UNF/UNFIP PROJECT DOCUMENT
Item
- Title
- UNF/UNFIP PROJECT DOCUMENT
- extracted text
-
RF_COM_H_54_SUDHA
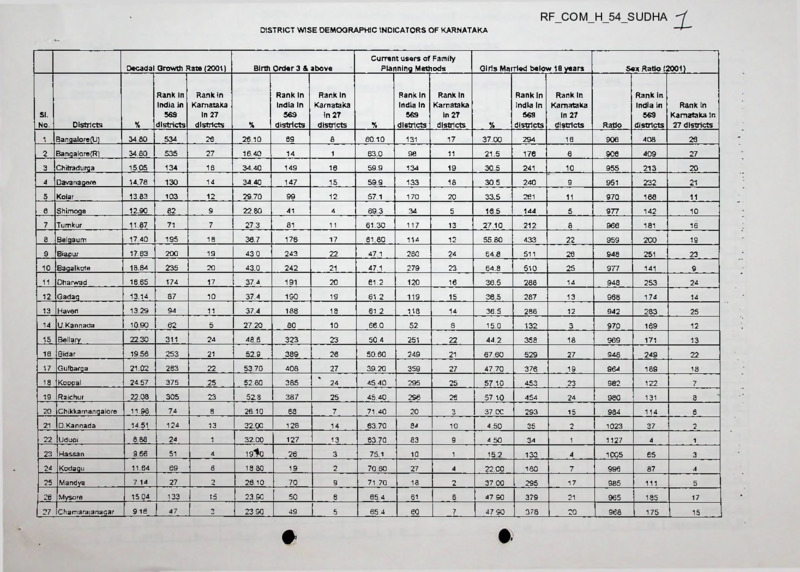
DISTRICT WISE DEMOGRAPHIC INDICATORS OF KARNATAKA
Decadal Growth Rate (2001)
Rank In
Rank In
India In Karnataka
569
In 27
districts districts
Current users of Family
Planning Methods
Birth Order 3 & above
Rank in
Rank In
India In Karnataka
569
In 27
districts districts
Girls Married below 18 years
Sex Ratio (2001)
Rank In
Karnataka
In 27
districts
Ratio
SI.
No.
Districts
%
Rank In
India In
569
districts
%
Rank In
India In
569
districts
1
Bangalore(U)
34 80
534
26
26 10
69
8
60.10
131
17
37.00
294
16
906
408
26
2
Bangalore (R)
34.80
535
27
16.40
14
1
63.0
98
11
21.5
176
6
906
409
27
3
Chitradurga
15.05
134
16
34.40
149
16
59.9
134
19
30 5
241
10
955
213
20
4
Davanagere
14.78
130
14
34.40
147
15
59 9
133
18
30.5
240
9
951
232
21
5
Kolar
13.83
103
12
29 70
99
12
57.1
170
20
33.5
261
11
970
168
11
6
Shimoga
12.90
82
9
22.80
41
4
693
34
5
165
144
5
977
142
10
7
Tumkur
11.87
71
7
27 3
81
11
61.30
117
13
27.10
212
8
966
181
16
8
Belgaum
17 40
195
18
36.7
176
17
61.80
114
12
55.80
433
22
959
2C0
19
9
Biapur
17.63
200
19
43.0
243
22
47.1
280
24
64 8
511
26
948
251
23
10 Bagalkote
18.84
235
20
43.0
242
21
47.1
279
23
64.8
510
25
977
141
9
Dharwad
16.65
174
17
37.4
191
20
61.2
120
16
36.5
288
14
948
253
24
12 Gadaq
13.14
87
10
37.4
190
19
61.2
119
15
365
287
13
968
174
14
13 Haven
13.29
94
11
37.4
188
18
61 2
118
14
36.5
286
12
942
283
25
10.90
62
5
27 20
80
10
66.0
52
6
150
132
3
970
169
12
15 Bellary
22 30
311
24
48 6
323
23
50 4
251
22
44.2
358
18
969
171
13
16 Bidar
19 56
253
21
52.9
389
26
50.60
249
21
67 60
529
27
948
249
22
17 Gulbarga
21.02
283
22
53 70
408
27
39.20
359
27
47 70
376
19
964
189
18
18 Koopal
24.57
375
25
52.80
385
24
45 40
295
25
57 10
453
23
982
122
7
19 Raichur
22.08
305
23
52.8
387
25
45.40
296
26
57 10
454
24
980
131
8
20 Chikkamangalore
11 98
74
8
26.10
68
7
71.40
20
Q
37 00
293
15
984
114
6
D. Kannada
14.51
124
13
32.00
128
14
63.70
84
10
4 50
35
2
1023
37
2
22 Udupi
6.88
24
1
32.00
127
13
63 70
83
9
4 50
34
1
1127
4
1
23 Hassan
9 66
51
4
19^0
26
3
75.1
10
1
152
133
4
1005
65
3
24 Kodagu
11.64
69
6
18.80
19
2
70 60
27
4
22. CO
180
7
996
87
4
25 Mandya
7 14
27
2
26.10
70
9
71 70
18
2
37 CO
295
17
985
111
5
26 Mysore
15 04
133
15
23 90
50
6
65 4
61
8
47 90
379
21
965
185
17
27 Chamaraianagar
9 16
47
3
23 90
49
5
65 4
60
7
47 90
378
20
968
175
15
11
14
21
U. Kannada
%
Rank In
Karnataka
In 27
districts
%
Rank in
India In
Rank In
Karnataka In
569
districts 27 districts
DISTRICT WISE DEMOGRAPHIC INDICATORS OF KARNATAKA
Complete Immunisation
Safe Delivery
Rank in
Karnataka
in 27
districts
Female Literacy Rate (2001)
Villages not connected with
pucca road (2000-01)
Estimated Coverage of safe
drinking water (2000)
SI.
No.
Districts
%
Rank in
India in
569
districts
%
Rank in
India in
569
districts
•/.
Rank In
India In
563
districts
1
Banaalore(LT)
90.60
41
3
77.70
139
16
78.98
29
1
0.00
64
11
67.56
320
8
2
BangalorefRI
79 10
92
7
83 70
96
14
78 98
30
2
0 00
65
12
71.30
288
4
3
Chitradurga
53 80
233
21
88.40
65
9
54.62
261
15
0.00
58
10
72.62
281
3
4
Davanaaere
53 80
231
20
88 40
63
8
58 45
209
11
0.00
26-
3
72 62
280
2
5
Kolar
59.20
202
18
90 60
48
6
52.61
289
16
23 10
208
27
74 00
275
1
6
Shimoga
83 00
70
5
92.90
30
2
67 24
111
7
4 67
134
21
54.60
437
18
7
Tumkur
63.50
183
16
88.00
66
10
57.18
226
13
21.47
201
26
66.59
335
12
8
Belaaum
68 60
150
12
64 80
226
20
52.53
296
18
0.00
42
6
52 94
452
21
9
Biaour
50 10
253
24
53 20
315
22
46 19
360
21
0 00
20
2
60 42
402
15
10
Bagalkote
50.10
252
23
53.20
314
21
44.10
404
23
0.00
7
1
60.42
401
14
11
Dharwad
65.30
172
15
74.80
162
19
62 20
157
9
0 00
55
9
67 18
328
11
12
Gadaa
65 30
170
14
74 80
161
18
52.58
295
17
0 00
45
7
67 18
327
10
13
Haveri
65 30
169
13
74 80
160
17
57.60
220
12
000
28
5
67.18
326
9
14
U. Kannada
86.10
54
4
89.90
57
7
68.48
91
6
18.55
191
25
24 89
543
25
15
Bellary
54,00
229
19
52.60
320
23
46 16
381
22
0 00
27
16
Bidar
52.50
237
22
50 30
336
24
50 01
328
20
2.86
123
17
Gulbarga
47.70
262
27
25.30
494
27
38 40
471
26
0.65
18
Koooal
48.00
258
25
37.20
418
25
40.76
441
25
12 32
19
Raichur
48.00
260
26
37.20
419
26
36 84
484
27
20
Chikkamangalore
78 00
97
8
83.50
97
15
64.47
135
21
D. Kannada
91.50
38
2
86 00
78
13
77.39
22
Udupi
91.50
37
1
86.00
77
12
23
Hassan
69.70
145
11
92.80
31
3
24
Kodagu
79 40
90
6
94&0
17
25
Mandva
61.90
185
17
88 00
26
Mysore
69.70
144
10
92.70
27
Chamarajanagar
69 70
143
9
92.70^|.
Rank in
Karnataka
In 27
districts
%
Rank in
Rank In
India in Karnataka
569
in 27
districts districts
Rank In
Karnataka
In 27
districts
7.
'
Rank in
Rank in
India in Karnataka
569
in 27
districts districts
4
69 41
301
5
20
49 84
471
23
113
19
51 92
456
22
174
23
53.91
442
19
12.32
175
24
53.91
443
20
8
4.97
136
22
57.25
424
17
34
3
000
78
16
16 49
557
27
74.02
49
4
0.00
70
15
16.49
556
26
59.32
200
10
0.00
88
18
65.55
351
13
1
72.53
63
5
0 00
85
17
36 95
524
24
67
11
51.62
306.
19
0.00
69
14
58.65
417
16
34
5
55 81
246
14
0.00
67
13
68.16
315
7
33
4
43.02
419
24
_^P_oo_
53
8
68.16
314
6
DISTRICT WISE DEMOGRAPHIC INDICATORS OF KARNATAKA
Births registered
Deaths registered
Composite Index
Rani; in
Rank In
India In 569 Karnataka In
districts
27 districts
Rank In
Rank In
India In 569 Karnataka In
districts
27 districts
Rank In India
Rani; In
In 563
Karnataka in 27
districts
districts
SI.
No.
Districts
1
Sanqaiore(U)
86.87
145
19
91.17
42
18
75.19
73
2
Eangalore(R)
64.88
264
24
82 03
79
19
75.34
72
9
a
Chitradurga
93.84
82
7
95 11
23
9
73 98
84
11
4
Davanagere
50.56
316
27
32.27
371
27
65.43
173
21
5
Kolar
84.01
154
20
95.11
<b
1
71.92
106
16
6
Shimoga
93.84
88
13
95.11
29
15
80.37
29
2
7
Tumkur
90.53
119
18
94.66
31
17
73.97
85
12
8
Belgaum
93.84
80
5
95 11
21
7
68 75
135
18
9
Biapur
93.84
78
3
95.11
19
5
62.86
206
22
%
%
%
10
10
Bagalkote
54.77
307
26
34.95
358
26
54 71
299
26
11
Dharwad
93.84
81
6
95.11
22
8
73.03
96
13
12
Gadag
93.10
103
15
59 42
207
21
69 72
124
17
13
Haven
62.93
276
25
40 17
321
25
65.66
170
19
14
U.Kannada
93.84
85
10
95.11
26
12
76.11
61
5
15
Bellary
93.84
79
4
95 11
20
6
65.54
171
20
23
16
Bidar
91 10
115
17
95.11
18
4
60 55
230
17
Gulbarga
92.70
1C5
16
95.11
16
2
5831
255
25
18
Koppal
75.82
202
23
48 39
258
24
53 09
323
27
19
Raichur
93.84
77
2
95.11
17
3
58.34
253
24
20
Chikkamangalore
79.44
181
22
50 70
240
23
72.13
102
15
21
D.Kannada
93.84
86
11
95.11
27
13
78.77
41
4
22
Udupi
81.56
167
21
52.05
233
22
75.97
64
6
23
Hassan
93.84
89
14
95.11
30
16
81 55
25
1
24
Kodagu
93.84
87
12
95.11
28
14
80.06
30
3
25
Mandya
93 84
84
9
95.11
25
11
75.86
66
7
26
Mysore
93.84
83
8
95.11
24
10
75.70
68
8
27
Chamarajanagar
93.84
76
1
59.89
205
20
72.18
101
14
Source: National Population Commmission
HIN India Annex III - Project Budget
Implementing Partner:
Project Title:
WHO
Health InterNetwork, India Pilot
Start Date:
Completion Date:
Agency Project ID code:
IMIS Project ID:
UNFIP Project Reference No.:
07/01/01
12/31/02
Q
Revision:
(Explain reason for
revision, i.e„ "new start
date", "extension", etc.I
WHO-GLO-00-15OB
Project Budget
CCAQ
codes
UNDP
codes
Project
II
Object of Expenditure
Budge:
Work-rr.orins
Lines
011
11
040/060
030
330
030
12
18
15
14
1 Salaries
a
International Professionals
d
Consultants
c
National Professionals
d
UN Volunteers
e
Administrative assistants
Total
2 Travel
Evaluation
Other mission travel
16
17
21
21
22
810
820
32
33
600
45
45
45
49
830
79
620
640
350
=f)0
III
0
5,200
64,500
0
15,500
85,200
0
1
6
0
6
13
Year 2
USS
|
Wort-monlhs
0
1,300
21,500
0
5,200
28,000
0
3
12
0
12
27
Year 4
|
Work-monUts
USS
0
3,900
43,000
0
10,300
57,200
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
OSS
0
13,600
18.100
0
0
0
0
3 Contractual services
International
National
Total
183,200
183,200
0
131,000
131,000
0
52,200
52,200
0
0
0
0
4 Meetings and training
Fellowships
Seminars, workshops, meetings
Total
0
61,100
61,100
0
28,900
28,900
0
32,200
32,200
0
0
0
0
5 Acquisitions
a
IT equipment
b
Transport equipment
c
Other acquisitions
Total
237.400
2,500
1,100
241,000
237.400
2,500
1,100
241,000
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
10.000
18,100
12,700
40,800
600
9,800
6,300
16,700
9,400
8,300
6.400
24,100
0
0
0
___ 0_
0
719,000
535,200
183,800
0
0
7 Miscellaneous
Reporting costs
Supplies
Sundry
Total
8 Total Project Cost
99
0
4
18
0
18
40
|
WwA-monlhs
USS
4,200
85,400
89,600
6 Grants
Total
53
53
53
|
Year 1
8,700
99,000
107,700
Total
360
370
300
Total
4,500
9 Support Cost @ 5%
35,950
26,760
9,190
0
0
10 UNF Contribution Total
754,950
561,960
192,990
0
0
561,960
192,990
___ 0
0
11 Cost Sharing
0
12 Grand Total
754,950
Notes:
i
2
3
4
5
All line items should be rounded off to the nearest hundred dollar or nearest dollar, as applicable.
Each line item should have detailed supporting justification and/or information.
Operating Expenses include bank charges, expendable office supplies, telephone lines/fax charges, freight, etc..
Training includes workshops, seminars, fellowships and similar activities.
’UNF Contribution Total" comprises cost sharing provided through UNFIP
Use this sheet for one agency. See "Project total" sheet for more guidance
Implementing Partner:
(Name of agency for this portion of grant)
Project Title:
Health InterNetwork. India Pilot
Start Date:
Revision:
Completion Date:
37621
Agency Project ID code:
IMIS Project ID:________________
|UNFIP Project Reference No.:
[
(Enter specific agency project number)
0
(Explain reason for
revision, i.e., "new start
date", "extension", etc.)
□
WHO-GLO-OO-1508
Project Budget
CCAQ
codes
UNDP
codes
°ro;ecl
II
Object of Expenditure
Si-dgc!
Worii-mont/is
Lines
011
040/060
030
330
030
1 Salaries
a
International Professionals
b
Consultants
c
National Professionals
d
UN Volunteers
e
Administrative assistants
Total
11.01
11 96
17.99
14,99
13.99
2 Travel
Evaluation
Other mission travel
e
242
15 99
16.99
Total
360
370
300
21.01
810
820
31.99
32.99
|
0
0
0
0
0
0
USS
Work-months
0
0
0
0
0
0
|
0
Year 4
USS
WorK'/nonths
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
5 Acquisitions
a
IT equipment
b
Transport equipment
c
Other acquisitions
Total
0
0
0
0
0
0
6 Grants
Total
0
0
0
0
0
0
0
0
0
0
8 Total Project Cost
0
0
0
3 Contractual services
International
National
21.02
21.99
Year 1
Total
Total
0
0
4 Meetings and training
620
640
45.01
600
45.02
45.03
49
830
79
350
wo
Fellowships
Seminars, workshops, meetings
Total
7 Miscellaneous
Reporting costs
Supplies
Sundry
52.99
53.01
53 02
Total
99
9 Support Cost @ 5%
0
0
0
10 UNF Contribution Total
0
0
0
11 Cost Sharing
0
12 Grand Total
_____0_
____ 0
___ 0
Notes:
1
2
3
4
5
All line items should be rounded off to the nearest hundred dollar or nearest dollar, as applicable.
Each line item should have detailed supporting justification and/or information.
Operating Expenses include bank charges, expendable office supplies, telephone lines/fax charges, freight, etc...
Training includes workshops, seminars, fellowships and similar activities
"UNF Contribution Total" comprises cost sharing provided through UNFIP
|
USS
Use this sheet for one agency. See "Project total" sheet for more guidance
Implementing Partner:
(Name of agency for this portion of grant)
Project Title:
Health InlerNetwork, India Pilot
37073
Start Date:
Completion Date:
Revision:
37621
Agency Project ID code:
IMIS Project ID:________________
|UNFIP Project Reference No.:
|
(Enter specific agency project number)
0
WHO-GLO-OO-1508
Project Budget
CCAQ
codes
UNDP
codes
Pro;«!
011
040/060
030
330
030
11.01
1 *96
17 99
14.99
1 Salaries
a
International Professionals
b
Consultants
National Professionals
c
UN Volunteers
d
13.99
e
230
242
15.99
16.99
2 Travel
Evaluation
Other mission travel
Administrative assistants
Total
830
79
350
500
400
Worh-monlhs
|
________Year 2
Wcrk-months
USS
|
________Year 3
USS
0
0
0
0
0
0
3 Contractual services
International
National
Total
0
0
0
0
0
4 Meetings and training
Fellowships
Seminars, workshops, meetings
Total
0
0
0
0
0
5 Acquisitions
a
IT equipment
b
Transport equipment
c
Other acquisitions
Total
0
0
0
0
0
0
6 Grants
Total
0
0
0
0
7 Miscellaneous
Reporting costs
0
0
0
0
0
0
8 Total Project Cost
0
0
0
9 Support Cost @ 5%
0
0
0
10 UNF Contribution Total
0
0
0
________ 0_
________ 0_
52.99
53.01
53.02
Supplies
Sundry
Total
99
11 Cost Sharing
0
12 Grand Total
_________ 0_
Notes:
i
2
3
4
5
Work-morJhsJ
0
31 99
32.99
500
0
0
0
0
0
0
Year 1
USS
0
21.01
21 02
21.99
45.01
45.02
45.03
49
520
540
|
0
0
0
Total
810
820
Total
Work-monlhs
Unes
350
370
300
___________ iy_______
II
Object of Expenditure
Budgei
All line items should be rounded off to the nearest hundred dollar or nearest dollar, as applicable.
