WESTERN REGION PUBLIC HEARING ON THE RIGHT TO HEALTH CARE
Item
- Title
- WESTERN REGION PUBLIC HEARING ON THE RIGHT TO HEALTH CARE
- extracted text
-
RF_COM_H_87_SUDHA
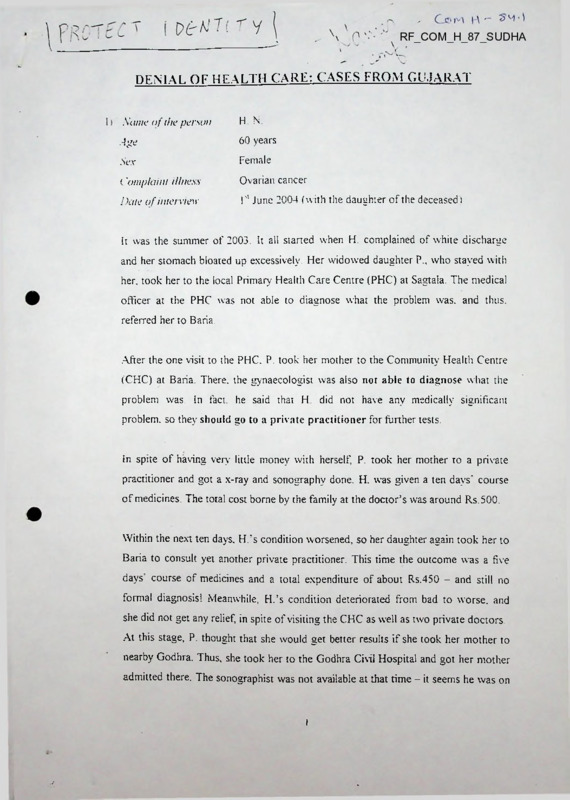
DEMAL OF HEALTH CARE: CASES FROM GUJARAT
Xante of the person
H N.
.4ge
60 years
.Sex
Female
('ontplaint illness
Ovarian cancer
Dene of interview
I'1 June 2004 (with the daughter of the deceased)
It was the summer of 2003. It all started when H. complained of white discharge
and her stomach bloated up excessively. Her widowed daughter P„ who stayed with
her, took her to the local Primary Health Care Centre (PHC) at Sagtala. The medical
officer at the PHC was not able to diagnose what the problem was. and thus.
referred her to Baria.
.After the one visit to the PHC. P. took her mother to the Community Health Centre
(CHC) at Baria. There, the gynaecologist was also not able to diagnose what the
problem was. In fact, he said that H
did not have any medically significant
problem, so they should go to a private practitioner for further tests.
In spite of having very little money with herself, P. took her mother to a private
practitioner and got a x-ray and sonography done. H. was given a ten days' course
of medicines. The total cost borne by the family at the doctor’s was around Rs.500.
Within the next ten days. H.’s condition worsened, so her daughter again took her to
Baria to consult yet another private practitioner. This time the outcome was a five
days course of medicines and a total expenditure of about Rs.450 - and still no
formal diagnosis! Meanwhile, H.’s condition deteriorated from bad to worse, and
she did not get any relief, in spite of visiting the CHC as well as two private doctors.
At this stage, P. thought that she would get better results if she took her mother to
nearby Godhra. Thus, she took her to the Godhra Civil Hospital and got her mother
admitted there. The sonographist was not available at that time - it seems he was on
vacation for twentv days - so the sonography could not be done at the Godhra Civil
Hospital H.'s desperate state made her daughter take her to a nearby private ciinic
for getting the sonography done. For this, she had to spend an additional Rs.300
After four days of being admitted at the Godhra Civil Hospital. H was forced to
move out. even though she was in no position to travel back Nevertheless, tired
and wom out and disappointed. P. and her mother went back home to Sagtala.
P. brought up the topic for discussion at the next meeting of the local womens
organisation. She expressed her anxiety for her mother's ill health and said that the
worst part was that thus far no one had been able to diagnose anything. The
organisation gave her a loan of Rs. 1000, out of which she spent Rs 500 to get a
private jeep to take H. to Godhra again - this time to a private nursing home - Lara
Hospital, of which the doctors were known to some of the organisation leaders This
was on 26th June 2003. P. spent almost Rs.800 on the consultation fee, blood tests.
urine tests and sonography (again from a private clinic), and was asked to get a
second opinion before the test results were confirmed.
P. took her mother to another private ciinic for a sonography, spending another
Rs.300 in the process. It was on 28th June 2003, after weeks of running around, and
of uncertainty that P. learnt that her mother was in the last stage of ovarian cancer.
She was also told that the swelling of the abdomen was due to problems related to
water retention. The doctors from Lara Hospital called a specialist from outside to
get the water removed from the abdominal area; around three kilograms of water
was removed. H. was kept in Lara Hospital for five days. By this time, P. had
already spent Rs.2000 that she had borrowed from the organisation and Rs. 1000
that her sister had sent to her for their mother's treatment. The doctors at Lara
Hospital advised P. to take her mother to Ahmedabad where her mother could get
specialized help at the government cancer hospital there. But P. was broke - she
had no money to go through with the journey, nor was she in a position to bear the
additional cost for her mother’s treatment. She and H. came back to Sagtala.
In about a week's time, one night. H.’s abdomen began swelling again and she
started vomiting violently. These symptoms were accompanied by diarrhea. H. was
in no position to walk. Some neighbours helped to earn- her to the road where thev
arranged for a jeep to go to Baria at the rate of Rs.200
At Baria. H. was admitted to the CHC. where she stayed for the next two davs
There also, she did not get any relief The CHC staff began telling P. to take her
mother away from there, they could find no solution to relieve her pain here at
Baria. When P. asked them if they could at least draw out the water from her
abdomen, the CHC staff asked her to sign an undertaking, saying that she would
take the responsibility for the outcome, and further, they asked for Rs.500 to carry'
out the exercise. “Otherwise”, they said, “you can go to Ahmedabad. because we
will not do anything about it."
P. took the decision to take her mother to Ahmedabad. She asked the CHC whether
they could give their vehicle to transport H. to Ahmedabad. The CHC staff asked
for Rs.800 for the use of the ambulance, saying that P. would get back Rs.500 on
her retum to Baria. When P. asked for written proof of this agreement. The CHC
staff refused. Finally, P. had to pay Rs.750 to take her mother to Ahmedabad in the
CHC ambulance.
It was at 6:00 p.m. on IO01 July 2003 when P. and her mother reached the Shah
Cancer Hospital at Ahmedabad accompanied by P.’s brother and a nephew. Even
when they got there, there was no respite from the harassment. They were asked
to get out, to stay with relatives in .Ahmedabad, and to come back the next day at
9:00 a.m. They pleaded with the doctor that they had no place to stay in
Ahmedabad, and no one that they knew there; could the doctor please consider
admitting H. that night itself? It was with a lot of pleading, groveling and begging
that H. was finally admitted to the hospital at around 8:00 p.m.
The first question that the doctor asked them was - "How much money do you
have’” The familv responded that they did not have any money with them; they
were poor and had alreadv spent a lot of money on H.'s treatment in the past month
or so The doctor then asked them whether they had brought along their ration card.
income certificate. and other documents that would help them to avail of
government schemes for families below poverty line (BPL). P. replied in the
negative, saxing that they had not been aware of these schemes and had. therefore.
not come prepared.
"Why have you come to Ahmedabad with no money? Don’t you know - only
those who earn and can spend money should come here to this cancer
hospital", the doctor scolded P. and her family. The family requested the doctor to
begin treatment, for which they would try to arrange for money P. sent her nephew
away immediately to his place of work and asked him to arrange for the money.
When he could not do so. he even went back to Baria to try and arrange for the
money back home
Meanwhile, in Ahmedabad. the doctor saw that the family was really poor and
desperate, so he began the treatment. There was. however, no help from the other
staff at the hospital. P. relates how the nurse would not help even to fix the saline
drip on to H.. When P. tried to do it herself, the blood started flowing in the
opposite direction and filled up the connecting pipe. It was only after some trial and
error that P. managed to fix the drip properly. The nurse merely looked on and
refused to help. While P. attended to her mother day in, and day out, the men had to
stay outside on the roads because they were not allowed inside the women's ward.
Finances were still in an uncertain stage. The family had to sell two of their 'simla'
trees for Rs.500 each, and then arranged for another Rs. 1000.
After nine days of being admitted to the cancer hospital at Ahmedabad, H. died at
6:00 p.m. on 19th July 2004. The family's troubles did not end here They had to
spend another Rs. 1500 to get back to Baria.
4
Type of denial
Lack of proper reference by CHC taken to District/Civil Hospital.
Sonography not done at District Hospital. Referred to pnvate.
Spent money for investigations and medicines/injections.
Absence of sonologist at District Hospital
Asking Rs. 500/- for removing fluid from ovarian cyst at District Hospital
No ambulance facility to transfer patient to Ahmedabad Cancer Hospital.
Denial of admission at cancer hospital, Ahmedabad
Demanding money for start treatment at cancer hospital, Ahmedabad.
Patient not attended in time.
(9) Insulting behaviour of staff of CHC, District Hospital and Cancer
Hospital, Ahmedabad.
(1)
(2)
(3)
(4)
(5)
(6)
(7)
(8)
Consequences
(1) Early death
(2) Severe financial loss
II) Name of the person
N.V.
Ape
35 years
.Sex
Female
Complaint illness
Uterine cancer
Date of interview
2nJ June 2004 (with the husband of the deceased person)
N.v.’s story illustrates a grave violation of the right to health care. About five years
before she fell seriously ill, N.v. had a tube pregnancy wherein the fallopian tube
burst because the foetus was lodged in the tube. This damaged the tube and caused
excessive bleeding, and she had to be hurried to the CHC at Baria. There she was
operated upon with twenty-three stitches and a tube was inserted.
After five years of this operation, N.v. complained of bleeding again. She again
went with her husband to the CHC at Baria. The doctor was not able to diagnose
what her condition was due to, but meanwhile he kept charging them for all the
medicines, saline drip bottles and tubes, etc. Therefore, Babubhai (N.v.’s
husband) took her to a private clinic in Baria, spending a lot of money in the
process, to see if some diagnosis could be got there But it was to no avail.
N v. was thus taken to the Godhra Civil Hospital The family had to spend Rs. 1150
to take her from Ruparel to Godhra. There they found out that N.v. was in the third
stage of uterine cancer. The staff at the Godhra Civil Hospital was very hostile.
They allowed N.v. to be admitted there only for a day and did not attend to the
medication
that
was
required
all.
at
Meanwhile.
N.v. s condition
was
deteriorating rapidly.
With no other place to go to, Babubhai took his wife to a private practitioner to get
her treatment so that she could get at least some relief. N.v was admitted at a
private clinic for fifteen days starting from 15lh January 2003. The sonography.
medicines, etc - all amounted to a total expenditure of Rs.2500 - maybe more. .After
those fifteen days. N.v.’s condition improved a little so she and her husband
returned home to Ruparel.
Within a few days of their return, a camp was organized by the Baria CHC at the
PHC near their house at Sevaniya. This w'as a camp for screening and treating those
with RTIs and STIs. N.v. and Babubhai went to attend this camp. There the doctor
from the Baria CHC confirmed that N.v. was suffering from cancer but said that he
could do nothing for her treatment.
The medical officer at the PHC was not helpful at all. He abused N.v. and her
husband and asked them to get out of the PHC premises. The pharmacist at the
Sevaniya PHC tried to help them out. He said that his brother was a civil surgeon at
Baroda, and could help them out if they w'ent there.
But how would they get there with the little money that thev had9 The ANM at the
PHC and a health worker from DMS tried to get some assistance from the
medical officer to arrange for to take N.v.
to
Baroda in
the PHC
jeep/ambulance, but they were rudely refused. They were asked to dish out
6
Rs.2100 Finally. Babubhai arranged a jeep from Baria with the help of a relative.
for which he ended up spending Rs. 900.
Once they reached Baroda, it was another series of struggles to even get a doctor's
consultation. They had reached on a Monday, and were asked to go back and come
on Wednesday With no one to stay with at Baroda, and hardlv am money on him.
Babubhai was at a. loss regarding what to do At Baroda, the fatniiv spent about
Rs. 1700 - and N v s condition omy got worse
r
Back in Ruparel. they made one more attempt to get medical attention at the
Sevaniya PHC, but to no avail. After a total of eight months of suffering and being
denied health care at every level, besides the additional cost of Rs. 137000 that the
family had to bear. N.v. died on 3rd July 2003.
Denial
(1)
(2)
(3)
(4)
(5)
(6)
Spent money for medicines at CHC, Baria
No ambulance facility for referral to Godhara District Hospital
Insulting behaviour by staff at Godhara and PHC doctor. Sevaniya
Corruption - asking Rs. 2100/- for PHC jeep to transfer the patient
Not attending patient in time at SSG Hospital, Baroda
No referral note given by special gynec. Camp
Consequences
(1) Death
(2) Severe financial loss
III) Atone of the person
Takhliben Rathwa
Age
25 years
.S'e.v
Female
Complaint illness
Maternal mortality
Address
Patel Falia, Village Kasatiya,
Devgadh Baria, District Dahod
7
29th Mav 2004 (with the Traditional Birth Attendant or
Dale of interview
TBA of the village, namely. Keslibenl
One-lakh women in India die every year due to complications before, after or
during pregnancy. Yet another lakh of women suffer from related conditions that
debilitate them in many wavs. According to a World Bank report (1996'). the
maternal mortality rate (MMR) of India is a huge 437 per 100.000 It has further
been reported that most of these deaths are due to infections caught at the time of
childbirth, due to nutritional deficiencies (like anemia),
early and frequent
pregnancies, etc. It is sad because these situations can be totally avoided by
registering
the
concerned
woman
at
the
neighbourhood
’anganwadi'.
bv
institutionalizing childbirth, by taking the necessary' tetanus toxoid (TT) vaccine
twice in the course of pregnancy, by taking a reasonably nutritious diet, and by
taking regular iron folic supplements
The national figures might be interesting, but we should also be asking ourselves.
“Who is dying, and why?", instead of focusing merely on the statistics. It will
clearly reveal that it is the women, children, and the elderly, the Dalits and the
adivasis who are at the receiving end.
Village Kasatiya lies in the remote and rocky area of Devgadh Baria taluka. It is
located on the periphery of the village Bara. Being around 25 km away from
Devgadh Baria. Kasatiya is very poorly connected even to the nearest PHC at
Sagtala. It is one of the regions wherein the FHW and MPHW hardly visit the
village. On visiting a nearby 'anganwadi', the service delivery unit for the Integrated
Child Development Services (ICDS) programme, the investigator also learnt that
the supplies of ORS packets and iron folic supplements had not reached the
'anganwadis' in the villages in the past year or so. Takhliben lost her life during
childbirth four months ago as a result of these systemic loopholes in the primary
health care system.
8
Takhliben used to live in the Patel falia of Kasatiya During the period of her
pregnancy she did not have access to either the iron folic supplement, nor did
she have access to the TT vaccine. The ANM never visits Kasatiya. and there are
no supplies at the 'anganwadi' either, so Takhliben never took iron folic
supplements. In spite of that, she made the effort to get at least one TT vaccine from
a private doctor in a place called Kadwal. Kadwal is not exactly near Kasativa. the
bus fare up to it being Rs. 10. But since there was no other option, Takhliben took
the trouble to get the vaccine.
Kasatiya is anyway very' inaccessible. At night, it is almost impossible to get a
vehicle to go anywhere. The night that Takhliben went into labour was no different.
The only person who was able to come to her assistance was the local 'dayan'. or
traditional birth attendant (TBA). ANAND1 has already facilitated the training of
several TBAs in the villages where it works. Unfortunately, this ‘dayan’ was not
one of the trained ones.
Takhliben went into labour and had a baby boy. But immediately after the delivery.
she began to bleed excessively. There was nothing the 'dayan' could do to stop her
suffering; Takhliben ultimately bled to death - another addition to the already large
number of maternal deaths in the country today.
Denial
(1) Non-availability of ante-natal care by ANM at village level, eg. Check up
Iron supplement, Injection TT, referral, etc.
(2) Delivery not attended by trained Dai (TBA)
(3) No access to PHC on CHC
Consequences
Death
ll') Name of the person
Age
Narmadaben Nayak
35 years
5
Xi'.v
Female
('omplaint illness
Case of tuberculosis (TB)
Address
Village Mithi Bor.
District Vadodra, Gujarat
Dale of interview
T‘ June 2004 (with the sister of the aggrieved person.
namely. Kusumben)
Narmadaben lives in the village called Mithi Bor. which lies in Baroda district.
When she came to visit her sister in Sagtala. she complained of cough and tever.
She began vomiting and her feet got swollen. Heavy breathing made it difficult for
her to even walk a single step.
Her sister Kusumben, one of the health workers of the DMS. took her to a nearby
PHC at Sevaniya. After three subsequent visits to the PHC. she was diagnosed as
suffering from TB. However, the medical officer at the PHC said that he could
not stan treatment because Mithi Bor lies in a taluka other than Devgadh
Baria, and he was not authorized to dispense medicines to residents of other
taiukas. Further, he said that Narmadaben should get a x-ray done at Baria
Kusumben took her sister to the CHC at Baria, where she got her admitted on 17lh
May 2004. There, it was confirmed that Narmadaben was indeed suffering from TB
(Category I). The doctor, however, repeated that he could not start treatment for
it because she is a resident of another taluka. and proper follow-up could not
be undertaken for the period of treatment. Kusumben assured the doctor she
would keep her sister at her own house for the next six months and take full
responsibility for her taking the medicines on time, as per schedule. The doctor
insisted that she should be taken to the PHC at Jhojh, where she would get the
appropriate treatment under the medical officer at that PHC, as per DOTS (Directly
Observed Treatment Short course). Meanwhile, Kusumben has to spend a lot of
money for the period that Narmadaben was admitted at the Baria CHC, and had to
get even the basic medicines like paracetamol from a medical store outside.
10
After going back from Baria, she tried again at the Sevaniya PHC. but was
disappointed again. After nine days. Narmadaben's condition improved slightly, so
her husband took her home to Mithi Bor
Once she got back home, her condition deteriorated again The previous symptoms
of coughing, vomiting and breathlessness appeared again. Narmadaben's husband
then took her to the PHC at Jhojh He explained that she had been diagnosed as
suffering from TB (Category I) and had been asked to seek treatment at the Jhojh
PHC. He asked them to begin her treatment immediately as she had already suffered
a great deal, and was now very ill
The medical officer at the Jhojh PHC. as well as the nurse, made a demand of
Rs.4000 for the treatment Narmadaben and her husband said that they were poor
and could not afford the treatment if it was so expensive; would the doctor please
reconsider? The doctor and the nurse said - ‘Do you think it comes for free? If
you want treatment here, you have to pay for it!’
Narmadaben and her husband turned away and returned home, disappointed and
unhappy. After all. they could not do anything about it. Narmadaben still gets
uncontrollable bouts of coughing and vomiting. She still gets breathless when she
walks a few steps. She still suffers, and no one is willing to help her.
(Update on 21a June 2004 - Narmadaben's sister Kusumben who is a health worker
in the DMS kept trying hard to get her sister some relief. Due to her efforts, it has
now been 10 days that Narmadaben's treatment has begun. She is receiving
treatment under DOTS at the Sevaniva PHC )
Denial
If
(1) Even though diagnosed at the SCM PHC/CHC, patient was denied
treatment on the ground that he belongs to other PHC area which is
situated far away from patient's village
(2) Corruption - demanding Rs. 4000/- for DGTs (TB) which is available at
no cost
(3) Insulting behaviour by 202 PHC
(4) Delay of treatment
Consequences
(1) Spending money for frequent uncalled for visits to PHCs/CHC
(2) Treatment delayed by more than one month
V) Name of the person
Kokilaben Nayak
Age
30 years
Sex
Female
Complaint illness
Complications in childbirth
Address
Maal Falia. Village Jhapatiya,
Devgadh Baria, District Dahod, Gujarat
Date of interview
2nd June 2004 (with Kokilaben and her husband namely.
Maheshbhai who was present at the time of childbirth.
Kokilaben
had
been
almost
unconscious
of
her
surroundings at the time, while her husband was there to
accompany her during childbirth.)
One can hear several cases as gruesome as that of Kokilaben's if one visits the tribal
villages of the Panchniahaals and Dahod districts. This story took place around four
years ago.
Kokilaben was pregnant with her first child. She had completed her term of
pregnancy, and would soon go into labour. Her husband Maheshbhai made
arrangements to take her to the CHC at Baria by hiring a private jeep from Jhapatiya
to Baria at the rate of Rs.500 Kokilaben was admitted there, and soon after, all the
CHC staff left for the day
The gynaecologist at the CHC (Dr Mahetra) told Maheshbhai that his wife would
have to undergo a caesarian operation, and unabashedly asked for Rs.4000-5000
for the same. Maheshbhai was suspicious of inducing childbirth through the
caesarian operation, as most people in the villages are However, he was further
apprehensive when the doctor asked for such a large sum of monev. It seemed to
Maheshbhai that the doctor was merely in the business of making monev. and there
was possibly no real need to earn.' out a caesarian operation.
Maheshbhai7s fears were only reinforced again and again. He was asked to buy all
the medicines from a medical store outside, and was told that the hospital store
could not provide any of the medicines. He was asked specifically to buy some
"labour-inducing7 medicines that would induce labour when injected. These
injections cost Rs. 150 each, and he was asked to buy three of them. However, when
it came to giving Kokilaben the injections, Maheshbhai observed that the nurse was
giving his wife some other injection. His doubts about the intentions of the CHC
staff multiplied.
Things only got worse One of the nurses in the ward manhandled Kokilaben and
injured her very seriously. She picked up one of her legs and turned it around so
hard that it caused the bone to crack. This caused irreversible damage. Even today
Kokilaben cannot walk straight, or carry heavy weights because it hurts her back
and legs to do so.
Soon after this incident happened. Maheshbhai decided that enough is enough. He
carried his almost unconscious wife out of the hospital, even though it was evening
and they had nowhere to go at that time. The guard tried to stop him, but he had
made up his mind that he would not see the birth of his firstborn in the corrupt and
callous government hospital. Kokilaben and he rested under a tree almost all night
long
In the early hours of the mominu. Maheshbhai took Kokilaben to a private clinic
(Maniben's) in Baria on the Dhanpur road There, Kokilaben was made to go
through a normal delivery. and little Raju was bom. The total expenditure at the
private clinic amounted to around Rs. 1500, and further. Maheshbhai had to spend
Rs.525 to book a jeep to return to Kokilaben's maternal home in Devirampura.
But the damage had already been done, and Kokilaben has to live with it everyday
of her life.
Denial
(1) Corruption/scandals - indicating ceasarian section - when it was not
indicated. Asking Rs. 5000/- for the same, when it is to be free
(2) Purchasing medicines from outside
(3) Insulting and injuhous behaviour by staff nurse to the patient
(4) Had to seek treatment from private clinic
Consequences
(1) Disability due to injuhous behaviour by the nurse (fracture and
permanent walking problem).
(2) Moderate financial loss
VI) Name of the patient
Jashodaben L'dabhai Baria
Age
28 Years.
Address
Godhar, Santarampur, Gujarat
Complaint
Complicated delivery.
Jashodaben L'dabhai Baria's family consists of her husband and a has girl child and
She registered under the local PHC for every basic immunization and other basic
treatment for her pregnancy and she also has been advised by the nurse of
Lunawada hospital to get in touch with the hospital in case she has any complaint
during her pregnancy
On 5/11/2003 she consulted at CHC Lunawada Hospital and the doctor told her that
she is carrying twins Later a ultra sonography in one private hospital indicated that
there is no second child but the position of the infant inside her uterus was not
normal
and it may be serious if she did not go for an operation immediately.
However, due to poor financial condition, she got back home without the operation.
On her way back home she felt the pain of delivery. Next day 6th of November her
husband decided to admit her in the government hospital for the delivery and finally
hospitalized her at the Godhra civil hospital instead of Lunawada Hospital at mid
night. The nurse of the Godhra civil hospital informed her husband that the doctor
was not available and could visit her only in the next dav morning. There was no
doctor for the emergency.
However, by mid night Jashodaben started labour. The nurse helped Jashodaben in
the emergency.
She started one saline intravenous infusion and informed that the
birth would be safe. This gave hope to Jashodaben's family. However, eventually
Jashodaben gave birth to a dead baby. Seeing the condition of Jashodaben, the nurse
prescribed four injections which cost Rs 90 per injection. She gave her some more
IV fluids and prescribed another two injections, that cost something like Rs. 7000/-.
Jashodaben husband could not find one of the prescribed injections at that early
hour, as the medical shop was yet to open and that cost Jashodaben’s life. Her
‘veins started straining’ and she died due to lack of the injections on time. The
hospital ambulance authority took Rs.650/- to carry home the dead body of
Jashodaben.
IV
Denial
(1)
(2)
(3)
(4)
(5)
Denied confirmation of twins (pregnancy) by CHC, Lunawala
Spent money for sonogarphy to confirm twin). It was not twin)
Doctor was not available at District Hospital, Godhra
Inadequate attention - as emergency was not attended by the
specialist doctor/ Nurse decided and gave treatment
Had to spend money for medicines
Consequences
(1)
(2)
Death of mother and foetus
Severe financial loss
: Sivkumari Chatur singh Tojaraf.
VII) Name of the Patient
: 35 years
Sex
: Female.
Address
: Saptarushi no Arro.Ramji Mandir. Bavalavlavinagar.
Opp.Flower Market, Jamalpur
/.
•
•
•
•
Date of interview: 15.6.04
Location of the PHC/Location and type of Hospital-Vadilal Sarabhai General
HospitafEllisbridge Ahmedabad city.
Illness/Complaints for which PHC/Hospital was visited-Accident. Severe
bum injuries due to bursting of stove.
Total number of visits to PHC/Hospital for this illness-1 Time
Date of last visit-11.3.04
1. History of last visits in the patients /attendants words(Here we want to collect information regarding the main symptoms of the patient.
who gave care and what kinds of examination, investigation and treatment were
given)
Shivkumari, a 35 year old school teacher met with a accident at her residence as she
was preparing the breakfast for her family -two children and her husband. Suddenly
her screams were heard aloud in the neighborhood and when the complainant
Ms.Gulshan Banu, her friend and colleague reached the spot along with the
16
neighbors they saw Shivkumari engulfed in flames along with her husband who
sustained bums too.when he tried to save her.
Neighbours and the complainant immediately rushed the victim to Vadilal Sarabhai
General Hospital run by Ahmedabad Municipal Corporation The doctor on duty
denied to admit the patient to the bums ward on the pretext that she does not have
any chances of survival. The staff out rightly said so. in front of the patient, which
added to her panic as she lost all hope of survival She is believed to have said to the
Ms.Gulshan Banu that now' that doctor has already declared her to be alive for onlv
few' hours, she needs to take care of her children.
Instead of starting the treatment the doctor asked the relatives to get the medicines
from outside only then they would take the case. They also added that if its too
urgent for them to get her treated, patient could be rushed to Civil Hospital, which is
a 30
min drive from the said hospital!
To add to the trauma, the nurse asks the relatives to cut open the clothes that were
almost stuck to the skin. As they tried they couldn't continue but the hospital did
not come forward to extend their hand, instead Ms.Banu had to remove the pieces
of cloth and break her bangles from the flesh which oozed blood and send out
unbearable stench. Still the mere thought of the entire episode makes her feel
drowsy and sends a chill shiver across her body She could not eat and sleep for
days together and ran high fever.
Having spend a handsome Rs. 1750/- for seven days which was collected from
various sources Shivkumari breathed her last on the seventh day struggling to
get a bed in the bums wards and some soothing words of relief from the
hospital stafT.
•
•
What were the perceived shortcomings or deficiencies in care? (As
perceived by the patient or attendants)
They did not start the treatment timely.
According to patient was there any adverse outcome because of
deficient care? (Death, Disability, continued or chronic health problem,
severely financial lose e.g. major loan or sale assets)
Death. Patient lost her life after 8 days.
2.
Medical attention received:
• Name of the doctor who attended to you-They don't know the name of
the doctor.
• If the doctor was not available at that time then who attended to you
I. Nurse/ANM
2. MPW
3. Pharmacist
NA
!7
4.
•
Any other person specify
How Ion® after you reach the PHC / Hospital did the medical
officer /doctor attend to you?
After 20 minutes
Was examination. Treatment, Operation delayed or denied
because of non-availability of a nurse, doctor or specialist?
Xo they intentionally denied starting the treatment on the pretext that
the patient would not survive.
•
•
In case of an emergency did the doctor immediately attend to
patient? During hospital stay, regarding conditions that required
immediate care was the doctor available to immediately attend to
the patient?
Xo. They attended the patient after 20 minutes.
•
•
Were nurses or Hospital staff available to attend the patient as
and when required?
Though the staff would be available in the nearby wards they would
come only after much persuasion.
Do you think that non-availability of any crucial equipment or
supply (oxygen, incubator, anasthetic eqipment, blood emergence
drugs etc) adversely affected the quality of care?
VS Hospital being one of General Hospitals of Abad city is equipped
with all the modern and crucial equipments for emergency and other
cases. The unwilling attitude of the staff was the only problem.
W'ere all the equipments required for the examination and
treatment of the patient available in the working condition in the
Hospital?
Yes
Diagnosis - (as told by the doctor)
3. Medicines:
• Did you get all the required medicines at the PHC /Hospital? Xo
• Did you have to go to any Private medical shop to buy some
medicines? Yes
• If so which medicines you had to buy from private medical shop?
Don’t know specific name of the medicine (injection and ointment)
• How much did it cost? Per container 251/ everyday.
•
18
•
4.
5.
Do you have the prescription? (If yes. obtain a Xerox of the same
and attach?)No
Expenditure:
• Case paper/ Card made - no
° Case paper fee /indoor fees charged-X.A
• Did you receive a receipt for the payment made? -NA
• Were you charged excess money at the PHC/ Hospital (more than
specified rates) Yes
o If yes. how much excess was charged? 2500/
o Did your family have to sell assets (land, cattle, jewelry etc) take
loans to pay for in the govt Hospital?
Yes. They had to take loans from others and they were in debt.
Referral:
® Was the patient refused admission or referred to another Hospital
without giving first aid care? NA
• If the patient was referred was ambulance or other vehicle made
available for the same? NA
• Did the govt doctor ask you to avail of any private sen ices (e. g
Laboratory services. sonography/Xray) while you were admitted in the
govt hospital? No
• In case you had to take the patient to private hospital, which
hospital?
(Name and address of the hospital?)
• What was the total expenditure on care at the private hospital
/private lab or imaging center?
• Did your family have to sell any assets (land, cattle, jewelry etc.)
or take loans to pay for the private hospital charges?
Yes. Her husband's friend spends the amount, which the deceased's
husband/relative not know.
Denial
1.
2.
3.
4.
5.
Doctor refused admission to bums ward on the pretext that survival chances
are nd.
Purchase medicines from outside then only treatment could be given.
Delay in treatment d extreme carelessness by the staff d doctor.
Was not admitted in burns ward.
Excess charges (Rs. 2500)
Consequences
I.
2.
self- confidence d- will to survive was shattered by the staff
Death
19
5.
4.
Moderate financial loss
Torture of relatives
VIII) Name of the Patient
: Rupaben Rajeshbhai Pathni.
: 24 vears
: Female
Address
: Boidivat Nagar. Saraspur Ahmedabad.
Date of interview
: 17.6.04
•
•
•
•
Location of the PHC/Location and type of Hospital -Shardaben Gosl
General Hospital, Saraspur Ahmedabad.
Illness/Complaints for which PHC/Hospital was visited -High fever coupled
with severe vomiting and Diarrhea
Total number of visits to PHC/Hospital for this illness-1 times
Date of last visit - 15.5.04
3. History of last visits in the patients /attendants words(Here we want to collect information regarding the main symptoms of the patient.
who gave care and what kinds of examination, investigation and treatment were
given)
Patient visited Shardaben General Hospital one of the largest and well-equipped
hospitals run by Ahmedabad Municipal Corporation as she complained of severe
diarrhea and vomiting. Unable to even stand firmly she requested the doctor to start
immediate treatment but he asked her to get an Injection from outside. When she
got the injection the nurse asked her to get on to the table which had blood stains
and dirty fluid with foul smell. She requested her to take her on to a clean table to
which the nurse reacted in a wild manner and said “You lower caste (vaghri) people
come her when you are at the verge of dying and disturb our sleep. If you want, you
lie down here or else go way.” Patient had no other option than to get herself
injected.
She did not get any relief from it and hence had to visit a private practitioner. After
a thorough examination she was diagnosed to have falcifarum malaria with edema
in the abdomen. She felt better after having undergone the treatment at the private
hospital.
2.0
What were the perceived shortcomings or deficiencies in care? (As
perceived by the patient or attendants)
Patient was not diagnosed properly and was ill treated by the para-medics.
Patient had to bypass the public health facility for a highly paid private
practitioner for the w ant of getting relief.
• According to patient was there any adverse outcome because of
deficient care? (Death, Disability, continued or chronic health problem.
severely financial lose e.g. major loan or sale assets)
Had she not consulted the private practitioner on time her condition would have
deteriorated further as the edema in the abdomen was causing severe pain.
•
.Medical attention received:
• Name of the doctor who attended to you-They don't know the name of
the doctor.
• If the doctor was not available at that time then who attended to you
1.
2.
3.
4.
Nurse/ANM
NA
MPW
Pharmacist
Any other person specify
How long after you reach the PHC / Hospital did the medical
officer /doctor attend to you?
After half an hour.
• Was examination, Treatment, Operation delayed or denied
because of non-availability of a nurse, doctor or specialist?
Medical and Para Medical staff though present did nor attend the
patient immediately even though she was extremely weak and
dehydrated and pleaded to attend her.
•
•
•
•
In case of an emergency did the doctor immediately attend
to patient? During hospital stay, regarding conditions that
required immediate care was the doctor available to
immediately attend to the patient?
No.
Were nurses or Hospital staff available to attend the patient as
and when required?
No.
Do you think that non-availability of any crucial equipment or
supply (oxygen, incubator, anasthetic eqipment, blood emergency
drugs etc) adversely affected the quality of care?
Patient was asked to buy an injection from outside only then they
would begin the treatment, it was told. Non-availability of essential
2J
druus even durinu emergency situation is a matter of serious
thinkin". Poor patients many of whom are not accompanied bv their
relatives find it difficult to run at different quarters for medicines.
Care should be taken that they are not harassed unnecessarily during
emergency situations.
• Were all the equipments required for the examination and
treatment of the patient available in the working condition in the
Hospital?
Yes
Diagnosis - (as told by the doctor)
3. Medicines:
o Did you get all the required medicines at the PHC /Hospital? -No
• Did you have to go to any Private medical shop to buy some
medicines? -Yes
• If so which medicines you had to buy from private medical shop?
She doesn't know the name of the injection
o How much did it cost? -40 Rupees for the purchase of one
injection.
• Do you have the prescription? (If yes, obtain a Xerox of the same
and attach9)No
4. Expenditure:
• Case paper/ Card made -no
• Case paper fee /indoor fees charged-NA
• Did you receive a receipt for the payment made? -NA
• Were you charged excess money at the PHC/ Hospital (more than
specified rates) NA
• If yes, how much excess was charged?
• Did your family have to sell assets (land, cattle, jewelry' etc) take
loans to pay for in the govt Hospital? No
5. Referral:
• Was the patient refused admission or referred to another Hospital
without giving first aid care? Yes
• If the patient was referred was ambulance or other vehicle made
available for the same? NA
• Did the govt doctor ask you to avail of anv private services (e. g
Laboratory services, sonography/Xray) while you were admitted in the
govt hospital? No
• In case you had to take the patient to private hospital, which
hospital?
(Name and address of the hospital?) Private Clinic. She doesn’t
know the clinic’s name.
• What was the total expenditure on care at the private hospital
/private lab or imaging center? She doesn’t know, her husband
paid the money.
2X
•
Did your family have to sell any assets (land, cattle, jewelrv etc.)
Or take loans to pay for the private hospital charges? No
Denial
1.
Delayed treatment only after getting medicines injections from the
market
2. Spent moneyfor the medicines
3. Insulting behaviour of the staff
4. Inadequate A low quality & care
5. Investigation & treatment by private doctor (]■'. Malarial
Consequences
1.
2.
Sufferingfor longer lime
Spent money to seek better care tn Pvt. Clinics
IX) Name of the Patient
: Rakshak Ghani Shah
Age
: 45 years
Sex
: Male
Address
: Sangam Bavalavlavinagar. Jamalpur.
Date ofinterview
:15.6.04
o
•
•
o
Location of the PHC/Location and type of Hospital-Vadilai Sarabhai General
Hospital, run by Ahmedabad Municipal Corporation.
Illness/Complaints for which PHC/Hospital was visited-V S Hospital
Total number of visits to PHC/Hospital for this illness- 2 Times.
Date of last visit-5.4.04
4. History of last visits in the patients /attendants words(Here we want to collect information regarding the main symptoms of the patient
who gave care and what kinds of examination, investigation and treatment were
given)
Patient had stomach ache at 12 am at night. Next day morning he had taken
medicine from the clinic in the chali .He was given antacid to reduce gas formation
but it did not help. Then he was taken to Dr. Amin's clinic, a private practitioner.
There it was told that his condition was critical. Immediately he was admitted to VS
hospital. After check-up and various x-rays test he was given medicines and sent
back home. His relatives were told that he is perfectly fine. Somehow after coming
home he could not bear the severe pain near his abdomen. He was again taken to
another clinic. There the doctor announced that his condition was critical. Then he
22
was taken to Chipa Welfare Trust. There, after taking sonography, they were told to
arrange 20,000/ immediately, for operation. Patient was not able to arrange 20,000/
and so he goes back with sonography report. Then again he goes to \ S hospital
with sonographv report, to get operated with lesser amount. Doctor operates the
patient and tells his relatives to arrange for medicines. Patient was not able to regain
his conciousness after the operation. Relatives were informed that he would have to
be operated on other kidney also. Patient expired after seven days.
This is a case of utter denial of the treatment at the right time. Had the patient been
diagnosed properly on his first visit itself he would have rescued.
•
•
What were the perceived shortcomings or deficiencies in care? (As
perceived by the patient or attendants)
Mentioned above.
According to patient was there any adverse outcome because of
deficient care? (Death, Disability, continued or chronic health problem.
severely financial lose e.g. major loan or sale assets)
Death.
5. Medical attention received:
• Name of the doctor who attended to you- Thev don’t know the name
of the doctor
• If the doctor was not available at that time then who attended to you
1.
2.
3.
4.
•
Nurse/ANM
NA
MPW
Pharmacist
Any other person specify
How long after you reach the PHC / Hospital did the medical officer
doctor attend to you?
Several visits to the hospital made it possible for the patient to get
treatment only to die needlessly.
•
Was examination, Treatment, Operation delayed or denied
because of non-availability of a nurse, doctor or specialist?
Even though Doctors and specialist was available the treatment wasn't
started on time.
•
In case of an emergency did the doctor immediately attend to
patient? During hospital stay, regarding conditions that required
immediate care was the doctor available to immediately attend to
the patient?
2ft
Please refer to the above-mentioned details.
• Were nurses or Hospital staff available to attend the patient as
and when required?
No they intentionally denied starting the treatment.
•
Do you mink that non-availability of any crucial equipment or
supply (oxygen, incubator, anasthetic eqipment. blood emergence
drugs etc) adversely affected the quality of care?
No, V.S Hospital is situated in Ahmedabad City. So any crucial
equipment or supply is available all time
«
Were all the equipments required for the examination and
treatment of the patient available in the working condition in the
Hospital?
Yes
Diagnosis - (as told by the doctor)
3. Medicines:
• Did you get all the required medicines at the PHC /Hospital? No
• Did you have to go to any Private medical shop to buy some
medicines? Yes
• If so which medicines you had to buy from private medical shop?
They don't know the name of medicine.
• How much did it cost? Total 3,000/ to 4,000/
• Do you have the prescription? (If yes, obtain a Xerox of the same
and attach?) No
4.
5.
Expenditure:
• Case paper/Card made-Yes
• Case paper fee /indoor fees charged -Rs 45/
•
Did you receive a receipt for the payment made? - No
• Were you charged excess money at the PHC/ Hospital (more than
specified rates) Yes
• If yes, how much excess was charged? 30/ more.
• Did your family have to sell assets (land, cattle, jewelry etc) take
Ioans to pay for in the govt Hospital?
Mortgaged the peddle rickshaw and got 3000/
Referral:
• Was the patient refused admission or referred to another Hospital
without giving first aid care? NA
• If the patient was referred was ambulance or other vehicle made
available for the same? NA
Z?
• Did the govt doctor ask you to avail of any private services (e. g
Laboratory services. sonography/Xray) while you were admitted in the
govt hospital? No
• In case you had to take the patient to private hospital, which
hospital?
(Name and address of the hospital?) Chipa welfare Trust Jamalpur
Ahmedabad.
• What was the total expenditure on care at the private hospital
/private lab or imaging center? NA
• Did your family have to sell any assets (land, cattle, jewelry etc.)
Or take loans to pay for the private hospital charges?
NA
Denial
1.
2.
3.
Inadequate investigations de care
Had to seek reference in private clinics & trust hospital
Purchase medicines from outside
Consequences
I.
2.
Death
Loss of livelihood - (mortgaged rickshaw)
X> Name of the Patient
Savita Ben Daya bhai Chavda
Age
30
Sex
Female
Address
Hanuman ki Chali. Khodiyamagar.
Behrampura.Ahmedabad City.
Date of interview
17.6.04
•
Location of the PHC/Location and type of Hospital - V.S Hospital Govt
general Hospital
•
Ulness/Compiaints for which PHC/Hospital was visited -Childbirth.
•
Total number of visits to PHC/Hospital for this illness-1 Tinies
•
Date of last visit- February 04
26
History of last visits in the patients /attendants words-
6.
(Here we want to collect information regarding the main symptoms of the patient.
who gave care and what kinds of examination, investigation and treatment were
given)
Patient started unbearable labor pain and she was taken to VS hospital by her
husband. When she reached nurse examined her and said there is still time for
childbirth and hence she should go back home and come the next day Savitaben
pleaded to get her admitted as she could not bear the pain, but the nurse was
adamant on her words and did not listen to the patient As they started to go to
Behrampura Municipal Hospital she had to be taken to a private nursing home on
the way as she delivered a baby boy.
This case is truly an example of denying the right treatment at the Municipal
Hospital for which the poor patient had to unnecessary get in trouble of running
from pillar to post just to get a safe childbirth. They had to bear the cost of getting
delivered at a private clinic too which would have been avoided had the nurse at VS
hospital examined her well and admitted her there itself.
•
What were the perceived shortcomings or deficiencies in care? (As
perceived by the patient or attendants)
Patient expresses her anguish over denying her the treatment even w'hen she
pleaded for it She had to over spend on account of the lack-luster attitude of the
staff. Not to mention of the panic and trauma they underwent at the last
moment.
• According to patient was there any adverse outcome because of
deficient care? (Death, Disability, continued or chronic health problem.
severely financial lose e.g. major Ioan or sale assets)
She had reached private hospital in time and was saved.
7.
Medical attention received:
• Name of the doctor who attended to you - Doctor was not there that
time they don’t know the name of the doctor.
• If the doctor was not available at that time then who attended to you
1, Nurse /ANM
2. MPW
3. Pharmacist
4. Any other person specify
•
How long after you reach the PHC / Hospital did the medical
officer /doctor attend to you?
Doctor and Medical officer not there that time. So they did not attend the patient.
2.7
Was examination. Treatment, Operation delayed or denied
because of non-availability of a nurse, doctor or specialist?
No. Nurse was there but intentionally denied to admit the patient.
•
In case of an emergency did the doctor immediately attend to
patient? During hospital stay, regarding conditions that required
immediate care was the doctor available to immediately attend to
the patient?
Doctor was not there so they did not attend the patient immediately and did
not provide the treatment
•
•
W ere nurses or Hospital staff available to attend the patient as
and when required?
Nurse was available but she not given the treatment and check up.
•
Do you think that non-availability of any crucial equipment or
supply (oxygen, incubator, anasthetic eqipment, blood emergency
drugs etc) adversely affected the quality' of care?
•
.
No, V.S Hospital is situated in Ahmedabad City. So any crucial
equipment or supply is available all time.
Were all the equipments required for the examination and
treatment of the patient available in the working condition in the
Hospital?
Yes.
Diagnosis - (as told by the doctor)
3. Medicines:
• Did you get all the required medicines at the PHC /Hospital? No
• Did you have to go to any Private medical shop to buy some
medicines? Yes
• If so which medicines you had to buy from private medical shop?
She don’t Know the name of medicine.
• How much did it cost? Don’t know
• Do you have the prescription? (If yes, obtain a Xerox of the same
and attach?) No
4.
Expenditure: The patient could not reach the public health center.
• Case paper/ Card made• Case paper fee /indoor fees charged• Did you receive a receipt for the payment made?
• Were you charged excess money at the PHC/ Hospital (more than
specified rates)
• If yes, how much excess was charged?
2S
Did your family have to sell assets (land, cattle, jewelry etc) take
loans to pay for in the govt Hospital?
Referral:
• Was the patient refused admission or referred to another Hospital
without giving first aid care? \es
• If the patient was referred was ambulance or other vehicle made
available for the same? NA
® Did the govt doctor ask you to avail of any private services (e g
Laboratory services, sonography/Xray) while you were admitted in the
govt hospital? No
® In case you had to take the patient to private hospital, which
hospital?
(Name and address of the hospital?)
Krishna Hospital. Behrampura
Ahmedabad City.
•
5.
o What was the total expenditure on care at the private hospital
/private lab or imaging center?
She Don't Know.
o Did your family have to sell any assets (land, cattle, jewelry etc.jor
take Ioans to pay for the private hospital charges ? No
Denial
I. Doctor not present
2. Nurse did nor examine properly even though patients was tn labour pain
3. Patients has to seek private service
4. Purchase medicines
Consequences
I. Delivery in Riskshaw
2. Had to spend for private service.
XI) Name
Mahefujabanu Mustaqali Syed
Age
30
Address
Akbarpur, Khambhat, Dist: Anand, Gujarat
Problem:
I was bom at Jaipur. My father was an industrial worker. I studied up to 10th standard.
When my marriage was proposed with Mustaqali. I refused because he was from
Khambhat. Through TV. I knew the problem of Silicosis in Khambhat But, I was
compelled to marry him. We married in I9S7. After our marriage, my husband settled
in Jaipur. But, on 20lh dav of the marriage he fell ill. He vomited blood. We started his
treatment. For few days, he would feel better and again he would be down. After 3
years, we left Jaipur and settled in Khambhat. Here he started grinding Agate stones
He used to do the work before our marriage. His condition deteriorated day by day and
he died in 1997.1 would take him to Jaipur whenever he is ill. I took him several time
But no one could save him. 1 do not why. He was only 31 years old when he died He
left behind him our four children, namely, Shabiabanu (13), Shayarabanu (11).
M.Taoufiqali(lO) and Samiulhaq (7)
I passed through verv bad period. 1 had four children to feed I had some problems in
claiming benefits offered by Government to the widows But, that heiped me a lot A
social organization helped me by giving machine for making holes in Agate stones I
earn my living by this work.
No one could save my husband from dieing. They say there is no treatment. So many
young people die here each year leaving behind widows like me No employer gives
any compensation. Even Government does not give any compensation When
Government cannot protect life of young people, should it not accept some
responsibility' to pay compensation so that we can lead respectable life’ Widows have
to send their children to work instead of school for want of money. When ever there is
train or plane accident Government pay compensation Government also pavs
compensation to the riot victims. When ever people die of taking illicit liquor.
Government pay compensation to the families of victims. It should be noted that liquor
is banned in Gujarat.
Health department has not succeeded in preventing the deaths caused bv Siiicosis. As a
result large numbers of people like us have to lead miserable life I want Government
and Health department to do some thing urgently and save agate workers.
Denial
(1) No preventive care at all. (inspection, safety measure and education)
(2) No counseling and guidance to patients suffering from occupational
problem.
XII) Name
Mahesh Karsanbhai Makawana
Address
At & Post: Shakarpur, Tai: Khambhat. Dist: .Anand.
Gujarat
Age\
34
Problem
Lack of quality health care, lack of health education
My father. Karsanbhai was earning his living by engaging himself in agriculture
labor and other petty labor jobs Income was not regular and enough for him to meet
both ends. So my Mother starred grinding Agate stones. She inhaled Silica dust at
work and as a result got Silicosis and /or TB She died after remaining in bed for
about one year in 1979. I was 6 years old and my younger brother Arvind was 5
years old when she died
Our grand mother then brought us up. My Mama (Mother's Brother) was
unmarried. When my mother died, he came to stay with us so that he can be of some
help to my father. He was working as grinder of Agate stones. He was earning w ell
Hence, my Father dared to continue our schooling
I failed in 9h standard, so I left school in 85-86 I had begun working on precious
stone, but later 1 switched to Agate grinding. Mama fell ill in the same year His
income stopped. He had helped us grow up. Now, he needed our help. My father
spent all his savings in giving treatment to Mama. He had to even sell some
ornaments. I started helping my father in land cultivation. Mama was cured and he
restarted his work He became ill once again. We had run out of our savings. We
needed money for his treatment So, I took Rs 4.000/- as advance from Kishan
Sheth, where my Mama was employed In lieu. I started working for Kishan Sheth.
The work place was a closed room where numbers of workers were grinding Agate
stones. The place used to be laden heavily with silica dust knowm as 'pH' in local
language. Amount of dust used to be so high that we would be covered completely
with dust by the end of the day. Our clothes, hair, nose would be full of dust I
worked there for 5 years .Then I went to another employer and then to third. In all I
worked for 9 years. Then I thought of doing something of my own. My father
helped me by lendingRs.3400/- to set up the unit.
I must mention here that two of my colleagues Sri.Prakash Parmar and Sri Ashok
Naran died at very’ young age of Silicosis. Both were unmarried. Prakash died at the
age of 32 and Ashok at the age of 35.
I bought machine and set up unit in front of my house. 1 was able to eam little more
now. My brother also could not continue his school. Soon, he was in the company
of bad boys He started drinking. He used to work as agate grinder. He would not
save anything. He would be under debt perpetually. I had to work hard to pay back
his debts. Had I not lost my mother at early age. my story would have been
different.
As other youngsters engaged in agate grinding in my village, I could not marry. No
one is ready to give us their girl as they know' that our life is fragile. When I am
sick, I was always think that, had I been married, my wife would have taken my
care. Today I feel lonely. In my home, now, we are all males. I have to prepare food
31
for me and my father. Mv brother is a vagabond Some times we do not see his face
for six months.
In February 2003. 1 became ill I had pain in chest, cough, sputum and
breathlessness. 1 went to TB Cetre- Mill Dawakhana. as popularly known- where
they do not have facility for X-ray. They ask to get the x-ray done I went to private
hospital for the X-ray Thev diagnosed TB In October. Ude! primary Health centre
put me on anti-TB drugs. In June 2004. they stopped medicines and noted on my
papers 'cured'1. They never diagnosed me to be suffering from Silicosis. The
Doctor did ask me mv occupation, which I told Why they can not diagnosis
correctly what I suffer from?
1 had to work on grinding wheel even when I was under treatment for TB Now. 1
have stopped working on wheels since last 2 months. Even now, 1 have occasional
chest pain. My father works and fills my belly. I feel ashamed.
I visited TB Centre at Khambhat on 9lh July accompanied by Prakash Parmar of
PTRC and requested Dr.David. In charge of the Centre, to issue me a certificate
regarding my correct diagnosis, particularly. Silicosis. He refused, saying they do
not have X-ray facility and even if there is X-ray their job is to only diagnose TB
and not Silicosis. He further clarified that he is 'empowered to make such
diagnoses. He also informed us that for X-ray we refer to CHC. Then. I went to
CHC. popularly known as Kennedy Hospital, where we met Dr Shastri. In charge.
and requested to issue me a certificate saying I suffer from Silicosis. He. too.
refused saying, he can not analyse the X-ray and hence he can not diagnose
'Silicosis'. He also offered us to refer me to Civil Hospital Ahmedabad for
diagnosis of Silicosis. Though this area is well known for the cases of Silicosis in
mass, not a single Government medical officer has made diagnosis to this effect I
Government health department has not given us any education about how this can
be prevented nor do they give any advice for healthy living and healthy work.
1 am not alone. In my village, people have been dieing of this disease since last so
many years. I lost my mother too in this disease. I do not understand why no one
can stop these deaths. There are so many orphans and single parent children.
Mahesh Makawana
Shakarpur
10/07/2004
Denial
(3) No preventive care at all. (inspection, safety measure and education)
(4) No counseling and guidance to patients suffering from occupational
problem.
XIII) Smita Sonawane (Vadodara)
Smita Dagdubhai Sonawane is 22 years old F.Y.B A. student and also a NonFormal Education teacher is residing in Shankamagar basti which is located in
Pratapganj. Vadodara
Her family includes her father who is handicapped, mother
who is a housewife, brother who is married and her sister-in-law
Whenever anyone from the basti is not feeling well, they have to visit the
dispensary located in Fatehgunj area which is quite close to their basti. Smita also
takes health senices from the same dispensary. Once when she had cough and
cold, she went for a checkup. Dr. Jayesh Prajapati made her lie down on the
examining table and examined her throat, chest and stomach and pelvic region.
Smita was puzzled as to why this thorough examination for minor ailment like
cough and cold, but she did not comment.
Again, after some days, she approached the doctor for obtaining a health certificate
for nursing course. She was accompanied by her mother but she was made to sit
outside the room. Again the doctor made her lie on the examination table and
examined her thoroughly He then told her that he would now have to check her
internally. She was scared and she lied that she was having her menses and
escaped the situation because she felt his touch was not one. a professional not
required.
The other women and people from Smita’s area and the nearby bastis. go to the
same dispensary for treatment. The women have similar experience with the
doctor. They go to the dispensary because the medicines that he gives are effective.
They are also scared to voice their feelings so this matter is only discussed among
women when they sit chatting in groups.
Denial
1.
Insulting, threatening & obnoxious behaviour on pan of doctor towards women
participants.
Consequence
1.
Women patients cannot use public healthcare service & are faced to use private
services, which cost heavily.
XIX) Pratibha Prakashbai Gliare
.-Age - 30 years. Residence: Shankamagar. Pratapganj. Vadodara
Interviewed on : 22.6.04
Pratibha had complaints of cold and cough and went to the Fatehganj Municipal
Dispensary on 9 6.04. The doctor there. Dr. Jayesh Prajapati. made her lie down
and felt her feet. legs, abdomen, chest etc on the pretense of examining her. The
patient. Pratibha felt unwarranted.
At the time of the interview, she and many other women in the basti complained
that this doctor behaves like this with all women and therefore they hesitate to go
for treatment to this Municipal Dispensary
This kind of indecent behaviour of a male doctor with female patients, in our
opinion constitutes sexual harassment and can be understood as a denial to health
care.
Denial
1.
Insulting, threatening & obnoxious behaviour on part of doctor towards women
participants.
Consequence
2.
Women patients cannot use public healthcare service & are faced to use private
services, which cost heavily.
JUSTICE FOR ALL- SAFIYA’S POST MORTEM
I met Safiya in a hospital. She lay in a comer, adjacent to die toilet. The stench was unbearable. She
was in no condition to talk. She tried but her mourii wide open, was filled with blisters. She was on
V drips unable to eat or dnnk ant-thing because her intestines had been ruptured. Suddenly
I.
somebody removed the sheet covering her body. Her intestines were exposed, raw and infected. I
felt faint. It took an effort to draw closer. As I stroked her head I saw the pus oozing from die
wounds. There was no skin. 1 felt helpless-frozen. Her daughters and familv were all beside her.
They told her story. I had no words then but I write for Safiva now.
Safiya lived in Jhalod, a town in Dahod district of Gujarat, seven hours drive from Alimedabad.
Hindus and Muslims - the majority of them landless agricultural labourers - had been living
togedier for years sharing dieir poverty and small joys. Living under die same voke of want had
blurred any differences of religion. Occasionally diere had been minor clashes between die two
communities but none too serious. They went to die fields togedier, celebrated each odiers’
festivals respectfully and pulled along as best diey could. March lJt, die dav after die Godlira
carnage changed all this forever.
31
Safiya’s brother Mohammadbhai tells the story. Returning home trom his dailv namaaz in the
afternoon he saw a well armed mob of about 500 people, in khaki shorts with saffron headbands
attacking his modest home. On second thoughts, it was not a mob. Their faces were familiar. Thev
all had names. Most of them were his neighbours. The door was being broken in. They entered his
house - his sole possession after a long and struggling life. As most of the mob left after looting
and burning, a few remained behind to perform more devious crimes. His mother, Bibiben, 80
years and too old to move, was beaten on die chest, kicked in die abdomen and then hacked to
deadi. His wife Khairoon was also stabbed in die abdomen. She collapsed. Thev left her for dead.
His eleven-vear-old niece was also stabbed in the abdomen and upper arm. Bv some luck she was
spared from furdier injure. A few men grabbed his widowed sister Safiya who had come home for
Eid and beat her till she could no longer stand. Then raped her, stabbed her repeatedlv in die
abdomen and pelvis, and for good measure beat her with metal pipes till her abdomen tore open
and her intestines spilled out. Thev left her for dead and moved on for more. Three long hours
passed. Mohammadbhai hid near die masjid, frozen, his senses not responding to anvdung that he
saw. He watched it all. Even today he asks himself why he did nothing as a son of 45, a husband, a
brodier and an uncle to protect his family?
The police arrived. By dien everv one had left save Mohammadbhai, and a disturbing calm had
settled down on his mohalla. He was taken away to anodier locality where he would be safe. But bv
some twisted official logic, die injured women were left behind. Hours later some villagers gadiered
courage to take Safiya and her mother to hospital. Her mother was declared dead on arrival but
Safiya was operated upon. Later die police came to record her statement. She could barelv speak
but she told her story. The FIR records “minor injuries”.
Complications developed from Safiya’s first operation and she was shifted to Baroda Civil Hospital
and operated upon for a second time. Still there was no improvement. After a mondi Safiva was
shifted to Dahod Anjuman Hospital, where I met her at the end of April 2(102. How she had
survived for 2 months amazed me. I knew that if she lav in diat hospital she would never make it. I
had to shift her to Ahmedabad. But it was not an easv task. We were up against a svstem. which
was proud of its deliberate and prolonged incompetence. Hindu owned private hospitals refused to
accept her. Odiers demanded impossible sums of monev. A Muslim owned pnvate hospital was
die last resort. The seven-hour joumev from Dahod to Alimedabad was a gamble. There were
chances of complications arising on the wav. The ride was a nightmare. The two doctors, her
daughters and I sat in silence as we all proved that nothing would go wrong.
Safiya was operated on for a dtird time die same dav. For die first time in two mondis she thought
she was going to live. When I was leaving she joined her hands. I thought she said ‘diank you’ and
‘come again.’ I promised I would. She died a week later on the 6th of May.
But Safiya’s story does not end with her life. The private hospital could not do a post mortem, so
Safiya had to return to Dahod. That meant another seven-hour journey, this time with a rotting
dead body. At Dahod District hospital the audiorities refused to do the post mortem. The body
had come from a private hospital in Ahmedabad; the history of die case was not clear, and diere
were no supporting papers - some reasons for refusing to do a post-mortem. No amount of
pleading could change dieir minds. No amount of questioning or pleading could change dieir
minds or give die family any reason. Authority needs never to explain anything. So poor dead
Safiva was taken to Jhalod hospital another hour’s journey awav and finally after six more hours of
haggling the doctors agreed to do the post mortem. The final report, which came two weeks later,
said it all. Deadi was due to ‘Renal Failure and Septicemia.
The FIR with its record of‘minor injuries’ and die cruel end-joke of‘deadi due to renal failure and
septicemia’ in die post-mortem made certain diat there will be no official record of die savagery
diat Safiya suffered; no recognition of the pain of those first hours; no punishment for her rapists
35
and tormentors; no compensation tor her family for all the neglect and agony of her months in
hospitals and ot course no investigation into her death.
Safiya was an Indian woman. She was raped, stabbed and beaten until she died of it. It took a long
time to accomplish all this. In life the State could nor protect her. Bur did it have to cheat her with
so much deliberate and premeditated care in death?
■\X ord count 1093)
Denial
(1) Inadequate attention at all levels
(2) Torture due to behaviour of medical staff
(3) Post mortem was denied at various hospitals
Consequences
(1) Death
(2) Harassment and torture to patient and her relatives
(3) Long term - mental stress to relatives
36
"Building a people's movement in mental health: creating mental health friendly prison.
Definitions of mental health:
" Health is not merely the absence of disease or infirmity' but rather, a state of complete physical.
mental and social well-being". (WHO constitution)
"Mental health is the capacity of the individual the group and the environment to interact with one
another in ways that promote subjective well-being, the optimal development and use of mental
abilities (cognitive, affective and relational), the achievement of individual and collective goals
consistent with justice the attainment and preservation of condition s ofjudgmental equality".
