GULBARGA VISIT-REGIONAL DISPARITIES
Item
- Title
- GULBARGA VISIT-REGIONAL DISPARITIES
- extracted text
-
RF_COM_H_69_1_SUDHA
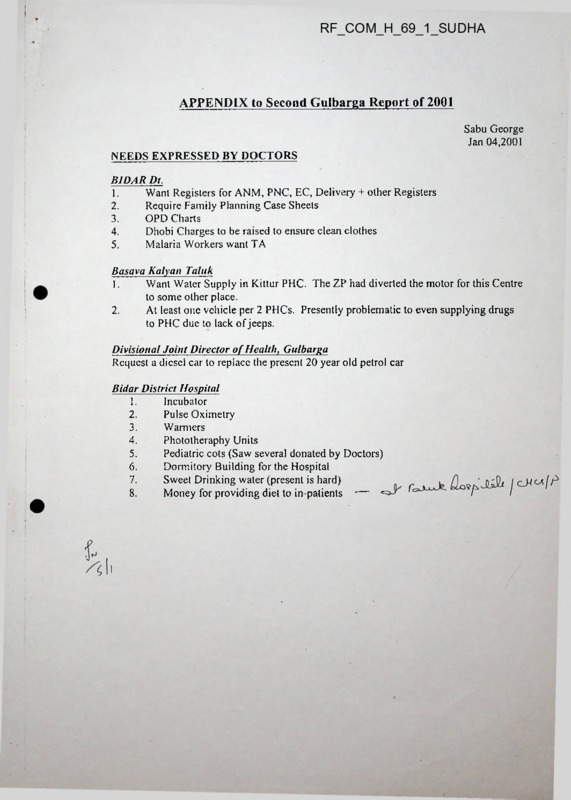
APPENDIX to Second Gulbarga Report of 2001
Sabu George
Jan 04,2001
NEEDS EXPRESSED BY DOCTORS
BIDAR Dt.
1.
Want Registers for ANM, PNC, EC, Delivery + other Registers
2.
Require Family Planning Case Sheets
3.
OPD Charts
4.
Dhobi Charges to be raised to ensure clean clothes
5.
Malaria Workers want TA
Basava Kalyan Taluk
1.
Want Water Supply in Kittur PHC. The ZP had diverted the motor for this Centre
to some other place.
2.
At least one vehicle per 2 PHCs. Presently problematic to even supplying drugs
to PHC due to lack of jeeps.
Divisional Joint Director of Health, Gulbarga
Request a diesel car to replace the present 20 year old petrol car
Bidar District Hospital
1.
Incubator
2.
Pulse Oximetry
3.
Warmers
4.
Phototheraphy Units
Pediatric cots (Saw several donated by Doctors)
5.
Dormitory Building for the Hospital
6.
7.
Sweet Drinking water (present is hard)
Money for providing diet to in-patients •— c
8.
Bagalkot Field visits
FIRST BAGALKOT REPORT OF 2001
January 5, 2001; Written in Trivandrum & revised at Bangalore
Sabu George
rime Spent and Places visited
Spent a total of 7.5 days over two visits in Bagalkot District in connection with the First
Pulse polio immunisation of 2000-1 (in end November and 2"d week of December). Went to 4
taluks. Met DHO, several senior Medical Officers at the taluk Headquarters including 2 Taluk
Medical Officers and few Health Education Officers. Visited villages in the 2 most backward
taluks of the Bagalkot District-Hungundu & Badami. Crossed the District border and visited 2
border PHCs in Raichur to assess the usually neglected borders of remote areas. Also met the
District 1CDS Programme Officer.
The significance of the Bagalkot visits is that it builds on the earlier visits (August) and
therefore we have more than a one time cross sectional glimpse of the Health System. Doctors
were more forthcoming despite the fact that the meetings occurred in the context of the Pulse
Polio.
Taluk Hospital
The Badami Taluk hospital is being renovated under KHSDP. The new Block
construction started belatedly unlike the few other Hospitals in the better off Taluks of the
District that were completed. The Senior Doctor complained that already the proposed wing has
been downsized. An X-ray room and another room has been removed from the original plans
due to lack of funds. The wall tiles will only be upto 2 feet instead of the proposed 6 feet. Only
after the construction is over will we know what else will be eliminated. The old building was
small and in bad condition.
Medical Officers: Corruption
The “new” Medical Officer I met in August apparently is no longer there. A Minister’s
son-in law has been appointed at the PHC. Apparently he rarely visits the PHC.
The "old" Doctor I met last time was absent at the PHC both the times I went. He was
out on field visits to monitor Pulse Polio. However, he met my friend from the Sugar Mill who
went on the following day and complained of corruption at the top District level. Medicines are
being sold privately and he is having problems with the District authorities in this regard. He
2
wanted public spirited individuals like us to take up this corruption. This Doctor has an unusual
in his previous background (see my August Report). He had just taken over the PHC that week.
11c had promised to stay in the PI IC quarters as soon as it was repaired by the Panchayat. This
visit he was still commuting 3 hours each way but since 1 could not meet this time find out why
he was not staying.
The District Health Officer
Shocked to know that the DHO did not know about the cunent situation of Poliomyelitis
cases from the Polio Surveillance System. He read if from the newspaper that there are now 6
wild virus cases and all in Northern Karnataka. I had contacted the Southern Surveillance In-
charge thru Prahalad just before I left for Bagalkot. As this information is useful to motivate the
Sugar mill volunteers to reach out to every unimmunised child left by the Government.
The DHO was unaware that there are another 4 more cases in Karnataka which are called
Compatible ones. I mention this as vertical systems like WHO polio surveillance though largely
dependant on the routine health delivery systems inevitably get a life of their own. Thus they do
not communicate and share the information with even the District Officials. The continued
persistence of poliomyelitis is also a reflection of the inadequacies of the WHO Polio eradication
strategy to understand field realities as much as of the routine health system to reach out to every
child. Just flooding vaccine around in repeated massive campaigns was presumed to be adequate
to eliminate polio (last year some of the Northern states had six rounds).
The DHO said that the Health Minister is largely interested in the Government Hospitals
and not that much on the primary health care infrastructure. He informed that the Commissioner
of Health had a meeting of the Belgaum region’s DHOs in November at Bijapur.
Pulse Polio Immunisation
Received excellent cooperation from the District and taluk Doctors this year. In the
beginning of the last year (May 1999) it was lukewarm, though they wanted the Sugar Mill just
to provide them money for hiring jeeps and buying food for the Booth staff. I had met the DHO
on a second Saturday evening. Despite being a holiday he took me to his Office and called up all
the 4 Taluk Medical Officers to remind them about the involvement of the Somaiya Sugar Mill
workers, Field staff, volunteers and Somaiya Nursing College students. Gave me several
thousand doses of vaccine, primarily to cover children of Maharastra migrant labour who cut
3
sugar cane in distant fields (away from villages) for the many mills who procure cane from the
Jamkhandi and Mudhol taluks. The Officials are feeling the heat from the top. All the six wild
virus poliomyelitis cases are in Northern Karnataka (2 each in Koppal, Gulbarga and 1 in
•
Raichur & Bagalkot).
Clearly there was fatigue in the field as there seems to be no end to Polior For last several
years the Government had been promising that it was the last time and polio would be eradicated.
The DHO told me that it was difficult for him to get jeeps requisitioned for 3 days from the other
Departments. I had received no such complaint last year from him. All the posters this year
mentioned only one day for both the rounds though the Government was actually committed to 3
days for completing pulse polio immunization. In at least two taluks the teachers did not
participate in the first day. Note last year they were involved in all the four rounds.
In one Raichur PI IC, 1 found booths closed by 2 pm on the first day. All the reports from
the sub-centres had arrived before 3 pm at the PHC. Either the PHC staff are very efficient or
that they were indifferent to the goal of polio eradication. Yes villages are nuclear and that there
are hardly any field huts in this region and therefore attaining complete immunization is easy.
But some families work in fields miles away and therefore the likelihood of ensuring complete
immunization by 2 pm is probably unlikely and the chances that the workers would traverse
miles on the next two for a few isolated children dispersed away in fields is remote. I wish I am
wrong but repeatedly 1 have found children left out in distant villages over the last 5 rounds in 4
taluks.
The 1CDS System
I had met the District Programme Officer of the ICDS. She said neither her nor the
Assistant Director of WCD have got their jeeps. Mr. Kanti, the Joint Director in charge had
J
■
• ••
earlier told me that the Jeeps for the newly formed will be given. When I met Mr. Kanti this
week in Bangalore he said had asked UNICEF Delhi to supply jeeps. This matter needs to be
followed with the ICDS Director as it might many months before the Jeeps do reach the new
Districts. (To be brief- Note previously in September, Mr. Kanti had given me another version).
Irrespective of the fact that whoever pays for the Jeep (UNICEF or GOI) it is important that the
jeeps be arranged soon. Too often there is cynicism and indifference to the well being of the
child at the sub-Dircctor levels in the ICDS Directorate. It may not be as bad as in the Health
4
Dept. Another instance, the previous Assistant Director of Gulbarga WCD and presently a
Deputy Director in WCD told me this week, that there is no hope that children in the 3 Blocks of
Gulbarga will be fed everyday (Presently they arc only fed officially only half the time-1 have
been to a village where feeding was disrupted for a whole month). Every body at the District
CEO, DC, ZP and at the State level- Director, Secretary are aware of this sad fact. Crores of
rupees have been diverted from children’s food to other heads with or without the connivance of
the Panchayats, WCD, Planning or Finance Departments over 3 years. In characteristic
bureaucratic style everybody blames somebody else. The Gulbarga DC said that the CEO should
take the initiative with the Panchayats. But a little later the DC said that he would do exactly
what the CEO would do- be indifferent to diversion from children’s food. He acknowledged that
PWD Contractors, Doctors who have strong lobbies have their self-interests protected while the
Anganwadi workers who arc the weakest suffer. The only thing on which all the officials agree
both in Gulbarga and in Bangalore is that this remains unresolved as the Northern people are not
empowered to protect their rights. Note this remains a problem of largely of Northern taluks.
I spoke to the Programme Officer of Bagalkot to identify neglected and remote villages of
Badami as she had served there for 6 years. Also enquired of Hungundu taluk. Offered to take
her in a jeep to Hungundu villages on the Pulse day as she had no Jeep. She wanted to be in
Badami as her boss was likely to be in Hungundu. She described the Assistant Director as a
serious person. 1 had not met the present AD after he had joined Bagalkot.
Raichur District Border villages
Visited 2 PHCs in the border. Situated in Lingsur Taluk. Villages in this remote area
alternate^ between Raichur & Bagalkot Districts. The first PHC was in a small village
Sajalagudda, and except for a Nurse who had the Polio vaccine nobody else was there. Running
water was there. Most of the rooms were kept locked. The Nurse had a key bunch of 20 keys or
so and took time to find the Doctor’s Office key. The Doctor’s room was dusty. No Doctor has
worked there for the past 6 years. In about 6 km on the Bagalkot side there was a PHC. The
adjacent PHC in Raichur was only 2 km away.
In fact, I did not even realize that the Building was a PHC till a School Employee told me
later. The local villagers had directed me to this Hospital but it looked tiny and was deserted
apart for a dog. 1 had taken it for a Sub-Centre and thought the lonely Nurse was there because it
5
was the Pulse Polio day. I was looking for a place for the hungry Bombay Nurses (who came for
Pulse Polio immunization) to have lunch at 2pm.
The second PHC I visited was a relatively new building and appeared clean. The PHC
is situated deep inside the village, far from the Main road of the village (to the locals- the PHC
was out of the village). Nagral PHC had no quarters and no vehicle. There was no approach
road and garbage heaps had to be crossed to reach the PHC. 1 was there before 3 PM. Only two
men staff were there. One ANM died and this has remained vacant. The Doctor had gone away
to his house in the village. 1 las been there for over 5 years. Started as a Contract Doctor. Was
told that there are 100+ patients every day. Though there was a village overhead tank just in
front of the PHC , the Centre had no running water. About six months ago a new Water Sump,
overhead tank (Sintex) and a pump were installed. But the contractor ran away without
connecting the pipes. The Pi 1C undertakes sterilization only once a month.
It is sad to see that in a PHC where there is water there is no Doctor and where there is a
Doctor that PHC docs not have running water. Should it take 6 months to get the pipes
connected when everything else has been installed?
The very location of PHCs is arbitrary. I believe it is helpful to do a survey of where the
PHCs are literally redundant- ie., that other PHCs are nearby and the PHC village is small &
isolated, and therefore unlikely to attract a Doctor. Such PHCs merely increase the numbers
without actually contributing to enhancing the health status of the population.
Costs
Several days over two hundred kms were covered. The entire costs- local travel, travel to
Bagalkot etc., exceeding eight thousand Rupees were not met by CHC.
Gulbarga Field visits
SECOND GULBARGA REPORT OF 2001
Nutrition, Epidemiology etc.
January 4, 2001; Written in Trivandrum & Bangalore
Sabu George
Nutrition Related
1. Assessment of Iron status of women after delivery
Thelma observed that Hemoglobin of the mothers were not being measured soon after
childbirth.