Each line item should have detailed supporting justification and/or information.
Operating Expenses include bank charges, expendable office supplies, telephone llnes/fax charges, freight, etc...
Training includes workshops, seminars, fellowships and similar activities.
*UNF Contribution Total" comprises cost sharing provided through UNFIP
USS
(Explain reason for
revision, i.e., “new start
date", “extension", etc )
□
Use this sheet for one agency. See "Project total" sheet for more guidance
Implementing Partner:
(Name of agency for this portion of grant)
Project Title:
Health InlerNetworfc, India Pilot
Start Date:
37073
Completion Date:
37621
Agency Project ID code:
IMIS Project ID:________________
|UNFIP Project Reference No.:
|
(Enter specific agency project number)
0
WHO-GLO-00-15OB
Project Budget
CCAQ
codes
UNDP
codes
Object of Expenditure
Budget
011
040/060
11.01
11.96
1 Salaries
a
International Professionals
b
Consultants
030
330
030
17.99
14.99
13 99
c
d
e
230
242
15 99
16.99
2 Travel
Evaluation
Other mission travel
21.01
370
300
21.02
21.99
810
820
31 99
32.99
620
45 01
640
600
45.02
45.03
49
830
79
|
VVoriiunonr/is
Lines
~360
i
Total
USS
National Professionals
0
0
o
0
0
o
UN Volunteers
Administrative assistants
Total
0
0
o
o
0
0
0
0
Total
0
Contractual services
International
National
Total
o
0
o
4 Meetings and training
Fellowships
Seminars, workshops, meetings
Total
5 Acquisitions
a
IT equipment
Transport equipment
b
c
Other acquisitions
Total
6 Grants
Total
0
o
0
o
0
o
0
0
0
7 Miscellaneous
350
500
400
Reporting costs
Supplies
Sundry
Total
52.99
53.01
53.02
0
0
0
0
8 Total Project Cost
9 Support Cost @ 5%
10 UNF Contribution Total
11 Cost Sharing
12 Grand Total
Notes:
i
2
3
4
5
All line items should be rounded off to the nearest hundred dollar or nearest dollar, as applicable
Each line item should have detailed supporting justification and/or information.
Operating Expenses include bank charges, expendable office supplies, telephone lines/fax charges, freight, etc.
Training includes workshops, seminars, fellowships and similar activities.
"UNF Contribution Total" comprises cost sharing provided through UNFIP
Use this sheet for one agency. See "Project total" sheet for more guidance
Implementing Partner:
(Name of agency for this portion of grant)
Project Title:
Health InterNetworfc. India Pilot
Start Date:
37073
Completion Date:
Agency Project ID code:
IMIS Project ID:
|UNFIP Project Reference No.:
(Explain reason for
revision, i.e., "new start
date”, "extension", etc.)
□
Revision:
37621
(Enter specific agency project number)
0
|
WHO-GLO-00-15OB
Project Budget
CCAQ
cooes
011
040/050
030
330
030
230
—^2
UNDP
codes
^oject
II
Object of Expenditure
BixJget
|
Work-norths
11.01
11 96
17.99
14 99
1 Salaries
a
International Professionals
b
Consultants
c
National Professionals
d
UN Volunteers
13.99
e
Administrative assistants
Total
2 Travel
Evaluation
Other mission travel
15.99
15 99
Total
IV
Year 1
Total
Work-tr,Orths
USS
0
0
0
0
0
0
0
0
0
0
0
0
|
0
Year 3
USS
VV<y><-n:on//)S
0
0
0
|
0
Year 4
USS
Work -norths
0
|
0
USS
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
3 Contractual services
360
370
300
21.01
2 V02
21 99
810
820
31.99
32 99
International
National
Total
0
0
0
4 Meetings and training
600
45.01
45 02
4503
49
830
79
620
540
350
500
400
•
Fellowships
Seminars, workshops, meetings
Total
5 Acquisitions
a
IT equipment
b
Transport equipment
c
Other acquisitions
Total
6 Grants
Total
7 Miscellaneous
Reporting costs
Supplies
Sundry
Total
52.99
53.01
53.02
99
8 Total Project Cost
0
0
0
0
0
0
0
0
0
0
0
0
9 Support Cost @ 5%
0
0
0
0
0
10 UNF Contribution Total
0
0
0
0
0
_____ 0
____ 0_
____ 0_
0
n Cost Sharing
12 Grand Total
Notes:
i
2
3
■i
5
0
____ 0_
All line items should be rounded off Io the nearest hundred dollar or nearest dollar, as applicable
Each line item should have detailed supporting justification and/or information.
Operating Expenses include bank charges, expendable office supplies, telephone lines/fax charges, freight, etc
Training includes workshops, seminars, fellowships and similar activities.
"UNF Contribution Total" comprises cost sharing provided through UNFIP
*
HealthlnterNetworklndiaPilot
| Duration
TaskName
Projectworkplan
Finish
Start
Odays
Thu8/9/01
Thu8/9/01
Jul
August _
Septembe
Aug
Sep
Define and identify main stakeholders, reference sites and access poi
1wk
Fri6/15/01
Thu6/21/01
Conduct detailed needs assessments at sites and determine requirem
6wks
Fn6/22/01
Thu8/2/01
2
Developworkplan(includingworkshopwithkeystakeholders)
1wk
Fri8/3/01
Thu8/9/01
3
Health ResearchlnformationSystem
Odays
Thu12/13/01
Thu12/13/01
Network key research institutions related to tuberculosis and tobacco
18wks
Fri8/10/01
Thu 12/13/01
4
8/1 (
Develop processes and templates for dissemination of research (incli
6wks
Fri8/10/01
Thu9/20/01
4
8/1(>[T
8/1 h
Odays
Thu12/13/01
Thu12/13/01
Review and adapt system for developing integrated Virtual Health Lib
9wks
Fri8/10/01
Thu 10/11/01
4
Network medical college libraries in reference states with National M(
9wks
Fri 10/12/01
Thu 12/13/01
11
NetworkMedicalCollegeLibraries
Odays
Thu 1/3/02
Thu1/3/02
Establishcontentselectioncriteria.standardsandprocesses
4 wks
Fri8/10/01
Thu9/6/01
4
e-publishing of selected journals and other key information (national
17wks
Fri9/7/01
Thu 1/3/02
15
Userinterfacedevelopment
20wks
Fri8/10/01
Thu 12/27/01
20
Connectivityandinfrastructureataccesspoints
Odays
Thu 1/3/02
Thu 1/3/02
21
Establishtechnicalspecifi cations, standardsandprocess
2wks
Fri8/10/01
22
Establishconnectivity (hard ware,software, intemetconnectivity)
19wks
Fri 8/24/01
24
Training/development
Odays
Thu1/3/02
Thu 1/3/02
25
Developtrainingmodules
17wks
Fri 8/10/01
26
Conductimtialtrainingprogramsatsites
4wks
Ongoingprojectmanagementandsupport
Trainingupdatesduringpilot
Electronicpublishingofkeyjournalsandotherkey information.
•n-18/2
>0
( :
10/
8/1 (>D
4
8/1 (> n
Thu8/23/01
4
8/1
Thu 1/3/02
21
'8/24
Thu 12/6/01
4
8/10>y~
Fri 12/7/01
Thu 1/3/02
25
52wks
Fri 1/4/02
Thu 1/2/03
22
52wks
Fri 1/4/02
Thu 1/2/03
22
8wks
Fri 1/3/03
Thu2/27/03
28
||----- 1|—j 8/23
23
27
28
29
30
31
32
|
Pilotevaluation
Task
Task Progress
u
Milestone
RolledUpMilestone
Summary
RolledUpProgress
CriticalTask
RolledUpTask
CriticalTaskProgress
RolledUpCriticalTask
II
Split
ExternalTasks
Pagel
Projectsummary
th9'6
HealthlnterNetworklndiaPilot
Task
1)____ ___ u
Milestone
CriticalTask
II____ _____ 0
RolledUpTask
CriticalTaskProgress
RolledUpCriticalTask
0____ _______ I)
u____ _______ |]
Rolled UpMilestone
xz
Split
1
1
□__________ J
ExternalTasks
Page2
Projectsummary
■----- 1
e"wo:k :/ esting at Ni ’ Sanglore
‘
■ >• ■?':: TS TTTftft. "r.ftcTTSftwrk Bfeefcg aft NT;' IBte’t.g
ft Cm. /00'' 17.//:'. 8 +053C
Thelma 1
S Sadagopar. T
•• Sudha
msiO’” <socha~a@vsr.'.csm>,
■ <ss@'iT2.ac.iT>,
<-ti~die@bjr.vs~..--et.in>,
^©ir.dsg^r.e. -.orr.”’ <sic@indegene.com>
Dear all.
Thank you very much taking out the time fir the meeting and your valuable thoughts/ suggestions/ comments
Will keep you posted with the developments, which should move quickly now.
Best Regards,
Ranjan
-C-ghai Message -Pwvgdj x
"hursday, October 04, 2001 5:19 PM
;ago:= (E--=‘ ); V-mala Murthy (E-mail); Thelma Narayan (E-mail); S Sadagopan (--ma;:), i-.dha v.-.—. (
- ee t- "rernstworx-Yeeting at NT; 3angiore,
‘ -a '.gs-".-.
:~z •"aeting at ths National TubercTosis mstitute, 3anga;:;m :
,-.'6C 2S CV
'
^’'.csrS;';''2:ng of the scops of the pilot.
' repsrstory ''3.x: steps.
:c;rg c*
and resource persons for different project compor.3’: s
4o:~er matte”.
tsk’-c 'cm/ara : me meeting
-<s"i an
j-’ .■
• T enders wou^d be joining iater
Ranjan Dwivea:
°rcject Manager- KeaSt”. nierNetwork India Project
•Aoric Health Organization
Rm 530 'A‘ Wing, \iman Bhawan, New Delhi
a
HEALTH INTERNETWORK INITIATIVE
TECHNOLOGY ADVISORY WORKSHOP
Date:
October 10-11, 2001
Venue: Pan American Health Organization / World Health Organization
525 Twenty-third Street, N W.
Washington, D C 20037
USA
The Health InterNetwork Initiative
In September 2000 UN Secretary-General, Kofi Annan, launched the Health
InterNetwork as a partnership to bridge the digital divide in health. Led by the World
Health Organization, the Health InterNetwork (HIN) brings together international
agencies, the private sector, foundations, non-governmental organizations and country
partners under the principle of ensuring equitable access to health information. The aim
of the initiative is to improve public health by improving the information environment of
health personnel, health-care providers, researchers and scientists, and policy makers
The core elements of the initiative are content, connectivity, and capacity building.
The Health InterNetwork site will help users find, organize, and share information for
public health. The information itself is produced and managed by different content
providers around the world Users will be able to access statistical data, scientific
publications and information for health policy and practice, as far as possible in their own
language. In addition, the site will make available a range of health information
technology applications such as geographical information systems and epidemiological
tools, as well as courses and training offered through distance learning. Particular
attention will be given to the production and publishing of local and regional healthrelated information that is currently unavailable electronically.
1.
Objectives of the Technology Advisory Workshop
The overall goal is to review technology options and provide recommendations for the
development and deployment of the Health InterNetwork site.
1.
Examine user scenarios, requirements, architecture, hardware and software
platforms, development process and software tools and resources,
knowledge/content management, connectivity implications and other technologyrelated issues which will impact site development and use.
2.
Consider implications, risks and potential cost and time requirements for
recommended options.
3
3.
Issues for Discussion by Workshop Participants
User and content requirements - Characteristics of the data in each content area,
global and local user requirements, and language implications.
Processes - Syndication of content from major content providers; publishing of local
content; authentication processes for restricted information; search, retrieval, and
display requirements, meta-data in building community and collaborative
environments; site architecture, navigation, and user interface design; development
options and associated implications, risks, and costs; updates and maintenance
issues.
Hardware options - Server platform, user devices, hardware options and
constraints; maintenance logistics; costs, risks, and implications
Software options - user device operating system, internet browser, email package,
office suite, proprietary and non-proprietary design tools; knowledge management
tools; search engines; databases; scalability; developer’s toolkits; management
interfaces; proprietary and non-proprietary applications for public health, authoring,
distance education, statistical packages, logistical support of health services
operations, peer-to-peer interactivity, etc; security
Connectivity - Constraints at country level e g. spectrum of options to access the
functionalities limited by existing telecommunication infrastructure, service level of
local ISP, and last-mile issues.
Technology resources - Identification of companies, experts, international and
national organizations, key national partners, academic institutions who could
contribute to HIN project
4.
Participants List - tentative
(See attachment)
5.
Background information on the Health InterNetwork Initiative
(See attachment)
HEALTH INTERNETWORK INITIATIVE
TECHNOLOGY ADVISORY WORKSHOP
Date:
October 10-11, 2001
Venue: Pan American Health Organization / World Health Organization
525 Twenty-third Street, N.W.
Washington, D.C 20037
USA
The Health InterNetwork Initiative
In September 2000 UN Secretary-General, Kofi Annan, launched the Health
InterNetwork as a partnership to bridge the digital divide in health. Led by the World
Health Organization, the Health InterNetwork (HIN) brings together international
agencies, the private sector, foundations, non-governmental organizations and country
partners under the principle of ensuring equitable access to health information. The aim
of the initiative is to improve public health by improving the information environment of
health personnel: health-care providers, researchers and scientists, and policy makers.
The core elements of the initiative are content, connectivity, and capacity building.
The Health InterNetwork site will help users find, organize, and share information for
public health. The information itself is produced and managed by different content
providers around the world. Users will be able to access statistical data, scientific
publications and information for health policy and practice, as far as possible in their own
language. In addition, the site will make available a range of health information
technology applications such as geographical information systems and epidemiological
tools, as well as courses and training offered through distance learning. Particular
attention will be given to the production and publishing of local and regional healthrelated information that is currently unavailable electronically.
1.
Objectives of the Technology Advisory Workshop
The overall goal is to review technology options and provide recommendations for the
development and deployment of the Health InterNetwork site.
1
Examine user scenarios, requirements, architecture, hardware and software
platforms, development process and software tools and resources,
knowledge/content management, connectivity implications and other technologyrelated issues which will impact site development and use.
2.
Consider implications, risks and potential cost and time requirements for
recommended options
2
3.
Outline strategy for site design, development, hosting, and testing, including phases,
timeline, milestones, priorities, partners, and options.
4.
Generate list of technology-related resources (products, corporations, institutions,
and individuals) for planning and resource commitment and to involve in follow-up
activities
2.
Proposed Content Areas
The particular strength and added value of the HIN site will be the rapid access to quality
assured public health information from multiple sources, as well as support for local and
locally/regionally-produced information - no site offers these features today. Earlier this
year a working group identified five content areas for the Health InterNetwork.
Content areas
Statistical
Data
Scientific
Publications
Information
Collections
Distance
Education
Numerical
information sets
- can include
raw, analyzed,
validated data
Peer-reviewed
primary
scientific
literature, and its
reviews and
indexes
Professional
and continuing
education and
training
packages
ICT tools for
public health
policy and
practice
Official
(international
organization,
national
government)
data and
statistics
Published
scientific
research (may
be priced)
Courses and
training products
for health
professionals at
all levels
Communication,
networking, and
publication tools
inc.
communities of
practice
applications
Epidemiological,
statistical,
program data
from different
sources
Major databases
(eg.
bibliographic,
evidence
compendia), text
books and
manuals
Information
packages.
created for
specific public
health
audiences and
purposes
Policies, reports.
guidelines,
protocols.
reference
material, and
authoritative
health
communication
material
' Gray" literature
and other
publications
Programmed
instruction
products
Public health
work
applications
(eg
Geographical
Information
Systems,
statistical
packages,
training and
diagnostic tools.
telemedicine)
Health IT
Applications
3
3.
Issues for Discussion by Workshop Participants
User and content requirements - Characteristics of the data in each content area;
global and local user requirements; and language implications.
Processes - Syndication of content from major content providers; publishing of local
content; authentication processes for restricted information, search, retrieval, and
display requirements; meta-data in building community and collaborative
environments; site architecture, navigation, and user interface design, development
options and associated implications, risks, and costs; updates and maintenance
issues.
Hardware options - Server platform, user devices, hardware options and
constraints; maintenance logistics; costs, risks, and implications.
Software options - user device operating system, internet browser, email package,
office suite; proprietary and non-proprietary design tools; knowledge management
tools; search engines, databases; scalability; developer’s toolkits; management
interfaces; proprietary and non-proprietary applications for public health, authoring,
distance education, statistical packages, logistical support of health services
operations, peer-to-peer interactivity, etc, security
Connectivity - Constraints at country level e g spectrum of options to access the
functionalities limited by existing telecommunication infrastructure, service level of
local ISP, and last-mile issues
Technology resources - Identification of companies, experts, international and
national organizations, key national partners, academic institutions who could
contribute to H1N project.
4.
Participants List - tentative
(See attachment)
5.
Background information on the Health InterNetwork Initiative
(See attachment)
UNF/UNFIP Project Document
Health InterNetwork (India Pilot)
12 June 2001
World Health Organization
HIN India
Health InterNetwork (India Pilot)
Project document
1.0
CoverPage
• Project title:
Health InterNetwork (India Pilot)
■
Project number:
WHO-GLO-00-150B
•
Project purpose:
To test scalable, sustainable approaches to bridging
the digital divide in health information and the gaps
between health research, policy and practice
■
Duration:
18 months
•
Expected start date:
1 July 2001
■
Location:
India, 2 states: Orissa - Deogarh district;
Karnataka - Bangalore rural district
•
Lead UN agency:
World Health Organization
(WHO country office, New Delhi)
•
UN cooperating agencies
UNDP and UNICEF country offices in India
■
Non-UN executing partners:
National: Ministry of Health and Family Welfare,
Ministry of Information Technology, National
Tuberculosis Institute, Tata Institute of Social
Sciences, Bharat Electronics Ltd., private
corporations (e.g. NIIT, TCS, Indegene Life Systems,
2 Streams Media), and NGOs (e.g. Sochara)
International: Harvard Center for International
Development and MIT Media Lab, Cornell
University, BIREME, Collexis Corp., Projecl.net Inc.