(WHO report 1981)
Mentally health & Law
The life of the mentally ill is totally governed by the existing law i.e. the Indian Mental Health Act
1987 which is repealed by the Old Lunacy Act 1912. The legislation's frameworks have primarily
actuated to protect society from the dysfunctional and dangerous manifestations of mental illness,
instead of protecting the status of the person with mental illness.
Limitations:
1. It is a custodial Act.
2. Mentally ill persons cannot stand trial. (Incapacity to stand trial due to unsoundness of mind.)
3. Discharge procedure is cumbersome.
4. The Act does not cover all aspects of Human Rights.
5. The Act does not address rehabilitation for the mentally ill.
When police perceives somebody as a "mental", they donot even file an FIR or complaint. If the
person is having a crime record, it automatically cancels the patient's right to voluntary treatment.
Mentally ill person shunting between different institutions e.g. police custody to jail to mental hospital
to beggars home is common. For "Shankar", he was transferred between jails twice without knowing
why. He was forcibly taken for psychiatric treatment at a hospital, before being finally transferred to
the state mental hospital. Force is used in the admission of patients, unlike other hospital: Physical
restrain and shackling was used to commit persons to the mental hospital. All commitments to the
hospital were involuntary.
Case studies document the humiliation of forced treatment {they had no right to bring me to a mental
hospital).
Human Right section:
Present Mental Health Act covers only one chapter on 'protection of human rights of mentally ill
person'. Further it addresses specifically on indignity and cruelty:
Section 81 (IMHA 1987) states:
No mentally ill persons shall be subjected during treatment to any indignity (whether physical or
mental) or cruelty.
Indignity & Cruelty in the form of:
1. E.C.T. (Electro convulsive therapy)
2. Solitary confinement
3. Involuntary treatment. {"They dragged me inside by my hair. Then they took away my clothes").
i
Treatment and Care:
1. The main forms of treatments are medication and shock treatment. Shock treatment without
anesthesia ("Receiving shock was the most painful of all"; "Shock has helped me to remember
my past") has been reported, with varying views on the impact of the treatment. Headaches and
memory loss are regularly reported after shock treatment. Shock treatment is used to calm
agitated patients, and regularly as an entry procedure into the hospital, without any regard for
consent procedure. This goes against all International human rights standards.
2. Solitary confinement is used in "therapy" context (for calming the patient).
Measures are used by force by parents, husband or relatives, police threat and use of sedative.
"Neeta", a long stay patient, became violent after being institutionalized. In her frustration to
go back home, she attacked and killed a fellow inmate in the mental hospital.
3. Some practices followed in mental hospital such as "shaving off the head", Women are not
given sanitary pads or underclothes. {"They dragged me inside by my hair. Then they took
away my clothes. They gave me these to wear".)
Advocacy issues:
I. Legal Aid:
2. Need for facilities in Pune city or in Maharashtra
i)
Half way home
,.j
ii)
Day care facilities and night care shelters.
iii)
Programme for wandering mentally ill patient.
3. Co-ordination between different inter-department levels e.g. Health = Disability = State mental
Health Authority
4. Specific modification in Beggary act
5. Community sensitization and working with families and carers
6. Prevention and promotion of mental health in all institutions and training for officials..
Bapu stand:
• Rationalizing procedures (involuntary commitment, transfer, escort, admission, discharge)
® Involving local authorities
• Role of NGO, working together
Conditions of the hospital- A view from below
“If there is hell on earth, then it is at this place. But I do not abuse anyone. I Just have to put up with whatever
situations are there. I do not like anyone here: neither do I like the living conditions here.
"The bed linen is distributed to everyone everyday on a rotational basis. So one always has dirty linen that other
people have soiled It is never cleaned The food is also very bad. It is half cooked. I can hardly eat myfood here. T
give it to others. Our clothes too are hardly changed. It is so dirty that we have body lice and eczema.
"AU of us have to bathe together at the taps, naked. We are not given underclothes. We have to wipe our bodies with
our clothes and wear the same wet clothes.
"Il is sheer hell to live over here. It is better to die. If one protests about anything, then one is shut into the solitary
cells. Those cells have no toilets. One has to urinate and defecate there itself, as well as eat and sleep over there. It
is the utmost form of torture. We are forced to obey all the attendant's orders. It is very unhygienic. We are
humiliated and tortured, if H'e refuse to do work that is degrading."
Center for Advocacy in Mental health
A Research Center of Bapu trust
Bl/11, B1/12, 6th floor, Konark Puram,
Kondhwa Khurd, Pune-411048
Ph#020-6837644/47, E-mail# wamhc@vsnl.net.in
Contact person: Vijay/Ramya
website #www.camhindia.org
Cnei ->(
£<•(• D_
BPL survey 2002
Some Learning from the Field
/fter the end of the BPL Survey 2002, delayed in Rajasthan till 2003 due to famine conditions in 2002-2003,
seme of our worst fears about the unsuitability of the design and administration of the survey have come
true. Some of the major findings are narrated below. The findings are drawn from our analysis of the Primary
Score Sheets for the Sheokar Gram Panchayat of Barmer District. Before narrating our findings it is
appropriate that we state the limitations of the method used by us.
Limitations
We have used the score sheets provided by the Government to the Gram Sabha for verification. Hence the
Government did provide scope for correction. However, there are a few reasons why we consider that the
Gram Sabha process initiated by the Government would not have been able to make the necessary changes.
1. Detailed score sheets were not displayed before the Gram Sabha. Only total points were provided
against the names of the households. This would not allow villagers to find out the specific
parameters under which the information depicted in the Score Sheets is untrue.
2. Gram Sabha proceedings do not last more than five-six hours. Hcwever, a detailed discussion on the
Score sheets would need much more time as scores for more than 1000 households would need to be
cEscussed with each household being evaluated against 13 different parameters. Even at the level of
Ward Sabha there would be about 70 Households, and a thorough discussion is likely to take more
than two days.
3. The Gram Sabha would be allowed to make corrections in case the Score Sheet has been filled
incorrectly. Hence, it would not be able to improve the selection process where the errors in selection
emanate from the faulty design of the Questionnaire itself.
4. A highly erroneous score sheet would discourage the village level processes.
Findings
The BPL identification process is based on the setting of a cut off point The cut off point would be set so as
to ensure that the percentage of households selected under the BPL category roughly approximate to the
Target provided by the central government to the state government The figure provided by the center to the
state of Rajasthan is 13.7% of the population. If we use the same cutoff method at the Panchayat level, the
sample Panchayat would have'a cut-off of 13 points. That is, all households getting 13 points or less would be
selected as BPL, while those obtaining 14 points or more would be left out of the list This would imply that
about .14.7% of the households in the Panchayat would be designated as BPL households. The following table
provides data regarding the caste wise details of the BPL selection.
Table 1:
If cut-off is 13 Points, implying coverage of 14.3% of the Households
Category
SC-:-:. ST.
OBC
Others
Total
Total Families
Number of Families that
Number of BPL families from
belonging to
would be selected as
% Selected as category as % of total number
Category
BPL
of BPL Families
BPL
.-c.
.135
.11
8%
6%
. -8
5%
27% 't-rvtaioT
. -L. 1019
89%
154
15%
30
0%
0%
0
1214
100%
14%
173
Table 2:_____ If cut-off is increased to 14 implying coverage of 18.7% of the Households
Category
SC
ST
OBC
Others
Total
Total Families
belonging to
Category
Number of BPL families from
Number of Families that % Selected category as % of total number of
BPL Families
would be selected as BPL as BPL
135
7%
12%
16
30
6%
13
43%
1019
87%
20%
201
30
0%
0
0%
1214
100%
19%
23°
In corr.iparEon, the actual figures from the BPL selection process carried out in 1997, gives us the following
figure. These figures have been used for targeting various Government welfare schemes from the year 1998
to date. The selection process in 1997 was carried out using a different questionnaire and used exclusion
criteria that could eliminate the better off households from the survey in the very beginning of the process.
However, the survey of 1997 itself was biased against the SC & ST households.
In comparison, the selection of BPL families in the 1997 BPL census gives us the
following figure.
Number of
Number of BPL families Change in number and % of Change .n number and % of
Families
from category as % of BPL households from 1997
BPL households from 1997
Census to 2002 Census.
selected as
total number of BPL
Census to 2002 Census.
Cut-off = 13
Category EPL
Families
Cut-off = 14
Number
%
Number
%
-33
sC
44
-75%
19%
-28
-64%
ST
0
4%
0%
8
5
63%
174
-20
OBC
77%
-11%
27
16%
0
Others
0%
Total
-53
226
100%
-23%
4
2%
Table 3:
From the above tables we can infer that:
1. A greater proportion of households belonging to the OBC category are likely to be selected while a
much lower proportion of SC households are likely to be selected. At a cut-off of 13 points about 15%
of OBC households would be selected while only 8% of the SC households will be selected. At a cut
off level of 14 points, about 20% of OBC households would be selected while only about 12% of the
SC households would be selected.
2. As compared to the last BPL census, the proportion of OBC BPL families to total BPL families will go
up. The proportion of OBC Households among the total BPL households was 77% in the 1997 census.
In the 2002 census, it is likely to be 89% at a cut-off level of 13 points and 87% at a cut-off level of
14 points.
3. As compared to the last BPL census, the proportion of SC families to total BPL families would come
down. The proportion of SC Households among the total BPL households was 19% in the 1997
census. In the 2002 census, it is likely to be 6% at a cut-off level of 13 points and 7% at a cut-off
level of 14 points.
4. In terms of absolute figures, the number of OBC BPL households was 174 in the 1997 census. This
figure would decrease by 20 (11%) if the cut-off level is set at 13. The figure would increase by 27
(16%) if the cut-off level is set at 14.
5. In terms of absolute figures, the number of SC BPL households was 44 in the 1997 census. This
figure would decrease by 33 (75%) if the cut-off level is set at 13. The figure would decrease by 28
(64%) if the cut-off level is set at 14.
In the sample Panchayat, thus, the current survey is likely to favor OBC households at the cost of SC
households. This in spite of the common knowledge - as well as the belief of the villagers - the proportion of
the poor is far greater among the SC communities than the OBC communities.
Apart from the households covered under the survey report, there are some households that have been left
out from the survey report. In the sample Panchayat all such households as have been left out from the BPL
Survey Report of the Government, belong to the Scheduled Caste Communities. The following is a list of left
out Families from the village 'Devanioyn ki Dhani' of the sample Panchayat. All these families belong to the SC
community.
1. Channaram s/o Hemaram
2. Bhagwanaram s/o Naggarama
3. Rekharam s/o Bhagwanaram
4. Bhuraram s/o Nimbaram
5.
6.
7.
8.
Paparam s/o Nimbaram
Hemi w/o Chatraram
Phuli w/o Pokraram
Herajram s/o Amrarram
Comparison between Score as collected by the Government Enumerator and score as enumerated through
participation of respondents.
o
Govt. Survey
Score Rank
19 10
1 Ajbaram S/o Keshraram Bhil ( Dhanne Ka Tala)
23 14
2 Chandanaram Malanaram Bhil (Dhanne Ka Tala)
17
8
3 Derajram S/o Gumanaram Garg ( Shivker)
17
9
4 Dcongraram S/o Neenuram Meqhwal (shivker)
25 15
5 Herajram S.o Durgaram Garg (Shivker)
20 11
Kara
ram
/
S/o
Udaram
Meqhwal
(shivker)
6
17
7
7 Kishnaram, s/o Haruram, Garg, Shivker
15
5
8 Ms. Jhamku, W/o Genaram, Shivker
23 13
9 Patita Ram, s/o Moolaram, Garg, Shivker
14
3
10 Prabhuram s/o Junjaram Bhil, Dhanne Ka tala
1
8
11 Sa.nkararam S/o Ghamuram Bhil ( Dhanne Ka Tala)
12
2
12 Sardara Ram s/o Gumanaram, Garg, Shivker
21 12
13 Sejuram S/o Pabudaan Bhil (Dhanne Ka Tala)
16 6
14 Shanti w/o Lt Tillaram Rana Rajpoot(Shivker)
14 4
15 Veeraram S/o JalaIram Bhil ( Dhanne Ka Tala)
Name
People's
People’s Score
Assessment
as % of Govt.
Score 1 Rank
Score
81
9
42% 1
7
7
30% ■
91
10
53%'
gj
13
53%:
9
11
36%
912
45% 1
7
4
41%;
8:
8
53% 1
7
3
30%:
7
5
50% 1
41
1
50%
7'
2
58%'
7
6
33%:
IB
16
63°/o\
IB
14
71°/o\
The households shown in bold letters are those who are likely to lose BPL status due to error in Government
survey. The households who are likely to get and advantage in getting BPL status over households that are
poorer than them are shown in bold italics.
Errors in the Questionnaire Design brought out during the BPL Survey 2002
Under the first point on Land, land ownership information should depict actual ownership. This has
not been the case. There have been the following errors:
a. In case of poor and less influential households staying and farming separately, but with land
papers being in the name of a common ancestor, the total land figure has been used for each
of the brothers. This has not been done for the influential families.
b. Even when poor families have mortgaged their land for loans from moneylenders, the land is
shown against their name and increases their points, thus, reducing their chances of getting
selected as BPL
c. Poor people have poor quality .land, but the quality of land has not been considered in the
survey.
2. Under the heading of house, poorest people who have obtained support under Indira Awaas Yojana
have been given higher points which reduces their chances of getting BPL status.
3. The question on dothing has led to large-scale misjudgment and nepotism. As such the question is
difficult to administer.
4. Misjudgment and nepotism is rampant also in the case of the question on Food Security. The
question, as administered, does not address the issue of amount of food available and only deals with
the number of times a family eats in a day.
5. The question on Sanitation has had a few misjudgments.
6. No Comments
7. Question on qualification of highest educated person in family gives higher points for educational
qualification irrespective of whether the higher qualification is enabling them to earn a higher income.
8. There has been large-scale misjudgment on this. Families sending children to school are penalized
while families sending children for work are rewarded. This can have adverse impact on the abolition
of child labor and enrolment in schools.
9. Families who have been given 4 points as falling under the 'Other' category are not necessarily better
off than families falling under the 'Salary' category. In some cases families with large landholdings
have been depicted as surviving on Wage Labor, while families, which have no land, have been
depicted as being dependent on subsistence cultivation.
10. The scoring pattern under the Status of children is incomplete. Thus -'amilies not having children havbeen aiven a score of 4. In fact this ~ :ec':on can be answered only •'?' famries with children in
1.
'fL
school-going age and hence can not be used as a scoring point. Further, families sending their
children to school are penalized while families not sending their children to school are rewarded.
11. Large scale misjudgment & nepotism has happened under this head with poorest families being
categorized as having no debts and being resource rich, while richer families have been shown as
being dependent on informal credit for daily needs.
12. The question on migration can be applicable to only such families, as have members able to migrate.
This discriminates especially against women headed households and households with old people
alone or with young children.
13. This question too has been the source of serious misjudgment & nepotism. Influential people
knowing that asking for TPDS and wage employment would give them lower scores, have asked for
the same. On the other hand poor people have often been persuaded to ask for housing so that they
get higher scores. In fact, seen in conjunction with the question on housing (Q2) this is a selfdefeating question. A family having a Pucca house and asking for TPDS and Wage Employment would
get 3 points on the two questions together. On the other hand a family having a Kutcha house and
asking for housing support would get 4 points on the two questions put together.
Annexure I
Case Studies
There have been severe malpractices in the BPL survey. Some of the better off households have received
much lower -scores implying greater poverty leading to greater probability of their being selected in the BPL
list- then the really poor families. Some of the cases of such households have been compared below:
Case: 1
Jugtaram s/o Bijaram , OBC, serial 34 Panchayat Shivkar has enough food throughout the year and has at
least one hectare of land. He has received 13 points meaning that he will be included in the BPL list on the
other hand Thanaram s/o Chutraram serial 192 in the same panchayat has less then one hectare of land and
he also does not get one square meal a day( as indicated in the government survey list} but his score is much
above Jugtaram i.e. 20. This is because one of the family member in Thanaram's family has studied up to
class 10m. And also because his children are studying in schools and not working. This has increased his score
tally by 4 points. He has got 4 points as he is not indebted and owns assets. Whereas a previous question of
the same survey clearly states that he doesn't own any assets( 0 score in question no 6). Also, the villagers
in his panchayat informed that he doses takes debts for daily consumption purposes. This clearly reflects a
case of misjudgment on part of the government surveyor.___________________________________________
Case n
Ruparam, Serial Number 78, Village Dhanne Ka Tala, Village Panchayat Shivkar has at least one hectare of
land and has two meals a day almost throughout the year has got 11 points. On the other hand Kaluram
Serial no 98 of village Shivkar has received 23 points because of following factors. The government survey
says that the average availability of normal wear dothing (per person) is 10 or more sets of doth. This has
fetched him 4 points. Whereas Ruparam has received no score for this question meaning average availability
is less than two. KAluram has also received one point more than Ruparam as one of the family members in
his family has studied up to class 5. The government list has given him a full score of 4 points saying that he
has enough food throughout the year. Whereas he himself and his neighbors informed that normally he gets
one square meal per day, but less than one square meal occasionally. This has increased his score by two
points as compared to Ruparam. Under the means of livelihood the government survey gives him a score of 4
but according to him and his villagers he is a casual labor and should have received no score for that. The
government survey further gives him 4 points as he isn't an indebted and own asset. On the other hand in a ;
previous question (NO.6) it says that he owns only one assets that in itself in contradictory. And according to i
his villagers he often takes loans for consumption purposes from non formal sources.
■
From this it is clear that there has been no cross verification of the survey done and individual bias of the
enumerator has played a key role in determining the BPL list.
I
Annexure n
Jtame
Sardara Ram s/o Gumanaram, Garg, Shivker
Sardara Ram s/o Gumanaram, Garg, Shivker
Patta Ram, s/o Moolaram, Gara, Shivker
Patta Ram, s/o Moolaram, Garg, Shivker
Ms. Jhamku, W/o Genaram, Shivker
I Ms. Jhamku, W/o Genaram, Shivker
|.<ishnaram, s/o Haruram, Garg, Shivker
|i<ishnaram, s/o Haruram, Garg, Shivker
Irierajram s/o Amraram, Dewaniyon Ki Dhani
|Herajram s/o Amraram, Dewaniyon Ki Dhani
I'Hemi w/o Lt_ Chutraram Meghwal, DKD
|Hemi w/o Lt Chutraram Meghwal, DKD
Prabhuram s/o Junjaram Bhil, Dhanne Ka tala
Prabhuram s/o Junjaram Bhil, Dhanne Ka tala
Sejuram S/o Pabudaan Bhil (Dhanne Ka Tala)
Sejuram S/o Pabudaan Bhil (Dhanne Ka Tala)
Ajbaram S/o Keshraram Bhil ( Dhanne Ka Tala)
Ajbaram S/o Keshraram Bhil ( Dhanne Ka Tala)
Chandanaram Malanaram Bhil (Dhanne Ka Tala)
Chandanaram Malanaram Bhil (Dhanne Ka Tala)
Veeraram S/o Jalalram Bhil ( Dhanne Ka Tala)
Veeraram S/o Jalalram Bhil ( Dhanne Ka Tala)
Sankararam S/o Ghamuram Bhil ( Dhanne Ka Tala)
Sankararam S/o Ghamuram Bhil ( Dhanne Ka Tala)
Derajram S/o Gumanaram Garg ( Shivker)
Derajram S/o Gumanaram Garg ( Shivker)
Herajram S.o Durgaram Garg (Shivker)
Herajram S.o Durgaram Garg (Shivker)
shanti w/o Lt Tillaram Rana Rajpoot( Shivker)
shanti w/o Lt Tillaram Rana Rajpoot( Shivker)
Kanaram / S/o Udaram Meghwal (shivker)
Kanaram / S/o Udaram Meghwal (shivker)
Doongraram S/o Neenuram Meghwal (shivker)
Doongraram S/o Neenuram Meghwal (shivker)
GS
PS
GS
PS
GS
PS
GS
PS
GS
PS
GS
PS
GS
PS
GS
PS
GS
PS
GS
PS
GS
PS
GS
PS
GS
PS
GS
PS
GS
PS
GS
PS
GS
PS
1 2 3 4 5 6 7 8 9 10 11 12 13 Total
1 1 1 4 0 0 1 3 1 0 0 0 0
12
1 1 0 0 0 0 1 3 0 0 1 0 0
7
2 3 1 4 0 0 1 3 1 4 3 1 0
23
1 1 0 0 0 0 1 3 0 1 0 0 0
7
1 3 1 3 0 0 1 1 1 4 0 0 0
15
2 1 0 0 0 0 0 2 0 0 0 3 0
8
1 2 1 3 0 0 1 3 1 4 0 1 0
17
0 1 0 0 0 0 1 3 0 1 1 0 0
7
1 1 0 0 0 0 1 1 0
1
0
3
0
1 1 0 0 0 0 1 1 1
3 1 0 2 0 0 0 3 1
3 1 0 0 0 0 0 3 0
4 0 1 3 0 0 0 3 1
4 0 0 0 0 0 0 3 0
2 1 1 3 0 0 1 3 1
2 1 0 0 0 0 1 3 0
2 1 2 3 0 0 1 3 1
1 1 0 1 0 0 1 3 0
3 2 0 2 0 0 1 3 1
3 1 0 0 0 0 1 3 0
3 1 0 0 0 0 0 2 1
1 0 0 0 0 0 0 3 0
1 2 1 4 0 0 1 3 1
1 1 0 0 0 0 1 2 0
2 3 1 4 0 0 1 3 1
1 1 0 0 0 0 1 3 1
0 1 1 3 0 0 1 2 1
2 1 0 2 0 0 0 2 0
2 2 1 3 0 0 1 3 1
3 2 0 3 0 0 0 1 0
2 1 1 3 0 0 1 3 1
4 1 0 1 0 0 1 0 2
1
0
0
0
0
1
1
0
0
1
1
0
0
4
1
4
1
4
0
4
0
4
0
0
1
0
4
0
0
0
4
0
0
1
1
0
0
0
3
1
0
0
2
0
0
0
3
3
0
2
0
3
0
3
0
1
0
0
0
0
3
1
0
3
3
1
0
1
0
0
9
0
14
0
7
21
3
0
7
3
19
0
8
3
23
0
7
0
14
0
10
0
8
0
4
0
17
0
9
2
25
0
9
0
16
0
10
0
20
0
9
0
17
0 —9
8
Explanation of Headings
GS: Govt. Survey, PS: People's Survey
1
2
3
4
5
6
Size group of operational holding of land
Type of house
Average Availability of normal wear
clothing (per person in pieces)
Food Security
Sanitation
Ownership of consumer durables
7 Literacy status of the highest literate adult
8 Status of the Household Labor Force
9 Means of livelihood
10 Status of children (5-14 years) [any child]
11 Type of indebtedness
12 Reason for migration from household
13 Preference of Assistance
CONVENTION ON RIGHT TO FOOD AND WORK
Bhopal, 11-13 June 2004
WORKSHOP ON PUBLIC DISTRIBUTION SYSTEM (PDS)
BACKGROUND NOTE
Kiran Moghc
The Beginning: The Public Distribution System (PDS) was set up in India originally as a
rationing system to cope with the food shortages during the Second World War period. From
1965, it was expanded into a universal system for delivering cheap foodgrain such as wheat
and rice and certain other essential commodities such as sugar, edible oil and kerosene. While
the major objective of the PDS has been to act as a welfare measure to provide these goods at
prices that are relatively lower than the market, it has also acted as a countervailing force to
prevent speculation in prices by profit-oriented private traders. Since the PDS constitutes a
major outlet for the sale of grain procured by the procurement agencies, it is an important link
in the support system provided to farmers by the government. Over the years, the buffer
stocks maintained by the PDS have served to ensure price stability and self-sufficiency in
food even in years of severe drought, and thereby helped to maintain the economic
sovereignty of the country.
Interstate Variations in Implementation: However, the implementation of the PDS has been
uneven across the country. There have been large interstate variations, with the four southern
states accounting for almost half (49%) of the total offtake of wheat and rice, while the
largely populated states of Bihar, Uttar Pradesh^ Madhya Pradesh and Rajasthan accounted
for only 10%. In terms of average per capita quantities, Kerela’s offtake was 53.3 kgs: in
Bihar it was only 2.3 kgs per person. Most importantly, there have been differences in the
coverage and utilization of the PDS by the public. For e.g., studies show that the PDS served
hardly 2% of the rural and 7% of the urban population in UP and Bihar, whereas it served
S7% of both the rural and the urban population in Kerela. In terms of serving the poor, XSS
consumption data indicates that poor families met between 8 to 20% of their needs from the
PDS. being dependent on the open market for the rest of their requirements. In general,
studies indicate that the access of the poor to the PDS by and large depended on the extent of
coverage in the state. Hence the poor in states with low coverage (such as Bihar and UP. MP.
etc.) lost out in comparison to states such as Andhra Pradesh and Kerela. In fact the Kerela
example proves that truly universal coverage, which consisted of a massive expansion of fair
price shops and the adequate and continuous availability of good quality' grain at prices lower
than the market, allowed the PDS to make a significant contribution to the purchases of poor
families and also enhance their nutritional status. On the other hand, large scale diversion of
toodgrain. wastage, poor quality, coupled with mismanagement and lack of sensitivity' of the
bureaucracy to meet the needs of the people in other states resulted in the failure of the PDS
to meet its avowed objective of enhancing the welfare of the poor.
NSS data indicates that average calorie intake in both rural and urban areas declined steadily
in the twenty-year period between 1972 and 1993, and that on an average, 44% of total
households were calorie deficient by normal nutritional standards. This called for a major
restructuring of the PDS to do away with the food insecurity of the majority of the Indian
people. Unfortunately, the kind of restructuring that was implemented with the advent of neo
liberal economic policies of structural adjustment since 1991 has furthered worsened the
situation.
Impact of Neo-Liberal Policies on the PDS: A key characteristic of these policies has been
their strong emphasis on reduction of public expenditure in order to reduce the fiscal deficit
This has taken the form of cutting back on several types of subsidies, particularly the ‘food
subsidy’. Although the food subsidy has remained virtually stagnant at around 0.6% of the
GDP over the last 20 years, reducing the ‘burden’ of food subsidy has been a central theme in
the policies of so-called economic reform. This has taken three forms; one has been a steep
increase in the prices of wheat and rice sold in the fair price shops, the second has been a
reduction in the quantum of foodgrain supplied to families through the PDS and finally there
has been a major policy shift from universal coverage to targeting the subsidy to selected
families that are identified as ‘poor’ on the basis of certain criteria laid down by the
government. Needless to say, such a ‘reform’ of the PDS has been one of the conditionalities
imposed by the World Bank while granting several types of loans to the central and several
state governments. The Andhra Pradesh Restructuring Project financed by the World Bank
for instance, required the state government to reduce the number of ration card holders
eligible for subsidised rice from 72% to 35%.
Increase in Prices of PDS Rice and Wheat: There has been a substantial increase in the issue
prices of rice and wheat supplied on the PDS over the last decade and a half, as seen in the
following tables.
Changes in Central Issue Prices of Rice and Wheat: Pre-Targeting
Year
June 1990
Dec 1991
Jan 1993
Feb 1994
1
Common Rice
(Rs/kg)
2.89
3.77
4.37
5.37
%Change
Wheat (Rs/kg)
%Change
30
16
23
2.34
2.80
3.30
4.02
20
18
22
Changes in Central Issue Prices of Rice: Post-Targeting
Year
|
June 1997
Feb 1999
July 2000
August 2002
Common R ice (Rs/kg)
APL
BPL
5.50
3.50
7.00
3.50
11.35
5.90
7.95
5.65
%Change
APL
BPL
27
62
68
-30
-04
Changes in Central Issue Prices of Wheat: Post-Targeting
Year
!
j
June 1997
Feb 1999
July 2000
August 2002
Wheat (Rs/kg)
APL
BPL
4.50
2.50
6.50
2.50
9.00
4.50
6.10
4.15
% Change
APL BPL
44
38
80
-32
-07
The steady increase in prices was done with a view to fix the central issue price as near the
'economic cost’ (the procurement and distribution costs) as possible, and bring down the food
subsidy bill. It also meant that any increase in procurement prices would automatically be
linked to an increase in issue prices. What is worse is that after targeting was introduced, the
price increase faced by the ‘poor’ BPL families was even higher the so-called ‘non-poor"
APL! As PDS prices approached the level of market prices, there was a corresponding
decline in the offtake from the PDS (from 20 million tonnes in 1996 to around 12 million
tonnes in 2000). As procurement continued and offtake declined, buffer stocks of wheat and
-ice rose to an unprecedented 60 million tonnes in the year 2000, around 5 times the required
norm. As a result the inventory carrying cost of the government went up to around Rs 14000
crores, which is around 44% of the total food subsidy. However per capita availability of
foodgrain declined from 505.5 gms per day in 1997 to 458.6 gms in 2000. In short, while
stains rotted and rats ran riot in government warehouses, millions of poor people in the
country faced growing starvation and malnourishment. In the face of a severe drought, prices
were somewhat reduced in 2002, but it was not enough to induce people to buy from the
PDS.
Reduction in quantities supplied: The massive increase in prices went hand in hand with a
reduction in quantities made available on the PDS. The allocation was changed from a per
capita basis to a per family basis. While the original monthly allocation was around 10 kg per
person (against an ICMR recommendation of 15 kg), the government brought down the
allocation to 20 kg per family (35 kg for BPL households), which is around 4 kg per person
in a family of 5. This meant that the poor had to increasingly depend on the open market for
meeting their requirements.
Targeting the Subsidy; The increase in prices and reduction in quantities went hand in hand
with the principle of ‘targeting’ the food subsidy; that is moving from universal access to a
system where only certain chosen families were entitled to rice and wheat at prices below the
market price. Initially targeting was introduced in 1992 for drought prone and backward areas
(Revamped PDS), but full-fledged targeting came in with the Targeted PDS (TPDS) in 1997.
The Planning Commission unilaterally determined the quota of families termed BPL (Below
the Poverty Line) who would be eligible for cheap food. These were in turn to be determined
by applying a criterion of annual household income of Rs 11000 per annum as per the IRDP
survey of 1996-97. The Planning Commission announced that only 36% of families in the
country were BPL and hence eligible for food subsidy, the others would henceforth have to
pay the ‘economic cost’ of rice and wheat.
Since the introduction of the TPDS was initially accompanied by a substantial reduction in
prices of rice and wheat for BPL families, it was welcomed by some quarters as a positive
measure in favour of the poor. However, it soon became clear that the purpose of targeting
was not to increase the welfare of the poor, but to eventually dismantle the entire PDS so that
the entire market for foodgrain could eventually be privatised.
The introduction of the Poverty Line criterion was essentially a masterstroke by the Central
government to abdicate its responsibility towards the food security of the people. For
example the Planning Commission determined that 32.65 lakhs (22.9%) of all households in
Andhra Pradesh were BPL, while the state government’s own survey indicated 113.02 lakhs
(68.67%) as BPL. Similarly for Karnataka, they assessed the level of BPL at 28.75 lakh
households (33.16%) whereas the state has determined the number of BPL ration cardholders
to be 64.83 lakh households (58.34%). For Kerela, the central government figure was 15.35
lakh (25.43%) and the state’s assessment was 20.59 lakhs. In Maharashtra the BPL quota was
65.45 lakhs against a state total of 77 lakhs only for rural areas. States that could not adjust
their previously high offtake to the new quotas of the Planning Commission had to find ways
of coping with the new situation. Each responded according to their commitment to the
people. States such as Kerela and West Bengal had to allocate additional state funds to meet
the cost of continuing to subsidise those families henceforth characterised as Above the
Poverty Line (APL). States such as Maharashtra, Uttar Pradesh and Andhra Pradesh simply
‘adjusted’ their poverty lines to accommodate the numbers determined by the Planning
Commission, while others such as Delhi simply abdicated their responsibility by declaring
that no BPL families existed.
Further, through successive surveys that use criteria such as possession of gas connections.
television sets, bicycles, permanent dwellings, etc. the government has successively reduced
the number of BPL families. For eg, in Pune district of Maharashtra, the number of BPL
beneficiaries identified at the outset of the TPDS was 59,340; it now stands reduced to
34,000. In one zone of Pune city, which incidentally has a large number of slums populated
by poor Dalit families, the number of BPL families was reduced from 12000 to 261!
This serves two purposes; one is to further reduce the food subsidy and the second is to
artificially deflate poverty figures and create a picture of growing prosperity when the
situation is in fact quite the reverse. The government s latest figures indicate an overall
poverty ratio of 26%, and the latest IRDP survey (for the 10lh Five Year Plan) that has been
conducted to determine poverty on the basis of consumption indicators will no doubt be
‘adjusted’ to this figure. That is precisely why the survey date has not yet been made public.
Since the IRDP survey has been conducted for rural areas there has been a genuine problem
of determining the poverty ratio in urban areas. For this purpose, some states have resorted to
using families selected for urban employment schemes, but the criteria are different and there
have been many difficulties; as a result, large numbers of the urban poor have been excluded,
the famous example being that of Dharavi, Mumbai’s largest slum where the number of BPL
families last counted was 128 (95 BPL and 32 Antyodaya) in a total of 83.855 ration card
holders!
Dividing the Poor: Large-scale criticism of the manner in which the poor were being
excluded led the government to announce the Antyodaya Anna Yojana for the ‘poorest of the
poor’ in 2001. This meant that from the BPL list, the lowest 10% of families was selected to
be eligible for rice and wheat at Rs 2 and Rs 3 per kg respectively. This has led to a further
division of the poor. Another scheme, the Annapurna Yojana, was introduced in the year
2000 to provide 10 kgs of foodgrain free to those who have no supporting families and are
not beneficiaries of other types of government schemes (eg widow pensions, etc.). It exists
virtually on paper because it is impossible to find the kind of destitute beneficiaries required
as per the rules of the scheme, who are literally the dispossessed. By creating a hierarchy of
beneficiaries within one system, the government has created further scope for corruption.
Since the grain is the same but priced differently, it can be easily diverted and sold for a
profit.
Most importantly, dividing the poor has disrupted their unity; each person hopes and strives
for the BPL card, because it gives much-needed relief, but in the bargain, loses sight of the
benefits of the universal system that actually needs to be conserved and strengthened. The
larger political implications of targeting should not be underestimated.
Targeted out of the System: The reason touted to justify targeting is to exclude the ’non
poor’ from the benefits of the subsidy. However, the experience of the universal PDS shows
that the non-poor usually practise self-exclusion, that is they voluntarily do not make use of
the system. In that sense, they do not benefit from the subsidy. In contrast, a system of faulty
targeting based on erroneous income and consumption poverty indicators ends up excluding
the poor who need the subsidy the most For e.g. a survey done by AIDWA in 2002 of 810
families in a Lucknow slum showed that 355 families (44%) did not possess a ration card,
BPL or otherwise. There were only 13 BPL cards, and not a single Antyodaya or Annapooma
beneficiary! In the entire state of Uttaranchal, only 216 families have been identified as
Antyodaya beneficiaries! The social costs of excluding the poor in a targeted system are
much higher than the administrative costs of including the non-poor in a universal system.
Eight years after the Targeted PDS has been in existence, there is growing evidence of
increasing food insecurity in terms of hunger, malnourishment and overall poverty. The
qualitatively negative impact on different vulnerable sections within the poor, particularly
single women. Dalits, Adivasis, minorities, project-displaced families, migrant workers, etc.
has also been raised and documented by different organizations and groups that have been
mobilizing people around the right to cheap food.
The present PDS as it stands today is characterised by • Frequent and bewildering changes in prices and lack of information in the public
about these changes
• Lack of availability of quotas in fair price shops at the appropriate time
• Arbitrary cancellation of BPL cards on the basis of flimsy criteria and subjective
opinions of fair price shop owners and ration officials
• Wrongful allotment of BPL and Antyodaya cards to the relatively better off due to
local political patronage
• Massive corruption in the issue of BPL cards
• Diversion of BPL and Antyodaya grain to the open market
• Lack of viability of fair price shops leading to further corrupt practices
All these factors have combined to throw needy families out the ambit of the PDS. To many
it has become virtually non-existent. Instead of restructuring it towards the poor, this is being
used as a rationale by the bureaucracy to justify the dismantling of the system. The food
stocks that accumulated two years ago as a result of these wrong policies were eventually
sold to exporters and private traders at Rs 4 per kg, a price well below the BPL price. The
food subsidy therefore ended up being targeted towards profiteers, not the poor.
What is even worse is that the BPL criterion has now become a tool to target other types of
social sector expenditure such as on health and education; It is now the BPL card which
determines the access of the poor to free health care or loans for self-help groups, housing
schemes, etc. It is becoming increasingly evident that the targeting of food subsidy is merely
the first step in the direction of bringing down total public expenditure meant for the poor.
There is also an additional issue of other items such as sugar and kerosene that are distributed
on the PDS. Despite large stocks of sugar, the PDS price of sugar was doubled; initially it
was restricted to BPL cardholders, but now sugar is no longer sold on the PDS. Similarly,
after the administered price system in the oil sector was dismantled, and the domestic prices
of petroleum products linked to the international market, the price of kerosene on the PDS
has risen from Rs 2.50 a litre to Rs 10 per litre. The quotas allotted to state governments have
been linked to the number of gas connections released to the state, and the resulting shortages
has provided the basis for a burgeoning black market in kerosene, which is available at Rs
20-25 per litre in the open market. This is a source of great hardship to common people, and
needs urgent attention. Any measures to strengthen the PDS must also include expanding the
number of essential commodities sold through it.
Political Consensus on Targeting: There has been a remarkable consensus within the two
major political parties, the BJP and the Congress on the issue of targeting food subsidy.
Despite pressure from Left parties who have been demanding a return to universalisation of
the PDS and a reduction in prices, the Common Minimum Programme of the recently elected
United Progressive Alliance states the intention of the government to “move towards
universal food security over time, iffoundfeasible" (emphasis added).
Urgency of the Situation: Several nutrition and other indicators point to the growing food
insecurity of the Indian people. The situation is urgent; it requires immediate attention by
policy makers. The right to cheap foodgrain through a strengthened public distribution
system must be made a fundamental right. As a first step, rice and wheat need to be made
available to all BPL households at highly reduced prices, (say Antodaya prices of Rs. 2 per
kg of wheat and Rs. 2 per kg rice. The BPL category needs to be extended to all vulnerable
sections including all agricultural labour, migrant workers, urban unorganised sector workers.
retrenched industrial workers, widows, single adult women, disabled persons, persons over
the age of sixty, female headed families, etc. Special attention needs to be paid to the food
security of Dalit and Adivasi households, The quantity of foodgrain supplied on the PDS
needs to be vastly increased and should be individual and not family based. The foodgrain
component of all employment-related schemes needs be calculated at current Antodaya
prices. A radical change is required in the methodology used to measure poverty.
Even amongst organisations that are mobilising people around the issue of cheap food, there
is still a debate about whether there should be a return to the universal PDS, or whether the
Targeted PDS should be further 'reformed’ to take care of the distortions introduced in the
system (for e.g.by rationalising the criteria for BPL selection, including more and more
categories of eligible households, etc).
It must be pointed out that the crucial issue is not one of better delivery and implementation,
but that of a basic policy choice of whether food security is a fundamental right that must be
available to all citizens regardless of their position (class, caste, region, gender, etc.) in
society. Targeting is not simply about ensuring that the poor get their due, but also about
excluding those whom the state believes does not have the right to access the subsidized
system, be it food or health of education. What is the basis for selecting some households and
excluding others in a country where more than half the population is impoverished, as evident
from several other social and economic indicators? What about crop failures, fluctuations in
input prices, crash in output prices, changing cropping patterns, closure of industries,
drought, floods etc, which can contribute to converting the ‘non-poor’ into the poor in a
matter of moments?
This workshop is intended to resolve some of these issues, and on the basis of concrete
experiences, formulate concrete demands that can form the basis for future struggles around
the Public Distribution System. In particular, it is intended to bring to:
•
•
•
•
•
Bring to the fore the experience of the TPDS, Antyodaya Anna Yojana and
Annapurna Yojana in different states
Share the experience of struggles built up around these schemes
Explore alternative forms of food security systems
Formulate tactical and strategic demands about the PDS
Discuss possible forms of future struggles around these demands
ALL INDIA DEMOCRATIC WOMEN’S ASSOCIATION, 121, V. P. HOUSE, RAFI MARG,
NEW DELHI 110 001
Tel: 23710476 email - aidwa@ndb.vsnl.net.in
Denial of Health Care
Testimonies from Rajasthan
A 65 year-old-man of village Dhirji -Ka [Cheda,- tehsil Bhadesar, district
Chittorgarh developed cough and breathlessness. He was taken to district hospital,
Chittorgarh where he was admitted. The doctors prescribed medicines that had to
be bought from private medical store. For one and a half years the patient took
treatment from the district hospital and spent around Rs.35000/-for the treatment
but still did not get well. He was taken to Udaipur referral hospital where he was
admitted for 15 days and told that he had liver problem. While he took medicines
he felt better but as soon as he stopped taking the medicines he would develop
swelling in the abdomen and legs. The treatment at Udaipur cost Rs.40,000/despite it being a Government hospital. The family had to mortgage and even sell
some off their land to arrange for the money. Yet the doctors at the referral
hospital told them to take the patient to Jaipur or Ahmedabad for further
treatment. The family had no more money left to take the patient and therefore
they were forced to bring the ill patient back home. For 2 months the patient
suffered lot of pain and discomfort and due to unavailability of proper treatment
eventually he died a very painful death.
Denial: Despite having a BPL card all the medicines had to be .bought from private
medical store
No proper diagnosis was done
Consequence: The patient lost his life due to lack of money
The family fell into heavy' debt
•
A 62-y'ear-old man of village Lakshmi Pura, district Nimach (adjacent to village
Vijaypur, district Chittorgarh) felt pain in his stomach in June 2001. He sought
treatment in Chittorgarh district hospital (which is closer than the district hospital
in Nimach). The patient was admitted in the hospital for 15 days during which
blood test, urine test and X-ray were done. In all these tests and medicines the
patient had to spend Rs.40,000/-. The doctor then told him that he needed an
operation for which blood would also have to be arranged and this would involve
an amount of R. 10,000/-. The patient is too poor to arrange for this much money
again. Thus he has not get the operation done., He has swelling in his abdomen
which is very painful. For temporary' relief he seeks treatment from a local private
doctor. The doctor charges Rs.200-300 every time and gives him 2 injections and
some tablets. This gives temporary relief and every month/ couple of months he
repeats this treatment. For 3 years the patient has been suffering in pain. In this
whole process he has had to sell off his 2 bullocks to arrange for the money.
Today he has no money for treatment and is extremely weak wit visible wasting
of muscles.
Denial: Denied operation due to lack of money
No free medicines form the government hospital.
Consequence: Patient has been suffering for the last 3 years and can die any day if he
does not receive immediate treatment.
•
He had to sell off his bullocks to arrange money for the treatment in the government
hospital.
In mav 1990. a 38 year old man of village Pithalwadi Khurd. tehsil Chhoti Sadri,
district chittorsarh. developed headache and suddenly became unconscious. The
family went to CHC, Chotti Sadri to call the doctor. Instead of coming himself the
doctor sent the compounder. The compounder gave 2 injections in the patient’s
head. After some time the patient recovered. After 3 days he again fell
unconscious. Then he was brought to the CHC & admitted. The doctor who had
admitted him went on a long leave after admitting the patient. The other doctor at
the CHC refused to treat the patient and scolded the family for consulting the
doctor earlier and then later approaching him. The patient remained admitted in
the CHC for 14 days without the doctors looking at him. The nurse and the
compounder kept giving some treatment for temporary relief. During this time the
family spent Rs. 15000/-. After 14 days the doctor came back from leave and told
the family to take the patient to Udaipur as he could not be treated at the CHC.
The family sold off thir land and jewellery and took the patient to Udaipur referral
hospital. He took treatment for 3 months but it did not help. Initially one of his
legs got paralysed and eventually both the legs got paralysed. The family
borrowed rs.4000/- from relatives and took him to a private hospital at Nimach
but it did not help either. Today the patient is paralysed below the waist and is
completely bedridden.
.
Denial: The doctor did not visit the patient himself and sent the compounder.
The doctor who had admitted the patient went, on leave and the other doctor refused to
see the patient.
••
. ..
All the tests and medicines had to be arranged from outside the hospital.
Consequence: Despite so much effort the patient is bedridden
The family has lost most of its assets
•
A 20-year-old woman of village Akhepur, tehsil Chhoti Sadri. district
Chittorgarh. was pregnant and wasiaken to the area CHC for delivery on 6:h June
2004. The patient reached the hospital at 12 o’clock in the night and nobody was
available at the CHC. Two doctors were on leave. The patient’s husband went to
the third doctor’s house to call him. The doctor answered from the window and
told the patient’s husband to call the LHV. He went to call the LHV but the LHV
did not answer. He came to back to CHC where he saw the wife’s pain had
increased. He went back to the LHV’s house. After knocking at the door for about
15 minutes the LHV came out. The LHV admitted the patient in the labour room,
gave a bottle of glucose, assured the husband that everything was fine and that
there was still some time for the delivery’ and she went back home. The patient’s
pain became unbearable and the husband went to the ward boy's house. By the
time the ward boy came it was 4-4.30 AM. At around 5 o’clock in the morning
the patient finally delivered but the child was born dead. The LHV came back and
told the family that the child had died two days ago in the womb itself.
Denial: There was nobody at the CHC in emergency.
The doctor did not come to attend the patient, instead asked the family to call the LHV
o
1 he LHV went back home without attending to the patient
The patient was left at the mercy of the ward boy.
All the service providers charged money
Consequence: The child did not survive.
The parents had to suffer lot of agony because of losing their child
A 21 year-old-woman of village Raju khera. tehsil Chhoti Sadri, district
Chittorgarh delivered a child in July 2003. She developed breast engorgement and
could not feed the child. The patient went to the area CHC where she was
suggested an operation to heal the breasts. She got scared of the operation and
took local treatment in the village itself. Since she was not able to feed the child
the child became very weak and developed vomiting/diarrhoea. She took the
infant to the CHC where medicines were prescribed. The patient bought the
medicines from private medical store but they did not help. Then they took the
child to the Nimach district hospital where he was admitted for 2 days and told
that it was necessan to breast-feed the child. The doctor suggested that they take
the child back to the village and get some other lactating woman to breast feed the
child. The family brought the child back but there was no other woman in the
village who could feed the child and eventually the child died after 3 days.
Denial: The patient was directly told for operation without giving any other alternatives.
The child was not given any supplementary' feed in the absence of mother’s milk.
Consequence: Pain in the patient’s breasts continued.
The child lost his life
»
«
3 years ago in August 2001, a 48-year-old woman of village Lader, tehsil
Bhadesar, district Chittorgarh felt pain in her right eye. She went to the area PHC
at Bhadesar where the doctors prescribed medicines and asked her to go to some
other hospital, as she could not be treated at the PHC. She went to district
hospital. Chittorgarh where she was given dressing for 5 day's but it did not help
and the pain continued. The patient also went to an eye camp held at SanvariyaJi
where she was given a "tube which brought no relief. In the hope to save her eye
the patient went to Udaipur referral hospital where she was told that eye
replacement could not be done. Instead if she arranged for around Rs.5000/-. she
could be given an artificial eye. The patient is too poor to arrange for this much
amount of money. She has already spent around Rs. 1500- in the treatment for
which she has had to mortgage her silver jewellery. Now the patient has lost her
right eye.
Denial: The patient was denied operation because she did not have money
Consequence: The patient has lost her eye.
•
Another woman of village Jaliya Peepliya, tehsil Nimbahera, Chittorgarh district
had itching/irritation and running water in her eyes in April 2002. She consulted
the doctors at eye camps held at SanvariyaJi and Chittorgarh where she was given
some medicines and tube but they did not help. Having got no relief in the
government camps the patient went to private doctors where she spent around
Rs.2000/- and was finally told that she needed an operation which would cost rs.
10.000/-. Being from a very poor family the patient does not have so much money
and today she remains without any treatment'with her eyes still paining and
reduced visibility.
Similar is the situation of another woman of Village Lader, tehsil Bhadesar.
district Chittorgarh.
Denial: In government facility proper examination& treatment was not given
Consequence: Patient suffered economic loss in private hospitals.
She now has reduced visibility due to lack of treatment in the government facilities and
money.
A 45 year old man of village Siyakhedi. tehsil Chhoti Sadri. district Chittorgarh.
developed fever, breathlessness and weakness in November 2001. He was taken
to the area CHC where blood, urine and sputum tests were prescribed. The tests
had to be done from private laboratory'. After seeing the reports the doctor
admitted the patient but after that did not visit the patient in the ward. The patient
went to the doctor's residence and the doctor prescribed some medicines. The
family bought these medicines from private medical store and the ward boy
administered these medicines. The treatment was not being-effective and the
patient was referred to Pratapgarh district hospital. At the district hospital, X-ray
was done and the patient was sent back' to the CHC after prescribing some
medicines. Since the treatment in government hospital was not helpful so the
patient consulted a private doctor. In the entire treatment the family spent about
Rs. 11,000/- for which the had to mortgage their land. Yet they were not able to
save the patient.
Denial: Doctor at the CHC did not visit the patient in the ward.
The patient was made to run from one hospital to the other.
Patient had to spend money in the government hospital and proper treatment was not
given either at CHC or at district hospital.
Consequence: The patient had to ultimately go to the private doctor.
Family suffered economic loss
Family and patient went through lot of mental agony and trauma in trying to seek
treatment from the Government facilities.
Despite all efforts the patient lost his life.
•
•
A 60-year-old man of village Jaliya P.eepliya, tehsil Nimbahera, district
Chittorgarh .has been suffering from white’ discharge 'for the last 6 years. The
extent of problem is such that he has to change his clothes thrice in a day.He took
treatment at Nimbahera CHC where he spent Rs.3000/- in treatment and
medicines. Gradually his condition kept deteriorating and he developed weakness,
breathlessness and cough. Having got no respite at the government hospital the
patient sought treatment at a private hospital in Mandsaur where he spent Rs.
6500/-. As the treatment was of no use, the patient went to another private clinic
in Nimach where he was given 5 injections and medicines for Rs.3500/-. Finally
he went back to the Nimbahera CHC as he had no more money for treatment in
private. Urine and sputum tests were done and he was referred to Udaipur referral
hospital. But by then the patient had exhausted all his resources and did not nave
any more money to go to Udaipur. So for the last one and a half years he has not
taken any treatment and continues to suffer.
Denial: Patient did not get any free medicines in the hospital.
Patient was not informed about the illness or given proper treatment.
Consequence: Patient kept running around from one hospital to the other.
Suffered economic loss
Did not get any relief and is still ill and suffering.
A 30-year-old man working in the stone mines in Jodhpur district developed TB
in November 1998 and sought treatment at Kamla Nehru TB hospital. Jodhpur.
The patient was admitted for 1 week during which X-ray and blood test were done
from private laboratory even including medications. After a week in the hospital
the patient was discharged. He took rest at home for a week and went back to
work. His condition deteriorated despite raking medicines and he went back to the
hospital and was again admitted. He continued taking medicines bought form
private medical store. This time the patient was discharged after 15 days but after
a week at home his condition started deteriorating severely and was again
admitted for 3 months. Once again examinations like X-ray and sputum were
done in private laboratory. In this entire treatment of 6 months the patient's family
spent an amount of about Rs. 20000/- by selling their land, jeweller}' and
borrowing money on interest. Despite all these efforts the family could not save
the patient, as they were unable to arrange for any more money. ■ .
Denial: X-ray, blood test & sputum test were done from .private laboratory.
The family spent huge amount of money on treatment. y
Consequence: Because of lack of adequate money the patient could not continue the
treatment and died.
Family suffered lot of mental anguish and distress.
Family's land and jewellery' were sold.
Family fell into heavy' debt. Now wife is the only earning member to repay the debt and
take care of children.
•
Another 29-year-old mineworker from Jodhpur was hurt while blasting the stones
on 31st march 1996. The patient was taken to Mahatma Gandhi hospital in
Jodhpur and admitted for a week. The patient spent around Rs. 7000/- on X-ray,
sonography & medicines all of which were arranged from outside the government
hospital. Treatment was not effective and the doctors told him to go to a private
hospital for better treatment. The patient was forced to seek treatment in private
hospital where he spent Rs. 20,000/-, which he arranged by borrowing form
relatives and taking loan on interest. Still the patient has not recovered completely
and finds it difficult to stand for more than half an hour at a stretch. He even
continues to repay the debt.
Denial: No test were done in the government hospital for detection of TB, insteac had to
be done from private laboratory.
No free medicines were provided from the Government hospital.
Consequences: The patient was forced to seek treatment in private hospital.
The family fell into heavy' debt which they are repaying even after eight years.
•
These are just two examples of thousands of-mine workers who continue to suffer in
Jodhpur stone mines. The work conditions in these mines provide little security to the
■workers. No security is being provided by the employer. Neither is the government health
system of any use to the poor and the resourceless. As a result of this thousands of
workers face numerous health hazards which lead to loss of life and money.
On 6th June 2004 a 25 year old woman from Tilawala village, Panchayat samiti, Sanganer. district
Jaipur, died due to ecxessive bleeding after delivering her second child (who survived) at the CHC,
Sanganer, Jaipur district. When the woman was beought in by her family at 4.00PM that evening
she was in labour. The LHV took her into the labour room. At 6.15 PM after delivering the child the
nurde came out and told the patient's husband to get an injection to stop the bleeding. FOr 45
minutes the nurse kept handling the serious matter on her own. The family kept asking her to call a
doctor, to call an expert. The hospital incharge is a gynaecologist. The nurse paid no heed. Then she
said mat the patient should be taken to the State Hospital or the Women's Hospital, 10 Km away in
the city. There was no ambulance. The family hired a private taxi. When the patient's condition
started deteriorating the nurse suggested the private hospital nearby. The private hospital said that
they could not do anything. By the time she was brought to the SMS State Medical College/Hopital
by 8.30PM she had died.
Denial:
The hospital did not have the injection to stop the bleeding and the patient was asked to get the
injection from outside.
The doctor was not called to attend the patient despite the patient repeatedly asking the nurse to do
so.
There was no ambulance in the hospital.
' •
consequences:
.The patient suffered in severe pain for a long time.
Family went through lot of mental agony in the whole process.
The patient lost her life.
The above matter shows how women's lives are treated with callousness in the CHC. This is also
significant that at this CHC during last 10 months 3 such incidents have taken place and this CHC
has shown no accountability to the people. On 6th August 2003 a labourer woman came to the CHC
for delivery. In this case midway during the operation the husbnad ws called and the doctors told
him that the child had died and since the child's bosywas half in the woman's body, which the doctor
did not know how to handle, she should be taken to the State medical college/hospital. The child's
head was wrapped ina polythene and tire patient was taken to a closeby private hospital where
fortunately the woman's life was saved. On 30th August 2003 in yet another delivery matter the
child died.
The CHC incharge who is a gynaecologist is never available. The other 2 doctors appointed are
dentists. There is no drinking water. Garbage lies all around. The ambulance is used personally by
doctors and other staff. The bedsheets are never washed. The CHC is in such a state of neglect
which is unavailable. There is no accountability inspite of protests. FIRs have been lodged in all the
above cases.
This CHC in such a pathetic state as above, is being used by people from 100 villages.
HEALTH STATUS OF
RAJASTHAN
Demography
■ Total Population
5.64,73122
2.93.51557
2,70,9’465
Male
Female
Jan Swasthya Abhiyan
Rajasthan Unit
B -8, Bapu Nagar, Senthi,
Chittorgarh 312 025 .
■ Sex Ratio
Urban
Rural
■ Juvenile sex ratio
■ Literacy rate
urban :
rural :
(Source: Census 2001)
Demography & infrastructure
(contd.)
■ Population density
■ Percent rural population
■ Percent with access to safe water
■ Percent with no toilet facility
■ Percent with access to electricity
165
76.62
49.6
71.8
64.4
Source: Census 2001
NFHS-II
(contd.)
Source:NFHS-II
82.3
52.0
.922
890
932
Urban
Rural
90S
SS5
914
M 76.46
M 87.10
M 72.96
F — 34
F 55.42
F 37.74
Health indices of Rajasthan
■ Infant mortality rate.
80.4
• Under five mortality.rate
114.9
« Maternal mortality rate
677
■ Total fertility rate
3.78
■ % of women with anaemia
48.5
■ % of women with severe anaemia 16.2
(contd.)
Status of health facilities
Health indices of Rajasthan
■ % of children with anaemia
■ % of children with chronic
undemutrition
■
CHCs
■ State norm: A CHC for every 1 lakh population
Total rural population to CHC ratio 1,45,680141 CHCs less than required
PHCs .
■ In tribal & desert areas
Population to PHC ratio
153 PHCs less than required
23758
■ In non-tribal areas
Population to PHC ratio
54 PHCs more than required
27951
(Cocxd.)
i
Percentage of vacant posts
Sub Centres
■ In tribal & desert areas
Population to sub-centre ratio
4118
1793 sub-centres less than required
■In non-tribal areas
Population to sub-centre ratio
4586
421 sub centres more than required .
.
•
■
■
■
•
«
MPW (14)..
Gynaecologists
Paediatricians
Anaesthetists
Surgeons
Medical officers
Medical officers Dental
63./
34.59
28.81
33.87
46.06
5.78
24.77
Health governance systems
■ The state does have an essential drug list but few
people are aware of it & it is hardly used. Over
medication is rampant.
■ A set of standard treatment guidelines has been
recently prepared
■ User fees is charged at CHCs & higher level hospitals
under DMRS.
Health sector budget
■ Annual health budget in relation to GDP
1998-1999
1999-2000
2000-2001
2001-2002
2002-2003
1.17%
1.12%
1.12%
1.12%
1.06% .
■ There is no such provision (except the 'Right to
Information ActQ whereby the public can mow what
drugs are available at the public health facility. People
are often denied medicines from the pubfc health
facilities and have to spend huge amounts of money
on drugs.
in
t
Qcm&u
fa'yecexJSvn
.
■ There is no functional system for people to lodge
complaints regarding negligence/poor quality services.
Complaint boxes may be existing but they are usually
placed in such a way that the public does not know
about them.
■ Annual health budget in relation to total population
Rs.158 per capita in 2002-03
Rs. 189 as per modified budget of 2004-05
■ Annual health budget for drugs
o A meagre 2.86% of total health budget rzas spent O'
drugs in 2002-03
o Per capjta population expenditure on drugs has bee'
abysmally low at
Rs.4.51 per capita in 2002-03
Rs.4.03 as pe'r BE for 2004-05
(contd.)
2
Policy Matters
| ■ The state does not have a health policy
• Neither is there any policy for regulating the private
medical sector
■ But what definitely exists & is practiced is the .
population policy
s Rajasthan has a very coercive population control
programme based on incentives & disincentives
(Contd.)
Externally funded projects
.
■ The state has an external aid of about
Rs.1913.47 crores for health related projects
■ These are supported by World Bank, UNICEF,
UNFPA, European Corhmision, GTZ
■ The World Bank grant of Rs.472 crores is in the
form of loan
■ There is no system for civil society monitoring of
these projects
- Target approach is being adopted S service providers
are penalised for not meeting targets
■ Standardised norms for sterilisation camps are
compromised in the zeal to achieve targets
l Two-child norm is applicable in the °anchayats,
Municipalities & State government
■ The civil society has no role in monitoring the
availability & delivery of health services
|
■ Despite the Regulation Gram Pancr.ayats too do
not have any effective role in planning &
implementation of local health services
I
Sip 5-
---------
i
Cases of Denial of Health Care from Maharashtra
Human rights violations to be presented to NHRC at Public Hearing, Bhopal
The Jan Arogya Abhiyan (JSA-Maharashtra) has documented over 80 cases of denial
of health care, from various regions of Maharashtra during the last several months. A
brief description of a sample of these cases, drawn from various parts of the state and
exemplifying various types of denial, are given below These cases would be
presented to the National Human Rights Commission during the Western region
public hearing on Right to Health Care at Bhopal on 29th July, 2004.
1. Place: Nandurbar District, Northern Maharashtra
In one of the Narmada Bachao Andolan’s ‘Jeevan Shala’ schools, a girl student
was bitten by a snake. The resident teacher hurriedly took her to the Rural
Hospital. Incidence of snakebite in this area is very high, especially in rainy
season. However, because of non-availability of snake anti-venin in that hospital,
the girl died after few hours. As it was a rainy season, activists from NBA tried to
persuade Rural Hospital authorities to make anti-venin available immediately so
that similar cases would not occur in the future. Unfortunately anti-venin remained
unavailable in the hospital for more than a fortnight. During this period, two more
girls died of snakebite due to non-availability of the life-saving anti-venin.
