COMMUNITY NEEDS ASSESSMENT APPROACH FOR FAMILY WELFARE IN INDIA
Item
- Title
- COMMUNITY NEEDS ASSESSMENT APPROACH FOR FAMILY WELFARE IN INDIA
- extracted text
-
RF_COM_H_71_SUDHA
Project "Enhancing nrenaredness formanas...f Enidemics in Bangalore" from Dr. Girish
:
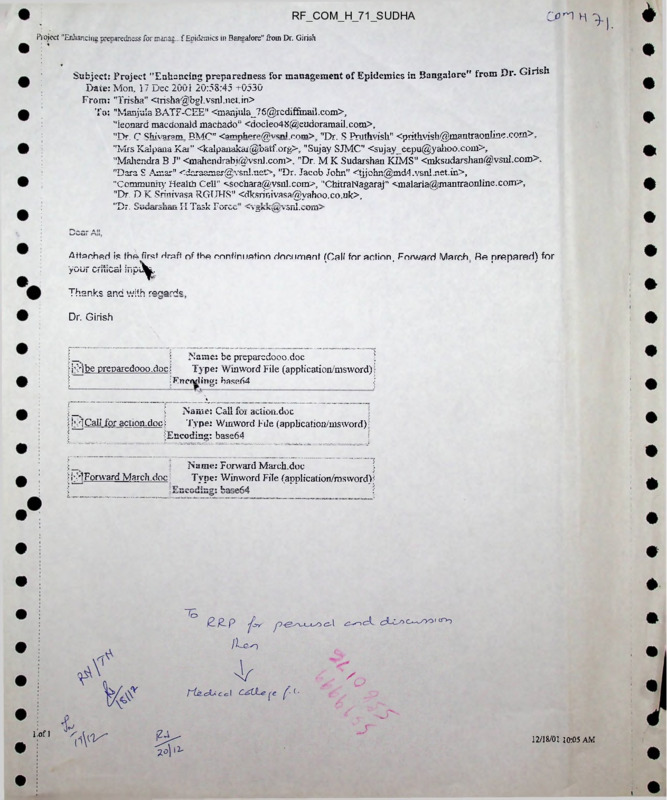
Subject: Project "Enhancing preparedness for management of Epidemics in Bangalore" from Dr. Girish
Date: Mon, 17 Dec 2001 20:58:45 -t-0530
From: "Trisha" <trisha@bgl.vsnl.net.in>
To: "Manjula BATE-CEE" <mar.jula_76@rcdiffinail.com>,
"leonard macdonald machado” <docleo48@eudoramail.com>,
"Dr. C ^hivaram BMC' <amnhpre@vsn1 c<->rn> "Dr. S Pruthvish" <prithiish@mantraonline.coni>,
"Mrs Kalpana Kai” <kalpanakar@batf.org>, "Sujay SJMC" <sujay_eepu@yahoo.com>,
"Mahendra B J" <mahendrabj@vsnl.com>, "Dr. M K Sudarshan KIMS" <mksudarshan@.vsnl.com>.
"Dara S Amar" <daraamar@vsnl.net>, "Dr. Jacob John" <tjjohn@md4.vsn!.net.in>,
“Community Health Cell" -ssochara@vsnl.com>, "ChitraNagaraj" <malaria@manrraonline.com>,
"Dr. D K Srinivasa RGTJHS" <dksrinivasa@yahoo.co.uk>,
"T>T.T T„„1. T?------ —1
x/i. o uuru oucm jl x laoniurvv
'y jruv^O roiu.cOrrt'
Attached is thA first draft of tho continuation document (Call for action, Forward March. Ra prepared) for
yo’uf critics! inpi^^.
Thonke
ond
. —....
.— u/ith ranarHc
Dr. Girish
•i
i
Name: be preparedooo.doc
i j</)be preparedooo.doc;
Type: WinWord File (application/msword);
iFncivling: base64
;
i
Name: Call for action.doc
i i'?>]CaIl for action.doci
Type: Wmword File (application/msword) ■
(Encoding: base64
!
H-IForward March.doc?
Name: Forward March.doc
Type: Winword File (application/msword):
1----r-aZA
Lofl
12/18/01 10:05 AM
Enhancing preparedness for management of Epidemics in Bangalore
<7 public health advocacy endeavour
be prey iireiooo
$ The city of Bangalore witnessed outbreak of
ti’ Gastroenteritis during the months of February and
Ij’ March 2001. During the consultation held by Of flee of
tif the Chief Health Officer, BIvfD it was decided to focus
on not just the immediate and short term but plan for
medium term as well as long term to combat: future
outbreaks. It was recognised that there was; a need to
initiate a systematic and co-ordinated effort at the city
level to monitor and forecast epidemics. Sanitsiry
$ vending of food and aspects of food hygiene: was
another key issue.
Adopting the “call for action’ and “marching forward’
to document the micro-epidemics and enhance the
preparedness of the health staff and heeilth care
facilities, the Core team has faciliiated the following
endeavours.:
a) Formaticon of the Epidemic Combat Task Force,
ECTF and the Joint Monitoring teams, JMT. The
perceived responsibilities and activities of the team
as agreed upon by the members lia.ve been
ir formulated.
b) Drafting the Epidemic Manual for die city cf
Bangalore.
% Effoits are currently on to delineate flic most
appropriate system for flow of information from the
different health care institutions ('Ihe Se ntinel
O J
u
Reporting Centres). This is necessary because the city
should be prepared to adequately respond to
outbreaks and ensure for its citizens a desirable A>
health status.
A preliminary planning interaction is scheduled on til
tire Tuesday, the 8th January 2002 at Juana Jyothi, “w
???Training Centre for Urban Affairs, adjacent V
Chowdiah Memorial hall, opposite Veidika Sablia,
Kodandaramapuram, Bangalore. Ihe agenda for til’
group discussion is finalising the Reporting formats, ti’
Flow of information, Case management stratejjies, til'
and Responsibilities of individual stakeholder.
tif
The major outcome of the deliberations would be to
arrive at the Calendar of events for the different a,
stakeholders. This would enable the city to anticipate S,
an outbreak aid appropriately respond to it.
□,
Concurrent efforts are on towards ensuring the Safe
vending of foods. Banning the vending is difficult;
conf.sca.ting and seizing the food snicks is
labourious. The lessons learnt from ihe ongoing
mcdel WHO-GOI project in Bangalore are' given
alongvrith.
More details of all the endeavour is available on ti’
request
til
Do not be part of the rumour.
o_>
tii
O >
tii
Cnii
,5x_-z
gfar
nJ'a 1A f*fin
O'G'^lt omi
w
Ij
1 ^?z7r>i'o-**<'>*r «««■/•
W**».*«*.
|
| In the wake of the outbreak of Gastroenteritis in the city during the months of February and March
I 2001 the Office of the Chief Health Officer and other concerned officials had scheduled an
I interaction with the facility from the departments of Community Medicine and Paediatrics from tne
I
Medical Colleges of Pangalore City, RWSSR officials, Superintendent of ED Hospital and select
j NGGs. The consultative group met on the if’ of March 2001 and 7"' of April 2001.The interaction
I focussed on the immediate, short term, medium term as well as long term plans to combat this and
future outbreaks.
The meeting analysed the existing situation as:
Reports in the media are usually the source ofinformation of the outbreaks.
The exact cause of the early outbreak in February 2001 could not be ascertained.
immediate measures undertaken included super-chlorination (apart from establishment of Help
fiiis siiH’ e fellb1.
cases being reported.
4. Enforcement ofSanitary vending offood needs to be publicised
5. A systematic and co-ordinated city level effort needs to be initiated.
1.
2.
3.
1
I
t t?o.o a r'TTfW.
I
I
I
a) Document the mici o-epidemics9 which precede the larger ones.
I
I
0 Set up a vigilant health inionnation gathering system utilising the sanitary health I
inspectors, health workers and Link workers with inputs from the local general I
I
practicitoners. nursing homes and hospitals. Lay reporting systems to be initiated. The I
mass media to be made a partner in the endeavour. An uniform, common, simple and II
I
comprehensible reporting format to be utilised.
I
❖ An. intersectoral emergency response team to assess the day to day situation and take
necessary intervention.
b) Enhance the preparedness of the health staff and health care facilities with proactive
support from the City fvledical Colleges.
b
Orient and sensitise the faculty at Isolation hospital regarding principles of
epidemiological investigation. Strengthen the available facilities including staff to
combat the epidemic.
o Make available module / protocol for standard case management and investigation at all
Offices of the MOH.
c) Immediately address the Hygiene and Sanitation of the street food vendors.
o Make available potable water and appropriate sanitary facilities at common street food
vending locations (FOOD COURTS).
♦ Orient and sensitise (Food Handlers; Food Inspectors') regarding hygienic food
handling and vending methods.
d) Undertake regular and frequent intersectoral meetings.
e) Delineate iong term solutions for water and sanitation problems.
Eiiiia.il cuts preparedness for management of Epidemics m Eangalorc
a nnhlic health advocacy endeavour
FOR W A* RD MARCH
Background:
In the wake of the outbreak of Gastroenteritis in the city during the months of February and
March 2001 a consultation was held by Office of the Chief Health Officer, BMP with the
faculty of medical Colleges in Bangalore City, BWSSB officials, Superintendent of ED
Hospital and select NGOs. The consultative group naa interactions and decided to rocus on
not just the immediate and short term but also plan for medium term as well as long term
pl2ns to combst future outbreaks.
The major lacunae in the existing reporting system was that it was not uniform nr complete If
not al! the health care settings, it did not cover even the major health care establishments in
the city. There was a need to initiate a systematic and co-ordinated effort at the city ievei to
monitor and forecast epidemics apart from publicising the enforcement of sanitary vending of
food and aspects of food hygiene
Adopting the call for action to document the micro-epidemics and enhance the preparedness
of the health staff and health care facilities with proactive support from the City Medical
Colleges and concerned NGOs a host of activities have been initiated.
The proposal to establish an Epidemic Management Col! for the city which has the
objective of not just to respond and function as the Information Ceil but also become a
barometer for the health status of the City.
The members drawn from multiple and broad based background constitute the health
intelligence input requirements in the City. When called for, due to an epidemic or out
break, they have overriding powers, enabling them to co-ordinate and execute the
p.scssssp' setion for s^idsmic control. The m.2’or h02lth coro institutions in ths citv to
bvCOiTiv Sentinel Surveillance Ui’iitS Shu the SysteiTi Of infonTiStiOH nOVv tO be
continuously monitored accoramg to a calendar of events.
2. The formotion of the Joint Inspection Teem, JIT 2nd the Epidemic Cornbet Tssk Force,
1.
Tho 5 JITc Aac.h comprising of a Deputy Health Officer of RMP and an Executive
Engineer each from tho Engineering departments of BMP and BWSSB would draw cut a
pioiocoi 1'01 inspection and rnoniioiing.
The FCTF comprising of the Zonal Health Officers of RMP, Additional Chief Engineers of
BWSSB and Zonal Chief Engineers of BMP would review the emerging situation and
take necessary action with technical support from the Medical Colleges, State and
National Institutions of Health, Professional Bodies and NGOs.
3.
A One-day workshop is to be scheduled on Friday, 21st December 2001 to arrive at the
consensus system that will be in place for the City with effect from 131 January 2002. The
convenors for the subgroups are as follows: Case Definition and Management Protocols
— Dr. Sujay, SJMC; Case 'investigation Protocols — Dr. Girish, MSRMC; Information
Dissemination - Dr. Mahendra, KIMS.
Enclosed alongwith is the name, address and contact for communication. The endeavour
is pan ot the Citizen - Government initiative to take Bangalore Forward.
Please do indicate your willingness to be a partner in the endeavour.
POLICY BRIEF
C.cw-> H - 3-1.
One oi the best ways to judge the well being of the
people of any nation is by examining the standards
oi health that ordinary people have attained.
Healthy living conditions and access to good quality
health care for all citizens are not only basic
human rights, but also essential prerequisites for
social and economic development. Hence it is high
time that people’s health is given priority as a
national political issue. The current health
policies need to be seriously examined so that new
policies can be implemented in the framework of
quality health care for all as a basic right. The
following sections first take a look at the hard
realities of people’s health in India today, and
examine some of the maladies of recent health
policies. Next the availability of various resources,
which could be utilised for an improved health care
system is discussed, finally followed by certain
recommendations to strengthen and reorient the
health system to ensure quality health care for
all. We hope these recommendations will be
Infant and Child mortality snuffs out the life
of 22 lakh children every year, and there has
Three completely avoidable child deaths
occur every minute. If the entire country were
been very little improvement in this situation
in recent years.'■ We are yet to achieve the
National Health Policy 1983 target to reduce
Infant Mortality Race to less than 60 per 1000
live births.-' More serious is the fact that the
rate of decline tn Infant Mortality, which was
significant in the 1970s and 80s, has slowed
down in the 1990s, (See graph below)
to achieve a better level of child health, for
example the child mortality levels of Kerala,1
then 18 lakh deaths of under-five children
could be avoided every year. The four major
killers (lower respiratory tract infection,
diarrheal diseases, perinatal causes and
vaccine preventable diseases) accounting for
over 60% of deaths under five years of age are
entirely preventable through better child health
care and supplemental feeding programs.-' The
most recent
estimate of complete
immunization coverage indicates that only
54% of all children under age three were fullyprotected.4
o
incorporated by political parties in their election
manifestos for the upcoming general election as
a demonstration of their commitment to public
health. Jan Swasthya Abhiyan, a national platform
working for people’s health, looks forward to such
a commitment from all political forces in the
countrv.
130,000 mothers die during childbirth every
year. The NHP 1983 target for 2000 was to
reduce Maternal Mortality Rate to less than 200
oer 100,000 live births. However, 407 mothers
die due to pregnancy related causes, for ever.'
100.000 live births even today.1 In fact, as per
the NFHS surveys in the last decade Maternal
Mortality Rate has increased from 424 maternal
deaths per 100.000 live births to 540 maternal
deaths per 100,000 live births.3
■ About 5 lakh people die from tuberculosis
every year18, and this number is almost
unchanged since Independence!19 20 lakh new
cases are added each year, to the burgeoning
number of TB patients presently estimated at
around 1.40 crore3 Indians !
•
India is experiencing a resurgence of various
communicable diseases including Malaria,
Encephalitis, Kala azar, Dengue and
Leptospirosis. The number of cases of Malaria
has remained at a high level of around 2
million cases annually since the mid eighties.
By the year 2001, the worrying fact has
emerged that nearly half of the cases are of
Falciparum malaria, which can cause the
deadly' cerebral malaria. The outbreak of
Dengue in India in 1996-97, saw 16,517 cases
1
such deaths might be prevented by tobacco
control measures2.
and claimed 545 lives3. Environmental and
social dislocations combined with weakening
public health systems have contributed to this
resurgence.
•
■
Diarrhea, dysentery, acute respiratory
infections and asthma continue to take their
toil because we are unable to improve
environmental health conditions. Around 6
every 5 minutes3!
lakh children die each year from an ordinary
illness like diarrhoea. While diarrhea itself
As a nation, today there is a need to look closely at
the deep problems in the health system, rather
than making exaggerated claims. There is a need
to recognize the growing health inequities, and
urgently implement basic changes in the health
system.
could be largely prevented by universal
provision of safe drinking water and sanitary
conditions, these deaths can be prevented by
timely administration of oral rehydration
solution, which is presently administered in
only 27% of cases3.
.
Estimates of mental health show about 10
million people suffering from serious mental
illness, 20-30 million having neuroses and 0.5
to 1 percent of all children having mental
retardation2. One Indian commits suicide
With political will and people’s involvement,
ensuring good quality health care for every Indian
is possible!
Cancer claims over 3 lakh lives per year and
tobacco related cancers contribute to 50% of
the overall cancer burden, which means that
The growing inequities in health and health care are unjust!
The Constitution of India guarantees the “Right to
Life’ to all citizens. However, the disparities relat
ing to survival and health, between the well off and
the poor, the urban residents and rural people, the
adivasis and dalits and others, and between men
and women are extremely glaring.
.
The Infant Mortality Rate in the poorest 20%
of the population is 2.5 times higher than that
in the richest 20% of the population. In other
words, an infant bom in a poor family is two
and half times more likely to die in infancy,
than an infant in a better off family3.
•
A child in the ‘Low standard of living' economic
group is almost four times more likely to die
in childhood than a child in the better off ‘High
standard of living' group. An Adivasi child is
one and half times more likely to die before
the fifth birthday than children of other groups3.
•
A girl is 1.5 times more likely to die before
reaching her fifth birthday, compared to a boy!
The female to male ratios for children are
rapidly declining, from 945 girls per 1000 boys
in 1991. to just 927 girls per 1000 boys in 200116.
This decline highlights an alarming trend of
discrimination against girl children, which
starts well before birth (in the form of sex
selective abortions), and continues into
childhood and adolescence (in the form of worse
treatment to girls)3L2
>
Dalit Women are one and a half times more
likely to suffer the consequences of chronic
malnutrition (stunted height) as compared to
women from other castes. Children below 3
years of age in scheduled tribes and scheduled
castes are twice as likely to be malnourished
than children in other groups.
a
A person from the poorest quintiie of the
population, despite more health problems, is
six times less likely to access hospitalization
than a person from the richest quintile. This
means that the poor are unable to afford and
access hospitalization in a very large proportion
of illness episodes, even when it is required.
•
The delivery of a mother, from the poorest
quintile of the population is over six times less
likely to be attended by a medically trained
person than the delivery of a well off mother,
from the richest quintile of the population. An
adivasi mother is half as likely to be deliuared
by a medically trained person3.
.
The ratio of hospital beds to population in rural
areas is fifteen times lower than that for urban
areas14.
•
The ratio of doctors to population in rural areas
is almost six times lower than the availability
of doctors for the urban population14.
•
Per person, Government spending on public
health is seven times lower in rural areas,
compared to Government health spending for
urban areas.
These health and health care inequities are
increasing, and are deeply unjust — a just health
system would ensure that all citizens, irrespective
of social background or gender, would get basic
quality health care in times of need.
Public health being w<eakened, people’s health being undermined
the most privatised in the world. Only five other
countries in the world are worse off than India
regarding public health spending (Burundi,
Myanmar, Pakistan, Sudan, Cambodia6). The
W.H.O. standard for expenditure on public health
is 5% of the GDP. The average spending today by
Less Developed Countries is 2.8 % of GDP, but India
presently spends only 0.9% of its GDP on public
health, which is merely one-third of the less
developed countries’ average6 !
The XDA Government has recently claimed that
one of its signal achievements has been the
allocation of 6% of GDP to Health care. In reality,
the government spends just 0.9 % of the GDP on
Health care and the rest is spent by people from
their own resources. Thus only 17% of all health
expenditure in this country is borne by the
government — this makes the Indian public health
system grossly inadequate to meet healthcare
demands of its people, and makes the health sector
The consequence of this dismally low allocation,
which stands at the lowest levels in the last two
decades, (in contrast to 1.3% of GDP achieved in
1985). is deteriorating quality of public health
services. For example, Primary health centers
(PHCs), meant to serve the needs of the poorest
and most marginalized people have the following
shocking statistics:
•
.
k
o
•
o
Only 38% of all PHCs have all the critical
staff
Only 31% have all the critical supplies
(defined as 60% of critical inputs), with only
Source: 7
3
3% of PHCs having 80% of all cntical inputs.
In spite of the high maternal mortality
ratio, 8 out of every 10 PHCs have no
Essential Obstetric Care drug kit!
Only 34% PHCs offer delivery services, while
only 3% offer Medical Termination of
Pregnancy!
A person accessing a community health
center would find no obstetrician in 7 out
of 10 centers, and no pediatrician in 8 out
of 10!
Private health, care and essential drugs are increasingly unaffordable !
The dominance of the private sector not only denies
access to poorer sections of society, but also skews
the balance towards urban biased, tertiary level
health services with profitability overriding equity.
and rationality of care often taking a back seat.
.
Irrational medical procedures are on the rise.
According to just one study in a community in
Chennai. 45% of all deliveries were performed
by Cesarean operations, whereas the WHO has
recommended that not more than 10-15% of
deliveries
would
require
Cesarean
operations17.
A growing proportion of Indians cannot afford
health care when they fall ill. National surveys
show that the number of people who could not
seek medical care because of lack of monev
increased significantly between 1986 and
1995:5. The proportion of such persons unable
Due to irrational prescribing, an average of
63 per cent of the money spent on prescriptions
is a waste. This means that nearly two-thirds
of the money that we spend on drugs may be
for unnecessary or irrational drugs-1!
to afford health care almost doubled.
increasing from 10 to 21 % in urban areas, and
growing from 15 to 24% in rural areas in this
decade15.
The pharmaceutical industry is rapidly
growing...yet only 20% of the population can
access all essential drugs that they require.
There is a proliferation of brand names with
over 70,000 brands marketed in India, but the
2002 Drug policy recommends that only 25
drugs be kept under price control13. As a result.
many drugs are being sold at 200 to 500 p^ent
profit margin, and essential drugs have bSrr.e
unaffordable for the majority of the Indian
population.
Forty percent of hospitalised people are forced
.
to borrow money or sell assets to cover
expenses15.
•
Over 2 crores of Indians are pushed below the
poverty line every year because of the
catastrophic effect of out of pocket spending on
health care-'"!
HeaTtfc policy developments: since the 1990s- have critically:
weakened! the: health; system
;
The effectiveness of the public health system and
access to quality health care, especially for the poor
has worsened since the decade of the 1990s. due
to a variety of policy developments, at both national
and state levels:
•
Stagnant public health budgets and
decreasing Government expenditure on
capital investment for public health
facilities.
•
introduction of user fees at various levels
of public health facilities.
•
Freezing of new recruitments and
inadequate budgets for supplies and
maintenance in the public health system.
•
Contracting out health services or
privatisation of health facilities.
•
Encouragement of growth of private
secondary and tertiary hospitals through
tax waivers, reduced import duties.
subsidized land etc. which have led to a
further expansion of the unregulated
orivate medical sector.
Promotion of ‘Health tourism’ for foreign
visitors, while basic health services remain
inaccessible for a large proportion of the
Indian population.
Conducting occasional, expensive and
largely ineffective ‘Health melas’ instead
of upgrading the public health system as a
sustainable solution.
Deregulation of the pharmace^cal
industry, lax price controls on drugs— the
list of drugs under price control being
proposed to be reduced to 25 drugs
(compared to 343 drugs under orice control
in 1979.)
Many bulk drug manufacturing units have
closed down due to liberalized import and
dumping as a result of the implementation
of the WTO agreement and autonomous
economic liberalization policies. Due to
reduction of customs duty and increase ot
excise duty, imported drugs will become
cheaper while local drugs will become more
expensive.
4
Indians need not accept poor health as their
inevitable fate! Many other developing countries.
’■vhich nave given a high priority to people’s health,
have achieved much better health outcomes
compared to India. As a country, we spend a higher
proportion or the GDP on health care compared to
these countries - but an overwhelming percentage
of this (83%) is private expenditure. As a result we
have a weak public health system with poor health
outcomes forcing families to spend a lot on private
medical care, which is expensive, and not always
appropriate, leaving us with ‘poor health at high
cost’! Here is how some other Asian countries are
doing in comparison with India...
Health Outcomes in Relation to Health Expenditures in some Asian countries10
Total Health
Expenditure
as % of GDP
L
Public Health
Expenditure
as % of total
Under 5
Mortality
Life Expectancy
Male
Female
India
5.2
17
95
59.6
61.2
Sri Lanka
3.0
45.4
19
65.8
73.4
Malaysia
2.4
57.6
14
67.6
69.9
Does India have tiie resources ta provide health care for all ?
As a country. Indians spend more on health care
than most other developing countries, but this is
mostly out-of-pocket spending. Health care
facilities have grown substantially, but these are
mostly in the private sector. The system is
producing more and more healthcare professionals.
but we lose them to the private sector, or to western
countries. To give some idea of the available health
care resources in India -
.
Compared to 11,174 hospitals in 1991 (57%
private), the number grew to 18.218 (75%
private) in 2000'7 In 2000. the country had
12.5 lakh doctors and 8 lakh nurses! At the
national level, there is one allopathic doctor
for every 1800 people, or one doctor from
systems including ISM and homeopathy for
SOO people. This means there are more
doctors than the required estimate of one
doctor for 1500 population-
•
Approximately 15.000 new graduate doctors
and 5.000 postgraduate doctors are produced
every year and one-fifth of them leave the
country for greener pastures-4.
o
We have an annual pharmaceutical
production of about 260 billion rupees--, and
we export a large proportion of these drugs
- Sadly, while our exports grow. 80% of our
people do not have access to all the drugs
they require.
In short, we have substantial health care
resources, but because of the privatised.
unregulated and inequitable nature of the health
care system, it is unable to ensure good quality
health care for a majority of citizens. Rather than
producing more doctors or setting up more private
hospitals, what we need is a reorganisation of the
health system, with substantial strengthening of
public health, greatly enhanced public expenditure.
regulation of the private medical sector and an
overall planned approach to make health care
resources available to all.
5
.What can be done as immediate steps ?
increased substantially, targeting the 5%
of GDP as public expenditure on health care
as recommended by the WHO.
. If the public health system fails to deliver
it should be treated as a legal offence.
remedy for which can be sought in the
courts of law. The public system must
ensure all elements of care like drug
prescriptions, diagnostic tests, child birth
services, hospitalization care etc. One way
to ensure this could be that in exceptional
situations, where patients who do not
receive these services from the public
facility they may be referred to seek them
from alternate facilities, which are
registered with the state agency. Such
registered and regulated facilities would
honour such referrals, for which the state
would reimburse them at a mutually agreed
rate. This would maintain pressure on the
public health system to provide all eleme^e
of care, and would ensure that the patiWt
is not deprived of essential care at time of
need.
o Various vulnerable and marginalised
sections of the population have special
health needs. There is a need for a range
of policy measures to eliminate
discrimination, and to provide special
quality' and sensitive services for women.
children, elderly persons, unorganised
sector workers, HIV-AIDS affected persons.
disabled persons, persons with mental
health problems and other vulnerable
groups. Similarly, situations of conflict.
displacement and migration need to be
addressed with a comprehensive approach
to ensure that the health rights of affected
people are protected. The People’s HetUfcb.
Charter deals with issues related to s'Wi
special sections of the population, and can
provide a basis for formulation of
appropriate policy initiatives, in
consultation
with
organisations
representing these social segments.
• Putting in place a National legislation to
regulate the private health sector, to adopt
minimum standards, accreditation.
standard treatment protocols, standardised
pricing of services etc.
. Adopting a rational and essential
medications-based drug policy. All States
must have an essential drugs and
consumables list and all the drugs and
consumables on this list must be under
price control. Further all state governments
must adopt procurement and distribution
The objective should be to make Health care a
Fundamental right and an operational
entitlement. This would require a National Public
Health Act, which mandates right to basic
healthcare services to all citizens through a
system of universal access to healthcare. The
Indian Constitution through its directive principles
provides the basis for the Right to health care, and
the Indian state has ratified the International
Covenant of Economic, Social and Cultural Rights
which makes it obligatory on its part to comply
with Article 12 that mandates right to healthcare.
Universal access to healthcare is well established
in a number of countries including not only
developed countries like Canada and United
Kingdom. but also developing countries such as
Cuba. Brazil. Costa Rica and Thailand. There is
no reason why this cannot be made a reality in
India. Hence we need to set in motion processes.
which will take us towards the goal of universal
access to health care, in a Rights-based framework
and with equity.
Some immediate steps related to the health care
system that need to be taken include:
Making healthcare a fundamental right by
suitable constitutional amendment. The
formulation of a National legislation
mandating the Right to Health care, with a
clearly defined comprehensive package of
health care, along with authorization of the
requisite budget, being made available
universally within one year.
■ Significant strengthening of the existing
public health system, especially in rural
areas, by assuring that all the required
infrastructure, staff, equipment, medicines
and other critical inputs are available, and
result in delivery of all required services.
These would be ensured based on clearly
defined, publicly displayed and monitored
norms.
• The declining trend of budgetary allocations
for public health needs to be reversed, and
budgets appropriately up-scaled to make
optimai provision of health care in the
public domain possible. At one level adopting
a fiscal policy of block funding or a system
of per capita allocation of resources to
different levels of health care, with an
emphasis on Primary Health Care will have
an immediate impact in reducing ruralurban inequities by making larger
resources available to rural health facilities
like Primary health centers and Rural
hospitals. Simultaneously, the budgetaryallocation to the heaith sector must be
.
6
policies similar to what has been done by
the Tamilnadu State Medical Services
Corporation and hence ensure that
essential drugs in the list are actually
available in every facility.
i he state should introduce a new
community-anchored health worker
scheme, and implement it in a phased
manner with involvement of people’s
organizations and panchayati raj
institutions, in both rural and urban areas,
through which first contact primary' care
and health education can be ensured.
Integration of medical education of all
systems to create a basic doctor ensuring
•
•
a wider outreach and improvement ot
access to health care services in all areas.
All state level coercive population control
policies, disincentives and orders should
be revoked. Disproportionate financial
allocation for population control activity
should not be allowed to skew funding from
other important public health priorities.
Integration of medical education of all.
systems to create a basic doctor ensuring
a wider outreach and improvement ot
access to health care services in all areas.
Effective regulation of the growth of
capitation based medical colleges.
Conclusion:
What is needed is a major restructuring and
strengthening of the health system. This involves
two major ingredients: popular mobilisation for
operationalising the Right to Health Care, and the
political will to implement policy changes
necessary to transform the health system. Jan
Swasthya Abhiyan is today involved in the former
task, by reaching out to people across the country.
enabling them to mobilise for their just health
rights. It calls upon political parties, which
recognise people's right to healthy lives, to address
the latter task, and to perform their historic duty
by establishing and operationalising the Right to
Health care as a Fundamental right.
The persistence of unacceptably large numbers of
avoidable deaths, resurgence of communicable
diseases, declining quality of public health services
and unaffordable, often inappropriate private
^edical care need not remain the lot of over a
Wilion ordinary Indians. Recent policy changes of
privatisation, declining public health budgets and
pro-drug industry measures need to be replaced by
strong public health initiatives, with the active
involvement of communities and civil society
organisations.
By and large. India today possesses the
humanpower, infrastructure, national financial
resources and appropriate health care know-how
to ensure quality health care for all its citizens.
This document focuses on the need for strengthening of the health care system, and certain immediate
steps required for this However, improvement of people's health requires equally importantly, provision
of other necessaiy facilities and conditions required for a healthy life, such as safe drinking water.
sanitation, food security, healthy housing, basic education and a safe environment. The People’s Health
Charter has dealt with these issues, and may be taken as a guideline tc develop effective policies and
improve people's living standard in order to achieve better health.
Published by CEHAT for JAN SWASTHYA ABHIYAN
7
Indian People’s Health Charter
> r?A /.■>■ •■
r^V. e - :cfr-
1 r. -;.
.
• -
■
■ ■
We the people of India, stand united in our condemnation of an iniquitous global system that, under the garb of
•Globalisation’ seeks to heap unprecedented misery and destitution on the overwhelming majority of the people on
this globe. This system has systematically ravaged the economies of poor nations in order to extract profits that
nurture a handful of powerful nations and corporations. The poor, across the globe, as well as the sections of poor
m the rich nations, are being further marginalised as they are displaced from home and hearth and alienated from
their sources of livelihood as a result of the forces unleashed by this system. Standing in firm opposition to such a
system we reaffirm our inalienable right to and demand for comprehensive health care that includes food security:
sustainable livelihood options including secure employment opportunities; access to housing, drinking water and
sanitation; and appropriate medical care for all; in sum - the right to Health For All, Now!
The promises made to us by the international community in the Alma Ata declaration have been systematically
repudiated by the World Bank, the IMF, the WTO and its'predecessors, the World Health Organization, and by a
government that functions under the dictates of International Finance Capital. The forces ‘Globalisation’ through
measures such as the structural adjustment programme are targeting our resources - built up with our labour.
sweat and lives over the last fifty years - and placing them in the service of the global “market' for extraction of
super-profits. The benefits of the public sector health care institutions, the public distribution system and other
infrastructure - such as they were - have been taken awav from us. It is the ultimate irony that we are now blamed
fcr our plight, with the argument that it is our numbers and our propensity to multiply that is responsible for our
poverty and deprivation. We declare health as a justiciable right and demand the provision of comprehensive health
care as a fundamental constitutional right of every one of us. We assert our right to take control of our health in our
own hands and for this the right to;
.
.
.
.
.
.
.
A truly decentralized system of local governance vested with adequate power and responsibilities, provided with
adequate finances and responsibility for local level planning.
A sustainable system of agriculture based on the principle of land to the tiller - both men and women - equitable
distribution of land and water, linked to a decentralized public distribution system that ensures that i^ine
goes hungry
universal access to education, adequate and safe drinking water, and housing and sanitation facilities
A dignified and sustainable livelihood
A clean and sustainable environment
A. drug industry geared to producing epidemiological essential drugs at affordable cost
A health care system which is gender sensitive and responsive to the people’s needs anc whose control is
vested in people’s hands and not based on market defined concept of health care.
Further, we declare our firm opposition to:
.
.
.
.
.
.
.
>
"
<
Agricultural policies attuned to the needs of the 'market’ that ignore disaggregated and equitaoie access to food
Destruction of our means to livelihood and appropriation, for private profit, of our natural resource bases and
appropriation of bio-diversity
The conversion of Health to the mere provision of medical facilities and care that are technology' intensive.
expensive, and accessible to a select few
The retreat, by the government, from the principle of providing free medical care, through reduction of public
sector expenditure on medical care and introduction of user fees in public sector medical institutions, that
place an unacceptable burden on the poor
The corporatization and commericializarion of medical care, state subsidies to the corporate sector in medical
care, and corporate sector health insurance
Coercive population control and promotion of hazardous contraceptive technology which are directed primarily
ar the poor and women
The use of patent regimes to steal our traditional knowledge and to put medical technology- and drugs Mtond
our reach
institutionalization of divisive and oppressive forces in society, such as communalism, caste, patriarchy, and
me attendant violence, yvhich have destroyed our peace and fragmented our solidarity.
.-. the light of the above we demand that:
1
The concept of comprehensive primary' health care, as envisioned in the Alma Ata Declaration should form the
fundamental basis for formulation of all policies related to health care. The trend towards fragmentation of
health delivery- programmes through conduct of a number of vertical programmes should be reversed. National
health programmes be integrated within the Primary- Health Care system with decentralized manning, decision
making and implementation with the active participation of the community. Focus be shifted from bio-medicai
and individual based measures to social, ecological and community based measures.
The primary health care institutions including trained village health workers, sub-centers, and the PHCs staffed
by doctors and the entire range of community health functionaries including the ICDS yvorkers. be placed under
me direct administrative and financial control of the relevant level Panchayati Raj institutions. The overall
infrastructure of the primary health care institutions be under the control of Panchayats and Gram Sabhas and
provision of free and accessible secondary and tertiary level care be under the control of Zilia Panshads, to be
accessed primarily through referrals from PHCs.
The essential components of primary' care should be:
. Village level health care based on Village Health Workers selected by the community and supported by
the Gram Sabha / Panchayat and the Government health services yvhich are given regulatory powers
and adequate resource support
S
•
•
•
•
o.
Primary Health Centers and sub-centers with adequate staff and supplies which provides quality curative
services at the primary health center level itself with good support from referral linkages
A comprehensive structure for Primary Health Care in urban areas based on urban PHCs, hqalth posts
and Community Health Workers under the control of local self government such as ward committees
and municipalities.
Enhanced content of Primary Health Care to include all measures which can be provided at the PHC
level even for less common or non-communicable diseases (e.g. epilepsy, hypertension, arthritis, preeciampsia. skin diseases) and integrated relevant epidemiological and preventive measures
Surveillance centers at block level to monitor rhe local epidemiological situation and tertiary care with
ail speciality services, available in every district.
A comprehensive medical care programme financed by the government to the extent of at least 5% of our GNP,
o: wnich at least half be disbursed to panchayau raj institutions to finance primary level care. This be accompanied
oy transfer of responsibilities to PRIs to run major parts of such a programme, along with measures to enhance
capacities of PRIs to undertake the tasks involved.
the policy of gradual privatisation of government medical institutions, through mechanisms such as introduction
oi user fees even for the poor, allowing private practice by Government Doctors, giving out PHCs on contract,
etc. be abandoned forthwith. Failure to provide appropriate medical care to a citizen by public health care
institutions be made punishable by law.
o.
.-. comprehensive need-based human-power plan for the health sector be formulated that addresses the requirement
:or creation of a much larger pool of paramedical functionaries and basic doctors, in place of the present trend
towards over-production of personnel trained in super-specialities. Major portions of undergraduate medical
ecucation. nursing as well as other paramedical training be imparted in district level medical care institutions,
as a necessary complement to training provided in medical/nursing colleges and other training insututions. No
more new medical colleges to be opened in the pnvate sector. No commodification of medical education. Steps
to eliminate illegal pnvate tuition by teachers in medical colleges. At least a year of compulsory rural posting for
undergraduate imedical, nursing and paramedical) education be made mandatory, without which license to
practice not be issued. Similarly, three years of rural posting after post graduation be made compulsory.
6.
Ti'.e unbridled and unchecked growth of the commercial pnvate sector be brought to a halt. Stnct observance of
standard guiaeiines for medical and surgical intervention and use of diagnostics, standard fee structure, and
periodic prescnption audit to be made obligatory. Legal and social mechanisms be set up to ensure observance
of minimum standards by ail pnvate hospitals, nursing/matemity homes and medical laboratones. Prevalent
practice oi offering commissions for referral to be made punishable by law. For this purpose a body with statutory
powers be constituted, which has due representation from peoples organisations and professional organisations.
7
A rational drug policy be formulated that ensures development and growth of a self-reliant industry for production
of ail essential drugs at affordable prices and of proper quality. The policy should, on a. priority basis:
.
.
.
.
.
.
.
.
8
•ij
Ban ail irrational and hazardous drugs. Set up effective mechanisms to control the introduction of new
drugs and formulations as well as periodic review of currently approved drugs.
Introduce production quotas & price ceiling for essential drugs
Promote compulsory use of generic names
Regulate advertisements, promotion and marketing of all medications based on ethical cntena
Formulate guidelines for use of old and new vaccines
Control the activities of the multinational sector and restrict their presence only to areas where they
are willing to bnng in new technology
Recommend repeal of the new patent act and bnng back mechanisms that prevent creauon of monopolies
and promote introduction of new drugs at affordable pnces
Promotion of the public sector in production of drugs and medical supplies, moving towards complete
self-reliance in these areas.
Medical Research prionties be based on morbidity and mortality profile of the country, and details regarding the
direction, intent and focus of all research programmes be made entirely transparent. Adequate government
funding be provided for such programmes. Ethical guidelines for research involving human subjects be drawn up
and implemented after an open public debate. No further experimentation, involving human subjects, be allowed
without a proper and legally tenable informed consent and appropriate legal protection. Failure to do so to be
cunisnabie by .aw. All unethical research, especially in the area of contraceptive research, be stooped forthwith.
men ianc mem who. without their consent and knowledge, have been subjected to experimentation, especially
wit.n nazarcous contraceptive technologies to be traced forthwith and appropriately compensated. Exemplary
carnages to oe awarded against the institutions (public and pnvate sector) involved in such anti-people, unethical
una illegal oractices in the past.
All . aercive measures including incentives and disincentives for limiting family size be abolished. The right of
famines anc women within families in determining the numoer of children they want should be recognized.
Concurrently. access to safe and affordable contraceptive measures be ensured which provides people, especially
me:'., the ..miity to make an informed choice. All long-term, invasive, systemic hazardous contraceptive
• c.-:inogies such as the mjectables (NET-EN, Depo-Provera. etc.), sub-dermal implants iNorplanti and'anti
■.
.tv -.accmes shouid be banned from both the public and private sector. Urgent measure be initiated to shift
• . tins of contraception away from women and ensure at least equal emphasis on men's responsibility for
■n:.-.:ception. Facilities for safe abortions be provided nght from the primary health center level.
'..court be crovided to traditional healing systems, including, local and home-based healing traditions, for
svsiematic research .and community based evaluation with a view to developing the knowledge base and use of
■ -,ese svstems Mong with modern medicine as part of a holistic healing perspective.
9
11.
Promotion of transparency and decentralization in the decision making process, related to health care, at all
levels as well as adherence to the pnnciple of right to information. Changes in health policies to be made only
after mandatory' wider scientific public debate.
*
12.
Introduction of ecological and social measures to check resurgence of communicable diseases. Such measures
should include:
.
.
.
Integration of health impact assessment into all development projects
Decentralized and effective surveillance and compulsorv notification of prevalent diseases like malaria,
TB by all health care providers, including private practitioners
Reonentation of measures to check STDs,/AIDS through universal sex education, promoting responsible
safe sex practices, questioning forced disruption and displacement and the culture of commodification
of sex. generating public awareness to remove stigma and universal availability of preventive and curative
services, and special attention to empowering women and availability of gender sensitive services in
this regard.
13.
Facilities for early detection and treatment of non-communicable diseases like diabetes, cancers, heart diseases,
etc. to be available to all at appropnate levels of medical care.
14.
Women-centered health initiatives that include:
.
.
.
•
15.
Child centered health initiatives that include:
.
.
•
.
16.
Awareness generation for social change on issues of gender and health, triple work burden, gender
discrimination tn upbringing and life conditions within and outside the family, preventive and curative
measures to deal with nealth consequences of women's work and violence against women
Complete maternity benefits and child care facilities to be provided in all occupations employing women,
be they in the organized or unorganized sector
Special support structures that focus on single, deserted, widowed women and minority women which
will include religious, ethnic and women with a different sexual orientation and commercial sex workers;
gender sensitive services to deal with all the health problems of women including reproductive health,
maternal health, abortion, and infertility
Vigorous public campaign accompanied by legal and administrative action against sex selective a'oo^Bns
including female feticide, infanticide and sex pre-selection.
A comprehensive child rights code, adequate budgetary allocation for universalisation of child care
services
An expanded & revitalized 1CDS programme. Ensuring adequate support to working women to facilitate
child care, especially oreast feeding
Comorehensive measures to prevent child abuse, sexual abuse and child prostitution
Educational, economic and legal measures to eradicate child labour, accompanied by measures to ensure
free and compulsory quality elementary education for all children.
Special measures relating to occupational and environmental health which focus on:
.
•
•
.
Banning of hazardous technologies in industry and agriculture
Worker centered monitoring of working conditions with the onus of ensuring a safe and secure workplace
on the management
Reorienting medical services for early detecuon of occupational disease
Special measures to reduce the likelihood of accidents and injuries in different settings, such as traffic
accidents, industrial accidents, agricultural injuries, etc.
17.
The approacn to mental health problems should take into account the social structure in India which makes
certain sections like women more vulnerable to mental health problems. Mental Health Measures that procure
a shift away from a bio-medical model towards a holistic model of mental health. Community support 8s ccmm^Jty
based management of mental health problems be promoted. Services for early detection os integrated management
of mental health problems be integrated with Primary Health Care and the rights of the mentally ill and the
mentally challenged persons to be sale guarded.
18.
Measures to promote the health of the elderly by ensuring economic security, opportunities for appropnate
employment, sensitive health care facilities and, when necessary, shelter for the elderiv. Services that cater to
the special needs of people in transit, the homeless, migratory workers and temporary settlement dwellers.
19.
Measures to promote the health of physically and mentally disadvantaged by focussing on the abilities rather
than deficiencies. Promotion of measures to integrate them in the community with special support rather than
segregating them; ensuring equitable opportunities for education, employment and special health care including
rehabilitative measures.
20.
Effective restriction on industries that promote addictions and an unhealthy lifestyle, like tobacco, alcohol, pan
masala etc., starting with an immediate ban on advertising, sponsorship and sale of their products to the
young, and provision of services for de-addiction
10
Constituents/of theJADFSWASTHYAABHIYAN
Fhe uan Swasthya Abhiyan at the national level is the coalition of the networks of voluntary organizations
and peoples movements involved in healthcare deliver.- and health policy, who made themselves a part of
ihe Peoples Health Assembly campaign in India in the year 2000, and have continued to participate in this
process. These national networks have numerous constituent organisations, which implies that a tew
hundred organizations are involved directly in the national process. Beyond these networks, several hundred
other organizations have been involved at state, district and block level activities across the country. The
networks that constitute the National Coordination Committee of Jan Swasthya Abhiyan are:
-•
3.
-.
=•
o.
S.
9.
10.
11.
12.
13.
I-.
15.
16.
17
IS.
19.
20.
21.
All India Peoples Science Network
All India Democratic Women’s Association
All India Drug Action Network
Asian Community Health Action Network
Bharat Gyan Vigyan Samiti
Catholic Health Association of India (CHAI)
Chrisuan Medical Association of India (CMAI)
Federation of Medical Representatives and Sales Associations of India (FMRAI)
Forum for Creche and Child Care Services (FORCES)
Joint Women’s Programme
Medico Friends Circle (MFC)
National .Alliance of People's Movements (NAPM)
National Alliance of Women’s Organisations (NAWO)
National Federation of Indian Women (NFIW)
Ramakrishna Mission
Voluntary Health Association of India (VHAI)
Association for Indian Development, India (AID-India)
Breastfeeding Promotion Network of India (BFPNI) National Resource Groups:
Centre for Ena.uiry into Health and Allied Themes (CEHAT)
Centre for Social xMedicine and Community' Health, Jawaharlal Nehru University
Community Health Cell (CHC)
ihe representatives of ail the above organisations constitute the National Coordination Committee of JSA.
which is the national decision making body of the coalition. N.H. Antia is the Chairperson and D. Banerjee
bs the Vice-Chairperson of JSA. National organisers of JSA include B. Ekbal as Convenor, Abhay Shukia.
Amit Sengupta, Amitava Guha, Thelma Narayan and T. Sundararaman as Joint convenors, with Vanaana
Prasad and N.B.Sarojini as National secretariat members.
Jan Swasthya Abhiyan presently has state units or contacts in the following states:
Andhra Pradesh, Assam, Bihar, Chhattisgarh, Delhi, Gujarat, Haryana, Himachal Pradesh,
Jharkhand, Karnataka, Kerala, Madhya Pradesh, Maharashtra, Orissa, Rajasthan, Tamil
Nadu. Tripura, Uttar Pradesh, West Bengal.
11
B. Ekbal,
National Convenor, JSA
Abhay Shukla
National Secretariat, JSA
Amit Sen Gupta
Jt. Convenor, JSA
Ph: 0471-2306634(0)
e. 2, j. ekbaLh~vsnI.com
Ph: 020-25451413 / 25452325
e-mail cehatounf2vsnl.com
Ph: 011-26862716/ 26524324
e-mail: ctddsEtZvsnl.com
Amitava Guha
Jt. Convenor, JSA
Thelma Narayan
Jt. Convenor, JSA
T. Sundararaman
Jt. Convenor, JSA
Ph: 033-24242862(0)
e-mail:
guhaamitava 2hotmail.com
Ph:080-5505924 / 5525372
e.mai]: socharaftZvsnl.com
Phone: 0771-2236104. 2236175
e-mail:
sunaar'2@ 123india.com
Sarojini
Member, National Secretariat
Vandana Prasad
Member, National Secretariat
Ph: 011-26968972 / 26850074
e-maii: samasaro@vsnl.com
Phone: 0120-2536578
e-mail: chaukhat@vahoo.com
SRS Bulletin. Government of India.1998
Planning Commission. Government of India. Tenth Five Year Plan 2002-2007. Volume II.
international Institute for Population Sciences and ORC Macro. National Family Health Surrey (NFHSII) 1998-99. India.
- International Institute for Population Sciences. RCH-RHS India 1998-1999.
5. National Crime Records Bureau. Ministry of Home Affairs. Accidental Deaths and Suicides In India
2000.
6. World Health Organization. The World Health Report 2003.
7 International Institute for Population Sciences. Facility Survey. 1999.
8. Misra. Chatterjee, Rao. India Health Report.Oxford University Press. New Delhi.2003
9. Morbidity and Treatment of Ailments. NSS Fifty' second round. Government of India. 1998.
10. Changing the Indian Heaith System - Draft Report, ICRIER. 2001
11. Shanff Abusaleh. India Human Development Report.Oxford University Press New Delhi.
12. Duggal.Ravi. Operationalizing Right to Healthcare in India. Right to Healthcare, Moving from Idea to
Reality.
CEHAT Mumbai.2003.
13. National Coordination Committee for the Jana Swasthya Sabha. Health for All NOW. 2004.
14. Central Bureau of Health Intelligence.Directorate General of Health Services. Ministry/ of Health and
Family Welfare. Health Information of India 2000 &2001.
15. National Sample Survey Organization. Department of Statistics.GOI.42nd and 52nd Round.
16. Census of India 2001: Provisional Population Totals.Registrar General and Census Commissioner GOI.
17. Pai M et al. A high rate of Cesaerean sections in affluent section of Chennai, is it a cause for concern?
Nat Med J India. 1999.12:156-158.
18. TB India 2003. RNTCP Stats Report.Central TB Division.DDHS GOI.
19. Heaith Survey and Development Committee. GOI 1946 (Bhore Report)
20 Mahal A www-woridbank.org
21. Phadke A. Drug Supply and Use. Towards a Rational Policy in India. Sage Publications New Delhi.
22. Ministry of Chemicals and Fertilizers.
1.
2.
3.
12
PROPOSAL FOR HEALTH CENTRES & MATERNITY HOSPITALS UNDER
LP.P.-VIII BANGALORE EXTENDING THE PROJECT TO 11 CITIES OF
KARNATAKA STATE.
A.
INTRODUCTION
The proposed Project is an extension of India Population Project-VEH, Bangalore,
to other Cities of Karnataka State. IPP-VIU is an IDA assisted Project. It provides IDA
with the opportunity to extend rapid but targeted assistance to the most vulnerable groups
through an agency which is already implementing the Project satisfactorily.
The special features of the Project are that:
a)
To assist the Govt, of India (GOI) in expanding the coverage of Family
Welfare (FW) and Reproductive and Child Health (RCH) services to
previously unserved urban slums.
b)
To act as a vehicle to improve the quality of services to be delivered to the
urban poor.
c)
Increase the demand for family welfare services by substantially
improving the participation of Private Voluntary Organisations and
Communities in the design, delivery and supervision of family welfare
services to be delivered to the slum communities by IEQ activities.
d)
Institute Innovative Scheme, under which investments in Female
Education and Vocation training, nutrition, awareness, environmental
sanitation through community participation, would be supported.
e)
In all 11 Cities, Health Centres are proposed on the basis of one Health
Centre for 50,000 population. Out of the 50,000 population around 20-30
thousand are expected to utilise the Health Centres facilities. In the case
of Hubli-Dharwad and Bhadravathi, the number of Health Centres
proposed is on the basis of one Health Centre for 40 thousand populations.
This is because the population is scattered and will not avail the health
facility if the distance is more than 3-5 K.M. from their residence.
,
..2..
g
GOALS AND OBJECTIVES
The goals set for various indicators under the National Health & Family Welfare
Programmes for the year 2000 to be attained in the Project Area are follows:
1.
Infant Mortality Rate
<60
2.
Perinatal Mortality Rate
<30-35
3.
Pre-school child mortality (1-5 years)
< 10
4.
Maternal Mortality Rate
<2
5.
Crude Birth Rate
<21
6.
Crude Death Rate
<9
7.
Effective Couple Protection Rate<%)
>60
8.
Pregnant Mothers receiving Antenatal Care 100%
9.
Immunisation Status (%)
a) TT for pregnant women
b) TT for school children
c) DPT (children 3 years)
d) Polio (infants)
e) BCG (infants)
100
100
85
85
85
Institutional deliveries (%)
95
10.
As per the National Health Policy, the services would be taken nearer to the door
steps of the people ensuring full participation of the community in the process of Health
Development.
..3..
The specific objectives of the project are to:
a) Improve maternal and child health, and
b) Reduce the fertility among the urban poor.
These objectives would be achieved by undertaking activities in five broad areas:
a)
Expanding service delivery to slum populations through improvements in
outreach services using volunteer female health workers selected from slum
communities, and upgrading of existing and construction of new health
facilities.
b)
Improving the quality of family welfare services provided to slum
populations, by upgrading the supervisory, managerial, technical and inter
personal skills at all levels of new and existing medical and para-medical
workers through pre-service, institutional in-service and on-the-job-recurrent
training; and increasing the availability of drugs, medicines and other
appropriate health supplies.
c)
Increasing the demand for family welfare services
through an expanded
programme of information, education and communication (DEC); increased
participation of the slum community through their representatives and groups
in the preparation and implementation of various project.
..4..
activities and the increased participation of Private Voluntary Organisations
and Private Medical Practitioners in the delivery of family welfare services to
slum communities.
d)
Strengthening the management and administration
of municipal Health
Departments through appropriate upgrading of Management Information
Systems (MIS), EEC, training, civil works, and audit and accounting functions,
as well as integrating and/or strengthening co-ordination of health services with
the provision of environmental sanitation and water supply services.
e)
Supporting Innovative Schemes which cover a range of additional services
including supplementary nutrition, creche programs, environmental sanitation
drives, education jind skill training programme for females, especially
adolescent girls, Non - Formal School and RCH interventions.
C.
Services to be delivered
Promotive and preventive health services specifically family welfare and maternal
and child care services would be delivered to the urban poor through a network of Health
Centres / Referral Health Centres of the Municipal Corporation.
..5..
The services planned to be provided by the Maternity Hospitals and Health Centres are listed
below:
Health Centre
Maternity Hospital
Health & Nutrition Education
Yes
No
Knowledge of vaccine
preventable diseases &
diarrhoea
Yes
No
Family Planning
Yes
Yes
Antenatal Care
Yes
Yes
Normal Deliveries
No
Yes
High Risk Deliveries
No
Post Natal Care
Yes
Yes
Immunisation of Mother & Child
Yes
Yes
Nutritional Care of children
upto the age of five
Yes
No
Medical check-up and followUp of school-going children
Yes
No
Treatment for minor ailments
Yes
Yes
Nor surgical care for children
needing specialist attention
No
Yes
Minor gynaecological procedures
No
Yes
Laboratory Tests: Basic
No
Yes
Service.
Promotive
Health Care
refered to major hospitals
..6..
Family Planning
Counselling and advice on appropriate
method
Yes
Yes
Supply of Condom/Oral Pill
Initial
Subsequent
Yes
Yes
Yes
Yes
Check up & insertion of IUD
Yes
Yes
Sterilization
No
Yes
M.T.P
Yes
Yes
Domicilliary follow-up of
Acceptors
Yes
No
The Health Centre will refer to the Maternity Homes pregnancies and cases
requiring gynaecological procedures, sterilization and M.T.P and attention by
Paediatrician.
The Maternity Hospital, in tum, will direct cases with major complications
requiring surgical intervention such as Caesarean Section, children with congenital
abnormalities to appropriate hospitals.
New Health Centres and renovation of existing centres is also part of the proposed
project. Actions will be initiated after rapid low cost base line survey by consultants.
D.
The Outreach Programme.
The Outreach Programme will be operated by each Health Centre with three
ANMs and ten Link Workers. The Link Workers will be selected from the slum dwellers
and will report to ANMs. They will be given requisite training by the specifically trained
Officer under I.P.P. - VIII. They will be paid a monthly honorarium of Rs.500/-.
..7..
The job responsibilities of the outreach workers are:
LHV
ANMS
Link Workers
1.
Detection of Antenatal cases
Yes
Yes
Yes
2.
Regn. of Antenatal cases
Yes
Yes
No
3.
Antenatal Care & Post Natal Care
Yes
Yes
Yes
4.
Immunization
Yes
Yes
No
5.
First aid services for mothers
and children
Yes
Yes
No
6.
Health Education
Yes
Yes
Yes
7.
Nutrition Education
Yes
Yes
Yes
8.
Motivation of cases for FP
Yes
Yes
Yes
9.
Depot Holders for Condoms,
Oral Pills and ORS Packets
Yes
Yes
Yes
10.
Supervision & Training of
Link Workers
Yes
Yes
11.
Referral to next level
H.C.
H.C.
ANM
12.
I.E.C. activity
Yes
Yes
Yes
The'outreach programme will provide different MCH & FW services according to
predetermined schedule at places in/or close to slums such as anganwadis, community
hails or other places owned by the Corporation/CMC.
The additional recurrent cost of the outreach programme is to be estimated.
..8..
E.
STAFF PROPOSED FOR A HEALTH CENTRE
1)
2)
3)
4)
F.
Lady Medical Officer
Lady Health Visitor
Auxiliary Nurse Midwife
Link Workers
-
1
1
3
10
JOB FUNCTIONS OF FIELD STAFF
The field staff will conduct Eligible Couple Survey in their allotted population.
The L.H.V. will have a population of 5000 in addition to supervision of the work of
A.N.M.s and Link Workers. Each A.N.M. will have a populatioon of 15,000. Each
Link worker will cater to a population of 5000.
They will prioritize the Eligible Couples according to the parity and age for F.W
Coverage.
They will register 100% Ante natal cases preferably in the first trimester.
They will ensure 100% immunisation of all pregnant, mothers and infants in
their juridiction
They will assist the Anemia Control Programme through distribution of FS
Adult and Children tablets.
They will ensure small and healthy family by acceptance of O.P.CC, IUD and
sterlization in their area.
They will conduct outreach programmes such as Antenatal immunization clinics,
awamess programmes, well baby show, clean hut competition. Health Check up Camps
in the slums.
They will identify innovative schcmes( to be conducted through NGOs), like
Creches Non Formal School, Vocational Training, Male Participation in H & FW
Programme.
The Health Centre Staff will identify and select Link workersf Selection Criteria
enclosed Annexure) They will conduct the relevant I.E.C. activities to create demand for
the FW & MCH programmes.
JOB FUNCTIONS OF THE LMO
She will be the overall responsible for effective implementation of FW & MCH,
RCH activities etc in the jurisdiction of the Health Centre to achieve the goals and
objectives. She will submit the periodical reports as per the norms.
G.
H.
EQUIPMENT /FURNITURE /DRUGS/ CONSUMABLES
Procurement of necessary modem equipments and replacement of unserviceable
equipments is proposed for all New Health Centres and existing U.F.W.C.s. Similarly
furniture will also be provided for New Health Centre and existing U.F.W.Cs. Drugs
and consumables is also to be provided for all New Health Centres. Partial support of
drugs will be provided for the existing U.F.W.Cs. (Details are given in Annexure)
H.
CIVIL WORKS
New Health Centre construction is proposed in all the 11 cities. The centres will
be located as close 'as possible to the slums . Building Plans approved for IPP-VIII
Bangalore will be utilised for the cities where Maternity Homes / Health Centres is
proposed. The tenders for all works will be advertised in National newspapers (NCB)
by EPP-VUI Office Bangalore. Thereafter evaluation will be done at the project office in
Bangalore, by for technical and financial bids.
One representative from each City will be a member of the evaluation committee,
where the lowest evaluated responsive bidder will be awarded the work order from the
Central Project Office IPP-VIII Bangalore. Supervision of work will be done by the
Engineering Department of the beneficiary City. Payment of bills will be made by
Project Co-ordinator IPP-VIII Bangalore after receipt of bills duly certified by concerned
CMCs & Corporation Commissioner. M/s. TOR Steel Research Foundation India who
are already appointed for quality control will be authorised to function as consultant for
quality control at five stages of civil construction for the beneficiary cities. Health Centre
Type design A,B & C, and type design for 12 bed maternity home is shown in annexure
will be utilised based on the availability of sites/area.
J.
TRAINING
All Medical, Paramedical Staff of Maternity Homes/ U.F.W.C.s/Health Centre., are to be
trained in the aims and objectives of I.P.P. - VIII also the implementation of programme.
The training will be taken up by the IPP-VIII Training Centre at Kodandaramapura,
Bangalore. For training Link Workers, each city will identity three persons (trainers)
who will be trained at Bangalore. Thereafter for Link Workers, training will be done at
the city level by these trained trainers.
The areas in which training is to be provided are:
1.
Management Development, Planning, Programming.
2.
NGO participation strategies.
..10..
3.
Monitoring & Supervision
4.
Communication, Motivation, and providing quality care.
5.
Clinical Update
6.
Health Care & FW Update
7.
Promotive and preventive Health Care & Family Welfare.
8.
Re-orientation practical training for Laboratory Technicians
9.
Maintenance of Stock Records & Collection & submission of periodical
reports.
10.
Orientation on Extension Approach, field training.
11.
Male Participation.
12.
Training Methodology
The training centre will be utilised for the training programmes. The cost of
training will be met out of the budget allocated to individual cities.
K.
I.E.C.
One community development officer is proposed for each city to co-ordinate,
I.
E.C.
and Women Development activities. Materials already produced by the IPP-VUI
Bangalore will be made available to all the cities. Budgetary provision is made to prepare
EEC materials according to local needs if necessary.
Materials already produced by the EPP-VIII, Bangalore will be made available to
all the cities as per budget provision made in proposal.
..II..
1,.
Innovative Schemes
The beneficary cities will identify the programmes to be taken up like Creches,
NFS, Vocational Training, Male Participation in F.W. programmes etc. The collabration
will various NGO's will be worked by the individual cities. The budget any allocation
for NGO's will be made based on the approval of the Project Implementation Committee
to the beneficiary cities. Selection Criteria for NGOs is given in the Annexure.
M.
MIES
Monthly Reporting Formats designed for IPP-VIII, Bangalore will be followed by
the beneficary cities. The compiled reports have to be sent to the IPP-VIII, Bangalore for
onward submission to GOK, GOI and World Bank authorities. Rapid low cost base line
surveys will be taken up for each city to enable planning, monitoring & evaluation of the
Project-End line survey will be conducted at the end of the project period.
N.
Community Participation:
The health personnel of the respective Corporation, Private Voluntary
Organisations and representatives from the slums would be involved in the decision
making process planning and co-ordination of programmes, and effective implementation
through a series of work shops.
"Social, Health & Environmental" Clubs "SHE" Clubs at the individual slum
level will be formed. These SHE Clubs at the gross root level form the nucleus for
effective community participation and are critical for the success of the Project.
Annexure .... Guide lines.
The LMO will promote the formation of SHE Club in each of the slums under the
jurisdiction of the health Centre. The families residing in the slums will be enrolled as
member of the SHE Club by collecting a monthly subscription of Rs. 5/- per family.