■
Total budget:
USS 754,950
■
UNF funding:
USS 754,950 (inch 5% programme support costs)
■
Summary project description:
- Facilitate an Internet-based network of health
service providers, researchers, and policy makers in
the tuberculosis and tobacco control programs
- Provide and test content, connectivity and training
options to enable optimal use of this network
- Enhance the capacity of local research institutions
and medical libraries to support and scale up the
Health InterNetwork
7
World Health Organization
HIN India
I.
2,0
Background and Analysis
Problem Statement/ Challenge/ Context
The Health InterNetwork Project
In September 2000, the UN Secretary-General launched a public-private initiative
to bridge the digital divide in health. Led by the World Health Organization, the Health
InterNetwork brings together international agencies, the private sector, foundations, non
governmental organizations and country partners under the principle of ensuring
equitable access to health information. The aim is to improve public health by facilitating
the flow of health infonnation, using the Internet. Health information - relevant, timely
and appropriate - must become unrestricted and affordable worldwide, so that all
communities can benefit from this global public good.
The focus of the Health InterNetwork (HIN) is on improving the information
environment of health personnel: professionals, researchers and scientists, and policy
makers. The core elements of the project are content, connectivity and capacity building.
I. Content: to deliver effective public health services
An Internet portal will provide a shortcut to high-quality, relevant and current
infonnation on public health. Users will be able to access statistical data, scientific
publications and information for health policy and practice, as far as possible in their own
language. In addition the portal will make available a range of infonnation technology
health applications such as geographical infonnation systems and epidemiological tools,
as well as courses and training offered through distance learning. Particular attention will
be given to the production and publishing of local and regional public health information
that is currently unavailable electronically.
II.
Connectivity: for information and communication
Starting on a small scale with 6-8 pilot projects and rolling out over a 7-year
period, the Health InterNetwork seeks to establish and equip up to 10,000 Internetconnected sites. The logistics of supplying, delivering and installing hardware and
software, Internet connectivity and providing maintenance will require working with non
governmental organizations and corporate and local private sector partners.
III.
Capacity building: to create an enabling information environment
Finding, evaluating, using and managing information is a significant challenge in
public health settings all over the world. Health InterNetwork training will concentrate on
building the skills needed to put infonnation into action: 1) infonnation access and use in
daily work, 2) basic computer and Internet skills, and 3) hands-on training to use
specialized public health tools.
3
World Health Organization
HIN India
HIN India pilot
India was selected as the one of the first HIN pilot countries because it has several
priority public health programs as well as valuable skills and resources that would
contribute to the development of the global Health InterNetwork project. Each HIN pilot
focuses on a particular facet of the overall Health InterNetwork. In the HIN India pilot,
the focus is on the gaps between health research, policy and practice.
Gaps between health research, policy and practice in India
These gaps exist throughout the world and have to be addressed to ensure that
relevant research reaches citizens in the form of effective, up to date health care.
Dr C.P. Thakur, the Union Minister for Health and Family Welfare, has
highlighted the gaps in the health research, policy and practice in India. In his 2001 status
report on TB in India, he points out that, as an example, most of the significant research
on the cure and control strategy for tuberculosis was carried out in India. Pioneering
research from the Tuberculosis Research Center, Chennai, and the National Tuberculosis
Institute, Bangalore, included:
the effectiveness of ambulatory treatment of tuberculosis, the effectiveness of intermittent
treatment regimes, the necessity of direct observation of treatment (DOT) by a trained
individual who is not a family member, the usefulness and practicability of AFB
microscopy as a diagnostic tool among patients reporting to health facilities and the
crushing burden of disease of tuberculosis on our society.
However, while several other countries benefited from these findings, India was
among the last countries to introduce this key life-saving research into its own health
policy and practice.
Regarding tobacco-related morbidity, the WHO Director-General observed last
year that it was in India, in 1964, that the first link between oropharyngal cancer and
chewing tobacco was identified. Studies from eastern India were the first in the world to
link palate cancer to the chewing of tobacco. Yet again, while other countries were able
to act decisively on this research, the tobacco control program in India is still in its
inception.
The implications of these gaps between health research, policy and practice must
be considered in the context of the magnitude of the two public health problems
discussed above - tuberculosis and tobacco use.
The burden of tuberculosis
In the 2001 report on tuberculosis, the Directorate General of Health Services in
India presents the effect of the disease on the country and its people, despite there being a
cure for the disease.
4
World Health Organization
HIN India
Everyday in India more than 20 000 people become infected with the tubercle bacillus.
more than 5 000 develop the disease, and more than 1 000 die from TB. India accounts
for nearly one third of the global burden of tuberculosis and the disease is one of India's
most important public health problems.
Tuberculosis is a major barrier to social and economic development. The direct and
indirect costs of tuberculosis to the country amount to Rs. 12 000 crore (US $3 billion)
per year. Every year, more than 17 crore (US $170 million) workdays are lost to the
national economy on account of tuberculosis, at a cost of Rs. 700 crore (US $200
million).
Every year, 300 000 children are forced to leave school because their parents have
tuberculosis, and 100 000 women lose their status as mothers and wives because of the
social stigma of tuberculosis. Tuberculosis kills more women than all causes of maternal
mortality combined (TB India 2001).
The Revised National Tuberculosis Program (RNTCP) has made a significant
impact on the burden of disease related to tuberculosis. Currently the program covers
more than one third of the country and 80% of the patients treated are being cured of the
disease compared with the 25% cure rate of a decade earlier. However there is still a lot
of effort needed to combat the disease and 'unless urgent action is taken more than 40
lakh (4 million) people in India will die of tuberculosis in the next decade'.
The tobacco threat
Tobacco has been established to be a risk factor in over 25 diseases, the first links
to cancer having been identified in India as mentioned earlier. In her address at the
International Conference on Global Tobacco Control Law in New Delhi, the WHO
Director-General Dr Gro Harlem Brundtland stated:
Today in India, tobacco kills 670,000 people every year. If unchecked and unregulated,
by 2030, tobacco will kill 10 million people each year. Seventy percent of those deaths
will occur in the developing world, with India and China in the lead. If nations do not act
individually and together, in the next 30 years, tobacco will kill more people than the
combined death toll from malaria, tuberculosis and maternal and child diseases. Every
tobacco related death is preventable. That is our message. That is our challenge.
The Framework Convention was introduced as a new legal instrument negotiated
by WHO, its member countries, and partners, including UNICEF and the World Bank, to
deal with the problem of tobacco use in a comprehensive manner.
The Framework Convention is expected to address issues as diverse as tobacco
advertising and promotion, agricultural diversification, product regulation, smuggling,
excise tax levels, treatment of tobacco dependence and smoke-free areas.
The Framework Convention process will activate all those areas of governance that have
a direct impact on public health. Science and economics will mesh with legislation and
litigation. Health ministers will work with their counterparts in finance, trade, labour,
agriculture and social affairs ministries to give public health the place it deserves.
5
World Health Organization
HIN India
Where are the gaps between health research, policy and practice?
There are several factors that contribute to the disjoint between research, policy
and practice. For instance, one important reason why research is not effectively utilized is
that it is often not perceived to be relevant to the priority health needs of the country. A
comparison of medical research carried out in India (as reflected by published literature)
with the country's healthcare needs (as reflected by morbidity and mortality statistics)
showed that there was a considerable mismatch between the two (Subbiah Arunachalam
1998). In addition the variability in reliability and validity of health research further
reduces its perceived utility.
The main objective of the Health InterNetwork project is to address the digital
divide in health information. Policy makers, researchers, health practitioners, information
scientists and librarians identified reasons for the current disjoint between research,
policy and practice in the context of the HIN project, access to research, dissemination of
research, and the environment for communicating research using information and
communication technologies.
I. Access to health research
India accounts for 23% of the global burden of disease from tuberculosis but only
for 5-6% of the world’s research output in this area as seen from papers indexed in three
international databases, viz. PubMed, Science Citation Index and Biochemistry and
Biophysics Citation Index over the ten years 1990-1999'. To improve the relevance of
health research the value of developing country research has to be recognized and
promoted.
In addition, access to these international databases is expensive and difficult.
Equitable and effective dissemination of health research information has to be ensured.
Currently in India it costs USS 12 to get one full text journal article from an international
database. It can take up to four months for a copy of this article to be delivered by surface
mail from the National Medical Library which has the single largest collection of
scientific and medical journals, both national and international, in the country. Most of
these journals are currently only available in hard copy.
Even when the research information is available it is often not in the form most
useful for the different stakeholder groups in health. Very few people, other than
researchers, read through multiple page reports or articles on research protocols and
findings. The appropriate formatting of research information is therefore crucial to
enhance the utilization of research for health policy and practice.
II.
Dissemination of research
There are various efforts related to dissemination of health research in India.
However, a huge amount of (valuable) unpublished information lies around in research
and medical institutions as raw or partially analyzed data. There is also considerable
6
World Health Organization
H1N India
duplication of effort across public, private and academic sectors involved in health care
and very little coordination between them.
Various agencies, donors, private and academic institutions all commission
research related to tuberculosis and tobacco control in India. However, there is no
network in the country to coordinate these efforts or to make this information available to
health policy makers, practitioners or other researchers. The flow of research information,
both international and national, leaves much to be desired and it can take several months
and even years for data to be analyzed and disseminated, all this reducing the perceived
utility of research for policy and practice.
III. The environment for the communicating health research using information and
communication technologies
Information and communication technologies offer cogent solutions to some of
the problems related to the access and dissemination of health research. These solutions
include tools for structuring health information networks, facilitating electronic
publishing, building searchable databases of local research, and enabling Internet-based
exchange of health information. However, these solutions have significant resource
implications and have to be situated in the larger social and political environment of the
country.
Infrastructure
An e-readiness assessment was conducted in five states that were initially
proposed for the Health InterNetwork India pilot. An e-readiness assessment tool
developed by the Harvard Center for International Development and the MIT Media Lab
(http://www.readinessguide.org ) was used for this purpose. The assessment showed that
even slates that were considered to be at the forefront of the information technology
revolution, in India and internationally, still faced many of the environment-related
problems outlined in the UN Administrative Committee on Coordination (ACC) 1998
statement:
The information technology gap and related inequities between industrialized and
developing nations are widening: a new type of poverty - information poverty - looms.
Most developing countries, especially the Least Developed Countries (LDCs), are not
sharing in the communication revolution, since they lack:
• affordable access to core information resources, cutting edge technology and to
sophisticated telecommunication systems and infrastructure;
■ the capacity to build, operate, manage, and service the technologies involved;
■ policies that promote equitable public participation in the information society as both
producers and consumers of information and knowledge; and
■ a work force trained to develop, maintain and provide the value-added products and
services required by the information economy.
Inequity
7
World Health Organization
HIN India
In addition to addressing these basic infrastructural issues care has to be taken that
the introduction of new technologies does not exacerbate existing inequities or create new
ones not only on an international level, but also within the country. For example, only 22
people in 1000 have telephone access in India and less than 2 in 1000 use the Internet. Of
Internet users in India more than 75% are males under the age of 30 from the higher
educated strata in the country (Eddie Cheung 2001). Facilitating equitable access has to
be paid particular attention when considering the use of technology in the health system
where professionals higher up in the health system hierarchy, like doctors and policy
makers, are predominantly male while the majority of the countries community health
workers are female.
Building up the basics
In considering the far-reaching and creative solutions offered by infonnation and
communication technologies, it is therefore important not to lose track of the foundations
on which these solutions must rest.
At a meeting to plan the Health InterNetwork India, Professor S. Vijaya, a
researcher currently working on genetics and tuberculosis at the Indian Institute of
Science, emphasized the importance of starting with the basics, and building up the
foundation of health research, policy and practice system in the country:
Research information needs to be compiled and made to reach the medical community as
well as the policy makers. In another 5 to 10 years, we should be able to see it making a
dent in the manner in which medical students are taught. I do believe that if we in India
can ensure that every medical graduate will come out and treat every TB patient he or she
sees with the standard, (current) WHO prescribed regimen of anti-TB drugs, we can
dramatically reduce the incidence of both TB as well as drug resistance.
I find the possibility exciting that we too, like some of the developed countries can make
a dent in our TB control programme without waiting for that miracle new drug that
everyone promises.
3.0
Relationship to UNF/UNFIP Programme Framework and Project Criteria
In 1998, ACC expressed profound concern at the deepening maldistribution of
access, resources and opportunities in the infonnation and communication field and
committed the organizations of the United Nations to assist developing countries in
redressing these alarming trends.
Through establishing new connectivity and infrastructure in developing countries
the Health InterNetwork responds to the ACC commitment to address the growing
inequities related to information and communication resources. In addition, the India pilot
aims to support priority health programs for tuberculosis and tobacco control where the
ultimate beneficiaries are the 'poorest of the poor1 who invariably bear the greatest burden
of these problems.
8
World Health Organization
HIN India
4.0
National/Government Commitment
The Government of India is firmly committed to the use of information and
communication technology for health. In 1986 the Indian Medlar Centre was set up as a
joint project of the Indian Council of Medical Research (ICMR) and the National
Informatics Centre (http://indmed.delhi.nic.in) to facilitate access across the country to
national and international bio-medical information. More recently, there have been two
major initiatives planned by the national government that correspond to the Health
InterNetwork objectives.
An expert committee on the Application of Information Technology in Medical
Education in India in its report dated January 2001, recommended that the following
projects be implemented through the Ministry of Health,
* School of Health Informatics at the Sanjay Gandhi Postgraduate Institute of
Medical Sciences, Lucknow,
■ Developing the use of IT for research, teaching and patient care at the
Postgraduate Institute of Medical Education and Research, Chandigarh,
" Knowledge network on Medicinal Plants and National Centre for Training and
Technology Transfer at the Regional Research Laboratory at Jammu,
■ Developing a National System of Flealth Research Information al the ICMR.
On March 22, 2001 the Prime Minister of India launched a national scheme for
linking 23 government medical college libraries. The scheme, with a budgetary provision
of over USS200,000, provides basic infrastructure, connectivity, and training to one
medical college library each in of 23 States. The libraries will be networked to share the
resources of the individual libraries as well as of the National Medical Library located in
Delhi.
The Health InterNetwork pilot will integrate with these national priority programs
and will thus also provide a means of integration between the individual national
programs.
Prerequisites and policy
The processes for logistic and policy procedures for implementation of the project
are in place. Representatives of the Ministry of Health and Family Welfare, Indian
Council of Medical Research, Ministry of Information Technology, National Institute of
Communicable Diseases, and the National Informatics Centre are key members of the
core team formed to facilitate planning, implementation and evaluation of the HIN pilot
project. The pilot project has evolved from discussions in the core team and the direct
involvement of the Ministry of Health and Family Welfare. The pilot will be coordinated
through a full time project manager in the office of the WHO Representative to India with
support from the HIN task force based at the WHO headquarters.
9
World Health Organization
I-IIN India
Integration and sustainability
The project responds to the needs of the government and integrates with the
government plans for ICT and health. The government has earmarked complementary
funding that augurs extremely well for the sustainability. For each component of the pilot
project a focal point has been identified from key governmental institutions to facilitate
project ownership, implementation and integration with the larger national infrastructure
and capacity building efforts.
5.0
Process followed in Project Identification/Formulation
In his announcement at the 2000 Millenium Assembly, the UN Secretary General
Kofi Annan described the Health InterNetwork in the following terms:
This network will establish... 10,000 on-line sites in hospitals, clinics and public health
facilities throughout the developing world. It aims to provide (tailored) access to relevant
up-to-date health and medical information...
The equipment and Internet access, wireless where necessary, will be provided by a
consortium... in co-operation with foundation and corporate partners.
Training and capacity-building... is an integral part of the project. The World Health
Organization is leading the United Nations in developing this initiative with external
partners.
Following this commitment from the Secretary-General, an inter UN agency
meeting was held in Geneva to define the specific objectives of the project. A small HTN
task force began working on the project at WHO, Geneva, with financial support from the
UN Foundation of USS 734,000. It was decided to develop the project up on the basis of
6-8 pilot projects conducted during the first year. India was selected as the first HIN
pilot country because it has several priority public health programs as well as the skills
and resources that would contribute to the development of the global Health
InterNetwork.
Over the next couple of months, meetings were held in India with key
stakeholders in health and information and communication technology in the country
(including the government, local UN agencies, NGOs, research institutions, policy
makers, health service providers, researchers, and the private sector) to discuss options
for the pilot project focus and scope. In addition, through a questionnaire the information
needs of over 600 policy makers, health service providers, researchers were assessed.
(The results of this assessment and other project related information is available on the
project development web site at www.hin.org.in).
10
World Health Organization
HIN India
Based on these inputs a draft project plan and logical framework were drafted
and circulated to some key experts and stakeholders. The consultations on this draft were
used to build up this proposal including the logical framework (Annex 1).
6.0
a.
Related Past and Current Activities
Lessons learned from past approaches to resolve the problem
There have been some very successful experiences related to the use of
information and communication technologies for development in India and there are four
main lessons to heed.
I.
Focus on need-based content
Mr Arunachalam, who coordinates an innovative, useful and used telecenter
project in rural Tamil Nadu advises, "The first thing we should do is to shift our focus
from the technology part of IT to the information (or content) part. (People's) information
needs are different. It is only on the basis of their current needs and how they get those
needs satisfied (that) one can think of meaningful technological interventions."
Dr C.A.K. Yesudian, head of the Department of Health Services at the Tata
Institute of Social Sciences, also emphasizes that the key to the success of the FUN India
project will be an in depth understanding of the needs of the main stakeholders involved
in the project. In addition he notes that this understanding would need to inform building
up the capacity of local institutions to meet these and future needs past the project phase.
II.
Aim for broad access and resource sharing
Capacity building cannot be confined to central institutions. 'When resources are
limited and the population to be served is very large, then considering community-based
access (to affordable and appropriate technology) and resource sharing is the only choice.
That is precisely what Sam Pitroda did, when Prime Minister Rajiv Gandhi called for his
help in improving telecom services in India. Thanks to Pitroda’s plan, today virtually
every town in India has a public telephone booth within a short distance from where one
can make local, national and international calls' (Subbiah Arunachalam 1999).
III.
Use local solutions
Dr Ashok Jhunjhunwala of the Indian Institute of Technology, Madras, noticed
that if telephone coverage had to move from 1 per cent of Indian homes to 15 to 25 per
cent, the transition would cost an astronomical sum, way beyond the means of a
developing country. The only solution was to get rid of the expensive copper wires,
which need to be hooked to every home wanting a phone connection. The problem
identified, Dr Jhunjhunwala went ahead to make the breakthrough 'wireless local loop'
technology, that also enables Internet access. And at less than half the price of similar
methods developed elsewhere (Shobha Warner 1997).
