[Untitled]
Item
- extracted text
-
The New England
Journal of Medicine
©Copyright. 1997. bx the Maxsjchusetf. Medical Societx
VOLUME 337
Si 1' 1 EMBER 1«, 1997
number
7 *; r
12
9j
^SIS IN U^??M
A TRIAL OF THREE REGIMENS TO PREVENT TUBERCI
§An
ADULTS INFECTED WITH THE HUMAN IMMUNOD ^^gNCY VpA
Christopher C. Whalen, M.D., John L. Johnson, M.D., Alphonse Okwera, M.B.,
M.S.,
Robin Huebner, Ph.D., M.P.H., Peter Mugyenyi, M.B., Ch.B., Roy D. Mugerwa, M.B., Ch.B.,
and Jerrold J. Ellner, M.D., for the Uganda-Case Western Reserve University Research Collaboration
Abstract
Background Infection with the human immuno
deficiency virus (HIV) greatly increases the risk of re
activation tuberculosis. We evaluated the safety and
efficacy of three preventive-therapy regimens in a
setting where exposure to tuberculosis is common.
Methods \Ne performed a randomized, placebocontrolled trial in 2736 HIV-infected adults recruited
in Kampala, Uganda. Subjects with positive tubercu
lin skin tests (induration, 2=5 mm) with purified pro
tein derivative (PPD) were randomly assigned to one
of four regimens: placebo (464 subjects), isoniazid
daily for six months (536), isoniazid and rifampin
daily for three months (556), or isoniazid, rifampin,
and pyrazinamide daily for three months (462). Sub
jects with anergy (0 mm induration in reaction to
PPD and Candida antigens) were randomly assigned
to receive either placebo (323 subjects) or six months
of isoniazid (395). The medications were dispensed
monthly and were self-administered.
Results Among the PPD-positive subjects, the in
cidence of tuberculosis in the three groups that re
ceived preventive therapy was lower than the rate in
the placebo group (P = 0.002 by the log-rank test).
The relative risk of tuberculosis with isoniazid alone,
as compared with placebo, was 0.33 (95 percent con
fidence interval, 0.14 to 0.77); with isoniazid and ri
fampin, 0.40 (0.18 to 0.86); and with isoniazid, rifam
pin, and pyrazinamide, 0.51 (0.24 to 1.08). Among
the subjects with anergy, the relative risk of tubercu
losis was 0.83 (95 percent confidence interval, 0.34
to 2.04) with isoniazid as compared with placebo.
Side effects were more common with the multidrug
regimens, and particularly with the regimen contain
ing pyrazinamide. Survival did not differ among the
groups, but the subjects with anergy had a higher
mortality rate than the PPD-positive subjects.
Conclusions
six-month course of isoniazid con
fers short-term protection against tuberculosis among
PPD-positive, HIV-infected adults. Multidrug regimens
with isoniazid and rifampin taken for three months
also reduce the risk of tuberculosis. (N Engl J Med
1997;337:801-8.)
©1997, Massachusetts Medical Society
"W" NFECTION with Mycobacterium tuberculosis
|
niost C0inn1011 human infection worldL wide. As the epidemic ol human immunode-A^ticiency virus (HIV) infection continues to
evolve, the risk of dual infection with HIV and
M. tuberculosis may be substantial in young adults,
especially in developing countries.1 HIV Infection
confers the greatest known risk for the development
of tuberculosis, both tor the reactivation of latent in
fection and for progressive primary disease.2 5 More
over, once active tuberculosis develops in HIVinfected persons, mortality is high, despite good
clinical and microbiologic responses to antitubercu
lous therapy.611
Pre\enti\e therapy has been proposed as a strategy
to control tuberculosis in I llV-infectcd popula
tions.12 l4 The potential benefit of preventive therapv
w as first suggested by observational studies of injec
tion-drug users,2-31516 but these were uncontrolled
studies of selected populations at high risk.17 Data
on the efficacy of preventivc therapy in HIV-sero
negative persons1^22 cannot be readily extrapolated
to HIV-seropositive persons, because of the con
founding effects of progressive immunosuppression
related to HIX infection and concern about an in-
From the Division oi Inlectionc Diseases. Department of McJkiiu
I nixcrsiix Hospitals <>t ( lexeland ami ( ase Western Reserxe 1‘mxersitx
'<<"•11 I . D I H . I J.l .i. ami the Department ol Eptdemiologx and
Biostatisncs. Case Western Reserxe Unixersitx K ( W > — all in ( kx'eland.
the Lgandan Ministrx ol Health, Xation.il Tuberculosis ami Leprosy Pro
gramme lAO >. the Joint Clinical Research Center r I’M .. and MakeiVie
I mxersitx < H D M — all in Kampala. I ganda; ami the ( enters tor Disease
Control and ITcxcntion. Atlanta iR.H • \ddrvss reprint requests to Di
Whalen at the Dept ol Epidemiologx and Bitistatistics. WG 49. ( ase West
ern Reserxe Cnixcrsitx. 109(10 | uclid Bhd . ( lexeland. OH 44106 4945
Other authors were I’ctcr Xsubuga. M R . ( h B . Ministrx o| Health.
Kampala; Michael \ |ccha. M D.. I mxersitx Hospitals of ( Icxcl.’.iu! an«l
( ase Western Reserxe Cnixcrsitx. ( lexeland. Harriet Mxanja. M B . ( h I!
M Med. Makcrcrc Cnixcrsitx. Kampala. ( issx Kuxo. M B._ ( h l’. . Joint
( limcal Research < enter. Kampala, and \nita Loughlin. M S.. John Mil
berg. M PH . and \ ukosaxa 1’ckoxK, M D . Ph D .'all of Cnnersitx Hoc
pitalsot ( lexeland and ( ase Western Rescue I nixcrsnx. ( lexeland
\oltiinc 337
Xu nt he i
12
801
I hc Xcu Enei.ind loiirn.il <>! Medicine
creased risk of drug toxicity in HIX’ infected per
sons.2’-4 Because of the relevance of preventive ther
apy to the strategy tor eliminating tuberculosis in
the United States and the potential benefit of pre
ventive therapy in targeted populations in resource
poor countries, in March 1993 the Uganda-Case
Western Reserve University Research Collaboration
began a randomized, placebo-controlled trial of three
regimens of therapy to prevent tuberculosis in HIVinfected Ugandan adults w ho had positive skin tests
with purified protein derivative (PPD). In October
1993 enrollment was expanded to include HIVinfected persons with anergy with respect to PPD
and Candida antigens, on the basis of new informa
tion suggesting an increased risk of tuberculosis in
HIV-infected persons with anergy.’4
METHODS
Study Design
The objective of this randomized, placebo-controlled clinical
trial was to determine the efficacy of three daily, self-administered
regimens of preventive therapy for tuberculosis in HIX' infected
adults. The trial was designed to obtain at least three years <>f fol
low-up data on all enrolled subjects, with annual interim anahses
to ensure timely detection of risks and benefits to the partici
pants. All subjects gave oral informed consent before screening
and enrollment in the study. The study protocol was approved bv
the institutional review board at the L'niversitv Hospitals of
(’leveland and Case Western Reserve L'niversitv and bv the L’gandan National AIDS Research Subcommittee.
Study Population
Between March 1, 1993, and April 20, 1995, Ugandan adults
IS years or more of age were screened for enrollment at live med
ical clinics and counseling centers for persons with HIX' tvpe I
(HIX' 1) infection in Kampala, Uganda. Enrollment of subjects
with anergy was begun in October 1993. In the PI’l) positive co
hort, enrollment in the isoniazid and isoniazid-plus-ntampin groups
was continued beyond the predetermined sample size to allow us
to screen and enroll subjects in the anergy groups. The study's
inclusion criteria were HIX' infection documented by enzymelinked immunosorbent assay, a PPI") skin test showing at least
5 mm of induration after 48 to 72 hours or anergy. and a Kar
nofsky performance score of more than 50.-; Anergy w as defined
as 0 mm of induration in reaction to both PPD and Candida an
tigens. Candida antigens were used for skin testing because teta
nus-toxoid and mumps vaccinations are not routinely used in
Uganda. Only one control antigen was used, to enhance accept
ance bv the subject. The exclusion criteria were the presence of
active tuberculosis, previous treatment for tuberculosis, use of an
tiretroviral drugs, a vv hite-cell count under 3000 per cubic mill:
meter, a hemoglobin level under 80 g per liter, serum aspartate
aminotransferase level over 90 U per liter, serum creatinine level
over 1.8 mg per deciliter (160 jzmol per liter), a positive urinary
(i human chorionic gonadotropin test, residence more than 20
km from a project clinic, advanced HIX’ disease, or the presence
of major underlying medical illness unrelated to HIX' infection.
Before entry into the trial, all the subjects were screened lor active
tuberculosis bv a history taking and physical examination, chest
radiography, sputum microscopy with the Zichl-N’eelsen stain for
acid-fast bacilli, and sputum mycobacterial culture
Intervention and Randomization
The four study groups received placebo (250 mg of ascorbic
acid per day for six months); isoniazid I 300 mg per day for six
802
•
September 18, 1997
months); isoniazid <300 mg per day) and rifampin (600 mg per
dav i lor three months; or isoniazid (300 mg per day), rifampin
600 mg per day i. and pvrazinamidc (2000 mg per day) for three
months. Blocked randomization was used (in blocks of six) to as
sign eligible subjects to one of the study regimens. Sequentially
numbered, sealed envelopes containing the treatment assign
ments were drawn in numerical order by a data clerk. Subjects
with anergv were assigned only to the placebo and isoniazid groups
bv a se|varate, but identical, randomization process. Instruction
about HIX’ and tuberculosis and counseling on compliance were
given to all study subjects at enrollment and during follow-up
clinic visits. Study nurses dispensed the medication in prepack
aged envelopes containing one month of doses with oral and
written instructions. A team of five experienced home health vis
itors traced rhe subjects who did not keep scheduled appoint
ments and encouraged them to return to the clinic.
Assessment of Outcome
Hie primary outcome of the study was the development of tu
berculosis; secondary outcomes included adverse drug reactions
and mortality . The subjects were evaluated monthly during the
first six months of the study and every three months thereafter.
Active screening for tuberculosis was performed at all scheduled
and unscheduled visits by means of a standardized evaluation of
the symptoms and signs of tuberculosis; chest radiographs were
obtained every six months. If tuberculosis was suspected on the
basis of symptoms, signs, or the chest radiograph, three sputum
specimens were obtained for mycobacterial smear and culture.
Decisions to initiate antituberculous therapy for active tuberculo
sis were made by on-site investigators after reviewing the clinical,
radiographic, and microbiologic data.
( ases of suspected tuberculosis were referred for independent
review and classification by two ehest physicians who were blind
ed to the subjects' treatment group. Subjects were selected for re
view it they had at least one of the following: symptoms or signs
consistent with active tuberculosis, a sputum smear positive for
acid fast bacilli, a positive culture for M. tuberculosis, abnormal
findings consistent with tuberculosis on chest radiography, or
empirical therapy for tuberculosis. The reviewers independently
classified suspected cases of tuberculosis according to operational
definitions of the disease.-’'’ Definite tuberculosis was defined as
culture-confirmed disease (more than five colonies of M. tuber
culosis}. Probable tuberculosis was defined as a clinical illness
consistent with tuberculosis on the basis of at least two of the fol
low ing findings: results of chest radiography consistent with pulmonary tuberculosis, smear of tissue or secretions positive for
.Kid last bacilli, or a response to antituberculous therapy. Suspect
ed cases that did not fulfill the criteria for definite or probable
tuberculosis were not considered to Ise active tuberculosis.