(optional)
It shall be registered and the Management Committee will have atleast three
women members out of 5.
..12..
The members of the Committee will elect a Chairman from one among them.
The Functions of SHE Club may be as follows:
a)
b)
c)
d)
e)
f)
g)
h)
i)
Create awareness of environmental hygiene.
Chalk out hygiene and sanitation programme for the slum.
Create awareness of MCH and FW programmes.
Prepare a plan of activites for the health centre based on priority of the
inhabitants.
Co-ordinate with health centre to ensure availability of services.
Discourage child marriages and early motherhood.
Organise non-formal education for girls not in school.
Ensure availability of free medical aid to the needy, and
Manage the funds of the Club for the benefit of the Community for any of
the activites mentioned above.
The subscriptions and grants received will be banked in the name of the Club and
jointly operated by the Chairperson and LMO.
O•
Involvement of Private Medical Practitioners who are practising in and
around shim.
The Private Medical Practitioners would be involved in:
a)
Motivating for Family Planning, MCH activity also male participation.
b)
Immunising children and pregnant women.
c)
Providing patient care and emergency services on payment basis.
d)
Referring to hospital for specialized care.
e)
Helping in effective service utilisation.
The list of PMPs volunteering to participate in the programme will be made for
each Health Centre. The Health Centre will involve the PMPs attached to it by supplying
the following items free of cost:
..13..
a)
b)
c)
d)
e)
Vaccines and cold chain equipment for immunization.
IUD, Oral Pills and Condoms for insertion/distribution to acceptor.
Tetanus toxiod, Iron and Folic acid tablet for ANC & PNC.
ORS packets for treatment of dehydration and
Promotion literature for display and distribution.
MATERNITY HOSPITALS:
In Mysore, Gulbarga, Davangere, Bellary, Raichur & Shimoga, 12 bed maternity
Homes are planned. The type design approved by World Bank for IPP-VIII Bangalore
will be utilised. The procedure adopted for awarding contract will be similar to that
adopted for health centres.
The following staff are proposed for each maternity home.
1)
2)
3)
4)
5)
6)
Lady Medical Officer
Staff nurses
Peons
Ayahs cum Sweeper
Lab Technician
Driver
-
1
3
3
3
1
1
One ambulance is proposed for each maternity home. To provide essential
obstetric care round the clock staff quarters for LMO proposed.
REFERRAL:
The referral facilities have been built into the health care delivery system that is
planned for all the cities. The link worker will refer cases to the ANM who in tum refers
to the health centres. The health centres will refer antenatal for investigations, deliveries.
sterlisations etc., to the maternity homes or district hospital as the case may be. The
maternity home will refer cases to government major institution for any obstetric
emergency or specialised Obstetric care. Each maternity home is provided with an
ambulance for referral purpose and drivers quarters is proposed for each maternity
hospital.
MANAGEMENT:
The Project Office IPP-VIII Bangalore will be the nodal office for implement
ation of Extended EPP-VEH Project for 11 Cities of Karnataka.
The Project Co-ordinator LPP-VIII will be the ex-officio Nodal Officer will be
the member secretary for Project Implementation Committee for Extended IPP-VIII
Cities of Karnataka.
..14..
IPP-VIII Project Office level one Executive Engineer, one Assistant Executive
Engineer, one clerical staff, one Accounts Superintendent and one clerk for Accounts
Department will be appointed exclusively for Extended Cities Project. Each city will be
engaging one Accounts Superintendent and one clerk. One Community Development
Officer with MSW qualification will be appointed on contract basis till the end of Project
period. For each city the Municipal Commissioner/ Health Officer will be designated as
the Project Officer. He will be overall responsible for civil works & service delivery.
Committees to he constituted under the IPP-VIII , Extended Project
I.
State Level Project Advisory and co-ordination committee.
The existing SLPA & CC will continue in the extended Project of
IPP-VIII with the addition of the commissioners of the beneficiary cities
as members. Secretary to Govt. Health & FW will be the member
secretary of the committee.
II.
Extended Project Implementation Committee headed by the Health
Secretary-1, with the Project Co-ordinator, IPP-VIII as member secretary
and the Commissioners, Chief Engineers and Health Officers of the
beneficiary cities as members will be constituted.
Please sec the
JSIG.for details.
15..
COMMITTEES CONSTITUTED FOR MONITORING IPP-VIII PROJECT ACTIVITIES
Existing Committees
I. -
Proposed Inclusions
STATE LEVEL PROJECT ADVISORY GO ORDINATION
COMMITTEE. (EMPOWERED COMMITTEE)
1)
Chief Secretary to GOK
Chairman
2)
Secretary to Govt.
Finance Dept.
Member
3)
Secretary to Govt.
Health & FW Dept.
Member - Secretary
4)
Secretary to Govt.
Urban Devpt. Dept.
Member
5)
Secretary to Govt.
Planning Dept.
Member
6)
Jt. Secretary to GOI
Ministry of Health & FW
Member
7)
Project Administrator &
Addl. Secy to Govt.
Karnataka health Systems
Devpt. Project.
Member
8)
Project Co-ordinator IPP-VIII. .
Bangalore
Member
1) Commissioner of
Corporations, CMC
of Beneficiary Cities.
..16..
v II.
Existing Committees
Proposed Inclusions
Project Implementation
Committee (P.I.C.)
1) Commissioners of
Corporations of
Beneficiary Cities.
1)
Health Secretary,
Government of Karnataka.
2)
Dy. Secretary to Govt.
Urban Devpt. Dept.
3)
Health Officer, Benefeciary
Cities
Member
Chief Engineer, Bencficary
Cities
Member
4) •
Chairman
2) Health Officers of
Municipal Corpus.
of the Beneficiary
Cities.
Urban Devpt. Dept.
6)
Secretary,
Karnataka Slum Clearance
Board,
Invitee member
7)
Jt. Director,
Women & Child Devpt. Dept.
Invitee Member
8)
Project Co-ordinator
IPP - VIII. B.M.p.
Ex - OfficioMember - Secretary
-17-
R.
FUND FLOW
Funds would be released by the Govt, of India to the State Government and
thereafter to the IPP-VIII Bangalore. The proposal for sanction of expenditure under
various heads will have to be placed before the Project Implementation Committee for
necessary approval. Bills for having incurred expenditure will be paid by the
EPP-Vin Project Office Bangalore. Permanent advance will be placed at disposal of the
Project Officer designated for each city. This can be utilised for salaries and other
contingencies. Separate account will have to be maintained for the funds released in each
city and the funds shall not be diverted.
..18..
Statement Show inn the Slum population and General Population in the I 1 selected
cities with MCH & EW facilities.
Sl.No.
Name of Cities
Population as on
1991 census Project
2001
Slum
Population
(Notified Slum)
Existing
UFV.’C PPC
1
Mysore
6.53.345
8.95.067
23,872
7
2
1
Hubli / Dharwad
6.48,298
7.71.391
30.780
7
2
Q
Belgaum
3.26.399
5.16.278
19,301
2
1
3
Gulbarga
3.04.099
3.97.167
10.367
2
1
5
Tumkur
1.38.903
2,06,046
61.814
1
1
6
Davangerc
2.66,082
4.36.592
1.30.978
1
1
7
Bijapur
1.86.939
2.25.565
67.670
-
2
8
Bellary
2.45.931
2.84.1 14
85.234
1
1
9
Raichur
1.83.138
2,70,178
81,053
. -
1
10
Bhadravathi
55.475
66.747
20.398
-
-
11
Shimoga
1.75.258
2.15.682
64.705
-
-
.
Revsew of UmpSementetion of
Community Needs Assessment
approach for Family Welfare in India
POLICY is a five-year project funded by the
U.S. Agency for International Development under
Contract No: HRN-C-00-00006-00, beginning
July 7,2000. The project is implemented by The
Futures Group International in collaboration with
Research Triangle Institute (RTI) and The Centre for
Development and Population Activities (CEDPA).
April 2001
,
\
Policy Project II
^Tne Futures Group International
Contents
Foreword
V
Abbreviations
vii
Glossary of Indian Terms
IX
Implementation of the Community Needs Assessment Approach in India
I
Gadde Narayana, Naveen Sangwan
CNA Approach for Family Welfare in Andhra Pradesh
19
Gadde Narayana, A.Kameswara Rao
CNA Approach for Family Welfare in Bihar
3I
Daya Krishan Mangal, Gadde Narayana
CNA Approach for Family Welfare in Gujarat
41
C. VS. Prasad, Daya Krishan Mangal
CNA Approach for Family Welfare in Karnataka
57
Ramakrishna Reddy, P.Hanumantharayappa, K.M.Sathyanarayana
CNA Approach for Family Welfare in Madhya Pradesh
71
Ashok Das, K.M.Sathyanarayana
CNA Approach for Family Welfare in Maharashtra
87
SharadNarvekar, A.D.Pendse, K.M.Sathyanarayana
CNA Approach for Family Welfare in Orissa
105
K.M.Sathyanarayana, Ranjana Kir
CNA Approach for Family Welfare in Rajasthan
123
Hemant Dwivedi. Daya Kishan Mangal, Gadde Narayana
CNA Approach for Family Welfare in Uttar Pradesh
j.S.Deepak
133
Foreword
The nearly five years since India abolished its target system have been filled with both
confusion and innovation. Confusion, because of the uncertain trumpet that prevailed at
every level, and innovation, because states and districts have made sincere efforts to find
new ways to deliver services under a broadened set of objectives. This volume traces the
experiences of nine states in their overall programs and in their special trials. An excellent
synthesis chapter comes first that details the tribulations since 1996 and reviews the nine
state experiences.
This book is the successor to Targets for Family Planning in Indio: An Analysis of Policy Change,
Consequences, and Alternative Choices, which appeared in 1998. Its first chapter traces the
history of target setting and the consequences for the program, as well as the factors that
led to the 1996 policy reversal. Other chapters present the experience of certain states
in the first year or so of the transition.
The transition continues; it is by no means complete. The puzzles of how to blend enlarged
objectives with softened work rules, during a flow of top down directives that often
conflict with each other, have yet to be entirely resolved. In one sense the ambiguities will
never be resolved in such a complex and far flung set of programs, but the major adaptations
are likely to settle down after a few more years. A mosaic of program variations now
exists, each one in flux and moving toward something new. This evolution must continue,
not to a perfect end point but toward a system whose principle features lack the old rigid
targets and one that has widened its aims.
While some sympathy with the old system persists and the targets in some form have not
died easily, a few profound changes have occurred that seem irreversible:
•
The old worker-specific, method-specific, and month-specific quotas are largely out
of favour and gone.
•
The rhetoric of the field-the vocabulary of discourse-has been largely transformed, to
speak of the felt needs of the people, community interests, and multiple services.
•
Truly major changes have been made to move toward new work rules, toward other
methods to accompany sterilization, and toward other services than just contraception.
Foreword
These changes are necessarily embraced within an administrative structure that continues
v much as before. The line from Delhi, with its large share of total funding and its central
directives, down through the state managers and the districts, will not go away.
k
Moreover workers cannot simply be sent out to do good by their own lights and their
own motivations. The context now is an admixture of the new ideology with the inevitability
of top down budgets, staff allocations, and overall goals. Much of the enduring confusion
in these five years arises from that tension-how to forge a field program that allows for
worker judgment, community power, and local options, while simultaneously showing
real achievements for urgent national goals.
The nine state reviews in this volume show what is needed from the research side: a ceaseless
examination of experience from the general program and from trails of program variations.
Each review broadly examines the reproductive health program in the whole state, describes
creative projects there, and traces the transition toward a target-free approach that is adapted
to local conditions, while still setting achievement expectations at the grassroots level. If
reviews like those in this volume had not been done they would have been most urgently
needed, and it is vital that they be continued on a regular basis.
The present review is offered with appreciation to Victor Barbiero, Director of the
Population, Health, and Nutrition Office, and to Sheena Chhabra, Team Leader of the
PREM Division, both of USAID in India, for their encouragement and support. Partial
financial support was provided by the Rockefeller Foundation, which is gratefully
acknowledged.
Reproductive behaviour has changed over most of India since the national program began
50 years ago, and the program, with all of its problems, deserves a generous share of
credit. By 1992 fertility had fallen much below its traditional level: nine of the 15 largest
states had crude birth rates in the 20s and had total fertility rates below three. The
national averages were 29 and 3.4, and by the 1998-99 survey 48% of couples were using
contraception. Yet replacement fertility is a good way off, and state programs will emerge
only gradually that strike the right balance between operational effectiveness and sensitivity
to the persons they serve. That process will be informed and advanced by studies like the
ones provided in this volume.
John A. Ross
Senior Fellow
The Futures Group International
Review, of Implementation of CNA Approach for family Welfare in India
VI
Abbreviations
AD
AGTP
AIDS
AN
ANC
ANN
ANMTC
AVSC
ARI
AWW
CBD
Additional Director
Awareness-Generation Training Programme
Acquired Immuno Deficiency Syndrome
Antenatal
Antenatal care
Auxiliary nurse midwife
ANN training centre
Association for Voluntary Surgical Contraception
Acute respiratory infection
Anganwadi Worker
Community-based distribution
CBR
Crude Birth Rate
CC
CDMO
CDR
CEO
CHC
CMIE
CMHO
CMO
CMS
Condom
Chief district medical officer
Crude Death Rate
Chief executive officer
Community health centre
Centre for Monitoring Indian Economy
Chief medical and Health Officer
Chief Medical Officer
Chief Medical Superintendent
CNA
CPR
CSSM
Community needs assessment
Couple Protection Rate
Child survival and safe motherhood
Cu-T
DAP
DDMHO
DHFWO
DMHO
DIFPSA
Copper-T
District action plan
Deputy District Medical and Health Officer
District Health and Family Welfare Officer
District Medical and Health Officer
District Innovations in Family Planning Services Agency
DIO
DPC
District Immunization Officer
District Planning Committee
DPT
DUDA
Diptheria Pertussis Tetanus
District Urban Development Agency
•• • *
.Abbreviation*
vii
;
T ..
EC
ECR
ELA
FRU
FW
FWHC
GOO
GOI
GTZ
Eligible Couple
Eligible Couple Register
Expected Level of Achievement
First Referral Unit
Family Welfare
Family Welfare Health Centre
Government of Orissa
Government of India
Deutsche Gesellschaft fiir Technische
Zusammenarbeit ...
HDI
Human Development Index
HMIS
Health Management Information
Systems
ICDS
Integrated Child Development
Services
IEC
Information, education, and
communication
IFA
Iron and folic acid
IFPS
Innovations in Family Planning
Services
IMA
Indian Medical Association
IMR
Infant mortality rate
IPD
Integrated Population and
Development
IPP
Indian Population Project
ISM
Indigenous Indian System of Medicine
1TPD
Integrated Tribal Development
Programme
IUCD/IUD Intrauterine Contraceptive Device/
Intrauterine Device
KFW
Kreditanstalt fur Wiederaufbau (KFW)
LHV
Lady Health Visitor
MCH
Maternal and child health
MIM
Maternal and Infant Mortality
MMR
Maternal Mortality Rate
MIS
Management Information Systems
MO
Medical Officer
MHFW
Ministry of Health and Family Welfare
MPHA
Male-public Health Assistant
MPW
Multi-purpose Worker
MSS
MTP
Mahila Swasthya Sangh
Medical termination of pregnancy
NACO
NFHS
NGO
NIC
NID
NIHFW
NSS
OR
ORS
ORT
PBA
PHC
PLA
POL
PRC
PRI
PSM
PVO
RCH
RH
RMP
Rs.
RTI
SC
ST
STD
SIFPSA
National AIDS Control Organization
National Family Health Survey
Non-governmental organization
National Informatics Centre
National Immunization Days
National Institute of Health and
Family Welfare
National Swayam Sevika
Operations research
Oral rehydration salts
Oral rehydration therapy
Pregnancy-based approach
Primary health centre
Participatory Learning for Action
Petrol, oil, and lubricants
Population Resource Centre
Panchayati raj institution
Preventive & Social Medicine
Private voluntary organization
Reproductive and child health
Reproductive Health
Rural Medical Practitioner
Rupees
Reproductive tract infection
Scheduled Caste
Scheduled Tribe
SIHFW
STI
TBA
TFA
TFR
TT
UIP
UNFPA
UNICEF
Sexually transmitted diseases
State Innovations for Family Planning
Services Project Agency
State Institute of Health and Family
Welfare
Sexually transmitted infection
Traditional Birth Attendant
Target-free approach
Total fertility rate
Tetanus toxoid
USAID
Universal Immunization Programme
United Nations Population Fund
United Nations Children’s Fund
United States Agency for
WHO
International Development
World Health Organization
Rcxicw of Implemcntdtiuii of CNA Approach lot hirnih \XVH.in in India
Glossary of Indian Terms
Anganwadi
A village-level centre under the ICDS
Programme
Bal Kalyan Samitis
Children Welfare Committees
Crore
1 crore = 1,00,00,000
Dai
Traditional midwife
Dudugi
Local announcement
Gram Pradhan
Village headman
Gram Sabhas
Village Committees
Jowar
Millet
Lakh
1 lakh = 1,00,000
Mahila Sammelan
Women's conference
Mahila Swaschya Sangh
Women’s Health Group/Organization
Ma Raksha Mahotsara
Safe Motherhood Festival
Panchayati Raj
Body of local government at village level
Vanaspati ghee
Vegetable Oil
Tur
A type of pulse
Taluka
Territorial division below district
Pradhan/Gram Pradhan
Headman/Village Headman
Pucca
all-weather
Zilla Sarkar
District Planning Committee
Zilla Swasthya Samiti
District Health Committee
loss.uv ol Indian I'crnis
IX
Implementation of the Community Needs
Assessment Approach in India
Gadde Narayana
Naveen Sangwan
Background
Since its inception in 1951, the Indian Family Planning Programme has
undergone many changes to meet the varied challenges over the years.
At different times, the programme has been expanded either to integrate
services, as was done in the 1970s with the multi-purpose workers
scheme. In recent years, in order to focus on the range of services
critical for the health of women and children, the programme has been
expanded to include elements of new schemes such as Child Survival
and Safe Motherhood (CSSM), Universal Immunization, and Reproductive
and Child Health (RCH). '
Prior to 1996, the programme used a target approach as the means to
stabilize population growth. All services, planning, and financing were
geared to achieving the demographic goals of reducing the birth rate and
the rate of population growth. To achieve the long- and short-term
demographic goals, this approach set targets in terms of a couple protection
rate (CPR), which was further broken down into method-specific targets.
with special focus on sterilization. The central government prescribed
these targets annually for each state, which in turn passed the annual
targets through the system down to the facility level? Thus, achievement
------
Leela Visaria. Shireen Jejeebhoy and Tom Merrick, "From Family'Planning to
Reproductive Health: Challenges Facing India" in International Family Planning
Perspectives, January 25. 1999, p 844-49
Gadde Narayana. Shalini Kakkai and Venkatesh Srinivasan, Target Free Approach for
Family Planning In India in The POLICY Project (ed) Targets for Family Planning in
India: An Analysis of Policy Change. Consequences and Alternative Choices: The
Futures Group International. New Delhi. 1998
CNA Appio.ulr in lmli.i
of contraceptive targets became the principal
indicator of success for India’s population stabilization
effort. The target system placed little importance
on clients’ personal choices and did not encourage
the use of a wider range of family planning methods.
As the target system increasingly took its toll on
services and quality, criticism grew as well. By the
end of the 1980s, population experts, researchers,
academicians, donors, and non-governmental
women’s groups in India had all registered strong
objections to India’s family planning programme.
These factors, along with
n April 1996, the GOI
international developments
introduced a major
during the 1994 International
vision of its approach to
Conference on Population and
Development and the 1996
imary health care. The
International
Women’s
MOHFW abolished
Conference in Beijing, created a
nethod-specific family
need for a change in approach.
planning targets, and
tlaccd it with what was
In April 1996, the Government
of India (GOI) introduced a major
revision of its approach to family planning and primary
health care. The Ministry of Health and Family Welfare
(MOHFW) abolished method-specific family planning
targets, and replaced it with what was initially called
the Target-Free Approach (TFA).3 The main aim of
the TFA was to shift the focus to clients’ needs and to
improve the quality of services. This paradigm shift
0lled for planning to start at the basic facility level and
titially called theTFA.
to be based solely on identified client needs and
intentions. Health workers would conduct surveys
to ascertain these needs. In other words, the former
“top-down” approach was to be replaced by a genuine
"bottom-up” approach in which health workers’ case
loads would be determined by identified local needs.
At the same time that targets were abolished, however,
MOHFW provided minimal guidance to the states on
how to implement the new policy. As a result, in
1996 and 1997, most states lacked operational
methodologies to assess community needs, develop
realistic performance goals and plans, and
institutionalize quality in service provision, especially
at the district level and below. TFA at the operational
level was even misinterpreted in some states as “no
targets means no work." To avoid these unfortunate
misconceptions and direct the programme more
towards clients’ needs, the new programme was recast
into the “Community Needs Assessment” (CNA)
approach in September 1997/ The underlying
philosophy of the new approach, however, remained
the same as the TFA.
Objectives of the Paper
This paper synthesizes the results of nine case
studies carried out by the POLICY Project in the
states of Andhra Pradesh, Bihar, Gujarat, Karnataka,
Madhya Pradesh, Maharashtra, Orissa, Rajasthan, and
Uttar Pradesh. The objectives of the case studies
were to:
o
examine the transition from the original target
system to the TFA and subsequently to CNA
approach
• Analyze the countrywide implementation of CNA
and the impact of the new system on programme
performance
o
Identify programmatic shortcomings that affected
the transition, draw lessons from the experiences
of implementation, and identify steps that could
be taken to improve the management and
performance of the new client-oriented system.
Ministry of Health and Family Welfare. Manual on Community Needs Assessment Approach, Government of India, 1998
Ministry of Health and Family Welfare, Manual on Community Needs Assessment Approach, Government of India, 1998
Review of hnplcnu-nt.uion ol r ’X \ Appro.,,!, Io, I .noil, Welllue in Indi.,
The case studies for nine states follow this synthesis
chapter.
Introduction of the Target-Free
Approach
Starting in the 1960s, the Ministry of Health and
Family Welfare annually fixed method-specific
targets, which largely determined the character of
programme implementation, monitoring, and
evaluation at all levels. Over the years, this led to a
situation where the achievement of contraceptive
targets rather than client services became the major
objective of public providers.5 The obsession with
targets and emphasis on sterilization resulted in
poor coverage of younger and low-parity couples,
virtual neglect of modern spacing methods, and
inflated performance reports particularly for spacing
methods. These conditions combined to severely
limit the demographic impact of the programme.
Not surprisingly, informed contraceptive choice,
clients needs, and quality of services were
inadequately addressed. The centralized planning
and top-down target setting hindered management
innovation and flexibility.6 As a result, the overall
reproductive health situation in India remained
poor, and GOI found itself responding to
performance shortfalls by periodically adjusting the
timeframes for achieving programme objectives.
Population experts argued that focus on numerical
targets thwarted attainment of the desired
demographic impact and that excessive pressure
to achieve targets resulted in over-reporting and
mismanagement. Non-governmental Organizations
(NGOs) and women’s groups argued that the
central government's notion that India’s birth rate
must be reduced by vigorous promotion of
contraception was a violation of human rights. The
poor quality of care provided to women by service
providers was taken as a sign of how little regard
those providers had for women’s health. In the
1980s and early 1990s, several key stakeholders,
including donor agencies, stimulated discussion of
varied viewpoints and advocated for a shift from
the target-oriented approach to innovative ways of
meeting reproductive health needs using an
integrated approach.
There was a growing interest in replacing the target
system with an entirely different approach—one that
would shift programme emphasis from providers to
clients. In September 1995, GOI
In the 1980s and early
abolished targets in the states of
1990s, several key
Tamil Nadu and Kerala and
stakeholders, including
requested every state to select
one or two districts to test the
TFA.
The new approach
envisaged decentralized planning
at the sub-centre level, in
consultation
with
the
donor agencies, stimulate)
discussion of varied
viewpoints and advocatet
for a shift from the TFA V
innovative ways of mectin
reproductive health need
community, to determine annual
workloads based on local needs.
using an integrated
approach.
By shifting more explicitly to
identified client needs and involving the community,
the GOI also hoped to stimulate better quality
services. Expected levels of achievement (ELA),
instead of targets, were now to be set by workers at
the grassroot level—female auxiliary nurse midwives
(ANMs) and male multi-purpose workers (MPWs)—
in response to community needs.
Basic Characteristics of TFA
•
Provide services according to client needs and
eliminate centrally determined targets
Gadde Narayana, Shalini Kakkar and Venkatesh Srinivasan, Ibid, TFGI, New Delhi, 1998
Naveen Sangwan and Rishikesh M. Maru, "Target-Free Approach: An Overview" in Journal of Health Management, 1.1, 1999, p
71-96.
CNA Approach in India
3
o
Provide a wider choice of safe contraceptive
methods and greatly strengthen and expand
reproductive health services
o
Emphasize the quality of services and decentralize
programme planning and management to the
district level and below
e
Build partnerships with the community and make
the programme a “people’s programme."
Change from TFA to CNA
In April 1996, without rigorously addressing the
experiences gained by all the states in implementing
the TFA, the central government decided to abolish
targets throughout India, making the entire nation
target free. Targets were removed without adequate
preparation and without discussion of what would
replace the old system. No new
To convey' clearer
monitoring
system
was
guidelines to health
proposed to replace the target
workers and to simplify
die implementation of die
TFA concept and
philosophy, the
government renamed die
TFA as die Community'
Need Assessment
(CNA) approach.
system. At the policy level, the
shift to the TFA was recognized
as a necessary step for
enhancement of the quality of
services. At the implementation
level (state and district),
however, the only guidance
programme
implementers
received was in the form of a manual (written in
English) to orient them on decentralized planning.
starting at the sub-centre level.
In September 1997, the government realized that
the TFA manual was not proving to be useful in
implementing the new approach and that the term
TFA was a misnomer. Nany health workers equated
TFA with “no work" or “no more monitoring based
on targets" and became complacent. The formats
introduced to estimate community needs and
expected levels of achievement were too complex
to be followed by the workers. The training
provided to health workers in the use of these
formats was inadequate and lacked uniformity. To
convey clearer guidelines to health workers and to
simplify the implementation of the TFA concept
and philosophy, the government renamed the TFA
as the Community Need Assessment (CNA)
approach. In. 1998, .they developed and distributed
a CNA manual to replace the TFA manual.
Currently, the programme follows the CNA
approach.
Analysis of the Transition from
Targets to CNA
Moving away from targets to the TFA is a major
organizational change. Implementation of an
organizational change of this kind in a vast
bureaucratic system is a daunting task. The change
process involves three stages: planning,
implementation and stabilization. The main purpose
of planning is to develop a strategy for
implementation. It involves identifying critical
implementation issues and designing operational
strategies to implement the change.
Figure 1
The Shift from Targets to CNA
Driving Force
Orientation
Concern
Goal
Approach
Targets
Provider
Target Achievement
Demographic impact
Top-oown
->
Community needs
Client
Quality of care
Reproductive health status
Bottom-up
Experiences of Implementing TFA/CNA
On a pilot basis in 1995-96. GOI designated a
single district in 18 different states and two entire
states as “target free.” The objective was to learn
from experience and determine the feasibility of
adopting the TFA nationwide. In the absence of
guidelines, each state responded according to their
level of comprehension of the new policy. For
instance, Andhra Pradesh designed a very
comprehensive information and monitoring
system and was ready to test run the system in
the target-free districts of East Godavari and
Medak. The government of Rajasthan introduced
a new innovative information and service delivery
system in Dausa and Tonk districts. Uttar Pradesh
carried out operations research in Agra and
Sitapur districts. Tamil Nadu designed and
introduced a new information system at all levels.
Other states largely waited for further instructions
from the central government.
The initiatives taken by the states are an indication
of the recognition of the need to change or revamp
the information and monitoring systems of the
family welfare programme. GOI, without taking into
account the changes contemplated or implemented
and without a comprehensive review of experiences
gained in the first phase of implementation of the
TFA, imposed the TFA in all states in February
1996. Several states initially resisted the change
and wanted the old target system to continue with
some cosmetic changes. GOI responded to the
situation by directly instructing District Collectors
or District Magistrates to abolish targets and to
introduce the target-free system with the help of
centrally designed new formats. Guidelines and a
budget to train workers and medical officers were
given directly to district authorities. State-level
Directorates of Health and Family Welfare were
mere spectators to this process. The training was
conducted without supervision, it was not of
uniform quality, and many did not understand the
philosophy behind the new approach. The formats
provided were complex and many workers could
not understand how to calculate the ELAs based
on sample surveys. Training programmes involving
several hundred thousand workers throughout
the country could not be completed until the end
of 1997.
Family planning performance in most states
declined from 1996 to 1997, creating a negative
reaction, particularly among top-level managers who
answer directly to their immediate political bosses.
The decline in performance in traditionally high
performance states was marginal, but in states like
Uttar Pradesh and Bihar, it was sharp and
perceptible. After several consultation meetings
and workshops, GOI realized
the limitations of the TFA
In many states with
formats and manual and the
weak monitoring
negative effect of the term
systems, the workers
“target free.” The manual
stopped visiting villages
was subsequently revised,
and in a meeting held for
representatives of state
governments in September
1997, in New Delhi, the
to provide services and
expected villagers to visit
clinics that were located
far away with no
transport facility.
revised manual was approved
at the same time as the name of the approach
changed. In many states with weak monitoring
systems, the workers stopped visiting villages to
provide services and expected villagers to visit
clinics that were located far away with no transport
facility. The term CNA was chosen to convey the
message that the workers' responsibility is to assess
the needs of the community and provide services
as per the community needs. A senior GOI officer,
reflecting on the prevailing situation, stipulated, "We
may have adopted a target-free approach, but this
is with reference to numerical method-specific
targets. We are not in a goal-free situation. We still
..4 :
have our goals and objectives intact, and this needs
to be emphasized." 7
The CNA approach has modified formats for data
collection. The number of formats was reduced from
14 planning and reporting formats for the TFA to
nine formats for the CNA approach. GOI dispatched
the English version of the CNA manual and formats
to state governments in 1998, necessitating
reorientation of workers. In addition, GOI
instructions were not clear on whether the new
formats should replace the old ones or continue as
a parallel activity. Training of workers remained a
major issue. A uniform training programme
was designed to cover all workers in the country
without taking into account differences in capabilities
and skills, which turned out to
be a major obstacle to
In Andhra Pradesh, with
strong political backing
institutionalizing the new system.
available to the states
In many states, the printed
programme, the
formats for CNA were not made
Department of Health and
available. Implementation of the
FamilyWelfare initiated the
CNA approach was not uniform,
formulation of a
varying from district to district
comprehensive state
within a state as well as from state
population policy that
to state. Given this scenario,
included both demographic
states responded to the new
and RH goals.
system in different ways. Some
states have blended the old
approach with the new approach and designed new
monitoring systems. Some have tried to implement
the new system, completely replacing the old system.
A few others have neither the old nor the new
system in place. The TFA, however, succeeded in
making the lexicon, and the use of such terms as
‘quality of services’, 'community or client needs',
‘integrated approaches’, and ‘expected levels of
performance’ are used to reflect the new philosophy
of service delivery. The following sections of this
paper summarize the experience of nine states in
adopting the new system.
Andhra Pradesh
In the first phase of the TFA, Andhra Pradesh
abolished targets in East Godavari and Medak
districts. Even before selecting these districts for
the TFA, the Directorate of Family Welfare designed
a new information and monitoring system to
completely replace the old system. TFA districts
were selected to pretest the new system. This
process was discontinued, however, after an
enthusiastic beginning due to lack of support from
the central government.8 The performance in both
TFA districts declined considerably. Many at the
state level thought that the new approach would
present a major hurdle to achieving the state’s
demographic objectives. With strong political
backing available to the state’s programme, the
Department of Health and Family Welfare initiated
the formulation of a comprehensive state population
policy that included both demographic and R.H
goals.’
The legislature approved the state
population policy, the first of its kind in the country,
in_ 1997. In the mean-time, the state completed
CNA training at all levels. The workers generate
expected levels of performance after conducting
surveys, and these numbers are compiled at various
levels to arrive at expected levels of performance
Department of Health and Family Welfare, Government of Madhya Pradesh and IIHMR, Proceedings of the Workshop on
Population Policy for Madhya Pradesh: Identification of Issues and Challenges, The POLICY Project, The Futures Group Interna
tional, 1999
C.B.S. Venkata Ramana, "Target-Free Approach for Family Welfare: A Review of Experiences in Andhra Pradesh", in The
POLICY Project (ed) Targets for Family Planning in India: An Analysis of Policy Change, Consequences and Alternative Choices,
The Futures Group International, New Delhi, 1998, p 26-47.
Government of Andhra Pradesh. Andhra Pradesh State Population Policy: A Statement and A Strategy, 1997
Review of lniplcint-nt.it ion of CXA Appio.ub. tor l .nnily Welfare in India
6
at the district and state levels. At the end of this
exercise, in their meetings with district officers,
state officers compare the policy objectives and the
ELAs arrived at based on data collected from
below.10 After considerable discussion and
negotiation, the district and state officers reach a
consensus on the ELA for the year. The districts,
in turn, distribute these numbers to all health
institutions in the district. Performance monitoring
systems at both the political and administrative levels
in the state were strengthened, and additional
resources were provided to districts to achieve
results. Consequently, performance, particularly
sterilization performance, has significantly improved
while spacing method use has remained more or
less the same over the same period of time. Senior
administrators of Andhra Pradesh strongly believe
that the state government, given its structures and
administrators feel that they have a successful
model for others to follow.
systems, has no capacity to serve spacing method
users. So the programme strategy places major
emphasis on the public sector for sterilization
services and on the private sector for marketing of
spacing methods. Recently, the state government
has promoted male sterilization. An experimental
project conducted to promote male sterilization in
performance review meetings
at all levels. The department
could not train workers in the
use of the new formats, since
many in the department did
not comprehend the content
of the manuals themselves. In
1998, two years after
two districts was a major success, with the number
of male sterilizations conducted in a year exceeding
that of female sterilizations. According to the results
of National Family Health Survey II (NFHS II),
Andhra Pradesh’s achievements are especially
significant in family planning acceptance,
immunization coverage, and maternal health care
services—particularly antenatal care (ANC) and
institutional deliveries.1 1 Having achieved
replacement level fertility, Andhra Pradesh now
intends to concentrate its efforts on reducing infant
mortality and increasing age at marriage. Many state
Bihar
Bihar is one of India's large states with low
contraceptive prevalence and high fertility. Its
performance in regard to deliveries assisted by
trained providers and immunization coverage of
children is also a cause for concern. The Department
of Family Welfare introduced the TFA in one of the
relatively better performing districts in 1995-96. The
department reviewed the experiences in
implementing TFA in this district with the help of an
external agency. Even before discussing the issues
involved, GOI mandated introduction of the TFA in
the entire state. The state government stopped
providing
targets
and
discontinued
monthly
Many of the medical
officers in the state
considered the TFA as
the “tension-free
approach” because
there was no need for
accountability after die
introduction of die
new system.
introduction of the TFA, a
donor agency helped the state initiate the training of
workers. Even after training, few workers are in a
position to use the new formats. No annual surveys
are conducted to determine the ELA based on
community needs assessment. ELA are generated
in the beginning of each year based on the past year’s
performance or based on workers’ perceptions.
Many of the medical officers in the state considered
the TFA as the "tension-free approach” because there
was no need for accountability after the introduction
Gadde Narayana and A. Kameshwara Rao, Community Needs Assessment Approach in Andhra Pradesh, The POLICY Project,
The Futures Group International. New Delhi, 1999 (Mimeo)
'
International Institute for Population Sciences, Andhra Pradesh: National Family Health Sutvey-India, 1998-99, Bombay, 2000.
f-.w.
V •
’
CNA \pprnacli in India
7
of the new system.12 Performance of all methods,
particularly sterilization, sharply declined in 1996—
97 and remained low after that. Many in the
department felt that there was a perceptible
improvement in the quality of services offered after
introduction of the TFA, in terms of method
acceptance among low-parity and young couples.
However, there is no evidence to support this
assertion, and, therefore, it looks more like a
justification for poor performance. More intensive
efforts are required to build capacity and to improve
programme management to make the CNA approach
a success in the state.
Gujarat
The government of Gujarat introduced the TFA in
Valsad district in 1995-96. The workers were briefed
about the TFA and asked to
improve the quality of services. In
The TFA was introduced
the initial months, due to lack of
in all districts in April
1996 but only in
any guidelines about the new
November 1997 did the
approach, the performance of the
state receive clear
district declir ed drastically,
guidelines from the
sending panic signals to the
central government on
administration. Several review
how to implement the
meetings with Primary Health
new approach.
Centre (PHC) medical officers
and workers occurred that
emphasized the need for regularly updating registers
of workers to serve the community. Due to these
intensive efforts, method-specific performance at the
end of the year was only 17-20 per cent less than
what it was in the previous year. The TFA was
introduced in all districts in April 1996 but only in
November 1997 did the state receive clear guidelines
from the central government on how to implement
the new approach. The Health and Family Welfare
Department trained 2,422 medical officers and 16,890
workers by March 1998. Workers then carried out
a community-level survey with the help of formats
given to them and estimated the expected levels of
performance. Following this process, the estimated
workloads were unrealistically high in a large number
of districts and low in others. The Directorate advised
the districts to take past performance as a benchmark
and compare past performance with the estimated
expected levels of performance. In Gujarat, workers
prepare sub-centre plans based on surveys but these
numbers are scaled down or up based on past
performance.13 In general, reported performance
declined slightly in 1996-97 for all family planning
methods and subsequently remained stagnant at that
level. Monitoring of family planning performance is
now based on ELA. In addition, the state has indicators
to monitor quality of services. State officials were not
perturbed by the marginal decline in performance and
were confident that the new system would be fully
institutionalized within a couple of years and start
yielding results.
Karnataka
Based on instructions received from GOI in 1995,
the government of Karnataka selected Mandya
district to experiment with TFA. Mandya district
officers passed on the information to the PHCs and
workers. There was no decline in year-end
performance. One of the medical officers of
Mandya observed, “Performance in the district
remained more or less the same even without
targets because workers in this district do not have
to make much effort. People accept family planning
on their own. In such a situation, targets or lack of
D. K. Mangal and Gadde Narayana, The Target-Free Approach in Bihar: A Review of Experiences, The POLICY Project, The
Futures Group International, New Delhi, 2000 (Mimeo)
C.V.S. Prasad and D. K. Mangal, The Community Needs Assessment Approach in Gujarat, The POLICY Project, The Futures
Group International, New Delhi, 2000 (Mimeo)
them make no difference”.14 With the introduction
of TFA in 1996, the state made substantial changes
to the government-prescribed formats. Workers
conducted annual surveys with the help of the
of TFA. Reported performance on all spacing
methods showed a decline of 5-10 per cent after
1996-97.
eligible couple registers (ECRs), but this data
remained unutilized because the targets were
prescribed from the top. After the TFA was
mandated, the state realized the need to use these
data and the centrally prescribed coverage norms
to arrive at ELA at all levels. However, the centrally
prescribed formats were not useful for calculating
the expected levels of achievement for family
planning methods. The state directorate, therefore,
instructed districts to take past performance into
account to arrive at ELA for family planning
methods. Some districts considered the pastyear’s
performance and others took a three-year average
of past performance levels to arrive at the expected
Madhya Pradesh
level of achievement for family planning. Karnataka
also conducted training programmes to reorient
health workers as well as members of Panchayati
Raj Institutions (PRIs) and anganwadi workers
(AWWs). In fact, implementation of the new
system preceded the training programmes. In
general, workers, supervisors, and medical officers
welcomed the new approach and adhered to all
instructions provided in terms of training
programmes, use of survey formats, and preparation
of sub-centre-level workplans. However, many felt
that the new approach has not addressed and is
not helpful for addressing the tremendous variations
within the state. Absence of such differentiated
approaches makes micro-level planning a
theoretical rather than a practical exercise. The
state needs to develop different formulae for
different regions or districts to estimate expected
levels of performance. Sterilization performance
in the state improved slightly after introduction
Madhya Pradesh was one of the first states to
conduct elections to local bodies after the 73rd and
74,h amendment to the Constitution of India and
devolved significant authority and responsibility to
the elected bodies. The elected bodies became
responsible for implementation of PHC and family
welfare programmes, and all health workers were
transferred to PRIs. As a result of structural changes
in programme implementation, the previously major
role of Department of Health and Family Welfare
became marginal. At the same time, elected^^
representatives of PRIs had
Madhya Pradesh was on
little
knowledge
of
of the first states to
programmes and lacked the
conduct elections to loa
skills and experience to
bodies after the 73'd an.
govern. It is in this milieu that
74d’ amendment to the
the TFA was first introduced
Constitution of India ai
in Narsinghpur district.
devolved significant
Workers were asked to
authority and
conduct an eligible couple
responsibility to die
(EC) survey and set their own
elected bodies.
targets in order to improve
performance. The family planning performance of
the district dropped substantially in 1995-96. After
introduction of TFA in the entire state, workers
were instructed to follow the GOI guidelinwff
conduct eligible couple (EC) surveys, and set their
own ELA based on past performance. The state
completed the training of district officers in 1997—
98. Since workers did not receive any training
during the two-year period in which TFA was
implemented, the methodology followed to
calculate expected levels of achievement varied
P. Ramakrishna Reddy. P. Hanumantharayappa and K. M. Sathyanarayana, The Community Needs Assessment Approach in
Karnataka. The POLICY Project. The Futures Group International, New Delhi, 2000 (Mimeo)
CNA Approach in India
9
from one institution to another.15 Information
collected with the help of ECRs designed a few years
prior to the introduction of the TFA was not
sufficient to prepare micro-plans. Realizing this and
to be in tune with the requirements of the TFA
formats, the Madhya Pradesh government
completely modified the ECRs and made newly
printed registers available to all sub-centres. ANMs
collected the information but were not in a position
to process the information to identify unmet need
for family planning and RH services. Instead of
training ANMs, this responsibility was entrusted to
statistical officers at the PHC level. There was no
involvement of PRIs in the assessment of
community needs. The state government has,
however, prepared a blueprint for training elected
representatives about their roles and
responsibilities. The Madhya
Pradesh government formulated
Political commitment to
a state population policy in
the family welfare
programme in Madhya
January 2000, that clearly spells
Pradesh is very high, and
out its family planning and RH
the department is trying
objectives for the next decade.16
to implement mechanisms
Integrated approaches involving
to continuously evaluate
elected representatives of local
performance and review
bodies are essential for achieving
strategies for achieving
these objectives. Family planning
policy objectives.
performance in the state
declined considerably for all
methods except for oral contraceptives. Political
commitment to the family welfare programme in
Madhya Pradesh is very high, and the department
is trying to implement mechanisms to continuously
evaluate performance and review strategies for
achieving policy objectives.
Maharashtra
Maharashtra selected Satara and Wardha districts in
1995-96 to abolish targets. Satara district officials
prepared a district action plan that emphasized the
need for a maternal child health (MCH) approach
for family planning. Satara district implemented its
plan after conducting a baseline survey in the district
with the help of health workers. Wardha has not
made any attempt to prepare a plan. In 1996-97,
TFA was extended to all districts. After review of
the TFA manual provided by GOI, the Directorate
of Family Welfare modified the formats to suit local
conditions and termed the new approach “selfdetermination of targets.”17 The quality of training
varied by district, and community involvement was
negligible. More systematic efforts were made to
train workers on the CNA approach in 1997-98.
In addition to the material provided by the central
government, the Directorate introduced four data
collection formats to be used by sub-centre
functionaries to assess community knowledge and
to estimate ELA for Family Planning/RH services. By
March 1998, all health functionaries in the state were
trained in the CNA approach. Training programmes
were evaluated and strengths and weaknesses
identified. However, the implementation of the CNA
approach was beset with several problems. The
formats designed required several modifications to
capture the relevant information. While the need to
modify the formats was recognized, additional
resources necessary to make the modifications were
not available. Since the attempts to prepare micro
plans were not successful, the government of
Maharashtra decided to use the findings of each
district’s RCH survey to prepare district-level plans.
Ashok Das and K. M. Sathyanarayana, The Community Needs Assessment Approach for Family Welfare in Madhya Pradesh,
The POLICY Project, The Futures Group International, New Delhi, 2000 (Mimeo)
Government of Madhya Pradesh, Madhya Pradesh Population Policy. January 2000
Subhash Salunke and Sharad Narvekar, Target Free Approach for Family Welfare: A Review of Experiences in Maharashtra, in
The POLICY Project (ed) Targets for Family Planning in India: An Analysis of Policy Change, Consequences and Alternative
Choices, The Futures Group International, New Delhi, 1998, p 49-78
' ‘i
Renew of Implementation of CNA Apptoaeh for Pantilj Welfare in India
10
The draft plans prepared by the district officers
required several modifications and refinements,
which were never made. During this period, family
planning performance declined considerably, but
MCH services improved to a large extent.
Maharashtra has long been considered as a state with
clear vision for implementing innovative strategies
to achieve results. Several other states, particularly
in the south, have recently shown better
performance than Maharashtra, however. One of the
main reasons for this discrepancy is that half of
Maharashtra's population lives in urban areas, and
there is no PHC and family planning service delivery
system to cover urban populations, particularly those
living in slums.18 Senior officers of the Directorate
also believe that the department's complacency as a
result of past performance has led to stagnation.
Several attempts made to revamp service delivery
systems have not yet yielded results either due to
lack of systematic effort or resources. Maharashtra
recently introduced a series of disincentives that are
both harsh and unrealistic to improve performance
in order to reach replacement level fertility within a
short span of time.
Orissa
Orissa selected the newly formed Kurda district to
implement the TFA in 1995-96. The government
of Orissa introduced a new ECR in 1993-94 and
made printed registers available to all sub-centres.
Sub-centre workers conducted surveys in all villages
in 1994-95 and updated data in 1995-96 to identify
ECs. Method-specific targets given to the workers
were withdrawn after introduction of the TFA in
the district. The directorate toyed with the idea of
introducing a birth-based approach to improve
maternal and child health services, but these ideas
never took concrete shape. After the introducing
TFA in all districts, the Directorate issued
instructions to prepare district plans based on norms
set by the state.'’ These norms stipulated that the
ELA for each sub-centre should not be less than 30
sterilizations, and 30 IUDs, IS oral pill, and 65
condom acceptors. Districts generally followed these
norms in preparing the plans they submitted to the
Directorate. Performance was monitored weekly at
the sector level. Training of health functionaries in
the TFA was completed in all districts by the end of
1997. After introduction of the CNA approach, no
further training was conducted. The CNA formats
provided by the central government were sent to all
districts with instructions that the new formats
should replace the old TFA
formats. The Directorate
In the 1990s, Orissa
planned to conduct CNA
divided its 13 districts
training in 1999. Sterilization
into 30 districts. The
and condom performance in
the state declined sharply after
introduction of the CNA
infrastructure available in
27 of die new districts is
grossly inadequate, and
resources are not available
approach while users of oral
to improve the situation.
contraceptives and IUDs
increased considerably during
the same period. Orissa faces several unique
problems that are major obstacles for effective
programme management. In the 1990s, Orissa
divided its 13 districts into 30 districts. The
infrastructure available in 27 of the new districts is
grossly inadequate, and resources are not available
to improve the situation. Orissa also experiences
severe cyclonic storms almost every year, disrupting
the normal functions of all departments. The health
department spends most of its energy and resources
Tara Kanitkar (ed) Proceedings of the Workshop on Population Policy for Maharashtra: Issues and Challenges, Centre for
Health Policy and Research, Pune, 1999 (Mimeo)
”
K. M. Sathyanarayana and Ranjana Kar, The Target-free Approach for Family Welfare in Orissa: A Review of Experiences, The
POLICY Project, The Futures Group International, New Delhi, 1999
CNA Approach in India
1 I
to contain epidemics that follow natural calamities.
Still, the state has a relatively good database at the
sub-centre level, which could be used to provide
services based on client needs. This will only be
possible, however, when the state identifies and
formulates new strategies to provide quality RH
services.
Rajasthan
Even before introduction of the TFA in 1994-95,
the government of Rajasthan decided that the unmet
need for family planning services should be the focal
point for all programme implementation efforts. To
introduce the unmet need concept at the village level,
sub-centre registers and report formats were
completely redesigned and workers trained in their
use. Workers were instructed to conduct surveys
to identify unmet need for both
limiting and spacing methods in
Even before introduction
the month of May, and districts
oftheTFAin 1994—95,
die government of
were to consolidate all
Rajasthan decided that
information and prepare district
the unmet need for
plans in the month of June. The
family planning senices
extent to which the workers
should be the focal point
satisfy unmet need has become
for all programme
the basis for performance
implementation efforts.
monitoring and evaluation.20 In
addition, the Department of
Family Welfare introduced concurrent evaluation by
external survey research agencies to check for
inflated performance reporting at all levels. The new
system was introduced in two districts to begin with
and rapidly expanded to all districts. By the time the
central government decided to implement the TFA,
Rajasthan had its new system in operation in the
entire state. There was considerable reluctance on
Rajasthan’s part to replace its system with the one
suggested by GOL Rajasthan’s system, which
identifies needs every year in each household, was
considered far better than the approach suggested
by the central government, which involved a series
of calculations to arrive at estimates of client needs.
In 1997, the department further expanded its system
to identify unmet need for RH services. A monthly
feedback system based on reviews of reported
performance was established in 1998-99. To review
Family planning and RH performance, senior
directorate officers visit each district once every two
months. Identification of unmet need with the help
of household surveys and a revamped monitoring
system has helped Rajasthan to improve its family
planning performance considerably. It is the only
state that has not experienced a decline in family
planning performance after introduction of the TFA.
The Rajasthan government also formulated a state
populatior^pqlicy in 1999 that clearly articulates the
goals and strategies for the family welfare
programme.21 Rajasthan, for understandable
reasons, has not paid much attention to the CNA
approach and the new formats proposed by GOL |
Uttar Pradesh
Uttar Pradesh selected two districts—Agra, a high-
performance district and Sitapur, a low-performance
district—to experiment with the TFA. With the
help of resources from the USAID-funded
Innovations in Family Planning Services (IFPS) Project,
the pregnancy-based approach and the unmet need
for family planning services approach were
introduced in both districts. Registers were designed
and workers trained in the use of the new registers.
Though family planning performance in both districts
Ram Lubhaya, Target-Free Approach for Family Welfare: A Review of Experiences in Rajasthan, in The POLICY Project (ed)
Targets for Family Planning in India: An Analysis of Policy Change, Consequences and Alternative Choices, The Futures Group
International, New Delhi, 1998, p 70-101
Department of Family Welfare, Population Policy of Rajasthan, Government of Rajasthan. 1999
Review of linpleinenration ol (.’X'A Approach [or l.tnuly Welfare in India
12
declined drastically after introduction of the TFA, a
slight improvement in MCH services was observed.
In 1996-97, Uttar Pradesh extended the TFA to
the entire state, but the training given to workers to
implement the new approach was ineffective.
Moreover, the state government had deleted the
family planning programme from the 20-point
programme, and district magistrates were instructed
not to monitor family planning programme
performance.22 Overall programme performance
drastically declined. After this, the Department of
Family Welfare started systematic preparatory work
to strengthen the target-free system from 1997-98
onwards. Training was conducted in all PHCs in the
state with the help of facilitators and a guide
developed specially for that purpose. All workers'1
were trained by November 1997. Uttar Pradesh
received the CNA manual to replace the old TFA
manual from the central government in March 1998^
The Directorate of Family Welfare decided to
continue with the TFA formats rather than introduce
the CNA formats and retrain all workers. During
this period, the department took several decisive
steps to improve access to and the quality of a wide
range of RH services rather than solely concentrating
on family planning. These steps included provision
of quality reproductive and child health services
through RCH camps, tetanus toxoid (TT) campaigns
covering all pregnant women, dai training to increase
the proportion of deliveries conducted by trained
personnel, and decentralized planning at the district
level using a participatory approach. In addition,
contraceptive marketing of condoms and oral
contraceptives in rural areas is expected to increase
spacing method use. The Government of Uttar
Pradesh has recently formulated a population policy
with clear strategies to integrate services, decentralize
delivery systems, and improve service quality.23 To
realize the policy objectives, the CNA approach has
to be further strengthened in the state by conducting
annual household surveys to identify unmet need
for family planning and RH services. Uttar Pradesh
discontinued this practice in the mid-1970s. A
common feature in other states, the Department of
Family Welfare has decided to reintroduce annual
household surveys with the help of simple formats
to identify unmet need for RH
and family planning services in
The Government of
four districts on a pilot basis.
Uttar Pradesh has
At the same time, the
department will develop a
more
comprehensive
management information
system (MIS) to cover the
entire state in a phased
manner.
recently formulated a
population policy with
clear strategies to
integrate services, *
decentralize delivery™
systems, and improve
service quality.
Conclusions
Moving from targets to the target-free approach
represented a major organizational change, and an
enormous challenge to India’s public health system.
Planning for change involves consensus and clear
understanding among stakeholders on the reasons
for change, the direction of change, and processes
to be followed in introducing change. Due to poor
experience with targets, the reasons for the national
level change were clear and in tune with the thinking g|
of the international community on the subject. The
groundwork done by GOI to educate and build
consensus among stakeholders in support of the /
TFA, however, was grossly inadequate. Resistance
to a change of this magnitude was inevitable and.
therefore, strategies to overcome resistance should
have been planned well in advance.
J. S. Deepak, The Community Needs Assessment Approach for Family Welfare: A Review of Experiences in Uttar Pradesh, The
POLICY Project, The Futures Group International, New Delhi, 2000
'
Government of Uttar Pradesh, Population Policy of Uttar Pradesh, 2000.
CNA /Xpproavh in India
13
The GOI, instead, chose a shorter route by
announcing the decision and dealing directly with
districts without involving state directorates. The
delivery of critical instructions, manuals, and formats
to districts to reorient workers occurred several
months after the introduction of the TFA. Formats
prepared to estimate and plan workloads were very
complex and involved several calculations based on
many assumptions. Those who designed the formats
never thought about the capabilities of the primary
users of these formats (i.e„ health workers at the
sub-centre level). Workers in all states found it
uniformly difficult to use the
One of the basic
new formats. In addition, the
problems with the new
training
programmes
approach is that it was
conducted to familiarize
designed by the central
workers with the new
government for use at the
procedures did not convey the
sub-centre level. This
philosophy behind the new
centrally imposed,
system.
Workers
and
decentralized system goes
supervisors had their own
against the core tenet of a
interpretation of the new
decentralized approach
approach that was different
for assessing
from the original intent of the
community needs.
programme. Not surprisingly.
performance dropped substantially in many states.
Interestingly, the high-performance states with
strong monitoring systems experienced only a
marginal decline in performance while the lowperformance states with weak monitoring systems
could not avert significant declines in performance.
TFA, in effect, widened the gap between high- and
low-performance states.
One of the basic problems with the new approach
is that it was designed by the central government
for use at the sub-centre level. This centrally
imposed, decentralized system goes against the core
tenet of a decentralized approach for assessing
community needs. The formats introduced under
the new system again rely heavily on a series of
quantitative measures for the sake of quality
improvement. The way in which the CNA approach
has been implemented undercuts the philosophy
behind the new approach.
The CNA approach has achieved some notable
positive results, however. Resistance to the change
has declined. Those working for the family welfare
programme at various levels are now largely
convinced about the futility of the numbers game as
practiced earlier. There is growing recognition of
the need for a thorough review of the programme
and for introduction of integrated and decentralized
service delivery systems with more emphasis on RH
services. The recent formulation of integrated
population policies by some state governments is, in
a sense, an expression of this need. Several states
have also realized that community needs should take
precedence over programme needs. Change of this
magnitude cannot be accomplished in a short
timeframe. Realizing this, many state governments
have initiated steps to introduce the change in a
systematic and phased manner. The process of
change has just begun and will probably take a few
more years to achieve the desired results, pnstead
of believing that the TFA or CNA approach is already
in place in the country, GOI should encourage state
governments to develop their own approaches for
assessing community needs and help them to do this
by providing resources and technical assistance until
the new systems are fully institutionalizedj
Review of Implementation of CNA Appion.li lor l-'amily Welfare in India
14
Table 1
Sterilization Performance Based on Service Statistics
Before and After Introduction of the Target-Free Approach
Andhra Pradesh
Bihar
Gujarat
Karnataka
Madhya Pradesh
Maharashtra
Orissa
Rajasthan
Uttar Pradesh
575,728
206,188
301,928
371,535
401,855
582,454
162,085
203,118
516,970
513,127
82,421
241,945
384,056
371,731
518,897
134,825
200,711
266,350
630,043
196,000
241,364
395,624
367,092
571,476
127.046
224,140
307,799
730,976
125,000
250,379
371,275
357,243
532,714
NA
229,295
347,401
298,127
156,186
409,139
376,247
598,012
453,321
193,167
204,765
1,664,021
293,872
222,744
401,436
372,341
617,928
418,711
245,693
224,100
2,029,847
287,190
175,609
413,189
337,854
576,188
402,450
NA
232,685
2,084,468
242,987
43,582
160,123
157,545
494,196
375,537
106,472
484,067
514,525
254,499
56,377
161,914
156,494
560,167
375,187
107,722
402,489
764,044
224,705
44,940
172,980
148,931
577,126
358,821
NA
325,465
722,290
613,013
99,945
1,105.687
358,627
1,761,754
685.855
369.528
720,414
1.769.096
605,137
78,578
824,116
323,021
1.650.486
594,164
255,967
470.874
2.045,682
539,620
98,875
889,990
278,626
1,545,022
586.489
NA
374.345
1.923.835
520,552
264,927
289,054
381,571
384,342
566,168
148,659
168,245
519,399
Table 2
IUD Performance Based on Service Statistics
Before and After Introduction of the Target-Free Approach
Andhra Pradesh
Bihar
Gujarat
Karnataka
Madhya Pradesh
Maharashtra
Orissa
Rajasthan
Uttar Pradesh
338,289
206,551
473,800
299,504
857,822
476,283
193,582
156,060
2,194,522
282,933
269,889
452,180
345,937
797,548
470,630
209,074
168,239
2,193,488
Table 3
Oral Pills Performance Based on Service Statistics
Before and After Introduction of the Target-Free Approach
Andhra Pradesh
Bihar
Gujarat
Karnataka
Madhya Pradesh
Maharashtra
Orissa
Rajasthan
Uttar Pradesh
261,864
65,430
179,025
138,232
476,277
418,194
93,904
92,268
487,250
242,262
67,214
172,920
151,145
511,288
483,269
99,731
125,230
558,509
Table 4
Condom Performance Based on Service Statistics
Before and After Introduction of the Target-Free Approach
Andhra Pradesh
Bihar
Gujarat
Karnataka
Madhya Pradesh
Maharashtra
Orissa
Rajasthan
Uttar Pradesh
1,252,752
194,497
1,292,225
395,108
1,987,146
1,168,747
467,838
475,272
2.897,773
820.163
191,305
1,105,558
374,687
2,004,814
1,163.775
443.483
519.048
2,434.224
Table 5
Summary of Experience in Implementing the TFA/CNA Approach in India
TFAin
1995-96
lamily Welfare in India
Performance
in selected
districts in
1995-96
TFAin
1996-97
Approach
Current
Situation
Selected two
districts.
designed a
comprehensive MIS
but did not
implement the
MIS due to
lack of
positive
response
from GOI
Selected one
district but no
instructions
were given
to the district
officers by
the
Directorate
Performance
declined
considerably
in both
districts
Performance
declined
considerably
Introduced
TFA in all
districts and
also
continued
with the old
system
Introduced
target-free
training in all
districts and
the
department
stopped
targets at all
levels
Selected one
district and
series of
performance
review
meetings
were
conducted to
arrest
possible
decline in
performance
Performance
declined only
by 17 per
cent
Introduced
TFA in all
districts and
conducted
household
surveys with
the help of
health
workers
Selected on
highperforming
district but no
guidance
provided on
what needs
to be done
Selected one
district and
conducted
EC survey
Selected two
districts and
prepared
micro-plans
in one district
and no plans
in the other
Selected one
new district
with weak
infrastructure
and
conducted
EC survey
Performance
of the district
more or less
remained the
same
Performance
of the district
dropped
substantially
Performance
in the
selected
districts
declined
marginally
Performance
declined
significantly
TFA was
introduced in
all districts
and GOI
formats were
modified
considerably
Targets were
abolished in
all districts
but state
circulated
performance
norms per
sub-centre
Abolished
targets but
districts took
Into
consideration
past
performance
to arrive at
ELAs
Abolished
targets and
shifted
programme
implementation
to elected
bodies of
panchayats
Selected two
districts even
before TFA to
provide services
based on
identified unmet
need
Performance
improved
marginally in
both districts
.
.
■
Pregnancybased
approach
and unmet
need
approach
was
introduced in
two districts
in which
targets were
abolished
Performance
declined
considerably
in both
districts
■ s'
State pursued
its own system
of household
surveys to
identify unmet
need. Serving
couples with
unmet need was
the objective
Abolished
targets In all
districts and
family
planning
programme
was delinked
from 20-point
programme
ife
1
Table 5
Summary of Experience in Implementing the TFA/CNA Approach in India
.RalasthanJ?^
PradeSh
Training
was
conducted
after
introduction
Training
programmes
lacked quality
and uniform
understanding
of manuals.
Supervision
of training
nearly absent
Training was
done two
years after
introduction
of the new
approach
CNA
Approach
Introduced in
1998-99 and
workers
were given
training.
manuals and
formats
CNA training
was not
imparted
Completed
training all
Medical
Officers and
workers by
March 1998
Training
conducted
and formats
distributed
Training
conducted and
formats
distributed and
at the same time
completely
modified ECRs
supplied
Current
Situation
Objectives
set in Andhra
Pradesh
Population
Policy are
given more
importance
than numbers
generated
from below.
ELA is based
on
negotiations
with district
officers
Neither is the
old target
system nor
new CNA
approach
based on
client needs
Workload
identified with
CNA formats
was much
higher than
average
annual
performance
of districts.
Districts
compare past
performance
and expected
workload and
arrive at
realistic ELAs
Average
performance
for the past
three years
and
estimates
based on
GOI norms
are
compared
and ELA is
arrive at by
each
district.
Health workers
collect
information with
the help of
ECRs but do not
know how to
utilize the
information. The
collected data
remains
unutilized.