Type of Denial:
Nonavailability of snake anti-venin in the Rural Hospital, although incidence
of snakebite in this area is very high
Consequences:
Completely avoidable deaths of three girl students, studying in Jeevan Shala
2. Place: Nandurbar District, Northern Maharashtra
On 4th April 2\)04 Nagu Hadku Godse went to Akkalkuwa PHC along with his
daughter, in her ninth month of pregnancy. When they reached the PHC his
daughter was already in labour. Mr.Godse tried to call the Medical Officer on duty
but he was untraceable. Although the ANM was in the campus of the PHC, inspite
of pleas of Mr.Godse, she refused to see the daughter who was in labour. Sensing
that he will not get help, Mr. Godse rushed to hire a private vehicle to take his
daughter to a private clinic, which was around 15 Km away from this PHC. But in
the mean while the daughter delivered in the open ground of the PHC. Mr.Godse
again went to ANM to seek her help. She accompanied him very reluctantly but
after watching his daughter plainly refused to cut the umbilical cord and did not
bother to provide essential care to the new bom. More over she scolded her helper
for allowing Mr. Godse to enter in PHC campus. Mr.Godse at last took his
daughter to a private clinic where the Doctor had separated the placenta
Type of Denial:
Nonavailability of services of the Doctor or ANM in the PHC.
Denial to provide essential delivery care, in extremely insensitive manner.
Consequences:
Severe financial loss, health riskrand-nrental-onguish to patient and relatives.
Place: Khodala PHC, Thane District, Coastal Maharashtra
3.
In one of the villages under Khodala PHC, an epidemic of diarrhea and
vomiting occurred in October 2003. Sensing the danger, a villager Mr. Dattu Vad
rushed to inform about the epidemic to Block Development Officer (BDO) who
unfortunately ignored this warning. Mr.Vad then tried to contact concerned authorities
in the PHC. However in PHC on duty Medical Officer was not available to take a
stock of the situation. All efforts of Mr Vad to contact the MO were in vain so at last
he called the CEO of Thane District. Finally the CEO arranged for a doctor and
vehicle. In the mean while, one women lost her life in this epidemic where as 5 others
were taken seriously ill. Paradoxically rather than complimoiting the efforts taken by
Mr.Vad, PHC officials were furious that he had dared to contact the CEO directly. In
spite of specific instructions by the District authorities to PHC doctor to monitor the
situation regularly, he visited die epidemic area subsequently on only three occasions
in 2 months.
Type of denial:
Medical Officer was not on duty in the PHC. BDO ignored the information
about an epidemic. No proper surveillance system to monitor outbreak of epidemic.
Warning by the local resident was ignored locally.
Consequences:
One death and five others became seriously ill.
4.Place: Vashila PHC, Thane Distict, Coastal Maharashtra
One-year-old Pinty Bhanwar was taken to Vashila PHC with acute breathing
problems and swelling around the eyes. Although she was taken to the PHC during
working hours, the on duty Doctor was not present in the campus, compunder in the
PHC gave some local application for eyes. Pinty’s parent waited for the Doctor to
come for around four hours; when the doctor failed to appear at last they decided to
shift her to adjacent Nandgaon PHC. The Doctor in this PHC gave some injection and
tablets and assured her parents that everything would be all right within few hours,
and left the place. Inspite of repeated requests, nobody in the PHC bothered to tell
them what is wrong with their daughter, nor was the child admitted in the PHC. The
parents had to keep the patient in a nearby relative’s house. Unfortunately the child
died without proper care and in absence of the Doctor on the same day.
Type of denial:
No Doctor was available in the first PHC, where as in the second PHC
although Doctor was available, there was no provision for admitting the patient.
Doctor left the PHC, abandoning the patient.
Consequences:
Death of the child.
S.Place: Kurkheda Rural Hospital, Gadchiroli District, Vidarbha region,
Maharashtra
Mrs Uttara Rupchand Dakhane is about 25 years old woman residing at Village Ghati,
Taluka Kurkheda, Dist: Gadchiroli.
Mrs. Dakhane registered herself at Kurkheda PHC for Ante-natal care in mid-2003.
On 5th August 2003 she developed labour pains and was taken to Rural Hospital
Kurkheda Medical Officers were present in Hospital. Mr. Rupchand Dakhne asked
the Nurse to admit the patient in labour. The Nurse told him to first get the patient
registered. After that he went to the MO. He told to take her at labour room. Once the
patient was in labour room, the Nurse came and put the patient in position for
delivery, left the room and did not bother to revisit the patient again. In the meanwhile
Mr. Dakhane asked to meet another medical officer. He wrote something on paper
and again sent him to the previous MO. This MO had a look at the patient and warned
her husband that since the mother was very weak, this could be a complicated
delivery and could be dangerous to her life. Ironically in spite of understanding
complications associated with the delivery', the MO did not visit labor room again.
FinalN the delivery took place without medical assistance. When the patient’s
husband reported to the nurse about the delivery, she came and cut the cord. The only
thing the Nurse did was to take the weight of the baby, she did not even care to see
that the baby should cry. The baby cried only when the Dai cleaned her, nearly half an
hour after birth. The Doctor did not pay any attention even after that.
After four -five months, the mother and father of the baby realised that the
development of the child was not proper and they took her to a child specialist in
Nagpur. He diagnosed mental retardation, due to negligence at the time of birth.
Type of denial;
Although being present in the campus, neither Doctor nor Nurse came to
conduct the delivery. Essential care of the newborn was not taken.
Consequences:
Negligence at time of delivery resulted in the child developing lifelong mental
retardation.
6.
Place:
PHC Haveli, Pune District, Western Maharashtra
Mrs. Asha Shelar presented the plight of the women who were herded for tubectomy
in PHCs in Haveli taluka She reported an incidence where the women were given
anaesthesia many hours before the operating surgeon arrived al the PHC. Thus by
the time the doctor started operating, the effect of anesthesia had already worn off.
The women were screaming with pain during the operation. The doctor physically
hit one of the patients when she was screaming. On top of that, loud music was put
on to prevent the screaming of the woman from reaching outside.
Type of denial:
Absence of proper planning at the PHC level leading to performance of tubectomy
operations without anaesthesia Extremely inhuman and callous attitude of the
Doctors during Tubectomy camps.
Consequences:
Extreme physical pain, mental agony and humiliation to women undergoing
sterilisation at camps.
7. Place: Rural Hospital Osmanabad, Marathwada region, Maharashtra
Mrs. Kusum Mali was taken to the Osmanabad civil hospital with complaint of high
fever, numbness in the extremities, anorexia etc. She was diagnosed as having typhoid
(without laboratory test) and accordingly treatment was started. However since her
condition deteriorated, she was taken to a private hospital where she was diagnosed to
have not typhoid but much more serious illness, G.B. Syndrome. Since her family
could not afford to treat her in the private hospital, she was again shifted to the Civil
Hospital. In the mean while her condition deteriorated further and she had acute
respiratory problems. She was in urgent need of a respirator, which was not available
in this Civil hospital, furthermore it was not even available in the main hospital in
neighbouring district, Solapur Civil Hospital. Hence relatives of the patient had to rent
because the operation was not successful. Thus in addition to the financial burden, is
the added emotional strife of a new disability. A woman who injured her hand was
made to wait more than a week before being admitted for an operation, her husband
had to borrow a large sum of money to pay for this operation, which in the end, was
not effective. The woman now also has to deal with the physical and emotional
burden of having an amputated arm, while the family has to struggle with a major
financial loss and debt.
Type of denial:
Operative treatment was significantly delayed, forced to pay large sums of money in a
Government hospital.
Consequences:
Irreversible disability, severe financial loss.
10. Place: Civil Hospital, Parbhani, Marathwada region, Maharashtra
In the Civil hospital, Parbhani, a 16 years old girl was admitted with 15% bums on
25th November. On 14th December nobody was present in that ward, taking advantage
of the situation a ward boy tried to sexually assault the patient. The girl narrated this
incident to her mother who works as a domestic worker. Her mother lodged an FIR in
the police station. What happened next was unexpected and extremely inhuman.
According to reports, shortly later, die same ward boy raped this girl in the hospital.
Her mother wait to the police station again to lodge a new complaint The Police
demanded a medical report of the patient, to be given from same hospital, as a
condition to lodge the FIR. The Hospital refused to provide this report, hence FIR
could not be lodged. Despite the fact that the bums were not major in nature, the girl
died after 15 days. This matter needs to be investigated thoroughly and necessary
action needs to be taken.
Type of denial:
Gross Human Rights violation in the campus of the civil hospital.
Consequences;
Extreme violation of dignity, girl died after 15 days.
Draft Report
Public hearing on availability of basic health services
in Thane District, Maharashtra
Vulnerable and marginalized groups in societies tend to bear an undue pronortion of health .
problems. Overt or implicit discrimination violates a fundamental human rights princirie that often
lies at the root of poor health status. In practice, discrimination can manifest itseit in Inadequately
targeted health programmes and restricted access to health services.'
- WHO. 2002
Background
Health has been universally acknowledged as a basic human right, and health care has
been recognised as an essential public good that is required for the full realisation of the
Right to life and other basic human rights. India, as a signatory' to the UN Declaration of
Human Rights (1948), the International Covenant on Economic. Social and Cultural Rights
(1966) and the Alma Ata ‘Health for All" declaration (1978) has explicitly recognised the
right to health. Interpreting sections of the Indian Constitution, such as Article 47 of the
Directive Principles and Article 21 of the Fundamental Rights, various Supreme Court and
High Court judgements have further outlined the duty of the state to provide essential health
care, and have specified correlative health rights of citizens.
However, access to quality' health care remains elusive for a large proportion of the
Indian population, especially the Adivasis. Adivasi people today face an onerous triple
burden of unhealthy factors. The first is increased susceptibility to ill health in the context of
poverty, because of denial of access to traditional resources, displacement, and erosion of
sustainable livelihoods and lifestyles. The second is poor physical access to health services,
and limited provision of health services in adivasi areas. And the third is the discriminatory
attitude of health care providers and administrators, which constitutes a serious human rights
violation and effectively completes the circle of denial, depriving adivasis of their right to
health.
In this situation, organisations that have emerged from adivasi struggles for identity
and survival have begun to question this serious denial, and have started raising the issue of
their right to health and health care. Some such organisations, like Kashtakari Sanghatna in
Thane district of Maharashtra, have been involved in developing people's health initiatives.
w hile also demanding accountability of public health services in a Rights-based framework.
Meanwhile, in September 2003 the Jan Swasthya Abhiyan (Peoples Health Campaign), a
national level platform of health related networks and organisations, working on the issue of
Health rights and strengthening of public health systems, organized a National level
workshop presided by Justice Anand, former Chief Justice of the Supreme Court and
Chairman of the National Human Rights Commission on the Denial of Health Care.
Subsequently, District level Public Hearings on Denial of Health Care were planned. It is in
this context that a coalition of peoples’ organisations. Shoshit Jan Andolan. organised a
public hearing on health rights in Mokhada town of Thane district on 9th January 2004. This
report attempts to bring out the main issues raised during the public hearing, to facilitate
further advocacy and action.
Framework of the Public Hearing
The organisers of the public hearing held on 9lh January 2004 in Mokhada were
Shoshit Jan Andolan (SJA, Movement of oppressed people), a coalition of peoples'
organisations involved in organising the adivasi and rural poor population on various
livelihood issues, particularly in Thane and Raigad districts of Maharashtra. The hearing was
hosted by Kashtakad-Singhntana. a people's organisation which is one of the constituents of
SJA. and has been working with toiling adivasi people in the northern pan of Thane District
since the last 25 years. Representatives of the Sanghatna collected information about health
facilities and cases of denial of health care from Dahanu, Jawhar.Vikramgad and Mokhada
talukas. The peoples' organisations Shramik Mukti Sanghatana (Murbad and Shahapur
talukas) and Eklavva Kashtakari Sanghatana (Shahapur taluka) also actively participated in
collecting information from their talukas and in mobilising people for the public hearing.
Public health officials who were present as respondents on behalf of the Maharashtra
health department included Dr. T.M. Suryavanshi (Additional District Health Officer. Thane
Dist.) and Dr. Sabde (Medical superintendent Jawhar Cottage hospital. Taluka Jawahar and
Mokhada Rural Hospital. Taluka Mokhada) along with other medical officers.
Panelists for the public hearing included Justice B.G. Kolse Patil (Retd. Judge.
Mumbai High Court), Dr. Kamakshi Bhate (Asst. Professor, G.S. Medical College. Mumbai)
and Dr. Chhaya Datar (Head, Women’s Studies Unit, Tata Institute of Social Sciences.
Mumbai).
Health related technical inputs for the public hearing, including analysis of the survey
information, were given by CEHAT. a health sector organisation. Dr. Nilangi Nanai
represented the Jan Swasthya Abhiyan
The programme of the hearing consisted of:
► Presentation of issues by people's representatives (including survey findings and cases
of denial of health care)
> Response by Health officials
► Discussion on key issues and opinions by panelists
Issues presented by people's representatives
Representatives of Shoshit Jan Andolan presented the findings of the survey of six
PHCs and one Rural Hospital in Thane district, exemplifying the deficiencies in these
facilities (summary given below). Cases of denial of health care were also presented, where
individuals gave testimony of how they had been denied essential services from specific
public health facilities (some examples given below). These were the context in which health
officials were invited to respond and clarify as to how relevant improvements would be
made.
Summary findings of survey of public health facilities
A total of seven Primary health centers (PHCs) and one Rural hospital were surveyed as
ground preparation for the public hearing. Information about the infrastrucural facilities.
staffing position and availability of various services such as Reproductive and child health
services, laboratory services, emergency services etc. was collected during this survey.
Similarly specific cases where health care was denied and the denial of health care had led to
serious consequences were collected. Protocols developed by CEHAT were utilised for data
collection, and interviews with village representatives along with site visits to the health
facilities and interviews with health care providers were employed to collect the information.
The seven PHCs from which the data was collected were from Vikramgad (Vikramgad
PHC). Dahanu (Saiwan PHC. Dhundalwadi PHC) Mokhada AVashele PHC. Aase PHC).
Jawhar (Nandgaon PHC) and Shahapur (Vashind PHC) talukas of Thane District. Ke}
findings related to the various health facilities surveyed are as follows:
Issues related to coverage and infrastructure:
•
In tribal areas, there should be one PHC catering to a population of 20.000 people.
But in the present survey, it was seen that out of 7 PHCs. 5 ’.'.ere providing services to
a much larger population than stipulated, between 30.000 and 40.000 people. This
overburdening was found to be affecting the quality of the services provided.
•
In all of the PHCs, the ambulance was not regularly functional. An ambulance in
working condition was present only in the RH. which was given to the patients at the
rate of Rs. 5 per kilometer, not affordable to man} impoverished families. In some
places, patients had to even hire private vehicles to transport seriously ill patients.
The condition of the operation theatres was similar, with most of the PHCs being
without regularly functioning minor OTs. In one of the Rural hospitals, the staff even
reported that the operation theatre was not in use because the culture swab had been
found positive for presence of micro organisms.
•
*
The level of hygiene was found to be grossly deficient in most of the PHCs.
■
In most of the PHCs, indoor facility to admit six patients at any time was not full}
functional.
No toilet facility for patients was found to be existent in most of the PHCs.
■
Issues related to the number and availability of staff:
•
In some PHCs. there was only one Medical Officer. Thus he / she could not regularly
visit the Subcentres in the PHC area as required. Even the other PHC staff such as
ANMs and MPWs was found to be not visiting the remote hamlets regularly.
■
The staffing situation of the only Rural hospital which was surveyed, was reported to
be grossly deficient. There was no separate resident doctor for the Rural Hospital. It
was understaffed with only 3 people working there, most of them not resident there.
Most of the patients approaching the hospital were referred to other Government
facilities.
•
Since there were no adequate residential facilities for the staff, in most of the PHCs
the staff never stayed at the PHC campus.
Issues related to discrimination against Adivasi patients:
•
A large number of people surveyed reported that certain of the PHC staff had a
callous attitude towards tribal patients. The doctors often asked the nurses or the
peons to examine the patients. In one PHC, certain staff including the doctor was
often found under influence of alcohol during duty hours. In another PHC, the doctor
was found to be playing cards, and in a third PHC playing cricket, during duty hours.
■
Women complained of abusive language and ill treatment at the time of delivery.
Some PHC staff demanded 100 to 150 rupees for conducting the delivery.
Issues related to the provision of essential services at the PHC:
•
In most of the PHCs, delivery services were not available around the clock.
■
Since there were no women doctors in any of the PHCs. the treatment for women's
reproductive health problems was not available in these faci’ities. deny ing women
one of the basic services under the Reproductive and Child Health . RCH) programme;
•
In none of the PHCs was the facility to test haemoglobin levels to confirm anaemia
available.
In none of the PHCs was the facility for safe MTP (abortions) available.
■
•
Important services such as operations for cataract (under National Blindness control
programme) and Male / Female sterilisation operations were not being carried out in
any of the PHCs.
Issues related to the availability’ of the medicines and supplies:
•
In none of the PHCs, all medicines were being given free to the patients.
■
The PHC staff reported in some PHCs that they have adequate stock of medicines.
But in reality almost in all the PHC areas the villagers reported that they had to buy
many of the medicines from outside. In one of the PHCs, even basic medications like
ORSpackets had to be purchasedfrom medical stores.
Though Government officials claimed to have enough stocks of iron and Folic acid
tablets, in none of the PHCs, they were being regularly given to the non-pregnant
women.
Patients were asked to buy basic supplies like needles and antiseptic lotion etc. from
outside private medical stores.
■
•
Cases of Denial of Health Care
During the public hearing, thirteen cases were presented to the Panelists. These cases
are representative in nature. Out of these, the denial of health care was serious enough to
have been associated with the death of six patients. The cases of denial of health care are
summarised below:
Case 1
Tokavda PHC, Taluka Murbad, Dist. Thane
Soni Shiva Wagh, age 45 years, was suffering from low' grade fever and weakness for
3-4 months so she went to the Tokavde PHC for treatment. She was given some medicine but
did not feel any better so she went to a private doctor who diagnosed her as having T.B. He
then directed her to go back to the PHC as she could not afford to buy the expensive drugs
required for her treatment. She told the PHC doctor that she had been diagnosed for T.B. and
requested him to give her the medicine. The PHC doctor got irritated with her and gave her
medicine for Malaria. She then went to the Cottage Hospital in Murbad and told the doctor
that she had been diagnosed for T.B. Since the X-ray machine was not functional she was
asked to get a chest X-ray done in a private X-ray centre. She was then asked to return to the
hospital after four days for the blood and sputum examination, however the technician was
not available. On the fourth day when she went back to the hospital the technician was still
unavailable. She was asked to return to the hospital on three consecutive days for the tests
which were ultimately never done. After having spent a small fortune and considerable time
and energy on travelling to the Rural Hospital in the taluka place, the patient gave up hope for
treatment in a government hospital.
Basic investigations for diagnosis of Tuberculosis, expected under the National TB
Control Programme, could not be given by a taluka level Cottage Hospital.
Case 2
Tokavda PHC, Taluka Murbad, Dist. Thane
A girl aged 12 years was bitten by a scorpion on her finger. She was rushed to
Tokavda PHC but without giving her any treatment she was referred to Rural Hospital
Murbad. There she was not treated but referred to the Civil Hospital in Ulhasnagar. Even in
Ulhasnagar they refused to admit her, and referred her to Sion Hospital where the patient
died. The family then had to spend an additional Rs. 2500 to bring the dead body back to
their village as they were refused a hearse.
Neither the PHC. nor the Rural Hospital, nor the Civil Hospital could treat a case of
scorpion bile, with fatal consequences.
Case 3
Tokavda PHC, Taluka Murbad, Dist. Thane
Gurunath Madhukar Bangara, age 2 years, r/o Bangarwadi, Village Karponde. was
suffering from diarrohea and vomiting so he was taken to the Tokavda PHC by his mother on
the morning of December 25, 2003. The doctor did not examine the child and gave a packet
of ORS. A couple of hours later the mother informed the doctor that the child was running
temperature. The doctor did not examine the child but wrote out a prescription for medicine.
injection and disposable syringe, all to be purchased from outside. The child was
administered the medicines purchased from the private medical store and sent home. The next
day the mother returned with the child and she was once again asked to purchase medicines
from outside. On the third day the mother did not return with the child as she had no more
money to purchase medicines.
Adequate treatment for diarrhoea, one the simplest and commonest illnesses, could
not be given by the PHC.
Case 4
Saralgaon PHC, Taluka Murbad, Dist Thane
Narayan Ghude, age 40 years, suffered a snake bite in the very early morning of
1/8/03. He was rushed to the Saralgaon PHC where he was not given anti-snake venom and
rather was sent to the R.H. in Murbad. Two hours later he died. Later the doctor of Saralgaon
PHC threatened the relatives that if they try to make a complaint they will be sued for
defamation.
The PHC failed to treat a case of snakebite, leading to considerable delay and fatal
consequences.
Case 5
Vikramgad PHC cum R.H., Taluka Vikramgad, Dist. Thane
Santaram Laxman Malkari, age 8 months and Sagar Lahu Kunwra, age 1.5 years, both
r/o Village Khuded, Taluka Vikramgad, were suffering from diarrohea and vomiting and
were taken to the Vikramgad R.H..as it is nearest to their village on 7/11/03. The doctor on
duty examined them and prescribed ORS packet to be bought from the medical store. The
parents of the children were accompanied by a local activist, who confronted the doctor when
he save them a prescription ter ORS, rather than supplying this from the PHC. They then
took the children to the Cottage Hospital in Jawhar where they were given treatment.
Essential supplies such as ORS. to be given under the Diarrheal Diseases Control
Programme. have to be purchased by the adivasi patients.
Case 6
Kasa PHC cum R.H., Taluka Dahanu, Dist. Thane
Sevanti Shankar Baswat. age 45 years, r/o Chinch Pada. Pawan. taluka Dahanu had patches
on her body and a sore on her leg. She went to the Kasa R.H. for treatment for leprosy. She
was admitted for one night, illegally charged Rs. 25 and asked to go home the next morning.
She was told she could not be given any treatment as her name was not registered under the
leprosy programme. Even her repeated requests to dress her w ound w ent unheeded.
The Rural Hospital denied essential care to a leprosy patient, to which she was
entitled under the National Leprosy Control Programme.
Case 7
Kasa PHC cum R.H., Taluka Dahanu, Dist. Thane
Javram Balu Rawtya, age 62 years, r/o Chari- Pawan, taluka Dahanu. was suffering from
continuous cough and breathlessness so he approached the Multi Purpose Worker (MPW) of
his village working through Kasa PHC for help. The MPW did not give him any assistance so
he came to the Cottage Hospital in Dahanu where an X-ray was taken, they examined his
blood and sputum and directed him to go to the Kasa PHC to get his treatment for T.B. under
the DOTS programme. He was told that the MPW would come to his house and give him his
tablets daily, which he was supposed to consume in the presence of the MPW. After a few'
days the MPW went on leave for 15 days and the treatment stopped. The patient went to the
MPW’s house to ask for the tablets but he refused to give them to him and said that he would
personally administer them to him at his house. After repeated requests to the MPW, the
patient complained to the doctor about the abrupt stoppage of his treatment. The MPW made
only one visit, gave him tablets for a few days after which the treatment was stopped
completely.
Regular treatment for a case of tuberculosis, the core activity of the National TB
Control Programme, was denied despite his taking repeated initiative to obtain treatment and
the patient being enrolled under the much-publicised 'DOTS' programme.
Case 8
Khodala PHC, Taluka Mokhada, Dist. Thane.
In the month of October 2003. Dadu Chander Vad of Village Kurlod accompanied a small
boy of his village suffering from diarrhoea and vomiting to Pethechapada, a hamlet of the
same village where the doctor of Khodala PHC was supposed to be stationed as part of a
"Rescue Unit" under the Nav Sanjeevani Yojana. The doctor was unavailable. Dadu found
that there were four to five other patients also suTfering from diarrhoea and vomiting, so he
rushed to Mokhada to inform the authorities. By the time he reached the taluka place from his
remote village it was lunch time, the BDO therefore asked him to contact him after lunch. He
then w'ent to the Resident Tehsildar (RNT) who asked him for a written application. The RNT
then went to the Panchayat Samiti Office personally along with Dadu but no one except the
peon was available. The RNT tried calling the Khodala PHC but the phone kept ringing, with
no response. He called the Jawhar hospital but they did not assure any action. Finally, the
RNT asked Dadu to wait for the BDO. Dadu took initiative and went to an STD booth, and
directly phoned the CEO of Thane district. The CEO then instructed the staff in Jawhar
Cottage Hospital to go to the village. Ultimate!} by the time help reached the village. one
woman had died. Another child from the same village who was taken to the Nandgaon PHC
for treatment earlier was prematurely discharged by the doctor and died in the village the
same night.
While an epidemic of gastroenteritis had erupted in a village, the nearbv Rescue
unitsupposed to deal with such emergencies, was nonfunctional. The concerned PHC did
not respond to telephone calls, and the Cottage hospital of the taluka also failed to take
effective action, until an ordinary’ villager contacted the CEO of the district and managed to
activate the government machinery. Meanwhile, two persons lost their lives due to the
unresponsiveness ofthe health system.
Case 9
Khodala PHC, Taluka Mokhada, Dist. Thane.
Navsu Sajan Rathad, age 65 years, r/o Village Kurlod, taluka Mokhada had diarrohea.
On June 7, 2003 after four to five bouts of loose motions he got dizz>. broke into a cold
sweat and became semi-conscious. His wife and some other villagers carried him to the
Khodala PHC and the wife went to look out for the lady doctor. It was about 5.00 p.m. The
w’ife met the doctor and told her about her husband's condition. The doctor got ven irritated
and told the woman that her duty hours were over and she was about to go home. She then
asked her to move the patient to Mokhada Rural hospital and left the premises. The woman
then went to the residences of the three resident nurses and begged them to treat her husband.
The}- refused saying that they w’ere not on duty and the nurse on night duty w'ould attend to
him. The nurse on night duty never turned up so once again she went to the houses of the
resident nurses. Finally one nurse Ms. Zule took pity and came to the PHC. She gave the
patient an injection and administered a bottle of saline. The nurse told them the} could not
stay in the PHC as there was nobody to attend to them, and she could not stay any longer.
Finally the patient was taken to a private doctor, one Dr. Kadav in Khodala. He administered
another bottle of saline and asked them to go home and return the next day as there was no
facility to admit him. The patient spent a total of Rs. 300 for treatment with the private
doctor.
A patient with diarrhoea, requiring rehydration could not get admission in a PHC.
The doctor, supposed to be on call around the clock, refused to attend to the patient and no
nurse was available to attend to an admitted patient, forcing the relatives to pay for the
expensive services ofa private doctor.
Case 10
Mokhada Rural Hospital, Taluka Mokhada, Dist. Thane
Mahadu Jivlya Wagh, age 44 years, r/o Village Neelmati, Chinchutara. Taluka
Mokhada. fell from a tree on 15/11/03. He was brought to the Mokhada Rural hospital
immediately. The doctor admitted him and asked the relatives of the patient to purchase two
bottles of saline which were administered to him. They then asked them to shift the patient to
Nashik Civil Hospital and informed them to hire a private vehicle as no ambulance was
available. The next day the patient was taken to Nashik Civil hospital where he was admitted.
The doctors there advised the relatives to take him to a private hospital for a C.T. scan as the
equipment in the Civil hospital was out of order. The relatives could not afford a C.T. scan so
the patient was discharged after fourteen days and has now' become crippled due to lack of
proper treatment.
A taluka level Rural Hospital did not have intravenous fluids to be given to a patient
with a fracture. No ambulance was available to transport such a needy patient. The Civil
Hospital in a large city like Nashik could not provide the CT scan facility, resulting in a
person becoming perhaps permanently disabled due to denial ofhealth care.
Case 11
Nandgaon PHC, Taluka Jawhar, Dist. Thane.
Vimal Yeshwant Zugre. age 25, r/o Thakur Pada, Nandgaon. taluka Jawhar had three
fingers crushed while she was pounding rice with a pestle and mortar on 5/11/03 at about
8.30 p.m. Her husband rushed her to the PHC in the same village. The Multi Purpose Worker
of Bhuritek who resides in the PHC premises was present. A number of villagers gathered
around the PHC. They requested the MPW to open the PHC and give some first aid but he
refused. The angry villagers threatened to break the lock, following which he opened the
PHC. The villagers then located an ANM attached to the PHC and asked her for help. She too
did not administer the dressing, and asked a peon of the PHC to do the dressing. The patient
was advised to go to Jawhar or Mokhada hospital. The villagers begged for the vehicle, as
there was no other means to transport the patient. The vehicle was refused. Finally the MPW
dropped the patient back to her house in the PHC vehicle. The next day the patient was taken
to Jawhar Cottage Hospital where her fingers were sutured. She was asked to return after a
few days to remove the stitches. She has gone to the hospital on three occasions, but the
stitches have not been removed. The patient is still unable to use her fingers.
No doctor was available at a PHC to attend to an injured patient. Neither the MPW
nor the ANM obliged to apply a dressing, which was finally done by the peon. Despite a
vehicle being available to transport the patient, it was refused.
Case 12
Jawhar Cottage Hospital, taluka Jawhar, Dist. Thane.
Ujwalla Pandu Vad, age 12 years, r/o Village Alivmal, taluka Jawhar went to school
on 27/11/03 as usual, after an early lunch at about 10.00 a.m. She vomited three times in
school and then came home. She continued vomiting a number of times. At about 7.00 p.m.
when her parents returned from work they rushed her to the Jawhar Cottage Hospital. She
was admitted in the hospital, given one injection and some tablets but she continued
vomiting. Her father requested the nurse on duty to attend to her but she did not pay any heed
instead she scolded the parents, saying that the girl was dirtying the hospital. The parents
were asked to give her glucose water orally which they administered the whole night. The
child could not sleep, she had high fever and she was crying incessantly, however no medical
staff came to see her despite several requests. At about 6.00 a.m. the child's stomach began to
become distended. Even then no medical staff on duty attended the patient. At 11.00 the
doctor came on his routine round, examined her pulse and moved on. The parents requested
the doctor to give the child intravenous saline, since she was not able to swallow the glucose
water but he did not pay any heed. At about 12 noon the child became unconscious. The
father rushed to Dr. Marad and informed him. The doctor asked him to bring the patient to his
chamber. By the time they brought the patient to the chamber, she had expired. The doctors
then put tubes through her nose and mouth but it was of no use. They then insisted on doing a
post mortem to which the relatives took objection, saying what is the use of diagnosing her
illness after she is dead. They took the body of the child home without a post mortem
examination.
While in the Cottage hospital, the child was in severe distress for over 12 hours, but
was not given adequate attention required to diagnose or treat the underlying problem. The
child died, and adequate medical attention not being given in time was a likely contributory
cause.
Case 13
Washele PHC, Taluka Mokhada and Nandgaon PHC, Taluka Jawhar. Dist. Thane
A one-year old girl, daughter of Kashinath Bhovar. r/o Dhamanshet Pendkvachaw adi.
Taluka Mokhada. who had rapid breathing and swollen eyes was taken about 6 kins, away
to PHC Washale. taluka Mokhada for treatment in the morning. The medical officer was not
present. In the afternoon, the peon gave the father of the patient some eye applicabs for
application. The father of the patient waited till the evening, but as the medical officer
remained absent the patient was taken back to her village. The next day the patient was taken
to another PHC another 6-7 kms. away at Nandgaon. where despite the severity of the
illness, the child w'as treated but not admitted, apparently due to non-availabiiity of admission
facilities. The parents were however instructed by the Medical officer to keep the child in a
neighbouring house to continue the treatment there. The next day the Medical officer left
Nandgaon. leaving the PHC without any Medical officer. The child died the next morning.
denied of adequate medical attention.
.Vo doctor was available at the first PHC to treat a child patient suffering with
pneumonia. At the second PHC the patient was denied admission despite the severity of the
case. Here the doctor subsequently left the premises leaving the patient without any medical
attention, followed by her death.
In summary, the denial of health care brought forth in the various cases presented was
mainly of following types:
•
Non-availability of doctor at PHC to treat patients
•
*
Denial of admission of serious patients in PHC
Non-functioning of "Rescue Unit” when gastroenteritis epidemic spreads, non
response of taluka medical staff
*
■
Non-availability' of essential supplies like ORS at PHC
Non-availability' of essential life-saving drugs like Antidote to snake and scorpion
venom at PHC, Rural Hospital and Civil Hospital.
Non-diagnosis of diseases like tuberculosis and denial of, or irregular treatment under
National Tuberculosis Control Programme and National Leprosy Control Programme
■
■
Referring the patient to higher facility' (Rural hospital) even for elementary services
such as suturing of an ordinary wound
•
Non-availability of child health services.
■
•
■
Failure of nursing staff to dress a wound
Refusal of ambulance facilities to transfer patients
Significant delay in treatment forcing patient to access private medical facility'
■
Medical negligence by Doctor on duty
Note on unavailability of water in Mokhada hospital
On 5th, 6th and 7th January, 2004 there was not a drop of water available for
the patients of Mokhada hospital for drinking and washing. The residential staff on the
premises managed to procure water in a bullock cart for their personal use. but relatives of
the patients had to trudge more than a kilometre to the market place with plastic bottles and
request for water for the patients, from the local teashops. When an activist of the Kashtakari
Sanghatna went to the hospital and asked the doctors to submit a written complaint to the
tehsildar. and arrange for a tanker, the doctors refused to do so saying they had to get the
permission of the Medical Superintendent. Since the Medical Superintendent Dr. Sabde. is
holding the charge of two hospitals in two separate talukas. Jawhar and Mokhada. he could
not be contacted. This matter was also raised during the Jan Sunwai. since the Mokhada
Rural Hospital is often without water, being on a hill and having no independent water
source. Lack of water for drinking or other basic needs is a major obstacle to be overcome by
patients.
Summary of responses by officials, discussion on key issues and
opinions by panelists
Response by Health officials
The ADHO, Thane and the Medical Superintendent, Jawhar Cottage Hospital
responded to some of the issues that were raised. The ADHO, Thane opined that the cases
and issues raised were not serious in nature. However, he and the Medical Superintendent
admitted that many of the issues were structural in nature, and were related to policy level
deficiencies, such as lack of adequate buildings, intermittent water supply, insufficient
humanpower lack of vehicles, and lack of doctors. They also pointed out that the provisions
for diesel for the vehicle to transport patients is inadequate, and the rates need to be revised.
Similarly, they conceded that treatment for anaemia is focussed on pregnant women. They
claimed that only deserving patients are referred to higher facilities, and that records are
maintained in the various centres, to prove the same. The M.S. also claimed that medical
supplies were adequately available, and that immunization programmes were being well
implemented.
However, despite the obvious deficiencies in various health centres and the denial of
patient care that had been presented, there was no categorical assurance of improvements,
and many of the specific issues pointed out were not addressed. This led to some further
discussion followed by opinions being given by the panelists.
Discussion on key issues and opinions by public and panelists
Brian Lobo, Convenor, S.J.A. - Strongly objected to the statement by ADHO that the issues
raised were not serious It is improper to pass the entire buck for non-performance on to the
higher authorities. While conceding that some matters needed to be handled at the higher
levels, many issues raised can be remedied at the local level by the District level officials eg.
such as insulting behaviour towards patients, abdication of duty and callousness of medical
officers and other staff, cleanliness in health centre premises and siphoning off of essential
services and drugs. The officials have not stated as to what action they will take against
erring medical staff. Suggested that a meeting with the Andolan representatives be called by
DHO to discuss all relevant issues raised.
Dr. Kamakshi Bhate, Panelist - Are medical officers trained in dealing with shortages of
essential supplies like snake-bite antidotes?
Response of ADHO - No training received, forced to learn on the job.
Dr. Kamakshi Bhate, Panelist - Illtreatment and derogatory behaviour towards adivasi
patients by medical staff must be stopped.
Response of ADHO - It is more a case of non-communication because health staff are not
familiar with the local language, training is being evolved for the same. As far as behaviour
is concerned, it is an individual matter.
Dr. Chhaya Datar, Panelist - People prefer to approach private doctors, this points to
inadequacies in the public health system.
Response of M.S. Jawhar Cottage Hospital - We have less doctors and many more
patients, hence are unable to give adequate attention to individual patients. It is not always
possible to state what action will be taken against errant staff, some things are best left
unsaid.
Dr. Dravid
- Private medical practitioner visiting from Pune - Considering the status
of the Public Health facilities . if 1 were to set up private practice in Mokhada I would have a
prosperous future as everyone w ill flock to me. I have also worked in the government set-up.
Private doctors are accountable to their patients since non-delivery of services results in fail
in patients. However government doctors are not accountable or concerned about drop in
patients. Medicine is not a depersonalized profession devoid of ethics and attitudes.
Justice B.G. Kolse Patil - The economy is being influenced by World Bank, hence the
interests of the poor are being ignored. One should not expect too much from this health
system. It is therefore necessary' to revitalize traditional health practices and systems.
However, the state of the public health system is absolutely deplorable. The report and the
case studies presented exemplify' this. He strongly condemned the insensitive and inhuman
treatment meted out to adivasi patients. He urged the people to organise themselves and
demand services, and if necessary to resort to gheraoing of doctors and even elected
representatives if they fail to deliver the goods. He also suggested to the ADHO that a
meeting with the Andolan representatives should be immediately called by the DHO to
discuss all relevant issues raised.
Conclusions and Recommendations
A. Coverage and infrastructure
1.
Increase in number and upgradation of PHCs to conform to population and six-bed
norms.
2. Upgradation of all newly commissioned Rural Hospitals eg. Vikramgad RH.
3.
Construction of commissioned PHCs eg. Aase (Mokhada taluka), and sub-centres.
4.
5.
All non-functional essential facilities and equipment at PHCs and Rural Hospitals to
be made operational eg. minor OTs in PHCs, X-Ray machine at Mokhada Rural
Hospital.
Strict implementation of sanitation norms at all medical centres
Immediate provision of water facilities at all PHCs and Mokhada RH.
Construction of toilet facilities in every PHC.
Regular cleaning of premises of PHC and other medical centres.
B. Staffing pattern and facilities for staff
1. Filling up of all vacancies in all medical centres, especially vacant doctors’ posts.
2.
Provision of staff to newly commissioned Rural Hospitals eg. Vikramgad.
3.
Appointment of woman medical officers in every PHC or weekly visits bv
gynaecologist.
4.
Provision of adequate housing facilities at PHCs and sub-centres for staff.
5.
6.
Regular visits as per Advance Tour Programme by ANMs and MPWs to villases.
Regular weekly doctors' clinics at all sub-centres.
1.
2.
Provision of 24 hour delivery services at every PHC.
Provision of facilities to perform safe MTPs in every PHC.
3.
4.
Proper diagnosis and regular treatment of cases under the National Programmes.
Inquiry into alleged siphoning off of drugs from PHCs. RHs etc.
5.
Re-imbursement to patients for expenses incurred on essential drugs and other
items that are to be available at medical centres as per norms.
Provision of iron tablets to non-pregnant anaemic women patients.
24 hour availability of free Ambulance with driver at every' medical centre.
Changes in OPD timings to suit local needs eg. 9 a.m.to 3 p.m. in Mokhada RH.
Sterilisation of all equipment used wherever not done eg. Nandgaon PHC.
6.
7.
S.
9.
D.
Monitoring of services
1. Immediate inquiry into and strict action against all staff against whom complaints
of
callousness, discrimination against adivasi patients, abdication of duty.
demanding of monetary payments etc. are lodged.
2. Institution of Calendar Public Register Programme in all villages to ensure regular
visits by all PHC staff.
3. Regular (quarterly) PHC level. Rural Hospital and District level meetings between
village and peoples' organisations’ representatives and health staff.
• •<7;
' ■'t'
MOHAN FOUNDATION
Liver Patient Support Group
Date: I July 2004
To,
The Panelists.
NiHRC. Public Hearing
Sub: Covering letter and background of the petitioner.
Dear Sir or Madam:
I am a 37-vear-old woman suffering from end stage liver failure disease and
waiting for cadaver liver transplantation for last 5 months. One year before, 1
came to know that the only solution, which could give me an extra lease of
life, is cadaver liver transplantation. In my own interest and in the interest of
other end stage organ failure patients in the same situation, 1 started working
as a volunteer of MOHAN (Multi Organ Harvesting Aid Network)
Foundation in Pune.
For the last one year, we as a group are interacting with relevant government
officials and concerned doctors and thereby experiencing the various hurdles
in the process of cadaver organ donation. Fortunately, we could make
significant contribution towards one successful multiorgan cadaver donation
in Pune where the liver was shared with one of the hospitals in Andhra
Pradesh for a very critical patient. There, were also a few unsuccessful
attempts.
Our efforts have given us a good insight in to the various problems in this
field. The practical experiences gained in the fieldwork prompt us to make
this petition. It is a great opportunity for us to present this petition to you
where we have mentioned all the issues and proposed legal and structural
policy changes.
Looking forward to interact with you.
Thank you,
Yours truly,
Naxlah^ ^an^dhere
Member-in-charge
Enclosure: Petition document with annexure (2+1=3 pages), News paoer article
Liver Patient Support Group. MOHAN Foundation
Z-901. Le-Mirage. 16 Boat Club Road. Pune 4! 1001; Ph: 020-26129454. 020-33302775
nndhamdhere a hounail.com
MOHAN I Ql NDATION
*
Liver Patient Support Group
Date: July 1. 2004
PETITION
(Document to be forwarded to the NHRC, 3 pages)
Across the country, there are thousands of end stage organ (kidney, liver, heart lung,
pancreas) failure patients. Many of them are waiting for organs for transpiantaccn. Every
year, hundreds of them die due to unavailability of organs on time. The most ethical way
of getting the organs for them is by cadaver organ donation (donation of vital organs of a
brain dead person).
Majority of these end stage organ failure patients suffer from denial of their rignt to get
the cadaver organs on time and do not receive mandated help in this regarc mom the
medical fraternity and concerned government health officials, mainly due to the egal and
structural deficiencies. The issues are listed down as follows.
Brain deaths are often not diagnosed or diagnosed late by the locai teams of
treating doctors (neurologists, neurosurgeons, critical care doctors and
intensivists).
2. The families of brain dead persons are not informed immediately after the
occurrence of brain death. In most of the cases they are not counseled about
brain death and also are not given a chance to select the option of donating
the vital organs of their cadaver before terminating the ventilator.
3. Majority of the hospitals either do not have infrastructure for brain ceath and
organ donation counseling or often the counselors are not well trained.
Hospital managements and social work departments are often reluctant to
allow volunteers of NGOs to enter in to the brain death situations for
counseling and other coordination work. They are kept away by maintaining
unnecessary secrecy.
4. The law allows only the hospitals, which are registered transplant centers to
retrieve cadaver organs. These are very few in number and whilst there are
hospitals, which do not have their own transplant programs but nevertheless
fulfill the basic requirements for organ retrieval and are willing to support the
cadaver organ donation program. The cadaver organ donation program
needs the support of these hospitals, as there is a large scarcity of cadaver
organs. The alternative option of moving the brain dead cadaver on ventilator
to a registered retrieval center, is in practice very difficult, adds to the distress
of the donor family and there is a further risk of loosing the cadaver and
thereby the invaluable cadaver organs.
5. The hospitals that are recognized and registered as transplant centers show
interest in counseling for and retrieval of only the organs in whicn they are
interested. They do not care to counsel for other organs (muttiongan) as they
do not think of sharing the other organs with others hospitals, cities or states.
It is an extremely selfish and irresponsible approach, as the cadaver organs
wasted are lives lost
6. The end stage organ failure patients are counting down their lives minute-byminute, hour-by-hour and day-by-day. At the same time the relevant medical
fraternity and the relevant government departments do not understand the
importance of time to take the policy decisions. They delay the process by
pointing out to the lacunae in the laws, rules and regulations that are often
misinterpreted.
1.
Liver l'i:i:e-:: Support Group. MOUAS routidulion
Z-‘.>oi. Lc-Mintgi. !«» Ro:i'» mb Rond Piute 41 ItX'l: Ph.
iincihiinidiure.. Amun:! e
• Po.r:i .;
■
MOHAN FOUNDATION
2
Liver Patient Support Group
In reality, cadaver organ donation program is the only way to overcome malpractices like
organ trade and scandals in the field of organ transplantation. There are many coctors
and hospital managements who in principle agree with tne cadaver organ donation
program and wish to support it in earnest. But are reticent to do so for want of acequate
legislative enactments (support) as they fear allegations of maloractice from the oublic.
other hospitals and media.
We pray and plead that the following changes be made in law and policies.
Diagnosis and first brain death declaration on time should be made
mandatory for the local team of doctors. Likewise it must also be mandatory
for the government authorized committee to be available round the cock on
call to' visit the donor hospital and certify brain death (Second brain death
declaration) on time.
sVcxA<\ W MoloWceA2. Brain death counseling should also be made mandatory thereby provicing the
family with the option of cadaver organ donation. p.e.ccvAs £VeiAA be-VtfA-.
3. The counselors should counsel for muitiorgan donation and provide correct
information about all the organs that can possibly be donated. If there is lack
of manpower or any other difficulty in counseling, Relevant NGO workers
should be allowed to assist in counseling and coordination. G
4. All those hospitals which fulfill the basic requirements for being a multiorgan
retrieval center should be registered and be given the permission to retrieve
the cadaver organs instead of expecting the cadavers to be moved to a
transplant center.
5. The transplant centers must share the organs with the other hospitals, cities
and states if they are not having their own transplant program for that
particular organs. This sharing can be achieved by networking of all organ
procuring agencies in the country.
sVjsuXA be tYviAAtrlneA6. The concerned medical fraternity and the government health officials must
become proactive and take fast decisions and prepare quick protocols for
promoting the process of cadaver organ donation. We must realize that
organs wasted are lives lost and time wasted reduces the success rates of
transplantations that are otherwise miracles in the modem medicine giving
new lease of quality life to the end stage organ failure patients.
7. Government health department and hospital managements should take
initiative in public education about cadaver organ and tissue donation and
enthuse other hospitals and doctors in their jurisdiction to support the cadaver
organ donation program.
1.
As an NGO and a patient support group dedicated towards the noble cause of
cadaver organ donation, we expect proactive actions from the NHRC regarding
these issues and look forward to the process of change in law and policies. We
request you to help end stage organ failure patients suffering from denial of right to
get the cadaver organs and the families of brain dead patients who should not be
denied the satisfaction, solace and comfort to be had from donating the organs of
their loved ones due to legal and structural deficiencies.
Nayan Dhamdhere^
Member
charge
Ln er Patient Support Group. MOHAN i:oti!iC,iti<’r.
Z-vOI. Le-Mirage. i<> Born Chib Road. Pune 41 1001: Ph. -. iJ't-Z- 12'u
nndhanidherewhorniml coin
MOHAN FOUNDATION
Liver Patient Support Group
Annexure
Why declare the brain death?
“It is agreed that permanent functional death of the brain stem constitutes the brain
death and that once this has occurred further artificial support is fruitless and should be
withdrawn. It is good medical practice to recognize when brain death has occurred and
to act accordingly, sparing relatives from the further emotional trauma of sterile hope.”
Source: Brain stem death; Information for healthcare professionals; Written and Produced by the
UK Transplant Coordinators Association
Why ask (counsel) for cadaver organ donation?
“We know from past experiences and research that the act of donation can actually help
the family. They can feel comforted through the knowledge that they have given hope to
others. Donation may be the one positive thing that can come out of an otherwise tragic
situation and the family should always be given this option.”
Source: Approaching the family; Information for healthcare professional; Written and Produced by
the UK Transplant Coordinators Association.
NOW YOU KNOW!
Transplants are modem miracles. It only happens because people care about people
and share these priceless gifts.
Source: Be a part of something good; A public service publication from - South Carolina Organ
Procurement Agency, Inc.
Required request
A policy of "required request" or required referral is operated in the United
States. Required referral is defined "that it shall be illegal, as well as
irresponsible and immoral to disconnect a ventilator from an individual
who is declared dead following brain stem testing without first making
proper enquiry as to the possibility of that individual's tissues and organs
being used for the purposes of transplantation".
The policy means opportunities for donation are less likely to be
overlooked. Many individuals may be having their right to donate removed
if their relatives are not approached. The next of kin also have a moral
and legal right to know they can donate organs and tissue if they or the
family so wish. Many families report that such a donation was helpful
rather than harmful.
Source: UK transplant website.
Liver Patient Support Group. MOHAN Foundation
Z-901. Le-Mirage. 16 Boat Club Road. Pune 411001; Ph: 020-26120454. 020-33302775
nndhamdhereShotmail.com
4
----------------------------------------- | MOONSET 0323
'—
PUNE I TUESDAY I MARCH 2, 2004 I
load I Pune-411001 I India I E-MAIL punenewsline@expressindia.com & Ieliers-pune6exprasslndia.com I Phone:26131541-6 I Fax: 26131547
She lives in their eyes, liver & kidney
I LIVERAGING HOPE I Family of 28-year-old who died of thrombosis donates her organs
EXPRESS NEWS SERVICE
through
MARCH 1
transplant.
organ
of dedicated liver'
patients from the
j
Rekha’s cadaver
Multi Organ Har
TW
EKHAr Sar- liver was retrieved
vesting Aid Net
•, | 9 dar’s I Ifttle in Pune and transwork (MOHAN)
'i? I
: daughLr/wail planted on a paswung into action
to motivate the deevery nignt,m- y^ient in Hyderabad
/ .JL.
; ing out for /heir
a rare liver exceased’s family to
Helpless, ttfeir
dppfatlon was Rekha Sardar
donate the organs,
to console the children who ^jdttoNpjrd at Ruby
Raghu Ram,
fpil to-come to terms with Hall Clinic recently. What whose son died died a while
was remarkable was the ac back, tried to convince
thetjrmotherlrdcath.
p Rekha ha) died of curacy and speed with which Rekha’s family. "I told them
painful thRilnBtixrs. But she the operation was per how my son’s eyes went to
continue/Wlie J uY^HPday formed. Even before obtain an eight-month-old Infant
— in someone’s eyes, kid ing a sanction for the trans and a four-year-old child.
neys ari(i. liver. She.gav<^ a plant from the Directorate I lis kidneys and liver were
lease of life to five people of Health Services, a group also donated."
> Wiping away his tears,
Rekha’s father R Sandanshiv says at first he did not
understand the meaning of
the term ‘brain dead’. “But
they told me that Rekha
would continue to live and
so I couldn’t refuse them.”
ffence, Rekha’s body was
shifted to Ruby Hall Clinic
and on seeing the potential
of a cadaver liver trans
plant (the extraction of an
organ from a deceased
body for transplantation to
a needy patient), Dr SheetnLDhadphale did her bit to
get a team of liver trans
plant surgeons trained at
King’s College Hospital,
UK to be flown from
Global Transplant Hospi
tal, Hyderabad for the op
eration.
The team extracted the
liver and kidney and flew
back with the liver to Hy
derabad, implanting it in
the needy patient.
Both the kidneys and
liver were transplanted in
the bodies of three end
stage organ failure patients
The team who performed
while the eyes were re
trieved and donated to two
others.
information about liver transplantation.
EXORBITANT, BUT THERE’S HOPE
THERE are barely tourer five transplant'centres in India and the
cost of a transplant is Rs 25 lakh upwards. Keeping this in rnind.a^;
group of liver patients and doctors have formed P support OK*®)
create awareness about cadaver Organ dohatfoa-Tney
cess slories with patients and their relatives and provide accurate.^)!.
■
-'&T>2
7.'?
; dp||^<|cd) TORI I fed) TO'd RPRR 3RTO! TO PRR 'd'lfelcd
■•C; '
.1 cfrRl 3Rta? ?f) tjddl, eft) <fj Hl°l«, TOI’eRl^oi eft MSeM, TOTR1 TO
; ’■’. HT^)’ El TOR WdTO fdqi<0l?
'•■■.•
.
> jjjfed ’Til#) feTO^qf ‘4r 33' RPnjd TO? 3tqqq dil<gd d3>H $■
prtd trro 3to? pTOr totoi) wfedi wi- TOtoTO
■«biw4) (r $ yrote tarofa Yipfeqi.
fTOR 3^1
w) ara^i
., j TOTOfefa
qy$. quj
' ■
j?h ’hfSrraw tpl otPi
tH JjrfTOfl.' ."
*• ............ .......... . ....... ’I••
bv<r^
h rJ XJI r-R Xjl
rJ Hi UI
•
pferoR
gp tha. JTrH
wi LXIJ
to (frora)
wro
rtctR
$) J
^4 Hlfol^hlHI WTO TO. TOR ^TO. R^BTO TO) ^TPTO
,■••«<■•> ................................. ...................... . ... ..
cX?lchm*-XJ XU'JllrAiJIrT
ptosto .4UrJF7
rtor JjXc\ p'.lrl
(TO ifa ‘3g’ 3i*krqN RtjkfeK TOTO1 '4I$I< TO5. ^ebVIKSlcl
>h;
dTl0)) Ms^rdi 7?lyl,Ml^d) 3F^ TO? R><{?’• fcNud) .
7,
fn'fcfe ?TPW i^ate TO UTd'^l^l
, ■ ■ <flddiiio6 ^hn \ ^«=bic*5 cjd£iqi
*j4f TOui) toto r
ri
3TO RTR STR?.
HlcM
tor 4) to4i.-...‘
TO)
$dkrdl, ?R)/JiRh
VTORTSR PR TOTO 3ferta 3iRqq fefeg Hd)<M4d R>l4<d TO,
37^ TO dig)?1 3R1 ■Wd:FTO fddKd)...
5f|cbdlct. ^<si|xq| gldqiSchiq< STTHTOR cbl^cdrt TO. PR HR-f^tata
^erumi froR p?Mi rto
H<qn4fl
oSfeTOd' PRRPfTO^ HI3). ^^'d-WzTTT'i’i'i r r
i
■
<^<IH d!4) fild-io)') ptfi jjTd fe’if'fety)) •■ ;-Ay: vHII^I’n
• A<6RH? ■-.." PRIcWI^
dfdl'.'^ R'iaJ -Hlfild 6ld.
•:
PJTdl dld3)d MTO Riki^ld’ RI
TO TOR TOR
3W-
cRkdl Hol)- RRR SRg7
RlPfl^i)
wfe
^cTO
3TTO5)
WMcil.
RTO
hTORI
da!>d ‘pfj’H
iffeci TOQ>c&
<^dd TO) TOTFT dld^'i cd Hi
TO 4>c?l TOl. Vsild TO ^RR
4R<R 3nF»| d3lc5 TORH ^TOWd
did)$)
dtWvfeh
4)R RRRRc? (cbTFUil),
3^1 RTR 37ddd TO TOTO!
-biIhR^ ,
3n?n
■ Etfe
^tetw^n^wfeRi fadTdi
R^fewdl
FR7 W^/l RH1 uRlcf) '(^R
■TOnRTd) 4c3 (cold ischaemic
time) BTTO) 3JiB. dfrdiuidl ?)
3? 13d; PUcJd 3|ldc5 HTOd $fcfed
TO dTORIRl TOR TOtd PqiTORTO
I?
fFRfe^ sT. 4r, 3i.
fe’Wld. 3Ffe P,JllciHH) (|<dld)rtl
RRqfg 3]]fu| ^RTTOPH TOTO TO
TO thMlfawl &l&<
vjmjpfl ’jtllRclTcRl ?IpfedHcR VTOI
rRI d W1 TOTOTO1 PR ifB ^Tdl?
R1 ^>^1^
?^R7 Q^r^/c?/
3/ q'/a/Z^q 377^3^7
^d dldlfdR
3ttddfe-?l WIRR OTU ^TOTOTO)
'
TRTOH ferofel 3Hdqi<lHul TOFTO
. W?«TO» </?c7/q< dldl<<b(
• RfTOTI TOfTOB 3n??J, 3iqqqixj) TOd
■t‘3f '^I^lHli^l^
UldsTH
w Ptaf) tor to?. fafcnm,
tfifeliTO Rl^RRJH d 3RITO <HIT1
371^1. fytiw/l. d&Wltjc^ lldl^ll ■ tfquj cjRUTO 3{|c5. TO fpfeg 37lfR
3iRd>cqi PuiHl Rra' 4i <ilAcdfe&
qRRcT5 502^3 PRHl ’TOnR
Puli4l dl4)
3T&, •
Rfeife^ Hfcfjdl, ^f.
TOST Hl^)d
tmroT W ^o
fcM
UlMcM.
$UrdI
cdldl . ijlTO fdoidld
<n4» wp d4te Tnfen
.j.y,^.
3TO TH?
°3WTO^
• qbaFdWI R^TO.
c*7 wi. 'tisrf
^rf4r
....
s
■-3^1$
.■ ?
. s s? :pffl
- ■^-.; , w<iwfe wNiara .siyiiai hk
cFfen TO ^cR
^toTO
Pil^l t*H; 3J$
.
3rW^5
<4l4Id TOO ‘-6|j|dl,
’’TO?? 3{<W ^7, (7T rWI*9 ’ ’
*ak^c? ^^377^
T^i1 W/^ Wthi, fifa
^1^^..',, R°j
tyefq
i&fed 3RFR
3Ffife
TO
3{dRd
TOTT1 tTOTO TORirfe difid TOld.
ijMIq ‘^tyi-41 cRcfi W^l<
1 TO^p2/?3??5^(73/7^.,
••; j
^l R&T -
,
•
•
.
' #
•.dirtied TOd.”
TO^rRHeR rdldlrt TOI ffeid TITOTO1,
3{I^fe
if;;‘^ •■ 3f. t
TO 'd'fid
JdilMKrtl £Utlld- Rdi 3TTOR £ldT
-..
tiwro) dT^f (PdWljk 3fdR3 •
Fffe
TOR TOTOL
cTOTOF^tei
V’'T
•
VftvTc? H5uIKdd( . “Wl®«ltA'c4<l 4c£ldc5
PRR1 TOTO 3H TO? TOT
TOR
yjiRTRira) TOR TOcl 3RTOTO TOR3
F-RFTITOl TOR fed PTO T(^ PRRR
qpqgj
cl
lbl<j^H,Pll
(5^^
3]^ ^f
^3
tfiwld.
&n&i.
b^to
o tor)
(rtr
torto
. tpy^/ W/(/c/< Ulfa r^l ^tRJ chicUd. Vsiti 3ffljcl
^[dcldql • RTOR^I ’ TOfeTO 3TTc51 H’c^dl.- 4) (1TOF) , ‘
wfem
M'pf
RTE), d^d RTOTORl
J^}p a)
.••"^■di.
:. _ ___ -_.« ..
-
F?gTORl fePI TOFfaiq^ d^dfauilcR '/( ?) 4 mM (w t)
• £feR RftL..£;\T.\t.'j. •.;/;
*«^
•.# - •■
3?^ TO# 377^f7. (m.)
di-^TOH wfe WTO5I. ■gf.t?ftdc5 did)
^dd;^l
MMrdlddi
J'a\--.: i
^itor rcTO
(R
^7‘ .^J tflaisf;
'
TO2?? Wrf
PTOPlidte 3lfrft1cn fewd) RTOl
373?, TR7R^ ^UcSI; .
<?H-dd 3TO51, ?R R ?ITO 3TT3.”
TOflw tfoTTOJ????. „
Mt R^...TOTTOI....’
3?R 311cm W^^efflebf
HiitDiii^ ^fR 3J$... Iflife gives you thousand reasons to
Mfe
ctyt then you show, you have million reasons to smile.1
KF^feni
TO .TO
ng
‘TOll
TO-fe’
3fPR
(nh’.d)
•
J7TO eft? TOfe eft R? .
5fe7...'7>77TO7...''
)_! I W FOH NDATIO\
• er Patient Support Group
July 28, 2004
In reality, cadaver organ donation program is the only way to overcome malpractices like
organ trade and scandals in the field of organ transplantation. There are many doctors
'and hospital managements who in principle agree with the cadaver organ donation
program and wish to support it in earnest. But are reticent to do so for want of adequate
legislative enactments (support) as they fear allegations of malpractice from the public,
other hospitals and media
We pray, plead and suggest that the following amendments be made in law and policies.
1.
A local representative from NGOs like MOHAN FOUNDATION should be
included in ZTCC so as to implement Multi-Organ retrieval and Transplant
program for the region, in a true spirit.
2.
Local ZTCC should have balanced^lructure of all concerned Medical
discipline’ representatives; relevant to the various organ Transplant This is
again to implement Multi-Organ retrieval and Transplant program for the
region, in a true spirit.
3.
In case of unclaimed cadaver (Brain-Death) , whether in mass disaster
situation or in individual accident case, over a period of 36 Hours after the
declaration of brain-Death for a particular case, Local ZTCC should be
empowered to retrieve the relevant organs for the benefits of the suffering
patients. In such situation, the Cadaver maintenance expenses should be
borne by the state, as unclaimed cadavers are the national resource or the
national property. Any claim on the death body and subsequent denial .to
donate the organs, by the concerned claimants, after the elapse of 36 hours
from the declaration of brain- death; should legally be overridden.
