Zichl-Neelsen
technique of sputum microscopy, fluorescence microscopv, culture, cost of examinations, etc.
An animal house is under construction which will
open up research possibilities in the field of disease
caused by atypical mycobacteria.
(v) BCG studies concerned with the quality of vaccine,
technique of vaccination, assessment of the BCG vacci
nation campaign, etc.
(vi) Miscellaneous research connected
with radiological
equipment, technique of radiography, training methocisand the results achieved through programme tiaming,
PERT-CPM of programme implementation, monitor
ing and assessment of the programme, etc.
Apart from research, the Institute has full scale involve
ment in training of the programme workers as well as tubeicu' losis workers of other categories, from India as vyell as other
countries. This activity comprises the following national as well
well
as international training courses.
(i) Two national courses each of 13 weeks’ duration every
year for training of tuberculosis control teams in the
programme management. Each team comprises a me-
some developing countries.
•te ™°'
<»»
year for District icvei i
nrrventive medicine,
of tuberculosis and social and pre'cntne
senior tuberculosis workers, etc.
for the personnel of State Tuber(iv) One course every year
culosis Centres.
2 UNICEF sponsored international
(v) The participants of
for
paediatric
teachers.
training course I
of the WHO sponsored
<"■> s,
training
"™"s' ‘:==;
s workers from other countries visiting the
(viii) Tuberculosis
fellowship.
institute on WHO
\
paring for diplomas or degrees.
Achievements
Formulation of District'“'""'VoXlatTd
the District Tuberculosis Programme (DTP) vas {formula ea
ind recommended to the government as the ptvo
^^r^^^^pmme ftmX^in
different areas, new research studies are being constantly unto
taken to. improve the Tuberculosis programme m the country.
g •
■*
Li
E
!
56
57 •
Research: In the field of research, the Institute has already
conducted over 130 studies on pulmonarv tuberculosis, com
munity suffering and behaviour, BCG vaccine and the cost as
pect as well as utilisation of the provided senices by the people,
efficiency of the senices, monitoring and assessment of pro
gramme objectives. Over 140 technical reports and papers have
since been published in national and international journals
and periodicals. Besides, technical innovations in the form of
a portable vaccination kit, a daylight X-rav film loading and
developing box, electric and electronic circuitary in X-ray units
and simple staining techniques have been developed. The DTP
work manuals evolved bv the Institute are in great demand in
the country as well as outside.
The supply of BCG vaccine and tuberculin dilutions be
gan in Februarv, 1949. Subsequently, the laboratory was shifted
To Its own building near the King fnstitute and l^arge-scaie pi<>
duction of BCG vaccine and tuberculin dilutions was taken
up. Apart from meeting the full requirement of the “untn s
mass BCG programme, the laboratory also supplied he Wogicals to many of its neighbouring countries. It is the woild
largest BCG producing centre.
Training: In the 33 national training courses conducted
so far, 433 tuberculosis control teams have been trained, compris
ing 527 medical officers, 524 laboratory technicians, 466 statis
tical assistants as well as 107 foreign programme workers. In
the 13 training courses conducted for public health nurses 65
have been trained. The 12 seminars have attractetl 230 partf
cipants so far. The training effort is generally considerably
ahead of the programme needs, after taking care of the turn
over due to retirement, etc., and the wastage.
Miscellaneous: The Institute faculty has functioned as
WHO advisers in several countries of the world, as visiting
professors on international training courses, as members on
several national and international technical committees and as
participants in the international conferences, in order to present
research papers.
P
I
I
I
BCG Vaccine Laboratory, Guindy, Madras
The Government of India felt the necessity to sponsor a
nation-wide BCG Vaccination Programme in 1948, and, to
achieve this object, Madras was chosen to house a BCG Vaccine
Laboratory, as a building constructed bv the Government of
India for the production of Yellow Fever Vaccine was available
m the King Institute Campus. At the request of the Govern
ment of India, the WHO sent Dr. Poul Lind, a Danish BCG
Expert, with all essential 'equipment to start the Vaccine Pro
duction Centre, and in August, 1948 the Laboratory was opened
by the then Union Health Minister, the late Rajkumari Amrit
Kaur
As the life of the liquid BCG Vaccine is limited and the
vaccine has to be protected from heat and light, need for the
preparation of freeze dried BCG Vaccine, which is heat stable
and which can be kept for longer penods was
this object a freeze-drving plant capable of prepanno
.
ampoules of freeze-dried vaccine in one shilt. was procmed t
the vear 19.->7. Three more plants each capable of.‘■'"’"o >ampoules at a time were added in November, 1.6 .
After getting satisfactory results, from the experiments <m
the preparation of freeze-dried vaccine, it was plawned to g
into iX-scale production of freeze-dried vaccine to replace
liquid vaccine in the entire programme. Additional sterile an
conditioned accommodation was provided, a testing and q|Uality control section was added and the required equipment i ..procured The production of freeze-dried BCG vias inhauce .
?o about 5 million doses and was supplied for use in the m»s,
campaign
in 1969.
In the Fourth Plan “Expansion of the BCG \ accine Labo
ratorv for enhancement of production of freeze-dneu BCG va,,
cine” was taken up as a plan scheme. A large number of techn c<
and non-technical staff was added, equipment was procured and
an independent testing and quality contro
£ot tc..
ino- and certifying the vaccine was established at the Nation.
Institute of Communicable Diseases in Delhi. The production
was enhanced to 30 million doses by the end of theou th
Plan and liquid vaccine was entirely replaced ^ freeze dned
vaccine in the whole programme. Tuberculin dilutions yei .
also prepared and supplied for diagnostic use m the country.
The WHO and UNICEF have been taking active interest in
Ae expanln of the laboratory so as to develop this laboratory
as a reo-ional laboratory for supply of freeze-dried BCG to the
otherCountries of the region. The WHO^as been providing
several consultants and fellowships. The UNICEF have b.e
1
59
58
supplying equipment and necessary spare parts, etc. An auto
matic ampoule sealing machine procured by the UNICEF r\as
installed in the Laboratory in 1973.
In the Fifth Plan, the target is to double the present pro
duction of the laboratory and further expand it if necessary.
A large part of the vaccine will be supplied in small packings
of 20 doses for use by rural health workers and institutions. Foi
this, a semi-industrial type freeze drier with a capacity of 8.000
ampoules per run has been procured by the Covernment Ot
India and has been installed in the Laboratory. The WHO and
the UNICEF have been assisting with experts, equipments and
material. The Laboratory is also participating in the quality
control and assav of BCG vaccine produced in different Labo. ratories in the world under WHO auspices.
The Testing and Quality Control Laboratory at the Na
tional Institute of Communicable Diseases is also being further
developed.
Tuberculosis Chemotherapy Centre
The Tuberculosis Chemotherapy Centre was established
in Madras in 1956, under the joint auspices of the Indian Coun
cil of Medical Research, the World Health Organisation, the
British Medical Research Council and the Government of Tamil
Nadu as a temporary project to conduct controlled studies de
signed to provide information on domiciliary chemotherapy in
the treatment of pulmonary tuberculosis.
The Centre has three main divisions: (/) Laboratory Divi
sion consisting of bacteriology and biochemistry sections,
(h) Statistical Division and a Clinical division consisting of out
patient department, and (Hi) Radiographic section and a well
organised domiciliary' service. A W.H.O- Senior Medical Officer
acted as the Director of this Centre from 1956 to 1964. In
1964. the National Director was appointed by the Indian Coun
cil of Medical Research, and the Centre was made a permanent
establishment under the Indian Council of Medical Research.
The World Health Organisation continues to maintain active
interest in the Centre’s research work and provides expertise
and supplies not available in India.
Controlled studies carried out at the Tuberculosis Chemo
therapy Centre have revealed that ambulatory' chemotherapy for
tuberculosis, based on a well-organised clinic service for a
y’ear, virtually' equals sanatorium treatment with the same che-
aotherapy for the same period, not 0^t
reutic response in terms of ov-ra11 lad oe .p
thePlikelihood
tavitv closure and sputum cons
‘ fouow.up. Jurtherrelapse in a subsequent 4-year pe tot o foHo
p
e
srore, tire risk of contracttng
"han in those of
warily contacts of pattents seated a^home than
oatients treated tn sanatonm;ent bvfore treatment had
contacts was from the infect
P‘
, h
h traditionallv
SZt X—”d°‘1’"
countries of the world.
In dailv oral regimens, reliance has; to be placedi on the
at
in
the
as a
“X21
STS
and has the advantage that the Physlc‘anTV
'tl ere-
Centre Based on these studies, the Centre has projected suPe
Sed intermittent chemotherapv as an ^^natn. system of
chemotherapy especially in
countries where the otgan sa
tion of standard oral regimens has already failed i P™c
’
Recentlv the Centre undertook a series of studies with a slo
rHease preparation of isoniazid for evolving effective onceweeklv reHmens which would considerably simplify the or a. nization of chemotherapy programme. Current research is dire
-d towards evolving effective short-course regimens.
*
\
I
61
60
i
The Centre also undertook studies on other chemothera
peutic regimens for treatment of tuberculosis with different
standard and reserve drugs and chemoprophylaxis studies. The
clinical studies were all supported by bacteriological and bio
chemical investigations in depth. Notable among other studies
conducted at the Centre are studies on metabolism of anti-tuber
culosis drugs, tests for detection of anti-tuberculosis drugs in
urine, biological characteristics of Indian strains of tubercle
bacilli and the comparative studies on different measures of
sensitivity of tubercle bacilli to various anti-tuberculosis drugs.
Many of lhe findings of the Centre have received a worldwide acknowledgement and indeedl some of them have had a
great impact on the formulation of tuberculosis control pro
grammes in Asia,. Africa,, South America and some parts of
Europe. Though the main aim of the studies at this Centre is
to evolve practical and effective methods of treatment for tuberotdosis patients in India, the logical sequence of the investigamns undertaken, together with supporting laboratory inxestigatksns, has resulted in invaluable knowledge of the principles of
chemotherapy. The Centre is recognised by the Inter bniversity
Board for Post-Graduate Study leading to Ph.D. degree in bac
teriology and bio-chemistry.
The training activities of the Centre include lecture de
monstrations to senior medical students, interns and post-gradu
ate medical students from the National Tuberculosis Insti
tute, Bangalore and for the International Course in Tubercu
losis. In addition, two I.C.M.R. fellowships are awarded anntally for training in the methodology of controlled clinical
trills and laboratory methods.
Tuberculosis Prevention Trial
A number of controlled
BCG trials have given very
conflicting results. Developing countries are dependent to a
veyr grent extent on BCG vaccination for the control of
tuberculosis, becau^
the shortfalls in diagnosis and treat
meat of tuberculosis.
has become essential to assess
precisely the value of BCG vacciner;on
our o^-n context.
Tlse Project Tuberculosis Trial was, therefore, ^rted in 1964
unsaer the auspices of the ICMR, the U.S. Public Heaiiu
lhe WHO.
i
After a preliminary feasibility study, the BCG trial vvas
started in 1968 in Chingleput District, Tamil Nadu. A sample
.urvev showed that this area had
high prevalence on non
specific sensitivity as well as of pulmonary tuberculosis, lhe
initial examination included complete census, tuberculin tests
with PPD-S and PPD-B. vaccinations with BCG or an injection
with a placebo, examination by X-ray of persons over 10 years
of age and bacteriological examination of - specimens ot
sputum from persons with X-ray abnormality. This P^3^ ®
the work was completed bv the end of March 19/1, coven o
32 months. Of the 3,66,265 persons registered, 2,8-,-4/ were
vaccinated with BCG or placebo.
. i of the area including the populaThe entire population
initiallv
surveillance.
lion examined
i.;.:;a!’.'’ is
:: under continuous
"
bv
the
studv
teams
are being
Tuberculosis patients diagnosed by
treated on domiciliary basis.
About 2’. months after the vaccination a random sample
of the vaccinated population was retested with tuberculin and
was also examined for BCG scars. It was found that . /0
and 6 0^ of those vaccinated with the strong and weak doses
;.f vaccine respectively had no scars and 2.7% of those injected
with placebo had scars. Among children aged (1-14) years and
reacting with induration measuring (0-7) mm to the tuberculin
test the mean size of post-vaccination allergy was found to be
16.S mm for the strong vaccine and 12.8 mm for tnc weak
vaccine. In the same group the mean size of scar uas 5— mm
for the strong vaccine and 3.4 mm for the weak vaccine.
Other Activities of the Project
Tuberculin testing of samples of population in certain
areas of North India with PPD-S and PPD-B, was done to
asxe« prevalence of non-specific sensitivity. It has been found
that only the hills of the Uttar Pradesh, Kashmir Valley and
Himachal Pradesh have verv much lower prevalence of nonqxcilir senritivitv. It has been found that the Nilgiri hills also
have a low prevalence of non-specific sensitivity. The study
suggested
that non-specific sensitivity was associated
with
alutude and not with the geographical location nF the area.
Retesting of random samples of the IB Prevention Trial
population with tuberculin was carried out at 2| years and
£'■111 r vears after the initial examination. It was observed that
X
63
62
W.H.O. and the UNICEEi^e^’i^,^Sthed^-
three months to -I
post-vaccination allergs had waned from
further waning from 2.1, years to
years and that there wz> no
4 years.
significance of this waning is not
- The reason for or the
clear.
to have gone
The prevalence of infection does not seem
patients have been the ma
;
to its own domiciliary
‘clinical section, patients
^°^onDo£ about S lakhs and also
treatment area coveun0 1 P ‘
frOjn neighbouring States
of patients.
down at four years.
BCG in the prevenUpn of
A Trial for the »alue of
So far, about 2.a-,000
----Leprosy was started from October 19/3.
about 1,73,000 persons
Srib^^eLite-as weil as suspicious cases of
respect of methods aiming
leprosy have been diagnosed so tar.
tuberculosis patients
The effect of BCG vaccination on
L..3
beten
studied. Long term
and tuberculin positive children has L_.
of 15 months in patients and
follow-up results over a period g. —
that BCG vaccination
over 21 vears in children have shown . of pulmonary tuberdid not' increase mortality among patienu,
’ i children or
culosis or among strong reactors 10 uMrcubn i
It can safely
:: that BCG
children did
BCC
vaccination was initiated.
Results of the Main Study
tuberculosis only among those
BCG can protect against
^uxu.. O:- /..e total number o
who are non-reactors to tuberculin.
tuberculosis that have developed
new culture positive cases ott..-.-' "T
during the first 21 years of the trial, only
./o are among this
that
group? The study is being continued so t--- adequate cases are
so that the
obtained from among the tubeiculm
O‘
protective effect of BCG can be studies.
State TB Training m
Demonstration Centres
New Delhi TB Centre
The New 1
Ihi Tul i
is
Centre, originally know;
’ isried bv the Tubei
- country to be upgraded ‘•fr/:n\hc Gove
in 1951 with assistance
•
“o^di^efficiencyPof domici-
Research in various
as
..-.aaiion Centre
of India, the
i
_
,.P
been one of the main
functions of the Centre.
nihprruiosis drug schedules, BCG
miology .and time trend o
The Centre. The
vaccination, etc., ha\e
^d-ai international coopcratixe
Centre has Parllt,Pa!a •
' aspects of tuberculosis and in
studies in respect of vano
d bv thc I.C.M.R.
several other cooperative stu'1 CS a .ic^cc o[ this Centre on
More than 100 papers base
e. pc
prescntcd at national
Trrt,?g o,
personnel has been one
include students for D.T.C.D.
Centre since its inccP^
p0Stgradaute medical students,
course and ,l>'lder;5r_ad^^„“"C1 ^Tuberculosis Health Visitors,
Para-medical workers ^lude
io
hers laboratory techmntirses, medical social «orke , d
p°
courses arc
cians, BCG technicians, etc A
is running th
S’the Oto tohrng IMitos of Ddk.is located in this CenThe Northern Regional TB Centre
supervision
tre ; nd works under ,the technical guidance and
0[ c Director of the Centre.
w Delhi
bnlk of the running expenditure of t1
Other
i ne
. provided by the Government c
TB
’ B Centre i
fuberculosis Association of Inai
txlxx statutory local boo.i
Association and certain
mstialso contribute toward:
. tary organisation a-— tutions.
I
f'
f
NATIONAL
PROGRAMME FOR
CONTROL OF
TUBERCULOSIS
L: TT
i L
■
-.
ffic '•
K?¥r
NATIONAL HEALTH
PROGRADE SERIES 10
-■
J
X<;
i
fcac
I
I
iK*S
i
-3
i
1
VHAl
'
>A-
Ae^tioa
,- ■-
NATiO^AL S^STiTUTE OP HEALTH AND FAMILY WELFARE
NEW MEHRAUU ROAD, BUNK■-.^WEW DELHM10 037
-tr'W.fiT - - .
.
NATIONAL HEALTH PROGRAMME SERIES 10
NATIONAL HEALTH PROGRAMMES SERIES
This series of publications is intended to promote the continuing
education, dissemination of information as well as the study of
health problems and major diseases in India for those who have
concern for the health and well-being of the people. It is also
intended to foster the development of an efficient system of health
care service delivery in the country on the basis of such up-dated
publications on the national programmes for the prevention and
control of health problems. In this task, the practitioners and
trainers/teachers of health systems, as also the policy-makers and
those affected by their policy, must be brought together. The
publications, issued in this series, will strive to bring them together
in thought, so that they might work together in action.
A
NATIONAL
PROGRAMME FOR
CONTROL OF
TUBERCULOSIS
e
l
1
Dr. A.K. Suri
Additional Director General (TB)
Directorate General of Health Services
Nlrman Bhavan, New Delhi
1
i
NATIONAL INSTITUTE OF HEALTH AND FAMILY WELFARE
NEW MEHRAULI ROAD, MUNIRKANEW DELHI-110 067
CONTENTS
introduction
I
I
Magnitude of the Problem
9
Aims and Principles
10
Infrastructure of the Programme
12
International Assistance to the TB Programme
15
Expansion of the Programme During the VI and VII Plans
15
Short Course Chemotherapy Drug Regimens
18
Schemes During the Vllth Plan Period
21
Financial Outlays
O
e
9
22
Evaluation of the Programme
23
Recommendations of the Evaluation
23
Present Position of NTP and Shortfalls/Problems
tn the Implementation of the Programme
26
Summary
31
References
33
[
LIST OF ABBREVIATIONS
T.B.
Tuberculosis
N.T.P.
National Tuberculosis Programme
D.T.P.
District Tuberculosis Programme
N.T.I.
National Tuberculosis Institute
I.C.M.R.
Indian Council of Medical Research
B.M.R.C.
British Medical Research Council
P.H.I.
Peripheral Health Institute
P.H.C.
Primary Health Centre
D.T.C.
District Tuberculosis Centre
M.P.W.
Multipurpose Worker
A.F.B.
Acid Fast Bacilli
S.I.D.A.
Swedish International Development Agency
R1, R2, R3, etc.
Regimen No. 1, 2, 3, etc.
2 SjHjRjZj
2 months regimen with Streptomycin,
Sulphate, Isoniazid, Refampicin and
Pyrazinamid on twice a twice a week.
2E.H.R.Z./
6 T H or 6 E H
Ethambutol, Isoniazid, Refampicin and
Pyrazinamid are given daily for 2 months
followed by Thiacetazone and Isoniazid given
daily for 6 months, or Ethambutol and Isoniazid
given daily for 6 months.
S.C.C.
Short Course Chemotherapy
G.P.
General Practitioners
U.T.
Union Territory
S.T.O.
State TB Officer
A.N.M. Auxiliary
A.N.M.
Auxiliary Nurse Midwife
E.P.I.
Expanded Programme on Immunization
FOREWORD
One of the cardinal factors for achieving Health for All by 2000 A.D. is the ability
of the individual and the organisation to recognise and respond to changes in
advancing technology for health maintenance and promotion, new pattern of
disease, disability, etc. new social policies, expectations and programmes for
better health services. Towards this end, the education of the people
concerning prevailing health problems and methods of preventing and
controlling them is the first requisite of Primary Health Care. This is more so in
the case of public welfare personnel and professionals through whom the
knowledge and skills should percolate to the grassroot level.
In adhering to the above perspective, the National Institute of Health and
Family Welfare conducts nearly fifty training courses/workshops annually
towards requirements of a system of continuing education for health
administrators of States and Districts, teachers of medical college, and also
the members of Indian Administrative Service. However, the problem of
updating the knowledge and skills of these personnel, already on the job, still
remains. It has proved arduous to have them re-trained at institutions.The
snail-like pace of implementation reflects in many instances the fact that this is
an area where most professionals feel unprepared. It is, therefore, essential to
initiate a programme to get relevant information out to individual participant. As
such, the development of self-learning resource materials to keep abreast of
scientific advances in research as well as in programme strategies is an
enviable task which the NIHFW has undertaken with large-scale efforts.
These resource material present an assiduous expatiation of various
National Health Programmes and Schemes currently in operation in the health
services system. Each of these expatiates the genesis, strategy, current
status, and the outcome of the evaluation of individual programme. Thus, the
primary aim of this Series would be to share and utilise the available resources
to update the knowledge and skills of programme personnel at their own place.
I fervently hope that this publication will provide orientation on the use of
such self-learning materials to learners/participants. I also wish to asseverate
that these resource materials will be updated periodically and as such, I am
sure, they should be a valuable aid in overcoming the lag.
O'
Much of the positive value in this Series originated with one or another of
our associates, sincerely thank these Programme Officers who had so kindly
undertaken the onerous task of compilation and completion of these
documents.
New Delhi
December, 1988
- Ik
J.P. Gupta
Director
-
Series Editors
INTRODUCTION
J.P. Gupta
S. Bhatnagar
Tuberculosis is a communicable, bacterial disease which results from
infection with TB bacilli. The TB bacilli is a rod-shaped organism, discovered
by Robert Koch in 1882. Tuberculosis can be traced back to the early history of
mankind. In our country, it has been known since the Vedic ages, that is, about
5000 years ago. It is world-wide in distribution and strikes both the rich and
poor, all races and both sexes. Tuberculosis affects all parts of the human
body, but, most commonly, the lungs. The patient with lung TB excretes
Tuberculosis bacilli with sputum through coughing, sneezing, etc. The germs,
thus excreted, can enter, mainly with the help of air currents, another healthy
human body while the person breathes in. On entering the lung, the bacilli
generally get a foothold on the peripheral part of the lung and this process is
called infection. The entry of the Tuberculosis germ into the body and its
gaining a foothold does not always lead to disease, immediately or later. Only a
few infected persons suffer with the disease process due to a number of
factors which are both intrinsic and extraneous. The intrinsic factor is poor
natural resistance or poor inborn immunity, which is a genetic one. Extraneous
factors are many, like poor living conditions, low social and educational status,
inadequate food or nourishment of the body, psychological and
temperamental status of the person and affliction by some other diseases like
diabetes, measles, cancer, etc. Today. Tuberculosis is treatable, curable and
© 1988, by the NIHFW, New Delhi
o
The views expressed in this publication are those of
author and do not necessarily represent the decisions of
the stated policy of the National Institute of Health and
Family Welfare. New Delhi..
!
preventable.
MAGNITUDE OF THE PROBLEM
Improvements in diet, housing and living conditions in modern times have
contributed to a decline in both TB mortality and new cases. The advent of
chemotherapy during the last four decades has accelerated these trends. But
Tuberculosis still ranks among the major health problems in the world,
specially in the developing countries. There are about 15 to 20 million cases
and three million deaths every year in the world due to Tuberculosis.
e
Printed and Published by the Department of Publications, National institute of Health and
Family Welfare, New Mehrauli Road, Munirka, New Delhi-110 067.
June 1989/2000
IN INDIA: The results of pre-tuberculine tests in mass BCG vaccination
campaigns indicated, for the first time, that the problem of Tuberculosis was
not limited to the urban areas only, in contrasttothe earlier belief. The National
Tuberculosis Survey during 1955-58 and subsequent limited surveys have
confirmed these findings.
Tuberculosis is a major public health problem in India and number one
killer among diseases. The National Tuberculosis Survey which was
conducted by the iCMR in the year 1955-58, revealed that nearly 1.5 per cent
of the total population above five years of age is estimated to be suffering from
TB of the lungs, of whom one fourth, or 0.4 per cent are infectious. Subsequent
limited surveys conducted in different parts of the country have confirmed
these findings. As per the 1981 census the total population of the country was
about 680 million and it was estimated that about 10 million people were
suffering from radiologically active pulmonary Tuberculosis disease of the
9
only 20-25 patients, can pay for the establishment of clinics which can handle
lungs, out of which about 2.5 million people were infectious. Few lakhs of new
Tuberculosis cases are added to the population every year but at the same
time, an equal number of cases are removed, on account of death,
spontaneous healing or treatment. This results in a state of near balance in the
number of Tuberculosis patients from year to year. It is further estimated that
nearly 50 per cent of the total population is infected with the TB bacilli, though
they are apparently healthy. The annual infection rate (that is about 1.6 per
cent) has remained almost constant for the last three decades.
Nearly 80 per cent of the people in our country live in about 6 lakh villages.
It is estimated that at least 2-3 sputum positive cases can be found in each
village of the country, and nearly 10-12 persons would be suffering from
radiologically active Tuberculosis of the lung. In an average district with a
population of 1.5 million, it is estimated that there will be about 5000 active
pulmonary cases who are infectious and about 20,000 radiologically active
pulmonary Tuberculosis cases. As per the recent study conducted by the NTI,
Bangalore, in their field area, the mortality rate has come down to 53 per lakh
population, and as per the study conducted by the New Delhi TB Centre, the
mortality rate in their population area is around 40 per lakh population. Since
the prevalence rate of pulmonary Tuberculosis cases is of the same order in
the rural areas as in the urban ones, and nearly 80 percent of the people of our
country live in villages, the problem of Tuberculosis in our country is really a
rural one.
AIM AND PRINCIPLES OF NATIONAL TB PROGRAMME
(NTP) - BACKGROUND INFORMATION
The mass BCG vaccination campaign and the National TB survey conducted
during 1955-58 led to the conclusion that Tuberculosis services had to be
provided on a country-wide and long-term basis.
The NTP aims at the methods by which the systematic reduction of
Tuberculosis in the community may be made within the available resources of
the country and within a reasonable time. The method of treating the patients
on a domiciliary basis was initially a compromise between the scientific idea
for the few, and the economically and practically feasible one for the many.
The short-term object of the programme is to diagnose and treat the patients at
places nearest to their homes and also to give preventive services to the bulk
of TB patients, specially those living in rural areas with the view of meeting their
‘felt needs', and to reduce their suffering and prevent disability and deaths to
the extent possible. The long-term objective of the programme is to reduce the
problem gradually till it ceases to be a public health problem.
From the economic point of view, we have, at present, got a few thousand
TB beds. To treat only the sputum positive cases, we need a few hundred crore
rupees for constructing hospitals and another few hundred crore rupees as
recurring expenditure annually. The money that would provide TB beds for
1000 to 1500 patients annually.
The cost of treating a Tuberculosis patient in a sanitorium for one year is
equal to that of treating 15 patients on domiciliary basis. So, from the economic
point of view, domiciliary treatment is the practical solution for tackling the
Tuberculosis problem with limited resources.
From the scientific point of view regarding treatment of patients on
domiciliary basis, it has been observed that the results of treating the’ P^en‘s
in a hospital and at home are more or less the same. There is hard y a y
difference between the hospital patients and those treated at home, as regar^
the immediate therapeutic response in terms of radiological improvem
,
sputum conversion and closure of cavity at the.end of one year, as also the
danger of relapse in the future, and infection to the contacts, provided
adequate chemotherapy is prescribed and taken regularly for the prescribed
01 <
period by the patient.
It has already been mentioned that Tuberculosis is equally prevalent in
rural and urban areas. For a developing country like India it would be a gigantic
task to identify all the Tuberculosis cases living in hundreds and thousands o
distant villages and to offer them regular treatment for a period of one to one
and a half years.
The studies conducted by the NTI, Bangalore, have revealed that nearly
95 per cent of the infectious Tuberculosis patients are conscious of their
symptoms and St least 50 per cent of them report to the nearest medical and
health institutions to seek medical aid.
Another research study conducted by the ICMR (1955-56), conclusively
proved that the Tuberculosis cases can be as effectively treated on
domiciliary basis as in hospitals.
Based on the results of these two studies, the country-wide district
Tuberculosis programme was evolved for the entire country by the NTh
Bangalore, in 1962. Under the programme, a district Tuberculosis centre is
being established in every district of the country to organise a community-wide
district Tuberculosis programme in association with all the existing medical
and health institutions. In an average district of our country.there are about 50
such peripheral health institutions. The main aim of the programme is to detec
as large a number of patients (sufferig from Tuberculosis) as poss.ble, nearest
to their homes and treat them effectively so that the infectious patients are
rendered non-infectious and the active and non-infectious cases do not
become infectious.
In doing so, priority is given to sputum positive Tuberculosis patients.
The patients are treated mostly on domiciliary basis because it is as
effective as institutional treatment and more acceptable to TB patients since
their domestic life lis not disrupted.
11
10
In addition, there are about 300 ordinary I uberculosis cr-r/cs which are
functioning in the country and are mostly located in big towns
cities. These
are equipped with either static X-ray unit or Fluoroscopy and laboratory
facilities and look after the needs of the local population living nearby.
Each district Tuberculosis centre is staffed by a team of medical and
paramedical personnel trained at the NTI, Bangalore, in X-ray and laboratory
diagnosis. treatment organisation and community control of Tuberculosis, and
is equipped with a static 100 M A X-ray unit fitted with an Odelca camera for
miniature radiography, and laboratory equipment for direct smear
miscroscopy.
There are about 46,000 TB beds available in the country to cater mainly to
the needs of the selected group of patients, i.e. those who are seriously sick or
suffering from some emergency or need surgical treatment or are social
destitutes, etc. We are making efforts to establish sufficient numbers of
Tuberculosis beds, as per the needs in every district of the country.
The d.strict Tuberculosis centre functions as a referral centre for the
entire Tuberculosis control proc'amme of the district. Its key personnel tour
the existing peripheral medical and health institutions, including the primarv
. health centres which cater to the health needs of the rural population, train the
. medical and paramedical personnel of such institutions in various essential
activities under the Tuberculosis programme, supervise their working, ensure
proper record keeping and reporting of the whole district and give advice also
at the TB clinic in the town or city of its location.
Thus, the district TB centre serves as a base for carrying out the case
finding and treatment programme throughout the district with the help of the
network of general health services of the district, so that these facilities are
brought nearer to the homes of the patients at minimum expenditure, and a
permanent case finding and treatment programme is developed. The
treatment is offered on an out-pat;ent and mainly self-administered basis. The
patients are encouraged to collect drugs from the PHCs nearest to their
homes. The minimum duration of tne uninterrupted chemotherapy is one year.
The optimal duration of treatment is one to one and a half years and the
extended period of treatment is upto a maximum of two years. All efforts are
made to ensure that the patient receives uninterrupted treatment for at least 12
months. Defaulter actions are taken, both at the district Tuberculosis centre
and at the peripheral health institutions, by way of letters to the individual
patient, letters to the head of the village or by sending the health
visitors/multipurpose health workers and village health guides, etc. In addition
to this, under the NTP, additional district Tuberculosis centres are being
established in those districts where the population is more than 2 million.
The additional district Tuberculosis centres are established in another
sub-divisional town of the district To cater to the needs of a small population of
a district, a mini district TB centre is being established. It is not necessary to
provide the full complement of key personnel at these mini district TB centres
and these centres are not provided with any X-ray facilities. Instead, the X-ray
facilities at the general hospital in the district are used.
INFRASTRUCTURE OF THE PROGRAMME
Out of the 434 districts in the country, the district TB programme has been
implemented in 371 districts.
On an average, in a district there are about 50 implementable PHCs and
other institutions (PHIs) and till now about 75 per cent of the PHIs have been
brought under the National Tuberculosis Programme.
12
01 ©
The Tuberculosis Institute, Bangalore, was established in 1959 with the
aim of evolving nationally applicable methods of Tuberculosis control and
training of key personnel for the Tuberculosis programme. Till now, about
4,600 key personnel of different categories have been trained. The Institute
holds reorientation/training seminars for senior health administrators and
professors of medical colleges, etc. Trainees from abroad also attend various
international courses at the Institute. This Institute is also carrying out
epidemiological, sociological, bacteriological and operational research
connected with the Tubercufosis programme. It has also been selected to
monitor the National Tuberculosis Programme on the basis of reports received
from the DTCs and to provide suitable technical guidance to the district
Tuberculosis centres to improve their performance.
This Institute is also carrying out short course chemotherapy regimen
trials under operational conditions in the field area.
The Tuberculosis Research Centre, Madras, was established in 1956 for
studying the feasibility and efficacy of domiciliary treatment of patients
suffering from pulmonary Tuberculosis, and evaluation of inexpensive,
effective chemotherapy regimens on mass application. The centre is at
present engaged in conducting control clinical trials on chemotherapy in 18
districts of the country, clinical trials on Tuberculosis meningitis.Tuberculosis
of the spine, etc. It has established a cardio-pulmonary physiology laboratory
and epidemiology unit.
0) B
Seventeen Tuberculosis training and demonstration centres are
functioning in the country to undertake the training of the medical and para
medical personnel required for manning the Tuberculosis centres; to give
technical guidance to the district TB centres; to undertake the cultural and
sensitivity tests; to give technical guidance to the complicated TB cases, etc.
The State TB demonstration centre acts as a model TB centre for the State.
CONVENTIONAL DRUG REGIMENS RECOMMENDED UNDER THE
PROGRAMME FOR SPUTUM POSITIVE PATIENTS (ADULTS)
Code No.
R1
Drugs and Doses Mode and Rhythm of
administration
Isoniazid 300 mg
+ Thiacetazone
150 mg
Both drugs in a single
dose or two divided
doses, orally, daily
Instructions
Self-administered
at home after meals
R2
R3
R4
R5
Bi-weekly regimen Intra-muscularly
Inj. Streptomycin
orally
0.75 gm/1 gm 4Isoniazid 600 to
700 mgm (15 mgm/
kg body weight) with
Pyridoxine
Both drugs given at
the same time
under supervision
of the treating
physician twice
weekly at intervals
of 3 to 4 days
Isoniazid 300 mg+
PAS 10 gms.
Self-administered
after meals
In a single dose
in two divided doses
both drugs orally, daily
Isoniazid 300 mg
F
" drugs
'
Both
in a single
+ Ethambutol 20 mg dose; orally, daily/
/kg body weight
i.e. 800 mg per
patients weight
^■50 kg and 1000
mg to 1200 mg >50
kg
For the Negative Tuberculosis Patients (Suspected Cases)
Tuberculosis paitents in whose sputum A F B are not seen, are advised
Regimen R1; i.e. Isoniazid 300 mg +Thiacetazone 150 mgm in single dose
orally, daily for one to one and a half years. Patients allergic to Thiacetazone
can be treated with R4.
Note:
INTERNATIONAL ASSISTANCE TO THE TB PROGRAMME
Self-administered
at home after meals
I
Biphasic regimen
a. Intensive phase
For first two months
Inj. Streptomycin
In a single dose,
0.75 mg/1 gm +
orally, daily,
Isoniazid 300 mg
(PAS and Thiaceta+Thiacetazone
zone should be given
150 mgm
in two divided doses)
orEthambutol200 mg
per kg body weight
i.e. 800 mg for
patients L 50 kg and
1000 to 1200 mg for
those more than
50 kg
or PAS 10 gms.
b. Continuation phase
With R1, R2, R3 or
R4
Inj. given under
supervision and
rest to be self
administered at
home
As per each regimen As per each regimen
The Drug PAS is gradually being withdrawn from the programme due
to cost, non-availability, etc.
O') t
By Swedish International Development Agency (SIDA): The Swedish
International Development Agency has been supporting the case finding and
treatment activities of the programme by supplying X-ray units with Odelca
cameras, miniature X-ray film rolls, drugs needed for conducting the short
course chemotherapy trial under pilot study, etc. since 1979. These X-ray
machines with Odelca cameras are supplied to the unequipped district TB
centres of the States/Union Territories, and as replacements to those district
TB centres where the X-ray machines with Odelca cameras have outlived
their utility. They are also are supplied to the additional TB centres, wherever
created. The miniature X-ray film rolls are supplied to the district TB centres.
Till now, the SIDA authorities have supplied about 175 X-ray machines with
Odelca cameras. The short course chemotherapy trial under pilot study is
being conducted in 18 districts of the country since 1983-84. The SIDA have
also agreed to give additional assistance within June 1989 for supply of
another 25 X-ray machines with Odelca cameras, miniature X-ray film rolls
and 100 vehicles. These vehicles would be supplied to the different districtTB
centres of the country where either the vehicles have outlived their utility or to
the newly created district TB centres for proper implementation and
supervision of the programme by the DTCs. The SIDA is also helping the
National Tuberculosis Institute, Bangalore, in various ways.
Assistance by the WHO: The WHO has been assisting the NTI,
Bangalore, since its inception in 1959 and the TB Research Centre, Madras
(ICMR) since 1956 by providing short-term consultants, fellowships, and
essential supplies and equipment. They are also providing assistance to these
two institutions for conducting short-term reorientation courses/seminars for
senior health administrators of the States/Union Territories, teachers of
medical colleges and refresher courses for the medical and paramedical
personnel of the district TB centres.
EXPANSION OF THE PROGRAMME DURING THE VI^AN^fPi^S
Expansion Under the 20-point Programme: A new^thrbst has been givefeoX
Remarks:
Drug regimens comprising. Inj. Streptomycine 0.75 gm/1 gm
twice or even thrice a week + INH 200 mg or 300 mg daily is not
sufficiently effective and, hence, not recommended.
case finding activities of the NTP under the 20-ppint proqr^tnaVUnder the,
20-point programme, targets for new TB case detection’TiHve been laid dowjr
14
15
'rational
P'
I’Ii
r
I
!
p
since 1982-83 and these targets are being increased every year. The
achievement of the targets of new TB case detection has been satisfactory
from the beginning.
routine rounds in the villages, should identify the ches: symptomatics
suspected to be suffering from pulmonary Tuberculosis and motivate them to
go to the nearest health institutions for necessary investigations, motivate the
diagnosed Tuberculosis cases to continue the anti-TB drugs uninterruptedly
• for the prescribed period, and take defaulter action on the patients who have
defaulted in continuing the drugs. The MPWs also involve themselves in health
educational activities on TB amongst the villagers and ■ B patients. For
conducting these activities, the MPWs in the PHCs and in the sub-centres are
gradually trained in. case finding, domiciliary treatment, BCG vaccination and
also in health-education activities.
i
Prior to the laying down of targets, only about 7 lakh new TB cases under
the programme had been detected, but at the present moment more than 1.4
mil ion new Tuberculosis cases have been detected under the programme. To
involve the primary health centres in more and more case finding activities in
tne rural areas, targets for new sputum examinations have been laid down
since 1983-84. With this, the PHCs are being more actively involved than
before in case finding activities, and a target for 600 new sputum examinations
per year by each PHC has been laid down. Initially, the achievement of targets
of new sputum examinations at PHCs was not very satisfactory but
considerable improvements are being noticed gradually.
The village health guides are also being involved in essential health
educational activities under the programme including motivation of chest
symptomatics to avail of all the diagnostic facilities of the health institutions,
and in motivation of the Tuberculosis patients living in their areas to take the
uninterrupted treatment for the prescribed period as per tne advice of tne
treating physician.
TARGETS AND ACHIEVEMENTS SINCE 1982-83
UNDER THE PROGRAMME
i
Year
82-83
10.00
10.80 (100%)
Expansion of the Programme in Urban Areas Under the City
Tuberculosis Programme: The district Tuberculosis programme was
planned mainly with rural India in mind. It has been observed mat the prob ems
in metropolitan and other big cities with a population over five lakhs are
different and the district TB programme would not be able to serve the needs of
these cities effectively. As such, it has been recommended that advantage
should be taken of the newly created health posts in the big cities and towns
with a population over five lakhs, for implementing the city TB programme,
which is already functioning in some cities like Delhi, Bombay.
No target laid
down
83-84
12.50
12.00 (96%)
34.00
12.00 (35%)
8~-85
13.75
12.54 (91%)
34.00
17.31 (50.2%)
85-86
14.00
13.58 (97%)
34.00
20.3 (59.5%)
85-87
14.50
14.13(97.5%)
34.00
21.69 (63.9%)
87- 88
15.00
15.62 (104%)
34.00
24.11 (71%)
88- 89
15.00
34.00
Expansion of the Programme in Rural Areas: To intensify the case
finding and case holding activities under the programme in rural areas, it has
been recommended that all the health workers of the peripheral health
institutions are to be involved in case finding and domiciliary treatment of the
Tuberculosis patients and also to be engaged in BCG vaccination of the
newborns and infants. It has been recommended that the MPWs, during their
16
To expand the treatment activities further for the rural people living in the
far-flung villages, it has been recommended that all the sub-centres which
have the necessary buildings for storage of drugs, and have me requisite staff,
should be involved in the distribution of drugs to the Tuberculosis patients.
Target for
Achievements
Target for
Achievements
detection
(in lakhs)
conducting new
(in lakhs)
of newTB cases
sputum exa
(in lakhs)
minations at
at PHCs
(in lakhs)
o
I
Extension of Short Course Chemotherapy Regimens (SCC): Under
the clinical trial conditions, the conversion and relapse rates with the
conventional drug regimens are 82 to 96 per cent and ■ to 15 per cent
respectively, at the end of one year.
In a study conducted by the National Tuberculosis Institute, Bangafore, it
was revealed that only 30 per cent of the cases completed treatment at the end
of one year under programme conditions with the conventional regimens and
the patients defaulted mostly after the first or second collection of drugs. It was
further revealed that in spite of poor completion of treatment rate, the
conversion rate of sputum was about 65 per cent at the end of one year.
But under the clinical trial conditions, there is about 100 per cent sputum
conversion in six to eight weeks and the relapse rate is only around 2 percent
with the short course chemotherapy drug regimens. The duration of treatment
17
I.1
I
1
with these drugs is only six to eight months. The main handicap in using the
short-term chemotherapy drugs was cost, but at the present moment, the cost
of these drugs, specially of Refampicin has gone down considerably and it is
expected that it will go down further.
In this regimen, the total duration of treatment is only six months. In the first
two months (intensive phase), the patient is given Streptomycin. Isoniazid.
Rifampicin and Pyrazinamide in the dosage mentioned above,twice a week. In
the remaining four months (continuation phase). INH 600 m9-^a^P'cln °°°
mg are given
given twice
twice aa week.
week. The
The patient
patient has
has to
to report
report to
to the
the DTC/PHI and all
drugs should be swallowed by the patient under the supervision or the
doctor/health staff. In case of non-availability of SM or intolerance to
Streptomycin, Ethambutol in the dosage of 12.6 gm (bi-weekly) may be
i
The long duration of the treatment, for a period of one to two years, with the
conventional anti-Tuberculosis drugs is believed to be one of the important
causes for the irregularity and discontinuation of treatment. Hence, to cut short
the duration of the treatment, achieve early conversion of the sputums,
thereby, preventing the spread of the disease and also to lower the relapserate
etc., the short course chemotherapy drug regimens have been introduced on a
pilot study basis since 1983-84 in 18 districts of the country to find out the
feasibility of introducing these drugs under the programme conditions. With
the encouraging results gained in the study, these regimens were introduced
in another 101 districts by 1987-88 for the sputum positive newly detected
Tuberculosis cases, excluding the 18 districts where these regimens were
introduced under the pilot study.’The short course chemotherapy regimens
are going to be introduced in another 75 districts of the country during 198889 It is expected that the majority of the districts of our country would be
covered with these regimens by the end of the Vllth Plan period.
I
substituted for Streptomycin.
Regimen B: Daily self-administered regimen
2EHRZ/6TH OR 6 EH
Ethambutol
(El 9)
(H 300 mg)
Isoniazid
(R 450 mg)
Rifampicin
Pyrazinamide (Z 1.5 g)
Thiacetazone (T 150 mg)
In this regimen, the total duration of treatment is eight months. During the
In this
eight months of treatment, the drugs have to be consumed daily by the patient.
In the first two months (intensive phase), the patient is given Ethambutol,
Isoniazid. Rifampicin and Pyrazinamide in the dosage mentioned above.
During the remaining six months (continuation phase). INH 300 mg ano
Thiacetazone 150 mg daily have to be given. If the patient cannot tolerate
Thiacetazone. Ethambutol 800 mg should be given daily.
It is hoped that by introducing these regimens, the defaulter rate of
treatment will go down further.
SHORT COURSE CHEMOTHERAPY DRUG
REGIMENS RECOMMENDED UNDER THE
NATIONAL TUBERCULOSIS PROGRAMME
All sputum positive cases aged 15 years and above, irrespective of history and
previous anti-TB treatment, are offered either of the following two drug
regimens:
Suitability of Patients for Appropriate Drug Regimen
Drug Regimens
The patients who express their inability to come to the centre twice a week
or who repeatedly fail to come to the centre twice a week for one month for
consumption of drugs are offered Regimen B, of eight months duration.
The patients who reside near the centre, and who are willing to attend the
centre twice a week for six months should be offered Regimen A.
These regimens have two phases:
■>
i. Intensive phase of the first two months with four drugs.
ii. Continuation phase of four to six months with two drugs.
Regimen A: Bi-weekly, intermittent supervised regimen
2S H R Z/ 4 H R
2222
22
Regimen containing
Streptomycin
Isoniazid
Rifampicin
Pyrazinamide
18
(S 0.75 g)
(H 600 mg)
(R 600 mg)
(Z 2 g)
Patient ‘Lost’ from Treatment
A patient who does not come for drugs for one month from the due date even
after two defaulter actions, is considered to be ‘lost’ from treatment. If t e
patient returns after becoming 'lost' he should be started on any one of the five
standard drug regimens (R1 to R5). It is important to ensure that every patient
put on short course regimens (either Regimen A or Regimen B) should have
collected 75 per cent of the required doses of the intensive phase within three
months from the start of treatment. Those patients who fail to complete this will
not be eligible for the continuation phase and will be offered the standard drug
regimen.
19
I
Compensatory Phase
Zilla Parishad, community leaders, youth leaders, etc. Ninety-five per cent of
the infectious sputum positive cases are already conscious of their chest
symptoms and a country-wide health education campaign must be carried out
to educate this group of chest symptomatics so that they get themselves
investigated and utilise the facilities available at the institutions nearest to their
homes.
Every effort has to be made to ensure that each patient put on SCC Regimen A
or B, completes treatment within the stipulated period. However, due to
unavoidable reasons, if any patient defaults, the compensatory phase may be
allowed. For the intensive phase of chemotherapy, an extension of one month
may be given to the patient to complete the required number of doses. That
means that under drug Regimen A. 17 doses should be taken in two months.
This may be allowed to be completed in three months. Under drug Regimen B,
four fortnightly collections of drugs should be made in two months. This may be
completed in three months.
A vast majority of patients suffering from Tuberculosis either report first to
the general practitioners or to the Governmept hospitals/dispensaries. As
such, the active participation of these health institutions and general
practitioners is a must for the success of the programme. The most important
point is to create active interest in the minds of general practitioners/medical
practitioners regarding the problem and the NTP and also to up-date their
knowledge about the present philosophy, diagnosis and treatment of
Tuberculosis through refresher courses. These courses are being conducted
by the Tuberculosis Association of India.
Similarly, an extension of one month in the continuation phase may be
allowed to compensate for the missing doses. However, the total duration of
chemotherapy, including the compensatory phase, should not exceed eight
months in drug Regimen A and ten months in drug Regimen B.
<))
Termination of SCC
Keeping this in mind, much stress has already been given to various
health educational aspects of the Tuberculosis programme by bringing out TV
spots, radio spots, advertisements in newspapers, material for medical
practitioners and the general population, etc. under the programme during the
Vllth Plan period.
For any patient remaining sputum positive after six months from the time of
initiating SCC on either of the regimens, the SCC is terminated and the
treatment card is closed.
For such patients, a new treatment card is to be opened (prolonged
treatment card) and the patient is put on INH and Thiacetazone (or
Ethambutol) for one year. This is called prolonged treatment. Any patient
remaining sputum positive after six months of prolonged treatment has to b^1
referred to specialised institutions for management of treatment failure.
Follow-up Examination
Every patient should be followed up strictly with sputum smear examinations once at the end of six months after starting treatment and another at the end of
chemotherapy (inclusive of compensatory period, if any).
Completion of Treatment
I
The funds provided on health education activities till, now, duringthe Vllth
Plan period, are as follows:
1985- 86
1986- 87
1987- 88
1988- 89
Rs.lakhs
Rs.40.00 lakhs
Rs.60.00 lakhs
Rs.50.00 lakhs
SCHEMES DURING THE VIITH PLAN PERIOD
As in the Vlth Plan period, the schemes of establishment of more district
Tuberculosis centres, TB beds. etc. have been included in the State plan
sector.
A patient who has completed 75 per cent or more doses of the required
number, during the intensive phase (including compensatory phase), is
considered to have completed the intensive phase and is eligible to enter the
continuation phase.
Centrally Sponsored Sector: Under the Centrally sponsored sector, the
following schemes are being implemented:
A patient who has completed 75 per cent or more of the required number
tre^tm63^thS COntinuatlon phase is considered to have completed optimum
b. Supply of anti-TB drugs/equipment to the Union Territories as a 100
per cent Centrally sponsored scheme.
Expansion of Health Education Activities: Any health programme
specially the NTP, a programme of great magnitude, cannot succeed without
the active involvement and cooperation of the community, village Panchayats
20
a. Supply of anti-TB drugs/equipment to the States on 50:50 sharing
basis between the Centre and the States.
c. Supply of anti-TB drugs to the TB clinics run by voluntary bodies as a
100 per cent Centrally sponsored scheme.
d. Expenditure on health education activities as a 100 per cent Centrally
sponsored scheme.
21
I
i
bacilli except in the developed countries where a few cases of i B were due to
the bovine type of infection. In India, the TB due to bovine type of infection is
rare as milk is boiled before use. In the developed countries, TB due to the
bovine type of infection has been controlled by pasteurising milk and other
measures.
FINANCIAL OUTLAYS AND ACTUAL EXPENDITURE INCURRED
DURING THE VITH AND VIITH PLAN PERIODS
Vlth Plan Period
Against the actual allotment of Rs.700 lakhs, the actual expenditure was
Rs.2040.00 lakhs.
EVALUATION OF THE PROGRAMME
Vllth Plan Period
Financial outlays
Rs.5500.00 lakhs
Actual expenditure incurred during the first three years of the Vllth Plan:
1985- 86
1986- 87
1987- 88
Rs.1112.00lakhs
Rs.1125.00lakhs
Rs.1415.00 lakhs
ce
BCG Vaccine, Its Efficacy and Current Status NTP vs EPI
From time to time, the experts of the Swedish International Development
Agency (SIDA) evaluate the functioning of the programme before signing the
agreement for aid to the programme and also during the agreement period.
Recently, the programme has been evaluated by the expen team of the SIDA
which has recognised the soundness of the programme and has also
observed that the programme is working more or less satisfactorily and in the
right direction.
The BCG vaccination programme has been in operation since 1951. However,
as the coverage of the susceptible population was not found to be very
satisfactory, it was decided that instead of carrying out the campaign through
BCG teams alone, the activity was to be integrated with the general health
services so that the newborns and infants, specially in tne vast rural areas,
may be covered expeditiously under the EPI programme The present BCG
teams (available in the States and Union Territories) in add tion to their current
duties under the vaccination programme, are also engaged in proper training
of the health workers in the technique of vaccination.
They have, however, made some recommendations to improve upon the
case detection and case holding activities of the programme, specially for the
rural regions.
A study of the integration of the BCG vaccination crogramme with the
general health services indicated that the services of Auxiliary Nurse
Midwives (ANMs) who are now designated as Female Health Workers, could
be utilised for BCG vaccination of infants without detriment to the ANMs' other
functions. (Baily, Kulbhushan, etc. Ind. J. Tub. XX, 4. 155 (1973).
