Blood-based PCR assay to detect Pulmonary Tuberculosis
Item
- Title
- Blood-based PCR assay to detect Pulmonary Tuberculosis
- extracted text
-
DOB
many northern people, there are references to di.se
transmitted by lemmings (lemming fever). One ;
lemming year, 1942, coincided with epidemics of hunt
of cases of fever with renal manifestations and occasio
myopia in German and Finnish troops stationed in Lap|
Whether these epidemics were due to Puumala or TOP •
and whether this phylogenetically old virus is pathoj
remains to be solved. Notably, from all hantaviruses ciw
by Arvicolinae rodents, only the European Puumala vir
known to be pathogenic, so far, in human beings.
HTN
^Alexander Plyusnin, Olli Vapalahti, Ake Lundkvist,
Heikki Henttonen, Antti Vaheri
RIOS
ELMO
^-BCC
PH
BAY
NY
95
SN
TUL/Tula
TUL/Mor
<21
TUL/Mal
TOP
5%
ILV
PUU/Sotk
/ i \ PUU/Vind
PUU/Udm
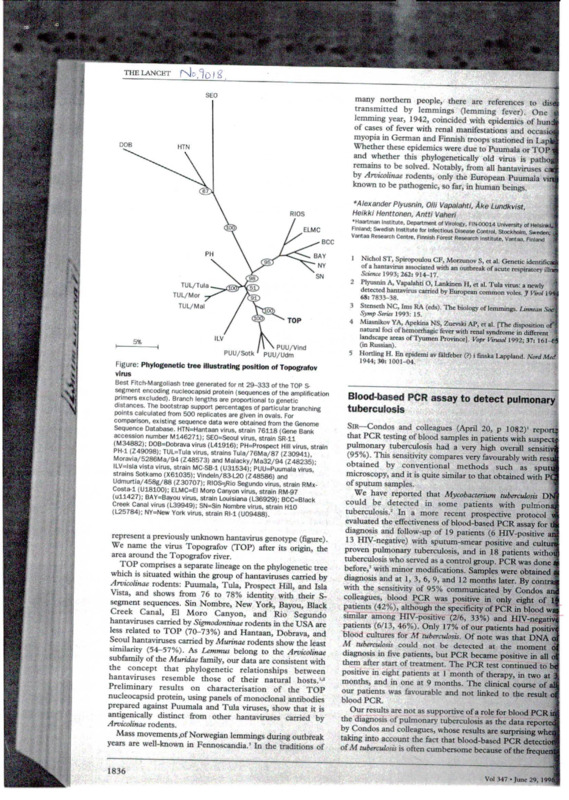
Figure: Phylogenetic tree illustrating position of Topografov
virus
Best Fitch-Margoliash tree generated for nt 29-333 of the TOP Ssegment encoding nucleocapsid protein (sequences of the amplification
primers excluded). Branch lengths are proportional to genetic
distances. The bootstrap support percentages of particular branching
points calculated from 500 replicates are given in ovals. For
comparison, existing sequence data were obtained from the Genome
Sequence Database. HTN=Hantaan virus, strain 76118 (Gene Bank
accession number M146271); SE0=Seoul virus, strain SR-11
DOB=Dobrava virus (L41916); PH=Prospect Hill virus, strain
PH-1 (Z49098); TUL=Tula virus, strains Tula/76Ma/87 (Z30941),
Moravia/5286Ma/94 (Z48573) and Malacky/Ma32/94 (Z48235)ILV=lsla vista virus, strain MC-SB-1 (U31534); PUU=Puumala virus,’
strains Sotkamo (X61035): Vindeln/83-L20 (Z48586) and
Udmurtia/458g/88 (Z30707); RI0S=Rio Segundo virus, strain RMxCosta-1 (U18100); ELMC=EI Morp Canyon virus, strain RM-97
(U11427); BAY=Bayou virus, strain Louisiana (L36929): BCC=Black
Creek Canal virus (L39949); SN=Sin Nombre virus, strain H10
(L25784); NY=New York virus, strain Rl-l (U09488).
represent a previously unknown hantavirus genotype (figure).