Process
followed to
arrive at ELAs
varied from one
institution to the
other
Training for
TFA system
Training for
TFA system
was not
effective and
done without
systematic
planning
No training In
the first two
years
of new
system
Uttar
■ Pradesh
Training was
conducted in
all districts and
manualsand
formats were
distributed
Training was
conducted but
more to satisfy
GOI than to
introduce the
new approach
•Training was
given for TFA
system - ’.
systematically
with
facilitators
and
guidelines in
place
Four new
formats were
introduced in
addition to GOI
formats and
training
conducted
more
systematically
No training
was given on
CNA approach
No training was
given and the
department
followed its own
approach and
expanded unmet
need concept to
RH services
No training
was imparted
on CNA
approach
New formats
introduced
were not
useful to
calculate ELA.
District tried to
use survey
data to
prepare district
plans but could
not succeed.
Largely
follows a
combination of
old and new
approaches
Most of the
districts follow
the method
specific norms
given by the
state
government.
EC surveys
are conducted
on annual
basis to
identify eligible
couples that
need services
Workers
conduct annual
survey in May to
identify unmet
need for Family
Planning and RH
services.
Workers are
asked to contact
couples with
unmet need and
provide services
based on
method choice
of client
Workers
estimate the
ELA and
consolidated
numbers are
submitted to
Directorate.
Then
Directorate
negotiates
with districts
to arrive at a
number that
is realistic
and
achievable
Training was
imparted and
TFA was
renamed as'
“self determination
of targets
. approach”
Table 5
Summary of Experience in Implementing the TFA/CNA Approach in India
7
uto.-'-.v-
*
.......
<
Monitoring
Systems
Performance
monitoring
systems are
strong with
high level of
political
commitment
Monitoring
systems
were weak
before TFA
and further
deteriorated
after TFA
Performance
monitoring
systems are
in place but
need to be
strengthened
Monitoring
systems are
in place and
no changes
introduced
after TFA
Monitoring
systems are
generally
weak due to
lack of
awareness
among
elected
representatives
about health
systems
Monitoring
systems are
strong for
rural health
institutions
but urban
service
delivery
systems are
weak
Monitoring
systems are
weak mainly
due to
formation a
large number
of new
districts. The
newly formed
districts do
not have
necessary
infrastructure
Monitoring
systems
were
strengthened
further at all
levels
Monitoring of
performance
is weak
largely due to
political
interference
Family
Planning
Performance
Sterilization
performance
improved
considerably
while
performance
of spacing
methods
fluctuated.
Family
planning
performance
of all
methods
declined
significantly.
Family
planning
performance
declined by
5- 10 per
cent for
different
methods over
a period of
three years.
Sterilization
and IUCD
performance
marginally
increased,
oral pill users
remained
same and
condoms
users
declined.
Sterilization,
IUCD and
condom
performance
declined
considerably
and oral pill
performance
improved
significantly.
Sterilization
and IUCD
performance
marginally
declined and
oral pill and
condom
performance
declined
significantly.
Sterilization
and condom
performance
declined but
oral pill and
IUCD
performance
improved
significantly.
Sterilization
and IUCD
performance
consistently
improved but
the oral pill
and condom
performance
fluctuated.
Sterilization
performance
declined by
40 per cent in
1996-97 and
marginally
improved
after that.
IUCD
performance
remained the
same and oral
pill
performance
improved
considerably.
Condom
performance
declined.
ft
C_C
Page 1 of i
From:
2- ■ - r-
Ats-iss
.- ■2 s;,
Sinba <A-Smha@DFiD GOV UK>
.
w§ hay® had son'? mor? deliberations around the proposed Public Report on Health over th® last few months.
: here is oe-haps greater clarity on how ws want to taka it forward I am attaching a revised version of the draft proposal for your suggestions
We look forawrd to your working as part of this group.
Ameneel
Community hteaiui C/c'l ^socnara^^vsrii.com^ Ot/OI/Oo 0! ■*Spm >>>
DearAmarjcct %>-nr.a.
Greetings from Community Health. Ceil!
My apologies for not replying to your mail of '2th November - travel,
iji-heaith ano vnri.-.us cam.-Him.er.?' •.■.rm
nf rhe. rnp.sann if it in
Dr 1 nelma Narayan
Coordinator.
i nis e-iTiaM nas ~een scameQ tor a > vtiuses oy ^<.af iruemet. Tne
Gc”-v’0c is OG’.'-'S’£ '.• oy 'vicoScvcLaijs. ror i'iioic iFnorination on a proacuve
3/18'03
H
ties oj India. where
bui the politica.
•ouiai io
ers io Hie
;c
A’c almost s;
he 1990s.
iea bv n
one ana vv
r
unci'
often limits th;
to wen
'r
ana iocus
by equaling ii
Io irix iah’zalion
!ci of pubb
unt
mu.
f economic inequality hj the 1990s is
is.’ poor
>s ui’alm.’ health care m die absence of
and
focus T]
ii oa the nation on
n
a
rt onJ’
:11 - be;
Health svstem co;
1
■
:
though nromotion of Indian S-*-."stems of Medicine has been
Hie Primap/ Health Svstem does not seem to address the
'•i health needs
camr-azons.
re^istorintz limited success, jeopardise the sustamablc delivery from tlte
hh svsre.m PersisTe.nce of hj?h incidence, of Tuberculosis and Malaria is symptomatic of
the health s"
io deliver health care of satisfactory qualify in a sustainable way. i he
'Tb? r-rrr-^^d Public Report on Health. would like to present an alternative Perspective
based
people's righr to heafrh. i he Riehi to Health is seen as a holistic right Thar focuses on
good health as a means to well- being. While dealins with health in its holistic dimension as a
multi-sectora'i issue, this Report '.viii specially focus on understanding poor people’s perceptions
•.■■f ". ci! - being and health as also the deliver', of health and medical services io the marginalized
and most disadvantaged sections of the society. This has been lite most neglected area so far in
the design ot health policies and programmes.
ITlE i±.A5i
A few mehmmaiv meetings. have been held to develop a team to undertake tins study.
Jeo.n Drez? ■ Development Economist\ K.B. Saxena ■ retired civil servant with interest in
'ip-c'f-i
iss’ies1’' 1
(' Smhvamal? I with considerable field experience m Public
outre for Social Medicine and Communitv Health
Gakar Mittal ■' independent worker with experience in the NGO and development agency
experience, in me iieaim seclor c zkiTi Ahuja ( irom kHSNAA IVfuesoorie with cm mteresi
in health issues'. Thelma Naravan < from the Commtmiiv Health Cell. Bangalore I.
on :■■■-
' also been evinced in working together by Health
Watch. ( rH*. ■ .
the JSA. Pusiipetidra. Dr. Manin Rani ant! Dr. B. Sekhar have also
XV.. .
•
-
■
.?••-
■ -V
_. .
4j.
c ■ ■: 1
: • kkw V '•
CJ.’.V
X ;..tv
ICcUli "ill
continue to into act with more and more people in various states to identify persons who
would like to associate with this work in any manner. As in the case of the Public Report
on Basic Education i PROBE), the Group would seek the support of a large number of
activists. organizations. academics arid institutions in lite course of doing the Report.
Special efforts will be ntade to draw noon the sunnort of field investisators with
.
-
I7c-.SC•.!
c----- -----
••.I
-
1
—-
‘
l-i r i/n
.j r f. ;th
OtllCf fidd
.
SXJPPOK.T FOS. T12E STUlJY7
In the course Oi picliniiiiary discussions. Dr. II. Rxuiiachadniii. Director. Institute oi
■•.
hns in nrineinjf! .'mr^efi in pnn’uie in^jiiJiiionni sunpori for
b
f.f *ni! 2;’’
g
. .
fji he v.’orhsd out in the course of the next few
i.G.
v-iivny.
l.t
J?:
.?wi..
Oj.a.iiiu
ch
c.ki
udv
TA.\fR coukl lie u-eveloped under his leadership. Besides;
ion with identified Faculty at IAMR will enrich the
perspective oi mis :_froup.
uuliv Report Oil ilcClitil IS IO prcseiil I«il alter nallv C
•
p. : <- ; / e a? Me
commodified and productivity~oriented(?)
Rishi io Heahh wnhin a hoiisiic iramework. The reoon will
.'1'
's,S7o
Hjif
- XiC
RutP'; r;f r'-->K?h tqv
---------------------------- ---------------- --
.-•
involving
noiicy optinns
,.r
-i.-• :11
-J. ,J.L- .■-■.'.J j
U; UlvWU^.
»s. r iziziplorinu people s pci'ccpiioiis oi iicaili*i iiiKi Vv'Ciitzcinu and iiicir CiOtcrniinaiiis
Sirj-iikd <>y S128 and gender (and inier-generaiionai •
tsi.nl
-■
■ -
C-Cto’'"T-c*ii’‘Oiicrc-
•” . w* rctioi"!
iHCtig-HvUS and U’loptiihlC syslciiiS
- Source of treatment* Private, public, their profiles.
Primary/secondary, tertiary'
•
Expenditure on treatment — how much and how the expenses were met
nhou*
«.
ul v ■•.
I
z L‘-
• ■
i
1!ness treatmen* /public
and
Private
health
service
•- -* 'i ■
LiStiiig Oi iicaiui Sci’ViCcS duCi SciViCc iJiOVKiCi'S. pliOiiC tiiiCi piiVaiu
Vn c
01 SCrviC-- CfOVldfirS
* <i ‘ z'xxiCii • Jiiiei x OiiC » z kiJ jJi
a
Perceptions of policy makers planners administrators
®
Exploring options lor civil society'professional body led regulation of private
providers ( for ethical practice)
i*r.’FOjtxi’ ■■ !>« 1 »,vii!.■». pei'ccpiiun oi linivss. iticir treatment secKins; oenaciout anu tne iicaith
si'Vicr
>viuc>s as mteiactive and integrated phenomena. The perception oi well being
,,
spr^'ices of the community, is to be viewed in relation
different providers of health care.
The field study would therefore collect data for
objectives a. b c< c. taitiiig districts witliin selected states as the units oi study within each
lieu.
lor. The elicit
.. Himachal Pradesh. Uilar Pradesh. Madhva Pradesh.
liiages Hl
identiiied in the course oi the sur
niiienta!.
'.Vitii
.11
L'td other civil
of
Cotieelina data on perceptions of '.veilbeing, and health, morbidilv and treatment
seekinc in. each of the villaaes and colonies of The urban ooor would be accotnoanied bv
•i irr'-1 of JicslxTi service *^i*oviclei*s resorted to fortruil and informal iVt district level a
h.wmu. •and
lions. both public and pii\ate. can be undertaken. Through
indepm ces< suun^s. provider perceptions regarding health, well being and quality
<cr<i ? '> can ’“••/ ziiciied as web ?> prescribing practices documented.
Rcconsnucimg me process of adoption of Health Sector Reform policies at center
and slate lev el.
-cuiG i:iv
I..
. __ 'RA31i
service
R I HE STUD
1’. is cxdccicg iiiai ilic i>tudv will take between 12-18 mon ills.
i tie R110201 is very tentative and based on the assumption tnal die institutional
narlncTshiH with I AMR will work out. Che Project office could then be located in the
LAMR premises and some of the administrative costs for the study will be lower as
x’Ci.ii
i
i: i>
«JiiC iOi
lilC z kviiii iil • c> ii U Li v C Stall. O1 iC xOi
tllw iv«JSC3i vii bcholaiS. OBC 1O1 Ociivl
entry and rbi meetings Group members, etc.
■ ■> ■
f to be oro^idedbv
1 wc -iden tai expanses
Stationary, library books. POL. Travel reimbursements, etc. As far as possible, train
travel f H ('’:«ss> will be provided for. Total Rs. 5 Lakhs .
I
■< d • > • > ■' ’ nr.
»v‘
iric i iiit/i idl US.
/Li t Ct t
IS Ct/'lCi i\.CDUi! Vi i'l t !>'tQ
4 r e-'.■'" ■■•. ■->.t■■<:■■<. 2 's’< ■.c momm and the other two for 12 months. [wo ot them will
be Senior Research Scholars with emoluments of Rs. 20000 - 25000 per month and two
"c-
' ei’ov.s with emoluments of Rs. 12000 - 15000 per month
The
......'.c..■ > c. .':C <.■■./ • dev ln?.c up specific memes for liicrulurc Survey. N'lcmbcrs of
the- group v. ;11 cifix be paid travel costs, unless they decide to join on a full lime basis.
■~y~ ■?.;?/ OM-’ys'ronj rr, nresettt ftfidillgS of tilt' HliCFO Stlldv tli~d to dssit'll Slll^'SV
workshop. ReQuirement - Rs. r lakhs
Seieciion i.-'.ci
oi Investigators
10 day training programme for 70 investigators - ?7'; Rs. 200 per day ( including travel
costs ) Recniirmenl Rs 1 40 lakhs
nacn iiu vStig.-iior to t>c oaiG ks. B.uOv per month plus t-A/LtA.. Survcv ‘Aork m about 1320 Milages wifi be done bv members of the Core (rroinr Project. Team Members.
fo’?' Reoairement Rs. 10 lakhs.
IVoi'ksnops and s'narin" sessions with Field Investigators
Provision oi lour truexi workshops (onco ^vory six months) mid shoring sessions with
Investigators. Requirement - Rs. 2 lakhs.
■
ivcuiiifcnjcni — Rs. 14 lakhs.
, - - n ■> • . . .' Ml-.'-.'
< j
Liio.
i
-'-»■> .> ■> ’ -. - • ->
«<’
a ( ToCc:. C.s.j
.W.;.:o.
\cC; .-.iai'uru also.
o’ zv
5
c’-y mv
\
•I
. ■• . .■ J
.
-'.xitr«v:
’
-
n«. -5
alikt
.-ran *»<’o i
gCiii
.% t-z-Ii
4 .-\n
uvUHiliia-uvIi
i WO Zv.ss)S;1 arsis Will SiiffiCc
/.’iCn't O-Oii
'
'
r?o
svs■• ii.J s.’irsLrv
\. I. '
c »’> i .-‘Lz v'Li \ i I t» >'<J Oi
. ■■
-
-V-V J;/
C'OSi /
1\jS.
iCiririS.
-■■(Ki -
nviK.
L/xlC
(To he |>< o\ joji 1
■'■/ty.'kshops
■ ■ l
llcivvl
Ke AJ jQ
Co-tvn H-9-h
Page 1 of7
Community Heaiin Cgii
rrom:
To:
uNnIKkIsHnAN m.v. (ur) <unnikru(gjyahoo.com>
<PH,A-Europe@vahooqroups.com>: "Health NOWI" <infoOhealth-now.orq>:
"IPHCWORLDW'DEY" <IPHCWORLDWIDE@yahoogroups.com>: <pha——• «
i
Sent:
Subject:
tOviyi
>
<Pt-In
4
............. •—------------ -
Qrnnn nO.H'^/^i/ahnnnmi
rnm>,- <nha.
r..—
•Q—— • — “ f"——'-xSp-J1—_a. _ _r------- -
11-"
Saturday, June IS, 2004 10:00 Prvi
[pha-ncc] People's Health Movement media coverage: THE LANCET- Volume 363, Number 9426
19 June 2004
—1a*r Ua'b 14-5, n-^4 <*ga jsgjjga nwrr.e-^f-af
f
^r_1...___ oc-> -.r_____ 1____ nnne
in T.__. nnn*
a,
ia ft ft ITT - ------ *M W 'VXM.'V***
W ~* «••••— XMJW.WM.*
< Uiumo UUU, ilUUlLTOl JUJ.V
X» ULUlQ^vi^
1. 2_l._ . f •________ 4.1____ t________a _ _____ /!___________ i >------ o
t £. .11 /11_._ nt: n n> a m.c . .1 Jx - ..! _ 1 __.i ..___!___________ onnr'n 1
LlLUp. I I W WYV . U1C4OUVCL. lUlH/JUUllltU/ VU1OUO/ 10^7140/ 4 Uli/ 11CU1.0UO, 7TZ,U.CUXlUUtU O11U 1CV1CW.477 I V, X
Viewpoint : Robert Beaglehole, Ruth Bonita, Richard Horton, Orvill Adams, Martin McKee
".......... This partnership has iong been neglected, although it did flourish briefly—at
lr,^e*4A^IAVJV 1 ± A WWX
___ 4-lnz- U/'■•*', 14'1", H'z',** All
-r-,
,4 -rv,-,rr1^4- r',rr',,iv, r'n'.l’Y' —,-r.
IAAAV4VA VXX<s AAVCA1.UA.A X X^X X XXX MCAjLlAAVA j XV XXXX^XXV Cl^CAAA X XI ACX 1XV CXX X
.->»-»
imorcssion under the influence of the Fennie's Health Bffove«ient.':>u
A
X
A L*
.
II
g 1 ' rx ‘ 41a
'Fhe practice of public health
Defining public health
The public health response to the global health challenges
Key themes of modern public-health theory and practice
Public health for the new era
References
The world is entering a new era in which, paradoxically, improvements in some health indicators and major
reversals in other indicators are occurring simultaneously. Rapid changes in an already complex global
health situation1,2 are taking place in a context in which the global public-health workforce is unprepared
In rnnfmTif Ihnse <4>Hl1f*Tiges. This luck of nrepHralinn is purity been use the challenges ere terne hti<1
anti tlie faxiuic Lu cvnuvut euiu work wiux vested uileicsts, wlucii piuiuuLC ouu sustain uimcuiuiy ucnavium
patterns.
If public-health practitioners are to ad dress national and global health challenges effective.!v; the way they
v, 4- 4«11« « ;y««4 gg-ZII
«
ft»*Z ftv «
A .-.1 AA h
--f
«« VIA XX CXAXXX rnuxiv TL^:„^„l
U1VXA IIVJXAr AUlUVCAAll.
UV-I UL1VOV VJKAUVUgVO
II AXA IV^UAIA <A AXXCXJWX X V.VZAniJV1H.UUUJ1,
IX
VXVC44 VAOXVIXX VIX
what public health iS, olid what it Cail Oxici, IS ictpiiicu. To be achievable, the ViSiOil illuSt thcil be
comiuuiucuieu not only io its prucuLioiiers, but also to the wider' policy community, whose uctious are
necessary to improve the health of the public. Here, we propose a reformulation of public health appropriate
for the global and national health challenges m this new era.
Approaches to the practice of public health are contingent on time and place. They are distinguished mainly
by the amount of authority vested in the state and their main disciplinary base. Tn terms of state
Involvement and resnnnsibilitv there e_re two extreme annrnnohesr the state medicine model and the market
model. The practice of public health in the USA is an
of the
approach. The p,,yy> of this
model is to limit governmer.t reaper ei hi Hty for public health and to encourage individual responsibility for
i......... i.t. .•________ _____ _______ t
____ it..................................... .t._,i n _________ _________ 1...« ..J11 _____________ J •- -•-..J-’.J.i. ...I..* .1___________ 1-- r.._ .......J.. «v..»
HCCUUl Ull^mvr-uir.l 11, VZA1 U1C 0.00 UAAiy UU11 Ulial. LXXVA UACUnCt will ACOpVAAU IV XX AVAX V XXX UCUO UCAAACUAUD AVA gvrvrvxo UAXtXU
promote health." The state medicine model, by contrast, envisages a strong roie for the state, encroaching in
many areas mat some might, consider private life. A particular version was transposed to the Soviet. Union,
where public health became a central part of state policy, summarised by Lenin’s comment that "if
communism does not destroy the louse, the louse will destroy communism".6 Another version was seen in
China for several decades after the re^/olution of 1949.?
6/2 i /04
1 of 7
Page2 of7
The disciplinary base of public health can be narrow—mainly the medical sciences—or broad and inclusive,
bringing together a wide range of disciplines including the political sciences. The medical model has
traditionally been identified with the UK, where public health was, until recently, regarded as a specialist
branch of clinical medicine.® The broad multidisciplinary approach to public health, sometimes referred to
as the social justice model, has a long tradition in several European countries, beginning with Virchow in
Prxissis. s.t tlic cnrt of tlio lOtH. century, with s. brief
n—e in some universities in Englonii in the
Hxidulc of tile last CciltuLfy.^ TlliS appi’Oadl to public llcaltll 11 aS bccil CSpcCially Su'Oilg iil Latiil Aillti'iCa
since the middle of the last century,10 and has echoes in both the Alma-Ata model of primary health care
and the new public health of the 1980s. The practice of social medicine has tocused on the social and
environmental determinants of health and disease and the effects of social and economic policies on health
status: this approach has rarelv been able to bridge the divide between rhetoric and policy.
▲
The definition of public health has changed as public health has evolved.1 ’ Common to most definitions is a
x«nx« of lh« gHTiHT-Hl public inlcrcxf. h fbc.iix on (lie browder d«(«rTninHTt(x oCbcHKb. wrjd h desire fo improve
the heelth of the entire nooulation. EJerlier definitions olso top*de explicit reference to the o.dministr3.tion of
Vi 05a]rh
services The ^letbors of definitions suggests ths.t o short ?nd succinct definition of public
xlCcxxtxl IS ilCCdcd th. ext io both bl’Gcid 111 SCOpO ckild vif Wide cippOcd*
We suggest that a suitable definition of public health is:
'Collective action for sustained population-wide health improvement"
Tin's defiriilioTi eTnpbexixex (be bwlIrriHrks of publir.-beHlfb prectire: (be forux on hcIi'otjs end in (erven (ions
that need collective (or collaborative or organised) actions;
iMin
?vAin ability (ie, the need to embed policies
ide health improv
The ethical underpinning of public health is of equal importance to its definition,12 but ethical frameworks
for public health 3re new.
Our view of the ethic?] basis for public ben 1th stems from knowledge of the
pervasive cfTect of the onvironmental and sooiueeonumic circumstances that constrain the decisions
uiuivxuucus iucurkC auuut nctuui. mis pOSiuOii auiiulS ulc positive OOuguuOiis Dy ^OVcrniliciits uiiu
communities io protect and improve the health oi all their citizens and is based on trie assumption that all
lives are of equal worth.
* fexp
Ths public-health response to ths global health challenges
To Tackle rhe major global health challenges effectively. the practice of public health wifi need to change, it
is not sufficient to focus only on urgent health priorities, for example, HIV/AIDS, tuberculosis, and malaria
in subSaharan Africa, or the narrowly focused Millennium Development Goals.13 Programmes and policies
are required that respond to poverty—the basic cause of much of tbe global burden of disease—prevent tbe
emerging epidemics of non-communicable disease, and address global environmental change, natural, and
man-made disasters, and the need for -sustainable health development. The justification for action is that
health is botii an end m itself—a human right—as well as a prerequisite for human development. 1B
Public health as practised now is not in a position to respond effectively to these challenges, mostlv because
the capacity of the public-health workforce has not kept pace with changing needs. The neglect of the
niiblic-hewllh infrastriml ure end (lie weakness of many heallh sysfems have compounded Ibis problem. Tn
most developed countries, nuhlic health has nm-mwed fn focus and, to a large extent, is driven by the
_ .
s
r
i
•
• i
i
■ i
j i •
i'i
•
i" i
icocixivii o^cliixd. Gi «iCci<xexIilC cpl<x&iiiiUiUgloi.S culU MlUiiiiJiilCiii oCitlivioto.
17 n
r
i
o
t
i .
no luvlio xi<xo Uxucli Geel! Uli Wxicii
can be meaauml easily, sucll as cholesterol or blood pressure, rather than ml tile immensely mole complex
issues of the broader social forces that also affect health, directly or indirectly, such as economic
transitions. The senism between research and health policy has widened and the focus of health reforms on
clinical services has further marginalised public health.1B The combination of increased attention to
bioterrorism and slowing economic growth, with their inevitable squeeze on public-health research in favour
6/21/04
Page 3 of7
The global health challenges require a workforce with a broad view of public health, an ability to work
collaboratively across disciplines and sectors, and with skills to influence policy-making at the. local,
national, and global levels. In view of the importance of politics to the development of public-health policy.
pv.hlic-hw.lth practitioners should be closely connected with the communities they serve to build the longfr>
fn ctIqVjctI chsllc7^ orr»o T'h/' /*r»rvnmJfy
£lnr'<?r» r>V»a11or»rv/'c mnnrc
if- tirill
be necessary for all members of the health workforce to adopt a public health perspective in their daily
iituvlucS.
* top
Key themes of modem public-health, theory and practice
xViod'cxxx public health has xiVC key LiiCxxxCiS (pcilid), Cavil of wllich IS all CSSelitial featuxe Oi Ixiudcixi publiU-
lieulth practice. Regi’ettably themes ore rareiy reflected in the reality of public-health practice or in public
health educational activities.
Mealth systems leadership
This oversight function is a central feature of efforts to improve the performance of health systems.20 It
requires a long-term perspective and involves several specific activities, the most important of which is
dofining slralegie <1ir«clw>Tls for honlfh systems. DefiTjinn these direefums is m central public-health
responsibility, as is the monitoring of progress towards the designated goals and
of the system. This
requires strong H rm m.from the govern m rm t to act Although man.,r other sectors pla,T a
part, responsibility for the legislative and regulatory framework for public health rests with governments.
Neglected aspects of health system leadership include failures of auVOCaCy Of accountability fui" improving
the health of entire populations, with most ministries of health continuing io focus on immediate issues
pertaining to health care.21
Collaboration in partnership with a wide range of groups from many sectors has been the central feature of
public-health practice since the mid 19th century. At first, collaborative action was justified as a way of
keeping to a minimum the effect of poverty and its associated ill health on earlv welfare systems.
Collaboration. across sectors is even more crucial now. In the
actions, the benefits of public health science will continue to be more fully taken up by the already
advantaged sections of society, as has happened with tobacco control.22
Gov**TTiTr>f*Tils are k«v Io ensuring* collaboraliva Hclionx Io nroTnolf* nonnlHlion-wide benllh iTriT>rov«Tn«Til
because the,r ^re ultimately responsible for the health of their populations. When the state downplays this
pp,--' ^n favour of individualism and market forces, the practice of public health is inevitably vraaken?d,
slowing progress towards health goals. The public-health ’workforce, because of its broad mandate and
skills uaSC, is uniquely placed to impi*OVc health through foi'ulatiOii of policy-led Sti'atcgieS olid delivery of
interventions that embrace collective actions.23
*■-. e*4 e*«4
4 —j «s
q- orvTi—.nil
On the basis of the technical developments in epidemiology from the middle of the last century, public
h«Hll}» Iihn been doTninHled by Ibf* qiiHulilHliva .sciences hI the expense of oilier public bewllb sciences,
Tl
is now recognised that many disciplines are needed to understand the links between the underlying and
or well a s to provide the evidence
policy mailing by use of
appropriate methods to answer appropriate questions to inform policyPublic-health training programmes
should include opportunities 10 study the full range of quantitative and qualitative sciences as well as
related sciences such as public-health law,20 demography, anthropology, and ethnography. Regrettably,
only a few institutions, mostly in developed countries, can offer the relevant courses.
A major ncgiecteu area of research has been the translation of evidence into effective policies and
programmes. Tiiis neglect is exemplified by the failure to capitalise on the compelling evidence trial trie
epidemics of cardiovascular disease are mostly preventable.26 It is rarely appreciated that every year an
6/2 i z04
Page 4 of 7
estimated b*3 million adults jmunger than 70 years die prematurely from cardiovascular dise^s** compared
.•♦I. er r.__ .•11*—
r______ Aino
___ __________ j «..t____ ....i.
•.............__.t. .• ...j /..ii ......
_____> 3 o •
<t
,VIU1 O \J 1U1UXV1X UOauxXO XXVXXX r\X£>K7, XJUOXCUXA, CU1U IUUC1 VU.XMOXO vmxxuxxidx ^<xu txge-gx VILXyoj.
kjCiCIitlllC
knowledge is cleoily only one of flic essential ingr edients of effective public-licaitil practice; knowledge must
be combined with engagement with civii society and social movements to compel effective action by ail those
who can make a difference if we are to achieve sustained improvements in population health.2'
cu^agcxucMt iu public-health pulley
Public-health practitioners need to understand the political nature of the process of developing health policy
HTifi hc| Hrcordniply. Despite the exhorlHlion by Virrhow in 1848 for Tne<1i<’ine Io heroine oolificHl. noblir-
health Practitioners have lon^ neglected, or even rejected, this crucial connection. The reasons for such
exclusion include the myrhea! dnm-nance of public health practice, the pryv.a111ng conser»rative neoliberal
Cv>lo^y cUivi. its effect on hccLitli xCaoIxxio, xaiovaxxiCicnv cXitciitiGix to the politics of public hcaltli in ti'ainmg
programmes, insufficient researcu into the ueterminants of effective policies and programmes, the power of
commercial interests, and above ail, the lack of confidence of many public-health practitioners. Of course,
what is politically feasible is often constrained, but strong pubiic-heaith science and leadership together
with close civil engagement—including working with the media-can shift the boundaries of what is
feasible.28
Community partnerships
Working with and in close association to the many communities being served is the most important of all
pcLx'tncroliipo for public-hccuui px<AK»utiO^Avxo. * xixio j^/cU'tiici'shlp is essential for buildmg tlic long-term
commuixiuy" aixu puxiuicai suppoi l ior CxxvCuve iieaiui policies, m uie sa>r<e Lime it proviu.es an oppox tumuy sor
population groups io negotiate their inclusion in health systems mid to demand the full range of public-
health and health services. This partnership has long been neglected, although it. did
rt______ .’..I.
1__ .‘..Cl..
-.4
I.......... 4 -1.-4------- II-
___________ J.___ 4 I... TT-... l4l. r?_____ All L,,_____________ -'4
.1.4
liic ncaiui rut mi utmiici, il aih^iil
ixociiioii Miicxiy—<a.L icaoi iiictoiivetiiy— unuci
MOMm
im impression under Lite influence of tlie People’s Healtli Movement.
*W
Public health lor the new era
S?fTf'n£r*‘hf‘’T’*^£F
+
nn Y
fxr2. LXAKA.V W.4V rnrj.r)
nn 1-1 z-» IAV1UIV
r-1 r.I.-T' I-ITV-I
<n-r->z-l W.VI.VV
r->n+f\rl V1X) VUXVfc
nn rl
11WAV11
jyilAVvrVV
1 ’f*ni'.XT‘1,0
X1XVCX&X 4-tiz\TTn
UliC.HVO
X> 17-r z-l rrnri M-llV
Lxiat they be xaugxxt bvtlx tv xlcW otudelito cilid tv txxc eXxotixig WvFrifvFCc. A SUppOrliVc xFiixIicVv’vrk xOF pUvxxU
lieoltli requires suviig and responsive government leaueisliip and adequate resources for personnel and
infrastructure, complemented by pubiic-heaith research, teaching, and services that use the full range of
pubiic-heaith sciences.
The reinvigoration of the public-health workforce <rili require —oenmitme^f to its fundamental phiinonpl.tr.pl
underpinning and clearly defined competencies for each of the main themes. It will then be in a better
positivii to auvucate for new resources fo± public-health practice, including atuavtmg a sliaxe of tlie extra
resources tor pruiuulmg health security and from tlie new global healtli funds. Some of these extra
resources should be directed into building the necessary pubiic-heaith infrastructure. Assessing public
health training programmes and ensuring mat new graduates are equipped in the necessary competencies
tor all thematic areas are the responsibility of public-health academics. Only a strong public-health
workforce will be able to respond to the global and national health challenges. Finally, strengthening public
health on an explicit ethical basis and a sound evidence base will promote the role of the state and
contribute, to building democracy worldwide. Health protection of the workers of the Soviet Union. Moscow,
Medgiz. 1947).
Conflict of interest statement
XlSSXXV^ WV1UUVU,
Acknovjledgments
this research had no specinc funding source.
6/2 i /04
Page 5 of?
References
1 Elcagleliole I\, ed. Global public health: a new era. Oxford: Oxfoid University Press, 2003.
2
McKee M, Garner P, Stott R, eds. International co-operation and health. Oxford: Oxford University Press,
2001.
3 WriO. world Health Keport, 2002: reducing risks, promoting healthy life. Geneva: world health
Organization, 2002.
1 The Lancet. The EUs answer to future public healtli challenges. Lancet 2002; 359: 2211.
5 Scutch field FD, Ijist.IM. Public health in North America, Tn Beaglehole R, p.d. Global public health: a new
era. Oxford: Oxford University Press, 2003.
6 Vinogradov NA, strashun Id. Health protection of the workers of the Soviet union. Moscow; Medgiz, 1947.
' Lee L, Lin V, nz<mn R, Ehao H. Public health L, China: histor,r and ccntcnv'orarv rbcUlonrreo tr, Bca^cholc
R, cd. Global public health: a new era. Oxford: Oxford University Press, 2003.
S The Lancet. Putting public health back into epidemiology. Lancet 1997; 350: 229.
9 Forcer D. Changing disciplines: John Ryie and the making of social medicine in twentieth century Britain.
Hist Science 1992; 30: 119-47. |PiibMed|
10 Woitzltin 11, Iriart C, Estrada A, Lomadrid S. Social medicine in Latin America: Productivity and dangers
facing tlie major national groups. Lancet 2001; G33; 315-23. [Text]
11 Hamlin C. The history and development of public health in developed countries. Tn Detels R, McEwen J,
Beaglehole P., Tanaka H, eds. Oxford textbook of public health, 4th edn. Oxford: Oxford University Press,
2002.
12 Wikler D, Cash R. Ethical issues in global public health. In Beaglehole R, ed. Global public health: a
new era. Oxford: Oxford University Press, 2003.
13
Kass NE. An ethics framework for public health. Am u Public Health 2001; 91: 1776-S2. [Pubivied]
14
Roberts M-7, Reich MR. Ethical analysis in nubile health. Lancet 20021 -359: 1055 59. ffextl
15 Sahn De, Stifel DC. Progress toward the millenium development goals in Africa. World
Development 2003; 31: 23-25. [PubMcdl
io Sen A. Development as freedom. Oxford: Oxford University Press, 2001.
17 McMichael A-J. Prisoners of the proximate. Am J Ppidemiol 1999' 149: 887 97. [PuhMedl
18 Beaglehole R, Bonita R. Public Health at the Crossroads: Achievements and prospects. Second edition.
Cambridge: Cambridge University Press, 2004.
19 Bui and Meluida Gules Foundation. 5200 million giant to accelerate research on 'giund vliulleiiges' in
global health, press release, http://www.gaiesfoundation.org/giobal health/announcements (accessed Feb
4, 2003).
20 WUO. World. Health Report, 2000. Health ■oyoterno* iuiprovitDg performance. Geneva: World. Health
6/21/04
- --O- n• nf 7.
21 Milburn A. Tackling health inequalities, improving public health, ttpeecn to the Kacuity of Public Health
Medicine. London: Nov 20, 2002.
lygJ'Lav.lur DA, Proiiltcl S, Sliow M, ct al. Smolmig and health: doos lay epidemiology explain the Lulu ■V'. of
Siuiukuifc ceosatiun among ucpiiveu populations. Ain J Public Health 2003; 93; 2GG-70. [PubMcd |
23 Milin N. Public. Hcwllb in fbe rriHrkel: pH<nng niHTiHged r.Hre. Ihhti government, end benltb dispHrificx, Ann.
Arbor, MI: University of Michigan Press, 2000.
24
McKinlay JB, Marceau LD. A tale of two tails. Am J Public Health 1999; 89: 295.
25
Gustin LG. Public health law xcfoim. Am J Public Health 2001; 91; 13G5-G8. [PubMed]
26
K '5
27
Beaglehole R. Global cardiovascular disease prevention: time to get serious. Lancet 2001; 358: 661PTa-trf-l
• 1 * —~~J
Powles J. Public health in developed countries. In Detels R, McEwen J, Beaglehole R, Tanaka H, eds.
28 Hamlin C. Commentary: John Sutherland's epidemiology of constitutions. hd J Epidemiol
2w2; 31: 915-19. (PubMed'i
Raeburn
29
? S. Putting the public into public health: towards a more people centred
pc*-,'?
approach. In Rcaglcnolc R, cd. Global public health: u. new era. Oxford: Oxford University Press, 2003.
Pconlc’s Health Movement, http://www.pha2000.org (accessed Jan 28, 200'1).
30
++++++++++++++++
Dr.Unnikrishnan PV
Yahoo’ Groups Sponsor
ADVERTISEMENT
Yahoo ■ Groups Links
o
io visit your qroup on the web, qo to:
hucp: /’/ groups . yahoo . com/qroup/pha-ncc/
6/2i/04
Page 7 of7
o
xour use of lahooi Groups is subject to the lahoo! Terms of service.
Go-^n
E PUBLIC HEALTH
.
h - ^-i.
'G
A life-saving order
While pharmaceutical companies try to persuade the government to reduce the number of drugs
under price control, a Supreme Court order directs the government to ensure that the prices of life
saving drugs are kept under strict control.
SIDDARTH NARRAIN
VEN as pressure from pharmaceutical
companies to reduce the number of
drugs that are under price control in India
increased, the Supreme Court, in an order
issued during the proceedings of a pet
ition, said clearly that the government
ild ensure that the prices of essential
life-saving drugs were kept under con
trol. The petition was filed by die All India
Drug Action Network (AIDAN), die
Medico Friends Circle (MFC), the Low
Cost Standard Therapeutics (LOCOST)
and the Jan Swasthya Sahyog. Says Colin
Gonsalves, the advocate representing these
organisations in the Supreme Court: “Any
move to reduce the number of drugs in
the DPCO [Drug Price Control Order]
E
*
will be in contravention of the Supreme
Court order in the K.S. Gopinadi case
where rhe court made an order on March
10, 2003, directing die government to en
sure that essential and life-saving drugs do
not fall out of price control.”
According to the World Health Orga
nisation (WHO), essential medicines are
those that satisfy the priority health care
needs of the population. The medicines
arc selected keeping in mind their public
health relevance, evidence of safety and
efficacy, and cost-effectiveness. Essential
medicines are intended to be available in
the context of a functioning healdi system
at all times in adequate quantities, in ap
propriate dosage forms with assured qual
ity and reliable information, and at a cost
diat the community and individual can
afford.
The history of price control in India
dates back to the Essential Commodities
Act of 1955, which kept a check on prices
of essential commodities including drugs.
In 1979, there was a list of 347 drugs in
the DPCO that were under price control.
Over a period of time, as a result of sus
tained lobbying by the Indian pharmaceu
tical industry, the number of drugs listed
in the DPCO fell to 142 in 1987 and to
76 in 1995. The problem is the absence of
a regulatory agency diat is empowered to
keep a check on the prices pharmaceutical
companies decide on and the profit mar
gins they think are acceptable. The Na
tional Pharmaceutical Pricing Authority
(NPPA), set up in 1997, is supposed to
monitor the prices of drugs to ensure that
A drug store in Bangalore. The criteria for price control in India do not seem to be working. While drugs such as quinine and
primaquinine used to combat malaria do not come under price control, analgin, which is banned in many countries because It
can cause serious blood disorders, is listed as essential.
FRONTLINE, JULY 30, 2004
103
pocket, making price regulation of phar
they do not flout the maximum price al
maceutical products unavoidable.” '
lowed if the}' are under price control.
According to Pharmaceutical Policy
In the European Union (E.U.) and
2002, which is formulated by the Ministry
Australia, governments have tried comple
of Chemicals and Fertilizers, the criteria
menting pharmaceutical licensing proce
for price control of bulk drugs are based on
dures with the ability of a company to
the sales figures of drugs, that is, the Mov
demonstrate the cost effectiveness of the
ing Annual Total value or MAT value of
drug. For example, the Pharmacy Benefits
the drugs concerned. These are calculated
Scheme (PBS) in Australia and die Na
by adding up the MAT values of single
tional Institute of Clinical Excellence
ingredient formulations of bulk drugs
(NICE) in England require companies to
submit evidence of the costs and effects of from the retail store audit data published
by the market research company ORGnew products. In the United Kingdom,
MARG. The idea is to identify bulk drugs
the U.K Pharmaceutical Price Regulation
of mass consumption, which do not have
Scheme (PPRS) regulates profits to a band
enough competition for the market ro
of 17 to 21 per cent on historical capital or
bring down the prices.
the initial capital used to
Bulk drugs are kept un
begin the venture with a
der price regulation if the
25 per cent variation on
the
total MAT value in re
either side. Companies
of
spect of any particular
are free to set prices, pro
bulk drug is more than
vided the rate of return is
Rs.25 crores and the per
within the band. If the
smdes* price
centage share of any of
profits are higher, the
wiii h© m
the formulatprs is 50 per
companies have to re
cent or more or the total
duce profits the next year
cerstirrn'eartiora of
MAT value arrived at in
and if the profits are low
the Supreme
respect of any particular
er, they can raise die
©mart’s orders
bulk drug is less than
prices. In France, Italy
Rs.25 crores but more
amid coimtairy to
and Belgium, prices are
than Rs. 10 crores and
set in relation to relative
the UFA
the percentage share of
cost, prices elsewhere in
government
’
s
any of the formulators is
the E.U., and die contri
90 or more. Since MAT
bution made to the na
CMP.
figures decide which
tional economy.
drugs will go out of price
In India, the author
control, there are many instances of life
ity in charge of drug pricing is not the
Ministry of Health and Family Welfare saving drugs that are not controlled by
drug pricing. According to ORG-MARG,
but the Ministry of Chemicals and Fertil
in March 2001, the life-saving diuretic and
izers. The Government of India appointed
anti-hypertensive, frusemide, had a total
the Committee on Drug Pricing in 1999;
MAT value of Rs.9.48 crores and though
its members included representatives from
the leading brand Lasix manufactured by
the pharmaceutical industry, the Secretary
of the NPPA, the Drug Controller of India Avantis had a market share of over 97 per
and the Secretary to the Ministry of cent, it escaped price control.
A cursory look at the drugs that are on
Chemicals and Fertilizers. In its summary
the DPCO shows that the criteria for price
recommendations, the Committee said:
“...In most other countries the regulation control are not working. While drugs such
of drug prices is considered necessary to
as quinine and primaquinine used to com
bat malaria do not come under price con
contain public expenditure due to the gov
trol, analgin, which is banned in many
ernment’s role in funding social health and
countries because it can cause serious
insurance schemes that cover hospital and
blood disorders, is listed as essential. Says
out-parient drugs.... In these countries, a
substantial portion of the popularion is Amit Sen Gupta, co-convener ofJan Swascovered through health insurance and thya.Abhiyan, a network of organisations
that works in the area of health: “The crite
public health schemes. As a result, con
ria for drug pricing have little to do with
sumers are not affected direcdy by the high
the country’s health policy, the availability
prices of drugs or the high costs of medical
of health care or the diseases that are preva
services but are made to pay for the in
lent. For example, tuberculosis often leads
creased costs through a high insurance pre
to complications when patients do not
mium. As opposed to this, a substantial
comply with the prescribed regimes for
portion of the population in India is mar
treatment because drugs are not available
ket-dependent and have to meet all their;
to the patient. When this happens, second
expenses on this account out of their own
104
and third line drugs are used, but none of
these are under price control.”
Says S. Srinivasan, from LOCOST, a
Vadodara-based trust that manufactures
low-cost drugs on a no-profit basis, “If one
looks at drug prices in terms of wages, that
is, if you look at the costs of drugs for a
person earning a minimum wage of Rs.60
in a State like Chhattisgarh, she/he has to
spend one month’s salary to afford immu
nisation for hepatitis A and nearly one and
a half month’s salary to afford treatment
for tuberculosis. The difference between
the prices of the Tamil Nadu Medical Ser
vices Corporation (TNMSC), set up to
ensure the availability of essential drugs, to
government medical institutions in the
Stare, and those charged in the market is
glaring. For instance, the daily cost of
treatment of tuberculosis using the least
expensive brands available in the markers
Rs.7.70 while the TNMSC rate is
Rs.2.49.”
Pharmaceutical companies have been
arguing that the number of drugs on the
DPCO should be reduced as adequate
competition will ensure reasonable prices.
But a close look ar the prices of drugs
shows that dais is not true. Often, the topselling brand of a particular category is also
the higher priced one; in other words, the
brand leader is often the price leader too.
Says Anurag Bhargav, a founding member
of the Jan Swasthya Abhiyan and a physi
cian: “If true competition and free market
characteristics were present, the brand
leaders that would sell the most would be
the lowest priced. In reality, the brand
leader is often the highest priced. For ex
ample, cefuroxime, a broad-spectrum anti
biotic, produced under the.brand name
ceftum, is priced the highest although the
brand has a share of 38 per cent, the
est in the market.”
Although Finance Minister P. Chi
dambaram has indicated that the govern
ment will reduce the rigours of price
control where it has become counter-effec
tive, reducing the number of essential
drugs on the DPCO will not only be in
contravention of the Supreme Court’s or
ders but also be contrary to the United
Progressive Alliance government’s Com
mon Minimum Programme, which has
promised to “take all steps to ensure the
availability of life-saving drugs at reason
able prices”. The government also has to
worry about the coming into force of
trade-related aspects of intellectual proper
ty rights or TRIPS in January 2005, which
will mean that the generic equivalents of
all drugs patented from that date onwards
can no longer be produced in the
country. ■
FRONTLINE, JULY 30, 2004
*
Go
H - T I•
■ PUBLIC HEALTH
An unhealthy trend
The quality of public health care delivery in India remains woeful while the private health care sector
attains impressive heights thanks to the government's privatisation drive.
ASHA KRISHNAKUMAR
A
RECENT story in 77;r
1 \.Po$t narrated how 53-year- old Ho
ward Staab travelled al! the vav from
Institute and Research Centre tb" «•. ■ .e ..a a!
operation that saved him from a ’in- 2. ... ■
enir.g heart problem Thu proc.tG :• ; <
Imk Si0.000. a mere ' per cent <
WP*ould have had to pay bad: md.<
some 23,000 primary health centres
(PHCs) 1,37,000 sub-centres and 3,000
community health centres, serving the
semi-urban and rural areas. Bur, according
to Ravi Duggal of the Centre for Enquiry
into • i .^Jth and Allied Them.is (CEHAT),
xri •
■ ihh at:a<count > 70 percent
pri.m .; awdicai care and 'l0 er cent of
•’
■ in India. 1: ..
ws 80 per
;onnel. In
•
of rhe .\« : :v<- _■! Health
.
50 crores
(Rs.
bdlion), while ti
sector
spent Rs.69,000 crores.
C liina, with which India is often com
pared. spends 2 per cent ol its GDP on
health; even Nepal (1.5 pur cent), Bangla
desh (1.6 per cent) and Pakistan (1 per
cent) spend more on public health than
Staab is but one of the 150,000 fowig-p who visited India last year seeking urnnp
arively cheap medical solutions, “if we dthis, we cm heal die world,” Apollo Hospi
tals' rounder-chairman Dr. C. Prarhap
Reddy said. But who will heal die people of
India, while the country waits for the
crumbs from medical tourism, which is
projected to grow into a
S2.2 billion industry by
2012?
The United Nations
Development Programme’s
(UNDP) latest Human De
velopment Report (HDR)
puts India’s public spend
ing on health among the
lowest in the world - S4 a
person a year or 0.9 per cent
GG".
of its gross domestic prodA(GDP). Of the 175
Smtries documented by
the HDR, only four have a
lower public spending on
health than India.
In sharp contrast, India
ranks an impressive 18th in
private health care spending
(4.2 per cent of GDP). The
contrast is so stark for very
few countries.
India’s health care sys
tem, comprising govern
ment and private sectors,
barely covers half its pop
ulation. The public sector
health infrastructure has
about five lakh doctors, 7.4
lakh nurses, 3.5 lakh chem
ists, 15,000 hospitals and
8,70,000 beds. It is a threetier structure comprising
FRONTLINE. DECEMBER 3, 2004
At a government hospital in Bhopal.
India in percentage point terms. In the
matter of basic health care infrastructure
and facilities, the country is far behind in
ternational standards. It has 94 beds per
100,000 people, compared to the World
Heal th Organisation norm of333. Accord
ing to some estimates, there are only 43
doctors for 10,000 people in India; exclude
the private sector and it becomes an abys
mal 1:30.000. Government hospitals need
at least 40,000 more doctors and a large
number of paramedics.
The demand-supply gap for public
health care delivery is large and on the rise,
and this gap is increasingly being filled by
private health care institutions. The urban
health care industry is booming, with a
host of private hospitals offering state-ofvices for die rich and die
the-art scrmiddle class. A 2002
study, “Health care in In
dia: The Road Ahead” by
the Confederation of In
dian
Industry
and
McKinsey & Company,
put the total value of the
health sector in India at
over Rs. 1,500 billion or 6
per cent of GDP. Of this,
15 per cent is publicly fi
nanced, 4 per cent is fi
nanced through social
insurance, 1 per cent
through private insurance
and the remaining 80 per
cent is out-of-pocket user
fees. Two-thirds of all us
ers fall into the last cate
gory, and 90 per cent of
them are from the poorest
sections. National data re
veal that 50 per cent of the
bottom quintile sold assets
or took loans to access pri
vate hospital care. An an
nual interest rate of 1,200
per cent on loans is not
uncommon; hence many
poor people end up in the
vicious cycle of bonded
ness, from which they do
not dream to escape dur
ing their lifetime - or even
123
over generations.
Says Union Health Secretary J.V.R.
Prasad Rao: “With health funding being so
low, the government can either hind doc
tors or get medicines or provide support
senices. Not all of these.” In its Common
Minimum Programme, the United Pro
gressive Alliance (UPA) government has
promised to spend 2 per cent of GDP on
health. So far, it has not indicated from
where the funds would come nor how they
would be spent. But a Health Ministry spo
kesperson has said that the emphasis would
be on enhancing public-private partnership
to improve health care delivery. Says Dr.
Rama Vaidyanathan Bam of the Jawaharlal
National University’s Centre for Social
Medicine and Community Health: “In its
1947 resolution, the government proposed
to spend 12 per cent of GDP or hedrl
every year. Even in the best of da;. -. it : .
never been anywhere close to this figiu.
The quality of public health
■. de i.
ery is woeful. The health ca/e svsrcm
only cash-strapped but also fiaug'-t vMinefficiency, it is prone to misj-.v, c. ■
abuse. According to Dr. K. Nagarai, Seni- •:
Professor, Madras Institute of Dcvekoment Studies, Chennai, comprehensive
public health care system is to be provided
with PHCs at the base and referrals to pro
vide secondary and tertiary care. Bur the
system is hardly effective, making compre
hensive health care delivery impossible.
First, the system of primary health care is
only an infrastructural intervention that
does nor take into consideration the local
needs. Second, the referral system almost
never works owing to infrastructural prob
lems such as lack of medical professionals,
medicines, transport and so on. According
to him, the situation is only worsening with
the government’s privatisation drive.
In a survey of 100 Rajasthan villages,
researchers from the Massachusetts Insti
tute of Technology and Princeton Univer
sity found an absenteeism rate of 44 per
cent among medical professionals in public
clinics. The absenteeism was cited to be
because of meetings and other work-related
problems. Apart from that, the PHCs re
mained closed half the time. Most rural
PHCs did not have running water, electric
ity or emergency medicines, leave alone
phones or vehicles. Some did not even have
routine medicines to treat children for fe
ver, cough and the common cold. The sur
vey showed that 65 per cent of households
in India go to private hospitals for treat
ment while only 29 per cent use the public
medical, sector. Even among poor house
holds, only 34 per cent used PHCs. They
are increasingly turning to amateur private
“doctors” and frith healers, even to treat
124
such infectious diseases as tuberculosis (TB)
and malaria.
According to Nirupam Bajjpai, Senior
Development Adviser and Director, South
Asia Programme Centre on Globalisation
and Sustainable Development, Columbia
University, the resurgence of communica
ble diseases such as malaria and TB in India
is partly because of the low levels of public
expenditure on health care and the com
mercialisation of medical care. The country
accounts for a third of the TB incidence
globally and has the largest number of ac
tive TB patients. An estimated 20-30 mil
lion episodes of malaria occur in India each
year, mortality on account of malaria is the
highest in India. Profit-oriented curative
care is therefore on rhe rise, 80 per cent of
which is in the private sphere. This has
: isvlted in spiralling medical care costs and
!'j.a! indebtedness.
Tuberculosis is the bit: kilk= Haiming
'
0»0( 0 live
• •
Mil? Shiva of the Vo'urtai • ■
ation of India: “Medical
' a<
as the second major cause
indebted
gcd.
,s
in rhe country next to dowiy."
Public health care spending has been
systematically shot down since rhe early
1990s with health care reforms following
die polity of structural adjustment. Even if
not explicit, the 2002 National Health Pol
ity’s support and encouragement to the pri
vate health sector further accentuated the
gradual withdrawal of the state from the
responsibility of public health care. The
state offers subsidies, loans, tax waivers and
other benefits for the setting up of private
practice, hospitals and diagnostic centres.
While about Rs. 10 lakhs (at current prices)
of public money is spent on the education
and training of each doctor, over 80 per
cent of those who pass our of public med
ical schools either joins the private sector or
migrate abroad. The country loses
Rs.4,000-5,000 million every year as a re
sult of such migration. The private health
sector has grown into a giant - in fret the
largest in the world - thanks to die support
of die state. Its mammoth size notwith
standing, this sector has remained com
pletely unregulated.
Says Ravi Duggal of CEHAT: “All over
the world there is a tendency to move to
wards more organised national healdi sys
tems and an increased share of public
finance in healdi care. Several countries
have universal health care systems where
the public sector’s share of the fiscal burden
is 60-100 per cent. This trend is inevitable
in the pursuit of equity and universal cov
erage.”
But what of health care coverage for
workers in the organised sector in India? Of
the 400 miUion employed people in the
country, hardly 28 million are in the orga
nised sector and covered by comprehensive
social security legislation, including social
health insurance. The largest of this is the
Employees State Insurance Scheme (ESIS),
which covers eight million employees; in
cluding their family members, it provides
health security to 33 million people In
2002-03, the ESI Corporation spent Rs. 12
billion (Rs. 1,200 crores) on health care for
its member-beneficiaries, averaging Rs.365
per capita. This effectively covers a mere 3.2
per cent of the population. About 0.5 per
cent of the population is covered through
the Central Government Health Scheme
(CGHS), which spends Rs.2 biltat
(Rs.200 crores) averaging at Rs.450
beneficiary.
According to Ravi Duggal, while these
social insurance plans have been around for
• long time, dieir credibility is now ar stake
owing to the large-scale outsourcing to the
private sector. For instance, in large cities,
die ESIS has panels of private doctors, who
provide ambulatory care to those covered
under the scheme. Similarly, under the
CGHS, the beneficiaries have the ‘choice’
of accessing private health care, with die
cost reimbursed. A senior bureaucrat can
get reimbursement for a bypass surgery up
to a maximum amount of Rs. 150,000. To
tally, less than 5 per cent of the population
has some form of social insurance cover for
health through employment.
Says Ravi Duggal: “The limited social
insurance coverage is also declining and get
ting privatised. There is a systematic decline
in the role of the state in public he^^
finance. This is conrraiy to the experie^?
elsewhere, which shows that universal ac
cess to health care can only be achieved
with financing mechanisms that are largely
of a public nature such as social insurance,
tax revenues or a combination of these.”
Experts argue that even from the point of
view of economics - labour hours lost and
productivity decline resulting from sickness
and disease - diere is a strong case for pro
viding public health care.
Clearly, seen from die social, economic
or political perspective, there is an urgent
need to universalise access to basic health
care and social insurance. This needs appro
priate legislation and a constitutional man
date. By generating the political will to
achieve diis end and activating civil society
to demand health care as a right, the coun
try can take positive steps to strengthen
public health care services. ■
FRONTLINE, DECEMBER 3, 2004
Cor-A H -
traditional Systems of)-' ,....'.
Medicine and Public frteaith j?1
ii
i
Status of Acceptance of Traditional Systems
this is limited to a few clinics, which have been
Although, the use of indigenous (traditional) sys
opened in Central Government Hospitals in Delhi.
tems of medicine is widespread and growing, there
ners or the public health community in the efficacy
Increasing use of herbal medicine and food
supplements
of the systems or the drugs. Coordination between
WHO, Geneva have reported that in 1998, 60 per
Alternative and Complementary Systems, as they
cent of the Australian population used alternative
has been little faith expressed by medical practitio
are called in different parts of the world, and the
medicine and 17000 herbal products, accounting for
conventional medical care (Allopathy) has not been
one billion Australian Dollars, have been registered.
organized so far except for a few minor examples.
In Belgium, according to a 1998 poll survey, almost
Most of the people who avail of alternative medi
40 per cent of the population have used comple
cal care, whether in India or abroad, are not re
mentary medicine and 59 per cent of doctors are
ferred by allopathic physicians but are mostly self
also using this, and in particular homeopathy medi
referred. According to a paper on Medical Malprac
cines. In France 49 per cent of the people have used
tice Implications of Alternative Medicine, published
complementary medicine and homeopathy. Herbal
in the Journal of the American Medical Association
medicines are particularly popular. According to the
in November 1998, the improvement in the quality
WHO the global market for medicinal herbs and
of care has been frustrated by long-standing pro
herbal products is estimated to touch US$ 5 tril
fessional rivalry between organized medicine and
lion by 2050.
non-allopathic health practitioners.
In the above
journal, it was also reported that financial analysts
have suggested that consumer spending on alterna
tive medicine may have surged to 69 per cent since
1989, and the market may be growing as fast as 30
per cent annually. Employers and insurers, includ
ing several major managed care organisations such
as Oxford Health Plans and Health Net, have re
cently begun to respond to this demand by adding
alternative therapies to their insurance products.
Some State legislatures in the US have enacted laws
that require health insurers to include alternative
treatments in the benefits they cover.
El
In Germany, there are 10,000-13,000 alternative
medicine practitioners and 75 per cent of the
physicians use complementary medicine. In the
United Kingdom, 90 per cent of the population
use complementary medicine and there are 8000
non-allopathic practitioners. In the United States,
a National Follow-up Survey has shown that, use
of alternative therapies have increased from 4(1
per cent to 42 per cent and
the growth is expected to
increase to 60 per cent.
In India, the Central Government Health Scheme
Indian Systems of Medicine
already extends reimbursement to government ser
The Indian Systems of Medicine (ISM) as referred
vants who prefer to avail of treatment under the
in India covers systems which originated in India as
indigenous systems.The increasing popularity world
wide of complementary, alternative, indigenous or
well as from other countries and got assimilated
over the course of time. These systems are
traditional medicine reflects the changing attitudes
Ayurveda, Siddha, Unani, Yoga & Naturopathy. Ho
and needs of the population. While in the US, 60%
meopathy, originated in Germany, is also covered by
of Medical Schools have begun to teach about al
the newly created Department of Indian Systems
ternative medical practices, in India, the Medical
Council of India, shuns the idea of even introduc
of Medicine & Homeopathy under the Ministry of
Health & Family Welfare in the Government of In
ing an introductory course. Again, in many hospi
dia, which has recognized these systems as they
tals abroad, while conventional and integrated medi
have to be differentiated from unrecognized systems
cine programmes are offered side by side, in India,
and folk medicine.
HEALTH FOR THE MILLIONS / May - June 2000
Ayurveda
and India. It has its origin in 5,h & 4lh Century B.C.
The documentation of Ayurveda is referred in the
under the patronage of Hippocrates and Galens of
Vedas (5000 B.C.). Ayurveda was comprehensively
Greece. (377-460 BC).The System is well documented
documented by Charak Samhita and Sushruta Samhita.
in the Quanum or Medical Bible and the writings of
According to Ayurveda, Health is considered a pre
Al Razi (850-953 AD). The system is based on the
requisite for achieving the goals of life, dharma, artha,
humoural theory i.e., presence of blood, phlegm, yel
kama & Moksha (salvation). Ayurveda takes an inte
low bile and black bile and the temperament of the
grated view of the physical, mental, spiritual and so
person is analysed as sanguine, phlegmatic, choleric
cial aspects of human beings. The philosophy of the
and melancholic. The system has had special success
physical, mental, spiritual and social aspects of human
in treating malaria Jeucoderma, filaria, live disorders,
beings.The philosophy of Ayurveda i.e., the 5 elements
jaundice, eczema, metabolic disorders and arthritis.
theory representing Tridosha vi.,Vata (Ether+Air),
Pittta (Fire) and Kapha (Water+Earth) covers the
Homeopathy
physical entities known as the 3 humors. The mental,
Homeopathy is a specialized method of drug therapy
spiritual attributes are described as Satva, Rajas and
curing a natural disease by administration of drugs
Tamas constitute human temperament (prakrati) and
which have been experimentally proved to process
personality. Ayurveda considers the human being as a
the power of producing similar artificial symptoms on
combination of three doshas, (Panch-indriyas) with
healthy human beings. In late 1700, a German Physi
sensory and motor functions, Mind (Manas), intellect
cian, Dr. Hahnemann examined this observation, dis
(Budhi) and Soul (Atman). The doctrine of Ayurveda
covering the fundamental principles of what has now
aims to keep these structural and functional entities
become Homeopathy. In Homeopathy, it is claimed
in a functional state of equilibrium which signifies good
that symptoms are capable of producing artificial
health.Any imbalance due to internal or external fac
symptoms on healthy individuals which can cure the
tors causes disease and restoring the equilibrium
same symptoms encountered in the course of natu
through various techniques, procedures, regimen, diet
ral disease. In treatment, primary emphasis is given to
and medicine signifies the treatment. In Ayurveda, di
increasing the defense mechanism of the individual
agnosis is done by questioning and by undertaking 8
through a holistic approach and treatment is directed
investigations including pulse, urine, faeces, tongue,
to correcting the imbalances in the immune mecha
eyes, visual/sensual examinations and inference.
nism. In this system, the choice of medication is sel
Ayurveda considers the human being as a microcosm,
dom identical although the disease may be the same.
for
treating each individual as separate, keeping in mind
Homeopathy has definite and effective treatment
the condition of the body, mind, temperament, sex,
chronic diseases such as diabetes, arthritis, bronchial
age, metabolic fire, work-rest pattern, sleep pattern
asthma, immunological disorders, behavioural disor
and diet.
ders and mental disorders.