The Chingleput study on BCG vaccination clearly indicated that the BCG
vaccination did not give any protections against the development of adult type
TB. Several animal studies and several controlled trials (BMRC, 72, Rosenthal61) had clearly shown that BCG vaccine almost always conferred a
measurable degree of protection more closely to the childnood form of TB and
its associate complications like meningeal and milliary type of TB. Hence, the
present policy of BCG vaccination is to vaccinate the child soon after birth. I n
urban areas, the newborns are vaccinated just after birth in Maternity
Hospitals and Child Welfare Clinics. In the rural areas, under the EPI
programme, multipurpose health workers, vaccinate all the newborns before
they are one year old alongwith other immunization.
The programme was evaluated by the expert committee formed by the ICMR
in the year 1975. The committee concluded that while the concept of the
programme was sound, there was considerable scope for improvement in the
implementation of the programme, specially at the peripheral health service
levels. The committee made certain recommendations for further
improvements which were then examined by an empowered committee
appointed by the Ministry of Health and Family Welfare and the detailed
guidelines for further improvement of the programme were given to the States
for implementation.
!
e
The NTI, Bangalore, has been entrusted with monitoring and evaluating
the programme on the basis of the performance reports of the DTPs.
The programme is reviewed from time to time at the meetings of the
Health Secretaries of the States/Union Territories and also during the meeting
of the Central Council of Health, at the Central level.
The programme is also reviewed every month by the Ministry of Health
and Family Welfare at the Central level and often at the levels of Health
Secretaries/Ministry.
At the State level, the programme is reviewed and evaluated regularly at
the State and district headquarters.
Recently, an independent organisation has been appointed by the
Ministry of Health and Family Welfare to evaluate the programme
independently.
RECOMMENDATIONS OF THE EVALUATION
Bovine Type of Bacilli and the Infection
A seminar held a! the NTI, Bangalore, on 5th and 6th January, 1988, which was
A majority of the TB cases in the world are due to infection with human type of
22
23
I
!
7. The MPWs and ANMs while receiving their basic training in the training
institutes should be imparted the requisite training in the essential aspects of
the TB programme.
attended by the health authorities of States/Union Territories, made some
suggestions/recommendations for improvement of the programme. The
salient recommendations/suggestions made by the ICMR committee and at
the seminar held at Bangalore are as follows:
8. Ever since the MPWs were entrusted the duty of collecting the sputum of
the chest symptomatics in the field, making slides and sending them for
examination through the microscopic centres, the quality of the work has
deteriorated considerably. It has been recommended that the MPWs, instead
of collecting sputums in the field during their home visits and preparing smear
slides of such patients, may motivate the chest symptomatics to.report to the
nearest PHC for investigation. The group was of the view that MPWs should not
be entrusted with the duty of supplying anti-TB drugs at me homes of the
patients.
1. For the speedy expansion and intensification of the activities under the
programme, the essential schemes which have a direct bearing on the
expansions of the case finding activity and treatment programme should be
taken up as a 100 per cent Centrally sponsored scheme. Due to financial
constraints, the State/ Union Territory health authorities are not able to provide
‘ sufficient funds for establishment of DTCs and for the procurement of anti-TB
drugs, etc. out of their share. As such, it has been recommended that the
scheme of establishment of DTCs in those districts where they are not
available at all and the scheme of establishment of additional DTCs for the
thickly populated districts be taken up as 100 per cent Centrally sponsored
schemes and cash assistance be provided to the States/Union Territories fcr
9. In a large number of PHCs, functioning microscopes are not available. It
has been recommended that the microscopes may be supplied by the
Government of India for the use of PHCs. It has been further recommended
that oil immersion lenses may also be supplied by the Government to bring
back into use the non-functioning microscopes available at the PHCs.
a. provision of essential medical/paramedical staff;
b. recurring expenditure for running of DTCs; and
c. provision of essential equipment.
10. Additional district TB centres may be established in th:ckly populated
districts or in those districts which are very large in area, it has been further
recommended that the additional district TB centre should not be located in
the city or town where a district TB centre is already functioning and it may be
established in another town or city of the district so that tne referral and
supervision activities can be properly developed.
2. The performance under the programme should be reviewed regularly on a
monthly basis at every level, just like the review of activities under the family
welfare or MCH programme, etc.
3. Over half of the cases of PTB requiring treatment are sputum negative and
cannot be diagnosed either due to non-availability of X-ray facilities at the
PHCs or due to the distance of the PHCs and DTCs from the patients home.
Under the minimum needs programme, it has been proposed to upgrade some
of PHCs to community centres and rural dispensaries to health centres which
would be equipped with general purpose X-ray units. The case finding
activities under the TB programme can be substantially increased by the
establishment of such equipped community health centres, etc. under the
Minimum Needs Programme.
4. In about 30 per cent PHCs either no multipurpose laboratory technicians
have been posted, or if posted, they are overloaded with work like malaria
work, etc. It has been recommended that the admission capacity of the
Laboratory Technicians Training School may be enlarged so that the existing
PHCs and newly established PHCs are provided with multipurpose trained
laboratory technicians.
I
11. For improvement of case holding activities under the- programme, the
medical and paramedical personnel of the district TB centre and peripheral
medical and health institutions have to play a vital role. Reputed motivation of
the patients and members of their families would considerably reduce the
defaulter rates. The multipurpose health workers should keep a list of TB
patients living in their area so that during their visits to the field, the patients and
their families are repeatedly educated about the need to take regular and
uninterrupted treatment for the prescribed period of time, as advised by the
medical attendant.
5. Full-time NTI trained medical and paramedical personnel should be
posted at the DTCs throughout the year for proper implementation and
supervision of the programme.
12. Voluntary organisations are playing an important role under the NTP. It
has been recommended that existing provisions made for the supply of antiTB drugs to such organisations be enhanced so that their total requirement of
anti-TB drugs for domiciliary treatment can be met. It has been further
recommended that those voluntary run TB institutions, which have already
been provided with an X-ray unit with Odelca camera, may be supplied with
miniature X-ray films for the expansion of case finding activities.
6. A vehicle alongwith suitable POL charges should be provided in each
district TB centre for proper implementation and supervision of the
programme.
Requests for cash assistance for purchase of essentia! X-ray/laboratory
equipment as well as for construction of buildings for TB institutions by such
voluntary organisations should be suitably considered by the Government.
24
25
country, as we could not keep pace with the carving out of new districts out of
bigger districts. At least 75 per cent of the implementable PHIs have been
brought under the DTPs in the implemented DTPs. About 4600 key personnel
have been trained by the NTI, Bangalore, for the uniform implementation and
development of the programme throughout the country. With the inclusion of
NTP under the 20-point programme, about 14 lakh new TB cases are being
detected at the present moment as against about 7 lakh cases detected few
years back. In addition to that, it is estimated that about 5 lakh newTB cases
are being detected and treated by the GPs, voluntary organisations, general
hospitals as well as by other agencies like Railways, ESI, Defence Services,
etc. which usually do not notify the cases under their care to the district TB
Section 35 CCA of the Income Tax Act may be amended to include
donors for the establishment of TB hospitals and clinics.
13. The attitude and behaviour of the medical officers of the health
institutions towards TB patients has to be more effective. Therefore, it has
been recommended that continued medical education programmes from the
grassroots to the State level for all medical and health personnel are essential.
Medical colleges should be more actively involved in the implementation of the
programme and undergraduate students may be sent for training at the DTCs.
. 14. The possibility of involving volunteers, Youth Clubs, Mahila Mandals for
health education of the community should be explored.
15. The poor and the deserving indigent TB patients may be granted some
cash assistance by the voluntary organisations to meet the expenses and
other essential needs.
16. It has been recommended that in every major State, the posting of trained
State TB officers alongwith requisite infrastructure is a M UST for improvement
of the programme.
centres.
e c
17. The drugs should be made available not only in the primary health
centres, but also in the sub-centres where facilities of storage and distribution
are available.
18. The TB clinic and demonstration centre/State TB centres should play a
more active role in the implementation of the TB programme in the region.
Besides running a district TB programme in the district, in which it is located,
this training centre should also undertake the culture examination work and be
a key referral centre for the entire State. The centre should also undertake the
reorientation training of the CMO/DMO/Civil Surgeons of the State, conduct
reorientation training of the X-ray technicians, laboratory technicians, etc. so
that such functions which are being undertaken by the NTI, Bangalore, at
present, can be transferred to the TB training and demonstration centre. It has
been recommended that from 1.1.1990, the NTI may conduct only two regular
training courses for the district medical and paramedical personnel.
But even with the extension of facilities and allocation of more and more
funds, the programme has not progressed asexpected earlier.The reasons for
this are many and varied. In spite of more and more new sputum examinations
being done at the PHCs, the quality of the sputum examinations has
deteriorated. The achievements of case detection and case holdings have
been below expectation.
0
19. It has been recommended that short course chemotherapy regimens
may be extended to more districts in the country so that by the end of the VII th
Plan period, a majority of the districts can be covered by these regimens.
PRESENT POSITION OF NTP AND SHORTFALLS/PROBLEMS
IN THE IMPLEMENTATION OF THE PROGRAMME
1
Since Independence, there have been considerable improvements in the
developments of anti-TB measures, in our country. Prior to 1947, we had only
about 85 ordinary TB clinics and about 6000 TB beds in the country. Against •
these, we have, at present, more than 600 TB clinics, which include district TB
centres, and about 46,000 TB beds. A total of 371 districts have been covered
under the district TB programme till now, out of the existing 434 districts of the
26
As a result of the active involvement of PHCs.the number of new sputum
examinations are increasing year by year. To cut short the duration of
treatment, short course chemotherapy drug regimens have already been
introduced for the newly detected sputum positive Tuberculosis cases in 119
districts of the country and the same is going to be introduced in another 75
districts during 1988-89. There has been substantial augmentation of the
financial allocation and expenditure as a Central share for the expansion of the
activities of the programme. In spite of financial constraints, shortage of
technical manpower, illiteracy, population explosion and poor socio
economic conditions etc., of the country, the achievements are by no means
negligible.
The operational research study conducted by the NTI, Bangalore, on the
POTENTIAL YIELD OF BACILLARY CASES IN NTP showed that each DTP
can detect about 2000 bacillary cases annually, whereas actually, on an
average, each DTP diagnosed only about 700 bacillary cases annually, that is.
about 35 per cent of the potential yield. Irregularity of drug intake and
inadequate duration of chemotherapy are the two major operational problems
in the case holding activity of the programme. Only about 30 to 35 per cent
cases complete the treatment with conventional regimens under the
programme conditions.
In another study conducted by the NTI, Bangalore, investigating the
efficacy of two standard regimens under programme conditions, the initial as
well as subsequent motivation of the patients was done exactly according to
the recommendation made in the programme which revealed similar
completion rates at the end of one year. In all probability, the DTPs are not
achieving results very close to the potentials.
27
I
But even with such defaulter rates, the conversion rate of sputums at the .
end of one year is about 65 per cent. Indeed, in the programme, neither the.
case finding nor the treatment activity are considered to be satisfactory. But
there appears to be a much larger gap i the case finding achievements than in
the treatment achievements.
From the operational study on DTP by the NTI, Bangalore, it is observed
that there is enough scope for improvement in the case finding activities of the
programme but this cannot possibly influence the treatment which could
probably be improved by technical considerations and, to a certain extent, by
modifying the operational conditions.
The reasons for the shortfall of the achievements of the NTP are many
and varied. But the two major reasons are the poor and slow development of
the general health services and poor socio-economic conditions/population
explosion of the country.
The NTP has been rightly integrated with the general health services.
Without the proper development of the general health services, the
programme cannot improve and function in the right direction. Unfortunately,
the primary health care facilities have not developed to the extent envisaged.
In 1946, the Bhore Committee recommended that each PHC should cater to
the needs of 30,000 population but due to the financial constraints, etc. this
was not found to be feasible. So in the early 50s, it was initially planned to
establish one PHC to caterto the needs of about 1,00,000 population, covering
an area of about 200 to 900 sq. kms. The studies conducted by the National
Institute of Health and Family Welfare and A.P. Jain’s Committee report have
indicated thatthe ACTIVE AREA OF INFLUENCE of a PHC does not go beyond
the radius of 8 to 10 kms. Obviously, only the TB patients who are living close to
these institutions have been availing of the facilities of the PHCs. This is an
important reason for the poor performance of the programme due to the
inadequate development of general health services.
Even before the advent of chemotherapy, the problem of TB could be
controlled due to improved socio-economic conditions in the developed
countries. It is estimated that about 35 per cent of the people in our country are
living below the poverty line, which is one of the main hurdles to be faced.
Health being a State subject, the scheme of implementation and
supervision of the NTP has been classified as a State Plan Activity and the
following difficulties are often encountered in the States in the proper
implementation and supervision of the programme:
1.
Due to lack of financial resources, the State/Union Territory health
authorities cannot implement and supervise the programme effectively.
2.
In some of the States, there exist different administrative controls of the
personnel working at the district TB centres and at the peripheral levels of the
same district causing difficulty in the implementation and smooth running of
the programme.
28
3.
Equal priority has not been given to the TB programme as to the other
3.
programmes like Malaria, Family Planning, by the States/Union Territories
health authorities.
4.
The proper status has not been given to the district TB officers by many
States/Union Territories authorities which hinders the proper implementation
and supervision of the programme at the PHC level.
5.
Non-availability of trained whole time State TB Officers in many of the
major States is a big problem. A trained whole time STO is absolutely essential
for the proper implementation and supervision of the DTP in the State.
6.
The apathetic attitude of the medical and paramedical, personnel
specially at the peripheral levels is another hurdle for the programme.
7.
DTPs have to be implemented in about 66 districts of the country.
Additional district TB centres are to be established in all the thickly populated
districts. Twenty-five per cent of PHIs are yet to be brought under the ambit of
the DTP.
8.
In many of the district TB centres, trained key personnel and vehicles are
not available throughout the year. This is a serious drawback since they are
absolutely essential for the proper implementation and supervision of the
programme.
9.
In a good number of districts in some of the States either there are no TB
bed or if there are, the number is less than ten.
10. In about 30 per cent of the PHCs either no NTI trained lab technician has
been posted or if posted, the lone technician is overburdened with work like
malaria work, etc. and findslittie time for sputum slide examinations.
11. The potentialities of the MPWs in case finding and case holding activities
of the programme have not been fully exploited.
12. Great difficulties are often encountered in the case finding programme
due to non-availability of essential materials and equipment like microscopes,
glass slides, chemicals, etc. at the peripheral levels.
13. The potential of the case holding activities of the sub-centres that have
sufficient staff and storage facilities for drugs, are not being fully exploited.
14.
Poor development of health education activities on Tuberculosis.
Present Trends of Tuberculosis in India
In the opinion of many experienced clinicians in the country, the Tuberculosis
disease has undergone a considerable change in its clinical presentation,
specially over the last quarter of the century.
Many retrospective studies (TAI, 1958, 1968), despite their scientific
weakness, have clearly brought out the gradual change in profile from a
29
prevalence of more acute and extensive disease among the young to a more
chronic, or a less severe disease among the elderly people. The near
consensus of these reports has been on a marked decrease of concomitant
complications of pulmonary Tuberculosis as, for example, Enteritis, Laryngitis,
Amyloid diseases, matted lymph glands with discharging sinuses, etc. It is very
significant that very similar changes were noticed in countries where
.Tuberculosis has definitely declined.
Available epidemiological information signifies no change in the
prevalence of bacillary Tuberculosis in the country, at least during the last
three decades and that equal prevalence in urban and rural areas means that
we are truly in the endemic phase of the disease and that there is a gradual but
slow natural decline of Tuberculosis in the country. The reason for the slow
and natural decline of Tuberculosis in the country, is probably the continued
poverty, malnutrition, overcrowding, etc.
As already stated, the epidemiology indicates that TB situation is almost
constant in India, and, if at all, shows a very slow downward trend. The
downward trend is evidenced by the apparent shift in the age of first infection
during the later decades of life and a gradual reduction in the incidence of the
childhood form of Tuberculosis resulting from the first infection. Indications are
also available that where the programme is functioning well, the problem, of
Tuberculosis in the community does show a downward trend.
lakhs.
Since continued motivation and education of the masses in various
aspects of the case finding, treatment and preventive activities under the
programme is necessary to enlist their cooperation, an intense/ > heath
education campaign must be carried out and the necessary public ty a
brought out periodically.
Mortality Trend
Tuberculosis is not a notifiable disease and the exact cause of deathi in each
case cannot be ascertained. As such, it is not possible to spell out the exact
©
0
SUMMARY
About 50 per cent of the people in our country are already infected with TB
germs, and about 1.5 per cent of the people above five years of age are
suffering from radiologically active pulmonary Tuberculosis; of these, 0.4 per
cent are infectious. The mortality rate has come down from 80 to 100 per
100,000 population to 53 and 40 per 100,000 population in Bangalore and
Delhi respectively where the programme is working satisfactorily. As 80 per
cent of the people in our country are living in the rual areas; the Tuberculosis
Prospects of TB Control in India
The present epidemic in India might have started in the 17th century and there
is evidence to indicate that the epidemic has been declining since the turn of
the 20th century. All available knowledge about the epidemiology indicates
that the Tuberculosis situation is almost constant in our country and, if at all,
shows a very slow downward decline.
At present, when the case finding activity is functioning at about 35 per
cent of the potential, and treatment efficacy is about 65 per cent, it can be
shown that per unit of investment in resources, improvement in case finding
would give higher dividends than the improvement in the treatment activities.
The District TB Programme, even at the present level of efficacy, has the
potential of enhancing the natural decline. Improved programme efficiency,
specially under case finding, is likely to produce a quicker decline. Rapid
socio-economic development and improved standards of living would lead to
a more spectacular decline in Tuberculosis, but that would not fall strictly
within the ambit of the control programme.
TB Programme for Urban Areas
The DTP was planned mainly with rural India in mind. However, the problems
of metropolitan and other large cities with a population of over 5 lakhs are
different and the DTP would not be able to serve the cities effectively. It is,
therefore, imperative to have different programme for these cities. Such city
30
number of deaths due to TB.
In a longitudinal study conducted by the NTI. Bangalore, in the Bangalore
district, where no anti-TB services were conducted, the mortality rate during
the period 1961 to 1968 was found to be 80 to 100 per lakh population. It has
been found recently that the mortality rate has come down where the
programme is functioning satisfactorily. As per the recent studies conduc ed
by the NTI Bangalore, and the New Delhi TB Centre in their field areas, the
mortality rates were found to be 53 and 40 per lakh population respect.vely.
0
I
I
problem in this country is really a rural one.
The National Tuberculosis Programme, as envisaged by the National
Tuberculosis Institute, Bangalore, has been functioning since 1962, and is a
permanent country-wide programme, integrated with the general healt
services. It is based on epidemiological, sociological and economical
conditions prevailing in the country. The objectives of the programme are to
diagnose, treat and give preventive services to the bulk of the TB patients and
to the community, nearest to their homes with a view to meet their ‘felt needs
and also to reduce their suffering and prevent disability and death, with the
ultimate objective of reducing the problem to such an extent that it ceases to
be a public health problem.
Under the programme, a District TB Programme, is being implemented in
every district of the country in association with all the existing general health
institutions of the district. Emphasis has been laid mainly on microscopic
31
examination or sputum. Radiological examinations are restricted for oatientc
wose sputum is repeatedly negative. Patients are treated primarily on
St PH tSIS W!,hKlhe flVe regimens of conventional anti-TB drugs To cut
hav“ pr T r
,reatme"t. short course chemotherapy drua?egimens
The involvement of the general practitioners and voluntary organisations,
and community participation in the programme is a MUST for the development
of the programme. A health education campaign in the community should
develop along with the proper functioning of our health and medical
institutions. Rapid socio-economic developments and improved standards of
living could lead to a more spectacular decline in Tuberculosis.
ave recently been introduced, or are going to be introduced in 1S4 dis'ricts of
the country by 1988-89. By the end of the VIIth Plan period most districts will
.n ams b^n"6''
BCG vaccination is give^oSy to
tmmu’nisX"
,he ex« Programmed
At present, our country is truly in the endemic phase of the disease and
there is a gradual and slow natural decline of Tuberculosis.
finrtin^UltiPTP°Se workers/vil|age health guides are beino involved in case
finding and case holding activities. The drug delivery’system is beino
expanded to the farthest corners of the districts by involving the sub-centres9
REFERENCES
1.
Salient Recommendations of the Task Force under ICMR on NTP-Mid-term
Appraisal.
2.
NATIONAL TUBERCULOSIS INSTITUTE (1988) Salient Suggestions/Recommendations for Implementation by the State/Union Territory Authorities
made in the Seminar. 5!h and 6th January, Bangalore. National Tuberculosis
Institute.
3.
BAILY (1974) Operational Study on Conversion Rate of Sputum with Anti-TB
Drug Regimens.
4.
'NATIOnSl TUBERCULOSIS INSTITUTE Mortality Rate due to TB Longitudinal
Study. Bangalore. National Tuberculosis Institute.
he la t few years. Considerable augmentation of funds to the programme as
Centres share has been made during the Vlth and Vllth Plan periods.
5.
6MRC & ROSENTHAL eta/. (1972) Controlled Clinical Trials on Protective Value
of BCG.
oroorPsVh SP'le ? extension of 'aerifies and augmentation of funds the
progress has not been as expected.
'
6.
NAGPAL, D.R. (1978) TB in India - A Perspective. IM^ Jr. 71 (2), July 16.
7.
BAILY (1983) TB Control of India - Current Problems and Possible Solutions. Ind.
Jr. T.B. XXX(2). Nov. 2, April.
8.
MINISTRY OF HEALTH AND FAMILY WELFARE (1987) Guidelines for
Introduction of SCC Regimens in DTP. Ministry of Health and Family Welfare.
July.
9.
BAILY (1976) Operational Study on the Conversion Rate by Standard
Chemotherapy. Bangalore, National Tuberculosis Institute.
10.
ANEJA & SAMMUEL, RUPENT (1982) Organisational Effort on a Clinical Trial
and its Relevance to Applicability of SCC in NTP. Ind. Jr. TB XXIX (1). January.
11.
ANEJA (1982) Chemotherapy in NTP. Newsletter 19(58). Bangalore, National
Tuberculosis Institute.
= Za^6rS r aCtiVe,y inwlved in -Sated moSi6nU'o;
12.
ANEJA SCC-Retrospect and Prospect.
prescribedf oe iod tVndhcotmmunities t0 take regular treatment for the
ed perl0d' The short course chemotherapy regimens alreariv
,he
13.
BAILY & JAGATA (1985) Chemotherapy of TB. Newsletter 21 (3): 64,
Bangalore, National Tuberculosis Institute.
14.
Presidential Address in 41st National Conference on TS and Chest Diseases 1986.
is evalumed t*5
°n the health education activities. The programme
IS evaluated at various levels regularly.
P uyamme
J'nce 'dependence, considerable improvements in anti-TB measures
have been noticed. The major districts of the country have already been
Di®triCl Tuberculosis Programme. About 300TB clinics ahd
46,000 TB beds are functioning, and about 76 per cent of the .mplemen able
cent J^he oSoeefnt?a?%effJCienCy Of the DiStriCt TB Pr°9ramme is about 35 per
cent o the pu.ential. Studies conducted at the National Tuberculosis In^tituto
Bangalore, revealed that 82 per cent of the sputum posXeX cThP
dtagnosed by examining the sputum twice. If the mXal/paramPdi^
c©
centTmey™aSte
effiCienCy °f the Pro9ram^e is about 30 per
modi i/ ~ xPectation- The condition can improve considerably if the
medical/paramedical personnel of the health institutions and also multi
32
33
k
-
<
a
15.
16.
DIRECTORATE GENERAL OF HEALTH SERVICES (1987) Circular on
Guidelines for Introduction of SCC in DTP. July 7. Directorate General of Health
Services.
Results of Relapse - Retrospective 5 years with SCC for 6 months and with
Standard Regimens for 18 months. American Review on Respiratory
Diseases. 1977. 116.
BMRC (1977) Trial on BCG and Vole Vaccination in the Prevention of TB in
Adolescents and Early Adults Life. B.M. Jr. 2.
18.
NATIONAL TUBERCULOSIS INSTITUTE Efficacy of two Standard Drug
Regimens under Programme Conditions. Bangalore, National Tuberculosis
Institute.
19.
NATIONAL TUBERCULOSIS INSTITUTE Operational Study on DTP. Bangalore,
National Tuberculosis Institute.
NATIONAL INSTITUTE OF HEALTH AND FAMILY WELFARE
(NIHFW) came into existence on 9th March, 1977, after {.the
Government of India, realising the commonality of objectives of the
two former institutions • National Institute of Health Administration
and Education (NIHAE) and National Institute of Family Planning
(NIFP) - and in pursuance of its policy to integrate health and family
planning services, decided to merge these two instituticns into an
Apex Technical Institution.
I
•
As an Apex Technical institute of its own kind in the country, the
NIHFW has been actively engaged in the promotion of health and
family welfare programmes through education, training, research,
evaluation and advisory-consultancy and other specialised services
ce
(
In order to achieve these objectives, the NIHFW, apart from its
regular M.D. Courses in Community Health Administration, also
conducts 30-35 in-service training courses/workshcps and seminars
every year, which are attended by a variety of personnel ranging from
high-ranking policy making officials and key trainers to the grassroot
level workers.
!.
Other activities of cardinal importance are research and
evaluation in the field of health and family welfare. NIHFW conducts
various research and evaluation studies at its own or in collaboration
with other national and international agencies. The results of these
studies are fed to the programme planners, administrators and
managers.
NIHFW also provides advisory and consultancy services to the
Ministry of Health and Family Welfare, to the States, voluntary
organisations and international agencies in matters related to health
and family welfare.
The Institute provides specialised services as a part of its
education, training and '3search activities. These include clinical
services, documentation, publication, audio-visual services and dat*
processing services.
(
-orr^
V^v;u ^sscciarion
T (a ’ '
i
/a ^d;A
-Vi-?
>■/
V.V.-T---''
A.r.'.t-
.. .v V-
‘-■u
uco:o.
.
1
34
u
1
s
lu«
Ip-«z- ?z- z
-JLzzr.:
■OK V'.
WWOBSI
lOBIilliSi
sftswaawfl
isa®wzwMs»sH^s
F'-
‘
r.
8
$
AfiiriNAillIGNAIs
H
B
Bl!
P^SS?R
NATIONAL HEALTH S>
PROGRAMME SERIES 10
»!
- --------------------
w wl
3|
Si
/
j
I
II
NATIONAL
PRQGRAMME FOR
CONTROL OF
TUBERCULOSIS
f
I
J
I
I
TUBERCULOSIS
i
!
.-ga
i
HL
p|si
w
IF'-3g
'A.-f-F. lrV-
i
■' F-
F\.-."•A'-7 ■'■:■■
'
-■
®oS|jV
/ '-•<<<
Ww-
1
1
><-
'
•■'•.■:
-
■
'-
- ■.
__ _
F- • '
-Z- ■
^-‘Z-zz ■■’F^'S z .
'-—F:z:\;ZZZ-?Z
teW4^-'
z:||| 1 ^Weie^ie^i u4
®i‘zz.-
^"VX
v.r,M LI?"
•\
Z '"--Z
otsi
r - ,jr.O ° .
Arna.^"
NATIONAL INSTITUTE OF HEALTH AND FAMILY WELFARE
NEW MEHRAULI ROAD, MUNIR..'\NEW DELHI-110 OSL
- - 'ZZ
‘
nz; ;., ZZ 'ZF.
■ ■
_
-
-3
NATIONAL HEALTH PROGRAMME SERIES 10
NATIONAL HEALTH PROGRAMMES SERIES
This series of publications is intended to promote the continuing
. education, dissemination of information as well as the study of
health problems and major diseases in India for those who have
concern for the health and well-being of the people. It is also
intended to foster the development of an efficient system of health
care service delivery in the country on the basis of such up-dated
’ publications on the national programmes for the prevention and
control of health problems. In this task, the practitioners and
trainers/teachers of health systems, as also the policy-makers and
those affected by their policy, must be brought together. The
publications, issued in this series, will strive to bring them together
in thought, so that they might work together in action.
i
A
i
NATIONAL
PROGRAMME FOR
CONTROL OF
TUBERCULOSIS
i
I
Dr. A.K. Suri
Additional Director General (TB)
Directorate General of Health Services
Nlrman Bhavan, New Delhi
'I
I
emeeei u4 ulrwiecbcew ersew
NATIONAL INSTITUTE OF HEALTH AND FAMILY WELFARE
NEW MEHRAULI ROAD. MUMIRKA^NEW DELHI-110 067
CONTENTS
Introduction
Magnitude of the Problem
I
Aims and Principles
Infrastructure of the Programme
International Assistance to the TB Programme
Expansion of the Programme During the VI and VII Plans
Short Course Chemotherapy Drug Regimens
Schemes During the Vllth Plan Period
Financial Outlays
Evaluation of the Programme
Recommendations of the Evaluation
Present Position of NTP and Shortfalls/Problems
in the Implementation of the Programme
Summary
References
9
9
10
12
15
15
18
21
22
23
23
26
31
33
FOREWORD
LIST OF ABBREVIATIONS
T.B.
Tuberculosis
N.T.P.
National Tuberculosis Programme
D.T.P.
District Tuberculosis Programme
N.T.I.
National Tuberculosis Institute
I.C.M.R.
Indian Council of Medical Research
B.M.R.C.
British Medical Research Council
P.H.I.
Peripheral Health Institute
P.H.C.
Primary Health Centre
D.T.C.
District Tuberculosis Centre
M.P.W.
Multipurpose Worker
A.F.B.
Acid Fast Bacilli
S.I.D.A.
Swedish International Development Agency
R1, R2, R3, etc.
Regimen No. 1, 2, 3, etc.
2 S^H^RiZi
2 months regimen with Streptomycin,
Sulphate, Isoniazid, Refampicin and
Pyrazinamid on twice a twice a week.
2E.H.R.Z7
6 T H or 6 E H
Ethambutol, Isoniazid, Refampicin and
Pyrazinamid are given daily for 2 months
followed by Thiacetazone and Isoniazid given
daily for 6 months, or Ethambutol and Isoniazid
given daily for 6 months.
s.c.c.
Short Course Chemotherapy
G.P.
General Practitioners
U.T.
Union Territory
S.T.O.
State TB Officer
One of the cardinal factors for achieving Health for All by 2000 A.D. is the ability
of the individual and the organisation to recognise and respond to chanoes in
advancing technology for health maintenance and promotion, new panern ot
disease, disability, etc. new social policies, expectations and programmes tor
better health services. Towards this end. the education of the people
concerning prevailing health problems and methods of preventing and
controlling them is the first requisite of Primary Health Care. This is more so in
the case of public welfare personnel and professionals through whom the
knowledge and skills should percolate to the grassroot level.
In adhering to the above perspective, the National Institute of Health and
Family Welfare conducts nearly fifty training courses/workshops annually
towards requirements of a system of continuing education for health
administrators of States and Districts, teachers of medical college, and also
the members of Indian Administrative Service. However, the problem o
updating the knowledge and skills of these personnel, already on the job. still
remains. It has proved arduous to have them re-trained at institutions.The
snail-like pace of implementation reflects in many instances the fact that this is
an area where most professionals feel unprepared. It is, therefore, essential to
initiate a programme to get relevant information out to individual participant. As
such, the development of self-learning resource materials to keep abreast of
scientific advances in research as well as in programme strategies is an
enviable task which the NIHFW has undertaken with large-scale efforts.
S''
These resource material present an assiduous expatiation of various
National Health Programmes and Schemes currently in operation in the health
services system. Each of these expatiates the genesis, strategy, current
status, and the outcome of the evaluation of individual programme. Thus, the
primary aim of this Series would be to share and utilise the available resources
to update the knowledge and skills of programme personnel at their own place.
I fervently hope that this publication will provide orientation on the use of
such self-learning materials to learners/participants. I also wish to asseverate
that these resource materials will be updated periodically and as such, I am
sure, they should be a valuable aid in overcoming the lag.
&
A.N.M. Auxiliary
A.N.M.
Auxiliary Nurse Midwife
E.P.I.
Expanded Programme on Immunization
Much of the positive value in this Series originated with one or another of
our associates, sincerely thank these Programme Officers who had so kindly
undertaken the onerous task of compilation and completion of these
documents.
New Delhi
December, 1988
•V
J.P. Gupta
Director
1.
I
I
INTRODUCTION
Tuberculosis is a communicable, bacterial disease which results from
infection with TB bacilli. The TB bacilli is a rod-shaped organism, discovered
by Robert Koch in 1882. Tuberculosis can be traced back to the early history o
mankind In our country, it has been known since the Vedic ages, that is, about
5000 years ago. It is world-wide in distribution and strikes both the rich and
poor all races and both sexes. Tuberculosis affects all parts of the human
body, but. most commonly, the lungs. The patient with lung TB excretes
Tuberculosis bacilli with sputum through coughing, sneezing, etc. The germs, t
thus excreted, can enter, mainly with the help of air currents, another healthy
human body while the person breathes in. On entering tne lung, the bacilli
generally get a foothold on the peripheral part of the lung and this process is
called infection. The entry of the Tuberculosis germ into the body and its
gaining a foothold does not always lead to disease, immediately or later, n y a
few infected persons suffer with the disease process due to a number of
factors which are both intrinsic and extraneous. The intrinsic factor is poor
natural resistance or poor inborn immunity, which is a genetic one. Extraneous
factors are many, like poor living conditions, low social and educational status,
inadequate food or nourishment of the body, psychological and
temperamental status of the person and affliction by some other diseases like
diabetes, measles, cancer, etc. Today, Tuberculosis is treatable, curable and
Sor/es Editors
J.P. Gupta
S. Bhatnagar
© 1988, by the NIHFW, New Delhi
The views expressed in this publication are those of
author and do not necessarily represent the decisions of
the stated policy of the National Institute of Health and
Family Welfare, New Delhi..
preventable.
MAGNITUDE OF THE PROBLEM
I
Improvements in diet, housing and living conditions in modern times have
contributed to a decline in both TB mortality and new cases. The advent of
chemotherapy during the last four decades has accelerated these trends. But
Tuberculosis still ranks among the major health problems in the world,
specially in the developing countries. There are about 15 to 20 million cases
and three million deaths every year in the world due to Tuberculosis.
IN INDIA' The results of pre-tuberculine tests in mass BCG vaccination
campaigns indicated, for the first time, that the problem of Tuberculosis was
not limited to the urban areas only, in contrast to the earlier belief. The National
Tuberculosis Survey during 1955-58 and subsequent limited surveys have
confirmed these findings.
Tuberculosis is a major public health problem in India and number one
killer among diseases. The National Tuberculosis Survey which was
conducted by the ICMR in the year 1955-58, revealed that nearly 1.5 per cent
of the total population above five years of age is estimated to be suffering from
TB of the lungs, of whom one fourth, or 0.4 per cent are infectious. Subsequent
limited surveys conducted in different parts of the country have confirmed
these findings. As per the 1981 census the total population of the country was
about 680 million and it was estimated that about 10 million people were
suffering from radiologically active pulmonary Tuberculosis disease of the
Printed and Published by the Department of Publications, National Institute of Health and
Family Welfare. New Mehrauli Road, Munirka, New Delhi-110 067.
June 1989/2000
g
i
«
i
only 20-25 patients, can pay for the establishment of clinics which can handle
lungs, out of which about 2.5 million people were infectious. Few lakhs of new
Tuberculosis cases are added to the population every year but at the same
time, an equal number of cases are removed, on account of death,
spontaneous healing or treatment. This results in a state of near balance in the
number of Tuberculosis patients from year to year. It is further estimated that
nearly 50 per cent of the total population is infected with the TB bacilli, though
they are apparently healthy. The annual infection rate (that is about 1.6 per
cent) has remained almost constant for the last three decades.
Nearly 80 per cent of the people in our country live in about 6 lakh villages.
It is estimated that at least 2-3 sputum positive cases can be found in each
village of the country, and nearly 10-12 persons would be suffering from
radiologically active Tuberculosis of the lung. In an average district with a
population of 1.5 million, it is estimated that there, will be about 5000 active
pulmonary cases who are infectious and about 20,000 radiologically active
pulmonary Tuberculosis cases. As per the recent study conducted by the NTI,
Bangalore, in their field area, the mortality rate has come down to 53 per lakh
population, and as per the study conducted by the New Delhi TB Centre, the
mortality rate in their population area is around 40 per lakh population. Since
the prevalence rate of pulmonary Tuberculosis cases is of the same order in
the rural areas as in the urban ones, and nearly 80 per cent of the people of our
country live in villages, the problem of Tuberculosis in our country is really a
rural one.
i
equal to that of treating 15 patients on domiciliary basis. So fromi the• ^onomi
point of view, domiciliary treatment is the practical solution for tackling
oi e
f
i
From the economic point of view, we have, at present, got a few thousand
TB beds. To treat only the sputum positive cases, we need a few hundred crore
rupees for constructing hospitals and another few hundred crore rupees as
recurring expenditure annually. The money that would provide TB beds for
period by the patient.
It has already been mentioned that Tuberculosis is equally prevalent in ,
rural and urban areas. For a developing country Hket ind.a‘^,d be 3^9na of
task to identify all the Tuberculosis cases living in hundreds and thousanos or
distant villages and to offer them regular treatment for a period of one to one
health institutions to seek medical aid.
Another research study conducted by the ICMR (1955-56). conclusively
proved that the Tuberculosis cases can be as effectively treated^on
The mass BCG vaccination campaign and the National TB survey conducted
during 1955-58 led to the conclusion that Tuberculosis services had to be
provided on a country-wide and long-term basis.
The NTP aims at the methods by which the systematic reduction of
Tuberculosis in the community may be made within the available resources of
the country and within a reasonable time. The method of treating the patients
on a domiciliary basis was initially a compromise between the scientific idea
for the few, and the economically and practically feasible one for the many.
The short-term object of the programme is to diagnose and treat the patients at
places nearest to their homes and also to give preventive services to the bulk
of TB patients, specially those living in rural areas with the view of meeting their
'felt needs’, and to reduce their suffering and prevent disability and deaths to
the extent possible. The long-term objective of the programme is to reduce the
problem gradually till it ceases to be a public health problem.
Tuberculosis problem with limited resources.
From the scientific point of view regarding treatment of patients on
domiciliary basis, it has been observed that the results of treat.ng, the paber
in a hosoital and at home are more or less the same. There is hardly any
difference between the hospital patients and those treated at home, as rega rds
the immediate therapeutic response in terms of
'^^^e
qnutum conversion and closure of cavity at the.end of one year, as also the
danger of relapse in the future, and infection to the contacts,
adequate chemotherapy is prescribed and taken regularly or e pre c
and a half years.
The studies conducted by the NTI, Bangalore, have revealed that nearly
95 per cent of the infectious Tuberculosis patients are conscious of their
symptoms and it least 50 per cent of them report to the nearest medical
AIM AND PRINCIPLES OF NATIONAL TB PROGRAMME
(NTP) - BACKGROUND INFORMATION
i
1000 to 1500 patients annually.
The cost of treating a Tuberculosis patient in a sanitorium for one year is
0? >
domiciliary basis as in hospitals.
Based on the results of these two studies, the country-wide district
Tuberculosis programme was evolved for the entire country by the NTI,
Bangalore, in 1962. Under the programme, a district Tuberculosis centre i
being established in every district of the country to organise a commun^w de
district Tuberculosis programme in association with all the existing med ca
and health institutions. In an average district of our country,there are about 50
such peripheral health institutions. The mam aim of the programme is tcide te
as large a number of patients (sufferig from Tuberculosis as Poss'b'®. n®3
to their homes and treat them effectively so that the infectious patients are
rendered non-infectious and the active and non-mfectious cases do not
become infectious.
In doing so, priority is given to sputum positive Tuberculosis patients.
The patients are treated mostly on domiciliary basis because it is as
effective as institutional treatment and more acceptable to TB patients sine
their domestic life lis not disrupted.
11
10
In addition, there are about 300 ordinary Tuberculosis clinics which are
functioning in the country and are mostly located in big towns and cities. These
are equipped with either static X-ray unit or Fluoroscopy and laboratory
facilities and look after the needs of the local population living nearby.
Each district Tuberculosis centre is staffed by a team of medical and
paramedical personnel trained at the NTI, Bangalore, in X-ray and laboratory
diagnosis, treatment organisation and community control of Tuberculosis, and
is equipped with a static 100 M A X-ray unit fitted with an Odelca camera for
miniature radiography, and laboratory equipment for direct smear
miscroscopy.
.
There are about 46,000 TB beds available in the country to cater mainly to
the needs of the selected group of patients, i.e. those who are seriously sick or
suffering from some emergency or need surgical treatment or are social
destitutes, etc. We are making efforts to establish sufficient
of
Tuberculosis beds, as per the needs in every district of the country.
The d strict Tuberculosis centre functions as a referral centre for the
entire Tuberculosis control proc'amme of the district. Its key personnel tour
the existing peripheral medical and health institutions, including the primary
. health centres which cater to the health needs of the rural population, train the
. medical and paramedical personnel of such institutions in various essential
activities under the Tuberculosis programme, supervise their working, ensure
proper record keeping and reporting of the whole district and give advice also
at the TB clinic in the town or city of its location.
Thus, the district TB centre serves as a base for carrying out the case
finding and treatment programme throughout the district with the help of the
network of general health services of the district, so that these facilities are
brought nearer to the homes of the patients at minimum expenditure, and a
permanent case finding and treatment programme is developed. The
treatment is offered on an out-patient and mainly self-administered basis. The
patients are encouraged to collect drugs from the PHCs nearest to their
homes. The minimum duration of tne uninterrupted chemotherapy is one year.
The optimal duration of treatment is one to one and a half years and the
extended period of treatment is upto a maximum of two years. All efforts are
made to ensure that the patient receives uninterrupted treatment for at least 12
months. Defaulter actions are taken, both at the district Tuberculosis centre
and at the peripheral health institutions, by way of letters to the individual
patient, letters to the head of the village or by sending the health
. visitors/multipurpose health workers and village health guides, etc. In addition
to this, under the NTP, additional district Tuberculosis centres are being
___ established in those districts where the population is more than 2 million.
The additional district Tuberculosis centres are established in another
sub-divisional town of the district To cater to the needs of a small population of
a district, a mini district TB centre is being established. It is not necessary to
provide the full complement of key personnel at these mini district TB centres
and these centres are not provided with any X-ray facilities. Instead, the X-ray
facilities at the general hospital in the district are used.
INFRASTRUCTURE OF THE PROGRAMME
Out of the 434 districts in the country, the district TB programme has been
implemented in 371 districts.
•) l <
The Tuberculosis Institute. Bangalore, was established in 1959 with the
aim of evolving nationally applicable methods of Tuberculosis control and
training of key personnel for the Tuberculosis programme. Till now, about
4,600 key personnel of different categories have been trained. The Institute
holds reorientation/training seminars for senior health administrators and
professors of medical colleges, etc. Trainees from abroad also attend various
international courses at the Institute. This Institute is also carrying out
epidemiological, sociological, bacteriological and operational research
connected with the Tubercufosis programme. It has also been selected to
monitor the National Tuberculosis Programme on the basis of reports received
from the DTCs and to provide suitable technical guidance to the district
Tuberculosis centres to improve their performance.
This Institute is also carrying out short course chemotherapy regimen
trials under operational conditions in the field area.
The Tuberculosis Research Centre. Madras, was established in 1956 for
studying the feasibility and efficacy of domiciliary treatment of patients
suffering from pulmonary Tuberculosis, and evaluation of inexpensive,
effective chemotherapy regimens on mass application. The centre is ^t
present engaged in conducting control clinical trials on chemotherapy in 18
districts of the country, clinical trials on Tuberculosis meningitis, Tuberculosis
of the spine, etc. It has established a cardio-pulmonary physiology laboratory
and epidemiology unit.
0) >
Seventeen Tuberculosis training and demonstration centres are
functioning in the country to undertake the training of the medical and para
medical personnel required for manning the Tuberculosis centres; to give
technical guidance to the district TB centres; to undertake the cultural and
sensitivity tests; to give technical guidance to the complicated TB cases, etc.
The State TB demonstration centre acts as a model TB centre for the State.
CONVENTIONAL DRUG REGIMENS RECOMMENDED UNDER THE
PROGRAMME FOR SPUTUM POSITIVE PATIENTS (ADULTS)
Code No.
On an average, in a district there are about 50 implementable PHCs and
other institutions (PHIs) and till now about 75 per cent of the PHIs have been
brought under the National Tuberculosis Programme.
12
R1
Drugs and Doses Mode and Rhythm of
administration
Isoniazid 300 mg
+ Thiacetazone
150 mg
Both drugs in a single
dose or two divided
doses, orally, daily
Instructions
Self-administered
at home after meals
R2
R3
R4
R5
Bi-weekly regimen Intra-muscularly
Inj. Streptomycin
orally
0.75 gm/1 gm +
Isoniazid 600 to
700 mgm (15 mgm/
kg body weight) with
Pyridoxine
Isoniazid 300 mg+
PAS 10 gms.
in a single dose
in two divided doses
both drugs orally, daily
Isoniazid 300 mg
F
" drugs
‘ w in a single
Both
+ Ethambutol 20 mg dose; orally, daily/
/kg body weight
i.e. 800 mg per
patients weight
4-50 kg and 1000
mg to 1200 mg >50
kg
With R1, R2. R3 or
!
I:
to cost, non-availability, etc.
INTERNATIONAL ASSISTANCE TO THE TB PROGRAMME
Sell-administered
after meals
t
I
Self-administered
at home after meals
Inj. given under
supervision and
rest to be self
administered at
home
O') >
As per each regimen As per each regimen
Drug regimens comprising Inj. Streptomycine 0.75 gm/1 gm
twice or even thrice a week + INH 200 mg or 300 mg daily is not
sufficiently effective and, hence, not recommended.
I
can be treated with R4.
Note: The Drug PAS is gradually being withdrawn from the programme due
For first two months
Inj. Streptomycin
In a single dose,
0.75 mg/1 gm +
orally, daily,
Isoniazid 300 mg
(PAS and Thiaceta4-Thiacetazone
zone should be given
150 mgm
in two divided doses)
or Ethambutol 200 mg
per kg body weight
i.e. 800 mg for
patients Z.50 kg and
1000 to 1200 mg for
those more than
50 kg
or PAS 10 gms.
b. Continuation phase
*
Tuberculosis paitents in whose sputum A F B are not seen, are advised
Regimen R1; i.e. Isoniazid 300 mg +Thiacetazone 150 mgm in single dose
orally, daily for one to one and a half years. Patients allergic to Thiacetazon
Biphasic regimen
a. Intensive phase
Remarks:
For the Negative Tuberculosis Patients (Suspected Cases)
Both drugs given at
the same time
under supervision
of the treating
physician twice
weekly at intervals
of 3 to 4 days
By Swedish International Development Agency (SIDA): The Swedish
International Development Agency has been supporting the case finding and
treatment activities of the programme by supplying X-ray units with Odelca
cameras, miniature X-ray film rolls, drugs needed for conducting the short
course chemotherapy trial under pilot study, etc. since 1979. These X-ray
machines with Odelca cameras are supplied to the unequipped district TB
centres of the States/Union Territories, and as replacements to those district
TB centres where the X-ray machines with Odelca cameras have outlived
their utility. They are also are supplied to the additional TB centres, wherever
created. The miniature X-ray film rolls are supplied to the district TB centres.
Till now, the SIDA authorities have supplied about 175 X-ray machines with
Odelca cameras. The short course chemotherapy trial under pilot study is
being conducted in 18 districts of the country since 1983-84. The SIDA have
also agreed to give additional assistance within June 1989 for supply of
another 25 X-ray machines with Odelca cameras, miniature X-ray film rolls
and 100 vehicles. These vehicles would be supplied to the different district TB
centres of the country where either the vehicles have outlived their utility or to
the newly created district TB centres for proper implementation and
supervision of the programme by the DTCs. The SIDA is also helping the
National Tuberculosis Institute, Bangalore, in various ways.
Assistance by the WHO: The WHO has been assisting the NTI.
Bangalore, since its inception in 1959 and theTB Research Centre, Madras
(ICMR) since 1956 by providing short-term consultants, fellowships, and
essential supplies and equipment. They are also providing assistance to these
two institutions for conducting short-term reorientation courses/seminars for
senior health administrators of the States/Union Territories, teachers of
medical colleges and refresher courses for the medical and paramedical
personnel of the district TB centres.
EXPANSION OF THE PROGRAMME DURING THE Vl^
Expansion Under the 20-point Programme: A newjhriist has been give^oX^
I..
!
case finding activities of the NTP under the 20-ppint progr^rrim^Dnder th&
20-point programme, targets for new TB case deiection’I^ave been laid dowij
14
15
,fytional Atca>
I
rI
Ii
II;
•
Prior to the laying down of targets, only about 7 lakh new TB cases under
lie programme had been detected, but at the present moment more than 1.4
mil ion new Tuberculosis cases have been detected under the programme. To
involve the primary health centres in more and more case finding activities in
t.ne rural areas, targets for new sputum examinations have been laid down
since 1983-84. With this, the PHCs are being more actively involved than
before in case finding activities, and a target for 600 new sputum examinations
per year by each PHC has been laid down. Initially, the achievement of targets
of new sputum examinations at PHCs was not very satisfactory but
considerable improvements are being noticed gradually.
10.00
10.80 (100%)
No target laid
down
83-84
12.50
12.00 (96%)
34.00
12.00 (35%)
8--85
13.75
12.54 (91%)
34.00
17.31 (50.2%)
85-86
14.00
13.58 (97%)
34.00
20.3 (59.5%)
85-87
14.50
14.13(97.5%)
34.00
21.69 (63.9%)
87-88
15.00
15.62 (104%)
34.00
24.11 (71%)
63-89
15.00
34.00
Expansion of the Programme in Rural Areas: To intensify the case
finding and case holding activities under the programme in rural areas, it has
been recommended that all the health workers of the peripheral health
institutions are to be involved in case finding and domiciliary treatment of the
Tuberculosis patients and also to be engaged in BCG vaccination of the
newborns and infants. It has been recommended that the MPWs, during their
16
treating physician.
To expand the treatment activities further for the rural people living in the
far-flung villages, it has been recommended that all the sub-centres which
have the necessary buildings for storage of drugs, and have me requisite staff,
should be involved in the distribution of drugs to the Tuberculosis patients.
Target for
Achievements
Target for
Achievements
detection
(in lakhs)
conducting new
(in lakhs)
of new TB cases
sputum exa
(in lakhs)
minations at
at PHCs
(in lakhs)
82-83
I
!
The village health guides are also being involved in essential health
educational activities under' the programme including mobvation of chest
symptomatics to avail of all the diagnostic facilities of the health institutions,
and in motivation of the Tuberculosis patients living in their areas to take the
uninterrupted treatment for the prescribed period as per tne advice of tne
TARGETS AND ACHIEVEMENTS SINCE 1982-83
UNDER THE PROGRAMME
Year
I
routine rounds in the villages, should identify the ches: symptomatics
suspected to be suffering from pulmonary Tuberculosis and motivate them to
go to the nearest health institutions for necessary investigations, motivate the
diagnosed Tuberculosis cases to continue the anti-TB drugs uninterruptedly
• for the prescribed period, and take defaulter action on the patients who nave
defaulted in continuing the drugs. The MPWs also involve themselves in health
educational activities on TB amongst the villagers and TB patients. For
conducting these activities, the MPWs in the PHCs and in thesub-centres are
gradually trained iacase finding, domiciliary treatment, BCG vaccination and
also in healtlveducation activities.
since 1982-83 and these targets are being increased every year. The
achievement of the targets of new TB case detection has been satisfactory
from the beginning.
