COMMUNITY HEALTH FELLOWSHIP SCHEME - ANNUL COMMUNITY HEALTH FELLOWS WORKSHOP 2005. MARCH 6-8 AT NAVASPOORTJHI KENDRA, BANGALORE
Item
- Title
- COMMUNITY HEALTH FELLOWSHIP SCHEME - ANNUL COMMUNITY HEALTH FELLOWS WORKSHOP 2005. MARCH 6-8 AT NAVASPOORTJHI KENDRA, BANGALORE
- extracted text
-
RF_COM_H_90_SUDHA
c2o
v\—
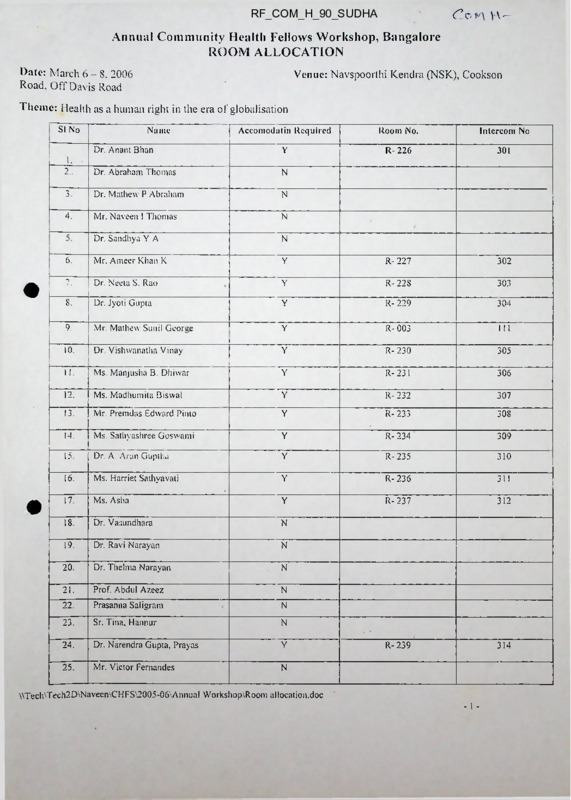
Annual Community Health Fellows Workshop, Bangalore
ROOM ALLOCATION
Venue: Navspoorthi Kendra (NSK), Cookson
Date: March 6 - 8. 2006
Road. Off Davis Road
Theme: Health as a human right in the era of globalisation
SI No
•
•
Name
Acconiodatin Required
Room No.
Intercom No
R- 226
301
Dr. Anant Bhan
Y
1.
2..
Dr. Abraham Thomas
N
3
Dr. Mathew P Abraham
N
4-
Mr. Naveen I Thomas
N
Dr. Sandhya Y A
N
6-
Mr. Ameer Khan K
Y
R- 227
302
7.
Dr. Neeta S. Rao
Y
R-228
303
8.
Dr. Jyoti Gupta
Y
R- 229
304
9.
Mr. Mathew Sunil Georoe
Y
R- 003
111
10.
Dr Vishwanatha Vinay
Y
R-230
305
11.
Ms. Manjusha B. Dhiwar
Y
R-231
306
12.
Ms. Madhumita Biswal
Y
R- 232
307
13.
Mr. Premdas Edward Pinto
Y
R-233
308
14.
Ms. Sathyashree Gcswami
Y
R- 234
309
15.
Dr. A. Arun Guptha
Y
R- 235
310
16.
Ms. Harriet Sathyavati
Y
R- 236
311
17.
Ms. Asha
Y
R-237
312
18.
Dr. Vasundhara
N
19.
Dr. Ravi Narayan
N
20.
Dr. Thelma Narayan
21.
Prof. Abdul Azeez
N
22.
Prasanna Saligram
N
23.
Sr. Tina, Hannur
N
24.
Dr. Narendra Gtipta, Prayas
Y
R- 239
314
25.
Mr. Victor Fernandes
N
.
N
\\Tech\Tech2D\Naveen\CHFS\2005-06\Annual Workshop\Room alloeation.doc
-1 -
COMMUNITY HEALT H CELL
Annual Community Health I'cllow Workshop, Bangalore
Date: 6lh to 8lh March - 2006
Venue: Nava Spoorthi Kendra, Bangalore
REQUISITION FORM FOR TRAVEL SUPPORT
NAME
ADDRESS
DETAILS OF TRAVEL EXPENSES
Mode
Date
Front
To
Amount
GRAND TOTAL (in Figures)
Rupees (in words):
Approved by:
Please attach supporting bills lor the claims mentioned above
Signature oC person
receiving the amount
C-O'M "Y 1 -
AGENDA ITEM NO. 5
Suggesting a global 'Right to Health campaign' by PHM
which could be launched at PHA-2
We thus find ourselves at a crossroads: health care can be considered a commodity to be sold,
or it can be considered a basic social right. It cannot comfortably be considered both of these
at the same time. This, I believe is the great drama of medicine at the start of this century.
And this is the choice before all people of faith and good will in these dangerous times.
- Paul Farmer
The context
The large scale weakening of public health systems, unchecked privatisation in various forms
and erosion of universal healthcare access systems are phenomena seen across the globe in
the current phase of liberalisation-hegemonic globalisation. The global health sector
discourse seems to be dominated by vertical, selective, urban and technocratic approaches, as
well as by 'public-private partnerships' of different kinds —at global, national and local
levels— as the preferred mode of implementation of services. Today there is an urgent need
for a process that will replace this dominant discourse by a 'Right to health and health care'
approach needed to achieve truly 'universal and comprehensive health care systems both in
developing and developed countries. To counter and reverse the current trend that
commoditizes health, there is thus a need to reach a strong global consensus on 'Health care
as a right', as well as a need to begin using the existing international and national provisions
that support this Right in an effective manner; we need to fight for strengthening public
health in an accountable manner. It is in this context that the possibility of launching a global
initiative to strengthen the 'Right to Health', with a focus on defending and operationalising
the 'Right to Health Care', is presented here below.
The justification
The majority of countries around the world (over 150) are party to the International Covenant
on Economic, Social and Cultural Rights. The General Comment 14 of CESCR, adopted in
the year 2000, elaborates on and goes into the details of the Right to Health and clearly
defines its broad characteristics, methods of operationalisation and current violations, and
suggests the means to monitor the implementation of this Right. We are nearing five years of
the launching of General Comment 14 —the most comprehensive internationally adopted
instrument that rules the understanding we ought to have of the Right to Health. However,
there is still a need to launch a global process that will raise the demands for the provisions of
GC 14 to be seriously implemented in all signatory countries. This stresses the paramount
importance of operationalising the 'Right to Health', and calls for reviewing, revisioning
and remissioning all global and national health sector initiatives in the light of the
overarching framework of health rights (such as, for example, MDGs).
A suggested content focus of the campaign
The 'Right to Health' framework provides us with an internationally agreed-upon consensus
structure based on which a strong argument should be constructed. However, within this
broad framework, we suggest that the campaign should, in its first phase, focus on the 'Right
to health care'. This is a burning issue in the context of current weak and weakening health
systems and it is amenable to actions from within the health sector. This, of course,
involves arriving at a broadened vision of health care, one that includes not only the entire
range of preventive, promotive and curative health services, but also services like nutritional
supplementation, ensuring drinking water quality, health related education and information —
all activities carried out with the primary and express purpose of improving health
comprehensively. It need not be emphasised that specific important aspects of this Right,
such as Women's right to health care, Children's health care rights, Mental health rights,
Health care rights of HIV-AIDS affected persons, Worker's health rights, The right to
essential drugs and other will be woven together, bringing diverse strands of the health
movement into a broad coalition that will work to strengthen public health systems and a
universal access to health care.
At the same time, some other key social determinants of health adversely affected by policy
changes that are having negative impacts on the health of the poor —and where PHM
members are in a position to document and push for policy changes-can and will be identified
at the country level and taken up as part of the campaign. This focus could be broadened in
the subsequent phase of the campaign.
Possible organisational collaboration (networking)
The United Nations Special Rapporteur on Right to Health is entrusted with the
responsibility of reviewing the status of implementation of this Right the world over. There
has been some communication with the present Rapporteur, Prof. Paul Hunt, who has shown
interest in the idea of such a global process. WHO has a division dealing with Ethics and
Human Rights, and there are persons in other divisions such as the Poverty and Health
Policies Division who also seem to be willing to lend support to such a process. Given our
aim to shift the focus of WHO towards a Rights-oriented approach, and given its global
potential to influence national health systems, we see WHO as an important collaborator in
such a process. Most countries have National human rights commissions or similar official
bodies, which we hope to involved to varying extents in monitoring the Right to Health.
Human rights groups have the potential to take interest in this issue, especially in issues like
access to care for HIV-AIDS affected persons. Of course, present strategic allies of PHM
will need to take a lead with us in the different countries helping us involve a broader range
of civil society organisations in this campaign (including women's organisations and
networks, coalitions of HIV-AIDS affected persons, trade unions of health sector personnel,
people's movements).
Suggested process to advance this discussion
To move towards a concrete campaign start-up process, we suggest a possible
sequence of activities as per below, which will be modified and refined based
on suggestions from the PHM global steering group and PHM activists across the
world.
a. During the upcoming PHM steering group meeting at Bangalore on 11-12 April,
a discussion is planned on the various aspects and feasibility of such a campaign. This will
provide the basis for concretising the next steps.
b. Sometime during the World Health Assembly in May, we plan a meeting co-organised by
the Poverty and Health Policies Division of WHO, PHM and other strategic allies, on 'Global
efforts for operationalising the Right to Health1. Paul Hunt will be invited to this meeting. In
this meeting, we will brainstorm on the possibilities of a Global Right to Health initiative,
and the possible roles of WHO, the Special Rapporteur on Health and of PHM and
other partners. At this point we foresee working out an outline of a larger event during PHA2 as suggested below. (Based on preliminary communications, it appears that both persons
from the Poverty and Health Policies Division of WHO and Paul Hunt are interested in such a
meeting).
Also during WHA, a PHM group will meet Dr. Lee and, while inviting him for PHA-2, we
will discuss this idea with him, since his endorsement is crucial for WHO co-sponsoring and
supportinng Regional consultations on 'Operationalising the Right to Health' in various WHO
regions and sponsoring the follow-up workshop on this during PHA-2 (as discussed below).
c. During PHA-2, we are thinking of having a well planned large workshop on 'Global action
for the Right to Health', involving WHO and PHM delegates from various regions and all
other partners who will have joined us by then.
Dr. Lee and Paul Hunt will be invited to co-chair this workshop, and there we will work out a
concrete outline of a 'Global Right to Health Campaign' focussing on ensuring widespread
social support, official recognition, delineation and operationalisation of the Right to Health
Care and Right to key health determinants. By then we will try to crystallise an agreement
among WHO, Paul Hunt and PHM to organise Regional events on the 'Right to Health' in
various regions of the world, which will be fed into by PHM country level reports or papers
and will be based on the stipulations in CESCR General Comment 14.
d. If such an agreement emerges, we plan to collaborate with WHO to organise a series of
Regional assemblies on 'Right to Health - Universal Access to Health Care', say from end
2005 to end 2006. Each regional assembly will be preceded by country level workshops,
wherever possible, involving national human rights bodies, to analyse the state of the 'Right
to health' in their country (based on GC 14 and national constitutional and legal obligations)
and to concretely delineate gaps in health rights, while raising the need for a mechanism to
address violations. The Regional assemblies will be attended by senior country health
officials, national human rights bodies and PHM delegations, and will discuss the
operationalisation of health rights and developing redressal and monitoring mechanisms in
each country.
e. This series of regional assemblies may culminate in some kind of resolution being adopted
al WHA-2007, calling for time-bound complete implementation of the Right to Health, and
putting in place mechanisms for monitoring and redressal of this right in all countries of the
world, while appealing for an end to all forms of violations of this Right based on a content
clearly defined by the CESCR general Comment 14. PHM partner organisations will use
this as a concrete opportunity to draw in many more organisations into their network, to
dialogue with their country governments, to engage with national human rights bodies and to
build a consensus on the need to end violations of health rights in various forms and to
reverse policies responsible for such violations.
The process will be used to try to shift the discourse from the preoccupation with globally
directed vertical programmes and privatisation-oriented measures, by talking about
widespread denial and violation of the Right to Health, by demanding a global consensus on
implementing this Right, and asking that all programmes and measures must now be critically
evaluated from a Health Rights perspective.
What can realistically be achieved in such a process?
There is no illusion that systematically raising the issue of'Right to Health' itself will lead to
actual complete implementation of this Right in countries across the globe. The universal
provision of even basic health services involves major budgetary, operational and systemic
changes; providing these in a definite Rights-based framework also involves major political
and legal reorientations; and such major changes cannot be expected in the near future, given
the political economy of health care in most countries of the world today.
However, we can expect and work for certain more achievable objectives, which will take us
towards the larger goal. Some such 'achievables' to be expected from a campaign may be explicit recognition of the Right to health care at country level; formation of health rights
monitoring bodies, with PHM and civil society participation in some countries; clearer
delineation of health rights at both global and country levels; shifting the focus of WHO
towards health rights / universal access systems and strengthening a group within WHO
to continue working for the same; bringing Right to health care into the global agenda and
making it a reference point in the global health discourse; and strengthening PHM networks
in various countries around a common, broad rallying point.
PHM organisation - PHM campaign; an iterative process of building both
An obvious and valid response to this suggestion may be that the development of PHM is
highly uneven in different countries, and that in many countries the PHM groups are not in a
position to take up such an activity. While accepting this situation, we also need to reckon
with the fact that PHM country circles, which were formed during or after PHA based on a
shared concern and broad understanding about health and the health sector, need to move
beyond communication and discussion to develop common advocacy activities, if they
are to develop further and to draw in more groups. Moving forward from the basis created by
the 'Million signature campaign' and the 'Health -Now! No to war, no to WTO' campaigns,
there is a need to develop shared effective advocacy initiatives at the country level. These
could directly engage with decision makers and could try to bring about certain changes in
the ground level situation based on people's awareness and initiative. A 'Right to Health'
campaign can be such a process, which can bring together existing and new PHM groups
towards defined country' level advocacy objectives, and hence can strengthen and expand the
PHM organisation while developing a common activity. Of course, assessing the overall
practicability, and ascertaining the existence of a minimum critical mass of PHM in a
substantial number of countries which is necessary to develop the campaign, is something
that would need to be done collectively by the People's Health Movement to concretely
evaluate the feasibility of this approach. Our appeal is that such a process of discussion
should be initiated, and that some first steps be planned to explore the potential of such a
campaign. If there is a basic consensus on taking this forward, then given the approaching
People's Health Assembly, we should make use of this major event to work out, crystallise
and plan the further process.
We are concretely asking Steering Group members to react to this so that the Secretariat can
give the green light to this exciting process. We ask you to respond before April 5th.
- Abhay Shukla and Claudio Schuftan
8
Viewpoint
Pushing the international health research agenda towards
equity and effectiveness
Lancet 2004; 3&4:1630-31
David McCoy, David Sanders, Fran Baum, Thelma Narayan, David Legge
Peoples Health Movement,
c/o Community Health Cell,
Bangalore, India (D McCoy,
D Sanders. F Baum, T Narayan.
D Legge)
Correspondence to:
Dr David McCoy
davidmccoy@xyx.demon.co.uk
1630
Despite substantial sums of money being devoted to
health research, most of it does not benefit the health of
poor people living in developing countries—a matter of
concern to civil society networks, such as the People’s
Health Movement.' Health research should play a more
influential part in improving the health of poor people,
not only through the distribution of knowledge, but also
by answering questions, such as why health and health
care inequities continue to grow despite greatly
increased global wealth, enhanced knowledge, and more
effective technologies.
Previous Editorials in this journal, and other reports,
have already highlighted three important issues.2-* First,
that the 10:90 gap—whereby only 10% of worldwide
health research funds are allocated to the problems
responsible for 90% of the world's burden of disease,
mainly in poor countries—needs to be reversed. Second,
that greater emphasis should be placed on research in
the social, economic, and political determinants of ill
health, relative to clinical and biological research. Third,
that the barriers to the transfer of knowledge from
research into policy and practice need to be overcome.
The 10.90 gap largely represents a funding gap shaped
by commercial interests, and inadequate funds being
provided through the public budgets of poor countries,
development assistance grants, charitable foundations,
and non-government organisations who have an interest
and a mandate to invest in public or noncommercial
research activities that are orientated towards addressing
the health needs of poor people.
Part of the solution to addressing this overall deficit in
funding includes continuing with current efforts to
increase development assistance, hasten the cancellation
of unfair debt and reform unjust trade structures. But
we also need creative thinking and bold action around
new proposals, such as raising funds through an
international authority that is able to effectively tax
global corporate profits/ or applying levies against global
financial transactions (eg, the Tobin tax).6-7
With respect to research on the social, political, and
economic determinants of health, we draw attention to
three points. The first is the need for more research into
the effects of globalisation on poor health and growing
health inequities, and on the development of proposals
to reform the current global, political, and economic
institutional order. In addition to research on more
effective mechanisms for global resource redistribution,
research should focus on how health equity can be
protected from the market failures of economic
globalisation and the operation of transnational
commercial interests. Second, we want more research
applied to the question of why the cancellation of the
odious debt of many poor countries has not been
forthcoming, why many rich countries' development
assistance still falls short of the UN’s 0-7% gross
domestic product target,’* and why bilateral and
multilateral trade agreements continue to be
unfavourable and even punitive towards the poorest and
sickest people. Third, more research is needed into the
design and financing of systems and basic services and
into how these factors determine access to good quality
care and other health inputs (eg, water and adequate
nutrition). As health systems become increasingly
inequitable and fragmented, research on the drivers and
effects of the liberalisation, segmentation, and
commercialisation of health-care systems is essential.
These three points complement the call for more
research on why available and affordable technology and
knowledge are not used, for example, to prevent millions
of children from dying of diarrhoeal disease and acute
respiratory infections. Appropriate research would
indicate how the mainly social and political barriers to
application of existing technologies might be overcome.
This achievement could be aided by country' case studies
that combine an analysis of the political economy of
poverty and ill health together with the health systems
factors that help or obstruct access to effective health
care. Such research would bring together political and
social scientists, health economists, public health
professionals, ethicists, and civil society organisations.
To promote the transfer of knowledge from research
into policy and practice, several issues should be
examined. Presently, there is a research culture and
incentive system that encourages researchers to be more
concerned with publishing their results in academic
journals than with ensuring that their research leads to
improved policy and practice. Furthermore, policy
makers and programme implementers in developing
countries are either sceptical about the value of research,
or do not have the skills to appraise and use new
information? The scarcity of capacity in the public sector
has been further aggravated by the steady brain drain of
capable health professionals to richer countries or from
the public sector to the domestic private or non
government sectors (including the health research
sector)."’
These difficulties could be overcome by changing the
incentive system and allocating a greater share of health
research funding to academic and non-government
research institutions in poor countries that work closely
with policy makers, health managers, service providers,
and communities. This allocation of funding needs to
www.thelancet.com Vol 364 October 30,2004
Viewpoint
be complemented with more investment in developing
research capacity within the health systems of poor
countries.
Research geared towards practical health systems
development is also often qualitatively different from
research that is geared towards the imperatives of
academia and the medical industry. For example,
research on the efficacy of interventions in a controlled
environment is different from that on the practicability
of applying effective interventions in the real world.
More action research that involves service providers can
help to bridge the gap between research and
implementation, and ensure that research is embedded
within the day-to-day realities and constraints of under Figure: People's Health Assembly rally, Dhaka, Bangladesh, 2000
resourced health-care systems. The use of participatory
research methods can also help poor communities will need to be exerted at all levels and by many different
shape health systems to meet their needs."1'
actors. The Peoples Health Movement is committed to
Research findings are also more successfully being increasingly influential.
implemented when researchers include mobilised Conflict of interest statement
citizen constituencies.1' Successful implementation is We declare dial we have no conflict of interest.
aided first by ensuring a vigorous community of civil Acknowledgments
society organisations with a mandate to keep a watch on D McCoy was funded by the Global Equity Gauge Alliance to attend a
health policy development and implementation; second, WHO consultation on health research that contributed to the final
production of this article.
by use of research funds to actively foster the capacity of
these organisations to change the commissioning and References
1
Peoples Health Movement, http://www.phmovemcnt.org (accessed
priority setting for research; and third, by including civil
Sept 21. 200-1).
society organisations in research production and 2 The Lancet. Kickstarting the revolution in health systems research.
Lancet 2004, 363: 1745.
’ encouraging partnerships that link them with academic
3
The Lancet. Mexico, 2004 research for global health and security
researchers.14
Lancet 2003; 362: 2033.
Finally, the imbalance in power between researchers 4 Global Forum for Heald) Research. 10/90 report on health research
2003-2004. Geneva. Switzerland: Global Forum for Health Research,
in rich and poor countries must be bridged. Many
2004. http://www.globalforumhealth.org/pagcs/index.asp (accessed
academic and non-government institutions in more
Sept 21, 2004).
developed countries benefit disproportionately from 5 Tax Justice Network. Declaration of the Tax Justice Network, 2003.
the meagre research funds that are focused on poor
http://www. taxjustice.net/e/e_declaration.pdf (accessed Sept 21.
2001).
health in developing countries. This imbalance is in a
6
Slecher H. Time for a Tobin Tax? Some practical and political
context where academic and research institutions in
arguments. Great Britain; Oxfam, May 1999. hltp://www.oxfam.
developing countries are struggling to gam their own
org.uk/what_we_do/issues/lTade/dowmloads/trade_tobintax.rlf
(accessed Sept 21, 2004).
funding and find it difficult to retain good staff.
7
Michalos AC. Good taxes: the case for taxing foreign currency
Practical ways of addressing the inequities within the
exchange and otiier financial transactions. New York: Duncan Press,
health research community might include mapping
1997.
out the distribution of research funds for health 8 Labonte R. Schrecker T. Sanders D. Mecus W, Fatal indifference- the
G8. Africa and global health Cape Town; University of Cape Town
problems between research institutions in rich and
Press, 2004.
poor countries, documenting the obstacles to the 9 Lomas, J. Using Linkage and exchange to move research into policy
at a Canadian Foundation. Health Affairs 2000; 19: 236-40.
development of research capacity in developing
countries and conducting in-depth case studies of the 10 Padaradi A. Chamberlain C, McCoy D, Ntuli A, Rowson M.
Loewenson R. Circulation or convection? Following die flow of
health-research funding policies and patterns of
health workers along the hierarchy of wealth. EQUINET- Network for
selected donor and international agencies.
Equity in Health in Southern Africa, 2003. http://www.gdnet.org/cf/
search/display.cfm?search-GDNDOCS&act-DOC&docnum-DOCl
Global conferences and summits on health research,
2980 (accessed Sept 22, 2004).
such as the two that are due in Mexico this November, by 11 Winter R, Munn-Giddings C. Action Research as an approach to
themselves are unlikely to substantially affect die
enquiry and development. In: A handbook for action research in
health and social care. London: Routiedge, 2001; 9-26.
challenges we present. The current pattern and use of
Martin K. de Koning K, eds. Participatory research in health- issues
health research shows the balance of prevailing global 12 and
experiences. Loudon: Zed Books, 1996; 1-18.
power, perspectives, and interests. Redressing 13 Minkler M, Wallerstein N, eds. Community-based participatoryresearch for health. San Francisco: Jossey-Bass, 2003.
the
imbalance
will
require
consciousnessraising, mobilisation, and pressure at many different 14 Sanders D. Labonte R. Baum F, Chopra M. Making research matter;
a civil society perspective on health research. WHO Bulletin
points in the global health research system and in
(in press).
health-care systems more broadly. Pressure for change
www.thelancet.com Vol 364 October 30, 2004
1631
low Y\ —
Peoples’ Forum against ADB
Call for Action!
ADB and World Bank, Quit Asia! Quit India!
Mobilise against the Asian Development Bank Annual Governors’ Meeting
3-6 May 2006 Hyderabad
The Asian Development Bank (ADB) is the third largest source of development finance in the AsiaPacific region, next to the World Bank Group and the Japanese Government. Every year, ADB moves huge
amounts of money across the Asia-Pacific region in a bid to foster rapid economic growth and market
capitalism. In 2004, the ADB’s total lending was US $ 5.3 billion which was used -to promote 64 projects
covering mostly road transport, communications, energy, law, economic management in the public policy
sectors Private sector assistance was to the tune of US S 807.2 million. The ADB’s largest borrowers in 2004
were China and India, each receiving USS 1.3 billion, about 24 per cent of the total lending. India is the fourth
largest shareholder in the ADB overall.
Despite its name, the management and operations of the ADB are greatly influenced by the USA and
the non-Asian capitalist powers. Although, Japan enjoys the most powerful status in the ADB, at par with the
USA, the non-Asians are powerful enough to manipulate the institution's directions to suit their own interests. In
promoting privatisation and private sector investments, the ADB routinely dole out lucrative contracts to favour
international firms and consultants.
Destructive and unaccountable
The ADB is an extremely secretive, non-transparent and unaccountable institution, despite its rhetoric
on good governance Its founding Charter of Principles provides the bank and its staff with immunity from local
and national laws. The ADB is thus not legally liable to communities, governments or individuals for any
wrongdoing, material harm or violation of rights.
Evaluation of ADB projects by independent researchers, citizen's groups, movements, NGOs and by its
own Operations Evaluation Department indicate that most ADB supported projects are poorly designed
implemented and managed. ADB does not facilitate public participation in development planning and access to
information while weakening local and national governance through undemocratic, non-transparent and nonconsultative methods of project implementation. ADB projects have continued to displace hundreds of
thousands of people across the region with little or no compensation, have resulted in negative environmental
and social impacts. The ADB, is therefore, charged with creating “development refugees" and “manufacturing
poverty" by the civil society organisations and movements.
The ADB, like the World Bank, has become the custodian of private investment and the promoter and
protector of corporate interests and profits. It follows the neo-liberal policy by imposing policy conditionalities the reform agenda and privatisation - on borrowing countries, and facilitates foreign companies to grab
contracts for research work, consultancy, project development, construction and management.
India Incorporated!
The ADB, in its Country Strategy and Programme (CSP) for India, 2003-2006, claims that the 10,h Plan
strategy is a sound one and is similar to its own poverty reduction strategy founded on pro-poor growth, social
development and good governance. India's strategy seems to fit well with the Banks! The CSP further says that
the most important role that India's development partners can play is in introducing international best practices
to strengthen fiscal and other structural reforms in the 10s' Plan' The Indian Government is playing second
fiddle by indicating that it looks to ADB, to play a leading catalytic role in supporting the next generation of
policy reforms. Since India can no longer access concessional loans from ADB, high risk loans at market rates
are taken for sectors focusing on high growth, reforms and private sector development.
During current CSP period, the ADB loans, starting from US $ 1.67 billion in 2003 is slated to increase
to US $ 2.05 billion in 2006, totaling US S 7.5 billion Projects financed by the ADB range from energy and
power sector reform and restructuring to road transport, water, irrigation, flood control, tourism, urban
development and administrative and fiscal reform. These projects are located across Jammu & Kashmir,
Uttaranchal, West Bengal and the North East, to Madhya Pradesh, Chhattisgarh, Gujarat, Rajasthan, Karnataka
and Kerala. The ADB’s array of policy conditions include, a) adopting legislations and regulations that favour
private sector involvement in key sectors, b) market-friendly restructuring, c) corporatisation and privatisation of
public enterprises and utilities, d) creating a flexible labour force, e) commercialization of agriculture and f) trade
and investment liberalization.
Mobilising against the Annual Governors’ Meeting
The ADB is holding its 39th Annual Governors' Meeting (AGM) from 3-6 May 2006 in Hyderabad.in the
State of Andhra Pradesh in southern India The Governors are the highest level of decision makers in the ADB.
Appointed by the ADB member countries, they are high-ranking national officials such as Finance Ministers or
Secretaries of National Treasuries. The current Chair of the AGM is Indian Finance Minister P Chidambaram.
Since 2000, peoples’ movements, communities affected by the ADB projects, progressive academics,
intellectuals, labour unions, activists and NGOs have used this opportunity to successfully mobilise themselves
at the AGM venues and protest against the institution and its development policies.
In 2000 and 2001, the ADB was shocked by the intensity of protests and strong messages sent to the
ADB by peoples' movements in Thailand and the US. The last AGM was in Turkey in 2005 where local
movements and organisations lent great support to the project affected and protest organisations that gathered
for the AGM.
In 2006, the eyes of the movements and struggles in Asia will be on Hyderabad and India. Peoples'
struggles against destructive development and oppressive economic and political structures are legendary in
India and particularly in Andhra Pradesh. Andhra Pradesh does not have any ADB supported projects, but it is
already a victim of the World Bank conditionalities - the power sector workers, the road transport workers, the
displaced tribals and the rural poor. In the recent past, the people of Hyderabad and Andhra Pradesh gave a
befitting reply to the Chandrababu Naidu Government that tried to foist a World Bank dictated reform agenda.
Thousands have marched in the streets of the city calling for a rejection of the World Bank's AP economic
restructuring loans. The Government that refused to listen to its people was comprehensively voted out of
power. The present Government, unfortunately, continues on the same path, eager to bring in foreign
investment at any cost.
The Hyderabad AGM offers us the opportunity to work with the groups in Andhra Pradesh; movements,
communities, organisations and activists in India and across Asia should come together and raise a collective
and unified voice against neo-liberalism. Whether through World Bank or ADB projects, the net impacts on
communities and societies are the same, especially on the poor, vulnerable and the marginalised, the workers,
dalits, tribals, women, peasants, the fishworkers or the urban poor, the hawkers and slum dwellers.
Come May 2006, let us give the ADB, the World Bank and all the other corporates who covet India's
resources and wealth, encroach upon the sovereignty of countries across the globe and in Asia, a unified
message:
Enough is Enough!
No to ADB, World Bank and the marauding corporates!
Governments listen to the voices of the peoples!
Peoples’ Forum against ADB comprises of the following groups from India and Asia:
•>
National Alliance of Peoples Movements, Narmada Bachao Andolan, Asia Pacific Movement on Debt and Development
(APMMD), Freedom from Debt Coalition, Philippines Rural Reconstruction Movement (PRRM), Karnataka Rajya Raitha
Sangha (KRRS), Equations. Nadi Ghati Morcha, River Basin Friends, Environment Support Group, ADB Quit Kerala
Campaign. INSAF. CORE. Urban Research Centre, Focus on the Global South. Citizens Concern for Dams & Development.
Delhi Forum, Samata, National Forum of Forest People & Forest Workers, mines minerals & People, Shaheen Centre,
Consumer Protection Forum, Water Initiatives, Consumer Protection Forum, Civil Society Initiative on IFIs (NE), Intercultural
Resources, NGO Task Force on ADB, Nagarika Hitharakshana Samithi, Balakedarara Hitharakshana Vedike, Anikethana
Trust, India Centre for Human Rights end Law (ICHRL), Palni Hills Conservation Council, National Fishworkers Forum,
Polavaram Project Andolana Samithi, Naga Peoples Movement for Human Rights, Movement Against Uranium Projects,
Centre for Environment Concerns, Aman Vedika, ITDS, Peoples Alliance Central East India, Japan Centre for a Sustainable
Environment and Society (JACSES), Center for Economic Justice, PAIRVI, Jharkhand Jangal Bachao Andolan, Bureau for
Human Rights. Adivasi Mukthi Sangathan. Peoples Movement in Subansiri Valley, Krishak Mukti Sangram Samithi.
Arunachal Citizens Rights. Indigenous/Tribal Peoples Development Center, Rural Volunteers Centre, Human Rights Tamil
Nadu Initiative.Parisava Badokidara Vedika, Human Rights Law Network, SAKSHI Human Rights Watch, Chatri, Jharkand
Labour Union. Dalit Women Forum. National Hawkers Federation, Net Work of Persons with Disabilities Organisation
(NPDO), Lok Raj Sangathan, Consumer Protection Council, Manthan Adhyayan Kendra, South Asia Network of Dams.
Rivers & People, Grassroot Options. FIMCOTN, Dwarf People’s Organisation. Chatn, New Trade Union Initiative. SEVA.
SABALA, National Campaign on Dalit Human Rights, Women's Collective, Bangla Praxis, Nagarik Udyog, Corporate
Accountability Desk of The Other Media, Chasma Lok Sath, National Centre for Advocacy Studies, Open Space. Peoples
Voice. Gangpur Adivasi Forum, Dalit Mukti Morcha, Plachimada Solidarity Committee, Pani Committee, Keselu Palu Group
(PNG). Uttaran, AOSED, Save Chara River Campaign, Gono Udyog Forum. Green Movement of Sri Lanka
Secretariat: 8-2-590/B, Road No. 1, Banjara Hills, Hyderabad, Andhra Pradesh, INDIA,
Tel No. 91 40 55637974, Email: forumce: rdina'.iontaqmail.com
People’s Health Movement [ \ y
Coi^a \a-
CtUMEE
0» Hiv Aira Ai-ds
FREAKS5'
'•’
Ith
joc’ai.et y ?mi and political issue and, above all, a fundamental human
: .
■
ill
. ,!k:c are at the root of
\ ests working against
on I las to be opposed
•’.nd
priorities have
i • J w.x '.july cr-anged.
' political action. It is
ilso .
intervention
that requires ps pi. oriented health and medical
•• .
. ,
people inter-sectoral policies,
good governanc-?. people’s participation t,nd effective communication.They should
be rooted in internationally accepted human rights and humanitarian norms.
The special needs of women and children as infected persons, their dependents
and caregivers should be addressed.
In the current context, People's Charter on HIV and AIDS recognises the devastating
impact of war and conflict on health systems and how it amplifies the vulnerabilities
of people to HIV and AIDS.
People's Charter on HIV and AIDS draws upon perspectives of communities affected
and infected with HIV and AIDS and those vulnerable to the infection. It encourages
people to develop their own solutions and hold accountable local authorities, national
governments, international organisations and corporations to their promises and
responsibilities.
VISION
As stated in the People's Charter for Health: 'Equity, ecologically sustainable
development, social justice and peace are at the heart of our vision of a better
world - a world in which a healthy life for all is a reality; a world that respects,
appreciates and celebrates all life and diversity; a world that enables the flowering
of people's talents and abilities to enrich one another; a world in which people’s
voices guide the decisions that shape our lives'.
PERSPECTIVES
The AIDS pandemic is one of the greatest humanitarian crises of all times. I t has caused
death and misery, destroyed families and communities, derailed development and reversed
health gains achieved over decades in one stroke. HIV and AIDS is already wiping out
a generation in Africa.Two decades after it began its onslaught, the disease is still spreading
fast, gaining a firm foothold in all parts of the world.
HIV and AIDS spreads along migration routes charted out by globalised trade. Social
and economic distress due to conflict, war; disasters, skewed international trade and unjust
economic policies make more and more people vulnerable to the infection.
The landmark Alma Ata Declaration of 1978 promised Health for All by 2000 through
primary health care. Verticalisation, changing economic priorities, invasion of pri^^
interests into political decision-making and a lack of political will led to a total breakdown
of the public health and primary health care systems during the 1980s and 1990s.The
spread of HIV and AIDS also contributed to the non-achievement of these goals.
Poverty, hunger and ill health are increasing because of neo-liberal economic policies.
In this context, integrated, adequately-resourced health systems based on primary health
care and public health are urgently required.
Lack of sensitisation and training of health personnel have created negative attitudes
towards persons living with HIV and AIDS. Such attitudes and practices lead to stigma
and discrimination that impede interventions.
It is essential to ensure that health care is safe and that people undergoing treatment
at health care facilities are not exposed to HIV or other infections.
A CALL FOR ACTION
People and Social Movements
People’s Charter on HIV and AIDS
Mobilise and strengthen capacities of communities in health promotion,
prevention and care.
*
W
Empower women and youth as key players in HIV interventions.
Build alliances among positive peoples networks, women's movements, health and
social activists, trade unions, student groups, academics and other progressive
constituencies.
Intensify the campaign for equitable and universal access to anti-retroviral (ABV)
treatment through comprehensive primary health care.
Facilitate legal measures and mass campaigns to change intellectual property rights
regimes that escalate drug prices.
Oppose policies dictated by multilateral financial and trade institutions that disregard
people's right to health and health care.
Expose links between the spread of HIV and AIDS and the underlying societal
determinants such as poverty, war and displacement, and participate in efforts to
redress these injustices.
09 Health Professionals and Health Workers
Provide responsible care and quality treatment to persons living with HIV and AIDS.
Stop stigma and discrimination in institutions of care and treatment.
Respect patients' right to dignity and privacy.
Follow ethical and regulatory principles in drug trials.
^kProvide adequate preventive measures to avoid transmission of infection in health
care institutions.
Support People's Health Movement initiatives that address the larger social, political
and economic issues.
JJ| Governments
Develop and strengthen comprehensive approaches based on primary health care
to include HIV and AIDS interventions.
Enhance involvement of people and civil society in planning and implementation.
Ensure greater involvement of persons living with HIV and AIDS at all levels.
Ensure occupational safety of health workers.
Increase access to basic services to people living with HIV and AIDS
Ensure easy, affordable and sustained availability of quality generic ARV and other
essential drugs.
Implement guidelines for transparent, scientific and ethical clinical trials.
Make nutritional inputs and psycho-social support part of HIV and AIDS care
Develop programmes for life skill education and women’s health empowerment
Promote traditional systems of medicine with enough resources.
Promote harm reduction policies and programmes for all vulnerable sections, including
sex workers, drug users, sexual minorities and street children.
[Tfl Corporates
Place people above profits.
Make available diagnostic and prognostic tests that are affordable.
Ensure the availability of ARV and essential medicines at affordable rates.
People’s Charter on HIV and AIDS '
Allocate adequate resources for public health.
^WHO and UNAIDS
Evolve a comprehensive approach that strengthens primary health care-and health
systems, with built-in indicators of progress.
Stop narrowly-focused vertical programmes.
Urge all governments to follow the UN's International Guidelines on HIV infection
and AIDS and Human Rights.
Include non-pnority countries in the 3x5 initiative.
Take appropriate action in ‘low prevalence countries'.
Start immediate action for sub-Saharan African countries.
Monitor the impact of trade agreements on health.
World Bank, International Monetary Fund and
World Trade Organization
Be accountable for social disasters caused by anti-poor macroeconomic policies.
Cancel debts of all poor countries, especially those identified as vulnerable to HIV
and AIDS.
Stop free trade agreements, privatisation of essential services, and the
commercialisation of health care.
Finance HIV and AIDS interventions with grants instead of loans.
Remove pharmaceutical patents that adversely affect availability of generic drugs.
Q.
a.
o
<u
Largely based on the People’s Charter for Health of the
People’s Health Movement.
1
Developed through an active participatory process involving
people from various walks of life, including persons living with
HIV and AIDS.
For more information contact:
People's Health Movement Secretariat:
CHC, 367, Jakkasandra 1st Main, 1st Block,
Koramangala, Bangalore - S60 034, India
Tel: +91 80 5128 0009; Fax: +91 80 25525372
Email: secretariat@phmovment.org
www.phmovement.org
Deigned by Books for Change. Bangaioto, India
lie’s Charter on HIV and AIDS
We call upon all individuals and organisations to endorse
and implement the People’s Charter on HIV and AIDS and
join the People’s Health Movement (PHM).
PHM has an active presence in about 100 countries.
The Rights Based Framework - Which Way To Go?
Anant Phadke
As a preparation for the discussion on 'right to health care’ in the forthcoming MFC meet,
in this note I would attempt three thingsI. To put the rights based framework in a larger, historical context so that there is more clarity
on the meaning of the issue of rights and human rights
II.
To argue that limiting ourselves purely in the rights based framework, without analysing the
political economy of health and health-care would not take us forward.