We name the virus Topografov (TOP) after its origin, the
area around the Topografov river.
I OP comprises a separate lineage on the phylogenetic tree
which is situated within the group of hantaviruses carried by
Arvicolinae rodents: Puumala, Tula, Prospect Hill, and Isla
Vista, and shows from 76 to 78% identity with their Ssegment sequences. Sin Nombre, New York, Bayou, Black
Creek Canal, El Moro Canyon, and Rio Segundo
hantaviruses carried by Sigmodontinae rodents in the USA are
less related to TOP (70-73%) and Hantaan, Dobrava, and
Seoul hantaviruses carried by Murinae rodents show the least
similarity (54-57%). As Lemmus belong to the Arvicolinae
subfamily of the Muridae family, our data are consistent with
the concept that phylogenetic relationships between
hantaviruses resemble those of their natural hosts.1,2
Preliminary results on characterisation of the TOP
nucleocapsid protein, using panels of monoclonal antibodies
prepared against Puumala and Tula viruses, show that it is
antigenically distinct from other hantaviruses carried by
Arvicolinae rodents.
Mass movements .of Norwegian lemmings during outbreak
years are well-known in Fennoscandia.’ In the traditions of
lnst,,ute’ Department of Virology, FIN00014 University of Helsinki,
Finland; Swedish Institute for Infectious Disease Control, Stockholm. Sweden;,
Vantaa Research Centre, Finnish Forest Research Institute, Vantaa, Finland
1
Nichol ST, Spiropoulou CF, Morzunov S, er al. Genetic identifier
9i J-Cj7with an outbreak °f acutc
>nn
2 Plyusnin A, Vapalahti O, Lankincn 11, et al. Tula virus: a newly 1
detected hantavirus carried by European common voles. J Virol 199<J
68: 7833—38.
3 Stenseth NC, Ims RA (eds). The biology of lemmings. Limuan .Snci
Symp Series 1993: 15.
4 Miasmkov YA, Apekina NS, Zuevski AP, et al. [The disposition, ofi
natural foa of hemorrhagic fever with renal syndrome in different 5
landscape areas of Tyumen Province). Vopr Vtrusol 1992; 37: lol-M
(in Russian).
5 Hording H. En epidemi av faltfeber (?) i finska Lappland. Nord Med
1944; 30: 1001-04.
Blood-based PCR assay to detect pulmonary
tuberculosis
Sir—Condos and colleagues (April 20, p 1082)’ repon
that PCR testing of
ot blood samples in patients with suspect;
suspect
pulmonary tuberculosis had a very high overall sensitivi
(95%). This sensitivity compares very favourably with resu
obtained by conventional methods such as sputq
microscopy, and it is quite similar to that obtained with PC
of sputum samples.
We have reported that Mycobacterium tuberculosis I)N'
could be detected in some patients with pulmona
tuberculosis.2 In a more recent prospective protocol v
evaluated the effectiveness of blood-based PCR assay for d
diagnosis and follow-up of 19 patients (6 HIV-positive ai
13 HI\-negative) with sputum-smear positive and cultufl
proven pulmonary tuberculosis, and in 18 patients withot
tuberculosis who served as a control group. PCR was done i
before, with minor modifications. Samples were obtained i
diagnosis and at 1, 3, 6, 9, and 12 months later. By contra
with the sensitivity of 95% communicated by Condos an
colleagues, blood PCR was positive in only eight of 1
patients (42%), although the specificity of PCR in blood wa
similar among HIV-positive (2/6, 33%) and HIV-negativ
patients (6/13, 46%). Only 17% of our patients had positiv
blood cultures for M tuberculosis. Of note was that DNA oi
M tuberculosis could not be detected at the moment of
diagnosis in five patients, but PCR became positive in all o|
them after start of treatment. The PCR test continued to be|
positive in eight patients at 1 month of therapy, in two at %
months, and in one at 9 months. The clinical course of al
our patients was favourable and not linked to the result o
blood PCR.