11
World Health Organization
HIN India
Researchers at the Indian Institute of Science and Bharat Electronics Limited who
are developing the cost-efficient, local language and Internet enabled Simputer have also
made significant advances in this respect.
IV.
Foster an enabling environment
Mrs S.L. Chinnappa (who was responsible for developing the Indian Medlars
Centre, bringing Medline to India, and developing library databases for several key
institutions in India) noted that,
WHO while starting a Health Information Network in India should ensure right from the
beginning, that the best practices of sharing, exchange of ideas and reciprocal contracts
are fostered among the participating institutions - whether Governmental or non
governmental - it should truly be a collaborative network. There should be very low or no
regulatory barriers to join the network.
If WHO wishes to avoid the risk of lapsed time in health care delivery, it should pursue
only an 'alliance strategy'. This will broaden the products/ service channels, improve
quality of information (especially clinical) and achieve more rapid penetration down to
the district and PHC or grass root levels.
...The cost benefits to society will be immeasurable depending on the speed with which
the project is planned, monitored and executed. The key to the success of the project is
the pin-pointing of responsibilities, accountability for delays and equal/mutual
cooperation among all players whether public or private sector, small or large institutions.
The key to the sustainability of the project will be a pilot designed so that it can be
replicated right across the board.
b.
Government/civil society efforts underway to address this problem
The Indian Government schemes, outlined in section 4.0 of this document,
highlight some of the main national efforts in this area. There are several health-related
portals in the country mainly targeted at consumers. Some health portals do address the
professional medical community (e.g. www.indegene.com). There are have been very
few attempts to integrate research information dissemination using Internet technologies,
beyond the individual databases and web sites of institutions like the Indian Medlars
Centre, the Indian Council for Medical Research and the National Tuberculosis Institute
for tuberculosis control. For tobacco control, there is currently an expressed need to
collate national and international research information on the subject. The Health
InterNetwork aims to integrate with these various efforts and build on the potential
synergies between them.
12
World Health Organization
HIN India
II.
Programme/Project Objectives, Activities and Anticipated Results
7.0
a.
Objectives and Strategy
Specify goals and objectives
The overall goal of the HIN India pilot is to test scalable, sustainable approaches
to bridging the digital divide in health information and between health research, policy
and practice. The specific objectives are to,
■ Facilitate an Internet-based network of health service providers, researchers and
policy makers in the tuberculosis and tobacco control programs
■ Provide and test content, connectivity and training options to enable optimal use
of this network
■ Enhance the capacity of local research institutions and medical libraries to support
and scale up the Health InterNetwork
b.
Major programnie/project activities
The major pilot project activities include
Finalizing the project work plan with national and international partners
Facilitating development of the Health Research Information System by
networking key research institutions related to tuberculosis and tobacco control
with the Indian Council for Medical Research
3. Networking key medical college libraries in the two reference states with the
National Medical Library
4. Supporting electronic publishing of key medical journals, health research reports
and policy documents related to tuberculosis and tobacco control and creating
integrated electronic databases of the same
5. Developing interfaces to allow integrated access to various health data sources
6. Establishing Internet connectivity at the selected access points
7. Developing training modules and conducting the initial training for the pilot
project participants
8. Managing the project and providing ongoing support
9. Establishing benchmarks to measure the impact of the pilot and providing optimal
training towards the same
10. Evaluating the pilot
1.
2.
c.
Indicators to measure progress in quantified and measurable terms
Overall the India pilot aims at a 75% increase in the access to health research
information and a 50% increase in the use of this research for policy and practice as
documented related to the tuberculosis and tobacco programs at the pilot sites in 18
months.
The broad indicators listed below will be refined at the time the project work plan
is finalized:
13
World Health Organization
HIN India
Access indicators
■ Inventory of research information, related to tuberculosis and tobacco control,
available at the pilot sites before and after the HIN pilot.
■ Pilot participant rating of access related needed health research information before
and after the HIN pilot (including availability, ease and speed of access, usability
and perceived usefulness).
Use indicators
At the selected pilot sites, before and after the pilot, review and compare:
■ Workflow related to health research, policy and practice, including collaboration
■ Users perceptions of project impact on health service delivery and policy
d.
Changes that the project will facilitate and highlight any innovative, catalytic aspects
■
•
■
■
Formatting health research information for maximal utility for different
stakeholders
Enabling key linkages and networking between health researchers, policy makers
and service providers
Developing scalable models for the use of information and communication
technologies and networking in the public health system
Testing appropriate and affordable technologies that can be used in a sustainable
manner at the community level (e.g. Simputer, solar power, health kiosks,
Wireless in Local Loop or radio-based connectivity)
e. Provisions being made to ensure that the project is sustainable (economically, financially,
socially, culturally)
The project contributes to long-term national government plans for the use of ICT
for health. Focal points have been identified from key national institutions and the private
sector to facilitate project ownership and implementation and integration with national
infrastructure and capacity building efforts. In addition, as the national government is
committed to funding for the use of ICT for health (section 4.0) the potential for
sustainability is encouraging.
With regard to the social and cultural aspects, local language and work
environments will be key considerations in the project and the project itself will be
developed in close consultation with the pilot participants.
f.
Gender and equity considerations
It is observed that over 75% of the Internet users are males under the age of 30
from the higher educated strata in the country (Eddie Cheung 2001). This project relates
to Internet use in the health system where, in general, professionals higher up in the
health system hierarchy, like doctors and policy makers, are predominantly male while
the majority of the village and community health workers are female.
14
World Health Organization
HIN India
Therefore, a dedicated effort is being made in this project to include the
community level public health services in the project as well as to have the health
reference kiosks in the health centers for easier access for village health workers the
majority of whom, as mentioned above, are women.
Currently most of the recognized expert consultants related to the project are
women and an effort will be made to have a gender balance in all the key decision
making and expert groups.
8.0
Beneficiaries
Primary beneficiaries
The primary beneficiaries are health service providers, researchers, and policy
makers and institutions in the public health system in India. The pilot project further
focuses on public health services related to tuberculosis and tobacco control.
a.
Health Service Providers
Medical Officer TB Control (8), TB program and lab supervisors (8), Community Health
Centers (5), Primary Health Centers (10), Doctors (15), Nurses (15), Multipurpose health
workers (15)
Benefits: Desktop PCs at each health center along with a common area health reference
kiosk; Simputers with Internet and Smart Card access, Indian language capabilities, forms
and decision support applications.
Researchers
Researchers at key tuberculosis and tobacco-control research institutions and at the Indian
Council of Medical Research
Benefits: A Health Research Information System; access to electronic publications and
databases of key journals and other related information; collaborative tools for research;
Internet connectivity where required.
Policy makers
Sub-district, district, state and national levels
Benefits: Training in Internet based information access and use and in the optimal use of
health research for policy and practice; Internet connectivity where required for the
project.
Libraries
Medical colleges libraries (4); National Medical Library
Benefits: Virtual Health Library system and associated training.
The main target groups for this project were consulted using an information needs
questionnaire. Over 600 health service providers, researchers and policy makers
responded. The results of this assessment contributed to the development of this proposal.
In addition, the representatives from these groups will be on the decision-making and
implementation bodies of the project.
15
World Health Organization
HIN India
Secondary beneficiaries
The general public will be the secondary beneficiaries of this project. A lot of the
information will be available in the public domain on line so anyone with Internet access
will be able to benefit from this key information on health.
In addition the public will benefit from improvements in health services catalyzed
through the project.
b.
Programme Strategy and Risks
9.0
a. Strategies for achieving the specific goals, objectives and anticipated results
Three principal considerations have been kept in mind while designing the
project:
■
■
■
Responding to user needs
Building on synergies between related projects
Fostering scalability and sustainability
The project plan has been designed in full consultation with the stakeholders and
takes into account the long-term strategy of the Government for the use of information
and communication technologies for health. At the same time, care has been taken to
incorporate elements that address some of the key concerns particular to the Health
InterNetwork (e.g. scalable solutions for the strategic use of ICT in health, global
standards for equity of access).
b. Identified risks
1. The biggest challenge for the project may be in facilitating and supporting the
associated cultural and attitudinal changes
2. A principal risk is the potential unpredictability of the time and effort required to
establish this virtual network through collaboration of the various stakeholders. This
could be due cultural reasons, complexity of project coordination, limited availability
of quality content over the pilot period and the technical challenge of setting up errorminimized, user-friendly networks and application software to meet the needs of the
various stakeholders.
3. In previous projects related to the use of the Internet for health the biggest challenge
has been getting doctors, policy makers and senior mangers to adopt and use new
technology.
4. Connectivity, especially low bandwidth and slow connections, remains a major
impediment to the acceptance and use of IT.
5. The bulk of Internet users are urban people who belong to the upper middle strata of
society. Addressing the functionaries in rural areas and lower socioeconomic groups,
like the village health workers, remains a challenge.
6. Local language content is sparse, but crucial for access and ease of use of the
network.
16
World Health Organization
HIN India
c.
Measures required to minimize these risks
Activities have been incorporated to enhance the adoption ofthe project through
targeted publicity and interaction amongst the stakeholders to hasten the required cultural
and attitudinal environment for collaboration. A careful needs analysis and the inventory
of available content is planned to address the problem of content relevance. Engaging the
best technology partners and adapting proven technologies for the systems to be built, is
expected to minimize the risks related to the technology used. Some of the other
identified risks and the action to minimize them are summarized in the table that follows.
RISK ANALYSIS (Note: ‘H’ stands for ‘High’, ‘M’ for ‘Medium’ and 'L' for Low)
Rating
Action / Contingency
Risk
H
Use standard interfaces to systems which have
New systems can’t be developed,
been previously established
because of time and resources, to meet
the specific requirements of HIN
Usage may vary' fluctuate from
H
Employ scalable architecture
Monitor usage levels during pilot
anticipated levels OR Pilot traffic runs
Control and monitor usage after launch
out of control
M
Support fast resolution through inter-agency
Authorization level required for each
working group to define authorization levels
specific service may not be fully
defined
Private partner branding may not
L
Relevant WHO guidelines on potential conflict
of interest apply
match WHO/HIN objectives
Half-hearted launch may lead to poor
H
Elave some quick-win applications; Ensure
targeted publicity and controlled launch
user perceptions
H
Clarify that the services provided through HIN
Participants may be unable to access
pilot are primarily those which relate to
the full range of needed services
through HIN
tuberculosis and tobacco control
Expected impact of the Health
Clearly define and discuss HfN objectives,
M
expected impact and relationship with related
InterNetwork project not clearly
understood
projects with stakeholders
Late joiners are precluded because the
standards have been defined by those
participating at the beginning
Increased access may lead to more
demand and greater than expected
resource requirements
Partners’ services are not available in
time for the pilot
Network becomes known externally
through press, etc, causing congestion,
or misunderstanding of pilot status
Participants’ expectations not met
because of the scope of the pilot
M
Keep architectures and processes open
M
Acknowledge and take into account for scale-up
phase
H
Define up front scope of requirements and
implementation times; Identify a “long list'' of
potential services; Prioritize services which are
already available in electronic, format
Ensure that knowledge of the network is
restricted during pilot stage
H
H
Need to raise awareness that this is only a 'pilot'
network, which does not portray the full
“network” when all content and countries linked
17
World Health Organization
HIN India
10.0
Value Added from Joint UN Intervention
The Health InterNetwork is a UN project and the different UN agencies have to
play synergistic roles based on their core competencies in order for the project to have
maximal impact.
■ WHO - Public health strategy, health content, and related field experience in the
country office (Coordinated with WHO Headquarters and the WHO South East
Asia Regional Office - SEARO)
■ UNDP - Country level infrastructure development and capacity building
• UNICEF - Extensive country level experience and field support staff; health
content
11.0
Value Added from NGO and Civil Society Partnerships
The Health InterNetwork is a public-private initiative that brings together
international agencies, the private sector, foundations, non-governmental organizations
and country partners to bridge the digital divide in health.
Partner interventions
International partners
■ Harvard Center for International Development and MIT Media Lab - expertise on
e-readiness, connectivity and technology; collaboration on connecting primary
health centers and on development of health kiosks
■ Cornell University - expertise on development communication and research on
the same
■ B1REME - Provision of the Virtual Health Library System and consultation on the
same
■ Collexis International Data Corporation - Technology for structuring the
collaborative research environment
■ Project.net Inc. - integrated web-based system for project management and
coordination
National partners
■ Ministry of Health and Family Welfare - responsible for public health in the
country including coordination of health research, policy and practice
■ Ministry of Information Technology - policy and infrastructure related to Internet
access and telecommunications in the country
■ National Tuberculosis Institute - lead agency for coordination of HIN India pilot
project as related to the tuberculosis control program
■ Tata Institute of Social Sciences - expertise in project evaluation and strategy
■ Bharat Electronics Ltd. - Production of Simputer, have radio enabled Internet
access, solar photo-voltaic cells (first developed for national defense systems now
available for development use)
* NUT - Information technology training; research and development of community
health kiosks
18
World Health Organization
I-IIN India
■
•
■
■
Tata Consultancy Services - Consultancy on computer software and systems
integration
Indegene Life Systems - have leading health portal for the medical community in
India (www.indegene.com). create health content for several digital devices,
including WAP and Simputer
2 Streams Media - integration of ICT with mass media techniques for
development of innovative audio and visual user interfaces
NGOs (e.g. Sochara) extensive field experience and networks related to
tuberculosis and other public health programs
As the project moves forward, space will be created for engaging more civil
society institutions. The partner institutions and projects across the country using Internet
technologies for health are presently poorly networked. The convergence created by
bringing these leading institutions and initiatives together will build on existing
synergies, optimize use of resources and skills and enhance the impact much beyond the
immediate gains from the HIN pilot project.
12.0
Charitable Purposes Justification for UNF
This project can be deemed an exclusively charitable project because, as
described in the project objective, it furthers the advancement of education and science
with the specific objective of improving health amongst the people of developing
countries in an equitable manner.
19
World Health Organization
I-I1N India
III
13.0
Program Management and Implementation
Management and Administration
a, b. Management structure
The management structure for the HIN India pilot is illustrated below.
i Health
1 InterNetwork
I Global
I" Office of the WHO
1
I
1
[
j
Representative to India I
Responsible for
,
administration and
I
coordination
I Core coordination team
! Coordination between
; representatives of ma jor
j stakeholder institutions in
i national public health
' includes Ministries of Health
; and Family Welfare and
1 Information technology.
1 Includes key stakeholders
; from pilot sites.
|
]
I
;
;
I
<
c.
Implementation
WHO will be accountable for the implementation of the project with support from
UNDP and UNICEF through their representative offices in India.
Administration
The administration of this project will be coordinated through the office of the
WHO representative to India. The implementation group in consultation with the core
coordination team and experts will make the financial decisions.
d.
Funding, accounting and reporting arrangements
The project is expected to be financed with extrabudgetary funds administered
through WHO headquarters. The current accounting and reporting procedures for UNF
funded projects will be followed.
e.
Administrative cost charges
The Program Support Costs @ 5% have been added to the project cost to meet the
costs of administering the program.
f.
20
World Health Organization
I-IIN India
g.
Co-financing and matching arrangements
The project has complementary objectives to the programs of the Government of
India for application of information technology to health. There are several investments
the government has made or is planning that will supplement the HIN project. For
example, the Government of India has already launched a scheme for networking 23
medical college libraries in the country with an outlay of INR 10 million. In addition the
Indian Council for Medical Research will co-finance the National Health Research
Information System component.
Several international and national institutions are also providing technology and
training support to the project. Three principal examples are the Latin American and
Caribbean Center on Health Sciences Information (BIREME) for the Virtual Health
Libraries Network, Collexis International Data Corporation for the National Health
Research Information System, and the Harvard Center for International Development and
MIT Media Labs for technical assistance.
In the course of the pilot planning process and its implementation, effort will be
made to engage other private sector partners and civil society institutions as required.
This India Pilot of the Health InterNetwork project is being submitted for funding
consideration to the Bill and Melinda Gates Foundation in follow-up to the global
planning funds provided by the UN Foundation in September 2000. Similar co-funding
arrangements from the public and private sectors are envisaged for the other pilots.
14.0
■
*
■
•
•
■
■
Inputs
The funds received from UNF will support the following inputs for the project,
Detailed requirements assessments and workshop for finalizing the project work
plan along with partners
Systems analysis, development and implementation of the National Health
Research Information system
Establishment of the virtual health library system and network of the medical
college libraries
System of on-line full text publication of research information and dissemination
Design of the most appropriate user interfaces for the different target groups,
including local language content
Provision of hardware, software and Internet connectivity to selected users
Development of training modules and training of the target users for access and
use of research information for health policy and practice
21
World Health Organization
HIN India
15.0
Reporting
Periodic financial reports, annual progress reports and final project reports for the
Health InterNetwork Pilot will be provided in accordance with existing UNF/UNFIP
arrangements.
The Project Manager of the HIN India Pilot, situated in the Office of the WHO
Representative to India, will be responsible for the reporting. The reports will be
transmitted through WHO headquarters in Geneva.
The pilot project will be implemented over the period July 2001 to December
2001. It will be operational for a period of one year from January 2002 to December
2002. The following reporting schedule is proposed:
Period
July 1, 2001 to December 31, 2001
January 1, 2002 to December 31,2002
July 1,2001 to December 31,2002
16.0
Report by
January 31, 2002
January 31, 2003
May 15,2003
Type of report
Annual report
Annual report
Final project report
Monitoring and Evaluation
The baseline data/benchmarks, which define the starting point at the outset of
project activities, will be determined by the detailed site assessments.
The project milestones detailed in the Gantt chart (Annex II) are discreet and
quantifiable and refer to specific activities that have an implementation duration and
budget. The progress of the project implementation will be measured against these
milestones:
■
■
■
■
"
■
■
■
■
■
■
Detailed needs analysis completed:
Project work plan finalized along with partners:
Training modules developed:
Key research institutions connected with ICMR:
Key medical college libraries and NML connected:
User interfaces and tools for accessing information operational:
Electronic publishing of key journals and documents in place:
Connectivity established at pilot district access sites:
Initial training conducted:
Pilot begins:
Evaluation of HIN India pilot completed:
2 August 2001
9 August 2001
6 December 2001
13 December 2001
13 December 2001
27 December 2001
3 January 2002 •
3 January 2002
3 January 2002
4 January 2002
27 February 2003
Quarterly evaluations and an end of project evaluation are envisaged. The expert
advisors, HIN task force in Geneva and the local UN offices will together decide who
performs the evaluations. This could include contractual assistance where needed
especially for the technology evaluations.