In the current situation where the iron status of both women and pre-school
children are poor; assessment and where required supplementation; at every instance when
women are at hospitals is necessary. Supplementation at the post-natal stage will improve
the iron status of the anemic and iron deplete women and also improve through breast milk
the status of iron deficient children. Note the iron levels of the mother immediately after
birth depends on her pre-pregnancy levels, diet and on the extent of blood losses during
delivery. Thus better quality of obstetric care has a role in averting reduction of iron levels
of a certain proportion of women.
The proposed hemoglobin assessment and supplementation should be made mandatory at
all 1’1 It s mid (iovl. I Inspitals.
2. Birth weights
At the CHC the birth weight data was suspicious as almost weights were rounded off to
500 grams. Several of the weights were 3.5 kg and one even 4 kg. The weighing balance
had 50 gram sub-division. This indifference to recording birth weights accurately is
common. Even in Kerala where over 95% births take place at Hospitals, trends on birth
weights are not available because of negligence in recording weights properly. As presently,
Karnataka is in a steep phase of increase in institutional deliveries, attention to recording
birth weights can help us to obtain good baselines on low birth weight incidence. Birth
weight is one of the most sensitive indicators of maternal nutritional status.
NATIVE EPIDEMIOLOGY; Gulbarga District Hospital Statistics
Surprised to find a detailed Annual Report of the District Hospital for the year 1999. The
statistics have been compiled with pride by the Medical Records Officer and the Hospital Staff.
Even a graph has been drawn. At one level the Report provide comprehensive information on
utilization of the beds, services and by whom.
Obviously, 1 looked for the existence of gender bias based on other knowledge, visits etc.
This data again confirms gender discrimination. For instance the number of boys using the
Hospital as inpatients are nearly 50% more than girls (1558 boys vs 1082 girls). This could not
be ascertained for out-patients as there was no disaggregation of children by sex. Just like in
Bangalore, Gulbarga women of marriageable age are several times more likely to be burnt to
death then men. This is likely to be the pattern over the last ten years (in the graph there is no
age disaggregation; only sex distribution). This excess risk for women is not occupational but
due to social causes as we know elsewhere from Bangalore, Dharwar, Mangalore etc. Therefore
the modem evil of dowry deaths is also present even in the most backward part of the State.
Not surprisingly almost all the sterilizations are on women (603 vs 2). Disturbingly, the
number of cataract surgeries done was only 346. Note that there is at least one Ophthalmologist
among the senior Medical Staff. Gross underutilization of Ophthalmic facilities is obvious even
when one looks at the OPD numbers. There is evidence that the hospital birth information is
probably credible. As seasonality is seen in the current year and the patterns are consistent over
the years.
Another useful purpose these statistics serve is to set up targets for improvements over
the next few years. Credible targets arc extremely important for motivating the system to
perform better. It needs to be kept in mind that the Health & Family Welfare system have aterrible record of manipulation in the country. In the routine health information system-Family
planning, immunization, mortality data have been cleverly made up for decades. Therefore even
to have reasonable estimates for targets has sometimes been difficult.
Targets have become common in developmental planning for about 3 decades. They
were borrowed from Management practice. Initially targets were pious dreams - mere statement
of intentions and too general. For instance, the 1974 World Food Conference had the goal:
“Within a decade no child will go to bed hungry, that no family will fear for its next bread, and
that no human being’s future and capacities will be stunted by malnutrition”. Regrettably targets
are often chosen without much thought. This defeats the very purpose of targets- to mobilise
public support & generate political will, and to raise resources. I deliberately elaborate on this as
some of the targets in the HNP Draft Proposal are problematic (For instance the MMR estimate
2
is absurd- Such figures will only spawn fraud). Given the sad reality that many past targets have
not been achieved in Karnataka and therefore such elusive figures are not likely to be taken
seriously. As Maxwell has said about food security targets- Targets have been repeatedly set,
repeatedly not achieved and repeatedly, so to speak repeated. This would be true of Karnataka
targets for the child. Therefore, I hope we will have credible targets that are achievable in a
definite time period. We cannot use targets like slogans (‘Health for AH’):
Measles Immunisation and ANMs
When Doctors were asked about Measles immunisation coverage the general response
was that children are all fully immunised. This was the same response during the last visit. The
independent Survey data like RCH reveal that coverage is poor. Therefore measles
immunisation is not taken seriously. In the Border Area District areas (some specific taluks of
the Gulbarga region) the DJD is planning to organise special efforts to improve coverage. It is
worth monitoring to see how much of the promises made at the visits will be implemented over
the next year.
In Bidar there were 30 vacancies of ANMs (total of 234). The shortage is not as acute as
in Gulbarga but the challenges are formidable. As the ante-natal coverage is among the lowest in
the State as per the RCH Survey.
Conclusion
Our visit in December was a short one. Merely a day in each District. Thanks to the
support of the DJD and the DHO Bidar we accomplished a lot. That Thelma being a Task Force
Member helped in getting attention of the Officials. The DC & CEO gave time.
This visit was largely confined to Hospitals and meeting District Officials. Thus
complementing the earlier visit where I went to several distant villages and met Nutrition Staff at
various levels. Krishnan, Thelma and myself y/e practically covered most of the taluks of the
large Gulbarga District. Due to lack of time we were confined to the Southern part of Bidar
District.
We were informed that the local MLA took interest in the Taluk Hospital in Basava
Kalyan taluk of Bidar. The Health Minister has improved the functioning of the Gulbarga
District Hospital. Perhaps, we can enlist the support of interested MLAs to improve the Public
Health System and resist the Bank influenced privatisation of the Government Health
Infrastructure.
3
Gulbarga Field visits
FIRST GULBARGA REPORT OF 2001
Version dated January 2, 2001; Written in Trivandrum & final revision in Bangalore
Sabu George
Note
From this report onwards observations of both the visits would be included for brevity
(Sept & Dec). Nutrition and Epidemiology related matters will be in a separate report.
Details of the Visit in December
Thelma and I spent one day each in Gulbarga and Bidar Districts. Had discussions with
the Divisional Joint Director of Health, Gulbarga region, DHO Bidar, Gulbarga’s CEO, Deputy
Commissioner andLGiiy Commissioner. Primarily visited Government Hospitals including
District Hospitals and 2 Taluk ones in Bidar. One PHC and CHC was reviewed by Thelma.
Visited the Hyderabad Karnataka Development Board Office. Briefly met with Medical
Missionaries Dr. Abraham and the Salins Family at Aurad village, Gulbarga and Bidar city
respectively.
Note that the DJD came with us to the PHC at Kamlapur in Gulbarga District near the
Bidar border. Kamlapur was chosen as it was on the way to Bidar. The DHO Bidar received us
at the Border and was with us till 9.45 pm. The specific Hospitals visited were decided largely
by him (Thelma indicated that she wanted to see a CHC & the District Hospital).
Hospitals
The physical condition of the majority of the hospitals visited was.pathetic. The Basava
Kalyan taluk hospital is an exceptional one in that the Chief Doctor (26 years service) took
genuine interest in serving people. The very ambience of the Hospitals and the number of
patients present were indicative of the interest the concerned Doctors took in their Government
job. The Gulbarga District Hospital has over 750 beds and is even larger than the Hubli
Hospital. We reached the Bidar District Hospital at about 9.15 pm and saw two Doctors in there.
Malnutrition, diarrhea were seen in the District hospitals. The specific needs expressed by the
Doctors will be reported in a subsequent report.
2
All PHCs in Bidar have Doctors. The 5 vacancies are being filled by the DC. In a few
days they will be on duty. The DHO wants sanction for direct recruitment of Nurses in Govt.
Hospitals.
Drugs did not seem to be a major problem. There was supply despite lack of adequate
vehicles for distribution to every PHC. The KHDSP apparently dumps the Drugs into taluk
Hospitals without ascertaining what the particular needs are. Thelma enquired and found that
Pediatric Doses of TB drugs were unavailable at all the Hospitals.
In construction of new Buildings the concerned Engineers do not actively involve the
Doctors in the Planning and Execution.
In the CHC we visited the Construction was going on without the least concern for
patients admitted. They had no toilets or water.
In all the sub-District Hospitals we visited we were informed that they got only a few
cases of TB every month unlike in St. Luke’s where they see 2 new cases every day. TB hardly
could be a St. Luke outreach area problem. Either the Govt. Doctors are not recognising TB or
the patients are unhappy with the treatment provided.
The neglect of DJD
Nobody had told me either in Bangalore or in Gulbarga in September about meeting the
DJD. Note 1 met the CEO, DC and other medical officials at the District. All referred me to the
DHO only and not to the DJD. Dr. Pranesh appeared to be serious about his responsibilities. A
native of Gulbarga had spent 17 years in Raichur. Did know several of the good Doctors I met in
my last visit. He lamented about his serious limitations. He is provided with a 20 year old petrol
vehicle. Other Divisional Heads have vehicles that they can requisition. He has no powers to
purchase even a battery. To get sanction from the Director in Bangalore can take a year.
The diversity of controls of Hospitals was evident in Gulbarga. The District Hospital is
under the DME as it is a teaching Hospital and thus the DJD has no responsibility for the largest
1 lospital in his region.
Of course, DJD was not pleased with the bossism of the IAS Officers. They take
decisions without understanding the Health System. When Thelma asked how the present
Commisioner and Secretary are- They are better as they listen.
3
He said under the Border Area Scheme they are going to initiate measles immunization.
They have received disposable syringes for this purpose.
DC , CEO & Municipal Commissioner’s Perspectives
The Doctors and IAS views of the Health System were of course different. These are
well known. Nevertheless, the IAS perspectives will be critically reviewed in a separate report.
Certainly there was some truth in the concerns expressed by the Doctors but clearly there is a real
lack of will on the part of the majority of the Doctors to get the Health system functioning
properly. The Administrators have rightly attributed this indifference to the private practice of
the Doctors. The DC highlighted the fact that Health Dept, is unique among Government
Departments in that majority of its vehicles are never in working condition. Most Doctors do not
stay in their PHC. They do not maintain the Hospitals. There is little discipline among the
Doctors. No surprise that they have found that even Compounders practice and the ANMs take
bribes. The Government should ban private practice and provide compensatory allowance for
the Doctors to improve the functioning of the Health System. There does not appear to be
financial decentralization in the Health Dept. The Medical Officers claim that they have no
financial powers. While even a Gram Panchayat Secretary spent two lakhs a year. The DC
believes that the Doctors can utilize the Panchayat System if the Doctors actively work with the
members. The Medical Officer at the PHC should be given an Annual Maintenance Grant.
There are only 3 Laprascopic Surgeons in the Gulbarga District which has a population of
35 lakhs. Nobody at the top levels monitor the functioning of the Doctors at the PHC and taluk
level. Specific directives should be issued so that sterilisations are dohe every week rather than
once a month. All those who have received Post Graduation should be mandated to participate in
sterilizations. All PHCs should conduct institutional deliveries. Careful monitoring of each
Centre is required. The Health Department should give priority for these areas as it gives to
Pulse Polio.
There are few Lady Doctors and he is now giving priority for their recruitment. He felt
that the Training provided to the Panchayat members is routine. 100 people are called for a
session and are made to listen to 4 to 5 long speeches. Smaller groups are required for
meaningful interaction.
4
The CEO said that the Contract Doctors do not have powers to take action against erring
officials. Felt that in-service training of the Contract Doctors in public Health is important.
Asserted that there is money with the panchayats for maintenance. All the Doctors had told that
this was a problem. The CEO said that there was 5 lakhs per GP and that Doctors should take
the initiative. Corruption cannot occur without the connivance of the Doctors, therefore blaming
only the Panchayats is not fair. Informed that a young ZP member, Sherin Prakash from Sedam
is himself a Doctor- Lecturer in the Medical College.
The urban areas are not under the CEO. They come under the DC. There are 3000 Self
Help Groups including that promoted by DWCRA. These could be used for health promotion
activities. The Group Insurance Programmes of the GIC etc. could be used to provide better
economic security for the poor by covering some Health care needs.
The Municipal Commissioner did not appear knowledgeable about health matters. Was
unaware of Mahila Samakya. Claimed that Malaria did not exist. But said that they were
fogging insecticide regularly. The Gulbarga Municipality covers 5 lakh people. 32 slums exist
including 10 unregistered ones. There are 5 to 6 other Municipal towns and 3 town panchayats
in Gulbarga District. IPP8 has not yet started. Sanctioned and will function from January. The
DC will recruit Staff for 7 Health Centres and 1 male and female Doctor. He said that the IPP
bosses do not take our suggestions. They impose what they like.
The major health problems he saw were lack of health care for slums and no Hospital
waste management for the City. There are more than 50 Clinics and Hospitals in the City. He
said a Delhi based NGO- Environment Education Centre under one Suresh are planning a Waste
Management Programme. This is funded by the State & Central Govt, and will start in 6 months.
The Hospitals have to pay for collection, disposal and incineration. The Health Cess collected by
the Corporation is given to the State Govt. Acknowledged that there are many street children but
no organisation working on this issue
Medical Missions in Bidar: The Salins Family
I was very keen on meeting with Dr. Salins as I had heard of them from Dr. Benjamin.
The Doctor couple are Vellore alumni and evangelical Christians. By the time we finished with
the Bidar taluk hospitals it was 8 pm. After dinner al DHO’s house, went to Dr. Salins’s house.