Our results are not as supportive of a role for blood PCR it
the diagnosis of pulmonary tuberculosis as the data reponet
by Condos and colleagues, whose results are surprising whei
taking into account the fact that blood-based PCR detection
of M tuberculosis is often cumbersome because of the frequen
1836
Vol 347 - June 29, 1996;
la
r
THE LANCET
•es to disea.,,
t). One sue:
cs of hundred
nd occasional.\
ed in Lapland,
a or TOP virus
is pathogenic
iviruses carried
.lumala virus is
igs.
ist,
4ty of Helsinki,
>olm. Sweden;
taa, Finland
itic identification
ispiratory illness.
cnee of inhibitors in the sample.’ By contrast with our
:udy, only 37% of their patients with pulmonary
berculosis were sputum-smear positive, and less than 4%
t
comparison with 17% in our series) had
cobacteraemia, which could reflect a low bacterial burden
majority of them, and this makes it difficult to
.stand the enormous (95%) sensitivity of blood PCR.
ily, it would be useful to know whether they found any
discrepancy in their results when the samples of PCR positive
patients were processed in duplicate.
If Condos and colleagues’ data are confirmed by other
groups, many concepts in the pulmonary tuberculosis will
need to be re-written, and blood-based PCR would then
serve as an efficient substitute for conventional
micr biological methods based in the study of sputum for the
diagnosis of pulmonary tuberculosis.
infection in Somalia at the time. Recreational drug
consumption in Somalia was limited to harmless Xat. In the
Eastern Cape, alcohol and marijuana are popular but there is
no intravenous drug culture in either environment. At
Nkqubela the incidence of HIV infection is unknown, since
patients often refuse to be tested.
In neither of these two very different environments does
drug resistance seem to have any relationship to erratic or
previous treatment. All the evidence suggests that the
resistance or sensitivity of the infecting organism is defined
before treatment begins, does not alter thereafter, and is not
altered subsequently by HIV infection or repeated treatment.
*Jos6 M Aguado, Maria J Rebollo, Elia Palenque, Lola Folgueria
HHV8 DNA in angiolymphoid hyperplasia of
the skin
Unit of Infectious Diseases and Department of Microbiology, Hospital 12 de
Octubre. 28041 Madrid. Spain
s: a newly
es. J Virol 1994;
1
. Linnean Soc
lisposition of
in different
92; 37: 161-65
nd. Nord Med
Condos R, McClune A, Rom WN, Schluger NW. Peripheral-blood
based PCR assay to identify patients with active pulmonary
tuberculosis. Lancet 1996; 347: 1082-85.
2 Folgueira L, Delagado R, Palenque E, Aguado JM, Noriega AR. Rapid
diagnosis of Mycobacterium tuberculosis bacteremia by PCR. J Clin
Microbiol 1996; 34: 512-15.
3 Folgueira L, Delagado R, Palenque E, Noriega AR. Detection of
Mycobacterium tuberculosis DNA in clinical samples by using a simple
lysis method and polymerase chain reaction. J Clin Microbiol 1993; 31:
1019-21.
ilmonary
32)1 reported
ith suspected
all sensitivity
y with results
as sputum
ed with PCR
Multidrug resistant tuberculosis in South
Africa
Sir—Nkqubela Chest Hospital in the Eastern Cape province
of South Africa, admits over 2000 patients with tuberculosis
(TB) annually. Short course chemotherapy including
rifampicin has been standard treatment since 1980. The
multidrug resistance (MDR) rate is low and does not change
significantly from year to year.
culosis DNA
pulmonary
protocol we
assay for the
positive and
and cultureents without
was done as
obtained at
By contrast
Condos and
eight of 19
n blood was
TV-negative
had positive
tat DNA of
moment of
ive in all of
inued to be
in two at 3
□urse of all
le result of
>od PCR in
ta reported
ising when
< detection
le frequent
Sensitive to all drugs
Resistant to INH and rifampicin
Resistant to INH
July-Dec 1993
1994
1995
331
7 (2-1%)
39(11-8%)
657
14 (2-1%)
629
14 (2-2%)
63 (9-6%)
54 (8-5%)
During 1995, two resistant patients were admitted after
failed treatment at other centres. All the others started
treatment at Nkqubela, had no history of previous treatment,
and were therefore resistant at their first admission. None
were known to be HIV seropositive; routine testing is not
undertaken, but none had evidence of HIV infection.