22
World Health Organization
HIN India
The indicators to be measured are outlined in section 7 c. of this document.
Details on how the evaluations will be conducted will be defined at the time of finalizing
the project work plan.
A provision of USD 33,660 (4.5% of the total budget) has been made for
monitoring and evaluation and a common format for all monitoring and evaluation
reports will be established after the needs assessments.
A system of program review by the administrative groups (Section 13 a, b) as well
as by the stakeholders and beneficiaries has been planned. The outcome of these reviews
will inform the progress of the project.
23
World Health Organization
HIN India
References
Dr Gro Harlem Brundtland, WHO's International Conference on Global Tobacco Control
Law: Towards a WHO Framework Convention on Tobacco Control, New Delhi, India.
Dr.C.P.Thakur 2001, TB India 2001: RNTCP status report, New Delhi, India.
Eddie Cheung. Profiling Indian Internet Users: Part 1. eMarketer . 4-1-2001.27-5-2001.
International Telecommunication Union 1998, World Telecommunications Development
Report 1998. Universal Access. Executive Summary.
Shobha Warrier. The Negroponte switch: An interview with Dr Ashok Jhunjhunwala of
1IT Madras. Rediff on the Net. 5-6-1997.
Subbiah Arunachalam 1999, "Information and Knowledge in the Age of Electronic
Communication: A Developing Country Perspective", Journal ofInformation Science,
vol. 25, no. 6, pp. 465-476.
Subbiah Arunachalam & Subbiah Gunasekaran, 2001, "Tuberculosis research in
India and China as reflected by the literature: From scientometrics to health care policy",
Paper under submission.
TB India 2001. Central TB Division, Directorate General of Health Services, Ministry of
Health and Family Welfare. TB India 2001: RNTCP status report New Delhi, India.
'We the Peoples’- The Role of the United Nations in the 21st Century: Millennium Report
of the United Nations Secretary-General.
In addition to UN partners and the Ministry of Health and Family Welfare in
India, Tata Consultancy Services, NUT and the following experts contributed
significantly to this proposal: Mr Subbiah Arunachalam, Dr Michael Best, Mrs S.L.
Chinnappa, Dr Shiban Gangu, Dr Nirmala Murthy, Mrs Sudha Murthy, Dr Thelma
Narayan, Professor. S. Vijaya and Dr C.A.K. Yesudian.
Special acknowledgement of Dr Jagota, Dr Suryanarayana and the staff at the
National Tuberculosis Institute in Bangalore who have taken on the lead role for
implementing the HIN India pilot.
Annexes
ANNEX I
Logical Framework I Project Summary
ANNEX II
Implementation plan
ANNEX III
Budget
24
World Health Organization
Identify 3 youth volunteers ^preferably women
from Kanakapura
Liih Volunteers will be computer literates
coordinating with the leaders of
various groups in the dissemination of
information
Will coordinate with the leaders of
various groups in the dissemination of
information
® Will be the only persons authorized to
operate the computer system at its
location
Will report to CHC on a regular
basis
The dissemination of information will be
carried out with bi-monthly Newsletters in
English and Kannada
&^5oo Joe sro £ o
WToST
Sift. >ciL,Hy4^
4j *> •
'lo4;cjj.
noyM/a^'
'To$r^^b*^)«o >
•
^*^8/
¥'**
w
S 6 W® ■ffj -S'J 0 i5
J^^ec-Xj
-B^I5 er®rcv>
y ^JT*
Y
V
-
V">$ ■% WJ ■
a^)tf^ ^d^S'Ftn**
SZoV*3^^^ -^’^>‘^'5
O0
r-
->^?fc3o A/a^ £ ^>aij H y’Aij
-8>^d> er&rv»
i*bdo3A _, ri./a d-8 A^c^o^eio ,
rtodo3AA
f<Odo3^6X>
^^3.
eA>3^<K&ae^
^<^it^l>ci&>
Acp^S .
Ox&aeT^
->
Ajya<J^"
?fe^ ToHftJSoJS^&Ttf
■/
io 3^f<^3^'5* ^✓J^.3' z^€.®JZ5jf*v
I
-? ajowi/^«C5is
J5oJ5<?
-?> ^V€asi?
tA v&
p» 3«jb
c4^>^&5U3uS
9/^ VJ
%o%, ^o^v*
*
- ^-g1 J^jd S^u/rfe
-" ,'§$&»'&
-
5J1.
a ^°- <$• ^CoA)
tSoXJhT*
.
- siza-d.A>S-t*S®a ^.^••tfe«i)
a
- vddeb 3y- a -BeoA)
^>^ORraa3b
Scx/tHaKMAf (2^d4’^-ztfS’°
C? ^oTc) E^
4^^
- ^osa(9 .
-
^0j cro o .
o^s'So <8^.;^
520636 zfeJ^H&G’oti
t\^8 ‘p ^5 &'a<2.*ic J?v7r &o B
—>
g&ae’Aj^o^^^3>J
£/
£,ccb
^O UTyfc
3^ Svislf? fe s ej£
ti?itJ^g, 4/a 0^3,0?.
■&,•■$
Io
,
zo^o
H s
&§ x<x
ij
_ 2><a^0&. S8t?8)
^-OOI
.
Methodology (Objective 2)
Identify existing networks among
doctors, school & college teachers,
Panchayati Raj members,
Anganwadis, NGOs, Junior Health
Assistants (F), and local Dais etc, if
any or create the need for a network
among these groups an d involve the
formal/informal leaders with
community preparatory workshops
Nominate a leader in each of the
Identified groups
Women
and
departments
child
development/RDPR
Agriculture department regarding information
on Tobacco/pesticides etc
O Beedi rolling -factories/cottage industry etc
0 Tobacco board
O Relevant studies/awareness on public health
programs conducted in schools and colleges in
Kanakapura Taluk
Literature sear.-h of relevant studies in
public/institutional/private libraries pertaining
to Kanakpura
Methodology (Objective 1)
Networking and snowballing with groups in
voluntary, institutions/colleges, public and
private sector
• Voluntary sector
BELAKU, Sri Ramana Maharshi Academy for Blind etc
• Institutions/Colleges
B R Ambedkar Medical College, V S Dental College etc
“7
•
- - - •• *5 .
Public Sector
NIMHANS, KIDWAI, Indira Gandhi Institute of Child
Health etc
EuroHealth Net
the European network for public health,
health promotion and disease prevention
HEALTH AND SOCIAL INCLUSION
IN THE CONTEXT OF LISBON
WORKING PAPER:
October 2004
www.eurohealthnet.org
HEALTH AND SOCIAL INCLUSION
IN THE CONTEXT OF LISBON
WORKING PAPER:
October 2004
Contents:
I. The European Social Model
II. The Lisbon Strategy
III. Components of the Lisbon Strategy
A. Economic Policy
B. European Policy/European Employment Strategy
C. Social Policy/Social Protection
1. Pensions
2. Social Inclusion
3. Health and Long Term Care
Streamlining
IV.
V. Evaluation
VI. Health and Social Inclusion in the context of Lisbon
Introduction
This briefing describes the nature and discusses the Lisbon Strategy and its objectives.
The aim is to place the EU Social Inclusion Strategy, and EuroHealthNet’s projects on
Health Inequalities and Health and Social Inclusion, into its wider policy context. (This can
clarify how the health sector can contribute to advancing social objectives within the EU.)
I.
THE EUROPEAN SOCIAL MODEL
The European Union was founded upon the idea that economic integration would lead to
greater prosperity and generate peace and security. The Treaty on European Union
states that its objective is to promote peace, its values and the well being of people. In
addition, Article 1-2 of the Treaty notes that the Community shall have as its task:
... to promote throughout the Community a harmonious, balanced and sustainable
development of economic activities, a high level of employment and of social
protection, equality between men and women, sustainable and non-inflationary growth,
a high degree of competitiveness and convergence of economic performance, a high
degree of protection and improvement of the quality of the environment, the raising of
the standard of living and quality of life, and economic and social cohesion and
solidarity among Member States.
This Article indicates that the aims and objectives of the European Union go beyond
economic integration, and also aim at achieving social development. Indeed, economic
and social development are tightly interlinked. Without sound economies, no sustainable
progresses can be achieved in social protection. Economic development and integration
are not a goal in itself but a means to increase the well being of society and the majority
of the population.
EU Member States are, however, hesitant to give the EU too many powers on issues
relating to social protection and want to maintain the right to structure their welfare states
according to their national traditions and politics. The EU therefore only has shared
(rather than exclusive) competence' in certain areas of social policy, and the principle of
subsidiarity2 persists in this area. The way Member States have organised their
societies, their tax-benefit regimes and their social welfare policies differ widely.
Despite the fact that there is no homogenous legal framework of social welfare in Europe,
terms like ‘Social Dimension of the EU’ and the ‘European Social Model’ are widely
used in both academic research and policy debates, when a unifying concept is sought to
identify the European Union, its way of life and its approach to society, as distinct from
' The principle of conferral of competencies states that the European Union shall act within the limits
conferred upon it by Member States in the Constitution.
’ This principle holds that in areas which do not fall within its exclusive competence, the Community shall
take action, in accordance with the principle of subsidiarity, only if and in so far as the objectives of the
proposed action cannot be sufficiently achieved by the Member States and can therefore, by reason of the
scale or the effects of the proposed action, be better achieved by the Community. Any action by the
Community shall not go beyond what is necessary to achieve the objectives of the Treaty. A more
descriptive analysis of the principle can be found in Protocol 30 to the EC Treaty.
2
the world. These terms allude to common values held by EU Member States (and, in
many cases, to distinguish the EU from models applied within the US or Asia).
The big difference between the European economic and social model and models found
in other developed countries is the extent to which the role of the state is used to mitigate
the social effects of free-market capitalism. European populations generally pay higher
taxes, thereby indicating a greater willingness to pool risk through the state, both to
ensure that it will provide for them when they need it, and to ensure that a degree of
social cohesion is maintained. This unique balance between state, individual and market
is embedded in European Treaties and policy-making traditions.3
The Barcelona European Council of March 2002 adopted the following definition of the
European social model: “(it) is based on good economic performance, a high level of
social protection and education and social dialogue’’.4 According to the High Level Group
on the Future of Social Policy in an Enlarged EU, the European social model thus stands
for the parallel development of economic and social prosperity and rests on the
consistency between economic efficiency and social progress. It aims to maintain
continually rising productivity and living standards across the Union, while helping to
ensure that the benefits are widely shared.5
Although the term ‘European Social Model’ is commonly applied, one cannot speak of a
single European ‘economic and social model’. There are a number of different models
that can be categorised into very different types of ‘sub-models’ (Liberal/Anglo Saxon,
Conservative/Continental, Nordic/Universal/Social Democratic, Southern
European/Mediterranean). All of these models have their strong and weak points.
Noteworthy is that Nordic countries are leading in most global competitiveness surveys,
such as the IMD World Competitiveness Report, with three of these economies, Finland,
Sweden and Denmark, emerging among the top five most competitive economies in the
world.6 The Nordic model, in particular, thereby serves as an example that economic,
social and environmental performance can go together, and that the role of the state is
crucial in achieving competitiveness.7
Nor should the European Social Model be regarded as a simple extrapolation of the
models of individual Member States to a European level. The 'EU level' model has,
rather, been described as a set of constitutional policies and principles, a basic floor of
social guarantees upheld by pan-European regulations, a fairly articulated co-ordination
regime that forces national systems to communicate with each other through forms of
mutual recognition, and a wider collection of aspirations, objectives and concerns.8
Thus, while EU Member States share common principles, the EU does not have the
competency to ‘harmonize’ social policy. EU Member States nevertheless face many of
the same tough challenges, which affect their ability to maintain existing balances
between the state, individuals and the market and to generate economic growth while
3 EPC. 2004, pg. 11
4 DG EMPLOI. Report of the High Level Group on the future of social policy in an enlarged European Union. May
2004,page 5
5 ibid.
6 EPC, 2004, pg.46
7ibid. pg.21
8 Ferrera in de la Porte, C. and Pochet, P. 2001, pg. 134
3
retaining social cohesion. They face common internal challenges, such as demographic
change and the need to alter the structures of government to address contemporary
realities. They also face common external challenges, such as the rise of a knowledge
based economy and greater competition generated by the processes of globalisation.
These developments are eroding Member State’s abilities to maintain the fiscal basis of
their social models. They require Member States to develop appropriate policy
responses, to introduce policies and programmes that aim to restructure their societies,
and find new optimal balances between economic efficiency and social progress.
II.
LISBON STRATEGY
In the face of, and in response to these challenges, the European Council in Lisbon of
March 2000 set out a new paradigm, or ambition, for the EU. European governments
committed themselves to work towards a new strategic goal for the next decade: “to
become the most competitive and dynamic knowledge-based economy capable of
sustainable economic growth with more and better jobs and greater social cohesion”. The
objectives of Lisbon constitute a ‘virtuous’ policy triangle, where economic policy,
employment policy and social inclusion interact in a mutually supportive manner. Social
policy underpins economic policy, and employment has not only economic but also a
social value.9
Social policy
Social Protection/Social Cohesion
Competitiveness/Dynamism of work
Economic Policy
Ouality/quantity of work
Employment policy
The Commission notes that if any one of the corners of this triangle were missing, the
Union would not reach its fundamental objectives, nor would it have legitimacy in the
eyes of the citizens. The Strategy touches on almost all of the EU's economic, social and
environmental activities.
The European Social Policy Agenda, launched by the Commission in June 2000, and
endorsed by the European Council of Nice in December 2000, bring together the various
initiatives and policy strands in the area of social policy within the Lisbon Strategy. It is a
large work programme, providing a comprehensive and coherent approach for the EU to
confront the new challenges to social policy which result form the radical transformation
of Europe’s economy and society, such as those generated by the new knowledge-driven
economy. It is, in this sense, a strategic response to modernise the European social
model and to translate the political commitments made at the Lisbon Summit into
concrete action.10
9
Social Policy Agenda, pg. 13
10 The EU also launched a Sustainable Development Strategy in May 2001. The Strategy recognizes the
'triangle' between social, economic and environmental aspects and the importance of balancing all three. It
contains a number of concrete proposals on how the European Union can improve its policy making to make
4
Implementation
The EC has a number of instruments that it can use to take forward the Lisbon Strategy.
The most powerful of these is (1) the development of legislation, which Member States
must implement nationally. As noted, however, the EU can only act in those areas where
the Member States have agreed to give it competency. These areas, or the so-called
acquis communautaire, are set out in the Treaties. The EU also uses (2) financial
instruments in the form of Structural Funds to promote common objectives. In addition it
engages in a number of (3) ‘accompanying' activities such as research, the development
of common indicators, dissemination of information, networking and training activities to
support policies developed in the social policy and other fields."
Open Method of Coordination (OMC)
An important mechanism that the EU has developed in order to achieve the Lisbon
objectives is the Open Method of Coordination (OMC). Lisbon aimed to limit as far as
possible new legislation at a European level and to achieve the established objectives
within the parameters of existing legislation.11
12 The Lisbon European Council therefore
developed the OMC, which was modelled after the European Employment Strategy
(discussed further below.) The OMC is built on the recognition that different approaches
within Europe can be very instructive for policy development and that there is strong
added value in co-ordinating and developing common policies and addressing common
problems and challenges.
Through the OMC, Member States decide what goals they aim to achieve in a policy
area, and develop a list of common objectives. Each Member State works this out in a
national action plan, which involves fixing guidelines with specific timetables for short,
medium and long terms. Member States also establish, where appropriate, quantitative
and qualitative indicators and benchmarks as a means of comparing best practices.
They should, then, translate the guidelines into national and regional policies by setting
specific targets and adopting measures. Member States comment on one another’s plans
and exchange good practices. The European Commission coordinates this process and
compares countries with one another. This process of periodic monitoring, evaluation and
peer review aims to stimulate excellence, achieve greater convergence on EU goals and
strengthen the learning process of those involved.
Under the OMC, key competences remain at the Member State level. The process is
founded on the belief that governments and other stakeholders will take the process
seriously and address shortcomings by adapting their own systems and methods in line
with best European practice.13 The approach, sometimes referred to as ‘soft law', is
essentially voluntary, and helps to expand policy activities beyond legally limited spheres.
It also seeks to enhance policy integration and linkage (e.g. between economic and social
policies, pensions, employment, immigration, etc.)14
it more coherent and focussed in the long term, as well as a number of specific headline objectives and
measures required to achieve them. The Strategy was reviewed in 2004.
11 The European Commission’s annual Spring Report examines (he Strategy in detail. The Spring Report is the only
document on the agenda of the Spring European Council, where EU Heads of State and Government assess the progress
of the strategy and decide future priorities in order to realize the Lisbon targets.
12 EPC (2004) pg. 37
13 ibid., pg. 13
14 de la Porte. C. and Pochet, P. pg. 3
5
111.
COMPONENTS OF THE LISBON STRATEGY
The following sections briefly discuss the components of the Lisbon triangle and the
mechanisms that have been developed under each of them to take forward the Lisbon
process. These policy tools have been designed at separate times, and ‘grafted' on to
one other. The final section will therefore discuss steps that are being taken to
‘streamline’, or ensure a better coordination of these activities, so that they can reinforce
one another in the effort to achieve the Lisbon goals.
A. Economic Policy (Competitiveness/Dynamism)
The real driving force of the European Union is economic integration. Without sound
economies, no sustainable progress can be achieved in social protection. Coordination at
European level in this area aims to achieve sustained economic growth with low inflation
and sound public finances.
Broad Economic Policy Guidelines
The 1993 Maastricht Treaty first introduced a system for co-ordinating the economic
policies of EU Member States. Articles 98-104 of the Treaty Establishing the European
Community set out the process used for the co-ordination of economic policy. Article 99
of the Treaty states that Member States “shall regard their economic policies as a matter
of common concern and shall co-ordinate them." This coordination takes place through
the Broad Economic Policy Guidelines (BEPG), which lay down the EC’s medium-term
economic policy strategy. The guidelines provide a benchmark enabling economic
developments in Member States to be monitored and compared.15 The guidelines are
concentrated around three main themes: growth and stability-oriented macroeconomic
polices; economic reforms to raise Europe’s growth potential; and strengthening
sustainability.