111. To locate the need and importance of a detailed discussion on right to health care in the
health-care movement in India.
I
Needs and rights
Let us begin with a simple, elementary question: why do we talk in terms of rights and not
in terms of needs? Food, water, health-care, education etc. are human needs in the modern world.
There are enough resources in the world to meet these basic needs of everyone. But this does not
happen because there are ■ huge wastages on preparations for wars, nuclear or otherwise;
• massive inefficiency in use of resources (for example use of individualised transport instead
of mass transport);
• mind-boggling creation of false needs like unnecessary medical interventions;
All this is basically a product of profit mongering and power mongering capitalist system. Add
to this, the greatest ever inequality in human history fuelled by the shameless greed of a few in the
new phase of globalization and complete sway of speculative finance capital. All this together
makes it impossible to fulfill even the basic needs of the vast-majority of the people inhabiting this
unique globe. Therefore, unless human needs are couched in the form of rights, these cannot be fulfilled
in our today’s society and there is a necessity to talk in terms of basic human rights, the fulfillment of
which has to be ensured by the state. This conversion of basic human needs into rights is not exactly a
very desirable thing. Our ultimate goal should be to build a society wherein basic human needs are
fulfilled without involving the language of rights.
Unlike animals, human needs change and expand. There is nothing like human rights, which
are valid for all times. The content of human needs and of human rights would develop as society
develops. For example, the content of‘Right to education’ would change as society develops.
Professional Rights and Human Rights
Today’s society is divided into various social groups whose interests are opposed to each
other- employers versus employees; landlords’ versus servants; people being benefited by
developmental project versus those displaced by it or suffering from it; men versus women, one
caste - group versus other etc. etc. Each of these social groups is competing with the other to gain
more wealth and prestige. Since resources are limited and especially in view of huge wastages,
inefficiencies, false needs mentioned above, they cannot suffice to meet all these competing needs,
the specific interests and needs of each of these groups have to be protected from others by
converting these needs into rights. In situations where interests of different groups are not opposed
to each other, there is no need to involve the discourse on rights. Thus generally we do not talk
about rights of mothers versus those of their infants. While rights of members of one foot ball
teams are guarded against those of the rival team members by the match referee, there is no
question of any rights of any team member within the team being pitted against those of others. The
point being made here is that the discourse of rights in today’s society is premised on opposed social
groups and their interests.
Human rights belong to a different category of rights. Out interest, needs as human beings, and
not as members of a particular class with particular interests also need to be protected from
violalions from the society in general. If I am old man, my interests, needs arise not out of
belonging to any professional group but arise out of my being an old person. Similar is the case of
not only groups like infants, pregnant mothers who have special needs but is also of many of our
needs as human beings and not as^part of a professional class. However, in today’s society human
interests take the form of interests of a professional class or are intrinsically bound by it. For example,
my interest as tenant-farmer lies in reducing the rent. 1 have to pay my landlord and the fulfillment
of my human interests as an old man partly depends on the protection of my interests as tenant
farmer. If the latter are violated, the former gets threatened. But nevertheless theses two have
different trajectories of development. My interests as tenant farmer are bound up with the existence
of tenant-land lord relationship. With the dissolution of this relationship my interests as tenant farmer will also disappear whereas, my human interests as an old man would continue in any
society.
Our long-term aim should be to build a society not based on antagonistic or opposed
professional interests but based on harmonious co-operative interests. In such a society, particular
class interests and rights will gradually wither away. There will not be a need for a powerful class
state to ensure that the rules of competition between opposed professional classes are observed.
However, there will be some contradiction between human interests of individuals and those of the
society as a whole. This is because the earlier Marxian vision of withering away of scarcity with the
unfettered development of productive forces no more seems to be realistic; energy and other natural
resources no longer seem to be limitless. Hence some amount of limited scarcity would continue, so
also the need to ration resources.' Even though complete plenty and hence a good bye to the
rationing of resources will never be achieved, if exploitation, inequality, ecological-sociaily
destructive use of resources is overcome, modern productive powers can reach a stagq when there
is less and less need to encroach on somebody else's needs in order to fulfill my needs.
To decide how much resources individuals would be entitled to from the common societal
pool would require the presence of a state power to ration the resources. The rights framework and
the state will be required to ensure the fulfillment of human needs of all. This state would not guard the
interests of any particular class or social layer. It would not be a state in the classical sense of the
word but will balance the human rights of individuals with those of the society as a whole. The
point is - the rights framework would be needed even after the withering away of class interests.
II
Political economy and human rights
Protection of civil and political rights is in a sense one of the fundamental principles of the
capitalist society. If the market is to function properly, each buyer or seller in the market has to be
political independent and free. This political equality is no obstacle to the inequality generated by
the logic of the market i.e. the logic of the purchase and sale of different commodities, including
the sale of human labor power. Hence political equality has been guaranteed by constitution in all
capitalist countries. A fair degree of observance of civil and political rights in advance countries
has been quite compatible with great socio-economic inequalities in these countries. However,
people’s organizations/human rights organizations have to be vigilant and fight for consistent
observance of civil and political equality. This is because, though the rulers as a whole have agreed
to recognize political rights, some times individual money bags, blinded by short-term interests and
profits, tend to violate these rights. The altitude of the rulers towards political rights is thus
inconsistent, whereas that of the people’s organizations, civil rights groups is of consistently
upholding of these rights. The US government raises the issue of violation of political rights when
it suits its interests, whereas for us, its a matter of basic principle.
As regards the socio-economic rights, the position of the rulers is much more inconsistent.
Here, it is more of paying lip service to these rights. The rulers are wedded to the interests of
propertied people and not to the interests of the vast majority of the laboring population. Hence
they cannot afford to guarantee the socio-economic rights of the people - right to livelihood, water,
health-care, etc. But there are different sections within the rulers. If health-care becomes very
costly and thereby leads to the demand for higher wages, many employers would like health-care to
become a right to be fulfilled through public funds so that the their wage-bill would not rise an
account of spiraling health care costs. They may thus support the demand for health-care as a right.
But overall, taken together, the rulers are not in favor of granting socio-economic rights, whatever
may be the international declarations. Unlike the civil-political rights, granting the socio-economic
rights is not compatible with the existing social order, at least in the developing countries. When we talk
of fulfillment of socio-economic rights, we have to keep this is mind.
Since some leading United Nation’s organizations talk about economic, social rights also,
we can use these declarations to put pressure on our governments, and we can make some progress
in harnessing some of these rights. But we have to be clear that demand for complete fulfillment of
all the socio-economic rights is actually a revolutionary demand. Just appealing the rulers or
merely demanding from them the socio-economic rights is not going to make any substantial
progress in achieving these rights. Neither is it adequate to keep merely monitoring the violations
of these rights. We have to find out concretely, who would be opposed to our concrete demands
like right to food, right to essential drugs and to health-care, etc. We will have to strategise how to
overcome this opposition; to what extent the existing state can ensure fulfillment of which demand
and why. If we keep away from the political economy of socio-economic rights, we would be merely
indulging into a sterile repetition of nicely worded international declarations or making a list of various
rights or would be kept busy with mere monitoring of their violations. We also need to go into the
political economy of the concerned issue and reveal the forces, which would be in favor of or would
be opposed to this demand, put forward an alternative policy of how things can be done differently if
balance of power is changed. For example, in health care, we have to point out what are the siciopolitical obstacles in achieving the right to health care and how to struggle against these forces.
This point brings us to the third, last issue of my note- the need and importance of a detailed
discussion on the right to health care in the ongoing health movement in India.
Ill
What is our alternative?
The new challenging situation
I would argue that today we are in a challenging, somewhat fluid socio-political situation
and we have to make efforts to shape the changes in health-care policies. The rulers are
restructuring the world. The post-war strategy of state capitalism or welfarism in which the state
played a leading role in the economy, in which the provision of basic social services was
considered the responsibility of the state, is now being abandoned. In India, the Nehruvian path of
development is being left behind. Thanks to the Nehruvian model of state capitalism in India, there
was a relatively very rapid development after independence. But this development has unleashed
new problems, which cannot be solved by merely continuing the Nehruvian policies. The economy
needs restructuring.
The rulers are trying to restructure the economy with their trinity formula of Globalisation,
Liberalisation, Privatisation (GLP), which suits the rulers but spells disaster for the ordinary people.
We need to formulate and press for an alternative strategy of restructuring in opposition to the GLP
strategy. In the field of health-care it is not adequate to oppose the various elements of ‘GLP in
health care’ in a piecemeal manner. Nor can we demand going back to the Nehruvian era. Our
opposition should be based on an alternative plan for restructuring of the health care system in India.
‘Right to health care’ can be the rallying slogan, theme of this alternative framework. Thus the
direct, indirect privatisation of public health services should be opposed on the basis of an
alternative framework of Universal Health Insurance of which a very much reformed, efficient,
accountable, expanded public health services would be a part. Our alternative policy could be
‘reform the public sector and regulate the private sector.’ (Instead of giving a call of ‘Save the
Public sector’ it will be more appropriate to give a call - “reform and expand the public sector;
regulate the private sector'.) In our plan for reforming the public health services, by way of
example, on the issue of accessibility of Primary Health Care we can argue for * a much more important role for Community Health Workers and their much better
integration into the public health services;
• much more accountability of the health services to the community and to the patients;
• a more rational use of the PHC staff by introducing multi-tasking wherever possible.
The point is. the current system is obsolete, the rulers are restructuring it with their GLP
strategy and our opposition to it has to be based on an alternative policy, which goes beyond the
Nehruvian model of development. Whether one is part of the system or want to reform it or
revolutionise it. today, one needs to go into the debates about strategic, policy issues. MFC offers a
broad platform for such debates.
The MFC debates
In the earlier MFC - annual meets, we have discussed in some detail various policy-issues
ranging from medical education to drug policy to women’s health. The People’s Health Charter of
the Jan Swasthya Abhiyan, of which MFC is a part, summarises our alternative on 20 crucial
aspects of a comprehensive alternative policy. Amongst us there can be differences of opinion
about some of these measures in this ‘twenty point programme’. But this Charter is an indication
that the Right to Health Care movement in India has not confined to a conventional ‘rights based
approach’ but has also involved itself in formulating alternative policies and'has time and again
pointed out specific changes in the current policies. We have thus not confined ourselves to merely
making a list of various health-rights of the people, but have argued for concrete policy-measures
needed to make health-care accessible to all. Now what needs to be done is to show concretely that
India has the resources to implement the various policy measures we have been arguing for. This is
necessary because officials, politicians say that they agree with the measures we have been
suggesting but say that “However, the state does not have the resources.” We need to work out at
least to a certain extant, how much funds would be required to institute the measures we are
suggesting and how the state can raise the resources to meet these funding requirements. This is
necessary to delegitimise the existing system and to move from a purely oppositional to a hegemonistic
politics. People will come forward to fight for these rights and there will be broader support to such
struggles if we are able to show that Indian economy has the resources, but the existing rulers are
not ready to harness these resources as this would involve harming the interests of those sections to
which they are wedded.
1 hope that the MFC meet would recognize the need to overcome the “there is no
alternative” (TINA) syndrome. Let us realise that policy-measures that we discussed in earlier
meets have acquired new significance as we have entered the era of restructuring of the economy
and society. In this new context let us revisit various policy measures we had debated. Let us
decide, how as part of the JSA, in this new situation we can contribute to pushing forward measures
which we had formulated earlier. MFC provides an open space for detailed discussions on the
content of various policy measures. Let us use this space more productively in the new situation.
The election results during the last few months have shown that people are expecting an
improvement in their daily lines. Emotional issues have been pushed back. The rulers are under
pressure to show results. In this fluid situation, policy - level interventions are likely to be much
more productive than hitherto. Now is the more opportune time to put pressure on the system, to
expose it. But we need to raise the quality and quantity of our efforts in this direction. Can MFC do
this?
2814 words
A statement from the People’s Health Movement prepared for presentation at
Making Partnerships Work for Health, a workshop at the
World Health Organization, Geneva, 26-28 October, 2005.
*
PHM identifies exploitation and marginalization of the poor as root causes of preventable
disease, malnutrition and death and in this and many other respects, women and children
are particularly vulnerable. This awareness guides all of our work including our position
on partnerships for health.
We start with a simple observation. Partners in any endeavour must genuinely share
a common goal. If they do not. the interaction is not a partnership and its precise nature
must be made clear for its real value and the real risks it may pose to public health, to be
properly evaluated.
With that in mind, we look first at interactions that are called ‘public private
partnerships’, because they are increasingly portrayed not just as a possible
arrangement - but as an innovative and unavoidable policy paradigm - to address
global health problems.
The Cuenca Declaration, issued at the Second People’s Health Assembly in July 2005 in
Ecuador, states: “We oppose public-private partnerships because the private sector has
no place in public health policy making”. We will elaborate on this here.
The extraordinary power of the private sector, and in particular of transnational
corporations (TNCs) and pharmaceutical houses under the neoliberal, corporate-led
globalization process, has been identified as the major obstacle to achieving social and
economic justice and therefore, also, Health for All.
TNCs already exert enormous power over governments and International Financial
Institutions (IFIs). Through PPPs, they are becoming major players in many areas of
public policy making, including health.
Let us clarify some fundamental democratic principles. All citizens are involved and
concerned in health matters as individuals (including employees and Chief Executive
Officers of TNCs). However, until recently it has been considered an unacceptable
conflict of interest to include TNCs as decision makers in public policy.
WHO has always interacted - and often collaborated - with private sector and other non
state actors. What is currently subsumed under the term partnerships with the private
sector includes such diverse activities as corporate donation, sponsorship, research
collaboration, negotiation or public tenders, and contracting out of selected health
services. It also includes global health alliances, such as GAVI, GAIN and the Global
Fund for AIDS, TB and Malaria which involve high level policy interactions between
UN agencies, corporations, and private foundations which propagate a business
philosophy.
Many of these interactions are not fundamentally new; others are social experiments.
Some, such as the outsourcing of public health services, the funding of international
public health and UN agencies through corporate charity and the GAVI style health
alliances are highly problematic.
What is new - and of serious concern in most current PPPs - is that industry is
invited as a ‘full partner’ in decision making processes on public issues.
Today, the UN Secretary-General’s Report on Enhanced cooperation between the United
Nations and all relevant partners, in particular the private sector, states that it offers to the
private sector through engagement in governmental processes “opportunities to have its
voice heard.”1'11
PHM argues that, in terms of both process and outcome, these developments are
incompatible with democratic decision making, economic justice, emancipatory
development, human rights including the right to health - and therefore the
achievement of Health for All.
A second simple observation is that TNCs have a legal obligation to make a profit for
shareholders. The raison d'etre of private companies is completely different from
that of organizations and groups working for Health for All and the meeting of
people's basic needs for health as a human right.
We have only time to present tlie briefest summary of some of the risks to public health
that this difference implies.
Public private partnerships:
•
•
•
•
•
•
Allow private interests to set/influence the public health agenda.
Sacrifice broad public health goals of prevention of disease, protection and
promotion of health, and tackling of the underlying social and economic
determinants of avoidable disease and death.
Prioritize technological interventions, cosmetic and unsustainable, which generate
profit for a minority.
Favour short term, vertical approaches and privatization of essential public
services rather than horizontal, comprehensive and sustainable public services.
Provide legitimacy to corporations' activities through association with UN
agencies (blue-washing); blur roles and real interests.
Compromise public agencies, including UN agencies, and make them ‘call the
tune’ for private interests of a tiny privileged minority rather than for 6 billion
people.
1111 UN (2005). Enhanced cooperation between the United Nations and all relevant partners, in
particular the private sector. Report of the Secretary-General, A/60/150,10 August, para 20
As a policy paradigm, then, the PHM regards PPPs as fundamentally flawed. It thus
follows that the actual evaluatiqn of the effectiveness of particular PPPs in practice is of
limited interest. PHM cautions that almost any project can demonstrate "effectiveness"
within a narrow context using a specific set of indicators - if enough money is thrown at
it by powerful actors, over a short space of time.
Evaluations of selected PPPs have been undertaken - though few of these have
considered risks and harm in the widest sense - and the results have been variable. PHM’s
conclusion is that PPPs arc ideology-driven rather than evidence-based. If one takes
privatization of health services as an example (as this is prominently promoted through
PPPs), no serious studies have yet shown that privatization of health services is either
efficient or effective. A wealth of evidence exists, however, to show that national,
universal, publicly run and funded health services are significantly cheaper and produce
far better health outcomes.
So what kind of partnerships does PHM recommend? PEIM promotes a broad based
holistic approach to health which involves common struggles in a spirit of solidarity.
Individuals and groups with whom WHO could work as partners need to share
goals and represent people's interests in terms of their right to health.
This would include health workers, public service workers, trade unions, teachers,
community workers, indigenous people's movements, landless peasants' movements,
community groups, solidarity movements, public interest NGOs, civil society
organizations, social justice political parties, professional associations and many more.
We support solidarity between groups and organizations serving the public interest
within, across and beyond the health sector in order to address the major determinants of
preventable disease, malnutrition and death because it is through such arrangements
that human rights and the right to health, which only some of us enjoy, have been
won.
We must never forget that these rights have been won painfully and slowly, with much
suffering and loss of life for the poor - and against formidable obstacles in the form of
powerful, private interests.
We cite as examples the efforts undertaken by various groups working in solidarity
towards Health for All to address the lack of food and water, bearing in mind that:
a) these two factors together account for well over 60% of preventable disease and death,
b) mothers and children are always the primary victims in times of shortage, and
c) that women are largely responsible for the provision of these daily essentials.
• Access to water and to essential services has been won through partnerships
between public sector workers, their unions, local community groups and health
workers in countless places the world over, most notably in Cochabamba, Bolivia.
• The struggle for food sovereignty, critical to adequate consumption of high
quality food, is the joint struggle of landless peasants' movements’, opponents of
liberalization of the agricultural sector, and the tremendous worldwide movement
for social and economic justice that has been meeting at the World Social Fora.
Such solidarity struggles involving collaboration between public interest groups confront
the formidable and overwhelming power of TNCs that are behind the neoliberal
restructuring of our world and increasing poverty and inequality - the first causes of poor
health.
Referring now to this meeting at the World Health Organization:
Why are agencies and organizations with public responsibilities adopting these
arrangements? For the simple reason that, today, the private sector is considered the
only untapped source of funds. The term PPP encompasses essentially the hope to
access funds of corporations and some hyper-rich. Under neoliberal economic regimes,
public sector budgets have been slashed and tax bases destroyed. These developments are
themselves the result of the influence of TNCs on governments and the international
financial institutions.
The solution to this problem is not for public bodies to go knocking at the doors of
the private sector, nor of the foundations of celebrity philanthropists from industry. The
solution is economic justice, including an adequate tax base, both nationally and
internationally, to cover all public services, as well as proper funding of public
institutions such as WHO through regular budgets so that it may fulfill its international
responsibilities unimpeded by corporate interests.
In relation to ‘Making Partnerships Work for Health’, we urge the World Health
Organization to keep to the founding principles set out in its Constitution. In particular
the following parts of the preamble:
"Informed opinion and active cooperation on the part of the public are of the utmost
importance in the improvement of the health of the people."
"Governments have a responsibility for the health of their peoples which can be fulfilled
only by the provision of adequate health and social measures."
The PHM urges WHO to claim its rightful place as the international health
authority and to ensure, with governments, accountability to the people, not to private
interests - in all matters of health. Our message is simple: Work with the people, for the
people!
Together, we can achieve Health for All.
*: For reasons beyond PHM control, the statement was not read at this workshop.
Policy lessons from comparing mortality from two global
forces: international terrorism and tobacco
George Thomson Sand Nick Wilson '33
Department of Public Health, Wellington School of Medicine and Health Sciences, University of
Otago, PO Box 7343, Wellington South, New Zealand
Globalization and Health 2005, 1:18
doi:10.1186/1744-8603-1-18
The electronic version of this article is the complete one and can be found online at:
http://www.qlobali2atonandhealth.com/conten t/1/1/18
Received
Accepted
Published
23 August 2005
15 December 2005
15 December 2005
© 2005 Thomson and Wilson; licensee BioMed Central Ltd.
This is an Open Access article distributed under the terms of the Creative Commons Attribution
License (htto-.//creativecommons.orq/licenses/bv/2.0'). which permits unrestricted use, distribution,
and reproduction in any medium, provided the original work is properly cited.
Abstract
Background
The aim of this study was to compare the mortality burdens from two global impacts
on mortality: international terrorism and the major cause of preventable death in
developed countries - tobacco use. We also sought to examine the similarities and
differences between these two causes of mortality so as to better inform the policy
responses directed at prevention.
Methods
Data on deaths from international terrorism were obtained from a US State
Department database for 1994-2003. Estimates for tobacco-attributable deaths were
based on Peto et al 2003. The countries were 37 developed and East European
countries.
Results and discussion
The collective annualized mortality burden from tobacco was approximately 5700
times that of international terrorism. The ratio of annual tobacco to international
terrorism deaths was lowest for the United States at 1700 times, followed by Russia
at 12,900 times. The tobacco death burden in all these countries was equivalent to
the impact of an 11 September type terrorist attack every 14 hours.
Different perceptions of risk may contribute to the relative lack of a policy response
to tobacco mortality, despite its relatively greater scale. The lack is also despite
tobacco control having a stronger evidence base for the prevention measures used.
Conclusion
This comparison highlights the way risk perception may determine different policy
responses to global forces causing mortality. Nevertheless, the large mortality
differential between international terrorism and tobacco use has policy implications
for informing the rational use of resources to prevent premature death.
Background
International terrorism, or aspects of it, have been argued to be a reaction to
globalization and/or to be aided by many of its features [1,2]. In the last twenty or
more years, there has been a substantial focus on terrorism-related policies in many
jurisdictions, particularly since the attacks of 11 September 2001 in the United
States. This focus has included spending and legislation, and has included public
health measures relating to bioterrorism protection [3,4]. The focus is
understandable, considering the political significance of attacks by non-state
organisations, and the economic and psychological effects on the societies which may
consider themselves attacked [5-71. However, it is important for policy makers to
know of the opportunity costs of the response to international terrorism, relative to
addressing other causes of premature death, and to better understand how
differences in risk perception influence policy making. Therefore, we contrasted the
mortality impacts of international terrorism with another major cause of preventable
death - tobacco use [8] (which is also exacerbated by globalization [9,10]). This
work is part of a wider attempt to put international terrorism into a public health
context [11,121.
Methods
As part of a study to describe the epidemiology of international terrorism [111 we
extracted data for 1994-2003 on international terrorist attacks involving any deaths
among non-perpetrators from United States (US) Department of State reports. The
definition of terrorism used by the Department is: 'Premeditated, politically motivated
violence perpetrated against noncombatant targets by subnational groups or
clandestine agents', with international terrorism meant as 'terrorism involving citizens
or the territory of more than one country'. These data were supplemented with
findings from more detailed published studies (see: [11]). Countries included were 21
'established market economy' countries and 16 'former socialist economies of Europe'
(as per the classification in an international mortality study) [13]. These two groups
of countries were selected because there was better quality data available for both
terrorism and tobacco. From these data, an average annual mortality burden was
calculated for each country.
Data on tobacco mortality was based on the updated estimates for the year 2000 by
Peto et al [ 141. This method involves country-specific rates of lung cancer mortality
together with corresponding rates from the American Cancer Society's Cancer
Prevention Study II to derive 'smoking impact ratios' by age and sex. The burden
includes tobacco-related: respiratory diseases, vascular diseases and other tobaccorelated cancers. This methodology has been shown to be a robust indicator of the
accumulated hazards of smoking [151.
Rates were calculated using the most recent population data for each country from
the World Health Organization website http://www.who.int/countrv/en/.
Results
For the selected countries collectively, the annual mortality burden from tobacco was
approximately 5700 times that of the average annual mortality burden from
international terrorism (Table 1). For 26 of the countries, there were no deaths from
international terrorism. Within the other 11 countries, the ratio of annual tobacco to
international terrorism deaths was lowest for the US at 1700 times, followed by
Russia at 12,900 times.
The absolute annual burden from tobacco was highest for the US at 514,000 deaths
per year in 2000 (Table 1). This is equivalent to the impact of an 11 September type
terrorist attack every 2.1 days. For all of these 37 countries collectively, the tobacco
mortality burden was equivalent to the impact of an 11 September type terrorist
attack every 14 hours.
Discussion
Definitions of terrorism are highly contended f 16-181. Furthermore, we have
identified some limitations with the US State Department dataset, including with the
definition used [111. Indeed, if a tighter definition of international terrorism was
used, then this would substantially reduce the number of deaths categorised in this
way (eg, relative to domestic terrorism or other types of homicide [111). Therefore
this analysis may over-represent the mortality burden from international terrorism to
some degree.
In contrast, the tobacco mortality estimates may be underestimates of the true
mortality burden. This is because the estimates by Peto et al ignore all deaths in
those aged under 35 years (including neonatal deaths and deaths from sudden infant
death syndrome attributable to smoking), and the methodology was one of
‘conservative underestimation,of tobacco hazards' [19]. More recent data also
suggests that the long-term hazards of smoking on health are probably higher than
previously thought [20], Nevertheless, methodologies for assessing the tobaccorelated mortality burden differ and for the US a more recent analysis [21] indicates a
lower mortality burden attributable to tobacco (ie, 438,000 versus the 514,000
calculated by Peto et al and used in this analysis).
Despite these various limitations, the findings of this analysis suggest that the
mortality burden from tobacco use is at present vastly greater than from
international terrorism in all the selected countries studied. This is even the case for
the US, which has suffered the worst mortality burden from international terrorism
out of these countries in the last decade.
Why does tobacco mortality not receive a proportionate response? Some may find
comparisons between 'catastrophic' and 'normal' deaths misplaced [22]. We
recognise the subjectivity of risk perception [23,24], and the tendencies of
populations to: (i) overestimate risks stemming from visible, well publicised sudden
violence with collective results, particularly where the cause is not well understood,
compared to risks with results dispersed over place and time; and (ii) to overestimate
risks from causes were there is little apparent control by the individual, compared to
risks from causes which appear to many to be voluntarily undertaken [25-27],
This tendency may be exacerbated by disproportionate media coverage of certain
causes of mortality which involve low risk at the individual level [28,29]. There is also
the political problem of giving priority to long-term issues, compared to dealing with
emotive immediate concerns [30,311. However, we have also demonstrated
elsewhere that even for another cause of mortality which results in visible, well
publicised sudden death (road crashes), policymaking does not appear to take into
account the disproportionate mortality burden, compared to that from international
terrorism [12],
International terrorism and the harm from tobacco use have similarities, in that they
both involve discrete perpetrators - international terrorist groups and the globalized
tobacco industry - against which governments can take action. Also, many tobacco
deaths globally are due to the'actions of foreigners - policymakers and company
officials in tobacco manufacturing and exporting countries. Both international
terrorism and tobacco use can substantially harm national economies and the
international economic fabric in many ways [32,331. Similarly, both can have
widespread impacts on the way society functions and on its institutions eg, terrorism
on security arrangements, and tobacco via the tobacco industry on the functioning of
political processes [34,35]. The costs from both are largely or totally preventable,
and investment in long-term prevention for both, as opposed to containment, may
not necessarily be mutually exclusive (eg, if military budgets are diverted to
terrorism prevention).
Despite these similarities, there are substantive differences. One is that the tobacco
industry, unlike terrorists, is generally described as 'a legal industry' ie, an industry
taking part in legal activity. This is despite the fact that the deliberate sale of a highly
addictive, commonly lethal substance, and the routine denial of some harms (eg, of
secondhand smoke) may be considered reckless criminal behaviour under the laws of
some countries [36]. This presumed 'legality' contributes to the societal acceptance
and political strength of the tobacco industry in developed countries, relative to
international terrorist groups.
Secondly, there is considerable evidence about the preventability of tobacco-related
harm using current methods, and of their cost-effectiveness [37-40], compared to
the high uncertainty about the effectiveness of particular measures to prevent
international terrorism or its health impacts [41.421. From a public health
perspective, anti-terrorism efforts tend to focus on immediate containment, rather
than addressing the possible root causes of terrorism [43-461. The cost-effectiveness
of public health measures related to potential terrorism impacts has had little
conclusive research [47,481.
A further difference, as this analysis indicates, is the vastly different scale of the
consequent mortality burdens. The policy implications of this include the relative
extent, effectiveness and cost-effectiveness of the resources used to address the two
problems [49-52], A public health and evidence-based approach may suggest a
greater relative emphasis on tobacco control both nationally and internationally.
While public health budgeting will always have to take into account public concerns
that are not based on the evidence of relative risks, we argue that such policy moves
should be as rigorously examined, as is the budgeting for tobacco control. A further
possible implication is to learn from the response to international terrorism, so as to
inform the way that tobacco marketing can be reframed as a serious threat to the
social and economic well-being of individual countries and to international social and
economic development.
Conclusion
This analysis suggests a very large mortality differential between these two problems
exacerbated by globalization, international terrorism and tobacco use. Different
perceptions of risk may contribute to the relative lack of a policy response to tobacco
mortality, despite its greater scale. The lack of an appropriate response is also
despite tobacco control having a stronger evidence base for the prevention measures
used. National and international policy makers need to consider these issues if they
are to make more rational use of resources to prevent premature mortality.
Competing interests
Both authors have undertaken contract work for tobacco control-related non
government agencies, and NW has undertaken contract work in tobacco control for
the New Zealand Ministry of Health.
Authors' contributions
Both authors contributed to the design of the study, the data collection and the
drafting and final write up of the manuscript. NW undertook the data analysis.
Acknowledgements
We thank two anonymous reviewers for helpful comments on the draft. There were
no funding sources for this study.
References
1. Cronin A: Behind the Curve: Globalization and International Terrorism.
International Security 2002, 27:30-58. [Publisher Full Text]
Return to citation in text: [1]
2. Campbell K: Globalization's First War?
The Washington Quarterly 2002, 25:7-14. [Publisher Full Text]
Return to citation in text: [1]
3.
Frist B: Public health and national security: the critical role of increased federal
support.
Health Affairs (Millwood) 2002, 21:117-130. [Publisher Full Text]
Return to citation in text: [1]
4.
Coignard B: Bioterrorism preparedness and response in European public health
institutes.
European Surveillance 2001, 6:159-166.
Return to citation in text: [1]
5.
Galea S, Vlahov D, Resnick H, Ahern J, Susser E, Gold J, Bucuvalas M, Kilpatrick D: Trends
of probable post-traumatic stress disorder in New York City after the September
11 terrorist attacks.
American Journal of Epidemiology 2003, 158:514-524. [PubMed Abstract][Publisher Full
Text]
Return to citation in text: [1]
6.
Dhooge L): A previously unimaginable risk potential: September 11 and the
insurance industry.
American Business Law Journal 2003, 40:687-780.
Return to citation in text: [1]
7. Fremont WP, Pataki C, Beresin EV: The impact of terrorism on children and
adolescents: terror in the skies, terror on television.
Child and Adolescent Psychiatric Clinics of North America 2005, 14:429-51, viii. [Publisher
Full Text]
Return to citation in text: [1]
8. Yach D, Hawkes C, Gould CL, Hofman KJ: The global burden of chronic diseases:
overcoming impediments to prevention and control.
JAMA 2004, 291:2616-2622. [PubMed Abstract][Publisher Full Text]
Return to citation in text: [1]
9. Taylor AL, Bettcher DW: WHO Framework Convention on Tobacco Control: a global
"good" for public health.
Bulletin of the World Health Organization 2000, 78:920-929. [PubMed Abstract]
Return to citation in text: [1]
10.
Chaloupka FJ, Nair R: International issues in the supply of tobacco: recent changes
and implications for alcohol.
Addiction 2000, 95 Suppl 4:S477-89. [PubMed Abstract][Publisher Full Text]
Return to citation in text: [1]
11.
Wilson N, Thomson G: The epidemiology of international terrorism involving fatal
outcomes in developed countries (1994-2003).
European Journal of Epidemiology 2005, 20:375-381. [PubMed Abstract][Publisher Full
Text]
Return to citation in text: [1] [2] [3] [4] [5]
12.
Wilson N, Thomson G: Deaths from international terrorism compared to road crash
deaths in OECD countries.
Injury Prevention 2005, 11:332-333. [PubMed Abstract][Publisher Full Text]
Return to citation in text: [1] [2]
13.
Murray CJL, Lopez AD: The global burden of disease. Annex table 1. State or territories
included in the Global Burden of Disease Study, by demographic region.
Geneva, Switzerland, World Health Organization; 1996.
Return to citation in text: [1]
14.
Peto R, Lopez AD, Boreham J, Thun M, Heath C: Mortality from smoking in developed
countries 1950-2000 (2nd edition).
Oxford, Oxford University Press; 2003.
Return to citation in text: [1]
15.
Ezzati M, Lopez AD: Measuring the accumulated hazards of smoking: global and
regional estimates for 2000.
Tobacco Control 2003, 12:79-85. [PubMed Abstract][Publisher Full Text]
Return to citation in text: [1]
16.
Arnold JL, Ortenwall P, Birnbaum ML, Sundnes KO, Aggrawal A, Anantharaman V, Al
Musleh AW, Asai Y, Burkle FMJ, Chung JM, Cruz-Vega F, Debacker M, Della Corte F, Delooz
H, Dickinson G, Hodgetts T, Holliman CJ, MacFarlane C, Rodoplu U, Stok E, Tsai MC: A
proposed universal medical and public health definition of terrorism.
Prehospital and Disaster Medicine 2003, 18:47-52.
Return to citation in text: [1]
17. Whitaker B: The definition of terrorism.
[http://www. guardian, co. uk/elsewhere/journalist/story/0,7792,487098,00. htm I ]Guard/an
2001., 7 May:
Accessed 17 August 2005
Return to citation in text: [1]
18. United Nations Office of Drugs and Crime: Definitions of terrorism.
[http://www.unodc.org/unodc/terrorism_definitions.htmllVienna , United Nations Office of
Drugs and Crime; 2004.
Accessed 17 August 2005
Return to citation in text: [1]
19. Peto R, Lopez AD, Boreham J, Thun M, Heath CJ: Mortality from tobacco in developed
countries: indirect estimation from national vital statistics.
Lancet 1992, 339:1268-1278. [PubMed Abstract][Publisher Full Text]
Return to citation in text: [1]
20. Doll R, Peto R, Boreham J, Sutherland I: Mortality in relation to smoking: 50 years'
observations on male British doctors.
BMJ 2004, 328:1519. [PubMed Abstract][Publisher Full Text] [PubMed Central Full Text]
Return to citation in text: [1]'
21. Centers for Disease Control and Prevention: Annual smoking-attributable mortality,
years of potential life lost, and productivity losses—United States, 1997-2001.
Morbidity and Mortality Weekly Report 2005, 54:625-628.
Return to citation in text: [1]
22. Shatenstein S, Chapman S: The banality of tobacco deaths.
Tobacco Control 2002, 11:1-2. [PubMed Abstract][Publisher Full Text]
Return to citation in text: [1]
23. Lerner JS, Gonzalez RM, Small DA, Fischhoff B: Effects of fear and anger on perceived
risks of terrorism: a national field experiment.
Psychological Science 2003, 14:144-150. [PubMed Abstract][Publisher Full Text]
Return to citation in text: [1]
24. Slovic P: Public perception of risk.
Journal of Environmental Health 1997, 59:22-24.
Return to citation in text: [1]
25. Slovic P: Perception of risk.
In The Earthscan Reader in risk and modern society. Edited by: Lofstedt R and L. Frewer L.
London, Earthscan; 1998.
Return to citation in text: [1]
26. Jamieson P, Romer D: What do young people think they know about the risks of
smoking?
In Smoking: Risk, perception and policy. Edited by: Slovic P. Thousand Oaks Ca, Sage
Publications; 2001.
Return to citation in text: [1]
27. Vaughan P: Perceiving risks.
In The World Health Report 2002 - Reducing Risks, Promoting Healthy Life. Edited by:
Campanini B. Geneva, World Health Organization; 2002.
Return to citation in text: [1]
28.
Russell C: Living can be hazardous to your health: how the news media cover
cancer risks.
Journal of the National Cancer Institute Monographs 1999, 167-170. [PubMed
Abstract][Publisher Full Text]
Return to citation in text: [1]
29.
Harrabin R, Coote A, Allen J: Health in the news: Risk, reporting and media influence.
London, Kings Fund Publications; 2003.
Return to citation in text: [1]^
30.
Berke PR: Reducing natural hazard risks through state growth management.
Journal of the American Planning Association 1998, 64:76-87.
Return to citation in text: [1]
31. Moser SC, Dilling L: Making climate hot.
Environment 2004, 46:32-48.
Return to citation in text: [1]
32. Jha P, Chaloupka FJ: The economics of global tobacco control.
Bmj 2000, 321:358-361. [PubMed Abstract][Publisher Full Text] [PubMed Central Full
Text]
Return to citation in text: [1]
33. Peck R, Chaloupka FJ, Jha P, Lightwood J: A welfare analysis of tobacco use.
In Tobacco Control in Developing Countries. Edited by: Jha P and Chaloupka FJ. Oxford,
Oxford University Press; 1999.
Return to citation in text: [1]-.
34. Saloojee Y, Dagli E: Tobacco industry tactics for resisting public policy on health.
Bulletin of the World Health Organization 2000, 78:902-910. [PubMed Abstract]
Return to citation in text: [1]
35. Muggli ME, Hurt RD, Repace J: The tobacco industry's political efforts to derail the
EPA report on ETS.
American Journal of Preventive Medicine 2004, 26:167-177. [PubMed Abstract] [Publisher
Full Text]
Return to citation in text: [1]
36. Liberman J, Clough 3: Corporations that kill: The criminal liability of tobacco
manufacturers.
Criminal Law Journal 2002, 26:223-237.
Return to citation in text: [1]
37. Hopkins DP, Briss PA, Ricard CJ, Husten CG, Carande-Kulis VG, Fielding JE, Alao MO,
McKenna JW, Sharp DJ, Harris JR, Woollery TA, Harris KW: Reviews of evidence
regarding interventions to reduce tobacco use and exposure to environmental
tobacco smoke.
American Journal of Preventive Medicine 2001, 20:16-66. [PubMed Abstract][Publisher Full
Text]
Return to citation in text: [1]
38. Ranson MK, Jha P, Chaloupka FJ, Nguyen SN: Global and regional estimates of the
effectiveness and cost-effectiveness of price increases and other tobacco control
policies.
,
Nicotine and Tobacco Research 2002, 4:311-319. [Publisher Full Text]
Return to citation in text: [1]
39.
VicHealth Centre for Tobacco Control: Tobacco control: A blue chip investment in public
health.
Melbourne, VicHealth Centre for Tobacco Control; 2003.
Return to citation in text: [1]
40.
Collins D, Lapsley H: Counting the costs of tobacco and the benefits of reducing smoking
prevalence in New South Wales.
Sydney, New South Wales Department of Health; 2005.
Return to citation in text: [1]
41.
Richardson L: Buying biosafety—is the price right?
New England Journal of Medicine 2004, 350:2121-2123. [PubMed Abstract][Publisher Full
Text]
Return to citation in text: [1]
42.
Elworthy S, Rogers P: The 'War on Terrorism': 12 month audit and future strategy
options.
[http://www.oxfordresearchgroup.org.uk/publications/briefings/waronterrorism.pdfJOxford,
Oxford Research Group; 2002.
Accessed 4 December 2005
Return to citation in text: [1]
43.
Gaddis JL: Grand Strategy in the Second Term.
Foreign Affairs 2005, 84:2-15.
Return to citation in text: [1]
44.
Frey BS: Dealing With Terrorism: Stick or Carrot?
Northampton, Edward Elgar; 2004.
Return to citation in text: [1]
45.
Klarevas L: Political realism: A culprit for the 9/11 attacks.