C
dunoj-rAc. \n V\me. Acmoln)
As an NGO and a patient support group dedicated towards the noble cause of
cadaver organ donation, we expect proactive actions from the NHRC regarding'
these issues and look forward to the process of change in law and policies. We
request you to help end stage organ failure patients suffering from denial of right to
get the cadaver organs and the families of brain dead patients who should not be
deni
the satisfaction, solace and comfort to be had from donating the organs of
ir lov^fii ones due to legal and structural deficiencies.
Prashant P. Joshi.
July 29, 2004 @ Bhopal
Member - in - charge .MOHAN FOUNDATION Nagpur.
Liver I ..;:cnl Support Group. MOHAN Foundation
Z-901. Le-Mirage. 16 Bo:r <. lub Rond, Pune 411001; Ph: 020-26120454,020-33302775
nndhamdhere/Whotmail.com
-6
GOA CASES OF DENIAL OF HEALTH CARE
On 11/7/2004. Mrs H (name changed) went to Chicalim Cottage Hospital complaining of
pain in her abdomen. The doctors at CCH referred her case to Goa Medical College
(GMC) for surgery, as they did not have the proper facilities and equipment to handle her
case. She was then admitted to Ward No 106 at the GMC and was diagnosed as having
fluid in her stomach. As she required surgery, the ELISA test was done. After her results
tested positive, the doctors were unwilling to perform surgery and instead have been
keeping her on drips. As on 23/7/04 she is still in hospital without surgery having been
performed.
On 2/7/2004, Ms Mahadevi who is an orphan was admitted into TB Hospital Margao due
to severe cough and chest pain. Sputum tests conducted revealed signs of activated
tuberculosis. On 14.07.2004, following her discharge the doctors issued her a prescription
to purchase Rifompicin, Ehambitol and Septromycin (Injectable), drugs that should have
been made available as part of the National TB programme. Being poor, she could not
afford the drugs and had to be referred (by a social worker) to an NGO run shelter for the
medicines.
NB: We have two more similar incidences reportedfor the same hospital and three for
TB Hospital, Taleigao about non-availability of drugs and prescription for their
purchase issued to the clients.
At GMC, Mrs S (name changed) who was diagnosed and admitted for meningitis was put
on drips due to her severe and weak condition. Being HIV positive, improper treatment
was meted out to her. Her drips were adjusted for “slower speed” to maintain as minimal
contact as possible. On 13.07.2004 following her discharge, it was reported by a social
worker that the scalp vein used to administer drips was still intact on her forearm. The
social worker then referred the case to a care home for PLHIV were she was promptly
attended to.
In October 2002, a commercial sex worker was referred to the STD Clinic, Baina (located
in the red light area) for diagnosis and treatment. She was accompanied to the clinic by a
peer educator from one of the local NGOs at 11.00pm. At the doctor was not present,
they decided to await his arrival. The doctor (male) did not turn up that day and was also
reported as being regularly absent from his duties during official working hours. As a
result of this, the sex worker had to be referred to a private doctor to seek timely
treatment for her worsening condition.
As a result of regular absenteeism and discrimination against sex workers at the STD
clinic, an NGO working in the area established a free medical services clinic for the
sex workers and the community.
In May 2004, Ajay, a 6yr old orphan staying in a care home for children was taken to
GMC after a bout of severe coughing. The doctors diagnosed him as having TB. On his
discharge, the doctors gave him a prescription for the purchase of Rifompicin and
Ehambitol. When he along with the “guardian” went to the pharmacy to collect the drugs.
they were informed that the stock was over and that they would have to purchase the
drugs themselves. The caretaker of the children shelter than had to seek donations to
purchase the required drugs for Ajay.
On 02.09.2002, Mr John Gonsalves was admitted to the Goa Medical College with
complaints of vomiting, fever and blurred vision. On developing breathing problems, he
was transferred to the intensive care unit of the hospital. Due to non-availability of a
ventilator (all machines were in use), he was kept on hold. The doctors than told the
parents to hire a ventilator from a private hospital. When the ventilator was brought, the
doctors declined to use it and preferred to opt for artificial respiration with the help of a
hand manned pump that was inserted through the larynx. This continued on for
approximately 16- 18 hrs after which he was put on a ventilator on the 4th of Sept. Also
during the time he was in GMC, the doctors told the family to conduct a series of
expensive tests that were not available at the GMC or in Goa. Costs to transport and test
samples of Cerebro spinal fluid (CSF) and another to tests various microorganism had to
be bome by the family. This not only resulted in additional expenses but also in delayed
diagnosis to discern the cause of infection and to seek timely treatment. His final report
stating cause of infection due to Enthrovirus arrived only after his death on 11.09.2002.
Additional costs bome by parents for services that were unavailable, insufficient
infrastructure to deal with intensive care cases, lack of proper testing facilities
resulting in delay in diagnosis of cause of infection.
In September 2003, Ms PD a person living with HIV who was prescribed ARV (anti
retrovirals) was required to do a CD4 test to determine her CD4 cell count prior to her
commencing therapy. GMC being the only place providing CD4 facilities in Goa at a
subsidised rate of Rs 500.00 she was shocked to discover that the machine was not
working (had not been working for the past one month). As it was imperative for her to
commence ARV due to her deteriorating condition, she went to Bangalore to do the test
where she had to pay Rs 1800.00. In the following year January-February 2003, she
accompanied two other persons to GMC to do the CD4 test only to find out that the
machine was still not repaired.
Non availability and lack of concern to repair essential equipment resulting in outside
investigations.
RECOMMENDATIONS
1,
2.
3.
4.
5.
6.
7.
8.
All essential drugs to be stocked at all government hospitals and to be provided free
of charge.
The government should provide free ARV therapy to persons living with HIV.
The GMC should purchase another CT scan .
All hospital equipment should be serviced regularly to avoid breakdown. Other
essential testing equipment and sophisticated labs have to be incorporated into the
current hospital set-up so as to negate the need for sending samples for testing out of
state.
The number of beds in the intensive care unit to be doubled. The district hospitals at
Hospicio, Margao should be improved and provided with increased facilities so as to
avaoid over dependency on the GMC.
Taking into account the various National Health programmes being implemented, all
drugs should be made available free and regular stock monitoring ensured.
The facilities at the PHC's have to be improved. Despite having a good health care
system, the PHC are understaffed, have no doctors and lack the basic amenities.
Prompt treatment to be given to all persons irrespective of their HIV status.
9. Universal precaution kits be made available in all hospitals for health care
workers.
Cases of denial of basic health care in Madhya Pradesh
Health for all by 2000, health as a basic right seems to be mere a slogan when we look at the status of
health at the village level. Even elementary, primary health-care is not available. On the basis of the
protocol prepared at the national level, we have documented these cases from Bar warn district of
denial of basic health care.
Women's health care
Case No 1M is a 30 year women residing in A village of B district. She was persuaded by Anganwadi worker to
undergo Laparoscopic Tubectomy (LTT) operation. She has 8 children and went to the camp only get
a checkup regarding fitness to undergo the LTT operation. But in the camp she was not only told that
she is fit to undergo LTT operation but also was immediately operated even though she had been 3
months pregnant and she had specifically told then that she has missed her cycle for 3 months ion
4/5/04). There was no kit for testing pregnancy and no ultrasound machine in the camp. She was also
discharged the same day.
In her village there are few more women, who have.had children after LTT operation and the entire
village is now afraid to undergo an LTT operation. ■
TYPE OF DENIAL:
1. Gross negligence by the health staff.
2. Non availability of the essential simple test required for detection of pregnancy.
CONSEQUENCES OF DENIAL
Extreme financial Loss on account of bringing up a 9th Child.
Case No-2
The only family planning service that is mostly provided in the PHC is tubectomy. It is generally
conducted in overcrowded camps held occasionally by the government at the PHCs. The main aim of
doctors and ANMs in these camps is to fulfill the set target and therefore the operations are often done
insensitively and in unhygienic conditions. No attempt is made to explain to the women what is being
done to them. Often women from the interior villages are forced to walk long distances to gel home the
same day.
In one of these types of camps, Ms. M, a 30 year old women from K village, went to the family
planning camp held at So PHC in So block. After her operation, which was conducted in overcrowded
conditions, she returned home the same day. A week later she went to the PHC to get the stitches
removed and returned home the same day. Two days later she developed severe abdominal pain and
was admitted to the civil hospital in Al. Here she was diagnosed with tetanus and was also told that
treatment will not be possible in that hospital and she would have to be taken elsewhere. Since the
family did not have the money for further expenses they took her back home where she died three days
later.
Here is a case of gross negligence by the government health facility and reflects the obsession of its
personnel to fulfill their agenda and targets rather than provide quality health sendees. Also there is
denial of health care and extreme insensitivity’ when she was detected to have developed. Tetanus, thev
simply’ referred her case abdicating themselves of all moral responsibility of a heath care provider.
TYPE OF DENIAL1. Negligence of the health staff leading to the deadly Tetanus to a patient.
2. Non-availability of the treatment for tetanus in a civil hospital.
3. Unavailability of transport facility to refer the patient to.higher facilitv.
CONSEQUENCES OF DENIAL
Death
Coriiinunicajblc diseases- •
Case no 3’ .
■
■
M 23 years is a old of D village of B district. He was suffering from body ache, fever and t.ood in
sputum. He was treated for 9 months for T.Bi by private doctors and incurred large am:uni of
expenditure but no improvement occurred. He was referred to B.districtdiospital. where again he was
put on anti-T.B. treatment without any sputum examination and referred to PHC. S for wheeling
medicines where all his investigations were again gotdone from private hospital. He paid mone;. to the
government doctor and'he was given T B treatment for 6 months. All this while his symptoms did not
change at all. He is a poor man but incurred a total expenditure of Rs. 26,000 in 2 years. He has
mortgaged his 3 acre land & pawned all his wife’s jeweller)' to pay for his medical treatment. He
visited 8 doctors (Pvt and Govt.) in all but now he has no money left and no will to fight with the
health bureaucracy.
TYPE OF DENIAL:
1. Patient referred outside for doing basic investigations.
2. Medicines not available & he was asked to replace the medicines used for the patient during
his stay in the hospital.
3. The Health Department was'insensitive.
’
# CONSEQUENCES OF DENIAL
Extreme financial loss and risk from a killer disease.
Case no 4
H is a 45 year old man of village L (J) having problem of cough with blood in sputum. Initially treated
at PHC & later referred CHC where he was diagnosed as patient of TB on the basis of sputum and Xray examination. He was given anti-T.B. medicines for 1 month, but thereafter had to discontinue the
treatment because of non availability of medicines in the CHC. For next 1 month he visited the CHC a
number of'occasions but did not get the medicines, Since his symptoms became worst he v_sited a
number of private hospitals in Gujarat, He had to sell off his wife’s jewellery, his goats; mortgaged his
land. The high expenditure of private treatment broke his back, Left with no money, .he again came
back to CHC, P. But here again he was refused treatment saying he has no problem.
TYPE OF DENIAL:
1. Medicines not available even at CHC for TB.
2. Negligence of the health staff.
'
.
• CONSEQUENCES OF DENIAL
Extreme financial Loss and risk to life due to lack of treatment.Child health problems-
Case no 5R is two and half years old child of Mr. V of village D of a block of Badwani district,M.P. He hai
fever & vomiting for which he was taken to a private doctor for two days. Later because of no
improvement, he was taken to G PHC where after treatment of 2-3 days he developed dropping of
the left eyelid (pitosis). He was referred to CHC, P where was treated by the doctor for 5 days, By this
time the child had developed rigidity of limbs, and the doctor gave eye drops & ointment for rigid
mussels for massage. He even took treatment from Jan Swasthya Rakshak of P block,.He was finally
referred to Badwani District hospital. Here no proper treatment was given to the child even though he
remained there for 8 days. Since condition of his eye worsened, he was asked to get admitted to the eye
ward. Child was taken to eye department again;The eye doctor without treating him referred him back
to the Pediatric department. Me was again kept in the Pediatric department for 6 days & his both eves
became infected. When his father protested he was referred to a private eye doctor.
From the prescription of private eye doctor (Part 01 case record) it is clear that the child had developed
complete paralysis of all the mussels of both eyes (complete opthalmoplegia) and very little could be
done to save his eye sight.
’
••
After seeing the prescription of private eye doctor the hospital instead of treating him. immediately
discharged the child.The unfortunate child became blind for life due to continued denial of health
services at the all levels (Jan swasthya Rakshak. PHC.CHC.District hospital)
TYPE OF DENIAL:
'•
1. Continued denial of health services at the all levels (Jan swasthya Rakshak.
PHC.CHC,District hospital) for a serious eye condition.
-- Negligence of the health staff.
CONSEQUENCES OF DENTAL
1. Permanent damage leading to a major handicap of blindness
2. Moderate financial loss.
Case no 6K is a 3 year old child of village J, The child was suffering from diarrhea, vomiting, was taken to the
MPW who gave ORS but since condition of child worsened, he was taken to the PHC where the doctor
administered saline, He was referred to bigger PHC where the child was given injections & medicines
which had to be purchased, Later the child was referred to Civil hospital B in a serious condition. No
ambulance was available at that time. The father spent a lot of time in arranging money for the private
vehicle to take him to. B, The child died op the way to B.
’
TYPE OF DENIAL
1. Non availability of the essential treatment of diarrhea and it’s complications.
2. Non availability ambulance
GENERAL EMERGENCIESI
_z
•
_<
Case no 7M is 25 years man of village S, was bitten by a rabid dog, He went to nearest PHC R, which did not
have any Anti Rabies vaccine, He was asked to purchase vaccine from the market. But due to lack of
money he couldn't do so. Having been denied this life saving, essential treatment at PHC level he
went to the District hospital R where only two doses of injection were administered and he was asked
to purchase the rest from market. M died after few months leaving behind two children, widowed wife
& old parents.
TYPE OF DENIAL:
1. Life saving, essential medicine for dog.bite not available at PHC and even at the district
hospital.
3. Negligence of the health staff.
CONSEQUENCES OF DENIAL
Death
Chronic illncss-
Casc No 8Mr. R was a resident of village R. near district headquarter D in Jharkhand state. In May 2002 Dr. J.
the cardiologist in Ranchi diagnosed him as a case of ischaemic heart disease due to high BP. He was
taking prescribed medicines regularly since then. In second week of January 2004 he complained fever
and vomiting which persisted for nearly two months in spite of treatments by doctors of D and R.
Finally some disease related to kidneys was detected by Dr. A.K S of D. His son decided to seek
treatment for him at Indore in CHL Apollo hospital. He approached Dr. NJ, Gastro -entomologist in
CHL Apollo Hospital at the evening of 12lh March 2004. After scrutinizing all the previous medical
records the doctor told him to discontinue all the medicines prescribed by Dr. S.C.J (Cardiologist),
because according to him Mr. R was not having any heart disease. Dr. J also told him to undergo some
investigations the next morning. Accordingly Mr. R went again to the hospital at 8 am on 13lh march
for investigation prescribed by Dr. J. After the investigations the doctor advised him to get admitted
into the hospital because he was having a bleeding oesophageal ulcer and his kidney had stated failing.
He was advised to undergo dialysis and accordingly did so in the Apollo Hospital on 14Ih March. After
the dialysis though his blood pressure showed a fall it was not monitored hourly, Relatives got restless
as the patient seemed to be sinking. After about three hours, the patient was checked properly on
repeated requests by the relatives. It was discovered that his BP has gone down very much and his
heart has developed a complication (atrial fibrillation). He was treated for this complication, shined to
the ICU but his BP was not monitored hourly, nor was any treatment given for this very' low BP (80/60
mm of Hg) bordering on shock. No cardiologist visited him till his death on 15th March morning
despite his critical heart condition since 14lh March evening.
He walked into the hospital at 10.30am on 13th March and was dead within 48 hours i.e. in the
morning of 15lh March 2004.
TYPE OF DENIAL: - Gross negligence in a tertiary care hospital
CONSEQUENCES OF DENIAL -Death
Case no-9
.
'
M. Suffering from TB for the last 3 years. Registered in the govt, hospital at A. However, not
cured due to lack of regular supply'of medicines. He has spent Rs.-2000e , so'far and sold his
goat. Now can not spend more as he is very poor.
TYPE OF DENIAL:
1. Life saving, essential anti-TB not regularly available at PHC and even at the district
hospital.
Madhya Pradesh
Undemutrition and
Starvation Deaths
An Inquiry
An investigation of undernutrition and suspected starvation deaths
in a few selected villages of Barwani district in Madhya Pradesh, a
chronically drought-prone region, has thrown up a number of
issues impinging on the concepts, methods and processes used for
measuring of malnutrition and starvation.
The analysis of this data has yielded the
results in Table 1. Some 84 per cent of the
children in these villages were found to
be malnourished and nearly 22 per cent
were found to be suffering from severe
malnutrition. It should be noted that these
severely malnourished children areal sig
nificant risk of succumbing to fatal infec
tions if malnutrition is not corrected. For
comparison, Tabic 2 gives the nutritional
status of children in tribal areas of MP as
per NNMB survey, 2000.
This data from National Nutrition
Monitoring Bureau (NNMB) Diet and
Nutritional Status of Tribal Population
Report on Birst Repeat Survey is according
to Gomez classification and hence has a
arwani district in western Madhya
Pradesh is one of the less deve
loped districts of the state, with a
large tribal population. This district with
a total population of 10.8 lakhs (2001
Census) has a tribal population of about
65 per cent. The district has suffered the
effects of severe drought during the last
three years, which is a part of the larger
scenario of failure of rains, which have
affected many regions of western India.
The SATHI team of CEHAT has been
children) in the age range of 1 to 5 years.
The swasthya sathis were given a brief
training in the use of the ‘mid arm circum
ference tape’ and were shown how to record
the findings for each child on a specially
prepared record sheer This was necessary
because all of the swasthya sathis are non
literate and could not write, but could
record the status of each child (red, yellow
or green) on the coloured record sheet.
They measured the mid arm circumference
of children and all those falling in the red
higher cutoff point for normalcy (>90 per
cent expected weight for age) which re
sults in this extremely high prevalence of
malnutrition (92 per cent). Here it may be
noted that if we use the Gomez classifi
cation, about 98 per cent children in the
Barwani sample would be classified as
malnourished.
However the figures for severe under
nutrition found in Barwani district (22 per
cent) seem comparable to the figures found
forthe general tribal population of Madhya
Pradesh according to NNMB (20.4 per
cent). Here the cut-off points in both clas
sification systems are the same, i e, <60
collaborating with n people's organisation,
zone, i c, with mid arm circumference less
per cent of expected body weight, and
Jagrit Adivasi Dalit Sangalhan, a broad
based health committee, Jan Swasthya
Satniti and an NGO, Ashagram Trust in
than 12.5 cm were classified as malnour
ished. The results when collected and
analysed,showed that 1,260 (75.7 percent)
children were malnourished. However, it
was felt that this was a comparauvely less
sensitive method, and a more accurate
estimation of the grade of undemutrition
was needed. Therefore certain hamlets were
selected from Pati and Barwani blocks for
a weight-for age survey. These hamlets
were randomly selected from clusters where
'.here were ongoing activities of local
organisations involved in the Jan Swasthya
Samiti. In this way 10 hamlets from Pati
and nine hamlets from Barwani block were
selected. All the children in these 19 hamlets
- a total of 712 children between age 1
to 5 years - were weighed, their age in
months was obtained and nutritional status
determined based on weight-for-agc. This
included recording of age in months,
measurement of weight, recording of
presence of edema and skin/hair changes
and taking a brief dietary history. The
standard TAP criterion - weight of-the
child being less than 80 per cent of the
expected weight - was used to define
undemutrition.
hence the proportions are directly compa
rable.
Table 3 shows detailed agewisc analysis
B
Barwani to develop a health initiative.
Given the prevailing drought situation,
these local organisations with inputs from
CEHAT carried out an investigation of
undemutrition in selected villages of Pati
and Barwani blocks and conducted a survey
of deaths in a few selected villages.
The study involved a survey of under
nutrition among one to five-year old
childem; a study of undemutrition among
adults; an asscssmentof suspected increase
in death rates; and verbal autopsy to as
certain the causes of deaths occurring
during a threc-month period.
Given the context of lowered food in
take, the first step was a survey of nutri
tional status of children. The first stage of
this survey was completed by ‘swasthya
sathis’ (community health workers, all
women), in 25 hamlets of nine villages in
Pati block. The hamlets were basically
those where swasthya sathis were based
and hence it was a convenience sample.
This survey covered all children in these
hamlets who could be contacted (1,663
Economic and Political Weekly
May 3, 2003
of nutritional status of under-five children.
however it is a sub sample of 311 chi Idrcn
in five villages of Pati block which have
been analysed in detail. Severe under
nutrition was found to be commonest
amongthereccntly wcaned( 12-23 months)
group-as high as 42.1 per cent-and less
common in higher age groups.
Undemutrition among Adults
Adults were also examined for under
nutrition in selected villages as part of the
study. Adult undemutrition was assessed
based on the Body Mass Index (BMI) or
(weight in kg/height in metres) with the
following standard classification.
BMI Analysis
Grade o( Undemutrition
BMI <16
BMI 16-17
BMI 17-18.5
BMI 18.5 to 20
BMI 20 to 25
BMI >25
III degree *CED
II degree CED
1 degree CED
Low normal
Normal
Overweight
' Chronic Energy Deficiency.
175!
taken place in the last one year. The fami
lies of the deceased were visited, the date/
month of death were recorded for ail deaths
in the past one year. In all, 70 deaths during
the last year were documented in these
three villages. To confirm the time span
of these deaths and in order not to miss
any deaths, an attempt was made to com
pare this data with the mortality records
maintained by the ANM. However this
additional corroborative data could not be
obtained from two of the three villages as
the local health authorities refused to
cooperate in giving this information.
Therefore the actual number of deaths is
actually likely to be higher than what we
could document
Local calendar, local festivals, phases of
the moon and local market days were used
to ascertain the date of death in case of
all deaths in the last three months. The
exact number of deaths in these three
occurring in the selected villages during
the last three months. This meant a detailed
investigation of the symptoms and signs,
bodily appearance, history of food intake,
family food supply and other relevant
factors in case of each death.
Although a standardised verbal autopsy
questionnaire for childhood deaths,
standardised by WHO along with John
Hopkins School and London School of
Hygiene and Tropical Medicine is avail
able, such was not the case with the VA
questionnaire for adults. So taking a
general-purpose VA questionnaire from
an article in WHO Bulletin as the basis,
a modified VA form was prepared which
could take care of 'starvation related
deaths’. Questions relating to food intake
and family food supply were added to this
questionnaire. This was done based on
.suggestions from C S Kapsc (head of
department forensic medicine, D Y Patil
slightly greater prevalence of undernutri-
months was used for llic calculation of
Medical College, Pune), VecnaShairugltiia
tion among women in MP (50 per cent)
as compared to men (47 per cent). Severe
undernutrition too is greater among women
(9 per cent) than men (6 per cent).
Severe undernutrition in Barwani in
adults (15 percent) is double that of tribal
areas of Madhya Pradesh in general (7.9
per cent), at the same time overall adult
undernutrition is significantly greater here
(63 per cent) than the NNMB data (49 per
cent). Undernutrition in men at Barwani
(73 per cent) seems to be much worse than
MP tribals in general (47 per cent) and
severe undernutrition among men in
Barwani (12 per cent) is double that of
NNMB data (6.3 per cent). On the other
hand the prevalence of undernutrition in
women seems to be comparable in Barwani
and tribal areas of MP (54 per cent and
50 per cent respectively), while severe
undernutrition is again somewhat higher
in Barwani (12 per centjahan the MP tribal
population (9.3 per cent). Overall tribal
areas in MP do not score well on nutrition
parameters, but the drought situation pre
vailing in Barwani seems to have taken an
additional toll and may be responsible for
the higher level of undernutrition.
death rates, as this being a short recall
period, the date of deaths could be as
sessed fairly accurately. This data, based
on the population of the village and con
cerning three month’s span was extrapo
lated for a population of 1,000 and a span
of a year and the death rates were cal
culated. It was found that the three monthly
death rate of Semli village was 3.5 deaths
per 1,000 population, of Verwada it was
2.65 and of Sipahiduwali it was 5.33 deaths
per 1,000 population.This brings the annual
rate of death per 1,000 population in these
villages to 14, 10.6 and 21.3 respectively.
The total annual death rate in these three
areas combined was 14.15.
The average death rate in the three vil
lages during these three months (14.15
deaths per 1,000 population per year) is
somewhat higher than the crude death
rate of MP (11 deaths per 1,000 population
per year, SRS). However, given the small
population base and time period in this
sample, it was not considered possible
to draw definitive conclusions from this
information.
(jt director, National Institute of Nutrition,
Hyderabad), and H H Trivedi (ex-profes
sor, department of medicine, M G Medical
College, Bhopal) who gave their detailed
and valuable inputs to modify this ques
tionnaire and also agreed to be the expert
panelists for analysing the results. The VA
questionnaire had the following major
sections.(l) Personal identification details.
(2) Family food supply related information
including irrigated and non-irrigated land
owned, state of the harvests, wages earned
and ongoing government fblief work,
Suspected Increase
in Death Rates
It was felt that more definitive investi
gation of the cause of all deaths occurring
in these villages in the recent period was
required in order to ascertain whether these
were starvation deaths. This exercise was
also considered essential to develop a
methodology to study and diagnose star
vation deaths. It was decided to conduct
a verbal autopsy (VA) on each death
132 adults (above age IS) were examined
in two villages for weight and height and
their BMI was calcullcd. The findings were
in Tables 4 and 5.
According to the findings, 63 per cent
of adults were undernourished, 15 per cent
adults had a BMI of less than 16 which
is indicative of chronic hungcr/cnergy
deficiency and severe undernutrition, which
can contribute to the development of lifethreatening illnesses. Undernutrition
among men seems to be more (73 percent)
than women (54 per cent). Severe under
nutrition among men (18 per cent) is also
somewhat greater than among women (12
per cent).
According to the NNMB data collected
from the tribal areas of Madhya Pradesh
in general, 49 per cent of the adults are
undernourished and 8 percent are severely
undernourished. As against the findings in
the Barwani study, the NNMB data shows
Anecdotal reports were received about
unusually high death rates in certain vil
lages. Three villages in one cluster, from
where there had been some reports of
suspected starvation deaths, were taken up
for investigation of all the deaths that had
1752
Use of Verbal Autopsy
Table 1: Undernutrition in Pati and
Badwanl
Grade
Criteria
(PerCent)
Normal
>80
Mild to moderate
undernutrition
1
71-80
11
61-71
Severe
undernutrition
111
51-60
IV
50<
Total
Total
Percentage
114
16
442
62.1
156
21.9
712
100
Pad and Badwani block combined. Total 19 hamlets.
712 children (IAP classification).
Table 2: Nutritional Status of 1-5 Year
Old Children in Tribal Areas
(Gomez classification)
Nutritional Grades
Madhya Pradesh • Tribal
N = 1514
Normal
Mild
Moderate
Severe
8.1
25.8
45.6
20.4
Economic and Political Weekly
May 3. 2003
catcgorywisc status of food items being
consumed by the family. (3) Individual
dietary history during the week and the
month before death. Calorific value of
each food item consumed was calculated
deaths were investigated, seven of which
were children, and 18 were adults.
The questionnaire was translated into
Hindi. Bhausaheb Aher who administered
the questionnaire and Amulya Nidhi who
in order to analyse this data. (4) Unnatural
assisted him (both MSWs) were both
food consumption patterns such as beg
ging or borrowing food, consumption of
unusual foods such as leaves of plants,
forest tubers, etc. (5) Signs and symptoms
during the last illness, as well as any medical
records and prescriptions. (6) Physical ap
pearance at the time of death.
Establishing the case of death - at the
end of the questionnaire there were sec
tions to record (a) immediate cause of
death; (b) underlying cause of death; and
(c) contributory cause of death. This di
agnosis was to be made by each panelist
based on the findings of the Verbal Au
topsy. For this the complete sets of copies
of all the filled questionnaires were sent
to each of the three panelists for analysis.
Their opinion about immediate, underly
ing and contributory causes of death were
taken and collated.
trained and acquainted with the medical
phrases and clinical conditions that appear
in the questionnaire. This was pre-tested,
by investigating the deaths of five children
and four adults in these villages, and then
finalised for use. Both the questionnaires
were used to investigate all the deaths in
the selected three villages - Semli.
Sipahiduwali and Verwada.
So far the verbal autopsy forms for all
the adult deaths have been analysed (18
deaths). The completed forms were sent
to all three panelists who gave their in
dependent opinions, which were then
compiled in a table. If at least two of the
three panelists stated starvation or malnu
trition as the underlying cause of death,
this was taken as the probable underlying
cause of death. A similar definition was
used for a probable contributory cause of
A drawback noticed in the process was
death. Among (he 18 adult deaths, in cnsc
that the currently available verbal autopsy
questionnaires are quite medicalised.
Although good quality training was im
parted regarding it's administration, and
the help of locally available doctors was
taken wherever necessary, it was felt that
a qualified doctor would have been better
suited for the job. This again brings us into
the realm of over-medicalising an essen
of three adult deaths, starvation was iden
tified as the probable underlying cause of
death. Apart from these, in an additional
three deaths, starvation or undemutrition
has been identified as the probable con
tributory cause of death.
Some of the many issues, which emerged
in the course of this study are:
(A) Though the phenomenon of starvation
tially social problem, Not only that ‘death
related to starvation’ almost neverappears
is widely discussed and reported, we cou Id
not find a very clear definition of starva
in the death certificate of a doctor certi
fying a death, but even undernutrition
seldom appears as an underlying cause. To
add to this we could not obtain any clear
guidelines about how to define a starva
tion death, or the parameters to certify
such a death (see discussion). A tool less
medical in nature, and one that can be
administered with minimal training is
tion and especially no clear definition of
a ‘starvation death’. However some indi
cators which were pointed out by Veena
Shatrughna and which helped to initially
guide us when we were grouping for some
working definitions, were as follows: a
dietary intake in adults of less than 500
kcal per day is starvation (NIN report on
drought in Gujarat); doubling of the pro
definitely needed. Our modified verbal
portion of adults with a BMI of less than
autopsy form might be seen as one step
in the direction of developing such a tool.
All the deaths (19 deaths), which oc
curred during March 2001 to May 2001,
in the villages of Semli, Sipahiduwali and
Verwada were investigated.These villages
were purposively selected, where local
activists suspected an unusually large
number of deaths. Six deaths during the
six months prior to this period (September
2000 to February 2001), which were
strongly suspected to be starvation deaths
were also analysed. Thus a total of 25
16, compared to the baseline, is indicative
of starvation; and consumption of abnor
mal or unusual foods (forest leaves/tubers/wild fruits not usually eaten, etc) is
Economic and Political Weekly
indicative of starvation. Howevcr.thc first
two of these criteria seemed problematic
when we started actually applying them
to the situation. The third seems useful but
may not be a sufficient criterion in itself.
The NIN criteria of starvation (men
tioned in passing in its report on drought
and malnutrition in Gujarat) of ‘less than
500 kcal intake perday’ seems inadequate.
Those having such low consumption lev
els would definitely be starving. But what
about those adults consuming between
500 and 1,400 kcal per day? They are
consuming below the amount required for
basal metabolic functions, and consider
ing the additional fact that they would be
doing some physical activities to obtain
food, they would he continuously and
Table 4: Nutritional Data for All Adults
(BMI) In Two Villages
BMI Analysis
Alt Adults (132)
BMI <16
BM116-17
BM117-18.5
BMI 18.5 to 20
BMI 20 to 25
BMI >25
Total
Females (65)
BMI <16
BMI 16-17
BM117-18.5
BMI 18.5 to 20
BMI 20 to 25
BMI >25
Total
Males (67)
BMI <18
BM116-17
BM117-18.5
BMI 18.5 to 20
BMI 20 to 25
BMI >25
Total
No
Percenter?e
20
19
45
26
21
01
132
15
14
34
20
16
01
100
111 degree CEO*
11 degree CED
1 degree CED
Low normal
Normal
Overweight
8
7
20
15
14
01
65
12
31
23 ,
22
02
100
lit dogree CED*
11 degree CED
1 degree CED
Low normal
Normal
Overweight
12
12
25
12
06
00
67
18
18
37
18
09
00
100
n
Grade of
Under
nutrition
111 degree CED‘
II degree CED
I degree CED
Low normal
Normal
Overweight
* CEO - Chronic energy deficiency.
Adults with BMI below 18.S (undernourished) -> 84
(63 per cent).
Adults with BMI below 16 (severe undernutrition)
-»20 (15 percent).
Women with BMI below 18.5 (undernourished)
-< 35 (54 percent).
Woman with BMI below 10 (severe undornutrIlion)
-» 8 (12 per cent).
Men with BMI below 18.5 -r (undernourished) 49
(73 per cent).
Men with BMI below 16 (severe undemutrition)
-> 12 (18 per cent).
Table 3: Agewise Analysis of Nutritional Status of Under-Five Children in Pati Block
Age (Months)
Normal
Mild/Mod Main
Severe Main
Tolal
12 to 23
24 to 35
36 to 47
48 IO 60
Total
7(3.2)
5 (A3)
11(13.7)
14(14.7)
37 (11 J)
37 (48.6)
38 (63.3)
59 (73.7)
63(66.3)
197 (63.3)
32 (42.1)
17(28.3)
10(12.5)
18(18.9) .
77(24.7)
76
60
80
95
311
Percentages in parentheses.
May 3, 2003
1753
perhaps rapidly losing body weight (prob
ably muscle mass since fat reserves would
be long gone). This is clearly an unsus
tainable situation. Given the fact that con
tinuing such a low level of dietary intake
will in the course of time inevitably lead
to fatal results, what distinguishes this
from starvation?
There seems little sense in talking of the
‘baseline’ for a community that is already
chronically undernourished. If statewise 9
universal undemutrition in rural and tribal
areas. However, the paradox is that the
government can ignore or downplay the
fact that hundreds of millions of children
and adults lead lives of severe, lifelong
undemutrition since it does not provoke
any public outcry. But a few starvation
deaths reported in the press make the entire
government machinery go into overdrive
to ‘deny’ such an event and take some
emergency measures. Even civil society
dividing line between malnutrition and
starvation? When exactly does the situa
tion change from 'a chronic problem’ to
‘an alarming situation’? Our figures for
severe malnutrition in Barwani (22 per
cent) are only minimally higher than the
NIN figures for severe malnutrition in tribal
areas of MP (20.4 per cent). One interpre
tation could be that the drought-induced
situation in Barwani is close to ‘normal’
- after hearing of our results of 84 per cent
percent tribal adults have a BMI <16, then
and middle class opinion which starts
malnutrition, one official in Barwani rather
wringing hands at the mention of starva cynically said, if this malnutrition thing is
tion deaths, remains impervious to the so common, isn’t it ‘normal’?
Or do we interpret this as a silent yet
implications of findings such as NIN data
according to which around 90 per cent of alarmingly widespread situation of chronic
children in rural areas are undernourished! severe undemutrition, with drought as an
So what do we do - focus on the near additional aggravating factor, a last straw
universal community undemutrition/star- which breaks the camel’s back and leads
vauonoronthefewstarvationdeaths? One to obvious deaths?
In summary, there seems to be an urgent
emerges as the main problem from a public
health perspective while theotherisan emer need to be able to utilise the wealth of
gency with the advocacy impact of moving existing data on widespread malnutrition
public opinion and the government sys for effective advocacy, to enable people
tem. Can we develop an approach to to access the right to food security. At the
adequately understand and document both? same time, there is a specific value of
Low prevalence
5-9 per cent population with
(C) Generally prevalent ‘baseline’ malnutri documenting starvation, or a state of
BMI <18.5
tion, gradually worsening severe malnu extremely reduced food intake which in
Medium prevalence
1O-19percertpopuiationwith
trition and starvation merge with each other due course is incompatible with life, both
BMI <18.5
High prevalence
20-39 per cent popciation with
along a seamless continuum. In a commu because it is a humanitarian emergency
(serious situation)
BMI <18.5
nity which is used to barely subsistence and because it may help to shake an other
Very high prevalence ■> = 40 per cent population
intake, three years of drought reduce this wise complacentstate and civil society into
(critical situation)
with BMI <185
further and then some families start eating some action. The challenge is to develop
By this classification, the situation in MP once aday, some individuals get to eat only an approach, which has both breadth and
tribal areas in general is already ‘critical’ once in two days... where exactly is the depth, which views malnutrition and
(49 per cent population with BMI <18.5)
Table 5: Comparative Table of Undemutrition In Selected Villages of Barwani
and the situation in Barwani can only be
called ‘supercritical’ (63 percent popula BMI Analysis
Proportion of MaiProportion of Mal
Percentage of Men
nourished Females
nourished Males
and Women Together
tion with BMI <18-5)1
(B) Starvation emerges more and more as 1 BMI <16 CED III degree
12
18
15
54
63
73
a public health problem requiring commu 2 BMI <18.5 CED all degrees
nity diagnosis. In this sense starvation
Table 6: NNMB Nutritional Data for All Adults (BMI), Madhya Pradesh (Tribal)
deaths differ from classical ‘disease re
lated mortality’. The diagnosis of a death BMI Analysis
Proportion Out of
Graded
3,209 Females
due to tuberculosis might be considered
Undemutrition
2,788 Males
All Adults
an individual diagnosis. But the diagnosis BMI <16
9.3
III degree CED*
6.3
7.9
12.4
of a ‘starvation death’ cannot be just an BM116-17
II degree CED
10
11.3
17-18.5
28.4
30.9
I degree CED
29.6
individual diagnosis; we have to document BM1
BMI 18.5 to 20
24.4
28.2
Low normal
26.2
the circumstances prevailing in the family BMI 20 to 25
24.2
23.1
23.7
Normal
BMI >25
1.3
1.5
1.4
Overweight
and community along with the individual Total
100
100
100
to reach such a conclusion, for the simple
CEO - Chronic energy deficiency.
reason that starvation is a deeply social •Source:
NNMB Technical Report No 19.
phenomenon. In fact, looking at the scale
why should ‘doubling’ of this to 18 per
cent be a criteria for starvation? By this
criterion, worse-off states would have a
higher cut-off point for starvation! If at all
we have to make a comparison, should it
not be with a general standard rather than
with a ‘baseline’ of an already unaccept
ably poor nutritional status? In this context
we can refer to the criteria laid down in
the WHO expert committee report on
Anthropometry (WHO TRS 854, 1995)
related to classifying low BMI as a public
health problem:
and depth of malnutrition in tribal and
rural areas of our country, making indi
vidual diagnosis of ‘starvation deaths’ may
seem almost incidental to the main issue.
These deaths, though tragic and extremely
unfortunate especially since they could
have been so easily prevented, arc just the
tip of the iceberg of a situation of near
1754
Table 7: Comparative Table of Undemutrition: MP Tribal Areas and Barwani
BMI Analysis
BMI <16
BMI <18.5
Females
Males
Pooled
Females
Malos
Pooled
Madhya Pradesh Tribal
Areas (Per Cent of Persons)
Barwani Villages
(Per Cent of Persons)
9.3
6.3
7.9
50.1
47.2
48.8
12
18
15
54
73
63
Economic and Political Weekly
May 3. 2003
starvation as public health problems with
a social dimension, and to wield such a
tool effectively to establish the entitlement
of all for basic food security.(HZl
collccling data and conducting interviews for this
[The study was undertaken by the SATHI team
Adivasi Dalit Sangathan and Ashagram Trust,
at the Centre for Health and Allied Themes
(CEHAT). Bhausaheb Aher has been involved in
Barwani contributed in various ways during ail
study as part of his block placement with CEHAT.
Abhay Shukla, Amulya Nidhi and Amita Pitre of
the SATHI team have participated in various
aspects of design and analysis. Activists of Jagrit
stages of the study.]
Jharkhand
of basic economic entitlements through
land reform, education and training, essen
tial medical facilities and credit that al
lowed for a wider sharing of social oppor
tunities, thus leading to the participation
of a majority of the people in the process
of economic expansion and social change.
While poverty still prevailed, this strat
egy led to an expansion of human capa
bilities, facilitated economic and indus
trial expansion by improving people’s
productive capacities, while at the same
time leading to an improvement in the
quality of life. Even the World Bank, with
its focus on the ‘market’ to boost growth,
has acknowledged the role of state-led
public action, particularly education, in
Dazzled, by the east Asian economic ‘miracle’, the newly created
leading to ‘the Asian economic miracle'
state of Jharkhand has drawn up a Vision 2010 document for
(1993).1 It has admitted that these are the
only economies that have “high growth
development that seeks to turn it into another Singapore. However,
and declining inequality” [ibid:3].
the document lacks clarity and commitment and also suffers from
In the case of Singapore, in thq decade
skewed priorities that will severely impede the state's progress
of 1972-82, poverty declined from 31 per
towards the goals of growth and poverty eradication.
cent to 10 per cent, in India from 54 per
cent to 43 per cent During this period, the
Nitya Rao
jective, but perhaps it is time to reflect on Singapore government had to demonstrate
the key ingredients of Singapore’s success to its people that the benefits of growth
harkhand, created as an independent and ask whether these are reflected in the would be shared. Attempts to reduce in
state in November 2000, has produced actions oreven in Jharkhand’s vision docu equalities in basic wealth were an impor
Vision 2010 - a statement of policy ment What have been the measures taken tant component of this development strat
directions for the new state. Former chief to counter the human costs in terms of dis egy. Thus, workers’ cooperatives were
minister Babulal Marandi had identified placement and shrinking access to natural formed to give workers a stake in the
increasing socio-economic disparities with, resources that would accompany a process economy, such as the ‘ fairprice supermarket
more than 56.8 per cent of the population of rapid growth? With many thousands cooperative' with over 2,40,000 members,
living below poverty line (as against 36 starving to death or dying of diarrhoea and ‘comfort taxis’, and many others. Simi
per cent for India in 1996-97), lack of road malaria, the answer sadly is predictable. larly, amassivepublichousing programme
connectivityinmorethan60percentof the
I discuss briefly in this paper the key was undertaken. The National Wages
villages, 54 per cent literacy rate (42 per elements of the east Asian ‘miracle’, and Council was set up in 1972 with represen
cent in the tribal sub-plan area that in then point towards the lack of both clarity tation from both the government and trade
cludes 112outof221 blocks in Jharkhand, and commitment in the Vision 2010 docu unions to keep the inter-industry wage
spread in 11 districts out of 22) and 85 per ment as well as in the actions of the state structure stable. By the early 1980s, pro
cent of villages having no electricity, as government, in terms of these key elements. vision of child care services was expanded
the key problems confronting the state,
to enable women to participate equally in
along with the challenge of extremism.
Development Strategies in Asia
the economy [Phongpaichit 1988]. The
Marandi, in the last several months, had
building of a merit-based and competent
seemed increasingly attracted by the ‘Asian
Remarking on Singapore’s achievements civil service as well as improving relations
strategy’ fordevelopment, particularly that in the introduction to his lecture at the between business and the state (including
adopted by Singapore. Along with an 11- Institute of Southeast Asian Studies in encouragement to small and medium
member team, he undertook a tour of Singapore, Amartya Sen said, “This enterprises) assisted the rapid economic
Singapore, Malaysia and Thailand in country's success in economic develop growth and demographic transition.
December 2002 [Prasad 2002b]. There ment as well as in building a vibrant and
By the mid-1980s, 5 per cent of GNP
after he proposed a trip for Jharkhand harmonious multicultural society has been was allocated to education, a bulk of it for
legislators to China and south-east Asia: exceptional” (1999:3). The success of the basic education. Universal, high quality
■'Legislators will be sent to foreign coun region lies not just in enhancing the pro basic education helped close gender gaps
tries to observe the developments there to ductivity of international trade, but rather in education. In the late 1990s, an increase
change their mindset” [IANS 2003]. These in its emphasis on basic education as a in income inequalities has become visible.
trips have been funded from the state’s prime mover of change as well as con Higherincomes are clearly linked to higher
exigency fund, meant for emergency pur scious measures for cultural integration of education; therefore, in order to stabilise
the Malays, Chinese and Tamils [Seen- income inequalities, there may now be a
poses [Prasad 2002b].
Turning Jharkhand into another Kong 1983]. The new features of the‘Asian need for the state to intervene in maintain
Singapore is indeed a commendable ob- strategy’ included the wide dissemination ing equal educational opportunities at the
Vision 2010
Chasing Mirages
J
Economic and Political Weekly
May 3, 2003
1755
Coivi }t • '2m'4I
fc(5lH
<1Hla
lfEI-O1 W 3WIct2, ferra
^-7, 3RVT cMcitHt, 'hHh.
H.5f.-16. PJTn : 0751-461086
5HH— mpbgvs@yahoo.co.in
1
cf>
HR oM MMTM <4t (qMRlcl fkifct <4 fciR R’twid HM
3TcqmM HR; RH
MMT "i^a - MntW - ^Hlfl’' 3 jjf Hiot
MTRH RM MR RM ^^ci
t1
sft? HHT fkeTT 4 4w
MR 2-3 HTs <4 MRTH HTcT MT MT cTM fqRVTT,
W q? ant-;?. Ma I MT MH HRd Mel fMRit 4t HHTM Mt Mei Im a MRH e4 feiR Mill'd
5 | <^<p OXS’ eft 3IIH 41ii4Md'l HR H^t
HE?) RXitl STIR eil'il <pI 4ld <4
cpivM HR MTH RTMnfcTM MM? H MMT IchPim SHlt RTMdfaM aH 4 lei'ei vldt
Hft gdHslHM Mt WdRid MRat 8 I RTMnfaM eMMT 4 $Hl4t Hla'l HR MTxt ei-diaiR
3HRPT - HcMxTH 3RR RMTM^tHTHRT 4 4o MR <pt MTat RfM HR nexi f<Pti aR? <4t
tiMal Mt wqRIa MRat 8 M? MTTHT MxTxt del I
fqcpHftMRH SitR T1IH RHRTM <4t U I8dI $ <4t y4i HR
HR 4 fsTRMat R-iRMIR
M h4IjIuI Mq a<p HH <4 41 Mil RT Hadid <pt MxTeT xPTTMR Mica xe'l ? RM dXM
4 8 eft <RXixi aRM 4 MfcftR 4t 8 f<P (vidM fed di $tild <4t Mln Rt HsMR did <4t
MPT 8 I Rl<PXiei RMT Rt HTHt 4 M$ Hi4 <jd"la HR Ret £• I MRT Ms I MTnT Mrf^R
Sn 4t— xcTMT M f<P
Rpan cH MRT HIM <4 leiT! HIM 4 H^MM ?
fqjq xai£l MTHMH gKI RTMTfeia RM Rti4 <pt RmIc HMJ HMM MT MqMtMR
xsIejim Si-QxlaTa
TIM! tilRd MRat t? eiRpd H.H. RTRMTR
<481 3Tq 4t ’Jxa M 3flR
cpHldul 4 dial MT 8tdI d4l x4i<Plxai I MT tin 4t It ftp uiq TTM RtRMTR H x4ImR
aq aM H aT RJR3T 8 34r H e4 ’JxR k Hl ci | 3TlR eft 3TtR 4 RTRMRT fxrfqRRiM 3mA
tils din tileil fnicpctiMfil Slid MT VTTHMR McRld Mr4 ?TR Msa ? f<P
MMMT 4 HsT 4tH14t 4t
st 1 RTTHM (4[<PeHI Rsild fqT Rbaiqi H <g4mul 3tTR
4ihiR4Im stthrtT tintil nicA Hia hmrh ?t hr 1? i
He ftPddl fdeiMHT 4 44 HMf r4m 4 tiIei Id I 1.6 MRPS MH <aitll"i <PI TScHTMT
MaT 11 RH^tH HMR RMTM 4 MxM 90 HER MH M1MM H.H. 4 et MTcTT 8 I ?RT
HM1R yla MTqM dlaRd 473.33 4Id 3THTM 3Meiq? 1?, vjqRb 37r?.Rit.RH.3TTR. <4
^aliqM ulaiqd fvtM 420 TTTH 3THTM ^T nfa Mina <4 feTR MTHp 11 ?HTx TTqRT 4
Wiaidd Hfa Mf4a 32 TTTH MTeT '□MedET t? MhI<p RI^H OTTHcT 22 TTTH MT s | ^cTn
Hx 4t MT xTRMR 3m4l Mdcll Mt M vjn <4t <41ei RTcft dM *^841 H MRT ti<p| eft
MHaT MR aM 3TTR W - M4T RIHat Rpft ? ^Rf HR ?H RfAt Mt qRHT st MM RTTH
Mx 46ei MRHT 3liq^4M t? M4IMI ’JET EJ3H H^t TlfeM 3TTH 8 I
fqf^TT
.■£ rft -iisRqt, ^xt, frert sfk fhiRht h
Rib'll
aft? erttw
7$ feTR HR. TO 5TIR fqRTR RftfcT EFT gEp RFT fqRTEF 13 REFER 2002
fft fttcft EFT 41441
EM x£ST wrfftcT ftef 3 qgRT | HR. RT.^TT. fcTRT. Eft WT-WT gH RFT H RRR-Rs 7ft
Jilifaei £ I RHrfftci ftnt 3 W7T ?ftt Rt qtf HrEIRTRT Eft ST^qaioi 3 f^lfcp<x-iepi R 3-trrt R W3H
ferfa EFT MlNvll Ri^l RHT I 'IR41Rkl EFT ER FRHciTFT ^Lpxei RcF 11 ERT Eft g-Reft faRb'^i
3^0)1'?! ^T. 4oHei
^101 Ejft RRRTT Rft HREfft TJRJ Eft EFRutf Eft <nt if MlHcpjfl qf | fc^q,] ERRT
f-FR 11
Rqiq> 7.8.02 - 28.8.02 qEF -igiRqi H 5 RTnr -qft Ejcg I
RhTEF 30.9.02 - 25.9.02 ckF E^yFft tJ 6 eftnf Eftt RR 1
FlFTR 21.10.02 - 24.10.02 cTM FiRMFF H 2 eftRT Ejft
|
f^RIEF 23.10.02 - 25.10.02 W FRtRT 3 2 cfm Ejft gR I
RHTEF 20.9.02 — 5.11.02 clcp ffteilHI'E H 9 eft'ft Ept ijFg (<4 61 xqixRF vjqcp-q ft)
f^RTR 6.11.02 EFT IIH cftcn-tl
(ftftpRTcp'i Eft
1 EJcg I
^xi|< qx-i qicj'l R EJETRTFR
TFT TFFT°T Rfcbcdcp'i Ep 3FJCTR
vi-rfi 'flHlR'Ui 2ft I <FW ^TfEFT—ETEfEFT MHcl'l
3TT7 cKj'f ST |
Het, EptfrW tT H^T eiPpn ci.<?i. 3TR 'xJHlPtTli
et <FLTiqul 4lci Tp fetq RiRfK FF7 |
*llvl tft «Ti •H.l'Ci ■'& Tpf <?i fcb -4 kh} wiq'iq'edl <F4'i T ul
VeTT
Epf Hl ci 4ai<H FTT
— TfEF RR>e«<p (5<FVei ^jcR 4wi<s(l'ti'kl)
SRHcITeT T& Rcpi^ e£ Sl^j'FK Rn|cp 11.11.02 cFF 41 H-fivi 2atrcUd H qlRaeii ci F,<F st [win
^ElRTcR «rScT st |
el'IF41 ir<J cTRsf E}?[ 34iq|qi tR ETgT HH 1 R|[cpetiq> 11
HTStReF ■RTR-EZJ <p-qi/viMcp-q'i Tpt 7TE3TT qfl ETgET <FH 6 I
O’^qFffRT 3 3IFT
$ RTTgTF Ejff fcRRT 4<|TRT Ep II l4iun
c ntfld eFI |
gF
4x414ci H feRRT, F4R'l<i, 4EJR cT2JT -1 FlP4l WT FTTct 6 I eR7 9F14d Ef?[ EFci cmv.-.sll 1500—2000
E$ HFZT t I H^TfW 7TTTr vTgT 5 efFTT Ef?| tjfJ gg ERT TFFi 46 4R4R t
25'0-300 En
F^ReTT SIlRqlFl RgFf 11 ZfF 7TTET ggT wRrn 3JlRc||l<l4f EFT ? I EJ^T eJtT <1x44 FT Reft 'i'lctiftqi^
qcftt 4r yRicTici ? 1 RicFftEng ->ft RfRft str Rjrft E?ft hr 7t ftFR efrr mhiRg ? grr ejtg eft
3FJHFT ftpHP W7
eWIT EFT REFcTT t
FREFT ERF EfcT SRtRef efhWT SIT I 5? 3141-1 <p ERF
Rr cftcT RR 3 EFftlft eTHT, WT eR 3 RFI Rtwft ?T Rtft sfr. FRTsft qg
RFT 3TH FIR RTE TI?
FTR ERR RT E3RFT FPIT I 3TRT4HT EFT? REIR«q Ep^R R^i ^iR <F EFRR Rift ssqHgx E?ft fRRRRft
3
H te
te fci^ ete TOTO ?te? TO? TO TOT $(Ril? TO ?R £ cT'ft
TOTOR te fnete v^cTO cRPTf te 3ft? TOTO ft ’j?9 te RH atTO ft
tout
1 srote te
H<J<^ H TOH ?te fTOTOT | ^j]
1
^^4, 3 cTgfteTOT
^R i fftrote tea ht? te ttoto te te tot Rr tea to tot? V-TO.to./vate.
■s^ te TOT ft Hte TOTO |
TOTO ft TO31TOT fte fft»ft TOTOf ft TOITO te TOg te TOTOsH TO<lTO; TOcIR'I TO?qlR HTOT
fTOTOTO Rq TORT TOHTOTTOT R1 Rote 31 Id R da Vjte te fdMcn te fed? TORTOT? ft TOITO te tetR
TOTOTOTT TO fntel nRT fteft 11 R?T TOT ft RlTOT TORct TOTTOnT TOT TOTO 1998 te TOTTO.d R1 TOT
70 dte R I ci [ten \3d<41 aMfttecT dgd TOH ?ate R I te4?? q> HTTOn ft *4 61 ‘I
TOidl TOkTT ft I TO
TO^it TOte a TOH a'lci TO? RTO xn In I ft I
“TOTO te TOTO TOTO" - telte TOlR ('TO WTO HTftelT, TORTO)
3TTOT—3TTOT 4 tl*j? ft illtete te TOcTte TO?ft TO Mdl TOeiT fte RH stte ft TOTO? te q>R TOTOTn
R I Rte tete 35 ate te ateter toto? tete to toth (tear tort te i fte d ft ft u (ft ten 50-100 arte
oTO TOTT fcTTOT TOTO te I ate TOT? ?TO 3TTO1HTO TOiqid'l te TOTO TO? (tel TOI I teft ate dintei'l ft TO^)
fte? ftrote fte? Rtf te cthtto ft tort te ftter [ft ft tear to?t toiai R tjtottot TOtterr a xifcai ate
TOT I TOTT ft TOtR te MITO dcq del fttft TOTT TO HTOdId ftt MgTOcil R I te?—fttt Uldte'l te ?Rt?