Dr. Christopher Salins and his wife Dr. Sushila served in hospitals in Karnataka for 3 years and
5
finally came to Bidar in 1969. Served only 2 years in the Methodist Hospital as they were
removed for their evangelical zeal. Then established the Good News Society Hospital in the
City. They do Leprosy rehabilitation and also urban & rural outreach work and run a rural
hospital. Dr. Salins has done several thousand Cataract surgeries with Lions. Their daughter has
specialised in Ophthalmology and has done research on diabetic retinopathy. The exemplary
devotion of the Salins family has kept their Hospitals and outreach work going for three decades
in Bidar. They had to close clinics in adjacent towns of Maharastra and Andhra due to lack of
Christian Doctors. We were informed that the old Methodist Hospital in the city has been
revived by a Doctor couple who joined recently.
Like Dr. Abraham, we could talk about the isolation of Salins (see earlier Gulbarga
report). But this also reflects on others in the Community Health sector, who have not taken the
trouble to get them involved in active partnerships to further the health status of the people in the
most remote parts of Karnataka.
Learnt that Xerophthalmia in pre-school children remains endemic in the rural areas in
Bidar.
Roads are more important than Health for the HKD Board
The Hyderabad Kamatak Development Board was constituted in 1991 and the 39 MLAs
from the 5 Districts of the Gulbarga region are members. This gives the local MLAs effective
control over the large Budget. Annual budget is of the order of 100 crores. Proposals for
projects directly emanate from these members. Thus construction activities like Roads &
Irrigation get overwhelming importance while Health receives a low priority. Such priorities are
because of the profits for local level politicians. The DC said funds for Roads are available from
multiple sources- MLA’s fund, MP fund, Panchayat allocations etc. and therefore does not
provide money if he can for roads from sources under his control.
Told that Flourosis is a problem in some parts of Koppal, Gulbarga and Raichur.
Rationale for the HNP and for World Bank money
The Hospital facilities are grossly inadequate in the Gulbarga region. For instance, the
Bidar District Hospital has less than 30 beds for women after delivery. Several of the existing
Hospitals are dilapidated. Therefore given that the State is spending almost all its resources on
Irrigation and Power there is no choice but to seek World Bank money for the benefit of the
6
poor. The eagerness of the State Health officers is understandable. The Bank officials are also
keen on lending to Karnataka. Therefore, we have to be extremely determined to ensure that the
project priorities are decided on the basis of the people’s needs rather than on the current
ideological predilections of the Bank. Similarly, we do not have to oblige ambitious World Bank
staff who often distort projects to test favourite hypotheses so as to further their personal careers.
These concerns are not theoretical. Rather, this was very evident in the recent mission of the
Bank to Karnataka in November.
Hopeful Future for the poor and the disadvantaged
> fl
The only affordable hope for the poor is the Govt. System for health care and public
health. Therefore, we have to resolutely oppose the privatisation of tht/Health Sector. The
institution of the user fees has resulted in reduction of the Out Patients at the Bidar District
Hospital (1100 to 700). There is need for a detailed study to assess the consequences of various
c
kinds of user fees to the poor in the most backvyard region of the State. Uniform policies for the
v.
whole state in these matters may have to be challenged as it would most adversely affect the least
empowered sections of the Karnataka population.
At the same time we have to get the Government Health structures to be more responsive
to the people (importantly increase access, coverage, equity and quality). This is the challenge
for the proposed HNP Project. Just as in the earlier field visits to the Districts, this time also we
found dedicated Doctors working under adverse circumstances in isolated areas. Identifying
such exceptional individuals, motivating and supporting them is one way to strengthen the
existing system. The optimal functioning of few sincere Doctors in an otherwise indifferent
Government Health infrastructure can make a difference in the long run to empower some people
to demand similar quality standards in more Government hospitals.
1»
It is of utmost importance that CHC strive to build networks in each of the backward
Districts to safeguard the interests of the poor. Sincere Government Doctors, well meaning
private sector practitioners, non-fundamentalist Christian medical missionaries, good NGOs etc.,
can be the partners. Obviously, such alliances require a lot of nurturing to fructify (just the
j organisation of the State PHA was a herculean effort). This World Bank project process should
be used to create and foster such alliances. Cells and individuals have roles; but only collective
It ■
. -.-.t-CS.A
Hi
t
tr-., . ci, !
><■ . c-?7 ■'o .A,' -2-e. V.r
->d
/tcc'-
c (tJJ.xxuJled) .
efforts of organisations and alliances can take on the forces of privatisation; particularly when the
State is more than willing to accept World Bank’s prescriptions.
Towards a holistic understanding of the Gulbarga region
^$.0 J
The present visit covered the Health sector while my earlier visit focused on the
Anganwadi sector. We still have not touched upon the District or Taluk Panchayats^The
hostility of both the Health Department and the WCD staff to the Panchayat Raj is well known
and we were repeatedly told by the Doctors and the CDPOs about their difficulties with the local
Panchayals. Panchayat Raj has been blamed for interference in appointments and transfers;
corruption, nepotism, non-functioning of the Departments etc. The inadequate democratisation
of the society in this backward area is well known but still we need to meet with the elected
representatives to know their side of the story. For instance the Gulbarga DC said the Health
Department just does not want to be accountable. If the Doctors did their work, then they would
have less problems with the Panchayats.
Our impression of the Northern region after field visits is much better then the scenario
which was painted from the South. Things are not hopeless in the North and much better than
what we were led to believe. If improvements in the staffing and infrastructure do take place in
the next two years in the Health and Nutrition sectors then this itself may reduce the differentials
in the Health indicators over the next five years between the North and the South.
I believe an unexplored area that remains is the prejudice against Gulbarga people in the
->^j^XSouth of the State. Social backwardness, including a pernicious feudal past of course creates
cultural stereotypes but does that explain the prejudice of even well meaning officials and
Doctors? We have been told that the same officials who do well in the South fail to do well in
the North. The Northern people are lazy and do not work hard! Even the extreme climate has
been blamed for the underdevelopment.
The political causes of backwardness need also to be understood better. Right from the
1950s Northern Karnataka had its share of political power. Chief Ministers like BD Jatti (from
Savalagi, Bagalkot); Veerendra Patil (Chincholi, Gulbarga) etc. were from the North. The great
Nigilinjappa himself had to go to the North when he was defeated from South to enter the
Assembly. Several times the Gulbarga region had large number of Ministers. Two senior
ministers from Gulbarga- Dharam Singh and Kharge, representing disadvantaged castes have a
8
nearly three decade uninterrupted tenure in the Assembly. Influential Congress stooges like CM
Stephen, Sonia etc. who would not have won elections elsewhere from the South have used the
Northern Karnataka people to further their political careers. Now that CHC has given priority to
North Karnataka perhaps it will make some efforts to better understand the political economy
and social history of this neglected region. Health is Politics and therefore this larger project is
necessarily related to the task of enhancing the well being of the Northern people.
ICcvxel'etCc
iJuoKic-tn h j <-f~ r <_ .
he
.
AaVeeh
■ 1J
/b
SG
cKsvf c HC
if Ke cz> cnx.I<S;e-Le
,c"^y
ictt’c-
/<-K
AcCy zte yW<-A> L.-.- e "> t ly
5Aov/d Z2?
c+fx-)
REPORT ON VISIT TO GULBARGA DIVISION ON 21-22"d DECEMBER 2000
PHC GOBBUR (AFZALPUR TALUK, GULBARGA DIST)
The PHC is located on the main road itself 25 Km from Gulbarga (map attd). The PHC
covers a population of 288442 in 21 villages. It has 8 Sub-centres -Gobbur, Havenur,
Bidamer, Chowdapur, Chinamgera, Banderwal, Hassergundagi, Sagnur (30 Kms away)
with 8 ANM’s all residing in these villages. Old building with many patients in
attendance on time of visit (1130Hrs). Has three doctors- Dr Nagendra (since 7 1/2 years
living in campus, belongs to Mandya Dist), Dr Premalatha (since 8 yrs living in campus)
both present , and Dr Vijayalakshmi (51/2 yrs shuttles daily from Gulbarga) who was
away at the sub-centre (where I met her also). On an average OPD attendance 50-60
patients mostly fever, URTI, LRTI and Dysentry. During the month of November,
2049 OPD patients treated and 37 inpatients (tubectomy, delivery, post-cataract surgery)
and during October 1760 OPD and 41 inpatients were treated. Electricity erratic , average
3-4 hrs cuts. Stand-by generator available (kerosene run, 1988 vintage, Honda).
Family planning achievements during the year -155 tubectomies and 140 IUD insertions
(performed by all three though only Male Dr trained ).Cataract operations done by
visiting Eye surgeon -12.Two AFP cases reported ( Sangapur and Sagnur- both
negative). 170 deliveries in the year. Whole year 90 cases of malaria (Pv 80, Pf 10) 1999
130 cases (Pv 124, Pf 6). Total 7 cases of TB, 1 sputum positive being treated at DTC.
Others on TZ only. Filariasis one positive.
One Mahindrajeep (IPP III, 1983 vintage) on road.
Training -Dr Nagendra underwent the following training
CSSM trg
one week
1995 RHWTC,Gulbarga
RCH trg
one week
1997
(learnt tubectomy himself)
1998
FP trg
two weeks
Mgment( IPP IX)two weeks 1999
Admin trg
1999 Nazir Ahmed Rural Trg Centre Mysore.
Feels all this training is required but with better resource persons. Also feels the necessity
for CME’s.
Private sector- No MBBS doctors available locally, but 7 BHMS practicing in his area.
Two medical shops function at Gobbur and Chowdapur.
Drug supplies- All medicines from Taluka stores now since two years (earlier from Dist.)
Slight short supply in this PHC (all other PHC’s/CHC’s visited had adequate
quantity).Supply is twice a year (60% and 40%) apart from FP drugs and vaccines which
are indented monthly. Kit A and Kit B are directly issued to sub-centres. Under RCH
only four SC’s repaired 3 yrs back. Two SC’s (Hassergundagi and Chowdapur) do not
have own building and functioning from ANM’s rented house.
Voluntary Agencies- SOSVA (3yrs back from two villages) now 8 villages . Only link
workers keep in touch with ANM’s in RCH activities.
Anganwadis- 28 AW’s; visit 8-9 AW’s monthly (3 monthly all to be covered)
CDPO/Supervisor contacts.
During rainy season, the accessibility of the villages to the PFIC is almost nil due to mud
roads which are only accessible by bullock carts / tractors.
Monthly / Quarterly meetings of gram panchayats are held and the MOs attend (5 GPs)
The PHC has 3 HW (M) against 8. Telephone is available.
IMPRESSlONS:This PHC seemed to have been informed of our visit and appeared to
give a conducted tour. The MO even wore a lab coat. Since it has two LMOs, one could
be deputed to PHC Atanur.
SUB CENTER CHERANGERA
Was located about 15 kms away from the PHC Gobbur. The LMO Dr. Vijaylakshmi,
ANM Uma and HW (M) P.R. Diradhar were available. The SC building was good but
had no electricity supply to the non-living portion. The ANM had managed to get an
illegal connection to her residence portion. There were 52 cases registered for ANC of
which 36 had yet to deliver out of 2525 population. There was no BP apparatus available.
Kit A & Kit B were available and well stocked with RCH medicines. The HW (M) only
has to collect 22 slides for MP every month and chlorinate 2 GP wells.
IMPRESSIONS: Furniture, electricity and water should be available at the SCs. The
duties of HW (M) needs to be well defined.
ANGANWADI - CHOWDAPUR TANDA
Met AWW Shivleela and helper Thipamma. The AW had 68 children registered of which
18 were below 1 year of age, 20 between 1-2 years and 38 were 3-6 years. Average
attendance was 20 per day. The AW functioned between 9-12 pm only and the children
had left when I visited at 12:30 pm. Twice a week energy food (60 gram, one handful) is
given to the children. Mothers also collect for the other children. There were no toys, no
registers, no medical kit, no weighing machine. Growth chart was poorly maintained.
Nice building. Doctor had last visited on 18th October and done medical check up. ANM
had given immunization to 8 children and 2 mothers on that day.
IMPRESSIONS: The AW was typically of what we had expected.
PHC ATANOOR (AFZALPUR TALUK) GULBARGA DISTRICT
PHC located on main Afazalpur -Chandapur road and at one end. Another PHU now
updated to PHC Revoor with three sub-centres (Dr. Raghunath Kulkami) taken over
some of the villages from this PHC.
Only one doctor, Dr. Shivakumar K Manakar, who lives in the village in a two roomed
house (pays Rs.400/- rent and gets HRA of Rs. 222/- per month) was employed on
contract basis 5 years back and confirmed only one year back. (Contract salary Rs. 40006000, regular salary 7400 basic consolidated Rs. 10,400/-). Doctor belongs to Gobbur.
PHC building in good condition and compact design, built by HKD Board under MLA
fund (approximate 24 lacs) in 4 Acre land. No water source as bore-well failed after 6
months. One hand-pump located nearby. Building does not have meeting hall or
mortuary.
PHC covers two villages - Bhoganahalli and Sidanur and covers a population of 14,185
through 3 sub-centres at Atanoor, Malabad and Chinchur. Two ANMs and two HW (M)
(One ANM on deputation). All ANMs residing in the villages. Requirement of LMO felt
to handle the female patients. The gram panchayat of Atanoor village has all women
members and has hence been requesting for an LMO (which could be easily deputed
from Gobbur). The PHC has no vehicle, no generator and electricity is erratic. The
average OPD attendance is 40 patients.