Harvard International Review 2004, 26:18-23.
Return to citation in text: [1]
46. Falkenrath RA: Problems of Preparedness.
International Security 2001, 25:147-186. [Publisher Full Text]
Return to citation in text: [1]
47.
Florig HK: Public health. Is safe mail worth the price?
Science 2002, 295:1467-1468. [PubMed Abstract][Publisher Full Text]
Return to citation in text: [1]
48.
Fowler RA, Sanders GD, BravSta DM, Nouri B, Gastwirth JM, Peterson D, Broker AG, Garber
AM, Owens DK: Cost-effectiveness of defending against bioterrorism: a comparison
of vaccination and antibiotic prophylaxis against anthrax.
Annals of Internal Medicine 2005, 142:601-610. [PubMed Abstract][Publisher Full Text]
Return to citation in text: [1]
49.
Wipfli H, Stillman F, Tamplin S, da Costa e Silva VL, Yach D, Samet J: Achieving the
Framework Convention on Tobacco Control's potential by investing in national
capacity.
Tobacco Control 2004, 13:433-437. [PubMed Abstract][Publisher Full Text]
Return to citation in text: [1]
50.
Beaglehole R, Yach D: Globalisation and the prevention and control of noncommunicable disease: the neglected chronic diseases of adults.
Lancet 2003, 362:903-908. [PubMed Abstract][Publisher Full Text]
Return to citation in text: [1]
51.
Perry WJ: Preparing for the Next Attack.
Foreign Affairs 2001, 80:31. *
Return to citation in text: [1]
52. Drozdiak W: The North Atlantic Drift.
Foreign Affairs 2005, 84:88-98.
Return to citation in text: [1]
H'
/x/ £->\
PUm je-H-c
Perspectives on Global Development and Technology
Volume 3, no. 1-2 (2004)
Special Issue:
Globalization and Health
Guest Editors: Richard L. Harris and Melinda J. Seid
CONTENTS
Editors’ Preface...........................................................
Acknowledgements....................................................................
List of Contributors....................................................................
iii
v
vii
1
Globalization and Health in the New Millennium..................
Richard L. Harris and Melinda J. Seid
1
2
Globalization, Health, and the Free Trade Regime: Assessing
the Links......................................................................................
47
Ronald Labonte
3
The Social Dimension of Globalization and Health..............
73
Aboubakr A. Badawi
4
Globalization and Health: The Paradox of the Periphery ....
91
Christine McMurray
5
Health Transition and Globalization in the Pacific: Vestiges of
Colonialism?...............................................................................
109
SlTALEKI A. FlNAU, IRIS L. WAINIQOLO AND GIUSEPPE
G. CUBONI
6
Globalization and Health Policy in South Africa....................
Di McIntyre, Stephen Thomas and Susan Cleary
7
Global Challenges to Equity in Safety and Health at Work:
Struggles for Fair Work in Southern Africa.............................
131
153
Rene Loewenson
8
Reproductive Health in Post-Transition Mongolia: Global
Discourses and Local Realities..................................................
Kimberley Rak and Craig R. Janes
171
9
Access to Healthcare via Telehealth: Experiences from the
Pacific..........................................................................................
197
Roy Smith
10
Globalization of Risks for Chronic Diseases Demands Global
Solutions......................................................................................
213
Derek Yach and Robert Beaglehole
11
The People’s Health Movement: A People’s Campaign for
“Health for all - Now!”.............................................................
235
Ravi Narayan and Claudio Schuftan
12
The Globalization of Health: Risks, Responses, and Alterna
tives .............................................................................................
Richard L. Harris and Melinda J. Seid
245
Editors’ Preface • iii
Editors’ Preface
This international collection of essays on globalization and health examines
the global health issues associated with the economic, technological,
political, social, cultural and environmental effects of globalization. These
essays analyze the complex linkages between globalization and health, the
health effects of globalization at all levels (global, national, and local),
and the policy and institutional responses associated with the health
consequences of globalization.
Tills collection combines essays that are global or broadly comparative in
scope with those that focus on health issues in a single country or region.
The contributors of these essays are international experts, officials, and
scholars who are deeply concerned about the global health problems and
issues addressed in this collection. They provide important information,
insights, and conclusions about the linkages between globalization and
health, the health effects of globalization, the major global health issues
faced by humanity, and the responses that have been and need to be
developed to these issues.
The health risks and challenges faced by humanity today are enormous.
The global increase in chronic diseases as well as the spread of new and
reemerging communicable diseases is unprecedented. The globalization
of contemporary economic, technological, political, social and cultural
forces and the healdt effects of these forces are increasing the risks to
population health around the world. This collection of essays was organized
to contribute to the global search for effective responses to the global health
problems confronting humanity at the outset of the twenty-first century'.
Hopefully, it will contribute to increasing awareness about these problems
and to the ongoing efforts to resolve them.
Richard L. Harris and Melinda J. Seid
Perspectives on Global Development and Technology, Volume 3, issue 1-2
© 2004 Koninklijke Brill NV, Leiden
Ute People’s Health Movement • 235
The People’s Health Movement:
A People’s Campaign for
“HEALTH FOR ALL—NOW!”
Ravi Narayan* and Claudio Schuftan**
Abstract
The People’s Health Assembly and the People’s Flealth
Movement have been a civil society effort to counter the
ill effects of globalization on health and health care. The
Assembly, dtrough an interactive dialogue, developed the
People’s Charter for Flealth as a tool for advocacy and a
call for radical action. Consisting of a wide range of action
initiatives, the People’s Charter for Health, now translated into
over forty languages, is helping to promote a movement that
involves geograpltical circles of health professionals and activists
dial organize street-level rallies, policy debates and dialogues,
and public education. The movement’s advocacy efforts with
the WHO and other major international health players and
health campaigns arc all focused on the goal of “Health for
All—Now!”
Background
In 1978, an International Health Assembly at Alma-Ata in USSR, co
sponsored by the World Health Organization (WHO), United Nations’
Children’s Fund (UNICEF); and others, gave the World a slogan “Health
for All by 2000” and endorsed the famous Alma-Ata Declaration, which
brought people and communities to the center of health planning and
health care strategies, and emphasized the role of community participation,
' People’s Health Movement Global Secretariat, Bangalore, India.
" People’s Health Movement, Hanoi, Vietnam.
Perspectives on Global Development and Technology, Volume 3, issue 1-2
© 2004 Koninklijke Brill NV, Leiden
236 • Narayan & Schuftan
appropriate technology, and intersectoral coordination. The declaration
was endorsed by most of the governments of the world and symbolized a
significant paradigm shift in the global understanding of health and health
care (WHO—UNICEF 1978).
Twenty-two years later, after much policy rhetoric, some concerted but
mostly ad hoc action, misplaced euphoria, assault and distortions by the
growing market economy of medicine, and a lot of governmental and
international health agency amnesia, this declaration remains unfulfilled
and mostly forgotten. As the world comes to terms with the new economic
forces of globalization, liberalization, and privatization, the dream of
providing health for all is receding. The People’s Health Assembly in
Savar, Bangladesh, on December 4-8, 2000, and the People’s Healdi
Movement that evolved from it represent a civil society effort to counter
this global amnesia and challenge health policymakers around the world
with a people’s health campaign for “Health for All—Now!”
The People’s Health Assembly
The glob.al People’s Health Assembly held at Savar, Dhaka, from
December 4-8, 2000, brought together 1453 people from 92 countries, in
an unusual five-day event, sharing people’s concerns about the unfulfilled
Health for All initiative launched in Alma-Ata two decades earlier
(Narayan 2000). The assembly included a variety of interactive dialogue
opportunities for all the health professionals and activists who gathered for
this significant event. These activities included the following:
• A march for health.
• Meetings at which testimonies on the health situation from many
parts of the world and struggles of people were shared and com
mented upon by multidisciplinary resource persons (People’s Healdi
Movement 2002).
• Parallel workshops to discuss a range of health and health-related
challenges.
• Cultural programs to symbolize the multiregional, multicultural, and
multiethnic diversity of the peoples of the world; also exhibitions and
video/film shows.
• Dialogue, in small and big groups, using formal and informal
opportunities.
The assembly in Savar was preceded by a series of preassembly events
all over the world. The most exceptional of these was the mobilization
in India. For nearly nine months preceding the assembly, there wengrassroots, local, and regional initiatives of people’s health enquiries
and audits; health songs and popular theater; subdistrict and district
level seminars; policy dialogues and the translation of national consensus
The People’s Health Movement • 237
documents on health into regional languages; and campaigns to challenge
medical professionals and the health system to become more Health for
All-oriented.
Finally, over 2000 delegates arrived in Kolkata, mostly by five people’s
health trains, bringing ideas and perspectives from 17 state conventions
and 250 district conventions. At Kolkata, the assembly endorsed tire Indian
People’s Health Charter, after two days of conferences, parallel workshops,
exhibitions, a march for health, a public rally, and cultural programs.
About 300 delegates from this assembly then traveled to Bangladesh,
mostly by bus, to attend the global People’s Health Assembly. Similar
activities, though less intense, took place in Bangladesh, Nepal, Sri Lanka,
Cambodia, the Philippines, Japan, and other parts of the world, including
Latin America, Europe, Africa, and Australia.
The People’s Charter for Health
Finally, at the end of a whole year of mobilization and five days of
a very intense and interactive assembly at Savar, Bangladesh, a global
people’s health charter emerged, which was endorsed by all the participants
(People’s Health Assembly 2000a). This charter provides:
• an expression of common concerns;
® a vision of a better and healthier world;
• a call for radical action;
• a tool for advocating people’s health; and
• a rallying point for global health movements, networks, and coalition
building.
The global people’s health charter is a significant development for many
reasons. First, it endorses health as a social, economic, and political issue
and a fundamental human right. Second, it identifies inequality, poverty,
exploitation, violence, and injustice as the roots of ill health. Third, it
underlines the imperative that Health for All means challenging powerful
economic interests, opposing globalization in its existing iniquitous model,
and drastically changing political and economic priorities. Fourth, it
includes perspectives and voices of the poor and marginalized (rarely heard)
people, and encourages them to develop their own local solutions. Finally,
it encourages people to hold accountable their own local authorities,
national governments, international organizations and corporations.
The vision and the principles of the charter, more than any other
document preceding it, extricate health from the myopic biomedicaltechno-managerialism of the last two decades, with its vertical, selective
magic bullets approach to health, and centers squarely in the context of
today’s global social, economical, political, cultural, and environmental
realities. However, the most significant gain of the People’s Health
238 • Narayan & Schuftan
Assembly and the Charter is that, for the first time since the Alma-Ala
Declaration (1978), a Health For All action plan unambiguously endorses
a call for action that tackles the broader determinants of health. These
include health as human right; economic challenges for health; social and
political challenges for health; environmental challenges for health; tackling
war, violence, conflict, and natural disasters; evolving a people-centered
health sector; and encouraging people’s participation in creating a healthy
world.
In a nutshell, the People’s Health Movement promotes a wide range
of approaches and initiatives to combat the ill-effects on health, health
systems, and health care initiatives of the triple assault by the forces of
globalization, liberalization, and privatization. These approaches include
the following:
• Combating the negative impacts of globalization as a worldwide
economic and political ideology and process.
• Significantly reforming the international financial institutions and the
WTO to make them more responsive to poverty alleviation and the
Health for All Now movement.
• Forgiveness of the foreign debt of the least developed countries and
the use of its equivalent for poverty reduction, health, and education
activities.
• Greater checks, restraints, and mechanisms to ensure their compliance
on the freewheeling powers of the transitional corporations, especially
pharmaceutical firms.
In addition to these initiatives aimed at the existing institutional framework
of the global economic system, the movement promotes a large number <>l
more specific initiatives aimed at tire following:
• Greater and more equitable household food security.
• Some type of a Tobin tax that will tax runaway international financial
transfers.
• Unconditionally supporting the emancipation of women and respect
ing their full rights.
• Putting health higher in the development agenda of governments.
• Promoting the health (and other) rights of displaced people.
• Halting the privatization of public health facilities and working
towards greater controls on the already installed private health sector
• More equitable, just, and empowered people’s participation in health
and development matters.
• A greater focus on poverty alleviation in national and international
development plans.
• Greater and unconditional access of the poor to health services and
treatment regardless of their ability to pay.
The People’s Health Movement • 239
• Strengthening public institutions, political parties, and trade unions
involved in the struggles of the poor.
• Opposing restricted and dogmatic fundamentalist views of the devel
opment process.
• Greater vigilance and activism in matters of water and air pollution,
the dumping of toxics, the disposal of waste, climate changes and
CO2 emissions, soil erosion, and other attacks on the environment.
• Militant opposition to the unsustainable exploitation of natural
resources and the destruction of forests.
• Protecting biodiversity and opposing biopiracy and the indiscriminate
use of genetically modified seeds.
• Holding violators of environmental crimes accountable.
• Systematically applying environmental assessments of development
projects and people-centered environmental audits.
Moreover, the movement has taken a position on a number of critical
global political issues such as the following:
• Opposing war and tire current USA-led, blind “anti-terrorist” cam
paigns.
• Categorically opposing the Israeli invasion of Palestinian towns,
having, among others, a sizeable negative impact on the health of
the Palestinian people.
• The democratization of the UN bodies and especially the Security
Council.
Finally, the movement promotes a large number of initiatives aimed at
transforming health in the most comprehensive manner possible. These
include the following:
• Making a renewed call for a comprehensive, a more democratic
people’s health care that is given the resources needed and that holds
governments accountable in this task.
• Independent national drug policies focused on essential, generic drugs.
• The transformation of WHO, supporting and actively working with
its new Civil Society Initiative (CSI) and making sure it remains
accountable to civil society.
• Assuring WHO stays staunchly independent from corporate interests.
• Sustaining and promoting the defense of effective patient’s rights.
• Expanding and incorporating traditional medicine.
• Changing the training of health personnel to assure that it covers the
great issues of our time as depicted in the People’s Charter for Health.
• Public health-oriented (and not for-profit) health research worldwide.
• Strong people’s organizations and a global movement working on
health issues.
240 • Narayan & Schujlan
• More proactive countering of the media that are at the service of the
globalization process.
• Promoting people’s empowerment leading to their greater control of
the health sendees they need and get.
• Creating the bases for more effective analysis and concerted actions by
the PHM’s members through their greater involvement in the PHM’s
website and listserve.
• Fostering a global solidarity network that can support and mobilize
fellow members when facing disasters, emergencies, or acute repressive
situations.
• Getting more actively involved in actions addressing the silent
epidemic of violence against women.
• Assuring more prompt responses and preventive/rehabilitative mea
sures in cases of natural disasters.
The decision to pursue this comprehensive combination of health initia
tives, as we enter the new millennium, is probably the most significant
achievement of the People’s Health Assembly and the evolving People’s
Health Movement (Schuftan 2002).
i
the
Tot
for
Coi
and
Tai
glol
■
'
:
;
3
poll
inst
are
glol
for
of i
issu
and
hav
nati
con
Significant Gains of the People’s Health Assembly
and the PHM
The mobilization process at the global level, the assembly, and the
development of the movement have already made many significant gains.
For the first time in decades, health and non-health networks have come
together to mobilize global solidarity and act collectivity for health. The
main organizations that have taken the lead in this effort include the
International People’s Health Council (IPHC), Health Action International
(HAI), Consumer International (CI), Asian Community Health Action
Network (ACHAN), Third World Network (TWN), Women’s Global
Network for Reproductive Rights (WGNRR), Gonoshasthya Kendra (GK),
and the Dag Hammaeskjold Foundation (DHF). More recently, new
networks such as the Global Equity Gauge Alliance (GEGA) and the Social
Forum Networks have joined the effort.
At the country level similar developments are beginning to happen.
In India, for instance, the movement has gained the support of various
scientific groups, women’s movements, the alliance of people’s movements,
health networks and associations, research and policy networks, and some
trade unions. Another significant development has been the development of
solidarity between national movements. This solidarity has found symbolic
expression in various collective documents at the global level (People’s
Health Assembly 2000b, 2000c). These documents have included themes
such as Health in the Era of Globalization: From Victims to Protagonists;
3
■
Thi
hea
of
of
incl
Fre:
Ma
Sinl
pro
Vie
Bra
volt
slid,
utet
foci
mui
e-gi
brie
vari
P
nati
The People's Health Movement • 241
tlie Political Economy of the Assault on Health; Equity and Inequity
Today; die Medicalization of Health Care and the Challenge of Health
for All; the Environmental Crisis: Threats to Health and Ways Forward;
Communication as if People Mattered: and Adapting Health Promotion
and Social Action to the Global Imbalances of the Twenty-First Century.
Taken together, these documents represent an unprecedented, emerging,
global consensus on a wide range of critical issues.
These kinds of “consensus documents” to support public education and
P'^^-’ advocacy have also been evolving at the country level. In India, for
instance, five small booklets, now translated into most Indian languages
are now being widely distributed on the following five issues: (1) what
globalization means for people’s health; (2) whatever happened to health
for all by 2000 .AD: (3) making life worth living by meeting basic needs
of all; (4) a world where we all matter by focusing on the health care
issues of women, children, street kids, the diflerendy abled and die aged;
and (5) confronting the commercialization of health care. These booklets
have been published by 18 national networks that together form the
national coordination committee in India and represent an unprecedented
consensus on these issues, the first of its kind in five decades.
The People’s Health Assembly itself was an unprecedented achievement.
This international health gathering expresses and symbolizes an alternative
health and development culture based on dialogue and the celebration
of people’s health. Another significant gain has been the translation
of die People’s Charter for Health into nearly 40 languages. These
include Arabic, Bangla, Chinese, Danish, English, Farsi, Finnish, Flemish,
Fr^ch, German, Greek, Hindi, Indonesian, Italian, Japanese, Kannada,
M^yalam, Ndebele, Nepalese, Philippine, Portuguese, Russian, Shona,
Sinhala, Spanish, Swahili, Swedish, Tamil, Urdu, Ukrainian, and in the
process are Tonga, Lithuanian, Norwegian, Welsh, Thai, Cambodian,
Vietnamese, Pastun, Dhari, and Creole. An audio tape in English with
Braille tides is also available. All these translations have been translated by
volunteers who are committed to the People’s Health Movement.
"Audio visual aids, including videos for public education, exhibitions,
slides, and other forms of communication, are being developed and distrib
uted. There is a new BBC Life Series video on the Health Protesters, which
focuses on the PHM movement. The movement itself has evolved a com
munication strategy, which includes a website (www.phmovement.org); an
e-group exchange/discussion group (PHA-Exchange@kabissa.org); news
briefs (nine since January 2001) and a host of press releases on a wide
variety of themes, special events, and crises.
Presentations of the People’s Health Charter have taken place at
national, regional, and international fora. They have included the World
242 • Narayan & Schujlan
Health Organization, the Global Forum for Health Research (GFHRForum 5 & 6), and the World Health Assembly. The relationship that
has developed between the PHM and WHO is particularly interesting.
In April 2001, a very effective and assertive lobbying effort by a visiting
PHM consultant to a WHO research seminar resulted in the formation
of the WHO Civil Society Initiative (WFIO CSI) announced at the World
Health Assembly in May 2001. Six PHM leaders were subsequently invited
to meet and dialogue with the WHO Director General. In May 2002,
WHO CSI invited PHM to present the People’s Charter for Health as
a Technical Briefing to the World Heath Assembly. Thirty-five PHM
members participated in this event. In May 2003, over 80 PHM delegate.^^
from 30 countries attended the 2003 World Health Assembly and mad<^^
statements on primary health care, TRIPS and other issues and were
invited to meet the new Director General designate, who welcomed greater
dialogue with PHM members at all levels of the WHO so that the
organization can be in touch with the realities of the lives of the poor and
the marginalized. The 2003 World Health Assembly was preceded by a
PHM Geneva meeting on the Alma-Ata Anniversary, which was attended
by some WHO staff, including the Pan-American Health Organization
Regional Director. These developments represent small but incremental
movements towards a critical collaboration between PHM and the WHO.
In many countries of the world, country-level PHM circles are beginning
to organize public meetings and local campaigns that include taking health
to the streets as a human rights issue. Discussions on the charter held with
professional associations and public health schools, articles and editorials
in medical/health journals are also beginning to increase. Policy dialogues
and action research circles are also being developed on the WHO/WHA,
Poverty and AIDS, Women’s Access to Heath, Health Research, Access to
Essential Drugs, Macroeconomics and Health, Public Private Partnerships,
and Food and Nutrition Security issues. Everyday the list of actions
increases.
Conclusion
The People’s Health Assembly and the People’s Health Movement that
have emerged from it have been an unprecedented development in the
journey towards the goal of Health for All. The PHM movement:
• is a multiregional, multicultural, and multidisciplinary mobilization
effort;
• brings together the largest collection of activists and professionals, civil
society representatives, and people’s representatives themselves;
• develops global instruments of concern and action; and
The People’s Health Movement • 243
• expresses solidarity with the health struggles of people around the
world, especially the poor and the marginalized who are affected by
the current global economic order.
Recognizing that we need a continous, sustained, collective effort, the
People’s Health Movement process reminds us, through the People’s
Health Charter, that a long road lies ahead in the campaign for Health
for All.
References
Narayan, Ravi
2000
“The People’s Health Assembly—A People’s Campaign for Health for All
Now.” Asian Exchange 16' 6-17.
People’s Health Assembly
2000a
,
2000b
2000c
-
“People’s Charter for Health.” People’s Health Assembly. December 8, GK
Savar, Bangladesh.
Discussion Papers Prepared by PHA Drafting Group, PHA Secretariat. GK
Savar, Dhaka, Bangladesh.
“Health in the Era of Globalization: From Victims to Protagonists.” Discussion
Paper by PGA Drafting Group, PHA Secretariat. GK Savar, Dhaka—
Bangladesh.
People’s Health Movement
2002
“Voices of the Unheard—Testimonies from the People’s Health Assembly.”
December 2000, GK Savar, Bangladesh.
Schuftan, Claudio
“The People’s Health Movement (PH1M) in 2002: Still at the Fore Front of the
Struggle for Health for All Now.” Issue Paper 2 for World Health Assembly.
Mav 2002, People’s Health Movement.
WHO/UNICEF
1978
“Primary Health Care.” Report of the International Conference on Primary
Health Care, September 6-12, Alma Ata, USSR.
2002
Globalization: Health Risks & Responses • 245
The Globalization of Health: Risks,
Responses, and Alternatives
9
Dr. Richard L. Harris* and
Dr. Melinda J. Seed**
Abstract
“
This essay provides a summary and synthesis of the wealth
of information, analysis, and conclusions provided by the other
contributors to this collection of essays on globalization and
health. The major themes addressed are the health risks and
health effects of globalization, the responses to these risks and
effects at the national and global levels, and the alternatives
to the present patterns of globalization in which the health of
billions of people around the world and the planet’s ecological
sustainability are threatened.
Introduction
In the introduction to this collection of essays on globalization and health,
we pointed out that, according to the existing literature on globalization
^Pd health, it is generally accepted that certain aspects of globalization
have “enhanced health and life expectancy in many populations,” while
other aspects of globalization “jeopardize population health via the erosion
- of social and environmental conditions, the global division of labor, the
exacerbation of the rich-poor gap between and within countries, and the
accelerating spread of consumerism” (McMichael and Beaglehole 2000).
' These threatening aspects of globalization present major challenges for
’ Global Studies Program, California State University, Monterey Bay, Seaside, California,
USA.
" Health Science Program, California State University, Sacramento, Sacramento,
California, USA.
Perspectives on Global Development and Technology, Volume 3, issue 1-2
© 2004 IConinklijke Brill NV, Leiden
246 • Hams & Seid
health researchers, practitioners, and policymakers today, and they are the
major focus of this collection of essays.
The contributors to this collection of essays on globalization and health
provide a wealth of information, analyses and conclusions on many of
the health risks and health effects of globalization, on the responses to
these risks and effects, and on the search for alternatives to how the
contemporary forces of globalization affect health around the world today.
In the pages that follow, we provide a summary and synthesis of the major
findings on these themes that the contributors to this collection of essays
have reported in the preceding pages.
The Health Benefits and Risks Associated with Globalization
Most of the contributors to this collection of essays agree that there have
been some significant health benefits from globalization. For example,
Badawi, Labonte, McMurray, Smith, and Yach and Beaglehole acknowl
edge in their essays that the global diffusion of new health-related knowl
edge and technologies as a result of international trade and investments
has contributed to disease surveillance, treatment and prevention around
the world as well as the spread of sanitation and vaccines that have greatly
reduced the threat of many deadly diseases.
McMurray states in her essay that “there is no doubt the spread of
Western medicine through out the world and the implementation of
global health programs has brought numerous benefits”; however, she also
points out that “at the same time, globalization has promoted patterns
of dependency, development, settlement and lifestyles that have been
detrimental to health.” Smith’s essay reveals how new information and
communication technologies (ICT) are being applied to healthcare in some
of the more remote areas of the Pacific islands, and he argues that these
technologies have the potential to provide “a remarkable expansion of the
medical expertise available to act in a curative manner” and to advance
preventative healthcare in these remote areas of the world. However,
Smith’s essay also reveals how these technologies, which are a central
feature of globalization, are a “two-edged sword.”
On the one side of the sword, the new information technologies and
Internet connectivity enhance the provision of healthcare to people in
remote and marginalized areas, but on the other side, they reinforce
the neocolonial ties and unequal power relationship that exist between
these areas and the developed core economies. They also transmit the
more negative aspects of the consumerist life-styles associated with dtese
economies.
The essay by Finau, Wainiqolo, and Cuboni focuses on how the
“changes in health of Pacificans are about the power imbalances brought
Globalization: Health Risks & Responses • 247
about by globalization, imperialism and colonialism.” They see “the
continuance of colonialism and imperialism in different forms” in the
present context of globalization. They also argue that many contemporary
“technologies and ideologies contribute to the reproduction and the
strengthening of the pattern of power relations that feed imperialism.”
In their essay on women’s reproductive health in post-transition Mongolia,
■ Rak and Janes proride an example of how this works. Their research
shows how the global discourse on family planning and reproductive health
as well as global reproductive health policies are based on assumptions
that “fail to consider die local cultural context of reproductive decision: ^^naking, do not meet women’s needs, and are therefore seriously flawed.”
Nevertheless, external donors and consultants who are in a very real sense
the agents of globalization in this case are imposing these global norms
'
and policies on women in Mongolia.
Most of the contributors to this collection of essays reveal either explicitly
or implicidy that, in fact, what is generally referred to as “globalization”
j* is none other than the global expansion and integration of contemporary
i
forms of capitalist production, distribution, and consumption. Their essays
reveal that the global expansion and integration of twenty-first century
1
capitalism involves not only the global diffusion of certain technologies,
;i
products, and practices, it also involves the global dissemination of certain
I
ideologies and cultural norms.
Together, these forces of capitalist globalization have inadvertently or
purposively promoted the follotring types of global health risks:
• The global spread of various communicable and noncommunicable
diseases.
• The global promotion of unhealthy products and practices.
• The global diffusion of a wide range of technologies and production
processes diat are hazardous both to human health and to the health
of the natural environment.
• The global promotion of inequitable forms of private health care and
.
the commercialization of health services and medicines diat place
them beyond the reach of large sectors of the world’s population.
• The global diffusion of Western norms, practices, and ideological
models/paradigms of health care that often conflict with local values
5 1
and needs and diat create/reinforce inequitable power relationships
j
and social inequities.
1 As we learn more about these and other adverse health effects of the global
1 expansion and integration of modern capitalism, it is clear that many of the
I a
contemporary' effects of the globalization of twenty-first century capitalism
1 are a serious threat to not only the health of billions of people around the
: sf
world but also to the sustainability of the planet’s entire biosphere.
248 • Hanis & Seid
As Labonte points out in his essay, we have now lived through
more than twenty years in which the global diffusion of knowledge
and technology has taken place under a neoliberal capitalist regime
of trade liberalization and global economic integration; yet. the health
impacts of this process of liberalization and globalization have been largely
negative, especially the effects of this process on what Labonte refers
to as the two fundamental health-determining pathways of globalization:
poverty/inequality and environmental sustainability.
The liberalization and globalization of die economies of many developj
ing countries have been accompanied by a corresponding increase in the
poverty, environmental degradation, and poor health of a large proportion
of the population. Loewenson notes in her essay that the incomes of a
quarter of the world’s population declined at the end of the last millen
nium when globalization was going at top speed. Even many of the positive
effects of the global expansion and integration of capitalism have adverse
consequences. Labonte’s essay gives the example of how the opening of the
economies of many developing countries to international trade and invest
ment has increased the access of women to wage-earning employment and
contributed to their empowerment in gender relations. However, he points
out that more often than not they are employed in low-paid, unhealthy and
insecure jobs, frequently in so-called free trade export zones where labor
organizations are prohibited and only single young women are employed
under hazardous working conditions (and often exploited and sexually ha
rassed). Loewenson reports in her essay that these young women have
been documented to experience high levels of job stress and reproductive
health problems, including miscarriages, problems with pregnancies, and
poor fetal health.
McMurray’s essay illustrates how the globalization of capitalism inten
sifies disparities in health between and within nations and also how it
can create paradoxical health outcomes in the most peripheral areas of
the global capitalist economy. Her essay reveals tliat in the smallest and
most remote countries within the global system, such as the Pacific island
countries, the negative health effects of capitalist globalization impact the
population more in the globalized (Westernized) and urbanized core areas
than in the thinly populated and more peripheral rural areas that have less
access to modem health services but relatively better environmental health
conditions. McMurray focuses on how globalization affects these societies
through, “first, its impact on environmental quality, second, its impact on
the quality and accessibility of health services, and third, its promotion of
unhealthy lifestyles.”
As Labonte’s essay and our own introductory essay in this collection
indicate, the extent to which the forces of globalization affect the health
Globalization: Health Risks & Responses • 249
of the population in individual countries depends upon the prevailing
economic, social, and political conditions in these countries; their level of
technological and economic development; and their natural endowments
(Comia 2001; Drager, Labonte, and Torgerson 2002; Woodward et aL
2001). These indigenous factors mediate most of the direct effects of
globalization on the national/domestic level as well as many of the indirect
effects of globalization on the community and household levels.
Labonte’s essay reveals that the forces of capitalist globalization affect
population health at the national level through various channels or
-.pathways, such as externally imposed macroeconomic policies (e.g., IMF
^kructural adjustment programs and monetary policies), the enforcement
of trade agreements, the flows of trade associated with these agreements,
official development assistance (from the United States and other major
“donor” countries), the international transfer of health-related knowledge
and information, and the influence of the global communications and
entertainment media. There are also “environmental pathways” through
which capitalist globalization affects health. These pathways include crossborder pollution, the depletion/contamination of natural resources (water,
- tire soil, fish stocks, and forests), and the destruction of the biodiversity
in local ecosystems. Many of the essays in this collection touch upon the
health effects of these environmental pathways of globalization.
Globalization and Life Style Changes
Most of the essays in this collection support the thesis that certain
contemporary patterns of death and disability are caused by the lifestyle
changes promoted by globalization, particularly the increased consumption
g^f unhealthy processed foods and products. These lifestyle changes and
^Particularly the unhealthy consumption patterns they entail are, as Yach
and Beaglehole demonstrate in their essay, contributing to an alarming
global increase in chronic and noncommunicable diseases (NCDs)—the
■ so-called diseases of affluence (although they are increasingly suffered by
the poor). McMurray, Smith, and Finau and his colleagues all address
the negative health impact of these lifestyle changes and the increased
consumption of unhealthy foods, especially in the island nations of the
Pacific.
All three essays on the Pacific call attention to the health effects of both
the disruptive changes and the uneven pattern of economic and social
development that have been promoted in the developing countries by
contemporary forms of capitalist investment, trade and production. Finau,
Wairtiqolo and Cuboni emphasize the disruptive and destructive nature
of many of these changes and attribute them to the Western capitalist
250 • Harris & Seid
model of development that has been imposed on the Pacific peoples by
colonialism, imperialism, and globalization.
According to Yach and Beaglehole, an unprecedented epidemiologic.il
or “health transition” is taking place in the world, and this transition is
responsible for the global increase in NCDs and the “double burden of
disease” (both communicable and noncommunicable diseases) suffered by
the populations of most of the developing countries. They cite data, which
indicate that NCDs have become the main cause of death and disability
throughout the world. They attribute this development to both the positive
aspects of globalization, which have contributed to the aging of the world’s
population through the diffusion of modern medicine and sanitation, and
to the negative aspects of globalization, which have promoted the adoption
of unhealthy lifestyles.
They' also note that the uneven development and social inequalities
associated with globalization are largely responsible for the fact that many
communicable diseases continue to be a major cause of death and disability
in the least developed areas (e.g., in sub-Saharan Africa and South Asia)
and in the poorer sectors of the population throughout the developing
countries. Thus, the poor in these areas suffer the so-called double burden
of disease (both communicable and NCDs) caused by the uneven patterns
of development and “poverty gaps” associated with the global expansion
of capitalism.
However, Finau, Wainiqolo, and Cuboni question the validity of the
“health transition” paradigm that Yach and Beaglehole and other global
health researchers use in their work. They question how much of the
so-called heath transition or what they call the “mortality transition” in
the Pacific countries is really due to the spread of NCDs as opposed
to underlying infectious risk factors, such as the emerging evidence that
certain NCDs may be caused by Heliocobacler pylori, Chlamydia pneumoniae,
and oral bacterial diseases. They also note that, for many Pacificans, the
quality of life they are now living “due to various transitions, may as well
mean that they are dead long before the certification of the expiry of life.”
Finau and his colleagues argue that it is in fact a cluster of various types
of transitions (religious, economic, environmental, political, social, etc.) and
particularly inequitable power relationships established by colonialism and
imperialism that are responsible for the poor health, dependency, and lack
of control over their own socio-economic development suffered by the
Pacific peoples. They blame the contemporary forces of globalization for
reinforcing and masking these determinants of health in the Pacific.
McMurray’s contribution to this collection of essays calls our attention to
the fact that one of the effects of capitalist globalization in the developing
countries is the migration of large numbers of people to the urban areas
................................................ ....................... ■
i. .
Globalization: Health Risks & Responses * 251
ill these countries, where they hope to find wage-earning employment
mid access to modern consumer goods. However, most urban migrants
iirr exposed to poor nutrition, substandard housing, and unsanitary
environments in these urban areas. As McMurray indicates in her essay,
llic limited employment and the low incomes that these migrants generally
earn leave them “no choice but to purchase the cheapest food, which tends
Io be the least nutritious.” Moreover, their consumption of unhealthy foods
is generally combined with their exposure to unsanitary environmental
conditions.
I he problem is that there are very few employment opportunities in the
urban areas and most jobs do not provide an adequate income. As a result,
(here is widespread unemployment, and most people'who are employed
do not earn enough income to maintain a nutritious dietary intake or
healthy lifestyle. McMurray also reveals that under these circumstances
ol urbanization without adequate employment, young people generally
have little incentive to maintain a healthy lifestyle and often engage in
various types of substance abuse and other unhealthy forms of behavior.
Based on her research in the Pacific, McMurray has found that “the
negative impact of urban lifestyles on health is clearly evident in that
l he incidence of early onset NCDs” in the Pacific “is lower in the outer
islands and remote areas ... where traditional foods are consumed and
people are engaged in subsistence agriculture and food gathering.” She
contends that similar conditions “can be observed in peripheral areas
everywhere, including remote and economically depressed areas within
most industrialized countries.”
According to McMurray, the rising incidence of early onset NCDs
among the urban population in the Pacific is “a direct consequence
of global forces that have led to urbanization without industrialization,
idealization of Western lifestyles and imports of cheap food, alcohol and
cigarettes.” She argues that no real improvements in the population health
of the Pacific island nations and other developing countries can be achieved
under these conditions “until their people are empowered and have the
means to choose healthy lifestyles.”
As indicated, Yach and Beaglehole also hold globalization responsible
for the lifestyle changes that have produced the rapid increases in
chronic diseases (especially cardiovascular disease, coronary heart disease,
stroke, cancer, chronic respiratory disease and diabetes) in the developing
countries and the fact that these diseases are now the major components
of the global burden of disease in all regions of the world. Moreover,
they argue that “policy makers and the donor community have neglected
l he rapidly growing burden of chronic diseases” even though they are the
252 • Harris & &id
major cause of death and ill-health in most of the developing as well as the
developed countries of the world.
Yach and Beaglehole contend that these diseases “predominate among
poor populations largely because of inequalities in the distribution of
major chronic disease risk factors.” They claim these risk factors are
“driven by the more fundamental causes of ill health in the socio-economic
environment.” They blame “global forces in trade and marketing” for
promoting “the entrenchment of the causes of these chronic diseases in all
regions.” The health risks they identify are tobacco consumption, unhealthy
diet/nutrition, physical inactivity and alcohol use, as well as the failure
to invest in appropriate prevention and health promotion measures. They
indicate that “most of these risk factors are common to the main categories
of chronic diseases and all are modifiable, albeit with some difficulty.”
According to Yach and Beaglehole, the aging of most populations due
to declining fertility rates and increasing child survival rates (one of the
health benefits of globalization), and the “nutrition transition” to diets that
are high in saturated fats and sugars but low in fruits and vegetables, as
well as smoking and alcohol usage, are being promoted by the forces ol
globalization. They also note that the nutrition transition to unhealthy
diets is generally combined with lower levels of physical activity and
regular tobacco and alcohol consumption. In fact, they cite WHO data
that indicate tobacco and alcohol consumption, high blood pressure, and
high cholesterol levels are the major contributors to the global burden ol'
chronic diseases.
Yach and Beaglehole say that globalization has contributed to the
rise in chronic diseases through a complex array of both direct and
indirect factors. They focus on “the direct negative effects of globalization,”
which they claim are best “illustrated by the increasingly globalized
production, promotion and marketing of tobacco, alcohol and other
products with adverse effects on population health status.” They blame
major transnational corporations and the global communications media
for “the marketing of tobacco, alcohol, sugary and fatty foods” in nearly
all parts of the world. They indicate that “a significant portion of all global
marketing is now targeted at children under the age of 14,” since the
companies that market high sugar and high fat fast foods, cigarettes and
alcoholic beverages seek “to foster brand-loyalty among pre-teens, as young
as six years, and teenagers.”
They give particular emphasis to what they call the “globalization of
die tobacco pandemic,” and the “strong link between increased tobacco
consumption and free trade and tobacco-related foreign direct investment."
Based on their research for the WHO, they have found that “tobacco
companies aggressively exploit the potential for growth in tobacco sales
Globalization: Health Risks & Responses • 253
in developing countries.” They claim this practice is “not surprising since
they are motivated only by their obligations to shareholders.” According to
Yach and Beaglehole, “the main targets of the industry and the associated
marketing campaigns are now young people and women, most of whom
do not smoke.”
Having been closely associated with the WHO’s tobacco control efforts
and the international campaign on behalf of the Framework Convention on
Tobacco Control, Yach and Beaglehole know a great deal about the tactics
that have been used by the transnational tobacco corporations to subvert
and oppose “any effective international regulatory regime” dealing with the
marketing, sale, and consumption of tobacco products. Included among
these tactics are the companies’ frequent public refutation or denial of the
evidence about the harmful effects of smoking and their practice of “paying
scientists to carry out spurious research aimed at confusing the public and
delaying action” to control tobacco marketing and consumption.
Yach and Beaglehole’s research also leads them to conclude that the
“alcohol industry is becoming as globally integrated and pervasive as the
tobacco industry.” They claim that there is a direct link between the
consumption of alcohol and certain cancers, cirrhosis of the liver, and most
injuries, especially motor vehicle-related injuries and injuries resulting from
violence. For this reason, they argue that there is a pressing need for global
action to control the marketing of alcohol to young people, “especially
through its association with sporting events and with gender specific roles.”