Expansion of the Programme in Urban Areas Under the City
Tuberculosis Programme: The district Tuberculosis programme was
planned mainly with rural India in mind. It has been observed that the problems
in metropolitan and other big cities with a population over five lakhs are
different and the district TB programme would not be able to serve the needs of
these cities effectively. As such, it has been recommended that advantage *
should be taken of the newly created health posts in the big cities and towns
with a population over five lakhs, for implementing the city TB programme,
which is already functioning in some cities like Delhi, Bomoay.
1
Extension of Short Course Chemotherapy Regimens (SCC): Under
the clinical trial conditions, the conversion and relapse rates with the
conventional drug regimens are 82 to 96 per cent and • to 15"mci *-ent
respectively, at the end of one year.
In a study conducted by the National Tuberculosis Institute, Bangatore, it
was revealed that only 30 per cent of the cases completed treatment at the end
of one year under programme conditions with the conventional regimens and
the patients defaulted mostly after the first or second collection of drugs. It was
further revealed that in spite of poor completion of treatment rate, the
conversion rate of sputum was about 65 per cent at the end of one year.
But under the clinical trial conditions, there is about 100 per cent sputum
conversion in six to eight weeks and the relapse rate is only around 2 percent
with the short course chemotherapy drug regimens. The duration of treatment
17
I
with these drugs is only six to eight months. The main handicap in using the
short-term chemotherapy drugs v/as cost, but at the present moment, the cost
of these drugs, specially of Refampicin has gone down considerably and it is
expected that it will go down further.
The long duration of the treatment, for a period of one to two years, with the
conventional anti-TubercuIosis drugs is believed to be one of the important
causes for the irregularity and discontinuation of treatment. Hence, to cut short
the duration of the treatment, achieve early conversion of the sputums,
thereby, preventing the spread of the disease and also to lower the relapse rate
etc., the short course chemotherapy drug regimens have been introduced on a
pilot study basis since 1983-84 in 18 districts of the country to find out the
feasibility of introducing these drugs under the programme conditions. With
the encouraging results gained in the study, these regimens were introduced
in another 101 districts by 1987-88 for the sputum positive newly detected
Tuberculosis cases, excluding the 18 districts where these regimens were
introduced under the pilot study.’The short course chemotherapy regimens
are going to be introduced in another 75 districts of the country during 198889. It is expected that the majority of the districts of our country would be
covered with these regimens by the end of the Vllth Plan period.
It is hoped that by introducing these regimens, the defaulter rate of
treatment will go down further.
SHORT COURSE CHEMOTHERAPY DRUG
REGIMENS RECOMMENDED UNDER THE
NATIONAL TUBERCULOSIS PROGRAMME
—: sm
substituted for Streptomycin.
--
Regimen B: Daily self-administered regimen
2EHRZ/6TH OR 6 EH
$))
Ethambutol
(E 1 9)
(H 300 mg)
Isoniazid
(R 450 mg)
Rifampicin
Pyrazinamide (Z 1.5 g)
Thiacetazone (T 150 mg)
In this regimen, the total duration of treatment is eight months During the
eight months of treatment, the drugs have '^^^^^^"'^Xhlmbutol
In the first two months (intensive phase), the patient is given Elharnbutol,
isoniazid. Rifampicin and Pyrazinamide in the dosage mentioned above^
During the remaining six months (continuation phase), INH 300 mg a d
Thiacetazone 150 mg daily have to be given. If the patient cannot tolerate
Thiacetazone, Ethambutol 800 mg should be given daiy.
All sputum positive cases aged 15 years and above, irrespective of history and
previous anti-TB treatment, are offered either of the following two drug
regimens:
Suitability of Patients for Appropriate Drug Regimen
Drug Regimens
The patients who express their inability to come to the centre twice a week
or who repeatedly fail to come to the centre twice a week for one month
consumption of drugs are offered Regimen B, of eight months duration.
These regimens have two phases:
i. Intensive phase of the first two months with four drugs.
ii. Continuation phase of four to six months with two drugs.
Regimen A: Bi-weekly, intermittent supervised regimen
2S H R Z/ 4 H R
2222
22
Regimen containing
Streptomycin
Isoniazid
Rifampicin
Pyrazinamide
18
(S 0.75 g)
(H 600 mg)
(R 600 mg)
(Z 2 g)
The patients who reside near the centre, and who are willing to attend The
centre twice a week for six months should be offered Regimen A.
Patient ‘Lost’ from Treatment
A patient who does not come for drugs for one month from the due date even
after two defaulter actions, is considered lobe lost from treatme •
patient returns after becoming 'lost' he should be started on any one of the hve
standard drug regimens (R1 to R5). It is important to ensure that every pat e
put on short course regimens (either Regimen A or Regimen B) shoe d have
collected 75 per cent of the required doses of lhe intensive phase wi hiri three
months from the start of treatment. Those patients who fail to completei th's w
not be eligible for the continuation phase and will be offered the standard drug
regimen.
19
I
Zilla Parishad, community leaders, youth leaders, etc. Ninety-five per cent of
the infectious sputum positive cases are already conscious of their chest
symptoms and a country-wide health education campaign must be carried out
to educate this group of chest symptomatics so that they get themselves
investigated and utilise the facilities available at the institutions nearest to their
Compensatory Phase
Every effort has to be made to ensure that each patient put on SCC Regimen A
or B, completes treatment within the stipulated period. However, due to
unavoidable reasons, if any patient defaults, the compensatory phase may be
allowed. For the intensive phase of chemotherapy, an extension of one month
may be given to the patient to complete the required number of doses. That
means that under drug Regimen A, 17 doses should be taken in two months.
This may be allowed to be completed in three months. Under drug Regimen B,
four fortnightly collections of drugs should be made in two months. This may be
completed in three months.
Similarly, an extension of one month in the continuation phase may be
allowed to compensate for the missing doses. However, the total duration of
chemotherapy, including the compensatory phase, should not exceed eight
months in drug Regimen A and ten months in drug Regimen B.
Termination of SCC
For any patient remaining sputum positive after six months from the time of
initiating SCC on either of the regimens, the SCC is terminated and the
treatment card is closed.
For such patients, a new treatment card is to be opened (prolonged
treatment card) and the patient is put on INH and Thiacetazone (or
Ethambutol) for one year. This is called prolonged treatment. Any patient
remaining sputum positive after six months of prolonged treatment has to b(*
referred to specialised institutions for management of treatment failure.
4)) ®
I
(I
A patient who has completed 75 per cent or more doses of the required
number, during the intensive phase (including compensatory phase), is
considered to have completed the intensive phase and is eligible to enter the
continuation phase.
As in the Vlth Plan period, the schemes of establishment of more district
Tuberculosis centres. TB beds. etc. have been included in the State plan
sector.
Centrally Sponsored Sector: Under the Centrally sponsored sector, the
following schemes are being implemented:
a. Supply of anti-TB drugs/equipment to the States on 50:50 sharing
basis between the Centre and the States.
b. Supply of anti-TB drugs/equipment to the Union Territories as a 100
per cent Centrally sponsored scheme.
A patient who has completed 75 per cent or more of the required number
of doses of the continuation phase is considered to have completed optimum
treatment.
20
Rs.10<X) lakhs
Rs.40.00 lakhs
Rs.60.00 lakhs
Rs.50.00 lakhs
SCHEMES DURING THE VIITH PLAN PERIOD
Completion of Treatment
Expansion of Health Education Activities'. Any health programme,
specially the NTP, a programme of great magnitude, cannot succeed without
the active involvement and,cooperation of the community, village Panchayats,
Keeping this in mind, much stress has already been given to various
health educational aspects of the Tuberculosis programme by bringing out TV
spots, radio spots, advertisements in newspapers, material (or medical
practitioners and the general population, etc. under the programme during the
Vllth Plan period.
1985- 86
1986- 87
1987- 88
1988- 89
Every patient should be followed up strictly with sputum smear examinations once at the end of six months after starting treatment and another at the end of
chemotherapy (inclusive of compensatory period, if any).
c. Supply of anti-TB drugs to the TB clinics run by voluntary bodies as a
100 per cent Centrally sponsored scheme.
L
!
homes.
A vast majority of patients suffering from Tuberculosis either report first to
the general practitioners or to the Governmeql hospitals/dispensaries. As
such, the active participation of these health institutions and general
practitioners is a must for the success of the programme. The most important
point is to create active interest in the minds of general praciitioners/medical
practitioners regarding the problem and the NTP and also to up-date their
knowledge about the present philosophy, diagnosis and treatment of
Tuberculosis through refresher courses. These courses are being cu..Juried
by the Tuberculosis Association of India.
The funds provided on health education activities till. now. during the Vllth
Plan period, are as follows:
Follow-up Examination
1*1
d. Expenditure on health education activities as a 100 per cent Centrally
sponsored scheme.
21
I
bacilli except in the developed countries where a few cases of TB were due to
the bovine type of infection. In India, the TB due to bovine type of infection is
rare as milk is boiled before use. In the developed countries. TB due to the
bovine type of infection has been controlled by pasteurising milk and other
FINANCIAL OUTLAYS AND ACTUAL EXPENDITURE INCURRED
DURING THE VITH AND VIITH PLAN PERIODS
Vlth Plan Period
measures.
Against the actual allotment of Rs.700 lakhs, the actual expenditure was
Rs.2040.00 lakhs.
EVALUATION OF THE PROGRAMME
The programme was evaluated by the expert committee formed by the ICMR
in the year 1975. The committee concluded that while the concept of the
programme was sound, there was considerable scope for improvement in the^
implementation of the programme, specially at the peripheral health service
levels. The committee made certain recommendations for further
improvements which were then examined by an empowered committee
appointed by the Ministry of Health and Family Welfare and the detailed
guidelines for further improvement of the programme were given to the States
for implementation.
Vllth Plan Period
Financial outlays
Rs.5500.00 lakns
Actual expenditure incurred during the first three years of the Vllth Plan:
1985- 86
1986- 87
1987- 88
Rs.1112.00 lakhs
Rs.1125.00 lakhs
Rs.1415-00 lakhs
BCG Vaccine, Its Efficacy and Current Status NTP vs EPI
From time to time, the experts of the Swedish International Development
Agency (SIDA) evaluate the functioning of the programme before signing the
agreement for aid to the programme and also during the agreement period.
Recently, the programme has been evaluated by the expert team of the SIDA
which has recognised the soundness of the programme and has also
observed that the programme is working more or less satisfactorily and in the
right direction.
The BCG vaccination programme has been in operation since 1951. However,
as the coverage of the susceptible population was not found to be very
satisfactory, it was decided that instead of carrying out the campaign through
BCG teams alone, the activity was to be integrated with the general health
services so that the newborns and infants, specially in me vast rural areas,
may be covered expeditiously under the EPI programme The present BCG
teams (available in the States and Union Territories) in add lion to their current
duties under the vaccination programme, are also engaged in proper training
of the health workers in the technique of vaccination.
They have, however, made some recommendations to improve upon the
case detection and case holding activities of the programme, specially for the
rural regions.
A study of the integration of the BCG vaccination programme with the
general health services indicated that the services of Auxiliary Nurse
Midwives (ANMs) who are now designated as Female Health Workers, could
be utilised for BCG vaccination of infants without detriment to the ANMs’ other
functions. (Baily, Kulbhushan, etc. Ind. J. Tub. XX, 4. 155 (1973).
The Chingleput study on BCG vaccination clearly indicated that the BCG
vaccination did not give any protections against the development of adult type
TB. Several animal studies and several controlled trials (BMRC, 72. Rosenthal61) had clearly shown that BCG vaccine almost always conferred a
measurable degree of protection more closely tothechildhood form of TB and
its associate complications like meningeal and milliary type of TB. Hence, the
present policy of BCG vaccination is to vaccinate the child soon after birth. In
urban areas, the newborns are vaccinated just after birth in Maternity
Hospitals and Child Welfare Clinics. In the rural areas, under the EPI
programme, multipurpose health workers, vaccinate all the newborns before
they are one year old alongwith other immunization.
The NTI. Bangalore, has been entrusted with monitoring and evaluating
the programme on the basis of the performance reports of the DTPs.
The programme is reviewed from time to time at the meetings of the
Health Secretaries of the States/Union Territories and also during the meeting
of the Central Council of Health, at the Central level.
<1
The programme is also reviewed every month by the Ministry of Health
and Family Welfare at the Central level and often at the levels of Health
Secretaries/Ministry.
At the State level, the programme is reviewed and evaluated 'cgularly at
the State and district headquarters.
Recently, an independent organisation has been appointed by the
Ministry of Health and Family Welfare to evaluate the programme
independently.
RECOMMENDATIONS OF THE EVALUATION
Bovine Type of Bacilli and the Infection
A seminar held at the NTI, Bangalore, on Sth and 6th January. 1988, which was
A majority of the TB cases in the world are due to infection with human type of
22
23
7. The MPWs and ANMs while receiving their basic train,ng in the training
institutes should be imparted the requisite training in the essential aspects of
the TB programme.
attended by the health authorities of States/Union Territories, made some
suggestions/recommendations for improvement of the programme. The
salient recommendations/suggestions made by the ICMR committee and at
the seminar held at Bangalore are as follows:
i
j
•i
1. For the speedy expansion and intensification of the activities under the
programme, the essential schemes which have a direct bearing on the
expansions of the case finding activity and treatment programme should be
taken up as a 100 per cent Centrally sponsored scheme. Due to financial
constraints, the State/Union Territory health authorities are not able to provide
' sufficient funds for establishment of DTCs and for the procurement of anti-TB
drugs, etc. out of their share. As such, it has been recommended that the
scheme of establishment of DTCs in those districts where they are not
available at all and the scheme of establishment of additional DTCs for the
thickly populated districts be taken up as 100 per cent Centrally sponsored
schemes and cash assistance be provided to the States/Union Territories fcr.
a. provision of essential medical/paramedical staff;
b. recurring expenditure for running of DTCs; and
c. provision of essential equipment.
!
2. The performance under the programme should be reviewed regularly on a
monthly basis at every level, just like the review of activities under the family
welfare or MCH programme, etc.
1
I
]
i
3. Over half of the cases of PTB requiring treatment are sputum negative and
cannot be diagnosed either due to non-availability of X-ray facilities at the
PHCs or due to the distance of the PHCs and DTCs from the patients home.
Under the minimum needs programme, it has been proposed to upgrade some
of PHCs to community centres and rural dispensaries to health centres which
would be equipped with general purpose X-ray units. The case finding
activities under the TB programme can be substantially increased by the
establishment of such equipped community health centres, etc. under the
Minimum Needs Programme.
4. In about 30 per cent PHCs either no multipurpose laboratory technicians
have been posted, or if posted, they are overloaded with work like malaria
work, etc. It has been recommended that the admission capacity of the
Laboratory Technicians Training School may be enlarged so that the existing
PHCs and newly established PHCs are provided with multipurpose trained
laboratory technicians.
5. Full-time NTI trained medical and paramedical personnel should be
posted at the DTCs throughout the year for proper implementation and
supervision of the programme.
6. A vehicle alongwith suitable POL charges should be provided in each
district TB centre for proper implementation and supervision of the
programme.
24
8. Ever since the MPWs were entrusted the duty of collecting the sputum of
the chest symptomatics in the field, making slides and sending them for
examination through the microscopic centres, the quality of the work has
deteriorated considerably. It has been recommended that the MPWs. instead
of collecting sputums in the field during their home visits and preparing smear *
slides of such patients, may motivate the chest symptomatics to.report to the
nearest PHC for investigation. The group was of the view that MPWs should not
be entrusted with the duty of supplying anti-TB drugs at the homes of the
patients.
(.f
9. In a large number of PHCs, functioning microscopes are not available. It
has been recommended that the microscopes may be supplied by the
Government of India for the use of PHCs. It has been further recommended
that oil immersion lenses may also be supplied by the Government to bring
back into use the non-functioning microscopes available at the PHCs.
10. Additional district TB centres may be established in thickly populated
districts or in those districts which are very large in area, it has been further
recommended that the additional district TB centre should not be located in
the city or town where a district TB centre is already functioning and it may be
established in another town or city of the district so that tne referral and
supervision activities can be properly developed.
11. For improvement of case holding activities under the programme, the
medical and paramedical personnel of the district TB centre and peripheral
medical and health institutions have to play a vital role. Rep^ed motivation’bf
the patients and members of their families would considerably reduce the
defaulter rates. The multipurpose health workers should keep a list of TB
patients living in their area so that during their visits to the field, the patients and
their families are repeatedly educated about the need to take regular and
uninterrupted treatment for the prescribed period of time, as advised by the
medical attendant.
12. Voluntary organisations are playing an important role under the NTP. It
has been recommended that existing provisions made for the supply of antiTB drugs to such organisations be enhanced so that their total requirement of
anti-TB drugs for domiciliary treatment can be met. It has been further
recommended that those voluntary run TB institutions, which have already
been provided with an X-ray unit with Odelca camera, may be supplied with
miniature X-ray films for the expansion of case finding activities.
Requests for cash assistance for purchase of essential X-ray/laboratory
equipment as well as for construction of buildings for TB institutions by such
voluntary organisations should be suitably considered by the Government.
25
counliy as we could nut keep pace with Hie caiviny out ul new districts out of
bigger districts. At least 75 per cent of the implementable PHIs have been
brought under the DTPs in the implemented DTPS. About 4600 key personnel
have been trained by the NTI, Bangalore, for the uniform implementation and
development of the programme throughout the country. With the inclusion of
NTP under the 20-point programme, about 14 lakh new TB cases are being
detected at the present moment as against about 7 lakh cases detected few
years back. In addition to that, it is estimated that about 5 lakh new TB cases
are being detected and treated by the GPs, voluntary organisations, general
hospitals as well as by other agencies like Railways, ESI, Defence Services,
etc. which usually do not notify the cases under their care to the district TB
Section 35 CCA of the Income lax Act may be amended to include
donors for the establishment of TB hospitals and clinics.
13. The attitude and behaviour of the medical officers of the health
institutions towards TB patients has to be more effective. Therefore, it has
been recommended that continued medical education programmes from the
grassroots to the State level for all medical and health personnel are essential.
Medical colleges should be more actively involved in the implementation of the
programme and undergraduate students may be sent for training at the DTCs.
. 14. The possibility of involving volunteers, Youth Clubs, Mahila Mandals for
health education of the community should be explored.
15. The poor and the deserving indigent TB patients may be granted some
cash assistance by the voluntary organisations to meet the expenses and
other essential needs.
16. It has been recommended that in every major State, the posting of trained
State TB officers alongwith requisite infrastructure is a MUST for improvement
of the programme.
centres.
As a result of the active involvement of PHCs, the number of new sputum
examinations are increasing year by year. To cut short the duration of
treatment, short course chemotherapy drug regimens have already been
introduced for the newly detected sputum positive Tuberculosis cases in 119
districts of the country and the same is going to be introduced in another 75
districts during 1988-89. There has been substantial augmentation of the
financial allocation and expenditure as a Central share for the expansion of the
activities of the programme. In spite of financial constraints, shortage of
technical manpower, illiteracy, population explosion and poor socio
economic conditions etc., of the country, the achievements are by no means
negligible.
I
0
17. The drugs should be made available not only in the primary health
centres, but also in the sub-centres where facilities of storage and distribution
are available.
18. The TB clinic and demonstration centre/State TB centres should play a
more active role in the implementation of the TB programme in the region.
Besides running a district TB programme in the district, in which it is located,
this training centre should also undertake the culture examination work and be
a key referral centre for the entire State. The centre should also undertake the
reorientation training of the CMO/DMO/Civil Surgeons of the State, conduct
reorientation training of the X-ray technicians, laboratory technicians, etc. so
that such functions which are being undertaken by the NTI, Bangalore, at
present, can be transferred to the TB training and demonstration centre. It has
been recommended that from 1.1.1990, the NTI may conduct only two regular
training courses for the district medical and paramedical personnel.
i
Since Independence, there have been considerable improvements in the
developments of anti-TB measures, in our country. Prior to 1947, we had only
about 85 ordinary TB clinics and about 6000 TB beds in the country. Against •
these, we have, at present, more than 600 TB clinics, which include district TB
centres, and about 46,000 TB beds. A total of 371 districts have been covered
under the district TB programme till now, out of the existing 434 districts of the
26
been below expectation.
©
19. It has been recommended that short course chemotherapy regimens
may be extended to more districts in the country so that by the end of the VII th
Plan period, a majority of the districts can be covered by these regimens.
PRESENT POSITION OF NTP AND SHORTFALLS/PROBLEMS
IN THE IMPLEMENTATION OF THE PROGRAMME
But even with the extension of facilities and allocation of more and more
funds, the programme has not progressed as expected earlier .The reasons for
this are many and varied. In spite of more and more newsputum examinations
being done at the PHCs, the quality of the sputum examinations has
deteriorated. The achievements of case detection and case holdings have
>
The operational research study conducted by the NTI. Bangalore, on the
POTENTIAL YIELD OF BACILLARY CASES IN NTP showed that each DTP
can detect about 2000 bacillary cases annually, whereas actually, on an
average, each DTP diagnosed only about 700 bacillary cases annually, that is,
about 35 per cent of the potential yield. Irregularity of drug intake and
inadequate duration of chemotherapy are the two major operational problems
in the case holding activity of the programme. Only about 30 to 35 per cent
cases complete the treatment with conventional regimens under the
programme conditions.
In another study conducted by the NTI, Bangalore, investigating the
efficacy of two standard regimens under programme conditions, the initial as
well as subsequent motivation of the patients was done exactly according to
the recommendation made in the programme which revealed similar
completion rates at the end of one year. In all probability, the DTPs are not
achieving results very close to the potentials.
27
3.
Equal priority has not been given to the TB programme as to the other
programmes like Malaria, Family Planning, by the States/Union Territories
But even with such defaulter rates, the conversion rate of sputums at the .
end of one year is about 65 per cent. Indeed, in the programme, neither the
case finding nor the treatment activity are considered to be satisfactory. But
there appears to be a much larger gap i the case finding achievements than in
the treatment achievements.
health authorities.
4.
The proper status has not been given to th« district TB officers by many
States/Union Territories authorities which hinders the proper implementation
and supervision of the programme at the PHC level.
From the operational study on DTP by the NTI, Bangalore, it is observed
that there is enough scope for improvement in the case finding activities of the
programme but this cannot possibly influence the treatment which could
probably be improved by technical considerations and, to a certain extent, by
modifying the operational conditions.
The reasons for the shortfall of the achievements of the NTP are many
and varied. But the two major reasons are the poor and slow development of
the general health services and poor socio-economic conditions/population
explosion of the country.
The NTP has been rightly integrated with the general health services.
Without the proper development of the general health services, the
programme cannot improve and function in the right direction. Unfortunately,
the primary health care facilities have not developed to the extent envisaged.
In 1946, the Shore Committee recommended that each PHC should cater to
the needs of 30,000 population but due to the financial constraints, etc. this
was not found to be feasible. So in the early 50s, it was initially planned to
establish one PHC to cater to the needsofabout 1,00,000 population,covering
an area of about 200 to 900 sq. kms. The studies conducted by the National
Institute of Health and Family Welfare and A.P. Jain's Committee report have
indicated that the ACTIVE AREA OF INFLUENCE of a PHC does not go beyond
the radius of 8 to 10 kms. Obviously, only the TB patients who are living close to
these institutions have been availing of the facilities of the PHCs. This is an
important reason for the poor performance of the programme due to the
inaoequate development of general health services.
Even before the advent of chemotherapy, the problem of TB could be
controlled due to improved socio-economic conditions in the developed
countries. It is estimated that about 35 per cent of the people in our country are
living below the poverty line, which is one of the main hurdles to be faced.
Health being a State subject, the scheme of implementation and
supervision of the NTP has been classified as a State Plan Activity and the
following difficulties are often encountered in the States in the proper
implementation and supervision of the programme:
1.
Due to lack of financial resources, the State/Union Territory health
authorities cannot implement and supervise the programme effectively.
2.
In some of the States, there exist different administrative controls of the
personnel working at the district TB centres and at the peripheral levels of the
same district causing difficulty in the implementation and smooth running of
the programme.
28
5.
Non-availability of trained whole time State TB Officers in many of the
major States is a big problem. A trained whole time STO is absolutely essential
for the proper implementation and supervision of the DTP in the State.
6.
The apathetic attitude of the medical and paramedical, personnel
specially at the peripheral levels is another hurdle for the programme.
©
7.
DTPs have to be implemented in about 66 districts of the country.
Additional district TB centres are to be established in all the thickly populated
districts. Twenty-five per cent of PHIs are yet to be brought under the ambit of
the DTP.
8.
In many of the district TB centres, trained key personnel and vehicles are
not available throughout the year. This is a serious drawback since they are
absolutely essential for the proper implementation and supervision of the
programme.
9.
Ina good number of districts in some of the States either there are no TB
bed or if there are, the number is less than ten.
10. In about 30 per cent of the PHCs either no NTI trained lab technician has
been posted or if posted, the lone technician is overburdened with work like
malaria work, etc. and findslittie time for sputum slide examinations.
11. The potentialities of the MPWs in case finding and case holding activities
of the programme have not been fully exploited.
12. Great difficulties are often encountered in the case finding programme
due to non-availability of essential materials and equipment like microscopes,
glass slides, chemicals, etc. at the peripheral levels.
13. The potential of the case holding activities of the sub-centres that have
sufficient staff and storage facilities for drugs, are not being fully exploited.
14.
Poor development of health education activities on Tuberculosis.
Present Trends of Tuberculosis in India
In the opinion of many experienced clinicians in the country, the Tuberculosis
disease has undergone a considerable change in its clinical presentation,
specially over the last quarter of the century.
Many retrospective studies (TAI, 1958, 1968), despite their scientific
weakness, have clearly brought out the gradual change in profile from a
29
I
i
prevalence of more acute and extensive disease among the young to a more
chronic, or a less severe disease among the elderly people. The near
consensus of these reports has been on a marked decrease of concomitant
complications of pulmonary Tuberculosis as, for example, Enteritis, Laryngitis,
Amyloid diseases, matted lymph glands with discharging sinuses, etc. It is very
significant that very similar changes were noticed in countries where
.Tuberculosis has definitely declined.
TB programmes
programmes l..lakhs.
Since continued motivation and education of the imasses in various
aspects of the case finding, treatment and prevents acttes under the
programme is necessary to enlist their cooperation, an mtens^ , heath
education campaign must be carried out and the necessary publicity material
i
brought out periodically.
Available epidemiological information signifies no change in the
prevalence of bacillary Tuberculosis in the country, at least during the last
three decades and that equal prevalence in urban and rural areas means that
we are truly in the endemic phase of the disease and that there is a gradual but
slow natural decline of Tuberculosis in the country. The reason for the slow
and natural decline of Tuberculosis in the country, is probably the continued
poverty, malnutrition, overcrowding, etc.
Mortality Trend
Tuberculosis is not a notifiable disease and the exact cause of death in each
case cannot be ascertained. As such, it is not possible to spell out the exact
As already stated, the epidemiology indicates that TB situation is almost
constant in India, and, if at all, shows a very slow downward trend. The
downward trend is evidenced by the apparent shift in the age of first infection
during the later decades of life and a gradual reduction in the incidence of the
childhood form of Tuberculosis resulting from the first infection. Indications are
also available that where the programme is functioning well, the problem, of
Tuberculosis in the community does show a downward trend.
■
SUMMARY
About 50 per cent of the people in our country are already infected with TB
germs, and about 1.5 per cent of the people above five years o. aget are
suffering from radiologically active pulmonary Tuberculosis, of these 0.4 pe
cent are infectious. The mortality rate has come down from 80 to 100 per
100.000 population to 53 and 40 per 100,000 population in Bangalore add
Delhi respectively where the programme is working satisfactorily. As 80 pe
cent of the people in our country are living in the rual areas; the Tuberculosis
Prospects of TB Control in India
The present epidemic in India might have started in the 17th century and there
is evidence to indicate that the epidemic has been declining since the turn of
the 20th century. All available knowledge about the epidemiology indicates
that the Tuberculosis situation is almost constant in our country and, if at all,
shows a very slow downward decline.
At present, when the case finding activity is functioning at about 35 per
cent of the potential, and treatment efficacy is about 65 per cent, it can be
shown that per unit of investment in resources, improvement in case finding
would give higher dividends than the improvement in the treatment activities.
The District TB Programme, even at the present level of efficacy, has the
potential of enhancing the natural decline. Improved programme efficiency,
specially under case finding, is likely to produce a quicker decline. Rapid
socio-economic development and improved standards of living would lead to
a more spectacular decline in Tuberculosis, but that would not fall strictly
within the ambit of the control programme.
number of deaths due to TB.
In a longitudinal study conducted by the NTI, Bangalore, in the Bangalore
district, where no anti-TB services were conducted, the mortality ratei during
the period 1961 to 1968 was found to be 80 to 100 per lakh population, ha
been found recently that the mortality rate has come down where
e
programme is functioning satisfactorily. As per the recent. studies ccindiic ed
bv the NTI Bangalore, and the New Delhi TB Centre in their field a e ,
mortality rates were found to be 53 and 40 per lakh population respectively.
I
I
I
problem in this country is really a rural one.
The National Tuberculosis Programme, as envisaged by the National
Tuberculosis Institute, Bangalore, has been functioning since 1962, and is a
permanent country-wide programme, integrated with the general health
services. It is based on epidemiological, sociological and economical
conditions prevailing in the country. The objectives of the programme are to
diagnose, treat and give preventive services to the bulk of the TB patients and
to the community, nearest to their homes with a view to meet their felt needs
and also to reduce their suffering and prevent disability and death, with the
ultimate objective of reducing the problem to such an extent that it ceases to
be a public health problem.
Under the programme, a District TB Programme, is being implemented in
every district of the country in association with all the existing general hea
institutions of the district. Emphasis has been laid mainly on microscopic
TB Programme for Urban Areas
The DTP was planned mainly with rural India in mind. However, the problems
of metropolitan and other large cities with a population of over 5 lakhs are
different and the DTP would not be able to serve the cities effectively. It is,
therefore, imperative to have different programme for these cities. Such city
31
30
1;
I
examination of sputum. Radiological examinations are restricted for patients
whose sputum is repeatedly negative. Patients are treated primarily on
domicihary basis with the five regimens of conventional anti-TB drugs. To cut
s on the duration of the treatment, shod course chemotherapy drug regimens
have recently been introduced, or are going to be introduced, in 194 districts of
the country by 1988-89. By the end of the VII th Plan period, most districts will
have been covered with these regimens. BCG vaccination is given only to
“i" “
The involvement of the general practitioners and voluntary organisations,
. and community participation in the programme is a MUST for the development
of the programme. A health education campaign in the community should
develop along with the proper functioning of our health and medical
institutions. Rapid socio-economic developments and improved standards of
living could.lead to a more spectacular decline in Tuberculosis.
At present, our country is truly in the endemic phase of the disease and
there is a gradual and slow natural decline of Tuberculosis.
un‘,“ “
Multipurpose workers/village health guides are being involved in case
finding and case holding activities. The drug delivery system is beino
expanded to the farthest corners of the districts by involving the sub-centres
Much stress has been laid on the health education activities. The programme
is evaluated al various levels regularly.
y
Since independence, considerable improvements in anti-TB measures
h^e„K.een n0!LCe^. The maior districts of the counlry have a^ady been
an non to0D'stricl Tubeteulosis Programme. About 300 TB clinics a6d
46 000 TB beds are functioning, and about 76 per cent of the implementable
run t H6 ?ee.rTn0U9h' Under the DTP' Aboul 4600 keV Personnel required to
run the district TB centres have been trained.
H
I..
REFERENCES
ce
The detection of new TB cases has more than doubled and the sputum
examination dl new cases in rural areas has increased considerabJy during
he last few yearsXonsiderable augmentation of funds to the programme as
e Centre s share has been made during the Vlth and Vllth Plan periods.
But in spite of extension of facilities and augmentation of funds the
progress has not been as expected.
I
i
!
n fT?^CaSe findin9 e^icier»cy of the District TB Programme is about 35 per
cent of the potential. Studies conducted at the National Tuberculosis Institute
Bangalore, revealed that 82 per cent of the sputum positive cases can be
diagnosed by examining the sputum twice. If the medical/paramedical
personnel including the multipurpose workers are trained properly effective
supervision of their working is provided, additional laboratory technicians are
posted wherever required and if a static miniature radiography equipment is
considerably '
h0SpitalS'the case f'ndin9 activi>ies would improve
Similarly, the case holding efficiency of the programme is about 30 per
cent of the expectation. The condition can improve considerably, if the
medical/paramedical personnel of the health institutions and also multi
purpose health workers are actively involved in repeated motivation of
patients their families and communities to take regular treatment for the
krtrodueZd Pe^d' The Sh°rl C°UrSe chemolheraPy regimens already
introduced in the programme, are likely to reduce the defaulter rate
considerably.
32
1.
Salient Recommendations of the Task Force under ICMR on NTP-Mid-term
Appraisal.
2.
NATIONAL TUBERCULOSIS INSTITUTE (1988) Salient Suggestions/Recommendations lor Implementation by the State/Union Territory Authorities
made in the Seminar. 5’h and 6th January, Bangalore. National Tuberculosis
Institute.
3.
BAILY (1974) Operational Study on Conversion Rate of Sputum with Anti-TB
Drug Regimens.
4.
NATIONAL TUBERCULOSIS INSTITUTE Mortality Rate due to TB Longitudinal
Study. Bangalore. National Tuberculosis Institute.
5.
BMRC & ROSENTHAL etal. (1972) Controlled Clinical Trials on ProtectiveValue
of BCG.
6.
NAGPAL, D.R. (1978) TB in India - A Perspective. IM^ Jr.
l,j'y 16^
BAILY (1983) TB Control of India - Current Problems and Possible Solutions. Ind.
Jr. T.B. XXX(2). Nov. 2. April.
(
8.
MINISTRY OF HEALTH AND FAMILY WELFARE (1987) Guidelines lor
Introduction of SCC Regimens in DTP. Ministry of Health and Family Welfare.
July.
9.
BAILY (1976) Operational Study on the Conversion Rate by Standard
Chemotherapy. Bangalore, National Tuberculosis Institute.
10.
ANEJA & SAMMUEL, RUPENT (1982) Organisational Effort on a Clinical Trial
and its Relevance to Applicability of SCC in NTP. Ind. Jr. TBMAX (1). January.
11.
ANEJA (1982) Chemotherapy in NTP. Newsletter 19(58). Bangalore. National
Tuberculosis Institute.
12.
ANEJA SCC-Retrospect and Prospect.
13.
BAILY & JAGATA (1985) Chemotherapy of TB. Newsletter 21 (3): 64,
Bangalore, National Tuberculosis Institute.
14.
Presidential Address in 41s! National Conference on TB and Chest Diseases 1986.
33
15.
DIRECTORATE GENERAL OF HEALTH SERVICES (1987) Circular on
Guidelines for Introduction of SCC in DTP. July 7. Directorate General of Health
. .
Results of Relapse - Retrospective 5 years with SCC for 6 months and with
Standard Regimens for 18 months. American Review on Respiratory
Diseases. 1977. 116.
17.
BMRC (1977) Trial on BCG and Vole Vaccination in the Prevention of TB in
Adolescents and Early Adults Life. B.M. Jr. 2.
18.
NATIONAL TUBERCULOSIS INSTITUTE Efficacy of two Standard Drug
Regimens under Programme Conditions. Bangalore, National Tuberculosis
Institute.
19.
I
NATIONAL TUBERCULOSIS INSTITUTE Operational Study on DTP. Bangalore,
National Tuberculosis Institute.
(0
i
I
j
i
i
!
I
I
r
€®
Afscciariofl
-■a r
ri. '■ ■
V? '-- r
Aiea, ^>'?J
• •■ fe; •' • >
I
I
I
As an Apex Technical Institute of its own kind in the country, the
NIHFW has been actively engaged in the promotion of health and
family welfare programmes through education, training, research,
evaluation and advisory-consultancy and other specialised services.
In order to achieve these objectives, the NIHFW, apart from,
regular M.D. Courses in Community Health Administration, also
conducts 30-35 in-service training courses/workshops and seminars
every year, which are attended by a variety of personnel ranging from
high-ranking policy making officials and key trainers to the grassrdot
level workers.
Other activities of cardinal Importance are research and
evaluation in the field of health and family welfare. NIHFW conducts
various research and evakuation studies at its own or in collaboration
with other national and international agencies. The results of these
studies are fed to the programme planners, administrators and
managers.
J.
NIHFW also provides advisory and consultancy services to the
Ministry of Health and Family Welfare, to the States, voluntary
organisations and international agencies in matters related to health
and family welfare.
The Institute provides specialised service’
a part of its
education, training and research activities. These include clinical
services, documentation, publication, audio-visual services and d'
processing services.
pen. r--n
1 Cc-mf
. I
■
NATIONAL INSTITUTE OF HEALTH AND FAMILY WELFARE
(NIHFW) came into existence on 9th March, 1977, after |4he
Government of India, realising the commonality of objectives of^the
two former institutions - National Institute of Health Administration
and Education (NIHAE) and National Institute of Family Planning
(NIFP) - and in pursuance of its policy to integrate health and family
planning services, decided to merge these two institutions into an
Apex Technical Inst-iiuticn.
Services.
16.
• ■
i
111.*
5 r - a.
O'
I
34
!
I
e»
SERIOUS IMPLICATIONS OF THE WORLD BANK'S REVISED
NATIONAL TUBERCULOSIS CONTROL PROGRAMME
FOR INDIA
(A POSITION PAPER FOR DISCUSSIONS AMONG CONCERNED SCHOLARS OF THE
COUNTRY. THE AUTHOR WELCOMES COMMENTS AND CRITICISM )
DEBABAR BANERJI
PROFESSOR EMERITUS
JAWAHARLAL NEHRU UNIVERSITY
i
i
NUCLUES FOR HEALTH POLICIES AND PROGRAMMES
B-43 PANCHSHEEL ENCLAVE, NEW DELHI -110017
TEL. 646 2S51
Cornniisioned by
Voluntary Health Association of India
40. Institutional Area, South of III
Ne^ Delhi - 110 016
I
i
I
SERIOUS IMPLICATIONS OF THE WORLD BANK'S REVISED
NATIONAL TUBERCULOSIS CONTROL PROGRAMME FOR INDIA
(A POSITION PAPER FOR DISCUSSIONS AMONG CONCERNED
SCHOLARS OF THE COUNTRY. THE AUTHOR WELCOMES COMMENTS
AND CRITICISM)
DEBABAR BANERJI
PROFESSOR EMERITUS
JAWAHARLAL NEHRU UNIVERSITY
NUCLEUS FOR HEALTH POLICIES AND PROGRAMMES
B—43 PANCHSHEEL ENCLAVE, NEW DELHI-110017
TEL. 646 2851
1
CHAPTER 1
AN OVERVIEW
The proposal of the World Bank for what they call ’’Revised
National Tuberculosis Control Programme” (RNTCP) for India is
going to have very damaging consequences for development of the
health services of the country, as it suffers
from serious
infirmities. The Voluntary Health Association of India and the
Nucleus for Health Policies and Programmes have got together to
produce this document, which contains a scientific analysis of
the RNTPC to draw attention to its infirmities and to formulate
an alternative proposal for strengthening the National
Tuberculosis Programme (NTP) of India. While the RNTCP will be
analysed in detail at a later stage, it will be worthwhile here
to note that the infirmities belong to three categories. The most
important among them is that the RNTCP has been developed without
paying adequate attention to the process of formulation of the
NTP and the factors which have come in the way of its
implementation over the more than three decades since it was
adopted by the Government of India. Secondly, in considering the
an
of
conceptualisation
of
the RNTCP as
an
outcome
interdisciplinary study, adopting a systems approach, there are
very serious flaws in project formulation in terms of system
analyses,
optimisation,
epidemiological and sociological
coverage f
managerial
and
technological
perspectives,
epidemiological impact, repayment of the World Bank loan,
replicability of the RNTCP, and other such considerations.
Thirdly, the World Bank promoted RNTCP is a part of the sequence
of what are termed as "International Initiatives" thrust on the
country from outside at the instance of international agencies,
backed up by strong support from many powerful western countries,
which make substantial contributions to the budgets of the
former. Ironically, as will be demonstrated later on, it is these
international initiatives which have been proved to be the major
hurdles in the way of implementation of the NTP all these years.
The RNTCP
thus appears as a not well thought out operation
performed by persons from the very same group who, in the first
place, have been responsible for the damage done to the NTP.
Even from this very broad mention of the RNTCP it is possible to
discern an underlying deep streak of dogmatism among the
exponents of the RNTCP, which has impelled them to 'forget' the
enormous and very substantial public health research in
tuberculosis conducted within the country and put enormous
pressure on the national
authorities to submit to 'models'
developed by them outside the country. Apart from very serious
conceptual flaws, these western models are technocentric, imposed
on the people from above and make the country dependent on
assistance
from
outside.
'Forgetting'
ideas
developed
indigenously has thus become almost a prerequisite for taking
international initiative in health fields; the fields gets closed
to scientific discussions and only those 'natives' who do not do
question them, or are incapable of doing so, are allowed entry
into the privileged group by the international syndicate.
Soon
after the poor countries of the world
had dared to make a
declaration of self-reliance in health in the Alma-Ata
Declaration of 1978 (WHO 1978), the affluent countries 'invented'
what they called ’’Selective Primary Health Care"
Care” (Walshe and
Warren 1979) , which was almost immediately followed by the
unleashing of a series of international initiatives in health,
This provides a frightening example of the extent to which the
more affluent countries of the world are prepared to go in
imposing their will on the countries that are economically and
politically dependent on them. Significantly, there has been
little protest from the concerned community of public health
scholars even in the affluent countries to such brazen forms of
manipulation of science to impose programmes on 'defenceless'
countries, from outside. The World Bank backed RNTCP is a
particularly unfortunate example of imposition of such
international initiatives.
The drive towards globalisation of the economy and polity has
made the poor countries even more vulnerable to manipulation by
the rich countries. In the so-called global village, the poor
countries are condemned to serve as bonded hirelings of the rich
kulaks and cowboys. A 'dialectical' outcome of this form of
international relations is for the oppressed peoples to make
conscious efforts to prevent the dominant powers to 'forget'
their historical heritage. To adapt a quotation from Milan
Kundera, it becomes a struggle between memory and forgetfulness.
Just as ahistoricity becomes an important weapon in the hands of
those who would fight to continue to monopolise the control over
the bulk of the resources of the world, breaking into their
consciousness to 'remind' them about the history they try to
forget becomes a weapon in the hands of the oppressed to fight
oppression.
At a time when a concerted effort is being made by World Bank
officials to promote RNTCP in this country, this document may be
considered as a modest effort to 'remind' them as well as the
concerned authorities in the country about the very significant
work that has been done in India to deal with tuberculosis as a
Zl~
public health problem. No apologies will be offered here for
consciously taking the side of the people by bringing out well
researched data which had formed the basis of the NTP some three
and a half decades ago. A very deliberate effort is made here to
describe the work rather extensively. The 'battle lines' are
clear: on one side are the indigenous research efforts made to
formulate a nationally applicable, socially acceptable and
epidemiologically effective tuberculosis programme, and on the
other side is a 'foreign inspired', prepackaged programme that is
sought to be thrust on the country by powerful countries and
international organisations.
./
CHAPTER 7
CONCLUSIONS AND AN ALTERNATIVE FFAJ4EWORK FOR ACTION
The above account shows how a well researched and reasonably
simple and straight forward programme can get hopelessly
confounded due to interplay of a variety of social, political and
economic forces. NTP essentially involved offering diagnosis and
treatment to the very substantial portion of tuberculosis
patients who were actively seeking treatment in various health
institutions, both in rural and urban areas.
These institutions
were offered a referral support system which extended right up to
the super-specialists in post-graduate teaching hospitals. State
Tuberculosis Centres and NTI and other tuberculosis research and
teaching institutes were meant to provide support to the
programme in the form of training, monitoring, evaluation and
operational research.
But as pointed out by Halfdan Mahler, 'even the simplest
technology, if it is not properly deployed and utilised by the
infrastructure,
just will
not move,
will
not control
tuberculosis, will not meet people's felt-needs.'
This is what
has befallen on NTP.
The infrastructure has been grievously
damaged because of sharp decline in the quality of public health
practice and research,
filling up of key public health posts by
the persons who do not have technical competence, by imposition
of target oriented specialised programmes on an already weak
infrastructure and a correspondingly sharp fall in the quality of
administrators and research personnel in the field of
tuberculosis.
From the basic premises presented
suggestions are being made below:
above t
some
important
1.
While tuberculosis workers cannot take on themselves the
onerous task of rejuvenating the moribund health and family
planning services systems, the crisis has become so profound
that there are good chances that the political leaders will
have to wake up to it.
A detailed
programme for
rejuvenation of the health services is given in the author's
B.C.Dasgupta Oration of the Indian Public Health Association
in 1988 (Banerji 1988b; 1984b).
Some important components
are:
a.
Building up a critical mass of public health workers in the
fields of education, training, research and practice.
1
b.
Restructuring the cadre structure to place competent public
health specialists in key public health positions.
c.
Concurrent removal of the square pegs in the round holes of
the system.
d.
Making "conditional” integration of the special target
oriented
family
planning
and
other
programmes
’'unconditional”.
This will lead to according much higher
priority to NTP as the problem is responsible for a
substantial part of the total suffering caused by health
problems as a whole.
2.
Tuberculosis workers can help in the process of rejuvenation
of the health and family planning service systems by
insisting that this process is critical for providing good
tuberculosis services to be suffering masses of the country.
3.
On its own, even considering the constraints of the general
health services as given, there is still considerable scope
for improving the NTP system through use of operational
research and systems analysis.
The Surajkund Conclave
recommendations can serve as a starting point.
4.
The very improvement in the NTP system might stimulate
improvement in the wider health and family planning services
systems, by providing an example.
5.
NTI can be rejuvenated by bringing together a competent
interdisciplinary team of workers, so that it can play a
role in strengthening the NTP.
It can even extend its
activities to serve as one of the many institutions which
would be necessary to strengthen the general health
services.
6.
Concurrently, competent tuberculosis workers are placed as
heads of tuberculosis wings of the central and state health
services.
7.
Other tuberculosis institutions, such as TRC, should be
tuned to serve the NTP, i.e., the problems they deal with
must emerge from the field situation, and not the other way
round, as is often the case at present.
8.
The idea of Task Force (Editorial 1990), or a similar set up
(Fox 1990), which is vested with power and resources to act
as a watchdog for the implementation of NTP, very well
blends with the other suggestions for improving NTP given
here.
2
*
9.
Again, there is considerable scope for optimising the urban
components of the NTP.
10.
Tuberculosis Association of India and its branches can be
revamped to perform a complementary role in strengthening of
NTP - e.g., conducting independent evaluation, offering
technical assistance,
providing logistical
support,
providing training, and so forth.
In sum, the suggestion is that we take steps to unleash the
social forces which ensure that simple and efficacious technology
developed in India is made accessible to the hundreds of
thousands of sputum positive cases, who are actively seeking
relief for suffering but who are still being thrown out of the
health institutions with a bottle of useless cough mixture.
Sociologically, it is contended that the very meeting of the felt
need generates more needs, and, if that does not happen, active
educational steps are taken to generate more needs to reach a
level when it starts having an epidemiological impact.
This
epidemiological impact will occur in consonance with the impact
that might occur as a result of changes in the natural history of
tuberculosis in India.
3
1
Dr. K.K. Datta
Dy. Director (TB Control)
Min. of Health & Family Welfare.
' 'ojOv's SPT
TB CONTROL PROQRAMME IN INDIA
BY DR.K.K.DATTA
!
The National TB Control Programme has been in operation in
India since 1962.
India was among the pioneers in discovering
and testing the efficacy of ambulatory treatment which obviated
the requirement of prolonged hospitalisation in most TB cases.
Treatment through prolonged stay in sanatoria of the 40s was
replaced by domiciliary management of cases for a period of 18
months or so.
This has been replaced by a technical break
through in the nature of short course multi-drug therapy consist
ing of INH, Rifampicin, Pyrazinamide and Etharzbutol.
The Short
Course Chemotherapy was incorporated into the programme in 1982,
for a limited number of cases.
India is a very large country with a current estimated
population of around 900 million. It has 32 provinces and 459
districts.
A district has an average population of 1.7 million
(Annex
1) •
f
The organization structure of the programme consists of (i)
390 District TB Centres having the composite function of case
detection through clinical examination of symptomatics, sputum
and x-ray examinations, case management and follow-up, epidemio
logical services including monitoring, supervision and reporting;
(ii) 330 TB clinics with diagnostic and case management services,
in the urban areas.
47,300 TB beds are also available for
treatment of seriously ill TB cases (Annex - 2) .
TB case detec
tion and management services are also available in general health
facilities like general hospitals. Medical College hospitals,
etc.
In India a large number of medical professionals are work
ing in the private Sector (hospitals, clinics etc) and it is
estimated that an almost similar number of TB cases as under the
NTP seek treatment in the private sector. However they are not
notified.
It is also important to note that the infrastructure
for TB was more organised and efficient in terms of domiciliary
management in rural areas compared to urban areas.
In many
municipalities the infrastructure for TB is very inadequate and
poor.
o
(?)
In India the population has been growing at the rate of over
2% per annum and the urban population has grown from around
17.97% in 1961 to 25.73% in 1991.
The number of new TB cases
detected per 1000 population under the NTP has increased from
1.13/1000 in 1981 to 1.80/1000 in 1991. However, the rate of new
smear positive TB cases recorded no increase or only a marginal
increase was seen (Annexure - 3) .
It clearly indicates that the
1
NATIONAL CONSULTATION ON TUBERCULOSIS
ORGANISED BY VHAI
programme did not function as efficiently as expected.
It may be
stated here that the supervised Short Course Chemotherapy is
available in 253 districts.
It has a very low coverage because
of non availability^of adequate quantum of drugs.
It is also
clear that though the existing
National TB Control Programme
laid an emphasis to detect more number of TB cases but the rate
of smear positive case detection is very low (less than 25% of
the diagnosed of TB are one smear positive).
This is due to
continued over reliance on x-ray diagnosis.
In fact often cases
are diagnosed on clinical and x-ray investigations and put on
treatment without sputum examinations being done.
Case holding is very poor, with only about one quarter of
the cases notified completing the course of therapy.
Therefore
the existing National TB Control Programme strategy has been
revised with the objective of achieving a high cure rate (85%)
and treating at least 100 sputum positive patients per 100,006
population thereby reducing morbidity and mortality and cutting
down
j
- the transmission.
----------------------j-t £s eXpected that about 100 smear
positive cases per 100,000 will be detected of which about two
thirds will be new and the rest will be relapses. failure etc.
The broad strategy of the revised NTP are:
(Annex 4
5)
1.
To change the current emphasis on radiological diagnosis to
sputum microscopy diagnosis.
2.
To treat with SCC, directly supervised in the intensive
phase, all sputum positive and seriously ill sputum negative
cases, and to involve the
peripheral health functionary in
supervised treatment administration .
3.
To make available all categories of anti-TB drugs in appropriate multi-drug blister packs, uninterrupted to all peripheral points.
4.
To strengthen the capability of DTC and State TB Centres for
effective implementation, monitoring and evaluation of the
programme including cohort analysis.
5.
To augment and improve the training capabilities both at the
national and state level
6.
Professionally managed IEC campaign.
7.
Operational Research.
2
l
The revised strategy is in line with the
recommendations
made by WHO.
The Government of India is also committed to main
tain the strengthened revised National TB Control Programme as a
permanent health system activity integrated into the existing
health
structure with strong leadership from a central unit.
The Governments commitment is evident from enhanced central plan
budgetary allocation from 150 million Indian rupees per annum 3
years ago to 460 million Indian rupees during the current finan
cial year.