During the treatment phase, the subjects were screened for ad
verse events at all scheduled monthly visits or unscheduled visits.
Medical of ficers recorded the type and grade of reaction with a
standard grading system for drug toxicity in HIV-infected per
sons.’ 1 he medical officers and study subjects could not be formallv blinded to the treatment because of the discoloration of
body fluids produced by rifampin; however, the medical officers
were instructed to perform the clinical examination and record
the findings without reference to the treatment code, and they
did not have access to the results of urinary testing. Mortalitywas
assessed through interviews with family members or review of
hospital records when available. Autopsies were not performed.
I hc date of death and reports of prominent symptoms at the time
of death were also obtained from family members.
Measurements
Demographic and clinical information was obtained through
standardized interviews and physical examination. At the time of
screening, venous blood was collected for enzyme linked immu
nosorbent assay testing lor HIX' I, complete blood and differen
tial counts (Coulter T540 svstem. Coulter Electronics, Hialeah,
/
THREE REGIMENS TO PREVENT TUBERCULOSIS IN UGANDAN ADULTS WITH HIV INFECTION
Fla.), and serum creatinine and aspartate aminotransferase meas
urements. HIX’ infection was documented by enzyme-linked im
munosorbent assay (Recombigen HIX’ 1 env and gag ELISA,
Cambridge BioScience, XVorcester, Mass.); 1 in 10 HIX-1-positive and l in 25 HIX’-1-negative scrum samples, according to
enzyme-linked immunosorbent assay, underwent confirmatory
testing bv HIX’-1 Western immunoblotting (BioRad Novapath,
Hercules, Calif). At the time of screening, all the subjects under
went Mantoux skin testing with 5 tuberculin units of PPD (Tu
bersol, Connaught Laboratories, Swiftwatcr, Pa.) and 0.1 ml of
Candida antigeif (Candida albicans allergic extract, Berkeley Bio
logics, Berkeley, Calif; 1:50 final concentration). After 48 to 72
hours, experienced observers recorded the results ol each skin test
in millimeters. Posteroanterior chest radiographs were obtained at
base line and at six month intervals during follow-up.
Before randomization, at least one sputum specimen was col
lected if the subject was able to produce sputum. All sputum spec
imens were digested, concentrated, and stained for acid-fast bacilli
by the Ziehl-Neelsen method at the Uganda Tuberculosis Inves
tigations Bac etiological Unit in Wandegeva. Sputum smears were
graded according to the number of acid-fast organisms seen on
light microscopy." Specimens were cultured for A/, tuberculosis on
Lowenstein-Jensen slants, incubated at 37°C in air, and examined
weeklv for eight weeks or until positive results were seen.
Compliance with the prescribed regimen was assessed by the
subject’s attendance at scheduled visits, urinary testing for isoniazid
metabolites (Mycodyn Uritec, DynaGen, Cambridge, Mass.), and
self-reports. Ninety-seven subjects in the three treatment groups
were randomlv selected for unscheduled tests for urinary isoniazid
metabolites performed at home between clinic appointments at the
beginning of the third month of preventive therapy.
Statistical Analysis
The intention-to-treat approach was used to analyze the data
for the primary and secondary end points of tuberculosis, adverse
drug reactions, and mortality. The incidence of tuberculosis w as
estimated bv the person-year method; the cumulative proportion
was estimated for adverse drug reactions and death. Efficacy was
estimated as the relative risk (with 95 percent confidence inter
vals) of tuberculosis in the treatment groups as compared w ith
the placebo group. The sample size was calculated separately for
the PPD-positive and anergy cohorts to achieve a power of 80
percent to detect a reduction of 67 percent in the incidence of
tuberculosis with an overall type I error of 5 percent. The sample
size was adjusted for expected mortality and losses to follow up.
The target sample size tor each treatment or placebo group was
410 for the PPI') positive cohort and 500 tor the anergy cohort.
A global test of significance was performed with the log-rank
statistic to compare the cumulative incidence of tuberculosis in
the treatment groups with that in the placebo group. The nomi
nal significance level, according to the Lan-DcMcts error-spend
ing function,-”' was 0.032 when adjusted for a second interim
analysis in which 47 of 56 expected events (84 percent) had oc
curred in the PPD-positive subjects. Three pairwise comparisons
were then made between each active treatment group and the
placebo group. The tvpe I error for these pairwise comparisons
was adjusted for multiple comparisons by using the nominal sig
nificance level from the global test to obtain an adjusted tvpe 1
error of 0.011 lor each comparison, preserving the overall, studywide tvpe I error of 0.05. A similar procedure was used to adjust
the significance level lor the subjects with anergy.
following reasons: active tuberculosis (smear- or cul
ture-positive; 185 subjects), HIV-seronegative or in
determinate (703), failure to return for skin testing
(28), PPD-negative (374), abnormal chest radio
graph (884), previous history of tuberculosis or use
of preventive therapy (96), poor performance status
(233), pregnancy (160), age greater than 50 years
(223), or residence more than 20 km from project
clinic (226). Information on the progress of subjects
through follow-up is available elsewhere.*
In both the PPD-positive and the anergy cohorts,
the treatment groups were balanced at base line in
terms of demographic factors, performance status,
and the results of laboratory tests (Table 1). During
follow-up, the numbers of subjects who withdrew
from the study, moved out of the study area, or
could not be located for unknown reasons did not
differ significantly among the study groups. The
mean number of scheduled visits, unscheduled visits
due to illness, and chest radiographs per person did
not differ significantly among the groups. Urine
tests for isoniazid metabolites were performed in
1754 subjects in the treatment groups (90 percent),
and 75 percent of the results were positive; the re
sults did not differ significantly among the treat
ment groups. Of the 97 subjects randomly selected
for a single spot check at home between clinic ap
pointments, 78 (80 percent) tested positive for iso
niazid metabolites. The subjects with positive re
sults on the spot test had a higher proportion of
positive tests at the regular monthly visits than the
subjects with negative tests (82 percent vs. 46 per
cent, P<0.001).
At the second interim analysis, in December 1995,
isoniazid alone was found to reduce the risk of tu
berculosis bv 67 percent in HIV-infected adults with
positive tuberculin skin tests, although there was no
significant difference in mortality among treatment
groups. Because the benefit of preventive therapy
with isoniazid satisfied conservative criteria for statis
tical significance, the study investigators and officials
at the Centers for Disease Control and Prevention,
the funding agency for the study, concurred that pre
ventive therapv with isoniazid should be offered to
the subjects randomly assigned to the placebo group.
Tuberculosis
In the PPI') positive cohort, 138 subjects met the
criteria for new cases of tuberculosis after a mean
RESULTS
Between March 1, 1993, and April 20, 1995, 9095
subjects were screened and 2736 were enrolled in the
study. Of the 9095 persons screened for the study,
4306 did not complete the base line evaluation and
2053 were ineligible for the study. Persons screened
for the study were not eligible for one or more of the
‘Sec XAl’S document no 054 IS lor 2 pages of supplemental\ material
Order from XAl’S. e/o Microfiche Publications. P.O Box 3513. <>rand
C'cntral Station. Xe« York. XV 10163 3513 Remit in advance 'in I' S
funds onlvi S7.75 tor photocopies or S5 tor microfiche. Outside the l^s .
add postage of S4 50 for up to 20 pages, and SI.00 lor each 10 pages ol
material thereafter, or SI 75 lor the first microfiche and SO.50 lor cash mi
crotiche thereafter There is a SI5 imoicmg charge on all orders lillcst be
fore payment
Volume 337
X umber 12
803
I lie Xcw England Journal of Medicine
Table 1. Chakai ii rimk \ 01 ihi Sii py Si hik is.*
Characteristic
PPD-Positive Cohort
iMisiAZin,
■ \=464l
iMixiAZin
‘S = 556<
kii virix
is = 556i
I’lRAZIX VMIIM
Is = 462 I
,s - 525
51
50
91
51
29
91
29
29
91
54
29
91
51
50
90
14
22.1
14
22 6
15
22 5
14
25
25
2200
2500
2500
126
616
S9
125
645
SS
127
6S0
S6
n m 11:< i
Male M.-X i ".i i
Mean age ivri
Kamiitkkv performance
score
Bodv-mass indexj
1’1’11 skin test i mm ofindu
ration i
Previous herpes zoster or
thrush i
Absolute lymphocyte count
< per mm!i
Hemoglobin ig/htcri
Person-years of observation
C. ompletion of trial i’Vi
Anergy Cohort
Im >\l V.ll',
KII VMH.S.
ri v i ini
iMisivzin
. s 595
52
50
9(1
21 9
o
55
55
2200
2ooo
2ioo
12o
125
52"
S5
125
SO
so
*CJtcgoric.il x.ikies were compared by the chi square test lor honiogcncm . omiiniioii- x.ilucs were
compared by analysis ot\ anance. I’l’D denotes a tuberculin skin test unh punlicsl proiem slcni.urc.
•fThe body mass index xvascalculated as the Height in kilograms divides! In the sspiarc <■! the height
in meters.
\
follow-up of 15 months. Forty-seven cases of tuber
culosis (24 definite and 23 probable) were observed.
In this cohort, the cumulative incidence of tubercu
losis was greater in the placebo group than in the
treatment groups (P = 0.002 by the log-rank test)
(Fig. 1A). In separate pairwise comparisons of indi
vidual treatment regimens with placebo (Table 2),
the relative risk of tuberculosis with isoniazid alone
was 0.33, a statistically significant value. A similar ef
fect was found with the isoniazid and rifampin
group as compared with the placebo groups; the rel
ative risk was 0.40, but in this comparison, the effect
narrowly failed to meet the prespecified adjusted lev
el of significance. The relative risk of tuberculosis
with the three-drug regimen was 0.51, and the esti
mate of the effect was of borderline statistical signif
icance. The relative risks of tuberculosis in the treat
ment groups as compared with the placebo groups
remained unchanged for isoniazid and isoniazid
with rifampin in a proportional-hazards regression
model after adjustment for age, sex, body-mass in
dex, hemoglobin level, white-cell count, Karnofsky
performance score, history of HIV-related infection,
and presence of chronic diarrhea or weight loss. Af
ter this adjustment, the relative risk with the threedrug regimen decreased to 0.43 and was of border
line statistical significance (P = ().O3).
When the analysis was restricted to definite, cul
ture-confirmed cases of tuberculosis among the
PPD-positive cohort, the relative risk of tuberculosis
with isoniazid was 0.22 (95 percent confidence in
terval, 0.06 to 0.77) and with isoniazid and rifam-
804
•
September 18. 1997
pin, 0.14 (95 percent confidence interval, 0.03 to
0.62), w hercas the efficacy with isoniazid, rifampin,
and pyrazinamide was unchanged.
In the anergy cohort, 66 subjects met the criteria
tor the blinded, independent review after a mean of
12 months of observation. Nineteen cases of definite
(9 cases) or probable ( 10 cases) tuberculosis were de
tected. The cumulative incidence of tuberculosis was
similar in the placebo and isoniazid groups (P = 0.68
by the log-rank test) (Eig. 1 B). The relative risk of tu
berculosis in the isoniazid group was 0.83 (Table 2),
but the wide confidence intervals did not exclude the
hypothesis of no difference in incidence rates. In a
proportional-hazards regression analysis adjusted for
age, sex, body-mass index, hemoglobin level, white
cell count, Karnofsky performance score, historv of
HIX’-rclatcd infection, and presence of diarrhea, the
relative risk of tuberculosis in the isoniazid group as
compared with the placebo group declined to 0.75,
but the confidence intervals remained wide. The rel
ative risk of definite tuberculosis was 0.75 (95 per
cent confidence interval, 0.20 to 2.79).