While this process of establishing and monitoring Member States adherence to guidelines
resembles that of the OMC, it can be considered ‘hard’ (rather than ‘soft’) coordination,
since these activities are justified under Article 99 of the Treaty. The BEPG are, in
addition, linked to the Economic Monetary Union (EMU) and the Stability and Growth
Pact, which are in theory exclusive EU competencies, which must be applied in 12 of the
25 EU Member States that are currently participating in the EMU. The recommendations
issued by the Commission are therefore much more influential than those issued through
the OMC processes that take place in the area of social protection, discussed further
below.
B. Employment Policy / European Employment Strategy
Beyond coordinating economic policies in order to optimise economic growth, it is also
important to ensure that this growth occurs in a way that generates higher levels of
15 The process begins when lhe Commission adopts recommendations for the guidelines, which are used by the
Economic and Financial Council (ECOF1N) to formulate a draft of BEPG. The guidelines contain two parts: a set of
horizontal recommendations and a set of country-specific recommendations. Member Slates report to the Commission
about important measures taken by them in the field of economic policy, lhe Commission prepares reports on lhe
consistency of economic policies of MS with BEPG. The Council may then, acting on a qualified majority, make the
necessary recommendations to the Member Slates concerned (mutual surveillance), the Commission publishes a report
making an overall assessment of lhe implementation of lhe BEPG’s. The process leads to both general and country
specific recommendations. The guidelines are produced on a multi-annual basis, with changes in intervening years only
taking into account major new developments. A full review of lhe guidelines is foreseen for 2006.
6
employment - since this is of importance to social stability and social cohesion. The
Amsterdam Treaty (1997) therefore brought employment formally on the agenda of the
European Union and aimed at a closer co-ordination of Member States’ employment
policies, as a part of the economic policy co-ordination process. This led to the
establishment of the European Employment Strategy (EES). The Strategy, launched by
the Luxembourg European Council in 1997 (and therefore also known as the
‘Luxembourg Process’) was designed as the main tool to give direction to and ensure co
ordination of the employment policy priorities to which Member States should subscribe
at EU level.
While the strategy was implemented prior to the Lisbon Council of 2000 (and a five year
evaluation was conducted in 2002), the Lisbon and subsequent Councils set the following
strategic goals: to raise the overall EU employment rate to 70% and to increase the
number of women in employment from an average to more than 60%, and that of older
workers to 50% by 2010. The aim is also to raise the overall employment rate to 67%,
and that of women to 57%, by 2005.16
Naps/Employment
Each year following the proposal from the Commission, the European Council agrees on
a yearly basis on a series of guidelines setting out common priorities for Member States'
employment policies. These are structured around four pillars: (1) employability, (2)
entrepreneurship, (3) adaptability and (4) equal opportunities. Member States draw up
NAPs/employment that describe how these guidelines have been put into practice
nationally. The Commission and the Council examine each Member State’s
NAP/employment and present a Joint Employment Report. The Commission then
presents a new proposal to revise the Employment Guidelines for the following year. The
Council may then decide, by qualified majority, to issue country specific
recommendations upon a proposal by the Commission.
Employment is considered an integral part of economic policies. These processes were
therefore streamlined in 2002, and certain outcomes of the employment process are now
incorporated in the Broad Economic Policy Guidelines. This gives the EU an important
degree of influence in the shaping of Member State’s employment policies.
C. Social Policy / Social Protection
The European Social Model’ aims, as noted above, to balance economic and social
considerations, since the two are mutually reinforcing. Economic growth is necessary to
achieve social protection, while a cohesive, well trained and healthy society is more likely
to generate growth. Since the creation of the European Communities, however, social
policy has always been lagging behind economic policy. One of the major achievements
of the Lisbon Strategy is therefore to try to put economic and social policy on an equal
footing.
The European Councils have given the following areas the highest priority in the area of
Social Protection: 1) Making pensions safe and pension systems sustainable 2)
16 Currently the EU wide employment rate is only at 64.3%, meaning the Lisbon Target of 67% for 2005 and the 2010
target of 70% are likely to be missed.
7
Promoting social inclusion, and 3) Ensuring a high quality and sustainable health care
throughout Europe. Making work pay by providing a secure income is regarded as a
cross cutting theme. These main axes were first identified in a Commission
Communication of 1999 on modernising Social Protection.
The Communication also suggested ‘enhanced mechanism for exchanging information
and monitoring policy developments’to implement the strategy and provide it with
visibility and political profile. This led to the establishment of the Social Protection
Committee (SPC) in 2000, whose main tasks are to monitor the social situation and the
development of social protection policies in the Member States and the Community and
to promote exchanges of information, experience and good practice between Member
States and the Commission. The establishment of the SPC is important, since it provided
for the first time a forum where serious and fundamental discussion could take place in a
well-prepared fashion between MS and ELI institutions on issues such as social
protection challenges in general and the inter-linkage between economic and social
integration. This would lead to tangible and concrete outcomes in the area of social
policy. This means that new analysis, exchanges of opinions, discussions and
recommendations will have a fair chance of leading to results and political decisions.17
1) Pensions
An important issue with far reaching implications with respect to Member State’s social
and economic policies is Europe’s ageing population.18 The Open Method of Coordination
has therefore been applied to this area in order to address the potential challenges that
this poses. In 2001, the Social Protection Committee and the Economic Policy Committee
produced a joint text in which they agreed on eleven objectives that centred around three
particular areas:
•
•
•
The Adequacy of pensions (ensuring that the capacity of Member State’s pension
systems is enough to meet future social objectives.)
Financial Sustainability of Pensions (ensuring that Member States have a multi
faceted strategy to place pension systems on a sound financial footing.)
Modernisation of pension systems in response to the changing needs of the
economy, society, and individuals.
National Strategy Reports (NSR/Pensions)
In September 2002, Member States submitted their first National Strategy Reports (NSR)
for pensions, in which they presented the measures that they have undertaken and are
undertaking in view of these European-level objectives. A peer-review session took place,
and the Commission adopted a draft Joint Report that evaluates the national strategies.
The Council is currently in the process of assessing these outcomes and of deciding
upon the objectives, methods and timetables for the future of the pension strategy. The
agreed upon guidelines are integrated into the BEPG’s, giving the EU more influence in
this area.
17 de la Porte, C. and Pochet. P. pg. 89
18 Women in Europe have on average only 1.4 births. Governments are concerned about too few workers in
future years to support the growing retirees in the population. Ageing population strains social security
systems and pension plans and puts pressure on health budgets because of high health care costs for the
elderly.
8
2) Social Inclusion
Articles 136 and 137 of the Amsterdam Treaty provide the European Community with the
legal competence to play an active role in supporting and complementing the activities of
Member States in combating social exclusion. The Lisbon European Council of March
2000 also agreed, on this basis, to take steps to make a decisive impact on the
eradication of poverty by 2010.19
In December 2000 the Nice European Council decided to launch the CMC in the field of
combating poverty and social exclusion and defined the following set of common
objectives:
1. To facilitate participation in employment and access to resources, rights, goods
and services for all
2. To prevent the risks of exclusion
3. To help the most vulnerable
4. To mobilize all relevant bodies
The Commission and Member States also agreed, in 2001, on 18 common indicators to
approach the measurement of poverty and social exclusion. These indicators cover a
variety of domains, such as income poverty, long-term unemployment, health and lifelong
learning, to reflect the multidimensional nature of poverty and social inclusion, which
cannot be reduced to a single variable. The indicators serve as a basis for the EU and
individual Member States to assess the progress of the social inclusion process on the
basis of verified outcomes.
National Action Plans for Social Inclusion (NAPs/inclusion)
The 15 EU Member States submitted their first round of National Action Plan for Social
Inclusion (NAPs/inclusion), which indicate how they will take forward the common
objectives mentioned above, in 2001. The NAPs/inclusion translate the common
objectives into national policies, while taking into account individual circumstance and the
particular nature of national social protection systems and social policies. The
Commission drew up its first Joint Report on Social Inclusion, which was endorsed by the
Council, summarising the results of the examination of the NAPs. Member States
submitted their second round of NAPs (2003-2005) in July 2003, which were also
summarised in a Commission/Council Joint Report and are currently in the process of
implementing these.20 Accession countries where also asked to submit Joint Inclusion
19
The Joint Report on Social Inclusion (2003) summarises the current situation in the EU with regard to
social inclusion. 15% of the EU population is living at risk of poverty in 2001. There were more than 55
million people al risk, of whom more than half live persistently on low relative income. The situation with
respect to Social Inclusion varies greatly between countries: lowest levels of exclusion can be found in
Sweden (10%) while the highest can be found in Ireland (21%). New EU Member States also fall within this
range, although the results of individual indicators differ greatly compared to that of the ‘old’ Member
Stales: while these countries face high levels of unemployment and low levels of perceived integration, there
are high levels of lifelong learning and income equity.
20 Member Stales have also been urged to give particular attention to the following six policy priorities in the
current round of NAP’s (2003-2005). since these are regarded to be especially relevant in the context of a
continuing uncertain global economic and political climate:
I. Promote investment in and tailoring of active labour market measures and education and training
systems to meet the needs of those who have the greatest difficulties in accessing employment
9
Memorandums (JIMs) outlining the situation and policy priorities in relation to poverty and
social exclusion in their countries. They submitted their first round of NAPs/inclusion
(2004-2006) in July 2004.
Action Programme
The Commission is also implementing an Action Programme (2001-2005) as part of its
Social Inclusion Strategy. Based on the OMC, it aims to encourage co-operation among
Member States, to strengthen the effectiveness and payoff of policies combating social
exclusion. The Action Program has three objectives:
-to improve the understanding of social exclusion
-to organise co-operation and reciprocal training in the context of the NAPs/inclusion
-to develop the capacity of players to address social exclusion effectively
EuroHealthNet's project on Health and Social Inclusion is funded under Strand 2 (Trans
national Exchange Program) of the Action Program. The project focuses on the
contribution that health related policies, programmes and interventions can make to
tackling social exclusion. This is taking place through a cross-national exchange and
comparison of effective policies and integrated, transferable good practices in Europe in
this field. Phase I of the project was successfully completed in 2003 and led to two
reports: Health, Poverty and Social Inclusion in Europe: Literature review on concepts,
relations and solutions, and Health, Poverty and Social Inclusion in Europe: Health
analysis of national action plans on social inclusion. Project partners are now engaged in
Phase II of the project (2004-2005), which involves the exchange of good practices, field
visits and a a final exhibit and conference to highlight the contribution that the health
sectors can make to social inclusion.
3) Health and Long Term Care
Health care systems remain the competence of Member States, and governments have,
traditionally, renounced EU interference in this area. The development of the Internal
Market has, however, had important implications for the stability and sustainability of
Member States health care systems since it has and will continue to lead to increased
patient and professional mobility, and affects national policies with respect to, for
example, advertising and the pricing of pharmaceuticals. Such policies have been
developed from an economic approach, while health and social considerations may not
be sufficiently taken into account when drafting them. The need for greater involvement
from policy makers in the health and social sector at EU level, as well as greater
coordination between Member States in this area is becoming more apparent.
In December 2001 the Commission therefore issued a Communication on the future of
health care and care for the elderly, which spells out the common objectives for the
European health care systems: accessibility, quality and financial viability, and provides
details of the problem of maintaining these principles. This was followed by a report from
2.
3.
4.
5.
6.
Ensure lhat social protection schemes are adequate and accessible for all and that they provide effective
work incentives for those who can work:
Increase the access of the most vulnerable and those most at risk of social exclusion, including disabled
people, to decent housing, quality health and lifelong learning opportunities;
Prevent early school leaving and promote smooth transition from school to work;
Develop a focus on eliminating child poverty and social exclusion among children;
Make a drive to reduce poverty and social exclusion of immigrants and ethnic minorities
I0
the Social Protection Committee (SPC) and the Economic Policy Committee (EPC) which
led the Council to conclude that 'useful lessons could be drawn from the sharing of
information and best practice regarding actions being taken by Member States to secure
the core social objectives of care and healthcare systems while ensuring their long term
sustainability.'
National Reports on Health and Long Term Care
In 2002. EU Member States filled out questionnaires in which they were asked to identify
and analyse the difficulties and challenges they faced that could block access to high
quality care and long-term care. Agreement will be reached, in 2004, on objectives and
indicators in this area. Member States will then submit national reports on Health and
Long Term Care by Spring 2005. These will be analysed in the broader context of other
Open Method of Coordination in the area of social protection and in relation with the
Lisbon strategy. DG EMPLOI and DG SANCO will coordinate work in this area. The
Social Protection Committee (SPC), the Economic Policy Committee (EPC) as well as a
new High Level Group on Health Services and Medical Care that was recently
established by DG SANCO, will be jointly responsible for this process.21 This group is
comprised of representatives of Health Ministries of the EU Member States.
While the focus of this process appears to be on health care of the quality and
accessibility of health care services for the elderly, this will automatically lead to an
assessment of health care services in general. Eventual future guidelines will be
integrated into the Broad Economic Policy Guidelines (BEPGs).
IV. Streamlining Process
The mechanisms that have been developed to take forward the Lisbon objectives have all
developed independently, making it a rather complex task to monitor all of these
processes as well as to ensure that they all send out similar political messages. It is,
however, vital that Member States ensure coherence between their economic,
employment and social protection policies.22 There is therefore a need to move towards a
more integrated approach that acknowledges the interdependence and complementarity
of these policies.
Economic and employment policies were already, accordingly, streamlined in 2002. The
social processes underway in the field of social protection will now also be synchronized
with the employment and economic processes. This involves creating a standardised
process based on a common set of objectives -concerning social inclusion, pensions and
healthcare, - and simplifying the procedures for submitting reports. The different reports
of the Social Protection Strategy (NAPs/incluson, NSR/Pensions, National Reports on
Health and Long Term Care) will still be produced by Member States and provide the
basis for a Commission Joint Report on each of these topics. The different reports will
then be synthesized into a single, triennial Joint Synthesis Report that will be an official
Council and Commission document. By 2006 the social process will therefore be in step
with those of the European Employment Strategy and the Broad Economic Policy
Guidelines, so that all three reports can be compared to one another to ensure a
_l The High Level Group on Health Services and Medical Care is a Permanent Committee that first met on 1
July 2004. Il will also be involved in the Recommendations of the High Level Process of Reflection on
Patient Mobility.
~ Joint Report. 2003, pg. 11
11
consistent approach. The first Joint Report on Social Protection and Inclusion will be
published in 2005.
V. Evaluation
2005 will be an important year for the Lisbon Strategy. In 2004, the Commission as well
as the 'High Level Group’ chaired by Former Dutch Prime Minister Wim Kok are
undertaking Mid-Term reviews of the Lisbon Agenda. The Commission evaluation will
focus on progress made within the OMC processes, while the High Level ‘Kok Group' will
focus on the extent to which the Lisbon objectives are being met and what needs to be
done to achieve further progress. This Group is, in theory, a Commission-led process,
although members have been nominated by the Member States. Both Mid-Term Review
processes will be completed by the end of 2004. The results of these evaluations will be
significant, since they will establish the future nature of the strategy and where emphasis
will be placed. This will be determined at the 2005 Spring Council.23
Work is also underway on a new Social Policy Agenda.24 A High Level Group that was
set up by the Commission in 2003 has just released its report with recommendations in
the future Social Policy Agenda (2006 - 2010). The report’s underlying philosophy is the
need to keep the balance between economic and social policy. It defines three major
challenges for the next social policy agenda: enlargement, population aging and
globalisation. Amongst the main messages conveyed is the need to foster social
inclusion and invest in children and young people in order to convey a positive perception
of the future and to develop a new intergenerational balance. The Group also reported,
however, that social policy development is currently running behind economic policy
development. This must be redressed if the balances represent by the Lisbon triangle are
to be maintained.
VI.
Health, Health Inequalities and Social Inclusion in the context of Lisbon
Health, as an individual’s most valuable resource, and therefore a society's most
important collective resource, should play a central role in achieving the Lisbon
objectives. The focus should, in this respect, be on increased cooperation to reduce
health inequalities between and within Member States as part of initiatives to improve
social inclusion and social cohesion.
EuroHealthNet’s Literature Review on Health, Poverty and Social Inclusion, which was an
outcome of the Phase I of the project on Health and Social Inclusion, illustrates how
23 The conclusions of the High Level ‘Kok Group’ (expected in early November 2004) arc likely to be
influential in determining the future of the Lisbon Strategy. Many civil society groups are critical of the
Group, and claim that the process lacks transparency and does not include any consultation procedures.
There is a fear that the conclusions of the High Level Group will focus exclusively on Economic and
Employment Policy, stressing employment and job creation over of quality of employment and
competitiveness over cohesion in general. There currently appears, for example, to be a strong focus on
’attracting people to the labour market’. This emphasis stigmatizes the unemployed, who very often want to
work, but can’t, due to a shortage of good (quality) jobs, or because they are unable to for reasons of ill
health. There is a fear that Social Policy in general and the Social Inclusion Strategy in particular are being
subordinated to other components of the Lisbon Strategy. (Social Platform. Contribution to Troika meeting
preceding the Informal Employment and Social Affairs Council, July 2004.)
24 The Report is available at:
http://europa.eu.int/comm/employment_social/social_policy_agenda/social_pol_ag_en.html
12
health, poverty and social exclusion are strongly interlinked. Ill health can lead to social
exclusion, while the experience of being excluded can lead to or compound ill health.
Investing in health can therefore be an important way of combating social exclusion.
This project also involved a ‘health audit’ of NAPs/inclusion, which revealed that health
related initiatives that were incorporated into the NAPs tend to focus on health care,
rather than on health promotion. These were, in addition, initiatives that were carried out
at the national, rather than at the local and community level. This reflects a failure to
recognise and mobilise an important body of actors that can contribute to efforts to
promote social inclusion and generate greater social cohesion.
The Lisbon Strategy has almost reached its half-way mark, and it will take a great deal of
political commitment to ensure that the EU gets closer to achieving its objectives, whilst
ensuring that a good balance is maintained between social and economic policy. (EU
Member States, for example, have only fully ratified and implemented seven of the over
forty Directives that relate to the Lisbon objectives.) Nevertheless, some positive
developments have taken place regarding the incorporation health related issues. The
new OMC process on Health and Long Term Care, for example, indicates increasing
focus on health related issues in the area of social protection (although this should focus
not only on health care but also on public health and health promotion.) Another positive
development is the imminent introduction of ‘healthy life years’ as a structural indicator in
the Strategy.
The establishment of the new EU Constitutional Treaty, which contains new provisions
relating to social policy, could also support and strengthen future EU actions in this area.