H tete TO ci-sn te STTOiT qte Rial TOf 3fr? ddtei
Rin cite I ^te <lte ste TOJT TOTO
teddtecl Rte 6 I TOT: R" TOTO aKK 3 dte cte I
q|R\l n Rte te ?TO TOT
ftefte TOT TO <tte te
tet fterte <tei §$ R | eiten ?JTO TO?a
tej tei4 Mee to Mate dRi Rte ate i
§dte TOT jJcnlter te <JTO te TOTO aTO tiSiaal TOTTO TOT tel? x^-TO TaTTOT ate R I eTFT TOa
at TO? ?R R I TOTSTO TO? TOdR TOTO ?R R I Rutte ^TOTO TO TO? ten TO? TOT 10 ftecit 3TOTTO (TO?)
fte? ?TO R"l ci Rte TO? TOTO TOTO factel tetR W nlRf | ??T TOTO? TOTOTO? gTTOT TOft TOTTO te TOTOte 3TTOTTO
qtetea to?to fteror roror R to? to?tt Rt 3t?totottotto R i toto TOrtete to toto ??t? te terro? totete
sate ter aRt aicja fte te? qdin te totto, totot tetR tet? totot tero toi^ 11r
tear?, qtelted 3ft? TOTOTO 'Jlhiult TOT TOTOTT TOT fqT TOTO ?TO? TOfte? te ?TOnt STOaT Rt n TOte W
terR toth to? ?rte te toth te TOrote tohtto totRtoh ftero totoh tot i date ate ?h tottoto te tot? te
fte TOTTn TO?H te lei? TOTOqT? TOT ?ite I TJTO TOHRT te VaRia
TO?T I
TOtete te toottot fte facte 15 ftefl te ate TOiate tete ter, crfteroiftete aft tototo to? toR R i
TOTO <siqc? ter 3TTV T?TO dlte TOTOTH TO nte I TO? TO? ?TO te TTOTOT ?te TO? ?HT? TORT at TOTOTO TOTdt nt
nRt
to?t te
ctete i ?jte te hr rosjte to? te toRt R i hhth ??jte te ’jtoj Rr toR toto te R i
TO 3TTO TOTO Hef t ?R R I
ate tototRtot rote tevim te srtot ?totht rorfR?" - toi^?ih (te.te. te tefte toth
dglltel)
TOitete te rote te torth htcjh roar fte TOirote tohitot rotent ?h after n ate tortor te ttotto
te TOnTOnviTO tj?2tt tetet h iter te a i ?jter toRR te totR ctete te tottoto^to ?h ■ropfite te ftetet tet
4
ftvIRI WF RTR oft R? RH ft Rft qft | Tnftft ft 3RTRT
RRTRF In ZJTx ft 3n5 W
fq, RPR 4—5 fqR 46ci fW 40—50 eft ft 3ft 3R5 4>l^ ftc RR ofR 3>RT RR] fft
tp
3HTR
Ptcrii I ?RFRF <Jq, RT3 ft 4-5 eftft ft RTRF ^F- 3Rs ft | ftfftR FJR Rrft ft RRf qy^RT f 35R R^T
3nR fftcnl St-ilvi Ptei 4II ^4??
cp'i-ift
W ft 3FRFRRT <fr Rift ft ftt
RIRRT I
3FHH4I-SI Rftf ft1 3pft 8 fqR RRR R'e<4lfti if ^61^41
RTq ft et RR 3ii«n«||<^ ftfeFR’R RFRT RR 8 ftft 3Hlwl «sqni W vft 3T3 fftclRci ft RR ? I
Weft 3TR ft ftF 'M'xi RFR RR W 4<sll RR RF3RTT t fft cFRRR RFlft HfgcHlQ 3F7R RTx Rft
oiflciH RiR ft cgMlPci ft1
JIft ft ftf xxsn ft ftP (ft.ftF.Rei.) ft el'l4l'l <r>i xifftd ftft RR eifteRT Rft fftRT R3iT I ftf sfTs
vi-s—(1? | q §RF Rjft ft 3FT31R $ti0l cFTR ft Rft ft I q|«iiqcp Rftq ^Rlft fftR ftt Rft Rq ft1
Pl Wei 8 3TRRRF ft
e73FT fttdl RR RiciRlcil 3TR ctq> ^R ftft ft 20 ft
\xiiiqi oil•q'l Rft uil-l ft 4,4’I ft I fft-lP 5 Rft ft <PH 3| 1 R, ft 8 Rvft SqR 60
3TRn7 3W
Rft
5
oufqvl wf*w f |
Vq7 aft? 'WTW Rrt<f01 -IH
■5 | c,6etqixi,
1? W q'lxi ^RF Ref n Ppqi I FRF WiW ^F aH WF 3TTa
W ^XHXI I $'H U^l<ld <F?T v-rt —1
fvFR n' qciiqi Pn ^RF <iiq (xsjvjxl) ^F 7 c?l4i'I '3?F
Rktj W s>lxdl qJ?9' sfR q?iLl'lquI -igl qfcs5 41HIX1 &T WFRTFI
tTq -]
"*TT ?RF qlXH q>lci
<RW
RFTcF ^ciqFl ^F 3
Wf 3 q'cs
'’j? ^F tiHI 4I4I I
wt <n jji41iji'I A ■’fr ReF R^la «iaii cf?F vit wiR^i 4in
S<F qp|Xul 31'41'14’ Jl 14 qicFl W Rm4I 3FT
ciWi
wrf sft i wr qFF tswt
W qRqT R41 RF ’’ft Pi'll fqRn
^fq? cRF ’TRsFR 3 3TTcT sFF g'tifei^ ,W fq’TTT
f^rn cfrffF R?F "^cg
I WT <n RRW $ft 3TSR
I ci'l-H41 1500
|pf.I x-ixqnxl ’Him ^i q'lcicl
xj^nl <n I
I
ci STR RHR aF I Vq5 cTF 4^ fqHT RF HTRFR ^f c?R
cPM4! Rs? RF
3] pt 4 Held 14 sJF Pb< dV P rFT 4,<4R 3FTRT, 'dceTl
3TR '3’14’1 ^^4, f?F
1
WTW 3 ’ft RRWft illuF-113ft Rft RTWT Reft f^ftci t RTF ^4 3ft 44140 ft WT 3ft Rs
5 | W 104 cRRf 3lft ftW RRs Rft 6 ciftftf 3ft fttcR RRs RRFR
fciR fftft Rft 6 I cFftftR RRTR
qft R3RR RF3 ft RfjR ^R t ftF R7>ft-3Rft eft ^ci<ft t feRF 3R ?RRT RRTR RfF R?oi R3 R3RR3R
■ftr R6I CRT WRT W Rrftftft ft RRTRTI
Reft ft UlftlR "ft 3RR ft RRft 3FFR3 4’lftq’H 3ft fftRoT fti ftRR SUdifta ? I WnR SRT
Tjft 3Fft 04? RRR 3ft^ RRS 3TRRRFR nft fftRT RRT Fft R? 4’144’4 RRRT RR ft 4dl4l RFoT
R^ 3T§R 3ft Rtcft ft 3ft 3ft^ -(R3T 3^7 ftft ^R, R1R <4^1)
5
fftqjft fftft RR ftsft ftfr ftt fftcR ftRT ft 32 fft.ftt ^Y t.
ft fttqR RY RR 3Tlft ft1 V3TCI RTRlft ftt Sl^xei&T ft 3TRft
ft> 'epixRi 3TrfftRrfftR
ft 31lftM
ft fftq
-~l^
eieicRi (RR fftfteTT ftReft RTef). ftR’Jei 3ftx YTRT xsTR ftt fftSTT 6 I fft^ft
TRp RTR
ft § 50 ft yRTRT eflR W ft RTeT ft YTRT ~ ft1 RST ftt Yjft ftt ftftd R«ei 3 RRT xT qftt
qjw ftt ?ra ftt rtrt viiqjn rtr
rs
ft |
ti<*w ft Rvsftt ft ft ftd
fttRT - RRT YTYRTTft coft-qix! (Vfft RTR ft YTScT Wi ft ftlxinj
R.R. RTxeT STTR fqSTTR Yllftlft RRYTR-ys, YPTR xTRRT RR vft.3TR.qtT. ft y.c.-.itpft ft YTfftffteT
ftrv <R 20 rrry-02 ftt f^ra^ft ft Rtsft sftfcp ft vrft rtr rt ftxr fftqi rtt "-x=nxi ft
xwft
trt ftteft ft rtyr xraf ft ft1
RTRxt RRR ft 35 fft.ftt. R7 TJR RTS RlfftRTftt RSjeT t RST ti&R-Ul 311fqquftftI ft YTTR-YTTR
Styt^Rtei vn ifci fttY [ft wri sft R RTT YTTRFR RR eft etHl'l ft ftt RY g ISYT ■‘lift R RR YPft Rifftiel
RRT ft ft|-q RTlftR 3TIRTY RY 3TRTY f-l'xi. RyTY 31 let I 6 I
RS xiqro ReT RftjRR [ftei'l3TT RRTReT eft RtSYT -lift ft JI-UI I RS t#ft xT 16 fft.ftt. RSft g I
RST ft RR RT YTYeTT 3RTSfttR fttY RY RTYR g1 RST eft YRTRTR RTRlftt ft RRT ft ftiYiR RoTRT fft
[ft Wei 3 RRT ft RlfftST R gift ft cMXul RRRR YJY9T 6 I >461 e}T ep? eft'11 ft Mir. Mtilc| 314ftl yiftin
g ftfftR RR RY fttg epRei ftqi Rgl St RT Ytft ft I
RRTReT ftl 3flY ft qft UH VRYRT ftt ftcftt ft SYT RRq>V fxRfa RY ftlq RTdRid Rftt ftft RTTRi
q-ftifft YTYqRY ftt 3TR ft R eft fttft RfgTReTT ft 3ftY d ftt RRTReft ftt ftt? Aftei I
fftW 3—4 RTS ft RfftftT RST fteTRR, ftY eTRT 3ftqft ftt TO WTR R^RT qR Yft ft | RST
etep fft [ftuft 3—4 RRT ft ftlft ft Mlftl fti fxRlei ftfttY Rftt
ft | eftJft ft 3TRft Mleie^ R?J3ft ftt
RRft ftf glet RY Eft'S [ft<41 ft I efrft RRJ SYT ftlYTR RiTeT RR RTYT RR ^ft ft I
“SRTY RY qft RR eft Reid ^XU eft 3RTY Xsllft qft 4? W ffteT RTTR | 3Rft esl-xfl
Vslft <4 ft RY Rft ftX f*rar ft qftt ft I ?Yrft Rsft RR ftY RY fftYRR CftYT) 3ftY
eieiftdi (q<t> xjtsftftxT) RRYRfeT) YRTR5Y ftt ^yi IX Yft st [" — RR> RTHTR
RST
fftSlfftRf 3TTY RR|RelR>[ftqt RY RTSRT RT fqT SYT ftR ft Yjftt R5T RRTxT fwft 3TRYTT
RTS ft ftt St ‘141 RT ftftnR YTYRYY 3TTY ReTixTR eft fttftt eft S'RtyiH ft ft I
RTR fti eiftl RTRef ft RR> V3TYT RRYY Rft eTRRSi RTTcT RTY cTlft S I fvift "rRlft’’ RR?T RRTcTT
ft I ftYT eicpfti ft TTlfttR SfeTRT RRTRTY Yfft qlytix ft qRa ft | ftfft>R 3TR YRTxt '-ft Rftt ffteTeft RRlIft
RRT R fttft ft RRYR RYTftt ft<4IRIY ftt RRlfaei
ft |
ffteitsn RTR ft YTSR cRlft Rft el cox RScT fftcRR Rft fftRfft RR Yftt ft I Rift [ft YTYRYY RTR
eTRRR fftfft 15 [ft ft ft YTSeT RT]ft VpS fftq ft | ftfftR ft RFRRTR^ RR ft RST Ref RT Yft 6 I
HtleM RYR ft <lRel 3Mlvi chlfttfH ftt RTYR fftRT RRT ft | RYTft 3TRi'fei RHiftf RR Rl-ftt fttRR
TnT cplft [ft 41 ^TRI ft | fftR RY (VJRS 7.00 RRT ft RTR ft 5 qft (Ten) RTTO RiYft ft RTR xjft 10 [ft el I
6
(PfqRT 3pY
P RRRTY ORYptHtRRpRrRYtPSPPtSpRRP WRY fpTRT
PlaP RT Ypt PioT Rp RRR 3TH
fqRT RTR RRT fPP P Pt RRiRR. PiHlPiRT, R?Pt RYcT 3px RRT?
RRT TfTT ntct Rt Rd ci IA 4, dHlpRPt RTR 3<pY pYTTRR RpRT R> vW^<l RTR P Rp cRR Pla P HR
P ytrt rr i
H.TT. RTYa S1TR R$ilH xi AA, qq^H— RR Tp RR P 21 n<W
gHI ?P xHxi q/iq> Rt HI Pl
Rfq R7T RiYT fqTRT I RRn spR RTR P fqRtt At RtR Rp Rpp xaRY H 3TWRT P WRY R YRTPlR
t-; 11 Xi H Rp §XiqP v,iqq>|p Pt | CTpP'l 31 <p x~i I a 41X P 5i I Cl ^3R PP <P HIH c?l Xi STR c|cp $xi 'liq
P 5 RTR RniH gxjP 3tt? qcq p Rtcf Tp g6 P RP"i Pi’ilR'Ui 3ltx <phIHuI xi -ci RR |
UR rAPt 3RR Tfjpf Rp
pt gYT RTR Rp fMcT At I PtR fpRcF 2-3 W P YTRT qp PPt,
SiTRctT RRT hTRTR RY RRiTYT RTY Yp A I cPTRR 10-15 fqqxT gq pt Rgt YTRR RTR TTTYH |3R p |
Visa RRp Rp R? felPi (YTtRpt RTR P) t fP> 4 fRR fpRft RTR R> cPAt Rp hpY 4 fqR
3TRT Rfq p RRTT Rp XISa cpl4 RnI vilal P 1
Xisa RRR cp 31-vi‘ia vtiqpl Hid P aieiiq A Hl ul <5T cpW
fqPt Pi Pt vJxn §3TT P I ^Ts q>l4 fpRflp PlHlH
m cH VsT P I
q>iq fpRp 10—15
gRT qRqRIT RT TgT P I P<p ^R q>M qRp cfp
RHTpt <p caqwjq et'l H | Pi <Rp tR pt cblH fci a I RT TsT P I $vlq> qqyi R R7? q^kqpci 2 R 2 1/2
[cpei'l 31aiR yfa HRqN mARh RS Rt?T P I 'JiqR Mlqtlln 10 Rail 3TnTR RT p I -J lPldl RT cp|i|
P vtei'n P RRn P RR Pt R R? R'-l qRp <|P a<1H apt RT I PRa HR^xi H RR R? Rl<4
qpx-il Rs TFT P I
Riat hR
RTPtPt P 31<?al<<U 41RHI <p RlP Rxaiq Rt RRHH 2 Rp HRH q-i P PfqRT Rp
R1RR R? qPp RRR Rpf fqRT RRT P 3fk Rp RTpR R? 2 "P 8 HTs ?TR Pt 3RTR fpRT Pl
RP^IR ^TRRIT P?H RIRRT R?T Rp RRT^R RI Pl up p R^j
tjcR: ^TRt Pt RT Rp P
2 RT’4 W OR 150/- P?TR fPeP 2p I RiPW P RRRT Pp X3pt qR Pi RRH RY fpRT RW P
Rg" q^g RY fqj vi-iR fctq YlfPi YRRTY P apf Pr^ p |
^rt RTR <ot RRfRsRT 394 P R5T qp^ Pt RRRR qp YjfRRT RRRRT Rpt P I eTRHR 9 fqF.Pt.
R? 3IRxt cp YRTYSR R-S P I ReT <TR Rial RRT RRs? P |
^Yi RTR P IRH 5 cpRT Rp
4 Pt Reel. RYa
3RY RRtRR P pt Rx RR I
RTRYT RTR RT RRT P 15 (R.Pt. Hgci P RTR Rp YT5TR Rp RRRR RY ^YT =Tx P RRTPla qP I
ReT Xl^lH qP gRIH 8 MR Nell R 3JRTR Rp YPRTp RXdl p | Rgt YTYRRY qP 3Rx P fqfpR RtRRT3Ti
Pg 3TRTR R>R RRRRT RTYRTRT Rial P | RRT ’^RH RTfpRT R RRTRT I
TflP RpPt Rp P3T P PtR R RTRT P fcTR Rgt 438.60 fqRdei 3TRTR Rp RRYa P I clA>H
HIR 100 fqRdci 3TRTR-Pt YTYRTR Rp 3TTY P fpRT RT YeR P I
RYRI'S pTRR Pg 3TRTR 42 A £l I ci qt P RT YjR p | gYT Pg 70 PHdei 3TRTR 3TkTT P PR5-!
8
ZFC <<r>ci'i xi 3in IF vodl A
'itfl 31 Id I I
Tpi Jp 'Jew F|4mIcH 31f?TFTft 3ft *idlM fW 3-Fy -tcivcx 3fFcit fiFH
«iia41a'
4t Fxi Fcl n
I
^'■6in FTTF ftp Mc<lF Mxllild
Fe 4t ^Pii^ci Fxn ft WF
fcFJ cFPTT 1-3 ~ WJ 7F? fqTF FTFT cTF fwFI 11
Tn? t ff? FTR <o FcF 3FT3T
?? 5 f^.^ft.
H Fct vJST wfef firsft <4t MgdH ’WrT «p 3BW F? F v-y xst 11 <p^4t< A 4d|i|| fq,
xi'twix Fl ci'('-p X1
'”FF Httf 3fh ^iWt eft ?Tfw ft VgqT 5 sH FH ^cFu F’fkcil
Hft
ci ci" — <t><?i <TdX,
X|vr<4 XiX<p|X Fl 3HTF FH ft dMeia? FxqTFT •,mi f | F^FEx n F?T ftfr 3<<I<??| Fx<ixl
(2003) cTF crTHF 75000 FF Ft FFT fqF FFPTT I
9
1
\h4q2TH, ReRPtq> <PMi[s|a 31R qlHNRRl <41 Pm coH
5T?f v> RRR 3TTRR dRei<q c0X<4|i|l
Rl4 I
2.
RrRT cp q^ fcxn RR hwct oiR RR t RRTRT R714r RR tjf t WM RRT R% RJRST RRTfqd
til A a fqRT wiN I
3.
tj<ai fPiiiqa Sv5T 4 tiaa RR 41 *H <r> «mci R n I qi m14R>n RcilRI R14 I Rd q^iRqiH 4
Rvit RRT Rt tun RR 4f 3TRRR R4 Rl4 I
4.
H.R. <p tni RTRT 4 q>41qul <p RR qR dRia dq4iul q><qi RR d-d 41 Rmc-I tg q4a M6ei
qR vn I k> |
■ 5.
RRJTW-41dl4l
RRs-ll, Qiq^-d VR TpTT 4
^4 41 dl 44 RSReffTR uil’q q^qf^ vTR I
^pq v> Rin H KlidqqR 3lfS|qj|R41 v> RRT— RRT 9 q i q a M P P Pl 41, 4? dtqqtl trlcul R
ti&in'iqvi'u qq 41 dPdfeia fqRTT vir I
6.
taiEj RR tiiiiRiq’ tTpETr.’^pR-s; jFRqTR afq qIvinI3TT q? fqRTTRRH 4 HR RT Tet [qqjfaql
qq acqqei SPiTq vi cY fq>4l vTR 1 qq'iRp qlv.-iiaff qq qdHIn fx-SjfcT R^hTH -qIqtci<n
3ilq<! qq titltix SiqHHnl 6 I
7.
tl41'cq -qiqiciq 7p gHI
tRqqt qff tslltl ^8TT -4441 q|vini<fll tR fq4 RU Sil.cRl
RRcR TRRf qq cqqnl, tqyn) R 3FR Rqi'll *R ciqii' viik;. V[4 ^R{
qi41ul'Jinl q?I -wiI.'^d
[q>qi vqq |
;
8.
?7 RRT H oRpTcT RHRT 41 31iq^qq> RTRSR
9.
3TRTR RsRRI 4 R’TeRI 3THTR
'eM'C al'! HV ^eiiviI PbqI RT
9aqn Rdtul
14 q^qi <JRRT^ RR |
TTRR fqRt RT
SUM qq HT^T RT(
I [qatul 4 3TT <61 R-sq-q qq otRlei 5PW 4t R? PbqI
I
10.
' IR q I til q I 4 Rc2R q?I is! c I q] cp 3TqTRp RR 6 in cp RRS RRul RaR RR | Rfcf vRR
73RTR Rp tiitiiqc: RHTRR Rd efiR R< 4 Ri RR, RTalRT 7R 41 Rift ^1
11.
RT
6 I
'14141 qq RRT H RR TRi RTHT <41 <jql RR RRdTRRRTT <p 3RRR tR qqfleJRR fqRR RTR I
10
cn
J,
•
shuh qft R7rTO 7® ns TOTOh
IlTO'lUi-b : TOfrJ
aftw irf- w w stRfw fciw ir
11-13
Oilqiei,
TOTOIH 1 7) 2 «lTO TITO : TOTOFI
qp)
TOuC-7 2 71 3 ?bft dTO : fcJSITH
w
TOrITO 3 TO
?II'I 6
-bi)
d-b
:
71HT7TTOTV TOTlfTOTTOiq
•
•llftcIHl') TO i|Ri)w ft iflbl.-I nil 3||fti|iR
1.
tiTOtoiip - 3iT?rr fftn
•
’flTOR 3lh di IF <bl 3|f?m?
ipi-^I’I
ibiftmTO
TO TOTO 7i7<bR 'TO
qfTOl <pf qft VETO TO) GftTOdlTO
W^fZrfzJfT : TTFfTOjT vHvilf? TO
ciciciR (TiT.qTO.) tITOto TOra (-bisidTO tftto) i
2.
f^\ |<)
TO qn.TO. rtTOrh (TO.TO.q71. swan ft ui^iRi* TiFufTOn) &rt TO
fTOd TO) 71H l *11917
wft 1 TO.TO.q71. iTOTO viTOTO ttTO TO 37399; TOTOTO (TOeft), TOr-bn
TOciqTOe TitTTTUTO (3JTEJ9^?T), Rd 77JT7-27J 3jfTOjR
<bl4?lleil3jf TO) RmIcI 77 y^lel<b7ul
TOTO 8:30 TO 9'30 TOTO d<b : TOWF
TITO 9:30 -iTO TO
:
TTIT^fcRJ,
tftlRJ
8 TO
10 uTO
VICTOR,
:
717177 TITO
13 vjjl 2004
qTO
3.
qc?PT bsivh (qq.q.TO.qn., heri^) TO ^rurq tTO (h.h. TOth Ton) i
VJTT7I 1319197, -TO TO =91917: $71 TlTOUell ft Kiel ft RITTOr ^Ift.
laltl dcMI-ld TO 17n9R ft gq 9fTOTO7 TO TOuRT q>r UHtTOiR 97 glbb
wTO TO TO ft
TOTO I TOfTOn irTO ft vttTOj
tTOs. OTOTOTO nfTOTOi
tot>
TJ7F 10:30 TO
71977 1
■
(q.q.), 7171*1 Cpfci 71 (ft let (96171-$;). 3lf<sl ci 9l7<ftd vt*19l<ft TOTOefT H’ld'l,
tpitTO cTOTOvWi 97 TOTO i TOra®-3iTO TOja (uh trrwj 3jTOfi),
<J5t4jFH
TO® : tTOrI 3141 did
TOrr jpTO (TO^T.qri.) : 371 -biTOieii -pt ■gro rTO
TOT tfTO.qrr. torrt TO geR TO 9lib<11 TO 5x 1 -pi ngieft -ft
WdRi 1 RiRiijs gt 571 m-pix gt: gft.TO.q7j. gcR TO j-u*n-i, TO.TO.q7f. TO
TO-ITO* TOcJ 1 TjTJanTO uTgfft fTOn TO (TO.TO.q71. TO ?TO TO TOTOn)
tttTOTOf
t, 51 cd
TO *9 97 3®<bH qft 'ltd'll 97 3lfTOl77
7lTOlv1<b : RRael
$<Mld TOfTTO TO TOeJ7 W W
3IFRI7J: TOleH 9lTO
trTO tTOtr gRTOw stTOTOt' 4) cnTO
qci.). RTO 3 (tpi.TOqTTO.), 7J1117 eiiTO (qTOTOrR.siv’j.). st^iuf
TOP cZiPki A ell <sH cllei 71^919 TO
^geTT TITO—
7^' TOT to pit vron TO 3,
wjfci ?to
trp! 3 TOTOnr 97 fTOf 1 tiTO TOTO'iui : Tym totor (9TO.TO
719 I Vi <b : tTO Hq< s-l) el I, R*lTO, -I-I 1719,
TOcf 7 TO 8 -jTO cfTO:
7'1’1 q<7 dlR-ftPl-lif -bl 3|l?l-bR: iHl -bl'lvilell ’bl IJW( uftv’l ft uft-bl
TOft) in^i -jpti ftg -i>lT fftRlft t)ui’IR qjl-TO^fifii ailtjfftqq ift ?n(ftef ft 1
fftfYlH jjt 571 9U7R §: W?F5 7TTOR <17| 4mI'IH TjPlflTOtn 3lft)pTTO
Ulef 7> TO) ’) i[7T-fi SFFlTjfl. ROel 7II6I 71-771 TOlft-tff SRI rl’IR
TO
proq aiRPran n5) urga.- TO
d>Hd, VrTOtT, 719^9, fftqrr
\z^*
fTO^r
tttotot 3 TOptr TjRftTOdi arfTOm tg TO aTOro
TOlW : 3JW
.
toTOTOtot
571 m TO 35ft 97
trtTO trit TO?9 wtr tptch TO fTOTO ns
TOh T
o 3l(TOlR 97 91J19 I TTOf TOTOn®:- 7(79 TTgOR (TOTO TOTOu). q.
irraei (TOtTOti). TO. 3i?iTO tri (q7.qft.31Yq.-7ft.TO.q71.1j.). trit ftsur (Tinft.
TOTO?) qft qri.TO. girai (7T>nfft<i) tiTOutto: TOftqr quira (suh $(TOijt TOgerj
7TT$71 ftcb-b) I
-------------------- ----------- ©--------------------------------
3 Fl TOT 6 :
cbl<Jsb<H
Rki
sftV
’
TOT
ct>H
•
FTHTm-FTR TO^TTcTH
TOTH TOT 3lfeTOV TO 3JTvflfeTOT
FWPjTTO—^flFTHT
cfTT 3TfiWR'
. ^TOTFcfTOfeTO fecTTOT HTOefl
<141 vi 47— sf. 3i Ro tI-i hhtt 3rtv
T? Tn^Td—^pReTH
1ST. 3TTOT TOT
11 d 13
•
2004
^TTE-fr ’-■RFT, ’-frwr
•
<pfe TO TOTHTT
44lvi<b : 1ST. fe4?T 3TsfTeT
3IRtTOTF 3t1t TOTO FTOMfaTOUT
FTHtTOTO : vYhT
qgjg fen
vjtottt.
TOT: 8 FT 10 TOT deb
tj<tb
fedlTO 11 FJd 2004
FTTH 6 TT TOT 8 TOl HTO :
10 vi <fn. 1 to! tiro TO^Tren to
TTOrad
:
3TOTT fSTO
7flcT
:
H.IT. HTTOT STH 14$IH TlRfcl
TOTOcT i-TOPT
TOT 8 Fl 9 TOT deb : HlvH
TOT 9 TOT Ft
:
FTTF^feTO TOT^TOH
TOTTOTO- TOTO 3TTOTOT
:
TPJS
'bRdl 41'111'1'1. 't’lfeld ‘ll”<llfc<l'<t TO MleT
dbll'IH
TOTO
:
FTTH 6 FT TOT 10 TOH TOT '•JTO Ft gfad 3rf>TTOH
TOIdR<b TOT TO TOlt
eWI I TOlcTO 4 f^TOfeT^r TO V# TOhb TOTO
3rj?W t far TOTO TO>
nferfefe STO
1ST. jTlTd TOT! TO^I.
31TOST H.5J VITO 3TOTTOT TOplfcT
<fld
TOF^rfeTO TOJg gTVT HWeT 4
fefero too 41 to m <i ?!*i
: MvU'b?0!
4 TOTO toPTO ?f I
^TOT fed
:
?tRto, 12
TITO 8:30 Tt
:
VTIeTT TTd
H«l*l ITO 3lHlll">ld TOI'll’d?
9:16 6|<fl d'b
3TTTO dlRfel gTVT
Tbni?IIeI13n efl feffef TO STTOjfvTTOTO
<bldl
si. TO.41. TO>1TOTO, efel TOdcT, 3TTW TRI
7f)d
H.U. HRd STH RsIH 'dRfcl
:i
2004
RFJ? gTVT
■■! ■l-'i '•I-'
TJTO 9:30 71 dTO? : TTdinTTOV TO4?TTTOTJ
12:30 TO5( TOT
1 • z^TOl
HtTOI TO 3lftWTV
tiqlviep: igj. UfFT
TO 1ST. TOTOTT TTOTO
•
d.'-l'l 'lIx'TO'I 'I 'll-H-i .|,|
Tfe'lvTeb : 3T?l'lc|> HR?!)
■.lli'I.ITO
1
2 TOf cTO : ^wH
• snferofi nftilCT 4 4ito to 3t1Wr ' ‘
effagV 2
3 dt TO : fa^TTH
: to I TOT : igf. ^feidl TH
------------- @--------------------
-------------------------------- @--------------------------------
& jrfdvT 3?fc cfiTJT cftT
1.
uH 3lteeEH TO Vl^te TOFTOI (NAPM)
2.
HKtl STH PlSlH Tlftfcl (BGVS)
3.
TOT WTOd 3lPHH (JSA)
4.
31 Ry el ’dl-idlil vHqte df^ell SlWcT (AIDWA)
5.
-1?Hc1 tested 3HTO ?fe?H gH (NFIW)
6.
TOpH dfeH TOTO SlftelTO 3TpHH (NCDHR)
7.
F£H SpITO eff dPeH
8.
^KHd tete-i tor dtera (nccrw)
9.
f?lgel gpm TOR fWel fteftel (PUCL)
10.
SpHT TO 3ll?ITOR TO VFpH 3rfteH (NCPRT)
3if$cfrrv’ vv
(NACDOR)
11
13 vfjT 2004
VFteJ Wrr^FT
1.
31paei ’TOR 4'Wl'Sl Hfjdl flfaffi (HJI.)
aflq, ?fte? gte (h.sj.)
16.
ftefte 3?ft ten tete aw
17.
TO ml^d H^dl dtel ti'ldd
18.
H.n. teitel tei teitetn
2.
Piro
3.
dHdl
4.
UfH
19.
5.
m sfte
20.
6.
H.JI. "HKrl sIH Pl slid dfte
2i.
tel TOitetero3!, ster
iJijto tera teitei
7.
q.n. ten urn
22.
8.
H (<IR^ 3lf'*l4H
23.
9.
TH d’J 4 HHI
24.
(idl'd Jl'lld detei ted
10.
diFjfe hM
25.
S"tel PdOdfl
11.
■Jl'WI'Jl vim
26.
TOlte
12.
M'llrl?fe elm ITO
27.
TOEfl HTO
28.
HPT te (iPhRi, terteIR
13.
(1414
3nRciidl ■di’jRi tero
4>l4sbH
^TTEft Htete, HtqieT, H»TPP^?T
14.
msy
29.
tetetei m teitpr ten, terra
15.
tel
30.
to ’rite dster tef teifa
: fiW jfrttld, dn
xaptef
•• 25557B9
cp^p vte?p arra)3ph
<-8/4, Rftei-'TI, HtqTH.
: 5294378
[I
I
i
ainWFL H.TL
i
Vpflupl >'bPlleUl : ‘li-’IU <i ?I l<HlI-l '!PT1
a—<?. r-tilllC'f
u'qX'Hl U.lelbn. ’H'llH
: 2z">Sr:8l.
: 2G6C352
•
41k3Fcpf?r f^eA <ncTl
^qTTSff
3TWFT
vTicM
W27 3?MH TMT WscI ■U’lvPiT, H.Vl. Wl mi< £KT 11
faz)
Ri^c;i-Tl f |
TcP^a ^trra wq 25W V7W WR
<-c|K-2ZI u?|q-| <|q| <n<<T|
2001 2fR tf<?T H
3Tf?j25R 11 ^rfeftl W?«ZJ
sfil W5 VeHT ?V ^rf^vT 251
3?r
Mi ci I W< T?
illuiHI 2$ clgd
T-ciR-ZZJ
fviell
•<<«H <-( Pi Pi 257 RcM ^37- cTsn y i4lul 'rtl'i HY — 'JlH xOH^ RTTtRT <Hl41 "'T? 'jTT R>
'IM H ^-qi<227 <5 cp|q$|>*{ cRT IMqIMq"1 <nVH
*-ic;c; cj^fl I
TTg 2} ftp Rf5’-$fl<5Tul 25R, Rleil <<11 <22} 3ITR ,{Jl41ul
q'lvUI 257 RR54
'i-iplpl gTRI <i^|ui ij x-qlx'-SZ] cf; C|>H cbxiI■£) wil^ I Ril'dH
§ Ri ’ficl H ^TR-aq c£l ^jcPJyT 'yRtlI''Tg^H <f5 feR
X5H 73R221 V5Rp
■'HgHcbiafi
WI
■'H^JIIcHcb
vIWp
cj XTcR
RTT2T ’IT’fPT Wq Tfftirl 3WW^I
cpT FmT 31 M W? f |
3 HT<
c41d HV '□t'l'I Ri|l Tl'm
7ffa H
WR2ZJ ^W3n 3TR TTWTfi WR22J qRPWff TH
I
tflvHI 2Rt w fWlcl
VRM RRW
^T[I R 'jy'r
zpt
cn<G TfFHI
will 2n | fvl'dcp 31 Tl' i c —
vjji 2002 d<T> F? 'IK ~ W vH WRW VSRp
>
2002 cT? g? W; i
>
tjyi Cl<?|cp'Ml dT 'IjfcRi
r- 7rfcj?fl 'if^cii
dlH <JR 3’ITT]
M<M
> fwj. cfH Hra ?W
1
TTSl. TpfcRft hRhI M SJT^ hRhi t£ ftfZ) rftm 3TT?R
xJMcl£RTT
<-
q?ST—<p?C M
WT? 2^ Aeppli ^Wfl wryrtl cRWpH TTlPlcI 11
i-K'-Plx fiixl ■cleiiS <■'■ Re?T <<R2J vficR ^7 'IHcTi 4iv--IJ <p >3c;^2M 257 Rpn-ii
wn HT 7R5T 11 ?H25T 3T3TIH
hw? Sii33n. ’i.q.cii?!^ i-.-^
wi
ql^fTH ^E2TW5I
w 3H5 Rncl'r 3
3H Rimxi 4?<
TR2JT ^WR.
^fi\' gr<i Rmi
> 755 Tim 31 cfH 7i2lfft35 777723 eft^
7ftI fftiTift
TTHTT 'eft
ww<fti
SFvFRT zH3 fcuft - 6|<c|Ffr, 57^311. TsH'lld 3fi3 <-317 eft 3PJ7T, $Ccil<K Tlc17l<SI 7
5^3 ift >#s wfsq
73 31ft
trit i
r- TTeftftql 77R27 ejft^ eft OffT 311ft Tift ft ft) Old TT' KTTH ft 373ft j^ft
7ft fft> 775
nra yi-’il^ 37112-1 773 ft 73ift7 ft 3iii ^vm uplifts u<ir<«-ti ftft7 ft fti ?11
ftTI ?R? 31 serratf 7ft fWft
1.
ft-EITT
deicll^l 712lfft75 731323 ftftT 35 ft ftft 33eft 3113 ^NlMIdl
"IKlefl UP1P137 13I<°-3 7|ft4 ft ft 'Ibl 31331 3lk 3113-lft
77131 313h35 771727 3^3 31 31 373 7717351 3113 fftft ^Heft
2.
5TT3.3TT 3cpc<i 3RlfH35 33WI 33^
■fii'i-D 3124Pl<3 73R23 3>-3
31 313 333RT 333 ^dRUIdl
37 Tff3 d'leid^i 333 3l*i4l '
3133Rq I 312TP135 >131-<23 333 35 31 JHc| 3Hl3397 333 <113 R31
3.
3333'13
4.
^"313
3i^3:&| 3T21Pl75 335327! <3^ 3;
TffH ■u.^iriRi afft 3FT33
Mlc4<4! 3I21Pi35 331322J ct'>< co 37 373 313731 3571
=31 015 8 3124ft<0 x-d|<2ZJ cp-3
r- Mc73> 7TT3 H 31 371 337 H3
16 J|1 cjI 351 333 cpx 313<?1 C «^1 q?t TT§ I
J
^73 vl6l 73 Rltiei ^75 37137 3 77^ 751
§71 Jlcpll 16 7771 7?5 141 3f^cil3lf 7?f 7117575 viHcbRl 77$ 773 7>
^37 27 |
3} 7ft 7^ I
> 77735 773 7> 15 31 30 H^cil 7 ^377 TTJ? 1ft 3727 771^ Tpeft 753 37ft W7 PWTcft
gill uiMcpi'ft ^cpccJl qft 7^
>
773
eft 33SJ
ft7fcr35
vi 1 'I cp 1 -ft
oqfcM
Tift 777
3IW17I eft Tift ft 317 371 C
vpft
73373,
eft H1KP1 31
Tlsj,
3f3
eft 7§
3771253
727
35735,
\333ft
31777714)
377-2J ftfftH
iftftTH
3t
3771 JITRfeft
vfitin ft!ui ’nftcft Jilt'll ‘iH 'JiH^r'H ftft P^vci^Yii xprieii uD
Znft>T RiV 'R
t-u Rrvi41 el tvR MV
____ ______________________________________________________
3lHHq|<ft ftiftepl,
'Hxft'il <J
'!<l 1 X-'^I ^STeH ft dLici<y 'Jl|'iv>:ft
■Sivex 'ft >3l4e1<y <41c|?|ft
MWlftcp
<-cj|X-aZI
■ft
(flT!
oti
ft vr'j? <rar
———-----------------------v4IQriJld
Jhc| qft
xd4 MX 5X
libeiioft ft
<4cj|c; <n?
'0^ci£J
'onnti vt|-1Q,|< cp'i fftftft ft WX-cjd Pb-UT -11<41 t? I
1-
ft
'ThsTHT qYf uii’i<t>i'fi eft
TlftM VxR MR
Mll’bblft -lt?i £t
xn fi <jh ft
!
<lftsf \K(R
Hift'
uftlSId
Ml I *1 <t> I ft jt
-
100 MpRld
XK'H-q
xFft gft vIHIcbft
_
■411-l’IVl'Sl
8
6
2
50 ufftyid
^7,6 ddl eft <JR
11
2
1
80 Uiciyici
WftdMd RR
03
| 134
<j f; i
VTgziin ft
2.
3^J
q
-I I cl
I 2.12 sfaw
^P'xCl 1? f^b '3 M
\ft *4 ] ~j
cf^ ft_j ]
yj ;
W®J Vllftfft ’RFT ^Rft ft V1R-F ft'
vifftRf t'
ftftftl Htfl’ t
tlXH^
3.
-j j cjCJ vj* ••{ q> •
3TRR 3TTcTT ft I (Me? ftl HfftH13ft ft RR <R HWI ft)
15
1
93.75
11
2
78.57
'TFT RPRWJ ■'fffftfa ftt W>H4 VTSm pft H'QR
TFR '■dfftfft ft MJR
3LR.R. /sft.tft/ftT <iI<-|d
j xravu ft^n
I
^uf
7R? xRH
2
fcTeT? HfiYeTT 3RR1 U fYdifti’H 3t.Ul./
XRR} 12 f^Rlft
Piilftl eft 34lx! 7Tpj?f ORdT dlfed I
3|t^uf
(10
ft
M>H
uRisift tjyf ’req
'H'tsill)
8
14.28
i
4.
TFrfWr
t
3cf47
fr
TrftV
ufcfsicf ftf
wu'd
5
9
35.71
7446 WT
3-
7
21.42
> TWWl 4llft(ft eft 434 4,1 4>'|il <H44J) <lft) 'lift] ft ^ui ftl *JQ>1 ft cilft’-f SW»)
<t>i<4yulie?l qft ci w cp'i <4i|-tft 3j[ftilHdlft 4 318.^144 <<s4H 4ft fftdcll ft I fvRT4> 4TRR
3Ni'bvlCll fft-Mlif M.?hD
5.
ft
|
W742] ^rPrfvT sFRT
^r4 47r[
WfkTT
TRq'rl :
'Tm WR q cY4,|4RU| 45 44444) H 3R1^ cTRJT 47 W
TJETR §3n ft I
nra 7TH wt 3 fWe) V47 WT H ^ict>l4Rui Wf TTOT? WIjpH 4ft H4R ^4T7
§3TT ft |
11 Wi ft oft? T^TR Hftl ^3TT I -Hcleiej 78.57 Ufcl^ld 3RF5eRn I
Hiftt <ft H0RH eft fftlft qddd'ET gWlT ftnTfl 474 ft 4ft] 4 4^ Yft4lefil 44lft 4^
6 I dcieis! gft 3RTOcTdT I
Tiiftfft cr; 464 q 4<5q> 4 <Pi44uITeft qft «fjp4T 4R 73TT4igfft 4<ftcT ifttft ft I
6.
<p-£
*r
gftlf&cl RH RTT2R
VEF5
3I-dJfcl 3TT^ <4lel
ifrat 3?T 'HTsill
toitsTj
I <5cpc<I
ufWrei
48
18
20
51
43
51
23
• 7 It hr-41
23
11
OlciH'SI
74
26
16
11
—
—
4ie<l
f' snv/ w w?n t
ariiPto rir^ /•£ qfi
nra
uI-spr
spft ?iQ5 £Prt tr
<*>10 xjyr -igi ■gsn ? i
FPfRl RR <R
7.
3jRlfi£17T
vi-l
uftieror
a
7<iit27j 7ffrai
«.
4
8
3
9
^ra
r?t
28.57
-
9
-j Ji
___________________________
21.42
_________
_______ J
RH W3 7Ew cfH WTEFT UH wJ 3TR wftw RR F? RRRSRn 7RR7R R RR
TR 50 Ufcl^lci, RTHFT RR
ir
29 nfcTUra RR H RWR if, feRKl R HIR 21.42
■£!ici^ici R? Ria'i ? |
g.
nitir/ra ^r< xrf^reRT
r- yia?Rjcf> RIRWJ
7717 IR
- 110/196 - 56.12 gfvRrd
TTPfW TxR IR
;
■' •
U^IEFI
: xFje 7RK
5
: •et'iMxi
4
t
Ii
|i______
i
ufcTSTU
i 8
56.12
I 8
31.71
cTT? OT^iSRT W1 ipT W vH RTR-ezj 7SW pf^TEFT 7^ 57TR RR YFI ? I R Wl
iR xiHlETT cRj cfl
<oT ^2-TTH
Wlxlcftft
eft)
Vl'lg
OiVHClici
UT^FqPl ’eft
utopia
^cT
137
97.16
4
2.83
uRlfefi cFI^ TlP ^iRajfo
; \3nfWftr
y fiisra
■ Hb!
ulxj-cjn ift -c^M ?,!’4 Ph'S *l>l
46
33.57
91
66.42
uRltfild '<1^ SRI
Hicr
uRi^ld
eH
38
26.95
|nfr
97
68.99
6
4.25
415
80
enje xioix Heft
.<
5TmTiii ^eTran h 3ii<n HI oiri'HI <J>| cppj tlV iR g'nfl g | jR-ffciZi yf$lf£i<T <T5 eft
~~ •■:?; - I’!'::
H;j <m|| bl Wft?151ul qm 75TH H) tjq Hf?l § | qf^iapj 5b ylchlRI ?
hV
HI? col viHcn<2TcTT <ft Ib'iiiq ?ft 31.71 5Tk1 «:d ? I
HRmRcp Hi? cJpF'T q5T ticjlei *1101 q> WJ22I
tii^j ch'id e q?I <]"=[ ycPT 0>l4
He Hi He ^rii^qa iff cjj<HT $Pll
icne cfH vSm4ijI FTffT t HI Heft I
vJST 1?3TT t, 3TT^ TH? W eft
TrfcF 7ft 7JH V?T
cT2IT rJ°f Heft ftft HV HH2T
uRiaPT <ft «JK vlrjcb) eft nftvH
eftft
cj
L
1
seb
60
laik ppa »|Ch "
8P7S
VL
Hl-*
89
P^
£
Et'LV
i
mAtyb
bpc^J
(tp
9 I0 ,lUQ-b <
^4^ A
|Jb inAckJty^
£. JJ22J9
i
i
'6
H& PIP
.
?JP I£
,. ..
---------
Mb <bh
P9fe
fell?. 1M2. Ithkh’h kl^k <fe ItBb.bJJjJt
ZO'Ob
S3
P 09
ZZ'BZ
81
91U 09-i.e
>9'08
61
cblj 0£—i-
Pit
ln>P^j
4>!t||fr £ kHMJK <
ln>-P|3j life
...
88’9
60
99’99
P6
96'92
88
a mpy £k
M3I1C kdalh
P<U
M 2.118 lahlh IP IP. |±PitJ J4> jJglP^jk
L__ _
19 P
80
06’89
i
29
9Z
pikiyti
;
Pik
Z.O ht'
£ (>lPPkUg <
Shfr
|
£
|
|nX4> l<b(J3
lnl^l<P|J> P1>^P £ Lt&mHk <
>_h MHl DJtUyte
>12118 Loih|.h £ ln><M<b(P- pul
"
. 14
4 q\>?|<bd grnft 41 msm 30 4 4 3ifsfta t 4f4a wa 41 uplift ft |
r-
3UGT\’ faim-l ;i f^lell-ft 4 R-14 4«l'l,41 jJvIH-x1 Ml-ll ll<MI H I ll4hl>d 'I'4h11
Httaraft g yraft qfteibii4 $ 4ft mr4
r-
? i
3inr-igii) asifSwn hh4 ft 14 apjfil q m-i 45 3pihi 4; ^iwi qum u7i «c|k\i |
W1 4a VTCJT wdft gftam 4 ggcf tjyi tlQJiavui 41 ^I4m, 7FW11 Hlfttfl q1,)
mra n4
<tr am, fcrej.
ara na 4 n4. mimTi nfftai g m41 qfftai 4
44 4m, 3H&T? qn ^TcHErai TJTfi 45 feP) ^Fifcgci 411
3R«i gicf ?4 ^4&wt 45 4kn rT^reigiv 3n4) gRT
3 et>t4 |3n t gg'i
vavig 11
^iiq,3i,r q <i«-i0
gm gi^i ^41 £ptji 45 Tr? ? i nH 'H w-m gm fmm45
M'l 3lkfi b I
cfkii'I/m 3j|< Mi.iq';; xYjijiI q <jE||>! IIJII ft I
^t4t
U fdfeil!
nri 4iq n g.^.vn. gm 441 <P7 4m fgmi m? 41
gh
4 gq; ma 4 44pmn am amig wnrm 4ft mm vjmv ^3n i
m gm msj 45 q;iq q ?jqa 3ipii 3irmlftmm 4 >jl’.4
41
qm!i41 g I
Tgrrnq vir~,ici gm ■<<11'1^1 g>i-i-qqi 4i f^rmi'ftft wh m ci'T'mi >4^ f4> viikict 4
q
x-qiX-3ZI c<>i4jp4i 4 mri "lungm ■1’^4 •<’;
m<4cic aa 4 ^<r«i 4rar ji i4cTl 4mm 4 mggw 4 aft ''jmjci af4rr4 amn
4r mct4i rjr%4 gg 3iwa 11
X
O-'/v,
I
STATUS OF PUBLIC HEALTH SERVICES IN BARWANI DISTRICT OF
MADHYA PRADESH
STUDY REPORT1
2003-2004
By
Jan Swasthya Samiti, Barwani / Sendhwa
Jan Swasthya Abhiyan, Madhya Pradesh
' This investigation was done by Jan Swasthya Samiti for Jan Swasthya Abhiyan to document the situation of public
health services. The study was done in collaboration with the organizations of JSA, MP, which includes Centre for
Enquiry into Health and Allied Themes (CEHAT) Indore, Ashagram Trust (AT). Jagrit Adivasi Dalit Sangathan (JADS)
and Adivasi.Mukti Sangathan (AMS).
ACKNOWLEDGEMENT
This study has been conducted by Jan Swasthya Abhiyan, Madhya Pradesh. The Jan Swasthya Samiti
acknowledges the people of the villages, staff of PHCs, CHCs and District Hosp.tai. Barwani who have
responded to the survey. The people have had much belief and conviction that this report would help
activate a dialogue between the people and the district health system.
The Samiti acknowledge individuals, M.S.W students from Barwani school of socia: work. Ashagram trust,
CEHAT, Indore, who have extended their support towards this endeavor. We are thankful to Dr Abhay
Shukla for his invaluable inputs. The Samifi recognises-the contribution of Mr. Laxmfnar'ayan Sohner ahd
Mr. Vijay for publication of this report. Kajal and Anand have done the Hindi translation of the summary
report.
Coordinated by:
Amulya Nidhi
Report Compiled by:
Amulya Nidhi
Ashish Gupta
, Sanjay Tirkey
With assistance from:
Shelley Saha
Kajal Jain
Investigation Team:
Main investigator.
Sanjay Tirkey
Field investigators'.
Anand Verma
Manish Dixit
Chetan Atre
Hridesh Singh
Pankaj Babu Agrawal
EXECUTIVE SUMMARY
Status of Public health services in Barwani district of Madhya Pradesh
PHCs in Barwani district:
There is a shortfall ci 15 PHCs in the district! One PHC is serving an average population of more than
29000 instead of 20,000.
None of the PHCs fulfill the 2-6 beds norm; all PHCs have less number of beds and 8 out of 31 (26 %}
have no admission facilities.
11 cut of the 31 PHCs (36 %) building are in very bad condition.
15 out of 31 PHCs (48 %) do not have normal delivery facilities and 13 (42%) PHCs do .not even have
a delivery room.
Out of 31 PHCs, 8 PHCs do not have connection of electric supply. In 40 % PHC the fans and the tube
i
i
liohts are not workino. Not a single PHC had a generator backup.
6 (19%) PHCs did not have any source of water. 13 (41%) PHCs have water supply by hand pump and
most of these run dry in summer months. Only 12 (42 %) of the PHCs had facility for running water.
26 PHCs (84%) do not have ambulance facilities. Only 5 PHCs (16%) had an ambulance facility and
even in these 5 PHCs the drivers do not reside in PHCs.
13% PHCs are running without regular doctors. Only 3 PHCs had lady doctor. In 70 % percent of the
PHC LHVs and MPWs were not posted.
-.. ■.
In 29 % of PHCs, doctors were not available in scheduled timings. Even for other staff in 20 % PHCs,
staffs are not present at scheduled timings.
CHCs-in Barwani district'
i
;
The district has less than half of the required number of CHCs. Instead of 1 CHC per 80,000 population
the district has 1 CHC for 1,84,612 population.
None of the CHCs fulfill the 30-bed norm; all CHCs have 10 beds or less.
40% CHCs do not have running water facility.
There is no functioning Operation Theatre in 60% CHCs; certain CHCs do not even have a delivery1
room
80% of the CHCs have no specialists, the single CHC with specialists has only half of those required
Only one CHC has a female doctor
In 40% CHCs, doctors are not present during scheduled timings
80% CHCs do not have neonatal resuscitation equipment or ECG machine; 40% do not have oxygen
cylinder, incubator or adequate operation equipment
None of the CHCs provide services for caesarean delivery.
40% CHCs do not provide treatment to severely anemic women or children with severe respiratory / :
gastrointestinal infections: 60% do not have STD clinics.
District Hospital in Barwani district
When admitted, some patients have to lie on floor and even in corridors. This was observed i
especially in Pediatric and orthopedic wards. Similar conditions exist in Mahila Hospital also where j
most of patients were seen to be lying on the floor.
The water facility in the hospital is erratic and unhygienic. The district hospital has only one water
tank but the water is likely to be contaminated as it is situated beside the septic tank.
Only one ambulance in the District Hospital is in good condition.
Many patients have to purchase medicines such as drugs/syrups/saline from private medical
stores.
j ROGI KALYAN SAMITI of Barwani District Hospital (Data for 2002-2003)
RKS iSrnot utilising almost 25 % of its collection even though the -hospital is seriously lacking in
many of the essential services due to lack of funds.
75% of the total money collected by RKS is earned from general patients. However, only 11% of
the total expenditure is spent on services for general patients.
Out of the total expenditure of Rs 15,26,201/- the major expenditure of (81.3%) RKS has been
incurred on items not related directly to patient services like new installation of AC, coolers,
grass cutter and water pump for lawn, building repair, electric expense of CMHO office and for
salary of staff employed by RKS.
4
INTRODUCTION:
‘.'p.-hya Pradesh is located a: the geographical centre of India with Bhopal as the capital. It snares its
borders with five states, viz. Maharashtra, Gujarat. Rajasthan, Uttar Pradesh and Chhaitishgarh. Erstwnile
Madhya Pradesh was the largest Indian state in terms of area (spread over 443.000 sq. kmst, and had
accounted for 14% of India's land mass. According to 2001 census, Madhya Pradesh had a population of
60,385,118(male 314,568,73. female 28,928,245). The population sex ratio number of females per 1000
males was 920 in 2001. The state, has the highest population of Schedule Tribes (23% of the country)
outside northeastern states. The literacy rate of the state is 64.11%. It is one of the most economically
backward states with more than 42 percent population living below the poverty line (NCAER 2002) It is also
one of the low literacy states in the country. Most of the villages in the state do net have an ail season
approach road. Tribal regions are mostly in hilly areas, where people have to walk nearly 15-20 Kilometers
to get basic services.
>
■*
■”
:
4
>
In the western region of Madhya Pradesh, Barwani is one of the less developed districts. Ninety percent
tribal population, mainly by Barelas, Bhilalas, and the Bhils, inhabits it.
According to 2001 Census the total population is 10,81,039. with 547837 males and 533202 females. The
female literacy is 19.01% and
the male literacy is 36.77%.
Barwani
district
has
7
development
blocks,
714
villages, 383 Gram Panchayat
and 1121 AWW. The maternal
mortality rate is 5 per 1000. In
terms of health facilities it has 1
district hospital, 5 Community
Health
Centre
(CHC),
31
Primary Health Centres (PHCs),
235 sub centers (SCs). At the
village level, ANM/MPW are
deputed to provide basic health
services to people.
The declaration of Alma-Ata
Conference in 1978, setting the goal of Health for All by 2000 AD has ushered in a new philosophy of
equity, the new primary health care approach. The National Health Plan (1983) proposed reorganization of
primary health centres on the oasis of one PHC for every 30000 rural population in me plains, and one
PHC for every 20000 population in hilly, tribal and backward areas for more effective coverage.
Health problems like tuberculosis and Malaria in tribal communities are compounded by difficult terrain,
mutual disbelief and mistrust between the community and health workers and non-availability of
essential/life saving medicines in the area. Poor child and maternal health status, prevalence of infectious
anc diseases are common causes of early deaths in this area and the state has to improve the situation by
improving its health services aoopting an appropriate developmental plans and by co-operation with social
anc voluntary organisations.
Madhya Pradesh Government has given a Guarantee to provide all basic Health services through Swastha
Jeevan Seva Guarantee Ycma, which was initiated in the year 2001. But over 2 years after the
implementation of the Yojna, re failure of the public heath services in several districts of Madhya Pradesh
continues to be a stark reality. This prompted the Jan Swasthya Samiti to initiate an investigation of Public
Health Services in Barwani district.
OBJECTIVES:
1. To assess the level and limitations regarding availability of the health care services in the
government health facilities.
To recommend improvements in organisation and delivery of public health care services
2.
METHODOLOGY:
Sample selection:
The data was collected from all the 5 Community Health Centers (CHCs), all the 31 Primary Health
Centres (PHCs), and the District Hospital from Barwani District.
?
■*
?
-Ji
:
*
>
Sources of Information Gathering:
1. The data was collected using the M.P. government checklist, which is used to monitor the public health
services. We decided to use the government checklist so as to demonstrate how the public healthy
services are functioning even according to their own guidelines. The checklist for'CHC had 131
parameters and PHCs had 65 parameters. A similar checklist was used for the Civil Hospital with 152
2.
3.
parameters.
All the checklists were filled, observed and crosschecked with interviews from doctors, other staff,
patients and villagers.
Beside the checklist, observation was also done to substantiate the data gathered by checklist.
The data was collected from doctors and other staff present at the health care facilities. The data was
collected between mid July to September 2003.
In the following sections, we would be presenting the findings of the data collected from PHC, CHCs and
district hospitals.
PRIMARY HEALTH CENTRES
REPORT CARD OF PRIMARY HEALTH CENTRES
.
I
There is a shortfall of 15 PHCs in the district! One PHC is sewing an average population of more than
29000 instead of 20,000.
I
l
None of the PHCs fulfill the 2-6 beds norm; all PHCs have less number of beds and 8 out of 31 (26 %)
have no admission facilities.
11 out of the 31 PHCs (36 %) building are in very bad condition.
I
15 out of 31 PHCs (48 %) do not have normal delivery facilities and 13 (42%) PHCs do not even have
a delivery room.
Out of 31 PHCs, 8 PHCs do not have connection of electric supply. In 40 % PHC the fans and the tube
lights are not working. Not a single PHC had a generator backup.
6 (19%) PHCs did not have any source of water. 13 (41%) PHCs have water supply by hand pump and
most of these run dry in summer months. Only 12 (42 %) of the PHCs had facility for running water.
26 PHCs (84%) do not have ambulance facilities. Only 5 PHCs (16%) had an ambulance facility and
even in these 5 PHCs the drivers do not reside in PHCs.
«
X
13% PHCs are running without regular doctors. Only 3 PHCs had lady doctor. In 70 % percent of the
PHC LHVs and MPWs were not posted.
In 29 % of PHCs, doctors were not available in scheduled timings. Even for other staff in 20 % PHCs,
staffs are not present at scheduled timings.
Findings of the PHCs:
1.
Adequacy of PHC:
A PHC is supposed to serve an area of 30000 population in plains and to 20000 population in remote and
tribal areas. Our area of study, Badwani district is a tribal area and thus a single PHC is supposed to serve
20000 rural population. According to 2001 census, the district had 9,23,063 rural population (Provisional
Population Total, Directorate of Census Operations, Census of India 2001, MP). So according to the
population criteria the district should have 46 PHCs but in reality the district have 31 PHCs. It means a
shortfall of 15 PHCs in a district! Thus in effect a PHC in the district is serving an average population of
more than 29000 instead of 20,000.
2.
Infrastructure arrangements:
2.1
Condition of building:
Of the 31 PHCs, 24 PHCs had their own building, whereas the rest 7 PHC are situated either in donated
place (21, place given by Gram Panchayat (2), rented place (1) and in subcentre (2). As shown in the table
below physical conditions of 11 PHCs are very bad.
Name of
block
% of government building
Bad
condition
33.1 (1)
0.0
0.0
0.0
66.7 (2)
100.0 (1)
66.7 (2)
0.0
33.1 (1)
50.0(1) ,
.0.0
0.0
. 2
4
Bad
condition
66.7 (2)
Badwani
100.0 (3)
Raipur
Newaii
50.0(1)?
33.1 (1)
■
Total PHC in
the block
Satisfactory
condition
Satisfactory
condition
Pati
% of non government building
3
4
6
Pansemal
Sendhwa .
100.0 (4)
0.0
71.4 (5)
0.0
0.0
28.6 (2)
0.0
0.0
7
Thikri
100.0 (2)
0.0
66.7 (2)
33.1 (1)
5
15
9
5
2
31
TOTAL of
PHCs
(Figures in pa.'Bninesis inacate number ol PHCs.)
In Rosar PHC the entire roof leaks. PHCs of Ojhar, Balwadi, Julwania, Dhawli, Wada and Sendhwa have
very bad leaking roofs and water easily gets into the building and damages the walls, door^and windows,
furniture, medical equipments and medicines. Leaking roofs affects other conditions of the building like
electricity. A large number of the PHCs have new buildings under construction since long and the PHCs
are being carried out from the old dilapidated buildings eg Julwania, Nagalwadi, ojhar,etc
2.2
Furniture:
As per norm every PHC is required to have admission facilities of minimum 4 to 6 beds. Our observation
show that in large number of PHCs there are 1-2 beds and in some PHCs there is not even a single bed
available ancf it is interesting to note that patients have to bring their own beds in case they want admission
in Balwadi or Dhauli PHC. In some of the PHCs there are no wards but beds are there in corridor and in
other PHCs there are wards but no beds. In Balwari PHC there is ward but no beds are there whereas in
Nagalwadi even though beds are there no ward is there.
’
Those PHCs that have beds do not have clean and adequate linen like cushions, pillows and bed sheets
for example in Dhanora and Rosar PHC. Either they are tom and in bad condition or they are extremely
dirty and have not been washed for a long time which is the condition in Jhopali, Chachriya, Nagalwadi.
Dawana, waria PHC.
Some PHCs lack basic furniture like chairs, tables and benches, examination tables etc. Lack of basic
furniture hampers efficient performance of the medical staff. In many PHC patients had to stand while they
wait for their turn to meet the doctor. Many PHCs did not have almirah which is needed to store medicines,
linens, bandages, injections and equipments etc. In many of the PHCs medicines were either left on
shelves or dumped on the floor or tied in bundles using clothes. Proper storage is essential for maintaining
the efficacy of medicines and injections. In Chachriya the medicines are not stored properly in absence of
almirah. In most of these PHCs the drugs supplied are without cover.
S
2.3
Delivery Room:
Forty two percent PHC (13) did not have a delivery room, and of the rest 18 PHC where there is a delivery
room delivery facility is not available in 6 PHCs for all 24 hours and in another 2 PHCs it is not available at
all. No delivery facility in Balwari, Moida, rakhi Bajurg, Bandha Bajurg, Chatley PHC.
This non-availability of basic health service like delivery needs to be seen in the light that charges for
normal delivery in private hospital vary from Rs 300 to Rs 1000 depending on the capacity of the individual
to pay.
2.4
Indoor facility:
PHC by its norm is supposed to have admission facility. The study show that in 8 PHCs (26%) there is no
indoor facility and only outpatient facility is available.
2.5
Electricity:
a
x
Out of 31 PHCs, 8 PHCs have powefcable connected but the supply has not been connected at*the time
of data collection e.g. Rosar, Moida, Dhanora, Chchariya etc. Even the PHCs with power connections have
very erratic power supply (4-6 hours per day). The electricity wiring is also very bad. For patient
examination and carrying our other routine activities availability of adequate light is very important.
Unfortunately in all the PHCs it was observed that in many rooms have dim lights. In 40 % PHC the fans
and the tube lights are in non working order. For sterilization, kerosene stoves are used by many PHCs
by which one can only boil needles, syringes and metal equipments, but a large number of items need dry
heat like gauze, cotton, plastic items etc. that cannot be heated in absence of electricity. Certain vaccines
like polio vaccine, anti-rabies vaccine and certain essential injections and reagents need continuous
refrigeration to maintain their potency. Even the ice packs for cold chain maintenance are required to be
refrigerated, to carry polio vaccine into far of villages. Lack of electricity even in presence of a refrigerator,
hampers the vaccination programmes.
Despite a poor erratic supply not a single PHC has a generator backup. Probably government has never
thought of providing modern equipments like auto analyzer, auto-claves etc. to the rural areas.
2.6
Water supply:
As evident from the table below 6 PHCs did not have any source of water (e.g. Dhauli.Talwara, Bajurg).
Thirteen PHCs have water supply by hand pump and most of these run dry in summer months. In Talwara
Deb water has to be fetched from more than half a kilometer away from the PHC. Only 42 percent of the
PHCs had facility for running water. As explained earlier, absence of water hampers cleanliness of the
facility. Therefore it is not surprising that our survey found that cleaning is unsatisfactory in 12 PHCs (39%).
Source of water
No water Facility
No of PHC
6
Percent
.19.4
Tap
12
38.7
Hand pump
Total
13
41.9
31
100.0
2.7
Toilet:
Most of the PHCs, did not have a functioning toilet facility!
3.
Ambulance:
Only 5 PHCs (16%) had an ambulance facility and even in these 5 PHCs the drivers do not reside in the
PHCs and take some time to reach the hospital in case of emergency loosing vital minutes in case of
emergency. In the absence of some basic emergency facilities at PHCs at least ambulance can be handy
during emergency cases, and proper transportation facility can be life saving. The charges for ambulance
is Rs. 4.00 per kilometers, but in some places double the amount are being unofficially charged.
o
However, in most PHCs the patients have to hire private taxis at very high cost if they are available, and if
they are not available or too expensive then in case of emergencies the patients' relatives becomes
helpless and many patients die because of lack of transportation facility. For instance, in Sendhwa block
there is only one ambulance attached to the Sendhwa PHC, which has to cater the needs of 6 other PHC
of the block which do not have any ambulance.
| Case Study 1:
i A clear example of 'denial of health care' is from Jhirijamli village of Sendhwa block of Barwani district,
where Nawalsingh, a poor adivasi, was residing with his family of 6 members. In the night of 23rd June his
son Kuwarsingh had a severe problem of vomiting and loose motions. Next day the MPW gave him an
ORS packet.
When no improvement was observed in the child's condition, it was suggested that he be taken to Dhanora
i PHC, where the MO treated him. But, after sometime bleeding started from inside the mouth and nose of
I the child. At another doctor's suggestion, Nawalsingh had to shift his child to Sendhwa PHC. Due to lack of
! money he had to bring the critically sick child by a brick loaded truck just because Dhanora PHC didn't
i have ambulance for this emergency situation.
■
Even in Sendhwa hospital, he had to purchase injections and syringes worth over hundred rupees.
Afterwards when the condition became more serious, it was suggested that he take the child to Barwani
district hospital. But Nawalsingh, a poor adivasi, did not have money for the transport and further treatment,
and ultimately decided to come back to home. On the way back home the child died.
This case study demonstrates how a PHC is not able to provide essential health services, not even an
ambulance in an emergency condition, to save the life of an ill child.
4.
Adequacy of staff:
A PHC as per norms is to have a medical officer in charge, two sector supervisors - one male and female,
a staff nurse, a laboratory technician, a compounder cum pharmacist and a dresser, a watchman and
atfeast one another class IV staff.