Adverse Drug Reactions
A total of 304 adverse events were reported in 279
subjects during the course of therapy in all studv
groups, including the placebo groups. The frequen
cy of any reported adverse event in the PPD-positive
cohort was greater in the treatment groups than in
the placebo group, and it was greatest in the group
receiving the regimen containing pyrazinamide (Ta
ble 3). Treatment was discontinued in 43 subjects.
THREE REGIMENS TO PREVENT TUBERCULOSIS IN UGANDAN ADULTS WITH HIV INFECTION
PPD-Positive Subjects
O.IO-i
o
Placebo
5 0.08•o
co
_c
0.06
~
0.04-
E
0.02-
=
___ J
J
3RHZ
3RH
6H
O
0.00
0
2
1
Follow-up (yr)
Study
Group
464
536
556
462
Placebo
6H
3RH
3RHZ
288
280
104
306
109
282
87
88
Subjects with Anergy
0.10-1
o
c
<D
•u
0.08
Q
_C
0.06-
Placebo
<D
>
□
E
D
-6H~~
0.04-
0.02-
o
0.00-0
d
Mortality
2
1
Follow-up (yr)
Study
Group
Placebo
6H
323
395
The most common reason for stopping therapy was
the development of rash or pruritus (25 subjects),
followed by nausea and vomiting (8 subjects). The
frequency of rash increased from less than 1 percent
in the placebo group to 5.8 percent in the group re
ceiving three drugs (P<0.001 by chi-square test for
trend). No cases of Stevens-Johnson syndrome were
reported. Arthralgias were more common in the
treated groups than with placebo (1.5, 2.8, 3.1, and
10.8 percent of subjects in the groups receiving pla
cebo, isoniazid, isoniazid with rifampin, and isonia
zid with rifampin and pyrazinamide, respectively).
Paresthesias were more common in the group receiv
ing isoniazid, rifampin, and pyrazinamide than in
the placebo group (6.5 percent vs. 2.4 percent,
P<0.001) but were reported with similar frequency
in the groups receiving isoniazid and isoniazid with
rifampin (2.4 and 3.1 percent, respectively).
Seven cases of clinical hepatitis w'ere detected by
medical officers during the routine evaluations. Of
the 1631 subjects whose serum aspartate aminotrans
ferase levels were measured during therapy, 65 had el
evated levels. Fifty-two of these subjects had peak ele
vations of 135 U per liter or lower. Of the 13 subjects
with values greater than 135 U per liter, 6 were subl jects with anergy who were receiving isoniazid; 5 were
. PPD-positive subjects receiving isoniazid, rifampin,
and pyrazinamide; 1 was a PPD-positive subject re
ceiving isoniazid; and 1 was a PPD-positive subject
I receiving placebo.
167
155
8
13
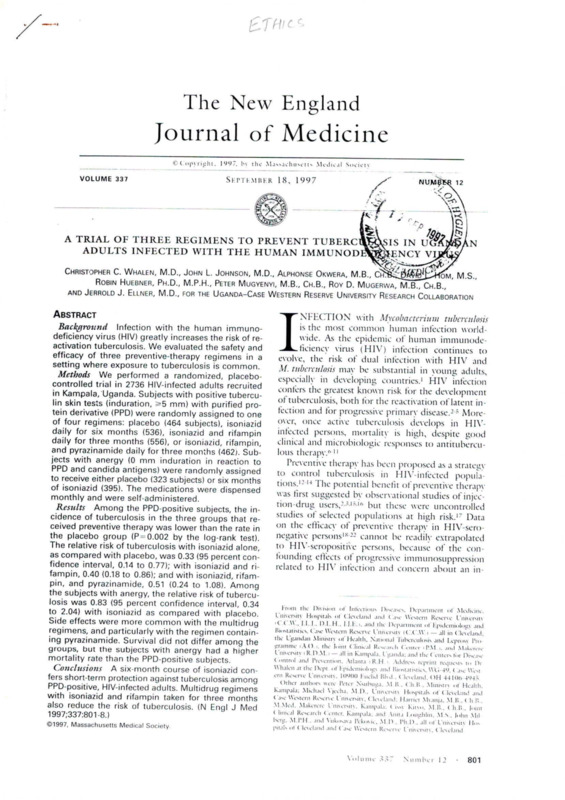
Figure 1. Cumulative Incidence of Tuberculosis among PPDPositive Subjects (Upper Panel) and Subjects with Anergy
(Lower Panel), According to Study Group.
For PPD-positive subjects, the incidence rates of tuberculosis
in the groups receiving preventive therapy were lower than the
rate in the placebo group (P = 0.002 by the log-rank test). For
subjects with anergy, the incidence rates of tuberculosis did
not differ between the placebo and isoniazid groups (P-0.68
by the log-rank test). 6H denotes patients receiving isoniazid
for six months, 3RH patients receiving isoniazid and rifampin
for three months, and 3RHZ patients receiving isoniazid, rifam
pin, and pyrazinamide for three months. The numbers below
the graphs are the numbers of subjects at risk.
During follow-up, there were 399 deaths: 237
among PPD-positive subjects and 162 among sub
jects with anergy. The overall mortality rate was
greater in the anergy cohort than in the PPD-positivc cohort (P = 0.001). The proportion surviving at
one year was 0.78 in the anergy cohort and 0.90 in
the PPD-positive cohort (P = 0.001 by the log-rank
test). When the analysis was stratified according to
the presence of anergy, there was no significant dif
ference between placebo and each treatment with
regard to cither the mortality rate or the cumulative
proportion of deaths (P>0.2 by the log-rank test)
in either the PPD-positive cohort or the anergy co
hort (Table 4). Of the 66 subjects in whom tuber
culosis developed, 13 died, for a cumulative mortal
ity rate of 20 percent.
DISCUSSION
In this randomized, placebo-controlled clinical
trial of therapy to prevent tuberculosis in HIVinfected Ugandan adults, self-administered isoniazid
taken daily for six months reduced the risk of tuber
culosis by 67 percent in subjects with positive PPD
skin tests (induration, ^5 mm). This level of short
term protection was achieved with a minimum of
adverse effects. The cfficacv of isoniazid in this studv
Vo I u inc 3 3 7
N u in b c r 12
805
I hc Xcw England Journal of Medicine
Table 2. Ixcidi xii oi Defixiif or Probable Tubeiu itoms A( <ordixg io
Study Group axd Ri iativf Risk of Tuber< itosis.‘
Group
Definite or
Probable
Tuberculosis
Crude
Relative Risk
(95% Cl)
Value!
Adjusted
Relative Risk
(95% Cl)t
9
10
3.41
1.08
1.32
1 73
1.0
0.33 (0.14-0.77)
0 40 id 18-0 Soi
0.51 10 24-I OS >
0.01
0 02
0 OS
1.0
0.32 (0.14-0.76)
0.41 (0 19-0.89)
0 43 (0.20-0.92)
10
9
3.06
2.53
1.0
0 S3 iO 34 2 04 i
<) os
10
0.75 <0.30- I 89i
P
ML < >1
< AsFs
PPD-positive cohortH
Placebo
Isoniazid
Isoniazid, rifampin
Isoniazid, rifampin, pyrazinamide
Ancrgy cohort
Placebo
Isoniazid
21
*CI denotes confidence interval The relative risk is as compared with the placebo group
fThc P sallies were determined with the Wald chi square Matisiic I hc nominal critical value was
0.011. adjusted for the second interim analysis and multiple comparisons with placebo.
{The relative risks have been adjusted for age. scs. white cell count, hemoglobin lesel. Karnobks
performance score, bodymass index, history of HIV related infection, and presence of chrome diar
rhea by Cox proportional-hazards regression anahsjs
§ The rate is the number of cases per 100 person vears
PPD-positive denotes a positive tuberculin skin test unit purified protein derivative
Table 3. Cvmltauxi: Ixcidexce oi- Aim km Evi xis, Gkade oi Ri.u nox ix Stldy
Sl BJECTS, AXD ErI-QI EXL Y OE DlSCOXI (XT Al IOX OF THERAPY ACCORDIXG IO STUDY
Group axd i hi Presexce or Abm x< i of Cui axeous Axergy.
Group
Cumulative
Incidence of
Reported
Adverse Events
Discontinuation
of Therapy
Grade of Reaction
Mil i>
M< >1'1 KA IF
MA FRF
number (percent)
PI’l) positive cohort*
Placebo
Isoniazid
Isoniazid, rifampin
Isoniazid, rifampin, pyra
zinamide
Ancrgy cohort
Placebo
Isoniazid
23 (5.01
60 i 1 1.2)
54 (9.7)
1 14 (24.7)
23 (5,0>
56 <10 4)
48 (8.6 >
101 (21 9i
22 (6.8)
31 (7.8)
22 (6.S)
29 (7.3)
0
4 (0.7)
o 11.11
12 (2.6)
0
0
0
1 (0.2)
13 (2.3)
26 (5.6)
0
2 (0.5)
0
0
0
0
1 (0.2)
3 (0.6)
•Pl’D positive denotes a positive tuberculin skin lest with purified protein derivative.
was similar to the efficacy of 71 percent found in a
randomized clinical trial of isoniazid in Haiti,-’0 but
the current study addressed some of the methodologic issues raised about the Haitian study.-’1 In
particular, the current analysis was based on a larger
number of cases of tuberculosis, with half the cases
confirmed by sputum culture. The incidence rates of
tuberculosis were lower in the current study than in
the Haitian study, perhaps as a result of the stricter
entry criteria used to exclude subjects with actixe tu
berculosis. Nevertheless, the consistent findings of
806
September 18, 1997
these two studies, in addition to the preliminary re
ports of other clinical trials,32-’-’ support the validity
of the observed protective effect. The duration of
this effect, however, remains to be established, since
variability in the annual risk of infection among
populations may affect the risk of tuberculosis after
preventive therapy has been completed, especially in
persons with advanced immunosuppression.
The current study extends previous observations
by evaluating the safety and efficacy of two multi
drug, three-month regimens, isoniazid and rifampin
/
THREE REGIMENS TO PREVENT TUBERCULOSIS IN UGANDAN ADULTS WITH HIV INFECTION
/
/
, paresthesias, were detected more frequently in the
treatment groups than in the placebo groups and
were more common in subjects receiving the regi
men containing pyrazinamide. Because medical offi
cers were not blinded to the subjects’ treatment as
P
Mortality
Relative Risk
Value
(95% cut
Rate*
Deaths
Group
signments, it is possible that this observed difference
resulted from detection or reporting bias. Nonethe
no. (%)
less, since these regimens arc intended to prevent tu
PI’D-positive cohort^
berculosis in asymptomatic or minimally symptomat1.0
64
(13.8)
10.2
Placebo
0 44 1 ic persons at risk, the treatment should not produce
0.9 (0.6-1.2)
58 (10.8)
8.9
Isoniazid
0.25
0.8 (O.5-1.2)
8.3
57 (10.3)
Isoniazid, rifampin
unacceptable side effects. Although the reported side
0.83
0.96 (0.7-1.4)
9.8
58 (12.6)
Isoniazid, rifampin,
effects
were not severe, they may have led to higher
pyrazinamide
rates of noncompliance or to the withdrawal of ther
Anergy cohort
22.3
1.0
76 (23.5)
Placebo
apy by physicians.