All EU Member States signed the Treaty on 29 October 2004, and have two years to
complete ratification. The Treaty increases the scope of EU action in social areas in a
number of ways. Part I of the Treaty, outlining the values and objectives of the EU,
incorporates human dignity and equality as values, and solidarity as an objective. While
these provisions are not binding, they can be invoked for political leverage. In addition,
Part III of the Treaty includes a new 'horizontal' article that will force those working in
other policy areas to consider the effects of their measures on, amongst other things,
social protection and social exclusion or to ‘mainstream’ exclusion issues. This article is
welcomed as an additional tool to tackle exclusion, although the extent to which it will be
put into effect remains to be seen. Another important development will be the
incorporation in Part II of the Charter of Fundamental Rights, which includes a chapter on
solidarity (eg. rights to social protection and heath care). The Charter will, if the Treaty
comes into force, have a binding legal force, and European Court of Justice decisions will
determine the extent to which it expands the regulatory reach of the EU. Provided that all
Member States ratify the Treaty, these provisions will increase the scope for action for
actors wishing to advance the ideals represented by the European Social Model.
Much more should currently be done, however, to strengthen the social protection
component of the Lisbon Process and to integrate health. Perhaps most important is to
raise recognition of the contribution of health as a productive factor. This requires more
evidence to highlight the exact cost-benefit of health expenditures and to advocate for
investment in health policies. This information should be integrated into the EC Economic
Guidelines and Member States should regularly report on this.
Achievement of the Lisbon objectives will also depend on the development of a more
cohesive strategy across EU competencies and on greater cooperation between different
13
policy sectors within the EU and in Member States. Policies relating to, for example, the
internal market, regional development, agriculture, education, transport, etc. all have
important implications for health and well-being. These sectors as well as all EU
institutions must take on the task of mainstreaming health and social issues in their work.
There is, in addition, the need for careful redistribution of resources from ‘Bads’ (for
example elements of agricultural or industrial production) to ‘Goods' (investment in health
and well-being for citizens.) This implies a major switch in attitudes in agreement of the
forthcoming EU financial perspectives 2007-2013.
Such measures should be taken forward to counteract the current tendency of
subordinating the social component of the Lisbon Strategy to economic and employment
considerations. Economic development and integration are not, as noted at the start of
this paper, a goal in itself but a means to increase the well being of society and the
majority of the population. Individual and collective health status can be considered a
good measure of whether the objectives of the Lisbon Strategy are being achieved.
Higher levels of good health, and reductions in health inequalities are both a means of
achieve these objectives, and a reflection of the Strategy's success.
14
EwroHeafithNet
the European network for public health.
health promotion and disease prevention
www.eurohealthnet.org
EuroHealthMet
(h<- Fnnip.vn nctW'-k for pubhc h-'alth.
htdltn
ailrf dk>e<1M ;»<■• C'U:on
Health Literacy and Internet
Recommendations to promote Health Literacy
by the means of the Internet
Silke Christmann, EuroHealthNet, April 2005
CONTENTS
INTRODUCTION...........................................................................................................3
1. HEALTH LITERACY............................................................................................... 3
1.1 Definition of health literacy..................................................................................... 3
1.2 Consequences of low health literacy....................................................................... 4
1.3 Levels of health literacy.......................................................................................... 5
2. INTERNET AND HEALTH COMMUNICATION................................................ 6
2.1 Internet and health information............................................................................... 6
2.2 Use of Internet among vulnerable groups...............................................................7
3. INITIATIVES OF THE EUROPEAN COMMISSION TOWARDS HEALTH
INFORMATION ON THE INTERNET........................................................................ 9
4. RECOMMENDATIONS TO PROMOTE HEALTH LITERACY BY
INTERNET.................................................................................................................... 12
4.1 Target Groups:........................................................................................................ 12
4.2 Possible set of recommendations:.......................................................................... 12
4.3 Detailed Recommendations to promote health literacy by the means of the Internet
(personal and community empowerment).................................................................... 13
4.3.1 Improve Access to the Internet for vulnerable groups (Public Internet Access Points 13
4.3.2 Development of a Regional/Local Health Portal, which offers information appropriate
to age, culture and language...............................................................................................14
4.3.3 Strengthen individual competence......................................................................... 16
4.3.4 Communication Strategy...................................................................................... 17
5. ANNEX................................................................................................................... 18
5.1 Quality' Criteria for Health Related Websites (EC 2002)........................................ 18
6.
SOURCES................................................................................................................19
INTRODUCTION
Due to a changing pattern in disease burdens from infectious diseases to chronic
diseases and the aging of the population in Europe health information becomes
increasingly important for citizens to act in a healthy way. Terms like empowerment
informed-shared-decision-making describe a
and
situation
that citizens
are
encouraged to take an active part and accountable role in their own health.
What about citizens, who don't have the ability to be informed? How can an equal
access and the ability to use health information in an effective way be assured? The
concept of health literacy offers a new approach to health promotion work.
This paper will explore in which way the use of Internet can contribute to improve
health literacy among European citizens, especially of those with low health status.
1.
HEALTH LITERACY
Primarily used in the context of medical care to help patients understanding health
care information, health literacy has recently become a topic in the field of health
promotion.
Health literacy is based on improved access to information and knowledge, informed
consent and negotiating skills and affects on health care utilization and the active
participation in health promotion activities (Kickbush 2001). Health literacy is clearly
dependant upon levels of fundamental literacy (Nutbeam 2000). While general
literacy and education are important determinants of health and inadequate literacy
is a risk factor for low health literacy, literate people are not consequently health
literate (Kickbush 2001).
The potential of Health literacy lies in its holistic approach, which takes into
consideration not only personal skills and environmental factors but requires tailored
information to develop the social and cognitive skills fundamental to act on health
determinants. Beside general strategies to promote literacy, stronger cooperation
between the health and education sector will therefore be essential so that people are
able to make healthy choices.
1.1
Definition of health literacy
The term health literacy is originally used in the United States and describes and
explains the relationship between patient literacy levels and their ability to comply
with prescribed therapeutic regimens (Ad Hoc Committee on Health Literacy 1999).
This approach defines health literacy as "the ability to read, understand and act on
health care information"(Center for Health Care Strategies 2000).
3
Most research and publications about health literacy concentrate on improving the
ability to read consent forms and other written health care information, understand
and act on written and oral information given by health care professionals (Kickbush
2001).
The US Healthy People 2010 objectives expand the patient-oriented approach of
health literacy towards health promotion by defining health literacy as "the capacity
to obtain, interpret and understand basic health information and services and the
competence to use such information and services to enhance health" (USDHHS
2000).
The broadest definition of health literacy is drawn by the World Health Organization
(WHO). Nutbeam describes health literacy in the WHO health promotion glossary as
follows: "Health literacy represents the cognitive and social skills which determine
the motivation and ability of individuals to gam access to, understand and use
information in ways which promote and maintain good health. Health literacy
means more than being able to read pamphlets and successfully make appointments.
By improving people's access to health information and their capacity to use it
effectively, health literacy is critical to empowerment."(Nutbeam 1998).
1.2
Consequences of low health literacy
Limited health literacy increases the disparity in health care access among
exceptionally vulnerable groups (Partnership for Clear Health Communication 2003).
Due to an unequal access to information technology, poor health literate people are
less informed and often produce supplementary costs to the healthcare system
because of inadequate or inappropriate use. Low health literacy is often linked to
chronic health problems because patients know less about their conditions and how
to handle symptoms.
According to the Center for Health Care Strategies, poor health literacy is
disproportionately more likely among older people, immigrants and those with low
incomes (CHCS 2003).
The health literacy of disadvantaged groups has therefore to be improved by
supporting access to health information, providing special information for people
with low health literacy skills and promoting their capacity to use information
effectively.
According to Nutbeam, the outcomes of high levels of health literacy will lead to
personal benefits, such as healthier lifestyle choices and effective use of the health
services. Furthermore, the ability to use information effectively, can lead to social
benefits, "e.g. by enabling effective community action for health" (Nutbeam 2000).
4
1.3
Levels of health literacy
Nutbeam classifies health literacy as a continuum with three levels: functional health
literacy, interactive health literacy and critical health literacy. These levels reflect
increasing degrees of autonomy and personal empowerment, dependant on
cognitive development and exposure to different information (Nutbeam 2000).
Level 1: functional health literacy: Functional health literacy means the "ability' to
apply literacy skills to health related materials such as prescriptions, appointment
cards, medicine labels" (Parker et al. 1995). By communication of factual information,
education in this field tends to promote knowledge of health risks, health services
and compliance with medical advice.
Examples of activities to improve functional health literacy: production of
information leaflets, traditional patient education. (Nutbeam 2000).
Level 2: interactive health literacy: Interactive health literacy is characterized by
personal skills like the capacity to act independently on knowledge as well as
motivation and self-confidence to provide information and interact with social
groups. Activities to improve interactive health literacy will result in individual
benefit by focussing on personal and social skill development as well as behavioural
outcomes
Examples of activities to improve interactive health literacy: school health education
programmes, tailored health communication regarding specific needs of different
groups (Nutbeam 2000).
Level 3: critical health literacy: Critical health literacy empowers individuals and
communities to critically analyse information and use it to exert greater control over
life events and situations. By improving individual and community capacity to act on
social, economic and environmental determinants of health, activities to promote
critical health literacy will be beneficial for the individual and the community.
Helping people to develop confidence to act on knowledge and the ability' to work
with and support others will best be achieved through community-based actions
Examples of activities to improve critical health literacy: Provision of technical advice
to support community action (Nutbeam 2000).
Health literacy is therefore a useful concept, which differs from Health Promotion
and Health Education approaches as it really focuses on communication and
empowerment of people to act upon the information they receive.
5
2.
Internet and health communication
Internet proposes an easy-to-use, universal access to information and provides
various possibilities to find the latest up-to-date, barrier free information that is
independent of location and time. Interactive services like online self-help-groups,
chats with experts and forums on special health topics can support active coping and
social support in a virtual community by anonymous contact.
Due to a wide-spread pool of information, which can be personalised, Internet can
enhance health literacy, health related knowledge and support people to become
responsible for their own health.
The paper will now focus on the role of Internet in providing health information as
well as the use of this media among vulnerable groups.
2.1
Internet and health information
Internet is increasingly becoming a key source of health information to most people
(Kickbush 2001). A majority of the population of the EU-15 (41.5 %) believed that the
Internet is a good source of health related information (European Opinion Research
Group 2003). About half of the people seeking health information on tire Internet
believe that the Internet has a major impact on their understanding of health
problems and on their interaction with their doctor (Wilson et al. 2004). The
proportion of users drops with age and increases with educational level: 35.3 % in
the 15-24 age group use Internet for health-related information, compared to 8.3 % in
the older age group (55+). Only 5.8 % among people who left full-time education at
the age of 15 use the Internet to get information about health.
Interestingly, health information is demanded both by Internet users and non-users
of all age groups (European Opinion Research Group 2003).
As with other media, there is a danger that the information provided via Internet is
false, of low quality or too complex for the average user. Information provided on
Internet is unfiltered, in that it does not always disseminate between user groups
(professionals, lay persons, etc.). The information could therefore generate emotional
reactions, if, for example, it discusses survival rates for specific diseases. Users may
not have adequate support to understand and process this information. Unequal
access to tire medium can also lead to a widening social gap ( Schmidt-Kaehler 2003).
Internet can be regarded as a pull-information1 source rather than a push
1 Pull-information require an actively search and selection process by the user to choose the information
he needs among a huge pool of information.
6
information2 source ( Television and printed media). Users may be overwhelmed by
the amount of information that they pull. Searching for "health" and "health
information" on Google (http://www.google.com), for example, results in 321,000,000
hits and 3,330,000 hits respectively.
In order to use Internet effectively, therefore, the general public must know how and
be supported in their efforts to manage this information. Health literacy is crucial to
use the Internet in an effective way and being capable to assess the available health
information.
2.2
Use of Internet among vulnerable groups
Internet is actually not very attractive and accessible to vulnerable groups. The
working
o document "eInclusion revisited: The Local Dimension of the Information
Society" from the European Commission (2005) emphasizes low Internet use among
housepersons (especially women), older citizens, retired people and people living in
rural areas. Education and income appear to be the most important variables to
digital exclusion. According to Eurobarometer 58.0 the subjectively identified
reasons for non-use of the Internet among European citizens are non availability of a
PC at home (high cost of PC ownership and internet connection); lack of access at
work or at Public Access Points, the complexity of technology and the lack of basic
skills (EC 2005 a).
While young people as well as people with a higher educational level mention costs
as main barrier for their non-use of the Internet, elderly (55+) and low educated (up
to 15) see the lack of training as main barrier (figure 1).
fig. 2. Why don't yon use the Internet ? (by Age group and Education level)
~ Push- information describes an information offer where media professionals have already selected
available information so that their reception occurs in a passive way, independently of the recipients'
special needs.
7
In general, the interest in Internet use among elderly and people of lower educational
level is significantly lower than among the general public (European Opinion
Research Group 2003). Regarding the results of the question "What would encourage
NON-users to use the Internet?", the low response rate of 31.7 % of the elderly and
38.4% respectively of low-educated could suggest that there is an additional cause
for the non-use, which is specific to vulnerable groups, that has not been identified.
fig. 2 What would encourage NON-users to use the Internet? (EU 15 by Age group and Terminal
Educational Level)
That additional cause for the low rate might be the inadequate sensitivity of the
value of Internet use in the life of disadvantaged populations as well as the mistrust
in technology in general (Chang et al. 2004).
Chang et al. see the digital divide prior in content-related barriers, such as lack of
local information, literacy barriers, language barriers and lack of cultural diversity.
On the one hand, disadvantaged people believe that Internet is of no use to them and
on the other hand they mention the high investment costs for hardware and
connection as well as the lack of training as the greatest barrier to using the Internet.
The underlying reason, however, could be that people don't use Internet because
they are not interested in the information provided (EC 2005 a).
The Internet requires basic skills, such as literacy and much of its content is
addressed to better educated people (EC 2005 a). On average, Internet health
information requires a 10lh grade (= age of 15) or higher reading level and only 10 of
1000 Web sites reviewed provided understandable content for low-literacy adults.
Zarcadoolas et al. explains that complex web features, such as animated links, may
be too complicated for low-literacy adults to identify and use. Concerning the use of
search engines, searching strategies, such as generation of specific search terms,
8
differentiation between sponsored and non-sponsored sites and the correct spelling
of the search terms were sub optimal (Birru et al. 2004).
The literacy level needed to read health information on the Internet appears to inhibit
information-seeking efforts of low-literacy adults (Birru et al. 2004). Birru also
reports that low-literacy adults who participated in a computer skill workshop felt
positive about continuing their online experiences and all expressed enthusiasm to
improve their skills (Birru et al. 2004).
These results show that a combined strategy of designing websites providing easy-
to-read health information, improving Computer- and Internet-skills and promoting
Computer and Internet access is necessary to improve health literacy among
vulnerable groups and to encourage them to use the Internet.
3.
Initiatives
of
the
European Commission
towards
HEALTH INFORMATION ON THE INTERNET
The European Commission, DG Information Society, declared E-Health as a priority
target in 2002. Since the inauguration of the eEurope action plan in 2002 by DG
INFO,
the
importance
of
Health
Information
is
mentioned
in
various
communications of DG SANCO and "improving health information and knowledge"
is the first strand of tire EC's current Public Health programme (2000-2006).
What is the role of online health information for the general public in the current
public health work programme as well as the eEurope 2005 Action Plan?
The Commissions' communications often refer to tire need for quality-proofed and
accessible health Information. In 2004, the EC mentioned that a "growing number of
people are looking proactively for information (..) and want to be actively involved
in decisions related to their own health"3. But how can the provision and accessibility
of this information for everyone be assured?
The "Health Information" strand deals with a wide range of issues such as
development of health indicators, analysis and reporting on health or dissemination
of health information, mostly focusing on health information for public health
professionals. Even in the area of E-health, the EC attaches only a little importance to
online health information for the general public. Previous activities of the European
Commission, like the establishment of standards for "Accessibility of Public Web
’ EC 2004 a, p.7
9
Sites and their Content"4 and "Quality criteria for Health related Websites"56
,
concentrate on establishing formal criteria for barrier-free access instead of ensuring
the provision of "barrier-free content". For example, the quality criteria for Health
related Websites (see Annex I) contains an entire paragraph on transparency and
regularity of updating the information, whereas important factors regarding the
content, such as usability and readability, are only enumerated under the point
"Accessibility".
The priorities of the EC in the area of e-Health, such as the published quality criteria,
are necessary but not sufficient to provide better health information to everyone,
including low health literate people. Proposed education campaigns to inform the
general public about the existence of quality codes and to educate site developers
about minimum quality standards as well as monitoring the member states actions to
make health information as accessible as possible to citizens, are useless if the
provided information (content) is neither understandable nor designed to answer the
information needs of the specific user.
In the context of its Public Health Programme the EC is preparing to establish a
European Union-wide public health portal with information "relevant to European
citizens"5, to be launched by the end of 2005. This Portal would be structured
thematically, mainly addressed to the general public, with a special section for
professionals. Concrete details about for example, what will be included in the
"citizens' section" or if the portal pays attention to the specific information needs of
different population groups (such as youth, elderly or men, women), have not yet
been communicated.
A paper produced in the context of the European Health Policy Forum (EHPF 2005),
a multi-stakeholder group of health actors, initiated by the Commission in 2001,
points out the importance of health information for the empowerment of citizens. In
their latest position paper of 9,h march 2005 "Recommendation Paper on Health
Information"), the working group on health information encourage the Commission
to develop a more coherent and comprehensive approach to health information
provided in the EU. For this purpose, the EHPF proposes a policy mapping exercise
to identify all EU initiatives and policies addressing health information, as well as a
consultation with key stakeholders (providers and user of health information).
This initiative, which takes the various aspects of health communication into
consideration and requires the improvement of general health literacy, could
4 EC 2001. http://europa.eu.int/eur-lex/en/com/cnc/2001 /coin2001 0529en01 ,pdf
5 EC 2002 a, http://europa.eu.int/eur-lex/en/com/cnc/2002/corn2002 0667en01.pdf
6 EC 2004 a, p.20.
to
contribute to the development of a user-relevant EU public health portal, also
accessible to low-health literate citizens.
11
4.
RECOMMENDATIONS
TO
PROMOTE
HEALTH
LITERACY BY INTERNET
To achieve functional health literacy, general literacy has to be improved to ensure
the ability to read and understand health materials. Existing initiatives in the health
care sector to promote functional health literacy among patients should be extended
to the general public.