Trade Liberalization and the Privatization of Health Care
The essays by Labonte, Badawi and McIntyre, Thomas and Cleary as well
as the contribution by Yach and Beaglehole reveal the adverse effects on
health of multilateral agreements such as the General Agreement on Tariffs
and Trade (GATT), the Technical Barriers to Trade (TBT) Agreement,
the Agreement on the Application of Sanitary and Phytosanitary Measures
(SPS), the Agreement on Trade-Related Intellectual Property Rights
(TRIPS), and the General Agreement on Trade in Services (GATS). The
essay by McIntyre, Thomas, and Cleary reveals how the GATS contributes
to the already existing problem of the migration of skilled health
professionals from South Africa (and other developing countries) to the
developed countries. Their essay also reveals the difficulties TRIPS imposes
on poorer countries that try to import or produce affordable medicines to
fight the disastrous effects of global diseases such as HIV/AIDS.
Badawi states that “access to low-cost, safe and effective essential
drugs is largely threatened by the agreement on TRIPS.” He argues
that “technology transfer, production and global movement of health
commodities are also threatened by the monopoly TRIPS gives to the
254 • Harris & Seid
companies who hold patents protected by the TRIPS agreement.” In fact,
as Labonte indicates, agreements such as TRIPS do not promote “free
trade”; rather they promote the protection and entrenchment of the socalled intellectual property rights and lucrative profits of companies and
individuals in the wealthier developed countries.
Labonte points out that the global “brain drain” of trained health
professionals from the developing to the developed countries has so far cost
the developing countries at least an estimated 500 million US dollars in
training costs. The GATS agreement is likely to accelerate this transfer of
skilled health practitioners from the developing to the developed countries.
Labonte notes that some 54 members of the WTO (including many
developing countries) have so far agreed to liberalize/privatize their health
care systems under the terms of the GATS agreement. The implementation
of the GATS provisions on the “progressive liberalization” of services will
contribute to the regressive privatization of health care systems, promote
the brain drain of health practitioners, and benefit the health of the
wealthier at the expense of the poorer sectors of the population.
The essays by Labonte, Yach and Beaglehole, Loewenson, and Badawi
indicate that the trade liberalization measures and the neoliberal economic
reforms associated with capitalist globalization have shifted a greater
burden of the costs of health care to those who can least afford to assume
these costs: low-paid workers in the export zones and industrialized urban
areas within the developing countries; self-employed and casual workers in
the growing “informal sector” of the economies of these countries; landless
peasants and agricultural workers; and the large numbers of unemployed,
Globalization: Health Risks & Responses • 255
to the population, especially under the “state shrinking” and fiscal
restraints imposed on them by the IMF, the World Bank, and the other
guardians and promoters of globalization. As Loewenson notes, under these
circumstances job-related injuries and ill health generally lead to not only
the loss of employment and household income, but to impoverishment
and the breakdown of the overburdened informal mechanisms of social
protection provided by the extended family and local community.
The privatization of health care has been particularly unkind to the poor
and to low-income households. As Badawi notes in his essay, many people
in the developing countries have been caught between the inability of their
governments to continue providing free public health services and their
own inability to pay the rising costs of basic health care. The forces of
globalization have led governments to reduce their spending on health
and other forms of social protection, to sell off many of their public
health facilities, and to encourage the privatization and commercialization
of health services and products. As a result, there has been a marked
deterioration in the health services of many of these countries and restricted
access to these services—both of which threaten the health of large sectors
of the population.
In the present context of increasing privatization and the promotion of
neoliberal policies at both global and the national levels by the IMF, World
Bank, and the WTO, national government responsibility for providing
basic health care for all members of the population has been replaced by
so-called selective primary health care, public-private partnerships, and the
privatization of health sendees and health care facilities. As the essay by
Narayan and Schuftan indicates, this shift in responsibility for providing
health care is considered by many critics of globalization and the current
trends in health to be a betrayal of the international commitment made
in the late seventies to provide primary health care for all by the year
2000. This was the official commitment made by most of die governments
represented at the 1978 International Health Assembly held at Alma-Ata
in the central Asian republic of what was then the Union of Soviet Socialist
Republics (PHA 2000:1).
The Alma-Ata declaration set forth the goal of achieving “Health for All
by the Year 2000” and charged the health ministries and health workers
around the world with the responsibility for providing comprehensive
primary health care to all the members of their societies by die beginning
of the new millennium. As Narayan and Schuftan indicate in their essay,
the global network of health activists and health advocacy organizations
involved in the People’s Health Movement (PHM) seek to halt the
privatization and commercialization of health care. The PHM holds that
health is a fundamental human right and that national governments have
256 • Harris & Seid
an obligation to ensure universal access to quality health care, education,
and other social services in accordance with people’s needs, not their ability
to pay. They are mobilizing broad-based popular movements around the
world in a global campaign to achieve the goal of “Health for All—Now!”
by pressuring governments to provide comprehensive primary health care
to their populations and incorporate health and other human rights into
their national constitutions and legal systems.
The Health Effects of Dependency, Neocolonialism, and
Western Ideological Paradigms
The essays by McMurray, Narayan and Schuftan, Rak and Janes, and
Finau and his colleagues reveal that Western medicine has been imposed
as the universal standard around the world, and that the health systems of
most developing countries are generally dependent upon the development
assistance they receive from the governments and NGOs of the developed
Western countries as well as international organizations such as the World
Bank and the World Health Organization (WHO). McMurray contends
that the health programs in the Pacific countries “are determined by
global health policies, set by tire World Health Organization and other
health sector donors.” Moreover, she argues that much of the assistance
these programs receive “fosters dependency and imposes conditions” on the
recipients that force them to accept donor policies, practices and medicines
as well as consultants from the donor countries.
Narayan and Schuftan indicate that the People’s Health Movemeni
believes that it has extricated health and health systems around the
world from the “myopic biomedical-techno-managerialism of the last two
decades, with its selective magic bullets approach to health.” The PHM’s
analysis of the political economy of health in the world today (PHA 2001)
lead its advocates to conclude that the most significant determinants ol
health in the world today are economic and political factors that have
colonial roots. Moreover, the movement’s analysis indicates that people’s
health around the world is under a triple assault from globalization,
liberalization, and privatization, which Narayan and Schuftan claim “have
ensured that health for all is a receding dream.” The PHM argues that
“health services today are inaccessible, unaffordable, inequitably distributed
and inappropriate in their emphasis and approach” (PHA 2001:3). The
movement also claims that “health care is increasingly used as a subtle and
widespread instrument of social control,” and that the Western model
or “ideology of medicine ... mystifies the real causes of illness, often
attributing disease to faulty individual behavior or natural misfortune,
rather than to social injustice, economic inequality and oppressive political
systems” (PHA 2001:18).
Globalization: Health Risks & Resporues ,
The essay by Finau, Wainiqolo, and Cuboni as well as the
by McMurray trace the current dependency and Western orientatioi^of
the health care systems in the developing countries to the imposition of
the Western curative model of health care on these societies by their
former Western colonial rulers. They attribute the continued dominance
of Western health policies, standards and practices in these societies
the development assistance they receive from the developed countries th
globalizing influence of Western education and training, and the economic
dependency of these countries on die developed Western countries (as well
as “Westernized” Japan). In fact, as Finau and his colleagues assert in tl
case of the Pacific island societies, many developing countries “are
practically colonies,” and as such they are still subjected to the racis
imperialist domination and exploitation they suffered under colonialism in the health field as well as in other fields.
Finau, Wainiqolo, and Cuboni argue that “imperialists control all pha
and determinants of the health transition” in the Pacific countries
<< ,
5
the
socialization of Pacificans, through foreign education, is another imperial' t
tool to enhance control” over the Pacific peoples. In fact, Fi,,„
fl.
’ mau and
his colleagues take the position that “globalization is the latest label f
capitalism, colonialism and imperialist expansion combined,” and I
regard the ideology of globalization as nothing more than an updated
version of the classic imperialist justification for the Western dominat'
of non-Western peoples formerly known as the “white man’s burde ”
According to Finau, Wainiqolo, and Cuboni most Western-trained healtl
personnel practice, reflect, and promote the Western emphasis on fi u ■
disease at the individual level rather than promoting community health
in a holistic manner. They argue most doctors and nurses are trained
disease fighters to save individuals ratiier than as health promoters to
communities. Imperialist ideologies and logics perpetuate and reproc]
the power imbalance and inequities of the past as well as strengthen tl
pattern of inequitable power relations associated with contemporary for
of imperialism under the guise of globalization.
Rak and Janes’ essay on reproductive health in Mongolia reveals ho
global reproductive health policies, promoted by international NGqs a ]
the governments of developed countries such as the United States i
family planning methods on women in countries such as Mongolia tl < t
often run counter to the beliefs, experiences, and needs of the jo
population. These imposed paternalistic and ethnocentric family plannmethods have ignored local cultural values and devalued the alto- -ln®
°
Lcrnatives
that exist at the local level. Rak and Janes reveal the contradiction '
this approach within the context of Mongolia’s rapidly deteriorating health
services caused by the adoption of market-based reforms, the reduction
258 • Harris & Seid
of the public budget for health care and the privatization of the health
sector.
The Health Effects of the Inequities Promoted by Globalization
At the outset of the new millennium, the WHO noted that “the greatest
burden of health risks is borne by the poor countries, and by the
disadvantaged in all societies” (WHO 2002:13). These sectors of the world’s
population have the misfortune of suffering the health effects of poverty as
well as well as the other social and economic inequities that characterize
the present era of capitalist global expansion and integration. Most of the
essays in this collection reveal that globalization is associated with economic
policies that create, reinforce, and intensify the inequities in health found
throughout the world. Thus, Loewenson states in her essay that “within
the current processes of globalization, inequality is not simply happening
but is being constructed by powerful economic and political interests and
public policies” that keep the benefits of globalization from reaching those
who need them the most. Finau, Wainiqolo, and Cuboni contend that the
economic and social inequities (including the health inequities) that the
Pacific peoples have inherited from colonial rule are reinforced today by
the contemporary forces of globalization, which they hold responsible for
the continuation of Western imperialism.
McIntyre, Thomas, and Cleary reveal in their essay how the struggle to
overcome the “legacy of massive inequalities in income, health status and
access to health and other social services” resulting from South Africa’s
colonial, racist, and repressive past has been hindered by the contemporary
forces of globalization. Moreover, they reveal that it is not just the obvious
forms of global intervention such as IMF loan conditions, externally
enforced compliance with the TRIPS Agreement on patented HIV/AIDS
medicines, and the World Bank’s privatization of health care programs that
exacerbate the existing inequities in South Africa. It is also the more subdc
and indirect influences of globalization that have led the post-apartheid
government in South Africa to adopt “self-imposed” structural adjustments
in order not to run afoul of die major forces in the global economy. These
self-imposed policies and practices tend to reinforce the health inequities
created by centuries of colonialism, racism, and European domination on
the African continent.
The essay by McIntyre and her colleagues reveals the extent to which
the global trend towards the privatization of health care and the indirect
impact of global health actors on the health sector in South Africa have
contributed to the “rapid and uncontrolled growth of the private sector,”
which in turn “has contributed to disparities in health service access
and the health of South Africans.” Today, less than 20 percent of the
Globalization: Health Risks & Responses • 259
population has access to more than 60 percent of the financial resources for
health care, while the remaining 80 percent of the population have access
to less than 40 percent of the financial resources devoted to health care
in the country. Moreover, only one-fourth of the doctors in the country
work in the public health sector, which serves the historically disadvantaged
majority of the population.
Rak and Janes premise their analysis of the global discourse on
reproductive health and its application to Mongolia on the assertion that
poverty in its modern sense was created in the developing countries by the
spread of the market economy and years of colonial rule, and they argue
that the current policies to “develop” these countries “have exacerbated the
divide between the rich and the poor.” Since the country adopted market
reforms, privatization, and the integration of its economy into the global
capitalist economic system, Mongolia has experienced a rapid deterioration
in its health services, increasing social inequality, and a high level of male
unemployment. Rak and Janes conclude that “it has taken the transition
from a socialist to a market economy, led by the intervention of the global
financial and policy institutions of the developed world, to create Mongolia
as a Third World country.”
The PHM, as Narayan and Schuftan’s essay explains, sees a direct re
lationship between existing health inequities and globalization. The mem
bers of this global movement consider inequality, poverty, exploitation,
violence and injustice as the root causes of ill health in the world today. As
Narayan and Schuftan make clear in their discussion of the People’s Char
ter for Health, achievement of the PHM’s goal of “Health for All—Now!”
requires “challenging the powerful economic interests that dominant the
existing global order, opposing globalization in its existing iniquitous form,
and drastically changing the political and economic priorities at all levels
of the global system.”
The Environmental Health Effects of Globalization
The wide variety and scope of globalization’s environmental effects make
it difficult to provide a sufficiently comprehensive analysis of these effects
in any single book or collection of essays. This collection of essays does
little more than scratch the surface of the health impact of some of the
more complex and far-reaching environmental effects of globalization,
such as global climate change, the depletion of the ozone layer, and the
contamination of oceans, lakes, and rivers around the world.
As we indicated in our introductory essay to this collection, there
is mounting evidence that the global diffusion of capitalist patterns of
production and consumption developed in the Western industrial societies
has created a multitude of environmental problems. In a research study
260 • Harris & Seid
undertaken by Diaz-Bonilla and his colleagues on the health risks of the
poor in developing countries, they claim that “poor environmental quality
has been calculated to be directly responsible for around 25 percent
of all preventable ill-health in the world today” (Diaz-Bonilla et al.
2002:38). They attribute much of this “poor environmental quality” to
the environmental “spill-over” effects of economic globalization.
Many of the essays in this collection recognize the threats to health posed
by the environmental effects of globalization. For example, Badawi notes
that environmental threats to health have resulted from the increasing
international trade in technology, capital, goods, services and labor. He
notes that many “environmentally unfriendly” industries have moved
from the developed to the developing countries, where there is generally
less concern about the health hazards caused by their technology and
often a lack of environmental health safeguards. Badawi also states
that the over exploitation of fishing licenses, deforestation, industrial
waste, and the dumping of health-hazardous materials are part of a
long list of environmental health threats confronting the populations of
the developing countries. Moreover, he warns that the indigenous germ
pool and medicinal plants in the developing countries are threatened
by the “commercial exploitation” of giant transnational corporations and
warns that “genetically modified organisms, microbiological pathogens and
hazards in animal production represent a real health risk for the developing
countries.”
Finau, Wainiqolo, and Cuboni contend that the cultivation of cash
crops, mining, and industrialization threaten the fragile environment of
the Pacific islands, and they say the “green house effect and rising sea
levels caused by metropolitan modern societies’ efforts to maintain their
consumption level are threatening the Pacificans’ habitat.” They also claim
that the environments in these societies “have become obesogenic, toxic
and insecure, due to crime and violence.” As a result, the Pacific countries
are undergoing what they refer to as an “environmental transition” that has
brought about “not only physical and social changes, but also developed
uncertainty and stress in the Pacific psyche.”
McMurray’s essay analyzes the effects of globalization on environmental
health in the Pacific and other developing countries. She notes that
“modernization” and globalization are responsible for the development
of urban areas and the increasing concentration of the population in
these areas. She cites United Nations data that indicate most developed
countries now have 70 percent or more of their population concentrated
in urban areas and that the number of these areas is increasing in most
countries. One of the environmental health problems created by this
increasing urbanization of the population and the globalization of these
Globalization: Health Risks & Responses • 261
societies is that they have adopted the costly portable water and sanitation
systems of the most developed countries in most of their urban areas, as
a result of their colonial legacy and/or the development assistance they
have received in recent decades. McMurray indicates that they now have
difficulty maintaining and extending these systems because they lack the
resources and technology needed to do this. She gives various examples of
the rising problems of pollution and contamination in the urban areas of
the Pacific resulting from the breakdown of their sewage and piped water
systems.
Loewenson’s essay on the health and safety aspects of working conditions
in Southern Africa reveals that most workers in this region of the
world “continue to experience work related hazards that have long been
controlled or even eliminated in high income countries.” According to
Loewenson, “the expansion of chemical, electronic and bio-technology
industries and of the service and transport sectors ... widened the spread of
work-related risks and their interaction with non work factors of ill health,
including environmental pollution.” Employment in the large informal
economy exposes workers in this sector to the health risks associated with
“poor access to clean water and sanitation, ergonomic hazards, hazardous
hand-tools and exposure to dusts and chemicals.” Loewenson also points
out that work in the agriculture, mining, and manufacturing sectors within
the southern African economies is associated with high rates of injury from
the mechanical, electrical, and physical hazards in their work environment.
The essays by Badawi, Labonte, Loewenson, McMurray, and Finau
and his colleagues acknowledge the fact that globalization and trade
liberalization have promoted the deregulation of production, health, and
die environment. These forces have seriously weakened the capacity of the
public sector to respond to the environmental and occupational health risks
posed by industry, mining, transportation/shipping, and commercialized
agriculture; they also have undermined the already inadequate forms of
worker protection and social protection (including health) in existence in
these countries.
Labonte’s essay argues that environmental issues are becoming “inher
ently global” and are no longer purely national or domestic issues. He
notes that the “environmental impacts of human activities are planetary in
scale and scope” and that “almost one-sixdi of humanity is on die move
to escape environmental or economic degradation and conflict.” Labonte
sees this situation as evidence of the need for global solutions to these
problems.
262 • Hams & Seid
Community Health Care, Grassroots Action, and Globalization
from below
As Finau, Wainiqolo and Cuboni contend in their essay, community
based, grassroots, and ethnic-specific health care has improved the access,
acceptability, availability, and affordability of the health care provided to
the communities it serves. This model of health care has also improved the
effectiveness, efficiency, efficacy, and equity of the health services provided
to these populations through changing the power relationships between the
health care providers and receivers. They argue that this model of health
care addresses the oppression and assimilation implanted by Western
colonialism and “borne by imperialism through globalization.” According
to Finau and his colleagues, community-based health care releases the
participants from the oppression of the Western health care model imposed
first by Western colonialism, and more recendy by contemporary forms
of imperialism under the guise of globalization (e.g., the globalization of
Western medical education and training, the transfer of Western medical
knowledge and technology, the bureaucratization and privatization of
health care along Western lines).
Narayan and Schuftan’s essay on the People’s Health Movement (PHM)
reveals the emphasis this new movement gives to community control of
health care, grassroots action, and global action based on the use of
international health advocacy networks. These are important elements in
the movement’s global campaign to combat the health inequities associated
with globalization and to make sure that universal access to comprehensive
primary health care is provided everywhere in the world. This movement
is engaged in what amounts to “globalization from below” as it builds
support for its global Health for All—Now strategy, lobbies at the global
level, and mobilizes a grassroots-based campaign to realize the vision and
achieve the goals of the People’s Charter for Health.
The Charter, which is the PHM’s visionary statement of goals and its
main tool for advocacy, calls for “a people-centered health sector that
is democratic and accountable” (PHA 2000:9). The Charter calls on the
people of the world to: (1) build and strengthen people’s organizations
as a basis for analysis and action; (2) promote, support, and engage in
actions that encourage people’s involvement in decision-making in public
services at all levels; (3) demand that people’s organizations be represented
in local, national and international fora that are relevant to health; and
(4) support local initiatives towards participatory democracy through the
establishment of people-centered solidarity networks across the world (PHA
2000:10). One of the primary principles of the Charter is the proposition
that “the participation of people and people’s organizations is essential to
Globalization: Health Risks & Responses • 263
the formulation, implementation and evaluation of all health and social
policies and programs” (PFIA 2000:4).
McIntyre, Thomas, and Cleary conclude in their essay that “the growth
in number, size and power of civil society organizations combined with the
increased networking of these organizations across national boundaries”
is having a “countervailing effect” on the negative health impacts of
globalization. They give the example of how civil society organizations in
South Africa gained the support of civil society groups in the Untied States
to pressure the US government into dropping its efforts to convince tire
South African government to change its policy relating to the importation
of medicines so that it would not contravene the TRIPS agreement. They
show how these groups in South Africa also teamed up with international
groups such as Medecins sans Frontieres and Health Action International
to oppose the efforts of the transnational pharmaceutical corporations
(with the support of their host governments) to pressure the South Africa
government and the governments of other developing countries (such as
Thailand) into restricting their use of certain provisions in the TRIPS
agreement that permit governments to obtain urgently needed patented
medicines at reduced prices.
The adverse effects of existing international trade agreements on health,
human rights, and the environment have been subjected to increasing
public criticism in recent years. As Labonte notes in his essay these
agreements have “become the focus for progressive social movements.”
The global networking and collaboration that have developed among these
social movements, such as the PHM, represent a form of “globalization
from below” that is rising up to challenge the “globalization from
above” imposed by the transnational corporations and their allies in
the IMF, World Bank, WTO, the Group of 8 governments (led by
the US government), and certain large international non-governmental
organizations that are closely associated with these forces.
Labonte notes in his essay that the WTO has been besieged by a broad
coalition of forces that are opposed to its global trade liberalization agenda.
He argues that there are several reforms in the global trade regime that
health activists in league with other progressive forces are promoting in
their efforts to change the current effects of the WTO’s trade liberalization
efforts. These reforms would:
• Extend “special and differential” trade agreement exemptions for
developing countries;
• Ban the patenting of life forms, exempt patent protection legislation
for poor countries indefinitely, decrease the patent protection period
and permit parallel importing under the TRIPS agreement;
264 • Harris & Seid
• Impose a Tobin Tax (named after the Nobel economist who first
proposed this idea) on international currency exchange transactions to
raise about US S150 billion annually for an international development
fund;
• Negotiate an overarching and enforceable rule in trade agreements
that would require, when there is any conflict, for environmental and
human rights agreements (including the right to health) to override
the trade agreements; and
• Exclude health, education and other essential services (such as water
and sanitation) from privatization since they are essential to human
life and health.
In addition, Labonte argues that the WTO needs to be overhauled by
making its decision-making more democratic and transparent. However,
he disagrees with those activists and social movements who are calling for
its abolition. He contends that this would be a mistake since “there is no
other vehicle where the unequal balance of economic power globally might
be subject to enforceable change.” Labonte believes that the struggles of
civil society organizations and the developing countries “to wrest reforms
from the WTO are giving rise to a new system of global governance for
the common good.”
The Current State of Global Health Governance
As Labonte points out in his essay, social, economic, environmental and
health issues are becoming “inherendy global” rather than purely national
or domestic. He argues that the evidence in favor of the need for global
solutions to these issues is irrefutable, including the evidence about the
rapid spread of infectious diseases, the increased adoption of unhealthy
lifestyles, and the increasing international promotion of unhealthy foods
and products such as tobacco and alcohol. Labonte concludes that “we live
in the most important historical moment of our species, [since] the planet
is dying, there is excessive affluence and poverty, [and] once far-away
conflicts and diseases are imperiling global health and security.” Faced
with this unprecedented situation, he optimistically contends that “we are
struggling forward to some system of global governance for our common
good.”
Yach and Beaglehole take a similar position. They conclude that the
global diffusion of the major risks of chronic diseases is now almost
complete and the prevalence of these diseases is increasing in most regions
of the world. They contend, however, that the prevention and control of
these diseases have not been able to keep pace with their globalization
and growth. Therefore, they conclude that sustained progress against these
diseases “will only occur when governments and influential international
Globalization: Health Risks & Responses • 265
bodies involved in health policy and funding acknowledge that the scope of
global public health must be rapidly broadened to include chronic diseases
and their risk factors.”
Based on their experience in the ongoing struggle over the international
control of tobacco, Yach and Beaglehole predict that “progress will
continue to be slow unless the response to the epidemics [of chronic
diseases] is scaled up in a manner commensurate with their burden on
both families and societies” around the world. They believe that global
solutions are needed to address the global health risks responsible for the
epidemics of chronic disease that are taking place around the world.
However, Yach and Beaglehole argue that the global health agenda is
currently dominated by what they call “the infectious disease paradigm.”
The main global health organizations and funding sources believe priority
should be given to the prevention and treatment of infectious or communi
cable diseases before addressing chronic diseases. Because most institutional
responses to disease prevention and control are based on this infectious dis
ease paradigm, Yach and Beaglehole argue that the global and national
responses to the spread of chronic diseases are “woefully inadequate and
few countries have implemented comprehensive prevention and control
policies.”
They contend that a comprehensive response that combats all the health
risks responsible for the global spread of chronic diseases is necessary,
and they argue this response must overcome the “powerful countervailing
forces” that presently stand in the way of changing the status quo.
According to Yach and Beaglehole, a successful global response to the
existing configuration of major health risks has to overcome the “many
powerful and persuasive commercial entities involved in the production
and promotion of unhealthy products.” They claim these entities “exert
an adverse influence on health policy developments” as well as on the
development and implementation of environmental policies.
Yach and Beaglehole conclude that “stronger and broader alliances of
major health professional bodies, consumer groups, enlightened industries
and academics are now needed to effectively prioritize the prevention of
the major risk factors” responsible for the global spread of chronic diseases.
They suggest that the global campaign for tobacco control provides a
successful model for how to organize a comprehensive response to the
global spread of chronic diseases.
Yach and Beaglehole ultimately conclude that there is an increasing
need to establish global norms on a wide range of global issues “to
balance the otherwise unrestrained influences of powerful actors.” They
argue that, if the WHO is strengthened it can be used to establish these
norms in the health sphere and then use the norms to resolve trade
266 • Harris & Said
disputes and other health-related global issues in a manner that promotes
positive health outcomes. However, they do not think the WHO and
national governments alone can address the challenges of chronic disease
prevention and control. As in the case of tobacco control, they believe
collaborative partnerships and interaction are needed with international
consumer advocacy groups, international and national sports federations,
sporting goods companies, transnational food corporations, retail food
businesses, and insurance companies to improve the quality and access
of people to healthy foods and increased physical activity. They advocate
a consultative and “multi-stakeholder approach” with all interested parties
as well as joint initiatives with the transnational food companies rather
than an adversarial relationship. However, they recognize the dangers and
difficulties that are involved in this approach.
Badawi’s essay urges the developing countries to make more effective
use of the provisions in the WTO agreements (the GATT, GATS, TBT,
and .Anti-Dumping agreement) that allow for “special and transitional
arrangements.” He contends that they can take the “compensatory
actions” allowed under these agreements to limit the negative effects
of globalization on their economies, environments, and protective social
services. Badawi says that, unfortunately, these agreements are not well
studied by policymakers and specialists in the developing countries. He
recommends that they develop their national capacity and expertise for
“expert reading” of the provisions of these agreements so that they can
use their special exemptions to protect what he and the International
Labor Organization refer to as the “social dimension” (social protection
and social services such as health) as well as the environmental health of
their populations.
Badawi also argues that the developing countries need to “cooperate
and consult with other developing and developed countries to influence
decision-making” at the WTO, the WHO, and other global institutions
as well as to negotiate multilateral and bilateral agreements that confront
the health hazards posed by globalization. Moreover, he argues that the
governments of the developing countries, contrary to the prevailing feeling
that [they] have lost control of their mandates, must, “adopt the measures
necessary to protect the public interests in the environment, public health
and nutrition.”
Loewenson argues in her essay that “there is a growing understanding
that global security and equity cannot be built on the significant burdens
of deprivation borne by communities in the south,” and that “globalization
has produced powerful tools, new communications technologies, more
widely connected social movements and an increasingly global recognition
of universal rights as fundamental to policy.” She contends that the full
Globalization: Health Risks & Responses * 267
potential of these tools can be used to create concerted global action
to protect workers’ health. The democratization and extension of the
enforcement powers of international agencies such as the ILO and WHO
would certainly help to improve die social protection of workers and
the many other sectors of the world’s population that are being harmed
and disadvantaged by the global expansion and integration of twenty-first
century capitalism.
Most global health advocates argue that a genuinely health-centered (and
people-centered) process of globalization can be achieved only by ensuring
that the interests of the developing countries and vulnerable populations are
fully represented in all international decision-making on global health issues
(Woodward et al. 2001:880). According to Badawi, Labonte, and Yach
and Beaglehole, the democratization of decision-making in the existing
international regulatory and financial organizations such as the WTO,
IMF, and World Bank is needed to transform these institutions into global
governance institutions that will advance the interests of the great majority
of the world’s population rather than the interests of the powerful economic
elites they now represent.
Alternatives to the Globalization of Health from above
The People’s Health Movement (PHM) is clear evidence that die existing
linkages between globalization and health are contestable. In fact, most
of die essays in this collection indicate that the adverse health effects
of globalization are being challenged at the global, national, and local
levels. The People’s Healdi Movement and the People’s Charter for Health
provide a significant expression of alternatives “from below” to the present
globalization, privatization and commercialization of health coming “from
above.” As Narayan and Schuftan state in their essay, this People’s Charter
for Health provides a vision of a better and healthier world, a call for
radical action, a tool for advocacy for people’s health, and a rallying point
for building a global health movement based on international networks
and coalition building.
The People’s Charter for Health lays out a blue print for the
transformation of the existing global order through democratization at
all levels of the existing system and through what some people in the
global social justice movement call “globalization from below” (Brecher,
Costello, and Smith 2000). It is based on the fundamental, but radical,
assumption that “to ensure health, people’s basic needs for food, water,
sanitation, housing, health services, education, employment and security
must be met” in the present time frame (PHA 2001:1). In addition, it
is based on the assumptions that global decisions must be democratized
and that people’s organizations and organized grassroots action can bring
268 • Harris & Setd
about an “alternative vision of development—one that promotes human
and environmental well-being” (PHA 2001:3). To achieve this vision, the
PHM is pursing the democratization of health decisions and outcomes at
all levels.
According to Narayan and Schuftan, the Charter for People’s Health
calls upon national governments and global institutions to recognize health
as a fundamental human right and as a social, economic, and political
issue deserving the highest priority. It also identifies inequality, poverty,
exploitation, violence, and injustice as the roots of ill-health, and it makes
clear that the achievement of universal access to primary health care
requires challenging powerful economic interests; opposing privatization
and globalization (in its present inequitable form); and drastically changing
the prevailing political and economic priorities at all levels in the global
order.
The Charter also makes it clear that the PHM wants the poor and
marginalized (rarely heard) peoples throughout tire world to participate in
health decision-making and develop their own local solutions to their health
problems. The movement encourages people to hold local authorities,
national governments, and international organizations and corporations
accountable for ensuring that the goal of Health for All is achieved
now, not at some distant point in the future. However, even though the
PHM firmly believes national governments have the primary responsibility
for promoting an equitable approach to health and human rights, the
movement knows that it will take pressure from people’s organizations to
force their governments to meet this responsibility. This statement reflects
one of the most important strategic assumptions held by the PHM: that
it will take organized grassroots action as well as concerted action at the
global level to bring about the profound social changes that are needed to
achieve the sweeping .vision and radical goals of the movement.
All the essays in this collection provide suggestions and/or proposals
for creating alternatives to the present conditions, in which the adverse
effects of globalization threaten the health of people around the world
and the planet’s ecological sustainability. In their essay Finau, Wainiqolo,
and Cuborti provide a series of models or strategies for thinking about
the management of change in the field of health. They are all based
on the assumption that change is inevitable and that the present power
imbalances in the world must be changed in order for substantial progress
to be achieved in the domain of health as well as in the other major
domains of human existence.
These models/strategies provide useful conceptual tools for thinking
about alternatives to the present global patterns and direction of change
in health. We hope that this entire collection of essays serves the same
Globalization: Health Risks & Responses *269
purpose as the models presented by Finau, Wainiqolo, and Cuboni—that
it contributes not only to the ongoing discourse on globalization and health
but also to the efforts that are being made around the world to find
alternatives to the adverse effects of globalization on the health of the
planet’s human population as well as the sustainability of its biosphere.
References
Brecher, Jeremy, Tim Costello and Brendan Smith
2000
Globalization from Below. Boston: South End Press.
Cornia, Giovanni
2001
“Globalization and Health: Results and Options.” Bulletin of the World Health
Organization 79: 834-841.
Diaz-Bonilla, Eugenio, Julie Babinard and Per Pinstrup-Andersen
2002
“Opportunities and Risks for the Poor in Developing Countries” (Working
Paper 83). Indian Council for Research on International Economic Relations,
New Delhi, India. Retrieved December 9, 2002 (http://www.icrier.res.in/
pdf/risk.pdf).
Drager, Nick, Ronald Labonte and Renee Torgerson
“Frameworks for Analyzing the Links Between Globalization and Health”
(Draft Document). Retrieved March 30, 2002 (http://dev.www.uregina.ca/
spheru/PDF%20Files/Labontc-Framcworks-Links.PDF).
People’s Health assembly (PHA)
2000
People’s Charter for Health. Bangalore, India: PHM Secretariat.
2001
“Health in the Era of Globalization: From Victims to Protagonists.” A Dis
cussion Paper prepared by the PHA drafting group. Savar, Bangladesh. PHA
Secretariat, Gonoshasthaya Kendra.
2002
Woodward, David, Nick Drager, Robert Beaglehole and Debra Lipson
2001
“Globalization and Health: A Framework for Analysis and Action.” Bulletin of
the World Health Organization 79: 875-880.
<Lo r-A V V —
Globalization: Health Risks & Responses • 215
The Globalization of Health: Risks,
Responses, and Alternatives
Dr. Richard L. Harris* and
Dr. Melinda J. Slid**
Abstract
This essay provides a summary and synthesis of the wealth
of information, analysis, and conclusions provided by the othui
contributors to this collection of essays on globalization and
health. The major themes addressed arc the health risks and
health effects of globalization, the responses to these risks and
effects at the national and global levels, and the alternatives
to the present patterns of globalization in which the health of
billions of people around die world and the planet’s ecological
susiainabilitv arc threatened.
Introduction
In the introduction to this collection of essays on globalizaiioi ;m<i health,
we pointed out (hat, according to the existing literature on. giobalizmion
and health, it is generally accepted that certain aspects ol globalization
have “enhanced health and life expectancy in many populations,’ whihother aspects of globalization “jeopardize population health \ia the ero.Tni
of social and environmental conditions, the global division of lai •>. thexacerbation ol the rich-poor gap between mid within cGi.in tries. .nd i h
accelerating spread of consumerism” (McMichael and Buaglrboic '.'l in1,.
These threatening aspects of globalization present rnajoi chailcng-s foi
* Glob.
*!
S'.uJ’f' Program. California Suite University. Monterey Ba.. Srasidv. (Mi::- -ik i.
’Health Scirm •
California. USA.
Program, California Slate I riversilv, S.irr:ri;«-s’«
Rtfsbedt:, ■ on Global 1 )ti'elo[mn:nt and Technology. I'alunie
© 2001 Idniiuklijh Brill JW, IHden
issue I 1'
Su
:.c •
246 • Hams c? Seid
health researchers, practitioners, and policymakers today, and they arc the.
major focus of this collection of essays.
The contributors to this collection of essays on globalization and health
provide a wealth of information, analyses and conclusions on many of
the health risks and health effects of globalization, on the responses to
these risks and effects, and on the search for alternatives to how the
contemporary forces of globalization affect health around the world today.
In the pages that follow, we provide a summary and synthesis of the major
findings on these themes that the contributors to this collection of essays
have reported in the preceding pages.
The Health Benefits and Risks Associated with Globalization
Most of the contributors to this collection of essays agree that there have
been some significant health benefits from globalization. For example,
Badawi, Labonte, McMurray, Smith, and Yach and Beaglehole acknowl
edge in their essays that the global diffusion of new health-related knowl
edge and technologies as a result of international trade and investments
has contributed to disease surveillance, treatment and prevention around
the world as well as the spread of sanitation and vaccines that have greatly
reduced the threat of many deadly diseases.
McMurray states in her essay that “there is no doubt the spread of
Western medicine through out the world and the implementation of
global health programs has brought numerous benefits”; however, she also
points out that “at the same time, globalization has promoted patterns
of dependency, development, settlement and lifestyles that have been
detrimental to health.” Smith’s essay reveals how new information and
communication technologies (ICT) are being applied to healthcare in some
of the more remote areas of the Pacific islands, and he argues that these
technologies have the potential to provide “a remarkable expansion of the
medical expertise available to act in a curative manner” and to advance
preventative healthcare in these remote areas of the world. However,
Smith’s essay also reveals how these technologies, which arc a central
feature of globalization, are a “two-edged sword.”
On the one side of the sword, the new information technologies and
Internet connectivity’ enhance the provision of healthcare to people ;n
remote and marginalized areas, but on the other side, they reinforce
the neocolonial ties and unequal power relationship that exist between
these areas and the developed core economies. They also transmit the
more negative aspects of the consumerist life-styles associated with these
economies.
The essay by Finau, Wainiqolo, and Cuboni focuses on how the
“changes in health of Pacificans are about the power imbalances brought
—
1
1
;
ab<
cot
pr<
“tc
'
str
In
i
Rt
!
j
■
sh
as •
th
I
'
m
N
i
va>
|
11‘
i
o
is
L
I
■
■
;■
>•
j
I
1
Globalization: Health Risks & Responses • 24 7
about by globalization, imperialism and colonialism.” They see “the
continuance of colonialism and imperialism in different forms” in the
present context of globalization. They also argue that many contemporary
“technologies and ideologies contribute to the reproduction and the
strengthening of the pattern of power relations that feed imperialism.”
In their essay on women’s reproductive health in post-transition Mongolia,
Rak and Janes provide an example of how this works. Their research
shows how the global discourse on family planning and reproductive health
as well as global reproductive health policies are based on assumptions
that “fail to consider the local cultural context of reproductive decision
making, do not meet women’s needs, and are therefore seriously flawed.”
Nevertheless, external donors and consultants who are in a very real sense
the agents of globalization in this case are imposing these global norms
and policies on women in Mongolia.
Most of the contributors to this collection of essays reveal either explicitly
or implicitly that, in fact, what is generally referred to as “globalization”
is none other than the global expansion and integration of contemporary
forms of capitalist production, distribution, and consumption. Their essays
reveal that the global expansion and integration of twenty-first century
capitalism involves not only the global diffusion of certain technologies,
products, and practices, it also involves the global dissemination of certain
ideologies and cultural norms.
Together, these forces of capitalist globalization have inadvertently or
purposively promoted the following types of global health risks:
o I’he global spread of various communicable and noncommunicable
diseases.
o The global promotion of unhealthy products and practices.
o The global diffusion of a wide range of technologies and production
processes that arc hazardous both to human health and to the health
of the natural environment.
• The global promotion of inequitable forms of private health care and
the commercialization of health services and medicines that place
them beyond the reach of large sectors of the world’s population.
c The global diffusion of Western nonns, practices, and ideological
models/paradigms of health care that often conflict with local values
and needs and that create/reinforce inequitable power relationships
and social inequities.
As we learn more about these and other adverse health effects of the global
expansion and integration of modern capitalism, it is clear that many of the
contemporary effects of the globalization of twenty-first century capitalism
are a serious threat to not only the health of billions of people around the
world but also to the sustainability of the planet’s entire biosphere.
As Labonte points out in his essay, we have now lived through
more than twenty years in which the global diffusion oh knowledge
and technology has taken place under a neoliberal capitalist regime
of trade liberalization and global economic integration; yet the health
impacts of this process of liberalization and globalization have been largely
negative, especially the effects of this process on what Labonte refers
to as the two fundamental health-determining pathways of globalization:
poverty/inequality and environmental sustainability.