- .. :-
Type of personnel
Doctor
% of PHCs
87.1
Compounder
16.0
Staff nurse
18.7
Others
30.7
No staff
1.3
As evident from the above table, 87 percent PHCs have a doctor but what is significant to note is that 13%
PHCs did not have doctors! For instance, Palsud and Roisar PHC do not have any doctor. In Moida and
Dhanora PHC, the doctor comes sometimes. Only 3 PHCs had lady doctor. The presence of compounder
and staff nurse is also very inadequate. In only around 30 percent of the PHCs, LHVs and MPWs were
found. One PHC (Inderpur) from Rajpur did not have any staff!
Functioning: Survey has shown that doctor stay in the Head quarter (HQ) in only 15 PHCs and in other 16
(52%) PHCs the doctor do not stay at the PHC. It is important for a PHC doctor to stay at the HQ in order
to attend to emergency cases. As evident from the table below in around 29 percent of PHCs, doctors were
not available in scheduled timings. Even for other staff in around 20 percent PHCs, staffs are not present at
scheduled timings.
Availability of service providers
Doctor available in scheduled timing
Other staff available in scheduled timing
% of PHCs
71 (22)
80.6 (25)
Figures in parenthesis indicates number ol PHCs.
10
6%>o /
%
/
/
/
5. Residence facility:
/
For doctor: Out of 31 PHC, 23 PHCs have residential facilities for doctors, but even these are ver; badly
maintained and as a result doctors don't stay there. It was found that doctor’s residences are occupied by
/
other staff. For instance, iln Mohda and Julvania they are occupied by compounders and dresse's.
/
For Staff: Out of 31 PHC, only 13 provides staff-quarters, 18 PHCs don't have any staff quarters.
Therefore LHVs, dresser and compounders working for 8-12 hours in a particular PHC are without a
residence and had to stay in rented accommodation.
6. Required Equipments:
The PHCs were surveyed for basic and essential instruments and equipments. These inciuced
stethoscope, B.P. apparatus, weighing machine, basic surgical instruments like scalpel, forceps etc..
microscope and oxygen cylinder. These equipments are either basic diagnostic tools even for routine and
emergency diagnosis or very essential equipments for conducting lab investigation or providing emergency
>
.-care. Out of 31 PHCs surveyed, 14 PHCs lacked essential supplies, and did not have more than 4 of these
items. In Rosar PHC, paper pin instead of needles is used for making blood slides. It is shock to find that in
a PHC needles are not available!
Case Study 2: Surgical Emergency:
Dhadgo is a 90 year old man of Kunjan village of Niwali block in Barwani district. Sometime ago he was j
not being able to pass urine and was suffering from acute urinary retention. Due to this problem he was i
taken to Sendhwa PHC for treatment, where Dr. Prajapati checked him and referred to Karuna Hospital I
(Private) by saying that he is not able to give him treatment here. Urinary retention is an acute surgical I
emergency and is simply treated by catherisation, which means a tube has to be inserted to drain the urine I
from the urinary bladder. This simple facility should be available at the PHC level.
In this emergency condition, the family'had to take Dhadgo to Karuna Hospital where the doctor was !
surprised that catherisation which is easy treatment, but was not given to this old man. Hence the person !
had to suffer and had to spend Rs. 1200/- on treatment, which could have been freely available.
7. Laboratory facilities:
One can find a mismatch between laboratory facilities, required instruments and human power. In some
PHCs there are labs equipped with microscope but there are no lab technicians and in others there are lab
technicians but no microscopes are there e.g. Moida, Rosar, Bhandara, Bajurg which do not have lab
technicians. In many PHCs there are microscope and lab technicians but in absence of reagents even
basic routine tests like blood, urine and sputum examination cannot be done.
8.
Type of services available (selected services):
Type of service
Immunization
% of PHCs
87.1
ANC/PNC clinic held
83.9
Referred new born cases treated
64.5
Treatment of communicable disease
61.3
Treatment of respiratory cases
Treatment of malaria
58.1
77.4
Laparoscope's
48.4
Female sterilization
54.8
As evident from the above table, none of the above essential services were available in all the PHCs.
Immunization services are available in 87 percent PHCs, though there is much scope to doubt whether all
the doses of immunization is provided to the children. If one goes by NFHS-2 data, complete coverage in
the state has come down from the earlier NFHS survey, the above figure seems doubtful. Many child
deaths happen due to respiratory problems, and one of the major barriers for seeking treatment is
unavailability of services. This is evident from this situational analysis of Badwam district, where only 56
percent PHCs are found treating respiratory cases. Little more than 61 percent PHCs were found to treat
communicable diseases. Even treatment of common illnesses like malaria is not available in more than 22
percent of the PHCs. Sterilisation services, which is very much emphasised in public health facilities that
too was not found inadequate in many PHCs, then one can imagine what can be the case for other
services. Sterilisation services were mostly provided through camps.
NATIONAL PROGRAMMES:
Malaria Control is a National Programme but in most PHCs there is no provision for testing of malaria
parasite e.g. Julwania PHC. In many PHCs even though slides are prepared, patients do not receive the
reports or the appropriate follow up treatment.
'
?
•”
12
COMMUNITY HEALTH CENTRES
Report card on CHCs in Barwani district
The district has less than half the required number of CHCs. Instead of 1 CHC per 80,000 1
population the district has 1 CHC for 1,84,612 population.
None of the CHCs fulfill the 30 beds norm, all CHCs have 10 beds or less.
40% CHCs do not have running water facility.
There is no functioning Operation Theatre in 60% CHCs; certain CHCs do not even have a
delivery room.
80% of the CHCs have no specialists,' the single CHC with specialist’s has only half of those
required.
Only one CHC has a female doctor.
In 40% CHCs, doctors are not present during scheduled timings.
80% CHCs do not have neonatal resuscitation equipment or ECG machine; 40% do not have
oxygen cylinder, incubator or adequate operation equipment.
None of the CHCs provide services for caesarean delivery.
Forty percent CHCs do not provide treatment to severely anemic.women or children with severe
respiratory / gastrointestinal infections; 60% do not have STD clinics.
1.Adequacy of CHCs:
The CHCs is conceived as a 30 bed secondary referral centre and the norm expected is 1 CHC per block
of 1 lakh population and for tribal areas is one CHC per 80000 population. At present Badwani district has
5 CHCs for a rural population of 9,23,063 (Provisional Population Totals, Rural-urban distribution, Census
of India 2001, Directorate of Census Operations, MP), which means instead of 1 CHC per 80,000
population (as per tribal area norm) it has 1 CHC for 1,84,612 population approximately. A shortfall of 4
CHCs! Two blocks, Sendhwa and Badwani do not have any CHC. This shortage of CHCs in the district
results in inadequacy of referrals services.
2.
Infrastructure arrangements:
CHCs of the district are all situated in government owned building but none of the CHCs have 30 beds
according to CHC norm. Only Rajpur and Pansemal CHC have 10 beds and the CHC at Pati has only 3
beds! Also 2 CHCs (Pati and Thikri) does not have the required furniture that a CHC is supposed to have.
In absence of required furniture, drugs and other medical instruments gets damaged.
2.1
Electricity:
Uninterrupted supply of electricity is an important requirement for any medical facility. One CHC (Thikri) at
the time of survey did not have electricity. In absence of electricity, drugs, and vaccines gets wasted and
loses its potency, it also affects the cold chain and can become fatal in cases of operations. Even in CHCs
where electricity is available, the wiring conditions are in bad shape. Alternative electric facility is available
in only one CHC (Rajpur).
I?
2.2 Water supply:
Three CHCs have facility for running water (i.e. tap) and for the rest two CHCs (Newali and Thikri), water is
stored in a earthen pot. But any facility with inpatient facility should have running tap water, bathing facility
and toilets. Even maintaining minimum cleanliness would be difficult to maintain in absence of such water
supply.
2.3
Delivery room:
Maternal death is very high in our country. It is quite unfortunate to find that the CHC in Pati did not have a
delivery room. Most of the villages in the district do not have trained birth attendants even, and therefore
for delivery many women had to take recourse to untrained traditional birth attendants. In 4 CHCs, delivery
room is present but it is in bad shape. It was observed that in Pansemal and Rajpur CHCs the deliver/
room is flooded with water during rains, and therefore become impossible to perform safe deliveries.
2.4
Operation theatre (OT):
There is no OT in 3 CHCs of the s5 CHCs in the district. It was .observed that only stitching of wdunds is
done' in OT, and due to lack of equipment, operations are not done and patients are referred to District
hospital.
2.5
Ambulance facility:
•
'
All the CHCs had an ambulance, but during emergency people are not able to avail this facility due to
variety of reasons like unavailability of drivers. According to the Rogi Kalyan Samiti norms people have io
pay Rs 4 per kilometer but interaction with people show that most of the people are illegally charged more
than that.
Vehicle for supervision: None of the CHCs had a vehicle for supervision, which in turns affects effective
monitoring of extension/outreach work of the CHC.
3.
Adequacy of staff:
Medical staff strength including availability.of specialists.at each CHC is important indicators of its provision'
of quality care. Of the CHCs studied, most did have medical officers but were found lacking in case of
specialists. The norm is that each CHC should have 4 specialists - surgery, obstetrics and gynaecology,
general medicine and paediatrics. Of the 5 CHCs only one CHC (Rajpur) had specialists that too only one
surgeon and paediatrician. Only one CHC had a female doctor. Presence of female doctors assumes
importance as women find it comfortable to share their health problems with female doctors especially
related to their reproductive problems.
In terms of other staff, all the CHCs had a computer operator (though some CHC donrf have computer!),
compounder, technician, radiographist and other 4th class staff. Two CHC did not have Block Extension
Educator (BEE) and clerk and one CHC did not have staff nurse. Absence of BEE means that supervision
and monitoring of extension workers are not done, which might mean no or less than required extension
services.
4.
Residence facility:
The checklist only had one question that is whether the doctor stays at head quarters. It was found that
doctors of all the 5 CHCs stay at the head quarters.
Functioning:
5.
Though the study found that the CHCs were open for full time, in 2 CHCs (Pati and Newali) doctors are not
present during scheduled timings. Also based on observation and with discussion with patients and
villagers it was found that beside regular timings doctors hesitate to come to hospitals to attend serious
cases and many of them are engaged in private practice during scheduled timings. This unavailability cf
doctors in health care facilities poses serious problems to patients in times of emergency in accessing
health care.
14
6. Required Equipments:
As evident from the table below, all the CHCs were found to have BP apparatus, microscope and X-ray
machine. Weiohino machines were found in 4 CHCs. In Pati CHC, x-ray facilities is available only once a
week, In Rajpur 3 days in a week. Only Rajpur CHC had a ECG machine. Newali ano Thikri were found to
have operation equipments but do not have a surgeon or an OT. There is thus a great mismatch of
equipments, facilities and human power. This mismatch forces people to seek medical care from private
oroviders. All the CHC had some of the equipments required for the cold chain, but none of them had all
the required (as per the checklist) instruments.
No of CHC
Required Instruments
Yes
No
I BP apparatus
5
0
Microscope
5
0
X-Ray machine ?
5?-
0
ECG machine
1
4
Weighing machine
4
1
Operation equipments
3
Equipments for cold chain
5
^2~
0
‘
■
Neo-natal Equipments
Resuscitation
1
4
Neonatal warmer
3
2
Incubator
3
2
Oxygen cylinder
3
2
Even life saving instrument like oxygen cylinder is absent in 2 CHCs (Pati and Rajpur). Important life saving
neonatal instruments like resuscitation, neonatal warmer and incubator is present Jn only one CHC
(Rajpur). No wonder neonatal mortality is high in Madhya Pradesh (According to NFHS - 2 MP,’neonatal
mortality is as high as 54.9 for 4 year period preceding the survey). Certain CHCs were found unable to
even perform a basic investigation such as estimation of Hemoglobin.
7. Type-of services available (selected list):
As evident from the table below, the services available as per the norms of a CHC are quite inadequate.
None of the CHCs provide services for caesarian delivery, which is an emergency service. Many maternal
deaths take place due to obstructed labour and these lives can be saved with timeiy interventions and
quality services.__________________ ____________________
Type of service
I
No of CHCs in which
it is available
Caesarian delivery
0
Treatment of severe anemic
3
pregnant women
Serious respiratory and diarrhea
3
cases
ANC and PNC clinic
5
Immunization services
5
Laparoscope's
4
Female sterilization
1
Non scalpel sterilization
1
Cuts
STD clinic
2
4
Though the data gathered show that all the CHCs organise ANC and PNC clinic but there s a large scope
of doubt about the range of services that are provided as ANC and PNC services.
As far as contraception services are concerned sterilisation services are available cn.y
camps. It is
reported that sterilisation follow-ups are done. CuT insertion services are available in - CHCs. All the
CHCs reported that temporary methods of family planning are available. It was also observed that in most
of the CHC,. tubectomy camps were organised merely to achieve the targets and these camps are
insensitive to the humane needs of the patients ignoring their basic rights and dignity. The most striking
feature of these camps is that the insuffolation procedure (a procedure in key hole surgery where air is
filled in abdomen to facilitate key hole surgery) is done using the cycle pump.
According to NFHS -2, more than 40 percent ever-married women in the state were fours to suffer from
any type of vaginal discharge or with symptoms of urinary tract infections (UTI). Our study found that only 2
CHCs have STD clinic, which is definitely quite inadequate with such' a high prevalence of STI/UTI
problems.
16
DISTRICT HOSPITAL (DH)
1.
INFRASTRUCTURE:
1.1 Furniture: Even though the hospital has 283 beds due to lack of mattresses some of them are unusec
and therefore some of the admitted patients have to lie on floor and even in corridors. This is the condition
especially in Paediatric and orthopedic wards and also Mahila Hospital where most of patients were seen
to be lying on the floor. Condition of beds and general hygienic conditions of '16 Palang ward' are found to
be in a bad state.
1.2
Beds Sheet and Linen: It was observed that those patents who are lucky to get a bed have to put up
with dirty bed-sheets and pillows which are not washed and are stained with blood and urine.
1.3
Electricity: It was observed that in many of the rooms the fans and lights are not working and the
wiring isjoose. As Barwani gets very hot-during summers it gets difficult for the staff and patients to" be
comfortable without a fan. Many patients are admitted and kept in the corridors, which have no fans.
1.4 Water: The patients especially the admitted patients need to have clean water for drinking, bathing and
toilet. However, the water facility is erratic and unhygenic. The district hospital has only one water tank but
the water is contaminated as it is situated beside the septic tank. Patients are thus not able to get safe
water for drinking and for other purposes.
1.5 Toilet facility: Though there is toilet attached with most wards they do not have water facility and
poses a threat to the overall hygiene of the hospital. The Sulabh Complex built with the money of RKS
charges Rs 21- per day per person and most admitted patients is not able to afford that.
' .□ Waiting facility: District Hospital caters for patients coming from far off places and many patients have
to be admitted for long period. There is no proper place for relatives of patients who are admitted. The
Ayushmati Bhawan is closed for the last 1 year and the Dhanwantri Dharamshala has broken doors and
windows and no beds'. In the last 1 year not even a single person has stayed in the Dharamshala.
Therefore water, toilet, bathing, food and residential facilities should be available for the relatives of those
patients.
2. Ambulances: There are three ambulances in the District Hospital. One is in good condition and used
regularly, the 2nd one has breakdowns and goes frequently for repair and the third is not used, as there is
no driver. According to people they don't find the service satisfactory, regular and affordable.
3. Availability of drugs: According to the norms, the district hospitals should have all essential drugs
including vaccines for dog bite and snakebite. But the study found that patients had to purchase medicines
from outside. This information was also corroborated from people who were admitted in the hospital. Many
patients said that they have to purchase at least some medicine drugs/syrups/saline from private medical
stores.
4. Blood Bank: Though there is a blood bank in the DH, people face difficulty when biood has to be
acquired. There is a need for proper monitoring of the services of the blood bank so that it can be optimally
used.
5. Diagnostic facilities: Though the DH is found to have facilities for basic diagnosis like a laboratory, X ray. but patients are charged for the tests that are conducted and most of the time the cost of these tests
are very high which a poor patients cannot afford.
I7
Mahila Hospital: "Prasuti ke nam par pratarna jhel rahi hain mahilain " Danik Bhaskar 1-102-2003. This
news and several other reporting in local dailies highlights the bad state of the Mahila Hospital but little has
been done to change the situation.
ROGI KALYAN SAMIT1 (RKS)
An initiative has been launched in the state under the Rogi Kalyan Samitis, where for the first time effort
was undertaken to bring in people’s participation in hospital and health centre management and to levy
user charges. Today there are 604 hospitals and health centres across Madhya Pradesh that has a RKS
(MP-HDR 2002). It was found that RKS is constituted in all the 5 CHCs but it was found that in 1 CHC
(Thikri) RKS do not have regular meetings. During one of the Health Dialogue in Pati, it was found that in
many PHCs under Pati CHC, RKS have formally not been constituted but staff is still collecting money from
patients without proper receipts, opening the way for gross financial irregularities.
ROGI KALYAN SAMITI (RKS),?DISTRICT HOSPITAL, BARWANI
RKS is saving almost 25 % of its collection even though it is seriously lacking in many of the
essential services due io lack of funds.
75% of the total money collected by RKS was earned from general patients but out of this 11% of
the total expenditure was spent on services to general patients.
Out of the total expenditure of Rs 15,26,201/- the major expenditure of (81.3%) has been incurred
on new installation of AC, Coolers and grass cutter and water pump for lawn, Repair, Electric
expense of CMHO office, salary of staff employed by RKS.
RKS of DH
As per the information procured from the District Hospital, during the Financial Year 2002-2003, the total
income of the RKS was Rs 20,07,762 and the total expenditure was Rs 15,26,201/- and a sum of Rs
4,81,5617- (24%) was saved in that financial year. RKS is saving almost 25 % of its collection even
though it is seriously lacking in many of the essential services due to lack of funds. It was also
gathered that the RKS has a large net saving lying as FDR in the bank amount, which was not disclosed.
On analysis of the accounts it was found that even though Rs 14,96,926 (75% of the total money out of
total Rs 20,07,762 collected by RKS)) was earned from general patients but out of this only Rs 2.14.634/(11% of the total expenditure made by RKS out of the total Rs 15,26,201) was spent on services for
general patients.
Earnings of Rs 14,96,926 (75%) from general patients include mainly collections in the form of
■ OPD (18.7%), collected @ Rs 2 per patient for case paper
■
■
■
■
■
Indoor (18.3%), collected @ Rs 5 per patient
Lab (10.2%), collected @ Rs 5-40 per patient
X-ray (3.1%) @ 20-40 per patient
Blood Bank (6.4%) collected - @ Rs50-100 per patient
Sonography (5.4%) @ 100 per patient
IS
Expenditure of Rs 2,14,634/- (11%) on services to general patients included:
Lab, Blood Bank, Chemicals, ARV (6.3%)
X-Ray Films (4.0%)
Blood Collection Exp. (1.9%)
.Eye (1.6)
Expenses on porridge for women who are admitted in delivery room (0.2%).
Out of the total expenditure of Rs 15,26,201/- the major expenditure of (81.3%) has been incurred on
New Installations of (Air Conditioners, coolers, grass cutter and water pump for lawn) -
22.3%
Repair-12.9%
Electric expenses for CMHO office -11.6%
Salary of staff employed by RKS - 7.8%
It shows that while the District Hospital is lacking in many of the essential services due to lack of
funds the moneyjs being spent on non essential repairs, installations etc.
'■
19
CONCLUSIONS
The investigation report shows that Barwani has a very public health delivery system. Given the fact mat
the state has a poor health status this lack of public health services becomes a major barrier in improving
health status. This poor state of health care services has been documented, published and presentee, a
number of health dialogues with the Government including Jan Sunwai's were held in Sendhwa and Pati,
but yet the Government has been very slow and reluctant in responding to these peoples' initiative to
improve public health.
'Health for all’, which initially became the target to be achieved by 2000, and also the 'Health Guarantee
Scheme' of M.P. Government which guarantees health care, the ground situation of today is very different.
The investigation shows that that the public health system is grossly lacking in preparedness to achieve
these objectives. Urgent action needs to be taken by the health bureaucracy for achieving these aims and
X3AURANTEE HEALTH SERVICES.
?
'
»
_>•
=
■
RECOMMENDATIONS
1.
District and Block level 'health coordination committees' should be formed immediately. These can
coordinate the efforts of the public health system and by the voluntary sector in the whole district. It
should include representatives of Jan Swasthya Samiti, NGOs, People's organisations and
representatives of the Health department at district and block level. These committees may conduct
review and planning meetings every two months to monitor improvement in health services.
2.
The services should be planned in such a way so as to give priority to areas which have difficult
accessibility, and have no health facility at all. For example Roisar, Palsud, Bokhrata, Balwadi, Dhauli
3.
4.
5.
etc.
'The outcome of the investigation shows that in Barwani-district, there is a shortage of 23 PHCs.
Therefore the Health department should ensure to adequate PHCs in every block. It should also
ensure at least one CHC per block. Some of the PHCs like Sendhwa should be upgraded to CHC.
All the public hospitals should immediately ensure regular water supply and power supply and also
ensure separate toilets and bathing facilities for men and women. Higher priority needs to be given
to waste disposal systems in all health care facilities.
All the public hospitals and health centers should have minimum number of beds according to the .
7.
norms. ■
In all hospitals (including PHCs, CHCs), ambulance with full-time drivers should be immediately
provided so that during emergencies they may be used for referral. The ambulance facility should be
made free for the people Below Poverty Line (BPL).
At every PHC/CHC/civil hospital a board giving information about the availability of various
8.
services and rates of services, should be put up.
Ail the primary and community health centers including district hospitals, should have all essentials
6.
<
drugs including Psychotropic Drugs. The emergency facilities like treatment for snakebites and
dog bites should be available in all the hospitals and health centres.
9. All the PHC, CHC and District hospital should adopt minimum norms of service delivery and
10.
11.
12.
provisioning for it.
It is also important that delivery room should be functional at PHC level.
In all hospitals basic laboratory set of tests should be provided. In district hospitals, the laboratory
should also be opened along with the OPD timings because people have to go for private laboratories
for certain tests. Sonography, X-ray and certain tests facility should be available on all days of the
week and timing should be user friendly.
The PHC staffing pattern needs restructuring to ensure utilization of manpower and better
functioning of the facility. PHCs may appoint two or three male/female multi-skilled employees.
All vacant posts in the health department should be filled immediately. With regard to this the most
important posts.are that of the lady doctor, ANM and medical officer.
14. The amount collected from the patients through the Rogi Kalyan Samiti should be made public and
displayed in the facility on regular basis. These funds should be used for better patient service by
providing enough medicines, disposable syringes, investigation facilities, beds and other facilities etc.
15. Public health system should support community level heath workers (Swasthya Sathis) working in
three blocks of Barwani and providing basic health services at village level, by providing them free
13.
drugs and referral support.
Report of Expert panelists concerning public hearing held on 4th September 03 at
Sendhwa, Madhya Pradesh
The Panel Consisted of Dr. Anant Phadke, CEHAT, Pune. Maharashra, Dr. Sunderraman .
Director, State Health Resource Centre, Chattisgarh, Dr. Rahul Sharma, Convenor. B.G.V.S. M.P.
(Bhopal).
The panel was quite impressed by the systematic reports presented PHC wise, for 31 PHCs,
CHC-wise for 5 CHCs and 1 District hospital. These oral and written submissions indicate that in the
eyes of the people, the services offered by the PHCs and CHCs are grossly deficient and of poor
quality. The State of buildings, equipment, availability of necessary staff, medicines are
unsatisfactory. There was considerable absence of doctors and casual attitude towards care.
Repeatedly we heard evidence that even with slight complications, doctors in these PHCs and
CHCs'send patients ^to Civil Hospital, Badwani, when they should have treated them locally itself.
Many PHC, CHC doctors and even some nurses have been illegally charging patients in govt.
dispensaries themselves.
We listened to the testimonies of some who had lost their children, mostly to diarrhoeal disease
and we are constrained to note that in every one of them there was palpable Negligence by the
concerned staff who referred the case to higher centre without giving the initial treatment which
would have been life saving. This kind of referring all sick cases and treating only trivial diseases,
that too if possible in their private clinics, is a complete rejection of the spirit of Health for All and
the national health policy.
Though they were duly invited by the organizers, unfortunately nobody from the health-officials
was present to respond to the issues raised and cases presented by the people. But even in absence of
the official explanation, the overall evidence presented by the people, very clearly showed the gross
deficiency and poor quality of services in PHCs and CHCs. The government of M.P. through its
Swasthya Jee.van Seva Gurantee Yojana has given a ‘guarantee’, to provide adequate health care to
the people. In practice, it seemed conspicuous by its absence.
We were shocked to know that appropriate treatment is not given even in simple cases of
diarrhoeas and no treatment is available in some areas for snakebite and dog-bite. Such gross deadly
deficiency is a matter of shame when we enter the 21st century.
Our-Recommendations1) The CMHO needs to seriously take note of these gross deficiencies and take up remedial
measures. A lot of additional attention, funds, human power and above all commitment is
needed to provide minimum health services, which we consider as the duty of the govt.
.
2) The various demands put forth by the Jana Swasthya Samiti by Sendhwa need to be taken
seriously.
3) The three cases presented by Rashtriya Satyagrahi Dal, very clearly show gross negligence
by the concerned govt, officials. Its very disturbing that despite the follow-up of these three
cases by the Rashtriya Satyagrahi Dal, so far, no justice has been done to the victims and no
action has been taken against the govt, officials. We strongly recommended that social
political leaders, thinkers, press take up these cases to mobilize public opinion to harness
justice in these cases.
4,h Sept. 03
*********
■
Annexure -1
BLOCK & POPULATION
Sector PHC
Villages
SubPHC
DHB Civil Hospital
Anjad (43222)
Acco. to
revenue
dept.
A.W.W.
Gram
Panchayat
Acco. to
survey
Bokrata
PATI (CHC) 100000
24
Rosar
110
10c
45
118
94
94
52
156
98
98!
64
256
76
\ 73'
42
117
Gandhawal
Bhawadi
34
Menimata
•>
SILAWAQ--(PHC) 134466
Talwada Bujurg
Palsud
40
Julwania
Nagalwadi
RAJPUR (CHC) 171026
Upla
Indrapur
Ojhar
Chatli
NIWALI (CHC) 85116
Jogwada
20
■
\ I
Khetia
Moyda
PANSEMAL (CHC) 129044
26
89
90
39
98
53
153
153.
90
228
51
148
383
1121
Bandhara Bujurg
Rakhi Bujurg
Balwadi
Jhopali
Dhavli
SENDHWA(PHC) 281824
Chacharia
Wada
1
Dhanora
Dawana
38
Baruphatak
THIKRI (CHC) 136341
94
93
Brahman gaon •
1
Uchawad
Talwada Deb
2+7=9
29
235
7141
707
Relevance of Land Reforms for Food SecurityPaper presented at National Conference on Food security and Right to work at BHOPAL
India has 70 million tones of surplus food grains in its food stores. Yet 27 percent of its
population is facing hunger and acute undemutrition. There are reports of “starvation"
deaths from various parts of the country. It is a matter of moral and political concern as
the depth of hunger is directly related to mortality rate, life expectancy and work
productivity.
Why are 350 million citizens living in the shadow of hunger amidst plenty? Who are
empty bellies and who are over fed and unnecessarily destroy food? Who is responsible
for this state of affairs? Lastly what must be done? This small paper tries to answer these
questions from the perspective of U.P. Campaign Committee for Land Reform and
Labour Rights.
Why the shadow of hunger?
•
.-.
: isw vann zrpusehoi .
The shadow of hunger is a manifestation of extreme inequalities in people’s income and
unjust distribution of economic resources in our country. At this juncture availability of
food is not the issue, the central issue is the people’s capacity to buy it or to produce it for
their substance. As per 1991 Agricultural census landless agricultural labour constitute
36.3 per cent households. Of. the land owning sections marginal farmers having less than
one hector of lanilubmpnse -59.4 per cent of farm holding population owning^.qnly.15 per.
xent-df-the opefat^Sioldings,-with average land holding size.of.039.hectos.|The small..
■farnieisjfhawing4;d®fa'^Z()0-hectors-of.lancL comprise'JL8.8.per cent_of.the&in'holding .
p^puLhdnj;btv-n2@i^4zp&!cen£ofilhelarea_operated!.witlLayerageJiol^n^^Jof .1 .43
.;Kectbre.'£rbgethe£i^^nM.and :smaU\farmers..constituteL78?P^SepL9tfl^fi^gJl;Xarming j
population- nwminoWfejier cent ofthe’area operated./Rest 21.8per cent semi- medium, ;
medium and larg'e?famibS'h^W67'?6:per cent- of the5dperated‘>a'rea;d
Land reform - equitable-distribution of land to the tiller-- is no! a political agenda now.
Access to land is privatized, it has become a marketable commodity - only those with
enough money have access to it. At the same time, die poor peasants are being lured or
sometimes c impelled to trade their land as commodity. 1 hey then migrate to the cities
and bcvi-me cheap labour for industry. It i< by hook or crook the land ot the poor peasants
is r'cine controlled In the net: Imrense in landless labour ana decrease in marginal and
small t.nmr- t- qtthc
wihle
'h.w is a ,»ic:?-tnenal grout! n -:!k
rate oi ■
(2)
W ho are empty bellies?
The landless, marginal and small fanners constitute the bulk of below poverty' line
population. The composition of the poor person consists of 22.5 per cent landless labour.
59.6 per cent marginal holders, 10.3 per cent small holders. 5.3 per cent medium and 2.0
per cent large holders. This clearly indicates that the poverty falls as land owning
increases.
Now enough data have been generated which relate the status of undernourished
population with the size of the farm household. Among the 223.2 million under nourished
persons the share of each category is: agricultural labour 19.1 per cent, marginal farmers
54.6 per cent, small farmers 12.9 per cent, medium 8.4 per cent and large farmers 4.9 per
cent. It is also closely associated with the status of calorie, protein and cereal intake.
Education and health are also associated with it.
Table One
Nutrition and Poverty Among Agricultural Labour and Fann Household
(1999-2000)
1—..................
Population under poverty %
Under nourished population %
Malnourished population
Calorie intake / person / day
Protein intake / person / day / gram
Cereal intake / kg / person / year
Agriculture Labour
39.7
45.5
48.7
1948
51.9
148.4
Farm Households
21.0
26.2
28.2
2278
62.7
161.7
Source - Chand et.al. Impact of Agricultural Trade and Related Reforms on Domestic
food securin' in India: Report of the study done for FAO, Rome Institute of Economic
Growth. Delhi. November.
These facts clearly points out the relationsliip of land holding and food securin' in our
countiy. People are starving because they do not have land or rights to resources. We
firmly believe’and reject all those policies, which commodify' land. Land is a source of
livelihood unless and until people don’t have livelihood there is no lasting solution to
hunger, under and mal nutrition
Whose Responsibility?
' ....... ~
...............•"* h':“n;r ;
direct concern <'•! ’he 'trne
icspoilsk'lljr. oi tile stale to wun allc: its liuZl:. >
»-• the cnmfirv"-' ■'•a'
............................
—....
_
..
!
(J)
citizen’s right to work for livelihood. The state is bound with international treaties and
commitments. The law of the land also holds state as responsible for creating conducive
conditions for food securin’.
However, the state has not preformed its’ duties satisfactorily. It failed miserably in
implementing its agenda of land reform. In the absence of economic democracy political
democracy is proving counter productive for resolving the problem of hunger. Right from
independence Indian state has served the interests of the upper classes. The globalization
of Indian economy has rendered the poor section of the population to more venerable
conditions. The poor masses have either harmonized themselves with the prevailing
conditions or adopting violence means to fulfill their requirements.
What can be done?
We feel the problem of hunger be resolved by the state through institutional methods and
agencies. People need to unite for food security. For this national level struggles and
mobilization need to incorporate new kind of agrarian reform - not just’of land
distribution. New agrarian reform needs to distribute land, set up cooperative agro
industries, defend the food sovereigntv’, right to produce using our own seeds, develop
new farming techniques adjusted to the scale of peasant economy and to the oquiHbriuni
of the environment, develop new social forms of production in agriculture matched with
education and schooling in rural areas. We must oppose corporatizing agriculture and
develop new terms of trade favouring landless labour and marginal and small farmers.
We must make moves for people cu:!t-.d hx!m.>logy and oppose chemicalization of
agiiculiuidl Dud. Wc must be united to make effective strategies for establishing people’s
customary rights over natural and common property resources. Natural resources should
be treated as sources of livelihood and not as a marketable commodity.
Recently, there is a significant change in the political scenario. Due to the pressure of the
people’s movement and assertions of deprived people as reflected in the general election
2004, peoples’ issues have come up very strongly in the political scenario. Although we
have a Right - Centrist Govt, coming to power, but the common minimum programme
(CMP) as adopted by the ruling coalition has mentioned the key issues of the deprived
sections, including Land Reform. This has created an opportunity for the peoples'
organizations and initiatives to strongly emphasize its perspective through democratic
struggles & follow up negotiations. An effective strategy has to be evoked to broaden the
movement base and also to make it more democratic and secular in the context of ciass.
caste & gender relationships.
Dr. S. Nischal
E-mail: S.nischal@india.cod.in
11,
S ft H AiZ ft M P y
_ -xq 7^ /
?k. 013^--
S-
CHC Fellowship
Experiences and Activities during the study on Right to Health Care as part of CHC Fellowship
Fellow: Shalini, Chhattisgarh
Mentor: DrT Sundararaman
1
CHC Fellowship Repoit
Chh®fifeg0]!rihi°S©me Vital Indicators
Indicators? W":
V,?
sIiidiaBS
V JHARKHAND
22000.- ^003i" )2000? 52003’
64
79
73
68
*IMR Total
74
69
*IMR Rural
95
85
Surgcija ’
Kortya'i
*IMR Urban
49
51
44
40
■ *Birth Rate Total
26.7
25
25.8
25
Ja&ti pur
’’ Birth Rate Rural
29.2
26.5
27.6
26.6
MADHYA PRADESH
’•Birth Rate Urban
22.8
22.6
20.7
19.9
*l)cath Rate Total
8
9.6
8.5
8.1
Bilaspur
’’'Death Rate Rural
11.2
9.7
9.3
8.7
Kowal dPa
[ja* igi'rXRaig'aitl
’■Death Rate Urban
7.2
7.1
6.1
6.3
Raipur
J.
r
1027
’•’'Population in million ( 2001)
20.79
urgl
’■• Population Share (%)
2.02
100
Rajnandgepn.i
’■■'Decadal Growth Rate during 1991-2001 (%) 18.06
21.34
Maha&umurtd
-7.67
’"'Change in decadal grow th rate (% points)
-2.52
['
Dhamtari
’■■'Female Literacy Rate 2001 (%)
52.4
54.28 MAHARASHTRA']
’■"■'Decadal Rise in Female Literacy (%points)
24.88
15
Kankcr* 1
ORISSA
’"'Decadal decline in illiterates (no. in million) 2.07
31.96
H
’■"'Sex Ratio
990
933
’ ’ Popn Density
154
324
Bastar
’■'■' Tribal Popula(ion(%)
34
’••'’■'C ouple Protection Ralc(%)
40.1
48.1
39.9
'■'’■’'( ouplc Protection Rate by Spacing
4.5
Danlewads
’■"■’■'('ouplc Protection Rate by Stei ilisation
35.4
***Full ANC
12.89
’■"'’■'Institutional Delivery
J21.O5
AMDIinA
PRADESH
22.4 ’ 42 13 41.9
Safe Delivery
’■’ ’■'C hildren Fully Immunized (%)
57.58 53.3
59.1
lVr.<d on *SRS -2002. "Census 2001 and ‘"IIPS-1999'
CMC Fellowship Report
Existing HeeaBth System and Gaps
Sub-centers:3818, sanctioned:4693, with own building: 1458.
■J- PHCs: 512, needed by norms: 720, currently sanctioned: 515,
with own building & adequate space in 327.
& CHCs:l 16, needed by norms 180, minimum need:130, with
adequate infrastructure: 34
■6- District hospitals: 16, with adequate infrastructure : 6
2 Govt. Run Medical Colleges_ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _ _
Facilities provided by Bhilai Steel Plants, mines hospitals,
Missionary hospitals/rural centres, NGO/Trade Union Run
Hospitals.
CIIC Fellowship Repoil
State-Civil Society Partnership Efforts At the Community Level—'•
Ml TAN IN PROGRAMME
■
■■
•'
■■
!:
i?--
"A trained woman health volunteer in every hamlet"
18 days of camp based training and 30 days of on the job
training over 18 months. Planned set of preventive and
promotive and curative tasks for each Mifanin.
Objectives:
Increase in health awareness
INCREASE IN HEALTH SERVICES UTILISATION
Community basing of disease control programmes and improved outreach
of first contact care
& Increased organisation and empowerment of women and increased
involvement and capability of panchayats
...................
.........
CHC Fellowship Repoil
Seven cardinal features of the;
Mitanin Programme
: i.cr.rvS’•,
c •':•••;
f"
a'"*:.,
7
.<»•;? ■ •
-
■
’•
<•
■ ";- J
i
1.
Woman as health volunteer and hamlet as the unit.
2.
Six month long process of selection- by the community but guided
by the trained facilitator
j
■ ■
3.
No honorarium (token compensation for work day loss)
||
4.
Sustained training and support over 18 months by a cadre of
trainers.
1
I
<1
• i
5.
Curative care - supplementary -not central to the programme
6.
State-Civil Society Partnership at all levels
7.
Parallel improvements in Health facilities to provide referral back
up to Mitanins.
■
CHC Fellowship Report
Current Status and Observations
on Mitanin Programme
& Programme ongoing in all 146 blocks in 3 phases.
& More than 54,000 Milanins selected.
& Around 20,000 have received 5 rounds of training, further 11000 to reach that stage.
& 23,000 recently got selected and 1st training is going on.
QQ
Programme evaluation completed in 25 blocks.
& Good Field Support and enthusiasm
Regular Interventions and Troubleshooting
,r.
Varying Strategies for varying situations-effective coordination established through thi$f>
Milanins started to respond to various health issues, local initiatives are seen.
■1
Massive Administrative tusk: Gaps in training and regular field support,
monitoring&reporting,
.'■’3
I*-
Q
,7}
Funds flow problems(negligence/corruption), Problems within dept, transfers, issues q!q
political support/commitment, issues of sustainability.
O
Local Specific lssues(tribal/remote areas)
J
CHC Fellowship Repott
©fher ongoing approaches
©n sfiretriig'a'heriing public health systems:
& Block by block approach on Enhancing Quality of Primary Health Care ■
(EQUIPJ-by closing gaps in terms of infrastructure, equipments,
manpower, skills and Motivation- launched in 32 blocks.
'& GRADED Essential Drug List(EDL) and Standard treatment guidelines
(STG)and State drug formulary(SDF) adopted.
STGs For primary health care doctor, For MPW/ANMs, For health
volunteer
Training of Doctors on the EDL, SDF and STGs. STG trainings for MPWs
and CHVs(Mitanins).
Reform in drug procurement and drug distributions systems
<J- Purchases only as per essential drug list and quality certification —both
GMP and quality testing.
& State Health Resource Centre(SHRC) formed to
initiate/sunnort/imolement these measures as an offshoot of
. ■
-i
w
.. ii
j
'.i
;l
CHC Fellowship Report
These Initiatives Count,
But quite eg Bott of problems still exist..... J
Denial of health care is prevalent in high degree.
-•I
Discrimination to poor, tribes and marginalised is a burning issue.
Within a very short period of 3-4 months study, a number of cases with
characters of serious denial or negligence identified- Cases of
malarial/maternal deaths, denial of treatment in TB, improper measures
to address/ control/ manage communicable diseases/epidemic
outbreaks, etc...
•1
lack of proper diagnosis and prescription, improper implementation of
programmes, Policy and governance issues, corruption within the
department, and many more reasons lead to these situations...
1
Without a statewide grassroots peoples movement which is keen on
regular advocacy and action, it is difficult to address these issues.
Political Interventions are also equally important, but
1. 1
'•J
QIC Fellowship Report
Role of State JSA/other giroops to address these issues I
and a brief on initiatives towards this direction]
'
,
■
pi
V ’.-S • i:
The coverage of initiatives for PHA-2000 was wide enough in the state and its follow up
activities could not be sustained for various reasons including absence of a vibrant state
group to lead it. Thus the Jan Swasihya Abhiyan in the state was not functional though
some efforts were made to sustain/revive the movement by some individuals/groups.
As the JSA state group was not functional at the initial stage of the project, establishing
individual level contacts to involve possible groups/individuals was a challenge. *
& Though a number of NGOs/CBOs work in the state, only a few got focus on grassroots
issues with a socio-political understanding. Activities of many are oriented around
issues with high funds availability, rather than around burning social issues. Also,
coverage of the positive groups is limited to small localities and their immediate
priorities vary.
& Now, as a result of constant efforts under this project and with support from many
activists/groups who are interested to build up the JSA in the state again, the JSA state
group which was stagnant has become reasonably active with added members from
new contacts. A number of state/zonal meetings and follow up activities towards raising
the issues of denial of health care are going on. So far, more than 10 organisations are
actively involved in case identification on denial of health care.____________________
CHC Fellowship Report
Activities initiated so far under the fellowship;
hn association with JSA on right to health care !
& Regular NGO/Activists contacts established and a number of local level meetings
held in May, June and July 2004. The Guiding principles and tools on documenting
denial of health care and Jan Swasthya Abhiyan has been translated/prepared and
widely circulated.
As a result, a state Jan Swasthya Abhiyan meeting with many new persons/
organisations held on Is’ Aug 2004 at Raipur.
>:■- A state JSA working group on right to health care has been formed and it has been
decided that the activities will be held in 4 Zones (Sarguja, Korba, Raipur, Bastar)
where public seminars would be organised to present the cases/testimonies.
In august first half, all the 4 zonal meetings were held and regional groups formed.
Tendative dates for zonal seminars finalised. Preparatory and review meetings
planned. Activities going on in all zones.
Attended the western region public hearing by NHRC at Bhopal
Preparations are on to move towards eastern region NHRC hearing to be held at
Ranchi on October 11.
r.-.i
1'1
CHC Fellowship Repoil
Chr©m©S©gy of individual activities
15 March-16 April 2004: Initid Orientation at CHC, Bangalore
A By May 15: translation/editing/preparation of tools, guidelines and basic
material on denial of health care. The PHA charter (India) also brought out in
Hindi as pail of Shis.
May-August:
- contacts established with various NGOs (both JSA and others) and individuals.
BiHiinj/oihiilalion of adivisls done.
JSA slate organiser on legular intervals
and briefed them about the progress.
- Regular follow up with all groups. Repeated visits and meetings wherever it was
necessary/possible.
- Attended Training Workshop of Bharat Gyan Vigyan Samiti community health team,
Raebareli, U.P, as a resource person on health centered self-help activities in self
help groups. Also covered right to health, right to food and right to health care.
- Assisted mentor in reviewing the functions and costs of public health facilities.
CHC Fellowship Repoit
Chronology of individual activities-2
■
.4:} .
I/...-.J'
- Attended review meetings of Milanin Programme and maintained regular
interaction with Mitanins and field functionaries wherever it was possible.
- Attended National Convention on Right to Food Campaign initiatives.
- Organised JSA state meeting, maintain regular interaction with JSA state group
members. Prepared meeting proceedings and circulated among member groups.
- Attended all the 4 zonal meetings held in the state on right to health care as a
resource person. Sensitised various groups/individuals attended the meeting on
right to health and right to health care. Assisted in formation of zonal working
groups, plans of action.
- Field Visits to support NGO activists/workers to guide them on case identification
and documentation. Regular follow ups maintained.
- Attended Western Region Public Hearing on denial of health care jointly organised
by National Human Rights Commission with JSA Support. Also attended JSA
national coordination committee meeting representing Chhattisgarh.
- Was invitee to National Consultation on right to health, organised by ActionAid
India,_as_pzirt ofdraftinqtheir countrystrategypaper.
.'•7.?.^.
CHC Fellowship Report
Meager Learning and Observations
During the Study
&
Right to Health/Right to Health Care: Need of constant alertness
preparations for events like NHRC hearing- challenges of case collection- strengthening
media advocacy- need of legislative/executive level lobbying.
& State and civil society joint initiatives : SHRC as an example of
institution and Mitanin as programme-strategies to sustain/replicate the innovations■ political and administrative bottlenecks- Human Resource Issues -need of parallel
community level advocacy and action which is not yet taken shape.
& Right to Food Campaign: Need of merger/joint action with JSA - importance
of community level action along with gaps identification and policy and
implemantational interventions with SC support- preparations for organising events.
& Chhattisgarh NGO Scenario: need of political education- importance of
reorganising groups of conceptually fit people- Jan Swasthya Abhiyan: A network
necessary for the time being-How to widen it through Mitanin- advocacy and action.
& Tribal Health Scenario: Problems with groups already working on the issue:
NGOs, Missionariesjboth Christian and Hindu), Health /Forest Depts - Issues of
comunalisation- Issues of health services outreach - Issues of Food and Nutrition.
CHC Fellowship Repoit
Remaining Activities as part of the study !
and Future Aspects;
The Project would continue till the eastern region NHRC-JSA public .
hearing proposed at Ranchi on 11th October, 2004. Following activities
would be completed before that:
- Proposed zonal public seminars on denial of health care in all 4 zones of
the state
- Review and final selection of cases for regional/national hearing
- Writing and presentation of cases
- Preparation of final Project Report/Publication.
■J/ After Completion of the tasks under this study, My future focus would be:
- Active involvement in Jun Swasthya Abhiyan
- Study and Support the tribal health scenario, with special attention to
nutrition aspects. This, I think, is one of the major areas needs attention of
community health programmes.
CH.C Fellowship Report
Groups involved in/ Supporting the study
A Abhivyakti SRC, Raipur.
A
ActionAid India Koria Initiative, Manedragarh.
j
A Adivasi Harijan Kalyan Samiti, Bastar.
A
A
Bharat Gyan Vigyan Samiti, Chhattisgarh.
CART, Raipur.
A
Chhattisgarh Kisan Mazdoor Andolan, Sarguja.
A
Lok Shakti Samiti, Raigarh.
A
Sahyogi Mitra Mandal, Durg.
A
SROUT, Raipur and Korba.
A
State Health Resource Centre, Chhattisgarh.
A
Vanvasi Chetna Ashram, Dantewada.
A
gg
•
And other Jan Swasthya Abhiyan member/Supporting Groups in Chhattisgarh.
S
R!
CHC Fellowship
STATUS OF PUBLIC
HEALTH SERVICES
IN BARWANI DISTRICT OF MADHYA PRADESH
Study Report
Jan Swasthya Samiti, Barwani / Sendhwa
2003 - 2004
Jan Swasthya Abhiyan, Madhya Pradesh
32
ANNEXURE- I
BLOCK & POPULATION
DH3 Civil Hoscital
Anjad 14322?)
PAP (CHCI10CCC0
Villages
Sector PHC
SuaPHC
Acco. to
revenue
dept.
Acco.to
sun-sy
Gram
Panchayat
A.V/.W.
STATUS OF PUBLIC HEALTH SERVICES
IN BARWANI DISTRICT OF MADHYA PRADESH
Bokrata
1
Rosar
24 |
TO
106
45
113
34
84
84
52
156
40
98
S3
64
256
2D
76
73
42
117
26
89
90
39
98
153
153
90
228
Gandhawal
[STUDY REPORT]
BhawatS
SILAWAD (PHC1134466
Menimata
Talwada Buturg
Palsud
Jtdwania
Nagahvadi
RAJPUR ICHC) 171026
Upla
Indrapur
Ojhar
Chatfi
NIWALI ICHC) 8SH6
Jogwada
Khetia
Moyda
PANSEMALICHC) 12S044 Bandhara Bujurg
1
Rakhi Bujurg
Balwadi
Jhopafi
53
DhavG
SENDHWA(PHC)2S1824
Chacharia
By
Warla
Jan Swasthya Samiti, Barwani / Sendhwa
2003 - 2004
Dhanora
Dawana
Barupathak
THiKRI ICHC) 13=341
2-7-3
33
94
93
51
148
Brahman Gaon
Uchawad
I
Talwada Dab
1
235 |
29
Jan Swasthya Abhiyan, .Madhya Pradesh
Published by CEHAT
714
707
383
1121
This investigation was done by Jan Swasthya Samiti for Jan Swasthya Aontyan to Document tne situation ot
public health services The study was done in collaboration with the organizations of JSA, MP, whicn induces
Centre for Enquiry into Health and Allied Themes (CEHAT) Indore. Ashag'am Trust (AGT). Jagrit Adtvasi Dalit
Sangathan (JADS) and Adtvasi Mukti Sangathan (AMS).
2
31
Our Recommendations-
This study has been conducted by Jan Swasthya Abhiyan, Madhya Pradesh. The Jan
Swasthya Samiti acknowledges the people ofthe villages, staffof PHCs, CHCs and District
Hospital, Barwani who have responded to the survey. The people have had much belief
and conviction that this report would help activate a dialogue between the people and the
district health system.
The Samiti acknowledge individuals, M.S.W students from Barwani school of social
work, Ashagram trust. CEHAT, Indore, who have extended their support towards this
endeavor. We are thankful to Dr Abhay Shukla for his invaluable inputs. The Samiti
recognises the contribution of Mr. Laxminarayan Sohner and Mr. Vijay for publication of
this report. Kajal and Anand have done the Hindi translation of the summary report.
Coordinated by:
Amulya Nidhi
Report Compiled by:
Amulya Nidhi
Ashish Gupta
Sanjay Tirkey
With assistancefrom:
Shelley Saha
Kajal Jain
Investigation Team:
Main investigator:
Sanjay Tirkey
Field investigators:
Anand Verma
Monish Dixit
Chelan A tre
Hridesh Singh
Pankaj Babu Agrawal
1.
The CMHO needs to seriously take note of these gross deficiencies and take
up remedial measures A lot of additional attention funds, human power and
above all commitment is needed to provide mini-urn health services, which
we consider as the duty of the govt.
2.
The various demands put forth by the Jana Swasthya Samiti by Sendhwa
need to be taken seriously.
3.
The three cases presented by Rashtriya Satyagrahi Dal. very clearly show
gross negligence by the concerned govt officials. Is very disturbing that despite
the follow-up of these three cases by the Rashtnya Satyagrahi Dal, so far, no
justice has been done to the victims and no action -as been taken against the
govt, officials. We strongly recommended that soci=-oolitical leaders, thinkers,
press take up these cases to mobilize public cordon to harness justice in
these cases.
4th Sept 03
30
3
Report of Expert panelists concerning public hearing held
on 4th September 03 at Sendhwa, Madhya Pradesh
The Panel Consisted of Dr. Anant Phadke, CEHAT, Pune, Maharashra,
Dr. Sunoerraman . Director, State Health Resource Centre, Cha'ttisgarh, Dr. Rahul
Sharma. Convenor. B.G.V.S. M.P. (Bhopal).
The panel was quite impressed by the systematic reports presented PHC
wise, for 31 PHCs, CHC-wise for 5 CHCs and 1 Distnct hospital. These oral and
written submissions indicate that in the eyes of the people, the services offered by
the PHCs and CHCs are grossly deficient and of poor quality. The State of buildings,
equipment, availability of necessary staff, medicines are unsatisfactory. There was
considerable absence of doctors and casual attitude towards care.
Repeatedly we heard evidence that even with slight complications, doctors in
these PHCs and CHCs send patients to Civil Hospital, Badwani, when they should
have treated them locally itself. Many PHC, CHC doctors and even some nurses
have been illegally charging patients in govt, dispensaries themselves.
We listened to the testimonies of some who nad lost their children, mostly to
diarrhoeal disease and we are constrained to note that in every one of them there
was palpable negligence by the concerned staff who referred the case to higher
centre without giving the initial treatment which would have been life saving. This
kind of referring all sick cases and treating only trivial diseases, that too if possible
in their private clinics, is a complete rejection of the spirit of Health for All and the
national health policy.
Though they were duly invited by the organizers, unfortunately nobody from
the health-officials was present to respond to the issues raised and cases presented
by the people. But even in absence of the official explanation, the overall evidence
presemed by the people, very clearly showed the gross deficiency and poor quality
of services in PHCs and CHCs. The government of M.P. through its Swasthya
Jeevan Seva Gurantee Yojana has given a ‘guarantee’ to provide adequate health
care to trie people, in practice, it seemed conspicuous by its absence.
We were shocked to know that appropriate treatment is not given even in
simple cases of diarrhoeas and no treatment is available in some areas for snakebite
and dog-bite. Such gross deadly deficiency is a matter of shame when we enter
the 21st century.
Status of Public health services in Barwani district of Madhya Pradesh
EXECUTIVE SUMMARY
PHCs in Barwani district:
■ There is a shortfall of 15 PHCs in the district' One =HC is serving an average
population of more than 29000 instead of 20,000.
• None of the PHCs fulfill the 2-6 beds norm; all PHCs nave less number of beds
and 8 out of 31. (26 %) have no admission facilities
• 11 out of the 31 PHCs (36 %) building are in very cad condition.
• 15 out of 31 PHCs (48 %) do not have normal delivery facilities and 13 (42%)
PHCs do not even have a delivery room
• Out of 31 PHCs, 8 PHCs do not have connection of electric supply. In 40 % PHC the
fans and the tubelights are not working Not a single PHC had a generator backup.
• 6 (19%) PHCs did not have any source of water. 13 (41%) PHCs have water
supply by hand pump and most of these run dry in summer months. Only 12
(42 %) of the PHCs had facility for running water.
• 26 PHCs (84%) do not have ambulance facilities. Only 5 PHCs (16%) had an
ambulance facility and even in these 5 PHCs the covers do not reside in PHCs.
• 13% PHCs are running without regular doctors. Only 3 PHCs had.lady doctor. In
70 % percent of the PHC LHVs and MPWs were not posted.
• In 29 % of PHCs, doctors were not available in scheduled timings. Even for
other staff in 20 % PHCs, staffs are not present at scheduled timings.
CHCs in Barwani district
• The district has less than half of the required number of CHCs. Instead of 1
CHC per 80.000 population the district has 1 CHC for 1,84.612 population.
• None of the CHCs fulfill the 30-bed norm: all CHCs have 10 beds or less.
• 40% CHCs do not have running water facility.
• There is no functioning Operation Theatre in 60% CHCs: certain CHCs do not
even have a delivery room
I
• 80% of the CHCs have no specialists, the single CHC with specialists has only
half of those required.
--------------------------------------------------------------------------------------------------------5. All the public hospitals and health centers should nave minimum number of
beds according to the norms.
6.
In all hospitals (including PHCs, CHCs), ambulance v:~ full-time drivers should
be immediately provided so that during emergencies tney may be used for
referral. The ambulance facility should be made
for the people Belov/
Poverty Line (BPL).
• 80% CHCs do not have neonatal resuscitation equipment or ECG machine;
40% do not have oxygen cylinder, incubator or adequate operation equipment.
7.
At every PHC/CHC/civil hospital a board giving information about the availability
of various services and rates of services, should be out up.
• None of the CHCs provide services for caesarean delivery.
8.
All the pnmary and community health centers including district hospitals, should
have all essentials drugs including Psychotropic Drugs. The emergency facilities
like treatment for snakebites and dog bites should be available in all the
hospitals and health centres.
9.
All the PHC, CHC and District hospital should adopt minimum norms of service
delivery and provisioning for it.
10.
It is also important that delivery room should be functional at PHC level.
11.
In all hospitals basic laboratory set of tests shou.c be provided. In district
hospitals, the laboratory should also be opened aiong with the OPD timings
because people have to go for private laboratories for certain tests. Sonography,
X-ray and certain tests facility should be available on all days of the week and
timing should be user friendly.
12.
The PHC staffing pattern needs restructuring to ensure utilization of manpower
and better functioning of the facility. PHCs may appoint two or three male/
female multi-skilled employees.
13.
All vacant posts in the health department should be filled immediately. With
regard to this the most important posts are that of the lady doctor, ANM and
medical officer.
14.
The amount collected from the patients through the Rogi Kalyan Samiti should
be made public and displayed in the facility on regular basis. These funds
should be used for better patient service by providing enough medicines,
disoosable syringes, investigation facilities, beds and other facilities etc.
15.
Puouc health system should support community level heath workers (Swasthya
Sathis) working in three blocks of Barwani and providing basic health services
at village level, by providing them free drugs and referral support.
• Only one CHC has a female doctor.
• In 40% CHCs, doctors are not present during scheduled timings.
• 40% CHCs do not provide treatment to severely anemic women or children with
severe respiratory I gastrointestinal infections; 60% do not have STD clinics.
District Hospital in Barwani district
• When admitted, some patients have to lie on floor and even in corridors. This was
observed especially in Pediatric and orthopedic wards. Similar conditions exist in
Mahila Hospital also where most of patients were seen to be lying on the floor.
• The water facility in the hospital is erratic and unhygienic. The district hospital
has only one water tank but the water is likely to be contaminated as it is situated
beside the septic tank.
• Only one ambulance in the District Hospital is in good condition.
• Many patients have to purchase medicines such as drugs/syrups/saline from
private medical stores.
ROGI KALYAN SAMIT! of Barwani District Hospital (Data for 2002-2003)
• RKS is not utilising almost 25 % of its collection even though the hospital is
seriously lacking in many of the essential services due to lack of funds.
• 75% of the total money collected by RKS is earned from general patients. However,
only 11% of the total expenditure is spent on services for general patients.
• Out of the total expenditure of Rs 15,26,201/- the major expenditure of (81.3%)
RKS has been incurred on items not related directly to patient services like new
installation of AC. coolers, grass cutter and water pump for lawn, building repair,
electric expense of CMHO office and for salary of staff employed by RKS.
5
CONCLUSIONS
The investigation report shows that Barwani has a very public health delivery
system. Given the fact that the state has a poor health status this lack of public
health services becomes a major barrier in improving health status. This poor
state of health care services has been documented, published and presented, a
number of health dialogues with the Government including Jan Sunwai's were
held in Sendhwa and Pati, but yet the Government has been very slow and reluctant
in responding to these peoples’ initiative to improve public health.
‘Health for All’, which initially became the target to be achieved by 2000, and
also the 'Health Guarantee Scheme’ of M.P. Government which guarantees health
care, the ground situation of today is very different. The investigation shows that
that the public health system is grossly lacking in preparedness to achieve these
objectives. Urgent action needs to be taken by the health bureaucracy for achieving
these aims and GAURANTEE HEALTH SERVICES.
RECOMMENDATIONS
1.
District and Block level ‘health coordination committees’ should be formed
immediately. These can coordinate the efforts of the public health system and
by the voluntary sector in the whole district. It should include representatives
of Jan Swasthya Samiti, NGOs, People's organisations and representatives
of the Health department at district and block level. These committees may
conduct review and planning meetings every two months to monitor
improvement in health'services.
2.
The services should be planned in such a way so as to give priority to areas
which have difficult accessibility, and have no health facility at all. For example
Roisar, Palsud, Bokhrata, Balwadi, Dhauli etc.
3.
The outcome of the investigation shows that in Barwani district, there is a
shortage of 23 PHCs. Therefore the Health department should ensure to
adequate PHCs in every block. It should also ensure at least one CHC per
block. Some of the PHCs like Sendhwa should be upgraded to CHC.
-
All the public hospitals should immediately ensure regular water supply and
power supply and also ensure separate toilets and bathing facilities for men
and women. Higher priority needs to be given to waste disposal systems in all
health care facilities.
INTRODUCTION
Madhya Pradesh is located at the geographical cerre of India with Bhopal as
the capital. It shares its borders with five states.
Maharashtra, Gujarat
Rajasthan, Uttar Pradesh and Chhattishgarh. Erstwhie Madhya Pradesh was the
largest Indian state in terms of area (spread over -*43.000 sq. kms), and had
accounted for 14% of India’s land mass. According to 2001 census, Madhya
Pradesh had a population of 60,385,118(male 314.5c3.73. female 28,928,245).
The population sex ratio number of females per 10OO males was 920 in 2001. The
state, has the highest population of Schedule Tribes 123% of the country) outside
northeastern states. The literacy rate of the state is 64.11%. It is one of the most
economically backward states with more than 42 percent population living below
the poverty line (NCAER 2002) It is also one of the low literacy states in the country.
Most of the villages in the state do not have an all season approach road. Tribal
regions are mostly in hilly areas, where people have to'walk nearly 15-20 Kilometers
to get basic services.
In the western region of Madhya Pradesh, Barwani is one of the less developed
districts. Ninety percent tribal population, mainly by Barelas, Bhilalas, and the Bhils,
inhabits it.
According to 2001 Census the total population is 10.81,039. with 547837 males
and 533202 females. The female
literacy is 19.01% and the male
Badwani
literacy is 36.77%. Barwani district (Madhya Pradesh)
has 7 development blocks, 714
villages, 383 Gram Panchayat and
1121 AWW. The maternal mortality
rate is 5 per 1000. In terms of health
facilities it has 1 district hospital, 5
Community Health Centre (CHC), 31
Primary Health Centres (PHCs), 235
sub centers (SCs). At the village
level. ANM/MPW.are deputed to
provide basic health services to
people.