2
FP operations earned out are 73/116 (November). IUD - 76 /125. 156 deliveries have
been conducted in the PHC by Jr. HA (I). 72 have been home deliveries under trained
Dais and only 19 deliveries have been by un-trained Dai. Average around 30 deliveries
per month. The Doctor has undergone adequate training courses but feels the requirement
of Tubectomy and MTP training.
There are 5-6 PPs in the area with BHMS /BAMS degrees.
Adequate supply of medicines with almost all antibiotics and no shortage of different
categories of drugs. (Supplied twice a year 60%, 40% ) Family Welfare indent as
required. No problem at sub-centres also.
There has been an epidemic of 36 cases of GE in one and a half months in Siddanur
village of which 4 were positive for Vibro Cholera. There have been 9 cases of Pv +
malaria and no sputum + case.
There is a good labour room (without tiling) but no delivery table. Mattresses having a
life of 1 -2 years only. There is a shortage of one pharmacist, one senior HI and two
group D employees. There is no telephone connection.
Doctor was highly motivated and had a beautiful brief of the activities and statistics of his
PFIC which he has given to the visitor.
IMPRESSIONS: The_PHC seemed to be a model compact PHC and even the building
could be the type of pattern for further constructions. Dedicated MOs should be
acknowledged and also contract service should be counted for their government service.
This would help them in getting their speciality.
TALUK HOSPITAL (AFZALPUR)
Was located on the main road and has two doctors. Dr. C.V. Takkalaki - the Taluk
Health Officer was supposedly away on tour and the other doctor Dr. Baburao Bellar had
reported for duty only at 3 pm. Presently 30 bedded but has hardly a few beds on the
verandah due to lack of space (supposed to be a 50 bedded hospital). Behind this
building, is a beautifully constructed 12 bedded hospital under HKD Board which is
under litigation since 5 years due to land encroachment. Recently IPP9 is looking out for
land to construct a new hospital. Phone is available. Average OPD 70 patients per day.
No admissions as no ward available. No toilet and no drinking water available. Ding
supply adequate. Surprisingly has no posted supervisory staff since three years and only
has deputed staff. Lab equipment satisfactory. X-Ray machine remained uninstalled for
one full year finally installed two months back, worked for few days and is again non
functional. X-Ray technician available. Deep-freezer and generator available.
IMPRESSIONS: The situation the hospital seems to be contrived to avoid providing
health services to the population who require it. Either the portion of the building
encroaching on the private land should be demolished (loss of a few lakhs) or a few lakhs
should be paid and out of court settlement done so that the building could be used by the
hospital. The proposal to construct another hospital seems quite ridiculous. Posting of
new set of staff could go a long way in reviving the collapsing hospital.
PHC ALMEL (SINDAGI TALUK, BIJAPUR DISTRICT, GOIP)
Three doctors were available of whom two are staying in the campus. Dr. S.S. Bajantri
(1995), Dr. Preeti S.J., LMO (5 months KHSDP regular) and Dr. Savitri Kinigi, LMO
3
(2 years). Have full staff except for shortage of 2 ANMs and pharmacist post vacant
since three years. Covers 8 villages through 5 sub-centres ( Bomanahalli, Devangam,
Kadni, Almel with two SCs and Mandanhalli which is vacant). Three HW (m) out of 6
available. PHC covers 34,000 population. Drug supply adequate, no standby generator,
vehicle condemned and transferred out. Has 15-20 deliveries every month. Malaria + 2-3
cases per month. 11 Sputum+ cases of which 4 under RNTCP and 10 under NTCP. Has
telephone. Has three gram panchayats of which Almel GP has one lady GP. Doctors
regularly attend GP meetings every month. Regular anganwadi medical check-ups are
earned out in the 21 anganwadis and CDPO meets regularly in the sector meetings.
Very old dilapidated building and roof leaking. Needs a new building urgently as doctors
residing in the campus itself and sufficient 5 acre land available. Also has an ANM
training centre in which 10 students are undergoing 4 month course. The hostel building
has become unsafe so they are residing in one of the staff quarters.
There are 4-5 MBBS doctors and 9-10 others in the area with 6 medical shops close by.
Doctors have had reasonable amount of training but feel the requirement of skill based
training in MTP, Tubectomy (including laparoscopic), anesthesia and medico-legal.
Doctor states that he has done 30-35 autopsies during his 5 years of service.
IMPRESSIONS: The PHC has dedicated staff staying in the campus and yet no proposal
to construct new buildings etc. are planned. Such PHCs should be given preference for all
major construction work. Re-distribution of LMOs by deputation should be done so that
no PHC / CHC I Hospital have more than one LMO. Training of all staff on MTP,
Tubectomy, Medico-legal, is a must to enable them to function more efficiently.
PHU STATION GANAGAPUR - AFZALPUR TALUK
PHU upgraded to CHC - 4 years back.
Dr. Suresh W Nayak ( 6years 6 months) is the present MO in charge. Shuttles daily by
Udayan Express from Gulbarga. Underwent training in management and orientation
training under IPPIX. Assists in Tubectomy. Feels he requires training in Administration,
Induction training and medico-legal training.
(Dr. M.S. Sangolikar now in CHC Nimbarga, Aland Taluk was earlier in this PHU for
10 years and lived in the campus.)
Has 3 SCs with 4 ANMs and 4 HW (m) covering 4 villages with about 10,000
population. One sub-cenrtre building ready but not handed over. All sub-centres have kit
A and B. No lab Technician but microscope available. Adequate quantity of drugs
available. 4 acre land available Average OPD 90-100,. 15-20 in-patients a month.FP 100
tubectomies achieved Malaria 6 cases per month. 6 Beds occupied with 6 Cases of
tubectomy were seen.
Village water supply pipe line not adequate. No independent supply. Requires a bore
well. No generator, PHC Devangangapur 10 Km away. No phone, no vehicle
ANMs living in quarters
IMPRESSIONS: Water supply and electricity should be a priority for all PHCs, SCs,
CHCs and hospitals. Communications like telephone and vehicle is a must to reach the
SCs.
4
PHC DHANGAPUR-ALAND TALUK (Not visited)
Spoken to the MO, Dr. Satish Patil (2-1/2 Years contract basis). Has 4 SCs. PHC
Building built under MLA fund 10 years back without plastering without electricity and
water supply. But were asked to occupy the same and has been functioning from it since
then. No repairs /additions / alterations possible since under controversy. Needs urgent
attention. Located 5 kras from CHC Nimbarga.
IMPRESSIONS: The government should evolve a policy to overcome such technical
snags and attend promptly to such functional PHCs rather than constructing in locations
where no doctor seems interested to work.
CHC NIMBARGA (ALAND TALUK), GULBARGA DISTRICT.
Dr. M.S. Sangolikar DCh. As mentioned earlier was in PHU Ganagapur, now recently
taken over the CHC. Shuttle daily from Gulbarga. (I collected all three doctors from the
Railway Station at 5 pm and visited all the above three medical units).
Good building with 30 beds. No Doctor earlier for 2 years. In 4 acres campus with 6
quarters except for MO all other staff are residing in the campus. 3 wards, no vehicle,
telephone available. Adequate medicines were available.
25-30 family welfare operations per month (only tubectomies), 32 malaria cases so far.
GE outbreak in village Nimbarga Tanda with 35 none positive for cholera. Immunization
adequate.
Beautiful operation theatre already available. One additional operation theatre and admin
block seems to have been sanctioned under IPPIX. Requirement of X-ray machine. X-ray
technician posted with CHC, presently under deputation out. No labour room available
which should have been the priority. Lab technician with two microscopes also available.
2 cases of TB detected and treated from other PHCs. Daily OPD attendance 90-100.
Since large OT already exists, only needs slight improvements. There is however a
requirement of labour room, admin room, post mortem room and X-ray plant.
IMPRESSIONS: It is typical of the CHC to have only one doctor and functioning only
as a PHC since its upgradation 3 years ago. Plans to construct additional OT etc. has no
meaning if no staff will be available to perform surgeries. The population also is too
small to have sufficient surgeries.
YADGIR TALUK GENERAL HOSPITAL(GULBARGA)
Taluk Health Officer P. Vijayakumar Paediatrician 1991 was not available.
Dr. R.N. Katti Surgeon 1995 briefed about the hospital.
Dr. G.D. Hunkunti surgeon 1990.
Dr. Thenga Kulkami LMO 1991
Dr. Neelamma LMO 2000
Dr. B.C. Patil Dental 2000.
Old 24 bedded hospital now shifted to new campus. Now supposed to be 50 bedded
hospital since 1992 further being upgraded to 100 bedded hospital under KHSDP. Bed
occupancy only 25-30 only tubectomy.
No anesthetist since 1992. Gynaecologist, Physician, Eye Surgeon post vacant. OPD
attendance 250-300 daily. 2 MOs quarters only.
5
Mobile vehicle ophthalmic unit (van) off road since 1 year due to burst tyre. Tempo Trax
of THO off road due to engine seize (lack of engine oil). Matador Ambulance on road.
Old X-ray machine functioning from old hospital 2 kms away. New X-ray machine
maybe installed through KHSDP. X-ray technician and Lab technician available. No
ECG machine available.
Malaria 500 slides per month examined. 190 positive of 5746 slides examined.
Operation Theatre in good condition with one working AC out of two. Used only for
Tubectomy operations. One more OT sanctioned recently. Surprising since no major
surgery performed since 10 years inspite of 2 surgeons being available. Also no cataract
surgeries being performed and figure of operations carried out by Mission Hospital are
reflected in the Government reports.
642 tubectomies performed (50-60 per month) includingl5 PHCs and 1 CHC covering a
population of 3,29000 of which closest PHC is Mudnar 4 kms away and the furthest
Kadechur 65 kms away. Adequate drugs are available.
Very old Dental chair available. Needs replacement.
IMPRESSIONS: This taluk hospital seems to have a very poor reputation with Doctors
not available most of the time. Even the team from KHSDP which had visited went back
without meeting anyone as they were offended as no one was available. Surprisingly the
2 surgeons only performed tubectomies in their long stint in the hospital. Construction of
an additional OT seems ridiculous and a waste of money. Since they have a dental
surgeon, it is logical that a good dental chair and equipment should be provided to
improve dental services. Lifting of cataract surgeries statistics from the Mission Hospital
nearby should be al some benefit to the NGO by providing lenses etc. The poor state of
vehicles shows the lack of concern by the Government staff. The workload seems to be
less for so many doctors and suggests that they are busy with their private practice.
HOLSTON MISSION HOSPITAL - YADGIR
Met Dr. M.C.Benjamin an eye specialist, who is the only doctor available in the hospital
with a handful of staff. The hospital had 100 beds and basic specialists like surgery,
medicine, Gynae, dental and eye earlier and was very popular. Since the locating of the
Taluk hospital nearby, the clients have reduced as Government facilities are totally free.
Also due to internal politics and poor management, the hospital has lost its capacity to be
a good hospital. The hospital gets another eye specialist trained in IOL from Gulbarga
city twice a month and performs cataract surgery. They have performed around 200
cataract operations. The hospital could be revived by support from the Government as it
has excellent facilities.
OPEC HOSPITAL RAICHUR
Dr. M.B. Karkenewar, Addl.Project Officer, KfW and Addl Director & Spl Officer
OPEC Hospital since 01 October 2000 was available and briefed about the hospital.
Hospital was inaugurated on 18th October 2000 and two teams from NIMHANS (1 neuro
physician and 1 neuro-surgeon)& Jayadeva Institute of Cardiology ( 1 cardiac surgeon, 1
cardiac anesthetist and 1 cardiologist) were attached for one month. Subsequently only 1
team from Jayadeva is functioning at the hospital. Also two new MBBS doctors (one son
of DJD Gulbarga) have been employed.
6
Super-speciality hospital with seven specialities- cardiology, nephrology, neurology,
bums, orthopaedics, plastic surgery and dental. Has latest generation of equipment
excluding MRI. One Lady Bio-medical engineer was available to show the equipment.
Has meager staff of 2 staff nurses, 1 clerk, 1 computer programmer, 1 pharmacist, 1
biomedical engineer, and 15 cleaning staff and 1 driver. Vehicle is from district hospital.
The operation theatres seem spacious but the doors do not close flush which is required in
an OT. Also AC vents are being installed as an afterthought showing that user interface
has not been taken into consideration.
Due to leaking roof of district hospital, about 100 beds are being transferred to this 350
bedded hospital. The project officer is due to retire on 1st March 2001. Work-load of the
hospital has been only to work up the cardiac patients and further referral to Bangalore.
IMPRESSIONS: A beautiful 350 bedded hospital gifted by OPEC to the Govt for the
poor people of Raichur and Gulbarga region. Due to inability of the State to run the
hospital (reqd budget 10 Cr /annually approx) seems to be a deliberate hurry to privatize
it defeating the very purpose of the gift. The very idea of keeping a low motivated person
to oversee the functioning speaks volumes. Ideally the hospital should start functioning as
a multi speciality hospital with all specialities like surgery, medicine, eye, ENT, dental
etc. and then build up into a super-speciality hospital once its bed occupancy increases
then automatically it can be reduced to only super-speciality beds. No attempt was made
to train local speacilists in super speciality to cater to the local need. It would not be
possible to sustain the hospital by importing specialists. Attempts should have also been
made to rope in philanthropic organizations even IT industry to raise 10 Cr. Annually and
run the hospital for the purpose for which it was originally designed.