The liberalization and globalization of the economies of many develop
ing countries have been accompanied by a corresponding increase in the
poverty, environmental degradation, and poor health of a large proportion
of the population. Loewenson notes in her essay that the incomes of a
quarter of the world’s population declined at the end of the last millen
nium when globalization was going at top speed. Even many of the positive
effects of the global expansion and integration of capitalism have adverse
consequences. Labonte’s essay gives the example of how the opening of the
economies of many developing countries to international trade and invest
ment has increased the access of women to wage-earning employment and
contributed to their empowerment in gender relations. However, he points
out that more often than not they are employed in low-paid, unhealthy and
insecure jobs, frequendy in so-called free trade export zones where labor
organizations are prohibited and only single young women are employed
under hazardous working conditions (and often exploited and sexually ha
rassed). Loewenson reports in her essay that these young women have
been documented to experience high levels of job stress and reproductive
health problems, including miscarriages, problems with pregnancies, and
poor fetal health.
McMurray’s essay illustrates how the globalization of capitalism inten
sifies disparities in health between and within nations and also how it
can create paradoxical health outcomes in the most peripheral areas of
the global capitalist economy. Her essay reveals that in the smallest and
most remote countries within the global system, such as the Pacific island
countries, the negative health effects of capitalist globalization impact the
population more in the globalized (Westernized) and urbanized core areas
than in the thinly populated and more peripheral rural areas that have less
access to modem health services but relatively better environmental health
conditions. McMurray focuses on how globalization affects these societies
through, “first, its impact on environmental quality, second, its impact on
the quality and accessibility of health services, and third, its promotion of
unhealthy lifestyles.”
As Labonte’s essay and our own introductory essay in this collection
indicate, the extent to which the forces of globalization affect the health
Globalization: Health Risks & Responses • 24 9
of the population in individual countries depends upon the prevailing
economic, social, and political conditions in these countries; their level of
technological and economic development; and their natural endowments
(Cornia 2001; Drager, Labonte, and Torgerson 2002; Woodward et al.
2001). These indigenous factors mediate most of the direct effects of
globalization on the national/domestic level as well as many of the indirect
effects of globalization on the community and household levels.
Labonte’s essay reveals that the forces of capitalist globalization affect
population health at the national level through various channels or
pathways, such as externally imposed macroeconomic policies (e.g., IMF
structural adjustment programs and monetary policies), the enforcement
of trade agreements, the flows of trade associated with these agreements,
official development assistance (from the United States and other major
“donor” countries), the international transfer of health-related knowledge
and information, and the influence of the global communications and
entertainment media. There are also “environmental pathways” through
which capitalist globalization affects health. These pathways include crossborder pollution, the depletion/coniamination of natural resources (water,
the soil, fish stocks, and forests), and the destruction of the biodiversity
in local ecosystems. Many of the essays in this collection touch upon the
health effects of these environmental pathways of globalization.
Globalization and Life Style Changes
j
|
1
Most of the essays in this collection support the thesis that certain
contemporary patterns of death and disability arc caused by the lifestyle
changes promoted by globalization, particularly the increased consumption
of unhealthy processed foods and products. These lifestyle changes and
particularly the unhealthy consumption patterns they entail are, as Yach
and Beaglehole demonstrate in their essay, contributing to an alarming
global increase in chronic and noncommunicable diseases (NCDs)—the
so-called diseases of affluence (although they arc increasingly suffered by
the poor). McMurray, Smith, and Finan and his colleagues all address
the negative health impact of these lifcstvlc changes and the increased
consumption of unhealthy foods, especially in the island nations of the
Pacific.
All three essays on the Pacific call attention to the health effects of both
the disruptive changes and the uneven pattern of economic and social
development that have been promoted in the developing countries by
contemporary forms of capitalist investment, trade and production. Finan,
Wainiqolo and Cuboni emphasize the disruptive and destructive nature
of many of these changes and attribute them to the Western capitalist
model of development that has been imposed on the Pacific peoples by
colonialism, imperialism, and globalization.
According to \ ach and Beaglehole, an unprecedented epidemiological
or “health transition” is taking place in the world, and this transition is
responsible for the global increase in NCDs and the “double burden of
disease” (both communicable and noncommunicablc diseases) suffered by
the populations of most of the developing countries. They cite data, which
indicate that NCDs have become the main cause of death and disability
throughout the world. They attribute this development to both the positive
aspects of globalization, which have contributed to the aging of the world’s
population through the diffusion of modern medicine and sanitation, and
to the negative aspects of globalization, which have promoted the adoption
of unhealthy lifestyles.
They also note that the uneven development and social inequalities
associated with globalization arc largely responsible for the fact that many
communicable diseases continue to be a major cause of death and disability
in the least developed areas (c.g., in sub-Saharan Africa and South Asia)
and in the poorer sectors of the population throughout the developing
countries. Thus, the poor in these areas suffer the so-called double burden
of disease (both communicable and NCDs) caused by the uneven patterns
of development and “poverty gaps” associated with the global expansion
of capitalism.
However, Finan, Wainiqolo, and Cuboni question the validity of the
“health transition” paradigm that Yach and Beaglehole and other global
health researchers use in their work. They question how much of the
so-called heath transition or what they call the “mortality transition” in
the Pacific countries is really due to the spread of NCDs as opposed
to underlying infectious risk factors, such as the emerging evidence that
certain NCDs may be caused by Heliocobacler pylori, Chlamydia pneumoniae,
and oral bacterial diseases. They also note that, for many Pacificans, the
quality of life they are now living “due to various transitions, may as well
mean that they are dead long before the certification of the expiiy of life.”
Finau and his colleagues argue that it is in fact a cluster of various types
of transitions (religious, economic, environmental, political, social, etc.) and
particularly inequitable power relationships established by colonialism and
imperialism that arc responsible for the poor health, dependency, and lack
of control over their own socio-economic development suffered by the
Pacific peoples. They blame the contemporary forces of globalization for
reinforcing and masking these determinants of health in the Pacific.
McMurray’s contribution to this collection of essays calls our attention to
the fact that one of the effects of capitalist globalization in the developing
countries is the migration of large numbers of people to the urban areas
Globalization: Health Risks & Responses • 251
in these countries, where they hope to find wage-earning employment
and access to modern consumer goods. However, most urban migrants
are exposed to poor nutrition, substandard housing, and unsanitary
environments in these urban areas. As McMurray indicates in her essay.
the limited employment and the low incomes that these migrants generally
earn leave them "no choice but to purchase the cheapest food, which tends
to be the least nutritious.” Moreover, their consumption of unhealthy foods
is generally combined with their exposure to unsanitarv environmental
conditions.
The problem is that there are very few employment opportunities in the
urban areas and most jobs do not provide an adequate income. As a result,
there is widespread unemployment, and most people who arc employed
do not earn enough income to maintain a nutritious dietan- intake or
healthy lifestyle. McMurray also reveals that under these circumstances
of urbanization without adequate employment, young people generally
have little incentive to maintain a healthy lifestyle and often engage in
various types of substance abuse and other unhealthy forms of behavior.
Based on her research in the Pacific, McMurray has found that "the
negative impact of urban lifestyles on health is clearly evident in that
the incidence o,f early onset NCDs” in the Pacific “is lower in the outer
islands and remote areas ... where traditional foods are consumed and
people arc engaged in subsistence agriculture and food gathering.” She
contends that similar conditions “can be observed in peripheral areas
everywhere, including remote and economically depressed anas within
most industrialized countries.”
According to McMurray, the rising incidence of early onset NGDs
among the urban population in the Pacific is “a direct consequence
of global forces that have led to urbanization without industrialization.
idealization of Western lifestyles and imports of cheap food, alcohol and
cigarettes.” She argues that no real improvements in the population health
of the Pacific island nations and other developing countries can be achieved
under these conditions “until their people arc empowered and haw- the
means to choose healthy lifestyles.”
As indicated, Yach and Beaglehole also hold globalization responsible
for the lifestyle changes that have produced the rapid increases in
chronic diseases (especially cardiovascular disease, coronary heart disease.
stroke, cancer, chronic respiratory disease anti diabetes) in the developing
countries and the fact that these diseases are now the major components
of the global burden of disease in all regions of (he world. Moreover.
they argue that “policy makers and the donor community have neglected
the rapidly growing burden of chronic diseases” even though they arc the
major cause of death and ill-health in most of the developing as well as the
developed countries of the world.
Yach and Beaglehole contend that these diseases “predominate among
poor populations largely because of inequalities in the distribution of
major chronic disease risk factors.” They claim these risk factors arc
“driven by the more fundamental causes of ill health in the socio-economic
environment.'' They blame “global forces in trade and marketing" for
promoting "the entrenchment of the causes of these chronic diseases tn till
regions.” The health risks they identify arc tobacco consumption, unhealthy
diet/nutrition, physical inactivity and alcohol use, as well as the failure
to invest in appropriate'prevention and health promotion measures. Thev
indicate that “most of these risk factors arc common to the main categories
of chronic diseases and all arc modifiable, albeit with some difficulty.”
According to Yach and Beaglehole, the aging of most populations due
to declining fertility rates and increasing child survival rates (one of the
health benefits of globalization), and the “nutrition transition” to diets that
are high in saturated fats and sugars but low in fruits and vegetables, as
well as smoking and alcohol usage, are being promoted by the forces of
globalization. They also note that the nutrition transition to unhealthy
diets is generally combined with lower levels of physical activity and
regular tobacco and alcohol consumption. In fact, they cite WHO data
that indicate tobacco and alcohol consumption, high blood pressure, and
high cholesterol levels are the major contributors to the global burden of
chronic diseases.
Yach and Beaglehole say that globalization has contributed to the
rise in chronic diseases through a complex array of both direct and
indirect factors. They focus on “the direct negative effects of globalization,”
which they claim are best “illustrated by the increasingly globalized
production, promotion and marketing of tobacco, alcohol and other
products with adverse effects on population health status.” They blame
major transnational corporations and the global communications media
for “the marketing of tobacco, alcohol, sugary' and fatty foods” in nearly
all parts of the world. They indicate that “a significant portion of all global
marketing is now targeted at children under the age of 14,” since the
companies that market high sugar and high fat fast foods, cigarettes and
alcoholic beverages seek “to foster brand-loyalty among pre-teens, as young
as six years, and teenagers.”
They give particular emphasis to what they call the “globalization of
the tobacco pandemic,” and the “strong link between increased tobacco
consumption and free trade and tobacco-related foreign direct investment.”
Based on their research for the WHO, they have found that “tobacco
companies aggressively exploit the potential for growth in tobacco sales
Globalization: Health Risks & Responses • 253
in developing countries.” They claim this practice is “not surprising since
they are motivated only by their obligations to shareholders.” According to
Yach and Beaglehole, “the main targets of the industry and the associated
marketing campaigns arc now young people and women, most of whom
do not smoke.”
Haring been closely associated with the WHO’s tobacco control efforts
and the international campaign on behalf of the Framework Convention on
Tobacco Control, Yach and Beaglehole know a great deal about the tactics
that have been used by the transnational tobacco corporations to subvert
and oppose “any effective international regulatory regime” dealing with the
marketing, sale, and consumption of tobacco products. Included among
these tactics are tire companies’ frequent public refutation or denial of the
evidence about the harmful effects of smoking and their practice of “paying
scientists to carry out spurious research aimed at confusing the public and
delaying action” to control tobacco marketing and consumption.
Yach and Beaglehole’s research also leads them to conclude that the
“alcohol industry' is becoming as globally' integrated and pervasive as the
tobacco industry'.” They claim that there is a direct link between the
consumption of alcohol and certain cancers, cirrhosis of the liver, and most
injuries, especially' motor vehicle-related injuries and injuries resulting from
violence. For this reason, they argue that there is a pressing need for global
action to control the marketing of alcohol to young people, “especially
through its association with sporting events and with gender specific roles.”
Trade Liberalization and the Privatization of Health Care
The essays by Labonte, Badawi and McIntyre, Thomas and Cleary as well
as the contribution by’ Yach and Beaglehole reveal the adverse effects on
health of multilateral agreements such as the General Agreement on Tariffs
and Trade (GATT), the Technical Barriers to Trade (TBT) Agreement,
the Agreement on the Application of Sanitary and Phylosanitaiy Measures
(SI’S), the Agreement on Trade-Related Intellectual Property Rights
(TRIPS), and the General Agreement on Trade in Services (GA I S;. The
essay' by' McIntyre, Thomas, and Cleary' reveals how the GATS contributes
to the already existing problem of the migration of skilled health
professionals from South Africa (and other developing countries) to the
developed countries. Their essay also reveals the difficulties TRIPS imposes
on poorer countries that try' to import or produce affordable medicines to
fight the disastrous effects of global diseases such as HIV/A1DS.
Badawi states that “access to low-cost, safe and effective essential
drugs is largely' threatened by' the agreement on TRIPS.” lie argues
that “technology transfer, production and global movement of health
commodities are also threatened by the monopoly TRIPS gives to the
254 • Harris & Seid
companies who hold patents protected by the TRIPS agreement.'' In fact,
as Labonte indicates, agreements such as TRIPS do not promote “free
trade”; rather they promote the protection and entrenchment of the socalled intellectual properly rights and lucrative profits of companies and
individuals in the wealthier developed countries.
Labonte points out that the global “brain drain” of trained health
professionals from the developing to the developed countries has so far cost
the developing countries at least tin estimated 500 million US dollars in
training costs. The GATS agreement is likely to accelerate this transfer of
skilled health practitioners from the developing to the developed countries.
Labonte notes that some 54 members of the WTO (including many
developing countries) have so far agreed to liberalize/privatize their health
care systems under the terms of the GATS agreement. The implementation
of the GATS provisions on the “progressive liberalization” of services will
contribute to the regressive privatization of health care systems, promote
the brain drain of health practitioners, and benefit the health of the
wealthier at the expense of the poorer sectors of the population.
The essays by Labonte, Yach and Beaglehole, Loewenson, and Badawi
indicate that the trade liberalization measures and the ncolibcral economic
reforms associated with capitalist globalization have shifted a greater
burden of the costs of health care to those who can least afford to assume
these costs: low-paid workers in the export zones and industrialized urban
areas within the developing countries; self-employed and casual workers in
the growing “informal sector” of the economies of these countries; landless
peasants and agricultural workers; and the large numbers of unemployed,
disabled and indigenous/tribal peoples around the world. They generally
do not have access to adequate health care and other forms of social
protection.
The IMF, World Bank, WTO and the main donors of official
development assistance have promoted the downsizing of the public sector
and the privatization of health care and other social sendees around
the world. Largely as a result of their influence, the governments of
the developing countries and the former socialist countries (“emerging
economies”) have privatized their health services and/or imposed socalled user fees and/or other types of “cost recovery” measures that have
raised the cost of such sendees above the capacity of large sectors of the
population to pay for them.
Badawi, Loewenson, and McIntyre and her associates call attention
to the fact that the poorer sectors of the population are not covered
by health insurance in most of the developing countries where health
care is being privatized. Moreover, the governments of these countries
generally do not have sufficient funds to provide adequate social protection
Globalization: Health Risks & Ra/miurt • 255
to the population, especially under the “state shrinking” and fiscal
restraints imposed on them by the IMF, the World Bank, and the other
guardians and promoters of globalization. As Locwenson notes, under these
circumstances job-related injuries and ill health generally lead to not only
the loss of employment and household income, but to impoverishment
and the breakdown of the overburdened informal mechanisms of social
protection provided by the extended family and local community.
The privatization of health care has been particularly unkind to the poor
and to low-income households. As Badawi notes in his essay, many people
in the developing countries have been caught between the inability of their
governments to continue providing free public health services and their
own inability to pay the rising costs of basic health care. The forces of
globalization have led governments to reduce their spending on health
and other forms of social protection, to sell off many of their public
health facilities, and to encourage the privatization and commercialization
of health services and products. As a result, there has been a marked
deterioration in the health services of many of these countries and restricted
access to these seivices—both of which threaten the health of large sectors
of the population.
In the present context of increasing privatization and the promotion ol
neoliberal policies at both global and the national levels by the IMF, World
Bank, and the WTO, national government responsibility for providing
basic health care for all members of the population has been replaced by
so-called selective primary health care, public-private partnerships, and the
privatization of health services and health care facilities. As the essay by
Narayan and Schuftan indicates, this shift in responsibility for providing
health care is considered by many critics of globalization and the current
trends in health to be a betrayal of the international commitment made
in the late seventies to provide primary health care for all by the year
2000. This was the official commitment made by most of the governments
represented at the 1978 International Health Assembly held at Alma-Ata
in the central Asian republic of what was then the Union of Soviet Socialist
Republics (PH A 2000:1).
The Alma-Ata declaration set forth the goal of achieving "I lealth T. .'.II
by the hear 2000” and charged the health ministries and health woiiar<
around the world with the responsibility for providing comprehensive
primary health care to all the members of their societies by the beginning
of the new millennium. As Narayan and Schuftan indicate in their essay.
the global network of health activists and health advocacv organizations
involved in the People’s Health Movement (Pl IM) seek to hall the
privatization and commercialization of health care. The PHM holds that
health is a fundamental human right and that national governments have
<■
’.‘iW
256 • Harris & Sari
an obligation to ensure universal access to quality health care, education,
and other social services in accordance with people’s needs, not their ability
to pay. They are mobilizing broad-based popular movements around the
world in a global campaign to achieve the goal of “Health for All -Now!”
by pressuring governments to provide comprehensive primary health care
to their populations and incorporate health and other human rights into
their national constitutions and legal systems.
The Health Effects of Dependency, Neocolonialism, and
Western Ideological Paradigms
The essays by McMurray, Narayan and Schuftan, Rak and Janes, and
Finan and his colleagues reveal that Western medicine has been imposed
as the universal standard around the world, and that the health systems of
most developing countries are generally dependent upon the development
assistance they receive from the governments and NGOs of the developed
Western countries as well as international organizations such as the World
Bank and the World Health Organization (WHO). McMurray contends
that the health programs in the Pacific countries “are determined by
global health policies, set by the World Health Organization and other
health sector donors.” Moreover, she argues that much of the assistance
these programs receive “fosters dependency and imposes conditions” on the
recipients that force them to accept donor policies, practices and medicines
as well as consultants from the donor countries.
Narayan and Schuftan indicate that the People’s Health Movement
believes that it has extricated health and health systems around the
world from the “myopic biomedical-techno-managerialism of the last two
decades, with its selective magic bullets approach to health.” The PHM’s
analysis of the political economy of health in the world today (PHA 2001)
lead its advocates to conclude that the most significant determinants of
health in the world today are economic and political factors that have
colonial roots. Moreover, the movement’s analysis indicates that people’s
health around the world is under a triple assault from globalization,
liberalization, and privatization, which Narayan and Schuftan claim “have
ensured that health for all is a receding drcam.” The PHM argues that
“health services today are inaccessible, unaffordable, inequitably distributed
and inappropriate in their emphasis and approach” (PHA 2001:3). The
movement also claims that “health care is increasingly used as a subtle and
widespread instrument of social control,” and that the Western model
or “ideology of medicine ... mystifies the real causes of illness, often
attributing disease to faulty individual behavior or natural misfortune,
rather than to social injustice, economic inequality and oppressive political
systems” (PHA 2001:18).
(ilohalizulion: 1 Itiillh Ri\k\ & Rcs/ioiim ■ ®
’ ■
The essay by Finan, Wainiqolo, and Cuboni as well as the essay
by McMurray trace the current dependency and Western orientation of
the health care systems in the developing countries to the imposition of
the Western curative model of health care on these societies by their
former Western colonial rulers. They attribute the continued dominance
of Western health policies, standards and practices in these societies to
the development assistance they receive from the developed countries, the
globalizing influence of Western education and training, and the economic
dependency of these countries on the developed Western countries (as well
as “Westernized” Japan). In fact, as Finau and his colleagues assert in the
case of the Pacific island societies, many developing countries “are still
practically colonies,” and as such they are still subjected to the racism,
imperialist domination and exploitation they suffered under colonialism—
in the health field as well as in other fields.
Finau, Wainiqolo, and Cuboni argue that “imperialists control all phases
and determinants of the health transition” in the Pacific countries, and “the
socialization of Pacificans, through foreign education, is another imperialist
tool to enhance control” over the Pacific peoples. In fact, Finau and
his colleagues take the position that “globalization is the latest label loi
capitalism, colonialism and imperialist expansion combined,” and they
regard the ideology of globalization as nothing more than an updated
version of the classic imperialist justification for the‘Western domination
of non-Wcstcrn peoples formerly known as the “white man’s burden.”
According to Finau, Wainiqolo, and Cuboni most Western-trained health
personnel practice, reflect, and promote the Western emphasis on fighting
disease at the individual level rather than promoting community health
in a holistic manner. They argue most doctors and nurses are trained as
disease fighters to save individuals rather than as health promoters to save
communities. Imperialist ideologies and logics perpetuate and reproduce
the power imbalance and inequities of the past as well as strengthen the
pattern of inequitable power relations associated with contemporary' forms
of imperialism under the guise of globalization.
Rak and Janes’ essay on reproductive health in Mongolia reveals how
global reproductive health policies, promoted by' international NGOs and
the governments of developed countries such as the United States, impose
family planning methods on women in countries such as Mongolia that
often run counter to the beliefs, experiences, and needs of the local
population. These imposed paternalistic and ethnocentric family planning
methods have ignored local cultural values and devalued the alternatives
that exist at the local level. Rak and Janes reveal the contradictions in
this approach within the context of Mongolia’s rapidly deteriorating health
services caused by the adoption of market-based reforms, the reduction
258 • Harris & Seid
of the public budget for health care and the privatization of the health
sector.
The Health Effects of the Inequities Promoted by Globalization
Al the outset of the new millennium, the WHO noted that “the greatest
burden of health risks is borne by the poor countries, and by. the
disadvantaged in all societies” (WHO 2002:13). These sectors of the world’s
population have the misfortune of suffering the health effects of poverty as
well as well as the other social and economic inequities that characterize
the present era of capitalist global expansion and integration. Most of the
essays in this collection reveal that globalization is associated with economic
policies that create, reinforce, and intensify the inequities in health found
throughout the world. Thus, Loewenson states in her essay that “within
the current processes of globalization, inequality is not simply happening
but is being constructed by powerful economic and political interests and
public policies” that keep the benefits of globalization from reaching those
who need them the most. Finau, Wainiqolo, and Cuboni contend that the
economic and social inequities (including the health inequities) that the
Pacific peoples have inherited from colonial rule are reinforced today by
the contemporary forces of globalization, which they hold responsible for
the continuation of Western imperialism.
McIntyre, Thomas, and Cleary reveal in their essay how the struggle to
overcome the “legacy of massive inequalities in income, health status and
access to health and other social services” resulting from South Africa’s
colonial, racist, and repressive past has been hindered by the contemporary
forces of globalization. Moreover, they reveal that it is not just the obvious
forms of global intervention such as IMF loan conditions, externally
enforced compliance with the TRIPS Agreement on patented HIV/AIDS
medicines, and the World Bank’s privatization of health care programs that
exacerbate the existing inequities in South Africa. It is also the more subtle
and indirect influences of globalization that have led the post-apartheid
government in South Africa to adopt “self-imposed” structural adjustments
in order not to run afoul of the major forces in the global economy. These
self-imposed policies and practices tend to reinforce the health inequities
created by centuries of colonialism, racism, and European domination on
the African continent.
The essay by McIntyre and her colleagues reveals the extent to which
the global trend towards the privatization of health care and the indirect
impact of global health actors on the health sector in South Africa have
contributed to the “rapid and uncontrolled growth of the private sector,”
which in turn “has contributed to disparities in health service access
and the health of South Africans.” Today, less than 20 percent of the
Globalization: Health Risks & Responses • 259
population has access to more than 60 percent of the financial resources for
health care, while the remaining 80 percent of the population have access
to less than 40 percent of the financial resources devoted to health care
in the country. Moreover, only one-fourth of the doctors in the country
work in the public health sector, which serves the historically disadvantaged
majority of the population.
Rak and Janes premise their analysis of the global discourse on
reproductive health and its application to Mongolia on the assertion that
poverty in its modern sense was created in the developing countries by the
spread of the market economy and years of colonial rule, and they argue
that the current policies to “develop” these countries “have exacerbated the
divide between the rich and the poor.” Since the country adopted market
reforms, privatization, and the integration of its economy into the global
capitalist economic system, Mongolia has experienced a rapid deterioration
in its health sendees, increasing social inequality, and a high level of male
unemployment. Rak and Janes conclude that “it has taken the transition
from a socialist to a market economy, led by the intervention of the global
financial and policy institutions of the developed world, to create Mongolia
as a Third World country.”
The PHM, as Narayan and Schuftan’s essay explains, secs a direct re
lationship between existing health inequities and globalization. The mem
bers of this global movement consider inequality, poverty, exploitation,
violence and injustice as the root causes of ill health in the world today. As
Narayan and Schuftan make clear in their discussion of the People’s Char
ter for Health, achievement of the PHM’s goal of “Health for All—Now!”
requires “challenging the powerful economic interests that dominant the
existing global order, opposing globalization in its existing iniquitous form,
and drastically changing the political and economic priorities at all levels
of the global system.”
The Environmental Health Effects of Globalization
The wide variety and scope of globalization’s environmental effects make
it difficult to provide a sufficiently comprehensive analysis of these effects
in any single book or collection of essays. This collection of essays docs
little more than scratch the surface of the health impact of some of the
more complex and far-reaching environmental effects of globalization,
such as global climate change, the depletion of the ozone layer, and the
contamination of oceans, lakes, and rivers around the world.
As we indicated in our introductory essay to this collection, there
is mounting evidence that the global diffusion of capitalist patterns of
production and consumption developed in the Western industrial societies
has created a multitude of environmental problems. In a research study
2 GO • Harris & Seid
undertaken by Diaz-Bonilla and his colleagues on the health risks of the
poor m developing countries, they claim that “poor environmental quality
has been calculated to be directly responsible for around 25 percent
of all preventable ill-health in the world today” (Diaz-Bonilla cl al.
2002:38). They attribute much of this “poor environmental quality” to
the environmental “spill-over” effects of economic globalization.
Many of the essays in this collection recognize the threats to health posed
by the environmental effects of globalization. For example, Badawi notes
that environmental threats to health have resulted from the increasing
international trade in technology, capital, goods, sendees and labor. He
notes that many “environmentally unfriendly” industries have moved
from the developed to the developing countries, where there is generally
less concern about the health hazards caused by their technology and
often a lack of environmental health safeguards. Badawi also states
that the over exploitation of fishing licenses, deforestation, industrial
waste, and the dumping of health-hazardous materials are part of a
long list of environmental health threats confronting the populations of
the developing countries. Moreover, he warns that the indigenous germ
pool and medicinal plants in the developing countries are threatened
by :he “commercial exploitation” of giant transnational corporations and
warns that “genetically modified organisms, microbiological pathogens and
hazards in animal production represent a real health risk for the developing
countries.”
Finau, Wainiqolo, and Cuboni contend that the cultivation of cash
crops, mining, and industrialization threaten the fragile environment of
the Pacific islands, and they say the “green house effect and rising sea
levels caused by metropolitan modern societies’ efforts to maintain their
consumption level are threatening the Pacificans’ habitat.” They also claim
that the environments in these societies “have become obesogcnic, toxic
and insecure, due to crime and violence.” As a result, the Pacific countries
an undergoing what they refer to as an “environmental transition” that has
brought about “not only physical and social changes, but also developed
uncertainty and stress in the Pacific psyche.”
McMurray’s essay analyzes the effects of globalization on environmental
health in the Pacific and other developing countries. She notes that
“modernization” and globalization are responsible for the development
of urban areas and the increasing concentration of the population in
these areas. She cites United Nations data that indicate most developed
c untries now have 70 percent or more of their population concentrated
in urban areas and that the number of these areas is increasing in most
c nmtries. One of the environmental health problems created by this
increasing urbanization of the population and the globalization of these
Globalization: Health Risks & Responses • 261
societies is that they have adopted the costly portable water and sanitation
systems of the most developed countries in most of their urban areas, as
a result of their colonial legacy and/or the development assistance they
have received in recent decades. McMurray indicates that they now have
difficulty maintaining and extending these systems because they lack the
resources and technology needed to do this. She gives various examples of
the rising problems of pollution and contamination in the urban areas of
the Pacific resulting from the breakdown of their sewage and piped water
systems.
Loewcnson’s essay on the health and safety aspects of working conditions
in Southern Africa reveals that most workers in this region of the
world “continue to experience work related hazards that have long been
controlled or even eliminated in high income countries.” According to
Loewcnson, “the expansion of chemical, electronic and bio-technology
industries and of the service and transport sectors ... widened the spread of
work-related risks and their interaction with non work factors of ill health,
including environmental pollution.” Employment in the large informal
economy exposes workers in this sector to the health risks associated with
“poor access to clean water and sanitation, ergonomic hazards, hazardous
hand-tools and exposure to dusts and chemicals.” Locwenson also points
out that work in the agriculture, mining, and manufacturing sectors within
the southern African economies is associated with high rates of injury from
the mechanical, electrical, and physical hazards in their work environment.
The essays by Badawi, Labonte, Loewcnson, McMurray, and Finau
and his colleagues acknowledge the fact that globalization and trade
liberalization have promoted the deregulation of production, health, and
the environment. These forces have seriously weakened the capacity of the
public sector to respond to the environmental and occupational health risks
posed by industry, mining, transportation/shipping, and commercialized
agriculture; they also have undermined the already inadequate forms of
worker protection and social protection 'including health) in existence in
these countries.
Labonte’s essay argues that environmental issues arc becoming "inher
ently global” and tire no longer purely national or domestic issues. He
notes that the “environmental impacts of human activities arc planetary in
scale and scope” and that “almost one-sixth of humanity is on the move
to escape environmental or economic degradation and conflict.” Labonte
secs this situation as evidence of the need for global solutions to these
problems.
262 * Harris o' Sad
Community Health Care, Grassroots Action, and Globalization
from below
As Finan, Wainiqolo and Cuboni contend in their essay, community
based, grassroots, and ethnic-specific health care has improved the access,
acceptability, availability, and affordability of the health care provided to
the communities it serves. This model of health care has also improved the
effectiveness, efficiency, efficacy, and equity of the health services provided
to these populations through changing the power relationships between the
health care providers and receivers. They argue that this model of health
care addresses the oppression and assimilation implanted by Western
colonialism and “borne by imperialism through globalization.” According
to Finau and his colleagues, community-based health care releases the
participants from the oppression of the Western health care model imposed
first by Western colonialism, and more recently by contemporary forms
of imperialism under the guise of globalization (e.g., the globalization of
Western medical education and training, the transfer of Western medical
knowledge and technology, the bureaucratization and privatization of
health care along Western lines).
.Narayan and Schuftan’s essay on the People’s Health Movement (PHM)
reveals the emphasis this new movement gives to community control of
health care, grassroots action, and global action based on the use of
international health advocacy networks. These are important elements in
die movement’s global campaign to combat the health inequities associated
with globalization and to make sure that universal access to comprehensive
primary health care is provided everywhere in the world. This movement
is engaged in what amounts to “globalization from below” as it builds
support for its global Health for All—Now strategy, lobbies at the global
level, and mobilizes a grassroots-based campaign to realize the vision and
achieve the goals of the People’s Charter for Health.
The Charter, which is the PHM’s visionary statement of goals and its
main tool for advocacy, calls for “a people-centered health sector that
is democratic and accountable” (PHA 2000:9). The Charter calls on the
people of the world to: (1) build and strengthen people’s organizations
as a basis for analysis and action; (2) promote, support, and engage in
actions that encourage people’s involvement in decision-making in public
sendees at all levels; (3) demand that people’s organizations be represented
in local, national and international fora that are relevant to health; and
(4) support local initiatives towards participator}' democracy through the
establishment of people-centered solidarity networks across the world (PHA
2000:10). One of the primary principles of the Charter is the proposition
that “the participation of people and people’s organizations is essential to
Globalization: Health Risks & Responses • 261
societies is that they have adopted the costly portable water and sanitation
systems of the most developed countries in most of their urban areas, as
a result of their colonial legacy and/or the development assistance they
have received in recent decades. McMurray indicates that they now have
difficulty maintaining and extending these systems because they lack the
resources and technology needed to do this. She gives various examples of
the rising problems of pollution and contamination in the urban areas of
the Pacific resulting from the breakdown of their sewage and piped water
systems.
Loewenson’s essay on the health and safety aspects of working conditions
in Southern Africa reveals that most workers in this region of the
world “continue to experience work related hazards that have long been
controlled or even eliminated in high income countries.” According to
Loewenson, “the expansion of chemical, electronic and bio-technology
industries and of the service and transport sectors ... widened the spread of
work-related risks and their interaction with non work factors of ill health,
including environmental pollution.” Employment in the large informal
economy exposes workers in this sector to the health risks associated with
“poor access to clean water and sanitation, ergonomic hazards, hazardous
hand-tools and exposure to dusts and chemicals.” Loewenson also points
out that work in the agriculture, mining, and manufacturing sectors within
the southern African economies is associated with high rates of injury from
the mechanical, electrical, and physical hazards in their work environment.
The essays by Badawi. Labonte, Loewenson, McMurray, and Finau
and his colleagues acknowledge the fact that globalization and trade
liberalization have promoted the deregulation of production, health, and
the environment. 1'hcsc forces have seriously weakened the capacity of the
public sector to respond to the environmental and occupational health risks
posed by industry, mining, transportation/shipping, and commercialized
agriculture; they also have undermined the already inadequate forms of
worker protection and social protection ,'including health) in existence in
these countries.
Labonte’s essay argues that environmental issues are becoming ‘'inher
ently global" and arc no longer purely national or domestic issues, lie
notes that the “environmental impacts of human activities arc planctaty in
scale and scope” and that “almost one-sixth of humanity is on the move
to escape environmental or economic degradation and conflict.” Labonte
sees this situation as evidence of the need for global solutions to these
problems.
262 • Harris
Seid
Community Health Care, Grassroots Action, and Globalization
from below
As Finau, Wainiqolo and Cuboni contend in their essay, community
based, grassroots, and ethnic-specific health care has improved the access,
acceptability, availability, and affordability of the health care provided to
the communities it serves. This model of health care has also improved the
effectiveness, efficiency, efficacy, and equity of the health services provided
to these populations through changing the power relationships between the
health care providers and receivers. They argue that this model of health
care addresses the oppression and assimilation implanted by Western
colonialism and “borne by imperialism through globalization.” According
to Finau and his colleagues, community-based health care releases the
participants from the oppression of the Western health care model imposed
first by Western colonialism, and more recently by contemporary forms
of imperialism under the guise of globalization (c.g., the globalization of
Western medical education and training, the transfer of Western medical
knowledge and technology, the bureaucratization and privatization of
health care along Western lines).
Narayan and Schuftan’s essay on the People’s Health .Movement (PH.M)
reveals the emphasis this new movement gives to community control of
health care, grassroots action, and global action based on the use of
international health advocacy networks. These are important elements in
the movement’s global campaign to combat the health inequities associated
with globalization and to make sure that universal access to comprehensive
primary' health care is provided everywhere in the world. This movement
is engaged in what amounts to “globalization from below” as it builds
support for its global Health for All—Now strategy, lobbies at the global
level, and mobilizes a grassroots-based campaign to realize the vision and
achieve the goals of the People’s Charter for Health.
The Charter, which is the PHM’s visionary statement of goals and its
main tool for advocacy, calls for “a people-centered health sector that
is democratic and accountable” (PHA 2000:9). The Charter calls on the
people of the world to: (1) build and strengthen people’s organizations
as a basis for analysis and action; (2) promote, support, and engage in
actions that encourage people’s involvement in decision-making in public
services at all levels; (3) demand that people’s organizations be represented
in local, national and international fora that are relevant to health; and
(4) support local initiatives towards participatory democracy through the
establishment of people-centered solidarity networks across the world (PHA
2000:10). One of the primary principles of the Charter is the proposition
that “the participation of people and people’s organizations is essential to
Globalization: Health Risks & Rcs/ionses • 263
the formulation, implementation and evaluation of all health and social
policies and programs'' (PHA 2000:4).
McIntyre, Thomas, and Cleary conclude in (heir essay that “the growth
in number, size and power of civil society organizations combined with the
increased networking of these organizations across national boundaries”
is having a “countervailing effect” on the negative health impacts of
globalization. They give the example of how civil society organizations in
South Africa gained the support of civil society groups in the Untied States
to pressure the US government into dropping its efforts to convince the
South African government to change its policy relating to the importation
of medicines so that it would not contravene the TRIPS agreement. They
show how these groups in South Africa also teamed up with international
groups such as Mcdccins sans Frontieres and Health Action International
to oppose the efforts of the transnational pharmaceutical coiporations
(with the support of their host governments) to pressure the South Africa
government and the governments of other developing countries (such as
Thailand) into restricting their use of certain provisions in the TRIPS
agreement that permit governments to obtain urgently needed patented
medicines at reduced prices.
The adverse effects of existing international trade agreements on health,
human rights, and the environment have been subjected to increasingpublic criticism in recent years. As Labonte notes in his essay these
agreements have “become the focus for progressive social movements.”
The global networking and collaboration that have developed among these
social movements, such as the PHM, represent a form of “globalization
from below” that is rising up to challenge the “globalization from
above” imposed by the transnational corporations and their allies in
the IMF, World Bank, WTO, the Group of 8 governments (led by
the US government), and certain large international non-governmental
organizations that are closely associated with these forces.
Labonte notes in his essay that the WTO has been besieged by a broad
coalition of forces that are opposed to its global trade liberalization agenda.
He argues that (here are several reforms in the global trade regime that
health activists in league with other progressive forces are promoting in
their efforts to change the current effects of the WTO’s trade liberalization
efforts. These reforms would:
o Extend “special and differential” trade agreement exemptions for
developing countries;
o Ban the patenting of life forms, exempt patent protection legislation
for poor countries indefinitely, decrease the patent protection period
and permit parallel importing under the TRIPS agreement;
J
o impose a Tobin Tax (named after the Nobel economist who first
proposed this idea) on international currency exchange transactions to
raise about US Si50 billion annually for an international development
fund;
s> Negotiate an overarching and enforceable rule in trade agreements
th.it would require, when there is any conflict, for environmental and
human rights agreements (including the right to health) to override
the trade agreements; and
o Exclude health, education and other essential services (such as water
and sanitation) from privatization since they arc essential to human
life and health.
In addition, Labonte argues that the WTO needs to be overhauled by
making its decision-making more democratic and transparent. However,
he disagrees with those activists and social movements who arc calling for
its abolition. He contends that this would be a mistake since “there is no
other vehicle where the unequal balance of economic power globally might
be subject to enforceable change.” Labonte believes that the struggles of
civil society organizations and the developing countries “to wrest reforms
from the WTO are giving rise to a new system of global governance for
the common good.”
The Current State of Global Health Governance
As Labonte points out in his essay, social, economic, environmental and
health issues are becoming “inherently global” rather than purely national
or domestic. He argues that the evidence in favor of the need for global
solutions to these, issues is irrefutable, including the evidence about the
rapid spread of infectious diseases, the increased adoption of unhealthy
lifestyles, and the increasing international promotion of unhealthy foods
and products such as tobacco and alcohol. Labonte concludes that “we live
in the most important historical moment of our species, [since] the planet
is dying, there is excessive affluence and poverty, [and] once far-away
conflicts and diseases are imperiling global health and security.” Faced
with this unprecedented situation, he optimistically contends that “we are
struggling forward to some system of global governance for our common
good.”
Yach and Beaglehole take a similar position. They conclude that the
global diffusion of the major risks of chronic diseases is now almost
complete and the prevalence of these diseases is increasing in most regions
of the world. They contend, however, that the prevention and control of
these diseases have not been able to keep pace with their globalization
and growth. Therefore, they conclude that sustained progress against these
diseases “will only occur when governments and influential international
il
Globalization: Health Risks & Responses • 265
bodies involved in health policy and funding acknowledge that the scope of
global public health must be rapidly broadened to include chronic diseases
and their risk factors.”