1.05 (0.77-1.42) 0.77
23.5
86 (21.6)
Isoniazid
In this study, short-term survival did not differ
•The monalitv rate is the number of deaths per 100 person-years. Total
significantly between the placebo and treatment
placebo, 625;
person-years for the PPD-positive cohort were as follows:
I "
groups in either the PPD-positive or the anergy coisoniazid, 652; isoniazid and rifampin, 689; and isoniazid, rifampin, and
hort. If the survival benefit of preventive therapy is
pvrazinamide, 589. Total person-years for the anergy cohort were as fol
lows: placebo, 340; and isoniazid, 367.
conferred through a reduction in the tuberculosis•fCI denotes confidence interval.
related case fatality rate, then the use of isoniazid in
JPPD-positive denotes a positive tuberculin skin test with purified pro
i the PPD-positive cohort prevented 14 cases of tu
tein derivative.
berculosis and approximately 3 deaths, assuming a
I case fatality rate of 20 percent. Thus, a large, ran
domized clinical trial of preventive therapy would be
and isoniazid, rifampin, and pyrazinamide. These regreduction in
imens substantially reduced the risk of tuberculosis, , needed to detect a clinically
. important
.
the relative risk of cause-specific mortality from tu
but the reduction did not reach the conservative level
berculosis. However, the absolute difference in the
of statistical significance. These regimens were in
mortality rates observed in this study between PPDcluded in the trial because of the greater sterilizing
positive subjects receiving isoniazid and those receiv
activity of rifampin,-’4 with or without pyrazinamide,
and because of the potential for improved compli- j ing placebo may indicate important public health
benefits in terms of survival if preventive therapy is
ance with shorter regimens.19 In addition, fixed-dose
combinations of these drugs arc available. The slight ! used widely in HIV-infected persons. The concluditference in efficacy between the two- and three- i sions regarding survival arc limited, however, be
cause the average duration of follow-up was short.
drug regimens may be due to the greater frequency
The implications of the findings of this study deof adverse events associated with the use of pyrazin- ;
pendI on the setting and the target population for
amide and its possible effect on compliance.
preventive therapy. In the United States, where the
nreve
In this study, there was evidence of a small benefit
annual risk of infection and the incidence of tuber
of preventive therapy with isoniazid in subjects with
culosis
are in general low, preventive therapy in du
anergy, but the confidence intervals were wide and
ally infected patients is both a standard medical
did not rule out the null hypothesis. The reason iso
practice and central to tuberculosis control. In deniazid did not confer the same degree of protection
in the subjects with anergy is unclear. We speculate_• J vcloping countries, where dual infection is common
that subjects with anergy may be at greater risk than | and continued exposure to infectious cases of tuberculosis is likely, preventive therapy provides benefit
PPD-positive subjects for primary failure of preven
to the individual patient, at least for a short time,
tive therapy because of drug malabsorption’5 37 or
but the effect on tuberculosis control remains to be
other host factors associated with advanced disease.
established.
Alternatively, exogenous reinfection with progressive
primary disease may occur because of the more ad
vanced degree of immunosuppression.
Supported by .1 cooperative agreement with the ( enters tor Disease
Control and Prevention (ADEPT/H1V Related Tuberculosis Demonstra
The safety of isoniazid as preventive therapy in
non Project, l’78/< ( 1'506716 ()4) and by a training grant from the
HIV-seronegative persons may not be readily extrap
1-ogartv International Center at the National Institutes ot Health (AIDS
olated to HIV-seropositive persons, because of the
International Training and Research Program, TW 00011 -08).
enhanced drug hypersensitivity associated with HIV
IVc arc indebted to the following members of the study team: ad
infection.4-1’-24 In the current trial, no serious toxic
ministration — I., (iaiy. M. Kasnjja, S Kibende, M. Manning,
effects were reported with six months of isoniazid,
,4. Nakayiza, and P biasitje; eoanselors and interviewers —
and the rate of clinical hepatitis was similar to that
(>'. Hwamikt, K Kyariihanjja. and K. (ialiwanijo: data manajjeis
observed in HIV seronegative persons of similar
— P. Bajaneza, 11 (Iwatndde, .S'. Katabalwa. /.B. Mtikasn. M. ()dii\
(.’. Opit, (>'. Olupot, and A. litryaninreba; dispenses — A. Abenage.-’K Other side effects, such as rash, arthralgias, ami
Table 4. Mori ai ity Kvi e and Cvmllative Proportion
oe Dea ms A< <orbing to Stvdy Group.
<
<
4
4
<
I
Volume 337
Number 12
807
The New England Journal of Medicine
i
/
I
/
aL-yn and L. X'dcncmtt; drii'crs — E. Kanniva. H. Kalninera. (>'. I.iinnnuba. R. .\hikasa, and L. Orycma;filing—G. linkmva. /L Mnlyabintu, and R. Nansnbiuyu health educators — IV. Rajiindirire
and .\f. Mwanje; home health visitors — K. Kataliwa, M. Kato.
/. Mnlabbi, and /. Nakibali; laboratory — K. Edmonds, P. Kataaba. .S’. Kabcnqera. ]. Okiror, E. Piwowar, H.S. Tnanme, and R.S.
Wallis; medical officers — IV. Ruknln, F. Byckwaso, A. Gasasira,
P. Kyambadde, H. Lttzzc, A. Matceyja, F. Mnbiru, C. Mnkuht, and
R. Odekc; microbiolotiy — T Aisu, E. Hatantja, and A. Morrissey;
nurses—J. Kaynnjjirizi, C. Kiramba, M. Mnlindwa, G. Nalnjiwa,
A. Rivamncece, and G. Tnmnsiimc; radiology — A. Adongo and
E. Katcndc; study coordinator — P. Langi; and tuberculin skin
testers — G. Mpalanyi, P. blasozzi, S. Nyolc, and G. IV/inii’n. II?
are also indebted to S. Okivare, Ministry of Health; M.G. AhvanoF-dycgn, director, AIDS Information Centre; F. Engwait-Adatn.
head of the Ugandan National Tuberculosis and Leprosy Pro
gramme; and the clients and staff of the following organizations:
AIDS Information Centre; Joint Clinical Research Center, the
AIDS Support Organization, Mulago Branch; the Post-HIV Test
Club, Kiscnyi; Good Samaritan Counseling Centre; HIV/AIDS
Clinics of St. John’s, Rubaga, and Nsambya Hospitals, Kampala,
Uganda; Drs. E. Villarino, A. Vernon, P. Smith, and R. O'Brien
and Mr. L. Gcitcr of the Centers for Disease Control and Prevention
for their scientific contributions to the study design and analysis; to
Drs. T.M. Daniel and F. van dcr Kuyp for their independent review
of incident cases of tuberculosis; and to the subjects who participated
in the trial.
REFERENCES
1. Narain IP, Raviglione M(’, Kochi A. HIV-associated tuberculosis in de
veloping countries: epidemiology and strategies for prevention. Tuberc
Lung Dis 1992;73:311 21.
2. Schvyn PA, Hancl D, Lewis VA, et al. A prospective study of the risk
of tuberculosis among intravenous drug users with human immunodefi
ciency virus infection. N Engl J Med 1989;320:545-50.
3. Schvyn PA, Sckcll BM, Alcabcs P, Friedland GH, Klein RS, Schoen
baum EE. High risk of active tuberculosis in HIV-infected drug users with
cutaneous anergv. JAMA 1992;268:504 9. [Erratum, JAMA 1992;268:
3434.1
4. Guclar A, Gatell JM, Verdejo I, et al. A prospective study of the risk of
tuberculosis among HIV-infected patients. AIDS 1993;7:1345-9.
5. Antonucci G, Girardi E, Raviglione MC, Ippolito G. Risk factors for
tuberculosis in HIV-infected persons: a prospective cohort studv. JAMA
1995;274:143-8.
6. Whalen C, Okwcra A, Johnson J, et al. Predictors of survival in human
immunodeficiency virus infected patients with pulmonary tuberculosis: the
Makercre University Case Western Reserve University Research Collabora
tion. Am J Respir Grit Care Med 1996;153:I977-81.
7. Pcrriens JH, Colebunders RL, Karahunga C, et al. increased mortality
and tuberculosis treatment failure rate among human immunodeficiency
virus (HIX') seropositive compared with HIV seronegative patients with
pulmonary tuberculosis treated with “standard" chemotherapy in Kinshasa,
Zaire. Am Rev Respir Dis 1991;144:750-5.
8. Nunn P, Brindle R, Carpenter L, et al. Cohort study of human imnni
nodeticiency virus infection in patients with tuberculosis in Nairobi, Kenya
analysis of early (6 month) mortality. Am Rev Respir Dis 1992,146:849
54. ’
9. Chaisson RE, Schecter GF, Theuer CP, Rutherford GW, Echcnbcrg DF,
Hopewell PC. Tuberculosis in patients with the acquired immunodcticien
cy syndrome: clinical features, response to therapy, and survival. Am Rev
Respir Dis 1987;136:570-4.
10. Small PM, Schecter GF, Goodman PC, Sandc MA, Chaisson RE,
Hopewell PC. Treatment of tuberculosis in patients with advanced human
immunodeficiency virus infection. N Engl J Med 1991;324:289 94.
11. Ackah AN, Coulibaly D, Digbcu H, et al. Response to treatment, mor
tality, and CD4 lymphocyte counts in HIV-infected persons with tubercu
losis in Abidjan, Cote d'Ivoire. Lancet 1995;345:607 10
12. Pitchcnik AE. Tuberculosis control and the AIDS epidemic in devel
oping countries. Ann Intern Med 1990;! 13:89-91.
808
September 18, 1997
,
I
13. O'Brien RJ. Pcrriens JH. Preventive therapy for tuberculosis in HIV
infection the promise and the reality. AIDS 1995;9:665-73.
14. Goodgamc RW. AIDS in Uganda — clinical ami social features
N Engl J Med 1990;323:383 9.
15. Moreno S, Baraia Etxaburu J. Bouza E. et al Risk for developing tu
berculosis among anergic patients infected with HIV Ann Intern Med
1993.1 19.194 8
16. Graham NMH, Galai N, Nelson KE, et al. Effect of isoniazid chemo
prophylaxis on HIX' related mycobacterial disease. Arch Intent Med 1996
156:889 94.
17. Rcichman LB. Felton CP. Edsall JR Drug dependence, a possiblc
nevv risk factor for tuberculosis disease. .Arch Intern Med 1979;! 39:337
9.
18. Fcrcbce SH. (Controlled chemoprophylaxis trials in tuberculosis: a gen
cral review. Adv Tubcrc Res 1970;17:28-i06.
19. Hong Kong Chest Serv icc/Tubcrculosis Research Centre, Madras/
British Medical Research Council. A double-blind placebo-controlled clin
ical trial of three antitubcrculosis chemoprophylaxis regimens in patients
with silicosis m Hong Kong. Am Rev Respir Dis 1992;145:36-41.
20. International Union Against Tuberculosis Committee on Prophylaxis.
Efticacv of various durations of isoniazid preventive therapy tor tuberculo
sis: five wars of'follow-up in the IUAT trial. Bull World Health Organ
1982.60:555 64.
21. (Comstock GW. Baum ( . Snider DE Jr. Isoniazid prophylaxis among
Alaskan Eskimos: a final report of the Bethel isoniazid studies. Am Rev
Respir Dis 1979;l 19 827 50.