7
<6
Sk/t
JZ- ,
7/«A/
REGIONAL DISPARITIES - GULBARGA DIVISION & BIJAPUR DISTRICT
Some of the impressions regarding regional disparities in Gulbarga Division and Bijapur
District after visiting the areas are outlined briefly below:
(I am not very certain that these observations would not be seen in other distr icts of
Karnataka also).
Roads:- Roads from Gulbarga on the Gulbarga Afzalpur -
Bijapur axis and roads
towards Yadgir taluk and from there to Raichur and within Gulbarga district itself were
of poor quality, uneven and full of deep pot holes. Further roads going into the taluks
were made of stone and very uneven. Roads leading into the villages were basically mud
roads and hence during rainy season the villages arc inaccessible by regular mode of
transport, which is practically for 3-4 months every year. This is quite in contrast to
many of the villages in Uttar Pradesh (BiMAROU state) where grampanchayats have
constructed brick roads to connect their villages to the main roads. These are long lasting
and easily repairable by local labour / shramadhan. Also brick kilns are found all along
the roads so bricks are cheap & easily available locally.
Transport:- Though state buses do fly on these roads they are infrequent and irregular.
Predominant nyftie of transport are pirate Mahindra Jeeps which cover short distances of
5-20 Kms and charge individuals accordingly. These Jeeps are over-crowded (more than
10 nasseneers) but seem to meet the needs of the neoole. Even the supervisory staff
infitodtog, MQ’o / L-AAO’q have to dapgnH an thio to visit SC’o and villages where no
tranOnOtt
ucUibpviL to Avuuuvic- nt
cU +Ur»
mv ittv o
vi ity ui
A i flic*
ono Jvvpo
Toano
rxv
wv vuu rs
vxf* tKcs
uiv zlorr
uaj f1-»
mvov
are available at the villages and the MO’s stated that they were used (without prejudice)
to transfer serious patients to the nearest hospital, whenever need arose. During rainy
season only bullock-carts and tractors could f)^ on the mud roads, otherwise villages
were virtually cut off from all services.
Electricity:- Electricity was only available in revenue and a few other villages. Most of
the PMC’s had no electricity supply during the time of visit. The MO’s stated that supply
was low voltage, erratic and with frequent unscheduled cuts varying form 2-8 hours a
day.
Water Supply:- Most of the PHC’s /CHC’s /few taluk hospitals did not have a proper
water connection and were dependent on the villages for their water requirement. They
had locked up the toilets to prevent patients from using the same in the absence of water
supply.
Epidemics:- During summer months out breaks of Gastro enteritis (many due to cholera)
were common. PHC Gobbur (Afzalpur Taluk) had 27 GE cases with 1 positive for
cholera this year (2000). PHC Atnoor (same taluk) had 36 GE cases with 4 positive for
cholera within 116 months in Siddanur village. CHC Ninibarga (Aland Taluk) reported
35 GE cases (nil positive for cholera) from village Ninibarga Tan da
Communicable Diseases:- Malaria seems to be a major problem in these areas though
under reporting is common. Raichur District is notorious for all types of Malaria
Benign mixed and Tertian Malaria, Urban Malaria, (cross-border) Migrant Malaria,
Tribal Malaria and chloroquine resistant Malaria. PHC Gobbur had 90 cases of malaria
(80Pv+10Pg) in 28,842 population of 21 villages (interestingly HW (M) at SC
Chirangera stated that he was required to collect 22 slides for fever cases in a month
under NMEP and chlorinate only two GP wells in his duties). PHC Atnoor had 9 cases of
Pv in 600 cases of fever in which slides were taken (Population 14,185 in 9 villages)
CHC Ninibarga reported 32 cases of Malaria and other PHC’s /CHC’s and taluk hospitals
reported 2-5 cases of malaria in a month (Gross under-estimate). Taluk hospital Yadgir
covering a population of 3,29,000 from 15 PHC’s and one CHC examines about 500
slides per month. They had 190 positive cases amesst-of 5,746 slides examined.
Tuberculosis:-was hardly being detected and this is a major concern. Most of the PHC’s
/CHC’s /Hospitals had detected nil to 10 cases ofTB in the whole year. This is inspite of
the fact that all of them had 1-2 microscopes and lab technicians. Only two drugs for
treatment of TB were available (]NH and thiacetazone).
Buildings:- Some of the PHC’s in Gobbur, PHC Almel (Bijapur district, Sindagi Taluk),
Taluk Hospitals Afzalpur were housed in dilapidated buildings and definitely need new
buildings. Many PHC’s /CHC’s and Taluk hospitals had good buildings and only needed
electricity, water supply and few minor repairs / maintenance. However, name of these
were comparable to the excellent PHC /CHC buildings of many of the districts of Uttar
Prjadesh which I had visited (constructed under IPP HI). Most of the PHC’s /CHC’s
Hospitals were on 4 acres of land with or without boundary walls.
Private Sector:- Most of these districts did not have private MBBS doctors near villages
or even in Taluks. A handful of quacks, BAMS, BHMS etc practiced in the taluks and
this was corroborated by the handful of Medical shops in these areas. Nursing homes and
specialist clinics were confined to the District Headquarters and many of these in
Gulbarga & Raichur were of a high standard.
(Hence I feel that task force could
recommend that licensing of practioners of other systems of medicine should be more
stringent and permission given for practice only at taluk & below levels^)
Position of Staff:- On the whole position of crucial staff at PHC’s /SC’s were adequate.
Most of the staff were residing in the staff quarters or villages for long durations. Staff
position in CHC’s & Taluk Hospitals were very poor with CHC’s being manned by
single doctors and with deficiency of most technical staff
Training of Staff:- Could determine only training needs of MO’s. Most of them had
underwent training for 1-2 weeks duration every year (especially under IPP IX).
However, they commented that the training was stereo-typed and unimaginative and
hardly skill-based.
They all felt the requirement of skill-based training in MTP,
Tubectomy (including Leparoscopic) and Medico legal. (This has also been identified by
RCH and other Trainers). Also need for CME’s (atleast twice a year) and involvement of
Medical Colleges/ Consultants as resource persons at RHWTC’s was felt would improve
their professional knowledge & skills.
Medicines:
Except Gobbur PHC all the other centres were well stocked with drugs
which arc received from GMS through District I Taluk stores in two allotments of 60%
and 40%. Also stocks received from other programmes especially RCH (kit A and B for
SC’s) ensured adequate stock of quality medicines.
Family Welfare:- Deliveries were being carried out in the PHC’s as well as in the
villages by trained and untrained Dais. . PHC Gobbur had conducted 170 deliveries and
155 Tubectomies (140 IVD insertions), PHC Atanoor 156 deliveries in PHC, 72 in
villages with trained Dais and 19 with untrained Dais. They had done 73 Tubectomies
and 76 IVD insertions. Vasectomy had a low priority. In fact a team from Regional
office of H & FW had organised camps of non -scalped vasectomy during the period of
our visit in Gulbarga region and succeeded in conducting only 7 cases. Taluk hospital,
Yadgir who had planned 4 cases could not get even one case. They conduct about 50 -60
tubectomies a month(642 during the year). CHC Station Ganagapur had conducted 100
tubectomies and CHC Ninabarga 25 -30 per month.
Cataract Operations:- Conduct of cataract
Gobbur had managed 12 cases.
operations have been discussed.
PHC,
Surprisingly, at Yadgir Taluk hospital no cataract
operation was conducted and they only reflect the cataract operations conducted in
Private Hospitals / Mission Hospitals locally.
The Holston Mission Hospital had
conducted 200 10L cataract surgeries by getting the Eye Specialist from Gulbarga city
twice a month. The mobile ophthalmic van (matador) of the Taluk hospital was offroad
since 1 year due to a burst tyre.
Immunization:- Routine immunization seems to be going on in a passive manner with
no extra effort to reach every infant in the village. There was adequate quantity of all
vaccines in all the PHC’s /CHC’s / Hospitals visited and records maintained. Cold chain
seemed adequate though many CHC’s / PHC’s had no stand by generator, (some of the
PHC’s visited would not open the deep freezers for inspection to avoid loss of cold,
which was appreciated).
At one anganwadi visited (Chandapur Thanda under PHC
Gobbur) 8 babies were given immunization including 2 measles and 1 booster dose and 2
pregnant mothers were given TT.
Taluk Health Officer:- Providing vehicles (Tata Sumo / Tempo Trax to THO’s seems
to be more a bane
than a boon to the provision of health services. 'They were absent
wherever we visited and teed back from the field indicate that they do not visit the PHC’s
CHC’s as frequently as they should.
:Skkre gio naldis p ari tie s
December 29, 2000
REPORT OF VISIT TO GULBARGA DIVISION - DECEMBER 2000.
Three CHC team members (TN, SKK, SG) who are part of the HNP team evolving the
Karnataka Integrated Health Nutrition and Family Welfare Services Development Project
proposal, with the Directorate of H & FW, GOK, spent two days, 21st and 22nd
December, 2000, visiting health institutions in Gulbarga Division and holding discussions
with Government officials and NGO’s regarding the proposed project.
The visit was facilitated by the Commissioner, H & FW and coordinated and organised
locally by the Divisional Joint Director of Health & FW, Gulbarga Division.
The team divided into two for greater coverage of field visits. Due to good
organizational support from the DJD and local officials and members were able to visit
institutions in Gulbarga, Bidar and Raichur districts and one in Bijapur district
Visits made included;
1.
PHC’s
a)
b)
c)
d)
e)
2.
CHC
a)
3.
Humnabad, Bidar district.
Basavakalyan, Bidar district.
Yadgir, Gulbarga district.
DISTRICT HOSPITAL
a)
b)
5.
Mannaekeli, Humnabad Taluk, Bidar district.
TALUK GENERAL HOSPITAL
a)
b)
c)
4.
Kami apur, Gulbarga district.
Gobbur
Afzalpur
Dangapur
Almel, Bijapur district
Bidar
Gulbarga
OTHER HOSPITALS
a)
b)
Raichur OPEC hospital.
Gulbarga cancer hospital, (linked to Kidwai Institute o Oncology,
Bangalore).
c)
6.
Gulbarga DTC (closed for lunch)
NGO INSTITUTIONS
a)
b)
c)
St. Luke’s Mission Hospital - rural Gulbarga (20 km away from town)
Bidar Methodist Hospital.
Mission Hospital, Yadgir.
Discussions held with:
1.
2.
3.
4.
5.
6.
7.
Dr. A. Pranesh, DJD, Gulbarga Division.
Dr. Nimbur, DHO, Bidar.
Mr. Maheswar Rao, CEO, Gulbarga
Mr. Lakshmi Narayan, DC, Gulbarga
Hyderabad, Karnataka Area Development Board Official.
Municipal Commissioner, Gulbarga
Doctors and some staff from institutions listed above.
Impressions, findings and suggestions for the HNP project.
1.
Development of detailed strategies for the special package for category ‘C’
districts, through consultation with local officials from health and related
departments is required and welcomed. It is preferable if a planning meeting is
held in Gulbarga to allow wider representation. Officials there also feel that the
meeting and its venue in Gulbarga would signify the importance given to the
region.
2.
The facility survey will need to be carefully and objectively carried out, with
physical verification. Duplication of facilities, OTs has been noted. Different
interpretations are sometimes given and certain items may be omitted by
- respondents, to suit their convenience, if not objectively done.
3.
There are a number of people with commitment and enthusiasm in the region who
need support and encouragement.
4.
Vacancies continue to be a problem e.g. of ANMs in Gulbarga district. Bidar
district is better placed. Recruiting more lady Medical officers may need to be a
priority. There are 24 LMO’s out of 100 in Gulbarga However, data about their
distribution in PHC’s is what is important Filling vacancies of common health
personnel, will help improve access to health care by women and to better the
performance in MCH and RCH, which is low for these districts.
5.
The DJD reportedly has inadequate resources and powers, both financial and
administrative. The DHO’s, technically under him, are administratively under the
ZP. Hence his role gets limited. For quality of care to be improved, supervision
and accountability for all aspects of technical work will need to be stronger. The
ZP does not have the capacity or expertise required to perform this role.
6.
Quality of work was variable in the institutions visited. Illustrative examples are
given.
6.1.
In Huinnabad Taluk General Hospital - There were hardly any patients. The only
patients in one ward were a mother with a newborn child. Their bed had no sheet
and the room was dirty. When asked for the chart - the baby was supposed to
weigh 3 kg. On verification, it was 2.4 kg. We were later told that the wrong
chart of a discharged patient was mistakenly shown to us, which indicated sloppy
work, considering there was only one patient. The mother’s hemoglobin, a
routine investigation, was not done, though she looked pale. This level of care
does not meet basic standards.
6.2.
We were told that there were 400 out patients everyday in the above hospital. The
registers recorded about 200 patients for that day. The column for diagnosis was
filled mainly by symptoms of fever, backache, GBA (generalised body ache).