Siddha
Yoga
The Siddha System is practised in the State of Tamil
Yoga is a way of life and consists of 8 components
Nadu in India. The diagnosis of the disease besides,
namely restraint, observance of austerity, physical
identifying the causes also examines the study of the
pcstures, breathing exercises, restraining the sense or
voice, colour of the body, tongue, status of the diges
gans, contemplation, meditation and samadhi. These
tive system and the person as a whole, as well as the
steps are believed to have a potential for the improve
disease. The Siddha System places emphasis on the
ment of physical health by encouraging better circu
patients environment, prevalent meteorological con
lation of oxygenated blood in the body, retraining the
siderations, age, sex, race, habits, mental frame, diet,
sense organs and thereby psychosomatic disorders/
appetite, physical condition and the physiological con
diseases and improves an individual’s resistance and
stitution. The Siddha system has been found to be
ability to endure stressful situations.
effective in treating chronic cases of liver, skin diseases,
anaemia, peptic ulcer and prostate.
Naturopathy
Naturopathy is not only a system of treatment but also
Unani
a way of life. It is often referred to as a drugless therapy.
The Unani Systems of medicine is a well-defined
Special attention is being given to eating habits using only
medical science and has grown out of a fusion of
natural, mostly uncooked food (fruits and vegetables,
devices, thought, experience and documentation de
adoption of purificatory practices, use of hydrotherapy,
rived through nations and countries with an ancient
cold-packs, mud-packs, baths, massage and a variety of
cultural heritage viz., Egypt, Arabia, Iraq, China, Syria
methods/measures to tone up the system, increase en
HEALTH FOR THE MILLIONS / May - June 2000
ergy levels aimed at producing a state of good health
for preserving the classical traditions and systemati
and happiness. It has many proponents among all chronic
cally using Ayurveda. Under the Unani System, 12 up
patients who found relief and sometimes cure where
graded Departments provided Postgraduate education.
conventional treatment failed.
A National Institute for Unani is under establishment.
Infrastructure available in India for ISM
& Kashmir and Uttar Pradesh.The Siddha System has
Unani has wide acceptance in Andhra Pradesh, Jammu
There is a vast parallel infrastructure available for ex
7 Post-graduate Departments and two undergradu
tending health services through the six indigenous
ate colleges. A National Institute for Siddha is pro
non-allopathic systems of medicine. There is a sepa
posed to be established. Undergraduate and Post
graduate Colleges as well as a National Institute of
rate Department of Indian Systems of Medicine & Ho
meopathy at the National level, headed by a Secre
Homeopathy are also functioning throughout the
tary to the Government of India with supporting tech
country.There is a high degree of acceptance for Ho
nical and administrative staff. With the establishment
meopathy in Maharashtra, Bihar, Tamil Nadu, Uttar
of a full fledged Department of Indian System of Medi
Pradesh, West Bengal and Orissa.
cine & Homeopathy, all these systems are receiving
undivided attention and are being actively propagated
Research and Development
and utilized in the delivery of health care. Emphasis
In the year 1969, the Government of India established
a Central Council for Research
is being placed on standard edu
cation, training and research. Sev
in Indian Medicine and Home
eral measures are being intro
opathy which was subsequently
duced to standardize the drugs
reorganized into separate Re
and establish their safety and ef
search Councils for Ayurveda
ficacy. In the States and Union Ter
and Siddha, Unani, Homeopathy
ritories, there are separate Direc
and Yoga & Naturopathy.The re
torates for dealing with these sys
search programmes being un
tems. In some of the States, there
dertaken by these Councils are
are separate Ministers for Indian
broadly categorized into Clinical
Systems & Homeopathy also. At
Research including Community
present, there are about 587,536
Health Care Research; Drug
practitioners of traditional medi
Research, covering Survey and
cines and homeopathy. There are
Cultivation of Medicinal Plants,
3,862 hospitals and 22,104 dis
Pharmacognosy, Phygto-chemistry,
pensaries in the Government
Pharmacology,Toxiocology, Drugs
Sector. In addition, there are a
Standarization, Literary Research
large number of other hospitals
for revival of the ancient classical
and dispensaries run by non-gov
literature and a Reproductive and
Child Health Programme, cover
ernmental agencies.
ing ante-natal and post-natal care
Education and Availability
of Practitioners in India
and the development of contra
ceptive drugs.
The education (under-graduate &
post-graduate) in the traditional
systems
of
medicine
i.e.,
' u a ii il u v
Ayurveda, Siddha, Unani and Homeopathy are regu
lated by the Central Councils for Indian System of
Medicine and Homeopathy.There are more than 300
Colleges of ISM & H conducting 5-1/2 year degree
courses. In addition, 45 Ayurvedic Colleges impart
The research findings are also
■publicised through the Councils
publications and periodicals.
Specialised monographs on the outcome of Clinical
Research, Drug Research and Literary Research have also
been published. The Research Councils can also be ac
cessed on E-mail at the following addresses:
Post-graduate Training, 3 major Institutions at the
Central Council for Research in Ayurveda & Siddha
Gujarat Ayurveda University, Jamnagar, Institute of
(CCRAS) ccras@del6.vsnl.net.in
Medical Sciences, Banarash Hindu University and the
National Institute ofAyurved, Jaipur, also impart Post
graduate Training and officer Doctoral Courses. The
Central Council for Research in Unani Medicine
(CCRUM) ccrum@del3.vsnl.net.in
largest number of practitioners are in Madhya Pradesh.
Central Council for Research in Homeopathy
Rajasthan and Uttar Pradesh. Kerala is also well-known
ccrh@del3. vsnl.net. in
HEALTH FOR THE MILLIONS / May - June 2000
C®mH' 'v').
Status of Acceptance of Traditional Systems
this is limited to a few clinics, which have been
Although, the use of indigenous (traditional) sys
tems of medicine is widespread and growing, there
opened in Central Government Hospitals in Delhi.
has been little faith expressed by medical practitio
ners or the public health community in the efficacy
of the systems or the drugs. Coordination between
Increasing use of herbal medicine and food
supplements
WHO, Geneva have reported that in 1998, 60 per
Alternative and Complementary Systems, as they
cent of the Australian population used alternative
are called in different parts of the world, and the
medicine and 17000 herbal products, accounting for
conventional medical care (Allopathy) has not been
one billion Australian Dollars, have been registered.
organized so far except for a few minor examples.
In Belgium, according to a 1998 poll survey, almost
Most of the people who avail of alternative medi
40 per cent of the population have used comple
cal care, whether in India or abroad, are not re
mentary medicine and 59 per cent of doctors are
ferred by allopathic physicians but are mostly self
also using this, and in particular homeopathy medi
referred. According to a paper on Medical Malprac
cines. In France 49 per cent of the people have used
tice Implications of Alternative Medicine, published
complementary medicine and homeopathy. Herbal
in the Journal of the American Medical Association
medicines are particularly popular.According to the
in November 1998, the improvement in the quality
WHO the global market for medicinal herbs and
of care has been frustrated by long-standing pro
herbal products is estimated to touch US$ 5 tril
fessional rivalry between organized medicine and
lion by 2050.
non-allopathic health practitioners.
In the above
journal, it was also reported that financial analysts
have suggested that consumer spending on alterna
tive medicine may have surged to 69 per cent since
1989, and the market may be growing as fast as 30
per cent annually. Employers and insurers, includ
ing several major managed care organisations such
as Oxford Health Plans and Health Net, have re
cently begun to respond to this demand by adding
alternative therapies to their insurance products.
Some State legislatures in the US have enacted laws
that require health insurers to include alternative
treatments in the benefits they cover.
in Germany, there are 10,600-13,000 alternative
medicine practitioners and 75 per cent of the
physicians use complementary medicine. In the
United Kingdom, 90 per cent of the population
use complementary medicine and there are 8000
non-allopathic practitioners. In the United States,
a National Follow-up Survey has shown that, use
of alternative therapies have increased from 4
per cent to 42 per cent and
the growth is expected to
■
4
increase to GO per cent.
In India, the Central Government Health Scheme
Indian Systems of Medicine
already extends reimbursement to government ser
The Indian Systems of Medicine (ISM) as referred
vants who prefer to avail of treatment under the
in India covers systems which originated in India as
indigenous systems.The increasing popularity world
well as from other countries and got assimilated
wide of complementary, alternative, indigenous or
over the course of time. These systems are
traditional medicine reflects the changing attitudes
Ayurveda, Siddha, Unani, Yoga & Naturopathy. Ho
and needs of the population. While in the US, 60%
meopathy, originated in Germany, is also covered by
of Medical Schools have begun to teach about al
the newly created Department of Indian Systems
ternative medical practices, in India, the Medical
of Medicine & Homeopathy under the Ministry of
Council of India, shuns the idea of even introduc
Health & Family Welfare in the Government of In
ing an introductory course. Again, in many hospi
dia, which has recognized these systems as they
tals abroad, while conventional and integrated medi
have to be differentiated from unrecognized systems
cine programmes are offered side by side, in India,
and folk medicine.
HEALTH FOR THE MILLIONS / May - lune 2000
Ayurveda
and India. It has its origin in 5,h & 4'1' Century B.C.
The documentation of Ayurveda is referred in die
under the patronage of Hippocrates and Galcns of
Vedas (5000 B.C.). Ayurveda was comprehensively
Greece. (377-460 BC).The System is well documented
documented by Charak Samhita and Sushruta Samhita.
in the Quanum or Medical Bible and the writings of
According to Ayurveda, Health is considered a pre
Al Razi (850-953 AD). The system is based on the
requisite for achieving the goals of life, dharma, artha,
humoural theory i.e., presence of blood, phlegm, yel
kama & Moksha (salvation). Ayurveda takes an inte
low bile and black bile and the temperament of the
grated view of the physical, mental, spiritual and so
person is analysed as sanguine, phlegmatic, choleric
cial aspects of human beings. The philosophy of the
and melancholic.The system has had special success
physical, mental, spiritual and social aspects of human
in treating malaria, leucoderma, filaria, live disorders,
beings.The philosophy of Ayurveda i.e., the 5 elements
jaundice, eczema, metabolic disorders and arthritis.
theory representing Tridosha vi.,Vata (Ethcr+Air),
Pittta (Fire) and Kapha (Water+Earth) covers the
physical entities known as the 3 humors.The mental,
Homeopathy is a specialized method of drug therapy
spiritual attributes are described as Satva, Rajas and
Tamas constitute human temperament (prakrati) and
which have been experimentally proved to process
Homeopathy
curing a natural disease by administration of drugs
personality. Ayurveda considers the human being as a
the power of producing similar artificial symptoms on
combination of three doshas, (Panch-indriyas) with
healthy human beings. In late 1700, a German Physi
sensory and motor functions, Mind (Manas), intellect
cian, Dr. Hahnemann examined this observation, dis
(Budhi) and Soul (Atman). The doctrine of Ayurveda
covering the fundamental principles of what has now
aims to keep these structural and functional entities
become Homeopathy. In Homeopathy, it is claimed
in a functional state of equilibrium which signifies good
that symptoms are capable of producing artificial
health.Any imbalance due to internal or external fac
symptoms on healthy individuals which can cure the
tors causes disease and restoring the equilibrium
same symptoms encountered in the course of natu
through various techniques, procedures, regimen, diet
ral disease. In treatment, primary emphasis is given to
and medicine signifies the treatment. In Ayurveda, di
increasing the defense mechanism of the individual
agnosis is done by questioning and by undertaking 8
through a holistic approach and treatment is directed
investigations including pulse, urine, faeces, tongue,
to correcting the imbalances in the immune mecha
eyes, visual/sensual examinations and inference.
nism. in this system, the choice of medication is sel
Ayurveda considers the human being as a microcosm,
dom identical although the disease may be the same.
treating each individual as separate, keeping in mind
Homeopathy has definite and effective treatment for
the condition of the body, mind, temperament, sex,
chronic diseases such as diabetes, arthritis, bronchial
age, metabolic fire,, work-rest pattern, sleep pattern
asthma, immunological disorders, behavioural disor
and diet.
ders and mental disorders.
Siddha
Yoga
The Siddha System is practised in the State of Tamil
Yoga is a way of life and consists of 8 components
Nadu in India. The diagnosis of the disease besides,
namely restraint, observance of austerity, physical
identifying the causes also examines the study of the
pcstures, breathing exercises, restraining the sense or
voice, colour of the body, tongue, status of the diges
gans, contemplation, meditation and samadhi. These
tive system and the person as a whole, as well as the
steps are believed to have a potential for the improve
of physical health by encouraging better circu
disease.The Siddha System places emphasis on the
ment
patients environment, prevalent meteorological con
lation of oxygenated blood in the body, retraining the
siderations, age, sex, race,'habits, mental frame, diet,
sense organs and thereby psychosomatic disorders/
appetite, physical condition and the physiological con
diseases and improves an individual’s resistance and
stitution. The Siddha system has been found to be
ability to endure stressful situations.
effective in treating chronic cases of liver, skin diseases,
anaemia, peptic ulcer and prostate.
Naturopathy
Unani
a way of life. It is often referred to as a drugless therapy.
The Unani Systems of medicine is a well-defined
Special attention is being given to eating habits using only
Naturopathy is not only a system of treatment but also
medical science and has grown out of a fusion of
natural, mostly uncooked food (fruits and vegetables,
devices, thought, experience and documentation de
adoption of purificatory practices, use of hydrotherapy,
rived through nations and countries with an ancient
cold-packs, mud-packs, baths, massage and a variety of
cultural heritage viz., Egypt, Arabia, Iraq. China, Syria
methods/measures to tone up the system, increase en-
HEALTH FOR THE MILLIONS / May - June 2000
orgy levels aimed at producing a state of good health
for preserving the classical traditions and systemati
and happiness. It has many proponents among all chronic
cally using Ayurveda. Under the Unani System, 12 up
patients who found relief and sometimes cure where
graded Departments provided Postgraduate education.
conventional treatment failed.
A National Institute for Unani is under establishment.
Infrastructure available in India for ISM
& Kashmir and Uttar Pradesh.The Siddha System has
Unani has wide acceptance in Andhra Pradesh, Jammu
There is a vast parallel infrastructure available for ex
7 Post-graduate Departments and two undergradu
tending health services through the six indigenous
ate colleges. A National Institute for Siddha is pro
non-allopathic systems of medicine. There is a sepa
rate Department of Indian Systems of Medicine & Ho
graduate Colleges as well as a National Institute of
posed to be established. Undergraduate and Post
meopathy at the National level, headed by a Secre
Homeopathy are also functioning throughout the •
tary to the Government of India with supporting tech
nical and administrative staff. With the establishment
of a full fledged Department of Indian System of Medi
country.There is a high degree of acceptance for Ho
meopathy in Maharashtra, Bihar, Tamil Nadu, Uttar
Pradesh, West Bengal and Orissa.
cine & Homeopathy, all these systems are receiving
undivided attention and are being actively propagated
Research and Development
and utilized in the delivery of health care. Emphasis
In the year 1969, the Government of India established
is being placed on standard edu
a Central Council for Research
cation, training and research. Sev
in Indian Medicine and Home
eral measures are being intro
opathy which was subsequently
duced to standardize the drugs
reorganized into separate Re
and establish their safety and ef
search Councils for Ayurveda
ficacy. In the States and Union Ter
and Siddha, Unani, Homeopathy
ritories, there are separate Direc
and Yoga & Naturopathy.The re
torates for dealing with these sys
search programmes being un
tems. In some of the States, there
dertaken by these Councils are
are separate Ministers for Indian
broadly categorized into Clinical
Systems & Homeopathy also. At
Research including Community
present, there are about 587,536
Health Care Research; Drug
practitioners of traditional medi
Research, covering Survey and
cines and homeopathy. Th.ere are
Cultivation of Medicinal Plants,
3,862 hospitals and 22,104 dis
Pharmacognosy, Phygto-chcmistry,
pensaries in the Government
Pharmacology,Toxiocology, Drugs
Sector. In addition, there are a
Standarization, Literary Research
large number of other hospitals
for revival of the ancient classical
and dispensaries run by non-gov
literature and a Reproductive and
Child Health Programme, cover
ernmental agencies.
ing ante-natal and post-natal care
Education and Availability
of Practitioners in India
and the development of contra
ceptive drugs.
The education (under-graduate &
post-graduate) in the traditional
systems
of
medicine
i.e.,
Ayurveda, Siddha, Unani and Homeopathy arc regu
lated by the Central Councils for Indian System of
Medicine and Homeopathy.There are more than 300
Colleges of ISM & H conducting 5-1/2 year degree
courses. In addition, 45 Ayurvedic Colleges impart
The research findings are also
publicised through the Councils
publications and periodicals.
Specialised monographs on the outcome of. Clinical
Research, Drug Research and Literary Research have also
been published. The Research Councils can also be ac
cessed on E-mail at the following addresses:
Post-graduate Training, 3 major Institutions at the
Central Council for Research in Ayurveda & Siddha
Gujarat Ayurveda University, Jamnagar, Institute of
(CCRAS) ccras@del6.vsnl.net.in
Medical Sciences, Banarash Hindu University and the
National Institute of Ayurved,Jaipur, also impart Post
graduate Training and officer Doctoral Courses. The
Central Council for Research in Unani Medicine
(CCRUM) ccrum@del3.vsnl.net. in
largest number of practitioners are in Madhya Pradesh.
Central Council for Research in Homeopathy
Rajasthan and Uttar Pradesh. Kerala is also well-known
ccrh@del3.vsnl.net.in
HEALTH FOR THE MILLIONS / May - June 2000
INDIA POPULATION PROJECT-Vlil
BANGALORE MAHANAGARPAL1KE
MULTI- INDICATORS STUDY
CENTRE FOR RESEARCH IN HEALTH AND SOCIAL WELFARE
MANAGEMENT
861, 18th Main Koad, Banashaukari II Stage, Bangalore 560070
December 1997
INDIA POPULATION PROJECT-VI11
BANGALORE MAHANAGARPAL1KE
MULTI- INDICATORS STUDY
CENTRE FOR RESEARCH IN HEALTH AND SOCIAL WELFARE
MANAGEMENT
861, 18th Main Road, Banashankari II Stage, Baugalore 560070
December 1997
Table of contents
Page No.
Executive Summary
1. Introduction
1.1. Topography of Bangalore and Slums
1
1.3. Methodology of the present study
1.4. Organisation of field work
1.5. Sample for the study
1.6. Analysis of data
9
9
10
11
12
12
2. Results of the study
2.1. Socio-demographic indicators
2.2. Nuptiality indicators
2.3. Fertility indicators
2.4. Family Planning indicators
2.5. Maternal and child health indicators
13
16
19
21
25
3. Conclusions
30
4. References
30
5. Tables
32
1.2. Background to the present study
6.
Appendix
List of Clusters
Map of the Area
Questionnaires used for the Survey
List of Tables
Table 1. Socio-demographic characteristics of the respondents
Table 2.
Age and sex stiectuie of the surveyed population
1'able 3.
Table 4.
Table 5.
Table 0.
Distribution of respondents according to age and marital status
Distribution of respondents according to religion and age at menarche
Distribution of xomen aged 15-44 years according to the age at marriage
Distribution of respondents according to present age and age at consummation
of marriage
Table 7. Age specific ferality rates in the community
Table 8. Distribution of respondents according to present age and age at first pregnancy
Table 9. Distribution of respondents according to present age and order of last pregnancy
Table 10 Distribution of respondents according to present age and length of open
intervals from last pregnancy
Table 11. Distribution of respondents according to knowledge of any FP method
Table 12. Distribution of respondents according to media exposure to family planning
messages
Table 13. Distribution of respondents according to religion and F.P. methods currently
practised
Table 14. Distribution of respondents according to present age and F.P. methods
currently practised
Table 15. Distribution of respondents according to parity of last birth and F.P. methods
currently practised
Table 16. Distribution of deliveries in the previous year according to ante-natal care
received
Table 17 .Distribution oi'caildren below five years according to the status of
breast feeding
Table 18. Distribution of-nderfive children according to mid ann circumference
Table 19. Distribution of children below five years according to management of diarrohea
episodes
Table 20. Distribution of-omen according to place of treatment for sickness
Table 21. Distribution of caildren aged 12-23 months according to immunisation status
EXECUTIVE SUMMARY
1. INTRODUCTION
1.1 Background
Government of India with the aid of World Bank have targeted to provide basic
health and family welfare services to the urban poor especially the slum dwellers by the
turn of the century. Consequently India Population Project-VIII (1PP-VH1) was
formulated and implemented in the slums of Bangalore Metropolitan Area. With the
ultimate goal of providing Family welfare (FW), Maternal & Child Health (MCH) care
services, the project is to focus on reduction of fertility levels in the area.
M/S General Automata Pvt. Ltd., Bangalore have been developing an efficient
Management Information System (MIS) for the present Project. As an initial task of this
assignment, indicators are being developed which not only felicitate the development of
Management Information System (MIS) but also help in monitoring the programmes
undertaken by the project. THE CENTRE FOR RESEARCH IN HEALTH AND
SOCIAL WELFARE MANAGEMENT, BANGALORE has been entrusted with the task
of collection of necessary data and assess the present level of the indicators which would
help in monitoring of the programme.
1.2.
Methodology of the present study
The methodology adopted for data collection in the present study consisted of
interview of currently married women in the reproductive age group 15 to 44 years troin
the households in thirty clusters randomly selected using the methodology of Probability
Proportional to Sample Size out of ail the slums of Bangalore Metropolitan Area- From
each of the selected clusters, fifty currently married women in the age group 15 to 44
were covered for the survey.
The survey was undertaken during the period 15 to 30, November 1997.
13. Sample for the study
A total of 1487 households were surveyed, from the thirty clusters to cover a sample
of 1500 married women in the age group 15-44 years. The households had a population
of 7796 consisting of 3995 males (51.2%) and 3801 females (48.8%). These households
provided a sample ot 2o2 women who had delivered during the previous year, i 180
children in the age group upto 5 years besides 141 children aged between 12-23 months.
In addition 30,400 population was uiiuinuiuied lor inlormuOou on births in the previous
year. .
2.
RESULTS OF THE STUDY
2.1. Socio-demographic indicators
2.1.1. Religion and caste
Of the total 1487 households surveyed, 76.1% were Hindus, 17.6% were Muslims
and 0.3% were Christians. Majority of the population in the slums were predominantly of,
under developed castes of the society.
2.1.2. Educational Status
The literacy rate of the population was 75.0%, with a male literacy rate of 79%
and female literacy rate of 09.1%. However in majority of them the educational status
was restricted only upto higher secondary level.
'flic dropout rate ;rom schools amongst children in the school going age group is
around 14.0% . The dropout rale amongst female children (10.0%) was higher than that
of male children (12.1%)
2.1.3. Economic condition
Only 34.9% of the population were gainfully employed, giving a dependency rate of
65.1%. Most of the women respondents were housewives (81.6%).
2.1.4. Mother tongue
Most of the population in the area were of mother tongue oilier than Kannada
(78.1%), indicating that they were from the neighbouring States migrated to the City in
m
search of employment.
2.1.5. Age and sex distribution
The households had a total population of 7796, consisting of 3995 males and
3801 females . The sex ratio in the population was 951.
The percentage of population aged between 0-14 years comprised of 39.8%,
which is higher than that of the state average of 36.7% observed by NFHS (1992-93).
However this percentage is much higher than the figure of 33.9% for urban areas of the
state. Further the proportion of female population in the age group 20-29, prime child
bearing age group, is very high ( 25.5%).
2.2. Nup tia lity In dica tors
2.2.1. Marital Status of women
Overall, only 13.3% of the women aged between 15-44 were not married., while
75.9% are currently married, 10.4% widowed and only 0.4% were either separated or
divorced. The proportion of currently married females in the age group 15-19 years is
41.1% which is very high as compared to only 26.7% in other urban areas of the state
(NFHS).
2.2.2. Age at menarche
More than half of women had attained their menarche between the age 13 to 14
years of age (51.7%)., while another 30.1% by 11 to 12 years. Only 18.3% had attained
their menarche beyond the age of 14 years. The mean age at attainment of menarche was
13.3
years.
2.2.3. Age at marriage
About 77% of the women had been married by the age of 18 years. The mean age
at marriage in the sample was. 16.9 years, with 16.8 years for Hindus, 16.7 years for
Muslims and 18.0 years for Christians. The age at marriage which had slightly increased
in the previous decade seems to have dnfted down in the recent years, as can be observed
from comparisons between respondents in different age cohorts.
2.2.4. Age at consummation of marriage
The mean age at consummation of marriage is 17.3 years and more than three
fourths (76.5%) of women had their consummation of marriage by 18 years of age. The
trend similar to the age at marriage is seen with the age at consummation of marriage also.
3
2.3. Fertility Indicators ■
2.3.1. Fertility levels
a. Crude Birth Rate
1 he crude birth rate in the population is 22.9 which is almost similar to the urban
rales ofKarnataka (NFIIS).
b. Fertility Rates
The General Fertility Rate in the sample was 87.0, while the TFR experienced by
the women in the sample is 2.53 . The Age Specific Fertility Rates indicate that the
fertility is highest in the age period 20-24 years with an ASFR of 0.2727 followed by 2529 years with an ASFR of 0.0975 and 15-19 years with ASFR of 0.0829. This indicates
that the prime child bearing in the community is amongst women aged 15-29 years, who
contribute lor 89.5% of the total births in the community.
2.3.2. Fertility trends
a. Age at first pregnancy
As a consequence of early age at marriage and consummation of marriage, the
age at first pregnancy was also low in the community. Majority of women had their first
pregnancy before completing the age of 18 years (58.4%). The mean age at first pregnancy
in the sample was 18.3 years.
b. Number of children ever born and Birth order of last pregnancy
On an average a women had conceived for three times. The proportion of women
with upto second paiily was only 42.0% in the community.
c. Open birth intervals
The average open birth interval in the community is about 30 months. The mean
birth interval was lower with younger mothers.
d. Age and parity of women delivered during previous one year
Nearly two thirds of the women in the community who had pregnancies in the
previous one year were young and in the age group 19 to 24 years. (66.0%). Further 9%
of these mothers were below the marriageable age of 18 years.
Paritywise, 41.3% of the births were of more than second para while 18.8% of over
third para.
4
2.4. Family planning indicators
2.4.1.
Knowledge on family planning sources
The knowledge of women in the sample on family planning is almost universal
with 96.3% of women being aware of different methods to prevent births. 47% of women
knew about three or more number of methods of family planning, while another 49% were
aware of one to two methods. The methods known in the order of percentages were
sterilisation of women (92.5%), oral pills (62.4%), IUD (49.8%) and Nirodh (27.7%).
Vasectomy was known only to a negligible proportion of women (1.6%).
However
the
communication between the couples on limiting the family size or on family planning
methods was restricted to only 34.6% of couples.
2.4.2.
Exposure to family planning messages through media
News paper reading was not very common with women and only 22% had access
to news papers.
Only 21 to 26% of women had accessed messages on family planning or health
tltrough radio broadcast, while the proportion of women who had watched some
programme related to family planning on television was around 56 to 58%.
2.4.3. Current Contraceptive Use
a. Couple protection rates
The couple protection rate through modem methods of contraception was 57.0%
in the community. Out them majority had adopted female sterilisation (48.9%) and the
proportion using spacing methods were very only 8.1%. Amongst the spacing methods
Oral pills were practised by 5.1% while IUD by 2.6%. Use of condoms was negligible
(1.5%).
b. Religion wise contraceptive use
Practice of contraceptive methods was slightly higher with Christian couples
(59.6%) as compared to Muslims (58.3%) or Hindus (56.5%). Practice of permanent
methods were more common with Christians (53.2%) as compared to Hindus (49.3%) and
Muslims (45.8%).
5
c. Age wise contraceptive use
The proportion of couples using contraceptives ranged from 9.8% amongst
women aged 15-19 years to 77.6% in the age group 35-39 years. However, only 49.1% of
women in the prime child bearing age of 15-29 years were using some method of
contraception as
compared to 72.8% in higher age groups (30+ years). A significant
number of couples in the prime child bearing age had undergone sterilisations (39.3%).
d. Paritywise contraceptive use
The contraceptive use rate with mothers upto first para was only 14.3%. The rates
gradually increased to 79.5% with mothers of fourth para, beyond which there was declin^
in the rates. Further, 75% of women of over second parity were practising family planning
while this percentage was only 35% with women upto second parity. However, only a
small proportion (9.5% of couples) of mothers upto second parity were using spacing
medtods. This clearly suggests that the programme has to propagate more on spacing
methods with younger couples with whom there is greater need for such methods.
2.5. Maternal and child health indicators
2.5.1. Aute-nutal care during pregnancy
Only about 5% of mothers did not have ante-natal check up.
About 01% of the
mothers hud initiated the check up in the first trimester while another 30.9% had initialed
during the second trimester. Significantly only a small proportion of Ute ante-natal check
up (7.2%) was carried out by the peripheral workers while the remaining were from
doctors (90.3%). A third of the mothers had utilised the services of private practitioners
for the purpose.
Only
7.6% of the mothers did not have tetanus toxoid immunisation during
pregnancy while only 17.6% had consumed a course of 60-90 IFA tablets.
Even though majority of the deliveries were institutional, there were still 14.5%
,home deliveries which were conducted mostly by unqualified personnel.
Availing of post-natal check up facilities was not very common as only 30.5% of
the mothers had such a care.
6
2.5.2. Child care during infancy and early childhood
a. Breast feeding and weaning
Even though almost all the children (98.7%) were breast fed during their infancy
only 53.2% of them were initiated on breast milk within one to two hours alter birth. Only
half of the mothers had continued breast feeding their babies beyond one year. Large
proportion of mothers had started supplementary feeding for infants within six months
(73.6%) of age.
b. Management of diarrhoea
About 9% of the children with diarrhoeal episodes did not avail of any medical
advice.
Private practitioners were the common source of treatment facilities for the
episodes (75.4%), while Government or Corporation health facilities were used for only a
quarter of episodes (24.7%). Food intake during the diarrhoeal episode was reduced in
45% of the cases while the rest had maintained the quantum of intake as usual.
Only 18.8% children were offered more fluids during the episode and in 30.0% of
the children the intake of fluids had reduced, which is not conducive in the management of
the episode. Further ORS was administered in only 51.2% of the episodes.
c. Malnourishment in children
In the community only 41.1% of the children aged 7 to 59 months were
nutritionally normal as per WHO standards of MAC (MAC >14.0 cms.). 35.6% of the
children were moderately malnourished (MAC between 12.6 to 14.0 cms.) while 24.0%
were severely malnourished (MAC< 12.5 cms). Although the prevalence of malnutrition
decreased with the age of the child, lite proportion of severely malnourished children were
as high as 30.2% with children aged above 4 years.
d. Immunisation status
Of the children aged 12-23 months, only 79.4% had completed the full schedule
of immunisations. The immunisation coverage for BCG was highest with 98.6% followed
by Measles (85.1%), DPT (82.3%) and Polio (79.4%).
7
3.0. CONCLUSIONS
The indicators as observed in the present study leads to the following conclusions.
The population in the slums consisted mostly of the underdeveloped castes, a
substantial proportion migrated from the neighbouring States and with low educational
attainments. The population has a high proportion of females in the prime child bearing ages.
Most of the women were married at early ages resulting in to early and repeated pregnancies.
Even though family planning acceptance rate is not low, the acceptance of F.P.
methods by young couples is very low. Use of spacing methods for contraception is
significantly low. There was a substantial proportion of unmet need for family planning which
can be met by sustained IEC programmes.
Ante-natal care is mostly provided by Private practitioners and is not complete in
many of the mothers and post natal care is not very common. There are still a considerable
proportion of home deliveries conducted mostly by untrained personnel.
Infant care lacks especially in the components of early initiation to breast milk
and provision of more fluids or ORS supplementation during diarrhoea. Immunisation
coverage is also not high. Prevalence of malnutrition amongst children aged below five years
is also high.
8
1. INTRODUCTION
1.1. Topography of Bangalore and the Slums
Bangalore City, the capital of Karnataka state is situated al 12° 50’ latitude in the
North and 77° 30’ longitude in the East at an altitude of 931 meters above the sea level.
The Urban agglomeration of the City is spread over 451 sq. kms. and has a population of
41.7 lakhs according to 1991 census. Population wise the City is the fifth biggest in the
Country ( 1991). The slums of Bangalore City are spread over entire length and breadth
and composed of all religions and castes. The slum population of the City is growing in
an unplanned and uncontained manner.
1.2.
Back ground to the present study
The family well-re programmes in India have been in operation for well over 40
years and despite additional inputs, the progress has been well below the targeted goals,
more so in the urban slums of the State. Various developmental programmes initiated by
the Government in the slums of the State have not been catching up due to accelerated
growth of the slums. Even in the family welfare programmes, the slums have been
lagging far below the levels of the stare.
Government of India with the aid of World Bank have initiated programmes to
provide basic health and family welfare services to the urban poor especially the slum
dwellers by die turn of the century. With this in view, India Population Project-VIH (1PP-
VIII) was formulated and implemented in the slums of Bangalore Metropolitan Area.
With the ultimate goal of providing Family welfare (FW), Maternal & Child Health
(MCH) care services, the project is to focus at the reduction of fertility levels in the area.
The objectives of India Population Project VIH are:
•
Reduction of crude birth rate to 21
•
Reduction of infant mortality rate to levels below 60
•
Reduction of maternal mortality rate to less than 2
•
Increasing couple protection rate to 60%
9
Management Information System (MIS) is the backbone of any Project to
effectively monitor and aid in the implementation of the activities. M/S General
Automata Pvt. Ltd., Bangalore, have been developing an efficient MIS for the present
Project. As an initial task of this assignment, indicators are being developed which not
only facilitate the development of MIS but also help in monitoring of the programmes
undertaken by the project. THE CENTRE FOR RESEARCH IN HEALTH AND
SOCIAL WELFARE MANAGEMENT, BANGALORE has been entrusted with the task
of collection of necessary data and assessment of the present level of the indicators
which would help in developing a Management Information System as well as in
monitoring of the programmes of the Project.
Methodology of the present study
1.3
The methodology adopted for data collection in the present study consisted of
interview of currently married women in the reproductive age group 15 to 44 years from
the households in randomly selected thirty clusters amongst the slums of Bangalore
Metropolitan Area. The Universe for the selection of the slums consisted of a list of all
the slums with their population obtained from the Slum Clearance Board at Bangalore
and updated with the IPP-VIH Project office. The sample of thirty clusters were drawn
from this list adopting the methodology of Probability Proportional to Sample Size. The
list of selected slums and their location are in Appendix 1 and 2.
From each of the selected clusters, fifty currently married women in the age group 15
to 44.
Thus a total of 1500 women currently married in the age group 15-44 were
included in the study sample. In order to provide representation of all segments of
population in the sample, the selected cluster was divided into five equal segments and
ten women were interviewed from each segment making up to fifty women in total for
each cluster. This method of selection of respondents was adopted from the methodology
of Pulse Polio Immunization Coverage Survey conducted by UNICEF (CRHSM.1996).
To have an adequate sample size for data on births, 200 households in each of the
selected clusters were covered. Thus 6000 households were enumerated for the purpose.
10
This was expected to cover a population of about 30,000 which is an adequate sample
size to estimate a birth rate of about 25 with an error limit of 10%.
From each of such segments a household was randomly selected and interview
conducted and continued in the subsequent household in a sequential manner till fifty
women were covered.
The set of variables included for the study are:
•
Socio-demographic variables pertaining to family members
•
Nuptiality and fertility history of women
o
Child rearing practices for the live births in the previous five years
°
Exposure of women to health education on family planning through media
°
Knowledge, attitude and practices of women on Family planning
•
Incidence of diarrhoea amongst under fives in the last one month and its management
o
Utilisation of health facilities
«>
Births in the household in the last one year and related particulars of the mother.
The above information was collected through interview technique on a pre
designed and pre-iested proforma
(Appendix 3). Currently married woman in the
reproductive age group 15-44 years was the respondent for all information pertaining to
women and her child. Some of the data were retrieved from the survey conducted in the
slums by the Centre in June 1997 (CRSHM.1977).
The age of an individual and dates pertaining to relevant variables were confirmed
by matching them with local events, fairs or festivals.
The survey was undertaken during the period 15 to 30, November 1997.
1.4. Organisation offield work in the study
The interviews were canvassed by trained investigators with good knowledge on
the subject matter of study and experience in similar capacity. They were further trained
for a period of one week including practical work in the field for the current survey. The
11
data colluclitin wa:. M.pct vised by it Supervisor ns well us Consultants of the study. 1'he
filled in questionnaires were-thoroughly field edited before data processing.
1.5. Sample for the study
A total of 1487 households were surveyed, in the thirty clusters to cover a sample
of 1500 eligible couples in the age group 15-44 years. These households provided a
sample of 262 women who had delivered during the previous year, 1180 children in the
age group below 5 years besides 141 children aged between 12-23 months. In addition
30,400 population was enumerated for information on births in the previous year.
1.6. Analysis of data
The data from the questionnaires were transferred on to the computer, edited and
analysed on SPSS package.
12
RESULTS OF THE STUDY
2.
The results of the study are outlined in the subsequent sections under the
following headings.
•
Socio-dcmographic indicators
•
Nuptiality indicators
»
Fertility indicators
•
Family planning Indicators
•
Maternal and child health indicators
o
Indicators on health facilities
2.1. Socio-demographic indicators
2.1.1. Religion and caste
Of the total 1487
households surveyed, 76.1%
were Hindus, 17.6%
were
Muslims and 6.3% were Christians. There were only 1.4% from Forward castes,. 25.8%
from Backward castes while Scheduled Castes and Tribes comprised of 48.9%. Thus it is
seen that the slums were predominantly inhabited by under developed castes of the
society (Table 1).
2.1.2.
Educational Status
The literacy rate of the population wise 75.0%, with a male literacy rate of 79%
and female literacy rate of 69.1%. However the educational status was restricted only to
higher secondary level, as only 1.4% of the population had school education beyond this
level. Further 39.8% of the males and another 37.6% of the females had education only
between primary and middle standards (Table 1).
11
Religion of households
□ HINDUS
□ MUSLIMS
□ CHRISTIANS
S B S fc 8 g
Caste of Hindus
Forward
Backward
8.C A ST
Casta
1 he school dropout rate amongst children in the age group 6-14 years is around 14.0%
The dropout rale amongst female children (16.0%) is higher than that of male children
(12.1%).
2.1.3. Economic condition
Out of the 7796 population in the sample, only 34.9% (2723) were gainfully
employed, giving a dependency rate of 65.1%. Amongst males 6.0% were engaged in
some type of professional jobs (Table 1).
Even though most of the women respondents were housewives (81.6%), 14.5%,
were engaged as coolie workers.
About a third of the households (34.6%) were of the of the opinion that their
economic condition over the last three years had improved, while 39.2% expressed that
their condition was same and the rest 26.2% thought the condition had worsened.
2.1.4. Mother tongue
Most of the population in the households had their mother tongue other than
Kannada (78.1%). Majority had Tamil (37.7%) as their mother tongue followed by Urdu
(24.6%) and Telugu (14.2%). This indicates that the population in the slums were mostly
from the neighbouring Stales migrated to the City in search of employment (Table 1).
2.1.5. Age and sex distribution
The households had a total population of 7796, consisting of 3995 males and
3801 females . The sex ratio which is an indicator of overall health status of a women was
951 which is higher than the sex ratio of 930 for urban areas of the stale (Census 1991).
The age and sex distribution of the population is shown in five year groups in
Table 2. The population aged between 0-14 years comprised of 39.8% higher than the
stale average of 36.7% observed by NEHS (1992-93). However this percentage is much
higher than the corresponding proportion in the urban areas of the state (33.9%). This
may be probably due to a higher birth rate in these slums as compared to other urban
15
areas. Further the proportion ot female population in the age group 20-29, prime child
bearing age group, is very high ( 25.5%) in contrast to males (19.2%).
2.2. Nuptiality Indicators
2.2.1.
Marital Status of woineu
Overall, only 13.3% of the women aged between 15-44 were not married., while
75.9% are currently married, 10.4% were widowed and only 0.4% were either separated
or divorced. The proportion of widows is on the higher side as compared to only 3,2% of
women aged 15-49 in NFHS survey( 1992-93) for urban areas. The proportion of
currently married females in the age group 15-19 years is 41.1% which is very high as
compared to only 26.7% in other urban areas of the state (NFHS), but similar to those of
rural areas. This high proportion of married women in the teen age group is a reflection of
prevalence of early marriages which has
repercussions on resulting into early
motherhood (Table 3).
2.2.2. Age at menarche
Majority of women had attained their menarche between the age of 13 to 14 years
(51.7%), while another 30.1% by the age 11 to 12 years. Only 18.3% had attained their
menarche beyond the age of 14 years. The mean age at attainment of menarche was 13.3
years in the sample. The proportion of Muslim women with early onset of menarche was
more than those of Hindu or Christian women. In fact this proportion was least amongst
Christian women. Early age at attainment of menarche has a bearing on the age at
marriage also, us the parents would be eager to get a girl married when once she attains
her menarche (Table 4).
2.2.3. Age at marriage
About 77% of the women had been married by the age of 18 years. The mean age
at marriage in the sample was 16.9 years, with 16.8 years for Hindus, 16.7 years for
Muslims and 18.0 years for Christians (Table 5)?
Comparison of age at marriage between the respondents in different age cohorts
would provide some information on the trends. As can be observed, the mean age at
marriage is lower amongst respondents aged over 30 years as compared to the respondents
aged below 30 years, except for the age group 15-19 years, with whom the mean is lowest.
16
Marital Status of Respondents
33?
ravojcsd
Marital Stauu of Kcipuadeati according to their age
|b36*
Percent
| IB 10-A4
Unmarried
Worrted
ftoporatosU
Divorced
Widowed
| 320-20
Percent
100
M
40
40
20
B 20-24
0
Unmarried
Married
Soperated/
Divorced
Widowed
A similar trend is observed even in the proportion of respondents married before the age
ot 18 years. This suggests that the mean age at marriage which had increased in the
previous decade might have drifted down wards amongst the slum dwellers, in the recent
years.
2.2.4.
Age at consummation of marriage
t he age al consummation of marriage i.e., the age at which tile couple starts
cohabiting together has a significant bearing on the number of children they give birth to
which in turn affects the health of the mother. More than three fourths (76.5%) of women
had their consummation of marriage by the age of 18 years (Table 6).
The mean age at consummation of marriage is 17.3 years, indicating that there is a
gap of about 4-6 months on an average between the age at marriage and age at
consummation of marriage.
Age cohorts depict similar trends with the age at consummation of marriage as
was observed with the age at marriage.
2.3. Fertility Indicators
2.3.1.
Fertility levels
The indicators of assessment of fertility in a community are crude birth rate,
general fertility rate, age specific fertility rate and total fertility rate. In the present study,
these rates are estimated from a sample of 30,400 population covering a period of one
year previous to the dale of survey.
a.
Crude Birth Rate
There were in all 696 births in the sample during the period of an year before the
date of survey while the population of the sample covered for the births is 30,400. Thus
the crude birth rate in the population is 22.9 which is almost similar to the urban rates of
Karnataka (NFHS). Even though no data is available for Bangalore City it may be
presumed that CBR of slums would be higher than that of the CITY.
b.
General Fertility Rate
With the number of births of 696 for a women population of 8004 in the age
group 15-44 in the sample, the General Fertility Rate is 87.0. This rate is similar to 89
19
observed for urban areas of the Stale (NFHS) during 1992-93, but much lower titan the
rural rate of 119.
c.
Age Specific and Total Fertility rates
Age Specific Fertility Rate (ASFR) and Total Fertility Rate (TFRj are refined
indicators of fertility as they take into account the differential age fertility patterns as well
as the age structure of the population. TFR is calculated as five times the sum of all the
age specific fertility rates, since in the present study ASFRs are calculated for five year
age intervals. This rate would provide an estimate of the number of children that would be
bom to a women during her reproductive span if she passes through the present fertility
level in the community (Table 7).
TFR experienced by the women in the sample is 2.53 . 'flic Age Specific Fertility
Rales indicate that the fertility is highest in the age period 20-24 years with an ASFR of
2727
0.
followed by 25-29 years with an ASFR of 0.0975 and 15-19 years with an ASFR
of 0.0829. This reflects that the prime child bearing in the community is in the age period
15-29 years, contributing for 89.5% of the total births in the community.
2.3.2. Fertility trends
The indicators which are used for understanding the fertility trends are the total
number of children ever bom, birth order of last pregnancy for mothers in different age
cohorts, age at first pregnancy and open birth interval of the last pregnancy. These rates
are discussed in the following paragraphs. Further the age and parity of women who had
delivered in the last on year is also analysed.
a. Age at first pregnancy
As a consequence of early age at marriage and consummation of marriage, the
age al first pregnancy was also low in the community. Majority of women had their first
pregnancy before the completion of 18 years of age (58.4%). These trends were similar
for
different religions in the community. The mean age at first pregnancy in the sample
was 18.3 years i.e. almost with in an year of consummation of marriage (Table 8).
b. Birth order of last pregnancy
The mean parity of women of the last birth was about 3.0. The proportion of
mothers with one or two parities was only 42.6% while those with over third parity was
32.3%. Even amongst younger mothers aged between 20-24 years, there were about 33%
20
with over third parity, while this proportion was as high as 63% with mothers over 25-29
years. This suggests that the community has a large proportion of young mothers who
have conceived for over three times. (Table 9).
c. Open birth intervals
The mean birth interval from the last pregnancy in the community was 30 months.
The means vary considerably between the mothers in the age groups below and above 30
years. The corresponding means in these two age groups were 25.7 and 37.2 months
respectively (Table 10).
d. Age and parity of women delivered during previous one year
Majority of the women who had delivered during the previous one year were
young and were in the age group 19 to 24 years. (66.0%). 9% of these mothers were below
the marriageable age of 18 years, which is a matter of concern.
Parity wise, 41.3% of the births were of over second para and 18.8% were of over
third para. Mothers with higher order parity were more amongst Muslims and Christians
(27%) as compared to Hindus (15.9%).
2.4. Family planning indicators
The main thrust of the process in the present project is on improving family
planning acceptance in the community. As such indicators on the knowledge, attitude and
practices of the slum dwellers pertaining to family planning, provides a clear idea to
monitor the over all impact of the programmes. The results obtained from the survey data
on these indicators along with indicators on
unmet demand for family planning are
presented below.
2.4.1. Knowledge on family planning sources
The knowledge of women in the sample on family planning is almost universal
with 96.3% of women being aware of methods to prevent the births. About 47% of the
women knew three or more methods of family planning, while another 49% were aware of
one or two methods. The methods known in the order of percentages were sterilisation of
women (92.5%), oral pills (62.4%), IUD (49.8%) and Nirodh (27.7%). Vasectomy was
known only to a negligible proponion of women (1.6%). However the communication
21
between the couples on limiting the family size or on family planning methods was very
much restricted as only 34.6% of couples communicated on the these topics (Table 11).
2.4.2.
Exposure to family planning messages through media
News paper reading was not very common with the women as only 22% had
access to news papers.
Only a little more than a third of the women had access to radio either regularly or
occasionally (35.2%). Christians are slightly better with the exposure to radio viewing
(39.4%h However, only around 21 to 26% of women had accessed some messages on
family planning or on health through radio broadcast (Table 12).
Television seems to be better accessible media than any of the other ones as
nearly three fourths (74.1%) of the women had an access to it either regularly or
occasionally. Christian women are belter off in the access to this media followed by
Muslims and Hindus. The percentage of women who had watched some programme
related to family planning on television was 56 to 58%.
2.4.3. Current Coutraceptive Use
a. Couple protection rates
The couple protection rale through modem methods of contraception was 57.0%
in the community. Majority of couples had adopted female sterilisation (48.9%) as method
of contraception while the proportion of couples using spacing methods was very small
(8.1%). Amongst the spacing methods. Oral pills were practised by 5.1% while IUD by
2.6%. Use of condoms was negligible (1.5%) (Table 13).
b. Religion wise contraceptive use
Practice of contraceptive methods was slightly higher with Christian couples
(59.6%) as compared to Hindus (56.5%)or Muslims (58.3%). Permanent methods were
more common with Cliristians (53.2%) followed by Hindus (49.3%) and Muslims (45.8%)
(Table 13).
c.
Age wise contraceptive use
The proportion of couples using contraceptives ranged from 9.8% amongst
women aged 15-19 years to 77.6% with the women in the age group 35-39 years. Only
49.1% of women in the prime child bearing age of 15-29 years were using some method of
22
Type of F.P. Methods used by age of Respondents
Type of F.P. Methods uaed by Parity of Lail pregnancy of Respondent*
3 3 a
contraception us compared to 72.8% in higher age groups (30f years). Only 39.3% of
couples in the prime child bearing age had undergone sterilisations besides the percentage
adopting spacing methods being meager (Table 14).
d.
Paritywise contraceptive use
Only 14.3% of the women upto first parity were using some method of
contraception. Even though this percentage gradually increased to 79.5% with women in
fourth para, the percentage decreased later. 75% of women of over second para were using
family planning methods while this percentage was only 35% with women upto second
parity. Of this 35%, the proportion adopting spacing methods was not much ( 9.5%
couples). This clearly suggests that the programme has to propagate more on spacing
methods with younger couples (Table 15).
e.
Unmet demand fur family planning
Out of 1500 couples 855 were practising one or the method of family planning. Of the
remaining 645 couples, 219 (34%) expressed a desire to plan their families by adopting
family planning methods in the near future. Of them 198 (30.2% of the total non users)
wanted to adopt a method with in a year. As such it is evident that there is about 34%
unmet need of family planning in the community. It is further implied that the couple
protection rate can be stepped up by about 13% if concerted efforts are made to motivate
and provide services to these 198 couples who are willing to adopt family planning in a
year’s period. Out of the 219 couples. 136 (62.1%) were desiring to go in for permanent
methods while the remaining were for adopting a spacing method.
Misconceptions or objections by family members or religion were the
prominent reasons for the non adoption of family planning methods. This indicates that
1EC programmes have to be stepped up to mouvate such couples.
2.5. Maternal and child health Indicators
Two of the objectives of the Project relate to reducing infant mortality and maternal
mortality in the area. Infant and maternal mortality can be reduced through provision of
effective maternal and child health care services, mainly ante-natal and natal care for
25
pregnant mothers and immunisation services for infants along with appropriate treatment
of diarrhoeal diseases of undcriive children. Information was collected to arrive at the
present levels of the indicators relevant to these activities and the results of the analysis
are presented below.
2.5.1.
Ante-natal care during pregnancy
As already stated, 262 women had delivered during the previous one year. Of
them except for about 5% of mothers all had ante-natal check up (ANC). However, only
61.5% of the ANCs were initiated in the first trimester while another 30.9% were initiated
during the second trimester. However those who did not have any checkup were those
without proper knowledge about the need for the same Table 16).
Significantly only a small proportion of the ANCs (7.2%) was carried out by the
peripheral workers while
the remaining were from doctors (90.3%). A third of die
mothers utilise private practitioners.
Only 7.6% of the mothers did not have tetanus toxoid immunisation during
pregnancy. About 84% of the mothers had iron and folic acid supplementation during
pregnancy. But only 17.o% had consumed a course of 60-90 of these tablets.
Even though majority of the deliveries were institutional, there were still 14.5%
home deliveries which were mostly conducted by unqualified personnel.
Availing of post-natal check up facilities was not very common as only 30.5% of
the mothers had availed of such a care.
2.5.2. Child care during infancy and early childhood
a. Breast feeding and weaning
Even though almost all the children (98.7%) were breast fed during their infancy
only 53.2% of them were initiated on breast milk within one to two hours after birth. As
many as 27.7% were initialed only after 12 hours.
continued breast feeding their babies
Only
half of the mothers had
for over one year. Prolonged breast feeding
increases the amenorrhoea period which may reduce the chance of onset of next
pregnancy (Table 17).
Large proportion of mothers had started supplementary feeding for infants within
six months (73.6%) of age.
26
b. Malnourishment in children
In the present survey malnutrition was assessed by the mid arm circumference
(MAC) of children. In the community only 41.1% of the children aged 7 to 59 months
were nutritionally normal as per WHO standards (MAC >14.0 cms.). There were 35.0%
of children moderately malnourished (MAC between 12.6 to 14.0 cms.) and 24.0%
severely malnourished (MAC< 12.5 cms). Even though the proportion of nutritionally
deficient children decreased with the age, the proportion severely malnourished was as
high as 30.2% with children over four years of age.
c. Management of diarrhoea
The prevalence of diarrhoea amongst children aged below five years was 14.4 %.
About 9% of these episodes did not avail of any medical advice. Most of the mothers
availed treatment facilities for the sickness from private health facilities (75.4%).
Government or Corporation health facilities were used only by about a quarter of mothers
(24.7%). As such it is desirable that these private practitioners are provided with
necessary background to initiate educational activities to mothers on various aspects of
health including family planning (Table 19 &20).
Nearly 45% of the mothers had reduced the food intake for the child during the
episode while the rest had the same quantum as usual. Only 18.8% children were offered
more tluids during the episode while in 30.0% of the children the quantum of fluid intake
had reduced, which is not conducive in the management of the episode. Further ORS
suppiimcnlalion was administered in only 5 1.2% of the episodes.
d. Immunisation status
There were 141 children aged 12 to 23 months in the sample. Out of them only
79.4% had completed the full schedule of immunisations. The immunisation coverage for
BCG was highest with 98.6% followed by Measles (85.1%), DPT (82.3%) and Polio
(79.4%). The drop out rate for DPT is 1.4% from first to second dose while it is 12.8%
from second to third dose. For Polio the drop out rate was 2.8% from first to second dose
and 13.5% for second to third dose (Table 21).
27
Personnel conducting antenatal checkup
2%
8%
■ ANM/LHV
■ Govammant doctor
□ Privata doctor
nUnquaified parson
Place of delivery
15%
15%
■ Homa
■ Corporation hospital
□ Other Govt hospital
28%
□ Private maternity homee
Person conducting home deliveries
■ Eberty lady
■ Dm
Food intake during diarrohea
Fluid intake during diarrhoea
El Less than usual
E) Sarno as usual
□ More than uaual
ORS administered during diarrhoea
3. CONCLUSIONS
The indicators as observed in the present study leads to the following conclusions.
The population in the slums consisted mostly of the underdeveloped castes, a
substantial proportion migrated
from the neighbouring Slates and with low educational
attainments. The population has a high proportion of females in the prime child bearing ages.
Most of the women were married at early ages resulting in to early and repeated pregnancies.
Even though family planning acceptance rate is not low, the acceptance of F.P.
methods by young couples is very low. Use of spacing methods for contraception is
significantly low. There was a substantial proportion of unmet need for family planning which
can be met by sustained IEC programmes.
Ante-natal care is mostly provided by Private practitioners and is not complete in
many of the mothers and post natal care is not very common. There are still a considerable
proportion of home deliveries conducted mostly by untrained personnel.
Infant care lacks especially in the components of early initiation to breast milk
and provision of more fluids or ORS supplimentation during diarrhoea. Immunisation
coverage is also not high. Prevalence of malnutrition amongst children aged below five years
is also high.
4. REFERENCES
Centre for Research in Health and Social Welfare Management:
1.
Coverage Evaluation Study, Pulse Polio Immunisation Programme, Karnataka State, 1996
Centre for Research in Health and Social Welfare Management:
2.
Baseline Study for IEC component, IPP-V11I, Bangalore Mahanagar Palike, 1977
3.
Institute for Socio-Economic Change and UPS: National Family Health Survey, Karnataka,
1995
4.
Registrar General. Govt, of India: Census of India, 1991, Quoted in SI. No. 3
30
Table 1, Socio-demouraphic Characteristics of the respondents
Socio-demographic
No.
%
characteristics
Religion
Hindu
Muslim
Christian
1132
261
94
76.1
17.6
6.3
5
17
180
606
120
204
0.3
1.1
12.1
40.8
8.1
13.7
1224
218
24
6
13
15
81.6
14.5
1.6
0.4
0.9
1.0
566
369
328
213
24
37.7
24.6
21.9
14.2
1.6
515
583
389
34.6
39.2
26.2
Caste of Hindus
Brahmins
Lingayat
Vokkaliga
S.C
S.T
Others
Occupation of respondent
Housewife
Coolie
Skilled worker
Unskilled worker
Professional
Service
Mother tongue
Tamil
Urdu
Kannada
Telugu
Others
Economic condition in last
three years
Better off
Same
Worse
32
Table 2. Age and sex structure of the surveyed population
Age in years
Males
Females
No.
%
No.
%
0-4
587
14.08
573
15.08
5-9
546
13.66
522
13.73
10-14
445
11.13
435
11.44
15-19
352
8.81
404
10.63
20-24
324
8.11
530
13.94
25-29
445
11.14
438
11.52
30-34
305
9.14
256
6.74
35-39
333
8.34
5.60
213
212
5.31
107
2.82
40-44
154
88
2.32
45-49
3.85
50-54
95
87
2.38
2.29
55-59
42
1.05
36
0.95
60-64
40
1.00
56
1.47
65+
55
1.40
56
1.50
Total
3995 _
100.0
3801
100.0
Both
No.
1160
1068
880
756
854
883
621
546
319
242
182
78
96
111
7796
%
14.8
13.7
11.3
9.6
11.0
11.3
8.0
7.0
4.1
3.1
2.3
1.0
1.2
1.5
100.0
Table 3. Distribution of respondents according to age and marital status
Marital
Status
Separated/ Widowed Total
Age in
Mamed
Unmarried
Divorced
years
166
3
. 404
15-19
No.
235
41.1
0.7
100.0
58.2
%
44
476
20-24
No.
2
8
530
89.8
8.3
0.4
1.5
%
100.0
423
4
25-29
No.
9
2
438
96.6
2.1
0.5
0.9
%
100.0
4
249
30-34
2
No.
1
256
1.6
97.3
0.8
0.4
100.0
%
410
4
220
643
No.
9
35+
0.6
63.8
34.2
100.0
1.4
%
1724
10
236
2271
301
No.
Total
75.9
0.4
10.4
100.0
13.3
%
33
Table 4. Distribution oi respondents according to religion and age at nicnarche
HINDU
MUSLIM
CHRISTIAN All
Age in years
No.
%
No.
%
No.
%
No.
%
11-12
322
28.2
109
41.3
21
22.3
452
30.1
13-14
589
51.6
129
48.9
58
61.7
776
51.7
15-16
208
18.2
23
8.7
14
14.8
245
16.5
More than 16
23
2.0
3
1.1
1
1.1
27
1.8
1142
100.0
264
100.0
94
100.0
1500
100.0
Total
*2= 52.58 P< 0.001
34
_Table 5. Distribution oi women aged 15-44 vears accordion to the age al marriaue
_________________________ ■
Age
at
Marr
iage
Age of the Upto 16192225+
Total
Mean S.D.
respondent 15
18 _ 2£
24_ __
13-19 No.
41
8
7
1
132
16.39 1.810
%
31.0
62.9
5.3
0.8
100.0
20-24 No.
%
115
225
49.9
102
22.6
9
2.0
-
451
100.0
17.06
2.258
25-29 No,
%
130
31.2
173
41.5
85
20.4
22
5.3
7
1.7
417
100.0
17,18
2,909
30-34 No.
94
40.5
90
38.8
32
13.8
10
4.3
6
2.6
232
100.0
16.63
2.932
%
35-39 No.
%
83
44.1
67
35.6
??
11.7
11
5.9
5
2.7
188
100.0
16.56
3.300
40+
No.
%
40
50.0
21
26.3
14
17.5
4
5.0
1
1.3
80
100.0
16.19
3.139
Total No.
0/
/u
503
33.5
659
43.9
262
17.5
56
3.7
20
1.3
1500
100.0
16.86
2.734
35
Table 6. Distribution ol respondents according to present age
_______ and age at consummation of marriage_____________
Age
at
consummation of marriaee
Age of the Upto 161922-24
25+
Total
respondent 15
18
21
15-19 No. 39
84
8
1
132
%
29.5
63.6
6.1
0.8
100.0
20-24 No. 110
224
107
10
451
% 24.4
49.7
23.7
2.2
100.0
25-29 No. 124
173
91
23
6
417
0/
/0
29.7
41.5
5.5
21.8
1.4
100.0
30-34 No.
89
93
34
10
6
232
%
38.4
40.1
14.7
4.3
2.6
100.0
35-39 No. 79
71
22
11
5
188
% 42.0
37.8
11.7
5.9
2.7
100.0
2
40+ No. 36
25
13
4
80
45.0
%
31.3
16.3
5.0
100 0
2.5
Total No. 477
670
275
58
20
1500
%
31.8
44.7
18.3
3.9
1.3
100.0
Table 7. Age specific fertility rates of women in the comn11.. my
Age
of No.
of No.
of Age specific
mothers
in mothers
births
in fertility rates
years
the year
15-19
1387
115
0.0829
20-24
1276
348
0.2727
25-29
1753
171
0.0975____
30-34
1439
36
0.0250
35-39
1313
8
0.0060
40-44
836
_18_
0.0215
TFR=2.53
CBR= 22.9
36
Tabic 8. Distribution of respondents according to present age
_______ and age at first pregnancy_______________________
Age of the
respondent
15-19 No.
%
20-24 No.
%
25-29 No.
%
30-34 No.
%
35-39 No.
%
40+ No.
%
Total No.
%
Upto
15
48
36.4
84
18.6
70
16.7
44
19.0
38
20.2
17
21.3
301
20.1
1618
65
49.2
162
35.9
146
35.0
90
38.8
82
43.6
30
37.5
575
38.3
Age
al
first
preg.
1921
18
13.6
2224
-
Total
Mean
19
4.2
138
33.1
61
26.3
43
22.9
20
25.0
466
31.1
46
11.0
22
9.5
13
6.9
7
8.7
107
7.1
132
100.0
451
100.0
417
100.0
232
100.0
188
100.0
80
100.0
1500
100.0
16.7
186
41.2
2527
1
0.8
17
4.1
15
6.5
12
6.4
6
7.5
51
3.4
18.2
18.7
18.6
18.3
18.5
18.3
37
Table 9. Distribution of respondents according to present age
_______ and order of last pregnancy______________________
Order of
last
preg-_______________
Age in
2
6+
Total
1
5
3
4
years
15-19
No.
71
20
96
4
1
0/0
74.0
20.8
1.0
100.0
4.2
419
20-24
No. 105
3
175
94
37
5
U/□
0.7
100.0
25.1
41.8
22.4
1.2
8.8
402
No. 33
11
115
148
60
35
25-29
2.7
100.0
8.7
28.6
36.8 14.9
%
8.2
27
229
No. 12
30-34
39
59
59
33
14.4
100.0
17.0
25.8 25.8
11.8
%
5.2
32
No. 3
21
37
37
185
35-39
55
0.