The declaration of Alma-Ata Conference in 1978. setting the goal of Health for
All by 2000 AD has ushered in a new philosophy of equity, the new primary health
27
6
care approach. The National Health Plan (1983) proposed reorganization of primary
health centres on the basis of one PHC for every 30000 rural population in the
plains, and one PHC for every 20000 population in hilly, tribal and backward areas
for more effective coverage.
Health problems like tuberculosis and Malaria in tribal communities are
compounded by difficult terrain, mutual disbelief and mistrust between the
community and health workers and non-availability of essential/life saving medicines
in the area. Poor child and maternal health status, prevalence of infectious and
diseases are common causes of early deaths in this area and the state has to
improve the situation by improving its health services adopting an appropriate
developmental plans and by co-operation with social and voluntary organisations
Madhya Pradesh Government has given a Guarantee to provide all basic Health
services through Swastha Jeevan Seva Guarantee Yojna, which was initiated in
the year 2001. But over 2 years after the implementation of the Yojna, the failure of
the public heath services in several districts of Madhya Pradesh continues to be a
stark reality. This prompted the Jan Swasthya Samiti to initiate an investigation of
Public Health Services in Barwani district.
OBJECTIVES:
1.
To assess the level and limitations regarding availability of the health care services
in the government health facilities.
2.
To recommend improvements in organisation and delivery of public health care
services.
METHODOLOGY:
Sample selection:
The data was collected from all the 5 Community Health Centers (CHCs), all the
31 Primary Health Centres (PHCs), and the District Hospital from Barwani District.
Sources of Information Gathering:
1
Tne data was collected using the M.P. government checklist, which is used to
monitor the puolic health services. We decided to use the government checklist
so as to demonstrate how the public health services are functioning even
according to tneir own guidelines. The checklist for CHC had 131 parameters
Expenditure of Rs 2,14,634/- (11%) on services to gernral patients included:
• Lab. Blood Bank. Chemicals, ARV (6.3%)
• X-Ray Films (4.0%)
• Blood Collection Exp. (1.9%)
• Eye (1.6)
• Expenses on porridge for women who are admittec r delivery room (0.2%).
Out of the total expenditure of Rs 15,26,201/- the macr expenditure of (81.3%)
has been incurred on
• New Installations of (Air Conditioners, coolers, grass cutter and water pump for
lawn) - 22.3%
• Repair-12.9%
• Electric expenses for CMHO office -11.6%
• Salary of staff employed by RKS - 7.8%
It shows that while the District Hospital is lacking in many of the essentiaJ
services due to lack of funds the money is being spent on non essential
repairs, installations etc.
-------------------------------------------------------------------------------------------------------------------------------------------------------------
26
ROGl KALYAN SAM1TI (RKS), DISTRICT HOSPITAL, BARWANI
• RKS is saving almost 25 % of its collection even though it is seriously lacking in
many of the essential services due to lack of funds.
• 75% of the total money collected by RKS was earned from general patients but
out of this 11% of the total expenditure was spent on services to general patients.
• Out of the total expenditure of Rs 15,26,201/- the major expenditure of (81.3%)
has been incurred on new installation of AC, Coolers and grass cutter and water
pump for lawn, Repair, Sectric expense of CMHO office, salary of staff employed
by RKS.
RKS of DH
As per the information procured from the District Hospital, during the Financial
Year 2002-2003, the total income of the RKS was Rs 20,07,762 and the total
expenditure was Rs 15.26.201/- and a sum of Rs 4.81,561/- (24%) was saved in
that financial year. RKS is saving almost 25 % of its collection even though it is
seriously lacking in many of the essential services due to lack of funds. It was also
gathered that the RKS has a large net saving lying as FDR in the bank amount,
which was not disclosed.
On analysis of the accounts it was found that eventhough Rs 14,96,926 (75%
of the total money out of total Rs 20,07,762 collected by RKS)) was earned from
general patients but out of this only Rs 2,14,634/- (11% of the total expenditure
made by RKS out of the total Rs 15,26,201) was spent on services for general
patients.
Earnings of Rs 14.96.926 (75%) from general patients include mainly collections
in the form of
• OPD (18.7%), collected @ Rs 2 per patient for case paper
<■ Indoor (18.3%), collected @ Rs 5 per patient
• Lab (10.2%), collected @ Rs 5-40 per patient
• X-ray (3.1%) @ 20-40 per patient
• Blood Bank (6.4%) collected - @ Rs50-100 per patient
• Sonography (5.4%) @ 100 per patient
and PHCs had 65 parameters. A similar checklist was _sed for the Civil Hospital
with 152 parameters.
2. All the checklists were filled, observed anc crosschecked with interviews from
doctors, other staff, patients and villagers.
3
Beside the checklist, observation was aiso done to substantiate the data
gathered by checklist.
The data was collected from doctors and ctner staff present at the health care
facilities. The data was collected between mid July to Sectember 2003.
In the following sections, we would be presenting the findings of the data
collected from PHC, CHCs and district hospitals.
7
25
8
PRIMARY HEALTH CENTRES
REPORT CARD OF PRIMARY HEALTH CENTRES
• There is a shortfall of 15 PHCs in the district! One PHC is serving an average
population of more than 29000 instead of 20,000.
• None of the PHCs fulfill the 2-6 beds nccm: all PHCs have less number of beds
and 8 out of 31 (26 %) have no admission facilities.
• 11 out of the 31 PHCs (36 %) building are in very bad condition.
• 15 out of 31 PHCs (48 %) do not have norma! delivery facilities and 13 (42%)
PHCs do not even have a delivery room.
• Out of 31 PHCs, 8 PHCs do not have connection of electric supply. In 40 % PHC
the fans and the tube lights are not working. Not a single PHC had a generator
backup.
• 6 (19%) PHCs did not have any source of water. 13 (41%) PHCs have water
supply by hand pump and most of these run dry in summer months. Only 12
(42 %) of the PHCs had facility for running water.
• 26 PHCs (84%) do not have ambulance facilities. Only 5 PHCs (16%) had an
ambulance facility and even in these 5 PHCs the drivers do not reside in PHCs.
2. Ambulances: There are three ambulances in the Dstrict Hospital. One is in
good condition and used regularly, the 2nd one has breaKccwns and goes frequently
for repair and the third is not used, as there is no driver. According to people they
don't find the service satisfactory, regular and affordabe
3. Availability of drugs: According to the norms, the district hospitals should
have all essential drugs including vaccines for dog bee and snakebite. But the
study found that patients had to purchase medicines from outside. This information
was .also corroborated from people who were admitted in tie hospital. Many patients
said that they have to purchase at least some medicine drugs/syrups/saline.from
private medical stores.
4. Blood Bank: Though there is a blood bank in the DH, people face difficulty
when blood has to be acquired. There is a need for proper monitoring of the services
of the blood bank so that it can be optimally used.
5. Diagnostic facilities: Though the DH is found to have facilities for basic diagnosis
like a laboratory, X - ray, but patients are charged for the tests that are conducted
and most of the time the cost of these tests are very high which a poor patients
cannot afford.
Mahila Hospital : "Prasuti ke nam par prata'ma jhel rani hain mahilain ’ Danik
Bhaskar 1-102-2003. This news and several other reporting in local dailies highlights
the bad state of the Mahila Hospital but little has been done to change the situation.
• 13% PHCs are running without regular doctors. Only 3 PHCs had lady doctor. In
70 % percent of the PHC LHVs and MPWs were not posted.
• In 29 % of PHCs, doctors were not available in scheduled timings. Even for
other staff in 20 % PHCs, staffs are net present at scheduled timings.
Findings of the PHCs:
1. Adequacy of PHC:
A PHC is supposed to serve an area of 30000 population in plains and to
20000 population in remote and tribal areas. Our area of study, Badwani district is
a tribal area and thus a single PHC is sumcosed to serve 20000 rural population.
According to 2001 census, the district nac 9,23.063 rural population (Provisional
Population Total, Directorate of Census Coerations, Census of India 2001, MP).
So accoroing to the population criteria tre district should have 46 PHCs but in
reality the district have 31 PHCs. It means a shortfall of 15 PHCs in a district! Thus
ROGl KALYAN SAMITI (RKS)
An initiative has been launched in the state under the Rogi Kalyan Samitis,
where for the first time effort was undertaken to bring in people's participation in
hospital and health centre management and to levy user charges. Today there are
604 hospitals and health centres across Madhya Pradesh that has a RKS (MPHDR 2002). It was found that RKS is constituted in all the 5 CHCs but it was found
that in 1 CHC (Thikri) RKS do not have regular meetings. During one of the Health
Dialogue in Pati. it was found that in many PHCs under Pati CHC, RKS have
formally not been constituted but staff is still collecting money from patients without
proper receipts, opening the way for gross financial irregularities.
■4
DISTRICT HOSPITAL (DH)
1.
INFRASTRUCTURE:
1.1 Furniture: Even though the hospital has 283 beds due to lack of mattresses
some of them are unused and therefore some of the admitted patients have to lie
on floor and even in comdors. This is the condition especially in Paediatric and
orthopedic wards and also Mahila Hospital where most of patients were seen to be
lying on the floor. Condition of beds and general hygienic conditions of'16 Palang
ward' are found to be in a bad state.
in effect a PHC in the district is serving an average poo-sron of more than 29000
instead of 20,000.
2. Infrastructure arrangements:
2.1 Condition of building:
Of the 31 PHCs, 24 PHCs had their own building, wrereas the rest 7 PHC are
situated either in donated place (2), place given by G-am Panchayat (2), rented
place (1) and in subcentre (2). As shown in the table becw physical conditions of
11 PHCs are very bad.
% of Non Go.emmentl
% of Government
Building
Building
Bad
Satisfactory
Bad
Satisfactory
Condition Condition Condition Condition
1.2 Beds Sheet and Linen: It was observed that those patents who are lucky to
get a bed have to put up with dirty bed-sheets and pillows which are not washed
and are stained with blood and urine.
Name of
Block
1.3 Electricity: It was observed that in many of the rooms the fans and lights are
not working and the wiring is loose. As Barwani gets very hot during summers it
gets difficult for the staff and patients to be comfortable without a fan. Many patients
are admitted and kept in the corridors, which have no fans.
Pati
66.7 (2)
33.1 (1)
0.0
00
3
Badwani
100.0(3)
0.0
100.0 (1)
0.0
4
Rajpur
33.1 (1)
66:7 (2)
66.7 (2)
33.1 (D
6
Newali
50.0(1)
50.0(1)
0.0
0.0
2
Pansemal
100.0 (4)
0.0
0.0
0.0
4
Sendhw'a
28.6 (2)
71.4 (5)
0.0
0.0
7
Thikri
100.0 (2)
0.0
66.7 (2)
33.1 (1)
5
15
9
5
2
31
1.4 Water: The patients especially the admitted patients need to have clean water
for drinking, bathing and toilet. However, the water facility is erratic and unhygenic.
The district hospital has only one water tank but the water is contaminated as it is
situated beside the septic tank. Patients are thus not able to get safe water for
drinking and for other purposes.
1.5 Toilet facility: Though there is toilet attached with most wards they do not
have water facility and poses a threat to the overall hygiene of the hospital. The
Sulabh Complex built with the money of RKS charges Rs 21- per day per person
and most admitted patients is not able to afford that.
TOTAL of
PHCs
Total PHC
in The Block
(Figures in parenthesis indicate number of PHCs.)
1.6 Waiting facility: District Hospital caters for patients coming from far off places
and many patients have to be admitted for long period. There is no proper place
for relatives of patients who are admitted. The Ayushmati Bhawan is closed for the
last 1 year and the Dhanwantri Dharamshala has broken doors and windows and
no beds. In the last 1 year not even a single person has stayed in the Dharamshala.
Therefore water, toilet, bathing, food and residential facilities should be available
for the relatives of those patients.
In Rosar PHC the entire roof leaks. PHCs of Ojhar. Baiwadi, Julwania, Dhawli,
Warla and Sendhwa have very bad leaking roofs and water easily gets into the
building and damages the walls, doors and windows, furniture, medical equipments
and med.cines. Leaking roofs affects other conditions of the building like electricity.
A large number of the PHCs have new buildings under construction since long
and the PHCs are being carried out from the old dilapidated buildings eg Julwania,
Nagalwadi, ojhar.etc
--------------------------------------------------------------------------------------------------------------------------------------------------------- ■------ 23
10
2.2
Furniture:
As per norm every PHC is required to have admission facilities of minimum
4 to 6 beds. Our observation show that in large number of PHCs there are
1-2 beds and in some PHCs there is not even a single bed available and it is
interesting to note that patients have to bring their own beds in case they want
admission in Balwadi or DhauB PHC. In some of the PHCs there are no wards but
beds are there in corridor and n other PHCs there are wards but no beds. In
Balwari PHC there is ward but no beds are there whereas in Nagalwadi even
though beds are there no ward is there.
Those PHCs that have beds do not have dean and adequate linen like cushions,
pillows and bed sheets for example in Dhanora and Rosar PHC. Either they are
tom and in bad condition or they are extremely dirty and have not been washed
for a long time which is the condition in Jhopali, Chachriya, Nagalwadi, Dawana,
warla PHC.
Some PHCs lack bask: fumcure like chairs, tables and benches, examination
tables etc. Lack of basic furniture hampers efficient performance of the medical
staff. In many PHC patients had to stand while they wait for their turn to meet
the doctor. Many PHCs did not have almirah which is needed to store
medicines, fmens, bandages, injections and equipments etc. In many of the PHCs
medicines were either left on shelves or dumped on the floor or tied in bundles
using clothes. Proper storage is essential for maintaining the efficacy of medicines
and injections. In Chachriya the medicines are not stored properly in absence of
almirah. In most of these PHCs the drugs supplied are without cover.
2.3
Delivery Room:
Forty two percent PHC (13) did not have a delivery room, and of the rest 18 PHC
where there is a delivery room, delivery facility is not available in 6 PHCs for all 24
hours and in another 2 PHCs it is not available at all. No delivery facility in Balwari,
Moida, rakhi Bajurg. Bandha Bajurg, Chatiey PHC.
This non-availability of basic health service like delivery needs to be seen in the
light that charges for normal deivery in private hospital vary from Rs 300 to Rs
1000 depending on the caoadrycfthe individual to pay.
insertion services are available in 4 CHCs. All the CKs reported that temporary
methods of family planning are available. It was also reserved that in most of the
CHC, tubectomy camps were organised merely to amieve the targets and these
camps are insensitive to the humane needs of the catients ignoring their basic
rights and dignity. The most striking feature of these camps is that the insuffolation
procedure (a procedure in key hole surgery where air is filed in abdomen to facilitate
key hole surgery) is done using the cycle pump.
According to NFHS -2, more than 40 percent ever-married women in the state
were found to suffer from any type of vaginal discharge or with symptoms of urinary
tract infections (UTI). Our study found that only 2 CHCs have STD clinic, which is
definitely quite inadequate with such a high prevalence of STI/UTI problems.
11
mortality is high in Madnya Pradesh (According to NFHS - 2 MP, neonatal mortality
is as high as 54.9 for 4 year period preceding the survey). Certain CHCs were
found unable to even perform a basic investigation such as estimation of
Hemoglobin.
7. Type of services available (selected list):
As evident from the table below, the services available as per the norms of a
CHC are quite inadequate. None of the CHCs provide services for caesarian
delivery, which is an emergency service. Many maternal deaths take place due to
obstructed labour and these lives can be saved with timely interventions and quality
services.
Type of service
No of CHCs in which
it is available
Caesarian delivery
0
Treatment of severe anemic pregnant women
3
Serious respiratory and diarrhea cases
3
ANC and PNC clinic
5
Immunization services
5
Laparoscope’s
4
Female sterilization
1
Non scalpel sterilization
1
Cuts
4
[ STD clinic
2
Though the data gathered show that al! the CHCs organise ANC and PNC
clinic but there is a large scope of doubt aocut tne range of services that are
provided as ANC and PNC services.
CASE NO 5 - CHILD HEALTH PROBLEMSR is 2 and half years old child of Mr. V of village D of azicck ofBadwani district,M.P.
He had fever & vomiting taken to private Doctor for twz days. Later because of no
improvement was taken to G PHC where treated by oicror. After treatment of 2-3
days his left eyelid dropped (pitosis) developed. He was referred to CHC, P where
treated by doctor for 5 days, by this time the child hac developed rigidity of limbs,
and the doctor gave eye drops & ointment for rigid mussels for massage. He even
took treatment from Jan Swasthya Rakshak of P block, vnere he was finally referred
to Badwani District hospital, here he was shown in eye department from where he
was referred to child (pediatric) department and admitted. Here no proper treatment
was given to the child even though he remained there iar 8days. Since condition of
his eye worsted, he was asked to get admitted to the ere ward. Child was taken to
eye department again; the eye doctor without treating am referred him back to the
Pediatric department He again was kept in the Pediatric department for 6days & his
both eyes became infected and when his father protested then he was referred to
private eye doctor.
From the prescription of private eye doctor (Part of case record) it is clear that the
child had developed complete paralysis of all the mussels of both eyes (complete
opthalmoplegia) and very little could be done to solve tis eye sight. After seeing the
prescription of private eye doctor the hospital instead cf treating him, immediately
discharged the child the unfortunate child became blind for life due to continued
denial of health services at the all levels (Jan swasthya Rakshak,
PHC,CHC,District hospital)
TYPE OF DENAIL:
1. Patient referred outside for doing investigations.
2. Negligence of the health staff.
3. Delay in treatment
CONSEQUENCES OF DENIAL
1. Permanent damage leading to handicap
2. Moderate financial loss.
2.4 Indoor facility:
PHC by its norm is supposed to have admission facility. The study show that
in 8 PHCs (26%) there is no indoor facility and only outoatien: facility is available.
2.5
As far as contraception services are concerned sterilisation services are
available only in camps. It is reported that sterilisation follow-ups are done. Cut
Electricity:
Out of 31 PHCs. 8 PHCs have power cable connected out the supply has
not been connected at the time of data collection e.c Rosar. Moida. Dhanora.
12
21
Chchariya etc. Even the PHCs with power connections have very erratic power
supply (4-6 hours per day). The electricity wiring is also very bad. For patient
examination and carrying our other routine activities availability of adequate light
is very important Unfortunately in all the PHCs it was observed that in many rooms
have dim lights. In 40 % PHC the fans and the tube lights are in non working order.
For sterilization, kerosene stoves are used by many PHCs by which one can only
boil needles, syringes and metal equipments, but a large number of items need
dry heat like gauze, cotton, plastic items etc, that cannot be heated in absence of
electricity. Certain vaccines like polio vaccine, anti-rabies vaccine and certain
essential injections and reagents need continuous refrigeration to maintain their
potency. Even the ice packs for cold chain maintenance are required to be
refrigerated, to cany polio vaccine into far of villages. Lack of electricity even in
presence of a refrigerator, hampers the vaccination programmes.
Despite a poor errabo supply not a single PHC has a generator backup.
Probably government has never thought of providing modem equipments like auto
analyzer, auto-claves etc. to the rural areas.
2.6
Water supply:
As evident from the table below 6 PHCs did not have any source of water
(e.g. Dhauli.Tatwara, Bajurg). Thirteen PHCs have water supply by hand pump
and most of these run dry in summer months. In Talwara Deb water has to be
fetched from more than half a kilometer away from the PHC. Only 42 percent of
the PHCs had facility for running water. As explained earlier, absence of water
hampers cleanliness of the facility. Therefore it is not surprising that our survey
found that cleaning is unsatisfactory in 12 PHCs (39%).
2.7
Source of water
No ofPHC
Percent
No water Facility
6
19.4
Tap
12
38.7
Hand pump
13
41.9
Total
31
100.0
Toilet:
Most of the PHCs, die not have a functioning toilet facility.
6.
Required Equipments:
As evident from the table below, all the CHCs were ~und to have BP apparatus,
microscope and X-ray machine. Weighing machines were found in 4 CHCs. In
Pati CHC, x-ray facilities is available only once a wee'. ~ Rajpur 3 days in a week.
Only Rajpur CHC had a ECG machine. Newali an: —nikri were found to have
operation equipments but do not have a surgeon or a* OT. There is thus a great
mismatch of equipments, facilities and human power. ~-is mismatch forces people
to seek medical care from private providers. All re CHC had some of the
equipments required for the cold chain, but none of rem had all the required (as
per the checklist) instruments.
Required Instruments
No of CHC
Yes
i
No
BP apparatus
5
|
0
Microscope
5 I
5 I
0
I
4
X-Ray machine
0
ECG machine
1
Weighing machine
4
1
Operation equipments
3
2
Equipments for cold chain
5
0
Resuscitation
1
4
Neonatal warmer
3
2
Incubator
3
2
Oxygen cylinder
3
2
Neo-natal Equipments
Even life saving instrument like oxygen cylinder is assent in 2 CHCs (Pati and
Rajpur) Important life saving neonatal instruments like resuscitation, neonatal
warmer and incubator is present in only one CHC (Rajpur). No wonder neonatal
20
13
avail this facility due to variety of reasons like unavailability of drivers. According to
tne Rogi Kaiyan Sam'ra norms people have to pay Rs 4 per kilometer but interaction
with people show that most of the people are illegally charged more than that.
Vehicle for supervision: None of the CHCs had a vehicle for supervision, which
in turns affects effective monitonng of extension/outreach work of the CHC.
3.
Adequacy of staff:
Medical staff strength including availability of specialists at each CHC is
important indicators of its provision of quality care. Of the CHCs studied, most did
have medical officers but were found lacking in case of specialists. The norm is
that each CHC should have 4 specialists - surgery, obstetrics and gynaecology,
general medidne and paediatrics. Of the 5 CHCs only one CHC (Rajpur) had
specialists that too only one surgeon and paediatridan. Only one CHC had a female
doctor. Presence of female doctors assumes importance as women find it
comfortable to share their health problems with female doctors especially related
to their reproductive problems.
In terms of other staff, all the CHCs had a computer operator (though some
CHC don't nave computer!), compounder, technidan, radiographist and other 4th
class staff. Two CHC did not have Block Extension Educator (BEE) and clerk and
one CHC did not have staff nurse. Absence of BEE means that supervision and
monitoring of extension workers are not done, which might mean no or less than
required extension services.
4.
Residence facility:
The checklist only had one question that is whether the doctor stays at head
quarters. It was found that doctors of all the 5 CHCs stay at the head quarters
5.
Functioning:
Though the study found that the CHCs were open for full time, in 2 CHCs (Pati
and Newalij doctors are not present during scheduled timings. Also based on
observation and with discussion with patterns and villagers it was found that beside
regular timings doctors nesitate to come to hospitals to attend serious cases and
many of them are engaged in private practice during scheduled timings. This
unavailability of doctors in health care facilities poses serious problems to patients
in times of emergency in accessing health care.
3.
Ambulance:
Only 5 PHCs (16%) had an ambulance facility an: even in these 5 PHCs the
dnvers do not reside in the PHCs and take some time:: -each the hospital in case
of emergency loosing vital minutes in case of emerge".?. In the absence of some
basic emergency facilities at PHCs at least ambuia'ce can be handy during
emergency cases, and proper transportation facility ca_ :e life saving. The charges
for ambulance is Rs. 4.00 per kilometers, but in some ciaces double the amount
are being unofficially charged. However, in most PHCs tne patients have to hire
private taxis at very high cost if they are available, ano f they are not available or
too expensive then in case of emergencies the patients miatives becomes helpless
and many patients die because of lack of transportation facility. For instance, in
Sendhwa block there is only one ambulance attached t: the Sendhwa PHC, which
has tocater the needs of 6 other PHC of the block which co not have any ambulance.
CASE STUDY 2:
A clear example of ‘denial of health care’ is from J village of a block of
Barwani district, where N, a poor adivasi, was residing with his family of 6
members, in the night of 23rd June his son K had a severe problem of vomiting
and loose motions. Next day the MPW gave him an ORS packet
When no improvement was observed in the child’s condition, it was
suggested that he be taken to nearest PHC, where the MO treated him. But,
aftersometime bleeding started from inside the mouth and nose of the child.
At another doctor's suggestion, N had to shift his child to Sendhwa PHC.
Due to lack of money he had to bring the critically sick child by a brick
loaded truck just because nearest PHC didn’t have ambulance for this
emergency situation.
Even in Sendhwa hospital, he had to purchase injections and syringes
worth over hundred rupees. Afterwards when the condition became more
serious, it was suggested that he take the child to Barwani district hospital.
But N, a poor adivasi, did not have money for the transport and further
treatment, and ultimately decided to come back to home. On the way back
home the child died.
This case study demonstrates how a PHC is not able to provide essential
health services, not even an ambulance in an emergency condition, to save
the life of an ill child.
19
14
This case study demonstrate how a PHC is not able to provide essential
health services, not even an ambulance in an emergency condition, to save
the life of an HI child. This case shows violation of Right to a set of basic
health services which is guarnteed to us by Article 21 of the Indian
Constitution and also Article 24 of the Convention on the Right of the Child.
4.
Adequacy of staff:
■ A PHC as per conns is to have a medical officer in charge, two sector
supervisors - one mae and female, a staff nurse, a laboratory technician, a
compounder cum pnamadst and a dresser, a watchman and atleast one another
class IV staff.
Type of personnel
% of PHCs
Doctor
87.1
Compounder
16.0
Staff nurse
18.7
Others
30.7
No staff
1.3
2.
Infrastructure arrangements:
CHCs of the district are all situated in government o.vned building but none of
the CHCs have 30 beds according to CHC norm. Only Raour and Pansemal CHC
have 10 beds and the CHC at Pati has. only 3 beds! As: 2 CHCs (Pati and Thikri)
does not have the required furniture that a CHC is sutzresed to have. In absence
of required furniture, drugs and other medical instrumsts gets damaged.
2.1
Electricity:
Uninterrupted supply of electricity is an important requirement for any medical
facility. One CHC (Thikri) at the time of survey did not rave electricity. In absence
of electricity, drugs, and vaccines gets wasted and loses its potency, it also affects
the cold chain and can become fatal in cases of operaccns. Even in CHCs where
electricity is available, the wiring conditions are in bac snape. Alternative electric
facility is available in only one CHC (Rajpur).
2.2
Water supply:
Three CHCs have facility for running water (i.e. tap' and for the rest two CHCs
(Newali and Thikri), water is stored in a earthen pot. But any facility with inpatient
facility should have running tap water, bathing facility and toilets. Even maintaining
minimum cleanliness would be difficult to maintain in absence of such water supply.
2.3
Delivery room:
• As evident from tne above table, 87 percent PHCs have a doctor but what is
significant to note istnat 13% PHCs did not have doctors! For instance, Palsud
and Roisar PHC do not have any doctor. In Moida and Dhanora PHC, the doctor
comes sometimes. Oray 3 PHCs had lady doctor. The presence of compounder
and staff nurse is also very inadequate. In only around 30 percent of the PHCs,
LHVs and MPWs were found. One PHC (Inderpur) from Rajpur did not have
any staff.
'
Maternal death is very high in our country. It is quite unfortunate to find that
the CHC in Pati did not have a delivery room. Most of tne villages in the district do
not have trained birth attendants even, and therefore for delivery many women
had to take recourse to untrained traditional birth attendants. In 4 CHCs, delivery
room is present but it is in bad shape. It was observed that in Pansemal and
Rajpur CHCs the delivery room is flooded with water during rains, and therefore
become impossible to perform safe deliveries.
Functioning:
2.4
Survey has shewn that doctor stay in the Head quarter (HQ)-in only 15 PHCs
and in other 16 (52% PHCs the doctor do not stay at the PHC. It is important for
a PHC doctor to stay a: the HQ in order to attend to emergency cases. .As evident
from the table below - around 29 percent of PHCs. doctors were not available in
scheduled timings. Even for other staff in around 20 percent PHCs, staffs are not
present at schedules tunings.
There is no OT in 3 CHCs of the 5 CHCs in the district. It was observed that
only stitching of wounds is done in OT, and due to lack of equipment, operations
are not done and patients are referred to District hospital.
2.5
Operation theatre (OT):
Ambulance facility:
All the CHCs had an ambulance, but during emergency people are not able to
19
14
• This case study demonstrate how a PHC is not able to provide essential
health services, not even an ambulance in an emergency condition, to save
the life of an HI chad. This case shows violation of Right to a set of basic
health services which is guarnteed to us by Article 21 of the Indian
Constitution and also Article 24 of the Convention on the Right of the Child.
4. Adequacy of staff:
■ A PHC as per norms is to have a medical officer in charge, two sector
supervisors - one mate and female, a staff nurse, a laboratory technician, a
compounder cum pharmacist and a dresser, a watchman and atleast one another
class IV staff.
Type of personnel
% of PHCs
Doctor
87.1
Compounder
16.0
Staff nurse
18.7
Others
30.7
No staff
1.3
2. Infrastructure arrangements:
CHCs of the district are all situated in government qwned building but none of
the CHCs have 30 beds according to CHC norm. Only Raipur and Pansemal CHC
have 10 beds and the CHC at Pati has. only 3 beds! Asst 2 CHCs (Pati and Thikri)
does not have the required furniture that a CHC is suotesed to have. In absence
of required furniture, drugs and other medical instruments gets damaged.
2.1 Electricity:
Uninterrupted supply of electricity is an important requirement for any medical
facility. One CHC (Thikri) at the time of survey did not nave electricity. In absence
of electricity, drugs, and vaccines gets wasted and loses its potency, it also affects
the cold chain and can become fatal in cases of operations. Even in CHCs where
electricity is available, the wiring conditions are in bad snape. Alternative electric
facility is available in only one CHC (Rajpur).
2.2
Water supply:
Three CHCs have facility for running water (i.e. tap) and for the rest two CHCs
(Newali and Thikri), water is stored in a earthen pot. But any facility with inpatient
facility should have running tap water, bathing facility and toilets. Even maintaining
minimum cleanliness would be difficult to maintain in absence of such water supply.
2.3
Delivery room:
. As evident from tne above table, 87 percent PHCs have a doctor but what is
significant to note is that 13% PHCs did not have doctors! For instance, Palsud
and Roisar PHC do net have any doctor. In Moida and Dhanora PHC, the doctor
comes sometimes. Oriy 3 PHCs had lady doctor. The presence of compounder
and staff nurse is asa very inadequate. In only around 30 percent of the PHCs,
LHVs and MPWs were found. One PHC (Inderpur) from Rajpur did not have
any staff.
•
Maternal death is very high in our country. It is quite unfortunate to find that
the CHC in Pati did not have a delivery room. Most of the villages in the district do
not have trained birth attendants even, and therefore for delivery many women
had to take recourse to untrained traditional birth attendants. In 4 CHCs, delivery
room is present but it is in bad shape. It was observed that in Pansemal and
Rajpur CHCs the delivery room is flooded with water during rains, and therefore
become impossible to perform safe deliveries.
Functioning:
2.4
Survey has shewn that doctor stay in the Head quarter (HQ)-in only 15 PHCs
and in other 16 (52% PHCs the doctor do not stay at the PHC. It is important for
a PHC doctor to stay at the HQ in order to attend to emergency cases. .As evident
from the table below - around 29 percent of PHCs. doctors were not available in
scheduled timings. Even for other staff in around 20 percent PHCs, staffs are not
present at schedules Linings.
There is no OT in 3 CHCs of the 5 CHCs in the district. It was observed that
only stitching of wounds is done in OT, and due to lack of equipment, operations
are not done and patients are referred to District hospital.
2.5
Operation theatre (OT):
Ambulance facility:
All the CHCs had an ambulance, but during emergency people are not able to
15
COMMUNITY HEALTH CENTRES
Availability of service providers
Report card on CHCs in Barwani district
- The district has less than half the required number of CHCs. Instead of 1 CHC
per 80.000 population the district has 1 CHC for 1,84,612 population.
% of PHCs
Doctor available in scheduled timing
71 (22)
Other staff available in scheduled timing
80.6 (25)
Figures in parenthesis indicates number of PHCs.
• None of the CHCs fulfill the 30 beds norm, all CHCs have 10 beds or less.
Residence facility:
• 40% CHCs do not have running water facility.
5.
• There is no functioning Operation Theatre in 60% CHCs; certain CHCs do not
even have a delivery room.
For doctor: Out of 31 PHC, 23 PHCs have residential facilities for doctors, but
even these are very badly maintained and as a result doctors don't stay there. It
was found that doctor’s residences are occupied by other staff. For instance, iln
Mohda and Julvania they are occupied by compounders and dressers.
• 80% of the CHCs have no specialists, the single CHC with specialists has only
half of those required.
o
• Only one CHC has a female doctor.
• In 40% CHCs. doctors are not present during scheduled timings.
• 80% CHCs do not have neonatal resuscitation equipment or ECG machine;
40% do not have oxygen cylinder, incubator or adequate operation equipment.
• None of the CHCs provide services for caesarean delivery.
Forty percent CHCs co not provide treatment to severely anemic women or
children with severe respiratory / gastrointestinal infections; 60% do not have STD
clinics.
1. Adequacy of CHCs:
The CHCs is conceived as a 30 bed secondary referral centre and the norm
expected is 1 CHC per peek of 1 lakh population and for tribal areas is one CHC
per 80000 population. At present Badwam district has 5 CHCs for a rural population
of 9,23,063 (Provisional Peculation Totals, Rural-urban distnbution, Census of India
2001, Directorate of Ce.~.s_s Operations, MP), which means instead of 1 CHC per
80,000 population (as per tribal area norm) it has 1 CHC for 1,84,612 population
approximately. A shortfai cf 4 CHCs! Two blocks, Sendhwa and Badwani do not
have any CHC. This s’erage of CHCs in the district results in inadequacy of
referrals services.
For Staff: Out of 31 PHC. only 13 provides staff-quarters, 18 PHCs don't have
any staff quarters. Therefore LHVs, dresser and compounders working for 8-12
hours in a particular PHC are without a residence and had to stay in rented
accommodation.
6.
Required Equipments:
The PHCs were surveyed for basic and essential instruments and equipments.
These included stethoscope, B.P. apparatus, weighing machine, basic surgical
instruments like scalpel, forceps etc., microscope and oxygen cylinder. These
equipments are either basic diagnostic tools even for routine and emergency
diagnosis or very essential equipments for conducting lab investigation or providing
emergency care. Out of 31 PHCs surveyed, 14 PHCs lacked essential supplies,
and did not have more than 4 of these items. In Rosar PHC, paper pin instead of
needles is used for making blood slides. It is shock to find that in a PHC needles
are not available!
CASE NO 3 - WOMEN HEALTH CARE
M is a 30 year women residing in A village of B district She was persuaded
by Anganwadi worker to undergo LTT operation, she has 8 children and
went to the camp where she only get a checkup regarding fitness to undergo
the LTT operation but in the camp she was not only told that she is fit to
undergo LTT operation but also immediately operated without giving any
local anesthesia even though she had been 3 months pregnant and she had
17
specifically told then that she has missing her cycle for 3 months (on 4J5/
04). There was no kit for testing Pregnancy and no Ultrasound machine in
the camp. She was also discharged the same day.
In her village there are few more women who have had children after LTT
operation and the entire village is now afraid to undergo an LTT operation.
Type of denial:
1. Negligence of the health staff.
2. Non availability of the essential equipment required for the treatment
Consequences Of Denial:
, Extreme financial Loss on account of bringing up a 9th Childs.
7.
Laboratory facilities:
One can find a mismatcn cetween laboratory facilities, required instruments and
human power. In some PHCs there are labs equipped with microscope but there
are no lab technicians anc in others there are lab technicians but no microscopes
are there e.g. Moida, Rosar. Bhandara, Bajurg which do not have lab technicians.
In many PHCs there are - croscope and lab technicians but in absence of reagents
even basic routine tests like blood, urine and sputum examination cannot be done.
• 8. Type of services available (selected services):
Type of service
% of PHCs
Immunization
87.1
ANC/PNC ctnic held
83.9
Referred new oom cases treated
64.5
Treatmen: r communicable disease
61.3
Treatment -’respiratory cases
58.1
Treatment tri malaria
77.4
Laparoscoce s
48 4
Female stemzation
54.8
As evident from the above table, none of the above essential services were
available in all the PHCs. Immunization services are available in 87 percent PHCs.
though there is much scope to doubt whether all the doses of immunization is
provided to the children. If one goes by NFHS-2 data, complete coverage in the
state has come down from the earlier NFHS survey, the above figure seems
doubtful. Many child deaths happen due to respiratory problems, and one of the
major barriers for seeking treatment is unavailability of services. This is evident
from this situational analysis of Badwani district, where only 58 percent PHCs are
found treating respiratory cases. Little more than 61 percent PHCs were found to
treat communicable diseases. Even treatment of common illnesses like malaria is
not available in more than 22 percent of the PHCs. Sterilisation services, which is
very much emphasised in public health facilities that too was not found inadequate
in many PHCs, then one can imagine what can be the case for other services.
Sterilisation services were mostly provided through camps.
NATIONAL PROGRAMMES:
Malaria Control is a National Programme but in most PHCs there is no provision
for testing of malaria parasite e.g. Julwania PHC. In many PHCs even though
slides are prepared, patients do not receive the reports or the appropriate follow
up treatment.
C
i )\ - jjM •
HEALTH IN GUJARAT:
A Brief Overview of Points of Concern
Prepared for the Western Region Public Hearing on Denial of Right to Health ('are.
.July 29. 2004. Bhopal
Introduction
We focus, in this report for the NHRC Public Hearing, on Maternal and Children's
Health and Occupational Health only. In Sections 2-8 we discuss the former and
Section 9 discusses Occupational Health Issues. We begin with giving salient
findings of the NFHS Survey 2 of 1998-99. Some of these figures are central to our
report of Gujarat’s health system (see annexure 1 for the NHFS Fact Sheet for
Gujarat)
Percent using govt, health facilities for sickness..................27 7
Current Contraceptive Use
Any modem method...................................................................53.3
Quality of Family Planning Services6
Percent told about side effects of method................................9 5
Percent of births3 whose mothers were assisted at
delivery by a:
Doctor......................................................................................... 37.4
ANM/nurse/midwife/LHV..................................................... 16.1
Traditional birth attendant...................................................... 42.4
Percents reporting at least one reproductive
health problem............................................................................ 28.6
Awareness of AIDS
Percent of women who have heard of AIDS........................ 29.8
Nutrition
Percent of women with anaemiall........................................... 46.3
Percent of women with moderate/severe anaemial 1............16.8
Percent of children age 6-35 months with anaemial 1 ........ 74.5
Percent of children age 6-35 months with moderate/
severe anaemial 1 ........................................................................ 50.4
Percent of children chronically undernourished
(stunted) 12.................................................................................... 43.6
Percent of children acutely undernourished (wasted)12...... 16.2
Percent of children underweight12........................................... 45.1
I
1. Background Characteristics of Population in Gujarat
About three-fifths (59 percent) of Gujarat's population lives in rural areas.
The age distribution is typical of populations that have recently experienced
a fertility decline, with relatively low proportions in the younger and older
age groups. Thirty-three percent of the population is below age 15, and 5
percent is age 65 and above. The sex ratio of the de facto population is 947
females per 1,000 males for Gujarat as a whole, and is lower in urban
areas (935) than in rural areas (955), suggesting that more men than
women have migrated to urban areas.
Missing Girl Children
The overall sex ratio is prone to migration from rural to urban area in search of
employment, education, etc The sex ratio in population category of 0-6 years is
relatively immune to such bias/aberrations and can be said to be relatively secular
indicator. On this account also, the State of Gujarat has fared badly as the 0-6 years
sex ratio has decreased from 928 in 1991 to only 878 in 2001.
In general this ratio is
poorer in urban areas compared to rural areas. In 2001 the 0-6 years sex ratio in urban
areas was only 825 compared to 905 in rural areas of the State. The district of Mahesana
fared worst in 0-6 years sex ratio having only 798 female children per 1000 male children
in this age group, while the district of The Dangs was the best having 974 female children
per 1000 male children.
While the Juvenile Sex Ratio is indicative of women’s status and the health status, it
also raises serious questions about the implementation of the Pre-natal Diagnostic
Techniques Act, 1994. Gujarat’s performance in the area is abysmal.
Twenty-seven percent of women age 15-19 are already married, including
5 percent who
are married but gauna has yet to be performed. In rural areas, 33 percent of women aee
15-19 have already married. Older women are more likely than younger women to have
married at an early age: 25 percent of women who are now age 45^19 married before
they were 15, compared with 7 percent of women who are now age 15-19. Although this
indicates that the proportion of women who marry young is declining rapidly, 41
percent of women in Gujarat still marry before reaching the legal minimum age of
18 years.
Z.
2. Malnutrition and Food Security
Annexure 2 (Tables 1-7) show the poor food and nutritional security status
of Gujarat, despite its image as a developed state. The percentage of
severely stunted and severely underweight children is the highest in the
country (see Table 7). The Food Insecurity Atlas1 has given the label of
extremely (food) insecure to Bihar, the sole claimant to that status; and
severely insecure States to Gujarat, Madhya Pradesh, Uttar Pradesh,
Rajasthan and Orissa - in that order. Moderately Insecure States are
W.Bengal, Maharashtra, Assam, Andhra Pradesh, Karnataka, and Haryana
while Moderately Secure States
are Tamil Nadu and Kerala with Punjab
being the Most Food Secure State.
Gujarat, as per the analysis of the Atlas, is the second most food insecure
State in India after Bihar, among the 16 states considered; while Tamil
Nadu despite its dismal calorie intakes fares third best after Punjab and
Kerala scoring because of relatively good health infrastructure.
Malnutrition among Women in Gujarat
Percent of women with anaemia...................................................... 46.3
Percent of women with moderate/severe anaemia.............. 16.8
Percent of children age 6-35 months with anaemia ...74.5
Percent of children age 6-35 months with moderate/
severe anaemia
Source: NHFS 2
•
•
50.4
Based on a weight-for-height index (the body-mass index), more
than one-third (37
percent) of women in Gujarat are
undernourished.
Nutritional deficiency is particularly serious for women in rural areas
and women in disadvantaged socioeconomic groups.
•
Women who are undernourished themselves are also much more
•
Overall, 46 percent of women in Gujarat have some degree of
anaemia, and 17 percent are moderately to severely anaemic.
Anaemia is a serious problem among women in every population
group, with prevalence rates ranging from 38 to 58 percent among
the various groups.
likely than other women to have children who are undernourished.
•
•
Pregnant women are much more likely than nonpregnant women to
be moderately to severely anaemic.
' rood Insecurity Alias of Rural India. MS Swaminathan Research Foundation and World Food Programme,
Chennai, April 2001
Child Malnutrition
NFHS-2 has used three internationally recognized standards to assess
children's nutritional status.weight-for-age, height-for-age, and weight-for-
height. Children who are more than two standard deviations below the
median
of an
international
reference
population
are
considered
underweight (measured in terms of weight-for-age), stunted (height-for
age), or wasted (weight-for-height). Stunting is a sign of chronic, long-term
undernutrition, wasting is a sign of acute, short-term undernutrition, and
underweight is a composite measure that takes into account both chronic
and acute undernutrition.
Malnutrition of Children in Gujarat________________________ _____________
Percent of children chronically undernourished
(stunted)
................................................................................... 43.6
Percent of children acutely undernourished (wasted)12...... 16.2
Percent
of
children
underweight
(weight
for
age)........................................... 45.1________________________________________
Source: NHFS 2
•
About
45 percent of children in Gujarat
under age three years are
underweight, a similar proportion (44 percent) are stunted, and 16
•
percent are wasted.
Child-nutritional status has improved in Gujarat since the time of
NFHS-1, when 48 percent of young children were underweight, but it
is still a serious problem.
•
Undernutrition is much higher in rural areas than in urban areas and
is
particularly
high
among
children
from
disadvantaged
socioeconomic groups.
•
The prevalence of undernutrition is somewhat greater for girls than
for boys.
•
Three-quarters of children age 6-35 months are anaemic, including a
large majority of children in every subgroup of the population.
3. Health Care Delivery System in Gujarat
•
Urban-rural difference in high order health facilities is quite high in the state
compared to all-India figures (Table 11). For example, the number of
hospitals per lakh population in urban areas in Gujarat is 16 times higher
than in rural areas. In India the difference is only six times. With respect to
beds per lakh population, urban-rural difference is 11 in Gujarat as well as in
India. Gujarat stands second (after Kerala) among 15 large states with respect to
hospitals per lakh population (based on Duggal et al 1995) and first with respect
to dispensaries per lakh population. Once again, their share is higher in urban
areas than in rural.
•
There is a non-availability of skilled personnel in the rural areas. 71.3% of
total doctors are in urban areas as against 65% population in rural areas.
(GOG Vision 2010).
•
The good spread of high order health facilities in Gujarat is supported by
public expenditure However, the private, voluntary sector, and charity
institutions also are playing an important role. A number of hospitals and
dispensaries have been set up in the past by princely states, especially the
Vadodara state and the states of the Saurashtra region. Many of these are either
run bv charitv trusts or have been handed over to the public sector.
Quality of Care Issues
•
•
Private sector is largely beyond the purview of legislation. Quality of care
and user fee remains largely unregulated. (Vision 2010 GOG)
There are no performance review systems of those working in the health
sector from the point of view of quality of services. (Vision 2010, GOG)
Urban health
•
Urban health for poor people is a problem. There is an uneven distribution
of health facilities and limited outreach to the poor.
o
There is inadequate infrastructure and insufficient facilities at the health
centers. (Vision 2010)
Resource allocations for health
As evident from the following table, over the last five years the allocation of resources
to the health and medical sector that outlay has declined from 4.81 percent to 2.87
percent.
i Plan and Non -Plan outlays of the Government of Gujarat over the last 5
years
Item
Unit
1999-2000 2000-2001 2001-02
2002-03
2003-04
Total State Annual Plan & Non Plan
Outlay
Plan & Non Plan Outlay for Medical
and Public Health (PM&PH)
% of PM & PH to Total Outlay
Crore
20673.57
24670.98
37792.84
31054.02
31998.03
Crore
995.40
973.08
953.83
948.74
919.41
%
4.81
3.94
2.52
3.06
2.87
PM&PH = Plan for Medical & Public Health
\ PM&PH = \on-Plan for Medical & Public Health
5
Source:
Government of Gujarat’s Vision 2010 (Health section)
•
Although GOG’s Vision 2010 statement mentions several areas of concern like
lack of Core Infrastructure, low utilization of PHCs. shortage of health staff.
skewed development of medical education and research, the V ision section per se
says little on how these areas of concern will be addressed. The Vision of GOG
is to develop Telemedicine. Interactive Health Communication System (G1HCS)
and a network of technologically sophisticated Mobile Dispensaries.
4. Government Policies and Programmes on Health as affecting Women
• Gujarat State Population Policy (2002)
The Population Policy statement was developed in 2000 as a step towards formulating a
State Population Policy, which came out in 2002. The Statement was a product of a high
level committee and a working group headed by the Health Minister. The Gujarat
Government set up a Social Infrastructure Development Board for achieving overall
development in the State. Population stabilisation was stated to be a priority of the Board.
Apart from population stabilization by 2008 being a priority, it would be useful to know
other priorities of the Board. This would help us to analyse the total context within which
Gujarat’s Population Policy was developed and to assess links for consistency7 in
approach.
The Goal of Gujarat’s Population Policy (GPP) has a focus on improving the quality
of life of people. However the paragraph on Objectives reveals a domination of
demographic objectives like Unmet Need for Contraception, reducing the Total
Fertility Rate (TFR) and increasing Contraceptive Prevalence Rate (CPR). Other
objectives like increasing safe Medical Termination of Pregnancies (MTPs),
providing quality maternal health services and so on, would better reflect the goal of
improving the quality of life of the people and a shift away from the demographic
orientation of all population policies.
One objective of the GPP is to reduce MMR to 100 per 100,000 live births bv 2010.
However, a reading of the policy does not clarify how this would be done.
• National Maternity Benefit Scheme
Under the Scheme, maternity benefit in the form of lumpsum cash assistance is provided
to women of households below the poverty line. Only pregnant women for up to the first
two live births provided they are of 19 years of age and above are eligible. Thus, younn
married girls who have to prove their fertility and become mothers at an early age are
excluded.
• Gender Equity Policy
In 2002 the Government of Gujarat initiated the process of formulating a Gender Equitv
Policy for the state The policy aims to narrow the gender gap and strive for an equitable
social structure. The Gender Equity Policy has recently been finalized by the state
government. .Among the broad objectives of this policy, the health related ones are
»
•
o
•
•
•
•
To promote best socio-cultural practices, and develop capacity in the societv to
eliminate gender discrimination;
To incorporate gender perspectives into various developmental programmes of the
State, and strengthen partnership between government organizations, professional
bodies, civil societv; national and international organizations.
To strengthen access to client-centered and good quality health services by women.
men and adolescents in order to ensure their survival and quality of life, including the
right to safe drinking water and sanitation;
To ensure access to and improve the quality of education for girls and women as a
prime vehicle for an egalitarian society;
To strengthen gender perspectives in the legislative framework to ensure gender
justice, and improve access to competent legal aid/support by women in need;
To advocate gender equity in all awareness programmes through various means
including media;
To strengthen advocacy and IEC from a gender equity perspective to impact upon
attitudinal changes and practices in society.
4.1 Government Programmes in Gujarat for Women
o
Maternal and Child Health (MCH) care services are being provided by the
Government of India since the 1950s by developing a network of PHCs and sub
centres staffed by doctors and ANMs.
®
Child Survival and Safe Motherhood Programme was initiated in 1992-93.
•
Reproductive and Child Health Programme launched in 1996, integrating maternal
and child health, family planning and reproductive health services. The important
elements of RCH programme for Safe Motherhood are:
•
•
Provision of antenatal care (ANC), ensuring at least three ANC visits, iron
and folic acid tablets for pregnant and lactating mothers, two doses of
tetanus toxoid vaccine, detection and treatment of anaemia in mothers,
management and referral of high-risk pregnancies
Encouraging institutional deliveries or home deliveries assisted by trained
health personnel.
7
•
•
•
Provision of post natal care, at least three postnatal visits
Providing the public health care system with critical inputs in terms of
infrastructure, staff, training supplv of various equipment, drugs, vaccines.
training of medical and paramedical staff for effective delivery of services.
Schemes under Safe Motherhood are:
•
•
•
•
•
Supplementary food, health education and essential care for women during
pregnancy and lactation from the village anganwadi centre.
Safe delivery services from the primary health centre
Emergency obstetric services form the First Referral Lnits/District
Hospital
Emergency transport fund for referral during obstetric emergencies from
the village panchayats.
The PHC/village panchayat provides Rs. 500/- as a monetary support to all
pregnant women from the disadvantaged sections of the society, upto two
births.
The Maternity Benefits Act, 1961, provides for 12 weeks’ maternity leave
for women alone and only to those who have put in 160 days of work within
12
months of the expected date of delivery.
As
most women
in the
organized sector never manage to retain continuous employment , this
does not benefit them (Qadeer, 2002).
Our recommendations
S.2 of the Act should be amended to include all industries including
home based industries. Hence, S.2 of the Act needs to be amended in
the following manner.
1.
The Act applies in the very’ first instance to every establishment
being a factory, mine or plantation, or an establishment covered by
Contract Labour Act or an establishment covered under Bombay
Shops and Establishment Act and also shall apply to all other
establishments whether industrial, commercial, agricultural or
otherwise
2.
Considering the fact that enforcement of Laws in small
establishments is very difficult it is suggested that the definition of
the employer be amended in the following manner;
Employer means
a. in relation to an establishment under the control of the
Government, a person appointed for the supervision and
control of employees
h. the person who has the ultimate control over the affairs of the
establishment and where such affairs are entrusted to any other
person whether called a manager or agent or contractor, such
person
c. In relation to an establishment covered by any law which
creates a separate body or a board for the welfare of the
employees, such board.
d In all other cases, the Government for the limited purpose of
payment of any dues under the Act.
3.
Rate of Maternity Benefit should not be less than minimum wage
prevalent under law at the time
4.
The penalty for violation of any of the benefits should be increased
to a minimum of Rs. 5000/- or more and imprisonment up to the
period of one year. 25% of the fine amount should be given to the
woman. S.21 of the Act needs to be appropriately amended.
The person incharge and contractor should be held responsible
jointly and severally. The ultimate responsible body must impose
terms and conditions with the contractor to ensure compliance with
the law.
The contractor should be responsible for fine and imprisonment
where as the person ultimately responsible should be liable for
compensation.
5.
The definition of miscarriage in the act excludes any miscarriage the
causing which is punishable under the I.P.C. this includes acts
leading to miscarriage to which the woman is not a party. Hence, the
definition of miscarriage in S.3(j) needs to be changed in the
following manner:
Miscarriage means expulsion of the contents of a pregnant
uterus at any period prior to or during the 26th week of
pregnancy.
6.
S 21 of the Act needs to be amended as follows
a)
S.21 (3) Where a claimant has a complaint regarding the
non-performance of the inspector, she has a right to
complain against him in appropriate forum. The inspector
should be made personally liable to pay the woman her dues
if the non-payment is due to his negligence.
b) S. 16 A should be added to read as follows - All Primary
Health Centers must keep the forms needed to be filled.
9
5. Maternal Mortality in Gujarat: A Continuing Problem
Though female death rates are higher than that of males in all age groups, it is especially
higher in between the 0-9 and 15-29. The high mortality rates among females can be
attributed to neglect of the girl child from birth onwards, high maternal mortality, less
access and use of health senices. Maternal mortality rate in India and Gujarat continue to
be high.
•
•
•
•
While infectious diseases cause nearly 65 percent of the deaths among women of
and only 2.5 percent are caused bv childbirth, among women in the reproductive
age group. 12.5 percent of the deaths are due to childbirth and related conditions
and only 2.6 percent deaths are caused by infectious diseases.
Complications such as bleeding, sepsis, eclampsia, obstructed labour and severe
anaemia account for at least three-fourths of obstetric deaths.
Many of these, for instance, anaemia and sepsis can be prevented by measures
such as therapeutic-prophylactic doses of iron, safe delivery trained health
personnel and regular antenatal check ups and referral support in times of
emergency/complication deliveries (Government of Gujarat, 2003).
Thus a large number of women continue to die of causes that can be prevented.
The maternal health indicators for Gujarat show that health services are reaching
more women during pregnancy than during delivery or after childbirth In Gujarat.
5.1
Percent of births whose mothers received:
•
•
•
•
•
antenatal check-up from a health professional - 86%;
antenatal check-up in the first trimester - 36%;
at least 3 check-ups from a medical professional - 60%
two or more tetanus toxoid injections - 73%;
iron and folic acid tablets or syrup -85%;
5.2
Percent of births whose mothers
had safe delivery (assisted by a trained health professional) - 54%
had delivery attended by a TBA - 42% (yet TBA training and continuing
support to TBAs have not received the attention that is required)
• had delivery attended by friends, relatives - 4%
• Majority of the institutional deliveries take place in the private medical sector
(low accountability of the private sector and inadequate controls of quality of
care)
• Non-institutional deliveries were followed by a postpartum check-up within 2 days 10%. (IIPS& ORC Macro, 2001).
•
•
io
5.3
Maternal Mortality and Morbidity
Various estimates of maternal mortality for Gujarat are:
• 398 per 100,000 (Government of Gujarat, 2000)
• 310 per 100.000 live births in 1993 (Bureau of Health Intelligence.
Commissionerate of Health Medical Services and Medical Education, 1996 cited
in Department of Women and Child Development, 2003)
• less than 400 per 100,000 live births in the early 1990s (UNFPA. 1997; Bhat et
al., 1995).
» 393 for 100.000 live births in 1998-99 (computed on the basis ofNFHS 1 and 2
data by IIHFW, 2003).
• 3.89 for every 1000 pregnancies (Health Monitor, 1998).
o 5 maternal deaths out of 992 live births during January 1996 to October 1999 in a
baseline household survey in rural Vadodara (PRC, 1999).
The State Population Policy Statement of Gujarat and the Vision 2010 document aim at
reduction of maternal mortality rate to less than 100 per 100,000 live births by 2010.
Morbidity
•
Twenty-nine percent of currently married women in Gujarat report
some type of reproductive-health problem, including abnormal
vaginal discharge, symptoms of urinary tract infections, and pain or
bleeding associated with intercourse.
•
Among these women, 67 percent have not sought any advice or
treatment. These results suggest a need to expand reproductive
health services and information programmes that encourage women
to discuss their problems with a health-care provider.
6. Programme and Policy Level Barriers: Women’s Health
Non-availability and accessibility of a trained health provider
•
the number of medical officers
living in the PHC or within the PHC
village
o only 55% PHCs have
quarters for MO/MO in
charge
(ORG-Marg,
1999)
o there is a huge backlog
(35%) in construction of
staff quarters at CHCs.
In December 1999 GOG
Non-availabilty of Staff - NGO
perspective
Village Tikkar in Halvad Taluka of Surendranagar
district is ven,’ well connected by transport it has a
high school, the community is very cooperative. Three
single women community workers of the NGO are
staying alone in the village. Personal safety is not an
issue. There is a quarter for the ANM. but she still
does not live there. The Tikkar PHC has a new
building and is well equipped , but not a single
delivery take place in this PHC.
1I
reports that there were 3359 quarters as against 5182 requires. (Vision
o
2010)
onlv 27% MOs are available and staying in the PHC compound and 10%
MOs staying within the PHC village (ORG-Marg, 1999)
The issue of adequacy' of medical health services was also addressed in Pascnim Baga
Khet Mazdoor Samiti vs. State of West Bengal{(l996)4 SCC 37}. Here the Supreme
Court held that the Medical Officers in government hospitals are duty bound to provide
medical assistance for preserving human life. Further the court ordered that Primary
Health Centers should be equipped to deal with medical emergencies. Failure on rhe part
of the government hospitals to provide timely medical treatment is violation of his Right
to Life.
•
number of ANMs living in the sub-centre village
o 70% PHCs have at least one quarter for ANM/health assistanr/nurse.
(ORG-Marg, 1999)
o 71% ANMs (range 48-93%) ANMs in rural areas of four districts live
within the sub-centre village, but only 30% of them (range lS-52%)
provided government accommodation and live in it, 35% not provided
government accommodation (Visaria, 1999).
•
The maternal health services under RCH continue to be focused on ANC and
have the high-risk approach. Provision of delivery care and provision of
emergency obstetric care are being neglected (Mavlankar, 2001).
•
PHCs, the most proximate health facilities after the sub-centre are not
designated to provide EmOC services
•
Emergency obstetric care continues to be inaccessible to many rural women due
to the following policies:
• Only postgraduate qualified obstetrician can perform obstetric surgical
procedures, basic doctors are restricted from performing these procedures
including cesarean section even in remote areas, where there is no specialist
obstetrician available. They can do only basic EmOC procedures, like manual
removal of placenta, suturing tears, assisted vaginal delivery etc.
• Para-medics - ANMs, lady health visitors - .are not allowed .to manage, or
stabilize obstetric emergencies, hke treating infection with annorotics,
stabilizing a case of eclampsia, and manual removal of placenta. All such cases
are referred to higher level facilities. Thus women have to travel long distances in
emergency and referrals add to the cost of treatment.
• Basic doctors and nurses cannot give anesthesia, though there are limited
number of anesthetists in rural areas, thus reducing access to emergency, life
saving surgery.
•
•
Access to blood transfusion in rural areas is reduced due to many unrealistic
infrastructure and staff requirements for licensing blood banks (Mavlankar, 2001)
With the aim of promoting safe deliveries, the R.CH programme there exists since
October 2000 a scheme of training of traditional birth attendants (TBAs) or
dais in 142 districts of India. In Gujarat, the Dangs district has been identified for
this scheme. .An evaluation of the programme, however showed that:
• Out of 426 enlisted dais, 398 were trained and passed the post trainin"
evaluation, however, none received a certificate and identification
card.
• .After the training, the quality of work of the trained dais was not
reviewed by the ANM or by the medical officer, as laid out in the
Scheme. (Das, Dey . Bhatt and Patel, no date)
GOI norms are 3 specialists for each CHC, in Gujarat there is onlv 1 specialist in
each CHC. 50% of specialist positions were vacant in 2000 Out of the 283
sanctioned posts only 142 were filled.
Barriers to Maternal Health
•
•
•
•
•
•
Importance of antenatal care is not sufficiently emphasized by the health care
system, as a result there most women who did not seek antenatal care did not
consider it necessary (70%) or customary (13%). (UPS and ORG Marg. 2001).
Lack of recognition of pregnancy complications. The concept of ‘pregnancy
gpmolicatipn; is .non-existent in the rural communities of Vadodara.,Mehsana.and
Rajkot. The problems (complications^ reiatea to pregnancy are considered a natural
part of childbearing. It appeared that the community recognised only those signs and
symptoms as serious and possibly fatal, which they had either heard or witnessed in
their villages. (Barge et al., 1994).
Lack of information about the danger signs, recognition of possible pregnancy
complications, the causes and consequences of pregnancy, delivery and post delivery
complications leads to delay in treatment seeking. (Barge et al., 1994)
Lack of awareness in the community that ANMs are trained and can be contacted
for assistance during delivery (Visaria, 1999).