22. I bc use of preventive therapy tor tuberculous infection in the United
States. MMWR 1990.39. RR Si:9 12
23. (Coopman SA. Johnson RA. Platt R. Stern RS. Cutaneous disease and
drug reactions m HIX’ infection. N Engl I Med 1993;328:1670-4.
24. Pozniak AL. MacLeod GA. Mahan M. Legg XX', Weinberg J. ’Hie in
fluence of HIX’ status on single and multiple drug reactions to antituber
culous thcrapv m Africa AIDS 1992:6:809 14.
25. Karnofsky DH. Burchcnal JH. I he clinical evaluation of chemothera
peutic agents in cancel. In: MacLeod (CM, cd. Evaluation of chemothera
peutic agents New York: Columbia University Press. 1949:191-205.
26. Bass JR Jr. l-arer I.S, Hopewell PC, Jacobs RE, Snider DE Jr. Diagnos
tic standards and classification of tuberculosis. Am Rev Respir Dis 1990;
142:725 35 | Erratum. Am Rev Respir Dis 1990;142:l470. |
27. AIDS ( linical I rials Group. Table for grading severity of adult adverse
experiences. XX'ashington, D.C.: Division ot AIDS, National institute of Al
lergy and Infectious Diseases, 1993.
28. International Union Against Tuberculosis and Lung Disease. Technical
guide tor sputum examination for tuberculosis by direct.microscopy. Bull
hit Union Against Tuberc Lung Dis 1986;61:1 16.
29. Lan KKG. DcMets DL. Discrete sequential boundaries tor clinical tri
als. Biometrika I983;7O:659 6.3.
30. Pape JW, Jean SS, Ho JL, Hafner A, Johnson XX'D Jr. Ertect of isoniazid
prophvlaxts on incidence of active tuberculosis and progression of HIV in
fection. Lancet 1993;342:268 72.
31. De Cock KM, Grant A, Porter JDH. Preventive therapy tor tubercu
losis m HIX’ infected persons: international recommendations, research,
and practice Lancet 1995;345:833-6.
32. Iialscv N, Cobcrly J, Atkinson J, et al. Twice weekly INH for I B pro
phviaxis. In. Abstracts of the 10th International Conference on AlDS/ln
icrnaiional Conference on STD, Yokohama, Japan, August 7-12, 1994:
167. abstract.
33. XX'adhawan D, Hira S, Mwansa N, Perine P. Preventive tuberculosis
chemotherapy with isoniazid among persons infected with human immu
nodeficiency virus. In: Abstracts of the Seventh International Conference
on AIDS. Florence, Italy, June 6-21, 1991. Vol. 2. Rome: Istituto Superiorc di Sanita, 1991:247 abstract.
34. l.ccoeur HF, rruffot-Pcrnot C, Grossct JH. Experimental short-course
preventive therapy of tuberculosis with rifampin and pvrazinamide. Am Rev
Respir Dis 1989;! 40:1189-93.
35. Peloquin CA, MacPhee AA, Berning SE. Malabsorption of antimycobactcrial medications. N Engl J Med 1993;329:1122-3. :
36. Berning SE, Hunt GA, Iseman MD, Peloquin CA. Malabsorption of
antitubcrculosis medications bv a patient with AIDS. N Engl J Med 1992;
327:1817-8.
37. Patel KB, Belmonte R, Crowe HM. Drag malabsorption and resistant
tuberculosis in HIX' infected patients. N Engl J Med 1995;332:336-7.
38. Comstock GXX', Edw ards PQ. The competing risks of tuberculosis and
hepatitis for adult tuberculin reactors. Am Rev Respir Dis 1975;! 11:573-7.
EDITORIALS
Editorials
The Ethics of Clinical Research
in the Third World
A N essential ethical condition for a randomized
Ik clinical trial comparing two treatments for a dis
ease is that there be no good reason for thinking one
is better than the other.1-2 Usually, investigators hope
and even expect that the new treatment will be better,
but there should not be solid evidence one way or the
other. If there is, not only would the trial be scientifi
cally redundant, but the investigators would be guilty
of knowingly giving inferior treatment to some partic
ipants in the trial. The necessity for investigators to be
in this state of equipoise2 applies to placebo-controlled
trials, as well. Only when there is no known effective
treatment is it ethical to compare a potential new
treatment with a placebo. When effective treatment
exists, a placebo may not be used. Instead, subjects in
the control group of the study must receive the best
known treatment. Investigators are responsible for all
subjects enrolled in a trial, not just some of them, and
the goals of the research are always secondary to the
well-being of the participants. Those requirements arcmade clear in the Declaration of Helsinki of the World
Health Organization (WHO), which is widely regard
ed as providing the fimdamcntal guiding priiicipfes of
research involving human subjects.3 It states, “In re
search on man |.ffr], the interest of science and so
ciety should never take precedence over consider
ations related to the w ellbeing of the subject,” and “In
any medical study, every patient — including those of
a control group, if any — should be assured of the best
proven diagnostic and therapeutic method.”
One reason ethical codes are unequivocal about in
vestigators’ primary obligation to care for the human
subjects of their research is the strong temptation to
subordinate the subjects’ welfare to the objectives of
the study. That is particularly likely when the research
question is extremely important and the answer
would probably improve the care of future patients
substantially. In those circumstances, it is sometimes
argued explicitly that obtaining a rapid, unambiguous
answer to the research question is the primarv ethical
obligation. With the most altruistic of motives, then,
researchers may find themselves slipping across a line
that prohibits treating human subjects as means to an
end. When that line is crossed, there is very little left
to protect patients from a callous disregard of their
welfare lor the sake of research goals. Even informed
consent, important though it is, is not protection
enough, because of the asymmetry in knowledge and
authority between researchers and their subjects. And
approval by an institutional review board, though also
important, is highly variable in its responsiveness to
patients’ interests when they conflict with the inter
ests of researchers.
A textbook example of unethical research is the
Tuskegee Study of Untreated Syphilis.4 In that study,
which was sponsored by the U.S. Public Health Service
and lasted from 1932 to 1972, 412 poor AfricanAmerican men with untreated syphilis were followed
and compared with 204 men free of the disease to de
termine the natural history of syphilis. Although there
was no very good treatment available at the time the
study began (heavy metals were the standard treat
ment), the research continued even after penicillin be
came widely available and was known to be highly ef
fective against syphilis. The study was not terminated
until it came to the attention of a reporter and the out
rage provoked by front-page stories in the Washington
! Star and New York limes embarrassed the Nixon
administration into calling a halt to it.5 The ethical
violations were multiple: Subjects did not provide
informed consent (indeed, they were deliberately de
ceived); they were denied the best known treatment;
and the study was continued even after highly effective
treatment became available. And what were the argu
ments in favor of the Tuskegee study? That these poor
African-American men probably would not have been
treated anyway, so the investigators were merely ob
serving what would have happened if there were no
study; and that the study was important (a “never-tobe-repeated opportunity,” said one physician after
penicillin became available).6 Ethical concern was even
stood on its head when it was suggested that not only
was the information valuable, bin it was especially so
for people like the subjects — an impoverished rural
population with a very high rate of untreated syphilis.
The only lament seemed to be that many of the sub
jects inadvertently received treatment bv other doctors.
Some of these issues arc raised by Lurie and Wolfe
elsewhere in this issue of the Journal. They discuss
the ethics of ongoing trials in the Third World of
regimens to prevent the vertical transmission of hu
man immunodeficiency virus (HIV) infection." All
except one of the trials employ placebo-treated con
trol groups, despite the fact that zidovudine has al
ready been clearly shown to cut the rate of vertical
transmission greatly and is now recommended in the
United States for all HIV-infected pregnant women.
I he justifications arc reminiscent of those for the
Tuskegee study; Women in the Third World would
not receive antiretroviral treatment anyway, so the
investigators arc simply observing what would hap
pen to the subjects' infants if there were no study.
And a placebo-controlled study is the fastest, most
efficient way to obtain unambiguous information
that will be of greatest value in the Third World.
1 hus, in response to protests from Wolfe and others
to the secretary of Health and Human Services, the
directors of the National Institutes of Health (NIH)
and the Centers for Disease Control anil Prevention
Volume 337
X umber 12
847
EDITORIALS
controlled, if at all possible. That rigidity may ex
plain the NIH’s pressure on Marc Lallemant to in
clude a placebo group in his study, as described by
Lurie and Wolfe.7 Sometimes journals are blamed
for the problem, because they are thought to de
mand strict conformity to the standard methods.
That is not true, at least not at this journal. We do
not want a scientifically neat study if it is ethically
flawed, but like Lurie and Wolfe we believe that in
many cases it is possible, with a little ingenuity, to
have both scientific and ethical rigor.
The retreat from ethical principles may also be ex
plained by some of the exigencies of doing clinical
research in an increasingly regulated and competitive
environment. Research in the Third World looks rel
atively attractive as it becomes better funded and
regulations at home become more restrictive. De
spite the existence of codes requiring that human
subjects receive at least the same protection abroad
as at home, they arc still honored partly in the
breach. The fact remains that many studies arc done
in the Third World that simply could not be done in
the countries sponsoring the work. Clinical trials
have become a big business, with many of the same
imperatives. To survive, it is necessary to get the
work done as quickly as possible, with a minimum
of obstacles. When these considerations prevail, it
seems as if we have not come very far from Tuskegee
after all. Those of us in the research community
need to redouble our commitment to the highest
ethical standards, no matter where the research is
conducted, and sponsoring agencies need to enforce
those standards, not undercut them.
Marcia Angell, M.D.
REFERENCES
1. Angell M. Patients' preferences in randomized clinical trials. N Engl J
Med 1984;310:1385-7.
2. Freedman B Equipoise and the ethics of clinical research. N Engl J Med
1987;317:141-5.
3. Declaration of Helsinki IV, 41st World Medical Assembly, Hong Kong,
September 1989. In: Annas GJ, Grodin MA, eds. The Nazi doctors and
the Nuremberg (’ode: human rights in human experimentation. New York:
Oxford L’niversity Press, 1992:339-42.
4. Twcntv vears after: the legacy of the Tuskegee syphilis study. Hastings
Cent Rep 1992;22(6):29-40.
5. Caplan AL. When evil intrudes. Hastings Cent Rep 1992;22(6):29-32.
6. The development of consent requirements in research ethics. In: Faden
RR, Beauchamp TL. A history and theory of informed consent. New York:
Oxford L’niversity Press, 1986:151 99.
7. Lurie P, Wolfe SM. Unethical trials of interventions to reduce perinatal
transmission of the human immunodeficiency virus in developing coun
tries. N Engl J Med 1997;337:853-6.
8. The conduct of clinical trials of'maternal-infant transmission of HIV
supported by the United States Department of Health and Human Sen ices
in developing countries. Washington, D.C.: Department of Health and
Human Sen ices, July 1997.
9. Whalen CC, Johnson JL, Okwera A, et al. A trial of three regimens to
prevent tuberculosis in L’gandan adults infected with the human immuno
deficiency virus. N Engl J Med 1997;337:801 8
10. I he use of preventive therapy for tuberculous infection in the Unites!
Stares: recommendations of the Advisors Committee for Elimination of'
Tuberculosis. MMWR Morb Mortal Wklv Rep 1990;39(RR 8):9 12.
11. Bass JB Jr, barer LS, Hopexsell PC, et al. Treatment of tuberculosis ami
tuberculosis infection in adults and children. Am J Respir Crit Care Med
1994;149:1359-74.
12. De Cock KM, Grant A, Porter JD. Preventive therapy for tuberculosis
in HIV-infected persons: international recommendations, research, and
practice. Lancet 1995;345:833-6.