11.4
17.3
100.0
1.6
20.0 29.7 20.0
No. 4
6
40-44
10
18
80
11
31
0/
7.5
0
5.0
12.5 22.5
13.8
38.8
100.0
No. 228
Total
376
1411
352
121
104
230
0/
/0
16.0
26.6
24.9 16.3
8.6
7.4
100.0
Table JO Distribution of respondents according to present age
and length of open intervals from last pregnancy
Open birth inter. in
months
Age of the -12
1925133137+
Total
respondent
18
24
30
36
15-19 No. 78
19
4
15
11
132
5
59.1
%
14.3
11.4
3.0
8.3
100.0
3.8
20-24 No. 128
74
47
73
42
87
451
%
25-29 No.
%
30-34 No.
%
35-39 No.
%
40+ No.
%
Total No.
%
16.4
16.2
10.4
9.3
19.3
100.0
12
5.2
7
3.7
-
24
5.8
12
5.2
2
1.1
-
37
8.9
7
3.0
1
0.5
-
25
6.0
3
1.3
-
-
53
12.7
12
5.2
5
2.7
-
282
18.8
131
8.7
133
8.9
79
5.3
123
8.2
221
53.0
186
80.2
173
92.0
80
100.0
752
50.1
417
100.0
232
100.0
188
100.0
80
100.0
1500
100.0
28.8
57
13.7
39
Tablel I. Distribution of respondents
according to knowledge of any FP method
No.
%
Particulars
Knowledge on FP
methods to limit
births
Yes
No
1445
55
96.3
3.7
Number of F.P.
Methods known
Nil
1
2
55
313
425
3.7
20.9
28.3
3
522
34.8
4
175
11.7
5
10
0.7
No.of Couples
1
1
Communicating
between themselves on
Spacing of children
519
34.6
40
Table 12 Distribution of respondents
according to media exposure
to family planning messages
Type of media
No.
0/
/o
/Ven's paper
Yes
No
331
1169
22.1
77.9
Kailio
973
64.9
Occasional
Regular
373
154
24.9
10.3
Television
389
25.9
Never
Occasional
Regular
366
745
24.4
49.7
Never
41
Tabic 13. Distribution ol respondents according to religion and F.P. methods currently
_________ practised_______ ;__________ ________________________________________
HINDU
MUSLIM
CHRISTIAN ALL
Methods practised
No.
%
No.
%
No.
%
No.
%
Nil
497
43.5
110
41.7
38
40.4
645
42.9
l-'cmalc sterilisation
563
49.3
121
45.8
50
53.2
734
48.9
Oral pills
30
2.6
7
2.7
2
2.1
39
2.6
IUD
47
4.1
25
9.5
4
4.2
76
5.1
Nirodh
5
0.4
1
0.4
-
-
6
0.4
Total
1142
100
264
100
94
100
1500
100
42
1 able 14. Distribution ol respondents according to present age and
_________ F.P. methods currently practised__________
F.P.
method
pract.
Age of the
respondent
Total
Women
Female
Sier.
IUD
Oral
Pills
Condoms
Total
praetisi
ng
15-19 No.
‘ u//1>
132
451
417
1
0.8
2
0.4
2
0.5
1
0.4
-
13
9.8
193
25-29 No.
4
3.0
32
7.1
28
6.7
8
3.4
4
2.1
-
4
20-24 No.
<) •
4
3.0
144
3 1.9
245
58.8
152
65.5
138
73.4
51
63.8
734
48.9
(>/
30-34 No.
232
0/
/0
35-39 No.
%
40+ No.
uy
/0
188
Total No.
0/
/0
1500
Age of lhe
Total
Women
respondent
15-29 No.
0/
/u
30+ No.
1)/1)
80
1000
500
76
5.1
Permanent
Method
393
39.3
341
68.2
3.0
15
3.3
10
2.4
5
2.2
4
2.1
1
1.2
39
2.6
Spacing
method
98
20.0
23
4.6
-
6
0.4
Total
Practising
491
49.1
42.8
285
68.3
166
71.6
146
77.6
52
65.0
855
57.0
364
72.8
43
1 able 15. Distribution ol respondents according to order of last pregnancy
and F.P. methods currently practised
F.P. '
method
pract.
Order of
Total
Female IUD
Oral
Condoms Total
last
Women Ster.
Pills
practising
pregnancy
0-1
No. 314
12
22
9
45
2
%
3.8
7.0
2.9
0.6
14.3
2
No. 371
163
22
10
195
%
43.9
5.9
2.7
52.6
240
3
No. 358
13
4
10
267
%
67.0
3.6
2.8
1.1
74.6
4
No.
%
5
No.
%
6+
No.
%
Total No.
224
123
110
1500
0/
/o
Order of
last
pregnancy
0-2 No.
o//II
Total
Women
3+
815
No.
11/
z II
685
162
72.3
91
74.0
66
11
4.9
4
3.3
4
60.0
3.6
734
76
5.1
48.9
Permanent
Method
5
2.2
-
175
25.5
559
65
9,5
56
68.6
(>.9
-
5
4.5
39
6
2.6
0.4
Spacing Total
method
Practising
178
79.5
95
77.2
75
68.2
855
57.0
240
35.0
615
75.0
44
Table 16. Deliveries in the previous year
according to ante-natal care received
Particulars of
ante-natal care
Had ante-natal
checkup
No.
%
249
95.0
1 bi trimester
2nd trimester
tot
81
61.5
30.9
3rd trimester
7
2.7
19
7.2
53.8
32.1
1.9
Time of starting ANC
Person providing care
ANM/LHV
Government doctor
Private doctor
Unqualified person
Doses of Tetanus
141
84
5
toxoid
Nil
1
2
20
11
105
3
126
7.6
4.2
40.0
48.1
1FA tablets consumed
Nil
Upto 30
31-60
61 -90
43
102
71
46
16.4
38.9
27.1
17.6
Place of delivery
Home
38
14.5
Corporation hospital
186
38
71.0
Elderly lady
24
Dai
14
63.2
36.8
80
182
30.5
69.5
Private maternity
homes
14.5
Person conducting
home deliveries
Post natal checkup
Yes
No
45
Table 17 . Distribution of children below five
years according to the status of
breast feeding ______________
Breast feeding pattern
No.
%
Breast feeding after
birth in hours
Never
1-2
3-6
7-12
13-24
24-r
11
440
112
35
88
141
1.3
53.2
13.5
4.2
10.6
17.1
182
22.3
8.6
19.2
23.3
26.6
B reast feeding
duration in months
1-6
7-9
10-12
13-18
18-r
70
157
190
217
Age al supplementary
feed in months
1-3
4-6
7-9
10-12
13-18
Not started
142
400
99
76
19
91
19.3
54.3
13.5
10.3
2.6
46
Table 18. Distribution of underfive children according to mid arm circumference of
children
Age
in
inont
hs
7-12
'1318
1924
2530
3136
37-48
49+
Total
Less No.
than. %
12.5 ems
12.6 No.
to
%
14 ems
More No.
than %
14 ems
37
24.1
95
17.5
34
23.4
16
19.0
36
23.5
57
25.4
48
30.2
254
24.0
77
50.3
73
51.0
67
46.2
32
38.1
44
28.8
57
25.5
20
12.6
370
35.6
39
25.5
45
31.5
44
30.3
36
42.9
73
47.7
110
49.1
90
56.6
437
41.1
Total No.
%
153
100.0
143
100.0
145
100.0
84
100.0
153
100.0
224
100.0
159
100.0
1061
100.0
Mid arm
circum fere
nee in ems
47
\
Tabic 19. Distribution ofchildrcn below five
years according to management of
__________ diarroliea during previous one month
Diarrhoea management
No.
%
Prevalence of
diarroliea
Yes
No
170
1010
14.4
85.5
No.
%
155
15
91.2
8.8
76
90
44.7
55.3
51
87
32
30.0
51.2
18.8
87
83
170
51.2
48.8
100.0
Management of
episode
History ofseeking
medical advice
Yes
No
Quantum offood
offered
Less than usual
Same as usual
Quantum offluids
offered
Less than usual
Same as usual
More than usual
OHS offered
Yes
No
Total
48
Table 20. Distribution of women according to
place of treatment for sickness
Place of treatment
No.
%
Corporation health
facility
Govt, health facility
Private health facility
25
1.7
345
1130
23.0
75.4
Total
1500
100.0
Table 21. Distribution of children aged 12-23 months
_________ according to immunisation status_________
Immunisation schedule
No.
%
139
B.C.G.
98.6
DPT - 3 Doses
116
82.3
134
- 2 Doses
95.1
136
- 1 Dose
96.5
Nil Dose
5
3.5
112
79.4
POLIO- 3 Doses
131
92.9
-2 Doses
135
95.7
-1 Dose
4.3
6
Nil Dose
120
85.1
Measles
141
No. of children aged 12-23
months
49
APPENDIX 3
QUESTIONNAIRES USED FOR THE SURVEY
BANGALORE MAHANAGAR PAT.TKR
INDIA POPULATION PROJECT - VIII
CENTRE FUR RKSKROi IN HEALTH AND SOCIAL WELFARE MANAGEMENT'
SURVEY OF SLUMS OF BANGALORE
GENERAL PARTICULARS
1.
Name of the Ward
3.
Name of the Area
4.
Name of the head of household
5.
Name of the respondent-mother
8.
Name of the interviewer
7.
Date of interview
8.
Identifioation No
2.
HH No
PROCESSING INFORMATION
Field Edited By
:--------------------------------------
Date
:--------------------------------------
Office Edited By
:---------------------------------------
Date
:---------------------------------------
Entered in Computer By
Date
:---------------------------------------
A.
HOUSEHOLD PARTICULARS
Please give the following particulars for all the eeibers of your faeily aha normally stay in the household.
SI.
No.
Naee
Age in
Sex
Harital statue Educational
Coipleted Hale 1 Harried
1
Status
Illeterate 1
years
Feaale 2 Nidowed
2
Separated 3
Prieary
2
Hiddle
3
Divorced
4
Relationship to
HOF
Unearned
5
Occupation
Higher Sec 4
If child
If child
> 5 Years nut going
going to
to School
to School Reasons
Yes 1
School far away
Ho
2
Susy in house wq/-|
Graduate
5
Child unwell
Technical
6
Rage earning
Post Grad. 7
No school for girl
Child
Others (Specify)
8
<5 Yrs
1
2
3
4
5
6
7
8
9
18
B.
1.
SOCIO-ECONOMIC INFORMATION OF THE HOUSEHOLD
What is the religion of the household?
Hindu
1
Muslim
2
Christian 3
2.
(
(
(
)
)
)
Jain
4
Sikh
5
Others 6
(specify)
If Hindu,what is the caste of the household?
Brahmin
Lingayath
Vokkaliga/Reddy
Scheduled Caste
Scheduled Tribe
Other Hindus
3.
)
)
)
(
(
(
1
2
3
4
5
6
(
(
(
(
(
(
)
)
)
)
)
)
Do you think that your family' s condition
during the last five years is
Better off
Sama
Worse
(
(
(
C. EXPOSURE TO HEALTH EDUCATION
1.
2.
3.
Have you ever attended any
orientation training course on
health in the last 3 years?
Yes 1 (
If yes, were any of these
topics discussed there?
Nutrition
Family planning
Child oare
Immunization
Disease prevention
Yes
Yes
Yes
Yes
Yes
Do you read news papers or
magazines?
4.
How often do you listen to
radio?
5.
If you listen to the radio,
can you tell us whether you
have heard any messages on:
Nutrition
Family planning
Child care
Immunization
Disease prevention
6.
How often do you watch TV?
)
No 2 (
(
(
(
(
(
)
)
)
)
)
No
No
No
No
No
Yes 1 (
)
No 2 (
1
1
1
1
1
2
2
2
2
2
(
(
(
(
(
Never
1 (
Occasionally 2 (
Regularly
3 (
(
(
(
(
)
)
)
)
Yes 1 (
)
Yes
Yes
Yes
Yes
1
1
1
1
No
No
No
No
2
2
2
2
No 2
Never
1 (
Occasionally 2 (
Regularly
3 (
)
)
)
(
(
(
(
(
)
)
)
7.
If you watch TV, cun you lull uu
whether you have watched any
programmes relating to:
Nutrition
Family Planning
Child care
Immunization
Disease prevention
Yes
Yes
Yes
Yes
Yes
1
1
1
1
1
(
(
(
(
(
)
)
)
)
)
2
2
2
2
2
No
No
No
No
No
(
<
(
(
<
D. MATERNITY HISTORY OF THE MOTHER
1. What was your age at puberty?.....................
2. What was your age at marriage?...................
3. What was your age at consummation of marriage?
4. What was your age at first pregnancy?...................
5. How many times you have conceived till now?
8 . Out of your conception how many were
Live births...................
Still births.................
Abortions........................
7 . Out of the live births how many were
Males................. females..................
8 . When did you have your last pregnancy?
.... months back
9 . What was the pregnancy order of this?...................
10 . Was the pregnancy
Wanted 1 (
)
Unwanted 2 (
)
E. OBSTERTICAL INFORMATION FOR THOSE WHO HAVE DELIVERED DURING
JUNE 1986 TO MAY 1897 ( Even if the child is not alive)
1. Name of the mother
2.
Age of the mother at pregnancy
3.
Order of pregnancy
4.
Date of delivery
5.
Sex of the child
8.
Is the child alive now ?
Yes 1 (
4
)
No 2 (
)
7. Did you have any checkup
during pregnancy from
a person from PHC/Subcentre
or Hospital or Doctor or
any other p erson
8. If did not have any
Why?
9.
Yes 1 (
Did not feel its
necessity
Did not know of
its necessity
Place of availability
not known
Place of availability
too far away
Workers not available
If you had checkup at what
period of pregnancy you had
the first checkup?
)
1 (
)
2 (
)
3 (
)
4 (
5 (
)
)
.... months
10. Who provided you the
checkup?
Dai
ANM
LHV
Govt.Doctor
Pvt. Doctor
Others(specify)
11.How many times did you have
the checkup?
12.
) No 2 (
1 (
2 (
3 (
4 (
5 (
6 (
)
)
)
)
)
)
a) Home
b) Clinic
Did you take tetanus toxoid
during pregnancy?
Yes 1 (
)
No 2 (
)
If yes, how many doses?
13.Were you given folic acid(iron)
tablets during pregnancy?
14.
15.
Yes 1 (
) No 2 (
If yes, how many pills did you cosume ? ------------Where was the place of delivery?
Home/House
Corporation Maternity
Hospital
Major Hospital
Pvt.Maternity Homes
Who assisted the delivery?
Elderly lady
Dai
ANM
5
Yes 1 (
3 (
4 (
1 (
2 (
5 (
Others (specify)
Did you have any checkup after
delivery within 40 days
from a health personnel?
1 (
2 (
3 (
4 (
LHV
Doctors
16.
)
) No 2 (
8 (
)
CHILD REARING PRACTICES FOR THE LAST LIVE BIRTH
F.
(Collect this information for deliveries in the last five years
irrespective of the fact, the child is alive or dead now).
Name of the child
1.
la. Age of the child(in months)
Did you breast feed this
child?
2.
Yes 1 (
No 2
)
3.
If no, why did you not
breast feed the baby?
4.
If yes, how many hours
after delivery you
started breast feeding?
... hours
How long did you breast
feed the child?
... months
At what age of the child you
started giving supplementary
feeding apart from breast nilk?
... months
5.
6.
(
Whether your child was
given the following immunisation?
(Collect information only for children aged 12 to 23 months)
7.
a.
b.
c.
h.
i.
BCG
DPT
Polio
Measles
Vit. A.
Yes
Yes
Yes
Yes
Yes
1
1
1
1
1
(
(
(
(
(
)
)
)
)
)
No
No
No
No
No
2
2
2
2
2
(
(
(
(
(
)
)
)
)
)
If yes no. of doses
If yes no. of doses
G.
KNOWLEDGE,ATTITUDE AND PRACTICES OF WIFE ON
POPULATION DYNAMICS AND FAMILY PLANNING
1.
Name of the respondent
2.
Age of the respondent
3.
What is your opinion regarding
the age at which your
children should be married?
Sons
....
Daughters
What is the legal at which
children should be married?
Sons
....
Daughters
According to you, how many
years after marriage a girl
should have her first baby?
.... Years
4.
6.
)
7.
8.
After how many years should
she have her second baby?
.... Years
How many children she should
give birth to?
a. Of them how many sons and daughters?
Sons
9.
....
Daughters
If yes, can you list those
methods?
11.
Have you used any of these
methods till now?
Yes 1 <
Yes 1 (
No 2 (
No 2 (
)
)
Yes 1 (
)
No 2 (
)
Yes 1 (
)
No 2 (
)
If yes, what method is it?
15. Are you satisfied with
this method?
IS.
)
)
If yes, what are they?
13. Are you still using any
method now?
14.
No sex preference
Do you know that there are
methods by which one can
avoid pregnancies?
10.
12.
....
If no, why?
17. Who motivated you to
adopt this method?
No
....
Undecided/upto God....
DK
....
19.When would you like to have your
(next) child ?
7
1
Yes
Within one year/soon
1-2 years
2+ years
DK
2
3
8
1
oo co ro
18.Apart from children you already have
do you want to have more children ?
20.Reasons for not having any (more)
child(ren)
?
No more/None
Currently Pregnant
Menopause
Sterile
Others
21.Why are you not using a FP method
to avoid pregnancy when you are not
interested ?
..........
.........
.........
..........
..........
1
2
3
4
7
(Specify)
Going to use soon
. . . .
Natural Sterility
....
Currently Pregnant
....
Lack of Knowledge
....
Afraid of
sterilisation
....
Cost too much
....
Can't work after
sterilisation
....
Worry about side
effects
....
Hard to get methods ....
Against religion
....
Opposed to FP
....
Husband opposed
....
Other people opposed....
Difficult to get
Pregnant
,...
Menopausal
....
Inconvenient
....
Don't like existing
methods
....
Others
. . ..
01
02
03
04
05
06
07
10
11
12
13
14
15
18
17
77
(Specify)
22.When are you planning to adopt a
FP method ?
23.Which method are you planning to
adopt
?
Within a year/soon
1-2 years
2+ years
DK
... . 1
.... . 2
. 3
. . . .
Male Sterilisation
.
Copper-T or IUD
Pill
Condom or Nirodh
...
Safe period for
periodic abstinence ...
W ithdrawal
Others
(Specify)
24.
Do you and your husband ever talk
about the spacing of children?
1
Female Sterilisation... . 2
Often
Some times
Rarely
Never
1
2
3
4
. 3
. 4
. 5
. 6
. 8
. 7
H.DIARROHEAL HISTORY OF CHILDREN BELOW FIVE YEARS
DURING THE LAST ONE MONTH AND FLACE OF TREATMENT FOR SICKNESS
1
SI. No. of the child
3
4
2
5
1. Name of the child
2. Age of the child in
months
3. Sex of the child
Male
1
Female 2
4.
Did the child suffer from
diarrohea in the last
one month?
Yes 1
No 2
5.
During the episode did
you seek any medical
consultation ?
Yes 1
No 2
8 . During the episode how
much of usual food was
offered?
Less than usual
Same as usual
More than usual
7. During the episode how
much of fluids wer
offered?
Less than usual
Same as usual
More than usual
8. During the episode was
the child given Oral
Rehydration solution?
Yes
No
1
2
3
1
2
3
1
2
9. Record the MUAC of
the child in mms.
10.
If someone is sick in the family where do you go for treatment ?
Corporation health centre
Government Hospital
Private practioner
Home remedies
None
1
2
3
4
5
(
(
(
(
(
)
)
)
)
)
11.
N.
What is the reason for seeking this particular
facility?
DETAILS OF BIRTHS IN THE FAMILY
SI.
No.
.
Family Size
Was there a
birth in the
Family during
June96-May 97
If Yes,
Sex of the
Child
Yes 1
No 2
Male 1
Female 2
Age of the Mother
at delivery
Order of birth
1
!
;
Page 1 of 4
Go
H'
Main Idet
From:
To:
Cc:
Sent:
Subject:
"rajan patil" <rajanpat i@yahoo.com>
"devika" <devika@xr.- eb.com>; "Centre for Resource Education" <hyd2_creind@sancharnet.in>;
"Toxics Link Chennai <tlchennai@vsnl.net>; "Madhumita Dutta" <mdutta@vsnl.net>; "Community
Health Cell" <chc@scchara.org>, "ravi" <ravig1@vsnl.com>; "Nitya" <nity68@vsnl.com>; "ananth
padmanabhan" <anar th@dialb.greenpeace.org>; <sambavna@sancharnet.in>; "Toxic Link delhi"
<t!delhi@vsnl com>: r>HM" <secretariat@phmovementorg>; <thanal@vsnl.com>; "Manu
Gopalan" <mangofori.@vsnl.net>; "Nimmi" <nirmala.karunan@dialb.greenpeace.org>
"disease surveillance <diseasesurveillance@yahoogroups.com>
Thursday, June 02 . 05 4:48 PM
Doctor who spoke ou; on public health issue is sued
Friends,
deja' vu' isn't it?
history' keeps repeating itself
regards,
rajan
£
again n again..
BMJ 2005;330:439 (26 February), doi: 10.1136/bmj.330.7489.439-a
Doctor who spoke cut on public health issue is sued
Sydney Christopher Zinn
A doctor who claims he was doing his job according to the tenets of the Hippocratic oath when he
spoke ou; about risks to health; from the operations of a major logging company in Tasmania is being
sued for causing alleged damage to the company’s business activities.
Dr Frank Nicklason, a staff specialist physician at the Royal Hobart Hospital, is one of 20 defendants,
including prominent environmentalists and another doctor, named in the writ by Gunns Ltd, which is
seeking almost $A6.3m (£2.6m; $5m; €3.8m) in damages.
fe
Dr Nicklason said the case mm slop doctors raising legitimate health concerns because of fear of
being i waived in prolonged and expensive legal action. He said that although the case would not
silence him it had already affected the forestry debate, which is dividing Tasmania.
7«-'s’ "It has succeeded in shutting other people up in Tasmania, mainly small local environmental and
G community groups," he said of the writ, which was served in December.
DrNick. :son faces years of k il action and a damages claim of SA250 000 for calling for an
indepe,. ent risk assessment <4 large piles of woodchips in the port of Burnie. He made the call in
2002, as a spokesman for the on-aligned lobby group Doctors for Forests.
He said ike Hippocratic oath required him to prevent illness not just in patients but in society as well,
and he .ieved, after talking ., ith experts, that the stockpiles of shredded wood on the wharf posed
potentia' ’tealth risks to Burnie s citizens.
6/3/2005
1-
Page 2 of 4
His res. . ch showed that legi. .ella bacteria, fungal organisms, and wood dust, all of which posed
health : ks, could have been i: the stockpiles, some of which had been undisturbed for years. The
local n ical community, however. had said nothing.
The n::
stock]'
gement at Gunns is fusing to comment on the case, but its own inquiries found that the
posed no danger to public health.
The st;,
Nickle
critics.
chairman of the Tasmanian Australian Medical Association Dr Michael Aizen said Dr
. had been caught up in Gunns "shotgun" approach, which was to sue a wide range of its
"In pi; Ale 1 feel that using the law to control the expression of concern about public health is
wrong. Gunns had any concerns they should have replied to Dr Nicklason with scientific
argum .
he said.
Re
’ Responses:
Read .
'apid Responses
Hea
.workers are speaking out in Wales too
.sanne mccabe
aj.com, 25 Feb 2005 [Full text]
corporate hegemony
chard Fielding
aj.com, 25 Feb 2005 [Full text]
1 Public Action Weeded to Prevent Gagging Public Health
ithony Lwegaba
Opp
Pea -
He;
tc
workers are speaking out in Wales
susanr.
retiree!
:cabe,
Send n
ise to
cf24 :
jourr
Reri
Spe
too
rkers_are
in Wales
c .
26 February
2005
In Wales they get suspended. A surgeon from Withy Bush
Hospital In West Wales actually dished out leaflets on the streets
of Have- ord West to highlight concerns about lack of beds in the
gynaecological ward. (This was Widely reported on TV last
month) i he Chair of the Community Health Council publicly
supported what the surgeon was claiming as the CHC had been
expressing the same concerns. Two weeks later ( a litle late in
the day maybe) a group of his colleagues wrote a collective
letter of support, theeir action was also made public).
People know all too well that the services are failing in Wales. A
week after he made his stand two senior nurses from University
College Hospital of Wales also spoke out on BBC Wales about the
6/3/2005
Page 3 of 4
state of ‘.he emergency services there..they claimed they were
unable to provide a safe service and that people were 'being
treated i:ke animals'.Ambulance drivers seem to feel more
intimidated because they tend to speak out anonymously about
ambulances lined up outside the hospital for lack of beds to
admit people. ~(Again publicised on BBC TV) A month ago the
spokesperson from BMA Wales stated that 'doctors are weeping
in despa.r' over the state of the services here.
It takes a lot for this sort of action to be taken by healthworkers
but here is a limit to how much stress anybody much less those
responsible for the well being of ill people, should be expected to
deal witfi on a daily basis.
Competing interests: None declared
Op P.
2 corporate Hegemony
Richar;! r
Senior
Univ.:.
ding,
:rer,
: Hong Kong
Send res
journal:
Re: Opp
he; ■
se to
-orjDorate
26 February 2005
AV " ‘
Sir, You; report on Dr. Nicklason who is being sued by a
corporat.on for raising health concerns (Doctor who spoke out on
health ccncerns is being sued, BMJ 2005, 330, 439) is yet
another example of a very worrying trend of corporate control
over freedom of expression. One section, 121, in the new
Serious Organized Crime and Police Bill about to be implemented
in the UK will oblige the police to arrest for harassment any
person handing out one leaflet to a person who has previously
been given a copy of that leaflet by a second person. This could
stifle most public protest in the UK. The MacDonald's Two would
not nave succeeded in protesting against MacDonalds foods had
this law ,een enacted then. Public complaint and protest against
corporate activities impacting health is being stifled worldwide
by tne co-option of increasingly repressive legal means, not least
by bankrupting whistleblowers trying to fight back. It is
imperative that those who desire a life and freedom that is not
subject to corporate control oppose repressive legislation like
this, speak out against this trend, and support those, like Dr.
Nick ason, who are victims of it.
Competing interests: None declared
Pe:.
G
Jul Putrt ic Ac Jon Needed to Prevent
g Publ ic Heaith
Anthon;
lecturer
•. gaba,
Health,
SCMR, I.
West In
Ba-.
Sc-
. rsityof
- -aveHUi,
28 February
2005
a
A
The action of Gunns Ltd to sue Dr Frank Nickloson and his
colleagues for raising up environmental health issues is very
disturbing as pointed out that it has sent a threat into health
conscious activists. However, this be seen as only the beginning
of a long struggle for which the following should be done:
r ? to
jOU:
Re:
ui Public
Act
Pre
He
p. d cq
1. Sensitise and mobilise professionals and the general public on
the issues at stake;
. ng_Public
2. Dem'....strate support for freedom of speech on public health
issues. Such campaigns should include - collection of signatures,
funos which will help the cause during the court process and
6/3/2005
Page 4 of 4
when possible police permitted (underlined) peaceful street
demonstrations.
3 Collect more evidence to document on the public health
impact of activities of such companies.
For ill these to occur a goal focused leadership must be in
charge.
The effect will be that no company functions without public
support and companies are or will be fully appreciative of that
fact.
All the best in the support for the cause of public health.
Competing interests: None declared
Do Y
Tired
http:/.
Yahoo!?
am? Yahoo! Mail has the best spam protection around
' .yahoo.com
6/3/2005
International Journal for Equity in
Health
BioMed Central
Open Access
Commentary
Self-help: What future role in health care for low and
middle-income countries?
KR Nayar*1, Catherine Kyobutungi2 and Oliver Razum2
Address: 'Centre of Social Medicine and Community Health, School of Social Sciences, Jawaharlal Nehru University, New Delhi 110 067, India
and department of Tropical Hygiene and Public Health, Heidelberg University, Im Neuenheimer Feld 324, 69120 Heidelberg, Germany
Email: KR Nayar’ - kmayar@mail.jnu.ac.in; Catherine Kyobutungi - c kyobutungi@urz.uni-heidelberg.de,
Oliver Razum - oliver.razum@urz.uni-heidelberg.de
• Corresponding author
Published: IS April 2004
International Journal for Equity in Health 2004, 3:1
Received: 17 October 2003
Accepted. 15 April 2004
This article is available from, http://www.equicyhealthj.com/content73/lll
© 2004 Nayar et al, licensee BroMed Central Ltd. This is an Open Access article: verbatim copying and redistribution of this article are permitted in all
media for any purpose, provided this notice is preserved along with the article's original URL.
Abstract
In the debate on 'Third options' for health care delivery in low- and middle-income countries it is
proposed that self-help should play a larger role. Self-help is expected to contribute towards
improving population health outcomes and reducing government health care expenditure. We
review scope and limitations of self-help groups in Europe and South Asia and assess their potential
role in health care within the context of health sector reform.
Self-help groups are voluntary unions of peers, formed for mutual assistance in accomplishing a
health-related purpose. In Europe, self-help groups developed out of dissatisfaction with a de
personalised health care system. They successfully complement existing social and health services
but cannot be instrumentalized to improve health outcomes while reducing health expenditure.
In South Asia, with its hierarchical society, instrumental approaches towards self-help prevail in
Non-governmental Organizations and government. The utility of this approach is limited as self
help groups are unlikely to be sustainable and effective when steered from outside. Self-help groups
are typical for individualistic societies with developed health care systems - they are less suitable
for hierarchical societies with unmet demand for regulated health care. We conclude that self-help
groups can help to achieve some degree of synergy between health care providers and users but
cannot be prescribed to partially replace government health services in low-income countries,
thereby reducing health care expenditure and ensuring equity in health care.
Background
The paradigm of health sector reforms currently under
taken at the global level, and especially in structurally
adjusting countries like India and elsewhere in the devel
oping world, enforces a move towards privatization of
medical care services. The State is often characterized as
inefficient and considered ill equipped to handle social
sectors such as health. This inefficiency argument is
applied to both issues of financing as well as the imple
mentation of health programs. The alternative suggested
is a mix of private and public, the primary care to the gov
ernment and the lucrative curative care to the private sec
tor [1], There are also certain options which fall between
completely state-oriented services and privatized care.
Page 1 of 10
(page number not for citation purposes)
International Journal for Equity in Health 2004, 3
One of the early such options was the Non-governmental
Organization. However, a number of recent impact stud
ies have shown that with regard to criteria such as reach
ing the poorest, coverage, cost-effectiveness, quality of
services or policy direction, non-governmental develop
ment organizations do not have any advantage over the
State [2] As concentration of funding and projects
increase, "NGOs become susceptible to bureaucratiza
tion, self-aggrandizement and imposition of standardized
solutions." |3|
Another approach discussed in this context is self-help
Self-help originates from industrialized countries and was
initially a bottom-up approach. Since the 1980s, however,
self-help has increasingly been "prescribed" by experts
with the explicit aim of reducing government health care
expenditure [4,5]. We argue that such instrumentalization
is about to occur again, this time in low- and middle
income countries with unmet demand for regulated
health care. The WHO report on Macroeconomics and
Health (2002) has identified investment in health as an
effective instrument for reducing poverty in low-income
countries. With their social and health systems cashstrapped, self-help is again being proposed as an allegedly
less costly but effective means of improving population
health.
However, the potentials and limitations of self-help in
health care for low- and middle- income countries have
not been sufficiently discussed. In this review paper we
provide a definition of self-help groups, briefly depict
their historical background, and assess scope as well as
limitations of the self-help movement in Europe where it
originated. In this section we demonstrate the inextricable
role of the political ideology of the day in the evolution of
the self-help movement and its subsequent instrumental
ization by the state in industrialized countries. Whether
and how this also applies to low- and middle- income
countries has not yet been discussed. In the main section,
we describe the political context, analyze experiences with
health-related self-help groups in Bangladesh and India,
and draw conclusions regarding the relevance of self-help
groups for improving population health. We restrict the
scope of this paper to the role of the self-help strategy in
health care, which encompasses the five categories of serv
ice provision in the health sector, namely: curative, pre
ventive, promotive, rehabilitative and palliative. Our
paper does not address the broader concept of health pro
motion as defined by the Ottawa Charter since this is a
result of inputs from various sectors, the individual effects
of which are difficult to evaluate [6|. Also, we address only
those aspects of self-help that have a direct effect on health
through service provision in the health sector. While the
self-help strategy is a long acknowledged tool for empow
erment, the latter is a much more complex process that
http7/www.equityhealthj.com/content/3/1/1
involves other methods of which self-help is just one Kar,
Pascual & Chickering (1999), for example, have aptly
described the dynamic and synergistic relationship
between health promotion, empowerment and quality of
life [7],
Methods
We obtained the material for this review from a search
covering the following databases: Medline advanced
(|Webspirs 4] 1966 -), PubMed (English), International
Bibliography of the Social Sciences (1BSS), Bibliography
of Asian Studies, Social Sciences (including Econ-Lit,
ERIC, Social Services Abstracts, Sociological Abstracts),
Popline, WHOL1S and other databases of UNDP, UNICEF
and UNR1SD. Apart from these databases, the review also
depended on government documents and conference
reports relevant to the topic.
The Self-help approach
The desirability of empowering communities to take care
of their health problems themselves has been raised since
long. Often it is argued that self-help is an ingredient of
the Primary Health Care strategy with its focus on "peo
ples' health in peoples' hands" |8|. The strong point could
be its orientation towards action and progress; people
would learn to be in the role of health care providers in
the process. One of the core principles of self-help is that
only those experiencing the problem can understand it
[9|. This is reflected in the comprehensive and still up-todate definition of self-help groups given by Katz & Bender
1976 [10] (cited in Katz, 1981, and in numerous other
review papers):
"Self-help groups are voluntary, small group structures for
mutual aid and the accomplishment of a special purpose.
They are usually formed by peers who have come together
for mutual assistance in satisfying a common need, over
coming a common handicap or life-disrupting problem,
and bringing about desired social and/or personal change.
The initiators and members of such groups perceive that
their needs are not, or cannot be, met by or through exist
ing social institutions. Self-help groups emphasize faceto-face social interactions and the assumption of personal
responsibility by members. They often provide material
assistance, as well as emotional support; they are fre
quently "cause"-oriented, and promulgate an ideology or
values through which members may attain an enhanced
sense of personal identity."
Katz highlights that self-help groups typically start from a
condition of powerlessness, and that the members spon
taneously (i.e. not urged by an outside authority) agree on
engaging in some actions in which they personally partic
ipate. Self-help groups create, and act within, a purpose
fully organized setting; this distinguishes them from
Page 2 of 10
(page number not for citation purposes)
International Journal for Equity in Health 2004, 3
http://www.equityhealthj.eom/content/3/1/1
self-care,
medical
which is practiced by individuals alone
or within a family [10].
Empowerment, on the other hand, is a process through
which individuals gain control over matters that concern
them most. It can be defined as a "multi-dimensional
social process that helps people gain control over their
own lives' [11]. Evidently, this concept is broader than
that of self-help in health care provision Empowerment is
distinct from self-help: While self-help is (or should be) a
spontaneous reaction by the affected individuals to an
undesirable situation, empowerment is by connotation a
proactive externally driven process. Although involve
ment in self-help may enhance personal empowerment,
community and organizational empowerment are
enhanced through other methods, as described by Kar
(1999). Empowerment can have indirect health effects
that are more difficult to quantify than the more direct
effects of self-help. In view of the broad concept and the
indirect effects, we restrict the scope of our review to self
help groups.
et
al.
Results
Self-help in industrialized countries
Historical background
By the mid-19lh century, population health in Victorian
England had deteriorated to an alarmingly low level; pov
erty, disease and death were wide-spread [12,13). It took
reformers inside and outside Government decades to
devise and implement reforms that would, towards the
end of the 19lh century, help to control infectious disease
and improve general living standards. Scientific and polit
ical debate on how to initiate social change and better
society had, by that time, come to rather dissimilar con
clusions. One group, the "social Darwinists", proposed to
apply Darwin's theory of natural selection in the evolu
tion of biological species to the improvement of human
society. The British philosopher Herbert Spencer, for
example, advocated what he called “true liberalism", an
extreme economic and social
He expected that
a massive restriction of the role of the state and a reliance
on the principles of the market (i.e. supply and demand),
laissez-faire.
would lead to the "survival of the fittest'1, and hence to
continuing improvement of the population. Spencer
expected that as his flavor of liberalism was mounting,
social altruism would increase, and "voluntary associa
tions” would replace government support and aid to the
"unfit" poor.
Other social researchers followed a rather different track.
Beatrice Potter (later married Webb) tried to learn from
organizations that members of disadvantaged population
segments themselves had created to alleviate their situa
tion; in 1891, she published
Peter Kropotkin, in his book
Great Britain.
The Co-operative Movement in
Mutual Aid
(originally 1902), did not deny the importance of Dar
win's theory of natural selection; yet he argued that co
operation, and not conflict, is the chief factor in the evo
lution ofspecies [14], According to Kropotkin, mutual aid
and self-help are the oldest and most natural systems to
improve the situation of human beings. Like Spencer,
Kropotkin reasoned against a centralized state (which he
thought should be replaced by voluntary associations of
mutual support), but from a libertarian rather than "truly
liberal" point of view. Thus, his core ideas embraced
empowerment of the weakest and not survival of the fit
test. Ultimately, however, it was neither social Darwinism
nor the self-help movement but the legislative work of
dedicated government officials and increasing investment
in water and sanitation that had brought about the major
improvement in population health by the end of the 19lh
century [12].
Many authors trace the history of "modern" self-help
Alcoholics Anonymous
groups to the foundation of
(AA) in
the US in 1935, a group that became active in a field in
which existing social and health services did not provide
adequate support. More recently, the 1960s civil rights
movement gave people the confidence to trust in their col
lective power, rather than in that of politicians or experts,
and empowerment became a core motive in the forma
tion of self-help groups. For example, people increasingly
felt that they were being pushed in a position of childlike
dependence once they became patients in the now hightech medical sector. They began to question medical clas
sifications of health and illness and the stigma attached to
certain conditions. With the advent of the women's move
ment, women began to oppose the medicalization of
birth and human reproduction and moved to "reclaim"
these from the male dominated medical sector [15,16].
People also began to criticize what they perceived as pro
fessionalization, fragmentation and specialization of
health care institutions, and started to look for alternative
ways of care that were holistic and allowed patients to par
ticipate in the decision making processes that concerned
their treatment. This trend was in part complimented in
the late 1960s by the emergence of the community devel
opment movement especially in Britain. The working
class was disillusioned with the welfare state, and had to
cope with increasing levels of poverty. The upper classes
thence advocated for social programs to "reach further
into the community." Self-help organizations sprung up
among the working class unemployed and this lay the
ground for alternative means of political expression
among Labour Party supporters frustrated with local state
functionaries. In the post Second World War period, racial
tensions arose in Britain because of unmet needs among
an increasing migrant population. The establishment of
the Community Development Project by the British gov
ernment was therefore catalysed by the need to resolve
Page 3 of 10
(page number not for citation purposes)
International Journal for Equity in Health 2004, 3
these growing tensions, cut spiraling welfare costs while
encouraging "community care” [17], These and other
related trends, encouraged and promoted the evolution of
the current self-help movement in Europe, the US, and
Japan in the 1970s. Initially, self-help groups in the health
field were considered as dangerous and rife with charla
tans. By the mid-1980s, the movement had gained wide
recognition and acceptance; national and international
networks of self-help groups were established, e.g. under
the auspices of WHO Europe [15-19],
In the early 1980s, the idea of self-help was again claimed
by politically opposing sides, this time in West Germany.
When the government cut back expenditure for health
and social services because of budgetary constraints, offi
cials proposed that self-help in groups, within families
and among neighbors, together with the work of unpaid
volunteers, should compensate for the resulting reduction
in services. They argued that this was in line with the
widely accepted principle of subsidiarity (meaning that
government should perform only tasks which cannot be
performed effectively at a more peripheral, local level).
There was even money set aside to support self-help
groups financially. The alternative health movement per
ceived self-help groups as a way to empower patients and
to reduce the influence of professionals and bureaucrats.
It soon became evident that government assistance to self
help groups tended to reduce their autonomy and could
not make up for the drop in quality of social services.
From this perspective, an instrument of empowerment
was being turned into a tool to trim down the welfare state
and promote conservative politics [4],
Scope and limitations of self-help
Self-help groups have dealt with a broad range of healthrelated problems where practical problems and psycho
logical sorrows of sufferers or their relatives need to be
tackled [18]. Examples are cancer post-care; addiction
(self or in family, e.g., AA); common conditions like
hypertension or diabetes; rare diseases (e g., Huntington's
chorea); support and social advocacy for family members
of psychiatric patients; etc. (15], There is broad agreement,
however, that self-help groups cannot replace existing
professional health services, but complement them [2022]. As Lock put it, "No self-help group has ever arisen to
provide a service that was already obtainable through the
medical system." [18] Another reason why self-help
groups cannot replace existing health services is that they
are not equally appropriate for al 1 population strata. Many
groups are run and attended largely by the white middle
class in distant middle class suburbs [18], Males, minori
ties, the aged, the working, and lower classes are underrepresented [10]. Overall, only 6-9% of potential partici
pants actually engage in self-help activities [23], Kropot
kin argued that self-help is a universal principle in nature
http://wwwequityhealthj.eom/content/3/1/1
114]; it should hence be practicable in all cultures. The
Western self-help groups, however, developed in a partic
ular social and historical context. Prerequisites for their
popularity were a well-educated middle class who no
longer wanted to trust the experts alone [17], and hightech medicine [24], Not all low- and middle-income
countries possess these attributes. There are examples of
successful transfer of the concept across cultures, however,
e.g. to Japan [25], Ultimately, it maybe more relevant that
self-help is appropriate only for a minority within a coun
try or society [23,241.
Self-help groups cannot be steered from the outside (by
politicians or health experts). Crucial for the functioning
of a self-help group is that its members are simultaneously
givers and receivers of help; and that the bureaucracy and
professionalism prevalent in the usual human service
organizations is absent. The chief reason for decline of
self-help groups is an autocratic leadership style of found
ers and a bureaucratization that preclude membership
participation. The natural history of self-help groups con
tains this risk: self-help groups tend to move from
via
and
to
[10] - which may
ultimately lead to their demise. Governmental funding
often accelerates this process, as there is a danger that self
help groups lose the necessary autonomy and self-deter
mination and are appropriated and instrumentalized by
state planning |17|. The same may happen when profes
sionals try to influence self-help groups. While mutual
respect and co-operation can be productive, competition
for clients, status, and power may arise [10]. As early as
1980, Jones wondered whether the self-help movement
will be "able to change aspects of modern medical practice
or whether groups will allow themselves to be controlled,
and submerged, by the professionals" [24|. On the other
hand self-help, like many other volunteerisms, is often
and unpredictable, and for that reason ultimately
unsustainable.
Informal Organization, Emergence of Leadership
mal Organization Professionalization
Origin
For
ad-
hoc
Enthusiasm about the perceived success of self-help
groups in the health field can be so infectious that it
replaces a systematic outcome evaluation: self-help
groups are said to "mobilize new resources to provide
health care" [22]; they are "the most exciting and least rec
ognized resource for improving public health" [5]; they
are a "success story" and even the "accepted fourth col
umn of health services" [19]. Collaboration with self-help
groups is deemed one of the "essential future tasks of
medical activity" for medical practitioners [20], Such
enthusiasm has been questioned by Badura
(2001).
They point out that since self-help groups obtain substan
tial amounts of public funds, their effect on the social and
physical wellbeing of members should be evaluated
together with the cost effectiveness, this being an
et al.
Page 4 of 10
(page number not for citation purposes)
International Journal for Equity in Health 2004, 3
approach that seems to cater for only a small percentage
of those who need it [23]. Proponents of the self-help
movement, however, largely reject attempts to make self
help "evidence-based", stressing instead the need to
understand health in a holistic way.
Studies of the outcomes of participation in self-help
groups are notoriously difficult, and evaluation has often
been less than rigorous. For example, the report "Self-help
and health in Europe'1 published by WHO Europe fre
quently alludes to "initial data" and results from "early
pilot studies" [13], When it comes to evaluation, Katz
observed that many self-help groups resist the involve
ment of outside researchers because the members ques
tion the appropriateness of outcome criteria set by
outsiders - especially so when empowerment is an impor
tant aim [10], This attitude, however, leads to criticism.
Oakley points out that various other social interventions
have actually been tested in a methodologically convinc
ing way in randomized controlled trials, and many have
been found to be ineffective. She worries that some
researchers abandoned randomized controlled trials
when they found that new "treatments" were no better
than old ones. They retreated to other methods of evalua
tion, allegedly to prove that their favored treatment works
[26],
Even proponents of self-help groups who carried out eval
uative studies in the 1980s conceded that the state of
research on the benefits of self help groups "is still rather
unsatisfactory” [21], a verdict that is being upheld 12
years later, in particular with respect to economic evalua
tion [23]. There are exceptions: within the German Cardi
ovascular Prevention Study, groups of community
members developed and implemented preventive activi
ties without a dedicated budget. As in the model described
by Moeller (1983), local doctors provided encouragement
and expertise on request, but did not organize or manage
the activities [20]. This approach was evaluated in a quasiexperimental design and shown to contribute towards
reducing the prevalence of cardiovascular risk factor levels
(27]. In summary, it is widely believed that in industrial
ized countries self-help groups contribute to improving
the health of, and providing care for, chronically ill and
disabled people [Additional File 1], But as a prescription
for improving health outcomes and saving money, self
help groups cannot yet be considered "evidence-based".
http7/www.equityhealthj.com/content/3/1/1
and empowerment of women. As governments and civil
society organizations of low- and middle income coun
tries, especially those in South Asia, have taken up the
concept of self-help, the agenda and to some extent the
social base have become broader and even more ambi
tious than in industrialized countries. Not only are self
help groups supposed to contribute towards income gen
eration of women members and thereby their empower
ment. They have to also provide psycho-social support
and information (prevention, promotion) to patients and
their relatives as they do in industrialized countries
[28,29]; and to perform some limited form of (curative
and rehabilitative) primary health care. Finally, they are
expected to improve financial accessibility to ensure sus
tainability of social services, thus, in effect, transforming
and expanding self-help groups into economically ori
ented co-operatives [Additional File 1]. Efforts are also on
to link such groups to people living with H1V/AIDS in
Asia-Pacific countries such as India, Cambodia, Nepal and
Malaysia [30].
In the following, we develop a typology of self-help
groups in Bangladesh and India in order to derive some
preliminary conclusions on the role of self-help groups
and what they have so far achieved within the health sys
tem of low-income countries, relative to the experience in
industrialized countries. We base this typology on 1) the
origin of self-help - did it develop from within the com
munity or was it an exogenous prescription? 2) the
approach followed by the self-help groups vis-a-vis their
purpose and targets, 3) the type of activities performed by
the self-help groups in health, and 4) the sustainability of
the groups.
Self-help in South Asia
Self-help under NGO sponsorship
The 1990s marked the arrival of Structural Adjustment
and economic liberalization in India. Concurrently, the
number of self-help groups linked with commercial banks
increased from 255 in 1992-93 to 2700 in 1995 [31],
Around eighty-five percent of these groups were formed
exclusively by women in production-oriented and income
generation activities such as garment making, food
processing, etc., and were following a
with a narrow economic focus. These self-help
groups were organized with tire help of outside agencies
and the support of social, religious or political leadership
and were seen as alternatives in rural development to
break away from the traditional bureaucracy and topdown management [32], A number of non-governmental
The background
Organizations based on the Gandhian philosophy of selfreliance had already been popularized during the freedom
movement in British India. In past years, self-help groups
in South Asia have been formed as part of a developmen
tal strategy with a primary focus on poverty alleviation
organizations started self-help groups mainly as savings
and credit groups without any emphasis on health. This
was an alternative movement due to the failure or absence
of a formal rural credit system [33]. The Grameen Bank of
Bangladesh is one of the earliest such movements. In most
of the above cases, women were the target group under an
approach
market-oriented
Page 5 of 10
(page number not for citation purposes)
International Journal for Equity in Health 2004, 3
http://www.equityhealthj.eom/content/3/1/1
approach to development, which advocated micro-enter
prises in the context of rolling back of the state, the
Some leading non-governmental organizations in Bihar,
which is one of the most backward states of India, have
removal of welfare provision and dismantling of labour
protection [34], However, available evidence shows that
such an approach has failed to make any significant
impact on the incomes of poor women over a sustained
initiated self-help groups primarily for income generation
activities. However, a substantial number of these groups
have been experimenting with activities in health, mostly
related to health campaigns and education [38], Many of
the groups have also been giving loans for medical treat
ment; the level of recovery however varies.
period and did not lead to any reduction in the gender
inequality [34]
The Self Employed Women's Association (SEWA) in
Gujarat, India, is a combination of self-help groups and
cooperatives of women workers in the informal sector. It
followed a multi-faceted
wherein
all economic activities of the groups were linked to health
and social issues, as against the market-oriented approach
[35] However, there continue to be intensive material
empowerment approach,
and managerial inputs from the apex association in the
organization and maintenance of the groups and co-oper
atives. SEWA has identified and trained midwives and
health workers from among the self-help groups. They
serve as health educators-cum-barefoot doctors to all the
women members of different groups and help the
women's groups in forging linkages with tire government
and private health care providers for specific services and
programs. The activities of these health workers include
health promotion and preventive health care through
health education, immunization, micro-nutrient supple
mentation, family planning, provision of rational drugs,
and low-cost traditional medicine [35]. Subsequently,
these health workers have formed their own co-operatives
in a move towards achieving sustainability. The evidence
from the SEWA experience is that lite self-help approach
as a community based insurance scheme can prevent
impoverishment through protection against catastrophic
health expenditure of poor households, given the finan
cial viability and strong administrative and management
capacity of the organization [36,37].
The Mahalir Association for Literacy, Awareness and
Rights (MALAR) was established in the Kanyakumari Dis
trict, Tamil Nadu, India, as a women's savings group with
the purpose of mobilizing women belonging to the
oppressed strata of the society through a structure inde
pendent of the government [31]. The MALAR experiment,
which followed an
is an entirely
self-reliant movement without any external funding, but
facilitated by external actors. Like SEWA, it has an organi
zational structure similar to co-operatives, with self-help
groups forming the basis. It is also running a health cam
paign, apart from trying to expand the activities to
empowerment approach,
women's library movement, legal aid activities, etc. Sev
eral districts in other states of India have also started such
initiatives.
Leading NGOs in Bangladesh have tried a self-help
approach for poverty alleviation by forming organizations
of poor women [39]. The activities, apart from income
and employment generation, included conscientization,
raising awareness for gender equity, and human resource
training.
A conference organized jointly by three Red Cross Socie
ties, UNDP and a number of other organizations revealed
the renewed interest in self-help, viewing it as a cost-effec
tive and sustainable approach to social development,
especially health [40]. The papers presented were based
on the experience of about 40 NGOs working in Bangla
desh. The NGOs considered the self-help approach largely
as a tool for community management, especially for
implementation of specific project-related activities. A
project approach is evident in this conceptualization of self
help groups: Self-help is utilized as a method of facilitat
ing community participation or as a way of enhancing
sustainability of projects conceived and implemented by
NGOs. Of special significance was that among the multi
tude of NGOs working in different sectors of the country,
some reported facing problems in phasing-out their activ
ities from the community. In these specific cases, for
example in developing a village health committee with
the aim of achieving self-reliance, self-help approach was
used as a phase-out strategy so that the NGOs could with
draw after the termination of the project.
Sustainability of NGO-sponsored self-help
There is limited evidence regarding the sustainability of
externally sponsored self-help groups especially after the
withdrawal of the mother NGOs which originally started
these groups. SEWA has been able to sustain its activities,
largely because of the intensive inputs and support pro
vided for the maintenance of the groups and due to the
evolution of the self-help groups to a more institutional
ized form similar to co-operatives. The experience from
Bihar suggests that the ability of a self-help movement to
become self-sustaining is rather limited, even with finan
cial strength and in the absence of organizational weak
nesses [38], It is premature to comment on the
sustainability of the MALAR experiment, which is still in
an early stage. In Bangladesh, one local NGO withdrew
from a primary health care project by using the Village
Health Development Committees formed in the begin
Page 6 of 10
(page number not for citation purposes)
International Journal for Equity in Health 2004, 3
http7/www.equityhealthj.com/content/3/1/1
ning of the project as a self-help mechanism |40|.
Although the consequences of the phasing out are not yet
clear, it is stated that a phasing out is not impossible if the
through a market-oriented strategy such as micro-enter
prises, thrift and credit societies, informal banks, etc.
people are told about it in the beginning of a project.
Another NGO promoted a self-reliance strategy because it
had previously experienced a sudden withdrawal of donor
The health component of Kudumbashree is limited to cre
ating awareness and facilitating access of members to
health services [44,45]. Weekly meetings of group mem
bers are organized to discuss issues related to hygiene,
mother and child care, nutrition, immunization, etc. A
Community Health Volunteer who is selected from
among the members performs convergence of various
programs under the Health and Social Welfare Depart
ments and helps the members, especially women, chil
dren and the aged, to access services.
support. The strategy adopted was the formation of health
and management committees with the participation of
people. The NGO reports that the task was difficult, as
people believed that government and non-government
organizations should provide health care free of cost |40|.
In a third case, where health was a major component, a
self-sustaining, payment-based card system for free serv
ices or a reduction of fees was introduced at the village
health posts [40] One of the significant limitations iden
tified was the inability to sustain community interest
when there were other priorities such as harvesting, or
when disasters occurred, for example floods. When self
help is implemented in a project mode, the motivation of
the project staff also becomes important. The project staff
may have apprehensions about loosing their job if the
self-help project becomes too successful. In yet another
case, self-help was visualized as a community support sys
tem for specific problems like obstetric care [40], The
project tried to link the support system with the local gov
ernment. Although it found that this approach would
potentially increase the access to health care and health
information, its sustainability could not be established.
Self-help under Government sponsorship
The Government of India has adopted the self-help
approach and micro-finance programs as tools for
women's empowerment, employment generation and for
achieving production-oriented goals. This is part of the
overall strategy within tire new economic policies to rede
fine the role of the government [41-43], A major initiative,
sponsored by the Government and known as 'Kudumbashree' (Welfare of the Family), is underway in the State
of Kerala. This new scheme, based on the mentioned
national strategy, is a highly formal and institutionalized
approach to self-help. Kudumbashree promotes income
generation activities for poor women by organizing
Neighborhood Groups (NHG), which will help them to
earn higher incomes, thereby enabling them to achieve
economic self-sufficiency. Several other state governments
in India have also initiated employment programs for
women (and even public-limited companies like
Women's Development Corporations) based on the con
cept of self-help. It is hoped that by building community
structures of women drawn from poverty-stricken families
and by helping them to overcome poverty, social and eco
nomic empowerment can be achieved. The empowerment
of women gets the central place in the conceptualization
of Kudumbashree, although it is operationalized largely
A typology of self-help in South Asia
In Bangladesh and India, three broad scenarios regarding
the structure of self-help groups involved in some form of
health activities are discernible. The characteristics are
given in [1], In the two countries, characterized by a hier
archical social structure and a substantial proportion of
poor, there is some degree of similarity in the origin of
self-help groups- they have not evolved endogenously or
as a spontaneous reaction to a common cause, but have
been initiated externally. The health-oriented groups in
India mainly target women for their programs, resembling
the purely market-oriented self-help groups. The NGOs in
Bangladesh, on tire other hand, are not targeted on
women alone The groups in the two countries follow dif
ferent approaches and have different emphasis on health
issues, from awareness campaigns and health education
to primary health care activities as in Bangladesh and the
SEWA initiative. However, none of the groups are
involved in provision of curative health care, and may not
be able to do so considering their composition and focus
(except supply of drugs, as in SEWA). The SEWA initiative
is characterized by its well-developed organizational
structure and intensive inputs, and probably these have
helped it to sustain its activities.
Evidence regarding the viability and cost-effectiveness of
the self-help approach in health care is limited, partially
because of its recent origin. Even SEWA, which has been
able to sustain its activities over a longer period, is not a
convincing example of alternate community financing in
health or provision of good quality clinical care. Moreo
ver, the evidence from Bangladesh shows that self-help
has only moderate success as a rollback or phase-out strat
egy. To some extent, however, self-help groups may be
able to increase access to, and facilitate the utilization of
existing health services [Additional File 1 ].
Successes of self-help In health care
Notable successful self-help groups in South Asia are
those which are run under huge organisations like BRAC
(Bangladeshi Rural Advancement Committee), SEWA,
Page 7 of 10
(page number not for citation purposes)
International Journal for Equity in Health 2004, 3
and Grameen Bank. They have in one way or another
engaged in health related activities ranging from health
education programs for child care by BRAC to training
"cum-barefoot doctors" by SEWA. Hadi argues that
involvement in these activities resulted in health benefits
for members of self-help groups and their families like
improved child care, and increased contraceptive use
146,47]. Other authors have also described a reduction in
domestic violence, increased health knowledge and better
disease prevention by women belonging to self-help
groups [48-51], Empowerment of women who participate
in self-help groups has also been described [52] but some
authors are sceptical about the reported successes in terms
of meaningful empowerment, and having an effect on
existing social structures that determine gender relations
and health [53,54], We found no examples where the
position of self-help group members has improved to
such an extent that they were capable of taking major deci
sions at community level in terms of resource allocation,
service provision, or influencing major policy changes in
health.
It is important to highlight that the few success stories
noted are in the context of large organizations that incor
porate self-help activities as just one component. It is
therefore hard to tease out the contribution of self-help
independent of other concurrent activities or the organisa
tional infrastructure. In addition, studies that tend to sub
scribe cause and effect relationships between membership
in self-help groups and changes in health status or health
behaviour have been criticised for not taking into account
sources of bias like choice based sampling and self-selec
tion into programs [55]. Thus, there is as yet no convinc
ing evidence that in societies with unmet demand for
regulated health care, self-help groups can become a
"third option" to replace ailing government health serv
ices.
Discussion and conclusions
http://www.equityhealthj.eom/content/3/1/1
Throughout the history of self-help, there has been a ten
dency to "usurp" this concept and put it to use in the inter
est of a conservative political agenda. The social
Darwinists of the 19th century envisioned a society based
on the principle of "survival of the fittest". They
demanded "no money for the unfit" and promoted self
help to ease the effect on the poor. In West Germany of
the mid-1980s, self-help groups were instrumentalized
under a revisionist interpretation of the principle of sub
sidiarity, again with the outspoken aim to reduce govern
ment expenditure, and in spite of missing evidence on
cost-effectiveness. Attempts like these ignore that self-help
does not come for free (neither for users, nor for the social
and health sector), and that it is appropriate only for a
small proportion of potential users. In some cases, as in
Britain, self-help groups were formed by the women's
movements, unemployed youth and migrants. Overall,
the aged, the working, the lower classes, the minority
groups are not reached, in other words, the very people
that are left most in need when funding of government
social and health services is reduced.
In the international health arena today, there are attempts
to appropriate the concept of self-help over again. Self
help groups are being prescribed to alleviate the effects of
a utilitarian approach to priority setting in the health sec
tor of low-income countries that resulted in "rationing by
exclusion" [56], Again, it is being overlooked that self
help is not free of cost. Potential users may not be able to
afford access to information, transport to reach meetings,
the required infrastructure, and clearinghouses to facili
tate the formation of new groups; etc. A successful self
help approach requires that lay people not only have
access to, but also learn to digest, health-related informa
tion (books, journals, Internet, etc.) that informs their
activities. In summary, self-help requires political accept
ance and financial support. Not only politicians, but also
health care professionals have to be compliant. Doctors
and nurses need to be prepared to co-operate with clients
on an equal basis. This means they need to be involved
early on, and be fully convinced of the advantages of self
help approaches, rather than be forced to participate.
People in Europe and the US form self-help groups to ful
fil a need that is not met by existing social and health serv
ices. Their aims are multiple and often divergent: to
empower themselves; to participate in decision-making;
to show concern and compassion for others in an increas
None of these prerequisites are met in South Asia to any
ingly individualistic society; and to feel being treated as a
dignified person, often in response to a health care system
that they perceive as high-tech but de-personalized. Given
the number and nature of these objectives (which, more
over, may be related to health outcomes only indirectly),
the cost-effectiveness of self-help groups has been difficult
to evaluate. In consequence, their role in health care pro
vision has not been promising. For proponents of self
help groups this is not a problem - they have always
insisted that this approach can complement, but never
replace, existing health services.
appreciable degree. In India [57) and Bangladesh, like in
many other low- and middle-income countries, vertical,
hierarchical social structures prevail, creating an environ
ment which is not very suitable for self-help groups. We
found that a prescriptive, instrumental approach to self
help is dominant, both in the NGO and the government
sector. Judging from experience in Europe, the utility of an
approach in which professionals attempt to steer self-help
groups from outside is very limited and unlikely to be sus
tainable, unless continuously supported by considerable
financial and organizational inputs. Self-help groups
Page 8 of 10
(page number not for citation purposes)
International Journal for Equity in Health 2004, 3
should be voluntary, have a convincing component of
service quality assurance, involve doctors early on, and
agree upon outcome measures (improved health? reduced
cost? equity? empowerment?) to assess cost-effectiveness.
In order to function, self-help groups require a basic ena
bling environment such as a stable social structure and a
functioning basic health care system offering a minimum
http.//www.equityhealthj.com/content/3/1/1
man Academic Exchange Service (DAAD) under the Innovatec program.
We thank Debora Landau for help with retrieving and reviewing literature.
References
I.
2.
3.
standard of quality. The presence of these two factors is a
prerequisite for self-help activities; they cannot be
expected to develop as a consequence of self-help in
health. Self-help groups can help to achieve some degree
of synergy between health care providers and users when
the prerequisites mentioned above are met. As long as this
is not the case, however, the transfer of a concept that orig
inated in Western, individualistic societies to a very differ
ent societal context will bring disappointing results. As a
part of the existing neo-liberal agenda, it might further
result in shifting the responsibility of health care from the
State to the individual, which would have serious implica
tions for equity and justice in health.
4.
5.
6.
7.
8.
9
10.
I I.
Competing interests
12.
None declared.
Authors' contributions
KRand OR were involved in the conceptualisation, frame
work, review and writing of the text. CK contributed addi
tional reviews, definitions, and towards developing
research questions. OR handled the section on industrial
ized countries and, KR and CK handled the sections on
low and middle-income countries. All the three were
responsible for the section on discussion and conclusions
Additional material
13.