Provisional and final diagnosis needs to be more professional, especially at this
referral level, where specialists ran the sendee. This database for any disease
surveillance system is inadequate and would produce misleading results.
6.3.
Hospital / health care waste management was a concept not understood or
practised in any of the institutions visited.
6.4.
Toilets were blocked in the CHC visited and environmental cleanliness was poor.
All 3 doctors in the CHC were MBBS and 1 on leave was an Auyurvedic
physician. There were no specialists as required at an FRU. However, they were
enthusiastic and eager to learn. There were 3 people from one family with high
fever, who had come in at about 4 pm that evening. By the time we reached a
little after 5 p.m. blood smears had been done by the CHC laboratory technician
and they were found to be positive for malaria (P.vivax). Treatment was being
initiated. This CHC had weekly F.P. operations performed by specialists who
come in. A number of post operative patients were admitted in the ward.
Registers revealed a fairly larger out- patients load. The number of sputum AFB
tests done was small, with very few TB patients on treatment The doctors were
keen to learn more about TB treatment and TB control.
They were also open to have a medicinal herbal garden in their vast compound.
6.5.
The Basavakalyan Taluk General Hospital was efficiently run and very busy. The
Gynecologist (LMO) was upto-date with all dimensions of work of the hospital,
including the renovations being undertaken under KFW. There were a large
number of patients at around 3 p.m when we visited. These appeared to be good
teamwork among the staff Records were well maintained. The institution looked
more cared for and clean.
ilc >(c afe sfe
POLICY BRIEF
Go^l H -Y/.
One of the best ways to judge the well being of the
people of any nation is by examining the standards
of health that ordinary people have attained.
Healthy living conditions and access to good quality
health care for all citizens are not only basic
human rights, but also essential prerequisites for
social and economic development. Hence it is high
time that people’s health is given priority as a
national political issue. The current health
policies need to be seriously examined so that new
policies can be implemented in the framework of
quality health care for all as a basic right. The
following sections first take a look at the hard
realities of people's health in India today, and
Infant and Child mortality snuffs out the life
of 22 lakh children every year, and there has
been very little improvement in this situation
in recent years.: We are yet to achieve the
National Health Policy 1983 target to reduce
Infant Mortality Rate to less than 60 per 1000
live births.- More serious is the fact that the
rate of decline in Infant Mortality, which was
significant in the 1970s and 80s, has slowed
down in the 1990s, (See graph below)
130.000 mothers die during childbirth every
year. The NHP 1983 target for 2000 was to
reduce Maternal Mortality Rate to less than 200
per 100,000 live births. However, 407 mothers
die due to pregnancy related causes, for every
100.000 live births even today.1 In fact, as per
the NFHS surveys in the last decade Maternal
Mortality Rate has increased from 424 maternal
deaths per 100,000 live births to 540 maternal
deaths per 100,000 live births?
examine some of the maladies of recent health
policies. Next the availability of various resources,
which could be utilised for an improved health care
system is discussed, finally followed by certain
recommendations to strengthen and reorient the
health system to ensure quality health care for
all. We hope these recommendations will be
incorporated by political parties in their election
manifestos for the upcoming general election as
a demonstration of their commitment to public
health. Jan Swasthya Abhiyan, a national platform
working for people’s health, looks forward to such
a commitment from all political forces in the
country.
•
Three completely avoidable child deaths
occur every minute. If the entire country were
to achieve a better level of child health, for
example the child mortality levels of Kerala,1
then 18 lakh deaths of under-five children
could be avoided every year. The four major
killers (lower respiratory tract infection,
diarrheal diseases, perinatal causes and
vaccine preventable diseases) accounting for
over 60% of deaths under five years of age are
entirely preventable through better child health
care and supplemental feeding programs? The
most
recent
estimate
of complete
immunization coverage indicates that only
54% of all children under age three were fully
protected?
, About 5 lakh people die from tuberculosis
every year18, and this number is almost
unchanged since Independence!19 20 lakh new
cases are added each year, to the burgeoning
number of TB patients presently estimated at
around 1.40 crore2 Indians 1
•
India is experiencing a resurgence of various
communicable diseases including Malaria,
Encephalitis, Kala azar, Dengue and
Leptospirosis. The number of cases of Malaria
has remained at a high level of around 2
million cases annually since the mid eighties.
By the year 2001, the worrying fact has
emerged that nearly half of the cases are of
Falciparum malaria, which can cause the
deadly cerebral malaria. The outbreak of
Dengue in India in 1996-97, saw 16,517 cases
such deaths might be prevented by tobacco
control measures2.
r
and claimed 545 lives3. Environmental and
social dislocations combined with weakening
public health systems have contributed to this
resurgence.
•
•
Diarrhea, dysentery, acute respiratory
infections and asthma continue to take their
toil because we are unable to improve
environmental health conditions. Around 6
every 5 minutes5!
lakh children die each year from an ordinary
illness like diarrhoea. While diarrhea itself
As a nation, today there is a need to look closely at
the deep problems in the health system, rather
than making exaggerated claims. There is a need
to recognize the growing health inequities, and
urgently implement basic changes in the health
system.
could be largely prevented by universal
provision of safe drinking water and sanitary
conditions, these deaths can be prevented by
timely administration of oral rehydration
solution, which is presently administered in
only 27% of cases3.
•
Estimates of mental health show about' 10
million people suffering from serious mental
illness, 20-30 million having neuroses and 0.5
to 1 percent of all children having mental
retardation2. One Indian commits suicide
With political will and people’s involvement,
ensuring good quality health care for every Indian
is possible!
Cancer claims over 3 lakh lives per year and
tobacco related cancers contribute to 50% of
the overall cancer burden, which means that
The growings inequities in health and. health care are unjust!
The Constitution of India guarantees the ‘Right to
Life’ to all citizens. However, the dispanties relat
ing to survival and health, between the well off and
the poor, the urban residents and rural people, the
adivasis and dalits and others, and between men
and women are extremely glaring.
•
The Infant Mortality Rate in the poorest 20%
of the population is 2.S times higher than that
in the richest 20% of the population. In other
words, an infant bom in a poor family is two
and half times more likely to die in infancy,
than an infant in a better off family3.
.
A child in the ‘Low standard of living’ economic
group is almost four times more likely to die
in childhood than a child in the better off ‘High
standard of living’ group. An Adivasi child is
one and half times more likely to die before
the fifth birthday than children of other groups3.
>
A girl is 1.5 times more likely to die before
reaching her fifth birthday, compared to a boy!
The female to male ratios for children are
rapidly declining, from 945 girls per 1000 boys
in 1991, to just 927 girls per 1000 boys in 2001 ‘6.
This decline highlights an alarming trend of
discrimination against girl children, which
starts well before birth (in the form of sex
selective abortions), and continues into
childhood and adolescence (in the form of worse
treatment to girls)3.
>
Dalit Women are one and a half times more
likely to suffer the consequences of chronic
malnutrition (stunted height) as compared to
women from other castes. Children below 3
years of age in scheduled tribes and scheduled
castes are twice as likely to be malnourished
than children in other groups.
o
A person from the poorest quintile of the
population, despite more health problems, is
six times less likely to access hospitalization
than a person from the richest quintile. This
means that the poor are unable to afford and
access hospitalization in a very large proportion
of illness episodes, even when it is required.
•
The delivery of a mother, from the poorest
quintile of the population is over six times less
likely to be attended by a medically trained
person than the delivery of a well off mother,
from the richest quintile of the population. An
adivasi mother is half as likely to be delisted
by a medically trained person3.
•
The ratio of hospital beds to population in rural
areas is fifteen times lower than that for urban
areas14.
•
The ratio of doctors to population in rural areas
is almost six times lower than the availability
of doctors for the urban population14.
•
Per person, Government spending on public
health is seven times lower in rural areas.
compared to Government health spending for
urban areas.
These health and health care inequities are
increasing, and are deeply unjust — a just health
system would ensure that all citizens, irrespective
of social background or gender, would get basic
quality health care in times of need.
the most privatised in the world. Only five other
countries in the world are worse off than India
regarding public health spending (Burundi,
Myanmar, Pakistan, Sudan, Cambodia1’). The
W H.O. standard for expenditure on public health
is 5% of the GDP. The average spending today by
Less Developed Countries is 2.8 % of GDP, but India
presently spends only 0.9% of its GDP on public
health, which is merely one-third of the less
developed countries’ average11 !
The NDA Government has recently claimed that
mu’ ol its iiigiml achievements has been the
allocation ol <j% ol GUI' to Health care. In reality,
the government spends just 0.9 % of the GDP on
Health care and the rest is spent by people from
their own resources. Thus only 17% of all health
expenditure in this country is borne by the
government— this makes the Indian public health
system grossly inadequate to meet healthcare
demands of its people, and makes the health sector
The consequence of this dismally low allocation,
which stands at the lowest levels in the last two
decades, (in contrast to 1.3% of GDP achieved in
1985), is deteriorating quality of public health
services. For example, Primary health centers
(PHCs), meant to serve the needs of the poorest
and most marginalized people have the following
shocking statistics:
•
A •
3% of PHCs having 80% of all critical inputs.
In spite of the high maternal mortality
ratio, 8 out of every 10 PHCs have no
Essential Obstetric Care drug kit!
Only 34% PHCs offer delivery services, while
only 3% offer Medical Termination of
Pregnancy!
A person accessing a community health
center would find no obstetrician in 7 out
of 10 centers, and no pediatrician in 8 out
of 10!
Only 38% of all PHCs have all the critical
staff
Only 31% have all the critical supplies
(defined as 60% of critical inputs), with only
Source: 7
3
Private health care and essential drugs are increasingly unaffordable !
-
The dominance of the private sector not only denies
access to poorer sections of society', but also skews
the balance towards urban biased, tertiary level
health services with profitability overriding equity,
and rationality of care often taking a back seat.
■
Irrational medical procedures are on the ijse.
According to just one study in a community in
Chennai, 45% of all deliveries were perfornjed
by Cesarean operations, whereas the WHO has
recommended that not more than 10-15% of
deliveries
would
require
Cesarean
operations1 T.
A growing proportion of Indians cannot afford
health care when they fall ill. National surveys
show that the number of people who could not
seek medical care because of lack of money
increased significantly between 1986 and
199513. The proportion of such persons unable
Due to irrational prescribing, an average of
63 per cent of the money spent on prescriptions
is a waste. This means that nearly two-thirds
of the money that we spend on drugs may be
for unnecessary or irrational drugs-1!
to afford health care almost doubled.
increasing from 10 to 21 % in urban areas, and
growing from 15 to 24% in rural areas in this
decade13.
.
The pharmaceutical industry is rapidly
growing...yet only 20% of the population can
access all essential drugs that they require.
There is a proliferation of brand names with
over 70,000 brands marketed in India, but the
2002 Drug policy recommends that only 25
drugs be kept under price control13. As a result.
many drugs are being sold at 200 to 500 p^ent
profit margin, and essential drugs have berome
unaffordable for the majority of the Indian
population.
Forty percent of hospitalised people are forced
to borrow money or sell assets to cover
expenses13.
.
Over 2 crores of Indians are pushed below the
poverty line every year because of the
catastrophic effect of out of pocket spending on
health care-"!
Health policy developments since the 1990s have critically
weakened the health system
The effectiveness of the public health system and
access to quality health care, especially for the poor
has worsened since the decade of the 1990s. due
to a variety of policy developments, at both national
and state levels:
•
Stagnant public health budgets and
decreasing Government expenditure on
capital investment for public health
facilities.
•
Introduction of user fees at various levels
of public health facilities.
.
Freezing of new recruitments and
inadequate budgets for supplies and
maintenance in the public health system.
•
Contracting out health services or
privatisation of health facilities.
•
Encouragement of growth of private
secondary and tertiary hospitals through
tax waivers, reduced import duties,
subsidized land etc. which have led to a
'■ further expansion of the unregulated
□rivate medical sector.
Promotion of ‘Health tourism’ for foreign
visitors, w'hile basic health services remain
inaccessible for a large proponion of the
Indian population.
Conducting occasional, expensive and
largely ineffective ‘Health melas’ instead
of upgrading the public health system as a
sustainable solution.
Deregulation of the pharmace^^cal
industry, lax price controls on drugs — the
list of drugs under price control being
proposed to be reduced to 25 drugs
(compared to 343 drugs under price control
in 1979.)
Many bulk drug manufacturing units have
closed down due to liberalized import and
dumping as a result of the implementation
of the WTO agreement and autonomous
economic liberalization policies. Due to
reduction of customs duy and increase, of
excise duty, imported drugs will become
cheaper while locaTdrugs will become more
expensive.
4
Indians need not accept poor health as their
inevitable fate! Many other developing countries.
which have given a high priority to people's health.
have achieved much better health outcomes
compared to India. As a country, we spend a higher
proportion o: the GDP on health care compared to
these countries - but an overwhelming percentage
of this (83%) is private expenditure. As a result we
have a weak public health system with poor health
outcomes forcing families to spend a lot on private
medical care, which is expensive, and not always
appropriate, leaving us with ‘poor health at high
cost’! Here is how some other Asian countries are
doing in comparison with India...