Annual risk of infection (Annex - 6)
The intensity of disease transmission in the community is
best reflected by the annual risk of infection which represents
the probability of a previously uninfected individual becoming
infected with TB during a one year period.
J
The estimated risk of infection ranges from 0.6 to 2.3%.
Epidemiological interpretation is difficult because of the varia
ble methods used in various studies.
However there is’ no evi
dence of a substantial decrease in the risk of infection over the
last 30 years.
The stagnant situation has been further corrobo
rated with 2 recent studies in the rural areas of South India.
One shows that the risk of infection has decreased from 1% in
1961 to 0.61-s in 1985.
The other did not show any change in the
risk of infection between 1969 to 1984 (risk of infection 1.7% in
both years).
This result is considered consistent with a poorly
functioning control programme leading to creation of chronic
cases and drug resistance.
In fact in clinical practice chronic
cases are often seen and resistance in tuberculosis is also
becoming a matter of concern.
Only a few laboratories are con
ducting drug sensitivity testing for TB in India.
Although data
on drug resistance is scarce & resistance is not systematically
monitored, available information (Annex - 7 & 8) is a cause for -r/-.
concern.
The very high rate of secondary resistance to both
Rifampicin and Isoniazid is particularly very serious, with long
term implications as these patients will transmit incurable form
of Tuberculosis in the community.
Because most adults were infected in their youth, a sma 11
decrease in RI would not have any rapid impact on the prevalence
of infection in the adult population.
It is safe to estimate
that at least 50% of the population above the age of 20 years is
infected and will remain at risk of disease and death from tuber
culosis for their lifetime.
A conservative estimate is that,
currently, the RI for India is 1.7 to 2%.
3
Notifications
Registration under the National Tuberculosis Control Pro
gramme highlights the problem of increasing over diagnosis of
smear negative and under diagnosis of smear positive cases.
During the period from 1980 to 1991, the number of District TB
Centres increased from 320 to 387.
However the trend reflects
(Annex 9)
an
9) an increased proportion of cases not confirmed by
smear examination,
The proportion of smear positive cases has
decreased from 25% in 1980 to about 20% in the late 80s.
lapses, failures, partially treated patients are often inappropriately included in these notifications.
Current TB rates
As per NTI estimates of 1974, about 8,70,000 new smear
positive TB cases have occured in 1992.
This number is very
similar to the 850000 estimated on the basis of incidence rate
from the Tuberculosis prevention trial undertaken by TRC Madras.
If the current average annual risk of infection is 1^7%, 1.6
million new TB cases occur annually of which 7,10,000 are smear
positive.
About l/3rd of the total Tuberculosis burden is borne
by the urban conglomeration (Annex - 10).
Age and Sex Distribution
The majority of tuberculosis cases in India occur below the
age of 45 years, with about 75% of the diagnosed cases between
15 and 44 years old.
Age-specific estimates of incidence during
1974 applied to the 1992 population, suggest that about 58% of
all cases today occur between 15 and 44 years old. Two thirds of
the cases are estimated to occur among males but tuberculosis
takes a proportionally larger toll on young females than among
young males.
More than 50% of female cases occur before age 34.
Mortality
Total mortality due to TB is uncertain but by any estimate
it poses a huge economic burden for India.
TB mortality is
estimated to be 420000 deaths every year (50/100000 population).
Cumulative mortality during the decade to the year 2000 will
probably exceed 3.5 million deaths, an enormous burden for the
society.
A large share of these premature deaths can be avoided
with a we 11-functioning programme.
Given the ages at which
deaths from tuberculosis are now occurring and the low costs for
tuberculosis programme inputs in India, it is probable that the
discounted cost per healthy year of life gained as a result of a
4
i
well-functioning tuberculosis control programme will be well
under $ US 10, making tuberculosis control one of the highest
priority interventions for the State and Central Governments.
HIV & Tuberculosis
HIV was first reported in Indian in 1986.
There is no
significant evidence yet available indicating its likely impact
on the TB situation in India.
As a large proportion of Indian
population (50% of the adult population) is already infected with
tuberculosis, it is most likely that with the spread of HIV, the
epidemiological situation of tuberculosis will detoriate.
Limit
ed data indicate that sero-positivity for HIV among TB patients
is much higher than that of the rest of the general population.
Upto the end of 1993 of the 559 AIDS patients 331 (60%) had
evidence of active tuberculosis.
As per the National AIDS Con
trol Programme currently there are about 0.75 million persons
infected with HIV.
Assuming half of these people are infected
with tuberculosis and that the break down rate from TB infection
to disease among dually infected individual is 10% per year, more
than 35000 HIV related TB cases are likely to occur annually.
With the spread of HIV renewed concern for tuberculosis made
authorities to look into the implementation of the programme
critically and the programme was nationally reviewed through a
group of national and international experts.
Some of the obser
vations of the review committee are (Annex - 11):
1.
Inadequate budgetary outlays and shortage of drugs
2.
Undue emphasis on X-ray instead of sputum testing for diag
nosis .
3.
Poor guality of microscopy.
4.
Emphasis on detection of new cases instead of achievement of
cure.
5.
Poor organisational set-up and support for T.B.
6.
Lack of consensus among practitioners regarding treatment
regimens.
As a follow up measure the National Technical Management
Group was strengthened through induction of senior level experts
and a revised strategy was drafted.
5
Several core-trainers were trained in the implementation of
the revised NTP at the national and international level with the
support of WHO and a large number of professionals were trained
to implement the revised NTP on a pilot basis in 5 sites namely
Delhi, Bombay, Calcutta, Bangalore and Gujarat.
These pilot
projects are being implemented with SIDA support.
The results
are found to be very encouraging; smear conversion rate after
having 3 months of treatment was around 85%.
During the coming
one year more pilot sites are being included for the
implementation of the revised NTP with World Bank Project Prepa
ration Facility Advance.
It has been proposed that during this
year one district in each of the 5 states and 1 site in each of
the 10 metropolitan cities will be covered with the revised
National Tuberculosis Control Programme on a pilot basis with
World Bank assistance, with a total population around 14 million.
Operational components of the revised NTP
Some of the important operational components of the revised
NTP will be (Annex 12 - 13) :
(1)
To strengthen the sputum microscopy facilities so that
quality sputum microscopy is available as close to the
people as possible through training of Laboratory Techni
cians and expanding the network of laboratory facilities and
diagnosing Tuberculosis cases at least on 3 sputum smear
examination instead of only one as it is done now.
(2)
To involve the most peripheral 1health functionary in supervised drug administration of anti-TB drugjs during the intensive phase.
(3)
To make available anti-TB drugs uninterrupted to all the
peripheral health facilities in multi-drug blister packs.
(4)
To create supervisory team at the sub-district level (0.5
million population) to improve the quality of supervision,
monitoring and evaluation.
(5)
To decentralise District
sub-district level.
(6)
To strengthen the epidemiological capability in cohort
analysis etc through proper training and strengthening of
the infrastructure.
(7)
To augment operational research activities to improve
programme implementation.
TB cases registration
6
at
the
the
(8)
To augment training facilities both at the National and
State level through expansion of the existing infrastrucfvture.
(9)
To establish professionally designed IEC activities to
support the implementation of the programme.
The initial results available from the pilot sites indicate
high sputum conversion rate around 85% and it appears that it
will be possible to achieve high cure rate through revised
strategy.
Under the revised strategy it is envisaged that the
new sputum positive cases and seriously ill sputum negative cases
will be on 4 anti-TB drugs nemely INH, rifampicin, pyrazinamide
and ethambutol for a period of 2 months and then during the
continuation phase of 4 months they will be given INH and Rifam
picin.
All the drugs will be administered 3 days in a week.
All
cases of sputum positive relapses, failures etc. will be given
the above mentioned 4 anti-TB drugs for a period of 3 months.
In
addition injection streptomycin will also be given.
During the
continuation phase these patients will receive 3 anti-TB drugs
nemely INH, Rifampicin and Ethambutol for a period of 5 months.
All the drugs will be administered 3 days in a week.
Sputum
negative less seriously ill cases will be either given standard
conventional chemotherapy for a period of 12 months with INH and
Ethambutol or INH and Thaicetazone or they may also be given if
resources are available 3 anti-TB drugs for a period of 2 months
like INH, Rifampicin and Pyrazinamide.
Subsequently they will
receive 2 drugs INH and Rifampicin for a period of 4 months.
Operational Research
Operational research activities are going to be augmented so
that the National Tuberculosis Control Programme gets appropriate
support for improving the efficiency of the implementation of the
programme.
Let me put on record the appreciation of our country for the
technical cooperation and guidance of WHO in implementing the
revised NTP on a pilot basis as well as the financial support of
the Government of Sweden.
Several operational studies to assist
in the formulation of the revised NTP and implementing the same
are under consideration.
Some of the operational studies which
are under progress and which are going to be initiated are
(Annex - 14):-
7
(1)
Studies on risk of infection in different parts of India.
(2)
Cohort analysis
(3)
Perception and attitude towards tuberculosis for profession
als and general population.
(4)
Revaluation of the reasons and level of delay in the diagno
sis of sputum positive pulmonary tuberculosis under pro
gramme conditions in South India.
(5)
Effectiveness of vi1lage-based health functionaries
improving treatment adherence of tuberculosis patients.
(6)
Minimising mis-diagnosis in smear negative Tuberculosis.
8
in
9
ANNEXURE
1
I
i
1
I
NATIONAL TUBERCULOSIS CONTROL PROGRAMME
IN INDIA
INDIA AT A GLANCE
POPULATION
(1991 CENSUS)
840 MILLION
PROVINCES
(INCLUDING UTS)
32
DISTRICTS
459
STANDARD DISTRICT
POPULATION
1.7 MILLION
I
annexure
national tuberculosis CONTROL PROGRAMME
IN INDIA
TUBERCULOSIS SERVICES
NO. OF DISTRICT TB
CENTRES
390
NO. OF TB CLINICS
330
NO. OF TB BEDS
47,300
NO. OF DISTRICTS
WITH S.C.C.
253
2
ANNEXURE
INDIA
YEAR
TUBERCULOSIS CONTROL PROGRAMME
RATE OF NEW TB CASES
DETECTED UNDER NTP
PER 1000 POPULATION
RATE OF SMEARS POSITIVE
TB CASES DETECTED UNDER
NTP PER 1000 POPULATION
1981
1.13
0.28
1982
1.32
0.31
1983
1.51
0.36
1984
1.52
0.36
1985
1.57
0.36
1986
1.68
0.37
1987
1.81
0.37
1988
1.85
0.37
1989
1.87
0.38
1990
1.84
0.38
1991
1.79
0.38
3
annexure
NATIONAL TUBERCULOSIS CONTROL PROGRAMME
IN INDIA
REVISED NTP
STRATEGY
1.
TO CHANGE THE CURRENT EMPHASIS ON
RADIOLOGICAL DIAGNOSIS TO SPUTUM
MICROSCOPIC DIAGNOSIS
2.
TO MAKE AVAILABLE DIRECTLY SUPERVISED
S.C.C. TO ALL SPUTUM POSITIVE AND
SERIOUSLY ILL SPUTUM NEGATIVE CASES
INVOLVING PERIPHERAL HEALTH FUNCTIONARY
3.
TO MAKE AVAILABLE ALL CATEGORIES OF
ANTI-TB DRUGS IN APPROPRIATE MULTIDRUG BLISTER PACKS, UNINTERRUPTED TO
ALL PERIPHERAL POINTS
1
4
1
ANNEXURE
NATIONAL TUBERCULOSIS CONTROL PROGRAMME
IN INDIA
REVISED NTP
STRATEGY
4.
TO STRENGTHEN EPIDEMIOLOGICAL CAPABILITY
OF DTC AND STATE TB CENTRES IN EFFECTIVE
IMPLEMENTATION/ MONITORING AND EVALUATION
INCLUDING COHORT ANALYSIS.
5.
PROFESSIONALLY MANAGED IEC CAMPAIGN
6.
OPERATIONAL RESEARCH
5
»
ANNEXURE -
national tuberculosis CONTROL PROGRAMME
IN INDIA
EPIDEMIOLOGICAL PICTURE
RISK OF INFECTION
PREVALENCE
OF
INFECTION
4.9%
9.6%
10.1%
10.4%
3.1%
9.0%
11.2%
6.7%
RI
YEAR
LOCATION
SOURCE
1.0%
1961
TUMKUR
NT I
2.0%
1969
TIRUVALLORE
TRC
2.1%
1983
BANGALORE
NT I
2.2%
1984
DHARMAPURI
NT I
0.6%
1985
BANGALORE
TRC
1.9%
1989
KADAMBATMUR
TRC
2.3%
1989
THIRUVELANGADU
TRC
1.4%
1989
NORTH ARCOT
TRC
ANNEXURE
NATIONAL TUBERCULOSIS CONTROL PROGRAMME
IN INDIA
DRUG RESISTANCE
DATA ON DRUG RESISTANCE SCARCE
RESISTANCE IS NOT SYSTEMATICALLY MONITORED
SOME STUDIES REVEAL THE FOLLOWING:
PRIMARY/INITIAL DRUG RESISTANCE
TYPE OF PATIENT
AND SAMPLE SIZE
S
% RESISTANCE TO
HR
RH
SRH
NEW CASES BY HISTORY
241
MADRAS
7.3
12.6
1.6
0.8
0.8
244
RAICHUR
11.0
19.1
3.2
2.0
1.2
324
DELHI
18.5
0.6
7
<
ANNEXURE
NATIONAL TUBERCULOSIS CONTROL PROGRAMME
IN INDIA
DRUG RESISTANCE
ACQUIRED DRUG RESISTANCE
TYPE OF PATIENT
AND SAMPLE SIZE
S
% RESISTANCE TO
HR
RH
SRH
PREVIOUSLY TREATED
37
MADRAS
35.0
62.0
13.5
5.4
8.1
111
RAICHUR
11.7
52.7
17.1
5.4
11.7
FAILURE
81
DELHI CENTRE
50.7
33.3
354
DELHI SUBURBS
78.8
61.5
560
NORTH ARGOT
30.0
65.0
16.0
Ind. J.Tub. Vol.39 No.2 pp 121-124.
WHO TB PrograMe Review - 19 9 2
6.0
9.0
8
ANNEXURE
Figure 1. India: Notifications of cases
of tuberculosis, 1980-1991
Thousands
1500 -
Sm«ar-po»itlv<
All pulmonary
1200 '
900 -
600
300
i________ j_________i________ i________ i________ i----------------1--------------- 1
O'—
1980 1981 1982 1983 1984 1985 1986 1987 1988 1989 1990 1991
Year
Extra-pulmonary casta art not raporttd
Sourca: NTU 1992
9
*
ANNEXURE
NATIONAL TUBERCULOSIS CONTROL PROGRAMME
IN INDIA
EPIDEMIOLOGICAL PICTURE
CURRENT A.R.I
NEW CASES
1.7%
(ALL FORMS)
- 1.6 MILLION PER YEAR
NEW SMEAR POSITIVE
CASES
- 0.71 MILLION PER YEAR
MORTALITY
- 0.42 MILLION PER YEAR
SOURCE: WHO REVIEW, 1992
1C
*
ANNEXURE
OBSERVATIONS OF THE REVIEW COMMITTEE
1.
INADEQUATE BUDGETARY OUTLAYS AND SHORTAGE
OF DRUGS
2.
UNDUE EMPHASIS ON X-RAY INSTEAD OF SPUTUM
TESTING FOR DIAGNOSIS
3.
POOR QUALITY OF MICROSCOPY
4.
EMPHASIS ON DETECTION OF NEW CASES INSTEAD
OF ACHIEVEMENT OF CURE
5.
POOR ORGANISATIONAL SET-UP AND SUPPORT FOR T.B.
6.
LACK OF CONSENSUS AMONG PRACTITIONERS REGARDING
TREATMENT REGIMENS
11
ANNEXURE
OPERATIONAL COMPONENTS OF THE REVISED NTP
1.
TO STRENGTHEN THE SPUTUM MICROSCOPY FACILITIES
SO THAT QUALITY SPUTUM MICROSCOPY IS AVAILABLE
AS CLOSE TO THE PEOPLE AS POSSIBLE THROUGH
TRAINING OF LABORATORY TECHNICIANS AND EXPAN
DING THE NETWORK OF LABORATORY FACILITIES AND
DIAGNOSING TUBERCULOSIS CASES AT LEAST ON 3
SPUTUM SMEAR EXAMINATION INSTEAD OF ONLY ONE
AS IT IS DONE NOW.
2.
TO INVOLVE THE MOST PERIPHERAL HEALTH FUNCTIO
NARY IN SUPERVISED DRUG ADMINISTRATION OF
ANTI-TH DRUGS DURING THE INTENSIVE PHASE.
3.
TO MAKE AVAILABLE ANTI-TB DRUGS UNINTERRUPTED
TO ALL THE PERIPHERAL HEALTH FACILITIES IN
MULTI-DRUG BLISTER PACKS.
4.
TO CREATE SUPERVISORY TEAM AT THE SUB-DISTRICT
LEVEL (0.5 MILLION POPULATION) TO IMPROVE THE
QUALITY OF SUPERVISION^ MONITORING AND EVALUA
TION.
12
ANNEXURE
>
OPERATIONAL COMPONENTS OF THE REVISED NTP
5.
TO DECENTRALISE DISTRICT TB CASES REGISTRATION
AT THE SUB-DISTRICT LEVEL.
6.
TO STRENGTHEN THE EPIDEMIOLOGICAL CAPABILITY
IN COHORT ANALYSIS ETC THROUGH PROPER TRAINING
AND STRENGTHENING OF THE INFRASTRUCTURE.
7.
TO AUGMENT OPERATIONAL RESEARCH ACTIVITIES TO
IMPROVE THE PROGRAMME IMPLEMENTATION
8.
TO AUGMENT TRAINING FACILITIES BOTH AT THE
NATIONAL AND STATE LEVEL THROUGH EXPANSION OF
THE EXISTING INFRASTRUCTURE.
9.
TO ESTABLISH PROFESSIONALLY DESIGNED IEC
ACTIVITIES TO SUPPORT THE IMPLEMENTATION
OF THE PROGRAMME.
13
■
ANNEXURE
OPERATIONAL RESEARCH
1.
STUDIES ON RISK OF INFECTION IN DIFFERENT
PARTS OF INDIA
2.
COHORT ANALYSIS
3. PERCEPTION AND ATTITUDE TOWARDS TUBERCULOSIS
FOR PROFESSIONALS AND GENERAL POPULATION.
4. REVALUATION OF THE REASONS AND LEVEL OF
DELAY IN THE DIAGNOSIS OF SPUTUM POSITIVE
PULMONARY TUBERCULOSIS UNDER PROGRAMME
CONDITIONS IN SOUTH INDIA.
5. EFFECTIVENESS OF VILLAGE-BASED HEALTH
FUNCTIONARIES IN IMPROVING TREATMENT
ADHERENCE OF TUBERCULOSIS PATIENTS.
6. MINIMISING MIS—DIAGNOSIS IN SMEAR NEGATIVE
TUBERCULOSIS
NATIONAL CONSULTATION ON TUBERCULOSIS
Venue
VHAI Conference Room.
PROGRAMME
13 July 1994
09.30
10.30 a.m.
Inauguration.
Mr.Alok Mukhopadhyay
Introduction of Objectives.
Dr.H.Sudarshan
Introduction of Participants.
10.30
10.45 a.m.
TEA
10.45
12.45 p.m.
Chairperson: Dr.Mira Shiva
National TB Control Programme.
Concept and bottlenecks.
Dr.B.T.Uke
Present status of TB in India
Revised National TB Control Programme
Dr.K.K.Datta
NTP- Past, Present and Future
Dr.D.Banerj ee
12.45
01.30 p.m.
LUNCH
01.30
02.30 p.m.
Chairperson: Dr.Thelma Narayanan
TB as part of Comprehensive Health Care
Dr.M.A.Seetha
Dr.Mukund Uplekar
Dr.Shavinder Singh
Dr.Narendra Gupta
TB in certain Occupations
Dr.J.R.Parikh
Mr.L.C.Tyagi
1
02.30
03.00 p.m.
Chairperson: Dr.P.K.Choudhari
General Practitioners in TB care.
Dr.S.N.Misra
Dr.Jagdish Sobti
Dr.Kalindi Thomas
Dr.Alfred Edwards
03.00
03.30 p.m.
Chairperson: Dr.M.A.Seetha
TB in Women and Children
Dr.Sarah Walters
Dr.Virender Singh
03.30 - 03.45 p.m.
03.45
05.00 p.m.
TEA
Chairperson: Dr.Anil P
Group Discussion:
Problems in TB care
2
14 July 1994
09.30
10.30 a.m.
Chairperson: Dr.Mukund Uplekar
TB and AIDS.
Dr.P.N.Sehgal
Dr.D.Banerjee
TB and Leprosy
Dr.Cornelius Walters
Dr.H.Sudarshan
10.30
10.45 a.m.
TEA
10.45
11.45 a.m.
Chairperson: Dr.H.Sudarshan
Drug therapy, Drug resistance
and Drug availability.
Dr.L.Suryanarayana
Dr.Mira Shiva
11.45
01.00 p.m.
Chairperson: Dr.S.P.Pamra
NGO experiences in TB care
Dr.H.Sudarshan
Dr.Prabir Chatterjee
Mr.Joseph Vazhakala
Mr.Sanjoy Ghosh
Dr.S.K.Singh
01.00
01.45 p.m.
LUNCH
01.45
03.00 p.m.
Chairperson: Dr.Mira Shiva
Group Discussion:
Solutions to Problems identified
03.00
04.00 p.m.
Chairperson:Dr.H.Sudarshan
Plan of action.
04.00
04.15 p.m.
TEA
04.15
05.30 p.m.
Valedictory session.
Dr.D.Banerjee
Dr.K.K.Datta
Dr.B.T.Uke
Dr.H.Sudarshan
Dr.Mira Shiva
Vote of Thanks
Dr.Anil P
*******
3
I
Name of the Paper
published at
:
MID-DAY
;
NEW DELHI
7 MpV ^4
I
Dated
Dm shortage adds to TB patients ' woes
: MIDWAY
DAY CORRESPONDENT
IW DELHI, May 17
However. organisms
ornanifimR and
and their
thoJr progeny
nrr»nonv to
tr» rero.
nddc the
the director. The patients disTB and Allied Diseases. However,
adds
Dr KK Datta, project manager of the main viable and multiply In the pres- continue the drug intake as soon as
National Tuberculosis Control ence of a concentration of the drug, they get well despite Instructions
ne shortage of essential drugs
Programme maintains that this prob that would normally destroy or In- from the doctors. Due to the prema
. e city hospitals has compounded
lem is not of much concern for TB is hibit the growth of these cells.
ture discontinuance of the medlCapital’s deteriorating tubercustill curable.
Following this drug failure the cines, the disease manifests Itself
problem. However the patients ’
In a recent study made by the second line of drugs like again within two years, explained
m to have found a new way of New Delhi TB Clinic Centre, the
----— ww.mw,
Kananmycln, Capreomycln ,
the
the director.
director. The
The chemotherapy
chemotherapy
Ijusting to this menace — by prevalence of acquired resistance Viomycin Amikacin, Cycloserine,
varies from six months to a year and
Mveloping drug resistance!
was found to be 50 per cent for Iso Ethionamide, Prothlonamltde are
varies
variesfrom
from individual
Individualto
toindividual
Individual
wording
Nicotonic
Addhydrazide
and- —
33 per prescribed which are more costly depending on the severity of
,
~ to health experts,
. ■
.’ fre,
.? A
v J—.J------nt shortage ofTB drugs in the
cent for Rifampdn, the first line of and
less
effective,
and
have
side
the
disease
caused
by
and less effective, and have side the disease caused by the
the bacbacdinics
chestdimes,
dinics, have drugs given to tuberculosis patients, effects, says Dr RC Jain, director of teria, MycobacteriumTubercu.;!tiics andchest
edpatients to developa resis- However, more cases of drug resis- the hospital. The first Gne of drugs
losis.
tance to the drugs. The discontinu
.u,. tance were noticed in Gujarat.
are streptomycin. Isoniazid,
Most of the hospitals at one time
ity in the Intake of drugs due to
Acquired resistance develops due Rifampcln,
Ethionamide,
or the other face a shortage of
irregular drug supply in the hospito Irregular intake of the drugs. Besides
Pyrazinamide and Thiacetazone.
drugs. Guru Teg Bahadur hospital,
!s has resulted in such a situation.
natural resistance, primary resistance
However, for matters to have which also has a chest clinic, was
rug resistance Is showing a Is also responsible for drug failure.
reached this level, the patients too
short of Rifampdn In March this
i trend
D ’, says Dr Rupak Singhla
Drug failure can be defined as the are to be blamed, «
M,OJ w
as they
do not year. The other TB dinics In the dty
a Ram Swaroop Institute for temporary or perman ent capacity of take the prescribed drugs regularly, are often short of drugs.
Printed and published by John Dayal for and on behalf of Special Protection Services (Pvt) Ltd, Herald House, 5-A, Bahadur
Printed at Herald Press,
Bahadur Shah Zafar Marg, New Delhi-1110002. Editor: John Dayal Tei. 3715581,37 {61^73715338.
Name of the Paper
1
THE HINDU BUSINESS LINE
Published at
s
NEW DELHI
Dated
I
/
(Delhi Edition)
1 7 APR mi
plans to make TB drugs
?•
presence felt in the conventional anti-TB that although it was believed that TB had
drugmarket
marketby
bymarketing
marketingrifampicin.
rifampicin.
drug
been eliminated, it had been proved wrong
Glaxo Pic, UK, had initiated a collaborative and that the World Health Organisation had
programme of research to combat TB, early
LAXO India Ltd has drawn up plans tok last year. Titled ’Action TB’, the programme once again declared TB a global public health,
emergency. One of the major reasons at
enter the anti-TB drug market in a big
big brought together research centres in the UK tributed to the resurgence of TB is its close
way. .■
and South Africa.
. .
Association with the HIV virus. Another facThe company has entered into a licensing
cdmmdnlv
arrangement with an Italian company for a , ioe lour UK-based research centres are tor is the emerging resistance to cdmmdnly
1 ! •*'» ’ ;'•■KI,
CUIUVIVVIVO. 0
■
" ?•
tong-acting compound which may be requir Glaxo group research, Middlesex, the London iiibd antibiotics?
at
longer
MW
«
Medic,n
^
St
,
’
«
Ave-year
^rograiiime
Initial'
Action
TB
Is
a
five-year
programme
Initlaled to be taken in lesser doses and i ‘
ventional •
a!\d &
? to ** fu.nded and managed by Glaxo
(Our Staff Correspondent
BOMBAY.
'BOMBAY,
°f
s a precursor to the introduction of this
have been formed into three groups centred
at the Universities of Capetown and
Stellenbosch as well
as the
Coindl
- South
9 ■ African
^ftiCan P3"/.5 co‘laboradve Programme and the two
Medical Research Council. ’
’ , ;r
^cuxc.
A statement issued by Glaxo pointed put company official
Name of the Papar
:
PATRIOT
Published at
;
NEW DELHI
Dated
The Health Ministry has
ear: Report
h’ Mult).Drug THernpy
10.52 lakh cases had been dis(MDT).In Hve years or more
charged as cured as Against the
nnd 16.6 per cent Increase In
target of 5.73 lakh. In 1993-94.
acceptors of family planning
methods over the last year,
The Ministry had a plan
mnrglnnl fall In Infunt mmoutlay
of Rs 483 crore for
cases was necessary, while the
tallty rate aft* iotn6
(he
■health for 1993-94, of which
non- Infectious cases could be
achievements highlighted In
more than 60 percent had been
treated with cheaper convcnthe annual report. .
used for national programmes
tional therapy.
On the health sector, the
tor the controland eradication
According to the report, the
report
says that |n the
of communicable diseases InMin slry has also approached
proposed World Bank project
eluding malaria, AIDS,
the World Bank for Rs 554
which odmlk lhnl (h(,rc nre
for leprosy eradication Rs 302
leprosy, TH and blindness.
ohout 500,000 death In the
crore assistance for on Intencrore would be provided to
S ve
kindness
control
On the faniliy
country annually on tiecountof
cover 66 endemic districts
tuberculosis.
program me in the seven Slates,
the report notes that under the
under MDToflhe 201 endemic
Tamilnndu, Andhra Pradesh,
The report expresses con
programme about 155 million
districts In the country, 135
Maharashtra,
Madhya
births had been averted so for.
cern that while 500,000 tubernave been covered by MDT
Pradesh, Uttar Pradesh,
culosls patients are cured every
It htis
succeeded in
in reuucfeduc- I
services.
.......
.. also »«w!«iea
Maslhan and Orissa.
year, this is being over
ende^lMHeiXtld
' ^0US,,nd ,p
The sanction of Rs 302
shadowed bynn addition ofone
crore World Bank aid for
million sputum positive cases
leprosy eradication, the ban by
annually.
from 5.97 to 3.8 during the
MDT programme which Invol.
23 Sutes on salt other than
The cost or drugs alone for
same
period, the Infant morWs treatment with the comodfsed salt to check Iodine
tallty rate from 146 to 79 and]
ensuring covernge of these
binatfon of three drugs —
Deficiency Disorders (IDD), a
Increasing the couple protec-/
sputum positive cases would
rifampicin, clofazimine and
90 per cent drop In leprosy
tlon
rote from 10.4 percent in’
come to about Rs 150 crore per
dapsone.
. .
cases in the 40 districts covered
1070-71 to 43.4 per cent bt^
—51e £cP°rt
more than
March 1993.
*• > ’
Prepared a project proposal
ror obtaining World Dank
nnancial assistance based on
short-term
course
chemotherapy f0r spu(lJni
positive tuberculosis cases.
This has been revealed In
the departments of health and
family welfare annual report
'°|r| J9”'94
•
w as Rs 50 crorc.
The Ministry Is of the view
that World Bank assistance for
tackling the sputum positive
Caplla)
■<
I
1
£
1
t
3|
■■
''r
to*1
'■
'J'3b
‘.'l,'?.' I. »1.-
IA..
■
‘.Wit l/SU»«»-
Dated
_
•
1 MAR 1994
-----
Lack of drugs
plagues MCD
TB clinics
Deshpande
valiker said. The manufacturers
concentrate on "producing the
more sophisticated drugs, which
IRREGULAR SUPPLY of drugs ai "AC/auUri,iy more e*Pensive.
And the TB medicine budgets
Municipal Corporation
of Delhi-run chest clinics in the arc so low that they are insufficient to even supply the cheannr
Capital has resulted in a I
^ l0RBTB
‘!!'he Patients." he saW.
mpli rV°idabJe pcriod of treal' drThe
. 3hc R.BTB Hospital has a
A randXhwUuheXst cli- ±geLl'?r fl
Rhs5 *°
6° ,al<h
,akh/or ™
medlcij Rs 2
nics revealed that manv oatipmc ?°S’ ...
wb 0 lb® hospital needs
have been visiting the clinics for tn?fr°i *2 supp,y aB lthe
be medic
medicines
"■•r.Wr. .h.Ig’hTBX;.?, "Dr
“SsuE!??-.
U Bhakta, in-charge of the
— programme, said though
’ the requirement was Rs 1 crore
the entire MCD health budget
was just Rs 35 lakh. The MCD
was
Shahdara.
®
° ^
as getting
galllng an aaid
>d of Rs 45 lakh
trom the
Central
The erratic supply of medic!
16 Ce
unlrai Government
Go''ern™n‘ for i'
.nes is a fallout of^faulty drug ficiem hT butththis
5,0too
° Was
' ij
wasinsuf
insufpurchasing policy and lack of ficient'he said
'
The National TB Control Pro- !
adequate funds. Because of this
irregular supply, the medication gramme is being run on the sampie survey, conducted by the Indlroutine of patients is getting
Medical R«earcii ,
upset, leading to drug resistance Lm nCil
in many cases. As a result, the dis (ICMR) way back in 1957 “No
ease-takes a longer time to get national survey has been conduc- ,
cured and patients suffer for lon led after this, though a couple of !
f00!3^5-!1-Veys ^ave been done up
ger period.
Mr Trilok Singh, a resident of °t?^’ Dr Bhakta admitted.
The 1957 survey showed that i
Kalyanpuri, has been visiting the
Shahdara chest clinic for the past .^ persons per 1.000 were ’
radiologically TB active”. And
lo months, but is still continuing
with medication. "Sometimes the only a fourth of these patients
medicines are not available and were high-risk cases, showing
we are asked to buy them from positive sputum results. “The
the market. But how can I afford number of TB cases has not
to buy (he tablet, which costs Rs increased since then." Dr Bhakta
maintained.
6, he said.
He blamed the patients for the
The Medical Superintendent of
the 1.200-bed Rajan Babu TB prolonged duration of the dis
Hospital. Dr J N Banvaliker, said ease. saying many of them defaul
tne national policy on TB had to ted on the prescribed course
After a month, when thev begin .
be radically changed, if TB were
to feel all right, they usually stop
to be contained.
The two drugs being supplied taking the medicines." Dr Bhaktato the MCD clinics, which were said It is hoping to bag a World
also part of the National TB Con Bank aid of Rs 900 crore for the
trol Programme. were not readily national programme. Till such
available in the market. Dr Ban- sulTe/^6 patients w,d conlinue to
New Delhi
I
FREE PRESS JOURNAL
Name of the Paper
:
Published at
: BOMBAY
Dated
2 7 MAR 1W .
~berciilosis becoming drug-resistant?.
ravin Kumar
Bj^Travin
SonSmS- .J™v
S&eXThS
in
TUBERCULOSIS (TB) has
..
£5±S5S1 weakened«immune
wfas
tfa
systems can-
^W^beUe^tha^
tury,lhankTtopcwfcrful dnigsilike
Niazid, rifampicin and the only treatment for TO was im- ststantTO. Multr-drug resrstant
TB is in fact pushing us back to
pyrazinamide. But since 1985, the proved sanitation and outdoor life,
microbe causing the disease,‘My- In I
,
cdbacteriumTuberculosis’, seems Camille Guerin showed that a Louis W. Sullivan, former US Sec
to be fighting back. For instance, non-viinlent strain of the bacte- retary of Health and Human Ser
vices. Since 1986, there has been
20.57 per cent of 588 patients at- rium could provide immunity
an overall increase of about 18 per
tending the Lady Willingdon State against the disease. The vaccine,
cent in TB cases in the US. The
1 TB Centre, Bangalore, were found BCG (Bacille Calmette Guerm) is
active transmission of the disease
resistant to one drug or another, now the most widely used vaccine is greater inhigh-risk groups like
WU11U. X>UWUV«r
t
** .
The team of scientists of the Na- in
in Uie
the world.
Effective tuvuuuvu.
reatment . * &* .
came with strepto- those living in homeless shelters
tional Tuberculosis Institute, Ban- for
— the
—- disease
-and isoniazid and prisons, in intravenous' drug
galore, conducted the study and mycin (1947)
.. users and health care workers, but
regard the findings as disquieting. (1952), which dramatically re it is feared that the disease is also
These come at a time when Short duced the number of TB deaths. spreading into the general popuCourse Chemotherapy, including ’
The bacteria usually spread lation. . *
rifempicin, is proposed to be in- through an infected person s
Sporadic treatment
troduced on a nationwide basis, cough. About 10 per cent of mThe
effect ofsporadic treatment
for similar results have been re- fected persons develop the active
lclv
disease.
The
main
symptoms
are
is
merely
to kill off microbe strains
■ported elsewhere.
of
the
many
bactefever,
night
sweats,
weight
loss,
jack
resistance to the drugs,
TB is one < ” '
rial1 infections like pneumonia, racking cough and spitting of enriching the population of resisblood. From the lungs, the initial tant ones, so that they eventually
tors in hospitals and clinics around
the world are losing the battle,
“We don’t have any more new efi
fective drugs in sight for manag
ing these resistant cases,” says Dr.
B.T.Uke, Director of the National
Tuberculosis Institute, Bangalore,
ever, comments Dr. Prabhakar, it
may be presumed that tuberculin
sensitivity in 6 HIV-infected indi
vidual could be used as an ihdica-"
tor of the progression of HIV. in
fection to full-blown cases.”
Losing battle
Medicine has so far kept one
step
_„
r ahead of bacterial mutations
e
with new drugs, but bacteria with
new resistance genes have been
appearing much more rapidly
just two years after the newest
batch ofantibiotics appeared in the
late 1980s. Drug companies have
lost interest m developing expen
sive TB drugs for patients in de
veloping countries (which can t
affqrd them). However, dis^over-
•x’Sir'SS.T.TZ,;.
throughthe lymphatic system and defences. Since each site of TB
of j^g resis.
the bloo^ to the bones gemto-un- infection in the patient s lungs
dnJg dc.
nary system
---------' contains 10 to
sitm Until
sign.new
Until
drugs
newcome
drugsup,
come
it up, it
crobes, this can happen m
in a matmat w^ujd
curs in about 15 per cent of pa- crobes>
worthwhile for health
tients.---------------------------------- ter of months.
care workers to pay more attention
The infected persons themThe AIDS connection
connection
to basic sanitation. Even more
The
selvesjlon’t notice the
WEat is worse, the AIDS epi- importantly, to educate doctors tp 1
aemrc uas givcu a wvot w ai_».
.
remains the leading cause of patients die. Treatment with . India, the link between TB and disease, particularly in hospitals, J
of isoniazid,
death Each year, there are an es- combination
----- AIDS has been noticed at various w here one-third of the patien are.
timated 8 million new cases of TB rifamp: cini and pyrazinamide for research centres. With a million on antibiotics and where selective
and' 2.9 million deaths from the
------- *k‘
■ identified HIV carriers in the pressure leading to drug-resistant ;
disease. In global terms, TB ac--- the threat of a TB epi- microbes is highest Patien ,
. t
in the developing world and for even to the combinaUon of two or
World^Hea^Ui LOrganisaiion
World Health Organisation
(WHO) declared tuberculosis a
\global emergency’
-------- .• < •
-- ---------million
lives in the
the next
next decane.
decade.
L
j
,
the
disease is
What is worse,
-king in tandem with AIDS, the
worl—^ _ that breaks down
‘
*the
’
disease
bddy’s immune system. In fact, TB
XSKX.maVo cure that they com-
*._t
Jk f
t te a coun;e of antibiotics in ordw ^wipe out all infecting tac
be eH« »
it will also be critical to iden-
5!taeal..l.C.n«omelCMK. W ! » 8^1^ ™ P-
strains ofbacteria. For this. WHO
. whoNET, which aims
20 per cent of TB patients f
^per
pjbhakar says to link hundreds of microbiology
I to
complete their course of drugs,
rate of TB could be laboratories,
IdVViavunvtf round
— the world to
according to the Centre for Dis- thatth ~
---------- rnv pool Information
about
dmg-res
information
about
dmg-resisease Control and Prevention 20 to 30 times higher among HIV tant strains of ba ctena and viruses^
cases than in normal individuals.
(CDC), Atlanta.
Name of the Paper
:
Published at
' guwahati
iDated
I
ASSAM TRIBUNE
2 7 MAR 1994
•
Spreading risk of tuberculosis
I
report of the World who persistently fail to complete world. He argues that the ratus for taking miniature films,
Health Organisation (WHO) their TB treatment course, But problem of TB is increasing the collection of specimens and
states that tuberculosis kills the situation is worse in the because of day by day increase in for conducting simple examina
tion. It will operate in such a way
around three million people a developing countries like India population.
Evidentally,government agen- that the villages and the slum,
year worldwide. The death rate who have poor tuberculosis
cise telling us that TB is under areas covered by the mobile^
is highest around the age of 30, programmes.
so those deaths represent a lot of
Earlier, TB was caused by control is not true. An expert clinic will be taken up a hew once
lost years. Now the chances of cramped living conditions, poor reacts strongly to some reports every two months, The work-;
sick people
dying, and of hygeine, lack of nutritious diet which appeared lately claiming ing of this clinic should be
infected people sickening, are and poverty but now AIDS have that TB has re-emerged in our attached with the National
quickly getting wprse. Yet those further triggered off this epi country. He says that TB was Tuberculosis Association ot
responsible for making funding demic in most part of the world. never controlled in India, so India (TAI) New Delhi.
decisions in the international
A survey conducted recently there is no question of its coming
The TAI is an organisation
community have failed to supply in Africa and other countries back. It . has always been a which iSjwholly devoted to the
the money needed to
serious--health problem in our ... eradication oi
of TB
In ■muia.^ine
India. ^The
w curtail the .^..where the prevalence of HIV and -------id in
four decades.
* ___ _»_xi_ '' was' founcied ' in
epidemic. Because little is being • ■ TB infection is very high, reveals -cnHntrvfnrthe
country for the last
last four
decades.;. I Associntion
J____ L.. •_*.________ .J.________________ •___
_____ i_____------------------------------ A
.
.*v !• ‘i
A study MM
on the epidemico-' '^^
”______
1939' as a voluntary
1
close link between these two
done
by international agencies 4.1the
of
tr
t
logical
aspects
the
TB,
to halt the rapid spread of tuber infections diseases. In Africa TB
culosis and that incurable forms is present in 50 per cent of the conducted for a period of 20 informed and fsustainedj^omof the disease will become more
T . ,
c,
:
' Paign agalMt.&h^dreaded
common and if it continues to be
Jaidev Sharma
,
j disease and to t^Auc^steps as
given low priority, the report *
----------- --------- -------- - ; are feasible by arrangin^roiifesays.
AIDS patients. While studies years in New Delhi Tuberculosis fences, establishinghioddTnstiAccording to experts, TB is carried out in Bombay show that Centre (1962-82), found no tutions and training tuberculosis
caused by a bacterium that can about 6 per cent of the TB appreciable change in the TB workers and carrying out ficalth
be passed through the air when patients also have HIV infection. graph of our country.--------------- education activitiesM^V., b '
someone with the disease Deadly association between HIV
So, if no adequate and
_•
“
h £ £
sneezes of coughs. While the infection and TB has also been immediate effective control
majority of the people with TB reported from Europe, America, measures are taken to combat i ™ h°3plt^had
. other uses because there^ere no
show no symptoms and are not Thailand and Australia.
the TB problem, our experts
doubt,''"'such
infections, they are at risks of
An expert of the Tuberculosis estunate that our country by the
India
g rosy
developing active TV throughout Association of India estimates year 2001 might have 20 million
their lives. And that TB, which is that in the next ten years or so TB patients of which over 4.21 dream, but where there isra will,
trated by giving patients medica the number of TB cases in India million would be spreading in there is a way. 4 "• * j-; ja • .
The science of modem warfare
tion over a six month period can will considerably go up. The infection to their fellow Indians
become resistant to drugs when Deputy Director of the New Delhi and more than 73,000 Indians gives the destruction of enemy
may die due to TB, every month. bases and of their lines of
the treatment is inadequate or TB centre also presents the grim
interupted.
In my view, there should be a communication avery high place
scenario in our country about
Surprisingly, the New York city this infectious disease in more concrete plan for running mobile in its operational repoitory. In
in order to combat prevalent revealing terms. He states that at clinidf in tuberculosis control our war against this disease we
epidemic of TB is given itself the present, India alone has 50 per measures. These clinics should m ust give it an equal importance.
?
he provided with X-Ray appa^ — INFA
right to lock away its TB patients cent of the TB population in the
Name of the Paper
:
BLITZ
Published at
I
BOMBAY
Dated
. I\»
:
-■<
f I
.r-l8 JAN
- 1994
Made for
EALIHFILE eacn otner
{
PRASHANT TRIKANNAD
A poor country like India can afford to
a country which has the misIgnore the deadly AIDS-TB combination at
Kam fortune of accounting for more
its own peril. The harsh reality is that
I than 6 lakh TB deaths out of an
treating a drug-resistant patient becomes
estimated worldwide mortality rate of
a hundred times more expensive than
3 million annually, India - where a TB
treating one v/ho adheres to the six to,
victim dies every single minute — is to
eight months anti-TB therapy. The'
tally unprepared to counter the global
resurgence of TB, especially through HIV
resurgence of a disease that was long
carriers, Is dangerous because an AIDS
thought of as vanquished. It Is not just
patient — whose defence mechanisms are
tuberculosis that Is looming up out of
already down — contracts TB that much
the darkness, but its menacing con
faster. While such a victim may not pass
on AIDS to one who has neither, he just
nection with HIV,
the
virus
that,
might transmit the TB virus to the
causes AIDS. While the World Health
unsuspecting victim. And the net result: a
Organisation wasted no time In labell' ing the disease as a “global public
killer epidemic that no one knows of.
; health enemy’’, the In! dlan
government,
which ought to have
taken the lead in
neutralising the new
and far deadlier threat,
did nothing. The Union
Health Ministry, it would seem, Is not
While TB Is actually going down in the
West, its resurgence, if any, in America, is
even aware of the TB-HIV nexus.
multifactorial with AIDS playing a large
While India is in an unenviable position •
to rattle off grim statistics on TB, it has no ~ part. "In my country, 5% of all TB cases
also HlV, positive or 5% of the AIDS
such data on the number of HIV patients ■’\-'are
patterns havekTB," Dr. Nardell disclosed.
who might have contracted the disease
The percentage of AIDS-TB victims In the'
too. "In Bombay alone, at least
US Is, no doubt, negligible, but it has40,000-50,000 HIV patients are believed to
nevertheless shaken America's medical
, have TB,” prominent member of The
fraternity Into doing something about it. 1
American College of Chest Physicians
Said Dr. Rao, "TB is transmitted In slow,
(Western India Chapter) Dr. V. S. J. Rao
motion. Add HIV and the
time for TB Infection
becomes shorter than
you would think."
TB has always
been 2 tune bomb»s
In many countries In.
Is either free or highly
said. The chest specialist cited a few case' ..subsidised. In the US, for example, TB
histories that could be a foretaste of the
victims, particularly those who refuse to
horrifying epidemic to come. Of the 920 z. abide by the therapy, are Isolated until
patients examined for the HIV virus at the
they are fully cured. In fact, the patient
Watumull Chest Hospital at Mahim in ... automatically becomes a state responsibility.
Bombay, 29 were diagnosed as having
In India, there is no such thing as health
• both AIDS and TB.
subsidy. What little free health care and
"AIDS with TB is almost always fatal,"1
subsidies the government has to offer Is
world-renowned chest physician Dr.
nothing short of a farce. In Bombay s
Edward A. Nardell told Butz. The Assistant • acclaimed KEM Municipal Hospital, TB
Professor of Medicine, Harvard Medical
patients have frequently complained of
School, who was on a Lupin-sponsored • being told to buy drugs from private
’ lecture tour to. India last month, feared——chemists. But, where Is the money?
AIDS has just shortened
that the revival of TB and Its link with the
"HIV positive patients risk a 5% to 10%
AIDS virus could hit India hardest. "In
chance of
™ ®*e7Xea^ shwma
New
intravenous Medical Director Dr. (Mrs) U. K. Sna m
New York
York City,
City, for
for instance,
Instance, intravenous
drug users and commercial sex workers said. In the course of he research. Dr.
u'uy have
u ’ AIDS are at gravest risk of
Sharma found that five Indians out of j
who
every 1,000 developed TB, many .at an ;
getting TB, too. When they shirk anti-TB
therapy, they develop drt^Tesistance . earlier stage. "Just one victim can infect
at least 12 others In his or her lifetime.” :
making curage for patients'difficult,’^ he
said adding; ~ 'There is no good treatment
It was keeping In mind these Important <
----------------that can wipe out TB in an AIDS patient. The - drawbacks kvour ‘health-care system
and1
the
resurgence of TB and AIDS that
case, thus, becomes complicated, Could
t
India fare any better?”
: prompted “Lupin Laboratories to sponsor
The
American College
cf
of Chest
Chee!
Dr. Nardell might have something
Physicians (Western India Chapter)-.
there. WHO has forecast as much as 5
crore AIDS patients In India by the year
2000 AD. Probably, even earlier than that.
J1
fl
Just imagine the Impact of AIDS with TB
JL|a
in a country which is the second most
|||f||||k’|J
populated nation In the world... where the •'
I 11I I ■
momentum of sex education has Just
begun to pick up... where the significance
of proper health care Is totally lost on the . organised lecture series of Dr. Edward A.
Ignorant public... where the government
Nardell
on
H
really doesn’t care a damn about health
Tuberculosis: Implications for the Present,
cars7Said Dr. Nardell: "Today, In New York ' . Strategies for the Future l_n_Bombay Jast ■
month. But are lectures, no matter how 7
' City, 20% of all HIV-positive cases having
TB are resistant to antl-TB drugs.” How ■ enlightening they are, merely enough to
shake a government out of its slumber?
long-will It be before Bombay Delhi,
- What do you think?
Madras and Calcutta follow suit?
I
—■■ -
—
—-
-
—
i iame of the Paper
:
THE HINDU
Published at
s
NEW DELHI .j
Dated
!
Not a history book disease
^■"Ep^HE number of cases of tuberculosis
B reported in the United Kingdom is on
B the increase especially among women
aged between 25 and 44, according to
the latest figures released.
Dr. Peter Davies, of the TB Research Unit and
the Cardiothoracic Centre, Liverpool, is urging
the doctors in England to be on the alert and
th°^
r°r
Predom*nant symPtoms among
(Delhi Edition)
infection, particularly AIDS victims.
Symptoms include coughing, often of blood,
chest pain.'shortness of breath, weight loss,
high temperature, especially in the evenings
and poor appetite.
and this does not necessarily either guarantee a
non occurrence or provide a cure definitely that
There are a number of antibiotics that can be
the disease will not affect them.
used to combat this disease successfully. But.
It all begins as a small inflamed area in the
lung, which turns into a cavity. This is caused according to the medical reports, now that
by the mycobacterium tuberculosis. However, in dangerous strains of TB have emerged, mainly
in the US complete drug resistance is
Britain, pulmonary TB is the most common
becoming a common feature in New York.
form of the disease. Droplets from the infected
Failure of treatment in Britain, where medical
patients are dispersed through coughing. The
treatment and care are totally free under the
‘TB is not a disease of the history books....the enhancing factor of this, however, is attributed National Health Service system, is usually
to
overcrowding,
malnutrition
and
immigration.
factors, such as poverty and immigration,
Admittedly, poverty, social depravation and bad because a doctor has either inadvertently
seemed to be responsible for the increase,” he
prescribed the wrong drugs or because the
housing
also add to the miser}'.
warned.
patient
has not taken the right ones. In some
The
WHO
(World
Health
Organisation)
h
ii
... ,, ,
.
*“v »»uu(»fuiiuneaiuiurganisaiioni
Instances, it is stated that the patients are
. hard,yofseems
believable,then'^e^nhe
but tuberculosis — recently
that threethis'yea"
million prople
scourge
the Victorians?
whid^inannounced
the"from'™
E*
themselves to blame for not taking the
II TT °f ..V,ctorians' then called by the will die in the world from TB this year alone,
prescribed antibiotics regularly for a period of
dJ5eaaded
the disease more than any other infectious disease. There
f name,
namp consumption" ~and
j u..
nearly one ye
year.
Admittedly, ltie
the admini
administration
olthe
♦--------.
01 me great depression —
- is making a”
are “two
engines
” driving the epidemic world- 7
.ar;
^uah22
nghtemng re-emergence in the capital city of wide — AIDS and poor TB control programmes. °f ant*blot,« m the drug management of the TB
ThXr v •
..
NearIy one in five tuberculosis deaths occurs in
T ever}tUa,Iy tobf
cured’is
Pn n h 2 ?C^ine ,8,ven to 3,1 .the chi,dren in P^P16 from Africa- TB will develop only in
3 susta,ned and a Prolonged affair. ■
ig is j schools is only a precautionary measure those whose bodies are unable to fight off the
P.