An analysis of the level of comprehension of written health materials (SMOG-
readability formula) revealed that only 3% of the available information is suitable for
people with a low educational level (Dierks et al. 2000).
The Internet is a developing and interactive media and has great potential to provide
understandable and useful health information, especially to people with low literacy
skills. New information technologies might address health information in a more
visual and interactive manner to make the information more accessible to those
having lower reading skills. Interactive tools like video streams and possibilities to
use technologies for disabled people like software that read Website content aloud,
could contribute to reduce the digital divide. New initiatives should be taken to
promote interactive and critical health literacy among vulnerable groups.
4.1
•
•
•
Target Groups:
Elderly
Immigrants
families in poverty' (esp. focus on house-hold women, youth)
4.2
Possible set of recommendations:
1.
Improve Internet access for vulnerable groups
2.
Ensure specific and high quality' online health information, which is
understandable and relevant to the target group.
3.
Provide skill training to develop the capacity of Computer/Internet-use
among vulnerable groups.
4.
Implementation of a broad communication strategy to promote the general
concept of health literacy among public, health professionals and politicians
at national level as well as specific projects among vulnerable groups at local
level.
5.
Further Research/Analysis on how to support vulnerable groups in the use of
computers/internet
12
4.3
Detailed Recommendations to promote health literacy by the means
of the Internet (personal and community empowerment)
4.3.1
Improve Access to the Internet for vulnerable groups (Public Internet Access
Points)
All citizens should have easy access to Public Internet Access Points, which could be
offered in two locations: Those that are highly frequented by the general population
on a daily basis (supermarkets, fast-food restaurants, phone-shops and libraries) and
social/health centres .The access points should provide long opening hours to ensure
accessibility after work and during the weekend and should integrated in existing
infrastructure.
Providing Public Internet Points in highly frequented central locations means that
people don't have to change their daily routine to get Internet Access.
Health centres offer a fixed location, additional information as well as assistance by
professional staff, but have the disadvantage of requiring a high budget for human
resources and office costs.
Developing collaboration with the private sector could promote the objective of
improving overall accessibility by contributing computers, and reduced or free
connection to Internet, as well as broadband access to poorer regions.
13
4.3.2
Development of a Regional/Local Health Portal, which offers information
appropriate to age, culture and language.
Regional/local authorities should develop health portals that are accessible through a
well-known site. The portal ensures quality information of regional relevance that is
written at a level that is easy to understand. Content is kept up-to-date by a network
of health professionals, social workers, communication and education specialists and
supervised by a independent team. This could stimulate multidisciplinary
collaboration between the different professions.
A barrier free and easy to handle health portal encourages person with low Internet
experience to start using this media. The most important barriers like having to use
search queries and search engines and to differentiate between good quality and
sponsored sites or incorrect information will be reduced by providing information on
a quality-proofed Portal. With growing media competence, people can leave the
easy-to-use and quality-assured area of the central portal.
The regional focus means that users can access relevant information about resources
available to them in their community. The aim is to foster social contacts between
citizens as well as professionals in the community and to improve knowledge about
available health information and services in the area.
The Health Portal should be based on 3 strands:
■
Health information (tailored and at a basic literacy level; nontextual messages
like video streams, graphics and audio should be developed to respond to
different learning styles (visual or audio learners)
•
Practical information about the Health System (regional Infrastructure +. a
interactive community map to see where the next doctor, hospital, self-helpgroup, health promoting activities (nutrition course, walking group, etc.,) is
located.
■
Interactive part (forum, thematically chat rooms, mail to experts, FAQ to share
the knowledge of the target group, possibility to valuate offers in the community)
To ensure useful and targetted information, health information needs of vulnerable
groups in the community "XY" should be examined through a social assessment.
This social assessment should take place in locations frequented by the specific target
group, such as schools for children of disadvantaged families, social welfare offices
(migrants) as well as hospitals, pharmacies or doctors offices (elderly people).
14
To guarantee a Health Portal which is oriented to the needs and interests of the
target groups7, representatives of the target group should be actively involved in the
designing process. It is strongly recommended that he portal be pre-tested among
individuals of the target group.
The Portal should be based on a set of new Guidelines, based on existing quality
instruments, such as the quality criteria of health-related websites (EC), afgis8, HONCode of Conduct9 or HIDDEL-vocabulary1011
. In order to ensure that the portal meets
the needs of low health literate people, the Guidelines should take into consideration
the content of the site, and ensure that the particular needs and abilities of specific
usergroups.
Main priorities could be a detailed description on important factors like "Usability"
(of the Site11, as well as the content12) as well as "Understandability"(didactics) of the
information provided for all citizens.
Additionally, a quality assessment tool (e.g. a short checklist) could be developed to
offer all citizens, especially members of the target group a easy-to-use tool to
critically use information.
' e.g. Elderly: The design of the information offered has to be adapted to their characteristics (decreased
attention span, simple and clear web pages, large buttons, large font sizes (14 points or more), high
contrast, no sound effects.
s The Health Information System Action Forum (afgis) provides criteria for the quality assurance of
health information in the new media like transparency, usability, accessibility, www.afcis.de
0 The Health on the Net Foundation sets an ethical standard for online health information. Provider,
commiting to these principles are allowed to put the HON-logo on their Website, www.hon.ch
10The Health Information Description, Disclosure and Evaluation Language (HIDDEL) enables the
Labeling of Websites based on the use of specific vocabulary to describe the information offer.
www.medcircle.org
11 is the navigation structure intuitive, does the site take into account the site specific needs of the target
group? e.g. elderly need simple pages, whereas young people are attracted by interactive tools)
12 is the provided information relevant to the specific target group
15
Strengthen individual competence
4.3.3
ICT- skills are nowadays an essential to individual development in our knowledge
based society. It is therefore of great importance that vulnerable groups, especially
immigrants and young people, develop these skills, in order to gain professional
qualifications and employment opportunities. The community-based trainings can
contribute to the building of a social network by learning together.
Modular trainings, focussing on problem-based learning, should therefore be
provided to improve the Computer/Internet-skills of vulnerable groups. To
overcome mental barriers such as mistrust of new technologies and the lack of useful
content, a focus of tine training should be on revealing the use amongst specific target
group by indicating how it can help facilitate interests or issues that are of real
concern to the participants (e.g. how they can use it to find out what specific health
promotion courses are offered in their community).
The trainings should be provided in different settings according to the specific target
group and preferably by a community member, who takes the role of a peer ("peer to
peer teaching"). Offering skill training in less formal circumstances by an instructor
from the same culture tends to be more motivating, especially for immigrants and
women.
The training programme should contain the following contents:
Providing computer and Internet- skills (how to use a computer/ what is the
Internet?)
b) How
to
manage
the
information
overload
(Pull-information)
(Finding information: How to use search engines (e.g. Google) and define
search strategies)
c) Critical reception of information provided (Communication of existing
quality criteria, development of a easy to use- tool specific to the needs of the
target group to judge the quality of information, exchange about the search
results in small groups).
a)
•
Additionally, the development of media-competence (in particular PC +
Internet) in school curricula should be strongly encouraged.
16
4.3.4
Communication Strategy
Promoting the strategies by a social marketing concept targeted at vulnerable
groups, which focuses on concrete values of the Internet use in their every-day-lives.
The communication strategy must address thus group's mistrust of technology in
general. The communication strategy should take into account the low use of Internet
among vulnerable groups by making use of non-digital communication to deliver the
message.
The Guidelines should be promoted among producers of health information to
ensure high quality information that is understandable to the whole European
Population, especially people with low health literacy skills. In addition, a universal
tool to facilitate the valuation of information should be promoted among the general
public through the use of different media.
17
5.
ANNEX
5.1 Quality Criteria for Health Related Websites (EC 2002 ).
Quality Criteria for Health Related Websites
Developed in widespread consultation with representatives of private and public eHealth websites and
information providers, other industrial representatives, public officials, and representatives of government
departments, international organisations, and non-governmental organisations.
These criteria should be applied in addition to relevant Community law
Transparency and Honesty
•
Transparency of provider of site - including name, physical address and electronic address of the
person or organisation responsible for the site (sec Article 5 and 6 Directive 2000/3 TEC on
Electronic Commerce).
•
Transparency of purpose and objective of the .site
•
Target audience clearly defined (further detail on purpose, multiple audience could be defined al
different levels).
• Transparency of all sources offunding lor site (grants, sponsors, advertisers. non-profit, voluntary
assistance).
Authority
•
Clear statement of sources for all information provided and date of publication of source.
•
Xante and credential of all human/institutional providers of information pul up on the site.
including dates al which credentials were received.
Privacy and data protection
•
Privacy and data protection policy and system for the processing of personal data, including
processing invisible to users, to be clearly defined in accordance with community Data Protection
legislation <Directives 95/46/EC and 2002-58 EC)
I'printing of information
•
Clear and regular updating of the site, with dale of up-date clearly displayed for each page and/or
item as relevant. Regular checking of relevance of information.
Accountability
• .■Iccountubihty - user feedback, mid appropriate oversight responsibility {such as a named quality
compliance officer for each site).
•
Responsible partnering - all efforts should be made to ensure that partnering or linking to other
websites is undertaken only with trustworthy individuals and organisations who themselves comply
with relevant codes of good practice.
•
Editorial policy - clear statement describing what procedure was used for selection of content.
Accessibility
•
,-k ce.v.s/bu'ny - attention io guidelines on physical accessibility as well as general findnbility,
searchability. readability, usability, etc.
Relevant Community Law is listed in footnote 3 Terms in italics arc further discussed in the Glossary of Terms
18
6.
SOURCES
Health literacy
Ad Hoc Committee on Health Literacy (1999). Health literacy: report of the Council on
Scientific Affairs, American Medical Association. Journal of the American Medical
Association, No. 281, 552-557.
Center for Health Care Strategies Inc. (CHCS) (2000). What is Health Literacy? Health
Literacy Fact Sheets, No. 1. CHCS,Princeton,NJ.
Online available: http://wwrv.chcs.org/usr doc/hll .pdf (02.03.2005).
Center for Health Care Strategies Inc. (CHCS) (2003). Who has Health Literacy Problems?
Health Literacy Fact Sheets, No. 2. CHCS,Princeton,NJ.
Online available: http://www.chcs.org/usr docZhl2.pdf (02.03.2005).
Duetz, M. & Abel, T. (2004). Health Literacy. Forderung und Nutzen von
Gesundheitskompetenzen in der Praxis. Managed Care, No. 5, 33-35.
Kickbusch, I. (2001).Health literacy: addressing the health and education divide.
Health Promotion International, Oxford. Vol.16, 289-297.
Nutbeam, D. (1998). WHO Health promotion glossary. Online available.
http://www.wpro.who.int/hpr/docs/glossary.pdf (02.03.2005)
Nutbeam, D.; Kickbusch, I. (2000). Advancing health literacy: a global challenge for
the 21st century. Health Promotion International, Oxford. Vol. 15,183 - 184.
Nutbeam, D. (2000). Health literacy as a public health goal: a challenge for
contemporary health education and communication strategies into the 21st century.
Health Promotion International, Oxford. Vol. 15, 259 - 267.
Partnership for Clear Health Communication (2003). Health Literacy. Statistics-at-aglance. Online available, http://www.askme3.org/pdfs/stats_at_a_glance.pdf (07.03.2005).
Pfizer (2003). Eradicating Low Health Literacy. The First Public Health Movement of
the 21st Century. Overview. White Paper. Online available.
http://www.askme3.org/pdfs/white_Paper.pdf (07.03.2005).
Rothschild, B. (2005): Health literacy: what the issue is, what is happening and what can be
done. In : Health Promotion Practice 6 (D.'S-ll
St. Leger, L. (2001). Schools, health literacy and public health. Possibilities and
challenges. Health Promotion International, Oxford, Vol.16,197 - 205.
United States Department of Health and Human Services, Office of Disease
Prevention and Health Promotion. (2000). Healthy People 2010. Online available:
h ttp://ww w.heal th.gov/heal thy people./11.03.2004).
19
Internet and health communication
Arnet, B.; Schaer, R. (2003).E-Health. In: Zenger, C.A.; Jung, T. (Editor).
Management im Gesundheitswesen und in der Gesundheitspolitik. Verlag Hans Huber,
Bern, 241- 254.
Birru, M.S., Monaco, V.M., Charles, L., Drew, H., Nije, V., Bierria, T.,Detlefsen E.,
Steinman, R.A. (2004). Internet usage by low-literacy adults seeking health
information: an observational analysis. Journal of Medical Internet Research. Vol.6.
Online available. http://www.jmir.Org/2004/3/e25/ (24.03.2005).
Casacuerta, D. (2005). An alternative Approach in the Use of e-Learning for Digital
Inclusion. Online available:
http://www.elearningeuropa.info/index.php?page=doc&doc id=5949&doclng=6&menuz
one=1 (22.02.2005)
Chang, B.L.; Bakken, S.; Brown, S.S.; Houston, T.K., Keeps, G.L.; Kukafa, R.; Safran, C.;
Stavri, P.Z. (2004). Bridging the Digital Divide : Reaching Vulnerable Populations.
Journal of the American Medical Informatics Association, Vol. 11. Online available.
http://www.pubmedcentral.gov/picrender.fcgi?tool=pmcentrez&blobtvpe=pdf&artid;=524
624 (22.02.2005).
Demiris, G.; Finkelstein, S.; Speedie, S.M.(2001). Considerations for the Design of a Web
based Clinical Monitoring and Educational System for Elderly Patients. Journal of the
American Medical Informatics Association. Vol.8. Online available.
http://www.pubmed central.gov/picrender.fcgi?tool=pmcentrez&blobtype=pdf&artid=131
044 (22.02.2005).
Dierks, M.-L.; Schwartz, F.W.; Walter, U. (2000). Patienten als Kunden.
Informationsbedarf und Qualitat von Patienteninformationen aus Sicht der Public
Health- Forschung. In: Jazbinsek, D. (Editor): Gesundheitskommunikation.
Westdeutscher Verlag, Wiesbaden, 150 - 163. Online available.
http://www.kommwiss.fuberlin.de/fileadmin/user upload/wissjour/Gesundheitskommunikation/l Dierks.pdf
(28.02.2005).
EC (2005 a).elnclusion revisited: The Local Dimension of the Information Society.
Commission staff working document. Part I. Brussels (4-02-2005). Online available:
http://europa.eu.int/comm/employment social/news/2005/feb/eincl local en.pdf
(03.03.2005).
EC (2005 b). Women and the elderly are crossing the digital divide, but the poor still
lag behind, says new EU report, Brussels (14-02-2005). Online available:
http://europa.eu.int/comm/employment social/news/2005/feb/einclusion en.html
(02.03.2005).
European Opinion Research Group (EORG) (2003). Eurobarometer 58.0. European Union
citizens and sources of information about health. Online available.
http://europa.eu.int/information society/eeurope/ehealth/conference/2003/doc/eb 58 en.
pdf (04.03.2005)
Lerch. M. (2001). Gesundheitskommunikation uber das Internet. In: Hurrelmann, K.
20
; Leppin, A. (Editor): Moderne Gesundheitskommunikation- vom Aufklarungsgesprach
zur E-Health. Verlag Hand Huber,Bern, 224-231.
Schmidt-Kaehler, S. (2003). Internetkompetenz fuer Menschen mit chronischen
Erkrankungen. Institut fuer Pflegewissenschaft an der Universitaet Bielefeld (IPW).
Wilson, P.;Leitner, C.; Moussalli, A. (2004). Mapping the potential of eHealth. Empowering
the citizen through ehealth tools and services. Presented at the eHealth conference, Cork,
Ireland,5-6 May 2004. Online available.
http://www.ehealthconference2004.ie/images/Mapping%20the%20Potential%20of%20eHe
alth.pdf (25.03.2005)
E-health and the European Commission
EC (2001). eEurope 2002. Accessibility of Public Web Sites and their Content.
Communication from the Commission to the Council, the European Parliament, the
Economic and Social Committee and the Committee of Regions. Brussels. Online
available, http://europa.eu.int/eur-lex/en/com/cnc/2001/com2001 0529en0'l .pdf
(28.03.2005).
EC (2002 a). eEurope 2002. Quality Criteria for Health Related Websites.
Communication from the Commission to the Council, the European Parliament, the
Economic and Social Committee and the Committee of Regions. Brussels. Online
available, http://europa.eu.int/eur-lex/en/coin/cnc/2002/com2002 0667en01.pdf
(25.03.2005).
EC (2002 b). eEurope 2OO5.An information society for all. An Action Plan to be presented in
view of the Sevilla European Council 21/22 June 2002. Communication from the
Commission to the Council, the European Parliament, the Economic and Social
Committee and the Committee of Regions,Brussels. Online available.
http://europa.eu.int/information society/eeurope/2002/news library/documents/eeurope
2005/eeurope2005 en.pdf (26.03.2005).
EC (2004 a). E-Health. Making healthcare better for European citizens: An action plan
for a European e-health Area. Communication from the Commission to the Council, the
European Parliament, the Economic and Social Committee and the Committee of
Regions,Brussels.Online available, http://europa.eu.inl/eurlex/en/com/cnc/2004/com2004 0356en01 .pdf. (26.03.2005).
EC (2004 b). Operating a European Union Public Health Information and Knowledge
System. Version 3. Document for the meeting of the Network of Competent Authorities
for Health and Knowledge, Luxemburg, 5lh and 6,h July 20004. Online available.
http://www.eu.int/comm/health/ph in forma tion/documents/ev20040705 rd 10 en.pdf
(29.03.2005).
EC (2005 a). EUROPA. Europe's Information Society Thematic Portal. eEurope 2005.
e-Health. Online available.
http://europa.eu.int/information society/eeurope/2005/all abotit/ehealth/index en.html
(25.03.2005)
EC (2005 b). EUROPA. Europe's Information Society. Thematic Portal. Quality of Life.
21
Health. Online available.
http://europa.eu.int/information Society/qualif/health/print en.htm (04.03.2005).
EC (2005 c). Community action in the field of public health. Work plan 2005. Online available.
http://vvww.eu.int/comm/health/ph programme/howtoapply/proposal docs/workplan20
05 en.pdf (28.02.2005).
EU Health Policy Forum (2005). Recommendations on Health information. 9 march 2005,
Brussels. Online available. http://forum.europa.eu.int/Public/irc/sanco/ehf/home
(29.03.2005)
22
- Media
 RF_COM_H_54_SUDHA.pdf
RF_COM_H_54_SUDHA.pdf
Position: 1656 (7 views)