Health Outcomes in Relation to Health Expenditures in some Asian countries10
Total Health
Expenditure
as % of GDP
Public Health
Expenditure
as % of total
Under 5
Mortality
India
5.2
17
Sri Lanka
3.0
Malaysia
2.4
Life Expectancy
Male
Female
95
59.6
61.2
45.4
19
65.8
73.4
57.6
14
67.6
69.9
Does India: have the resources to provide health care for all ?
•
•________________________
As a country. Indians spend more on health care
than most other developing countries, but this is
mostly out-of-pocket spending. Health care
facilities have grown substantially, but these are
mostly in the private sector. The system is
producing more and more healthcare professionals.
but we lose them to the private sector, or to western
countries. To give some idea of the available health
care resources in India •
Compared to 11,174 hospitals in 1991 (57%
private,!, the number grew to 18.218 (75%
private) in 200014. In 2000. the country had
12.5 lakh doctors and 8 lakh nurses! At the
national level, there is one allopathic doctor
for every 1800 people, or one doctor from
systems including ISM and homeopathy for
SOO people. This means there are more
doctors than the required estimate of one
doctor for 1500 population-.
•
Approximately 15,000 new graduate doctors
and 5,000 postgraduate doctors are produced
every year and one-fifth of them leave the
country for greener pastures14.
o
-_____________ ___ ______________________________________________________
We have an annual pharmaceutical
production of about 260 billion rupees-’, and
we export a large proportion of these drugs
- Sadly, while our exports grow. 80% of our
people do not have access to all the drugs
they require.
In short, we have substantial health care
resources, but because of the privatised.
unregulated and inequitable nature of the health
care system, it is unable to ensure good quality
health care for a majority’ of citizens. Rather than
producing more doctors or setting up more private
hospitals, what we need is a reorganisation of the
health system, with substantial strengthening of
public health, greatly enhanced public expenditure.
regulation of the private medical sector and an
overall planned approach to make health care
resources available to all.
5
increased substantially, targeting the 5%
of GDP as public expenditure on health care
as recommended by the WHO.
• If the public health system fails to deliver
it should be treated as a legal offence.
remedy for which can be sought in the
courts of law. The public system must
ensure all elements of care like drug
prescriptions, diagnostic tests, child birth
services, hospitalization care etc. One way
to ensure this could be that in exceptional
situations, where patients who do not
receive these services from the public
facility they may be referred to seek them
from alternate facilities, which are
registered with the state agency. Such
registered and regulated facilities would
honour such referrals, for which the state
would reimburse them at a mutually agreed
rate. This would maintain pressure on the
public health system to provide all eleme^h
of care, and would ensure that the patient
is not deprived of essential care at time of
need.
o Various vulnerable and marginalised
sections of the population have special
health needs. There is a need for a range
of policy measures to eliminate
discrimination, and to provide special
quality’ and sensitive services for women.
children, elderly persons, unorganised
sector workers, HIV-AIDS affected persons.
disabled persons, persons with mental
health problems and other vulnerable
groups. Similarly, situations of conflict,
displacement and migration need to be
addressed with a comprehensive approach
to ensure that the health rights of affected
people are protected. The People’s Heqflta.
Charter deals with issues related to sucn
special sections of the population, and can
provide a basis for formulation ot
appropriate policy initiatives, in
consultation
with
organisations
representing these social segments.
• Putting in place a National legislation to
regulate the private health sector, to adopt
minimum standards, accreditation.
standard treatment protocols, standardised
pricing of services etc.
• Adopting a rational and essential
medications-based drug policy. All States
must have an essential drugs and
consumables list and all the drugs and
consumables on this list must be under
price control. Further all state governments
must adopt procurement and distribution
The objective should be to make Health care a
Fundamental right and an operational
entitlement. This would require a National Public
Health. Act, which mandates right to basic
healthcare services to all citizens through a
system of universal access to healthcare. The
Indian Constitution through its directive principles
provides the basis for the Right to health care, and
the Indian state has ratified the International
Covenant of Economic, Social and Cultural Rights
which makes it obligatory on its part to comply
with Article 12 that mandates right to healthcare.
Universal access to healthcare is well established
m a number of countries including not only
developed countries like Canada and United
Kingdom, but aiso developing countries such as
Cuba. Brazil. Costa Rica and Thailand. There is
no reason why this cannot be made a reality in
India. Hence we need to set in motion processes.
which will take us towards the goal of universal
access to health care, in a Rights-based framework
and with equity.
Some immediate steps related to the health care
system that need to be taken include:
. Making healthcare a fundamental right by
suitable constitutional amendment. The
formulation of a National legislation
mandating the Right to Health care, with a
clearly defined comprehensive package of
health care, along with authorization of the
requisite budget, being made available
universally within one year.
• Significant strengthening of the existing
public health system, especially in rural
areas, by assuring that all the required
infrastructure, staff, equipment, medicines
and other critical inputs are available, and
result in delivery' of all required services.
These would be ensured based on clearly
defined, publicly displayed and monitored
norms.
• The declining trend of budgetary allocations
for public health needs to be reversed, and
budgets appropriately up-scaled to make
optimal provision of health care in the
public domain possible. At one level adopting
a fiscal policy of block funding or a system
of per capita allocation of resources to
different levels of health care, with an
emphasis on Primary Health Care will have
an immediate impact in reducing ruralurban inequities by making larger
resources available to rural health facilities
like Primary health centers and Rural
hospitals. Simultaneously, the budgetary
allocation to the health sector must be
6
•
•
policies similar to what has been done by
the Tamilnadu State Medical Services
Corporation and hence ensure that
essential drugs in the list are actually
available in every facility.
the state should introduce a new
community-anchored health worker
scheme, and implement it in a phased
manner with involvement of people's
organizations and panchayati raj
institutions, in both rural and urban areas,
through which first contact primary’ care
and health education can be ensured.
integration of medical education of all
systems to create a basic doctor ensuring
•
.
a wider outreach and improvement of
access to health care services in all areas.
All state level coercive population control
policies, disincentives and orders should
be revoked. Disproportionate financial
allocation for population control activity
should not be allowed to skew funding from
other important public health priorities.
Integration of medical education of all
systems to create a basic doctor ensuring
a wider outreach and improvement of
access to health care services in all areas.
Effective regulation of the growth of
capitation based medical colleges.
What is needed is a major restructuring and
strengthening of the health system. This involves
two major ingredients: popular mobilisation for
operationalising the Right to Health Care, and the
political will to implement policy changes
necessary to transform the health system, Jan
Swasthya Abhiyan is today involved in the former
task, by reaching out to people across the country.
enabling them to mobilise for their just health
rights. It calls upon political parties, which
recognise people's right to healthy lives, to address
the latter task, and to perform their historic duty
by establishing and operationalising rhe Right to
Health care as a Fundamental right.
The persistence of unacceptably large numbers of
avoidable deaths, resurgence of communicable
diseases, declining quality’ of public health services
and unaffordable, often inappropriate private
^edicai care need not remain the lot of over a
milion ordinary Indians. Recent policy changes of
privatisation, declining public health budgets and
pro-drug industry measures need to be replaced bv
strong public health initiatives, with the active
involvement of communities and civil societv
organisations.
By and large. India today possesses the
humanpower, infrastructure, national financial
resources and appropriate health care know-how
to ensure quality health care for all its citizens.
This document focuses on rhe need for strengthening of the heaith care system, and certain immediate
steps required for this. However, improvement of people's health requires equally importantly, provision
of other necessary facilities and conditions required for a healthy life, such as safe drinking water.
sanitation, food security, healthy housing, basic education and a safe environment. The People’s Health
Charter has dealt with these issues, and may be taken as a guideline to develop effective policies and
^nprove people's living standard in order to achieve better health.
Published by CEHAT for JAN SWASTHYA ABHIYAN
7
We the people of India, stand united in our condemnation of an iniquitous global system that, under the garfi of
Globalisation’ seeks to heap unprecedented miser.’ and destitution on the overwhelming majority of the people on
this globe. This system has systematically ravaged the economies of poor nations in order to extract profits that
nurture a handful of powerful nations and corporations. The poor, across the globe, as well as the sections of pbor
::: the rich nations, are being further marginalised as they are displaced from home and hearth and alienated from
their sources of livelihood as a result of the forces unleashed by this system. Standing in firm opposition to such a
system we reaffirm our inalienable right to and demand for comprehensive health care that includes food security:
sustainable livelihood options including secure employment opportunities; access to housing, drinking water and
sanitation: and appropriate medical care for all; in sum - the right to Health For All, Now!
The promises made to us by the international community in the Alma Ata declaration have been systematically
repudiated by the World Bank, the IMF, the WTO and its predecessors, the World Health Organization, and by a
government that functions under the dictates of International Finance Capital. The forces ‘Globalisation’ through
measures such as the structural adjustment programme are targeting our resources - built up with our labour.
sweat and lives over the last fifty years - and placing them in the service of the global “market'’ for extraction of
super-profits. The benefits of the public sector health care institutions, the public distribution system and other
infrastructure - such as they were - have been taken away from us. It is the ultimate irony that we are now blamed
for our plight, with the argument that it is our numbers and our propensity to multiply that is responsible for our
poverty and deprivation. We declare health as a justiciable right and demand the provision of comprehensive health
care as a fundamental constitutional right of ever.- one of us. We assert our right to take control of our health in our
own hands and for this the right to:
.
.
.
.
.
.
.
A truly decentralized system of local governance vested with adequate power and responsibilities, provided with
adequate finances and responsibility for local level planning.
A sustainable system of agriculture based on the principle of land to the tiller - both men and women - equitable
distribution of land and water, linked to a decentralized public distribution system that ensures that n^pne
goes hungry
Universal access to education, adequate and safe drinking water, and housing and sanitation facilities
A dignified and sustainable livelihood
A clean and sustainable environment
A drug industry geared to producing epidemiological essential drugs at affordable cost
A health care system which is gender sensitive and responsive to the people’s needs and whose control is
vested m people s hands and not based on market defined concept of health care.
Further, we deciare our firm opposition to:
.
.
.
•
.
.
.
.
Agricultural policies attuned to the needs of the ’market' that ignore disaggregated and equitable access to food
Destruction of our means to livelihood and appropriation, for private profit, of our natural resource bases and
appropriation of bio-diversity.
The conversion of Health to the mere provision of medical facilities and care that are technology’ intensive.
expensive, and accessible to a select few
The retreat, by the government, from the principle of providing free medical care, through reduction oi public
sector expenditure on medical care and introduction of user fees in public sector-medical institutions, that
place an unacceptable burden on the poor
The corporatization and commencialization of medical care, state subsidies to the corporate sector in medical
care, and corporate sector health insurance
Coercive population control and promotion of hazardous contraceptive technology which are directed primarily
at the poor and women
The use of patent regimes to steal our traditional knowledge and to put medical technology’ and drugs ^Jond
our reach
institutionalization of divisive and oppressive forces in society, such as communalism, caste, patriarchy, and
the attendant violence, which have destroyed our peace and fragmented our solidarity.
in the light of the above we demand that:
The concept of comprehensive primary health care, as envisioned in the Alma Ata Declaration should form the
fundamental basis for formulation of all policies related to health care. The trend towards fragmentation oi
health delivery programmes through conduct of a number of vertical programmes should be reversed. National
health programmes be integrated within the Primary Health Care system with decentralized planning, decision
making and implementation with the active participation of the community. Focus be shifted from bio-medicai
and individual based measures to social, ecological and community based measures.
2.
The primary health care institutions including trained village health workers, sub-centers, and the PHCs staffed
by doctors and the entire range of community health functionaries including the 1CDS workers, be placed under
the direct administrative and financial control of the relevant level Panchayati Raj institutions. The overall
infrastructure of the pnmarv health care institutions be under rhe control of Panchayats and Gram Sabhas and
provision of free and accessible secondary and tertiary level care be under the control of Zilla Parishads. to be
accessed primarily through referrals from PHCs.
The essential components of primary’ care should be;
.
Village level health care based on Village Health Workers selected by the community and supported by
the Gram Sabha / Panchayat and the Government health services which are given regulatory powers
and adequate resource support
S
•
•
•
•
•
Primary Health Centers and sub-centers with adequate staff and supplies which provides quality curative
services at the primary health center level itself with good support from referral linkages
A comprehensive structure for Primary Health Care in urban areas based on urban PHCs, health posts
and Community Health Workers under the control of local seif government such as ward committees
and municipalities.
Enhanced content of Primary Health Care to include all measures which can be provided at the PHC
leve: even for less common or non-communicable diseases (e.g. epilepsy, hypertension, arthritis, preeciampsia. skin diseases) and integrated relevant epidemiological and preventive measures
Surveillance centers at block level to monitor the local epidemiological situation and tertiary care with
all speciality services, available in every district.
3.
A comprehensive medical care programme financed by the government to the extent of at least 5% of our GNP;
o: watch at least half be disbursed to panchayati raj institutions to finance primary level care. This be accompanied
m. transier of responsibilities to PRIs to run major parts of such a programme, along with measures to enhance
capacities of PRIs to undertake the tasks involved.
-.
The policy of gradual privatisation of government medical institutions, through mechanisms such as introduction
oi user fees even for the poor, allowing private practice by Government Doctors, giving out PHCs on contract.
etc. be abandoned forthwith. Failure to provide appropriate medical care to a citizen by public health care
institutions be made punishable by law.