P. SURRAMANYAM
SUBRAMANYAM
Same of the Paper 5 THE HINDUSTAN TIMES
Publrehed at
I
Dated
1 1 4 JAN im
NEW DELHI
(Late City Edition)
Ptleas to tackle TB on priority i
• }h{r Correspondent
j.0™6. ^own to /our. per lakh in scribing three to four drugs. Howcv- •
--- —---------------israei, is gradually rising. Presently er, __| lrllePendin
V11 .S on
whmiuvii
u» i^n of ’
lhe cond
-------------------------------------------------------------------I ’v-M
NFW iSfi mt t
[ne nu™ber Js as much as ten per the patient, the trearmenVcontinues
' six months. If less than three
cen^nZ iktehISrael,iS barely CUl°SiS in ‘"diaSut ills a matter of shT5 are used and that too, for a
matter of short while, there is a risk of recurr
flndia (here a're threZmCS
ence and aggravation of the disease
jZy he said. Micro-bacterial TB ;
o.iild be resistant to one drug or
fcnd
TX
°^B
n
.L
Dis
“
ses
sev^ejf
o
9
?
8
"
T
“
WaS
are
land Tuberculosis: who decent"1
rIn
“InIsrael,
Israel,ioeffons
efforts
areonontor
forrere- i I |
disappointed b?
'988 “
work
fight the^se^elhh
,3 visit to India, is
< < ^nIy one drug in a short period of
jthe general health condition prevail
. t,me- Cooperation by immunologing in the country.
ists, epidemiologists and others is
J .piling an example, he says during
> required for the research work’’, he
this recent visit to Bombay for the
said.
Jfirst International Congress on HuIn his country, there are 200 HIV
jHian
Immunodeficiency
Virus
mHIV) and Tuberculosis, he was
active and 2,000 sero-positive cases.
Ltaken aback by the ignorant attitude
More than half of the HIV-positive
patients have also developed tuber
jpf 3 patient who spat blood conculosis. In the whole world, there
jlinuously while coughing but “never
soothered to ask for help”.
are 12 million HIV sero-positive
cases and the World Health Orga
5
Lliraz, as an international ex
nisation has predicted that it could
pert on lung diseases feels that un
less TB is taken up as a national
go up to 40 millionfjy the year 2,000.
Tn India, the‘suggested number till
gssue and given priority to prevent it
now is one million HIV sero
spreading further, it may be
positive cases,'* he said.
come impossible to live here.
Dr Eliraz feels that the intema5 Besides this, he emphasised that it
tional health community should
as necessary to make the people
; have handled the situation more
gware of their health and the facili
■
Dr Abraham Eliraz r’ . seriously in 1986 itself.
ties available for treatment. Howev
er, the need to motivate the medicos
Regarding lung diseases, the 55— HT photo
Js also a must.
year-old doctor from Jerusalem
J .He says before the jproblem dropped to four*per lakh.
stated that chronic obstructive pulReaches a saturation point, it is
is
Since Israel experienced such‘ a “,unary diseases
aiseases are caused due to
C
------ - --- J
VV111I lilt
Ll“ “^°™yab?Ja^
°w rate of incidence of tuberculosis smoke inhalationi and
and pollution
pollution
welo^ed
countries
in
the
health
sec* 1’? T® Past’ the present number is which destroy lungs and cause bronf ’ ••'’r';1 sec
lor iand’ cnllprt1 fundc
____
’ d • 1 ,nterna'' obviously a matter of concern. “I chitis and emphysema/ In Israel
.iional hhealth
"a,th community.
“T":1 ,V- u
had predicted that by the year 2,000, 2,000 new cases of lung c^cer are
* He ofthe
has noUdhn
doubtd^
about
lilkv
Ut !the
hVa2r ,TB k111 ?e el,minated fr°m my coun- reported every year and incidence of
IhJ. ci?n^ di
t° handle try but I was wrong,” he said.
lung cancer among women is also
Jieln hPm rn bUl Israe uCan a,so
fording to him, the rise in the high- Dr Eliraz feels that, cigarette
iinnP”
overcome the situa- number of TB cases is due to the smoking is the main cause of this
Skr
‘^'grants who after getting the ini- disease, as 30 per cent of the total
b ,nd to. the d,s‘ J1®1 treatment for a short while, van- population of five million is addicted >
pse, one is forcing a situation when ish from the scene. And since the to cigarettes.
|t would become difficult to live here disease is infectious, it spreads and Tn fact, ™
e children,
u-.u
I
20 per
perCen
cent
of
jeranse the disease will get spread, infects others. In Israel there is an k In
i
20
- of
chlldren’ ' j
ftNalready quite late but not too influx of immigrants from Ethiopia, ceirof^dTts8"?1’ °' If
'f P"
jatrijo control,
control,” he said.
|atrf;o
Russia and other countries Desoite n
f ?.du,ts’ ar,e s.uffenng from
!I PLE,Iraz
’ who specialises in In- all out efforts by doctors and social d-th!Ja' .Fo.^unate,y’ he ^ys. m InZll.... ........
UrnH. Medicine
--------workers, the immigrant ™? negli- dia the
d—ofr asthma is low
the —
incidence
lernhil
and Pulmonary
1
compared to other countries. In
pf&ficine and presently holds the gent about the preventive---and
J cura Israel lung diseases like bronchial
rank of a Major in the Israeli Army, tive measures.
fc conscious of the fact that the inci... given to TB patient asthma are more because of food
The treatment
habits than industrial pollution, he
pence of tuberculosis which had in Israel is initialFy confined to pre- said.
-
I. m
f ^JSSSSiS
cmssssss
........
fe !3J
_______ - '
I
Name of the Paper
i
INDIAN EXPRESS
Published
t
CHANDIGARH
Dated
. - 1 FEB 1994
—|
—•
n _____
_________
(City Edition)
-r.
VP/TB threat looms large in HP
; AshwIni Sharma
ZShimla ■
r. - -
/ .•
~
-
PREVENTION, it is said, is better than
cure. But what if preventive methods are
implemented in a casual, slow and ineffec
tive manner. That is one reason why the
shadow of tuberculosis, a dreaded disease
second only to AIDS, looms large over the
entire population of Himachal Pradesh, es
pecially those living in the tribal and back
ward areas.
f Health experts and medical scientists
are alarmed over the rise in TB cases in the
state during the past few years. Over two
from the disease and 20,000znew cases are
•reported every year.
<
Manygo
gounreported
unreportedas
aspeople
peoplein
inurban
urban
Many
areas
areas prefer
prefer to
to remain
remain secretive
secretive about
about it
it
"In
In fact,
fact, this
this section
section poses
poses more
more danger
danger
than the illiterates of backward areas '
areas,
• claims K. L. Kapoor, the state TB Control
:Officer
claims K. L. Kapoor,' the
state
TB
Control
J
J
control
Officer
.J------------ • /
Health Department
Department survey
survey shows
shows
:i> :’A Health
■
backward areas of Himachal "There is no anti-TB medicine available
Pradesh, where people live in congested for the past few months' in Sirmaut W?U it
dwellings, are more prone to the disease, notallow the disease to relapse incase of
or example, m the land-locked valleys of those already under treatment," questions
Dodra-Kawar, six to eight or even more a health volunteer. ;
,
members of a family live in single-room ■ According to Directoi'Health Slices,
T, ' , ,
j. K. Kakkar, the main thrust of the iiroc<?°k'
aind s£ay for days to grapune is on preventing transmission of
Xi.msi xisssss
There has been ». .hmrf
•
• .u
rat?r he feels.
‘
i
B
era esuedaH^ ° R
Mandi, Kan- been created in the district hospitals
Chamba ^Cullu ^Shimlaandtr83
Chamba' BHaspur and Mahan. Th|p‘
are asking- the hpahh a Fk ^in^ur‘
Department has also set up district '
^2X1S
to ^d a TB centres in 11 districts, excluding iW. i
oaHents in Pand"0?
survey of TB haul-Spiti, where a tuberculosis clin^tt .1
P« m Pang! says Rakesh Kanwar, working. The health officials are iStW. /
The Tuberculosis C<^trnl Pm
optimistic, of the eradication of this diseSe.
W"FF
““ 'raTd
by radiologically active IB of which 19,300
are bacillary cases. Of the 20,000 new cases
coming every year, one-fourth turn out to
r------- *—
-•
- am
.« form
,
.. L.
'
chief medical officers for effective impletransmitted to others. The other
of•--/
X- shnrfXp^f ? ,aUth
for
°2tieS, COmP ain of dentation of the programme, lAess the
i ray positive TB is equally dangerous ~~
fur Hpn?mgL
' rnhmeXand insuffi- state government mafcs a deteXied ef- .
: the infected persons as it mainly damages
" ’ p^Hv^»T7UPI?b.7and‘he "on-coop- forts, the disease may assumed serious 'I
lungs and other vital human organs.
erative attitude of the urban patients., dimension.
4
* >'
i
Dated
2° JAH 1994
/
^Alarming riseof TB through HIV
________ Staff Reporter
1990—with 2.1 million, or near among TB patients can also be
Apart from abstinence, safe HIV since the start of the epidely SOperceiiloflhein,in India — seen in India. In Manipur, more, sexual practice includes mutual mic. Approximately two million
to 12 million in 2005. Between than 11 per cent of reported TB fidelity, non-penelrative sex people were infected in 1995
IT IS a well-established fact 1990 and 1999, eight I1Illlllin
' sex people were infected in 1993.
million patients are HIV-positive. And and protected sexual inlercour•today that the Aids pandemic is people
• ■.’ r- expected" to have al the JJ Hospital HIV prevalen-. se, he pointed out. “We need to . I*1 India, the estimated
numbmiging nboul a resurgeiK-.- of (developed TH n.s a consequence
cc among TB patients rose from provide information about her of HIV infections has risen
tuberculosis. Most TB-infecled (‘
r‘'IIV
,v infection.
oil
<
through by 60 per cent over the past year
people go through their lives .• In African countries particu- 2 percent in 1989 to a 11 percent these safe sex options
this
year.
a 'i—.T’
Hds.year.
many different channels
J., to
.j to around l.G million. Many of
without suffering active tuber- Jarly 'iffonio/i
1 108 become essential today reach everyone,” he said,. Asia’s other HIV infections are
rulosis because the bacteria is annuali<nnmi.^ Y A,t. j miv
1? (,(,nd)at this dual epidemic.
“Condoms are a very
very highly in Thailand, where in the north
kept in (•heck by their immune oases line i ii 7!,)<)r
wiih?.
1
.
1
)
|F
<
’
i°
r
.
e
X
en
,
<
d)vious
way,
pointed
out
effective
means of prev
preventing one in five military recruits and
system.
tripled,
A»i«. in. K’.. .aS.!.)r ^e,s<?.r!’’s ,(> ‘d* we can to 1 IIV *transmission
and; we
we must
must one
one in
in 25
25 pregnant
pregnant women
women are
L...’
“But like the. cobras kitpl in years. in
In Asia the same picture is prevent HI V infection. Another, dispel all myths to the contra- now IIIV-pos ’live.
baskets, the bacteria quickly
(,
o to Mappear. Th'is
...o is 1IUI
starling
not isfor IB programmes to acceler- ry,” said Dr Merson. “Their use
By the year 2000 as many as
naiu isr jvivrsun. ineiruse
•nwHihc h11 r1. »IV .e!)I?es a,on^ very s”rPrisi»g» given the° fact ■...... - »'•
ate their efforts to interrupt TB needs to be promoted through half a million Asians each year
•ma bus the lid, said the execu- *'
*
*
’
tliat there are an estimated one'
by ...
the curative
----- ;; j social marketing campaigns are expected
.---------to develop Aids.
live director of the Global Pro billion people in Asia latently transmission i...
will ihave enormous congramme
on /i.ua
Aids,, i7i
Dr ivnunuej
Michael infected with the tubercle treatment of infectious tubercu- that make the condom as much This ...sii
•■•v w..
losis cases.
; rMerson,
'
- -his- keynote dress al bacilli.
a part of life as toothpaste and sequences for health care sysm
i
Dr Merson said that while the soaP*”
terns in some countries, includ' the Tirsl ImernaUonal £onfe”r-‘
Clinical and surveillance data
Dr Merson said that the ing ones which are currently
cnee on HlV/Aids Infection, suggest that in Thailand TB is two routes of infection, namely
Tuberculosis and Respiratory the most important life the sharing of needles and con- second method for preventing well developed and financed,
Diseases.’ The three-day confe threatening infection associat- laminated blood, are more easy, sexual transmission is the early
Dr Merson said thatin the abs
rence started in the city on ,ed with HIV. In one large Bang- to talk about, it is sexual inter-, diagnosis and treatment of
course which accounts for nine sexually transmitted diseases. ence of any cure for HIV infec
.hntiniryB.
a?1.4
three in five of all
tion and none foreseen in the
out often 111V infections among
According to recent Who cal- Aids patients’ adniilted bet.
■Uwecn adults and adolescents. “There
According
to Who
estimates, incur future, comjjassionate
.-n’
’
Hwoummcn,
culahons, the number of new 1-“' Hnd* 1991
“
lu,(l P’diBonary fore, the main focus must be UI1
on hy the end of 1993, 14 million care in a climate of understand
TB cases each year worldwide is I'B.
preventing the sexual transmis- adolescents and adults and.orie ‘ing and non-discrimination can
st-<
rise from 7.5 million in
Rising trends of HW infection sion ofl
million children worldwide prolong both the duration and
of 1IIV,
1IV,” he stressed.
would have been infected with Quality of life of those infected.
Bombay
- -• -
r
.
1
■
...
.
.
Name of the Paper : INDIAN EXPRESS
Published at ’
I NEW DELHI
Dated
I
1 5 FEB 1994
Nation-wide TB
control plan flops
by BM Kaura
CALCUTTA - The nation-wide
tuberculosis control programme,
launched with great fanfare 32
; years back, has come a cropper.
J 'In West Bengal alone, there are
, 14 lakh victims of TB.
'■
;
r
•••■
So disappointing has been the
TB control programme
that the
.
West Bengal government has had
to change its strategy altogether.
L.
yoJ, .*.*1
In a changed strategy,
the programme will now be funded by
■ —
---Bank
' under
' -----the
World
WHO auj spices. In the first phase six sta| tes and five metro cities
including Calcutta have been seT
ectecj
The main objective of the new
programme is to reduce mortality
rate, attack rate and to break the
transmission chain of infection at
the source on account of tuberculosis.
According to Abul Hasant, the
state tuberculosis control pro
gramme officer, the revised pro
gramme will be launched in the
state from Murshidabad district
from April 15, which is the most
affected district in the state. He
said the WHO has promised to
spend Rs 38 crore in West Bengal for treatment and training
the staff in five years, the target
period.
In the first phase six districts Jalpaiguri, Darjeeling, CoochBihar, Nadia, Murshidabad and
Maida have been selected for the
programme. The main emphasis
of the revised programme will be
to provide a short course chemo
therapy to all “smear positive
and cavity cases” and to detect
and treat at least 1500 petients
annually.
Hasant told ENS that short
course chemotherapy programme
has already been launched in
Calcutta from January. The state
Government has already given
training to ten state medical officers and 12 Calcutta Municipal
Corporation officers so for treating the patients. He said the need
for revamping the existing pro
gramme arose because of inad?quate coverage of TB services in
primary health centres and inadequate drug supply. This has re
sulted in the treatment of only
one-third of detected cases. Patient dropout after initial treat
ment has also hampered
treatment,
SN Sengupta, specialist at the
local SSKM hospital, said that
0.4 per cent of the total affected
people were the main carriers of
the disease, which is spreading
fast.
(City Edition)
Published at
I
Dated
; 12FEB1W
BOMBAY
I
. " patients out of a population of 8
crore, and put ’sputum positive
Patna
cases requiring close institutional
care at 3 lakh in Bihar.
OlHAR is, perhaps, a firstBihar Health Minister Sudha
. Department officials are now
Oclass example of high
Shrivastava admitted that the
sure that because of the laxity of
handed bureaucracy coupled
state was about to lose out on the
just one man — the Health Comwith shameless laxity. The TB
project, especially since there
. missioner — to initiate a move,
■ - ?’
'■’Wav
were other states ready with their
capital of India is on the point
Uhe -.grant could be diverted by
proposals
and
are
demanding
of losing out a World Bank aid
the Centre io some other needy'
additional allotment for their own
of Rs. 1,100 crore that was to
.r otate.
action programmes to be in
assist the Centrally-managed
All that World Bank; and
itiated next year.
nationwide ahti-Tuberculosis
. government required was a <
Health Commissioner K. project The reason? Bihar Health
detailed ‘ assessment of - the
Arumugam is not in the eye of
..ground situation onTB in '-Bihar
Commissioner K Arumugam, it
controversy. He is the “very point
- for a -sanctioned amount ef Rs.
seems, has failed to finalise the
of the controversy". The proposal
100 crore per year for the next 10 proposals, thus, forcing Worid . 5
and
■
years, and a further grant of Rs.
Bank authorities to reconsider
government was received by
100 crore for establishment char
the whopping grant.
Arumugam over three months
ges, vehicles purchase, etc.*., _
ago.
However,
he
failed
to
get
As per the Central plan, five
The total annual grant on
the proposal finalised and ac
states having comparatively
Tuberculosis which the Bihar
cepted
by
the
Centre.
higher number of TB cases were
government has been .able to.
selected by the World Bank for
Surprisingly, the proposal was
muster until now is around Rs. 8
implementation of the anti-TB Ac
not even put before Health Mini
VICTIM
OF
BUREAUCRATIC
LAXITY:
A
TB
patient
languishes
in
a
crore in the non-plan head and
tion Programme. Of the five
ster Sudha Shrivastava — a fact
Rs.' 1.5 crore in the plan head as
Bihar hospital
states, Bihar topped the Bank’s
that came to light only when the
against the Rs. 100 crore per
preference list and an unprece
minister convened a departmen
deem it fit to attend the three-day
infrastructure of its existing TB
year grant from the World Bank
dented Rs. 1,100-crore aid was
tal review meeting to assess the
review session, that too, at a time
hospitals or increasing the num
— a project which would have
sanctioned, and was there for
progress made towards control
ber of beds therein.
when the state department is al
come as a nutritive health dose
the state’s asking.
ling TB in the state.
ready strapped for cash, par
The Health Department es for an ailing state .if the proposal
But, as things stand today,
Worse still, Arumugam did not
ticularly, for strengthening the
timated as many as 1? lakh TB
had been finalised.
CHANDRA SHEKHAR YADAV
Name of the Paper
:
LOKMAT TIMES
Published at
i
NAGPUR
. Dated
x
, m'EB 19K
Tuberculosis: A social problem
/ herjXe are unable
V' /
control tubercuo losis despite the
” availability of effecJVC drugs to treat it,indicates
tnal tuberculosis is now a social
problem. The cause of a social
problem may be many and
involves different people includmg doctors, patients, paramedicals, relatives of patients and the
social worker. The rtfcst painful
attitude seen in the approach of
social workers towards tubercu
losis is, the admission of the patiin hosipital. Despite repeaterfandrnnti
.
ill"
Dr R F Jain
uuous health education at all
evels there is no satisfactory
response of patients to the proculosis and concomitant disj er treatment of tuberculosis. easesshouidgohZiXd
^gS
- us look at the problem and
If the anti-TB drugs are admi- Sd
,tS ^)angers and
_a •
.
LHJ11
leSCl tO fnA Hpvplnnmant
emedies available at various
nistered in the right combinalevels.
bon and doses the treatment resistance. These problems can
role of the doctor
be avoided by consulting a TB
1
he patient coming with symp- will be effective. It is necessary
to
explain
to
the
patient
the
regi
’
is suggestive of tuberculosis
Prolonged use of corticobe investigated, keeping in men and side effects
md the problem of tuberculou 8
in India. Once the investiga administered. Treatment by a nm and rn.iid
^®^>ecial.,sl rather than follow- lopment of cavities in°the hin^"
tions■ for
for detecting pulmonary
■
are not conclusive and wfam nnhHr^c npt,on of ^authorised
|t is a usual practice tn tSit
■ KSsdSTJSL. a!“«,*•?“^•■3*.'
SF— SsHSaS
treatment,
investigations
Eit°o^^
investigations for the other
lar
in
their
treatment
organs of the body which could
be affected.
Once the diagnosis of tubercuthe administration of improper
in f
^nt; L
'osis is confirmed, the symp doses
and duration and imoro
J S°^l Ca?^S 11 has been
toms pertaining to other dis- per combination of various °bserve.d 11131 ,niection Strepto^es like diabetes, enteric dmgs. It is not uncomm™ m E ’S
f<>r years
ever, hepatitis etc are not to be find some qualified medical
311(1
When
Patient
verlooked. Treatment of tuber- practitioners prescribing many
7?’S p^act,ce needs to
H eovnumg many be discontinued and if necessa-
ot^er inJectoble vitamin pre
parations could be prescri lid.
Before prescribing drugs to
patients whose sputum test pro
ves TB positive their case histo
ry should be reviewed, to avoid a
waste of time, money and health.
The patient:
_
ft’
Most often patients approach
the doctor for treatment in the
(advanced stages of TB. One way
of detecting TB early is to take
cognisance of symptoms like'
cough fever, pain in chest,'!
breathlessness which do not res
pond to usual treatment. Should!
this problem occur the patient
should gel himselfor herself trea
ted immediately at a TB hospital
er any other medical centreio
avoid damage to the lungs which
: is the most vital organ 'for
4 respiration.
Patients should not stop or
change their treatment without
the Jmowledge of the doctors. It
reasons for the abrupt intetnr '1
in treatment by patients j
attitude of tlie staff at i
the TB clinic, the general practi- I
boners and the social workers. I
The role of social worker:
I
Social workers have a major role I
to play in curbing the spread of i
TB through their involvement in i
health education programmes f
at the local and community level, f
Whilst it is easy to treat TB It f
is difficult to cure tuberculosis >•
for want of proper treatmentJpf-F
lowup and co-operation /ofpatients. Let us make it ouries-F
ponsibility to erradicate TB. . ’
..... '
Name of the Paper
Published st
Dated
:
MADHYA PRADESH CHRONICLE
:
BHOPAL
1
1 2 DEC 1993
(City Edition)
TBfunction
in women
'
Expterts discussovarian
occurs but only in {
I
-i
V vyZfur Staff Reporter
2 percent there is tuberculous in- 'j
BHOPAL: On^ of the important volvement of the ovaries. Re- ->;,
and emotionally most disturbing search has disclosed that the manifestation of .tuberculosis ,reproductive
WK(
v malfunction
,VW1W1I tw
lxz ■;
is due to
among women in the child bearing
hypothalmus in the brain in 31 /
i irnanrn in
__ _
age is Ihn
the Hiol
disturbance
in tho
the i < ipercent hyperlactemia
in 41 per- ;
reproduction function. Speaking cent ovarien hypofunction in 28 ■
■at the 48th National Conference percent, and is reversible in most
on Tuberculosis and Chest Dis cases with proper treatment.
...i
eases in Bhopal, Dr (Mrs) SN
Dr DDS Kulpati delivered the
Tripathy disclosed that in 84 per- prestigious
uyivwo ,Ranbaxy
lcl„uaAy MVMCI
WVI, ...
Robert„Koch
linrt Oic_
cent women* disturbance of the ■<1 ora{j0n r»r»
on InfarcKlial
interstitial ILunp
Dis- '
eases, based on his extensive ex
perience in the Lok Nayak
Jaiprakash Hospital in New Delhi.
He pointed out the problem in
volved in clinical assessment of
these cases, which mimic pul- ;
monary tuberculosis closely. Their 1
management with steroids and
immunsuppressants and poor '
, prognosis were stressed.
A ray of hope for the chronic ■
failure patients who have multiple
drug resistance but cannot be i
treated with the very costly and
mostly unavoidable reserve drugs
was given by Dr Baldev Raj from ■
Rohtak who showed very , en
couraging results with artificial
• pneumoperitoneum, a therapy
widely practical in the nineteen
fiftees and now largely given up.
u^s|fei
THURSDAY AUGUST 5 1993
Indian Express
afflicts poor Faniyas
1 and unremunefative areas here
with a predominantly tribal
A PPU AND his sister
concentration are being ,
ZA Koyma wonder which will
increasingly shunned by doctors:
-8*. kill them first: The
There are about 16 Primary
tuberculosis that has already
Health Centres in such locales still
gnawed them down to wheezing
abegging for doctors. Even the
bundles of skin and bones, or the
only Central Governmentspectre of starvation looming
sponsored Tribal Health Centre
closer each miserable day.
in Manantavady with 100 tribal
The lethal disease has ensured
patients a day, has ceased
that these two young Paniya
functioning for the same reason.
tribals ofNenmeni Kunnu never
Then there is sickle cell
again toil in a settler’s farm
anaemia, the crippling, killing
nearby, as they had been doing
genetic scourge which an
since childhood. Their sole
unestimated number of tribal
lifeline to survival now is the Rs
families reel under - in some
,
20 or so which Appu’s wife ekes
instances those hit by TB as well.
out, on her especially lucky days.
£Like that of Kannady, of
But in this poverty-stricken '
Noolpuzha: More than the pain
tribal hamjet in Wayanad, the
typical of the disease's peak that
plight of these two - condemned
has now permenantly confined
to he m their squalid, fly-infested
him to the damp mud floor of his
Si
hut - is nothing unique, not even
crumbling home, what breaks him
special. Men die a living death
is watching his.three-year-old
flies live on. And most do not ’
daughter, already a TB patient,
even know what better to expect.
withering by the day.
No one knows just how many
The only known medicine for
among the district’s roughly
sickle cell anaemia - albiet of
1,30,000 tribals have TB, or how
unconfirmed utility - is hydroxy
many it might have actually
urea, which costs a whopping Rs
decimated thus far. Guestimates
nrPP“„“n_lJl1S ®*Ster Koy["a’ boJh afflicted with tuberculosis^
251 per week’s course and is
vary sharply, while local
of starvation since the
are haunted by the spectre Sported. Many tribals now beg,
lethal disease has rendered them unfit
authorities scoff at apprehensions
or pawn“ their
U
’ ‘ lands
‘ to
to eke out a living. borrow
Express photo.
even as no comprehensive
enterprising settlers to buy this for j
four was found afflicted with the
screening has been done yet.
National Institute of
their stricken kin. Like
.' j
But available indications are, in disease.
ds severe as being apprehended:
Tuberculosis, has no lab, no
Mathevan, a Kuruma tribal of . ? j
The
district
TB
officer
told
this
any case ominous: Sources at a
time med’cines from the
aiagnostic equipment and not
Kottoor who lost his daughter to
correspondent that he was still to
chantable hospital, which
CGHS reached him was in March the disease last month and is now
even
the
compulsory
minimum
see
all
the
test
reports
of
this
concessionally screened 81 tribals
last, that too only a quarter of the trying to save his only son.
oiarr.
’
group, but added there was
ofNenmeni Kunnu as a
year’s needs.
Worse
still,
the
young
doctor
The proud owner of over an
precious little his office could do
humanitarian gesture last week
acre of paddy fields once, his
forrUeaStowhathewilldo
anj'way. He had never received
said that almost one out of every
But at least he is determined to
•or medicines m case the TB
children’s disease has already
his mandatory training at the
stay
put
and
try,
unlike
many
threat is eventually detected to be
reduced him to a famished
others. As a rule, impoverished
labourer
kalpetta
llllill
I wy
toHO .
The
Economist
MAY 2OTH-26TH 1995
DEINVENTING GOVERNMENT
MURDOCH'S MEDIA
page 15
pages 17 and 43
page 31
MENEM AGAIN
pages 18 and 50
?X2...
{Jirharns •!&
Ai^trw .
A^o OeninM .
CoXMW .OM?90 if«ianrf . iKr2M) Kenya
KjInlOO Ni^fia . Niitf.i’W) Pcxtuftdl
£xr.fc>20
.. ... PTASSSG (Uf
Bahrain .. i>Sh4f
eqypt......... U18 G»e*x.<?
C.R0900 IwkmO
iR.{7 ?« Uix<?wno-»*; LfrtSS ?4qrww.. ..
. .Riyal 35.00 Sweeten....... $fcK32 UK .
won
Bef<jiu;n . fiFtS? Finiand.
. HM24 Haiiond . Hfi8.75 iiWl .......... MlSt? MoMa
l.ml AS
. .IMS.SO Souci ArobaSwitwlsnri.5lr7.?O USA.
..Vicao south Afr«A.fU5 50 TutM>y . 71^.000 7ifr.Hatnw?. Z$23 00
Qpm. . <(2.20 Ft.sfo
FW6 Hs»nna*y.
HASO .’tau. ure 7.5W>
MAt zUTH 1995
Economist
Disease fights back
T? BOLA is a terrifying illness. It kills quickly.
JD Nine in every ten of those who become in
fected die, and it is an especially hideous
death. Thanks to its speed and gruesomeness,
this virus has commanded front-page head
lines all over the world in recent days. Sleeping
sickness—which can be just as deadly and
whose spread across large parts of Zaire is vir
tually unchecked—has commanded no such
attention. This is not so surprising: Ebola is
new and untreatable, sleeping sickness is old
and treatable—merely untreated. The outbreak
of Ebola in Kikwit has so fer claimed about 100 victims; sleep
ing sickness kills 200,000 Zairois a year.
Established and curable diseases are doing fer more harm
to people than new diseases. What is worse, their strength is
growing, not fading. These diseases do not, by and large, kill the
affluent westerners who now shudder at Ebola. But they
should, at least, prick their consciences. In due course, these
diseases may do far worse than that.
Never look away
The problem humans have with germs is that they work by
rules that humans find hard to deal with, rules so different that
before Pasteur no one knew what they were. Germs are quick;
humans are slow. Germs have no thought for the future;
humans plan. Germs have no technologies; humans are con
summate users of tools. Most important, germs never give up.
Humans do so all too readily.
For centuries staphylococcus bacteria made trivial wounds
fetal injuries. Then science came up with a tool to use against
them: penicillin. In 1952 staphylococcus bacteria were almost
100% susceptible to penicillin, and the scourge became an irri
tant. By 1982 90% of the strains had become resistant to the
drug. Clever humans, not unduly worried, changed tools. The
germs developed resistance to the new ones. Now, only one
safe drug can be relied upon to fight staphylococcus:
vancomycin. Other bugs are already resistant to it; their rele
vant know-how, bits of information encoded in dna, may be
all too easily transfened. Then the game will be back to square
one—except that fer more people undergo surgery now than
before antibiotics made it safe. In 1992 4% of Americans who
underwent surgery became infected. Most of those 920,000
people were infected with staphylococcus.
In late 18th century Europe, tuberculosis killed perhaps one
in five. Careful use ofantibiotics gradually put paid to it. After a
while, the world decided that the fight was over; but no one
told the tuberculosis bacillus. In New York city, spending on
tuberculosis fell from $40m in 1968 to $2m in 1989. The cuts hit
outpatient work, so no one was there to ensure that the sick—
often homeless drug addicts—took their medicine properly.
That let resistance bloom. By the beginning of
1991 almost half of New York’s new cases of tu
berculosis were resistant to the two main drugs
previously used, and the costs of hospitalising
people with tuberculosis in the city had
reached $50m a year.
Many problems fail to yield to public
spending. Tuberculosis in America is not one
of them. National surveillance worked well
until the 1970s. When, against expert advice,
responsibility for this work was given to the
states, the programme fell apart. In 1986, just as
the comeback was getting underway, the multi-drug-resistance
unit at the Centres for Disease Control in Atlanta was closed.
All told, cuts in tuberculosis programmes during the 1980s
saved America perhaps $200m. According to one estimate,
America spent more than $1 billion on multi-drug-resistant tu
berculosis in the five years up to 1994.
America stands out only because it is rich enough and
knowledgable enough to lack excuse. But similar stories, and
worse, have unfolded around the world. In developing coun
tries, most cases of tuberculosis could be cured with drugs that
cost as little as $13 a patient. Yet, worldwide, less than 50% of
detected cases are being cured. There seems no fundamental
reason why the world should not achieve a success rate of at
least 85%. Clinics in Somalia already do. The World Health
Organisation, itself in dire need of reform (see page 83), esti
mates that cheap, systematic interventions might save 12m of
the 30m likely to die from tuberculosis in the next ten years.
More surveillance and better use of resources is only part of
the answer. Some new diseases will need new treatments. Un
fortunately, work on these tends not to start unless the diseases
attack the rich. Antibiotic research has been neglected while
drug companies turned to chronic diseases of the old and
wealthy, which are far more profitable. Some perfectly good
antibiotics have even slipped out of production because only
the poor needed them. All the same, there are areas where
humans can fight back; and they may even learn to play by the
germs’ rules. Antibiotics may well in future be developed using
the same random but effective evolutionary techniques that
give germs the power to develop resistance; the harnessing of
such methods in the test tube is one of the most potent new
approaches to pharmacology. And new data networks could
make the infrastructure of surveillance possible to build even
where little physical infrastructure exists. That will let people
pool their knowledge, much as the germs transfer their villain
ous coils of DNA.
However, the wonderdrug mentality that allowed human
ity to see antibiotics as a once-and-for-all solution, rather than
a tactical victory that needed following through, should not be
allowed to return. Final victories, if any, will be few and far
between. This is a race with no foreseeable end.
Evolution is a response to changing environments, and the
human environment is changing with unprecedented rapid
ity. Ecosystems are being altered across the planet. Climate
may be changing too. People are cramming themselves into
vast cities, and travelling between confine with niiherto un
heard-of ease. These changes may not have much effect on hu
man evolution—at least not yet—bufthe evolution of germs is
vastly quicker.
New diseases like Ebola may be less threatening in them
selves than as harbingers of activity in the microbial world
within. The chance that a plague from Kinshasa will bring the
world to its knees may be small this time. But if the world fails
to pay attention, next time could be worse.
SCIENCE AND TECHNOLOGY
Perverse response
Deaths*
1990, $m
1990, m
11...
0.4
o.a
____________
1.6
AIDS
Leprosy
Leprosy
Tropical
diseases
—1
Malaria
TB
TB
nr WO years ago the World Health OrgaJL nisation (who) declared tuberculosis a
global emergency—an unprecedented step.
Tuberculosis was, by that time, killing more
adults than any other infectious disease.
Unfortunately efforts to halt its resurgent
spread have had only limited effects. In
1990 tuberculosis was responsible for 2.5m
deaths at all ages. By 2005 the figure is ex
pected to be nearer 4m. However, stemming
the problem is not seen as a high priority. As
the chart shows, tuberculosis is as easy for
foreign-aid donors to ignore as it is for poor
people to die of.
In rich countries, the discovery of antibi
otics and the spread of health-care systems
robbed tuberculosis of its terror from the
1940s onwards. Levels of the disease fell
steadily. Its return in the 1980s was due to a
number of different factors undermining
that progress: aids, fractured health-care
systems and drug resistance.
The tuberculosis bacillus thrives in peo
ple infected with the human immunode
ficiency virus (hiv) because they lack the
THE ECONOMIST MAY ZOTH 1995
immune cells to keep the tuberculosis bacte
ria at bay. People who are “immunocom
promised” are perhaps 25 times more likely
to contract tuberculosis. If they are already
infected but not sick (as many people are)
the erosion of their immune system will al
low the disease to take hold. Once people
are ill, the disease begins to spread—and it is
much easier to catch than hiv. A rise in lo
cal cases of tuberculosis is often the first clue
that hivhas arrived.
Poor health-care systems make it more
likely that people with tuberculosis will die.
They also increase the spread and potency
ofthe disease. Ifsick people are on the street,
not in the sanitorium, they are more likely
to infect others. And a lack of consistent
health care makes the disease grow hardier.
If the antibiotics that kill the bacterium are
not taken according to a strict regime, which
will often be the case if there is no supervi
sion, the bugs may develop resistance.
Many of them already have. This worsens
the prognosis for the patient and drives up
the costs of treatment. More analysis has to
be done to see which drugs will work in
which cases.
The who believes that if health workers
simply made sure that drug regimens were
strictly adhered to—in a programme the
who now describes as “directly observed
treatment, short-course” (dots)—the tuber
culosis crisis would be slowed down signifi
cantly, and drug resistance brought to some
extent under control. The logic seems cor
rect. But there have been few successes.
Tanzania offers one. In the late 1970s
Karel Styblo, a Dutch physician, convinced
the authorities to treat the disease with a
cocktail of antibiotics. This increased the
proportion of victims cured from 40% to
nearly 80% in 1990. When, in the early
1990s, tuberculosis looked like becoming a
serious problem again, the authorities were
quick to act, increasing their vigilance to
make sure infections were dealt with. It cost
Tanzania up to $10 per life saved and $3 per
new infection avoided.
China, home to a quarter of the world’s
tuberculosis cases, has recently stepped up
its supervision of patients and changed the
way treatment is paid for. Doctors now
make money by curing people, not by sell-
160
120
;
I
- - -~T\|
Diarrhoea
Malaria
Source World Bank
Join the DOTS
40
0
AIDS
Tropical
diseases
Diarrhoea
Tuberculosis
Fundingr
1
|
-
D
’Adutti and chiMran ow 5 y«ar»
ttxwnai aid flow*
ing drugs. Around halfof China has enterec
into the dots programme; 90% of patient
treated since 1993 have been cured, at a cos
of $100 per patient. Each sufferer so curec
might have infected 10-15 other people hat
the disease run its course.
In New York city the number of tubercv
losis cases soared in the 1980s as public
health services deteriorated and Hivbegar
to emerge. In 1991 the city started sendin
outreach workers to patients’ ho
anc
workplaces to make sure they c^..4pliec
with their prescriptions. Around 40% of th
city’s tuberculosis cases are now under th
dots regime. The caseload stands at 3,00C
a decline of 15% since 1992.
In the rest of the world, though, tubercu
losis continues to rage. Twenty of the 2
countries in central and eastern Europe anc
the former Soviet Union are seeing a resur
gence. In most of Africa and Asia rates of in
fection are increasing. In America dots ha.
been extended to only 17% of the caseloac
outside New York. And responses to the dis
ease that are less than helpful are still bein
practised in many places: the treatment c
infected people with anti-tuberculosi
drugs before they become sick, which is
good way to breed drug resistance; ventila
tion systems which, while providing pa
tients with fresh air, also spread the diseas
further; and x-rays to reduce the ; :tior.
which do no good.
The dots strategy is an improvemem
but it will certainly not eradicate tuberculc
sis. The only global eradication mankinc
has yet engineered has been of smallpo?
which was a much easier challenge. Ther
was an effective vaccine, and the paths of in
fection were relatively controllable. Th
bcg vaccine for tuberculosis is effective pn
marily, if not only, in preventing non-infec
tious forms ofthe disease in children. It can
not stop the spread of adult pulmonar
pneumonia. Yet eradication is not the onl
way to make the world better. According t<
the who, as many as 12m more people wii
die over the next decade from tuberculosi
without worldwide dots than would witi
it—and at the end of that grim decade, ther
will be yet more resistant strains ofthe virui
It sounds like something to avoid.
Slje ^'cw llork eimes
MONDAY, APRIL 3,1995
Editorial
Tuberculosis Resurgent
Health professionals are losing the struggle to
control tuberculosis, an infectious disease that will
kill some three million people this year, mostly in
poor nations but increasingly in wealthy societies as
well. The woefully underfinanced campaign has had
only scattered successes around the world. Worse
yet, skimpy or misdirected programs in many
countries may inadvertently be spreading the dis
ease, thus doing more harm than good.
That tragic development does not mean health
professionals should give up the fight and let nature
take Its devastating course. The only sensible re
sponse is to refashion tuberculosis control pro
grams and boost their funding by the modest
amounts needed to make them truly effective.
Tuberculosis, once a leading cause of death In
North America and Europe, had seemed on the run
since mid-century, thanks to improved living condi
tions and antibiotics. But recently it has resurged as
nations let down their guard, leaving tuberculosis
“the world’s most neglected health crisis,” in the
opinion of the World Health Organization.
The resurgence has been accelerated by AIDS,
which weakens the immune system and allows
tuberculosis to fulminate. It has also been fueled by
inadequate TB-control programs that fail to admin
ister the right mix of drugs over the prolonged, sixmonth course of treatment In many nations, pro
grams are just good enough to save many victims
from prompt death but not good enough to cure
most of them. They survive to spread the infection,
often in a new form resistant to antibiotics.
The most effective tactic for controlling the
spread is “directly observed treatment,” in which
health workers provide the required medicine to
Infected people and watch them take it That ap
proach has already succeeded in curing sick pa
tients and thus cutting the rate of transmission in
New York City, Tanzania and China.
W.H.O. estimates that $360 million a year is
needed to apply the same tactics widely. The devel
oping nations, with most of the cases, would be
expected to supply $250 million, either from new
money or money they currendy spend on lesseffective control strategies.
The industrialized nations would be asked to put
up about $100 million a year, mostly to buy drugs.
That wise investment would not only help the poor
countries, it would cut transmission to the rich
countries as well Already a third of this nation’s
new TB cases are among foreign-bom residents,
and the percentage is expected to rise. The best
place to defeat this epidemic is at the source, before
migration and international travel spread the dis
ease far and wide. This is one foreign aid program
that would clearly pay health dividends at home.
SCIENCE
VOL 267 • 24 MARCH 1995
News & Comment
INFECTIOUS DISEASE
WHO Calls for Action Against TB
In the movie Outbreak, an exotic virus
breaks out of Africa, killing everyone it in
fects. In real life, however, pathogens don’t
have to be exotic to cause a deadly epidemic.
In a report released on 20 March, the World
Health Organization (WHO) reveals that an
old scourge—tuberculosis—is still rampag
ing out of control despite the organization’s
2-year-old campaign to prevent its spread.
Even more chilling, drug-resistant strains of
Mycobacterium tuberculosis, the bacterium
that causes TB, are on the rise.
To combat these outbreaks, the WHO
report, entitled “Stop TB at the Source,” rec
ommends international adoption of a con
trol strategy called Directly Observed Treat
ment—Short-course (DOTS), which aims
to ensure that all patients complete their full
course of treatment. Without an effective
treatment program, WHO predicts that by
the year 2005, TB will kill 4 million people a
year—up from about 2.5 million. The toll
could be even worse if the multidrug-resistant strains continue to spread.
The upswing in incidence of TB is being
fueled by what WHO spokesperson Kraig
Klaudt calls “worldwide medical chaos.” In
the West, efforts to combat TB have largely
slackened off due to the mistaken belief that
the disease was brought under control with
the introduction ofeffective drugs in the 1940s.
In fact, the epidemic had simply been pushed
into the poorer reaches of society—the in
ner-city dwellers and the homeless—and is
now re-emerging with a vengeance, partially
fueled by the spread of the AIDS virus, which
increases susceptibility to TB. Governments
in developing countries, says WHO, have
been slow to channel resources into TB con
trol, even though studies show that in terms of
productive lives saved it’s cost-effective.
Because only patients with active TB can
transmit the disease, WHO argues that con
trol programs should focus on people with
symptoms—usually a chronic cough—rather
than waste resources on screening programs
that also pick up patients with inactive forms
of TB. “It’s the cough that spreads the dis
ease,” says Paul Nunn, WHO’s chief of TB
research and development. “The cough to
TB is the same as sex to HIV.”
But TB treatment requires taking antibi
otics for a full 6 months. Symptoms abate
within a few weeks, however, and patients,
thinking they are cured, may stop their treat
ment, allowing the disease to spread and en
couraging the emergence of drug-resistant
strains of TB. To stop that from happening,
WHO is campaigning for governments to
adopt the DOTS treatment strategy: Use
trained health workers to check that patients
take every pill, and supply free drugs and
4
■>
other incentives to en
sure that patients fin
ish their treatment. “TB
control is basically a
management problem,”
says Thomas Frieden.
< 2.5
head of the New York
2.5-10
City Health Depart- 2S2 10-35
ment’s Bureau of TB
35 “70
Control. Frieden should Ml 70-100
100+
know, because N ew York
is one of the few places
in the world that has
turned its current TB
epidemic around. In the past 2 years the
number of new TB cases has been reduced
more than 20% to about 3000 by using the
DOTS regimen, as well as treatment incen
tives such as free subwav tokens.
Despite New York’s best efforts, however,
“a handful of patients are resistant to all
[anti-TB] drugs,” savs Frieden. To curb the
resurgence of those lethal strains of TB, since
1993, the city health department has re
sorted to placing patients who persistently
refuse to complete treatment under “deten
tion until cured” in the hospital.
A xe-
WgE
'I
1
o
D
IX
3
z
£
<
TB breaks out... again. The map shows that
TB is re-emerging worldwide. (The scale num
bers indicate deaths per 100,000 people.)
In developing countries, says Nunn, “the
chances are that multidrug resistance is less
of a problem,” because patients are more
likely to go untreated than to receive par^1
treatment. Hot spots of resistant strains h
been identified in India, Brazil, and some
other developing countries, however. TB
strains have no respect for international bor
ders, notes Nunn, which is another reason
that “governments need to be made aware
that TB is a huge problem [for which] there is
a cost-effective treatment.”
-Rachel Nowak
Apnqs puw Bouejojoj x»uosjo<i anoA aoj noX 01
J»utoq oy Adoo oqotjd Him : OHO - XSO-IOOfl
2 0 Mar 1998
DSLH!
V/
.^(3 IT5
tuberculosis, the WHO estimated that three
1 million people died from the disease in 19 ).
-more than aPt the peak of the TB ep.dem.es m the
M
T'
'J (S’-. 5- 10
TB THOU
Tuberculosis kills a thousand Indians'every day, yet f
to check the alarming spread of the silent scourge,
ease the WHO has ever classified as a global emer
gpncy’
a classification which confirms that we are
at war with a terrible enemy.
;
USX... ngh.
«
less cured Infectious cases are considered to be those
amined under a microscope. These patient are
short course chemotherapy are at least 95 percent
effective in treating these sick fiatl‘!ntsm’l0WTp/aSt
ment is interrupted or incomplete, the bacilli in a
person’s lungs can survive, multiply, or form a more
dangerous form of TB known as Drug Resistant TB.
Such a person is very likely to have a relapse again
and infect others. Only, this time the same medicines
may not work.
Desperately seeking drugs
It has been more than thirty years since a new TB
drug has been brought to the market. There is no cure
for some multi-drug resistant strains. If the
ic continues to be neglected, the future generations
will remember this decade as the time when
ity allowed deadly bacilli swarming the air to become
drug resistant and incurable, throughout the world.
The n^om^oAhe world’s health care systems are
doing a poor job of curing TB patients. In many' C9U£’
tries patients are diagnosed only on the basis of X
Kay shadows. As a result, many people with other lung
diseases or those who have had TB in the past but are
now cured, have shadows on their X-rays and are in
correctly diagnosed with tuberculosis. WHO recom
mends that health workers should look for actual I B
bacilli rather than just shadows when diagnosing
•
Many countries are still not
of
course chemotherapy to treat their patient^ They^of
where treatment practices are accomplishing nothing
other than creating drug resistant TB F°r exampk
in a survey of 100 doctors in Mumbai, it was found
that up to 80 different drug combinations were being
used — most of which were inappropriate.
X.r.1 »e.kf worth of modloM-
T,«
too much public health money is spent on health expenditures in developing countries - such' as heart
^significant share of the health budgets in many
developing countries is spent on expensive medical
services that benefit only a few members of society.
The World Development Report, 1993, concluded that
on highly cost-effective health interventions that could
save tniilions of lives. One ol the findings of the re
port is that tuberculosis is among the most cos efit (live
diseases to control in adults over the age of 15 years.
The WHO estin
of donor governn
ed each year fronfight TB in poore
foreign aid progrt
8 million new TB
The American i
the United State
TP
TROUBLE
thousand Indians every day, yet precious little is done
■ing spread of the silent scourge, laments Dr MM Puri
5/
■s spent on health ex■ries — such as heart
oncers.
is left over to spend
erventions that could
e findings of the rethe most cost effective
r the age of 15 years.
cases cost the country approximately $700 million.
Nearly one third of these US cases were foreign born.
These figures have led the US Center for Disease
Control to stress the importance of investing in glob
al TB control as a means of eventually reducing the
number of domestic TB cases.
Bitter pill to swallow
The WHO’s strategy for curing TB patients is to use
directly observed treatment, short course (DOTs). DOTs
is a system where health workers watch as each pa
tient takes the correct medication. Health workers must
watch their patients actually swallow each dose of med
icines.‘This supervision must continue every day for
the first two months and, ideally, for all six months of
treatment.
By using DOTs one can almost be certain that TB
patients will be cured. It is the key to stopping the TB
epidemic. This also prevents the development of re
sistant TB germs to the few drugs available for treat
ment of TB.
In our country, the National Tuberculosis Control
Programme was started in 1962 but has not made
much impact on the epidemiology of Tuberculosis. An
evaluate ion of the National Tuberculosis Programme
(NTP) in collaboration with the WHO in September
1992, detected the following anomalies:
• Weakness of the Central level
• Diagnosis based mainly on X-ray shadows with
out bacteriological confirmation
• Lack of coverage of TB treatment in the primary
health care network
• Multiple and inadequate treatment regimens and
irregular supplies of drugs
The consequences of these factors were abysmally
low treatment completion rates of 25 per cent on an
average, a low proportion of infectious cases among
patients diagnosed with TB, and complicated health
seeking behaviour of patients — who hopped between
the public and private sectors. All these contributed
to high default rates, and to the emergence of drug
resistance.
Global red alert
In 1993, the World Health Organisation declared
Tuberculosis a global emergency. Operational targets
were pegged to cure at least 85 per cent of the cas
es diagnosed and to detect 70 per cent of the esti
mated incidence.
To achieve rapid progress towards these global tar
gets, technical support from the WHO Global TB
Programme was concentrated in priority countries —
those with large number of cases.
The Indian government adopted the global strate
gy for effective TB control and tested this strategy as
a development of the Revised National Tuberculosis
Programme (RNTP), both in metropolitan and rur
al areas, with directly observed short course intermittent regimen. The results were very encouragingCure or completion rates of over 808 and bacterio
logical confirmation of over 50 per cent among the
diagnosed cases of tuberculosis. The strategy now cov
ers a population^of 12 million and will expand to 20
Financial support for this is provided by the
Government of India, loans from the World Bank and
and ODA. It is-hoped that the
BNTP wiR cover all of India in less than ten ‘yearls!
India alone contributes to one third of the TB cas
es m the world. As in the past, the world is now fo
cused on tuberculosis control in India. The future of
tuberculo8!6 in India, and by extension in the world
foreign aid programme spent just $ 14 million to fight
8 million new 7 B cases in developing countries
1 he American Medical Association estimates that in
the United States alone that same year just 26 000
’ J
’
DOCl’OST-CBD: This photo copy is being supplieC
, _
_uu- nftrsonal reference and study
Patients and the community in general.
rrh
(The author is a Senior Specialist at the
^am SaJuP tnst^e of Tuberculosis
Allied Diseases, New Delhi)
I
I
26
P. JAGOTA ET AL
chemotherapy period and as against sputum
conversion rates of 82% and 94% respecti
vely, obtained in controlled trials of these
two regimens (TB Chemotherapy Centre,
Madras, 1966 and 1964) a difference in
bacteriological conversion of about 20-30%
being observed between clinical trials and
programme conditions.
Though the two studies may not be con
sidered strictly comparable, it is observed that
the acceptability and final result are far
superior with short course chemotherapy.
(TB), Karnataka at LWSTC, to Dr. S.
Hanumanthappa, Medical Officer and all the
other staff of LWSTC who assisted in conduct
ing the study, to Mr. B.K. Keshavamurthy,
Mrs. A. Korah, Mrs. Victoria Lalitha, Mr.
B.A. Eswara and Mr. N. Narahari Rao,
Health Visitors of NTI, Mr. M.V. Jaigopal
of the Statistical Section of NTI and all
the other staff of NTI who participated in
the study, to Mr. P. Perumal for the secretari
al assistance, and to Dr. Sudha Xirasagar,
Medical Officer, NTI who assisted in drafting
the report.
?