14.
15.
16.
17.
18.
19
20.
Additional File 1
Comparison of the ideal self-help model in health to the evidence from
industrialized and South-Asian countries
Click here for file
[hup://www.biomedcentral.com/content/supplementary/14759276-3-l-Sl.doc]
Additional File 2
Typology of self-help groups with a health orientation in Bangladesh and
India
Click here for file
[ hup.://www.biomedcentral.com/content/supplementary/14759276-3-l-S2.doc]
21.
22.
23.
24.
25.
26.
Acknowledgements
This work was partly funded by EU, INCO-DC Contract
ERBICI8CT980352 in Germany and partly by INCO-DC contract
ICA4CT-2000-30009 in India. K. R. Nayar received support from the Ger
27.
World Bank; World Development Report Investing in Health. Washington
1993.
UNRISD; Visible Hands: Taking Responsibility for Social Development.
Geneva 2000 Forum, the Next Step in Social Development Geneva 2000.
26-30 June 2000
Wolfe M: Social Integration: Institutions and Actors. Occa
sional Paper No. 4. -World Summit for Social Development.
Geneva: United Nations Research Institute for Social Development 1994.
Deppe HU: Selbsthilfe zwischen Subsidiaritat und Klassensolidaritat. Osterreichische Zeitschnft fur Soziologie 1985, 10:82-95.
Humphreys K, Ribisl KM; Viewpoint on Self-help groups - a case
for a partnership with Self-Help groups. Public Health Reports
1999,114:322-329.
World Health Organization; Ottawa Charter for Health Promotion. Inter
national Conference on Health Promotion, Ottawa. Geneva 1986.
Kar SB, Pascual CA, Chickening KL Empowerment of women for
health promotion: a Meta-analysis. Social Science and Medicine
1999, 49:1431-1460.
Robinson D: The self-help component of primary health care.
SocSci Med 1980, I4A:4I5-42I.
Robinson D; Self-help Groups in Primary Health Care. World
Health Forum 1981,2:185-191.
Katz AH: Self-help and mutual aid: An emerging social move
ment? Annual Review of Sociology 1981,7:129-155.
Page N, Czuba CE: Empowerment: What is It? Journal of Extension
1999, 37(5): I-5.
Szreter S: Rapid economic growth and 'the four Ds’ of disrup
tion, deprivation, disease and death: public health lessons
from nineteenth-century Britain for twenty-first-century
China? Tropical Medicine & International Health 1999, 4:146-152.
Wohl AS: Endangered Lives. Public Health in Victorian Britain London: JM
Dent; 1983.
Kropotkin PA: Gegenseitige Hilfe [Mutual Aid] Leipzig:Verlag von
Theod. Thomas; 1904.
World Health Organization: Self-help and health in Europe. New
approaches in health care. Copenhagen 1983.
Kickbusch I: Self-care in health promotion. Social Science and
Medicine 1989, 29:125-130.
Craig G: Community work and the State. Community Develop
mentjournal 1989, 24:3-18.
Lock S: Self help groups: the fourth estate in medicine? British
Medical Journal (Clinical Research Ed.) 1986, 293:1596-1600.
Matzat J; Self-help groups in West Germany. Developments of
the last decade. Acta Psychiatr Scand 1987, Suppl 337:42-51.
Moeller ML: Self-help and the medical practitioner. In Self-help
and health in Europe. New approaches in health care Edited by: Hatch S,
Kickbusch I. Copenhagen: WHO Regional Office for Europe;
1983:68-76.
Trojan A: Benefits of self-help groups: a survey of 232 mem
bers from 65 disease- related groups. Social Science and Medicine
1989,29:225-32.
Richardson A: Health promotion through self-help: the contri
bution of self-help groups. In Health Promotion Research. Towards a
New Social Epidemiology Edited by: Badura B, Kickbusch I. Copenhagen:
WHO Regional Office for Europe; 1991:467-75.
Badura B, Schaeffer D, von Troschke J: Versorgungsforschung in
Deutschland: Fragestellungen und Fbrderbedarf [Issues in
Health Services Research]. Zeitschnft Gesundheitswissenschaften
2001,9:294-311.
Jones P; The emergence of self-help groups. Health Education
Journal 1980,39:84-87.
Oka T, Borkman T: The history, concepts and theories of self
help groups: from an international perspective. Japanese Jour
nal of Occupational Therapy 2000, 37:718-722.
Oakley A: Experimentation and social interventions: a forgot
ten but important history. British Medical Journal 1998,
317:1239-1242.
Scheuermann W, Razum O, Scheidt R, Wiesemann A, von Frankenberg H, Topf G, Nussel E: Effectiveness of a decentralized, com
munity-related approach to reduce cardiovascular disease
Page 9 of 10
(page number not for citation purposes)
International Journal for Equity in Health 2004, 3
28.
29.
30.
31.
32.
33.
34.
risk factor levels in Germany. European Heart Journal 2000,
21:1591-1597.
Osborne K: Support to HIV-positive people, NAPWA South
Africa. AIDS Bulletin 1997, 6:38-39.
Jayaseelan J: Responding to local needs. Self-help groups. AIDS
Action 1993, 20:4.
UNDP: Micro-finance and HIV/AIDS: building partnerships. Report of the
session organized by UNDP and its partners for the Asia-Pacific region
micro-credit summit New Delhi 2002. 3 February 2001
Franco TD, Kalpana K: United We Sit New Delhi; Bharat Gyan Vigyan
Samiti; 1999.
Rajagopal: Empowering rural women’s groups for strengthen
ing economic linkages: Some Indian experiments. Develop
ment in Practice 1999, 9:327-341.
Karmakar KG: Rural Credit and Self-Help Groups: Micro-finance Needs
and Concepts in India New Delhi: Sage; 1999.
Mayoux L From Vicious to Virtuous Circles? Gender and
Micro-Enterprise Development. Occasional Paper Number 3, U N.
Fourth World Conference on Women 1995 [http;//www.unrisd,org/
http://www.equityhealthj com/content/3/1/1
54.
55.
56.
57.
Laxmi M: Micro credit, Macro hype [http://www.indiatogether.org/
women/finance/macrohype.htro].
Pitt MM, Khandker SR, Mckernan SM, Abdul Latif M: Credit pro
grams for the poor and reproductive health behaviour in
Low - income countries: Are the reported causal relation
ships the result of heterogeneity bias? Demography 1999,
36(I):I-2I.
Stefanini A; Ethics in health care priority-setting: a north
south double standard? Tropical Medicine & International Health
1999, 4:709-712.
Gupta D: Mistaken Modernity: India between Worlds New Delhi: Harper
Collins Publishers India; 2000.
80256B3G0Q5BGCF9/(httpPublicatiQns)Z
5901781754E7G? 1580256B67QQ5B6AF7?QpenD.ocument].
35.
36.
37.
38.
39.
40.
41.
42.
43.
44.
45.
46.
47.
48.
49.
50.
51.
52.
53.
Self Employed Women's Association: Promoting health security for
women in the informal sector. Ahemedabad 2000.
Kawabata K, Xu K, Carrin G: Preventing impoverishment
through protection against catastrophic health expenditure.
Bulletin of the World Health Organization 2002, 80(8):6l2.
Ranson MK: Reduction in catastrophic health care expendi
tures by a community-based health insurance in Gujarat,
India: current experiences and challenges. Bulletin of the World
Health Organization 2002, 80:613-621.
UNICEF Bihar Field Unit: Bihar SHG Mapping Study 2001-02 Bihar
2002.
Mushtaque A, Chowdhury R, Bhuiya A, Do Poverty alleviation
programmes reduce inequities in health? The Bangladesh
experience. In Poverty, Inequality and Health: An International Perspec
tive Edited by Leon DA, Walt G. Oxford; Oxford University Press;
2001:313-331.
Self-help Promotion Event Secretariat (Ed); Pre-prints of papers of the
Development through Self-Help: be a part of it. Self-Help Promotion Con
ference: Dhaka. ICDDRB Social and Behavioural Science Program 2001.
10-11 November 2001
Government of India: Approach Paper to the Tenth Five Year Plan (20022007). Planning Commission, New Delhi 2001.
Government of India: Department of Women and Child Development
National Policy on Women Empowerment [hccp;//wcd,nic,in].
Government of India: Ninth Five Year Plan [http://planningcommis
sion.nic.in/plans/planrel/fiveyr/default.html]Government of Kerala: State Poverty Eradication Mission. Kudumbashree
Media Division Trivandrum; undated .
Government of Kerala. State Poverty Eradication Mission [http://
www.kudumbashree.org].
Hadi Ac Diagnosis of pneumonia by community health volun
teers: experience of BRAG, Bangladesh. Tropical Doctor 2001,
31:75-77.
Hadi A: Effects of the productive role of Bangladeshi women
on their reproductive decisions. Asia-Pacific Population Journal
2001, I6(4):l-I4.
Schuler SR, Hashemi SM, Riley AP, Akhter S: Credit programs,
patriarchy and Men’s violence against women in rural Bang
ladesh. Social Science and Medicine 1996, 43(12): 1729-1742.
Hadi Ac Integrating prevention of acute respiratory infections
with micro credit programme: experience of BRAC, Bangla
desh. Public Health 2002, I 16(4):238-244.
Hadi A: Promoting health knowledge through micro credit
programmes: experiences of BRAC in Bangladesh. Health pro
motion International 2001, 16(3):219-227.
Bhuiya A, Hanifi SM, Hossain M, Aziz A: Effects of an AIDS aware
ness campaign on knowledge about AIDS in a remote rural
area of Bangladesh. International Quarterly of community health edu
cation 2000, 19(I ):51 -63.
Hashemi SM, Schuler SR, Riley AP: Rural credit programs and
empowerment in Bangladesh. World development 1996,
24(4):635-653.
Goetz AM, Gupta RS: Who takes credit? Gender, Power and
Control over Loan Use in Rural credit programs in Bangla
desh. World Development 1996, 24( I ):45-63.
Publish with Bio Med Central and every
scientist can read your work free of charge
'BioMed Central will be the most significant development for
disseminating the results of biomedical research in our lifetime.'
Sir Paul Nurse, Cancer Research UK
Your research papers will be:
• available free of charge to the entire biomedical community
• peer reviewed and published immediately upon acceptance
• cited in PubMed and archived on PubMed Central
• yours — you keep the copyright
J BioMedcentral
Submit your manuscript here:
if
http7/www.biomedcentral.com/info/publi$hlng adv.asp
’v—J
Page 10 of 10
(page number not for citation purposes)
Community Health Centre
Draft Guidelines
Recommendations of the Task Group-Ill
headed by Dr. S.P. Agarwal, DGHS
Directorate General of Health Sendees
Mfnktty of Health & Family Welfare
Government of India
Contents
Executive Summary
1
Introduction
3
Minimum Requirements in CHC
6
Quality Assurance in Service Delivery
12
Checklists
14
Annexures
17
Annexure 1: Revised National Tuberculosis Control Programme
Annexure 2: National AIDS Control Programme
Annexure 3: National Vector-borne Disease Control Programme
Annexure 4: National Leprosy Eradication Programme
Annexure 5: National Blindness Control Programme
Annexure 6: Integrated Disease Surveillance Project
Annexure 7: Referral Transport Model
Annexure 8: List of Equipment in CHC
Annexure 9: List of Drugs in CHC
Annexure 10: GOI Guidelines for Blood Storage
Annexure 11: GOI Guidelines for Waste Management
Annexure 12: Charter of Patients' Rights.
Annexure 13: Composition of Task Group III and Consultation Process
Executive Summary
The Community Health Centres (CHCs) which constitute the secondary level of
health care were designed to provide referral as well as specialist health care to
the rural population. These centres are however fulfilling the tasks entrusted to
them only to a limited extent. The launch of the National Rural Health Mission
(NRHM) gives us the opportunity to have a fresh look at their functioning.
In order to provide Quality Care in these CHCs Indian Public Health Standards
(IPHS) are being prescribed to provide optimal expert care to the community
and achieve and maintain an acceptable standard of quality of care. These
standards would help monitor and improve the functioning of the CHCs.
Service Delivery
«
•
•
All "Assured Services" as envisaged in the CHC should be available, which
includes routine and emergency care in Surgery, Medicine, Obstetrics
and Gynaecology and Paediatrics in addition to all the National Health
programmes.
Appropriate guidelines for each National Programme for management of
routine and emergency cases are being provided to the CHC.
All the support services to fulfil the above objectives will be strengthened
at the CHC level.
Minimum Requirement for Delivery of the Above-mentioned
Services
The following requirements are being projected based on an average bed
occupancy of 60%. It would be a dynamic process in the sense that if the
utilisation goes up, the standards would be further upgraded. As regards
manpower, 2 specialists namely Anaesthetist and Public Health Programme
Manager will be provided on contractual basis in addition to the available
specialists namely Surgery Medicine, Obstetrics and Gynaecology and
Paediatrics.
The support manpower will include a Public Health Nurse and ANM in addition
to the existing staff. An Ophthalmic Assistant will also be need to be provided
in centres where currently there is none.
Facilities
The equipment provided under the CSSM s deemed adequate. Physical
infrastructure will be remodelled or rearranged to make best possible use for
The child should be given only breast milk
from birth to six mouths
Executive Summaw | 1
c?t mal utiiisat or.,
''lew constructions will Fellow the specifications provided
ir this document.
..gs ..ill de as per the list provided with tire document. All the support
•Hees like laboratory, blood storage etc. will be strengthened.
Human Resource Management
Capacity Building will be ensured at all levels by periodic training of all
cadres.
Accountability
It is mandatory for every CHC to have "Rogi Kalyan Samiti" to ensure
accountability.
Every CHC shall have the Charter of Patients' Rights displayed prominently at
the entrance. A grievance mechanism under the overall supervision of Rogi
Kalyan Samitis would also be set up.
Quality of Services
Every CHC shall also have the Standard Operating Procedures and Standard
Treatment Protocols for common ailments and the National Health
Programmes.
Social audit by involvement of the community through Consumer Forum and
Rogi Kalyan Samitis is being recommended. To maintain quality of services,
external monitoring through Panchayati Raj Institutions and internal
monitoring at appropriate intervals will be advocated. Guidelines are being
provided for management of routine and emergency cases under the National
Health Programmes so as to maintain uniformity in management in tune with
the National Policy.
2 i IPHS - CHC Level
Opt for hospital delivery for
safety ofmother & baby
‘
Introduction
Health care delivery in India has been envisaged at three levels namely primary,
secondary and tertiary. The secondary level of health care essentially includes
Community Health Centres (CHCs), constituting the First Referral Units(FRUs)
and the district hospitals. The CHCs were designed to provide referral health
care for cases from the primary level and for cases in need of specialist care
approaching the centre directly. 4 PHCs are included under each CHC thus
catering to approximately 80,000 population in tribal/hilly areas and 1, 20,000
population in plain areas. CHC is a 30-bedded hospital providing specialist care
in Medicine, Obstetrics and Gynaecology, Surgery and Paediatrics. These centres
are however fulfilling the tasks entrusted to them only to a limited extent. The
launch of the National Rural Health Mission (NRHM) gives us the opportunity
to have a fresh look at their functioning.
NRHM envisages bringing up the CHC services to the level of Indian Public
Health Standards. Although there are already existing standards as prescribed
by the Bureau of Indian Standards for 30-bedded hospital, these are at present
not achievable as they are very resource-intensive. Under the NRHM, the
Accredited Social Health Activist (ASHA) is being envisaged in each village
to promote the health activities. With ASHA in place, there is bound to be a
groundwell of demands for health services and the system needs to be geared
to face the challenge. Not only does the system require upgradation to handle
higher patient load, but emphasis also needs to be given to quality aspects to
increase the level of patient satisfaction. In order to ensure quality of services,
the Indian Public Health Standards are being set up for CHCs so as to provide a
yardstick to measure the services being provided there. This document provides
the requirements for a Minimum Functional Grade of a Community Health
Centre.
Objectives of Indian Public Health Standards (IPHS) for CHCs
•
°
•
To provide optimal expert care to the community
To achieve and maintain an acceptable standard of quality of care
To make the services more responsive and sensitive to the needs of the
community
Service Delivery in CHCs
Every CHC has to provide the rollowing services whicn can be-known as the
Assured Services:
Health worker’s advice & care is
/.
C-,.
.... r_ ■' r
ar__
Intoduction I
«
Care of rautne and emergency cases in surgerye
r>
Tris includes incision and drainage, and surgery for Hernia. Hydrocele.
□
•
Appendicitis, Haemorrhoids, Fistula, etc.
Harding or emergencies like Intestinal Obstruction, Haemorrhage, etc.
Care of routine and emergency cases in medicine:
a
Specific mention is being made of handling of all emergencies in relation
to the National Health Programmes as per guidelines like Dengue,
Haemorrhagic Fever, Cerebral Malaria, etc. Appropriate guidelines are
already available under each programme, which should be compiled in
•
•
a single manual.
24-hour delivery services including normal and assisted deliveries
Essential and Emergency Obstetric Care including surgical interventions like
•
Caesarean Sections and other medical interventions
Full range of family planning services including Laproscopic Services
•
•
•
•
Safe Abortion Services
Newborn Care
Routine and Emergency Care of sick children
Other management including nasal packing, tracheostomy, foreign body
•
removal etc.
All the National Health Programmes (NHP) should be delivered through
the CHCs. Integration with the existing programmes like blindness control,
Integrated Disease Surveillance Project, is vital to provide comprehensive
services. The requirements for the important NHPs are being annexed as
separate guidelines with the document.
■
RNTCP: CHCs are expected to provide diagnostic services through the
microscopy centres which are already established in the CHCs and
treatment services as per the Technical Guidelines and Operational
guidelines for Tuberculosis Control. (Annexure 1)
■
HIV/AIDS Control Programme: The expected services at the CHC level are
being provided with this document which may be suitably implemented.
(Annexure 2)
4 | IPHS - CHC Level
■
National Vector-Borne Disease Control Programme: The CHCs are to
provide diagnostic and treatment facilities for routine and complicated
cases of Malaria, Filaria, Dengue, Japanese Encephalitis and Kala-azar
in the respective endemic zones. (Annexure 3)
■
National Leprosy Eradication Programme: The minimum services that
are to be available at the CHCs are for diagnosis and treatment of cases
and reactions of Leprosy along with advice to patient on Prevention of
Deformity. (Annexure 4)
■
National Programme for Control of Blindness: The eye care services that
should be available at the CHC are diagnosis and treatment of common
eye diseases, refraction services and surgical services including cataract
by I0L implantation at selected CHCs optionally. 1 eye surgeon is being
envisaged for every 5 lakh population. (Annexure 5)
Atleast three ante-natal checkup
must for pregnant women
Under Integrated Disease Surveillance Project, the related services
include services for diagnosis for Malaria, Tuberculosis, Typhoid and
tests for detection of faecal contamination of water and chlorination
level. CHC will function as peripheral surveillance unit and collate,
analyse and report information to District Surveillance Unit. In outbreak
situations, appropriate action will be initiated. (Annexure 6)
Others:
■
Blood Storage Facility
e
Essential Laboratory Services
o
Referral (transport) Services: (details given in Annexure 7)
■
•
Complete and correct knowledge
protects von from AIDS
Introduction | 5
•nmmum *
uremeau> nn tm
The following requirements are being projected based on the assumption that
there will be average bed occupancy of 60%. The strength may be further
increased if the occupancy increases with subsequent upgradation.
Certain suggestions for offsetting the deficiencies in the availability of required
manpower:
• Anaesthetists:
■
Diploma and MD seats for post graduation in Anesthesia to be increased
across the country. However, care should be taken to only include
institutions with assured quality and able to provide adequate clinical
■
training.
Certificate course for one year in Anesthesia by the National Board of
Examinations
•
Public Health Programme Manager:
■
Diploma and MD seats for post graduation in Public Health to be
increased across the country. However, care should be taken to only
include institutions with assured quality and able to provide adequate
field and community-based training.
■
Persons with DNB degrees in Family Medicine, Hospital Administration,
Public Health, Maternal and Child Health are to be recognised for the
■
post.
Persons who have completed the Professional Development Course of 3
months with a 9-month field training in recognised training institute
may also be eligible for the same. This may also be seen as a career
advancement avenue for Medical Officers serving in PHCs who may be
eligible for the post after a stint of 3-4 years in PHC and completion of
this course.
Equipment
•
•
6 | IPHS - CHC Level
The List of equipment provided under the CSSM may be referred to as they
are deemed to be adequate for providing all services in the CHC. (Annexure
8). Before ordering new sets, the existing equipment should be properly
assessed.
For ophthalmic equipment wherever the services are available and equipment
required under various National Health Programmes are given in respective
annexure (1, 2, 4, 5, 6), and Blood Storage Facilities (Annexure-10). Cold
chain equipment are supplied under Immunisation Programme.
The child should be given only breast milk
from birth to six months
•
•
•
Maintenance of equipment: It is estimated that 10-15% of the annual
budget is necessary for maintenance.
2 refrigerators, one for the ward and one for 0T should be available in the
CHC. Sharing of refrigerator with the lab should be possible.
Appropriate standards for equipments are already available in the Bureau
of Indian Standards. If standards for any equipment are not available,
technical specifications for the equipment may be prepared by the technical
committee for the process of tendering and procurement.
Drugs
The list of essential drugs and emergency drugs are provided as annexure 9.
Programme specific drugs are detailed in the guidelines under each
programme.
Clinical Manpower
Personnel
Minimum
requirement
Proposed
Desirable qualifications
General Surgeon
1
1
MS/DNB, (General Surgery)
Physician
1
1
MD/ONB, (General
Medicine)
Obstetrician/
Gynaecologist
1
1
MD/DNB/DGO (OBG)
Paediatrics
1
Justification
1
MD/DNB/DCh (Paediatrics)
Anaesthetist
1
MD/DNB/DA( Anesthesia)/
Certificate course in
Anaesthesia for one year
Essential if there is to
be utilisation of the
surgical specialities.
They may be on
contractual appointment
or hiring of services
from private sectors on
case-to case basis.
Public Health
Programme
Manager. He/
she will be also
designated
as Block
Surveillance
Officer.
1
MD/DNB/DPH/Social
science with public health
background/any other
recognised course
Will be responsible
for surveillance,
coordination of NHPs,
management of ASHAs,
training, etc. The
appointment will be on
contractual basis.
MD/MS/DOMS/DNB/
(Ophthal)
For every/ 5 lakh
population as per Visi m
2920 approved Plan
Action.
Eye surgeon
■
Total
4
Optfor hospital delivery for
safety ofmother dr habv.
_5/7______
Minimum Requirements in CHC I 7
Support Manpower
Personnel
Existing
■‘Nurse-midwife
7+ 2
Dresser (certified by Red Cross/St.Johns
Ambulance)
1
Pharmacist/compounder
1
Lab. technician
1
,
__________
Radiographer
1
“Ophthalmic Assistant
0-1
Ward boys/nursing orderly
2
Sweepers
3
Chowkidar
OPD attendant
Statistical assistant/Data entry operator
5“*
0T attendant
Registration clerk
Total essential
21/22+2
1 ANM and 1 PHN for family welfare will be appointed under the ASHA
scheme
*'
Ophthalmic assistant may be placed wherever it does not exist through
redeployment or contract basis.
*•’ Flexibility may rest with the state for recruitment of personnel as per
needs.
Investigative Facilities at the CHC
•
In addition to the lab facilities in the CHC, ECG should be made available in
the CHC with appropriate training to a nursing staff.
•
All necessary reagents, glassware and facilities for collecting and transport
of samples should be made available.
Physical Infrastructure
The CHC should have 30 indoor beds with one operation theatre, labour room,
x-ray facility and laboratory facility. In order to provide these facilities,
following are the guidelines:
• Location of the Centre: To the extent possible, the centre should be
located at the centre of the block headquarter in order to improve access
to the patients. This may be applicable only to centres that are to be newly
established.
However, priority is to be given to operationalise the existing CHCs.
8 | IPHS - CHC Level
Health worker’s advice & care is
best for your family’s welfare
The building should have areas/space marked for the following:
•
Entrance Zone
a
Prominent display boards in local language providing information
regarding the services available and the timings of the institute
e
Registration counters
Pharmacy for drug dispensing and storage
Clean public utilities separate for males and females
Suggestion/complaint boxes for the patients/visitors and also
information regarding the person responsible for redressal of
b
b
b
complaints.
•
Outpatient Department
b
c
n
■
Clinics for various medical disciplines: These clinics include
general medicine, general surgery, dental (optional), obstetric and
gynaecology, paediatrics and family welfare. Separate cubicles
for general medicine and surgery with separate area for internal
examination (privacy) can be provided if there are no separate
rooms for each. The cubicles for consultation and examination in
all clinics should provide for doctor's table, chair, patient's stool,
follower's seat, wash basin, examination couch and equipment for
examination.
Room shall have, for the admission of light and air, one or more
apertures, such as windows and fan Lights, opening directly to the
external air or into an open verandah. The windows should be in
two opposite walls.
Family Welfare Clinic: The clinic should provide educative,
preventive, diagnostic and curative facilities for maternal, child
health, school health and health education. Importance of health
education is being increasingly recognised as an effective tool of
preventive treatment. People visiting hospital should be informed
of environmental hygiene, clean habits, need for taking preventive
measures against epidemics, family planning, etc. Treatment room
in this clinic should act as operating room for IUCD insertion and
investigation, etc. It should be in close proximity to Obstetric and
Gynaecology OPD.
Waiting room for patients
■
The Drug Dispensary should be located in an area conveniently
accessible from all clinics. The dispensary and compounding room
should have two dispensing windows, compounding counters and
shelves. The pattern of arranging the counters and shelves shall
depend on the size of the room. The medicines which require cold
storage and blood required for operations and emergencies should
be kept in refrigerators.
U
Emergency Room/Casualty: The emergency cases ma.y be attended
by OPD during OPD hours and in inpatient units afterwards.
Atleast three ante-natal checkup
mustfor pregnant women
Minimum Requirements in CHC i '■
<•
"reattr. Room
Mmor OT
n
u
®
. ijccfon rocm ar d Dressing room
V/a.as: Separate for Males and Females
->
Nursing station- The nursing station shall be centered such that it
serves ail the clinics from that place. The nursing station should be
spacious enough to accommodate a medicine chest/a work counter
for preparing dressings, medicines, sinks, dressing tables with
screen in between and pedal operated bins to hold soiled material.
It should have provision for:
♦ Injections,
♦
Dressings,
♦
Examination and dressing table,
♦
Bins for waste material,
♦ Wash basins,
♦ Syringe destroyer
♦
Needle cutter
•
Patient Area:
■
■
■
•
Enough space between beds
Toilets; separate for males and females
Separate space/room for patients needing isolation
Ancillary Rooms:
Nurses rest room
■
»
•
There should be an area separating OPD and indoor facility
Operation Theatre/Labour Room:
■
■
■
■
Patient area:
♦
Pre-operative and Post-operative(recovery)room
Staff area:
♦
Changing room separate for males and females
Storage area for sterile supplies
OT/Labour room area:
♦ Operating room/labour room
♦ Scrub area
♦
♦
•
•
Instrument sterilisation area
Disposal area
Public Utilities: Separate for Males and Females
Physical infrastructure for Support Services:
■
CSSD:
■
♦ Sterilisation and Sterile storage
Laundry:
♦
Storage: Separate for dirty linen and clean linen
Outsourcing is recommended after appropriate training of washer
man regarding separate treatment for infected and non-infected
linen.
10 | IPHS - CHC Level
Complete and correct knowledge
protects you from AIDS
♦
Services: Electricity/Telephones/Water/Civil Engineering: May
be outsourced. Maintenance of proper sanitation in toilets and
other public utilities should be given utmost attention. Sufficient
funding for this purpose must be kept and the services may be
outsourced.
B
Water Supply : Arrangements shall be made to supply 10,000
litres of potable water per day to meet all the requirements
(including laundry) except fire fighting. Storage capacity
for 2 days requirements should be on the basis of the above
consumption. Round the clock water supply shall be made
available to all wards and departments of the hospital.
Separate reserve emergency overhead tank shall be provided
for operation theatre. Necessary water storage overhead
tanks with pumping/boosting arrangement shall be made.
The laying and distribution of the water supply system shall
be according to the provisions of IS: 2065-1983*. Cold
and hot water supply piping should be run in concealed
form embedded into wall with full precautions to avoid any
seepage. Geyser in O.T./L.R. and one in ward also should
be provided. Wherever feasible solar installations should be
promoted.
•
Emergency Lighting: Emergency portable/fixed light units
should also be provided in the wards and departments to
serve as alternative source of Light in case of power failure.
Generator back-up should be available in all facilities.
Generator should be of good capacity. Use of solar energy
wherever feasible may be used.
®
Telephone: minimum two direct lines with intercom facility
should be available.
•
Administrative Zone: Separate rooms should be available for:
■
■
Office
Stores
Capacity Building
•
Training of all cadres of worker at periodic intervals is an essential
component.
«
Multi-skill training for paramedical workers
The child should be given only b east milk
from birth to six months
Minimum Requirements in CHC | 11
Duality Assy ramcs
•
Sen/Ks Delivery
Quality of service should be maintained at all levels.
Standard treatment protocc. For all national programmes and locally common
diseases should be made available at all CHCs. Standard Treatment Protocol:
is the "Heart" of quality and cost of care. All the efforts that are being
made to improve "hardware i.e. infrastructure" and "software i.e. human
resources" are necessary but NOT sufficient. These need to be guided by
standard treatment protocols. Some of the states have already prepared
•
these guidelines.
Diet: Diet may either be outsourced or adequate space for cooking should
be provided in a separate space.
•
CSSD
■
Adequate space and standard procedures for sterilisation and sterile
storage should be available.
•
Laundry
Storage: Separate for dirty linen and clean linen
Outsourcing is recommended after appropriate training of washerman
regarding separate treatment for infected and non-infected linen.
Services: Electricity/telephones/water/civil engineering: may be
■
■
•
outsourced.
•
•
•
•
Blood Storage Units: The GOT guidelines as given in Annexure may be
referred to. (Annexure 10)
Waste Disposal: As per National guidelines on hospital waste management
as applicable to 30 bed CHCs (Annexure 11) or may be outsourced to
agencies trained in this.
Charter of Patient Rights: It is mandatory for every CHC to have the Charter
of Patient Rights prominently displayed at the entrance.
Details are provided in the Annexure 12.
Quality Control:
■
Internal monitoring:
Social Audit: Through
♦
Rogi Kalyan Samitis/Panchayati Raj
Institution, etc.
•
Medical audit
♦
Others like technical audit, economic audit, disaster preparedness
audit, etc.
♦
•
•
•
-
12 | IPHS - CHC Level
Patient care: This shall include:
Access to patients
Registration and admission procedures
Examination
Information exchange
Opt for hospital delivery for
safety ofmother & baby
«
Treatment
Other facilities: waiting, toilets, drinking water
c
Indoor patients:
Linen/beds
Staying facilities for relatives
Diet and drinking water
Toilets
External Monitoring:
n
•
•
c
Gradation by PRI (Zilla Parishad)/Rogi Kalyan Samitis
Monitoring of laboratory:
■
c
Internal Quality Assessment Scheme
External Quality Assessment Scheme
Record Maintenance
Computers are to be used for accurate record maintenance.
•
Suggested innovations:
o
Water harvesting should be introduced in all new buildings
■
Computerisation is a must and would be essential for record maintenance
and surveillance.
n
To maintain the hospital Landscaping, a room to store garden implements;
seeds, etc, should be provided.
Based on the above minimum requirements, the standards need to be developed
by a professional body.
Health worker’s advice & care is
best for yourfamily’s welfare ,
Qua 'ty Assurance in S rvice ueli- ery | i.-:
Checklists
Checklis for mini in urn requirement of CHCs
Services
Existing
Remarks
Population covered
Specialist services available
Medicine
Surgery
OBG
Paediatrics
NHPs
Emergency services
Laboratory
Blood storage
Infrastructure
Existing
Remarks
(As per specifications)
Area of the building
OPD rooms/cubicles
Waiting room for patients
No. of beds: Male
No. of beds: Female
Operation theatre
Labour room
Laboratory
X-ray room
Blood storage
Pharmacy
Water supply
Electricity
Garden
Transport facilities
14 i IPHS - CHC Level
At least three ante-natal checkup
must for pregnant women
Checklist for Equipment
Equipment
(As per list)
Available
Functional
Remarks
Checklist for Drugs
„
~
----------
Drugs
(As per Essential Drug list)
Available
Remarks
Available
Whether functional as
per norms
Checklist for Audit
Particulars
Patient’s charter
Rogi Kalyan Samiti
Internal monitoring
External monitoring
Availability of SOPs/STPs*
’Standard Operating Procedures/Standard Treatment Protocols
Complete and correct knowledge
protectsyou from AIDS
Checklist | i:>
Annexures
Armexure 1
Requirements with regard to Revised National TB Control
Programme for Indian Public Health Standards at CHC Level
Diagnostic Services
®
A Microscopy Centre (MC) is established for 1, 00,000 population. For hilly,
tribal and difficult areas MC is established for 50,000 populations. The
Microscopy Centres are established at PHC, CHC or District Hospital.
•
Inputs
i.
RNTCP has provided inputs to upgrade the infrastructure through minor
civil works of the existing laboratories to be able to come up to the
minimum standard required to carry out sputum microscopy. At present,
about 87% of the country is covered under RNTCP and it is envisaged to
cover the entire country by June 2005.
ii. Manpower: Existing Laboratory Technicians (LTs) are provided training
and they function as LTs to carry out sputum microscopy. For up to
20% of the requirements of the LTs at designated microscopy centres at
the District Level, LTs are provided by RNTCP on contractual basis.
iii. Equipment: Binocular Microscopes are provided to the Microscopy
Centres for sputum microscopy.
iv. Laboratory Consumables: Funds are provided to the District TB Control
societies for procurement and supply of all the consumables required
to carry out sputum microscopy. The list of laboratory consumables
required at MC is enclosed at Annexure-I.
Treatment Services
1. Medical Officers: All Medical Officers are trained in RNTCP to suspect chest
symptomatics, refer them for sputum microscopy and be able to categories
* -e ...atients and handle side effects of anti TB drugs.
'■■OTf Centres: All sub-centres, PHCs, CHCs an.! District Hospitals work as
S L’.'tr?'.. In addition, the community DO^S providers are also trained
r!.?'i'/er DOT. A room of the CHC is used to function as DOTS centre.
=C' es
seating and making available drinking water to the patients
f >r or.sun at on jf drugs are provided under h ■ prooramme.
. . c cbka si.o d,-l be given only breast milk
I'. om bi.tr i ■ A mi. nibs
3.
DOTS Providers: Ihe Multi Purpose Workers (MPWs), pharmacists and staff
r.urs.-s are "trained in to monitor consumption of anti TB drugs by the
pc. ticn us.
4.
AL me DOTS providers to deliver treatment as per treatment guidelines.
All the doctors to categories patients as per treatment guidelines (refer
Technical Guidelines).
5.
Drugs in patient wise boxes and Loose drugs are provided at DOT Centres
through District TB Centre (DTC). Details of the drugs given at Annexure-
II.
6.
Recording and reporting to be done as per Operational Guidelines (refer
Operational Guidelines).
Treatment of Complicated Cases
1. For patients who require admission (Pleural Effusion, Emphysema etc.)
drugs are provided in the form of prolongation pouches through District TB
Centre for indoor treatment.
2.
The common complications of TB can be treated by the medical officers/
specialists at CHC and side effects of drugs can also be handled by the
doctors at CHC.
Quality Assurance
1. Diagnosis: The diagnostic services are supervised by Senior TB Laboratory
Supervisor (STLS) for all the microscopy centres at the sub-district level
(5,00,000 population or 2, 50,000 population in the hilly, difficult and
tribal areas).
2. Treatment: All major drugs procured at the Centre through World Bank
recommended procedures and provided to the States, thereby assuring
quality of the drugs.
IPHS - CHC Level
Opt for hospital delivery for
safety of mother & baby
List of Anti-TB drugs procured under National TB Control Programme
Strength
SI.No
Product code
number
Product description
1-
Product Code-I
Treatment box for
Cat.I patient. Each
treatment box
containing 24 combipacks of Schedule-I
in one pouch and 18
multi-blister calendar
combi-pack of
Schedule-2 in another
pouch
Each combi-pack
of Schedule-I
containing
1 R Cap.of 450mg
2 II Tabs, of 300mg
each
2 E Tabs of 600mg
each
2 Z Tabs, of 750mg
each
Each multi-blister
calender combi-pack of
Schedule-2 containing
3 R Caps.of 450 mg
each
6 H Tabs, of 300mg
each
4 Pyrioxine Tabs of 5mg
each
Treatment box for
Cat.II patient. Each
treatment box
containing 36 combipacks of Schedule-I
in one pouch and 22
multi-blister calendar
combi-pack of
Schedule-3 in another
pouch
Each combi-pack
of Schedule-I
containing
1 R Cap.of 450mg
2 II Tabs, of 300mg
each
2 E Tabs of 600mg
each
2 Z Tabs, of 750mg
each
Each multi-blister
calender combi-pack of
Schedule-3 containing
3 R Caps.of 450 mg
each
6 H Tabs, of 300mg
each
6 E Tabs of 600mg each
4 Pyrioxine Tabs of 5mg
each
Treatment box for
Cat.III patient.
Each treatment box
containing 24 combipacks of Schedule-4
in one pouch and 18
multi-blister calendar
combi-pack of
Schedule-2 in another
pouch
Each combi-pack of
Schedule-4
containing
1 R Cap.of 450mg
2 H Tabs, of 300mg
each
2 Z Tabs, of 750mg
each
Each multi-blister
calender combi-pack of
Schedule-2 containing
3 R Caps.of 450 mg
each
6 H Tabs, of 300mg
each
4 Pyrioxine Tabs of 5mg
each
Treatment box for
prolongation of
intensive phase of
Cat.I & Cat.II patient.
Each box containing
5 pouches and each
pouch containing 12
blister comoi-pack of
Schedule-1
Each combi-pack of Schedule-I containing
1 R Cap.of 450mg
2 H Tabs, of 300mg each
2 E Tabs of 600mg each
2 Z Tabs, of 750mg each
Treatment box for
Cat-I patient
2.
Product Code-2
Treatment box for
Cat-II patient
3.
Product Code-3
Treatment box for
Cat-Ill patient
4.
Product Code-4
Treatment box for
prolongation of
intensive phase of
Cai-I &Cat. r
Health uoiaer's advice care ts
best foi ■year fa,nily’s welfare
Annexures | 19
Product Code-?
Loose packs of
Streptomycin vials
Each viai o' 75Cmg
Jut; Lt de-6
Blister strips pack
containing
10 Rifan pj.r ■ :p: le or :50rng each
Product Code-7
Blister strips pack
containing
10 INH Tablet of lOOmg
P-oduct Code-8
Blister strips pack
containing
10 Pyrazinanride Tablets of 500mg
9-
Product Code-10
Blister strips pack or
foil packs containing
10 E Tabs of 800mg each
10.
Product Code-11
Blister strips pack
containing
10 H Tabs of 300mg each
11.
Product Code-12
Blister strips pack
containing
10 Rifampicin Capsules of 450 mg each
P
7
i
R= Rifampicin; H= Isoniazid; E= Ethambutol; Z= Pyrazianamide; S.M= Inj. Streptomycin.
?<) | IPHS - CHC Level
Atleast three ante-natal checkup
must for pregnant women
Annexure 2
HIV Guidelines
At present the preventive and care interventions for the control of HIV/AIDS are
being provided below district level through Integrated Health Care System using
the available staff. There is also a provision of training of health care providers
and generating awareness through intensive IEC campaign. The programme is
being further strengthened by converging the activities under NACP with RCH
programme, which is underway. The following activities are being proposed to
be integrated at CHC Level.
■ S. No.
Activities
Proposed
1.
RTI/STD management services
Expansion of services up to CHC & 24 hours
PHC. Basic screening test for RTI?STD to be
made available at the CHCs
2
VCTC & youth information
centres
Expansion of services up to CHCs in all
States.
3.
Prevention of Parent-to-Child
Transmission(PPTCT)
Services to be provided at all CHCs
4.
Behaviour Change
Communication (BCC)
Joint communication strategy messages &
medium development to be done
5.
Condom promotion
Joint condom procurement & distribution
of condoms to meet the needs of sexually
active women and men as a method of dual
protection
6.
Blood safety
Blood storage centres planned at FRUs will
procure blood from licensed blood banks
but will be supported by RCH
7.
Trainings
A specific plan will be developed jointly
by both the departments to train the
peripheral staff at CHC
8
Management information
system
AU facilities to report service performance
on RTI/STI, VCTC, PPTCT as a part of routine
reporting
9.
Operationalisation
A convergence facilitator to be appointed
to ensure coordinated inputs between the
activities implemented by NACP and RCH
Complete and co; reel knowledge
protects you from A IDS
Annexme-..
Annexure 3
National Vercc. Borne Disease Control Programme
■'
feet
■
- Di ■ jas -■ Ct
■"
Prog . ■ .
I 7BD( ’ ,, e stw n’l ■
Nati nal \nti Mala a Programme (NAMP) is the country's ,r si rorr.prehensive
and mulri-faceted 'ublic health activity. Directoiate of NVBDCP is the nodal
agency for prevention ana control of major vector borne diseases of public
health importance namely Malaria, Filariasis, Japanese Encephalitis (JE), Kala-
azar and Dengue.
Following are the strategy for control of these diseases:
a) Malaria:
•
Early diagnosis and prompt treatment of Malaria cases
•
Integrated vector control
•
Early detection and containment of Malaria outbreak
•
Information, Education and Communication (IEC) for personal protection
and community involvement for Malaria control
•
Training and Capacity Building of Medical and Para-medical workers
•
Monitoring and evaluation of efficient Management Information System
(MIS)
b) Dengue:
•
Epidemiological surveillance of Dengue cases
•
Entomological surveillance of Aedes Aegypti mosquitoes
•
Clinical management of reported cases
•
Control of mosquitoes through Integrated Vector Management including
source reduction, use of larvivorous fishes, impregnated bednets and
selective fogging with Pyrethrum
•
Behaviour change communication to change behavior of the community
about prevention of breeding of mosquitoes
c)
Kala-azar:
•
Early diagnosis & complete treatment through Primary Health Care
System
•
Interruption of transmission through vector control by undertaking
•
d)
1PHS - CHC Level
residual insecticidal spraying in affected areas
Health education and community participation
Japanese Encephalitis:
»
Vector control by insecticidal spraying with appropriate insecticide for
outbreak containment
The child should be given only breast milk
from birth to six months
•
e)
EjS'. diagnosis and prompt clinical management to reduce fatality
•
Health education
«
Training of medical personnel and professionals
Filariasis:
For elimination of Lymphatic Filariasis following are the strategies:
•
Annual Mass Drug Administration (MDA) with single dose of DEC to all
•
eligible population at risk of Lymphatic Filariasis
Home-based .management of Lymphodema cases and
o
Hydroceloctomy
To provide the above services under NVBDCP the PHC Medical Officers are the
in-charge of PHC. The diagnosis, treatment and examination are performed at
CHCs as per the pattern of PHC. In addition, CHCs are the first referral units for
treatment of severe and complicated Malaria cases. To provide following services,
the CHCs should be equipped with the items as mentioned at Annexure:
1. Diagnosis of Malaria cases, microscopic confirmation and treatment.
2. Cases of suspected JE and Dengue to be provided symptomatic treatment,
hospitalisation and case managements.
3.
Complete treatment to Kala-azar cases in Kala-azar endemic areas.
4.
Complete treatment of micro-Filaria positive cases with DEC and participation
& arrangement of MDA along with preparedness of management of side
reactions.
Standards:
The CHC medical officer should be well-trained in the control programme of the
vector borne diseases and should carry out the following activities:-
a) He will, in consultation with District Malaria Officer and the community,
select FTD/DDC holders and Voluntary Link Workers for his PRIMARY HEALTH
CARE
b) He will refer all fever cases to Malaria laboratory for blood smear collection
and examination before giving final prescription/medicines.
c)
He will supervise all Malaria Clinics and PHC laboratory in his area, see
the quality of blood smear collection, staining, efficiency microscopic
examination and check whether the stain is filtered daily.
Opt for hospital delivery for
safety of mother & baby
Annexures
J) He -aill also easure/supervise that all positive cases get radical; treatment
In' r 48
.
’S CT £XcTC. iTCT'O'" .
e) He will also ensure that sufficient stocks of Anti-Malarials including Quinine
tablets and injectable Quinine and Artemisenine are available in CHC and
also PHCs
f)
He will ensure that Malaria laboratory is kept in proper condition along with
microscope and other equipments.
g)
He will provide referral services to severe cases of Malaria
h)
He will refer severe and complicated cases to District Hospital in case of
emergency and drug failure.
i)
He will also ensure that Filaria cases are managed at CHC and the Hydrocele
cases are operated.
1. Drugs
Chloroquine,
Primaquine,
Sulphadoxin
Pyremethamine
Combination,
Artemisinine Derivatives, Quinine Injections, Quinine Tablets and 5% Dextrose
saline and DEC tablets
2. Equipment
Microscope, Slides, Pricking Needles, Cotton, Stains, Staining Jars, Filter Paper,
Glass Marking Pencil, Lint Cloth and Glasswares for preparation of stains and
storage.
3. IEC Material
•
Display material like posters, banners and permanent hoardings etc.
•
Distribution material like handbills, pamphlets, booklets display cards etc.
•
Training materials like guidelines on programme strategies, dose-schedule
cards etc.
24 | IPHS - CHC Level
Health worker’s advice & care is
bestfor your family’s welfare
Annexure 4
National Leprosy Eradication Programme
Minimum services to be available at Community Health Centres (CHC) are:
«
Diagnosis of Leprosy
•
Treatment
®
Management of reactions
•
Advise to patient on POD Care
1. Leprosy Case Diagnosis
•
•
Manpower required
■
Medical Officer trained in Leprosy diagnosis
■
Pharmacist to issue medicine and manage MDT Stock
n
Health Worker trained to maintain records/reports
Methodology
By following Standard National Guidelines (Annexure-I).
b
2. Treatment of Cases
•
CHC should have MDT Blister Packs {MB(A), MB(C), PB(A), PB(C)} atleast 3
months stock against patients under treatment.
•
The CHC will classify and treat Leprosy which MDT as per National
Guidelines
3. Management of Reaction Cases
•
The CHC should have adequate stock of prednisolone tablets for management
of reaction cases as per National Guidelines (Annexure-III).
4. Advise to Patient for Prevention of Deformity and Ulcer Care.
•
CHC should have a Medical Officer, Pharmacist, Health Worker properly
trained for providing counselling to the patients. (Annexure-IV)
Atleast three ante-natal checkup
must for pregnant women
Annexurer. ,
eprosv Case Diagnosis
a:se Leprosy?
Signs of Leprosy
A Leprosy patient is someone who has a skin patch or patches with a definite
loss of sensation and has not completed a full course of treatment with multi
drug therapy.
Leprosy Patches
Can be pale or reddish or copper-coloured, can be flat or raised, do not
itch, usually do not hurt, lack sensation to heat, touch or pain, can appear
anywhere.
Other signs of Leprosy include
Reddish or skin-coloured nodules or smooth, shiny diffuse thickening of the
skin without a loss of sensation.
2. Which Signs is Not Leprosy?
Skin patches ....
• Present from birth (i.e. birth marks)
• Where there is normal feelings
• That itch
• That are white, black or dark red
• With scaling or skin
•
That appear or disappear suddenly and spread fast
3. How to Examine a Patient for Leprosy?
•
•
•
•
•
•
Examine the skin in daylight or in a well-lit room
Examine the whole body, taking care to respect the patient's privacy
Ask the patient if the patch itches. If so, it cannot be Leprosy
Test only one or two skin patches for sensory loss
If there is a definite loss of sensation, it is Leprosy
Ask about treatment received in the past
•
A person who has completed a full coursed of MDT very rarely needs further
treatment
•
Look for any visible disability of eyes, face, hands and feet
•
When in doubt about the diagnosis, always send the patient to the nearest
referral centre.
4. How to Test for Sensory Loss?
•
•
•
| 1PHS - CHC Level
Take a pointed object such as a pen
Show the person what you are going to do.
Lightly touch rhe skin with the pen
Complete and correct knowledge
AroMr/c no rj
Zi«r>7i»
A
•
Ask the person to point to where they felt the pen
Now ask them to close their eyes so that they cannot see what you are
doing
Lightly touch the centre of the most prominent skin patch and ask them to
•
•
point to where they felt the pen
Repeat the procedure on normal skin and on the same patch again.
If the person feels nothing on the skin patch, it is Leprosy. Start treatment
•
•
immediately.
5. How to Classify Leprosy?
Leprosy is classified into Paucibacillary or Multibacillary Leprosy based on the
number of patches.
> 1-5 patches?
•
It is Paucibacillary (PB) Leprosy
•
Treatment: 6 PB Blister Packs
> More than 5 patches?
o
It is Multibacillary (MB) Leprosy
Treatment: 12 MB Blister Packs
»
Treatment of Leprosy Cases
MDT Regimens
MDT supply in separate blister packs for MB (Adult), MB (Child), PB (Adult) &
PB (Child). Each blister pack contains treatment for 4 weeks.
1. PB Adult Treatment:
Once a month: 1 Day
2 Capsules of Rifampicin (300 mg X 2)
1 Tablet of Dapsone (100 mg)
•
•
Once a day: Days 2-28
•
1 Tablet of Dapsone (100 mg)
2.
MB Adult Treatment:
Once a month: 1 Day
°
»
*>
2 Capsules of Rifampicin (300 mg X 2)
3 Capsules of Clofazimine (100 mg X 3)
1 Tablet of Dapsone (100 mg)
r.;7Days 2-28
i. Capsule jt Clofazimine (50 mg)
TaL r~ Dapsone (100 mg)
■
■
■ 'he cij'nd should be given only breast milk
, . .
.
,
from bi; th to six months
r
Annexuies | 2
FULL COURSE: 12 MONTHS
It is crucial that patients unc :;snsc; which drugs they have to take once
month and which every day.
PB Child Treatment (10-14 years):
Once a month: 1 Day
3.
o
®
2 Capsules of Rifampicin (300 mg + 150 mg)
1 Tablet of Dapsone (50 mg)
Once a day: Days 2-28
•
1 Tablet of Dapsone (50 mg)
FULL COURSE: 6 Blister Packs
For children younger than 10, the dose must be adjusted according to body
weight.
MB Child Treatment (10-14 years):
Once a month: 1 Day
4.
•
•
•
2 Capsules of Rifampicin (300 mg + 150 mg)
3 Capsules of Clofazimine (50 mg X 3)
1 Tablet of Dapsone (50 mg)
Once a day: Days 2-28
•
•
1 Capsule of Cllofazimine every other day (50 mg)
1 Tablet of Dapsone (50 mg)
FULL COURSE: 12 Blister Packs
For children younger than 10, the dose must be adjusted according to body
weight.
Information for the Patient-Counselling Points
About Leprosy
•
They will be cured of Leprosy if they take the drugs in the blister packs as
advised
•
They must complete a full course of treatment : 6 blisters for PB patients
and 12 blisters for MB patients
The drugs stop the disease from spreading
•
•
28 I IPHS - CMC Level
Patients can lead normal lives. They can live at home, go to school, work,
and play, get married, have children, and participate in social events.
Opt for hospital delivery for
Their treatment
•
•
The MDT blister packs are free of charge
They should keep the blister packs in a dry, safe and shady place and out of
•
the reach of children
If the drugs are spoiled (changed colour, broken), the health worker will
replace them
Possible problems
«
•
•
•
•
The medicines will turn their urine red and their skin darker.
Patients should not worry : both will return to normal once the treatment
is completed
They must go immediately to a health centre if they have any problems
(pain, fever, malaise, new lesions, muscle weakness).
They should return for a check-up after they complete their treatment
If they already have disabilities, tell them how to protect themselves from
injuries
Important points about MDT
Safety
«
•
•
•
MDT is very safe and effective in curing Leprosy
MDT is safe during pregnancy
MDT is safe for patients being treated for Tuberculosis (TB) as well as those
who are HIV-Positive
Rifampicin is common to the treatment of Leprosy and TB and must be
given in the doses reguired for TB
Treatment
•
•
•
•
Give MDT free of charge to all Leprosy patients
Help ensure that patients complete their treatment
Give patients enough blister packs to Last until their next visit
Use accompanied MDT for all patients who find it difficult to visit the health
centre regularly
•
If a person cured of Leprosy presents new skin patches with definite loss of
sensation, consider this as a case of relapse. Re-treat with appropriate MDT
regimen
MDT Supplies
Do not use MDT blister packs
o beyond the expiry date
°
if the drugs are damaged, or have changed colour, or if a capsule is
broken
•
keep MD~ blister packs in a cupboard or a wooden box.
Health worker’s advice & care is
best for yourfamily’s welfare
Arnexures | 29
If MDT blister-packs for children are not available, remove tablets from an adult
psck or ths sppropnste cose.
Management of Reactions Cases
1. Leprosy Reactions
Patients can develop reactions, which are part of the natural course of the
disease. Reactions are not a side effect of MDT. They are the body's response
to Leprosy and do not mean that the disease is becoming worse or that the
treatment is not working.
2. Managing Reactions
If a patient has any of these symptoms, he or she must go immediately to a
health centre for treatment. Reactions require urgent treatment with special
medicines as they can Lead to irreversible deformities.
Give aspirin or paracetamol to reduce pain and fever. Advise the patients to
rest as that is essential.
3. Dose of Prednisolone
Maximum Dose of Prednisolone is 1 mg per kg of body weight
If you have a course of corticosteriods
(e.g. prednisolone), please administer :
40 mg daily for weeks 1 and 2,
30 mg daily for weeks 3 and 4,
20 mg daily for weeks 5 and 6,
15 mg daily for weeks 7 and 8,
10 mg daily for weeks 9 and 10,
5 mg daily for weeks 11 and 12.
30 I IPHS - CHC Level
Atleast three ante-natal checkup
Prevention of Deformity and Ulcer Care Services
Simple measures to prevent disabilities
Patients with insensitive hands or feet injure themselves without noticing it.
These wounds can get infected and over time, lead to irreversible deformities.
The patients with insensitive hands or feet should be advised as below :
a)
Inspect hand/feet daily looking for blisters, warm spots, red spots and
tender areas.
b)
Learn how to avoid injury
Hands
•
«
•
Feet
•
®
o
•
Use protective implements like gloves, towels, long sticks
Practice safe procedure while cooking
Bandage tool handles with cloth to make them safer
Walk slowly, avoid running
Do not stand at one place for long time
Do not walk long distances, rest in between
Use protective footwear - MCR
c)
If skin has become hard & dry, keep hands/feet soaked in water for 20
minutes. Apply oil over skin afterwards. Scrape off the callused skin.
d)
Do not use finger nails to remove nasal concretions.
Complete and correct knowledge
«... A ,■ . 4 ’r>e
Annexures | 21
Annaxure 5
National Programme for Control of Blindness
Services and Standards at Community Health Centres
(a)
(i)
Eye Care Services
Basic Services: Diagnosis and Treatment of Common Eye Diseases
(ii) Refraction Services
(iii) Surgical Services including Cataract Surgery (by I0L implantation) at
selected places (one per 5 lakh population)
(b)
Physical Structure for Eye Care at CHC
(i)
(ii)
Refraction Room
Eye OT with Eye Ward (number of beds dependent on workload)
(c) Equipment
For IOL Surgery
• Operating Microscope
• A-Scan Biometer
• Keratometer
•
•
•
•
•
•
Slit Lamp
Auto Refractometer
Flash Autoclave
Streak Retinoscope
Tonometers (Schiotz)
Direct Ophthalmoscope
For Primary Eye Care & Vision Testing
• Tonometers (Schiotz)
• Direct Ophthalmoscope
• Illuminated Vision Testing Drum
•
•
•
Trial Lens Sets with Trial Frames
Snellen & Near Vision Charts
Battery Operated Torch (2)
Eye Ointments
•
•
Atropine (1%)
Local antibiotic: Framycetin/Gentamicin etc.
•
Local antibiotic steroid ointment
32 I IPHS - CHC Level
The child should be given only breast milk
from birth to six months
Ophthalmic Drops
• Xylocaine 4% (30ml)
• Local antibiotic: Framycetin/Gentamicin etc.
» Local antibiotic steroid drops
» Pilocarpine Nitrate 2%
• Timolol 0.5%
• Homatropine 2%
• Tropicamide 1%
Injections
° Xylocaine 2% (30 ml)
« Inj Hyalase (Hyaluronidase)
• Gentamycin
o
®
o
®
Betamethasone/Dexamethasone
Inj. Maracaine (0.5%) (For regoinal anesthesia)
Inj. Adrenaline
Ringer Lacate (540 ml) from reputed firm
Surgical Accessories
<-■ Gauze
® Green shades
o
Blades (Carbon Steel)
® Opsite surgical gauze (10x14 c.m.)
• Double needle suture (commodity asstt. G0I )
o
Visco-elastics from reputed firm
(d) Human Resources
1.
2.
Eye surgeon (trained in I0L Surgery)
Ophthalmic assistant
Opt for hospital delivery for
safety ofmother & baby
Annexure
Integratsci Disease Surveillance Project
Services and Standards at Co nrcijn ;?/ Health Centres
(a) Services relating to Disease Surveillance:
(i) Laboratory services for diagnosis of Malaria, Tuberculosis, Typhoid and tests
for detection of faecal contamination of water and chlorination Level.
Existing peripheral laboratories at the PHC Level are capable of handling
microscopic examination of sputum and blood smears and are currently
undertaking this activity under TB and Malaria Control Programmes.
Typhoid can be diagnosed at the periphery using 'Typhi Dot' test, which
can be performed easily and has established validity and reliability. Kits are
available for detecting fecal contamination of water, which can be used at
the periphery and these will be made available.
Disease
Test
Tuberculosis
Sputum AFB smear
Malaria
Blood smear for Malaria
Typhoid
Rapid diagnostic test (Typhi Dot)
Water Quality
Kit for chlorination test
Water Quality
Rapid test kit for fecal contamination
(ii) Data Management: CHC will function as Peripheral Surveillance Unit and
coallate, analyse and report information to District Surveillance Unit. In
out-break situations, appropriate action will also be initiated.
(b) Physical Structure for Laboratory at CHC
| IPHS - CHC Level
Item
No. at CHC level
1
Marble/Stone Table Top for Platform
1
2
Wash-basins (Steel/Porcelain)
1
3
Water Tapes
1
4
Electric Fittings
As per requirement
5
Office Table
1
6
Office Chairs
3
7
Revolving Stools
2
8
AI m i r a h f St eel / Wooden)
1
9
Wooden Steel Racks
1
Health worker’s advice & care is
!>,><■/ h>e vnur fawilv’s welfare
(c)
Laboratory Equipment
I
Binocular microscope with oil immersion
2.
3.
4
5.
6.
7.
Lancet
Ice box
Stool transport carrier
Test tube rack
Table top centrifuge
Refrigerator
8.
9.
10.
Spirit lamp
Smear transporting box
Sterile leak proof containers
(d) Laboratory Supplies
1.
2.
3.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
Clean slides
Slide markers
Gloves
Transport medium (Cary Blair)
Sterile test tubes
Plastic vials
Sterile cotton wool swabs
Rapid diagnostic kit Typhoid
Rapid test kit for faecal contamination
Blood culture bottles with broth
Zeil Neelsen acid fast stain
Aluminium foil
Cotton
Sealing material
Extra plastic vials for transportation of serum
(e) Human Resources: Personnel trained in Disease Surveillance
1. Medical officer
2. Laboratory technician
Medical Record Keeper/Data Entry Operator
Aileast three ante-natal checkup
must for pregnant women
Ro.: rd the clock functional ambulance/rural transportation - Haryana model
1.
An advertisement is placed in local newspaper for leasing of ambulance
2.
3.
by the CMO office.
Preference is given to Ex-Army Defence/Services personnel.
Ambulance is given to the driver by the CMO office. No guarantee is
7.
required.
Charges of transportation are fixed at Rs. 5/km.
Driver is on a contract basis
Driver is required to deposit 50 paise/km in CMO office a monthly basis.
This money is kept for major repair.
Driver gets Rs. 4.50/km. This would cover petrol, salary and minor
8.
repairs.
Driver owns the ambulance after 5 years.
4.
5.
6.
36 I IPHS - CHC Level
Complete and correct knowledge
orntects von from AlIDS
Annexure 8
Equipment
Standard Surgical Set -1 (Instruments) FRU
1
12
1
|
12
|
1 4 Gloves surgeon, latex sterilisable, size 7 12
12
|
5 Gloves surgeon, latex sterilisable, 7-1/2 12
12
1
1 Tray, instrument/dressing with cover, 310 x 200 x 500 mm-ss 1
: 2 Gloves surgeon, latex sterilisable, size 5 12
1 3 Gloves surgeon, latex sterilisable, 6-1/2 12
!
1 6 Gloves surgeon, latex sterilisable, 8 12
12
7 Forceps, backhaus towel, 130 mm 4
4
8 Forceps, sponge holding, 228 mm 6
6
4
9 Forceps, artery, pean straight, 160 mm, stainless steel 4
10 Forceps hysterectomy, curved, 22.5 mm 4
4
11 Forceps, hemostatic, halsteads mosquito, straight, 125 mm-ss 6
5
12 Forceps, tissue, all/is 6x7 teeth, straight, 200 mm-ss 6
6
13 Forceps, uterine, tenaculum, 280 mm. stainless steel 1
1
14 Needle holder, mayo, straight, narrow jaw, 175 mm. ss 1
1
15 Knife-handle surgical for minor surgery #31
1
15 Knife-handle surgical for major surgery #41
1
17 Knife-blade surgical, size 11, for minor surgery, pkt of 5 3
3
18 Knife-blade surgical, size 15 for minor surgery, pkt of 5 4
*
j 19 Knife blade surgical, size 22, for major surgery, pkt of 5 3
3
- 20 Needles, suture triangular point, 7.3 cm, pkt of 6 2
2
1 21 Needles, suture, round bodied, 3/8 circle No. 12 pkt of 6 2
2
22 Retractor, abdominal, Deavers, size 3, 2.5 cm x 22.5 cm 1
1
, 23 Retactor, double-ended abdominal, Beltouis, set of 2 2
1
25 Retractor abdominal, Balfour 3 blade self-retaining 1
1
25 Scissors, operating, straight, blunt point, 170 mm 1
1
27 Scissors, gauze, straight, 230 mm, stainless steel 1
1
28 Suction tube, 225 mm. size 23 F 1
1
29 Clamp intestinal, Doyen, curved, 225 mm, stainless steel 2
2
!