Based on their experience in the ongoing struggle over the international
control of tobacco, Yach and Beaglehole predict that “progress will
continue to be slow unless the response to the epidemics [of chronic
diseases] is scaled up in a manner commensurate with their burden on
both families and societies” around the world. They believe that global
solutions are needed to address the global health risks responsible for the
epidemics of chronic disease that arc taking place around the world.
However, Yach and Beaglehole argue that the global health agenda is
currently dominated by what they call “the infectious disease paradigm.”
The main global health organizations and funding sources believe priority'
should be given to the prevention and treatment of infectious or communi
cable diseases before addressing chronic diseases. Because most institutional
responses to disease prevention and control arc based on this infectious dis
ease paradigm, Yach and Beaglehole argue that the global and national
responses to the spread of chronic diseases are “woefully inadequate and
few countries have implemented 'comprehensive prevention and control
policies.”
They contend that a comprehensive response that combats all the health
risks responsible for the global spread of chronic diseases is necessary,
and they argue this response must overcome the “powerful countervailing
forces” that presently stand in the way' of changing the status quo.
According to Yach and Beaglehole, a successful global response to the
existing configuration of major health risks has to overcome the “many'
powerful and persuasive commercial entities involved in the production
and promotion of unhealthy products.” They' claim these entities “exert
an adverse influence on health policy developments” as well as on the
development and implementation of environmental policies.
Yach and Beaglehole conclude that “stronger and broader alliances of
major health professional bodies, consumer groups, enlightened industries
and academics are now needed to effectively' prioritize the prevention of
the major risk factors” responsible for the global spread of chronic diseases.
They suggest that the global campaign for tobacco control provides a
successful model for how to organize a comprehensive response to the
global spread of chronic diseases.
Yach and Beaglehole ultimately conclude that there is an increasing
need to establish global norms on a wide range of global issues “to
balance the otherwise unrestrained influences of powerful actors.” They
argue that, if the WHO is strengthened it can be used to establish these
norms in the health sphere and then use the norms to resolve trade
266 ® Harris & Seid
disputes and other health-related global issues in a manner that promotes
positive health outcomes. However, they do not drink the WHO and
national governments alone can address the challenges of chronic disease
prevention and control. As in the case of tobacco control, they believe
collaborative partnerships and interaction are needed with international
consumer advocacy' groups, international and national sports federations,
sporting goods companies, transnational food corporations, retail food
businesses, and insurance companies to improve the quality and access
of people to healthy foods and increased physical activity. They advocate I
a consultative and “multi-stakeholder approach” with all interested parties
as well as joint initiatives with the transnational food companies rather
than an adversarial relationship. However, they recognize the dangers and i
difficulties that are involved in this approach.
Badawi’s essay urges the developing countries to make more effective
use of the provisions in the WTO agreements (the GATT, GATS, TBT, ;
and Anti-Dumping agreement) that allow for “special and transitional
arrangements.” He contends that they can take the “compensatory i
actions” allowed under these agreements to limit the negative effects
of globalization on their economies, environments, and protective social
services. Badawi says that, unfortunately, these agreements are not well '
studied by policymakers and specialists in the developing countries. He !
recommends that they develop their national capacity and expertise for
“expert reading” of the provisions of these agreements so that they can ‘
use their special exemptions to protect what he and the International ■
Labor Organization refer to as the “social dimension” (social protection ■
and social services such as health) as well as the environmental health of i
their populations.
Badawi also argues that the developing countries need to “cooperate
and consult with other developing and developed countries to influence i
decision-making” at the WTO, the WHO, and other global institutions j
as well as to negotiate multilateral and bilateral agreements that confront
the healdi hazards posed by globalization. Moreover, he argues that the
governments of the developing countries, contrary to the prevailing feeling ,
that [they] have lost control of their mandates, must, “adopt the measures
necessary to protect the public interests in the environment, public health
and nutrition.”
Loewenson argues in her essay that “there is a growing understanding
that global security and equity cannot be built on the significant burdens
of deprivation borne by communities in the south,” and that “globalization
has produced powerful tools, new communications technologies, more
widely connected social movements and an increasingly global recognition
of universal rights as fundamental to policy.” She contends that the full
Globalization: Health Risks & Responses • 267
potential of these tools can be used to create concerted global action
to protect workers’ health. The democratization and extension of the
enforcement powers of international agencies such as the ILO and WHO
would certainly help to improve the social protection of workers and
the many other sectors of the world’s population that are being harmed
and disadvantaged by the global expansion and integration of twenty-first
century capitalism.
Most global health advocates argue that a genuinely health-centered (and
people-centered) process of globalization can be achieved only by ensuring
that the interests of the developing countries and vulnerable populations are
fully represented in all international decision-making on global health issues
(Woodward et al. 2001:880). According to Badawi, Labonte, and Yach
and Beaglehole, the democratization of decision-making in the existing
international regulatory' and financial organizations such as the WTO,
IMF, and World Bank is needed to transform these institutions into global
governance institutions that will advance the interests of the great majority
of the world’s population rather than the interests of the powerful economic
elites they now represent.
Alternatives to the Globalization of Health from above
The People’s Health Movement (PHM) is clear evidence that the existing
linkages between globalization and health are contestable. In fact, most
of the essays in this collection indicate that the adverse health effects
of globalization are being challenged at the global, national, and local
levels. The People’s Health Movement and the People’s Charter for Health
provide a significant expression of alternatives “from below” to the present
globalization, privatization and commercialization of health coming “from
above.” As Narayan and Schuftan state in their essay, this People’s Charter
for FIcalth provides a vision of a better and healthier world, a call for
radical action, a tool for advocacy for people’s health, and a rallying point
for building a global health movement based on international networks
and coalition building.
The People’s Charter for Health lays out a blue print for the
transformation of the existing global order through democratization at
all levels of the existing system and through what some people in the
global social justice movement call “globalization from below” (Brecher,
Costello, and Smith 2000). It is based on the fundamental, but radical,
assumption that “to ensure health, people’s basic needs for food, water,
sanitation, housing, health services, education, employment and security
must be met” in the present time frame (PHA 2001:1). In addition, it
is based on the assumptions that global decisions must be democratized
and that people's organizations and organized grassroots action can bring
268 • Hanis 5? &id
about an "alternative vision of development—one that promotes human
and environmental well-being” (1’11A 2001:3). To achieve this vision, the
PHM is pursing the democratization of health decisions and outcomes at
all levels.
According to Narayan and Schuftan, the Charter for People’s Health
calls upon national governments and global institutions to recognize health
as a fundamental human right and as a social, economic, and political
issue deserving the highest priority. It also identifies inequality, poverty,
exploitation, violence, and injustice as the roots of ill-health, and it makes
clear that the achievement of universal access to primary health care
requires challenging powerful economic interests; opposing privatization
and globalization (in its present inequitable form); and drastically changing
the prevailing political and economic priorities at all levels in the global
order.
The Charter also makes it clear that the PHM wants the poor and
marginalized (rarely heard) peoples throughout the world to participate in
health decision-making and develop their own local solutions to their health
problems. The movement encourages people to hold local authorities,
national governments, and international organizations and cotporations
accountable for ensuring that the goal of Health for All is achieved
now, not at some distant point in the future. However, even though the
PHM firmly believes national governments have the primary responsibility
for promoting an equitable, approach to health and human rights, the
movement knows that it will take pressure from people’s organizations to
force their governments to meet this responsibility. This statement reflects
one of the most important strategic assumptions held by the PHM: that
it will take organized grassroots action as well as concerted action at the
global level to bring about the profound social changes that are needed to
achieve the sweeping vision and radical goals of the movement.
All the essays in this collection provide suggestions and/or proposals
for creating alternatives to the present conditions, in which the adverse
effects of globalization threaten the health of people around the world
and the planet’s ecological sustainability. In their essay Finau, Wainiqolo,
and Cuboni provide a series of models or strategies for thinking about
the management of change in the field of health. They are all based
on the assumption that change is inevitable and that the present power
imbalances in the world must be changed in order for substantial progress
to be achieved in the domain of health as well as in the. other major
domains of human existence.
These models/stratcgies provide useful conceptual tools for thinking
about alternatives to the present global patterns and direction of change
in health. We hope that this entire collection of essays serves the same
.j
q
t
j
'i
y
I
j
1
;
1
;
•
j
f
I
!
i
;
1
i
i
■,
Globalization: Health Risks & Responses • 269
purpose as the models presented by Finau, Wainiqolo. and Cuboni—that
it contributes not only to the ongoing discourse on globalization and health
but also to the cflbrts that are being made around the world to find
alternatives to the adverse effects of globalization on the health of the
planet’s human population as well as the sustainability of its biosphere.
References
Brecher, Jeremy, Tim Costello and Brendan Smith
2000
Globalization from Belon1. Boston: South End Press.
Cornia, Giovanni
2001
“Globalization and Health: Results and Options/’ Bulletin of the World. Health
Organization 79: 834-841.
Diaz-Bonilla, Eugenio, Julie Babinard and Per Pinstrup-Andersen
2002
“Opportunities and Risks for the Poor in Developing Countries” (Working
- Paper 83). Indian Council for Research on International Economic Relations,
New Delhi, India. Retrieved December 9, 2002 (http://www.icrier.rcs.in/
pdf/risk.pdf).
Drager, Nick, Ronald Labonte and Renee Torgerson
“Frameworks for Analyzing the Links Between Globalization and Health”
(Draft Document). Retrieved March 30, 2002 (http:/7de\ .www.urcgina.ca/
spheru/PDF%20Files/Labonte-Frameworks-Links.PDF».
People’s Health Assembly (PHA)
2000
Peoples Charter for Health. Bangalore, India: PHM Secretarial.
2001
'‘Health in the Era of Globalization: From Victims to Protagonists/’ A Dis
cussion Paper prepared by the PHA drafting group. Savar, Bangladesh- PHA
Secretariat. Gonoshasthava Kendra.
2002
Wood’a \rd. David, Nick Drager. Robert Beaglehole and Debra Lipson
2001
“Globalization and Health: A Framework for Analysis and Action.” Bulletin if
the World Health Organization 79: 875-880.
I-'
CONTENTS
VOLUME-I
I
Research studies conducted by the Task Force on Health and Family Welfare
1.
Proposal for Review of Organisation Structure and Design of Job Responsibilities for 1
Health and Family Welfare Department.
2.
Review of Externally Aided Projects in the context of their integration into the
Health Services Delivery in Karnataka.
137
3.
Training Programmes for Health Personnel in Government Service in Karnataka.
200
I 4.
Public Health Care Services under Panchayat Raj System in Karnataka.
321 •
5.
Disparities in Health and Health care Services.
360
6.
Review of Role of Private Sector in Health Services (Access and Quality).
381
VOLUME-n
7.
Health Expenditures in the State Budget.
1
8.
Peoples Perceptions of Public Health Care Services in Karnataka.
28
9.
Research Study on the Feasibility and Modalities of application of principles of 73
Health Promotion and its integration with Health Education.
II
Does Karnataka State need more Medical Colleges?
148
IH
Indian Systems of Medicine and Homoeopathy.
212
FV
Rational Use of Drugs.
234
V
Alcohol Use and Misuse in Karnataka.
289
000000000000000000000000000000000000000000.
GOVERNMENT OF KARNATAKA
0
0
0
0
0
0
TASK FORCE ON HEALTH AND FAMILY WELFARE
I
0
0
0
0
A Commissioned Research Study
0
0
I
0
0
0
0
’ 0
0
1
0
0
0
0
0
0
0
0
1
0
0
0
0
0
0
0
0
•i
0
0
1
0
0
0
0
0
0 REVIEW OF EXTERNALLY AIDED PROJECTS IN THE CONTEXT OF
0
S3
0
THEIR INTEGRATION INTO THE HEALTH SERVICE DELIVERY IN
ti
0
KARNATAKA
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
I
0
0
0
0
0
0
0
0
0
0
0
By
0
0
. 0
0
Dr. Ravi Narayan
0
0
Community Health Cell
0
0
367,1st Main, Jakkasandra
0
Koramangala, Bangalore - 34
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
000000000000000000000000000000000000000000
«
131
Content List
A - Introduction
1
B - General Description of Externally Aided Projects (EAP’s)
4
C - Project Goals, Focus and Distribution
7
D - Overview of Programmes and Activities
15
E - Overall Strengths and Weaknesses of EAP's
17
F - Lessons from some Case Studies
26
G - Some Policy Imperatives Including Integration and
Sustainability
30
H - Some Reflections on Financial / Economic Implication of
EAP’s
38
I - General policy concerns : Are we reinventing the wheel ?
43
J-Final Conclusions and Recommendations from a future
policy point of view
46
K - Limitations of the Review Exercise
50
L-Acknowledgements
51
M-Bibliography
.
„
52
N —Tables
I Externally Aided Projects - General Description
II Objectives / Focus / Regional Distribution
III Programmes and Activities by - Review of Budget Heading
IV Some Strengths and Weaknesses
5
8
15a
19
O - Case Studies
A. Training Experience in a Northern District
B. An Urban Health Centre
P — Appendices
i)
ii)
Project Proposal
Some issues and questions addressed in the review and
A conceptual framework for review - Diagrammatic
presentation.
!3£
27
29
G : Some Policy Imperatives Including Integration and Sustainability
The previous chapters provide an overall framework of the 10 EAP’s in Karnataka
and some of the quantifiable or qualitatively describable indicators and features of
these projects to help the project overview. As indicated in the project protocol this
exercise was primarily a critical policy review and not an evaluation exercise of
each of the EAP’s per se. Some of the finding in the previous chapters and tables
have addressed some of the questions that were included in our original list. In this
chapter we try to address those which have not been adequately covered by the
earlier one as well as provide some additional critical comments even on those that
have been covered, drawing primarily from the very candid and frank interactive
discussions we had with a wide variety of project directors. These policy issues and
imperatives are as follows:
1.
Scope of Projects
All the projects focus on Health System Development with varying degrees of
emphasis on Primary Health care. While some focus on secondary level (e.g.
KHSDP) there is a built in assumption that the secondary care support is with a
view to support through efficient referral systems - the primary health care network.
While in practice the links may not be so well established the conceptual framework
is well directed to this issue. It is at the ‘Public Health’ context level however that
tire projects show a general weakness inspite of the fact that unlike other states in
the country ‘public health expertise’ is available even among the senior leadership
of the state. One can only surmise that in the changing financial situation perhaps
financial management contingencies and bio-medically defined management
framework are inadvertently distorting public health concepts and priorities. The
focus on basic determinants of health is weak (nutrition, water supply, sanitation,
environment) both at content level, emphasis and linkages; key public health
components like surveillance and health promotion are inadequate; and the ‘new
public health’ emphasis on empowerment of the community and public at large in
health decision making is totally overshadowed by top down provision of specific
packages euphemistically called social marketing. This lacunae I weakness needs to
be seriously addressed.
2.
Project Planning
In the absence of a strong Strategic Planning Cell in the Directorate (inspite of a
provision in KHSDP for this) problems of project flexibility, design, long lead times
and delays, in preparation, complications in procedures and various ongoing
management and operational problems, all of which have been experienced in one
EAP or another - are a symptom of lack of adequate attention to building in-house
capacity for more realistic project planning and management. This has led to
compartmentalized planning, inadequate collection of field based data or evidence,
and adhocism in decision making further compounding the problem. Lessons are
not learnt from positive and negative experiences of a particular EAP or its success
-Ids
30
at some form of system development so the ‘wheel is reinvented’ each time by each
project and the system is not enriched by the collective experience. E.g. Different
EAP’s have had different experiences of dealing with the ‘NGO sector’ or the
private sector - some positive; some not so positive; some even disastrous in terms
of unreliable partners or even ‘fly by night’ operators but the whole system does not
learn from this to evolve a Directorates policy for NGO or Private sector
partnership. This situation may change with the Task Force recommendation on
state policy directives but for the present this is a lacunae to be urgently addressed.
3.
Who drives the projects?
This was a very difficult policy issue to address. On the face of it, the State
Government / State Health Directorate drives the project not the funding partners or
their external consultants and all sorts of mutual consultations / reviews are
organised. However two factors do affect the ‘driving’ of the project.
•
Absence of local homework
In the absence of rigorous ‘policy’ and evidence based homework on the
governments / directorate side due to a lack of strategic planning capacity as
mentioned earlier, external consultants of funding partners are often able to drive
the decision by just providing more options, more evidence based on data
marshalled from experience elsewhere and the state policy makers are then more
easily influenced or ready to accept them. e.g. During the study period an external
funding agency resource person provided more data and perspective on private
sector in Karnataka, than could be marshalled by local expertise thus inadvertently
pushing the private sector agenda. The reliability of this data or whether it was
extrapolated from quite different sources could not be commented upon, adequately
without local homework.
•
Conditionalities of funding partners
World Bank Ioans more than other agencies arc also usually supported by some
conditionalities that are clearly stated in their documents.
i.
The need for economic reforms.
ii.
The need to engage the private sector.
iii.
The need to promote user fees as a means of cost recovery.
iv.
The need to follow certain forms of ‘tender’ or ‘consultancy ‘laid down
by bank’ etc.
There does not seem to be adequate home work in-house on these and
implications especially long term options, before loan agreements are signed.
their
Some World Bank conditions
“The Country Approach Strategy (CAS) recommends focussing Bank-group
financed investments on states that are undertaking economic restructuring
programmes and supporting sectoral policy reforms. Karnataka is one of the state
that has initiated important fiscal, sectoral and governance reforms. Further more it
supports the CAS objectives by strengthening institutional capacity
,
engaging the private sector
....,
“Each project state
shall levy user charges in district and subdivisional
hospitals in accordance with a program and time schedule acceptable to the
Association(IDA)”.
“Goods and works shall be procured in accordance with provisions of section I of
the guidelines for procurement under IBRD loans and IDA credits” (International
competitive bidding, bid packages etc).
“Consultants services shall be procured under contracts awarded in accordance with
the provision of the Guidelines for the use of consultants by World Bank borrowers
and by the World Bank as executing agency - published by the Bank in August
1981”.
Source : Various reports of the Bank and Project Agreements
Both these factors lead to the continuing perception and the fact that indeed the
‘external agent’ does drive the project intentionally through general conditionalities
or ‘inadvertently through inadequate borrowers homework’. This needs to be
addressed urgently.
Even where conditionalities are inevitable, these should be closely monitored and
either reviewed if they have negative consequences or internalised into the system if
they have positive implications.
4.
Are there areas of overlap / duplication ?
•
Compartmentalized projects by the very fact of being developed independently
as ‘stand alone’ projects and not as components of a larger wholistic integrated
project are bound to produce overlap and duplication.
•
Not surprisingly the chairperson of the Task Force during one of his recent
inspection visits found ‘three operation theatres in a PHC compound’ built by
different EAP’s with no evidence from the MIS of local needs that warranted
such investment. In HMIS, IEC, and Training there are many overlaps and
duplications .
So different projects produce manuals and teaching aids or audio visual
aids for Health Education which are quite similar in content;
Health functionaries are expected to maintain a wide variety of registers
that cater to the needs of different HMIS of different EAP’s ; and
Doctors go for different training programmes organised by a wide
variety of EAP’s that add to variety but not to a coordinated training plan
at district or PHC level (see case study A)
•
An overall integrated planning and training exercise is therefore urgently
required. At the directorate / state level there are efforts to prevent this
duplication of input and efforts but systematic change to streamline this process
and prevent even accidental or inadvertent duplication is required since the
health sector functions under a constant financial resource constraint and any
effort to ensure more efficient deployment of available resources is welcome. A
good example of adhoc integration is the utilization of KHSDP Resources for
KfW project needs.
5.
Ownership and Leadership
•
In most projects the state level ownership is strong except perhaps in those
projects which are ‘package deals’ decided at the centre.
•
Because some of the EAP’s have established independent structural identities
e.g. KHSDP, IPP VIII, IPP IX, the links and feeling of shared ownership by the
parent directorate (in the case of KHSDP and IPP IX) and the parent Municipal
Corporation (in tire case of IPP VEH) is weak. E.g. no serious consideration
regarding sustainability issues and integration challenges relevant to KHSDP or
IPP IX projects have been addressed at the directorate or Health secretariat. Nor
is the Municipal Corporation adequately concerned about the very same issues
vis a vis IPP VIII project.
•
Another significant lacunae seen in the EAP’s as they are presently structured, is
that ownership at District level - at the point of implementation is quite weak vis
a vis District Health Officers and PHC MOs; and perhaps non-existent vis a vis
PRI institutions. All these three groups are crucial to ensure the integration and
long term sustainability of all these projects. Ownership can be enhanced by
involving all of them from the very inception and conceptual planning stage of
such projects.
•
Leadership of the project directors has been good as long as there have not been
frequent changes of leadership or the burdening of project directors by multiple
and additional responsibilities.
•
However the leadership and ownership are particularly crucial if EAP’s have to
become more complementary or supplementary to each other and the whole
health care delivery system.
promotes linkages is crucial.
Leadership that coordinates, networks and
•
Public Health orientation and socio-epidemiological orientation of the leadership
- whether generalist administrator or medical / technical leadership is an
important necessity to prevent inadvertent distortions due to extraneous lobbies
or market forces. This will also enhance capacity to negotiate with external
consultants and others as well.
6.
Intersectorality
While in many EAP’s the importance of this factor is mentioned, the intersectoral
coordination between departments and programme managers and decision makers
of different concerned ministries is still not given adequate priority. At the heart of
good ‘public health strategies’ is the emphasis on intersectoral coordination and
while EAP’s may have not seized the opportunity in this aspect so far, the evolving
Integrated Health, Nutrition and Population project (HNP) must focus on this aspect
urgently and significantly. Even at the grassroots level a better coordination
between PHC, ICDS centre, local schools, women credit cooperatives and
development workers would strongly strengthen programme performance aiid
outreach.
7.
Integration
There is urgent need to integrate Health with Family welfare; public health , primary
health care and the population agenda with each other to avoid not only duplication
by compartmentalization but also to reach the community and tackle the health
problems of people especially the poor in a more integrated way. Much lip service
has been paid to the issue of integration but the stand alone EAP’s have not tackled
this issue adequately. In fact different EAP’s focussed on different problems even
further disintegrate the work of the directorate.
DHO’s and MO’s are constantly preoccupied or distracted at ground level by
frequent visits of consultants, review teams, project teams asking for this and that
data or feed back; the more EAP’s the more such distraction from the normal
planning and management routine.
At the directorate level different EAP’s require different protocols to be filled,
(different MIS mechanisms) so quite a bit of directorate staff time is spent in filling
up questionnaires, schedules enhancing paper work but not necessarily enhancing
efficiency of planning and management.
Consultants for each EAP provide their own framework of ideas and decision
making. These do not allow for any inter-EAP consultant communication. One
EAP may appoint a consultant that suggests one type of ideas, another EAP another
type and all these have to function at the same PHC level or the same district level
or have to be operationalised by the same health functionary. This situation
necessarily leads to adhocism and anarchy especially in the absence of state policy
guidelines. Integration and coordinated communication is urgently required.
Another urgent area for integration to avoid wasteful duplication of time arid
procedure is the need for integrating all the single project related district level and
state level societies into one Health society at both levels to receive and disburse the
funds. Serious policy reflection also needs to be done to ensure that the District
society’s work under the purview of the Zilla Parishad and PRI.
8.
Equity
While overall the EAP’s do not have a well planned Equity focus some emphasis on
Northern disadvantaged districts and on women and SC/ST have been identified and
noted. HMIS of all EAP’s as well as the Directorate must begin to focus on Equity
in a more concerted way in the years to come. This ‘equity imperative’ must include
i.
ii.
iii.
iv.
Geographical - Within districts and between districts.
Gender - between male and female sections of the population and
especially focus on girl child.
Class / Caste - Between rich, middle class and poor or the so called
haves and have-nots or ‘landed’ and ‘landless’ etc.
Marginalisation - SC/ST or special groups such as child labour or rural
migrants to urban areas, street child, elderly, people with disabilities etc.
Unless the HMIS focusses on disaggregated data the equity principle cannot be
furthered by active policy or programmatic intervention. EAP’s could build this in
to their framework more concretely so that they go beyond policy rhetoric.
9.
Partnerships
All EAP’s have built some form of partnerships with the voluntary sector, NGO’s,
private sector, academic institutions or research institutions. But these do not build
on a larger policy framework of the state since guidelines on such partnerships are
not available. They tend to be some what adhoc. The directorate should actively
move towards some form of Resource Directory; Accreditation system; or
reviewing and registering system for such partners so that EAP’s and different
health departments can draw from pooled experience and pooled resource lists. A
partnership cell in the Directorate like the erstwhile Society for Coordination of
Voluntary Agencies (SCOVA) idea could build such directories, framework of
guidelines and linkages, of use to all departments and projects.
10.
Community Partnership and Empowerment
The resistance of the Health department to work with Panchayati Raj Institutions is
well known and though some of the reservations of the health leadership may be
verj' genuine and based on difficult or awkward situations of ‘interference’ or
extraneous push / pull factors in decision making - there is urgent need to review
this and get over the problem rather than ignore it. With increasing political
decentralization, PRIs will play an important part in local planning and
administration in the future and EAPs should promote this process and not distort it.
The district level societies which leave decision making in the hands of the
bureaucracy may be good for efficient disbursement of EAP funds but they
definitely mitigate against active community participation. EAP’s in particular must
begin to focus on human development more than infrastructure; and in this human
development component strengthening of community based organizations like PRI
institutions to contribute to local planning and ensure accountability and
transparency through capacity building will become as crucial as building health
teams to deliver tire programmes efficiently and effectively.
11.
Accountability / Transparency
EAP’s may develop their own monitoring system and evaluation systems, even
audit systems but they are not accountable to the people, the political system, the
legal system in the same way as the directorate and its regular programmes. While
bureaucrats and technocrats may be closely involved with the development of these
projects and the evolution of their frameworks of action there is still the danger of
creation of a parallel system of decision making and programme management which
may be seen as relevant in the short term but could become problematic in the long
term.
However it was noted that overall some of the guidelines and procedures of the
projects were able to immunize the project from the corruption and political
interference which affect the larger system all the time since it does prevent the
influence of extraneous ‘push’ and ‘pull’ factors due to clear cut guidelines that are
not easy to circumvent.
In the short term review we were not able to make clear cut judgement whether
extraneous interference’s were making any sort of affect on programme formulation
or implementation. The use of retired government personnel as consultants was
common (a sort of ‘old boy’ network) which affected the dynamics of the
programme and subsequently its performance in some cases but not necessarily to
integrity. On the whole it may be surmised that EAP’s are as subject to outside
interference as the rest of the system not necessarily more.
However in the matter of construction costs and delays and whether some
contractors were favoured rather than others - These areas were difficult to explore
in the time constraint. There was hearsay evidence of this type all the time
including architects inflating designs / and enhancing profit margins in other
ways, etc.
12.
Sustainability'
This was one area on which there was very little real focus or policy discussion or
planning in the projects at any level - project plans, project dialogue, project
implementation mechanisms and so on. It is important to emphasizes that
sustainability is often seen as being financial only. It is actually more than this and
includes staff and other policies as well.
The overall assumptions which ignored this imperative and the trends seen were as
follows:
i.
The projects were seen as filling lacunae in the existing system and not
creating additional structures or functions.
ii.
The parent unit or department like the BMP in the case of IPP VIII and
Health Directorate in the case of IPP IX, KHSDP etc were expected to take
over the project when the period of the project was over. There seemed to
be no contingency plans being evolved for this inevitable reality,
iii.
In some project documents there was mention of cost recovery usually
through user fees mechanism; or sustainability was to be made possible by
NGO - or private sector partnership or take over but this was not followed
up by serious operational guidelines or planning with the concerned parties.
iv.
Sustainability as an issue seemed to be considered in the last year of the
project as a knee-jerk reaction rather than as a serious plan evolved from the
very beginning.
v.
Unless the directorate estimates recurrent costs, running costs, maintenance
costs and other such definable entities seriously as the time for phasing out
of the project nears and unless these costs are budgeted for or recovery
planned in some sort of methodical way - Sustainability like cost recovery
will remain rhetorical and ultimately ignored or considered as someone
else’s problem at a later date.
vi.
In some cases there seemed to be a confidence that some project donor
would always step in to fill the lacunae if one donor phased out - so again
this complacency led to a fatalistic non-planning situation which was not at
all uncommon.
Sustainability of these relatively large EAP’s is a very serious policy issue that
needs urgent attention at the highest level and the active involvement of the finance
ministry as well.
II. Some Reflections on the Financial / Economic implications of EAP’s
Understanding the financial / economic implications of the increasing reliance on
EAP’s to support the health care delivery system in the state and the gradual shift
from grant giving funding partners to becoming ‘borrowers’ of loans, was not an
easy policy issue to review due to atleast two constraints.
• The financial management of the EAP’s are separate systems not easily listed to
the states own health budgeting / accounting system.
• The loan implications and the debt burden and debt servicing implications are
not easy to explore in a short time constraint under which the project functioned.
The reviewers studied some earlier analysis particularly the review document
(Analysis of Expenditure Medical and Public Health, Family welfare by
S.Subramanya) and the more recent study of Dr.Vinod Vyasulu and group and also
studied the credit agreements of various projects and the budget and account
statements as well as status of project tables from World Bank and other sources.
From a review of all these secondary sources of data the following conclusions and
policy concerns are listed out: (See also box items which are extracts from authentic
source and support our conclusions)
1.
While the overall expenditure on health and family welfare is gradually
decreasing and hovering between 1.1 and 1.4 of net state domestic product
which is itself an overall low investment (ICSSR / ICMR recommend 8%), the
reliance on EAP’s is increasing which means Non-plan expenditure is coming
down and Plan allocations are increasing. This is not a very healthy trend.
2.
Most of the expenditure in non-plan is now directed to salaries with less and less
available for programme / action components. EAP’s are tending to take over
more and more of this programme component - again not a healthy trend.
3.
Considering that EAP’s are now more and more loans rather than grants or long
term soft loans this is a worrisome development. If these loans are not utilized
with efficiency then we have the double burden of continuing ill health and a
‘debt burden’.
4.
Though all the projects talk about sustainability and cost recovery and user fees
mechanism is often mentioned as a long - term option there is no indication that
this mechanism is effective in reality.
While some recovery has been
demonstrated; and some efforts to identify those who cannot pay etc is being
experimented; and the decision to let the amount / revenue collected be kept at
the institutional level for local use rather than transferred to the general account
or treasury - none of the mid-term reviews show that this could be a major
option for sustainability even though in the short term they may help to improve
quality by enhancing consumer participation. Researchers and programme
evaluators are not unjustified in their concern that ‘user fees’ may ultimately
W6-
3-2
Health Financing - An Analysis
1.
“State Finances, Health Finances and Efficiency: Three key issues, with regard
to public sector finances at the state level need to be addressed. First the overall
fiscal situation in many states has deteriorated sharply since the early 1990s,
with a rise in the fiscal deficit, an increase in interest payments as a share of
total revenues, and an increase in debt outstanding as a share of state domestic
product. The deterioration in the overall financial situation faced by the states
has had a deleterious effect on the health sector. The share of health and family
welfare in the total state revenue budget has declined since the early 1990s
suggesting that past declining trends of health sector’s share in the budget has
been exacerbated, rather than reversed. The decline in the health sector’s share
occurred despite a rise in real per capita expenditures in all states up to 1991,
indicating that total government expenditures rose faster than health
expenditures. Total government spending is about USS 2-3 per capita for health
services and is inadequate to meet the government’s stated objectives. To
achieve the government’s objective of funding a basic package of health
services, substantially more resources for health care are required, but the
overall state finances noted above pose a serious problem. Second, within the
health sector in most states, resource allocation in the public sector is skewed in
favour of tertiary care services relative to needs at the primary and secondary
levels, particularly rural and community hospitals. Third, much of the resources
are absorbed by salary costs.
The recurrent budget for operations and
maintenance is chronically under-funded and the programs are not fully
effective”.
2.
“Alternative Methods of Health Care Financing : The resource constraints faced
in the health sector will required alternative methods of health care financing to
supplement budgetary allocations. Alternative methods of financing health care,
such as cost recovery, social and private insurance, and participatory schemes,
are limited. Reported revenue data indicate that cost recovery in the health
sector is about 3% on an average in India, although there are problems in
estimating the level. Some of the problems faced with cost recovery include:
a. Lack of an appropriate mechanism within the government to review user
charges;
b. Weak administrative mechanism for collecting user fees;
c. Difficulty in targeting the poor for exemption from user fees; and
d. Constraints to greater retention of funds generated through user charges at
the point of collection.
Based on international experience it should be noted, however, that a cost
recovery rate of 15-20% in the health sector is about the most that can be
expected in the public sector. In the long run, issues such as private insurance
and managed health care will need to be addressed, as the industrial and urban
sectors in India expand, and cost containment becomes increasingly important”.
Source : Analysis of Expenditure on Medical & Public Health, Family Welfare
State Health Finances
“Non Plan expenditure, which is met from resources raised internally by the state,
accounted for 63-69 percent of the total expenditure on health and family welfare
between 1990-91 and 1994-95; this came down to 57 percent in 1995-96.
Reduction in the proportion of non-Plan expenditure in 1995-96 is because of
increase in Plan allocations and capital outlays. One reason for this increase could
be the availability of funds from externally assisted population and health projects
and Central government aided projects such as the AIDS control programme”.
“With expenditure on health and family welfare accounting for only 1.21 percent of
the net State Domestic Product down to 1.14 percent in 1991-92, but up to 1.24
percent in 1992-93, decreasing again to 1.22 percent in 1993-94 before increasing to
1.37 percent in 1994-95. It is clear that fluctuations of this nature are undesirable
for the growth of the health sector as also that expenditure on health and family
welfare is, by any reckoning, inadequate. A study group on Health for All, set up
jointly by the Indian Council of Social Science Research and Indian Council of
Medical Research, recommended ‘a substantial increase in public expenditure on
health at about 8 or 9 percent per year (at constant prices) over the next 20 years”.
Source : Human Development in Karnataka - 1999
de-emphasize the need to focus on the marginalised. Other problems with this
mechanism are highlighted in the box items as well.
5.
There is a danger that increasing reliance on EAP’s will ensure that programme
costs in the regular non-plan health budgets will be ignored with a long - term
distortion in budgeting creeping in. (This will perpetuate long standing
budgetary imbalances with long term implications for health budgets).
6.
There seems also a tendency to be more extravagant with issues like
constructions, consultancies, equipment, vehicles, etc because EAP’s promote
unwittingly a more ‘private sector’ ethos so thrift, careful planning, basic
simplicity and other such values that would ensure ‘quality’ at low cost or a
more judicious use of resources so that more is available for grassroot needs is
being affected.
7.
Finally it may be important to caution that reliance on EAP’s should only be a
short term plan. Ultimately health budgets like the investment on education and
welfare (social sector) should be increased as a long term investment in quality
human development. Enough economic analysis and theory - including the
more recent endorsement by the work of economists like Amartya Sen and
others show this direction as the way ahead. This needs political will and
commitment and some courageous state development policy planning. Let short
term solutions like EAP’s not come in the way of concerted, action for sustained
development and higher investment in health.
J.
General Policy Concerns : Are we reinventing the wheel?
The key researcher for this study and some of Iris colleagues had reviewed the
World Bank activities in the Health Sector in India based on a case study on “The
World Bank’s role in the Health system in India” facilitated by the Sector and
Thematics Evaluation Group of the Operations Evaluation Department of World
Bank in August 1999.
That review had raised seven sets of questions / findings for a policy meeting
organised by the Bank with Planning Commission, Ministry of Health and Family
Welfare and others. The review of EAP’s in Karnataka was a good opportunity to
look at these propositions in a wider variety of project initiatives and with
partnerships beyond the one with the bank. Our findings suggest that many of these
concerns are very real ones even in the context of the current EAP’s in the state and
need to be given serious consideration by policy makers and project directors within
the state before these distortions and concerns become too systemic. They are
equally important for the funding partners. These concerns are enumerated as a set
of policy questions that project directors and partners should reflect upon as they
review their projects for long-term sustainability and integration within the larger
system.
1.
Is Public Health not being adequately emphasised in problem analysis
project planning and formulation?
-
2.
Is there a confusion in understanding public health?
Is economic or techno-managerial context taking precedence over socioepidemiological analysis?
Are the wider determinants of health like nutrition, water supply, sanitation,
and pollution not adequately addressed?
Is the focus on poor, indigent, marginalised not central?
Are regional diversities and differentials not central to decisions on focus of
programme?
Is Primary Health Care being given adequate emphasis and priority ?
-
Is there focus on selective ‘cost effective treatment strategies’ rather than
enabling / empowering processes?
Is there focus on first referral units rather than primary health centres,
subcentres and home based care?
Is community involvement in planning and organisation mostly
rhetorical with community capacity building made subservient to
exigencies of top down management systems.
Are Panchayati Raj institutions generally ignored and registered societies
promoted as an instrument of decentralization but under bureaucratic
control?
3.
Arc these partnerships adequately transparent and accountable ?
-
-
4.
Are the partners willing to share the costs of failure and distortions due
to poor programme design or planning which ultimately affects the poor?
Is long term sustainability or integration into existing health care system
being adequately addressed or followed up as an end of project after
thought?
Is there unhealthy competition between projects rather then collaboration
and sharing of expertise and experience?
Are accountability and transparency systems not clearly defined and
hence not actively monitored?
Some ethical issues and dilemmas ?
What is the ethics of promoting NGO-private sector partnership in the
absence of solid evidence that these are more efficient operational
options?
What is tire ethics of taking credit when an initiative is successful and
yield positive results while pointing a finger to the directorate or ministry
when the initiative is problematic?
What is the ethics of expanding quality at the cost of or absence of
adequate and operational quality control?
What is the ethics of promoting infrastructure and ‘hardware’ at the cost
of‘software ‘ that can more easily focus and reach the poor?
5.
Some management issues and dilemmas?
In spite of marshalling lots of expertise both local and foreign is there a
tendency to:
Develop ‘hardware’ rather than ‘software’?
Expect ‘training’ to get over needs for serious management reforms?
Little thought to social accountability and transparency?
- Inadequate attention to building ownership among different stake holders
particularly district level players?
Focussing on ‘user fees’ as the only primary fund enhancing option
rather than looking at diverse options?
Overall neglect of health human power issues like continuity, skill
development and promoting team concept?
6
Is the political economy adequately addressed?
-
Are the health projects adequately located in a broader, political, social,
institutional analysis and adequately based on evidence of how projects
run or do not run?
-ISo
Are issues such as political will; corruption and influence of lobbies
political interference; market economy; being given adequate emphasis
in the strategic planning exercises?
Without developing a strong ‘public health policy resource group’ within
the directorate is the free lancing, free floating, adhoc Consultancies and
commissioned studies not allowing the means of change to become
systemic?
7. Is cultural context being disregarded?
-
Inspite of a rich and diverse tradition of Indian and alternative systems of
medicine, including promotion and investment in health humanpower
development in these systems by government and private initiative; are
the EAP’s ignoring the local cultural context and these alternatives in
their formulation?
All these issues are relevant today and it was surprising to find that most of them
were applicable to all the EAPs in the state and not only for those supported by
World Bank. However it must be noted that the cun-ent health leadership both
bureaucratic and technocratic seemed much more alive to these policy, issues. That
was a positive finding, symbolizing future potential. However as was brought out
again and again in the interactive discussions local holistic problem analysis and
policy homework was inadequate in all these aspects. Strengthening of
strategic policy analysis and development was an urgent action imperative.
Policy makers and project managers need urgent orientation to Public Health
aspects of decision making and socio-economic politico - cultural aspects of
health situation analysis. Any strategic planning exercise in the future for the
continuation of the existing projects or the evolution of newer one must take these
crucial questions into account so that the projects can be implemented more
effectively and in a more realistic context with reduction in the implementation
gaps.