1
I
The authors are grateful to the Govern
The outcome of SCC in patients with
initial Isoniazid resistance (without histor of ment of Karnataka for having supplied the
previous anti-TB treatment) deserves a brief drugs required for the study.
mention. Over 60% of such patients were
REFERENCES
converted, most of them having also achieved
a satisfactory level of treatment compliance.
East African/BMRC; Controlled Clinical Trial of
four short-course regimens of chemotherapy for
Ignoring the initial drug sensitivity status,
two durations in the treatment of pulmonary
tuberculosis. Tubercle; 1980, 61, 59-69.
out of the 225 patients put on SCC and
assessed at the end of chemotherapy, 84% Daily, G.V.J. et al; A Concurrent Comparison of an
unsupervised self administered daily regimen
became bacteriologically negative, and of
and a fully supervised twice weekly regimen of
them, 16% relapsed over the next 16 months.
Chemotherapy in a routine out patient treatment
It is possible that other sturdier short
course regimens will achieve even higher
acceptability and sputum conversion and,
especially, lower relapse rates.
Acknowledgement
The authors are grateful to Dr .A Banerji
Dr. K.S. Aneja and G.E. Rupert Samuel who
initiated the study, to Dr. Iqbal Begum and
later Dr. B. Krishnacharya, Joint Directors
programme; Jnd. J. Tub.; 1974, 21, 152-167.
Tuberculosis Chemotherapy Centre, Madras;
Isoniazid plus thioacetazone compared with two
regimens of Isoniazed plus PAS in the domici
liary treatment of pulmonary tuberculosis in
South Indian patients. Bull. WHO.; 1966, 34,
483-575.
Tuberculosis Chemotherapy Centre, Madras; A
concurrent Comparison of intermittent (twice
weekly) Isoniazid plus streptomycin and daily
Isoniazid plus PAS in the domiciliary treatment
of pulmonary tuberculosis. Bull. WHO.; 1964,
31, 247-271.
/
T
THE ACCEPTABILITY AND EFFICACY OF TWO REGIMENS OF SHOT COURSE
r
f
Of the 94 patients on Regimen A and 107
patients on Regimen B, 76 and 90 respectively
who achieved bacteriological negativity at the
end of Sth month, were eligible for follow up
till the completion of 24th month after start
of chemotherapy. Patients who did not
report to the centre on their own for any
complaint, during the follow up period, were
actively followed up at the end of 12th, 15th
and 24th months after the start of chemo
therapy.
Of the 76 patients on Regimen A, 9
patients (11.8%) and of the 90 patients on
Regimen B, 15 (16.7%) had bacteriological
relapse during the sixteen months of follow
up. The difference did not attain statistical
significance.
15. Patients in the subsidiary analysis
Patients who were admitted to the core
group of the study but were found to excrete
Isoniazid resistant organisms, pre-treatment,
were analysed separately.
There were 44 cases, 24 on Regimen A
and 20 on Regimen B, who did not give any
history of treatment prior to intake, but ex
creted Isonazid resistant organisms at intake.
Comparison of these two groups for age, sex
and distance from home to Centre did not
show any differences.
Of the 24 patients on Regimen A, 22 and
all the 20 patients on Regimen B completed
either the 3rd or the 4th level of drug collection/intake. Of the 24 patients on Regimen
A, 23 were examined at the end of treatment
and of them, 15 (65.2%) were bacteriologically
negative. Similarly, of the 20 patients on
Regimen B, one died at the end of 7th month
(he was culture negative at 4th month), 17
were examined and 9 became bacteriologically
negative.
?
Thus, of the total 40 drug resistant pati
ents examined at end of treatment, 24 (60%)
showed bacteriological conversion.
Of the 15 patients on Regimen A and the
9 patients on Regimen B who were bacterio
logically negative at the completion of eight
months of treatment, two and five patients
respectively relapsed by the end of 24th
month. One patient (Regimen A) was re
ported dead at the 12th month follow up.
Discussion
The applicability of a treat n jat regime in
programme conditions depends upon a high
level of effieacy in controlled clinical trials,
25
a high degree of acceptability to the patients,
and the resilience of the regimen to withstand
its use under widely varying conditions
prevailing in the different district TB pro
grammes of the country. Hence a three step
evaluation of a regimen becomes necessary
firstly, to estimate its efficacy under ideal
conditions; secondly, to estimate its opera
tional efficacy and thirdly, to assess the
regimen through monitoring of several DTPs
under which it has been introduced on a pilot
basis.
This study presents the acceptability of
two 8-month short course drug regimens and
the consequent bacteriological conversions
observed under the operational constraints
of an urban tuberculosis programme, after
strictly following the recommendations in the
programme manuals. Thus, these findings
represent what can at best be achieved under
programme conditions—the potentials of
acceptability and resulting cure rates. The
operational aspects such as drug costs work
load, etc., in order to achieve this order of
treatment efficiency, will be reported in a
subsequent paper.
It is seen that around 80% of patients
starting on either drug regimen completed
optimum treatment (i.e. more than 80% of
drug intake or collection). Only a small pro
portion of patients did not complete satis
factory level of treatment. The bacteriologi
cal conversion in either regimen was of the
order of 91% as against almost 100% obtained
in controlled clinical trials. In this study
relapse rates within 16 months after stopping
chemotherapy were of the order of 12% and
17% respectively for Regimens A and B, the
difference failing to achieve statistical signific
ance. , These regimens had shown a relapse
ia
ic ui
rate
of about 7% under controlled trial conditions.. Thus it could be seen that both
bacteriological conversion and relapse rates
are quite close to rates observed in controlled
trials.
A similar study was conducted at the same
Centre, in 1973, in order to study the accepta
bility and bacteriological conversion of two
conventional drug regimens of one year dura
tion—the daily self-administered Isoniazid and
Thiacetazone (TH-Ri of DTP) and supervis
ed twice weekly Streptomycin and Isoniazid
(G.V.J. Baily et al 1971) (SHTW) In this
study only 56% of patients put on TH, and
31% of patients put on SH two completed
satisfactory treatment (i.e. more than 80% of .
treatment). Among the patients who initiated
treatment, 60% of those initiated on TH and
68% of those initiated on SHPW were ]
bacteriologically negitive at the end of
24
P. JAGOTA, et al
put on Regimen A and 92 patients (i.e. 87%)
on Regimen B were examined. The bacterio
logical status at the end of each period is
given in the Table.
them with an MIC of 5 p.gm or more). There
were no deaths.
14.6 Bacteriological response to treatment as
related to level of drug collection
There was radiological improvement in
93% of patients on either regimen. However,
lesions healed by complete clearing in 6% of
patients on Regimen A and 21% of patients
on Regimen B, the difference being statistic
ally significant.
Table 7 presents the bacteriological re
sponse to treatment as related to level of
drug collection.
It is observed that about 87% of patients
on Regimen A and 92% on Regimen B showed
a favourable response, judged bacteriologically. Of those that continued to remain
bacteriologically positive, only three patients
excreted Isoniazid resistant organisms (all of
Radiological response to chemotherapy :
14.7 Bacteriological relapses by the end of 24
months after the start of chemotherapy
Table 8 presents the bacteriological
relapses (among patients bacteriologically
negative at the end of chemotherapy).
Table 7
Bacteriological Response to Treatment as Related to Level of Drug Collection
Culture and
Sensitivity
Level of Drug collection
---------------------------------------------- 1----------------------------3
4
2
1
Total
Regimen A
Negative No.
%
Positive
Sensitive
Resistant
Dead
Not Examined
1
2
7
66
5
4
1
6
4
2
76
(87.4%)
11
8
3
6
1
7
94
Total
Negative No.
%
Positive
Sensitive
Resistant
Dead
Not Examined
Regimen B
10
4
4
2
2
2
2
90
(91.8%)
8
8
2
5
2
9
3
77
107
Total
Table 8
(Bacteriological Relapses among Patients with Culture Negative at the end of Chemotherapy)
initial Culture
Status
Regimen
No.
Eligible
Sensitive
A
B
Both
76
90
166
Resistant
A
B
Both
15
9
24
Sensitive &
Resistant
A
B
Both
91
99
190
Relapse
No.
%
9
15
24
2
5
7
11.8
16.7
14.5
11
20
31
29.2
12.1
20.2
61.3
23
THE ACCEPTABILITY AND EFCICACY OF TWO REGIMENS OF SHORT COURSE
It is observed that 73 (77.7%) patients on
Regimen A and 81 (75.7%) patients on
Regimen B completed the 4th level of drug
collection i.e. they completed more than 80%
drug intake in both the phases. Only 12 of
the total 201 patients on either regimen com
pleted only the 1st or 2nd levels of treatment.
I
14.5 Bacteriological response during and at the
end of treatment
Table 6 presents the bacteriological status
of patients during chemotherapy at the 4th,
7th and Sth months of treatment. At the end
of the eighth month, 84 patients (i.e. 89.4%)
Table 4
Levels of Drug Collection
Proportion of expected
No. of doses/collections
made during 8 months
Level
Regimen B
Regimen A
Intensive
phase
Continuation
phase
Intensive
phase Doses
Cont. Phase
collections
Intensive
phase Doses
Cont. Phase
collections
1
(50-79) %
< 80%
15-23
0-5
30-47
0-4
2
(50-79) %
> 80%
15-23
6-7
30-47
5-9
3
> 80%
< 80%
24-30
0-5
48-60
0-4
4
> 80%
> 80%
24-30
6-7
48-60
5-6
Table 5
Distribution of cases in the main analysis by the the level of Drug Collection
Regimen
Regimen A
Level
B
No.
%
No.
%
1
2
2.1
9
8.4
2
1
1.1
3
18
19.1
17
15.9
4
73
77.7
81
75.7
Total
94
100.0
107
100,0
Table 6
Bacteriological Status at the end of 4tht 7th and Sth months
Regimen A
Regimen B
Total
Negative
Positive
Not done
66
11
17
4th Month
83
3
21
149
14
38
Negative
Positive
Not done
73
4
17
7th Month
85
6
16
158
10
33
Negative
Positive
Not done
73
11
10
Sth Month
85
*
7
15
158
18
25
Total
94
107
201
Bact. Status (culture)
4
22
P. JAGoTA, J3T AL
Table 2
Comparison of Cases in the main analysis with respect to age, sex and
distance from Residence to Centre
Regimen A
Age
Sex
Regimen B
Total
No.
%
No.
%
No.
%
12 — 24
25 — 44
45 4-
32
46
16
34.0
48.9
17.0
43
54
40.2
50.5
9.3
75
100
26
37.3
49.8
Male
Female
M 4- F
55
39
94
58.5
41.5
68
39
107
63.6
36.4
123
61.2
38.8
35
43
16
37.2
45.7
17.0
39
54
14
36.4
50.5
13.1
74
97
30
36.8
48.3
14.9
94
100.0
107
100.0
201
100.0
KMs
< 4
Distance
5-8
9 4Total
10
78
I
12.9
201
Table 3
Coverages for Sputum Examination at Check-up
Month
of
Check-up
No.
%
No.
%
4
77
81.9
87*
81.3
7
79*
84.0
93*
86.9
8
84
89.4
93*
86.9
Total cases
94
100.0
107
100.0
Regimen A
Regimen
B
♦Includes sputum collected but found contaminated.
visits if necessary to collect sputum specimens
in order to obtain accurate information on
the bacteriological response to chemotherapy:
Such attempts were not made at the end of
the 4th month, as they would have influenced
the treatment compliance pattern.
14.3 Levels of drug collection
Patients in the main analysis were distribu
ted according to the criteria defined in Table
4. These criteria were adopted to assess the
relative role of intensive phase and continua
tion phase under different patterns of treat
ment compliance.
Compliance Level 1 comprises patients
who in their intensive phase have taken
<80% of the due doses and in the continua
tion phase, less than 80% of their due drug
collections. Thus, for Regimen A, a patient
making 15-23 visits for supervised drug
administration (as against the full 30) and
0-5 monthly collections (as against the full 7)
is classified as “Level 1” compliance. Similar
ly Levels 2, 3 and 4 are also shown in the
table.
14 4 Treatment Compliance
Table 5 presents the levels of drug collec
tion achieved by the 94 patients on Regimen
A and 107 patients on Regimen B according
to the levels of drug collection.
4
21
THE ACCEPTABILITY AND EFFICACY OF TWO REGIMENS OF SHORT COURSE
t
regimen, exclusions and drug sensitivity
pattern. Of the 150 patients allocated to
Regimen A, and 171 to Regimen B, 23 and 33
respectively were excluded from the study as
they did not complete even half the number
of the doses in intensive phase of chemother
apy. Of the 127 patients on Regimen A, 94
excreted organisms sensitive to Isoniazid, 24
excreted Isoniazid resistant strains, and 9
were negative on culture. Similarly of the 138
At the end of the 12th and 24th months, patients put on Regimen B, 107 had drug
patients were also eligible for a 70 mm sensitive organisms pre-treatment, and the
rest were either resistant or negative. The 94
photofluorogram of the chest.
and 107 drug sensitive patients on Regimen A
and B respectively are classified as patients in
All follow-up and check-up investigations the main analysis, and the rest for subsidiary
were done within a period of one week prior
to and two weeks after the exact due date of analysis.
follow-up.
14. Results—Patients in the main analysis
13. Classification of Patients Admitted to the
14.1 Comparison of patients allocated to the
Study
two regimens in the main analysis
The intake of patients lasted from January
Table 2 presents the comparison of the 94
’83 to May ’84. During this period 1,822
bacillary cases were diagnosed. Of these, patients allocated to Regimen A and 107
1,418 patients were excluded, of whom 696 patients allocated to Regimen B with regard
were residing outside the city limits, 695 to initial culture status, age, sex and distance
(38.1%) were not willing to attend the centre from residence to the Centre.
for treatment and 27 did not satisfy the other
criteria for admission to the study. Of the 14.2 Coverages for bacteriological check-up
404 patients admitted to the study, 322 were
classified as core group and the remaining 82
Table 3 presents the coverages for bacterio
patients with history of previous anti-TB logical check-up at the end of 4th, 7th and
treatment, as non-core group. One
C patient 8th month
of the core group was excluded by mistake, on
The 4th month check-up coverages are
grounds of allergy to Streptomycin.
lower than those of 7th and Sth months. This
Table 1 presents the distribution of the is because, at the end of chemotherapy period,
321 patients in the core group according to extra efforts were made by additional home
negative at the end of chemotherapy were
eligible for follow up investigations at the end
of the 12th, 15th and 24th months after admis
sion to the study. At each follow up, one spot
and one overnight/spot specimen of sputum
were collected for bacteriological investiga
tions; history of symptoms and subsequent
antitubercular treatment taken after the eight
month period were elicited.
Table 1
Distribution of Previously Untreated Patients by Allocation to Drug Regimen,
and Initial Drug Sensitivity Status
Total Cases
321
I
I
Reg. B
Reg. A 150
♦
r
I
I
I
I
138
Excluded
23
127
171
Excluded
33
I
I
I
I
J
I
Sens.
94
Resist.
24
Neg,
9
Sens.
107
Resist.
20
Neg.
11
P. JAGOTA, ET AL
20
6. Chemotherapy Regimens
Two 8 month regimens were studied :
(1) Regimen A i 1SHRZ+7TH i.e,
Streptomycin (S) 0.75 g.
Isoniazid (H)
300 mg.
Rifampicin (R) 450 mg. for patients
weighing<50 kgs. and
600 mg. for >50 kgs.
Pyrazinamide (Z) 1.5 g. for patients
weighing <50 kgs.
2 g. for 50 kgs.
Thioacetazone (T) 150 mg.
S+H + R+Zin daily doses as described
above was administered under supervision
for one month followed by H+T in doses as
mentioned above for the next seven months.
H+T was dispensed as monthly supplies,
and self administered by the patient on a
domiciliary basis.
(2) Regimen B : 2SHR-4-6TH
Regimen B differed from Regimen A in
that the initial intensive phase did not con
tain Pyrazinamide and that the period was
extended to two months. The continuation
phase was limited to six months.
7. Compensatory Period
Keeping in mind the crucial contribution
of the intensive phase to the success of an
SCC regimen, it was decided to provide a
reasonable period of time as “Compensatory
Period” to compensate for the missed doses.
To qualify for compensatory period, the
patient had to have completed at least 50%
of the prescribed number of doses within the
originally stipulated period. A compensatory
period of upto 15 days in case of Regimen A,
and 1 month in case of Regimen B was offe
red to patients to compensate for the missed
doses.
8. Defaulter Actions
A patient was considered a “defaulter” ii
he did not attend the clinic on the due date
for administration or for collection of drugs.
For each default, a patient was given a
maximum of two defaulter actions. The first
action was in the form of a letter written and
posted on the evening of the date of default.
If he failed to turn up within the next three
days, a second action i.e. a home visit, was
made. During compensatory phase, no defaul
ter actions were taken.
9. Exclusions from the Study
Patients who did not complete at least 50%
of the due daily doses in the originally stipu
lated period of intensive phase, were exclu
ded from the study. On exclusion from study,
the treatment cards were transferred to the
treatment section of LWSTDC for routine
management under DTP; no further check up
or follow up actions were undertaken for
them.
10. Check-up Examinations
(i) One specimen of sputum each, at the
end of the 4th month and 7th month,
and two specimens (one spot and
another overnight/spot) at the end of
the 8th month for direct smear, cul
ture and sensitivity tests.
(ii) One 70 mm photofluorogram at the
end of the Sth month of initiation of
chemotherapy.
(iii) Brief interview to elicit symptom
status and additional anti-tuberculosis
treatment from other sources, if any.
11. Criteria for Favourable and Unfavourable
Response at the end of Treatment
Death during the treatment period was
considered an unfavourable response. A
patient was also defined to have had an
unfavourable response if any one of three
specimens of sputum collected at the end of
the 7th and 8th months was bacteriologically
positive by culture. If, from any one of these
specimens, Isoniazid resistant organisms were
isolated, the patient was considered to have
developed drug resistance.
However, even if ail three specimens (at
the end of 7th and 8th months) were not
available, the result of the available (one or
two) specimens has been used to report the
response to treatment.
12. Follow-up Procedures After Sth Month of
Chemotherapy
Initial culture negatives were not eligible
for follow up after chemotherapy. Patients
with unfavourable response to treatment were
also not eligible for follow up at 12th and
15th months. They were put on a DTP
regimen and followed up only at 24th month
to ascertain their status.
Patients who
became bacteriologically
♦
THE ACCEPTABILITY AND EIFICACY OF 1WO REGIMENS OF SHORT COURSE
Further, no extra efforts were put in to re
trieve patients particularly for a check-up
examination, before the end of the chemothe
rapy period.
2. Objectives
The main objectives of the investigation
were to study :
(i) the acceptability of two eight-month
regimens of short course chemothe
rapy in terms of initial willingness to
attend clinic daily for two months,
and the actual pattern of drug collec
tion,
(ii) the response to treatment assessed in
terms of bacteriological status at the
end of 8 months after the start of
chemotherapy, and relapses by the
end of the 24th month after starting
treatment,
(iii)* the operational aspects of implemen
ting short course domiciliary chemo
therapy, in an urban tuberculosis
programme.
3.
Criteria for Admission of Patients to the
Study
Core group : All new patients diagnosed
at LWSTDC, Bangalore satisfying the follow
ing criteria were admitted to the study :
(a) Sputum positive on direct microscopy
(b) No previous treatment or not more
than two weeks of chemotherapy
(c) Aged 12 years or more
(d) Judged as bona fide residents of Ban
galore City
(e) Physically fit to attend the clinic daily,
in intensive phase
(f) Without clinically evident liver,
kidney or joint disease, advanced
pregnancy, or diabetes mellitus.
It may be noted that the above group of
patients, by and large, represents the type of
patients admitted to controlled clinical trials,
and as such, the efficacy of the regimen
observed under programme conditions among
such patients could be compared to the true
efficacy observed under conditions of a con
trolled clinical trial
Non-core group : Under programme con
ditions, however, patients who have had pre-
♦Will be reported separately.
19
vious chemotherapy have also to be put on
treatment despite the fact that the patient may
even have become drug resistant—a fact that
will not be known in a vast majority of TB
centres in the country, as drug sensitivity
tests are not undertaken at most centres.
Thus, patients who had been previously trea
ted for more than 15 days, were also included
in the study in a separate random allocation
and were termed the “Non-Core Group”.
Analysis of non-core group of patients
will be reported as part of the operational as
pects of the study, separately.
4. Pre-Treatnient Investigations
(a) One 70 mm PA photofluorogram of
the chest
(b) Two specimens of sputum —one su
pervised spot specimen and another
overnight specimen, (collected within
four days of admission to the study),
both examined by direct smear ZiehlNeilsen technique, and culture and
sensitivity tests to Isoniazid, Strepto
mycin and Rifampicin,
(c) Pre-treatment interview &
examinations
Pre-treatment interview consisted of :
(i) History of symptoms, with duration
(ii) Clinical examination
(iii) Willingness to attend the clinic daily
for two months and monthly for the
rest of the duration
(iv) History of previous chemotherapy.
(v) Careful re-elicitation of the conditions
listed under item 3.
5. Allocation to Regimen
As soon as the medical officer ensured
that all the conditions listed under item 3
were satisfied, and the patient was willing to
attend the clinic as required, allocation to
regimen was done on the basis of random
sampling numbers placed in serially numbered
sealed envelopes provided by the Statistical
Section of the National Tuberculosis Institute
(NT1), Bangalore. For each patient, the
next in the serially numbered envelopes was
opened and allocation made. Each envelope
contained a slip indicating the regimen.
Allocation of patients to the regimen in
the non-core group was done through a sepa
rate random allocation. But all other acti
vities' were the same for both groups.
Reprinted from the Indian Journal of Tuberculosis, January 1989
hid. J. Tub., 1989, 36, 18
THE ACCEPTABILITY AND EFFICACY OF TWO REGIMENS OF SHORT COURSE
CHEMOTHERAPY UNDER CONDITIONS OF AN URBAN
TUBERCULOSIS PROGRAMME
P. Jagota1, E.V. Venkatarama Gupta2, B.S. Nagaraja Rao2
N. Parimala3 & G.V.J. Daily4
Introduction
The availability of potent bactericidal
drugs such as Rifampicin, Pyrazinamide and
Isoniazid has made it possible to reduce the
duration of treatment of tuberculosis from
12 months in case of coventional regimens
to 6 months in Short Course Chemotherapy
(SCC) regimens. This development holds out
the promise of better treatment compliance
by patients, resulting in better cure rates
under programme conditions.
At this juncture, it would be pertinent to
recapitulate that, before a treatment regimen
is recommended for mass use under a pro
gramme, it undergoes evaluation in at least
3 stages. At the first tier, controlled clinical
trials of the drug regimen testify to its efficacy
under ideal conditions after ensuring that
every patient put on treatment consumes
most, if not all, of the doses of prescribed
chemotherapy within the stipulated period.
In the second and third tiers of evaluation,
regimens are studied for widespread applica
bility on a routine basis. The second tier
consists of an operational study of the poten
tial efficacy, when all the programme recomendations are satisfied ; the effort possible
under a routine tuberculosis service program
me is invested in an operational trial, no less
and no more. The “operational efficacy”
within the frame work of a programme comes
to be defined thus. Sputum conversion and
relapse rates under various treatment com
pliance patterns are observed.
In the third stage, the regimen is actually
introduced in a National Tuberculosis Pro
gramme (NTP) in several units of the NTP,
on a pilot basis, and, carefully monitored
with selected indices, over a period of time, to
assess its success and shortcomings, on a
large scale. At this stage, the regimen would
be applied under a broad range of conditions,
prevailing in the different district tuberculosis
programmes (DTP), where it is introduced.
The NTP in India consists of several hundred
1.
2.
3.
4.
DTPs. Though, in principle, they are expec
ted to function according to recommendations
in the manuals, the actual functioning may be
ideal in one DTP, and rather less than ideal
in another. For example, at one centre, a
patient may be carefully motivated about his
disease, intake of drugs etc, but at another,
motivation of the patient may be rather
casual. Many such factors could influence
the actual efficiency of the treatment program
me in a DTP.
This study attempts to evaluate the ope
rational efficacy of two short course chemo
therapy regimens when a certain, well-defined
amount of effort is invested, under conditions
of an urban tuberculosis programme.
These two regimens of eight months’ dura
tion had been studied under controlled trial
conditions (East African BMRC, 1980), in spu
tum smear positive patients, without history
of previous chemotherapy. Almost 100% of
patients, with drug sensitive strains pretreat
ment, had a favourable response at the end of
chemotherapy and the relapse rates over 30
months in the 2 regimens were : 6% for the
regimen with a two month intensive phase
with three drugs (2SHR/6TH), and 7% for
the regimen with a one month intensive phase
with four drugs (1SHRZ/7TH)
The acceptability and efficacies of the
above two regimens of SCC offered to tuber
culosis patients on a domiciliary basis, were
studied at the Lady Willingdon State TB
Demonstration and Training Centre (LWSTDC) in Bangalore City. In addition, it was
also planned to obtain data on various orga
nisational aspects of an urban domiciliary
chemotherapy programme.
The study design aimed at maximum sim
ulation of programme conditions, avoiding
any undue influence of the research effort on
patient compliance. For example, in the
attempt to study bacteriological response to
treatment, the number of interim check up
examinations were kept to the bare minimum.
Chief Medical Officer, National Tuberculosis Institute [NTI], Bangalore.
Deputy Directors, Lady Willingdon State TB Centre [LWSTC], Bangalore.
Statistical Assistant, NTI, Bangalore.
Farmer Director, NTI, Bangalore.
<
?(£ S-I4Ind. J. Tub., 1991, 38, 55
Original Article
OPERATIONAL FEASIBILITY OF AN UNSUPERVISED INTERMITTENT
SHORT COURSE CHEMOTHERAPY REGIMEN AT THE DISTRICT
TUBERCULOSIS CENTRE*
P. Jagota,1 E.V.V. Gupta,2 T.R. Sreenivas,3 N. Parimala4 and K. Chaudhuri5
Summary : The acceptability, treatment
compliance and efficacy of a self-administered
short course intermittent regimen were studied
under programme conditions. Of 244 smear
positive patients eligible for intake, 150
accepted the regimen. Results of 123 among
them, who had initial drug sensitive organisms,
are presented. At the end of chemotherapy, 86
were culture negative, irrespective of the
amount of treatment taken. Sputum conversion
was directly related to the level of drug
collection, 92.8% patients with > 80% drug
collection attaining bacteriological conversion.
Among the rest, who made < 80% drug
collection, 60% became sputum negative.
Relapses, over a period of three years from the
date of diagnosis, were 10%.
always been debatable, owing to low initial
acceptance and treatment completion rates,
resulting from the requirement of supervised
administration. It may be recalled that whereas in
daily regimens under the DTP, drugs can not only
be collected on monthly/fortnightly basis but by
proxy as well, in intermittent regimens it is
obligatory to have each dose consumed by the
patient under supervision at the centre.
This study attempts to investigate the
operational problems in the delivery of an
intermittent SCC regimen and its efficacy when
drugs are issued on fortnightly basis for self
administration at home.
The objectives of the study were to study
Proportion of patients who returned for
treatment following defaulter action was 90%
throughout the period of treatment. The
workload due to drug collection and defaulter
retrieval actions were within manageable limits
and there was no workload due to adverse
reactions.
The availability of many highly efficacious
intermittent Short Course Chemotherapy (SCC)
regimens can be viewed as a promising
development, considering reduced cost, lower
incidence of adverse reactions, reduction in the
total amount of drugs to be consumed and less
frequent administration of drugs. However, the
virtues of intermittent regimens notwithstanding,
feasibility of their use as a twelve month
conventional or a six month SCC regimen in the
District Tuberculosis Programme (DTP) has
Objectives
2.
(z) acceptability of an all oral self
administered six month intermittent
regimen of SCC in terms of initial
willingness to collect drugs,
(w) response to treatment assessed in terms of
bacteriological status at the end of six
months and relapses over a period of 36
months after starting the treatment,
(iii) operational aspects of implementation of
unsupervised intermittent SCC regimen in
terms of workload.
3.
Material and Methods
3.1
Method
The study was conducted at Lady Willingdon
State Tuberculosis Centre (LWSTC), Bangalore.
The intake period was one year (Jan. 1985 to
1. Chief Medical Officer, 3. Statistician, 4. Statistical Assistant, 5. Director, National Tuberculosis Institute,
Bangalore (NTI).
2. Deputy Director, Lady Willingdon State TB Centre, Bangalore.
* Paper presented at the 45th National Conference on TB and Chest Diseases held at Rohtak in January 1991.
Correspondence: Dr. P. Jagota, Chief Medical Officer, National TB Institute, Bangalore.
P. JAG OTA ET AL
56
Dec. 1985). The drugs were issued once weekly in
the intensive phase for 2 months initially and on
fortnightly basis for 4 months of continuation
phase.
3.2
Eligibility
All the patients diagnosed as sputum positive
on direct smear at LWSTC were eligible for
intake if the following criteria were satisfied :
(a)
Living within city limits of Bangalore
(b) Aged 12 years or more
(c) Willing to take treatment
(d)
Regimen
The regimen selected for the study was :
2EHR/4H2R2
(a)
Rifampicin (R) 600 mg
(а)
Both drugs taken
together twice weekly
for 4 months. Self
administered
at
home.
Pre-treatment investigations
One 70 mm PA photofluorogram of the
chest.
(б) Two specimens of sputum—one supervised
spot and another overnight (collected
within eight days of initiation of
treatment). Both were examined by direct
smear and culture. Sensitivity tests to
Isoniazid, Streptomycin and Rifampicin
were performed.
3.5
An adverse reaction was classified minor if it
subsided with or without symptomatic treatment.
It was classified as major if it warranted
modification of chemotherapy e.g., jaundice
disturbance in vision, etc.
Check up and follow up examination
Check up examinations were carried out
during chemotherapy at the end of second and
sixth months from start of treatment and follow
up examinations at the end of twelve and thirtysix months.
3.8
Continuation phase 4H2R2
Isoniazid (H) 600 mg
3.4
Adverse reactions and their management
Classification ofpatients during the intake
Intensive phase 2EHR
Ethambutol (E) 800 mg All drugs consumed
together daily for 2
Isoniazid (H) 300 mg
months. Self admini
Rifampicin (R) 450 mg stered at home.
(b)
3.6
No history of previous anti-tubercular
treatment
(e) No serious concomitant disease.
3.3
collection. The first defaulter action was taken in
the form of a letter on the due date (instead of
third day, as recommended under DTP). Second
defaulter action was taken on the fourth day of
default in the form of home visit. A patient not
collecting the drugs within one month from the
due date was considered ‘lost’.
Management of drug default
A patient was considered a ‘defaulter’ if he did
not attend the centre on the due date for drug
Out of the total 680 sputum positive
tuberculosis patients diagnosed at the centre
during the intake period (1.1.85 to 6.12.85), 244
were eligible for intake into the study and the
remaining 436 could not be offered this regimen
for reasons shown in chart 1.
Of the patients offered the regimen, 15
(61.5%) accepted it and the remaining 94 did not.
Of those who accepted, 123 had initial drug
sensitive organisms and 25 were drug resistant.
Remaining two cases were smear positive and
culture negative. The results of 123 patients with
initial drug sensitive organisms are reported in
this paper.
4.
Results
4.1
Level of drug collection
The patients were distributed according to the
extent of treatment received in the intensive and
continuation phase, as given in Table 1.
4.2
Treatment completion and default
Table 2 gives the distribution of cases by levels
of drug collection. It is observed that 70 (56.9%),
FEASIBILITY OF AN UNSUPERVISED INTERMITTENT SCC REGIMEN AT THE DTC
57
Total patients
680
~T~
^Willing^^
Outside
262
Resistant
Sensitive
123
25
I
Previously
treated
142
Criteria not
satisfied
32
Negative
2
Chart 1. Classification of sputum smear positive patients diagnosed during 1-1-1985 to 6-12-1985
Intensive
phase
Continuation
phase
1
< 80%
< 80%
2
< 80%
>80%
drug collection through the treatment period. Of
the 123 patients, 75 (61%) made all the
collections expected of them during the first
month. Between 46% and 41% of patients made
the collections due during each of the second
through the sixth month. Overall, only 84 patients
(68.3%) completed the intensive phase, 39
(35.5%) the continuation, and 39 (31.7%) the
entire period of treatment with one or no default.
3
> 80%
< 80%
4.4
4
> 80%'
> 80%
Table 1. Definition of levels of dmg collection
Level
Proportion of expected no. of doses/
collections made during six months
Table 2. Distribution ofpatients by the level of ding
collection
No.
%
1
23
18.7
2
5
4.1
3
25
20.3
4
70
56.9
Total
123
100.0
Level of drug collection
25 (20.3%) and 28 (2.8%) patients completed, 4,
3 and below 3 (2 and 1) levels of drug collection
respectively.
4.3
Regularity in drug collection
Figure 1 shows the pattern of regularity in
Defaults
Table 3 (a) shows distribution of expected
drug collections by month, defaults and retrievals
following defaulter action. Of 492 drug
collections due to be made during the first month
(excluding the 123 initial collections where
chance of default did not exist), 52 (10.6%)
defaults occurred. During the second month, of
the 448 collections expected to be made, 87
(19.4%) did not take place on the due date.
Similarly 19.1%, 33.2%, 32.5% and 29.8% of the
expected collections were missed during the third,
fourth, fifth and sixth months respectively,
showing a rising trend in defaults with time
(P < 0.001). However, return for drug collection
after defaulter action was of the order of 78.8%
and 81.4% at the first and sixth month
respectively, compared to over 90% during the
intervening period of second through fifth month,
the differences being statistically significant
(P < 0.01, 0.02 and 0.05) between the first month
and the second, third and fourth or fifth month
58
P.JAGOTA ETAL
1OO
(A
H
Z
w
H
CL
u_
O
UJ
0
<
H
Z
UJ
o
QL
UJ
W//////,
x^<<<
x X X
LOST Z/
X x XX X
x
X
x
x X X X X
X xx
X
80xx Xxxx'xX
X X Xx
XxX
X x;
X x^
xx X x X
xx
XX X y
x
yX
X X X x.
X
X x X*
X
X
X
X
X
X
x
X
X
X X x x y
X
xx X X X X XX X IRREGULAR X X*
60 \ x X X X X X X
X X X X X X x x
X x >
x X * X X X
XX x X * x
* X X x
X x X X X X X
*
X
X X X
X
X X X x * X x X
X X X :X >
40-
REGULAR
20-
(L
1
1
I
1
I
2
3
4
5
MONTH OF TREATMENT
6
Fig. 1. Pattern of monthly drug collections among 123 patients on an SCC Regimen
Table 3 (a). Distribution of drug collections by month
Month of treatment
1
2
3
4
5
6
492+
448
330
214
206
198
No. of defaults
52
87
63
71
67
59
Percent*
10.6
19.4
19.1
33.2
32.5
29.8
Returned for collection
41
85
60
67
63
48
Percent**
78.8
97.7
95.2
94.4
94.0
81.4
No. of expected collections
4 Excluding 123 initial collections. Percentages as follows :
*Out of expected collections; **Out of defaults
respectively.
Table 3 (i>) shows response to defaulter
actions. A total of 399 defaults i.e., 139 in
intensive and 260 in continuation phase, occurred
during the period of chemotherapy. In each of the
phases, the patient, in 90% instances of default,
returned. The defaulting patients reported that
the letters were not received by them in 169
instances and they visited the centre on their own
before receipt of letter.
Home visit was done for the remaining 186
instances (60 in intensive and 126 in continuation
phase), for patients who did not respond to the
letter. Patients in 36 such instances reported for
>9
FEASIBILI1Y OF AN UNSUPERVISED INTERMITTENT SCC REGIMEN AT THE DTC
Table 5. Bacteriological status at the end of second and
sixth month
Table 3 (b). Retrieval of defaults
Initial
phase
Continuance
phase
79
134
Bacteriological Level of drug collection
status (culture) —
4
3
2
1
—due to letter
19
25
Second month
—not due to letter
60
109
Retrieval
Drug collected (1-3) days—
Negative
Drug collected (4-9) days—
38
82
—due to home visit
27
57
—not due to visit
11
25
Drug collected 10+ days
9
22
Drug not collected
13
22
Total defaults
139
260
Patients lost
13
11
Negative
Percent
10.6
10.0
Percent
Coverages for bacteriological check up
51
90
79.6
78.9
1
18
24
24
69
114
1
1
9
17
64
92
85.0
92.8
86.0
5
23
H
1
76.0
Percent
drugs, when the team had just left for home
visiting. Thus in 62% instances of default drugs
were collected consequent to home visit.
4.5
11
I—
Positive
5
Total
16
Not done
7
5
Total
H
Sixth month
7
4
Positive
6
1
3
5
15
Total
13
5
20
69
107
Not done
10
5
1
16
Grand total
23
25
70
123
5
Table 4 presents the coverages for sputum
examination at the end of second and sixth
months, both of which were high.
of them excreting resistant organisms (not on
Table). No deaths were reported during the
period of chemotherapy.
Table 4. Coverages of sputum examinations at
check up
Considering only those patients who
completed level 4 of drug collection (> 80% in
both phase i.e., completed optimum treatment),
64 of the 70 patients (92.8%) became culture
negative by the end of chemotherapy.
Examined
Month of
check up
Treatment initiated
(drug sensitive)
(No.)
No.
%
2
123
115
93.5
6
123
107
87.0
Bacteriological conversion at the end of
intensive phase, being the early index, was similar
in both < 80% and 2: 80% of drug collection
(76.6% respectively).
4.7
Relapses
4.6 Bacteriological response during chemotherapy
Table 5 presents the bacteriological status of
patients at the end of second and sixth month of
chemotherapy, distributed according to the levels
of drug collection.
It is observed that of the 123 patients a total of
92 (86%) showed a favourable response judged
bacteriologically at the end of sixth month.
Fifteen patients were found to be positive, seven
Bacteriological relapses over a period of 12
and 36 months of the start of chemotherapy
among the 92 patients, who had achieved sputum
negativity at the end of sixth month, are
presented in Table 6. The relapse rates were
observed to be 5.4% and 4.6% at the end of
twelfth and thirty-sixth months respectively,
adding up to a total of 9.9% within a period of 36
months.
60
P. JAGOTA ETAL
Table 6. Bacteriological relapse among converted
patients
Relapse
Relapse at
No. eligible* No.
%
Death
12th month
92
5
5.4
1
36th month
86
4
4.6
1
Total
92
9
9.8
*Converted at 6 month
4.6 Fate of the total cohort over a period of 36
months
distribution to weekly and fortnightly distribution
in intensive and continuation phase respectively
increased the frequency of visits by each patient
but did not increase the workload as these 123
patients were treated for a period of six months
only.
4.10.2
For 123 patients 399 defaulter actions in the
form of letter posting or, on an average, 3.2
letters were posted per patient on treatment.
Home visits became necessary on 186 occasions
i.e. 1.5 home visits per patient on treatment.
4.10.3
Of the initial 123 patients, 95 (77.3%) could be
followed up at the end of thirty-sixth month
(Table 7). Of these, 7 (7.4%) were dead. Among
the remaining patients, sputum could be collected
from 74, of whom 69 (93.2%) were sputum
nevative and five were positive.
Out of 28 patients not available for the thirty
sixth month follow up, 19 and 16 were examined
at the sixth and twelfth months respectively. All of
them except 3 were negative (not on Table).
4.9
Adverse reactions
Minor adverse symptoms were reported by
seven patients in the intensive phase. No adverse
reaction of major type requiring modification or
stoppage of any anti-tuberculosis drugs was
reported in the study. The incidence of adverse
reactions of both minor and major type was
virtually nil in this regimen.
4.10
Workload in the centre
4.10.1
Due to drug distribution
A change of policy from monthly drug
Due to defaulter retrieval actions
Due to adverse reactions
There was no workload due to adverse
reactions as patients were free from any kind of
toxicity due to drugs.
5.
Discussion
Intermittent anti-tuberculosis regimens are
particularly recommended to be administered
only on supervised basis. This is intended to
guard against treatment failure due to irregular
or selective consumption of drugs, or toxicity
from inadvertent overdosage of a drug, which is
already prescribed at a higher dose compared to
that in daily regimens. Moreover, supervised drug
administration is supposed to take care of a
possible concealed default, which has been shown
to occur in self-administered regimens. On the
other hand, intermittent regimens require the
patient to pay frequent visits to the centre
imposing an extra burden on him. It is an
additional workload for the organization as well.
These factors seem to restrict the applicability of
intermittent regimens in the programme in spite
of its being less toxic and relatively cheaper. To
Table 7. Fate of 123 patients at 36 months
Total
patients
123
Patients
followed up
Sputum examination
Dead
95
*Out of station-2; No sputum-12
7
Not examined
14*
Positive
Sensitive
Resistant
2
3
Negative
Examined
69
(93.2)
74
FEASIBILFl’Y OF AN UNSUPERVISED INTERMITTENT SCC REGIMEN AT THE DTC
overcome the above hurdle and at the same time
retain the advantages of SCC regimens given
intermittently, the feasibility of an unsupervised
semi-intermittent all oral SCC regimen was
studied under operation conditions of a District
Tuberculosis Centre (DTC).
5.1
Initial willingness
The regimen was acceptable to the patients to
the extent of 61.5%, when they were required to
visit the centre weekly in the intensive phase and
fortnightly in the continuation phase for drug
collection. This is higher than the initial
willingness of 38% observed in an earlier report’,
vherein the patients were asked to attend DTC
daily for initial two months for supervised
administration of drugs in the intensive phase.
The present study, carried out in the same centre,
immediately following the earlier study,
therefore, represents an improvement in the
acceptability of self-administered intermittent
regimen, possible due to the reduced frequency
of attendance required of the patients.
5.2
Default
Default in drug collection is generally known
to affect the outcome of treatment results.
Besides, default increases the workload of the
treatment centre, since defaulters have to be
identified on a day to day basis and letters have to
be written or home visits made. In this study,
more than 31.7% of patients completed
•eatment with or without a defaulter action. The
Appendix-I. Bacteriological status at the end of 6th
month by level of d/ug collection
Bacteriological
status (culture)
61
remaining defaulters required two or more
actions, sometime or the other. The occurrence
of defaults out of collections due during a month
was significantly less during the first month and
appeared to rise thereafter. However, proportion
of those returned for collection, out of those due
but initially missed during a month was
significantly less during the first and sixth months.
Probably, defaulter actions were comparatively
less successful during the first month due to lack
of conviction among the newly diagnosed patients
regarding treatment offered at the centre. In the
sixth month, the higher drop out rate could be a
result of complacency developing among patients,
who were on the verge of achieving treatment
completion, leading to a comparatively response
to retrieval action.
It is seen that 56.8% of the patients completed
optimum treatment (80% of drug collection). It
could be achieved only due to defaulter actions,
as patients in 90% of the instances of default
were retrieved by letters or home visit. However,
letters on the same day appeared to be a little
premature, as a large number of defaulters
attended the centre for the drug collection before
the receipt of letter.
5.3
Therapeutic efficacy
Bacteriological conversion at the end of
treatment period in this study was 86% and there
was no death. Among the 95 patients who could
be followed up for 36 months, only 7 (7.4%) were
dead. Of the remaining 88, 69 were sputum
negative and a sample of sputum could not be
produced in 12 at thirty-sixth month. In all 81
patients could be considered to have a stable
Total
Appendix-II. Completion of treatment, conversion and
relapse according to initial culture status
Initial
culture
status
Completion Conversion Relapse
No. of treatment (end of (at 36th
%
chemo
chemomonth)
therapy) %
%
Level of drug collection
1
2
3
4
Negative
9
4
20
72
105
(80.8%)
Positive
7
2
5
11
25
Sensitive
3
5
3
11
Sensitive
123
56.9
86.0
9.8
Resistant
4
8
14
Resistant
25
52.0
57.1
16.7
Negative
2
(1)
(1)
(1)
150
56.0
80.8
11.5
2
Death
Exam not done
14
Total
30
6
5
1
20
Total
30
84
150
Figures in brackets are actual numbers
62
P. JAG OTA ETAL
bacteriologically converted status after 36 months
(92%). Thus, initial as well as the ultimate spu
tum conversion and low death rates observed in
the study, do not give scope for undue appre
hension regarding irregular or selective consump
tion of any drug even though unsupervised. On
the other hand, sputum conversions were directly
related to level of drug collections, thereby
strengthening the hypothesis that those who
collected the drugs generally consumed them as
per advice.2
As shown in the Appendix Tables, if all the 150
smear positive patients are assessed (culture
facilities not being available in DTP), 84(56%)
took at least 80% of the prescribed treatment and
105 (80.8%) became culture negative at end of
chemotherapy. Of the latter, 12(11.5%) relapsed
during a 30 month follow-up. Thus, the regimen
has an overall efficacy of 71.5%.
5.4
Workload
Workload on account of treatment activity at
any treatment centre can be envisaged due to the
number of visits required by a set of patients to
collect drugs, defaults necessitating retrieval
action, and occurrence of adverse reactions
calling for additional attention.
From data available in this study (not
presented), 10 patients were estimated to attend
DTC daily for drug collection on the average.
Nearly 400 defaulter actions were required in six
months, with the average of one action per
patient every two months. It amounted to not
more than three defaulter actions per working
day. Moreover, there was virtually no adverse
reaction requiring additional attention of the staff
during the period of study.
In conclusion, the unsupervised intermittent
regimen was found feasible for implementation in
a DTP, as it was initially acceptable and had high
treatment completion rate. These favourable
operational aspects, taken along with the
favourable outcome of chemotherapy, expressed
as stable bacteriological conversion in a high
proportion of cases and absence of adverse
reactions, make it a suitable regimen for
application in the programme.
Acknowledgement
The authors arc grateful to Dr B.S. Nagaraja
Rao, former Joint Director (TB), LWSTC,
Bangalore for permitting the study to be carried
out at the centre and for the continued
encouragement. Dr K.S. Aneja, former TB
Specialist, NTI, Dr G.V.J. Baily, former Director
NTI and Mr G.E. Rupert Samuel forme.
Statistical Asst., NTI were initially involved in
designing the study. Mrs V.N. Saroja, Public
Health Nurse and Mr M.V. Jaigopal, Computer
were associated in organizing the field work and
assisting in the statistical analysis respectively. A
large number of health visitors and other
categories of field staff both from LWSTC,
Bangalore and NTI conducted the field work and
made immense contribution in bringing the
investigation to a successful conclusion. Mr B.R.
Narayana Prasad, Draughtsman prepared the
drawing and Miss K.R. Prameela prepared the
typescript. The authors are grateful to them.
References
1.
Jagota, P., Sudha Xirasagar, Parimala, N., and
Chaudhuri,K. A study of operational factors
influencing the applicability of two regimens o
Short Course Chemotherapy under conditions
of an urban tuberculosis programme; Ind. J.
Tuber.; 1989,36, 213.
2.
Gothi G.D., Savic, D., Baily, G.V.J., Rao, K.P.,
Nair, S.S., and Samuel. R. Collection and
consumption of self-administered anti
tuberculosis drugs under programme conditions;
Ind. J. Tuber.; 1971,18, 107.
p I -S s •’ f
KARNATAKA STATE TUBERCULOSIS ASSOCIATION
3. UNION STREET, BANGALORE - 560 001 - Phone 564387
GUIDELINES FOR THE TREATMENT OF
TUBERCULOSIS
Compiled by
THE NATIONAL TUBERCULOSIS INSTITUTE
No. 8, Bellary Road,
Bangalore - 560 003
Phone 361192
COMMONLY USED ANTI TUBERCULOSIS DRUG REGIMENS IN THE TREATMENT OF TUBERCULOSIS
ABBREVIATIONS: H = Isoniazid; R = Rifampicin; S = Streptomycin; Z = Pyrazinamide; E = Ethambutol;
T = Thioacetazone
UNDER NATIONAL TUBERCULOSIS PROGRAMME
A. Standard drug regimens (12-18 months)
SI.
. No.
1.
Regimen & dosage
___________________________________________
Mode & Rhythm
Duration
(months)
Inj. S (IM) to be given five days in a week either
at Clinic/Home/Disp. DTC: Other two drugs as
per the regimens to be taken daily, orally.
2STH/ 10TH or 10EH Intensive
Phase (2 months)
S = 0.75 g.
Approx. Cost
Rs. 350/- to Rs.
1,050/- (Cost as per
the drugs used)
H = 300 mg
T = 150 mg or E = 1g
Continuation Phase (10 months)
12
Both drugs to be taken together daily, orally.
H = 300 mg
T = 150 mg or E = 800 mg
2.
E = 800-1200 mg (<50 - > 50 kg)
H = 300 mg
3.
Both drugs to be taken together daily in single
dose or in two divided doses orally.
EH
12
TH
Rs. 800/-
Collection: Monthly from Disp./Clinic/DTC/Shop.
- do -
Rs. 125/-
Twice weekly with three-four days interval. Both
drugs to be taken together under supervision at
the Clinic/DTC.
Rs. 550/-
T = 150 mg
H = 300 mg
4.
18
S2H2
S = 0.75 g.
H = 600 mg.
12
B. Short Course Chemotherapy (SCC) regimens (6-8 months)
1.
2EHRZ/6TH or 6EH
Intensive phase (2 months)
E = 1g
H = 300 mg
8
R = 450-600 mg (<50 - > 50 kg)
All drugs to be taken daily, orally at the same
time.
Rs. 745/-
Z = 1.5 to 2 g
Continuation phase (6 months)
H = 300 mg
- do -
T = 150 mg or E = 800 mg
2.
2S2H2R2Z2 / 4H2R2
Intensive phase (2 months)
S = 0.75 g or E = 1.6 g
H = 600 mg
R = 600 mg
6
Twice weekly with three-four days interval. All
drugs to be taken under supervision at the
Clinic/DTC.
Z = 2g
Continuation phase (4 months)
H = 600 mg
R = 600 mg.
- do -
Rs. 500/-
OTHER SHORT COURSE CHEMOTHERAPY (SCC) REGIMENS
1.
2SHRZ/4HR
Intensive phase (2 months)
S = 0.75 g
H = 300 gm
R = 450-600 mg (<50 - > 50 kg)
6
Inj. S(IM) to be taken five days in a week either
at the Clinic/Home/Disp./DTC. Other drugs to
be taken daily, orally at the same time.
Rs. 1,135/-
Z = 1.5 to 2 g
Continuation phase (4 months)
H = 300 mg
Both the drugs to be taken together daily, orally.
R = 450-600 mg
2.
2EHR/7HR
Intensive phase (2 months)
E = 800 mg
H = 300 mg
All the drugs to be taken daily, orally at the
same time.
R = 450-600 mg
Continuation phase
Rs. 800/-
months)
H = 300 mg
- do -
R = 450 - 600 mg
Corrigendum
Under Instructions
Please Read
*1 as
# All drugs may preferably be taken before breakfast,
’if not tolerated, one hour after the breakfast.
12 mg;S = 20 mg;Z = 30
*2 as :H = 5 mg;R = 10
*E 35 25 mg; 15 mg after 2 months; T = 4 mg.
35 mg;
•
Wherever necessary, Injection Streptomycin may be replaced with tablet Ethambutol or vice-versa.
•
Whenever patients have not been able to take all the prescribed doses in the stipulated time, a grace period of
15 days to one month may be allowed to complete the treatment in each phase.
•
Always do sputum examination for AFB to confirm the diagnosis of tuberculosis.
•
Avoid use of injection Streptomycin during PREGNANCY of any duration.
•
The recommended SCC regimens are of 100% efficacy as proved under controlled clinical trials against
different forms of tuberculosis viz., pulmonary, miliary and extra pulmonary disease.
COMMONLY OBSERVED ADVERSE REACTIONS TO ANTI TUBERCULOSIS DRUG REGIMENS
SI.
No.
Adverse reaction
Offending
drug(s)
Symptoms and management
1.
R
2.
Red Brown colour of urine and
other body fluids
Vestibular damage of VIII nerve
3.