13. Msamanga GI, Fasvzi WAV. The double burden of HIV infection and
tuberculosis in sub-Saharan Africa. N Engl J Med 1997;337:849-51.
14. Angell M. Ethical imperialism? Ethics in international collaborative
clinical research N Engl J Med 1988;319:1081-3.
15. Protection of human subjects, 45 CFR § 46 (1996).
16. International ethical guidelines for biomedical research involving hu
man subjects. Geneva: Council for International Organizations of Medical
Sciences, 1993.
17. Angell M. The Nazi hvpothermia experiments and unethical research
today. N Engl J Med 1990;322:1462-4
©1997, Massachusetts Medical Society.
The Double Burden of HIV
Infection and Tuberculosis
in Sub-Saharan Africa
I
r I ^HE World Health Organization (WHO) estiJL mated that by June 1996 14 million people were
living with human immunodeficiency virus (HIV) in
fection in sub-Saharan Africa. Although it contains
only 10 percent of the world’s population, subSaharan Africa is home to about 65 percent of all the
world’s HIV-infected people. In several urban cen
ters, more than 10 percent of the asymptomatic
adults and about 15 to 30 percent of the women at
tending prenatal-care clinics are infected. A 1994 pa
per reported that in rural Uganda more than 80 per
cent of the deaths among men and women 25 to 44
years of age were attributable to HIV infection.1 The
reported risk of perinatal transmission of HIV is gen
erally higher in African studies (30 to 45 percent)
than in European and American studies (7 to 30
percent). Although the median length of time from
seroconversion to the appearance of the acquired
immunodeficiency syndrome (AIDS) is approximate
ly 10 years in the United States, it is only 4.4 years
among female sex workers in Nairobi, Kenya.2
The death of one or both parents from HIV in
fection has left many African children without so
cial, emotional, or economic support. HIV infection
has also put additional strains on the already over
stretched health care systems. The average annual per
capita expenditure on health is $11 for the region,
and in several countries it is less than $4. Many areas
lack essential drugs and medical supplies, including
antibiotics, antiseptics, and gloves. With the increas
ing privatization of the health care sector, many
health services (excluding prenatal care and other pre
vention programs) arc available — but at a price. Al
though mechanisms have been developed to waive
the fees for those who cannot afford them, these may
be difficult to implement when the majority of pa
tients arc poor. In fact, over 50 percent of the adult
patients admitted to the hospital in Africa arc infected
Volume 337
Number 12
849
r
t*F
The Xc« England Journal of Medicine
with HIX', and many of them arc unable to pay for
care. Given that HIV infection is most prevalent
among the economically productive age groups, pa
tients’ families suftcr tremendously because of the fre
quent illnesses and eventual death of those infected.
A secondary epidemic of tuberculosis is accompany
ing the rise in the number of HIV-infected persons.
WHO estimates that worldwide nearly 5 million peo
ple are infected with both HIV and tuberculosis, and
three quarters of them live in Africa.' Prevention oP
tuberculosis among those with HIV infection is a log
ical public health goal, given that such patients arc at
high risk for tuberculosis, which in turn is associated
with an increased likelihood of death. Long before the
advent of AIDS, preventive therapy with isoniazid was
show n to reduce the occurrence of tuberculosis signif
icantly among contacts of patients with active disease
and among those with conversion of a tuberculin skin
test to positive.4 Because of concern about the in
creased adverse effects of antitubcrculosis therapy in
HIX'-positivc patients, a number of trials have exam
ined the safety and efficacy of chemoprophylaxis in
this population. Placebo-controlled studies were car
ried out in Haiti, Zambia, and Kenya with varying de
signs and results. In the Haitian study, a 12-month
course of isoniazid significantly reduced the incidence
of tuberculosis among HIV-positive subjects with
positive tuberculin skin tests. However, about 40 per
cent of the new cases were based on presumptive di
agnoses of tuberculosis? In the Zambian study, a sixmonth course of isoniazid reduced the incidence of
tuberculosis among patients with positive tuberculin
skin tests? But in the study from Kenya there was no
effect of six months of therapy with isoniazid among
HIV-positive subjects, although the number who had
positive tuberculin skin tests was too small to permit
the effect of therapy to be examined in this subgroup/
In this issue of the Journal, Whalen et al. report,
that a six-month course of isoniazid among HIVinfected Ugandans with positive tuberculin skin tests
reduced the risk of tuberculosis by about 70 percent
after a mean follow-up period of 15 months.8 Isonia
zid therapv may have reduced the risk of tuberculosis
among subjects with anergy as well. This study also
adds to our knowledge of the role of preventive ther
apies that include drugs other than isoniazid, such as
rifampin and pyrazinamide. For the subjects who re
ceived a three-month course of isoniazid and rifam
pin, there was about a 60 percent reduction in the
risk of tuberculosis as compared with those given pla
cebo. The reduction in the risk of tuberculosis for
those given isoniazid, rifampin, and pyrazinamide was
49 percent. Alternative regimens arc needed for those
infected with isoniazid-resistant strains, and the short
er courses arc likely to improve compliance. However,
thev arc also associated w ith a higher risk of adverse
events and arc most costly. Although none of the
treatments in this study reduced mortality significant-
850
•
September IS, 1997
Iv, the sample size and duration of follow-up were in
adequate for this question to be examined.
The results of the study from Uganda support the
administration of isoniazid as preventive therapy for
persons in sub-Saharan Africa who arc infected with
HIV and have positive tuberculin skin tests. Before
any such program can lx* implemented on a communitvwidc level, research on the operational and pro
grammatic questions is urgently needed. Is preventive
therapy feasible in sub-Saharan Africa? Is it cost effec
tive, as compared with other uses of scarce health care
dollars? The introduction of a program of preventive
therapy requires human resources, laboratory sup
plies, drugs, and transport facilities in order to carry
out voluntary counseling and testing for HIV infec
tion, to identify and exclude all those with active tu
berculosis, to perform tuberculin skin testing, and to
provide follow-up care. The exclusion of those with
active tuberculosis is important, since treatment with
isoniazid alone is insufficient and would lead to the
development of drug-resistant organisms. It is also
important to exclude people with liver problems at
base line and to terminate therapy among those in
whom hepatotoxicity develops during follow-up. In
one report, unsupcrv ised preventive therapy in Ugan
da was associated with poor compliance.9 On the oth
er hand, directly observed therapy for tuberculosis
given by nonmedical staff w as reported to be success
ful in a South African community,1" and a similar sys
tem could be instituted for preventive therapy.
A number of’ scientific issues still need to be ad
dressed. These include the question of how long the
protection afforded by preventive therapy lasts. The
protection afforded by 6 to 12 months of isoniazid
therapy is probably lifelong in the parts of the world
w here the risk of transmission of tuberculosis is low.
In sub-Saharan Africa, however, the duration of ef
ficacy may be much shorter because the risk of in
fection or reinfection is so high. The efficacy and
economics of providing long-term preventive thera
py or lifelong therapy and the risk of accelerating
drug resistance need to be examined.11 Given our
current state of knowledge, however, future studies
should not include a placebo group, since preventive
therapy should be considered the standard of care.
In sub-Saharan Africa, where there is little access
to antiretroviral drugs, preventive therapy for tuber
culosis may be the single most affordable interven
tion for the prolongation of a healthy life in HIVinfected persons. By preventing tuberculosis, these
regimens will also help reduce the transmission of
tuberculosis in African communities. Although we
agree with WHO that interrupting the transmission
of tuberculosis by curative treatment of infectious
cases should continue to be the priority for tuber
culosis programs,12 efforts need to be made to apply
these important findings about preventive therapy to
the community and the region where the study was
EDITORIALS
carried out. It is clear that African programs of tu
may lead to delusions. Negative symptoms involve the
berculosis and AIDS control will be unable to un , loss of normal functioning — the loss of will, range of
dertake this additional responsibility alone, since they
affect, pleasure, and fluency and content of speech,
rely largely on donor
<'
support. Extension of these proThe intensity of these symptoms and the residual dis
grams will be possible only through the cooperation
ability they cause may prevent people with schizophre
of many governments, pharmaceutical companies,
nia from beginning a career, completing an education,
and international agencies.
or enjoying a life that may once have been filled with
great promise. Rates of employment among people
Gernard I. Msamanga, M.D., Sc.D. i with schizophrenia rarely exceed 20 percent.
Muhimbili Medical Center
Schizophrenia is a chronic illness; less than 20 per
Dar es Salaam, Tanzania
cent of patients recover from a single episode of psy
chosis and return to the lives they knew before. More
Wafaie W. Fawzi, M.B., B.S., Dr.P.H.
frequently, patients have repeated episodes, with dec
Harvard School of Public Health
rements in base-line functioning accompanying each
Boston, MA 02115
one; a few never recover from the first episode and
REFERENCES
continue to have pervasive psychotic symptoms.
For 35 years, the pharmacologic approach to schizo
1. Mulder DW, Nunn AJ, Kamali A, Nakiyingi J, Wagner HU, KcngcyaKayondo JF. Two-year HIV-1-associated mortality in a Ugandan rural pop
phrenia involved antipsychotic medication based on
ulation. Lancet 1994;343:1021-3.
D2 dopamine-reccptor antagonism. The dopamine
2. Anzala OA, Nagclkcrke NJ, Bwayo JI, et al. Rapid progression to disease
in African sex workers with human immunodefieienev virus tvpe 1 infec
hypothesis of schizophrenia was proposed in 1963,'
tion. J Infect Dis 1995;171:686-9. (Erratum, J Infect Dis 1996;!73:1529 ]
10 years after the first antipsychotic medication was
\ 3./ The HIV/AIDS and tuberculosis epidemics: implications lor TB control.
introduced. This hypothesis was based on the ob
Geneva: World Health Organization, 1994. (WHO/TB/CARG(4)/94.4.)
4. O'Brien RJ. Preventive therapy for tuberculosis. In: Porter JDH,
servation that all antipsychotic drugs had a strong af
McAdam KPWJ, cds. Tuberculosis: back to the future. Chichester, Eng
finity for a particular dopamine receptor (D2) and
land: Wile)’, 1994:151, 66.
that dopamine agonists, such as methylphenidate and
5. Pape JW, Jean SS, Ho JL, Hafner A, Johnson WD Jr. Eflcct of isoniazid
prophylaxis on incidence of active tuberculosis and progression of HIV in
dextroamphetamine, could produce a psychotic con
fection. Lancet 1993;342:268-72.
dition. Standard antipsychotic drugs differed only in
6. Wadhawan D, Hira'S, Mwansa N, Perine P. Preventive tuberculosis che
motherapy with isoniazid among persons infected with HIV-1. Presented
their side effects, not in their mechanisms of action.
at the Eighth International Conference on AIDS/Third STD World Con
Consistent
side effects were those associated with D2
gress. Amsterdam, July 19-24, 1992. abstract.
antagonism, most likely in the nigrostriatal dopamine
7. Hawken MP, Meme HK, Elliott EC. et al. Isoniazid preventive therapy
for tuberculosis in HIX'-1 -infected adults: results of a randomized con
tracts, which led to extrapyramidal symptoms of stiff
trolled trial. AIDS 1997:11 875-82.
ness,
tremor,
pseudoparkinsonism,
and akathisia. Sub8. Whalen CC, Johnson JL, Okwera A, eti ai.
al. A trial
nidi of three
uircc regimens
rcginiciis to
io
’
* 1
I
• j
rv
in Ugandan
adults infected
immuno
i JCCtlVCly, tnCSC Side eirCCtS were unpleasant, leading
iprevent tuberculosis
.........................