J. Final Conclusion and Recommendations from a future Policy point of view.
The previous sections highlight the key findings and trends that emerged from the
review process. However taken as a whole set of project experiences the key issues
and conclusions that have emerged as significant for a concerted policy response are
the following
1.
While the EAP’s do focus on a large number of health problems and health
sector development issues, addressing various lacunae in the existing Health
care delivery system in the state at both primary and secondary level, they do
evolve, exist and function in relatively compartmentalized ways without
fitting cogently into a comprehensive, integrated strategic larger state
health policy I plan evidenced by -
•
The absence of any state health policy document that includes serious reviews or
details of all of them.
•
Any coordinating mechanism at directorate level that addresses them in a
collective context.
•
Any consistent and rigorous strategic planning exercise / document that was
used by programme designers when these EAPs were evolved.
Some
congruence / complementarity between / across projects has evolved since the
members of the project committees overlap with senior policy makers common
to all, but this is ‘adhoc’ and not always intentional.
[Probably the HDR Report, Karnataka Task Force in Health and the recently
evolving HNP project are fore-runners for this much needed paradigm shift from
selective compartmentalized programme planning to more comprehensive
integrated Health sector planning processes].
2. On tire other hand while compartmentalized evolution may have lead to some
problems of duplication and integration, especially in IEC and training, but also
sometimes
in
infrastructure
development,
the
very
feature
of
compartmentalization has also lead to a certain degree of project autonomy that
has lead to many interesting initiatives and innovations in structure, framework,
operational mechanisms, evaluation and monitoring, some of which have been
identified by this short-term review. These need to be rigorously documented,
objectively evaluated further and adopted / adapted by the whole system as the
projects phase out and get taken over and integrated by the ongoing larger
systems.
-Iga.
kc
3.
Overall the Directorate / EAP’s have shown
•
An ability to evolve laudable objectives for each EAP.
•
General lack of competence in the evidence based homework required to
translate objectives into implementable strategies leading to delays in starting up
times.
•
Diffidence in guidelines and systems development leading to operational and
execution delays.
•
While ability to handle the hardware (infrastructure construction - civil works,
equipment and transport) has been established, effective software development
(training, IEC and Quality Assurance) has remained a weak skill / capacity.
Also cost over runs have been many compounded with poor utilisation in other
areas showing in-different financial management capacity as well.
4.
Like the general health care services development, the projects have not shown
any evidence-based focus on equity, gender, regional disparity or other
policy imperatives like impact assessment, community partnership and
ownership, partnership building and decentralization and hence though there
are some successes and some failures as well, in none of these areas can EAP’s
be shown to have used their own programme / project autonomy to enhance the
health sector experience in these areas. This is partly a reflection also that at
the Ministry level there are no clearly circulated policies or programme
guidelines on these policy imperatives and hence project managers have had to
explore these dimensions if at all with diffidence rather than confidence and
clarity. Similarly the issues of corruption, political interference, transparency
and accountability seem to effect them just as much as they affect the larger
public health system- no less, no more though perhaps in the tendering /
purchase policies sometimes as conditionalities of the funding agencies, there
seems to be an overall feeling among programme managers that outside or local
interference is less!
5. Lack of continuity of key personnel has been an important handicap and lack
of systems to monitor quality of care and responsiveness to local needs had
handicapped the establishing or the enhancement of effectiveness. In addition
selection of consultants and senior project consultant need to be critically
reviewed and made more competence based and transparent. Apart from an oldboy network phenomena selection is not always focussed on skills for the job.
6.
While tlie general impression of the programme managers seemed to be that
■ these EAPs were not consciously donor driven and there was space and
opportunity for local technical opinion to evolve project formulation, the
impression of donor driven agenda was often attributed to lack of local
homework and evidence generation and hence a tendency to accept the
suggestions / frame work / ideas of working external consultants as an easy
option. This aspect again underlines the urgent need to develop and enhance the
strategic planning capacities of the Ministry / Directorate and making it multi
disciplinary as well [The KfW and OPEC experiences have however been good
examples of the need ‘to look at gift horses in the mouth’ seriously which could
have avoided all the problems that have followed. They have also shown the
absence of long term planning capacities especially in human resource
development for the hospitals being upgraded].
7.
Integration as an issue does not seem to have been seriously considered by any
of the projects since many projects were seen as stand alone or focusing on
infrastructure not process. [The absence of clarity in development of a referral
system complex between primary and secondary care (for example: IPP VIII,
IPP IX and KHSDP) is a case in point. Similarly IPP VIII, IPP IX and RCH
could have been more complementary, etc.] This leads to wasteful duplication
at the ground - level.
8.
Sustainability is another policy imperative that does not seem to have been
taken seriously by the whole system since in many ways this should be a long
term concern of the Directorate and not just of the EAPs. KfW project had some
serious options outlined in the project part which were not adequately
experimented with. [Efforts to evolve systems of user fees; efforts to identify
and hand-over (contract) out services to NGO’s and or private sector etc. are
being experimented with in KHSDP, IPP VIII, RCH but these experiments seem
adhoc and not within a clear-cut policy framework. Nor are they being
evaluated objectively to establish relevance or effectivity]. Overall the human
power development experience that is crucial for sustainability has often been
ignored or inadequately addressed.
9.
Overall EAPs do not seem to be adequately drawing upon the Public Health I
Community Medicine capacities of the state in any concerted or formal way
nor for that matter on the phenomenal inter-disciplinary capacities of institutions
such as IIM, ISEC, NLSUI and other resource centers of health, social
development or strategic planning expertise- many of which are also available in
other districts and regions. In fact there seems to be an overall lack of public
health / sociological orientation in problem identification, situation analysis
or programme planning in the EAPs evidenced by a sense the researchers got
of the dominance of:
Infrastructure over human resource development.
Bio medicine over socio-epidemiology.
Secondary care over primary health care (especially preventive
public health).
Centralization over decentralization.
Provision of services over enabling / empowerment strategies.
10.
Finally a review of EAPs undertaken by us, inspite of the time and
methodological constraints, lead us to suggest that there is urgent need to:a)
Develop strategic planning capacities in the Health sector of the
State to handle the complexities of Health sector development as
well as the challenges of negotiating sustainable projects with
external agencies and funding partners that develop not distort /
enhance capacities all round /and integrate not disintegrate.
This capacity should be multi-disciplinary, directorate-based and as
an immediate starting point should also become the integrated
evidence based monitoring unit for all the health programmes of the
state including EAPs.
b)
Develop mechanisms of integrated planning that would start as a
first step of all programme managers and programme implementers
being networked into a coordinated planning mechanism that from
time to time focuses on integration and sustainability issues beyond
the dynamics of compartmentalized projects / program. [The project
preparatory committee of the current HNP project could well become
the starting point of such a mechanism].
c)
Both these mechanisms should draw on multidisciplinary
professional expertise in the state especially public health and the
behavioral sciences from all the resource centres both public, NGO,
private and the professional colleges. (The HNP project is trying to
do this by involving a multi disciplinary group like Community
Health Cell (an NGO) but this needs to be done with greater clarity
and flexibility.
c)
A more detailed internal review and analysis of current EAPs
should be undertaken as an in-house exercise by both (a) and (b)
supported by (c) so that the positive lessons from EAP experience is
integrated into health sector development in the state and
distortions /problems handled by a more decentralized programme
implementation mechanism or countered through more effective
evidence based long term strategic programme planning.
K.
Limitations of the Review Exercise
The task of reviewing ten Externally aided projects in Health in the state in a
short term framework of 4-5 months was a very stupendous and exhaustive task
and perhaps quite unrealistic as well.
Hundreds of pages of reports, reviews and other documents had to be perused
and interactive interviews had to be arranged with a large number of very busy
government officials and project managers within this short term framework by
researchers who also had to work within a framework of complementary
demand and deadlines.
In two cases RNTCP and KSAPS interactive discussions with programme
directors could not be completed so we used reported information monthly both presentations at KTFH meetings and documents and one other programme
due to time constraint. NLEP (Leprosy control) was not included. Since this
review was trying to identify the broader policy issues relevant to Externally
aided projects in general all the nitty gritty’s of all the projects were not
focussed upon.
The study was also focussing on many issues that are neither easy to measure
nor always easy to elicit because qualitative judgements on qualitative issues
are often not easy to collect especially if the judgements are negative or critical.
We must record however that most of the people interviewed showed a
phenomenal degree of openness, frankness and willingness to discuss even
‘sensitive’ areas and this candidness is really appreciated.
We have tried to do our best integrating the rich, response and feedback that was
received in the interactive discussions supported by background notes and
papers and our own reading and critical analysis of all the documents that we
were able to access. The effort has been made to make this review a learning
experience as a partner not as a critical external reviewer.
We hope we have been able to collate and highlight the salient features — both
strengths and weaknesses of EAP’s when taken collectively. Much more needs
to be done to address all the questions originally listed out, some have been
answered, others only just considered. More time would definitely have helped.
However the experience has shown that full justification can only be done if this
review, both
in-house and external becomes part of the ongoing Strategic
Planning Cell of the Directorate / Ministry. If our study has helped to get this
message across we would have felt fully complimented by our efforts.
5'o
L.
Acknowledgements
To the Karnataka Task Force in Health for the opportunity to make an overview of
the externally aided Health projects of the state.
To all the project directors particularly Mr. Arvind Risbud (KHSDP, OPEC, KfW),
Mr. Krishna Rao (TPP VIII and IPP IX), Dr. G.V.Nagaraj (RCH) and Dr.
Jayachandra Rao (IPP VIII) Dr. Shamanna (NPCB-K) and all their consultants and
supportive staff for the frankness and openness with which they participated in the
review and made available reports and other documents.
To Dr. Thelma Narayan and Dr. C.M. Francis who shared insights as the Task Force
process continued; and all the CHC team members who encouraged and supported
tire project framework.
Finally to Mr. Anil Kumar (Secretarial cum Account Assistant) who typed the
manuscript, Mr. M.Kumar (Administrative Officer) and the rest of the CHC office
team, who particularly helped with all the operational aspects of the short term
project.
Dr. Sampath.K.Krishnan.
Policy Fellow &
Research Associate,
Community Health Cell,
Bangalore.
Dr. Ravi Narayan,
Community Health Adviser,
Community Health Cell,
Bangalore.
Dated: 28,h March 2001.
m-
5>
1-1^
Comments on "Case Study of World Bank activities
in the Health Sector in India"
Presented at the Consultative Meeting on "World Bank Activities in the Health Sector in
India" at World Bank Office, New Delhi, on 9th August 1999
The Sector and Thematic Evaluations Group and the Operations Evaluation Department of the
World Bank (India) prepared a case study on the World Bank's Health - Nutrition - Population
program in India based on review of literature, sector and project documents and the
proceedings of the workshop on "The World Bank's Role in the Health System in India"
which included 9 papers commissioned by OED.
This note by some of us from the Society for Community Health Awareness, Research and
Action, Bangalore, a multi-disciplinary professional resource group working for the last 15
years supporting community level health action and community oriented health policies by
the voluntary sector and government, brings to bear comments on this case study from a
Public Health, socio-epidemiological; management; ethical; and public policy perspective which are the disciplines represented among the four member group of the society, who
studied the document.
We had a little over a week to study this document and in spite of a request were able to get
copy of only one of the nine commissioned papers! So our comments are based on a rather
rushed analysis of tire document handicapped by the absence of access to the background
papers from which much of the perspectives and conclusions included in the case study, are
drawn. Notwithstanding this constraint we hope the concerns we raise will be taken seriously
by the Ministry of Health and Family Welfare and the World Bank India operations team.
We believe these are concerns that we along with so many other public health / community
health I health policy resource groups have been raising for over two decades now, but we are
emboldened once again to do so -because for once, the findings of this case study so strongly
endorse and support them. These comments are also based on insights that we have with
involvement with World Bank projects at Karnataka State levels in various ways.
We believe it is time that the Ministry of Health and Family Welfare at the Centre and State
and the International funding partners, particularly the World Bank ('who is now the largest
lender in health, nutrition and population with the largest programme in India') - who jointly
conceive, conceptualize, operationalise and monitor such large collaborative projects on
behalf of the people of this country - (emphasizing "poor and undeserved and concentrating
on children and mothers") took these concerns seriously.
This significant, rather short, but important Consultative Meeting could be a serious step in
that direction. However, a more detailed dialogue is required if these concerns must get
translated into constructive policy change.
Dr. Ravi Narayan
Dr. C.M. Francis
Dr. Thelma Narayan
Dr. N. Devadasan
Community Health Cell,
Society for Community Health Awareness, Research and Action,
No.367, 'Srinivasa Nilaya', Jakkasandra I Main,
I Block, Koramangala, Bangalore- 560034.
Phone : (080) 553 15 18; Telefax : (080) 552 53 72; Email: sochara@vsnl.com
Comments
The Case Study of World Bank Activities in the Health Sector in India brings together
findings from a variety of sources (mostly World Bank commissioned) and attempts a
comprehensive, critical, historical view of 23 projects undertaken by tire Bank in partnership
with the Ministry of Health and Family Welfare at Central and State levels and to which the
Bank "contributed over $2.6 billion plus studies and policy dialogue"
The case study is frank, introspective and 'as objective as possible under the circumstances'.
Though inadequately referrenced even from the commissioned studies, and perhaps
representing sets of opinions rather than 'evidence based analysis' it is still a sobering
indictment of what the Bank claims to be the "largest Health Nutrition and Population
programme" funded by it.
Appendix 1 of this note lists out in the report's words key findings and conclusions producing
a rather disturbing, disconcerting scenario and a rather frank admission of failure, and
distortion. If a SWOT analysis were to be done on the case study -then weaknesses
would far outweigh the strengths; and threats / distortions far outweigh the
opportunities!
In the absence of access to all the commissioned studies and reports / documents quoted in the
report, it would be unfair to attempt a comprehensive review of the document, but we raise
the following comments, reflections and questions from a Public Health; Epidemiological;
Management; Political Economy; Public Policy and Ethical perspective, keeping an overview
of the overall partnership between MOHFW and the World Bank in mind and not addressing
just the nitty gritty. Some of these are endorsed in the case study. Others are derived from the
findings presented.
1.
Public Health devalued
The whole partnership suffers from a disturbingly lack of 'public health' competence and
perspective and this chronic lacunae does not seem to have been overcome even when the
claim "the Bank is now on the right track" is made.
Throughout problem analysis, project planning and formulation, there is a confusion
between
public health system and public health care system
between socio-epidemiological context of a problem and its economic or techno
managerial context, the latter taking precedence over the former every time
the wider determinants of health status that need to be addressed by good public
health is totally ignored (devaluation of nutrition is admitted but other aspects like
water supply and sanitation, transport and communication, environment pollution
have not been addressed and even health education in this report is put outside the
confines of the health sector.
The focus on the poor, the indigent and the marginalised which should be the central
focus of an equitous public health system is ignored or if present in programme focus
is ignored in programme implementation
In fact both 'epidemiology' which is the sheet anchor of public health and 'political
economy1 which should be a important part of problem analysis is totally ignored.
The regional diversities and differentials -now known for a long term are ignored.
2
Between the generalist administrators who now manage India's Health System and
the 'economists and programme managers' that advise them from among the Bank's
staff and Consultants Public Health has been totally devalued and distorted both
due to a lack of public health orientation and public health competence among the
policy makers concerned.
Primary Health Care sidelined
2.
The World Bank projects evolved and developed when the country began to take the
Srivastava (1974) and Kartar Singh report (1973) seriously; commissioned the
ICSSR/ICMR Health for All : An alternative strategy document (1981) after becoming an
enthusiastic signatory of the Alma Ata declaration; enunciated the National Health Policy
guidelines of 1982; the National Education Policy of 1986 and the National Education
Policy for Health Sciences in 1989. In addition, the ICMR initiated its review of
Alternative Approaches in Health Care (1976) and the Evaluation of Alternative Primary
Health Care (1980). Preceding these documents but supplementing / complementing
them, there was a spate of micro-level and collective initiatives in Alternative Health Care
in the 1970s and 1980s which are now well documented and a host of very incisive,
evidence based, thought provoking analysis of India's health care systems from social,
economic, cultural, political, epidemiological and public policy perspectives from the mid
1980s to date. The World Bank project partnerships seem to be totally 'uninformed'
about all this and has not only ignored the Primary Health Care mandate but has actively
distorted the Primary Health Care agenda by focussing on
-
3.
'selective, cost effective treatment schedules' rather than enabling / empowering
health care processes
relying only on the now well debated and well established inadequacies of the GBD
study based on DALYS (WDR - 93 and the documents thatfollowed)
focussing now on secondary hospitals rather than primary health care
on first referral units rather than the Primary Health Centres
totally neglecting the people and community, whose involvement at all levels was
envisaged by the Alma Ata commitment and 'whose needs / capacities / aspirations
were to be emphasised' and not made subservient to needs of technology or the
exigencies of top down management systems.
Finally, it ignores PanchayatraJ, which has to be the focus of Public Health and
Primary Health Care in the 1990s (even cautions against it) and then creates
Registered Societies as a decentralization initiative without clarifying how they will
be made accountable, transparent, responsive to public need or the country's
democratic political system.
Unconstitutional partnership
The World Bank seeks to influence / health policy in India by (a) virtue of being the
largest lender to the sector, even though there is enough evidence that this forms a small
part of the entire country's budget; (b) by various conditionalities that overrule local
expertise and project formulations, (c) by thrusting on the country ideas from rather
different countries with different social, economic, cultural, political, ecological and
epidemiological context. (An example from Malaria Control will be given to substantiate
this)
What is the 'Constitutional validity' of this leverage which is greatly enhanced by use of
'funding muscle'? and which was established during a period of economic vulnerability of
the country (The big break' mentioned in page 18).
3
Considering that many of these are loans and not grants, is the World Bank willing to
bear the costs offailure and distortions due to poor programme planning that ultimately
affect the poor the most?
What is the long-term sustainability of such a leveraged process - often arrogant, top
down and externally inspired. What is the effect on local health system capacity
development?
Is it not leading to coercion? Distortion? Competition?
Who will bear the
responsibility? What is the accountability and transparency especially to civic society?
The MOHFW must seriously dialogue on these issues before the PAC, the legal
system, the political system and civic society begin to question and initiate informed
citizens' action against it. In Karnataka this process is already starting up.
4.
Ethical issues
The case study raises some major ethical issues
(a)
What are the ethics of promoting so enthusiastically the 'private sector1 when there is
no evidence even from Bank sources that the private sector either has the capacity to
provide 'low cost effective quality care' or has any commitment to 'public health' or to
the goal of equity (giving only the example of Apollo, Chennai, which is not even
among the best examples of corporate social responsibility is a case in point).
(b)
What is the 'ethics' of undertaking a partnership taking the credit when there is
success and then pointing a finger at the MOHFW when problems are identified and
not solved (the report calls the World Bank position 'cautious' but 'incompetence' is
what the report establishes). Does this make World Bank an unreliable partner?
(c)
What is the ethics of continuing to fund even after 1990 - a programme, when the
Bank is well aware of the flaws and distortions?
(d)
What is the 'ethics' of expanding 'quantity' at the cost of'quality' or 'infrastructure' at
the cost of'services focussing on the poor'.
Is it at all surprising that ever since the World Bank has become a lender of large amounts
of money -that the medical scams in the country have also gone up? There may be no
cause-effect relations but why does the report ignore corruption which is endemic in the
country; is now well documented by civic society; and is well accepted in problem
analysis, by serious policy researchers.
Has the World Bank ignored it by oversight? Is it aware that it may be inadvertently
supporting it or even facilitating it - international tenders and guidelines not
withstanding?
5.
Management issues
In terms of 'Management' perspectives, it is rather surprising that a partnership that claims
to be able to marshall international expertise has continued to:
4
i.
develop infrastructure quantity rather than quality;
ii.
expected 'training' inputs to get over needs ofmanagement reforms;
Hi.
iv.
given so little thought to accountability and transparency;
relied on internal monitoring / evaluation by in-house staffand consultants rather
than independent credible external evaluation;
v.
ignored health human power management issues;
vi.
focussed only on 'userfee' rather than diverse fund enhancing options including
health budget increase;
vii.
given so little thought to ownership
Directorate of Health Service staff at all levels often feel coerced by the conditionalities
/guidelines and lack of flexibility, and do not identify with it. There is also nil ownership
at the community / civic society level.
(This is probably the greatest failure of the World Bank projects and both MOHFW and
World Bank partnership cannot overlook this any longer).
All this may be changing now - the case study claims - but is this real change understood
at core policy level?
6.
Political Economy
The case study does not look adequately at the larger 'political economy1 issues against
which the analysis and the successes and failures should be contextualised. These include
the financial situation in the country and globally; the reduction / stagnation of public
sector budgets; the impact of rise in prices on drugs / diagnostics; the contraction of
public sector; the expansion ofprivate sector under LPG (Liberalization, Privatization
and Globalization) and its impact on public health and access by poor to medical care,
the potential impact of WTO and changes in Patent laws; the increasing corruption and
scams, etc., and thereby the policy researchers involved in the partnership constantly
under-estimate the political, social, institutional and other dimensions of the problem
analysis and hence offer recommendations that are general and not focussed on 'how and
why things run' or 'do not run'. The report admits this and hope the next phase will
address it. While this may be changing, of late is it still on the sidelines of the
partnerships planning and problem solving efforts and depends very much on the quality
and experience of consultancies and in-house expertise that is facilitated both inside the
MOHFW and the WB-India office.
Unless there is a strong 'public health policy resource group within the MOHFW' in the
next phase and this free-lancing, free floating, adhoc consultancies and commissioned
studies are institutionalised a real change in competence may not take place. The report
establishes rather well the inadequacies of the last two decades but its chapter on
implication for the future or how to develop an effective programme fails to grasp the
complexity of the situation. One does not know whether this naievity is intentional or
inadvertent?
5
7.
Building on strengths and new insights
While the above 6 comments may seem to focus mainly on weaknesses and distortions
that have plagued the framework of the World Bank Project partnerships, we do also
recognise some strengths and especially some of the new insights in the report which we
hope will find increasingly higher place on the agenda of problem analysis, project
formulation and project management in the future.
Some Strengths
i.
ii.
By focussing on 'private sector1 even though on the 'profit' rather than 'non-profit'
and 'corporate' rather than 'general practice', the Bank has brought into policy
focus the engagement with the private sector which has long been a 'blind spot' in
Indian health planning. It is time the GOI / MOHFW studied this sector
recognized, monitored, involved, regulated, evaluated and 'quality assured' in this
sector.
It has more recently supported the target free approach and the shift from Family
Planning, especially sterilization, to Mother and Child Health (RCH) but still has
a long way to go towards women's health and development.
Some New insights
iii.
It has also identified the following new thrusts in its section on policy
implications which are welcome
"need to focus on staff policies and practices regarding compensation,
assignment, transfer, promotion and demotion work rules and supervision"
"need to take more account of field conditions and to find solutions to
implementation problems"
"need to ensure that basic, simple services for the poor are not neglected in
the wake of attention paid to secondary hospitals"
All these are definitely steps in the right direction. In addition, we believe that if the
points 1-7 are considered not as negative judgements but as stimulus to change track and
be rooted in local social reality than these will add to important policy change as well.
8.
Some of blind spots continue even after two decades of w'ork in India, (a) One is
especially striking and that is the total disregard of Indian and alternative systems of
medicine and folk health traditions, in spite of the country having such a large network of
institutions, health centres and human resources in these systems, (b) Is the total lack of
understanding of people from a social / community point of view'. Reducing everyone to
a potential patient, client or stakeholder and taking about social marketing through IEC
rather than community involvement in planning, organising, monitoring and evaluation
continues and is another major lacunae.
9.
Our comments do not attempt a response to all the nitty gritty. In Appendix 2, we list out
an alternative framework of reference -a paradigm shift that is seriously required if the
World Bank and MOHFW want really to be on the right track. The Bhore Committee
recognised it in 1946; the WHO through Alma Ata in 1978, GOI in 1982 through the
NHP; and the ICSSR / ICMR earlier in their Health for All report in 1981;
How long can the poor and marginalised in our country wait for this shift to take place
in World Bank thinking. In the 1999, there is a some possibility - as seen in this report.
Will 'peoples health' needs finally prevail over the 'market economy of health'? Will
ethical concern for health of the poor prevail over neo-liberal economics? Will the
World Bank partnership with MOHFW be willing to make this paradigm shift?
6
Appendix - 1
SOME FINDINGS OF THE CASE STUDY
1.
Bank Project 1972 - 1988
a. "the projects did not make significant differential improvement in project districts
compared to non-project districts" (page v)
b. "Outputs other than infrastructure were largely neglected" (page v)
c. "No attempt was made to apply different delivery models in project districts"
d. "project districts continued to operate under the same personnel and recurrent budget
constraints.
2.
TINP
a. "less successful in reducing moderate malnutrition"
b. "Programme experience seems to have been lost on India' and with it the clear
emphasis on malnutrition as a leading risk for ill health".
3.
ICDS
a. "Only modest positive effects" (page vi)
b. "targetting essentially by self selection" rather than as originally envisaged "targetting
of the poor"
c. "no Bank support for revision or structural change", (page 11)
4.
Primary services
a. "efforts to improve quality have not accomplished much and it has devoted
inadequate attention to content, monitoring and evaluation, and feedback of
results".
5.
Before 1988
a. "Bank ill prepared to make practical, constructive suggestion for systems
improvements an alternative approach"
6.
Sector Studies 1988-98
a. "Tendency to make policy recommendation that are too general" (page 8)
b. "Tendency to draw judgements about facts without adequate comparisons to
experiences elsewhere" (page 5)
c. "Inadequate analysis of underlying political, institutional and sociological factors
that explain why things work the way they do" (page 8)
d. "Earlier studies tended to be designed and executed by Bank staff with limited
consultation" (Page 8)
7.
IPP-VI &IPP-VII
a. "More success in expanding the delivery and training systems than in improving their
functioning"
b. "quality and performance of the training programme remained weak" (page 9)
c. "Efforts to strengthen MCH & IEC not very productive" (page 9)
d. "Little progress in shifting contraceptive mix" (page 9)
e. "failure to involve stakeholders in significant ways in design of project"
8.
IPP-VIII (1992-97)
a. "The goals and design are appropriate and relevant but they are too new and
disbursing too slowly to judge their effectiveness or impact".
7
o
\ V ~~
GLOBALISATION: EFFECT ON HEALTH
Globalization is defined as the process of increasing economic, political and social
interdependence and integration.
The spectacular break-through in 'Information
Technology' has made the process of globalization significantly different, quantitatively
and qualitatively.
Globalization also means / or seems to be occurring:
When multinational corporations locate themselves anywhere they wish;
Western Financial Institutions influence and guide patterns of 'development'
everywhere; and
a)
b)
If:
National Governments cannot match the power of Transnational capital
The Labour of all regions is to be set in a competitive race with each other;
c)
d)
Then:
It is not through any existing forms of International Organizations that the poor are going
to be able to defend themselves
(Adapted from Jeremy Seabook's article in Third World Network Features)
Positive implications
♦ Information sharing: There is the possibility that more and varied information will be
available, which can be put to use by other countries. Such information will be useful
in improving.
❖
❖
❖
❖
❖
Services, standards and quality of care;
Policies;
Legislation;
Exchange of ideas;
Appropriate technology
♦ Increased awareness among people of issues and activities elsewhere;
♦ Better practices by health care professionals and workers.
Negative Implications
While there can be some such positive influences, the possibility of harmful effects on
health and health is much greater.
G:\OLD FILES\P850\P850 E\CHANDER\people's Health
Movement\Globalizatoin\GLOBALIsation 17.10.01 fromCMF.doc
1
Products patents
These patents give the holder the exclusive right to use the patented invention for a
specified period of time. GATT allows a product patent for 20 years from the date of
filing the patent application.
Process patents
These patents grant the holder the right s to use the process and product obtained by that
process.
Indian Patents Act, 1970, recognized only process patents. IPA states that the patent
should not be used as an important monopoly. It required making available the process
for manufacture of the product within the country recognizing the patent. TRIPS
agreement confers the right to import and does not require the production of the patented
invention in India.
TRIPS provisions
Inventions in all field s of technology, including drugs, chemicals, foods, agricultural
products, animals, plants, and micro-organisms are entitled to product and process
patents. We have witnessed the patenting of'basmati'.
The Indian Patent Act provided a duration of 14 years for patent protection. A patent for
process of manufacturing substances used or capable of being used as food, medicine or
drugs has a duration of seven years from the date of filing and five years from the date of
sealing of the patent, whichever is shorter.
GATT requires 20 years patent protection for all inventions in the field of technology,
17-20 years for pharmaceuticals, which can be further increased as process patent when
the product patent expires.
There is an obligation to set up production facilities in the country granting the patent.
Article 29 dilutes this provision. Patentee would be allowed to import the product in the
countries granting the patent; this is to be taken as on par with the obligation for
production in the country that grants the patent. This would make Third World Countries
merely markets for Transnational Corporations with no obligations.
According to all legal norms, when there is alleged violation, the accused is considered
to be innocent until proved otherwise. But in the new Patent rules, the burden of proof is
shifted to the accused. If a company files a suit against another of violation of copyright,
the accused will have to prove his / her innocence.
G:\OLD FILES\P850\P850 E\CHANDER\people's Health
Movement\Globalizatoin\GLOB ALIsation 17.10.01 fromCMF.doc
3
Patenting plant varieties
There are many herbs which have been traditionally used in India and other tropical
countries as medicines. Now, these are being taken by the affluent countries. When
genetic resources are taken from the tropical countries to the affluent countries, they are
treated as freely usable and knowledge of their characteristics is seen as belonging to all.
When the same is processed by mixing the traits, they are treated as private intellectual
property attached to them.
The same thing happens to food crops seeds. This has resulted in a few companies in the
North controlling the whole of the world seed markets and genetic resources. This can
affect food security.
Farmers' exemption had allowed them to keep seeds form the harvest for the next sowing.
In the revised system, the farmers' exemption has been removed. If a farmer is found
using a patented variety of seeds, which he does not buy, all that the agent of the patent
holder has to do is to file a complaint with the concerned authority.
Farmers will be forced to buy new seeds for every sowing. The local plant breeders will
have to pay royalty for using the patented variety.
TRIPS and pharmaceuticals
According to Article 70.8, pharmaceuticals and agro-chemical firms can file applications
for product patents within one year of signing the GATT accord. The applicants will be
given monopoly of marketing rights for five years from the date of application.
Drug prices in India were among the highest in the world before the Indian Patent Act,
1970. IPA reversed the trend. Indian companies have now become major bulk drug
producers. There are about 10,000 units engaged in the production of bulk drugs and
formulations. The producers could bring down the price drastically. But this situation
will change drastically with the new legislation.
G:\OLD FILES\P850\P850 E\CHANDER\people's Health
Movement\Globalizatoin\GLOBALIsation 17.10.01 fromCMF.doc
4
Globalisation; Effect on Health
Globalisation provides threats and opportunities to the health of the people. As it is
practised today, globalisation has more threats than opportunities. This is because
the competition far outstrips collaboration. The impact on health and health care
systems is broad and profound. Globalisation is the process of increasing economic,
political and social interdependence and global integration, Capital, goods, persons,
concepts, ideas and values diffuse across the boundaries of the countries.
Positive implications
0
Information sharing : There is the possibility that more and varied information
will be available, which can be put to use by other countries. Such information
will be useful in improving
* services, standards and quality of care
* ' policies
* legislation
* exchange of ideas
* appropriate technology
0
Increased awareness among people
0
Better practices by health care professionals and workers
While there can be many positive influences, the possibility of harm to health and
health is much greater.
Health technologies
Competition among health care providers will induce the spread of newer and not
fully tested technologies. This will lead to increasing investments in expensive,
sophisticated technologies, which may not be appropriate for the developing country.
Public sector:
To remain competitive in 'global markets, public expenditure has to minimized.
World bank and IMF.insist .that there should be a contraction of the public sector in
the health care services.
Dr.C.M.Francis and Dr.V.Benjamin
To be Published in, forthcoming issues of People.' s Reporter
Global factor and their consequences
eg ‘Downsizing’ and structural adjustment policies, leading to unemployment.
Marginalization, increased poverty, decreased social safety nets leading to
higher morbidity and mortality rates.
eg Increased promotion of tobacco, alcohol and psycho-active dings, dumping of
unsafe pharmaceuticals.
•
Increased addition, ineffective and harmful treatment
eg Promotion of cash crops at the expense of food crops.
Food security threatened; malnutrition increased
Cd Environmental degradation and unsustainable consumption by the rich: resource
depletion; water and air pollution; ozone depletion; accumulation of greenhouse
gases and global warming.
Epidemics; respiratory disorders; immunosuppression, skin cancers; cataracts;
effects of floods and storms; food shortages and malnutrition.
eg Patents
Patents
The GATT agreement on Trade Related Intellectual Property Rights (TRIPS) is meant
to protect intellectual property rights (IPR). It concerns mainly patents, which have
serious implications on health care.
There are two types of patents:
Product patents
These patents give the holder the exclusive right to use the patented invention for a
specified period of time. GATT allows a product patent for 20 years from the date of
filing the patent application.
Process patents
These patents grant the holder the exclusive rights to use the process and product
obtained by that process.
Indian Patents Act, 1970, recognised only process patents. IPA states that the patent
should not be used as an import monopoly.
TRIPS agreement confers the exclusive right to import and does not require
commercial production of the patented invention in India.
2
TRIPS’ provisions
Inventions in all fields of technology, including drugs, chemicals, foods, agricultural
products, animals, plants, and micro-organisms, are entitled to product and process
patents.
Duration of patent protection : Industrialized countries: 17-20 years
Indian Patent Act: 14 years.
According to IPA, a patent for process of manufacturing substances used or capable of
being used as food, medicine or drugs has a duration of seven years from the date of
filing and five years from the date of sealing of the patent, whichever is shorter.
GATT requires 20 years patent protection for all inventions in the field of
technology, 17-20 years for pharmaceuticals, which can be further increased as process
patent when the product patent expires.
There is an obligation to set up production facilities in the country granting the
patent. Article 29 dilutes this provision. Patentee would be allowed to import the
product in the countries granting the patent; this is to be taken as on par with the
obligation for production in the country that grants the patent. This would make
Third World countries merely markets for Transnational Corporations with no
obligations.
According to all legal norms, when there is alleged violation, the accused is considered
to be innocent until proved otherwise, but in the new Patent rules, the burden of
proof is shifted to the accused. If a company files a suit against another of violation of
copyright, the accused will have to prove his/her innocence.
Patenting plant varieties
There are many herbs which have been traditionally in India and other tropical
countries as medicines. Now, there are being taken by the affluent countries. When
genetic resources are taken format he tropical countries to the affluent countries, they
are treated as free and knowledge of their characteristics is seen as belonging to all.
When the same is processed by mixing the traits, they are treated as private intellectual
property attached to them.
The same thing happens to food crops seeds.
This has resulted in a few companies in the North controlling the whole of the world
seed markets and genetic resources. This can affect food security,
t
Fanners’ exemption had allowed them to keep seeds form the harvest for the next
sowing./ In the revised system, the farmers’ exemption has been renewed. If a farmer
is found using a patented variety of seeds, which he does not buy, all that the agent of
the patent holder has to do is to file a complaint with the concerned authority.
Farmers will be forced to buy new seeds for every sowing. The local plant breeders
will have to pay royally for using the patented variety.
TRIPS and pharmaceuticals
According to Article 70.8, pharmaceuticals and agro-chemical firms can file
applications for products patents within one year of signing the GATT accord. The
applicants will be given monopoly marketing rights for five years from the date of
application.
drug prices in India were among the highest in the world before the Indian Patent Act,
1970. IPA reversed the trend. Indian companies have now become major btdk drug
producers. There are about 10,000 units engaged in the production of bulk drugs and
formulations. The producers could bring down the price drastically.
According to the new rules, the products need not be produced here. They can be
imported and sold at very high prices; the Government will not have any control over
its price.
Values
Globalisation brings about changes In values. Profit-at-any-cost becomes the guiding
mantra (free market economy replacing the mixed economy). Consumerism spreads
itself, bringing on the newer fashions and technology. Craving for them depletes the
purchasing power. The amount available for the purchase of food materials becomes
reduced substantially.
J
lunk foods
■
I
A craze for junk foods is created, reducing the intake of wholesome food. This affects
the nutrition which is even otherwise poor.
Commercial crops
Cash crops are replacing food crops. Farmers in Punjab are growing tomato and
potato for Pepsi.
Karnataka shifted to sunflower cultivation to satisfy the
requirements of Cargill. Andhra Pradesh shifted to prawn and shrimp cultivation.
Kerala has been using its land more and more for the production of rubber, whose
price has come down. All these affect cereal production and food security.
4
Public Distribution System
The millions of the poor in India were being helped through the Public Distribution
System. GATT demands slashing down of the subsidies to the PDS. This would
result in the prices of food and other essential commodities going up beyond the
purchasing power of the poor.
Industries
Trade liberalisation is often accompanied by “decentralisation”
industrialised countries.
in
the less
“In India which has only in recent years opened up fully to the global
economy, international competition has already led some sectors if industry to
seek an advantage by recruiting cheap child labour---Increased child.labour is reported in sericulture, fish processing and genetic
engineering of seeds (UNICEF, 1996)”
With the competition due to globalization, many industries and business houses are
reducing their staff. Unemployment is staring at these people and the number of
people below poverty line is increasing.
Dumping 'duty' industries
Hazardous industries and poor technologies will be relocated in the developing
countries, leading to health hazards.
India has become a dumping ground for hazardous waste. The Supreme Court, on
February 6, 1998, directed the Customs and other authorities in charge of the
Tughlaqabad Container Depot and the Bombay Port Trust to neither auction nor
release till further orders several containers of hazardous waste (Indian Express,
February 7, 1998).
Supportive environment for health
The physical, social and economic environment must be supportive to health.
Globalisation threatens to damage the environment. The inequities are increasing
The ‘have’ resort to wasteful consumption of the world resources. There is need for a
more equitable distribution and utilization of the earth’s limited resources.'
5
Globalisation has provided an important new argument in favour of off-loading public
funding ns well as publicly operated provider institutions on to private sector and
household budgets.
Earlier efforts of multinationals to establish production operations in different local
markets - contemporary decisions to base production on exports from wherever
manufacturing can be done most cheaply.
Globalisation is the growing integration of the world economy, linked together by
large and increasing private sector financial and trade flows.
Desire of developing countries to attract multinational corporations and new jobs for
their people - increasingly fierce effects of developed countries to retain a larger share
of available investment capital and thereby to increase their own share of both jobs
and international trade - invest less in developing countries, provide fewer jobs in the
developing world but help developed countries fund jobs for their own unemployed.
“When barriers between advanced and backward economics
are destroyed, a new form of human exploitation can follow,
resembling that of colonialisom in the 19th and early 20th
centuries, complete with new forms of indentured labour”
- Plaff, 25 September, 1997
Equity
Equity will be absent when there are unequal players : the rich and the poor in the
country and the rich and poor nations. Action is needful for
*
*
*
equit)' in health and health care services;
access for all to essential health care;
reduction in the burden of diseases and suffering.
Lifestyles
Health requires healthy life styles. Globalisation often promotes harmful lifestyles
through advertisements and trade. One such is the promotion of tobacco.
Cost of health care
Globalization tends to bring costly,'sophisticated hospitals, beyond the capacity of the
people; so also the cost of diagnostic tests. Yet, by advertisements through various
media, people are made to go for these costly procedures, which may be standard in
affluent countries, whose per capita income is 100 or more times that of India.
6
People
The transnational movement of people is restricted by Visor regulations. There is
selection. Well-trained personnel of the developing countries are attracted by better
remuneration and working conditions in the affluent countries. This causes a drain of
qualified health personnel, who have been trained at great expense.