Gastro-Intestinal
Harmless: No treatment required: Assurance to be given to the
patient.
Giddiness & Vertigo: Can be prevented by giving Inj. S five days in
a week, in daily phase regimen, specially in elderly patients: If
symptoms persists, replace S with E.
Anorexia, vomiting, pain abdomen, mostly transient: Symptomatic
relief to be given: Drugs to be taken after meals.
4.
Clinical jaundice
5.
Cutaneous and hypersensitive
reactions
T,S: R, E
(Rarely)
6.
Retrobulbar neuritis
E
S
T or RH or
RHZ
combination
T or RH or
RHZ
combination
Nausea, vomiting, pain abdomen, fever, malaise, yellow colouration
of urine, skin and eyes: STOP ALL DRUGS till recovery: Advise
rest and symptomatic treatment: Later on, treat with EH or SH
(twice weekly) regimen.
Mild - itching all over the body with or without rashes. Symptomatic
treatment.
Moderate - Swelling of periorbital area, conjuctivitis, rigors, malaise,
headache, vomiting, lymphadenopathy, albuminuria - change the
drug.
Severe - (This stage should not be allowed to occur)
Rarely - Exfoliative dermatitis with involvement of mucus
membrane (Stevens-johnson syndrome) may occur particularly as
a reaction to T - terminate the drug and hospitalise.
Hypersensitive reaction - occur in early stage of treatment. Not
dose related - change the drug.
Anaphylactic shock - can occur rarely after a single large dose, if
patient is already hypersensitive to the drug.
Diminuition in acuity of vision and or colour vision. Terminate the
drug. Avoid if possible, the drug in myopic and child patient.
I
Global TB Epidemic Out of Control
http://abcnews.go.com/sections/living/DailyNews/tuberculosis0318. hlml
T> IS 5-' 1 C
ARCNFWSrnm
'74
SEARCH NOW: dffejgp
Choose a Medical Topic
- Di: <2. Lveretf Koop
home*
WHO Haases Awareness
Bv Edith Lederer
Global TB
The Associated Press
8WBIBiafy
Ik* li-S-
world
LONDON, March 18—A
Epidemic tuberculosis epidemic: is out of
.
Called Out
of Control
r
k Imslriess
► technology
9(.leil„
control in many countries and unless ►
> travel
action is taken nearly 1 billion more > espn sports
people will become infected and 70 > mr.showblz
dispatches
million will die in the next two
> abcnews shows
>- gsleiy
decades, the World Health
|k weather
Organization says.
> local
At a conference this week in London,
public health and tuberculosis experts
have been assessing whether 22 countries
which account for 80 percent of the
“This year, more people world’s TB cases are making progress
will die of TB than in any towards controlling the infectious disease.
“The TB epidemic is now increasing in
other year in history.”
many
countries, with devastating
— World Health Organization
consequences,” WHO said in a statement
summarizing a report to be released
Thursday. “This year, more people will
die of TB than in any other year in
history.”
Tuberculosis, which attacks mainly the
lungs, intestines, skin and brain, is a
bigger killer than malaria and AIDS
combined, and kills more women than all
the combined causes of maternal
mortality. Every year, between 2 and 3
million people die from TB, including
100,000 children, the Geneva-based U.N.
agency said.
> search
> famlly.com
RELATED
LINKS
Global
Infection
Threat
HEALTH &
LMNG
HEADLINES
An Unprecedented Step
/
I of3
In 1993, WHO took an unprecedented
step and declared tuberculosis a global
emergency. Between 1993 and 1996, TB
cases increased 13 percent worldwide.
Experts on the Ad Hoc Commission on
the Global Tuberculosis Epidemic have
been examining new data to see how well
the 22 worst-affected countries are
meeting WHO’s global targets of
detecting 70 percent of infectious TB
mail
fa
ABCNEW$.cam
> send this pa^e
to a friend
toolbox
8/19/99 5:13 Pb
GlobakTB Epidemic Out of Control
http://abcnews.go.com/sections/living/DailyNews/tuberculosis0318.hlinl
cases and curing 85 percent of those by
the year 2000.
The countries are Afghanistan,
Bangladesh, Brazil, China, Democratic
Republic of Congo, Ethiopia, India,
Indonesia, Iran, Mexico, Myanmar,
Nigeria, Pakistan, Peru, Philippines,
Russia, South Africa, Sudan, Tanzania,
Thailand, Uganda and Vietnam.
One-third of the world’s population is
infected with the TB bacillus, and
between 5 and 10 percent will become
sick with pulmonary TB during their
lifetime, the WHO said. Only those who
are sick are infectious, and they can
transmit the disease by coughing, talking
or spitting.
“It is estimated that between now and
2020, nearly 1 billion more people will be
newly infected, 200 million people will
get sick, and 70 million will die from
TB—if control is not strengthened,” the
group said.
Poor Program Management
According to the WHO, there are nearly 3
million new TB cases in southeast Asia
every year and nearly 2 million new cases
in sub-Saharan Africa.
More than a quarter of a million new
cases occur annually in Eastern Europe,
which is experiencing an increase in TB
deaths after almost 40 years of steady
decline, WHO said.
Since the 1940s, there have been drugs
to treat tuberculosis.
But WHO said poorly managed TB
treatment programs are causing
drug-resistant strains of tuberculosis to
emerge, “which could render TB
incurable.”
Up to 50 million people may be
infected with drug-resistant TB, either
because they did not take all their
medicines regularly for the required
period—often because they start to feel
better—or because they receive the wrong
drugs or don’t have a reliable drug supply,
WHO said.
TB treatment costs around $2,000 per
2 of 3
8/19/99 5:14 PN
Global <TB Epidemic Out of Control
http ://abcnews. go. com/sections/living/Dai lyNews/tuberculosi s0318.html
patient, but rises 100-fold to about
$250,000 for patients with drug-resistant
strains, WHO said. ■
Copyright 1998 Associated Press. All
rights reserved. This material may not be
published, broadcast, rewritten, or
redistributed.
s ra rwav e
3 of 3
Copyright 1800- A6C News and Slsrwava
Corporation. All rights reserved. Thia
roatertal may nol be publlBhed. broadcBBl.
re written, or redEstrsbuted in snytoffm.
8/19/99 5:16 I’M
r
! TB-controi project: Doorstep treatment yields residts
o*;
ISHA DAGA
| JUNE 20
do not complete their course. As each TB patient causes side-effects such as dizziness, so the patient haps the most important aspect of RNTCP is that nitynity
workers
who
actually
talktalk
to pati
workers
who
actually
to patients, said
can infect 10 or more persons, 100 patients back defaults.” "
By constantly interacting with the pa seeks to treat the patient at a time and place con BMC’s Deputy' Executive Health officer Dr
on treatment will mean a check on at least 1000 tient, reassuring him, and watching him take the venient to him/her, and each patient has his/her Ramesh Kathuria, at a recent discussion hosted by
WO non-governmental organisations new cases. ‘Case-holding, or prevention of de drugs, the programme has countered most of own marked treatment kit with the full course sup RC of Bombay Harbour. He mused? 1 don’t know
(NGOs) have succeeded in achieving cure fault, is also the goal of the new programme.
these problems.
plies. Member-Secretary of the Mumbai District how many of us would be willing to spend half an
of eight tuberculosis (TB) patients early
“Leaving a course midway often leads to multiNigama Mascarenhas, Director, FSC said, TB Control Society and Deputy Executive Health hour with an MDRTB case." Kathuria stressed
this month under a focused TB control pro drug-rcsitant (MDR) TB,” according to Dr A J “We focus on the social aspect of TB, reminding Officer of the BMC Dr K N Khcrgamkar said, that “different theories of motivation need to be
gramme launched in three civic wards in Mumbai. Desai, Director of RC Bombay Harbour’s TB pro- patients of the consequences for their family if he “We have set up 256 DOTS centres in Mumbai. applied, again and again, to ensure success.”
The Rotary' Club (RC) of Bombay Harbour ject. “The patient then spreads MDR bacteria, does not recover.” She says, “Our field worker The patient can visit the centre closest to him. And
Another critical neglected area is the private
and the Family Service Centre (FSC) traced and making it even tougher to control the disease,” he goes to their homes to ensure that he takes the the kit ensures that the patient is not told midway sector. According to Rangan, “ About 60 per cent
motivated 94 TB patients, who had stopped treat added. Out of 329 listed defaulters, the NGOs dose.“Though municipal workers do the same that there are no medicines.”
of the population still visits Private Medical Practi
ment halfway, to resume treatment which is based could follow up on only 303 cases but had to narrow thing, they have fixed hours ofwork, duringwhich
However, Dr Shecla Rangan, Consultant to tioners (PMP). RNTCP must build faith in the
on Directly Observed Treatment Short-course down to 94 cases to be taken up for DOTS treat the patient may not be home.”
the Foundation for Research in Community public health system. Mahashursays.“PMPs have
(DOTS) model approved under the Revised Na ment
A Central TB division document claims that Health points out that the programme fails to look to be taken into confidence and explained the effi
tional TB Control Programme (RNTCP)
On several reasons for default, Desai revealed, DOTS model ‘ensures cure by providing the most at some crucial social and economic factors. cacy of DOTS.”
launched by the Central government in July last
Most patients cannot afford to leave their work effective medicine and confirming that it is taken.’ “Many women are not allowed to travel alone to
Khcrgamkar assures that the BMC is planning
year.
and come for treatment. Many, on feeling better It is based on good diagnosis through lop quality the centres for treatment and cannot leave house workshops for PMPs in August. “We arc trying to
The control programme launched in A, B and after a month, stop coming, assuming they are microscopy, an uninterrupted supply'of high qual- hold work.”
establish a standardised treatment. Since we have
—J T_ _1_ _1_ _ .
1 •
C wards in January 1998 targets defaulters since f
cured.
In alcoholics, .1the. combination
of poor ity drugs, treatment that is directly observed and
Success in any TB project depends ultimately', enough supplies of drugs, we can give the GPs
i studies have shown that two thirds of TB patients nourishment, strong medication and alcohol systematically monitored by a health worker. Per on.the motivation levels of the health and commu treatment kits free of cost.”
CO
,3
A Controlled Clinical Trial of 3- and 5-Month Regimens in the
Treatment of Sputum-Positive Pulmonary Tuberculosis
in South India12
t
I
I
)
• TUBERCULOSIS RESEARCH CENTRE, MADRAS,3 and NATIONAL TUBERCULOSIS
INSTITUTE, BANGALORE4
1
Introduction
I
Several highly effective short-course reg
imens (6 to 9 months) have been evolved
for the treatment of smear-positive pul
monary tuberculosis (1). But the crucial
issue is to determine the shortest possi
ble duration of chemotherapy that would
be highly effective. The pioneer investi
gation of Kreis and associates (2) showed
that 3-month regimens of streptomycin
given daily,with 900 mg of isoniazid and
1,200 mg of rifampin given daily or ev
ery other 4ay to sputum-positive'patients
had a relapse rate of 13% in 91 patients
in a 12-month period of follow-up. The
preliminary findings of a 5-month regi
men at this Centre, with a 2-month in
tensive phase of streptomycin, isoniazid,
rifampin, and pyrazinamide daily fol
lowed by streptomycin, isoniazid, and
pyrazinamide twice a week, indicated that
the relapse rate was likely to be low.
Against this background, this Centre
planned a large-scale investigation of a
-egimen irf which all 4 drugs were given
daily for 3 months in standard dosages,
thus adding the important drug, pyrazin
amide, to the combination studied by
Kreis and associates (2). However, in case
this regimen proved to have a substantial
relapse rate, a second regimen, with the
addition of a 2-month continuation
phase of twice-weekly streptomycin, iso
niazid, and pyrazinamide was also stud
ied. Because rifampin was then very
costly, it was decided to evaluate its con
tribution to the second regimen. A 7month regimen of streptomycin, isonia
zid, and pyrazinamide given daily for 2
months and twice-weekly thereafter had
a low relapse rate (4%) in an earlier study
from this Centre (3). So a similar non
rifampin regimen, but for 5 months in
stead of 7 months, with the 3 drugs given
daily for 3 months and twice-weekly
thereafter, was also studied.
A controlled clinical trial of the 3 reg-
SUMMARY A controlled comparison of 3 short-course regimens was undertaken in patients with
newly diagnosed, sputum-positive, pulmonary tuberculosis in South India. The regimens were: (7)
R3: rifampin plus streptomycin plus isoniazid plus pyrazinamide daily for 3 months; (2) R5: the same
as regimen R3 followed by streptomycin plus isoniazid plus pyrazinamide twice weekly for 2 months;
(3) Z5: the same as regimen R5 but without rifampin. The distributions of various pretreatment char
acteristics were similar in the 3 series. At the end of treatment, 6 patients (3 R3, 3 Z5) of 694 (228
R3, 230 R5, 236 Z5) with drug-sensitive organisms initially were classified as having an unfavorable
response. By 24 months (21 months of follow-up for the R3 regimen and 19 months for the R5 and
Z5 regimens), a bacteriologic relapse requiring treatment occurred in 20% of 200 R3, 4% of 187
R5, and 13% of 199 Z5 patients, the difference between the R3 and R5 series being highly significant
(p = 0.00001). Considering patients with cultures initially resistant to isoniazid, 4 of 57 in the R3
and R5 series combined had an unfavorable response to treatment compared with 13 of 26 in the
Z5 series (p < 0.0001). Of the 4 patients with an unfavorable response in the R3 and R5 series com
bined, resistance to rifampin emerged in 2. Complaints of arthralgia were made by 45% of the R3
and R5 patients combined and 70% of the Z5 patients (p < 0.00001). However, chemotherapy was
modified in only 5 and 12%, respectively. Jaundice occurred in 7% of the R3 and R5 patients and
1% Of the Z5 patients (p < 0.00001).
AM REV RESPIR DIS 1986; 134:27-33
imens was carried out at the Tuberculosis
Research Centre, Madras, and at the Lady
Willingdon Tuberculosis Clinic, Banga
lore, in collaboration with the National
Tuberculosis Institute, Bangalore. The
amalgamated results during chemother
apy and the bacteriologic relapses up to
24 months from the start of treatment,
that is, a 21-month period of follow-up
for the 3-month regimen and a 19-month
follow-up for the 5-month regimens, are
presented in this report.
R3: daily chemotherapy with rifampin, 12
mg/kg body weight in 3 graded doses, plus
streptomycin sulphate, 0.75 g, plus isoniazid,
400 mg (incorporating pyridoxine, 10 mg),
plus pyrazinamide, 35 mg/kg in 5 graded
doses according to body weight. All the drugs
were given in a single dose; the duration of
chemotherapy was 3 months.
R5: the same las regimen R3, followed by
twice-weekly chemotherapy for 2 months with
streptomycin, 0.75 g, plus isoniazid, 15 mg/kg
body weight in 3 graded doses (incorporat
ing pyridoxine, 10 mg), plus pyrazinamide,
70 mg/kg in 5 graded doses according to body
Methods
Plan and Conduct of the Study
Patients. The patients were residents of ei
ther Madras or Bangalore City, came from
poor sections of these communities, and had
come to the outpatient ches£ clinics because
of symptoms. The criteria for admission were
similar to those in previous studies (4), that
is, the patients were 12 yr of age or older, had
newly diagnosed pulmonary tuberculosis, had
not had previous chemotherapy for more than
2 wk, and had 2 sputum cultures positive for
M. tuberculosis.
Chemotherapeutic regimens. The patients
were allocated at random to one of the fol
lowing 3 regimens.
(Received in originalform July 26, 1985 and in re
vised form January 7, 1986)
1 This report was prepared on behalf of the sup
porting institutions by Dr. R. Parthasarathy, Dr.
R. Prabhakar, and Mr. P. R. Somasundaram, in
collaboration with the other members of the scien
tific staff.
2 Requests for reprints should be addressed to
Dr. Prabhakar, Tuberculosis Research Centre, Chetput, Madras-600031, India.
3 Under the Indian Council of Medical Research,
New Delhi.
4 Under the Directorate General of Health Ser
vices, Government of India, New Delhi.
27
28
weight. The total duration of chemotherapy
was 5 months.
Z5: The same as regimen R5 but without
rifampin.
The dosages of drugs other than isoniazid
in the daily phase and streptomycin in both
phases were increased appropriately if the pa
tient gained weight but were not reduced for
weight loss.
Pretreatment investigations. The pretreat
ment investigations included a chest radio
graph, the examination of 2 overnight and
2 spot specimens of sputum by smear and cul
ture, sensitivity tests to streptomycin, isonia
zid, and rifampin on 2 positive cultures, and
identification tests on all positive cultures. In
the Madras patients, serum concentrations of
bilirubin, aspartate and alanine aminotrans
ferase activities, and a blood platelet count
were determined.
Investigations during treatment andfollow
up. Every month during treatment, the phy
sician recorded any departure from the
prescribed regimen and drug intolerance. Spu
tum specimens were examined every month
by microscopy and culture, 3 (2 overnight, 1
spot) from 1 to 6 months and 2 (1 overnight,
1 spot) from 7 to 24 months. One positive
culture was tested each month for sensitivity
to streptomycin and isoniazid and, in addi
tion, to rifampin during the first 3 months
for R3 and R5 patients. A chest radiograph
was taken at 1, 3, 12, and 24 months and, in
addition, at 5 months for R5 and Z5 patients.
To check whether the patient took isoniazid
from other sources, a clinic urine specimen
was tested for acetylisoniazid (5) at least once
a month.
General management. All the patients were
treated as outpatients. They attended the clinic
daily for 3 months (excepting holidays) and
received their chemotherapy under the close
supervision of a clinic nurse. The patients al
located to the 5-month regimens attended
twice a week for the next 2 months. If a pa
tient failed to attend, the home was visited
by the next day.
Bacteriologic procedures. Sputum smears
were examined by fluorescence microscopy
(6), and the specimens were cultured by a
modification of Petroffs method (4). Posi
tive cultures were screened for M. tuberculo
sis (7) and were tested for sensitivity to isonia
zid and rifampin by the minimal inhibitory
concentration method and to streptomycin by
the resistance ratio method (8). The defini
tions of drug resistance were the same as in
previous studies for isoniazid (3,4) and strep
tomycin (3). Resistance to rifampin was de
fined as a yield of 64 mg/L on both the cul
tures pretreatment and a yield of 64 mg/L
during treatment.
Change of chemotherapy. The progress of
each patient was reviewed regularly during
chemotherapy. The allocated regimen was
changed if the patient had clear-cut clinical
and/or radiographic deterioration in the pres
ence of a positive sputum, major drug toxic
ity, or an unfavorable bacteriologic response.
Extension of the duration of chemother
TUBERCULOSIS RESEARCH CENTRE/NATIONAL TUBERCULOSIS INSTITUTE
TABLE 1
CHARACTERISTICS ON ADMISSION TO TREATMENT
R3
All
Regimens
Z5
R5
(n)
(%)
(n)
(%)
(n)
(%)
0)
(%)
Slight
Limited
Moderate
Extensive
Gross
9
55
83
78
3
4
24
36
34
1
17
58
81
74
0
7
25
35
32
0
14
55
90
76
1
6
23
38
32
1
40
168
254
228
4
6
24
37
33
1
Extent of
cavitation
Nil
Slight
Moderate
Extensive
5
85
69
69
2
37
30
30
6
74
81
69
3
32
35
30
10
82
74
70
4
35
31
30
21
241
224
208
3
35
32
30
Direct smear
result of
1st collec
tion speci
men of
sputum
Negative
Positive
1 + (scanty)
2 + (moderate)
3 + (heavy)
18
8
20
9
17
7
55
8
62
114
34
27
50
15
63
119
28
27
52
12
70
114
35
30
48
15
195
347
97
28
50
14
228
100
230
100
236
100
694
10r
Total
radiographic
extent of
disease
Total patients
Definition of abbreviations: R3 = Rifampin (R) plus streptomycin (S) plus isoniazid (H) plus pyrazinamide (Z) daily for 3 months;
R5 = RSHZ daily for 3 months, then SHZ twice a week for 2 months; Z5 = SHZ daily for 3 months, then SHZ twice a week for
2 months.
apy. Patients who had missed 1 or more doses
or had had 2 or more drugs withheld had the
duration of daily and/or twice-weekly che
motherapy, with all the drugs extended ap
propriately at the end of each phase of treat
ment.
Patients in analyses. In all, 919 patients (303
R3, 310 R5, 306 Z5) were admitted. Of these,
114 were excluded; 43 from all analyses be
cause of ineligibility (7 had been infected by
mycobacteria other than M tuberculosis, 1
had spinal tuberculosis, 3 had less than 2 posi
tive cultures, 32 had had previous chemother
apy for more than 2 wk); 71 from efficacy
analyses (2 died of nontuberculous causes,
2 died of tuberculosis early in treatment, 3
had treatment changed on account of adverse
reactions, and 64 had missed or had inter
ruption of 25% or more of chemotherapy).
There remained for analyses 694 patients (228
R3, 230 R5, 236 Z5) with bacilli initially sen
sitive to isoniazid, streptomycin, and rifampin
and 111 (34 R3, 40 R5, 37 Z5) with bacilli ini
tially resistant to 1 or more drugs. The results
are presented separately for the 2 groups.
Results
Patients with Bacilli Initially Sensitive to
Isoniazid, Streptomycin, and Rifampin
Characteristics on admission. Of the 694
patients, 70% were males, 32% were
younger than 25 yr of age, and 19% were
45 yr of age or older. The mean weight
was 40 kg. The 3 series were similar with
respect to these factors. The distributions
of patients in the 3 series were similar
with respect to radiographic extent of dis
ease, extent of cavitation, and smear posi
tivity on admission (table 1). Most of the
patients had extensive, cavitary, smear
positive disease.
Tuberculosis deaths. Three patients (
R3,1 Z5) died of tuberculosis or its com
plications; 1 (R3) died on the second day
of chemotherapy, and another (R3) died
of hemoptysis on the twelfth day. Nei
ther of them can be considered failures
in antibacterial terms, and they have been
TABLE 2
CULTURE RESULTS BASED ON 3 SPECIMENS OF SPUTUM EACH MONTH
Z5
R3+R5
Month after
Start of
Treatment
1
2
3
4
5
Total
Patients
458
457
455
229t
2281
All
Cultures
Negative
Total
All
Cultures
Negative
(n)
(%)
Patients
(n)
(%)
p Value
169
415
439
223
226
37
91
96
97
99
236
236
235
234
236
45
175
218
226
230
19
74
93
97
97
0.001
* Contrast not significant (p > 0.05).
t Patients receiving the R5 regimen only.
0.001
NS*
NS
NS
29
3- AND 5-MONTH REGIMENS IN TREATMENT OF TUBERCULOSIS
TABLE 3
BACTERIOLOGIC RELAPSE DURING THE 24 MONTHS AFTER ADMISSION* REQUIRING TREATMENT
IN PATIENTS WHO COMPLETED THEIR CHEMOTHERAPY WITHIN 15 DAYS AFTER THE PRESCRIBED PERIOD
Patients
with a
Favorable
or Doubtful
Response^
Series
200
187
199
22
5
16
44
10
31
95%
Confidence
Limits
Total
(%)
(n)
R3
R5
Z5
Bacteriologic Relapses Requiring Treatment^
Total
Bacterio
logic
Relapses
Month of Relapse after Stopping
Chemotherapy
(n)
(%)
(%)
1-3
4-6
7-12
13-19
20 or 21
39
8
25
20
4
13
14-26
2-8
8-18
11
2
9
17
2
10
7
3
1
3
1
5
1
* That is, 21 months after stopping chemotherapy for the R3 regimen and 19 months for the R5 and Z5 regimens.
t Of the 11 patients (6 R3, 2 R5, 3 Z5) with a doubtful response, 2 (1 R3, 1 R5) had a bacteriologic relapse requiring treatment at 3 months and with
drug-sensitive cultures in both.
* Three other patients had treatment restarted for other reasons-1 (R3) for hydropneumothorax in the 2nd month, 1 (R5) for a radiographic deteriora
tion with positive smears in the 3rd month, and 1 (Z5) for tuberculous lymphadenitis in the 16th month.
Bacteriologic Relapse
Exclusionsfrom relapse analyses. Of the
above 225 R3, 230 R5, and 233 Z5 pa
tients who had a favorable or doubtful
response at the end of chemotherapy, 13
(6 R3, 1 R5, 6 Z5) have been excluded.
Of these, 2 (both R3) had chemotherapy
continued beyond 3 months because of
3 positive smears at 3 months, 7 died of
nontuberculous causes, 2 migrated, and
2 discharged themselves. Thus, there re
mained 675 patients (219 R3, 229 R5, 227
Z5) in the relapse analysis.
A bacteriologic relapse was defined as
a total of 2 or more cultures positive for
M. tuberculosis in any 3 consecutive
monthly examinations. Treatment was re
started if 1 of the cultures yielded 20'colonies or more and there was 1 positive
smear, or if a patient intermittently pro
duced positive cultures for several months.
The relapse rates in 586 patients (200
R3,187 R5,199 Z5) who completed their
chemotherapy within 15 days of the pre
scribed 3- or 5-month period are pre
sented in table 3.
A bacteriologic relapse occurred in 44
(22%) of the R3, 10 (5%) of theR5, and
tently positive culture results throughout
the 5 months, the organisms being drug
sensitive, and was retreated. Three others
(all R3), who had positive cultures at 1
and 2 months, each had a single positive
culture (1 or 2 colonies) at 3 months, the
bacilli being fully sensitive; 2 of them had
chemotherapy continued, but the third
was consistently culture negative from the
fifth month without further chemother
apy. The sixth patient (Z5) died of spon
taneous pneumothorax (listed in Tuber
culosis deaths above).
A patient was classified as having had
a doubtful response if 1 or 2 cultures were
positive in the last month of treatment
and all the cultures in the preceding
month were negative; 11 patients (6 R3,
2 R5, 3 Z5) had a doubtful response, 10
with 1 positive culture and 1 with 2 posi
tive cultures. Of the 12 cultures, the yield
was 1 colony in 8, 2 or 3 colonies in 2,
16 colonies in 1, and 20 to 100 colonies
in 1. The bacilli were resistant to isonia
zid but sensitive to streptomycin in 2, and
sensitive to both drugs in the rest. Che
motherapy was not continued for any of
them.
excluded from the analyses of efficacy.
The third patient (Z5), who was positive
by smear and culture at 1 month, died
of spontaneous pneumothorax in the sev
enth week.
Culture results. The proportions of pa
tients with all cultures negative month
by month are presented in table 2. At 1
and 2 months, the proportions were sig
nificantly higher in the R3 and R5 series
than in the Z5 series (p < 0.001, in both
instances). From the third month onward,
the rates were very high, and similar in
the rifampin and nonrifampin series.
Response at the end ofchemotherapy.
A patient was classified as having had
an unfavorable bacteriologic response if
1 or more of 3 cultures were positive at
each of the last 2 months of treatment,
irrespective of the number of colonies.
In all, 6 patients (3 R3, 3 Z5) were clas
sified as having had an unfavorable re
sponse. Two were clear-cut bacteriologiC failures; 1 (Z5) had persistently posi
tive smear and culture results, with the
emergence of resistance to streptomycin
and isoniazid, and had chemotherapy
changed, and the other (Z5) had persis-
TABLE 4
EXTENSION OF CHEMOTHERAPY BEYOND THE PRESCRIBED PERIOD AND RELATIONSHIP
WITH INCIDENCE OF RELAPSE REQUIRING TREATMENT
<j
Duration of
Treatment beyond
Prescribed
Period
Z5
R5
R3
Relapses
Requiring
T reatment
Patients
in
Analysis
Patients
in
Analysis
Patients
in
Relapses
Requiring
T reatment
Analysis
(%)
(n) (% of A)
(n) (B)
(%)
(n) (% of B)
102
98
47
45
53
134
23
59
11 )
53 *(
9
18
21
0
2
0
41
25 I
152 (‘
18
229
100
1
7
0
0
0
8
(days)
(n) (A)
Nil
< 15
> 15 but < 30
> 30 but < 60
> 60 but < 75
Total
219
100
18
21
11
19
Relapses
Requiring
Treatment
2
5
0
3
(n) (C)
(%)
(n) (% of C)
72
127
32
56
18
9
12
11 i
0 )
12
13
12
1
2
227
100
28
17 )
11
30
TUBERCULOSIS RESEARCH CENTRE/NATIONAL TUBERCULOSIS INSTITUTE
31 (16%) of the Z5 patients. However,
5, 2, and 6, respectively, became persis
tently culture negative without retreat
ment. The proportions of patients with
a bacteriologic relapse requiring treat
ment were 20% in the R3, 4% in the R5,
and 13% in the Z5 series. The relapse
rates in the R3 and Z5 series were signifi
cantly higher than that in the R5 series
(p = 0.00001 and < 0.01, respectively);
the difference between the relapse rates
in the R3 and Z5 series was not signifi
cant (p = 0.08).
In all, 72 patients had a bacteriologic
relapse requiring treatment; this occurred
within 6 months of stopping chemother
apy in 51 (71%). The sensitivity test re
sults of the different cultures tested at
the time of relapse were consistent in 55
patients; 53 (32 R3, 5 R5,16 Z5) had cul
tures sensitive to streptomycin and isonia
zid, 1 (R3) had cultures resistant to strep
tomycin and sensitive to isoniazid, and
the other (Z5) had cultures resistant to
both drugs.
The distribution of the 675 patients in
the analyses according to the period of
extension of the duration of chemother
apy and the relationship with bacterio
logic relapse requiring treatment is pre
sented in table 4. There was a suggestion
in the R3 and R5 series that prolonga
tion by more than 15 days reduced the
relapse rate.
Patients with Pretreatment Drug-Resistant
Organisms
There were 111 patients in the analyses
TABLE 5
RESPONSE TO CHEMOTHERAPY AND BACTERIOLOGIC RELAPSE DURING
THE 19 TO 21 MONTHS AFTER STOPPING CHEMOTHERAPY IN PATIENTS
WITH DRUG-RESISTANT BACILLI INITIALLY
Unfavorable
Response at
the End of
Series
Total
Patients
Chemotherapy
Relapses
Requiring
Treatment
Streptomycin only
R3
R5
Z5
7
9
11
0
0
1
1
1
1•
Isoniazid only
R3
R5
Z5
17
17
12
1
1
5
5
1
1
Streptomycin
and isoniazid
R3
R5
Z5
9
14
14
1
1
8
1
1
1
Streptomycin
and/or
isoniazid
R3
R5
Z5
33
40
37
2
2
14
7
3
3
Pretreatment
Resistance to:*
* One patient (R3) had resistance to rifampin (only); he had a favorable response at the end of
chemotherapy but had a bacteriologic relapse requiring treatment.
of efficacy with drug resistance initially
(table 5). The distributions in the 3 se
ries according to pretreatment character
istics were broadly similar. Of the 27 pa
tients with bacilli resistant to streptomy
cin alone, only 1 (Z5) had an unfavorable
response. Of the patients with strains
resistant to isoniazid alone, 2 of 34 in the
R3 and R5 series combined had an un
favorable response compared with 5 of
12 in the Z5 series (p < 0.01). Of the pa
tients with bacilli resistant to both strep
tomycin and isoniazid, 2 of 23 in the R3
and R5 series combined and 8 of 14 in
the Z5 series had an unfavorable response
(p < 0.01).
Concerning rifampin sensitivity tests
during treatment, of the 4 patients in the
R3 and R5 series who had unfavorable
responses, resistance to rifampin emerged
in 1 of the 2 with resistance to isoniazid
alone initially, and in 1 of the 2 with re
sistance to streptomycin and isoniazid;
the resistance emerged at 1 month in
both.
In all, 89 patients (30 R3, 37 R5, 22
Z5) with resistance to streptomycin and/
or isoniazid initially could be assessed
TABLE 6
INCIDENCE OF POSSIBLE ADVERSE REACTIONS TO ANTITUBERCULOSIS DRUGS
IN 908 PATIENTS (297 R3, 307 R5, 304 Z5) AND THEIR MANAGEMENT
Patients with Reactions
Chemotherapy Modification
Series
0) (A)
(%)
Onset in
Daily Phase
(% of K)
Any
R3
R5
Z5
186
203
238
63
66
78
100
92
98
53
51
48
18
17
16
17
24
16
25
21
26
11
6
6*
Arthralgia
R3
R5
Z5
137
133
212
46
43
70
100
94
99
15
13
36
5
4
12
2
3
12
10
8
22
3
2
2
Jaundice
R3
R5
Z5
18
26
2
6
8
1
93
18
25
2
6
8
1
10
15
2
6
8
0
2
2
0
Giddiness
R3
R5
Z5
42
54
50
14
18
16
100
81
84
15
10
10
5
3
3
3
1
1
8
8
4
4
1
5
Others
R3
R5
Z5
66
83
67
22
27
22
100
90
84
9
6
3
3
2
1
6
5
1
1
0
1
2
1
1
Adverse
Reaction
Total
Total
(”)
(%)
Interruption
Dosage
Reduction
Termination
• Two patients had streptomycin as well as pyrazinamide terminated because of giddiness and arthralgia in one and an anaphylactic reaction and
arthralgia in the other.
3- AND 5-MONTH REGIMENS IN TREATMENT OF TUBERCULOSIS
for relapse. Of these, 13 (7 R3, 3 R5, 3
Z5) had a bacteriologic relapse requir
ing treatment (table 5). Although the re
lapse rate in the R3 series was higher than
those in the other 2 series, it is similar
to that in patients with initially drug
sensitive organisms in that series.
Giddiness. Complaints of giddiness
were made by 146 (42 R3, 54 R5, 50 Z5)
patients. Streptomycin was interrupted
in 5, the dosage was reduced in 20 (ineluding 16 who had an interruption also),
and it was terminated in 10.
Other adverse reactions. Complaints
of other possible adverse reactions
(mainly gastrointestinal or cutaneous)
were made by 25 % in the rifampin series
and 22% in the nonrifampin series, but
only 2% and 1%, respectively, required
modification of chemotherapy. Serious
adverse reactions warranting termination
of drugs occurred in 4 (2 R3,1 R5, 1 Z5)
patients. One patient (R5) developed exfoliative dermatitis in the third month.
A second patient (Z5) developed a severe
anaphylactic reaction after the first dose
of streptomycin. The other 2 patients
(both R3) had severe episodes of
vomiting.
A dverse Reactions
Patients were not questioned about
symptoms of adverse reactions, but every spontaneous complaint was recorded
after careful questioning by a physician,
The 876 patients eligible for the study
and the 32 who had received previous
chemotherapy are considered in this section. Possible adverse reactions occurred
in 63% of 297 R3, 66% of 307 R5, and
78% of 304 Z5 patients (table 6). The
contrast between the incidence in the R3
and R5 series and that in the Z5 series
is highly significant (p < 0.001); it is at
tributable to the high incidence of ar
thralgia in the Z5 series. However,
modifications of chemotherapy were
Discussion
necessary in similar proportions of pa The most important finding of this study
tients, namely, 18% of the R3, 17% of was the high relapse rate with the 3the R5, and 16% of the Z5 patients. One month daily regimen of rifampin, strepor more of the drugs had to be termi tomycin, isoniazid, and pyrazinamide,
nated in 11 (4%) R3, 6 (2%) R5, and 6 namely, 20% during a 21-month period
(2%) Z5 patients.
of follow-up (i.e., after stopping chemoArthralgia. A complaint of arthralgia therapy) in 200 patients with drugwas made by 270 (45%) of 604 rifampin sensitive cultures initially, the 95% conpatients and by 212 (70%) of 304 non fidence limits being 14 to 26%. This findrifampin patients, a highly significant ing is in agreement with those of 4 other
difference (p < 0.00001). In all but 12 pa studies of 3- or 4-month regimens. Thus,
tients (1 R3, 8 R5, 3 Z5), the onset was Eule and associates (10, and personal
during the daily phase, particularly in the communication), using the same drugs
second month when 52% occurred. Che daily for 3 months, reported a relapse rate
motherapy was modified in 28 (5%) rif- of 20% in 61 patients during a 3- to 5-yr
ampin patients and in 36 (12%) non- period of follow-up. In a study in New
ifampin patients (p < 0.0001). Pyrazina- Delhi of rifampin, isoniazid, and
mide was terminated in 7 patients. Full pyrazinamide daily for 8 wk, followed by
details of the arthralgia have been rifampin plus isoniazid daily for 4 wk,
reported elsewhere (9).
the relapse rate in a follow-up period of
Jaundice. Jaundice occurred much 21 months was 23% in 52 patients (11).
more often in the rifampin series (7%) The on2y study reporting a low relapse
than in the nonrifampin series (1%) rate (6% of 53 patients in a 24-month
(p < 0.00001). The onset was during the period of follow-up) was that of
daily phase in 43 patients, 34 occurring Mehrotra and associates (12, 13) from
in the first month. In all but 1 (R5) the Agra, India. The drugs and duration were
chemotherapy was modified. The usual the same as in the present study, but the
policy was to interrupt all the drugs. The patients were classified as having relapsed
drug for which dosage was reduced or only if radiographic deterioration was obwhich was terminated was rifampin in all served, in addition to reversal to culture
the cases.
positivity for at least 2 consecutive
Hepatitis without clinical jaundice months. Considering 4-month daily reg(abnormal hepatic function test values, imens containing rifampin and isoniazid
with symptoms) was observed in 5 (4 R3, throughout and pyrazinamide for at least
1 R5) of the total of 532 (173 R3, 180 2 months, the relapse rates were 13% of
R5, 179 Z5) Madras patients. The onset 208 patients in East Africa (14) and 10%
was in the first month in 3 (all R3) and of 156 in Singapore (15), during 24 and
the third month in 2 (1 R3, 1 R5). Two 26 months of follow-up, respectively,
patients (both R3) had drugs interrupted. These findings suggest that short-course
I'
31
regimens (3 or 4 months) are inadequate
as the treatment for sputum-positive pul
monary tuberculosis.
Fox (1, 16) has presented information
on the influence of the duration of che
motherapy in smear-positive disease,
comparing bacteriologic relapse rates in
a number of studies with regimens all of
which contained daily streptomycin,
isoniazid, rifampin, and pyrazinamide,
at least in the initial phase (1); the updated figures (16) were 1% for the 6month regimens, 4% for the 4.5- to
5-month regimens, 12% for the 4-month
regimens, and 16% for the 3-month
regimens.
Even in patients who had consistently
smear-negative pulmonary tuberculosis
with small lesions, a study in Hong Kong
(17) showed that neither 2 nor 3 months
of daily chemotherapy with streptomycin, isoniazid, rifampin, and pyrazina
mide was adequate, the bacteriologic re
lapse rates in a 5-yr period being 23%
and lo^To, respectively, and the relapse
rates including patients with radiographic
deterioration but no bacteriologic confirmation being 32 and 13%, respectively,
Although the relapse rate with the 3month rifampin-containing regimen of
the present study is unacceptably high,
it is noteworthy that practically all the
patients with initially drug-sensitive
bacilli attained sputum conversion by 3
months, and nearly 80% remained bacteriologically negative for as long as 2
yr; most of the latter are likely to have
been cured. This finding is of interest in
the context of patient compliance, because the patients stand a good chance
of attaining a cure even if they discontinue treatment well before the completion of a 6-month regimen.
Considering next the 5-month rifampin-containing regimen (R5) in the present study, the findings were substantially
better than with the 3-month regimen;
none of 230 patients in the R5 series had
an unfavorable response, and only 4%
of 187 (95% confidence limits, 2 to 8%)
had a bacteriologic relapse requiring
treatment in 19 months of follow-up. An
earlier study (6) from this Centre had
shown that a similar regimen but with
a 2-month intensive phase and a 3-month
continuation phase also had no failures
and a low relapse rate (5%) in 19 months,
This suggests that in 5-month regimens
consisting of rifampin, streptomycin,
isoniazid, and pyrazinamide daily followed by streptomycin, isoniazid, and
pyrazinamide twice a week, a third month
of daily chemotherapy confers little additional benefit in patients with drug-
32
sensitive cultures initially. In contrast, the
5-month nonrifampin regimen in the
present study (Z5) was clearly inferior to
the R5 regimen (3 of 236 patients had
an unfavorable response, and 13% of 199
had a bacteriologic relapse requiring
treatment) and was only marginally bet
ter than the 3-month regimen —a clear
demonstration of the importance of rif
ampin in short-course chemotherapy.
The high relapse rate of 20% was ob
served in the R3 regimen of the present
study, with 90 doses of rifampin, isonia
zid, streptomycin, and pyrazinamide
given daily for a period of 3 months. A
similar number of doses (95) had been
prescribed by Snider and associates (18)
but had a relapse rate of 0% of 84 pa
tients during an 18-month period of
follow-up; the same 4 drugs had been
given daily for 2 months, followed by rif
ampin and isoniazid twice-weekly in the
next 4 months. This suggests that it would
be more profitable to spread out the 90
doses by giving them intermittently af
ter an initial daily phase. Indeed, inter
mittent chemotherapy from the begin
ning could be highly effective and also
result in a considerable reduction in the
number of doses, which would reduce the
cost and probably lower the incidence of
side effects. Thus, 78 doses of the 4 drugs
given thrice a week over 6 months in
Hong Kong (19) resulted in a relapse rate
of 1% in 151 patients. Eule and cowork
ers (10) gave 52 doses of the 4 drugs twice
a week for 6 months and reported a re
lapse rate of 0% in 61 patients in a 12month period (10), and 3.3% in 121 pa
tients during a 36- to 48-month period
(personal communication).
In patients with initial resistance to
isoniazid, the contribution made by rif
ampin is noteworthy. Thus, 13 (50%) of
26 such patients who received the non
rifampin (Z5) regimen had an unfavora
ble response, as compared with 4 (7%)
of 57 who received the rifampin regimens
(R3 and R5). This is in conformity with
our earlier findings (3) and those of
Mitchison and Nunn (20).
The incidence of jaundice was signif
icantly higher (p < 0.00001) in the 2 rif
ampin series (7%) than in the nonrifam
pin series (1%). Furthermore, its onset
was early, 34 (77%) of 44 in the rifampin
series developing it in the first month.
A higher incidence of clinical jaundice
in patients who received rifampin in ad
dition to isoniazid, streptomycin, and
thioacetazone (17% of 63 patients) than
in those who did not receive rifampin
(6% of 67 patients) has been reported
TUBERCULOSIS RESEARCH CENTRE/NATIONAL TUBERCULOSIS INSTITUTE
by Rao and associates (21), also from In
dia, the mean time of onset being 15.5
and 71 days, respectively. These findings
strongly suggest that adding rifampin to
isoniazid or isoniazid and pyrazinamide
substantially increases heptatotoxicity. In
contrast, there is evidence that when
pyrazinamide is added to isoniazid and
rifampin in daily chemotherapy, there is
no increase in hepatotoxicity (22-25).
However, a low incidence of hepatotox
icity (1% or less) in patients receiving rif
ampin, isoniazid, and pyrazinamide daily
for 2 months or more has been reported
from East Africa (14,26) and Hong Kong
(25). Various factors that probably in
fluence the occurrence of hepatitis in
South Indian patients (27) and the pos
sible mechanism by which combinations
of rifampin and isoniazid cause hepati
tis (28) are discussed in detail elsewhere.
Arthralgia, attributable to pyrazina
mide, was a common complaint, but che
motherapy had to be modified in only
4% in the rifampin and 12% in the non
rifampin series. As in the previous study
(3), the incidence in the rifampin series
(45%) was appreciably lower than in the
nonrifampin series (70%). This is prob
ably due to an increase in the renal ex
cretion of uric acid caused by rifampin,
which could lead to a decrease in the
deposition of uric acid in the joints (29).
In conclusion, this study has shown
that the 5-month rifampin-containing
regimen is highly effective both in pa
tients with drug-sensitive cultures initially
and in those with drug-resistant cultures.
Its limitations include the daily atten
dance for 3 months and a high incidence
of side effects. Hence this Centre is cur
rently investigating fully intermittent reg
imens that involve less frequent atten
dances by the patients, are likely to have
fewer adverse reactions, and are less ex
pensive.
Acknowledgment
The scientific staff with major responsibility
for the work are as follows. National Tuber
culosisinstitute, Bangalore: Dr. N. K. Menon,
succeeded by Dr. A. Banerji, Director; Dr.
K. S. Aneja, Dr. P. Jagota^and Dr. A. G.
Kurthkoti, MedicaFOfficersTDr. N. Naganathan, Bacteriologist; Mrs. Radha Narayanan;
Sociologist; and Mr. K. Srikantan, Statisti
cian. Tuberculosis Research Centre, Madras:
Dr. S. P. Tripathy, Director; Clinic: Dr. C. V.
Ramakrishnan, Dr. R. Parthasarathy, Dr. O.
Nazareth, Dr. T. Santha Devi, Dr. D. C. Arumainayagam, Dr. V. K. Vijayan, Dr. Rani
Balasubramanian, Dr. S. V. Rathnasabapathy, Dr. Manjula Datta, Dr. R. V. S. N. Sarma,
Dr. Rajeswari Ramachandran, Dr. V. Kuma-
raswami, Dr. M. S. Jawahar, Dr. S. Ramakrishnan, Dr. K. Rajaram, Mrs. M. Jeyalakshmi Monga, Mrs. Parvathy Raghavan,
Mrs. Sudah Ganapathy and Mr. K. N.
Gopilingam; Laboratory-Bacteriology: Dr. R.
Prabhakar, Mrs. S. Subbammal, Dr. C. N.
Paramasivan, Mr. P. Venkataraman, Dr. N.
Selvakumar, Mr. B. N. Gopalan, and Mr. C.
Alexander; Biochemistry: Dr. G. Raghupati
Sarma, Dr. Prema Gurumurthy, and Mr. S.
Kailasam; Immunology: Dr. P. R. Narayanan,
Dr. Raji Swamy, Dr. Ramesh Paranjape, and
Mr. A. Ravoof; Statistics: Mr. P. R. Somasundaram, Mr. M. S. Krishnamurthy, Mr. G. S.
Acharyulu, Mr. B. Janardhanam, Mr. A. S. L.
Narayana, Mr. S. Sivasubramanian, Mr. P. V.
Krishnamurthy, and Mr. D. Rajappa.
The writers thank the Superintendent, Lady
Willingdon Tuberculosis Demonstration and
Training Centre (Dr. H. Shivalingappa, suc
ceeded by Dr. Nanjundaswamy Rao) for
providing space for conducting the study in
Bangalore. Special thanks are due to Dr. K. V
Krishnaswami for assessment of radiographs,
and to Prof. Wallace Fox and Prof. D. A.
Mitchison, British Medical Research Coun
cil, London, who gave valuable advice on the
preparation of the report as well as the plan
ning of the study.
We are grateful to the entire staff of the
3 collaborating institutions for their en
thusiastic cooperation. The public health
nurses, health visitors, clinic nurses, and so
cial workers made particularly valuable con
tributions. The secretarial assistance of Mr.
R. S. Sen and Mrs. M. Vijayalakshmi is grate
fully acknowledged.
References
1. Fox W. Whither short-course chemotherapy?
Br J Dis Chest 1981; 75:331-57.
2. Kreis B, Pretet S, Birenbaum J, et al. Two threemonth treatment regimens for pulmonary tuber
culosis. Bull Int Union Tuberc 1976; 51:71-5.
3. Tuberculosis Research Centre, Madras. Stud
of chemotherapy regimens of 5 and 7 months’ du
ration and the role of corticosteroids in the treat
ment of sputum-positive patients with pulmonary
tuberculosis in South India. Tubercle 1983; 64:73-91.
4. Tuberculosis Chemotherapy Centre, Madras. A
concurrent comparison of isoniazid plus PAS with
three regimens of isoniazid alone in the domiciliary
treatment of pulmonary tuberculosis in South In
dia. Bull WHO 1960; 23:535-85.
5. Eidus L, Hamilton EJ. A new method for the
determination of 7V-acetylisoniazid in urine of am
bulatory patients. Am Rev Respir Dis 1964;
89:587-8.
6. Else Holst, Mitchison DA, Radhakrishna S. Ex
amination of smears for tubercle bacilli by fluores
cence microscopy. Indian J Med Res 1959; 47:495-9.
7. Allen B, Baker FJ, Mycobacteria: isolation,
identification and sensitivity testing. London: But
terworth, 1968.
8. Canetti G, Fox W, Khomenko A, et al. Advances
in techniques of testing mycobacterial drug sensi
tivity, and the use of sensitivity tests in tuberculo
sis control programmes. Bull WHO 1969; 31:21-43.
9. Nazareth O, Acharyulu GS, Janardhanam B,
etal. Arthralgia in South Indian patients with pul-
3- AND 5-MONTH REGIMENS IN TREATMENT OF TUBERCULOSIS
*
i
>
monary tuberculosis during treatment with
pyrazinamide and rifampicin. Lung (India) 1984;
3:231-6.
10. Eule H, Beck H, Evers H, et al. Daily and in
termittent short-course chemotherapy using four
drugs in recently detected bacillary pulmonary
tuberculosis. Bull Int Union Ibberc 1982; 57:63.
11. Research Committee of the Tuberculosis As
sociation of India. Short-course chemotherapy of
pulmonary tuberculosis. Second Tuberculosis As
sociation of India trial. Indian J TUberc 1984;
31:81-8.
12. Mehrotra ML, Gautam KD, Chaube CK.
Shortest possible acceptable, effective ambulatory
chemotherapy in pulmonary tuberculosis. Prelim
inary report. Am Rev Respir Dis 1981; 124:239-44.
13. Mehrotra ML, Gautam KD, Chaube CK.
Shortest possible acceptable effective chemother
apy in ambulatory patients with pulmonary tuber
culosis. Part II. Results during the 24 months after
the end of chemotherapy. Am Rev Respir Dis 1984;
129:1016-7.
14. East African/British Medical Research Coun
cils Study. Controlled clinical trial in five short
course (4-month) chemotherapy regimens in pul
monary tuberculosis. Second report of the 4th study.
Am Rev Respir Dis 1981; 123:165-70.
15. Singapore Tuberculosis Service/British Med
ical Research Council. Clinical trial of six-month
and four-month regimens of chemotherapy in the
treatment of pulmonary tuberculosis. The results
up to 30 months. TYibercle 1981; 62:95-102.
16. Fox W. Short-course chemotherapy for pul
monary tuberculosis and some problems of its
programme application with particular reference
to India. Lung India 1984; 2:161-74.
17. Hong Kong Chest Service/Tuberculosis Re
search Centre, Madras/British Medical Research
Council. A controlled trial of 2-month, 3-month,
and 12-month regimens of chemotherapy for
sputum-smear-negative pulmonary tuberculosis.
The results at 60 months. Am Rev Respir Dis 1984;
130:23-8.
18. Snider DE Jr, Ragowski J, Zierski M, Bek E,
Long MW. Successful intermittent treatment of
smear-positive pulmonary tuberculosis in six
months. A cooperative study in Poland. Am Rev
Respir Dis 1982; 125:265-7.
19. Hong Kong Chest Service/British Medical Re
search Council. Controlled trial of 4 three-timesweekly regimens and a daily regimen all given for
6 months for pulmonary tuberculosis. Second re
port. The results up to 24 months. Tubercle 1982;
63:89-98.
20. Mitchison DA, Nunn AJ. Influence of initial
drug resistance on the response to short-course che
motherapy of pulmonary tuberculosis. Am Rev
Respir Dis (In press).
21. Rao NK, Wadia RS, Karve SR, Grant KB.
Hepatotoxicity of antituberculosis drugs. J Assoc
Physicians India 1982; 30:295-8.
22. British Thoracic Association. A controlled trial
of six months chemotherapy in pulmonary tuber
culosis. First report. Results during chemotherapy.
Br J Dis Chest 1981; 75:141-53.
23. East African/British Medical Research Coun
cil Study. Controlled clinical trial of four short
course (6-month) regimens of chemotherapy for
33
treatment of pulmonary tuberculosis. Lancet 1974;
2:1100-6.