ANMs’ concern regarding their personal safety when called at night, antagonism
of the villagers towards them, fear of the risks involved in when called to attend a
complicated delivery (Visaria, 1999).
Affordability of health services
An analysis of the lending pattern of 30 women’s savings and credit groups (90%
belonged to BPL families) in the Panchamahals district, over 1996-98 shows that_after
agriculture, health is the next major expense for which women take loans (Source:
AN ANDI).
13
Why women do not go to PHC for services.
a) The clerk at the case registration window asks for a bribe to issue the case paper.
b) Doctors would not attend on the nomen and make them wait.
c) These women had been pinched bv the Doctors on their legs but would not examine them
for the complaint. At the CHC n omen were slapped on the thighs if they w ere a little shy to
completely take off their petticoat at the delivery table.
d) Doctors and particularly nurses use abusive language.
el At the OPD women are not given complete instructions about the medicines and the dosage.
often they do not complete the course and therefore do not completely heal. This leads to the
belief that PHC medicines do not really cure.
f) Women arc in general afraid that thev might be made unconscious through the intravenous
medicines and then they will be sterilized with out their know ledge.
Based on interview of women Galtbeh village ofGhogamba block Panchntaltaais district and
Fangio village - Devgadh Baria block Dahod district.
Source: A.\A.\'DI
H
Access to Services
•
The aim of 100% availability of the critical inputs in the public health facilities has '
been brought down to 60% as adequate/doable. However, oniv 54% FRUs and 18% ;
CHCs have adequate critical inputs, while 64% PHCs have adequate critical inputs.
•
33% PHCs. 25% CHCs and 8% FRUs were not conducting deliveries in the three
months preceding the facility survey.
•
85% CHCs and 75% FRUs not conducting any lower segment sterilization or Csection
®
Obstetrician gynaecologist available in only 17% FRUs and 18% CHCs
®
Anaesthesiologist available in none of the FRUs and 13% CHCs.
®
The post of obstetrician gynecologist sanctioned in only 11 of 24 FRUs and in 7 of
40 CHCs. but filled in only 4 FRUs and 6 CHCs.
•
Only 17% FRUs and 45% CHCs have separate aseptic labour room.
®
Normal delivery kit not available in 69% PHCs, 54% FRUs, 20% CHCs.
®
Emergency obstetric drug kit not available in 96% FRUs. 95% CHCs. essential
obstetric care drugs not available in 88% PHCs.
•
Sufficient stock of TT vaccine only in 13% FRUs. 10% CHCs. 71% PHCs.
®
Sufficient stock of 1FA tablets large and small in oniv 17% FRUs, 30% CHCs and
65% PHCs.
(Source: ORG-MARG. 1999).
•
Less than 30% ANMs in sub-centres report the equipment they regularly use for
ANC was in working condition.
•
Nurses do not stay in the village and cannot be called, or put to inconvenience, and
they do not come even if they are called.
(Source: Visaria. 1999).
•
In Vadodara district, due to non-availability of an obstetrician gynaecologist, none
of the 12 CHCs surveyed provided 24-hour EOC services. Even the 4 CHCs having
a gynecologist only partially treated EOC cases and referred them further. The non
availability7 of an anaesthetist in 11 CHCs, affected the provision of emergency
services. As none of the CHCs had any blood bank facilities, all cases requiring
blood transfusion were referred to higher level facilities.
(Source: Ansari and Patel. 2001)
Access to Secondary Health Care
•
The operation theatres (OT) in manv of the CHCs were ill-maintained Cracked
floors in the OT (n=7) and dirty floor (n=4), unclean, dusty and bloodstained
operation table (n=6) were observed in some of the CHCs. Only half of the CHCs
had any arrangement for uninterrupted power supply (tour had emergency light
and one had a generator).
•
The component of counselling in all reproductive health services like antenatal
and postnatal care. EOC. family planning, MTP. infertility and RTl.'STD. was
generally poor
•
Women with reproductive morbidities consult male doctors as the last resort:
since they have to undergo physical examination, they prefer a female doctor.
Few male doctors carried out pelvic or physical examination of their female
clients who came for services like IUD insertion, MTP. RTI/STD, antenatal or
postnatal care.
•
In the interaction between clients and providers, doctors seemed to be more
sympathetic to women who sought services for MTP and infertility, compared
with clients who came for ANC or FP services Clients' opinion about the
providers seemed to be influenced to a great extent by bow they were greeted bv
the providers
•
Exit interviews with 206 women patients at the CHC revealed
• Only 44% were explained about their health problem
• 43% were explained how to take the medicine
• 50% were advised on follow-up visit
• 57% said auditory and visual privacy was maintained during examination.
Source: Ansari and Patel. 2001
16
7. Domestic Violence
•
in
Gujarat,
there is widespread
acceptance among ever-married
women that the beating of wives by husbands is justified under some
•
circumstances.
Approximately one-third (36 percent) of women accept at least one
•
Ten percent of ever-married women in Gujarat have experienced
of six reasons as a justification for a husband beating his wife.
beatings or physical
mistreatment since age 15, and 6 percent
experienced such violence in the 12 months preceding the survey.
•
Most of these women have been beaten or physically mistreated by
their husbands.
•
Domestic violence against women is especially prevalent for women
who are not currently married and women living in households with a
low standard of living.
Violence against women is on the increase. The existing laws are not able to
address the situation Our recommendations in criminal law are as follows:
•
Sections 498-A (IPC) and 304-B of the Indian Penal Code (IPC) do not
seem to be enough to provide justice to women Section 306 (IPC), as per
the opinion of the Gujarat High Court cannot be seen as operative when
cruelty under section 498-A (IPC) is proved
The following ‘note7 could be appended to section 498-A (IPC)
The cruelty could be proved, inter alia, by (i) a medical certificate
showing that injury was inflicted and that treatment was taken in a
hospital or (ii) a complaint lodged at a police station by the victim of
mental / physical torture by husband or any relative of the husband or
(iii) the woman had to invite third party to intervene on her behalf in
the quarrels between her and her tormentors or (iv) that the woman was
completed to return to her natal home repeatedly
17
The changes are proposed to make the section applicable to unnatural
deaths on account of domestic violence.
•
Along with section 498-A a married woman has added (IPC) section 113A to the Indian Evidence Act in 1983 to raise a presumption regarding
abatement of suicide. From this section it is suggested that phrases
delimiting the section to seven years be deleted. The section amended as
per above comments will read as follows.
113-A. When the question is whether the commission of suicide by a
woman had been abetted by her husband or any relative of her husband
and it is shown that she had committed suicide and that her husband or
such relative of her husband had subjected her to cruelty, the court may
presume having regard to all the other circumstances of the case, that
such suicide had been abetted by her husband
18
8. HIV-AIDS Awareness
Only 30 percent of women in Gujarat have ever heard of AIDS.
.
Awareness of AIDS is particularly low among rural women, poor
•
women, scheduled-tribe women, and illiterate women.
Among women who have heard of AIDS, 86 percent learned about
•
disease
the
from
television
and
15
percent
from
the
radio,
suggesting that government efforts to promote AIDS awareness
through the electronic mass media have achieved some success.
Among women who have heard of AIDS, however, more than onethird (35 percent) do not know of any way to avoid infection. Survey
results suggest that health personnel could play a much larger role
in promoting AIDS awareness. In Gujarat, only 4 percent of women
who know about AIDS learned about the disease from a health
worker.
•
9. Infant and Child Health
NFHS-2
estimates
provides
associated
with
the survival
of
infant
and
child
of young children.
mortality and
factors
During the five years
preceding the survey,
®
the infant mortality rate was 63 deaths at age 0-11 months per
•
The child mortality rate declined more, from 38 deaths at age 1-4
1,000 live births, down from 69 per 1,000 live births in NFHS-1.
years per 1,000 children reaching age one to 24 per 1.000 in NFHS-
1.
•
The rates in NFHS-2 imply that 1 in 16 children still die in the first
year of life, and 1 in 12 die before reaching age five.
Immunisation
immunization is an
important component of child-survival
programmes in India, with efforts focussing on six serious but preventable
Child
diseases tuberculosis, diphtheria, pertussis, tetanus, polio, and measles.
The objective of the Universal Immunization Programme(UIP), launched in
1985-86, was to extend immunization coverage against these diseases to
at least 85 percent of infants by 1990.
•
In Gujarat,
53 percent of children age 12-23 months are fully
vaccinated, another 40 percent have received some but not all of the
recommended vaccinations, and 7 percent have not been vaccinated
at all.
19
•
Immunization coverage, although far from complete, has improved
somewhat since NFHS-1, when only 50 percent of children were fully
vaccinated and 19 percent had not been vaccinated at all.
•
of
children
Eighty-five
percent
vaccinated
against tuberculosis,
have
been
64 percent have received
three
age
12-23
months
doses of DPT vaccine, and 69 percent have received three doses of
polio vaccine.
The largest increase in vaccination coverage between NFHS-1 and
•
NFHS-2 is for Polio
1, where coverage increased from 78 to 90
percent.
Full immunization coverage is not as high as it might be, primarily because
only 64 percent have received three doses of DPT and only 64 percent of
children have been vaccinated against measles. Dropout rates for the series
of DPT and polio vaccinations are also a problem. Eightythree percent of
children received the first DPT vaccination, but, as already mentioned, only
64 percent received all three doses; 90 percent received the first polio
vaccination,
but only 69
percent received
all
three doses.
It is
also
recommended that children under age five years should receive oral doses
of vitamin A every six months starting at age nine months.
10.
Occupational Health in Gujarat: A Major Public Health Issue
Ignored Completely
10.1 Gujarat is considered one of the most developed states in India. It is
leader in manufacture and supply of Salt, Soda Ash, Dyes &
Intermediates, Spectacle Frames, Ceramics, diamonds, pesticide
formulations, fertilizers and other petrochemicals. It houses 25,000
registered factories.
•
•
•
•
•
Gujarat has the highest number of units identified as Major Accident
Hazard Units.
“Golden Corridor’ - From Umargam- Vapi in South to Mahesana in North houses
most of the chemical units.
Tata Chemicals. Reliance Refinery, Dhrangadhra Chemicals, Gujarat Heavy
Chemicals. GSFC. Saurashtra Chemicals, Indian Rayon are some of the major
units in Saurashtra area. Saurashtra also have major Cement Units.
There are large numbers of units, which do not get themselves registered
Gujarat has one of the biggest ship breaking yard in Asia, where more than 50,000
workers are engaged in ship breaking.
20
Gujarat has largest sea coast in the country (one third of India's sea-coast). On it
1600 km long cost, fishing is main business activity (Fish production second onlv
to Kerala) Kandala is second big port on western cost after Bombav. Now.
several small ports have come up,
•
10.2 Among its population of 50 million, 20-30 million are workers. Agriculture is
biggest sector employing about 3 million workers. Most agriculture workers do not get
full employment of 365 days. Though there is law for paying minimum wages, most
do not enjoy that right.
•
»
o
Most agricultural workers do not have any legal cover for protection of
health and safety at work.
They are exposed to toxic pesticides and physical, mechanical and biological
hazards like organic and inorganic dust, heat, bacteria etc.
Each year large numbers of workers die of Leptospirosis and pesticides.
In another Supreme Court judgement Dr. Ashok v/s Union of India {(1997) 5 SCC 10}
the Hon'ble Supreme Court held that insecticides are carcinogenic and so banned the
production, distribution and sale of such insecticides as it causes health hazard affecting
Article 21. Right to life enshrined in Article 21 means right to have something more than
survival and not mere existence.
10.3 Construction is another major industry employing about 1 million workers
Until recent past, there was no legal cover fro protection of health and safety of these
workers. Rules recently passed by Government of Gujarat may still take one year to get
implemented. Most construction workers are intra-state migrants. 70 % of .them
migrate with family and stay in open near site.
In Bandhiia Mukti Morch vs Union of India {AIR 1984 SC 802} the Supreme Court held
that workers should not be deprived of their Right to Life. They should be provided with
humane working and living conditions.
•
•
•
Large numbers of workers die in accidents at work.
Either they fall from height or struck with falling objects or get electrical
shock.
Cement dust and silica dust causes dermatitis, non-specific lung diseases or
fatal Silicosis. No reliable data is available for accidents or serious injuries.
10.4 In manufacturing sector, 0.8 million workers are employed in registered
factories while another 1 million are employed in small-scale manufacturing sector.
•
Workers are exposed to large number of toxic materials and hazards like
organic solvents, pesticides, dyes, and all sorts of organic and non-organic
dusts, noise. Factories Act and other Acts protect workers in registered
factories. Each year more than 200 workers die in fatal accidents and
2.1
•
thousands get injured. The rate of fatal accidents is 25 per 1,00,000 workers
employed which is much higher than ILO estimates of 11 per 10 .
By and by, more and more workers are compelled to work under contractor.
where thev do not get minimum wases or social security like insurance. Those
who are covered by the Employees State Insurance Act. get very' poor senices
Area in which this Act is not applicable, Workmen’s compensation Act applies.
Under this Act, few workers dare to claim compensation Those who dare do not
always get justice.
10.5 Occupational Health is a major public health issue but, neither the Health
Department nor the Labor Department take it seriously As a result, cases of
occupational diseases are neither diagnosed nor notified
•
There is legal provision for compensation of occupational lung diseases under ESI
Act as well as Workmen's Compensation Act. Since cases are not diagnosed no
compensation is paid. After independence, there is not a single case of
Occupational cancer though workers handle known human carcinogens like
Benzene, benzidine, chromium, Asbestos, Vinyl Chloride etc. There are no cases
registered of occupational nephritis or toxic jaundice. Until recently, there was not
a single case of dermatitis compensated. Large numbers of workers die of
Silicosis in Agate, Ceramic, Glass, construction and other industries, but do not
get any compensation After workers struggled they have been able to claim
compensation for Byssinosis and Silicosis (in Glass industry). We have only one
known case of Occupational Asthma compensation and one case of
dermatitis.
•
Thousands of workers in textile, Handloom, engineering, chemical, transport are
exposed to high noise, but few claim compensation and fewer get compensation.
Workers pay their contribution for these risks but they do not get benefit when
they deserve. Workplace environment remains unmonitored, though there is legal
provision for monitoring it.
In Kirloskar Brothers Ltd. v/s. Employees State Insurance Corporation {(1996) 2SCC
682} it has been held that right to health is the fundamental right of the workmen. Just
and favorable conditions of work imply to ensure safe and healthy working conditions
to the workmen.
10.7 Government of India has ratified many ILO resolutions but not the resolution
No. 155. If ratified, this would offer legal cover for health and safety for millions of
workers in primary and secondary' sectors like service sector and agriculture sectors. We
strongly demand ratification for this resolution.
10.8 Numbers of cases of occupational diseases registered in 1998 in India were 1963.
Among these 52 were from Gujarat and rest were from Orissa. No other states reported
22.
anv case of Occupational disease. (Report of working group on Occupational Health &
Safety for 10ih Five Year plan. 2002)
In the judgement of Consumer Education and Research Centre and others v/s Union
of India and others {(1995) 3 SCC 42} the Supreme Court has held that right to heath
and medical care to protect the health and vigor of the workmen while in service or
post retirement is a fundamental right of a worker. Under article 21 Supreme Court
directed that compensation he paid to the worker suffering from Lung cancer.
10.9 Dismal record of Compensation
• In a decade from 91-2001. ESIC paid compensation to 191 workers for various
diseases, out of which 149 were textile mill workers for Byssinosis. They also
paid compensation to 21 workers who died of occupational diseases. (KSSM
Bulletin, Feb 2002)
• In 1996, certifying Surgeon of Baroda Factory Inspectorate identified 53 cases of
Chromium toxicity. ESIC paid compensation to 5 workers among these and rest
were rejected. 21 petitions are pending before Medical Appeal Tribunal And ESI
Court at Baroda for hearing.
o In 1988, ESI paid compensation to about 100 workers of Glass Factors' in Baroda
for Silicosis. (Dhtiliafefsa\ Gujarati booklet; PRIA, 1995)
o Large numbers of cases have been reported of acute poisoning from chemical
units by Modi Hospital in Ankleshwar. In a period of two years, i.e. January' 93
to December 94. 1079 cases of industrial accidents were admitted in this hospital.
out of which 211 were that of chemical exposure. 33 cases of pesticide exposure
were brought to this hospital in the period from June 94 to October 94. In 93 the
Hospital received 34 cases of Aniline poisoning. In year 89-90, they received 65
cases of acute chemical exposure.(Behind Iron Gates; PRJA,Dec,95)
•
In the article titled “Epidemiology of poisoning in an industry based hospital of
South Gujarat”. Dr. R. Calton reports 521 cases of poisoning during the period
June’97 to June’2000. He writes, ‘A total of 521 cases were admitted with a
suspected poisoning between June 1997 to June 2000, out of which 439 cases met
the inclusion criteria and were included in the analysis. Majority of cases (157,
35.8%) suffered from Aniline poisoning, followed by the Organo-phosphorus
(OP) Compounds (135, 30.8%). A large majority of the cases were asphyxiated
by gases. Toxicity of known gases was found in 41 (9.3% cases while a large
majority of cases had toxicity to some unknown gases (48, 10.9%). (Indian
Journal of Industrial Medicine, Oct. 2002)
10.11 India has 1461 Major Accident Hazard (MAH) units. Gujarat state has
highest number of these units with 28% share followed by Maharashtra state with
22%. In Gujarat 416 Major Accident Hazard (MAH) units were identified, out of which
44 were closed and 372 were working. Bharuch district had maximum concentration of
such units (78 units) followed by Baroda (82 units), Ahmedabad (43), Valsad (46) and
Surat (32). These five districts have 75% of the total working units. This area is known as
"Golden Corridor”. Situation of fatal accidents may be summarized by following table:
23
Comparison of Industrial Accidents in 1998
Maharashtra
Gujarat
India
Fatal Accidents
223
163
Non-fatal accidents
11930
17120
1
_____ i
Incidence rate for fatal
0.56
0.16
0.34
Incidence rate for non-fatal
30.01
16.28
6.7
Frequency rate for fatal
0.18
0.05
0.09
Frequency rate for non-fatal
9.79
4.92
1.8
|
Fatal Accidents in Chemical Factories
No.of fatal accidents
2001
42
2002
68
2003
50
No. Year
1
2
3
Specific Demands
1.
2.
3.
4.
5.
6.
State Government should co-ordinate with Factory Inspectorate and Rural
Labor Commissioner to take stock of the situation of Occupational Health
State Government should give out budget for Health education for
Occupational diseases and injuries.
State Government should form a Commission for Occupational Safety and
Health for co-ordination between various departments.
Health department should take up research projects to know the status and
economical burden on Society.
Health department should create Industrial hygiene department and monitor
workplace environment
Health department should publish data and report of its efforts.
Z4
Source KSSM Bulletin. Feb 2002
' Source KSSM Bulletin. Feb 2002
No. of Cases Compensated by ESIC1
Disease/Condition
Byssinosis
Byssinosis
Byssinosis
Byssinosis
Asbestosis
Byssinosis
Byssinosis
Byssinosis
Byssinosis
Deafness
Silicosis
Byssinosis
Deafness
Dermatitis
Total
No.
of
cases
Year
8
3
10
35
1
26
7
16
31
8
6
13
26
1
191
1991
92
94
95
95
96
97
98
99
99
99
2001
2001
2001
No.of cases of compensation for deaths2
Disease
Byssinosis
Byssinosis
Byssinosis
Byssinosis
Byssinosis
Byssinosis
Byssinosis
Byssinosis
Deafness
Total
Numbers
2
1
10
3
1
1
1
1
1
21
Year
1991
94
95
96
97
98
99
2001
2001
Anncxure 1
FACT SHEET. GUJARAT
NATIONAL FAMILY HEALTH SURVEY. 1998-99
Sample Size
Households...............................................................
Ever-married women age 15-49...........................
3,9c*.
....... 3.S4s
Characteristics of Households
Percent with electricity........................................................ 8~ *
Percent within 15 minutes of safe water supplyi................ 7
Percent with flush toilet............................................ .......... 31 c
Percent with no toiler facility.................................... .......... 5- 9
Percent using govt, health facilities for sickness................ 27.7
Percent using iodized salt (at least 15 ppm)................... cc.l
Characteristics ofWomenz
Percent urban............................................................... .... 42.5
Percent illiterate................................................................... 50.3
Percent completed high school and above.......................... 20.1
Percent Hindu........................................................................ 89.7
Percent Muslim....................................................................... 8.2
Percent Jain.......................................... ................................. 1.1
Percent regularly exposed to mass media............. ............ 66 2
Percent working in the past 12 months.................. .............50 8
Status of Women’
Percent involved in decisions about own health..... ........... 71 4
Percent with control over some money . . ........................... 73 6
Marriage
Percent never married among women age 15-19.............. 73.5
Med.ian age at marriage among women age 20-49............17.9
Fertility and Fertility Preferences
Total fertility rate (for the past 3 years)................................. 2.7
Mean number of children ever born to women 40-49 ........ 4.0
Median age at first birth among women age 25-49 .......... 20.1
Percent of birthsaof order 3 and above.............................. 40 9
Mean ideal number of children*.............................................2 5
Percent of women with 2 living children wanting
another child........................................................................ 17.2
26
Current Contraceptive Lse
Any method........................................................................ 59 0
Any modern method.............................................................. 53,3
Ptll .................................
-................................................ 15
IUD ............ ............................................ -........................... 3 1
Condom................................................................. ............... 3.5
Female sterilization................................. ... .
43 0
Male sterilization.................................................................. 2 3
Any traditional method.......................................................... 5.6
Rhythm/safe period ........................................................... 4.8
Withdrawal............ ............... ............................................. 0.8
Other traditional or modern method...................................... 0 1
Unmet Need for Family Plannings
Percent with unmet need for family planning......... ........... 8.5
Percent with unmet need for spacing..................... .............. 4.8
'Water from pipes, hand pump, covered well, or tanker truck
’Ever-married women age 15-49
sFor births in the past 3 years
-Excluding women giving non-numeric responses
□Among currently married women age 15-49
Quality of Family Planning ServicesS
Percent told about side effects of method.............................9.5
Percent who received follow-up services.......... ................ 70.8
Childhood Mortality
Infant mortality rate?........................................................... 62.6
Under-five mortality rate?................... ............ ............... 85.1
Safe Motherhood and Women’s Reproductive Health
Percent of birthss within 24 months of previous birth ..... 31.9
Percent of birthss whose mothers received:
Antenatal check-up from a health professional................ 86.3
Antenatal check-up in first trimester................................. 35 8
Two or more tetanus toxoid injections..............................72.7
Iron and folic acid tablets or syrup.................................... 78.0
Percent of birthss-whose mothers were assisted at
delivery by a:
Doctor................................................................................. 37.4
ANM/nurse/midwife/LHV................................................. 16.1
Traditional birth attendant.................................................. 42.4
Percents reporting at least one reproductive
health problem...................................................................... 28.6
2T
Awareness of AIDS
Percent of women who have heard of AIDS...................... 29.8
Child Health
Percent of children age 0-3 months exclusively
breastfed............................................................................. 65.2
Median duration of breastfeeding (months) ..................... 22.0
Percent of children? who received vaccinations:
BCG.........................7........................................................ 84.7
DPT (3 doses)................................................................... 64.1
Polio (3 doses).................................................................. 68.6
Measles ....... ......................................................................63.6
All vaccinations................................................. ............ . 53 0
Percent of childrens with diarrhoea in the past
2 weeks who received oral rehydration salts (ORS)........ 28.9
Percent of childremowith acute respiratory infection in
the past 2 weeks taken to a health facility or provider...... 71.2
Nutrition
Percent of women with anaemiau....................................... 46.3
Percent of women with moderate/severe anaemiau........... 16.8
Percent of children age 6-35 months with anaemiau....... 74.5
Percent of children age 6-35 months with moderate/
severe anaemiau................................................................ 50.4
Percent of children chronically undernourished
(stunted)iz........................................................................... 43.6
Percent of children acutely undernourished (wastedlia......16,2
Percent of children underweights....................................... 45.1
aFor current users of modern methods
■For the 5 years preceding the survey (1994-98)
sFor births in the past 5 years (excluding first births)
sChildren age 12-23 months
loChildren under 3 years
nAnaemia-haemoglobin level < 11.0 grams/decilitre (g/dI)
for children and pregnant women and < 12.0 g/dI for
nonpregnant women. Moderate/severe anaemia
-haemoglobin level < 10.0 g/dl.
sStunting assessed by height-for-age, wasting assessed by
weight-for-height, underweight assessed by weight for age
22
Annexure 2
Table 1'
4
Pul
ses
0.36
0.6
0
0.3
1
0.5
7
0.8
2
0.5
8
0.50
23.
29
59.63
State
1
Cereals
1
Bihar
1.14
Cereals
Substitut
e
0.00
2.
Gujarat
0.85
0.00
1.07
3
Tamil
Nadu
Uttar
Pradesh
AH India
0 93
0.01
0 49
1.10
0.00
0 58
1 04
0.05
0.83
420
3.73
24.9
2
4
ICMR
Norm
gms
in
2
5
3
Suga
r
Sr.
No.
Vegeta
bles
0.60
0.54
0.45
0.48
6
Frui
ts
7
Fats
& Oils
8
Milk
9
Egg
s
10
Meat
11
Fish
0.3
5
0.3
5
0.7
1
0.3
6
0.4
5
0.44
0.4
8
1.0
1
0.4
2
1.0
9
0.9
7
0.0
1
0.0
2
0.1
0
0.0
2
0.0
6
0.09
0 16
0.07
0.03
0.23
0.23
0.15
0.05
0.15
0.28
22.
11.52
146
.23
2.7
6
3.69
7.04
60
0.98
0.39
0.58
0.52
Consumption Index with ICMR as the Base (=1) for Various Food Items
Source: Col. 1,2,4 NSSO, 50‘" Round (Report No.402), Level and Patterns of Consumer
Expenditure (1993-94)
Col. 3,5-11, NSSO, 50th Round, Quantity of Consumption of all Food Items (Rural)
1 Source: Table 3.2 of the Food Security of India Atlas, MSSRF, Chennai
Table 21
Calorie Intake among the States
Sr
No
State
1.
2.
3.
4.
Bihar
Gujarat
Tamil Nadu
Uttar Pradesh
All India
Average
Intake per
Consumer
Unit
Per day
Kcal
2
Average
Per
Capita
intake
Per day
Kcal
3
Calorie
Intake
Of
the
lowest
Decile
(Kcal)
Per cu/day
4
Average
Intake
Of lower Exp
Groups
<Rs.l90
Per cu/day
Kcal
2637.00
2470.00
2347.00
2899.00
2683.00
2115.00
1994.00
1884 00
2307.00
2153.00
1790.88
1788.34
1551.38
2103.15
1954.03
2142.75
1685.25
1683.75
2240.00
2049.25
Source: Col. 1-5, NSSO, Sarvekshana, Vol.XXI, No.2, 73rd Issue (1997)
1 Table 3.3 of the Atlas
30
5
Percentage
of
Households
in
The
lower
Exp
Groups <Rs.
190
39.53
12.93
22.99 ■
26.29
22.19
Table 31
Deficient Calorie Intake (per consumer unit per day)
Sr.
No.
1.
2.
3.
4.
State
1
Percentage of
- Households
Consuming
Less than
1890 Kcal
14 10
20.40
28 20
8 00
2
Percentage of
Households
Consuming
Less than
2400 Kcal
41.80
53.70
61 30
31 00
Bihar
Gujarat
Tamil Nadu
Uttar
Pradesh
13.40
42.00
All India
Source: Col. 1-2. NSSO, Sarvekshana, Vol. XXI. No.2. 73rd Issue (1997)
Table 42
Calorie Intake of Landless Labourers and Cultivators
1
Percentage
Of
landless
Labour
Household
s
To
total
HH
3
Percentage
of
Landless
labour
HH
consuming
<2300 Kcal
to total HH
4
Percentage
of
Submarginal
Cultivators
(with <0.40
ha)
to
total
holding
5
Percenta'
ge of
Sr.
State
Cultivate
No.
r
Consum
ing
<2300
Kcal
to total
cultivator
s
Bihar
19.00
52.03
27.00
1.
45.00
8.55
Gujarat
17.90
10.02
26.77
40.00
2.
56.00
Tamil Nadu
26.60
53.65
3.
17.29
43.00
65.00
Uttar Pradesh 7.60
4.
38.00
20.00
41.00
3 12
All India
14 20
37 71
49.00
6.96
29.00
Source: Col. 1-6, Kumar Praduman and Joshi, P.K., “Determinants of Food Intake and
Nutritional Status of Farm Households in Rural India" (2000), Mimeograph
1 Table 3.4 of the Atlas
2 Table 3.5 of the Atlas
2
Percentage of
Landless
labour
HH
consuming
<2300 Kcal
to
total
landless
labour HH
6
Percentag
e
Of hungry
Submargi
nal
Cultivators
To total
Cultivators
31.22
19.12
35 49
18.53
22.32
Column 3 clearly indicates that non-implementation of Minimum Wages Act badly
affects the health status of the landless labour. The minimum wages fixed by itself are
not based on the minimum calories requirement even if it were to be folloued.
Table 5l
Protein Calorie Inadequacy (Percentage of population with protein and/or calorie deficiency)
2
1
3
4
P-C+
P+C+
P+CPCSr.
State
No.
76 5
1.2
12.3
10 0
Bihar
1
2.5
0.0
60.3
37.3
Gujarat
2.
29.7
41.4
0.0
28 9
Tamil Nadu
3.
NA
NA
NA
NA
Uttar Pradesh
4.
P: Protein C:Calorie +: Adequate
Inadequate
Calorie Adequacy: 2425 Kcal per consumer unit per day. Protein Adequacy: 60 gms per
consumer unit per day
Source: Col 1-4, MHRD, India Nutrition Profile (1998)
Table 6: Life Expectancy at Age One2
Sr.
No.
1
2
3.
State
1
Life Expectancy
At the age one
(1992-96)
2
Rank
65.2
8
Andhra Pradesh
1
60.6
Assam
5
Bihar
63 2
65.1
7
4.‘
Gujarat
5
67.6
12
Haryana
13
6.
68.1
Himachal Pradesh
66 6
11
7.
Karnataka
16
8.
73 2
Kerala
2
9.
Madhya Pradesh
61.2
10
13
Maharashtra
68.1
4
11.
Orissa
62 6
15
12.
Punjab
70.5
13
6
Rajasthan
64.6
14
10
Tamil Nadu
66.1
15
3
Uttar Pradesh
62.2
16.
West Bengal
65.8
9
Source: GOI, Registrar General and Census Commissioner, Sample Registration
Surveys (1992-96)
' Table 4.1 of the Adas
‘ Table 4.6 of the Atlas
32>
Table 71
Child Health Indicators
1
1
Sr.
No
State
Percentage
Of severely
Stunted
Children
Under five
2
Percentage
Of severely
Undervveigh
t
Children
Under five
22.20
3
Percentag
e
Of severely
Wasted
Children
Under five
3.50
4
Child
Mortalit
y
Rate
(1990)
5
Infant
Mortalit
y
Rate
(1997)
70 00
17 00
27.00
Andhra
Pradesh
79 00
28 00
5 30
2
Assam
32.60
17.90
73.00
27.00
9.50
3.
Bihar
44.00
29.50
69.00
24.00
3.90
4.
Gujarat
54.20
36.27
70.00
23 00
3 70
Haryana
19.10
5.
34.70
64.00
16.00
2.00
Himachal
19.70
6.
38 90
Pradesh
20 00
63.00
1.10
7.
Karnataka
37 70
22.80
3 00
11.00
2.90
15.70
8.
Kerala
37.30
99.00
35 00
Madhya
4.20
9.
40.00
33.40
Pradesh
14.00
56.00
Maharashtra
1.10
28.60
10
43.30
29 00
100.00
3.10
Orissa
22.00
11.
26.50
16 00
54.00
Punjab
2.80
12.
38.20
19.10
3 90
32.00
89.00
13
Rajasthan
37.20
16.40
58.00
14
Tamil Nadu
1.70
15.00
16.10
21.50
89.00
15
Uttar Pradesh
40.50
24 60
3.80
32.00
West Bengal
18.40
1.20
18 00
58 00
16
37.60
All India
7.69
6.29
2.05
8.46
21.35
Source: Col. 1,2,3 NNMB 1996, MHRD, India Nutrition Profile (1998) and Shariff, A., (NCAER)
India Human Development Report (1999). Col. 4,5 GOI, Registrar General and Census
Commissioner, Sample Registration Surveys (1990 and 1997).
1
References
Ansari, R, A. & PateL B. C. (2001). Quality of reproductive health services at
Community Health Centres: An in-depth study in rural Gujarat. Baroda: Centre for
Operations Research and Training.
Bhat et al., (1995). Maternal mortality: Estimates from an econometric model. In Monica
Das Gupta, Linclon C. Chen and T. N. Krishnan (Eds ), Women s health in India: Risk
and Vulnerablity. Delhi: Oxford University Press, Delhi.
Department ofWomen and Child Development. (2003, January). Gujarat State Gender
Equity Policy: Formulation Process. Gandhinagar: Government of Gujarat, Department
ofWomen and Child Development.
1 Table 4.9 of the Atlas
Foundation for Research in Health Systems (FRHS) Health Monitor. 1998 Ahmedabad
FRHS.
Government of Gujarat. (1981) Health Statistics of Gujarat. 1980 Ahmedabad: Health
Secretariat. Government of Gujarat.
Government of Gujarat. Realising I'ision 2010. Gandhinagar
Hirway, 1., and Mahadevia D.
Indian Insitute of Health and Family Welfare (IIHFW). (2003). Estimates of maternal
mortality ratio. From a Regression modelfor major states of India Project Report. No 7.
Annual Report. 2002-2003. Hyderabad: IIHFW, Hyderabad.
International Institute for Population Sciences (UPS) Mumbai & ORC Macro. (2001)
National Family Health Survey (NFHS 2), 1998-99; India; Gujarat. Mumbai' UPS
Mavlankar, D._ Ramani, K. V., and Shaw, J. (2003, September). Management of RH
services in India and the needfor health system reform. Working Paper No. 2003-09-04
Ahmedabad: Indian Institute of Management Ahmedabad.
ORG Centre for Social Research. Division of ORG-MARG Research. (1999). Facility
survey (1999) under the Reproductive and Child Health Project; Gujarat (districts of
Ahmedabad, Gandhinagar. Kheda. Bharuch, Surat and Valsad). Baroda. Author.
Population Research Centre (PRC). 1999. Baseline survey under the Reproductive and
Child Health Sub-project in rural Baroda District, Baroda, PRC.
Qadeer, I. (2002). Women’s health policies and programmes: A critical
review.
In
R.
Khanna,
M.
Shiva
and
S.
Gopalan
(Eds.),
Towards
comprehensive women’s health programmes and policies (pp. 231-260).
Baroda: SAHAJ.
Visaria, L. (1999). The quality of reproductive health care in Gujarat: perspectives of
female health workers and their clients (pp. 143-168). In M. A. Koenig and M. E. Khan
(Eds.), improving quality of care in India's Family Welfare Programme. New Delhi:
Population Council.
Contributors
SAHAJ, WOHTRAC- WSRC ( MS University, Baroda), ANAND1, Deepak Charitable
Trust, Center for Social Justice, Sanchetana, SWATI, TRU
Jagdish Patel
35
PRESS RELEASE- 29/7/04
NHRC to hear cases of denial of healthcare in Western Region public hearing
National Human Rights commission taking cognizance of the denial of health care cases in the
•.ountry.Joday heard over 40 blatant cases of denial of health care in its Western Region public
hearing on Right to Health Care organized by NHRC and Jan Swasthya Abhiyan ( JSA).These
cases include avoidable deaths due to untreated snake bite, denial of delivery care leading to
women delivering in the open outside health centers, operating without anaesthesia in sterilization
camps resulting in severe anguish to the operated women, discrimination against persons with
IIIV and failure of the public health system to promptly respond to an outbreak leading to deaths.
These cases were reported from five states including Madhya Pradesh, Rajasthan, Gujarat.
Maharashtra and Goa.
In Madhya Pradesh, a 25-year-old man died of a dog bite as the nearest Ratlam civil hospital
• lid not have any anti-rabies vaccine. While in Maharshtra three girl students died of snake bite
because of non -availability of anti snake venom m the Rural Hospital.In anothercase in Madhya
Pradesh a two-an-a-half years .old child was referred to Badwani civil hospital after a long and
tedious process for treatment of his continuing eye-problem. However, the child was not treated
in tire eye department and did not receive adequate eye care finally resulting in both his eyes
becoming infected and complete loss of eye sight in both eyes.
<
In Gujarat , many such cases were reported where the doctors advise patients to go to private
hospital, if not they demand money for medicines and treatment. In fact Ahemdabad Cancer
1 lospital, did not even have an ambulance to transfer a patient leading to an early death of a
patient. In Rajasthan cases clearly highlight the infrastructural deficiencies and lack of access of
health care facilities. A stone quarry worker in Jodhpur developed silico-tuberculosis had to pay
for his treatment at the District Hospital and had to buy drugs from private medial stores. During
six month of treatment and after spending Rs 20.000 for which he had. to sell off all his land and
belongings he died leaving behind his family in heavy debt.Large-scale corruption in the district
and rural hospitals are the norm in all the states. The doctors oftenrdirectly charge money .from
poor people although they possesses the BPLcardsand do not provide treatment if their demands
in- not met.
/
.
-
-
'. . . ■ .
.
■"
-
.
This hearing is being attended by Justice Bhaskar Rao, Member. NHRC. Dr N.H_Antia,
Chairperson Health Committee NHRC, Dr B Ekbal, National Convenor, JSA, Health Secretaries
.'Health Commissioners of all five States and Secretaries of various State Human Rights
Commissions. Nearly 200 delegates from the JSA units rn the concerned States are also
participating in this hearing. .
:
.
,'•>
I he Western region public hearing is first of the series which will be followed by four more
hearings in other regions of the country (South, North, East and North-east) followed by a
iiatiniial public hearing on Right to health care in December 04 in Delhi.. Thus the Bhopal public
hearing acquires historic importance by inaugurating a process of highlighting and moving
towards establishing the right to health care in India. It is expected that the NHRC will direct
various state governments to implement a range of improvements in health services and greater
interaction with civil society in order to ensure the.health rights of all citizens. Jan Swasthya
Abhiyan would carry forward the campaign that has been strengthened by this process,-to demand
the making of right to health care a fundamental constitutional right
o '.i-.' •r;
lh \bhay Shukla National Joint Convenor (JSA) —I
Dr Ajay Khare, State Coordinator MP JSA :.
. - ■ ■'rhjJl’J
■
| lk > cb
1J W 4 > k 0 1 t? ^ ? t
/ ln h y i:
'Z
"I
lte » b tr > h ^ » lt> »
h ^ > lb » ^P lb ^ 1IA (b bX U >l,lbA P .
b j l<b |blk.K > b h X P 4 .< ^ |t P lb b ]R t? 7 ^ lb 4 ( P lb ^ ||r \ |b ^ |P IP h » K ;'X K b X F ? .
h io j
<3
2.
PfRR: ffoft ftgraftsWRR jRIsRT 2-6 qcftjj ftRR
<h-gl A f 8 Ml^lPiq> TOTFra4>~sl f
yqRracfT tf> 3PpjW qqqraq^'f^<HT 751$ I Tfft grafts
qf) HH1 di-tn <ft tjfttii ft qft $ I
3.
wi: jcf3i graft*'Wff®i^=gtA£ 11 ^RszjsfRgt'(36gft?Ri) ^’RiRbc^HIda"ho-i vMkarawffci
4.
gTia^ftw:^ jqaiRjcf 31 graft*-MiTwii-iffTfis (48 gRtsra) graft*
ifsraqf f, qffjHTtafrj 13 (42gftf?ia) graft~*4<i-t<ar^tfat
5.
‘^:gft^gqHq57f
7?q (g7rq*af) ft aft f i
toRt ; ja 31 graft* wr $5=gf f’ ft 8 graft* rarraq Rr ft ftqjftt 4h *tf awn
sjq
& I Rh^
Rft Rr
®
q< qft f i *fr a* ft> f*ftl r* ft ft Rvi<f) *t q*f?ft* ra*rar it? tr ft vn^d dMctsd *^t <c, *4pr> H.g. ft ftRftt <£t
yqcfradT *t f^fa **f, ?57reftfeaf 1OT*bft* dHd (Emergencies) ftfH graft* -Wffra^t^ftrifftt <ft *lf <zi qt^i aft'f |
6.
qftt: 6 graft* rarara fc^f (19 gfft?ia) ftftft
qfttift*tfra*rar ar raraaft’f i i3graft*7qi7=raiftgf (i4gfft?ia) ft
dcfJM qftt qjq*HT5<ftld * 7RftvlMcn^ f Rnd*t ft3lR<q|9RT: qftftt’ftTJR Riftf I
7.
Rjftft: JR 31 ftft 5 (l6gft?Ta)qraft*qqT7«T^ftfifR^ft7T^fcraTf, 31^26 (84 irfcfSTcT) ft *tf ra*rai aff t, qft'sa 5
graft* rarrazr f*ftt' ft ft *?a ain* graft* rarara
qftTR ft ftgra aff *7ft f’ 13n*Rf* Trra if a?ft wa ara* *V jaar
qaart, ftiaftygdaaacfaar^i
8.
13 gift?ia graft* 'Hit^ij ^f foai sftef & aa Rf f' i aft' * aa 3 graft* qarraa ^f if afteff faRbed* aaara f i
9,
7Oyfci?ia yi<uPiq>Rii-<d^4 cb-glft'q'O'f
qqfqiciiaft 1(4 LHVs^5qq'ift'5R*jtj
1 o. graft*rarvra^ftfcpprt29 gfft aaftf^cd*aaaqqaraqaiHftaqa^aaft'an?q^ iaft'3iraaftarfftffftftcPraa 2 o aft aa
graftq, -MIRUJ 4,-$; cbMtilYl RH-U q?3i Wdici SdMcW H ffif I
11. K>ft 31 g lPlm tq 1i'-slifdTilcid'yfcl'Mi vjMci^ nflf sfRluini)
1.
qi? <f>-sl ift ■Hiq^dfpdi: 4-sqinl Rncl
Jci d I (jq I ft 4> ■eqi’tssj <b-s;Y if
d'(6^4>l4-1^l 0'('<^ l
an^^lftqjq'-Hi^qiftcU'eqi+^q ^i^yqcicMf I vfffgft
80000RR5R^qq^7q^Tftq5raR^^ftRT:qTffqqfTf^4l,84J12^UH7t^qq^7njJrrf^WF?2lf)R^3qeWf I
2.
ftIRR:ftRtt->ft'til*J<lft<b-MIW4^-si^ftqHI^I'<30qciqdqcie4’lfftl lOqTgwfsfiqqRqffyqReyf I
3.
qftf: 40 yft^ld
4.
affqfcFf
■WIWJ
^'ft^ftd
^qT^fiftcbtf cZId-raTRfft I
: 60 qftraa ■Hiyqift* Wf+wj ^f if 3ffqY?FT WHft'f, qqqt f
ftfefiq f I vjqftj J5^<|ft<t>
■MI+W4 ^-sif^g-Hq 45«ttdMci*y dfl’t I
5.
80 gftraa 'tii^ift*'^rar^rA’ft^Msi sfee?qffw^<ift4> q^TBraft 3Rq?zraswftft?ta$ffifqf 3n^
yqR-ajf i
A’HftcIT ftft>cdq>yMci»M f I
6.
4>d<?i J8 tuyqiftm •Wi'HUI
7.
40Mft«ld ■dl^qiftq>tqit«-q^>-s;l AftPbcti<t>, SitMaici <F1 -ddqiqft ifdHci^M dfl <6cif I
8.
3nq?qq> tjftmqff
80 gft?ra tn^jqiftqi tqit^q
qs’fftqnsTHTqf 140 uRisid <ii*j<ift<t> ■Mi'Wi
a
dlH<t> yq4><ui qq STHiq f ?raf 80 ufcisra 4' ECG
q?
A' atfq^Hftictq^, ^RRjyteqqrqqfH 3ffqY^tgqqfHyqqjwHfff‘i
9.
<i>l f ■fttuyuftm tqiv^q ‘b-sRiviRdd f^clqxt^fci^ 3nq?qm^ftsift yqRra q>xii| if 3Rqpf f I
io.
40 gft?ra tiiyqiftq> «idx., <b-$; qftq jftftqrmICsci qferoff, ?qttn ?iq +i4'Jl fftrfeffq-w qiil tjq
4RR^t ■gfty i y cm
I
11.
60gft?TddItjqift* WI+AU4
1.
fcRR: ftFRRf ^t WqiHdii' q>RUT
ftXFT, nftcfT ftmq 1(4 ftlSJ ftRFT if’ <ft ^tftqf ^t vrfft q? ft
ftR^'qqqrqt^df^snftittqfd^ara^it^f'RHRqtsRqmHit'HTqi-Rq^^tf^J^^TWTqcraTf 1
2.
qpft: Rich 3itsai<?i qpft ^t tjftm3fi qqift yfta ran qff ftqr rt
3.
3ts?crar4’qqf crarcn$cftq>ttqqqq^t4Rqf fTrarq§?fTnraYt5^■gqnrftqffqqrf,
qffqTRT^f sRiiqff^f^'ir'H^tRt'TraTqsiqi^Rtqt'qqsRqHTHij'Y^qTgftqiH^tRTaTff
4.
tfWcPT : 3Rq?TTef 4> 57 <ndt & Tira 4 fid iciq eft vlMcl«u f 4<-c( 4>ft qftt <ft yfttfT Rft f eft ?>ff
rRtvffqq jcUR
tfJbftd YVI1& Rii**lf farift* dft’f I
113RqaiH A’
5cfra f^ETT snai f I
qftt ^rrycfj ft
?>,
r,
x‘t>«<§dft
Rftlft f f
oftrn ft Tjno ? frqiciq gorar nar ?. firoft’ ofi eoPf 2 aoft ofiffto orot crarar onar £ oft 35^ ofto safii gft 3go off 357 orft 1
5.
oftuft'45 HKI 3Tcft 45 ag?ft<^ftt 3ftt E33T=4TO£ft I 35I<J~5^ H3U fftuft 1 HIH ft 34 035^ 331 EHOOTft 030 45 3T3TGJ 3Tlf4
6.
GtT3
- <gt ?’ Tira d firar 3ttt4 ft! gocvh ogf11
: 3Ofi finer! 3574dlc5 ft fifftS vff^ TjiftEIlft' ddefey at £ tRTvj gru Uffat' d p35 gdft 3{fi35 gift £ fii ofto oftGT GOT 3gH
-I el *x 7i*ft i
7.
S<Tgft4i?Tt3{74dlc5ft>40c5»4^MT'xt
8.
srfft *a t ftsYcu 3ft o^a ?ft
*W4i?Jc<n§dft 35 Rl* gift ^'ffti’lftqH^vId-^’Og-l-5^1*7 75*ft 1
orgr otgitt ft 33if^t$*i'iY3 -axlo-Tl gteft ft1 wqaief ft'Trftl 35532335 33itat'35T srora ft i
ftftt *c*l|ui TiPtfd, fecTT 35700577, 3<$4l-ft
1.
ftftt *<-41* -eiPtfei 31001 3553 35T 25 OlftSTeT OTO 030 357 Tftt ft GTafii 3t7MdlclY ft 30 45 35053 ft 35537335 03 ’JePJeT 7j(4t| |if gq<Hot|
Oftt gt 31 Tftt ft I
2.
ftftt 350310 TiPlid di Jcl 3T53 355 cTOOO 75 Wfi?57T OTO (3/4) 7TIOF3 Oftvfl ft 0355 (4535 05505 ftGfdd UO3TT facift OTeft 7ffft3T3ft’
OTtlPiidci'lOO 11 UlcISld 75 4 *7 at ft I
3.
TftftfftsiNI Pbs'HT’ 15,26.2Ol/-f5qft35EZrat'ft'fteHHO81.3dft?TaT35HHft3n'ift7jfftaT3ftq77Ofta^t'357ft§0, 03735ftt?5O73
JHT cforft 0313^3 R1(4k75I 037357*3 3Tp|*lft 4l*|4|[ct*l 07 4'Tift 4435753505ftO?fto3Opft4tOfcT 03Tfavieft 07’071 351(4 07
333g3Otl
3330ftffticOft'7357*3dtTH7313ft4> 35*330sOTTfftfaaftotfto5J3OTOlftGf Tefft, M*lRld 03OTfja(45000ft', gOOTft!Oftt757^17
ftf TTPI PlPtst 5J35T7 ft ddi 314317
sOTT Pit cl ft 7017*3 -yftyioft ^t 3H3iHdl 03 TH 7313ft 3ft 773T ftl 03T ft fulTift ftST dt Tloft oftt OH
7}-iUl4 ftt TffcfttCTd ft Gft Olftt 0^ ^03T (431175 TSuftf ft Tfft Oft ftt 107^ ?7lft5 UOTId ft! 757*17 ?7T Tpft ft5 sOTT ^STO OO tjftf cO3T GH 73T7S3
ft> OfcT 3ftft357Tft3O?flHfftSTft Oftt'ftftt ft I
7*d7* 63 rnftdicio 7017*3 03TOI73z|'3I7u<D vlftq^-3d3O?qi7l’1 R4 vlld ftGfdRt>
d74iftdl fftf^TT35533-5 ft sTiafttcOft
O-SOI-ll Rneft ft 7017*3 ■giooioftdt (t*lfd 3td4d 30-ftOft I TPft 35 (eft* 7017*53ft5ijft?3dt ^(d 35 feit; XTT4>I7 3ft 3nft 3itr 3TpT3533T7T357ft
3Tdtft'702lfttciT’d JW303S3**<Hx)dlO*lA*7iftftl
7JS031.
3H33Hft 70e ft ft5 q-soi-ft I4ift ft epei 23 UlilPl* 7417*3 4>-ftl *T«4i0IO ftfvRT35T*5dcl0 ftft5 7417*3 (o *5HI sOTTftoft ft> gT ftoft 31
TITSlfftOT 7-477*3 q5=g 53OH&( 3571ft 03 fft*R5d 357ft 4ft 3514744x71 ft I UlilP)* 7477*4 ft^St'3TcO3T gT xft* ft 350 ft 350 03?
711 do I fo 01 7017*3 *-S T3l(od feft vSlft ^t 3tl0734>dl ft I Jt# UlOpI* 7017*4 *-O vift ftftoi !4l4p54> 7017*3 45-5 3ft Tll^Olfo*
T4T7*4 4>-545T5qft'l4*R7d 14*31 u5l-5I Olifto I
3.
MI4p50i 7017*3 4>-s ft StTMdlcI *ftoiftoT <St c4474i 07 ^ftfoo 17 4? 70*T
oftofto 357ft dt303?335cTT ft 31[4> xJ4e1<4 *51 -10 * I (rt> 35T
'JTT-tJTT 75^041’1 fftfOT GOo4i 35*RftgeTT WI7*4 ftoift'!JTTT gt lid I HTOfft* 7317*44s^ft 2 offtcO 3ft? 3 JTH 3Tft05 f?T3T3ff ft 3ST
350arft7^ft35T 303?335?TTft I
4.
3i7MdlcTl ftTTftt deco^uf MOcJTdOftvtlft Oliftd, XS175*7H[ftc1l (oI4k75*, oiftcil 74l7*3 *l4*di OO ectlwl ftlfcTO 'Sio’dftftTOOl
5.
Rncll 3t70dlc1 Tllftd TPft MI4p|* 0O Til^Ollo* 7017*3 4i-$ft ft Tiftt 3TT3?335 OOlij G4cl»4 el-ft Ollfto I
6.
TPft 75 7451 ft 3570dlciYftp54HI^I? Oc53 03 (ftTd? G0d<4 gift Ollfto I TTMfttTTRT3574dlc5Yft5TTT335JT03 3H3 M754 754^35Pf4l4
TjfftEIT3ft'4ft yqci^dl gift! 3Tf^01
7.
3t7MdlclYft Olftt00 fftofeft 4ft PtoPld dMd«3dl Tjptlsod dt wtlftl 4lffto 751*1 ft!7514offtciT03 JT50 U711*4-7 3531103 -5gift 3frfft 4ft
C307-4T gift! Olfftol 3tTMdlrtYft‘1<?1 4l4 Hlftl 04 4107 4ft PtOUXil 4ft C307-4TM7MI3piO>dl4> 7513 E3H 4ft 4ft 3TT3?0*dl
8.
I
Trftt3TTqaraYft7Tdtn35R^tGfhft'45fc50M4l,ISIIc5I^I:gf4ETT4tGn-ft4lflOlftraT3<'W<5IHft’MAlI’ISHc5l,3ft.ftt.^t. SJT?gift457503
ft tlf^d-ft Olifto *olTo> 3Tftt eftof 3ft 4TgT GIT ESTGfra 4574l-ft qSfftt I Xll-llyi4ft, 0375-4 03 JU Gftafdt TjfftHT g? 7503 GOePO
gtftt3TfftOI
9.
75ftt357O?TTc5t'ft3IT35f^f3>?5O4O7g7cT0I^:7T^tgf43T24 3uft5T4377Tfft<TGOc5«Odftl3Tfft0l75W^tGftcftu ’Tft4td3T45ftt4
Gfl4-5 4100 *7ft £d-g O^ftft flfam fa:?}?* 4ftl dlfeo I
H’Jlvil
10.
lul flftfcT sTRT eftdlftHTcftsRtZRyqqftq TOlfft', RssiMdS tjgdft, Mci*I RTfft 3TO?TOi 4W| qt qrqfa<MI ft
'(Pn
znt-ft qiif << l
11.
3ii»fPto hto qr sra? wTjfftTOJTfftft jft, siq, RSej<rft qroft to rtoT TOft to? w TORft qq 5vft<r?Hgt rbwh ftyqtfdj
glftdiff^i
12. HcftzsWKTO4TOTOftiRTR-WdlciTOSMcW^ftmaffz£tTfjfttqRTOTHTcftSftTzPlqq<ul tlted ’^’114ftSTOftfttnf^|
13. Rnft ft
-^ifttU-ift
R4fcl TO fft1klHl
Vpd (vtdl ’td'flU ^TF22J ’Hpilct ^T 4IcH Rb^ll vIMi
3?I
I
tdPlfcid Rb^l viHl^lf^k’l
^tvilnl ^if^'s’ I
^^dl4lRnftft> '5T' TOft’'S3THftqRdltft? SRTORTf1fasftfftftt'ssft>dRdRft? WIfttSTOTTSetTOTHTO.&TOfft'
4iH<i>< arrtroftt ftftf ft Miar(ft<f> torto 4jto, s^ift aRquieff afR wi-wzi 4t hth to sr TOt ftl«Miaif ^t nrRTf tftR 4t 11
'H' 4? qfftdR ft 6 RTOR ft fcrsft '& SH4t fttH Hsft if STOT ftlTO (3 STR) TOIT an I ftsft Hftft 23 ajH 2003 TOP qg f4c^R
TOST air I TO 3TSTTO SfttScf qgft uft 2-3 HR Seftt-qSTsft 3ft? R/TO ffts ’ft SRS-HST r4 | gsq Wlt-tt| q>r4<bdl
(’JH.’ft.SxHj.) gRTHftzft ORS Mid-st [4<u H<ii Mt-JiitidH ciqft Mts-ft 'S' MitiPiqi wlta-n 4>TdftviA4T fcRd»gi ’Idi I
q gi W<»|{I R-Wd IR ft'ST. 'Sftsft'ft^T3fRUHqT3TTft?TTOftlftftSRlfHTOT ftnf ISfiftt SRlfHS3TftftHq ft Hft4>«
q 55 ft S[R fftdTRft RHT §tifR4 vi-it ft’qqi ft vTlft qft <4t>6l Mdl I f m4 HT gift H
SHRsq HT gi’) ^t dvdg
’l$ld
arq4
qit fs ^t n4t nrft ^t wi 6.00 TOt tT4qt Rwr^t srhstr cImr 3udi 1 vtgi st. ‘r' ytl 4<ai 1 d§d HrtRisr to4 4t
TOTO^tS^RRlfHHffRHlf RTRz£t IRTHH-HTIHH^ 'H* ^tHTO’ft t^TRHRFt HS, ftM<6t<£lHd 100/ - Rapt aft I TOT
ft Sit feRTtRR RTfe 1ft HTO ’ft RFt
TORT Pl’is4 ft? 35RUT TOt HSTOft 3 RTn ^t HTgT WI iftft <fft
I TOT^T TO 4t
g5iftft5^RUT'H'3Tqftq^nftqSTOft?tRlftft‘3RTHafaiTITOTHqftfiT?tf^TO4t'H'3Tqftq^qTtHffTOTTO5T3fRTORTaR
^RTftq5RTOTOftft'ftTO8.00<nftRTOTTOT?Traft ’FTTI
-:-
^uMcRnSHlftTORTOTOTOTqnaTftqJTOTfcraTRRnHRHTfefttlftRrft ’RT^TOTOHTHfftqf^TORTOftHTn^t
RHft^tqRHftRTf rsrifHc^t-^RT^tHTOTTitftjRftftT^RlH’ft^TOTOftHTqftTTOTHftHHaT’RUtRTOHHTOTftRTft
qi IM Rd I id
qi ft'i ’iici 'b'Rqft gHlt'di'-i-q 3iic||f I
TOTOR^TOTnftSRTH^TOTftf fe’JqPcR’Tj^fftTOSft^anTOftHTft'g’JH^qjt^RTRftftftSRTHafTOlftTOTOTOftTO
gCi;.? W
?/: <<
'■::?z'C--;'?/-: :
••'-■■-
■
w':- 'A-
V ",
■ •?-’. -
.■ .'■ \ '>■. -
■
?<’"■“■ '-------------- ' ---------------
■
. -/ •
r -^*4^2:
■ -••,
■•■-::
:- ■ ■
,
;
'
WZd;.-
...
eit’lld ^1 g3JT!
“
V qrf qfcT V VRT 3 0 STR 4ft dffcll t Rt far TO ' 3T*, ftTRT -ftydi <6t ftroft f ISH HffRT ft> 8 «rft f’ I
STR f^dWt
2003 ftaiT’Hdlft 4>l4TOf 'S' ft 'R'vJ'Wi+aq Wfft'gtft dl<ft d-d44t &MT4ftRH4>lft ftft^’jqffRTft^tSRTSft I HffRT
3rqftqfciftTSTaT is/s/osqft^roft'nfttiqffsT. 's' (ht.tot.4to, ’ftrorJsTs LTTftTOftss^rsifqftsTHfftTOTOi
auMianftrqixlq 6HftftqR4/5/2004qft 's' qifqft d-s<i>i §-Jii I $tift tiiM> weftSTf fftr 8UM^h4>TOS'Ht nftqftaft I
d(fRl 44 S-d<b qfci 4> gixi vriid 4>TOftnftogtft HTTS’4g5Utf> fcbdl Rl Tjcbl an, TOlPb S-ft 2-3HftftftHgldlft dff 3TT^ft
aft 15Sftr didujc; 'H' qft nftqcil gift ^tqftf Minqutl dffftnf <hR y-ft 8 TOt ift TO' 9 ft'
<fc| <ft$r H SI gift gi> ftt SdHIMS
TOfl
g-d ’iTq ft 'S ft> 3icliqi 3TTOdff Rl-3il dft fttft> did «Itl
f I wigl <<ct> 3T11 ’lid 41eift'aSTfft?TOT LTT (<jt41d M^fft
ftfftTOTvnftqTRTHSftftt3udftiH) «bw ft'dO'jadf, qff<jtixl atRSTORHSftfttqTTSrftfc’^TTOftft R"ft§f f I
TO3TTOTOTmHTORTO tiftRl q-sqiftl/ftTOTcRTTwMTORTO3fft<iHH.q. 5RTRqwi+TO^fftsn3Tf4ttf?HTOTftfttqiTOf<JPbST
TOTf I TO3TTOTOSHTOKTO3TPTTOT, H.ST. 4t -TOdl'TI titTOft ft> tlgdlq ft (4*41 TOT f I fvTRft CEHAT, 5"Wit 3TRTBITH^TO, dddlft,
Vilbel Rlftqiftlqfcidtiddd, 3iiRqiftl
ti‘101 ti Alrtd fe'l RUIdd ft'^ttq tiqMq>ft>TOftftvTZTfcRfti, MSWfftuTfSftftft’anTOPHt.
nftlq fttftrcf, ftnd srft, ff tftar Rig, qq^vi sruqici q>i tisqft'i Rich I Rqftii ftqjcH ft'^<sq sqftft’TOfcRftr, apjRTTPrRi RraftHJJHT, zgRTH
vid TTOT ft eft tilgl ZgT Sgzftq tgl I
ft7cTfl'TOTff7Ry'»//?/d’
TO TORTO Htftfft, ^STOft/ftSn
- Media
 RF_COM_H_87_SUDHA.pdf
RF_COM_H_87_SUDHA.pdf
Position: 1702 (7 views)