,......................
---: with the human
...... -.................
deficiency virus. N Engl J Med 1997;337:801-8.
j to cycles of noncompliance and relapse. Estimates of
9. Aisu f, Raviglione MC. t ar. Praag E, et al. Preventive chemotherapv for
40 percent rates of noncompli;
. iance among patients
Hl\ -associates! tulx'rculosis in Uganda: an operational assessment at a vol
untary counselling and testing centre. AIDS 1995;9:267-73.
treated with antipsychotic agents were not unusual;
10. Wilkinson D, Davies GR, Connolly C. Directly observed therapv for
when noncompliance was combined with the thera
tuberculosis in rural South Africa, 1991 through 1994. .Am J Public Health
peutic limitations of the drugs, rates of relapse were
1996;86:1094-7.
11. De Cock KM, Grant A, Porter JD. Preventive therapy for tuberculosis
! quite high.
in HIV-infected persons: international recommendations, research, and
Clozapine, the first novel antipsychotic drug to
practice. Lancet 1995;345:833-6.
appear, was introduced in the United States in 1989.
12. Tuberculosis preventive therapv in HIV-infected individuals. Wklv Ep
idemiol Rec 1993;68:361-4.
A conventional antipsychotic drug, such as haloper
©1997, Massachusetts Medical Society.
idol, produced its antipsychotic effects after binding
to 80 percent of dopamine D2 receptors; clozapine
produced an antipsychotic effect after binding to
less than 20 percent of D2 receptors. Hypotheses
Pharmacologic Advances in the
about clozapines principal mechanism of action have
Treatment of Schizophrenia
been hotly debated, but without resolution. Pro
posed mechanisms of action have focused, separateh
\ LTHOUGH medications have dramatically imand in combination, on other dopamine receptors
XJL proved the li\es of many people with schizophre
(DI and D4) and on clozapine’s effects on the sero
nia, treatment resistance remains a serious problem.
tonin receptor 5-hydro.xytryptaminc. The initial in
Three quarters of patients with schizophrenia become
terest in serotonin receptors was stimulated bv ly
ill before the age of 25. The manifestations of the dis
sergic acid diethylamide (LSD), which has high
ease include two types of symptoms — “positive” and
serotonergic activity. Until clozapine was developed,
“negative.” Positive symptoms arc distortions of nor
however, investigation of serotonin receptors in the
mal functioning. Distortion of perceptions mav appear
context of schizophrenia had fallen oft'. This was be
as hallucinations; distortion of inferential thinking
cause the main psychotic symptoms associated with
Volume 337
Number 12
851
ji
I?'
I
!
t
L;.:'
2
I
SOUNDING BOARD
j document has been widely cited as justification for
subsequent trials in developing countries. In our view,
most of these trials arc unethical and will lead to hun
dreds of preventable HIV infections in infants.
Unethical Trials of
Primarily on the basis of documents obtained
from the Centers for Disease Control and Preven
Interventions to Reduce
tion (CDC), \vc have identified 18 randomized,
Perinatal Transmission of the
controlled trials of interventions to prevent perinatal
Human Immunodeficiency Virus
HIV transmission that cither began to enroll pain Developing Countries
i tients after the ACTG 076 study was completed or
have not yet begun to enroll patients. The studies
T has been almost three years since the Journal'
to evaluate a variety of interventions:
y
, arc
__ _ designed
---- o-----------------------published the results of AIDS Clinical Trials
antiretroviral
antiretroviral drugs
drugs such
such as
as zidovudine (usually in
Group (ACTG) Study 076, the first randomized,
regimens that are less expensive or complex than the
controlled trial in which an intervention was proved
ACTG 076 regimen), vitamin A and its derivatives,
to reduce the incidence of human immunodefi
intrapartum vaginal washing, and HIV immune glob
ciency' virus (HIV) infection. The antiretroviral drug
ulin, a form of immunotherapy. These trials involve
zidovudine, administered orally to HIV-positive prega total of more than 17,000 women.
nant women in the United States and France, admin
In the two studies being performed in the United
istered intravenously during labor, and subsequently
States, the patients in all the study groups have unadministered to the
newborn
infants,
reduced
die to
inzidovudine or other antiretroviral
-k........
►k^
restricted
access
cidence of HIV infection by two thirds.2 The regi
drugs. In 15 of the 16 trials in developing countries.
men can save the life of one of every seven infants
however, some or all of the patients arc not provid
born to HIV-infected women.
ed with antiretroviral drugs. Nine of the 15 studies
Because of these findings, the study was terminat
being conducted outside the United States are fund
ed at the first interim analysis and within two months
ed by the U.S. government through the CDC or the
after the results had been announced, the Public
National Institutes of Health (NIH), 5 are funded
Health Service had convened a meeting and con
by other governments, and 1 is funded by the Unit
cluded that the ACTG 076 regimen should be rec
ed Nations AIDS Program. The studies are being
ommended for all HIV-positive pregnant women
conducted in Cote d’Ivoire, Uganda, Tanzania, South
without substantial prior exposure to zidovudine
Africa, Malawi, Thailand, Ethiopia, Burkina Faso,
and should be considered for other HIV-positive
Zimbabwe, Kenya, and the Dominican Republic.
pregnant women on a case-by-case basis.3 The stand
These 15 studies clearly violate recent guidelines
aid of care tor HIV-positive pregnant women thus
designed specifically to address ethical issues pertain
became the ACTG 076 regimen.
ing to studies in developing countries. According
In the United States, three recent studies of clin
to these guidelines, “The ethical standards applied
ical practice report that the use of the ACTG 076
should be no less exacting than they would be in the
regimen is associated with decreases of 50 percent or
case of research carried out in [the sponsoring] coun
more in perinatal HIV transmission.4 6 But in devel
try.”9 In addition, U.S. regulations governing stud
oping countries, especially in Asia and sub-Saharan
ies performed with federal funds domestically or
Africa, where it is projected that by the year 2000,
abroad specify that research procedures must “not
6 million pregnant women will be infected with
unnecessarily expose subjects to risk.”10
HIV/ the potential of the ACTG 076 regimen re
The 16th study is noteworthy both as a model of
mains unrealized primarily because of the drug’s ex
an ethically conducted study attempting to identify
orbitant com in most countries.
less expensive antiretroviral regimens and as an indi
Clearly, a regimen that is less expensive than ACTG
cation of how strong the placebo-controlled trial or
076 but as effective is desirable, in both developing
thodoxy is. In 1994, Marc Lallcmant, a researcher at
and industrialized countries. But there has been
the Harvard School of Public Health, applied for
uncertainty about what research design to use in the
NIH funding for an equivalency study in Thailand
search for a less expensive regimen. In June 1994,
in which three shorter zidovudine regimens were to
the World Health Organization (WHO) convened a
be compared with a regimen similar to that used in
group in Geneva to assess the agenda for research on
the AGIG 076 study. An equivalency' studv is typi
perinatal HIV transmission in the wake of ACTG
cally conducted when a particular regimen has al
076. The group, which included no ethicists, con
ready been proved effective and one is interested in
cluded, “Placebo-controlled trials offer the best op
determining whether a second regimen is about as
tion for a rapid and scientifically valid assessment of
effective but less toxic or expensive.11 The NIH studv
alternative antiretroviral drug regimens to prevent
section repeatedly put pressure on Lallcmant and
[perinatal | transmission of HIV.”x This unpublished
the Harvard School of Public Health to conduct a
Sounding Board
I
Volume 337
N umber 12
853
The Xcw England Journal of Medicine
■w
placebo-controlled trial instead, prompting the di
rector ot Harvard s human subjects committee to re
ply, “The conduct of a placebo-controlled trial for
[zidovudine) in pregnant women in Thailand would
be unethical and unacceptable, since an active-con
trolled trial is feasible.”12 The NIH eventually relent
ed, and the study is now under way. Since the nine
studies of antiretroviral drugs have attracted the
most attention, we focus on them in this article.
ASKING THE WRONG RESEARCH
QUESTION
There arc numerous areas of agreement between
those conducting or defending these placebo-con
trolled studies in developing countries and those op
posing such trials. The two sides agree that perinatal
HIV transmission is a grave problem meriting con
certed international attention; that the ACTG 076 tri
al was a major breakthrough in perinatal HIX' preven
tion; that there is a role for research on this topic in
developing countries; that identifying less expensive,
similarly effective interventions would be of enormous
benefit, given the limited resources for medical care in
most developing countries; and that randomized stud
ies can help identify such interventions.
The sole point of disagreement is the best compar
ison group to use in assessing the effectiveness of lessexpensive interventions once an effective intervention
has been identified. The researchers conducting the
placebo-controlled trials assert that such trials repre
sent the only appropriate research design, implying
that they answer the question, ‘Ts the shorter regi
men better than nothing?” We take the more opti
mistic view that, given the findings of ACTG 076 and
other clinical information, researchers are quite capa
ble of designing a shorter antiretroviral regimen that
is approximately as effective as the ACTG 076 regi
men. The proposal for the Harvard study in Thailand
states the research question clearly: “Can we reduce
the duration of prophylactic [zidovudine] treatment
without increasing the risk of perinatal transmission
of HIV, that is, without compromising the demon
strated efficacy of the standard ACTG 076 [zidovu
dine] regimen?”1-’ We believe that such equivalency
studies of alternative antiretroviral regimens will pro
vide even more useful results than placebo-controlled
trials, without the deaths of hundreds of newborns
that arc inevitable if placebo groups are used.
At a recent congressional hearing on research eth
ics, NIH director Harold Varmus was asked how the
Department of Health and Human Services could
be funding both a placebo-controlled trial (through
the CDC) and a non-placebo-controlled equivalencv studv (through the NIH) in Thailand. Dr. Varmus
conceded that placebo-controlled studies arc “not the
onlv wav to achieve results.”14 If the research can be
satisfactorily conducted in more than one way, why
not select the approach that minimizes loss of life?
854
■
September 18. 1997
INADEQUATE ANALYSIS OF DATA FROM
ACTG 076 AND OTHER SOURCES
fhc NIH, CDC, WHO, and the researchers con
ducting the studies we consider unethical argue that
differences in the duration and route of administra
tion of antiretroviral agents in the shorter regimens,
as compared with the ACTG 076 regimen, justify the
use of a placebo group.1’’IH Given that ACl’G 076 was
a well-conducted, randomized, controlled trial, it is
disturbing that the rich data available from the study
were not adequately used by the group assembled by
WHO in June 1994, which recommended placebocontrolled trials after ACTG 076, or by the investiga
tors of the 15 studies we consider unethical.
In fact, the ACTG 076 investigators conducted a
subgroup analysis to identify an appropriate period
for prepartum administration of zidovudine. The ap
proximate median duration of prepartum treatment
was 12 weeks. In a comparison of treatment for 12
weeks or less (average, 7) with treatment for more
than 12 weeks (average, 17), there was no univari
ate association between the duration of treatment
and its effect in reducing perinatal HIV transmission
(P = 0.99) (Gelber R: personal communication). This
analysis is somewhat limited by the number of infect
ed infants and its post hoc nature. However, when
combined with information such as the fact that in
non-breast-feeding populations an estimated 65 per
cent of cases of perinatal HIV infection are transmit
ted during delivery and 95 percent of the remaining
cases are transmitted within two months of delivery,19
the analysis suggests that the shorter regimens may be
equallv effective. This finding should have been ex
plored in later studies by randomly assigning women
to longer or shorter treatment regimens.