2
31 Forceps, tissue spring type, 160 mm, stainless steel 2
2
32 Forceps , tissue spring type, 250 mm, stainless steel. 1
1
The child should, be given only breast milk
from birth to six months
i
2
24 Scissors, operating curved mayo-blunt pointed 170mm 1
' 30 Clamp intestinal, Doyen straight, 225 mm, stainless steel 2
|
Annexures | 37
Stangarc Suroica'. Set - II
1. Forceps, tissue, 5x7 teeth, Thomas-Allis, 200 mm- ss 1
2. Forceps, backhaus towel, 230 mm, stainless steel 4
1
:
4
3. Syringe, anaesthetic (control), 10 ml, luer-glass 1
i
4. Syringe, nypooermic, 10 ml glass, spare for item 3 4
4
5. Needles, hypocermic 20G x 1-1/2" box of 12 1
1
6. Forceps, tissue, spring type, 145 mm, stainless steel 1
1
7. Forceps, tissue soring tyoe 1x2 teeth, Semkins, 250 mm 1
1
8. Forceps, tissue spring tyoe, .250 mm, stainless steel 1
1
9. Forceps, hemostat curved mosquito halsteads, 130 mm 6
6
10. Forceps, artery', straight pean, 160 mm, stainless steel 3
3
11. Forceps artery, curved pean, 200 mm, stainless steel 1
1
12. Forceps, tissue, Babcock, 195 mm, stainless steel 2
2
13. Knife handle for minor surgery No. 3 1
1
14. Knife blade for minor surgery' No. 10, pkt of 5 8
8
15. Needle holder, straight narrow-jaw Mayo-Heger, 175 mm 1
1
16. Needle suture straight, 5.5 mm, triangular point, pkt of 6 2
2
17. Needle, Mayo, Vz circle, taper point, size 6, pkt of 6 2
.2
18. Catheter urethral Nelaton solid-tip one-eye 14 Fr 1
1
19. Catheter uretnral Nelaton solid-tip one-eye 16 Fr 1
1
20. Catheter uretnral Nelaton solid-tip one-eye 18 Fr 1
1
21. Forceps uterine tenaculum duplay dbl-cvd, 280 mm 1
1
22. Uterine elevator (Ranathlood), stainless steel 1
1
23. Hook, obstetric, Smellie, stainless steel 1
1
24. Proctoscope Mcevedy complete with case 1
1
25. Bowl, sponge, 600 ml, stainless steel 1
1
26. Retractor abdominal Richardson-Eastman, dbl-ended, set 2 1
1
27. Retractor abdominal Deaver, 25 mm x 3 cm, stainless steel 1
1
28. Speculum vaginal bi-valve graves, medium, stainless steel 1
1
29. Scissors ligature, spencer straight, 130 mm, stainless steel
1
30. Scissors operating straight, 140 mm, blunt/blunt ss 1
1
31. Scissors operating curved, 170 mm, blunt/blunt ss 2
2
32. Tray instrument curved, 225 x 125 x 50 mm, stainless steel 1
1
33. Battery cells for item 24 2
2
IUD Insertion Kit
1. Setal sterilisation tray with cover size 300 x 220 x 70 mm, S/S, Ref IS:
3993 1
1
2. Gloves surgeon, latex, size 6-1/2 Ref. 4148 6
6
3. Gloves surgeon latex, size 7-1/2 Ref. 4148 6
6
4. Bowl, metal sponge, 600 ml, Ref. IS: 5782 1
1
Optfor hospital delivery for
safety o~
■■
I 5. Speculum vaginal bi-valve cusco's graves small ss 1
1
| 6. Forceps sponge holding, straight 228 MMH Semken 200 mm 1
1
j 7. Sound uterine simpson, 300 mm graduated UB 20 mm 1
1
8. Forceps uterine tenaculum duplay DBL-CVD, 280 mm 1
1
j 9. Forceps tissue - 160 mm 1
1
| 10. Anterior vaginal wall retractor stainless 1
1
11. Torch without batteries 1
i 12. Gloves surgeon, latex, size 7, Ref: 4148 6
13. Gloves surgeon, latex size 6 Ref. IS: 4148 6
j 14. Battery dry cell 1.5 V 'D' Type for Item 7G 1
■
1
6
6
1
15. Speculum vaginal bi-valve cusco's/Grea Ves Medium ss 1
1
16. Forceps artery, straight, Pean, 160 mm 1
1
17. Scissors operating, straight, 145 mm, Blunt/Blunt 1
1
18. Forceos uterine vulsellum curved, Museux, 240 mm 1
i :
19. Speculum vaginal double-ended sime size #3 1
i
'
CHC Standard Surgical Set - III
Tray, instrument/dressing with cover, 310 x 195 x 63 mm 1
1
Forceps, backhaus towel, 130 mm, stainless steel 4
4
Forceps, hemostat, straight, Kelly, 140 mm, stainless steel 4
4
,
Forceps, hemostat, curved, Kelly, 125mm, stainless steel 2
2
,
Forceps, tissue Allis, 150 mm, stainless steel, 4x5 teeth 2
2
, Knife handle for minor surgery No. 3 1
1
Knife blade for minor surgery, size 11, pkt of 5 10
10
: Needle hypodermic, Luer 22G x 11/4", box of 12 1
1
Needle hypodermic, Luer 250G x 3/4", box of 12 1
1
Needle, suture straight 5.5 cm, triangular point, pkt of 6 2
2
Needle, suture, Mayo Vz circle, taper point No. 6, pkt of 6 2
2
■ Scissors, ligature, angled on flat, 140 mm, stainless steel 1
1
Syringe anaesthetic control, Luer - 5 ml, glass 4
4
Syringe 5 ml, spare for item 13 4
*
!
I
Steriliser, instrument 200 x 100 x 60 mm with burner ss 1
1
Syringe, hypodermic, Luer 5 ml, glass 4
4
'
Forceps, steriliser, Cheatle, 265 mm, stainless steel 1
1
1
Normal Delivery Kit
1 Trolley, dressing carriage size 76C, long x 46 cm wide and 84 cm high. Ref. IS
4769/1968 1
1
Towel, trolley 84 cm x 54 cm 2
2
Gown, operation, cotton 1
1
Cap. operation, surgeon's 36 x 46 cm 2
2
Health worker’s advice & care is
bestfor your family’s welfare
Annexures | 39
Gauze aDsoroe-.: -.on-sterile 200 mm x 6 m as per IS: 171/1985 2
2
Tray instrume~: • ttn cover 450 mm (L) x 300 mm (W) x 80 mm (H) 1
1
Macintosh, ooera cion, plastic 2
2
Mask, face. su*ge on s cao of rear ties: B) Beret type with elastic hem 2
2
Towel, glove _
3
Cotton wool a esc -cent non-sterilise 500G 2
2
Drum, sterilise.; cylindrical-275 mm Dia x 132 mm, ss as per IS: 3831/1979 2
2
Table instrument adjustable type with tray ss 1
1
Standard S.-rgicai. Set - IV
Vaccum extractor. Malastrom 1
1
Forceps obstetric. Wrigley's, 280 mm, stainless steel 1
1
Forceps, obstet-ic. Barnes-Neville, with traction, 390mm 1
1
Forceps, sponge nolding, straight 228 mm, stainless steel 4
4
Forceps, arter;.. Soencer-Wells, straight, 180mm-ss 2
2
Forceps, artery. Soencer-Wells, straight, 140mm-ss 2
2
Holder, needle straight, Mayo-Hegar, 175 mm-ss 1
Scissors, ligature. Soencer, 130 mm, stainless steel 1
1
1
Scissors, episiotomy, angular, Braun, 145 mm, stainless steel 1
1
Forceps, tissue, soring-type, 1x2 teeth, 160 mm-ss 1
1
Forceps, tissue, soring-type, serrated ups, 160mm-ss 1
1
Catheter, uretnra., rubber, Foley's 14 ER 1
1
Catheter, uretnra.. Nelaton, set of five (Fr 12-20) rubber 1
1
Forceps, backnaus towel -130 mm-ss 4
4
Soeculum, vag-na.. Sim's, double-ended # 3-ss 1
1
Soeculum, vagina.. Hamilton-Bailey 1
1
Standard S_-gicaL Set - V
Forceps, obstet.Neville-Barnes, W/traction 390 mm 1
1
Hook, decapitation, Braun, 300 mm, stainless steel 1
1
Hook, crochet, oostetric 300 mm, Smellie, stainless steel 1
1
Bone, forceps Mesnard 280 mm, stainless steel 4
4
Perforator, Smellie, 250 mm, stainless steel 1
1
Forceps, cranial. Gouss, straight, 295 mm-ss 1
1
. Cranioclast, Braun, stainless steel, 365 mm long 1
1
Scissors ligature Spencer 130 mm, stainless steel 1
1
Forceps sponge nolding, 22.5 cm straight - ss 1
1
Forceps, tissue, soring-type, 1x2 teeth, 160 mm, stainless steel 1
1
Forceps, tissue, soring-type, serrated tips, 160 mm-ss 1
1
Forceps, arter.. Soencer-Wells, straight, 180 mm-ss 2
2
Forceps, artery. Soencer-Wells, straight, 140 mm-ss 2
2
Forceps, scalp nap, Willet's 190 mm -ss 4
4
Atleast three ante-natal checkup
niitslforp-.
Forceps, Vulsellum, duplay double curved, 280 mm-ss 4
4
Forceps, Vulsellum, duplay double curved, 240 mm-ss 1
1
Catheter, urethral, 14 Fr. solid tip, one eye, soft rubber 3
3
Holder, needle, Mayo-Hegar, narrow jaw, straight, 175 mm-ss 1
1
Speculum vaginal bi-valve, Cusco-medium, stainless steel 1
1
Speculum, vaginal sim's double-ended, size tt 3-ss 1
1
Forceps, backhaus towel, 130 mm, stainless steel 4
4
Standard Surgical Set - VI
Forceps, sponge holding, straight, 225 mm, stainless steel 4
4
Speculum, vaginal, Sim's double-ended size # 3 - ss 1
1
Speculum, vaginal, weighted Auvard, 38 x 75 mm blade - ss 1
1
Forceps, tenaculum, Teale's, 230 mm-ss x 3 x 4 2
3x42
Sound, uterine, Simpson, 300 mm with 200 mm graduations 1
1
Dilator, uterine, double - ended hegar, set of 5 - ss 1
1
Curette, uterine, sim's blunt, 26 cm x 11 mm size tt 4-ss 2
2
Curette, uterine, sim's sharp, 26 cm x 9 mm size it 3-ss 2
2
Forceps, artery, Spencer-Well's straight, 140 mm-ss 1
1
Forceps, tissue, spring-type, serrated tips, 160 mm-ss 1
1
Forceps, ovum, Krantz, 290 mm, stainless steel 1
1
Equipment for Anaesthesia
Facemask, plastic w/rubber cushion & headstrap, set of 4 4
4
Airway Guedel or Berman, autoclavable rubber, set of 6 2
2
Laryngoscope, set with infant, child, adolescent blades 3
3
Catheter, endotracheal w/cuff, rubber set of 4 3
3
Catheter, urethral, stainless steel, set of 8 in case 2
2
Forceps, catheter, Magill, adult and child sizes, set of 2 1
1
Connectors, catheter, straight/curved, 3, 4, 5 mm (set of 6) 3
3
Cuffs for endotracheal catheters, spare for item 4 4
4
Breathing tubes, hoses, connectors for item 1, anti-static 4
4
Valve, inhaler, chrome-plated brass, Y-shape 3
3
Bag, breathing, self inflating, anti-static rubber, set of 4 2
2
Vaporiser, halothane, dial setting 2
2
Vaporiser, ether or methoxyflurane, wick type 2
2
Intravenous set in box 6
6
Needle, spinal, stainless set of 4 2
2
Syringe, anesthetic, control 5ml Luer mount glass 2
2
Cells for item 3 2
2
Complete and correct knowledge
protects you from AIDS
1
Annexures | 41
Equipment for Neo-nataL Resuscitation
Catheter, mucus, rubber, open ended tip, size 14FR 2
2
Catheter, nasal, rubber, open tip, funnel end, size 8Fr 2
2
, Catheter, endotracneal, open tip, funnel end rubber, 12Fr 3
3
Stilette, curved, for stiffening tracheal catheter SS 1
1
I Catheter, suction, rubber, size 8Fr 3
3
Laryngoscope, infant, w/three blades and spare bulbs. 1
1
Lateral mask, with ventillatory bag, infant size 2
2
Resuscitator, automatic, basinet type 1
1
Lamp, ultra-violet (heat source) with floor stand 1
1
Cells for item 6 (Laryngoscope) 2
2
Materials Kit for Blood Transfusion
Bovine albumin 20% testing agent, box of 10 x 5 ml vials 5
5
| Centrifuge, angle head for 6 x 15 ml tubes, 240 volt 1
1
l Bath, water, serological, with racks, cover, thermostate, 240 v 1
1
Pipette, volumetric, set of six 1 ml/2 ml/3 ml/5 ml/10 ml/20 ml 1
1
Test-tube without rim 75 x 12 mm HRG 12
12
1 Test-tube without rim 150 x 16 mm, HRG 12
12
Cuff, sphygmomanometer, set of two sizes - Child/Adult 1
1
Needle, blood collect'on disposable, 17G x 1-1/3 box of 100 1
1
Ball, donor squeeze, rubber, dia, 60 mm 1
1
: Forceps, artery, Spencer-Wells, straight 140 mm, stainless steel 1
1
' Scissors, operating, straight 140 mm, blunt/jpoints, ss 1
1
CPDA anti-coagulent, pilot bottle 350 ml for collection 20
20
Microscope, binocular, inclined, 10 x 40 x 100 x magnificant 1
1
Illuminator for item 14 (microscope) 1
1
Slides, microscope, plain 25 x 75 mm, clinical, box of 100 1
1
Equipment for Operation Theatre
Diathermy machine
Dressing drum all sizes,
Lamps shadowless:
a) ceiling Lamp
b) portable type
Steriliser
Suction apparatus
Stand with wheel for single
basin
Table operation, hydraulic:
a) Major
b) Minor
42 I IPHS - CMC Level
The child should be given only breast milk
from birth to six mouths
Trolley for patients
Trolley for instruments
X-ray view box
Wheel chairs
Equipment for Labour Room
Aprons rubber
Cradles baby
Wheel chair,
Cabinet, Instrument
Dressing drum
Shadowless lamps
Table for
a) Obstetric labour
b) Examination
Trolley for
a) Patients
b) Dressing
Torch (flash Light)
Trays
Vacuum extractor
Weighing machine baby
Wheel chairs
Equipment for Radiology
Aprons Lead rubber
Diagnostic X-ray Unit 200/300mA with automatic device
Dark room accessories
Dark room timer
Film clips
Lead sheets
X-ray view box
Xray protection screen
X-ray film processing tank
EQUIPMENTS under National Health Programmes ( as listed under each NHP),
Cold storage facility under Immunisation Programme and Blood Storage
equipment as at annexure- 10.
Optfor hospital delivery for
safety of mother & baby
Annexures | 43
Annexure 9
List of Essential Drugs for CHC
Name of the Drug
Route of
administration/dosage
form
1
Oxygen
Inhalation
2
Lignocaine Hydrochloride
Topical Forms
2-5%
Injection
1-2%
Tablets
2 mg, 5 mg, 10 mg
Injection
5 mg/ml
3
Diazepam
Strength
1
4
Acetyl Salicylic Acid
Tablets
75mg, 100 mg 300 mg 350 mg
5
Ibuprofen
Tablets
200 mg, 400 mg
6
Paracetamol
Injection
150 mg/ml
Syrup
125 mg/5ml
Tablets
500 mg
7
Pentazocine Lactate
injection
30 mg/ml
8
Chloroquine Phosphate
Tablets
150 mg
Injection
40 mg/ml
Syrup
50 ml/5 ml
9
Adrenaline bititrate
Injection
Img/ml
10
Chlorpheniramine Maleate
Tablets
4 mg
i
11
Prednisolone
Tablets
5 mg, 10 mg
1
12
Promethazine HCL
Tablet/syrup
!
1
13
Phenobarbitone
Tablets
30 mg. 60 mg
Injection
200 mg/ml
Capsules or Tablets
50 mg,100 mg
14
|
Phenytoin Sodium
15
Albendazole
16
Amoxicillin Powder
Syrup
25 mg/ml
Tablets
400 mg
Suspension
200 mg/5 ml
For suspension
125 mg/5 ml
Capsules
250 mg
500 mg
17
Ciprofloxacin Hydrochloride
Tablets
250 mg,500 mg
18
Co-Trimoxazole
Tablets
40 + 200 mg
80 + 400 mg
19
Norfloxacine
44 I IPHS - CHC Level
Suspension
40 +200 mg/5 ml
Tablet
400 mg
Health worker’s advice & care is
bestfor your family’s welfare
20
Doxycycline
Capsules
100 mg
21
Metronidazole
Tablets
200 mg,400 mg
22
Clotrimazole
Pessaries
100 mg, 200 mg
Gel
2%
23
24
Sulfadoxine + Pyrimethamine
Ferrous Salt
Tablets
500 mg +25 mg
Tablets
60 mg
Oral Solution
25 mg
25
Folic Acid
Tablets
1 mg, 5 mg
26
Isosorbide Mononitrate/Dinitrate
Tablets
10 mg, 20 mg
27
Amlodipine
Tablets
2.5 mg, 5 mg,10 mg
28
Digoxin
Tablets
0.25 mg
Injection
0.25 mg/ml
Elixir
0.05 mg/ml
6% + 3%
29
Benzoic Acid + Salicylic Acid
Ointment or Cream
30
Miconazole
Ointment or Cream
2%
31
Neomycin + Bacitracin
Ointment
5 mg + 500 IU
32
Silver Sulphadiazine
Cream
1%
33
Benzyl Benzoate
Lotion
25%
34
Acriflavin + Glycerin
Solution
35
Gentian Violet
Paint
0.5%, 1%
36
Hydrogen Peroxide
Solution
6%
37
Povidone Iodine
Solution
5%, 10%
38
Bleaching Powder
Powder
39
Potassium Permanganate
Crystals for Solution
40
Furosemide
41
Aluminium Hydroxide +
Magnesium
Injection,
10 mg/ml,
Tablets
40 mg
Tablet
Suspension
Hydroxide
42
Domperidone
43
Local Anaesthetic,Astringent and
Antiinflammatory Medicine
Ointment/Suppository
44
Dicyclomine Hydrochloride
Tablets
Injection
10 mg/ml
45
Oral Rehydration Salts
Powder for Solution
As per IP
46
Dexamithasone sodium
injection
4 mg/ml
47
Ciprofloxacin Hydrochloride
Drops/Ointment
0.3%
48
Tetracycline Hydrochloride
Ointment
1%
49
Alprazolam
Tab
0.25 mg
Atleast three ante-natal checkup
mustfor pregnant women
Tablets
10 mg
Syrup
1 mg/ml
10 mg
Annexures | 45
50
Salbutamol Sulphate
‘ Tablets
2 mg, 4 mg
; Syrup
2 mg/5 ml
; Inhalation
100 mg/dose
84.7 mg/ml
'
51
Etophyline Anhydrous
Injection
i
52
Glucose
Injection
5% isotonic
53
Glucose with Sodium Chloride
Injection
5% + 0.9%
54
Normal Saline
Injection
0.9%
55
Ringer Lactate
Injection
56
Plasma Volume Expander
Injection
57
|
i
i
1
!
1
I
1
50% hypertonic
Water for Injection
Injection
2 ml, 5 ml,10 ml
58
Ascorbic Acid
Tablets
100 mg, 500 mg
59
60
Calcium Salts
Tablets
250 mg, 500 mg
Multivitamins(As per Schedule V)
Tablets
61
Aten lol
Tablets
50 mg
Tablets
20 mg
52
Floxitin
63
Amitryptiline Hcl
Tablets
25 mg
64
Bisacodyl
Tablets
05 mg
65
General Anaesthetic Drugs
67
Tinidazole
Tablets
68
Daonil
Tablets
69
Haloperidol
Tablets
70
Sulpacetamide Eye Drops
Other Injections:
S. No.
if, | TPMS _ fur I owol
Injections
1.
Cryst. Penicillin
2.
Inj.Procaine Penicillin
3.
Inj.Benzathine Penicillin (1.2)
4.
Inj. Phenytoin Sodium 50mg/ml
5
Inj. Ampicillin
6
Inj. Gentamicin
7
Inj. Soda Bicarb
8
Inj. Calcium Gluconate
9
Inj. KCI
10
Inj. Atropine
11
Inj. Hyoscine N-butyl Bromide
12
Inj. Hydrocortisone
13
Inj. Syntocinon (synthetic oxytocin)
14
Inj. Methyl Ergometrine Maleate
Complete and correct knowledge
Protects von from AIDS
15
Inj. Isoxsuprine Hydrochloride
16
Inj. Aminophyllin
17
Inj. Chloramphenicol
18
Inj. Mannitol
19
Inj. Pethidine
20
Inj. Chlorpromazine
-Drugs under various National Health Programmes(as listed under each NHP)
-Vaccines as under Immunisation Programme
The child should be given only breast milk
Annexures | 47
Annexure 10
Extracts from National Guidelines on Blood Storage Facilities at FRUs.
1.
Requirements
Sauce : The area required for setting up the facility is only 10 square meters,
well-lighted, clean and preferably air-conditioned.
Manpower: One of the existing doctors and technicians should be designated
for this purpose. They should be trained in the operation of blood storage
centers and other basic procedures like storage, grouping, cross- matching and
release of blood.
The medical officer designated for this purpose will be responsible for overall
working of the storage center.
Electricity: 24 hours supply is essential. Provision of back-up generator is
required.
Equipment: Each FRU should have the following :
1.
2.
Blood bag refrigerators having a storage capacity of 50 units of blood.
Deep freezers for freezing ice packs required for transportation. The deep
freezers available in the FRUs under the Immunisation Programme can be
3.
utilised for this purpose.
Insulated carrier boxes with ice packs for maintaining the cold chain
during transportation of blood bags.
4.
Microscope and centrifuge: Since these are an integral part of any existing
Laboratory, these would already be available at the FRUs. These should be
supplied only if they are not already available.
Consumables: There should be adequate provision for consumables and
blood grouping reagents. The following quantities would suffice the annual
requirement of an FRU with up to 50 beds.
Consumables Quantity
Pasteur pipette 12 dozens/year
Glass tubes 7.5 to 10 mm - 100 dozens/year
Glass slides 1" x 2" boxes of 20 or 25 each/year
Test tube racks 6 racks, each for 24 tables
Rubber teats 6 dozens/year
Gloves disposable rubber gloves 500 pairs per year
Blotting tissue paper As required
Marker pencil (alcohol based) As required
IPHS - CHC Level
Optfor hospital delivery for
safety of mother & baby
Toothpicks as required
Reagents: All the reagents should come from the Mother Blood Bank.
Anti-A 2-vials each per month
Anti-B 2-vials each per month
Anti-AB 2-vials each per month
Anti-D (Blend of IgM & IgG) 2 vials each per month
Antihuman Globulin 1 vial per month
(Polyclonal IgG & Complement)
Since quality of the reagents is an important issue, the supplies of these should
be made from the same blood bank/center from where blood is obtained. For
this purpose, State Govemments/Union Territories should provide the additional
budgetary requirements to the mother blood bank/center.
Disinfectants: Bleach & Hypochlorite Solution - As required
2. Suggested quantities of Whole Blood Units to be available
at Blood Storage Units
5 units each of A, B, 0 (Positive)
2 units of AB (Positive)
1 units each of A, B & 0 (Negative)
This can be modified according to the actual requirement
3. Storage and Transportation
Cold chain: It is necessary to maintain the cold chain at all levels i.e. from
the mother center to the blood storage center to the issue of blood. This can
be achieved by using insulated carrier boxes. During transportation, the blood
should be properly packed into cold boxes surrounded by the ice packs. Ice,
if used should'be clean and should not come in direct contact with the blood
bags. The blood should be kept in blood bank refrigerator at 4°-6°c ± 2°c. The
temperature of the blood should be monitored continuously.
Storage: The storage center should check the condition of blood on receipt from
the mother center and also during the period of storage. The responsibility of
any problem arising from storage, cross matching, issue and transfusion will be
of the storage center. Any unit of blood showing hemolysis, turbidity or change
in colour should not be taken on stock for transfusion. Due care should be taken
to maintain sterility of blood by keeping all storage areas clean. The expiry of
the blood is normally 35/42 days depending on the type of blood bags used.
The Medical Officer in-charge should ensure that unused blood bags should be
returned to the mother center at Least 10 days before the expiry of the blood
and fresh blood obtained in its place. The blood storage centers are designed
to ensure rapid and safe delivery of whole blood in an emergency, the detail
of storage of packed cells, fresh frozen plasma and platelets concentrate are
Health worker’s advice dr care is
bestfor your family's welfare
therefore not given in these guidelines. In case, however, these are required to
be stored, the storage procedures of the mother blood bank should be followed.
4. Issue of Blood
Patients blood grouping and cross matching should invariably be carried out
before issue of blood. A proper record of this should be kept.
First In and First Out (FIFO) policy, whereby blood closer to expiry date is used
first, should be followed.
5. Disposal
Since all the blood bags will already be tested by the mother center, disposal
of empty blood bags should be done by landfill. Gloves should be cut and put
in bleach for at least one hour and then disposed as normal waste.
6. Documentation and Records
The center should maintain proper records for procurement, cross matching and
issue of blood and blood components. These records should be kept for at Least
5 years.
7. Training
Training of doctors and technicians, who will be responsible far ;.•<>
Storage Center, should be carried out for 3 days in an identified center as per
the guidelines. Training will include:
°
°
Pre-transfusion checking, i.e. patient identity and grouping
Cross matching
°
Compatibility
°
0
0
Problems in grouping and cross matching
Troubleshooting
Issue of blood
•
•
Transfusion reactions and its management
Disposal of blood bags
The states will have to identify the institutions where training of the staff
responsible for running the blood bank is to be held. These could be the blood
banks at Medical Colleges, Regional Blood Banks, Indian Red Cross Blood Banks,
or any other well set up, licensed Blood Bank, provided they have the necessary
infrastructure for undertaking training.
The training will be for three-days duration during which the Medical Officer and
the technician from the identified FRUs will be posted at the training institution.
A "Standard Operating Procedures Manual" (SOPM) has been developed and
is part of these guidelines. This SOPM will be used as the training material. A
50 I IPHS - CHC Level
Atleast three ante-natal checkup
mustfor pregnant women
copy of this SOPM will be made available to the Medical Officer for use in his
Blood Storage Center for undertaking storage, grouping, cross matching and
transfusion.
In addition to the training of the above Medical Staff, it is considered necessary
that the clinicians who will be responsible for prescribing the use of blood
are also sensitised on the various parameters of blood transfusion. For this
the "Clinician's Guide to Appropriate Use of Blood" has been developed. It
is suggested that one-day sensitisation programme for the clinicians may be
organised at the District Hospital/Medical College.
Government of India will make the expenditure for the above-mentioned
trainings, available as per the norms of training under the RCH Programme. This
training will, however, be coordinated by the Training Division of Department
of Family Welfare. The states are required to include training as part of the
overall State Action Plan for establishing Blood Storage Centers.
Equipments for Laboratory Tests & Blood Transfusion
Rod, flint-glass, 1000 x 10 mm dia, set of two 2
Cylinder, measuring, graduated W/pouring lip, glass, 50 ml 2
Bottle, wash, polyethylene W/angled delivery tube, 250 ml 1
Timer, clock, interval, spring wound, 60 minutes x 1 minute 1
Rack, slide drying nickel/silver, 30 slide capacity 1
Tray, staining, stainless steel 450 x 350 x 25 mm 1
Chamber, counting, glass, double neubauer ruling 2
Pipette, serological glass, 0.05 ml x 0.0125 ml 6
Pipette, serological glass, 1.0 ml x 0.10 ml 6
Counter, differential, blood cells, 6 unit 1
Centrifuge, micro-hematocrit, 6 tubes, 240v 1
Cover glass for counting chamber (item 7), Box of 12 1
Tube, capillary, heparinised, 75 mm x 1.5 mm, vial of 100 10
Lamp, spirit W/screw cap. Metal 60 ml 1
Lancet, blood (Hadgedorn needle) 75 mm pack of 10 ss 10
Benedict's reagent qualitative dry components for soln 1
Pipette measuring glass, set of two sizes 10 ml, 20 ml 2
Test tube, w/o rim, heat resistant glass, 100 x 13 mm 24
Clamp, test-tube, nickel plated spring wire, standard type 3
Beaker, HRG glass, low form, set of two sizes, 50 ml, 150 ml 2
Rack, test-tube wooden with 12 x 22 mm dia holes 1
Complete and correct knowledge
protects von from AJDS
Annexures | 51
Annexure 11
National Guidelines on Hospital Waste Management based on the BioMedical Waste(Management & Handling) Rules, 1998.
(Only relevant portions as applicable to a 30 bed CHC need to be taken in
to account from this guidelines)
The Bio-Medical Waste (Management & Handling) Rules, 1998 were notified under
the Environment Protection Act, 1986(29 of 1986) by the Ministry of Environment
and Forest, Government of India on 20th July, 1998. The guidelines have been
prepared to enable each hospital to implement the said Rules, by developing
comprehensive plan for hospital waste management, in terms of segregation,
collection, treatment, transportation and disposal of the hospital waste.
1. Policy on Hospital Waste Management
The policy statement aims to provide for a system for management of all
potentially infectious and hazardous waste in accordance with the Bio-Medical
Waste (Management & Handling) rules, 1998 (BMW,1998)
2. Definition of Bio-Medical Waste
Bio-Medical Waste means any waste, which is generated during the diagnosis,
treatment or immunisation of human beings or animals or in research activities
pertaining thereto or in the production or testing of biologicals, including
categories mentioned in the Schedule I of the Bio-Medical Waste (Management
&
Handling) Rules, 1998.
3. Categories of Bio-Medical Waste
Hazardous, toxic and Bio-Medical waste has been separated into the following
categories for the purpose of its safe transportation to a specific site for specific
treatment. Certain categories of infectious waste require specific treatment
(disinfection/decontamination) before transportation for disposal. These
categories of bio-medical waste are mentioned as below:
Category No. 1 - Human Anatomical Waste
This includes human tissues, organs, body parts.
Category No. 2 - Animal Waste
This includes animaltissues, organs, body parts, carcasses, bleeding parts, fluid,
blood and experimental animals used in research, waste generated by veterinary
hospitals and colleges, discharge from hospitals and animal houses.
52 | IPHS - CHC Level
The child should be given only breast milk
from birth to six months
Category No. 3 - Microbiology & Biotechnology Waste
This includes waste from laboratory cultures, stocks or specimens of micro
organisms live or attenuated vaccines, human and animal cell culture used in
research and infectious agents from research and industrial laboratories, wastes
from production of biological, toxins, dishes and devices used for transfer of
culture.
Category No. 4 - Waste Sharps
This comprises of needles, syringes, scalpels, blades, glass, etc. that may cause
puncture and cuts. This includes both used and unusable sharps.
Category No. 5 - Discarded Medicines and Cytotoxic drugs
This includes wastes comprising of outdated, contaminated and discarded
medicines.
Category No. 6 - Soiled Waste
It comprises of items contaminated with blood, and body fluids including cotton,
dressings, soiled plaster castes, linens, beddings, other material contaminated
with blood.
Category No. 7 - Solid Waste
This includes wastes generated from disposable items, other than the waste
sharps, such as tubings, catheters, intravenous sets, etc.
Category No. 8 - Liquid Waste
This includes waste generated from laboratory and washing, cleaning, house
keeping and disinfecting activities.
Category No. 9 - Incineration Ash
This contains of ash from incineration of any bio-medical waste
Category No. 10 - Chemical Waste
This contains chemicals used in production of biologicals and chemicals used
in.disinfection, insecticides etc.
4. Segregation of Waste
It should be done at the site of generation of bio-medical waste, e.g., all
patient care activity areas, diagnostic service areas, operation theatres,
labour rooms, treatment rooms.
4.2 The responsibility of segregation should be with the generator of bio
medical waste, i.e.. Doctors, Nurses, Technician etc.
4.3 The bio-medical waste should be segregated as per categories applicable.
4.1
Optfor hospital delivery for
sa etv o mother dr baby
Annexures | 53
5.
Collection of Bio-Medical Waste:
Collection of Bio-medical waste should be done as per Bio-Medical Waste
(Management & Handling) Rules, 1998 (Rule 6 - Schedule II). The collection
bags and the containers should be labelled as per guidelines of Schedule III,
i.e., symbols for bio-hazard and cytotoxic. A separate container shall be placed
at every point of generation for general waste to be disposed of through
Municipal Authority.
The trolleys which are used to collect hospital waste should be designed in
such a way that there should be no leakage or spillage of bio-medical waste
while transporting to designated site.
5.1 Type of container and colour for collection of bio-medical waste:
Category
Type of container
Colour coding
1. Human anatomical waste
Plastic bag
Yellow
2. Animal waste
Plastic bag
Yellow
3. Microbiology & Biotechnology
waste
Plastic bag
Yellow/Red
4. Waste sharp
Plastic bag, puncture
proof container
Blue/white/
Translucent
5. Discarded medicines &
Cytotoxic waste
Plastic bag
Black
6. Solid waste (Soiled)
Plastic bag
Yellow/Red
7. * Solid waste (Plastic)
Plastic bag
Blue/White
8. Liquid waste
------------
--------------
9. Incineration ash
Plastic bag
Black
10. Chemical waste (solid)
Plastic bag
Black
* Those plastics which contains liquid like blood, urine, pus, etc, should be put into red colour
bag for microwaving and autoclaving and other items should be put into blue or white bag
after chemical treatment and mutilation/shredding.
5.2
5.3
5.4
54 | IPHS - CMC Level
All the items sent to incinerator/deep burial(Cat 1, 2, 3, 6) should be
placed in yellow coloured bags.
All the bio-medical waste to be sent for microwave/Autoclave treatment
should be placed in red coloured bags.(Cat. 3, 6, & 7)
Any waste which is sent to shredder after autoclaving/microwaving/
chemical treatment is to be packed in blue/white translucent bag.
Health worker’s advice & care is
bestfor your familys tvelfare
5.5
5.6
Location of containers:
All containers having different coloured plastic bags should be located
at the point of generation of waste, i.e., near OT tables, injection rooms,
diagnostic service areas, dressing trolleys, injection trolleys, etc.
Labelling: All the bags/containers must be labelled bio-hazard or cytotoxic
with symbols according to the rules (Schedule III of bio-medical waste
rules, 1998)
5.7
Bags: It should be ensured that waste bags are filled up to three-fourth
capacity, tied securely and removed from the site of the generation to the
storage area regularly and timely.
5.8
The categories of waste (Cat. 4, 7, 8,& 10) which require pre-treatment
(decontamination/disinfection) at the site of generation such as plastic
and sharp materials, etc., should be removed from the site of generation
only after treatment.
The quantity of collection should be documented in a register. The colour
plastic bags should be replaced and the garbage bin should be cleaned
with disinfectant regularly.
5.9
6.
Storage of Waste
Storage refers to the holding of bio-medical waste for a certain period of time
at the site of generation till its transit for treatment and final disposal.
6.1 No untreated bio-medical waste shall be kept stored beyond a period of
48 hours.
6.2 The authorised person must take the permission of the prescribed authority, if
for any reason it becomes necessary to store the waste beyond 48 hours.
6.3 The authorised person should take measures to ensure that the waste does
not adversely affect human health and the environment, in case it is kept
beyond the prescribed Limit.
7.
Transportation
7.1
Transportation of waste within the hospitals
7.1.1 Within the hospital, waste routes must be designated to avoid the
passage of waste through patient care areas as far as possible.
7.1.2 Separate time schedules are prepared for transportation of bio
medical waste and general waste; it will reduce chances of their
mix-up.
Dedicated wheeled containers, trolleys or carts with proper label
(as per Schedule IV of Rule 6) should be used to transport the
waste from the site off storage to the site of treatment.
7.1.4 Trolleys or carts should be thoroughly cleansed and disinfected in
the event of any spillage.
7.1.5 The wheeled containers should be designed in such a manner that the
waste can be easily Loaded, remains secured during transportation,
does not have any sharp edges and easy to cleanse and disinfect.
7.1.3
Atleast three ante-natal checkup
An.i-ijayiirae
I
KC
7.2
Transportation of waste for disposal outside the hospital:
7.2.1. Notwithstanding anything contained in the Motor Vehicles Act,.
1988 or rules thereunder, bio-medical waste shall be transported
only in such vehicles as may be authorised for the purpose by the
competent authority.
7.2.2 The containers for transportation must be Labelled as given in
Schedule III and IV of BMW, 1998
8. Treatment of Hospital Waste (Please see Rule 5, Schedule V & VI)
8.1
8.2
General waste (Non-hazardous, non-toxic, non-infectious). The safe
disposal of this waste should be ensured by the occupier through Local
Municipal Authority.
Bio-Medical Waste
Monitoring of incinerator/autoclave/microwave shall be carried out once in
a month to check the performance of the equipment. One should ensure:
j)
The proper operation & maintenance of the incinerators/autoclave/
microwave
ii)
Attainment of prescribed temperatures in both the chambers of
incinerators while incinerating the waste.
iii)
Not to incinerate plastic materials
iv)
Only skilled persons operate the equipment
v)
Proper record book shall be maintained for the incinerators/
autoclave/microwave/shredder. Such record book shall have the
entries of period of operation, temperature/pressure attained while
treating the waste, quantity for waste treated, etc.
vi)
The scavengers shall not be allowed to sort out the waste
vii)
Proper hygiene shall be maintained at, both the waste treatment
plant site as well as the waste storage area.
viii)
Categories 4, 7, 8, and 10 should be treated with chemical
disinfectant like 1% hypochlorite solution or any other equivalent
chemical reagent to ensure disinfection.
8.1.1 Incineration: The incinerator should be installed and made
operational as per specifications under the BMW rules , 1998
(Schedule V) and an authorisation shall be taken from the prescribed
authority for the management and handling of bio-medical waste
including installation and operation of treatment facility as per
Rule 8 of Bio-Medical Waste (Management & Handling) Rules,1998.
Specific requirements regarding the incinerators and norms of
combustion efficiency and emission levels, etc. have been defined
in the Bio-Medical Waste (Management & Handling) Rules,1998.
In case of small hospitals, joint facilities for incineration can be
developed depending upon the local policies of the hospital and
feasibility. The plastic bags made of chlorinated plastics should not
be incinerated.
56 I IPHS - CHC Level
Complete and correct knowledge
protects you from AIDS
Deep Burial: Standard for deep burial are also mentioned in
the Bio-Medical Waste (Management & Handling) Rules 1998
(Schedule V). The cities having less than 5 lakh population can opt
for deep burial for wastes under categories 1 & 2.
8.1.3 Autoclave and Microwave treatment: Standards forthe autoclaving
and microwaving are also mentioned in the Bio-Medical Waste
(Management & Handling) Rules 1998 (Schedule V). All equipment
installed/shared should meet these specifications. The waste under
category 3, 4, 6, and 7 can be treated by these techniques.
8.1.4 Shredding: The plastics (IV bottle, IV sets, syringes, catheters, etc.)
sharps (needles, blades, glass, etc.) should be shredded but only after
chemical treatment/microwaving/autoclaving, ensuring disinfection.
8.1.5 Needles destroyers can be used for disposal of needles directly
8.1.2
without chemical treatment
Secured Landfill: The incinerator ash, discarded medicines,
cytotoxic substances and solid chemical waste should be treated by
this option(Cat. 5, 9, & 10)
8.1.7 It may be noted there are multiple options available for disposal of
certain category of waste, the individual hospital can choose the
best option, depending upon treatment facilities available.
8.1.8 Radioactive Waste: The management of the radioactive waste
should be undertaken as per guidelines of BARC.
8.1.9 Liquid (Cat. 8) & Chemical Waste (Cat. 10)
i) Chemical waste & Liquid waste from Laboratory: Suitable
treatment, dilution or 1% hypochlorite solution as required
shall be given before disposal.
ii) The effluents generated from the hospital should conform to
limits as laid down in the Bio-Medical Waste (Management &
Handling) Rules 1998 (Schedule V).
iii) The Liquid and chemical waste should not be used for any other
purpose.
iv) For discharge in to public sewers with terminal facilities, the
prescribed standard limits should be ensured.
8.1.6
9. Safety Measures
9.1
Personal protection: Hospitals and health care authorities have to ensure
that the following personal protective equipment is provided:
i) Gloves
a) Disposable gloves
b) Latex surgical gloves
c) Heavy duty rubber gloves(uptil elbows) for cleaners
ii) Masks: Simple and cheap mask to prevent health care workers against
aerosols, splashes and dust.
iii) Protective glasses
The child should be given only breast milk
rom birth to rzr months
Annexures | 57
iv) Plastic aprons
v) Special foot wear, e.g. gum boots for hospital waste handler.
9.2 Immunisation against Hepatitis B and Tetanus shall be given to all hospital
staff
All the generators of bio-medical waste should adopt universal precautions
and appropriate safety measures while doing therapeutic and diagnostic
activities and also while handling the bio-medical waste.
«
9.4 All the sanitation workers engaged in the handling and transporting should
be made aware of the risks involved in handling the bio-medical waste.
9.5 Any worker reporting with an accident/injifry due to handling of bio
medical waste should be given prompt first aid. Necessary investigations
and follow up action as per requirement may be carried out.
9.6 Reporting accident and spillages
The procedure for reporting accidents(as per Form III of BMW Rules, 1998)
should be followed and the records should be kept. The report should
include the nature of accidents, when and where it occurred and which
staff was directly involved. It should also show type of waste involved and
emergency measures taken.
9.3
10 Training
All the medical professional must be made aware of Bio-Medical Waste
(Management & Handling) Rules, 1998.
10.2 Each and every hospital must have well planned awareness and training
programmes for all categories of personnel including administrators to
make them aware about safe hospital waste management practices.
10.3 Training should be conducted category wise and more emphasis should be
given in training modules as per category of personnel.
10.4 Training should be conducted in appropriate Language/medium and in an
acceptable manner
10.5 Wherever possible audio-visual material and experienced trainers should
be used. Hands on training about colour coded bags; categorisation and
chemical disinfections can be given to concerned employees.
10.6 Training should be interactive and should include, demonstration sessions,
behavioural science approach should be adopted with emphasis on
establishing proper practices. Training is a continuous process and will
need constant reinforcement.
10.1
11. Management and Administration
11.1
58 | IPHS - CHC Level
The head of the hospital shall form a Waste Management Committee under
his chairmanship. The Waste Management Committee shall meet regularly
to review the performance of the waste disposal. This Committee should
be responsible for making hospital specific action plan for hospital waste
management and for its supervision, monitoring, implementation and
looking after the safety of the bio-medical waste handlers.
Optfor hospital delivery for
safety of mother & baby
The heads of each hospital will have to take authorisation for generation
of waste from appropriate authorities well in time as notified by the
concerned state/UT Government and get it renewed as per time schedule
laid in the rules. The application is to be made as per format given in form
I for grant of authorisation.(Please see page 18 of notified BMW rules)
11.3 The annual reports, accident reporting, as required under BMW rules should
be submitted to the concerned authorities as per BMW rules format(Form
II and Form III respectively) (Please see pages 19& 20 of BMW rules)
11.2
12. Coordination between Hospital and Outside Agencies
Municipal authorities: As quite a large percentage of waste (up to 90%)
generated in Indian hospital belong to general category (non-toxic and
non-hazardous), the hospital authorities should have constant interaction
with municipal authorities so that this category of waste is regularly
taken out of the hospital premises for further disposal
12.2 Coordinated efforts should be made by health authorities and municipal
authorities to involve private sector/NGOs for creation of common facilities
for treatment.
12.3 Health authorities in coordination with municipal authorities should
facilitate optimal utilisation of waste treatment facility in the area.
12.4 Coordination with NGOs and Environmental Groups, for public awareness
and education.
12.5 Sharing of facility: Hospital which is not on a possession of their own
facility for treatment may get their waste treated in a shared facility. The
hospitals having additional capacity may extend their facility to nearby
smaller hospital or health care units.
12.6 There should be coordinated agencies to take care of exigencies/disruption
of waste treatment equipment in a unit
12.1
Health worker’s advice & care is
Annexures | 59
Annexure 12
Model Citizens Charter for CHCs and PHCs
1. Preamble
Community Health Centres and Primary Health Centres exist to provide health
care to every citizen of India within the allocated resources and available
facilities. The Charter seeks to provide a framework which enables citizens to
know.
•
what services are available?
•
the quality of services they are entitled to.
•
the means through which complaints regarding denial or poor qualities of
services will be addressed.
2. Objectives
•
•
•
•
•
to make available medical treatment and the related facilities for
citizens.
to provide appropriate advice, treatment and support that would help to
cure the ailment to the extent medically possible.
to ensure that treatment is best on well considered judgment, is timely
and comprehensive and with the consent of the citizen being treated.
to ensure just awareness of the nature of the ailment, progress of treatment,
duration of treatment and impact on their health and lives, and
to redress any grievances in this regard.
3. Commitments of the Charter
•
•
•
to provide access to available facilities without discrimination,
to provide emergency care, if needed on reaching the CHC/PHC
to provide adequate number of notice boards detailing the location of all
•
the facilities.
to provide written
•
information
on
diagnosis,
treatment
being
administered.
to record complaints and designate appropriate officer, who will respond
at an appointed time, that may be same day in case of inpatients and the
next day in case of out patients.
4. Component of Service at CHCs
•
•
access to CHCs and professional medical care to all
making provision for emergency care after main treatment hour whenever
needed
•
informing users about available facilities, costs involved and requirements
expected of them with regard to the treatment in clear and simple terms.
informing users of equipment out of order
•
60 | IPHS - CHC Level
Atleast three ante-natal checkup
mustfor pregnant women
•
*
ensuring that users can seek clarifications and assistance in making use
of medical treatment and CHC facility.
Informing users about procedures for reporting in-efficiencies in services
or non-availability of facilities.
5. Grievance Redressal
°
•
•
•
grievances that citizens have will be recorded
there will be a designated officer to respond to the request deemed urgent
by the person recording the grievance
aggrieved user after his/her complaint recorded would be allowed to seek
a second opinion within the CHC
to have a public grievance committee outside the CHC to deal with the
grievances that are not resolved within the CHC.
6. Responsibilities of the Users
°
users of CHC would attempt to understand the commitments made in the
charter
0
user would not insist on service above the standard set in the charter
because it could negatively affect the provision of the minimum acceptable
level of service to another user.
instruction of the CHC's personnel would be followed sincerely, and
in case of grievances, the redressal mechanism machinery would be
addressed by users without delay.
•
•
7. Performance Audit and Review of the Charter
•
performance audit may be conducted through a peer review every two
or three years after covering the areas where the standards have been
specified
Complete and correct knowledge.
Annexure 13
Composition of the Task Group III and the
Consultation Process
Under the National Rural Health Mission, 8 Task Groups were constituted to
deliberate upon various issues concerning the operationalisation of National
Rural Health Mission. Task Group III under the chairmanship of DGHS comprised
the following members:
1.
Dr. S.P. Agarwal, Director General Health Services: Chairperson
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
Dr. Imrana Quader, JNU
Mrs. Brinda Karat
Mr. Satish Agnihotri, IAS
Dr. Ravi Narayan, CHC
Mrs. Sheela Rani Chungat, Secretary (Health, Tamil Nadu)
Mr. Ram Lubaya, IAS, Govt, of Rajasthan
Dr. Mohan Rao, JNU
Dr. Mira Shiva, VHAI
Dr. Jean Dreze, NAC
Mr. P.R. Krishna Kumar
Mr. Taradatt, JS, (AYUSH)
Dr. I.S.Pal, DG (FW), Uttaranchal
Mr. S.R. Mohanty, Madhya Pradesh
Dr. Abhay Shukla, CEHAT
Dr. S.K. Satpathy, DC (ID), Rapporteur
The first meeting of the Task Group III was held on 10th Feb.2005. The GroupIll was assigned the task of preparing status papers on the following four
issues:
•
Setting up of Indian Public Health Standards for health care delivery in
Community Health Centres
•
Strengthening Public Institutions for health delivery
•
Ensuring availability of doctors in rural areas
•
Mainstreaming of AYUSH
As a follow-up to the meeting the DG HS reviewed the progress on a daily
basis with some of the members from the Directorate and also experts from
outside who were invited to join the process. The 4 papers were prepared
and sent to all the members electronically and were also given print copies.
The second meeting of the Task Group III was held on 26th Feb. 2005, under
the Chairmanship of Dr. S.P. Agarwal, DGHS at Nirman Bhawan, New Delhi.
Secretary (Health & F.W.) also participated in the discussion briefly. The list
62 | IPHS - CHC Level
The child should be given only breast milk
from birth to six months
of Members/their representatives and various experts who participated in the
meeting was as follows:
•
Dr. S.P. Agarwal, Director General Health Services: Chairperson
•
Dr. Imrana Quader, JNU
•
Dr. Thelma Narayan, CHC
•
Dr. S. Murugan, Director(FW Tamil Nadu)
•
Dr. Mohan Rao, JNU
•
Dr. Mira Shiva, VHAI
•
Mr. S.R. Mohanty, Madhya Pradesh
•
Mr. B. Venkatraman, QCI
•
Dr. Abhay Shukla, CEHAT
•
Mr. B.P. Sharma., JS
•
Dr. S.K. Sharma, Adviser, AYUSH
•
Dr. C.S.Pandav, AIIMS
•
Dr. Ichhpujani (DDG (P)
•
Dr. D.C. Jain, DC (CH/T)
•
Dr. A.K. Harit, CMO, DGHS
•
Dr. A.N. Sinha, CMO (HA)
•
Dr. Sadhana Bhagwat, Consultant Cancer
•
Dr. Praveena Goel, AC (UH)
•
Dr. Himanshu Bhushan, AC (MH-II)
•
Mrs. Mridula Das ADG (N)
•
Mrs. Shubhra Singh, Director (P/RHM)
•
Mr. Babu Lal Dir, (ID)
•
Dr. S.K. Satpathy DC (ID), Rapporteur
These papers were discussed with the members present. Subsequent to the
meeting, inputs from the deliberations were added to the papers. Further
consultations were held on a daily basis with the members available at the
Directorate and external experts. Another meeting with the various National
Health Programme Officers and experts was also held on 7th March 2005.
The document on IPHS was prepared initially aiming at setting up Standards
for the CHCs. But after discussion with Director (P/RHM), the paper was scaled
down to discuss the requirements for minimum functional grading of CHCs with
scope for further upgradation. Inputs were taken from the Programme Officers of
National Health Programmes, consultants from accreditation agencies and also
from Dept, of Community Medicine, AIIMS for preparation of the.documents.
Opt for hospital delivery for
Annexures | 63
o m J-l - T | -
AGENDA ITEM NO. 2
Health civil society in east and southern
Africa:
Towards a unified agenda and action for
people’s health, equity and justice
REPORT OF A REGIONAL MEETING
February 17-19 2005
Lusaka, Zambia
*-APeople's Health Movemer
SATUCC
S Af SF
Southern and Eastern African Trade
Information and Negotiations Initiative
Regional Network for Equity in Health in Southern Africa
(EQUINET), People's Health Movement (PHM)
Treatment Action Campaign (TAC), Southern and Eastern
African Trade Information and Negotiations Initiative
(SEATINI), Community Working Group on Health (CWGH),
Health Action International (HAI), Southern African Social
Forum, Southern African Trade Union Co-ordinating Council
(SATUCC)
Z?
Meeting hosted by CHESSORE Zambia
Report produced by TARSC
Support from Dag Hammerskold Foundation
and Rockefeller
AGENDA ITEM NO.2
Table of contents
1. Background..................................................................................................... 2
2. Welcome, introductions.................................................................................. 3
3. Presentations: Current challenges, alternatives and issues for health civil
society................................................................................................................... 4
3.1. Challenges to common goals of health equity and social justice............ 4
3.2. Forging an alternative in east and southern Africa................................... 5
3.3. Agendas for global health....................................................................... 7
3.4. Agendas for regional health..................................................................... 9
4. Priorities for health and civil society action................................................... 10
5. Health in Brazil.............................................................................................. 13
6. Priorities for health and civil society action, continued..................................14
6.1. Organising people’s power for health..................................................... 14
6.2. Building a national people’s health system............................................ 14
6.3. Financing a more equitable health system............................................. 14
6.4.
Ensuring the Human resources for health........................................... 15
6.5. Challenging trade liberalization and encroachment on health............... 15
7.
Strengths, weaknesses, opportunities and threats for health civil
society................................................................................................................. 16
7.3. Organising people’s power for health..................................................... 16
7.2
Building national people’s health systems........................................... 16
7.3 Ensuring the human resources for health............................................... 16
7.4. Fair financing fora national people’s health system..............................17
7.4. Challenging trade liberalization and encroachment on health............... 17
8. Presentations from social movements.......................................................... 18
8.1. African Social Forum.............................................................................. 18
8.2. People’s Health Assembly..................................................................... 19
8.3. WTO Ministerial, Hong Kong December 2005.......................................20
9. Moving forward: Fundamental principles, values and issues for health civil
society................................................................................................................. 20
9.1. Guiding values....................................................................................... 20
9.2 Major areas of work................................................................................. 20
9.3 Organisational objectives........................................................................ 22
10. Moving forward: follow up actions............. .................................................22
10.1. Strengthening peoples power in health.............................................. 22
10.2. Improving the conditions of health workers.......................................... 23
10.3. Ensuring fair financing......................................................................... 23
10.4. Advancing health in trade.................................................................... 23
10.5 Building one struggle from many fronts................................................... 24
11. Closing........................................................................................................ 25
Appendix 1: List of Delegates............................................................................. 26
Appendix 3: Program........................................................................................... 28
Appendix 3: Useful Websites.............................................................................. 28
1
Health civil society in east and southern Africa:
Towards a unified agenda and action for people’s health,
equity and justice
REPORT OF A REGIONAL MEETING
February 17-19 2005
Lusaka, Zambia
1. Background
During 2002/3, EQUINET, Peoples Health Movement (PHM), International People's Health Council
(IPHC) and Community Working Group on Health (CWGH) identified a need for closer dialogue and
networking between health and related civil society in east and southern Africa to achieve common
health goals.
Civil society in this region has built strong platforms and made progress in advancing peoples
health in a number of areas, including around broad health rights, primary health care, patients
rights, treatment access, corporate responsibilities to protect workers health, resisting damaging
health impacts of globalisation, resistance to privatisation of essential services for health and
protecting rights of people living with HIV and AIDS. Civil society has also through broad networks
like EQUINET and PHM and through participation in the Social Forum processes, outlined policies
for building equity and social justice in health and health care, particularly through a strong public
sector health system. These wider platforms are, however, not strongly linked to the issue
campaigns, while the issue campaigns are not necessarily all informed by the same analysis of the
political and economic causes of ill health, of the health systems we are seeking to build or of the
wider changes needed to achieve health goals.
A meeting held in Johannesburg South Africa on November 26 2003 involving 14 networks of
health civil society (many of these with numerous individual health civil society members) identified
a number of common goals and values informing health civil society work, namely:
• Common aim for equity and justice and to realize the right to health
• We all seek to bring power to the people and to strengthen people's voice in decision
making through organising, uniting people and building public consciousness.
• We all work in areas that impact on health and on the wider health system
•
•
We are all working for an alternative to the current neoliberal system, and our perspective
and practice is for a system that is based on solidarity, equity, justice and public interest,
from local to global level
We act as a people’s watchdog and monitor the performance of government and private
sector against their commitments and the public interests, systems and values we are
promoting.
To take forward this consensus vision we agreed to:
• consolidate and strengthen our influence and role as health civil society through building
shared analysis and positions on health issues and strengthening our dialogue and
networking; and
• identify strategic issues that we need to take up jointly and across health civil society as a
whole to advance our common platform, while giving wider solidarity on specific campaign
issues within wider civil society platforms.
This was taken forward through health civil society participation in the June 2004 EQUINET
regional conference and by a planning committee made up of EQUINET (Secretariat at TARSC and
SEA i INI), PHM, Treatment Action Campaign (TAC) and CWGH. The planning committee was also
joined by the Southern African Trade Union Co-ordinating Council (SATUCC) and Health Action
International (HAI).
We developed a background document that outlined our common positions and analysis, and
proposed to hold a regional meeting in February 2005 in Zambia. The planning committee
2
proposed that the meeting bring together the leadership of health civil society organisations in east
and southern Africa to:
• review our current positions and analysis, identify areas where we share perspective and
analysis and debate and review areas where we differ;
• build a unified and shared analysis, perspective and goals across health civil society to
inform our individual and our joint platforms, strategies and campaigns;
• identify key and critical common goals and positions and the strategies for taking these
forward as health civil society in the region;
• identify and agree on mechanisms for strengthening linkages, resource sharing, solidarity
action and unified campaigns across health civil society in east and southern Africa; and
• identify and agree on mechanisms and processes that will strengthen and build our
capabilities for ensuring mandate from, voice and agency of and accountability to
communities in this process.
This report outlines the proceedings of the meeting and the resolutions and plans for future work
made by the health civil society groups at the meeting. The meeting was hosted by CHESSORE,
the theme co-ordinator in EQUINET on participation in health, with support from TARSC. The
meeting was supported by Rockefeller Foundation and Dag Hammerskold Foundation through
EQUINET, and travel contributions were made by Peoples Health Movement and Health Action
International. The delegate list for the meeting is shown in Appendix 1 and the programme in
Appendix 2. The report has been compiled by Rebecca Pointer and Rene Loewenson of
TARSC/EQUINET.
2. Welcome, introductions
Chosani Njobvu from CHESSORE welcomed everybody to the meeting and thanked them for
attending. Mwajumah Masaigana PHM and EQUINET steering committee member facilitated
the introductions and everyone introduced themselves to the group.
She noted that the delegates shared a common goal of working for health equity. The
meeting was designed to bring us together to strengthen ourselves, to build cohesion and
linkages, and to identify strategies for working together. We need to identify areas where we
agree so that we can build capacity and ensure that we are all going in the same direction.
Therefore, we need to identify who we are, what we think of ourselves, where we are now,
and where do we want to go - and how - to create a shared vision.
Mwajumah wished the meeting productive work in building a cohesive and strong movement.
Rene Loewenson TARSC/EQUINET introduced the purpose of the meeting, which was
fundamentally to enhance the collective unity and purpose of health civil society around a
common agenda, while enabling differences on focus in individual groups areas of action.
More specifically the meeting aimed to:
• review our current positions and analysis, identify areas where we share perspective and
analysis and debate and review areas where we differ;
• build a unified and shared analysis, perspective and goals across health civil society to
inform our individual and our joint platforms, strategies and campaigns; and
• identify key and critical common goals and positions and the strategies for taking these
forward as health civil society in the region.
Honesty, being self-critical and being mutually respectful are necessary to building trust
around a shared agenda, which taps different struggle styles in working together.
The major health civil society groups hosting the process were acknowledged as present
although there was still an agreed need to draw in people from the traditional health
movement and land lobbies. The meeting included groups from South Africa, Zambia,
Zimbabwe, Tanzania given the formative organisations noting that these networks do reach
into other countries in the region, however work would now need to be done to take the
dialogue to countries not represented at the meeting, including Mozambique, Namibia,
3
A single-issue campaign has implications for the health sector as a whole. We have had little
success with addressing weak health systems as a whole, while single-issue campaigns like
the Treatment Action Campaign (TAC) have had success. This raises the issue of how we
balance single-issue campaigns with a broader health systems approach?
To build solidarity, can we agree to disagree, sharpen contradictions, be tolerant of diversity
and share some values? We need to identify the point beyond which there is no common
ground. We also need to examine how donors determine what is done, aside from what we
feel is needed, and how it polarizes civil society. For example funders often have a rightsbased approach to governance, but this is in a context where investors are given more rights
than people, so you end up with a perverse rights-based approach. Funders also often opt for
a poverty-based approach with direct budget support. This gives donors direct access to
parliamentarians, and policies can become externally determined. There is also a lot of
debate with funders around debt cancellation and whether it is going to create more problems
than it solves.
With regard to strategies, should the state be a primary target of radicalism, or is an anti-state
approach divisive? And what is the place of indigenous knowledge systems, nutrition/
promoting food security? These issues call for us to develop a sophisticated approach to the
tactics and strategy we use.
3.2. Forging an alternative in east and southern Africa
Godfrey Kanyeze of LEDRIZ
observed that it is now generally
agreed by wide sections of
Southern African society that the
neo-liberal paradigm of
development has failed the
people. Poverty has not only
entrenched but also deepened,
and the gap between the rich and
the poor has increased. Members
of the broad trade union
movement and some intellectuals
in the region have been working
on an alternative paradigm, as a
serious effort aimed at providing
the people in the region with an
alternative development
programme that aims at being
both visionary and at the same
time practical.
7 Basic Principles of ANSA:-1. A Holistic Bottom-up
Worldvievy to Developing Alternatives to Neo-Liberalism
He presented the seven basic
principles and ten essential
elements for forging an alternative in east and southern Africa.
1.
A people-led strategy, as opposed to an IMF-WB-WTO-donor led strategy.
Liberations governments have appropriated people's right to determine alternatives,
seeing themselves as the voice of the people without consulting the people. People
should define the agenda, not the 'experts'.
2.
At an economic level, an alternative production system. In Africa, we have a formal
economic sector, which employs about 20% of the workforce. It was created by
destroying the livelihoods of the peasant sector to make men - and not women wage earners to subsidise production. Therefore poverty is a structural issue.
Peasant labour is a source of cheap labour for the formal economy and also fuels the
informal economy. While current economic strategies focus on trying to grow the
formal economy by selling commodities, the formal sector is actually contracting by
exporting raw materials at lower and lower prices to meet the needs of imperialism,
which requires declining terms of trade.
5
3.