The absconding rate at Nkqubela averages 7-8%; it is
actually lower, because a few patients abscond repeatedly.
They are admitted sick, leave when they feel better and
return when they relapse. Not one of these has developed
resistant organisms; not even one who has been admitted 8
times in less than 3 years. No MDR patient has a relative or
contact with MDR TB. The report of an MDR infection
arrives 3 months or more after admission. No incident of
crossinfection has been recorded, even among HIV
seropositive contacts.
TB clinics in a group of refugee camps in Somalia in
1986-89 recorded an incidence of 0-7% of failed treatment
in patients initially sputum positive—ie, still sputum positive
after 6 months of chemotherapy. The default rate was 17-8%
over one year. Many patients had previous treatment in other
camps, but they rarely admitted it. There was no HIV
Margaret L Westwater
Nkqubela Chest Hospital, Mdantsane, Eastern Cape. South Africa
Sir—Wc have reported Kaposi’s sarcoma-associated HHV8
DNA sequences in an angiosarcoma of the face in an HIV
negative patient, suggesting that this virus may be implicated
in the pathogenesis of an endothelial cell-derived cancer
other than Kaposi’s sarcoma (KS).' Benign angiogenic
lesions, on the other hand, have been found not to contain
HHV8 sequences.’’5 We report four cases of HHV8
sequences in patients with angiolymphoid hyperplasia and
eosinophilia (ALHE).
DNA was extracted from the paraffin-embedded tissue
specimens of four patients with histologically confirmed
diagnosis of ALHE. All patients were HIV-negative and had
no clinical signs of immunodeficiency. PCR with primers
specific for the 233 bp KS3302JJ fragment was carried out as
described by Chang et al.’ We detected 233-bp bands in each
of the four ALHE lesions. 'Die specificity of the bands were
confirmed by hybridisation to a previously sequenced HHV8
probe obtained from KS tissue.’
ALHE is an uncommon benign disorder characterised by
soft angiomatous tumours usually on the face, ear, or scalp.4
The main histological feature is proliferation of atypical
endothelial cells (as seen in KS and angiosarcoma of the
face) accompanied by an infiltrate of eosinophils and
lymphocytes. Vascular tumours characterised by the
proliferation of atypical epitheloid endothelial cells with
abundant eosinophilic hyaline cytoplasm span a broad
spectrum of histological appearances and behaviour. At the
benign end are the epitheloid haemangiomas such as ALHE
and at the malignant end are highly aggressive epitheloid
angiosarcomas. The presence of HHV8 sequences in both
benign and malignant proliferations of endothelial cells
suggests that the virus alone is not sufficient to produce a
specific lesion.
Rolland Gyulai, •Lajos Kemdny, Eva Addm, Ferenc Nagy,
Attila Dobozy
•Department of Dermatology. Albert Szent-Gyorgyi Medical University, aid
Biological Research Institute. Hungarian Academy of Sciences, H 6701 Szeged,
Hungary
Gyulai R, Kcnieny L* Kiss M. el al. Herpesvirus-like nucleic acid
sequence in angiosarcoma in a patient without HIV infection.
A Engl 7 M.d 1096; 334: 540-11.
2 Chang Y, Ccsannan F, Pcssin MS, ct al. Identification of new human
herpesvirus-like DNA sequences in AIDS-associated Kaposi’s
sarcoma. Science 1904: 266: 1865 69
3 Keineny L, Gyulai R, Kiss M, ct al. Herpesvirus like nucleic acid
sequences in patients with Eastern European sporadic Kaposi’s
sarcoma. ,7 Invest Eermotol 1996; 106: 381.
4 Olsen TG, Helwig EB. Angiolymphoid hyperplasia with eosinophilia.
J Am Acad Dermatol 1985; 12: 781-96.
I
- Media
 RF-TB-1.12.pdf
RF-TB-1.12.pdf
Position: 1453 (8 views)