What about the argument that the use of the oral
route for intrapartum administration of zidovudine in
the present trials (as opposed to the intravenous route
in ACTG 076) justifies the use of a placebo? In its
protocols for its two studies in -Thailand and Cote
d’Ivoire, the CDC acknowledged that previous “phar*
macokinetic modelling data suggest that [zidovudine]
scrum levels obtained with this [oral] dose will be similar to levels obtained with an intravenous infusion.”20
Thus, on the basis of the ACTG 076 data, knowl
edge about the timing of perinatal transmission, and
pharmacokinetic data, the researchers should have
had every reason to believe that well-designed short
er regimens would be more effective than placebo.
These findings seriously disturb the equipoise (uncertainty over the likely study result) necessary to justify
a placebo-controlled trial on ethical grounds.21
DEFINING PLACEBO AS THE STANDARD
OF CARE IN DEVELOPING COUNTRIES
Some officials and researchers have defended the
use of placebo-controlled studies in developing coun-
Vs-
SOUNDING BOARD
tries by arguing that the subjects arc treated at least
according to the standard of care in these countries,
which consists of unproven regimens or no treatment
at all. This assertion reveals a fundamental misunder
standing of the concept of the standard ofcarc. In de
veloping countries, the standard ofcarc (in this case,
not providing zidovudine to HIV positive pregnant
women) is not based on a consideration of alternative
treatments or previous clinical data, but is instead an
economically determined policy of governments that
cannot afford the prices set by drug companies. We
agree with the Council for International Organiza
tions of Medical Sciences that researchers working in
developing countries have an ethical responsibility to
provide treatment that conforms to the standard of
care in the sponsoring country, when possible.9 An
exception would be a standard of care that required
an exorbitant expenditure, such as the cost of build
ing a coronary care unit. Since zidovudine is usually
made available free of charge by the manufacturer for
use in clinical trials, excessive cost is not a factor in
this case. Acceptance of a standard ofcarc that does
not conform to the standard in the sponsoring coun
try’ results in a double standard in research. Such a
double standard, which permits research designs that
are unacceptable in the sponsoring countrv, creates
an incentive to use as research subjects those with the
least access to health care.
What arc the potential implications of accepting
such a double standard? Researchers might inject
live malaria parasites into Hl\’positive subjects in
China in order to study the effect on the progres
sion of HIV infection, even though the study pro
tocol had been rejected in the United States and
Mexico. Or researchers might randomly assign mal
nourished San (bushmen) to receive vitamin-forti
fied or standard bread. One might also justify trials
of HIV vaccines in which the subjects were not pro
vided with condoms or state of-thc-art counseling
about safe sex by arguing that they arc not custom
arily provided in the developing countries in ques
tion. These arc not simply hypothetical worst-case
scenarios; the first two studies have alrcadv been
performed,22 2-; and the third has been proposed
and criticized.24
Annas and Grodin recently commented on the
characterization and justification of' placebos as a
standard ofcarc: “'Nothing' is a description of what
happens; ‘standard of care’ is a normative standard
of effective medical treatment, whether or not it is
provided to a particular communitv.”2S
JUSTIFYING PLACEBO CONTROLLED
TRIALS BY CLAIMING THEY ARE
MORE RAPID
Researchers have also sought to justify placebo
controlled trials by arguing that they require fewer
subjects than equivalency studies and can therefore
be completed more rapidly. Because equivalency
studies are simply concerned with excluding alter
native interventions that fall below some preestab
lished level of efficacy (as opposed to establishing
which intervention is superior), it is customary to
use one-sided statistical testing in such studies."
The numbers of women needed for a placebo-controlled trial and an equivalency study are similar.26
In a placebo-controlled trial of a short course of zi
dovudine, with rates of perinatal HIV transmission
of 25 percent in the placebo group and 15 percent
in the zidovudine group, an alpha level of 0.05
(two-sided), and a beta level of 0.2, 500 subjects
would be needed. An equivalency study with a
transmission rate of 10 percent in the group receiv
ing the ACTG 076 regimen, a difference in efficacy
of 6 percent (above the 10 percent), an alpha level
of 0.05 (one-sided), and a beta level of 0.2 would
require 620 subjects (McCarthy W: personal com
munication).
TOWARD A SINGLE INTERNATIONAL
STANDARD OF ETHICAL RESEARCH
Researchers assume greater ethical responsibilities
when they enroll subjects in clinical studies, a precept
acknowledged by Varmus recently when he insist
ed that all subjects in an NIH-sponsored needle
exchange trial be offered hepatitis B vaccine.27 ResideBts_of impoverished, postcolonial countries, the
majority of whom are people of color, must be pro
tected from potential exploitation in research. Other
wise, the abominable state of healtlf care in these
countries can be used to justify studies that could
newer pass ethical muster in the sponsoring countrv.
With the increasing globalization of trade, govern
ment research dollars becoming scarce, and more at
tention being paid to the hazards posed by “emerging
infections” to the residents of industrialized coun
tries, it is likely that studies in developing countries
will increase. It is time to develop standards of re
search that preclude the kinds of double standards ev
ident in these trials. In an editorial published nine
years ago in the Journal, Marcia Angell stated, “Htb
man subjects in any part of the world should be pro
tected by an irreducible set of ethical standards.”28
Tragically, for the hundreds of infants who have need
lessly contracted HIV infection in the perinatal-trans
mission studies that have already been completed, anv
such protection will have come too late.
Peter Lurie, M.D., M.P.H.
Sidney M. Wolfe, M.D.
Public Citizen's Health Research Group
Washington, DC 20009
REFERENCES
1. < oniior EM. Sperling Rs. c.elbcr R.ct al. Reduction of maternal-infant
tranMnisMon of human iminunodcticiencv virus tvpe 1 with zidovudine
treatment X Engl I Med I994.SS1.I ITS 80.
Volume 337
Number 12
855
&
b
•
/.
/
The Neu England Journal of Medicine
2. Sperling RS. Shapiro DE. Coombs RIX', ct al Maternal viral load, zido
vudine treatment, anil the risk of transmission of human immunodelicicncv
virus type 1 from mother to infant. N Engl 1 Med 1996:335:1621 9.
3. Recommendations of the U.S. Public Health Service iask Force on the
use of zidovudine to reduce perinatal transmission of human immunodefi
ciency virus. MMW'R Morb Mortal Wkly Rep 19*74:431 RR 1 11:1 20.
4. Fiscus SA, Adimora AA. Schoenbach X’J, et al. Perinatal HIX' infection
and the effect of zidovudine therapy on transmission in rural and urban
counties. JAMA 1996;275:1483 8
5. (aioper E. Diaz C, Pitt J, ct al. Impact of ACIG 0/6: use of zidovudine
during pregnancy and changes in the rate of HIX’ vertical transmission. In:
Program and abstracts of the Third Conference on Retroviruses and Op
portunistic Infections, Washington. D.C., January 28-Fcbruary 1. 1996.
Washington, D.C.: Infectious Diseases Society of America, 1996:57.
6. Simonds RJ. Nesheim S, Matheson P, et al. Declining mother to child
HIX’ transmission following perinatal ZDX' recommendations. Presented at
the 11th International Conference on AIDS. X’ancouvcr. Canada, July
7-12, 1996. abstract.
7. Scarlatti G. Paediatric HIX’ infection. Lancet 1996,348:863 8.
8. Recommendations from the meeting on mothcr-to-infant transmission
of HIX' bv use of antiretrovirals, Geneva, World Health Organization. June
23-25, 1994.
9. World Health Organization. International ethical guidelines for bio
medical research involving human subjects. Geneva: Council tor Interna
tional Organizations of Medical Sciences, 1993.
10. 45 CFR46.il 1(a)(1).
11. Testing equivalence of two binomial proportions. In: Machin D.
Campbell MJ. Statistical tables for the design of clinical trials. Oxford,
England: Blackwell Scientific, 1987:35-53.
12. Brennan TA. Letter to Gilbert Meier, NIH Division of Research Eth
ics. December 28, 1994
13. Lallemant M, X'ithayasai X’ A short ZDX’ course to prevent perinatal
HIV in Thailand. Boston: Harvard School of Public Health, April 28,
1995.
14. X’armus H. Testimony before the Subcommittee on Human Resources.
Committee on Government Reform and Oversight, U.S. House of Reprcsentatives, May 8, 1997.
15. Draft talking points: responding to Public Citizen press conference.
Press release of the National Institutes of Health, April 22. 1997.
16. Questions and answers: CDC studies of AZT to prevent mother
,
to child HIV transmission in developing countries Press release of the
( enters t<>r Disease ( onirol and Prevention. Atlanta, (undated document.)
17. Questions and answers on the L'NAIDS sponsored trials for the pre
vention of mother to-child transmission: background brief to assist in re
sponding to issues raised by the public and the media. Press release of the
L'nitcd Nations AIDS Program, (undated document.)
18. Halsey NA. Mcincrt CL. Ruh Al. et al. Letter to Harold Varnuts, Di
rector of National Institutes of Health. Baltimore: Johns Hopkins Univer
sity. May 6. 1997.
19. Wiktor SZ, Ehounou E. A randomized placebo-controlled intersention study to evaluate the safety ami cflectivencss of oral zidovudine ad
ministered in late pregnancy to reduce the incidence of mothcr-lo child
transmission of HIV 1 in Abidjan, Cote D’Ivoire. Atlanta: Centers for Dis
case Control and Prevention, (undated document.)
20. Rouzioux C. Costagliola D, Burgard M, ct al. Timing of mother tochild HIV 1 transmission depends on maternal status. AIDS 1993;7:Suppl
2:S49 S52.
21. Ercedman B Equipoise ami the ethics of clinical research. N Engl J
Med 1987;317:141-5.
22. Heimlich HJ. Chen XP, Xiao BQ, et al. CD4 response in HIX’ positive
patients treated with malaria therapy. Presented at the 1 1th International
Conference on AIDS, Vancouver. B.C., July 7-12, 1996. abstract.
23. Bishop \VB, Laubscher 1, Labadarios D, Rehder P, Louw ME, Felling
ham SA. Eflect of vitamin enriched bread on the vitamin status of an iso
lated rural community — a controlled clinical trial. S Afr Med J 1996;86:
Suppl:458-62.
24. Lurie P, Bishaw M, Chesney MA, ct al. Ethical, behavioral, and social
aspects of' HIX’ vaccine trials in developing countries. JAMA 1994;271:
295-301.
25. Annas G. Grodin M. An apologv is not enough. Boston Globe. May
18, 1997:CLC2.
26. Freedman B, XX'cijer C, Glass K( . Placebo orthodoxy in clinical re
search. I. Empirical and methodological myths. J Law Med Ethics 1996;
24:243-51.
27. X’armus H. Comments at the meeting of the Advisorv Committee to
the Director of the National Institutes of Health, December 12, 1996.
28. Angell M. Ethical imperialism? Ethics in international collaborative
clinical research. N Engl J Med 1988;319:1081 3.
©1997, Massachusetts Medical Society.
RECEIVE THE JOURNAL'S TABLE OF CONTENTS EACH WEEK BY E-MAIL
To receive the table of contents of the Nfii’ Enjjlaud Journal of Medicine by e-mail
every Thursday morning, send an e-mail message to:
listscrv@massmed.org
Leave the subject line blank, and type the following as the body of your message:
subscribe TOC-L
You can also sign up through our website at: http://www.nejm.org
856
•
September IS, 1997
- Media
 RF-TB-1.9.pdf
RF-TB-1.9.pdf
Not viewed