Grassroots-led regional integration (as opposed to the current fragmentation in the
region by Empire). Currently regional integration - through SADC and NEPAD, etc. is being driven by the European Union and United States, which are trying got drive
the structures and determine the configurations.
4.
Selective de-linking with globalization by focusing on regional trade, instead of
international trade.
An alternative strategy of
science and technology,
The People, the Sta+e and the Empire
not just importing
technology from northern
A holistic analysis requires us to look at all the
countries, but using our
following three factors in an interconnected manner.
own raw materials to
the global (or the Imperial Factor), the State (or the
develop our own products.
5.
A strategy of alliance and
networking with national,
regional and global
progressive forces,
drawing on our previous
experiences of
mobilization.
Politically governed
redistribution on wealth
and opportunities.
Governance or Democratic Factor) and the people (or
the Social Factor).From this, three propositions
follow:• a) Ignore SF, and you have discontent and
rebellion
• b) Ignore DF, and you have suppression and
opposition.
• c) Ignore IF, and you have domination by the
Empire, and Resistance.
From these three, the following formula suggests
itself as a guiding principle to achieve peace and
justice. It may be written thus:
8.
A focus on women's
rights as the basis for a
healthy and productive
society.
9.
A strategy where education is linked with production.
10.
A strategy of peoples' mobilisation and visible demonstrations.
Peace and Justice = SF + DF - IF
The goal of all development is to enhance human centred values and human and social
welfare. It is customary to categorise human rights at three levels - the political or civil rights
(or "blue rights"), economic rights (or "red rights”), and social and cultural rights (or “green
rights"). However, a human rights approach on its own will not be effective; there are powerful
vested interests and a certain power configurations at the national and global levels that need
to be challenged in order to bring about necessary change.
Whilst a human rights approach is a useful starting point, important issues of distribution of
welfare and economic well being within and between nations remain as a significant aspect of
the overall value system. It is important, furthermore, to take a livelihood approach to human
rights, because human rights are not simply individual rights, but also community and national
rights. An important ingredient of this is the right to national self-determination, enshrined in
the United Nations Charter. Also important is the right of communities at the local level to
determine their own life-styles and destinies, and control over the technology and norms of
production and reproduction central to their livelihoods, within the broader parameters of
national and global environment. A people-oriented strategy needs to address issues of
concern to the people (such as land reform or food security or issues of sustaining livelihood)
district-by-district, village-by-village.
It is important in any alternative strategy to address the question of agency for change. The
issue of “agency", or the motive force for change, cannot be kept out of the analysis, or
deferred to a later date; it has to be integrated in a holistic manner into an alternative strategy.
6
He noted that within this the state is a creation of history, and it is a product of struggles. The
state is daily configured. It metamorphoses on a daily basis. It is a product of the struggle
between people on the one hand and the forces that control the state at a particular point in
time on the other. The creation of a developmental or ethical state, thus, is not an academic
exercise', nor is it one that can be postponed to some future date. It is matter of daily struggle.
And, when everything is said and done, it is the people who are defenders of their own rights;
it is they that are the agents of change
He further observed that "nations" as presently constituted are becoming inadequate political
geographic units for advancing the economic interests or security of the people within the
nations. How “nations” will evolve in the future nobody knows. What we do know is that there
is a powerful movement towards regionalism. He proposed a people and grassroots led
regional integration, in contrast to the "perverse integration” crafted not by the people within
the region, but externally imposed.
The ANSA-Strategy addresses a current challenge, the scenario that exists here and now,
and not something in a distant future. Struggle is a daily business; it is a continuous process.
The provision for example of the basic needs of the population and social services are not
battles of the future, postponed to some future date (such as, for example, to 2015 in the
MDG model) but parts of everyday battles. When these services are daily being privatised or
commercialised in Southern Africa at the behest of the state or the IMF or the World Bank or
individual donors, they become matters of concern to the people NOW, and not at some
future date. An example can be seen, in the current negotiations for an Economic Partnership
Agreement (EPA) between Africa and the European Union - it is not tomorrow’s battle. It is
today's battle. Tomorrow will already be too late.
In the discussion that followed delegates raised concerns about corruption undermining
positions that seek to reinforce the role of the state. It was acknowledged that this is a
collective problem that needs addressing, through tackling governance to ensure that our
issues are addressed and articulated by the sate and providing adequate checks and
balances. We also need to note that rich countries and powerful interests are involved in a lot
of the corruption and expose and deal with it at this level as well.
Delegates also raised the issue of how we operationalise power to the people. It was noted
that electoral and representative democracy where voting without the possibility of recall has
led to depoliticisation, demobilization and reliance on the state. It is critical to reclaim the role
of people who are the source of power and development for our leaders. We should institute
the right to recall. Services should remain in the public domain. Let us define for ourselves
what participation is, and push for participatory democracy, backed by the resources to
implement it.
It was further noted that we need to examine our own relative emphasis between anti
imperialism and anti-capitalism. Many of our states have anti-imperialist sentiments, but are
not anti-capitalist. This means that being anti-empire is not the end point for achieving social
justice. It was however also noted that in the current environment we need to be clear about
where the 'major determining contradictions are, so we focus on those and not undermine
ourselves by division.
3.3.
Agendas for global health
David Sanders, PHM, outlined recent decades of unequal progress in local health, with more
rapid improvements for the rich than the poor:
*
life expectancy increased from 46 years in the. 1950s to 65 years in 1995;
*
child deaths were reduced from 17.5 million a year to 11 million a year;
*
there was substantial control of disease poliomyelitis, diphtheria, measles,
onchocerciasis, dracunculiasis through immunisation and disease control
programmes; and
*
a decline in cardiovascular disease in males in industrialised countries.
7
Because of economic changes (e.g. SAPs) and the AIDS epidemic, we have seen massive
reversals of these gains, and now, for example, we have seen an increase in child deaths
since the 1990s. We have seen:
• the implementation of a selective PHC approach with money being pulled and programs
not being sustained;
•
inequitable globalization based on the trade liberalizations, removal of subsidies, currency
devaluations and the debt crisis which escalated from 1970s through unfair trade practice
and so SAPs were imposed, and
• health sector reform in the form of actions to improve the performance of the civil service,
decentralization, actions to improve the functioning of national ministries of health,
universal delivery of a core set of essential services, broadening health financing options,
working with the private sector, and adopting sector wide approaches to aid rational
planning.
While the World Bank denied the link between declining health and SAPs, it has now through
the Macroeconomic Commission on Health generally been conclude that the effect of SAPs
on health has been largely negative. However, the International Financial Institutions (IFIs)
have never been held to account for their errors.
SAPS opened up current phase of globalization in favour of Transnational Corporations
(TNCs) whose reach has expanded dramatically in the last decade, reinforced by WTO. Top
companies have turnovers higher even than middle-income countries and countries in this
region don't have negotiating clout. He quoted Henry Kissinger:
'The process of development begins by widening the gap between rich and poor in
each country ... What are developing countries to make of the rhetoric in favour of
rapid liberalisation when rich countries with full employment and strong safety nets
argue that they need to impose protection measures to help those of their own
citizens adversely affected by globalisation ? ...The basic challenge is that what is
called globalisation is really another name for the dominant role of the United
States...'
He outlined the Health sector reforms implemented in many countries and their lack of
success in achieving health equity or building health systems. Efficiency measures, through
more involvement of private sector and 'cost-effectiveness' has led to private health care as a
parallel system drawing on resources of the public health sector, “dual practice" of public
sector human resources: “moonlighting", competition for clients and time, internal migration,
and so on. Decentralization may improve democratic participation, but it is under-funded and
ill prepared, without the necessary resources, training and staff, so it often increases
inequities. The literature on low- and middle-income countries provides little evidence that
decentralisation has resulted in creation of new posts, job re-profiling, or an improved staff
mix”. Human resource planning responsibilities are often transferred to local managers
without providing them with adequate skills for these roles. The available literature is also
quite negative about the impact of decentralisation on professional development opportunities
or working conditions.
He noted that cost-effectiveness approaches had led to a range of selective primary health
care packages excluding areas obviously important for health, like public provision of safe
water. More recently vertical programs, such as those for HIV treatment can weaken overall
health systems and through this other PHC interventions like immunization. Within PHC the
role of social mobilization, civil society and the need for an intersectoral focus has often been
neglected.
He called in contrast for a comprehensive approach to health and outlined the work of the
People's Health Movement (PHM), guided by the People’s Charter for Health. PHM is a
network of civil society organizations, within which organizations can retain their own integrity.
The PHM "Call for action" includes demands from local to global around health as a human
right, tacklmg the broader determinants of health, social and political challenges, "
macroeconomic, environmental and a people-centred health system. The second People's
Health Assembly will be held in Ecuador in 2005.
8
3.4. Agendas for regional health
Rene Loewenson of TARSC/ EQUINET presented the outcomes from process of regional
work that was consolidated at June 2004 EQUINET conference. Health is not simply and only
a sector but rathe' an ourcome of how successfully we are addressing human needs and
issues of justice and equity in all other sectors and policies. Health is an expression of and
tool for organizing around other basic claims of society. Liberation movements in southern
Africa recognized this and delivery on health was a powerful organizing tool. There is a wide
constituency for health across the region reflected in post independence policies of equity and
justice in health. While there have been diversions on this platform we are staging our
struggle on active, not barren ground.
A regional agenda of equity and social justice in health means giving visibility and voice to
injustices in health, and building perspective and power in a purposive manner to deal with
these injustices. Visibility and profile is not an end point: we need to ensure that the issues
are not co-opted by other agendas - like cough medicine for a cough rather than dealing with
polluting smoke. We need to use visibility of injustice to drive a deeper agenda that goes to
the causes of the causes of these outcomes.
The EQUINET 2004 conference resolutions highlight areas of this agenda for the region:
I.
Calling for global relations that promote equity, social justice, people’s health
and public interests:
Governments, realising that poverty is a security and development threat have mobilized
around poverty reduction and the Millennium Development goals. It has been estimated that
S50bn annually is needed to meet these goals. This is the same amount spent each year on
cigarettes by Europeans and far less than the S740 billion a year spent on arms.
Box 1: International and global relations that promote equity, social justice, people’s health
and public interests
Basic Education for all
Cosmetics in the USA
$6 hillion
$8 billion
Water and Sanitation for all
$9 hillion
Ice cream in Europe
$11 billion
Reproductive Health for all Women
Perfumes in Europe and the USA
Basic Health and Nutrition
Pet Foods in Europe and the USA
Business Entertainment in Japan
Cigarettes in Europe
Alcoholic Drinks in Europe
Narcotic Drugs in the World
Military Spending in the World
$12 hillion
$12 billion
$13 hillion
$17 billion
$35 billion
$50 billion
$105 billion
$400 billion
$780 billion
Source: Human Development Report, 1993
Public interest over commercial interest in health, with rising investments in
the state and public sector in health
Responding to health needs calls for rising investment in public sector in health, with
collective, population-oriented strategies for health and comprehensive primary health care.
Rich countries and rich communities generally choose to invest more in their public sectors
when they have the resources. Southern African public sector health systems have been
seriously underfunded and need reinvestment for recovery. EQUINET has thus called for
increased progressive tax-based funding of health systems as the most equitable, universal
and efficient form of health financing where the rich contribute a greater share of their income
to health than the poor. At least 15% of government spending should be spent in the public
health sector, particularly to support the district and primary health care systems that address
priority health needs.
ii.
Fairer terms of trade and action around restitution for south-north flows
caused by debt, unfair trade rules and human resource flows.
We need to protect and use government authority in trade agreements to safeguard public
health, such as through use of full flexibilities of TRIPS, making no health sector commitments
iii.
9
under GATS, act as a watchdog trade agreements and ensure that the executive is
accountable to parliament and public on WTO and trade agreements. This means we need
democratic and accountable states, with full authority to exercise policy measures necessary
to protect the health of people. We also need to identify policies that will better retain the
human resource we have and shape the forms of compensation needed to meet for
regressive south-north subsidies incurred through health personnel migration. Nutrition,
fundamental to health and food security, calls for policies that increase household and
especially women's control over food production and consumption, including land
redistribution, investment in smallholder farming and confronting monopoly control of food
marketing.
Driving such policies calls for powerful and effective participatory and representative
mechanisms for public contribution to decision making in health backed by a concept of
human rights that addresses economic and social entitlements for health and affirms the
agency of communities in claiming these entitlements.
In many countries colonial health systems were largely unreformed, preserving rural-urban,
public-private segmentations, even thought these were narrowed for a period and PHC
programmes added. We need to make clear the deeper transformation of our health systems
needed, so that we have a comprehensive national and people's health system, that
addresses the health and health care needs of the whole population, backed by a unified
solidarity system of funding.
In the discussion that followed delegates raised debate on the role of the World Health
Organisation in the UN system and its ability to bring about a more radical change in health.
The fact that WHO is controlled by member states is important, but the fact that some wealthy
governments have withheld contributions to exert pressure on WHO weakens this potential
role. We also have the contradiction that governments themselves are buying into neoliberal
policies even when they rejected them while in the struggle. Can we win people to
progressive health position and understand and engage the contradictions inside the state?
Delegates observed that there is a lack of understanding among health workers and
communities about the role of the state, about their roles and their working conditions. Health
woikers largely see themselves as responsible to the state ratner than to the communities
they serve. Transforming the health system also means transforming the understanding of
health workers.
These wider issues need to be addressed while more immediate responses take place. We
cannot stop work on food relief or immediate work to bring curative relief to people, but such
campaigns need to be linked to structural changes, and ensure that they operate in a way that
support and do not undermine these structural changes. Hence for example relief food in
school feeding projects should aim to use local suppliers.
We need to strengthen the whole health system, including tertiary level care, and ensure that
the tertiary level does not become increasingly privatized and inaccessible to people, and
draw funds away from PHC. It is very important to look at how health care financing happens
and what impacts on this. Also we need to think about what constitutes a public health system
as often churches/ faith-based organizations have too much say in public health.
4. Priorities for health and civil society action
We then organised a participatory session to bring out the priority issues that people felt
needed to be the focus of our collective future work. People raised and carried out debates in
small groups recording these on flip charts in different parts of the room and moving between
debates. After a period of time a number of key issues emerged, with various debate points
raised around these issues:
10
HEALTH FINANCING
How is government going to tackle the private sector and finance national health
insurance?
How can government be involved in ensuring that policies are pro-poor?
World Bank etc. propose that public health services are 'inefficient' - what is the
evidence base of this and what is the 'efficiency' of the private sector?
Donor co-ordination required.
Global fund and replenishment conferences = predictable financing via an equitable
contributions framework
Global fund not sustainable and should not be relied upon
Establish rules for the global fund
STOP GLOBAL FUND NOW! Global funds are weakening health systems by providing
a vertical system and not co-ordinating with the people and governments.
We need to monitor financial (donor money) flows.
Industries are concerned with profit, not people!
"Africa has no skilled labour, not profitable!" - Is this true?
Government commitment to Abuja declaration - 15%
Mechanisms for protecting the vulnerable (advance risk sharing):
* national social health security must reach the targeted beneficiaries
* resources should be allocated for preventive and promotion (need driven)
National health interests vs. World Bank conditionalities and health budget ceilings.
Economic revival: how do we link this to debt?
2005 presents opportunities to get more money for healthcare: how do we engage and
how do we use it?
UNITY OF HEALTH CIVIL SOCIETY
Recognise that it is "one struggle with many fronts".
While there are many fronts we should not take our eyes of the long-term objective and
work to achieve that.
Single-issue campaigns give us a sense of urgency! Engage: EPAs, AGOA, Bilaterals,
TB, Malaria, HIV and AIDS!
Taking advantage of the health-related aspects of MDGs to advance our cause: Wait
for 2015? No, take advantage of the window of opportunity provided.
Poverty related goals interrelate with health aspects.
Without debt cancellation MDGs won't be achieved.
Reduction of maternal mortality is of the MDG goais - let us use it for advocacy on
health.
Advocacy for governance that puts people's demands in the priority agenda.
FOOD SOVEREIGNTY
Food is a uniting health, production, consumption, labour, etc. issue
We are talking about food not organizing around food!
The role of agriculture and health reform in promoting access to health care.
WTO on agriculture:
• increase production
• stop north subsidy
• say 'no' to GMOs
Agricultural policies contribute to healthcare problems
Elaborate what "food sovereignty" means
Give women land in their own right.
Women's access to health.
11
ORGANISING PEOPLE’S POWER FOR BETTER HEALTH
CSOs must start with their community, engage their district officials and move on to
national leaders. CSOs should have people's backing for their demands
Work with local communities, using local knowledge, traditional health systems.
Increase access to comprehensive PHC where communities interact with providers,
government and state.
CSOs role is to demystify trade agreements and other relevant policies.
Economic literacy for mass mobilization
Communities to be informed about policy and processes where they can participate
g. policy discussions, parliamentary hearings, etc.
e.
CSOs can facilitate logistical support such as childcare, transport, confidence building,
etc. to enable mobilization.
CSOs must increase people's awareness on health an human rights.
Are we alone where the government representatives, private hospitals and mission
hospitals are present? We need to hear about the problems they face.
Strengthen health civil society at all levels (local, regional, national and international) as
it is seen to be fragmented and need to explore why this is so.
CSOs have become the new elite and lost touch with the people. How do we mend that
bridge and remain relevant? We need to define who we are, remain accountable and
link up, respect and mobilize grassroots organizations.___________________________
HUMAN RESOURCES FOR HEALTH
The "Brain Drain" - staff exodus and human resources for health
Perverse subsidization of south to the north undermines and weakens our responses to
public health and health systems.
Which health workers do we want to support and retain? (PHC & district)
Recognition and better co-ordination of community health workers (CHWs), traditional
healers, etc.
Fragmented health workers organization.
Health worker organizations are not linked to other civil society organizations.
The north should put money into training in developing countries.
Private sector to channel resources to the public sector for human resources.
Campaign for compensation to poor countries whose HR is losts.
No to GATS type free movement of labour.
Lifelong education and training funded by governments.
Work with health workers within our countries to campaign for better working
conditions.
Government to narrow gaps in salary among top staff and community workers.
Funding for public health services.
Retain skilled health workers and improve conditions of employment.
Transformation of international institutions.
Promote and support the public health system.
Implementation and improvement of OH&S policies, strategies and systems.
Cost-sharing mechanisms are reducing access to healthcare for rural communities.
Trade unions should broaden their discussion beyond wage agreements/ increases
and focus on globalization affecting their well-being and including health.
Build solidarity with CBOs, CSOs, etc.__________________
The review in plenary of the flip charts and the debates that took place around them as
used to raise the priority issues to take forward:
1. How do we develop one struggle with many fronts - single-issue and broad fronts?
Can we use and advance on windows of opportunity that arise from issues to
advance structural and systems issues. What are those windows of opportunity and
how do we use them?
2. Civil society as an organizer of people’s power in various forms - how, where,
through what forms? This also calls for a clearer analysis of the strengths and
weaknesses of health civil society in these roles. We also need to strengthen the
12
links between labour, community based and civil society organizations to build
solidarity across these groups - What is the basis and processes of this solidarity?
3. Human resources are a strategic issue: There are parallel health service structures
with little integration and links between health workers and health civil society. Social
movements and civil society can only achieve goals by integrating the two. This has a
ripple effect on service provision, as workers are the producers of services. We also
need to tackle the internal brain drain
4. Health financing is a further strategic issue to address at global level, between
public and private sectors and within the public sector. We need to explore
approaches and mechanisms for funding a more equitable public health care system.
In this we need to engage in the debate and research the view - held by proponents
of neoliberalism - that a public health care system is inefficient. This raises focus on
our positions on stopping perverse resource flows from Africa vs increasing aid flows
into Africa.
5. Resisting and reversing trade liberalization and trade encroachment on health,
through WTO and bilateral negotiations. How do we defend the public sector within
trade?
6. Food sovereignty means addressing the role of women as producers, and issues
outside the health sector like trade, land distribution, GMOs and food production and
marketing.
7. National health systems: These areas all imply collaboration around building a
national health system. What kind of health systems do we want? How do we
integrate various issues and goals into this and how do we ensure the funding and
workers for it?
Within these broad issues we need to explore which struggles we take up as health civil
society, and how we work around these. What are our strengths and weaknesses around
these key issues and what are we currently doing around them.
5. Health in Brazil
To support the discussion of the way forward, Armando de Negri of ALAMES and WSF Brazil
outlined the policies and processes of health civil society in Brazil. In the 1980s Brazil was
confronting many of the challenges raised at the meeting facing southern and east Africa
today. Brazil had a general idea of the kind of programme we wanted to develop with a focus
on the right to health. This was strongly influenced by the health reforms in Italy in the 60s
and 70s. Therefore, we built a health system around a few simple ideas:
• health is a right of all citizens;
•
this universal right meant a right to all healthcare, not just primary health care (PHC);
with egalitarian access to health care; and
•
a strong statement about social participation in health, with real decision-making
power, health councils at a city level, state and national level regarding government,
health providers and health workers.
This permitted us to defend the National Health System (NHS) from privatization and gave us
clear ideas in managing the relationship with work in other sectors. Since health was a duty of
the state, legal actions were taken when health would be affected and the state could
intervene at any time that health is tread upon. If there are bed shortages in the public health
system, the state can access beds in the private health system. There is absolutely no
payment for services and the constitution establishes that it is forbidden to charge for health the same laws apply to the private health sector as the public health sector.
We have local organization of the NHS, avoiding the collapse induced by more neoliberal
forms of decentralization. The research and management components are decentralized, but
there is a unified system, supported by 9,8% of national tax collections: 12% of the health
budget goes to state governments and 15% to local governments. There were attempt to
include water and sanitation in the health budget, but we successfully prevented that.
13
City governments have high management responsibilities in terms of tying health planning
into integrated planning. We are also now developing family health programs that cover 3000
people and can tackle counseling, medication, special care for HIV and AIDS needs.
Brazil's health system is an exception in Latin America, as other Latin America countries have
not been able to face and take on global systems. However, we have proved that it is possible
to have a universal system, and it is much cheaper than the fragmented private sector.
Therefore we must struggle for a global right to a universal health system. We need to use
this example to negotiate with funders; civil society must express what they want in terms of
these programmes.
There is a need for Latin American and South American countries to build alliances to support
and exchange with each other and to fight to be, not just an economical block, but also have a
social agenda with a right to health, so as to eliminate inequities between countries.
6. Priorities for health and civil society action, continued...
Following through on the discussion of the first day the health civil society groups identified
further the major objectives and specific issues in the five major areas of common concern:
• organizing people's power, including labour;
• building a national people's health system.
• financing a more equitable health system;
• ensuring human resources for health.; and
» challenging trade liberalization and encroachment.
6.1.
Organising people’s power for health
Objective: Building a critical mass working together towards a common vision of the right to
health for all as a constitutional right.
Sites of struggle
•
Bringing unity across civil society organisations, while ensuring autonomy.
• Building an inclusive front of all stakeholders working in health and related areas.
• Demystifying and linking local, national and global struggles to co-ordinate action.
• Defining realistic priorities.
• Ensuring the survival of civil society organisations against external attacks and
challenges (state and donor).
6.2.
Building a national people’s health system
Objective: Publicly-funded comprehensive, participatory, equitable and universal health
systems.
Sites of struggle
• Lobby governments to promote, finance and provide comprehensive primary care
that is participatory and involves promotion, prevention, rehabilitation and curative
aspects.
• Oppose privatization of public health services.
•
Promote, support and engage in actions that encourage people's power and control in
decision-making on health at all levels including patient and consumer rights.
•
Pressure governments to adopt, implement and enforce national health and drug
policies.
• Support, recognize and promote traditional and holistic healing systems and
practitioners and their integration into health systems.
6.3.
Financing a more equitable health system
Objective: Increased fair, sustainable and equitable financing for health at national, regional
and global level in order to secure the universal right to health.
At a national level, rising investment that strengthens the national health system through the
public health sector, with mechanisms that ensure universality, solidarity and transparency
and that promote public over commercial interests.
14
Sites of struggle
• Abuja Declaration that African governments spend at least 15% of national budgets
on health, (but also need our own realistic target for funding a national health service).
• Unconditional debt cancellation.
• Increased aid for health to meet short term needs ways that strengthen health
systems and that are sustainable.
• Equitable allocation of national budgets for health, with promotion of tax funding for
health; national debates on health insurance; and scrapping of user fees at PHC
level.
• Lifting of IMF Medium Term Expenditure Frameworks ( METF) caps for increased
health spending.
• Ensuring these positions are adopted in WTO, MDGs, Commission for Africa, World
Bank PRSPs, SADC, EAC, etc.
6.4.
Ensuring the human resources for health
Objective: Adequate, well-trained, equitably distributed and motivated health workers.
Sites of struggle
• Improved working conditions for public health workers (incentives; wages, OH&S policies),
with emphasis at primary and community level.
• Lifelong training of health workers to become more problem-orientated, practice-based,
including management and self-evaluation skills.
•
Awareness campaign around the implications of migration of health workers, (public to
private health institutions; within and outside the region) and compensation issues.
•
Oppose GATS commitments that promote movement of health workers to private sector
and to wealthy countries, backed by positive measures to retain health workers, to
compensate for perverse south-north subsidies, and to implement codes on ethical
recruitment.
6.5.
Challenging trade liberalization and encroachment on health
Objective: Popular participation and transparency to ensure a fair international trade system,
where people are put before profits (health over commercial interests); and where our states
and governments maintain sovereignty through regulatory flexibility for development.
Sites of struggle
Access to medication
*
National level: regulatory and financing frameworks.
*
Regional level: make WTO powerless.
* Global level, fight against TRIPS.
Privatisation
*
National level: PRSPs, GEAR and SAPs.
*
Regional level: NEPAD issues and other regional trade agreements (RTAs).
* Global level: impact of GATs.
Food sovereignty
* National level: tackle GMOs, monocultures, cashcropping, and food security.
*
Regional level: WTO agreements, regional agreements on national level issues.
* Global level: subsidies, commodity prices, food aid and donors, market access.
Indigenous knowledge systems and national regulation
*
National level: regulation required.
*
Regional level: powerlessness in Regional trade agreements.
* Global level: bio-piracy, TRIPs
Watchdog trade measures that impact on health
'
National level: governments, parliaments, faith-based organizations, domestic capital,
social movements and CSOs and FBOs.
*
Regional level: European union EPA, United States AGOA and FTAs. Work with
African social forum processes, African RTAs such as SADC and Comesa to tackle
regional fragmentation.
* Global level: WTO, WIPD, WHO, WHA, UNDP, UNCTAD, WSF WEF, G8, etc.
7.
Strengths, weaknesses, opportunities and threats for health civil society
David Sanders PHM outlined the motivation for doing a SWOT analysis of health civil society.
He noted that those working to build and establish PHM in South Africa have found
mobilization difficult. The experiences from this indicated the need to do a reality check
around our strengths, weaknesses, opportunities and threats in building mobilization. This
SWOT analysis should be in relation to the key issues identified and reflect on our country
and organizational situations. A SWOT analysis will also help us prioritise a realistic set of
collective actions.
The delegates carried out the analyses in groups and identified key strengths and
weaknesses, opportunities and threats that need to be taken into account in shaping follow up
work:
7.1.
Organising people’s power for health
The major concern is to increase the capacities of civil society organisations.
Strengths: CSOs have a commitment to the issue, and embrace diverse experience, skills,
expertise and knowledge. There are many organisations working on health issues in the
region, and successful single-issue campaigns, able to mount a quick response to issues.
Weaknesses: Civil society is fragmented, with splintered effort and lack of a joint vision.
Organisations have limited resources and are donor dependent (and driven in some cases)
with more funding for vertical than comprehensive programmes. Some CSOs are losing focus
and lack the passion to fight for a cause. This leads to too many meetings and too little action.
There is also too much work and too few people weakening our capacity.
Opportunities: There are windows of opportunity: the WTO Cancun victory created the
possibility for alliance between NGOs and governments, the MDGs. The need to address
health system decline creates a mobilizing opportunity to push for national public health
system. Strategic alliances have formed across issues and across the region, such as the
National and African Social forums, this fourm.
Threats: Exist in some government policies, such as the Zimbabwe NGO Bill and
unsupportive governments. Global disasters result in the movement of policy attention and
funds away from Africa, e.g. Tsunami, Iraq, etc. Donors are focusing on vertical programs
such as vaccination, and prefer large established organizations over smaller ones. Civil
society organisations lack finance, human resources and time.
7.2.
Building national people’s health systems
Strengths: There is analytical experience and organizations are working in these areas in the
region.
Weaknesses: This is a complex area and patchy understanding of how to grapple with key
issues in unions, CSOs. It needs a lot of work to get unions and communities on board.
Ineffective and poorly resourced health committees, community organizations demobilize
communities.
Opportunities: A common understanding, an interested media, global funds and increased
resources, opportunities; opportunities for links with other organizations to build a popular
movement.
Threats: Weak public understanding of how the health system functions; Disinterested media
attitudes. Funds going to vertical programmes, over broader approaches. Unsupportive or
repressive policies to civil society and lack of autonomy of health civil society.
7.3.
Ensuring the human resources for health
The major concern is to improve the working conditions of health care worker, increase
training and capacity, believing this will also impact on the brain drain and as a way of
bringing health workers on board in fighting the brain drain and building health systems.
16
Strengths: Existing organisational capacity to build around this campaign by organizations
which represent workers interests. A lot of work is being done around improving working
conditions. It is an issue that is common across the region, from health workers to civil
society. There is a felt need from health workers to build a campaign around this.
Weaknesses: This is a single-issue campaign that may again neglect health systems. It costs
a lot of organizational resources, while capacity and energy are already stretched in terms of
capacity, resources. There is lack of co-ordination amongst the unions, and issue is not taken
up at a federation level. There are also issues of sectoral organization and conflict of
interests.
Opportunities: Communities are dissatisfied with current service delivery and there is a
window of opportunity through engaging around treatment access. HR has achieved a higher
profile with possibility of additional funds for HRH.
Threats: Conflict between communities and health workers and the impact of HIV and AIDS.
7.4.
Fair financing fora national people’s health system
The key goals are increased per capita spending on health, progressive tax funding for health,
debt cancellation, and appropriate external funding to support national health system
Strengths: There is consensus that current spending is inadequate. There is expertise and
information in this area in CSOs in the region, solidarity from Northern CSOs, e.g.: on debt
cancellation and CSOs in South America have researched models that could be adapted in
Africa, such as, the Brazilian model. CSOs have the ability to track health sector funding.
Weaknesses: There is a low level of civil society/ government engagement on the issue and
different opinions on strategies that could be used to address the issue e.g. tax-based
delivery, health insurance, debt cancellation with or without conditionalities, MDGs, etc. There
is poor SADC-CSO engagement on the issue and absence of a regional combined effort that
includes governments and CSOs. There is inadequate follow-up by CSOs of gains and
promises made at the global level and inadequate capacity to monitor and poor monitoring
and influence on use of saving created by debt cancellation. Too many unmet needs result in
disagreements on what funding should be used for.
Opportunities: All African union countries signed the Abuja declarations that African
governments should spend at least 15% to be sent on health. WHO has developed
recommendations on per capita spending on health. World Bank has upcoming meetings
with civil society, PRSP processes in countries are engaging CSOs, as is the Global Fund
replenishment conference, AU, Africa Commission and the G8 is now chaired by Britain,
which has been leading the push for debt. There is potential to increase awareness among
CSOs on the issue.
Threats: Low levels of public sector funding and misuse of funds weakens national advocacy,
reliance on external funding with conditionalities, and external influence from financiers
around, such as caps on health spending. Resistance may come from the private sector, who
see solidarity financing measures as some form of control.
International processes such as WTO, Commision for Africa, SADC, EAC, Comesa can be
used to dissipate energy, therefore we need to be careful what processes we engage in and
how. Global funding is not being used to strengthen health systems.
7.5.
Challenging trade liberalization and encroachment on health
The key issues were identified as access to medications, privatization and food sovereignty
and security.
Strengths: There are visible movements and campaigns; Already developed strong positions
against privatization in individual organizations; partners with an anti-orivatisation agenda.
Weakness: Single-issue campaigns. Few organizations working specifically on TRiPs and
health in the region. No regional programme of action, although PATAM, EQUINET initiating
work. Don't have clear articulation, requiring additional dialogue, for example anti-privatisation
is not articulated within EQUINET. Nutrition is not major issue that we are tackling and
therefore we are weak in this area.
Opportunities: Can use single issues to move onto other platforms and build on victory for
comprehensive health campaigns. Raise dialogue and campaigns around issues of orivate
and public sector and take advantage of the dialogue on the new perceptions on the role of
17
the state. Information dissemination can catalyse action. Need to get traditional healers on
board.
Threats: WTO, TRIPs, FTAs, EPAs, RTAs, national development plans, donors and IFIs, etc.
Control of supply impacts on trade and consumption. There is a perception that governments
are not efficient in delivering services and that the public health sector is weak. There is lack
of knowledge on how trade agreements such as TRIPs impact on our lives and a varied level
of dialogue on privatization. We are locally in conflict with government around issues that
governments are advancing that were rejected in Cancun.
8. Presentations from social movements
To give background to planning of future work delegates heard further input on three major
social movement processes that impact on health
8.1. African Social Forum
Thomas Deve noted that the WSF is an open space where we throw proposals and dialogue.
Anyone can participate without mandates from any organization. The entry point in Africa
started at the top and one of the biggest challenges we have is to explain the open space to
people who are used to more bureaucratized processes. WSF has a charter of principles and
is an initiative to challenge neo-liberal corporatisation and develop alternatives. WSF is for
movements and organizations that want to undermine work of Davos - and it is a parallel
process with those meetings.
Since it is an open space, there are many people and agendas, and debate alone will not
change the world. So there have been debates around methodology of WSF. It relies on
registration of organizations and events to announce their programs, but revolves around the
slogans: “Our world is not for sale’’; “Not in our name" and “Another world is possible”.
There is now an African Social Forum (ASF) that has identified thematic areas for work such
as labour, youth, gender, etc. Professional activists from NGOs are administering the process
as social movements are resource poor. The sub-regions of the ASF are Southern Africa,
Arab North, East Africa, and West Africa. The most vibrant region so far is southern Africa
and it has the most organizations involved, with labour movements (except South Africa,
students and AIDS activists. So SASF has a big niche in determining agenda of ASF. How do
we organize to make sure we are everyone participates in it? In the Social Movements Indaba
held in Johannesburg, organizations constantly demanded mandates, which is not how the
Social Forum process works, so how do we interact with it, to what extent do we show
solidarity and when do we break with it?
African attendance at previous WSFs has been disorganized, and you could easily get lost.
We need to prepare a program and agenda before we even get to the venue otherwise we
always face these challenges. Those of us involved in Trade issues have built people-topeople solidarity networks to bring alternative dialogue to the social forum. On the ground we
have a challenge to hold SASF in Zimbabwe in October 2005 and in 2006 to have regional
expressions of WSF (e.g. ASF - may be in Morocco).
The WSF on health was outlined by Armando De Negri., This meeting has a history at first
WSF in 2001 when we identified the need to put people together to prepare health agenda for
WSF as it is not a main issue of the WSF, although it was represented under neo-liberal
umbrella. In 2001 we proposed the health WSF to take place 3 days before main event and it
has been held for next 3 years until the 2004 international forum for people’s health.
In 2003 PHM joined the meeting, and in 2004 PHM was responsible for organizing it. This
year we ran WSF on health, as it's an important space to put together main agendas of
"Another world is possible". The health forum developed a group of general agreements to
develop and identify terms of about how:
* the struggle for health is linked to struggle against neoliberalism and war
* health is a fundamental human right
* this can be developed into national systems for health.
The final agreement was to generate an organizational process similar to WSF with
international council to generate permanent space for dialogue. We are proposing that we are
18
identified and linked to WSF and will follow the dynamics and organize a health WSF
wherever the WSF takes place to develop an exchange of information between regions.
Initial dialogue in health WSF sees the need to bring Africa on board, establish effective ways
to touch the bases of social movement’s etc in order to establish wider struggle and
internationalise as much as possible. The health WSF is a coalition of coalitions, meant to
reinforce wide coalitions to develop stronger international movement for human rights
program. The Health WSF called for participation in PHA in Ecuador to achieve good South
American participation around this event.
The dialogue on the format of WSF for 2006 is a confirmation of peoples' idea for expansion
of the process, but organizing it is taking too much of energy when we'd rather be in the
trenches and fighting. That is why a continental process was decided on for 2006. There are a
number of different positions being developed on future of WSF.
It is hard for 150 000 people to reach common agreement, but with thematic divisions there
were more that 300 different proposals as exchange of ideas within the forum. The main
purpose of WSF is to generate a broader perspective, make friends, know you are not alone
and know you have allies.
8.2.
People’s Health Assembly
Samuel Ochieng noted that the next PHA is in July 2005 in Ecuador. Civil society realized that
objectives of World Health Assembly were not being met and therefore we needed to have an
alternative forum to achieve the "Health for All" call. The first PHA was held in 2000 in
Bangladesh; about 1500 people attended from 93 countries.
Since then PHA has been involved in a number of international forums and campaigns for
health. After 5 years PHM will be holding PHA 2 in July 2005 in Ecuador. The process has
begun and we have an international organizing committee. The main objective of this is to;
• strengthen and expand the PHM as a network that struggles for the revival of the original
spirit and principles of "Health for All";
• launch a more concerted global action to achieve a full and universal recognition of the
Right to Health as a fundamental Human Right;
• widen the debate leading to a more proactive resistance to all the forces that oppose and
violate the right to health of the people-many of them enshrined in neoliberai reform
policies and in the overwhelmingly unfair move towards globalization with its shift towards
increasing militarisation; and
• share experiences and practices useful for the universalisation of our struggle to
implement alternative models of people-centered and beneficiary controlled health care
delivery systems
Preliminary themes have been developed and we are busy developing a programme. We
want to take people who have roots and who can make sufficient use of the knowledge and
help us establish the network. We have resources and we ask for support in identifying
candidates and developing process to ensure that Africa is well represented.
We are also seeking to develop a project called "African Dreams" within the PHC exchange.
We are collecting stories, poems, posters, photos or other artistic works to create an
exhibition. Please submit anything you have on this to Mwajuma Mwasaigana.
Armando extended an invitation for the southern African delegation going to Ecuador through
Johannesburg and Porte Allegre, to have a two-day stop in Brazil to find out more about
Brazil's health system.
19
8.3.
WTO Ministerial, Hong Kong December 2005
Riaz Tayob outlined the process to the WTO Ministerial conference of trade ministers meeting
every two years. The specific challenges we are facing at the next WTO are to review TRIPS
agreements to allow countries that do not have manufacturing capacity to import generics
This agreement comes up for review and may be held over, as rich countries want to hold it
over developing countries heads. Developing countries also want to prevent patenting of
discovery.
The strategy inside the WTO is that nothing's agreed until everything is agreed and the
GATS negotiations are also going to be included in this agenda. Key issues in the
negotiations are agriculture to limit northern countries tariffs and export rights for poor
countries. We are blocking out venues for African civil society and parliamentarians so that
they can call ministers to account Because Africa is underrepresented at the parallel event
trying to make sure that Africa speakers are represented We need to promote a
communications system that will work for activists in Hong Kong to organize people at home
and MPs.
The WTO co-ordinating group meeting - the Hong Kong People's Alliance Against WTO —
organized by Asian people will be meeting in March. The Africa Trade Network co-ordinates
around a combined assault on the WTO and we still need to work how we are going to
participate in this.
9. Moving forward: Fundamental principles, values and issues for health civil society
Following these discussions Rene facilitated a session that aimed to draw together the key issues
raised in the previous sessions and set the platform for defining a programme of follow up work
The summary below reflects the outcomes from the session.
9.1.
Guiding values
Health civil society in the region is guided by principles and values of:
•
«
o
•
•
9.2.
the fundamental right to health and to life
equity and social justice
people led and people centred health systems
public over commercial interests in health: Health before profits
people led and grassroots driven regional integration
anti-neoliberal policies.
Major areas of work
We are building a national people’s health system
Health civil society organisations in the region agreed that the central struggle to reflect these
values and principles in 2005 is for a national people's health system.
This is the unifying goal for our various areas of struggle and the common platform around
which we are all uniting, recognising the different areas of struggle around this. We
understand a national people's health system to be one that is universal, comprehensive,
equitable, participatory and publicly funded.
We built an understanding of how our different areas of struggle contribute and relate to this
uniting goal.
20
Health is organised around people's power. This
demands a critical mass of conscious and
organised people, with rights to meaningfully
participate in their health systems, working
collectively for their constitutional rights to
health
A NPHS demands sustained
A national people's health
system demands adequate,
well trained, appropriate,
equitably distributed and
motivated health workers.
This calls for improved
conditions and training for
health workers, and a
challenge to the trade in
and migration of health
oersonnel.
Underlying a NPHS is an
economy
that
widens
people's
access
to
productive wealth and to
essential services
We are building national
people's
health
system
(NPHS) - one that is
universal, comprehensive,
equitable,
participatory
and publicly funded.
The state is a site of struggle, nationally and
globally. It supports the national people's health
system by resisting privatisation and promoting
the public interest. It has and protects the
authority and policy space to advance health. It
protects the public in trade agreements (TRIPS,
GATS, FTAs) and contronts trade liberalisation.
increased fair financing of the
universal right to health, through
rising investment in the public
health sector, increased per
capita funding to health and
increased progressive tax
funding for health. This calls for
debt cancellation and sustainable
global / international funding to
reinforce the public health
system.
A NPHS provides universal
treatment
access
to
(prevention and care) and
protects food sovereignty,
and
indigenous
knowledge
systems.
Our different areas of struggle ano issue campaigns in health civil society can be located within
this wider unifying struggle. Each area demands and reinforces the other, once it is located within
this unifying framework. We therefore carry the unifying platform of building a national peoples
health system into all our issue platforms.
9.3.
Organisational objectives
Health civil society in the region is guided in its mode of work by objectives of.
0 Being people led and people-centred
0 Being organised at grassroots, national and global level
0 Having in one struggle with many fronts
0 Linking single issues to the broader vision
0 Being united organisationally across labour, community organisations and social movement
0 Scaling up and advancing on victories
0 Working in solidarity
0 Taking advantage of windows of opportunity.
10. Moving forward: Follow up actions
With these key principles, areas of action and organizational objectives defined, we identified as
groups and in plenary the major areas of follow up action These are summarized below.
We identified several major areas of action as focus for follow up:
« strengthening peoples power in health
• improving the conditions of health workers
• ensuring fair financing for health
• advancing health in trade.
We also identified that issues such as access to treatment embed in ail these areas of action and
present opportunities through the gains achieved to advance our wider health interests.
10.1.
Strengthening peoples power in health
Lead organisations for taking this area forward are: CWGH, EQUINET, MWENGO, MHEN, PHM.
• Civic education for a NPHS: We will develop, produce and with civil society organisations in
countries widen the use of civic education materials on health that promote the NPHS
(CWGH and EQUINET (TARSC) with national health civil society. We will training facilitators
in how to use participatory health training materials (CWGH) and run an activist learning
workshop open to health civil society in June 2005 (MWENGO).
• People to people links: We will make links with and strengthen community health workers
understanding (PHM) and make links with parliamentarians in our work (EQUINET, CWGH,
GEGA and local health civil society). We will strengthen national coalitions of health civil
society with a comprehensive focus on a NPHS (HEPS, MHEN, CWGH, TANGO). We will be
actively brought into, supported in and participate in social movement activities of the Social
Forum and the Peoples Health Movement (SaSF, PHM).
» Communication outreach: We will disseminate information on issues relating to the NPHS
in clear, understandeable and simple terms (PHM, MWENGO, CWGH).
> We will co-ordinate out mailing lists to share information and build common issue newsletters
where we send the same messages through our editorials (MWENGO, PHM, EQUINET,
PATAM). We will provide training on ICTs (MWENGO, EQUINET).
22
10.2.
Improving the conditions of health workers
Lead organisations for taking this area forward are: SATUCC and PHM.
• Building evidence on Health worker issues: We will gather research evidence on the
conditions of health workers including norms and losses across countries and the impact of
privatisation of services and analyse the policy directions from this. (MSP; PHM; EQUINET;
SATUCC, PATAM).
• Debating and developing policy options: We will bring our evidence from different
research processes into the EQUINET regional policy forum on health human resources to be
held in July 2005 to develop our policy positions and take these back to our organisations and
to our dialogues at national level with health workers (EQUINET, all).
• Advancing and engaging on our policies: We will hold a follow up meeting to discuss our
advocacy positions after the EQUINET conference and secure funding for a regional
campaign that we will take forward through existing campaigns and at country and regional
level (MSP, SAMWU, NEHAWU, SATUCC, PHM), Our first campaign day will be on May Day
2005. We will hold meetings in SA and in the region to build capacity on health worker issues
(SATUCC, SAMWU, NEHAWU).
• Information and media outreach: We will disseminate media statements on the issue, such
as in the SAMWU/MSP/ILRIG press conference on occupational health conditions of health
workers on 7 March 2005. We will use the MSP radio show on occupational health of health
workers distributed through 40 radio stations in SA and the website to take up these issues.
We will build solidarity with and disseminate each other's statements and positions in line with
our unified platform, including in our newsletters. We will fundraise for wider radio outreach on
health worker policy positions (MSP).
10.3.
Ensuring fair financing
Lead organisations for taking this area forward are: EQUINET, CIN, HAI, PHM.
• Sharing evidence and building alliances: We will share information through our mailing
lists and newsletters in fair financing issues (EQUINET) and on global funding issues
(TAC/PATAM). We will hold regional policy debates: on fair financing in April 2005
(EQUINET), in March/April in SA (TAC). We will examine how GPPIs strengthen health
systems (PHM, CIN, HST, CHESSORE), explore options for fair financing in Africa
(EQUINET, CIN) and investigate national health insurance schemes proposals (CIN) and
private sector regulation (PHM, TAC) for their impact on fair financing.
• Monitoring and tracking health financing: We will track how funds for AIDS are used
(HEPS; MHEN) and whether G8, Abuja and other commitments are met (EQUINET, PATAM).
We will track how PRSPs are operating (CIN).
• Campaign on fair financing and debt cancellation: We will campaign for debt cancellation
and advance this at the July G8 meeting (PATAM, TAC and all). We will advocate for an
increase in health financing (All) and campaign for the abolition of user fees (TANGO, all).
10.4.
Advancing health in trade
Lead organisations for taking this area forward are: ATN, SEATINI.
• Sharing information, building literacy and building alliances: We will share information
through monthly conference calls (HAI, Oxfam, MSF, TAC, AidsLaw Project); networking
meetings (SATUCC); economic literacy activities (CHESSORE, ACRN, MWENGO, ATN,
SEATINI) meetings with MPs (SEATINI, CHJESSORE, EQUINET, CWGH, HEPS, HAI) ’ We
will disseminate specific papers on issues, (HAI- medicines paper re: EPAs). We will build
capacities on trade and health isues at country and regional level (SEATINI, EQUINET, CHP)
• Campaign and engage on trade issues: We will campaign against EPAs (early March
ATN, MWENGO, LEDRIZ, SEATINI, ACRN), against AGOA (SATUCC); and on AU-IPr’
23
•
medicines access (March SEATINI, ATN, HAI). We will engage the AU on TRIPS (April
TAC/PATAM). We will participate in the Hong Kong ministers planning meeting (26-28 Feb,
SEATINI) ; the MPs preparation workshop for Hong Kong (ATN August) and in the Hong
Kong WTO Ministerial (MWENGO, LEDRIZ, SEATINI , EQUINET 13-18 Dec)
Promoting alternatives: We will contribute to the building of alternatives to neoliberalism
and locate the NPHS in the wider framework of economic and social policy for its
achievement (LEDRIZ; before June).
10.5 Building one struggle from many fronts
These areas of struggle will be integrated through:
• a common and uniting position
o united health civil society in agreed common platforms
• common/ joint processes and materials.
Our common and uniting position is for a national people’s health system.
The common platforms we will jointly aim at ensuring presence and engagement on the NPHS
and the specific issues relevant to that platform are:
o AU Ministers of Health meeting, April 2005: lobby on the NPHS, fair financing, TRIPS,
PATAM/TAC to lead in organizing.
o World Health Day April 7 2005: lobby on NPHS, link to mother and childcare (PHM to lead
in organising).
o May Day May 2005: lobby on NPHS and health worker conditions, SATUCC to lead in
organizing.
• G8 July 2005: mobilisation and social action on trade, financing and NPHS: Lead in
organising MWENGO, SASF, TAC).
• PHA2 July 2005: plenary from the region on the NPHS. PHM to lead in organizing.
• AU Ministers Meeting Sep-Dec 2005: lobby on trade-health issues, ATN to lead in
organizing.
• SASF October 2005: Zimbabwe, plenary on NPHS (Mwengo to lead in organising).
• UNGASS September 2005: lobby position on the NPHS and fair financing (lead to be
finalised EQUINET?).
• WTO Hong Kong Ministerial December 2005: lobby and social action on trade and health.
Lead in organising ATN, SEATINI).
• ASF January 2006: Morocco WSHF to lead in organizing.
• WSF Jan 2007: Nairobi WSHF to lead in organizing.
The point0 of co-ordination, planning and review for our work are:
•
April 2005, EQUINET: A meeting of the health civil society lead institutions on 18 April after
the EQUINET steering committee meeting in Johannesburg. EQUINET to ensure all
organisations are present.
•
June 2005, CWGH: A meeting of the health civil society institutions in June 2005 at the
CWGH National Conference in Zimbabwe. CWGH to ensure relevant health civil society
organisations are present.
•
July 2005 PHM: A meeting of the health civil society led institutions in July 2005 at the PHA2
in Equador. PHM SA to attempt to ensure all organisations are present.
September 2005 SATUCC: A meeting of the health civil society institutions at the SATUCC
regional labour forum in Sept/Oct 2005. SATUCC to ensure that relevant health civil society
organisations are present.
•
24
The processes we will use to strengthen our joint and common platforms are:
• Developing and producing materials for awareness and education on the NPHS.
• Producing and sharing materials for advocacy, lobbying etc.
• Ensuring organisations going to meetings take a joint mandate of the health civil society
network, obtain d=solidarity from the network and feed back to the network.
• Setting up a joint mailing list for the health civil society network.
The co-ordinating committee for the health civil society network includes CWGH, EQUINET, HAI,
PHM, TAC/ PATAM, SEATINI, SASF, and SATUCC. EQUINET will continue to provide
secretariat support (to be reviewed in April) and will set up the mailing list. The April meeting will
examine the secretariat roles and see how these can be devolved. EQUINET will gather existing
materials from health civil society organisations and disseminate to the network.
PHM will give feedback in March to all organisations in the co-ordinating committee on their
participation and support for attending PHA2 (PHM-SA to follow up) and to all organisations on
the outcome of the plenary on Africa at PHA2.
The April co-ordinating meeting will review and finalise the joint platform on the NPHS that is
integrated into issues platforms and discuss funding, proposals for cross cutting activities and
work. In the meantime all groups will explore funding for the programme of work.
11. Closing
Delegates used the ideas of the past days to brainstorm banners, campaign messages and key
messages for forums such as G8. While there was debate on the exact working there was
evidence on common purpose and common passion across the groups - the objective of the
workshop!
There is convergence across all groups of the key message of Building a national people’s health
system, and consensus on the key areas that this means engaging on.
Itai Rusike of CWGH thanked the delegates for their time and commitments, thanked
CHESSORE for hosting the meeting and EQUINET/ TARSC for organizing it, the sponsors for
their support and everyone who put work into the workshop. He wished everyone a good journey
home and energy in carrying out the work we have agreed to undertake.
25
Appendix 1: List of Delegates
DELEGATE NAME AND
institution
ADDRESS
EMAIL
PHONE/FAX
Christa Cepuch
HAI Africa
P 0 Box 73860 -00200
Nairobi, Kenya
christa@haiafrica.org
Tel:+254 -20 4444835
Fax: +254 -20 4441090
Cell:0733615189
Wellington Chela
SATUCC
P.O. Box 70751, Ndola
Zambia
nucvy@zamtcl.zm
02-611345-6
02-614679
Jennifer Chimlambe
MHEN
Box 1618
Lilongwe Malawi
healthequity@malawi.net
265 01 752 099.
Cell 265 09 205590.
Hameda Dedat
Researcher
MSP
PO Box 1213
Woodstock 7915
Cape Tcwn SouttrAfric.
Armando De Negri
PHM Brazil, ISEQH,
WSFH
Rua Anita Garibaldi
834/202 Porto Alegre-RS Brazil
armandon@portoweb.com.br
Tel 55 51 99960562
Fax: 55 51 33143690
Thomas Deve
Southern African Social
Forum / MWENGO
20 McChlery Ave
Eastlea
Harare
Zimbabwe
Thomas@mwenqo.orq.zw
Tel: +263 4 700090
Soraya Elloker
SAMWU
47 Beverley Street
Athlone 7945 Cape Town
South Africa
soraya.elloker@capetown.gov.za
Tel +27 021 633 2002
Fax. +27 021 633 5020
Godfrey Kanyenze
LEDRIZ
Box 3549 Harare
Zimbabwe
ledriz@africaonline.co.zw
Tel: +263 91948398
Tendayi Kureya
PATAM/SAfAIDS
SAFAIDS 17 Beveridge Road
Belgravia Harare
Zimbabwe
tendayi@safaids.orq.zw
Tel: +263-4-336193
Fax:+263-4-336195
Moheb Labib
PATAM
Coptic Hospital
Box 30220, Lusaka, Zambia
moheb@netafnca.co.zm
260-95757008
260-1-237584
Fax 260-1-230587
Rene Loewenson
Programme Manager
EQUINET /TARSC
47 Van Praagh Ave, Milton Park
Harare, Zimbabwe
rene@tarsc.org
+263 4 708835
Fax 737220
Bridget Lloyd
PHM
99 Balfour Street
Woodstock Cape Town 7925
South Africa
Mwajumah Masaigana
PHM/EQUINET
PO Box 240 Bagamoyo
Dar Es Salaam
Tanzania
masaiqana@africaonline.co.tz
Tel: +255 23 2440062
Fax:+255 23 2440021
Ednah Masiyiwa
CWGH / Womens Action
Group
11 Lincoln Rd
Avondale Harare
Zimbabwe
waq@waq.orq.zw
Tel: +263 4 308738
Fax: +263 4 339161
Njogu Morgan
TAC
135 Smit ST Auckland House
Braamfontein 2017 South Africa
njoqu@tac orq.za
Tel: +27-11-339842
Fax: .27-11-4031932
Matilda Moyo
Southern African Social
Forum / MWENGO
20 McChlery Ave
Eastlea
Harare
Zimbabwe
matilda(o)mwenqo.orq.zw
Tel: +263 4 700090
msp@ilriq.orq.za
Hameda 786@yahoo.com
Tel: 021 447 6375
Fax: 021 448 2282
0820553619
Tel: +27 021 447 5464
bridqetl@mweb.co.za
26
Godfrey Musuka
Programme Officer,
EQUINET/TARSC
47 Van Praagh Ave, Milton Park
Harare, Zimbabwe
qodfreym(3)tarsc.orq
+263 4 708835
Fax 737220
Andrew Mushi
TANGO
PO Box 31147
Shekilango
Dar Es Salaam, Tanzania
tanqo@africaonline.co.tz
amushi1@yahoo.com
Tel 255 22 2774581/2
Fax 255 22 2774581
Rosette Mutambi
National Coordinator
HEPS Uganda.
P.O Box 2426. Kisingiri Road.
Mengo,
Kampala .Uganda
heps@utlonline.co.uq
rmutambi@hotmail.com
Chosani Njobvu
CHESSORE
6th Floor TAZARA HOUSE, P.
O. Box 320168. Woodlands,
Lusaka Zambia
Josiah Ndhlovu
PATAM/ MSF/ TALC/
TPTC/ DATF
: 041 270970/078 371401,
chosaniniobu@yahoo.com
chessore@zamnet.zm
+260-1-228359
+260-95-704446
Fax: 228359
MSF
msfqr-kapiri@athens.msf.org
tulipamopic@yahoo.co.uk
+260-97670212
Samuel Ochieng
Consumer Information
Network
Consumer Information Network
[CIN]
P. 0. Box 7569, 00300 Nairobi
Kenya
cin@insiqhtkenya.com
Tel/Fax+254 20 781131
254-72255509
Nimla Pillay
SATUCC
P.O. BOX 1100
□urban 4000
South Africa
NPSWU
npswu@mweb.co.za
Tel: +27 31 3047563
Fax: +27 31 307 3306
Rebecca Pointer
EQUINET/MSP
9 Albertyn Road
Muizenberg, Cape Town
7945South Africa
reb(5)wfeet.za net
Tel: +27 21 788 3847
Fax: +27 21 788 3847
Itai Rusike
Community Working Group
on Health CWGH
114 McChlery Avenue Eastlea
Harare PO Box 1376 Belvedere
Harare, Zimbabwe
cwqh@rnweb.co.zw
+263-4-788100/788099
Fax 788134
David Sanders
PHM/IPHC
SOPH UWC P Bag 17 Belleville
7535
South Africa
Sthembiso Shezi
NEHAWU
11 Priscilla Street. Kensington.
Johannesburg. 2094 South
Africa
Riaz Tayob
SEATINI/ EQUINET
POBox 1558
Crown Mines 2025
South Africa
dsanders@uwc.ac.za
shezi@nehawuorq.za
Tel:+27 21 959 2132
Fax: +27 21 959 2872
Tel: 2711833 2902
Fax. 27118330757
•
riazt@iafrica.com
Tel: +27 83 778 7222
Fax: +27 83-118 7787222
27
Appendix 3: Program
Health civil society in east and southern Africa: Towards a unified agenda and action for people's health, equity
and justice
Day one: Thursday February 17
Aims for the day:
To review our current positions and analysis, identify areas where we share perspective and analysis and
debate and review areas where we differ, build shared analysis and joint platforms, strategies and
campaigns.
Welcome, introductions of delegates and groups represented
Background to the meeting
Current challenges, alternatives and issues for health civil society
Challenges to common goals of health equity and social justice - R Tayob, SEATINI
Forging an alternative in East and Southern Africa - G Kanyenze, SATUCC/LEDRIZ
Agendas for global health - D Sanders PHM
Agendas for regional health- R Loewenson EQUINET
Lunch
Group /plenary exercise on positions and priorities
Plenary review on priority issues
830-930am
930-10am
1030-1150am
1150-1 pm
1pm-2pm
2-330pm
345-445pm
Day two: Friday February 18
Aims for the day:
To understand and review the strength, co-ordination and connection of health civil society to broader social
movements nationally, regionally and globally. To assess the feasibility of significant co-ordinated regional
activity.
830-930am
Plenary (facilitated) mapping of the strength of health civil society around priorities identified on
day one. Where and in which issues is civil society pro-active? What is the strength of
mobilisation around the identified issues.
Group exercise: SWOT analysis
Plenary: report back
Lunch
Plenary discussion: Issues from the analysis
Group work on issues raised in plenary
Plenary feedback on group discussions. Discussion and review of common positions and
actions
1000-1130am
1130-1230pm
1230-145pm
145-300pm
315-415pm
415-600pm
Day three: Saturday February 19
Aims for the day:
To identify and agree on mechanisms for strengthening linkages, resource sharing, solidarity action and
unified campaigns across health civil society In east and southern Africa.
To identify and agree on mechanisms and processes that will strengthen and build our capabilities for this
To map the way forward
0830-1000am
1000-1200pm
1245-100pm
1pm-2pm
200-330pm
Group exercise: Development of a plan of action
Plenary: report and discussion
Closing
Lunch
Wrap up meeting of the planning committee
Appendix 3: Useful Websites
www.phmovement.org
www patam.org
www.cwqh.orq.zw
sa.indymedia.org
www.fsms.orq.br
www.queensu.ca/msp/
www.equinetafrica.org
www.mwengo.org
www.tac.org.za
www.haiafrica.org
www.samwu.org.za
28
Appendix 3: Program
Health civil society in east and southern Africa: Towards a unified agenda and action for people’s health, equity
and justice
Day one: Thursday February 17
Aims for the day:
To review our current positions and analysis, identify areas where we share perspective and analysis and
debate and review areas where we differ, build shared analysis and joint platforms, strategies and
campaigns.
830-930am
930-10am
1030-1150am
Welcome, introductions of delegates and groups represented
Background to the meeting
Current challenges, alternatives and issues for health civil society
Challenges to common goals of health equity and social justice - R Tayob, SEATINI
Forging an alternative in East and Southern Africa - G Kanyenze, SATUCC/LEDRIZ
Agendas for global health - D Sanders PHM
Agendas for regional health- R Loewenson EQUINET
Lunch
Group /plenary exercise on positions and priorities
Plenary review on priority issues
1150-1 pm
1pm-2pm
2-330pm
345~445pm
Day two: Friday February 18
Aims for the day:
To understand and review the strength, co-ordination and connection of health civil society to broader social
movements nationally, regionally and globally. To assess the feasibility of significant co-ordinated regional
activity.
830-930am
Plenary (facilitated) mapping of the strength of health civil society around priorities identified on
day one. Where and in which issues is civil society pro-active? What is the strength of
mobilisation around the identified issues.
Group exercise: SWOT analysis
Plenary: report back
Lunch
Plenary discussion: Issues from the analysis
Group work on issues raised in plenary
Plenary feedback on group discussions. Discussion and review of common positions and
actions
1000-1130am
1130-1230pm
1230-145pm
145-300pm
315-415pm
415-600pm
Day three: Saturday February 19
Aims for the day:
To identify and agree on mechanisms for strengthening linkages, resource sharing, solidarity action and
unified campaigns across health civil society in east and southern Africa.
To identify and agree on mechanisms and processes that will strengthen and build our capabilities for this.
To map the way forward
0830-1000am
1000-1200pm
1245-100pm
1pm-2pm
200-330pm
Group exercise: Development of a plan of action
Plenary: report and discussion
Closing
Lunch
Wrap up meeting of the planning committee
Appendix 3: Useful Websites
www.phmovement.org
www.patam.org
www.cwqh.orq.zw
sa.indymedia.org
www.fsms.orq.br
www.queensu.ca/msp/
www.equinetafrica.org
www.mwengo.org
www.tac.org.za
www.haiafrica.org
www.samwu.org.za
28
- Media
 RF_COM_H_71_SUDHA.pdf
RF_COM_H_71_SUDHA.pdf
Position: 1444 (8 views)