5.
A comprehensive need-based human-power plan for the health sector be formulated that addresses the requirement
tor creation of a much larger pool of paramedical funcuonanes and basic doctors, in place of the present trend
towards over-production of personnel trained in super-specialities. Major portions of undergraduate medical
education, nursing as well as other paramedical training be imparted in district level medical care institutions.
as a necessarv complement to training provided in medical/nursing colleges and other training institutions. No
more new medical colleges to be opened in the pnvate sector. No commodification of medical education. Steps
to eliminate illegal pnvate tuition by teachers in medical colleges. At least a year of compulsory rural posting for
undergraduate imedical, nursing and paramedical) education be made mandatory, without which license to
practice not be issued. Similarly, three years of rural posung after post graduation be made compulsory.
o.
The unbridled and unchecked growth of the commercial pnvate sector be brought to a halt. Strict observance of
standard guidelines for medical and surgical intervenuon and use of diagnostics, standard fee structure, and
periodic prescription audit to be made obligatory. Legal and social mechanisms be set up to ensure observance
jf minimum standards by all pnvate hospitals, nursing/matemity homes and medical laboratones. Prevalent
practice oi ottering commissions for referral to be made punishable by law. For this purpose a body with statutory
powers be constituted, which has due representation from peoples organisations and professional organisations.
T.
A rational drug policy be formulated that ensures development and growth of a self-reliant industry for production
•?: ail essential drugs at affordable prices and of proper quality. The policy should, on a. pnority basis:
.
.
•
.
.
.
.
.
Ban ail irrationai and hazardous drugs. Set up effective mechanisms to control the introduction of new
drugs and formulations as well as periodic review of currently approved drugs.
Intrcauce production quotas & price ceiling for essential drugs
Promote compulsory use of generic names
Regulate advertisements, promotion and marketing of all medications based on ethical criteria
Formulate guidelines for use of old and new vaccines
Control the activities of the multinational sector and restrict their presence only to areas where they
are •.wiling to bang in new technology
Recommend repeal of the new patent act and bring back mechanisms that prevent creation of monopolies
ana promote introduction of new drugs at affordable pnces
Promotion of the public sector in production of drugs and medical supplies, moving towards complete
seif-renance in these areas.
8.
Mec.ical Research priorities be based on morbidity and mortality profile of the country', and details regarding the
direction, intent and focus of all research programmes be made entirely transparent. Adequate government
funding be provided for such programmes. Ethical guidelines for research involving human subjects be drawn up
and implemented after an open public debate. No further experimentation, involving human subjects, be allowed
without a proper and legally tenable informed consent and appropriate legal protection. Failure to do so to be
cuntshabie oy .aw. All unethical research, especially in the area of contraceptive research, be stopped forthwith.
'. . men lane mem who. without their consent and knowledge, have been subjected to experimentation, especially
with hazarcous contraceptive tecnnologies to be. traced forthwith and appropriately compensated. Exemplary
carnages to oe awarded against the institutions (public and pnvate sector) involved in such anti-people, unethical
uM illegal practices in the past.
a.
All -ocrcive measures including incentives and disincentives for limiting family size be abolished. The right of
families anc women within families in determining the numoer of children they want should be recognized.
u jncurrenttv. access to safe and affordable contraceptive measures be ensured which provides people, especially
men. the ..miltv to make an informed choice. All long-term, invasive, systemic hazardous contraceptive
..-.miiogies >uch as the mjectables (NET-EN. Depo-Provera. etc.), sub-dermal implants (Norplanti and'anti
: •ru.itv vaccines shouid be canned from both the public and private sector. Urgent measure be initiated to shift
: ■. nus o;
ritraception away from women and ensure at least equal emphasis on men s responsibility for
..■mraception Facilities for safe abortions be provided nght from the primary health center level.
IU. '..court be provided to traditional healing systems, including.local and home-based healing traditions, for
'vsiematic research and community based evaluation with a view to developing the knowledge base and use of
•nese svstems along with modem medicine as part of a holistic healing perspective.
9
II.
Promotion of transparency and decentralization in the decision making process, related to health carp, at all
levels as '.veil as adherence to the principle of right to information. Changes in health policies to be made only
after mandatory wider scientific public debate.
12.
Introduction of ecological and social measures to check resurgence of communicable diseases. Such measures
should include:
.
.
.
Integration of health impact assessment into all development projects
•
Decentralized and effective surveillance and compulsory notification of prevalent diseases like malaria,
TS by all health care providers, including private practitioners
Reorientation of measures to check STDs/AIDS through universal sex education, promoting resoonsible
safe sex practices, questioning forced disruption and displacement and the culture of commodification
of sex. generating public awareness to remove stigma and universal availability of preventive and curative
services, and special attention to empowering women and availability of gender sensitive services in
this regard.
13.
Facilities for early detection and treatment of non-communicable diseases like diabetes, cancers, heart diseases.
etc. to be available to all at appropriate levels of medical care.
14.
Women-centered health initiatives that include:
•
•
•
.
15.
Child centered health initiatives that include:
.
.
.
.
16.
Awareness generation for social change on issues of gender and health, triple work burden, gender
discrimination in upbringing and life conditions within and outside the family; preventive and curative
measures to deal with health consequences of women s work and violence against women
Complete maternity benefits and child care facilities to be provided in all occupations employing women,
be they in the organized or unorganized sector
Special support structures that focus on single, deserted, widowed women and minority' women which
will include religious, ethnic and women with a different sexual orientation and commercial sex workers:
gender sensitive services to deal with all the health problems of women including reproductive health.
maternal health, abortion, and infertility
Vigorous public campaign accompanied by legal and administrative action against sex selective aboi^hs
including female feticide, infanticide and sex pre-seiection.
A comprehensive child rights code, adequate budgetary allocation for universalisation of child care
services
An expanded &. revitalized 1CDS programme. Ensuring adequate support to working women to facilitate
child care, especially breast feeding
Comprehensive measures to prevent child abuse, sexual abuse and child prostitution
Educational, economic and legal measures to eradicate child labour, accompanied by measures to ensure
free and compulsory quality elementary education for all children.
Special measures relating to occupational and environmental health which focus on:
•
.
.
•
Banning of hazardous tecnnoiogies in industry and agriculture
Worker centered monitoring of working conditions with the onus of ensuring a safe and secure workplace
on the management
Reonenting medical services for early detecuon of occupational disease
Special measures to reduce the likelihood of accidents and injuries in different settings, such as traffic
accidents, industrial accidents, agnculturai injuries, etc.
17 The approach to mental heaith problems should take into account the social structure in India which makes
certain sections like women more vulnerable to mental health problems. Mental Health Measures that prolate
a shift away from a bio-medicai model towards a holistic model of mental health. Community support & ccmmMny
based management of mental health problems be promoted. Services for early detection & integrated management
of mental heaith problems be integrated with Primary Health Care and the rights of the mentally ill and the
mentally challenged persons to be sale guarded.
18.
Measures to promote the health of the elderly by ensuring economic security, opportunities for appropriate
employment, sensitive heaith care facilities and. when necessarv, shelter for the elderly. Services that cater to
the special needs of people in transit, the homeless, migratory workers and temporary settlement dwellers.
19.
Measures to promote the health of physically and mentally disadvantaged by focussing on the abilities rather
than deficiencies. Promotion of measures to integrate them in the community with special support rather than
segregating them: ensuring equitable opportunities for education, employment and special health care including
rehabilitative measures.
20.
Effective restriction on industries that promote addictions and an unhealthy lifestyle, like tobacco, alcohol, pan
masala etc., starting with an immediate ban on advertising, sponsorship and sale of their products to the
young, and provision of services for de-addiction
10
The Jar. Swasthya Abhiyan at the national level is the coalition of the networks of voluntary organizations
and peoples movements involved in healthcare delivery and health policy, who made themselves a part of
the Peoples Health Assembly campaign in India in the year 2000, and have continued to participate in this
process. These national networks have numerous constituent organisations, which implies that a few
hundred organizations are involved directly in the national process. Beyond these networks, several hundred
other organizations have been involved at state, district and block level activities across the country. The
networks that constitute the National Coordination Committee of Jan Swasthya Abhiyan are:
1.
2.
3.
4.
5.
6.
7.
3.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
All India Peoples Science Network
All India Democratic Women’s Association
All India Drug Action Network
Asian Community Health Action Network
Bharat Gyan Vigyan Samiti
Catholic Health Association of India (CHAI)
Christian Medical Association of India (CMAJ)
Federation of Medical Representatives and Sales Associations of India (FMRAI)
Forum for Creche and Child Care Services (FORCES)
Joint Women’s Programme
Medico Friends Circle (MFC)
National .Alliance of People’s Movements (NAPM)
National Alliance of Women’s Organisations (NAWO)
National Federation of Indian Women (NFIW)
Ramakrishna Mission
Voluntary Health Association of India (VHAI)
Association for Indian Development, India (AJD-India)
Breastfeeding Promotion Network of India (BFPNI) National Resource Groups:
Centre for Enquiry into Health and Allied Themes (CEHAT)
Centre for Social Medicine and Community Health, Jawaharlal Nehru University
Community Health Cell (CHC)
The representatives of all the above organisations constitute the National Coordination Committee of JSA,
which is the national decision making body of the coalition. N.H. Antia is the Chairperson and D. Banerjee
Js the Vice-Chairperson of JSA. National organisers of JSA include B. Ekbal as Convenor, Abhay Shukla,
Amit Sengupta. Amitava Guha, Thelma Narayan and T. Sundararaman as Joint convenors, with Vandana
Prasad and N.B.Sarojini as National secretariat members.
Jan Swasthya Abhiyan presently has state units or contacts in the following states:
Andhra Pradesh. Assam, Bihar, Chhattisgarh, Delhi, Gujarat, Haryana, Himachal Pradesh,
Jharkhand, Karnataka, Kerala, Madhya Pradesh, Maharashtra, Orissa, Rajasthan, Tamil
Nadu, Tripura, Uttar Pradesh, West Bengal.
11
B. Ekbal,
National Convenor, JSA
Ph: 0471-2306634(0)
e_:naj[. ekbaigvsnl.com
Abhay Shukia
National Secretariat, JSA
Ph: 020-25451413 / 25452325
e-mail : cehatoungvsnl.com
Amit Sen Gupta
Jt. Convenor, JSA
Ph: 011-26862716/ 26524324
e-mail: ctddsr7vsnl.com
Amitava Guha
Jt. Convenor, JSA
Ph: 033-24242862(0)
e-mail:
guhaamitava Shotmail.com
Thelma Narayan
Jt. Convenor, JSA
Ph:080-5505924 / 5525372
e-mail' socharagvsnl.com
T. Sundararaman
Jt. Convenor, JSA
Phone: 0771-2236104. 2236175
e-mail:
sundar2g 123india.com
Vandana Prasad
Member, National Secretariat
Phone: 0120-2536578
e-mail' chaukhat@vahoo.com
Sarojini
Member, National Secretariat
Ph: 011-26968972 / 26850074
e-mail' samasarogvsnl.com
Sources:
1.
2.
3.
SRS Bulletin. Government of India.1998.
Planning Commission. Government of India. Tenth Five Year Plan 2002-2007. Volume !!.
international Institute for Population Sciences and ORC Macro. National Family Health Survey (NFHS-
II) 199S-99. India.
International Institute for Population Sciences. RCH-RHS India 1998-1999.
National Crime Records Bureau. Ministry of Home Affairs. Accidental Deaths and Suicides In India
2000.
6. World Health Organization. The World Heaith Report 2003.
7. International Institute for Population Sciences. Facility Survey. 1999.
8. Misra. Chatterjee, Rao. India Health Report.Oxford University Press. New Delhi.2003
9. Morbidity and Treatment of Ailments. NSS Fifty second round. Government of India. 1998.
10. Changing the Indian Health System - Draft Report, ICRIER, 2001
11. Shanff Abusaleh. India Human Development Report.Oxford University Press New Delhi.
12. Duggal.Ravi. Operationalizing Right to Healthcare in India. Right to Healthcare. Moving from Idea to
4.
5.
15.
16.
17.
Reality.
CEHAT.Mumbai.2003.
National Coordination Committee for the Jana Swasthya Sabha. Health for All NOW. 2004.
Central Bureau of Health Intelligence.Directorate General of Health Services. Ministry of Health and
Family Welfare. Health Information of India 2000 &2001.
National Sample Survey Organization. Department of Statistics.GOI.42"“ and 52"“ Round.
Census of India 2001: Provisional Population Totals.Registrar General and Census Commissioner GO1.
Pai M et al. A high rate of Cesaerean sections in affluent section of Chennai, is it a cause for concern?
18.
19.
20.
Nat Med J India. 1999,12:156-158.
TB India 2003. R.NTCP Stats Report.Central TB Division.DDHS GOI.
Heaith Survev and Deveioomenr Committee, GOI 1946 (Bhore Report)
Mahal A. www.woridbank.org
21.
Phadke A. Drug Supply and Use. Towards a Rational Policy in India. Sage Publications New Delhi.
22.
Ministry of Chemicals and Fertilizers.
13.
14.
12
- Media
 RF_COM_H_69_1_SUDHA.pdf
RF_COM_H_69_1_SUDHA.pdf
Position: 2598 (4 views)