24. Third East African/British Medical Research
Councils Study. Controlled clinical trial of four
short-course regimens of chemotherapy for two du
rations in the treatment of pulmonary tuberculo
sis. First report. Am Rev Respir Dis 1978; 118:39-48.
25. Hong Kong Chest Service/British Medical Re
search Council. Controlled trial of 6-month and
8-month regimens in the treatment of pulmonary
tuberculosis. First report. Am Rev Respir Dis 1978;
118:219-27.
26. East and Central African/British Medical Re
search Council Fifth Collaborative Study. Con
trolled clinical trial of 4 short-course regimens of
chemotherapy (three 6-month and one 8-month)
for pulmonary tuberculosis. Tubercle 1983;
64:153-66.
27. Parthasarathy R, Raghupati Sarma G, Janardhanam B, et al. Hepatic toxicity in South Indian
patients during treatment of tuberculosis with short
course regimens containing isoniazid, rifampin, and
pyrazinamide. Tubercle (in press).
28. Raghupati Sarma G, Immanuel C, Kailasam
S, Narayana ASL, Venkatesan P. Rifampin-induced
release of hydrazine from isoniazid: a possible cause
of hepatitis during treatment of tuberculosis with
regimens containing isoniazid and rifampin. Am
Rev Respir Dis 1986; 133:1072-5.
29. Raghupati Sarma G, Acharyulu GS, Kannapiran M, Krishnamurthy PV, Prema Gurumurthy,
Tripathy SP. Role of rifampicin in arthralgia in
duced by pyrazinamide. Tubercle 1983; 64:93-100.
TUBERCULOSIS CONTROL IN INDIA-CURRENT PROBLEMS AND POSSIBLE SOLUTIONS
G7V7J7 BAIL?
Attempts to reduce the problem of tuberculosis through
organised efforts had their beginnings in India in the late thirties.
With the introduction of chemotherapy, organised home treatment of
tuberculosis from the TB cliri.cs, situated mainly inncities and
district headquarter towns, was started. The mass BCG- campaign,
started in 2052, gave the first indications that the problems of
tuberculosis in rural areas could be as big as that in the urban
areas. .The/need ..ifor extebding case-finding and treatment of tuber
culosis to the rural areas, in addition to urban areas, was confirmed
by the sample survey J1J of tuberculosis conducted by the I.C.M.R.
The concept of offering tuberculosis services as a component of the
comprehensive health care delivered by the general health services
was evolved in the country over two decides age^ The concept has
been endorsed by the WHO (2) (3) and recommended for application
in its member countries in accordance with the developmental
situation in each country. In evolving this concept, cognisance
was taken not only of the size and extent of the problem of tuber
culosis but also of the fact that the rural areas continue to remain
ill served. In the words of Morley (4) ??Although three quarters
of the population in most developing countries live in rural areas,
three quarters of the spending on the medical care is in urban areas,
where three quarters of doctors live. Three quarters of the deaths
are caused by conditions that can be prevented at low cost, but
three quarters of the medical budget is spent on curative services,
manyof them provided for the elite at high cost'.
But, the picture is changing. Primary Health Care, as
enunciated by the WHO (5), and to which India is strongly committed,
holds the promise that a drastic reallocation of national resources
will be made, in an all out effort to provide essential health care
to the rural population. The report of Working Group appointed by
the Govt, of India on Health for All by 2000 AvB. (6; recognises
tuberculosis services as an important component of Primary Health’
care. The,inclusion of tuberculosis in the nation(s 30-point
programme is indeed the beginning of the realisation of the commit
ment.
In dealing with the tuberculosis problem and the National
Tuberculosis Programme, it is appropriate to realise that the past 9
and even,to-day, several organisations, notably the Tuhercuisis
Associations, institutions and private practitioners have contributed
considerably and continue to do so, for the alleviation of the
suffering caused by tuberculosis. However, in this presentation
on the problems of and projects for tuberculosis control in India,
the rural areas as also the National Tuberculosis Programme have
been selected for'the main emphasis. It is probably appropriate
to do so as that is where most of the problems exist.
I. THE PROBLEM OE TUB^RCULOS IS
J)]? OOMBAT:
1.
epidemiological dimensions of the tuberculosis problem in
India;
“
~
~
’
India is one tf the few developing countries of the world
where epidemiology of pulmonary tuberculosis has been studied for
a relatively long time. In recent years, a large amount of docu
mentation has come to bo available mainly through epidemiological
studies conducted in different parts of the country. In most of
these studies, either one or more of the three main epidemiological
tools, viz., tuberculin test,9 chest X-ray examinations and
(—2
A9
NATIONAL TUBERCULOSIS PROGRAMME
,
-- - , —.
-M—1
I. —■ IW- —*—■ • — —I. ■—« I
Iiw
I
■
—
I
5
-
gsome problems and issuess
Binayak Sen, CMSS, Dalli Rajhara, xMP 491228
1, conceptual problems
IN THEIR seminal 1962 paper on symptom awareness in
tuberculosis, Banerjee and Anderson, re-emphasized the
probelm of tuberculosis as a problem of human suffering,
and outlined a strategy for tuberculosis control based on
this concept. This strategy, abjured a policy of active case
finding. Instead, it concentrated its attention on greater
diagnostic sensitivity towards and adequate treatment for
those people suffering from symptoms suggestive of tuberculosis
who presented themselves at the existing hospitals and clinics.
Together with the Madras Chemotherapy Centre study on domiciliary
treatment, it forms the theoretical basis of our present day
tuberculosis programmeo
THE CREDIBILITY of this system rests on the adequacy
with which the entire range of presenting symptoms is
handled. The logical corrolary of the adoption of this approach
would, therefore, be the development of an integrated and
well-defined system for tackling the entire range of tuberculosis
symptomatology.
INSTEAD, THE National Tuberculosis programme has set its
sights on a Mirage - the interruption of bacterial transmission.
To this end, it defines a* case1 of tuberculosis as. a. person
excreting tubercle bacilli,, in his sputum. This approach is
unscientific because it is only at a much later stage along
the exponential curve of falling prev ’lencc that the interruption
of transmission becomes even a remote possibility. It also
ignores the fact that never in the history of human tuberculosis
has a reduction in transmission been brought about by a
specifically medical intervention.
AS A result of my four years experiepce of working in
voluntary institutions participating in district tuberculosis
control programmes — in Hoshangabad and in Durg - I am familiar
with the way in which this approach works in practice. A person
who presents himself at a Public Health Institution with symptoms
suggestive of tuberculosis is not regarded as a person suffering
from a disability and consequently in need of help but simply
as an entity to be categorised, ie., TB or not TB. After a
cursory physical examination he is sent for a sputum test. If
he obliges by producing a positive sputum, that is. the end of
the matter. He can then be placed on a standard treatment
regime.(1 y inh and Thiacotazone daily) and forgotten
anout. Once in a way his sputum may be checked but the treatment
regime is not affected thereby. I have documented evidence
of"patients, sputum positive after a year's treatment with INH.
and thacetazone, being continued on the same drug. When challenged,
the government doctor has explained, "that is the only regime
available". In point of fact, in practice this is often true.
BUT WE will come to problems of chemotherapy later. The
point I am trying to make is that from the point of view’ of
of a despamtely sick man, frightened by a dreaded diagnosis,
it is cold comfort to be given 30 tablets -and told to come
back again after a month's treatment and assured that ho will
get well in 18 months time. This is particularly so since
oooooooooooooooooooooooooo.>.0000000
888888fie88888888888888fi9888888»8e8S
• T_ n
_
A note prepared for the mfc core group meeting (July 84)
at Wardha..
^.19’71’934
e
"
o
,2
2
there are doctors at every
(
’
street corner assuring
patients
(with considerable honesty) that they will get well withi seme
private treatment in six months or less.
LET US now come to the case of those who were sputum
negative* The cost of a ’free’ MMR X-ray from Durg to.
a person in Rajhora, is well over Rs.50-00* The cost of
a local private X-ray is Rs* 35-00. Which should the patient
choose?
IT SHOULD be noted that I have been talking all along of
the ideal case* We have not taken any account of the
government doctor nudging the patient towards his private
clinic; the laboratory technician asking fo.r his 'fee1; the
X-ray technician’s rudeness, or the irregularity in drug
supply.
THE PATIENT of tuberculosis- is basically a suffering
person* It is the least of his concern that he is
excreting M tuberculosis in his sputum* What he is much more
worried.about is the fact that he has cough, chest pain,
fever, body ache, and nausea* He cannot work* He feels weak. He
loses his sexual potency* His children starve and often fall >
ill in their turn* A physically distant and emotionally remote
health centre can offer him nothing* It is well to remember
that the Madras Chemotherapy Centre study on domiciliary
treatment had weekly home visits as part of their protocol.
It is a great pity that this investigation has formed the
basis for a programme that thinks it sufficient to throw
some tablets once a month at a desperately sick man*
2o primary tb and extra-pulmcnary tb
4 TREATING THE problem of tuberculosis as a problem of
suffering people, rather than as a pr blem of successfully
eliminated parasitic myco-bacteria brings us t\ two sets of
illnesses often neglected in the current programmes*
ao
primary tuberculosis
Between 10 & 20 percent of Indian children are tuberculin
sensitive by the time they are five years old, though seme
surveys (Raj Narayan) yield a lower estimate* The popular
(medical) conccpti n of primary tuberculosis is of a mild
intercurrent illness that is only incidentally detected in
a chest X-ray and attains clinical significance cnly in the
’progressive’ form. This is not true* In malnourished children
not cnly is infection itself accompanied by significant
morbidity but it is the 1 interaction’ between infection and
nutrition—that is the factor that needs to be considered*
When we consider that, according to ICMR, 65% of Indian children
an severely malnourished,
the dimension of the problem
become a little more plain.
It is a common misc. ncoption (even, as I have discovered,
among TB ’Specialists’), that clinically apparent primary
tuberculosis can safely be treated by a short ccurse of INH
alone* This is a nation that goes against all bacteriological
logic. One only creates a population of INH resistant bacteria
strategically situated to subsequently produce reactivation
disease*
o .3
f
3
<
bo
Extra Pulmonary Tuberculosis
The chapter on Epidemiology in the Text Bock.of Tuberculosis
(by the Tuberculosis Association of India) has ncthing tc
say about extra pulmonary disease. In my experience this forms
a significant proportion of c^ses of tuberculosis. In particular,
scrofula burnt cut tuberculous cervical lymphadenitis is still
a common finding in backward areas of the country.
3. staff problems
SUCH CASES of ignorance among people working in- the field
of tuberculosis are not rare. This is because almost the
entire field level medical staff of the tuberculosis progrmmc
are 'dead-beats' people who have been promoted t. an admini
strative position because their seniority has become an
administrative embarassment.
IN A Government District Hospital, .despite all the other
problems one can atleast meet de ctors whr are inter.stedin their work in the medical, su.r. ical, gynaecological and other
specialist departments. Not sc in tuberculosis. The. department
which should, by all epidemiological logic, claim the most
brilliant and dedicated of our technical manpewer, is invariably
academically dead. In Hcshangabad, the District Tuberculosis
Officer was simply absent for a long period of time.
THE PARA-MEDICAL staff on the other hand ar often
exceptionally dedicated and able. They often run the
programme practically independentally. Hcwcverr they have tc
pay the price for their competence. In Durg, the statistical
assistant—a key person and in this case extremely competent
and dedicated—has been on full time deputation to the Civil
Surgeon's office, helping to administer the hospital.
4O chem^therapy
a.
Existing patterns
In thccryz the National Tuberculosis pre gramme pr< ■viclus
a wide choice among several alternative rcgimcso These include
daily INH and thiacetazcne with or without an initial period
of intensive treatment with daily streptomycin .and/or PASO
The bi-weekly supervised regimes consisting of INH/SM and
INH/PASZ have been designed specially to ensure patient
compliance.
Even according tc the treatment manual supplied to the
district Tuberculosis Officers, only sputum positive patients
are eligible for all these regimes. X-ray positive, sputum
negative: patients often just as sick as their 'positive’
brethren and about 5 times as numerous, are eligible only
for the daily self-administered INH/-TH regime. Presumably
compliance isnot a consideration where they arc concerned.
r
In actual practice, the- < nly regime available, with any
regularity is daily INH/TH. (incidentally, pyridoxine tablets
necessary tc c untcract INH induced pyridoxin deficiency
arc practically unheard of. Patients arc told to eat lots of
peanuts!, ) PAS I have net seen in the past one year.
Streptomycin is constantly in short supply so that pate, .mts
arc often randomly shuffled back and f- rth between regimes
containing SM and these without. The effect of such regime
changes in 'midstream1, on treatment offactivity, bacteria
. . o -4
i
»
sensitivity, and patient compliance remains, as t.iey say.
a subject for research.
Coming to the INH/TH regime, rTH
^” is
’ by no means an
uncontroversial drug, its use is banned~in
some countries
but let that pass. The incidence of ’maior' toxicity in
MadraS Sh°Wed the followin^fcidence offside
Cutaneous hypersensitivity reactions - 7%;
Jaundice
3%;
Intractable vomiting - 3%
Apart from these, there are minor side effects such as
anorexia, nausea, vomiting and head ache. Weight gain and
rise m haemoglobin level arc less in patients' on^PH al
compared with those on PAS. The effect of such minor side
effects on patient compliance, especially in the absence of
imagined medlCal suPervision and reassurance, can only 'be
prOblems Wlth the bi-weekly INH/SM regime not
■ c. able for sputum negative patients, : and limited and
irregular supply of SMO In addition, there is a rul<_ that
SM injections can only be given at the PHC level
o In other
words, this rc~
cgime is effectively available only to those
who live within
“a about
at _ _ i 5 kms of a PHC o
bo
Drug resist'inc c
Coming now to the problem of resistant
:
tuberculosis
there- .arc a number of problems .in the
-- ? existing frameworko
(1) Drug
resistance. in tuberculosis is not a rare
,
phenomenono Existing studies show that the
prevalence of primary drug resistance to both INH
and SM m India are (individually) of the order of
5 to 10 percent. The provalence of oeguired drug..
t no^ -^nown to mc„ But the success rate
of th. standard first lino treatment regime is of the
order of 80 to 85 percent under ideal conditions.
(2) There is evidence to show that pre-tr^utmont drug
sensitivity tests do not <affect
:
the outcome of
treatment provided standard
~d two phase regimes are
used, with an initial intensiv------ phase using throe
drugso However in my experience such regimes are
only to a... very small pxuperuion
proportion or
of patients even
diprict centres, and to practically
none in the
■
;
p ripheral centres. Most patients go on a standard
cwo drug regime (general INH-TH).
(3) Whena patient fails to respond clinically to a
particular regime, there ar no facilities for druo
sensitivity testing even in these selected cases.
heoretically, in the existing- model, they can be
referred to Tuberculosis Sanatoria for treatment with
2nd line drugs. In practice,. however, (a)' practically
th&se patients do get referred to Sanatoria;
i1'
, even among those who arestarted on second
Imo drugs at such centres, there are no facilities
to
such drugs after the patient is discharged.
in
l°ne P-tient 1 managed to get referred to a Sanatorium
JJ Bhopal emerged after , two months looking much better and
clutchingj a prescription for rifampicin and 'ethambutol.
o . o o .5
b
Co
Possiblc Alternatives
It is well known that there now exists a wide variety
of alternative drug regimes, for the treatment cf tuberculosis
many of which , result- in
cure of proportion of patients
a higher
in a imuch shorter period of time than existing'standard regimes,
The conventional wisdom is that these alternative regimes
regimes
comprise a ‘second l.ine’ of treatment for patients resistant
to the standard regimes.
The factthat the government itself does not take this
argument seriously is shown by the free availability of the
so called ‘second line’ drugs in the open market. Of cours^,
the price is far beyond the reach cf the ordinary tuberculosis
p^ti<_nt. As a result, wc have in India the ir< nic situation,
where the District Tuborcuiosj_s officer and the PHC Medical
Officers are the only medical practiticncrs who (in their
official capacity) have no access to the newer drugs for
the treatment of tuberculosis.
In effect there are today,
today. in tuberculosis, ias in every
other field of medical and indeed of public life,r two sets
of policies in operation—one for the pocr and one set for
those
Lh;— who
..ho can (even if only with difficulty) pay.
The argument against the newer regimes can now be seen
plainly for what it is a question cf cost, It is worth
going into this question in seme details.
5, the question of cost
a. o
How much?.
lhe cost of a complete course cf treatment with the
newer drugs at current market prices is cf the order of
Rs.500-00 to Rs.1000-00., Regimes containing Streptomycin
arc liable tc cost more because of the administrative cost
of giving the injection.
We are not talking of enormous sums of money. The cost
<.f bi-weekly INH/SM with, an initial intensive phase,
phase. is not
much less. Neither is the cost Of INH/PAS regimes. The logic
of the exclusive dependence on INH/TH new become clear.
Put another way, the cost of treating a case of
tuberculosis with the newer <drugs and the cost of treating a
case cf intestinal obstruction or pyogenic meningitis is
about the same. The cost of treatingf a case cf ischaemic
heart disease or lung cancer or brain tumor :.r diabetes
mellitus or chronic renal failure is several times higher.
The comparison becomes ridiculous when one carries the contrast
to fields outside medicine—say, to defence or CHOGM.
bo
Cost
•c. whom?
The second aspect cf the cost equation. Whatis the ‘cost’
c f a.twenty percent relapse rate which is the best result
cbtainablo with standard 'first line1 regime? What is the ’cost’
of a. c se <of thiacetazcne induced agranulocytosis or StevensJohnson Syndrcme? What is the 1 cost' of travelling up and down
from village to PHC, village to District centre,, village te
wherever, for 18 months as a .ninst the six me nths with newer
regimes? What is the 'cost1 in bus fare? What is the ’cost'
in lost income? What is the ’cost* in the suffering of a
poor man? This is
‘ ' n which the policy makers of
•--.uesti
tuberculosis mu£t answer.
’ “ • 6 (objectives -f the meet)
6
A note on the objectives of
an. mfc annual meeting .^n tubercu 1 csis
(1) The objectives <Of'T the
_1_ conference Should not Include the'
framing ci alternative
Thu existing policies
n-ilirr
t government programmes.
The^existing
-- Any
alternative
t< fcrmulato will
Lv
Stc » - ■
Y
“ m°Y bo ablc
involve a restructuring too radical"'
fd their acceptance to be feasible,' <
other factors militating
ilitating against
against their
their acceptance.
(2) An important
part cf the prcgrnnync. fcr. the c.- nfareneu
should be the. understanding of the problem of-tuberculosis
in its national
- have much
an underst-ndingtPeSX"tlVe‘ NCt mQnf mfc
1
Sharc
q
c-.mmvn
understanding
of the problem," it is useless to 'try to devise programmes
of action.
HY bct?ln =ncept
in
Possible-programme •■cutccmds cf the conferences
a.
l/cnce£ted effort tc work out a 'solid critique
ana
VykStitl-in.
with
b.
Working out and executing pilct projects based
cn
alternative’ rg‘uppro
■'.ches tc the problem ■'■■■ f tuberculosis#
utilising newer
..- tcchhclogical as well ns s-ciclogical
insights. These would include
intensive small scale
field level1 studies.
Surveying
the problems '
the much'neglOcioPptdi.
Sis' . deluding
Cf AStvTtCte'i erbiological impiicPb^ "
primary
’ f)l
t-iimc.ry tuberculosis in forc-sch
-i
axto„
ta„a impli„tl;ns
s
_cns r. f drug resistance
ii. in”Of^dd'VCr!?m‘Snt '“’■-Witlos lnt,.nslv<!ly
Ol™SUtlY3 °£
etc.
1
.1-1110-
-ncc ln government programmes
iiio Wc.rking • ut alternative
•approaches including
newer ways to impr ve aticnt compliance, newer
treatment regimes, newt^ diagnostic approaches
including newer approaches
to diagnosing drug
resistanceo
f
Z-€
i
L
7>l$ 5 •' 4R -51
■NTI Newsletter (1938) 24/1 &2, 3
CURRENT TOPICS
PRIMARY HEALTH CARE AND TUBERCULOSIS PROGRAMME*
I
P. Chandrasekhar**
I
I
I am grateful to the Tuberculosis Association of Andhra Pradesh for selecting
me to deliver ”Dr P.V.Benjamin Memorial Oration for 1988”.
To be asked to deliver an oration in memory of the ‘Late Dr P.V.Benjamin,
is in itself a great honour and privilege, most challenging and I accept it with
. utmost humility, dedication and devotion.
Dr Benjamin, has been a powerful personality in the field of Tuberculosis
and has been regarded as ’’Father of Anti-Tuberculosis movement in India and
an elder statesman among International Experts”. To talk about Dr Benjamin
is like describing a multi-dimensional and multifaceted individual. It is obr
good fortune that we have encountered this remarkable man who had the unique
power of presenting novel ideas in the control of tuberculosis and at the same
time a genial and practical man. He was a symbol of hard and dedicated work
• and his forceful and persuasive personality is a thing worth remembering and
emulating.
/
r
I
I had the unique experience and privilege to avail of his guidance and I owe
my speciality - ’Tuberculosis’, to his advice and initiative. He had shown that
one should have a cause to pursue, have sufficient motivation to pursue the
cause, and should be willing ‘to make sacrifices to achieve the cause to which
one is deeply committed.
In the early part of the century, it became very clear to Dr Benjamin that •
the ’western model’ of dealing with the problem of tuberculosis viz., training ,
of thousands of specialists, creating number of beds and running several vehicles
would not be in consonance with the realities existing in our country like meagre
resources and huge size of problem of tuberculosis. He strongly felt that we
should forcefully repudiate the western model totally, if we have to move forward
and generate a National Tuberculosis Programme, in the spirit of social equity
and this was the basis and the background why the National Tuberculosis Institute,
Bangalore was established in early 1960s. And, being an impatient man, a tvtfo
♦Dr P.V.Benjamin Memorial Oration delivered at the. 15th Andhra Pradesh
Tuberculosis & Chest Disease Workers’ Conference, Hyderabad - 9th &
10th April, 1988.
J
**Ep!dorriiologist, National Tuberculosis
Bangalore 580 003
Institute,
a,
Bellary
Road,
/
o
4
&
4
years time was given to NTI to formulate and evolve a programme, although
many of us would have liked to continue research for 5 to 10 years. The challenge
was to develop a suitable and appropriate technology which would be subservient
to the people, applicable and acceptable to the community.
HEALTH SCENARIO OF INDIA
I wish to briefly review the health scenario of our country. The Constitution
of India envisages the establishment of a new social order based on equality,
freedom, justice and dignity of the individuals. It aims at elimination of-poverty,
ignorance and ill health and makes the States responsible in raising the level
of nutrition and the standard of living of its people. The improvement of public
health is among its primary duties and forms the main thrust of our health policy.
It was felt during the early stages that an integrated comprehensive approach
in health services, medical education and research should be established in order
to serve the health needs and the priorities of the country.
/
•
OUR HERITAGE
. India has rich, centuries old heritage of medical and health sciences. The
philosophy of ayurveda and surgical skills enunciated by Charaka and Shushruta
bear testimony to our ancient tradition in the scientific health care of our people.
The approach of this ancient medical system was of a holistic nature and took
account of all aspects of human health and disease. Over centuries, this system
of medicine continued to be practised widely. However, the allopathic system
of medicine has in a relatively short period of time made a major impact on
the natural approach to health care and' the pattern of development of health
services in our country.
PAST ACHIEVEMENT
During the last few decades since the attainment of independence,
considerable progress has been achieved in improving the health status of our
people/ Smallpox has been eliminated, Plague is no longer a problem, mortality
from Cholera and related diseases have declined and Malaria has been brought
under control to a great extent.
In spite of such impressive gains, the health scene of our country constitutes
a serious threat and urgent concern. The high .rate of population growth continues
to have an adverse impact on the health of our people and the quality of their
lives. The mortality rate for women and children «re still distressingly high.
Communicable and non-communicable diseases are yet to be brought under
the effective control. Blindness, Leprosy and Tuberculosis continues to have
a high incidence. Hardly 30% of our rural population have access to potable
water supply and 5% enjoy basic sanitation. /
.
The existing situation is largely endangered by the development policies
and the establishment of curative centres based on ’western models’ which are
5
inappropriate and totally irrelevant to the real needs of our people and entirely
out of context to the socio-economic conditions prevailing in the country. The
hospital based and the cure oriented approach have benefited >only the upper
crust of our society specially those residing in the urban areas,. The uncontrolled
proliferation of this approach lias been at the cost of providing comprehensive
primary health care services to the entire population both in the urban and rural
areas.^ The high technology boom which our country is passing through is
responsible for distorting the picture of the actual health needs of the community.
"It is easy for a developing country to go from ox cart
to the jot age; but in the process it leaves 90% of its
people behind".
- John Balcomb, World Health
Forum, Vol.5, 1984
Further, continued high emphasis on curative services have lead to the neglect
of the /essentials of health care viz., preventive, promotive, curative and
. rehabilitative aspects of health care. The prevailing policies with regard to
medical education and training of medical and para-medical personnel at various .
levels have resulted in a wide gap between the consumers and the providers of
health care. Present day doctors whom we train are not fully qualified to deliver
or participate in the primary health care activities, because they are not^v
adequately trained to meet the concepts of primary health care. The vast majority
are still narrowly focussed on ’curative care’, i,e., removing symptoms rather '
than eliminating the causes that lead to symptoms. It is said that:
"Trying to promote primary health care through medical
profession is like trying to promote land reforms through
big landlords/owners"
- Dr David Werner, Director
of Californian Foundation
NATIONAL HEALTH POLICY
1
Over years, the planning process has become oblivious of the fact that the,
ultimate goal of achieving a satisfactory health status for our people • cannot
be secured without involving the community. In other words, community
participation is essential and depends upon proper identification of their health
needs,, their priorities as well as in the proper implementation and management
of various health and related programmes.
A national ^health policy, has to be necessarily within the integrated planning
frame workz which seeks to provide universal, comprehensive health services
relevant to the actual needs and priorities of the community at a cost people can afford ensuring at every stage total involvement and participation of the
community. Health policy has’to go in search of equity - oriented components
'o
of
oi other
oiner sectors to form
iorm part of a movement towards the integrated improvement
ot well being. Equity in health is above all equity in development. It implies
that foremost attention to those who are in the lowest segment of national
health profile. The health of these vulnerable groups will reveal how and why
the national health strategy*fails to reach persons of this group, often due to
multisectoral complexityz^
’’It must be borne in mind that the tragedy of life doesn’t
lie in not reaching your goal.. The tragedy lies in having
• no goal to reach, It isn’t a calamity to die with dreams
unfulfilled, Ibut' it
“ is a calamity not to drcam. It is not
a disaster to be unable to capture- your
but .itv .j
is a
—-ideal,
---------- , —
disaster to Jiaye no ideal to capture. It is not a disgrace
not to reach the stars, but it is a disgrace to have no "stars
to reach for. Not failure, but low aim is sin”
Dr Benjamin .Mays, Former
President of Morehouse College
in Atlanta, Georgia, U.S.A.
c v ^ornPre^ens^vtc health care’ is the key stone to community health and consists
oi hoalth care delivery system at the primary, secondary and tertiary levels.
Primary Health Care
Primary health care does not mean the first contact only, but it is the very
essence of all health activity. It is the prime and central core of health and
underlines primacy. Figs. 1 and 2 show the basic components of primary health
care and includes disease prevention, health promotion, curative and rehabilitative
aspects of health. The main emphasis shifts from curative aspect to health
ca_r.c activities. The idea of reaching out to people is a laudable one but extremely
or£Gnis?-z n suggests that.all health efforts should emerge from
within the community and directed to the community. Briefly, the emphasis
m primary health care is a shifts
P
Fig. 3
(See next page)
s^ongly advocates the use of enlightened and highly motivated individuals
W’ thin the community as the first contact health personnel, in the total national
health system.
The concept of primary health care depends upon the relative roles of primary,
secondary and tertiary levels of health care and has been depicted in Fig.4,
and is based fundamentally on the triad of:
b
(1) Community involvement (2) Intersectoral co-ordination, and (3) Appropriate
technology.
7
Fig* 3
To,
From
Illness
Health
Cure
Care
Health promotion
Treatment
Episodic treatment
Continuous treatment
General physicians, para-professionalsSocial Workers, Health Visitors, etc.
Specialists & Physicians
Specific problem
2
Comprehensive health care
Single handed
Physician/Doctor
. Health Teams
Health Sector alone
Collaboration among all sectors - housing,
economy etc. Intersectoral collaboration
!
Clinical decision making
:
Community participation
In other words, primary health care means essential, necessary and relevant
to the individual, the family and the community. It does not mean a diluted or
second rate service for the poor. The usual definition and which is a comprehensive
one, is as follows: Fig-5
’’Essential health care made universally available to individuals
and. families in the community by methods acceptable to them
through full participation and at a cost that the community and
country can afford”
The essence of this concept s the involvement of the community and the
use of appropriate technology.whic.i would be subservient to the community.
Components of primary healtl rare are:
1. Comprehensiveness; includes t prevention, promotion, curative
rehabilitative services. .
2. Regionalisation - peripheralisation of services - reaching out to
people.
3. Stress on rural areas.
4. Appropriate technology - o x pies’ oriented technology.
5. Universally acccssible/acuf ptable.
6. Community participation-
and
3
708.
9.
Two-way referral system.
Evolution through evaluation.
Intersectoral co-ordination - in planning, programming, other areas
of education, housing, sanitation, socio-economic conditions leading
to overall development.
Secondary Health Caro-
Secondary health care is essentially delivered at the subdistrict and district
levels. Essential prerequisite is m interlinkage between Primary Health Centre,
subdistrict and district levels. Unless there is functional and well organised
two-way referral system, it is not likely to be successful. There should be a
continuous interaction between doctors of Primary Health Centro and the
Specialists at the district hospital. Such interaction will necessarily improve
the knowledge and skills of those involved in the delivery of primary health
.. care./
•
'
Tertiary Health Care
/ The main objective at this level is to provide Specialists1 services in all Hie
disciplines with supportive laboratory as well as appropriate facilities. Concept
of tertiary health care is through medical colleges, regional institutions or
specialised care. They should be responsible for organising refresher courses
for medical professionals in peripheral areas. The concept of different levels
of health care and their interlinkages have been shown in Figs. 1 and 2. For
a final'level of comprehensive health care, better understanding of co-ordination
and/Tinkage’ have to be firmly established.
/
The Shore Committee of 1946 recognised this intersectoral efforts and
linkages. - The Primary Health Centre was conceived as a nucleus from which
primary health care services would radiate through subcentres over to the country
side - a process of complete decentralisation of all activities. The Primary
Health Centre was conceived as an institutional, structure to provide integrated»
comprehensive services to the rural population of our country i.e. preventive,
promotive, curative and rehabilitative aspects of health care. This was a response
of the political leadership of the freedom movemenVto meet the rising aspirations
of the masses of people. The first batch of Primary Health Centres was set
up in 1952. Quantitatively there has been a significant increase in the number
of medical and para-medical personnel in Primary Health Centres. Qualitatively
there has been major changes viz., many mass campaigns have been integrated
with Primary Health Centres, both in terms of their staff as well as function.
There has been national programmes which were developed as an integrated
component of Primary Health ’ Centre for e.g. tuberculosis, integrated child
development programme and blindness.
Kartar Singh Committee of 1973, however, extended the outreaches of
Primary Health Centres by the introduction of Multi-purpose Health Workers
Scheme and establishment of a subcentre for over 5,000 rural population. The
9
Community Health Workers Scheme launched in 1977 is structured around the
central philosophy of ’’placing peoples’ health in their hands” by providing one
Community Health Volunteer/Guide for every 1,000 population. The Community
Health Volunteer/Guide Scheme was of profound social and political significance.In effect it meant going directly to the people to strengthen their capacities
to cope up with their health problems themselves and seek and demand services
from the Primary Health Centres and other referral health institutions. The
infrastructure described.. above was considered adequate to provide primary
health, care to the rural population and it would require proper back up by
providing two-way referral services.
FiS-S
»
I
.
«
■
"
. ' V4
■'
-I
•
The success of comprehensive health care is very well illustrated by the
Chinese example, where China’s grnat achievement in public health has been
due to total political commitment ;at all levels of Government and society,
and regards health as an integral part of social equity. Health is everyone’s
right and Responsibility and the- !bare foot doctor’ became only a feasible symbol
of this approach.
,
■ .t
>
.
..•j (,
A Chinese dictum says:.
. Go in search of your people •
Love thqm
. Learn from them Z , w.
Plan with them ;
Serve them
Begin with what they have
Build on what they know
' ‘
P4ao
•
■
r
I
i
Many a developing countries have tried to follow this approach by training a
large cadre of para-professionals viz., Multi-purpose Workers, Village Health
Guides, but without makirig adequate provision for referrals, technical back
up and administrative support.
•
■
I
.
’’The greatest tragedy of all Is when a developing
country builds a health plan for the needs of tomorrow
on the imported solutions of yesterday"
'(
Dr David Morley
/ The desirability of training large number of auxiliary health workers is very
much a political decision than a technical one. India’s conscious decision to
train a large number of para-professionals is an expression of this political
decision.
,
.
’
10
’’Therapeusis of social imedicine is not social action
but political action based1 on medical recommendation ”
Francis Crew
Professor of Social Medicine
ALMA ATA PLEDGE .
“-
=
22SS
StSS?
"t0° i‘cr tteWs
the^goal 'of0-’Health1 fOr ^iTy
™
/b C0,nrnitted to attaining
comprehensive primarv h^niih /a.
•
through the universal provision of
health promotion, curative and rehah^Ht^r W111Ch- !ncludcs disease prevention,
objective i<5 n hi<r
? d rehabilitative services. Achievement of this
that each country has to^oVonr^f001*11^ W‘th a hugC P°Pulation ar>d demands
on the prevaS Slth orXL 7° tstrate^ and P1™
action depending
herculean task, if is'not PO-sSt 7nr
“nd a,vailable resources.^-In this
responsibility as it needs'th f°r.h 7 sarviCeS a °ne to undcrtQ,<e tin’s heavy
departments^ concerned 2th L“SS
aiid/^^ation of all the
overall socio-economic improvement
°f the country leading to
collaboration is based on tl^efS
Wh° e concePt of intersectoral
has been tried in countries\iko%- VTCn7S na multi sectoral approach and which
in India. Cuba vaccTnated the
’ r’
China’ C°Sta Rica and Ker^
^'”‘totedP0uqwUchIn(Ucatea^,^^te^^«^t^ 72 hour, a„d
of heS’rT.d0™1!165’
politlcal
“'lol »iu .
■
14.
■ ----------- ”**1 resulted in the development
sub^caulnrrtppf”'111011’ - Water
programs
”a'“. Qnd
- sanitation> and other
when cXared dechne.in mortality and which is considered
remarkable
X
d
socio-economic situation.
Simultaneous
development of
an
exccUenj
St
h
7
Q
s
y
ner
&
isti
d
c«ect
on health,
He al. th .is
development. The importance of multi
fs.ect<?ral HPPr°ach to overall
dependence of ’basic needs’- satiafvinw
1 Tf actlcn 1S exPlained by the inter
to satisfy others.
*
’ '
% Q nee<^
strengthen peoples’ capacity
provXXX0
XWX* ,'’e
This declaration emphasised that^ime^/thT 0
dimension of 2000 AD.
tackled . not by training moro dnnf me °£ the w<?rst health problems could be
wXmge^
water and ade^te sanitation, then im^XJ0^^
ft
11
i
I
become a priority. With severe malnutrition, both adults and children become
more vulnerable to disease and hence, nutrition forms an important component..
On the medical front, simple vaccination could prevent 6 communicable diseases
which has defied all attempts so far, hence Expanded Programme of Immunisation .
forms yet another avenue^/
i
It is exactly a decade since the Alma Ata Declaration was made and accepted
by the member States. •'’During this period, several important events have taken
place, for e.g?
'
1«
World economy underwent severe economic shock waves in the form
of prolonged recession.
2U
World population swept past 4,800 million mark.
Urbanisation grow at a disturbing rate, creating new challenges
for health and developmental plans.
3»
4.
In such an alarming scenario of adversity, it needs lot of courage,foresight
and,efforts for member States to pursue programmes for human development.
Despite many set backs, the gains during the past decade has been quite
substantial. There is now a dense net work .of health services in rural areas.
One Community Health Volunteer/Guide for 1,000 population, a sub centre
with male and female health workers.for every 5,000 population, a Primary
Health Centre for 30,000 people, a community health centre for 1,00,000 people
and a 25 bod hospital for 40,000 population. No other country in the third world
with similar resource constraints can claim to have such an infrastructure of
health services for its rural population.
.
/ India’s political commitment was .made in the form of 20 Point Programme.
It is the agenda given to the nation in 1982 which pinpoints special areas of
thrust to produce tangible results./it is the nation’s commitment and calls for '
hard work,yelped, by a clear sense of purpose and discipline. The intension is
to move the whole economy of the nation and it is left to us to maintain the
momentum. The whole nation is on the rhove. on several fronts (20 Point). It
has generated a . wave of commitment and‘there is no stopping till the targets
are acnieved. It - has created an awareness, urgency and accountability among
all the health workers at all levels to complete the targetSo/Tuberculosis has
been one of the programmes included in this agenda.
t
jr •
I
/
1
Rise in absolute number of children and old people adding to the
burden, of work force, unemployment aggravating the situation
together., with a variety of political conflicts, threat of nuclear
accident/war, violation of human e rights, growing environmental
pollution, selfgenerating and self-expanding* poverty leading to
malnutrition, and the spectre of starvation in the form of severe
floods and drought in the areas of cultivable lands, all seem to
proclaim approaching world catastrophe.^/
.
12
TUBERCULOSIS & PRIMARY HEALTH CARE
Tuberculosis continues to be a public health hazard in dur country despite
several outstanding research in the field of tuberculosis/It still continues to
bo.her the health planners despite the fact that it is preventable, and definitely
and ^’t
reaS10n? 10r °Ur failure C0lild be medicai> organisational, economical
It is almost scandalous having tc witness millions of cases of tuberculosis
dying without the benefit of modern drugs and simpler methods of diagnosis.
In spite of several scientific break throughs, we still find the problem of
tuberculosis haunting us., ■'
tuberculosis through centuries have been considered as an affliction of the
mdiyidual rather than a public health problem, not being endemic to territorial
distinctions and not being absorbable in epidemic proportions, it has been regarded
d,lseose’ t’lOUfJb its main symptom ’cough1 is by no means silent,
luberculosis does not provoke communities to get together to fight it nor does
dL?1nVlde#LCaUSe WziCh readily attract3 attention of those who guide the
destinies of the nation/
ab0Ut 30 years after the discovery of Mycobacterium
tuberculosis, the Sanitary Commissioner to the Government of India urged that
deait Wlth M a-Public henlth Problem. The immediate response
■
Government was to open Sanatoria and institutions for treatment
?»artS °-f thS cot!ntpy- This approach emphasised more on
n vMuabsing the patient and his treatment and isolate him from his physical
md social environment. During the crucial years immediately after the
uicependence, it seemed possible to embark on an effective programme which
would have a marked influence on the problem of tuberculosis.
;n
Ind'? launched a massive National BCG Programme, the biggest
th?^TOTW m tterm.S of P°Pulation covered. The ’50s was also the time when
'rnhr.nr.Oi'mGlLV?0tentlQ1
dru®s on domiciliary basis was demonstrated by the
Tuberculosis Chemotherapy Centre, Madras. This created a sense of euphoria
esultmg in the firm conviction that the control of tuberculosis was still within
-ho foreseeable future and the end of tuberculosis was in sight.
o bOf<' AW°p decades aK° National Tuberculosis Institute made a giant stride
a Um field of public health in formulating the tuberculosis programme within
General Health Services. Right from the start, the programme
the GenS Heafth sTrXs?
C°n®®^ °f
inteBration at a11 levels
Prr3^LhlghKSexrS<l-Of ^Ptimism lead to the formulation of National Tuberculosis
?me by Natlonal Tuberculosis Institute in 1960s based on the clear dictum
imolement^d Winer+h the p®0Ple are' and a peoples’ oriented programme was
implemented in the country. The emphasis was on changing and developing
13
General Health Services and the concept of integration was an added dimension
along with other national health programmes, dove tailing with other socio□mic priorities of the country. Reaching out.to the people through the
Multi-purpose Workers/Community Health Guides is an added feature of National
Tuberculosis Programme. In other words, tuberculosis programme fitted very
well with the concepts of primary health care.-
i
Soon this optimism became hazy and distorted not because of any upward
trend in the disease, but because of the country’s sagging commitments to the
cause. This malaise took various forms such as dislocation of trained personnel,
improper utilisation of resources, haphazard and disproportion of supplies.
The tuberculosis programme is so structured that it provides greater resilience a
so that it eah change and modify according to the General .Health. Serrices^
It would swim or sink with General Health Services. The clarion call to provide
primary health care found a response in the National Tuberculosis Programme
as well. In 1980s, it had the expectation to see the tuberculosis programme
unfurled to the full extent through the Primary Health Care, a strategy that
would make health services available to those who need them specially in rural
areas and in 1990s it should be possible to mako it a component in a package
for Health for All by 2000 AD.
'I
TECHNOLOGY
J
• Zi peoples* oriented technology was the main stay in the formulation and
implementation of the tuberculosis programme of India, during the early T60s
at the National Tuberculosis Institute, Bangalore uiid was^-based on the following
premise:
’
’ .
.
,
.
I
;
j
•
.
About two thirds of. all cases of tuberculosis in a district was found
to be worried about the disease and half of the cases had actually
gone to the nearby Government institutions to seek relief of their
symptoms. And what was more revealing was the fact.that ho serious
attempt was made to diagnose them at these health institution^^This
finding was crucial in formulating a "peoples’ oriented" National
Tuberculosis Programme of India which ensured that:
I
?
z/ Top priority is given to tuberculosis patients who are actually seeking
relief of their symptoms, i.e.’felt need’ (social priority)
As patients seek treatment at the health institutions which is part
of the General Health Services, tuberculosis services is made available
to them within the frame work of General Health Services themselves
with proper back up of referral services (choice of a peoples1' oriented
health service delivery system)
Since all sputum positive cases have cough, they could easily be
diagnosed at any or all the rural institutions by simply examining the
I
.I
/
.... ru™
5-
4
14
sputum of cough cases for tubercle bacilli. Once the case is diagnosed,
these cases.,are offered domiciliary treatment by these very same
health institutions (peoples' oriented technology)
Meeting the-existing felt need will generate further felt needs and
this will persuade others who have not sought treatment to seClrrolicf
because of this spread effect of 'satisfied customer', it is possible
to cover most of the^cases'in the community.
Fig. 7
<•
Tom the above, it. would be seen that the tuberculosis programme us
conceived, planned and implemented in the country has taken care of all the
principles and concepts of primary health care. The emphasis right from the
beginning has b.een on peoples' participation.; which .is a process in which the
ielt need of the community is duly taken care. of. Communities have always
shown enough potential to be self-reliant. Village knowledge, village skills
and rural wisdom have to be appreciated while planning a health programme.
rhrrai>nCfdPt
com'?u.nity Participation is not at all a new one, since the dawn
\^,man
lnL’ ’ living participatory life, facing odds together^slmrmF
common problems and objectives, i.e., collective hunting and stared gaHTEsTrta need for this concept is totally reflected in the 1st Five Year Plan where
the emphasis was ,,qn . community developmental programmes in the form of
green revolution.
11
FUTURE PERSPECTIVES
riwnrberC-n0S^ P^ramme has the potential and the flexibility to adapt mid
change with the General Health Services, This is a unique fktaurc and has
sustained the programme all along in its-full potential,. The time .for empty
slogans is over and it is now time for prompt and'effective action, so that these
slogans could be converted into more meaningful and purposeful action. •
■arv^1^ At» has provided the prescription and pledge - "Health for All by 2090
‘ rin-C° luhCn’ scores of Planning committees have met and pious resolutions
and policies have been made. Now is the time for action. Action must be in
rifjni earnest.
,
;
Future
h’?D onSthPirre
^If of the infectious cases are seeking medicfll
aX? on.fheir own initiative for relief of their suffering, most of them , are turned
for Ubm'cXs^rOPetbdltSn°S1S’ R iS indeed a great crime t0 treQt an individual'
for tuberculosis without proper diagnosis and to withhold treatment when the
■ tiMtment1Lflau1rfeS^bhShed"''1IgnOranCe °f drUgS’ d0Sage nnd duration of
treatment by qualified personnel cannot any more be tolerated. Expensive
S
./
/
’
■
?
15
second lino drugs are being pushed into market and are being prescribed often
in sub-therapeutic doses with irrational combination, leading to emergence
of drug resistance. Resistance to Rifampicin is already assuming alarming
proportions due-to indiscriminate use, and it is a clear warning and indication
of the extent to which there is a complete anarchy in the treatment of
tuberculosis in the country. ' .
!
i
In the words of Dr J.R.BIgnall,/?the stbry of tuberculosis during the past
30 years has been one of great^triumph and tragedy - the triumph of the scientist
who has provided the means to control and ultimately eradicate tuberculosis
and the tragedy of the widespread failures- to exploit these discoveries. Each
and every discovery in the field of tuberculosis has been fully exploited by the
technically advanced countries, so much so that some of these countries will
reach the limit of eradication by 2000 AD, while in developing and underdeveloped
countries, the problem of tuberculosis has increased in terms of absolute numbers
because of sheer Increase in population. This dismal tuberculosis scene has
some redeeming features.
■
■
a pmgnosis and treatment of tuberculosis is now no longer the domain of the
Tuberculosis Specialist - This is mainly due to tho availability of standardised
tochhique of sputum microscopy for diagnosis and standard drug regimens of
long and short duration - The position today is that any quattflod doctor .can
confidently diagnose and treat tuberculosis, is an accepted fact. Still sadly
it is not practised widely due to lack of dissemination of knov/ledge in this
regard".
:
Let us pledge ourselves today and make the slogan ’'Defeat tuberculosis
now and for ever" a reality^ . Time has come when our actions and performances
would be audited by the people. There is no excuse whatsoever in allowing a
patient to go undiagnosed and untreated when we have the appropriate technology
with us. This is perhaps the last chance we have and Tat us not throw it away
in the midst of committees and seminars.
REFERENCES
1. Bajaj JS: Role of specialization in comprehensive health care, Indian
J Med Education 1980, 19/1, 45.
2. National Health Policy, DGHS Chronicle, January 1983, 19/1, 1-21.
3. India, Ministry of Health <3c Family Welfare: Report of the working
group on "Health for All by 2000 A.D.", Ministry of Health 6c Family
Welfare, New Delhi, 1981.
4. Horder J: General practice in 2000: Alma Ata Declaration, Brit Med
Journal 1983, 286, 191.
<
■
J
15
/
!»-
•J
Structeal orgsmisatian «& organisational frame work in
. • comprehensive health care
• .
•.
•.
■
i
Secondary
. Health
Cara
z
j-*
r..-.
Primary
Health
Care
■
<4
v
'X?^
Clock
■
I
Ir
Bqs’ig HuoUk Units
"k
i
J
Oiskict
a
X
>
Taluka or
Svb-OisUIcU
>■
VillOOO
7-1
Family & Ccmmuntly
tridlvIcJuat
,}..,
‘
COCnP^hf'nU^O#
lUotth
Cor«
/':
.
T ertlary
Ke al In Cant
pobcy
National
vV
plonft’nS
>•
Regional
rC^
C°v
DisIhcU/Zonol
1
■
u
Fig-2
Pyramid of health services
Ministry'
of
Health 7'
f Specialized
/
national
( • institutes
\
\
\
University hospitals
Specifliizea neaith care using increasingly
■ - sophisticated technology.
Regional health sendees
District health services
Rural (or local) hospital:
and related services
A Hmiled number of commurthy-onenled
professionals who manage primary health
care services end form tha first-referral level
Rural (or Iocs!) health centres
intermediate health care using intermediate .
technology, delivered by a corps ofintermediatedevel health workers who
complement end supervise field activities
£ fi
<-_>
CJ
II
"e3
S
*^3
cn
rj
ra
t
J
c
*:
i
I
s
*
Community dispensaries end village health posts
f
c-j
■
Primary health care using primary
technology, delivered by front-line
workers at the community level,,
who constitute the bulk of
health-service personnel.
\
t
1C
(A
o
Is
>}
s
o
1
' i4
K-a
h
b &
I E°
?n.
F«? •
•*C3 .t3
SH
. 3
. XO
•o
co
<iWC’
s
’
£
tn
'
p
u
.
Q
•
frs
E?
H r|
M
q O
•d B
• Pu t-
‘ p
tl—
£>
r*r
o
Q
J e<
<
,
<Sj
&
G/
CO
•\—M
I
.<»<J-M|
1'
o
Cl? •
il
o
o
$
•rf'O
□
•SM
b 9
-4(
/X'
1 B
c/
C 3
'd
)
o
5
M
in
I
u-
a •«
e
tj P-sJ
Ga
I
19
*
Fig. 5
primary health care
DEFINITION:
essential HEALTH CARE MADE
UNIVERSALLY AVAILABLE TO
INDIVIDUALS AND FAMILIES in THE'
acceptable TO THEM THROUGH FULL COMMUNITY BY METHODS
a cost that .the COMMUNITY AND COUNTRY PARTICIPATION AND AT
CAN AFFORD
PRINCIPLES of:
1.COMPREHENSIVENESS,
-kehunsivENESS,
PREVENTION
AND REHABILITATIVE SERVICES
'
PROMOTION,
2. regionalisation
REACHING OUT TO PEOPLE PERIPHERALISATION
3.STRESS ON RURAL AREAS
^.APPROPRIATE TECHNOLOGY
5. UNIVERSALLY
|
OF
CURATIVE
SERVICES
- PEOPLE'S ORIENTED TECHNOLOGY
ACCESS IBLE/aCCEPTABLE
6. COMMUNITY
participation
7. TWO WAY REFERRALS
coordination
IN
F'
PROGRAMM iN-G
SAN TArnME
DEVELOPMENTAL AREAS OF PLANNING,
EDUCATION,.
,• HOUSING,
TATITAn°N'
SOCIO-ECONOMIC CONDITIONS
'
ETC.
LEADING
TO
TOTAL DEVELOPMENT '
9.EVOLUTION THROUGH EVALUATION
.20
o.a
s«^
o
o .
. o ■?
JJ-^
4?
U
O’
'o
<$. <!>
«<
&» *«?
. <V)
■ •HJ
■S
s?u> 5:•
/*•£
*c^,
VI
<£ tj
t!
»J '^“j
■. Wi
•jo
' r«b
£
■
o
•^»
Cm -
'
'
k «i\&a>
■
I
I
V?
3
5
<d)
S'*
U
i
/
^5
Sm
■■57
: e^*.- H, .
■ ■ o
^-!
w
ir'j.
Q
V.
*^0 ’
VI
'
Qj
*ts^.
VJ
v ■
■
If
K
«3 :
E
£
S’
‘■/’J
■
<3
h---- I-
».
,«J
•**
'
W
e Q
,t <
■' -•
rwj.'vn..... , -.-.pr.
5
.
*
21.
Fig.7
♦
DISTRICT ■ TUBERCULOSIS PROGRAMME ■
(DIAGRAMMATIC REPRESENTATION)
Z^S^X-
A
'*
ol
n ______ tn
’.
■** ***• I **
X.*" “ * ••
/
s
r
t
I
I
T U S
CLIMCaT'
I
\
Or 3
/
i
O
■
J. •
on
' ’a
to
O
a
sV^y /
i
c Ant ^5
O.
A—,'
let
X‘.
£■
i.
&
,*Mt-***- REFERRED FOR CHEST X-RAY
HISUUTS OF X-RAY INTIMATED
TRAINING,SUPERVISION t SUPPLIES
REPORTING, SEEKING TECHNICAL ADVICE
•r.«—<j>
—O
Position: 1654 (7 views)