Many of the health personnel go to the richer countries to get better training but do
not return. Further the training there may not match the needs of the home country.
If they do return, they derm and a duplication of the health care facilities found in the
affluent country.
■
7
C_G F\ V\ '
ORIGIN OF HIV
*
Three of the earliest known instances of HIV infection are as follows:
1. A plasma sample taken in 1959 from an adult male living in what is now the
Democratic Republic of Congo.
2. HIV found in tissue samples from an American teenager who died in St. Louis in
1969.
3. HIV found in tissue samples from a Norwegian sailor who died around 1976.
A 1998 analysis of the plasma sample from 1959 has suggested that HIV-1 was
introduced into humans around the 1940s or the early 1950s; much earlier than
previously thought. Other scientists have dated the sample to an even earlier period perhaps as far back as the end of the 19th century.
2
In January 2000 however, the results of a new study presented at the 7th Conference on
Retroviruses and Opportunistic Infections, suggested that the first case of HIV-1 infection
occurred around 1930 in West Africa . The study was carried out by Dr Bette Korber of
the Los Alamos National Laboratory. The estimate of 1930 (which does have a 15 year
margin of error) was based on a complicated computer model of HIV's evolution. If
accurate, it means that HIV was in existence before many scenarios (such as the OPV and
conspiracy theories) suggest.
Theories for the Origin of HIV
It has been known for a long time that certain viruses can pass between species. Indeed,
the very' fact that chimpanzees obtained SIV from two other species of ape shows just
how easily this crossover can occur. As animals ourselves, we are just as susceptible.
When a viral transfer between animals and humans takes place, it is known as zoonosis.
Below are some of the most common theories about how this 'zoonosis' took place, and
how SIV became HIV in humans:
2
The 'Hunter' Theory
The most commonly accepted theory is that of the 'hunter1. In
this scenario. SIVcpz was transferred to humans as a result of
chimps being killed and eaten or their blood getting into cuts or
wounds on the hunter. Normally the hunter's body would have
fought off SIV, but on a few occasions it adapted itself within
its new human host and become HIV-1. The fact that there were
several different early strains of HIV, each with a slightly
different genetic make-up (the most common of which was
HIV-1 group M), would support this theory: every time it
passed from a chimpanzee to a man, it would have developed in
a slightly different way within his body, and thus produced a slightly different strain.
An article published in The Lancet in 2004 also shows how retroviral transfer from
primates to hunters is still occurring even today. In a sample of 1099 individuals in
*A Background Note for session at Snehadan by Sunil George
Cameroon, they discovered to ten (1%) were infected with SFV (Simian Foamy Virus),
an illness which, like SIV. was previously thought only to infect primates. All these
infections were believed to have been acquired through the butchering and consumption
of monkey and ape meat. Discoveries such as this have lead to calls for an outright ban
on bushmeat hunting to prevent simian viruses being passed to humans.
The Oral Polio Vaccine (OPV) theory
Could production of the oral polio vaccine have
contributed to the spread of HIV? Some other rather
controversial theories have contended that HIV was
transferred iatrogenically (i.e. via medical experiments).
One particularly well-publicised idea is that polio
vaccines played a role in the transfer.
In his book. The River, the journalist Edward Hooper
suggested that HIV could be traced to the testing of an oral polio vaccine called Chat,
given to about a million people in the Belgian Congo, Rwanda and Burundi in the late
1950s. To be reproduced, live polio vaccine needs to be cultivated in living tissue, and
Hooper's belief is that Chat was grown in kidney cells taken from local chimps infected
with SIVcmz. This, he claims, would have resulted in the contamination of the vaccine
with chimp SIV. and a large number of people subsequently becoming infected with
HIV-1.
However, in February 2000 the Wistar Institute in Philadelphia (one of the original places
that developed the Chat vaccine) announced that it had discovered in its stores a phial of
polio vaccine that had been used as part of the program. The vaccine was subsequently
analysed and in April 2001 it was announced that no trace had been found of either HIV
or chimpanzee SIV. A second analysis confirnjed that only macaque monkey kidney
cells, which cannot be infected with SIV or H1V, were used to make Chat. While this is
just one phial of many, most have taken its existence to mean that the OPV vaccine
theory is not possible.
The fact that the OPV theory accounts for just one (group M) of several different groups
of HIV also suggests that transferral must have happened in other ways too. The final
element that suggests that the OPV theory is not credible as the sole method of
transmission is the argument that HIV existed in humans before the vaccine trials were
ever carried out. More about when HIV came into being can be found below.
The Contaminated Needle Theory
This is an extension of the original 'hunter' theory. In the 1950s, the use of disposable
plastic syringes became commonplace around the world as a cheap, sterile way to
administer medicines. However, to African healthcare professionals working on
inoculation and other medical programmes, the htige quantities of syringes needed would
have been very costly. It is therefore likely that one single syringe would have been used
to inject multiple patients without any sterilisation in between. This would rapidly have
2
transferred any viral particles (within a hunter's blood for example) from one person to
another, creating huge potential for the virus/to mutate and replicate in each new
individual it entered, even if the S1V within the original person infected had not yet
converted to HIV.
The Colonialism Theory
The colonialism or 'Heart of Darkness' theory, is one of the more recent theories to have
entered into the debate. It is again based on the basic 'hunter' premise, but more
thoroughly explains how this original infection could have lead to an epidemic. It was
first proposed in 2000 by Jim Moore, an American specialist in primate behaviour, who
published his findings in the journal AIDS Research and Human Retroviruses. During the
late 19th and early 20 th century, much of Africa was ruled by colonial forces. In areas
such as French Equatorial Africa and the Belgian Congo, colonial rule was particularly
harsh and many Africans were forced into labour camps where sanitation was poor, food
was scare and physical demands were extreme. These factors alone would have been
sufficient to create poor health in anyone, so SI V could easily have infiltrated the labour
force and taken advantage of their weakened inlmune systems to become HIV. A stray
and perhaps sick chimpanzee with SIV would have made a welcome extra source of food
for the workers.
Moore also believes that many of the labourers would have been inoculated with unsterile
needles against diseases such as smallpox (to keep them alive and working), and that
many of the camps actively employed prostitutes to keep the workers happy, creating
numerous possibilities for onward transmission. A large number of labourers would have
died before they even developed the first symptoms of AIDS, and those that did get sick
would not have stood out as any different in an already disease-ridden population. Even if
they had been identified, all evidence (including medical records) that the camps existed
was destroyed to cover up the fact that a staggering 50% of the local population were
wiped out there.
One final factor Moore uses to support his theory, is the fact that the labour camps were
set up around the time that HIV was first believed to have passed into humans - the early
part of the 20th century.
The Conspiracy Theory
Some say that HIV is a 'conspiracy theory' or that it is 'man-made'. A recent survey
carried out in the US for example, identified a significant number of African Americans
who believe HIV was manufactured as part of a biological warfare programme, designed
to wipe out large numbers of black and homosexual people. Many say this was done
under the auspices of the US federal 'Special Cancer Virus Program' (SCVP), possibly
with the help of the CIA. Some even believe that the virus was spread (either deliberately
or inadvertently) to thousands of people all over the world through the smallpox
inoculation programme, or to gay men through Hepatitis B vaccine trials. While none of
these theories can be definitively disproved, the evidence they are based on is tenuous at
best. and often ignores the clear link between SIV and HIV, or the fact that the virus has
been identified in people as far back as 1959. They also fail to take into consideration the
lack of genetic-engineering technology available to 'create' the virus at the time that
/\IDS first appeared.
WHERE?
The question of exactly where the transfer took place, and where the 'epidemic' officially
first developed has always been controversial. Given the evidence we have already
looked at. it is likely that Africa was indeed the continent where the transfer of HIV to
humans first occurred (monkeys from Asia and South America have never been found to
have SI Vs that could cause HIV in humans). However, who exactly spread the virus from
Africa, to America and beyond remains a mystery. It is quite possible that separate
'pockets' of the virus could have been developing in a number of different countries years
before the first cases were ever officially identified, making it virtually impossible to
trace one single source.
What did cause the epidemic to spread so suddenly then?
There are a number of factors that may have contributed to the sudden spread of HIV.
most of which occurred in the latter half of the twentieth century.
Travel
?
Both national and international travel undoubtedly had a major role in the initial spread of
HIV. In the US. international travel by young men making the most of the gay sexual
revolution of the late 70s and early 80s would certainly have played a large part in taking
the virus worldwide. In Africa, the virus would probably have been spread along truck
routes and between towns and cities within the continent itself. However, it is quite
conceivable that some of the early outbreaks in African nations were not started by
Africans infected with the 'original' virus at all, but by people visiting from overseas
where the epidemic had been growing too. The process of transmission in a global
pandemic is simply too complex to blame on any one group or individual.
The Blood Industry'
As blood transfusions became a routine part of medical practice, an industry to meet this
increased demand for blood began to develop Aapidly. In some countries such as the
USA. donors were paid to give blood, a policy that often attracted those most desperate
for cash; among them intravenous drug users. In the early stages of the epidemic, doctors
were unaware of how easily HIV could be spread and blood donations remained
unscreened. This blood was then sent worldwide, and unfortunately most people who
received infected donations went on to become HIV positive themselves. In the late
1960's haemophiliacs also began to benefit from the blood clotting properties of a product
called Factor VIII. However, to produce this coagulant, blood from hundreds of
individual donors had to be pooled. This meant that a single donation of HIV+ blood
4
could contaminate a huge batch of Factor VIII. This put thousands of haemophiliacs all
over the world at risk of HIV. and many subsequently contracted the virus.
Drug Use
The 1970s saw an increase in the availability of heroin following the Vietnam War and
other conflicts in the Middle East, which helped stimulate a growth in intravenous drug
use. This increased availability and together with the development of disposable plastic
syringes and the establishment of 'shooting galleries' where people could buy drugs and
rent equipment, provided another route through which the virus could be passed on.
Structure and types of the virus
f
HIV belongs to the family of retroviruses. There are two types of HIV viruses: Type 1
and Type 2. Both Types are prevalent in India, Type 1 is more frequently reported. HIV
Type 1 is a more virulent pathogen than Type 2 HIV Type 2 is generally milder, slower
to progress and poorly transmitted vertically. The virus is found in almost all body fluids
and organs, but they are present in large numbers in the semen, vaginal and cervical
secretions and blood. The highest concentration of HIV among body fluids is found in the
cerebrospinal fluid.
HIV attacks the white blood cells, in particular a group of cells know as the CD4 cells.
Cd4 cells coordinate the response of our immune system to any foreign agent in our body
such as bacteria or viruses by enabling the production of antibodies that neutralise and
eliminate them from our body. When the CD4 cells are infected then our body’s defence
mechanism begins to crumble and we become prone to infections that a healthy person is
able to ward off.
}
Modes of Transmission
S.No.
Modes of
Transmission
Efficiency
Source of infection
1
2
3
Sexual Intercourse
Blood transfusion
Perinatal (Parent
to Child)
Injecting Drug use
Needle stick in jury
0.14.0%
90-95%
20-40%
80-86%
3-5%
2-3%
0.54.0%
Less than 0.1%
3-5%
4
5
Stages of HIV Infection
Generally we can divide the stages of HIV infection in an individual as follows
1. Window Period
It usually lasts from 6 weeks to 12 weeks. Routine tests like ELISA, Western Blot,
RAPID will turn to be negative during this period. Few people develop what is
5
known as ‘seroconversion illness’. Most people are unaware that they have been
infected. The person continues to be healthy and do all types of normal work. The
person is a carrier of the virus and can transmit it to others by all the routes that have
been mentioned.
2.
Period of Latency
This can last from anywhere between 3 months to 10 years and more. The person who
is infected is a carried of the virus. He/She has no symptoms of the disease at this
stage. The person is considered HIV positive as revealed by a positive test. A person
can be in this stage for several years before the virus has destroyed much of the
immune system and he/she falls ill.
3.
AIDS Case
This can be from anywhere between two years from the time of infection to ten years
or more. As immunesuppression develops, the CD4 count falls and viral load
increases. Signs and symptoms of the disease begin to manifest itself. These diseases
are classified as minor (wasting, minor skid and oral problems, recurrent sinusitis
etc.) and major (TB, bacterial pneumonia, chronic diarrhoea, prolonged unexplained
fever). Multiple diseases and clinical problems are common in AIDS patients and in
the absence of specific therapy death occurs.
Current rates/statistics
The following statistics taken from the latest UNAIDS report show us our current state
with regard to our fight against HIV &AIDS.
People with HIV/AIDS in 2004
Total
Adults
Women
Children
39.4 million (35.9 - 44.3 million)
37.2 million (33.8-41.7 million)
17.6 million (16.3-19.5 million)
2.2 million (2.0-2.6 million)
People newly infected with HIV in 2004
Total
Adults
Children under 15 years
4.9 million ^4.3 - 6.4 million)
4.3 million (3.7 - 5.7 million)
640,000 (570,000-750,000)
AIDS Deaths in 2004
Total
Adults
Children under 15 years
3.1 million (2.8-3.5 million)
2.6 million (2.3-2.9 million)
510,000 (460,000-600,000)
Diagnosis
HIV infection is diagnosed by blood tests that detect the HIV antibodies.
HIV antibody tests usually done are
& ELISA Test
RAPID Test
6
<%“ Western Blot
All the above tests turn positive only three months after the HIV infection has occurred.
The following tests detect the virus directly instead of the antibodies
Polymerase Chain Reaction (PCR) test
NASBA (Viral Load assessment) test
P24 antigen test
Both PCR and NASBA turn positive after 72 hours of infection while P24 turns positive
after 2 weeks of infection. While these tests have shrunk the window period they are
extremely expensive and available only in few places.
Treatment regimes and positive living
A person infected with HIV does not require any special treatment for a long period
depending upon the progression of the illness in the body. Once someone comes to know
that he/she is infected with HIV, it is more important to take care of basic hygiene and
nutrition. Of great importance is the psychological support that a HIV -i-ve person
receives from the community.
While HIV was not treatable a few years ago today HIV is a treatable manageable illness
though a complete cure has not yet been found.
The drugs that are used to treat HIV infection are know as Anti retroviral drugs or ARVS.
These are required only after a certain stage of progression, prolong the life, and improve
the quality of life of the infected person.
t
Anti retroviral drugs are of different types. The common clinical criterion that is used to
start Antiretroviral Therapy (ART) is the level of the CD4 count in an infected person.
The current guideline is when the CD4 count falls below 200 or the viral load increases
above 50.000-100,000 copies/ml. The assessment whether Antiretroviral therapy should
be started is to be done only by a qualified medical practitioner.
Common Interventions
1. Prevention and Awareness Building
This is one of the common interventions that is done. It focuses primarily on people
indulging in high-risk behaviour and how they can be helped not to contract the virus.
2.
Care and Support
Interventions under care and support focus on People already infected or affected by
HIV&AIDS.
;
3.
Campaigns against Stigma and Discrimination
This refers to all efforts aimed at removing the stigma and discrimination faced by
People Living with HIV&AIDS.
Social and Ethical issues in HIV/AIDS
1. HIV and its consequences
Acquired Immune Deficiency syndrome (AIDS), which is a consequence of HIV
infection is not merely a disease as its impact on the general population goes far
7
beyond health. It involves social and developmental issues. People with HIV &
AIDS often fail to get timely and appropriate medial care because of the social
stigma and reluctance among a large number of doctors to treat such patients. Its
association with sexuality, illness and death often produces strong feelings in the
community. As a result, HIV positive people often fail to get their due rights, both
as a patient and as a human being.
2.
Social issues in relation to HIV infected persons
Society has overreacted to the epidemic, mainly because HIV is transmitted
primarily through a behaviour which is private, secret, often hidden and in
many places illegal, l.e. through sexual intercourse and through needle
sharing for intravenous drug use.
}
Worldwide, many people infected with HIV &AIDS are denied of their
human rights.
Stigma and Discrimination are major obstacles to effective HIV & AIDS
prevention and care.
Fear of discrimination may prevent people from seeking treatment for HIV &
AIDS or from acknowledging their HIV status publicly. Some are put into
quarantine, imprisoned or forcibly tested.
<%>" The details of HIV positive individuals have found prominent media coverage
exposing them to social identification and subsequent abuses.
<=>■ People with or suspected of having HIV may be turned away from health care
service, denied housing and employment, , shunned by their friends and
collegues, turned down for insurance coverage and refused entry into foreign
countries. In some cases they are evicted from home by their families,
divorced by their spouses and suffer physical violence or even murder.
It is, therefore, important that respecting, promoting and protecting human rights
are as important as providing care to HIV positive persons.
3.
General emotional problems of the infected
People living with HIV & AIDS go through a myriad of human emotions, such as
o” Fear of dying particularly alone
<%» Loss of livelihood and ambitions and physical distress
Grief, losses they have experienced or anticipating
Guilt of having infected others, sadness of family
<■>■ Depression -absence of a cure
Denial of status and social responsibility
Anxiety-prognosis, rejection and concern about confidentiality
<%» Anger- unlucky to catch the infection
Suicidal activity- as a way to avoid pain
8
*>
<%
Loss of self-esteem- rejection by colleagues, family members
Spiritual concerns about impending death, loneliness etc
4. Important ethical issues
The most important are in relation to ethical issues has been in terms of testing for
HIV status. Testing for HIV infection involves a simple test but the results have a
profound significance for both the individual and the community. The development of
a test in 1985 to detect HIV infection in individuals has had two aspects
1. It has opened the way to protect blood supply and allowed the identification of
people, who while apparently healthy could transmit the infection.
2.
It also exposed HIV positive people to stigmatization, discrimination and even
loss of freedom.
There are three ethical aspects in testing for HIV infection
Mandatory' testing- should not be done, w/th exceptions like blood donation
<?>” Voluntary testing - can be done after obtaining informed consent from the person
to be tested.
*> Pre and post test counseling- must be done to ensure that the person being tested,
<%
has the knowledge of the significance of the test results and options available in
case of a positive status.
Note:
Screening for safety purposes is not allowed.
It is important to remember that professional misconduct and negligence can lead to
legal liability.
Judgment of the Supreme Court of India
"Without permission of the patient, a doctor shall not inform the details of the
treatment to anybody, except the doctor to wfiom the patient is being referred to for
further opinion or management. However a ‘doctor may consider it a duty to ensure
that the sexual partner of a known HIV +ve patient is informed of the risk, regardless
of the patients own wishes ”.
9
(So f'A VV
Proposal for a global ‘Right to Health and Health Care Campaign’
to be launched by the People’s Health Movement.
[Short Version. December 2005]
The context
1. There is an urgent need to replace the dominant discourse in health by a process aimed at
universally achieving the ‘right to health and to health care’ as the main objective to achieve
more equitable health care systems in both developing and developed countries.
2. The People’s Health Movement (PHM) is launching a global initiative to strengthen the
‘Right to Health’ (RTH) with a focus on defending and operationalising the ‘Right to Health
Care’.
3. Since it is predictable socio-pblitical forces at work that determine the risk of most forms
of human rights violations, this Campaign looks at what additional measures have to be taken
now. 8. It grounds our understanding of human rights violations in the broader analyses of
power and social inequality. Knowing carries obligations -thus the proposed Campaign.
4. Poverty is the world’s greatest killer. It is thus not enough to improve the situation of the
poor within the existing social relationships. Structures and not just individuals must be
changed if the RTH of the marginalized in the world is to be achieved.
5. Rights are realised by changing the prevailing power relations. Rights cannot be advanced
but through the organised efforts of the state and of civil society.
6. Public health must be linked to a return to social justice and equity; this is the central
challenge for the future of public health. The Campaign here proposed by PHM thus seeks
the social transformations indispensable to resolve the inequities found in health.
The justification
7. There is now a need to launch a global process of mobilization to actually implement the
provisions of General Comment 14
*
in all countries. The ‘Right to Health’ will be
operationalized by changing global and national health sector reform initiatives.
Nearly 150 countries around the world are parties to the International Covenant on Economic, Social and Cultural Rights. General
Comment 14 (GC 14) of the Committee on Economic, Social and Cultural Rights (CESCR) adopted in the year 2000 elaborates on and
clarifies the Right to Health by defining the content, the methods of operationalization, the violations and the suggested means to monitor
the implementation of this right. GC14 is the most authoritative interpretation of international law relating to the right to health.
(http://www.unhchr.ch/tbs/doc.nsf/('svmbol)/E.C . 12.2000,4.En?OpenDocument)
8. But why do we need a global campaign on the Right to Health? Much is wrong with the
neo-liberal model of global restructuring in the world. This process is unchecked either by
national or global mechanisms.'It is in this context that there is growing recognition of the
need for a global initiative to address health systems issues in a rights-based framework.
What will this entail?:
A. Neo-liberal policies restrict the revenue of the state for use for welfare purposes so
that governments find themselves unable to finance health security systems. To put in
place mechanisms of effective redistribution of resources is only possible through a
globally coordinated effort, thus the Global Campaign.
B. We need to establish universal norms regarding a basic standard of essential health
care services that must, be ensured. Further, health care workers distribution must be
based on need rather than on the ability of richer countries to pay more for human
resources from poorer countries.
C. There is also a need to challenge the dominant global discourse of 'Health care as a
commodity’ and ‘safety nets for those left outside the benefits’ wherein health services
1
are increasingly marketized and governments retreat from the provision of health care.
We need to counter this with a ‘Health care as a human right ’ discourse.
A Campaign focusing on the Right to Health Care
9. PHM struggles for and demands the respect of all aspects of health rights.
10. This right includes both the Right to health determinants such as water, food security,
housing, sanitation, education, a safe and healthy working and living environment, etc., and
the Right to health care (the right to the entire spectrum of preventive, curative and
rehabilitative services plus health education and selected promotive activities/
11. Naturally, the global health movement has an important role to play regarding both of the
above components of the Right to Health. However, in practice, this suggests two types of
tasks for the global health movement:
I. Tackling the right to health determinants
12. Supporting campaigns on water, food security, housing, etc. There are existing initiatives
already working for these rights. This recognition places the obligation on PHM activists to
actively support such initiatives though not necessarily to take up the responsibility of
primary' leadership of such groups.
13. A specific role that has to be played by PHM activists is to document violations of the
Right to Health and its underlying determinants. Health-based arguments can indeed
significantly strengthen the demands to tackle these determinants.
II. Strengthening the right to health care
14. This is a task for which the global health movement has an unquestionable responsibility
to take the lead on.
We suggest the following overall strategy for PHM:
15. Regarding the strengthening the Right to health determinants, PHM country circles would
continue to expand their involvement in these initiatives in their countries and regions. PHM
may even co-initiate specific international campaigns on a particular health determinant (e.g.,
the Right to Water). However, it is not strategically possible for a global health movement
like PHM to launch a single campaign encompassing all health determinants on a global
scale.
16. We suggest launching a Global Right to Health and Health Care Campaign. PHM has
a primary responsibility regarding this issue. However, during this campaign, the
documenting of violations will not be restricted to those in the sphere of health care, but will
encompass denouncing violations of health rights related to the various determinants of
health.
17. These two types of activities should be combined as part of a comprehensive approach to
the Right to Health. This differentiated strategy does not reflect any judgement on the relative
importance of health care vs. the underlying and basic determinants of people’s health; it is
rather a question of the strategic approach chosen.
What is the added value of adopting this focus?
18. A RTH Campaign has a big social mobilization potential; the HR approach is backed by
international legislation; the RTH approach demands that decision-makers take
responsibility; HR imply correlative duties that are universal and indivisible; and (Unlike the
MDGs) the HR approach is focused on processes that lead to concrete outcomes.
What does the RTH imply?
7
2
19. In every development process there are two types of actors: claim holders and duty
bearers. When the State does not respect human rights, claim holders have to demand their
rights from the duty bearers in government.
20. The marginalized are being denied their rights, in part because, as claim holders, they do
not have the capacity to effectively demand (claim) their rights; rights are also violated
because duty bearers do not have the capacity or the will to fulfil their obligations (called
"correlative duties’).
21. Therefore, in the HR-based approach (HRBAP) one has to carry out two types of
analyses: a) situation analyses in which one determines the causes of the problems placing
them in a hierarchical causality chain of immediate, underlying and basic determinants, and
b) capacity’ analyses in which one determines who are the individuals/institutions that bear
the duty to do something about the above causes calling on them to fulfil their duties as per
their country’s obligations as signatory of the United Nations HR covenants.
22. These two types of analyses have to be carried out with the community and the
beneficiaries of the health system so that the rights being violated can be identified jointly
and those responsible can be confronted —for them to do something about the problems
identified.
• 1
23. Asa PHM ultimate goal, we do NOT look for health policies that favour the poor... We
seek significant poverty reduction policies that directly address the social determinants of the
inequitable distribution of resources, as much as we seek to end the exiting violations to the
RTH. The Campaign gives us the possibility of advancing PHM’s political agenda that
strives for equity and for the structural changes that will do away with the social, economic
and political determinants of health.
24. We are no longer going to go to beg for changes to be implemented; we are now going to
demand them based on existing international law already in force in most of the countries
where we work. Disseminating this concept is in itself empowering and is part and parcel of
this Campaign.
25. We have to overcome the culture of silence and apathy about the HR violations in health
we all know are happening. This, because HR and the RTH will never be given to poor,
marginalized, discriminated and indigenous persons. Repeat: rights are never given, they
have to be fought for! And this is what the RTH Campaign will attempt to do.
Suggested focus of the Campaign
26. It does not need to be emphasised that specific important aspects of this Right, such as
women’s and children’s right to health care, mental health rights, HIV and AIDS-affected
persons health care rights, workers’ health rights, the right to essential drugs, etc. need to
(and will) be woven into the Campaign, bringing diverse branches of the global health
movement into a broad coalition working for public health systems that strengthen universal
access to health care.
y
27. PHM will document violations, which can help push for changes in the key wider
determinants of health; they Will also denounce and act upon adverse existing and new
policies that are having negative impacts on the Right to Health (such as the privatisation of
services, the weakening of universal access systems, vertical programmes that fragment
health systems, the cun-ent 90/10 gap in research funding, the unjust international trade
regimes —to name just but a few).
Possible organizational collaboration
'
28. The United Nations Special Rapporteur on the Right to Health has already shown interest
in the idea of this global Carripaign. WHO will need to be strongly influenced, and could be a
3
potential collaborator. PHM has been a key actor in the launching of the Commission on the
Social Determints of Health (CSDH) of WHO which we see having a real potential in the
fight for the RTH care. Most countries have National Human Rights Commissions or official
bodies that can be involved in monitoring the Right to Health. Present PHM-member
organizations will also involve a broader range of civil society organizations in our network
including women’s organizations, coalitions of HIV and AIDS-affected persons, trade unions
of health sector personnel, people’s movements, etc.; in this sense the campaign would be led
by PHM-and-partners.
Suggested process to launch the Campaign
29. To move towards implementing ther Campaign process, we here propose a sequence of
activities.
I.
Preparatory phase (early to mid 2006)
1. Creation of a broad consensus on the Campaign idea. Formation of a ‘Core
Campaign Steeririg Group’ of about 6-8 organizations who are willing to help
coordinate the Campaign globally. This team will actively support a host of
regional organizers and will lead the international networking work, plus the fundraising and advocacy work for the Campaign. To support this team, a global
campaign secretariat (of about three to four .persons) will need to be formed to
coordinate the campaign.
2. Identification of specific (existing PHM or newly associated) groups that will take
regional responsibilities. If possible, at least one consultation within each region
to discuss the campaign will have to be held.
3. Identification of short and long-term sources of funding.
4. Ensure local campaign ownership and active involvement throughout the process.
A mechanism for regular consultation with allies will be set up.
5. Completion of guidelines for the preparation of status papers on ‘The State of the
Right to Health’ in each country (early 2006).
6. Contribution to the next (2007) edition of the Global Health Watch.
30.This phase will culminate in'a restricted consultation of the Steering Group in the first
quarter of 2006 in which the developments so far will be reviewed and plans made for the
next phase of the Campaign.
II. Documentation and analysis phase (the last three quarters of 2006).
31. During this period, country, regional and global reports will be prepared as follows:
1. Country papers or reports on the Status of the Right to Health Care will be
completed in the countries of at least two regions; in the other regions, the process
will be started and’ brought to as an advanced stage as possible. Options are as
follows:
• Full blown Country Reports: These will be the most extensive and will
analyse all or most aspects of the health care system in the country and report
on their current status with facts and figures, documenting why and how
General Comment 14 has (not) been fulfilled five years after its adoption
(within the framework of a ‘progressive realization of the right to health’).
• Country Status Papers: These will be less detailed and may not coyer all
components of the health sector, but will be based on country level
information and statistics that bring out major health care system gaps.
4
Country Overviews: These will only contain a listing of major issues of
concern from the Right to Health perspective (e.g., declining health budgets,
unregulated privatization, imposition of user fees, dismantling of the social
security system).
32. The aim is that about 40-50 countries will prepare these country reports or status papers aiming at a minimum of 5 in each region.
2. A Global Health .Watch Report chapter on the Right to Health could be
drafted focused on how the various global agencies and actors are infringing the
Right to Health in different ways. It will also focus on the minimum obligations
developed countries have to contribute to health care development in poorer
countries and to stop the northward migration of health professionals.
33. This phase will culminate with the concrete planning of Regional Assemblies on the
Right to Health in the seven or eight regions (to be determined) .of the world: Dates, venues,
financial arrangements, major agenda contents and organising agencies will be identified and
given concrete mandates. For .this, a pre-planning meeting to finalise the program of these
regional assemblies may be held at the end of 2006.
•
III. Regional Assemblies and subsequent action phase (after the World Health Assembly
of May 2007)
34: Plans are as follows:
1.
Sequential Regional assemblies on the Right to Health will be held in all
regions of the world: one assembly in each of the seven or eight regions,
spaced about. 2 .months apart. These would be called by PHM, with
involvement of the UN Special Rapporteur on the Right to Health and WHO,
and will be attended by national health officials, national human rights
committees and PHM, as well as other health and human rights activists.
Available country reports/country performance report cards on the Right to
Health will be presented and discussed. These assemblies will attract wide
media coverage. Action plans to implement the Right to Health will be drawn,
discussed and presented in the second half of the assemblies.
2.
This series of-regional assemblies may culminate in some kind of a resolution
being proposed for adoption at, say, the World Health Assembly in Geneva in
2008. Such a resolution will call for the time-bound implementation of the
Right to Health. This will include demanding governments progressively
incorporate RTH principles and standards into their national laws. Further, the
resolution will put in place mechanisms for monitoring and redressal of this
right in all countries of the world. PHM partner organizations will also use this
as a concrete opportunity to draw-in many more organizations into the
network, to dialogue with their country governments, and to engage with
national NGOs and human rights bodies.
3.
Finalisation of the Global Health Watch report on the Right to Health is
envisioned for April 2007. The same could include summaries of all the
regional analysis papers and a one-page standardized abstract of the available
country Right to Health reports.
4.
Preparation of a ‘Global Action Plan on the Right to Health Care’. Such a
document will convincingly show how quality essential health care services
could be made- available NOW to every human being on earth, provided
certain key reallocation of priorities and resources are enacted. This Global
assessment will be accompanied by practical recommendations for the
5
countries in each region; the latter will form the basis of a Concrete Agenda to
achieve the goals set out in the People’s Charter for Health.
5.
The 2008 World Health Assembly will be asked to adopt a ‘Declaration on
the Right to Health for All’ for implementation by member countries, The
same will have time-bound, specific and monitorable goals and contain the
basic principles of a bottom-up health sector reform. The aim will be to
sponsor effective community involvement and monitoring in health thus
operationalizing the Right to Health. A shift in policies of all the international
agencies working in the health sector will be demanded so that they
progressively move towards a human rights-based approach to health
planning.
35. Some shift in the focus of WHO towards the Fluman Rights-based Approach to Health
will be needed: a shift that puts universal access systems at the center and that strengthens a
group inside WHO that will continue to work and provide leadership on this work.
36. The strengthening and broadening of the PHM network in various countries across the
globe will be both an outcome, and also an imperative to take the Movement forward around
this rallying point.
A few conceptual and strategic points
37. i- The Campaign will challenge the commoditization of health, asserting the inalienable
role of the state in public health systems with the public at the center.
ii- The Campaign makes health rights operational, and thus requires demanding specific
commitments and norms thhf provide measurable parameters for monitoring and for the
enforcement of redressal mechanisms.
iii- The Campaign builds a broad strategic alliance involving various special health rights
movements that already (or not yet) claim the Right to Health as a key human right.
iv- The Campaign is deeply rooted in national initiatives, yet also addresses key global
processes and counters powerful strategic opponents.
v- The Campaign vies for putting the RTH more at the center of attention in the health
discourse, and engages major actors making them take an explicit stand on the Right to
Health.
’ ' '
vi- For today, the Campaign represents a strategy of resistance (i.e., preventing a further
weakening of public health systems) and, for tomorrow, it offers a whole new alternative
vision (i,e., universal access to comprehensive health care plus the tackling of the key
negative determinants of health).
vii- The Campaign will be used to shift the discourse from the preoccupation with vertical
programmes and privatisation-oriented measures to focusing more on widespread denial and
violations of the Right to Health, on demanding a global consensus on the implementation of
this right, and on asking that all programmes and measures now be critically evaluated
according to the tenets of health as a right.
What may be realistically achieved through the proposed process?
38. We have no illusion that systematically raising the issue of the ‘Right to Health’ will by
itself lead to an actual complete implementation of this right in countries across the globe.
The universal provision of even basic health care services 'involves major budgetary,
operational and systemic changes; in addition to shifting to a rights-based framework, major
political and legal reorientations are thus needed -and such major changes cannot be
expected to happen in full in the near future.
6
39. However, we can expect and can work on a number of more achievable objectives that
can take us towards the larger Human Rights goal. Some of these ‘achievables’ to be
considered in our Campaign are: the explicit recognition of the Right to Health Care at
country level; the formation, in some countries, of health rights monitoring bodies with PHM
and civil society participation; a clearer delineation of health rights at both global and country
level; the shifting of the focus of WHO towards health rights/universal access systems and
the strengthening of groups within WHO that will work along these lines; and, finally, the
strengthening of the PHM network in as many countries as possible so all its members work
around a common and broad rallying point.
Organization of PHM and of partners and the Campaign
40. Recognizing that PHM country circles —which were formed during or after the first
People's Health Assembly (PHA1) need to move beyond discussions to develop forceful,
shared advocacy activities; this is crucial if they are to develop further and to draw-in more
groups into our movement. There is now a need to develop and carry out shared and more
effective advocacy actions at country level. These are to be directed at engaging both claim
holder groups and decision-makers (duty-bearers) in an effort to bring about needed changes
in the existing (and often deteriorating) situation. A ‘Right to Health and Health Care’
Campaign can be such a catalyst and unifying process bringing together existing and new
PHM circles, as well as involving new partner groups and networks. The campaign has the
potential to give space to new organizations and networks, which have so far not been active
in PHM. Assessing the campaign’s viability will start by ascertaining the existence of a
minimum critical mass of PHM-and-partners strength and power in a substantial number of
countries. Our appeal is for such a process to start as early as possible. As a first step, we plan
to explore the potential of this global Right to Health and Health Care Campaign. We have to
make use of the momentum achieved at PHA2 to crystallise and plan the future courses of
action of the Campaign —understanding that each country will move at its best (individual)
pace.
. .
-Abhay Shukla and Claudio Schuftan, People’s Health Movement India and Vietnam.
abhavseemafcbysnl. com: claudio&.hcmc. netnam. vn
7
Co AA W —
Community Health Cell
Community Health Fellowship Scheme
Annual Community Health Fellows’ Workshop 2006
Dates : March 6 - 8, 2006
•
:
Venue: Navaspoorthi Kendra, Bangalore.
Health as a Human Right in the Era of Globalisation
6th March 2006 (Monday)
9.00 - 10.00a.rn
- Informal Fellowship
10.00 - 10.30 a.m
- Tea Break
10.30 -11.30 a.m
- Introductions
* Objectives/ Schedule of Workshop
® Expectation Inventory
11.30 - 12.00 noon
- Demystifying Globalisation
» Pooling ideas and perspectives - Premdas and Naveen
12.00 - 1.00 p.m
- Session I - Facilitator: Thelma Narayan & CHC Team
o Reflections on Field realities of Globalization effects on Health
and Health Care at local level.
a. Did 1 observe any trends/ changes in my area of field work
that could be attributed to new economic policies or forces
of globalization
b. Were there any impacts of these on Health and Health Care
of local people.
1.00 - 2.00 p.m
Lunch
2.00 - 3.30 p.m
- Session 11 - Reflections ( continued )
3.30 - 4.00 p.m
- Tea Break
4.00 - 5.30 p.m
- Session III
• Reflections ( continued )
• Synthesis (Anant, Sathyashree)
a. Forces of Globalization visible at Community level
b. Effects of these on Peoples Health and Access to Health Care
5.30 - 7.00 p.m
-
7.00 - 8.00 p.m
- Group Discussion : i) CHFS Bulletin
ii) MFC meeting and Dec 2006 request
Free time
(Post Dinner Sing-song)
~lh March ( Tuesday )
9.30- 11.00 a.m
- Impact of globalization on social and economic life of people
Resource Person: Prof. Abdul Aziz (ISEC)
(45 minutes presentation, 45 minutes interactive discussion)
11.00 - 11.30 a.m
- Tea Break
11.30 - 1.00 p.m
- Health Human Resource Development in the era of globalization
(challenges and response)
Resource person: Thelma Narayan
1.00 - 2.00 p.m
- Lunch
2.00 - 3.00 p.m
- Travel to Snehadhan or other agencies
3.00 - 6.00 p.m
- Observation/ Interaction visit followed by Reflection session at Snehadan
• The realities of HIV/AIDS
• Globalisation and the challenge of Access to ARVs for patients as
a Human Right
Resource Persons : Sunil George/ Sr. Sylvia/ Ms. Manjula
7.00 - 10.00 p.m
- Informal dialogue
- Preparation of Presentations
8lh March 2006 (Wednesday): Women’s Day
9.00 - 11.00 a.m
- Health Rights : What are they/What are the obstacles/What can be done
Chair person: Narendra Gupta (Prayas, JSA/ NAPM)
•
Women’s Health (Facilitators: Madhumita, Sathyashree)
o Activity
o Study on ANC (Sr. Tina/ Vinay)
•
Dalits, Adivasis, Children, Disaster situations, Workers, Street
children, etc.
(Fellows should choose subgroups and prepare 5-7 minutes presentation on Rights of socially
excluded groups and the challenges to meet them. Not more than 9-10 groups of 2 fellows each)
11.30 - 1.00 p.m
- International Health Financing and Health Systems - Issues and
Challenges
Resource person: Ravi Narayan, PHM Global Secretariat
(Will cover study on External funded projects in Karnataka for Task Force and WB Evaluation, and
PHM critique of report of Commission on Macroeconomics and Health)
1.00 - 2.00 p.m
- Lunch
2.00 - 4.00 p.m
- Informal Discussion with External Review team conducting end review of
the CHFS - Exclusively for interns/ fellows (Dr. Vasundhara / Dr.
Narendra Gupta)
4.00-4.30 p.m
- Tea
4.30 - 5.30 p.m
- CHFS - Next Steps and the Way Ahead
Facilitator: Dr. Thelma Narayan & CHC team
Additional
i)
ii)
iii)
Display of books, documents and other materials
Bulletin Board
Cultural programs - to be organized by fellows
9"' lo 15"' March
Will evolve in discussion with die present batch on 6lh March
Will include
i)
ii)
iii)
Session with Dr. Shekar Seshadri on life skills education
Time for discussion with Mentors
Time for Reports
iv)
v)
Visits
Informal Group discussion
- Media
 RF_COM_H_90_SUDHA.pdf
RF_COM_H_90_SUDHA.pdf
Position: 1903 (6 views)